Kidney stone breakthrough procedure at UW called 'game changer' for patients
by Preston Phillips, KOMO News Anchor
SEATTLE — A groundbreaking medical procedure for those with kidney stones will soon be offered at the University of Washington after more than two decades of research. It will also give astronauts the go ahead they need from NASA to travel to Mars.
It's a groundbreaking procedure to get rid of painful stones while you're awake, no anesthesia needed.
"This has the potential to be game changing," said Dr. Kennedy Hall with UW Medicine.
Still being run through clinical trials at UW Medicine, the procedure called burst wave lithotripsy uses an ultrasound wand and soundwaves to break apart the kidney stone.
Ultrasonic propulsion is then used to move the stone fragments out, potentially giving patients relief in 10 minutes or less.
"It would really kind of revolutionize the treatment of kidney stones in the sense that you could come to the clinic and have a stone treated before its a problem," said Dr. Jonathan Harper with UW Medicine.
Seattle resident Mark Mackenzie will tell you first hand, the treatment works. He got a chance to take part in the clinical trial just days before he was to be operated on.
"Nothing else in your life matters when you're experiencing kidney stone pain. I wrote an email to the folks that had done the treatment and just thanked them from the bottom of my heart for saving me from that ordeal," Mackenzie said. "It's not a cure-all for everybody, but in some cases, as in mine, it can be, almost what amounts to a miracle cure."
Dr. Kennedy Hall, an emergency medicine doctor at Harborview Medical Center, said this will also change how future patients are treated in the emergency room, who show up, having no idea they have a kidney stone.
"There are a lot of patients with kidney stones, over a million visits a year to emergency departments," said Hall. "Many of them would have stones that we could intervene on at that point of care in the emergency department, so it's potentially groundbreaking."
This technology is also making it possible for astronauts to travel to Mars, since astronauts are at a greater risk for developing kidney stones during space travel.
It's so important to NASA, the space agency has been funding the research for the last 10 years.
"They could potentially use this technology while there, to help break a stone or push it to where they could help stay on their mission and not have to come back to land," said Harper.
Right now this technology is only available through clinical trials, but according to UW Medicine, it may be available to be used on patients in a regular office setting within the next year or so.
Suggestions or feedback?

MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
New treatment could ease the passage of kidney stones
Press contact :, media download.
*Terms of Use:
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."
Previous image Next image
Every year, more than half a million Americans visit the emergency room for kidney stone problems. In most cases, the stones eventually pass out of the body on their own, but the process can be excruciatingly painful.
Researchers at MIT and Massachusetts General Hospital have now devised a potential treatment that could make passing kidney stones faster and less painful. They have identified a combination of two drugs that relax the walls of the ureter — the tube that connects the kidneys to the bladder — and can be delivered directly to the ureter with a catheter-like instrument.
Relaxing the ureter could help stones move through the tube more easily, the researchers say.
“We think this could significantly impact kidney stone disease, which affects millions of people,” says Michael Cima, the David H. Koch Professor of Engineering in MIT’s Department of Materials Science and Engineering, a member of MIT’s Koch Institute for Integrative Cancer Research, and the senior author of the study.
This kind of treatment could also make it easier and less painful to insert stents into the ureter, which is sometimes done after a kidney stone is passed, to prevent the tube from becoming blocked or collapsing.
Christopher Lee, a recent PhD recipient in the Harvard-MIT Division of Health Sciences and Technology, is the lead author of the study , which appears today in Nature Biomedical Engineering .
Local drug delivery
Kidney stones are made from hard crystals that accumulate in the kidneys when there is too much solid waste in the urine and not enough liquid to wash it out. It is estimated that about one in 10 people will have a kidney stone at some point in their lives.
Several years ago, Cima and Brian Eisner, who co-directs the Kidney Stone Program at MGH and is also an author of the paper, began thinking about ways to improve the treatment of kidney stones. While some larger stones require surgery, the usual treatment plan is simply to wait for the stones to pass, which takes an average of 10 days. Patients are given painkillers as well as an oral medication that is meant to help relax the ureter, but studies have offered conflicting evidence on whether this drug actually helps. (There are no FDA-approved oral therapies for kidney stones and ureteral dilation.)
Cima and Eisner thought that delivering a muscle relaxant directly to the ureter might offer a better alternative. Most of the pain from passing a kidney stone arises from cramps and inflammation in the ureter as the stones pass through the narrow tube, so relaxing the muscles surrounding the tube could help ease this passage.
Around this time, Lee, then a new student in MIT’s Health Sciences and Technology program, met with Cima to discuss possible thesis projects and became interested in pursuing a kidney stone treatment.
“If you look at how kidney stones are treated today, it hasn’t really changed since about 1980, and there’s a pretty substantial amount of evidence that the drugs given don’t work very well,” Lee says. “The volume of how many people this could potentially help is really exciting.”
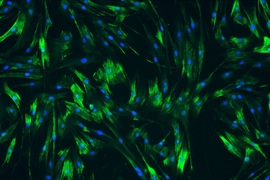
The researchers first set out to identify drugs that might work well when delivered directly to the ureter. They selected 18 drugs used to treat conditions such as high blood pressure or glaucoma and exposed them to human ureteral cells grown in a lab dish, where they could measure how much the drugs relaxed the smooth muscle cells. They hypothesized that if they delivered such drugs directly to the ureter, they could get a much bigger relaxation effect than by delivering such drugs orally, while minimizing possible harm to the rest of the body.
“We found several drugs that had the effect that we expected, and in every case we found that the concentrations required to be effective were more than would be safe if given systemically,” Cima says.
Next, the researchers used intensive computational processing to individually analyze the relaxation responses of nearly 1 billion cells after drug exposure. They identified two drugs that worked especially well, and found that they worked even better when given together. One of these is nifedipine, a calcium channel blocker used to treat high blood pressure, and the other is a type of drug known as a ROCK (rho kinase) inhibitor, which is used to treat glaucoma.
The researchers tested various doses of this combination of drugs in ureters removed from pigs, and showed that they could dramatically reduce the frequency and length of contractions of the ureter. Tests in live pigs also showed that the treatment nearly eliminated ureteral contractions.
For these experiments, the researchers delivered the drugs using a cystoscope, which is very similar to a catheter but has a small fiber optic channel that can connect to a camera or lens. They found that with this type of delivery, the drugs were not detectable in the animals’ bloodstream, suggesting that the drugs remained in the lining of the ureter and did not go elsewhere in the body, which would lessen the risk of potential side effects.
Ureteral relaxation
More studies are needed to determine how long the muscle relaxing effect lasts and how much relaxation would be needed to expedite stone passage, the researchers say. They are now launching a startup company, Fluidity Medicine, to continue developing the technology for possible testing in human patients.
In addition to treating kidney stones, this approach could also be useful for relaxing the ureter to help doctors insert a ureteral stent. It could also help when placing any other kind of instrument, such as an endoscope, in the ureter.
“The platform pairs drug delivery to the ureter. We are eager to first target muscle relaxation, and as offshoots of that, we have kidney stones, ureteral stents, and endoscopic surgery,” Lee says. “We have a bunch of other urological indications that would go through different developmental pathways but can all be hit and all have meaningful patient populations.”
The research was funded by the MIT Institute of Medical Engineering and Science Broshy Fellowship, the MIT Deshpande Center for Technological Innovation, the Koch Institute Support (core) Grant from the National Cancer Institute, and the National Institutes of Health.
Share this news article on:
Press mentions.
MIT researchers have developed a new treatment that could help ease the pain caused by passing kidney stones, reports CBS Boston. The researchers found that “delivering a combination of two muscle relaxants directly to the ureter, the tube that connects the kidneys and bladder, can make passage faster and less painful.”
Previous item Next item
Related Links
- Paper: "Identification and local delivery of vasodilators for the reduction of ureteral contractions"
- Michael Cima
- Koch Institute
- Department of Materials Science and Engineering
Related Topics
- Materials science and engineering
- National Institutes of Health (NIH)
- Health sciences and technology
Related Articles
Hydration sensor could improve dialysis

Big step in battling bladder disease

Successful human tests for first wirelessly controlled drug-delivery chip
More mit news.

A biomedical engineer pivots from human movement to women’s health
Read full story →
MIT tops among single-campus universities in US patents granted
A new way to detect radiation involving cheap ceramics

