We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


Chapter 5: 10 Real Cases on Acute Heart Failure Syndrome: Diagnosis, Management, and Follow-Up
Swathi Roy; Gayathri Kamalakkannan
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Full Chapter
- Supplementary Content
Case 1: Diagnosis and Management of New-Onset Heart Failure With Reduced Ejection Fraction
A 54-year-old woman presented to the telemetry floor with shortness of breath (SOB) for 4 months that progressed to an extent that she was unable to perform daily activities. She also used 3 pillows to sleep and often woke up from sleep due to difficulty catching her breath. Her medical history included hypertension, dyslipidemia, diabetes mellitus, and history of triple bypass surgery 4 years ago. Her current home medications included aspirin, atorvastatin, amlodipine, and metformin. No significant social or family history was noted. Her vital signs were stable. Physical examination showed bilateral diffuse crackles in lungs, elevated jugular venous pressure, and 2+ pitting lower extremity edema. ECG showed normal sinus rhythm with left ventricular hypertrophy. Chest x-ray showed vascular congestion. Laboratory results showed a pro-B-type natriuretic peptide (pro-BNP) level of 874 pg/mL and troponin level of 0.22 ng/mL. Thyroid panel was normal. An echocardiogram demonstrated systolic dysfunction, mild mitral regurgitation, a dilated left atrium, and an ejection fraction (EF) of 33%. How would you manage this case?
In this case, a patient with known history of coronary artery disease presented with worsening of shortness of breath with lower extremity edema and jugular venous distension along with crackles in the lung. The sign and symptoms along with labs and imaging findings point to diagnosis of heart failure with reduced EF (HFrEF). She should be treated with diuretics and guideline-directed medical therapy for congestive heart failure (CHF). Telemetry monitoring for arrythmia should be performed, especially with structural heart disease. Electrolyte and urine output monitoring should be continued.
In the initial evaluation of patients who present with signs and symptoms of heart failure, pro-BNP level measurement may be used as both a diagnostic and prognostic tool. Based on left ventricular EF (LVEF), heart failure is classified into heart failure with preserved EF (HFpEF) if LVEF is >50%, HFrEF if LVEF is <40%, and heart failure with mid-range EF (HFmEF) if LVEF is 40% to 50%. All patients with symptomatic heart failure should be started on an angiotensin-converting enzyme (ACE) inhibitor (or angiotensin receptor blocker if ACE inhibitor is not tolerated) and β-blocker, as appropriate. In addition, in patients with New York Heart Association functional classes II through IV, an aldosterone antagonist should be prescribed. In African American patients, hydralazine and nitrates should be added. Recent recommendations also recommend starting an angiotensin receptor-neprilysin inhibitor (ARNI) in patients who are symptomatic on ACE inhibitors.
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
- Search Menu
- Author videos
- ESC Content Collections
- Supplements
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About European Heart Journal Supplements
- About the European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, case presentation.
- < Previous
Clinical case: heart failure and ischaemic heart disease
- Article contents
- Figures & tables
- Supplementary Data
Giuseppe M C Rosano, Clinical case: heart failure and ischaemic heart disease, European Heart Journal Supplements , Volume 21, Issue Supplement_C, April 2019, Pages C42–C44, https://doi.org/10.1093/eurheartj/suz046
- Permissions Icon Permissions
Patients with ischaemic heart disease that develop heart failure should be treated as per appropriate European Society of Cardiology/Heart Failure Association (ESC/HFA) guidelines.
Glucose control in diabetic patients with heart failure should be more lenient that in patients without cardiovascular disease.
Optimization of cardiac metabolism and control of heart rate should be a priority for the treatment of angina in patients with heart failure of ischaemic origin.
This clinical case refers to an 83-year-old man with moderate chronic obstructive pulmonary disease and shows that implementation of appropriate medical therapy according to the European Society of Cardiology/Heart Failure Association (ESC/HFA) guidelines improves symptoms and quality of life. 1 The case also illustrates that optimization of glucose metabolism with a more lenient glucose control was most probably important in improving the overall clinical status and functional capacity.
The patient has family history of coronary artery disease as his brother had suffered an acute myocardial infarction (AMI) at the age of 64 and his sister had received coronary artery by-pass. He also has a 14-year diagnosis of arterial hypertension, and he is diabetic on oral glucose-lowering agents since 12 years. He smokes 30 cigarettes per day since childhood.
In February 2009, after 2 weeks of angina for moderate efforts, he suffered an acute anterior myocardial infarction. He presented late (after 14 h since symptom onset) at the hospital where he had been treated conservatively and had been discharged on medical therapy: Atenolol 50 mg o.d., Amlodipine 2.5 mg o.d., Aspirin 100 mg o.d., Atorvastatin 20 mg o.d., Metformin 500 mg tds, Gliclazide 30 mg o.d., Salmeterol 50, and Fluticasone 500 mg oral inhalers.
Four weeks after discharge, he underwent a planned electrocardiogram (ECG) stress test that documented silent effort-induced ST-segment depression (1.5 mm in V4–V6) at 50 W.
He underwent a coronary angiography (June 2009) and left ventriculography that showed a not dilated left ventricle with apical dyskinesia, normal left ventricular ejection fraction (LVEF, 52%); occlusion of proximal LAD, 60% stenosis of circumflex (CX), and 60% stenosis of distal right coronary artery (RCA). An attempt to cross the occluded left anterior descending (LAD) was unsuccessful.
He was therefore discharged on medical therapy with: Atenolol 50 mg o.d., Atorvastatin 20 mg o.d., Amlodipine 2.5 mg o.d., Perindopril 4 mg o.d., oral isosorbide mono-nitrate (ISMN) 60 mg o.d., Aspirin 100 mg o.d., metformin 850 mg tds, Gliclazide 30 mg o.d., Salmeterol 50 mcg, and Fluticasone 500 mcg b.i.d. oral inhalers.
He had been well for a few months but in March 2010 he started to complain of retrosternal constriction associated to dyspnoea for moderate efforts (New York Heart Association (NYHA) II–III, Canadian Class II).
For this reason, he was prescribed a second coronary angiography that showed progression of atherosclerosis with 80% stenosis on the circumflex (after the I obtuse marginal branch) and distal RCA. The LAD was still occluded.
After consultation with the heart team, CABG was avoided because surgical the risk was deemed too high and the patient underwent palliative percutaneous coronary intervention (PCI) of CX and RCA. It was again attempted to cross the occlusion on the LAD. But this attempt was, again, unsuccessful. Collateral circulation from posterior interventricular artery (PDL) to the LAD was found. The pre-PCI echocardiogram documented moderate left ventricular dysfunction (EF 38%), the pre-discharge echocardiogram documented a LVEF of 34%. Because of the reduced LVEF, atenolol was changed for Bisoprolol (5 mg o.d.).
At follow-up visit in December 2012, the clinical status and the haemodynamic conditions had deteriorated. He complained of worsening effort-induced dyspnoea/angina that now occurred for less than a flight of stairs (NYHA III). On clinical examination clear signs of worsening heart failure were detected ( Table 1 ). His medical therapy was modified to: Bisoprolol 5 mg o.d., Atorvastatin 20 mg o.d., Amlodipine 2.5 mg o.d., Perindopil 5 mg o.d., ISMN 60 mg o.d., Aspirin 100 mg o.d., Metformin 500 mg tds, Furosemide 50 mg o.d., Gliclazide 30 mg o.d., Salmeterol 50 mcg oral inhaler, and Fluticasone 500 mcg oral inhaler. A stress perfusion cardiac scintigraphy was requested and revealed dilated ventricles with LVEF 19%, fixed apical perfusion defect and reversible perfusion defect of the antero-septal wall (ischaemic burden <10%, Figure 1 ). He was admitted, and an ICD was implanted.
Clinical parameters during follow-up visits
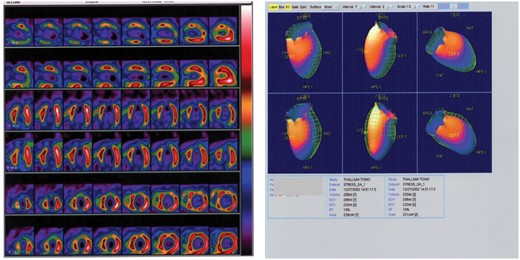
Myocardial perfusion scintigraphy and left ventriculography showing dilated left ventricle with left ventricular ejection fraction 19%. Reversible perfusion defects on the antero-septal wall and fixed apical perfusion defect.
In March 2013, he felt slightly better but still complained of effort-induced dyspnoea/angina (NYHA III, Table 1 ). Medical therapy was updated with bisoprolol changed with Nebivolol 5 mg o.d. and perindopril changed to Enalapril 10 mg b.i.d. The switch from bisoprolol to nebivolol was undertaken because of the better tolerability and outcome data with nebivolol in elderly patients with heart failure. Perindopril was switched to enalapril because the first one has no indication for the treatment of heart failure.
In September 2013, the clinical conditions were unchanged, he still complained of effort-induced dyspnoea/angina (NYHA III) and did not notice any change in his exercise capacity. His BNP was 1670. He was referred for a 3-month cycle of cardiac rehabilitation during which his medical therapy was changed to: Nebivolol 5 mg o.d., Ivabradine 5 mg b.i.d., uptitrated in October to 7.5 b.i.d., Trimetazidine 20 mg tds, Furosemide 50 mg, Metolazone 5 mg o.d., K-canrenoate 50 mg, Enalapril 10 mg b.i.d., Clopidogrel 75 mg o.d., Atorvastatin 40 mg o.d., Metformin 500 mg b.i.d., Salmeterol 50 mcg oral inhaler, and Fluticasone 500 mcg oral inhaler.
At the follow-up visit in January 2014, he felt much better and had symptomatically, he no longer complained of angina, nor dyspnoea (NYHA Class II, Table 1 ). Trimetazidine was added because of its benefits in heart failure patients of ischaemic origin and because of its effect on functional capacity. Ivabradine was added to reduce heart rate since it was felt that increasing nebivolol, that was already titrated to an effective dose, would have had led to hypotension.
He missed his follow-up visits in June and October 2014 because he was feeling well and he had decided to spend some time at his house in the south of Italy. In January and June 2015, he was well, asymptomatic (NYHA I–II) and able to attend his daily activities. He did not complain of angina nor dyspnoea and reported no limitations in his daily activities. Unfortunately, in November 2015 he was hit by a moped while on the zebra crossing in Rome and he later died in hospital as a consequence of the trauma.
This case highlights the need of optimizing both the heart failure and the anti-anginal medications in patients with heart failure of ischaemic origin. This patient has improved dramatically after the up-titration of diuretics, the control of heart rate with nebivolol and ivabradine and the additional use of trimetazidine. 1–3 All these drugs have contributed to improve the clinical status together with a more lenient control of glucose metabolism. 4 This is another crucial point to take into account in diabetic patients, especially if elderly, with heart failure in whom aggressive glucose control is detrimental for their functional capacity and long-term prognosis. 5
IRCCS San Raffaele - Ricerca corrente Ministero della Salute 2018.
Conflict of interest : none declared. The authors didn’t receive any financial support in terms of honorarium by Servier for the supplement articles.
Ponikowski P , Voors AA , Anker SD , Bueno H , Cleland JG , Coats AJ , Falk V , González-Juanatey JR , Harjola VP , Jankowska EA , Jessup M , Linde C , Nihoyannopoulos P , Parissis JT , Pieske B , Riley JP , Rosano GM , Ruilope LM , Ruschitzka F , Rutten FH , van der Meer P ; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the Special Contribution of the Heart Failure Association (HFA) of the ESC . Eur J Heart Fail 2016 ; 18 : 891 – 975 .
Google Scholar
Rosano GM , Vitale C. Metabolic modulation of cardiac metabolism in heart failure . Card Fail Rev 2018 ; 4 : 99 – 103 .
Vitale C , Ilaria S , Rosano GM. Pharmacological interventions effective in improving exercise capacity in heart failure . Card Fail Rev 2018 ; 4 : 1 – 27 .
Seferović PM , Petrie MC , Filippatos GS , Anker SD , Rosano G , Bauersachs J , Paulus WJ , Komajda M , Cosentino F , de Boer RA , Farmakis D , Doehner W , Lambrinou E , Lopatin Y , Piepoli MF , Theodorakis MJ , Wiggers H , Lekakis J , Mebazaa A , Mamas MA , Tschöpe C , Hoes AW , Seferović JP , Logue J , McDonagh T , Riley JP , Milinković I , Polovina M , van Veldhuisen DJ , Lainscak M , Maggioni AP , Ruschitzka F , McMurray JJV. Type 2 diabetes mellitus and heart failure: a position statement from the Heart Failure Association of the European Society of Cardiology . Eur J Heart Fail 2018 ; 20 : 853 – 872 .
Vitale C , Spoletini I , Rosano GM. Frailty in heart failure: implications for management . Card Fail Rev 2018 ; 4 : 104 – 106 .
- myocardial ischemia
- cardiac rehabilitation
- heart failure
- older adult
Email alerts
More on this topic, related articles in pubmed, citing articles via.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1554-2815
- Print ISSN 1520-765X
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Case report
- Open access
- Published: 09 February 2021
Clinical judgement in chest pain: a case report
- Mishita Goel ORCID: orcid.org/0000-0003-1540-2910 1 ,
- Shubhkarman Dhillon 1 ,
- Sarwan Kumar 1 &
- Vesna Tegeltija 1
Journal of Medical Case Reports volume 15 , Article number: 49 ( 2021 ) Cite this article
3878 Accesses
2 Altmetric
Metrics details
Cardiac stress testing is a validated diagnostic tool to assess symptomatic patients with intermediate pretest probability of coronary artery disease (CAD). However, in some cases, the cardiac stress test may provide inconclusive results and the decision for further workup typically depends on the clinical judgement of the physician. These decisions can greatly affect patient outcomes.
Case presentation
We present an interesting case of a 54-year-old Caucasian male with history of tobacco use and gastroesophageal reflux disease (GERD) who presented with atypical chest pain. He had an asymptomatic electrocardiogram (EKG) stress test with intermediate probability of ischemia. Further workup with coronary computed tomography angiography (CCTA) and cardiac catheterization revealed multivessel CAD requiring a bypass surgery. In this case, the patient only had a history of tobacco use but no other significant comorbidities. He was clinically stable during his hospital stay and his testing was anticipated to be negative. However to complete workup, cardiology recommended anatomical testing with CCTA given the indeterminate EKG stress test results but the results of significant stenosis were surprising with the patient eventually requiring coronary artery bypass grafting (CABG).
As a result of the availability of multiple noninvasive diagnostic tests with almost similar sensitivities for CAD, physicians often face this dilemma of choosing the right test for optimal evaluation of chest pain in patients with intermediate pretest probability of CAD. Optimal test selection requires an individualized patient approach. Our experience with this case emphasizes the role of history taking, clinical judgement, and the risk/benefit ratio in deciding further workup when faced with inconclusive stress test results. Physicians should have a lower threshold for further workup of patients with inconclusive or even negative stress test results because of the diagnostic limitations of the test. Instead, utilizing a different, anatomical test may be more valuable. Specifically, the case established the usefulness of CCTA in cases such as this where other CAD diagnostic testing is indeterminate.
Peer Review reports
Heart disease is one of the most commonly encountered medical conditions in the world. Individuals seeking medical help because of chest pain frequently require further testing for heart disease. Cardiac stress testing is a validated diagnostic tool commonly used to assess symptomatic patients with intermediate pretest probability of coronary artery disease (CAD). Baseline electrocardiogram (EKG) findings and ability to exercise are important factors to determine the most appropriate cardiac stress test. Exercise EKG stress test is preferred in patients who have normal baseline EKGs and are able to exercise. Patients found to have positive test results with chest pain usually undergo cardiac catheterization, while those with negative test results are usually considered to have non-cardiac chest pain. In some cases, the cardiac stress test may provide inconclusive results. The decision for further workup typically depends on the clinical judgement of the physician and the results may greatly affect patient outcomes. We present an interesting case of a healthy man who presented with chest pain and had an inconclusive EKG stress test, but further workup was performed and revealed multivessel CAD requiring a bypass surgery.
A 54-year-old, overweight (BMI 29), Caucasian man with a history of tobacco smoking and gastroesophageal reflux presented to the emergency department with chest pain. He described it as sudden in onset, while he was working on his laptop. Location was substernal, radiating to his left arm and jaw. Initially, the pain was 7/10 in intensity but it improved spontaneously even before he reached the hospital or received any medications. On further probing, he reported that he had experienced intermittent episodes of chest pain for the last 3 weeks but it was mostly exertional and was relieved with rest. The pain was not associated with shortness of breath, diaphoresis, or nausea/vomiting. He denied any fever, chills, cough, abdominal pain, urinary or bowel complaints. He did not have any family history of significant cardiac events.
On presentation, the patient was hemodynamically stable with a blood pressure of 139/85 mmHg and heart rate of 81 beats per minute. His EKG did not show any ischemic changes, no left ventricular hypertrophy, or left bundle branch block. Three sets of serial troponin enzyme were less than 0.010. Lipid panel showed total cholesterol of 235, triglycerides 408, HDL 26, and LDL could not be calculated. His pretest probability of CAD was intermediate on the basis of age and sex. Since the patient was chest pain free since admission and was able to exercise, an exercise treadmill EKG stress test was ordered. The patient achieved 95% of maximum predicted heart rate and 10 METs of exercise with normalization of slight T wave inversions that were seen in leads V2, V3, and V4 at rest. Thus, it was read as maximum asymptomatic stress test with intermediate probability of ischemia. Echocardiogram was obtained which showed normal left ventricular function and no significant valvular or wall motion abnormalities. At this point, cardiology was consulted to evaluate the patient and they recommended coronary computed tomography angiography (CCTA) for further risk stratification.
Diagnosis and management
CCTA results showed approximate 70% stenosis of the origin of the left anterior descending artery (LAD) secondary to noncalcified plaque extending over a length of approximately 4 mm (Fig. 1 ), approximate 40–50% stenosis of the proximal ramus intermedius branch secondary to mixed calcified and noncalcified plaque and scattered calcified and noncalcified plaque along the circumflex and obtuse marginal branches with 30–40% luminal diameter stenosis. Fractional flow reserve–computed tomography (FFR-CT) revealed a high likelihood of flow-limiting stenosis with a value of less than 0.5 secondary to the significant stenosis at the origin of the LAD and a low likelihood of flow-limiting stenosis in the left circumflex, ramus intermedius, and right coronary arteries.
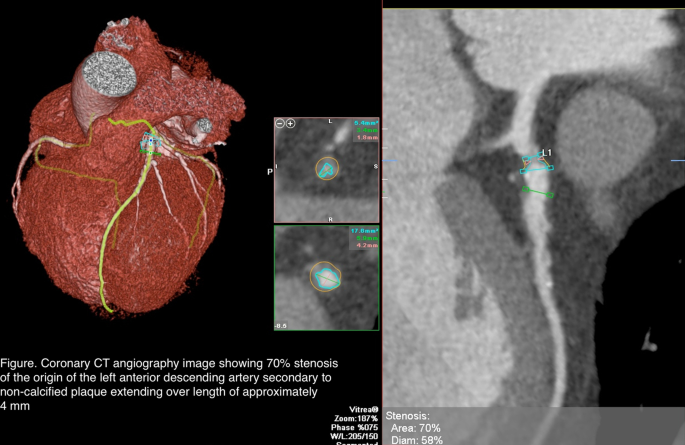
Coronary computed tomography angiography image showing 70% stenosis of the origin of the left anterior descending artery to secondary to non-calcified plaque extending over a length of approximately 4 mm
The patient was then taken for cardiac catheterization which showed a 95% stenotic lesion of LAD with partial perfusion (TIMI grade 2 flow) giving rise to diagonal 1, which has an ostial and proximal 70% stenosis; ramus intermedius with proximal 70% segmental stenosis; circumflex, nondominant vessel, which has mild disease in proximal distal segments, giving rise to obtuse marginal 1, which has proximal 70% stenosis. Cardiothoracic surgery was consulted and the patient underwent bypass graft surgery.
Outcome and follow-up
The patient did well after the surgery. He stayed in the hospital for 4 days post-op without any complaints and was discharged home in stable condition. A referral to home care was made to provide for monitoring of the patient's progress and detection of any complications during the immediate post-op period. Cardiac rehabilitation referral was also provided and the patient was instructed to follow up with a cardiologist and cardiothoracic surgeon.
Cardiac stress testing is usually performed for diagnosis of CAD in patients with intermediate pretest probability of CAD. Appropriate history, physical examination, and baseline EKG findings are crucial in determining the most appropriate and cost-effective stress test for these patients. According to the American College of Cardiology (ACC)/American Heart Association (AHA) guidelines, exercise stress EKG is recommended as an initial diagnostic test among patients at intermediate pretest risk who are able to exercise and who have an interpretable resting EKG [ 1 ]. In the presence of baseline EKG abnormalities, including ST depression greater than 1 mm, left ventricular hypertrophy, left bundle branch block, paced rhythm or pre-excitation, functional tests with imaging or anatomical tests including CCTA are preferred. Studies have shown that exercise EKG test is adequate for risk stratification of cardiac events which are found to be very low in patients with a negative EKG stress test [ 2 ].
Our case describes a commonly encountered scenario of a patient with few risk factors for CAD who presented to the hospital with chest pain and requires further diagnostic testing for CAD. Treadmill EKG is one of the most utilized CAD testing methods in our practice and the results guide further management of patients presenting with chest pain. A meta-analysis including 22 years of research revealed the pooled sensitivity of EKG stress test in detecting CAD to be 68% and specificity to be 77% [ 1 ]. Despite this, EKG stress tests continue to be one of the most commonly used and trusted tools in our clinical practice.
A cohort study comparing usefulness of dipyridamole echocardiography, dobutamine-atropine echocardiography, and exercise stress testing revealed similar sensitivity for diagnosis of CAD in patients presenting with chest pain [ 3 ]. In fact even in cases of multivessel CAD, studies have shown similar sensitivity of all three tests [ 4 ]. Studies have shown low prevalence of significant ischemia and CAD mortality in patients achieving more than 10 METs on exercise stress test [ 5 ]. In a 2014 randomized controlled trial, all cause mortality was found to be similar in patients with suspected CAD and normal resting EKG who underwent EKG stress test with imaging compared to those without imaging [ 6 ].
Physicians seldom see reports of indeterminate stress test results which is when they depend on expert opinion for further evaluation. In this case, the patient was an overweight 54-year-old man who had a history of tobacco use but no other significant comorbidities were known. He was clinically stable during his hospital stay. We anticipated his testing would be negative. To complete workup, cardiology recommended anatomical testing with CCTA given the indeterminate EKG stress test results and this was performed immediately. The results of significant stenosis were surprising to the care team. CCTA is a relatively newer non-invasive anatomical test that has a high diagnostic accuracy to identify the presence of coronary plaques and stenosis. Since it can also determine the extent of stenosis, it is being used for CAD risk stratification. In patients with low to intermediate probability of acute coronary syndrome (ACS), it can be used as an initial test to rule out ACS owing to its high negative predictive value. It is also being utilized as an alternative to invasive coronary angiography in patients with equivocal stress test results.
Our case demonstrates a situation where CCTA proved to be a more accurate diagnostic tool than EKG stress testing. The results significantly altered management as the patient concluded his hospital stay with coronary artery bypass grafting (CABG). Alternatively, if CCTA was not performed and the cardiologist deemed the indeterminate stress test results as negative, the patient may have been discharged and may have had a deleterious cardiac outcome. Recent guidelines from the National Institute of Health and Care Excellence recommend CCTA as the initial diagnostic test in patients with suspected CAD [ 7 ]. However, contrast-related side effects, availability of test, and cost are the main barriers to this recommendation at this time. CCTA has also been shown to have limited diagnostic accuracy in patients with intracoronary stents. The PROMISE trial showed no significant difference in clinical outcomes of patients with suspected CAD who underwent anatomical stress testing with CCTA compared to those who underwent functional stress testing [ 8 ]. However it may be worthwhile to utilize CCTA as the initial CAD diagnostic test if no contraindications are noted.
As a result of the availability of multiple noninvasive diagnostic tests with almost similar sensitivities for CAD, physicians often face this dilemma of choosing the right test for optimal evaluation of chest pain in patients with intermediate pretest probability of CAD. Optimal test selection requires an individualized patient approach. Our case describes a patient with intermediate probability of CAD presenting to the hospital with chest pain that resolved on admission and having a treadmill EKG stress test with indeterminate results. Decision to proceed with anatomical testing using CCTA was made and the patient was found to have significant CAD requiring CABG. Our experience with this case emphasizes the role of history taking, clinical judgement, and the risk/benefit ratio in deciding further workup when faced with inconclusive stress test results. Physicians should have a lower threshold for further workup of patients with inconclusive or even negative stress test results because of the diagnostic limitations of the test. Repeating the same test may result in uncertainty and indeterminate stress test should not be presumed as negative. Instead, utilizing a different, anatomical CAD test may be more valuable. Specifically, the case established the usefulness of CCTA in cases such as this where other CAD diagnostic testing is indeterminate.
Availability of supporting data
Data that supports this study have been referenced here.
Bourque JM, Beller GA. Value of exercise ECG for risk stratification in suspected or known CAD in the era of advanced imaging technologies. JACC Cardiovasc Imaging. 2015;8(11):1309–21.
Article Google Scholar
Christman MP, Bittencourt MS, Hulten E, et al . Yield of downstream tests after exercise treadmill testing. J Am Coll Cardiol. 2014;63(13):1264–74. https://doi.org/10.1016/j.jacc.2013.11.052 .
Article PubMed PubMed Central Google Scholar
Alberto J, Román S, Vilacosta I, et al . Dipyridamole and dobutamine-atropine stress echocardiography in the diagnosis of coronary artery disease: comparison with exercise stress test, analysis of agreement, and impact of antianginal treatment. Chest. 1996;110(5):1248–54.
Previtali M, Lanzarini L, Fetiveau R, et al . Comparison of dobutamine stress echocardiography, dipyridamole stress echocardiography and exercise stress testing for diagnosis of coronary artery disease. Am J Cardiol. 1993;72(12):865–70.
Article CAS Google Scholar
Bourque JM, Charlton GT, Holland BH, Belyea CM, Watson DD, Beller GA. Prognosis in patients achieving ≥10 METS on exercise stress testing: Was SPECT imaging useful? J Nucl Cardiol. 2011;18(2):230–7. https://doi.org/10.1007/s12350-010-9323-2 .
Article PubMed Google Scholar
Duvall WL, Lane Duvall W, Savino JA, et al . Prospective evaluation of a new protocol for the provisional use of perfusion imaging with exercise stress testing. Eur J Nucl Med Mol Imaging. 2015;42(2):305–16. https://doi.org/10.1007/s00259-014-2864-x .
Overview | Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis | Guidance | NICE. https://www.nice.org.uk/guidance/cg95 . Accessed 18 Apr 2020.
Douglas PS, Hoffmann U, Patel MR, et al . Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372(14):1291–300.
Download references
Acknowledgements
We would like to acknowledge contribution of Dr. Nishit Choksi and Dr. Nishtha Sareen, who were the cardiologists involved in care of this patient. All the above stated authors have contributed significantly in writing and editing the manuscript.
No funding received.
Author information
Authors and affiliations.
Department of Internal Medicine, Ascension Providence Rochester Hospital/Wayne State University School of Medicine, 1101 W University Drive, Rochester, MI, 48307, USA
Mishita Goel, Shubhkarman Dhillon, Sarwan Kumar & Vesna Tegeltija
You can also search for this author in PubMed Google Scholar
Contributions
We confirm that all authors have contributed in writing and drafting, obtaining images, editing and reviewing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mishita Goel .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval or formal consent not required for this type of study.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
No competing interests to disclose.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Goel, M., Dhillon, S., Kumar, S. et al. Clinical judgement in chest pain: a case report . J Med Case Reports 15 , 49 (2021). https://doi.org/10.1186/s13256-021-02666-z
Download citation
Received : 20 November 2020
Accepted : 06 January 2021
Published : 09 February 2021
DOI : https://doi.org/10.1186/s13256-021-02666-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Stress test
- Coronary artery disease
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
Heart Failure Center Patient Cases

