This site uses essential cookies. We'd also like to set additional cookies . | Manage preferences
Call for more information and costs or if you are enquiring for yourself or a family member you can use our online cost guide for individuals.

Case Study: Neurological rehabilitation
by Joanna Bresi-Ando
Lucas was a 49 year old male, who ran his own business as an IT consultant. He lived with his wife and 2 adult children in their own home. Lucas was previously fully independent with all his daily activities and had no significant past medical history.
Lucas fell down the stairs at work and sustained a sub arachnoid haemorrhage, a fractured skull, facial lacerations and 2 fractured ribs. He was admitted to the nearest hospital with a trauma centre, where he underwent surgery to debride and evacuate the depressed skull fracture and debride and repair the lacerations.
As a result of the brain injury, Lucas was left with the following impairments;
- Left sided lower limb weakness
- Reduced balance
- Cognitive difficulties - particularly working memory, reduced attention and executive function skills
- Expressive and receptive language difficulties
- Increased fatigue.
Following his acute admission, Lucas was transferred to a rehab unit, however his low mood deteriorated and he was increasingly agitated. Lucas made very little progress on the unit, so it was decided in his best interests for his rehab to be continued at home.
NHS community services in his borough did not provide neuro specific rehab and Lucas’ Case Manager began the search for a neuro Occupational therapist.
Reason for referral
Lucas was referred to occupational therapy for an assessment of his physical and cognitive needs, to allow him to reach his optimal level of function.
Initial assessment
Lucas was independently mobile indoors and short distances outdoors using a walking stick with supervision.
He was independent with personal care and able to prepare simple meals such as breakfast and a hot drink, however he struggled with complex meal prep tasks. He previously enjoyed cooking and this had been the main household task he would participate in prior to his accident. Lucas’ goal was be able to independently cook a complex meal for his family.
Lucas required support to manage his daily routine; he required supervision to access the community and was dependent for financial management. He fatigued easily and struggled to join in with group conversations, so was increasingly socially isolated.
Recommendations for occupational therapy intervention were to
- Develop meaningful roles and a routine focusing on productivity and structure.
- Develop fatigue management, pacing and energy conservation techniques.
- Use relaxation techniques to help manage his fatigue.
- Develop memory aid strategies, such as using his phone as a reminder and a notebook to write down prompts and lists.
- Explore vocational pursuits
Other recommendations were;
- To continue with physiotherapy treatment
- To be assessed by a speech and Language therapist for continuing communication issues.
- To be assessed by a neuropsychologist for further assessment of his cognitive function and work collaboratively with the occupational therapist in the areas of vocational rehab and mood management.
Goal setting
Lucas was able to come up with an overall cooking goal with support from the occupational therapist; he wished to prepare spaghetti bolognese safely and independently without getting distracted from the task.
The occupational therapist then worked with Lucas and his family on the following short term goals:
- To be able to produce a shopping list with minimal assistance,
- To be able to access his local shops with distant supervision and
- To shop for the ingredients with distant supervision.
The short term goals were incorporated into a structured weekly timetable for Lucas to follow.
Assessment/Intervention
Assessment and treatment was completed simultaneously, through the use of functional tasks and repetitive practice of that task.
Although Lucas had an overall cooking goal, in order to achieve it, meant that he was required to work on other functional skills at the same time, such as searching for and locating items in his kitchen in order to work out what was missing and would need to go on a shopping list, safely accessing the community to get to the local shops and making his way around a supermarket, as well as paying for shopping and transporting it home.
Occupational therapists are very aware of how frustrating it can be for clients to achieve what seems to them to be the simplest of tasks and how this frustration can turn into a negative mind set and demoralise the client. In order to avoid this and empower the client to gain a sense of achievement, a graded approach to activities is often used.
In Lucas’ case he was initially given one step of the overall task to complete, i.e. cooking the mince independently and then would be assisted with the other steps. Over time he was encouraged to complete more of the steps on his own. Discussion with Lucas before starting a task and getting him to rate himself on how well he thought he would perform and then reflecting back at the end of the session on his actual performance also served as a method of encouraging self-monitoring and helped him to realise he could manage better than he thought.
Lucas was taught a strategy of using simple worded checklists for each step of the task and checking them off, before moving on to the next step.
The OT would intervene each time he deviated from the task and bring him back to the checklist.
To address attentional difficulties, the OT began to introduce distractions into the environment, i.e. radio on in the background or talking to Lucas when he was completing a task.
By the end of 12 weeks of rehab Lucas was able to make Spaghetti Bolognese with distant supervision.
Lucas had taken on board the strategies of using checklists to help him through the task, but was unable to recognise when he had deviated from a task and always required a prompt to return to his checklist. Lucas’ safety awareness during meal prep improved and family were happy for him to make them a meal with minimal support from themselves.
As Lucas had been required to regularly walk to his local shops, his confidence with community access improved along with confidence to speak with strangers and articulate his needs.
Lucas has not yet been able to return to work and is unsure of whether he wishes to do so, but he is interested in volunteering with a local charity as a means of further occupying his time and increasing his social interactions.
He continues to work with the occupational therapist on managing his fatigue.
Related topics
View articles by topic.
- Industry news
- Professional guides
- Press release
- Our clients
- Daily Living Skills
- Military charities
- Royal Visit
- Fatigue management
- Networking event
- Assistive technology
- Remote Services
- Catrin Pugh
- Returning to work
- Clinical governance
- Educational Series for Charities
- Psychological trauma
- pain-management
- Workplace assessments
- Paediatrics
- Financial management
- Educational Needs
- Mental Health
- Disabled Facilities Grant (DFG)
- Speech and Language
- Recruitment
Problems we solve
- Self care skills
- Complex needs
- Fine motor skills
- Gross motor skills
- Memory problems
- Planning activities
- Organisation skills
- Cooking & household activities
- Getting out & about
- Handwriting
- Seating & wheelchairs
- Moving around the home
- Personal care & dressing
- Access in & out of the home
- The work place
- Standing & self-support
- Mobility & falls
Conditions we treat
- Developmental delay
- Sensory Processing Disorder
- Attention Deficit Hyperactivity Disorder (ADHD)
- Brain injury
- Motor Neurone Disease
- Spinal injury
- Multiple Sclerosis
- Learning difficulties
- Scar management
- Amputations
A professional’s guide to functional rehabilitation
Manage your cookie preferences..
You can learn more about the cookies we set in our cookie policy .
Essential cookies
These cookies are essential for the website to function and are always on.
Analytics Cookies
These cookies are used to collect information about how visitors use our site.
Profile Cookies
Whilst we do not show advertising on our site, we may collect data to sign-post our services elsewhere.
Cognitive approach to improving participation after stroke: two case studies
Affiliation.
- 1 Washington University School of Medicine, St. Louis, MO, USA.
- PMID: 21309372
- DOI: 10.5014/ajot.2011.09010
Despite the need for occupational therapy to emphasize client-specific occupational performance, primary emphasis in stroke rehabilitation continues to be on the remediation of client factors and self-care. Such practice leaves many survivors of stroke with continuing performance deficits. Two case studies demonstrate a novel, alternative approach. The Cognitive Orientation to Daily Occupational Performance (CO-OP) treatment is a performance-based, problem-solving approach to developing functional skills that are client centered. CO-OP was used to guide treatment with 2 older women. The findings suggest that the approach has the potential to successfully help clients with stroke achieve their everyday occupational goals and support continued research in this area. This work will lead to a pilot randomized controlled trial.
Publication types
- Case Reports
- Research Support, Non-U.S. Gov't
- Occupational Therapy / methods*
- Problem Solving
- Stroke / psychology*
- Stroke Rehabilitation*

- About SSNAP
- What is SSNAP?
- Patient guidelines
- Information sheets
- Plain Language Summary reports
- Fair Processing Statement
- Research using SSNAP data
- National data opt-out
- SSNAP Artists
- Resources for providers
- Dataset and helpnotes
- Data analysis and methodology
- Domains, key indicators and scoring
- Results and reports
- Data collection deadlines
- Reporting outputs- frequency
- Reporting outputs- forthcoming dates
- Clinical and groups
- Data requests
- Published papers
- Posters and oral presentations
- SSNAP collaboration
- Using SSNAP reports
- Using SSNAP tools
- Case studies
- Health economics
- Newsletters
- Regional - ISDN
- ICB/LHB/LCG
- CCG/LHB/LCG
- Stroke PREMs 2022/23
- Enhancing service quality for patients requiring bed-based rehabilitation
- Effective intermittent pneumatic compression (IPC) management at Worthing Hospital
- Establishing nutritional risk in all acute stroke patients
- How the correct calculation of mRS from the acute setting reflects the rehab given by ESD service
- Identifying and supporting patients with mood disturbance after stroke at Charing Cross Hospital
- Improving occupational therapy provision at St Thomas’ Hospital
- Increasing access to Speech and Language Therapy on an acute stroke unit
- Developed an assessment tool for families to complete home assessments themselves to reduce the need for occupational therapists to travel to patients' homes, and thereby increase therapy time delivered to patients as a result;
- Divided up therapy time during the day to incorporate 45 minute therapy target for those individuals who may not be able to tolerate a single session;
- Embedded daily rehabilitation timetabling across the whole in-patient pathway embedded within ‘team timetabling’. This ensured capacity and priorities were managed across whole team.
- Piloted a research project to demonstrate feasibility of home environment assessment using information technology (iPads);
- Prioritised new admissions within 24 hours to establish rehabilitation plans and increase the number of days which patents are treated by OT;
- Developed creative group therapy sessions to ensure daily intensive rehabilitation through “Brunch and Lunch” groups thereby ensuring therapeutic and social interactive benefits.
- Collaborative joint working between social services and OT resulting in a seamless referral process avoiding bureaucratic processes;
- Monthly ‘working group’ led by OT, ensuring service delivery and quality improvement projects are highlighted, prioritised and enacted.
Sentinel Stroke National Audit Programme Kings College London Addison House Guy's Campus London SE1 1UL
0116 464 9901 [email protected]
Cookie policy Privacy policy Built by Net Solving Limited Designed by Itineris Limited

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10388505

Exploring the contribution of case study research to the evidence base for occupational therapy: a scoping review
Leona mcquaid.
Glasgow Caledonian University, Glasgow, UK
Katie Thomson
Katrina bannigan, associated data.
The datasets generated and analysed during the current study are available in the UK Data Service ReShare repository, [10.5255/UKDA-SN-855706].
Case study research is generating interest to evaluate complex interventions. However, it is not clear how this is being utilized by occupational therapists or how feasible it is to contribute to the evidence base. This scoping review explores case study research within occupational therapy in terms of how it is defined, the methodological characteristics adopted, such as data collection and analysis, and the range of practice contexts in which it is applied. We consider the viability of case study research for contributing to our evidence base.
Opinion, text and empirical studies within an occupational therapy practice context were included. A three-step extensive search following Joanna Briggs Institute methodology was conducted in June 2020 and updated in July 2021 across ten databases, websites, peer-reviewed and grey literature from 2016 onwards. Study selection was completed by two independent reviewers. A data extraction table was developed and piloted and data charted to align with research questions. Data extraction was completed by one reviewer and a 10% sample cross checked by another.
Eighty-eight studies were included in the review consisting of ( n = 84) empirical case study and ( n = 4) non-empirical papers. Case study research has been conducted globally, with a range of populations across different settings. The majority were conducted in a community setting ( n = 48/84; 57%) with populations experiencing neurodevelopmental disorder ( n = 32/84; 38%), stroke ( n = 14/84;17%) and non-diagnosis specific ( n = 13/84; 15%). Methodologies adopted quantitative ( n = 42/84; 50%), mixed methods ( n = 22/84; 26%) and qualitative designs ( n = 20/84; 24%). However, identifying the methodology and ‘case’ was a challenge due to methodological inconsistencies.
Conclusions
Case study research is useful when large-scale inquiry is not appropriate; for cases of complexity, early intervention efficacy, theory testing or when small participant numbers are available. It appears a viable methodology to contribute to the evidence base for occupation and health as it has been used to evaluate interventions across a breadth of occupational therapy practice contexts. Viability could be enhanced through consistent conduct and reporting to allow pooling of case data. A conceptual model and description of case study research in occupational therapy is proposed to support this.
Systematic review registration
Open Science Framework 10.17605/OSF.IO/PCFJ6.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-023-02292-4.
Developing evidence informed occupational therapy practice is a priority across international practice standards and research agendas [ 1 , 2 ]. The challenge in achieving this, however, is multifaceted. Occupational therapists report a lack of research knowledge, time, resources and organizational support as barriers in the conduct of research [ 3 – 5 ]. Implementing findings from a research environment to the reality of clinical practice also presents a challenge despite knowledge translation and implementation strategies [ 6 ]. In practice, therapists use reasoning, experience and the client’s perspectives in addition to research [ 7 , 8 ]. This holistic approach to service provision can be difficult to capture, but the need to demonstrate impact and quality outcomes remains.
