Hormonal contraception: practice-based case studies
The wide range of hormonal contraception available means that patients can present with a range of problems or concerns that require advice or assessment

Burger/Phanie/REX
Combined oral contraceptives are contraindicated in patients who have migraines and smokers aged over 35 years.
‘Quick start’ regimens, in which regular contraception is started before the woman’s next ‘normal’ period, are available if the woman needs to start contraception immediately. These are also useful for women with irregular menstrual cycles, where such a wait is impractical. Quick start regimens are outside the product licences for hormonal contraception products.
Any woman with unscheduled vaginal bleeding needs to check whether she is pregnant, have a risk assessment or tests for sexually transmitted infections, and a vaginal examination, which should include a cervical smear to rule out cancer.
Most methods of contraception are safe and effective but some may have troublesome side effects. It is therefore important to have a woman’s preferences in mind when recommending a method of contraception, and inform her of the trade-offs of each option so that she can make a choice that is right for her and her circumstances.
This article will use theoretical case studies to illustrate common problems associated with contraception and treatment options to consider.

Case study 1: smoker with headaches
Agnetha Perry is 36 years old and she has been taking Ovranette (ethinylestradiol 30µg and levonorgestrel 150µg; Pfizer) for six months. She has no personal or family history of heart disease or venous thromboembolism (VTE). She stopped smoking over a year ago, but has recently started to smoke again because of stress at work. She now smokes 20 cigarettes a day. She has noticed some bad headaches; sometimes she has to take time off work because of them. She is not sure what is causing her headaches. She has just seen the practice nurse at her GP surgery to get a repeat prescription. Her blood pressure at check-up was 120/67mmHg and her body mass index (BMI) was 27. Should she continue on Ovranette?
Ovranette is a combined oral contraceptive (COC). According to the UK Medical Eligibility Criteria (UK MEC), a history of non-migrainous headache is not a contraindication to starting or continuing with the COC [1] . However, if she were to have migraine with aura, it may no longer be safe for her to continue as this is a UK MEC category 3 condition for COCs, where the theoretical or proven risks generally outweigh the advantages of using the method (See ‘Hormonal contraception: methods and patient eligibility’).
Agnetha has a lso started smoking again. This would not be a problem if she were aged under 35 years, which would be UK MEC 2 for COCs. However, this has put her in UK MEC 4 for COCs, as it would increase her risk of cardiovascular d isease.
Agnetha should be advised to speak to her GP or a specialist to discuss changing from a COC to an oestrogen-free method of contraception, all of which would be suitable for this patient.
Case study 2: regular EHC use
Bethany Chang is 19 years old and requests the ‘morning after pill’ from you. Your records show she has had two prescriptions for emergency hormonal contraception (EHC) dispensed in the past three months. She is not on regular contraception as she says she is too forgetful to take the pill and, since she is not with a regular partner, she does not feel she needs to go on a long-term method. What would you cover in your discussion?
There are three issues that might need to be covered: immediate need for emergency contraception; future contraception; and risk of sexually transmitted infections.
First, establish if Bethany is suitable for levonorgestrel, ulipristal acetate or copper intrauterine device for emergency contraception. If her last unprotected sexual intercourse was <72 hours ago and she has not had sex since her last normal menstrual period, she can be given levonorgestrel as emergency contraception. If she last had sex more than 72 hours but less than 120 hours ago, ulipristal acetate might be suitable. Copper intrauterine device is the only option if she had sex more than five days ago [2] .
Bethany is at risk of sexually transmitted infections (STIs) as she is young, does not have a regular partner and may have unprotected sex. No method of contraception apart from condoms protects against STIs., and she may need a check-up at a sexual health clinic. In 2013, more than 1.7 million chlamydia tests were carried out in England among young people aged 15–24 years, with over 139,000 chlamydia diagnoses made [3] . In addition, the intrauterine device is contraindicated in women with a current chlamydial or gonorrhoeal infection (UK MEC 4).
Bethany may wish to try long acting reversible contraceptives (LARCs) such as the progestogen-only injection, progestogen-only implant, and either of the intrauterine methods. If she chose the copper intrauterine device for emergency contraception, she could keep it in situ for regular contraception.
If Bethany does want to start regular contraception, she may be eligible for a ‘quick start’ regimen, in which regular contraception is started before the woman’s next ‘normal’ period. These are also useful for women with irregular menstrual cycles, where such a wait is impractical. Quick start regimens are outside the product licences for hormonal contraception products.
The UK Faculty of Sexual and Reproductive Healthcare has produced clinical guidance on quick start regimens [4] . Most contraceptives (with the exception of the levonorgestrel intrauterine device), can be used in a quick start regimen [3] .
These patients need to take extra contraceptive precautions; for seven days if using levonorgestrel EHC (two days if starting a progestogen-only pill), or 14 days if using ulipristal acetate (nine days if starting a progestogen-only pill). This longer period is required because ulipristal acetate is a progestogen antagonist, and in theory could reduce the efficacy of progestogen-containing contraceptives.
As pregnancy cannot be reasonably excluded when quick starting at the time of using EHC, healthcare professionals should ensure that the woman is:
- Likely to continue to be at risk of pregnancy or she has requested to start contraception immediately;
- Aware that EHC is not totally effective and she may be pregnant;
- Informed that there may be a theoretical risk to a foetus from exposure to contraceptive hormones, but evidence suggests no harm;
- Aware that a pregnancy test has to be taken no sooner than three weeks after last unprotected sexual intercourse to reliably exclude pregnancy and knows where to obtain test kits;
- Offered alternative forms of contraception (e.g. condoms);
- Invited to return if she has any concerns or problems with the contraception.
Case study 3: risk of venous thromboembolism
Caroline Pelton is 35 years old and has been using Marvelon (ethinylestradiol 30µg and desogestrel 150µg; MSD) for a few years. She was started on doxycycline for her acne by her GP and she is concerned about it interfering with her contraceptive. Caroline is also taking sodium valproate for epilepsy, and has not had a seizure for five years. She read online that Marvelon increases her risk of blood clots. She is now very concerned and wonders if she should change her contraception.
Marvelon contains desogestrel, a third-generation progestogen. Some newer generations of progestogens are associated with increased risk of VTE but the absolute risk is still small. The risk of VTE in women not using contraception and who are not pregnant is 2 per 10,000 healthy women a year (see ‘Risk of venous thromboembolism with combined hormonal contraceptives’); this rises to 5–7 per 10,000 for women who use combined hormonal contraception (CHC) containing levonorgestrel, and 9–12 per 10,000 in women who use CHC containing desogestrel [5] .
Her absolute risk of VTE while taking Marvelon is still small. Her risk would increase further if she were to become pregnant, have surgery, have a period of immobilisation, malignancy and if she had inherited conditions (e.g. factor V Leiden mutation). Given the potential risks and benefits, she can be advised to continue with Marvelon.
There are some anticonvul sants and antibiotics (e.g. rifampicin and rifabutin) that reduce the efficacy of CHCs, progestogen-only pills and contraceptive implants due to their effect as enzyme inducers. Anticonvulsants that are strong enzyme inducers include carbamazepine, phenytoin and primidone; sodium valproate has no significant effects on the efficacy of CHC and Caroline does not need to change her treatment. Enzyme inducers are not known to effect depot medroxyprogesterone acetate or intrau terine devices, but may affect the etonogestrel implant.
Doxycycline does not affect the efficacy of CHCs, and Caroline can continue her treatment as prescribed. Alternatively, the CHC co-cyprindiol (ethinylestradiol and cyproterone acetate) is licensed for the treatment of acne that has not responded to oral antibiotics. It is associated with higher VTE risk so patients should be switched to another contraceptive three to four months after the acne has resolved [6] .
Case study 4: concern about irregular bleeding
Debbie Winger is a 33 year old woman who has been using the depot medroxyprogesterone acetate injection for contraception for almost a year. She is not happy with it because she thinks it is causing her a lot of irregular bleeding. She is a non-smoker with no personal or family history of VTE or cardiovascular disease. She had a repeat dose two months ago. At that time her blood pressure was 110/55mmHg and her weight had increased by 13kg since starting, making her BMI almost 30. She was prescribed a pack of Microgynon (levonorgestrel 150µg) to help with the irregular bleeding (to ‘add back’ oestrogen). She had no side effects with Microgynon and asks if it is possible to switch.
Unscheduled bleeding is not uncommon [7] with progestogen-only contraception, including depot medroxyprogesterone acetate. Up to 70% of women using depot medroxyprogesterone acetate can become amenorrhoeic after one year. It is the only form of hormonal contraception associated with weight gain, but only in women under 18 years with a BMI >30 [8] .
Any woman with unscheduled vaginal bleeding needs to check whether she is pregnant, have a risk assessment or tests for STIs, and a vaginal examination, which should include a cervical smear to rule out cancer. A COC with 30–35µg of ethinylestradiol with levonogestrel or norethisterone enanthate may be used for up to three months continuously or in the usual cyclical regimen to regulate bleeding; this is an unlicensed indication [9] .
Debbie does not have contraindications for use of a COC so she can discontinue her injections and continue using Microgynon; a BMI of 30–34 is a UK MEC category 2 for COCs. She does not need to take extra precautions when she stops her injections as she is covered by the COC.
Richard Ma is a GP principal in London, and NIHR In-Practice Fellow at Imperial College, London.
How to have effective consultations on contraception in pharmacy
What benefits do long-acting reversible contraceptives offer compared with other available methods?
Community pharmacists can use this summary of the available devices to address misconceptions & provide effective counselling.
Content supported by Bayer
[1] Faculty of Sexual and Reproductive Healthcare. UK Medical Eligibility Criteria for contraceptive use. London: Faculty of Sexual and Reproductive Healthcare 2009.
[2] Faculty of Sexual and Reproductive Healthcare. Faculty of Sexual and Reproductive Healthcare Clinical Guidance — emergency contraception. London: Faculty of Sexual and Reproductive Healthcare, 2012.
[3] Public Health England. Sexually transmitted infections. Annual data tables 2013 . London: PHE 2013.
[4] Faculty of Sexual and Reproductive Healthcare. Faculty of Sexual and Reproductive Healthcare Clinical Guidance — quick starting contraception. London: Faculty of Sexual and Reproductive Healthcare; 2010.
[5] Faculty of Sexual and Reproductive Healthcare. Venous thromboembolism (VTE) and hormonal contraception. London: Faculty of Sexual and Reproductive Healthcare 2014.
[6] Faculty of Sexual and Reproductive Healthcare. Faculty of Sexual and Reproductive Healthcare Clinical Guidance — combined hormonal contraception. London: Faculty of Sexual and Reproductive Healthcare 2011.
[7] Kovacs G. Progestogen-only pills and bleeding disturbances. Hum Reprod 1996;11(Suppl 2):20–23.
[8] Faculty of Sexual and Reproductive Healthcare. Faculty of Sexual and Reproductive Healthcare Clinical Guidance — progestogen-only injectable contraception . London: Faculty of Sexual and Reproductive Healthcare 2015.
[9] Faculty of Sexual and Reproductive Healthcare. Management of unscheduled bleeding in women using hormonal contraception. London: Faculty of Sexual and Reproductive Healthcare, Royal College of Obstetricians and Gynaecologists 2009.
You might also be interested in…
Hormonal contraception: methods and patient eligibility

Half of all trusts could be using electronic prescription service by 2026, says NHS England

Pharmacy regulator to consider supporting surveys of registrants’ wellbeing
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
Contributor Disclosures
Please read the Disclaimer at the end of this page.
INTRODUCTION — The choice of a contraceptive method is a complex decision; medical providers have an important role in providing information and supporting patients' decision-making about contraceptive methods through contraceptive counseling. In this topic, we will review the goals of quality contraceptive counseling, review different approaches to this counseling and their relationship to health equity, and provide a step-by-step guide to providing high-quality, patient-centered counseling. Information specific to each contraceptive method is presented in detail separately.
In this topic, we will focus on the counseling needs of those with the potential for pregnancy; specifically, all individuals with a uterus and ovaries, regardless of gender. We encourage the reader to consider the specific counseling needs of transgender and gender expansive individuals [ 1 ]. Clinicians should ask all patients who identify as male about their contraceptive needs as well. (See 'Special populations' below.)
GOALS — In broad strokes, the provision of family planning care is designed to help individuals achieve their reproductive goals. However, data suggest that family planning care should not have a singular focus of preventing unintended pregnancy, as this is not consistent with all patients' preferences or necessary to optimize health outcomes. Rather, providers can focus on people reach their desired reproductive outcomes by supporting them to make informed decisions about their fertility and contraceptive use that are aligned with their preferences and reproductive goals ( table 1 ).
HOW TO DO CONTRACEPTIVE COUNSELING — The steps for providing patient-centered contraceptive counseling using shared decision-making are laid out in the figure ( figure 1 ) and detailed below.
Personalized counseling with shared decision-making — Contraceptive counseling has evolved from either 1) providing clinical data on methods with no decision support or 2) directive counseling for specific methods to a shared conversation between patient and clinician that incorporates patient preferences into the selection process.
● Shift to shared decision-making – Contraceptive counseling has evolved from either clinician-level directive counseling toward the mostly highly effective methods or provision of education to personalized counseling using shared decision-making [ 2-5 ]. This approach, which is considered ideal for preference-sensitive decisions that are highly dependent on individual values and needs, is designed to assist patients in making the best decision for themselves [ 6,7 ].
In shared decision-making, patients are acknowledged as the experts on their preferences, while providers contribute their medical knowledge about the different options and the ways in which they relate to patients' preferences [ 5 ]. In this way, patient autonomy and the diversity of preferences for contraceptive method characteristics can be respected, while at the same time, patients are offered support in aligning their preferences with the available options ( table 1 ).
Interventions to promote shared decision-making have been reported to improve patients' ability to make decisions that are informed and consistent with their values and to increase patient knowledge [ 8,9 ]. Research in contraception specifically has found that patients are more satisfied with the counseling experience and their method when they experience shared decision-making [ 10 ]. Initial studies suggest that telehealth visits can be as effective as in-person ones for contraceptive care [ 11 ].
● Incorporation of patient-centered care – A shift toward personalized counseling is consistent with the increasing emphasis on providing patient-centered care, which is defined by the National Academy of Medicine as care that is "respectful of, and responsive to, individual patient preferences, needs, and values" [ 12 ]. In addition to the ethical reasons for providing this type of care [ 13 ], in the context of family planning, the receipt of patient-centered care is also likely to positively impact patients' long-term health care engagement and outcomes. Evidence of long-term impact is provided by studies reporting that receiving patient-centered contraceptive counseling focused on individual preferences is associated with continuing a chosen contraceptive method and using a highly or moderately effective method six months after the visit [ 14 ]. Conversely, patients who felt pressured during contraceptive counseling reported being less likely to engage with future reproductive health care [ 15 ].
● Earlier counseling models – Prior counseling approaches focused on patient autonomy and contraceptive efficacy. These points have been incorporated into the shared decision-making model.
• Menu-based approach – An alternative approach to contraceptive counseling that is frequently discussed, especially in the context of low- and middle-income countries [ 16 ], is a menu, or consumer-driven, approach, in which the provider's role is only to provide education and not to influence decision-making [ 2 ]. While this approach is focused on patient autonomy, research has found that many women in fact value receiving support from providers in the decision-making process, as opposed to being left to make the decision on their own [ 17-21 ].
• Highly effective methods – Over the last decade, there has also been a movement toward directive models of counseling focused on promoting use of the most highly effective methods. These approaches have included applying motivational interviewing, a patient-centered directive counseling model developed in the context of addiction medicine, to contraceptive counseling designed to motivate use of specific methods [ 22 ]. Another prominent model has been a "tiered effectiveness" approach, which structures counseling according to the effectiveness of methods, with a corresponding emphasis on those that are most effective [ 23 ]. These approaches are not ideally patient-centered in that they do not prioritize patients' preferences for method characteristics and they make assumptions about the relative importance of effectiveness at preventing pregnancy.
Establish rapport — While a positive interpersonal relationship is essential for all aspects of medical care, it is of particular relevance in contraceptive counseling given its personal and sensitive context [ 17 ]. Communication behaviors, such as greeting patients warmly and making small talk, have been associated with contraceptive continuation [ 14 ], further indicating that this is an essential component of the contraceptive counseling encounter. We advise all providers to consciously incorporate small talk into the beginning of their visit to establish a positive therapeutic relationship with their patient.
Identify patient-centered reproductive goals — The first step in providing patient-centered contraceptive counseling is identifying patients for whom this counseling is appropriate [ 5 ]. In our practice, we ask patients if they wish to discuss contraception or pregnancy prevention ( table 2 ).
● Identify patients who wish to discuss contraception or pregnancy prevention – To address the limitations of the approaches below, we encourage the use of the question "Do you want to discuss contraception or pregnancy prevention at your visit today?" as means of identifying those who may become pregnant and who would wish to discuss contraceptive options. Follow-up discussion could address those patients with unsure or ambivalent answers to help them receive the care that best meets their needs, as well as those patients who already have their pregnancy needs meet, whether through sterilization or other means of pregnancy prevention.
● One key question – A modified version of the Centers for Disease Control and Prevention's (CDC) reproductive life plan approach (bullet below) is the commonly cited "One Key Question" in which patients are asked if they would like to become pregnant in the next year [ 24 ]. This is responsive to some criticisms of the CDC's reproductive life planning model (bullet below) because it limits the time frame under consideration and also incorporates the possibility that patients may not have defined intentions through response options of "okay either way" or "unsure." However, it is not ideal for identifying patients' current need for contraceptive counseling, as someone who wishes to become pregnant in the next year may still desire birth control now, those who do not actively desire pregnancy may prefer not to use contraception, and individuals who do not wish to become pregnant may not be at risk for pregnancy due to previous sterilization or not having sex that could result in pregnancy (eg, having sex with an individual who does not produce sperm).
● Reproductive life plan – The CDC has promoted the use of a "Reproductive Life Plan" approach, in which individuals of reproductive age define how many children they wish to have, and when, as a means of determining which services (eg, preconception care, contraceptive care) are appropriate for an individual [ 25 ]. This approach has been criticized as being overly proscriptive and not reflecting the ways in which people develop and modify their reproductive goals over time, including the potential of welcoming an unintended pregnancy [ 26 ].
Opportunity for preconception counseling — In addition to identifying those who wish to use contraception, family planning providers have the opportunity to identify those in need of counseling related to the impact of their health and health behaviors on future pregnancies (eg, "preconception care"). Recommendations from the CDC and others encourage providing preconception counseling at all visits with women of reproductive age [ 27-29 ]. As this can be difficult in time-limited encounters, such assessments can be prioritized for those with chronic medical conditions or with social or environmental risks or exposures. (See "The preconception office visit" .)
Providers can ask additional questions beyond the immediate need for contraception to identify those for whom counseling related to future reproduction may be appropriate. One approach that has been suggested is using the "PATH" questions [ 26 ], which address pregnancy attitudes and timing in a patient-centered way that acknowledges that many patients will not have a well-defined plan. The PATH questions are:
● P regnancy A ttitudes – Do you think you might like to have (more) children at some point?
● T iming – If the patient is considering future parenthood: When do you think that might be?
● H ow important is prevention – How important is it to you to prevent pregnancy (until then)?
Document medical history/potential contraindications — Once a patient is identified as being appropriate for and desirous of contraceptive counseling, providers can then assess for medical conditions that could affect the safety of specific methods. Common medical conditions to consider include smoking status, cardiovascular conditions (eg, hypertension or history of venous thrombosis), and history of migraine with aura [ 30 ].
Both the World Health Organization (WHO) and the CDC maintain evidence-based recommendations for use of contraceptive methods in the context of a range of medical conditions and personal characteristics [ 31,32 ]. The World Health Organization Medical Eligibility Criteria for Contraceptive Use and the US Medical Eligibility Criteria for Contraceptive Use are freely available, easy to use, and provide contraceptive prescribers with definitive guidance on safety across a broad range of conditions for different patient populations. Both label contraceptive methods as category 1, 2, 3, or 4 for each identified condition; those in categories 1 and 2 are considered generally safe and category 4 methods are contraindicated. For those classified as category 3, the recommendations state that the "method is usually not recommended unless other more appropriate methods are not available or acceptable." Importantly, this guidance takes into account whether another method that may be class 1 or class 2 is "acceptable" to the individual patient, and therefore, a category 3 rating should not discourage prescribing that method for a patient who has been informed of the risks and who determines that this method is the most acceptable for them.
Related topics on contraception selection in patients with specific health issues include:
● (See "Contraception: Counseling for women with inherited thrombophilias" .)
● (See "Contraception: Counseling for females with obesity" .)
● (See "Pregnancy and contraception in patients with nondialysis chronic kidney disease" .)
● (See "Pregnancy in patients on dialysis", section on 'Contraception' .)
● (See "Bipolar disorder in women: Contraception and preconception assessment and counseling" .)
● (See "Approach to the patient following treatment for breast cancer", section on 'Contraception after breast cancer' .)
● (See "HIV and women" and "HIV and women", section on 'Choice of contraception' .)
● (See "Overview of the management of epilepsy in adults" and "Overview of the management of epilepsy in adults", section on 'Contraception' .)
THE SHARED DECISION-MAKING PROCESS — After identifying that a patient should receive contraceptive counseling and identifying any conditions that may limit the range of methods available to her, providers of contraceptive counseling can then begin the process of selecting the method through a shared decision-making process [ 5 ]. Examples of how a shared decision-making interaction can proceed can be found in the table ( table 3 ).
Initiate the conversation — We advise beginning the conversation with a question that explicitly lets patients know that their preferences will be respected in the counseling process, such as "Do you have a sense of what is important to you about your method?"
We acknowledge, and have experienced, that many patients will not have an answer to this question, in part because they may have experienced past counseling approaches that did not prioritize their preferences. Patients' lack of experience with this type of question underscores the importance of leading the conversation with the patient's values, communicating that their preferences will be at the forefront of the discussion, and beginning the process of them considering what in fact those preferences are. As discussed above, common approaches that highlight only specific methods or immediately attempt to narrow down the options do not engage patients in discussions of their preferences. (See 'Personalized counseling with shared decision-making' above.)
Of note, this question is also distinct from another commonly used approach, in which providers ask "Which method are you interested in?" While on the surface, this question appears to prioritize the patient's preferences, it also assumes that patients are aware of their options and how those options relate to their preferences for different method characteristics, such as changes in bleeding patterns or efficacy. This question then drives the conversation to specific methods, rather than opening the conversation around the patient's preferences. Keeping the conversation open is particularly important given that patients may not feel empowered to ask questions of providers if not explicitly given the opportunity [ 2,33 ].
When opening the conversation by asking patients if they have a sense of their preferences, some patients may, in their responses, communicate explicitly or implicitly a desire for a non-shared decision-making approach. For example, some may immediately indicate that they know which method they wish to begin and convey a lack of interest in further discussion (autonomous decision-making). By contrast, other patients may respond by asking providers which method they think is best is or which method they think they should use (provider-driven decision-making). In both cases, patient-centered clinicians need to be aware of and responsive to those decision-making preferences ( table 3 ) [ 34 ]. However, given the personal nature of contraceptive use, as well as the complexity of contraceptive selection, clinicians should take care to ensure patients' decision-making ability is maintained. In the case of the patient who wishes to make an autonomous decision, clinicians can offer to discuss other contraceptive methods and thus maintain the patient's option of receiving further education. For the (less common) patients who wish to defer some or all of the decision-making to the clinician, clinicians can facilitate a preference-concordant decision by eliciting patient preferences, as described below, and then taking a more active role in mapping those preferences on to specific methods. (See 'Facilitate decision-making' below.)
Elicit informed preferences — Once the conversation has been opened by stating a focus on the patient's preferences, the next step in the shared decision-making process is to help individuals identify those preferences. These decisions should be informed by evidence, which necessitates an interactive educational conversation between the clinician and patient about the different ways that methods vary, including [ 35 ]:
● How they are taken
● How often they are taken
● Effect on menstrual bleeding (including regularity and flow)
● Other side effects
● Noncontraceptive benefits
● Effect on future fertility
We begin with a general overview of how the contraceptive methods vary and use language-appropriate visual aids to provide additional information and start the conversation ( figure 2 ) [ 36 ]. When starting this process, it is important to first respond to any priorities expressed in response to the initial question about preferences. For example, if a patient indicates that the most important thing about a method is that they do not have to remember it all the time, clinicians can acknowledge this preference, provide the range of options described above, and ask which of these options for frequency of remembering a method would be acceptable to them.
Next, we review general characteristics (eg, efficacy, how often the method is used, and resultant menstrual changes) and discuss the range of options within each characteristic. To avoid triggering preconceptions about specific methods, we advise using general descriptions, rather than identifying specific methods, with language such as "There are methods you take every day, every week, every month, every three months, or even less often. How do you feel about these different options?"
The degree to which the clinician should elicit patient preferences prior to moving to the next step will vary by patient. While ideally a clinician will ask about all of the above method characteristics, in many cases, a few strong preferences will be expressed which adequately narrow down the options. In that case, it may be appropriate to begin the decision-making process without reviewing all method characteristics, while being aware that additional preferences may emerge during the decision-making process that change the course of the conversation. As an example, for a patient who prioritizes getting regular periods and desires a method that will decrease acne, a clinician can begin the decision-making process by focusing on methods that align with these preferences, such as short-acting hormonal contraceptives (eg, oral contraceptive pill, contraceptive ring, and contraceptive patch). (See 'Facilitate decision-making' below.)
Discuss method characteristics — Below, we provide specific tips for how to discuss method efficacy, changes in menstrual bleeding, other side effects, noncontraceptive benefits, and effect on future fertility in order to elicit informed preferences for these characteristics.
● Efficacy – Misconceptions about both the absolute and relative efficacy of different methods to prevent pregnancy are common [ 37 ]. Therefore, understanding a patient's preferences around method efficacy, which is a high priority for many, is essential [ 38,39 ]. One data-supported strategy to improve patient knowledge is to review a tiered efficacy chart, such as that created by the United States Family Planning National Training Center ( figure 2 ) [ 40 ]. In addition to the use of visual aids, best practices for risk communication include stating natural frequencies rather than percentages (eg, stating "with typical use, method efficacy varies from 1 in 100 to 20 in 100 women getting pregnant in one year of use"). While tiered efficacy charts are commonly used, they are not the only approach.
● Changes in menstrual bleeding – Available prescription methods all have some effect on menstrual bleeding ( figure 2 ), and individuals have strong and varied preferences related to these changes [ 41,42 ]. Importantly, the same change, such as amenorrhea, can be viewed as a benefit by some individuals yet a negative side effect by others [ 43 ]. Therefore, we recommend specifically eliciting preferences about bleeding by asking a nondirective question such as "How do you feel about your method causing changes in your period, such as making it less regular, making it more or less heavy, or making it go away entirely?" Importantly, some patients' preferences are due to misconceptions about the safety of changes in their bleeding patterns, specifically with respect to amenorrhea [ 44-46 ]. Therefore, expressed preferences to avoid amenorrhea should be nonjudgmentally explored to determine whether this preference is based on misconceptions, while providing education to dispel any misinformation ( table 3 ).
● Other side effects – People frequently receive information about contraceptive methods from their social networks, and negative information is more commonly communicated than positive [ 47-50 ]. Therefore, many patients have concerns about potential negative impacts on contraceptive methods that will influence their choice of method. While it is not possible to systematically go through all evidence for side effects for all methods in a standard contraceptive visit, we advise directly asking patients if they have concerns about side effects of specific methods. This approach will allow clinicians to both understand patients' preferences and to address any misconceptions. When providing evidence-based information, clinicians should be aware of, and sensitive to, how much people value and trust information received through social networks about the lived experience with a contraceptive method [ 48 ]. Clinicians should avoid being dismissive of such experiences, acknowledge that "everyone is different," and emphasize the evidence for what is common ( table 3 ). By not discounting the experience relayed through peer networks, clinicians avoid triggering distrust and allow patients to hear the evidence and consider how it may relate to their experience with that method.
● Noncontraceptive benefits – In addition to preventing pregnancy, contraceptives have numerous noncontraceptive benefits that may influence patient selection ( table 4 ).
● Impact on sexual experience – A prospective study of over 1800 female individuals initiating a no-fee contraceptive of their choice reported that positive sexual experience while using the contraceptive method was strongly correlated with patient satisfaction [ 51 ]. Sexual experience was a stronger correlate of satisfaction than reduction or elimination of vaginal bleeding. In presenting contraception selection, clinicians are encouraged to ask patients to consider whether specific method characteristics (such as whether or not the method is coitally dependent and whether the method causes irregular bleeding) may have an effect on their sexual satisfaction.
● Effect on future fertility – If not previously elicited, clinicians can assess whether pregnancy is desired in the short or long term. Such a conversation provides clinicians the opportunity to address common misconceptions about the effect of contraceptive methods on fertility [ 37,52 ]. We review that only sterilization has a permanent effect on fertility, while the contraceptive injection has a shorter term impact.
Facilitate decision-making — The goal of this phase of counseling is to help patients identify the most appropriate method for them given their preferences and the contraceptives' characteristics. Clinicians should be aware that preferences and planned contraceptive may change over time [ 53 ]. Specific scenarios that may be encountered during the decision-making process include:
● One strong preference – For a patient who has identified one dominant preference, such as the desire to use a highly effective method, this process can be as simple as informing the patient that given their preference, intrauterine devices (IUD), implants, and sterilization may be the best choices and asking follow-up questions to help them determine which of these is most appropriate.
● More than one expressed preference – In cases where patients have identified more than one preference, clinicians can educate them about how these values overlap with the characteristics of available methods. Again, visual aids ( figure 2 ) can be helpful in this process, as can pelvic models or samples of contraceptive methods. For patients with preferences that align with one method (such as the desire to minimize acne and to have lighter, regular periods), clinicians can help patients choose among the appropriate methods (in this case, the contraceptive pill, patch, and ring) using follow-up questions. When preferences are in conflict (eg, the desire for the most highly effective method and the desire to have a method that is not placed into the body), clinicians can discuss how these preferences do not overlap and ask patients to consider how to weigh their preferences relative to each other. An example of this conversation is provided in the table ( table 3 ).
● Newly disclosed preference – When patients reveal a new contraceptive preference during the process of decision-making, it may be necessary to move back and forth between determining preferences and facilitating decision-making in response to those preferences. These new preferences can then be incorporated into the decision-making process, as described in the previous bullet.
Specific issues that can arise during the decision-making process:
● Clinician preference or bias – In facilitating the decision-making process, we avoid expressing any partiality that does not reflect the patient's own expressed preferences. Indicating such a bias is not consistent with the preference-sensitive nature of contraceptive decision-making and is particularly problematic given that the priorities of clinicians around contraceptive methods have been found to vary significantly from those of patients [ 54 ]. In addition, as patients who feel their clinician had a method preference are less likely to be satisfied with their method [ 10 ], and those who felt pressured to use a contraceptive implant are more likely to discontinue their method [ 55 ], counseling in this way can interfere with patients' contraceptive use. Phrases such as "Based on what you are telling me, these methods may be a good fit" can help to avoid any appearance of partiality.
● Discussion of personal experience other than the patient's – The question of whether or not clinicians should disclose personal experience with contraceptive methods during the course of counseling can arise, either because patients directly ask clinicians or because clinicians want to use their lived experience as part of the educational process. In other areas of health care, whether or not clinicians should disclose personal information is a source of controversy, and the ethical issues are heightened in contraceptive counseling given its personal and social context [ 56 ]. However, one study using audio recordings of contraceptive counseling visits found that brief incidences of self-disclosure were not disruptive to the clinical encounter and did not elicit negative reactions from patients [ 56 ]. Whether or not such disclosures were beneficial to the patients' decision-making process could not be determined. One study did report that clinicians sharing personal experiences of IUDs was associated with increased uptake of this method [ 57 ]. As this suggests that self-disclosure has the potential to be influential, clinicians should be cautious when giving personal information to ensure that it does not inappropriately bias decision-making.
● Avoidance of less available or familiar methods – Clinicians should be conscious of a tendency to be less likely to counsel about methods with which they have less experience or do not provide in their clinics. Such selective counseling may lead to patients being less likely to be offered methods requiring procedures (such as IUDs, implants, and female and male sterilization) or nonprescription methods (such as fertility awareness-based methods) even if they are a good fit for the expressed preferences. Clinicians should be aware of resources in their communities to provide these methods and make appropriate referrals as needed. Detailed reviews of these contraceptive methods are presented in individual discussions.
• (See "Intrauterine contraception: Background and device types" .)
• (See "Contraception: Etonogestrel implant" .)
• (See "Overview of female permanent contraception" .)
• (See "Vasectomy" .)
• (See "Fertility awareness-based methods of pregnancy prevention" .)
Selecting a method — While the process of eliciting preferences and mapping them to the available methods is shared, the ultimate decision about which method to use should be made by the patient, unless they explicitly ask for guidance from the clinician. In those cases, clinicians can rely on their knowledge of the patient's preferences to identify the method that is likely to be the best fit. Clinicians can precipitate the final decision by asking questions such as "Given what we talked about, and what is important to you about your method, what do you think would be the best choice for you at this time?"
Starting a method — We follow the Centers for Disease Control and Prevention (CDC) US Selected Practice Recommendations for Contraceptive Use ( US SPR ) to guide start time, assess the patient's need for contraceptive back-up, and identify any necessary preinitiation testing [ 58 ]. Most contraceptives can be started on the same day as the visit and require minimal examination or testing prior to initiation ( table 5 ). Screening for sexually transmitted infections (STIs) is done per the CDC Sexually Transmitted Diseases Treatment Guideline [ 59 ]. The US SPR also provides guidance to reasonably exclude pregnancy prior to method initiation and to assess the need for back-up contraception ( table 6 ). When it is not possible to reasonably exclude pregnancy, contraceptive methods other than the IUD can still be initiated immediately with appropriate counseling and consent ( algorithm 1 ). The need for emergency contraception should be considered for all patients. If the patient is a candidate for emergency contraception and interested in the copper IUD , this method will provide emergency contraception and then can remain in place for continued contraception (the levonorgestrel-releasing IUDs do not provide emergency contraception). (See "Emergency contraception" .)
New-start counseling should also include information and support to optimize the patient's correct use of the method in the context of their unique life circumstances (eg, how to best remember to take a pill every day given their life's demands). Additionally, the US SPR provides information about what to do if one or more doses of a short-acting contraceptive method is late or missed [ 58 ].
Counseling about side effects is a continuous process; we revisit this discussion once a method is chosen and at follow-up visits. Anticipatory counseling about potential side effects has been associated with both method satisfaction and method continuation [ 60,61 ]. We next discuss how to arrange timely follow-up visits and obtain contraceptive refills, if relevant. Lastly, we specifically inform patients of the acceptability of method switching (eg, that patients are welcome to come back at any time for a different method for any reason). Rather than framing discontinuation as a failure, we recognize that method discontinuation and switching is a normal occurrence among contraceptive users that helps ensure that individuals are comfortable accessing care when they need it [ 62 ].
Assess risk of sexually transmitted infections — We assess a patient's risk of acquiring an STI as a routine part of contraceptive counseling. All patients at risk for acquiring an STI are advised to use condoms (internal or external) in addition to their chosen method for pregnancy prevention. Detailed information on the prevention of STIs is presented separately. (See "Prevention of sexually transmitted infections" .)
Additionally, concern has been raised that hormonal contraception, and particularly the contraceptive injection, could increase the risk of acquiring HIV infection. In the absence of definitive data, we agree with the World Health Organization (WHO) and CDC assessments that individuals at high risk of and living with HIV can continue to use all existing hormonal contraceptive methods, as the benefits generally outweigh the risk [ 63 ]. Although still a subject of debate, progestin-only contraceptive injection does not appear to increase the risk of HIV acquisition. (See "HIV and women", section on 'Risk factors for HIV acquisition' .)
SPECIAL POPULATIONS
● Adolescents – Adolescents and young adults have unique contraceptive needs that reflect variations in individual development, barriers to contraceptive access, and lack of information [ 37,64,65 ]. While there may be a tendency toward more directive counseling with adolescents because of their perceived higher risk for adverse reproductive health outcomes, adolescents are also resistant to authority, and counseling viewed as overbearing has the potential to interfere with engagement with reproductive health services in the short and long term. The contraceptive issues specific to adolescents are reviewed separately. (See "Contraception: Issues specific to adolescents" .)
● Postpartum individuals – Best practices for the provision of peripartum contraceptive counseling include discussing contraceptive options multiple times over the course of prenatal care, providing patients with information about the safety of different contraceptive methods in the immediate postpartum period, and including the potential effect on lactation [ 31,66 ]. Patients should be provided with the option of immediate postpartum contraception, including insertion of intrauterine devices (IUDs; within ten minutes of delivery), and should be informed about the increased risk of expulsion when provided in this manner [ 67 ]. In addition, clinicians should discuss potential increased risks associated with a short interpregnancy interval and simultaneously recognize that each individual will weigh these risks differently with respect to their own reproductive goals.
• (See "Contraception: Postpartum counseling and methods" .)
• (See "Interpregnancy interval: Optimizing time between pregnancies" .)
● Individuals who have recently had an abortion – Surveys of patients receiving abortion care have found that over 60 percent do not wish to discuss contraception at the time of their abortion [ 68,69 ]. Therefore, while contraceptive methods should be available to all patients having an abortion, clinicians should be responsive to individual patients' preferences for information and decision support in the context of providing this care. Insisting on providing counseling when not desired by patients has the potential to contribute to further stigma associated with receiving abortion care. (See "Contraception: Postabortion" .)
● Individuals who request IUD or implant removal – When individuals seek IUD or implant removal for reasons other than desiring a pregnancy, some clinicians may promote continued use of the IUD or implant because of high efficacy, despite the patient's expressed desire for removal [ 70-72 ]. We strongly advise against this practice as it has the potential to result in mistrust of family planning clinicians and impinges on the patient's autonomy. Instead, we first assure the patient that we will remove the method at their request. We then ask them if they would like to discuss their concerns or experiences of side effects prior to removal. This approach allows us to address any issues and provide additional education when appropriate and acceptable to the patient. For patients who still desire method removal, we then proceed as requested. (See "Intrauterine contraception: Management of side effects and complications" and "Evaluation and management of unscheduled bleeding in individuals using hormonal contraception" .)
● Individuals with chronic medical conditions – As described above, the World Health Organization Medical Eligibility Criteria for Contraceptive Use and the US Medical Eligibility Criteria for Contraceptive Use review the safety of specific contraceptive methods in patients with chronic medical conditions [ 31,32 ]. While clinicians may wish to promote the most effective contraceptive methods for those at risk of medically complicated pregnancy, patient reproductive autonomy must be maintained. Careful education and detailed counseling about contraceptive efficacy, risks associated with pregnancy, possible role of emergency contraception, and the availability and safety of abortion in case an undesired pregnancy occurs can support patients in making autonomous, informed decisions.
● Individuals with obesity – Individuals with obesity can be offered all contraceptive options, including combined estrogen-progestin contraceptives [ 30,31 ]. (See "Contraception: Counseling for females with obesity" .)
● Individuals with substance use disorders – As there is a documented unmet need for family planning services among patients with substance use orders, those providing care to these individuals should ensure they have access to quality contraceptive counseling and services [ 73-75 ]. Clinicians caring for these patients may be biased toward specific methods given the higher risk for pregnancy complications in this population [ 76 ]. However, this tendency can trigger the heightened mistrust of the medical community by those with substance use disorders and has the potential to interfere with reproductive autonomy [ 77 ]. Therefore, a shared decision-making model grounded in the patient's preferences can both build trust and help patients identify a method of contraception that is best suited to their social and medical contexts.
In giving decision support, providers should be aware of the association between use of opiates with menstrual disturbances, including prolonged amenorrhea [ 78 ]. As this amenorrhea may lead women to underestimate their risk of pregnancy, education about the possibility of ovulation and resulting pregnancy, even when menstruation is irregular or absent, should be provided. In addition, given the frequent co-occurrence of substance use disorders with experiences of intimate partner violence and other forms of trauma, as well as posttraumatic stress disorder, providing trauma-informed care can be particularly important for this population [ 79,80 ]. A discussion of trauma-informed care is presented separately. (See "Health care for female trauma survivors (with posttraumatic stress disorder or similarly severe symptoms)" .)
● Individuals with intellectual or physical disability – Individuals with intellectual or physical disabilities have unique needs. The contraceptive selection process may involve a guardian as well as the patient. Data to guide the decision-making process are often lacking, and the benefits, risks, side effects, and consequences of an undesired pregnancy must be balanced against one another. As an example, the magnitude of thrombotic risk from estrogen-containing hormonal contraceptives in those with limited mobility (eg, patient in wheelchair) is not known. However, hormonal contraceptives can be desirable for these patients because they reduce menstrual frequency or flow in addition to preventing pregnancy. (See "Hormonal contraception for menstrual suppression" .)
Additional challenges can include the patient's limited capacity (intellectual, physical, or both) to use a method, problems with menstrual hygiene, and inability to undergo an office-based examination or procedure. Some patients with intellectual disabilities cannot tolerate pelvic examinations, which makes pelvic examination or placement of an IUD in an office setting unrealistic.
Sterilization in patients with intellectual or physical disabilities raises the ethical issues of patient autonomy and informed consent [ 81 ]. Sterilization in patients with disabilities is reviewed separately. (See "Overview of female permanent contraception", section on 'Vulnerable populations' .)
● Individuals with history of cancer – In 2012, the Society of Family Planning (SFP) published clinical guidelines for contraception in patients with cancer [ 82 ]. While the subsequent World Health Organization Medical Eligibility Criteria for Contraceptive Use and the US Medical Eligibility Criteria for Contraceptive Use approved hormonal contraception for most non-hormone-dependent cancers (ie, except for breast cancer), the SFP guidelines contain additional considerations that we believe are important.
For the following groups, the SFP advised:
• Those with active cancer or who have been treated for cancer within six months – Avoid estrogen-progestin contraceptives because both cancer and combined hormonal contraception are risk factors for venous thrombosis. (See "Combined estrogen-progestin contraception: Side effects and health concerns", section on 'Effects on cancer development' .)
• Those with a history of breast cancer – Consider use of a copper IUD , unless they are taking tamoxifen . In the latter case, off-label use of a levonorgestrel-releasing IUD can reduce the risk of tamoxifen-induced endometrial changes without increasing the risk of breast cancer recurrence. (See "Approach to the patient following treatment for breast cancer", section on 'Contraception after breast cancer' and "Intrauterine contraception: Candidates and device selection", section on 'Endometrial protection' .)
• Those at risk of breast cancer or recurrence – Emergency contraceptive pills are not contraindicated. (See "Emergency contraception" .)
● Transmasculine individuals – Not all people capable of pregnancy identify as women; transmasculine individuals have specific counseling needs [ 1 ]. These include considerations related to taking a gender-affirming sexual history and preferences for side effect profiles [ 1 ]. (See "Primary care of transgender individuals" .)
MYTHS OF CONTRACEPTIVE COUNSELING — Over the past few decades, the goal of family planning has been interpreted as equivalent to helping individuals avoid unintended pregnancy; the assumption has been that unintended pregnancies are uniformly negative outcomes for individuals and for society [ 83-86 ]. To this end, many family planning programs and policies have prioritized use of the most highly effective methods [ 87,88 ]. Over time, the appropriateness of this focus has been questioned based on the diverse perspectives people have about the potential for pregnancy in their lives, data about the health impacts of pregnancy intention for mothers and babies, and what is known about people's preferences for contraceptive methods.
● Unintended pregnancy is not always unwelcome – Research on women's feelings about pregnancy intention in the current literature has advanced the assumption that an unintended pregnancy is an inherently bad outcome [ 89 ]. Rather, women have varying perspectives about whether, and to what degree, an unintended pregnancy would be a positive or negative experience in their lives [ 89-92 ]. In fact, some women embrace the lack of predictability of their fertility and consider unintended pregnancies to be welcome surprises [ 93 ].
● Unintended pregnancies are not necessarily unhealthy pregnancies – It is also increasingly understood that the literature about the association between pregnancy intention and poor maternal and child health outcomes is not as robust as previously thought, especially in developed countries [ 84,94 ]. This is consistent with the understanding that an unintended pregnancy does not result in the same negative reactions in all individuals [ 89 ]. In addition, it is likely that other factors (such as socioeconomic status) could confound the relationship between pregnancy intention and outcomes when attempting to assess the impact of pregnancy intention [ 94 ].
● Contraceptive efficacy is only one important contraceptive characteristic – Commensurate with the above findings about people's views on pregnancy, research has revealed that people have diverse and strong preferences for contraceptive methods [ 38,39,95 ]. Data indicate that efficacy is not the only, or always the most important, characteristic for people choosing a contraceptive method. For example, one study stated that, on average, those surveyed reported 11 characteristics that were important to them, with the following percentages noting these characteristics were "extremely important" [ 39 ]:
• Very effective at preventing pregnancy – 89 percent
• Easy to use – 80 percent
• Few or no side effects – 74 percent
• Woman has control over when and whether to use the method – 71 percent
• No one can tell that the woman is using the method – 55 percent
• No change in menstrual periods – 44 percent
PROMOTION OF HEALTH EQUITY — Contraceptive counseling occurs in an historical and social context in which family planning providers and services have participated in coercive and unethical practices designed to limit the fertility of specific populations, including women of color, poor women, and women with disabilities [ 96 ]. Examples include nonconsensual sterilization and targeted marketing of the contraceptive injection Depo-Provera [ 97,98 ]. This history remains in the consciousness of the communities impacted, with one study reporting that over 40 percent of Black and Hispanic Americans think that the government promotes birth control to limit minorities [ 37 ]. A different study documented that over one-third of Black women believe "medical and public health institutions use poor and minority people as guinea pigs to try out new birth control methods" [ 81 ].
While this history has the potential to affect how patients perceive contraceptive counseling regardless of the counseling provided, there is also evidence from studies of ongoing bias in counseling according to the race/ethnicity of the patient. These include findings that women of color are more likely to report being advised to limit their childbearing than are White women in the context of prenatal care [ 99 ], and that Black women are more likely than White women to report having been pressured by a clinician to use contraception [ 100 ]. In addition, studies using standardized case scenarios have found that providers are more likely to recommend the intrauterine device (IUD) to low-income Black and Hispanic women than to low-income White women [ 101 ], and are more likely to agree to sterilize women of color and poor women than White women or non-poor women [ 102 ]. These findings are consistent with the broader literature on health care disparities in the United States, which has documented that patients of color receive different, lower quality care than do White patients, even with identical clinical presentations and access to care [ 103 ]. (See "Racial and ethnic inequities in obstetric and gynecologic care and role of implicit biases" .)
Given this history, the recent emphasis on directive counseling toward methods of contraception that require a provider to both insert and remove a device (ie, IUDs and implants) has raised concerns about the potential to recreate, or appear to recreate, historical injustices related to reproductive control [ 96 ]. This is particularly relevant given that women of color have been found to be less likely to desire a contraceptive method that they are unable to remove or discontinue on their own [ 39 ]. Therefore, directive counseling toward these methods is more poorly aligned with their preferences than it is for White patients, while also having the potential to heighten preexisting mistrust of family planning providers.
In contrast to directive counseling, shared decision-making provides a structure for counseling, described above, that protects against perceived or actual bias in counseling by explicitly focusing on women's expressed preferences. Given that bias can influence how decision support is provided, however, those practicing shared decision-making should be aware of the potential for bias to influence their counseling in subtle ways and should work to guard against overemphasizing specific methods based on assumptions about what women do or should want [ 5 ].
● (See 'Personalized counseling with shared decision-making' above.)
● (See "Racial and ethnic inequities in obstetric and gynecologic care and role of implicit biases", section on 'Mitigation of implicit bias' .)
RESOURCES FOR PATIENTS AND CLINICIANS
● bedsider.org : A free website developed by the National Campaign to Prevent Teen and Unplanned Pregnancy, a private nonprofit group
● The Family Planning National Training Center : The website for federally funded contraceptive resources developed with the support of the Office of Population Affairs
● Center for Young Women's Health : A free website run by Boston Children's Hospital that addresses reproductive health needs of teens and young adults
● Beyond the Pill : A free website run by the University of California San Francisco
● SexandU.ca : An educational site run by the Society of Obstetricians and Gynaecologists of Canada that includes descriptions of various methods and a tool to help with selection of birth control
● PICCK.org is a clinical and public health program designed to promote contraceptive choice and effective contraceptive counseling across the Commonwealth of Massachusetts with an emphasis on patient-centered care rooted in principles of autonomy, equity, and justice.
● Planned Parenthood : A nonprofit organization dedicated to reproductive health with resources for patients and clinicians
● ACOG Contraceptive FAQs : American College of Obstetricians and Gynecologists addresses frequently asked questions (FAQs) about contraception
● ACOG LARC Program : American College of Obstetricians and Gynecologists Long-Acting Reversible Contraception Program
● United States Medical Eligibility Criteria for Contraceptive Use
● United States Selected Practice Recommendations for Contraceptive Use
● World Health Organization Medical Eligibility Criteria for Contraceptive Use
SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. (See "Society guideline links: Contraception" .)
INFORMATION FOR PATIENTS — UpToDate offers two types of patient education materials, "The Basics" and "Beyond the Basics." The Basics patient education pieces are written in plain language, at the 5 th to 6 th grade reading level, and they answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. (You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword(s) of interest.)