A crossroads for computing at MIT

Growing our donated organ supply

New AI method captures uncertainty in medical images
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
Clinical Trials
Kidney stones.
Displaying 37 studies
Percutaneous nephrolithotomy (PCNL) is a surgical procedure that is standard of care for the removal of large kidney stones. PCNL involves removal of the stone(s) from the kidney through a temporary tract that is percutaneously placed through the patient's back during surgery. There is a significant risk of urinary tract infection after PCNL but wide clinical variation in use of prophylactic antibiotics in the days leading up to surgery. For patients who had already agreed to undergo PCNL, we plan to randomize them either to 1 week of preoperative antibiotic prophylaxis plus < 24 hours of perioperative IV antibiotics or ...
The primary focus of this minimal risk study will be to assess and refine the ability of DE CT to accurately determine kidney stone composition.
The purpose of the study is to compare the effects, good and/or bad, of a treatment for removing kidney stones called the SURE procedure for stone evacuation to the standard treatment using a basket for stone removal.
A prospective study to determine if the removal of non-obstructing renal calculi can reduce or eliminate participant's pain and/or improve their quality of life.
The purpose of this trial is to investigate the impact of increased fluid intake and increased urine output on the recurrence rate of urinary stone disease (USD) in adults and children. The primary aim of the trial is to determine whether a multi‐component program of behavioral interventions to increase fluid intake will result in reduced risk of stone disease progression over a 2‐year period.
The purpose of this study is to determine if the use of preoperative antibiotics given to prevent infection actually decreases the postoperative risk in patients having surgery to remove kidney stones.
We hypothesize that clinical studies to investigate the role of individual proteins in kidney stone pathogenesis have likely been confounded by an unknown variety of underlying renal pathologies. Therefore, we propose to examine urinary protein crystallization inhibitors in patient populations that have been carefully phenotyped relative to renal stone precursor lesions by direct endoscopic visualization. In collaboration with Project #1, our second major goal is to use these accurately phenotyped patients in order to adapt modern dual-energy CT technology to develop a reliable noninvasive technique to accurately and noninvasively determine stone composition and visualize the earliest kidney stone precursor lesions. ...
90 genes related to Monogenic Stone Disease will be determined via DNA analysis by the Mayo Rare Kidney Stone Consortium (RKSC) research staff.
The purpose of this study is to determine if the performances of two types of scopes that are used to treat kidney stones are equivalent. This will help guide institutions in the future to purchase the best scopes for their patients.
The purpose of this study is to compare the operative outcomes and complications of mini-percutaneous nephrolithotomy (mini-PCNL) versus standard PCNL for renal stones.
The purpose of this study is to evaluate the potential of Moses laser technology to reduce operative time compared to non-Moses settings for ureteroscopic treatment of nephrolithiasis.
Assessment of Health-related Quality of Life in Rare Kidney Stone Formers in the Rare Kidney Stone Consortium
A Study of the ability for CT imaging to accurately predict the fragility (quality of being easily broken) of kidney stones during surgical intervention.
The purpose of this study is to determine if models predicting symptomatic recurrence (Recurrence of Kidney Stones score) in the prospective cohort study (IRB #08-006541) also predict radiographic stone formation and growth among 300 incident stone formers at Mayo Clinic Rochester and 55 incident stone formers at Mayo Clinic Florida in our current prospective cohort.
In this study the investigators propose to use a daily dose of 45 mg (30 mg at 8 AM and 15 mg at 4 PM). This relatively small well-tolerated dose is likely to persistently increase urine volume and reduce urine supersaturation and to be well tolerated by patients with kidney stone disease and normal renal function. The twice-daily (8 AM and 4 PM) regimen is designed to produce a maximal AVP inhibition on waking with a gradual fall-off of effect during the night. To this end, a higher dose is used in the morning, with a lower dose in the ...
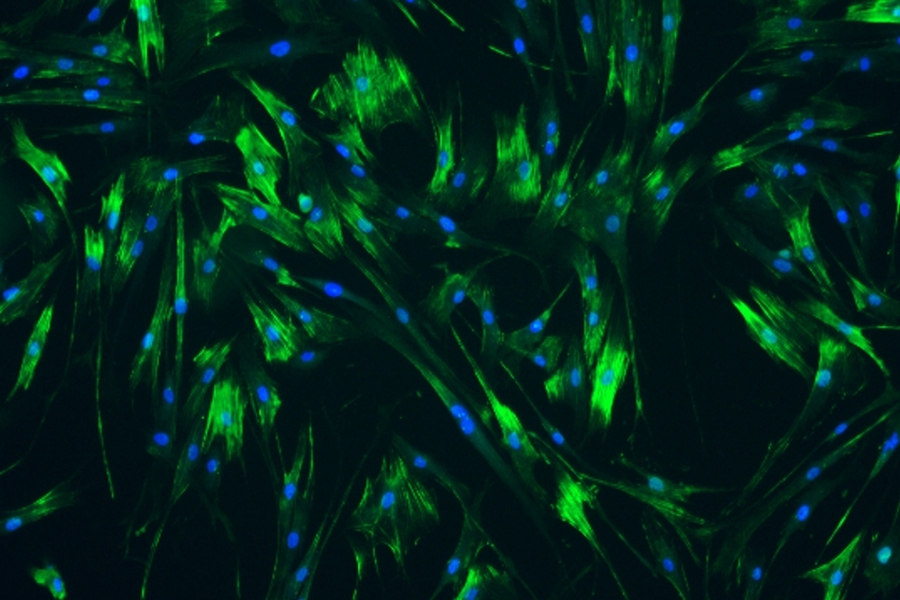
The purpose of this study is to assess the effectiveness of the Smart Water Bottle technology to monitor and increase fluid intake in patients with kidney stones and low urine output.
To characterize the microbiome in 4 groups of subjects (primary hyperoxaluria type I (PH1), idiopathic CaOx stone, enteric hyperoxaluria (EH) and healthy participants) by comparing the number of species and diversity of the microbial populations and pathway for oxalate metabolism by paralleling the gene expression of enzymes involved in oxalate degradation by gut bacteria.
The purpose of this study is to collect real-world evidence on the performance of the SOLTIVE™ Premium SuperPulsed Laser System for laser lithotripsy in ureteroscopy, PCNL or mini PCNL for kidney and ureteral stones.
Due to the ongoing opioid epidemic in the United States, there is increased attention and interest in reducing the use of opioid medication after surgery to minimize the risk of opioid tolerance and addiction, decrease the pool of unused opioids available for misuse, and maximize the use of alternative pain management medications and techniques. The purpose of this study is to implement and assess a standard way of prescribing opioids following percutaneous nephrolithotomy.
The purpose of this study is to measure how well two different devices work to break up and remove kidney stones. We are comparing a newer device to an older one to see which one is faster at breaking up kidney stones. We hypothesize that the Trilogy device will increase the stone clearance rate by 25% compared to the Shockpulse-SE device.
Patients with Dent disease have suppressed levels of FGF 23 which contributes to hypercalciuria, kidney stones, nephrocalcinosis and renal failure. Supplementation with phosphorus may reduce hypercalciuria.
The purpose of this study is to establish a database to collect and analyze information on metabolic and environmental risk factors for kidney stone formation in children.
The purpose of this study is to compare the ability to identify uric acid renal stones between alternate CT scanning techniques and the current dual-source CT scanning technique.
The purpose of this study is to compare the frequency of occurance of kidney stone formation in liver disease patients compared to the general population.
The purpose of this study is to determine if CBD oil has any effect on decreasing postoperative pain control following ureteroscopy for urinary stone disease, and to determine if CBD oil has any effect in decreasing the amount of postoperative opioids (commonly used drug) used by patients after undergoing ureteroscopy for urinary stone disease.
By comparing people who have kidney stones to people who do not have kidney stones, we hope to learn what causes kidney stones to form and determine if kidney stones lead to loss of kidney function or kidney disease.
The objective of this study is to collect data on stone formation and the degree of nephrocalcinosis in patients (≥ 2 years of age) with genetically confirmed PH3 and relatively intact renal function and to explore the potential relationship between Uox and new stone formation.
This is a natural history study of adults, adolescents, and children (≥ 2 years of age) with genetically confirmed primary hyperoxaluria type 3 (PH3) who have a history of stone events during the last 3 years and/or the presence of pre-existing stones detected by renal ultrasound at Screening.
The relationship between the level of Uox and the ...
The objective of this study is to compare the effectiveness of (A) a standardized general risk information sheet only, (B) a standardized general risk information sheet plus a probabilistic risk tool, (C) standardized sheet plus narrative enhanced probabilistic risk tool on a variety of patient reported and patient centered outcomes related to pain treatment and the risks and benefits of opioid prescriptions for common, acute pain conditions.
This study will help us determine whether certain genetic mutations, more than others, are a cause of more severe disease in Primary Hyperoxaluria.
The purpose of this study is to collect medical information from a large number of patients in many areas of the world with primary hyperoxaluria (PH), Dent disease, Cystinuria and APRT deficiency. This information will create a registry that will help us to compare similarities and differences in patients and their symptoms. The more patients we are able to enter into the registry, the more we will be able to understand the Primary Hyperoxalurias,Dent disease, cystinuria and APRT and learn better ways of caring for patients with these diseases.
The purpose of this study is to evaluate the safety, tolerability, and effectiveness of different doses of ALLN 177 for reducing urinary oxalate excretion in patients with secondary hyperoxaluria and recurrent kidney stones.
Evaluate the safety, tolerability, and efficacy of 28 days of treatment with ALLN-177 for reducing urinary oxalate excretion in patients with secondary hyperoxaluria and kidney stones.
The purpose of this study is to determine the effectiveness, durability, and long-term safety of Reloxaliase in patients with Enteric Hyperoxaluria.
This study is being done to obtain samples from patients with primary hyperoxaluria, cystinuria, adenine phosphoribosyl transferase (APRT) deficiency, and Dent disease, and from their family members, for use in future research.
The purpose of this study is to obtain post-market safety and effectiveness data for FlexivaTM Pulse High Power Single-Use Laser Fibers during lithotripsy and soft tissue procedure of holmium laser enucleation of the prostate (HoLEP).
This study aims to evaluate the mechanisms leading to hyperoxaluria and increased risk of kidney stone formation after bariatric surgery.
The purpose of this study is to determine the natural history of the hereditary forms of nephrolithiasis and chronic kidney disease (CKD), primary hyperoxaluria (PH), cystinuria, Dent disease and adenine phosphoribosyltransferase deficiency (APRTd) and acquired enteric hyperoxaluria (EH). The investigator will measure blood and urinary markers of inflammation and determine relationship to the disease course. Cross-comparisons among the disorders will allow us to better evaluate mechanisms of renal dysfunction in these disorders.
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
September 1, 2021
New Tool Shows Geology behind Kidney Stone Crystallization
Rather than crystallizing all at once, kidney stones dissolve and re-form over and over
By Harini Barath
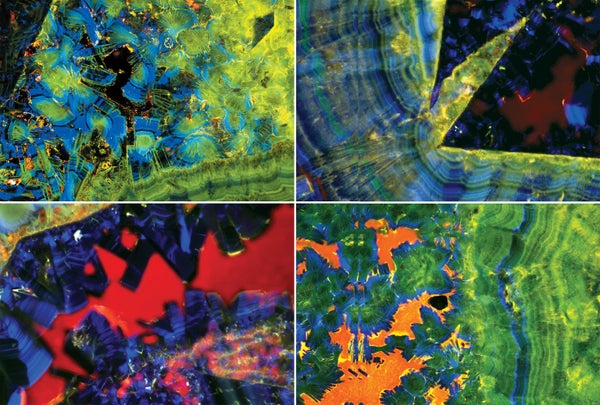
Kidney stone cross-sections hint at their complex formation process.
Mayandi Sivaguru and Bruce Fouke
Medical researchers are poised to map the entire process of kidney stone formation for the first time, thanks to insights from an unlikely source: geology. Combining this framework with a suite of cutting-edge microscopic tools and a new device that grows kidney stones in the laboratory, they are developing novel ways to stop or slow down the stones’ growth.
Stone disease occurs when jagged mineral crystals form in urine within the kidney. This excruciating problem affects roughly one in 10 adults and is steadily rising, especially in women and adolescents. “It’s common, debilitating and costly, both to the health-care system as well as individuals. To top it off, it’s also recurrent—if you’ve had one, there’s about a 50 percent chance of having another soon,” says urologist Margaret Pearle, who treats stone disease at the University of Texas Southwestern Medical Center and did not participate in the new research.
Geobiologist Bruce Fouke turned his microscope lens from coral reefs to kidney stones about a decade ago. Working with biologists and doctors at the Mayo Clinic and the University of Illinois at Urbana-Champaign, he found that kidney stones form similarly to many other stones in nature: they partially dissolve and re-form many times rather than crystallizing all at once. “That’s when we realized that stones are quite dynamic and have phases where they’re dissolving, so maybe there’s a way to harness that dissolution phase and treat stones,” says Fouke’s collaborator Amy Krambeck, a urologist at Northwestern Medicine.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
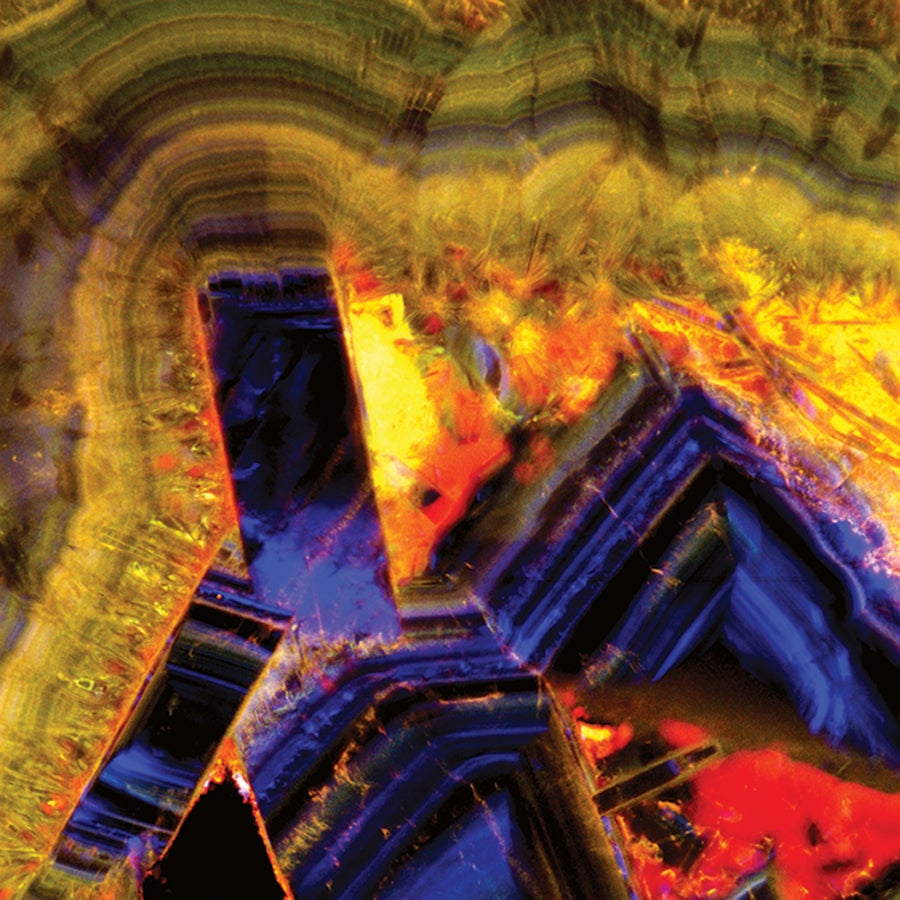
Section of a kidney stone. Credit: Mayandi Sivaguru and Bruce Fouke
There have been few good animal or lab models to study kidney stone formation, Krambeck says. So the team developed a new device called the GeoBioCell, a cartridge designed to mimic the kidney’s intricate internal structures. It lets scientists measure and link how various factors—including kidney cell activity, as well as the urinary microbiome, chemistry and flow—can affect stone growth. Varying any one factor can make stones develop and dissolve differently.
In their recent research, summarized in Nature Reviews Urology , the researchers primarily used GeoBioCell to study growing calcium oxalate crystals, which account for about 70 percent of kidney stones. Until Fouke’s preliminary work, these crystals were thought to be almost impossible to dissolve—but he and his colleagues found the stones do, in fact, partially dissolve in the body before regrowing. The scientists are now using GeoBioCell to examine precisely how stones form, and they hope to identify ways of initiating or prolonging the dissolution phase with drugs. They are also using the new device to test a variety of proteins (including the bone-related osteopontin) that could potentially inhibit growth if administered as a drug. Additionally, they are investigating the impact that specific microorganisms and microbial communities might have on stone formation.
This research has tremendous potential to identify kidney processes that can be targeted with drugs or other interventions, Pearle says, and will likely improve doctors’ ability to predict and treat stone recurrence.
VISE team works to develop 3D navigation system to better treat kidney stones
William Snyder
Aug 9, 2023, 11:11 AM
by Jill Clendening
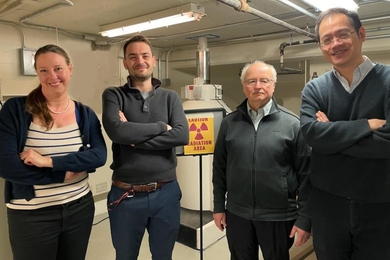
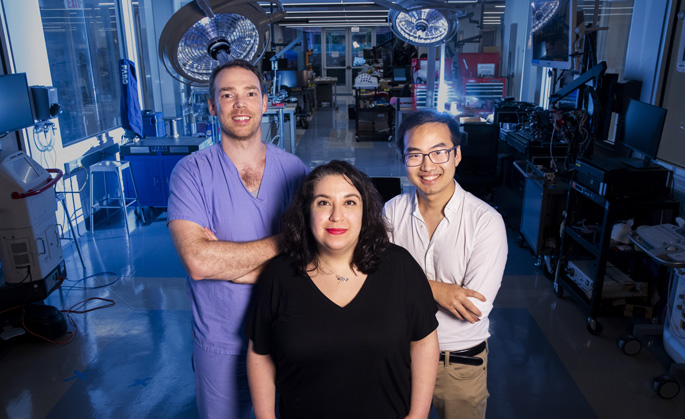
A multidisciplinary team at the Vanderbilt Institute for Surgery and Engineering (VISE) is working to create a real-time navigational system to decrease residual stone fragments left behind after kidney stone surgery.
Of the 100,000 patients who undergo an endoscopic kidney stone removal each year in the United States, 25% will require a repeat stone surgery within 20 months. This is nearly always due to stone fragments left behind, which can lead to ureteral obstruction, urinary tract infection and kidney injury. According to the National Kidney Foundation, it is estimated that 1 in 10 people will have a kidney stone at some time in their lives.
“We hope to transform the surgical care of kidney stone patients,” said co-principal investigator Nicholas Kavoussi, MD, assistant professor of Urology at Vanderbilt University Medical Center. “Endoscopic stone surgery requires the surgeon to visualize the entire renal collecting system to locate every kidney stone, and there are many challenges in this. During surgery, blood or debris can obscure the already limited field of view. Also, successfully navigating through the renal collecting system requires the surgeon to mentally create a 3D model of the patient’s anatomy from preoperative 2D computerized tomography (CT) images.
“During a surgical procedure, kidney stones can fragment and scatter, further complicating intraoperative tracking. We believe that a navigational system during stone surgery can improve stone-free rates, reducing recurrent surgeries and complications from residual fragments.”
By overlaying a 3D model of a patient’s preoperative imaging and updating it during the surgery, the resulting navigational map will allow the surgeon to more accurately track stones and stone fragments. The first-of-its-kind navigational system is expected to identify stone fragments less than 250 micrometers in diameter, a size typically considered to be dust, which can then be removed to alleviate future problems. The navigational system is being designed to work with existing endoscopic surgical cameras, allowing integration with any surgical system in use.
Co-principal investigator Ipek Oguz, PhD, assistant professor at the Vanderbilt University Department of Computer Science, is an expert in machine learning/deep learning methods for medical image segmentation. She and her team will analyze the videos and images obtained during the study to determine the new system’s effectiveness and the impact on patient outcomes.
“At the conclusion of our two-year study we expect to have collected the data needed to justify a large-scale, multicenter trial to evaluate outcomes of kidney stone removal surgeries with and without the navigational system,” Oguz said. “Additionally, our system is generalizable so future researchers developing automated tracking and video segmentation systems could potentially apply our basic approach for other endoscopic surgeries.”
The Department of Urology has an active kidney stone practice, seeing more than 60 patients with kidney stones each week. In the region, VUMC serves as the tertiary referral center for complex kidney stone patients.
“I’ve seen firsthand the impact repeat surgeries have on patients when residual kidney stone fragments cause complications,” Kavoussi said. “They are usually frustrated, often in pain, and the last thing they want is another procedure. Add to that their lost time at work and from their daily activities, and it’s easy to see why this is a surgical challenge we need to resolve.”
VISE is an interdisciplinary, trans-institutional structure designed to facilitate interactions and exchanges between engineers and physicians. Its mission is the creation, development, implementation, clinical evaluation and translation of methods, devices, algorithms and systems designed to facilitate interventional processes and their outcomes.
This research is supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R21DK133742). VISE provided initial support for this project via a physician-in-residence award to Kavoussi and Oguz, which was leveraged to conduct preliminary studies.
Explore Story Topics
- Computer Science
- Home Features
- News Sidebar
- endoscopic surgeries
- kidney stone surgery
- real-time navigational system
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
March 31, 2022
New way to blast kidney stones can be done in doctor's office
by Amy Norton

