

The Ultimate Guide to Nursing Assignments: 7 Tips and Strategies
Nursing assignments are a critical component of every nursing student’s academic journey. They serve as opportunities to test your knowledge, apply theoretical concepts to real-world scenarios, and develop essential skills necessary for your future nursing career. However, tackling nursing assignments can often be overwhelming, particularly when you’re juggling multiple responsibilities. In this comprehensive guide, we provide valuable tips, strategies, and expert assignment help services to help you excel in your nursing assignments. Whether you’re struggling with research, structuring your assignment, or proofreading, we’re here to support you every step of the way.
Understanding the Nursing Assignments
To excel in nursing assignments , it’s crucial to start by thoroughly understanding the requirements. Take the time to carefully read the assignment prompt, paying close attention to the topic, word count, formatting guidelines, and any specific instructions provided by your instructor. Understanding these key components will ensure that you meet all the necessary criteria.
Conducting Thorough Research
Once you have a clear understanding of the assignment, it’s time to conduct thorough research. Solid research forms the foundation of any successful nursing assignment. Begin by gathering relevant and credible sources, such as nursing textbooks, scholarly articles, reputable websites , and academic databases specific to nursing. These resources will provide you with evidence-based information to support your arguments and demonstrate your understanding of the topic.
Creating a Well-Structured Outline
A well-structured outline is essential for organizing your thoughts and ensuring a logical flow in your nursing assignment. An effective outline acts as a roadmap, guiding you through the writing process and ensuring that you cover all the necessary points.
At [Your Service Name], our expert writers can assist you in creating a comprehensive outline tailored to your specific assignment. By collaborating with us, you can receive personalized guidance in organizing your ideas effectively and structuring your assignment in a logical manner. Our writers understand the nuances of nursing assignments and can help you identify the most important concepts and supporting evidence to include.
Using a Professional Tone
Maintaining a professional tone throughout your nursing assignment is crucial. As aspiring healthcare professionals, it’s essential to communicate your ideas with clarity, conciseness, and professionalism. Use clear and concise language, avoiding jargon or slang that may hinder the reader’s understanding. Present your arguments and supporting evidence in a logical and coherent manner, demonstrating your ability to think critically and apply nursing principles.
Our expert writers have extensive experience in academic writing within the field of nursing. They possess a deep understanding of the professional tone required for nursing assignments and can ensure that your assignment is written to the highest standards. By collaborating with us, you can receive guidance in maintaining a professional tone and effectively conveying your ideas.
Incorporating Practical Examples
In addition to a professional tone, incorporating practical examples into your nursing assignment can greatly enhance its quality. Practical examples bring theoretical concepts to life, illustrating their application in real-life scenarios. They demonstrate your understanding of nursing principles and showcase your ability to bridge the gap between theory and practice.
Our team consists of experienced nursing professionals who can assist you in incorporating relevant practical examples into your assignment. Drawing from their extensive knowledge and expertise, they can provide you with real-life scenarios or case studies that strengthen the impact and credibility of your work. By collaborating with us, you can elevate the quality of your assignment by demonstrating your ability to apply nursing concepts in practical settings.
Proofreading and Editing
Proofreading and editing are essential steps in the assignment writing process. They ensure that your nursing assignment is polished, error-free, and effectively communicates your ideas. After completing the initial draft, it’s crucial to take a break and return to your work with fresh eyes. During the proofreading stage, carefully review your assignment for grammar, spelling, punctuation, and sentence structure. Correct any errors and inconsistencies that may affect the clarity and professionalism of your writing.
At nursingresearchhelp.com , we have a dedicated team of proofreaders and editors who specialize in nursing assignments. They meticulously review your work, ensuring that it adheres to formatting guidelines and meets the highest standards of academic writing. Our proofreaders and editors will help you refine your assignment, ensuring that it is polished and error-free. By collaborating with us, you can rest assured that your assignment will be thoroughly reviewed and refined before submission.
Seeking Help When Needed
In addition to proofreading and editing, it’s important to seek help when needed. Nursing assignments can be challenging, and it’s perfectly normal to require assistance. Whether you’re facing difficulties in understanding the assignment prompt, need guidance in specific areas, or simply want a fresh perspective on your work, don’t hesitate to reach out for support.
Our friendly and knowledgeable support team is always available to address any questions or concerns you may have. We understand the unique challenges faced by nursing students and can provide you with the guidance and clarification you need. By seeking help when needed, you can overcome obstacles and ensure the successful completion of your nursing assignments.
Mastering nursing assignments is within your reach with the right tips, strategies, and expert assignment help services. At nursingresearchhelp.com we are committed to supporting nursing students in excelling in their academic pursuits. Our experienced writers, proofreaders, and editors can provide personalized assistance throughout the assignment writing process, ensuring that your assignments meet the highest standards of quality and professionalism.
With our help, you can confidently tackle your nursing assignments and overcome any challenges you may face. Visit our website nursingresearchhelp.com to learn more about our services and how we can support you in achieving academic excellence. Whether you need guidance in understanding the assignment, conducting thorough research, creating a well-structured outline, using a professional tone, incorporating practical examples, or ensuring a polished final product, we are here to assist you. Trust us for reliable and professional assignment help tailored to your needs.
Don’t let the challenges of nursing assignments hold you back—reach out to us for reliable and professional assignment help tailored to your needs.
You might also like

Nursingresearchhelp.com is the fastest, easiest and most reliable way to have content written for your website. You’ll be able to post a project and 1000s of freelance writers from across the globe will have instant access to write your content quickly, professionally, and affordably.
QUICK LINKS
- HOW IT WORKS
- OUR SERVICES
- TERMS OF USE