● Basics topics (see "Patient education: Choosing birth control (The Basics)" and "Patient education: Vasectomy (The Basics)" and "Patient education: Barrier methods of birth control (The Basics)" )
● Beyond the Basics topics (see "Patient education: Birth control; which method is right for me? (Beyond the Basics)" and "Patient education: Vasectomy (Beyond the Basics)" )
SUMMARY AND RECOMMENDATIONS
● Personalized counseling and shared decision-making – Data suggest that family planning care should not have a singular focus of preventing unintended pregnancy, as this is not consistent with all individual's preferences or necessary to optimize health outcomes. Contraceptive counseling has evolved from clinician-led directive counseling and provision of education to personalized, patient-centered counseling that includes shared decision-making. (See 'Goals' above and 'Personalized counseling with shared decision-making' above.)
● Identify contraceptive need – The first step in providing patient-centered contraceptive counseling is identifying patients for whom this counseling is appropriate. In our practice, we ask patients if they wish to discuss contraception or pregnancy prevention ( table 2 ). (See 'Identify patient-centered reproductive goals' above.)
● Assess medical conditions – Once a person is identified as being appropriate for and desirous of contraceptive counseling, providers can then assess for medical conditions that could affect the safety of specific methods. (See 'Document medical history/potential contraindications' above.)
Guidance on safety across a broad range of individual and medical conditions for different patient populations is available through:
• World Health Organization Medical Eligibility Criteria for Contraceptive Use and the
• US Medical Eligibility Criteria for Contraceptive Use
● Elicit patient preferences – Patient-centered contraceptive counseling using shared decision-making should first elicit informed preferences for method characteristics, and then support patients in considering how these characteristics relate to the available methods, while leaving the ultimate decision up to the patient. (See 'The shared decision-making process' above.)
• Method characteristics to consider – Preferences for characteristics of contraceptive methods to consider when providing counseling include those related to method effectiveness, how often the method is taken/used, how the method is taken/used, menstrual changes, other side effects, noncontraceptive benefits, return to fertility, and privacy. (See 'Elicit informed preferences' above.)
• Address misinformation – Providers can address misconceptions and misinformation about methods, especially those transmitted through social networks, in a respectful way that does not dismiss these concerns but provides evidence-based information about the known effects of specific methods. (See 'Discuss method characteristics' above.)
• Role of visual aids – Use of visual aids, such as the Title X contraceptive method options chart ( figure 2 ), can help to structure and guide counseling. (See 'Facilitate decision-making' above.)
● Educate on use of selected method – Counseling after method selection should provide each individual with information about how to start their method, how to optimize their use of the method, side effects they may experience, how to access necessary follow-up care including refills, and how to access care if they wish to discuss discontinuation and/or method switching. Emergency contraception and protection from sexually transmitted infections are also discussed. (See 'Selecting a method' above and 'Starting a method' above and 'Assess risk of sexually transmitted infections' above.)
● Special populations – Counseling for specific populations, including adolescents, gender-expansive individuals, and/or individuals with substance use disorders, chronic medical conditions, and/or mental or intellectual disability, should prioritize these patients' reproductive autonomy and provide tailored education to support their informed decision-making. (See 'Special populations' above.)
● Potential impact of unconscious bias – Providers should be aware of the potential for unconscious bias about patients' race/ethnicity to influence their counseling. Use of a shared decision-making model explicitly focused on patient preferences can limit the impact of such bias. (See 'Promotion of health equity' above.)
ACKNOWLEDGMENT — The UpToDate editorial staff acknowledges Mimi Zieman, MD, and Andrew Kaunitz, MD, who contributed to earlier versions of this topic review.
- Krempasky C, Harris M, Abern L, Grimstad F. Contraception across the transmasculine spectrum. Am J Obstet Gynecol 2020; 222:134.
- Dehlendorf C, Kimport K, Levy K, Steinauer J. A qualitative analysis of approaches to contraceptive counseling. Perspect Sex Reprod Health 2014; 46:233.
- Schivone GB, Glish LL. Contraceptive counseling for continuation and satisfaction. Curr Opin Obstet Gynecol 2017; 29:443.
- Thompson R, Manski R, Donnelly KZ, et al. Right For Me: protocol for a cluster randomised trial of two interventions for facilitating shared decision-making about contraceptive methods. BMJ Open 2017; 7:e017830.
- American College of Obstetricians and Gynecologists’ Committee on Health Care for Underserved Women, Contraceptive Equity Expert Work Group, and Committee on Ethics. Patient-Centered Contraceptive Counseling: ACOG Committee Statement Number 1. Obstet Gynecol 2022; 139:350.
- Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997; 44:681.
- Elwyn G, Dehlendorf C, Epstein RM, et al. Shared decision making and motivational interviewing: achieving patient-centered care across the spectrum of health care problems. Ann Fam Med 2014; 12:270.
- Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017; 4:CD001431.
- Goueth RC, Maki KG, Babatunde A, et al. Effects of technology-based contraceptive decision aids: a systematic review and meta-analysis. Am J Obstet Gynecol 2022; 227:705.
- Dehlendorf C, Grumbach K, Schmittdiel JA, Steinauer J. Shared decision making in contraceptive counseling. Contraception 2017; 95:452.
- Effectiveness of Telehealth for Women’s Preventive Services, Cantor A, Nelson HD, Pappas M, Atchison C, Hatch B, Huguet N, Flynn B, McDonagh M. (Eds), Agency for Healthcare Research and Quality (US), Rockville (MD) 2022.
- Crossing the Quality Chasm: A New Health System for the 21st Century, Institute of Medicine (US) Committee on Quality of Health Care in America (Ed), National Academies Press (US), Washington (DC) 2001.
- Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med 2011; 9:100.
- Dehlendorf C, Henderson JT, Vittinghoff E, et al. Association of the quality of interpersonal care during family planning counseling with contraceptive use. Am J Obstet Gynecol 2016; 215:78.e1.
- Gomez AM, Wapman M. Under (implicit) pressure: young Black and Latina women's perceptions of contraceptive care. Contraception 2017; 96:221.
- Upadhyay U. Informed Choice in Family Planning: Helping People Decide. Johns Hopkins University Bloomberg School of Public Health, Population Information Program, Baltimore 2001.
- Dehlendorf C, Levy K, Kelley A, et al. Women's preferences for contraceptive counseling and decision making. Contraception 2013; 88:250.
- Sober S, Shea JA, Shaber AG, et al. Postpartum adolescents' contraceptive counselling preferences. Eur J Contracept Reprod Health Care 2017; 22:83.
- Carvajal DN, Gioia D, Mudafort ER, et al. How can Primary Care Physicians Best Support Contraceptive Decision Making? A Qualitative Study Exploring the Perspectives of Baltimore Latinas. Womens Health Issues 2017; 27:158.
- Dehlendorf C, Diedrich J, Drey E, et al. Preferences for decision-making about contraception and general health care among reproductive age women at an abortion clinic. Patient Educ Couns 2010; 81:343.
- Fox E, Reyna A, Malcolm NM, et al. Client Preferences for Contraceptive Counseling: A Systematic Review. Am J Prev Med 2018; 55:691.
- Whitaker AK, Terplan M, Gold MA, et al. Effect of a brief educational intervention on the attitudes of young women toward the intrauterine device. J Pediatr Adolesc Gynecol 2010; 23:116.
- Madden T, Mullersman JL, Omvig KJ, et al. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception 2013; 88:243.
- Bellanca HK, Hunter MS. ONE KEY QUESTION®: Preventive reproductive health is part of high quality primary care. Contraception 2013; 88:3.
- Gavin L, Moskosky S, Carter M, et al. Providing quality family planning services: Recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep 2014; 63:1.
- Callegari LS, Aiken AR, Dehlendorf C, et al. Addressing potential pitfalls of reproductive life planning with patient-centered counseling. Am J Obstet Gynecol 2017; 216:129.
- Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care--United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep 2006; 55:1.
- ACOG Committee Opinion No. 762: Prepregnancy Counseling. Obstet Gynecol 2019; 133:e78. Reaffirmed 2021.
- Contraception. Quality Standard [QS129]. National Institute for Health and Care Excellence (NICE). September 2016. www.nice.org.uk/guidance/qs129 (Accessed on January 22, 2019).
- ACOG Practice Bulletin No. 206: Use of Hormonal Contraception in Women With Coexisting Medical Conditions. Obstet Gynecol 2019; 133:e128. Reaffirmed 2022.
- Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep 2016; 65:1.
- Medical eligibility criteria for contraceptive use, Fifth edition. World Health Organization. 2015. www.who.int/reproductivehealth/publications/family_planning/Ex-Summ-MEC-5/en/ (Accessed on January 22, 2019).
- Frosch DL, May SG, Rendle KA, et al. Authoritarian physicians and patients' fear of being labeled 'difficult' among key obstacles to shared decision making. Health Aff (Millwood) 2012; 31:1030.
- Chewning B, Bylund CL, Shah B, et al. Patient preferences for shared decisions: a systematic review. Patient Educ Couns 2012; 86:9.
- Hatcher RA, Trussell J, Nelson AL, et al. Contraceptive Technology, 21st ed, Ayer Company Publishers, Inc., New York 2018.
- Anderson S, Frerichs L, Kaysin A, et al. Effects of Two Educational Posters on Contraceptive Knowledge and Intentions: A Randomized Controlled Trial. Obstet Gynecol 2019; 133:53.
- Craig AD, Dehlendorf C, Borrero S, et al. Exploring young adults' contraceptive knowledge and attitudes: disparities by race/ethnicity and age. Womens Health Issues 2014; 24:e281.
- Madden T, Secura GM, Nease RF, et al. The role of contraceptive attributes in women's contraceptive decision making. Am J Obstet Gynecol 2015; 213:46.e1.
- Jackson AV, Karasek D, Dehlendorf C, Foster DG. Racial and ethnic differences in women's preferences for features of contraceptive methods. Contraception 2016; 93:406.
- Steiner MJ, Trussell J, Mehta N, et al. Communicating contraceptive effectiveness: A randomized controlled trial to inform a World Health Organization family planning handbook. Am J Obstet Gynecol 2006; 195:85.
- Polis CB, Hussain R, Berry A. There might be blood: a scoping review on women's responses to contraceptive-induced menstrual bleeding changes. Reprod Health 2018; 15:114.
- Nappi RE, Fiala C, Chabbert-Buffet N, et al. Women's preferences for menstrual bleeding frequency: results of the Inconvenience Due to Women's Monthly Bleeding (ISY) survey. Eur J Contracept Reprod Health Care 2016; 21:242.
- Newton VL, Hoggart L. Hormonal contraception and regulation of menstruation: a study of young women's attitudes towards 'having a period'. J Fam Plann Reprod Health Care 2015; 41:210.
- Andrist LC, Arias RD, Nucatola D, et al. Women's and providers' attitudes toward menstrual suppression with extended use of oral contraceptives. Contraception 2004; 70:359.
- Andrist LC, Hoyt A, Weinstein D, McGibbon C. The need to bleed: women's attitudes and beliefs about menstrual suppression. J Am Acad Nurse Pract 2004; 16:31.
- Rose JG, Chrisler JC, Couture S. Young women's attitudes toward continuous use of oral contraceptives: the effect of priming positive attitudes toward menstruation on women's willingness to suppress menstruation. Health Care Women Int 2008; 29:688.
- Anderson N, Steinauer J, Valente T, et al. Women's social communication about IUDs: a qualitative analysis. Perspect Sex Reprod Health 2014; 46:141.
- Yee L, Simon M. The role of the social network in contraceptive decision-making among young, African American and Latina women. J Adolesc Health 2010; 47:374.
- Gilliam ML, Davis SD, Neustadt AB, Levey EJ. Contraceptive attitudes among inner-city African American female adolescents: Barriers to effective hormonal contraceptive use. J Pediatr Adolesc Gynecol 2009; 22:97.
- Gilliam ML, Warden M, Goldstein C, Tapia B. Concerns about contraceptive side effects among young Latinas: a focus-group approach. Contraception 2004; 70:299.
- Kramer RD, Higgins JA, Everett B, et al. A Prospective Analysis of the Relationship Between Sexual Acceptability and Contraceptive Satisfaction Over Time. Am J Obstet Gynecol 2021.
- Payne JB, Sundstrom B, DeMaria AL. A Qualitative Study of Young Women's Beliefs About Intrauterine Devices: Fear of Infertility. J Midwifery Womens Health 2016; 61:482.
- Thornton M, Ascha MS, Arora KS. Addressing Fluidity in Contraceptive Decision-Making: A Key Component of Patient-Centered Contraceptive Counseling. Am J Obstet Gynecol 2022.
- Donnelly KZ, Foster TC, Thompson R. What matters most? The content and concordance of patients' and providers' information priorities for contraceptive decision making. Contraception 2014; 90:280.
- Berenson AB, Wiemann CM, Rickerr VI, McCombs SL. Contraceptive outcomes among adolescents prescribed Norplant implants versus oral contraceptives after one year of use. Am J Obstet Gynecol 1997; 176:586.
- McLean M, Steinauer J, Schmittdiel J, et al. Provider self-disclosure during contraceptive counseling. Contraception 2017; 95:161.
- Benson LS, Perrucci A, Drey EA, Steinauer JE. Effect of shared contraceptive experiences on IUD use at an urban abortion clinic. Contraception 2012; 85:198.
- Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for Contraceptive Use, 2016. MMWR Recomm Rep 2016; 65:1.
- Workowski KA, Bolan GA, Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015; 64:1.
- Backman T, Huhtala S, Luoto R, et al. Advance information improves user satisfaction with the levonorgestrel intrauterine system. Obstet Gynecol 2002; 99:608.
- Canto De Cetina TE, Canto P, Ordoñez Luna M. Effect of counseling to improve compliance in Mexican women receiving depot-medroxyprogesterone acetate. Contraception 2001; 63:143.
- Simmons RG, Sanders JN, Geist C, et al. Predictors of contraceptive switching and discontinuation within the first 6 months of use among Highly Effective Reversible Contraceptive Initiative Salt Lake study participants. Am J Obstet Gynecol 2019; 220:376.e1.
- Tepper NK, Curtis KM, Cox S, Whiteman MK. Update to U.S. Medical Eligibility Criteria for Contraceptive Use, 2016: Updated Recommendations for the Use of Contraception Among Women at High Risk for HIV Infection. MMWR Morb Mortal Wkly Rep 2020; 69:405.
- Stidham Hall K, Moreau C, Trussell J. Discouraging trends in reproductive health service use among adolescent and young adult women in the USA, 2002-2008. Hum Reprod 2011; 26:2541.
- Bender SS, Fulbright YK. Content analysis: a review of perceived barriers to sexual and reproductive health services by young people. Eur J Contracept Reprod Health Care 2013; 18:159.
- Yee L, Simon M. Urban minority women's perceptions of and preferences for postpartum contraceptive counseling. J Midwifery Womens Health 2011; 56:54.
- Moniz MH, Spector-Bagdady K, Heisler M, Harris LH. Inpatient Postpartum Long-Acting Reversible Contraception: Care That Promotes Reproductive Justice. Obstet Gynecol 2017; 130:783.
- Matulich M, Cansino C, Culwell KR, Creinin MD. Understanding women's desires for contraceptive counseling at the time of first-trimester surgical abortion. Contraception 2014; 89:36.
- Cansino C, Lichtenberg ES, Perriera LK, et al. Do women want to talk about birth control at the time of a first-trimester abortion? Contraception 2018; 98:535.
- Amico JR, Bennett AH, Karasz A, Gold M. "I wish they could hold on a little longer": physicians' experiences with requests for early IUD removal. Contraception 2017; 96:106.
- Amico JR, Bennett AH, Karasz A, Gold M. "She just told me to leave it": Women's experiences discussing early elective IUD removal. Contraception 2016; 94:357.
- Higgins JA, Kramer RD, Ryder KM. Provider Bias in Long-Acting Reversible Contraception (LARC) Promotion and Removal: Perceptions of Young Adult Women. Am J Public Health 2016; 106:1932.
- Griffith G, Kumaraswami T, Chrysanthopoulou SA, et al. Prescription contraception use and adherence by women with substance use disorders. Addiction 2017; 112:1638.
- McNeely CA, Hutson S, Sturdivant TL, et al. Expanding Contraceptive Access for Women With Substance Use Disorders: Partnerships Between Public Health Departments and County Jails. J Public Health Manag Pract 2019; 25:229.
- Handy CJ, Lange HLH, Manos BE, et al. A Retrospective Chart Review of Contraceptive Use among Adolescents with Opioid Use Disorder. J Pediatr Adolesc Gynecol 2018; 31:122.
- Black KI, Day CA. Improving Access to Long-Acting Contraceptive Methods and Reducing Unplanned Pregnancy Among Women with Substance Use Disorders. Subst Abuse 2016; 10:27.
- Merrill JO, Rhodes LA, Deyo RA, et al. Mutual mistrust in the medical care of drug users: the keys to the "narc" cabinet. J Gen Intern Med 2002; 17:327.
- Schmittner J, Schroeder JR, Epstein DH, Preston KL. Menstrual cycle length during methadone maintenance. Addiction 2005; 100:829.
- Bonomi AE, Anderson ML, Reid RJ, et al. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med 2009; 169:1692.
- Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatr Clin North Am 2010; 33:339.
- Thorburn S, Bogart LM. Conspiracy beliefs about birth control: barriers to pregnancy prevention among African Americans of reproductive age. Health Educ Behav 2005; 32:474.
- Patel A, Schwarz EB, Society of Family Planning. Cancer and contraception. Release date May 2012. SFP Guideline #20121. Contraception 2012; 86:191.
- Finer LB, Zolna MR. Declines in Unintended Pregnancy in the United States, 2008-2011. N Engl J Med 2016; 374:843.
- Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann 2008; 39:18.
- Birgisson NE, Zhao Q, Secura GM, et al. Preventing unintended pregnancy: The contraceptive CHOICE project in review. J Womens Health (Larchmt) 2015; 24:349.
- Centers for Disease Control and Prevention. The 6/18 Initiative: Evidence Summary: Prevent Unintended Pregnancy 2016. http://www.cdc.gov/sixeighteen/pregnancy/index.htm. (Accessed on November 26, 2018).
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol 2011; 118:184.
- Secura GM, Allsworth JE, Madden T, et al. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol 2010; 203:115.e1.
- Aiken AR, Borrero S, Callegari LS, Dehlendorf C. Rethinking the Pregnancy Planning Paradigm: Unintended Conceptions or Unrepresentative Concepts? Perspect Sex Reprod Health 2016; 48:147.
- Aiken AR. Happiness about unintended pregnancy and its relationship to contraceptive desires among a predominantly Latina cohort. Perspect Sex Reprod Health 2015; 47:99.
- Aiken AR, Dillaway C, Mevs-Korff N. A blessing I can't afford: factors underlying the paradox of happiness about unintended pregnancy. Soc Sci Med 2015; 132:149.
- Gomez AM, Arteaga S, Ingraham N, et al. It's Not Planned, But Is It Okay? The Acceptability of Unplanned Pregnancy Among Young People. Womens Health Issues 2018; 28:408.
- Zeal C, Higgins JA, Newton SR. Patient-Perceived Autonomy and Long-Acting Reversible Contraceptive Use: A Qualitative Assessment in a Midwestern, University Community. Biores Open Access 2018; 7:25.
- Hall JA, Benton L, Copas A, Stephenson J. Pregnancy Intention and Pregnancy Outcome: Systematic Review and Meta-Analysis. Matern Child Health J 2017; 21:670.
- Lessard LN, Karasek D, Ma S, et al. Contraceptive features preferred by women at high risk of unintended pregnancy. Perspect Sex Reprod Health 2012; 44:194.
- Gomez AM, Fuentes L, Allina A. Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health 2014; 46:171.
- Roberts D. Killing the black body: Race, Reproduction, and the Meaning of Liberty, Pantheon Books, New York 1997.
- Stern AM. Sterilized in the name of public health: race, immigration, and reproductive control in modern California. Am J Public Health 2005; 95:1128.
- Downing RA, LaVeist TA, Bullock HE. Intersections of ethnicity and social class in provider advice regarding reproductive health. Am J Public Health 2007; 97:1803.
- Becker D, Tsui AO. Reproductive health service preferences and perceptions of quality among low-income women: racial, ethnic and language group differences. Perspect Sex Reprod Health 2008; 40:202.
- Dehlendorf C, Ruskin R, Grumbach K, et al. Recommendations for intrauterine contraception: a randomized trial of the effects of patients' race/ethnicity and socioeconomic status. Am J Obstet Gynecol 2010; 203:319.e1.
- Harrison DD, Cooke CW. An elucidation of factors influencing physicians' willingness to perform elective female sterilization. Obstet Gynecol 1988; 72:565.
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR (Eds), National Academies Press 2003.

SCOTT L. PARADISE, MD, CORINNE A. LANDIS, MD, AND DAVID A. KLEIN, MD, MPH
This is an updated version of the article that appeared in print.
Am Fam Physician. 2022;106(3):251-259
Related editorial: Contraception Recommendations: Updates for the Busy Clinician
Related letter to the editor: Physicians Need Education About Fertility Awareness–Based Methods
Published online May 27, 2022.
Author disclosure: No relevant financial relationships.
Primary care clinicians are uniquely situated to reduce unintended pregnancy in the context of a patient's medical comorbidities, social circumstance, and gender identity. New evidence regarding contraception use has emerged in recent years. The copper intrauterine device is the most effective option for emergency contraception, with similar effectiveness found for the levonorgestrel-releasing intrauterine system, 52 mg, and both offer extended future contraception. Ulipristal given within 120 hours after unprotected intercourse is the most effective oral emergency contraceptive. Oral levonorgestrel, 1.5 mg, is slightly less effective than ulipristal, and is less effective in patients with a body mass index of more than 30 kg per m 2 and if administered after 72 hours. The Yuzpe method, which uses a combination of oral contraceptives, is less effective than ulipristal or oral levonorgestrel, 1.5 mg, and has high risk of nausea and vomiting. Contraception methods based on fertility awareness are safe and have similar effectiveness as condom use and the withdrawal method. Patients who have migraine with aura have a higher risk of ischemic stroke, and combined oral contraceptives appear to increase this risk. Therefore, the Centers for Disease Control and Prevention recommends avoiding their use in these patients. Studies support the extended use of the levonorgestrel-releasing intrauterine system, 52 mg, for eight years, the copper intrauterine device for 12 years, and the etonogestrel subdermal contraceptive implant for five years. One levonorgestrel-releasing intrauterine device, 52 mg, (Mirena) was recently approved by the U.S. Food and Drug Administration (FDA) for eight years of use to prevent pregnancy. However, the intervals for the copper intrauterine device and the etonogestrel subdermal contraceptive implant are longer than approved by the FDA, and patient-clinician shared decision-making should be used. Subcutaneous depot medroxyprogesterone acetate, 104 mg, a newer formulation with prefilled syringes, can be safely self-administered every 13 weeks. Because bone density loss appears to be reversible, the American College of Obstetricians and Gynecologists recommends considering use of depot medroxyprogesterone acetate beyond two years despite an FDA boxed warning about increased fracture risk. Testosterone does not prevent pregnancy but is safe to use with hormonal contraception; thus, transgender and gender-diverse patients with a uterus can be offered the full range of contraceptive options.
In the United States, 45% of pregnancies in 2011 were unintended. 1 Primary care clinicians are uniquely situated to provide holistic contraceptive care in the context of a patient's medical comorbidities, social circumstance, and gender identity. This article addresses recent updates on the topic of contraception and answers common questions for clinicians. Table 1 includes comprehensive family planning resources provided by the Centers for Disease Control and Prevention (CDC). 2
What Forms of Emergency Contraception Are Effective?
The copper intrauterine device (IUD; Paragard) is the most effective intervention for emergency contraception when placed within 120 hours of unprotected intercourse. A large single study suggests that the levonorgestrel-releasing intrauterine system, 52 mg, (Mirena, Liletta) is similarly effective. Oral ulipristal (Ella); oral levonorgestrel, 1.5 mg, (Plan B One-Step); and the Yuzpe method are also effective if started within 120 hours. Emergency contraception should be started as soon as possible . 3 – 5 Oral emergency contraception may have decreased effectiveness with increasing body mass index . Table 2 summarizes emergency contraception options . 5 – 8
EVIDENCE SUMMARY
When placed within 120 hours after unprotected intercourse, the copper IUD is 99.9% effective at preventing pregnancy. 9 A recent study suggests that the levonorgestrel-releasing intrauterine system, 52 mg, is similarly effective. 6 In 317 patients who received the levonorgestrel-releasing intrauterine system, 52 mg, within 120 hours of unprotected intercourse, only one pregnancy occurred. This was similar to the group using the copper IUD. 6 Both methods offer reliable long-term contraception after placement, high continuation rates, high user satisfaction, and consistent effectiveness regardless of body mass index. 4 – 6
Ulipristal is the most effective oral emergency contraceptive, with a 1.3% pregnancy rate when started within 120 hours. Oral levonorgestrel, 1.5 mg, is slightly less effective than ulipristal with a 2.5% pregnancy rate. 7 Oral levonorgestrel, 1.5 mg, is approximately twice as effective if given within 72 hours than when given at 72 to 120 hours, and it is less effective for obese patients. 7 , 8 Pregnancy rates may also increase for obese patients using ulipristal, but data are conflicting. 8 The Yuzpe method uses a combination of oral contraceptives (0.1 to 0.12 mg of ethinyl estradiol and 0.5 to 0.6 mg of levonorgestrel) repeated after 12 hours. It is a low-cost, widely available method but is less effective than oral levonorgestrel, 1.5 mg, or ulipristal. 7 The Yuzpe method is associated with high rates of nausea and vomiting. 4 , 5 , 7
Oral emergency contraception does not affect an existing pregnancy, and a pregnancy test is unnecessary before use. 3 , 5 Because ulipristal may interact with the progestin component of hormonal contraceptives, it is recommended to wait at least five days before starting hormonal contraception after using ulipristal to preserve emergency contraception effectiveness. 4 Hormonal contraception may be started on the same day as oral levonorgestrel, 1.5 mg, administration. 5 If a patient does not have a withdrawal bleed within three weeks of using oral emergency contraception, a pregnancy test should be performed. 4
Are Fertility Awareness Methods of Contraception Effective?
Fertility awareness methods, which predict timing of ovulation so that intercourse can be avoided, have varying rates of effectiveness that are comparable to barrier and withdrawal methods . 10 Smartphone-based applications that aid in fertility awareness are advertised as improving effectiveness but may not be subject to peer review .
Fertility awareness methods track fertility intervals and physiologic changes, including body temperature, presence and consistency of cervical mucus, and urinary hormone excretion, to predict ovulation for the purpose of avoiding intercourse during that time. 5 , 11 , 12 These methods were previously reviewed in American Family Physician ( https://www.aafp.org/afp/2012/1115/p924 ). Although 4% of women report using fertility awareness methods, clinicians may not counsel patients on these methods because of perceived ineffectiveness, lack of training, insufficient time, or poor reimbursement. 12 , 13
A systematic review that excluded low-quality studies found that typical use of fertility awareness methods results in 2.0 to 33.6 pregnancies per 100 person-years ( Table 3 11 ) , depending on the method used, and is comparable to typical condom use and the withdrawal method. 5 , 11 Smart-phone applications that aid in fertility awareness improve adherence and ease of use, but effectiveness studies may not be subject to peer review. 14 , 15 The U.S. Food and Drug Administration (FDA) permitted marketing of the smart-phone applications Natural Cycles and Clue Birth Control to prevent pregnancy, noting a 6.5% failure rate over one year with typical use. 16 , 17
Fertility awareness methods should be avoided if patients have irregular menstrual cycles or partners who do not support abstinence or alternative contraceptive methods during fertile windows. They are a safe and reasonable alternative for patients who prefer to avoid hormonal contraception. 11
What Contraceptive Methods Are Less Safe for People With Migraines?
Migraine with aura is associated with an increased risk of ischemic stroke, whereas the risk for those who have migraine without aura is less clear . 18 , 19 Use of combined hormonal contraceptives, including oral contraceptives, transdermal patch, or vaginal ring, in patients who have migraine with aura appears to increase stroke risk . 19 – 21 The CDC's U.S. Medical Eligibility Criteria for Contraceptive Use (USMEC) recommend against prescribing combined hormonal contraceptives for patients who have migraine with aura . 20
In patients with migraines, use of combined hormonal contraceptives has been associated with a two- to fourfold increase in ischemic stroke risk; however, most studies do not differentiate between migraine subtypes. 19 , 20 Early studies suggested that the increased risk of ischemic stroke was common to all migraines, but more recent meta-analyses suggest the increased risk is limited to those who have migraine with aura. 18 , 22
In a case-control study using a nationwide database, the presence of migraine with aura and the use of combined hormonal contraceptives appear to increase risk of ischemic stroke, and risks may be additive. 21 Risk of stroke in patients who had migraine without aura was approximately twice as high as patients without migraine, regardless of combined hormonal contraceptive use. 21 Another study suggests that migraine with aura is associated with 1.5 times greater odds of ischemic stroke compared with no migraine, regardless of combined hormonal contraceptive use. 23 Although ischemic stroke risk from the use of combined hormonal contraceptives is theorized to be dependent on estrogen dose, evidence is limited. 19 The CDC and American College of Obstetricians and Gynecologists recommend avoiding the use of estrogen-containing contraceptives in patients who have migraine with aura but note that clear evidence of harm is limited. 20 , 24
All patients with headaches should be evaluated for migraines and the presence of aura. 24 Migraine subtypes were discussed previously in American Family Physician ( https://www.aafp.org/afp/2019/0101/p17.html and https://www.aafp.org/afp/2020/0401/p419.html ).
The USMEC has four categories of medical eligibility for contraceptive use. 20 Combined hormonal contraceptives are USMEC category 2 (i.e., advantages generally outweigh the risks) for patients who have migraines without aura, including menstrual migraine, and category 4 (i.e., unacceptable health risks) for those who have migraines with aura. Nonhormonal and progestin-only contraceptives are category 1 (i.e., no restrictions for use). Category 3 indicates that the theoretical or proven risks usually outweigh advantages. More information on the USMEC recommendations can be found at https://www.cdc.gov/reproductivehealth/contraception/mmwr/mec/summary.html .
How Long Does Long-Acting Reversible Contraception Remain Effective?
Data support continued contraceptive benefit from the levonorgestrel-releasing intrauterine system, 52 mg, for eight years; the copper IUD for 12 years; and the etonogestrel subdermal contraceptive implant (Nexplanon) for five years . 25 , 26 In 2021, the FDA approved use of one levonorgestrel-releasing intrauterine system, 52 mg, (Mirena) for eight years to prevent pregnancy. Extending use of other forms of long-acting reversible contraception (LARC) beyond the FDA-approved duration requires shared decision-making for off-label use .
LARC, including the levonorgestrel-releasing intrauterine system, copper IUD, and etonogestrel subdermal implant, reliably prevents pregnancy with typical use (less than one pregnancy per 100 patient-years over 12 months). 5 LARC is user independent and cost-effective, resulting in high patient satisfaction and high rates of continuation for 12 months. LARC can be used safely and effectively in adolescents and nulliparous patients. 5 , 27 – 29 Table 4 summarizes the key characteristics of LARC methods. 5 , 25 , 26 , 30 , 31
The levonorgestrel-releasing intrauterine system, 52 mg, was initially certified by the FDA for five years of use, whereas the copper IUD was initially certified for 10 years. However, studies demonstrate that the levonorgestrel-releasing intrauterine system continues to be highly effective for at least eight years, and the copper IUD is effective for at least 12 years. 25 , 32 – 34
A systematic review showed that the levonorgestrel-releasing intrauterine system had a lower pregnancy rate during the sixth and seventh year of use than in the first year. 25 Small studies support longer duration of effectiveness for the levonorgestrel-releasing intrauterine system, with no pregnancies in 776 patients over 10 years in one study. 32 The FDA recently certified Mirena for eight years and Liletta for six years of use to prevent pregnancy. 33 , 34
The copper IUD also appears to be effective during extended use. In two studies with 314 patients, use of the copper IUD for 12 years instead of 10 years did not result in additional pregnancies. 25 The FDA has not addressed extending the duration of copper IUD use.
The etonogestrel subdermal contraceptive implant is approved by the FDA for three years of use, but data suggest that it remains effective for at least five years. Serum etonogestrel levels have been shown to remain above contraceptive levels at five years. 35 In observational studies with more than 1,000 participants, no pregnancies occurred between three and five years of use. 26 , 35
The CDC recommends that clinicians be reasonably certain that a patient is not pregnant before IUD placement ( Table 5 ) . 4 This does not necessarily require a negative pregnancy test, which may be inaccurate in early pregnancy. The growth in telemedicine may increase the opportunity for counseling patients on the use of LARC options. Counseling should be based on noncoercive shared decision-making through patient-centered, reproductive-justice principles. 36 , 37
Can Depot Medroxyprogesterone Acetate Be Self-Administered Subcutaneously? What Are the Effects on Bone Mineral Density?
Subcutaneous depot medroxyprogesterone acetate (DeposubQ Provera) can be safely and effectively self-administered, potentially leading to fewer missed injections and unintended pregnancies. Depot medroxyprogesterone acetate may lead to loss of bone mineral density, which should be a consideration in those with relevant medical conditions . 19 , 20 , 38 , 39
Self-Administration of Subcutaneous Injections . Similar to 150-mg intramuscular depot medroxyprogesterone acetate (Depo-Provera), 104-mg subcutaneous depot medroxyprogesterone acetate is a progestin-only contraceptive that can be administered every 12 to 15 weeks. 39 – 43 However, the subcutaneous method uses a smaller needle and injection volume. 39 – 43 Self-administration of subcutaneous depot medroxyprogesterone acetate has been shown to be effective in clinical trials. In a meta-analysis of 3,851 participants, self-administered subcutaneous injections improved adherence compared with injections administered by a clinician, with comparable pregnancy rates and adverse effects other than injection site reactions. 31
Subcutaneous depot medroxyprogesterone is certified by the FDA for administration by a clinician. Self-administration is off-label use. 43 To reduce COVID-19-related barriers to care, some states have expanded telemedicine coverage for self-administration of subcutaneous depot medroxyprogesterone acetate. 44 The World Health Organization and CDC recommend self-administration of the subcutaneous injections as an additional approach to deliver injectable contraception to improve health equity, particularly among youth and marginalized populations. 40 , 43
Subcutaneous administration of depot medroxyprogesterone acetate has the same indications, risks, and benefits as intramuscular administration. 4 , 20 , 43 Instructions for self-administration of the subcutaneous injection are available at https://www.reproductiveaccess.org/wp-content/uploads/2017/08/2021-04-english-depo-sub-q.pdf .
Effect of Depot Medroxyprogesterone Acetate on Bone Mineral Density . Unlike other commonly used contraceptives, depot medroxyprogesterone acetate decreases pituitary gonadotropin secretion, leading to reduced estrogen production and possibly loss of bone mineral density. 38 In 2004, the FDA issued a boxed warning indicating that fracture risk may increase after two years of use. 38 Subsequent studies have shown that the loss of bone mineral density is substantially recoverable after stopping the medication, suggesting that there may be less risk of fracture with prolonged use than previously thought. 20 , 38 , 45 , 46
The American College of Obstetricians and Gynecologists recommends shared decision-making for extending the use of depot medroxyprogesterone acetate beyond two years in healthy patients, including review of the FDA warning and subsequent evidence; however, concerns about bone mineral density should not prevent continuing use beyond two years. 38 According to the CDC, there are no restrictions on the use of depot medroxyprogesterone acetate in healthy patients between 18 and 45 years of age. 20 Depot medroxyprogesterone acetate may have a higher risk of bone mineral density effects for patients younger than 18 years and older than 45 years, and when conditions such as cystic fibrosis, inflammatory bowel disease, or multiple sclerosis predispose the patient to lower bone mineral density. 20 For these special conditions, the CDC suggests that advantages of depot medroxyprogesterone acetate generally outweigh the risks. 20
Table 4 summarizes the key characteristics of depot medroxyprogesterone acetate. 5 , 25 , 26 , 30 , 31
What Are Contraception Considerations in Transgender and Gender-Diverse People With a Uterus?
Transgender and gender-diverse people with a uterus, including those assigned female sex at birth who have transgender or nonbinary masculine-spectrum identity or expression, can safely be offered the full range of contraceptive options, including emergency contraception. Contraception is effective for pregnancy prevention or menstrual suppression with gender-affirming hormone treatments . 30 , 47 Unintended pregnancies occur in transgender people taking testosterone, demonstrating that testosterone is not effective for contraception .
Even in the presence of amenorrhea, testosterone treatment does not prevent ovulation. 48 In addition to the family planning benefit, contraception has a safety function for transmasculine patients. Testosterone is a known teratogen that requires a washout period to prevent abnormal genital development in the fetus if the patient becomes pregnant. 30 Because pregnancy or menstruation may cause significant distress for transmasculine people, regular reproductive health counseling, including family planning and preferences for fertility preservation, is important. 36 Counseling should include discussing sexual behavior that may result in pregnancy. 47 , 49
Combining testosterone therapy with contraceptives containing estrogen does not appear to increase the risk of venous thromboembolism. 30 Transmasculine people may prefer to avoid oral contraceptives because of their associations with cisgender women and their perceived, but unlikely, feminizing effects. 30 , 47 , 50 Continuous use of contraceptives containing estrogen effectively suppresses uterine bleeding, and these contraceptives are easily discontinued when desired. Daily oral norethindrone acetate can suppress menses but has not been proven effective for contraception. 30
LARC is approximately 20 times more effective than daily oral contraceptives, making them appropriate options for transmasculine people. 27 IUD placement may be uncomfortable and distressful for transgender patients, which can be attenuated by anticipatory counseling, anxiolytics, sedation, smaller speculums, and short-term vaginal estradiol (Estrace) before the procedure. 30 Among progestin-only options, depot medroxyprogesterone acetate and the levonorgestrel-releasing intrauterine system, 52 mg, are most likely to lead to long-term amenorrhea. 30 Oophorectomy and hysterectomy are considered medically necessary for trans-masculine people who desire permanent sterilization. 47 , 51 , 52
When a transmasculine person with amenorrhea uses emergency contraception, a pregnancy test should be performed within four weeks. If a patient experiences bleeding after having amenorrhea or develops new pelvic pain, earlier evaluation including testing for pregnancy and sexually transmitted infections should be performed. 30
To mitigate stigma and barriers to care, clinicians can create welcoming environments by using gender-neutral language (e.g., people who menstruate, external pelvic area, chest instead of breasts, and absorbent products instead of menstrual pads or tampons). 30 , 53 Creating an inclusive clinical practice was discussed previously in American Family Physician ( https://www.aafp.org/afp/2018/1201/p645.html ).
Data Sources: A PubMed search was completed using the MeSH terms natural family planning methods, long-acting reversible contraception, hormonal contraception, migraine disorders, contraception, postcoital, or transgender persons. The reference lists of three cited manuscripts, guidelines by the American College of Obstetricians and Gynecologists and the World Health Organization, and two relevant reviews were searched for additional studies of interest. Other queries included Essential Evidence Plus, UpToDate, and the Cochrane Database of Systematic Reviews. Search dates: April 6 to June 6, 2021, and February 18, 2022.
Editor's Note: In August 2022, the U.S. Food and Drug Administration extended the recommended duration of use for the levonorgestrel-releasing intrauterine system, 52 mg, (Mirena) to eight years based on a demonstration of more than 99% effectiveness between six and eight years of use. This change is not reflected in the print edition of this article.—Sumi Sexton, MD, Editor-in-Chief
The views expressed in this publication are those of the authors and do not reflect the official policy or position of the Departments of the Navy and Air Force, the Department of Defense, or the U.S. government.
Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374(9):843-852.
Klein DA, Arnold JJ, Reese ES. Provision of contraception: key recommendations from the CDC. Am Fam Physician. 2015;91(9):625-633.
Practice bulletin no. 152: emergency contraception. Obstet Gynecol. 2015;126(3):e1-e11.
Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. selected practice recommendations for contraceptive use, 2016. MMWR Recomm Rep. 2016;65(4):1-66.
Hatcher RA. Contraceptive Technology . 21st ed. Ayer Company Publishers, Inc.; 2018.
Turok DK, Gero A, Simmons RG, et al. Levonorgestrel vs. copper intrauterine devices for emergency contraception. N Engl J Med. 2021;384(4):335-344.
Shen J, Che Y, Showell E, et al. Interventions for emergency contraception. Cochrane Database Syst Rev. 2019(1):CD001324.
Jatlaoui TC, Curtis KM. Safety and effectiveness data for emergency contraceptive pills among women with obesity: a systematic review. Contraception. 2016;94(6):605-611.
Cleland K, Zhu H, Goldstuck N, et al. The efficacy of intrauterine devices for emergency contraception: a systematic review of 35 years of experience. Hum Reprod. 2012;27(7):1994-2000.
- Contraceptive Technology. Comparing typical effectiveness of contraceptive methods. Accessed February 18, 2022. http://www.contraceptivetechnology.org/wp-content/uploads/2013/09/Contraception-Effectiveness.pdf
Peragallo Urrutia R, Polis CB, Jensen ET, et al. Effectiveness of fertility awareness-based methods for pregnancy prevention: a systematic review [published correction appears in Obstet Gynecol . 2019; 133(2): 382]. Obstet Gynecol. 2018;132(3):591-604.
Brewer M, Stevens L. Use of fertility awareness-based methods of contraception: evidence from the National Survey of Family Growth, 2013–2017. Contraception. 2021;104(2):183-187.
Webb S, Cheng A, Simmons R, et al. A mixed-methods assessment of health care providers' knowledge, attitudes, and practices around fertility awareness-based methods in Title X clinics in the United States. Womens Health Rep (New Rochelle). 2020;1(1):354-365.
Polis CB. Published analysis of contraceptive effectiveness of Daysy and DaysyView app is fatally flawed. Reprod Health. 2018;15(1):113.
Duane M, Contreras A, Jensen ET, et al. The performance of fertility awareness-based method apps marketed to avoid pregnancy. J Am Board Fam Med. 2016;29(4):508-511.
U.S. Food and Drug Administration. FDA allows marketing of first direct-to-consumer app for contraceptive use to prevent pregnancy. August 10, 2018. Accessed June 8, 2021. https://www.fda.gov/news-events/press-announcements/fda-allows-marketing-first-direct-consumer-app-contraceptive-use-prevent-pregnancy
U.S. Food and Drug Administration. 510(k) premarket notification. Clue Birth Control. February 18, 2021. Accessed June 8, 2021. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K193330
Spector JT, Kahn SR, Jones MR, et al. Migraine headache and ischemic stroke risk: an updated meta-analysis. Am J Med. 2010;123(7):612-624.
Tepper NK, et al. Safety of hormonal contraceptives among women with migraine: a systematic review. Contraception. 2016;94(6):630-640.
Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep. 2016;65(3):1-103.
Champaloux SW, Tepper NK, Monsour M, et al. Use of combined hormonal contraceptives among women with migraines and risk of ischemic stroke. Am J Obstet Gynecol. 2017;216(5):489.e1-489.e7.
Etminan M, Takkouche B, Isorna FC, et al. Risk of ischaemic stroke in people with migraine: systematic review and meta-analysis of observational studies [published corrections appear in BMJ . 2005; 330(7487): 345 and BMJ . 2005; 330(7491): 596]. BMJ. 2005;330(7482):63.
MacClellan LR, Giles W, Cole J, et al. Probable migraine with visual aura and risk of ischemic stroke: the stroke prevention in young women study. Stroke. 2007;38(9):2438-2445.
ACOG practice bulletin no. 206: use of hormonal contraception in women with coexisting medical conditions [published correction appears in Obstet Gynecol . 2019; 133(6): 1288]. Obstet Gynecol. 2019;133(2):e128-e150.
Ti AJ, Roe AH, Whitehouse KC, et al. Effectiveness and safety of extending intrauterine device duration: a systematic review. Am J Obstet Gynecol. 2020;223(1):24-35.e3.
Thaxton L, Lavelanet A. Systematic review of efficacy with extending contraceptive implant duration. Int J Gynaecol Obstet. 2019;144(1):2-8.
Curtis KM, Peipert JF. Long-acting reversible contraception. N Engl J Med. 2017;376(5):461-468.
Secura GM, et al. Provision of no-cost, long-acting contraception and teenage pregnancy [published correction appears in N Engl J Med . 2014; 372(3): 297]. N Engl J Med. 2014;371(14):1316-1323.
ACOG committee opinion no. 735: adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol. 2018;131(5):e130-e139.
Krempasky C, Harris M, Abern L, et al. Contraception across the trans-masculine spectrum. Am J Obstet Gynecol. 2020;222(2):134-143.
Kennedy CE, Yeh PT, Gaffield ML, et al. Self-administration of injectable contraception: a systematic review and meta-analysis. BMJ Glob Health. 2019;4(2):e001350.
Bahamondes L, Fernandes A, Bahamondes MV, et al. Pregnancy outcomes associated with extended use of the 52-mg 20 μg/day levonorgestrel-releasing intrauterine system beyond 60 months: a chart review of 776 women in Brazil. Contraception. 2018;97(3):205-209.
- FDA News. FDA expands approval of Mirena IUD device. August 25, 2022. Accessed August 29, 2022. https://www.fdanews.com/articles/209140-fda-expands-approval-of-mirena-iud-device
Liletta (levonorgestrel-releasing intrauterine system). Allergan, Inc.; 2019. Accessed May 31, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/206229s008lbl.pdf
McNicholas C, Swor E, Wan L, et al. Prolonged use of the etonogestrel implant and levonorgestrel intrauterine device: 2 years beyond Food and Drug Administration-approved duration. Am J Obstet Gynecol. 2017;216(6):586.e1-586.e6.
- American College of Obstetricians and Gynecologists' Committee on Health Care for Underserved Women, Contraceptive Equity Expert Work Group, and Committee on Ethics. Patient-centered contraceptive counseling: ACOG committee statement number 1. Obstet Gynecol. 2022;139(2):350-353.
Brandi K, Fuentes L. The history of tiered-effectiveness contraceptive counseling and the importance of patient-centered family planning care. Am J Obstet Gynecol. 2020;222(4S):S873-S877.
Committee opinion no. 602: depot medroxyprogesterone acetate and bone effects. Obstet Gynecol. 2014;123(6):1398-1402.
Burke HM, Chen M, Buluzi M, et al. Effect of self-administration versus provider-administered injection of subcutaneous depot medroxyprogesterone acetate on continuation rates in Malawi: a randomised controlled trial. Lancet Glob Health. 2018;6(5):e568-e578.
World Health Organization. WHO consolidated guideline on self-care interventions for health: sexual and reproductive health and rights. 2019. Accessed May 27, 2021. https://apps.who.int/iris/bitstream/handle/10665/325480/9789241550550-eng.pdf
Kohn JE, Simons HR, Della Badia L, et al. Increased 1-year continuation of DMPA among women randomized to self-administration: results from a randomized controlled trial at Planned Parenthood. Contraception. 2018;97(3):198-204.
- National Family Planning and Reproductive Health Association. DMPA-SQ and self-administration procedures clinical protocol. November 2020. Accessed May 27, 2021. https://www.nationalfamilyplanning.org/covid-19-resource-hub
Curtis KM, Nguyen A, Reeves JA, et al. Update to U.S. selected practice recommendations for contraceptive use: self-administration of subcutaneous depot medroxyprogesterone acetate. MMWR Morb Mortal Wkly Rep. 2021;70(20):739-743.
State of California Health and Human Services Agency. Information regarding the use of subcutaneous depot medroxyprogesterone acetate during the 2019 novel coronavirus public health emergency. Accessed March 21, 2021. https://www.dhcs.ca.gov/Documents/COVID-19/Medi-Cal-FFS-Depo-Provera-SQ-Temp-Policy.pdf
Lopez LM, Chen M, Mullins Long S, et al. Steroidal contraceptives and bone fractures in women: evidence from observational studies. Cochrane Database Syst Rev. 2015(7):CD009849.
Kyvernitakis I, Kostev K, Nassour T, et al. The impact of depot medroxyprogesterone acetate on fracture risk: a case-control study from the UK. Osteoporos Int. 2017;28(1):291-297
Health care for transgender and gender diverse individuals: ACOG committee opinion summary, number 823. Obstet Gynecol. 2021;137(3):554-555.
Taub RL, Ellis SA, Neal-Perry G, et al. The effect of testosterone on ovulatory function in transmasculine individuals. Am J Obstet Gynecol. 2020;223(2):229.e1-229.e8.
Light A, Wang L, Zeymo A, et al. Family planning and contraception use in transgender men. Contraception. 2018;98(4):266-269.
Agénor M, Cottrill AA, Kay E, et al. Contraceptive beliefs, decision making and care experiences among transmasculine young adults: a qualitative analysis. Perspect Sex Reprod Health. 2020;52(1):7-14.
Deutsch MB, ed. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2nd ed. June 2016. Accessed May 27, 2021. https://transcare.ucsf.edu/guidelines
Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline [published corrections appears in J Clin Endocrinol Metab . 2018; 103(2): 699 and J Clin Endocrinol Metab . 2018; 103(7): 2758–2759]. J Clin Endocrinol Metab. 2017;102(11):3869-3903.
Klein DA, Paradise SL, Goodwin ET. Caring for transgender and gender-diverse persons: what clinicians should know. Am Fam Physician. 2018;98(11):645-653.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2022 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Research article
- Open access
- Published: 17 January 2019
Family planning among undergraduate university students: a CASE study of a public university in Ghana
- Fred Yao Gbagbo ORCID: orcid.org/0000-0001-8441-6633 1 &
- Jacqueline Nkrumah 1
BMC Women's Health volume 19 , Article number: 12 ( 2019 ) Cite this article
35k Accesses
12 Citations
6 Altmetric
Metrics details
Globally, the rate of unplanned pregnancies among students at institutions of higher education, continue to increase annually despite the universal awareness and availability of contraceptives to the general population. This study examined family planning among undergraduate university students focusing on their knowledge, use and attitudes towards contraception in the University of Education Winneba.