A noninvasive ultrasound technique is capable of quickly pulverizing kidney stones, an early study shows—in what researchers call a first step toward a simpler, anesthesia-free treatment for the painful problem.
The study reports on the first 19 patients who've had kidney stones treated with the ultrasound "bursts." So far, it's been able to completely, or nearly completely, break up stones within 10 minutes.
Much more research lies ahead, but experts not involved in the study called the early results "exciting." If it pans out, they said, the ultrasound technique could make noninvasive treatment for kidney stones more readily available to patients.
Kidney stones are common, affecting about 10% of people at some point, according to the National Kidney Foundation.
Often, a stone can be passed in the urine without too much agony. In other cases—such as when a larger stone is causing a blockage or unbearable pain—treatment is necessary.
Right now, many kidney stones can be treated with a procedure called shock wave lithotripsy . It delivers high-energy sound waves through the skin to break the stone into tiny fragments that can then be passed.
But there are downsides, said Dr. Mathew Sorenson, of the University of Washington School of Medicine in Seattle, one of the researchers on the new work.
Shock wave therapy can be painful, so it's typically done in the operating room, with patients under anesthesia, in the United States.
Sorenson and his colleagues have been developing an alternative approach called burst wave lithotripsy. They say it has the potential to blast kidney stones in a shorter amount of time, and possibly without anesthesia.
The ultimate goal, the researchers said, is to perform the procedure on fully awake patients, during an office visit with a urologist—or even in the emergency room when patients arrive in severe pain.
Unlike shock wave therapy, the burst wave approach uses "short harmonic bursts" of ultrasound energy, according to the research team. Previous research has suggested it can break up stones more quickly, and with less pain, than shock waves.
In the new study, the researchers tested the burst wave technique in 19 patients who were undergoing kidney stone treatment with a procedure called ureteroscopy . It involves threading a thin scope through the urethra, up to the location of the kidney stone; instruments are used to either snare the stone or break it into fragments that can be removed.
Because ureteroscopy requires anesthesia, the study patients were under when the ultrasound bursts were applied, for up to 10 minutes.
Overall, the researchers found, that was enough to fragment 21 of 23 stones. Half of the stones had at least 90% of their volume pulverized to pieces of no more than 2 millimeters (mm). And nine stones (39%) were completely broken down to that degree.
The findings were published recently in The Journal of Urology .
Two urologists who were not involved in the study called that effectiveness impressive, considering the short duration of treatment (which was chosen to limit patients' time under anesthesia).
Kidney stones broken down to 2 mm or less should be relatively easy to pass, said Dr. Mantu Gupta, director of the Kidney Stone Center at Mount Sinai, in New York City.
Gupta noted that the study did not actually test the hoped-for, real-world scenario: Using the technique without anesthesia. But previous work by the team has indicated patients can tolerate it.
"This is very exciting," Gupta said, adding that the safety data so far looks good, too.
Some patients showed mild bleeding, with small amounts of blood in the urine.
Dr. William Roberts, a professor of urology at the University of Michigan, also described the work as exciting.
"This certainly looks as safe, or safer than, shock wave lithotripsy," he said.
Whether burst waves could be more effective is unclear, but Roberts said that if the procedure can, in fact, be done in the urologist's office, that would be a big advantage.
None of that means the technology would help everyone with kidney stones . Roberts noted that while 19 patients were treated, a similar number entered the study but could not receive the ultrasound treatment: Some had stones that were too deep, for instance, or were obstructed by a rib or the bowel.
Still, Roberts said, even if only certain patients could have the procedure, its potential to be "more accessible" would be a boon.
But Dr. Joseph Vassalotti, chief medical officer of the National Kidney Foundation, said that while the procedure is "promising," most of the study patients were of normal body mass index ( BMI ), which makes breaking up stones with shock wave therapy easier.
"Low enrollment of obese patients is important not only because obesity is common in the U.S., but also because obesity is a technical limitation to performance of [ultrasound burst and shock wave therapy]," Vassalotti said.
Since earlier work suggests the burst wave approach is tolerable, patients might not need pain medication afterward to deal with the procedure itself, Roberts said—though they might need a pain reliever like acetaminophen (Tylenol) if passing the fragments proves uncomfortable.
The study team said it has begun studies to test the approach in patients who arrive in the emergency department with kidney stone pain. The technology has also been licensed to SonoMotion Inc., which is developing a commercial version and conducting its own clinical trials.
Copyright © 2022 HealthDay . All rights reserved.
Explore further
Feedback to editors

Newly found rare cells could be a missing link in color perception
7 minutes ago

New vaccine strategy may mean the end of the line for endless boosters
16 minutes ago

Research explores why we remember what we remember
43 minutes ago

Epilepsy drug prevents brain tumors in mice with neurofibromatosis type 1
45 minutes ago

New way found to treat early relapse in leukemia

Researchers discover cause of a new rare genetic condition: Glutamine synthetase stabilization disorder
2 hours ago

Microplastics make their way from the gut to other organs, researchers find

Researchers identify brain region involved in control of attention
3 hours ago

Boosting the brain's control of prosthetic devices by tapping the cerebellum

Breakthrough aerosol human infection model gives hope for future TB vaccine development
Related stories.

First human study using sound waves to break up kidney stones shows promising results
Mar 22, 2022

Why are kidney stones so painful?
Mar 21, 2017
More urinary tract stones are being treated with surgery
May 12, 2016

Study links kidney stones with bone problems
Mar 3, 2021
New insights on sex differences in kidney stone risk
Nov 5, 2021

Extracorporeal shock wave lithotripsy best at 90 pulses/min
Jul 16, 2015
Recommended for you

Specific nasal cells found to protect against COVID-19 in children
10 hours ago

Large study finds antibiotics aren't effective for most lower tract respiratory infections
4 hours ago

COVID-19 poses greater risk of death to those with cancer, large study finds
6 hours ago

Kidney disease intervention outcomes encouraging, despite null result
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

New tech gives kidney stone patients options
Media Contact: Barbara Clements - 253-740-5043, [email protected]

Patients dealing with small kidney stones that persist after surgery may soon have options to “push” the stones from their body, rather than face another more invasive procedure.
A clinical trial at the Kidney Stone Center at UW Medical Center – Northwest is testing the ability of ultrasound waves to dislodge and move small fragments left behind after surgery so they can naturally be expelled. A team representing the University of Washington's Applied Physics Laboratory and the Department of Urology hopes to finalize trial results and submit the process to the U.S. Food and Drug Administration for approval next year.
So far the results have been good, said Dr. Mathew Sorensen , a UW Medicine urologist.
“All the surgeries that we do to treat stones have the potential to leave fragments behind,” Sorensen noted. “Some of those fragments, especially if they're small, usually clear pretty quickly. But the ones that stay and hang out, especially if they stay in the bottom of the kidney, they have the potential to grow and ... lead to another event such as surgery or an unpleasant [emergency room] visit down the road.”
The ultrasound procedure being tested does not require anesthesia, just one or two clinic visits of about 30 minutes each. Then the fragments have a better chance of clearing, sometimes with a few hours, Sorensen said. So far 55 patients have been enrolled in this trial, and Sorensen’s team hopes to enroll 12-16 more .
NASA is particularly interested in this technology. For astronauts on long missions in a weightless environment, kidney stones are a real concern because no surgical option exists to treat the condition in flight, Sorensen said. More than 30 astronauts have reported kidney stones within two years of space flight, so NASA assumes a similar situation could develop during a trip to Mars or the moon. Kidney tissue samples from UW Medicine were recently flown to the International Space Station to observe kidneys' function in space.
Sorensen’s group also is exploring using ultrasound to break larger stones into small pieces, and then use this handheld device to push and expel the fragments to help resolve a painful event. This may allow treatment of stones without anesthesia and pose an attractive option for at-risk patients, such as those with spinal cord injuries.
“Imagine a scenario where you get diagnosed with a stone and you come in and you see us in clinic, and it's a small or modest-sized stone that we normally would talk about treating with a surgical procedure, but instead we might offer a 30-minute, no-anesthesia procedure to break the stone and move it so it can be expelled,” he said. This technology is also of interest to NASA, he added.
Back down on Earth, Sorensen can relate personally to this new technology.
“I've had three stones myself, including one procedure to treat a stone, so I'm definitely familiar with the discomfort and pain that they cause,” he said. “Anything we can come up with that is going to be as effective as and less invasive than some of the technologies we have now, and not require anesthesia, I think that's a really exciting future,” he said.
Every year, more than 600 people in the throes of a kidney-stone episode seek emergency care at Harborview and UW Medical Center in Seattle. Kidney stones become symptomatic if they become stuck in the urinary tract, causing debilitating pain. In addition, obstruction of urine flow causes a backup, which can result in kidney swelling and cramping, and set the stage for infection or lasting damage.
More information on the trial described above can be found here. Information on the breaking trial, can be found here .
For details about UW Medicine, please visit http://uwmedicine.org/about .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.2018; 2018

Kidney Stone Disease: An Update on Current Concepts
Tilahun alelign.
1 Department of Microbial, Cellular and Molecular Biology, College of Natural Sciences, Addis Ababa University, P.O. Box 1176, Addis Ababa, Ethiopia
2 Department of Biology, Debre Birhan University, P.O. Box 445, Debre Birhan, Ethiopia
Beyene Petros
Kidney stone disease is a crystal concretion formed usually within the kidneys. It is an increasing urological disorder of human health, affecting about 12% of the world population. It has been associated with an increased risk of end-stage renal failure. The etiology of kidney stone is multifactorial. The most common type of kidney stone is calcium oxalate formed at Randall's plaque on the renal papillary surfaces. The mechanism of stone formation is a complex process which results from several physicochemical events including supersaturation, nucleation, growth, aggregation, and retention of urinary stone constituents within tubular cells. These steps are modulated by an imbalance between factors that promote or inhibit urinary crystallization. It is also noted that cellular injury promotes retention of particles on renal papillary surfaces. The exposure of renal epithelial cells to oxalate causes a signaling cascade which leads to apoptosis by p38 mitogen-activated protein kinase pathways. Currently, there is no satisfactory drug to cure and/or prevent kidney stone recurrences. Thus, further understanding of the pathophysiology of kidney stone formation is a research area to manage urolithiasis using new drugs. Therefore, this review has intended to provide a compiled up-to-date information on kidney stone etiology, pathogenesis, and prevention approaches.
1. Introduction
1.1. overview of kidney stones.
Kidney stones are mainly lodged in the kidney(s) [ 1 ]. Mankind has been afflicted by urinary stones since centuries dating back to 4000 B.C. [ 2 ], and it is the most common disease of the urinary tract. The prevention of renal stone recurrence remains to be a serious problem in human health [ 3 ]. The prevention of stone recurrence requires better understanding of the mechanisms involved in stone formation [ 4 ]. Kidney stones have been associated with an increased risk of chronic kidney diseases [ 5 ], end-stage renal failure [ 3 , 6 ], cardiovascular diseases [ 7 , 8 ], diabetes, and hypertension [ 9 ]. It has been suggested that kidney stone may be a systemic disorder linked to the metabolic syndrome. Nephrolithiasis is responsible for 2 to 3% of end-stage renal cases if it is associated with nephrocalcinosis [ 10 ].
The symptoms of kidney stone are related to their location whether it is in the kidney, ureter, or urinary bladder [ 11 ]. Initially, stone formation does not cause any symptom. Later, signs and symptoms of the stone disease consist of renal colic (intense cramping pain), flank pain (pain in the back side), hematuria (bloody urine), obstructive uropathy (urinary tract disease), urinary tract infections, blockage of urine flow, and hydronephrosis (dilation of the kidney). These conditions may result in nausea and vomiting with associated suffering from the stone event [ 12 ]. Thus, the treatment and time lost from work involves substantial cost imposing an impact on the quality of life and nation's economy.
1.2. Epidemiology of Kidney Stones
Globally, kidney stone disease prevalence and recurrence rates are increasing [ 13 ], with limited options of effective drugs. Urolithiasis affects about 12% of the world population at some stage in their lifetime [ 14 ]. It affects all ages, sexes, and races [ 15 , 16 ] but occurs more frequently in men than in women within the age of 20–49 years [ 17 ]. If patients do not apply metaphylaxis, the relapsing rate of secondary stone formations is estimated to be 10–23% per year, 50% in 5–10 years, and 75% in 20 years of the patient [ 15 ]. However, lifetime recurrence rate is higher in males, although the incidence of nephrolithiasis is growing among females [ 18 ]. Therefore, prophylactic management is of great importance to manage urolithiasis.
Recent studies have reported that the prevalence of urolithiasis has been increasing in the past decades in both developed and developing countries. This growing trend is believed to be associated with changes in lifestyle modifications such as lack of physical activity and dietary habits [ 19 – 21 ] and global warming [ 16 ]. In the United States, kidney stone affects 1 in 11 people [ 22 ], and it is estimated that 600,000 Americans suffer from urinary stones every year. In Indian population, about 12% of them are expected to have urinary stones and out of which 50% may end up with loss of kidney functions [ 23 ].
2. The Urinary System and Stones
The urinary filtrate is formed in the glomerulus and passes into the tubules where the volume and content are altered by reabsorption or secretions. Most solute reabsorption occurs in the proximal tubules, whereas fine adjustments to urine composition take place in the distal tubule and collecting ducts. The loop of Henle serves to concentrate urine composed of 95% water, 2.5% urea, 2.5% mixture of minerals, salts, hormones, and enzymes. In the proximal tubules, glucose, sodium, chloride, and water are reabsorbed and returned to the blood stream along with essential nutrients such as amino acids, proteins, bicarbonate, calcium, phosphate, and potassium. In the distal tubule, the salt and acid-base balance of blood is regulated [ 24 ]. The location of stones may vary as indicated in Figure 1 .