HOME | HF CENTER HOME | FAQ | ABOUT
Heart Failure: Ask the Expert – Patient Cases
Welcome to the GCVI HF Center’s Ask the Expert – Patient Cases channel! On this channel you will have access to multiple heart failure patient cases published by leading ACC experts. We also encourage you to engage and consult with ACC global experts on cases specific to your practice. Ask the Expert through the online portal below!
Engage with ACC global experts!
Heart Failure Patient Case Quizzes
- Unrecognized HFpEF in a Type 2 DM Patient – Reducing CV and HF Risk
- Untreated HFrEF/Ischemic Cardiomyopathy in Type 2 DM – How to Optimize Medical Therapy to Improve Heart Failure Outcomes
- Restrictive Cardiomyopathies Series: Advanced HF Therapies in ATTR Cardiac Amyloidosis (Certified Patient Case Study)
- ECG of the Month: Variable QRS Morphologies in Heart Failure
- Untreated HFrEF/Ischemic Cardiomyopathy in Type 2 DM
- Unrecognized HFpEF in a Type 2 DM Patient
Regional Patient Case Quizzes Select your region to view available courses.

JACC Journals on ACC.org
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 4: 10 Real Cases on Valvular Heart Disease: Diagnosis, Management, and Follow-Up
Nikhitha Mantri; Puvanalingam Ayyadurai; Marin Nicu
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Clinical Symptoms
- Full Chapter
- Supplementary Content
Case 1: Management of Patent Foramen Ovale
A 26-year-old woman presented to the emergency department (ED) with chest pain for 1 day. The chest pain started suddenly, was nonradiating, and was associated with arm movement. She did house cleaning 1 day prior to presentation. The pain was not relieved by taking over-the-counter medication. She denied palpitations, dizziness, shortness of breath, and trauma. Her family history and social history were unremarkable. On presentation to the ED, her vital signs were stable. On physical examination, she did not have any significant findings except chest wall tenderness. Her ECG showed first-degree atrioventricular block. Initial laboratory findings were unremarkable. She was given analgesics. The patient was transferred to the telemetry floor, where an echocardiogram was performed, which showed a normal left ventricular ejection fraction with no wall motion or valvular abnormality and a small patent foramen ovale (PFO). How would you manage this case?
This patient is a young asymptomatic woman who presented with musculoskeletal chest pain. Incidentally, she was noted to have a PFO, which is asymptomatic and does not require any treatment.
PFO is an opening in the atrial wall at the location of the fossa ovalis that remains open beyond 1 year of life. After birth, when the pulmonary circulation develops, the foramen ovale closes due to the increase in left atrial pressures, which takes up to 1 year.
PFO is usually asymptomatic and is often found incidentally. However, it carries a risk of paradoxical embolism in high-risk patients. Some patients present with systemic embolism causing organ infarcts and even myocardial infarction.
The diagnostic test of choice is echocardiography. PFO can be detected using color flow Doppler, contrast echocardiography, and transmitral Doppler.
Isolated PFO does not usually require any treatment unless it is associated with an unexplained neurologic event. Such conditions are treated with antiplatelet drugs and anticoagulation therapy. Percutaneous closure of the PFO is an option when there is contraindication to medical management and anticoagulant treatment, in the setting of paradoxical embolism or cryptogenic stroke. Surgical closure is indicated when the opening is >25 mm or when there is failure of a percutaneous device.
PFO is usually asymptomatic and is often found incidentally.
Isolated PFO does not usually require any treatment unless it is associated with an unexplained neurologic event.
Case 2: Management of Aortic Stenosis
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Complete Your CE
Course case studies, external link, this link leads outside of the netce site to:.
While we have selected sites that we believe offer good, reliable information, we are not responsible for the content provided. Furthermore, these links do not constitute an endorsement of these organizations or their programs by NetCE, and none should be inferred.
Women and Coronary Heart Disease
Course #33224 - $90 -
#33224: Women and Coronary Heart Disease
Your certificate(s) of completion have been emailed to
- Back to Course Home
- Review the course material online or in print.
- Complete the course evaluation.
- Review your Transcript to view and print your Certificate of Completion. Your date of completion will be the date (Pacific Time) the course was electronically submitted for credit, with no exceptions. Partial credit is not available.
CASE STUDY 1
The following case studies offer an opportunity for healthcare professionals to test or improve their skills in observation and diagnosis. While the outcome in each has already been determined, the information and scenarios may be used to help in day-to-day patient interaction. Analyses of all of the case studies are presented following this section.
Read through the following clinical vignettes and take time to review each woman's cardiovascular risk factor profile. Then, refer to the questions at the end of the case study to analyze each female patient's current health status.
Patient S is a White woman, 43 years of age, and mother of three small children. She has a long-standing history of significant obesity with little success in dieting over the years. At 5'3", she is obese, weighing 220 pounds. Her fat distribution is "apple-shaped" and consequently, her waist-hip ratio is more than the 0.8 normal range. In addition, Patient S lives a fairly sedentary lifestyle and does not have a regular exercise program. Her dietary habits do not take into account basic recommendations for cardiac nutrition.
Patient J is 55 years of age and teaches high school English. Her cardiovascular risk factor profile includes a 30-pack-year history of cigarette smoking and altered lipid levels. Her HDL is only 35 mg/dL and her LDL is 145 mg/dL. Patient J has tried with little success to control her cholesterol with diet. Recently, she began taking gemfibrozil as prescribed by her family physician, but has not followed his recommendation to quit smoking and enroll in a smoking cessation program at a local hospital. Rather, she continues to smoke one pack of cigarettes per day.
Patient V is a woman, 47 years of age, who has a family history of CHD. Although she denies ever experiencing cardiac symptoms, her brother suffered a nonfatal MI at 46 years of age and her father had an MI at 53 years of age. Both of these cardiac events were medically managed. However, her father's disease did progress to the point that he underwent CABG surgery five years ago. He had three coronary artery lesions bypassed. In addition to her family history, Patient V is approximately 30 pounds overweight and does not exercise on a regular basis. She drinks approximately two to three glasses of red wine per day and has never smoked.
Patient D is 67 years of age and lives in an assisted living retirement community. An insulin-dependent diabetic since adolescence, Patient D is unable to care for herself due to the effects of the diabetes on her eyesight, as well as the development of peripheral neuropathies. In addition to the diabetes, Patient D continues to smoke. By now, she has a 40-pack-year history of smoking.
Patient F is an African American woman, 36 years of age, with a history of mild hypertension. Her blood pressure has been fairly well controlled on an ACE inhibitor over the past two years. Patient F eats a well-balanced, nutritious diet, exercises three to five times a week, and does not have a history of smoking or alcohol use. However, she does exhibit excessive competitiveness, being harried, and rushing to complete more and more tasks in an ever-shrinking period of time. In addition to these characteristics, she exhibits a somewhat cynical or negative outlook with occasional expression of hostile or angry thoughts and feelings.
In analyzing these clinical vignettes, consider the following questions:
Which of these women is at greatest risk for CHD?
Who is at least risk?
What recommendations would you make in counseling each patient regarding her cardiovascular health?
Case Study 1 Analyses
All five of these women have risk factors for CHD. However, Patients J and D possess three of the most significant cardiovascular risk factors: cigarette smoking, diabetes, and hyperlipidemia. Therefore, based on the data available in the vignettes, Patients J and D are at greatest risk for CHD. If further information was available about each woman's cardiac risk factor profiles, we might be able to differentiate even further to determine which of these two women is at greater risk.
Patient F appears be in the best cardiovascular state among the group. Her mild hypertension is well controlled; she is not overweight, eats a sensible diet, and sees that she gets some form of aerobic exercise at least three times a week.
What specific recommendations would you make in counseling each woman about her cardiovascular health?
Counseling recommendations for Patient S would primarily focus on cardiac nutrition aspects and developing an exercise program for cardiovascular fitness. Because she is more than 30% overweight, she is at a tremendously increased risk of CHD due to the added stress on her heart and the changes that occur in lipid metabolism when fat is distributed in the abdominal versus gluteal region. Therefore, patient teaching should emphasize good nutrition and reading nutrition labels to manage caloric intake, as well as limiting intake of fat and cholesterol. In addition to changes in diet, Patient S should be counseled on incorporating some form of aerobic exercise, such as walking, three to five times a week to achieve cardiovascular fitness. The exercise will also have the added benefit of helping her modify her weight level.
Two major concerns become evident in assessing Patient J's health status—her smoking history and her hyperlipidemia. Recommendations would focus on encouraging and motivating the patient to quit smoking, through the use of the nicotine patch or gum with the additional support of bupropion and/or a smoking cessation program to increase her chances of successfully quitting. These programs are essential because they teach the patient behavioral and psychologic techniques to utilize at various stages of the quitting process and help the person identify specific problem situations and how these can be realistically managed. Patient J's lipid profile should be closely monitored to determine the effectiveness of gemfibrozil in lowering her LDL levels. In addition, patient teaching should focus on the deleterious effects of smoking on lipid profiles, specifically HDL levels. Smoking tends to decrease levels of HDL, which could be used as another health information tidbit to motivate Patient J to quit smoking.
Recommendations for cardiac health for Patient V would primarily focus on the alterable factors rather than her significant family history, which cannot be changed. As a result, patient teaching and counseling would be geared toward getting her weight into a more desirable range by paying attention to nutrition and getting some form of regular aerobic exercise. Patient V would also benefit from more health teaching regarding alcohol consumption. While a moderate intake of alcohol may be associated with positive antioxidant effects that can impart some protection against the development of CHD, the key is moderation. One drink per day is the recommendation for alcohol consumption in women.
In assessing Patient D's health history, her diabetes and smoking habit are big concerns. In terms of her diabetes, she is in need of strict control to prevent further progression and significant complications associated with the disease, such as CHD. Another major factor that would help prevent a major cardiac event is for her to quit smoking. Remember that many cardiovascular risk factors are synergistic. In other words, risk factors work together in increasing an individual's risk of developing CHD. Cigarette smoking and diabetes are both powerful independent risk factors for CHD, and together, they significantly elevate the chances of developing the disease.
Patient counseling recommendations for Patient F are twofold: continued control of her hypertension and stress management. Patient F and all of the women should be applauded regarding the positive habits they have incorporated into their lifestyle. In this patient's case, these positive aspects include attention to nutrition, aerobic exercise, and staying away from smoking or alcohol use. She does, however, need assistance with stress management. While her regular exercise program is most likely one avenue for her to deal with this stress, it obviously is not singly effective. In other words, additional stress management strategies could be added to her repertoire.
CASE STUDY 2
Patient M is a White woman, 75 years of age, who presented to her local emergency department with sudden complaints of chest pain. She described the pain as a severe substernal burning sensation that radiated across the chest to her shoulders bilaterally and then to the neck and jaw region. Although not brought on by exertion, the chest pain was associated with dyspnea, pallor, diaphoresis, nausea, and epigastric discomfort. Patient M had taken one nitroglycerin tablet with partial relief. When the chest pain recurred 10 to 15 minutes later, her family dialed 911 and the local emergency medical service responded. Once transported to the emergency department, her pain persisted. She received two additional doses of nitroglycerin and was placed on 2 L of oxygen per nasal cannula.
Following stabilization, she was admitted to a telemetry floor for further observation and medical management. Nursing assessment revealed the following cardiovascular risk factors: 50-pack-year history of smoking, hypertension, and mild-to-moderate obesity. As part of the medical workup, Patient M was scheduled for a coronary angiogram the following day. The angiogram revealed an 80% blockage of the right coronary artery and the cardiologist recommended Patient M consider a PCI to open the coronary artery blockage.
The following day, Patient M underwent a PCI to the right coronary artery. The procedure was progressing uneventfully until she had an episode of bradycardia as her heart rate dropped to 38 beats per minute. The patient received a 0.5 mg dose of IV atropine, which was repeated in 10 minutes. Other than this episode, Patient M did not experience any other postprocedure complications, such as hypotension, or other technical-related problems.
The day after the PCI, Patient M was receiving her discharge instructions from her nurse when she began noticing a return of the dull epigastric pain. The pain did not appear to be related to her food intake because she was progressing on her diet. Later that day, as the pain persisted, Patient M had an ultrasound of her abdomen, which showed multiple walnut-sized gallstones. The gastroenterologist referred her to a general surgeon who recommended that she undergo a cholecystectomy for further relief of her gastrointestinal symptoms. The surgeon advised her of the risks and benefits of laparoscopic versus traditional surgery, and Patient M opted for the laparoscopic procedure. Four small incisions were made in her abdomen, and the cholecystectomy was performed without any complications. Three days postoperatively, she complained again of moderate-to-severe epigastric pain and became jaundiced. An endoscopic retrograde cholangiopancreatography revealed retained stones in the common bile duct, which were removed. Patient M subsequently recovered and was discharged home after a total of nine days in the hospital.
In analyzing this case study, consider the following questions:
What cardiovascular risk factors are present? What risk factors are negative?
Is the patient's chest pain syndrome typical or atypical for women? Why or why not?
What tests would you anticipate in the diagnostic workup of women experiencing angina?
What nursing diagnoses would be appropriate for this patient during hospitalization? What special implications do these diagnoses have in women?
Case Study 2 Analyses
What coronary risk factors are present? What risk factors are negative?
The cardiovascular risk factors known for Patient M include her age, postmenopausal status, smoking history, and hypertension.
The chest pain syndrome experienced by Patient M is typical for women. She described the chest pain as a substernal burning sensation that radiated across her precordium to her shoulder region bilaterally and then to her neck and jaw. In addition, her chest pain was accompanied by dyspnea, diaphoresis, nausea, and epigastric distress, all of which may or may not be associated with anginal episodes in women. In contrast, chest pain in men often begins substernally and spreads across the left precordium down the left arm.
What tests would you anticipate to be in the diagnostic workup of women experiencing angina?
The diagnostic phase for women with angina often begins with a resting 12-lead ECG. This test is useful in women due to their higher proportion of silent or unrecognized infarctions. Conversely, the exercise ECG is not considered a good test in women due to high false-positive rates and other problems associated with women exercising at adequate intensity levels. Other noninvasive cardiac diagnostic tests might include nuclear myocardial perfusion scans and exercise echocardiogram. Of these three tests, the exercise echocardiogram is the best test for women. It is associated with the highest accuracy rates and is especially sensitive to single vessel disease, which occurs more frequently in women than in men.
Decreased Cardiac Output : With the sudden onset of angina and need to undergo a PCI to open a blockage of the right coronary artery, Patient M is at risk for decreased cardiac output. Women should be taught to take angina seriously and to have it evaluated by a physician as soon as possible. This is especially critical in women because they have an unfavorable prognosis post-MI. After PCI, women also have higher mortality rates and, therefore, should be carefully assessed. Complications must be recognized early in their course so they can be corrected and managed successfully.
Pain : Patient M really has two etiologies of her pain: chest pain and epigastric discomfort referred from her biliary tract disease. It is important to recognize that angina is often more severe in women than men (and both stable and unstable angina are more frequent in women), and therefore, necessary pharmacologic therapy may be more intense. In women, angina is managed best by either nitrates or calcium channel blockers, although the dosage may not be the same as it is in men. Because women have been excluded from many clinical drug trials testing cardiac medications, the optimal dose of various medications to treat women is less well known. Further research is needed to guide this area of clinical practice.
Knowledge Deficit : Like any other patient undergoing diagnostic testing and an invasive cardiac procedure, not to mention the cholecystectomy, Patient M should be taught about various components of her illness and hospitalization. These components include her disease process, diagnostic tests, medications, risk factor modification, and the recovery process, with emphasis on the long-term positive outcomes associated with PCI in women. In addition, when teaching female cardiac patients, it is vital to search for patient teaching materials that discuss the unique concerns of women with CHD.
CASE STUDY 3
Patient Y, a woman 76 years of age, was seen in the Women's Cardiac Center for a personalized health and risk factor assessment. Assessment findings included a heart rate of 84 beats per minute, blood pressure 172/68 mm Hg, height 5'5", and weight 171 pounds. Waist-hip ratio was 0.75, and skin fold calipers measured 42% body fat. Lipid profile included total cholesterol of 239 mg/dL, HDL 40 mg/dL, LDL 159 mg/dL, ratio 5.9 mg/dL, and triglycerides 248 mg/dL. Fasting glucose was 79 mg/dL. Past medical history included hiatal hernia, cholecystectomy, hypothyroidism, arthritis, insomnia, and a long-standing history of ankle edema. The patient also reported symptoms suspicious of sleep apnea.
Based on this assessment, cardiovascular risk factors were identified and the patient was instructed on risk factor modification. Four months later, she phoned the Women's Cardiac Center with complaints of anterior chest discomfort that radiated to her neck, jaw, and back, accompanied by shortness of breath. She was referred to Cardiology and seen three days later.
The diagnostic workup included a 12-lead ECG and nuclear myocardial perfusion scan, followed by an angiogram. She was not considered a candidate for the exercise EKG due to her advanced age and other comorbidities, specifically arthritis, which would limit her ability to exercise at adequate intensity levels. The 12-lead ECG revealed nonspecific T-wave changes in the inferior leads, and the nuclear scan was positive, suggestive of single-vessel disease of the left circumflex artery. An angiogram was then performed and showed triple vessel disease with significant left main disease. Her occlusions were 50% to 60% of the left main, 90% of the circumflex, and 60% of the right coronary artery. EF was estimated at 60%, indicating preserved left ventricular function. Based on these diagnostic findings, the patient was referred for CABG surgery.
Two weeks later, Patient Y underwent CABG surgery with internal mammary grafting. During surgery, she required inotropic support with dobutamine and epinephrine and atrioventricular sequential pacing. An intra-aortic balloon pump (IABP) was also placed via the right femoral artery due to right heart failure. On the first postoperative day, the patient remained in the intensive care unit on the IABP and ventilator. Lab values showed a creatine phosphokinase of 3113 IU/L and creatine kinase isoenzyme MB of 169.4 IU/L. A bedside echocardiogram confirmed an inferior-posterior and right ventricular infarct.
The patient was transferred to the cardiac surgical stepdown unit on the third postoperative day where she developed atrial fibrillation and was digitalized. Oxygen was administered at 5 L per nasal cannula and her ambulation was significantly limited. In addition, a bruit was noted in her right groin. An echo-Doppler revealed a two-chamber pseudoaneurysm which was unsuccessfully compressed. On the sixth postoperative day, the patient went in and out of atrial fibrillation/flutter and converted to sinus rhythm on postoperative day 7. As a result, she was weaned from oxygen and progressed with independent ambulation. However, she remained hospitalized until postoperative day 12 for observation of her heart rhythm and right groin pseudoaneurysm.
Two days after discharge, the patient received a follow-up telephone call from the Cardiac Liaison Nurse to assess her condition. Patient Y stated she was "feeling pretty good," yet indicated some difficulty with incisional pain, anorexia, fluid loss, insomnia, and confusion about her medications. After recuperating at home, the patient enrolled in a phase II cardiac rehabilitation program. At this time, the patient reports no angina or chest discomfort. She is progressing in her exercise program and tolerating activity. Problems experienced since discharge include a urinary tract infection, depression, and increasing heart failure. Her furosemide dosage has been increased, and she has obtained good relief of her symptoms.
What is the common picture of a woman's general health and cardiac status when referred for CABG surgery?
What significance does this patient's perioperative MI have for her long-term prognosis?
Identify ways to assess both short- and long-term outcomes of women post-CABG surgery.
Case Study 3 Analyses
Patient Y has the following cardiovascular risk factors:
Age: Older than 60 years of age
Positive family history: Both parents died from CHD
Hypertension: 172/68 mm Hg
Hypercholesterolemia: Total cholesterol 239 mg/dL; HDL 40 mg/dL; LDL 159 mg/dL; ratio 5.9; triglycerides 248 mg/dL
Body composition: Percentage of body fat is 42%
Menopause: Received HRT for 20 years
Stress: Rated as a 5 on a 0 to 10 scale
The following cardiovascular risk factors are negative:
Personal history of cardiovascular or cerebrovascular disease
Smoking history
History of alcohol consumption
Sedentary lifestyle (Reports walking one mile per day)
As in the previous case study, Patient Y's chest pain syndrome is fairly typical for women. She experienced chest discomfort in the anterior region of her chest, which then radiated to her neck, jaw, and back. The chest pain was also accompanied by shortness of breath, which may or may not occur in women, just like other associated symptoms such as nausea, diaphoresis, or lightheadedness.
What is the common picture of a woman's general health and cardiac status when referred for CABG?
Like Patient Y, women who are referred for CABG surgery tend to be older with more comorbidities or multiple health problems, including hypertension, hypothyroidism, sleep apnea, arthritis, hiatal hernia, and sciatica. In terms of cardiac status, women tend to be referred more often for unstable angina, in comparison to men who usually are referred on the basis of a positive exercise ECG. In addition, women tend to have a lower incidence of prior MI before surgery and thus have better EFs, fewer diseased arteries or more single vessel disease (50% have single-vessel disease versus 25% two-vessel and 25% three-vessel disease), and more left ventricular hypertrophy and mitral regurgitation.
What significance does the patient's perioperative MI have for her long-term prognosis?
Women who suffer an MI have a worse prognosis than men, which is why timely diagnosis with an appropriate workup and treatment is so important in women experiencing anginal symptoms. When women go on to infarct, they have a much greater chance of not surviving, both in the early postinfarct period as well as later in their clinical course.
Decreased Cardiac Output : Patient Y was a woman with complaints of angina who underwent CABG surgery. During the surgical procedure, she suffered an inferior-posterior and right ventricular infarct. Despite the fact that her left ventricular EF was preserved at 60% post-MI, she should be carefully observed for early signs of heart failure, as well as any other complications during the postoperative period.
Pain : Again, prior to surgical intervention, Patient Y's angina should be carefully assessed and treated with nitrates or calcium channel blockers to prevent an acute MI, which would significantly impact her prognosis and long-term outcome. While postsurgical pain is most likely incisional, it is still important to assess for the return of angina, which could signal reocclusion of one of the bypass grafts.
Activity Intolerance : Patient Y is 76 years of age with multiple health problems, including arthritis. She will likely be slow to mobilize in the postoperative phase to begin with, which is compounded by the problems she developed with postoperative atrial fibrillation. After her ventricular rate was controlled and the pseudoaneurysm was addressed, her cardiac rehabilitation activity and exercise program was appropriately resumed.
Body Image Disturbance : This is a potential nursing diagnosis for Patient Y given her feelings of depression in the postdischarge phase. These feelings could be considered a normal part of recuperation and a reflection of perceived changes in body image due to the sternotomy and leg incisions. After being discharged home, she did complain of continued incisional pain that could be partially alleviated by wearing a supportive bra to decrease tension from the breasts.
Knowledge Deficit : As with Patient M in Case Study 2, Patient Y has a knowledge deficit regarding her cardiac disease and surgical procedure. Patient teaching for Patient Y should incorporate elements such as disease process, cardiac medications, activity restriction, caring for the surgical incision, risk factor modification, outpatient cardiac rehabilitation, and the recovery process. She would also benefit from gender and sex-specific patient teaching aids, if available, so she could relate to the unique concerns and needs of women who have faced CHD and CABG surgery.
Patient outcomes may be measured both during the hospitalization and postdischarge phases. During the hospitalization phase, examples of clinical outcomes to be assessed for a population of female cardiac patients include complication rates (e.g., perioperative MIs, dysrhythmias, pseudoaneurysms); length of stay (both intensive care unit and hospital length of stay); and readmissions (both intensive care units and hospital readmissions), along with the clinical reasons.
After the hospitalization phase, patient outcomes may be assessed again. Examples of outcomes to be measured in the early discharge phase include pain, appetite, wound healing (incisions in surgical patients), rest/sleep patterns, psychologic comfort, and exercise patterns. Teaching and learning outcomes are also important to assess, including whether the female cardiac patient understood her discharge instructions related to activity and exercise, cardiac medications, diet, and when to return to work. Quality of life becomes an important consideration for this population. Research suggests that women experience more days of restricted activity due to continuing cardiac symptomatology, such as recurring chest pain and dyspnea. Ability to return to work and previous hobbies and pastimes would be an important area to assess in this regard.
CASE STUDY 4
Patient A was a woman, 88 years of age, who lived in an assisted living retirement home. She had been a widow for 20 years, after losing her husband to long-term complications associated with diabetes. Until approximately seven years ago, Patient A had been in relatively good health with no major health problems, but she suffered a mild stroke at 81 years of age. At that time, she decided to quit her 50- to 60-year smoking habit. Other than her smoking history, she did not have any other significant cardiovascular risk factors.
After recuperating from her stroke, Patient A decided to leave her apartment and move into the assisted living facility where she would not only have some companionship but also receive assistance with meals and transportation to doctor's appointments and other activities. About six years after suffering the cerebrovascular accident, she had a bout of heart failure. She was admitted to the local hospital and received oxygen per nasal cannula, IV furosemide, and digoxin. After two weeks in the hospital, the patient was discharged home in apparently better condition. However, two days after returning home Patient A suffered a sudden cardiac death event at the breakfast table. Efforts at resuscitation were unsuccessful.
Case Study 4 Analyses
Positive cardiovascular risk factors for Patient A include the nonalterable factors of age and menopause and the alterable factor of smoking history. The risk factors that were negative in her history include family history of CHD, hypertension, hyperlipidemia, obesity, sedentary lifestyle, or psychosocial concerns.
Patient A's cardiac event is atypical for women in terms of initial presentation of the disease process. MI and sudden cardiac death are more commonly a first manifestation of CHD in men, while angina is the most common presenting scenario for women. Women tend to lag behind men in both the occurrence and incidence of CHD, as well as sudden cardiac death events. In terms of Patient A's history, it is possible that she initially suffered an MI, which was not recognized, and went on to develop heart failure as a post-MI complication. This then explains her increased risk for earlier reinfarction and higher mortality.
CASE STUDY 5
Patient H, a White woman 60 years of age, suddenly began complaining of chest pain one evening. The pain was substernal, spread down both arms bilaterally, and radiated to her neck and jaw region. Patient H also complained of shortness of breath, nausea, and diaphoresis. Never having witnessed these symptoms before, Patient H's husband and daughter transported her to the local emergency department.
When she arrived in the emergency department, immediate priorities focused on obtaining a brief yet comprehensive history of symptomatology and past medical problems, as well as instituting appropriate treatments. The health assessment revealed numerous cardiovascular risk factors. Patient H's increasing age is one nonalterable risk factor present. In addition, she has a significant family history of CHD. Her mother and grandmother both suffered fatal heart attacks in their late 50s or early 60s. While Patient H does not have a history of smoking, she does have hypertension, hyperlipidemia, and diabetes. She is also obese, with a height of 5'2" and weight of 240 pounds and does not report engaging in a regular exercise program.
In terms of supportive treatment, Patient H was placed on 3 L of supplemental oxygen per nasal cannula and given sublingual nitroglycerin. She rated her pain an 8 on a 0 to 10 scale and did not report an appreciable decrease in her pain level after the first nitroglycerin dose. A second sublingual dose was given, after which she obtained relief. In the diagnostic workup phase, Patient H had a 12-lead ECG that revealed signs of ischemia in leads II and III and a ventricular dysrhythmia. Serial cardiac enzymes were drawn to rule out MI. Patient H was admitted to the coronary care unit (CCU) for treatment of an inferior MI.
Once transferred to the CCU, the patient was placed on the bedside monitor and a left radial arterial line and left subclavian Swan Ganz catheter were inserted for hemodynamic monitoring purposes. A bedside echocardiogram was performed to assess left ventricular EF and overall function of the chambers of the heart. The exam revealed that left ventricular EF was not preserved, estimated at only about 40% pumping function. Positive inotropes were started to increase the contractility of the heart and improve cardiac output. Intravenous nitroglycerin that was started in the emergency department was continued to improve coronary perfusion and for afterload reduction. After two days, Patient H was transferred out of the CCU to the cardiology stepdown unit. Telemetry showed slight sinus bradycardia at a rate of 56 beats per minute without ectopy. Other vital signs included blood pressure 102/56 mm Hg and a respiratory rate of 26 breaths per minute. Patient H remained on supplemental oxygen at 2 L per nasal cannula.
Cardiac rehabilitation was initiated when Patient H was in the stepdown unit. Rehabilitation activities first focused on identifying her risk stratification level, from low to high on a continuum, to guide initial activity and further exercise prescriptions. Because the patient's left ventricular EF was approximately 40%, her risk stratification level was identified as moderate and she was instructed that her cardiac rehabilitation activity would entail ambulating three times a day, first with monitored assistance in the hallway, working eventually toward the goal of independent ambulation. Prior to her first ambulation, Patient H's nurse took orthostatic blood pressure readings with the following results: lying 120/68 mm Hg; sitting 116/64 mm Hg; and standing 112/62 mm Hg. Heart rate pre-exercise was 58 beats per minute. As a result of these data, Patient H was assisted into the hallway for monitored ambulation. After walking for approximately two minutes, her heart rhythm converted from sinus bradycardia into a fast atrial fibrillation, with a ventricular rate of 180 beats per minute. Her blood pressure was 102/56 mm Hg. The patient was assisted back to bed, and a cardiology consult was requested.
The consulting cardiologist ordered a diltiazem drip. After her ventricular rate was under control, the patient was digitalized with 1 mg of digoxin followed by a maintenance dose of 0.125 mg IV. Other cardiac medications added to the regime included a beta blocker, furosemide, and potassium.
On the day of discharge, Patient H's family was present for discharge teaching. Her nurse explained the list of medications, including the dose and frequency, as well as her activity limitations. Patient H was instructed not to drive a car for two weeks and to increase her walking each day by one minute until she arrived at the goal of approximately 30 to 45 minutes at least three times a week. In addition, Patient H was informed about the nearest outpatient cardiac rehabilitation program. It was explained to her that the primary benefits of attending an outpatient program would be that the staff would assist her in developing an activity and exercise program individualized to her needs and physical capabilities. In addition, they would teach her and her family other components of heart healthy living, such as cardiac nutrition, managing diabetes, and stress.
After discharge, the patient did enroll in an outpatient cardiac rehabilitation program and had attended three sessions when she began developing symptoms of heart failure, including orthopnea, shortness of breath, and weight gain. On physical examination, crackles were auscultated bibasilarly and dependent pitting edema was present in her ankles bilaterally. On being seen in the heart failure clinic, she was restarted on a diuretic, furosemide, and an ACE inhibitor and her digoxin was kept at the same dosage.
What special implications exist with regard to dosing cardiac medications in women?
Describe the common response of women with CHD to activity.
What factors influence women's involvement in cardiac rehabilitation programs?
Case Study 5 Analyses
Patient H has the following cardiovascular risk factors:
Age: 60 years of age
Positive family history: Mother and grandmother both died prematurely from an MI
Hypertension
Hyperlipidemia
Obesity: Weight 240 pounds; height 5'2"
Sedentary lifestyle
Postmenopausal
Perceived stress
Patient H's chest pain was located substernally and radiated down both arms and to her neck and jaw. In addition, she was short of breath, diaphoretic, and nauseated. This clinical picture is fairly typical in women. Unlike the usual presentation in men, women may complain of no chest pain or chest pain that does or does not radiate. The pain may also be accompanied by other cardiac symptoms such as diaphoresis, dyspnea, or lightheadedness, but not necessarily so; in some cases, these symptoms are absent altogether.
Nursing diagnoses that would apply in this case study include decreased cardiac output, pain, activity intolerance, and knowledge deficit. The nursing implications that these diagnoses have in women have been discussed in previous case studies. In women who have suffered an MI, it is important to assess for other health problems or conditions that could impact their recovery because their morbidity and mortality rates are already higher than women with angina or those who have undergone a revascularization procedure.
Historically, research did not include women in clinical trials on the efficacy of cardiac medications. The optimal dose of these medications in women requires further study because, for the most part, they were tested on men. It may be that women need less, more, or the same dose as men. Further research including women is needed to determine the therapeutic dosage ranges for various cardiac medications, such as nitrates, beta blockers, or calcium channel blockers.
Describe the common response to activity of women with CHD.
In general, women with CHD tend to be older than their male counterparts. As a result, women presenting with cardiac problems may also have other significant comorbidities such as diabetes, hypertension, and arthritis which may slow their activity progression. Therefore, during the acute phase, it is essential to involve either physical therapy and/or cardiac rehabilitation to begin mobilizing the patient and progressing with activity as appropriate to the patient's condition.
Many factors have been studied regarding women's participation in formal outpatient cardiac rehabilitation programs. Some of the most common reasons women give for decreased attendance include family commitments, financial concerns, and medical problems, such as increasing angina and/or other cardiac symptoms.
CASE STUDY 6
The following vignettes describe women with cardiac symptomatology who received either medical or surgical treatment. Read through these vignettes and analyze them using the questions that are presented at the end of the case studies.
Patient R, an African American woman 52 years of age, recently underwent a CABG procedure. An angiogram revealed three-vessel disease. As a result, she had bypasses to her right coronary artery, left circumflex artery, and obtuse marginal artery.
Patient B is a White woman, 65 years of age, with a long-standing history of stable angina. She has been medically managed for the past several months on nitrates (sublingual nitroglycerin) and an ACE inhibitor.
Patient L is 45 years of age. She experienced a sudden onset of chest and arm pain while driving to a family affair with her husband. Because the pain did not subside, her husband drove her directly to the local emergency department, where she was evaluated and underwent several diagnostic tests, including a 12-lead ECG, serial cardiac enzymes, and a dipyridamole echocardiogram. The 12-lead ECG and cardiac enzyme elevations suggested an evolving MI. As a result, Patient L was treated with thrombolytic therapy in the emergency department, then admitted to the CCU for further treatment and observation.
Patient E, an Asian American woman 52 years of age, had been experiencing episodes of pain that spread across her chest and occasionally radiated down one or both arms and/or to her jaw region. Over the last week or so, the chest pain episodes increased in frequency to the point she thought she should have a medical evaluation. Patient E saw a cardiologist, who suggested the patient undergo an angiogram. The procedure revealed a 60% lesion of the right coronary artery that the cardiologist believed could be treated successfully with angioplasty.
Based on the information, which woman has the best prognosis? The worst prognosis? Why?
What are some of the complications associated with each of these medical and surgical therapies?
Case Study 6 Analyses
Patient B has the best prognosis. She has a long-standing history of stable angina that has been adequately managed with nitrates and an ACE inhibitor. Women with angina have a better prognosis than those who suffer an MI, one of the main reasons why it is so important to accurately assess a woman's cardiovascular risk factors and work on modifying those areas possible to prevent an MI from ever happening. After a woman has an MI, the mortality rates are significantly higher.
On the other hand, Patient R and Patient L have the worst prognoses of the women presented in this vignette. Women who undergo CABG surgery have double the perioperative mortality rate of men and also fare poorer in the early postoperative period, generally complaining of more angina, dyspnea, and reduced mobility. These findings may be due to the fact that women tend to be older at the time of surgery, have more advanced disease, and significant comorbidities. However, five- and 10-year survival rates between men and women are comparable.
Medical Management : A possible complication or adverse effect associated with medical management focuses on the dosage of cardiac medications used to treat women with CHD. Women may have a different vasomotor tone compared to men and, thus, may require less nitrates. Only further research will give us the answers to guide clinical practice decisions.
Thrombolytic Therapy : The main complication associated with thrombolytic therapy in women is bleeding, especially intracranial bleeding. The reason for this increased incidence in women may be dose related.
PCI : The most common reported complications associated with angioplasty include bradycardia, hypotension, bleeding, and vascular complications. However, dissection is becoming less common as advances and improvements are made in angioplasty catheters.
CABG Surgery : During the operative phase, incomplete revascularization (resulting in angina, dyspnea, and sub-sequent restricted activity) may occur due to women's smaller coronary arteries and difficulty in anastomosis. However, improved surgical tools and techniques have minimized the difficulties. Reports have also shown that women have longer hospital stays, greater complication rates, and higher postoperative morbidity (as previously suggested), but similar long-term outcomes.
- About NetCE
- About TRC Healthcare
- Do Not Sell My Personal Information
Copyright © 2024 NetCE · Contact Us

