

The Ultimate Patient Case Presentation Template for Med Students
- April 6, 2024
- Reviewed by: Amy Rontal, MD

Knowing how to deliver a patient presentation is one of the most important skills to learn on your journey to becoming a physician. After all, when you’re on a medical team, you’ll need to convey all the critical information about a patient in an organized manner without any gaps in knowledge transfer.
One big caveat: opinions about the correct way to present a patient are highly personal and everyone is slightly different. Additionally, there’s a lot of variation in presentations across specialties, and even for ICU vs floor patients.
My goal with this blog is to give you the most complete version of a patient presentation, so you can tailor your presentations to the preferences of your attending and team. So, think of what follows as a model for presenting any general patient.
Here’s a breakdown of what goes into the typical patient presentation.
Looking for some help studying your shelf/Step 2 studying with clinical rotations? Try our combined Step 2 & Shelf Exams Qbank with 5,500 practice questions— free for 7 days!
7 Ingredients for a Patient Case Presentation Template
1. the one-liner.
The one-liner is a succinct sentence that primes your listeners to the patient.
A typical format is: “[Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y].
2. The Chief Complaint
This is a very brief statement of the patient’s complaint in their own words. A common pitfall is when medical students say that the patient had a chief complaint of some medical condition (like cholecystitis) and the attending asks if the patient really used that word!
An example might be, “Patient has chief complaint of difficulty breathing while walking.”
3. History of Present Illness (HPI)
The goal of the HPI is to illustrate the story of the patient’s complaint. I remember when I first began medical school, I had a lot of trouble determining what was relevant and ended up giving a lot of extra details. Don’t worry if you have the same issue. With time, you’ll learn which details are important.
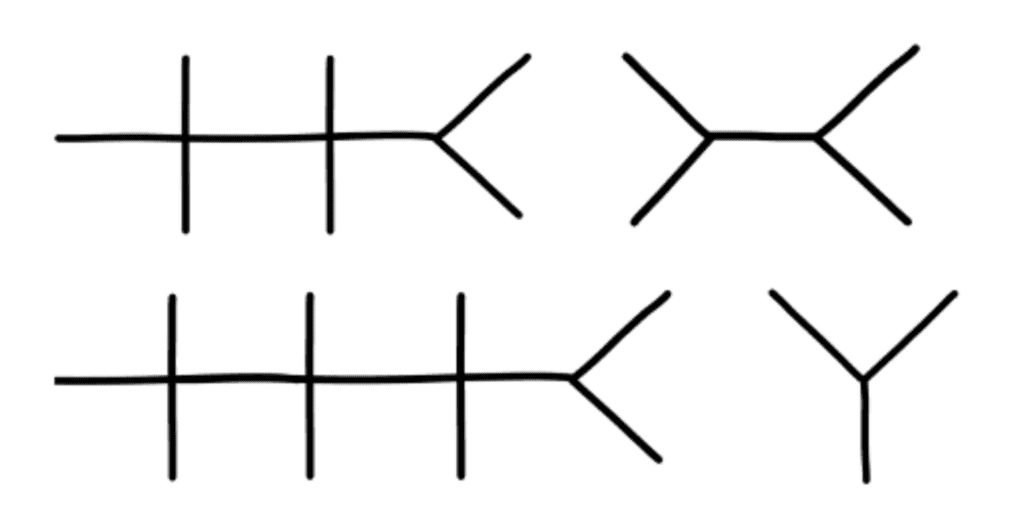
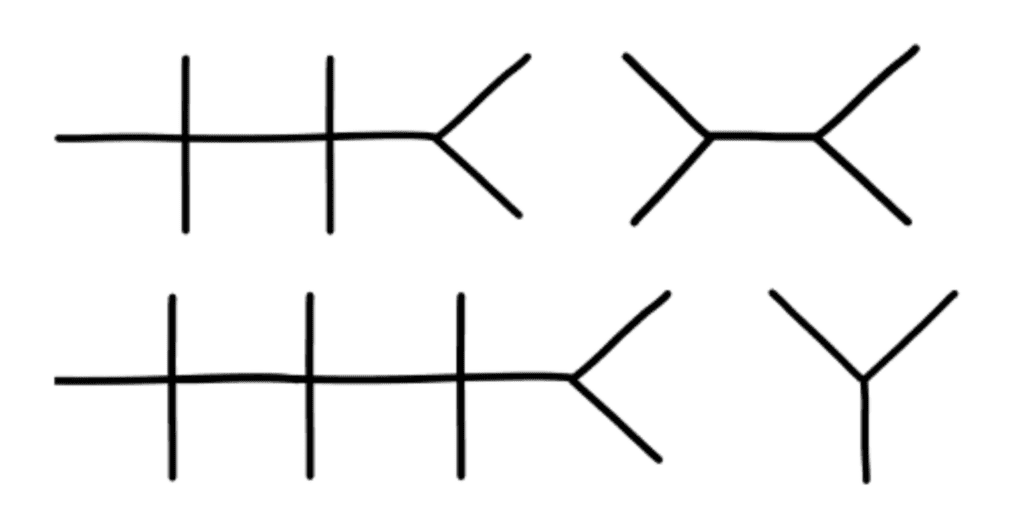
The OPQRST Framework
In the beginning of your clinical experience, a helpful framework to use is OPQRST:
Describe when the issue started, and if it occurs during certain environmental or personal exposures.
P rovocative
Report if there are any factors that make the pain better or worse. These can be broad, like noting their shortness of breath worsened when lying flat, or their symptoms resolved during rest.
Relay how the patient describes their pain or associated symptoms. For example, does the patient have a burning versus a pressure sensation? Are they feeling weakness, stiffness, or pain?
R egion/Location
Indicate where the pain is located and if it radiates anywhere.
Talk about how bad the pain is for the patient. Typically, a 0-10 pain scale is useful to provide some objective measure.
Discuss how long the pain lasts and how often it occurs.
A Case Study
While the OPQRST framework is great when starting out, it can be limiting. Let’s take an example where the patient is not experiencing pain and comes in with altered mental status along with diffuse jaundice of the skin and a history of chronic liver disease. You will find that certain sections of OPQRST do not apply.
In this event, the HPI is still a story, but with a different framework. Try to go in chronological order. Include relevant details like if there have been any changes in medications, diet, or bowel movements.
Pertinent Positive and Negative Symptoms
Regardless of the framework you use, the name of the game is pertinent positive and negative symptoms the patient is experiencing. I’d like to highlight the word “pertinent.” It’s less likely the patient’s chronic osteoarthritis and its management is related to their new onset shortness of breath, but it’s still important for knowing the patient’s complete medical picture. A better place to mention these details would be in the “Past Medical History” section, and reserve the HPI portion for more pertinent history.
As you become exposed to more illness scripts, experience will teach you which parts of the history are most helpful to state. Also, as you spend more time on the wards, you will pick up on which questions are relevant and important to ask during the patient interview. By painting a clear picture with pertinent positives and negatives during your presentation, the history will guide what may be higher or lower on the differential diagnosis.
Some other important components to add are the patient’s additional past medical/surgical history, family history, social history, medications, allergies, and immunizations.
The HEADSSS Method
Particularly, the social history is an important time to describe the patient as a complete person and understand how their life story may affect their present condition.
