Long Covid explanation in new study possibly paves way for tests and treatments
Scientists have identified a persistent change in a handful of blood proteins in people with long Covid that indicates that an important part of their immune system remains on high alert for months after an acute infection.
The findings , published Thursday in the journal Science, could help explain what causes the persistent fatigue, brain fog and other debilitating symptoms of long Covid , as well as pave the way for diagnostic tests and potentially, a long-awaited treatment, experts say.
The study followed 113 Covid patients for up to one year after they were first infected, along with 39 healthy controls. At the six-month mark, 40 patients had developed long Covid symptoms .
Repeated blood samples turned up important differences in their blood: A group of proteins indicated that a part of the body’s immune system called the complement system remained activated long after it should have returned to normal.
“When you have a viral or bacterial infection , the complement system becomes activated and binds to these viruses and bacteria and then eliminates them,” said Dr. Onur Boyman, a professor of immunology at the University of Zurich in Switzerland and one of the study’s investigators. The system then returns to its resting state, where its regular job is to clear the body of dead cells, he said.
But if the complement system remains in its microbe-fighting state after the viruses and bacteria are eliminated, “it starts damaging healthy cells,” he said.
“These can be endothelial cells that line the inner layers of blood vessels, the cells of the blood itself, and cells in different organs, like the brain or the lungs,” he continued. The result is tissue damage and microclots in the blood.
Previous studies have documented blood clotting and tissue damage in people with long Covid. “But this research gets at the molecular mechanism of how that might be initiated,” said Akiko Iwasaki, a professor of immunobiology and molecular, cellular and developmental biology at the Yale School of Medicine, who was not involved with the new study.
Tissue damage along with blood clots can lead to the disabling symptoms of long Covid, including an intolerance to exercise.
During exercise, the heart pumps more blood and agitates the endothelial cells inside blood vessels, which are everywhere in the body, Boyman said.
“In healthy people, normal endothelial cells can take these changes, but the inflamed endothelial cells in long Covid patients cannot,” he said.
Iwasaki noted that microclots can reduce the level of oxygen and nutrients delivered to different organs.
“If your brain, for example, isn’t getting enough oxygen, obviously there will be a lot of issues with memory, brain fog and fatigue,” she said.

A possible path to tests and treatments
A little more than 14% of adults in the United States report ever having experienced long Covid, according to the most recent data from the U.S. Census Bureau’s Household Pulse Survey .
Dr. Monica Verduzco-Gutierrez, chair of rehabilitation medicine at the University of Texas Health Science Center at San Antonio and head of its long Covid clinic, praised the new study.
“Understanding the mechanisms of long Covid is how we’re going to figure out treatments,” she said.
Other studies have also identified potential mechanisms. In one study , published in the October issue of the journal Cell, researchers suggested that remnants of the virus lingering in the gut of long Covid patients triggered reductions in the neurotransmitter serotonin. Lower serotonin levels, they said, could explain some neurological and cognitive symptoms. Another study , published in the journal Nature in September by Iwasaki and her colleagues, found that long Covid patients had significantly lower levels of the hormone cortisol than other Covid patients and healthy controls. Cortisol helps people feel alert and awake.
Verduzco-Gutierrez, Iwasaki and Boyman agree that the new research points the way toward developing diagnostic tests and treatment by focusing on the proteins of the complement system.
However, Boyman and his colleagues used cutting-edge, complicated methods for detecting the differences in these proteins that could not be used in a routine diagnostic lab.
“We need companies already active in diagnostics that have sufficient manpower and financial power” to develop a simplified test, he said.
Once a test is developed, or with rigorous screening for long Covid patients, pharmaceutical companies could begin clinical trials of potential treatments, Boyman said. Drugs already exist to modulate and inhibit the complement system for very rare immune diseases that affect the kidneys, muscles or nervous system, and they could be tested in long Covid patients, he said.
New drugs could also be developed, Iwasaki said.
“I think there are a lot of things that we can try in the future,” she said. But first, the results of this study need to be replicated, as with any research, she added.
Verduzco-Gutierrez said she would like to see any future studies follow patients for a longer period of time. “What about people who have had long Covid for three years? We don’t know what their blood looks like,” she said.
Barbara Mantel is an NBC News contributor. She is also the topic leader for freelancing at the Association of Health Care Journalists, writing blog posts, tip sheets and market guides, as well as producing and hosting webinars. Barbara’s work has appeared in CQ Researcher, AARP, Undark, Next Avenue, Medical Economics, Healthline, Today.com, NPR and The New York Times.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
June 28, 2022
Long COVID symptoms linked to inflammation
At a glance.
- Prolonged inflammation after SARS-CoV-2 infections caused permanent damage to lungs and kidneys, affected the brain, and correlated with behavioral changes in hamsters.
- The results suggest a mechanism for the symptoms of Long COVID in people.

The effects of COVID-19 can persist long after the initial symptoms of the illness are gone. These effects, called post-acute sequelae of COVID-19 (or PASC), can include brain fog, fatigue, headaches, dizziness, and shortness of breath. Long COVID—when symptoms last weeks or months after the acute infection has passed—affects about 2.5% of COVID patients. While patients who were hospitalized are more susceptible, even those with mild cases can experience Long COVID.
A research team led by Drs. Benjamin tenOever at the NYU Grossman School of Medicine and Venetia Zachariou at the Icahn School of Medicine at Mount Sinai set out to understand the underlying biology of Long COVID. The researchers, who were supported in part by NIH, studied the golden hamster, a widely used small animal model for respiratory infections. The hamsters were exposed to SARS-CoV-2 via their nostrils. For comparison, another group was exposed to a flu virus, influenza A. Various samples were taken for analysis after 3, 14, and 31 days of infection.
Tissues from human donors who had COVID-19 at the time of death or had recovered from COVID-19 but died from other causes were also sampled and analyzed. Results appeared on June 7, 2022, in Science Translational Medicine.
Both SARS-CoV-2 and influenza A infections were largely cleared within two weeks, similar to the course of recovery in humans. Following SARS-CoV-2 infection, however, animals showed much more extensive lung damage and slower recovery than those exposed to influenza A. Those exposed to SARS-CoV-2 also had more kidney damage.
When the scientists sampled different parts of hamster brains to analyze gene activity, they found that SARS-CoV-2 had unique effects on the hamster olfactory system—the parts of the nose and brain responsible for smell. The olfactory epithelium, the lining inside the nose, showed signs of extensive inflammation long after the virus could be detected. SARS-CoV-2 also caused high levels of inflammation in the olfactory bulb, a part of the brain involved in processing smell as well as in emotion and learning. Inflammation in these areas persisted long after the infection was cleared.
Interestingly, chronic inflammation in the olfactory system correlated with behavioral changes in the hamsters thought to reflect mood disorders like depression and anxiety. Although olfactory bulb tissue from people who recovered from COVID-19 and died of other causes is difficult to obtain, the few samples studied were comparable to that of the hamsters. This suggests that the inflammation seen in the hamsters may explain the mechanism responsible for symptoms of Long COVID in people. Further research is needed to fully understand the link between brain inflammation, brain activity, and behavioral changes.
“[T]his study suggests that the molecular mechanism behind many Long COVID-19 symptoms stems from this persistent inflammation while describing an animal model close enough to human biology to be useful in the design of future treatments,” tenOever says.
—by Larisa Gearhart-Serna, Ph.D.
Related Links
- T Cells Protect Against COVID-19 in Absence of Antibody Response
- Intranasal Proteins Could Protect Against COVID-19 Variants
- Antibodies Recognize New SARS-CoV-2 Omicron Variant After Booster
- COVID-19 Immune Response Improves for Months After Vaccination
- How COVID-19 Affects the Brain
- Long COVID or Post-COVID Conditions
References: SARS-CoV-2 infection in hamsters and humans results in lasting and unique systemic perturbations post recovery . Frere JJ, Serafini RA, Pryce KD, Zazhytska M, Oishi K, Golynker I, Panis M, Zimering J, Horiuchi S, Hoagland DA, Møller R, Ruiz A, Kodra A, Overdevest JB, Canoll PD, Borczuk AC, Chandar V, Bram Y, Schwartz R, Lomvardas S, Zachariou V, tenOever BR. Science Translational Medicine . 2022 Jun 7:eabq3059.
Funding: NIH’s National Institute of Neurological Disorders and Stroke (NINDS) and National Institute on Deafness and Other Communication Disorders (NIDCD); Zegar Family Foundation; New York Genome Center.
Connect with Us
- More Social Media from NIH
- Português Br
- Journalist Pass
Study identifies risk factors for long-haul COVID disease in adults
Lynda De Widt
Share this:

Mayo Clinic researchers have identified risk factors that can cause adult COVID-19 patients to suffer symptoms that linger for months or years. The condition is often referred to as long-haul COVID . The findings are reported in the Journal of Investigative Medicine .
Researchers surveyed more than 3,000 adults over the age of 18 who were treated via Mayo Clinic's virtual COVID-19 clinics in Florida, Arizona and Minnesota between March 2020 and March 2021. They reviewed the patients' symptoms, the incidence of long-haul COVID in the group and how many were hospitalized due to COVID-19. The patients were also asked to rate their perception of the severity of their symptoms, whether they received a diagnosis of long-haul COVID, how long it took for them to resume their usual activities, and how much time they missed from work.
Study Findings
"We found that patients with severe COVID-19 symptoms were more likely to have long-haul COVID than those who had mild symptoms," says Bala Munipalli, M.D., an internist at Mayo Clinic in Florida and co-senior author of the study. "A majority of these were women who had been hospitalized, suffered from psychological impacts from COVID-19 such as anxiety and depression, and required more than one month to return to their normal activities after the illness."

The average age of the respondents in the study was 54 and most were women, including 57% of the patients surveyed who reported severe symptoms; 60% with mild symptoms; and 65% with moderate symptoms. Most patients (92%) with mild symptoms were able to resume their usual schedules within four weeks after COVID-19 infection, but 23% of these patients with mild acute infection developed long-haul COVID. Significantly more (37.4%) patients with severe symptoms were hospitalized than those with mild (0.9%) or moderate symptoms (4.8%). Hospitalized patients also reported having persistent symptoms of long-haul COVID (67%), needing a month or more to resume their usual activities, missing work for at least three weeks, and having negative psychological side effects.
Most respondents in the study reported long-haul COVID symptoms that lasted three to six months, with those symptoms ranging in severity. The most common symptoms in the study group were fatigue, loss of smell, altered taste, shortness of breath and poor sleep.
More to learn
"The inability to resume normal activities within one month after acute COVID-19 may be a predictive factor for long-haul COVID. As we continue to study this disease, we hope to gain a better understanding of who is susceptible to it, the symptoms that remain persistent, and how to best manage these patients in the early course of their illness," says Dr. Munipalli. "Additional studies may help guide the standardization of future assessment tools to evaluate impairment and also provide valuable information to employers, educators, policymakers and patients."
The researchers note that a multidisciplinary approach to long-haul COVID is needed and that healthcare personnel should recognize key symptoms, obtain a careful medical history and physical examination, as well as pay close attention to comorbid medical conditions in patients with persistent symptoms.
Dr. Munipalli says her team plans additional research focusing on treatments for long-haul COVID.
Other Mayo Clinic researchers on this paper include Abd Moain Abu Dabrh, M.B., B.Ch., M.S. ; Dacre Knight, M.D. ; Ilana Logvinov, M.D.; Stefan Paul; Troy Delaney, Yaohua Ma; Zhuo Li; and Ravindra Ganesh, M.B.B.S., M.D.
- Mayo Clinic in Florida opens downtown Jacksonville site focused on education, research Mayo Clinic expert answers questions about the new COVID-19 vaccine
Related Articles

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 08 April 2024
Large-scale phenotyping of patients with long COVID post-hospitalization reveals mechanistic subtypes of disease
- Felicity Liew 1 na1 ,
- Claudia Efstathiou ORCID: orcid.org/0000-0001-6125-8126 1 na1 ,
- Sara Fontanella 1 ,
- Matthew Richardson 2 ,
- Ruth Saunders 2 ,
- Dawid Swieboda 1 ,
- Jasmin K. Sidhu 1 ,
- Stephanie Ascough 1 ,
- Shona C. Moore ORCID: orcid.org/0000-0001-8610-2806 3 ,
- Noura Mohamed 4 ,
- Jose Nunag ORCID: orcid.org/0000-0002-4218-0500 5 ,
- Clara King 5 ,
- Olivia C. Leavy 2 , 6 ,
- Omer Elneima 2 ,
- Hamish J. C. McAuley 2 ,
- Aarti Shikotra 7 ,
- Amisha Singapuri ORCID: orcid.org/0009-0002-4711-7516 2 ,
- Marco Sereno ORCID: orcid.org/0000-0003-4573-9303 2 ,
- Victoria C. Harris 2 ,
- Linzy Houchen-Wolloff ORCID: orcid.org/0000-0003-4940-8835 8 ,
- Neil J. Greening ORCID: orcid.org/0000-0003-0453-7529 2 ,
- Nazir I. Lone ORCID: orcid.org/0000-0003-2707-2779 9 ,
- Matthew Thorpe 10 ,
- A. A. Roger Thompson ORCID: orcid.org/0000-0002-0717-4551 11 ,
- Sarah L. Rowland-Jones 11 ,
- Annemarie B. Docherty ORCID: orcid.org/0000-0001-8277-420X 10 ,
- James D. Chalmers 12 ,
- Ling-Pei Ho ORCID: orcid.org/0000-0001-8319-301X 13 ,
- Alexander Horsley ORCID: orcid.org/0000-0003-1828-0058 14 ,
- Betty Raman 15 ,
- Krisnah Poinasamy 16 ,
- Michael Marks 17 , 18 , 19 ,
- Onn Min Kon 1 ,
- Luke S. Howard ORCID: orcid.org/0000-0003-2822-210X 1 ,
- Daniel G. Wootton 3 ,
- Jennifer K. Quint 1 ,
- Thushan I. de Silva ORCID: orcid.org/0000-0002-6498-9212 11 ,
- Antonia Ho 20 ,
- Christopher Chiu ORCID: orcid.org/0000-0003-0914-920X 1 ,
- Ewen M. Harrison ORCID: orcid.org/0000-0002-5018-3066 10 ,
- William Greenhalf 21 ,
- J. Kenneth Baillie ORCID: orcid.org/0000-0001-5258-793X 10 , 22 , 23 ,
- Malcolm G. Semple ORCID: orcid.org/0000-0001-9700-0418 3 , 24 ,
- Lance Turtle 3 , 24 ,
- Rachael A. Evans ORCID: orcid.org/0000-0002-1667-868X 2 ,
- Louise V. Wain 2 , 6 ,
- Christopher Brightling 2 ,
- Ryan S. Thwaites ORCID: orcid.org/0000-0003-3052-2793 1 na1 ,
- Peter J. M. Openshaw ORCID: orcid.org/0000-0002-7220-2555 1 na1 ,
- PHOSP-COVID collaborative group &
ISARIC investigators
Nature Immunology volume 25 , pages 607–621 ( 2024 ) Cite this article
25k Accesses
1 Citations
2140 Altmetric
Metrics details
- Inflammasome
- Inflammation
- Innate immunity
One in ten severe acute respiratory syndrome coronavirus 2 infections result in prolonged symptoms termed long coronavirus disease (COVID), yet disease phenotypes and mechanisms are poorly understood 1 . Here we profiled 368 plasma proteins in 657 participants ≥3 months following hospitalization. Of these, 426 had at least one long COVID symptom and 233 had fully recovered. Elevated markers of myeloid inflammation and complement activation were associated with long COVID. IL-1R2, MATN2 and COLEC12 were associated with cardiorespiratory symptoms, fatigue and anxiety/depression; MATN2, CSF3 and C1QA were elevated in gastrointestinal symptoms and C1QA was elevated in cognitive impairment. Additional markers of alterations in nerve tissue repair (SPON-1 and NFASC) were elevated in those with cognitive impairment and SCG3, suggestive of brain–gut axis disturbance, was elevated in gastrointestinal symptoms. Severe acute respiratory syndrome coronavirus 2-specific immunoglobulin G (IgG) was persistently elevated in some individuals with long COVID, but virus was not detected in sputum. Analysis of inflammatory markers in nasal fluids showed no association with symptoms. Our study aimed to understand inflammatory processes that underlie long COVID and was not designed for biomarker discovery. Our findings suggest that specific inflammatory pathways related to tissue damage are implicated in subtypes of long COVID, which might be targeted in future therapeutic trials.
Similar content being viewed by others

Immunopathological signatures in multisystem inflammatory syndrome in children and pediatric COVID-19
Keith Sacco, Riccardo Castagnoli, … Luigi D. Notarangelo

In COVID-19, NLRP3 inflammasome genetic variants are associated with critical disease and these effects are partly mediated by the sickness symptom complex: a nomothetic network approach
Michael Maes, Walton Luiz Del Tedesco Junior, … Andréa Name Colado Simão