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics
Coronary Heart Disease Research
Language switcher.
For almost 75 years, the NHLBI has been at the forefront of improving the nation’s health and reducing the burden of heart and vascular diseases . Heart disease, including coronary heart disease, remains the leading cause of death in the United States. However, the rate of heart disease deaths has declined by 70% over the past 50 years, thanks in part to NHLBI-funded research. Many current studies funded by the NHLBI focus on discovering genetic associations and finding new ways to prevent and treat the onset of coronary heart disease and associated medical conditions.

NHLBI research that really made a difference
The NHLBI supports a wide range of long-term studies to understand the risk factors of coronary heart disease. These ongoing studies, among others, have led to many discoveries that have increased our understanding of the causes of cardiovascular disease among different populations, helping to shape evidence-based clinical practice guidelines.
- Risk factors that can be changed: The NHLBI Framingham Heart Study (FHS) revealed that cardiovascular disease is caused by modifiable risk factors such as smoking, high blood pressure , obesity , high cholesterol levels, and physical inactivity. It is why, in routine physicals, healthcare providers check for high blood pressure, high cholesterol, unhealthy eating patterns, smoking, physical inactivity, and unhealthy weight. The FHS found that cigarette smoking increases the risk of heart disease. Researchers also showed that cardiovascular disease can affect people differently depending on sex or race, underscoring the need to address health disparities.
- Risk factors for Hispanic/Latino adults: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) found that heart disease risk factors are widespread among Hispanic/Latino adults in the United States , with 80% of men and 71% of women having at least one risk factor. Researchers also used HCHS/SOL genetic data to explore genes linked with central adiposity (the tendency to have excess body fat around the waist) in Hispanic/Latino adults. Before this study, genes linked with central adiposity, a risk factor for coronary heart disease, had been identified in people of European ancestry. These results showed that those genes also predict central adiposity for Hispanic/Latino communities. Some of the genes identified were more common among people with Mexican or Central/South American ancestry, while others were more common among people of Caribbean ancestry.
- Risk factors for African Americans: The Jackson Heart Study (JHS) began in 1997 and includes more than 5,300 African American men and women in Jackson, Mississippi. It has studied genetic and environmental factors that raise the risk of heart problems, especially high blood pressure, coronary heart disease, heart failure , stroke , and peripheral artery disease (PAD) . Researchers discovered a gene variant in African American individuals that doubles the risk of heart disease. They also found that even small spikes in blood pressure can lead to a higher risk of death. A community engagement component of the JHS is putting 20 years of the study’s findings into action by turning traditional gathering places, such as barbershops and churches, into health information hubs.
- Risk factors for American Indians: The NHLBI actively supports the Strong Heart Study , a long-term study that began in 1988 to examine cardiovascular disease and its risk factors among American Indian men and women. The Strong Heart Study is one of the largest epidemiological studies of American Indian people ever undertaken. It involves a partnership with 12 Tribal Nations and has followed more than 8,000 participants, many of whom live in low-income rural areas of Arizona, Oklahoma, and the Dakotas. Cardiovascular disease remains the leading cause of death for American Indian people. Yet the prevalence and severity of cardiovascular disease among American Indian people has been challenging to study because of the small sizes of the communities, as well as the relatively young age, cultural diversity, and wide geographic distribution of the population. In 2019, the NHLBI renewed its commitment to the Strong Heart Study with a new study phase that includes more funding for community-driven pilot projects and a continued emphasis on training and development. Read more about the goals and key findings of the Strong Heart Study.
Current research funded by the NHLBI
Within our Division of Cardiovascular Sciences , the Atherothrombosis and Coronary Artery Disease Branch of its Adult and Pediatric Cardiac Research Program and the Center for Translation Research and Implementation Science oversee much of our funded research on coronary heart disease.
Research funding
Find funding opportunities and program contacts for research on coronary heart disease.
Current research on preventing coronary heart disease
- Blood cholesterol and coronary heart disease: The NHLBI supports new research into lowering the risk of coronary heart disease by reducing levels of cholesterol in the blood. High levels of blood cholesterol, especially a type called low-density lipoprotein (LDL) cholesterol, raise the risk of coronary heart disease. However, even with medicine that lowers LDL cholesterol, there is still a risk of coronary heart disease due to other proteins, called triglyceride-rich ApoB-containing lipoproteins (ApoBCLs), that circulate in the blood. Researchers are working to find innovative ways to reduce the levels of ApoBCLs, which may help prevent coronary heart disease and other cardiovascular conditions.
- Pregnancy, preeclampsia, and coronary heart disease risk: NHLBI-supported researchers are investigating the link between developing preeclampsia during pregnancy and an increased risk for heart disease over the lifespan . This project uses “omics” data – such as genomics, proteomics, and other research areas – from three different cohorts of women to define and assess preeclampsia biomarkers associated with cardiovascular health outcomes. Researchers have determined that high blood pressure during pregnancy and low birth weight are predictors of atherosclerotic cardiovascular disease in women . Ultimately, these findings can inform new preventive strategies to lower the risk of coronary heart disease.
- Community-level efforts to lower heart disease risk among African American people: The NHLBI is funding initiatives to partner with churches in order to engage with African American communities and lower disparities in heart health . Studies have found that church-led interventions reduce risk factors for coronary heart disease and other cardiovascular conditions. NHLBI-supported researchers assessed data from more than 17,000 participants across multiple studies and determined that these community-based approaches are effective in lowering heart disease risk factors .
Find more NHLBI-funded studies on preventing coronary heart disease on the NIH RePORTER.

Learn about the impact of COVID-19 on your risk of coronary heart disease.
Current research on understanding the causes of coronary heart disease
- Pregnancy and long-term heart disease: NHLBI researchers are continuing the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-be (nuMoM2b) study to understand the relationship between pregnancy-related problems, such as gestational hypertension, and heart problems. The study also looks at how problems during pregnancy may increase risk factors for heart disease later in life. NuMoM2b launched in 2010, and long-term studies are ongoing, with the goal of collecting high-quality data and understanding how heart disease develops in women after pregnancy.
- How coronary artery disease affects heart attack risk: NHLBI-funded researchers are investigating why some people with coronary artery disease are more at risk for heart attacks than others. Researchers have found that people with coronary artery disease who have high-risk coronary plaques are more likely to have serious cardiac events, including heart attacks. However, we do not know why some people develop high-risk coronary plaques and others do not. Researchers hope that this study will help providers better identify which people are most at risk of heart attacks before they occur.
- Genetics of coronary heart disease: The NHLBI supports studies to identify genetic variants associated with coronary heart disease . Researchers are investigating how genes affect important molecular cascades involved in the development of coronary heart disease . This deeper understanding of the underlying causes for plaque buildup and damage to the blood vessels can inform prevention strategies and help healthcare providers develop personalized treatment for people with coronary heart disease caused by specific genetic mutations.
Find more NHLBI-funded studies on understanding the causes of coronary heart disease on the NIH RePORTER.

Recent findings suggest that cholesterol-lowering treatment can lower the risk of heart disease complications in people with HIV.
Current research on treatments for coronary heart disease
- Insight into new molecular targets for treatment: NHLBI-supported researchers are investigating the role of high-density lipoprotein (HDL) cholesterol in coronary heart disease and other medical conditions . Understanding how the molecular pathways of cholesterol affect the disease mechanism for atherosclerosis and plaque buildup in the blood vessels of the heart can lead to new therapeutic approaches for the treatment of coronary heart disease. Researchers have found evidence that treatments that boost HDL function can lower systemic inflammation and slow down plaque buildup . This mechanism could be targeted to develop a new treatment approach for coronary heart disease.
- Long-term studies of treatment effectiveness: The NHLBI is supporting the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial EXTENDed Follow-up (EXTEND) , which compares the long-term outcomes of an initial invasive versus conservative strategy for more than 5,000 surviving participants of the original ISCHEMIA trial. Researchers have found no difference in mortality outcomes between invasive and conservative management strategies for patients with chronic coronary heart disease after more than 3 years. They will continue to follow up with participants for up to 10 years. Researchers are also assessing the impact of nonfatal events on long-term heart disease and mortality. A more accurate heart disease risk score will be constructed to help healthcare providers deliver more precise care for their patients.
- Evaluating a new therapy for protecting new mothers: The NHLBI is supporting the Randomized Evaluation of Bromocriptine In Myocardial Recovery Therapy for Peripartum Cardiomyopathy (REBIRTH) , for determining the role of bromocriptine as a treatment for peripartum cardiomyopathy (PPCM). Previous research suggests that prolactin, a hormone that stimulates the production of milk for breastfeeding, may contribute to the development of cardiomyopathy late in pregnancy or the first several months postpartum. Bromocriptine, once commonly used in the United States to stop milk production, has shown promising results in studies conducted in South Africa and Germany. Researchers will enroll approximately 200 women across North America who have been diagnosed with PPCM and assess their heart function after 6 months.
- Impact of mental health on response to treatment: NHLBI-supported researchers are investigating how mental health conditions can affect treatment effectiveness for people with coronary heart disease. Studies show that depression is linked to a higher risk for negative outcomes from coronary heart disease. Researchers found that having depression is associated with poor adherence to medical treatment for coronary heart disease . This means that people with depression are less likely to follow through with their heart disease treatment plans, possibly contributing to their chances of experiencing worse outcomes. Researchers are also studying new ways to treat depression in patients with coronary heart disease .
Find more NHLBI-funded studies on treating coronary heart disease on the NIH RePORTER.

Researchers have found no clear difference in patient survival or heart attack risk between managing heart disease through medication and lifestyle changes compared with invasive procedures.
Coronary heart disease research labs at the NHLBI
- Laboratory of Cardiac Physiology
- Laboratory of Cardiovascular Biology
- Minority Health and Health Disparities Population Laboratory
- Social Determinants of Obesity and Cardiovascular Risk Laboratory
- Laboratory for Cardiovascular Epidemiology and Genomics
- Laboratory for Hemostasis and Platelet Biology
Related coronary heart disease programs
- In 2002, the NHLBI launched The Heart Truth® , the first federally sponsored national health education program designed to raise awareness about heart disease as the leading cause of death in women. The NHLBI and The Heart Truth® supported the creation of the Red Dress® as the national symbol for awareness about women and heart disease, and also coordinate National Wear Red Day ® and American Heart Month each February.
- The Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC) facilitates access to and maximizes the scientific value of NHLBI biospecimen and data collections. A main goal is to promote the use of these scientific resources by the broader research community. BioLINCC serves to coordinate searches across data and biospecimen collections and provide an electronic means for requesting additional information and submitting requests for collections. Researchers wanting to submit biospecimen collections to the NHLBI Biorepository to share with qualified investigators may also use the website to initiate the application process.
- Our Trans-Omics for Precision Medicine (TOPMed) Program studies the ways genetic information, along with information about health status, lifestyle, and the environment, can be used to predict the best ways to prevent and treat heart, lung, blood, and sleep disorders. TOPMed specifically supports NHLBI’s Precision Medicine Activities.
- NHLBI population and epidemiology studies in different groups of people, including the Atherosclerosis Risk in Communities (ARIC) Study , the Multi-Ethnic Study of Atherosclerosis (MESA) , and the Cardiovascular Health Study (CHS) , have made major contributions to understanding the causes and prevention of heart and vascular diseases, including coronary heart disease.
- The Cardiothoracic Surgical Trials Network (CTSN) is an international clinical research enterprise that studies heart valve disease , arrhythmias , heart failure, coronary heart disease, and surgical complications. The trials span all phases of development, from early translation to completion, and have more than 14,000 participants. The trials include six completed randomized clinical trials, three large observational studies, and many other smaller studies.