Kidney stone locations in the urinary system. (a) Adopted from [ 25 ]. (b) Adopted from [ 26 ].
3. Types of Kidney Stones
The chemical composition of kidney stones depends on the abnormalities in urine composition of various chemicals. Stones differ in size, shape, and chemical compositions (mineralogy) [ 27 ]. Based on variations in mineral composition and pathogenesis, kidney stones are commonly classified into five types as follows [ 28 ].
3.1. Calcium Stones: Calcium Oxalate and Calcium Phosphate
Calcium stones are predominant renal stones comprising about 80% of all urinary calculi [ 29 ]. The proportion of calcium stones may account for pure calcium oxalate (CaOx) (50%), calcium phosphate (CaP, termed as apatite) (5%), and a mixture of both (45%) [ 30 ]. The main constituent of calcium stones is brushite (calcium hydrogen phosphate) or hydroxyapatite [ 31 , 32 ]. Calcium oxalate is found in the majority of kidney stones and exists in the form of CaOx monohydrate (COM, termed as mineral names: whewellite, CaC 2 O 4 ·H 2 O), and CaOx dihydrate (COD, weddellite, CaC 2 O 4 ·2H 2 O), or as a combination of both which accounts for greater than 60% [ 33 ]. COM is the most thermodynamically stable form of stone. COM is more frequently observed than COD in clinical stones [ 34 ].
Many factors contribute to CaOx stone formation such as hypercalciuria (resorptive, renal leak, absorptive, and metabolic diseases), hyperuricosuria, hyperoxaluria, hypocitraturia, hypomagnesuria, and hypercystinuria [ 35 ]. Mostly, urinary pH of 5.0 to 6.5 promotes CaOx stones [ 36 ], whereas calcium phosphate stones occur when pH is greater than 7.5 [ 11 ]. The recurrence of calcium stone is greater than other types of kidney stones.
3.2. Struvite or Magnesium Ammonium Phosphate Stones
Struvite stones occur to the extent of 10–15% and have also been referred to as infection stones and triple phosphate stones. It occurs among patients with chronic urinary tract infections that produce urease, the most common being Proteus mirabilis and less common pathogens include Klebsiella pneumonia , Pseudomonas aeruginosa, and Enterobacter [ 1 , 28 , 29 ]. Urease is necessary to split/cleave urea to ammonia and CO 2, making urine more alkaline which elevates pH (typically > 7). Phosphate is less soluble at alkaline versus acidic pH, so phosphate precipitates on to the insoluble ammonium products, yielding to a large staghorn stone formation [ 37 ]. Women's are likely to develop this type of stone than the male. Escherichia coli is not capable of splitting urea and is not associated with struvite stones [ 38 ].
3.3. Uric Acid Stones or Urate
This accounts approximately for 3–10% of all stone types [ 1 , 29 ]. Diets high in purines especially those containing animal protein diet such as meat and fish, results in hyperuricosuria, low urine volume, and low urinary pH (pH < 5.05) exacerbates uric acid stone formation [ 11 , 28 , 39 ]. Peoples with gouty arthritis may form stones in the kidney(s). The most prevalent cause of uric acid nephrolithiasis is idiopathic [ 38 ], and uric acid stones are more common in men than in women.
3.4. Cystine Stones
These stones comprise less than 2% of all stone types. It is a genetic disorder of the transport of an amino acid and cystine. It results in an excess of cystinuria in urinary excretions [ 1 , 29 ], which is an autosomal recessive disorder caused by a defect in the rBAT gene on chromosome 2 [ 40 ], resulting in impaired renal tubular absorption of cystine or leaking cystine into urine. It does not dissolve in urine and leads to cystine stone formation [ 11 ]. People who are homozygous for cystinuria excrete more than 600 millimole insoluble cystine per day [ 28 ]. The development of urinary cystine is the only clinical manifestation of this cystine stone disease [ 40 ].
3.5. Drug-Induced Stones
This accounts for about 1% of all stone types [ 1 ]. Drugs such as guaifenesin, triamterene, atazanavir, and sulfa drugs induce these stones. For instance, people who take the protease inhibitor indinavir sulphate, a drug used to treat HIV infection, are at risk of developing kidney stones [ 28 ]. Such lithogenic drugs or its metabolites may deposit to form a nidus or on renal calculi already present. On the other hand, these drugs may induce the formation of calculi through its metabolic action by interfering with calcium oxalate or purine metabolisms [ 38 ].
4. Kidney Stone Compositions
The chemical compositions of urinary stones include crystals and noncrystalline phases or the organic material (the matrix). The organic matrix of urinary stones consists of macromolecules such as glycosaminoglycans (GAG's), lipids, carbohydrates, and proteins. These molecules play a significant role by promoting or inhibiting the processes of kidney stone development ( Table 1 ). The main components of the stone matrix are proteins (64%), nonamino sugars (9.6%), hexosamine as glucosamine (5%), water (10%), and inorganic ash (10.4%). The matrix acts as a template participating in the assembly of kidney stones. The matrix of all stones contains phospholipids (8.6%) of the total lipid, which in turn represents about 10.3% of stone matrix. Cell membrane phospholipids, as part of organic matrix, promote the formation of calcium oxalate and calcium phosphate stones [ 41 ]. Albumin is the major component of the matrix of all stone types [ 42 ].
Urinary stone matrix protein modulators of crystallization in nephrolithiasis [ 34 , 41 ].
I: inhibitor; P: promoter; “—”: no effect.
Brushite stone is a hard phosphate mineral with an increasing incidence rate, and a quarter of calcium phosphate (CaP) patients form stones containing brushite [ 43 ]. In the urinary tract, CaP may be present in the form of hydroxyapatite, carbonate apatite, or brushite (calcium monohydrogen phosphate dihydrate, CaHPO4·2H2O). Brushite is resistant to shock wave and ultrasonic lithotripsy treatment [ 44 ].
4.1. Etiology of Kidney Stones
Formation of kidney stones (calculogenesis) is a complex and multifactorial process including intrinsic (such as age, sex, and heredity) and extrinsic factors such as geography, climate, dietary, mineral composition, and water intake [ 15 ]. A summary of possible causes of kidney stone formation is shown in Table 2 .
Risk factors associated with kidney stone formations.
5. Mechanisms of Renal Stone Formation
The pathogenesis of kidney stone or biomineralization is a complex biochemical process which remains incompletely understood [ 41 ]. Renal stone formation is a biological process that involves physicochemical changes and supersaturation of urine. Supersaturated solution refers to a solution that contains more of dissolved material than could be dissolved by the solvent under normal circumstances [ 34 ]. As a result of supersaturation, solutes precipitate in urine leads to nucleation and then crystal concretions are formed. That is, crystallization occurs when the concentration of two ions exceeds their saturation point in the solution [ 55 ]. The transformation of a liquid to a solid phase is influenced by pH and specific concentrations of excess substances. The level of urinary saturation with respect to the stone-forming constituents like calcium, phosphorus, uric acid, oxalate, cystine, and low urine volume are risk factors for crystallization [ 1 , 56 ]. Thus, crystallization process depends on the thermodynamics (that leads to nucleation) and kinetics (which comprises the rates of nucleation or crystal growth) of a supersaturated solution [ 57 ]. Therefore, lithiasis can be prevented by avoiding supersaturation.
However, it should be noted that stone formation is usually dependent on the level of imbalance between urinary inhibitors and promoters of crystallization. All stones share similar events with respect to the mineral phase of stone formation. But, the sequence of events leading to stone formation differs depending on the type of stone and urine chemistry. For instance, crystallization of calcium-based stones (calcium oxalate or calcium phosphate) occurs in supersaturated urine if it is with low concentrations of inhibitors. Uric acid interferes the solubility of calcium oxalate and promotes CaOx stone formation. In healthy controls, crystallization process is opposed by inhibitory substances and gets safe [ 1 ]. The sequence of events that trigger stone formation includes nucleation, growth, aggregation, and retention of crystals within the kidneys [ 27 , 58 ].
5.1. Crystal Nucleation
The first step in the formation of kidney stone begins by the formation of nucleus (termed as nidus) from supersaturated urine retained inside the kidneys [ 11 , 42 ]. In a supersaturated liquid, free atoms, ions, or molecules start forming microscopic clusters that precipitate when the bulk free energy of the cluster is less than that of the liquid. For example, charged soluble molecules such as calcium and oxalate combine to form calcium oxalate crystals and become insoluble [ 34 ]. Nucleation may be formed in the kidney through free particle or fixed particle mechanism [ 26 , 34 ]. In supersaturated solutions, if promoters exceed that of inhibitors, nucleation starts [ 34 ].
Once a nucleus is created (and/or if it is anchored), crystallization can occur at lower chemical pressure than required for the formation of the initial nucleus. Existing epithelial cells, urinary casts, RBCs, and other crystals in urine can act as nucleating centers in the process of nuclei formation termed as heterogeneous nucleation [ 41 ]. The organic matrix, mucopolysaccharide acts as a binding agent by increasing heterogeneous nucleation and crystal aggregation [ 59 ]. On the other hand, nanobacteria is claimed to form apatite structures serving as a crystallization center for stone formation [ 60 ]. The whole process potentiates stone formation. The role of oxalate-degrading bacteria, such as Oxalobacter formigenes , in CaOx stone formation is a subject of current research [ 61 ]. Thus, treatment which targets the process of nucleation intervention is one of the best approaches to control kidney stone.
5.2. Crystal Growth
Crystals in urine stick together to form a small hard mass of stone referred as crystal growth. Stone growth is accomplished through aggregation of preformed crystals or secondary nucleation of crystal on the matrix-coated surface [ 62 ]. Once a nidus has achieved, the overall free energy is decreased by adding new crystal components to its surface. The total free energy of the cluster is increased by the surface energy. The process of stone growth is slow and requires longer time to obstruct the renal tubules [ 34 ]. From organic matrix, mainly Tamm–Horsfall protein and osteopontin are promoters of CaOx stone formation [ 13 ]. Under in vitro study, crystals induced in human urine demonstrated an intimate association between calcium-containing crystals and organic matrix (lipids and proteins). Lipids of cellular membranes are basically believed to involve in nucleation of crystals [ 63 ].
5.3. Crystal Aggregation
The process whereby a small hard mass of a crystal in solution sticks together to form a larger stone is called aggregation. All models of CaOx urolithiasis concede that crystal aggregation is probably involved in crystal retention within the kidneys [ 41 ]. Crystal aggregation is considered to be the most critical step in stone formation.
5.4. Crystal-Cell Interaction
The attachment of grown crystals with the renal tubule lining of epithelial cells is termed as crystal retention or crystal-cell interaction [ 41 , 64 ]. In individuals with hyperoxaluria, renal tubular epithelial cells were injured due to exposure to high oxalate concentrations or sharp calcium oxalate monohydrate (COM) crystals [ 10 , 65 , 66 ]. Crystal-cell interaction results in the movement of crystals from basolateral side of cells to the basement membrane [ 10 ]. Then, crystals could be taken into cells and anchored to the basement membrane of the kidneys [ 66 ]. The interaction of COM crystals with the surface of renal epithelial cells could be a critical initiating event in nephrolithiasis. An increased retention force between the crystal and injured renal tubule epithelium cells promotes CaOx crystallization [ 67 ]. Most of the crystals attached to epithelial cells are thought to be digested by macrophages and/or lysosomes inside cells and then discharged with urine [ 66 ].
Following renal tubular cell injury, cellular degradation produces numerous membrane vesicles which are nucleators of calcium crystals as supported by in vitro and in vivo studies [ 41 ]. Injured cells release substances like renal prothrombin fragment-1 or other anionic proteins which induce COM crystal agglomeration [ 68 ]. Reactive oxygen species is thought to be one of the factors involved in renal cell injury [ 69 ]. Thus, reduction of renal oxidative stress could be an effective treatment option.
Injured cells potentiate to invert its cell membrane which is anionic to the urinary environment and acts as site of crystal adherence. COM crystals have stronger affinity of attachment towards the inverted anionic membrane [ 69 ], than calcium oxalate dihydrate (COD) crystals [ 70 ]. On the other hand, deposition of COM crystal was observed in Madin–Darby canine kidney epithelial cells (MDCK cells), than at proximal tubular epithelial cells derived from pig kidney (LLC-PK1 cells) study models [ 71 ]. This preferential difference may be due to the presence of a binding molecule such as hyaluronan on Madin–Darby canine kidney epithelial cells for COM crystal attachment [ 67 ]. Although the detailed mechanisms of crystal-cell interaction remain unexplored, one of the best ways to treat urolithiasis is to control crystal-cell retentions.
5.5. Endocytosis of CaOx Crystals
Endocytosis or engulfment of crystals by renal tubular cells is the earliest process in the formation of kidney stones. Studies on tissue culture crystal-cell interactions indicated that COM crystals rapidly adhere to microvilli on the cell surface and subsequently internalized. Polyanion molecules present in tubular fluid/urine such as glycosaminoglycans, glycoproteins, and citrate may coat crystals and inhibit the binding of COM crystals to cell membrane [ 41 ]. For example, Tamm–Horsfall glycoproteins (THP) have a dual biological role in stone formation. Lieske et al. [ 72 ] reported that THP may promote renal stone formation by initiating the interaction of COM crystals with distal tubular cells of the nephron. Another study revealed that, upon lowering pH and raising ionic strength, THP's viscosity increases which exhibits high tendency of polymerization and fails to inhibit crystallization. Moreover, THP becomes a strong promoter of crystallization in the presence of additional calcium ions [ 73 ]. In contrast, THP is thought to protect against COM stone formation by inhibiting COM aggregation when it is at high pH and low ionic strength as reported by Hess [ 73 ]. COM aggregation assays revealed that desialylated THP promoted COM aggregation, while normal THP inhibited aggregation [ 74 ]. Similar reports revealed that THP may inhibit calcium oxalate crystal aggregation, whereas uromodulin may promote aggregation [ 75 ]. Inactivating the THP gene in mouse embryonic stem cells results in spontaneous formation of calcium crystals in adult kidneys. This is a convincing evidence that THP is a critical urinary inhibitor of human nephrolithiasis [ 76 ].
Various cellular and extracellular events are involved during stone formation. Modulators targeting the steps from supersaturation to crystal retention may be a potential means to block stone formation. Similarly, the blockage of crystal binding molecules (such as osteopontin, hyaluronic acid, sialic acid, and monocyte chemoattractant protein-1) expressed on epithelial cell membranes may be an alternative approach to prevent stone formation [ 41 ]. Experimental findings demonstrated that stone calcification is triggered by reactive oxygen species (ROS) and the development of oxidative stress [ 77 ]. In vitro [ 78 , 79 ] and in vivo [ 80 , 81 ] studies have demonstrated that CaOx crystals are toxic for renal epithelial cells that produce injury and renal cell death. Similarly, an exposure to hypercalciuria produces cellular injury and ROS-induced lipid peroxidation which stimulates calcium oxalate deposition [ 82 ]. The pathophysiology of urinary stone formation is incompletely understood. A summary of the various steps involved in stone formation is shown below ( Figure 2 ).