Epidemiology, clinical presentation, pathophysiology, and management of long COVID: an update
Sizhen Su, Yimiao Zhao, … Lin Lu
One in ten severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections results in post-acute sequelae of coronavirus disease 2019 (PASC) or long coronavirus disease (COVID), which affects 65 million people worldwide 1 . Long COVID (LC) remains common, even after mild acute infection with recent variants 2 , and it is likely LC will continue to cause substantial long-term ill health, requiring targeted management based on an understanding of how disease phenotypes relate to underlying mechanisms. Persistent inflammation has been reported in adults with LC 1 , 3 , but studies have been limited in size, timing of samples or breadth of immune mediators measured, leading to inconsistent or absent associations with symptoms. Markers of oxidative stress, metabolic disturbance, vasculoproliferative processes and IFN-, NF-κB- or monocyte-related inflammation have been suggested 3 , 4 , 5 , 6 .
The PHOSP-COVID study, a multicenter United Kingdom study of patients previously hospitalized with COVID-19, has reported inflammatory profiles in 626 adults with health impairment after COVID-19, identified through clustering. Elevated IL-6 and markers of mucosal inflammation were observed in those with severe impairment compared with individuals with milder impairment 7 . However, LC is a heterogeneous condition that may be a distinct form of health impairment after COVID-19, and it remains unclear whether there are inflammatory changes specific to LC symptom subtypes. Determining whether activated inflammatory pathways underlie all cases of LC or if mechanisms differ according to clinical presentation is essential for developing effective therapies and has been highlighted as a top research priority by patients and clinicians 8 .
In this Letter, in a prospective multicenter study, we measured 368 plasma proteins in 657 adults previously hospitalized for COVID-19 (Fig. 1a and Table 1 ). Individuals in our cohort experienced a range of acute COVID-19 severities based on World Health Organization (WHO) progression scores 9 ; WHO 3–4 (no oxygen support, n = 133 and median age of 55 years), WHO 5–6 (oxygen support, n = 353 and median age of 59 years) and WHO 7–9 (critical care, n = 171 and median age of 57 years). Participants were hospitalized for COVID-19 ≥3 months before sample collection (median 6.1 months, interquartile range (IQR) 5.1–6.8 months and range 3.0–8.3 months) and confirmed clinically ( n = 36/657) or by PCR ( n = 621/657). Symptom data indicated 233/657 (35%) felt fully recovered at 6 months (hereafter ‘recovered’) and the remaining 424 (65%) reported symptoms consistent with the WHO definition for LC (symptoms ≥3 months post infection 10 ). Given the diversity of LC presentations, patients were grouped according to symptom type (Fig. 1b ). Groups were defined using symptoms and health deficits that have been commonly reported in the literature 1 ( Methods ). A multivariate penalized logistic regression model (PLR) was used to explore associations of clinical covariates and immune mediators at 6 months between recovered patients ( n = 233) and each LC group (cardiorespiratory symptoms, cardioresp, n = 398, Fig. 1c ; fatigue, n = 384, Fig. 1d ; affective symptoms, anxiety/depression, n = 202, Fig. 1e ; gastrointestinal symptoms, GI, n = 132, Fig. 1f ; and cognitive impairment, cognitive, n = 61, Fig. 1g ). Women ( n = 239) were more likely to experience CardioResp (odds ratio (OR 1.14), Fatigue (OR 1.22), GI (OR 1.13) and Cognitive (OR 1.03) outcomes (Fig. 1c,d,f,g ). Repeated cross-validation was used to optimize and assess model performance ( Methods and Extended Data Fig. 1 ). Pre-existing conditions, such as chronic lung disease, neurological disease and cardiovascular disease (Supplementary Table 1 ), were associated with all LC groups (Fig. 1c–g ). Age, C-reactive protein (CRP) and acute disease severity were not associated with any LC group (Table 1 ).
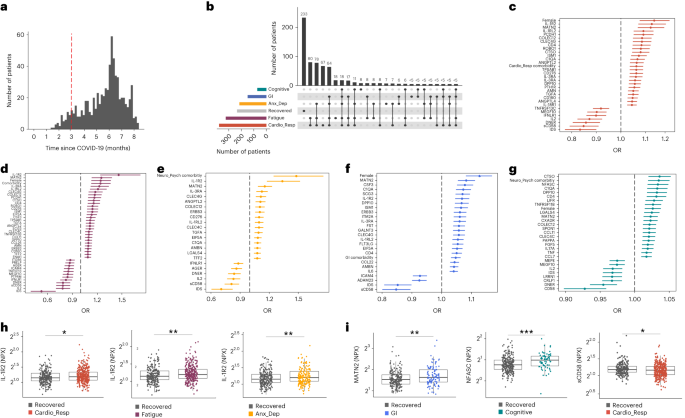
a , Distribution of time from COVID-19 hospitalization at sample collection. All samples were cross-sectional. The vertical red line indicates the 3 month cutoff used to define our final cohort and samples collected before 3 months were excluded. b , An UpSet plot describing pooled LC groups. The horizontal colored bars represent the number of patients in each symptom group: cardiorespiratory (Cardio_Resp), fatigue, cognitive, GI and anxiety/depression (Anx_Dep). Vertical black bars represent the number of patients in each symptom combination group. To prevent patient identification, where less than five patients belong to a combination group, this has been represented as ‘<5’. The recovered group ( n = 233) were used as controls. c – g , Forest plots of Olink protein concentrations (NPX) associated with Cardio_Resp ( n = 365) ( c ), fatigue (n = 314) ( d ), Anx_Dep ( n = 202) ( e ), GI ( n = 124) ( f ) and cognitive ( n = 60) ( g ). Neuro_Psych, neuropsychiatric. The error bars represent the median accuracy of the model. h , i , Distribution of Olink values (NPX) for IL-1R2 ( h ) and MATN2, neurofascin and sCD58 ( i ) measured between symptomatic and recovered individuals in recovered ( n = 233), Cardio_Resp ( n = 365), fatigue ( n = 314) and Anx_Dep ( n = 202) groups ( h ) and MATN2 in GI ( n = 124), neurofascin in cognitive ( n = 60) and sCD58 in Cardio_Resp and recovered groups ( i ). The box plot center line represents the median, the boundaries represent IQR and the whisker length represents 1.5× IQR. The median values were compared between groups using two-sided Wilcoxon signed-rank test, * P < 0.05, ** P < 0.01, *** P < 0.001 and **** P < 0.0001.
To study the association of peripheral inflammation with symptoms, we analyzed cross-sectional data collected approximately 6 months after hospitalizations. We measured 368 immune mediators from plasma collected contemporaneously with symptom data. Mediators suggestive of myeloid inflammation were associated with all symptoms (Fig. 1c–h ). Elevated IL-1R2, an IL-1 receptor expressed by monocytes and macrophages modulating inflammation 11 and MATN2, an extracellular matrix protein that modulates tissue inflammation through recruitment of innate immune cells 12 , were associated with cardioresp (IL-1R2 OR 1.14, Fig. 1c,h ), fatigue (IL-1R2 OR 1.45, Fig. 1d,h ), anxiety/depression (IL-1R2 OR 1.34. Fig. 1e,h ) and GI (MATN2 OR 1.08, Fig. 1f ). IL-3RA, an IL-3 receptor, was associated with cardioresp (OR 1.07, Fig. 1c ), fatigue (OR 1.21, Fig. 1d ), anxiety/depression (OR 1.12, Fig. 1e ) and GI (OR 1.06, Fig. 1f ) groups, while CSF3, a cytokine promoting neutrophilic inflammation 13 , was elevated in cardioresp (OR 1.06, Fig. 1c ), fatigue (OR 1.12, Fig. 1d ) and GI (OR 1.08, Fig. 1f ).
Elevated COLEC12, which initiates inflammation in tissues by activating the alternative complement pathway 14 , associated with cardioresp (OR 1.09, Fig. 1c ), fatigue (OR 1.19, Fig. 1d ) and anxiety/depression (OR 1.11, Fig. 1e ), but not with GI (Fig. 1f ) and only weakly with cognitive (OR 1.02, Fig. 1g ). C1QA, a degradation product released by complement activation 15 was associated with GI (OR 1.08, Fig. 1f ) and cognitive (OR 1.03, Fig. 1g ). C1QA, which is known to mediate dementia-related neuroinflammation 16 , had the third strongest association with cognitive (Fig. 1g ). These observations indicated that myeloid inflammation and complement activation were associated with LC.
Increased expression of DPP10 and SCG3 was observed in the GI group compared with recovered (DPP10 OR 1.07 and SCG3 OR 1.08, Fig. 1f ). DPP10 is a membrane protein that modulates tissue inflammation, and increased DPP10 expression is associated with inflammatory bowel disease 17 , 18 , suggesting that GI symptoms may result from enteric inflammation. Elevated SCG3, a multifunctional protein that has been associated with irritable bowel syndrome 19 , suggested that noninflammatory disturbance of the brain–gut axis or dysbiosis, may occur in the GI group. The cognitive group was associated with elevated CTSO (OR 1.04), NFASC (OR 1.03) and SPON-1 (OR 1.02, Fig. 1g,i ). NFASC and SPON-1 regulate neural growth 20 , 21 , while CTSO is a cysteine proteinase supporting tissue turnover 22 . The increased expression of these three proteins as well as C1QA and DPP10 in the cognitive group (Fig. 1g ) suggested neuroinflammation and alterations in nerve tissue repair, possibly resulting in neurodegeneration. Together, our findings indicated that complement activation and myeloid inflammation were common to all LC groups, but subtle differences were observed in the GI and cognitive groups, which may have mechanistic importance. Acutely elevated fibrinogen during hospitalization has been reported to be predictive of LC cognitive deficits 23 . We found elevated fibrinogen in LC relative to recovered (Extended Data Fig. 2a ; P = 0.0077), although this was not significant when restricted to the cognitive group ( P = 0.074), supporting our observation of complement pathway activation in LC and in keeping with reports that complement dysregulation and thrombosis drive severe COVID-19 (ref. 24 ).
Elevated sCD58 was associated with lower odds of all LC symptoms and was most pronounced in cardioresp (OR 0.85, Fig. 1c,i ), fatigue (OR 0.80, Fig. 1d ) and anxiety/depression (OR 0.83, Fig. 1e ). IL-2 was negatively associated with the cardioresp (Fig. 1c , OR 0.87), fatigue (Fig. 1d , OR 0.80), anxiety/depression (Fig. 1e , OR 0.84) and cognitive (Fig. 1g , OR 0.96) groups. Both IL-2 and sCD58 have immunoregulatory functions 25 , 26 . Specifically, sCD58 suppresses IL-1- or IL-6-dependent interactions between CD2 + monocytes and CD58 + T or natural killer cells 26 . The association of sCD58 with recovered suggests a central role of dysregulated myeloid inflammation in LC. Elevated markers of tissue repair, IDS and DNER 27 , 28 , were also associated with recovered relative to all LC groups (Fig. 1c–g ). Taken together, our data suggest that suppression of myeloid inflammation and enhanced tissue repair were associated with recovered, supporting the use of immunomodulatory agents in therapeutic trials 29 (Supplementary Table 2 ).
We next sought to validate the experimental and analytical approaches used. Although Olink has been validated against other immunoassay platforms, showing superior sensitivity and specificity 30 , 31 , we confirmed the performance of Olink against chemiluminescent immunoassays within our cohort. We performed chemiluminescent immunoassays on plasma from a subgroup of 58 participants (recovered n = 13 and LC n = 45). There were good correlations between results from Olink (normalized protein expression (NPX)) and chemiluminescent immunoassays (pg ml −1 ) for CSF3, IL-1R2, IL-3RA, TNF and TFF2 (Extended Data Fig. 3 ). Most samples did not have concentrations of IL-2 detectable using a mesoscale discovery chemiluminescent assay, limiting this analysis to 14 samples (recovered n = 4, LC n = 10, R = 0.55 and P = 0.053, Extended Data Fig. 3 ). We next repeated our analysis using alternative definitions of LC. The Centers for Disease Control and Prevention and National Institute for Health and Care Excellence definitions for LC include symptoms occurring 1 month post infection 32 , 33 . Using the 1 month post-infection definition included 62 additional participants to our analysis (recovered n = 21, 3 females and median age 61 years and LC n = 41, 15 females and median age 60 years, Extended Data Fig. 2c ) and found that inflammatory associations with each LC group were consistent with our analysis based on the WHO definition (Extended Data Fig. 2d–h ). Finally, to validate the analytical approach (PLR) we examined the distribution of data, prioritizing proteins that were most strongly associated with each LC/recovered group (IL-1R2, MATN2, NFASC and sCD58). Each protein was significantly elevated in the LC group compared with recovered (Fig. 1h,i and Extended Data Fig. 4 ), consistent with the PLR. Alternative regression approaches (unadjusted regression models and partial least squares, PLS) reported results consistent with the original analysis of protein associations and LC outcome in the WHO-defined cohort (Fig. 1c–g , Supplementary Table 3 and Extended Data Figs. 5 and 6 ). The standard errors of PLS estimates were wide (Extended Data Fig. 6 ), consistent with previous demonstrations that PLR is the optimal method to analyze high-dimensional data where variables may have combined effects 34 . As inflammatory proteins are often colinear, working in-tandem to mediate effects, we prioritized PLR results to draw conclusions.
To explore the relationship between inflammatory mediators associated with different LC symptoms, we performed a network analysis of Olink mediators highlighted by PLR within each LC group. COLEC12 and markers of endothelial and mucosal inflammation (MATN2, PCDH1, ROBO1, ISM1, ANGPTL2, TGF-α and TFF2) were highly correlated within the cardioresp, fatigue and anxiety/depression groups (Fig. 2 and Extended Data Fig. 7 ). Elevated PCDH1, an adhesion protein modulating airway inflammation 35 , was highly correlated with other inflammatory proteins associated with the cardioresp group (Fig. 2 ), suggesting that systemic inflammation may arise from the lung in these individuals. This was supported by increased expression of IL-3RA, which regulates innate immune responses in the lung through interactions with circulating IL-3 (ref. 36 ), in fatigue (Figs. 1d and 2 ), which correlated with markers of tissue inflammation, including PCDH1 (Fig. 2 ). MATN2 and ISM1, mucosal proteins that enhance inflammation 37 , 38 , were highly correlated in the GI group (Fig. 2 ), highlighting the role of tissue-specific inflammation in different LC groups. SCG3 correlated less closely with mediators in the GI group (Fig. 2 ), suggesting that the brain–gut axis may contribute separately to some GI symptoms. SPON-1, which regulates neural growth 21 , was the most highly correlated mediator in the cognitive group (Fig. 2 and Extended Data Fig. 7 ), highlighting that processes within nerve tissue may underlie this group. These observations suggested that inflammation might arise from mucosal tissues and that additional mechanisms may contribute to pathophysiology underlying the GI and cognitive groups.
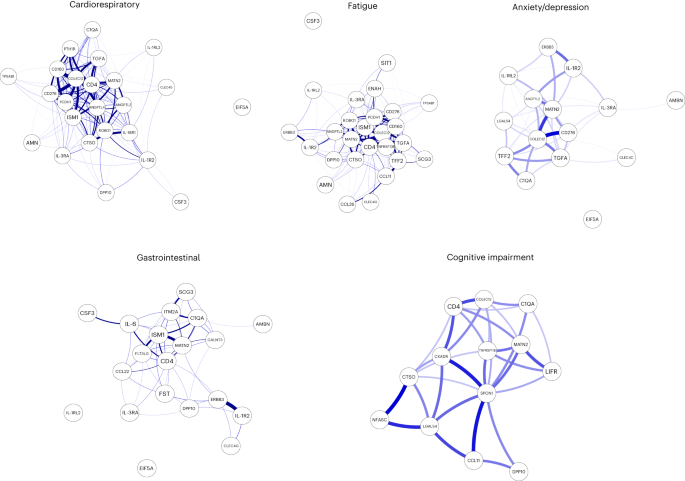
Network analysis of Olink mediators associated with cardioresp ( n = 365), fatigue ( n = 314), anxiety/depression ( n = 202), GI ( n = 124) and cognitive groups ( n = 60). Each node corresponds to a protein mediator identified by PLR. The edges (blue lines) were weighted according to the size of Spearman’s rank correlation coefficient between proteins. All edges represent positive and significant correlations ( P < 0.05) after FDR adjustment.
Women were more likely to experience LC (Table 1 ), as found in previous studies 1 . As estrogen can influence immunological responses 39 , we investigated whether hormonal differences between men and women with LC in our cohort explained this trend. We grouped men and women with LC symptoms into two age groups (those younger than 50 years and those 50 years and older, using age as a proxy for menopause status in women) and compared mediator levels between men and women in each age group, prioritizing those identified by PLR to be higher in LC compared with recovered. As we aimed to understand whether women with LC had stronger inflammatory responses than men with LC, we did not assess differences in men and women in the recovered group. IL-1R2 and MATN2 were significantly higher in women ≥50 years than men ≥50 years in the cardioresp group (Fig. 3a , IL-1R2 and MATN2) and the fatigue group (Fig. 3b ). In the GI group, CSF3 was higher in women ≥50 years compared with men ≥50 years (Fig. 3c ), indicating that the inflammatory markers observed in women were not likely to be estrogen-dependent. Women have been reported to have stronger innate immune responses to infection and to be at greater risk of autoimmunity 39 , possibly explaining why some women in the ≥50 years group had higher inflammatory proteins than men the same group. Proteins associated with the anxiety/depression (IL-1R2 P = 0.11 and MATN2 P = 0.61, Extended Data Fig. 8a ) and cognitive groups (CTSO P = 0.64 and NFASC P = 0.41, Extended Data Fig. 8b ) were not different between men and women in either age group, consistent with the absent/weak association between sex and these outcomes identified by PLR (Fig. 1e,g ). Though our findings suggested that nonhormonal differences in inflammatory responses may explain why some women are more likely to have LC, they require confirmation in adequately powered studies.
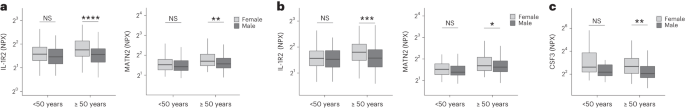
a – c , Olink-measured plasma protein levels (NPX) of IL-1R2 and MATN2 ( a and b ) and CSF3 ( c ) between LC men and LC women divided by age (<50 or ≥50 years) in the cardiorespiratory group (<50 years n = 8 and ≥50 years n = 270) ( a ), fatigue group (<50 years n = 81 and ≥50 years n = 227) ( b ) and GI group (<50 years n = 34 and ≥50 years n = 82) ( c ). the median values were compared between men and women using two-sided Wilcoxon signed-rank test, * P < 0.05, ** P < 0.01, *** P < 0.001 and **** P < 0.0001. The box plot center line represents the median, the boundaries represent IQR and the whisker length represents 1.5× IQR.
To test whether local respiratory tract inflammation persisted after COVID-19, we compared nasosorption samples from 89 participants (recovered, n = 31; LC, n = 33; and healthy SARS-CoV-2 naive controls, n = 25, Supplementary Tables 4 and 5 ). Several inflammatory markers were elevated in the upper respiratory tract post COVID (including IL-1α, CXCL10, CXCL11, TNF, VEGF and TFF2) when compared with naive controls, but similar between recovered and LC (Fig. 4a ). In the cardioresp group ( n = 29), inflammatory mediators elevated in plasma (for example, IL-6, APO-2, TGF-α and TFF2) were not elevated in the upper respiratory tract (Extended Data Fig. 9a ) and there was no correlation between plasma and nasal mediator levels (Extended Data Fig. 9b ). This exploratory analysis suggested upper respiratory tract inflammation post COVID was not specifically associated with cardiorespiratory symptoms.
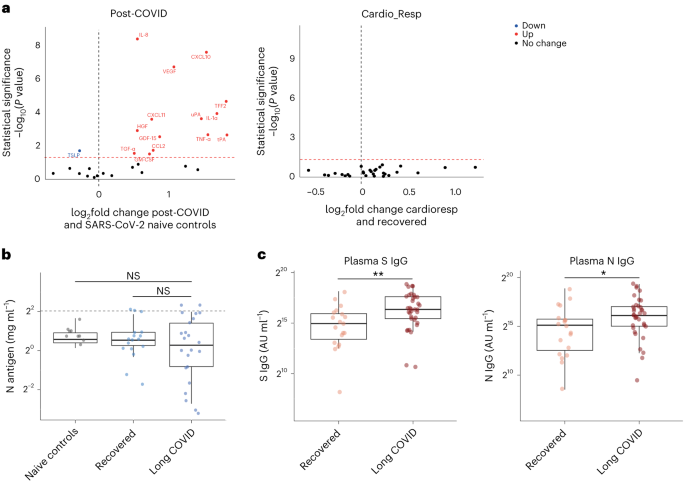
a , Nasal cytokines measured by immunoassay in post-COVID participants ( n = 64) compared with healthy SARS-CoV-2 naive controls ( n = 25), and between the the cardioresp group ( n = 29) and the recovered group ( n = 31). The red values indicate significantly increased cytokine levels after FDR adjustment ( P < 0.05) using two-tailed Wilcoxon signed-rank test. b , SARS-CoV-2 N antigen measured in sputum by electrochemiluminescence from recovered ( n = 17) and pooled LC ( n = 23) groups, compared with BALF from SARS-CoV-2 naive controls ( n = 9). The horizontal dashed line indicates the lower limit of detection of the assay. c , Plasma S- and N-specific IgG responses measured by electrochemiluminescence in the LC ( n = 35) and recovered ( n = 19) groups. The median values were compared using two-sided Wilcoxon signed-rank tests, NS P > 0.05, * P < 0.05, ** P < 0.01, *** P < 0.001 and **** P < 0.0001. The box plot center lines represent the median, the boundaries represent IQR and the whisker length represents 1.5× IQR.
To explore whether SARS-CoV-2 persistence might explain the inflammatory profiles observed in the cardioresp group, we measured SARS-CoV-2 nucleocapsid (N) antigen in sputum from 40 participants (recovered n = 17 and LC n = 23) collected approximately 6 months post hospitalization (Supplementary Table 6 ). All samples were compared with prepandemic bronchoalveolar lavage fluid ( n = 9, Supplementary Table 4 ). Only four samples (recovered n = 2 and LC n = 2) had N antigen above the assay’s lower limit of detection, and there was no difference in N antigen concentrations between LC and recovered (Fig. 4b , P = 0.78). These observations did not exclude viral persistence, which might require tissues samples for detection 40 , 41 . On the basis of the hypothesis that persistent viral antigen might prevent a decline in antibody levels over time, we examined the titers of SARS-CoV-2-specific antibodies in unvaccinated individuals (recovered n = 19 and LC n = 35). SARS-CoV-2 N-specific ( P = 0.023) and spike (S)-specific ( P = 0.0040) immunoglobulin G (IgG) levels were elevated in LC compared with recovered (Fig. 4c ).
Overall, we identified myeloid inflammation and complement activation in the cardioresp, fatigue, anxiety/depression, cognitive and GI groups 6 months after hospitalization (Extended Data Fig. 10 ). Our findings build on results of smaller studies 5 , 6 , 42 and are consistent with a genome-wide association study that identified an independent association between LC and FOXP4 , which modulates neutrophilic inflammation and immune cell function 43 , 44 . In addition, we identified tissue-specific inflammatory elements, indicating that myeloid disturbance in different tissues may result in distinct symptoms. Multiple mechanisms for LC have been suggested, including autoimmunity, thrombosis, vascular dysfunction, SARS-CoV-2 persistence and latent virus reactivation 1 . All these processes involve myeloid inflammation and complement activation 45 . Complement activation in LC has been suggested in a proteomic study in 97 mostly nonhospitalized COVID-19 cases 42 and a study of 48 LC patients, of which one-third experienced severe acute disease 46 . As components of the complement system are known to have a short half-life 47 , ongoing complement activation suggests active inflammation rather than past tissue damage from acute infection.
Despite the heterogeneity of LC and the likelihood of coexisting or multiple etiologies, our work suggests some common pathways that might be targeted therapeutically and supports the rationale for several drugs currently under trial. Our finding of increased sCD58 levels (associated with suppression of monocyte–lymphocyte interactions 26 ) in the recovered group, strengthens our conclusion that myeloid inflammation is central to the biology of LC and that trials of steroids, IL-1 antagonists, JAK inhibitors, naltrexone and colchicine are justified. Although anticoagulants such as apixaban might prevent thrombosis downstream of complement dysregulation, they can also increase the risk of serious bleeding when given after COVID-19 hospitalization 48 . Thus, clinical trials, already underway, need to carefully assess the risks and benefits of anticoagulants (Supplementary Table 2 ).
Our finding of elevated S- and N-specific IgG in LC could suggest viral persistence, as found in other studies 6 , 42 , 49 . Our network analysis indicated that inflammatory proteins in the cardioresp group interacted strongly with ISM1 and ROBO1, which are expressed during respiratory tract infection and regulate lung inflammation 50 , 51 . Although we were unable to find SARS-CoV-2 antigen in sputum from our LC cases, we did not test for viral persistence in GI tract and lung tissue 40 , 41 or in plasma 52 . Evidence of SARS-CoV-2 persistence would justify trials of antiviral drugs (singly or in combination) in LC. It is also possible that autoimmune processes could result in an innate inflammatory profile in LC. Autoreactive B cells have been identified in LC patients with higher SARS-CoV-2-specific antibody titers in a study of mostly mild acute COVID cases (59% WHO 2–3) 42 , a different population from our study of hospitalized cases.
Our observations of distinct protein profiles in GI and cognitive groups support previous reports on distinct associations between Epstein–Barr virus reactivation and neurological symptoms, or autoantibodies and GI symptoms relative to other forms of LC 49 , 53 . We did not assess autoantibody induction but found evidence of brain–gut axis disturbance (SCG3) in the GI group, which occurs in many autoimmune diseases 54 . We found signatures suggestive of neuroinflammation (C1QA) in the cognitive group, consistent with findings of brain abnormalities on magnetic resonance imaging after COVID-19 hospitalization 55 , as well as findings of microglial activation in mice after COVID-19 (ref. 56 ). Proinflammatory signatures dominated in the cardioresp, fatigue and anxiety/depression groups and were consistent with those seen in non-COVID depression, suggesting shared mechanisms 57 . The association between markers of myeloid inflammation, including IL-3RA, and symptoms was greatest for fatigue. Whilst membrane-bound IL-3RA facilitates IL-3 signaling upstream of myelopoesis 36 its soluble form (measured in plasma) can bind IL-3 and can act as a decoy receptor, preventing monocyte maturation and enhancing immunopathology 58 . Monocytes from individuals with post-COVID fatigue are reported to have abnormal expression profiles (including reduced CXCR2), suggestive of altered maturation and migration 5 , 59 . Lung-specific inflammation was suggested by the association between PCDH1 (an airway epithelial adhesion molecule 35 ) and cardioresp symptoms.
Our observations do not align with all published observations on LC. One proteomic study of 55 LC cases after generally mild (WHO 2–3) acute disease found that TNF and IFN signatures were elevated in LC 3 . Vasculoproliferative processes and metabolic disturbance have been reported in LC 4 , 60 , but these studies used uninfected healthy individuals for comparison and cannot distinguish between LC-specific phenomena and residual post-COVID inflammation. A study of 63 adults (LC, n = 50 and recovered, n = 13) reported no association between immune cell activation and LC 3 months after infection 61 , though myeloid inflammation was not directly measured, and 3 months post infection may be too early to detect subtle differences between LC and recovered cases due to residual acute inflammation.
Our study has limitations. We designed the study to identify inflammatory markers identifying pathways underlying LC subgroups rather than diagnostic biomarkers. The ORs we report are small, but associations were consistent across alternative methods of analysis and when using different LC definitions. Small effect sizes can be expected when using PLR, which shrinks correlated mediator coefficients to reflect combined effects and prevent colinear inflation 62 , and could also result from measurement of plasma mediators that may underestimate tissue inflammation. Although our LC cohort is large compared with most other published studies, some of our subgroups are small (only 60 cases were designated cognitive). Though the performance of the cognitive PLR model was adequate, our findings should be validated in larger studies. It should be noted that our cohort of hospitalized cases may not represent all types of LC, especially those occurring after mild infection. We looked for an effect of acute disease severity within our study and did not find it, and are reassured that the inflammatory profiles we observed were consistent with those seen in smaller studies including nonhospitalized cases 42 , 46 . Studies of posthospital LC may be confounded by ‘posthospital syndrome’, which encompasses general and nonspecific effects of hospitalization (particularly intensive care) 63 .
In conclusion, we found markers of myeloid inflammation and complement activation in our large prospective posthospital cohort of patients with LC, in addition to distinct inflammatory patterns in patients with cognitive impairment or gastrointestinal symptoms. These findings show the need to consider subphenotypes in managing patients with LC and support the use of antiviral or immunomodulatory agents in controlled therapeutic trials.
Study design and ethics
After hospitalization for COVID-19, adults who had no comorbidity resulting in a prognosis of less than 6 months were recruited to the PHOSP-COVID study ( n = 719). Patients hospitalized between February 2020 and January 2021 were recruited. Both sexes were recruited and gender was self-reported (female, n = 257 and male, n = 462). Written informed consent was obtained from all patients. Ethical approvals for the PHOSP-COVID study were given by Leeds West Research Ethics Committee (20/YH/0225).
Symptom data and samples were prospectively collected from individuals approximately 6 months (IQR 5.1–6.8 months and range 3.0–8.3 months) post hospitalization (Fig. 1a ), via the PHOSP-COVID multicenter United Kingdom study 64 . Data relating to patient demographics and acute admission were collected via the International Severe Acute Respiratory and Emerging Infection Consortium World Health Organization Clinical Characterisation Protocol United Kingdom (ISARIC4C study; IRAS260007/IRAS126600) (ref. 65 ). Adults hospitalized during the SARS-CoV-2 pandemic were systematically recruited into ISARIC4C. Written informed consent was obtained from all patients. Ethical approval was given by the South Central–Oxford C Research Ethics Committee in England (reference 13:/SC/0149), Scotland A Research Ethics Committee (20/SS/0028) and WHO Ethics Review Committee (RPC571 and RPC572l, 25 April 2013).
Data were collected to account for variables affecting symptom outcome, via hospital records and self-reporting. Acute disease severity was classified according to the WHO clinical progression score: WHO class 3–4: no oxygen therapy; class 5: oxygen therapy; class 6: noninvasive ventilation or high-flow nasal oxygen; and class 7–9: managed in critical care 9 . Clinical data were used to place patients into six categories: ‘recovered’, ‘GI’, ‘cardiorespiratory’, ‘fatigue’, ‘cognitive impairment’ and ‘anxiety/depression’ (Supplementary Table 7 ). Patient-reported symptoms and validated clinical scores were used when feasible, including Medical Research Council (MRC) breathlessness score, dyspnea-12 score, Functional Assessment of Chronic Illness Therapy (FACIT) score, Patient Health Questionnaire (PHQ)-9 and Generalized Anxiety Disorder (GAD)-7. Cognitive impairment was defined as a Montreal Cognitive Assessment score <26. GI symptoms were defined as answering ‘Yes’ to the presence of at least two of the listed symptoms. ‘Recovered’ was defined by self-reporting. Patients were placed in multiple groups if they experienced a combination of symptoms.
Matched nasal fluid and sputum samples were prospectively collected from a subgroup of convalescent patients approximately 6 months after hospitalization via the PHOSP-COVID study. Nasal and bronchoalveolar lavage fluid (BALF) collected from healthy volunteers before the COVID-19 pandemic were used as controls (Supplementary Table 4 ). Written consent was obtained for all individuals and ethical approvals were given by London–Harrow Research Ethics Committee (13/LO/1899) for the collection of nasal samples and the Health Research Authority London–Fulham Research Ethics Committee (IRAS project ID 154109; references 14/LO/1023, 10/H0711/94 and 11/LO/1826) for BALF samples.
Ethylenediaminetetraacetic acid plasma was collected from whole blood taken by venepuncture and frozen at −80 °C as previously described 7 , 66 . Nasal fluid was collected using a NasosorptionTM FX·I device (Hunt Developments), which uses a synthetic absorptive matrix to collect concentrated nasal fluid. Samples were eluted and stored as previously described 67 . Sputum samples were collected via passive expectoration and frozen at −80 °C without the addition of buffers. Sputum samples from convalescent individuals were compared with BALF from healthy SARS-CoV-2-naive controls, collected before the pandemic. BALF samples were used to act as a comparison for lower respiratory tract samples since passively expectorated sputum from healthy SARS-CoV-2-naive individuals was not available. BALF samples were obtained by instillation and recovery of up to 240 ml of normal saline via a fiberoptic bronchoscope. BALF was filtered through 100 µM strainers into sterile 50 ml Falcon tubes, then centrifuged for 10 min at 400 g at 4 °C. The resulting supernatant was transferred into sterile 50 ml Falcon tubes and frozen at −80 °C until use. The full methods for BALF collection and processing have been described previously 68 , 69 .
Immunoassays
To determine inflammatory signatures that associated with symptom outcomes, plasma samples were analyzed on an Olink Explore 384 Inflammation panel 70 . Supplementary Table 8 (Appendix 1 ) lists all the analytes measured. To ensure the validity of results, samples were run in a single batch with the use of negative controls, plate controls in triplicate and repeated measurement of patient samples between plates in duplicate. Samples were randomized between plates according to site and sample collection date. Randomization between plates was blind to LC/recovered outcome. Data were first normalized to an internal extension control that was included in each sample well. Plates were standardized by normalizing to interplate controls, run in triplicate on each plate. Each plate contained a minimum of four patient samples, which were duplicates on another plate; these duplicate pairs allowed any plate to be linked to any other through the duplicates. Data were then intensity normalized across all cohort samples. Finally, Olink results underwent quality control processing and samples or analytes that did not reach quality control standards were excluded. Final normalized relative protein quantities were reported as log 2 NPX values.
To further validate our findings, we performed conventional electrochemiluminescence (ECL) assays and enzyme-linked immunosorbent assay for Olink mediators that were associated with symptom outcome ( Supplementary Methods ). Contemporaneously collected plasma samples were available from 58 individuals. Like most omics platforms, Olink measures relative quantities, so perfect agreement with conventional assays that measure absolute concentrations is not expected.
Sputum samples were thawed before analysis and sputum plugs were extracted with the addition of 0.1% dithiothreitol creating a one in two sample dilution, as previously described 71 . SARS-CoV-2 S and N proteins were measured by ECL S-plex assay at a fixed dilution of one in two (Mesoscale Diagnostics), as per the manufacturers protocol 72 . Control BALF samples were thawed and measured on the same plate, neat. The S-plex assay is highly sensitive in detecting viral antigen in respiratory tract samples 73 .
Nasal cytokines were measured by ECL (mesoscale discovery) and Luminex bead multiplex assays (Biotechne). The full methods and list of analytes are detailed in Supplementary Methods .
Statistics and reproducibility
Clinical data was collected via the PHOSP REDCap database, to which access is available under reasonable request as per the data sharing statement in the manuscript. All analyses were performed within the Outbreak Data Analysis Platform (ODAP). All data and code can be accessed using information in the ‘Data sharing’ and ‘Code sharing’ statements at the end of the manuscript. No statistical method was used to predetermine sample size. Data distribution was assumed to be normal but this was not formally tested. Olink assays and immunoassays were randomized and investigators were blinded to outcomes.
To determine protein signatures that associated with each symptom outcome, a ridge PLR was used. PLR shrinks coefficients to account for combined effects within high-dimensional data, preventing false discovery while managing multicollinearity 34 . Thus, PLR was chosen a priori as the most appropriate model to assess associations between a large number of explanatory variables (that may work together to mediate effects) and symptom outcome 34 , 62 , 70 , 74 . In keeping with our aim to perform an unbiased exploration of inflammatory process, the model alpha was set to zero, facilitating regularization without complete penalization of any mediator. This enabled review of all possible mediators that might associate with LC 62 .