Learn how heart disease may be different for women than for men.
Explore more NHLBI research on coronary heart disease
The sections above provide you with the highlights of NHLBI-supported research on coronary heart disease. You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 14 December 2021
A case control study of occupation and cardiovascular disease risk in Japanese men and women
- Kota Fukai 1 ,
- Yuko Furuya 1 ,
- Shoko Nakazawa 1 ,
- Noriko Kojimahara 2 ,
- Keika Hoshi 3 , 4 ,
- Akihiro Toyota 5 &
- Masayuki Tatemichi nAff1
Scientific Reports volume 11 , Article number: 23983 ( 2021 ) Cite this article
5287 Accesses
10 Citations
6 Altmetric
Metrics details
- Epidemiology
- Occupational health
We aimed to investigate the risks of cardiovascular diseases associated with specific occupations, using a nation-wide, multicentre, hospital-based registry data from the Inpatient Clinico-Occupational Survey. The analysis included 539,110 controls (non-circulatory disease) and 23,792 cases (cerebral infarction, intracerebral/subarachnoid hemorrhage, acute myocardial infarction) aged ≥ 20 years who were initially hospitalized during 2005–2015. The participants’ occupational and clinical histories were collected by interviewers and medical doctors. Occupations were coded into 81 categories according to the Japanese standard occupation classification. Multivariable logistic regression analysis adjusted for age, admission year and hospital, smoking, alcohol consumption, hypertension, and shift-work was conducted by sex using general clerical workers as the reference. Increased risks of cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction, were observed in 15, 20, 25, and 1 occupation(s) in men, and 9, 2, 2, and 10 occupations in women. Motor vehicle drivers, food and drink preparatory workers, fishery workers, cargo workers, civil engineer workers, and other manual workers in men and other manual workers in women faced increased risks of all three stroke subtypes. Our findings demonstrate associations between specific occupations and the risk of cardiovascular disease incidence and suggest that the risk may vary by occupation.
Similar content being viewed by others

The effects of genetic and modifiable risk factors on brain regions vulnerable to ageing and disease
Jordi Manuello, Joosung Min, … Gwenaëlle Douaud
Risk of COVID-19 death in adults who received booster COVID-19 vaccinations in England
Isobel L. Ward, Chris Robertson, … Vahé Nafilyan