One way of organizing the social history is the HEADSSS method: – H ome living situation and relationships – E ducation and employment – A ctivities and hobbies – D rug use (alcohol, tobacco, cocaine, etc.) Note frequency of use, and if applicable, be sure to add which types of alcohol consumption (like beer versus hard liquor) and forms of drug use. – S exual history (partners, STI history, pregnancy plans) – S uicidality and depression – S piritual and religious history Again, there’s a lot of variation in presenting social history, so just follow the lead of your team. For example, it’s not always necessary/relevant to obtain a sexual history, so use your judgment of the situation.
4. Review of Symptoms
Oftentimes, most elements of this section are embedded within the HPI. If there are any additional symptoms not mentioned in the HPI, it’s appropriate to state them here.
5. Objective
Vital signs.
Some attendings love to hear all five vital signs: temperature, blood pressure (mean arterial pressure if applicable), heart rate, respiratory rate, and oxygen saturation. Others are happy with “afebrile and vital signs stable.” Just find out their preference and stick to that.
Physical Exam
This is one of the most important parts of the patient presentation for any specialty. It paints a picture of how the patient looks and can guide acute management like in the case of a rigid abdomen. As discussed in the HPI section, typically you should report pertinent positives and negatives.
When you’re starting out, your attending and team may prefer for you to report all findings as part of your learning. For example, pulmonary exam findings can be reported as: “Regular chest appearance. No abnormalities on palpation. Lungs resonant to percussion. Clear to auscultation bilaterally without crackles, rhonchi, or wheezing.”
Typically, you want to report the physical exams in a head to toe format: General Appearance, Mental Status, Neurologic, Eyes/Ears/Nose/Mouth/Neck, Cardiovascular, Pulmonary, Breast, Abdominal, Genitourinary, Musculoskeletal, and Skin. Depending on the situation, additional exams can be incorporated as applicable.
Now comes reporting pertinent positive and negative labs. Several labs are often drawn upon admission. It’s easy to fall into the trap of reading off all the labs and losing everyone’s attention. Here are some pieces of advice:
You normally can’t go wrong sticking to abnormal lab values.
One qualification is that for a patient with concern for acute coronary syndrome, reporting a normal troponin is essential. Also, stating the normalization of previously abnormal lab values like liver enzymes is important.
Demonstrate trends in lab values.
A lab value is just a single point in time and does not paint the full picture. For example, a hemoglobin of 10g/dL in a patient at 15g/dL the previous day is a lot more concerning than a patient who has been stable at 10g/dL for a week.
Try to avoid editorializing in this section.
Save your analysis of the labs for the assessment section. Again, this can be a point of personal preference. In my experience, the team typically wants the raw objective data in this section.
This is also a good place to state the ins and outs of your patient (if applicable). In some patients, these metrics are strictly recorded and are typically reported as total fluid in and out over the past day followed by the net fluid balance. For example, “1L in, 2L out, net -1L over the past 24 hours.”
6. Diagnostics/Imaging
Next, you’ll want to review any important diagnostic tests and imaging. For example, describe how the EKG and echo look in a patient presenting with chest pain or the abdominal CT scan in a patient with right lower quadrant abdominal pain.
Try to provide your own interpretation to develop your skills and then include the final impression. Also, report if a diagnostic test is still pending.
7. Assessment/Plan
This is the fun part where you get to use your critical thinking (aka doctor) skills! For the scope of this blog, we’ll review a problem-based plan. It’s helpful to begin with a summary statement that incorporates the one-liner, presenting issue(s)/diagnosis(es), and patient stability.
Then, go through all the problems relevant to the admission. You can impress your audience by casting a wide differential diagnosis and going through the elements of your patient presentation that support one diagnosis over another. Following your assessment, try to suggest a management plan. In a patient with congestive heart failure exacerbation, initiating a diuresis regimen and measuring strict ins/outs are good starting points.
You may even suggest a follow-up on their latest ejection fraction with an echo and check if they’re on guideline-directed medical therapy. Again, with more time on the clinical wards you’ll start to pick up on what management plan to suggest.
One pointer is to talk about all relevant problems, not just the presenting issue. For example, a patient with diabetes may need to be put on a sliding scale insulin regimen or another patient may require physical/occupational therapy. Just try to stay organized and be comprehensive.