The study was a descriptive cross-sectional survey using a structured self-administered questionnaire. One hundred undergraduate students from the University of Education Winneba were selected using a multistage simple random sampling technique. A Likert scale was used to assess the attitude of the respondents towards family planning methods.
Findings show that the respondents had a positive attitude towards family planning with an average mean score of about 4.0 using a contraceptive attitude Likert scale. Knowledge of contraception, awareness and benefits however do not commensurate contraceptive use among undergraduate students since availability, accessibility and preference influence usage. Emergency Contraception (Lydia) was reported as easy to get contraceptive, hence the most frequently used contraceptive (31%) among young female students aged 21-24 years who appeared as the most vulnerable in accessing and using contraceptives due to perceived social stigma.
The observation that levels of Family Planning awareness levels do not commensurate knowledge and usage levels calls for more innovative strategies for contraceptive promotion, and Education on the various university campus. The study recommends that public Universities in Ghana should consider a possible curriculum restructuring to incorporate family planning updates. In this regard, a nationwide mixed method study targeting other tertiary institutions including colleges of education in Ghana is required to explore the topic further to inform policy and programme decisions.
Peer Review reports
The global incidence of unplanned pregnancies amongst students at higher educational institutions every year continues to increase despite the high awareness and knowledge on regular modern contraceptives and emergency contraceptives among students in higher educational institutions [ 1 , 2 ]. Despite the immense contraceptive benefits for students in higher educational institutions [ 3 ], there is no direct positive correlation between the universal awareness, knowledge and use of contraceptives which challenges global health efforts. The poor utilisation of contraceptives in tertiary institutions is associated with many interrelated factors ranging from personal to institutional setbacks [ 4 ]. This eventually contributes to high unplanned pregnancy rates which is estimated to have contributed to about 8 to 30 million annual pregnancies worldwide [ 5 ]. Global estimates have also shown that about 210 million pregnancies occur annually across the world. 75 million (or about 36%) of the 210 are unplanned or unwanted pregnancies [ 6 ]. Students between 18 and 24 years report the highest rates of unplanned pregnancies in the world’s tertiary institutions [ 7 , 8 ]. A situation associated with multiple challenges across the world for countries, academic institutions and the individuals involved [ 9 ].
Studies in Africa, have generally documented low knowledge and awareness levels of effective contraceptive use amongst higher educational students [ 10 ]. Several factors including age, culture, ethnicity, religion, poor access to contraceptive services, peer pressure and lack of partner support were identified as contributing to the non-utilisation of contraceptives in tertiary institutions [ 11 ]. In a study amongst 15 to 24 year old South African women, it was estimated that only 52.2% of sexually experienced women are using contraceptives [ 12 ]. Because 80% of undergraduate students at higher educational institutions are sexually active, it is important that they have access to safe, accessible and adequate contraceptive services [ 13 ].
Although national surveys on family planning [ 14 ] have extensively looked at contraceptive uptake in Ghana, little is known about contraceptive up take among students in Ghanaian Universities. This study therefore examines family planning acceptance among students of the University of Education, Winneba in Ghana to compliment national data on family planning.
A descriptive cross-sectional study design using a quantitative approach of data collection was adopted. This design was chosen because it fits studies in natural setting, explains phenomena from the view point of persons being studied and produces descriptive data from the respondent own written or spoken words [ 15 ].
The study was conducted in the main campus of the University of Education, Winneba. The university was established in 1992 to train middle and top-level manpower for the educational sector of Ghana. It has four main satellite campuses, (Winneba and Ajumako in the Central Region of Ghana, Kumasi, and Mampong campuses in Ashanti Region of Ghana). The Winneba campus has three smaller campuses with five faculties (Faculty of social science education, Faculty of languages, Faculty of science education, Faculty of educational studies and School of creative Arts).
The study population comprised134 ‘non-resident’ undergraduate students of the University of Education Winneba, between ages 17–36 years in 2017 who were registered with an accommodation agent in Winneba that looks for accommodation for students who are unable to obtain university accommodation on campus. This population and age group was selected because anecdotal evidence shows that being a ‘non-resident’ student has the likelihood of making one vulnerable to sexual exploitations whilst seeking accommodation off campus. This age group was considered to be the reproductive age group of the undergraduate students. Because the University only guarantees on campus residential accommodation for only selected first year students, those who do not get the university’s residential accommodation are likely to be victims of sexual exploitations in the Effutu Municipality where the university is situated. This challenge is due to the scarcity of accommodation coupled with the high rent charges for rented accommodation. As per the estimated sample size calculated, a total of one hundred respondents comprising twenty from each of the five faculties were sampled at random to include both male and female students from the various course levels. This was done to ensure a true representation of the student population for the study.
A multistage sampling technique was used to select these respondents for the study. The first stage involved half day orientation of 2 field assistants (male and female) the estimation of the undergraduate students’ population who falls in this category during the period of the study. The second stage involved sample size calculation using an online Raosoft sample size calculator at 95% confidence interval, 5% margin of error and 50% response distribution [ 16 ]. In terms of the figures, the sample size n and margin of error E are given by:
Where N is the population size (134), R is the fraction of responses that the study is interested in, and Z(c/100) is the critical value for the confidence level c. The estimated number of respondents were then randomly sampled and contacted for participating in the in the third stage of the study. The fourth stage of the study involved distributing the developed questionnaires to consented students.
A Structured Questionnaire (See Additional file 1 ), designed by the authors was used to solicit responses from respondents. The questionnaire was exploratory in nature with both opened and closed ended questions to help respondents easily share their views. The questionnaire was pre-tested among 20 potential respondents from a different university. The Contraceptive Attitude Likert scales was used to measure attitudes by asking people to respond to series of statements about the topic, in terms of the extent to which they agree or disagree with them. Thus, tapping into the cognitive and affective components of attitudes [ 17 ]. The Contraceptive Attitude Scale presented positive and negative statements to elicit for responses that portray participants’ attitudes relating to contraception.
One hundred questionnaires were administered, and all the answers to a particular question were arranged, numbered and responses were coded. The responses were again listed and grouped, putting those with the same code together. Data analysis was done after data had been collected and checked for completeness and accuracy. The Statistical Package for Social Sciences (SPSS) software version 23 was used for data analysis. Frequencies, percentages and bar charts were used to describe the data in multivariable tables.
Ethics approval and consent to participate
An approval was obtained from the University prior to data collection. Written consent for participation and publication of findings were also obtained from respondents after the purpose, objectives and potential risk and benefits inherent in the study had been explained to them. Prior to the commencement of the study, the research protocol was presented at the bi-weekly academic research seminars of the Faculty of Science Education, University of Education, Winneba. The seminar brought together lectures of the Faculty (equivalent to an ethical review meeting) who critiqued and reviewed the study protocol for ethical suitability and sound methodology. All participants in the study were given the opportunity to ask questions about the study at any stage, and to withdraw from the study at any time. All data collected were kept confidential and data was analysed anonymously to ensure that results were not traceable to individual respondent.
The overall response rate for the study was 100%. Table 1 presents the background characteristics of respondents. A large number of the respondents were within the age categories of 21 to 24 years and 25 to 28 years. Most of the respondents were single (86.0%) and have no children (86.0%).
Table 2 present results of students’ knowledge, information sources and reasons for accepting or not accepting family planning. Family planning awareness and knowledge among students was a key consideration in the study.
About 94% of respondents answered yes to whether they have ever heard about family planning. Although majority (61%) of the respondents believed FP is helpful, about (67.0%) knew that one could get pregnant by relying on the withdrawal method. It appears most students would be committed to family planning uptake if services are made available. This is evident by 69% of them responding in the affirmative when asked whether they will encourage their family or friends to use family planning services in the University.
Having knowledge of family planning does not necessarily translate into utilization since the respondents had varied reasons for and against using family planning. Respondents who were of the view that FP was not helpful (25.0%) had either not used any family planning method before (28.0%) or had ever suffered unpleasant negative side effects (20.0%) following family planning usage or believed the bible is against family planning (2.0%).
Figure 1 presents respondents’ attitudes towards family planning as estimated using the Contraceptive Attitude Scale. The overall population surveyed had a positive attitude towards family planning (average mean attitude score was about 4.0 out of 5.0).
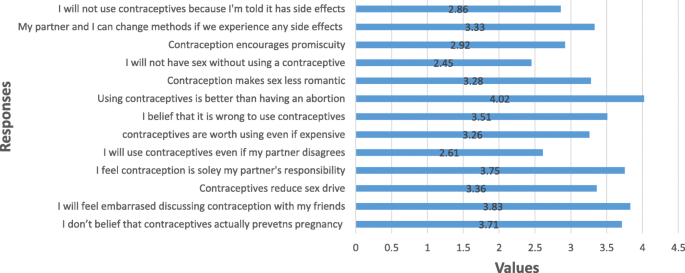
Attitude towards Family Planning
There were however some divergent responses to the questions relating to contraceptive use. Some of these include:
‘I will not have sexual intercourse if no contraceptive method was available’
‘I will use contraceptives even if my partner does not want me to use it’
‘I will not use contraceptives because they encourage promiscuity’
When the respondents were asked if they have ever used any FP method before, the majority of the respondents (67.0%) mentioned that they had never used any FP method. Regarding availability of family planning service when needed, about 64.0% of the respondents indicated that family planning services are always available in chemical shops and from colleges on campus when needed. About 58% will use FP methods in the future. Regarding information on source of family planning services if required, most of the respondents (85%) knew where to get family planning services in their communities (Table 3 ). Young Female students aged 21-24 years were the most vulnerable in accessing and using contraceptives due to perceived social stigma relating to a female student buying a contraceptive.
Table 4 documents the various family planning choices and reasons for the choices. About 65.0% of respondents reported that they primarily use contraceptives to prevent pregnancy and usually use a contraceptive before sexual intercourse (34.0%). When asked to select the primary methods of contraception frequently used, Emergency Contraception was the most reported frequently used (51%) contraceptive followed by male condoms (34.0%). Various side effects associated with some FP methods were also reported. Some respondents were of the view that there should be education for students on the risk and benefits of FP methods for effective use. Others believed FP should not be tolerated among students because it can be abused leading to major health problems that could affect studies. Knowledge of contraception, awareness and benefits however do not commensurate contraceptive use among undergraduate students since availability, accessibility, preference and cost of contraceptives hinders use.
This study examined family planning among undergraduate university students focusing on their knowledge, use and attitudes towards family planning in the University of Education Winneba. The study was a descriptive cross-sectional survey using a structured self-administered questionnaire for data collection. Various findings obtained from the study had reproductive health programme and policy implications. Informal sources of family planning information such as friends, peers and relatives were common information sources for young people [ 18 ] but yet prone to misconceptions, distortions and half-truths. Other studies ranked the family (parents, brothers and sisters) as the lowest source of information on sexuality [ 19 , 20 , 21 ]. These findings are similar to those reported in the current study that high level of awareness (94.0%) of contraceptives is noted among university students.
An observation that a large number of the respondents were within the age categories of 21 to 24 years and 25 to 28 years of which most (86.0%) were single and have no children (86.0%), is an indication that current university students are relatively young and unmarried. A situation that predisposes them to sexual exploitations and requires knowledge on family planning methods to enable them make informed decision and choices regarding their reproductive intentions. Family planning awareness and knowledge among students was a key consideration in the study. The majority (94%) of respondents indicating that they have ever heard about family planning shows a near universal awareness of family planning methods. This is in line with national reports on family planning awareness in Ghana and a significant departure from many other studies which tended to focus on awareness alone or translate awareness to knowledge [ 22 , 23 ]. Understanding the methods and benefits of contraception are critical to having motivated users. It has also been noted that motivation is one of the important factors in minimizing failure rates in the utilization of contraception [ 24 ]. From previous research findings [ 25 , 26 , 27 ] it was established that the most commonly used Family Planning methods among students were short term methods predominantly, condoms, oral contraceptives and withdrawal methods. This confirms finding of other studies that students had little knowledge about effective contraceptive methods [ 28 ]. In the current study, a remarkable percentage (25%) did not know that pregnancy could occur when one relying solely on withdrawal method. Also about 21.0% of respondents did not know what oral contraceptive pills do, and some 3% also said oral contraceptive pill prevents Sexually Transmitted Infections (STIs). It was surprising to note in this era of increasing STIs that about 2% of respondents’ from a tertiary institution belief a single condom can be reused many times if washed and dried.
At the tertiary level, one would have expected that all respondents would have known the implications of unprotected sexual intercourse. However the study finding that about (61%) of the respondents believed family planning is helpful implies that there are some other students who don’t belief in family planning hence having unprotected sexual intercourse. Although accessibility to family planning methods on campus in this study was very high (66.0%), results from other similar studies were to the contrary [ 29 , 30 ]. This therefore suggests that if students know the benefits and how to use contraceptives, they will not experience unwanted pregnancies and its associated consequences of unsafe abortion complications, disruption in academic work and possible death. Contraceptive education is a component of sex education and is one of the proven approaches to prevent risky sexual behaviour and must be introduced on university campuses to guide students’ family planning choices.
Additionally, findings also shows that there are some students about (67.0%) at the university who knew that one could get pregnant by relying on the withdrawal method yet that is their preferred family planning methods. Various studies [ 31 , 32 ] have explained this observation further by indicating that some adolescents girls feel that a partner’s use of condom suggest that they (the girls) might be classified as unclean, likened to commercial sex workers or seen as engaging in extra-relationship sexual activities if they negotiate for condom use during sexual intercourse. The perception of ‘ I trust my partner so no need for condom use’ further explains the frequency of withdrawal methods being a regular family planning method on campus.
Generally, it appears most students were committed to family planning uptake if services are made available as evident by about 69% of them responding in affirmative when asked whether they will encourage their family or friends to use family planning services in the University. This observation is positive for enhanced family planning service delivery on university campuses to meet the needs of students. Contrary to this observation are those of similar studies which reported that Student frown on invasive family planning methods [ 33 , 34 ]. The distinction between invasive and non-invasive methods bothers on factors such as availability of method, ease of use and adherence to instructions of a health professional to use the method.
Respondents outlined various sources of family planning information of which television adverts constituted the most reported (31%) source of information. This observation is quite worrying since anecdotal evidence from university campuses shows that majority of student rarely have and watch televisions whist on the various campuses. It will therefore be very important and useful to devise innovative ways of educating students on family planning methods whilst on campus.
A finding that having knowledge of family planning does not necessarily translate into usage is very revealing and of public health importance. As it would have been expected, using a method is the surest way of explaining its relevance. However in this study, respondents who were of the view that family planning was not helpful had never used any family planning method before (28.0%). It is there important to use of family planning satisfied client for contraceptive education and promotion on University campuses to ensure the desired positive results. These are students who are likely to positively influence their sexually active peers on contraceptive use since they are likely to say: ‘ I will not have sexual intercourse if no contraceptive method was available’ or ‘I will use contraceptives even if my partner does not want me to use it’ as reported in the study.
Regarding information on source of family planning services if required, most of the respondents (85%) knew where to get family planning services in their communities. For availability of family planning services when needed, about 64.0% of the respondents indicated that family planning services are always available in chemical shops and from colleges on campus when needed. The obvious indicated sources of contraceptives on campus (i.e., chemical shops and peers) do not provide varying choice of services there by limiting students to short term and less effective family planning methods. It is encouraging noting that about 58% of respondents will use FP methods in future. This is an indication of them understanding the importance of family planning to studies as about 65.0% of respondents reported primarily using contraceptives to prevent pregnancy and usually use a method before sexual intercourse (34.0%) despite the various side effects associated with some FP methods reported.
Knowledge of contraception, awareness and benefits however do not commensurate contraceptive use among undergraduate students since availability, accessibility and preference influence usage. Emergency Contraception (Lydia) was reported as easy to get contraceptive, hence the most frequently used contraceptive (31%) among young female students aged 21-24 years who appeared as the most vulnerable in accessing and using contraceptives due to perceived social stigma. This observation shows that Students always have a unique view on issues especially those in youthful ages. It is therefore important to incorporate their views in family planning programming. The observation that some respondents were of the view that there should be education for students on the risk and benefits of family planning methods for effective use is in the right direction and worth exploring. There are also concerns of values clarification as observed by the findings that some respondents believed family planning should not be tolerated among students because it can be abused leading students to becoming promiscuous or suffering major health problems that will affect their studies.
The following recommendations are therefore being suggested to chart a way forward:
Public Universities in Ghana should consider a possible curriculum restructuring to incorporate family planning lessons in the academic programme for students to acquire current knowledge in this area. The reproductive health education programs should include the importance of using dual contraceptive methods as a means to prevent HIV transmission and pregnancy, as well as information on how to make an informed decision relating to contraceptive choices.
The Winneba Municipal Health Directorate should incorporate family planning education on campuses into their public health programs.
The university health service should also create friendly environment for student to access family planning services and also collaborate with the student body to organise programmes to educate the students on family planning methods.
The student representative council (SRC) should also make family planning education a part of their programs and in collaboration with the university health services organise free STI testing and family planning counselling at least once yearly.
A nationwide mixed method study targeting other tertiary institutions particularly colleges of education in Ghana is required to explore the topic further for a national decision on contraceptive security in tertiary institutions in Ghana.
Conclusions
Findings of this study showed that the awareness of family planning among the students was high. However, levels of contraceptive usage were low and restricted to the short term, Emergency Contraceptives and redrawal methods. The perception by a cross-section of respondents (although by a small group) that condoms can be reused more than once confirms the gross ignorance of contraception practices and the potential risk to STIs and Pregnancy. Additionally, Emergency Contraception (Lydia) being reported as easy to get contraceptive, hence the most frequently used contraceptive (31%) among young female students aged 21-24 years, is an indication that this student population appeared as the most vulnerable in accessing and using contraceptives due to perceived social stigma and must therefore be the prime focus of contraception education and services on the University. The University of Education being a tertiary institution mandated to train teachers, is expected to ensure that its students have accurate and current information on family planning methods relevant to educate others. This is an obvious gap that requires policy decisions at all levels and FP education interventions at the tertiary level of education in Ghana.
Abbreviations
- Family planning
Statistical Package for Social Sciences
Sexually Transmitted Infections
University of Education Winneba
World Health Organization (WHO). (2013): Family planning fact sheet. Retrieved from http://www.who.int/mediacentre/factsheets/fs351/en / United Nations. (2011). The millennium development goals report. Retrieved from www.un.org/millenniumgoals/11_MDG%20Report_EN.pdf
Maja TMM, Ehlers VJ. Contraceptive practices in northern Tshwane, Gauteng Province. Health SA Gesondheid. 2004;9(4):42–52 https://doi.org/10.4102/hsag.v9i4.179 .
Article Google Scholar
Ersek, J.L., Brunner Huber, L.R., Thompson, M.E. & Warren-Findlow, J., (2011):‘Satisfaction and discontinuation of contraception by contraceptive method among university women’, Matern Child Health J 15, 497–506. PMID: 20428934, https://doi.org/10.1007/s10995-010-0610-y
Hubacher, D., Ifigeneia, M. & McGinn, E., (2008): ‘Unintended pregnancy in sub-Saharan Africa: magnitude of the problem and potential role of contraceptive implants to alleviate it’, Contraception 78, 73–78. PMID: 18555821, https://doi.org/10.1016/j.contraception.2008.03.002
Adhikari, R., (2009): ‘Factors affecting awareness of emergency contraception among college students in Kathmandu, Nepal’, BMC Women’s Health 9, 27. PMID: 19761598, https://doi.org/10.1186/1472-6874-9-27
Singh, S., Sedgh, G., & Hussain, R. (2010) “Unintended pregnancy: worldwide levels, trends, and outcomes”Studies in family planning 41, no. 4:241–250.
Esere MO. Effect of sex education programme on at-risk sexual behaviour of school going adolescents in Ilorin, Nigeria. Africa health science. June. 2008;8(2):120–5.
Google Scholar
Trieu, S.l., Shenoy, D.P., Bratton, S. & Marshak, H.H., (2011): ‘Provision of emergency contraception at student health centers in California community colleges’, Womens Health Issues 21(6), 431–437. PMID: 21703870, https://doi.org/10.1016/j.whi.2011.04.011
Vermaas, L., (2010). ‘Dealing with unplanned pregnancies and abortions amongst tertiary students’, paper presented at the 6th African Conference on Psychotherapy in Uganda, Kampala, Uganda, 14–16 December, viewed 13 February 2013, from http://www.tut.ac.za/News/Pages/pregnancies.aspx .
Ahmed, F.A., Moussa, K.M., Petterson, K.O. & Asamoah, B.O., (2012), ‘Assessing knowledge, attitude, and practice of emergency contraception: A cross sectional study among Ethiopian undergraduate female students’, BMC Public Health, 12, 110, viewed 06 March 2015, from http://biomedcentral.com/1471 –2458/12/110 Page 7 of Original Research http://www.curationis.org.za doi: https://doi.org/10.4102/curationis.v38i2.1535 .
Golbasi Z, Tugut N, Erenel AS. Knowledge and opinions of Turkish University students about contraceptive methods and emergency contraception. Sex Disabil. 2012;30:77–87 https://doi.org/10.1007/s11195-011-9227-3 .
MacPhail, C., Pettifor, A.E., Pascoe, S. & Rees, H.V., (2007): ‘Contraception use and pregnancy among 15–24 year old south African women: a nationally representative cross-sectional survey’, BMC Med 5, 31. PMID: 17963521, https://doi.org/10.1186/1741-17015/5/31
Bryant, K.D., (2009): ‘Contraceptive use and attitudes among female college students’, Journal of ABNF 20(1), 12–16. PMID: 19278182.
Ghana Statistical Service (2014). Ghana Demographic and Health Survey Report.
Akintade OL, Pengpid S, Peltzer K. Awareness and use of and barriers to family planning services among female university students in Lesotho’, south African journal of Gynaecology 17(3), 72–78.McNab C, (2009): what social media offers to health professionals and citizens. Bull World Health Organ. 2011;87:566.
Raosoft Sample Size Calculator Accessed on 2 nd July, 2012 from http://www.raosoft.com/samplesize.html
Tilahun D, Assefa T, Belachew T. Knowledge, attitude and practice of emergency contraceptives among Adama University female students. Ethiopia Journal of Health Sciences November. 2010;20(3):195–202.
Sigereda G., (2004): Barriers to use contraceptive among adolescents in the city of Addis Ababa. Master’s theses.
Abiodun MO, Olayinka PB. Sexual activity and contraceptive use among female students of tertiary educational institutions in Illorin. Nigeria Contraception. 2009;79(2):146–9.
Mehra, D., Agardh, A., Petterson, K.O. & Ostergren, P.O., (2012): ‘Non-use of contraception: determinants among Ugandan university students’, Glob Health Action 5, 18599. PMID: 23058273, https://doi.org/10.3402/gha.v5i0.18599
Tayo A, Akinola O, Babatunde A, Adewunmi A, (2011): Contraceptive knowledge and usage among female school students in Lagos, south-West Nigeria. Journal of public health and epidemiology January, 3 (1), pg. 34–37.
Bafana T. Factures influencing contraceptive use and unplanned pregnancy in a South African population. MA thesis: Witwatersrand University; 2010.
Egarter C, Grimm C, Ahrendt KNH-J, Bitzer J, Ehlers VJ, Zvavemwe Z. Experiences of a community based contraceptive programme. Int J Nurs Stud. 2009;46(3):302–9.
World Health Organization, WHO. Programming for adolescent health and development: report of a WHO/UNFPA/UNICEF study group on programming for adolescent health. Technical report. Geneva: WHO; 1999. p. 886.
Cadmus E, Owoaje E. Patterns of contraceptive use among female undergraduates in the University of Ibadan, Nigeria. The Internet Journal of Health. 2009;10(2).
John, H. Contraceptive Knowledge, Perceptions and use among adolescents journal of Sociol Res 2012; 3(2):170–180. 25–34.
Appiah-Agyekum, N.N. & Kayi, E.A. (2013). Students’ Perceptions of Contraceptives in University of Ghana, 7(1): 39–44. Beware of AIDS (BAWA), Offinso-Ashanti, Ghana International Conference on AIDS. International Conference of AIDS 12: 1005 (abstract number 60018).
Roberts, C., Moodley, J. & Esterhuizen, T., (2004): Emergency contraception: knowledge and practices of tertiary students in Durban, South Africa’, Journal of Obstetrics and Gynaecology 24(4), 441–445. PMID: 15203588, https://doi.org/10.1080/0144361040001685619
Canadian Statistics, (2010): Trends in the Age Composition of College and University Students and Graduates www. Statcan.gc.ca Accessed 1/4/14.
Dreyer G. Contraception: a south African perspective. Pretoria: Van Schaik Publishers; 2012.
Adegoke AA. Adolescents in Africa: Revealing the problems of teenagers in contemporary African society. Ibadan, Hadassah Publishing; 2003.
Omo-Aghoja LO, Omo-Aghoja VW, Aghoja CO, Okonofua FE, Aghedo O, Umueri C, Otayohwo R, Feyi-Waboso P, Onowhakpor EA, Inikori KA. Factors associated with the knowledge, practice and perceptions of contraception in rural southern Nigeria. Ghana Med J. 2009;43(3):115–21.
CAS PubMed PubMed Central Google Scholar
McMahon S, Hansen L, Mann J, Sevigny C, Wong T, Roache M. Contraception. BMC Womens Health. 2004;4(Suppl1):S25.
Clements S, Madise N. Who is being served least by family planning providers? A study of modern contraceptives use in Ghana, Tanzania and Zimbabwe. Afr J Reprod Health. 2004;8:124.
Download references
Acknowledgements
The authors are grateful to the University of Education Winneba, Faculty of Science Education for the valuable inputs in shaping the manuscript. Many thanks also to the respondents for their corporation during data collection.
The entire study was jointly funded by the authors.
Availability of data and materials
The raw data and any material related to the study is available upon reasonable request from the corresponding author.
Author information
Authors and affiliations.
Department of Health Administration and Education, University of Education Winneba, Faculty of Science Education, P.O. Box 25, Winneba, Ghana
Fred Yao Gbagbo & Jacqueline Nkrumah
You can also search for this author in PubMed Google Scholar
Contributions
FYG conceptualized and designed the study. JN supervised the data collection, analysis and drafted the initial report. Both authors discussed the report, edited it together and approved the manuscript for final submission.
Corresponding author
Correspondence to Fred Yao Gbagbo .
Ethics declarations
The research protocol was first presented at the Faculty of Science Education, University of Education, Winneba periodic academic seminars for review and approval for methodology and ethical suitability. This seminar, brings together senior members and research fellows of the University to review research protocols and papers meant for publication and conferences. Approval for data collection and publication were subsequently granted following the full incorporation of comments received from the seminar presentation.
Prior to data collection, verbal and written permissions were sought from the respondents to participate in the study. The permission was granted after the objectives and nature of the study were satisfactorily explained to the respondents.
Consent for publication
The respondents consented for the study to be published but assured of anonymity before administering the questionnaire. The respondents were also given the opportunity to ask questions about the study at any stage, and to withdraw from the study at any time.
Competing interests
The authors declare that they have no competing interests in this study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Appendix I-Questionaire. The appendix I contains the structured question developed by the authors and used for data collection in the study. (DOCX 23 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Gbagbo, F.Y., Nkrumah, J. Family planning among undergraduate university students: a CASE study of a public university in Ghana. BMC Women's Health 19 , 12 (2019). https://doi.org/10.1186/s12905-019-0708-3
Download citation
Received : 01 August 2017
Accepted : 02 January 2019
Published : 17 January 2019
DOI : https://doi.org/10.1186/s12905-019-0708-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Undergraduate students
- University of Education
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Contraception for...
Contraception for women: an evidence based overview
- Related content
- Peer review
- Jean-Jacques Amy , editor in chief 1 ,
- Vrijesh Tripathi , lecturer 2
- 1 European Journal of Contraception and Reproductive Health Care, Opalfeneweg 3, B-1740 Ternat, Belgium
- 2 Faculty of Science and Agriculture, University of West Indies, St Augustine, Trinidad and Tobago, West Indies
- Correspondence to: J-J Amy, Florencestraat, 62, B-1050 Brussels, Belgium jeanjacques.amy{at}skynet.be
Summary points
Combined oestrogen and progestogen contraceptives inhibit ovulation. Their biological effects and safety profiles are similar regardless of route of administration
Progestogen-only methods act by various mechanisms and can be used by women in whom oestrogens are contraindicated
Copper bearing intrauterine devices combine the highest efficacy with the lowest cost. The levonorgestrel releasing intrauterine system reduces menstrual blood loss
When used correctly, the lactational amenorrhoea method prevents conception in more than 98% of women during the first six months after childbirth
Levonorgestrel-only emergency contraceptive pills and copper bearing intrauterine devices are valuable methods of emergency contraception
Emergency contraceptive pills prevent pregnancy; they should be taken as soon as possible, and not later than 72 hours after unprotected intercourse
Contraception allows parents to choose the number and spacing of children. Each year, family planning programmes prevent an estimated 187 million unintended pregnancies, including 60 million unplanned births and 105 million abortions, and avert an estimated 2.7 million infant deaths and 215 000 pregnancy related deaths. 1
The prevalence of contraceptive use differs across the world owing to differences in desired number of children, awareness, funding, and service delivery, with an overall prevalence of use worldwide of 63%. Female sterilisation and intrauterine devices account for nearly 40% in less developed regions, and pills, intrauterine devices, and condoms for the same proportion in more developed regions. 2 This article reviews evidence based information on contraceptive methods currently available for women.
Sources and selection criteria
We prepared this review by searching Cochrane reviews, PubMed, and our personal archives of references.
The family planning consultation
Counselling.
Counselling is thought to enable clients to make contraceptive choices that best fit their values and needs; it should lead to greater satisfaction and more correct and longer use of contraception, particularly when partners are involved. However, a Cochrane review of randomised controlled trials that acknowledged heterogeneity between studies found no conclusive evidence that counselling improves adherence to, and continuation of, the use of contraceptives. 3
The World Health Organization identifies four types of clients according to their counselling needs: returning clients with no problems, returning clients with problems, new clients with a method in mind, and new clients with no method in mind. 4 Family planning providers must therefore be both knowledgeable and skilled in communicating information. Ideally, family planning counselling is holistic and encompasses sexual and reproductive health, but prevention of sexually transmitted infections is outside the scope of this review.
Clinical aspects
According to WHO international guidelines, the minimum requirements before starting contraception with a combined oestrogen-progestogen product consists of asking for a personal and family history of deep vein thrombosis and measuring blood pressure at baseline and follow-up. 5 Combined agents are best avoided by women over 35 years who smoke. 5 Progestogens only can be started in healthy non-pregnant women without screening procedures. 5
A recent Cochrane review found little evidence to support the idea that immediately starting hormonal contraception is associated with greater effectiveness, continuation, and acceptance than starting the contraception after the onset of the next menses. 6
How do hormonal contraceptives work?
Combined oestrogen-progestogen products.
Table 1 ⇓ lists the currently available combined oestrogen-progestogen contraceptives. These products release an oestrogen (mostly ethinylestradiol) and a progestogen, which act systemically to inhibit ovulation. All, except the sequential pill, also increase the viscosity of cervical mucus—which inhibits migration of sperm to the uterine cavity—and suppress endometrial growth. Combined oral contraceptives, patches, and combined vaginal rings may be used cyclically, according to an extended regimen (with a medication-free interval), or continuously. According to WHO guidelines, 4 return to fertility on discontinuation of treatment is immediate, with the exception of monthly injectable preparations, which require five months on average after the last injection for fertility to return.
Combined oestrogen-progestogen preparations
- View inline
Progestogen-only products
Progestogen-only preparations (table 2 ⇓ ) may be given to women in whom oestrogens are contraindicated. Progestogen-only pills are taken each day at the same time, with no pill-free interval. Progestogen-only pills and implants that release levonorgestrel act primarily by thickening the cervical mucus; ovulation is not always prevented. In addition to their effect on cervical mucus, desogestrel pills, depot medroxyprogesterone acetate, and etonogestrel releasing implants inhibit ovulation in most cycles. Fertility returns as soon as pills are discontinued, whereas it takes an average of 10 and six months to return after the last injection of depot medroxyprogesterone acetate and norethisterone enantate, respectively. 4
Progestogen-only preparations
How effective are hormonal contraceptives?
Effectiveness is related to the acceptability of the contraceptive method and to compliance. “Typical use” is considerably less effective than “perfect use” (correct and consistent use). A recent Cochrane review found that combined oral contraceptive pills, transdermal patches, and vaginal rings were equally efficacious 7 : they have a failure rate of 0.3 per 100 women per year with perfect use and 8 with typical use. 7 8 Maintaining a regular schedule is more important for progestogen-only pills than for combined oral contraceptives—more than a three hour delay in taking the progestogen-only pill can cause failure of contraception. Implants, injectable preparations, and intrauterine contraceptives do not depend on daily compliance and have lower failure rates. 8 Implants (failure rate of 0.05 per 100 women per year with typical use) and injectable preparations (3) are among the most effective reversible contraceptives. 8 According to recently updated WHO recommendations, depot medroxyprogesterone acetate may be given up to four weeks late without pregnancy needing first to be ruled out. 5
How is the effectiveness of hormonal contraceptives affected by drug interaction?
The efficacy of hormonal contraceptives may be reduced when liver enzyme inducing drugs are taken simultaneously. 5 Box 1 lists several drugs that interact with hormonal contraceptives. Certain antibiotics without liver enzyme inducing activity alter the enterohepatic recirculation of sex steroids and thereby reduce the efficacy of combined oral contraceptives. Additional contraceptive protection, such as a barrier method, should be used concurrently and for four weeks after discontinuing such drugs. Interactions of antiretrovirals with hormonal contraceptives are specific to the type of antiretroviral and hormonal contraceptive being used. HIV positive women should use a dual method of hormonal and barrier contraception. 9
Box 1 Drugs that interact with hormonal contraceptives 5 9
Liver enzyme inducing drugs that reduce the efficacy of hormonal contraceptives.
Barbiturates
Carbamazepine
Oxcarbazepine
Griseofulvin
Certain antiretrovirals (such as ritonavir and nevirapine)
Other drugs
Non-liver enzyme inducing antibiotics (various interactions)
Lamotrigine (concentrations lowered by the contraceptive)
Ciclosporin (concentrations raised by the contraceptive)
Potassium sparing diuretics (risk of hyperkalaemia with pills containing drospirenone)
What are the non-contraceptive benefits of combined contraceptive pills?
Analysis of data from 45 observational studies from 21 countries showed that the overall relative risk of ovarian cancer decreased by 20% for each five years of use. 10 In women who had used combined oral contraceptives for 15 years the risk was halved. A protective effect with regard to both endometrial and ovarian malignancy can be detected in ex-users of contraceptives for up to 15 years.
Hormonal contraceptives may be used to treat dysfunctional uterine bleeding, dysmenorrhoea, and menorrhagia; their use is associated with a lower incidence of functional ovarian cysts, benign breast disease, and colorectal cancer. w1 Their effect on bone mineral density depends on the dose of oestrogen and the age of the woman.
What are the adverse effects and complications of hormonal contraceptives?
The side effects and complications of combined oral contraceptives have been well investigated. A nationwide prospective study carried out in the United States showed that after six months of using an oral contraceptive 16% (switchers) to 32% (starters) of women had stopped taking their pill. Nearly half (46%) of the women who discontinued did so because of side effects, such as breakthrough bleeding and headache. 11
Case-control studies have shown an increased relative risk of deep venous thrombosis and pulmonary embolism, ranging from 2.1 to 4.4. 12 This risk is related to the dose of oestrogen and the type of progestogen. Pills containing desogestrel or gestodene are associated with a twofold greater risk than those containing levonorgestel or norethisterone; those containing cyproterone acetate have a four times greater risk. 12 The data are insufficient to make conclusions about combined oral contraceptives containing other progestogens. 12 Women with thrombophilia are particularly at risk of thromboembolic events. A systematic review and meta-analysis of seven studies of women taking combined oral contraceptives found significant associations of the risk of thromboembolism with deficiencies of antithrombin, protein C, or protein S; raised concentrations of factor VIIIc; and the presence of factor V Leiden and prothrombin G20210A. 13
Use of combined oral contraceptives is associated with an increased risk of myocardial infarction, stroke, gallbladder disease, hypertension, glycometabolic imbalance in people with diabetes, carcinoma of the cervix, hepatocellular carcinoma, and—to a lesser degree—breast cancer in current users. These risks are not modified when ethinylestradiol is given parenterally, or by the use of new progestogens not derived from 19-nortestosterone. 5 A Cochrane review found that transdermal patches cause more, and the vaginal ring causes fewer (except for vaginal discharge and vaginitis), side effects than combined oral contraceptives. 7 A cohort study found a more than twofold increase in deep venous thrombosis and pulmonary embolism in users of transdermal contraceptives compared with women taking a combined oral contraceptive containing 35 µg ethinylestradiol and norgestimate. 14 Box 2 lists contraindications to the use of combined hormonal contraceptives.
Box 2 Contraindications to combined hormonal contraceptives 4 5
Absolute contraindications (class 4 in the who classification).
Undiagnosed genital bleeding
Breast cancer
Past or present circulatory disease (for example, arterial or venous thrombosis, ischaemic heart disease, and cerebral haemorrhage)
Thrombophilia
Pill induced hypertension
Migraine with aura
Active liver disease, cholestatic jaundice, Dubin-Johnson syndrome, acute porphyria
Systemic lupus erythematosus
Haemolytic-uraemic syndrome
Thrombotic thrombocytopenic purpura
Relative contraindications (class 2 or 3 in the WHO classification)
Smoker aged over 35 years
Hypertension (blood pressure above 140/90 mm Hg)
Hyperprolactinaemia
Gall bladder disease
Migraine without aura
Otosclerosis
Sickle cell disease
The use of a progestogen only is commonly associated with altered bleeding patterns. w2 w3 Use of depot medroxyprogesterone acetate decreases bone mineral density, but this returns to baseline values after discontinuation of treatment. w4
How do intrauterine contraceptives work?
Copper bearing intrauterine devices act by immobilising sperm in the uterine cavity and preventing fertilisation. Of all contraceptive methods, these devices combine the highest efficacy with the lowest cost. w5 The TCu-380A is approved for 10 years but could be effective for 12.
The levonorgestrel releasing intrauterine system causes marked (but reversible) atrophy of the endometrium. A Cochrane review of contraception trials found this system to be as effective as the TCu-380A. 15 It is approved for five years of use and is successful in treating menorrhagia and dysmenorrhoea. A systematic review of nine studies showed that menstrual bleeding over time is reduced by 74-97%. 16 A systematic overview of observational studies found limited evidence that this system benefits women with endometriosis, adenomyosis, fibroids, endometrial hyperplasia, and early stage endometrial cancer (in women unfit for surgery). 17 WHO guidelines state that fertility returns immediately after removal of all intrauterine contraceptives. 4
What are the adverse effects and complications of intrauterine contraceptives?
Insertion of intrauterine devices can be painful. Rarely, uterine perforation occurs. Immediate postpartum or postabortum insertion has the advantages of high motivation, assurance that the woman is not pregnant, and convenience, but it is associated (particularly postpartum and after a second trimester abortion) with a higher expulsion rate than after interval insertion (box 3). 5
Box 3 Contraception for special groups
Adolescents.
When accessible, adolescents mostly use pills (less often patches or rings) or male condoms. Dual protection with a condom and another contraceptive should be encouraged. Easy access to emergency contraception is a priority. Long acting reversible contraceptives protect more effectively against unwanted pregnancy; injectable preparations and implants are preferable to copper bearing intrauterine devices in this age group.
Post partum
Because of the higher risk of thrombosis during the first weeks after childbirth, combined oestrogen-progestogen preparations should not be used until 21 days after delivery. Progestogen-only pills may be started at once. Progestogen-only injectable preparations may cause heavy metrorrhagia if given before six weeks post partum. Intrauterine contraceptives may be inserted immediately after delivery or any time from six weeks post partum onwards (to lessen the risk of perforation). Diaphragms and cervical caps should not be fitted until six to 12 weeks post partum.
Lactating mothers
Breast feeding is a contraindication for the use of all hormonal methods except for progestogen-only pills, which have no known adverse effect on the infant or lactation.
Older (perimenopausal) women
Contraceptives (including 20 µg pills) that are well tolerated, effective, and not contraindicated should not be discontinued until menopause is confirmed or the age of 51. The levonorgestrel intrauterine system is particularly useful for premenopausal women with menorrhagia. Because of diminishing fertility, less effective methods (such as diaphragms and cervical caps) may provide sufficient protection in this age group.
Copper bearing intrauterine devices increase menstrual flow by 30% on average and may aggravate dysmenorrhoea. According to a recent Cochrane review, non-steroidal anti-inflammatory drugs reduce bleeding and pain associated with the use of intrauterine devices; tranexamic acid is a second line treatment for excessive bleeding. 18 A case-control study found that intrauterine devices do not raise the risk of tubal occlusion in nulligravid women, 19 and a meta-analysis of case-control studies showed that ectopic pregnancy is not more common in women who conceive with an intrauterine device in place. 20 According to observational evidence, intrauterine devices do not increase the risk of pelvic inflammatory disease unless inserted in women with pre-existing gonorrhoea or Chlamydia infection. w6
Women using a levonorgestrel releasing intrauterine system may have spotting and bleeding during the first months, acne (if already prone to it), mastalgia, or mood changes and they may develop functional ovarian cysts. The recurrence or persistence of side effects may require the removal of the device. Amenorrhoea occurs in about 20% of women one year after insertion of the levonorgestrel releasing intrauterine system. Women may consider it a reason for discontinuation if they were not counselled about the beneficial effect this may have on their health.
How useful are barrier methods?
All barrier methods offer the convenience of contraception “when needed,” but their success rate depends on correct and consistent use. Typical use is associated with high failure rates (from 15 for the male condom to 32 per 100 women per year for the cervical cap used by multiparous women), 8 and all may cause allergy.
The female condom is a single-use polyurethane sheath, which is placed into the vagina. To insert the condom into the vagina, the movable and flexible inner ring at its closed end is compressed and introduced much like a diaphragm. The larger, fixed outer ring remains outside the vagina to cover part of the introitus. The penis should be manually placed (by either partner) into the sheath to prevent it from becoming wrongly positioned between the condom and the vaginal wall. The condom is removed immediately after intercourse.
The diaphragm is particularly suited for women over the age of 35, whose fertility is progressively decreasing and who show greater compliance. It should be inserted less than three hours before intercourse and left in situ for at least six hours afterwards. Its use increases the risk of urinary tract infections.
The cervical cap may be inserted up to 48 hours before coitus. Both the diaphragm and the cap must be coated with spermicide before insertion. Neither should be fitted within six to 12 weeks after childbirth or second trimester abortion, and neither protects against HIV. Women with a history of toxic shock syndrome should not use a diaphragm or a cap.
How useful are spermicides, used alone?
Spermicides are usually used with barrier devices, and they are not reliable if used alone, except in women whose natural fertility is reduced, particularly with increasing age. Their use many times a day (for example, by professional sex workers) may cause damage of the vaginal wall and facilitate HIV transmission. w7
Does evidence support the use of natural contraceptive methods?
Methods based on fertility awareness involve identifying “fertile days” of the cycle by observing changes in the basal body temperature or cervical secretions, or by monitoring cycle days, and abstaining from coitus or using a barrier contraceptive on those days. A Cochrane review, in which the authors searched five computerised databases for randomised controlled trials of these methods, concluded that—because of poor methodology and reporting—pregnancy rates could not be determined. 21 Although these methods may be the only ones deemed acceptable for personal or religious reasons, or the only ones available in resource poor settings, they are difficult to apply; couples who use them should be informed about the lack of evidence regarding their effectiveness and, where possible, counselled about other options they might consider.
Is the “lactational amenorrhoea method” reliable?
The lactational amenorrhoea method is an efficient physiological tool for spacing births. Suckling an infant reduces the release of gonadotrophins, which suppress ovulation and cause amenorrhoea. Reduced suckling leads to the return of ovulation.
For this method to be successful three conditions must be met: the baby must be exclusively or nearly exclusively breast fed on demand, day and night; the mother must be amenorrhoeic; and the method must not be relied on for more than six months. Another contraceptive method must be used as soon as these criteria are no longer fulfilled.
A Cochrane review established that the lactational amenorrhoea method, when correctly applied, is 98% effective. 22 The beneficial effects of exclusive breast feeding on the infant are important additional advantages. w8
When and how to use emergency contraception
Emergency contraception includes all methods that act after intercourse but before implantation. For maximal efficacy it should be used as soon as possible. Combined oral contraceptives, progestogen-only pills, mifepristone, and copper bearing intrauterine devices may be used. Hormonal emergency contraceptives can be offered at any time during the menstrual cycle, and even twice in a given cycle, if necessary.
Currently, the levonorgestrel-only emergency contraceptive is the most widely used. A recent Cochrane review found it to be more effective and better tolerated than the combined oral contraceptive, with no adverse effect on pregnancy. 23 A single 1500 µg dose regimen is simpler than 750 µg taken twice, 12 hours apart. When dedicated emergency contraceptive pills are not available, the Yuzpe method may be used: two tablets of a combined oral contraceptive, each containing 50 µg ethinylestradiol and 250 µg levonorgestrel, are taken twice at a 12 hour interval. The selective progesterone receptor modulator mifepristone (10 mg taken within five days of unprotected coitus) is also effective, but it may cause the next menstruation to be delayed, 24 which may increase anxiety.
A WHO multicentre randomised trial found that a single low dose of mifepristone and both the single and the two dose regimens of levonorgestrel are equally efficacious. 25 A Cochrane review using information from eight randomised controlled trials found that advance provision of hormonal emergency contraceptives had no negative effect on sexual and reproductive health behaviours and outcomes. 26 Another systematic review showed that increased access to emergency contraceptive pills enhances use but does not reduce rates of unintended pregnancy. 27
Postcoital (up to five days) insertion of a copper intrauterine device prevents implantation. The method is effective, even after multiple coital exposures during a short interval, and it has the advantage of providing ongoing contraception.
What are the drawbacks of sterilisation?
According to the guidelines of the International Planned Parenthood Federation, voluntary sterilisation should be available to all people who do not request it under duress, who are certain that they want no more children, and who understand the nature of the procedure after counselling. Verbal counselling must be backed by printed information to be read by the patient before the operation. w9
Female sterilisation is more risky than vasectomy. A large prospective multicentre cohort study showed that the cumulative probability of regret within 14 years after tubal sterilisation was considerably higher (20% v 6%) for women sterilised at the age of 30 or less than for those over 30. 28 Regret is more common after sterilisation immediately post partum or after an abortion than at a less emotional time. Unpredicted life events, like a change in marital status or the death of a child, are also sources of regret. Counsellors must mention that tubal occlusion is permanent and irreversible, and that it carries a low failure rate.
At what age can a woman stop using contraception?
Women who smoke and those with other cardiac risk factors should discontinue use of combined oral contraceptives at age 35 and switch to another method. In healthy non-smokers, any method that is well tolerated, including low dose (20 µg ethinylestradiol) combined oral contraceptives, can be used up to age 51, after which the risk of conceiving is negligible. Women who prefer to stop using hormonal or intrauterine contraceptives at an earlier age can use a barrier method until menopause is confirmed.
Tips for non-specialists
The best contraceptive method for a given woman is the one that is medically safe, that she uses consistently, and that she feels happy with
Contraceptives containing an oestrogen (such as combined oral contraceptives) should not be used by women with hypertension or a history of deep vein thrombosis. Hormonal methods should not be used by women with breast cancer or serious liver disease
For contraceptives that rely on compliance (such as pills and barrier methods), the failure rate with “typical use” is considerably higher than that associated with “perfect use”
Long acting reversible contraceptives like intrauterine devices, injectable preparations, and implants depend least on the user and are as efficacious as sterilisation
Return of fertility after use of contraceptive injectable preparations takes longer than after discontinuation of other methods
After use of an emergency contraceptive a reliable method of contraception should be initiated
Areas of ongoing and future research
Replacing ethinylestradiol, which has many side effects, with natural oestrogens (such as oestradiol and estetrol) in certain circumstances
Developing new progestogens that bind specifically to the progesterone receptor and will replace those currently used in certain applications
Expanding the range of applications of progesterone receptor modulators such as mifepristone (for example, as oestrogen-free contraceptives given orally or by means of intrauterine systems or vaginal rings)
Blocking the expression of newly identified genes implicated in gametogenesis, follicular rupture, development of the corpus luteum, sperm motility, or capacitation to create therapeutic modalities with few side effects
Elucidating the mechanism of action of the levonorgestrel intrauterine system
Investigating the effect of hormonal contraceptives on indicators of the progression of HIV infection and the mechanism whereby they increase genital shedding of virus in HIV positive women
Additional educational resources
Resources for healthcare professionals.