A 50 repeats tenfold nested cross-validation was used to select the optimal lambda for each model and assess its accuracy (Extended Data Fig. 1 ). The performance of the cognitive impairment model was influenced by the imbalance in size of the symptom group ( n = 60) relative to recovered ( n = 250). The model was weighted to account for this imbalance resulting in a sensitivity of 0.98, indicating its validity. We have expanded on the model performance and validation approaches in Supplementary Information .
Age, sex, acute disease severity and preexisting comorbidities were included as covariates in the PLR analysis (Supplementary Tables 1 and 3 ). Covariates were selected a priori using features reported to influence the risk of LC and inflammatory responses 1 , 39 , 64 , 75 . Ethnicity was not included since it has been shown not to predict symptom outcome in this cohort 64 . Individuals with missing data were excluded from the regression analysis. Each symptom group was compared with the ‘recovered’ group. The model coefficients of each covariate were converted into ORs for each outcome and visualized in a forest plot, after removing variables associated with regularized OR between 0.98 and 1.02 or in cases where most variables fell outside of this range, using mediators associated with the highest decile of coefficients either side of this range. This enabled exclusion of mediators with effect sizes that were unlikely to have clinical or mechanistic importance since the ridge PLR shrinks and orders coefficients according to their relative importance rather than making estimates with standard error. Thus, confidence intervals cannot be appropriately derived from PLR, and forest plot error bars were calculated using the median accuracy of the model generated by the nested cross-validation. To verify observations made through PLR analysis, we also performed an unadjusted PLR, an unadjusted logistic regression and a PLS analysis. Univariate analyses using Wilcoxon signed-rank test was also performed (Supplementary Table 8 , Appendix 1 ). Analyses were performed in R version 4.2.0 using ‘data.table v1.14.2’, ‘EnvStats v2.7.0’ ‘tidyverse v1.3.2’, ‘lme4 v1.1-32’, ‘caret v6.0-93’, ‘glmnet v4.1-6’, ‘mdatools v0.14.0’, ‘ggpubbr v0.4.0’ and ‘ggplot2 v3.3.6’ packages.
To further investigate the relationship between proteins elevated in each symptom group, we performed a correlation network analysis using Spearman’s rank correlation coefficient and false discovery rate (FDR) thresholding. The mediators visualized in the PLR forest plots, which were associated with cardiorespiratory symptoms, fatigue, anxiety/depression GI symptoms and cognitive impairment were used, respectively. Analyses were performed in R version 4.2.0 using ‘bootnet v1.5.6 ’ and ‘qgraph v1.9.8 ’ packages.
To determine whether differences in protein levels between men and women related to hormonal differences, we divided each symptom group into premenopausal and postmenopausal groups using an age cutoff of 50 years old. Differences between sexes in each group were determined using the Wilcoxon signed-rank test. To understand whether antigen persistence contributed to inflammation in adults with LC, the median viral antigen concentration from sputum/BALF samples and cytokine concentrations from nasal samples were compared using the Wilcoxon signed-rank test. All tests were two-tailed and statistical significance was defined as a P value < 0.05 after adjustment for FDR ( q -value of 0.05). Analyses were performed in R version 4.2.0 using ‘bootnet v1.5.6’ and ‘qgraph v1.9.8’ packages.
Extended Data Fig. 10 was made using Biorender, accessed at www.biorender.com .
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
This is an open access article under the CC BY 4.0 license.
The PHOSP-COVID protocol, consent form, definition and derivation of clinical characteristics and outcomes, training materials, regulatory documents, information about requests for data access, and other relevant study materials are available online at ref. 76 . Access to these materials can be granted by contacting [email protected] and [email protected].
The ISARIC4C protocol, data sharing and publication policy are available at https://isaric4c.net . ISARIC4C’s Independent Data and Material Access Committee welcomes applications for access to data and materials ( https://isaric4c.net ).
The datasets used in the study contain extensive clinical information at an individual level that prevent them from being deposited in an public depository due to data protection policies of the study. Study data can only be accessed via the ODAP, a protected research environment. All data used in this study are available within ODAP and accessible under reasonable request. Data access criteria and information about how to request access is available online at ref. 76 . If criteria are met and a request is made, access can be gained by signing the eDRIS user agreement.
Code availability
Code was written within the ODAP, using R v4.2.0 and publicly available packages (‘data.table v1.14.2’, ‘EnvStats v2.7.0’, ‘tidyverse v1.3.2’, ‘lme4 v1.1-32’, ‘caret v6.0-93’, ‘glmnet v4.1-6’, ‘mdatools v0.14.0’, ‘ggpubbr v0.4.0’, ‘ggplot2 v3.3.6’, ‘bootnet v1.5.6’ and ‘qgraph v1.9.8’ packages). No new algorithms or functions were created and code used in-built functions in listed packages available on CRAN. The code used to generate data and to analyze data is publicly available at https://github.com/isaric4c/wiki/wiki/ISARIC ; https://github.com/SurgicalInformatics/cocin_cc and https://github.com/ClaudiaEfstath/PHOSP_Olink_NatImm .
Davis, H. E., McCorkell, L., Vogel, J. M. & Topol, E. J. Long COVID: major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 21 , 133–146 (2023).
Article CAS PubMed PubMed Central Google Scholar
Antonelli, M., Pujol, J. C., Spector, T. D., Ourselin, S. & Steves, C. J. Risk of long COVID associated with delta versus omicron variants of SARS-CoV-2. Lancet 399 , 2263–2264 (2022).
Talla, A. et al. Persistent serum protein signatures define an inflammatory subcategory of long COVID. Nat. Commun. 14 , 3417 (2023).
Captur, G. et al. Plasma proteomic signature predicts who will get persistent symptoms following SARS-CoV-2 infection. EBioMedicine 85 , 104293 (2022).
Scott, N. A. et al. Monocyte migration profiles define disease severity in acute COVID-19 and unique features of long COVID. Eur. Respir. J. https://doi.org/10.1183/13993003.02226-2022 (2023).
Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Nature https://doi.org/10.1038/s41586-023-06651-y (2023).
Article PubMed PubMed Central Google Scholar
Evans, R. A. et al. Clinical characteristics with inflammation profiling of long COVID and association with 1-year recovery following hospitalisation in the UK: a prospective observational study. Lancet Respir. Med . 10 , 761–775 (2022).
Article CAS Google Scholar
Houchen-Wolloff, L. et al. Joint patient and clinician priority setting to identify 10 key research questions regarding the long-term sequelae of COVID-19. Thorax 77 , 717–720 (2022).
Article PubMed Google Scholar
Marshall, J. C. et al. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis. 20 , e192–e197 (2020).
Post COVID-19 condition (long COVID). World Health Organization https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition#:~:text=Definition,months%20with%20no%20other%20explanation (2022).
Peters, V. A., Joesting, J. J. & Freund, G. G. IL-1 receptor 2 (IL-1R2) and its role in immune regulation. Brain Behav. Immun. 32 , 1–8 (2013).
Article CAS PubMed Google Scholar
Luo, Z. et al. Monocytes augment inflammatory responses in human aortic valve interstitial cells via β2-integrin/ICAM-1-mediated signaling. Inflamm. Res. 71 , 681–694 (2022).
Bendall, L. J. & Bradstock, K. F. G-CSF: from granulopoietic stimulant to bone marrow stem cell mobilizing agent. Cytokine Growth Factor Rev. 25 , 355–367 (2014).
Ma, Y. J. et al. Soluble collectin-12 (CL-12) is a pattern recognition molecule initiating complement activation via the alternative pathway. J. Immunol. 195 , 3365–3373 (2015).
Laursen, N. S. et al. Functional and structural characterization of a potent C1q inhibitor targeting the classical pathway of the complement system. Front. Immunol. 11 , 1504 (2020).
Dejanovic, B. et al. Complement C1q-dependent excitatory and inhibitory synapse elimination by astrocytes and microglia in Alzheimer’s disease mouse models. Nat. Aging 2 , 837–850 (2022).
Xue, G., Hua, L., Zhou, N. & Li, J. Characteristics of immune cell infiltration and associated diagnostic biomarkers in ulcerative colitis: results from bioinformatics analysis. Bioengineered 12 , 252–265 (2021).
He, T. et al. Integrative computational approach identifies immune‐relevant biomarkers in ulcerative colitis. FEBS Open Bio. 12 , 500–515 (2022).
Sundin, J. et al. Fecal chromogranins and secretogranins are linked to the fecal and mucosal intestinal bacterial composition of IBS patients and healthy subjects. Sci. Rep. 8 , 16821 (2018).
Kriebel, M., Wuchter, J., Trinks, S. & Volkmer, H. Neurofascin: a switch between neuronal plasticity and stability. Int. J. Biochem. Cell Biol. 44 , 694–697 (2012).
Woo, W.-M. et al. The C. elegans F-spondin family protein SPON-1 maintains cell adhesion in neural and non-neural tissues. Development 135 , 2747–2756 (2008).
Yadati, T., Houben, T., Bitorina, A. & Shiri-Sverdlov, R. The ins and outs of cathepsins: physiological function and role in disease management. Cells 9 , 1679 (2020).
Taquet, M. et al. Acute blood biomarker profiles predict cognitive deficits 6 and 12 months after COVID-19 hospitalization. Nat. Med. https://doi.org/10.1038/s41591-023-02525-y (2023).
Siggins, M. K. et al. Alternative pathway dysregulation in tissues drives sustained complement activation and predicts outcome across the disease course in COVID‐19. Immunology 168 , 473–492 (2023).
Pol, J. G., Caudana, P., Paillet, J., Piaggio, E. & Kroemer, G. Effects of interleukin-2 in immunostimulation and immunosuppression. J. Exp. Med. 217 , e20191247 (2020).
Zhang, Y., Liu, Q., Yang, S. & Liao, Q. CD58 immunobiology at a glance. Front. Immunol. 12 , 705260 (2021).
Demydchuk, M. et al. Insights into Hunter syndrome from the structure of iduronate-2-sulfatase. Nat. Commun. 8 , 15786 (2017).
Wang, Z. et al. DNER promotes epithelial–mesenchymal transition and prevents chemosensitivity through the Wnt/β-catenin pathway in breast cancer. Cell Death Dis. 11 , 642 (2020).
Bonilla, H. et al. Therapeutic trials for long COVID-19: a call to action from the interventions taskforce of the RECOVER initiative. Front. Immunol. 14 , 1129459 (2023).
Wik, L. et al. Proximity extension assay in combination with next-generation sequencing for high-throughput proteome-wide analysis. Mol. Cell. Proteomics 20 , 100168 (2021).
Measuring protein biomarkers with Olink—technical comparisons and orthogonal validation. Olink Proteomics https://www.olink.com/content/uploads/2021/09/olink-technical-comparisons-and-orthogonal-validation-1118-v2.0.pdf (2021).
COVID-19 rapid guideline: managing the long-term effects of COVID-19. National Institute for Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN) and Royal College of General Practitioners (RCGP) https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742 (2022).
Long COVID or post-COVID conditions. Centers for Disease Control and Prevention https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html#:~:text=Long%20COVID%20is%20broadly%20defined,after%20acute%20COVID%2D19%20infection (2023).
Firinguetti, L., Kibria, G. & Araya, R. Study of partial least squares and ridge regression methods. Commun. Stat. Simul. Comput 46 , 6631–6644 (2017).
Article Google Scholar
Mortensen, L. J., Kreiner-Moller, E., Hakonarson, H., Bonnelykke, K. & Bisgaard, H. The PCDH1 gene and asthma in early childhood. Eur. Respir. J. 43 , 792–800 (2014).
Tong, Y. et al. The RNFT2/IL-3Rα axis regulates IL-3 signaling and innate immunity. JCI Insight 5 , e133652 (2020).
Wu, Y. et al. Effect of ISM1 on the immune microenvironment and epithelial-mesenchymal transition in colorectal cancer. Front. Cell Dev. Biol. 9 , 681240 (2021).
Luo, G. G. & Ou, J. J. Oncogenic viruses and cancer. Virol. Sin. 30 , 83–84 (2015).
Klein, S. L. & Flanagan, K. L. Sex differences in immune responses. Nat. Rev. Immunol. 16 , 626–638 (2016).
Gaebler, C. et al. Evolution of antibody immunity to SARS-CoV-2. Nature 591 , 639–644 (2021).
Bussani, R. et al. Persistent SARS‐CoV‐2 infection in patients seemingly recovered from COVID‐19. J. Pathol. 259 , 254–263 (2023).
Woodruff, M. C. et al. Chronic inflammation, neutrophil activity, and autoreactivity splits long COVID. Nat. Commun. 14 , 4201 (2023).
Lammi, V. et al. Genome-wide association study of long COVID. Preprint at medRxiv https://doi.org/10.1101/2023.06.29.23292056 (2023).
Ismailova, A. et al. Identification of a forkhead box protein transcriptional network induced in human neutrophils in response to inflammatory stimuli. Front. Immunol. 14 , 1123344 (2023).
Beurskens, F. J., van Schaarenburg, R. A. & Trouw, L. A. C1q, antibodies and anti-C1q autoantibodies. Mol. Immunol. 68 , 6–13 (2015).
Cervia-Hasler, C. et al. Persistent complement dysregulation with signs of thromboinflammation in active long Covid. Science 383 , eadg7942 (2024).
Morgan, B. P. & Harris, C. L. Complement, a target for therapy in inflammatory and degenerative diseases. Nat. Rev. Drug Discov. 14 , 857–877 (2015).
Toshner, M. R. et al. Apixaban following discharge in hospitalised adults with COVID-19: preliminary results from a multicentre, open-label, randomised controlled platform clinical trial. Preprint at medRxiv , https://doi.org/10.1101/2022.12.07.22283175 (2022).
Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185 , 881–895.e20 (2022).
Branchfield, K. et al. Pulmonary neuroendocrine cells function as airway sensors to control lung immune response. Science 351 , 707–710 (2016).
Rivera-Torruco, G. et al. Isthmin 1 identifies a subset of lung hematopoietic stem cells and it is associated with systemic inflammation. J. Immunol. 202 , 118.18 (2019).
Swank, Z. et al. Persistent circulating severe acute respiratory syndrome coronavirus 2 spike is associated with post-acute coronavirus disease 2019 sequelae. Clin. Infect. Dis. 76 , e487–e490 (2023).
Peluso, M. J. et al. Chronic viral coinfections differentially affect the likelihood of developing long COVID. J. Clin. Invest. 133 , e163669 (2023).
Bellocchi, C. et al. The interplay between autonomic nervous system and inflammation across systemic autoimmune diseases. Int. J. Mol. Sci. 23 , 2449 (2022).
Raman, B. et al. Multiorgan MRI findings after hospitalisation with COVID-19 in the UK (C-MORE): a prospective, multicentre, observational cohort study. Lancet Respir. Med 11 , 1003–1019 (2023).
Fernández-Castañeda, A. et al. Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation. Cell 185 , 2452–2468.e16 (2022).
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W. & Kelley, K. W. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat. Rev. Neurosci. 9 , 46–56 (2008).
Broughton, S. E. et al. Dual mechanism of interleukin-3 receptor blockade by an anti-cancer antibody. Cell Rep. 8 , 410–419 (2014).
Ley, K., Miller, Y. I. & Hedrick, C. C. Monocyte and macrophage dynamics during atherogenesis. Arterioscler. Thromb. Vasc. Biol. 31 , 1506–1516 (2011).
Iosef, C. et al. Plasma proteome of long-COVID patients indicates HIF-mediated vasculo-proliferative disease with impact on brain and heart function. J. Transl. Med. 21 , 377 (2023).
Santopaolo, M. et al. Prolonged T-cell activation and long COVID symptoms independently associate with severe COVID-19 at 3 months. eLife 12 , e85009 (2023).
Friedman, J., Hastie, T. & Tibshirani, R. Regularization paths for generalized linear models via coordinate descent. J. Stat. Softw. 33 , 1–22 (2010).
Voiriot, G. et al. Chronic critical illness and post-intensive care syndrome: from pathophysiology to clinical challenges. Ann. Intensive Care 12 , 58 (2022).
Evans, R. A. et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir. Med 9 , 1275–1287 (2021).
Docherty, A. B. et al. Features of 20,133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. BMJ https://doi.org/10.1136/bmj.m1985 (2020).
Elneima, O. et al. Cohort profile: post-hospitalisation COVID-19 study (PHOSP-COVID). Preprint at medRxiv https://doi.org/10.1101/2023.05.08.23289442 (2023).
Liew, F. et al. SARS-CoV-2-specific nasal IgA wanes 9 months after hospitalisation with COVID-19 and is not induced by subsequent vaccination. EBioMedicine 87 , 104402 (2023).
Ascough, S. et al. Divergent age-related humoral correlates of protection against respiratory syncytial virus infection in older and young adults: a pilot, controlled, human infection challenge model. Lancet Healthy Longev. 3 , e405–e416 (2022).
Guvenel, A. et al. Epitope-specific airway-resident CD4+ T cell dynamics during experimental human RSV infection. J. Clin. Invest. 130 , 523–538 (2019).
Article PubMed Central Google Scholar
Greenwood, C. J. et al. A comparison of penalised regression methods for informing the selection of predictive markers. PLoS ONE 15 , e0242730 (2020).
Higham, A. et al. Leukotriene B4 levels in sputum from asthma patients. ERJ Open Res. 2 , 00088–02015 (2016).
SARS-CoV-2 spike kit. MSD https://www.mesoscale.com/~/media/files/product%20inserts/s-plex%20sars-cov-2%20spike%20kit%20product%20insert.pdf (2023).
Ren, A. et al. Ultrasensitive assay for saliva-based SARS-CoV-2 antigen detection. Clin. Chem. Lab. Med. 60 , 771–777 (2022).
Breheny, P. & Huang, J. Penalized methods for bi-level variable selection. Stat. Interface 2 , 369–380 (2009).
Thwaites, R. S. et al. Inflammatory profiles across the spectrum of disease reveal a distinct role for GM-CSF in severe COVID-19. Sci. Immunol. 6 , eabg9873 (2021).
Resources. PHOSP-COVID https://phosp.org/resource/ (2022).
Download references
Acknowledgements
This research used data assets made available by ODAP as part of the Data and Connectivity National Core Study, led by Health Data Research UK in partnership with the Office for National Statistics and funded by UK Research and Innovation (grant ref. MC_PC_20058). This work is supported by the following grants: the PHOSP-COVD study is jointly funded by UK Research and Innovation and National Institute of Health and Care Research (NIHR; grant references MR/V027859/1 and COV0319). ISARIC4C is supported by grants from the National Institute for Health and Care Research (award CO-CIN-01) and the MRC (grant MC_PC_19059) Liverpool Experimental Cancer Medicine Centre provided infrastructure support for this research (grant reference C18616/A25153). Other grants that have supported this work include the UK Coronavirus Immunology Consortium (funder reference 1257927), the Imperial Biomedical Research Centre (NIHR Imperial BRC, grant IS-BRC-1215-20013), the Health Protection Research Unit in Respiratory Infections at Imperial College London and NIHR Health Protection Research Unit in Emerging and Zoonotic Infections at University of Liverpool, both in partnership with Public Health England, (NIHR award 200907), Wellcome Trust and Department for International Development (215091/Z/18/Z), Health Data Research UK (grant code 2021.0155), MRC (grant code MC_UU_12014/12) and NIHR Clinical Research Network for providing infrastructure support for this research. We also acknowledge the support of the MRC EMINENT Network (MR/R502121/1), which is cofunded by GSK, the Comprehensive Local Research Networks, the MRC HIC-Vac network (MR/R005982/1) and the RSV Consortium in Europe Horizon 2020 Framework Grant 116019. F.L. is supported by an MRC clinical training fellowship (award MR/W000970/1). C.E. is funded by NIHR (grant P91258-4). L.-P.H. is supported by Oxford NIHR Biomedical Research Centre. A.A.R.T. is supported by a British Heart Foundation (BHF) Intermediate Clinical Fellowship (FS/18/13/33281). S.L.R.-J. receives support from UK Research and Innovation (UKRI), Global Challenges Research Fund (GCRF), Rosetrees Trust, British HIV association (BHIVA), European & Developing Countries Clinical Trials Partnership (EDCTP) and Globvac. J.D.C. has grants from AstraZeneca, Boehringer Ingelheim, GSK, Gilead Sciences, Grifols, Novartis and Insmed. R.A.E. holds a NIHR Clinician Scientist Fellowship (CS-2016-16-020). A. Horsley is currently supported by UK Research and Innovation, NIHR and NIHR Manchester BRC. B.R. receives support from BHF Oxford Centre of Research Excellence, NIHR Oxford BRC and MRC. D.G.W. is supported by an NIHR Advanced Fellowship. A. Ho has received support from MRC and for the Coronavirus Immunology Consortium (MR/V028448/1). L.T. is supported by the US Food and Drug Administration Medical Countermeasures Initiative contract 75F40120C00085 and the National Institute for Health Research Health Protection Research Unit in Emerging and Zoonotic Infections (NIHR200907) at the University of Liverpool in partnership with UK Health Security Agency (UK-HSA), in collaboration with Liverpool School of Tropical Medicine and the University of Oxford. L.V.W. has received support from UKRI, GSK/Asthma and Lung UK and NIHR for this study. M.G.S. has received support from NIHR UK, MRC UK and Health Protection Research Unit in Emerging and Zoonotic Infections, University of Liverpool. J.K.B. is supported by the Wellcome Trust (223164/Z/21/Z) and UKRI (MC_PC_20004, MC_PC_19025, MC_PC_1905, MRNO2995X/1 and MC_PC_20029). The funders were not involved in the study design, interpretation of data or writing of this manuscript. The views expressed are those of the authors and not necessarily those of the Department of Health and Social Care (DHSC), the Department for International Development (DID), NIHR, MRC, the Wellcome Trust, UK-HSA, the National Health Service or the Department of Health. P.J.M.O. is supported by a NIHR Senior Investigator Award (award 201385). We thank all the participants and their families. We thank the many research administrators, health-care and social-care professionals who contributed to setting up and delivering the PHOSP-COVID study at all of the 65 NHS trusts/health boards and 25 research institutions across the United Kingdom, as well as those who contributed to setting up and delivering the ISARIC4C study at 305 NHS trusts/health boards. We also thank all the supporting staff at the NIHR Clinical Research Network, Health Research Authority, Research Ethics Committee, Department of Health and Social Care, Public Health Scotland and Public Health England. We thank K. Holmes at the NIHR Office for Clinical Research Infrastructure for her support in coordinating the charities group. The PHOSP-COVID industry framework was formed to provide advice and support in commercial discussions, and we thank the Association of the British Pharmaceutical Industry as well the NIHR Office for Clinical Research Infrastructure for coordinating this. We are very grateful to all the charities that have provided insight to the study: Action Pulmonary Fibrosis, Alzheimer’s Research UK, Asthma and Lung UK, British Heart Foundation, Diabetes UK, Cystic Fibrosis Trust, Kidney Research UK, MQ Mental Health, Muscular Dystrophy UK, Stroke Association Blood Cancer UK, McPin Foundations and Versus Arthritis. We thank the NIHR Leicester Biomedical Research Centre patient and public involvement group and Long Covid Support. We also thank G. Khandaker and D. C. Newcomb who provided valuable feedback on this work. Extended Data Fig. 10 was created using Biorender.
Author information
These authors contributed equally: Felicity Liew, Claudia Efstathiou, Ryan S. Thwaites, Peter J. M. Openshaw.
Authors and Affiliations
National Heart and Lung Institute, Imperial College London, London, UK
Felicity Liew, Claudia Efstathiou, Sara Fontanella, Dawid Swieboda, Jasmin K. Sidhu, Stephanie Ascough, Onn Min Kon, Luke S. Howard, Jennifer K. Quint, Christopher Chiu, Ryan S. Thwaites, Peter J. M. Openshaw, Jake Dunning & Peter J. M. Openshaw
Institute for Lung Health, Leicester NIHR Biomedical Research Centre, University of Leicester, Leicester, UK
Matthew Richardson, Ruth Saunders, Olivia C. Leavy, Omer Elneima, Hamish J. C. McAuley, Amisha Singapuri, Marco Sereno, Victoria C. Harris, Neil J. Greening, Rachael A. Evans, Louise V. Wain, Christopher Brightling & Ananga Singapuri
NIHR Health Protection Research Unit in Emerging and Zoonotic Infections, Institute of Infection, Veterinary and Ecological Sciences, University of Liverpool, Liverpool, UK
Shona C. Moore, Daniel G. Wootton, Malcolm G. Semple, Lance Turtle, William A. Paxton & Georgios Pollakis
The Imperial Clinical Respiratory Research Unit, Imperial College NHS Trust, London, UK
Noura Mohamed
Cardiovascular Research Team, Imperial College Healthcare NHS Trust, London, UK
Jose Nunag & Clara King
Department of Population Health Sciences, University of Leicester, Leicester, UK
Olivia C. Leavy, Louise V. Wain & Beatriz Guillen-Guio
NIHR Leicester Biomedical Research Centre, University of Leicester, Leicester, UK
Aarti Shikotra
Centre for Exercise and Rehabilitation Science, NIHR Leicester Biomedical Research Centre-Respiratory, University of Leicester, Leicester, UK
Linzy Houchen-Wolloff
Usher Institute, University of Edinburgh, Edinburgh, UK
Nazir I. Lone, Luke Daines, Annemarie B. Docherty, Nazir I. Lone, Matthew Thorpe, Annemarie B. Docherty, Thomas M. Drake, Cameron J. Fairfield, Ewen M. Harrison, Stephen R. Knight, Kenneth A. Mclean, Derek Murphy, Lisa Norman, Riinu Pius & Catherine A. Shaw
Centre for Medical Informatics, The Usher Institute, University of Edinburgh, Edinburgh, UK
Matthew Thorpe, Annemarie B. Docherty, Ewen M. Harrison, J. Kenneth Baillie, Sarah L. Rowland-Jones, A. A. Roger Thompson & Thushan de Silva
Department of Infection, Immunity and Cardiovascular Disease, University of Sheffield, Sheffield, UK
A. A. Roger Thompson, Sarah L. Rowland-Jones, Thushan I. de Silva & James D. Chalmers
University of Dundee, Ninewells Hospital and Medical School, Dundee, UK
James D. Chalmers & Ling-Pei Ho
MRC Human Immunology Unit, University of Oxford, Oxford, UK
Ling-Pei Ho & Alexander Horsley
Division of Infection, Immunity and Respiratory Medicine, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, UK
Alexander Horsley & Betty Raman
Radcliffe Department of Medicine, University of Oxford, Oxford, UK
Betty Raman & Krisnah Poinasamy
Asthma + Lung UK, London, UK
Krisnah Poinasamy & Michael Marks
Department of Clinical Research, London School of Hygiene and Tropical Medicine, London, UK
Michael Marks
Hospital for Tropical Diseases, University College London Hospital, London, UK
Division of Infection and Immunity, University College London, London, UK
Michael Marks & Mahdad Noursadeghi
MRC Centre for Virus Research, School of Infection and Immunity, University of Glasgow, Glasgow, UK
Antonia Ho & William Greenhalf
Institute of Systems, Molecular and Integrative Biology, University of Liverpool, Liverpool, UK
William Greenhalf & J. Kenneth Baillie
The Roslin Institute, University of Edinburgh, Edinburgh, UK
J. Kenneth Baillie, J. Kenneth Baillie, Sara Clohisey, Fiona Griffiths, Ross Hendry, Andrew Law & Wilna Oosthuyzen
Pandemic Science Hub, University of Edinburgh, Edinburgh, UK
J. Kenneth Baillie
The Pandemic Institute, University of Liverpool, Liverpool, UK
Malcolm G. Semple & Lance Turtle
University of Manchester, Manchester, UK
Kathryn Abel, Perdita Barran, H. Chinoy, Bill Deakin, M. Harvie, C. A. Miller, Stefan Stanel & Drupad Trivedi
Intensive Care Unit, Royal Infirmary of Edinburgh, Edinburgh, UK
Kathryn Abel & J. Kenneth Baillie
North Bristol NHS Trust and University of Bristol, Bristol, UK
H. Adamali, David Arnold, Shaney Barratt, A. Dipper, Sarah Dunn, Nick Maskell, Anna Morley, Leigh Morrison, Louise Stadon, Samuel Waterson & H. Welch
University of Edinburgh, Manchester, UK
Davies Adeloye, D. E. Newby, Riinu Pius, Igor Rudan, Manu Shankar-Hari, Catherine Sudlow, Sarah Walmsley & Bang Zheng
King’s College Hospital NHS Foundation Trust and King’s College London, London, UK
Oluwaseun Adeyemi, Rita Adrego, Hosanna Assefa-Kebede, Jonathon Breeze, S. Byrne, Pearl Dulawan, Amy Hoare, Caroline Jolley, Abigail Knighton, M. Malim, Sheetal Patale, Ida Peralta, Natassia Powell, Albert Ramos, K. Shevket, Fabio Speranza & Amelie Te
Guy’s and St Thomas’ NHS Foundation Trust, London, UK
Laura Aguilar Jimenez, Gill Arbane, Sarah Betts, Karen Bisnauthsing, A. Dewar, Nicholas Hart, G. Kaltsakas, Helen Kerslake, Murphy Magtoto, Philip Marino, L. M. Martinez, Marlies Ostermann, Jennifer Rossdale & Teresa Solano
Royal Free London NHS Foundation Trust, London, UK
Shanaz Ahmad, Simon Brill, John Hurst, Hannah Jarvis, C. Laing, Lai Lim, S. Mandal, Darwin Matila, Olaoluwa Olaosebikan & Claire Singh
University Hospital Birmingham NHS Foundation Trust and University of Birmingham, Birmingham, UK
N. Ahmad Haider, Catherine Atkin, Rhiannon Baggott, Michelle Bates, A. Botkai, Anna Casey, B. Cooper, Joanne Dasgin, Camilla Dawson, Katharine Draxlbauer, N. Gautam, J. Hazeldine, T. Hiwot, Sophie Holden, Karen Isaacs, T. Jackson, Vicky Kamwa, D. Lewis, Janet Lord, S. Madathil, C. McGee, K. Mcgee, Aoife Neal, Alex Newton-Cox, Joseph Nyaboko, Dhruv Parekh, Z. Peterkin, H. Qureshi, Liz Ratcliffe, Elizabeth Sapey, J. Short, Tracy Soulsby, J. Stockley, Zehra Suleiman, Tamika Thompson, Maximina Ventura, Sinead Walder, Carly Welch, Daisy Wilson, S. Yasmin & Kay Por Yip
Stroke Association, London, UK
Rubina Ahmed & Richard Francis
University College London Hospital and University College London, London, UK
Nyarko Ahwireng, Dongchun Bang, Donna Basire, Jeremy Brown, Rachel Chambers, A. Checkley, R. Evans, M. Heightman, T. Hillman, Joseph Jacob, Roman Jastrub, M. Lipman, S. Logan, D. Lomas, Marta Merida Morillas, Hannah Plant, Joanna Porter, K. Roy & E. Wall
Oxford University Hospitals NHS Foundation Trust and University of Oxford, Oxford, UK
Mark Ainsworth, Asma Alamoudi, Angela Bloss, Penny Carter, M. Cassar, Jin Chen, Florence Conneh, T. Dong, Ranuromanana Evans, V. Ferreira, Emily Fraser, John Geddes, F. Gleeson, Paul Harrison, May Havinden-Williams, P. Jezzard, Ivan Koychev, Prathiba Kurupati, H. McShane, Clare Megson, Stefan Neubauer, Debby Nicoll, C. Nikolaidou, G. Ogg, Edmund Pacpaco, M. Pavlides, Yanchun Peng, Nayia Petousi, John Pimm, Najib Rahman, M. J. Rowland, Kathryn Saunders, Michael Sharpe, Nick Talbot, E. M. Tunnicliffe & C. Xie
St George’s University Hospitals NHS Foundation Trust, London, UK
Mariam Ali, Raminder Aul, A. Dunleavy, D. Forton, Mark Mencias, N. Msimanga, T. Samakomva, Sulman Siddique, Vera Tavoukjian & J. Teixeira
University Hospitals of Leicester NHS Trust and University of Leicester, Leicester, UK
M. Aljaroof, Natalie Armstrong, H. Arnold, Hnin Aung, Majda Bakali, M. Bakau, E. Baldry, Molly Baldwin, Charlotte Bourne, Michelle Bourne, Nigel Brunskill, P. Cairns, Liesel Carr, Amanda Charalambou, C. Christie, Melanie Davies, Enya Daynes, Sarah Diver, Rachael Dowling, Sarah Edwards, C. Edwardson, H. Evans, J. Finch, Sarah Glover, Nicola Goodman, Bibek Gooptu, Kate Hadley, Pranab Haldar, Beverley Hargadon, W. Ibrahim, L. Ingram, Kamlesh Khunti, A. Lea, D. Lee, Gerry McCann, P. McCourt, Teresa Mcnally, George Mills, Will Monteiro, Manish Pareek, S. Parker, Anne Prickett, I. N. Qureshi, A. Rowland, Richard Russell, Salman Siddiqui, Sally Singh, J. Skeemer, M. Soares, E. Stringer, T. Thornton, Martin Tobin, T. J. C. Ward, F. Woodhead, Tom Yates & A. J. Yousuf
University of Exeter, Exeter, UK
Louise Allan, Clive Ballard & Andrew McGovern
University of Leicester, Leicester, UK
Richard Allen, Michelle Bingham, Terry Brugha, Selina Finney, Rob Free, Don Jones, Claire Lawson, Daniel Lozano-Rojas, Gardiner Lucy, Alistair Moss, Elizabeta Mukaetova-Ladinska, Petr Novotny, Kimon Ntotsis, Charlotte Overton, John Pearl, Tatiana Plekhanova, M. Richardson, Nilesh Samani, Jack Sargant, Ruth Saunders, M. Sharma, Mike Steiner, Chris Taylor, Sarah Terry, C. Tong, E. Turner, J. Wormleighton & Bang Zhao
Liverpool University Hospitals NHS Foundation Trust and University of Liverpool, Liverpool, UK
Lisa Allerton, Ann Marie Allt, M. Beadsworth, Anthony Berridge, Jo Brown, Shirley Cooper, Andy Cross, Sylviane Defres, S. L. Dobson, Joanne Earley, N. French, Kera Hainey, Hayley Hardwick, Jenny Hawkes, Victoria Highett, Sabina Kaprowska, Angela Key, Lara Lavelle-Langham, N. Lewis-Burke, Gladys Madzamba, Flora Malein, Sophie Marsh, Chloe Mears, Lucy Melling, Matthew Noonan, L. Poll, James Pratt, Emma Richardson, Anna Rowe, Victoria Shaw, K. A. Tripp, Lilian Wajero, S. A. Williams-Howard, Dan Wootton & J. Wyles
Sherwood Forest Hospitals NHS Foundation Trust, Nottingham, UK
Lynne Allsop, Kaytie Bennett, Phil Buckley, Margaret Flynn, Mandy Gill, Camelia Goodwin, M. Greatorex, Heidi Gregory, Cheryl Heeley, Leah Holloway, Megan Holmes, John Hutchinson, Jill Kirk, Wayne Lovegrove, Terri Ann Sewell, Sarah Shelton, D. Sissons, Katie Slack, Susan Smith, D. Sowter, Sarah Turner, V. Whitworth & Inez Wynter
Nottingham University Hospitals NHS Trust and University of Nottingham, London, UK
Paula Almeida, Akram Hosseini, Robert Needham & Karen Shaw
Manchester University NHS Foundation Trust and University of Manchester, London, UK
Bashar Al-Sheklly, Cristina Avram, John Blaikely, M. Buch, N. Choudhury, David Faluyi, T. Felton, T. Gorsuch, Neil Hanley, Tracy Hussell, Zunaira Kausar, Natasha Odell, Rebecca Osbourne, Karen Piper Hanley, K. Radhakrishnan & Sue Stockdale
Imperial College London, London, UK
Danny Altmann, Anew Frankel, Luke S. Howard, Desmond Johnston, Liz Lightstone, Anne Lingford-Hughes, William Man, Steve McAdoo, Jane Mitchell, Philip Molyneaux, Christos Nicolaou, D. P. O’Regan, L. Price, Jennifer K. Quint, David Smith, Jonathon Valabhji, Simon Walsh, Martin Wilkins & Michelle Willicombe
Hampshire Hospitals NHS Foundation Trust, Basingstoke, UK
Maria Alvarez Corral, Ava Maria Arias, Emily Bevan, Denise Griffin, Jane Martin, J. Owen, Sheila Payne, A. Prabhu, Annabel Reed, Will Storrar, Nick Williams & Caroline Wrey Brown
British Heart Foundation, Birmingham, UK
Shannon Amoils
NHS Greater Glasgow and Clyde Health Board and University of Glasgow, Glasgow, UK
David Anderson, Neil Basu, Hannah Bayes, Colin Berry, Ammani Brown, Andrew Dougherty, K. Fallon, L. Gilmour, D. Grieve, K. Mangion, I. B. McInnes, A. Morrow, Kathryn Scott & R. Sykes
University of Oxford, Oxford, UK
Charalambos Antoniades, A. Bates, M. Beggs, Kamaldeep Bhui, Katie Breeze, K. M. Channon, David Clark, X. Fu, Masud Husain, Lucy Kingham, Paul Klenerman, Hanan Lamlum, X. Li, E. Lukaschuk, Celeste McCracken, K. McGlynn, R. Menke, K. Motohashi, T. E. Nichols, Godwin Ogbole, S. Piechnik, I. Propescu, J. Propescu, A. A. Samat, Z. B. Sanders, Louise Sigfrid & M. Webster
Belfast Health and Social Care Trust and Queen’s University Belfast, Belfast, UK
Cherie Armour, Vanessa Brown, John Busby, Bronwen Connolly, Thelma Craig, Stephen Drain, Liam Heaney, Bernie King, Nick Magee, E. Major, Danny McAulay, Lorcan McGarvey, Jade McGinness, Tunde Peto & Roisin Stone
Airedale NHS Foundation Trust, Keighley, UK
Lisa Armstrong, Brigid Hairsine, Helen Henson, Claire Kurasz, Alison Shaw & Liz Shenton
Wrightington Wigan and Leigh NHS Trust, Wigan, UK
A. Ashish, Josh Cooper & Emma Robinson
Leeds Teaching Hospitals and University of Leeds, Leeds, UK
Andrew Ashworth, Paul Beirne, Jude Clarke, C. Coupland, Matthhew Dalton, Clair Favager, Jodie Glossop, John Greenwood, Lucy Hall, Tim Hardy, Amy Humphries, Jennifer Murira, Dan Peckham, S. Plein, Jade Rangeley, Gwen Saalmink, Ai Lyn Tan, Elaine Wade, Beverley Whittam, Nicola Window & Janet Woods
University of Liverpool, Liverpool, UK