A Note About Patient Presentation Skills
When you’re doing your first patient presentations, it’s common to feel nervous. There may be a lot of “uhs” and “ums.”
Here’s the good news: you don’t have to be perfect! You just need to make a good faith attempt and keep on going with the presentation.
With time, your confidence will build. Practice your fluency in the mirror when you have a chance. No one was born knowing medicine and everyone has gone through the same stages of learning you are!
Practice your presentation a couple times before you present to the team if you have time. Pull a resident aside if they have the bandwidth to make sure you have all the information you need.
One big piece of advice: NEVER LIE. If you don’t know a specific detail, it’s okay to say, “I’m not sure, but I can look that up.” Someone on your team can usually retrieve the information while you continue on with your presentation.
Example Patient Case Presentation Template
Here’s a blank patient case presentation template that may come in handy. You can adapt it to best fit your needs.
One-Liner:
Chief Complaint:
History of Present Illness:
Past Medical History:
Past Surgical History:
Family History:
Social History:
Medications:
Immunizations:
Objective:
Vital Signs :
BP ___ /___
O2 sat ___
Physical Exam:
General Appearance:
Mental Status:
Neurological:
Eyes, Ears, Nose, Mouth, and Neck:
Cardiovascular:
Genitourinary:
Musculoskeletal:
Most Recent Labs:
Previous Labs:
Diagnostics/Imaging:
Impression/Interpretation:
Assessment/Plan:
One-line summary:
#Problem 1:
Assessment:
#Problem 2:
Final Thoughts on Patient Presentations
I hope this post demystified the patient presentation for you. Be sure to stay organized in your delivery and be flexible with the specifications your team may provide. Something I’d like to highlight is that you may need to tailor the presentation to the specialty you’re on. For example, on OB/GYN, it’s important to include a pregnancy history.
Nonetheless, the aforementioned template should set you up for success from a broad overview perspective. Stay tuned for my next post on how to give an ICU patient presentation. And if you’d like me to address any other topics in a blog, write to me at [email protected] !
Looking for more (free!) content to help you through clinical rotations? Check out these other posts from Blueprint tutors on the Med School blog:
- How I Balanced My Clinical Rotations with Shelf Exam Studying
- How (and Why) to Use a Qbank to Prepare for USMLE Step 2
- How to Study For Shelf Exams: A Tutor’s Guide
About the Author
Hailing from Phoenix, AZ, Neelesh is an enthusiastic, cheerful, and patient tutor. He is currently an Integrated Cardiothoracic Surgery Resident at The Ohio State University. He graduated from the Keck School of Medicine of the University of Southern California and served as president for the Class of 2024. He also graduated as valedictorian of his high school and the USC Viterbi School of Engineering, obtaining a B.S. in Biomedical Engineering in 2020. He discovered his penchant for teaching when he began tutoring his friends for the SAT and ACT in the summer of 2015 out of his living room. Outside of the academic sphere, Neelesh enjoys surfing and camping. Twitter: @NeeleshBagrodia LinkedIn: http://www.linkedin. com/in/ neelesh -bagrodia