Arguably, the challenge in evidencing the value of occupational therapy reflects the complexity of practice where the ‘the active ingredient’ is difficult to stipulate [ 9 ]. This is comparable to the ‘complexity turn’ of wider health and social care which acknowledges that interventions are not always linear processes with predictable outcomes [ 10 ]. In recognition of this, debate exists in occupational therapy about how best to develop the evidence base [ 11 ]. Whilst the need for large-scale inquiry and randomized controlled trials is evident, there is also a growing perception that this may not be appropriate to answer the full spectrum of practice-based questions [ 10 ]. Instead, the research method adopted should respond appropriately to the question being asked and often a range of methods may be necessary. In particular for occupational therapy, researchers should consider designs carefully, particularly when testing interventions, so the holistic nature of practice is not compromised [ 11 ]. A shift to a pluralistic approach which best serves the decision-making needs of practitioners may be more appropriate [ 12 , 13 ].
Case study methodology—an in-depth analysis of a phenomenon within its real-world context [ 14 ]—has become increasingly popular in social sciences and is beginning to generate greater interest in occupational therapy [ 11 , 15 ]. Focus on a single case in context presents a familiar and therefore potentially feasible approach to research for practitioners. As a methodology, it relies on the collection of multiple sources of data to gain an in-depth understanding of the case [ 14 ], resembling multiple sources of evidence informing decision making in practice [ 11 ]. Flyvberg [ 16 ] argues this detailed contextual knowledge is necessary for understanding human behaviours when there can be no absolutes. It therefore provides an alternative methodology where large-scale inquiry is not appropriate or feasible [ 14 ].
Confusion surrounds case study methodology in terms of how it is conducted, reported and consequently identified in the literature. Previous reviews have noted inconsistencies between methodology and design, mislabeling of case study research and a lack of clarity defining the case and context boundaries [ 15 , 17 ]. It is often associated with qualitative origins, evolving from the natural and social sciences where disciplines such as anthropology, sociology and psychology demonstrate early application of the methodology and have since used it to grow their evidence base [ 18 , 19 ]. However, case study research can be shaped by paradigm, study design and selection of methods, either qualitative, quantitative or mixed. Its flexibility as a methodology and variation in approach by seminal authors may add to the confusion. For instance, Stake [ 20 ] and Merriam [ 21 ] align to a qualitative approach whereas Yin [ 14 ] adopts more of a positivist approach with a priori design to examine causality. The language around case studies can also be synonymous with ‘non-research’ case reports, anecdotes about practice or educational case studies which do not include data collection or analysis [ 22 ]. However, case study methodology is research involving systematic processes of data collection with the ability to draw rigourous conclusions [ 17 ]. Hence, there is a need to better understand this methodology and bring clarity in defining it for research use in occupational therapy practice.
There are misconceptions that case study research can provide only descriptive or exploratory data and it is regarded as poorer evidence in the effectiveness evidence hierarchy [ 10 ]. However, in a meta-narrative review of case study approaches to evaluate complex interventions, Paparini et al. [ 15 ] noted diversity in epistemological and methodological approaches from narrative inquiry to the more quasi-experimental. As such, case study research offers flexibility to answer a range of questions aiding a pluralistic approach to research. Yin [ 14 ] suggests three purposes of case study research; (i) descriptive; describes a phenomenon such as an intervention; (ii) explorative; explores situations where there is no single outcome, and (iii) explanatory; seeks to explain casual relationships. Stake [ 20 ] on the other hand describes case study research as (i) intrinsic; to understand a single case, (ii) instrumental; where the case is of secondary interest to facilitate understanding to another context and (iii) collective; when multiple cases are studied around a similar concept. Whilst it has been criticized for lack of rigour and external validity [ 22 ], one case can be sufficient to make causal claims, similar to a single experiment [ 15 ]. A particular case can disprove a theory and prompt further investigation or testing [ 16 ]. Furthermore, Yin [ 14 ] reasons the accumulation of case studies may offer greater rigour, reliability and external validity of findings as a larger dataset is created. Through case replication and organized accessible storage, there is potential for data to be mined to conduct rigourous practice-based research [ 11 , 23 ].
Some contention exists around the classification of single-case designs, including N-of-1 observational and experimental designs. Rice, Stein and Tomlin [ 24 ] argue the single-case experimental design (SCED) is not the same as a case study; however, Paparini [ 10 ] maintains this is coterminous with Yin’s explanatory case study aims. The International Collaborative Network of N-of-1 Trials and Single-Case Designs (ICN) articulates these designs broadly as the study of a single participant in a real-world clinical application [ 25 ]. This singular and contextual focus makes these designs appropriate to consider under the umbrella term case study research for the purposes of this review and exploring how N-of-1 may be a viable means to develop the occupational therapy evidence base.
Case study research has previously been advocated for in occupational therapy. Ottenbacher [ 26 ] originally described the small ‘N’ study as a tool for practitioners to address their responsibilities of documenting service provision effectiveness. Others have provided support for case study methodology to demonstrate clinical impact, overcome challenges of investigating complex phenomena and develop the occupational therapy evidence base [ 27 – 29 ]. It is presented as a good ‘fit’ for occupational therapy with untapped potential for contributing to the evidence base [ 11 , 30 ]. Whilst these studies offer a justification for the use of case study research in occupational therapy and call for greater uptake of the method, no extensive review of empirical case study methodology in occupational therapy practice has been conducted. It therefore remains unclear if, and how, the methodology is being utilized, or how feasible it is to contribute to the evidence base. A scoping review was deemed the most appropriate methodology for this review as it has recognized value for researching broader topics [ 31 ]. It will identify all available, eligible evidence and chart key information from the literature to answer the research questions and identify any gaps in the knowledge base.
A preliminary search of PROSPERO, MEDLINE, the Open Science Framework and JBI Evidence Synthesis was conducted. A similar scoping review was published in 2020 but focused solely on the use of qualitative case studies in occupational therapy, therefore providing a restricted view of case study methodologies [ 32 ]. Equally, the literature search was conducted in 2017 and interest in this methodology has grown since; hence, there may have been a change in the use of qualitative case study research methods within occupational therapy in recent years.
This scoping review explores case study research within occupational therapy in terms of how it is defined, the methodological characteristics adopted, such as data collection and analysis, and the range of practice contexts in which it is applied. By reviewing case study research within the field, it will be possible to assess the viability of case study research for contributing to the evidence base for occupation and health. The enriched understanding of case study research within occupational therapy could identify areas for future research and strategies to improve evidence-based clinical outcomes for those accessing services.
Review questions
This review aims to understand how case study research methodologies are used to contribute to the evidence base for occupational therapy practice. Specifically, it will identify and chart data to address the following sub-questions:
- How is ‘case study’ defined as a research methodology in occupational therapy literature?
- What are the methodological characteristics of case study research used in occupational therapy practice?
- What are the contexts and recorded implications of case study research undertaken in occupational therapy practice?
This scoping review was conducted in accordance with the Joanna Briggs Institute (JBI) methodology for scoping reviews [ 33 ] and, in line with best practice, used the updated Preferred Reporting Items Systematic Reviews and Meta-Analyses Extension for Scoping Reviews checklist (PRISMA-ScR) (See Additional File 1 for PRISMA-ScR checklist) [ 34 – 36 ]. It was conducted in accordance with an a priori protocol [ 37 ], and any deviations from this are reported and justified.
Inclusion criteria
Participants.
This review considered studies where occupational therapy input is provided as the object of study or the ‘case’ within the case study; therefore, the inclusion criteria was not limited by participant characteristics. It is possible that included studies may not involve participants given the nature of case study research and non-empirical study types are also eligible for inclusion. This allowed the potential for a representative picture of who and what occupational therapists have studied using case study methodology.
Empirical studies using case study research methodology were included. Literature reviews, text or opinion pieces which discuss the value of case study research within occupational therapy practice were also included to ascertain how others have used or conceptualized the use of case study research to achieve evidence-based practice. Papers were excluded where a case study research design was not explicit, for example, a descriptive case report without data collection and analysis.
Any area of occupational therapy practice was considered which spans health and social care, criminal justice, education and other diverse areas [ 38 ]. An a priori decision was made to exclude studies where the occupational therapy context could not be clearly defined, for example, multidisciplinary input or where practice was not the focus of the study, for example, describing an occupation only. All geographical locations were considered; however, as only articles written in English language were included, this may have created a geographical restriction through language limitations.
Types of sources
This scoping review included studies, as well as thesis and book chapters, if they involved empirical quantitative, qualitative and mixed method case study designs. Opinion, text or other articles which discuss the use of case study research in an occupational therapy practice context were also included. Case studies that are descriptive with no data collection and analysis were excluded. This was identified through reviewing the methods undertaken rather than how a study self-identified.
Search strategy
The search strategy aimed to locate both published and unpublished primary studies, reviews and text and opinion papers. To support the development and accuracy of the search strategy, a health systems librarian and occupational therapy profession specialist librarian were consulted in the early development stages. As per the JBI recommended three-step approach, an initial limited search of MEDLINE (EBSCO) and CINAHL (EBSCO) was undertaken to identify articles on the topic. The text words contained in the titles and abstracts of relevant articles, and the index terms used to describe the articles were used to develop a full search strategy. The scoping review process is iterative [ 33 ] so it was noted in the protocol that the search strategy may need to be adapted as the review evolved. As a result of the preliminary searches, a change was required through the addition of the search term ‘occupational science’. Without its inclusion, a valuable review on the use of case study research in occupational science which also included occupational therapy practice was missed [ 39 ]. Therefore, the addition of this term ensured a thorough search, recognizing the influence of occupational science on occupational therapy practice.
The search strategy, including all identified keywords and index terms, was adapted for each included information source and a second search was undertaken in June 2020 and updated on 7th July 2021. The full search strategies are provided in Additional file 2 . The reference lists of articles included in the review were screened for additional papers plus a key author search to ensure all relevant studies were identified [ 33 ]. Studies published in English were included as the resources for translation were not available within the scope of this review.
The databases searched included MEDLINE (EBSCO), CINAHL (EBSCO), AMED (EBSCO), EMBASE (Ovid), PsychINFO (ProQuest) and Web Of Science. Sources of unpublished studies and grey literature searched included OpenGrey, Google and Google Scholar, OTDBASE, EthOS and OADT. To identify occupational therapy-specific literature, the content pages of practice publications Occupational Therapy News (UK), Occupational Therapy Now (Canada) and Occupational Therapy Practice (USA) were also screened from 2016.
Despite running preparatory searches, an unmanageable amount of papers were returned and on inspection many were dated in their approach to practice and language. For example, Pinkney [ 40 ] referred to ‘senile dementia’ and Pomeroy [ 41 ] referred to ‘handicap goals’. Therefore, to keep the review feasible as well as contemporary, a decision was made by the team to limit date parameters to 2016 onwards. This also meant that the OTSeeker database was omitted as a change from a priori as it has not remained comprehensive from this date due to lack of funding.
Study/source of evidence selection
Following the search, all identified records were collated and uploaded into Mendeley V1.19.4 (Mendeley Ltd., Elsevier, Netherlands) and duplicates removed. A decision was made not to use the JBI System for the Unified Management, Assessment and Review of Information (JBI SUMARI; Adelaide, Australia) as JBI SUMARI does not offer modifiable data extraction templates which was needed for this review [ 33 ]. Instead, studies were transferred to Rayyan QCRI (Qatar Computing Research Institute [Data Analytics], Doha, Qatar), a systematic review web application to manage the independent relevance checking process [ 42 ].
A screening tool was developed and piloted on a sample of studies by all three reviewers (LMQ; KT; KB) and adjusted until consensus reached to enhance clarity before continuing the full screening process. The screening tool served as a memory aid to ensure reviewers were being consistent in how the inclusion criteria was applied and all decisions were recorded on Rayyan QCRI. Titles and abstracts were screened by two independent reviewers for assessment against the inclusion criteria (LMQ; KT and KB reviewed half each). Due to the broad nature of the question and a lack of clarity in reporting case study research methodology in the title or abstract, where there was doubt, articles were included for full-text review to be as inclusive as possible. Potentially relevant papers were retrieved in full and assessed in detail against the inclusion criteria by two independent reviewers (LMQ; KT and KB reviewed half each). Full-text studies that did not meet the inclusion criteria were excluded, and reasons for their exclusion recorded. Any disagreements that arose between reviewers were resolved through discussion or with a third reviewer. Where required, the screening tool was refined following these discussions to create an audit trail and further enhance consistency in how inclusion criteria was applied in the screening process. Studies were not quality assessed, as per scoping review guidance [ 33 ], as the purpose of this scoping review was to map available existing evidence rather than consider methodological quality.
Data extraction
Data were extracted from papers using a data extraction tool developed by the reviewers into a Microsoft Excel spreadsheet (Redmond, Washington, USA). The tool was piloted by two independent reviewers initially on fourteen papers, an increase from the suggestion at protocol stage given the high number of included studies, and subsequently modified and revised. This clarified that only study designs stated, rather than conjected, would be extracted to reflect how authors self-categorize and define case study methodology. Additionally, it presented the need for a separate data extraction tool for non-empirical papers as some of the detail in the original tool was not relevant to review or discursive paper designs. The new tool captured details on reported strengths, limitations and explanations of data collection/analysis for the use of this methodology in occupational therapy practice. The updated data extraction tools are presented in Additional files 3 and 4 .