M. Ashworth, D. Cuthbertson, G. Kemp, Anne McArdle, Benedict Michael, Will Reynolds, Lisa Spencer, Ben Vinson, Katie A. Ahmed, Jane A. Armstrong, Milton Ashworth, Innocent G. Asiimwe, Siddharth Bakshi, Samantha L. Barlow, Laura Booth, Benjamin Brennan, Katie Bullock, Nicola Carlucci, Emily Cass, Benjamin W. A. Catterall, Jordan J. Clark, Emily A. Clarke, Sarah Cole, Louise Cooper, Helen Cox, Christopher Davis, Oslem Dincarslan, Alejandra Doce Carracedo, Chris Dunn, Philip Dyer, Angela Elliott, Anthony Evans, Lorna Finch, Lewis W. S. Fisher, Lisa Flaherty, Terry Foster, Isabel Garcia-Dorival, Philip Gunning, Catherine Hartley, Karl Holden, Anthony Holmes, Rebecca L. Jensen, Christopher B. Jones, Trevor R. Jones, Shadia Khandaker, Katharine King, Robyn T. Kiy, Chrysa Koukorava, Annette Lake, Suzannah Lant, Diane Latawiec, Lara Lavelle-Langham, Daniella Lefteri, Lauren Lett, Lucia A. Livoti, Maria Mancini, Hannah Massey, Nicole Maziere, Sarah McDonald, Laurence McEvoy, John McLauchlan, Soeren Metelmann, Nahida S. Miah, Joanna Middleton, Joyce Mitchell, Ellen G. Murphy, Rebekah Penrice-Randal, Jack Pilgrim, Tessa Prince, P. Matthew Ridley, Debby Sales, Rebecca K. Shears, Benjamin Small, Krishanthi S. Subramaniam, Agnieska Szemiel, Aislynn Taggart, Jolanta Tanianis-Hughes, Jordan Thomas, Erwan Trochu, Libby van Tonder, Eve Wilcock & J. Eunice Zhang
University College London, London, UK
Shahab Aslani, Amita Banerjee, R. Batterham, Gabrielle Baxter, Robert Bell, Anthony David, Emma Denneny, Alun Hughes, W. Lilaonitkul, P. Mehta, Ashkan Pakzad, Bojidar Rangelov, B. Williams, James Willoughby & Moucheng Xu
Hull University Teaching Hospitals NHS Trust and University of Hull, Hull, UK
Paul Atkin, K. Brindle, Michael Crooks, Katie Drury, Nicholas Easom, Rachel Flockton, L. Holdsworth, A. Richards, D. L. Sykes, Susannah Thackray-Nocera & C. Wright
East Kent Hospitals University NHS Foundation Trust, Canterbury, UK
Liam Austin, Eva Beranova, Tracey Cosier, Joanne Deery, Tracy Hazelton, Carly Price, Hazel Ramos, Reanne Solly, Sharon Turney & Heather Weston
Baillie Gifford Pandemic Science Hub, Centre for Inflammation Research, The Queen’s Medical Research Institute, University of Edinburgh, Edinburgh, UK
Nikos Avramidis, J. Kenneth Baillie, Erola Pairo-Castineira & Konrad Rawlik
Roslin Institute, University of Edinburgh, Edinburgh, UK
Nikos Avramidis, J. Kenneth Baillie & Erola Pairo-Castineira
Newcastle upon Tyne Hospitals NHS Foundation Trust and University of Newcastle, Newcastle upon Tyne, UK
A. Ayoub, J. Brown, G. Burns, Gareth Davies, Anthony De Soyza, Carlos Echevarria, Helen Fisher, C. Francis, Alan Greenhalgh, Philip Hogarth, Joan Hughes, Kasim Jiwa, G. Jones, G. MacGowan, D. Price, Avan Sayer, John Simpson, H. Tedd, S. Thomas, Sophie West, M. Witham, S. Wright & A. Young
East Cheshire NHS Trust, Macclesfield, UK
Marta Babores, Maureen Holland, Natalie Keenan, Sharlene Shashaa & Helen Wassall
Sheffield Teaching NHS Foundation Trust and University of Sheffield, Sheffield, UK
J. Bagshaw, M. Begum, K. Birchall, Robyn Butcher, H. Carborn, Flora Chan, Kerry Chapman, Yutung Cheng, Luke Chetham, Cameron Clark, Zach Coburn, Joby Cole, Myles Dixon, Alexandra Fairman, J. Finnigan, H. Foot, David Foote, Amber Ford, Rebecca Gregory, Kate Harrington, L. Haslam, L. Hesselden, J. Hockridge, Ailsa Holbourn, B. Holroyd-Hind, L. Holt, Alice Howell, E. Hurditch, F. Ilyas, Claire Jarman, Allan Lawrie, Ju Hee Lee, Elvina Lee, Rebecca Lenagh, Alison Lye, Irene Macharia, M. Marshall, Angeline Mbuyisa, J. McNeill, Sharon Megson, J. Meiring, L. Milner, S. Misra, Helen Newell, Tom Newman, C. Norman, Lorenza Nwafor, Dibya Pattenadk, Megan Plowright, Julie Porter, Phillip Ravencroft, C. Roddis, J. Rodger, Peter Saunders, J. Sidebottom, Jacqui Smith, Laurie Smith, N. Steele, G. Stephens, R. Stimpson, B. Thamu, N. Tinker, Kim Turner, Helena Turton, Phillip Wade, S. Walker, James Watson, Imogen Wilson & Amira Zawia
University of Nottingham, Nottingham, UK
David Baguley, Chris Coleman, E. Cox, Laura Fabbri, Susan Francis, Ian Hall, E. Hufton, Simon Johnson, Fasih Khan, Paaig Kitterick, Richard Morriss, Nick Selby, Iain Stewart & Louise Wright
Wirral University Teaching Hospital, Wirral, UK
Elisabeth Bailey, Anne Reddington & Andrew Wight
MRC Human Genetics Unit, Institute of Genetics and Cancer, University of Edinburgh, Western General Hospital, Edinburgh, UK
University of Swansea, Swansea, UK
University of Southampton, London, UK
David Baldwin, P. C. Calder, Nathan Huneke & Gemma Simons
Royal Brompton and Harefield Clinical Group, Guy’s and St Thomas’ NHS Foundation Trust, London, UK
R. E. Barker, Daniele Cristiano, N. Dormand, P. George, Mahitha Gummadi, S. Kon, Kamal Liyanage, C. M. Nolan, B. Patel, Suhani Patel, Oliver Polgar, L. Price, P. Shah, Suver Singh & J. A. Walsh
York and Scarborough NHS Foundation Trust, York, UK
Laura Barman, Claire Brookes, K. Elliott, L. Griffiths, Zoe Guy, Kate Howard, Diana Ionita, Heidi Redfearn, Carol Sarginson & Alison Turnbull
NHS Highland, Inverness, UK
Fiona Barrett, A. Donaldson & Beth Sage
Royal Papworth Hospital NHS Foundation Trust, Cambridge, UK
Helen Baxendale, Lucie Garner, C. Johnson, J. Mackie, Alice Michael, J. Newman, Jamie Pack, K. Paques, H. Parfrey, J. Parmar & A. Reddy
University Hospitals of Derby and Burton, Derby, UK
Paul Beckett, Caroline Dickens & Uttam Nanda
NHS Lanarkshire, Hamilton, UK
Murdina Bell, Angela Brown, M. Brown, R. Hamil, Karen Leitch, L. Macliver, Manish Patel, Jackie Quigley, Andrew Smith & B. Welsh
Cambridge University Hospitals NHS Foundation Trust, NIHR Cambridge Clinical Research Facility and University of Cambridge, Cambridge, UK
Areti Bermperi, Isabel Cruz, K. Dempsey, Anne Elmer, Jonathon Fuld, H. Jones, Sherly Jose, Stefan Marciniak, M. Parkes, Carla Ribeiro, Jessica Taylor, Mark Toshner, L. Watson & J. Worsley
Loughborough University, Loughborough, UK
Lettie Bishop & David Stensel
Betsi Cadwallader University Health Board, Bangor, UK
Annette Bolger, Ffyon Davies, Ahmed Haggar, Joanne Lewis, Arwel Lloyd, R. Manley, Emma McIvor, Daniel Menzies, K. Roberts, W. Saxon, David Southern, Christian Subbe & Victoria Whitehead
Nottingham University Hospitals NHS Trust and University of Nottingham, Nottingham, UK
Charlotte Bolton, J. Bonnington, Melanie Chrystal, Catherine Dupont, Paul Greenhaff, Ayushman Gupta, W. Jang, S. Linford, Laura Matthews, Athanasios Nikolaidis, Sabrina Prosper & Andrew Thomas
King’s College London, London, UK
Kate Bramham, M. Brown, Khalida Ismail, Tim Nicholson, Carmen Pariante, Claire Sharpe, Simon Wessely & J. Whitney
Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK
Lucy Brear, Karen Regan, Dinesh Saralaya & Kim Storton
South London and Maudsley NHS Foundation Trust and King’s College London, London, UK
G. Breen & M. Hotopf
London School of Hygiene and Tropical Medicine, London, UK
Andrew Briggs
Whittington Health NHS Trust, London, UK
E. Bright, P. Crisp, Ruvini Dharmagunawardena & M. Stern
Cardiff and Vale University Health Board, Cardiff, UK
Lauren Broad, Teriann Evans, Matthew Haynes, L. Jones, Lucy Knibbs, Alison McQueen, Catherine Oliver, Kerry Paradowski, Ramsey Sabit & Jenny Williams
Yeovil District Hospital NHS Foundation Trust, Yeovil, UK
Andrew Broadley
University of Birmingham, Birmingham, UK
Mattew Broome, Paul McArdle, Paul Moss, David Thickett, Rachel Upthegrove, Dan Wilkinson, David Wraith & Erin L. Aldera
BHF Centre for Cardiovascular Science, University of Edinburgh, Edinburgh, UK
Anda Bularga
University of Cambridge, Cambridge, UK
Ed Bullmore, Jonathon Heeney, Claudia Langenberg, William Schwaeble, Charlotte Summers & J. Weir McCall
NIHR Leicester Biomedical Research Centre–Respiratory Patient and Public Involvement Group, Leicester, UK
Jenny Bunker, Rhyan Gill & Rashmita Nathu
Imperial College Healthcare NHS Trust and Imperial College London, London, UK
L. Burden, Ellen Calvelo, Bethany Card, Caitlin Carr, Edwin Chilvers, Donna Copeland, P. Cullinan, Patrick Daly, Lynsey Evison, Tamanah Fayzan, Hussain Gordon, Sulaimaan Haq, Gisli Jenkins, Clara King, Onn Min Kon, Katherine March, Myril Mariveles, Laura McLeavey, Silvia Moriera, Unber Munawar, Uchechi Nwanguma, Lorna Orriss-Dib, Alexandra Ross, Maura Roy, Emily Russell, Katherine Samuel, J. Schronce, Neil Simpson, Lawrence Tarusan, David Thomas, Chloe Wood & Najira Yasmin
Harrogate and District NHD Foundation Trust, Harrogate, UK
Tracy Burdett, James Featherstone, Cathy Lawson, Alison Layton, Clare Mills & Lorraine Stephenson
Newcastle University/Chair of NIHR Dementia TRC, Newcastle, UK
Oxford University Hospitals NHS Foundation Trust, Oxford, UK
A. Burns & N. Kanellakis
Tameside and Glossop Integrated Care NHS Foundation Trust, Ashton-under-Lyne, UK
Al-Tahoor Butt, Martina Coulding, Heather Jones, Susan Kilroy, Jacqueline McCormick, Jerome McIntosh, Heather Savill, Victoria Turner & Joanne Vere
University of Oxford, Nuffield Department of Medicine, Oxford, UK
University of Glasgow, Glasgow, UK
Jonathon Cavanagh, S. MacDonald, Kate O’Donnell, John Petrie, Naveed Sattar & Mark Spears
United Lincolnshire Hospitals NHS Trust, Grantham, UK
Manish Chablani & Lynn Osborne
Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Trudie Chalder
University Hospital of South Manchester NHS Foundation Trust, Manchester, UK
N. Chaudhuri
University Hospital Southampton NHS Foundation Trust and University of Southampton, Southampton, UK
Caroline Childs, R. Djukanovic, S. Fletcher, Matt Harvey, Mark Jones, Elizabeth Marouzet, B. Marshall, Reena Samuel, T. Sass, Tim Wallis & Helen Wheeler
King’s College Hospital/Guy’s and St Thomas’ NHS FT, London, UK
A. Chiribiri & C. O’Brien
Barts Health NHS Trust, London, UK
K. Chong-James, C. David, W. Y. James, Paul Pfeffer & O. Zongo
NHS Lothian and University of Edinburgh, Edinburgh, UK
Gaunab Choudhury, S. Clohisey, Andrew Deans, J. Furniss, Ewen Harrison, S. Kelly & Aziz Sheikh
School of Cardiovascular Medicine and Sciences. King’s College London, London, UK
Phillip Chowienczyk
Lewisham and Greenwich NHS Trust, London, UK
Hywel Dda University Health Board, Haverfordwest, UK
S. Coetzee, Kim Davies, Rachel Ann Hughes, Ronda Loosley, Heather McGuinness, Abdelrahman Mohamed, Linda O’Brien, Zohra Omar, Emma Perkins, Janet Phipps, Gavin Ross, Abigail Taylor, Helen Tench & Rebecca Wolf-Roberts
NHS Tayside and University of Dundee, Dundee, UK
David Connell, C. Deas, Anne Elliott, J. George, S. Mohammed, J. Rowland, A. R. Solstice, Debbie Sutherland & Caroline Tee
Swansea Bay University Health Board, Port Talbot, UK
Lynda Connor, Amanda Cook, Gwyneth Davies, Tabitha Rees, Favas Thaivalappil & Caradog Thomas
Faculty of Medicine, Nursing and Health Sciences, School of Biomedical Sciences, Monash University, Melbourne, Victoria, Australia
Eamon Coughlan
Rotherham NHS Foundation Trust, Rotherham, UK
Alison Daniels, Anil Hormis, Julie Ingham & Lisa Zeidan
Salford Royal NHS Foundation Trust, Salford, UK
P. Dark, Nawar Diar-Bakerly, D. Evans, E. Hardy, Alice Harvey, D. Holgate, Sean Knight, N. Mairs, N. Majeed, L. McMorrow, J. Oxton, Jessica Pendlebury, C. Summersgill, R. Ugwuoke & S. Whittaker
Cwm Taf Morgannwg University Health Board, Mountain Ash, UK
Ellie Davies, Cerys Evenden, Alyson Hancock, Kia Hancock, Ceri Lynch, Meryl Rees, Lisa Roche, Natalie Stroud & T. Thomas-Woods
Borders General Hospital, NHS Borders, Melrose, UK
Joy Dawson, Hosni El-Taweel & Leanne Robinson
Aneurin Bevan University Health Board, Caerleon, UK
Amanda Dell, Sara Fairbairn, Nancy Hawkings, Jill Haworth, Michaela Hoare, Victoria Lewis, Alice Lucey, Georgia Mallison, Heeah Nassa, Chris Pennington, Andrea Price, Claire Price, Andrew Storrie, Gemma Willis & Susan Young
University of Exeter Medical School, Exeter, UK
London North West University Healthcare NHS Trust, London, UK
Shalin Diwanji, Sambasivarao Gurram, Padmasayee Papineni, Sheena Quaid, Gerlynn Tiongson & Ekaterina Watson
Alzheimer’s Research UK, Cambridge, UK
Hannah Dobson
Health and Care Research Wales, Cardiff, UK
Yvette Ellis
University of Bristol, Bristol, UK
Jonathon Evans
University of Sheffield, Sheffield, UK
L. Finnigan, Laura Saunders & James Wild
Great Western Hospital Foundation Trust, Swindon, UK
Eva Fraile & Jacinta Ugoji
Royal Devon and Exeter NHS Trust, Barnstaple, UK
Michael Gibbons
Kettering General Hospital NHS Trust, Kettering, UK
Anne-Marie Guerdette, Melanie Hewitt, R. Reddy, Katie Warwick & Sonia White
NIHR Leicester Biomedical Research Centre, Leicester, UK
Beatriz Guillen-Guio
University of Leeds, Leeds, UK
Elspeth Guthrie & Max Henderson
Royal Surrey NHS Foundation Trust, Cranleigh, UK
Mark Halling-Brown & Katherine McCullough
Chesterfield Royal Hospital NHS Trust, Calow, UK
Edward Harris & Claire Sampson
Long Covid Support, London, UK
Claire Hastie, Natalie Rogers & Nikki Smith
King’s College Hospital, NHS Foundation Trust and King’s College London, London, UK
Department of Oncology and Metabolism, University of Sheffield, Sheffield, UK
Simon Heller
NIHR Office for Clinical Research Infrastructure, London, UK
Katie Holmes
Asthma UK and British Lung Foundation Partnership, London, UK
Ian Jarrold & Samantha Walker
North Middlesex University Hospital NHS Trust, London, UK
Bhagy Jayaraman & Tessa Light
Action for Pulmonary Fibrosis, Peterborough, UK
Cardiff University, National Centre for Mental Health, Cardiff, UK
McPin Foundation, London, UK
Thomas Kabir
Roslin Institute, The University of Edinburgh, Edinburgh, UK
Steven Kerr
The Hillingdon Hospitals NHS Foundation Trust, London, UK
Samantha Kon, G. Landers, Harpreet Lota, Mariam Nasseri & Sofiya Portukhay
Queen Mary University of London, London, UK
Ania Korszun
Swansea University, Swansea Welsh Network, Hywel Dda University Health Board, Swansea, UK
Royal Infirmary of Edinburgh, NHS Lothian, Edinburgh, UK
Nazir I. Lone
Barts Heart Centre, London, UK
Barts Health NHS Trust and Queen Mary University of London, London, UK
Adrian Martineau
Salisbury NHS Foundation Trust, Salisbury, UK
Wadzanai Matimba-Mupaya & Sophia Strong-Sheldrake
University of Newcastle, Newcastle, UK
Hamish McAllister-Williams, Stella-Maria Paddick, Anthony Rostron & John Paul Taylor
Gateshead NHS Trust, Gateshead, UK
W. McCormick, Lorraine Pearce, S. Pugmire, Wendy Stoker & Ann Wilson
Manchester Centre for Clinical Neurosciences, Salford Royal NHS Foundation Trust, Manchester, UK
Katherine McIvor
Kidney Research UK, Peterborough, UK
Aisling McMahon
NHS Dumfries and Galloway, Dumfries, UK
Michael McMahon & Paula Neill
Swansea University, Swansea, UK
MQ Mental Health Research, London, UK
Lea Milligan
BHF Centre for Cardiovascular Science, Usher Institute of Population Health Sciences and Informatics, University of Edinburgh, Edinburgh, UK
Nicholas Mills
Shropshire Community Health NHS Trust, Shropshire, UK
Sharon Painter, Johanne Tomlinson & Louise Warburton
Somerset NHS Foundation Trust, Taunton, UK
Sue Palmer, Dawn Redwood, Jo Tilley, Carinna Vickers & Tania Wainwright
Francis Crick Institute, London, UK
Markus Ralser
Manchester University NHD Foundation Trust, Manchester, UK
Pilar Rivera-Ortega
Diabetes UK, University of Glasgow, Glasgow, UK
Elizabeth Robertson
Barnsley Hospital NHS Foundation Trust, Barnsley, UK
Amy Sanderson
MRC–University of Glasgow Centre for Virus Research, Glasgow, UK
Janet Scott
Diabetes UK, London, UK
Kamini Shah
British Heart Foundation Centre, King’s College London, London, UK
King’s College Hospital NHS Foundation Trust, London, UK
University Hospitals Birmingham NHS Foundation Trust and University of Birmingham, Birmingham, UK
Institute of Cardiovascular and Medical Sciences, BHF Glasgow Cardiovascular Research Centre, University of Glasgow, Glasgow, UK
University College London NHS Foundation Trust, London and Barts Health NHS Trust, London, UK
Northumbria University, Newcastle upon Tyne, UK
Ioannis Vogiatzis
Swansea University and Swansea Welsh Network, Swansea, UK
N. Williams
DUK | NHS Digital, Salford Royal Foundation Trust, Salford, UK
Queen Alexandra Hospital, Portsmouth, UK
- Kayode Adeniji
Princess Royal Hospital, Haywards Heath, UK
Daniel Agranoff & Chi Eziefula
Bassetlaw Hospital, Bassetlaw, UK
Darent Valley Hospital, Dartford, UK
Queen Elizabeth the Queen Mother Hospital, Margate, UK
Ana Alegria
School of Informatics, University of Edinburgh, Edinburgh, UK
Beatrice Alex, Benjamin Bach & James Scott-Brown
North East and North Cumbria Ingerated, Newcastle upon Tyne, UK
Section of Biomolecular Medicine, Division of Systems Medicine, Department of Metabolism, Digestion and Reproduction, Imperial College London, London, UK
Petros Andrikopoulos, Kanta Chechi, Marc-Emmanuel Dumas, Julian Griffin, Sonia Liggi & Zoltan Takats
Section of Genomic and Environmental Medicine, Respiratory Division, National Heart and Lung Institute, Imperial College London, London, UK
Petros Andrikopoulos, Marc-Emmanuel Dumas, Michael Olanipekun & Anthonia Osagie
John Radcliffe Hospital, Oxford, UK
Brian Angus
Royal Albert Edward Infirmary, Wigan, UK
Abdul Ashish
Manchester Royal Infirmary, Manchester, UK
Dougal Atkinson
MRC Human Genetics Unit, Institute of Genetics and Cancer, University of Edinburgh, Western General Hospital, Crewe Road, Edinburgh, UK
Section of Molecular Virology, Imperial College London, London, UK
Wendy S. Barclay
Furness General Hospital, Barrow-in-Furness, UK
Shahedal Bari
Hull University Teaching Hospital Trust, Kingston upon Hull, UK
Gavin Barlow
Hillingdon Hospital, Hillingdon, UK
Stella Barnass
St Thomas’ Hospital, London, UK
Nicholas Barrett
Coventry and Warwickshire, Coventry, UK
Christopher Bassford
St Michael’s Hospital, Bristol, UK
Sneha Basude
Stepping Hill Hospital, Stockport, UK
David Baxter
Royal Liverpool University Hospital, Liverpool, UK
Michael Beadsworth
Bristol Royal Hospital Children’s, Bristol, UK
Jolanta Bernatoniene
Scarborough Hospital, Scarborough, UK
John Berridge
Golden Jubilee National Hospital, Clydebank, UK
Colin Berry
Liverpool Heart and Chest Hospital, Liverpool, UK
Nicola Best
Centre for Inflammation Research, The Queen’s Medical Research Institute, University of Edinburgh, Edinburgh, UK
Debby Bogaert & Clark D. Russell
James Paget University Hospital, Great Yarmouth, UK
Pieter Bothma & Darell Tupper-Carey
Aberdeen Royal Infirmary, Aberdeen, UK
Robin Brittain-Long
Adamson Hospital, Cupar, UK
Naomi Bulteel
Royal Devon and Exeter Hospital, Exeter, UK
Worcestershire Royal Hospital, Worcester, UK
Andrew Burtenshaw
ISARIC Global Support Centre, Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Gail Carson, Laura Merson & Louise Sigfrid
Conquest Hospital, Hastings, UK
Vikki Caruth
The James Cook University Hospital, Middlesbrough, UK
David Chadwick
Dorset County Hospital, Dorchester, UK
Duncan Chambler
Antimicrobial Resistance and Hospital Acquired Infection Department, Public Health England, London, UK
Meera Chand
Department of Epidemiology and Biostatistics, School of Public Health, Faculty of Medicine, Imperial College London, London, UK
Kanta Chechi
Royal Bournemouth General Hospital, Bournemouth, UK
Harrogate Hospital, Harrogate, UK
Jenny Child
Royal Blackburn Teaching Hospital, Blackburn, UK
Srikanth Chukkambotla
Edinburgh Clinical Research Facility, University of Edinburgh, Edinburgh, UK
Richard Clark, Audrey Coutts, Lorna Donelly, Angie Fawkes, Tammy Gilchrist, Katarzyna Hafezi, Louise MacGillivray, Alan Maclean, Sarah McCafferty, Kirstie Morrice, Lee Murphy & Nicola Wrobel
Torbay Hospital, Torquay, UK
Northern General Hospital, Sheffield, UK
Paul Collini, Cariad Evans & Gary Mills
Liverpool Clinical Trials Centre, University of Liverpool, Liverpool, UK
Marie Connor, Jo Dalton, Chloe Donohue, Carrol Gamble, Michelle Girvan, Sophie Halpin, Janet Harrison, Clare Jackson, Laura Marsh, Stephanie Roberts & Egle Saviciute
Department of Infectious Disease, Imperial College London, London, UK
Graham S. Cooke & Shiranee Sriskandan
St Georges Hospital (Tooting), London, UK
Catherine Cosgrove
Blackpool Victoria Hospital, Blackpool, UK
Jason Cupitt & Joanne Howard
The Royal London Hospital, London, UK
Maria-Teresa Cutino-Moguel
MRC-University of Glasgow Centre for Virus Research, Glasgow, UK
Ana da Silva Filipe, Antonia Y. W. Ho, Sarah E. McDonald, Massimo Palmarini, David L. Robertson, Janet T. Scott & Emma C. Thomson
Salford Royal Hospital, Salford, UK
University Hospital of North Durham, Durham, UK
Chris Dawson
Norfolk and Norwich University Hospital, Norwich, UK
Samir Dervisevic
Intensive Care Unit, Royal Infirmary Edinburgh, Edinburgh, UK
Annemarie B. Docherty & Seán Keating
Institute of Infection, Veterinary and Ecological Sciences, Faculty of Health and Life Sciences, University of Liverpool, Liverpool, UK
Cara Donegan & Rebecca G. Spencer
Salisbury District Hospital, Salisbury, UK
Phil Donnison
National Phenome Centre, Department of Metabolism, Digestion and Reproduction, Imperial College London, London, UK
Gonçalo dos Santos Correia, Matthew Lewis, Lynn Maslen, Caroline Sands, Zoltan Takats & Panteleimon Takis
Section of Bioanalytical Chemistry, Department of Metabolism, Digestion and Reproduction, Imperial College London, London, UK
Gonçalo dos Santos Correia, Matthew Lewis, Lynn Maslen, Caroline Sands & Panteleimon Takis
Guy’s and St Thomas’, NHS Foundation Trust, London, UK
Sam Douthwaite, Michael MacMahon, Marlies Ostermann & Manu Shankar-Hari
The Royal Oldham Hospital, Oldham, UK
Andrew Drummond
European Genomic Institute for Diabetes, Institut Pasteur de Lille, Lille University Hospital, University of Lille, Lille, France
Marc-Emmanuel Dumas
McGill University and Genome Quebec Innovation Centre, Montreal, Qeubec, Canada
National Infection Service, Public Health England, London, UK
Jake Dunning & Maria Zambon
Hereford Count Hospital, Hereford, UK
Ingrid DuRand
Southampton General Hospital, Southampton, UK
Ahilanadan Dushianthan
Northampton General Hospital, Northampton, UK
Tristan Dyer
University Hospital of Wales, Cardiff, UK
Chrisopher Fegan
University Hospitals Bristol NHS Foundation Trust, Bristol, UK
Liverpool School of Tropical Medicine, Liverpool, UK
Tom Fletcher
Leighton Hospital, Crewe, UK
Duncan Fullerton & Elijah Matovu
Manor Hospital, Walsall, UK
Scunthorpe Hospital, Scunthorpe, UK
Sanjeev Garg
Cambridge University Hospital, Cambridge, UK
Effrossyni Gkrania-Klotsas
West Suffolk NHS Foundation Trust, Bury St Edmunds, UK
Basingstoke and North Hampshire Hospital, Basingstoke, UK
Arthur Goldsmith
North Cumberland Infirmary, Carlisle, UK
Clive Graham
Paediatric Liver, GI and Nutrition Centre and MowatLabs, King’s College Hospital, London, UK
Tassos Grammatikopoulos
Institute of Liver Studies, King’s College London, London, UK
Institute of Microbiology and Infection, University of Birmingham, Birmingham, UK
Christopher A. Green
Department of Molecular and Clinical Cancer Medicine, University of Liverpool, Liverpool, UK
William Greenhalf
Institute for Global Health, University College London, London, UK
Rishi K. Gupta
NIHR Health Protection Research Unit, Institute of Infection, Veterinary and Ecological Sciences, Faculty of Health and Life Sciences, University of Liverpool, Liverpool, UK
Hayley Hardwick, Malcolm G. Semple, Tom Solomon & Lance C. W. Turtle
Warwick Hospital, Warwick, UK
Elaine Hardy
Birmingham Children’s Hospital, Birmingham, UK
Stuart Hartshorn
Nottingham City Hospital, Nottingham, UK
Daniel Harvey
Glangwili Hospital Child Health Section, Carmarthen, UK
Peter Havalda
Alder Hey Children’s Hospital, Liverpool, UK
Daniel B. Hawcutt
Department of Infectious Diseases, Queen Elizabeth University Hospital, Glasgow, UK
Antonia Y. W. Ho
Bronglais General Hospital, Aberystwyth, UK
Maria Hobrok
Worthing Hospital, Worthing, UK
Luke Hodgson
Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Peter W. Horby
Rotheram District General Hospital, Rotheram, UK
Anil Hormis
Virology Reference Department, National Infection Service, Public Health England, Colindale Avenue, London, UK
Samreen Ijaz
Royal Free Hospital, London, UK
Michael Jacobs & Padmasayee Papineni
Homerton Hospital, London, UK
Airedale Hospital, Airedale, UK
Paul Jennings
Basildon Hospital, Basildon, UK
Agilan Kaliappan
The Christie NHS Foundation Trust, Manchester, UK
Vidya Kasipandian
University Hospital Lewisham, London, UK
Stephen Kegg
The Whittington Hospital, London, UK
Michael Kelsey
Southmead Hospital, Bristol, UK
Jason Kendall
Sheffield Childrens Hospital, Sheffield, UK
Caroline Kerrison
Royal United Hospital, Bath, UK
Ian Kerslake
Department of Pharmacology, University of Liverpool, Liverpool, UK
Nuffield Department of Medicine, Peter Medawar Building for Pathogen Research, University of Oxford, Oxford, UK
Paul Klenerman
Translational Gastroenterology Unit, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Public Health Scotland, Edinburgh, UK
Susan Knight, Eva Lahnsteiner & Sarah Tait
Western General Hospital, Edinburgh, UK
Oliver Koch
Southend University Hospital NHS Foundation Trust, Southend-on-Sea, UK
Gouri Koduri
Hinchingbrooke Hospital, Huntingdon, UK
George Koshy & Tamas Leiner
Royal Preston Hospital, Fulwood, UK
Shondipon Laha
University Hospital (Coventry), Coventry, UK
Steven Laird
The Walton Centre, Liverpool, UK
Susan Larkin
ISARIC, Global Support Centre, COVID-19 Clinical Research Resources, Epidemic diseases Research Group, Oxford (ERGO), University of Oxford, Oxford, UK
James Lee & Daniel Plotkin
Centre for Health Informatics, Division of Informatics, Imaging and Data Science, School of Health Sciences, Faculty of Biology, Medicine and Health, University of Manchester, Manchester Academic Health Science Centre, Manchester, UK
Gary Leeming
Hull Royal Infirmary, Hull, UK
Patrick Lillie
Nottingham University Hospitals NHS Trust:, Nottingham, UK
Wei Shen Lim
Darlington Memorial Hospital, Darlington, UK
Queen Elizabeth Hospital (Gateshead), Gateshead, UK
Vanessa Linnett
Warrington Hospital, Warrington, UK
Jeff Little
Bristol Royal Hospital for Children, Bristol, UK
Mark Lyttle
St Mary’s Hospital (Isle of Wight), Isle of Wight, UK
Emily MacNaughton
The Tunbridge Wells Hospital, Royal Tunbridge Wells, UK
Ravish Mankregod
Huddersfield Royal, Huddersfield, UK
Countess of Chester Hospital, Liverpool, UK
Ruth McEwen & Lawrence Wilson
Frimley Park Hospital, Frimley, UK
Manjula Meda
Nuffield Department of Medicine, John Radcliffe Hospital, Oxford, UK
Alexander J. Mentzer
Department of Microbiology/Infectious Diseases, Oxford University Hospitals NHS Foundation Trust, John Radcliffe Hospital, Oxford, UK
MRC Human Genetics Unit, MRC Institute of Genetics and Molecular Medicine, University of Edinburgh, Edinburgh, UK
Alison M. Meynert & Murray Wham
St James University Hospital, Leeds, UK
Jane Minton
Arrowe Park Hospital, Birkenhead, UK
Kavya Mohandas
Great Ormond Street Hospital, London, UK
Royal Shrewsbury Hospital, Shrewsbury, UK
Addenbrookes Hospital, Cambridge, UK
Elinoor Moore
Institute of Infection, Veterinary and Ecological Sciences, University of Liverpool, Liverpool, UK
Shona C. Moore, William A. Paxton & Georgios Pollakis
East Surrey Hospital (Redhill), Redhill, UK
Patrick Morgan
Burton Hospital, Burton, UK
Craig Morris & Tim Reynolds
Peterborough City Hospital, Peterborough, UK
Katherine Mortimore
Kent and Canterbury Hospital, Canterbury, UK
Samuel Moses
Weston Area General Trust, Bristol, UK
Mbiye Mpenge
Bedfordshire Hospital, Bedfordshire, UK
Rohinton Mulla
Glasgow Royal Infirmary, Glasgow, UK
Michael Murphy
Macclesfield General Hospital, Macclesfield, UK
Thapas Nagarajan
Derbyshire Healthcare, Derbyshire, UK
Megan Nagel
Chelsea and Westminster Hospital, London, UK
Mark Nelson & Matthew K. O’Shea
Watford General Hospital, Watford, UK
Lillian Norris & Tom Stambach
EPCC, University of Edinburgh, Edinburgh, UK
Lucy Norris
Section of Biomolecular Medicine, Division of Systems Medicine, Department of Metabolism, Digestion and Reproduction, London, UK
Michael Olanipekun
Imperial College Healthcare NHS Trust: London, London, UK
Peter J. M. Openshaw
Division of Systems Medicine, Department of Metabolism, Digestion and Reproduction, Imperial College London, London, UK
Anthonia Osagie
Prince Philip Hospital, Llanelli, UK
Igor Otahal & Andrew Workman
George Eliot Hospital – Acute Services, Nuneaton, UK
Molecular and Clinical Cancer Medicine, Institute of Systems, Molecular and Integrative Biology, University of Liverpool, Liverpool, UK
Carlo Palmieri
Clatterbridge Cancer Centre NHS Foundation Trust, Liverpool, UK
Kettering General Hospital, Kettering, UK
Selva Panchatsharam
University Hospitals of North Midlands NHS Trust, North Midlands, UK
Danai Papakonstantinou
Russells Hall Hospital, Dudley, UK
Hassan Paraiso
Harefield Hospital, Harefield, UK
Lister Hospital, Lister, UK
Natalie Pattison
Musgrove Park Hospital, Taunton, UK
Justin Pepperell
Kingston Hospital, Kingston, UK
Mark Peters
Queen’s Hospital, Romford, UK
Mandeep Phull
Southport and Formby District General Hospital, Southport, UK
Stefania Pintus
St George’s University of London, London, UK
Tim Planche
King’s College Hospital (Denmark Hill), London, UK
Centre for Clinical Infection and Diagnostics Research, Department of Infectious Diseases, School of Immunology and Microbial Sciences, King’s College London, London, UK
Nicholas Price
Department of Infectious Diseases, Guy’s and St Thomas’ NHS Foundation Trust, London, UK
The Clatterbridge Cancer Centre NHS Foundation, Bebington, UK
David Price
The Great Western Hospital, Swindon, UK
Rachel Prout
Ninewells Hospital, Dundee, UK
Nikolas Rae
Institute of Evolutionary Biology, University of Edinburgh, Edinburgh, UK
Andrew Rambaut
Poole Hospital NHS Trust, Poole, UK
Henrik Reschreiter
William Harvey Hospital, Ashford, UK
Neil Richardson
King’s Mill Hospital, Sutton-in-Ashfield, UK
Mark Roberts
Liverpool Women’s Hospital, Liverpool, UK
Devender Roberts
Pinderfields Hospital, Wakefield, UK
Alistair Rose
North Devon District Hospital, Barnstaple, UK
Guy Rousseau
Queen Elizabeth Hospital, Birmingham, UK
Tameside General Hospital, Ashton-under-Lyne, UK
Brendan Ryan
City Hospital (Birmingham), Birmingham, UK
Taranprit Saluja
Department of Pediatrics and Virology, St Mary’s Medical School Bldg, Imperial College London, London, UK
Vanessa Sancho-Shimizu
The Newcastle Upon Tyne Hospitals NHS Foundation Trust, Newcastle Upon Tyne, UK
Matthias Schmid
NHS Greater Glasgow and Clyde, Glasgow, UK
Janet T. Scott
Respiratory Medicine, Institute in The Park, University of Liverpool, Alder Hey Children’s Hospital, Liverpool, UK
Malcolm G. Semple
Broomfield Hospital, Broomfield, UK
Stoke Mandeville, UK
Prad Shanmuga
University Hospital of North Tees, Stockton-on-Tees, UK
Anil Sharma
Institute of Translational Medicine, University of, Liverpool, Merseyside, UK
Victoria E. Shaw
Royal Manchester Children’s Hospital, Manchester, UK
Anna Shawcross
New Cross Hospital, Wolverhampton, UK
Jagtur Singh Pooni
Bedford Hospital, Bedford, UK
Jeremy Sizer
Colchester General Hospital, Colchester, UK
Richard Smith
University Hospital Birmingham NHS Foundation Trust, Birmingham, UK
Catherine Snelson & Tony Whitehouse
Walton Centre NHS Foundation Trust, Liverpool, UK
Tom Solomon
Chesterfield Royal Hospital, Calow, UK
Nick Spittle
MRC Centre for Molecular Bacteriology and Infection, Imperial College London, London, UK
Shiranee Sriskandan
Princess Alexandra Hospital, Harlow, UK
Nikki Staines & Shico Visuvanathan
Milton Keynes Hospital, Eaglestone, UK
Richard Stewart
Division of Structural Biology, The Wellcome Centre for Human Genetics, University of Oxford, Oxford, UK
David Stuart
Royal Bolton Hopital, Farnworth, UK
Pradeep Subudhi
Department of Medicine, University of Cambridge, Cambridge, UK
Charlotte Summers
Department of Child Life and Health, University of Edinburgh, Edinburgh, UK
Olivia V. Swann
Royal Gwent (Newport), Newport, UK
Tamas Szakmany
The Royal Marsden Hospital (London), London, UK
Kate Tatham
Blood Borne Virus Unit, Virus Reference Department, National Infection Service, Public Health England, London, UK
Richard S. Tedder
Transfusion Microbiology, National Health Service Blood and Transplant, London, UK
Department of Medicine, Imperial College London, London, UK
Queen Victoria Hospital (East Grinstead), East Grinstead, UK
Leeds Teaching Hospitals NHS Trust, Leeds, UK
Robert Thompson
Royal Stoke University Hospital, Stoke-on-Trent, UK
Chris Thompson
Whiston Hospital, Rainhill, UK
Ascanio Tridente
Tropical and Infectious Disease Unit, Royal Liverpool University Hospital, Liverpool, UK
Lance C. W. Turtle
Croydon University Hospital, Thornton Heath, UK
Mary Twagira
Gloucester Royal, Gloucester, UK
Nick Vallotton
West Hertfordshire Teaching Hospitals NHS Trust, Hertfordshire, UK
Rama Vancheeswaran
North Middlesex Hospital, London, UK
Rachel Vincent
Medway Maritime Hospital, Gillingham, UK
Lisa Vincent-Smith
Royal Papworth Hospital Everard, Cambridge, UK
Alan Vuylsteke
Derriford (Plymouth), Plymouth, UK
St Helier Hospital, Sutton, UK
Rachel Wake
Royal Berkshire Hospital, Reading, UK
Andrew Walden
Royal Liverpool Hospital, Liverpool, UK
Ingeborg Welters
Bradford Royal infirmary, Bradford, UK
Paul Whittaker
Central Middlesex, London, UK
Ashley Whittington
Royal Cornwall Hospital (Tresliske), Truro, UK
Meme Wijesinghe
North Bristol NHS Trust, Bristol, UK
Martin Williams
St. Peter’s Hospital, Runnymede, UK
Stephen Winchester
Leicester Royal Infirmary, Leicester, UK
Martin Wiselka
Grantham and District Hospital, Grantham, UK
Adam Wolverson
Aintree University Hospital, Liverpool, UK
Daniel G. Wootton
North Tyneside General Hospital, North Shields, UK
Bryan Yates
Queen Elizabeth Hospital, King’s Lynn, UK
Peter Young
You can also search for this author in PubMed Google Scholar
PHOSP-COVID collaborative group
- Kathryn Abel
- , H. Adamali
- , Davies Adeloye
- , Oluwaseun Adeyemi
- , Rita Adrego
- , Laura Aguilar Jimenez
- , Shanaz Ahmad
- , N. Ahmad Haider
- , Rubina Ahmed
- , Nyarko Ahwireng
- , Mark Ainsworth
- , Asma Alamoudi
- , Mariam Ali
- , M. Aljaroof
- , Louise Allan
- , Richard Allen
- , Lisa Allerton
- , Lynne Allsop
- , Ann Marie Allt
- , Paula Almeida
- , Bashar Al-Sheklly
- , Danny Altmann
- , Maria Alvarez Corral
- , Shannon Amoils
- , David Anderson
- , Charalambos Antoniades
- , Gill Arbane
- , Ava Maria Arias
- , Cherie Armour
- , Lisa Armstrong
- , Natalie Armstrong
- , David Arnold
- , H. Arnold
- , A. Ashish
- , Andrew Ashworth
- , M. Ashworth
- , Shahab Aslani
- , Hosanna Assefa-Kebede
- , Paul Atkin
- , Catherine Atkin
- , Raminder Aul
- , Hnin Aung
- , Liam Austin
- , Cristina Avram
- , Nikos Avramidis
- , Marta Babores
- , Rhiannon Baggott
- , J. Bagshaw
- , David Baguley
- , Elisabeth Bailey
- , J. Kenneth Baillie
- , Steve Bain
- , Majda Bakali
- , E. Baldry
- , Molly Baldwin
- , David Baldwin
- , Clive Ballard
- , Amita Banerjee
- , Dongchun Bang
- , R. E. Barker
- , Laura Barman
- , Perdita Barran
- , Shaney Barratt
- , Fiona Barrett
- , Donna Basire
- , Neil Basu
- , Michelle Bates
- , R. Batterham
- , Helen Baxendale
- , Gabrielle Baxter
- , Hannah Bayes
- , M. Beadsworth
- , Paul Beckett
- , Paul Beirne
- , Murdina Bell
- , Robert Bell
- , Kaytie Bennett
- , Eva Beranova
- , Areti Bermperi
- , Anthony Berridge
- , Colin Berry
- , Sarah Betts
- , Emily Bevan
- , Kamaldeep Bhui
- , Michelle Bingham
- , K. Birchall
- , Lettie Bishop
- , Karen Bisnauthsing
- , John Blaikely
- , Angela Bloss
- , Annette Bolger
- , Charlotte Bolton
- , J. Bonnington
- , A. Botkai
- , Charlotte Bourne
- , Michelle Bourne
- , Kate Bramham
- , Lucy Brear
- , Jonathon Breeze
- , Katie Breeze
- , Andrew Briggs
- , E. Bright
- , Christopher Brightling
- , Simon Brill
- , K. Brindle
- , Lauren Broad
- , Andrew Broadley
- , Claire Brookes
- , Mattew Broome
- , Vanessa Brown
- , Ammani Brown
- , Angela Brown
- , Jeremy Brown
- , Terry Brugha
- , Nigel Brunskill
- , Phil Buckley
- , Anda Bularga
- , Ed Bullmore
- , Jenny Bunker
- , L. Burden
- , Tracy Burdett
- , David Burn
- , John Busby
- , Robyn Butcher
- , Al-Tahoor Butt
- , P. Cairns
- , P. C. Calder
- , Ellen Calvelo
- , H. Carborn
- , Bethany Card
- , Caitlin Carr
- , Liesel Carr
- , G. Carson
- , Penny Carter
- , Anna Casey
- , M. Cassar
- , Jonathon Cavanagh
- , Manish Chablani
- , Trudie Chalder
- , James D. Chalmers
- , Rachel Chambers
- , Flora Chan
- , K. M. Channon
- , Kerry Chapman
- , Amanda Charalambou
- , N. Chaudhuri
- , A. Checkley
- , Yutung Cheng
- , Luke Chetham
- , Caroline Childs
- , Edwin Chilvers
- , H. Chinoy
- , A. Chiribiri
- , K. Chong-James
- , N. Choudhury
- , Gaunab Choudhury
- , Phillip Chowienczyk
- , C. Christie
- , Melanie Chrystal
- , Cameron Clark
- , David Clark
- , Jude Clarke
- , S. Clohisey
- , G. Coakley
- , Zach Coburn
- , S. Coetzee
- , Joby Cole
- , Chris Coleman
- , Florence Conneh
- , David Connell
- , Bronwen Connolly
- , Lynda Connor
- , Amanda Cook
- , Shirley Cooper
- , B. Cooper
- , Josh Cooper
- , Donna Copeland
- , Tracey Cosier
- , Eamon Coughlan
- , Martina Coulding
- , C. Coupland
- , Thelma Craig
- , Daniele Cristiano
- , Michael Crooks
- , Andy Cross
- , Isabel Cruz
- , P. Cullinan