Schematic representation of the various events of kidney stone formation.
5.6. Cell Injury and Apoptosis
Exposure to high levels of oxalate or CaOx crystals induces epithelial cellular injury, which is a predisposing factor to subsequent stone formation [ 83 , 84 ]. CaOx crystal depositions in the kidneys upregulate the expression and synthesis of macromolecules that can promote inflammation [ 85 ]. Crystals may be endocytosed by cells or transported to the interstitium. It has been suggested that injured cells develop a nidus which promotes the retention of particles on the renal papillary surface [ 86 ]. In individuals with severe primary hyperoxaluria, renal tubular cells are injured and crystals become attached to them [ 66 ]. The addition of CaOx crystals onto Madin–Darby canine kidney (MDCK) cell lines showed an increase in the release of lysosomal enzymes, prostaglandin E2, and cytosolic enzymes [ 87 ]. A study on animal models also revealed that the administration of high concentrations of CaOx crystals or oxalate ions appears to be toxic causing renal tubular cell damage [ 41 ]. It has been suggested that oxalate increases the availability of free radicals by inhibiting enzymes responsible for their degradation. For instance, reactive oxygen species can damage the mitochondrial membrane and reduce its transmembrane potential. These events are known features of early process in apoptotic pathways [ 88 ].
The activation of p38 mitogen-activated protein kinase (p38 MAPK) signaling pathway regulates the expression of cellular proteins. The various extracellular stimuli or stresses like ultraviolet radiation and proinflammatory cytokines may activate p38 MAPK which results in phosphorylation and activation of transcription factors [ 89 ]. The exposure of renal cells to oxalate increases an altered gene expression that induces apoptosis signaling cascades [ 88 ]. A study revealed that the exposure of HK-2 cells to increased oxalate levels results in an increased transcriptional activation of IL-2R beta mRNA and consequently increases IL-2R beta protein levels which drive cellular changes like induction of inflammation. Oxalate-induced activation may trigger p38 MAPK signaling by acting on cell membranes, although the exact mechanisms have not been established [ 90 ].
Apoptosis at the level of renal tubular cells may lead to stone formation through cellular demise and postapoptotic necrosis which could promote calcium crystal aggregation and growth. This fact has been supported by in vitro study on MDCK cells being exposed to oxalate ions [ 91 ]. However, it has to be noted that some cells did not respond to oxalate injury. This may be due to the fact that changes in gene expression could protect from apoptosis and then inhibit from lithiasis [ 35 ]. These findings highlight the need for future studies clarifying novel biochemical targets of kidney stone formation and the utility of p38 MAPK inhibitors in preventing stone formation.
5.7. Genetic Basis of Kidney Stone Formation
Environmental factors interacting with underlying genetic factors cause rare stone disease [ 92 ]. The production of promoters and inhibitors of crystallization depends on proper functioning of the renal epithelial cells. Cellular dysfunction affects the supersaturation of urinary excretion by influencing ions such as calcium, oxalate, and citrate [ 93 ]. Some genetic defects which lead to stone formation are shown in Table 3 .
Gene involved in hypercalciuria, gene products, and renal phenotype [ 93 ].
5.8. Randall's Plaques
Randall's plaques appear to be the precursor's origin of urinary stone development although it is unclear whether it involves in all stone types or not [ 62 ]. Moreover, the pathogenesis of Randall's plaque itself is not clearly known [ 94 ]. The majority of CaOx stones are found to be attached with renal papillae at the sites of Randall's plaque [ 26 ]. It is located at the interstitial basement membrane in loop of Henle [ 95 , 96 ]. Calcium phosphate (apatite), and purine crystal compositions were identified in plaques, whereas apatite is dominant [ 97 ]. Initially, calcium phosphate crystals and organic matrix are deposited along the basement membranes of the thin loops of Henle and extend further into the interstitial space to the urothelium, constituting the so-called Randall plaques. Evidence suggests that a primary interstitial apatite crystal formation secondarily leads to CaOx stone formation [ 13 ]. In supersaturated urine, crystals adhere to the urothelium which may enhance subsequent stone growth [ 98 ].
Due to renal cell injury, plaque is exposed to supersaturated urine. Renal epithelial cell damage (degradation) products promote heterogeneous nucleation and promotes crystal adherence in renal cells. Randall plaque calcification is triggered by oxidative stress. Cells may express molecules at distal and collecting tubules which act as crystal binding sites such as phosphatidylserine, CD44, osteopontin, and hyaluronan [ 27 , 99 ]. Renal epithelial cells of the loop of Henle or collecting ducts produce membrane vesicles at the basal side which leads to plague formation [ 77 ]. Thus, apatite crystal deposits have been proposed to act as nidus for CaOx stone formation by attachment on further matrix molecules [ 13 , 77 ]. However, the driving forces in plaque formation and the involved matrix molecules remain elusive.
Kidney stones are either attached to the renal papillae or found freely [ 100 ]. According to the fixed particle pathway, the beginning of calcium phosphate (CaP) deposition in the interstitium establishes a nucleus for CaOx formation. CaP formed in the basement membrane of the loops of Henle, the inner medullary collecting ducts, and ducts of Bellini serves as an attachment site for stone development. Idiopathic stone formers develop CaOx attached to fixed sites of interstitial plaque [ 26 ]. Stones of the distal tubular acidosis attach to plugs protruding from dilated ducts of Bellini, whereas cystinuria stones do not attach to the renal plagues (found freely) [ 26 ]. CaP, uric acid, or cystine crystals formed in the renal tubules plug at the terminal collecting ducts. When mineralization reaches the renal papillary surface, plaques rupture exposing CaP crystals to the pelvic urine. Then, urinary macromolecules deposit over the exposed CaP crystals and promote CaOx deposition on CaP [ 4 ].
5.9. Kidney Stone Inhibitors and Promoters
Inhibitors are substances which decrease the initiation of supersaturation, nucleation, crystal growth, rate of aggregation, or any other processes required to stone formation [ 34 ]. Normally, urine contains chemicals that prevent crystal formation. Inhibitors in urine includes small organic anions such as citrate, small inorganic anions such as pyrophosphates, multivalent metallic cations such as magnesium, or macromolecules such as osteopontin, glycosaminoglycans, glycoproteins, urinary prothrombin fragment-1, and Tamm–Horsfall proteins [ 41 , 62 ]. These inhibitors do not seem to work equally for everyone; therefore, some people form stones. But, if crystals formed remain tiny, usually it travels through the urinary tract and passes out from the body with urine splash without being noticed. Inhibitors may act either directly by interacting with crystal or indirectly by influencing the urinary environment [ 42 ]. When inhibitory compounds adsorb onto the surface of the crystal, it inhibits nucleation, crystal growth, aggregation, or crystal-cell adherence.
In contrast, promoters are substances which facilitate stone formation by various mechanisms [ 62 ]. Some of the promoters include cell membrane lipids (phospholipids, cholesterol, and glycolipids) [ 42 ], calcitriol hormone enhancement via parathyroid hormone stimulation [ 101 ], oxalate, calcium, sodium, cystine, and low urine volume [ 34 ]. Among recurrent stone formers, urinary oxalate excretion was found to be higher, whereas citrate excretion was lower [ 102 ]. Studies indicated that oxalate can increase chloride, sodium, and water reabsorption in the proximal tubule and activate multiple signaling pathways in renal epithelial cells [ 103 ]. In general, an imbalance between urinary stone inhibitors and promoters has been suggested to be the cause for stone formation [ 34 ]. A list of substances generally considered to inhibit or promote stone formation process is shown in Table 1 .
6. Preventive Options for Urolithiasis
Effective kidney stone prevention depends upon addressing the cause of stone formation. Generally, to prevent the first episodes of kidney stone formation or its secondary episodes, proper management of diet and the use of medications is required. Primary prevention of kidney stone disease via dietary intervention is low-cost public health initiative with massive societal implications. Thus, nutritional management is the best preventive strategy against urolithiasis [ 104 ].
Regardless of the underlying etiology and drug treatment of the stone disease, patients should be instructed to increase their water intake in order to maintain a urine output of at least 2 liter per day [ 49 ]. A simple and most important lifestyle change to prevent stone disease is to drink more water/liquids. Enough fluid intake reduces urinary saturation and dilutes promoters of CaOx crystallization. Dietary recommendations should be adjusted based on individual metabolic abnormalities. For absorptive hyperoxaluria, low oxalate diet and increased dietary calcium intake are recommended [ 61 ].
A high sodium intake boosts stone risk by reducing renal tubular calcium reabsorption and increasing urinary calcium [ 105 ]. Restriction of animal proteins is also encouraged since animal proteins provide an increased acid load because of its high content of sulfur-containing amino acids. Thus, high protein intake reduces urine pH and the level of citrate and enhances urinary calcium excretion via bone reabsorption. Therefore, if you have very acidic urine, you may need to eat less meat, fish, and poultry and avoid food with vitamin D [ 106 ]. Instead, an increase intake of fruits and vegetables rich in potassium is recommended [ 49 ].
People who form calcium stones used to be told to avoid dairy products and other foods with high calcium content. However, persons with a tendency of kidney stone formation should not be advised to restrict calcium intake unless it has been known that he/she has an excessive use of calcium [ 107 ]. A reduced intake of calcium leads to an increased intestinal absorption of oxalate, which itself may account for an increased risk of stone formation. Calcium supplements may reduce oxalate absorption because the calcium binds dietary oxalate in the gut lumen. However, the benefit of taking calcium pills is controversial. Vitamin C has been implicated in stone formation because of in vivo conversion of ascorbic acid to oxalate. Therefore, a limitation of vitamin C supplementation is recommended [ 105 ].
For prevention of calcium oxalate, cystine, and uric acid stones, urine should be alkalinized by eating a diet high in fruits and vegetables, taking supplemental or prescription citrate, or drinking alkaline mineral waters. For uric acid stone formers, gout needs to be controlled, and for cystine stone formers, sodium and protein intakes need to restricted. For prevention of calcium phosphate and struvite stones, urine should be acidified. For struvite stones, acidifying the urine is the single most important step [ 108 ]. Patients must receive careful follow-up to be sure that the infection has cleared. However, the current treatment modalities are not efficient to prevent urolithiasis, and further research is required.
7. Conclusion
Despite considerable improvements in the development of new therapies for the management of urinary stones, the incidence of urolithiasis is increasing worldwide. Many aspects of renal stone formation remain unclear. However, it is certain that renal cell injury, crystal retention, cell apoptosis, Randall's plaque, and associated stone inhibitors or promoters play important roles for kidney stone formation. These seem to be critical targets that lead to developing a novel strategy to prevent kidney stone disease and drugs against kidney stones. In addition, the identification of novel treatment targets on the basis of molecular and cellular alterations in relation to stone formation will help develop better drugs. Moreover, better understanding of the mechanisms of urolithiasis associated with stone inhibitors or promoters will be critical for stone-removing medications. Furthermore, understanding the underlying pathophysiology, pathogenesis, and genetic basis of kidney stone formation will hopefully lead to discover novel drugs and strategies to manage urolithiasis in the near future.
Conflicts of Interest
The authors declare that they have no conflicts of interest.

Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Management of Kidney Stones in 2020
- 1 Division of Nephrology and Hypertension, Mayo Clinic, Rochester, Minnesota
- 2 Division of Epidemiology, Mayo Clinic, Rochester, Minnesota
- 3 Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota
- 4 Division of Urology, Geisel School of Medicine at Dartmouth, Hanover, New Hampshire
- JAMA Diagnostic Test Interpretation Evaluation and Management of Nephrolithiasis Li Song, MD; Naim M. Maalouf, MD JAMA
- Comment & Response Diagnostic Imaging for Kidney Stones Ralph C. Wang, MD, MAS; Marshall L. Stoller, MD; Rebecca Smith-Bindman, MD JAMA
- Comment & Response Diagnostic Imaging for Kidney Stones—Reply Andrew D. Rule, MD, MSc; John C. Lieske, MD; Vernon M. Pais Jr, MD JAMA
- JAMA Patient Page Patient Information: Kidney Stones Kristin Walter, MD, MS JAMA
- Review Trends, Evaluation, and Management of Pediatric Nephrolithiasis Joel D. Hernandez, MD; Jonathan S. Ellison, MD; Thomas S. Lendvay, MD JAMA Pediatrics
- JAMA Pediatrics Patient Page Kidney Stones in Children and Adolescents Megan A. Moreno, MD, MSEd, MPH JAMA Pediatrics
Kidney stones are common, painful, and frequently recur. Although precise estimates of the incidence of symptomatic kidney stones for the entire US are unavailable, a Minnesota population-based study reported that between 1984 and 2012, the incidence of symptomatic kidney stones that required treatment increased from 51 to 217 per 100 000 person-years in women and from 145 to 299 per 100 000 person-years in men. 1
Read More About
Rule AD , Lieske JC , Pais VM. Management of Kidney Stones in 2020. JAMA. 2020;323(19):1961–1962. doi:10.1001/jama.2020.0662
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Kidney disease ends here .

New research explains link between body shape and risk of developing kidney stones
New results from researchers at the University of Oxford published i n the Journal of the American Society of Nephrology suggest that carrying excess fat around your middle (often referred to as an ‘apple’ body shape) increases your risk of kidney stones by raising blood calcium levels.
What is kidney stone disease?
Kidney stone disease is a common condition affecting around one in ten people where by hard ‘stones’ made of minerals and salts form in the kidneys. They can often be tiny, but if they get too big or if they move into the tubes connecting the kidney to the bladder, they can cause severe pain and can potentially lead to further complications.
Although many people will only get one kidney stone in their lifetime, around half of patients who develop a kidney stone will go on to develop more in the future. For some, there is a known genetic cause, but in many cases, we don’t fully understand why kidney stones form, or why they come back.

Leaving no stone unturned to understand causes of kidney stones
We know from previous studies that people with more body fat are more likely to develop kidney stones but until now it has been unclear why.
With funding from Kidney Research UK, the National Institute for Health Research and the Wellcome Trust, Dr Sarah Howles and her team used data from the UK Biobank – a collection of health and genetic information from around 500,000 participants – to investigate the link between fat and kidney stone disease.
The team found that people with a higher body mass index (BMI), and people with a high waist-to-hip ratio (a measure of how much fat tissue is carried around the middle) develop more kidney stones. They then used genetic techniques using data from the UK Biobank and a biobank in Finland called ‘FinnGen’ to show that having a higher BMI or high waist-to-hip ratio directly causes an increased risk of developing kidney stones.
“ This new knowledge will help healthcare providers to give better advice to patients as we now know that, even if a patient has a normal BMI, if they are carrying excess fat around their middle , this might increase their risk of developing kidney stones , and they could benefit from lifestyle changes . Our results also suggest that therapies that target fat tissue stores might affect blood calcium levels and prevent patients from developing kidney stones ." Dr Sarah Howles
Finding the missing link between fat and kidney stones
By analysing genetic data, the team found that carrying excess fat tissue around your middle increases the risk of developing kidney stones by raising the levels of calcium in the blood. This in turn can enter the urine and mix with other substances to form solid crystals that can grow into stones.
What does this mean for the future?
The team are now working on understanding exactly how body fat can change blood calcium levels as knowledge of these pathways will open the door to developing new treatments to prevent kidney stones from forming.
Research news

Can we support new approaches to kidney care by looking more closely at personalised care? The NURTuRE perspective

Pregnancy and Alport syndrome: a new way to look at the kidney filters

Study highlights potential early intervention for diabetic patients at risk of kidney disease

Study suggests rare kidney diseases treatments could dramatically reduce the burden of kidney disease on patients and the NHS

Survey highlights gaps in mental health care for UK kidney patients

Study shows promise of creating mini kidneys for personalised prenatal care

Unravelling inherited kidney diseases: an International Women’s Day conversation with Dr Melanie Chan

New results from the MELODY study highlight the variations in care experienced by transplant patients at different hospitals

Can sugar patterns help to predict kidney disease?

Unlocking the potential of kidney blood vessels in the treatment of childhood kidney disease

Can diabetic eye disease treatments affect kidney function?

Understanding the link between genetics and the immune system in the development of idiopathic nephrotic syndrome

Can stem cells help us improve the condition of donor kidneys?

Diabetes and kidney research charities team up to tackle diabetic kidney disease

Ground-breaking clinical trial offers treatment hope for IgA nephropathy

Meet Professor Claire Sharpe

Identifying a new drug target for diabetic kidney disease

Understanding the genetic causes of common childhood kidney disease

Exploring the role of BK virus in kidney transplant patients’ cancer risk: a World Cancer Day conversation with Dr Simon Baker

Kidney patients help trial world’s first blood potassium self-testing device
Why not make a donation now.
(Every £ counts)
Privacy Overview
- Log in

Stones in 2023: New treatment options and ‘cooked kidneys’
Urologists have no lack of new treatment options for stones, but sometimes the difference between the dozen or so Thulium fiber laser systems that have come to market since 2018 lies only in the graphical user interface. The actual capabilities and underlying technology are identical. This was one helpful piece of advice from Prof. Olivier Traxer (FR) during his state-of-the-art lecture “Beyond Holmium Laser: A new laser technology every year?”.
Prof. Traxer spoke at the Plenary Session on urinary stones on the final day of EAU23 in Milan. A core urological topic, the session covered a lot of ground, from medical to surgical treatment and the multidisciplinary approach that can come when urologists and nephrologists join forces in the analysis and treatment of kidney stones.
Traxer also cautioned the audience about the manufacturers’ presets on machines: a poll of some stone experts’ preferred settings for their thulium fibre systems shows no consensus at all, each having his or her own preferred presets. “As urologists we should also warn manufacturers to stop advertising the high frequencies that their products can achieve. This might work well in lab settings, but in real life we cannot maintain these high-frequency regimes on our patients.”
Distilling his lecture to three take-home messages, Prof. Traxer impressed on the audience the formula Energy x Frequency = Power, or J x Hz = Watts, emphasising the importance of energy and power, over frequency.
Second, when evaluating the effectiveness of new laser technology, the real-life application should be leading as laboratory settings cannot always be reproduced bedside. Finally, Prof. Traxer presented a useful rule of thumb for the audience: for kidney stones, work from surface to centre and always use 20-25W or less. For ureteral stones, from centre to surface and using a lower frequency range of 12-15W.
Dangers of overheating
Earlier in the session, Ass. Prof. Panagiotis Kallidonis (GR) and Dr. Thomas Tailly (BE) traded a few friendly barbs about the risk of overheating kidneys during the debate “Temperature rise by laser application: Fact or myth?”
With the possibilities of high-wattage machines, certainly the possibility and risk is very real. Combined with access sheaths, a manual pump and intermittent use of laser, power of 40W can safely be applied, argued Prof. Kallidonis. Dr. Tailly instead pointed that other than using more energy, there was very little evidence to suggest high-power use yielded better results than 10-20W. Chilled irrigation would be even better.
In the subsequent discussion, led by EULIS Chairman Prof. Christian Seitz (AT), the three discussed the impact of irrigation and how this could even best be measured in the first place, as well as proper use of sheaths.
Share this page
Highlights from day 4 at eau24, urothelial cancer: practice-changing results.
- EAU24 Resource Centre
- EAU23 Resource Centre
- EAU22 Resource Centre
- EAU Homepage
- EAU Privacy Policy
Certificate of Attendance
Available as of Wednesday 10 April 2024
Privacy Overview
Shedding light on the microbiome and kidney stones
A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones.
The human microbiome comprises trillions of microorganisms, including healthy bacteria. In recent years, research has begun to uncover its role in health and numerous diseases.
The research team examined the gut, urinary and salivary microbiomes in 83 patients who had kidney stones and compared them to 30 healthy controls. They found changes in all three microbiomes were linked to kidney stone formation.
"Kidney stone disease has been rising in recent years, affecting roughly 10 per cent of people," says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph's Health Care London (St. Joseph's). "While previous research has shown a connection between the gut microbiome and kidney stones in those who have taken antibiotics, we also wanted to explore the connection to other microbiomes in the hopes we can advance understanding and potential treatments."
Study participants included people who had formed kidney stones, had not had antibiotic exposure in the last 90 days and were having the stones removed surgically at St. Joseph's.
"Our testing -- called shotgun metagenomic sequencing -- allowed us to discover which bacteria were present in the gut and the genetic capabilities of those bacteria, or how it functions. We also did a simpler sequencing of the oral and urinary samples," explains Dr. Kait Al, lead author on the study and Postdoctoral Research Fellow at Western's Schulich School of Medicine & Dentistry.
Kidney stones are most commonly formed from calcium oxalate, which is a waste product produced by the body. Historically, it was thought people with specific gut microbes, like one bacterium called Oxalobacter formigenes that breaks down oxalate, were less likely to form kidney stones. This study suggests there are other factors.
"It's a more complex story. The microbes form a kind of network that's stable and beneficial in healthy people, but in those with kidney stones, that network is broken down. They're not producing the same vitamins and useful metabolites, not just in the gut but also in the urinary tract and oral cavity," Dr. Al explains.
There was also evidence that those with kidney stones had been exposed to more antimicrobials, as they had more antibiotic-resistant genes.
"We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant," explains Dr. Burton, also an Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine & Dentistry.
The research team says that although more research is needed, these initial findings shed light on the overall importance of a person's microbiome and keeping it as healthy as possible, with a microbiome-friendly diet and minimal antibiotic use potentially part of the solution.
The study was funded in part through the Weston Foundation and supported by the American Urological Association.
- Kidney Disease
- Bladder Disorders
- Diseases and Conditions
- Microbes and More
- Veterinary Medicine
- Kidney stone
- Excretory system
- Inflammation of the kidney
- Kidney transplantation
- Renal cell carcinoma
- Developmental biology
Story Source:
Materials provided by Lawson Health Research Institute . Note: Content may be edited for style and length.
Journal Reference :
- Kait F. Al, Benjamin R. Joris, Brendan A. Daisley, John A. Chmiel, Jennifer Bjazevic, Gregor Reid, Gregory B. Gloor, John D. Denstedt, Hassan Razvi, Jeremy P. Burton. Multi-site microbiota alteration is a hallmark of kidney stone formation . Microbiome , 2023; 11 (1) DOI: 10.1186/s40168-023-01703-x
Cite This Page :
Explore More
- Quantum Effects in Electron Waves
- Star Trek's Holodeck Recreated Using ChatGPT
- Cloud Engineering to Mitigate Global Warming
- Detecting Delayed Concussion Recovery
- Bonobos: More Aggressive Than Thought
- Brightest Gamma-Ray Burst
- Stellar Winds of Three Sun-Like Stars Detected
- Fences Causing Genetic Problems for Mammals
- Ozone Impact On Fly Species
- Parkinson's: New Theory On Origins and Spread
Trending Topics
Strange & offbeat.
- Português Br
- Journalist Pass
Preventing kidney stones before they form
Mayo Clinic Staff
Share this:

Kidney stones are small, hard deposits made of minerals and reoccurring materials inside the kidneys. Stones often go unnoticed in the kidney until they move into the ureter —the tube connecting the kidney and bladder.
If a stone leaves the kidney and blocks urine from exiting, usually while in the ureter, it can cause urine to back up and lead to intense pain.
Kidney stones are common, affecting about 12% of the U.S. population. Kidney stone development usually begins when people are in their 20s or 30s, and the problem can continue for years.
Many things can increase your risk for stones, including family history, health factors like diabetes, dietary habits or if your urine lacks substances to prevent crystals from sticking together.
Types of kidney stones
There are four types of kidney stones. Knowing the type of your kidney stone will help determine its cause and give you clues on how to reduce your chance of developing more stones. If you pass a kidney stone, try to save it to give to your healthcare team for analysis.
Types of kidney stones include:
- Calcium stones This is the most common type of kidney stone. About 70% to 80% of kidney stones are calcium stones, which are usually made of calcium and oxalate. Oxalate is a substance produced by the liver and also absorbed from your diet. Certain fruits and vegetables, like spinach, have high oxalate content. Taking high doses of vitamin D and vitamin C, gastric surgery and several metabolic disorders can increase the concentration of calcium or oxalate in your urine.
Calcium stones can also be made of calcium phosphate. This type of stone is more common in people with metabolic conditions like renal tubular acidosis. It may also be associated with some medications used to treat migraines (topiramate) or blood pressure (furosemide or triamterene).
- Struvite stones Struvite stones can form after a urinary tract infection. These stones can grow quickly and become large, sometimes with few symptoms or little warning.
- Uric acid stones Uric acid stones can form in people who lose too much fluid because of chronic diarrhea or malabsorption, eat a high-protein diet or who have gout. Certain genetic factors also may increase your risk of uric acid stones.
- Cystine stones These stones form in people with a hereditary disorder called cystinuria, which causes the kidneys to excrete too much of a specific amino acid.
Preventing kidney stones
Nearly 50% of people who have developed kidney stones will develop another stone in 10 years if they do not take steps to prevent a recurrence. Usually, this includes a combination of lifestyle changes and medications.
Lifestyle changes
You may reduce your risk of kidney stones if you:
- Drink water throughout the day. People with a history of kidney stones should drink enough fluids to pass about 80 oz (2.5 liters) of urine every day. This is the most effective therapy available to prevent future kidney stones. Your healthcare team may ask you to measure your urine output to ensure you drink enough water.
- Eat fewer oxalate-rich foods. Switching to a diet low in oxalates can reduce your risk of calcium oxalate stones. Foods that are highest in oxalates include spinach, rhubarb, baked potatoes, lentils, navy beans, bran, grits and almonds.
A high amount of salt and animal protein in your diet can also increase your kidney stone risk. A diet lower in sodium and higher in potassium — contained in many fruits and vegetables — can reduce the risk of stone formation.
- Continue eating calcium-rich foods, but use caution with calcium supplements. Calcium in food can actually lower your risk of kidney stones. Continue eating calcium-rich foods unless your healthcare team recommends otherwise. Talk with your healthcare team before taking calcium supplements, however, because these may be linked to an increased risk of kidney stones.
- Take steps to reduce urinary tract infections. Some people are more susceptible to developing recurrent urinary tract infections. Fewer infections can reduce the risk of developing struvite stones. Get tips for preventing urinary tract infections .
Medications
Medications can control the amount of minerals and salts in the urine and may be helpful in people who form certain kinds of stones. The type of medication your doctor prescribes will depend on the type of kidney stones you have and the specific makeup of your urine, which is determined by testing. Some medications can reduce uric acid levels in the blood and reduce your risk of uric acid stones, while others increase the solubility of cystine in your urine and lower your risk of cystine stones.
Kidney stone formation is specific to each person, so it's important to work with your healthcare team to develop a personalized treatment plan . That plan should consider what kind of kidney stones you have, possible causes for their formation and specific steps to prevent them.
Spencer Bershow, M.D. , cares for patients in Urology in Mankato and New Prague , Minnesota.
- Mayo Clinic prepares to biomanufacture a new CAR-T cell therapy for recurring B-cell blood cancers Mayo Clinic Minute: Why you and your family need a flu shot
Related Articles

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 03 April 2024
Time to sound the alarm about the hidden epidemic of kidney disease
You have full access to this article via your institution.

Kidney disease is growing worldwide. The secretariat of the World Health Organization has welcomed the call to include it as a non-communicable disease that causes premature deaths. Credit: Vsevolod Zviryk/SPL
A quiet epidemic is building around the world. It is the third-fastest-growing cause of death globally. By 2040, it is expected to become the fifth-highest cause of years of life lost. Already, 850 million people are affected, and treating them is draining public-health coffers: the US government-funded health-care plan Medicare alone spends US$130 billion to do so each year. The culprit is kidney disease, a condition in which damage to the kidneys prevents them from filtering the blood.
And yet, in discussions of priorities for global public health, the words ‘kidney disease’ do not always feature. One reason for this is that kidney disease is not on the World Health Organization (WHO) list of priority non-communicable diseases (NCDs) that cause premature deaths. The roster of such NCDs includes heart disease, stroke, diabetes, cancer and chronic lung disease. With kidney disease missing, awareness of its growing impact remains low.
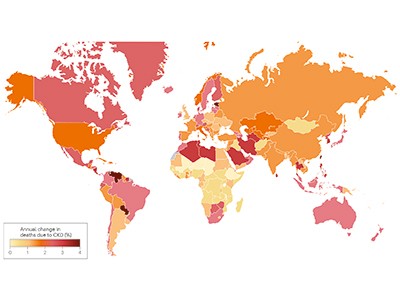
Chronic kidney disease and the global public health agenda: an international consensus
The authors of an article in Nature Reviews Nephrology this week want to change that ( A. Francis et al. Nature Rev. Nephrol . https://doi.org/10.1038/s41581-024-00820-6; 2024 ). They are led by the three largest professional organizations working in kidney health — the International Society of Nephrology, the American Society of Nephrology and the European Renal Association — and they’re urging the WHO to include kidney disease on the priority NCD list.
This will, the authors argue, bring attention to the growing threat, which is particularly dire for people in low- and lower-middle-income countries, who already bear two‑thirds of the world’s kidney-disease burden. Adding kidney disease to the list will also mean that reducing deaths from it could become more of a priority for the United Nations Sustainable Development Goals target to reduce premature deaths from NCDs by one-third by 2030.
As of now, rates of chronic kidney disease are likely to increase in low- and lower-middle-income countries as the proportion of older people in their populations increases. Inclusion on the WHO list could provide an incentive for health authorities to prioritize treatments, data collection and other research, along with funding, as with other NCDs.
Kidney disease often accompanies other conditions that do appear on the NCD list, such as heart disease, cancer and diabetes — indeed, kidney-disease deaths caused specifically by diabetes are on the list. But the article authors argue that “tackling diabetes and heart disease alone will not target the core drivers of a large proportion of kidney diseases”. Both acute and chronic kidney disease can have many causes. They can be caused by infection or exposure to toxic substances. Increasingly, the consequences of global climate change, including high temperatures and reduced availability of fresh water, are thought to be contributing to the global burden of kidney disease, as well.
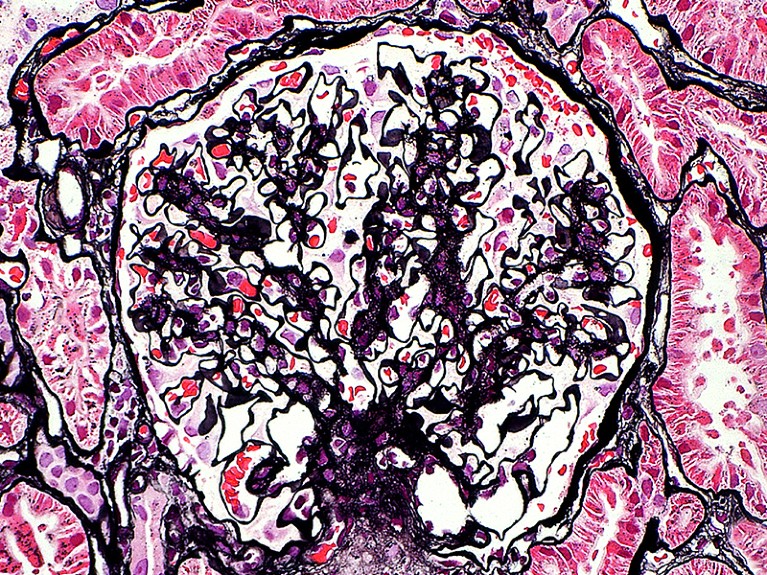
The kidney glomerulus filters waste products from the blood. In people with damaged kidneys, this happens through dialysis. Credit: Ziad M. El-Zaatari/SPL
The WHO secretariat, which works closely with the nephrology community, welcomes the call to include kidney disease as an NCD that causes premature deaths, says Slim Slama, who heads the NCD unit at the secretariat in Geneva, Switzerland. The data support including kidney disease as an NCD driver of premature death, he adds.
The decision to include kidney disease along with other priority NCDs isn’t only down to the WHO, however. There must be conversations between the secretariat, WHO member states, the nephrology community, patient advocates and others. WHO member states need to instruct the agency to take the steps to make it happen, including providing appropriate funding for strategic and technical assistance.
Data and funding gaps
Three reports based on surveys by the International Society of Nephrology since 2016 highlight the scale of data gaps ( A. K. Bello et al. Lancet Glob. Health 12 , E382–E395; 2024 ). In many countries, screening for kidney disease is difficult to access and a large proportion of cases go undetected and therefore uncounted. For example, it is not known precisely how many people with kidney failure die each year because of lack of access to dialysis or transplantation: the numbers are somewhere between two million and seven million, according to the WHO. Advocates must push public-health officials in more countries to collect the data needed to monitor kidney disease and the impact of prevention and treatment efforts.
Even with better data, treatments for kidney disease are often prohibitively expensive. They include dialysis, an intervention to filter the blood when kidneys cannot. Dialysis is often required two or three times weekly for the remainder of the recipient’s life, or until they can receive a transplant, and it is notoriously costly. In Thailand, for example, it accounted for 3% of the country’s total health-care expenditures in 2022, according to the country’s parliamentary budget office.

End chronic kidney disease neglect
These costs could come down if people who have diabetes or high blood pressure, for example, could be routinely screened for impaired kidney function, because they are at high risk of developing chronic kidney disease. This would enable kidney damage to be detected early, before symptoms set in, opening the way for treatments that do not immediately require dialysis or transplant surgery.
New drugs that boost weight loss and treat type 2 diabetes could also help to prevent or reduce stress on the kidneys, but these, too, are too expensive for many people in need. That is why something needs to be done to make drugs more affordable. The pharmaceutical industry, which has become extremely profitable, has a crucial role. In Denmark, for example, the industry’s profits helped to tip the national economy from recession into growth in 2023, according to the public agency Statistics Denmark. The COVID-19 pandemic showed that making profits and making drugs available, and affordable, to a wide population need not be mutually exclusive. Similarly innovative thinking is now needed. “The whole world needs to reckon with this kidney problem,” says Valerie Luyckx, a biomedical ethicist at the University of Zurich in Switzerland.
The WHO adding kidney disease to its priority list could also attract funding for treatment, research and disease registries. That could jump-start the development of new treatments and help to make current treatments more affordable and accessible.
NCDs are responsible for 74% of deaths worldwide, but the world’s biggest donors to global health currently devote less than 2% of their budgets for international health assistance to NCD prevention and control, and not including kidney disease. Drawing more attention to the quiet rampage of kidney disease among some of the most vulnerable people would be one important step in turning these statistics around.
Nature 628 , 7-8 (2024)
doi: https://doi.org/10.1038/d41586-024-00961-5
Reprints and permissions
Related Articles

- Developing world
- Health care

AI can help to tailor drugs for Africa — but Africans should lead the way
Comment 09 APR 24

Rwanda 30 years on: understanding the horror of genocide
Editorial 09 APR 24

Africa’s postdoc workforce is on the rise — but at what cost?
Career Feature 02 APR 24

What the India election means for science
News 10 APR 24

Brazil budget cuts could leave science labs without power and water
News 08 APR 24

Will the Gates Foundation’s preprint-centric policy help open access?
News 04 APR 24

Lethal dust storms blanket Asia every spring — now AI could help predict them
News 15 APR 24