Call/Text: +1 608 912 3884

The Nursing Process: A Comprehensive Guide

In 1958, Ida Jean Orlando began developing the nursing process still evident in nursing care today. According to Orlando’s theory, the patient’s behavior sets the nursing process in motion. Through the nurse’s knowledge to analyze and diagnose the behavior to determine the patient’s needs.
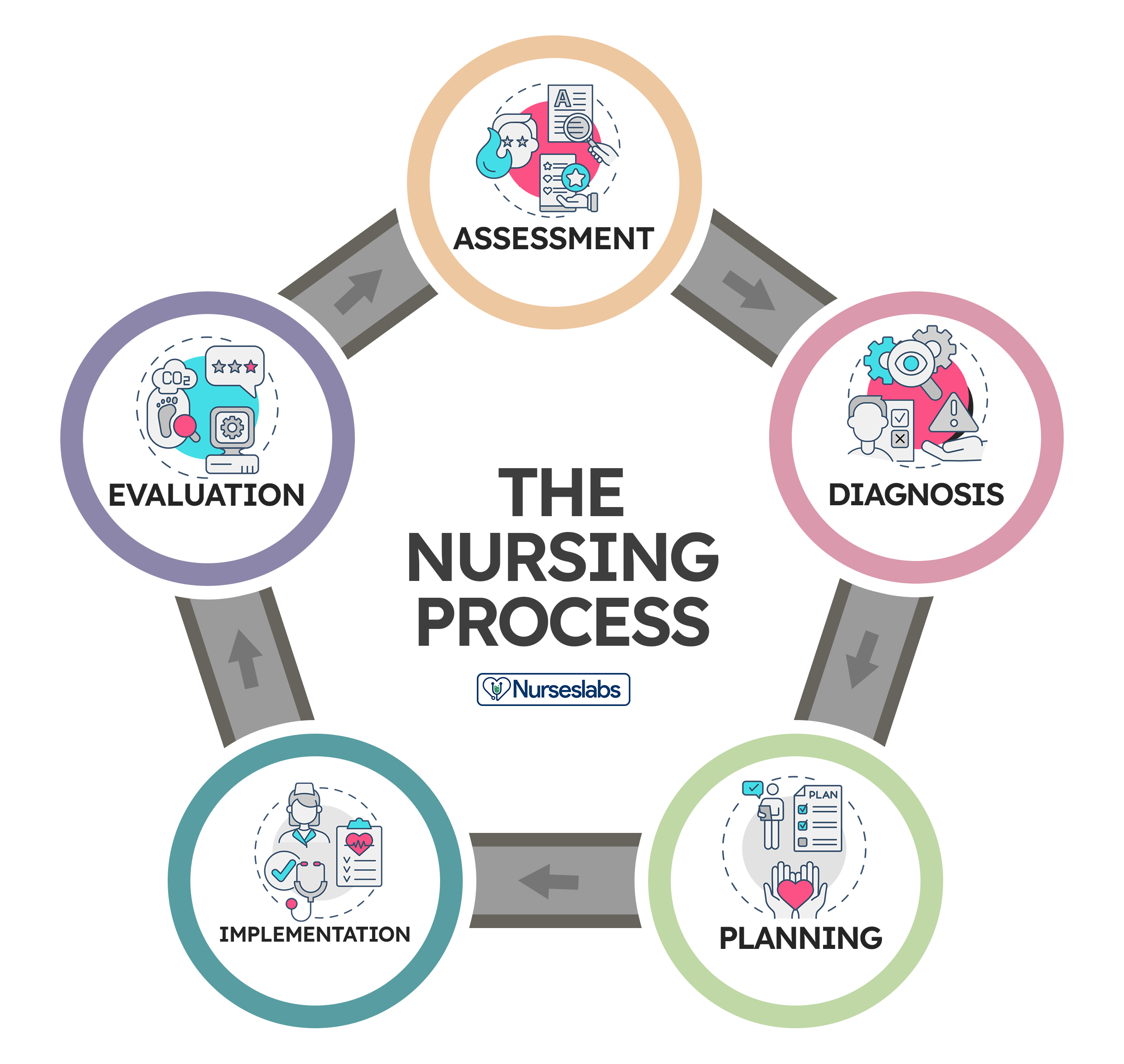
Application of the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EBP) recommendations, and nursing intuition, the nursing process functions as a systematic guide to client-centered care with five subsequent steps. These are assessment , diagnosis, planning, implementation, and evaluation ( ADPIE ).
Table of Contents
What is the nursing process.
- What is the purpose of the nursing process?
Characteristics of the nursing process
Nursing process steps, collecting data, objective data or signs, subjective data or symptoms, verbal data, nonverbal data, primary source, secondary source, tertiary source, health interview, physical examination, observation, validating data, documenting data.
- 2. Diagnosis: “What is the problem?”
Initial Planning
Ongoing planning, discharge planning, developing a nursing care plan, behavioral nursing interventions, community nursing interventions, family nursing interventions, health system nursing interventions, physiological nursing interventions, safety nursing interventions, skills used in implementing nursing care, 1. reassessing the client, 2. determining the nurse’s need for assistance, nursing intervention categories, independent nursing interventions, dependent nursing interventions, interdependent nursing interventions, 4. supervising the delegated care, 5. documenting nursing activities, 1. collecting data, 2. comparing data with desired outcomes, 3. analyzing client’s response relating to nursing activities, 4. identifying factors contributing to success or failure, 5. continuing, modifying, or terminating the nursing care plan, 6. discharge planning.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse’s critical thinking to provide the best care possible to the client.
What is the purpose of the nursing process?
The following are the purposes of the nursing process:
- To identify the client’s health status and actual or potential health care problems or needs (through assessment).
- To establish plans to meet the identified needs.
- To deliver specific nursing interventions to meet those needs.
- To apply the best available caregiving evidence and promote human functions and responses to health and illness (ANA, 2010).
- To protect nurses against legal problems related to nursing care when the standards of the nursing process are followed correctly.
- To help the nurse perform in a systematically organized way their practice.
- To establish a database about the client’s health status, health concerns, response to illness, and the ability to manage health care needs.
The following are the unique characteristics of the nursing process:
- Patient-centered . The unique approach of the nursing process requires care respectful of and responsive to the individual patient’s needs, preferences, and values. The nurse functions as a patient advocate by keeping the patient’s right to practice informed decision-making and maintaining patient-centered engagement in the health care setting.
- Interpersonal . The nursing process provides the basis for the therapeutic process in which the nurse and patient respect each other as individuals, both of them learning and growing due to the interaction. It involves the interaction between the nurse and the patient with a common goal.
- Collaborative . The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care.
- Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
- Requires critical thinking . The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation. The acronym ADPIE is an easy way to remember the components of the nursing process. Nurses need to learn how to apply the process step-by-step. However, as critical thinking develops through experience, they learn how to move back and forth among the steps of the nursing process.
The steps of the nursing process are not separate entities but overlapping, continuing subprocesses. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps of the nursing process are detailed below:
1. Assessment: “What data is collected?”
The first phase of the nursing process is assessment . It involves collecting, organizing, validating, and documenting the clients’ health status. This data can be obtained in a variety of ways. Usually, when the nurse first encounters a patient, the nurse is expected to assess to identify the patient’s health problems as well as the physiological, psychological, and emotional state and to establish a database about the client’s response to health concerns or illness and the ability to manage health care needs. Critical thinking skills are essential to the assessment, thus requiring concept-based curriculum changes.
Data collection is the process of gathering information regarding a client’s health status. The process must be systematic and continuous in collecting data to prevent the omission of important information concerning the client.
The best way to collect data is through head-to-toe assessment. Learn more about it at our guide: Head to Toe Assessment: Complete Physical Assessment Guide
Types of Data
Data collected about a client generally falls into objective or subjective categories, but data can also be verbal and nonverbal.
Objective data are overt, measurable, tangible data collected via the senses, such as sight, touch, smell, or hearing, and compared to an accepted standard, such as vital signs, intake and output , height and weight, body temperature, pulse, and respiratory rates, blood pressure, vomiting , distended abdomen, presence of edema , lung sounds, crying, skin color, and presence of diaphoresis.
Subjective data involve covert information, such as feelings, perceptions, thoughts, sensations, or concerns that are shared by the patient and can be verified only by the patient, such as nausea , pain , numbness, pruritus, attitudes, beliefs, values, and perceptions of the health concern and life events.
Verbal data are spoken or written data such as statements made by the client or by a secondary source. Verbal data requires the listening skills of the nurse to assess difficulties such as slurring, tone of voice, assertiveness, anxiety , difficulty in finding the desired word, and flight of ideas.
Nonverbal data are observable behavior transmitting a message without words, such as the patient’s body language, general appearance, facial expressions, gestures, eye contact, proxemics (distance), body language, touch, posture, clothing. Nonverbal data obtained can sometimes be more powerful than verbal data, as the client’s body language may not be congruent with what they really think or feel. Obtaining and analyzing nonverbal data can help reinforce other forms of data and understand what the patient really feels.
Sources of Data
Sources of data can be primary, secondary, and tertiary . The client is the primary source of data, while family members, support persons, records and reports, other health professionals, laboratory and diagnostics fall under secondary sources.
The client is the only primary source of data and the only one who can provide subjective data. Anything the client says or reports to the members of the healthcare team is considered primary.
A source is considered secondary data if it is provided from someone else other than the client but within the client’s frame of reference. Information provided by the client’s family or significant others are considered secondary sources of data if the client cannot speak for themselves, is lacking facts and understanding, or is a child. Additionally, the client’s records and assessment data from other nurses or other members of the healthcare team are considered secondary sources of data.
Sources from outside the client’s frame of reference are considered tertiary sources of data . Examples of tertiary data include information from textbooks, medical and nursing journals, drug handbooks, surveys, and policy and procedural manuals.
Methods of Data Collection
The main methods used to collect data are health interviews, physical examination, and observation.
The most common approach to gathering important information is through an interview. An interview is an intended communication or a conversation with a purpose, for example, to obtain or provide information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. One example of the interview is the nursing health history, which is a part of the nursing admission assessment. Patient interaction is generally the heaviest during the assessment phase of the nursing process so rapport must be established during this step.
Aside from conducting interviews, nurses will perform physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Establishing a good physical assessment would, later on, provide a more accurate diagnosis, planning, and better interventions and evaluation.
Observation is an assessment tool that depends on the use of the five senses (sight, touch, hearing, smell, and taste) to learn information about the client. This information relates to characteristics of the client’s appearance, functioning, primary relationships, and environment. Although nurses observe mainly through sight, most of the senses are engaged during careful observations such as smelling foul odors, hearing or auscultating lung and heart sounds and feeling the pulse rate and other palpable skin deformations.
Validation is the process of verifying the data to ensure that it is accurate and factual. One way to validate observations is through “double-checking,” and it allows the nurse to complete the following tasks:
- Ensures that assessment information is double-checked, verified, and complete. For example, during routine assessment, the nurse obtains a reading of 210/96 mm Hg of a client with no history of hypertension . To validate the data, the nurse should retake the blood pressure and if necessary, use another equipment to confirm the measurement or ask someone else to perform the assessment.
- Ensure that objective and related subjective data are valid and accurate. For example, the client’s perceptions of “feeling hot” need to be compared with the measurement of the body temperature.
- Ensure that the nurse does not come to a conclusion without adequate data to support the conclusion. A nurse assumes tiny purple or bluish-black swollen areas under the tongue of an older adult client to be abnormal until reading about physical changes of aging.
- Ensure that any ambiguous or vague statements are clarified. For example, a 86-year-old female client who is not a native English speaker says that “I am in pain on and off for 4 weeks,” would require verification for clarity from the nurse by asking “Can you describe what your pain is like? What do you mean by on and off?”
- Acquire additional details that may have been overlooked. For example, the nurse is asking a 32-year-old client if he is allergic to any prescription or non-prescription medications. And what would happen if he takes these medications.
- Distinguish between cues and inferences. Cues are subjective or objective data that can be directly observed by the nurse; that is, what the client says or what the nurse can see, hear, feel, smell, or measure. On the other hand, inferences are the nurse’s interpretation or conclusions made based on the cues. For example, the nurse observes the cues that the incision is red, hot, and swollen and makes an inference that the incision is infected.
Once all the information has been collected, data can be recorded and sorted. Excellent record-keeping is fundamental so that all the data gathered is documented and explained in a way that is accessible to the whole health care team and can be referenced during evaluation.
2. Diagnosis: “What is the problem?”
The second step of the nursing process is the nursing diagnosis . The nurse will analyze all the gathered information and diagnose the client’s condition and needs. Diagnosing involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements about a patient’s potential or actual health problem. More than one diagnosis is sometimes made for a single patient. Formulating a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care.
The types, components, processes, examples, and writing nursing diagnosis are discussed more in detail here “ Nursing Diagnosis Guide: All You Need To Know To Master Diagnosing ”
3. Planning: “How to manage the problem?”
Planning is the third step of the nursing process. It provides direction for nursing interventions. When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome.
The planning phase is where goals and outcomes are formulated that directly impact patient care based on evidence-based practice (EBP) guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual’s unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement, and continuity of care across the healthcare continuum.
Types of Planning
Planning starts with the first client contact and resumes until the nurse-client relationship ends, preferably when the client is discharged from the health care facility.
Initial planning is done by the nurse who conducts the admission assessment. Usually, the same nurse would be the one to create the initial comprehensive plan of care.
Ongoing planning is done by all the nurses who work with the client. As a nurse obtain new information and evaluate the client’s responses to care, they can individualize the initial care plan further. An ongoing care plan also occurs at the beginning of a shift. Ongoing planning allows the nurse to:
- determine if the client’s health status has changed
- set priorities for the client during the shift
- decide which problem to focus on during the shift
- coordinate with nurses to ensure that more than one problem can be addressed at each client contact
Discharge planning is the process of anticipating and planning for needs after discharge. To provide continuity of care, nurses need to accomplish the following:
- Start discharge planning for all clients when they are admitted to any health care setting.
- Involve the client and the client’s family or support persons in the planning process.
- Collaborate with other health care professionals as needed to ensure that biopsychosocial, cultural, and spiritual needs are met.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database .
4. Implementation : “Putting the plan into action!”
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect. It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This typically begins with the medical staff conducting any needed medical interventions.
Interventions should be specific to each patient and focus on achievable outcomes. Actions associated with a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks such as medication administration , educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
A taxonomy of nursing interventions referred to as the Nursing Interventions Classification (NIC) taxonomy, was developed by the Iowa Intervention Project. The nurse can look up a client’s nursing diagnosis to see which nursing interventions are recommended.
Nursing Interventions Classification (NIC) System
There are more than 550 nursing intervention labels that nurses can use to provide the proper care to their patients. These interventions are categorized into seven fields or classes of interventions according to the Nursing Interventions Classification system.
These are interventions designed to help a patient change their behavior. With behavioral interventions, in contrast, patient behavior is the key and the goal is to modify it. The following measures are examples of behavioral nursing interventions:
- Encouraging stress and relaxation techniques
- Providing support to quit smoking
- Engaging the patient in some form of physical activity , like walking, to reduce the patient’s anxiety, anger, and hostility
These are interventions that refer to the community-wide approach to health behavior change. Instead of focusing mainly on the individual as a change agent, community interventionists recognize a host of other factors that contribute to an individual’s capacity to achieve optimal health, such as:
- Implementing an education program for first-time mothers
- Promoting diet and physical activities
- Initiating HIV awareness and violence-prevention programs
- Organizing a fun run to raise money for breast cancer research
These are interventions that influence a patient’s entire family.
- Implementing a family-centered approach in reducing the threat of illness spreading when one family member is diagnosed with a communicable disease
- Providing a nursing woman support in breastfeeding her new baby
- Educating family members about caring for the patient
These are interventions that designed to maintain a safe medical facility for all patients and staff, such as:
- Following procedures to reduce the risk of infection for patients during hospital stays.
- Ensuring that the patient’s environment is safe and comfortable, such as repositioning them to avoid pressure ulcers in bed
These are interventions related to a patient’s physical health to make sure that any physical needs are being met and that the patient is in a healthy condition. These nursing interventions are classified into two types: basic and complex.
- Basic. Basic interventions regarding the patient’s physical health include hands-on procedures ranging from feeding to hygiene assistance.
- Complex. Some physiological nursing interventions are more complex, such as the insertion of an IV line to administer fluids to a dehydrated patient.
These are interventions that maintain a patient’s safety and prevent injuries, such as:
- Educating a patient about how to call for assistance if they are not able to safely move around on their own
- Providing instructions for using assistive devices such as walkers or canes, or how to take a shower safely.
When implementing care, nurses need cognitive, interpersonal, and technical skills to perform the care plan successfully.
- Cognitive Skills are also known as Intellectual Skills are skills involve learning and understanding fundamental knowledge including basic sciences, nursing procedures, and their underlying rationale before caring for clients. Cognitive skills also include problem-solving, decision-making, critical thinking, clinical reasoning, and creativity.
- Interpersonal Skills are skills that involve believing, behaving, and relating to others. The effectiveness of a nursing action usually leans mainly on the nurse’s ability to communicate with the patient and the members of the health care team.
- Technical Skills are purposeful “hands-on” skills such as changing a sterile dressing, administering an injection, manipulating equipment, bandaging, moving, lifting, and repositioning clients. All of these activities require safe and competent performance.
Process of Implementing
The process of implementing typically includes the following:
Prior to implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even if an order is written on the care plan, the client’s condition may have changed.
Other nursing tasks or activities may also be performed by non-RN members of the healthcare team. Members of this team may include unlicensed assistive personnel (UAP) and caregivers , as well as other licensed healthcare workers, such as licensed practical nurses/licensed vocational nurses (LPNs/LVNs). The nurse may need assistance when implementing some nursing intervention, such as ambulating an unsteady obese client, repositioning a client, or when a nurse is not familiar with a particular model of traction equipment needs assistance the first time it is applied.
3. Implementing the nursing interventions
Nurses must not only have a substantial knowledge base of the sciences, nursing theory , nursing practice, and legal parameters of nursing interventions but also must have the psychomotor skills to implement procedures safely. It is necessary for nurses to describe, explain, and clarify to the client what interventions will be done, what sensations to anticipate, what the client is expected to do, and what the expected outcome is. When implementing care, nurses perform activities that may be independent, dependent, or interdependent.
Nursing interventions are grouped into three categories according to the role of the healthcare professional involved in the patient’s care:
A registered nurse can perform independent interventions on their own without the help or assistance from other medical personnel, such as:
- routine nursing tasks such as checking vital signs
- educating a patient on the importance of their medication so they can administer it as prescribed
A nurse cannot initiate dependent interventions alone. Some actions require guidance or supervision from a physician or other medical professional, such as:
- prescribing new medication
- inserting and removing a urinary catheter
- providing diet
- Implementing wound or bladder irrigations
A nurse performs as part of collaborative or interdependent interventions that involve team members across disciplines.
- In some cases, such as post- surgery , the patient’s recovery plan may require prescription medication from a physician, feeding assistance from a nurse, and treatment by a physical therapist or occupational therapist.
- The physician may prescribe a specific diet to a patient. The nurse includes diet counseling in the patient care plan. To aid the patient, even more, the nurse enlists the help of the dietician that is available in the facility.
Delegate specific nursing interventions to other members of the nursing team as appropriate. Consider the capabilities and limitations of the members of the nursing team and supervise the performance of the nursing interventions. Deciding whether delegation is indicated is another activity that arises during the nursing process.
The American Nurses Association and the National Council of State Boards of Nursing (2006) define delegation as “the process for a nurse to direct another person to perform nursing tasks and activities.” It generally concerns the appointment of the performance of activities or tasks associated with patient care to unlicensed assistive personnel while retaining accountability for the outcome.
Nevertheless, registered nurses cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to unlicensed assistive personnel include assessment and evaluation of the impact of interventions on care provided to the patient.
Record what has been done as well as the patient’s responses to nursing interventions precisely and concisely.
5. Evaluation : “Did the plan work?”
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened.
Steps in Evaluation
Nursing evaluation includes (1) collecting data, (2) comparing collected data with desired outcomes, (3) analyzing client’s response relating to nursing activities, (4) identifying factors that contributed to the success or failure of the care plan, (5) continuing, modifying, or terminating the nursing care plan, and (6) planning for future nursing care.
The nurse recollects data so that conclusions can be drawn about whether goals have been fulfilled. It is usually vital to collect both objective and subjective data. Data must be documented concisely and accurately to facilitate the next part of the evaluating process.
The documented goals and objectives of the nursing care plan become the standards or criteria by which to measure the client’s progress whether the desired outcome has been met, partially met, or not met.
- The goal was met , when the client response is the same as the desired outcome.
- The goal was partially met , when either a short-term outcome was achieved but the long-term goal was not, or the desired goal was incompletely attained.
- The goal was not met.
It is also very important to determine whether the nursing activities had any relation to the outcomes whether it was successfully accomplished or not.
It is required to collect more data to confirm if the plan was successful or a failure. Different factors may contribute to the achievement of goals. For example, the client’s family may or may not be supportive, or the client may be uncooperative to perform such activities.
The nursing process is dynamic and cyclical. If goals were not sufficed, the nursing process begins again from the first step. Reassessment and modification may continually be needed to keep them current and relevant depending upon general patient condition. The plan of care may be adjusted based on new assessment data. Problems may arise or change accordingly. As clients complete their goals, new goals are set. If goals remain unmet, nurses must evaluate the reasons these goals are not being achieved and recommend revisions to the nursing care plan.
Discharge planning is the process of transitioning a patient from one level of care to the next. Discharge plans are individualized instructions provided as the client is prepared for continued care outside the healthcare facility or for independent living at home. The main purpose of a discharge plan is to improve the client’s quality of life by ensuring continuity of care together with the client’s family or other healthcare workers providing continuing care.
The following are the key elements of IDEAL discharge planning according to the Agency for Healthcare Research and Quality:
- I nclude the patient and family as full partners in the discharge planning process.
- Describe what life at home will be like
- Review medications
- Highlight warning signs and problems
- Explain test results
- Schedule follow-up appointments
- E ducate the patient and family in plain language about the patient’s condition, the discharge process, and next steps throughout the hospital stay.
- A ssess how well doctors and nurses explain the diagnosis, condition, and next steps in the patient’s care to the patient and family and use teach back.
- L isten to and honor the patient’s and family’s goals, preferences, observations, and concerns.
A discharge plan includes specific components of client teaching with documentation such as:
- Equipment needed at home. Coordinate home-based care and special equipment needed.
- Dietary needs or special diet . Discuss what the patient can or cannot eat at home.
- Medications to be taken at home. List the patient’s medications and discuss the purpose of each medicine, how much to take, how to take it, and potential side effects.
- Resources such as contact numbers and addresses of important people. Write down the name and contact information of someone to call if there is a problem.
- Emergency response: Danger signs. Identify and educate patients and families about warning signs or potential problems.
- Home care activities. Educate patient on what activities to do or avoid at home.
- Summary. Discuss with the patient and family about the patient’s condition, the discharge process, and follow-up checkups.
38 thoughts on “The Nursing Process: A Comprehensive Guide”
This article is helpful
So helpful And easy to understand A very good guide for nurses
I’m a clinical instructor teaching Fundamentals this semester. The article will be very helpful to give an in-depth explanation of “The Nursing Process” to students. Thank you.
Very detailed and easy to understand. Thx
Am a student I find it very educative
This is so helpful
Excellent information that is clearly outlined and user friendly.
This is so wonderful thank you
So helpful thank you
this is very helpful thank you
Helpful. So grateful
Is the nursing process the same as “critical thinking”?
Great information! Thanks!
This is very helpful. Thank you
Great explanation, in the understanding of Nursing process
Very Helpful to students, thank you for sharing
Excellent job. A great help to all nursing students. Thank you for sharing. God bless you.
Hi Joycelyn, Thank you so much for your kind words! It’s really rewarding to hear that it’s helping nursing students out there. We’re all about sharing knowledge and making things a bit easier. 😊 If there’s anything else you’d like to see or know, just let me know. And blessings right back at you!
Thank you so much…It’s a very comprehensive reference.
You’re very welcome, A.C! I’m glad you found the nursing process reference comprehensive and useful. Just out of curiosity, is there a particular step in the nursing process you’d like to explore more deeply, or do you have any specific areas where you’d like more detailed information?
I am a nursing student and I see this as a helpful tool, very detailed and easy to understand thanks for sharing
Hi Mawuli, I’m delighted to know that you’re finding our resources helpful! If you have any specific questions or if there’s a particular topic you’d like more information on, please feel free to ask. I’m here to assist you with any nursing-related inquiries you may have. Keep up the great work in your studies! 🩺📚🌟
Keep updating me about Nursing pdfs. You guys are really good at your work!!
Hey Mokete, Thank you so much for the kind words! We’re thrilled to hear that you’re finding our nursing resources helpful. We’ll do our best to keep you updated with more valuable nursing PDFs and information. If there’s anything specific you’d like to see or if you have any questions, feel free to let us know. Keep up the great work in your nursing journey! 👩⚕️📚🌟
Thanks it really helps alot
Glad to be of help! Thank you!
This guideline very useful for Nurses building their competency and practice quality of care of Nursing to use as reference please allow to download free especially to Nurses who live in developing countries since it is not affordable to buy it
You can download the articles by printing them as PDF :) You can use a service called printfriendly (google it) to make PDFs of our webpages.
Excellent work done I’m very happy to see this stuffs
Thank you so much…It’s a very comprehensive reference. God bless you
Hello Theophilus, You’re very welcome, and thank you for the blessings! 😊 I’m glad you found the reference on the nursing process comprehensive. Just out of curiosity, is there a particular part of the nursing process you’re most interested in, or any aspect you’d like to explore more deeply?
God bless you too, and if you have any more questions, feel free to ask!
Very helpful information. Thank you.
Thank you so much, Alisa. If you need more information or help regarding this, let us know.
You’re doing a great job here. Please can you do it in such a way for us to download it as a pdf?
Hi Millicent, Thank you so much for the kind words! 😊 I’m really glad you’re finding the site useful.
Regarding your request to download content as a PDF, a neat trick you can use is the “print” function in your web browser. Here’s how you can do it:
Open the page you want to save as a PDF. -Go to the “File” menu in your browser and select “Print,” or simply press Ctrl+P (Cmd+P on Mac). -In the print window, look for a destination option and select “Save as PDF” or something similar. -Adjust any settings as needed, then click “Save” or “Print,” and choose where you want to save the file on your computer.
This way, you can turn any page into a PDF for your personal use. If you have any more questions or need further assistance, feel free to ask. Always here to help!
Leave a Comment Cancel reply
opens in a new window
- South Dakota Nurse November 2018 issue is now available.