Data extraction was completed by the first author and a 10% sample checked by a second reviewer. As recommended in the data extraction process [ 34 ], multiple reports from the same study were linked. The data extracted for empirical studies included specific details about the definitions, justification and citations of case study research, the methodological characteristics, the context in terms of practice setting and population and key findings and implications relevant to the review question [ 37 ]. Authors of papers were contacted to request missing or additional data, where required.
Data presentation
As specified in the protocol and recommended in the JBI scoping review guidance, the extracted data is presented in diagrammatic and tabular form. A narrative summary accompanies the charted results and describes how the results relate to the scoping review questions. A mapping approach to analysis was adopted as the objective of this scoping review was to collate the range of existing evidence and describe the methodological characteristics of case study research, rather than synthesis or appraise the evidence.
In total, database and secondary searching returned 8382 studies (Fig. 1 ). After duplicates were removed, 5280 underwent title and abstract screening with 4080 articles excluded at this stage. Full-text screening and application of the updated 2016 date parameters led to a further 1108 articles excluded. This left 92 articles eligible for inclusion. This included seven reports linked to three studies which were subsequently combined [ 43 ] and four non-empirical papers consisting of a discussion piece and three literature reviews. Three of these reviewed the use of case study research in occupational therapy and/or occupational science prior to 2016, further justifying the decision to provide a more contemporary review. A final total of 88 records were included in the review; 84 empirical studies, and four non-empirical papers. The characteristics of included studies are presented in Additional files 5 and 6 . The majority of studies were excluded due to not having an occupational therapy practice focus, for example, multidisciplinary or a description of the meaning of an occupation rather than in a practice context (see Additional File 7 for more detail).

Search results and study selection and inclusion process [ 34 ]
After an initial dip from 2016, publication of empirical case study research shows a consistent trend from 2017 onwards; the lower number in 2021 is attributed to the search stopping mid-way through the year (July 2021) (Table (Table1). 1 ). Across the 88 included studies, there is greater representation of the Global North with the USA ( n = 24/88; 27%), Canada ( n =12/88; 14%) and UK ( n = 11/88; 13%) publishing the most case study research. Case study research has been adopted to address exploratory and explanatory aims, and as such, it has been used to understand the outcomes of interventions, to explore elements of practice such as theoretical models, and to understand occupation and occupational science concepts to inform practice. Empirical case study research was identified in journal articles ( n = 77/88; 87%), predominantly in occupational therapy-specific journals ( n = 56/88; 63%), theses ( n = 6/88; 7%), abstracts ( n = 4/88; 5%) and a book chapter ( n = 1/88; 1%). The majority of case study research adopted a multiple case design ( n = 64/84; 76%); however, single-case designs were also published ( n = 19/84; 23%). Included studies have used multiple data collection methods including interviews, observation and outcome data and have been used in a range of practice settings across the life span. The empirical studies will now be mapped to answer each question of this review followed by mapping of the non-empirical studies.
Summary of included studies
Mapping of empirical studies
There did not appear to be a consistent approach adopted across studies to define case study methodology. Figure 2 captures the various ways studies self-reported their methodological design (the more prominent the text, the more a word or phrase was featured in the data). Of the 84 empirical studies, 57% ( n = 48/84) provided a definition or justification for the chosen case study research methodology. The most common cited explanations for adopting case study methodology were as follows: (i) to gain a deep understanding of the case ( n = 28/84; 33%); (ii) to achieve this using multiple data sources, perspectives or baseline measures ( n = 21/84; 25%) and (iii) to study the case in the real-world environment or context ( n = 17/84; 20%). A need for comprehensive understanding was linked to the complexity of the case, such as a social interaction or human behaviour, e.g. Carrol [ 44 ] and Soeker & Pape [ 45 ]. Case study methodology was also justified as more suitable or practical when the phenomena was too complex or too little was already known for other data collection approaches, such as experiments or surveys to be used, e.g. Nilsson et al. [ 46 ] and Stickley & Hall [ 47 ]. Consequently, 10 studies specifically justified case study research as appropriate for early efficacy and feasibility studies, e.g. Peters et al. [ 48 ]. Case study methodology was described as a form of empirical enquiry or research by a small number of studies ( n = 13/84; 15%), and in some instances, this was justified as being closely aligned to the principles of occupational therapy practice or a way to provide clinically relevant information, e.g. Kearns Murphy & Sheil [ 49 ] and Verikios et al. [ 50 ]. To a lesser extent ( n = 6/84; 7%), case study methodology was described as a way to test theory.

Phrase cloud illustration of study design as self-identified in included empirical studies. Size of the word illustrates frequency of use
Less than half of studies ( n = 41/84; 48%) referred to seminal authors or included relevant case study methodological citations. Table Table2 2 provides a summary of cited author explanation of case study research. Yin’s work was most commonly cited followed by Stake and Merriam whom were more associated, but not limited to, qualitative case studies. Dibsdall [ 51 ] and Hurst [ 52 ] justified their choice of Yin’s approach to case study methodology because it provided a clearer structure to follow.
- a Study design.
Summary of cited author explanation of case study research
Congruence between description of study design and the methods undertaken was not always consistent, and reporting of ethical approval to distinguish case study research from case reports was not always reliable. For example, two studies classified as case reports by the American Journal of Occupational Therapy [ 56 , 57 ] include a methods section with data collection and analysis and have received ethical approval which would be more consistent with case study research methodology rather than a descriptive, non-research case report [ 14 ]. In contrast, Longpre et al. [ 58 ] documented that, after seeking guidance from three university review boards, ethics was not required for a case study approach despite including interview and document review data collection and an appropriate research citation.
- b Methods of data collection
Quantitative data collection methods accounted for the majority of methods ( n = 42/84; 50%), but mixed methods ( n = 22/84; 26%) and qualitative ( n = 20/84; 24%) approaches were also used. As such, studies appeared to represent different research paradigms, although the authors positioning is only stated in two studies; critical realism [ 52 ] and constructivism [ 59 ]. Data collection methods varied dependent on practice setting with quantitative methods dominant in inpatient and outpatient settings whereas third sector only used qualitative methods (Fig. 3 ). Community settings used a mixture of quantitative, qualitative and mixed methods.

Number of studies per practice setting and data collection approach
Quantitative data was used to evaluate effectiveness with testing pre and post intervention, and as such, they adopted explanatory, N-of-1, single-case experimental or observational designs. In contrast, qualitative designs were used in studies with an exploratory or descriptive purpose. Here, qualitative data added further understanding of the effects or acceptability of an intervention from a variety of perspectives. Data collection methods across qualitative studies included the use of semi-structured interviews, observation, document review, field diaries and focus groups. Observation was also evident in quantitative methods but for the purpose of gathering performance data and applying objective measures rather than descriptive or thematic purposes. Mixed methods case study research included a range of designs such as the single-case experimental design [ 60 ], multiple case study [ 61 ] and descriptive case study [ 62 ].
- iii Outcome measures.
None of the included quantitative studies used exactly the same measures. However, the Canadian Occupational Performance Measure (COPM) was the most commonly used occupation-based outcome measure ( n = 20/84; 23%) and to a lesser extent, the Assessment of Motor and Process Skills (AMPS) was used ( n = 3/84; 4%). The Goal Attainment Scale (GAS) was also used ( n = 5/84; 6%) and Kearns Murphy and Sheil [ 50 ] in particular advocated for its use in occupational therapy case study research, particularly in mental health settings. Non-occupation-specific measures of function were also used such as Range of Movement, Fugl-Meyer assessment, Sensory profiles and other condition-specific measures, e.g. Hospital Anxiety Depression Scale [ 63 ], Stroke Impact Scale [ 64 ] and Modified Checklist for Autism in Toddlers [ 65 ].
- iv Methods of analysis.
Descriptive analysis and visual analysis to compare data graphed over time was used in quantitative experimental designs. Statistical analysis in the form of Rasch and frequency analysis was also employed in some instances [ 66 – 68 ] but this was largely in conjunction with visual analysis. Both Gustaffson et al. [ 69 ] and Gimeno et al. [ 70 ] suggested in their studies that visual analysis is preferable for single-case designs rather than statistical hypothesis testing due to the small number of participants. Thematic and content analyses were commonly used in qualitative studies in addition to descriptive statistics. For multiple case designs, within and cross case analysis was described [ 59 , 64 , 71 – 74 ]. Specifically, Yin’s approach to pattern matching [ 51 , 73 , 75 , 76 ], explanation building [ 45 ] and matrix coding [ 77 ] was used. Two studies referred specifically to Stake’s approach to data analysis [ 59 , 78 ].
- e The case.
Few studies ( n = 10/84; 11%) made the case explicit in terms of description, selection or boundaries. In particular, quantitative case study designs appeared not to define the case; therefore, the participant receiving occupational therapy was assumed to be the case. In these studies, the inclusion criteria, time and location of intervention appear to be the boundary. Alternatively, the provision of occupational therapy input as a process could be the case of interest. Fields [ 78 ] and Pretorious [ 79 ] exemplify a clearly defined case as an individual and both were bounded by the context of time and location. Haines et al. [ 78 ] and Hyett et al. [ 59 ] demonstrate a defined case as a process, occupational therapy provision and a social network respectively. Across the studies, the case, either stated or conjected, was predominately an individual ( n = 72/84; 85%). Groups, namely families ( n = 5/84; 6%) and organizations were also identified as the case ( n = 4; 5%). The case was stated as a process in a small number of studies ( n = 3/84; 4%); however, without a clear description of the case and boundary, it is challenging to accurately identify this within the included studies.
- a Practice contexts
Occupational therapy case study research were conducted with various client groups across a range of practice settings (Additional files 8 and 9 ). The majority were based in the community ( n = 48/84; 57%); however, the practice context or setting where the research was carried out was not always clearly reported ( n = 11/84; 13%). Interventions adopting therapeutic use of occupation and activity were apparent, such as feeding [ 80 ], gaming [ 81 , 82 ], gardening [ 83 ] and play [ 84 – 86 ]. This was more prevalent in outpatient or community settings with inpatient settings adopting more of a compensatory approach [ 87 ] to facilitate engagement in occupations as an end, rather than the therapeutic use of occupation itself as a means. Across all practice settings, the most common occupational therapy interventions were sensory-based interventions ( n = 10/84; 12%) for example Giencke Kimball et al. [ 88 ], Go & Lee [ 89 ] Hejazi-Shirmard et al. [ 90 ], and provision of assistive equipment ( n = 9/88; 11%) for example Cruz et al. [ 91 ], Golisz et al. [ 92 ] and Teixeira & Alves [ 93 ]. In other instances ( n = 4/84; 5%), provision of occupational therapy was described as the intervention, subsequently involving a range of input rather than a single defined intervention, for example Kearns Murphy & Sheil [ 49 ], Haines et al. [ 78 ] and Pretorius [ 79 ].
Although all studies had a practice focus, not all were intervention specific but investigated a broader aspect of practice and so did not always include participants ( n = 11/84; 13%). For example, Carey et al. [ 94 ] conducted an instrumental case study on the case of occupational therapy practice in the broad context of mental health services in Saskatchewan, Canada. This involved reviewing documentation and records from practice rather than including a population group or specific intervention. Others focused on particular assessments used in practice [ 95 , 96 ] using conceptual frameworks in practice [ 52 , 59 ] and practice at the organization or community level [ 47 , 71 , 97 , 98 ].
For studies that included a population group, case study methodology was used across the life span; adults ( n = 27/84; 32%) children ( n = 24/84; 29%) and to a lesser extent, older adults ( n = 6/84; 7%). It was also used with mixed age populations ( n = 21/84; 25%) for instance, with families. Across all age groups, case study research was conducted largely with populations experiencing neurodevelopmental disorder ( n = 32/84; 38%), stroke ( n = 14/84; 17%) and ill mental health ( n = 9/84; 11%) but was not always diagnosis specific ( n = 13/84; 15%) (Additional file 9 ). For example, in Dibsdall’s [ 51 ] case study of a reablement service, occupational therapists provided a service to individuals with a range of diagnoses. Similarly, Fischl et al. [ 72 ] supported older adults with digital technology-mediated occupations irrelevant to a particular diagnosis.
- b Recorded implications for practice.
As the majority of studies had an intervention focus ( n = 73/84; 87%), they were able to draw conclusions in terms of how and why an intervention works. However, implications for practice in terms of intervention efficacy were often presented as preliminary or pilot with recommendations for further research including larger sample size studies. Through multiple data collection methods, some studies incorporated participant, family or therapist views to triangulate data and draw conclusions about the acceptability of an intervention [ 50 , 62 , 99 ]. As an example, Peny-Dahlstand et al. [ 99 ] includes a clear diagram illustrating how multiple data sources are collected from the patient, the therapist and the organizational perspective to analyse feasibility in terms of acceptability, efficacy, adaptation and expansion. Details of the Cognitive Orientation to daily Occupational Performance intervention are aligned to a protocol giving the reader a sense of how this can be implemented in practice. Similarly, a detailed description of the intervention, case and/or context can aid transferability [ 14 ] as in Carlsedt et al.’s [ 64 ] overview of the BUS TRIPS intervention.