WHO ( www.who.int/reproductive-health/ )— Medical eligibility criteria for contraceptive use , 3rd ed. Geneva: Reproductive Health and Research, 2004 (type title into the search box)
WHO ( www.who.int/reproductive-health/publications/spr/spr_2008_update.pdf )— Selected practice recommendations for contraceptive use: 2008 update (click on “Family planning” first)
Faculty of Sexual and Reproductive Healthcare ( www.ffprhc.org.uk )—Provides method specific guidance (first click on “Good medical practice”)
International Planned Parenthood Federation. Medical and service delivery guidelines. ( www.ippf.org/en/Resources/Guides-toolkits/ )—These guidelines offer up to date evidence based guidance on various issues, including family planning
Royal College of Obstetricians and Gynaecologists ( www.rcog.org.uk/index.asp?PageID=699 )— Male and female sterilisation . Evidence-based clinical guideline no 4. 2004 (type title in the search box)
Resources for patients
Association of Reproductive Health Professionals ( www.arhp.org/patienteducation/index.cfm )—Series of booklets on various reproductive health matters, including contraception
Family Planning Council ( www.familyplanning.org/ )—Information on birth control methods
Contraceptive.org.uk ( www.contraceptive.org.uk/ )—Refers to other sources of information
Emergency Contraception Website ( www.not-2-late.com )—Provides information on emergency contraception for “the morning after”
Royal College of Obstetricians and Gynaecologists ( www.rcog.org.uk/index.asp?PageID=703 )—Patient information leaflet on sterilisation for women and men
Society of Obstetricians and Gynaecologists of Canada ( www.sexualityandu.ca )—Information adapted to different target groups, such as teenagers, adults, parents, teachers, and healthcare professionals
Cite this as: BMJ 2009;339:b2895
Contributors: J-JA wrote the first draft of the article and both authors helped review the evidence on which the paper is based. Both authors are guarantors.
Competing interests: J-JA has been paid by Bayer Schering Pharma and by Organon, part of Schering-Plough, for organising education.
Provenance and peer review: Commissioned; externally peer reviewed.
- ↵ Singh S, Darroch JE, Vlassoff M, Nadeau J. Adding it up: the benefits of investing in sexual and reproductive health care. New York: Alan Guttmacher Institute, 2003 . www.guttmacher.org/pubs/addingitup.pdf .
- ↵ United Nations Department of Economics and Social Affairs Population Division. World contraceptive use. 2007 . ww.un.org/esa/population/publications/contraceptive2007/contraceptive_2007_table.pdf .
- ↵ Lopez LM, Steiner M, Grimes DA, Schulz KF. Strategies for communication effectiveness. Cochrane Database Syst Rev 2008 ;(4):CD006964.
- ↵ WHO. Selected practice recommendations for contraceptive use: 2008 update. 2008 . www.who.int/reproductive-health/publications/spr/spr_2008_update.pdf (click on “Family planning” first.
- ↵ WHO. Medical eligibility criteria for contraceptive use. 3rd ed. 2004 . www.who.int/reproductivehealth/publications/family_planning/9789290215080/en/index.html .
- ↵ Lopez LM, Newmann SJ, Grimes DA, Nanda K, Schulz KF. Immediate start of hormonal contraceptives for contraception. Cochrane Database Syst Rev 2008 ;(2):CD006260.
- ↵ Lopez LM, Grimes DA, Gallo MF, Schulz KF. Skin patch and vaginal ring versus combined oral contraceptives for contraception. Cochrane Database Syst Rev 2008 ;(1):CD003552.
- ↵ Trussell J. Contraceptive efficacy. In: Hatcher RA, Trussell J, Stewart F, Nelson A, Cates W, Guest F, et al, eds. Contraceptive technology. 18th ed. New York: Ardent Media, 2004 :355-63.
- ↵ El-Ibiary SY, Cocohoba JM. Effects of HIV antiretrovirals on the pharmacokinetics of hormonal contraceptives. Eur J Contracept Reprod Health Care 2008 ; 13 : 123 -32. OpenUrl CrossRef PubMed Web of Science
- ↵ Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and oral contraceptives: collaborative reanalysis of data from 45 epidemiological studies including 23 257 women with ovarian cancer and 87 303 controls. Lancet 2008 ; 371 : 303 -14. OpenUrl CrossRef PubMed Web of Science
- ↵ Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: a prospective evaluation of frequency and reasons. Am J Obstet Gynecol 1998 ; 179 : 577 -82. OpenUrl CrossRef PubMed Web of Science
- ↵ Martinez F, Avecilla A. Combined hormonal contraception and venous thromboembolism. Eur J Contracept Reprod Health Care 2007 ; 12 : 97 -106. OpenUrl CrossRef PubMed Web of Science
- ↵ Wu O, Robertson L, Langhorne P, Twaddle S, Lowe GD, Clarke P, et al. Oral contraceptives, hormonal replacement therapy, thrombophilias and risk of venous thromboembolism: a systematic review. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) Study. Thromb Haemost 2005 ; 94 : 17 -25. OpenUrl PubMed Web of Science
- ↵ Cole JA, Norman H, Doherty M, Walker AM. Venous thromboembolism, myocardial infarction, and stroke among transdermal contraceptive system users. Obstet Gynecol 2007 ; 109 : 339 -46. OpenUrl CrossRef PubMed Web of Science
- ↵ Grimes DA, Lopez LM, Manion C, Schulz KF. Cochrane systematic reviews of IUD trials: lessons learned. Contraception 2007 ; 75 (suppl): S55 -9. OpenUrl CrossRef PubMed Web of Science
- ↵ Hubacher D, Grimes DA. Noncontraceptive health benefits of intrauterine devices: a systematic review. Obstet Gynecol Surv 2002 ; 57 : 120 -8. OpenUrl CrossRef PubMed Web of Science
- ↵ Varma R, Sinha D, Gupta JK. Non-contraceptive uses of levonorgestrel-releasing hormone system (LNG-IUS)—a systematic enquiry and overview. Eur J Obstet Gynecol Reprod Biol 2006 ; 125 : 9 -28. OpenUrl CrossRef PubMed Web of Science
- ↵ Grimes DA, Hubacher D, Lopez LM, Schulz KF. Non-steroidal anti-inflammatory drugs for heavy bleeding or pain associated with intrauterine-device use. Cochrane Database Syst Rev 2006 ;(3):CD006034.
- ↵ Hubacher D, Lara-Ricalde R, Taylor DJ, Guerra-Infante F, Guzman-Rodriguez R. Use of copper intrauterine devices and the risk of tubal infertility among nulligravid women. N Engl J Med 2001 ; 345 : 561 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Xiong X, Buekens P, Wollast E. IUD use and the risk of ectopic pregnancy: a meta-analysis of case-control studies. Contraception 1995 ; 52 : 23 -34. OpenUrl CrossRef PubMed Web of Science
- ↵ Grimes DA, Gallo MF, Halpern V, Nanda K, Schulz KF, Lopez LM. Fertility awareness-based methods for contraception. Cochrane Database Syst Rev 2007 ;(3):CD004860.
- ↵ Van der Wijden C, Kleinen J. Lactational amenorrhea for family planning. Cochrane Database Syst Rev 2003 ;(4):CD001329.
- ↵ Cheng L, Gülmezoglu AM, van Oel CJ, Piaggio G, Ezcurra E, van Look PF. Interventions for emergency contraception. Cochrane Database Syst Rev 2007 ;(4):CD001324.
- ↵ Task Force on Postovulatory Methods of Fertility Regulation. Comparison of three single doses of mifepristone as emergency contraception: a randomised trial. Lancet 1999 ; 353 : 697 -702. OpenUrl CrossRef PubMed Web of Science
- ↵ Von Hertzen H, Piaggio G, Ding J, Chen J, Song S, Bártfai G, et al. Low dose mifepristone and two regimens of levonorgestrel for emergency contraception: a WHO multicentre randomised trial. Lancet 2002 ; 360 : 1803 -10. OpenUrl CrossRef PubMed Web of Science
- ↵ Polis CB, Schaffer K, Blanchard K, Glasier A, Harper C, Grimes DA. Advance provision of emergency contraception for pregnancy prevention. Cochrane Database Syst Rev 2007 ;(2):CD005497.
- ↵ Raymond EG, Trussell J, Polis CB. Population effect of increased access to emergency contraceptive pills: a systematic review. Obstet Gynecol 2007 ; 109 : 181 -8. OpenUrl CrossRef PubMed Web of Science
- ↵ Hillis SD, Marchbanks PA, Ratliff Tylor L, Peterson HB. Poststerilization regret: findings from the United States Collaborative Review of Sterilization. Obstet Gynecol 1999 ; 93 : 889 -95. OpenUrl CrossRef PubMed Web of Science
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 46, Issue 4
- A systematic review of the effectiveness of counselling strategies for modern contraceptive methods: what works and what doesn’t?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-9641-8780 Francesca L Cavallaro 1 ,
- Lenka Benova 2 , 3 ,
- Onikepe O Owolabi 4 ,
- http://orcid.org/0000-0001-6949-8976 Moazzam Ali 5
- 1 University College London , London , London , UK
- 2 Institute of Tropical Medicine , Antwerp , Belgium
- 3 London School of Hygiene and Tropical Medicine , London , UK
- 4 Guttmacher Institute , New York , New York , USA
- 5 World Health Organization , Geneva , Switzerland
- Correspondence to Dr Moazzam Ali, Reproductive health and research, World Health Organization, 1211 Geneva, Switzerland; alimoa{at}who.int
Aim The aim of this systematic review was to synthesise the evidence on the comparative effectiveness of different counselling strategies for modern contraception on contraceptive behaviour and satisfaction, and to examine their advantages and disadvantages.
Methods Six electronic databases (Medline, Embase, Global Health, Popline, CINAHL Plus, and Cochrane Library) were searched to identify publications comparing two or more contraceptive counselling strategies and reporting quantitative results on contraceptive use, uptake, continuation or switching, or client satisfaction. Studies of women or couples from any country, published in English since 1990 were considered.
Results A total of 63 publications corresponding to 61 studies met the inclusion criteria. There was substantial heterogeneity in study settings, interventions and outcome measures. Interventions targeting women initiating a method (including structured counselling on side effects) tended to show positive effects on contraceptive continuation. In contrast, the majority of studies of provider training and decision-making tools for method choice did not find evidence of an effect. Additional antenatal or postpartum counselling sessions were associated with increased postpartum contraceptive use, regardless of their timing in pregnancy or postpartum. Dedicated pre-abortion contraceptive counselling was associated with increased use only when accompanied by broader contraceptive method provision. Male partner or couples counselling was effective at increasing contraceptive use in two of five studies targeting non-users, women initiating implants or seeking abortion. High-quality evidence is lacking for the majority of intervention types.
Conclusions The evidence base and quality of studies are limited, and further research is needed to determine the effectiveness of many counselling interventions in different settings.
- modern contraceptives
- counselling
- contraceptive behaviour
- method continuation
- client satisfaction
- family planning service provision
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/bmjsrh-2019-200377
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Key messages
Detailed counselling on side effects for users initiating new methods may be effective at improving continuation (evidence of effect in three of four studies).
Additional counselling sessions in pregnancy or postpartum may increase postpartum contraceptive uptake (evidence of effect in four of five studies).
Caution is required in interpreting the evidence, due to a lack of high-quality evidence for most interventions, and substantial heterogeneity in study settings, interventions, and outcome measures.
There is a need to improve reporting of studies, and to develop and evaluate novel interventions in different settings.
Ensuring access to contraception is fundamental to human rights and contributes to improved health outcomes, as recognised in Sustainable Development Goal 3.7 (universal access to sexual and reproductive healthcare services). 1 Despite increases in contraceptive use in the last several decades, an estimated 214 million women of reproductive age have an unmet need for contraception in developing regions. 2 Women in need of contraception or their male partners may not use a method for multiple reasons, including poor geographical or financial access, health concerns or side effects, and low decision-making power. 3–6 Meeting the unmet need for contraception in developing regions would avert an estimated 67 million unintended pregnancies, 36 million induced abortions, and 76 000 maternal deaths each year. 2 In addition, effective contraceptive coverage among users can be improved, as illustrated by suboptimal use 7 8 and high discontinuation rates. 3
Contraceptive counselling can help clients choose a method meeting their needs and preferences, manage side effects, and support method continuation or switching. High-quality counselling therefore has a high potential to strengthen efforts to reduce unmet need for contraception. The Bruce framework identified six dimensions for quality family planning (FP) services, including choice of methods, information given to clients, and interpersonal relations. 9 Recent efforts have outlined key components for quality contraceptive counselling, including needs assessment, tailored communication, and shared decision-making. 10 11 Attention has been called to the specific needs of adolescents, including for dual protection against pregnancy and sexually transmitted infections (STIs) and respect for adolescents’ autonomy. 12
Despite these multiple frameworks, no clear consensus exists on how best to deliver contraceptive counselling to meet client needs and satisfaction. The WHO 2016 Selected Practice Recommendations include guidelines for counselling content for each method – primarily side effects and protection against STIs 13 – while the WHO 2018 Global Handbook for Family Planning Providers further includes recommendations on interpersonal qualities (including respect and confidentiality). 14 Guidance on the best mode for counselling delivery, such as face-to-face versus digital support, is limited.
Several reviews have examined counselling strategies to improve contraceptive use, finding mixed or limited effects on contraceptive behaviour and pregnancy outcomes. 15–18 However, they focused on specific subgroups (such as adolescents) and included comparison groups with no counselling. The objective of this systematic review is to synthesise the evidence on the comparative effectiveness of contraceptive counselling strategies on contraceptive behaviour and satisfaction, and examine their advantages and disadvantages.
The protocol for this systematic review is included in online supplementary appendix 1 . We defined contraceptive counselling as the provision of contraceptive information and support for decision-making regarding contraceptive method selection (new or switching clients) or for continued use of contraceptive method (continuing clients).
Supplemental material
Inclusion and exclusion criteria.
We included studies comparing two or more counselling interventions and reporting quantitative findings on contraceptive behaviour (uptake, use, or continuation of a modern method, or switching modern methods at the time of counselling), or on client satisfaction with method or services. We used the WHO definition of modern methods; 19 interventions or outcomes focused solely on barrier methods were excluded. Long-acting reversible contraception (LARC) includes contraceptive implants and intrauterine devices (IUDs).
Only studies where the comparison group received contraceptive counselling were included. We included studies of women or couples, including postabortion, postpartum and breastfeeding women, but excluded studies of women with medical conditions affecting contraceptive eligibility (such as breast cancer). 14 Randomised controlled trials (RCTs) and non-randomised studies, as well as peer-reviewed and grey literature publications, were considered.
We considered evidence from all countries, published in English since the publication of the Bruce framework 9 in 1990.
Search strategy
We manually searched the key journal Contraception between January 2010 and October 2018 to identify keywords. Six databases (Medline, Embase, Global Health, Popline, CINAHL Plus, and Cochrane Library of Systematic Reviews) were searched for eligible studies published from 1 January 1990 to 31 October 2018, using keywords related to contraception, counselling and outcomes of interest (full search strategy in online supplementary appendix 1 ). Manual searches of reference lists of included studies and relevant systematic reviews identified in the search were additionally conducted.
Article selection
All unique identified publications were screened by one author (FC) based on title and abstract. A random 20% of excluded records were double-screened by a second reviewer (LB or OO) to ensure no relevant studies were missed; any differences in decisions between reviewers were resolved through discussion with a third reviewer (MA). All retrieved full texts were screened by one author (FC), and reason for exclusion was documented based on a hierarchical list ( figure 1 ). Data were extracted from included studies by one author (FC) in an Excel data extraction sheet. Four included full-text articles (7%) were extracted in duplicate by a second reviewer (LB or OO), and any differences reconciled by consultation with MA.
- Download figure
- Open in new tab
- Download powerpoint
PRISMA flow diagram.
Data synthesis
We reported results according to intervention type and target population, with specific attention paid to adolescents and young women. The substantial variability in contraceptive counselling interventions and outcome measures prevented us from conducting a meta-analysis. We summarised findings on the effectiveness of contraceptive counselling narratively and in summary tables, and described the advantages and disadvantages of reviewed interventions based on information reported by study authors and subjective assessment of review authors.
In this review we followed PRISMA reporting guidelines, with the exception of risk of bias which was not assessed systematically.
Systematic search results
In total, 2307 publication records were identified in the search and 968 duplicate records removed, leaving 1339 unique publications ( figure 1 ). Based on title and abstract screening, 142 were retained for full-text review; double-screening of 20% (n=240) of excluded publications did not identify any missed publications. Forty-three reviewed publications met the inclusion criteria, with most studies excluded as duplicate publication of results (including literature reviews). Twenty additional publications were identified through reference lists of included articles and 29 literature reviews.
In total, 63 publications referring to 61 studies identified in the systematic and manual searches were included in this review. Two studies published initial 20 21 and follow-up outcomes 22 23 in separate articles; we report short- and long-term outcomes as a single study.
Study characteristics and intervention typology
Characteristics of included studies are summarised in online supplementary appendix 2, table 1 . Approximately half of the included studies were conducted in the WHO Americas region (n=29), including 22 in the USA. Around half of studies were RCTs (n=29 individual and n=4 cluster RCTs), followed by uncontrolled pre-post studies (n=14) and non-randomised observational studies (n=9). Four studies were described by their authors as having a quasi-experimental design. 24–27
Table 1 summarises the different types of counselling interventions in included studies according to target population. Fouteen of the 61 included studies targeted adolescents or young women (including three each postpartum and postabortion).
- View inline
Mapping of study interventions (reference numbers) across target populations in included studies (n=61)
The most commonly reported outcomes were contraceptive use among all women (n=32), continuation among women who had initiated a method (n=23) and method uptake among women not using at the time of counselling (n=15). Only one study reported information on contraceptive switching at the time of counselling. Nineteen of the 61 studies reported satisfaction outcomes, including eight on method satisfaction and 13 on satisfaction with counselling and/or services. Only 25 of the 61 studies (41%) included more than one of the six outcomes assessed in this review.
Association with outcomes
Online supplementary table 2 describes the 61 included studies; the intervention effects on outcomes of interest is summarised in table 2 .
Summary of intervention effects
Interventions targeting women choosing a contraceptive method
Eleven studies targeted women choosing a method, including seven studies of digital decision-making aids in the USA. Two targeted young women, with mixed results on immediate contraceptive uptake and no effect on longer-term use. 28 29 Among women of all ages, computer-based algorithms with tailored printout were associated with increased choice of effective method and use at follow-up. 21 23 Other studies found no or negative effect on contraceptive behaviour. 30 31 Digital tools were associated with lower counselling satisfaction compared with health educators, 31 but higher than pamphlets only. 32
Studies of paper-based decision aids for face-to-face counselling found increased method selection and satisfaction with services after training on WHO Decision-Making Tool in Iran, 33 and increased LARC uptake with shared decision-making brochures in the USA. 34 However, Balanced Counselling Strategy training – using method-specific counselling cards 35 – had no effect on contraceptive use, continuation or clinic satisfaction in Peru 36 or Egypt. 25

Interventions targeting women requesting or initiating a chosen method
Nine studies examined counselling strategies to improve continuation among women requesting a method. Among young women using oral contraceptives, daily text messages improved continuation, 37 but evidence was inconclusive for health belief model-based counselling. 38 Among women of all ages, continuation increased with detailed counselling on side effects in China 39 and Mexico, 39 but not Brazil. 40 Counselling addressing IUD-related beliefs halved discontinuation in rural India, 41 and tubal ligation scoring was associated with fewer requests for reversal in Turkey. 42 Introducing the WHO Decision-Making Tool did not affect continuation among pill and injectable initiators in Nicaragua. 26 Women with husband counselling had higher continuation in Bangladesh. 43
The two studies reporting satisfaction outcomes found no or negative effects. 38 43
Interventions targeting all FP service users to improve quality of care
Nine studies examined interventions to improve the quality of FP services among all clients. In the USA, training on LARC clinical skills and client-centred counselling produced an increase in LARC uptake among adolescents aged 18–19 years, but not among 18–25-year-olds as a whole. 44 Broad-ranging clinical, counselling and logistical training in Senegal 45 and the Philippines 24 found no difference in short- or long-term contraceptive use. Training in the Balanced Counselling Strategy or GATHER approach was associated with increased contraceptive use in some settings but not others. 27 46–48 No intervention had a positive effect on client satisfaction, except for one in China. 49
Patient coaching prior to initial consultation did not affect continuation in Indonesia. 50
Interventions targeting women undergoing abortion
Eleven studies focused on women undergoing abortion, including three RCTs among young women. In the USA, additional motivational interviewing increased LARC initiation and satisfaction with counselling, with no effect on overall method satisfaction or use. 51 In China, individual counselling, male partner involvement, and free contraception increased modern contraceptive use at 6 months postabortion (adjusted OR 2.03, 95% CI 1.04 to 3.98) compared with group education only. 52 However, a video on LARC information did not have any effect on contraceptive or satisfaction outcomes in the USA. 53
Studies of women of all ages found additional physician counselling and expanded contraceptive provision in the UK, 54 automated messages and access to telephone counselling in Cambodia, 55 and personalised individual counselling in Brazil 20 22 did not increase contraceptive use after the first few months postabortion. In the UK, women who opted for advance telephone counselling rather than face-to-face counselling during abortion consultation had 60% higher adjusted odds of receiving LARC or sterilisation. 56 In Russia, provider training was followed by higher contraceptive use at 12 months; satisfaction results were mixed. 57 Additional interview with a FP nurse in Iceland, 58 husband counselling in Egypt, 59 and WHO Decision-Making Tool in the USA 60 had no effect on contraceptive behaviour.
Interventions targeting postpartum women
Thirteen studies examined interventions for postpartum initiation. Two studies among adolescents and young women found higher LARC uptake with additional pre-discharge counselling in Thailand 61 and intensive motivational interviewing in a non-randomised study in the USA. 62
Among women of all ages, additional antenatal or postpartum counselling was associated with increased postpartum use in two RCTs and one non-randomised study in Nepal, 63 Nigeria 64 and Turkey, 65 but tailored antenatal counselling did not increase use in the UK, China or South Africa. 66 Structured counselling increased LARC uptake after a preterm birth in the USA, 67 and counselling on lactational amenorrhea increased modern method use by 10% 1 year postpartum in Brazil. 68 Physician counselling was associated with higher satisfaction in a RCT in the USA, 69 but did not increase postpartum use in Turkey, 70 compared with leaflet/video counselling. Refresher provider trainings in Bangladesh 71 and intensive counselling in Kenya 72 were not associated with postpartum IUD uptake, continuation, or satisfaction.
Systematic contraceptive counselling for women attending services other than FP
Four pre-post studies found evidence of increases in contraceptive use after interventions systematising the provision of contraceptive counselling to all women attending non-FP outpatient services, including adolescents in juvenile detention in the USA, 73 voluntary counselling and testing (VCT) clients in Ethiopia, 74 women seeking pregnancy testing at a walk-in clinic in the USA, 75 and women attending an abortion clinic in the UK. 76 However, these interventions also included expanded method provision.
Community-based interventions
In four community-based counselling interventions, couples counselling for non-users was associated with higher uptake and continuation in Ethiopia, 77 but not in Jordan 78 or Malawi. 79 A study of peer counselling had a small sample and high non-response, limiting interpretation. 80
Advantages and disadvantages of different types of counselling interventions
Advantages and disadvantages of interventions included in this review are summarised in figure 2 and online supplementary table 3 .
Summary of advantages and disadvantages of different counselling intervention types
Only a few studies measured impact on consultation length, reporting increases 46 51 or no change. 50 Authors highlighted the implications of additional and longer consultations for patient volume and staffing, and associated costs of increases in staff, resources or contraceptive products. In contrast, interventions during waiting times prior to consultation (including digital tools) were described as potentially saving provider time. 31 50 81
Development of custom digital tools was highlighted as expensive, but client population input was considered critical for success in several studies. 29 81 Their potential for reaching digitally literate adolescents more widely, including in community contexts, was emphasised. 28 Counselling satisfaction with digital tools alone was low, and these are best used in addition to, rather than instead of, face-to-face counselling. 31 Telephone-based interventions have the advantage of providing access to many women at low cost, but they cannot reach women without phones, 55 and can require many attempts to reach participants. 38
Counselling up to the time of birth or abortion can reach women who may not access services at a later time and provide time for a fuller discussion of different methods, 56 64 although some women may be reluctant to initiate contraception immediately, therefore effective follow-up mechanisms are needed. 55 Conversely, routine postpartum counselling at 3–6 weeks may reach some women after they have resumed sexual activity. 64 Involving male partners in counselling may target the main contraceptive decision-maker in some settings, although partner availability posed important logistical challenges. 52 59 78 79
With the end of the FP2020 period in sight, this systematic review provides a timely synthesis of the effectiveness of different counselling interventions on contraceptive behaviour and client satisfaction. In our review, detailed counselling for women initiating contraception was associated with increased contraceptive continuation in non-randomised studies and one of two RCTs. Most studies of digital decision-making tools and provider training (including paper-based decision-making aids) did not find evidence of effect on contraceptive behaviour or satisfaction. Exceptions included training in the Population Council’s Balanced Counselling Strategy 35 and WHO Decision-Making Tool, 82 effective in some – but not other – settings. Interventions to systematically counsel women outside of FP services were associated with increased contraceptive use in contexts of expanded contraceptive provision; it is therefore not possible to attribute changes to counselling alone. Additional counselling sessions in pregnancy or postpartum appeared to increase postpartum contraceptive use, regardless of their timing. Non-randomised studies found evidence of effectiveness for several other postpartum and postabortion interventions. Male partner counselling was associated with increased contraceptive use in two of five studies.
Due to concerns with data quality and heterogeneity, caution is required in interpreting the evidence. Half (n=33) of 61 identified studies were RCTs, and although we did not assess study quality systematically, many non-randomised studies were prone to selection bias and few reported adjusted estimates. There was wide heterogeneity in intervention types, study designs, client populations, settings, and outcome measures across studies, and the evidence base is limited to a small number of studies for each of many interventions. Notable gaps include evidence on interventions targeting continuing users and women experiencing side effects, postpartum and postabortion decision-making tools, and community-based interventions other than couples counselling.
To our knowledge, this is the first systematic review to summarise the available evidence on comparative effectiveness of different counselling strategies across different client populations (including adolescents, postpartum and postabortion women). Our focus on comparing counselling strategies is critical to help identify successful interventions to improve contraceptive services. We examined outcomes directly affected by counselling (contraceptive behaviour and client satisfaction); however, preventing unmet need for contraception and unwanted pregnancies (influenced by multiple other factors) is the ultimate objective from a public health standpoint, and counselling process indicators such as client participation and knowledge are also important.
Our review has some limitations. Keywords for counselling interventions are not well defined; we maximised identification of relevant studies through a wide range of search synonyms and extensive manual searches. Advantages and disadvantages of different intervention types were assessed based on information reported by authors and a subjective assessment by reviewers, to facilitate assessment of intervention suitability to individual contexts.
There are also limitations to the evidence base. First, study quality was variable, particularly among non-randomised studies (almost half of the included studies). We did not assess risk of bias systematically, however, there was no or weak evidence for most intervention types in non-randomised studies. Selection bias is likely to overestimate the strength of association, with women opting into the intervention being more likely to use contraception, and a lack of effect is unlikely to hide a 'true' population effect. Non-randomised studies finding evidence of intervention effect – including structured counselling on side effects for women initiating a method – should be assessed in RCTs before recommendations can be made. We were unable to build forest plots because most studies reported percentages rather than effect estimates with confidence intervals, and we acknowledge the limitations of conclusions based on dichotomised p values. 83
Second, substantial heterogeneity in study settings, interventions and outcomes limits the comparability of studies. Similar interventions were effective in some – but not all – settings, highlighting the importance of context as well as implementation intensity and fidelity. Effectiveness on contraceptive behaviour may be limited by contraceptive provision at the time of counselling (restricted in some abortion and postpartum clinics), cost of methods (particularly LARC as mentioned in the USA 30 34 44 and Thailand 61 ), availability of providers and resources, and quality of care. Findings are therefore unlikely to be generalisable to all settings, with a particularly limited evidence base outside of high-income countries (26 of 61 studies were conducted in the USA or UK).
Third, many included studies did not clearly state whether the intervention targeted women initiating, switching and/or continuing contraception, and women switching methods were often grouped with initiators. Furthermore, multiple studies referred to 'continuation' among all clients (not all of whom had initiated a method at the time of intervention), and most studies reported contraceptive use at follow-up among all women (including those no longer in need of contraception).
Several recommendations for programmes emerge from our findings. Where possible, repeated counselling throughout pregnancy and postpartum can contribute to maximising access to information and contraceptive uptake. Interventions seeking to improve contraceptive counselling need to be tailored to the patient flow, record flow and contraceptive methods available in each setting, and embedded within broader quality of care improvements (including clinical training, where necessary). Facilities implementing counselling interventions should monitor the impact on consultation duration, patient volume and method mix to ensure necessary staffing and resources.
Despite inconclusive evidence relating to contraceptive continuation, women initiating hormonal methods should receive detailed counselling on side effects and the possibility of changing methods if desired. Counselling on LARC should ensure respect for women’s informed choice. 84 85 Contraceptive provision at abortion services is recommended as best practice in developing regions: 86 87 where not possible, referrals should be optimised to ensure contraceptive needs are met. Male partner counselling should ensure strict consent procedures. 59
There is a need for increased conceptual clarity in the literature (see recommendations in box 1 ). Appropriate denominators for contraceptive uptake (women not using a method at baseline) and continuation (women with a need for contraception at follow-up) should be used. Moreover, fertility intentions are fluid, 88–90 and research is needed to identify reasonable length of follow-up for measuring counselling effect on contraceptive behaviour, including after abortion and childbirth.
Recommendations for reporting of studies of contraceptive counselling interventions
Intervention and participant characteristics.
Clarify whether the intervention targets women initiating or switching contraception, continuing users, or a combination of these, and report results stratified according to these categories
Specify whether women already using contraception and/or satisfied with their method are eligible for inclusion, and if so report the acceptance rate and percentage of participants in these groups
Outcome measures
Report contraceptive use and continuation among women with a need for contraception (rather than all women) at each follow-up time point
Report contraceptive behaviour outcomes within reasonable time frames during which fertility preferences may remain constant, including postpartum and postabortion (additional research will be needed to identify these time frames; shorter time frames may be more appropriate)
Report switching outcomes for interventions targeting women undergoing abortion
Where possible, report pregnancy outcomes (unwanted pregnancy and abortion) in addition to contraceptive behaviour outcomes
Report measures of experience of contraceptive care; better measures of client satisfaction will need to be developed (including client-centredness and perceived quality of care) 91
Future research should identify and evaluate interventions supporting contraceptive continuation, including identifying users with lower satisfaction over time and supporting method switching where required. Alternative interventions to counsel women before or after abortion, and mechanisms for referral and follow-up for those not wanting to initiate contraception at the time of abortion, are also needed. Lastly, improved measurement of satisfaction with counselling are needed; recent efforts to develop measures of perceived quality or client-centredness of care 91 may represent promising avenues.
Conclusions
Contraceptive counselling has a key potential to improve effective use of contraception and reduce unmet need. This review indicates that additional sessions during pregnancy or postpartum may increase uptake and detailed counselling on side effects for women initiating a method may be effective at improving continuation. However, there was at best limited evidence for effectiveness of other contraceptive counselling interventions, and the evidence should be interpreted with caution given low-quality evidence and substantial heterogeneity. Improved reporting of studies of contraceptive counselling and novel effective interventions are needed.
Additional educational resources
Brief educational strategies for improving contraception use in young people (Cochrane review)
Education for contraceptive use by women after childbirth (Cochrane review)
Effectiveness of contraceptive counselling of women following an abortion (systematic review and meta-analysis)
Mobile phone-based interventions for improving contraception use (Cochrane review)
Acknowledgments
The authors gratefully acknowledge Isa Bogaert and the Library from the Institute of Tropical Medicine in Antwerp, Belgium for their help retrieving full texts. They would also like to extend their thanks to Mr Tomas Allen, World Heath Organization Library, Geneva, Switzerland for his input and in helping find a number of articles for this review. The authors based the protocol for this systematic review on several prior reviews, including Lopez and colleagues and Smith and colleagues.
- United Nations
- Guttmacher Institute
- Cleland J ,
- Haider TL ,
- Campbell M ,
- Sahin-Hodoglugil NN ,
- Bradley S ,
- Dehlendorf C ,
- Krajewski C ,
- Kaneshiro B
- World Health Organization
- World Health Organization and Johns Hopkins Bloomberg School of Public Health
- Ferreira ALCG ,
- Figueiroa JN , et al
- Tolley EE , et al
- Hiller JE , et al
- Ngo TD , et al
- Carneiro Gomes Ferreira AL ,
- Impieri Souza A ,
- Evangelista Pessoa R , et al
- Garbers S ,
- Meserve A ,
- Kottke M , et al
- Boa-Viagem MM ,
- Ramarao S ,
- Kim J , et al
- Kharboush I ,
- Chin-Quee DS ,
- Janowitz B ,
- Otterness C
- Winnard K , et al
- Chewning B ,
- Wilson D , et al
- Hebert LE ,
- Quinn M , et al
- Wilson EK ,
- Sridhar A ,
- Forbes ER , et al
- Kofinas JD ,
- Sapra KJ , et al
- Farrokh-Eslamlou H ,
- Aghlmand S ,
- Eslami M , et al
- George TP ,
- DeCristofaro C ,
- Dumas BP , et al
- Castano PM ,
- Andres R , et al
- Berenson AB ,
- Canto De Cetina TE ,
- Ordoñez Luna M
- Modesto W ,
- Bahamondes MV ,
- Bahamondes L
- Patel A , et al
- Kadayifçi O
- McMahan J , et al
- Bednarek P , et al
- RamaRao S ,
- Jones H , et al
- Brambila C ,
- de la Cruz M
- Mullersman JL ,
- Omvig KJ , et al
- Sapkota S ,
- Rajbhandary R ,
- Basuki E , et al
- Whitaker AK ,
- Munroe E , et al
- Zhang W-H ,
- Cheng Y , et al
- Davidson AS ,
- Martins SL , et al
- Schunmann C ,
- Gold J , et al
- Aiken ARA ,
- Forsyth T , et al
- Savelieva I ,
- Bender SS ,
- Geirsson RT
- Abdel Tawab N ,
- Huntington D ,
- Hassan EO , et al
- Langston AM ,
- Rosario L ,
- Westhoff CL
- Kaewkiattikun K
- Bambulas T ,
- Sutton M , et al
- Manandhar DS ,
- Shrestha P , et al
- Adanikin AI ,
- Onwudiegwu U ,
- Cakiroglu Y
- van der Spuy ZM ,
- Cheng L , et al
- Torres LN ,
- Clark EAS , et al
- Santos LC ,
- Osis MJ , et al
- Proctor A ,
- Jenkins TR ,
- Loeb T , et al
- Uzuner A , et al
- Antora AH ,
- Dewan F , et al
- Ndegwa SW ,
- Gichuhi JW ,
- Qureshi Z , et al
- Eissa MA , et al
- Gillespie D ,
- Bradley H ,
- Woldegiorgis M , et al
- Baldauf E , et al
- Yassin AS ,
- El-Khoury M ,
- Thornton R ,
- Chatterji M , et al
- Kopp D , et al
- Ferguson SL
- Fitzpatrick J ,
- Steinauer J , et al
- Amrhein V ,
- Greenland S ,
- Fuentes L ,
- Hendrixson A
- Irani L , et al
- High Impact Practices in Family Planning (HIP)
- Bhrolchain M ,
- Beaujouan E
- Speizer IS ,
- Calhoun LM ,
- Hoke T , et al
- Keesara S ,
- Harper CC , et al
- Henderson JT ,
- Vittinghoff E , et al
- Garceau RJ , et al
- Gilliam M ,
Twitter @CescaCava, @Moazzam2000
Contributors MA initiated the study and defined the research question. All authors contributed to developing the detailed methodology. FC carried out the literature review, LB and OO acted as second reviewers and data extractors, and MA provided reconciliation in case of any discrepancies. FC drafted the protocol and manuscript. All the other authors edited the draft and approved the final version for publication.
Funding This review was conducted with financial support from the Bill and Melinda Gates Foundation. The funding source did not play a role in the study design, analysis or interpretation of data, or in the writing of the report. The conclusions and opinions expressed here are those of the authors and not necessarily those of the funder.
Disclaimer This paper contains the collective views of an international group of experts, and does not necessarily represent the decisions or the stated policy of the World Health Organization.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Open access
- Published: 17 January 2022
Assessing the cost-effectiveness of contraceptive methods from a health provider perspective: case study of Kiambu County Hospital, Kenya
- James Kiragu Ngacha ORCID: orcid.org/0000-0001-8874-9179 1 &
- Richard Ayah 1
Reproductive Health volume 19 , Article number: 11 ( 2022 ) Cite this article
5517 Accesses
2 Citations
4 Altmetric
Metrics details
Kenya’s contraceptive prevalence rate at 53% is low, with wide disparity among the 47 counties that make up the country (2–76%). Significant financial investment is required to maintain this level of contraceptive use and increase it to levels seen in more developed countries. This is in the context of a growing population, declining donor funding, limited fiscal space and competing health challenges. Studies have shown that long-term contraceptive methods are more cost-effective than short-term methods. However, it is unclear if this applies in Sub-Saharan Africa; with limited financial resources, lower social economic status among users, and publicly managed commodity supply chains, in vertical programs largely dependent on donor funding. This study assessed the cost-effectiveness of contraceptive methods used in Kenya.
A cross-sectional study was undertaken in a county referral hospital in mid-2018. Purposive sampling of 5 family planning clinic providers and systematic sampling of 15 service delivery sessions per method was done. Questionnaire aided interviews were done to determine inputs required to provide services and direct observation to measure time taken to provide each method. Cost per method was determined using activity based costing, effectiveness via couple year protection conversion factors, and cost-effectiveness was expressed as cost per couple year protection.
The intra-uterine copper device was most cost-effective at 4.87 US dollars per couple year protection followed by the 2-Rod Implant at 6.36, the 1-Rod Implant at 9.50, DMPA at 23.68, while the combined oral contraceptive pills were least cost-effective at 38.60 US dollars per couple year protection. Long-term methods attracted a higher initial cost of service delivery when compared to short-term methods.
Long-term contraceptive methods are more cost-effective. As such, investing in long-term contraceptives would save costs despite higher initial cost of service delivery. It is recommended, therefore, that Sub-Saharan Africa countries allocate more domestic financial resources towards availability of contraceptive services, preferably with multi-year planning and budget commitment. The resources should be invested in a wide range of interventions shown to increase uptake of long-term methods, including reduction of cost barriers for the younger population, thereby increasing contraceptive prevalence rates.
Plain language summary
The proportion of women of reproductive age using a contraceptive method in Kenya, at 53% is low. More funding is required to ensure women who need contraceptives have access and continue using them. Previous research has shown that contraceptives that protect a woman from getting pregnant for an extended period utilize less resources. This study assessed the potential of contraceptives used in Kenya to produce results at less cost.
This study was undertaken in a sub-national referral hospital in mid-2018. A sample of 5 family planning clinic providers were interviewed while 15 contraceptive service sessions per method were observed. The interviews were conducted to determine the supplies required to offer services. Observation was used to measure time taken to provide each contraceptive method. The cost associated with providing each contraceptive per year was determined using activity based costing. Effectiveness of each method was determined using the rate of protection from pregnancy during one-year. Cost-effectiveness was the money utilized to achieve protection from pregnancy in one year of use.
The Copper-T coil was found to achieve greater results at a lesser cost of 4.87 US dollars for one year of protection from pregnancy, followed by the 2-Rod Implant at US dollars 6.36, the 1-Rod Implant at 9.50, DMPA at 23.68, and The Pill at 38.60 US dollars.
Contraceptive methods that protect a woman from getting pregnant for a longer period utilize less resources. Investing in such would save costs despite requiring higher initial cost of service provision.
Peer Review reports
Introduction
In 2017, it was estimated that of the 1.6 billion women of reproductive age in developing countries, about 885 million needed contraception [ 1 ]. The unmet need for contraception in developing countries stood at about 214 million women with the unmet need being highest in Sub-Sahara Africa at 21% [ 1 ]. According to the Kenya Demographic and Health Survey (KDHS) 2014/15, Kenya had a contraceptive prevalence rate (CPR) of 58% for all methods (and 53% for modern methods—mCPR) among married women, up from 46% in 2009 [ 2 ]. The 2019 estimated mCPR among married women was 61.4 [ 3 ]. The KDHS 2014/15 put the unmet need for contraception in Kenya at 18% for married women (26% for all women of reproductive age) down from 26% (married women) in 2009 [ 2 ]; 2019 estimate is 16.9% [ 3 ]. The 2014/15 mCPR was dominated by Depot Medroxy-Progesterone Acetate (DMPA) contributing 26%, followed by implants at 10%. Pills contributed 8% while intrauterine copper devices (IUCDs) and sterilization contributed about 3% each. The rest was contributed by condoms and traditional methods among others [ 2 ]. Kiambu County, one of the 47 counties in Kenya, had a CPR that is higher than the national average at 74% for all methods and 68% for modern methods among married women [ 2 ]. In this county, DMPA contributed 22%, followed by pills at 19%. Implants contributed 12%, IUCDs contributed 9%, female sterilization contributed 3%, while condoms and non-modern methods contributed the rest [ 2 ].
Contraceptive programmes are some of the most cost-effective tools available for tackling public health challenges of our day [ 4 , 5 ], and also contribute to economic growth and development [ 1 , 6 ]. Contraceptives are known to significantly reduce maternal and child mortality, over and above directly reducing the number of unwanted pregnancies and unsafe abortions [ 1 ]. Contraceptives have also been shown to contribute positively to factors of economic growth and development especially in relation to women and children [ 6 ]. From an economic point of view, the use of contraceptives is clearly more beneficial than failure to use; with cost-benefit ratios of 1:9 in UK [ 4 ], 1:7 in USA [ 5 ], 1:2 in Sierra Leone [ 7 ], and 1:4 in Kenya [ 8 ] among other studies that show similar trends [ 9 , 10 , 11 , 12 ]. However, questions persist regarding which methods are more cost-effective.
Long-acting contraceptive methods appear to be more cost-effective than short-acting methods from all perspectives [ 13 , 14 , 15 , 16 , 17 ]. This can be explained by long-acting methods being more efficacious [ 18 ], that is, have a lower failure rate when used correctly and consistently. Therefore, each service results into higher benefit when viewed from health provider perspective and less visits to the health facilities for the same level of effectiveness from clients’ perspective. Further, long-acting methods are less dependent on user compliance and their efficacy is close to or similar to typical use effectiveness [ 18 ]. There is, therefore, less cost associated with their failure and consequences of failure [ 13 , 14 , 15 ]. From clients’ perspective, this means less costs associated with unwanted pregnancies, and reduced workload in form of antenatal, postnatal and peri-natal healthcare needs from provider’s and health system’s perspectives. From the society perspective, less contraceptive failure results into better population management and associated economic benefits. Published data shows that implants are the most efficacious method with about 0.05 unintended pregnancies per 100 women per year; IUCDs 0.6, while DMPA and Combined Oral Contraceptive Pills (CoCs) have a failure rate of 0.3 [ 18 ]. This is in contrast to male condoms that have a failure rate of 2 unintended pregnancies per 100 women per year, 5 for female condoms, 6 for cycle beads, 18 for spermicides, and use of no method would result into about 85 pregnancies [ 18 ].
A number of studies have shown some short-term methods dominating their long-term counterparts in cost-effectiveness for the entire or part of the study period [ 13 , 19 , 20 , 21 ]. This could be explained by some studies having only considered fixed costs [ 21 ], or considered a period of less than 2 years [ 13 , 19 ], or differing market dynamics (context) for example cost of commodities [ 20 ]. Some studies showed implants as the least cost-effective method [ 19 , 20 , 21 ]. This could be explained by differing market dynamics and high cost of implants at the time of the studies.
Several factors affect real-world effectiveness of contraceptives. Short-term methods are not only less efficacious than long-term methods, but also their effectiveness (CoCs and DMPA) is highly dependent on correct and consistent use [ 14 , 18 ]. Although user compliance is not a major factor in determining effectiveness of long-acting reversible contraceptives (LARCs), continuation/discontinuation of use, which is user-dependent, has an impact on effectiveness. The mean 1-year continuation rate of etonogestrel implants, for example, was higher among women in middle-income countries during clinical trials than in developed countries [ 22 ]. Subsequent studies showed higher continuation rates in lower income countries (98% in Nigeria) [ 23 ] than in developed countries (87% in USA [ 24 ] and 75% in the UK) [ 25 ]. Drug interactions and general health status of users also determine effectiveness of contraceptives [ 18 ]. Various drugs especially protease inhibitors used as part of Antiretroviral Therapy (ART) in treatment and prophylaxis of HIV/AIDS are known to reduce effectiveness of hormonal contraceptive methods [ 18 ]. Age of users affect effectiveness of some contraceptive methods with younger users having higher number of pregnancies prevented in the case of sterilization [ 13 ]. Frequency of sexual intercourse determines effectiveness of methods that are dependent on sexual activity for example diaphragm, spermicides and condoms [ 26 ]. From the above, it is clear that contextual factors have an effect on effectiveness of various contraceptive methods (both long and short acting methods) due to varying socio-economic status of users, prevalence of infectious disease and lifestyle factors.
Various studies evaluated cost from different perspectives—clients, health system and wider society perspectives. From the clients’ perspective, costs included user fee and transport, consequences of method failure as well intangible costs like psychological impact of methods failure [ 27 , 28 ]. From health system perspective, costs were either fixed (capital and overheads at facility and health system management levels) or recurrent (labour, commodities and equipment) [ 17 , 20 , 21 ] or determined via cost modeling [ 13 ]. Societal perspective would include all the above costs plus opportunity cost of providing the services and costs to the society due methods failure [ 14 , 27 ]. The choice of cost perspective depended on study objectives, resources (financial, time and human), and availability of data.
In summary, long-term contraceptive methods are expected to attract higher cost of service delivery (from provider perspective) when compared to short-term methods [ 13 , 14 ] and more cost-effective in the long run. This can be attributed to higher cost of commodities especially for implants [ 29 ], cost of labour, training, and equipment required to provide the long-term methods [ 13 , 30 ]. Due to lower cost of service delivery, short-term methods are therefore likely to be more cost-effective in 1 to 2 year horizon [ 13 , 14 , 15 ]. ‘Decisions of value’ that would affect the cost of providing healthcare services are influenced by a wide range of ‘inner and outer context’ [ 31 ] that range from information, organizational culture, governance, economic and political conditions [ 32 ]. The cost associated with each method is, therefore, expected to vary with cost perspectives, but also, from country to country, region to region of each country, and even from facility to facility given their unique contextual factors. Irrespective of the cost-effectiveness profile of the available methods, informed clients’ choice is paramount and family planning programs should always have a wide range of methods in all service delivery points.
Research problem
Kenya’s mCPR at 53% [ 2 ] (2019 estimate is 61% [ 3 ]) among married women remains low. A lot of investment is required to sustain this CPR in the face of growing population, and increase it to the levels seen in more developed countries (77% in N. Europe, 82% in Eastern Asia, and 75% in N. America) [ 33 ]. This is in an environment of reducing donor funding that has been the backbone of the FP program in Kenya and inadequate local resources allocation by both the national and county governments. Efficient use of resources is, therefore, critical.
Several studies have shown that long-acting contraceptive methods are more cost-effective than short-term methods [ 13 , 14 , 15 ]. However, most of these studies have been carried out in more developed countries where healthcare and contraceptive programmes have differing dynamics compared to Kenya and therefore Kiambu County. Some of the possible contextual differences include: involvement of the private sector, social economic status of providers and clients, health insurance coverage (including other forms of risk pooling), commodities’ supply chain management, and levels of unmet need. Unique country (and in this case county) specific data is critical for prudent decision making. This study was, therefore, designed to assess cost-effectiveness of various contraceptive methods in the context of Kiambu County.
Research question and objectives
This study sort to answer the question; “What is the cost-effectiveness of contraceptive methods available in Kenya?” The objective of this study was to determine the cost-effectiveness of contraceptive methods used in Kenya.
Study design
This research was a cross-sectional study to determine the cost-effectiveness of contraceptive methods offered in Kiambu County Hospital in Kenya. This was a full economic evaluation encompassing assessment of cost, effectiveness and several alternative courses of action.
Study site and population
Kiambu County Hospital was chosen because of convenience (about 15 kilometres from Nairobi City) and the County has a higher mCPR (68%) than the national average of 53%, and higher contribution of long-term methods than the national average [ 2 ]. Kiambu County Hospital is a Public Hospital and one of the 45 Level 4 (Kenya Essential Package for Health classification) hospitals in Kenya—36 of the hospitals (80%) being private (for profit and not for profit) while 9 (20%) are public (owned and managed by the Kiambu County Government) [ 34 ]. In 2016/17 financial year, Kiambu County Hospital had a total work load of 355,910 (outpatient visits plus number of bed days) [ 35 ]. The study population consisted of the healthcare providers who offer family planning services in the hospital.
Selection of alternatives
The following contraceptive methods were selected for this study because they contributed 89% of mCPR in Kenya and 91% of mCPR among married couples in Kiambu County [ 2 ]:
Intra-uterine copper devices (IUCDs)—Copper T® 380
Contraceptive implants;
2-Rods Contraceptive Implants, each containing 75 mg levonorgestrel—Jadelle®
1-Rod Contraceptive Implants, each containing 68 mg etonogestrel—Implanon NXT ®
Depot Medroxy-Progesterone Acetate (DMPA) 150 mg, Intramuscular
Combine Oral Contraceptive Pills (CoC—Pills)—a cycle of 28 pills having 21 pills each containing Ethinylestradiol 30 mcg, and Levonogestrel 150 mcg and an extra 7 Ferrous Sulfate pills that are supplied in a pack of 3 cycles under an MoH, Kenya owned brand called ‘Chaguo Langu’
Cost of providing each method (dependent variables)—sample, sampling and data collection
Cost was estimated through Activity Based Costing model [ 36 , 37 ] as shown in the study’s conceptual framework (Fig. 1 ).