Cardiovascular disease and cancer: shared risk factors and mechanisms
Nicholas S. Wilcox, Uri Amit, … Bonnie Ky
Introduction
The incidence of cardiovascular disease (CVD), including stroke and coronary heart disease (CHD), has exhibited a decreasing trend in Japan since the late twentieth century 1 . However, CVD remains associated with a high disease burden and major concerns in workers.
Previously, socio-epidemiological studies suggested that the occupational grade or class, a known social determinant of health, may also be a risk factor for CVD 2 . In the Whitehall study, Marmot et al. classified 17,530 British civil servants into four occupational grades (administrator, professional and executive, clerical, and other) and reported that the 10-year CHD mortality rate was three times higher in the lowest grade (other) relative to the highest grade (administrator) 3 . In Japan, Zaitsu et al. recently reported the risks of CHD and stroke incidence associated with broad occupational categories (manager, professional, service, and blue-collar) in combination with industrial clusters (white-collar, service, and blue-collar) 4 . Compared to the study in Britain 3 , the study in Japan identified a stronger pattern of CHD risk in higher occupational classes 4 . Other studies have also reported an association between CVD and occupational classes 5 , 6 , however, the results have been inconsistent. Therefore, it is difficult for clinicians to apply the findings in actual practice, even if they collected past occupational histories.
We hypothesized that there might be hidden hazards in various subcategorized occupations that may contribute to the risk of developing CVD. This research background suggests a need to focus on the specific occupation as epidemiological evidence rather than as a feature that can be represented by occupational grades or classes 7 . Generally, occupational classification schemes are not sufficiently detailed to enable a fine-scale analysis of associations with health measures 8 . One recent study demonstrated that the use of a detailed classification of occupations more accurately predicted health measures than did a broader classification or various combinations of socio-economic factors 7 . This may also be due to unknown occupational-related potential factors besides the effects of individual health status factors such as hypertension, smoking, or alcohol consumption, which are risk factors for CVD. In other words, it is important to examine the association between an individual’s detailed occupation and the risk of CVD onset from the viewpoint of occupational medicine. Roles may be different between men and women in the same occupation. To the best of our knowledge, no previously published study has explored this relationship. Therefore, we aimed to examine whether the incidence of CVD differs depending on the specific occupation among adults who participated in a nation-wide large-scale inpatient registry in Japan.
Study design and participants
This is a nation-wide multi-hospital-based case–control study. The present study was conducted using data from the Inpatient Clinico-Occupational Survey, which has been conducted by the Rosai Hospital Group since 1984. The details of this survey have been described elsewhere 4 , 9 , 10 . Briefly, the Inpatient Clinico-Occupational Survey collects clinical and occupational history information for all inpatients older than 15 years who were admitted to facilities belonging to the nation-wide Rosai Hospital Group (> 13,000 beds in 34 hospitals as in the year 2015) and remained alive at 24 h after admission. The clinical history data of each patient were combined with a summary of inpatient treatment recorded by physicians. Definitive diagnoses for admission were coded using the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) 11 . Lifestyle habits (e.g., smoking and alcohol consumption) and history of hypertension were also included in the clinical history. All information was registered in the Inpatient Clinico-Occupational Database by the health information manager and a trained occupational history surveyor at each hospital. Data were collected at each admission for patients who were hospitalized multiple times during the study period. The clinical and occupational history registry rates were nearly 100% and 66%, respectively.
For the present study, we used data collected during 2005–2015, when the clinical and occupational data of 829,926 participants were subjected to analysis. For patients who were hospitalized multiple times, only the first hospitalization data were used. We excluded participants younger than 20 years (n = 18,094); those whose occupation were unclassifiable (n = 303); those for whom were unemployed as the longest-held occupation (n = 77,895), student (n = 18,993), homemaker (n = 118,973). Furthermore, we excluded those admitted for diseases of the circulatory system except CVD (n = 32,825). Finally, 562,902 participants remained for analysis.
This study was performed according to the tenets of the Declaration of Helsinki. Written informed consent was obtained from each patient prior to completion of all the questionnaires. Access to the dataset was provided under a research agreement between the study authors and the Japan Organization of Occupational Health and Safety. This study was approved by the Research Ethics Committees of Tokai University School of Medicine, Kanagawa, Japan (Protocol Number 18R-309) and the Japan Organization of Occupational Health and Safety (Protocol Number R1-006).
Cases and controls
CVD cases were defined as patients with a diagnosis at admission of cerebral infarction (ICD-10, I63; n = 12,826), intracerebral haemorrhage (ICD-10, I61; n = 4905), subarachnoid haemorrhage (ICD-10, I60; n = 1641), and acute myocardial infarction (ICD-10, I21; n = 4420). Consistent with the methodology used in previous studies 12 , the controls were defined as patients who were admitted at the same hospital and during the same period for reasons other than diseases of the circulatory system (ICD-10, I00 to I99 except for I21, I60, I61, I63; n = 65,591). The final analysis included 23,792 cases and 539,110 controls. The participant flowchart is outlined in S1 Fig.
Occupation assessment
The participants were interviewed regarding their current and three previous occupations, as well as the duration of each. Occupational history information was coded according to the Japan Standard Occupational Classification, which was published by the Japanese Ministry of Internal Affairs and Communications 13 by a trained occupational history surveyor. To accommodate the revision of the Japan Standard Occupational Classification which was published by the government during the survey, the Japan Organisation of Occupational Health and Safety created an original unified code of 81 occupations that would cover the revision. This unified classification is roughly compliant with the sub-major (two-digit codes, 43 groups) and minor (three-digit codes, 130 groups) categories of the International Standard Classification of Occupations 2008 (ISCO-08) 14 . For each participant, the longest-held of the four most recent occupations was adopted as the exposure variable. Information about shift-work history was also collected. The list of occupations and numbers of controls and cases in detail are presented in S1 Table.
Statistical analyses
The odds ratios (ORs) and 95% confidence intervals (95% CIs) of the incidence of CVD (cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction) were estimated using multivariable logistic regression analysis. We used general clerical workers as the reference group in all analyses because it was the most frequent category for both men and women and was considered to have less effect of various occupational hazards. Lifestyle habits (e.g., smoking and alcohol consumption) and history of hypertension were also included in the clinical history. Model 1 was the unadjusted model. Model 2 was created by adjusting for age (in years, continuous), admission date (in years, categorical), and admitting hospital (34 hospitals, categorical). We the adjusted admission date to explore potential heterogeneity introduced by changes in the environment within the occupation and by secular changes in diagnostic practices or treatment. Also, we adjusted the admission hospital to account for differences by region, despite the same occupation, such as rural and urban areas, since this database was nationwide database. Model 3 was further adjusted for smoking (never smoker, former smoker, current smoker), alcohol consumption (non-drinker, former drinker, current drinker), and hypertension (yes/no). In Japan, hypertension has a high prevalence and the outcome (CVD) is not only caused by the exposure (occupation). Since hypertension is both associated with occupation and CVD, we adjusted hypertension in model 3 as a potential cofounder. Model 4 was further adjusted for shift-work (yes/no). No missing values for confounders in the dataset for this analysis existed due to a standard protocol by trained interviewers.
While CVD is chronically affected by the cardiovascular system, it is a sudden-onset disease, and to account for acute effects, we conducted a sensitivity analysis using the current occupation as an exposure variable. A two-sided p value < 0.05 was considered statistically significant. All analyses were performed using the Statistical Analysis System (SAS) Software version 9.4 (SAS Institute, Cary, NC, USA).
The characteristics of the cases and controls are presented in Table 1 . Notably, the distributions of age and smoking status differed between these groups. Cases of subarachnoid hemorrhage included younger patients and tended to include large proportions of current smokers and alcohol drinkers.
Cerebral infarction accounted for the largest number of cases among both men and women, and the ORs of various occupations for the incidence of cerebral infarction were calculated using each model. The statistically significant results corresponding to occupations resulting from any of the four models are described in Fig. 1 a (men) and Fig. 1 b (women), and the full results are available in S2 Table. In the fully adjusted model (Model 4), high ORs of cerebral infarction were observed in 15 occupations among men (doctors, dentists, veterinarians, pharmacists; other health care workers; authors, journalists, editors; other managerial workers; merchandise sales workers; domestic hygiene service workers; food and drink preparatory workers; other service workers; fishery; motor vehicle drivers; other transport workers; electro-mechanic assembly workers; civil engineer workers; cargo workers; and other manual workers), as well as 9 occupations among women (other engineers; other managerial workers; customer service workers; residential facilities management personnel; agriculture; other mechanical assembly; food manufacturing; construction machinery operators; and other manual workers). Low ORs of cerebral infarction were observed in management staff of government officials and forestry among men, and none among women. The results of the unadjusted model (Model 1) differed somewhat from those of the other models. After adjusting for age (Model 2), however, the results remained consistent even with further adjustments (e.g., admission date, hospital, smoking, drinking, hypertension, and shift-work). The full results of cases of intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction are available in S3 – S5 Tables. These results were similar to those of cases of cerebral infarction, although smoking and alcohol consumption also appeared to affect the incidence of subarachnoid hemorrhage and acute myocardial infarction. Shift-work had no apparent effect on the associations of occupations with CVD.
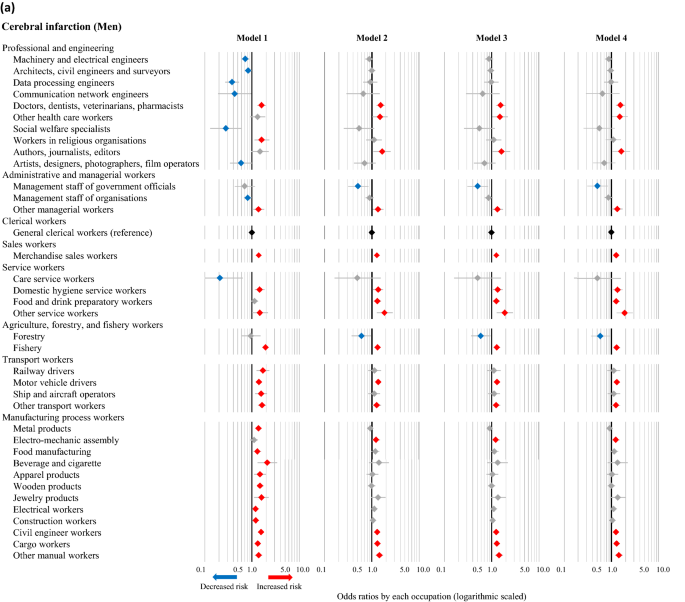
Odds ratios of cerebral infarction associated with occupations among men ( a ) and women ( b ) based on different models. The odds ratios (symbols) and 95% confidence intervals (bars) were estimated using univariate and multivariable logistic regression analyses, with general clerical workers as the reference. Red and blue symbols indicate statistically significant increases and decreases in risk, respectively. Model 1: Unadjusted. Model 2: Adjusted for age, admission date, and hospital. Model 3: Adjusted for the factors in Model 2 plus smoking, alcohol consumption, and hypertension. Model 4: Adjusted for the factors in Model 3 plus shift-work.
The fully adjusted ORs (Model 4) for cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction in association with various occupations were also calculated, using general clerical workers as the reference group. The statistically significant results corresponding to specific occupations in any of the four disease categories are presented in Fig. 2 a (men) and Fig. 2 b (women), while the full results are available in S2 – S5 Tables. The number of categories that were significantly associated with increased risks of cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction were, 15, 20, 25, and one occupation(s) among men, respectively, while two, zero, zero, and six occupations were associated with decreased risks of the respective conditions. Moreover, among men, increased risks of all three subtypes of stroke were observed in food and drink preparatory workers, fishery, motor vehicle drivers, civil engineer workers, cargo workers, and other manual workers. Among women, nine, two, two, and ten occupations were associated with a significantly increased risk of cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction, respectively, while one, zero, zero, and zero occupations were associated with decreased risks of the respective conditions. Moreover, female participants classified as other manual workers had increased risks of all three subtypes of stroke. Female food and drink preparatory workers also exhibited an increasing trend in the risk of all three subtypes of stroke, although these associations were not statistically significant.
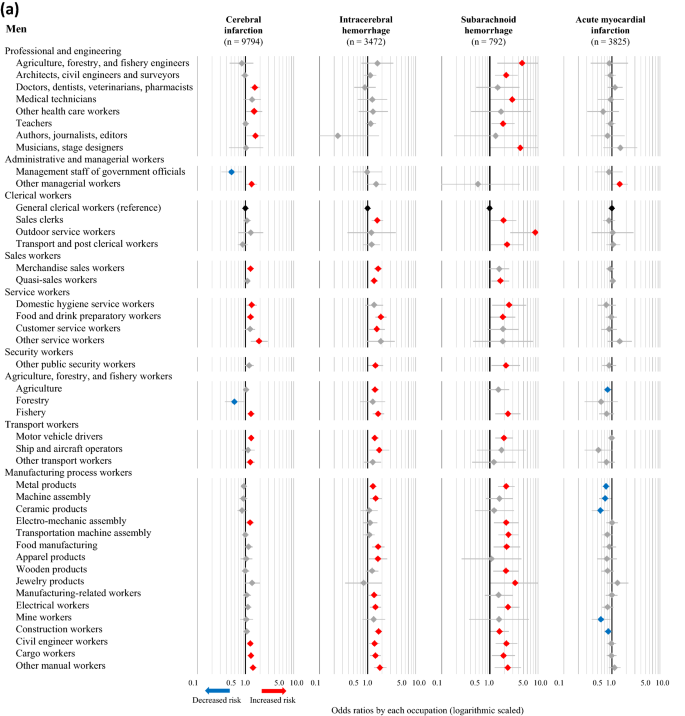
Odds ratios for CVD associated with occupations among men ( a ) and women ( b ). The odds ratios (symbols) and 95% confidence intervals (bars) were estimated using multivariable logistic regression analysis, with general clerical workers as the reference. The analysis was adjusted for age, admission date, hospital, smoking, alcohol consumption, hypertension, and shift-work. Red and blue symbols indicate statistically significant increases and decreases in risk, respectively.
The results of the sensitivity analysis, which included only participants whose current occupation was also the longest-held occupation, are presented in Fig. 3 a (men) and Fig. 3 b (women) as fully adjusted ORs (Model 4) of the incidence of CVD. Among men, two, 17, and 19 occupations were associated with an increased risk of cerebral infarction, intracerebral hemorrhage, and subarachnoid hemorrhage, respectively, to the same degree observed in the full population analysis, while two occupations were associated with a decreased risk. Consistent with the full analysis, male motor vehicle drivers continued to face increased risks of all three subtypes of stroke. Among women, two, one, and four occupations were associated with an increased risk of cerebral infarction, intracerebral hemorrhage, and acute myocardial infarction, respectively, to the same degree observed in the full population analysis.
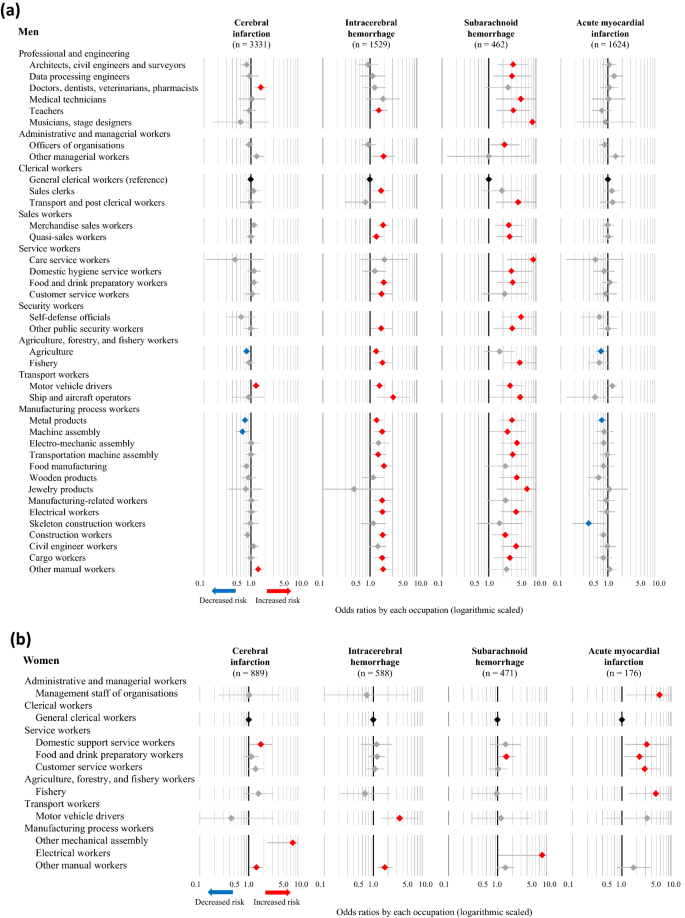
Odds ratios for CVD associated with occupations among men ( a ) and women ( b ) whose current occupation was also the longest-held occupation. The odds ratios (symbols) and 95% confidence intervals (bars) were estimated using multivariable logistic regression analysis, with general clerical workers as the reference. The analysis was adjusted for age, admission date, hospital, smoking, alcohol consumption, hypertension, and shift-work. Red and blue symbols indicate statistically significant increases and decreases in risk, respectively.
In this study, based on a data set from a nation-wide large-scale inpatient survey in Japan, we explored the potential associations between specific occupations and CVD. Although some previous studies have demonstrated associations between occupational classes or grades and CVD 3 , 4 , 15 , 16 , 17 , ours is one of the first to provide descriptive results associated with specific occupations. Interestingly, there were clear differences in the association of specific occupations with a risk for CVD between men and women, cerebral versus coronary, and between cerebral infarction and hemorrhage. There was one specific occupation that increased the risk for CHD in men, but ten occupations showed a significantly increased risk in women. On the other hand, men had many occupations that increased the risk for cerebrovascular diseases, but women had few.
Among men, only other management workers increased the risk for CHD. On the other hand, motor vehicle drivers, food and drink preparatory workers, and other manual workers exhibited a robust increase in the risk of all three subtypes of stroke when compared with the reference group of general clerical workers. However, in our sensitivity analysis (Fig. 3 a), only doctors, motor vehicle drivers, and other manual workers showed a slightly increased risk for cerebral infarction. While quasi-sales workers (i.e. other sales workers), food and drink preparatory workers, fishery workers, and manufacturing process workers (e.g., metal producers, skeleton construction workers, civil engineers, and cargo workers) faced increased risks of both intracerebral and subarachnoid hemorrhage, but not cerebral infarction. Hypertension plays a pivotal role in stroke, particularly hemorrhage 18 , although we conducted model-based adjustment for hypertension based on information of the present illness. We consider that these specific occupations with an increased risk for hemorrhage may temporarily and markedly elevate blood pressures in workers by mental or physical stresses. In addition, the ‘physical activity paradox’ is recently emphasized, and occupational physical activity (OPA) is considered to play an important role in CVD 19 . According to Steeves’s classifications 20 , the occupations that were found to be associated with intracerebral hemorrhage were classified as occupations with high OPA levels. The occupations with high odds ratios of intracerebral haemorrhage such as agriculture, forestry, and fishery engineers (OR = 4.72), outdoor service workers (OR = 8.86), communication workers (OR = 3.60) are considered to be high OPA level. Further investigation of OPA levels and CVD risk is needed.
In women, there were significant occupations associated with an increased risk of CHD, such as management staff of organizations, domestic support service workers, customer service workers, and fishery workers. These findings were different from those in men suggesting that it might be more mentally stressful for women than men, resulting in the development of coronary arterial atherosclerosis. However, the associations between specific occupations and cerebral hemorrhages were less clear. Three types of manufacturing process workers (food manufacturing, construction machinery operators, and other mechanical assembly workers) had a strongly increased risk of stroke. Orthostatic hypotension is an important risk factor for stroke 21 . Thus, among workers with these occupations, they stand all day, and chronic orthostatic hypotension might be a risk factor. Other engineers and other managerial workers also showed an increased risk for stroke. However, this classification was not clear, and the reason was unknown.