- , D. Cuthbertson
- , Luke Daines
- , Matthhew Dalton
- , Patrick Daly
- , Alison Daniels
- , Joanne Dasgin
- , Anthony David
- , Ffyon Davies
- , Ellie Davies
- , Kim Davies
- , Gareth Davies
- , Gwyneth Davies
- , Melanie Davies
- , Joy Dawson
- , Camilla Dawson
- , Enya Daynes
- , Anthony De Soyza
- , Bill Deakin
- , Andrew Deans
- , Joanne Deery
- , Sylviane Defres
- , Amanda Dell
- , K. Dempsey
- , Emma Denneny
- , J. Dennis
- , Ruvini Dharmagunawardena
- , Nawar Diar-Bakerly
- , Caroline Dickens
- , A. Dipper
- , Sarah Diver
- , Shalin Diwanji
- , Myles Dixon
- , R. Djukanovic
- , Hannah Dobson
- , S. L. Dobson
- , Annemarie B. Docherty
- , A. Donaldson
- , N. Dormand
- , Andrew Dougherty
- , Rachael Dowling
- , Stephen Drain
- , Katharine Draxlbauer
- , Katie Drury
- , Pearl Dulawan
- , A. Dunleavy
- , Sarah Dunn
- , Catherine Dupont
- , Joanne Earley
- , Nicholas Easom
- , Carlos Echevarria
- , Sarah Edwards
- , C. Edwardson
- , Claudia Efstathiou
- , Anne Elliott
- , K. Elliott
- , Yvette Ellis
- , Anne Elmer
- , Omer Elneima
- , Hosni El-Taweel
- , Teriann Evans
- , Ranuromanana Evans
- , Rachael A. Evans
- , Jonathon Evans
- , Cerys Evenden
- , Lynsey Evison
- , Laura Fabbri
- , Sara Fairbairn
- , Alexandra Fairman
- , K. Fallon
- , David Faluyi
- , Clair Favager
- , Tamanah Fayzan
- , James Featherstone
- , T. Felton
- , V. Ferreira
- , Selina Finney
- , J. Finnigan
- , L. Finnigan
- , Helen Fisher
- , S. Fletcher
- , Rachel Flockton
- , Margaret Flynn
- , David Foote
- , Amber Ford
- , D. Forton
- , Eva Fraile
- , C. Francis
- , Richard Francis
- , Susan Francis
- , Anew Frankel
- , Emily Fraser
- , N. French
- , Jonathon Fuld
- , J. Furniss
- , Lucie Garner
- , N. Gautam
- , John Geddes
- , J. George
- , P. George
- , Michael Gibbons
- , Rhyan Gill
- , Mandy Gill
- , L. Gilmour
- , F. Gleeson
- , Jodie Glossop
- , Sarah Glover
- , Nicola Goodman
- , Camelia Goodwin
- , Bibek Gooptu
- , Hussain Gordon
- , T. Gorsuch
- , M. Greatorex
- , Paul Greenhaff
- , William Greenhalf
- , Alan Greenhalgh
- , Neil J. Greening
- , John Greenwood
- , Rebecca Gregory
- , Heidi Gregory
- , D. Grieve
- , Denise Griffin
- , L. Griffiths
- , Anne-Marie Guerdette
- , Beatriz Guillen-Guio
- , Mahitha Gummadi
- , Ayushman Gupta
- , Sambasivarao Gurram
- , Elspeth Guthrie
- , Kate Hadley
- , Ahmed Haggar
- , Kera Hainey
- , Brigid Hairsine
- , Pranab Haldar
- , Lucy Hall
- , Mark Halling-Brown
- , Alyson Hancock
- , Kia Hancock
- , Neil Hanley
- , Sulaimaan Haq
- , Hayley Hardwick
- , Tim Hardy
- , Beverley Hargadon
- , Kate Harrington
- , Edward Harris
- , Victoria C. Harris
- , Ewen Harrison
- , Paul Harrison
- , Nicholas Hart
- , Alice Harvey
- , Matt Harvey
- , M. Harvie
- , L. Haslam
- , Claire Hastie
- , May Havinden-Williams
- , Jenny Hawkes
- , Nancy Hawkings
- , Jill Haworth
- , A. Hayday
- , Matthew Haynes
- , J. Hazeldine
- , Tracy Hazelton
- , Liam Heaney
- , Cheryl Heeley
- , Jonathon Heeney
- , M. Heightman
- , Simon Heller
- , Max Henderson
- , Helen Henson
- , L. Hesselden
- , Melanie Hewitt
- , Victoria Highett
- , T. Hillman
- , Ling-Pei Ho
- , Michaela Hoare
- , Amy Hoare
- , J. Hockridge
- , Philip Hogarth
- , Ailsa Holbourn
- , Sophie Holden
- , L. Holdsworth
- , D. Holgate
- , Maureen Holland
- , Leah Holloway
- , Katie Holmes
- , Megan Holmes
- , B. Holroyd-Hind
- , Anil Hormis
- , Alexander Horsley
- , Akram Hosseini
- , M. Hotopf
- , Linzy Houchen-Wolloff
- , Luke S. Howard
- , Kate Howard
- , Alice Howell
- , E. Hufton
- , Rachel Ann Hughes
- , Joan Hughes
- , Alun Hughes
- , Amy Humphries
- , Nathan Huneke
- , E. Hurditch
- , John Hurst
- , Masud Husain
- , Tracy Hussell
- , John Hutchinson
- , W. Ibrahim
- , Julie Ingham
- , L. Ingram
- , Diana Ionita
- , Karen Isaacs
- , Khalida Ismail
- , T. Jackson
- , Joseph Jacob
- , W. Y. James
- , Claire Jarman
- , Ian Jarrold
- , Hannah Jarvis
- , Roman Jastrub
- , Bhagy Jayaraman
- , Gisli Jenkins
- , P. Jezzard
- , Kasim Jiwa
- , C. Johnson
- , Simon Johnson
- , Desmond Johnston
- , Caroline Jolley
- , Ian Jones
- , Heather Jones
- , Mark Jones
- , Don Jones
- , Sherly Jose
- , Thomas Kabir
- , G. Kaltsakas
- , Vicky Kamwa
- , N. Kanellakis
- , Sabina Kaprowska
- , Zunaira Kausar
- , Natalie Keenan
- , Steven Kerr
- , Helen Kerslake
- , Angela Key
- , Fasih Khan
- , Kamlesh Khunti
- , Susan Kilroy
- , Bernie King
- , Clara King
- , Lucy Kingham
- , Jill Kirk
- , Paaig Kitterick
- , Paul Klenerman
- , Lucy Knibbs
- , Sean Knight
- , Abigail Knighton
- , Onn Min Kon
- , Samantha Kon
- , Ania Korszun
- , Ivan Koychev
- , Claire Kurasz
- , Prathiba Kurupati
- , Hanan Lamlum
- , G. Landers
- , Claudia Langenberg
- , Lara Lavelle-Langham
- , Allan Lawrie
- , Cathy Lawson
- , Claire Lawson
- , Alison Layton
- , Olivia C. Leavy
- , Ju Hee Lee
- , Elvina Lee
- , Karen Leitch
- , Rebecca Lenagh
- , Victoria Lewis
- , Joanne Lewis
- , Keir Lewis
- , N. Lewis-Burke
- , Felicity Liew
- , Tessa Light
- , Liz Lightstone
- , W. Lilaonitkul
- , S. Linford
- , Anne Lingford-Hughes
- , M. Lipman
- , Kamal Liyanage
- , Arwel Lloyd
- , Nazir I. Lone
- , Ronda Loosley
- , Janet Lord
- , Harpreet Lota
- , Wayne Lovegrove
- , Daniel Lozano-Rojas
- , Alice Lucey
- , Gardiner Lucy
- , E. Lukaschuk
- , Alison Lye
- , Ceri Lynch
- , S. MacDonald
- , G. MacGowan
- , Irene Macharia
- , J. Mackie
- , L. Macliver
- , S. Madathil
- , Gladys Madzamba
- , Nick Magee
- , Murphy Magtoto
- , N. Majeed
- , Flora Malein
- , Georgia Mallison
- , William Man
- , S. Mandal
- , K. Mangion
- , C. Manisty
- , R. Manley
- , Katherine March
- , Stefan Marciniak
- , Philip Marino
- , Myril Mariveles
- , Michael Marks
- , Elizabeth Marouzet
- , Sophie Marsh
- , M. Marshall
- , B. Marshall
- , Jane Martin
- , Adrian Martineau
- , L. M. Martinez
- , Nick Maskell
- , Darwin Matila
- , Wadzanai Matimba-Mupaya
- , Laura Matthews
- , Angeline Mbuyisa
- , Steve McAdoo
- , Hamish McAllister-Williams
- , Paul McArdle
- , Anne McArdle
- , Danny McAulay
- , Hamish J. C. McAuley
- , Gerry McCann
- , W. McCormick
- , Jacqueline McCormick
- , P. McCourt
- , Celeste McCracken
- , Lorcan McGarvey
- , Jade McGinness
- , K. McGlynn
- , Andrew McGovern
- , Heather McGuinness
- , I. B. McInnes
- , Jerome McIntosh
- , Emma McIvor
- , Katherine McIvor
- , Laura McLeavey
- , Aisling McMahon
- , Michael McMahon
- , L. McMorrow
- , Teresa Mcnally
- , M. McNarry
- , J. McNeill
- , Alison McQueen
- , H. McShane
- , Chloe Mears
- , Clare Megson
- , Sharon Megson
- , J. Meiring
- , Lucy Melling
- , Mark Mencias
- , Daniel Menzies
- , Marta Merida Morillas
- , Alice Michael
- , Benedict Michael
- , C. A. Miller
- , Lea Milligan
- , Nicholas Mills
- , Clare Mills
- , George Mills
- , L. Milner
- , Jane Mitchell
- , Abdelrahman Mohamed
- , Noura Mohamed
- , S. Mohammed
- , Philip Molyneaux
- , Will Monteiro
- , Silvia Moriera
- , Anna Morley
- , Leigh Morrison
- , Richard Morriss
- , A. Morrow
- , Paul Moss
- , Alistair Moss
- , K. Motohashi
- , N. Msimanga
- , Elizabeta Mukaetova-Ladinska
- , Unber Munawar
- , Jennifer Murira
- , Uttam Nanda
- , Heeah Nassa
- , Mariam Nasseri
- , Rashmita Nathu
- , Aoife Neal
- , Robert Needham
- , Paula Neill
- , Stefan Neubauer
- , D. E. Newby
- , Helen Newell
- , J. Newman
- , Tom Newman
- , Alex Newton-Cox
- , T. E. Nichols
- , Tim Nicholson
- , Christos Nicolaou
- , Debby Nicoll
- , Athanasios Nikolaidis
- , C. Nikolaidou
- , C. M. Nolan
- , Matthew Noonan
- , C. Norman
- , Petr Novotny
- , Kimon Ntotsis
- , Jose Nunag
- , Lorenza Nwafor
- , Uchechi Nwanguma
- , Joseph Nyaboko
- , Linda O’Brien
- , C. O’Brien
- , Natasha Odell
- , Kate O’Donnell
- , Godwin Ogbole
- , Olaoluwa Olaosebikan
- , Catherine Oliver
- , Zohra Omar
- , Peter J. M. Openshaw
- , D. P. O’Regan
- , Lorna Orriss-Dib
- , Lynn Osborne
- , Rebecca Osbourne
- , Marlies Ostermann
- , Charlotte Overton
- , Jamie Pack
- , Edmund Pacpaco
- , Stella-Maria Paddick
- , Sharon Painter
- , Erola Pairo-Castineira
- , Ashkan Pakzad
- , Sue Palmer
- , Padmasayee Papineni
- , K. Paques
- , Kerry Paradowski
- , Manish Pareek
- , Dhruv Parekh
- , H. Parfrey
- , Carmen Pariante
- , S. Parker
- , M. Parkes
- , J. Parmar
- , Sheetal Patale
- , Manish Patel
- , Suhani Patel
- , Dibya Pattenadk
- , M. Pavlides
- , Sheila Payne
- , Lorraine Pearce
- , John Pearl
- , Dan Peckham
- , Jessica Pendlebury
- , Yanchun Peng
- , Chris Pennington
- , Ida Peralta
- , Emma Perkins
- , Z. Peterkin
- , Tunde Peto
- , Nayia Petousi
- , John Petrie
- , Paul Pfeffer
- , Janet Phipps
- , S. Piechnik
- , John Pimm
- , Karen Piper Hanley
- , Riinu Pius
- , Hannah Plant
- , Tatiana Plekhanova
- , Megan Plowright
- , Krisnah Poinasamy
- , Oliver Polgar
- , Julie Porter
- , Joanna Porter
- , Sofiya Portukhay
- , Natassia Powell
- , A. Prabhu
- , James Pratt
- , Andrea Price
- , Claire Price
- , Carly Price
- , Anne Prickett
- , I. Propescu
- , J. Propescu
- , Sabrina Prosper
- , S. Pugmire
- , Sheena Quaid
- , Jackie Quigley
- , Jennifer K. Quint
- , H. Qureshi
- , I. N. Qureshi
- , K. Radhakrishnan
- , Najib Rahman
- , Markus Ralser
- , Betty Raman
- , Hazel Ramos
- , Albert Ramos
- , Jade Rangeley
- , Bojidar Rangelov
- , Liz Ratcliffe
- , Phillip Ravencroft
- , Konrad Rawlik
- , Anne Reddington
- , Heidi Redfearn
- , Dawn Redwood
- , Annabel Reed
- , Meryl Rees
- , Tabitha Rees
- , Karen Regan
- , Will Reynolds
- , Carla Ribeiro
- , A. Richards
- , Emma Richardson
- , M. Richardson
- , Pilar Rivera-Ortega
- , K. Roberts
- , Elizabeth Robertson
- , Leanne Robinson
- , Emma Robinson
- , Lisa Roche
- , C. Roddis
- , J. Rodger
- , Natalie Rogers
- , Gavin Ross
- , Alexandra Ross
- , Jennifer Rossdale
- , Anthony Rostron
- , Anna Rowe
- , J. Rowland
- , M. J. Rowland
- , A. Rowland
- , Sarah L. Rowland-Jones
- , Maura Roy
- , Igor Rudan
- , Richard Russell
- , Emily Russell
- , Gwen Saalmink
- , Ramsey Sabit
- , Beth Sage
- , T. Samakomva
- , Nilesh Samani
- , A. A. Samat
- , Claire Sampson
- , Katherine Samuel
- , Reena Samuel
- , Z. B. Sanders
- , Amy Sanderson
- , Elizabeth Sapey
- , Dinesh Saralaya
- , Jack Sargant
- , Carol Sarginson
- , Naveed Sattar
- , Kathryn Saunders
- , Peter Saunders
- , Ruth Saunders
- , Laura Saunders
- , Heather Savill
- , Avan Sayer
- , J. Schronce
- , William Schwaeble
- , Janet Scott
- , Kathryn Scott
- , Nick Selby
- , Malcolm G. Semple
- , Marco Sereno
- , Terri Ann Sewell
- , Kamini Shah
- , Ajay Shah
- , Manu Shankar-Hari
- , M. Sharma
- , Claire Sharpe
- , Michael Sharpe
- , Sharlene Shashaa
- , Alison Shaw
- , Victoria Shaw
- , Karen Shaw
- , Aziz Sheikh
- , Sarah Shelton
- , Liz Shenton
- , K. Shevket
- , Aarti Shikotra
- , Sulman Siddique
- , Salman Siddiqui
- , J. Sidebottom
- , Louise Sigfrid
- , Gemma Simons
- , Neil Simpson
- , John Simpson
- , Ananga Singapuri
- , Suver Singh
- , Claire Singh
- , Sally Singh
- , D. Sissons
- , J. Skeemer
- , Katie Slack
- , David Smith
- , Nikki Smith
- , Andrew Smith
- , Jacqui Smith
- , Laurie Smith
- , Susan Smith
- , M. Soares
- , Teresa Solano
- , Reanne Solly
- , A. R. Solstice
- , Tracy Soulsby
- , David Southern
- , D. Sowter
- , Mark Spears
- , Lisa Spencer
- , Fabio Speranza
- , Louise Stadon
- , Stefan Stanel
- , R. Steeds
- , N. Steele
- , Mike Steiner
- , David Stensel
- , G. Stephens
- , Lorraine Stephenson
- , Iain Stewart
- , R. Stimpson
- , Sue Stockdale
- , J. Stockley
- , Wendy Stoker
- , Roisin Stone
- , Will Storrar
- , Andrew Storrie
- , Kim Storton
- , E. Stringer
- , Sophia Strong-Sheldrake
- , Natalie Stroud
- , Christian Subbe
- , Catherine Sudlow
- , Zehra Suleiman
- , Charlotte Summers
- , C. Summersgill
- , Debbie Sutherland
- , D. L. Sykes
- , Nick Talbot
- , Ai Lyn Tan
- , Lawrence Tarusan
- , Vera Tavoukjian
- , Jessica Taylor
- , Abigail Taylor
- , Chris Taylor
- , John Paul Taylor
- , Amelie Te
- , Caroline Tee
- , J. Teixeira
- , Helen Tench
- , Sarah Terry
- , Susannah Thackray-Nocera
- , Favas Thaivalappil
- , David Thickett
- , David Thomas
- , S. Thomas
- , Caradog Thomas
- , Andrew Thomas
- , T. Thomas-Woods
- , A. A. Roger Thompson
- , Tamika Thompson
- , T. Thornton
- , Matthew Thorpe
- , Ryan S. Thwaites
- , Jo Tilley
- , N. Tinker
- , Gerlynn Tiongson
- , Martin Tobin
- , Johanne Tomlinson
- , Mark Toshner
- , T. Treibel
- , K. A. Tripp
- , Drupad Trivedi
- , E. M. Tunnicliffe
- , Alison Turnbull
- , Kim Turner
- , Sarah Turner
- , Victoria Turner
- , E. Turner
- , Sharon Turney
- , Lance Turtle
- , Helena Turton
- , Jacinta Ugoji
- , R. Ugwuoke
- , Rachel Upthegrove
- , Jonathon Valabhji
- , Maximina Ventura
- , Joanne Vere
- , Carinna Vickers
- , Ben Vinson
- , Ioannis Vogiatzis
- , Elaine Wade
- , Phillip Wade
- , Louise V. Wain
- , Tania Wainwright
- , Lilian Wajero
- , Sinead Walder
- , Samantha Walker
- , S. Walker
- , Tim Wallis
- , Sarah Walmsley
- , Simon Walsh
- , J. A. Walsh
- , Louise Warburton
- , T. J. C. Ward
- , Katie Warwick
- , Helen Wassall
- , Samuel Waterson
- , L. Watson
- , Ekaterina Watson
- , James Watson
- , M. Webster
- , J. Weir McCall
- , Carly Welch
- , Simon Wessely
- , Sophie West
- , Heather Weston
- , Helen Wheeler
- , Sonia White
- , Victoria Whitehead
- , J. Whitney
- , S. Whittaker
- , Beverley Whittam
- , V. Whitworth
- , Andrew Wight
- , James Wild
- , Martin Wilkins
- , Dan Wilkinson
- , Nick Williams
- , N. Williams
- , B. Williams
- , Jenny Williams
- , S. A. Williams-Howard
- , Michelle Willicombe
- , Gemma Willis
- , James Willoughby
- , Ann Wilson
- , Imogen Wilson
- , Daisy Wilson
- , Nicola Window
- , M. Witham
- , Rebecca Wolf-Roberts
- , Chloe Wood
- , F. Woodhead
- , Janet Woods
- , Dan Wootton
- , J. Wormleighton
- , J. Worsley
- , David Wraith
- , Caroline Wrey Brown
- , C. Wright
- , S. Wright
- , Louise Wright
- , Inez Wynter
- , Moucheng Xu
- , Najira Yasmin
- , S. Yasmin
- , Tom Yates
- , Kay Por Yip
- , Susan Young
- , Bob Young
- , A. J. Yousuf
- , Amira Zawia
- , Lisa Zeidan
- , Bang Zhao
- , Bang Zheng
- & O. Zongo
- , Daniel Agranoff
- , Ken Agwuh
- , Katie A. Ahmed
- , Dhiraj Ail
- , Erin L. Aldera
- , Ana Alegria
- , Beatrice Alex
- , Sam Allen
- , Petros Andrikopoulos
- , Brian Angus
- , Jane A. Armstrong
- , Abdul Ashish
- , Milton Ashworth
- , Innocent G. Asiimwe
- , Dougal Atkinson
- , Benjamin Bach
- , Siddharth Bakshi
- , Wendy S. Barclay
- , Shahedal Bari
- , Gavin Barlow
- , Samantha L. Barlow
- , Stella Barnass
- , Nicholas Barrett
- , Christopher Bassford
- , Sneha Basude
- , David Baxter
- , Michael Beadsworth
- , Jolanta Bernatoniene
- , John Berridge
- , Nicola Best
- , Debby Bogaert
- , Laura Booth
- , Pieter Bothma
- , Benjamin Brennan
- , Robin Brittain-Long
- , Katie Bullock
- , Naomi Bulteel
- , Tom Burden
- , Andrew Burtenshaw
- , Nicola Carlucci
- , Gail Carson
- , Vikki Caruth
- , Emily Cass
- , Benjamin W. A. Catterall
- , David Chadwick
- , Duncan Chambler
- , Meera Chand
- , Kanta Chechi
- , Nigel Chee
- , Jenny Child
- , Srikanth Chukkambotla
- , Richard Clark
- , Tom Clark
- , Jordan J. Clark
- , Emily A. Clarke
- , Sara Clohisey
- , Sarah Cole
- , Paul Collini
- , Marie Connor
- , Graham S. Cooke
- , Louise Cooper
- , Catherine Cosgrove
- , Audrey Coutts
- , Helen Cox
- , Jason Cupitt
- , Maria-Teresa Cutino-Moguel
- , Ana da Silva Filipe
- , Jo Dalton
- , Paul Dark
- , Christopher Davis
- , Chris Dawson
- , Thushan de Silva
- , Samir Dervisevic
- , Oslem Dincarslan
- , Alejandra Doce Carracedo
- , Cara Donegan
- , Lorna Donelly
- , Phil Donnison
- , Chloe Donohue
- , Gonçalo dos Santos Correia
- , Sam Douthwaite
- , Thomas M. Drake
- , Andrew Drummond
- , Marc-Emmanuel Dumas
- , Chris Dunn
- , Jake Dunning
- , Ingrid DuRand
- , Ahilanadan Dushianthan
- , Tristan Dyer
- , Philip Dyer
- , Angela Elliott
- , Cariad Evans
- , Anthony Evans
- , Chi Eziefula
- , Cameron J. Fairfield
- , Angie Fawkes
- , Chrisopher Fegan
- , Lorna Finch
- , Adam Finn
- , Lewis W. S. Fisher
- , Lisa Flaherty
- , Tom Fletcher
- , Terry Foster
- , Duncan Fullerton
- , Carrol Gamble
- , Isabel Garcia-Dorival
- , Atul Garg
- , Sanjeev Garg
- , Tammy Gilchrist
- , Michelle Girvan
- , Effrossyni Gkrania-Klotsas
- , Jo Godden
- , Arthur Goldsmith
- , Clive Graham
- , Tassos Grammatikopoulos
- , Christopher A. Green
- , Julian Griffin
- , Fiona Griffiths
- , Philip Gunning
- , Rishi K. Gupta
- , Katarzyna Hafezi
- , Sophie Halpin
- , Elaine Hardy
- , Ewen M. Harrison
- , Janet Harrison
- , Catherine Hartley
- , Stuart Hartshorn
- , Daniel Harvey
- , Peter Havalda
- , Daniel B. Hawcutt
- , Ross Hendry
- , Antonia Y. W. Ho
- , Maria Hobrok
- , Luke Hodgson
- , Karl Holden
- , Anthony Holmes
- , Peter W. Horby
- , Joanne Howard
- , Samreen Ijaz
- , Clare Jackson
- , Michael Jacobs
- , Susan Jain
- , Paul Jennings
- , Rebecca L. Jensen
- , Christopher B. Jones
- , Trevor R. Jones
- , Agilan Kaliappan
- , Vidya Kasipandian
- , Seán Keating
- , Stephen Kegg
- , Michael Kelsey
- , Jason Kendall
- , Caroline Kerrison
- , Ian Kerslake
- , Shadia Khandaker
- , Katharine King
- , Robyn T. Kiy
- , Stephen R. Knight
- , Susan Knight
- , Oliver Koch
- , Gouri Koduri
- , George Koshy
- , Chrysa Koukorava
- , Shondipon Laha
- , Eva Lahnsteiner
- , Steven Laird
- , Annette Lake
- , Suzannah Lant
- , Susan Larkin
- , Diane Latawiec
- , Andrew Law
- , James Lee
- , Gary Leeming
- , Daniella Lefteri
- , Tamas Leiner
- , Lauren Lett
- , Matthew Lewis
- , Sonia Liggi
- , Patrick Lillie
- , Wei Shen Lim
- , James Limb
- , Vanessa Linnett
- , Jeff Little
- , Lucia A. Livoti
- , Mark Lyttle
- , Louise MacGillivray
- , Alan Maclean
- , Michael MacMahon
- , Emily MacNaughton
- , Maria Mancini
- , Ravish Mankregod
- , Laura Marsh
- , Lynn Maslen
- , Hannah Massey
- , Huw Masson
- , Elijah Matovu
- , Nicole Maziere
- , Sarah McCafferty
- , Katherine McCullough
- , Sarah E. McDonald
- , Sarah McDonald
- , Laurence McEvoy
- , Ruth McEwen
- , John McLauchlan
- , Kenneth A. Mclean
- , Manjula Meda
- , Alexander J. Mentzer
- , Laura Merson
- , Soeren Metelmann
- , Alison M. Meynert
- , Nahida S. Miah
- , Joanna Middleton
- , Gary Mills
- , Jane Minton
- , Joyce Mitchell
- , Kavya Mohandas
- , James Moon
- , Elinoor Moore
- , Shona C. Moore
- , Patrick Morgan
- , Kirstie Morrice
- , Craig Morris
- , Katherine Mortimore
- , Samuel Moses
- , Mbiye Mpenge
- , Rohinton Mulla
- , Derek Murphy
- , Lee Murphy
- , Michael Murphy
- , Ellen G. Murphy
- , Thapas Nagarajan
- , Megan Nagel
- , Mark Nelson
- , Lisa Norman
- , Lillian Norris
- , Lucy Norris
- , Mahdad Noursadeghi
- , Michael Olanipekun
- , Wilna Oosthuyzen
- , Anthonia Osagie
- , Matthew K. O’Shea
- , Igor Otahal
- , Mark Pais
- , Massimo Palmarini
- , Carlo Palmieri
- , Selva Panchatsharam
- , Danai Papakonstantinou
- , Hassan Paraiso
- , Brij Patel
- , Natalie Pattison
- , William A. Paxton
- , Rebekah Penrice-Randal
- , Justin Pepperell
- , Mark Peters
- , Mandeep Phull
- , Jack Pilgrim
- , Stefania Pintus
- , Tim Planche
- , Daniel Plotkin
- , Georgios Pollakis
- , Frank Post
- , Nicholas Price
- , David Price
- , Tessa Prince
- , Rachel Prout
- , Nikolas Rae
- , Andrew Rambaut
- , Henrik Reschreiter
- , Tim Reynolds
- , Neil Richardson
- , P. Matthew Ridley
- , Mark Roberts
- , Stephanie Roberts
- , Devender Roberts
- , David L. Robertson
- , Alistair Rose
- , Guy Rousseau
- , Bobby Ruge
- , Clark D. Russell
- , Brendan Ryan
- , Debby Sales
- , Taranprit Saluja
- , Vanessa Sancho-Shimizu
- , Caroline Sands
- , Egle Saviciute
- , Matthias Schmid
- , Janet T. Scott
- , James Scott-Brown
- , Aarti Shah
- , Prad Shanmuga
- , Anil Sharma
- , Catherine A. Shaw
- , Victoria E. Shaw
- , Anna Shawcross
- , Rebecca K. Shears
- , Jagtur Singh Pooni
- , Jeremy Sizer
- , Benjamin Small
- , Richard Smith
- , Catherine Snelson
- , Tom Solomon
- , Rebecca G. Spencer
- , Nick Spittle
- , Shiranee Sriskandan
- , Nikki Staines
- , Tom Stambach
- , Richard Stewart
- , David Stuart
- , Krishanthi S. Subramaniam
- , Pradeep Subudhi
- , Olivia V. Swann
- , Tamas Szakmany
- , Agnieska Szemiel
- , Aislynn Taggart
- , Sarah Tait
- , Zoltan Takats
- , Panteleimon Takis
- , Jolanta Tanianis-Hughes
- , Kate Tatham
- , Richard S. Tedder
- , Jo Thomas
- , Jordan Thomas
- , Robert Thompson
- , Chris Thompson
- , Emma C. Thomson
- , Ascanio Tridente
- , Erwan Trochu
- , Darell Tupper-Carey
- , Lance C. W. Turtle
- , Mary Twagira
- , Nick Vallotton
- , Libby van Tonder
- , Rama Vancheeswaran
- , Rachel Vincent
- , Lisa Vincent-Smith
- , Shico Visuvanathan
- , Alan Vuylsteke
- , Sam Waddy
- , Rachel Wake
- , Andrew Walden
- , Ingeborg Welters
- , Murray Wham
- , Tony Whitehouse
- , Paul Whittaker
- , Ashley Whittington
- , Meme Wijesinghe
- , Eve Wilcock
- , Martin Williams
- , Lawrence Wilson
- , Stephen Winchester
- , Martin Wiselka
- , Adam Wolverson
- , Daniel G. Wootton
- , Andrew Workman
- , Nicola Wrobel
- , Bryan Yates
- , Peter Young
- , Maria Zambon
- & J. Eunice Zhang
Contributions
F.L. recruited participants, acquired clinical samples, analyzed and interpreted data and cowrote the manuscript, including all drafting and revisions. C.E. analyzed and interpreted data and cowrote this manuscript, including all drafting and revisions. S.F. and M.R. supported the analysis and interpretation of data as well as drafting and revisions. D.S., J.K.S., S.C.M., S.A., N.M., J.N., C.K., O.C.L., O.E., H.J.C.M., A. Shikotra, A. Singapuri, M.S., V.C.H., M.T., N.J.G., N.I.L. and C.C. contributed to acquisition of data underlying this study. L.H.-W., A.A.R.T., S.L.R.-J., L.S.H., O.M.K., D.G.W., T.I.d.S. and A. Ho made substantial contributions to conception/design and implementation of this work and/or acquisition of clinical samples for this work. They have supported drafting and revisions of the manuscript. E.M.H., J.K.Q. and A.B.D. made substantial contributions to the study design as well as data access, linkage and analysis. They have supported drafting and revisions of this work. J.D.C., L.-P.H., A. Horsley, B.R., K.P., M.M. and W.G. made substantial contributions to the conception and design of this work and have supported drafting and revisions of this work. J.K.B. obtained funding for ISARIC4C, is ISARIC4C consortium co-lead, has made substantial contributions to conception and design of this work and has supported drafting and revisions of this work. M.G.S. obtained funding for ISARIC4C, is ISARIC4C consortium co-lead, sponsor/protocol chief investigator, has made substantial contributions to conception and design of this work and has supported drafting and revisions of this work. R.A.E. and L.V.W. are co-leads of PHOSP-COVID, made substantial contributions to conception and design of this work, the acquisition and analysis of data, and have supported drafting and revisions of this work. C.B. is the chief investigator of PHOSP-COVID and has made substantial contributions to conception and design of this work. R.S.T. and L.T. made substantial contributions to the acquisition, analysis and interpretation of the data underlying this study and have contributed to drafting and revisions of this work. P.J.M.O. obtained funding for ISARIC4C, is ISARIC4C consortium co-lead, sponsor/protocol chief investigator and has made substantial contributions to conception and design of this work. R.S.T. and P.J.M.O. have also made key contributions to interpretation of data and have co-written this manuscript. All authors have read and approve the final version to be published. All authors agree to accountability for all aspects of this work. All investigators within ISARIC4C and the PHOSP-COVID consortia have made substantial contributions to the conception or design of this study and/or acquisition of data for this study. The full list of authors within these groups is available in Supplementary Information .
Corresponding authors
Correspondence to Ryan S. Thwaites or Peter J. M. Openshaw .
Ethics declarations
Competing interests.
F.L., C.E., D.S., J.K.S., S.C.M., C.D., C.K., N.M., L.N., E.M.H., A.B.D., J.K.Q., L.-P.H., K.P., L.S.H., O.M.K., S.F., T.I.d.S., D.G.W., R.S.T. and J.K.B. have no conflicts of interest. A.A.R.T. receives speaker fees and support to attend meetings from Janssen Pharmaceuticals. S.L.R.-J. is on the data safety monitoring board for Bexero trial in HIV+ adults in Kenya. J.D.C. is the deputy chief editor of the European Respiratory Journal and receives consulting fees from AstraZeneca, Boehringer Ingelheim, Chiesi, GSK, Insmed, Janssen, Novartis, Pfizer and Zambon. A. Horsley is deputy chair of NIHR Translational Research Collaboration (unpaid role). B.R. receives honoraria from Axcella therapeutics. R.A.E. is co-lead of PHOSP-COVID and receives fees from AstraZenaca/Evidera for consultancy on LC and from AstraZenaca for consultancy on digital health. R.A.E. has received speaker fees from Boehringer in June 2021 and has held a role as European Respiratory Society Assembly 01.02 Pulmonary Rehabilitation secretary. R.A.E. is on the American Thoracic Society Pulmonary Rehabilitation Assembly program committee. L.V.W. also receives funding from Orion pharma and GSK and holds contracts with Genentech and AstraZenaca. L.V.W. has received consulting fees from Galapagos and Boehringer, is on the data advisory board for Galapagos and is Associate Editor for the European Respiratory Journal . A. Ho is a member of NIHR Urgent Public Health Group (June 2020–March 2021). M.M. is an applicant on the PHOSP study funded by NIHR/DHSC. M.G.S. acts as an independent external and nonremunerated member of Pfizer’s External Data Monitoring Committee for their mRNA vaccine program(s), is Chair of Infectious Disease Scientific Advisory Board of Integrum Scientific LLC, and is director of MedEx Solutions Ltd. and majority owner of MedEx Solutions Ltd. and minority owner of Integrum Scientific LLC. M.G.S.’s institution has been in receipt of gifts from Chiesi Farmaceutici S.p.A. of Clinical Trial Investigational Medicinal Product without encumbrance and distribution of same to trial sites. M.G.S. is a nonrenumerated member of HMG UK New Emerging Respiratory Virus Threats Advisory Group and has previously been a nonrenumerated member of the Scientific Advisory Group for Emergencies (SAGE). C.B. has received consulting fees and/or grants from GSK, AstraZeneca, Genentech, Roche, Novartis, Sanofi, Regeneron, Chiesi, Mologic and 4DPharma. L.T. has received consulting fees from MHRA, AstraZeneca and Synairgen and speakers’ fees from Eisai Ltd., and support for conference attendance from AstraZeneca. L.T. has a patent pending with ZikaVac. P.J.M.O. reports grants from the EU Innovative Medicines Initiative 2 Joint Undertaking during the submitted work; grants from UK Medical Research Council, GSK, Wellcome Trust, EU Innovative Medicines Initiative, UK National Institute for Health Research and UK Research and Innovation–Department for Business, Energy and Industrial Strategy; and personal fees from Pfizer, Janssen and Seqirus, outside the submitted work.
Peer review
Peer review information.
Nature Immunology thanks Ziyad Al-Aly and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Ioana Staicu was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended data fig. 1 penalized logistic regression performance..
Graphs show classification error and Area under curve (AUC) from the 50 repeats tenfold nested cross-validation used to optimise and assess the performance of PLR testing associations with each LC outcome relative to Recovered (n = 233): Cardio_Resp (n = 398), Fatigue (n = 384), Anxiety/Depression (n = 202), GI (n = 132), ( e ) Cognitive (n = 6). The distributions of classification error and area under curve (AUC) from the nested cross-validation are shown. Box plot centre line represents the Median and boundaries of the box represent interquartile range (IQR), the whisker length represent 1.5xIQR.
Extended Data Fig. 2 Associations with long COVID symptoms in full study cohort.
( a ) Fibrinogen levels at 6 months were compared between pooled LC cases (n = 295) and Recovered (n = 233) and between the Cognitive group (n = 41) and Recovered (n = 233). Box plot centre line represent the Median and boundaries of the box represent interquartile range (IQR), the whisker length represents 1.5xIQR, any outliers beyond the whisker range are shown as individual dots. Median differences were compared using two-sided Wilcoxon signed-rank test *= p < 0·05, **= p < 0·01, ***= p < 0·001, ****= p < 0·0001. Unadjusted p-values are reported. b ) Distribution of time from COVID-19 hospitalisation at sample collection applying CDC and NICE definitions of LC (n = 719) ( c ) Upset plot of symptom groups. Horizontal coloured bars represent the number of patients in each symptom group: Cardiorespiratory (Cardio_Resp), Fatigue, Cognitive, Gastrointestinal (GI) and Anxiety/Depression (Anx_Dep). Vertical black bars represent the number of patients in each symptom combination group. To prevent patient identification, where less than 5 patients belong to a combination group, this has been represented as ‘<5’. The Recovered group (n = 250) were used as controls. Forest plots show Olink protein concentrations (NPX) associated with ( d ) Cardio_Resp (n = 398), ( e ) Fatigue (n = 342), ( f ) Anx_Dep (n = 219), ( g ) GI (n = 134), and ( h ) Cognitive (n = 65). Error bars represent the median accuracy of the model.
Extended Data Fig. 3 Validation of olink measurements using conventional assays in plasma.
Olink measured protein (NPX) were compared to chemiluminescence assays (ECL or ELISA, log2[pg/mL]) to validate our findings, where contemporaneously collected plasma samples were available (n = 58). Results from key mediators associated with LC groups were validated: CSF3, IL1R2, IL2, IL3RA, TNFa, TFF2. R = spearman rank correlation coefficient and shaded areas indicated the 95% confidence interval. Samples that fell below the lower limit of detection for a given assay were excluded and the ‘n’ value on each panel indicates the number of samples above this limit.
Extended Data Fig. 4 Univariate analysis of proteins associated with each symptom.
Olink measured plasma protein levels (NPX) compared between LC groups (Cardio_Resp, n = 398, Fatigue n = 384, Anxiety/Depression, n = 202, GI, n = 132 and Cognitive, n = 60) and Recovered (n = 233). Proteins identified by PLR were compared between groups. Median differences were compared using two-sided Wilcoxon signed-rank test. * = p < 0·05, ** = p < 0·01, *** = p < 0·001, ****= p < 0·0001 after FDR adjustment. Box plot centre line represent the Median and boundaries of the box represent interquartile range (IQR), the whisker length represents 1.5xIQR, any outliers beyond the whisker range are shown as individual dots.
Extended Data Fig. 5 Unadjusted Penalised Logistic Regression.
Olink measured proteins (NPX) and their association with Cardio_Resp (n = 398), Fatigue (n = 342), Anx_Dep (n = 219), GI (n = 134), and Cognitive (n = 65). Forest plots show odds of each LC outcome vs Recovered (n = 233), using PLR without adjusting for clinical co-variates. Error bars represent the median accuracy of the model.
Extended Data Fig. 6 Partial Least Squares analysis.
Olink measured proteins (NPX) and their association with Cardio_Resp (n = 398), Fatigue (n = 342), Anx_Dep (n = 219), GI (n = 134), and Cognitive (n = 65) groups. Forest plots show odds of LC outcome vs Recovered (n = 233), using PLS analysis. Error bars represent the standard error of the coefficient estimate.
Extended Data Fig. 7 Network analysis centrality.
Each graph shows the centrality score for each Olink measured protein (NPX) found to have significant associations with other proteins that were elevated in the Cardio_Resp (n = 398), Fatigue (n = 342), Anx_Dep (n = 219), GI (n = 134), and Cognitive (n = 65) groups relative to Recovered (n = 233).
Extended Data Fig. 8 Inflammation in men and women with long COVID.
Olink measured plasma protein levels (NPX) between men and women with symptoms, divided by age (<50 or >=50years): (a) shows IL1R2 and MATN2 in the Anxiety/Depression group (<50 n = 55, >=50 n = 133), (b) shows CTSO and NFASC in the Cognitive group (<50 n = 11, >=50 n = 50). Median values were compared between men and women using two-sided Wilcoxon signed-rank test. Box plot centre line represent the Median and boundaries represent interquartile range (IQR), the whisker length represents 1.5xIQR.
Extended Data Fig. 9 Inflammation in the upper respiratory tract.
Nasal cytokines measured by immunoassay in the CardioResp Group (n = 29) and Recovered (n = 31): ( a ) shows IL1a, IL1b, IL-6, APO-2, TGFa, TFF2. Median differences were compared using two-sided Wilcoxon signed-rank test. Box plot centre line represents the Median and boundaries of the box represent interquartile range (IQR), the whisker length represent 1.5xIQR. ( b ) Shows cytokines measured by immunoassay in paired plasma and nasal (n = 70). Correlations between IL1a, IL1b, IL-6, APO-2, TGFa and TFF2 in nasal and plasma samples were compared using Spearman’s rank correlation coefficient ( R ). Shaded areas indicated the 95% confidence interval of R.
Extended Data Fig. 10 Graphical abstract.
Summary of interpretation of key findings from Olink measured proteins and their association with CardioResp (n = 398), Fatigue (n = 342), Anx/Dep (n = 219), GI (n = 134), and Cognitive (n = 65) groups relative to Recovered (n = 233).
Supplementary information
Supplementary information.
Supplementary Methods, Statistics and reproducibility statement, Supplementary Results, Supplementary Tables 1–7, Extended data figure legends, Appendix 1 (Supplementary Table 8), Appendix 2 (PHOSP-COVID author list) and Appendix 3 (ISARIC4C author list).
Reporting Summary
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Liew, F., Efstathiou, C., Fontanella, S. et al. Large-scale phenotyping of patients with long COVID post-hospitalization reveals mechanistic subtypes of disease. Nat Immunol 25 , 607–621 (2024). https://doi.org/10.1038/s41590-024-01778-0
Download citation
Received : 11 August 2023
Accepted : 06 February 2024
Published : 08 April 2024
Issue Date : April 2024
DOI : https://doi.org/10.1038/s41590-024-01778-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Immune dysregulation in long covid.
- Laura Ceglarek
- Onur Boyman
Nature Immunology (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
New long COVID study uncovers high inflammation in patients as Senate calls for more research on 'crisis'
The study followed 113 patients at four different hospitals in Switzerland.
A new study in Science is shining a light on the continuing impact of long COVID, with research revealing further and continuing health concerns for some of the 16 million sufferers in the U.S.
Long COVID is a syndrome, or collection of symptoms, that continue or develop after an acute COVID-19 infection and can last weeks, months or years. There is no test to confirm if symptoms are related to long COVID. Some scientists suggest that long COVID is caused by overactive immune cells, but the exact cause remains unclear.
The study followed 113 patients at four different hospitals in Switzerland with mild and severe COVID-19 and found that 40 had symptoms of long COVID at six months, 22 of whom had persistent symptoms at 12 months.
Researchers looked at blood samples from the 40 who experienced long COVID symptoms, compared them to controls who were not infected with COVID-19, and found that those who had long COVID had evidence of inflammation (increased complement activity), blood cell dysregulation (hemolysis and platelet activation) and tissue injury in their blood.
MORE: Long COVID research opens door for further exploration on post-viral illness
The specific details from the small study may help provide "a basis for new diagnostic solutions," according to the researchers, for the condition with no known cure or FDA-approved treatments.
While these results finding evidence of inflammation in patients with long COVID symptoms are not entirely surprising nor specific to long COVID, they are a step forward in identifying the cause of long COVID.
It's more than just researchers, though, looking into developments in our understanding of the syndrome. The condition received renewed attention from the federal government last week, as the U.S. Senate Committee on Health, Education, Labor and Pensions convened a group of patients and experts to testify about the impacts of long COVID before a bipartisan group of Senators.