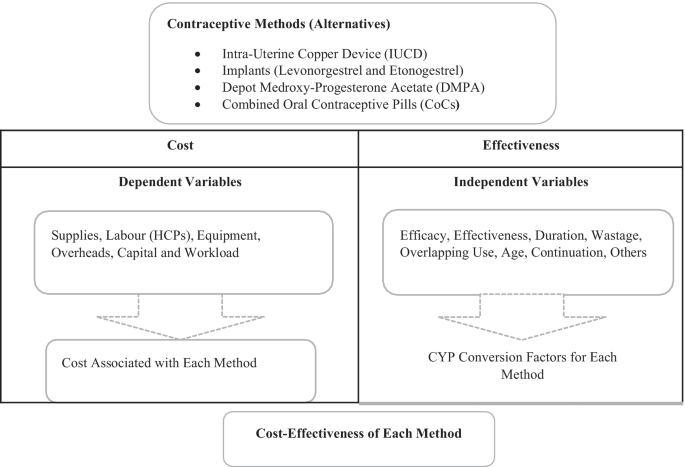
Conceptual framework
Inputs required to provide each method were classified into; supplies, labour, equipment overheads, and capital. A purposeful sampling of all healthcare providers manning the FP clinic on day one of the study was done. The study was carried out between July and October 2018. Questionnaire aided interviews (5 respondents) was carried out to determine supplies, equipment, capital, and overheads required to provide IUCDs; implants; DMPA and CoC Pills, and number of routine follow-up visits per method. This was followed by in-depth interviews (2 respondents) to clarify the client’s pathway and exact identity of inputs identified above; for example, the brand and pack size of glove, the brand name and other specifications of the Blood Pressure machine used and so forth for the purposes of costing. Information from the in-depth interviews and questionnaires was validated through procurement records and observation of available supplies, equipment and capital in the facility. The hospital workload for 2017/17 was used to distribute cost of capital, shared equipment, and overheads among the studied methods. Time taken to provide each method was used to estimate labour cost and was collected via direct observation of at least the first 15 service deliver sessions per method, selected via systematic sampling. The time at entering and leaving the service delivery room was noted on pre-designed tally sheets.
Sample size of the number of services to be observed was calculated as follows [ 38 ]; n = ((Z 1/2 α) 2 x SD 2 ) ÷ d 2 : where Z 1/2 α = 1.96 (α = 5%), expected standard deviation = SD (5 min), and acceptable level of error = d (3 min). The slowest method to provide was assumed to take an average of 40 min
Secondary data was collected from various sources as shown in Table 1 .
Effectiveness of each method (independent variables)
Effectiveness was estimated from Couple Years Protection (CYP) conversion factor associated with each method—that translates services into common impact (prevention of pregnancy). CYP conversion factors take into account the efficacy of each method, duration of use, effectiveness, coital frequency for coitus dependent methods, wastage (for self-administered methods), misreporting (accounts for data quality), age (for sterilization), consistency of use, non-contraceptive use (for condoms), and overlapping coverage (use of more than one method at a time) that influence effectiveness of contraceptive services [ 26 ]. This measure of effectiveness is easy to use and requires the number of services offered or volume of commodities distributed as the only input. Data used to construct conversion factors often include data from developing countries on factors that affect effectiveness of contraceptive services [ 26 ]. A study conducted in Iran used Adjusted CYP conversion factors as the measure for effectiveness of various methods [ 20 ] and quoted its robustness and ease of use as the reasons for choosing it. A study conducted in Kenya [ 21 ] also used CYP as the measure of effectiveness. In summary, the use of CYP conversion factors as a measure of effectiveness is simple, uses service data as the only input, considers the context of developing countries and is appropriate for use in studies like this one. Conversion factors used in this study were obtained from USAID website [ 41 ].
Data from primary or secondary sources was entered in a pre-designed Microsoft Excel sheet, cleaned and processed for further analysis.
Calculations
The study utilized an Activity Based Costing model to determine the cost of providing the various contraceptive services to clients [ 36 , 37 ]. Calculations were done using Microsoft Excel sheets. The following steps were followed to estimate cost: identification of inputs needed per activity and per method, quantification of inputs per method, costing of inputs per method, computation of cost per method, and finally calculation of cost per couple years of protection.
Price was used to estimate the cost of inputs. Cost of supplies was determined from the average prices by public sector suppliers (for a few products that were not available through public sector supply chain, private sector prices were used) at the time of the study. Cost of FP commodities supplied to the hospital as donations was estimated from average price to the donors plus 10% cost freight, customs clearance, storage and in-country distribution. Cost of labour was determined from time taken to provide each method, job groups of the providers, and average salary of each job group (as set by salaries and Remuneration Commission of Kenya). Cost of equipment was determined from the prices of procuring new equipment at the time of the study, amortized as per their useful life years and then distributed among various methods using the workload. Cost of overheads was determined from 2016/17 FY facility expenditure and hospital workload. Capital cost was determined from space utilized and amortized cost of putting up new building, and cost of procuring new furniture and other required installations at the time of study (amortized as per their useful life years) distributed to each method using workload.
Cost of each method was then divided by CYP conversation factor for each method that as available on USAID website [ 41 ] accessed on 5th August 2017 to determine cost-effectiveness of each method. The various methods were then ranked according to their cost-effectiveness with the method showing the lowest cost per CYP being deemed the most cost-effective as shown in Table 2 .
Ethical considerations
Ethical approval was obtained from Kenyatta National Hospital/University of Nairobi Ethical Review Committee (KNH/UoN-ERCA210). Further approval was received from the Kiambu County Health Research Development Unit and the Kiambu County Hospital management before commencement of the study.
Inputs required to provide services
The IUCD was found to be the most cost-effective method at 4.87 USD (CI 4.16–5.60) per CYP (exchange rate 103KeS to the USD), followed by the 2-Rod Implant at 6.36 (CI 5.85–6.87), the 1-Rod Implant at 9.50 (8.72–10.28), DMPA at 23.68 (CI 21.39–24.86), and CoC Pills at 38.60 (CI 0.40–46.82) was the least cost-effective. The cost-effectiveness ratio when compared to IUCD was as follows; 2-Rod Implant 1.3, 1-Rod Implant 1.95, DMPA 4.86, and COC Pills 7.92. The 2-Rods Implant attracted the highest initial cost of services delivery per client at 24.19 (70% recurrent i.e. supplies and equipment), followed by 1-Rod Implant at 23.78 (70% recurrent), while IUCD was the least expensive long-term method to provide at 22.41 (46% recurrent) per client. On the other hand, short-term methods attracted less initial cost of service delivery with DMPA costing 5.91 (55% recurrent) and CoC Pill at 2.57(50% recurrent) per client. On average, labour, supplies and overheads were the main cost drivers accounting for 92% of the cost, each contributing about 30% of the total cost. Cost of FP commodities alone contributed 40% for the 2 Rod Implant, 42% for the 1-Rod Implant, 2.5% for the IUCD, 19% for DMPA and 10% for CoC Pills.
Seventeen (17) individual supplies items were needed to provide services of the contraceptive methods studied. The CoC pills required only the FP commodity while DMPA required syringe and needle and alcohol swab as well. The IUCD required chlorhexidine, sterilized gloves, surgical masks and gauze swabs while the implants required lidocaine, syringe and needle, povidone iodine solution, gauze swabs, adhesive plaster, sterile gloves, non-sterile gloves and pressure bandage. All the clients needed triage equipment notably blood pressure (BP) machine, thermometer, weighing scale and stethoscope. Long-term methods required more of the 24 pieces of equipment identified due to sterile/aseptic procedures required to insert and remove the methods. The IUCD and implants required the most provider time among long-term methods (IUCD 46 min (n = 33, CI 28–63), 2-Rod Implant 35 min (n = 23, CI 25–46) and 1-Rod Implant 29 min (n = 39, CI 19–38). On the other hand, among the short-term methods, DMPA required 6.50 min (n = 27, CI 5.5–7.5) and an average of 2 cycles of CoC Pills 7.10 min (n = 19 CI 3.5–10.8). Implants and IUCD attracted more overhead costs than the short-term methods since they required sterilization of insertion and removal equipment. The capital cost was evenly distributed (per visits) among all the methods as shown in Table 3 .
Discussion and conclusion
The results of this study were generally consistent with findings of similar studies [ 13 , 14 , 15 , 16 , 17 , 28 ] where long-term methods dominated short-term methods; with the IUCD attracting lowest cost per CYP, followed by the 2-Rod Implant (1.3 times more than IUCD), the 1-Rod Implant (1.95 times), DMPA (4.86 times), and finally CoC Pills (7.92 times). The difference with findings of deviating studies may be attributed to differing market dynamics (contextual factors such as price of commodities especially implants in the country the studies were carried out [ 19 , 20 ] or time of the study [ 21 ] ) as well as a drastic reduction in the price of implants in FP 2020 Countries in 2013 [ 42 , 43 ]. Some studies showed a number of short-term methods dominating their long-term counterparts, for entire time of the study or part of the study period [ 13 , 19 , 20 , 21 ]which can be explained by failure to consider fixed costs [ 21 ] or considering short period (less than 2 years) [ 13 , 19 ]. In our study, fixed costs accounted for 38% on average—54% for IUCD, 50% for CoC Pills, 45% for DMPA and 30% for implants. In agreement with other studies, we found that long-term methods attracted higher initial cost of service delivery when compared to short term methods. The 2-Rods Implant attracted the highest cost of services delivery 24.19 USD, followed by 1-Rod Implant at 23.78, IUCD at 22.41, DMPA at 5.91 and CoC Pill at 2.57 per client. This can be explained by higher cost of procuring commodities [ 13 , 17 , 20 , 21 ], higher cost of labour (HCP time) [ 13 , 17 , 20 , 21 ], and cost of equipment and supplies [ 13 , 44 ] required to provide long-term methods. Over and above this, long-term methods attract additional cost to the health system in form of training the HCP [ 42 , 44 ] to offer services. We, therefore, can conclude that long-term contraceptive methods are more cost-effective than short-term methods, but require more initial investment in terms of commodities, equipment, labour, and training of service providers.
These results should be interpreted with caution given the following limitations. First, this was a case study carried out only in one hospital and reflects the unique context within the hospital, for example, the skills mix of the healthcare provider (HCP) manning the FP clinic. Second, only the cost of labour was subjected to statistical analysis. Other costs were based on secondary data and actual measurements, and workload was used to distribute cost among the methods. Changes in the hospital workload and that of various contraceptive methods could affect the results [ 20 ]. Third, the study only considered cost from provider perspective. Costs from other perspectives could have changed the total cost per method without changing the cost-effectiveness pattern observed since the same fundamentals (less utilization of services per unit of effectiveness and lower failure rate) drive cost-effectiveness. Several studies from client and societal perspectives shows the same pattern; long-acting methods are more cost effective [ 15 , 28 ]. Fourth, the study did not include costs associated with contraceptive method failure and management of adverse effects. These costs would most likely enhance cost-effectiveness seen among long-term methods since they have less failure rates.
Increasing the use of long-term contraceptive methods involves investing both in the supply side (training, support supervision and mentoring, commodity security, multiple service delivery models (including outreaches) and demand generation for FP services [ 43 , 44 , 45 ]; while putting the clients’ right to make informed choice at the centre. This kind of investment requires long-term planning with possibility of multi-year budgets. Long-term planning and budgeting are currently possible with donor funded vertical FP programs given multi-year commitment by donors. Donor funding has been the main source of financial resources for FP programs in SSA since their inception [ 46 , 47 ]. However, this has been on decline in the recent years and it is likely to reduce even more with the reintroduction of the Global Gag Rule in 2017 with expanded interpretation [ 48 ]. For Kenya, the decline is likely to be even more pronounced due to attainment of lower-middle income status since 2014 [ 49 ]. There is need to mobilize more domestic funding to ensure adequate service delivery and long-term sustainability [ 47 , 50 ]. Unfortunately, domestic resources which are based on government annual budgets may not promote long-term planning. Such annual budgets run the risk of being based on costs of providing various contraceptive methods other than their long-term cost effectiveness.
Some African countries, including Kenya, have budgetary allocation (though inadequate) for FP programs including for procurement of FP commodities [ 46 , 47 ]. Whether the budgets are ring-fenced for FP commodities and services is subject for a separate discussion. For Kenya, utilization of the inadequate domestic funds is complicated by devolution of health services where policy direction is a function of the national government while service delivery is at the county level (sub-national level) [ 47 , 50 ]. Some counties in Kenya have FP budgets [ 50 , 51 ] but unfortunately, the budgets are inadequate and much of the FP related expenditure at the county level only cater for FP commodities and service delivery [ 51 ] other than the comprehensive investment that has been shown to increase utilization of long-term contraceptive methods. Having up-to-date FP Costed Implementation Plans (CIP) at both the Central Government and each of the 47 counties could be one of the ways to ensure long-term planning as well as coordinated investment to increase use of long-term methods. The central government has a 2017-20 FP CIP [ 52 ] but only a few counties have FP CIPs [ 51 ].
Whereas cost of contraceptives has been identified as a barrier to accessing FP services [ 53 ], (especially LARCs [ 54 , 55 ]) by all women, it is one of the most important barriers to youth and adolescent access to long-term contraceptive methods [ 30 , 56 , 57 , 58 , 59 ]. Removing cost barriers among other investment was found to increase uptake of long-term methods [ 30 ] by youth and adolescents; which is a growing demography in almost all developing countries including Kenya. FP services in FP 2020 countries is heavily subsidized through vertical donor funded programs [ 46 , 47 , 60 ]. With declining donor funding, domestic sources of financial resources would again be required to continue subsidizing FP services. Innovative solutions within Universal Health Coverage framework where financially vulnerable groups like the youth and adolescent access services for free could be one solution that removes cost barriers to accessing long-term contraceptive methods. This would have the overall effect of increasing the proportion of CPR contributed by long-term methods—since young people form a very large proportion of the populations in Africa (20% of all global youth (15-24 years), which is expected to rise to 42% by 2030) [ 61 ].
Recommendations
In the current environment of declining donor funding, it is important for each country in Sub-Saharan Africa to allocate adequate financial resources to ensure continued availability of FP services and sufficiently invest in long-term methods. Adequate resource allocation is especially important for long-term methods that not only attract a higher initial cost of service delivery, but also require further investments in form of training services providers and procurement of equipment. Budget commitments should be multi-year in nature to enable long-term planning based on long-term cost saving other than initial cost of providing the services and capacity building. The budgetary allocation should cover all the investments that have been shown to increase use of long-term contraceptive methods such as; training of service providers, multiple and responsive service delivery options, commodity security, equipping facilities and demand creation. Funds for procuring FP commodities need to be in their specific budget lines. This is because FP commodities account for a very significant proportion of the overall cost of providing FP services but also form a very critical input to the services.
Resource allocation at the national level alone may unfortunately not result into availability of FP services or increased use of long-term methods. Adequate resource allocation at the sub-national levels for example local municipal governments that are responsible for health service delivery is also vital. Unlike in the current donor funded vertical FP programs, it is difficult to have domestic funds allocated to sub-national authorities that can only be used to deliver FP services. Unless local authorities and health care managers at the local level prioritize FP, services could continue to be inadequate at the local level despite resources commitment at the national level because of the following reasons. First: in some regions, the demand for FP services may be low and, local authorities and healthcare managers may allocate resources to more pressing healthcare needs. Second: local authorities are less likely to feel the pressure to meet international commitments to the same extent as national government. For example, many countries in SSA have made commitments to improve access to family planning services through the FP 2020 movement. The national governments may align their budgets to such global and other regional commitments only for the funds to be diverted at the local level. Third; local authorities and healthcare managers’ interests may not align with family planning objectives since higher populations may often translate to higher resource allocation to their regions.
Lastly, it is important for the current subsidies that are inbuilt in most FP programs in SSA to continue or where possible be enhanced, even in the face of declining donor funding, economic challenges and competing priorities. Justice, as an ethical principle clearly support subsidizing FP services given that there are many positive externalities associated with use of contraceptives. Women (even those of high economic status and can afford) should not fully meet the cost of using contraceptives when the entire society benefit from the use. The principle of equity, both as a desirable goal of the health system and an ethical principle also support subsidies in the Family Planning services. Women the world over and even more so in the SSA are considered to be less economically endowed when compared to men while they consume the highest proportion of contraceptive services. Further, youth and adolescents are considered economically vulnerable and removing cost barriers for this demography has been associated with improved uptake of FP services. Continuing to make FP commodities available, free of charge, to all service delivery points (both public and private) is one way that would ensure subsidies continue in an equitable way—where those of lower economic status access service without any user fee (or minimal user fee at public facilities to cover other costs of service delivery) while those of higher economic status pay more user fee in private facilities. Market segmentation hence total market approach to providing FP services would be achieved without putting undue burden on women or incurring huge administrative cost of trying to keep free commodities in the public facilities only. Removing all cost barriers for the most economically vulnerable, especially youth and adolescents, for example through vouchers covering transport cost and user fee would further improve equity and promote use of long-term methods.
Availability of data and materials
The datasets generated and analysed during this study are in the possession of the authors and are available for sharing.
Abbreviations
Acquired immuno-deficiency syndrome
Adjusted couple years protection
Ante-natal clinic
Antiretroviral treatment
Blood pressure/British pharmacopeia
Bachelor of Science in Nursing
Cost-effectiveness analysis
Choosing interventions that are cost-effective
Community Health Workers
Combined Oral contraceptive pills
Contraceptives prevalence rate
Costed Implementation Plan
Central Sterilization Services Department
Couple years protection
Children wellness clinic
Depot medroxy-progesterone acetate
District Health Information System 2
Etonogestrel
Family planning
Financial year
British Pound Sterling
Government of Kenya
Healthcare providers
Human immunodeficiency virus
Intra-muscular
Integrated management of childhood illness
Intra-uterine copper device
Intra-uterine device
Intra-uterine systems
Kenya Demographic and Health Survey
Kenya Essential Package for Health
Kenya Shillings
Kenya Medical Supplies Authority
Kenya Health Policy 2012–2030
Kenya Health Sector Strategic and Investment Plan
Kenya National Bureau of Statistics
Kenyatta National Hospital
Long-acting and reversible contraceptive
Levonorgestrel intra-uterine system
Maternal Child Health
Mission for Essential Drugs and Supplies
Post natal care
Prevention of mother-to-child transmission
Standard deviation
Tuberculosis
United Kingdom
United Nations Family Planning Agency
United States of America
United States Agency for International Development
United States Dollar
World Health Organization
Guttmacher Institute. ADDING IT UP: investing in contraception and maternal and newborn health. New York; 2017. http://www.gatesfoundation.org/What-We-Do/Global-Development/Family-Planning%0A https://www.guttmacher.org/fact-sheet/adding-it-up-contraception-mnh-2017 .
Kenya National Bureau of Statistics (KNBS). KDHS 2014. Nairobi, Kenya; 2014.
FP 2020. Family Planning 2020—Kenya. Track 20 Project—Data. https://www.familyplanning2020.org/kenya . Published 2020. Accessed 18 Feb 2020.
Jayatunga W. Contraception: economic analysis estimation of the return on investment (ROI) for publicly funded contraception in England. London; 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/730292/contraception_return_on_investment_report.pdf .
Frost J, Sonfield A, Zolna MR, Finer LB. Return on investment: a fuller assessment of the benefits and cost savings of the US publicly funded family planning program. Milbank Q. 2014;92(4):667–720. https://doi.org/10.1111/1468-0009.12212 .
Article PubMed Central Google Scholar
Canning D, Schultz TP. The economic consequences of reproductive health and family planning. Lancet. 2012;380:165–71.
Article Google Scholar
Keen S, Begum H, Friedman HS, James CD. Scaling up family planning in Sierra Leone: a prospective cost–benefit analysis. Women’s Health. 2017. https://doi.org/10.1177/1745505717724617 .
Article PubMed PubMed Central Google Scholar
Warira D. The African Institute for Development Policy (AFIDEP). Family planning in Kenya: saving lives, saving money. https://www.afidep.org/family-planning-in-kenya-saving-lives-saving-money/ . Published 2015. Accessed 10 Dec 2018.
Trussell J. Contraceptive efficacy. In: Hatcher RA, Trussell J, Srewart F, Nelson A, Cates W, Guest F, Kowal D, editors. Contraceptive technology. Eighteenth. New York: Ardent Media; 2004. p. 773–845.
Google Scholar
Udeh B, Losch M, Spies E. The cost of unintended pregnancy in Iowa: a benefit-cost analysis of public funded family planning services. 2009. http://ir.uiowa.edu/cgi/viewcontent.cgi?article=1047&context=ppc_health .
Lanzona LAJ. Family planning as an investment in human capital: cost-benefit analysis of the programme in Malaybalay, Bukidnon, the Philippines. Millenn Asia. 2013;4(1):41–66.
Mugo MG, Muriithi PJ. Cost effectiveness analysis of family planning programs. J Afr Dev. 2017;19:13–22.
Mavranezouli I. The cost-effectiveness of long-acting reversible contraceptive methods in the UK : analysis based on a decision-analytic model developed for a National Institute for Health and Clinical Excellence (NICE) clinical practice guideline. Hum Reprod. 2008;23(6):1338–45. https://doi.org/10.1093/humrep/den091 .
Article PubMed Google Scholar
Lipetz C, Phillips CJ, Fleming CF. The cost-effectiveness of a long-acting reversible contraceptive (Implanon ®) relative to oral contraception in a community setting. Contraception. 2009;79(4):304–9. https://doi.org/10.1016/j.contraception.2008.11.003 .
Henry N, Hawes C, Lowin J, Lekander I, Filonenko A, Kallner HK. Cost-effectiveness analysis of a low-dose contraceptive levonorgestrel intrauterine system in Sweden. Acta Obstet Gynecol Scand. 2015;94:884–90. https://doi.org/10.1111/aogs.12679 .
Lafuma A, Agostini A, Linet T, Robert J, Levy-Bachelot L, Godard C. Cost-effectiveness of Nexplanon® (Etonogestrel Implant) compared to other reimbursed contraceptive methods in France based on real life data. Value Health. 2015;18(8):735–6. https://doi.org/10.1016/j.jval.2015.09.2818 .
Ssewanyana S, Kasirye I. The cost effectiveness of family planning services in Uganda. J Afr Dev. 2017;19:1–11.
WHO. Family planning: a global handbook for providers (2011 Update). Baltimore and Geneva; 2011. http://apps.who.int/iris/bitstream/10665/44028/1/9780978856373_eng.pdf .
Sauer DLH, Ann K. Estimating the relative cost effectiveness of four contraceptive methods in the prevention of unwanted pregnancies within Departmènt of Defense Active-Duty Women. J Manag Care Pharm. 1999;5(2):131–6.
Nakhaee N, Gorji AMHA, Mohammadi M. Assessing the cost-effectiveness of contraceptive methods in Shiraz, Islamic Republic of Iran. East Mediterr Health J. 2002;8(1):55–63.
Article CAS Google Scholar
Futures Group. The cost of family planning in Kenya. Washington, DC; 2010. http://www.healthpolicyinitiative.com/Publications/Documents/1189_1_1189_1_Kenya_Brief_FINAL_7_12_10_acc.pdf .
Palomba S, Falbo A, Cello AD, et al. Nexplanon: the new implant for long-term contraception. A comprehensive descriptive review. Gynecol Endocrinol. 2012;3590(August 2017):710–21. https://doi.org/10.3109/09513590.2011.652247 .
State P. One-year experience with implanon sub-dermal implants in Jos. Nigeria. 2010;13(March):28–31.
Wilson S, Tennant C, Sammel MD, Schreiber C. Immediate postpartum etonogestrel implant: a contraception option with. Contraception. 2014;90(3):259–64. https://doi.org/10.1016/j.contraception.2014.05.006 .
Article CAS PubMed Google Scholar
Lakha F, Glasier AF. Continuation rates of Implanon R in the UK: data from an observational study in a clinical setting. Contraception. 2006;74:287–9. https://doi.org/10.1016/j.contraception.2006.05.072 .
Stover J, Bertrand JT, Shelton JD. Empirically based conversion factors for calculating couple-years of protection. Eval Rev. 2000;24(1):3–46.
Trussell J, Shochet T. Cost-effectiveness of emergency contraceptive pills in the public sector in the USA. Expert Rev Pharmacoecon Outcomes Res. 2003;3(4):433–40. https://doi.org/10.1586/14737167.3.4.433 .
Sweileh WM, Barham AM. Contraceptive methods: cost/effectiveness ratio from a customer’s perspective in Palestine. An-Najah Univ J Res (N Sc). 2003;17(1):43–51.
Espey E, Ogburn T. Long-acting reversible contraceptives. Obstet Gynecol. 2011;117(3):705–19. https://doi.org/10.1097/AOG.0b013e31820ce2f0 .
Kavanaugh ML, Jerman J, Ethier K, Moskosky S. Meeting the contraceptive needs of teens and young adults: youth-friendly and long-acting reversible contraceptive services in US family planning facilities. J Adolesc Health. 2013;52(3):284–92. https://doi.org/10.1016/j.jadohealth.2012.10.276 .
Pettigrew AM. The awakening giant: continuity and change in imperial chemical industries. Chichester: Wiley-Blackwell; 1985. http://eureka.sbs.ox.ac.uk/id/eprint/1610 .
Williams I, Brown H, Healy P. Contextual factors influencing cost and quality decisions in health and care: a structured evidence review and narrative synthesis. Int J Health Policy Manag. 2018;7(8):683–95. https://doi.org/10.15171/ijhpm.2018.09 .
United Nations. Trends in contraceptive use worldwide 2015. New York; 2015. https://doi.org/10.1016/j.contraception.2012.08.029 .
Ministry of Health. Kenya Master Health Facility List.
Ministry of Health. Kenya Health Information System. DHIS2. https://hiskenya.org/dhis-web-commons/security/login.action;jsessionid=E54DC6FD2379988937FA75DA43 1E68F0. Published 2018. Accessed August 15, 2018.
Cooper R, Kaplan RS. Profit priorities from activity-based costing. 1991:130–135. http://disa.uniroma3.it/wp-content/uploads/2016/09/588_3931.pdf .
Kaplan RS, Anderson SR. Time-driven activity-based costing. SSRN J. 2003. https://doi.org/10.2139/ssrn.485443 .
Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013;35(2):121–6. https://doi.org/10.4103/0253-7176.116232 .
Ministry of Health. Family planning commodities quantification 2018–2020 technical report. Nairobi; 2018.
WHO. Cost effectiveness and strategic planning (WHO-CHOICE). Capital item—useful lives reported by country experts. https://www.who.int/choice/costs/prices_t4/en/ . Published 2018. Accessed 1 Nov 2018.
USAID. USAID Website. Couple years of protection (CYP). https://www.usaid.gov/what-we-do/global-health/family-planning/couple-years-protection-cyp . Published 2014. Accessed 5 Aug 2017.
Christofield M, Lacoste M. Accessible contraceptive implant removal services: an essential element of quality service delivery and scale-up. Glob Health Sci Pract. 2015;4(3):366–72.
Jacobstein R, Stanley H. Contraceptive implants: providing better choice to meet growing family planning demand. Glob Health Sci Pract. 2013;1(1):11–7. https://doi.org/10.9745/GHSP-D-12-00003 .
Muthamia M, Owino K, Nyachae P, et al. The Tupange Project in Kenya: a multifaceted approach to increasing use of long-acting reversible contraceptives. Glob Health Sci Pract. 2016;4:44–59.
Ngo TD, Nuccio O, Pereira SK, Footman K, Reiss K. Evaluating a LARC Expansion Program in 14 Sub-Saharan African Countries: a service delivery model for meeting FP2020 goals. Matern Child Health J. 2016. https://doi.org/10.1007/s10995-016-2014-0 .
May JF. The politics of family planning policies and programs in sub-Saharan. Popul Dev Rev. 2017;43:308–329. https://www.jstor.org/stable/26622884 .
Bongaarts J, Hardee K. The role of public-sector family planning programs in meeting the demand for contraception in Sub-Saharan Africa. Int Perspect Sex Reprod Health. 2017;43(2):41–50. https://www.jstor.org/stable/ https://doi.org/10.1363/43e3917 .
Mavodza C, Goldman R, Cooper B. The impacts of the global gag rule on global health: a scoping review. Glob Health Res Policy. 2019;4(26):1–21. https://doi.org/10.1186/s41256-019-0113-3 .
Jonah CMP, Sambu WC, May JD. A comparative analysis of socioeconomic inequities in stunting: a case of three middle-income African countries. Arch Public Health. 2018;76(77):1–15. https://doi.org/10.1186/s13690-018-0320-2RESEARCH .
Keyonzo N, Korir J, Abilla F, et al. Changing face of family planning funding in Kenya: a cross-sectional survey of two urban counties. Afr J Reprod Health. 2017;21(December):24–32. https://doi.org/10.29063/ajrh2017/v21i4.3 .
Deutsche Stiftung Weltbevölkerung (DSW). County family planning budget county family planning budget. Nairobi; 2016.
MOH. National Family Planning Costed Implementation Plan 2017–2020. Nairobi; 2018. http://familyhealth.go.ke/wp-content/uploads/2018/02/National-FP-Costed-Imlementation-Plan-2017-2020.pdf .
Muanda M, Ndongo PG, Taub LD, Bertrand JT. Barriers to modern contraceptive use in Kinshasa, DRC. PLoS ONE. 2016;11(12):1–13. https://doi.org/10.1371/journal.pone.0167560 .
Adedini SA, Omisakin OA, Somefun OD. Trends, patterns and determinants of long-acting reversible methods of contraception among women in sub-Saharan Africa. PLoS ONE. 2019;14(6):1–16. https://doi.org/10.1371/journal.pone.0217574 .
Parks C, Peipert JF. Eliminating health disparities in unintended pregnancy with long-acting reversible contraception (LARC). Am J Obstet Gynecol. 2016;214(6):681–8. https://doi.org/10.1016/j.ajog.2016.02.017 .
Brittain AW, Williams JR, Zapata LB, Pazol K, Romero LM, Weik TS. Youth-friendly family planning services for young people: a systematic review. Am J Prev Med. 2015;49(2):S73–84. https://doi.org/10.1016/j.amepre.2015.03.019 .
Eisenberg D, McNicholas C, Peipert JF. Cost as a barrier to long-acting reversible contraceptive (LARC) use in adolescents. J Adolesc Health. 2013;52(4 SUPPL.):59–63. https://doi.org/10.1016/j.jadohealth.2013.01.012 .
Hall KS, Ela E, Zochowski MK, et al. “I don’t know enough to feel comfortable using them:” women’s knowledge of and perceived barriers to long-acting reversible contraceptives on a college campus. Contraception. 2016;93(6):556–64. https://doi.org/10.1016/j.contraception.2016.02.007 .
Hardee K, Harris S, Rodriguez M, Kumar J, Bakamjian L, Newman K, Brown W. Achieving the goal of the London summit on family planning by adhering to voluntary, rights-based family planning: what can we learn from past experiences with coercion? Int Perspect Sex Reprod Health. 2014;40(4):206–214. http://www.jstor.org/stable/ https://doi.org/10.1363/intsexrephea.40.4.206 .
Grollman C, Cavallaro FL, Duclos D, Borghi J, Bakare V, Martı M. Donor funding for family planning: levels and trends between 2003 and 2013. Health Policy Plan. 2018;33(4):574–82. https://doi.org/10.1093/heapol/czy006 .
United Nations. Youth Empowerment. United Nations, Office of the Special Advisor on Africa (OSAA), Peace, security and development. https://www.un.org/en/africa/osaa/peace/youth.shtml . Published 2015. Accessed 16 Jul 2020.
Download references
Acknowledgements
I wish to acknowledge with gratitude my supervisor, Dr. Richard Ayah, for the support he gave to me towards completion of this research project. I wish to thank the staff in the School of Public Health for their support and guidance. The Kenyatta National Hospital/University of Nairobi Ethical Review Committee is thanked for approving the research. I acknowledge the support given by management and staff of Kiambu County Hospital. My gratitude goes to the data collection, processing and analysis team. Finally, the encouragement and support of my family is greatly appreciated. Neither the research nor the manuscript was sponsored
The authors utilized personal funding for the study.
Author information
Authors and affiliations.
Department of Public & Global Health, University of Nairobi, Nairobi, Kenya
James Kiragu Ngacha & Richard Ayah
You can also search for this author in PubMed Google Scholar
Contributions
All the authors participated in all the phases of the study which include conception of the study, protocol development, data collection, analysis and manuscript preparation. Both the authors read and approved the final manuscript.
Corresponding author
Correspondence to James Kiragu Ngacha .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from Kenyatta National Hospital/University of Nairobi Ethical Review Committee (KNH/UoN-ERCA210). Further approval was received from the Kiambu County Health Research Development Unit and the Kiambu County Hospital management before commencement of the study. Written consent was obtained from all respondents in this study prior to the start of each data collection activity.
Consent for publication
The authors hereby give consent for the publication of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ngacha, J.K., Ayah, R. Assessing the cost-effectiveness of contraceptive methods from a health provider perspective: case study of Kiambu County Hospital, Kenya. Reprod Health 19 , 11 (2022). https://doi.org/10.1186/s12978-021-01308-3
Download citation
Received : 09 November 2020
Accepted : 06 November 2021
Published : 17 January 2022
DOI : https://doi.org/10.1186/s12978-021-01308-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Contraceptive methods
- Contraceptive prevalence rate
- Cost-effectiveness
- Couple year protection
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
Assessing the cost-effectiveness of contraceptive methods from a health provider perspective: case study of Kiambu County Hospital, Kenya
Affiliations.
- 1 Department of Public & Global Health, University of Nairobi, Nairobi, Kenya. [email protected].
- 2 Department of Public & Global Health, University of Nairobi, Nairobi, Kenya.
- PMID: 35039047
- PMCID: PMC8762951
- DOI: 10.1186/s12978-021-01308-3
Background: Kenya's contraceptive prevalence rate at 53% is low, with wide disparity among the 47 counties that make up the country (2-76%). Significant financial investment is required to maintain this level of contraceptive use and increase it to levels seen in more developed countries. This is in the context of a growing population, declining donor funding, limited fiscal space and competing health challenges. Studies have shown that long-term contraceptive methods are more cost-effective than short-term methods. However, it is unclear if this applies in Sub-Saharan Africa; with limited financial resources, lower social economic status among users, and publicly managed commodity supply chains, in vertical programs largely dependent on donor funding. This study assessed the cost-effectiveness of contraceptive methods used in Kenya.
Methods: A cross-sectional study was undertaken in a county referral hospital in mid-2018. Purposive sampling of 5 family planning clinic providers and systematic sampling of 15 service delivery sessions per method was done. Questionnaire aided interviews were done to determine inputs required to provide services and direct observation to measure time taken to provide each method. Cost per method was determined using activity based costing, effectiveness via couple year protection conversion factors, and cost-effectiveness was expressed as cost per couple year protection.
Results: The intra-uterine copper device was most cost-effective at 4.87 US dollars per couple year protection followed by the 2-Rod Implant at 6.36, the 1-Rod Implant at 9.50, DMPA at 23.68, while the combined oral contraceptive pills were least cost-effective at 38.60 US dollars per couple year protection. Long-term methods attracted a higher initial cost of service delivery when compared to short-term methods.
Conclusion: Long-term contraceptive methods are more cost-effective. As such, investing in long-term contraceptives would save costs despite higher initial cost of service delivery. It is recommended, therefore, that Sub-Saharan Africa countries allocate more domestic financial resources towards availability of contraceptive services, preferably with multi-year planning and budget commitment. The resources should be invested in a wide range of interventions shown to increase uptake of long-term methods, including reduction of cost barriers for the younger population, thereby increasing contraceptive prevalence rates.
Keywords: Contraceptive methods; Contraceptive prevalence rate; Cost-effectiveness; Couple year protection.
Plain language summary
The proportion of women of reproductive age using a contraceptive method in Kenya, at 53% is low. More funding is required to ensure women who need contraceptives have access and continue using them. Previous research has shown that contraceptives that protect a woman from getting pregnant for an extended period utilize less resources. This study assessed the potential of contraceptives used in Kenya to produce results at less cost.This study was undertaken in a sub-national referral hospital in mid-2018. A sample of 5 family planning clinic providers were interviewed while 15 contraceptive service sessions per method were observed. The interviews were conducted to determine the supplies required to offer services. Observation was used to measure time taken to provide each contraceptive method. The cost associated with providing each contraceptive per year was determined using activity based costing. Effectiveness of each method was determined using the rate of protection from pregnancy during one-year. Cost-effectiveness was the money utilized to achieve protection from pregnancy in one year of use.The Copper-T coil was found to achieve greater results at a lesser cost of 4.87 US dollars for one year of protection from pregnancy, followed by the 2-Rod Implant at US dollars 6.36, the 1-Rod Implant at 9.50, DMPA at 23.68, and The Pill at 38.60 US dollars.Contraceptive methods that protect a woman from getting pregnant for a longer period utilize less resources. Investing in such would save costs despite requiring higher initial cost of service provision.
© 2022. The Author(s).
- Contraception*
- Cost-Benefit Analysis
- Cross-Sectional Studies
- Family Planning Services
- Hospitals, County*
- Open access
- Published: 27 July 2022
Barriers for multiparous women to using long-term contraceptive methods in Southeast Asia: case study in Philippines and Indonesia
- Agung Dwi Laksono ORCID: orcid.org/0000-0002-9056-0399 1 ,
- Nikmatur Rohmah 2 &
- Hario Megatsari ORCID: orcid.org/0000-0001-6555-319X 3
BMC Public Health volume 22 , Article number: 1425 ( 2022 ) Cite this article
3787 Accesses
2 Citations
Metrics details
Multiparous women are supposed to be able to end their reproductive cycle to decrease population growth. This study aimed to analyze barriers for multiparous women to use long-term contraceptive methods (LTCM) in the Philippines and Indonesia.
The study population was women aged 15–49 years old who have given birth to a live baby > 1 in the Philippines and Indonesia. The weighted sample size was 12,085 Philippines women and 25,543 Indonesian women. To identify variables associated with the use of LTCM, we analyzed place of residence, age group, education level, marital status, employment status, and wealth status. The final step employed multinomial logistic regression.
In both countries, the results showed that variables associated with non-user LTCM were younger women, living in rural areas with poor education. Women without partner and unemployed had higher probability to not use LTCM. Finally, low wealth status had a higher probability than the richest multiparous to not use LTCM.
The study concluded that there were six barriers for multiparous women to use LTCM in the Philippines and Indonesia. The six obstacles were living in rural areas, being younger, poor education, single, unemployed, and low wealth.
Peer Review reports
Introduction
Population growth in Southeast Asia has outpaced growth in the U.S., U.K., and China in the last 5 years. Meanwhile, the population growth rate in Southeast Asia is 5.8%. Philippines population growth of 8.2% is the highest growth compared to other Southeast Asian countries. Indonesia’s population grows by 5.9%, just below Malaysia’s at 7.9% [ 1 ].
Southeast Asia’s current population is 672,082,017, equivalent to 8.58% of the world’s total population. Southeast Asia is ranked number 3 in the Asian region. The population density in Southeast Asia is 154 per km2, and 50% reside in urban areas. The mean age of the Southeast Asian population was 30.2 years. Based on population, Indonesia is ranked first in the Southeast Asia region and fourth globally, with 273,523,615 people. The Philippines is in second place in the Southeast Asia region and 13 globally, with 109,581,078 people. The rapid population growth in Indonesia and the Philippines indicates that the number of pregnancies that reach proper delivery in both countries is high [ 2 , 3 ].
The number of pregnancies that achieve a viable delivery referred to as parity [ 4 ]. Women who have given birth more than two times are called multiparous and have given birth ≥ four times called grand multiparous. The more often a woman gives birth, the more it has the potential to increase population growth. The crude birth rates in the Philippines and Indonesia are ranked 4th and 5th in the Southeast Asia region, namely 20.2 and 17.7 live births per 1000 population [ 5 ]. The family size in the Philippines also allows a woman to give birth more than two times. The Philippines’ average ideal family size is 2.7 children for all women and 3.0 children for currently married women [ 6 ].
The high proportions of multiparous and grand multiparous cause population growth to occur rapidly. The distribution of currently married women in Indonesia is 25.57% multiparous and 4.27% grand multiparous. The remaining 62.58% were primiparous, and 7.57% never gave birth based on parity [ 7 ]. In some countries, the proportion of multiparous shows a higher number than primiparous. Among them are Nigeria, Uganda, Northwestern Ethiopia, and North Carolina [ 8 , 9 , 10 , 11 ]. This situation is different when we compare it to China. The proportion of multiparous women is 15.5%, primiparous 29.1, and 55.4% childless [ 12 ].
The utilization of LTCM is related to many factors, several studies showed that facts [ 13 , 14 , 15 ]. One of the factors is related to pregnancy, both planned and unplanned pregnancies. For example study conducted by Pasundani in 2020 [ 15 ] in Indonesia, age, education, parity, and information are all variables that have been linked to the usage of LTCM. Other study revealed the same messages that unplanned pregnancy was also factors for women utilize the LTCM [ 16 ].
Meanwhile, women who give birth more than two times have the risk of various complications of pregnancy and childbirth and even death. The risk of death from maternal causes is related to pregnancy risk and complications during birth [ 17 ]. The three causes of maternal death in the Philippines include complications of delivery, pregnancy-related hypertension, and postpartum hemorrhage [ 18 ]. Multiparous women have less time to recover their reproductive organs and less time to rest. Multiparous has an increasing burden as the number of children born. In general, the history of miscarriage and gestational diabetes was higher in the grand multiparous [ 19 ].
Previous studies found a significant association between grand multiparous and pregnancy outcome. Among them include cesarean section, fetal macrosomia, diabetes mellitus, hypertension in pregnancy caused [ 20 ]. Multiparity is still a threat to women’s health problems. This threat is mainly related to the various complications that can occur during pregnancy and childbirth. Efforts to minimize this threat are to carry out pregnancy and birth control.
Long-term contraceptive methods (LTCM) are the most effective method for controlling pregnancy and birth [ 21 ]. Including the LTCM are an intrauterine device (IUD), female sterilization, and implant/Norplant. LTCM can prevent unwanted pregnancy up to 20 times better than pills and vaginal rings [ 22 ]. LTCM is a form of birth control that is very effective and has the lowest maintenance costs (most economical) [ 9 , 23 ]. Unfortunately, women attracted to LTCM but did not use it are more likely to be multiparous women [ 11 ]. Although LTCM is proven to reduce pregnancy effectively and is effective regardless of user compliance, its absorption is still low [ 24 , 25 ].
A previous study in seven countries found that the widespread use of LTCM was still low, namely 16% [ 26 ]. IUDs and implants’ use is still low, 1.8 and 10.4%, respectively [ 9 ]. Policymakers need to know more information about the various challenges in women’s access to use LTCM. Moreover, we need to investigate this further. This study analyzes the obstacles for multiparous women to use LTCM in the Philippines and Indonesia based on the background description.
Materials and methods
Availability of data and materials.
The author is unable to share the data publicly because a third party and the ICF, who own it, do not have permit to do so. The author requested The 2017 IDHS and 2017 PDHS data set to the ICF (data set of childbearing age women) and the ICF gave the access to confidential data through https://dhsprogram.com .
Data source
The report used secondary data as research materials from the 2017 Philippines Demographic and Health Survey (PDHS) and 2017 Indonesian Demographic and Health Survey (IDHS). The PDHS and IDHS are part of the Inner City Fund’s (ICF) Global Demographic and Health Survey (DHS) survey collection. The sample population was women aged 15–49 years who had given birth in Indonesia to a live baby of over 1 (multiparous). The sampling procedure used stratification and multi-stage random sampling. The method yielded a weighted sample size of 12,085 Filipino women and 25,543 Indonesian women. The study period was from July 24th – September 30th 2017.
Data analysis
The dependent variable in this study was the use of long-term contraceptive methods (LTCM). In this study, LTCM is a modern contraceptive type consisting of IUD, female sterilization, and implant/Norplant. The study divides the use of LTCM into 2 categories, namely “Yes” and “No.”
There were six independent variables involved in the analysis of this study. The six variables are a type of place of residence, age group, education level, marital status, employment status, and wealth status. The residence type consists of 2 categories, namely “urban” and “rural.” The urban-rural criteria refer to Statistics Indonesia. Age group is divided into 7 categories in 5 years, namely “15–19”, “20–24”, “25–29”, “30–34”, “35–39”, and “40–45”. Education level is the respondent’s recognition of the last diploma they have. Education level is divided into 4 categories, namely “no education”, “primary”, “secondary”, and “higher”. The study also divided marital status into two categories: “single” and “married/living with a partner.” The study divided into two categories for employment status, namely “unemployed” and “employed.”
The study determined wealth status based on the quintile of wealth owned by a household. Households were scored based on the number and type of items they have, from televisions to bicycles or cars, and housing characteristics, such as drinking water sources, toilet facilities, and primary building materials for the house’s floor. This score calculated using principal component analysis. National wealth quintiles were arranged based on household scores for each person in the household and then divided by the distribution into the same five categories, accounting for 20% of the population [ 27 ].
In the first step, the authors conducted a collinearity test. The action is to ensure no multicollinearity between the independent variables. Furthermore, the study carried out a bivariate test between the dependent and independent variables using the Chi-Square test. The study used the binary logistic regression to analyze barriers for multiparous women to use LTCM in Indonesia and Philippines in the final stage, and we used the significancy p < 0.05. We used 95% confidence interval in the binary logistic regression. All stage statistical analyzes carried out using SPSS 22 software.
Ethical statement
The 2017 PDHS and the 2017 IDHS have received ethics approval from the national ethics commission at the Ministry of Health, Philippines, and Indonesia. The authors deleted the respondents’ identities from the dataset. Besides, respondents have provided written approval for their involvement in the study. The author has obtained permission to use Inner City Fund International’s data through its website: https://dhsprogram.com/data/new-user-registration.cfm .
Table 1 showed the results of the co-linearity test. The analysis results displayed the tolerance value for all independent variables was > 0.10, and the variance inflation factor (VIF) value for all independent variables was < 10.00. The results of this analysis informed that there were no symptoms of multicollinearity between the independent variables.
Descriptive analysis
Table 2 showed descriptive statistics of multiparous women in the Philippines and Indonesia. Based on the type of place of residence, Philippines multiparous women who live in rural areas dominated the two categories of the use of LTCM. Meanwhile, multiparous Indonesian women who use LTCM were dominated by those who live in urban areas. Meanwhile, multiparous Indonesian women who do not use LTCM were dominated by those who live in rural areas.
Based on the age group, women in the 40–44 age group occupied the multiparous Philippines and Indonesian women who use LTCM. On the other hand, the Philippines and multiparous Indonesian women who do not use LTCM are dominated by the younger age group, namely 35–39. According to the education level, the Philippines and multiparous Indonesian women with secondary education dominated the two categories of the use of LTCM.
Based on marital status, the Philippines and multiparous Indonesian women who are married/living with partners dominated the two categories of the use of LTCM. Meanwhile, based on employment status in both types, the use of LTCM is dominated by the Philippines and Indonesian employed women.
Finally, according to wealth status, multiparous Philippines women who use LTCM are dominated by the wealthy class with the lower category. On the other side, multiparous Philippines women who do not use LTCM are dominated by those with the most deficient wealth status category. Moreover, the wealthiest overwhelmed multiparous Indonesian women who use LTCM. On the other hand, the more decadent wealthy status category dominated multiparous Indonesian women who do not use LTCM.
Multivariate analysis
Table 3 showed binary logistic regression results. In this final stage, the study involved all independent variables. The binary logistic regression uses “The use of LTCM: Yes” as references.
Table 3 showed that multiparous Philippines women living in rural areas are more likely to live in urban areas 1.070 times not to use LTCM (AOR 1.070; 95% CI 1.070–1.070). Meanwhile, multiparous Indonesian women living in rural areas were 1061 times more likely than those residing in urban areas not to use LTCM (AOR 1.061; 95% CI 1.061–1.062). This analysis indicates that living in rural areas is a risk factor for multiparous women in the Philippines and Indonesia for not using LTCM.
According to the age group, Philippines multiparous women in the age group 35–39 and under have a higher likelihood of not using LTCM than the 45–49 age group. Philippines multiparous women in the 40–44 age group are less likely to use LTCM than the 45–49 age group. Meanwhile, multiparous Indonesian women with the age group 30–34 and under have a higher likelihood of not using LTCM than the 45–49 age group. Multiparous Indonesian women in the age group over 35–39 and above are less likely to use LTCM. This information shows that younger multiparous women in the Philippines and Indonesia have a higher risk of not using LTCM.
Based on the education level, multiparous Philippines women with no education have a higher chance of not using LTCM than those with higher education. Multiparous Philippines women with primary and secondary education have a lower possibility of not using LTCM than those with higher education. On the other hand, multiparous Indonesian women with any education level have a higher probability of not using LTCM than those with higher education. This analysis indicates that inadequate education is a risk factor for multiparous women in the Philippines and Indonesia for not using LTCM.
According to marital status, the Philippines and multiparous Indonesian women with a single group (never in a union, widowed, divorced) have a higher probability than those with status married/living with partners not to use LTCM. The result shows that not having a partner is a risk factor for multiparous women in the Philippines and Indonesia for not using LTCM.
On the other side, unemployed multiparous women in the Philippines and Indonesia have a higher probability of not using LTCM than those employed. This analysis shows that the unemployed are a risk factor for multiparous women in the Philippines and Indonesia for not using LTCM.
Finally, based on wealth status, the poorest Philippines multiparous women have a higher likelihood of not using LTCM than the richest one. Multiparous Philippines women with other wealthy groups were less likely not to use LTCM than the richest. On the other hand, multiparous Indonesian women with any wealthy status have a higher chance of not using LARC than the richest. This analysis indicated that low wealth status has a higher probability than the richest multiparous in the Philippines and Indonesia not to use LTCM.