Motor vehicle drivers and food and drink preparatory workers exhibited a robust increase in the risk of all three subtypes of stroke. As for other possibilities, we may point out the risk of passive smoking. This is a major public health issue that is considered a risk factor for CVD 22 , 23 , 24 . In Japan, the Health Promotion Law enacted in 2003 obligated administrators of public facilities to make efforts to prevent passive smoking. However, restaurants and taxicabs were the least developed areas for passive smoking prevention. Until the late 2000s, Japanese taxi drivers were exposed to second-hand cigarette smoke due to passengers 25 . Many restaurants that employ food and drink preparatory workers do not impose restrictions on smoking, which was allowed in 95.9% of the customer areas and 85.0% of the employee work areas in restaurants in 2007 26 . According to the Japanese National Health and Nutrition Survey in 2013, 50.9% of people were exposed to second-hand smoke at restaurants 27 . The evidence suggests that second-hand smoke may have contributed to the increased risk of CVD among subjects employed in workplaces without smoking restrictions.
Although it is difficult to compare our findings with those of previous studies that focused on occupational classes or grades, our results generally appear to be consistent with those of earlier analyses. Particularly, socioeconomically advantaged groups tend to have a lower risk of CVD 6 , whereas so-called manual workers have a higher risk 16 , 28 . Our results demonstrate that several occupations in the categories of manufacturing process, service, and sales were associated with a high risk of CVD even after adjusting for age, smoking and alcohol consumption habits, hypertension, and shift work. Thus, our results indicate that information on the occupation of patients is important for physicians to prevent the onset of CVD.
One strength of this study is the use of an extensive set of detailed information about previous and current occupations which was collected by professionally trained investigators. An analysis of the relationships between occupations and CVD risk requires a large population for which specific occupation data are available. Although hypertension and smoking are the risk factors most strongly associated with CVD 29 , an assessment focused on the occupational histories of participants in a clinical population at risk of CVD is important from the viewpoint of occupational medicine. We noted that in our survey, the association between occupation and CVD remained even after other factors were adjusted, suggesting the involvement of hidden occupation-related factors.
Our study had limitations. First, the study may have been subject to selection bias regarding the controls (i.e., Berkson’s bias) 30 . The hospital admission probability is defined as the probability that the members of a community group will be admitted to the hospital 31 , and we selected controls from among patients admitted to the same hospitals as the cases. The distribution of the occupational profiles of our controls were nationally representative 4 , 9 . Yet, bias towards or away from null association may exist in the selection of hospital controls, who may be more biased toward risk factors for being hospitalized for any disease than the general population. Second, data regarding other clinical risk factors for CVD, such as blood pressure, total cholesterol, and glucose intolerance, were unavailable. However, we used self-reported data adjusted for a history of hypertension. Third, other socioeconomic covariates such as working hours or income which were examined in other relevant studies 6 , 32 were not assessed due to the lack of data. Employees who worked long hours had a higher risk of stroke than those working standard hours; the association with CHD was weaker 32 . Future studies should consider the effects of long working hours on the difference of onset of stroke and CHD. No strong association between the income level and CVD risk has been observed in Japan 6 . For available factors, we adjusted shift work as a work-related factor and achieved consistent results. Fourth, we considered only the longest-held occupation as the risk factor, and we did not consider the impact of a change nor sequence in employment. There is a possibility that they may have changed jobs or become unemployed depending on their health conditions. Further assessment is needed to address this variable.
In conclusion, the present study has clearly demonstrated the difference between long-held specific occupations and the risk of CVD. From the viewpoint of occupational medicine, our results may be valuable to investigate key factors among these potentially high-risk occupations in terms of the risk of CVD.
Data availability
The datasets are not publicly available due to restrictions used under the license for the current study. There are available on reasonable request from the corresponding author.
Hata, J. et al. Secular trends in cardiovascular disease and its risk factors in Japanese: Half-century data from the Hisayama Study (1961–2009). Circulation 128 , 1198–1205. https://doi.org/10.1161/CIRCULATIONAHA.113.002424 (2013).
Article PubMed Google Scholar
Havranek, E. P. et al. Social determinants of risk and outcomes for cardiovascular disease: A scientific statement from the American Heart Association. Circulation 132 , 873–898. https://doi.org/10.1161/CIR.0000000000000228 (2015).
Marmot, M. G., Shipley, M. J. & Rose, G. Inequalities in death-specific explanations of a general pattern?. Lancet 323 , 1003–1006. https://doi.org/10.1016/S0140-6736(84)92337-7 (1984).
Article Google Scholar
Zaitsu, M. et al. Occupational class and risk of cardiovascular disease incidence in Japan: Nationwide, multicenter, hospital-based case-control study. J. Am. Heart Assoc. 8 , e011350–e011350. https://doi.org/10.1161/JAHA.118.011350 (2019).
Article PubMed PubMed Central Google Scholar
Chen, R., McKevitt, C., Rudd, A. G. & Wolfe, C. D. A. Socioeconomic deprivation and survival after stroke findings from the prospective south london stroke register of 1995 to 2011. Stroke 45 , 217–223. https://doi.org/10.1161/Strokeaha.113.003266 (2014).
Marshall, I. J. et al. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 14 , 1206–1218. https://doi.org/10.1016/S1474-4422(15)00200-8 (2015).
Eyles, E., Manley, D. & Jones, K. Occupied with classification: Which occupational classification scheme better predicts health outcomes?. Soc. Sci. Med. 227 , 56–62. https://doi.org/10.1016/j.socscimed.2018.09.020 (2019).
Clougherty, J. E., Souza, K. & Cullen, M. R. Work and its role in shaping the social gradient in health. Ann. N. Y. Acad. Sci. 1186 , 102–124. https://doi.org/10.1111/j.1749-6632.2009.05338.x (2010).
Article ADS PubMed PubMed Central Google Scholar
Kaneko, R., Zaitsu, M., Sato, Y. & Kobayashi, Y. Risk of cancer and longest-held occupations in Japanese workers: A multicenter hospital-based case-control study. Cancer Med. 8 , 6139–6150. https://doi.org/10.1002/cam4.2499 (2019).
Fukai, K., Kojimahara, N., Hoshi, K., Toyota, A. & Tatemichi, M. Combined effects of occupational exposure to hazardous operations and lifestyle-related factors on cancer incidence. Cancer Sci. 111 , 4581–4593. https://doi.org/10.1111/cas.14663 (2020).
Article CAS PubMed PubMed Central Google Scholar
World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: 10th revision , 2nd ed. https://apps.who.int/iris/handle/10665/42980 (2004).
Wacholder, S., Silverman, D. T., McLaughlin, J. K. & Mandel, J. S. Selection of controls in case-control studies: II. Types of controls. Am. J. Epidemiol. 135 , 1029–1041. https://doi.org/10.1093/oxfordjournals.aje.a116397 (1992).
Article CAS PubMed Google Scholar
Japanese Ministry of Internal Affairs and Communications. Japan Standard Occupational Classification http://www.soumu.go.jp/english/dgpp_ss/seido/shokgyou/index-co.htm (2009).
International Labour Organization. International Standard Classification of Occupations . https://www.ilo.org/public/english/bureau/stat/isco/isco08/ (2016).
Marmot, M. G. & Shipley, M. J. Do socioeconomic differences in mortality persist after retirement? 25 year follow up of civil servants from the first Whitehall study. BMJ 313 , 1177–1180. https://doi.org/10.1136/bmj.313.7066.1177 (1996).
McFadden, E., Luben, R., Wareham, N., Bingham, S. & Khaw, K. T. Social class, risk factors, and stroke incidence in men and women a prospective study in the european prospective investigation into cancer in norfolk cohort. Stroke 40 , 1070–1077. https://doi.org/10.1161/STROKEAHA.108.533414 (2009).
Min, Y. I. et al. Cardiovascular disease burden and socioeconomic correlates: Findings from the Jackson Heart Study. J. Am. Heart Assoc. 6 , e004416–e004416. https://doi.org/10.1161/JAHA.116.004416 (2017).
Andalib, S. et al. Blood pressure variability: A new predicting factor for clinical outcomes of intracerebral hemorrhage. J. Stroke Cerebrovasc. Dis. 29 , 105340. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105340 (2020).
Holtermann, A., Schnohr, P., Nordestgaard, B. G. & Marott, J. L. The physical activity paradox in cardiovascular disease and all-cause mortality: The contemporary Copenhagen General Population Study with 104 046 adults. Eur. Heart J. 42 , 1499–1511. https://doi.org/10.1093/eurheartj/ehab087 (2021).
Steeves, J. A. et al. Daily physical activity by occupational classification in US adults: NHANES 2005–2006. J. Phys. Act Health https://doi.org/10.1123/jpah.2017-0465 (2018).
Min, M. et al. The association between orthostatic hypotension and cognition and stroke: A meta-analysis of prospective cohort studies. Blood Press. 29 , 3–12. https://doi.org/10.1080/08037051.2019.1689808 (2020).
Saito, J. et al. ‘Only Fathers Smoking’ contributes the most to socioeconomic inequalities: Changes in socioeconomic inequalities in infants’ exposure to second hand smoke over time in Japan. PLoS ONE 10 , e0139512–e0139512. https://doi.org/10.1371/journal.pone.0139512 (2015).
Öberg, M., Jaakkola, M. S., Woodward, A., Peruga, A. & Prüss-Ustün, A. Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. Lancet 377 , 139–146. https://doi.org/10.1016/S0140-6736(10)61388-8 (2011).
Barnoya, J. & Glantz, S. A. Cardiovascular effects of secondhand smoke: Nearly as large as smoking. Circulation 111 , 2684–2698. https://doi.org/10.1161/CIRCULATIONAHA.104.492215 (2005).
Kobayashi, F. et al. Acute effects of cigarette smoking on the heart rate variability of taxi drivers during work. Scand. J. Work. Environ. Health 31 , 360–366. https://doi.org/10.2307/40967516 (2005).
Sakamoto, R. et al. Second-hand smoke in restaurants after enforcement of a health promotion law in Japan. J. Public Health Policy 28 , 156–161. https://doi.org/10.1057/palgrave.jphp.3200120 (2007).
Japanese Ministry of Health Labour and Welfare. The National Health and Nutrition Survey in Japan https://www.mhlw.go.jp/bunya/kenkou/eiyou/h25-houkoku.html (2013).
Novak, M. et al. Occupational status and incidences of ischemic and hemorrhagic stroke in Swedish men: A population-based 35-year prospective follow-up study. Eur. J. Epidemiol. 28 , 697–704. https://doi.org/10.1007/s10654-013-9833-8 (2013).
Ueshima, H. et al. Cardiovascular disease and risk factors in Asia: A selected review. Circulation 118 , 2702–2709. https://doi.org/10.1161/CIRCULATIONAHA.108.790048 (2008).
Schwartzbaum, J., Ahlbom, A. & Feychting, M. Berkson’s bias reviewed. Eur. J. Epidemiol. 18 , 1109–1112. https://doi.org/10.1023/B:EJEP.0000006552.89605.c8 (2003).
Berkson, J. Limitations of the application of fourfold table analysis to hospital data. Int. J. Epidemiol. 43 , 511–515. https://doi.org/10.1093/ije/dyu022 (2014).
Kivimäki, M. et al. Long working hours and risk of coronary heart disease and stroke: A systematic review and meta-analysis of published and unpublished data for 603 838 individuals. Lancet 386 , 1739–1746. https://doi.org/10.1016/S0140-6736(15)60295-1 (2015).
Download references
Acknowledgements
We would like to express gratitude to all the study staff in JOHAS for their commitment to data collection. We would like to thank Editage ( http://www.editage.com ) for editing and reviewing this manuscript for English language.
This work was supported by Research Project on Inpatient Clinico-Occupational Database of Rosai Hospital Group (2021).
Author information
- Masayuki Tatemichi
Present address: Department of Preventive Medicine, Tokai University School of Medicine, Isehara, Japan
Authors and Affiliations
Department of Preventive Medicine, Tokai University School of Medicine, Isehara, Japan
Kota Fukai, Yuko Furuya & Shoko Nakazawa
Department of Public Health, Shizuoka Graduate University of Public Health, Shizuoka, Japan
Noriko Kojimahara
Center for Public Health Informatics, National Institute of Public Health, Wako, Japan
Keika Hoshi
Department of Hygiene, School of Medicine, Kitasato University, Sagamihara, Japan
Chugoku Rosai Hospital Research Center for the Promotion of Health and Employment Support, Japan Organization of Occupational Health and Safety, Hiroshima, Japan
Akihiro Toyota
You can also search for this author in PubMed Google Scholar
Contributions
N.K., K.H., A.T., and M.T. received funding acquisition and collected data. Y.F., K.F., and S.N. designed this study and analysed the data. Y.F., K.F., and M.T. wrote the paper. K.F., N.K., K.H., A.T., and M.T. supervised this study and provided critical comments. All authors reviewed the manuscript.
Corresponding author
Correspondence to Masayuki Tatemichi .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary figure s1., supplementary table s1., supplementary table s2., supplementary table s3., supplementary table s4., supplementary table s5., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Fukai, K., Furuya, Y., Nakazawa, S. et al. A case control study of occupation and cardiovascular disease risk in Japanese men and women. Sci Rep 11 , 23983 (2021). https://doi.org/10.1038/s41598-021-03410-9
Download citation
Received : 15 June 2021
Accepted : 30 November 2021
Published : 14 December 2021
DOI : https://doi.org/10.1038/s41598-021-03410-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Incidence of coronary heart disease among remote workers: a nationwide web-based cohort study.
- Masayoshi Zaitsu
- Tomohiro Ishimaru
- Yoshihisa Fujino
Scientific Reports (2024)
Alcohol use patterns and risk of incident cataract surgery: a large scale case–control study in Japan
- Ryo Terauchi
Scientific Reports (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Case Report: Congestive Heart Failure
The patient's heart failure needs to be classified to determine the appropriate treatment strategy.
Case Presentation
WC is a 67-year-old man with hypertension, hyperlipidemia, and coronary artery disease, and had triple bypass surgery 17 years ago. His current home medications include amlodipine 10 mg once daily, atorvastatin 80 mg once daily, and aspirin 81 mg once daily. He presents to the clinic with shortness of breath (SOB), which occurs when performing simple tasks such as sweeping the floor. He reports sleeping in a recliner at night due to orthopnea. Physical examination reveals elevated jugular venous pressure and 1+ pitting lower extremity edema (LEE). An echocardiogram demonstrates systolic dysfunction, mild mitral regurgitation, a dilated left atrium, and an ejection fraction (EF) of 30%. Laboratory results show a pro-B-type natriuretic peptide level of 1302 pg/mL, a troponin level of <0.34, and an unremarkable basic metabolic panel (BMP). Measurement of vital signs shows blood pressure (BP) of 156/92 mm Hg, a heart rate of 80 beats/min, an Spo 2 of 94%, a temperature of 36.5 °C, a pain level of 2 on a scale of 10, and a weight of 185 lb (84.1 kg). WC’s pharmacy coverage is Medicare Part D. The medical team would like assistance in optimizing the medication regimen for WC’s new diagnosis.
First, the patient’s heart failure needs to be classified to determine the appropriate treatment strategy. The patient’s EF is ≤40%; therefore, per the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) 2013 Guideline for the Management of Heart Failure, WC’s condition will be categorized as heart failure with reduced ejection fraction (HFrEF), also known as systolic heart failure. 1 The atrial dilation and systolic dysfunction seen on the echocardiogram are evidence of structural heart disease. The patient is also exhibiting symptoms that limit his daily activities. These 2 findings together categorize the patient’s condition as ACCF/AHA stage C. 1 Further, the patient has SOB with normal activity, but is comfortable at rest, so his condition has a functional classification of II, according to the New York Heart Association (NYHA) . 1
The following are indicated for stage C HFrEF: an angiotensin-converting enzyme (ACE) inhibitor (or angiotensin receptor blocker if the patient cannot tolerate an ACE inhibitor) and beta blocker (specifically metoprolol succinate, bisoprolol, or carvedilol). 1 In addition, for NYHA functional classes II through IV, an aldosterone antagonist is recommended if the estimated creatinine clearance is >30 mL/min and the potassium level is <5.0 mEq/dL. 1 In clinical trials, these medication classes have demonstrated a decrease in mortality and morbidity when used in patients with HFrEF. 2-4 Non-dihydropyridine channel blockers, such as verapamil and diltiazem, are not recommended due to their negative inotropic effects, which may cause harm in patients with HFrEF. 1 Despite a lack of mortality benefit, loop or thiazide diuretics are recommended for symptomatic management of hypervolemia in patients with normal renal function. 5 A diuretic is also recommended with initiation of a beta blocker in hypervolemic patients, due to increased fluid retention caused by beta blockers. It is important not to delay initiation of a beta blocker in these patients, due to the significant benefit demonstrated in clinical trials. 1
Because amlodipine is an antihypertensive that may contribute to LEE and has no proven functional or mortality benefit in HFrEF, it is reasonable to discontinue this medication in this patient. Hypertension is an important modifiable risk factor for all classifications of heart failure. 1,6,7 Per the 2014 American Society of Hypertension and the International Society of Hypertension (ASH/ISH) guidelines for the management of hypertension, WC’s goal BP is <140/90 mm Hg. 7 It would be acceptable to restart this medication at a later date if target doses of the ACE inhibitor, beta blocker, and aldosterone antagonist do not achieve the patient’s BP goal.
Based on guideline recommendations and evidence-based medicine, the following are reasonable recommendations for WC: discontinue amlodipine; initiate lisinopril 5 mg once daily, titrating it to the BP goal or a target dose of 40 mg, as tolerated; initiate furosemide 20 mg once daily, titrating it to the patient’s goal dry weight; initiate metoprolol succinate 25 mg once daily, titrating it, as tolerated, to a target dose of 200 mg once daily over 8 weeks; initiate spironolactone 25 mg once daily; return to the clinic in 3 to 7 days to reassess volume status, BP, and BMP to monitor renal function and electrolytes.
Heather Steelman Coleman, PharmD, is a PGY1 Ambulatory Care Pharmacy Resident at University of North Carolina (UNC) Health Care. She earned her doctor of pharmacy degree from UNC Eshelman School of Pharmacy.
- Writing Committee Members, Yancy CW, Jessup M, Bozkut B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation . 2013;128(16):e240-e327. doi: 10.1161/CIR.0b013e31829e8776.
- Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure: Collaborative Group on ACE Inhibitor Trials. JAMA .1995;273(18):1450-1456.
- Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet . 1999;353(9169):2001-2007.
- Pitt B, Zannad F, Remme WJ, et al; Randomized Aldactone Evaluation Study Investigators. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med . 1999;341(10):709-717.
- Leto L, Aspromonte N, Feola M. Efficacy and safety of loop diuretic therapy in acute decompensated heart failure: a clinical review. Heart Fail Rev . 2014;19(2):237-246. doi: 10.1007/s10741-012-9354-7.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA . 2014;311(5):507-520. doi: 10.1001/jama.2013.284427.
- Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens . 2014;32(1):3-15. doi: 10.1097/HJH.0000000000000065.
GLPs Are the Latest Example of the Shift to Alternative Purchasing Models