Bird flu outbreak in US cows: why scientists are concerned
News Explainer 08 APR 24
Adopt universal standards for study adaptation to boost health, education and social-science research
Correspondence 02 APR 24
Energy AI / Grid Modernization / Hydrogen Energy / Power Semiconductor Concentration / KENTECH College
21, Kentech-gil, Naju-si, Jeollanam-do, Republic of Korea(KR)
Korea Institute of Energy Technology
Professor in Macromolecular Chemistry
The Department of Chemistry - Ångström conducts research and education in Chemistry. The department has 260 employees and has a turnover of 290 mil...
Uppsala (Stad) (SE)
Uppsala University
Postdoctoral research fellow focused on generative modelling of synthetic cohorts in brain research
Lunds universitet, Institutionen för kliniska vetenskaper Malmö Lund University was founded in 1666 and is repeatedly ranked among the world’s top ...
Lund (Stad), Skåne (SE)
Lund University
Junior Group Leader Position at IMBA - Institute of Molecular Biotechnology
The Institute of Molecular Biotechnology (IMBA) is one of Europe’s leading institutes for basic research in the life sciences. IMBA is located on t...
Austria (AT)
IMBA - Institute of Molecular Biotechnology
Research Group Head, BeiGene Institute
A cross-disciplinary research organization where cutting-edge science and technology drive the discovery of impactful Insights
Pudong New Area, Shanghai
BeiGene Institute
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Patient Care & Health Information
- Diseases & Conditions
- Kidney stones
If your doctor suspects that you have a kidney stone, you may have diagnostic tests and procedures, such as:
- Blood testing. Blood tests may reveal too much calcium or uric acid in your blood. Blood test results help monitor the health of your kidneys and may lead your doctor to check for other medical conditions.
- Urine testing. The 24-hour urine collection test may show that you're excreting too many stone-forming minerals or too few stone-preventing substances. For this test, your doctor may request that you perform two urine collections over two consecutive days.
Imaging. Imaging tests may show kidney stones in your urinary tract. High-speed or dual energy computerized tomography (CT) may reveal even tiny stones. Simple abdominal X-rays are used less frequently because this kind of imaging test can miss small kidney stones.
Ultrasound, a noninvasive test that is quick and easy to perform, is another imaging option to diagnose kidney stones.
- Analysis of passed stones. You may be asked to urinate through a strainer to catch stones that you pass. Lab analysis will reveal the makeup of your kidney stones. Your doctor uses this information to determine what's causing your kidney stones and to form a plan to prevent more kidney stones.
- Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your kidney stones-related health concerns Start Here
More Information
Kidney stones care at Mayo Clinic
- Computerized tomography (CT) urogram
- Intravenous pyelogram
Treatment for kidney stones varies, depending on the type of stone and the cause.
Small stones with minimal symptoms
Most small kidney stones won't require invasive treatment. You may be able to pass a small stone by:
- Drinking water. Drinking as much as 2 to 3 quarts (1.8 to 3.6 liters) a day will keep your urine dilute and may prevent stones from forming. Unless your doctor tells you otherwise, drink enough fluid — ideally mostly water — to produce clear or nearly clear urine.
- Pain relievers. Passing a small stone can cause some discomfort. To relieve mild pain, your doctor may recommend pain relievers such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve).
- Medical therapy. Your doctor may give you a medication to help pass your kidney stone. This type of medication, known as an alpha blocker, relaxes the muscles in your ureter, helping you pass the kidney stone more quickly and with less pain. Examples of alpha blockers include tamsulosin (Flomax) and the drug combination dutasteride and tamsulosin (Jalyn).
Large stones and those that cause symptoms
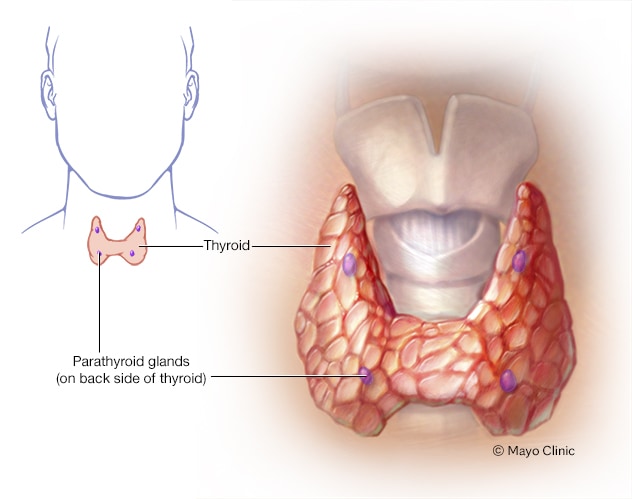
Parathyroid glands
The four tiny parathyroid glands, which lie near the thyroid, make the parathyroid hormone. The hormone plays a role in controlling levels of the minerals calcium and phosphorus in the body.
Kidney stones that are too large to pass on their own or cause bleeding, kidney damage or ongoing urinary tract infections may require more-extensive treatment. Procedures may include:
Using sound waves to break up stones. For certain kidney stones — depending on size and location — your doctor may recommend a procedure called extracorporeal shock wave lithotripsy (ESWL).
ESWL uses sound waves to create strong vibrations (shock waves) that break the stones into tiny pieces that can be passed in your urine. The procedure lasts about 45 to 60 minutes and can cause moderate pain, so you may be under sedation or light anesthesia to make you comfortable.
ESWL can cause blood in the urine, bruising on the back or abdomen, bleeding around the kidney and other adjacent organs, and discomfort as the stone fragments pass through the urinary tract.
Surgery to remove very large stones in the kidney. A procedure called percutaneous nephrolithotomy (nef-row-lih-THOT-uh-me) involves surgically removing a kidney stone using small telescopes and instruments inserted through a small incision in your back.
You will receive general anesthesia during the surgery and be in the hospital for one to two days while you recover. Your doctor may recommend this surgery if ESWL is unsuccessful.
Using a scope to remove stones. To remove a smaller stone in your ureter or kidney, your doctor may pass a thin lighted tube (ureteroscope) equipped with a camera through your urethra and bladder to your ureter.
Once the stone is located, special tools can snare the stone or break it into pieces that will pass in your urine. Your doctor may then place a small tube (stent) in the ureter to relieve swelling and promote healing. You may need general or local anesthesia during this procedure.
Parathyroid gland surgery. Some calcium phosphate stones are caused by overactive parathyroid glands, which are located on the four corners of your thyroid gland, just below your Adam's apple. When these glands produce too much parathyroid hormone (hyperparathyroidism), your calcium levels can become too high and kidney stones may form as a result.
Hyperparathyroidism sometimes occurs when a small, benign tumor forms in one of your parathyroid glands or you develop another condition that leads these glands to produce more parathyroid hormone. Removing the growth from the gland stops the formation of kidney stones. Or your doctor may recommend treatment of the condition that's causing your parathyroid gland to overproduce the hormone.
Prevention of kidney stones may include a combination of lifestyle changes and medications.
Lifestyle changes
You may reduce your risk of kidney stones if you:
Drink water throughout the day. For people with a history of kidney stones, doctors usually recommend drinking enough fluids to pass about 2.1 quarts (2 liters) of urine a day. Your doctor may ask that you measure your urine output to make sure that you're drinking enough water.
If you live in a hot, dry climate or you exercise frequently, you may need to drink even more water to produce enough urine. If your urine is light and clear, you're likely drinking enough water.
- Eat fewer oxalate-rich foods. If you tend to form calcium oxalate stones, your doctor may recommend restricting foods rich in oxalates. These include rhubarb, beets, okra, spinach, Swiss chard, sweet potatoes, nuts, tea, chocolate, black pepper and soy products.
- Choose a diet low in salt and animal protein. Reduce the amount of salt you eat and choose nonanimal protein sources, such as legumes. Consider using a salt substitute, such as Mrs. Dash.
Continue eating calcium-rich foods, but use caution with calcium supplements. Calcium in food doesn't have an effect on your risk of kidney stones. Continue eating calcium-rich foods unless your doctor advises otherwise.
Ask your doctor before taking calcium supplements, as these have been linked to increased risk of kidney stones. You may reduce the risk by taking supplements with meals. Diets low in calcium can increase kidney stone formation in some people.
Ask your doctor for a referral to a dietitian who can help you develop an eating plan that reduces your risk of kidney stones.
Medications
Medications can control the amount of minerals and salts in the urine and may be helpful in people who form certain kinds of stones. The type of medication your doctor prescribes will depend on the kind of kidney stones you have. Here are some examples:
- Calcium stones. To help prevent calcium stones from forming, your doctor may prescribe a thiazide diuretic or a phosphate-containing preparation.
- Uric acid stones. Your doctor may prescribe allopurinol (Zyloprim, Aloprim) to reduce uric acid levels in your blood and urine and a medicine to keep your urine alkaline. In some cases, allopurinol and an alkalizing agent may dissolve the uric acid stones.
- Struvite stones. To prevent struvite stones, your doctor may recommend strategies to keep your urine free of bacteria that cause infection, including drinking fluids to maintain good urine flow and frequent voiding. In rare cases long-term use of antibiotics in small or intermittent doses may help achieve this goal. For instance, your doctor may recommend an antibiotic before and for a while after surgery to treat your kidney stones.
- Cystine stones. Along with suggesting a diet lower in salt and protein, your doctor may recommend that you drink more fluids so that you produce a lot more urine,. If that alone doesn't help, your doctor may also prescribe a medication that increases the solubility of cystine in your urine.
- Percutaneous nephrolithotomy
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get the latest health information from Mayo Clinic delivered to your inbox.
Subscribe for free and receive your in-depth guide to digestive health, plus the latest on health innovations and news. You can unsubscribe at any time. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Your in-depth digestive health guide will be in your inbox shortly. You will also receive emails from Mayo Clinic on the latest health news, research, and care.
If you don’t receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Preparing for your appointment
Small kidney stones that don't block your kidney or cause other problems can be treated by your family doctor. But if you have a large kidney stone and experience severe pain or kidney problems, your doctor may refer you to a doctor who treats problems in the urinary tract (urologist or nephrologist).
What you can do
To prepare for your appointment:
- Ask if there's anything you need to do before your appointment, such as limit your diet.
- Write down your symptoms, including any that seem unrelated to kidney stones.
- Keep track of how much you drink and urinate during a 24-hour period.
- Make a list of all medications, vitamins or other supplements that you take.
- Take a family member or friend along, if possible, to help you remember what you discuss with your doctor.
- Write down questions to ask your doctor.
For kidney stones, some basic questions include:
- Do I have a kidney stone?
- What size is the kidney stone?
- Where is the kidney stone located?
- What type of kidney stone do I have?
- Will I need medication to treat my condition?
- Will I need surgery or another procedure?
- What's the chance that I'll develop another kidney stone?
- How can I prevent kidney stones in the future?
- I have other health conditions. How can I best manage them together?
- Do I need to follow any restrictions?
- Should I see a specialist? If so, does insurance typically cover the services of a specialist?
- Is there a generic alternative to the medicine you're prescribing?
- Do you have any educational material that I can take with me? What websites do you recommend?
- Do I need a follow-up visit?
Besides the questions you prepare in advance, don't hesitate to ask any other questions during your appointment as they occur to you.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Has anyone else in your family had kidney stones?
- Goldman L, et al., eds. Nephrolithiasis. In: Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Jan. 20, 2020.
- Kidney stones. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/kidney-stones. Accessed Jan. 20, 2020.
- McKean SC, et al., eds. Kidney stones. In: Principles and Practice of Hospital Medicine. 2nd ed. McGraw-Hill Education; 2017. https://accessmedicine.mhmedical.com/. Accessed Jan. 20, 2020.
- What are kidney stones? American Urological Association. https://www.urologyhealth.org/urologic-conditions/kidney-stones. Accessed Jan. 20, 2020.
- Kellerman RD, et al. Nephrolithiasis. In: Conn's Current Therapy 2020. Elsevier; 2020. https://www.clinicalkey.com. Accessed Jan. 20, 2020.
- Braswell-Pickering EA. Allscripts EPSi. Mayo Clinic. Nov. 3, 2021.
- Curhan GC, et al. Diagnosis and acute management of suspected nephrolithiasis in adults. https://www.uptodate.com/search/contents. Accessed Jan. 20, 2020.
- Yu ASL, et al., eds. Diagnostic kidney imaging. In: Brenner & Rector's The Kidney. 11th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Jan. 20, 2020.
- Fontenelle LF, et al. Kidney stones: Treatment and prevention. American Family Physician. 2019. https://www.aafp.org/afp/2019/0415/p490.html. Accessed Jan. 20, 2020.
- Preminger GM. Options in the management of renal and ureteral stones in adults. https://www.uptodate.com/search/contents. Accessed Jan. 20, 2020.
- Preventing Kidney Stones
Associated Procedures
News from mayo clinic.
- Preventing kidney stones before they form Oct. 11, 2023, 01:59 p.m. CDT
- Mayo Clinic Minute: Where is the kidney stone belt? July 03, 2023, 02:00 p.m. CDT
- Mayo Clinic Minute: What can you eat to avoid kidney stones? March 30, 2023, 03:30 p.m. CDT
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

Consuming processed foods and drinks raises risk of kidney stones: study
By Stephen Beech via SWNS
Processed food and drink - such as cookies, cakes and soda - increase the risk of kidney stones, warns a new study.
Researchers have shown for the first time that a greater intake of added sugars commonly found in processed consumables raises the chances of developing the painful condition.
Kidney stones affect more than one in 10 people. Common symptoms include severe pain, nausea, vomiting, fever, chills, and bloody urine.
But doctors say kidney stones don’t just reduce the quality of life as, in the long run, they may lead to infections, swollen kidneys and potentially fatal renal disease.
Known risk factors for developing the condition include being an adult male, obesity, chronic diarrhea, dehydration, and having inflammatory bowel disease (IBD), diabetes, or gout.
The new study, published in the journal Frontiers in Nutrition , has shown for the first time that elevated consumption of added sugars should probably be added to the list of risk factors for kidney stones.
The Chinese research team say added sugars occur in many processed foods, but are especially common in sugar-sweetened pop, fruit drinks, chocolate, ice cream, biscuits and cakes.
Study lead author Dr. Shan Yin said: “Ours is the first study to report an association between added sugar consumption and kidney stones.
“It suggests that limiting added sugar intake may help to prevent the formation of kidney stones.”
Dr. Yin and his colleagues analyzed health data from more than 28,000 American adults. Participants self-reported if they had a history of kidney stones.
Each participant’s daily intake of added sugars was estimated from recall of their most recent consumption of food and drinks, given twice: once in a face-to-face interview, and once in a telephone interview between three and 10 days later.
The participants also received a healthy eating index score which summarised their diet in terms of the adequacy of beneficial diet components such as fruits, veg, and whole grains, and moderation of potentially harmful foods, such as refined grains, salt, and saturated fats.
The research team adjusted the odds of developing kidney stones per year during the trial for a range of factors including gender, age, race or ethnicity, relative income and body mass index (BMI).
At the start of the study, participants with a higher intake of added sugar tended to have a higher current prevalence of kidney stones, a lower healthy eating score, and a lower education level.
The overall average intake of added sugars was 272.1 calories per day, which corresponded to 13.2 percent of the total daily energy intake.
The research team showed that the percentage of energy intake from added sugars was "positively and consistently" correlated with kidney stones.
For example, participants whose intake of added sugars was among the 25 percent highest had 39 percent greater odds of developing kidney stones over the course of the study.
Similarly, participants who derived more than 25 percent of their total energy from added sugars had an 88 percent greater odds than those who derived less than five percent of their total energy from added sugars.
Dr. Yin, a researcher at the Affiliated Hospital of North Sichuan Medical College, said the mechanisms of the relation between consuming more added sugars and a greater risk of developing kidney stones is not yet known.
He added: “Further studies are needed to explore the association between added sugar and various diseases or pathological conditions in detail.
“For example, what types of kidney stones are most associated with added sugar intake? How much should we reduce our consumption of added sugars to lower the risk of kidney stone formation?
"Nevertheless, our findings already offer valuable insights for decision-makers.”
The post Consuming processed foods and drinks raises risk of kidney stones: study appeared first on Talker .

- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- 2023 in medicine
- Why exercise is key to living a long and healthy life
- What do we know about the gut microbiome in IBD?
- My podcast changed me
- Can 'biological race' explain disparities in health?
- Why Parkinson's research is zooming in on the gut
- Health Hubs
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- Our Editorial Process
- Content Integrity
- Conscious Language
- Health Conditions
- Health Products
Does cannabis increase or reduce the risk of kidney stones?