In the Senate's first-ever hearing on this topic, Sen. Tammy Baldwin said researchers and government officials need to "increase the sense of urgency" over understanding and treating the condition.
For Sen. Bernie Sanders, chairman of the committee, more needs to be done.
"We think we haven't done anywhere near enough, and we hope to turn that around," he said.
Medical experts testified at the hearing, telling the committee that the condition can emerge in patients of all ages and backgrounds, that the risk increases with multiple infections, and rates of long COVID are higher in minority communities.
"The burden of disease and disability from long COVID is on par with the burden of cancer and heart disease," Dr. Ziyad Al-Aly, M.D., a clinical epidemiologist at Washington University, said. "We must develop sustainable solutions to prevent repeated infections with SARS-CoV-2 and long COVID that would be embraced by the public."
Patients and Caregivers
Angela Meriquez Vazquez , a long COVID patient from California, testified that she has helped over 15,000 sufferers through online advocacy.
"We are living through the largest mass destabilizing event in modern history," she told the Senators.
MORE: America's gun violence problem by the numbers
As she told her own story, Meriquez Vazquez, a former runner, said she is currently on 12 medications. Although she said she has managed to continue working, and she has health care, the condition has forced her to work from home, lying down to minimize her symptoms.
Related Stories

Group urges new packaging of melatonin products
- Apr 16, 5:31 PM

Counterfeit Botox causing harmful reactions in US
- Apr 16, 4:01 PM

Hundreds of drugs in short supply: Pharmacists
- Apr 12, 1:08 PM
"Not since the emergence of the AIDS pandemic has there been such an imperative for large-scale change in healthcare, public health, and inequitable structures that bring exceptional risks of illness, suffering, disability, and mortality," Meriquez Vazzque said.
One of the Senators -- Republican Roger Marshall -- shared his own testimony, revealing to the committee that one of his loved ones "is one of the 16 million people" who has "suffered for two years" with the condition.
He told the committee his family member's illness is "like mono(nucleosis) that does not go away," adding that the person has seen 30 doctors in an attempt to find help.
Marshall said there needs to be more focus on treatments for long COVID at the Centers for Disease Control and Prevention.
"I'm frustrated that our CDC is more focused on vaccines than they are on treatments," he said.
Epidemiologists and Researchers weigh in
Dr. Al-Aly, while testifying, repeatedly called on our country's leaders and medical experts to come together to tackle the ongoing health crisis.
"We are the best nation on earth, and we can solve this," he said.
One of his proposed solutions is establishing a new multidisciplinary research institute to address infection-associated chronic conditions.
Research into the condition has been "slow," Dr. Charisse Madlock-Brown, Ph.D. from the University of Iowa, said at the hearing. She noted clinical trials are in the "experimental medicine" phase and pushed for more investment to identify proven treatments.
Sen. Tim Kaine said the National Institutes of Health has been provided more than $1 billion since 2020 to study long COVID, and he urged representatives from NIH to testify before the committee. In 2021, the NIH launched the Researching COVID to Enhance Recovery initiative to identify further risk factors and causes of long COVID.
"We can't take two years just to get 'geared up,'" he said.
According to the most recent information from the CDC , long COVID can cause up to 200 symptoms , including chronic fatigue, blood clots, gastrointestinal issues, brain fog and heart issues. Symptoms can last from months to years following a COVID infection. Risk factors for developing long COVID after a COVID-19 infection that have been identified include severe COVID-19 illness, underlying health conditions (such as asthma, diabetes, obesity or autoimmune diseases) and not getting the COVID-19 vaccine.
While the interest from the Senate and the new study in Science are promising, more research needs to be done to find the specific cause of why some people get long COVID from COVID-19, and others do not, and to find effective treatments.
Erin Hannon, MD, contributed to this report. Hannon is a resident physician in pediatrics from Columbia University/New York-Presbyterian Hospital, and a member of the ABC News Medical Unit.
Related Topics
- Coronavirus

US lawmakers urge release of Russia critic Kara-Murza on the anniversary of his imprisonment
- Apr 9, 12:04 PM
ABC News Live
24/7 coverage of breaking news and live events
Advertisement
Supported by
Scientists Offer a New Explanation for Long Covid

By Pam Belluck
- Share full article
A team of scientists is proposing a new explanation for some cases of long Covid, based on their findings that serotonin levels were lower in people with the complex condition.
In their study , published on Monday in the journal Cell, researchers at the University of Pennsylvania suggest that serotonin reduction is triggered by remnants of the virus lingering in the gut. Depleted serotonin could especially explain memory problems and some neurological and cognitive symptoms of long Covid, they say.

Why It Matters: New ways to diagnose and treat long Covid.
This is one of several new studies documenting distinct biological changes in the bodies of people with long Covid — offering important discoveries for a condition that takes many forms and often does not register on standard diagnostic tools like X-rays.
The research could point the way toward possible treatments, including medications that boost serotonin. And the authors said the biological pathway that their research outlines could unite many of the major theories of what causes long Covid: lingering remnants of the virus, inflammation, increased blood clotting and dysfunction of the autonomic nervous system.
“All these different hypotheses might be connected through the serotonin pathway,” said Christoph Thaiss, a lead author of the study and an assistant professor of microbiology at the Perelman School of Medicine at the University of Pennsylvania.
“Second of all, even if not everybody experiences difficulties in the serotonin pathway, at least a subset might respond to therapies that activate this pathway,” he said.
“This is an excellent study that identifies lower levels of circulating serotonin as a mechanism for long Covid,” said Akiko Iwasaki, an immunologist at Yale University. Her team and colleagues at the Icahn School of Medicine at Mount Sinai recently published a study that identified other biological changes linked to some cases of long Covid, including levels of the hormone cortisol. These studies could point to specific subtypes of long Covid or different biological indicators at different points in the condition.
The Back Story: A series of disruptions set off by bits of virus in the gut.
Researchers analyzed the blood of 58 patients who had been experiencing long Covid for between three months and 22 months since their infection. Those results were compared to blood analysis of 30 people with no post-Covid symptoms and 60 patients who were in the early, acute stage of coronavirus infection.
Maayan Levy, a lead author and assistant professor of microbiology at the Perelman School of Medicine, said levels of serotonin and other metabolites were altered right after a coronavirus infection, something that also happens immediately after other viral infections.
But in people with long Covid, serotonin was the only significant molecule that did not recover to pre-infection levels, she said.
The team analyzed stool samples from some of the long Covid patients and found that they contained remaining viral particles. Putting the findings in patients together with research on mice and miniature models of the human gut, where most serotonin is produced, the team identified a pathway that could underlie some cases of long Covid.
Here’s the idea: Viral remnants prompt the immune system to produce infection-fighting proteins called interferons. Interferons cause inflammation that reduces the body’s ability to absorb tryptophan, an amino acid that helps produce serotonin in the gut. Blood clots that can form after a coronavirus infection may impair the body’s ability to circulate serotonin.
Depleted serotonin disrupts the vagus nerve system, which transmits signals between the body and the brain, the researchers said. Serotonin plays a role in short-term memory, and the researchers proposed that depleted serotonin could lead to memory problems and other cognitive issues that many people with long Covid experience.
“They showed that one-two-three punch to the serotonin pathway then leads to vagal nerve dysfunction and memory impairment,” Dr. Iwasaki said.
There are caveats. The study was not large, so the findings need to be confirmed with other research. Participants in some other long Covid studies, in which some patients had milder symptoms, did not always show depleted serotonin, a result that Dr. Levy said might indicate that depletion happened only in people whose long Covid involves multiple serious symptoms.
What’s Next: A clinical trial of Prozac.
Scientists want to find biomarkers for long Covid — biological changes that can be measured to help diagnose the condition. Dr. Thaiss said the new study suggested three: the presence of viral remnants in stool, low serotonin and high levels of interferons.
Most experts believe that there will not be a single biomarker for the condition, but that several indicators will emerge and might vary, based on the type of symptoms and other factors.
There is tremendous need for effective ways to treat long Covid, and clinical trials of several treatments are underway. Dr. Levy and Dr. Thaiss said they would be starting a clinical trial to test fluoxetine, a selective serotonin reuptake inhibitor often marketed as Prozac, and possibly also tryptophan.
“If we supplement serotonin or prevent the degradation of serotonin, maybe we can restore some of the vagal signals and improve memory and cognition and so on,” Dr. Levy said.
Pam Belluck is a health and science writer whose honors include sharing a Pulitzer Prize and winning the Victor Cohn Prize for Excellence in Medical Science Reporting. She is the author of “Island Practice,” a book about an unusual doctor. More about Pam Belluck

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
HHS Announces the Formation of the Office of Long COVID Research and Practice and Launch of Long COVID Clinical Trials Through the RECOVER Initiative
C urrent analysis estimates that 7.7 million to 23 million Americans have developed Long COVID.
Today, U.S. Department of Health and Human Services (HHS) Secretary Xavier Becerra released the following statement applauding the formation of the Office of Long COVID Research and Practice to lead the Long COVID response and coordination across the federal government and, in addition, the National Institutes of Health (NIH) launch of the Long COVID clinical trials through the RECOVER Initiative.
“As our nation continues to make strides in combating COVID-19, it is crucial that we address the impact of Long COVID and provide resources to those in need,” said HHS Secretary Becerra. “Last year President Biden called on HHS to coordinate the response to Long COVID. The Official establishment of the Long COVID Coordinating office and the launch of the RECOVER clinical trials solidifies this issue as an ongoing priority.”
“The Office of Long COVID Research and Practice will enhance efforts being undertaken across the U.S. government to improve the lives of those who continue to experience the long-term impacts of the worst public health crisis in a century,” said Adm Rachel Levine, M.D. “Bringing together the resources and expertise of federal, state, and local partners, patients, providers, researchers, and the business sector to answer the American peoples most urgent calls to action.”
Background on the Office of Long COVID Research and Practice:
The Office of Long COVID Research will be located within HHS’s Office of the Assistant Secretary for Health under the leadership of the HHS Assistant Secretary for Health, Admiral Rachel Levine. The Office is charged with on-going coordination of the whole-of-government response to the longer-term effects of COVID-19, including Long COVID and associated conditions and the implementation of the National Research Action Plan on Long COVID and the Services and Supports for Longer-Term Impacts of COVID-19 . Currently 14 federal departments engage on Long COVID, including over a dozen HHS Operating and Staff Divisions with a goal to reduce the impacts of Long COVID by improving quality of life for people living with Long COVID and reducing disparities related to Long COVID.
Background on the RECOVER Initiative:
The NIH RECOVER Initiative is a $1.15 billion nationwide research program designed to understand, treat, and prevent long COVID, which describes long-term symptoms following infection by SARS-Cov-2, the virus that causes COVID-19. More than 200 symptoms are associated with long COVID, and the condition can cause problems throughout the body, affecting nearly all body systems including the nervous, cardiovascular, gastrointestinal, pulmonary, autonomic, and immune systems.
Launched in 2021, RECOVER established one of the largest, most diverse study group of patients with Long COVID in the world. The initial stage of the initiative involved launching large observational multi-site studies examining and following people through their experience with COVID-19 to learn why some people develop long-term symptoms while others recover completely. These studies are ongoing and have recruited more than 24,000 participants to date. Researchers also are analyzing 60 million electronic health records and conducting more than 40 pathobiology studies on how COVID-19 affects different body tissues and organs. This study cohort participated in RECOVER observational studies that allowed researchers to characterize the condition in great detail, which is critical for informing the development of clinical trials to test interventions. The clinical trials are designed so multiple treatments and therapies can be studied across five focus areas. Platform protocols for two of these areas were posted today, July 31, with enrollment for these trials beginning the end of July and throughout the summer. To learn more about the RECOVER clinical trials visit: https://trials.RECOVERCovid.org .
Through collaboration with federal partners, researchers, clinicians, patient advocacy organizations, and the business sector, the Biden-Harris Administration remains committed to addressing the longer-term impacts of the worst public health crisis in a century. We will continue to listen and learn from patients, caregivers, frontline workers, and those with lived experience, so we can accelerate understanding and breakthroughs together.
Sign Up for Email Updates
Receive the latest updates from the Secretary, Blogs, and News Releases
Subscribe to RSS
Receive latest updates

Related News Releases
Hhs, dhs, and fema announce completion of multi-year review of state efforts to provide language access during the covid-19 public health emergency, readout of hhs secretary becerra’s meeting with pharmacy ceos on covid-19 therapeutics commercialization, readout of hhs meeting with health care providers on covid-19 therapeutics commercialization, related blog posts.

Calling innovators! HHS Long COVID Healthathon launches with $25K in prizes
Reflections from the deputy director of the hhs office of long covid research and practice.

Driving Long COVID Innovation with Health+ Human-Centered Design
Media inquiries.
For general media inquiries, please contact [email protected] .
Subscribe or renew today
Every print subscription comes with full digital access
Science News
Finally, scientists are making progress on long covid.

By Nancy Shute
Editor in Chief
March 31, 2024 at 7:15 am
Share this:
I’ve been thinking about the old-fashioned term “invalid.” In the 19th century, popular literature was awash with characters like Beth in Little Women , who patiently knitted away in her sickbed until she succumbed to long-term damage from scarlet fever. Characters like Beth were a prettied-up version of reality. Many children died or were disabled by diseases that we can now fend off with antibiotics and vaccines.
My mother could have been one of those grim true-life stories. As a child in the 1930s, she almost died from an infection of the mastoid bone, which is typically caused by ear infections. In the pre-antibiotics era, it was a leading cause of childhood death. Mom remembered long, lonely weeks lying in bed, staring out the window at children playing, and then many more months of being a weak, sickly child. She recovered and grew up to become a nurse specializing in pediatrics. I still have her copy of Little Women .
COVID-19 may seem a long way from Little Women , but in an odd way we’re also stuck in the part of the plot where people suffer and languish. Researchers around the world are trying to figure out how the SARS-CoV-2 virus causes lasting damage to the human body, and what treatments could restore health to those suffering from long COVID.
It’s a huge challenge, in part because there’s no test yet to determine if someone has long COVID. Instead, there’s an unruly bundle of symptoms that can include problems thinking, exhaustion, heart issues and joint aches. These ailments are common to many diseases. That makes it difficult to get a diagnosis, let alone treatment.
But recent advances in unraveling long COVID’s mysteries are exciting researchers, senior writer Meghan Rosen reports. Immunologist Akiko Iwasaki told Rosen that it’s as if there’s a “picture being revealed from the fog.”
That includes new findings on cognitive problems that are a persistent symptom of long COVID. In March, researchers reported that patients with what’s commonly called brain fog can have a leaky blood-brain barrier , which may allow viruses, cells and other intruders into brain tissue. The brains of patients without brain fog aren’t similarly affected.
Researchers are also searching more broadly, looking for clues to how the virus plays havoc with the immune systems of long COVID patients.
Rosen, an ace journalist with a Ph.D. in biochemistry and molecular biology, had her own reasons for wanting to find out the state of long COVID research. After catching the virus, she suffered for months with exhaustion and leg pain. Her doctor tested for all sorts of illnesses, including Lyme and thyroid disease, but the tests came back negative. So, probably long COVID, but who knows? Rosen kept trying to manage work and family, only to find herself wiped out if she pushed a bit too much.
Fortunately, Rosen’s now feeling much better, pretty much back to her usual energetic self. But many long COVID patients, she notes, are not so lucky. They’re waiting and hoping that science will help them move on from this wretched chapter in their lives.
Subscribers, enter your e-mail address for full access to the Science News archives and digital editions.
Not a subscriber? Become one now .
New Long COVID Findings Offer Fuller Picture of Condition
Research published this week suggests that a test for long COVID could be possible.
Study: 1 in 14 Hit With Long COVID

Seth Wenig | AP
A woman walks through a door with a sign asking shoppers to wear masks in New York on Feb. 9, 2022.
COVID-19 isn’t going away – and neither is long COVID. But new data about its prevalence as well as research into biomarkers of long COVID published this week are helping researchers understand what to look for when it comes to the condition.
Data published by the Centers for Disease Control and Prevention’s National Center for Health Statistics on Tuesday was a stark reminder that, while not widespread, some children are affected by long COVID.
Pulling from the 2022 National Health Interview Survey, the data shows that 1.3% of children ever had long COVID as of last year, according to reports from their parents.
The researchers defined long COVID as the “presence of symptoms for at least 3 months after having COVID-19 among those who received either a positive test or a doctor’s diagnosis of COVID-19.”
The rate of long COVID is significantly higher among adults than in children. The survey found that in 2022, about 7% of adults – or about 1 in 14 – reported ever having long COVID. More women reported having had long COVID than men – a trend also observed in children.
Adults ages 35-49 were most likely to have had long COVID, according to the data. Hispanic adults were more likely than Black and white adults to have it.
The Best Cartoons on Health Care

The survey also found a higher prevalence of long COVID among Americans living in more rural areas compared with those living in large central metropolitan areas.
There are no approved treatments or tests for the condition. Its cause (or, more likely, causes) remains unknown, though studies have made some progress .
Research published Monday in the journal Nature found that people with long COVID have clear differences in their hormone and immune function when compared to people without the condition. The findings offer hope that a test for the condition is possible.
“These findings are important – they can inform more sensitive testing for long COVID patients and personalized treatments for long COVID that have, until now, not had a proven scientific rationale,” David Putrino, principal investigator of the study, said in a statement . “This is a decisive step forward in the development of valid and reliable blood testing protocols for long COVID.”
The study looked at survey results and blood samples from 270 individuals. It found that the blood of those experiencing long COVID had specific biomarkers, like abnormal T cell activity, reactivation of dormant viruses and low cortisol levels.
“These markers need to be validated in larger studies, but provide a first step in dissecting the disease pathogenesis of long COVID,” Akiko Iwasaki, co-principal investigator of the study, said in a statement.
Coronavirus metrics are increasing in the U.S., underscoring that COVID-19 – as well as long COVID – will be a lasting problem. Health officials have moved away from trying to prevent coronavirus infections, instead shifting their focus to preventing hospitalizations and deaths. Still, many Americans are dealing with repeat infections of COVID-19, which can come with increased risk for a myriad of health problems.