Related Posts
How to Study For Shelf Exams: A Tutor’s Guide
- May 6, 2024

The Ultimate ICU Patient Presentation Template for Med Students
- May 3, 2024

Quiz: Which “Scrubs” Character Are You in Your Clinical Rotations?
- March 26, 2024

Clinical Case Study
Ai generator.

In 1970, the world first got acquainted with Genie. It was also the little girl’s first time to see a world beyond the potty chair where she was often bound to. Barely a contact outside for most of her life, she was a ripe case for studying the effects of extreme isolation in young children. Clinical case studies shed light on rare and specific circumstances, like Genie’s ordeal, that help us understand the bigger picture. Largely qualitative research , these case studies are an attempt to understand a subject and the case, usually in relation to a general concept.
8+ Clinical Case Study Templates and Examples
Clinical case studies can focus on a person, group, or community. In contrast to case reports , these studies don’t end in reporting about the diagnosis, treatment, and follow-up of patients. Case studies abide by the research methodology and design to understand an experience. During a case study analysis, both subjective and objective accounts of the events are deemed valid data. By focusing on a pixel of the picture, you can learn something that you would have otherwise overlooked. We have prepared the following case study templates that you can use in your research. For your reference, we added examples of scenarios where clinical case studies are being used.
1. Case Study Analysis Template
- Google Docs
Size: A4 & US Letter Sizes
Case studies are a common method of research in medical and psychological sciences. They are vivid narratives about undocumented cases that strike researchers as irregular and interesting. Their highly descriptive content are valuable information to the respective scientific community. They also open new avenues of inquiry and offer an in-depth treatment of a topic that empirical research cannot give. Its comprehensive nature helps make case study a popular research option, even if it falls short of evidence-based data. Thinking of using this research method? Get started with this template!
2. Clinical Case Study Template
Size: 49 KB
Since the studies contain detailed accounts, you have to format all the information into categories. The defined structure of the article makes all the information easy to absorb. A case study generally contains the following sections: abstract, introduction, patient information, review of related literature, methodology , findings, then the conclusion. The comprehensive nature of this research method might deter novice researchers, while veteran medical writers might just need a reminder. In either case, this sample outline is for you!
3. Clinical Case Study Sample

Size: 939 KB
This research method is usable in answering different inquiries. It is notable that case studies are heavy on the qualitative data. Researchers can obtain relevant data from interviews, questionnaires , personal and patients’ observations, journals, clinical reports, and existing literature. However, as seen in this attached example, quantitative data can also be collected as the researchers deem fit. Because the goal is not to derive data that can represent a population, researchers can use a smaller sample size. Study how to make both numbers and descriptions work to your advantage in preparing your clinical case study with this example!
4. Medical Case Study Example