April Is Stress Awareness Month: A Little Humbling Self-Awareness May Go a Long Way

Empowering Oncology Pharmacists: Driving Innovation and Advancement Through Pharmacist-Led Research

OTC Contraception Hits Shelves

Continuing Education Programming Focuses on Specialty Pharmacy Skills

Pharmacy Policy Updates, March 2024
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Br J Clin Pharmacol
- v.47(3); 1999 Mar

Clinical case studies in heart failure management
Robert j macfadyen.
1 Department of Clinical Pharmacology, University of Dundee, Ninewells Hospital and Medical School, Dundee DD1 9SY, United Kingdom
2 Department of Cardiology, University of Dundee, Ninewells Hospital and Medical School, Dundee DD1 9SY, United Kingdom
Paul Shiels
Allan d struthers, therapeutic aspects of heart failure management.
The outlook for patients with cardiac failure has improved substantially in the last 15 years. This is largely due to the application of the results of multicentre clinical trials of new and older drugs and a better understanding of outcomes for individual patients. Interest has focused on systolic dysfunction in both symptomatic and asymptomatic patients. Less is known about the definition and management of diastolic dysfunction.
The following case studies have been chosen to illustrate the basis for therapeutic management of systolic heart failure and outline the remaining gaps in knowledge, of which there are several. The issues apply across the spectrum of patients seen in clinical practice.
Acute stabilization and chronic management of systolic failure
Case history.
A 74-year-old female patient was admitted from home with progressive increase in breathlessness, orthopnoea and ankle oedema over the previous 3 weeks. Her general practitioner had prescribed oral coamoxiclav and coamilofruse (substituting the latter for bendrofluazide). She had suffered from dyspepsia, increasing over recent weeks, and the general practitioner had noted a new murmur.
She was apyrexial yet tachypnoeic (25 beats min −1 ); with a low volume pulse. Sitting blood pressure was 110/70 mm Hg. The apex beat was in the anterior axillary line and a parasternal lift was prominent. A pansystolic murmur was audible and late inspiratory crackles were heard throughout both lung fields. There was sacral oedema.
The ECG confirmed sinus tachycardia (110 beats min −1 ) with antero-lateral Q waves of previous infarction and the chest X-ray confirmed cardiomegaly and interstitial oedema. Routine chemistry showed Na + 128 mmol l −1 ; K + 5.8 mmol l −1 ; urea 9 mmol l −1 ; creatinine 155 mmol l −1 . A creatine kinase series was unremarkable. Echocardiography showed a dilated heart (left ventricular end diastolic distension (LVEDD) 650 mm) with anterior and septal hypokinesis and apical dilatation compatible with previous anterior infarction. The posterior wall was contracting vigorously. A high velocity jet (4.7 m s −1 ) of mitral regurgitation was noted but the left atrial size was normal.
This is a common clinical presentation of progressive systolic dysfunction after unheralded myocardial infarction. A number of therapeutic and general management steps should be considered for all such patients. Whereas in stable patients clinical identification or grading of the severity of heart failure is unreliable [ 1 ], recent studies suggest that in acute heart failure clinical diagnosis is much more secure [ 2 ]. Any abnormality of the ECG in a breathless patient is supportive evidence for a cardiac cause of dyspnoea. A normal ECG usually suggests another diagnosis [ 3 ]. Radiological cardiomegaly is also supportive of a diagnosis of heart failure [ 4 ]. This is not the case for more subtle radiological signs, even in the hands of experienced radiological staff [ 5 ] where the clinical context can significantly affect the interpretation. Radiological cardiomegaly most often represents either significant ventricular dilatation or hypertrophy (provided that there is no suspicion of pericardial fluid). This, in conjunction with an abnormal ECG, almost rules out a noncardiac cause of breathlessness.
Echocardiography provides definitive diagnosis. Although a lack of quantitative images is a frequent practical problem, this may not be of importance to clinical management [ 6 ].
Immediate therapeutic strategies
While there is a lack of controlled clinical trial evidence to support the use of diuretics as initial therapy, effective diuresis and consequent adjustment of the loading conditions of the failing heart is generally regarded as essential [ 7 ]. Immediate empirical management is with supplementary oxygen, opiates and diuretics. Vasodilatation appears to be an important effect of intravenous diuretics although clear evidence for this is scant. However, relief of symptoms appears to precede diuresis and natriuresis.
Intravenous nitrate infusion provides balanced arterio- venous dilatation and is widely employed, supported by beneficial central haemodynamic changes in small studies [ 8 ], although little is known about its effects on either morbidity or mortality [ 9 ]. Intravenous ACE inhibitors also produce beneficial haemodynamic effects [ 10 ]. These drugs are not used routinely intravenously due to difficulties with appropriate dosage regimens, unpredictable and protracted hypotensive effects and concerns over an adverse effect on survival in haemodynamically unstable patients in the early stages after myocardial infarction [ 11 ]. More recent data suggest that there may yet be a role for intravenous administration of ACE inhibitors in unstable patients [ 12 ].
Long-term therapeutic issues
ACE inhibitors It is now clear that patients with either symptomatic or asymptomatic left ventricular dysfunction benefit from ACE inhibitor drugs. Morbidity is reduced with symptomatic improvement, improved exercise duration and improved quality of life indices. Mortality is reduced at all stages of the illness with greater absolute benefit the greater the degree of left ventricular impairment. Treatment is effective regardless of age, gender or aetiology of cardiac impairment. Further coronary events are also reduced in patients with ischaemic cardiomyopathy [ 13 ] although the reasons for this are obscure.
Research now focuses on the reasons why ACE inhibitors remain under used in the management of heart failure [ 14 ]. They are cost-effective in comparison with other cardiovascular treatments [ 15 ] (e.g. lipid lowering in patients with ischaemic heart disease; control of mild hypertension) even when used for treatment of mild (NYHA Grade I/II) heart failure. The reasons why individual patients do not receive an ACE inhibitor need to be clearly defined but may relate to unfounded concerns about side effects. The implications for such patients are a significantly worse prognosis for symptom control, repeated hospitalization and survival.
The degree of neurohormonal suppression by the ACE inhibitor is linked to survival in individual patients [ 16 ]. Some patients taking long-term ACE inhibitor therapy still have normal or elevated levels of the key mediator hormones aldosterone and angiotensin II. The reasons for this are unclear. It may be due to the secondary rise in active renin in response to treatment, failure of compliance, the use of short-acting agents (although these are undoubtedly better than placebo) or to alternative control pathways for generating angiotensin II (the tissue chymase system) and aldosterone (K + or ACTH).
Despite 20 years of study the minimum effective dose of an ACE inhibitor to treat heart failure remains unknown [ 17 ]. It is possible that the symptomatic and mortality benefits occur at different doses and are achieved through a combination of haemodynamic, hormonal or structural effects on the heart and/or the kidneys. One large but short-duration study of enalapril (NETWORK) [ 18 ] has suggested that high dosages may be unnecessary to reduce mortality. The results of a larger study with lisinopril (ATLAS) [ 19 ] suggest high doses may provide additional benefits.
The need for long-term loop diuretic treatment in stable patients taking an ACE inhibitor is unclear and has received little attention. Few studies address the effects of ACE inhibition alone compared with those of an ACE inhibitor plus diuretic, either in the short or long-term. Patients treated with and without a loop diuretic after myocardial infarction in the SAVE study appeared to benefit from captopril [ 20 ]. Those requiring a loop diuretic might have more significant impairment of left ventricular systolic function but this is by no means always the case. Although the left ventricular ejection fraction is an accurate predictor of mortality, it is poorly correlated with exercise capacity. Discontinuation of frusemide in patients with stable heart failure appears to be feasible in a minority of patients, usually those with lesser degrees of impairment of left ventricular function [ 21 ]. In practice this is rarely attempted and chronic diuretic therapy is usual for patients who have had one episode of overt heart failure requiring hospital admission.
Newer agents to suppress the renin angiotensin aldosterone system
Other agents that block the tissue and circulating RAS have been widely studied. Inhibitors of renin have been available for many years but there are few published data from controlled trials [ 22 ]. Low oral bioavailability has seriously compromised the value of this drug class although they are undoubtedly active biochemically and haemodynamically after intravenous administration [ 23 ].
More promising are the selective orally active nonpeptide antagonists of the angiotensin II AT 1 receptor (ARAs) of which there are now several [ 24 ]. Haemodynamic activity is predictable and all produce prolonged hormone suppression. These drugs have a significant advantage for some patients, since they do not produce the dry cough which results from potentiation of kinins during treatment with an ACE inhibitor [ 25 ].
A recent trial has shown a useful improvement in short-term survival with the AT 1 ARA losartan compared with thrice daily captopril in elderly patients with grade II/III heart failure [ 26 ]. This study was designed to examine the safety of losartan with respect to renal function. The reasons for reduced mortality in the group receiving losartan are unclear. The large body of experimental work suggesting that potentiation of the effects of kinins by ACE inhibitors has an important adjuvant role in the therapeutic effects of ACE inhibitors in heart failure [ 27 ] now appears to be in doubt. Before the use of ARAs can be recommended in preference to ACE inhibitors for the management of heart failure, this result must be confirmed in outcome trials. At present, ARAs are a useful alternative for patients intolerant of ACE inhibitors.
Other therapeutic options in systolic heart failure
Combination high dose oral nitrate and hydralazine therapy was shown in the mid 1980s to be effective in relieving symptoms of heart failure [ 28 ] although the impact on survival was less than that achieved by an ACE inhibitor [ 29 ]. The efficacy of nitrates or hydralazine alone has not been tested. The combination should be considered when an ACE inhibitor is contraindicated, e.g. in bilateral reno-vascular stenosis. The main limitation to this therapy is intolerable vasodilator side-effects in a substantial proportion of patients. Nitrate tolerance must be avoided by ensuring an 8 h wash-out phase overnight.
Management and course of the illustrative case
The patient was symptomatically improved by initial intravenous diuretics and supplemental oxygen correction of the fluid imbalance (1.5 l fluid restriction; oral coamilofruse twice daily) resulted in a weight loss of 4.5 kg over 5 days. Although supine blood pressure remained low (≈100 mmHg), an ACE inhibitor (perindopril 2 mg daily) was introduced without difficulty and she experienced no postural symptoms. Renal function improved in response to the changes in therapy. No other therapy was required long-term and diuretic dose was subsequently reduced to coamilofruse one daily). While remaining functionally limited at discharge, she was able to live independently. Having remained well during out-patient review and with no further cardiac admissions, she died suddenly at home some 18 months after presentation.
Optimization of therapy in established cardiac failure
A 53-year-old man who had sustained previous inferior and anterior myocardial infarctions presented with gradually increasing fatigue and oedema despite increasing diuretic therapy. He was being treated with frusemide 80 mg three times daily, captopril 50 mg three times daily, aspirin 150 mg once daily, isosorbide mononitrate SR 60 mg once daily and amlodipine 10 mg once daily.
On examination he had dependent oedema to the mid thigh and basal fine crepitations. He had a resting tachycardia of 105 beats min −1 in sinus rhythm. Mitral and tricuspid regurgitation were evident and the supine blood pressure was low at 95/48 mmHg. Laboratory investigation revealed a reduced serum sodium (125 mmol l −1 ) with impaired renal function (urea 12.8 mmol l −1 ; creatinine 189 μmol l −1 ). The chest radiograph showed minimal interstitial oedema, a right sided pleural effusion and marked cardiomegaly. A 24-h ECG shows repetitive but nonsustained ventricular tachycardia (4 episodes of 10–20 beats with rate >150 beats min −1 ) and multifocal ventricular ectopy (>15 000 aberrant beats/24 h). Repeat echocardiography revealed poor left ventricular contractility with global impairment, marked dilatation (LVEDD 750 mm) and functional mitral regurgitation. Radionuclide scintigraphy indicated a left ventricular ejection fraction of 11%.
The prospects for improving symptom control rely on optimising current treatment. Multiple drug therapy involves the risk of patient confusion over the medicines and a failure of compliance. This is a neglected area in the care of patients with heart failure [ 30 ] yet well known to be associated with poor clinical outcome in cardiac patients [ 31 ]. Most decompensated patients require hospital admission for assessment and observation although community based care is increasingly being studied to reduce costs (see below).
Isolated dependent oedema may be drug-related. Although amlodipine does not appear to cause deterioration in heart failure [ 32 ] unlike some calcium antagonists [ 33 ], marked oedema can occur in some patients. Unless active myocardial ischaemia is present and there are no other management options, withdrawal should be considered.
Diuretic resistance and optimising diuretic therapy
Initiating more effective diuresis and overcoming diuretic resistance is the first goal. Increasing the dosage or frequency of dosing with an oral loop diuretic has limited value for diuretic resistance. Improved efficacy can be achieved by a variety of means [ 34 ]. Oral combination diuretic therapy with the addition of a thiazide drug such as bendrofluazide is one option. Although metolazone is often used, it offers no greater benefit and may cause a greater incidence of adverse effects [ 35 ]. The combination of a loop diuretic with a potassium sparing diuretic is another possibility. If the patient is taking an ACE inhibitor, such an approach is not generally advised but can be used with success given careful control (see below). Combination diuretic treatment requires close monitoring. Once a diuresis is established, it may be possible to stop the additional drug. Long-term combination therapy has not been shown to be beneficial and the risks of electrolyte depletion and induction of dysrhythmia (although this remains controversial) raises concerns. If a combination of diuretics is continued, regular biochemical monitoring is desirable.
Another method to overcome resistance to loop diuretic therapy is intravenous administration either by bolus dosing or by continuous infusion [ 36 ]. The latter is particularly effective as it delivers a constant efficient concentration of frusemide at the tubular lumen. Careful monitoring of renal function and the extent of the diuresis are desirable.
Diuresis can also be enhanced by the addition of low-dose dopamine infusion to facilitate renal vasodilatation [ 37 ]. This may be used in combination with intravenous or oral loop diuretic. Oral dopamine agonist drugs have not been demonstrated to be useful [ 38 ].
Improving neurohormonal blockade of aldosterone and angiotensin II
Failure to suppress plasma angiotensin II and/or aldosterone concentrations may be associated with an adverse outcome in heart failure [ 39 ]. Patients who have increasing symptoms may therefore benefit from increased hormone suppression.
The short-acting agent captopril provides incomplete hormone suppression over 24 h unless used in multiple daily doses. Nevertheless, it is widely used in heart failure. The case for using a longer-acting ACE inhibitor in preference is poorly documented. Comparative studies of long and short-acting ACE inhibitors are few and do not address improvement in symptoms or mortality. Short-acting drugs are sometimes used on the pretext of a lower risk of producing significant biochemical renal dysfunction [ 40 ]. However, adverse renal effects induced by the combination of loop diuretic and ACE inhibitor are generally predictable, minor and are probably unrelated to the duration of action of the ACE inhibitor selected [ 41 ]. Increased dosage or increased dose frequency of the ACE inhibitor might be useful for some patients, although the optimal dose of ACE inhibitor remains uncertain.
Due to the strength of the evidence suggesting that neurohormonal activation in heart failure is integral both to the progression of symptoms and pathology [ 42 ] the combination of ACE inhibitor and ARA is being examined as an option. By blocking the negative feedback loop promoting renin release following treatment with an ACE inhibitor and in addition by providing receptor blockade, levels of bioactive angiotensin II are markedly reduced [ 43 ]. This strategy is currently under investigation using enalapril and valsartan in a multicentre outcome study (ValHeFT).
As aldosterone has control systems independent of the renin-angiotensin axis and since it may be independently detrimental in heart failure, the use of additional aldosterone blockade may have a role. Spironolactone has a variety of beneficial effects on surrogate markers of prognosis in heart failure [ 44 ]. Whether this can be translated to an improved outcome will be demonstrated by the multicentre RALES study [ 45 ]. Preliminary reports of this study suggest that mortality is significantly reduced by this combination. The combination of loop diuretic, ACE inhibitor and spironolactone increases the risk of renal dysfunction and significant electrolyte imbalance, particularly potassium retention. In small trials it is not possible to assess the frequency of such potential adverse events in routine clinical practice, since treatment and biochemical changes are closely monitored.
Additional therapies
Digoxin The role of digoxin in patients with heart failure already treated with an ACE inhibitor and diuretics and who are in sinus rhythm has been a matter of controversy for many years. However, digoxin withdrawal was demonstrated to be detrimental in the PROVED trial [ 46 ]. Recent studies have confirmed that there is no adverse effect on mortality in heart failure [ 47 ] when digoxin is added to patients on diuretics and ACE inhibitors. However, there were useful reductions in recurrent hospitalization after the addition of digoxin. Digoxin should be considered in patients with persistent symptoms despite optimal dosage of a diuretic and an ACE inhibitor. Care should be exercised when there is impairment of renal function and/or suspicion of impaired AV conduction or sinus node disease, in view of the effects of digoxin on cardiac conduction.
β-adrenoceptor blockade
More recently considerable interest has arisen in the use of β-adrenoceptor blockade in heart failure. Importantly these studies have been conducted in patients who were already receiving an ACE inhibitor and diuretic. The combination of data from several studies using carvedilol, a non selective β-adrenoceptor antagonist with additional α 1 -adrenoceptor blocking effects, show its efficacy in unselected patients with heart failure. Carvedilol improves survival in patients already receiving an ACE inhibitor and diuretic [ 48 ]. Worsening heart failure was not more frequent in the β-adrenoceptor blocker treated patients and benefits only emerge over weeks, with a vaguely defined period of increased symptoms during the early phase of treatment. Cardioselective (β 1 )-adrenoceptor blockade has been studied for some years in the management of idiopathic dilated cardiomyopathy. Recently preliminary data from a multicentre trial of bisoprolol in unselected heart failure have shown unequivocal evidence of further reductions in mortality. Although the overall mortality reductions appear small, significant reductions in symptomatic decompensation were evident [ 49 ]. A retrospective (though nonrandomised) analysis of the SAVE study database [ 50 ] suggested that in patients with asymptomatic left ventricular dysfunction after myocardial infarction there is a 30% reduction in cardiovascular death and a 21% reduction in the development of heart failure with the addition of any β-adrenoceptor blocker to captopril.
Small scale studies suggest greater improvements in central haemodynamics and a more significant impact on cardiac adrenergic tone with carvedilol in comparison with metoprolol [ 51 ]. Overall the impact of β-adrenoceptor blockade on exercise capacity is variable, positive in some studies but negative or insubstantial in others dependent on the method of testing [ 52 ].
If β-adrenoceptor blockade is to be widely accepted as a treatment for heart failure, significant practical issues remain to be addressed. There is no clear definition of those patients who stand to benefit most. The treatment appears to be well tolerated in small studies (7–8% intolerance for cardioselective and/or vasodilating β-adrenoceptor blockers; [ 53 ]) but many patients in routine clinical practice will have occult peripheral vascular disease or airways obstruction related to smoking which may complicate the use of these drugs.
The best methods for initiation of treatment is uncertain. Large doses of a β-adrenoceptor bocker can induce hypotension, bradycardia and shock due to the withdrawal of myocardial adrenergic support. As the benefits of β-adrenoceptor blockade appear to emerge gradually during chronic therapy [ 54 ] slow dosage titration is desirable. In most instances weekly medical reviews including daily weight records and regular blood pressure and renal function assessment are recommended for safe treatment [ 53 ]. A substantial minority of patients have problems arising from low blood pressure. As with the ACE inhibitors the optimal dose of β-adrenoceptor blockers is unknown and titration to the ‘maximum tolerated’ dose is currently recommended.
The mechanism of action of β-adrenoceptor blockers in heart failure is unclear. As many patients have overt or covert coronary disease they may simply reduce the impact of ischaemia in otherwise stable cardiac failure. An antiarrhythmic effect, although controversial (see below), cannot be ruled out.
Balanced vasodilator therapy
The use of diuretics can be guided by clinical assessment and body weight. For other treatments, the use of invasive pressure measurements can be valuable. Optimal use of vasodilator/vasoconstrictor agents and inotropic drugs in conjunction with diuretics can sometimes be guided by readings from a central haemodynamic monitoring catheter. This is particularly helpful for patients who have uncontrolled breathlessness and oedema or as a prelude to cardiac transplantation [ 55 ]. This approach can be effective in restoring a compensated state to an otherwise decompensated and deteriorating patient. Most patients who develop major haemodynamic and symptomatic decline despite an ACE inhibitor and effective diuresis are in an almost intractable position. Intensive intravenous therapy, more commonly employed in North America and in younger patients, is not widely used in Europe. Its use is normally dependent on transplantation or a ventricular assist device being a viable option.
Anti-arrhythmic therapy
Control of dysrhythmia in heart failure remains a major concern. Many patients die suddenly, usually attributed to some form of dysrhythmia (both tachydysrhythmias and bradydysrhythmias are common). The numbers who die in this way may be increasing with the increasing use of therapies that reduce uncontrolled pump failure as the mode of death.
The use of antiarrhythmic therapy in left ventricular dysfunction is restricted following the results from the CAST studies which demonstrated increased mortality with some treatments in patients with coexistent left ventricular (LV) dysfunction [ 56 ]. A particular concern reflects the use of potent drugs with the potential for pro-arrhythmic effects in patients who had minimal levels of electrical instability. Amiodarone appears to be an exception. Although results from four major trials have not shown consistent improvement in survival in established LV dysfunction [ 57 , 58 ], amiodarone is the best available drug for overt dysrhythmia in the face of impaired LV function. In general it can be used without preliminary electrophysiological testing [ 59 ].
Nonsustained ventricular tachycardia (VT) is common in symptomatic heart failure and is an independent marker of increased risk of sudden death in severe heart failure [ 60 ]. Whether amiodarone should be prescribed in all patients with heart failure who have non sustained and asymptomatic VT is not yet clear.
The role of drug therapy in comparison with electrical devices allowing sophisticated pacing detection and including the implantable cardioverter/defibrillator remains an important area for study [ 61 ]. At present these devices are generally restricted to patients with documented syncopal dysrhythmia or resuscitated arrest. Patients who survive arrhythmogenic cardiac arrest generally have significant pre-existent heart failure and structurally abnormal hearts. In Europe the application of such technology remains relatively limited and adequate trials comparing this therapy with drug treatments, although underway, are not yet available for guidance. These devices may play a significant role in heart failure in the management of selected patients.
Pulsed inotropic therapy and inotropic-vasodilator drugs
The use of inotropic agents in heart failure has encountered many problems. In the 1980s and early 1990s many agents were developed with effects on the heart and vascular tree combining a central inotropic stimulus with peripheral arterial vasodilatation. These have been uniformly unsuccessful during chronic dosing and often result in increased mortality [ 62 – 64 ] (e.g. flosequinan; ibopamine) As a result, the development of new drugs in this class has been all but halted. The major problems have been selection of appropriate patients and the narrow therapeutic index for such treatments. However, these drugs may have a role in the short term to relieve symptoms without the increase in mortality that occurs during protracted use [ 65 ].
In a different approach to inotropic therapy, Adamopoulos and colleagues employed intermittent dobutamine infusion in 20 patients with severe heart failure in an attempt to up-regulate myocardial β 1 -adrenoceptors [ 66 ]. In the short term, there were no clinical complications of treatment, but also no increase in diuresis. Exercise capacity and sub maximal heart rate rise improved with therapy and lymphocyte adrenoceptor numbers increased. This result is in contrast to the adverse effects of chronic inotropic therapy [ 64 ]. A fine balance may have be struck to improve adrenoreceptor responsiveness but to avoid excessive stimulation or adrenoceptor down-regulation.
Multidisciplinary care and hospitalization
Despite high annual mortality rates a substantial proportion of patients with heart failure face an uncertain yet chronic illness. Many patients are elderly and need repeated hospital admission. These admissions are both psychologically and financially taxing. In common with many chronic diseases, management of these patients can be improved by contact with many varied health professionals concerned not only with cardiac care but social circumstances; promotion of drug compliance and psychological support [ 67 , 68 ]. Non-pharmacological approaches such as increased exercise and training within limits has important and demonstrable physical [ 69 ] as well as psychological effects [ 70 ]. There are few instances where a supervised increase in physical exercise is not of benefit to the patient with heart failure.
Surgical management
Surgical treatment need not be considered as a final line of therapy. Increasingly important is the application of surgical revascularization for occult or overt ischaemia in patients with heart failure. This is often the best way to improve contractility although the operative management may be complicated and associated with increased perioperative mortality. Less well demonstrated are the benefits of scar reduction; cardiomyoplasty or the most recent and most dramatic innovation of ventricular reduction/ventriculotomy. As yet these procedures are limited in their application to a few selected patients and with generally no agreed role.
Cardiac transplantation is a proven therapy but restricted by organ availability and delay prior to intervention. Assessment is usually based on the severity of cardiac impairment on objective testing during treatment with maximal therapies. It is increasingly recognized that many patients with very poor left ventricular function can survive for many years without transplant. Functional exercise capacity is seen as the main delineator of those patients who should be entered onto an urgent transplantation waiting list or those who can safely remain on drug therapy [ 71 , 72 ]. The long-term problems of rejection and accelerated atherosclerosis and their effects on survival after transplantation will not be considered here. The outlook for the transplanted patient is dramatically better than those who await transplantation.
Following emergency admission, initiation of diuresis required bolus doses of intravenous frusemide combined with continuous intravenous infusion of dopamine and fluid and sodium restriction. Although he was considered a good candidate for invasive pulmonary pressure monitoring, this proved unnecessary. Following temporary withdrawal of captopril during stabilisation of renal function and diuresis, an ACE inhibitor was subsequently reintroduced without difficulty (lisinopril 10 mg daily). Renal function improved and blood pressure stabilised. Following discharge he remained symptomatic. Oral digoxin was introduced with only modest benefit. Repeat outpatient ambulatory ECG recording confirmed persistent episodes of non-sustained ventricular tachycardia. He was treated with prophylactic oral amiodarone despite his lack of symptoms. Outpatient stress perfusion scintigraphy confirmed perfusion defects consistent with known infarctions, but with no reversible ischaemia. Maximal cardiopulmonary exercise testing confirmed severe functional incapacity and very poor maximal oxygen consumption at peak exertion (13 ml kg −1 min −1 ). He was therefore referred for consideration of orthotopic cardiac transplantation.
Key therapeutic points
Case 1 acute stabilization and chronic management of systolic failure.
- Establishing aetiology must be part of diagnosis but does not importantly affect therapeutic strategies
- Diuretic therapy is a key element although formally untested in symptomatic patients. Diuretics were given to nearly all the patients in trials assessing the efficacy of ACE inhibitors.
- ACE inhibition must be considered in all patients and failure to provide this treatment requires clear justification. Morbidity and mortality benefits are unequivocal and generally greater the more significant the impairment of LV function. Minor or relative contraindications to use (e.g. asymptomatic hypotension; minor pretreatment renal impairment) should be weighed against the significant consequences of failure to treat.
- Angiotensin receptor antagonists may be an effective substitute for patients unable to tolerate an ACE inhibitor.
Case 2 Optimization of therapy in established heart failure
- In-hospital stabilization is usually necessary if the patient is already taking diuretics and an ACE inhibitor.
- Optimising diuretic therapy may involve:
- intravenous treatment
- combination therapy
- and/or haemodynamic (Swan Ganz catheter) monitoring
- Consider adjuvant digoxin for symptom control even in sinus rhythm
- Consider adjuvant β-adrenoceptor blockade
- dose titration may be protracted and complex
- the effects of selection bias (patient tolerance to treatment) on clinical trial results is unclear and may be important when considering treatment in routine practice
- Pulsed inotropic therapy or balanced vasodilator/inotropic therapy may be useful in selected patients
- Surgical revascularization or myocardial reconstruction may be feasible and useful options but are unproven in formal clinical trials
- Transplantation is effective when available but ‘survivors’ live to receive transplants