The study results found that living in rural areas was a risk factor for multiparous women in the Philippines and Indonesia for not using LTCM. Empirically, rural areas are often left behind compared to urban areas in development in all fields, including the health sector [ 28 ]. This situation impacts the availability of information and services to access LTCM for multiparous women [ 29 , 30 ].
The study found that younger multiparous women in the Philippines and Indonesia had a higher risk of not using LTCM. This finding is in line with studies in India [ 31 ]. This condition is likely because older multiparous women tend to want to stop their reproductive period. Meanwhile, those who are young still have the desire to have more children [ 32 , 33 ].
The research found low education to be a risk factor for multiparous women in the Philippines and Indonesia for not using LTCM. Women with better education levels better understand their needs. Moreover, with better education, women also better understand the risk factors for any action or decision they take [ 34 , 35 ], including better understanding the myths circulating about LTCM [ 36 ]. This reason is why multiparous women with higher education prefer to use LTCM [ 37 , 38 , 39 ]. Higher education levels have been found in several previous studies to positively determine health performance [ 38 ]. Conversely, several studies found poor education to be a barrier to higher-quality implementation in the health sector [ 40 , 41 , 42 ].
On the other hand, not having a partner was a risk factor for multiparous women in the Philippines and Indonesia for not using LTCM. In the context of countries with Eastern customs such as the Philippines and Indonesia, sexual activity for women who do not have a partner is a disgrace [ 43 , 44 ]. This condition encourages women to control their sexual activity. This situation is likely to suppress the need for LTCM in unmarried multiparous women.
Meanwhile, the unemployed was a risk factor for multiparous women in the Philippines and Indonesia for not using LTCM. This situation may be due to employed multiparous women who prefer practical and effective contraceptive methods [ 45 , 46 ]. Previous studies have shown the higher effectiveness of LTCM than non-LTCM methods [ 47 ]. On the other hand, LTCM is more effective for employed multiparous women than the forgetfulness factor caused by being busy. Other study revealed that women empowerment factors, one of it is employment, related to the utilization of LTCM [ 13 ].
Finally, the study found low wealth status to have a higher probability than the richest multiparous in Indonesia not to use LTCM. The previous studies saw poverty as a barrier to performance output in many health sectors, especially those related to and requiring costs [ 27 , 48 ]. This situation also applies to poor multiparous women’s access to LTCM [ 49 , 50 ]. This cost is a barrier that should encourage the government to realize the financing mechanism through insurance for LTCM [ 38 , 51 , 52 ].
In summary, this research shows that six variables prevent a multiparous woman from using LTCM, namely: living in the rural area, younger age, poor education, single, unemployed and poor. The implication of this situation for a country is an uncontrolled population explosion, leading to repeated unfavorable conditions in society, including poverty, ignorance, and high unemployment [ 53 ]. Another negative situation is the risk of an unqualified future generation because their parents cannot optimally carry out child care [ 54 ].
Previous research has recommended strategies to increase the use of LTCM, including reducing costs to get LTCM services, increasing public understanding of LTCM [ 55 ], and increase the skill capacity of health workers [ 56 ]. We can develop a strategy by cooperating with relevant stakeholders to make the LTCM program a success in an area [ 57 ]. From the findings above, appropriate policy recommendations include: providing subsidies for LTCM services for the poor, initiating an insurance model for LTCM, educating the public massively, being innovative, creative, and measurable, and periodically updating the skills capacity of health workers.
Study limitation
This study has a limitation: the study’s variable is limited and depends on the availability of secondary data (DHS data). However, the study has a positive impact on the maternal and child health programs in Indonesia, such as this study can be estimated to the national level with correct weight to describe the level of the problem at the national level. Furthermore this study can be used by the government to develop policy based on the scientific evidence, especially related to LCTM and how the strategy of the government to deliver it to the specific population in the country.
Conclusions
The research results concluded that there were six barriers for multiparous women to using LTCM in the Philippines and Indonesia. The six obstacles are living in rural areas, being younger, poor education, single, unemployed, and low wealth. Based on the findings of the research, the author recommend to the Philippines and Indonesia government to integrate the public health program and family planning program that can addres to the rural areas, teenagers, low education, unemployed group and poor people.
The authors cannot publicly share the data because a third party and authors do not have permission to share it. The 2017 IDHS data set name requested from the ICF ‘data set of childbearing age women’ is available from the ICF contact https://dhsprogram.com/data/new-userregistration.cfm for researchers who meet the criteria for access to confidential data.
Abbreviations
- Long-term contraceptive methods
Intrauterine device
Philippines Demographic and Health Survey
Indonesian Demographic and Health Survey
Inner City Fund
Variance inflation factor
Adjusted odds ratio
Pusparisa Y. Southeast Asia’s rapid population growth (Pesatnya Pertumbuhan Populasi Asia Tenggara); 2019. p. 1–2.
Google Scholar
Worldometer. South-Eastern Asia Population (LIVE). 2020.
Worldometer. Current world Population. 2020.
Creinin M, Simhan H. Can we communicate gravidity and parity better? Obstet Gynecol. 2020;113(3):709–11.
Article Google Scholar
Moore M. Crude birth rate in Southeast Asia in 2019, by country (in births per 1,000 population); 2020.
Philippine Statistics Authority and Inner City Fund. Key Findings from the Philippine National Demographic and Health Survey 2017. 2018. 1–20.
Gafar A, Suza DE, Efendi F, Pramono AP, Susanti IA, Mishbahatul E. Determinants of contraceptive use among married women in Indonesia [ version 1 ; peer review : 2 approved]. F1000Research. 2020;6(APR):1–9.
Solanke BL, Banjo OO, Oyinloye BO, Asa SS. Maternal grand multiparity and intention to use modern contraceptives in Nigeria. BMC Public Health. 2018;18(1):1–15.
Anguzu R, Sempeera H, Sekandi JN. High parity predicts use of long-acting reversible contraceptives in the extended postpartum period among women in rural Uganda. Contracept Reprod Med. 2018;3(1):1–7.
Gashaye KT, Tsegaye AT, Abebe SM, Woldetsadik MA, Ayele TA, Gashaw ZM. Determinants of long acting reversible contraception utilization in Northwest Ethiopia: an institution-based case control study. PLoS One. 2020;15(10 October):1–19.
Zerden ML, Tang JH, Stuart GS, Norton DR, Verbiest SB, Brody S. Barriers to receiving long-acting reversible contraception in the postpartum period. Women’s Heal Issues. 2015;25(6):616–21.
Luo Z, Gao L, Anguzu R, Zhao J. Long-acting reversible contraceptive use in the post-abortion period among women seeking abortion in mainland China: intentions and barriers. Reprod Health. 2018;15(1):1–9.
Yaya S, Uthman OA, Ekholuenetale M, Bishwajit G. Women empowerment as an enabling factor of contraceptive use in sub-Saharan Africa: a multilevel analysis of cross-sectional surveys of 32 countries. Reprod Health. 2018;15(1):214. https://doi.org/10.1186/s12978-018-0658-5 .
Article PubMed PubMed Central Google Scholar
Ontiri S, Ndirangu G, Kabue M, Biesma R, Stekelenburg J, Ouma C. Long-acting reversible contraception uptake and associated factors among women of reproductive age in rural Kenya. Int J Environ Res Public Health. 2019;16(9):1–11.
Nita Adhani Pasundani1 KB. Determinant of the use of long-term contraceptive method: an analysis of 2017 Indonesian demographic health survey. Indian J Public Heal Res. 2020;11(5 SE):739–45 Available from: https://medicopublication.com/index.php/ijphrd/article/view/9426 .
Getahun DS, Wolde HF, Muchie KF, Yeshita HY. Utilization and determinants of long term and permanent contraceptive methods among married reproductive age women at Janamora district, Northwest Ethiopia. BMC Res Notes. 2018;11(1):836 Available from: https://pubmed.ncbi.nlm.nih.gov/30477564 .
World Health Organization. World health statistics overview 2019: monitoring health for the SDGs, sustainable development goals. Geneva; 2019.
Papp L, Kleiman M. Maternal Morbidity and Mortality Why do Filipino Mothers Die? 2020. p. 1.
Al-Shaikh GK, Ibrahim GH, Fayed AA, Al-Mandeel H. Grand multiparity and the possible risk of adverse maternal and neonatal outcomes: a dilemma to be deciphered. BMC Pregnancy Childbirth. 2017;17(1):1–7.
Alsammani M, Ahmed S. Grand multiparity: risk factors and outcome in a tertiary hospital: a comparative study. Mater Socio Medica. 2015;27(4):244.
Li L, Tran D, Zhu H, Balimane P, Willett G, Zhao P, et al. Use of model-informed drug development to streamline development of long-acting products: can these successes be translated to long-acting hormonal contraceptives? Annu Rev Pharmacol Toxicol. 2021;61:745–56.
Article CAS PubMed Google Scholar
Ilmiyah DE, Budihastuti UR, Nurhaeni IDA, Mudigdo A. Determinants of Women’s choice of a long-acting reversible contraceptive in Boyolali. Central Java J Matern Child Heal. 2018;03(03):225–32.
Olson EM, Kramer RD, Gibson C, Wautlet CK, Schmuhl NB, Ehrenthal DB. Contraception in Wisconsin. WMJ. 2019;117(4):149–55.
Mazza D, Bateson D, Frearson M, Goldstone P, Kovacs G, Baber R. Current barriers and potential strategies to increase the use of long-acting reversible contraception (LARC) to reduce the rate of unintended pregnancies in Australia: an expert roundtable discussion. Aust New Zeal J Obstet Gynaecol. 2017;57(2):206–12.
Garrett CC, Keogh LA, Kavanagh A, Tomnay J, Hocking JS. Understanding the low uptake of long-acting reversible contraception by young women in Australia: a qualitative study. BMC Womens Health. 2015;15(1):1–10.
Article CAS Google Scholar
Faustmann T, Crocker J, Moeller C, Engler Y, Caetano C, Buhling KJ. How do women and health care professionals view hormonal long-acting reversible contraception? Results from an international survey. Eur J Contracept Reprod Heal Care. 2019;24(6):422–9.
Wulandari RD, Qomarrudin MB, Supriyanto S, Laksono AD. Socioeconomic disparities in hospital utilization among elderly people in Indonesia. Indian J Public Heal Res Dev. 2019;10(11):1800–4.
Laksono AD, Wulandari RD, Efendi F. Determinants of hospital utilisation among urban poor societies in Indonesia. Int J Innov Creat Chang. 2020;12(9):375–87.
Seran AA, Antaria MD, Haksama S, Setijaningrum E, Laksono AD, Prahastuti Sujoso AD. Disparities of the use of hormonal and non-hormonal contraceptive drugs in urban and rural areas in Indonesia and the world. Syst Rev Pharm. 2020;11(9):66–73.
Seran AA, Laksono AD, Sujoso ADP, Masruroh II, Marasabessy N, et al. Does contraception used better in urban areas?: an analysis of the 2017 IDHS (Indonesia demographic and health survey). Syst Rev Pharm. 2020;11(11):1892–7.
Yadav K, Agarwal M, Shukla M, Singh JV, Singh VK. Unmet need for family planning services among young married women (15-24 years) living in urban slums of India. BMC Womens Health. 2020;20(1):187.
Yadav K, Agarwal M, Singh JV, Singh VK. Determinants of non-use of family planning methods by young married women (15-24 years) living in urban slums of Uttar Pradesh. Indian J Community Heal. 2017;29(1):55–66.
Paul R, Huysman BC, Maddipati R, Madden T. Familiarity and acceptability of long-acting reversible contraception and contraceptive choice. Am J Obstet Gynecol. 2020;222(4):S884.e1–9.
Wulandari RD, Laksono AD. The association of socioeconomic status on early marriage among women in rural Indonesia (Hubungan status ekonomi terhadap pernikahan dini pada perempuan di perdesaan Indonesia). J Kesehat Reproduksi. 2020;11(2):115–24.
Onyowo UG, Namo IS. Effect of Early Marriage on Girl- Child ’ s Furthe r Education in Okpokwu Local Government Area , Nigeria : Implications for Counseling. KIU J Humanit. 2019;4(1):65–72.
Richards MJ, Coleman-Minahan K, Sheeder J. Long-acting reversible contraceptive attitudes and acceptability in adolescents and young adults: a key to patient-centered contraceptive counseling. J Pediatr Adolesc Gynecol. 2020;33(6):673–80.
Aduloju OP, Akintayo AA, Adefisan AS, Aduloju T. Utilization of Long-Acting Reversible Contraceptive (LARC) Methods in a tertiary hospital in southwestern Nigeria: A Mixed Methods Study. J Obstet Gynecol India. 2021.
Eeckhaut MCW, Sweeney MM, Feng L. Desire for sterilization reversal among U.S. females: increasing inequalities by educational level. Perspect Sex Reprod Health. 2018;50(3):139–45.
Hayford SR, Kissling A, Guzzo KB. Changing educational differentials in female sterilization. Perspect Sex Reprod Health. 2020;52(2):117–27.
Laksono AD, Wulandari RD. The Barrier to Maternity Care in Rural Indonesia. J Public Heal From Theory to Pract. 2020.
Wulandari RD, Laksono AD, Rachmawaty T, Rukmini. Barriers to antenatal care utilization in Indonesia. Medico-Legal Updat. 2021;21(1):828–34.
Rohmah N, Yusuf A, Hargono R, Laksono AD, Masruroh II, et al. Determinants of teenage pregnancy in Indonesia. Indian J forensic. Med Toxicol. 2020;14(3):2080–5.
Himawan KK, Bambling M, Edirippulige S. What does it mean to be single in Indonesia? Religiosity, social stigma, and marital status among never-married Indonesian adults. SAGE Open. 2018;8(3).
Himawan KK. Singleness, sex, and spirituality: how religion affects the experience of being single in Indonesia. Ment Heal Relig Cult. 2020;23(2):1–12.
Bahamondes L, Fernandes A, Monteiro I, Bahamondes MV. Long-acting reversible contraceptive (LARCs) methods. Best Pract Res Clin Obstet Gynaecol. 2019;66:28–40.
Article PubMed Google Scholar
Raccah-Tebeka B, Plu-Bureau G. Long-acting reversible contraception. Rev Prat. 2018;68(4):387–91.
PubMed Google Scholar
Allen S, Barlow E. Long-acting reversible contraception. Pediatr Clin N Am. 2017;64(2):359–69.
Wulandari RD, Putri NK, Laksono AD. Socioeconomic Disparities in Antenatal Care Utilisation in Urban Indonesia. Int J Innov Creat Chang. 2020;14(2):498–514.
Beshar I, So J, Chelvakumar M, Cahill EP, Shaw KA, Shaw JG. Socioeconomic differences persist in use of permanent vs long-acting reversible contraception: An analysis of the National Survey of Family Growth, 2006 to 2010 vs 2015 to 2017. Contraception. 2021.
Laksono AD, Matahari R, Wulandari RD. Factors related to the choice of contraceptive methods among the poor in Indonesia. Syst Rev Pharm. 2020;11(9):195–200.
Krashin JW, Stuart GS, Garrett J, Spector H, Bryant AG, Charm S, et al. Contraception insurance coverage and receipt of long-acting reversible contraception or depot medroxyprogesterone acetate on the day of abortion. Obstet Gynecol. 2017;130(1):109–17.
Fuerst MF, George KE, Moore JE. Long-Acting Reversible Contraception in Medicaid: Where Do We Go From Here? Women’s Heal Issues. 2020.
Gerland P, Raftery AE, Ševčíková H, Li N, Gu D, Spoorenberg T, et al. World population stabilization unlikely this century. Science. 2014;346(6206):234 LP–237 Available from: http://science.sciencemag.org/content/346/6206/234.abstract .
Laksono AD, Wulandari RD. “Children are assets”: Meta synthesis of child values in the Lani and Acehnese (“Anak adalah Aset”: Meta Sintesis Nilai Anak pada Suku Lani dan Suku Aceh). J Kesehat Reproduksi. 2019;10(1):11–20.
Shoupe D. LARC methods: entering a new age of contraception and reproductive health. Contracept Reprod Med. 2016;1(1):4. https://doi.org/10.1186/s40834-016-0011-8 .
Cleland J, Ali M, Benova L, Daniele M. The promotion of intrauterine contraception in low- and middle-income countries: a narrative review. Contraception. 2017;95(6):519–28 Available from: http://www.sciencedirect.com/science/article/pii/S0010782417300975 .
Kroelinger CD, Morgan IA, DeSisto CL, Estrich C, Waddell LF, Mackie C, et al. State-Identified Implementation Strategies to Increase Uptake of Immediate Postpartum Long-Acting Reversible Contraception Policies. J Women’s Heal. 2018;28(3):346–56. https://doi.org/10.1089/jwh.2018.7083 .
Download references
Acknowledgments
The author would like to thank Inner City Fund International, who has agreed to allow the authors to analyze the 2017 PDHS and the 2017 IDHS data in this article.
Not applicable.
Author information
Authors and affiliations.
National Research and Innovation Agency, The Republic of Indonesia, Jakarta, Indonesia
Agung Dwi Laksono
Faculty of Health Science, Muhammadiyah University of Jember, East Java, Indonesia
Nikmatur Rohmah
Faculty of Public Health, University of Airlangga, Surabaya, Indonesia
Hario Megatsari
You can also search for this author in PubMed Google Scholar
Contributions
ADL developed the proposal, analyzed and interpreted the data. NR and HM was a significant contributor in conducting the study, interpreting the data and writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Hario Megatsari .
Ethics declarations
Ethics approval and consent to participate.
The 2017 IDHS has passed ethical clearance from the National Ethics Committee. The authors delete all respondents’ identities from the dataset. Respondents have provided written approval for their involvement in the study through filling the informed concent. The author has obtained permission for the use of data for this study through the website: https://dhsprogram.com/data/new-user-registration.cfm . All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Laksono, A.D., Rohmah, N. & Megatsari, H. Barriers for multiparous women to using long-term contraceptive methods in Southeast Asia: case study in Philippines and Indonesia. BMC Public Health 22 , 1425 (2022). https://doi.org/10.1186/s12889-022-13844-z
Download citation
Received : 20 March 2021
Accepted : 14 July 2022
Published : 27 July 2022
DOI : https://doi.org/10.1186/s12889-022-13844-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Multiparous women
- Contraception
- Public health
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Research Council (US) Committee on Population; Parnell AM, editor. Contraceptive Use and Controlled Fertility: Health Issues for Women and Children Background Papers. Washington (DC): National Academies Press (US); 1989.

Contraceptive Use and Controlled Fertility: Health Issues for Women and Children Background Papers.
- Hardcopy Version at National Academies Press
Health Effects of Contraception
Nancy C. Lee, Herbert B. Peterson, and Susan Y. Chu
- Introduction
Until the 1960s rhythm and barrier contraceptives were the only methods of birth control widely available to couples desiring to plan the number and spacing of their children. In the 1960s oral contraceptives (OCs) were introduced and new efficacious intrauterine devices (IUDs) became widely available, so that the choice of effective methods of contraception increased substantially. Later, in the 1970s, female and male sterilization techniques became much more widely accepted and used. Couples were then able to choose from several different temporary and permanent methods of contraception and to switch from one to another. Worldwide, family planning programs expanded, and the prevalence of contraceptive use increased.
As these methods of contraception became more widely used, anecdotal reports of adverse health effects associated with their use began to appear. Since the late 1960s and early 1970s, epidemiologic studies have more rigorously evaluated the health effects associated with the use of different contraceptive methods. Most of these studies have been conducted in the United States and Europe. In the process researchers have recognized that different contraceptive methods have important beneficial health effects, in addition to the desired effect of preventing pregnancy. Although much research is still needed, especially targeted to the developing world, a large body of information is now available to assess the health effects of the various contraceptive methods.
The various contraceptive methods have health risks, but pregnancy itself has attendant risks of morbidity and mortality. In 1983, Ory et al. attempted to quantify the mortality risks associated with using the various methods of contraception. Those risks were compared with the risks associated with using no method of contraception, which are actually the mortality risk associated with pregnancy. These estimates are presented in Table 1 . Using no method of contraception carries a higher cumulative risk of death than using any contraceptive method except that of OCs by older women who smoke. The mortality risks associated with using no contraception and with using OCs are higher in older women than in younger women. For all other contraceptive methods, the mortality risk does not appear to vary by age. Although the estimates are not presented in Table 1 , vasectomy involves no mortality risk for women and virtually none for the male partner (Ory et al., 1983).
Estimated Cumulative Number of Deaths per 100,000 Nonsterile Women Aged 17–44, Attributable to Contraceptive Method, by Age Group.
Below we will present in detail the health effects of the various widely available methods of contraception, limiting our discussion to those methods that are considered moderately to highly effective. Most epidemiologic and clinical studies of the health effects of contraceptives have been carried out in developed countries. We recognize the difficulty in generalizing these results to the special health and cultural situations in the less developed countries. Furthermore, the effects of the various contraceptive methods on the risk of diseases generally limited to less developed countries have had very little characterization. Because of the expanding role of family planning programs and contraceptive use in these countries, studies to evaluate the health effects of contraceptives in various regions and cultures are needed.
Modern contraceptive methods vary substantially in how effectively they prevent pregnancies. Because pregnancy itself has attendant health risks and benefits, the rates of accidental pregnancy associated with the various methods of contraception are one important aspect to consider when measuring the health effects of these methods. In 1987 Trussell and Kost published their comprehensive review assessing failure rates for each method of contraception. After reviewing all available studies, they estimated the rate of failure (i.e., accidental pregnancy) in the first year of use associated with ''perfect'' use of each contraceptive. They called this estimate the "lowest expected" failure rate; this rate should reflect the frequency of failures caused by the contraceptive itself. They also reported for each method a "typical" failure rate, defined as the rate of accidental pregnancy in the first year of use among typical couples who use that method. The typical failure rate is determined both by failures as a result of imperfect use of a contraceptive and by failures directly related to the method itself. Most of the typical failure rates were derived from national surveys of U.S. women. The authors summarized these rates, by contraceptive method, in a single table (Trussell and Kost, 1987, p. 271). We present a modified version of that table here ( Table 2 ). In our table and throughout the text we have substituted the term method failure rate for lowest expected failure rate and user failure rate for typical failure rate to follow more closely the terminology used in much of the existing literature. Note that the method failure rates are consistently low for most modern contraceptives. However, user failure rates vary widely, a function of the degree of acceptability and compliance required for successful use of each method.
Method Failure and User Failure Rates During the First Year of Use of a Contraceptive Method, United States.
- Oral Contraceptives
OCs, a highly effective method of birth control, are available in two types. Combination OCs, the most widely used, consist of both an estrogen and a progestin component. Most combination OCs contain a fixed daily dose of an estrogen and progestin and are taken for 21 of 28 days of each menstrual cycle (Hatcher et al., 1988). Recently introduced, phasic combination OCs contain varying doses of the estrogen and progestin components throughout the menstrual cycle. The second type of OC is the progestin-only pill (often called the minipill), which contains only a progestin. Combination OCs with fixed doses of estrogen and progestin have been used much more frequently than phasic or progestin-only pills; hence, most epidemiologic studies on the health effects of OCs are essentially studies of the effects of this type of OC.
OCs prevent pregnancy chiefly by inhibiting ovulation in almost all menstrual cycles, although OC-related changes in the cervical mucus and endometrium may also have contraceptive effects. Failure rates associated with OC use are low. The method failure rate for combination OCs is 0. 1 percent per year and for progestin-only OCs is 0.5 percent per year ( Table 2 ). The user failure rate cannot be readily determined for the two types of OCs separately, but it is about 3 percent per year for any type of OC. Because this user failure rate was derived from data where the vast majority of women used combination OCs, the figure probably is closest to the user failure rate for combination OCs. Most experts believe that the progestin-only pill has a higher user failure rate.
The health risks and benefits of OC use have been extensively studied and documented (Ory, 1982; Ory et al., 1983; Stadel, 1986; Prentice and Thomas, 1987). For a recent extensive review and list of references, see Stadel (1986) or Prentice and Thomas (1987).
Because OCs are highly effective at preventing any pregnancy, they appear to decrease greatly the risk of ectopic pregnancy. Results from a large case-control study of ectopic pregnancies conducted in the United States showed that current OC users had a relative risk of ectopic pregnancy of 0.1 (95 percent confidence interval, 0.1–0.2) compared with women who were using no contraceptive method (Ory, 1981).
Noncontraceptive Benefits
An important benefit from OC use is a reduction in risk of two serious reproductive system cancers, endometrial and ovarian cancers. This reduction has been documented in at least 9 and 11 epidemiologic studies, respectively (The Cancer and Steroid Hormone Study [CASH], 1987a, 1987b). Although the theoretical mechanisms that may explain these protective effects are quite different for the two types of cancer, the magnitude and characteristics of the protective effects are similar. The most detailed characterization of these protective effects comes from the CASH Study, a large case-control study conducted in the United States by the Centers for Disease Control, with support from the National Institute of Child Health and Human Development (CASH, 1987a, 1987b). OC use was associated with a 40 percent reduction in the risk of endometrial cancer as well as a 40 percent reduction in the risk of ovarian cancer, regardless of the specific formulation of combination OC used. The effect appeared to persist long after OC use had been discontinued; furthermore, protection increased with increasing cumulative duration of OC use.
The protective effect of OCs on endometrial cancer is most likely related to direct effects on the endometrium. Among current OC users the carcinogenic effect of unopposed estrogen on the endometrium is probably reduced because combination OCs contain both estrogen and progestin. The continued protection seen among past OC users is less well understood. Perhaps the combination of estrogen and progestin irreversibly changes endometrial cells so that they are not susceptible to carcinogens or to malignant transformation (CASH, 1987a).
Suppression of ovulation and suppression of pituitary secretion of gonadotropins have both been postulated as mechanisms by which OCs protect against ovarian cancer (Weiss, 1982). Two other factors that provide protection from ovarian cancer, increasing parity and breastfeeding (Gwinn et al., submitted), may also derive their protective effects from one of these two proposed mechanisms. Available epidemiologic studies do not provide sufficient information to choose one of these postulated mechanisms over the other.
Fourteen epidemiologic studies have found a decreased risk of benign breast disease (BBD) associated with OC use, including both case-control and cohort studies (Stadel, 1986). Evidence suggests that OCs decrease the risk of fibrocystic disease and fibroadenoma diagnosed by biopsy as well as the risk of breast lumps observed clinically but not biopsied. Results from a large cohort study conducted in the United Kingdom by the Oxford Family Planning Association have provided especially useful information about the relationship between OC use and BBD (Brinton et al., 1981). The decreased risk of BBD seen among women who use OCs occurs primarily among current or recent users who have used them for 2 years or longer. The relative risk among women who have used OCs for more than 2 years compared with nonusers is about 0.6 for fibrocystic disease and about 0.5 for unbiopsied breast lumps. The relative risk of fibroadenoma among women who have used OCs for less than 2 years is about 0.4, which is essentially the same as the relative risk of 0.3 among women who have used OCs for 2 or more years. The decreased risk of BBD does not persist among past OC users who have not used OCs for more than 1 year.
Many epidemiologic studies have found that a history of BBD increases a woman's risk of breast cancer. Even though OCs decrease the risk of BBD, epidemiologic studies have not found that OCs decrease the risk of breast cancer, as might be suggested by the OCs-BBD relationship. The most likely explanation for this paradox is that OCs probably decrease the risk of the large proportion of BBD that is not closely linked to breast cancer risk but do not decrease the risk of the types of BBD that increase a woman's risk of breast cancer (Stadel, 1986). Clearly, more information about the interrelationship between OC use, histologic types of BBD, and breast cancer is needed.
Seven epidemiologic studies have found that current or recent OC use reduces the risk of pelvic inflammatory disease (PID) (Stadel, 1986). On average, these studies have found that the risk of PID among OC users is about 40 percent lower than the risk among women using no contraceptive method.
The most detailed analysis of this issue comes from the U.S.-based Women's Health Study, a large hospital-based case-control study conducted from 1976 to 1978 (Rubin et al., 1982). This study found that the overall relative risk of PID among current OC users was about 0.5 compared with women using no contraception. However, this protective effect was limited to women who had been using OCs for at least 1 year. Furthermore, women not currently using OCs but who had used them in the past were no longer protected.
Two mechanisms have been proposed to explain how OCs protect against the development of PID. First, OCs may change cervical mucus so that it prevents pathogenic organisms from ascending into the upper genital tract. Second, because OCs reduce menstrual blood flow, a decreased amount of medium may be available for bacterial growth (Rubin et al., 1982).
Most of the studies of the relationship between OCs and PID have been hospital-based studies, so that case groups in these studies consisted of women hospitalized for PID. Because many women diagnosed with acute PID are not hospitalized, findings about women who are may not be generally extended to women who develop asymptomatic PID or symptomatic PID that does not require hospitalization (Washington et al., 1985). Specifically, gonorrhea may be an important cause of PID that requires hospitalization, whereas other bacterial etiologies such as chlamydia may cause much of the PID among women who do not require hospitalization. If OCs only protect against the bacterial etiologies of PID that are likely to require hospitalization, using OCs may not protect against some important causes of PID. Little epidemiologic evidence exists to clarify this question.
Results from a large cohort study in the United Kingdom have provided clear evidence that OC use decreases the risk of iron-deficiency anemia, in both current and past OC users (Royal College of General Practitioners, [RCGP], 1970). The protective effect provided by current OC use is probably due to the decrease in menstrual blood flow routinely seen among OC users. An increase in iron reserves probably accounts for the persistence of the decreased risk in past users. In countries where the prevalance of iron-deficiency anemia is high, this benefit to OC users may be especially important (Stadel, 1986).
Three epidemiologic studies have found that OC use decreases the risk of functional ovarian cysts, including follicular, granulosa lutein, and theca lutein cysts (Stadel, 1986). Decrease in risk appears to be confined to current OC users and is probably related to the suppression of ovulation that occurs during OC use.
Evidence from a case-control study that used data collected from the Oxford Family Planning Association cohort study suggests that OC use protects a woman from developing uterine fibroids (Ross et al., 1986). The risk of fibroids decreased with increasing duration of OC use: each 5 years of OC use contributed another 17 percent reduction in fibroid risk. The mechanism of the protective effect is still speculative. The authors proposed that circulating estrogens, either exogenous or endogenous, may promote the formation of fibroids and that the decreased risk associated with OC use may be explained by the modifying effect of the progestins in OCs.
Adverse Health Effects
Cardiovascular effects.
Most epidemiologic evidence suggests that OC use increases the risk of cardiovascular disease, in particular the risk of venous thromboembolism, myocardial infarction (MI), and stroke (Stadel, 1986). However, the risk of serious illness or death from cardiovascular disease that can be attributed to OC use is apparently concentrated among certain groups of women, primarily older women and women who smoke cigarettes.
At least 11 case-control and 4 cohort studies have found that OC use increases the risk of venous thromboembolism (Vessey, 1980). Results from those studies have shown that current OC use increases the risk of venous thromboembolism, although the increased risk does not appear to persist among past users. Furthermore, the risk among current users remains constant with increasing duration of OC use. The risk of both superficial and deep vein thrombosis among current OC users is directly related to the estrogen content of OCs: the higher the estrogen content of the OC, the greater the risk of venous thromboembolism (Stadel, 1986). The pathogenesis of venous thromboembolism among OC users probably involves an increase in the size of intravascular clots formed in response to thrombotic stimuli, most likely a result of estrogen-induced decreases in antithrombin III and plasminogen activators. Unlike the associations between OC use and MI and stroke, available studies have not found any interrelationship between OCs, venous thromboembolism, and cigarette smoking. The increased risk of venous thromboembolism is an important source of illness attributable to OC use but is a very infrequent cause of mortality (Stadel, 1986).
In contrast to the low attributable risk of death from venous thromboembolism associated with OC use, the increased risk of MI and stroke observed in women currently using OCs has been demonstrated to be an important source of the mortality risk attributable to OCs (Stadel, 1986). Current OC use increases the risk of MI, thrombotic stroke, and hemorrhagic stroke. The risk of MI and stroke associated with current OC use is strongly influenced by age and by the presence of other cardiovascular risk factors, such as cigarette smoking, hypertension, and diabetes. For example, the risk of MI that is attributable to OCs among nonsmoking women 30 to 39 years of age is about 4 cases per 100,000 current users per year, but it increases to about 185 cases per 100,000 current users per year among women aged 40 to 44 years who smoke heavily ( Table 3 ). The risk attributable to past OC use appears also to be concentrated among older women and older women who smoke heavily. The risk of adverse cardiovascular events among current OC users appears to be directly related to the estrogen content of the OCs; although less conclusive, risk may also be related to progestin content. The pathogenesis of MI and stroke among current OC users may be related both to the intravascular coagulation system and to the effects of increased blood pressure and metabolic changes.
Current Use of Oral Contraceptives (OCs), Cigarette Smoking, and Risk of Myocardial Infarction (MI).
Current OC use has been found to elevate blood pressure slightly in most women—about 1 to 2 mm Hg diastolic and 5 mm Hg systolic (Stadel, 1986). OC use leads to approximately a threefold to sixfold increased risk of overt hypertension. This risk has been observed to increase with increasing age and with increasing duration of OC use. Whether other risk factors for hypertension may be related to the increased risk attributable to OC use has not be established.
Metabolic Effects
The progestin component of OCs has been found to decrease the concentration of high-density lipoprotein-cholesterol (HDL-C), whereas the estrogen component has been found to increase HDL-C concentration (Stadel, 1986). Hence, the effects of different OC formulations on HDL-C concentration apparently depend on the specific estrogen-progestin content. A U.S. study provided information about 10 combination OCs: 3 lowered HDL-C concentrations, 2 had no effect, and 5 increased HDL-C levels (Bradley et al., 1978). If the progestin component has a strong anti-estrogen effect, the tendency of the estrogen component to increase HDL-C concentration may be overpowered (Stadel, 1986).
Current OC use has been found to decrease glucose tolerance among most women, although this decrease appears to be small, unrelated to duration of use, and only additive to the effects of other risk factors for impaired glucose tolerance (Stadel, 1986). This decrease in glucose tolerance is directly related to the estrogen content of the OCs, although there may be a relationship to the progestin content also. More important, OCs containing relatively small amounts of estrogen— < 50 micrograms of ethinyl estradiol—do not appear to decrease glucose tolerance to any appreciable extent.
Neoplastic Diseases
Epidemiologic studies clearly indicate that OC use increases the risk of hepatocellular adenoma (HCA), a rare, benign neoplasm of the liver. Although benign, HCA can cause serious abdominal hemorrhage and death, with a death-to-case ratio of approximately 8 percent (Rooks et al., 1979). Among women of reproductive age who have never used OCs or who used them for a short time, HCA develops at an annual rate of about 1.0 to 1.3 per million women 16 to 44 years of age. However, OC use is a strong risk factor for HCA, with a relative risk greater than 100 among women who have used OCs for 3 or more years compared with women who have used OCs for 1 year or less. The increased risk appears to be directly related to the duration of use, the age of the user, and the estrogen content of the OC. However, the absolute risk of HCA associated with OC use is small because of the rarity of the tumor. Among women who have used OCs for 5 years or longer, the attributable risk is estimated to be about 2 cases of HCA per 100,000 users per year (Stadel, 1986).
Epidemiologic studies have well demonstrated that OC use protects women from developing endometrial and ovarian cancers. However, the effect OCs may have on the risk for developing certain other malignancies remains unclear. Hepatocellular carcinoma and malignant melanoma have both been associated with OC use, although the strength of the associations has not been great. For this reason as well as the fact that those tumors are quite rare, the public health impact of a true positive association would not be great for either type of malignancy. Conversely, the debate about whether OC use increases the risk of cervical and breast cancers remains heated; some studies have found no effect on cancer risk, while others have found disturbing increases in risk. Because breast and cervical cancers are two of the most common cancers affecting women, contraceptive providers and epidemiologists feel an urgent need to resolve these discrepant results. However, as will be discussed subsequently, the possibility of a quick resolution to the controversies is unlikely.
Both case-control and cohort studies have assessed the relationship between OC use and malignant melanoma. Generally, they have not found substantial increases in the risk of melanoma associated with OC use (Stadel, 1986). Certain studies do suggest that OCs may increase the risk among certain subgroups of women, especially those who have used OCs for a long time (Ramcharan et al., 1981; Bain et al., 1982; Holly et al., 1983; Beral et al., 1984). Few studies have adequately addressed the risk by histologic type of melanoma. Future studies of this association will have several issues to consider, including the rarity of the tumor among women, the different histologic subtypes of melanoma, and the potentially confounding effects of exposure to sunlight.
The association between OC use and benign liver tumors, as well as a number of case reports of liver cancer among OC users, have led to theoretical concerns that OC use might increase the risk of malignant liver tumors. Three case-control studies published since 1983 have found increased risks of hepatocellular carcinoma among OC users (Henderson et al., 1983; Forman et al., 1986; Neuberger et al., 1986). Generally, the increased risk has been confined to women with a history of long-term OC use. However, each of the studies had few women in the case group ( < 30) and had methodological problems that may have biased the results.
In developed countries hepatocellular carcinoma is extremely rare among reproductive-aged women. In the United States in 1982 only 59 women died from liver cancer among approximately 52 million women aged 15 to 44 years (National Center for Health Statistics, 1982). Hence, even if OC use substantially increases the relative risk of liver cancer, the attributable risk would still be very low.
In many developing countries liver cancer is a much more common problem, primarily because of the relationship between hepatocellular carcinoma and chronic hepatitis B virus infection, which has a high prevalence in some regions. In those areas the possible interrelationships between OC use, hepatitis B infection, and liver cancer are more troublesome. Currently, the World Health Organization (WHO) is conducting a multicenter case-control study to address the relationship between OC use and liver cancer. Data are being collected from three developing countries with high rates of hepatitis B infection and liver cancer. It is hoped that results from this study will shed light on the relationship between OC use and this serious malignancy.
The potentially positive association between OC use and cervical cancer has added importance when considered in the setting of less developed countries. Surveillance information from developing countries, although sometimes fragmentary and incomplete, suggests that cancer of the cervix is the most frequent malignancy among women in those countries (Lunt, 1984). Unfortunately, screening efforts in those countries usually reach very limited segments of the female population. Unlike the situation in developed countries where provision of contraceptive services is usually accompanied by routine Papanicolaou (Pap) screening for cervical cancer, family planning programs in developing countries often do not have the resources to provide Pap screening for their clients.
To date, no definite causal relationship has been established between OC use and cervical cancer. Of 15 major epidemiologic studies, 8 have found no increased risk of cervical neoplasia and 7 have found significantly increased risks overall or increases among certain subgroups of users (Piper, 1985; Brinton et al., 1986; Ebeling et al., 1987; Irwin et al., 1988). At least some of the discrepancies may be due to methodological problems encountered in the various study designs, including (1) confounding bias caused by the effects of certain sexual behaviors that are well-recognized risk factors for cervical cancer; (2) overdiagnosis (by Pap screening) of cervical neoplasia among OC users; (3) a detection bias caused by increased Pap screening of OC users compared with nonusers; and (4) inappropriate comparison groups that include women who have used barrier methods, which are thought to protect against cervical cancer. (Swan and Pettiti, 1982; Piper, 1985) One recent case-control study from Costa Rica that considered the effects of sexual activity, history of sexually transmitted diseases (STDs), and the enhanced detection of cervical neoplasia among OC users found no elevated risk of invasive cervical cancer associated with OC use (Irwin et al., 1988). Although women who had used OCs had an increased risk of carcinoma in situ compared with never-users in the study, this increased risk was confined to women who had recently used OCs. Further, no increased risk of carcinoma in situ was found among subgroups in whom a history of Pap screening was not strongly linked to OC use. Both findings suggest that any elevated risk of carcinoma in situ among OC users may have been due to a bias caused by enhanced detection of disease. Another study of invasive cervical cancer from Maryland found no association with OC use (Celentano et al., 1987). However, two other recent studies, which also controlled for potentially confounding factors, found a 50 percent increased risk of invasive cervical cancer among women who had ever used OCs; women who used OCs for 5 or more years had about a twofold increase in risk (Brinton et al., 1986; Ebeling et al., 1987).
Results from these recent studies of the OC—cervical cancer relationship remain conflicting, even though most of the potential methodological problems were considered. OCs probably do not dramatically increase the overall risk of cervical dysplasia or cancer, although long-term use or use by specific subgroups of women may increase the risk. Furthermore, little is known about the relationship between OC use and human papillomavirus infection, which is thought to have an important role in cervical carcinogenesis. Further research is needed to clarify these complex relationships. Certainly, OC users, both current and past, need to be screened regularly with Pap smears. Whether or not using OCs is a risk factor for cervical cancer, it provides an ideal opportunity to screen sexually active women for this serious reproductive system cancer.
More than 15 published studies have reported that, overall, use of OCs does not appear to increase or decrease a woman's risk of breast cancer (Prentice and Thomas, 1987). However, many of those investigations were conducted in the 1970s, little more than 10 to 15 years after OCs were introduced. In these earlier investigations researchers had limited ability to study the long-term effects of OC use, particularly the effects of long duration of use, of distant time since first use, of use at specific ages, and of use in relation to other key reproductive events related to a woman's risk of developing breast cancer. Additionally, many of the studies of the OC–breast cancer relationship were not large enough to examine the relationship according to specific OC formulations and among certain high-risk subgroups of women.
To date, the CASH Study is the largest study designed to assess the risk of breast cancer associated with OC use (CASH, 1986). The study was a population-based case-control study conducted in eight regions of the United States from 1980 to 1982. Detailed information about reproductive history, contraceptive use, family history of cancer, and personal characteristics and habits was collected from 4,711 women with newly diagnosed breast cancer and from 4,676 control women. Case and control women were from 20 to 54 years of age. Compared with women who had never used OCs, women who had used OCs had a relative risk of breast cancer of 1.0 (0.9–1.1); even women who had used OCs for 15 or more years had no increased risk. None of the 12 OC formulations most commonly used in the United States were associated with a statistically significant increased risk of breast cancer. Analyses also showed no increase in risk among high-risk subgroups of women, including women with a history of BBD or a family history of breast cancer or those who were nulliparous or older at first term pregnancy.
Nonetheless, despite many studies indicating that OC use apparently does not increase the overall risk of breast cancer, controversy remains concerning whether long-term OC use, use at an early age, or use before the first term pregnancy might increase breast cancer risk (Skegg, 1988). Several recent studies have found increases in risk among certain subgroups of women. An analysis published in 1983 suggested that women who used certain OC formulations classified as ''high progestin'' before the age of 25 appeared more likely to develop pre-menopausal breast cancer than women who did not use OCs before age 25 (Pike et al., 1983). In the same year a report from England suggested that women with long-term OC use before their first child was born had an increased risk of premenopausal breast cancer compared with women who did not use OCs before the birth of their first child (McPherson et al., 1983). A 1985 report described results from an analysis using a subset of data from the CASH Study that replicated the analyses from the two 1983 reports (Stadel et al., 1985). In this analysis 2,088 women who had breast cancer and were from 20 to 44 years old were compared with 2,065 control women in the same age group. No significant increase or decrease in risk was observed among women who used high-progestin OCs before age 25, even when duration of use exceeded 6 years. Similarly, women who used OCs before their first term pregnancy did not have an increased risk, even when duration of use exceeded 4 years.
In 1986 two additional conflicting reports were published (Meirek et al., 1986; Paul et al., 1986). Analyses from a case-control study conducted in Scandinavia found a risk of premenopausal breast cancer among women with long-term OC use and use before the first term pregnancy (Meirek et al., 1986). The investigators reported a twofold increase in risk of breast cancer among women who used OCs for as long as 12 years. In contrast, analyses from a New Zealand case-control study did not find elevations in risk associated with OC use, even among women who had used OCs for a long time and who started taking them at an early age or among women who used OCs before their first term pregnancy (Paul et al., 1986).
A recently published analysis from the CASH Study examined in detail the risk of breast cancer in relation to early use of OCs (Schlesselman et al., 1988). The study found no evidence that use of OCs in the distant past increased breast cancer risk through age 54. Parous women who had used OCs for more than 6 years before their first term pregnancy, at 10–14 years after that pregnancy, were found to have a risk of breast cancer relative to nonusers of 1.1 (0.3–3.9). Among nulliparous women with more than 6 years of OC use, the relative risk of breast cancer at 10–14 years after they last used OCs was 0.6 (0.1–3.7).
Epidemiologists continue trying to disentangle the reasons for the discrepancies among the published studies (McPherson et al., 1986; McPherson and Drife, 1986; Anonymous, 1986; Schlesselman et al., 1987; Skegg, 1988). McPherson et al. (1986) have suggested that any possible risk of breast cancer associated with OC use at early ages may not become apparent for at least 20 years. Women born in the 1940s who used OCs in the 1960s will reach the ages of highest risk for breast cancer by the year 2000. If OC use at young ages is a risk factor for breast cancer, and if at least 20 years is required between exposure to OCs and the diagnosis of breast cancer, then these women might be expected to be diagnosed with breast cancer some time during the next 20 years. Under these assumptions, researchers may not be able to detect such a relationship at the present time.
The conflicting reports about the possible relationship between OC use and breast cancer risk, particularly use at an early age and before first term pregnancy, are confusing and troublesome. However, the preponderance of epidemiologic studies suggests that, overall, OCs do not increase the risk of breast cancer. If they do increase the risk in certain subgroups of women, the increase is not great and is generally confined to long-term users. Most experts believe that current recommendations for OC use should not be changed because of the continuing OC-breast cancer controversy. As women who used OCs in the 1960s reach the ages of highest risk for breast cancer, investigators should vigorously pursue opportunities to continue studying the long-term effects of OC use on breast cancer risk.
Other Effects
Several epidemiologic studies published in the 1970s reported that using OCs increased a woman's risk of gallbladder disease. Results from two large cohort studies from the United Kingdom published in 1982 better clarified the relationship between OCs and gallbladder disease (Layde et al., 1982; RCGP, 1982). Each study found that the increased risk appeared to be confined to recent users and to short-term users. No differences in risk were found with differing estrogen or progestin doses. The authors of both studies concluded that using Ocs apparently accelerated the development of gallbladder disease among susceptible women, rather than increased the overall lifetime risk.
A twofold to threefold increase in the prevalence of chlamydia trachomatis infection of the cervix among OC users has been demonstrated in 12 epidemiologic studies (Washington et al., 1985). Three reasons for this increase in risk have been suggested: (1) greater sexual activity among OC users than nonusers, (2) enhanced detection of chlamydial infection because of increased cervical ectropion induced by OC use, and (3) a direct effect of OC use on the risk of chlamydial infection. Three of the epidemiologic studies measured sexual activity and found no increase among OC users; furthermore, several epidemiologic studies have not found an increased risk of gonococcal infection among OC users (Washington et al., 1985). Whether or not it is merely easier to detect chlamydia infection among women who use OCs cannot be easily assessed and remains unresolved.
- Intrauterine Devices
The first IUDs that were widely used, such as the Lippes Loop TM and Saf-T-Coil TM , were made of inert plastic. In the 1970s a second generation of IUDs was introduced in which the plastic IUD acted as a carrier for metal or hormonal substances (Piotrow et al., 1979). These medicated devices included the Copper-7, Copper-T series, and the Progestasert TM . More recently a new and improved copper IUD, the Copper-T 380A, was developed; it may soon be the major IUD available in most countries (Treiman and Liskin, 1988).
The IUD is a highly effective contraceptive, with method failure rates of about 1 percent per year for medicated IUDs and 2 percent per year for nonmedicated ones ( Table 2 ). Because of undetected IUD expulsion, the user failure rate for IUDs is estimated to be somewhat higher, about 6 percent per year.
Because IUDs apparently prevent both intrauterine and ectopic pregnancies, the overall risk of ectopic pregnancy among IUD users is probably decreased compared with women who use no contraception. A 1981 study reported that current IUD users had a relative risk of ectopic pregnancy of 0.4 (0.3–0.6) compared with women using no contraception (Ory, 1981). However, about 5 percent to 15 percent of IUD-associated pregnancies are ectopic as IUDs seem to be more effective at preventing intrauterine pregnancies.
No major noncontraceptive health benefits are linked to IUD use. Progesterone-elaborating IUDs tend to decrease menstrual blood loss and dysmenorrhea, which can be viewed as a benefit for those women in whom it occurs (Hatcher et al., 1988).
Four major health risks have been associated with IUD use: (1) spontaneous abortion, which may rarely progress to septic abortion; (2) uterine perforation; (3) PID; and (4) tubal infertility. Based on information from studies done primarily in the United States and other developed countries, estimates for the annual mortality risk attributable to IUD use are between 1 and 2 deaths per 100,000 women (Ory et al., 1983). Mortality rates from IUD use may be somewhat higher in developing countries because of delays in treating complications or lack of access to medical facilities.
Although pregnancy rates are low among IUD users, complications may occur in women who do become pregnant. If the IUD is left in place, the chance of spontaneous abortion is 50 percent. If the IUD is removed, this rate drops to 25 percent (Hatcher et al., 1988). Septic abortion is a rare but sometimes fatal complication (10 per 100,000) that may occur if the IUD is left in place after the first trimester of pregnancy (Ory et al., 1983). If the IUD is removed as soon as the pregnancy is diagnosed, most instances of septic abortion can be prevented.
Perforation of the uterus may occur when an IUD is inserted, although this injury is often undetected and usually not serious. The incidence of perforation is unknown but is probably less than 1 percent (Hatcher et al., 1988). Very rarely the IUD is extruded into the abdominal cavity, requiring laparotomy to remove it. The risk of perforation during insertion increases substantially in two subgroups of women: lactating women and women within 8 weeks of delivery, because they have softer uterine musculature; at these times the risk of perforation may be increased substantially (Heartwell and Schlesselman, 1983).