Join the Conversation
Tags: Coronavirus , public health
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

The Implications of Trump Legal Wins
Lauren Camera April 16, 2024

The Week in Cartoons April 15-19
April 16, 2024, at 3:47 p.m.

Justices Weigh Jan. 6 Obstruction Charge

Johnson Draws New Threats With Aid Bill
Aneeta Mathur-Ashton April 16, 2024

New Home Construction Slumps
Tim Smart April 16, 2024

High Court to Consider Jan. 6 Charges


An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To NHLBI Information & Resources on COVID-19
- Research Funding
- Research Strategy
- For Clinicians
- For the Public
Many people recover fully within a few days or weeks after being infected with SARS-CoV-2, the virus that causes COVID-19. However, others have symptoms that linger for weeks, months, or even years after their initial diagnosis. Some people seem to recover from COVID-19 but then see their symptoms return, or they develop different symptoms within a few months. Even people who had no symptoms when they were infected can develop them later. Either mild or severe COVID-19 can lead to long-lasting symptoms.
Long COVID, long-haul COVID, post-COVID-19 condition, chronic COVID, and post-acute sequelae of SARS-CoV-2 (PASC) are all names for the health problems that some people experience a few months after a COVID-19 diagnosis. Symptoms of Long COVID may be the same as or different than symptoms of COVID-19 . Long COVID can also trigger other health conditions such as diabetes or kidney disease.
For more information on Long COVID, check out these U.S. government resources:
National Institutes of Health (NIH)
- Explore Long COVID information, news , and more on the COVID-19 research website
- Learn about NIH’s RECOVER initiative and find clinical trials on Long COVID
- Read how this NIH-funded RECOVER study developed a new symptom scoring system that will improve future Long COVID treatments
- Read this NHLBI news story about how obstructive sleep apnea increases risks for Long COVID
- Read this NHLBI news story about how lingering symptoms are common after COVID hospitalization
- Read how an NIH-funded RECOVER study identified potential long COVID disparities
- Read this NHLBI news story about how Long COVID may be less common in children
- Read how an NHLBI-funded study found that exercise lags are common after Long COVID
- Read this NIH Director’s Blog post about using artificial intelligence to advance the understanding of Long COVID
- Read this NHLBI news story about how Long COVID impacts children.
Centers for Disease Control and Prevention (CDC)
- Find tips for talking with your healthcare provider about Long COVID
- Check out this fact sheet about caring for people living with post-COVID conditions
This White House fact sheet provides information about comprehensive government efforts to prevent, diagnose, and treat Long COVID.

What are Long Covid Symptoms?
Check out this interactive graphic from NIH to learn how Long COVID affects different parts of the human body.

RECOVER Research Review (R3) Seminar Series
The NIH RECOVER initiative’s R3 Seminar Series promotes a shared understanding of the scientific research on Long COVID. This forum speeds up discovery by allowing experts to
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- Health & Well-being
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Funding Opportunities
- Join Our Voluntary Faculty
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Embryonic Stem Cell Research Oversight
- COVID-19 Vaccinations in CT
- COVID-19 in Connecticut Schools
- Connecticut Towns COVID-19 Impact Dashboard
- Connecticut Town 14-Day Cases Time Lapse
- CT Correctional Facilities with COVID Cases Dashboard
- Connecticut COVID Presence Map
- CT Nursing Homes with COVID-19 Cases
- U.S. COVID Presence Map
- COVID-19 Case Density by US County
- Global Cases Dashboard
- Time-Lapse of Global Spread
- US Racial and Ethnic Disparities in COVID-19 Mortality
- Childcare Survey and Data Display
- Risk of Complications Conditional on COVID-19 Infection
- Travel Time to COVID Testing Sites in Connecticut
- Travel Time to COVID Testing Sites in the US
- Project Team
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Study Uncovers Drivers of Lingering Symptoms in COVID-19 Long-haulers
Covid-19 patient.
A Yale-Duke collaborative research team may have identified some of the first biomarkers linked to impaired lung function in long-term COVID-19 patients.
Since the early months of the pandemic, scientists have tried to determine why some patients experience symptoms such as shortness of breath, cough, fever, fatigue, or chest pain weeks to months after their initial COVID-19 infection. What may drive or predict the persistence of long-term symptoms, also known as “post-acute sequelae of COVID-19,” remains poorly understood. A study published June 10 in the journal JCI Insight may provide answers about this mysterious condition.
The study, led by Hyung J. Chun, MD , an associate professor of cardiovascular medicine and pathology and co-director of the Yale Cardiovascular Research Center, examined the predictors of persistent illness.
“We wanted to get a better understanding of what is driving the disease process in patients who had persistent symptoms after their COVID-19 infection,” said Chun.
The researchers used patient data collected from the post-COVID-19 clinics to analyze whether the severity of the COVID-19 illness could impact the likelihood of persistent symptoms later — specifically worsening lung function — and if proteins in the blood were linked to increased likelihood of symptoms in post-COVID-19 patients.
Chun and the Yale team partnered with colleagues at Duke University School of Medicine for the study. The team enrolled 61 participants from post-COVID-19 clinics. The researchers used a pulmonary function test to track two key parameters for lung function, including the amount of air a person could exhale after taking a deep breath, and the ability to transfer inhaled oxygen from the lungs to the red blood cells.
We wanted to get a better understanding of what is driving the disease process in patients who had persistent symptoms after their COVID-19 infection. Hyung J. Chun, MD
The results showed that almost 70 percent of patients continued to report persistent difficulty breathing during their follow-up visits. The data also confirmed that those with more severe illness during their acute COVID infection were more likely to have impaired lung function at the time of the follow up.
Next, the team analyzed patients’ blood samples to identify biomarkers or biological markers that may be associated with persistent lung symptoms. They identified three proteins (lipocalin 2, matrix metalloproteinase 7, and hepatocyte growth factor) that were strongly associated with impaired lung function.
“These are markers of activation of a specific immune cell type called neutrophils, as well as factors that may promote lung injury when elevated. While we previously found them to be strongly associated with severe illness during acute COVID-19 illness, it is interesting that they appear to remain elevated in those who continue to have poor lung function during their recovery,” said Chun.
The findings support a Feb. 26 study published in the journal Blood Advances , where Chun and his colleagues discovered that lipocalin 2 and hepatocyte growth factors predicted which patients were more likely to suffer severe COVID-19 illness and require intensive care. Chun believes that these biomarkers may not only be associated with the severity of COVID-19 symptoms, but may also be driving the disease process — which could be targeted by future therapies.
The study’s co-authors are Alexander Pine, Alfred I. Lee, Vanessa Yu, and Marcus Shallow from the Yale School of Medicine, and Elias Coutavas, Coral X. Giovacchini, Anne Mathews, Brian Stephenson, Loretta G. Que, and Bryan D. Kraft of the Duke University School of Medicine.
Featured in this article
- Hyung Chun, MD, FAHA Associate Professor Adjunct
- Alexander B. Pine, MD, PhD Assistant Professor of Medicine (Hematology); Assistant Professor of Medicine, Hematology
- Alfred Lee, MD, PhD Professor of Medicine (Hematology); Director, Hematology/Oncology Fellowship Program; Chief, Classical Hematology Program
- Skip to main content
- Keyboard shortcuts for audio player
Goats and Soda
- Infectious Disease
- Development
- Women & Girls
- Coronavirus FAQ
A new clue to the reason some people come down with long COVID

Max Barnhart

Protesters march outside the White House to call attention to those who have long COVID and those who have the disabling disease Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Nathan Posner/Anadolu Agency via Getty Images hide caption
Protesters march outside the White House to call attention to those who have long COVID and those who have the disabling disease Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Stéphanie Longet is an immunologist and a COVID researcher at the University of Saint-Etienne in France, and just like 10-20% of adults who were infected with the virus , she continues to have symptoms well after her infection has resolved – a condition known colloquially as long COVID.
"I got COVID one year ago and I developed some persistent symptoms," she says. "I cannot work too long. My legs are quickly exhausted. In the morning it feels like I had run a marathon during the night, and I didn't do anything, I just slept."
Longet and other scientists don't exactly know why some people develop long COVID while others don't, but preliminary research released in medRxiv in July suggests that genetics plays a role.
The new research, which was an international collaboration between dozens of scientists, describes how some people carry a version of a single gene, FOXP4 , that is associated with developing long COVID. Longet calls the new research an "important element" in understanding why some people's COVID symptoms seemingly never resolve.
A surprising finding about long COVID
Long COVID only affects a small percentage of people who are infected with SARS-CoV-2, but the scope of the pandemic means that many millions of people are suffering. Roughly 25 million people in the U.S. and over 17 million people in Europe have long COVID symptoms, with many more in other parts of the world.
There isn't a universally agreed upon definition for what is considered long COVID – people experience a range of different symptoms including "fatigue, muscle pain, intestinal disorders and brain fog" and for different periods of time according to Longet, who was not involved in the new research. That's made the disease difficult for scientists to fully understand.
But the new research adds to the growing body of work showing that genetics can influence COVID outcomes. It was only a few weeks ago when NPR reported that genetics might make some people resistant to developing any COVID symptoms at all.
Jill Hollenbach , an immunologist at the University of California, San Francisco, was one of the scientists who led the research on asymptomatic COVID. She says she was "surprised and excited" about the new long COVID findings.
"The fact that the authors were able to detect this association [between the FOXP4 gene and long COVID], I think, is spectacular," Hollenbach says.
Hollenbach also thinks that the new research on long COVID is refreshing because "there's a lot of frustration on the public's part around progress" of understanding the disease and how to treat it. "There can be a perception out there amongst some people who are involved in advocacy for long COVID that it's being dismissed [by the scientific community] and I don't think that's true."
The gene that may be connected
The new study looked at DNA from 6,450 people who developed long COVID and compared it to the DNA of those who did not. Not everyone who reported long COVID symptoms in the study had a clinical diagnosis so the research team used a broad definition of long COVID as self-reported symptoms of COVID that affect day-to-day life three months after the initial infection.
When that data was analyzed, only one connection between a person's genes and whether they developed long COVID stood out – the FOXP4 gene.
The FOXP4 gene is what biologists call a "transcription factor," meaning that it helps regulate processes throughout the body but isn't responsible for any one thing in particular. The new research shows that the gene is active in the lungs and mentions that other studies have found an association between FOXP4 and lung cancer.
However, the research does not point to FOXP4 as a smoking gun. "If you have the variant of FOXP4, in theory, you could have a higher probability to develop long COVID," Longet says. "But it doesn't mean if you have the variant that you will have long COVID."
Hollenbach, who published similar work on asymptomatic COVID in the journal Nature , says the new work is "methodologically extremely sound" and that "the result appears to be really clear."
But Hollenbach is also quick to point out that the genetic effect of the FOXP4 gene is relatively small – though that's not entirely surprising. "It's uncommon to see extremely strong genetic effects," she says. "What we find in studies like this gives us insights into what the underlying pathophysiology is."
The new research hints at "some underlying immune dysregulation in the lung itself," Hollenbach says, suggesting an abnormal immune response to COVID might be causing the long-term harm. "We need to just continue to follow these breadcrumbs and see where they lead us."
That might partially explain why so many people with long COVID are having lung problems, but for other common long COVID symptoms, like brain fog and fatigue, the activity of FOXP4 doesn't provide much of a clue, meaning there's more work to be done in order to understand all facets of the disease.
Why your genes may not fully dictate your COVID destiny
The latest research shows that there are clear connections between a person's genetics and how they respond to COVID. So does this mean that every individual's COVID fate was set in stone from the day they were born?
Hollenbach doesn't think so. "I don't believe that we are unnecessarily subjected to some kind of pre-destiny according to our genes," she says. "There's going to be many genetic and non-genetic factors that are going to be in play here."
One thing that Hollenbach says the scientific community agrees upon, and that this new research reinforces, is that, "you're more likely to have long COVID If you've had a very severe bout of COVID."
Which is why, according to Hollenbach, "vaccination is still our greatest tool" in the fight against COVID because it can prevent or reduce the severity of a COVID infection, reducing the chance someone develops long COVID.
In the meantime, however, there doesn't seem to be any imminent relief for those who are already dealing with the effects of long COVID. Longet suggests that people, "find different ways to organize your life. It's what I've done a little bit."
Working different hours, making diet modifications and trying light breathing exercises are all little things researchers have found to help manage symptoms .
Despite the lack of immediate help, Longet still believes that scientists will soon figure out a way to help resolve her symptoms and the symptoms of others with long COVID. "I'm hopeful because now there are quite a lot of studies and a lot of researchers who are working on this," she says. "I believe in science, so I'm quite hopeful."
Three studies spotlight long-term burden of COVID in US adults

Jikaboom / iStock
Three new studies shed new light on long COVID in the United States, with one finding that two thirds of severely ill patients reported persistent impairments for up to 1 year, another showing that US veterans were at three times the risk of preventable hospitalization in the month after infection, and the last revealing that one third of COVID-19 survivors had lingering symptoms at one time.
57% of very ill had persistent physical problems
Today in Critical Care Medicine , University of California San Francisco (UCSF) researchers describe their study of 156 critically ill COVID-19 patients transferred to long-term acute-care hospitals in Georgia, Kentucky, Nebraska, and Texas for weaning from ventilation and rehabilitation from March 2020 to February 2021.
Patients completed online or phone interviews 1 year after hospital release. The average patient age was 65, and average hospital stay was 2 months. Most spent an average of 1 month on mechanical ventilation and were healthy before their infection.
Of the 156 patients, almost two-thirds (64%) said they had a persistent impairment, including physical (57%), respiratory (49%), psychiatric (24%), and cognitive (15%) problems, 1 year later. Nearly half (47%) reported more than one type of impairment, and 19% still needed supplemental oxygen.
"We have millions of survivors of the most severe and prolonged COVID illness globally," first author Anil Makam, MD, said in a UCSF news release . "Our study is important to understand their recovery and long-term impairments, and to provide a nuanced understanding of their life-changing experience."
About 79% of patients said they hadn't fully recovered at 1 year, 99% were back at home, and 60% of the previously employed had returned to work. Many patients said they were more affected by hospital-related issues such as bedsores and nerve damage that limited use of their extremities than by COVID-related problems. Participants attributed improvement to exercise and rehabilitation, support, and time.
"The long-lasting impairments we observed are common to survivors of any prolonged critical illness, and not specific to COVID, and are best addressed through multidisciplinary rehabilitation," Makam said.
Veterans at much higher risk for 1 year
Today in JAMA Network Open , a team led by researchers from the Veterans Affairs (VA) Portland Health Care System in Oregon used an emulated-target randomized trial design with monthly sequential trials to compare the risk of potentially preventable hospitalization among COVID-infected veterans to those of matched uninfected controls.
The study enrolled 189,136 veterans diagnosed as having COVID-19 from March 2020 to April 2021 and 943,084 controls. The average patient age was 60.3 years, 89.1% were men, 69.4% were White, and 23.4% were Black. The primary outcome was a potentially preventable hospitalization at a VA facility, VA-purchased community care, or Medicare fee-for-service care.
"Delayed or inadequate treatment of ambulatory care–sensitive conditions (acute or chronic conditions that can be treated effectively through quality ambulatory care [ACSCs]) can result in hospitalization," the study authors wrote.
An increased risk of preventable hospitalization in veterans with SARS-CoV-2 ... highlights the need for research on ways in which SARS-CoV-2 shapes postinfection care needs and engagement with the health system.
"Thus, hospitalizations for ACSCs (hereinafter referred to as potentially preventable hospitalizations) are widely recognized as an indicator of ambulatory care access and quality. They are also increasingly used as a measure of health system performance during public health emergencies."
A total of 3.1% of participants (3.8% of COVID-19 survivors and 3.0% of controls) had a potentially preventable hospitalization during the 1-year follow-up. The risk of hospitalization was higher among COVID-19 survivors at 0 to 30 days (adjusted hazard ratio [AHR], 3.26), 0 to 90 days (AHR, 2.12), 0 to 180 days (AHR, 1.69), and 0 to 365 days (AHR, 1.44).
"In this cohort study, an increased risk of preventable hospitalization in veterans with SARS-CoV-2, which persisted for at least 1 year after initial infection, highlights the need for research on ways in which SARS-CoV-2 shapes postinfection care needs and engagement with the health system," the researchers wrote. "Solutions are needed to mitigate preventable hospitalization after SARS-CoV-2."
17 million adults currently have long COVID
Yesterday, KFF reported its latest long-COVID data, which show that rates of the condition have remained relatively steady for a year, suggesting that the burden will persist unless new methods of prevention and treatment are developed.
The data follow the March 2024 release of updated Centers for Disease Control and Prevention (CDC) COVID-19 recommendations, which don't instruct people to isolate after testing positive.
" The new CDC guidance brings a unified approach to the risks from respiratory viruses and reflects the nation’s progress against severe illness from COVID-19," wrote author Alice Burns, PhD, KFF associate director of the Program on Medicaid & Uninsured.
Although rates of long COVID have stabilized, the 17 million adults with long COVID may experience many employment and material hardships.
"However, as the nation moves further from the COVID-19 pandemic, rates of long COVID remain steady and 7% of all adults—roughly 17 million people—reported currently having long COVID in March 2024."
Among the findings:
- Of adult COVID-19 survivors (60%), 3 in 10 report having long COVID at one time, and about 1 in 10 say they still have it.
- Roughly 17 million adults currently have long COVID.
- A total of 79% of adult with long COVID say their condition has limited their participation in activities, with 25% reporting it limits their activities "a lot."
- Persistent symptoms occur most often among people who are transgender or have disabilities.
- Regarding COVID-19 as just another respiratory virus may make accessing healthcare more difficult for groups disproportionately affected by persistent symptoms.
- A total of 5% to 10% of adults may continue to have long COVID at any point, and research to improve diagnosis and treatment takes time.
"Although rates of long COVID have stabilized, the 17 million adults with long COVID may experience many employment and material hardships, with 4 in 10 reporting food insecurity, 2 in 10 reporting difficulty paying rent or mortgage, and 1 in 10 reporting that they had to stop working for a period of time because of their symptoms," Burns wrote.
Related news
Nasal cells offer clues about why covid-19 is typically milder in children.

Many healthcare workers unsure about COVID vaccine boosters for themselves, kids

Study finds no evidence COVID-19 causes childhood asthma

Oregon data: COVID vaccines not tied to sudden cardiac death in young people

Minority healthcare workers experienced COVID testing delays in first 2 years of pandemic

Bernie Sanders calls for $10 billion for long-COVID moonshot

Study identifies inflammation and symptom patterns in long COVID
Blood donor study finds 21% incidence of long-term symptoms attributed to COVID-19

This week's top reads
Wisconsin confirms another county affected by cwd in deer.
The 3-year-old buck was found dead in the town of Wautoma, within 10 miles of the Marquette and Portage county borders.
Avian flu virus detected in more Michigan dairy herds and on another large layer farm
Along with multiple detections now in dairy cows, avian flu has also hit 2 massive farms housing egg-laying hens in the state.

Vietnam reports its first human infection from H9 avian flu virus
The patient lived adjacent to a poultry market, but there were no reports of bird illnesses or deaths.
Avian flu detected in North Carolina dairy herd
Seven states have now reported the virus in dairy herds, with detections at 21 facilities.

Study: Pathogens that cause surgical infections may be coming from patients' skin
The study authors say the findings could have implications for infection-prevention strategies.
Among blood donors with prior SARS-CoV-2 infection, 23.6% reported long-term neurologic symptoms.

Inflammation of myeloid cells and activation of immune proteins that are part of the complement system stood out blood from long COVID patients, but it's not clear if that applies to all types of long COVID.
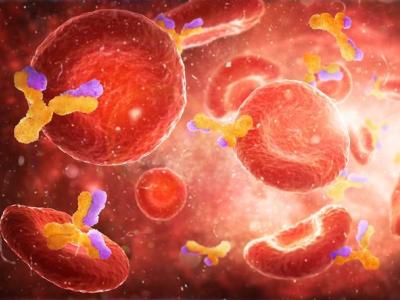
Avian flu virus detected in South Dakota dairy herd
Today's announcement raises the number of affected states to 8.
One study found that veterans were at 44% higher risk of a preventable hospitalization in the year after infection.

Healthcare worker vaccine reluctance can compromise patient care, the authors say.

Our underwriters
Unrestricted financial support provided by.

- Antimicrobial Resistance
- Chronic Wasting Disease
- All Topics A-Z
- Resilient Drug Supply
- Influenza Vaccines Roadmap
- CIDRAP Leadership Forum
- Roadmap Development
- Coronavirus Vaccines Roadmap
- Antimicrobial Stewardship
- Osterholm Update
- Newsletters
- About CIDRAP
- CIDRAP in the News
- Our Director
- Osterholm in the Press
- Shop Merchandise
- Nebraska Medicine
- Give to GCHS
New Study Finds Potential Cause of Long COVID Symptoms—Experts Explain
- Published Jan 23, 2024
Prevention Researchers say this could lead to diagnostic tests and treatments.
Long COVID has mystified the medical community for years, making it a tough condition to diagnose, let alone treat. However, a growing body of research has found more information on what may be behind long COVID , with the hope of eventually finding an effective treatment. Now, a new study has made an interesting discovery on what may cause long COVID symptoms : a change in the immune system that may be detected via a blood test.
That’s the major takeaway from a new study published in the journal Science . For the study, researchers followed 113 patients with COVID-19 and 39 healthy patients as controls. After six months, 40 of the COVID-19 patients developed symptoms of long COVID.
The researchers analyzed blood samples from those patients and found that they had a group of proteins that showed that a portion of the immune system called the complement system was ramped up well after the patients recovered from COVID-19.
The study analyzed 6,596 proteins across 268 blood samples, which were collected during patients’ acute phase and again six months later. Researchers found several differences in the blood of people with long COVID compared to the healthy patients, including an imbalance in proteins involved in blood clotting and inflammation. Researchers also found that those with long COVID had a group of proteins that showed that a portion of the immune system, called the complement system, was ramped up well after the patients recovered from COVID-19.
Leave a comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Disclaimer: This translation was last updated on August 2, 2022. For up-to-date content, please visit the English version of this page.
Disclaimer: The Spanish COVID-19 site is currently undergoing significant updates which may lead to a delay in translated content. We apologize for any inconvenience.
Long COVID or Post-COVID Conditions
Some people who have been infected with the virus that causes COVID-19 can experience long-term effects from their infection, known as Long COVID or Post-COVID Conditions (PCC). Long COVID is broadly defined as signs, symptoms, and conditions that continue or develop after acute COVID-19 infection. This definition of Long COVID was developed by the Department of Health and Human Services (HHS) in collaboration with CDC and other partners.
People call Long COVID by many names, including Post-COVID Conditions, long-haul COVID, post-acute COVID-19, long-term effects of COVID, and chronic COVID. The term post-acute sequelae of SARS CoV-2 infection (PASC) is also used to refer to a subset of Long COVID.
What You Need to Know
- Long COVID is a real illness and can result in chronic conditions that require comprehensive care. There are resources available .
- Long COVID can include a wide range of ongoing health problems; these conditions can last weeks, months, or years.
- Long COVID occurs more often in people who had severe COVID-19 illness, but anyone who has been infected with the virus that causes COVID-19 can experience it.
- People who are not vaccinated against COVID-19 and become infected may have a higher risk of developing Long COVID compared to people who have been vaccinated.
- People can be reinfected with SARS-CoV-2, the virus that causes COVID-19, multiple times. Each time a person is infected or reinfected with SARS-CoV-2, they have a risk of developing Long COVID.
- While most people with Long COVID have evidence of infection or COVID-19 illness, in some cases, a person with Long COVID may not have tested positive for the virus or known they were infected.
- CDC and partners are working to understand more about who experiences Long COVID and why, including whether groups disproportionately impacted by COVID-19 are at higher risk.
In July 2021, Long COVID was added as a recognized condition that could result in a disability under the Americans with Disabilities Act (ADA). Learn more: Guidance on “Long COVID” as a Disability Under the ADA .
About Long COVID
Long COVID is a wide range of new, returning, or ongoing health problems that people experience after being infected with the virus that causes COVID-19. Most people with COVID-19 get better within a few days to a few weeks after infection, so at least 4 weeks after infection is the start of when Long COVID could first be identified. Anyone who was infected can experience Long COVID. Most people with Long COVID experienced symptoms days after first learning they had COVID-19, but some people who later experienced Long COVID did not know when they got infected.
There is no test that determines if your symptoms or condition is due to COVID-19. Long COVID is not one illness. Your healthcare provider considers a diagnosis of Long COVID based on your health history, including if you had a diagnosis of COVID-19 either by a positive test or by symptoms or exposure, as well as based on a health examination.
Science behind Long COVID
RECOVER: Researching COVID to Enhance Recovery
People with Long COVID may experience many symptoms.
People with Long COVID can have a wide range of symptoms that can last weeks, months, or even years after infection. Sometimes the symptoms can even go away and come back again. For some people, Long COVID can last weeks, months, or years after COVID-19 illness and can sometimes result in disability.
Long COVID may not affect everyone the same way. People with Long COVID may experience health problems from different types and combinations of symptoms that may emerge, persist, resolve, and reemerge over different lengths of time. Though most patients’ symptoms slowly improve with time, speaking with your healthcare provider about the symptoms you are experiencing after having COVID-19 could help determine if you might have Long COVID.
People who experience Long COVID most commonly report:
General symptoms ( Not a Comprehensive List)
- Tiredness or fatigue that interferes with daily life
- Symptoms that get worse after physical or mental effort (also known as “ post-exertional malaise ”)
Respiratory and heart symptoms
- Difficulty breathing or shortness of breath
- Fast-beating or pounding heart (also known as heart palpitations)
Neurological symptoms
- Difficulty thinking or concentrating (sometimes referred to as “brain fog”)
- Sleep problems
- Dizziness when you stand up (lightheadedness)
- Pins-and-needles feelings
- Change in smell or taste
- Depression or anxiety
Digestive symptoms
- Stomach pain
Other symptoms
- Joint or muscle pain
- Changes in menstrual cycles
Symptoms that are hard to explain and manage
Some people with Long COVID have symptoms that are not explained by tests or easy to manage.
People with Long COVID may develop or continue to have symptoms that are hard to explain and manage. Clinical evaluations and results of routine blood tests, chest X-rays, and electrocardiograms may be normal. The symptoms are similar to those reported by people with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and other poorly understood chronic illnesses that may occur after other infections. People with these unexplained symptoms may be misunderstood by their healthcare providers, which can result in a delay in diagnosis and receiving the appropriate care or treatment.
Review these tips to help prepare for a healthcare provider appointment for Long COVID.
Health conditions
Some people experience new health conditions after COVID-19 illness.
Some people, especially those who had severe COVID-19, experience multiorgan effects or autoimmune conditions with symptoms lasting weeks, months, or even years after COVID-19 illness. Multi-organ effects can involve many body systems, including the heart, lung, kidney, skin, and brain. As a result of these effects, people who have had COVID-19 may be more likely to develop new health conditions such as diabetes, heart conditions, blood clots, or neurological conditions compared with people who have not had COVID-19.
People experiencing any severe illness may develop health problems
People experiencing any severe illness, hospitalization, or treatment may develop problems such as post-intensive care syndrome (PICS).
PICS refers to the health effects that may begin when a person is in an intensive care unit (ICU), and which may persist after a person returns home. These effects can include muscle weakness, problems with thinking and judgment, and symptoms of post-traumatic stress disorder (PTSD), a long-term reaction to a very stressful event. While PICS is not specific to infection with SARS-CoV-2, it may occur and contribute to the person’s experience of Long COVID. For people who experience PICS following a COVID-19 diagnosis, it is difficult to determine whether these health problems are caused by a severe illness, the virus itself, or a combination of both.
People More Likely to Develop Long COVID
Some people may be more at risk for developing Long COVID.
Researchers are working to understand which people or groups of people are more likely to have Long COVID, and why. Studies have shown that some groups of people may be affected more by Long COVID. These are examples and not a comprehensive list of people or groups who might be more at risk than other groups for developing Long COVID:
- People who have experienced more severe COVID-19 illness, especially those who were hospitalized or needed intensive care.
- People who had underlying health conditions prior to COVID-19.
- People who did not get a COVID-19 vaccine.
Health Inequities May Affect Populations at Risk for Long COVID
Some people are at increased risk of getting sick from COVID-19 because of where they live or work, or because they can’t get health care. Health inequities may put some people from racial or ethnic minority groups and some people with disabilities at greater risk for developing Long COVID. Scientists are researching some of those factors that may place these communities at higher risk of getting infected or developing Long COVID.
Preventing Long COVID
The best way to prevent Long COVID is to protect yourself and others from becoming infected. For people who are eligible, CDC recommends staying up to date on COVID-19 vaccination , along with improving ventilation, getting tested for COVID-19 if needed, and seeking treatment for COVID-19 if eligible. Additional preventative measures include avoiding close contact with people who have a confirmed or suspected COVID-19 illness and washing hands or using alcohol-based hand sanitizer.
Research suggests that people who get a COVID-19 infection after vaccination are less likely to report Long COVID, compared to people who are unvaccinated.
CDC, other federal agencies, and non-federal partners are working to identify further measures to lessen a person’s risk of developing Long COVID. Learn more about protecting yourself and others from COVID-19 .
Living with Long COVID
Living with Long COVID can be hard, especially when there are no immediate answers or solutions.
People experiencing Long COVID can seek care from a healthcare provider to come up with a personal medical management plan that can help improve their symptoms and quality of life. Review these tips to help prepare for a healthcare provider appointment for Long COVID. In addition, there are many support groups being organized that can help patients and their caregivers.
Although Long COVID appears to be less common in children and adolescents than in adults, long-term effects after COVID-19 do occur in children and adolescents .
Talk to your doctor if you think you or your child has Long COVID. Learn more: Tips for Talking to Your Healthcare Provider about Post-COVID Conditions
Data for Long COVID
Studies are in progress to better understand Long COVID and how many people experience them.
CDC is using multiple approaches to estimate how many people experience Long COVID. Each approach can provide a piece of the puzzle to give us a better picture of who is experiencing Long COVID. For example, some studies look for the presence of Long COVID based on self-reported symptoms, while others collect symptoms and conditions recorded in medical records. Some studies focus only on people who have been hospitalized, while others include people who were not hospitalized. The estimates for how many people experience Long COVID can be quite different depending on who was included in the study, as well as how and when the study collected information. Estimates of the proportion of people who had COVID-19 that go on to experience Long COVID can vary.
CDC posts data on Long COVID and provides analyses, the most recent of which can be found on the U.S. Census Bureau’s Household Pulse Survey .
CDC and other federal agencies, as well as academic institutions and research organizations, are working to learn more about the short- and long-term health effects associated with COVID-19 , who gets them and why.
Scientists are also learning more about how new variants could potentially affect Long COVID. We are still learning to what extent certain groups are at higher risk, and if different groups of people tend to experience different types of Long COVID. CDC has several studies that will help us better understand Long COVID and how healthcare providers can treat or support patients with these long-term effects. CDC will continue to share information with healthcare providers to help them evaluate and manage these conditions.
CDC is working to:
- Better identify the most frequent symptoms and diagnoses experienced by patients with Long COVID.
- Better understand how many people are affected by Long COVID, and how often people who are infected with COVID-19 develop Long COVID
- Better understand risk factors and protective factors, including which groups might be more at risk, and if different groups experience different symptoms.
- Help understand how Long COVID limit or restrict people’s daily activity.
- Help identify groups that have been more affected by Long COVID, lack access to care and treatment for Long COVID, or experience stigma.
- Better understand the role vaccination plays in preventing Long COVID.
- Collaborate with professional medical groups to develop and offer clinical guidance and other educational materials for healthcare providers, patients, and the public.
Related Pages
- Caring for People with Post-COVID Conditions
- Preparing for Appointments for Post-COVID Conditions
- Researching COVID to Enhance Recovery
- Guidance on “Long COVID” as a Disability Under the ADA
For Healthcare Professionals
- Post-COVID Conditions: Healthcare Providers
Search for and find historical COVID-19 pages and files. Please note the content on these pages and files is no longer being updated and may be out of date.
- Visit archive.cdc.gov for a historical snapshot of the COVID-19 website, capturing the end of the Federal Public Health Emergency on June 28, 2023.
- Visit the dynamic COVID-19 collection to search the COVID-19 website as far back as July 30, 2021.
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
COVID-19: Long-term effects
Some people continue to experience health problems long after having COVID-19. Understand the possible symptoms and risk factors for post-COVID-19 syndrome.
Most people who get coronavirus disease 2019 (COVID-19) recover within a few weeks. But some people — even those who had mild versions of the disease — might have symptoms that last a long time afterward. These ongoing health problems are sometimes called post- COVID-19 syndrome, post- COVID conditions, long COVID-19 , long-haul COVID-19 , and post acute sequelae of SARS COV-2 infection (PASC).
What is post-COVID-19 syndrome and how common is it?
Post- COVID-19 syndrome involves a variety of new, returning or ongoing symptoms that people experience more than four weeks after getting COVID-19 . In some people, post- COVID-19 syndrome lasts months or years or causes disability.
Research suggests that between one month and one year after having COVID-19 , 1 in 5 people ages 18 to 64 has at least one medical condition that might be due to COVID-19 . Among people age 65 and older, 1 in 4 has at least one medical condition that might be due to COVID-19 .
What are the symptoms of post-COVID-19 syndrome?
The most commonly reported symptoms of post- COVID-19 syndrome include:
- Symptoms that get worse after physical or mental effort
- Lung (respiratory) symptoms, including difficulty breathing or shortness of breath and cough
Other possible symptoms include:
- Neurological symptoms or mental health conditions, including difficulty thinking or concentrating, headache, sleep problems, dizziness when you stand, pins-and-needles feeling, loss of smell or taste, and depression or anxiety
- Joint or muscle pain
- Heart symptoms or conditions, including chest pain and fast or pounding heartbeat
- Digestive symptoms, including diarrhea and stomach pain
- Blood clots and blood vessel (vascular) issues, including a blood clot that travels to the lungs from deep veins in the legs and blocks blood flow to the lungs (pulmonary embolism)
- Other symptoms, such as a rash and changes in the menstrual cycle
Keep in mind that it can be hard to tell if you are having symptoms due to COVID-19 or another cause, such as a preexisting medical condition.
It's also not clear if post- COVID-19 syndrome is new and unique to COVID-19 . Some symptoms are similar to those caused by chronic fatigue syndrome and other chronic illnesses that develop after infections. Chronic fatigue syndrome involves extreme fatigue that worsens with physical or mental activity, but doesn't improve with rest.
Why does COVID-19 cause ongoing health problems?
Organ damage could play a role. People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. Inflammation and problems with the immune system can also happen. It isn't clear how long these effects might last. The effects also could lead to the development of new conditions, such as diabetes or a heart or nervous system condition.
The experience of having severe COVID-19 might be another factor. People with severe symptoms of COVID-19 often need to be treated in a hospital intensive care unit. This can result in extreme weakness and post-traumatic stress disorder, a mental health condition triggered by a terrifying event.
What are the risk factors for post-COVID-19 syndrome?
You might be more likely to have post- COVID-19 syndrome if:
- You had severe illness with COVID-19 , especially if you were hospitalized or needed intensive care.
- You had certain medical conditions before getting the COVID-19 virus.
- You had a condition affecting your organs and tissues (multisystem inflammatory syndrome) while sick with COVID-19 or afterward.
Post- COVID-19 syndrome also appears to be more common in adults than in children and teens. However, anyone who gets COVID-19 can have long-term effects, including people with no symptoms or mild illness with COVID-19 .
What should you do if you have post-COVID-19 syndrome symptoms?
If you're having symptoms of post- COVID-19 syndrome, talk to your health care provider. To prepare for your appointment, write down:
- When your symptoms started
- What makes your symptoms worse
- How often you experience symptoms
- How your symptoms affect your activities
Your health care provider might do lab tests, such as a complete blood count or liver function test. You might have other tests or procedures, such as chest X-rays, based on your symptoms. The information you provide and any test results will help your health care provider come up with a treatment plan.
In addition, you might benefit from connecting with others in a support group and sharing resources.
- Long COVID or post-COVID conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html. Accessed May 6, 2022.
- Post-COVID conditions: Overview for healthcare providers. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html. Accessed May 6, 2022.
- Mikkelsen ME, et al. COVID-19: Evaluation and management of adults following acute viral illness. https://www.uptodate.com/contents/search. Accessed May 6, 2022.
- Saeed S, et al. Coronavirus disease 2019 and cardiovascular complications: Focused clinical review. Journal of Hypertension. 2021; doi:10.1097/HJH.0000000000002819.
- AskMayoExpert. Post-COVID-19 syndrome. Mayo Clinic; 2022.
- Multisystem inflammatory syndrome (MIS). Centers for Disease Control and Prevention. https://www.cdc.gov/mis/index.html. Accessed May 24, 2022.
- Patient tips: Healthcare provider appointments for post-COVID conditions. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/post-covid-appointment/index.html. Accessed May 24, 2022.
- Bull-Otterson L, et al. Post-COVID conditions among adult COVID-19 survivors aged 18-64 and ≥ 65 years — United States, March 2020 — November 2021. MMWR Morbidity and Mortality Weekly Report. 2022; doi:10.15585/mmwr.mm7121e1.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Post-COVID Recovery & COVID-19 Support Group - Related information Post-COVID Recovery & COVID-19 Support Group
- Rehabilitation after COVID-19 - Related information Rehabilitation after COVID-19
- Post-COVID-19 syndrome could be a long haul (podcast) - Related information Post-COVID-19 syndrome could be a long haul (podcast)
- COVID-19 Coronavirus Long-term effects
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