The remaining studies ( n = 11/84; 13%) added to the understanding of non-intervention aspects of practice such as the use of models, frameworks and assessment tools within the practice context or recommended policy changes. For example, Soeker and Pape [ 45 ] explored the experiences of individuals with a brain injury of the Model of Self-Efficacy (MOOSE) as it was used by occupational therapists to support their return to work journey. Using an exploratory multiple case design, the authors were able to conclude that the MOOSE is a useful model in this area of practice as well as increasing understanding of how and why it supported work retraining.
Mapping of non-empirical papers
Four non-empirical papers that reviewed the use of case study research related to occupational therapy were included in this review. These were integrative reviews of case study research in occupational therapy [ 100 ], occupational science [ 39 ] and a scoping review of qualitative case study research [ 32 ] together with a discussion of the applicability of single-case experimental designs to occupational therapy [ 101 ]. The literature review searches were conducted in either 2016 or 2017 and identified 32 [ 100 ], 27 [ 32 ] and 18 studies [ 39 ]. Results reflect the findings of the empirical studies in the current review, suggesting a global uptake of case study research in occupational therapy across a diversity of practice settings used to understand interventions as well as broader concepts related to practice.
Together, the reviews present the defining features of case study methodology as investigating a phenomenon (i) in depth, (ii) in its real-life natural context, and (iii) using multiple sources of data for triangulation. Jonasdittor et al. [ 39 ] and Carey [ 100 ] both suggest case study methodology can cross research paradigms and therefore can be qualitative, quantitative or mixed methods in nature. Lane [ 101 ] somewhat contradicts this stating that case studies are a form of descriptive qualitative inquiry and therefore described the quantitative single-case experimental design (SCED) as distinct and separate from case study research. However, Lane [ 101 ] also acknowledged that multiple sources of data may be used including narrative records but this should be considered secondary to observing trends in data because the primary focus is to determine the effect of the intervention. In the SCED, multiple data collection points are used for in-depth understanding to measure change and make appropriate intervention responses. Hercegovac et al. [ 32 ] did not make a distinction about data collection methods but sought only qualitative case study research. Reflective of this, the majority of studies identified by Jonasdottir et al.’s [ 39 ] and Hercegovac et al.’s [ 32 ] reviews were qualitative but in Carey’s review [ 100 ] they were mixed methods. Quantitative studies were less common.
All four papers comment that generalizations cannot be made from a single case. Instead, providing a thick description of characteristics and information about the case was deemed necessary to help the reader understand the context and determine transferability of the case. Collecting and comparing across cases was also noted to provide greater validity [ 101 ]. Despite this, Hercegovac et al. [ 32 ] identified only 18% of studies that had adequately defined the case. All review and discussion papers conclude that case study or single-case experimental designs are appropriate in the study of occupation and health. They support the wider adoption of this methodology to advance the occupational therapy evidence base because it offers a rigourous but flexible approach to study complexity in the real-world practice environment. It is presented as a ‘familiar, appropriate tool’ ([ 100 ]; p.1293) to develop evidence informed practice.
The findings of this review, in conjunction with the wider literature knowledge base, are integrated in Fig. 4 as a proposed conceptual model to illustrate how case study research can be applied in occupational therapy practice. It highlights the three important elements of the methodology as the ‘Case’ of interest, the rationale for the ‘Study’ design and that it is a ‘Research’ method. Central to the application of this methodology is the aim to achieve an in-depth understanding of a phenomenon within the occupational therapy practice context. To compliment Fig. 4 , a description of case study research within occupational therapy is proposed as;
‘a flexible methodology that can cross research paradigms where the focus is to gain an in-depth understanding of a case in the real-life practice context. The case and context can reflect any aspect of occupational therapy, but must be clearly defined and described within a given boundary. A comprehensive understanding of the case or cases should be gained through triangulation of data collection either through multiple data sources or multiple time points.’

Proposed conceptual model describing case study research in occupational therapy practice
This scoping review explored the use of case study research within the occupational therapy evidence base from 2016 to 2021. A large number of studies ( N = 88) were identified across a variety of practice settings and following a dip after 2016, publication trends appeared consistent over this period. This suggests that case study research has potential viability for contributing to the evidence base of occupation and health. However, the findings of this review identified inconsistencies in how case study research was defined and variation in the methodologies adopted. Therefore, to maximize its potential as an evidence building tool, further clarity on case study methodology is needed. It is hoped that this review, in particular the proposed definition and conceptual model, will help achieve this.
A key issue highlighted was the lack of consistent or easily identifiable terms used to describe the methodology. Some studies defined the design by number of cases (e.g. single/multiple), by purpose (e.g. exploratory, descriptive, experimental) or by data collection (e.g. quantitative, qualitative, mixed). Other terms were also used such as ‘almost experimental’, ‘case series’, ‘changing criterion’ and ‘case report’. Hyett [ 17 ] suggested case study, as a research approach, has been confused with the non-research-based case report and this is supported by the findings of the current review. Self-identified ‘case studies’ were excluded, in line with the inclusion criteria, if they did not report data collection or analysis. In addition, journal classification of study type was at times incongruent with the methodology taken, e.g. Proffitt et al. [ 57 ]. Alpi & Evans [ 102 ] highlight this lack of distinction not only in journal classification but also in database indexing. They propose that case study is a rigourous qualitative research methodology and case report is a patient or event description. Based on this, the Journal of Medical Library Association updated classification of descriptive manuscripts previously known as case studies to case reports and case studies as a research methodology are now identified as original investigations. Despite this effort at clarification, there is still room for debate. Where Alpi & Evans [ 102 ] suggest N-of-1 single subject studies fit the case report label, Paparini et al. [ 10 ] aligns this to the explanatory case study. Therefore, this review adopted Yin’s [ 14 ] term ‘case study research’ as a common language that can be used by occupational therapists in the conduct and reporting of this methodology. It is suggested this will make the distinction clear from case report or non-research.
The issues highlighted in this review reflect current debate about case study research methodology. A key issue identified with empirical case study research was the inadequate description of the case and boundary so that it could be easily identified by the reader. Other reviews of case study research in occupational therapy included in this review [ 32 , 39 , 100 ] also identified this as a concern pre-2016 and Hyett [ 17 ] identified this more broadly in the literature, but particularly a concern for health and social science case studies. A clearly identifiable case, with detailed description including the boundary and context, is necessary for practitioners to understand how it may translate to their own practice. A case is not synonymous with participant and, whilst it can be an individual of interest, it can also take a more intangible form of a process such as intervention delivery, practice networks or other practice areas of interest such as theory.
As a form of inquiry, case study research provides context-specific, practice-based evidence, so the practice context must be understood. This in-depth, contextual understanding provides an alternative to studies seeking breadth of knowledge or generalizations and is thus the unique characteristic of case study research [ 11 ]. For this reason, ‘in-depth’ inquiry and ‘occupational therapy practice context’ are positioned at the core of the proposed descriptive model, encapsulated by the ‘case and context boundary’ as essential elements to case study research methodology (Fig. 4 ).
Case study research has been shown to be a flexible methodology both in design and purpose. Of particular interest to evidence building is its use to explore the efficacy and feasibility of an intervention in the real-life practice context. These findings support the assertions of previous authors who have suggested that case study research can be used to demonstrate clinical impact of interventions and to investigate complex multifactorial phenomena [ 11 , 27 – 29 ]. Particularly in areas of innovative or emerging practice, case study research can provide a way to capture impact when participant numbers or resources are not available to conduct larger-scale inquiry. Stickley and Hall [ 47 ], for instance, specifically state that their study is the first known investigation into social enterprise in occupational therapy. As a first step to building evidence, a descriptive or single-case account can therefore provide an important grounding on which to build upon. The need for timely evidence during the Covid-19 pandemic demonstrated an acute awareness of this but it has also been recognized as a process of cumulative evidence building in occupational science [ 103 ] and more broadly across other disciplines [ 104 ]. Of note however is Flyvbjerg’s [ 16 ] argument that the case study holds value beyond pilot or preliminary data. Whilst it may be difficult to generalize from a case study, particularly in terms of process, the outcomes can contribute to knowledge when used to test a theory or data pooled across cases.
By mapping the findings of this review, case study research appears to mirror the broad and varying nature of occupational therapy. It reflects occupational therapy as a direct service provided to individuals or groups, but also to others on a client’s behalf [ 105 ]. Organization, population and system-level practice is also recognized as an important aspect of occupational therapy practice [ 38 ] and was reflected in the included cases [ 71 , 97 ]. Case study research therefore not only has the potential to evidence impact through intervention outcomes, but also has wider health and well-being impact potential by exploring and advocating for occupational therapy across the full spectrum of practice including diverse areas.
Occupational therapy was provided in a range of settings including hospital, community and industry sectors. Interventions adopted illustrate the global variation in occupational therapy practice. For instance, compression bandaging [ 69 , 106 ] and electrical stimulation [ 107 , 108 ] are not aspects of standard practice in the UK but reflect other international practice standards [ 109 , 110 ]. Interventions were wide ranging and reflective of those described in the American Occupational Therapy Process and Domain Framework [ 38 ]. This included therapeutic use of occupation [ 83 ], interventions to support occupation [ 111 ], education and training-based [ 112 ], advocacy-based [ 76 ], group-based [ 113 ] and virtual interventions [ 114 ]. Narrowing the intervention to a single entity was not always possible or appropriate reflecting the complexity of occupational therapy practice and several authors, for example Kearns Murphy & Sheil [ 49 ] and Pretorious [ 79 ] instead reported occupational therapy as the intervention involving a range of activities and approaches that were meaningful and goal directed for the client.
A suggested strength of case study research identified by the findings is the similarity between the research process and clinical practice. Fleming [ 115 ] had suggested that practitioners generate hypothesis in clinical practice to test theory and problem solve elements of the therapy process for example, why an intervention may not be working as expected. Similarly, case study research has been used to test theory in evaluative or explanatory designs. Methods of data collection (e.g. observation, outcome measurement, document review, interview, client feedback) and analysis (e.g. descriptive, visual, pattern-matching outcomes) bear resemblance to how evidence is collected in practice to inform the intervention process [ 116 ]. The term ‘pattern matching’ is an analytic strategy adopted by Yin [ 14 ] in case study research to compare patterns in collected data to theory. However, pattern matching is also evident in occupational therapy clinical reasoning literature, particularly in relation to how practitioners utilize tacit knowledge to inform decision making [ 117 , 118 ]. This insight into case study research supports the perspective that it may be a more familiar and therefore achievable approach to evidence building for practitioners.
The challenge of capturing the complexity of practice has previously been cited as a barrier to research engagement and evidence-based practice in occupational therapy [ 11 ]. In contrast to this, case study research was largely justified as the chosen methodology because it allowed for individual tailoring of the intervention to the case and context [ 72 , 74 , 75 ]. The ability to provide a narrative description of the case, context, intervention and how it was implemented or adapted was seen across case study research, including single-case experimental designs (SCED). This idea of ‘individualization’ of treatment is also noted by Fleming [ 119 ] to differentiate occupational therapy clinical reasoning from medical procedural reasoning. The effectiveness of occupational therapy is not solely based on a prescriptive treatment, but is also influenced by the interactions between the therapist and service user and the particulars of that context. Therefore, if thinking on clinical reasoning has evolved to capture the important nuances of interactive reasoning [ 115 ] and furthermore embodied practice [ 118 ] then it would seem appropriate that the research approach to building evidence should also. A pluralistic approach whereby there is a valued position for both case study research and larger-scale inquiry to capture both the depth and breadth of practice would seem fitting. Collecting and pooling case study research data from practice can capture these important elements and allow for pattern matching or synthesis. In this way, case study research can hold value for evidence building, just as the randomized controlled trial, or other larger-scale inquiry, does for generalizability with the potential to inform policy and practice.
Based on the findings from this review, collecting case studies from practice to develop an evidence base is potentially viable given its uptake across practice areas and relatively consistent publication. In psychotherapy, Fishman [ 23 ] advocated for a database of cases which follow a systematic structure so they can be easily understood, recognized and data compared. Journals dedicated to publishing case data using a methodical format have since evolved in psychotherapy [ 120 ]. In occupational therapy, the Japanese Association of Occupational Therapists [ 121 ] collects practical case reports from members using dedicated computer software to host a collective description of occupational therapy practice. There is potential then to adopt this even on an international basis, where occupational therapy practice can be shared and measured. The challenge however is in achieving a systematic approach to how case study research data is collected and recorded to allow for meaningful comparisons and conclusions to be drawn.
In this review, quantitative and mixed method designs used a range of different outcome measures which is not conducive to pooling cross case data. Goal Attainment Scaling (GAS) is an outcome measure that defines individualized goals and relative outcomes to determine therapeutic effectiveness [ 122 ]. It is a measure advocated for its applicability across areas of practice but also for research, both large-scale inquiry and case study research [ 123 ]. In this review, it was used across age groups, in the community, outpatient settings and schools and in the areas of neurodevelopmental disorder, stroke, brain injury and ill mental health.