Most epidemiologic studies of the issue have found that IUD users have an increased risk of PID (Grimes, 1987). This finding contrasts with all other modern methods of temporary contraception, which seem to protect a user from developing PID.
PID is usually but not always the result of an STD, such as gonorrhea or chlamydial infection. The overall incidence of PID varies greatly in different populations and depends mainly on sexual behaviors. The incidence of PID among IUD users also varies substantially. In a Scandinavian study of women with gonorrhea, 24 percent of IUD users developed PID (Ryden et al., 1979). Results from a large cohort study of married women in the United Kingdom showed a PID rate of 0.15 per 100 woman-years (Vessey et al., 1981). Clinical trials that determined rates of IUD removal because of PID found rates about eight times greater than the study from the United Kingdom, up to 1.22 per 100 woman-years (Siven and Stern, 1979).
The Dalkon Shield TM , an IUD used in the 1970s but no longer available, has been associated with a high risk of PID in several studies (Grimes, 1987). Women using IUD types other than the Dalkon Shield have been found to have about 1.5 to 2.0 times greater risk of PID than women using no contraceptive method. Most studies that have looked at the relationship of PID risk to the timing of IUD insertion have found that much of the increased risk is probably confined to the first few months after insertion. A recently published analysis has found that IUD users who are in mutually monogamous sexual relationships probably have little increased risk of PID associated with their IUD use (Lee et al., 1988). Much of the increased risk of PID seen among IUD users may be confined to women who are at increased risk for developing STDs.
One of the most important and serious sequellae of PID is tubal infertility. Results from a large cohort study of women with surgically confirmed PID have demonstrated that these women have an increased risk of subsequent tubal infertility (Westrom, 1987). The data showed that, among the women with PID who were subsequently exposed to a chance of pregnancy, infertility occurred in 11 percent after one episode of PID, 23 percent after two episodes, and 54 percent after three episodes.
Until recently little epidemiologic evidence directly linked IUD use with infertility. Results from most clinical trials of IUDs found that more than 70 percent of women conceive within 12 months of IUD removal (Liskin and Fox, 1982).
A large cohort study from the United Kingdom found that within 2 years of removal 92 percent of former users had given birth (Vessey et al., 1978). However, two U.S. case-control studies reported that the risk of tubal infertility among nulliparous women who had ever used IUDs was about twice that of those who had never used them (Daling et al., 1985; Cramer et al., 1985).
Both of these case-control studies found different risks of tubal infertility associated with different types of IUDs (Daling et al., 1985; Cramer et al., 1985). Women who had used the Dalkon Shield had the highest risk of tubal infertility. The lowest risk was seen among women who had used copper IUDs, while women who used the Lippes Loop or Saf-T-Coil IUDs had intermediate risks. Although these findings were consistent between the two studies, the numbers of users of specific IUD types were small, and the differences may have been due to chance alone.
The incidence of IUD-associated infertility is unknown, although it is probably less than the incidence of IUD-associated PID. The increased risk of infertility is presumably related to the increased PID risk associated with IUD use, even if PID is never recognized clinically. Cramer et al. (1985) found that women who reported having only one sexual partner had no increased risk of tubal infertility associated with IUD use.
- Barrier Methods
Because of the potential for preventing transmission of STDs, such as acquired immune deficiency syndrome, researchers are focusing new attention on barrier methods of contraception—condoms, diaphragms, spermicides, and sponges. Generally, barrier methods are less effective at preventing pregnancy than are OCs, IUDs, sterilization, injectables, and implants. Further, the effectiveness of barrier methods is extremely user dependent; improper use by unmotivated users can result in high failure rates. Side effects are minimal; consequently, the main risks associated with barrier methods are complications from unintentional pregnancy (Ory et al., 1983).
Discontinuation of use of barrier methods is common, both because they have higher risks of failure and because they may be obtrusive and less convenient to use (Sherris et al., 1984). But an important advantage of barrier methods is their protection against various STDs. Barrier methods also protect against acute PID and the resulting tubal infertility by keeping organisms that cause PID—such as Neisseria gonorrhoeae and Chlamydia trachomatis—from infecting the lower genital tract and from ascending into the upper genital tract (Kelaghan et al., 1982; Cramer et al., 1987).
Condoms are a safe, reversible method of birth control increasingly being used to prevent both pregnancy and STDs. The estimated method failure rate for condom use (without spermicide) is 2 percent per year, while the user failure rate is 12 percent ( Table 2 ). The effectiveness of condoms as both a contraceptive and a disease prophylactic depends on consistent and proper use. If couples begin to rely solely on condoms for protection against both pregnancy and infection, they could experience a substantial increase in the number of accidental pregnancies from incorrect or inconsistent use (Trussell and Kost, 1987). As condom use increases, acceptability and compliance will be important to monitor.
In vitro studies have demonstrated that latex condoms are effective barriers to herpes simplex virus type 2 (Conant et al., 1984; Judson et al., in press), Chlamydia trachomatis (Judson et al., in press), cytomegalovirus (Katznelson et al., 1984), and human immunodeficiency virus (HIV) (Conant et al., 1986; Rietmeijer et al., 1988). Natural membrane condoms may give less protection against viral STDs than latex ones, which contain smaller pores (Centers for Disease Control, 1988). Because using condoms prevents semen deposition, their use should also reduce transmission of organisms that may be present in semen, such as Neisseria gonorrhoeae, hepatitis B virus, Trichomonas vaginalis, and HIV (Stone et al., 1986).
Epidemiologic data relating to condom use and the prevention of STDs are limited. Several studies have shown that condom users, their partners, or both have a lower frequency of gonorrhea (Barlow, 1977; Hooper et al., 1978). Preliminary epidemiologic data suggest that using condoms may protect against sexual transmission of HIV infection (Fischl et al., 1987; Centers for Disease Control, 1987). Recent studies of prostitutes have also suggested a protective relationship between condom use and HIV infection (Smith and Smith, 1986; Centers for Disease Control, 1987; Mann et al., 1987).
However, these studies were based on observational data, and condom users are likely to differ from nonusers in important characteristics that may be related to the risk of acquisition of STDs (Feldblum and Fortney, 1988). Although conclusive epidemiologic evidence is lacking, available data suggest that the use of condoms is an effective preventive measure against STDs (Horsburgh et al., 1987). Failure of condoms to protect against STDs is probably explained by user failure more often than by product failure (Centers for Disease Control, 1988). The use of spermicides is considered a useful adjunct to condoms because spermicides can inhibit in vitro the growth of a broad range of sexually transmitted pathogens (Cramer et al., 1987; Francis and Chin, 1987).
Spermicides and the Contraceptive Sponge
Spermicides are chemical agents that inactivate sperm in the vagina before the sperm can move into the upper genital tract. Spermicides in use today include nonoxynol-9, octoxynol-9, and menfegol, although the latter is not available in the United States. Spermicides containing mercuric compounds, rejected as unsafe by the U.S. Food and Drug Administration (FDA), are still marketed in some Latin American countries and elsewhere (Sherris et al., 1984). Inert carriers of the spermicide include foams, jellies, creams, and suppositories; newer carriers include foaming suppositories (Neo Sampoon TM ) and spermicide-impregnated sponges (Today TM ).
The type of spermicidal agent or carrier has little effect on failure rates. The method failure rate is estimated to be about 3 percent per year; however, the user failure rate, at 21 percent per year, is much higher ( Table 2 ), largely because use must be premeditated. Furthermore, because spermicides are messy and can be irritating to mucous membranes, women often stop using them (Sherris et al., 1984). Protection from pregnancy, however, can be increased considerably if spermicides are used in conjunction with other barrier methods such as diaphragms or condoms.
Among nulliparous women the failure rates for the contraceptive sponge are comparable to the failure rates for the diaphragm; the method failure rate is 5 percent per year and the user failure rate is 18 percent per year ( Table 2 ). However, among parous women the method failure rate is 8 percent and the user failure rate is 28 percent.
Both laboratory evidence and clinical evidence suggest that spermicides protect against various STDs (Stone et al., 1986). In vitro studies have shown that spermicides inhibit the growth of Neisseria gonorrhoeae (Singh et al., 1972; Cowan and Cree, 1973) and inactivate herpes simplex virus type 2 (Singh et al., 1976) and HIV (Hicks et al., 1985). Although epidemiologic evidence is sparse, the virucidal effects of spermicides may provide some protection against cervical cancer, since the cancer may be initiated or promoted by a sexually transmitted virus such as human papilloma virus (Spring and Gruber, 1985). Several epidemiologic studies have found that spermicides protect users from gonorrhea infections (Jick et al., 1982; Quinn and O'Reilly, 1985), especially when used with condoms or diaphragms (Austin et al., 1984). A clinical trial among high-risk women using contraceptive sponges impregnated with nonoxynol-9 demonstrated protection against chlamydial and gonorrheal infections (Rosenberg et al., 1987).
One epidemiologic study suggested a connection between spermicides used near the time of conception or during pregnancy and the risk of congenital defects (Jick et al., 1981). Since that report, several larger and better designed studies have failed to confirm the association (Huggins et al., 1982; Mills et al., 1982; Shapiro et al., 1982; Cordero and Layde, 1983).
Additional health risks have been associated with the contraceptive sponge, a newer type of spermicidal carrier. Sponge users may be at increased risk of vaginal candidiasis, possibly because nonoxynol-9 allows candidal overgrowth (Rosenberg et al., 1987). Of greater health consequence is a possible association between using the contraceptive sponge and developing toxic shock syndrome (TSS); sponge users have a relative risk of 10.5 (2.1–52.7) compared with women using no barrier method (Schwartz et al., 1989). Because TSS is an extremely rare disease, the absolute risk of sponge users developing TSS is quite small; however, because TSS is a serious illness, physicians and sponge users should be aware of the symptoms and alert to the possibility (Faich et al., 1986; Schwartz et al., 1989). Postpartum women and women who have had TSS should not use the sponge, and women should never leave the sponge in the vagina for more than 30 hours (Reingold, 1986).
Diaphragm with Spermicide
Diaphragms used with spermicidal cream or jelly are a safe method of contraception and, when used correctly and consistently, can be an effective contraceptive. Because diaphragms/spermicides are inconvenient to use, only highly motivated women will experience low failure rates. Although the method failure rate is estimated to be about 3 percent per year, the user failure rate is much higher, about 18 percent per year ( Table 2 ). Clinicians should consider how motivated their patients are before advising diaphragm use (Sherris et al., 1984).
As with other barrier methods, diaphragm/spermicide use may have several noncontraceptive health benefits. This method appears to protect against gonorrhea, PID, and tubal infertility (Jick et al., 1982; Kelaghan et al., 1982; Cramer et al., 1987). Several case-control studies found cervical dysplasia and cervical neoplasia less common among diaphragm users than among other women (Wright et al., 1978; Harris et al., 1980; Celentano et al., 1987). Because diaphragms are almost always used with spermicides and spermicides alone may protect against various STDs, the separate protective effects of diaphragms on specific conditions may be difficult to measure (Stone et al., 1986).
As with the contraceptive sponge, diaphragms have been associated with a significantly higher risk of TSS (Hymowitz, 1981; Baehler et al., 1982; Schwartz et al., 1989). In one case-control study diaphragm users had a relative risk of TSS of 11.7 (2.5–56.1) compared with nonusers; however, the estimated absolute risk of TSS associated with diaphragm use was low, about 2.25 cases per 100,000 users per year (Schwartz et al., 1989). A less serious but more frequent complication associated with diaphragm use is urinary tract infections; the relative risks for diaphragm users developing a urinary tract infection compared with nonusers ranges from 2.0 to 3.0 (Foxman and Frerichs, 1985; Fihn et al., 1985; Vessey et al., 1987). Better fitted diaphragms and urination after intercourse may reduce the risk of urinary tract infections (Foxman and Frerichs, 1985). Women at particular risk for urinary tract infections, such as those with recurrent infections, should probably consider other contraceptive methods.
Cervical Caps
Cervical caps are cup-shaped devices, held in place by suction, that fit over the cervix (Hatcher et al., 1988). When used with spermicides, their effectiveness is comparable to that of diaphragms, with a method failure rate of about 5 percent per year and a user failure rate of 18 percent per year ( Table 2 ). Cervical caps have not been widely used; hence, little published research is available. Reports from small studies suggest that about half the women who want to use the cap cannot be fitted. Many other women discontinue use because of odor problems, difficulty in insertion or removal, or dislodgement during intercourse (Ory et al., 1983). Advantages are that the cap can be left in place longer than 24 hours and that it can be inserted many hours or even a day or two before coitus (Sherris et al., 1984). Although potential health risks and benefits associated with the cervical cap are probably similiar to those associated with the diaphragm, available data are too limited to document them (Hatcher et al., 1988).
- Long-Acting Methods
Several long-acting contraceptive methods now available are highly effective, convenient to use, and give protection from pregnancy for 1 month to 5 years. All contain some kind of progestin. Disturbance of the menstrual cycle is the most common side effect of all progestin-containing contraceptives and is the major reason women stop using them.
Injectables
Two long-acting injectable progestins—depot-medroxprogesterone acetate (DMPA; Depo-Provera TM ) and norethindrone enanthate (NET; Noristerat TM )— are the most widely used and studied of several injectable contraceptives available. DMPA is approved for contraception in at least 90 countries, NET in more than 40 (Liskin et al., 1987). At present neither is licensed for use as a contraceptive in the United States.
Injectables are highly effective: the estimated method failure rate is 0.3 percent per year for DMPA, given every 90 days, and 0.4 percent per year for NET, given at 8-or 12-week intervals ( Table 2 ). Because minimum compliance is necessary, the user failure rates are approximately equal to the method failure rates. Injectables prevent pregnancy in several ways. Possible mechanisms include inhibiting ovulation; thickening cervical mucus; and altering the endometrial lining, which inhibits implantation (Liskin and Quillin, 1982).
Considerable controversy regarding possible cancer risks has been associated with DMPA and NET, chiefly stemming from data from animal studies suggesting that DMPA use could increase the risk of breast and endometrial cancers (WHO, 1986a). Although the applicability of these animal models is debatable and human studies have either failed to demonstrate these relationships or are inconclusive (Liang et al., 1983; WHO, 1986a; Lee et al., 1987), the possibility of increased risk of cancer among DMPA users was one reason the FDA did not approve DMPA for contraceptive use in the United States (Sun, 1984).
In 1986 preliminary results were published from an ongoing case-control study conducted by WHO concerning the relationship between DMPA and breast cancer (WHO, 1986a). This is the largest epidemiologic study of the DMPA-breast cancer relationship published to date. Women who had ever used DMPA had a risk of breast cancer of 1.0 (0.7–1.5); no increase in risk was seen even for long-term users. Conversely, a recent study in Costa Rica found that DMPA users had an elevated risk of breast cancer of 2.6 (1.4–4.7); however, no dose-response effect was found (Lee et al., 1987). Because of the small number of DMPA users in the study and the lack of a dose-response relationship, the authors considered the results to be inclusive.
Another analysis from the same WHO study found that the risk of invasive cervical cancer was slightly higher for long-term DMPA users than for never-users (relative risk of 1.4 [0.9–2.2]); however, results were considered inconclusive because of the small number of long-term DMPA users as well as the lack of a consistent trend with duration of use (WHO, 1986a). Results from the Costa Rica study showed no increase in risk of either invasive cervical cancer or carcinoma in situ associated with DMPA use (Oberle et al., 1988).
Although DMPA and NET have yet to be conclusively linked to any human cancer, epidemiologic studies have been hindered by small sample sizes and short durations of exposure. Whether injectable contraceptives are associated with any cancer will be resolved only after additional data have accumulated (WHO, 1986a).
Reported metabolic effects of DMPA and NET use include changes in blood pressure as well as changes in insulin, cholesterol, and triglyceride levels; however, the findings are inconsistent and have shown no clear clinical significance (WHO, 1986b; Liskin et al., 1987). Concern over cholesterol levels among women who use DMPA or NET is mainly due to the reported cardiovascular problems associated with OC use, generally thought to be caused by the estrogen component of the pill (Rosenfield et al., 1983). Lower levels of HDL-C have been reported among women who were taking OCs with a high progestin potency or a progestin alone (Bradley et al., 1978). Most studies of DMPA users have found either no change in total cholesterol and triglycerides or a decrease, a possibly beneficial effect (Liskin et al., 1987). However, a few studies have reported an increase in cholesterol with longer use of DMPA or a decrease in HDL-C, both possibly adverse effects. The only study involving NET also found a decrease in HDL-C (Fotherby et al., 1982). The clinical significance of these decreases in HDL-C is uncertain; to date, no associations between DMPA or NET use and increased incidence of cardiovascular disease have been reported. Trials are under way in five countries to measure changes in lipid metabolism in DMPA and NET users (Liskin et al., 1987).
Unlike combination OCs, DMPA and NET appear to have little effect on the coagulation system (Liskin et al., 1987). Most laboratory studies have found little change in the coagulation and fibrinolytic systems that affect blood clotting.
The most consistently reported side effect of DMPA and NET use is a change in menstrual pattern: more than two-thirds of DMPA users and one-half of NET users have no regular menstrual cycles during the first year they use these contraceptives (Liskin et al., 1987). Amenorrhea or irregular, unpredictable bleeding episodes are the most common problems (WHO, 1978, 1987) and the principal reasons that women stop using injectables. Amenorrhea, more frequent with DMPA than NET, is probably the most upsetting change because women cannot be sure they are not pregnant (Liskin et al., 1987). Prolonged bleeding or spotting can be disturbing, especially if local customs restrict the activities of menstruating women. The occurrence of heavy bleeding requiring medical attention is rare, found among about 0.5 percent of users. In fact, because bleeding is often lighter than normal, increased hemoglobin levels among some users have been reported (WHO, 1986b).
Studies of children exposed to DMPA from breast milk have found no measurable consequences, even when followed up to 10 years after exposure (Liskin et al., 1987). This is not an unexpected finding, for very little of the hormone is transmitted in breast milk.
Neither DMPA nor NET appears to have any permanent effect on fertility (Liskin et al., 1987). However, resumption of ovulation and fertility is delayed; ovulation can be inhibited for 4 to 9 months or more after the last injection (Pardthaisong et al., 1980; Affandi et al., 1987). Although return to fertility is comparable to that seen with OC and IUD use, because of fears about permanent infertility, some family planning programs use injectables only among higher-parity women (Liskin et al., 1987). In fact, injectable progestins may protect women from PID, a major cause of infertility, by causing changes in cervical mucus (Gray, 1985).
Injectable progestins may also protect against endometrial and ovarian cancers. Excess estrogen is known to increase the risk of endometrial cancer, while progestins mitigate this effect (Rosenfield et al., 1983). Further, several studies have demonstrated a negative association between the use of combination OCs and endometrial cancer, a protective effect thought to be caused by the progestin component. Preliminary results from a WHO case-control study found that DMPA users had a relative risk of 0.3 (0.04–2.4) compared with never-users; however, data were based on just 52 women with endometrial cancer, only one of whom had ever used DMPA (WHO, 1986a).
Even fewer data exist on the association between ovarian cancer and DMPA use. However, several studies have demonstrated a negative association between OC use and ovarian cancer, perhaps due to the effects of an ovulation (Rosenfield et al., 1983). Because injectable progestins usually prevent ovulation, there is at least a theoretical possibility that use of DMPA or NET might reduce the risk of ovarian cancer. Preliminary results from the WHO study support this possibility: DMPA users had a relative risk of ovarian cancer of 0.7 (0.3–1.7) compared with never users, based on 7 exposed cases and 74 exposed controls (WHO, 1986a).
Several new types of injectables are currently in use or under development. Injectable microspheres and microcapsules release hormone at a more constant rate, and preliminary trials have found fewer side effects than with DMPA or NET (Liskin et al., 1987). However, as with all progestational agents, irregular menstrual bleeding is a common side effect. Estrogen-progestin combinations that are injected monthly are being used in Latin America and China; preliminary results have shown highly effective protection and fewer problems with bleeding irregularities.
The NORPLANT® subdermal implant system is another highly effective, long-acting progestational contraceptive method (Liskin et al., 1987). It is currently being considered by the FDA for use in the United States. Developed by the Population Council, NORPLANT® implants come in two forms. The first and more widely used system, NORPLANT® consists of six silastic rods, each about 1 inch long and 0.1 inch in diameter, containing 35 milligrams of the progestin levonorgestrel. The newer system, NORPLANT-2®, consists of two rods, each containing 70 milligrams of levonorgestrel. With both systems, rods are implanted under the skin, usually in the upper arm; the hormone is then released at a continuous, slow rate. Insertion and removal require a minor surgical procedure performed by trained health care personnel; however, once implanted, no further action is required for several years.
Both systems provide long-term protection from pregnancy. NORPLANT® is highly effective for 5 years, NORPLANT-2® for at least 3 years. In the first year of use the average reported failure rate is 0.2 percent ( Table 2 ). However, the failure rate may be slightly higher among obese women. The mechanisms for pregnancy prevention are probably similar to those for the injectable contraceptives.
The rate of ectopic pregnancy among NORPLANT® users, about 1.5 per 1,000 woman-years, is about the same as the rate among women using copper and unmedicated IUDs (Liskin et al., 1987). Because the rate is lower than that for women using no contraception, NORPLANT® users can be considered to be protected from ectopic pregnancy.
As with injectables, the most common side effect of implants is disturbance of the menstrual cycle. Bleeding irregularity, the most frequent reason that women discontinue use of the method (Salah et al., 1987; Pasquale et al., 1987), causes 2 percent to 7 percent of women to stop using implants in the first year (Liskin et al., 1987). However, episodes of abnormal bleeding diminish with duration of use (Salah et al., 1987; Diaz et al., 1987), and the implants can be removed immediately if there are any disturbing side effects.
Transient ovarian cysts occur in a small percentage of women using NORPLANT® (Salah et al., 1987; Diaz et al., 1987); although the cysts regress eventually, they have been a reason for implant removal (Pasquale et al., 1987). Permanent infertility does not appear to be a concern; several studies have shown that fertility quickly returns after implants are removed (Diaz et al., 1987; Affandi et al., 1987).
Generally, no changes in several metabolic indicators have been found secondary to NORPLANT® use, including liver function, carbohydrate metabolism, blood coagulation, blood pressure, or body weight (Liskin et al., 1987). Studies of lipid metabolism in NORPLANT® users have produced conflicting results. However, no epidemiologic studies of cardiovascular complications among NORPLANT® users have been completed.
- Tubal Sterilization
Since the 1930s more than 95 million women worldwide have undergone tubal sterilization, making it the most widely used contraceptive method in the world (Liskin et al., 1985). The popularity of tubal sterilization continues to grow rapidly in many countries, which suggests that the estimate of the number of women who have had the procedure may be a conservative one. Currently, more than 15 percent of married women of reproductive age have undergone tubal sterilization in countries as diverse as Brazil, Panama, South Korea, Thailand, and the United States. In China an estimated 27 percent of women have undergone tubal sterilization. Tubal sterilization has been very popular in the United States, Latin America, the Caribbean, and in much of Asia. Africa and the Middle East have the lowest prevalence of tubal sterilization.
Tubal sterilization procedures can be characterized by (1) timing with respect to pregnancy, (2) the surgical approach to the fallopian tubes, and (3) the method of tubal occlusion. Tubal sterilization can be performed shortly after vaginal delivery, concurrently with cesarean section, at the time of induced abortion, or remote from pregnancy termination. In the latter instance the procedure is known as interval tubal sterilization.
Surgery for most tubal sterilizations requires an abdominal incision. For either postpartum or interval sterilizations, an abdominal incision 2 to 5 centimeters long, termed a minilaparotomy, allows the surgeon access to the fallopian tubes (Ross et al., 1985).
Laparoscopic tubal sterilization is becoming increasingly popular, particularly in developed countries. For laparoscopic procedures the abdominal incision is usually only about 1 centimeter long. Two general methods of inserting the laparoscope are used. In the first, termed closed laparoscopy , a surgeon uses an insufflating needle, a sharp trocar, or both to enter the abdominal cavity before inserting the laparoscope. An alternative technique called open laparoscopy attempts to minimize the risk of intra-abdominal injury caused by the insufflating needle or trocar by combining features of minilaparotomy and closed laparoscopy. Although open laparoscopy requires more time than closed laparoscopy, it reduces the chance of trauma to major blood vessels and the gastrointestinal tract and thus is inherently safer, especially for facilities that do not have the equipment and personnel necessary to handle serious surgical complications.
Alternative surgical approaches include the vaginal approach and the transcervical approach. Although the vaginal approach produces no visible scar, it is used less frequently because of the increased risk of pelvic infection (Ross et al., 1985). A transcervical approach, involving instillation of a sclerosing agent into the fallopian tubes, is widely used only in China.
The fallopian tubes can be occluded by ligation (with or without resection), by coagulation using unipolar or bipolar current, or by mechanical occlusion with silastic bands or clips. Tubal occlusions for postpartum laparotomies are generally done by ligation. All of these techniques can be used for interval sterilization, but the methods of occlusion for laparoscopy are limited to the use of coagulation or mechanical devices. Unipolar coagulation involves use of an electrical current that passes into the tube and through the patient to a ground plate attached to the patient. This system, which has resulted in fatal thermal bowel injuries (Peterson et al., 1981a), has largely been replaced in the United States by a bipolar coagulation technique that includes only the tissue in the grasping forceps as an integral part of the electrical circuit, thereby reducing the risk of serious thermal injuries (Hulka et al., 1987).
With the exception of conventional laparotomy, all surgical approaches and methods of tubal occlusion can be safely and effectively performed using local anesthesia. Because of the hazards inherent in the use of general anesthesia, the World Federation of Health Agencies for the Advancement of Voluntary Surgical Contraception (1984) advocates using local anesthesia for uncomplicated procedures.
A pregnancy that is identified after sterilization may have occurred because of conception before sterilization or because the operation was not successful. Conception before sterilization, called a luteal-phase pregnancy, is estimated to occur in about 2 to 3 per 1,000 interval tubal sterilizations (Chi and Feldblum, 1981). The most effective means of reducing the risk of luteal-phase pregnancy is to perform the sterilization before the estimated date of ovulation (Grubb and Peterson, 1985).
Rates of true sterilization failure vary by method of tubal occlusion, surgical expertise, and other factors, such as whether a woman has tubal disease. Overall rates are estimated to be between 0.2 percent and 0.4 percent per year ( Table 2 ). No studies currently available permit rigorous comparison of failure rates by method of tubal occlusion, though one such study with the potential to do so is in progress in the United States. Since 1978 a multicenter cohort study conducted by the Centers for Disease Control has enrolled approximately 12,000 women undergoing tubal sterilization. These women are currently in various stages of a planned 5-year follow-up. Final study results will not, however, be available until the early 1990s.
When sterilization fails, the relative likelihood of ectopic gestation appears to be increased. Further, the risk seems to vary by method of tubal occlusion, with highest risk of ectopic pregnancy following electrocoagulation (Bhiwandiwala et al., 1982). The absolute likelihood of ectopic pregnancy after sterilization is actually reduced, however, relative to the risk a woman would incur when not using any contraception or using an IUD (DeStefano et al., 1982).
Studies from around the world suggest that tubal sterilization is a remarkably safe surgical procedure; however, more women die from tubal sterilizations than men die from vasectomies. Case-fatality rates for tubal sterilization have been estimated in reports from Europe, the United States, India, and Bangladesh. A French survey of approximately 100,000 laparoscopic procedures (including those for purposes other than sterilization) estimated a case-fatality rate of 20 per 100,000 procedures (Mintz, 1977). A prospective study of laparoscopic procedures from the United Kingdom reported a case-fatality rate of 10 per 100,000 procedures (Chamberlain and Brown, 1978). The case-fatality rate of tubal sterilization in U.S. hospitals has been estimated to be approximately 4 per 100,000 procedures (Peterson et al., 1982a). In a report from India the case-fatality rate from postpartum tubal sterilization was 7 per 100,000 procedures (Indian Council of Medical Research, 1982). In two studies from Bangladesh the case-fatality rate was estimated to be between 12 and 19 per 100,000 procedures (Grimes et al., 1982a, 1982b).
Worldwide, most sterilization-attributable deaths are caused by complications related to use of anesthesia, although deaths have occurred from hemorrhage and thermal injury (Peterson et al., 1983). In the United States 11 of 29 women whose deaths were attributable to sterilization suffered complications of general anesthesia (Peterson et al., 1983). Other reports from the United Kingdom and France have also identified complications of general anesthesia as the leading cause of laparoscopic-associated, sterilization-attributable death (Mintz, 1977; Chamberlain and Brown, 1978). Even in countries where general anesthesia is not often used, complications of anesthesia are still a major cause of sterilization-attributable death (Grimes et al., 1982a; Ross et al., 1985).
Reports regarding nonfatal complications attributable to tubal sterilization have varied by study design, definition, and classification of complications. Although comparing complication rates between studies is difficult, such studies indicate that major morbidity associated with tubal sterilization is uncommon and that safety varies with surgical and anesthetic technique. One large multicenter study, which included data from 23 countries, reported a complication rate of 2.0 percent for the approximately 7,000 women undergoing laparoscopy with silastic band application (Mumford et al., 1980). This rate was approximately twice that experienced by the approximately 5,000 women undergoing minilaparotomy procedures (0.8 percent). The WHO has reported the only randomized multicenter, multinational study. In that study approximately 800 women had minilaparotomies, and approximately 800 underwent laparoscopy using electrocoagulation. Major complications occurred in 1.5 percent of women undergoing minilaparotomy and in 0.9 percent of women undergoing laparoscopy. Minor complications were reported in 11.6 percent and 6.0 percent, respectively (WHO, 1982a).
The WHO also reported on a multicenter study of postpartum sterilization in which major complications occurred in only 0.3 percent of the patients (WHO, 1982b). This rate is identical to that reported from a large multicenter study of postpartum minilaparotomy conducted in India (Indian Council of Medical Research, 1982). In that study major complication rates associated with minilaparotomy did not substantially vary between those minilaparotomy procedures performed postpartum, those performed in association with early pregnancy termination, or those performed as an interval procedure. By contrast, women undergoing interval laparoscopy had a complication rate of 1.2 percent, and women undergoing interval colpotomy (via a vaginal incision) had an overall complication rate of 5.7 percent.
In a U.S. multicenter prospective study of laparoscopic tubal sterilization, 1.7 percent of women experienced at least one of six standard intra-operative or postoperative complications (DeStefano et al., 1983a). The most frequent major complication (1.1 percent) was unintended major surgery. In some instances this unintended surgery occurred because of incidental pathology identified during laparoscopy or because of technical limitations of laparoscopy itself. Thus, not all complications were directly caused by the laparoscopic procedure per se. The risk of complications was increased twofold or more by the following factors: obesity, lung disease, diabetes mellitus, previous abdominal or pelvic surgery, and a history of PID.
Although the overall major complication rate attributable to tubal sterilization is less than 2 percent, such complications can result in serious injury or death. The likelihood of serious injury appears to vary somewhat by surgical approach and tubal occlusion technique. Most minilaparotomy complications are not serious, with minor hemorrhage, minor wound infections, and uterine perforations reported most frequently (Liskin et al., 1985). By contrast, laparoscopy is more likely to result in serious complications. While rare, perforation injuries to major blood vessels or the gastrointestinal tract can occur (Peterson et al., 1982b). Open laparoscopy should markedly reduce the risk of these complications. One comparative study assessing complications among 1,112 women undergoing open laparoscopy and 288 women undergoing conventional laparoscopy failed to demonstrate a difference in complication rates (Bhiwandiwala et al., 1985). However, to detect a difference between open and closed laparoscopy, an epidemiologic study would have to involve thousands of women to have sufficient study power to detect a difference.
Complication rates also may vary with respect to method of tubal occlusion. For example, mesosalpingeal hemorrhage occurs more often from silastic band application than from alternative techniques. Unipolar coagulation increases the risk of thermal bowel injury. Although this type of injury likely occurs in fewer than 1 per 1,000 cases, more than 100 nonfatal thermal bowel injuries and 3 deaths from the use of unipolar instruments have been reported in the United States (Peterson et al., 1981a).
Because of the number of women involved, any important long-term sequelae of tubal sterilization would have major impact. On balance, the existing literature has failed to demonstrate any important negative long-term health effects of tubal sterilization. Most concerns regarding potential long-term sequelae have dealt with four issues: (1) menstrual abnormalities, (2) hysterectomy following tubal sterilization, (3) regret, and (4) ectopic pregnancy. We addressed the last concern previously in the section on sterilization efficacy.
Before 1980 most studies found an increase in menstrual abnormalities following tubal sterilization, the so-called post-tubal syndrome. Such studies, however, had major methodological limitations, including: (1) failure to identify and account for biases inherent in their retrospective design, (2) failure to use comparison groups, (3) failure to consider the effects of prior contraceptive use, (4) failure to consider women without menstrual changes or with improvements in menstrual symptoms, and (5) failure to evaluate information regarding presterilization menstrual patterns. Since 1980 most reports have had fewer methodological limitations and have failed to support the existence of a post-tubal syndrome.
One study has reported data from a series of approximately 10,000 women undergoing tubal sterilization at 64 institutions in 27 countries (Bhiwandiwala et al., 1983). Six menstrual symptoms were evaluated before and after sterilization, with most women reporting no changes 1 year after sterilization. When menstrual changes did occur, about as many women experienced improvement in symptoms as experienced deleterious change. A substantial percentage of the observed changes were attributable to cessation of OC or IUD use rather than to the sterilization procedure per se. No significant differences in menstrual patterns after sterilization were found among the various tubal occlusion techniques reviewed.
Another report concerned a sample of approximately 1,500 women selected from 45 centers in 24 countries (Fortney et al., 1983). The most important determinants of menstrual patterns after sterilization were the patterns at the time of sterilization. Women with abnormal patterns before sterilization were three times more likely to experience change than women with normal cycles; many of these women experienced change toward more normal cycles.
Several other reports from the United States and the United Kingdom that assessed menstrual patterns 1 or 2 years after sterilization failed to find support for the existence of a post-tubal syndrome. In the United States the Centers for Disease Control used data from a multicenter prospective study in which approximately 2,500 women were followed for 2 years after sterilization (DeStefano et al., 1983b). Each woman served as her own control; her menstrual function at the follow-up interview was compared with her menstrual function at the preoperative interview. Except for menstrual pain among women who underwent unipolar electrocoagulation, the prevalence of adverse menstrual function after tubal sterilization did not increase. Further, approximately 50 percent of women with adverse menstrual function preoperatively had an improvement by 2 years after tubal sterilization.
In a report from England 551 women undergoing interval sterilization were studied (Foulkes and Chamberlain, 1985). No increase in menstrual abnormalities among sterilized women compared with nonsterilized women was found after a year of follow-up. Both sterilized and nonsterilized women were more likely to experience heavy and prolonged menstrual bleeding if they had been using OCs before sterilization. Thus, discontinuation of OCs was more likely to result in abnormalities of menstruation than was sterilization per se.
Two studies, one from the United Kingdom (Vessey et al., 1983) and one from the United States (DeStefano et al., 1985), reported on menstrual function among women more than 2 years after their sterilizations. The study from the United Kingdom compared the experience of 2,243 women undergoing tubal sterilization with 3,551 women whose husbands underwent vasectomy. Three years after sterilization hospital referral or hospitalization for menstrual complaints was nearly equal for women undergoing sterilization and for the comparison group. After 6 years, sterilized women had a slight, but not statistically significant, increased risk for hospital referral or admission for menstrual complaints.
The study from the United States was principally designed to assess the long-term impact of OC use (DeStefano et al., 1985). In that analysis 719 women who underwent tubal sterilization were compared with 1,083 women whose partners underwent vasectomy. At follow-up, with intervals longer than 2 years, the tubal sterilization group had a significantly increased risk of abnormal menstrual cycles and combinations of two or more adverse menstrual outcomes. The likelihood of menstrual abnormalities was greatest, however, among the group of sterilized women who had presterilization menstrual complaints.
To date, no study has been reported that includes long-term follow-up for sterilized and nonsterilized women in a manner that allows comparison of specific menstrual symptoms and specific methods of tubal occlusion. The Centers for Disease Control in the United States is conducting such a study, but it will not be completed until the early 1990s.
Whether tubal sterilization increases the risk of subsequent hysterectomy is uncertain. Concerns that it does have been based, in part, on the possible existence of the post-tubal syndrome we noted earlier. Whether or not a post-tubal syndrome exists, the perception that it does may increase the likelihood that menstrual abnormalities after sterilization are managed surgically. Further, once a woman has been sterilized, either she or her physician may resort more quickly to surgical management of any gynecologic problem. These possibilities were assessed in the previously mentioned cohort study from the United Kingdom (Vessey et al., 1983). After both 3 years and 6 years of follow-up, hospital referrals leading to hysterectomy were equally likely in women who had undergone tubal sterilization and in wives of men who had undergone vasectomy. In Canada a population-based study using data from a health insurance plan studied 4,374 women aged 25 to 44 who underwent tubal ligation in 1974 (Cohen, 1987). As a comparison group, a random sample of 10,000 women registered in the insurance plan in 1974 was chosen. After 2 years of follow-up, no difference was found in adverse gynecologic outcomes between the two groups. However, beginning with the 2-year follow-up and increasing for up to 9 years, women ages 25 to 29 undergoing tubal sterilization had a statistically significant 60 percent increase in the probability of subsequent hysterectomy, even after controlling for other risk factors. For women aged 30 and over, tubal sterilization did not increase the likelihood of subsequent hysterectomy. The results from the two cohort studies with longer-term follow-up argue for continuing surveillance of sterilization sequelae beyond a 1-or 2-year period.
Published reports indicate that most women are satisfied with their decision to undergo sterilization. An overview of recent worldwide studies indicates that 2 percent to 13 percent of women interviewed 6 months to 6 years postoperatively expressed regret at having been sterilized; only 1 percent to 3 percent of those women seriously considered or underwent sterilization reversal procedures (Liskin et al., 1985). However, the prevalence of regret is likely to vary substantially by definition of regret. One survey of U.S. women found that 26 percent responded affirmatively when asked, ''If it were possible for you to have another baby, would you, yourself, like to have one?'' (Henshaw and Singh, 1986). In that same survey 10 percent of women responded affirmatively when asked, "As things look to you just now, if the operation could be safely reversed, that is changed back, would you want to have it reversed?"
Careful presterilization counseling is likely to minimize the chance of poststerilization regret. To maximize effectiveness, such counseling should focus on the reasons women might regret having been sterilized. A variety of studies have indicated that younger women, usually reported as less than 30 years of age, are more likely to regret having been sterilized (Grubb et al., 1985). In many developed countries divorce and remarriage are common reasons women regret sterilization and request its reversal.
A multicenter prospective study conducted by the Centers for Disease Control in the United States has found that only 2 percent of women regretted having a tubal sterilization I year after the procedure, compared with 2.7 percent after 2 years (Grubb et al., 1985). Five years after the procedure approximately 4 percent regretted it (unpublished data). Because the possibility for major life changes (e.g., death of a spouse or child) increases as women age, the longer the time since the procedure, the more likely women may be to regret having been sterilized. Thus, length of follow-up must be considered when comparing rates of regret in various studies.
In another study conducted in the United States, Shain et al. (1986) compared the likelihood that women undergoing tubal sterilization will regret it relative to the likelihood that women whose husbands underwent vasectomy will have regrets. At 1-year follow-up, only 2 of 234 (0.9 percent) women who had undergone tubal ligation compared with 2 of 154 (1.3 percent) women whose husbands underwent vasectomy expressed regret at having had the procedure. As the authors indicated, however, dissatisfaction with sterilization may involve various degrees of intensity, ranging from occasional concerns to desire for reversal. Further, these feelings are not static. When the authors used a broader measure of satisfaction/dissatisfaction as an outcome, women who had undergone tubal sterilization expressed significantly more positive feelings during follow-up interviews than did women whose husbands underwent vasectomies. This was attributed to a disproportionate prevalence of female control over reproductive decision making among women undergoing tubal sterilization. The authors concluded that counseling of the couple and the ability to exercise control over one's body are important predictors of sterilization regret.
Sterilization Reversal
The proportion of sterilized women who seek reversal is small but nontrivial (Ross et al., 1985). Highly sophisticated microsurgical techniques for tubal reanastomosis that increase the likelihood of successful reversal have been developed. These techniques are generally limited to developed countries. When available, such procedures are expensive and require laparotomy under general anesthesia. The likelihood of successful reversal depends on the method of tubal occlusion originally used. In general, 50 percent to 70 percent of women undergoing reversal surgery achieve intrauterine pregnancy (Liskin et al., 1985). However, most reports are from the selected series of highly skilled surgeons using sophisticated microsurgical techniques.
Vasectomy is cutting and occluding the vas deferens to prevent sperm transport in semen. Although generally considered to be safe, simple, and highly effective, vasectomy is not widely popular in most of the world. In fact, the majority of the estimated 41 million men currently using vasectomy for contraception reside in four countries—the United States, United Kingdom, China, and India (Gallen et al., 1986). By comparison, more than 95 million women worldwide have undergone tubal sterilization. Among regions, Africa is the least active in providing vasectomy services, Asia the most active, and Latin America moderately active (Ross and Huber, 1983). The limited popularity of vasectomy has been attributed to motivational factors and access to services (Gallen et al., 1986). In addition, female sterilization has become more popular than male sterilization in some countries (Ross and Huber, 1983).
Vasectomy is a minor surgical procedure that usually takes 5 to 10 minutes to perform (Ross et al., 1985). The procedure consists of isolating the vas deferens and then using one of three methods to occlude it: ligation, coagulation, or clip application. Ligation is the most widely used approach. If ligatures are tied too snugly, resulting in vas transection, or too loosely, resulting in incomplete occlusion, sperm can leak into surrounding tissues, resulting in sperm granuloma formation. Coagulation of the vas mucosa is an alternative method of occlusion that minimizes damage to the vas muscularis. Some believe that this method reduces the likelihood of sperm granuloma formation. Clips are rarely used for vas occlusion. Several clips must be applied to achieve maximum effectiveness, and, because they are not absorbable, the vasectomized man can sometimes feel the clips.
Local anesthesia without premedication is the anesthetic technique of choice for most vasectomies (Association for Voluntary Sterilization, 1983). The strong preference for local anesthesia is based on the higher risk of morbidity and mortality associated with general anesthesia (Peterson et al., 1981b, 1983). A survey of selected outpatient facilities conducted in the United States in 1980 indicated that the type of anesthesia used varied substantially by facility type (Kendrick et al., 1985). Freestanding surgical facilities reported performing 29 percent of their vasectomies using general anesthesia; conversely, 96 percent of the facilities not classified as freestanding reported using local or regional anesthesia. Outside the United States, particularly in developing countries, almost all vasectomies are performed using local anesthesia (Ross et al., 1985).
Vasectomy failure rates have ranged from 0 percent to 2.2 percent, with most studies reporting fewer than I percent (Liskin et al., 1983) ( Table 2 ). However, few data are available that allow for a comparative assessment of failure rates associated with the various methods of vas occlusion. Most vasectomy failures can be attributed to unprotected coitus shortly after vasectomy or spontaneous reanastomosis of the vas. Unprotected coitus before sperm has been cleared from the male reproductive tract can result in pregnancy, although the duration of male fertility following vas occlusion remains uncertain (Lewis et al., 1984). Sperm may be absent within I to 10 weeks or more after vasectomy, depending in part on the frequency of ejaculation (Liskin et al., 1983). The Association for Voluntary Sterilization recommends using contraceptives for the first 15 ejaculations or 6 weeks after vasectomy (Ross et al., 1985).
Most true vasectomy failures occur when fistulous tracks develop through a sperm granuloma, resulting in a spontaneous reanastomosis of the vas (Liskin et al., 1983). The reanastomosis usually occurs within several months after vasectomy, although late reanastomosis up to 3 years after vasectomy has been documented, both after ligation and coagulation methods. In a study of 14,047 men the wives of 6 men became pregnant between 16 months and 3 years after vasectomy (Philp et al., 1984). Other causes of vasectomy failure include operating on the wrong structure and congenital duplication of the vas (Liskin et al., 1983).
The risk of death attributable to vasectomy is quite low. A detailed review of sterilization-attributable deaths in Bangladesh occurring in 1979 and 1980 identified seven deaths attributable to vasectomy, for a vasectomy-attributable mortality rate of 31 per 100,000 procedures (Grimes et al., 1982a). Scrotal infection and sepsis caused most of the deaths. Subsequently, the use of sterile gloves during all vasectomies was recommended. Follow-up surveillance in 1981 identified no vasectomy-attributable deaths among approximately 14,000 men (Grimes et al., 1982b). The Association for Voluntary Sterilization has recorded only two vasectomy-attributable deaths associated with more than 160,000 procedures performed in the international programs it has supported (Ross et al., 1985). Vasectomy-attributable deaths in the United States are quite rare. While there has been no systematic effort to identify such deaths in the United States, at least one vasectomy-attributable death is known to have occurred (District Court of Appeals of Florida, Dunn v. Campbell, 1964).
The most common complications of vasectomy are swelling of the scrotal tissue, bruising, and pain. As many as 50 percent of men undergoing the procedure may experience these complaints, which generally subside within I to 2 weeks without treatment (Liskin et al., 1983). Hematoma formation and infection, which can be serious but generally are not, occur much less frequently.
Hematoma formation generally occurs in fewer than I percent of vasectomized men, but it has been reported in as many as 4 percent. Physicians surveyed in the United States in 1983 reported a hematoma rate of 2 percent (Kendrick et al., 1987). In that survey the hematoma rate was significantly higher among physicians performing I to 10 vasectomies per year (4.6 percent) than among those performing 11 to 50 vasectomies (2.4 percent) or more than 50 vasectomies (1.6 percent).
Infection after vasectomy is uncommon, usually occurring in fewer than 2 percent of men, although rates of infection as high as 6 percent have been reported (Liskin et al., 1983). Most infections occur at the site of skin incisions or around skin sutures. In rare instances, such as those reported in Bangladesh, infection can result in sepsis and death (Grimes et al., 1982a). Careful aseptic technique and sterile gloves are likely to reduce the risk of infection (Association for Voluntary Sterilization, 1983).
Epididymitis, manifested as swelling and tenderness of the epididymis, is generally reported in fewer than I percent of men undergoing vasectomy (Liskin et al., 1983). This complication has been attributed to a hydrostatic pressure increase within the epididymis after vas occlusion (Association for Voluntary Sterilization, 1983). Bacterial infection as an etiology of the epididymitis is uncommon (Schmidt, 1975). Epididymitis may develop several months after vasectomy, but it is most likely to occur soon after the procedure. Symptoms usually subside within a week (Ross et al., 1985). One report (Massey et al., 1984) compared vasectomized and nonvasectomized men with respect to the likelihood of developing epididymitis. After vasectomy, 2.6 percent of men experienced epididymitis versus 1.1 percent of men who had not had the procedure. However, differences between the two groups in the rate of epididymitis occurred only within the first year after vasectomy.
Sperm granulomas—nodules containing sperm, epithelial cells, and lymphocytes—represent an inflammatory response to sperm leaking into surrounding tissue. Most such granulomas are small and clinically not important, but they can result in pain at the site of vas occlusion or in the epididymis. The incidence of sperm granulomas is not known. However, granulomas at the vasectomy site have been found in 15 percent to 40 percent of sterilization reversal procedures; granulomas in the epididymis have been found in 10 percent to 50 percent of these procedures (Liskin et al., 1983). Symptomatic sperm granulomas are substantially less frequent. Follow-up studies report symptomatic granulomas in only 0 percent to 3 percent of vasectomies (Ross et al., 1985). In such instances a tender nodule at the site of vas occlusion or in the epididymis may cause discomfort, although the discomfort usually subsides spontaneously (Schmidt and Morris, 1973). As already noted, sperm granulomas can cause vasectomy failure if fistulous tracks develop through the granuloma. Ligation for vas occlusion is more likely to result in sperm granuloma formation than use of coagulation (Schmidt and Free, 1978). However, coagulation results in more complete occlusion of the vas, and this occlusion may increase the likelihood of an epididymal granuloma with resultant epididymal obstruction (Silber, 1978).
Long-Term Safety
A series of major epidemiologic investigations have been conducted in the 1980s to assess the long-term safety of vasectomy. In general, those studies are remarkably consistent in failing to identify any long-term health risks attributable to vasectomy.
Studies of long-term complications associated with vasectomy were stimulated primarily by two concerns: (1) evidence that 50 percent to 70 percent of men develop antisperm antibodies following vasectomy (Ansbacher, 1971; Schulman et al., 1972) and (2) reports of increased atherosclerosis in cynomolgus monkeys after vasectomy compared with nonvasectomized monkeys (Alexander et al., 1974). These findings are the basis for the hypothesis that antisperm antibodies form circulating immune complexes that might collect in arterial walls and contribute to the development of atherosclerosis (Alexander and Anderson, 1979). At least six epidemiologic studies specifically designed to assess this hypothesis have since indicated that vasectomy does not increase the incidence of MI in the 10 years following vasectomy (Goldacre et al., 1978, 1979; Walker et al., 1981; Petitti et al., 1982; Massey et al., 1984; Perrin et al., 1984). Subsequent to these reports, Rosenberg et al. (1986) evaluated data from a hospital-based, case-control study to assess whether vasectomy was associated with a subsequent increase in the risk of MI 10 or more years after surgery and whether any effect was more pronounced in men already predisposed to MI. The analysis supported findings from previous reports indicating that vasectomy did not increase the risk of MI within 10 years after surgery. Further, the authors found no overall increase in risk 10 or more years after surgery and no additional risk among men already predisposed to MI because of the presence of other risk factors for coronary artery disease. In summary, the available epidemiologic studies provide strong evidence that vasectomy does not increase the likelihood of MI.