The Many Reasons for Hope in Long Covid
A cnn reporter's new book tells how long covid patients make democracy work..
Updated April 13, 2024 | Reviewed by Gary Drevitch
- What Is a Career
- Find a career counsellor near me
- Long Covid patient-led innovations are changing the way healthcare is delivered.
- Patient advocacy has led to political support for Long Covid research.
- The new book "The Long Haul" is about the little guy finding a way to make democracy work to solve a problem.

To the millions of patients with Long Covid, who have lived with up to four years of debilitating or disabling symptoms, the disease is a disaster. Yet, in the midst of all the suffering, CNN Reporter Ryan Prior sees a story of community, advocacy, and democracy at its best. This week alone, U.S. Sen. Bernie Sanders has responded to the cries of Long Covid patients by announcing a legislative proposal for $10 billion in research funding for Long Covid over the next 10 years.
I talked with Prior, a fellow writer for Psychology Today , about his book, The Long Haul: How Long Covid Survivors Are Revolutionizing Health Care. In the book, Prior weaves his own life, the stories of activist patients, and the latest science into a captivating tale of regular people crying out for care that actually works. Scientists and public officials, who expected Covid-19 to be an infection that cleared up in a matter of weeks, were caught off guard by the tens of millions around the world who got sick and stayed sick. These Long Covid patients often found solace only with one another, organizing support groups across oceans and continents while ill in bed.
The Long Haul is now out in paperback from MIT Press.
Alison Escalante: Your own story was part of the inspiration for the book. What happened?
Ryan Prior: I got sick in 2006 on the weekend of my 17th birthday. I was a cross-country runner and a soccer player and taking AP classes. And then within two weeks, I had to drop out of school for about seven months. And I went to 16 different doctors who ultimately gave me the diagnosis of chronic fatigue syndrome. I attribute it to a tick-borne illness, likely Lyme disease due to a tick bite I had at a Boy Scout camp. I took 15 pills a day and got an IV infusion every month for about 12 years. But at this point I am entirely recovered, barring a relapse .
AE: What is the focus of your book and how has your view changed since it was published?
RP: I wanted to build the story around regular people who were able to stand up for a specific problem that they were having, and then to alert the powers that be to that problem: The story of regular citizens in a democracy to guide the process for how we solve problems. But when I finished this book in February 2022 I was dismayed, because I felt the story was half finished, and I really wanted to have a triumphal ending.
Even in the last few days, my feeling toward the book has changed because Senator Bernie Sanders, the Chair of the Senate Health, Education , Labor, and Pensions (HELP) Committee, has proposed a bill calling for the Long COVID moonshot and $10 billion over 10 years for research.
In 2021, I contacted Lisa McCorkell, and Hannah Davis from the Patient Led Research Collaborative to make them a part of this book showing how small groups of people can make a huge difference. Lisa wrote a piece in Nature, and then Sen. Sanders proposed the bill for the Long Covid Moonshot. It all proves my book’s underlying hypothesis: that when this huge number of people suffers, the powers that be can and do respond. And that makes me feel more optimistic ; this is what we learned in ninth-grade civics about how democracy is supposed to work.
AE: Is there bipartisan support for Long Covid research funding?
RP: Yes. There are two important Republicans on the HELP committee who are doctors. One of them is Kansas Senator Roger Marshall , who has a close loved one with Long COVID who has been to dozens of doctors, and been mostly bed-bound for a couple of years. Similarly, Louisiana Senator Bill Cassidy sees Long Covid as a very real problem and has called for research into solutions. The greatest amount of hope I have yet felt about Long COVID has happened in the last couple months.
AE: What have you seen in the last couple months that can give hope to patients?
RP: First, there’s a lot of phenomenal work being done in the startup world. For example, RTHM is a medical group designed to treat patients with Long Covid. I'm on the advisory board for a startup called COVID Blue Health, developing an AI -empowered virtual patient-centered care platform for patients with infection-associated chronic illness .
In the philanthropic sector, Vitalik Buterin, the co-founder the cryptocurrency Ethereum, is funding the Patient Led Research Collaborative. He’s also funding the Polybio Research Foundation , which is doing some incredible work on looking into the long-term effects of pathogens.
AE: How else are patients innovating ways to help themselves?
RP: With Long Covid comes despair and anguish. The severity of the symptoms and of the disability is exactly as bad as we [the pre-existing community with post-viral illnesses] had feared, especially for a specific subset of patients who are more moderate-to-severe and can't work anymore.
And there is also an exciting part: that so many people who have Long Covid are creatively building on the knowledge that that's largely been curated by patients with post-infectious Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS ). There is the generosity and willingness of patients to share their experience in online forums, which could be Slack, Facebook , Twitter, Reddit, etc. So many Long Covid patients know exactly what to expect, not because they've learned that from their doctors, but because they learned it from fellow patients. So there's a really important story here about peer-to-peer health.

When somebody gets a new diagnosis, they should be prescribed not just a treatment plan, but also be prescribed a peer support group who can walk them through it. This is how new Long Covid patients learn which supplement to put into your water for electrolytes, or what kind of compression stockings to wear and which brands are better or worse for dealing with postural orthostatic tachycardia syndrome (POTS). And those really specific aspects of patient wisdom are very important.
AE: What else are Long Covid patients doing to change health care?
RP: It’s been incredibly exciting to see patients creating startups, several of which involve using wearables to track and manage symptoms. Chicago-based Pathize is one of those groups. And Visible is a group that's run out of the UK, which has a lot of users on their platform. A community has evolved around these platforms, where patients can share data and compare what works for them. They are taking technology, and they're building new ways of doing research.
AE: What would you say to the naysayers who claim that Long Covid is psychosomatic? For example, some naysayers insist that support groups make things worse by “reinforcing an identity ." Others claim that the very act of measuring heart rate with a wearable causes anxiety and thus elevated heart rate.
RP: People who are well don't join support groups because they don't need them. Obviously, correlation doesn't guarantee causation. You could easily make a different inference based on that same data.
But for doctors struggling to separate these symptoms from anxiety or depression , there are numerous studies showing all kinds of different detectable objective data [that Long Covid is a biological disease]; for example, studies showing off-the-charts amounts of inflammation.
I think that some of the most important inferences come from the HIV doctors who come into Long Covid and see it under the exactly the same framework. You've got researchers who are veterans of looking at HIV, who are moving into the Long Covid world and translating all of their knowledge and finding similarities.
AE: What are your thoughts on Long Covid patient complaints about medical gaslighting ?
RP: Many health-care providers are under extreme pressure from the system that they are in to label something quickly, even if it's not correct, because of the lack of time that they have and the lack of tools that they have. And they have to figure out some other specialists to shuffle that patient onto. The number of options that the primary-care doctor has are severely limited and so patients get put into psychiatric areas due to the overall lack of knowledge.
Many patients rightly accused their doctors of gaslighting them. The other side of it is that many physicians are experiencing moral injury : When you see somebody suffering and you cannot do anything about it, that's traumatizing for doctors. As the actual possibilities for treating these patients increase, I hope to see better performance among health providers.
It takes 90 minutes to do a medical visit with a Long Covid patient, because of all the body systems involved. But if you could design a clinic where you've got the five or six relevant specialists, you can get it done in three hours.
AE: Is there a takeaway you'd like to leave with us?
RP: So many parts of these new ways of doing healthcare can be patient-centered and patient-led. There's an entirely new entrepreneurial ecosystem being built up, in addition to new ways of doing science. There really is hope for Long Covid patients and those with other post-infectious illnesses.

A pediatrician and writer, Dr. Escalante is on a mission to help parents out of the Shouldstorm that disconnects them from their kids. She is raising her own rambunctious boys.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

The tell-tale sign of long COVID—and 7 more common symptoms
Posted: March 22, 2024 | Last updated: March 22, 2024

Eight long-haul symptoms of COVID-19
Most people who get infected with the coronavirus recover within a few weeks. However, some continue to experience symptoms weeks or even months after they are infected. They have what are known as long-haul symptoms of COVID-19 . As such, they are sometimes called COVID-19 long-haulers. Sometimes, even patients who had a mild or asymptomatic coronavirus infection can become long-haulers.
Scientists want to learn more about who becomes a long-hauler and why. This knowledge can help shape public policy, and determine the best standards of care and precautions to prevent viral transmission of the disease.
An advocacy group called Patient-Led Research for COVID-19 released its first report in May 2020, to provide an in-depth look at the experiences of more than 600 COVID-19 long-haulers. Susannah Fox, who studies online communities of patients with chronic conditions, told MIT Technology Review in August 2020 that such patient groups will be more important to health professionals, particularly during crises such as the coronavirus, that cause health professionals to be overwhelmed.
"The future of health care and technology is being built on such communities," Fox said. She added that some of the earliest users of online bulletin boards and other online communities were patients with chronic diseases.
Stacker compiled a list of long-term COVID-19 symptoms based on research and data from experts at institutions across the world, including the Centers for Disease Control and Prevention, Mayo Clinic, Northwestern University, and New York-Presbyterian/Columbia University.

Altered sense of smell and taste
Among 100 people who presented to Northwestern Memorial Hospital's Neuro-COVID-19 clinic in Chicago, with symptoms compatible with the Infectious Diseases Society of America COVID-19 guidelines, 59% reported dysgeusia, or an impaired sense of taste, and 55% reported anosmia, or an altered sense of smell. The patients were seen at the hospital, which operates in a partnership with Northwestern University's Feinberg School of Medicine, an average of five to six months after the onset of COVID-19 symptoms. Dysgeusia and anosmia may be the result of viral invasion of the olfactory cortex, the part of the brain associated with the sense of smell and taste.

Difficulty breathing
Dyspnea, or difficulty breathing, is the most common long-haul symptom of COVID-19. More than 40% to almost 70% of patients with COVID-19 report having trouble breathing 60 to 100 days after diagnosis or hospitalization. Dyspnea has been linked to viral damage of the alveolar and epithelial cells in the lungs, and inflammatory damage to vascular cells. Researchers have found corticosteroids may help some long-haul COVID-19 patients with residual lung inflammation or persistent inflammatory interstitial lung disease.

Memory issues
Cognitive impairment after COVID-19 recovery can present as trouble with concentration, memory, understanding words and language, and/or executive function. These cognitive difficulties may be the result of damage to the hippocampus, the part of the brain that plays an important role in learning and memory. Damage to the hippocampus may put people with COVID-19 long-haul symptoms at risk for the hippocampal-related degeneration characteristic of Alzheimer's disease.

More frequent blood clots
The coronavirus that causes COVID-19 can make blood cells more likely to coagulate , or clump and form clots. Specifically, heart damage caused by COVID-19 is likely the result of clots in the small vessels, or capillaries, in the heart. The risk of blood clots in those with long-haul COVID-19 may be associated with damage from severe inflammation, although scientists don't know how long the inflammation can persist. Doctors might want to treat blood clots in those with long-haul COVID-19 with low-molecular weight heparin and direct oral anticoagulants versus vitamin K antagonists , because patients taking vitamin K antagonists need frequent blood tests to monitor medication levels.

Trouble sleeping
Patients with long-haul COVID-19 may develop or will continue to experience neuropsychiatric symptoms, including insomnia, or sleeplessness, for months after they are initially infected. These symptoms may be the result of nerve cell damage due to inflammation . Levels of immune system activation are directly associated with cognitive and behavioral changes. Although little compelling evidence exists that the coronavirus that causes COVID-19 infects neurons, autopsies have found evidence that the virus causes changes in the brain that promote inflammation in nerve cells and blood vessels in the brain. Inflammaging, the chronic low-level brain inflammation that develops with age, may also play a role in the persistent psychiatric effects of COVID-19.
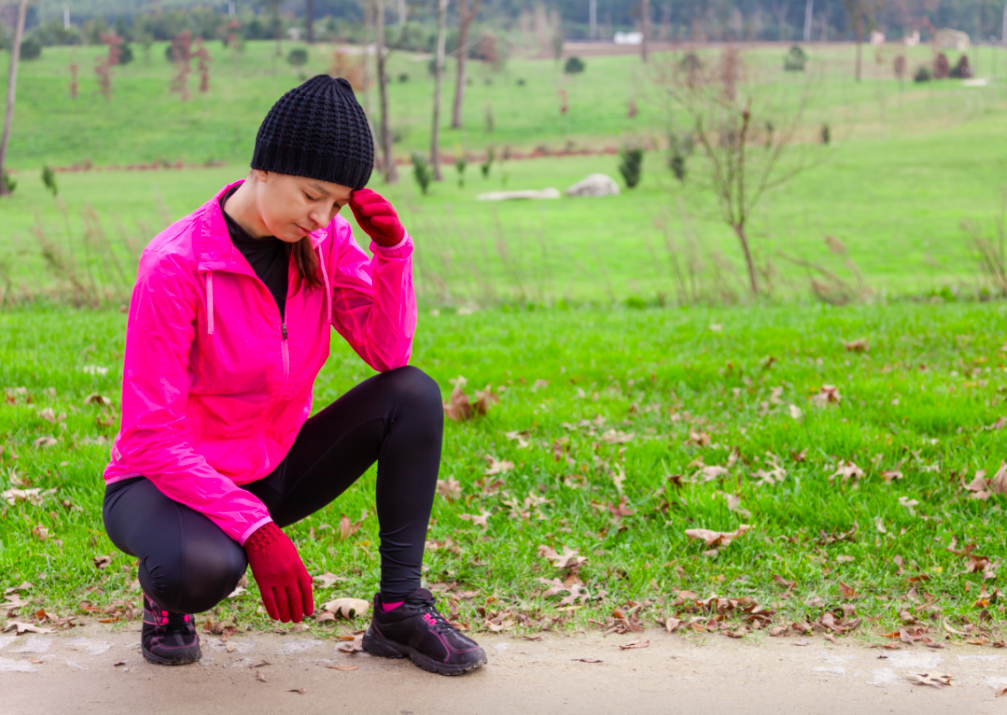
Lightheadedness
Dizziness, sometimes called vertigo, has long been associated with viral infections . So researchers are not really surprised that studies from around the world have found vertigo is one of the most common symptoms of COVID-19. Scientists in Pakistan believe that the coronavirus enters the nervous system via the circulatory system, and binds to the angiotensin-converting enzyme 2 receptors in the lining of the capillaries in the brain. Hypoxia, or insufficient oxygen delivery, and damage caused by blood clots and inflammation are other possible ways nervous system damage can cause vertigo in those with long-haul COVID-19.
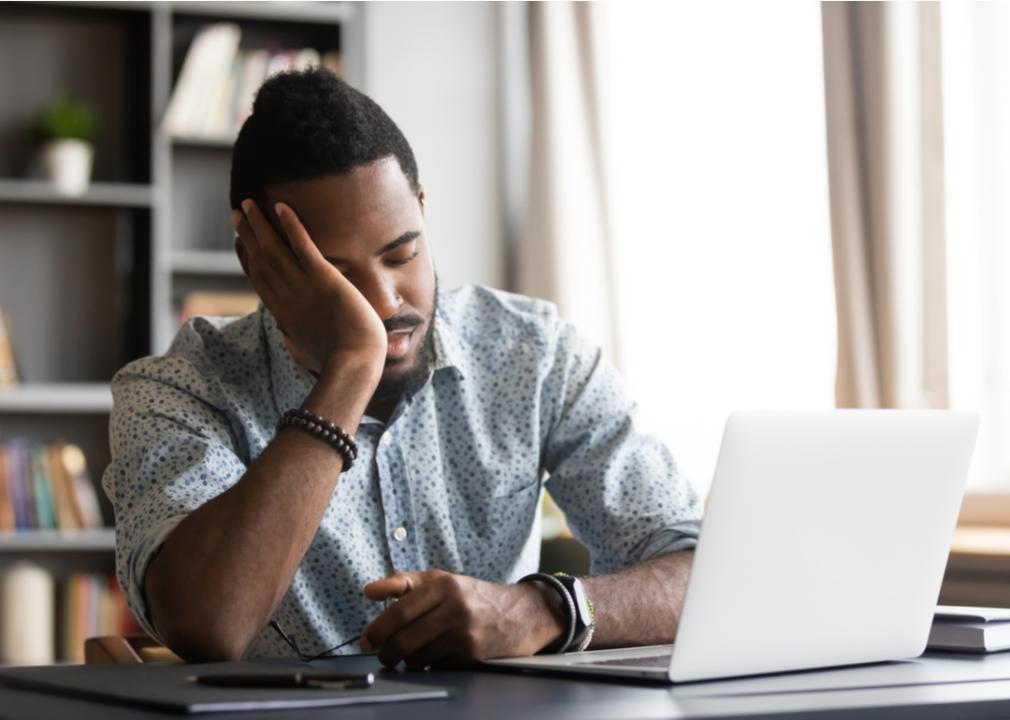
Strain after physical or mental work
Scientists do not know much about what causes post-COVID-19 fatigue, also called post-exertional malaise or chronic fatigue/myalgic encephalopathy, following viral infection. One possible explanation is that while the body fights off the coronavirus, the immune system releases proteins that promote inflammation and can stimulate the immune response. These proteins are called cytokines, and they are also responsible for the symptoms of post-COVID-19 fatigue. However, cytokine levels sometimes do not return to normal and cause ongoing symptoms.

Chest pain and heart palpitations
Viral infection, inflammation and the immune response, and a decrease in the number of, or downregulation of, angiotensin-converting enzyme 2 receptors may be the root cause of chest pain and heart palpitations in those with long-haul COVID-19. Infection, inflammation, and the downregulation of ACE2 receptors damage the heart muscle; the pericardium, or the sac around the heart; and the conduction system that controls the heartbeat by conducting electrical impulses through the heart. Scarring of the heart muscle can lead to palpitations, or arrhythmias, as can cytokines, which are proteins that stimulate the immune response and promote inflammation.
More for You
Israeli strikes in Lebanon kill three including Hezbollah commander - army video
Water Bears' 'Incredible Response' to Radiation Surprises Scientists
Patrick Mahomes explains why he avoided calling for tight gun-control laws after shooting, endorsing president
Illinois woman hits Target with class action lawsuit for collecting biometric data without her consent
12 safest places if World War 3 breaks out
Top 20 Saturday Night Live Sketches That Broke the Whole Cast
KFC Is Changing Its Menu—Here’s What to Expect
US Ally Detects China Spy Ship Near Coast
10 pairs of movies with strikingly similar plots that came out the same year
How Do I Know If My Dog Is Happy? 12 Signs of a Happy Dog
Tech trick: How to tell who’s calling when you don’t recognize the phone number
This Type Of Fencing Might Be The Answer To Your Snake Problem
The Coolest Car From the Year You Were Born (1945-1995)
Top 10 Times Bill Hader Broke The SNL Cast
Spire collapses on one of Europe’s most iconic buildings in huge fire
78 Riddles for Adults That Will Test Your Smarts
Wendy's Is Selling Almost Its Entire Menu for $1 This Week
Woman who accused Trevor Bauer of sexual assault indicted for fraud in Arizona
Cellphone nightmare leads to ported numbers, identity theft and fight for recovery
50 of the most memorable TV lines ever written

IMAGES
COMMENTS
Scientists have identified a persistent change in a handful of blood proteins in people with long Covid that indicates that an important part of their immune system remains on high alert for ...
Although the long COVID research has been difficult, she sees no other option but to stay involved. "We're driven by desperation, out of improving our own quality of life." Nature 628 , 26 ...
The RECOVER clinical trials will be conducted using "platform protocols," under which multiple treatments for a single disease can be tested simultaneously. As of August 2023, two protocols are active. RECOVER-VITAL will test whether a longer course of Paxlovid, an antiviral drug used to treat acute SARS-CoV-2 infection, is also effective ...
During the early stages of the Covid-19 pandemic, reports emerged that persons who had been infected with SARS-CoV-2 were having lingering health problems. Such long-term issues were collectively r...
News Release. Thursday, May 25, 2023. Large study provides scientists with deeper insight into long COVID symptoms. NIH-funded research effort identifies most common symptoms, potential subgroups, and initial symptom-based scoring system - with aim of improving future diagnostics and treatment.
Long COVID is an often debilitating illness that occurs in at least 10% of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections. More than 200 symptoms have been identified with ...
Symptoms associated with autonomic nervous system dysfunction have been among those that patients with long COVID say are most burdensome. The trials are part of the National Institutes of Health's Researching COVID to Enhance Recovery (RECOVER) Initiative, a nationwide research program to fully understand, diagnose and treat long COVID.
The Centers for Disease Control and Prevention (CDC) estimates that more than 114 million Americans had been infected with Covid-19 through March 2021. Factoring in new infections in unvaccinated ...
Many people recover quickly from COVID-19, but some do not. NIH has launched a new initiative to study long-term symptoms. The goals of the research include finding better treatments for long COVID. Chimére Smith felt her first symptoms of COVID-19 on a Sunday morning in March 2020. "It almost felt like I could feel the virus entering into ...
These effects, called post-acute sequelae of COVID-19 (or PASC), can include brain fog, fatigue, headaches, dizziness, and shortness of breath. Long COVID—when symptoms last weeks or months after the acute infection has passed—affects about 2.5% of COVID patients. While patients who were hospitalized are more susceptible, even those with ...
The Long Haul of Long Covid — ITT Episode 19 31m 41s Download. This podcast episode explores long Covid, an often-disabling but unexplained syndrome of post-acute sequelae of SARS-CoV-2. How is ...
New Long Covid trials aim to clear lingering virus—and help patients in dire need. 11 Apr 2024. 11:00 AM ET. By Jennifer Couzin-Frankel. Jaxson Riley, 9 years old, has Long Covid and is enrolled in a clinical trial. On good days, he likes to ride his motorized bike in the neighborhood with his father. Sofia Aldinio.
Mayo Clinic researchers have identified risk factors that can cause adult COVID-19 patients to suffer symptoms that linger for months or years. The condition is often referred to as long-haul COVID.The findings are reported in the Journal of Investigative Medicine.. Researchers surveyed more than 3,000 adults over the age of 18 who were treated via Mayo Clinic's virtual COVID-19 clinics in ...
One in ten severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections results in post-acute sequelae of coronavirus disease 2019 (PASC) or long coronavirus disease (COVID), which ...
A new study in Science is shining a light on the continuing impact of long COVID, with research revealing further and continuing health concerns for some of the 16 million sufferers in the U.S ...
The News. A team of scientists is proposing a new explanation for some cases of long Covid, based on their findings that serotonin levels were lower in people with the complex condition. In their ...
What is the treatment for long-haul COVID? Doctors and therapists can work with you to address symptoms. The Johns Hopkins Post-Acute COVID-19 Team (JH PACT) is a special multidisciplinary clinic to support the recovery of people who have had COVID-19, and similar clinics are emerging at other hospitals. Breathing exercises, physical therapy, medications and other treatments appear to be helpful.
Current analysis estimates that 7.7 million to 23 million Americans have developed Long COVID.. Today, U.S. Department of Health and Human Services (HHS) Secretary Xavier Becerra released the following statement applauding the formation of the Office of Long COVID Research and Practice to lead the Long COVID response and coordination across the federal government and, in addition, the National ...
Finally, scientists are making progress on long COVID. By Nancy Shute. Editor in Chief. March 31, 2024 at 7:15 am. I've been thinking about the old-fashioned term "invalid.". In the 19th ...
The survey found that in 2022, about 7% of adults - or about 1 in 14 - reported ever having long COVID. More women reported having had long COVID than men - a trend also observed in children ...
Either mild or severe COVID-19 can lead to long-lasting symptoms. Long COVID, long-haul COVID, post-COVID-19 condition, chronic COVID, and post-acute sequelae of SARS-CoV-2 (PASC) are all names for the health problems that some people experience a few months after a COVID-19 diagnosis. Symptoms of Long COVID may be the same as or different than ...
What may drive or predict the persistence of long-term symptoms, also known as "post-acute sequelae of COVID-19," remains poorly understood. A study published June 10 in the journal JCI Insight may provide answers about this mysterious condition. The study, led by Hyung J. Chun, MD, an associate professor of cardiovascular medicine and ...
The new research hints at "some underlying immune dysregulation in the lung itself," Hollenbach says, suggesting an abnormal immune response to COVID might be causing the long-term harm.
Three new studies shed new light on long COVID in the United States, with one finding that two thirds of severely ill patients reported persistent impairments for up to 1 year, another showing that US veterans were at three times the risk of preventable hospitalization in the month after infection, and the last revealing that one third of COVID-19 survivors had lingering symptoms at one time.
Prevention Researchers say this could lead to diagnostic tests and treatments.. Long COVID has mystified the medical community for years, making it a tough condition to diagnose, let alone treat. However, a growing body of research has found more information on what may be behind long COVID, with the hope of eventually finding an effective treatment.. Now, a new study has made an interesting ...
Long COVID is broadly defined as signs, symptoms, and conditions that continue or develop after acute COVID-19 infection. This definition of Long COVID was developed by the Department of Health and Human Services (HHS) in collaboration with CDC and other partners. People call Long COVID by many names, including Post-COVID Conditions, long-haul ...
Organ damage could play a role. People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. Inflammation and problems with the immune system can also happen. It isn't clear how long these effects might last. The effects also could lead to the development of new conditions, such as ...
Rates of long COVID have begun to flatten. About 1 in 10 adults with COVID have reported having long COVID since rates fell in 2023, according to a KFF analysis of the latest data from the Centers ...
The new book "The Long Haul" is about the little guy finding a way to make democracy work to solve a problem. To the millions of patients with Long Covid, who have lived with up to four years of ...
An advocacy group called Patient-Led Research for COVID-19 released its first report in May 2020, to provide an in-depth look at the experiences of more than 600 COVID-19 long-haulers.