8 Steps for Making Effective Nurse-Patient Assignments
This article appears on page 14 of
South Dakota Nurse November 2018
Reprinted from American Nurse Today
Successful assignments require attention to the needs of both nurses and patients.
YOUR MANAGER wants you to learn how to make nurse patient assignments. What? Already? When did you became a senior nurse on your floor? But you’re up to the challenge and ready to learn the process.
Nurse-patient assignments help coordinate daily unit activities, matching nurses with patients to meet unit and patient needs for a specific length of time. If you are new to this challenge, try these eight tips as a guide for making nurse-patient assignments.
1. Find a mentor
Most nurses learn to make nurse-patient assignments from a colleague. Consider asking if you can observe your charge nurse make assignments. Ask questions to learn what factors are taken into consideration for each assignment. Nurses who make assignments are aware of their importance and are serious in their efforts to consider every piece of information when making them. By asking questions, you’ll better understand how priorities are set and the thought that’s given to each assignment. Making nurse-patient assignments is challenging, but with your mentor’s help, you’ll move from novice to competent in no time.
2. Gather your supplies (knowledge)
Before completing any nursing task, you need to gather your supplies. In this case, that means knowledge. You’ll need information about the unit, the nurses, and the patients. (See What you need to know.) Some of this information you already know, and some you’ll need to gather. But make sure you have everything you need before you begin making assignments. Missing and unknown information is dangerous and may jeopardize patient and staff safety. The unit and its environment will set the foundation for your assignments. The environment (unit physical layout, average patient length of stay [LOS]) defines your process and assignment configuration (nurse-to-patient ratios). You’re probably familiar with your unit’s layout and patient flow, but do you know the average LOS or nurse-to-patient ratios? Do you know what time of day most admissions and discharges occur or the timing of certain daily activities? And do other nursing duties need to be covered (rapid response, on call to another unit)? Review your unit’s policy and procedures manual for unit staffing and assignment guidelines. The American Nurses Association’s ANA ‘s Principles for Nurse Staffing 2nd edition also is an excellent resource.
Review the assignment sheet or whiteboard used on your unit. It has clues to the information you need. It provides the framework for the assignment-making process, including staff constraints, additional duties that must be covered, and patient factors most important on your unit. Use the electronic health record (EHR) to generate various useful pieces of patient information. You also can use the census sheet, patient acuity list, or other documents of nursing activity, such as a generic hospital patient summary or a unit-specific patient report that includes important patient factors.
Depending on your unit, the shift, and the patient population, you’ll need to consider different factors when making assignments. Ask yourself these questions: What patient information is important for my unit? Does my unit generate a patient acuity or workload factor? What are the time-consuming tasks on my unit (medications, dressing changes, psychosocial support, total care, isolation)? Which patients require higher surveillance or monitoring? Finally, always talk to the clinical nurses caring for the patients. Patient conditions change faster than they can be documented in the EHR, so rely on the clinical nurses to confirm each patient’s acuity and individual nurses’ workloads. Nurses want to be asked for input about their patients’ condition, and they’re your best resource.
Now ask yourself: How well do I know the other nurses on my unit? This knowledge is the last piece of information you need before you can make assignments. The names of the nurses assigned to the shift can be found on the unit schedule or a staffing list from a centralized staffing office. If you know the nurses and have worked with them, you’ll be able to determine who has the most and least experience, who’s been on the floor the longest, and who has specialty certifications. You’ll also want to keep in mind who the newest nurses are and who’s still on orientation.
3. Decide on the process
Now that you’ve gathered the information you need, you’re ready to develop your plan for assigning nurses. This step usually combines the unit layout with your patient flow. Nurses typically use one of three processes–area, direct, or group–to make assignments. (See Choose your process.)
4. Set priorities for the shift
The purpose of nurse-patient assignments is to provide the best and safest care to patients, but other goals will compete for consideration and priority. This is where making assignments gets difficult. You’ll need to consider continuity of care, new nurse orientation, patient requests and satisfaction, staff well-being, fairness, equal distribution of the workload, nurse development, and workload completion.
5. Make the assignments
Grab your writing instrument and pencil in that first nurse’s name. This first match should satisfy your highest priority. For example, if nurse and any other returning nurses are reassigned to the patients they had on their previous shift. If, however, you have a complex patient with a higher-than-average acuity, you just assigned your best nurse to this patient. After you’ve satisfied your highest priority, move to your next highest priority and match nurses with unassigned patients and areas.
Sounds easy, right? Frequently, though, you’ll be faced with competing priorities that aren’t easy to rate, and completing the assignments may take a few tries. You want to satisfy as many of your priorities as you can while also delivering safe, quality nursing care to patients. You’ll shuffle, move, and change assignments many times before you’re satisfied that you’ve maximized your priorities and the potential for positive outcomes. Congratulate yourself–the nurse-patient assignments are finally made.
6. Adjust the assignments
You just made the assignments, so why do you need to adjust them? The nurse-patient assignment list is a living, breathing document. It involves people who are constantly changing–their conditions improve and deteriorate, they’re admitted and discharged, and their nursing needs can change in an instant. The assignment process requires constant evaluation and reevaluation of information and priorities. And that’s why the assignments are usually written in pencil on paper or in marker on a dry-erase board. As the charge nurse, you must communicate with patients and staff throughout the shift and react to changing needs by updating assignments. Your goal is to ensure patients receive the best care possible; how that’s accomplished can change from minute to minute.
7. Evaluate success
What’s the best way to evaluate the success of your nurse-patient assignments? Think back to your priorities and goals. Did all the patients receive safe, quality care? Did you maintain continuity of care? Did the new nurse get the best orientation experience? Were the assignments fair? Measure success based on patient and nurse outcomes.
Check in with the nurses and patients to get their feedback. Ask how the assignment went. Did everyone get his or her work done? Were all the patients’ needs met? What could have been done better? Get specifics. Transparency is key here. Explain your rationale for each assignment (including your focus on patient safety) and keep in mind that you have more information than the nurses. You’re directing activity across the entire unit, so you see the big picture. Your colleagues will be much more understanding when you share your perspective. When you speak with patients, ask about their experiences and if all their needs were met.
8. Keep practicing
Nurse-patient assignments never lose their complexity, but you’ll get better at recognizing potential pitfalls and maximizing patient and nurse outcomes. Keep practicing and remember that good assignments contribute to nurses’ overall job satisfaction.
What you need to know
Before you make decisions about nurse-patient assignments, you need as much information as possible about your unit, nurses, and patients.
Common patient decision factors Demographics • Age • Cultural background • Gender • Language
Acuity • Chief complaint • Code status • Cognitive status • Comorbidities • Condition • Diagnosis • History • Lab work • Procedures • Type of surgery • Vital signs • Weight
Workload • Nursing interventions • Admissions, discharges, transfers • Blood products • Chemotherapy • Drains • Dressing changes • End-of-life care • I.V. therapy • Lines • Medications • Phototherapy • Treatments • Activities of daily living • Bowel incontinence • Feedings • Total care
Safety measures • Airway • Contact precautions • Dermatologic precautions • Fall precautions • Restraints • Surveillance
Psychosocial support • Emotional needs • Familial support • Intellectual needs
Care coordination • Consultations • Diagnostic tests • Orders • Physician visit
Common nurse decision factors Demographics • Culture/race • Gender • Generation/age • Personality
Preference • Request to be assigned/not assigned to a patient
Competence • Certification • Education • Efficiency • Experience • Knowledge/knowledge deficit • Licensure • Orienting • Skills • Speed • Status (float, travel)
Choose your process
Your nurse-patient assignment process may be dictated by unit layout, patient census, or nurse-to-patient ratio. Most nurses use one of three assignment processes.
Area assignment This process involves assigning nurses and patients to areas. If you work in the emergency department (ED) or postanesthesia care unit (PACU), you likely make nurse-patient assignments this way. A nurse is assigned to an area, such as triage in the ED or Beds 1 and 2 in the PACU, and then patients are assigned to each area throughout the shift.
Direct assignment The second option is to assign each nurse directly to a patient. This process works best on units with a lower patient census and nurse-to-patient ratio. For example, on a higher-acuity unit, such as an intensive care unit, the nurse is matched with one or two patients, so a direct assignment is made.
Group assignment With the third option, you assign patients to groups and then assign the nurse to a group. Bigger units have higher censuses and nurse-to-patient ratios (1:5 or 1:6). They also can have unique physical features or layouts that direct how assignments are made. A unit might be separated by hallways, divided into pods, or just too large for one nurse to safely provide care to patients in rooms at opposite ends of the unit. So, grouping patients together based on unit geography and other acuity/workload factors may be the safest and most effective way to make assignments.
You also can combine processes. For example, in a labor and delivery unit, you can assign one nurse to the triage area (area process) while another nurse is assigned to one or two specific patients (direct process). Unit characteristics direct your process for making assignments. Your process will remain the same unless your unit’s geography or patient characteristics (length of stay, nurse-patient ratio) change.
Stephanie B. Allen is an assistant professor at Pace University in Pleasantville, New York.
Selected references Allen SB. The nurse-patient assignment process: What clinical nurses and patients think. MEDSURG Nurs. 2018;27(2):77-82. Allen SB. The nurse-patient assignment: Purposes and decision factors. J Nurs Adm. 2015;45(12):628-35. Allen SB. Assignments matter: Results of a nurse-patient assignment survey. MEDSURG Nurs [in press]. American Nurses Association (ANA). ANA‘s Principles for Nurse Staffing. 2nd ed. Silver Spring, MD: ANA; 2012.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Nursing admission assessment and examination.
Tammy J. Toney-Butler ; Wendy J. Unison-Pace .
Last Update: August 28, 2023 .
- Definition/Introduction
The initial nursing assessment, the first step in the five steps of the nursing process, involves the systematic and continuous collection of data; sorting, analyzing, and organizing that data; and the documentation and communication of the data collected. Critical thinking skills applied during the nursing process provide a decision-making framework to develop and guide a plan of care for the patient incorporating evidence-based practice concepts. This concept of precision education to tailor care based on an individual's unique cultural, spiritual, and physical needs, rather than a trial by error, one size fits all approach results in a more favorable outcome. [1] [2] [3]
The nursing assessment includes gathering information concerning the patient's individual physiological, psychological, sociological, and spiritual needs. It is the first step in the successful evaluation of a patient. Subjective and objective data collection are an integral part of this process. Part of the assessment includes data collection by obtaining vital signs such as temperature, respiratory rate, heart rate, blood pressure, and pain level using an age or condition appropriate pain scale. The assessment identifies current and future care needs of the patient by allowing the formation of a nursing diagnosis. The nurse recognizes normal and abnormal patient physiology and helps prioritize interventions and care. [4] [5]
Nursing Process
- Assessment (gather subjective and objective data, family history, surgical history, medical history, medication history, psychosocial history)
- Analysis or diagnosis (formulate a nursing diagnosis by using clinical judgment; what is wrong with the patient)
- Planning (develop a care plan which incorporates goals, potential outcomes, interventions)
- Implementation (perform the task or intervention)
- Evaluation (was the intervention successful or unsuccessful)
- Issues of Concern
The function of the initial nursing assessment is to identify the assessment parameters and responsibilities needed to plan and deliver appropriate, individualized care to the patient. [6] [7] [8] [9]
This includes documenting:
- Appropriate level of care to meet the client's or patient’s needs in a linguistically appropriate, culturally competent manner
- Evaluating response to care
- Community support
- Assessment and reassessment once admitted
- Safe plan of discharge
The nurse should strive to complete:
- Admission history and physical assessment as soon as the patient arrives at the unit or status is changed to an inpatient
- Data collected should be entered on the Nursing Admission Assessment Sheet and may vary slightly depending on the facility
- Additional data collected should be added
- Documentation and signature either written or electronic by the nurse performing the assessment
Summary Nursing Admission Assessment
- Documentation: Name, medical record number, age, date, time, probable medical diagnosis, chief complaint, the source of information (two patient identifiers)
- Past medical history: Prior hospitalizations and major illnesses and surgeries
- Assess pain: Location, severity, and use of a pain scale
- Allergies: Medications, foods, and environmental; nature of the reaction and seriousness; intolerances to medications; apply allergy band and confirm all prepopulated allergies in the electronic medical record (EMR) with the patient or caregiver
- Medications: Confirm accuracy of the list, names, and dosages of medications by reconciling all medications promptly using electronic data confirmation, if available, from local pharmacies; include supplements and over-the-counter medications
- Valuables: Record and send to appropriate safe storage or send home with family following any institutional policies on the secure management of patient belongings; provide and label denture cups
- Rights: Orient patient, caregivers, and family to location, rights, and responsibilities; goal of admission and discharge goal
- Activities: Check daily activity limits and need for mobility aids
- Falls: Assess Morse Fall Risk and initiate fall precautions as dictated by institutional policy
- Psychosocial: Evaluate need for a sitter or video monitoring, any signs of agitation, restlessness, hallucinations, depression, suicidal ideations, or substance abuse
- Nutritional: Appetite, changes in body weight, need for nutritional consultation based on body mass index (BMI) calculated from measured height and weight on admission
- Vital signs: Temperature recorded in Celsius, heart rate, respiratory rate, blood pressure, pain level on admission, oxygen saturation
- Any handoff information from other departments
Physical Exam
- Cardiovascular: Heart sounds; pulse irregular, regular, weak, thready, bounding, absent; extremity coolness; capillary refill delayed or brisk; presence of swelling, edema, or cyanosis
- Respiratory: Breath sounds, breathing pattern, cough, character of sputum, shallow or labored respirations, agonal breathing, gasps, retractions present, shallow, asymmetrical chest rise, dyspnea on exertion
- Gastrointestinal: Bowel sounds, abdominal tenderness, any masses, scars, character of bowel movements, color, consistency, appetite poor or good, weight loss, weight gain, nausea, vomiting, abdominal pain, presence of feeding tube
- Genitourinary: Character of voiding, discharge, vaginal bleeding (pad count), last menstrual period or date of menopause or hysterectomy, rashes, itching, burning, painful intercourse, urinary frequency, hesitancy, presence of catheter
- Neuromuscular: Level of consciousness using AVPU (alert, voice, pain, unresponsive); Glasgow coma scale (GCS); speech clear, slurred, or difficult; pupil reactivity and appearance; extremity movement equal or unequal; steady gait; trouble swallowing
- Integument: Turgor, integrity, color, and temperature, Braden Risk Assessment, diaphoresis, cold, warm, flushed, mottled, jaundiced, cyanotic, pale, ruddy, any signs of skin breakdown, chronic wounds
Initial Assessment [10] [11] [12]
Steps in Evaluating a New Patient
- Record chief complaint and history
- Perform physical examination
- Complete an initial psychological evaluation; screen for intimate partner violence; CAGE questionnaire and CIWA (Clinical Institute Withdrawal Assessment for Alcohol) scoring if indicated; suicide risk assessment
- Provide a certified translator if a language barrier exists; ensure culturally competent care and privacy
- Ensure the healthcare provider has ordered the appropriate tests for the suspected diagnosis, and initiate any predetermined protocols according to the hospital or institutional policy
Which provides the diagnosis most often: history, physical, or diagnostic tests?
- History: 70%
- Physical: 15% to 20%
- Diagnostic tests: 10% to 15%
History Taking Techniques
Record chief complaint
History of the present illness, presence of pain
P-Q-R-S-T Tool to Evaluate Pain
- P: What provokes symptoms? What improves or exacerbates the condition? What were you doing when it started? Does position or activity make it worse?
- Q: Quality and Quantity of symptoms: Is it dull, sharp, constant, intermittent, throbbing, pulsating, aching, tearing or stabbing?
- R: Radiation or Region of symptoms: Does the pain travel, or is it only in one location? Has it always been in the same area, or did it start somewhere else?
- S: Severity of symptoms or rating on a pain scale. Does it affect activities of daily living such as walking, sitting, eating, or sleeping?
- T: Time or how long have they had the symptoms. Is it worse after eating, changes in weather, or time of day?
S-A-M-P-L-E
- S: Signs and symptoms
- A: Allergies
- M: Medications
- P: Past medical history
- L: Last meal or oral intake
- E: Events before the acute situation
Pain Assessment
Pain, or the fifth vital sign, is a crucial component in providing the appropriate care to the patient. Pain assessment may be subjective and difficult to measure. Pain is anything the patient or client states that it is to them. As nurses, you should be aware of the many factors that can influence the patient's pain. Systematic pain assessment, measurement, and reassessment enhance the ability to keep the patient comfortable. Pain scales that are age appropriate assist in the concise measurement and communication of pain among providers. Improvement of communication regarding pain assessment and reassessment during admission and discharge processes facilitate pain management, thus enhancing overall function and quality of life in a trickle-down fashion.
According to one performance and improvement outpatient project in 2017, areas for improvement in pain reassessment policies and procedures were identified in a clinic setting. The study concluded compliance rates for the 30-minute time requirement outlined in the clinic policy for pain reassessment were found to be low. Heavy patient load, staff memory rather than documentation, and a lack of standardized procedures in the electronic health record (EHR) design played a role in low compliance with the reassessment of pain. Barriers to pain assessment and reassessment are important benchmarks in quality improvement projects. Key performance indicators (KPIs) to improve pain management goals and overall patient satisfaction, balanced with the challenges of an opioid crisis and oversedation risks, all play a role in future research studies and quality of care projects. Recognition of indicators of pain and comprehensive knowledge in pain assessment will guide care and pain management protocols.
Indicators of Pain
- Restlessness or pacing
- Groaning or moaning
- Gasping or grunting
- Nausea or vomiting
- Diaphoresis
- Clenching of the teeth and facial expressions
- Tachycardia or blood pressure changes
- Panting or increased respiratory rate
- Clutching or protecting a part of the body
- Unable to speak or open eyes
- Decreased interest in activities, social gatherings, or old routines
Psychosocial Assessment
The primary consideration is the health and emotional needs of the patient. Assessment of cognitive function, checking for hallucinations and delusions, evaluating concentration levels, and inquiring into interests and level of activity constitute a mental or emotional health assessment. Asking about how the client feels and their response to those feelings is part of a psychological assessment. Are they agitated, irritable, speaking in loud vocal tones, demanding, depressed, suicidal, unable to talk, have a flat affect, crying, overwhelmed, or are there any signs of substance abuse? The psychological examination may include perceptions, whether justifiable or not, on the part of the patient or client. Religion and cultural beliefs are critical areas to consider. Screening for delirium is essential because symptoms are often subtle and easily overlooked, or explained away as fatigue or depression.
Safety Assessment
- Ambulatory aids
- Environmental concerns, home safety
- Domestic and family violence risk, human trafficking risks, elder or child abuse risk
- Suicidal ideation (initiate suicide precautions as directed by institutional policy)
Therapeutic Communication Techniques Used to Take a Good History
Multiple strategies are employed that will include:
- Active, attentive listening
- Reflection, sharing observations
- Share hope
- Share humor
- Therapeutic silence
- Provide information
- Clarification
- Paraphrasing
- Asking relevant questions
- Summarizing
- Self-disclosure
- Confrontation
What are examples?
- Active, attentive listening: Attention to the details of what the patient is saying either in a verbal or nonverbal manner
- Reflection, share observations: Repeat the patient’s words to encourage discussion, state observations that will not make the patient angry or embarrassed; i.e., " You seem tired today, sad...," " You have hardly eaten anything this morning."
- Empathy: Demonstrate that you understand and feel for the patient, recognition of their current situation and perceived feelings, and communicating in a nonjudgmental, unbiased way of acceptance
- Share hope: Ensure in the patient a sense of power, hope in an often hopeless environment, and the possibility of a positive outcome
- Share humor: Fosters a relationship of emotional support, establishes rapport, acts as a positive diversion technique, and promotes physical and mental well being. Cultural considerations play a role in humor
- Touch: Touch may be a source of comfort or discomfort for a patient, wanted or unwanted; observe verbal and nonverbal cues with touch; holding a hand, conducting a physical assessment, performing a procedure
- Therapeutic silence: Fosters an environment of patience, thought and reflection on difficult decisions, and allows time to observe any nonverbal signs of discomfort (the patient typically breaks the silence first)
- Provide information: During an assessment and care, inform the patient as to what is about to happen, explain findings and the need for further testing or observation to promote trust and decrease anxiety
- Clarification: Ask questions to clear up ambiguous statements, ask the client or patient to rephrase or restate confusing remarks so wrong assumptions are clarifiable and a missed opportunity for valuable information forgone
- Focusing: Brings the focus of the conversation to an essential area of concern, eliminating vague or rambling dialogue, centers the assessment on the source of discomfort and pertinent details in the history
- Paraphrasing: Invites patient participation and understanding in a conversation
- Asking relevant questions: Questions are general at first then become more specific; asked in a logical, consecutive order; open-ended, close-ended, and focused questions may be useful during an assessment
- Summarizing: Provides a review of assessment findings, offers clarification opportunities, informs the next step in the admission and hospitalization process
- Self-disclosure: Promotes a trusting relationship, the feeling that the patient is not in this alone, or unique in their current circumstances; provides a framework for hope, support, and respect
- Confrontation: You may have to confront the patient after a trustful rapport has been established, discussing any inconsistencies in the history, thought processes, or inappropriate behavior
Cultural Assessment
The cultural competency assessment will identify factors that may impede the implementation of nursing diagnosis and care. Information obtained should include:
- Ethnic origin, languages spoken, and need for an interpreter
- Primary language preferred for written and verbal instructions
- Support system, decision makers
- Living arrangements
- Religious practices
- Emotional responses
- Special food requirements, dietary considerations
- Cultural customs or taboos such as unwanted touching or eye contact
Physical Examination Techniques
Initial evaluation or the general survey may include:
- Overall health status
- Body habitus
- Personal hygiene, grooming
- Skin condition such as signs of breakdown or chronic wounds
- Breath and body odor
- Overall mood and psychological state
- Initial vital sign measurements: temperature recorded in Celsius in most institutions, respiratory rate, pulse rate, blood pressure with appropriate sized cuff, pulse oximetry reading and note if on room air or oxygen; accurately measured weight in kilograms with the proper scale and height measurement, so body mass index (BMI) is calculable for dosing weights and nutritional guidelines
Secondary Assessment
- Cardiovascular
- Gastrointestinal
- Musculoskeletal
- Neurological
- Genitourinary/Pelvic
- Integumentary
- Mental status and behavioral
- Look at all areas of the skin, including those under clothing or gowns
- Ensure patient is undressed, allowing for privacy, uncover one body part at a time if possible
- Lighting should be bright
- Be alert for any malodors from the body including the oral cavity; fecal odor, fruity-smell, odor of alcohol or tobacco on the breath
- Compare one side to the other, and ask the patient about any asymmetrical areas
- Observe for color, rashes, skin breakdown, tubes and drains, scars, bruising, burns
- Grade any edema present
- Document pertinent normal and abnormal findings
- Consistency
- Tenderness
- Temperature and moisture (warm, moist or cool, and dry)
- Tactile fremitus
- Good hand and finger technique
- Good striking and listening technique
- Especially important in the pulmonary and gastrointestinal systems
- Dull, flat, resonance, hyper-resonance, or tympany sounds
- Percussion is an advanced technique requiring a specific skill set to perform. Therefore, it is a skill practiced by advanced practice nurses as opposed to a bedside nurse on a routine basis
Auscultation
- Listening to body sounds such as bowel sounds, breath sounds, and heart sounds
- Important in examination of the heart, blood pressure, and gastrointestinal system
- Listen for bruits, murmurs, friction rubs, and irregularities in pulse
What are important things to remember about the physical exam?
- Physical exam length can vary depending on complexity
- Physical exam extends from passive observation to hands-on
- Be systematic and thorough
- Ensure privacy and comfort
- Warm hands for patient comfort
- Avoid long fingernails to prevent patient injury during the exam
- Palpate areas that are tender or painful last
- Be alert for any signs of maltreatment or abuse, and follow mandatory reporting guidelines
- Abdominal assessment follows the techniques in this sequence: inspection, auscultation, percussion, and palpation
- Auscultate bowel sounds for at least 15 seconds in each quadrant using the diaphragm of the stethoscope, starting with the lower right-hand quadrant and moving clockwise
- If a fistula is present for hemodialysis, assess for a thrill or bruit, document presence or absence. Notify managing healthcare provider immediately if absent
- Steps in a comprehensive lung exam include PIPPA; Positioning of the patient, Inspection, Palpation, Percussion, Auscultation
Diagnostic Studies
Driven by findings on the history and physical examination; options include:
- Blood tests (CBC, chemistry, bedside glucose, pregnancy test, urinalysis, cardiac enzymes, coagulation studies)
- Imaging studies (X-rays, CT, MRI, ultrasound)
- Other diagnostic studies (ECG, EEG, lumbar puncture, etc.,)
Discharge Planning
- Document mode of transport
- Who is accompanying the patient?
- Transfer forms/EMTALA considerations
- Functional status
- Financial considerations
- Discharge medications and instructions
- Follow up information, referrals, hotline numbers, shelter information
- Barriers to learning
- Document verbalization that discharge instructions were understood by caregiver or surrogate
- Provide translators and language appropriate discharge instructions or paperwork
- Clinical Significance
Often the initial history and physical examination lead to the identification of life- or limb-threatening conditions that can be stabilized promptly, ensuring better patient outcomes. The sooner the patient is correctly assessed, the more likely a life-altering condition is recognizable, nursing diagnosis formulated, appropriate intervention or treatment initiated, and stabilizing care rendered. Physiological abnormalities manifested by changes in vital signs and level of consciousness often provide early warning signs that patient condition is deteriorating; thus, requiring prompt intervention to forego an adverse outcome, decreasing morbidity and mortality risk. In the fast-paced, resource-challenged healthcare environment today, thorough assessment can pose a challenge for the healthcare provider but is essential to safe, quality care. The importance of a head-to-toe assessment, critical thinking skills guided by research, and therapeutic communication are the mainstays of safe practice. [13] [14] [15]
Assessment findings that include current vital signs, lab values, changes in condition such as decreased urine output, cardiac rhythm, pain level, and mental status, as well as pertinent medical history with recommendations for care, are communicated to the provider by the nurse. Communicating in a concise, efficient manner in rapidly changing situations and deteriorating patient conditions can promote quick solutions during difficult circumstances. Healthcare providers communicate and share in the decision-making process. The SBAR model facilitates this communication between members of the healthcare team and bridges the gap between a narrative, descriptive approach and one armed with exact details.
Communication using the SBAR Model
- Recommendation
Assessment Tools
- Activities of daily living scale
- Cough assessment
- Health questionnaires such as those that address recent travel and exposure risks
- Waterlow or Braden scale for assessing pressure ulcer risk
- Glasgow coma scale/AVPU for assessment of consciousness
- Pain scales such as the Faces Pain Scale (FPS), Numeric Rating System (NRS), Visual Analogue Scales (VAS), Wong-Baker Faces Pain Rating Scale (WBS), and the (MPQ) McGill Pain Questionnaire
- CAGE assessment/CIWA scoring
- Morse Fall Risk
- Standard vital sign flow charts for different age groups
- NIH Stroke Scale (NIHSS)
- Dysphagia Screen
- 4AT Assessment for Delirium
- The nurse should be familiar with the otoscope, penlight, stethoscope (bell and diaphragm), thermometer, bladder scanner, speculum, eye charts, cardiac and blood pressure monitors, fetal doppler and extremity doppler, and sphygmomanometer
- Stretcher or bed for proper positioning during a physical exam
- Hand hygiene products, personal protective equipment if required
- Alcohol swabs, sanitizer, or soapy water to clean equipment after use, such as with stethoscopes, to decrease the likelihood of cross-contamination of pathogens from inanimate objects (follow any manufacturer guidelines or institutional policies)
- Computer or paper chart to document findings
- Calculation devices for BMI, conversion from pounds to kilograms, kilograms to pounds, Celsius to Farenheight
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Tammy Toney-Butler declares no relevant financial relationships with ineligible companies.
Disclosure: Wendy Unison-Pace declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Toney-Butler TJ, Unison-Pace WJ. Nursing Admission Assessment and Examination. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. [JBI Libr Syst Rev. 2012] A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. Truglio-Londrigan M, Slyer JT, Singleton JK, Worral P. JBI Libr Syst Rev. 2012; 10(58):4633-4646.
- Student and educator experiences of maternal-child simulation-based learning: a systematic review of qualitative evidence protocol. [JBI Database System Rev Implem...] Student and educator experiences of maternal-child simulation-based learning: a systematic review of qualitative evidence protocol. MacKinnon K, Marcellus L, Rivers J, Gordon C, Ryan M, Butcher D. JBI Database System Rev Implement Rep. 2015 Jan; 13(1):14-26.
- Medical Error Reduction and Prevention. [StatPearls. 2024] Medical Error Reduction and Prevention. Rodziewicz TL, Houseman B, Hipskind JE. StatPearls. 2024 Jan
- Review Deprescribing medicines in older people living with multimorbidity and polypharmacy: the TAILOR evidence synthesis. [Health Technol Assess. 2022] Review Deprescribing medicines in older people living with multimorbidity and polypharmacy: the TAILOR evidence synthesis. Reeve J, Maden M, Hill R, Turk A, Mahtani K, Wong G, Lasserson D, Krska J, Mangin D, Byng R, et al. Health Technol Assess. 2022 Jul; 26(32):1-148.
- Review The impact of empirical studies of spirituality and culture on nurse education. [J Clin Nurs. 2006] Review The impact of empirical studies of spirituality and culture on nurse education. Narayanasamy A. J Clin Nurs. 2006 Jul; 15(7):840-51.
Recent Activity
- Nursing Admission Assessment and Examination - StatPearls Nursing Admission Assessment and Examination - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Open access
- Published: 17 April 2024
Deciphering the influence: academic stress and its role in shaping learning approaches among nursing students: a cross-sectional study
- Rawhia Salah Dogham 1 ,
- Heba Fakieh Mansy Ali 1 ,
- Asmaa Saber Ghaly 3 ,
- Nermine M. Elcokany 2 ,
- Mohamed Mahmoud Seweid 4 &
- Ayman Mohamed El-Ashry ORCID: orcid.org/0000-0001-7718-4942 5
BMC Nursing volume 23 , Article number: 249 ( 2024 ) Cite this article
203 Accesses
Metrics details
Nursing education presents unique challenges, including high levels of academic stress and varied learning approaches among students. Understanding the relationship between academic stress and learning approaches is crucial for enhancing nursing education effectiveness and student well-being.
This study aimed to investigate the prevalence of academic stress and its correlation with learning approaches among nursing students.
Design and Method
A cross-sectional descriptive correlation research design was employed. A convenient sample of 1010 nursing students participated, completing socio-demographic data, the Perceived Stress Scale (PSS), and the Revised Study Process Questionnaire (R-SPQ-2 F).
Most nursing students experienced moderate academic stress (56.3%) and exhibited moderate levels of deep learning approaches (55.0%). Stress from a lack of professional knowledge and skills negatively correlates with deep learning approaches (r = -0.392) and positively correlates with surface learning approaches (r = 0.365). Female students showed higher deep learning approach scores, while male students exhibited higher surface learning approach scores. Age, gender, educational level, and academic stress significantly influenced learning approaches.
Academic stress significantly impacts learning approaches among nursing students. Strategies addressing stressors and promoting healthy learning approaches are essential for enhancing nursing education and student well-being.
Nursing implication
Understanding academic stress’s impact on nursing students’ learning approaches enables tailored interventions. Recognizing stressors informs strategies for promoting adaptive coping, fostering deep learning, and creating supportive environments. Integrating stress management, mentorship, and counseling enhances student well-being and nursing education quality.
Peer Review reports
Introduction
Nursing education is a demanding field that requires students to acquire extensive knowledge and skills to provide competent and compassionate care. Nursing education curriculum involves high-stress environments that can significantly impact students’ learning approaches and academic performance [ 1 , 2 ]. Numerous studies have investigated learning approaches in nursing education, highlighting the importance of identifying individual students’ preferred approaches. The most studied learning approaches include deep, surface, and strategic approaches. Deep learning approaches involve students actively seeking meaning, making connections, and critically analyzing information. Surface learning approaches focus on memorization and reproducing information without a more profound understanding. Strategic learning approaches aim to achieve high grades by adopting specific strategies, such as memorization techniques or time management skills [ 3 , 4 , 5 ].
Nursing education stands out due to its focus on practical training, where the blend of academic and clinical coursework becomes a significant stressor for students, despite academic stress being shared among all university students [ 6 , 7 , 8 ]. Consequently, nursing students are recognized as prone to high-stress levels. Stress is the physiological and psychological response that occurs when a biological control system identifies a deviation between the desired (target) state and the actual state of a fitness-critical variable, whether that discrepancy arises internally or externally to the human [ 9 ]. Stress levels can vary from objective threats to subjective appraisals, making it a highly personalized response to circumstances. Failure to manage these demands leads to stress imbalance [ 10 ].
Nursing students face three primary stressors during their education: academic, clinical, and personal/social stress. Academic stress is caused by the fear of failure in exams, assessments, and training, as well as workload concerns [ 11 ]. Clinical stress, on the other hand, arises from work-related difficulties such as coping with death, fear of failure, and interpersonal dynamics within the organization. Personal and social stressors are caused by an imbalance between home and school, financial hardships, and other factors. Throughout their education, nursing students have to deal with heavy workloads, time constraints, clinical placements, and high academic expectations. Multiple studies have shown that nursing students experience higher stress levels compared to students in other fields [ 12 , 13 , 14 ].
Research has examined the relationship between academic stress and coping strategies among nursing students, but no studies focus specifically on the learning approach and academic stress. However, existing literature suggests that students interested in nursing tend to experience lower levels of academic stress [ 7 ]. Therefore, interest in nursing can lead to deep learning approaches, which promote a comprehensive understanding of the subject matter, allowing students to feel more confident and less overwhelmed by coursework and exams. Conversely, students employing surface learning approaches may experience higher stress levels due to the reliance on memorization [ 3 ].
Understanding the interplay between academic stress and learning approaches among nursing students is essential for designing effective educational interventions. Nursing educators can foster deep learning approaches by incorporating active learning strategies, critical thinking exercises, and reflection activities into the curriculum [ 15 ]. Creating supportive learning environments encouraging collaboration, self-care, and stress management techniques can help alleviate academic stress. Additionally, providing mentorship and counselling services tailored to nursing students’ unique challenges can contribute to their overall well-being and academic success [ 16 , 17 , 18 ].
Despite the scarcity of research focusing on the link between academic stress and learning methods in nursing students, it’s crucial to identify the unique stressors they encounter. The intensity of these stressors can be connected to the learning strategies employed by these students. Academic stress and learning approach are intertwined aspects of the student experience. While academic stress can influence learning approaches, the choice of learning approach can also impact the level of academic stress experienced. By understanding this relationship and implementing strategies to promote healthy learning approaches and manage academic stress, educators and institutions can foster an environment conducive to deep learning and student well-being.
Hence, this study aims to investigate the correlation between academic stress and learning approaches experienced by nursing students.
Study objectives
Assess the levels of academic stress among nursing students.
Assess the learning approaches among nursing students.
Identify the relationship between academic stress and learning approach among nursing students.
Identify the effect of academic stress and related factors on learning approach and among nursing students.
Materials and methods
Research design.
A cross-sectional descriptive correlation research design adhering to the STROBE guidelines was used for this study.
A research project was conducted at Alexandria Nursing College, situated in Egypt. The college adheres to the national standards for nursing education and functions under the jurisdiction of the Egyptian Ministry of Higher Education. Alexandria Nursing College comprises nine specialized nursing departments that offer various nursing specializations. These departments include Nursing Administration, Community Health Nursing, Gerontological Nursing, Medical-Surgical Nursing, Critical Care Nursing, Pediatric Nursing, Obstetric and Gynecological Nursing, Nursing Education, and Psychiatric Nursing and Mental Health. The credit hour system is the fundamental basis of both undergraduate and graduate programs. This framework guarantees a thorough evaluation of academic outcomes by providing an organized structure for tracking academic progress and conducting analyses.
Participants and sample size calculation
The researchers used the Epi Info 7 program to calculate the sample size. The calculations were based on specific parameters such as a population size of 9886 students for the academic year 2022–2023, an expected frequency of 50%, a maximum margin of error of 5%, and a confidence coefficient of 99.9%. Based on these parameters, the program indicated that a minimum sample size of 976 students was required. As a result, the researchers recruited a convenient sample of 1010 nursing students from different academic levels during the 2022–2023 academic year [ 19 ]. This sample size was larger than the minimum required, which could help to increase the accuracy and reliability of the study results. Participation in the study required enrollment in a nursing program and voluntary agreement to take part. The exclusion criteria included individuals with mental illnesses based on their response and those who failed to complete the questionnaires.
socio-demographic data that include students’ age, sex, educational level, hours of sleep at night, hours spent studying, and GPA from the previous semester.