Kearns-Murphy & Sheil [ 49 , 123 , 124 ] adopted Goal Attainment Scaling in their longitudinal case study and explored the different methods of analysis of the measure. They concluded that charting GAS scores at multiple timepoints is beneficial to case study research as it adds to the ‘in-depth’ analysis providing insight into the fluctuations of therapy and outcomes in the real-life context. Visual analysis of charted scores is then an appropriate analytic technique for intervention-based case study research. Two time points, before and after, are more suited to large-scale inquiry for generalization but in the case study, only the performance of an individual on a particular day is highlighted which may be influenced by several contextual factors. Given these assertions, adopting a consistent outcome measure across practice such as GAS, would allow for in-depth, case and context-specific understanding that could also be comparable and pooled across cases.
Strengths and limitations of the scoping review
This review searched published and grey literature using a variety of terms that have been used interchangeably with case study research with the aim of conducting a comprehensive overview. It followed a peer-reviewed protocol with systematic and transparent processes. JBI methodology for the conduct of scoping reviews was followed and bibliographic software (Mendeley) and systematic review software (Rayyan) was used to manage citations and the screening process. Additionally, an updated search was completed in July 2021 to enhance the timeliness and relevance of findings.
Ten databases were searched and no further relevant articles were identified through websites or citation searching, affirming that a thorough search had been conducted. However, to balance a comprehensive search with the practicality of resources, some decisions were made which may impact the inclusivity of the review. Western dominant databases and English language limits were applied because of translation resource availability within the research team. The search algorithm was developed and tested with an academic health librarian at the protocol stage; however, as case study methodology was not always clear from the title and abstract, an unmanageable amount of data was presented at full-text stage. To manage the number of records, inclusion criteria was changed to provide a contemporary overview from 2016 rather than 1990. This may introduce some bias to the review, where relevant articles pre-2016 or in other languages were omitted. However, the narrower focus allowed for in-depth data mapping to maximize the value of findings for informing future practice and research. Without taking this step, the output would likely have been more superficial. As a large number of 88 studies were still included in total, it was felt an appropriate balance had been achieved.
Findings suggest that case study research is a viable methodology to contribute to the evidence base for occupation and health as it has been used to evaluate interventions across a range of occupational therapy practice contexts. It has been used for cases of complexity, early intervention efficacy and feasibility, theory testing or when small participant numbers are available, in other words, when large-scale inquiry is not appropriate.
Inconsistencies were identified that mirror findings of case study research methodology in other disciplines. In particular, case study design and description of the case and boundary were poorly reported. Therefore, this review proposes that a common language is used—case study research—to define this flexible methodology. A description and conceptual model are proposed to assist in clarifying how case study research can be applied and reported in occupational therapy. Consistent reporting as a research form of inquiry improved description of the case and boundary and reference to seminal authors would help differentiate research from non-research cases and enhance viability for pooling cases together through more consistent, systematic conduct and reporting.
Implications for research and practice
There is a need to distinguish case study as a research method, separate from the illustrative case report and from purely qualitative inquiry, for it to be identifiable in the literature to reduce confusion and capability concerns. Therefore, the term ‘case study research’ is proposed when referring to the research methodology specifically. Citation of seminal authors alongside this description of study design would aid visibility of case study research as distinct from non-research and could also support appropriate journal classification. Greater clarity in reporting case description, including a narrative summary of the case, context and boundary of study is also an area for development. The development of a systematic template for the collection and reporting of case study data, ideally mirrored internationally, would likely be an ideal solution. This would potentially build capability for the conduct of rigourous case study research, help make it more identifiable in the literature and support pooling data across studies for synthesis and generalization, thereby overcoming the criticisms of case study research. Through accurate and detailed description of case context and boundary, practitioners would more easily be able to identify if the information is relevant to their own practice context.
Case study research has been shown to be appropriate for use across settings and populations, therefore pooling data could enable services to benchmark. Practitioners seeking to explore research within their practice are encouraged to consider the case study approach for its flexible nature and suitability to the person-centred values of occupational therapy. Use of a consistent outcome measure would support pooling of data and, as GAS is specific to the individual rather than practice setting, services may want to explore it as a measure suitable for intervention-based case study research.
Acknowledgements
Acknowledgements and thanks are extended to the Elizabeth Casson Trust for individual funding awarded to the corresponding author and to the Case Study International Think Tank for their professional support.
Abbreviation
Authors’ contributions.
All authors (LMQ; KT; KB) were involved in the conceptualization of the idea for this review. LMQ developed the search strategy and conducted database searching. All authors contributed to the screening and selection of studies and piloted the data extraction tool. LMQ completed data extraction and KT cross checked a 10% sample of these. LMQ charted the results and completed the first draft of the paper with input from the other authors. LMQ critically revised the draft paper and all authors read and approved the final draft before submission.
No grant funding has been provided for this review.
Availability of data and materials
Declarations.
Not applicable.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Study protocol
- Open access
- Published: 11 April 2024
Effects of task-based mirror therapy on upper limb motor function in hemiplegia: study protocol for a randomized controlled clinical trial
- Hongzhen Liu 1 ,
- Yangjie Xu 1 ,
- Wei Jiang 1 ,
- Fangchao Hu 2 ,
- Yi Zhou 1 ,
- Feng Zhou 1 ,
- Ying Yin 1 &
- Botao Tan ORCID: orcid.org/0000-0001-8513-3416 1
Trials volume 25 , Article number: 254 ( 2024 ) Cite this article
105 Accesses
Metrics details
Background and purpose
Research to date has lacked definitive evidence to determine whether mirror therapy promotes the recovery of upper extremity function after stroke. Considering that previous studies did not stratify patients based on structural retention, this may be one of the reasons for the negative results obtained in many trials. The goal evaluates the efficacy of TBMT (utilizing an innovatively designed mirror) versus standard occupational therapy for stroke patient’s upper limb functionality.

Methods and analysis
This single-center randomized controlled trial will involve 50 patients with stroke. All patients will be randomly assigned to either the task-based mirror therapy or the control group. The interventions will be performed 5 days per week for 4 weeks. The primary outcomes will be the mean change in scores on both the FMA-UE and modified Barthel Index (MBI) from baseline to 4 weeks intervention and at 12 weeks follow-up between the two groups and within groups. The other outcomes will include the Action Research Arm Test (ARAT), the Nine Hole Peg Test (9HPT), the Functional Independence Measure, and MRI.
This trial will not only to establish that task-based mirror therapy (TBMT) could improve the recovery of hand function after stroke but also to explore the underlying mechanisms. We expect that this finding will clarify the brain activation and brain network mechanisms underlying the improvement of hand function with task-oriented mirror therapy and lead to new ideas for stroke hand function rehabilitation.
Trial registration
URL: https://www.chictr.org.cn ; Unique identifier: ChiCTR2300068855. Registered on March 1, 2023
Peer Review reports
Introduction
The severe consequences of stroke often result in residual motor, sensory, cognitive, urinary, and fecal dysfunction, making it challenging for survivors to reintegrate into their families and society [ 1 , 2 ]. Recent research indicates that approximately 85% of stroke patients experience hemiparesis in their upper or lower extremities, while 55 to 75% of stroke survivors face limited upper extremity function [ 3 ]. Upper extremity function accounts for 60% of total body function, and hand function alone comprises 90% of upper extremity function. Therefore, effective hand rehabilitation is essential to successfully reintegrate patients into their families and enhance their independence [ 4 ].
Although rehabilitation training is the primary treatment method for stroke patients, the current results of rehabilitation for poststroke hand dysfunction are not satisfactory [ 1 ]. There is an urgent need to develop more effective and inexpensive rehabilitation techniques for hand function. Mirror therapy (MT) has emerged as a promising new rehabilitation intervention in recent years [ 5 , 6 ]. MT typically involves placing a flat mirror on the unaffected side of the body, allowing the patient to “embody” their paralyzed limb through the optical illusion created by the mirror. This technique effectively “tricks” the brain into perceiving movement in the affected limb, potentially aiding in the recovery of motor function. MT has shown particular efficacy in the treatment of phantom limb pain [ 7 , 8 , 9 ] and has also begun to show promise as a therapeutic approach for stroke [ 5 ]. Research has demonstrated that MT is an effective adjunctive therapy for improving upper extremity motor function and daily living among stroke patients [ 7 , 10 , 11 , 12 ]. A study found that MT combined with bilateral arm training and graded activities was effective in improving motor performance of the paretic upper limb after stroke compared with conventional therapy without MT [ 13 ]. We have also done previous studies demonstrating that the combination of conventional rehabilitation therapy and TBMT is an effective way to improve functional recovery in upper limb stroke patients [ 14 ] (Fig. 1 ). However, to date there has been little agreement on the facilitative effect of MT. A randomized controlled trial by Antoniotti et al. found no significant difference between actual and sham MT for functional recovery of the upper extremity in early stroke [ 15 ]. There is a strong link between acquisition of motor skills and neuronal plasticity at cortical and subcortical levels in the central nervous system [ 16 ]. Therefore, it is possible that these limitations arise from the fact that patients exhibit varying degrees of structural preservation at the injury site, and the treatment of MT effect on upper limb motor function of hemiplegia is somehow dependent on the severity of the lesion, which ultimately resulted in contradictory findings.

Conventional mirror therapy
The corticospinal tract (CST) is the primary descending motor pathway that connects cortical motor regions with spinal cord neurons, and it plays a crucial role in human upper limb mobility. Consequently, maintaining the structural integrity of the CST is crucial for determining the upper limits of upper limb recovery in patients. Studies have shown that the extent of CST injury is the optimal biomarker for successful rehabilitation of the upper extremity after stroke [ 17 ]. Baseline anatomical integrity assessment is essential to ensure patient balance and uniformity. Furthermore, this approach can predict functional recovery in chronic stroke for more effective neurological rehab treatment. Because there is a significant correlation between functional recovery and the preserved structural basis of the lesion [ 18 ]. Diffusion tensor imaging (DTI) is an MRI imaging technique that can detect lesions and display nerve fiber bundles in three dimensions [ 19 ]. Previous research has established that extracting CST bundle FA values from DTI data can yield valuable insight into their integrity and provide useful information about individualized rehabilitative strategies in stroke patients [ 20 ]. For this study, in an attempt to ensure the consistency of treatment efficacy irrespective of patient disease characteristics, we will employ DTI to assess the severity of CST degeneration in our subject patients. Post-enrollment, we will conduct a subgroup analysis to ensure balanced rehabilitation potential across various patient populations.
On the other hand, imaging evaluation can also help us understand the mechanisms by which mirror therapy [ 21 , 22 , 23 ]. For example, during MT, stroke patients showed increased functional magnetic resonance imaging (fMRI) activities across widely distributed brain regions [ 24 , 25 ]. Camera-based visual input from the start-up mirror facilitated motor recovery, daily functioning, and brain network separation in subacute stroke patients [ 26 ]. However, few authors have been able to provide a systematic account of the mechanisms of mirror therapy. This new clinical trial is unique due to the following factors: the innovative utilization of DTI imaging which considers CST integrity as a fundamental measure, reduces variables that may impact the randomization process; the implementation of a novel therapeutic apparatus that improves the effectiveness of TBMT; to investigate the mechanism, the project proposes to use the BOLD-fMRI technique to reflect the active level of brain regions and whole-brain functional network connections to reveal the spontaneous activity patterns, connectivity patterns, and brain network characteristics, thus providing new theoretical support for the study of the neural mechanisms of mirror therapy.
Methods/design
Study design.
This is a single-center, prospective, single-blinding, randomized controlled superiority trial. The objective will be used to evaluate the effectiveness of TBMT (using a newly designed mirror) compared to conventional occupational therapy on upper extremity functions of stroke patients. Patients will be randomly allocated in a 1:1 ratio into a control ( N = 25) or TBMT group ( N = 25), with the control group receiving conventional occupational therapy intervention and TBMT group receiving task-based mirror therapy in addition to CG. A professional team will measure relevant outcomes at baseline and 4 weeks after treatment.
Sample size estimation
The sample size was derived from pre-existing research using G Power v.3.1, considering significance level ( α ) = 0.05, power (1 − β) = 0.95, and given that the minimal clinically significant difference in patient’s hand function improvement, as per prior study data, is 9 points in the FMA-UE with an effect size of d = 1.13 [ 14 ]. Estimation via G Power software yielded a requirement of 44 samples. Considering potential subject attrition or termination, the sample size could be augmented by 10–15%, resulting in the adjusted sample size of N = 50, or 25 patients in each group. Consequently, the total sample size for both groups was formulated as 50.
Participants
Fifty eligible patients with upper limb motor dysfunction in stroke will be recruited from the outpatient and inpatient departments of the Department of Rehabilitation Medicine, Department of Neurology, and Department of Neurosurgery of the Second Hospital of Chongqing Medical University. Eligible patients had to satisfy the inclusion, exclusion criteria, and termination criteria (Table 1 ). Information about this trial will be posted via posters in the waiting area of the Rehabilitation Department and the Rehabilitation Medicine Clinic so that interested patients can contact the program director through their therapist. If an applicant meets the study criteria, then they will be invited to participate
Randomization and blinding
A total of 50 patients who meet the inclusion criteria will be randomly assigned to either the task-based mirror group or the control group. The randomization sequence will be generated by an independent statistician using SPSS Version 19.0. Patients will be assigned randomization numbers based on the order of enrollment. To maintain blinding, opaque sealed envelopes will be utilized to conceal group assignments. Patients will only become aware of their group after opening the envelope, which will be securely stored in a separate cabinet. Blinding of evaluators will be employed in this study to avoid bias stemming from subjective factors. The same investigator, who will be blinded to the treatment assignment, performed all the assessments. Additionally, statisticians will conceal the groupings and their significance, and the code will remain undisclosed until the analysis is finalized. In case of a severe incident during a trial, blinding may need to be undone for proper treatment. This decision must be endorsed by the trial’s lead researcher/medic, and recorded in the protocol, with utmost consideration given to minimizing bias and ensuring data quality.