Size: 563 KB
In a physician’s life, he or she is bound to come across a case that medical school and textbooks did not warn him or her. Clinical case studies are a form of communication about novel findings or observations in practice. Sort of like a medical buzz, the studies contain information like unreported health complications, adverse response to treatment, or new remedial methods. These case studies can also branch into new research directions. This case study illustrates how misdiagnosis can be harmful to the patient. Because some diseases can have overlapping symptoms, it can be hard to identify which is which. The case study alerted the medical community that a seemingly mundane skin condition can point to something more serious.
5. Psychological Case Study Example
Size: 425 KB
In the field of psychology, clinic psychologists and therapists can report about their interactions with the patient. Some of these cases can stand out as rare and unusual. Others may also serve as a useful reference. Practitioners can obtain information through semi-structured interviews wherein the patient talks with a mental health professional. After the sessions, the practitioner can interpret his or her findings into diagnosis and recommend a treatment plan . Psychology is not entirely removed from medicine. The specialist can incorporate the medical history of the patient in his or her interpretation. This sample case study shows medicine and psychology can work together in the prevention of stress-induced asthma attacks.
6. Sample Clinical Case Study

Size: 85 KB
The descriptive take of clinical case studies on a situation presents an exhaustive analysis that is not available in empirical research. However, the qualitative nature of these studies is a double-edged sword. The combination of subjective and objective analysis makes the content susceptible to personal biases. Because the case is unique to an individual or a group, researchers cannot replicate the result. The replicability of findings is a hallmark of reliable research. Therefore, clinical case studies have a low-reliability measure. The attached case study is an example of the use of descriptive analysis in the diagnosis and treatment of a patient with depression and adjustment disorder with mixed anxiety.
7. Medical Case Study Guide

Size: 266 KB
Another point raised against clinical case studies is the issue of memory distortion. The human memory is not a machine that can record and retrieve information at command. It is fallible, and it will make mistakes. The patients can emphasize a few parts of their history and overlook otherwise important pieces of the puzzle. Reliance on memory recall when writing the study can also fail the researchers. The sample clinical case study added here shows how a patient’s recollection of events in her life can be used in the presentation of the case. If the patient failed to recall important details, the researchers might have a different interpretations of the case.
8. Student Medical Case Study

Despite criticisms regarding susceptibility to biases and low-reliability measure, clinical case studies have been an indispensable tool for learning. Studies have reported a significant improvement in the academic performance of students after the integration of case studies into the learning ecosystem. Case studies are situation-based narratives about a textbook principle. Application-motivated learning is effective because the theoretical framework isn’t removed from the real-world experience. This case study is an example of those that are used in the classroom. The students are presented with a problem and series of follow up questions that will help them understand and address the issues exhibited.
9. Clinical Case Study Article
Size: 171 KB
Unlike empirical investigations, the goal is not to come up with results that can represent a population. Case studies focus on understanding an unusual plight through subjective and objective analysis. Understandably, such situation might not hold for most people. They are also the method of choice for understanding circumstances that cannot be reproduced in controlled testing environments, like Genie’s case earlier or the case discussed in the attached case study sample. Therapy for anorexia nervosa and obsessive personality disorder is hard to come by using quantitative research. Replicating such conditions will constitute a criminal offense. What case studies lack in the universality of the results, they make up for the richness of the insights obtained. It acknowledges that the human experience will always have a degree of subjectivity. This defense of clinical case studies makes them significant in their own right.
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting

IMAGES
VIDEO
COMMENTS
Presenting patient cases is a key part of everyday clinical practice. A well …
Presentation of Case. Dr. Daniel A. Zlotoff: A 44-year-old woman was admitted to this hospital because of shortness of breath and chest pain.
Enhance medical presentations with our Case Presentation Templates. …
Here are the 7 parts of a patient case presentation template, plus some advice …
Define a patient case presentation. List the typical information included in a patient case …
clinical case presentation – guidelines ‘He who studies medicine without books sails an …
Clinical case studies are a form of communication about novel findings or observations in practice. Sort of like a medical buzz, the studies contain information like unreported health complications, adverse response to …