Tool two: the perceived stress scale (PSS)
It was initially created by Sheu et al. (1997) to gauge the level and nature of stress perceived by nursing students attending Taiwanese universities [ 20 ]. It comprises 29 items rated on a 5-point Likert scale, where (0 = never, 1 = rarely, 2 = sometimes, 3 = reasonably often, and 4 = very often), with a total score ranging from 0 to 116. The cut-off points of levels of perceived stress scale according to score percentage were low < 33.33%, moderate 33.33–66.66%, and high more than 66.66%. Higher scores indicate higher stress levels. The items are categorized into six subscales reflecting different sources of stress. The first subscale assesses “stress stemming from lack of professional knowledge and skills” and includes 3 items. The second subscale evaluates “stress from caring for patients” with 8 items. The third subscale measures “stress from assignments and workload” with 5 items. The fourth subscale focuses on “stress from interactions with teachers and nursing staff” with 6 items. The fifth subscale gauges “stress from the clinical environment” with 3 items. The sixth subscale addresses “stress from peers and daily life” with 4 items. El-Ashry et al. (2022) reported an excellent internal consistency reliability of 0.83 [ 21 ]. Two bilingual translators translated the English version of the scale into Arabic and then back-translated it into English by two other independent translators to verify its accuracy. The suitability of the translated version was confirmed through a confirmatory factor analysis (CFA), which yielded goodness-of-fit indices such as a comparative fit index (CFI) of 0.712, a Tucker-Lewis index (TLI) of 0.812, and a root mean square error of approximation (RMSEA) of 0.100.
Tool three: revised study process questionnaire (R-SPQ-2 F)
It was developed by Biggs et al. (2001). It examines deep and surface learning approaches using only 20 questions; each subscale contains 10 questions [ 22 ]. On a 5-point Likert scale ranging from 0 (never or only rarely true of me) to 4 (always or almost always accurate of me). The total score ranged from 0 to 80, with a higher score reflecting more deep or surface learning approaches. The cut-off points of levels of revised study process questionnaire according to score percentage were low < 33%, moderate 33–66%, and high more than 66%. Biggs et al. (2001) found that Cronbach alpha value was 0.73 for deep learning approach and 0.64 for the surface learning approach, which was considered acceptable. Two translators fluent in English and Arabic initially translated a scale from English to Arabic. To ensure the accuracy of the translation, they translated it back into English. The translated version’s appropriateness was evaluated using a confirmatory factor analysis (CFA). The CFA produced several goodness-of-fit indices, including a Comparative Fit Index (CFI) of 0.790, a Tucker-Lewis Index (TLI) of 0.912, and a Root Mean Square Error of Approximation (RMSEA) of 0.100. Comparative Fit Index (CFI) of 0.790, a Tucker-Lewis Index (TLI) of 0.912, and a Root Mean Square Error of Approximation (RMSEA) of 0.100.
Ethical considerations
The Alexandria University College of Nursing’s Research Ethics Committee provided ethical permission before the study’s implementation. Furthermore, pertinent authorities acquired ethical approval at participating nursing institutions. The vice deans of the participating institutions provided written informed consent attesting to institutional support and authority. By giving written informed consent, participants confirmed they were taking part voluntarily. Strict protocols were followed to protect participants’ privacy during the whole investigation. The obtained personal data was kept private and available only to the study team. Ensuring participants’ privacy and anonymity was of utmost importance.
Tools validity
The researchers created tool one after reviewing pertinent literature. Two bilingual translators independently translated the English version into Arabic to evaluate the applicability of the academic stress and learning approach tools for Arabic-speaking populations. To assure accuracy, two additional impartial translators back-translated the translation into English. They were also assessed by a five-person jury of professionals from the education and psychiatric nursing departments. The scales were found to have sufficiently evaluated the intended structures by the jury.
Pilot study
A preliminary investigation involved 100 nursing student applicants, distinct from the final sample, to gauge the efficacy, clarity, and potential obstacles in utilizing the research instruments. The pilot findings indicated that the instruments were accurate, comprehensible, and suitable for the target demographic. Additionally, Cronbach’s Alpha was utilized to further assess the instruments’ reliability, demonstrating internal solid consistency for both the learning approaches and academic stress tools, with values of 0.91 and 0.85, respectively.
Data collection
The researchers convened with each qualified student in a relaxed, unoccupied classroom in their respective college settings. Following a briefing on the study’s objectives, the students filled out the datasheet. The interviews typically lasted 15 to 20 min.
Data analysis
The data collected were analyzed using IBM SPSS software version 26.0. Following data entry, a thorough examination and verification were undertaken to ensure accuracy. The normality of quantitative data distributions was assessed using Kolmogorov-Smirnov tests. Cronbach’s Alpha was employed to evaluate the reliability and internal consistency of the study instruments. Descriptive statistics, including means (M), standard deviations (SD), and frequencies/percentages, were computed to summarize academic stress and learning approaches for categorical data. Student’s t-tests compared scores between two groups for normally distributed variables, while One-way ANOVA compared scores across more than two categories of a categorical variable. Pearson’s correlation coefficient determined the strength and direction of associations between customarily distributed quantitative variables. Hierarchical regression analysis identified the primary independent factors influencing learning approaches. Statistical significance was determined at the 5% (p < 0.05).
Table 1 presents socio-demographic data for a group of 1010 nursing students. The age distribution shows that 38.8% of the students were between 18 and 21 years old, 32.9% were between 21 and 24 years old, and 28.3% were between 24 and 28 years old, with an average age of approximately 22.79. Regarding gender, most of the students were female (77%), while 23% were male. The students were distributed across different educational years, a majority of 34.4% in the second year, followed by 29.4% in the fourth year. The students’ hours spent studying were found to be approximately two-thirds (67%) of the students who studied between 3 and 6 h. Similarly, sleep patterns differ among the students; more than three-quarters (77.3%) of students sleep between 5- to more than 7 h, and only 2.4% sleep less than 2 h per night. Finally, the student’s Grade Point Average (GPA) from the previous semester was also provided. 21% of the students had a GPA between 2 and 2.5, 40.9% had a GPA between 2.5 and 3, and 38.1% had a GPA between 3 and 3.5.
Figure 1 provides the learning approach level among nursing students. In terms of learning approach, most students (55.0%) exhibited a moderate level of deep learning approach, followed by 25.9% with a high level and 19.1% with a low level. The surface learning approach was more prevalent, with 47.8% of students showing a moderate level, 41.7% showing a low level, and only 10.5% exhibiting a high level.
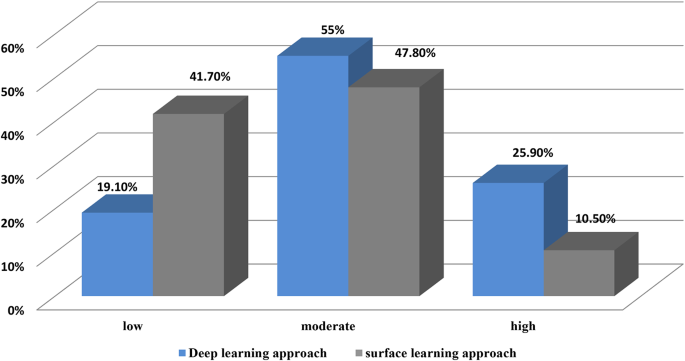
Nursing students? levels of learning approach (N=1010)
Figure 2 provides the types of academic stress levels among nursing students. Among nursing students, various stressors significantly impact their academic experiences. Foremost among these stressors are the pressure and demands associated with academic assignments and workload, with 30.8% of students attributing their high stress levels to these factors. Challenges within the clinical environment are closely behind, contributing significantly to high stress levels among 25.7% of nursing students. Interactions with peers and daily life stressors also weigh heavily on students, ranking third among sources of high stress, with 21.5% of students citing this as a significant factor. Similarly, interaction with teachers and nursing staff closely follow, contributing to high-stress levels for 20.3% of nursing students. While still significant, stress from taking care of patients ranks slightly lower, with 16.7% of students reporting it as a significant factor contributing to their academic stress. At the lowest end of the ranking, but still notable, is stress from a perceived lack of professional knowledge and skills, with 15.9% of students experiencing high stress in this area.
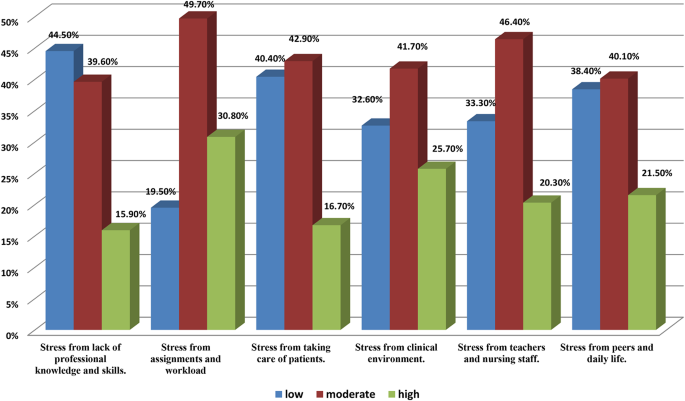
Nursing students? levels of academic stress subtypes (N=1010)
Figure 3 provides the total levels of academic stress among nursing students. The majority of students experienced moderate academic stress (56.3%), followed by those experiencing low academic stress (29.9%), and a minority experienced high academic stress (13.8%).
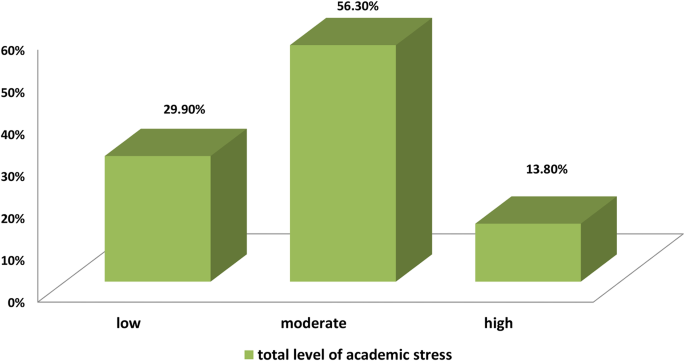
Nursing students? levels of total academic stress (N=1010)
Table 2 displays the correlation between academic stress subscales and deep and surface learning approaches among 1010 nursing students. All stress subscales exhibited a negative correlation regarding the deep learning approach, indicating that the inclination toward deep learning decreases with increasing stress levels. The most significant negative correlation was observed with stress stemming from the lack of professional knowledge and skills (r=-0.392, p < 0.001), followed by stress from the clinical environment (r=-0.109, p = 0.001), stress from assignments and workload (r=-0.103, p = 0.001), stress from peers and daily life (r=-0.095, p = 0.002), and stress from patient care responsibilities (r=-0.093, p = 0.003). The weakest negative correlation was found with stress from interactions with teachers and nursing staff (r=-0.083, p = 0.009). Conversely, concerning the surface learning approach, all stress subscales displayed a positive correlation, indicating that heightened stress levels corresponded with an increased tendency toward superficial learning. The most substantial positive correlation was observed with stress related to the lack of professional knowledge and skills (r = 0.365, p < 0.001), followed by stress from patient care responsibilities (r = 0.334, p < 0.001), overall stress (r = 0.355, p < 0.001), stress from interactions with teachers and nursing staff (r = 0.262, p < 0.001), stress from assignments and workload (r = 0.262, p < 0.001), and stress from the clinical environment (r = 0.254, p < 0.001). The weakest positive correlation was noted with stress stemming from peers and daily life (r = 0.186, p < 0.001).
Table 3 outlines the association between the socio-demographic characteristics of nursing students and their deep and surface learning approaches. Concerning age, statistically significant differences were observed in deep and surface learning approaches (F = 3.661, p = 0.003 and F = 7.983, p < 0.001, respectively). Gender also demonstrated significant differences in deep and surface learning approaches (t = 3.290, p = 0.001 and t = 8.638, p < 0.001, respectively). Female students exhibited higher scores in the deep learning approach (31.59 ± 8.28) compared to male students (29.59 ± 7.73), while male students had higher scores in the surface learning approach (29.97 ± 7.36) compared to female students (24.90 ± 7.97). Educational level exhibited statistically significant differences in deep and surface learning approaches (F = 5.599, p = 0.001 and F = 17.284, p < 0.001, respectively). Both deep and surface learning approach scores increased with higher educational levels. The duration of study hours demonstrated significant differences only in the surface learning approach (F = 3.550, p = 0.014), with scores increasing as study hours increased. However, no significant difference was observed in the deep learning approach (F = 0.861, p = 0.461). Hours of sleep per night and GPA from the previous semester did not exhibit statistically significant differences in deep or surface learning approaches.
Table 4 presents a multivariate linear regression analysis examining the factors influencing the learning approach among 1110 nursing students. The deep learning approach was positively influenced by age, gender (being female), educational year level, and stress from teachers and nursing staff, as indicated by their positive coefficients and significant p-values (p < 0.05). However, it was negatively influenced by stress from a lack of professional knowledge and skills. The other factors do not significantly influence the deep learning approach. On the other hand, the surface learning approach was positively influenced by gender (being female), educational year level, stress from lack of professional knowledge and skills, stress from assignments and workload, and stress from taking care of patients, as indicated by their positive coefficients and significant p-values (p < 0.05). However, it was negatively influenced by gender (being male). The other factors do not significantly influence the surface learning approach. The adjusted R-squared values indicated that the variables in the model explain 17.8% of the variance in the deep learning approach and 25.5% in the surface learning approach. Both models were statistically significant (p < 0.001).
Nursing students’ academic stress and learning approaches are essential to planning for effective and efficient learning. Nursing education also aims to develop knowledgeable and competent students with problem-solving and critical-thinking skills.
The study’s findings highlight the significant presence of stress among nursing students, with a majority experiencing moderate to severe levels of academic stress. This aligns with previous research indicating that academic stress is prevalent among nursing students. For instance, Zheng et al. (2022) observed moderated stress levels in nursing students during clinical placements [ 23 ], while El-Ashry et al. (2022) found that nearly all first-year nursing students in Egypt experienced severe academic stress [ 21 ]. Conversely, Ali and El-Sherbini (2018) reported that over three-quarters of nursing students faced high academic stress. The complexity of the nursing program likely contributes to these stress levels [ 24 ].
The current study revealed that nursing students identified the highest sources of academic stress as workload from assignments and the stress of caring for patients. This aligns with Banu et al.‘s (2015) findings, where academic demands, assignments, examinations, high workload, and combining clinical work with patient interaction were cited as everyday stressors [ 25 ]. Additionally, Anaman-Torgbor et al. (2021) identified lectures, assignments, and examinations as predictors of academic stress through logistic regression analysis. These stressors may stem from nursing programs emphasizing the development of highly qualified graduates who acquire knowledge, values, and skills through classroom and clinical experiences [ 26 ].
The results regarding learning approaches indicate that most nursing students predominantly employed the deep learning approach. Despite acknowledging a surface learning approach among the participants in the present study, the prevalence of deep learning was higher. This inclination toward the deep learning approach is anticipated in nursing students due to their engagement with advanced courses, requiring retention, integration, and transfer of information at elevated levels. The deep learning approach correlates with a gratifying learning experience and contributes to higher academic achievements [ 3 ]. Moreover, the nursing program’s emphasis on active learning strategies fosters critical thinking, problem-solving, and decision-making skills. These findings align with Mahmoud et al.‘s (2019) study, reporting a significant presence (83.31%) of the deep learning approach among undergraduate nursing students at King Khalid University’s Faculty of Nursing [ 27 ]. Additionally, Mohamed &Morsi (2019) found that most nursing students at Benha University’s Faculty of Nursing embraced the deep learning approach (65.4%) compared to the surface learning approach [ 28 ].
The study observed a negative correlation between the deep learning approach and the overall mean stress score, contrasting with a positive correlation between surface learning approaches and overall stress levels. Elevated academic stress levels may diminish motivation and engagement in the learning process, potentially leading students to feel overwhelmed, disinterested, or burned out, prompting a shift toward a surface learning approach. This finding resonates with previous research indicating that nursing students who actively seek positive academic support strategies during academic stress have better prospects for success than those who do not [ 29 ]. Nebhinani et al. (2020) identified interface concerns and academic workload as significant stress-related factors. Notably, only an interest in nursing demonstrated a significant association with stress levels, with participants interested in nursing primarily employing adaptive coping strategies compared to non-interested students.
The current research reveals a statistically significant inverse relationship between different dimensions of academic stress and adopting the deep learning approach. The most substantial negative correlation was observed with stress arising from a lack of professional knowledge and skills, succeeded by stress associated with the clinical environment, assignments, and workload. Nursing students encounter diverse stressors, including delivering patient care, handling assignments and workloads, navigating challenging interactions with staff and faculty, perceived inadequacies in clinical proficiency, and facing examinations [ 30 ].
In the current study, the multivariate linear regression analysis reveals that various factors positively influence the deep learning approach, including age, female gender, educational year level, and stress from teachers and nursing staff. In contrast, stress from a lack of professional knowledge and skills exert a negative influence. Conversely, the surface learning approach is positively influenced by female gender, educational year level, stress from lack of professional knowledge and skills, stress from assignments and workload, and stress from taking care of patients, but negatively affected by male gender. The models explain 17.8% and 25.5% of the variance in the deep and surface learning approaches, respectively, and both are statistically significant. These findings underscore the intricate interplay of demographic and stress-related factors in shaping nursing students’ learning approaches. High workloads and patient care responsibilities may compel students to prioritize completing tasks over deep comprehension. This pressure could lead to a surface learning approach as students focus on meeting immediate demands rather than engaging deeply with course material. This observation aligns with the findings of Alsayed et al. (2021), who identified age, gender, and study year as significant factors influencing students’ learning approaches.
Deep learners often demonstrate better self-regulation skills, such as effective time management, goal setting, and seeking support when needed. These skills can help manage academic stress and maintain a balanced learning approach. These are supported by studies that studied the effect of coping strategies on stress levels [ 6 , 31 , 32 ]. On the contrary, Pacheco-Castillo et al. study (2021) found a strong significant relationship between academic stressors and students’ level of performance. That study also proved that the more academic stress a student faces, the lower their academic achievement.
Strengths and limitations of the study
This study has lots of advantages. It provides insightful information about the educational experiences of Egyptian nursing students, a demographic that has yet to receive much research. The study’s limited generalizability to other people or nations stems from its concentration on this particular group. This might be addressed in future studies by using a more varied sample. Another drawback is the dependence on self-reported metrics, which may contain biases and mistakes. Although the cross-sectional design offers a moment-in-time view of the problem, it cannot determine causation or evaluate changes over time. To address this, longitudinal research may be carried out.
Notwithstanding these drawbacks, the study substantially contributes to the expanding knowledge of academic stress and nursing students’ learning styles. Additional research is needed to determine teaching strategies that improve deep-learning approaches among nursing students. A qualitative study is required to analyze learning approaches and factors that may influence nursing students’ selection of learning approaches.
According to the present study’s findings, nursing students encounter considerable academic stress, primarily stemming from heavy assignments and workload, as well as interactions with teachers and nursing staff. Additionally, it was observed that students who experience lower levels of academic stress typically adopt a deep learning approach, whereas those facing higher stress levels tend to resort to a surface learning approach. Demographic factors such as age, gender, and educational level influence nursing students’ choice of learning approach. Specifically, female students are more inclined towards deep learning, whereas male students prefer surface learning. Moreover, deep and surface learning approach scores show an upward trend with increasing educational levels and study hours. Academic stress emerges as a significant determinant shaping the adoption of learning approaches among nursing students.
Implications in nursing practice
Nursing programs should consider integrating stress management techniques into their curriculum. Providing students with resources and skills to cope with academic stress can improve their well-being and academic performance. Educators can incorporate teaching strategies that promote deep learning approaches, such as problem-based learning, critical thinking exercises, and active learning methods. These approaches help students engage more deeply with course material and reduce reliance on surface learning techniques. Recognizing the gender differences in learning approaches, nursing programs can offer gender-specific support services and resources. For example, providing targeted workshops or counseling services that address male and female nursing students’ unique stressors and learning needs. Implementing mentorship programs and peer support groups can create a supportive environment where students can share experiences, seek advice, and receive encouragement from their peers and faculty members. Encouraging students to reflect on their learning processes and identify effective study strategies can help them develop metacognitive skills and become more self-directed learners. Faculty members can facilitate this process by incorporating reflective exercises into the curriculum. Nursing faculty and staff should receive training on recognizing signs of academic stress among students and providing appropriate support and resources. Additionally, professional development opportunities can help educators stay updated on evidence-based teaching strategies and practical interventions for addressing student stress.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to restrictions imposed by the institutional review board to protect participant confidentiality, but are available from the corresponding author on reasonable request.
Liu J, Yang Y, Chen J, Zhang Y, Zeng Y, Li J. Stress and coping styles among nursing students during the initial period of the clinical practicum: A cross-section study. Int J Nurs Sci. 2022a;9(2). https://doi.org/10.1016/j.ijnss.2022.02.004 .
Saifan A, Devadas B, Daradkeh F, Abdel-Fattah H, Aljabery M, Michael LM. Solutions to bridge the theory-practice gap in nursing education in the UAE: a qualitative study. BMC Med Educ. 2021;21(1). https://doi.org/10.1186/s12909-021-02919-x .
Alsayed S, Alshammari F, Pasay-an E, Dator WL. Investigating the learning approaches of students in nursing education. J Taibah Univ Med Sci. 2021;16(1). https://doi.org/10.1016/j.jtumed.2020.10.008 .
Salah Dogham R, Elcokany NM, Saber Ghaly A, Dawood TMA, Aldakheel FM, Llaguno MBB, Mohsen DM. Self-directed learning readiness and online learning self-efficacy among undergraduate nursing students. Int J Afr Nurs Sci. 2022;17. https://doi.org/10.1016/j.ijans.2022.100490 .
Zhao Y, Kuan HK, Chung JOK, Chan CKY, Li WHC. Students’ approaches to learning in a clinical practicum: a psychometric evaluation based on item response theory. Nurse Educ Today. 2018;66. https://doi.org/10.1016/j.nedt.2018.04.015 .
Huang HM, Fang YW. Stress and coping strategies of online nursing practicum courses for Taiwanese nursing students during the COVID-19 pandemic: a qualitative study. Healthcare. 2023;11(14). https://doi.org/10.3390/healthcare11142053 .
Nebhinani M, Kumar A, Parihar A, Rani R. Stress and coping strategies among undergraduate nursing students: a descriptive assessment from Western Rajasthan. Indian J Community Med. 2020;45(2). https://doi.org/10.4103/ijcm.IJCM_231_19 .
Olvera Alvarez HA, Provencio-Vasquez E, Slavich GM, Laurent JGC, Browning M, McKee-Lopez G, Robbins L, Spengler JD. Stress and health in nursing students: the Nurse Engagement and Wellness Study. Nurs Res. 2019;68(6). https://doi.org/10.1097/NNR.0000000000000383 .
Del Giudice M, Buck CL, Chaby LE, Gormally BM, Taff CC, Thawley CJ, Vitousek MN, Wada H. What is stress? A systems perspective. Integr Comp Biol. 2018;58(6):1019–32. https://doi.org/10.1093/icb/icy114 .
Article PubMed Google Scholar
Bhui K, Dinos S, Galant-Miecznikowska M, de Jongh B, Stansfeld S. Perceptions of work stress causes and effective interventions in employees working in public, private and non-governmental organisations: a qualitative study. BJPsych Bull. 2016;40(6). https://doi.org/10.1192/pb.bp.115.050823 .
Lavoie-Tremblay M, Sanzone L, Aubé T, Paquet M. Sources of stress and coping strategies among undergraduate nursing students across all years. Can J Nurs Res. 2021. https://doi.org/10.1177/08445621211028076 .
Article PubMed PubMed Central Google Scholar
Ahmed WAM, Abdulla YHA, Alkhadher MA, Alshameri FA. Perceived stress and coping strategies among nursing students during the COVID-19 pandemic: a systematic review. Saudi J Health Syst Res. 2022;2(3). https://doi.org/10.1159/000526061 .
Pacheco-Castillo J, Casuso-Holgado MJ, Labajos-Manzanares MT, Moreno-Morales N. Academic stress among nursing students in a Private University at Puerto Rico, and its Association with their academic performance. Open J Nurs. 2021;11(09). https://doi.org/10.4236/ojn.2021.119063 .
Tran TTT, Nguyen NB, Luong MA, Bui THA, Phan TD, Tran VO, Ngo TH, Minas H, Nguyen TQ. Stress, anxiety and depression in clinical nurses in Vietnam: a cross-sectional survey and cluster analysis. Int J Ment Health Syst. 2019;13(1). https://doi.org/10.1186/s13033-018-0257-4 .
Magnavita N, Chiorri C. Academic stress and active learning of nursing students: a cross-sectional study. Nurse Educ Today. 2018;68. https://doi.org/10.1016/j.nedt.2018.06.003 .
Folkvord SE, Risa CF. Factors that enhance midwifery students’ learning and development of self-efficacy in clinical placement: a systematic qualitative review. Nurse Educ Pract. 2023;66. https://doi.org/10.1016/j.nepr.2022.103510 .
Myers SB, Sweeney AC, Popick V, Wesley K, Bordfeld A, Fingerhut R. Self-care practices and perceived stress levels among psychology graduate students. Train Educ Prof Psychol. 2012;6(1). https://doi.org/10.1037/a0026534 .
Zeb H, Arif I, Younas A. Nurse educators’ experiences of fostering undergraduate students’ ability to manage stress and demanding situations: a phenomenological inquiry. Nurse Educ Pract. 2022;65. https://doi.org/10.1016/j.nepr.2022.103501 .
Centers for Disease Control and Prevention. User Guide| Support| Epi Info™ [Internet]. Atlanta: CDC; [cited 2024 Jan 31]. Available from: CDC website.
Sheu S, Lin HS, Hwang SL, Yu PJ, Hu WY, Lou MF. The development and testing of a perceived stress scale for nursing students in clinical practice. J Nurs Res. 1997;5:41–52. Available from: http://ntur.lib.ntu.edu.tw/handle/246246/165917 .
El-Ashry AM, Harby SS, Ali AAG. Clinical stressors as perceived by first-year nursing students of their experience at Alexandria main university hospital during the COVID-19 pandemic. Arch Psychiatr Nurs. 2022;41:214–20. https://doi.org/10.1016/j.apnu.2022.08.007 .
Biggs J, Kember D, Leung DYP. The revised two-factor study process questionnaire: R-SPQ-2F. Br J Educ Psychol. 2001;71(1):133–49. https://doi.org/10.1348/000709901158433 .
Article CAS PubMed Google Scholar
Zheng YX, Jiao JR, Hao WN. Stress levels of nursing students: a systematic review and meta-analysis. Med (United States). 2022;101(36). https://doi.org/10.1097/MD.0000000000030547 .
Ali AM, El-Sherbini HH. Academic stress and its contributing factors among faculty nursing students in Alexandria. Alexandria Scientific Nursing Journal. 2018; 20(1):163–181. Available from: https://asalexu.journals.ekb.eg/article_207756_b62caf4d7e1e7a3b292bbb3c6632a0ab.pdf .
Banu P, Deb S, Vardhan V, Rao T. Perceived academic stress of university students across gender, academic streams, semesters, and academic performance. Indian J Health Wellbeing. 2015;6(3):231–235. Available from: http://www.iahrw.com/index.php/home/journal_detail/19#list .
Anaman-Torgbor JA, Tarkang E, Adedia D, Attah OM, Evans A, Sabina N. Academic-related stress among Ghanaian nursing students. Florence Nightingale J Nurs. 2021;29(3):263. https://doi.org/10.5152/FNJN.2021.21030 .
Mahmoud HG, Ahmed KE, Ibrahim EA. Learning Styles and Learning Approaches of Bachelor Nursing Students and its Relation to Their Achievement. Int J Nurs Didact. 2019;9(03):11–20. Available from: http://www.nursingdidactics.com/index.php/ijnd/article/view/2465 .
Mohamed NAAA, Morsi MES, Learning Styles L, Approaches. Academic achievement factors, and self efficacy among nursing students. Int J Novel Res Healthc Nurs. 2019;6(1):818–30. Available from: www.noveltyjournals.com.
Google Scholar
Onieva-Zafra MD, Fernández-Muñoz JJ, Fernández-Martínez E, García-Sánchez FJ, Abreu-Sánchez A, Parra-Fernández ML. Anxiety, perceived stress and coping strategies in nursing students: a cross-sectional, correlational, descriptive study. BMC Med Educ. 2020;20:1–9. https://doi.org/10.1186/s12909-020-02294-z .
Article Google Scholar
Aljohani W, Banakhar M, Sharif L, Alsaggaf F, Felemban O, Wright R. Sources of stress among Saudi Arabian nursing students: a cross-sectional study. Int J Environ Res Public Health. 2021;18(22). https://doi.org/10.3390/ijerph182211958 .
Liu Y, Wang L, Shao H, Han P, Jiang J, Duan X. Nursing students’ experience during their practicum in an intensive care unit: a qualitative meta-synthesis. Front Public Health. 2022;10. https://doi.org/10.3389/fpubh.2022.974244 .
Majrashi A, Khalil A, Nagshabandi E, Al MA. Stressors and coping strategies among nursing students during the COVID-19 pandemic: scoping review. Nurs Rep. 2021;11(2):444–59. https://doi.org/10.3390/nursrep11020042 .
Download references
Acknowledgements
Our sincere thanks go to all the nursing students in the study. We also want to thank Dr/ Rasha Badry for their statistical analysis help and contribution to this study.
The research was not funded by public, commercial, or non-profit organizations.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and affiliations.
Nursing Education, Faculty of Nursing, Alexandria University, Alexandria, Egypt
Rawhia Salah Dogham & Heba Fakieh Mansy Ali
Critical Care & Emergency Nursing, Faculty of Nursing, Alexandria University, Alexandria, Egypt
Nermine M. Elcokany
Obstetrics and Gynecology Nursing, Faculty of Nursing, Alexandria University, Alexandria, Egypt
Asmaa Saber Ghaly
Faculty of Nursing, Beni-Suef University, Beni-Suef, Egypt
Mohamed Mahmoud Seweid
Psychiatric and Mental Health Nursing, Faculty of Nursing, Alexandria University, Alexandria, Egypt
Ayman Mohamed El-Ashry
You can also search for this author in PubMed Google Scholar
Contributions
Ayman M. El-Ashry & Rawhia S. Dogham: conceptualization, preparation, and data collection; methodology; investigation; formal analysis; data analysis; writing-original draft; writing-manuscript; and editing. Heba F. Mansy Ali & Asmaa S. Ghaly: conceptualization, preparation, methodology, investigation, writing-original draft, writing-review, and editing. Nermine M. Elcokany & Mohamed M. Seweid: Methodology, investigation, formal analysis, data collection, writing-manuscript & editing. All authors reviewed the manuscript and accept for publication.
Corresponding author
Correspondence to Ayman Mohamed El-Ashry .
Ethics declarations
Ethics approval and consent to participate.
The research adhered to the guidelines and regulations outlined in the Declaration of Helsinki (DoH-Oct2008). The Faculty of Nursing’s Research Ethical Committee (REC) at Alexandria University approved data collection in this study (IRB00013620/95/9/2022). Participants were required to sign an informed written consent form, which included an explanation of the research and an assessment of their understanding.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dogham, R.S., Ali, H.F.M., Ghaly, A.S. et al. Deciphering the influence: academic stress and its role in shaping learning approaches among nursing students: a cross-sectional study. BMC Nurs 23 , 249 (2024). https://doi.org/10.1186/s12912-024-01885-1
Download citation
Received : 31 January 2024
Accepted : 21 March 2024
Published : 17 April 2024
DOI : https://doi.org/10.1186/s12912-024-01885-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Academic stress
- Learning approaches
- Nursing students
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
College of Nursing, Lexington Medical Center partnership aims to address state nursing shortage