Interventions
The study protocol is illustrated in Fig. 2 . All participants who fulfil the inclusion criteria will be assessed. This research protocol conforms to the CONTORT 2010 guidance, adheres to the Revised Standards for Reporting Intervention trials (SPIRIT) protocols, and satisfies the SPIRIT checklist criteria (online supplementary additional file 2 ) [ 27 ]. This trial will investigate the TBMT versus a control intervention and accords with the SPIRIT Figure (Table 2 ). Patients will be randomized to a conventional and task-based mirror treatment group for 5 consecutive days per week for 4 weeks, ensuring a total of 40 min of treatment time per day for each group. A trained and professional occupational therapist will be assigned to conduct this trial, and each patient will sign an informed consent form (online supplementary additional file 1 ) before treatment.
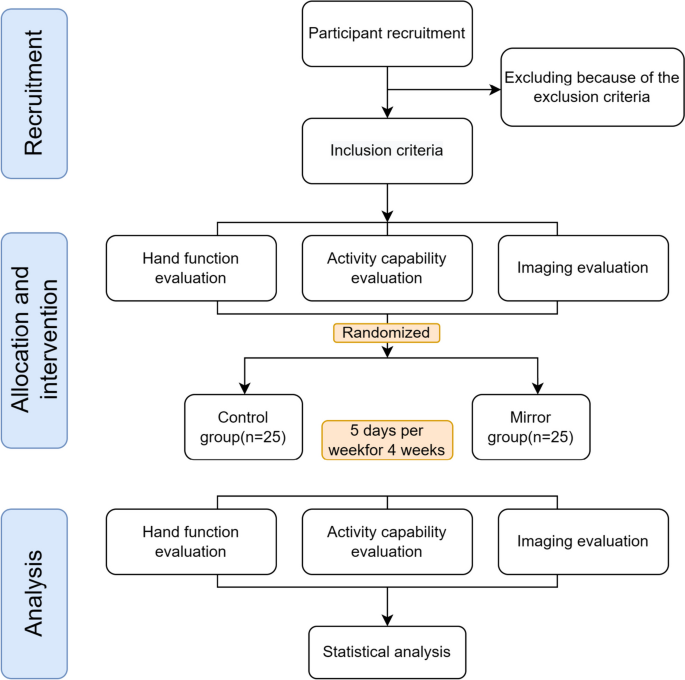
Proposed participant flow
Control group (CG)
Depending on the patient’s condition, 20 min of occupational therapy without the mirror will be conducted alongside 20 min of conventional treatment, resulting in a total duration of 40 min. The above training will be performed unassisted by a mirror therapy rehabilitator 5 days a week for 4 weeks.
Task-based mirror therapy (TBMT)
Patients in the TBMT group will receive 20 min of conventional therapy followed by 20 min of TBMT. We designed an ergonomic mirror therapy device (patent number: Z120212 2278905.3) (Fig. 3 ). Patients will be seated facing the mirror device, with both hands in the box under the screen that substitutes the conventional mirror. The high-definition LCD can display the mirrored image of the healthy hand. Both hands can move freely in the box. By looking at the image on the LCD screen, the patient may create an “optical illusion” that activates mirror neurons and triggers the active activity of the affected hand. The task orientation is as follows: the patient moves with the healthy limb while observing the mirror image and using the affected hand as much as possible to perform the following movements together: elbow flexion and extension, ulnar and radial deviation, wrist flexion and extension, finger flexion and extension, finger adduction, and abduction, as well as the use of sponge balls, water cups, rags, chopsticks, cups, tubes, and wooden blocks. Patients will use their healthy upper limbs to move objects such as watches and rings to promote imagination. This process focuses on placing an object on the affected limb while exercising on the healthy side to facilitate stimulation. The affected upper limb may not have any allowed voluntary activity [ 14 ].

Ergonomic mirror therapy device
Appropriate care is permitted during the trial period, including pain management, defecation assistance, and posture management. Hand function interventions are prohibited during non-treatment periods to ensure the effectiveness of the trial.
Outcome measurements
Patients will undergo clinical outcome measurements at baseline, 4 weeks into treatment, and immediately after 12 weeks of treatment. Evaluations will encompass basic information, indicators of hand function, daily activity, and imaging techniques (DTI, CST integrity assessment, including FA, rFA, ROI, and FC values). Specialized training will be provided to evaluators to ensure the credibility of the evaluation.
Primary outcomes
The Fugl-Meyer Assessment for upper extremity (FMA-UE) will be utilized to evaluate the level of upper limb motor function impairment, with a maximum score of 66 points [ 28 , 29 ]. This assessment includes 23 different movements grouped into four categories (shoulder/elbow/forearm, wrist, hand/finger, and coordination), whereby 33 items are assessed. Rated on a 3-point scale, task completion is scored as 0 for inability, 1 for partial ability, and 2 for near-normal ability. The reliability, validity, and responsiveness of the FMA-UE assessment for stroke patients are well recognized [ 30 ]. Therefore, FMA-UE will be considered as the primary outcome.
Secondary outcomes
Brunnstrom is a motor function and muscle spasticity assessment method for the affected upper extremity [ 31 ]. It includes six stages: Grade 1: absence of random movement, no upper or lower extremity movement; Grade 2: joint response, comovement, and minimal random movements; Grade 3: random comovement with the ability to grasp but not extend; Grade 4: separation of movement, including the ability to pinch and make minor extensions; Grade 5: gradual restoration of muscle tone with fine movements, simultaneous yet independent extension of fingers; and Grade 6: motor ability approaching normalcy but speed and accuracy are suboptimal.
The Modified Barthel Index (MBI) assesses the mobility of stroke patients concerning their ability to carry out specific activities of daily living. These activities include eating, bathing, dressing, bowel and urinary control, toileting, bed and chair transfer, level walking, and stair walking [ 32 , 33 ]. A total score of 100 can be achieved, and scores of 60 or higher indicate self-sufficiency. Independence positively correlates with the score.
We commonly use the Action Research Arm Test (ARAT) to assess the ability of the affected upper extremity and hand to handle objects of different sizes, weights, and shapes. The test assesses 19 tests of arm motor function, both distal and proximal. Each test is given a score of 0, 1, 2, or 3, with higher scores resulting in better function. The total ARAT score is the sum of the 19 tests, resulting in a maximum score of 57 [ 34 ]. Nine Hole Peg Test (9HPT): assesses the patient’s whole hand dexterity. The assessment requires the patient to take nine pegs from the container and insert them into a small pegboard, then remove and place them back into the container. The patient’s score depends on the speed of insertion and removal, with the faster the time, the higher the score [ 35 ].
Imaging outcome measures
Subjects will undergo Rs-fMRI scans utilizing a gradient echo EPI sequence (repetition time = 2000 ms, echo time = 30 ms, FOV = 220 × 220mm 2 , flip angle = 90°, matrix size = 64 × 64, 30 transverse slices, slice thickness = 4 mm, gap = 0.8 mm). Each Rs-fMRI acquisition will yield 240 volumes [ 36 ]. High-resolution T1-weighted 3D anatomical images will be obtained in the sagittal orientation using a fast field echo sequence, repetition time (TR) = 7.4 ms; echo time (TE) = 3.6 ms; flip angle = 8 ◦ ; field of view (FOV) = 250 × 250 mm 2 ; matrix = 228 × 227; 150 slices; slice thickness = 1.1 mm with no gap and voxel size = 1.1 × 1.1 × 1.1 mm 3 . DTI parameters were a spin echobased echo-planar imaging sequence in contiguous axial planes that included 16 volumes with diffusion gradients applied along 15 noncollinear directions ( b = 800 s/mm 2 ) and one volume without diffusion weighting ( b = 0 s/mm 2 ). Each volume consisted of 65 contiguous axial slices covering the entire brain (TR = 6973 ms; TE = 75 ms; flip angle = 90 ◦ ; FOV = 224 × 224 mm 2 ; matrix = 112 × 112 and voxel size = 2 × 2 × 2 mm 3 ). All MRI scans need to be performed by a specialized imaging physician, with the patient being scanned for both fMRI and DTI sequences in a single session, with the fMRI scan taking approximately 15–20 min, followed by the DTI scan taking approximately 5–10 min. The DTI and fMRI scanning workflow diagram is shown in Fig. 4 .
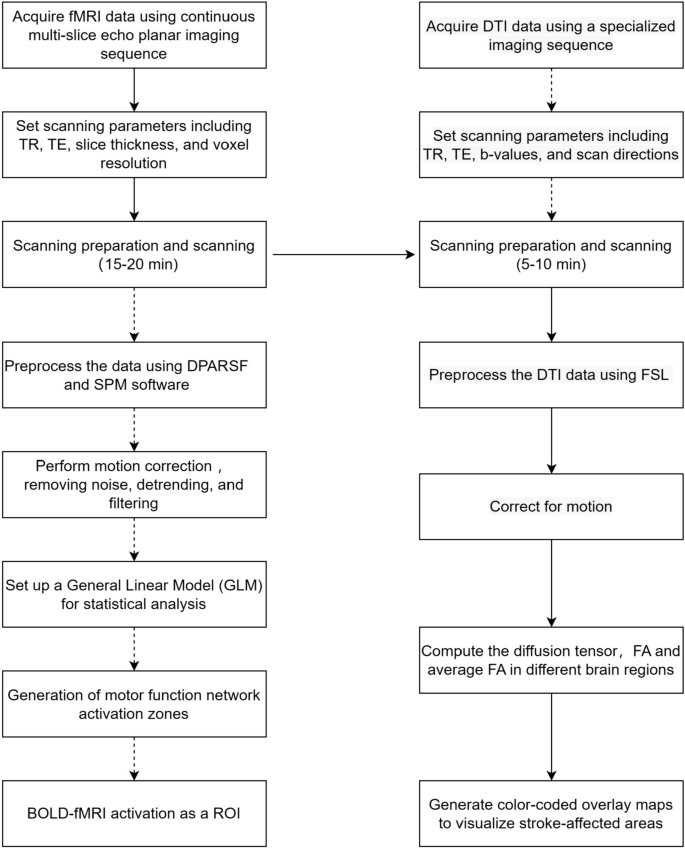
The DTI and fMRI scanning workflow diagram
Image data acquisition and preprocessing
For fiber tract identification, we will use automated fiber quantification (AFQ) software to identify 20 WM tracts in each participant’s brain [ 37 ]. The identification procedure included three primary steps: (1) whole-brain deterministic fiber tractography, (2) waypoint ROl-based tract segmentation, and (3) probability map-based fiber refinement. Twenty fiber tracts will be identified according to the predefined ROls and probability maps: bilateral thalamic radiation CST, cingulum cingulate, cingulum hippocampus callosum forceps major, callosum forceps minor, bilateral inferior front-occipital fasciculus (IFOF), bilateral inferior longitudinal fasciculus(lLF), superior longitudinal fasciculus (SLF), bilateral uncinate, bilateral arcuate. Then, each fiber bundle will be divided into 100 segments. Finally, the FA, MD, AD, and RD of each segment of each fiber bundle will be calculated. The automated calculation will be performed by MATLAB 2011b. First, the effective self-diffusion tensor will be computed from the movement and distortion-corrected dataset [ 38 ]. The unit-less FA is an anisotropy index and ranges from 0 in fully isotropic diffusion to 1 in fully anisotropic diffusion [ 39 ]. Mean FA will be calculated for the affected and unaffected sides of each patient within a 5-mm radius of the posterior limb of the internal capsule. For methods, see Radlinska et al. [ 40 ]. Based on this, the diffusion indicators of rFA and FAasy are calculated for both participant groups using the following formula:
The values of rFA and FAasy ranged from 0 to 1. The lower the rFA and the higher the FAasy, the more significant the decrease in ipsilateral CST anisotropy of the lesion, i.e., the more severe the impairment of CST integrity.
The fMRI is an imaging technology without intervention and employs magnetic resonance for quantifying hemodynamic alterations triggered by neuronal activity, indicating brain region activation. On patient readiness, full brain scans commence during rest-state scanning, instructing them to unwind, occlude vision, and refrain from intentional cognitive tasks. Images of the patients with left‐sided lesions will be flipped before preprocessing. After flipping, the right hemisphere will be tagged as the ipsilesional side and the left hemisphere as the contralesional side. fMRI preprocessing will be carried out using DPARSF, which provides a pipeline workspace based on Statistical Parametric Mapping (SPM; Wellcome Trust Centre for Neuroimaging, London) [ 41 ]. First, volumes from each run will be realigned to their first volume to estimate motion artifacts. The head motion will be then corrected using a six‐parameter rigid body spatial transformation. Functional mean images will be obtained and co‐registered to the corresponding individual structural image before normalization to the standard Montreal Neurological Institute (MNI) template. Finally, images will be smoothed with an 8‐mm isotropic Gaussian kernel.