As noted, much of the concern regarding the relationship between vasectomy and atherosclerosis was precipitated by reports of worsening atherosclerosis among vasectomized monkeys. Recently, the investigators who first reported this finding have presented data that do not support their first report. Their new data suggest that vasectomy does not increase the extent of atherosclerosis among cynomolgus monkeys, even in those found to be hyperresponsive to an atherogenic diet (Clarkson et al., 1988).
Several epidemiologic studies have assessed the relationship between vasectomy and a variety of other diseases associated with alterations of the immune system. In a historical cohort study conducted in the United States, 10,590 vasectomized men from four cities were interviewed, along with a neighborhood control for each vasectomized man (Massey et al., 1984). Any report of disease potentially related to vasectomy via an immunopathologic mechanism was validated by medical record review. Except for epididymitis/orchitis, the incidence of diseases, including those with a known or suspected immunopathologic basis, was similar for vasectomized men and paired controls. This finding was true not only for individual diseases but also for broader categories of diseases in which immunopathologic mechanisms might operate. Two other studies have failed to show an increase in the incidence of hospitalized illness for vasectomized men compared with nonvasectomized men (Walker et al., 1981; Petitti et al., 1982). The sole exception was that in one of the studies vasectomized men had higher rates of hospitalization for diseases of the genito-urinary system during the early postvasectomy period (Walker et al., 1981).
One recent report (Kronmal et al., 1988) raises additional concern regarding the relationship between vasectomy and subsequent genito-urinary tract disease by suggesting that vasectomy may increase the likelihood of urolithiasis. The age-adjusted relative risk for calculi among men who had undergone vasectomy was statistically significantly increased by approximately 70 percent. Although based on a study designed to evaluate the relationship between vasectomy and coronary artery disease, these findings are supported by another report mentioned previously (Walker et al., 1981). By contrast, another study found that the incidence of hospitalization for genito-urinary diseases was not significantly different between vasectomized and nonvasectomized men (Petitti et al., 1983). One possible biologic explanation for a relationship between vasectomy and urolithiasis centers around the production of antisperm antibodies. Whether antibody production might increase the tendency for formation of urinary calculi is not known. The possibility that vasectomized men may have an increased risk for genito-urinary disease warrants further evaluation, but available data are generally reassuring.
Vasectomy Reversal
Changes in life situation may lead men to regret their decision to undergo vasectomy. Surveys indicate that the prevalence of such regret worldwide is low (Liskin et al., 1983). Vasectomy reversal requires a high level of surgical expertise, is expensive, and is relatively unavailable in many parts of the world. Microsurgical techniques are necessary for optimal results. Furthermore, the original vasectomy technique may affect the likelihood of success of any subsequent reversal attempt. Because of the wide variety of factors influencing the likelihood of successful reversal, the success rate in the aggregate is difficult to estimate. Most surgeons report 30 percent to 60 percent success rates for vasectomy reversal, whereas some report even higher rates (Liskin et al., 1983). Even if the theoretical reversal rate remains consistently high, the technical difficulty of the surgery, with the attendant requirements for skilled microsurgeons, makes reversal impractical or unavailable for men in much of the world (Ross et al., 1985).
- Affandi, B., S. S. I. Santoso, Djajadilaga, et al. 1987. Pregnancy after removal of Norplant® implants contraceptive . Contraception 36:203–209. [ PubMed : 3123134 ]
- Alexander, N. J., and D. J. Anderson. 1979. Vasectomy: consequences of autoimmunity to sperm antigens . Fertility & Sterility 32:253–260. [ PubMed : 114428 ]
- Alexander, N. J., B. J. Wilson, and B. D. Patterson. 1974. Vasectomy: immunological effects on rhesus monkeys and men . Fertility & Sterility 25:149–156. [ PubMed : 4129871 ]
- Anonymous. 1986. Oral contraceptives and breast cancer . Lancet 2:665–666. [ PubMed : 2876138 ]
- Ansbacher, R. 1971. Sperm-agglutinating and sperm-immobilizing antibodies in vasectomized men . Fertility & Sterility 22:629–632. [ PubMed : 5115099 ]
- Association for Voluntary Sterilization. 1983. Minutes prepared for a Vasectomy Seminar . Science Committee, New York, June 6.
- Austin, H., W. C. Louv, and W. J. Alexander. 1984. A case-controlstudy of spermicides and gonorrhea . Journal of the American Medical Association 251:2822–2824. [ PubMed : 6716608 ]
- Baehler, E. A., W. P. Dillon, T. J. Cumbo, et al. 1982. Prolonged use of a diaphragm and toxic shock syndrome . Fertility & Sterility 38:248–250. [ PubMed : 7106318 ]
- Bain, C., C. H. Hennekens, F. E. Speizer, et al. 1982. Oral contraceptive use and malignant melanoma . Journal of the National Cancer Institute 68:537–539. [ PubMed : 6951070 ]
- Barlow, D. 1977. The condom and gonorrhea . Lancet 2:811–813. [ PubMed : 71612 ]
- Beral, V., S. Evans, H. Shaw, et al. 1984. Oral contraceptive use and malignant melanoma in Australia . British Journal of Cancer 50:681–685. [ PMC free article : PMC1976969 ] [ PubMed : 6498066 ]
- Bhiwandiwala, P. P., S. D. Mumford, and P. J. Feldblum. 1982. A comparison of different laparoscopic sterilization occlusion techniques in 24,439 procedures . American Journal of Obstetrics and Gynecology 144:319–331. 1983. Menstrual pattern changes following laparoscopic sterilization with different occlusion techniques: a review of 10,004 cases . American Journal of Obstetrics and Gynecology 145: 684–694.
- Bhiwandiwala, P. P., S. D. Mumford, and K. I. Kennedy. 1985. Comparison of the safety of open and conventional laparoscopic sterilization . Obstetrics and Gynecology 66:391–394. [ PubMed : 3160988 ]
- Bradley, D. D., J. Wingerd, D. B. Petitti, et al. 1978. Serum high density lipoprotein cholesterol in women using oral contraceptives, estrogens, and progestins . New England Journal of Medicine 299:17–20. [ PubMed : 207983 ]
- Brinton, L. A., M. P. Vessey, R. Flavel, et al. 1981. Risk factors for benign breast disease . American Journal of Epidemiology 113:203–214. [ PubMed : 7468579 ]
- Brinton, L. A., G. R. Huggins, H. F. Leham, et al. 1986. Long-term use of oral contraceptives and risk of invasive cervical cancer . International Journal of Cancer 38:339–344. [ PubMed : 3744592 ]
- The Cancer and Steroid Hormone Study of the Centers for Disease Control and the National Institute of Child Health and Human Development. 1986. Oral-contraceptive use and the risk of breast cancer . New England Journal of Medicine 315:405–411. [ PubMed : 3736618 ]
- The Cancer and Steroid Hormone Study of the Centers for Disease Control and the National Institute of Child Health and Human Development. 1987. a. Combination oral contraceptive use and the risk of endometrial cancer . Journal of the American Medical Association 257:796–800. [ PubMed : 3027423 ]
- The Cancer and Steroid Hormone Study of the Centers for Disease Control and the National Institute of Child Health and Human Development. 1987. b. The reduction in risk of ovarian cancer associated with oral-contraceptive use . New England Journal of Medicine 316:650–655. [ PubMed : 3821795 ]
- Celentano, D. D., A. C. Klassen, C. S. Weissman, et al. 1987. The role of contraceptive use in cervical cancer: the Maryland cervical cancer case-control study . American Journal of Epidemiology 126:592–604. [ PubMed : 3631051 ]
- Centers for Disease Control. 1987. Antibody to human immunodeficiency virus in female prostitutes . Morbidity and Mortality Weekly Report 36:157–161. 1988. Condoms for prevention of sexually transmitted diseases . Morbidity and Mortality Weekly Report 37: 133–137. [ PubMed : 3102921 ]
- Chamberlain, G., editor; , and J. C. Brown, editor. , eds. 1978. Gynaecological Laparoscopy: The Report of the Working Party of the Confidential Inquiry into Gynaecological Laparoscopy . London: The Royal College of Obstetricians and Gynaecologists.
- Chi, I.-C., and P. J. Feldblum. 1981. Luteal phase pregnancies in female sterilization patients . Contraception 23:10. [ PubMed : 7285577 ]
- Clarkson, T. B., N. J. Alexander, and T. M. Morgan. 1988. Atherosclerosisof cynomolgus monkeys hyper-and hyporesponsive to dietary cholesterol: lack of an effect of vasectomy . Arteriosclerosis 8:488–498. [ PubMed : 3190556 ]
- Cohen, M. M. 1987. Long-term risk of hysterectomy after tubal sterilization . American Journal of Epidemiology 125:410–419. [ PubMed : 3812448 ]
- Conant, M. A., D. W. Spicer, and C. D. Smith. 1984. Herpes simplex virus transmission: condom studies . Sexually Transmitted Diseases 11:94–95. [ PubMed : 6087482 ]
- Conant, M., D. Hardy, J. Sematinger, et al. 1986. Condoms prevent transmission of AIDS-associated retrovirus . Journal of the American Medical Association 255:1706. [ PubMed : 3005677 ]
- Cordero, J. F., and P. M. Layde. 1983. Vaginal spermicides, chromosomal abnormalities and limb reduction defects . Family Planning Perspective 15:16. [ PubMed : 6680698 ]
- Cowan, M. E., and G. E. Cree. 1973. A note on the susceptibility of N. gonorrhoeae to contraceptive agent Nonyl-P . British Journal of Venereal Diseases 49:65–66. [ PMC free article : PMC1044854 ] [ PubMed : 4632811 ]
- Cramer, D. W., I. Schiff, S. C. Schoenbaum, et al. 1985. Tubal infertility and the intrauterine device . New England Journal of Medicine 312:941–947. [ PubMed : 3974684 ]
- Cramer, D. W., M. B. Goldman, I. Schiff, et al. 1987. The relationship of tubal infertility to barrier method and oral contraceptive use . Journal of the American Medical Association 257:2446–2450. [ PubMed : 3573242 ]
- Daling, J. R., N. S. Weiss, B. J. Metch, et al. 1985. Primary tubal infertility in relation to the use of an intrauterine device . New England Journal of Medicine 312:937–941. [ PubMed : 3974683 ]
- DeStefano, F., H. B. Peterson, P. M. Layde, et al. 1982. Risk of ectopic pregnancy following tubal sterilization . Obstetrics and Gynecology 60:326–330. [ PubMed : 7121914 ]
- DeStefano, F., J. R. Greenspan, R. C. Dicker, et al. 1983. a. Complications of interval laparoscopic tubal sterilization . Obstetrics and Gynecology 61:153–158. [ PubMed : 6218431 ]
- DeStefano, F., C. M. Huezo, H. B. Peterson, et al. 1983. b. Menstrual changes after tubal sterilization . Obstetrics and Gynecology 62:673–681. [ PubMed : 6633993 ]
- DeStefano, F., J. A. Perlman, H. B. Peterson, et al. 1985. Long-term risk of menstrual disturbances after tubal sterilization . American Journal of Obstetrics and Gynecology 152:835–841. [ PubMed : 4040707 ]
- Diaz, S., M. Pavez, P. Miranda, et al. 1987. Long-term follow-up of women treated with Norplant TM implants . Contraception 35:551–567. [ PubMed : 3117490 ]
- District Court of Appeals of Florida. 1964. Dunn v. Campbell , Florida, 166 SO. 2d217. July 1, Second District.
- Ebeling, K., P. Nischan, and C. Schindler. 1987. Use of oral contraceptives and risk of invasive cervical cancer in previously screened women . International Journal of Cancer 39:427–430. [ PubMed : 3557701 ]
- Faich, G., K. Pearson, D. Fleming, et al. 1986. Toxic shock syndrome and the vaginal contraceptive sponge . Journal of the American Medical Association 255:216–218. [ PubMed : 3001376 ]
- Feldblum, P. J., and J. A. Fortney. 1988. Condoms, spermicides, and the transmission of human immunodeficiency virus: a review of the literature . American Journal of Public Health 78:52–54. [ PMC free article : PMC1349207 ] [ PubMed : 3276230 ]
- Fihn, S. D., R. H. Latham, P. Roberts, et al. 1985. Association between diaphragm use and urinary tract infection . Journal of the American Medical Association 254:240–245. [ PubMed : 3999367 ]
- Fischl, M. A., G. M. Dickinson, G. B. Scott, et al. 1987. Evaluation of heterosexual partners, children, and household contacts of adults with AIDS . Journal of the American Medical Association 257:640–644. [ PubMed : 3467077 ]
- Forman, D., T. J. Vincent, and R. Doll. 1986. Cancer of the liver and the use of oral contraceptives . British Medical Journal 292:1357–1361. [ PMC free article : PMC1340367 ] [ PubMed : 3011186 ]
- Fortney, J. A., L. P. Cole, and K. I. Kennedy. 1983. A new approach to measuring menstrual pattern change after sterilization . American Journal of Obstetrics and Gynecology 147:830–836. [ PubMed : 6650607 ]
- Fotherby, K., I. Trayner, I. Howard, et al. 1982. Effect of injectable norethisterone oenanthate (Norigest) on blood lipid levels . Contraception 25:435–446. [ PubMed : 6955136 ]
- Foulkes, J., and G. Chamberlain. 1985. Effects of sterilization on menstruation . Southern Medical Journal 78:544. [ PubMed : 3992301 ]
- Foxman, B., and R. R. Frerichs. 1985. Epidemiology of urinary tract infections. I: Diaphragm use and sexual intercourse . American Journal of Public Health 75:1308–1313. [ PMC free article : PMC1646718 ] [ PubMed : 4051066 ]
- Francis, D. P., and J. Chin. 1987. The prevention of acquired immunodeficiency syndrome in the United States . Journal of the American Medical Association 257:1357–1366. [ PubMed : 3546744 ]
- Gallen, M. E., L. Liskin, and N. Kak. 1986. Men—new focus for family planning programs . Population Reports Series J, No. 33. [ PubMed : 3582720 ]
- Goldacre, M. J., J. A. Clarke, M. A. Heasman, et al. 1978. Followup of vasectomy using medical record linkage . American Journal of Epidemiology 108:176–180. [ PubMed : 707485 ]
- Goldacre, M., M. Vessey, J. Clarke, et al. 1979. Record linkage study of morbidity following vasectomy . Pp. 567–579 in I. H. Lepow, editor; and R. Crozier, editor. , eds. Vasectomy: Immunologic and Pathophysiologic Effects in Animals and Man . New York: Academic Press.
- Gray, R. H. 1985. Reduced risk of pelvic inflammatory disease with injectable contraceptives . Lancet 1:1046. [ PubMed : 2859496 ]
- Grimes, D. A. 1987. Intrauterine devices and pelvic inflammatory disease: recent developments . Contraception 36:97–109. [ PubMed : 3311628 ]
- Grimes, D. A., H. B. Peterson, M. J. Rosenberg, et al. 1982. a. Sterilization-attributable deaths in Bangladesh . International Journal of Gynaecology and Obstetrics 20:149–154. [ PubMed : 6125437 ]
- Grimes D. A., A. P. Satterthwaite, R. W. Rochat, et al. 1982. b. Deaths from contraceptive sterilization in Bangladesh: rates, causes, and prevention . Obstetrics and Gynecology 60:635–640. [ PubMed : 7145254 ]
- Grubb, G. S., and H. B. Peterson. 1985. Luteal phase pregnancy and tubal sterilization . Obstetrics and Gynecology 66:784–788. [ PubMed : 4069479 ]
- Grubb, G. S., H. B. Peterson, P. M. Layde, et al. 1985. Regret after decision to have a tubal sterilization . Fertility & Sterility 44:248–253. [ PubMed : 4018280 ]
- Gwinn, M. L., N. C. Lee, P. H. Rhodes, et al. n.d. Pregnancy, breast feeding, and oral contraceptives and the risk of epithelial ovarian cancer . Journal of Clinical Epidemiology . (Submitted for publication) [ PubMed : 2348208 ]
- Harris, R. W. C., L. A. Brinton, R. H. Cowdell, et al. 1980. Characteristics of women with dysplasia or carcinoma in situ of the cervix uteri . British Journal of Cancer 42:359–369. [ PMC free article : PMC2010409 ] [ PubMed : 7426342 ]
- Hatcher, R. A., F. Guest, F. Stewart, et al. 1988. Contraceptive technology: 1988–1989 . New York: Printed Matter, Inc./Irvington Publisher, Inc.
- Heartwell, S. F., and S. Schlesselman. 1983. Risk of uterine perforation among users of intrauterine devices . Obstetrics and Gynecology 61:31–36. [ PubMed : 6823347 ]
- Henderson, B. E., S. Preston-Martin, H. A. Edmondson, et al. 1983. Hepatocellular carcinoma and oral contraceptives . British Journal of Cancer 48:437–440. [ PMC free article : PMC2011476 ] [ PubMed : 6311235 ]
- Henshaw, S. K., and S. Singh. 1986. Sterilization regret among U.S. couples . Family Planning Perspectives 18:238–240. [ PubMed : 3803559 ]
- Hicks, D. R., L. S. Martin, J. P. Getchell, et al. 1985. Inactivation of HTLV-III/LAV-infected cultures of normal human lymphocytes by nonoxynol-9 in vitro . Lancet 1422–1423. [ PubMed : 2867413 ]
- Holly, E. A., N. S. Weiss, and J. M. Liff. 1983. Cutaneous melanomain relation to exogenous hormones and reproductive factors . Journal of the National Cancer Institute 70:827–831. [ PubMed : 6573527 ]
- Hooper, R. R., G. H. Reynolds, O. G. Jones, et al. 1978. Cohort study of venereal disease. I. The risk of gonorrhea transmission from infected women to men . American Journal of Epidemiology 108:136–144. [ PubMed : 707474 ]
- Horsburgh, C. R., J. M. Douglas, and F. M. LaForce. 1987. Preventive strategies in sexually transmitted diseases for the primary care physician . Journal of the American Medical Association 258:815–821. [ PubMed : 3039185 ]
- Huggins, G., M. Vessey, R. Flavel, et al. 1982. Vaginal spermicides and outcome of pregnancy: findings in a large cohort study . Contraception 25:219. [ PubMed : 7075194 ]
- Hulka, J. F., H. B. Peterson, M. Surrey, et al. 1987. American Association of Gynecologic Laparoscopists' 1985 membership survey . Journal of Reproductive Medicine 32:732–735. [ PubMed : 2960806 ]
- Hymowitz, E. E. 1981. Toxic shock syndrome and the diaphragm . New England Journal of Medicine 305:834. [ PubMed : 7266642 ]
- Indian Council of Medical Research. 1982. Collaborative Study on Sequelae of Tubal Sterilization . Monograph. New Delhi.
- Irwin. K. L., L. Rosero-Bixby, M. W. Oberle, et al. 1988. Oral contraceptives and cervical cancer risk in Costa Rica: Detection bias or causal association? Journal of the American Medical Association 259:59–64. [ PubMed : 3334773 ]
- Jick, H., A. M. Walker, K. J. Rothman, et al. 1981. Vaginal spermicides and congenital disorders . Journal of the American Medical Association 245:1329–1332. [ PubMed : 7206132 ]
- Jick, H., M. T. Hannan, A. Stergachis, et al. 1982. Vaginal spermicides and gonorrhea . Journal of the American Medical Association 248:1619–1621. [ PubMed : 6809970 ]
- Judson, F. N., J. M. Enret, G. M. Bodin, et al. in press. In vitro evaluations of condoms with and without nonoxynol-9 as physical and chemical barriers against Chlamydia trachomatis, herpes simplex virus type 2, and human immunodeficiency virus . Sexually Transmitted Diseases (Suppl.) [ PubMed : 2545003 ]
- Katznelson, S., W. L. Drew, and L. Mintz. 1984. Efficacy of the condom as a barrier to the transmission of cytomegalo virus . Journal of Infectious Diseases 150:155–157. [ PubMed : 6086770 ]
- Kelaghan, J., G. L. Rubin, H. W. Ory, et al. 1982. Barrier-methodcontraceptives and pelvic inflammatory disease . Journal of the American Medical Association 248:184–187. [ PubMed : 7087109 ]
- Kendrick, J. S., E. P. Rhodenhiser, G. L. Rubin, et al. 1985. Characteristics of vasectomy performed in selected outpatient facilities in the United States, 1980 . Journal of Reproductive Medicine 30:936–938. [ PubMed : 4078830 ]
- Kendrick, J. S., B. Gonzales, D. H. Huber, et al. 1987. Complications of vasectomy in the United States . Journal of Family Practice 25:245–248. [ PubMed : 3625140 ]
- Kronmal, R. A., J. N. Krieger, J. W. Kennedy, et al. 1988. Vasectomy and urolithiasis . Lancet 1:22–23. [ PubMed : 2891890 ]
- Layde, P. M., M. P. Vessey, and D. Yeates. 1982. Risk factors for gallbladder disease: a cohort study of young women attending family planning clinics . Journal of Epidemiology and Community Health 36:274–278. [ PMC free article : PMC1052232 ] [ PubMed : 7166683 ]
- Lee, N. C., L. Rosero-Bixby, M. W. Oberle, et al. 1987. A case-control study of breast cancer and hormonal contraception in Costa Rica . Journal of the National Cancer Institute 79:1247–1254. [ PubMed : 2961909 ]
- Lee, N. C., G. L. Rubin, and R. Borucki. 1988. The intrauterine device and pelvic inflammatory disease revisited: new results from the Women's Health Study . Obstetrics and Gynecology 72:1–6. [ PubMed : 3380496 ]
- Lewis, E. L., C. K. Brazil, and J. W. Overstreet. 1984. Human sperm function in the ejaculate following vasectomy . Fertility & Sterility 42:895–898. [ PubMed : 6542030 ]
- Liang, A. P., A. G. Levenson, P. M. Layde, et al. 1983. Risk of breast, uterine corpus, and ovarian cancer in women receiving medroxypro-gesterone injections . Journal of the American Medical Association 249:2909–2912. [ PubMed : 6842804 ]
- Liskin, L., and G. Fox. 1982. IUDS: an appropriate contraceptive for many women . Population Reports Series B, No. 4. [ PubMed : 7117675 ]
- Liskin, L., and W. F. Quillin. 1982. Long-acting progestins: promise and prospects . Population Reports Series K, No. 2.
- Liskin, L, J. M. Pile, and W. F. Quillin. 1983. Vasectomy—safe and simple . Population Reports Series D, No. 4.
- Liskin, L., W. Rinehart, R. Blackburn, et al. 1985. Minilaparotomy and laparoscopy: safe, effective and widely used . Population Reports Series C, No. 9. [ PubMed : 3158564 ]
- Liskin, L., R. Blackburn, and R. Ghani. 1987. Hormonal contraception: new long-acting methods . Population Reports Series K, No. 3. [ PubMed : 3111901 ]
- Lunt, R. 1984. Worldwide early detection of cervical cancer . Obstetrics and Gynecology 63:708–713. [ PubMed : 6717875 ]
- Mann, J., T. C. Quinn, and P. Piot. 1987. Condom use and HIV infection among prostitutes—Zaire (Letter) . New England Journal of Medicine 316:345. [ PubMed : 3807969 ]
- Massey, F. J., G. S. Bernstein, W. M. O'Fallon, et al. 1984. Vasectomy and health: results from a large cohort study . Journal of the American Medical Association 252:1023–1029. [ PubMed : 6748206 ]
- McPherson, K., and J. O. Drife. 1986. The pill and breast cancer: Why the uncertainty? British Medical Journal 293:709–710. [ PMC free article : PMC1341438 ] [ PubMed : 3094619 ]
- McPherson, K., A. Neil, M. P. Vessey, et al. 1983. Oral contraceptives and breast cancer . Lancet 2:1414–1415. [ PubMed : 6140506 ]
- McPherson, K., P. A. Coope, and M. P. Vessey. 1986. Early oral contraceptive use and breast cancer: theoretical effects of latency . Journal of Epidemiology and Community Health 40:289–294. [ PMC free article : PMC1052548 ] [ PubMed : 3655620 ]
- Meirik, O., E. Lund, H.-O. Adami, et al. 1986. Oral contraceptive use and breast cancer in young women . Lancet 2:650–654. [ PubMed : 2876135 ]
- Mills, J. L., E. E. Harley, G. F. Reed, et al. 1982. Are spermicides teratogenic? Journal of the American Medical Association 248:2148. [ PubMed : 7120641 ]
- Mintz, M. 1977. Risk and prophylaxis in laparoscopy: a survey of 100,000 cases . Journal of Reproductive Medicine 18:269–272. [ PubMed : 141517 ]
- Mumford, S. D., P. P. Bhiwandiwala, and I.-C. Chi. 1980. Laparoscopic and minilaparotomy female sterilization compared in 15,167 cases . Lancet 2:1066–1070. [ PubMed : 6107689 ]
- National Center for Health Statistics. 1982. Vital Statistics of the United States . Vol. 2. Mortality Part A. Hyattsville, Md.: NationalCenter for Health Statistics.
- Neuberger, J., D. Forman, R. Doll, et al. 1986. Oral contraceptives and hepatocellular carcinoma . British Medical Journal 292:1355–1357. [ PMC free article : PMC1340366 ] [ PubMed : 3011185 ]
- Oberle, M. W., L. Rosero-Bixby, K. L. Irwin, et al. 1988. Cervical cancer risk and use of depot-medroxyprogesterone acetate in Costa Rica . International Journal of Epidemiology 17:718–723. [ PubMed : 2976059 ]
- Ory, H. W. 1981. The Women's Health Study. Ectopic pregnancy and intrauterine contraceptive devices: new perspectives . Obstetrics and Gynecology 57:137–144. [ PubMed : 7465116 ]
- 1982. The noncontraceptive health benefits from oral contraceptive use . Family Planning Perspective 14:182–184. [ PubMed : 7117506 ]
- Ory, H. W., J. D. Forrest, and R. Lincoln. 1983. Making Choices: Evaluating the Health Risks and Benefits of Birth Control Methods . New York: The Alan Guttmacher Institute.
- Pardthaisong, T., R. H. Gray, and E. B. McDaniel. 1980. Return of fertility after discontinuation of depot-medroxyprogesterone acetate and intra-uterine devices in Northern Thailand . Lancet 1:509–512. [ PubMed : 6102234 ]
- Pasquale, S. A., V. Brandeis, R. I. Cruz, et al. 1987. Norplant TM contraceptive implants: rods versus capsules . Contraception 36:305–316. [ PubMed : 3119287 ]
- Paul, C., D. C. G. Skegg, G. F. S. Spears, et al. 1986. Oral contraceptives and breast cancer: a national study . British Journal of Medicine 293:723–726. [ PMC free article : PMC1341446 ] [ PubMed : 3094626 ]
- Perrin, E. B., J. S. Woods, and N. Tsukasu, et al. 1984. Long-term effect of vasectomy on coronary heart disease . American Journal of Public Health 74:128–132. [ PMC free article : PMC1651398 ] [ PubMed : 6691522 ]
- Peterson, H. B., H. W. Ory, J. R. Greenspan, et al. 1981. a. Deaths associated with laparoscopic sterilization by unipolar coagulating devices, 1978–1979 . American Journal of Obstetrics and Gynecology 139:141. [ PubMed : 6450536 ]
- Peterson, H. B., D. A. Grimes, W. Cates, et al. 1981. b. Comparative risk of death from induced abortion at 12 weeks gestation performed with local vs. general anesthesia . American Journal of Obstetrics and Gynecology 141:763. [ PubMed : 7315903 ]
- Peterson, H. B., F. DeStefano, J. R. Greenspan, et al. 1982. a. Mortality risk associated with tubal sterilization in United States hospitals . American Journal of Obstetrics and Gynecology 143:125–129. [ PubMed : 7081321 ]
- Peterson, H. B., J. R. Greenspan, and H. W. Ory. 1982. b. Death following puncture of the aorta during laparoscopic sterilization . Obstetrics and Gynecology 59:133. [ PubMed : 6210865 ]
- Peterson, H. B., F. DeStefano, G. L. Rubin, et al. 1983. Deaths attributable to tubal sterilization in the United States, 1977–1981 . American Journal of Obstetrics and Gynecology 146:131–136. [ PubMed : 6846428 ]
- Petitti, D. B., R. Klein, H. Kipp, et al. 1982. A survey of personal habits, symptoms of illness, and histories of disease in men with and without vasectomies . American Journal of Public Health 72:476–480. [ PMC free article : PMC1649776 ] [ PubMed : 7065336 ]
- Petitti, D. B., R. Klein, H. Kipp, et al. 1983. Vasectomy and the incidence of hospitalized illness . Journal of Urology 129:760–762. [ PubMed : 6842696 ]
- Philp, T., J. Guillebaud, and B. Budd. 1984. Late failure of vasectomy after 2 documented analyses showing azoospermic semen . British Medical Journal 289:77–79. [ PMC free article : PMC1441962 ] [ PubMed : 6428685 ]
- Pike, M. C., B. E. Henderson, M. D. Krailo, et al. 1983. Breast cancerin young women and the use of oral contraceptives: possible modifying effects of formulation and age at use . Lancet 2:926–930. [ PubMed : 6138501 ]
- Piotrow, P. T., W. Rinehart, and J. C. Schmidt. 1979. IUDs—update on safety, effectiveness, and research . Population Reports Series B, No. 3.
- Piper, J. N. 1985. Oral contraceptives and cervical cancer . Gynecologic Oncology 22:1–14. [ PubMed : 3894173 ]
- Prentice, R. L., and D. B. Thomas. 1987. On the epidemiology of oral contraceptives and disease . Advances in Cancer Research 49:285–401. [ PubMed : 3314396 ]
- Quinn, R. W., and K. R. O'Reilly. 1985. Contraceptive practices of women attending the sexually transmitted diseases clinic in Nashville, Tennessee . Sexually Transmitted Diseases 12:99–102. [ PubMed : 4035523 ]
- Ramcharan, S., F. A. Pellegrin, R. Ray, et al. 1981. The Walnut Creek contraceptive drug study. A prospective study of the side effects of oral contraceptives , Vol. III. Washington, D.C.: U.S. Government Printing Office. [ PubMed : 7205804 ]
- Reingold, A. L. 1986. Toxic shock syndrome and the contraceptive sponge . Journal of the American Medical Association 255:242–243. [ PubMed : 3941504 ]
- Rietmeijer, C. A. M., J. W. Krebs, P. M. Feorino, et al. 1988. Condoms as physical and chemical barriers against human immunodeficiency virus . Journal of the American Medical Association 259:1851–1853. [ PubMed : 2830416 ]
- Rooks, J. B., H. W. Ory, K. G. Ishak, et al. 1979. Epidemiology of hepatocellular adenoma: the role of oral contraceptive use . Journal of the American Medical Association 242:644–648. [ PubMed : 221698 ]
- Rosenberg, L., P. J. Schwingel, D. W. Kaufmann, et al. 1986. The risk of myocardial infarction 10 or more years after vasectomy in men under 55 years of age . American Journal of Epidemiology 123:1049–1056. [ PubMed : 3706275 ]
- Rosenberg, M. J., W. Rojanapithayakom, P. J. Feldblum, and J. E. Higgins. 1987. Effect of the contraceptive sponge on chlamydial infection, gonorrhea, and candidiasis . Journal of the American Medical Association 257:2308–2312. [ PubMed : 3033339 ]
- Rosenfield, A., D. Maine, R. Rochat, et al. 1983. The Food and Drug Administration and medroxyprogesterone acetate . Journal of the American Medical Association 249:2922–2928. [ PubMed : 6221125 ]
- Ross, J. A., and D. H. Huber. 1983. Acceptance and prevalence of vasectomy in developing countries . Studies in Family Planning 14:67–72. [ PubMed : 6845390 ]
- Ross, J. A., S. Hong, and D. H. Huber. 1985. Voluntary Sterilization: An International Fact Book . New York: Association for Voluntary Sterilization.
- Ross, R. K., M. C. Pike, M. P. Vessey, et al. 1986. Risk factors for uterine fibroids: reduced risk associated with oral contraceptives . British Medical Journal 293:359–362. [ PMC free article : PMC1341047 ] [ PubMed : 3730804 ]
- Royal College of General Practitioners. 1970. Oral contraceptives and health . London: Pitman Medical.
- Royal College of General Practitioners Oral Contraception Study. 1982. Oral contraceptives in gallbladder disease . Lancet ; 2:957–959.
- Rubin, G. L., H. W. Ory, and P. M. Layde. 1982. Oral contraceptives and pelvic inflammatory disease . American Journal of Obstetrics and Gynecology 144:630–635. [ PubMed : 7137247 ]
- Ryden, G., L. Fahraeus, L. Molin, et al. 1979. Do contraceptives influence the incidence of acute pelvic inflammatory disease in women with gonorrhea? Contraception 20:149–157. [ PubMed : 114354 ]
- Salah, M., A. M. Ahmed, M. Abo-Eloyoun, et al. 1987. Five-year experience with Norplant TM implants in Assiut, Egypt . Contraception 35:543–550. [ PubMed : 3117489 ]
- Schlesselman, J. J., B. V. Stadel, P. Murray, et al. 1987. Consistency and plausibility in epidemiologic analyses: application to breast cancer in relation to use of oral contraceptives . Journal of Chronic Diseases 40:1033–1039. 1988. Breast cancer in relation to early use of oral contraceptives: no evidence of a latent effect . Journal of the American Medical Association 259: 1828–1833. [ PubMed : 3654903 ]
- Schmidt, S. S. 1975. Complications of vas surgery . Pp. 78–88 in J. J. Sciarra, editor; , C. Markland, editor; , and J. J. Speidel, editor. , eds. Control of Male Fertility . Hagerstown, Md.: Harper & Row.
- Schmidt, S. S., and N. J. Free. 1978. The bipolar needle for vasectomy . 1. Experience with the first 1,000 cases. Fertility & Sterility 29:676–680. [ PubMed : 658480 ]
- Schmidt, S. S., and R. R. Morris. 1973. Spermatic granuloma: the complication of vasectomy . Fertility & Sterility 24:941–947. [ PubMed : 4758641 ]
- Schulman, S., E. Zappi, U. Ahmed, et al. 1972. Immunologic consequences of vasectomy . Contraception 5:269–278. [ PubMed : 4650652 ]
- Schwartz, B., S. Gaventa, C. V. Broome, et al. 1989. Nonmenstrual toxic shock syndrome associated with barrier contraceptives: report of a case-control study . Review of Infectious Diseases 11(Suppl. 1):S43–S49. [ PubMed : 2928652 ]
- Shain, R. N., W. B. Miller, and A. E. C. Holden. 1986. Married women's dissatisfaction with tubal sterilization and vasectomy at first-year follow-up: effects of perceived spousal dominance . Fertility & Sterility 45:808–819. [ PubMed : 3709829 ]
- Shapiro, S., D. Slone, O. P. Heinonen, et al. 1982. Birth defects and vaginal spermicides . Journal of the American Medical Association 247:2381. [ PubMed : 6279895 ]
- Sherris, J. D., S. H. Moore, and G. Fox. 1984. New developments in vaginal contraception . Population Reports Series H, No. 7. [ PubMed : 6321270 ]
- Silber, S. J. 1978. Vasectomy and vasectomy reversal . Fertility & Sterility 29:125–140. [ PubMed : 342283 ]
- Singh, B., J. C. Cutler, and A. M. Utidjian. 1972. II. Effect in vitro of vaginal contraceptive and noncontraceptive preparation on Treponema pallidum and Neisseria gonorrhoeae . British Journal of Venereal Diseases 48:57–64. [ PMC free article : PMC1048272 ] [ PubMed : 4622671 ]
- Singh, B., B. Postic, and J. C. Cutler. 1976. Virucial effect of certain chemical contraceptives on type 2 herpes virus . American Journal of Obstetrics and Gynecology 126:422–425. [ PubMed : 984103 ]
- Sivin, I., and J. Stern. 1979. Long acting, more effective Copper T IUD's: a summary of U.S. experience, 1970-1975 . Studies in Family Planning 10:263–281. [ PubMed : 516121 ]
- Skegg, D. C. 1988. Potential for bias in case-control studies of oral contraceptives and breast cancer . American Journal of Epidemiology 127:205–212. [ PubMed : 3276164 ]
- Smith, G. L., and K. F. Smith. 1986. Lack of HIV infection and condom use in licensed prostitutes (Letter) . Lancet 2:1392. [ PubMed : 2878245 ]
- Spring, S. B., and J. Gruber. 1985. Relationship of DNA viruses and cervical carcinoma . Journal of the National Cancer Institute 75:589–590.
- Stadel, B. 1986. Oral contraceptives and the occurrence of disease: clinical overview . Pp. 3–41 in A. T. Gregoire, editor; and R. G. Blye, editor. , eds. Contraceptive Steroids—Pharmacology and Safety . New York: Plenum Press.
- Stadel, B. V., G. L. Rubin, L. A. Webster, et al. 1985. Oral contraceptives and breast cancer in young women . Lancet 2:970–973. [ PubMed : 2865503 ]
- Stone, K. M., D. A. Grimes, and L. S. Magder. 1986. Personal protection against sexually transmitted diseases . American Journal of Obstetrics and Gynecology 155:180–188. [ PubMed : 3524240 ]
- Sun, M. 1984. Panel says Depo-Provera not proved safe . Science 226:950–951. [ PubMed : 6239373 ]
- Swan, S. H., and D. B. Petitti. 1982. A review of problems of bias and confounding in epidemiologic studies of cervical neoplasia and oral contraceptives . American Journal of Epidemiology 115:10–18. [ PubMed : 7034529 ]
- Swenson, I., A. R. Khan, and F. A. Jahan. 1980. A randomized, single blind comparative trial of norethindrone enanthate and depot-medroxyprogesterone acetate in Bangladesh . Contraception 2:207–215. [ PubMed : 6446442 ]
- Treiman, K., and L Liskin 1988. IUDs—a new look . Population Reports Series B, No. 5.
- Trussell, J., and K. Kost. 1987. Contraceptive failure in the United States: a critical review of the literature . Studies in Family Planning 18:237–283. [ PubMed : 3318006 ]
- Vessey, M. P. 1980. Female hormones and vascular disease—an epidemiological overview . British Journal of Family Planning 6:1–12.
- Vessey, M. P., N. H. Wright, K. McPherson, et al. 1978. Fertility after stopping different methods of contraception . British Medical Journal (6108) February:265–267. [ PMC free article : PMC1602681 ] [ PubMed : 620301 ]
- Vessey, M. P., D. Yeates, R. Flavel, et al. 1981. Pelvic inflammatory disease and the intrauterine device: findings in a large cohort study . British Medical Journal 282:855–857. [ PMC free article : PMC1504676 ] [ PubMed : 6783202 ]
- Vessey, M., G. Huggins, M. Lawless, et al. 1983. Tubal sterilization: findings in a large prospective study . British Journal of Obstetrics and Gynaecology 90:203–209. [ PubMed : 6830727 ]
- Vessey, M. P., M. A. Metcalfe, K. McPherson, et al. 1987. Urinary tract infection in relation to diaphragm use and obesity . International Journal of Epidemiology 16:441–444. [ PubMed : 3667045 ]
- Walker, A. M., H. Jick, J. R. Hunter, et al. 1981. Vasectomy and nonfatal myocardial infarction . Lancet 1: 13–15. [ PubMed : 6109049 ]
- Washington, A. E., S. Gove, J. Schachter, et al. 1985. Oral contraceptives, chlamydia trachomatis infection, and pelvic inflammatory disease: a word of caution about protection . Journal of the American Medical Association 253:2246–2250. [ PubMed : 3974117 ]
- Weiss, N. S. 1982. Ovary . Pp. 871–880 in D. Schottenfeld, editor; and J. F. Fraumeni, Jr., editor. , eds. Cancer Epidemiology and Prevention . Philadelphia: W. B. Saunders.
- Westrom, L. 1987. Pelvic inflammatory disease. Bacteriology and sequelae . Contraception 36:111–128. [ PubMed : 3311621 ]
- World Federation of Health Agencies for the Advancement of Voluntary Surgical Contraception. 1984. Safety of Voluntary Surgical Contraception . New York.
- World Health Organization Task Force on Long-Acting Systemic Agents for the Regulation of Fertility. 1978. Multinational comparativeclinical evaluation of two long-acting injectable contraceptive steroids: norethisterone oenanthate and medroxyprogesterone acetate. 2. Bleeding patterns and side effects . Contraception 17:395–406. [ PubMed : 657807 ]
- World Health Organization Task Force on Female Sterilization. 1982. a. Minilaparotomy or laparoscopy for sterilization: a multicenter, multinational randomized study . American Journal of Obstetrics and Gynecology 143:645–652. [ PubMed : 6211987 ]
- World Health Organization Task Force on Female Sterilization. 1982. b. Randomized comparative study of culdoscopy and minilaparotomy for surgical contraception in women . Contraception 26:587–593. [ PubMed : 6762946 ]
- World Health Organization. 1986. a. Depot-medroxyprogesterone (DMPA) and cancer: memorandum from a WHO meeting . Bulletin of the World Health Organization 64:375–382. [ PMC free article : PMC2490874 ] [ PubMed : 2945666 ]
- World Health Organization Task Force on Long-acting Agents for Fertility Regulation. 1986. b. Metabolic side-effects of injectable depot-medroxyprogesterone acetate, 150mg three-monthly, in undernourished lactating women . Bulletin of the World Health Organization 64:587–594. [ PMC free article : PMC2490899 ] [ PubMed : 3490928 ]
- World Health Organization Task Force on Long-Acting Systemic Agents for Fertility Regulation. 1987. A multicentered phase III comparative clinical trial of depot-medroxyprogesterone acetate given three-monthly as doses of 100mg or 150mg: II . The comparison of bleeding patterns. Contraception 35:591–610. [ PubMed : 2959448 ]
- Wright, N. H., M. P. Vessey, B. Kenward, et al. 1978. Neoplasia and dysplasia of the cervix uteri and contraception: a possible protective effect of the diaphragm . British Journal of Cancer 38:273–279. [ PMC free article : PMC2009729 ] [ PubMed : 698042 ]
Nancy C. Lee and Herbert B. Peterson are deputy chief and chief, respectively, of the Epidemiologic Studies Branch, Division of Reproductive Health, Center for Chronic Disease Prevention and Health Promotion of the Centers for Disease Control. Susan Y. Chu is epidemiologist in the Special Projects Section, Surveillance Branch, AIDS Program, Center for Infectious Diseases, of the Centers for Disease Control.
- Cite this Page National Research Council (US) Committee on Population; Parnell AM, editor. Contraceptive Use and Controlled Fertility: Health Issues for Women and Children Background Papers. Washington (DC): National Academies Press (US); 1989. Health Effects of Contraception.
- PDF version of this title (2.5M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Health Effects of Contraception - Contraceptive Use and Controlled Fertility Health Effects of Contraception - Contraceptive Use and Controlled Fertility
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
The AMPOWER study was a multicenter, single-arm, open-label, phase 3 study of 1,384 women, of which 1,114 were included in the primary efficacy analysis. 7 In this study, the intravaginal gel demonstrated 86.3% contraceptive efficacy with typical use (as opposed to preliminary studies submitted to the US Food and Drug Administration [FDA] that ...
No method of contraception apart from condoms protects against STIs., and she may need a check-up at a sexual health clinic. In 2013, more than 1.7 million chlamydia tests were carried out in England among young people aged 15-24 years, ... Invited to return if she has any concerns or problems with the contraception. Case study 3: risk of ...
Contraception is widely used in the United States, with an estimated 88.2% of all women ages 15 to 44 years using at least one form of contraception during their lifetime. 1 Among women who could become pregnant but don't wish to do so, 90% use some form of contraception. 2 Thus, nurses in various settings are likely to encounter patients who are using contraception while presenting for a ...
2. In the 65% of women aged 15 to 49 years using contraception, sterilization is used by 18.6%, oral contraceptive pill by 12.6%, and male condoms by 8.7%. 14. Injections and CHC (including estrogen and progestin pills, ring, and patch) have failure rates of 6% to 9% with typical use. 2.
Contraception for adolescents. Objectives. The rate of births among adolescents in the United States is four times higher than in western Europe, accounting for 13% of all births in the United States. 1, 2 Between 1985 and 1990 the cost to the public of teenage child-bearing was $120 billion. 3 The age-specific levels of sexual activity are ...
INTRODUCTION — The choice of a contraceptive method is a complex decision; medical providers have an important role in providing information and supporting patients' decision-making about contraceptive methods through contraceptive counseling. In this topic, we will review the goals of quality contraceptive counseling, review different approaches to this counseling and their relationship to ...
Case Studies. We presented 10 case studies with standardized descriptions of a female patient requesting a method of birth control (see Table 1). Patients in the case studies varied systematically by age (either 23- or 36-years-old), and race/ethnicity, specifically White, Chinese, Filipina, Native Hawaiian, and Micronesian.
A systematic review that excluded low-quality studies found that typical use of fertility awareness methods results in 2.0 to 33.6 pregnancies per 100 person-years (Table 3 11), depending on the ...
studies of women or couples, including postabortion, postpartum and breastfeeding women, but excluded studies of women with medical conditions affecting contraceptive eligibility (such as breast cancer).14 Randomised controlled trials (RCTs) and non- randomised studies, as well as peer-reviewed and grey literature publications, were considered.
Background Globally, the rate of unplanned pregnancies among students at institutions of higher education, continue to increase annually despite the universal awareness and availability of contraceptives to the general population. This study examined family planning among undergraduate university students focusing on their knowledge, use and attitudes towards contraception in the University of ...
Contraception allows parents to choose the number and spacing of children. Each year, family planning programmes prevent an estimated 187 million unintended pregnancies, including 60 million unplanned births and 105 million abortions, and avert an estimated 2.7 million infant deaths and 215 000 pregnancy related deaths.1 The prevalence of contraceptive use differs across the world owing to ...
Aim The aim of this systematic review was to synthesise the evidence on the comparative effectiveness of different counselling strategies for modern contraception on contraceptive behaviour and satisfaction, and to examine their advantages and disadvantages. Methods Six electronic databases (Medline, Embase, Global Health, Popline, CINAHL Plus, and Cochrane Library) were searched to identify ...
The Contraceptive CHOICE Project was a large prospective cohort study designed to promote the use of long-acting, reversible contraceptive (LARC) methods to reduce unintended pregnancy in the St ...
The dominance of one contraceptive method in some locations raises the question of whether family planning policies should aim to expand method mix or invest in making existing methods more accessible. Lower rates of demand satisfied among women aged 15-24 years are also concerning because unintended pregnancies before age 25 years can forestall or eliminate education and employment ...
PIP: Presented and discussed are 3 cases illustrating the need for individualized decision-making in contraceptive prescription. In the 1st case, a 34-year-old woman with multiple sclerosis requested a contraceptive method with a lower failure rate than that associated with barrier methods. After discussion about potential risks and side ...
Contraceptive use has numerous health benefits such as preventing unplanned pregnancies, ensuring optimum spacing between births, reducing maternal and child mortality, and improving the lives of women and children in general. This study examines the level of contraceptive use, its determinants, reasons for non-use of contraception among women in the reproductive age group (18-49 years ...
Background Youth ages 15 to 24, who comprise a large portion of sub-Saharan Africa, face a higher burden of unmet contraceptive need than adults. Despite increased international and national commitments to improving young people's access to contraception, significant barriers impede their access to a full range of methods. To further explore these barriers among youth in Kenya, Nigeria, and ...
Background Kenya's contraceptive prevalence rate at 53% is low, with wide disparity among the 47 counties that make up the country (2-76%). Significant financial investment is required to maintain this level of contraceptive use and increase it to levels seen in more developed countries. This is in the context of a growing population, declining donor funding, limited fiscal space and ...
Nonuse of contraceptive methods, ... a structure by which to explore whether efficacy is a priority for a given patient and to emphasize highly effective methods if this is in fact the case, ... as shown in multiple studies regarding the contraceptive injection and its associated menstrual changes. 25,60 In addition, ...
Abstract. Increasing choice and introducing new contraceptive methods in the National Family Welfare Program in India could play a significant role in increasing adoption of contraception and meeting the unmet need of a large proportion of couples. However, inclusion of any new contraceptive method in India has to face many challenges at ...
Long-term contraceptive methods are more cost-effective. As such, investing in long-term contraceptives would save costs despite higher initial cost of service delivery. ... Assessing the cost-effectiveness of contraceptive methods from a health provider perspective: case study of Kiambu County Hospital, Kenya Reprod Health. 2022 Jan 17;19(1 ...
Background Multiparous women are supposed to be able to end their reproductive cycle to decrease population growth. This study aimed to analyze barriers for multiparous women to use long-term contraceptive methods (LTCM) in the Philippines and Indonesia. Methods The study population was women aged 15-49 years old who have given birth to a live baby > 1 in the Philippines and Indonesia. The ...
Methods. The patient-pharmacist consult includes a blood pressure check, contraindication screen, and contraceptive counseling. The pharmacist can prescribe up to a year's supply of the pill, patch, ring, injection, gel, and/or diaphragm. Referrals are made if long-acting reversible contraception is desired.
Until the 1960s rhythm and barrier contraceptives were the only methods of birth control widely available to couples desiring to plan the number and spacing of their children. ... 1981; Baehler et al., 1982; Schwartz et al., 1989). In one case-control study diaphragm users had a relative risk of TSS of 11.7 (2.5-56.1) compared with nonusers ...