The College of Nursing is getting a new building, but it won't be on USC's campus.
The 52,000-square-foot facility is being built next to Lexington Medical Center to instruct students alongside one of USC's medical partners. The facility is on track to be completed by fall 2024, university architect Derek Gruner said.
South Carolina is projected to have one of the most acute nursing shortages in the country by 2030, College of Nursing Dean Jeannette Andrews said. The partnership hopes to address the need by training more nurses.
"I t's a creative partnership and a win-win for both organizations to be able to meet a mutual need in our state," Andrews said. "And we were both at the place and time of readiness to move forward to do something," .
The space is being constructed as "built to suit," meaning that it is built specifically for its future nursing occupants.
The three-floor building features new classrooms, space for 40 faculty and staff and an upgraded simulation lab. It will also include a student lounge and study spaces , something the USC nursing building lacks.
The simulation lab is one of the key features of the building, t aking up the entire second floor. This makes it three times larger than the current lab at USC.
Fourth-year nursing student Alyssa Massey said the simulation lab is the biggest benefit of the new building due to the updated equipment it provides.
"We did our ACLS code and it was a different type of defibrillator than we see," Massey said. "We're still able to learn from it, but it's just not necessarily the same equipment (in hospitals) since nursing is always progressing."
Moving the simulation lab to the Lexington Medical campus will allow the current lab to be remodeled into a bio behavioral research space for graduate programs, Andrews said.
"It's really transformative in a lot of ways because (it's) just giving us more space, creates more opportunity, so it's a win-win for everybody," Andrews said.