Functional connectivity analysis
In this study, seed-based analysis will estimate brain region connectivity strengths by calculating correlation coefficients of each brain area’s time series. ROIs will be identified from brain areas differing between healthy and stroke patients with impaired hand function. Pearson correlations between ROIs and all brain voxel time series will be assessed, transforming them into normal distributions through Fisher’s z transformation. A whole-brain functional connectivity analysis, seeding on the abnormal brain area, will identify the post-mirror therapy functional connectivity differences between the control and experimental groups [ 36 ].
Whole-brain functional network analysis
Following preliminary processing, the representative time series of each region of interest (ROI) will be acquired by extracting and averaging the time series of all the voxels within the specified ROI. An asymmetric correlation matrix will be generated by computing Pearson’s correlation coefficient of all conceivable pairs of the representative time series. Sparsity (Sp) will be used to set the threshold value and calculate the brain network topology properties. Finally, the differences in the topological properties and connections of brain networks between the intervention and control groups will be explored by analyzing the whole-brain functional network.
Experiments consider conducted employing the SPM8-compliant DPARSFV2.2 suite on MATLAB 2011b. Paired t -tests will analyze data sets from individual groups before and after intervention, with p < 0.05 defining significance. Later, a two-sample t -test will assess differences in functional connectivity between the study and control cohorts post-therapy. A p < 0.05 cut-off will be utilized for substantial functional connectivity alterations, followed by AlphaSim multiple comparison corrections. Relevant observation zones consist of activated areas with ≥ 82 active voxels.
Safety and adverse event monitoring
There will be a low probability of adverse events in this study. Potential risks are skin irritation, redness, scratching, dizziness, and seizures. Any adverse events during the study should be recorded, observed, and followed up in detail, including whether the adverse event is quantitatively related to mirror therapy, whether symptoms resolve or disappear after stopping treatment, and whether appropriate treatment has been administered. The questionnaires will be administered to the participants after every treatment, and the results will be recorded and analyzed. The outcome assessors will judge the severity (mild, moderate, or severe), seriousness, and causality (definitely related, probably related, possibly related, possibly not related, definitely not related to the intervention, or not assessable). In severe cases, more moderate interventions are required to prevent overwhelming the patient’s body. In the event of severe adverse reactions or worsening of the condition, immediate termination of the experiment and prompt reporting to the ethics committee are essential. In addition, a Data Monitoring Committee (DMC) will help finalize interim analyses or stop rules. The DMC is composed of clinicians and statisticians, independent of the sponsor and study team. It scrutinizes accumulated data and recommends modifications for future trials, ensuring risks to participants remain within limits. The DMC can discontinue a trial if significant protocol infractions transpire or large patient dropouts occur. Should any participants suffer any harm from the trial, they will receive necessary medical treatment for the injury or complication, free of charge, as a public patient within the Second Affiliated Hospital of Chongqing Medical University. This safeguard aims to protect the health and safety of participants and provide necessary medical care.
Statistical analysis
Data management and analysis will be conducted in SPSS version 23. Groups will be compared at baseline using the t test for independent samples for the continuous variables, and the chi-square test for categorical data. The differences of the outcomes, including the FMA-UE, MBI, ARAT, and the 9HPT, between the groups at each of the trial time points will be analyzed using mixed-design 2-way repeated-measures analysis of variance (ANOVA), taking time (4 levels: preintervention, after 2 weeks, after 4 weeks of intervention and 3 months at the end of the trial for follow-up) as the within-subject factor and group (2 levels: TBMT and CG) as the between-subject factor. If participants drop out during the intervention period, they will not be excluded due to the principle of intention to treat (ITT). Furthermore, in instances of missing data, the continuation of observations (LOCF) method will be employed, whereby the last recorded observation preceding the gap in data will serve as a substitute. Unfavorable stroke outcomes correspond to lower FA values for corticospinal tracts, while robust functional recovery denotes elevated FA values. Subgroup analyses of FA values will be conducted based on the interquartile spacing (< 25% interval; 25–75% interval; > 75% interval) method post the inclusion of all individuals to standardize the baseline conditions of the patients. We will use linear regression model outcomes at 4 weeks post-treatment cessation as the dependent variable (FMA-UE). This model will include treatment assignment (TBMT vs. CT) and baseline outcome measure as fixed-effects, as well as patient characteristics (low or high impairment severity at baseline). We will examine differential impacts by fitting separate models with treatment-impairment severity. We will report relevant point estimates and standard errors for these models and conduct 5% level tests for interaction terms with two-sided alternative hypotheses. A p -value < 0.05 is deemed a statistically significant discrepancy.
Patient and public involvement
Although patients cannot directly participate in the design process of clinical trials, they can offer valuable input during the recruitment and informed consent phase. Their views can enhance transparency and fairness, ensuring that patients fully understand the purpose, risks, and advantages of the trial. We prioritize regular feedback and evaluation from patients and assess their satisfaction with the trial process each time to ensure that their voices are heard and to identify necessary improvements. The outcome measures to be evaluated in this study will potentially be influenced by the sociodemographic characteristics and preferences of the patients. Therefore, we use a comprehensive assessment. The result of our study will be published in a peer-reviewed journal.
Modification of the protocol
Any modifications to the protocol, including changes in objectives, design, patient population, sample size, and study procedures will require a formal application from the Institutional Review Board (the Board) and Hospital Research Ethics Committee (the Committee) of the Second Affiliated Hospital of Chongqing Medical University. Based on safety assessment data, if research is changed to eliminate an apparent immediate danger(s) to the subject, the investigator will promptly notify the Board and the Committee on Change(s). Review by the Board and Committee at the next meeting convened to determine whether the proposed change(s) are consistent with the subject’s continued welfare.
Data management and quality
Only researchers who participated in this study can access the data. Each participant will receive an ID number for privacy during the trial period. Details are captured on custom case report forms (CRFs) that undergo double checking for accuracy and completion. Associated documents obtain unique code numbers then securely stored within the Rehabilitation Medicine Division of the hospital. Hard copies are transferred to an Excel spreadsheet for review by two doctors before storage on a password-protected computer. Only the lead researcher and statistician hold passwords to this document cabinet, adhering to medical record retention laws and GCP principles. Two additional healthcare professionals will undertake periodic physical site audits to confirm meticulous adherence to the investigative protocol and data accuracy. Through these strategies, we augment patient cooperation and decrease instances of dropout.
Hand function is a key issue in stroke rehabilitation. While there are various treatment options, the availability of precise and effective methods remains a major challenge. Mirror therapy is a relatively effective therapeutic intervention [ 14 ]. However, previous studies have not linked functional recovery to the structural basis preserved by the lesion. This may be a potential reason why different teams in the current mirror therapy study have reached opposite results [ 42 ]. Therefore, it is imperative to establish high-quality evidence to support the use of mirror therapy in stroke rehabilitation. To address this gap, this is the first study to incorporate comprehensive patient baseline data while considering structural preservation and utilized a customized ergonomic therapeutic device. The primary aim of this study is to assess how effective MT is in rehabilitating stroke patients.
MT is based on the mirror neuron system and uses the plane mirror imaging principle for the contralateral activity images projected on the affected side. It also combines optical illusions, visual feedback, and virtual reality [ 43 ]. This visual stimulus supports motor rehabilitation by capitalizing on the strong connection between visual input and the pre-motor cortex [ 44 ]. A recent clinical study concluded the neural mechanisms of motor imagery training (MIT) in stroke rehabilitation by fMRI. The conclusion was drawn that MIT helps reduce compensatory activation in both hemispheres in stroke patients, remodels FC in the ipsilateral hemisphere, and promotes functional recovery [ 45 ]. However, there is a relatively small body of literature that is concerned with the neural mechanisms of mirror therapy in depth. In this study, we will focus on analyzing the Pearson correlation coefficients between two specific brain regions. We will also investigate the differences in topological properties and lateral connections within the brain network of both intervention and control groups. By doing so, we aim to identify any characteristic manifestations of brain network changes resulting from mirror treatment. This will enable us to better understand the neurological mechanism behind improved hand function through mirror treatment. Meanwhile, we will use an array of assessment techniques to determine the effectiveness of TBMT, including autonomic control (FMA), arm and hand motor recovery (Brunnstrom phase), manual dexterity (9HPT), and daily activities. This study is extremely comprehensive, as you can observe.
In conclusion, this will be a well-controlled, high-quality clinical study, and the findings may be used to update evidence-based protocols in postacute stroke care planning and to translate evidence into practice and medical decision-making.
Availability of data and materials
Not applicable.
Abbreviations
- Diffusion tensor imaging
Fugl-Meyer Assessment Upper Extremity Scale
Modified Barthel Index
Action Research Arm Test
Nine Hole Peg Test
- Task-based mirror therapy
Mirror therapy
Corticospinal tract
Functional magnetic resonance imaging
Blood oxygenated level dependent functional magnetic resonance imaging
Occupational therapy
Fractional anisotropy
Relative fractional anisotropy
Region of interest
Functional connectivity
Echo-planar imaging
Data Processing Assistant for Resting-State fMRI
Statistical Parametric Mapping
Montreal Neurological Institute
Good Clinical Practice
Motor imagery training
Stinear CM, Lang CE, Zeiler S, Byblow WD. Advances and challenges in stroke rehabilitation. Lancet Neurol. 2020;19:348–60.
Article CAS PubMed Google Scholar
Wu S, Wu B, Liu M, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18:394–405.
Article PubMed Google Scholar
Jorgensen HS, Nakayama H, Raaschou HO, Vive-Larsen J, Stoier M, Olsen TS. Outcome and time course of recovery in stroke. Part II: time course of recovery. The Copenhagen Stroke Study. Arch Phys Med Rehabil. 1995;76:406–12.
Parker VM, Wade DT, Langton HR. Loss of arm function after stroke: measurement, frequency, and recovery. Int Rehabil Med. 1986;8:69–73.
CAS PubMed Google Scholar
Yavuzer G, Selles R, Sezer N, et al. Mirror therapy improves hand function in subacute stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2008;89:393–8.
Sutbeyaz S, Yavuzer G, Sezer N, Koseoglu BF. Mirror therapy enhances lower-extremity motor recovery and motor functioning after stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2007;88:555–9.
Altschuler EL, Wisdom SB, Stone L, et al. Rehabilitation of hemiparesis after stroke with a mirror. Lancet. 1999;353:2035–6.
Thieme H, Morkisch N, Mehrholz J, et al. Mirror therapy for improving motor function after stroke. Cochrane Database Syst Rev. 2018;7:CD008449.
PubMed Google Scholar
Rothgangel A, Braun S, Winkens B, Beurskens A, Smeets R. Traditional and augmented reality mirror therapy for patients with chronic phantom limb pain (PACT study): results of a three-group, multicentre single-blind randomized controlled trial. Clin Rehabil. 2018;32:1591–608.
Dohle C, Puellen J, Nakaten A, Kuest J, Rietz C, Karbe H. Mirror therapy promotes recovery from severe hemiparesis: a randomized controlled trial. Neurorehabil Neural Repair. 2009;23:209–17.
Pomeroy V, Aglioti SM, Mark VW, et al. Neurological principles and rehabilitation of action disorders: rehabilitation interventions. Neurorehabil Neural Repair. 2011;25:33S–43S.
Article PubMed PubMed Central Google Scholar
Thieme H, Mehrholz J, Pohl M, Behrens J, Dohle C. Mirror therapy for improving motor function after stroke. Stroke. 2013;44(7):CD008449.
Google Scholar
Samuelkamaleshkumar S, Reethajanetsureka S, Pauljebaraj P, Benshamir B, Padankatti SM, David JA. Mirror therapy enhances motor performance in the paretic upper limb after stroke: a pilot randomized controlled trial. Arch Phys Med Rehabil. 2014;95:2000–5.
Madhoun HY, Tan B, Feng Y, Zhou Y, Zhou C, Yu L. Task-based mirror therapy enhances the upper limb motor function in subacute stroke patients: a randomized control trial. Eur J Phys Rehabil Med. 2020;56:265–71.
Jo S, Kim H, Song C. A novel approach to increase attention during mirror therapy among stroke patients: a video-based behavioral analysis. Brain Sci. 2022;12(3):297.
Dayan E, Cohen LG. Neuroplasticity subserving motor skill learning. Neuron. 2011;72:443–54.
Article CAS PubMed PubMed Central Google Scholar
Boyd LA, Hayward KS, Ward NS, et al. Biomarkers of stroke recovery: consensus-based core recommendations from the stroke recovery and rehabilitation roundtable. Neurorehabil Neural Repair. 2017;31:864–76.
Boden-Albala B, Carman H, Southwick L, et al. Examining barriers and practices to recruitment and retention in stroke clinical trials. Stroke. 2015;46:2232–7.
Acosta-Cabronero J, Williams GB, Pengas G, Nestor PJ. Absolute diffusivities define the landscape of white matter degeneration in Alzheimer’s disease. Brain. 2010;133:529–39.