IMAGES
VIDEO
COMMENTS
On examination, the temperature was 36.4°C, the heart rate 103 beats per minute, the blood pressure 79/51 mm Hg, the respiratory rate 30 breaths per minute, and the oxygen saturation 99% while ...
A 67-year-old woman sought emergency medical care due to prolonged chest pain. In April 2009 the patient had prolonged chest pain and at that time she sought medical care. She was admitted at the hospital and diagnosed with myocardial infarction. The patient had hypertension, diabetes mellitus, dyslipidemia and was a smoker.
Dr. Amy A. Sarma: A 54-year-old man was evaluated at this hospital because of new heart failure. One month before this evaluation, a nonproductive cough developed after the patient took a business ...
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by ...
In this case, a patient with known history of coronary artery disease presented with worsening of shortness of breath with lower extremity edema and jugular venous distension along with crackles in the lung. The sign and symptoms along with labs and imaging findings point to diagnosis of heart failure with reduced EF (HFrEF).
Presentation of Case. Dr. Jacqueline B. Henson (Medicine): A 54-year-old man was evaluated at this hospital after cardiac arrest associated with ventricular fibrillation. The patient had been in ...
The main causes of heart failure are hypertension, coronary artery disease, Chagas disease, cardiomyopathies, endocrinopathies, toxins, and drugs, among others 1. The cardinal manifestations of heart failure are dyspnea and fatigue, and may include exercise intolerance, fluid retention, and pulmonary and systemic congestion 3. The patient in ...
That risk was confirmed in a study with 2285 patients diagnosed with stable coronary artery disease and diabetes mellitus (female sex, 34.9%; age range, 55 to 68 years; mean age, 61 years), and followed up for five years 14. Cardiovascular death, non-fatal acute myocardial infarction or non-fatal stroke occurred in 12.9% (178/1388 patients) of ...
Introduction. This clinical case refers to an 83-year-old man with moderate chronic obstructive pulmonary disease and shows that implementation of appropriate medical therapy according to the European Society of Cardiology/Heart Failure Association (ESC/HFA) guidelines improves symptoms and quality of life. 1 The case also illustrates that optimization of glucose metabolism with a more lenient ...
Background Cardiac stress testing is a validated diagnostic tool to assess symptomatic patients with intermediate pretest probability of coronary artery disease (CAD). However, in some cases, the cardiac stress test may provide inconclusive results and the decision for further workup typically depends on the clinical judgement of the physician. These decisions can greatly affect patient ...
Welcome to the GCVI HF Center's Ask the Expert - Patient Cases channel! On this channel you will have access to multiple heart failure patient cases published by leading ACC experts. We also encourage you to engage and consult with ACC global experts on cases specific to your practice. Ask the Expert through the online portal below!
Another diagnostic hypothesis for the clinical case is pulmonary embolism. The absence of pulmonary symptoms, mainly dyspnea, makes this hypothesis less likely. It is the most common symptom of this disease, occurring in over 78% of the patients 4. Sudden chest pain of sudden onset and very often pleuritic, affects up to 44% of patients 4 ...
Read chapter 4 of Patient Management in the Telemetry/Cardiac Step-Down Unit: A Case-Based Approach online now, exclusively on AccessCardiology. AccessCardiology is a subscription-based resource from McGraw Hill that features trusted medical content from the best minds in medicine.
Enriching the American Heart Association COVID‐19 Cardiovascular Disease Registry Through Linkage With External Data Sources: Rationale and Design, Journal of the American Heart Association, 11 ...
CASE STUDY 1. Read through the following clinical vignettes and take time to review each woman's cardiovascular risk factor profile. Then, refer to the questions at the end of the case study to analyze each female patient's current health status. Patient S is a White woman, 43 years of age, and mother of three small children.
Read international case studies of cardiovascular disease prevention in a joint report by the BHF and Public Health England. The UK has made progress on bringing down the premature death rate associated with cardiovascular disease (CVD) in recent years. But CVD still affects around seven million people in the UK, is responsible for one in five ...
On examination, the temperature was 37.6°C, the blood pressure 157/74 mm Hg, the heart rate 124 beats per minute, the respiratory rate 40 breaths per minute, and the oxygen saturation 94% while ...
The questions raised in this chapter include queries regarding the Jonathan's risk factors for heart disease, main considerations of a cardio-protective diet, definition of troponin, the nutrition and dietetic diagnosis, and aim and implementation of the dietetic intervention.
Heart disease, including coronary heart disease, remains the leading cause of death in the United States. However, the rate of heart disease deaths has declined by 70% over the past 50 years, thanks in part to NHLBI-funded research. Many current studies funded by the NHLBI focus on discovering genetic associations and finding new ways to ...
A subsample of 10 patients were selected for within-case analysis to further explore mechanisms by which the risk calculators may lead to changes in patient or practitioner behaviour. Selection was on the basis of evidence of positive intentions and/or behaviours to reduce CVD risk following the health check, to provide balance across QRISK2 and JBS3 groups, to cover a range of general ...
Kivimäki, M. et al. Long working hours and risk of coronary heart disease and stroke: A systematic review and meta-analysis of published and unpublished data for 603 838 individuals. Lancet 386 ...
Case Presentation. WC is a 67-year-old man with hypertension, hyperlipidemia, and coronary artery disease, and had triple bypass surgery 17 years ago. ... heart failure. 1 The atrial dilation and systolic dysfunction seen on the echocardiogram are evidence of structural heart disease. The patient is also exhibiting symptoms that limit his daily ...
Case Presentation. The patient is a 60-year-old white female presenting to the emergency department with acute onset shortness of breath. Symptoms began approximately 2 days before and had progressively worsened with no associated, aggravating, or relieving factors noted. She had similar symptoms approximately 1 year ago with an acute, chronic ...
Case 2 Optimization of therapy in established heart failure. In-hospital stabilization is usually necessary if the patient is already taking diuretics and an ACE inhibitor. 1. Remes J, Miettinen H, Reunanen A, Pyorala K. Validity of diagnosis of heart failure in primary health care. Eur Heart J. 1991;12:315-321.