A sign at Lexington Medical Center directs patients to different areas of the hospital in Columbia, South Carolina on April 14, 2024. The College Nursing is partnering with the hospital to fix the state's nursing shortage.
Lexington Medical approached USC about two years ago to ask how the university's program could expand to help address the nursing shortage in the state . The nursing program has almost doubled in size in the last 10 years, but space and faculty limitations have prevented more growth.
Andrew said there are three things needed to expand the program — physical space, clinical space and faculty.
"Because there's a nursing shortage, there's a nursing faculty shortage," Andrews said. "I need physical space to train (students) in the classroom and train them — we also train them in our simulation center ... Then I need physical space. I need clinical sites."
Rather than expand the on-campus nursing building, the hospital offered land next to the hospital . USC's nursing program designed the interior of the building to its specification , with Lexington Medical Center fronting most of the money to build it.
"What we have with Lexington Medical Center is called an academic services agreement where the two parties have this understanding of what each one will do for one another ," Gruner said. "Lexington's responsibility primarily is to build this building ... there are Lexington staff that will be actually participating in the teaching of our students. "
The medical center will staff students during clinical rotations. Nursing students are required to go through rotations at different acute care wards , which is where training from hospitals comes in.
"It's more than a building to us because we are working with Lexington nursing staff and nursing leadership to really think about how we train nurses in the hospital," Andrews said.
Third and fourth-year nursing students and graduate nursing students will have classes there next semester, Andrews said.
Students will travel to Lexington Medical Center for classes and simulations , with free parking being provided next to the buildin g. Andrews said the partnership will help set an example for the future.
"We hope this is a model for others to help meet the different needs of our state and be creative with how we partner with people," Andrews said.
More Like This
South carolina commission for minority affairs holds first minority self-publishing authors roundtable, column: picklegarden on the river is a unique, promising recreational spot for all, usc unveils monument honoring 60th anniversary of desegregation, trending now, efforts ramp up across south carolina to ban dei programs, books in higher education, public k-12 schools, column: the university needs to improve accessibility on campus for students with disabilities, competing beyond the field: how club sports obtain funding, homecoming, family ties, hopes of personal growth bring the 2024 football transfer class to south carolina.
Antique Icons of the Mother of God from the Rostov Kremlin State Museum
Founded by Rostov merchants A. Titov and I. Shlyakov in 1883, the Rostov Kremlin State Museum is now recognized as one of the most valuable objects of cultural heritage in Russia . Located on the territory of the Archbishop’s Yard, a beautiful architectural ensemble of the 17 th century, it currently possesses approximately 92,000 exhibits, including antique icons, porcelain, oil paintings, decorative arts, and archeological findings.
While there are many unique pieces of religious art in the collection of the Rostov Kremlin State Museum, from precious church utensils to wood carvings, antique Russian icons have always occupied a very special place in it. For this reason, we want to draw your attention to a stunning selection of antique icons of the Mother of God, dating back to the 14 th – 15 th century.
- Our Lady of Tenderness (late 14 th century)
This piece of antique icons depicting the renowned Orthodox image of the Mother of God Eleusa came from the Church of St. John the Evangelist on the Ishna River, not far from Rostov. The most interesting thing about it is that the reverse side of this antique icon (see photo above) depicts the Holy Martyrs Eustathius and Thekla. This image was painted in the late 13 th century, which is almost a hundred years earlier than the image of Our Lady of Tenderness.
- The Mother of God Hodegetria (mid-15 th century)
As you already know, the Mother of God Hodegetria is one of the most beloved and revered Eastern Orthodox icons of the Theotokos in Russia. This particular antique icon came from the Church of St. Dmitry of Solun in the Ponikarovo village, Rostov region.
- Deesis icon of the Mother of God (late 15 th century)
Created in the second half of the 15 th century, this beautiful piece of antique icons of the Mother of God was part of a Deesis (a set of Orthodox Christian icons depicting Christ, the Virgin Mary, and St. John the Baptist). It came from the Church of the Intercession in the Gumenets village, Rostov region.
- Our Lady of Tenderness (late 15 th century)
This hand-painted icon of Our Lady of Tenderness represents one more example of two-sided antique icons in the Museum’s collection. Its reverse side depicts another popular in Russia image – St. Nicholas, the Wonderworker . It came from the Church of St. Dimitry of Rostov in the Pesoshnya village.
These were only several examples of unique Marian icons you can find in the Rostov Kremlin State Museum. Its collection is truly impressive, with a whole range of incredible antique icons that are definitely worth seeing.
Photo credit: Christian art/icon-art.info
Preserving icons: an interview with an icon expert, review of oleg kushnirskiy’s russian icon catalog received from uglich, saint catherine’s monastery in sinai: the treasury of byzantium, russian orthodox icons and animal images depicted in them, our russian icon book was reviewed by the radishchev art museum, candlemas: the history and traditional russian icon of the feast.
- Photographers