Lee J, Chang WH, Kim Y-H. Relationship between the corticospinal and Corticocerebellar tracts and their role in upper extremity motor recovery in stroke patients. J Pers Med. 2021;11(11):1162.
Rong J, Ding L, Xiong L, et al. Mirror visual feedback prior to robot-assisted training facilitates rehabilitation after stroke: a randomized controlled study. Front Neurol. 2021;12:683703.
Veldsman M, Cumming T, Brodtmann A. Beyond BOLD: optimizing functional imaging in stroke populations. Hum Brain Mapp. 2015;36:1620–36.
Altamura C, Reinhard M, Vry M-S, et al. The longitudinal changes of BOLD response and cerebral hemodynamics from acute to subacute stroke. A fMRI and TCD study. BMC Neurosci. 2009;10:151.
Michielsen ME, Smits M, Ribbers GM, et al. The neuronal correlates of mirror therapy: an fMRI study on mirror induced visual illusions in patients with stroke. J Neurol Neurosurg Psychiatry. 2011;82:393–8.
Saleh S, Adamovich SV, Tunik E. Mirrored feedback in chronic stroke: recruitment and effective connectivity of ipsilesional sensorimotor networks. Neurorehabil Neural Repair. 2014;28:344–54.
Ding L, Wang X, Chen S, et al. Camera-based mirror visual input for priming promotes motor recovery, daily function, and brain network segregation in subacute stroke patients. Neurorehabil Neural Repair. 2019;33:307–18.
Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2012;10:28–55.
Bushnell C, Bettger JP, Cockroft KM, et al. Chronic stroke outcome measures for motor function intervention trials: expert panel recommendations. Circ Cardiovasc Qual Outcomes. 2015;8:S163–9.
See J, Dodakian L, Chou C, et al. A standardized approach to the Fugl-Meyer assessment and its implications for clinical trials. Neurorehabil Neural Repair. 2013;27:732–41.
Hsieh YW, Wu CY, Lin KC, Chang YF, Chen CL, Liu JS. Responsiveness and validity of three outcome measures of motor function after stroke rehabilitation. Stroke. 2009;40:1386–91.
Brunnstrom S. Motor testing procedures in hemiplegia: based on sequential recovery stages. Phys Ther. 1966;46:357–75.
Ohura T, Hase K, Nakajima Y, Nakayama T. Validity and reliability of a performance evaluation tool based on the modified Barthel Index for stroke patients. BMC Med Res Methodol. 2017;17:131.
Yang CM, Wang YC, Lee CH, Chen MH, Hsieh CL. A comparison of test-retest reliability and random measurement error of the Barthel Index and modified Barthel Index in patients with chronic stroke. Disabil Rehabil. 2022;44:2099–103.
Daghsen L, Fleury L, Bouvier J, et al. Evaluation of a shortened version of the Action Research Arm Test (ARAT) for upper extremity function after stroke: the Mini-ARAT. Clin Rehabil. 2022;36:1257–66.
Metrot J, Froger J, Hauret I, Mottet D, van Dokkum L, Laffont I. Motor recovery of the ipsilesional upper limb in subacute stroke. Arch Phys Med Rehabil. 2013;94:2283–90.
Wang H, Xu G, Wang X, et al. The reorganization of resting-state brain networks associated with motor imagery training in chronic stroke patients. IEEE Trans Neural Syst Rehabil Eng. 2019;27:2237–45.
Yeatman JD, Dougherty RF, Myall NJ, Wandell BA, Feldman HM. Tract profiles of white matter properties: automating fiber-tract quantification. PLoS One. 2012;7:e49790.
Basser PJ, Mattiello J, LeBihan D. Estimation of the effective self-diffusion tensor from the NMR spin echo. J Magn Reson B. 1994;103:247–54.
Basser PJ, Pierpaoli C. Microstructural and physiological features of tissues elucidated by quantitative-diffusion-tensor MRI. 1996. J Magn Reson. 2011;213:560–70.
Radlinska B, Ghinani S, Leppert IR, Minuk J, Pike GB, Thiel A. Diffusion tensor imaging, permanent pyramidal tract damage, and outcome in subcortical stroke. Neurology. 2010;75:1048–54.
Chao-Gan Y, Yu-Feng Z. DPARSF: a MATLAB toolbox for “pipeline” data analysis of resting-state fMRI. Front Syst Neurosci. 2010;4:13.
PubMed PubMed Central Google Scholar
Antoniotti P, Veronelli L, Caronni A, et al. No evidence of effectiveness of mirror therapy early after stroke: an assessor-blinded randomized controlled trial. Clin Rehabil. 2019;33:885–93.
Ramachandran VS, Rogers-Ramachandran D, Cobb S. Touching the phantom limb. Nature. 1995;377:489–90.
Hebert D, Lindsay MP, McIntyre A, et al. Canadian stroke best practice recommendations: stroke rehabilitation practice guidelines, update 2015. Int J Stroke. 2016;11:459–84.
Wang H, Xiong X, Zhang K, et al. Motor network reorganization after motor imagery training in stroke patients with moderate to severe upper limb impairment. CNS Neurosci Ther. 2023;29:619–32.
Download references
Acknowledgements and Funding
Both BTT, YY, and WJ have acquired the rewards of the Kuanren Talents Program of the Second Affiliated Hospital of Chongqing Medical University. This work is supported by the Chongqing Medical Scientific Research Project (Joint Project of Chongqing Health Commission and Science and Technology Bureau), No. 2023MSXM037. The funders had no role in the study design, data collection, or analysis of the manuscript.
Trial status
At the time of submission of this publication, we are recruiting patients and expect to complete this in December 2024. This is protocol version 1. Recruitment began on July 1, 2023.
Author information
Authors and affiliations.
Department of Rehabilitation Medicine, The Second Affiliated Hospital of Chongqing Medical University, 74 Lin Jiang Road, Chongqing, 40010, China
Hongzhen Liu, Yangjie Xu, Wei Jiang, Yi Zhou, Lu Pan, Feng Zhou, Ying Yin & Botao Tan
Department of Mechanical Engineering, Chongqing University of Technology, No. 69 Hongguang Avenue, Chongqing, 400054, China
Fangchao Hu
You can also search for this author in PubMed Google Scholar
Contributions
WJ and BTT developed the initial idea of the trial, and BTT is the principal investigator. BTT, HZL, YJX, WJ, YZ, LP, and FZ conceived the study, and BTT and HZL wrote the manuscript. All authors commented on drafts of this paper and read and approved this final manuscript.
Corresponding author
Correspondence to Botao Tan .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Institutional Review Board and Hospital Research Ethics Committee of the Second Affiliated Hospital of Chongqing Medical University on Dec 30, 2022 (approval No. 2022-314, date and version identifier: 30 December 2022/V1.0) and will be conducted at the Department of Rehabilitation Medicine, the Second Affiliated Hospital, Chongqing Medical University, Chongqing, China. The Chinese Clinical Trial Registry granted full approval of the study protocol, recruitment materials, and consent form (URL: https://www.chictr.org.cn ; unique identifier: ChiCTR2300068855; date of registration: March 1, 2023). All methods will be carried out in accordance with the principles of the Declaration of Helsinki and relevant ethical guidelines covering informed consent, confidentiality and data storage. Written informed consent will be provided by all patients after providing a detailed description of the study with them. The results will be distributed to patients, researchers, healthcare providers, and sponsors.
Consent for publication
Consent will be obtained directly from patient(s).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Liu, H., Xu, Y., Jiang, W. et al. Effects of task-based mirror therapy on upper limb motor function in hemiplegia: study protocol for a randomized controlled clinical trial. Trials 25 , 254 (2024). https://doi.org/10.1186/s13063-024-08081-1
Download citation
Received : 24 August 2023
Accepted : 29 March 2024
Published : 11 April 2024
DOI : https://doi.org/10.1186/s13063-024-08081-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hand function rehabilitation
ISSN: 1745-6215
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Three years poststroke: A case study . Madison K. Walston, Volume 29 • Issue 2 • February 2024, pp. 39-41 02/01/2024. Olivia experienced a left-side stroke more than 3 years ago and currently resides in an assisted living facility. After the stroke, Olivia had hemi paresis on her right and dominant side and only minimal movement in the ...
Case Study: Neurological rehabilitation. by Joanna Bresi-Ando. Lucas was a 49 year old male, who ran his own business as an IT consultant. He lived with his wife and 2 adult children in their own home. Lucas was previously fully independent with all his daily activities and had no significant past medical history.
The aim of this paper is to provide an overview of occupational therapy practice in stroke patients. ... Case Study Continued. Daily occupational therapy treatment involved improving awareness of the impact of left neglect on daily tasks, systematic visual scanning training, and practical strategies for daily task completion to overcome the ...
Abstract. Background and Purpose— Occupational therapy (OT) is an important aspect of stroke rehabilitation. The objective of this study was to determine from the available literature whether OT interventions improve outcome for stroke patients. Methods— An extensive search in MEDLINE, CINAHL, EMBASE, AMED, and SCISEARCH was performed.
The purpose of this case study was to describe the longitudinal management and outcomes for OT and PT for a patient with a cerebellar stroke with surgical excision over a 14-month treatment course. This patient had an exceptionally long and complex continuum of care that required close coordination and facilitation between disciplines and care ...
Case Study | Stroke Rehabilitation: Assessment and Upper Limb Intervention. Updated: Nov 8, 2020. By Jamie Grant - Director, The Occupational Therapy Hub. Originally written in 2016. UK stroke discharge service. ... Neurology; Stroke; Placements; Case Studies (Plus+) 4,248 views. Related Posts See All. Case Study | Paediatric Disability: OT ...
Methods. We performed a retrospective cohort study using the 2005-2016 Japan Rehabilitation Database, from which we identified patients with stroke (n = 10,270) who were admitted to acute care hospitals (n = 37).We defined active OT (AOT) and non-AOT as OT intervention times (total intervention time/length of hospital stay) longer or shorter than the daily physical therapy intervention time ...
1Department of Occupational Therapy, Eastern Kentucky University, Camille, Richmond, USA. 24867352. 10.3109/07380577.2014.921751. This descriptive case study illustrates the experiences of a 55-year-old male with a chronic disability resulting from a stroke, living in the community and a clinician's trial using occupation-based interventions ...
Abstract. Background and Purpose— Occupational therapy (OT) is an important aspect of stroke rehabilitation. The objective of this study was to determine from the available literature whether OT interventions improve outcome for stroke patients. Methods— An extensive search in MEDLINE, CINAHL, EMBASE, AMED, and SCISEARCH was performed.
The Open Journal of Occupational Therapy Volume 4 Issue 2 Spring 2016 Article 7 April 2016 Use of Occupational Performance Coaching for stroke survivors (OPC-Stroke) in late rehabilitation: A descriptive case study Danika Belliveau University of Ottawa - Canada, [email protected] Isabelle Belliveau
Case Study | Stroke Rehabilitation: Constraint Induced Movement Therapy Updated: Nov 8, 2020 By Jamie Grant, Occupational Therapist; Director, The Occupational Therapy Hub
Keywords: case study, depression, stroke, occupational therapy, elderly; 1. Introduction Occupational therapy (OT) is based on the idea that health and well-being are affected by and affect the nature and pattern of occupations in which persons engage and rich life satisfaction.
Despite the need for occupational therapy to emphasize client-specific occupational performance, primary emphasis in stroke rehabilitation continues to be on the remediation of client factors and self-care. Such practice leaves many survivors of stroke with continuing performance deficits. Two case studies demonstrate a novel, alternative approach.
There are approximately 1% referral rates to tertiary neuro-rehabilittaion inpatient beds due to efficiency working between inpatient and stroke community services lead by OT. The case study was written by Dr Ajay Bhalla (Consultant Stroke Physician), and Nicole Walmsley, (Occupational Therapist) at Guys and St Thomas' NHS Foundation Trust.
Stroke is the major cause of disability globally. This disease can affect the patient's independence and functional mobility severely. Community-based occupational therapy is expected to improve the post-stroke patient's movement and independence to perform daily activities. This study aims to evaluate the effectiveness of community-based occupational therapy, providing assistive ...
Occupational therapy. Similar to physical therapy, occupational therapy (OT) ... Facial Nerve Therapy. A stroke may cause some level of temporary facial paralysis. This can affect a person's daily functions, communication with others, self-esteem, and quality of life. UPMC Rehabilitation Institute's facial nerve therapists have advanced ...
This scoping review explores case study research within occupational therapy in terms of how it is defined, the methodological characteristics adopted, such as data collection and analysis, and the range of practice contexts in which it is applied. We consider the viability of case study research for contributing to our evidence base.
Study design. This is a single-center, prospective, single-blinding, randomized controlled superiority trial. The objective will be used to evaluate the effectiveness of TBMT (using a newly designed mirror) compared to conventional occupational therapy on upper extremity functions of stroke patients.
Management of fatigue and depression. Development of new/meaningful occupations. Study with Quizlet and memorize flashcards containing terms like What is human occupation?, What is occupational therapy?, What are the main aspects of stroke assessment and rehabilitation that occupational therapists are responsible for? [7] and more.