Urban Soundtracks: Rostov-on-Don According to Motorama
For reasons unknown to me, Russian music has never broken into the Western consciousness, beyond that brief t.A T.u phase in the 2000’s. Americans just never caught on to the wonder that is Philipp Kirkorov, I suppose. Nonetheless, Motorama has carved out a small niche for themselves as an underground hit. Maybe this is down to their lyrics being in English, or perhaps it’s the fact that they have a near-perfect capacity to summarize our twisted emotional landscape with their own brand of Post Punk.
Hailing from Rostov, Russia, they were formed outside the Moscow and Saint Petersburg cultural centers, which produce the bulk of the nation’s cultural exports. Known for being a far more rough city, Rostov appears to be the ideal backdrop for Motorama’s amazing capacity to engender emotions, like disappointment and anxiety. However, little writing is produced about the city and it attracts few tourists from outside Russia. As such, we spoke to Vladislav Parshin from the band, and he kindly put together a bit of a mix to understand the place a bit more.
For most people anything outside of Russia, the country is a complete mystery. How did being from Rostov shape your musical tastes and you guys as artists?
For me the main influence was my father who showed me tons of great music from the Soviet Union and abroad and all these songs formed my tastes. Rostov-on-Don is also an important part of shaping the taste, as I knew personally the members of the New Wave/Post-Punk 90’s bands like Elen and Matrosskaya Tishina , they influenced me in the beginning of the 2000’s.
It is interesting looking at musical scenes that are outside the centers of arts like Manchester, Seattle, and Louisville. It is as if being removed from the mainstream conversation allows you to produce something completely unique and personal. To a certain degree, do you think that your band was almost blessed to be outside the major cities of mainstream culture?
I won’t say that it was a blessing, but it was fine for us as a band. I think that living outside the big cultural spots is a good chance for creating something by yourself, you have more free time, instead of visiting never ending exhibitions, concerts and parties. But at the same time it’s harder to meet people who share the same ideas and who can help you in what you are doing. In general I feel comfortable living in Rostov-on-Don, we are flying to Moscow and St. Petersburg from time to time only because of the concerts.
The mix is fantastic. It is very Post Punk/synth-inspired. However, it is hardly the most ‘sunshine and rainbows’ mix. You’ve said in other interviews that there is nothing exciting about your home city of Rostov. Does that contribute to the sound of the mix?
I like such music and I think it suits our city.
In many articles, your work has been compared to British post-punk bands but I think it is fair to say that you’re part of a broader Soviet/post-Soviet tradition of bands like Kino. What is it about this darker style of music that continues to attract people across different generations in the former USSR?
I think that there’s a specific side in Russian character that is connected with such dark or sorrowful music. For example, lots of traditional folk songs from different parts of Russia are based on metaphysical stories connected with faith and death. All these existential problems are reflected in different art genres here, not only with music, but also literature.
- Yekaterinburg
- Novosibirsk
- Vladivostok
Rostov-on-Don
- Tours to Russia
- Practicalities
- Russia in Lists
Rusmania • Deep into Russia
- Rostov Region

Rostov-on-Don is the largest city in South Russia and the centre of Russia's Southern Federal District. Although officially known as Rostov-on-Don to distinguish it from the ancient city of Rostov , in speech it is usually just called Rostov as the bigger of the two Rostovs (the orginal Rostov is confusingly then often called Rostov-Veliky). Rostov-on-Don is closely associated with the Cossacks and is also referred to as the 'Gateway to the Caucasus'. In 2018 the city served as a FIFA World Cup venue.
Plan your next trip to Russia
Ready-to-book tours.
Your holiday in Russia starts here. Choose and book your tour to Russia.
REQUEST A CUSTOMISED TRIP
Looking for something unique? Create the trip of your dreams with the help of our experts.
Newsletters

DP Daybreak
Our daily newsletter rounding up all of the top headlines from the DP. Get it Monday-Friday in your inbox. Free.

34th Street Magazine's "Toast" is a semi-weekly newsletter with the latest on Penn's campus culture and arts scene. Delivered Monday-Wednesday-Friday. Free.

Penn, Unbuttoned
Penn, Unbuttoned is Penn's only intentionally satirical newsletter, giving you your weekly dose of comedy from Under the Button every Wednesday. Free.

Quaker Nation
Quaker Nation is a weekly sports newsletter covering all things Penn sports. Delivered Monday mornings to your inbox. Free.

Recruiter's Row
Recruiter's Row is a biweekly recruitment newsletter that keeps you up-to-date on all things employment related. Get it in your inbox every other Wednesday. Free.
Print Edition of The Daily Pennsylvanian
Get our award-winning print editions of The Daily Pennsylvanian delivered to your doorstep every week.
I've already signed up
The Daily Pennsylvanian is a student-run nonprofit.
Please support us by disabling your ad blocker on our site.
Penn community holds memorial ceremony honoring legacy of former Interim President Claire Fagin

Penn community members gathered for a memorial ceremony on April 17 in honor of Claire Fagin who served as Penn’s interim president from 1993 to 1994, and as dean of the School of Nursing from 1977 to 1992.
Friends, former colleagues, and family members spoke about Fagin's life and impact during the memorial celebration, which took place in the Zellerbach Theatre in the Annenberg Center for the Performing Arts. Fagin, who died in early 2024 at the age of 97, was one of the first women to lead an Ivy League university, and the first woman to lead Penn.
The program speakers included Interim President Larry Jameson, former Penn President Judith Rodin, and former President Amy Gutmann, among others. Members of the Penn Glee Club performed an opening musical selection, and Krista Pinola, chair of the Nursing School Board of Advisors, performed the closing vocals alongside Nursing School student singers.
Nursing Dean Antonio Villarruel began the memorial service with an anecdote of a phone call between her and Fagin that occurred in 2022. According to Villarruel, Fagin had told her that she was “getting ready to go”, and spoke with her about the details of the memorial service she wanted to have after her death.
Four months after Magill’s resignation, Penn yet to announce search for next president
Former Penn Board of Trustees Chair Scott Bok warns of difficult upcoming presidential search
Villarruel said that during the phone conversation, Fagin nominated her son, Charles Fagin, as well as Villarruel herself, to emcee the event. Fagin also identified students, colleagues, and friends who she wanted to speak at the event.
“Whether you’re sharing our reflections today or not, whether you knew Claire or not, you are here because Claire had an impact on you and this university and beyond,” Villarruel said. “I know many of you in turn had an impact on her.”
Following Villarruel was University Chaplain Reverend Charles “Chaz” Howard, who spoke on Fagin's legacy. He praised Fagin's “remarkable” leadership skills, referring to her as “The Healer” — a nickname she earned from restoring Penn’s sense of community in a difficult time.
“An inspiring example set by Dr. Fagin not only endures but is richly instructive,” Howard said. “As we honor her legacy and memory, we also listen closely to her teachings. The Healer has lessons for us still.”
Former President Judith Rodin served as president after Fagin, and went on to lead the school for a decade. She reflected on Fagin's dedication to Penn, specifically her efforts to “heal the campus” both structurally and financially.
“No placeholder, no caretaker was Claire Fagin,” Rodin said. “And I must say it was both wondrous and challenging to follow because Claire loved the role, and Penn loved her back.”
She said that Fagin understood the significance of creating pathways for women at Penn, especially in fields dominated by men. Fagin implemented many initiatives to foster women's success during her time as a University leader, including mentorship programs, leadership seminars, and advocacy efforts.
Gutmann, who was Penn’s president after both Rodin and Fagin, recalled feeling “supported” by Fagin during her term.
“I cannot count the number of messages I received from Claire out of the blue, always uplifting and on the pulse beat of what was happening on Penn’s campus,” Gutmann said.
The next six speakers were all close friends of Fagin who she had designated before her death to speak at the memorial. These included former colleagues from Penn — such as professor emerita Neville Strumpf, and current professor Linda Aiken — as well as from the New York University Rory Meyers College of Nursing, where Fagin earned her doctorate, and taught as a professor until 1969.
Former Nursing School Dean Afaf Meleis, who was unable to attend the ceremony, appeared through a video projected onto a screen. Meleis said that she first met Fagin when Fagin was invited to the University of California San Francisco as a visiting professor. Years later, Meleis accepted Penn’s offer to be the dean of the Nursing School.
“It is [at Penn] that I experienced firsthand [Fagin's] deep influence, her incredible legacy, and her fabulous mentorship,” Meleis said.
Other speakers also shared personal stories from their experiences working with Fagin. Jodi Sarkisian, who was Fagin's assistant during her term as interim president, recounted an anecdote of seeing her walk into College Hall to accept her presidency.
“She wore a bright green knit dress, and laughed easily,” Sarkisian said. “Her strides were long and purposeful, and I remember how confident she was when she met with Sheldon Hackney in the president’s office, and how confident she was that day when he handed over the reins as he departed for the [National Endowment for the Humanities].”
Sign up for our newsletter
Get our newsletter, DP Daybreak , delivered to your inbox every weekday morning.
Sarkisian said that Fagin became interim president in a time when the work was “voluminous and complex”, and was able to “calm” the University while continuing to build onto its strong foundation.
The final speaker of the ceremony was Charles Fagin, who thanked students and faculty for attending the event.
“Claire would have loved this, and wanted us all together to continue gathering and making a difference in the world, and to take care of each other, and to love each other, and to remember to use your voice,” he said. “And she would’ve loved that.”
The Daily Pennsylvanian is an independent, student-run newspaper. Please consider making a donation to support the coverage that shapes the University. Your generosity ensures a future of strong journalism at Penn.
PennConnects
More like this.

SNF Paideia Program hosts event honoring founding faculty director Michael Delli Carpini

Africana Studies class studies history of Black students, faculty, and staff at Penn

Sarah Light named inaugural presidential professor at Wharton for work on business, climate change

Penn's Wellness and Resilience Summit teaches stress management skills, elicits positive reactions

"Little Fires Everywhere" author Celeste Ng reflects on heritage, literature at memorial lecture

COMMENTS
1.1: Aims Of Nursing. Nursing involves independent, cooperative, person-centered care for people of all ages, families, groups, and communities. Nurses assist the sick or the well person in all settings. Nursing includes promoting health, preventing illness, and caring for ill, disabled, and dying people. Health promotion encourages people to ...
The Ultimate Guide to Nursing Assignments: 7 Tips and Strategies. Nursing assignments are a critical component of every nursing student's academic journey. They serve as opportunities to test your knowledge, apply theoretical concepts to real-world scenarios, and develop essential skills necessary for your future nursing career.
Similarly, the ability for nurses to predict change, employ improvement strategies, and exercise fiscal prudence are critical skills. System awareness, innovation, and design also are needed to address such issues as structural racism and systemic inequity. Entry-Level Professional Nursing Education.
It has clues to the information you need. It provides the framework for the assignment-making process, including staff constraints, additional duties that must be covered, and patient factors most impor-tant on your unit. Use the electronic health record (EHR) to generate various useful pieces of patient in-formation.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care ...
Nurses do this activity every shift. They know how to find pertinent information and use the nursing process as a critical thinking model to guide patient care. The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients' well-being and health. This chapter will explain how to use the nursing process as standards of professional ...
This article describes the ongoing, hospital-wide effort to evaluate and implement a nursing assignment tool based on electronic health record (EHR) functionality and auto-calculated nursing workload scores. EHR records of individual patient workload scores from all hospital units were collected from August 2017 to June 2018.
You'll need to consider continuity of care, new nurse orientation, patient requests and satisfaction, staff well-being, fairness, equal distribution of the workload, nurse development, and workload completion. 5. Make the assignments. Grab your writing instrument and pencil in that first nurse's name.
Background. Nursing leadership is essential during times of rapid change. A strong association between competent nursing leadership and system quality and safety has been shown in scholarly literature by Adams (2018) and Akbiyik et al. (2020).The COVID-19 pandemic challenged nursing leadership to provide high quality and safe care delivery within an ever-changing health care system and ...
The nurse-patient assignment is a complex process driven by the patient, nurse, and environment, and further study is needed to identify factors linked to patient safety, nurses, and environmental outcomes. OBJECTIVE: Identify purposes and decision factors of the nurse-patient assignment process. BACKGROUND: Nurse-patient assignments can positively impact patient, nurse, and environmental ...
Qualitative Health Research (10 citations) and Journal of Pediatric Nursing (6 citations) were the journals where citations to the analysis were most frequent. The earliest citation was in 1989 and the most recent came in 2016. ... the analysis was not cited in the background section of the manuscript as informing the aims or design of the ...
articles suggested patterns of practice to improve the overall nurse patient assignment process. Each of the 18 publications explained the contextual evidence of underlining activities within the. practice environments that contributed to strengths and weaknesses of the assignment steps and. practices (Reavy, 2016).
The specific aims were to learn who makes nurse-patient assignments, how they learn to make them, and if satisfaction with an assignment affects absenteeism and turnover.
1. Concept, philosophy, aims & objectives of nursing education - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online.
KNOWLEDGE AIM • Nursing education aims at imparting scientific and up-to- date knowledge in the area of biological, behavioural, social and medical science. 7. • Nursing education's primary focus is to inculcate the appropriate nursing skills and the right attitude among the student nurses.
AI-enhanced description. Nursing Path. The document discusses the aims, objectives, vision, and mission of nursing management. It provides definitions of vision as the strongly felt aim or calling that defines where the profession wants to be in the future, and mission as defining where the profession is currently going and its purpose.
Post basic B.Sc Nursing INC prescribes the syllabus which has been revised three times, the last revision was done in 1981. It was done on basis of the 10+3+2 system of general education. At present the B.Sc Nursing programme which is recommended by the INC is of four years and has foundations for future study and specialization in nursing.
Aims and Objectives of Nursing Management, Vision and Mission Statement - Free download as PDF File (.pdf), Text File (.txt) or read online for free. Nursing Administration and Management,
The initial nursing assessment, the first step in the five steps of the nursing process, involves the systematic and continuous collection of data; sorting, analyzing, and organizing that data; and the documentation and communication of the data collected. Critical thinking skills applied during the nursing process provide a decision-making framework to develop and guide a plan of care for the ...
The third subscale measures "stress from assignments and workload" with 5 items. The fourth subscale focuses on "stress from interactions with teachers and nursing staff" with 6 items. ... Nursing education also aims to develop knowledgeable and competent students with problem-solving and critical-thinking skills. The study's findings ...
In 1939, there were 27,039 Jews living in Rostov (totaling 5.4% of the population). In the summer and fall of 1941 the town was inundated with refugees; about 20,000 Jews were able to evacuate. The German army occupied the town twice, in November 1941 and from July 1942 to February 1943. The Nazis murdered 13,000 Jews on 11 August 1942.
The College of Nursing is getting a new building, but it won't be on USC's campus. The 52,000-square-foot facility is being built next to Lexington Medical Center to instruct students alongside one of USC's medical partners. The facility is on track to be completed by fall 2024, university architect Derek Gruner said.
January 21, 2018 Antique Icons of the Mother of God from the Rostov Kremlin State Museum. Founded by Rostov merchants A. Titov and I. Shlyakov in 1883, the Rostov Kremlin State Museum is now recognized as one of the most valuable objects of cultural heritage in Russia.Located on the territory of the Archbishop's Yard, a beautiful architectural ensemble of the 17 th century, it currently ...
Known for being a far more rough city, Rostov appears to be the ideal backdrop for Motorama's amazing capacity to engender emotions, like disappointment and anxiety. However, little writing is produced about the city and it attracts few tourists from outside Russia. As such, we spoke to Vladislav Parshin from the band, and he kindly put ...
Rostov-on-Don is the largest city in South Russia and the centre of Russia's Southern Federal District. Although officially known as Rostov-on-Don to distinguish it from the ancient city of Rostov, in speech it is usually just called Rostov as the bigger of the two Rostovs (the orginal Rostov is confusingly then often called Rostov-Veliky).Rostov-on-Don is closely associated with the Cossacks ...
Members of the Penn Glee Club performed an opening musical selection, and Krista Pinola, chair of the Nursing School Board of Advisors, performed the closing vocals alongside Nursing School student singers. Nursing Dean Antonio Villarruel began the memorial service with an anecdote of a phone call between her and Fagin that occurred in 2022.