Kidney stones are hard masses that can form in the kidneys and cause pain. While evidence notes that smoking is a risk factor, no research suggests cannabis increases the risk of kidney stones.
Kidney stones describe hard deposits of dissolved minerals that can accumulate in the kidneys. If the stones become large enough, they can lodge themselves in the urinary tract, causing pain. Without removal, they can lead to complications such as infection and kidney damage.
Cannabis is a plant containing compounds that may have medicinal benefits. The most abundant substances in cannabis are cannabidiol (CBD) and delta-9-tetrahydrocannabinol (THC). People can use the cannabis plant in a variety of ways, such as by smoking or consuming it.
While smoking tobacco can increase the risk of kidney stone formation, no evidence suggests smoking cannabis increases the risk. Instead, some research suggests it may actually lower the risk. However, more research is still necessary.
Can cannabis use result in kidney stones?
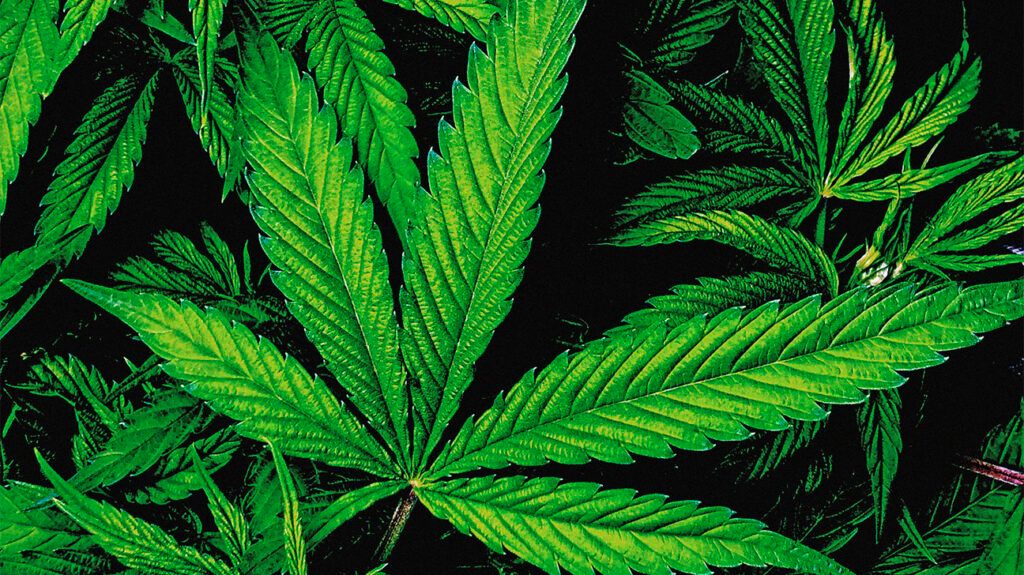
Kidney stones are a common health problem. Evidence notes that smoking can greatly contribute to the risk of kidney stones.
A 2023 analysis and 2023 presentation both suggest smoking tobacco increases the risk of kidney stones due to increasing the concentration of cotinine in the blood. This is a by-product that forms after nicotine enters the body. A 2022 study notes that cotinine can decrease kidney function, while a 2023 study indicates secondhand smoke is also a risk factor for kidney stones.
While smoking tobacco is a direct risk factor, and smoking anything can be harmful, there is currently no association between cannabis use and kidney stones. However, possible complications from chronic cannabis use may increase the risk.
Cannabinoid hyperemesis syndrome (CHS) describes when a person experiences nausea, vomiting, and abdominal pain after long-term and frequent cannabis use. A 2023 case study proposes a link between CHS and kidney stones due to dehydration and electrolyte imbalances. However, the authors highlight that the link is unclear and that further research is necessary.
Can cannabis reduce kidney stone risk?
A 2020 article notes that there is little guidance or evidence regarding the effects of cannabis use on kidney health. However, it adds that possible links between smoking cannabis and kidney disease are more likely to relate to tobacco use. It further mentions that using cannabis in other ways, such as oral consumption, may avoid possible health risks.
The article concludes that the possible link warrants further research.
According to a 2023 study , cannabis use in males has an inverse relation to kidney stones. This suggests that cannabis use may reduce the risk of kidney stones. However, the study found no significant difference in females or the overall population.
Kidney stone causes and risk factors
Kidney stones typically occur when high levels of certain substances accumulate in the urine. These substances can include calcium , oxalate , and phosphorus .
Anyone can develop kidney stones, though certain factors may increase the risk. Causes and risk factors of kidney stones can include :
- not drinking a sufficient amount of water, known as dehydration
- a diet rich in protein, sodium, or sugar
- having obesity
- previous surgery on the intestines
- a personal or family history of kidney stones
- having polycystic kidney disease
- taking certain medications, such as diuretics or calcium-based antacids
- health problems that may cause substances, such as calcium, to build up in the urine
- health problems that can cause swelling in the digestive system or joints
Read on to learn more about natural remedies for kidney stones and how to speed up the process of passing stones .
Kidney stone prevention tips
Although kidney stones are common, people can take preventive steps to reduce the risk of them developing. Typically, this involves making some lifestyle changes .
Tips to prevent kidney stones can include :
- drinking sufficient amounts of water
- limiting foods and beverages containing excessive sugar or high fructose corn syrup
- consuming more fruits and vegetables
- consuming more plant-based proteins and less animal proteins
- reducing excess salt in the diet
- maintaining a moderate weight
- trying to reduce oxalate intake
- consuming calcium-rich foods, as they can actually help prevent stone formation
Read on to learn more about preventing kidney stones .
Can cannabis benefit health?
Research into the possible health benefits of cannabis and cannabinoids is ongoing, though it can be difficult to evaluate the safety of these substances accurately. This is due to the variety of ways people can use them and the varying levels of different compounds such as CBD and THC .
Many people may consider using cannabis recreationally due to its euphoric or psychoactive effects. Currently, there is a lack of evidence investigating the benefits of recreational cannabis.
At present, components of the cannabis plant are the active ingredient in a number of medications. This includes drugs that may be beneficial for individuals with cancer , AIDS , multiple sclerosis (MS) , and epilepsy .
Evidence suggests possible health benefits of cannabis may include :
- reducing inflammation
- treating anxiety disorders
- preventing seizures
- managing gastrointestinal disorders
- helping with addictive behaviors
- lowering blood pressure
- alleviating the side effects of chemotherapy
- anticancer properties
Currently, it is advisable only to take cannabis, cannabinoid-containing products, or medications as a healthcare professional advises.
Read on to learn more about the health benefits of cannabis .
Evidence notes that smoking is a risk factor for developing kidney stones. However, research notes that this relates to tobacco products containing nicotine. As such, there are currently no direct links between cannabis and the development of kidney stones. Instead, some evidence suggests that cannabis may reduce this risk.
Research is still ongoing into the potential health benefits of cannabis, including its effects on the kidneys. Therefore, further research is still necessary.
Tips for preventing kidney stones can include drinking water, dietary changes, and maintaining a moderate weight.
Last medically reviewed on April 12, 2024
- Urology / Nephrology
- Marijuana / Cannabis / CBD
How we reviewed this article:
- 7 urological conditions impacted by smoking. (2018). https://www.urologyhealth.org/healthy-living/care-blog/2018/7-urologic-conditions-impacted-by-smoking
- Chen Y-H, et al. (2023). The impact of secondhand smoke on the development of kidney stone disease is not inferior to that of smoking: A longitudinal cohort study. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-023-16116-6
- Chu F, et al. (2023). Cannabinoid hyperemesis syndrome. https://www.ncbi.nlm.nih.gov/books/NBK549915/
- Cotinine factsheet. (2017). https://www.cdc.gov/biomonitoring/Cotinine_FactSheet.html
- Di X, et al. (2023). Association between marijuana use and kidney stone: A cross-sectional study of NHANES 2009 to 2018. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10513173/
- Fu Y-C, et al. (2022). The association between smoking and renal function in people over 20 years old. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9205397/
- Huang Y, et al. (2023). Associations between smoke exposure and kidney stones: Results from the NHANES (2007–2018) and Mendelian randomization analysis. https://www.frontiersin.org/articles/10.3389/fmed.2023.1218051/full
- Is marijuana safe and effective as medicine? (2020). https://nida.nih.gov/publications/research-reports/marijuana/marijuana-safe-effective-medicine
- Isles C. (2021). 7 potential health benefits of cannabis. https://www.jwu.edu/news/2021/09/7-potential-health-benefits-of-cannabis.html
- Kidney stones. (2017). https://www.niddk.nih.gov/health-information/urologic-diseases/kidney-stones
- Kidney stones. (n.d.). https://www.kidney.org/atoz/content/kidneystones
- Kidney stones. (n.d.). https://www.urologyhealth.org/urology-a-z/k/kidney-stones
- Kidney stones: Causes, symptoms and treatment options. (2022). https://www.kidneyfund.org/all-about-kidneys/other-kidney-problems/kidney-stones
- Patel M, et al. (2023). A case of a patient with cannabis hyperemesis syndrome along with recurrent nephrolithiasis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10163339/
- Rein, JL. (2020). The nephrologist's guide to cannabis and cannabinoids. https://journals.lww.com/co-nephrolhypertens/fulltext/2020/03000/the_nephrologist_s_guide_to_cannabis_and.15.aspx
- Tang J, et al. (2023). Cigarette smoking and prevalent kidney stone: The National Health and Nutrition Examination Survey 2011-2018. https://www.asn-online.org/education/kidneyweek/2023/program-abstract.aspx?controlId=3938045
Share this article
Latest news
- Plant-based, low-sugar diet linked to lower heart failure risk in large study
- Swapping table salt for salt substitutes may lower the risk of dying early
- GLP-1 drugs for diabetes and weight loss unlikely to affect thyroid cancer risk
- Exercising between 6 p.m. and midnight may be more beneficial for people with obesity
- Stopping aspirin a month after stent implant may not increase blood clot risk
Related Coverage
Cannabis is a plant that people use as a medicinal and recreational drug. Its ingredient may help treat chronic pain and other conditions. Learn more…
Kidney stones are crystalized minerals that form in the kidneys. They can cause a lot of pain and discomfort. In this article, we discuss 10 ways to…
Kidney stones form when minerals build up in the kidneys, usually due to not drinking enough fluid. Learn about the types, causes, and symptoms, as…
Smoking can cause weight changes. Quitting smoking may cause moderate weight gain. Learn more here.
Some evidence shows that smoking cannabis may interact with blood-thinning medication and bleeding during surgery. Learn more here.
You are here
Acute kidney injury (aki), table of contents, about acute kidney injury (aki), signs and symptoms, complications, preparing for your appointment.
Acute kidney injury (AKI) is the sudden loss of kidney function. Learn more about the symptoms to watch for and ways to lower your risk.
Acute kidney injury (AKI) is a term used to describe when your kidneys are suddenly not able to filter waste products from the blood. This can happen within a few hours or a few days. For most people, AKI develops within 48 hours, but sometimes it can take as long as 7 days.
This replaces an older term “acute renal failure” (or ARF) which you may still see or hear occasionally.
The signs and symptoms of AKI can differ depending on many factors like the cause, severity, and your other health conditions. If symptoms do happen, they may include one or more of the following:
- Making less urine (pee) than usual or no urine
- Swelling in legs, ankles, and/or feet
- Fatigue or tiredness
- Shortness of breath (trouble breathing)
- Confusion or mood changes
- High blood pressure
- Decreased appetite (low desire to eat)
- Flank pain (pain on the side of your back - between your ribs and hips)
- Chest pain or pressure
- Seizures or coma (in severe cases)
In some cases, AKI causes no symptoms and is only found through other tests done by your healthcare professional.
AKI can have many different causes. Many people get AKI when a related disease or condition puts extra stress on your kidneys. Another common cause for AKI is when your body is reacting to an urgent or emergent health concern (such as heart surgery or COVID-19 infection). Lastly, AKI can be caused by medications or other substances that you may consume. Examples for each of these scenarios are provided below.
Usually, AKI happens because of a combination of factors. This is especially true for older adults who are at higher risk given their age.
Related disease or condition
- Autoimmune kidney disease, such as glomerulonephritis , lupus , or IgA nephropathy
- Cancer (especially bladder, cervical, ovarian, or prostate cancer)
- Chronic kidney disease
- Diabetes flare-up (also known as diabetes-related ketoacidosis or DKA)
- Heart disease (e.g. heart attack, heart failure, or other condition leading to decreased heart function)
- Kidney infection
- Kidney stones
- Liver disease or cirrhosis
- Multiple myeloma (a specific type of blood cancer)
- Vasculitis (long-term inflammation and scarring in your blood vessels)
Urgent or emergent health concerns
- Acute tubular necrosis (ATN), a situation causing very low blood flow to the kidneys
- Anaphylaxis (severe allergic reaction)
- Blood clot or cholesterol blocking a blood vessel in your kidney(s)
- Hypotension (very low blood pressure) or shock
- Hemorrhage (severe loss of blood)
- Major surgery
- Pregnancy complications
- Severe dehydration (not getting enough water or fluids for your body’s needs)
- Severe diarrhea and/or vomiting
- Severe skin burns
Medications and other substances
Items in this list may not cause AKI by themselves, but when combined with other factors from the other 2 categories above, your risk of AKI goes up significantly.
- Certain antibiotics, especially ones given for severe infections
- Certain blood pressure medicines, like ACE inhibitors/ARBs or diuretics (water pills)
- ibuprofen (Motrin, Advil)
- indomethacin (Indocin)
- naproxen (Aleve, Naprosyn)
- diclofenac tablets or capsules (Cataflam, Zipsor)
- celecoxib (Celebrex)
- meloxicam (Mobic)
- aspirin (only if more than 325 mg per day)
- Iodine-based contrast dye (used for CT scans and other forms of medical imaging)
- Recreational drugs, such as heroin or cocaine
- Some medicines used for cancer or HIV
- Toxic alcohols, such as methanol, ethylene glycol (antifreeze), or isopropyl/isopropanol (rubbing alcohol)
AKI can cause a build-up of waste products in your blood and make it hard to keep the right balance of fluid and minerals in your body. It can also cause permanent damage to your kidneys, leading to chronic kidney disease (CKD) . Without treatment, AKI can also affect other organs such as the brain, heart, and lungs. So, it is important to know what to watch for and how to lower your risk.
If your healthcare professional suspects AKI, they will perform an assessment to identify its potential cause (or causes). This may include performing a physical exam, reviewing your medical conditions and medication use history in the past week (including over-the-counter products and herbal supplements), asking about recent events and experiences (e.g. symptoms, water intake, recreational drug use, relevant travel), and ordering blood and/or urine tests.
Some of the most common tests used to check for AKI, include:
- Serum (blood) creatinine – a blood test used to check how well your kidneys are filtering this waste product from your blood
- Estimated glomerular filtration rate (eGFR) – this is calculated based on your serum (blood) creatinine level, age, and sex to estimate your kidney function
- Blood urea nitrogen (BUN) – similar to creatinine, this test can be used to measure another waste product in your blood to see how well your kidneys are filtering the blood
- Other blood tests , such as sodium, potassium, and bicarbonate (to see if anything is out of balance)
- Urine output – your healthcare professional may track how much urine (pee) you pass each day, especially if you are having AKI in the hospital
- Urine test (urinalysis) – a general urine test may be used to find more clues about the cause of AKI
- Imaging tests , like an ultrasound, may be helpful in some cases
- Kidney biopsy – in some less common situations, your healthcare professional may need to look at a tiny piece of your kidney under a microscope to get a better idea about the cause
Other tests may be ordered based on what your healthcare professional thinks might be causing your AKI.
Treatment for AKI depends on what caused it in the first place. This is why finding the cause is so important. Some most common approaches to treating AKI include:
- Stopping any medicines that may be causing or contributing to your AKI
- Giving you fluids (either by mouth or through your veins)
- Antibiotics (if AKI is caused by a bacterial infection)
- Placing a urine catheter (a thin tube used to drain your bladder, useful if AKI is caused by a blockage)
- In most cases, dialysis treatments are only temporary until the kidneys can recover.
Most people with AKI will need to spend some time in the hospital to be monitored while receiving treatment.
After having AKI, you have a higher risk for other health problems, such as chronic kidney disease (CKD), heart disease, or stroke). You are also at a higher risk of getting AKI again in the future. So, it is important to have regular follow-up visits with your healthcare professional and check your kidney health, starting with two simple tests (ideally within 3 months of finishing treatment for your AKI).
Questions to ask
- What are my biggest risk factors for AKI?
- What can I do to help lower my risk for AKI?
- Are there any medications I should avoid (either now or in the future) due to my kidneys?
- [If having potential symptoms of AKI] Should I go to the emergency room for my symptoms?
- Was the cause of my AKI preventable? If so, what can I do to prevent it from happening again?
- When should I follow up after my AKI treatment is done to check my kidney health?
This content is provided for informational use only and is not intended as medical advice or as a substitute for the medical advice of a healthcare professional.
Save this content:
Share this content:
Is this content helpful?
Back to top:

IMAGES
VIDEO
COMMENTS
Observations from the authors and other research groups suggest that there are five entirely different main mechanisms for kidney stone formation. Urinary supersaturation and crystallization are the driving force for intrarenal crystal precipitation. Randall's plaques are recognized as the origin of calcium oxalate stone formation.
In this double-blind trial, 416 patients with recurrent calcium-containing kidney stones were randomly assigned to receive hydrochlorothiazide at a dose of 12.5 mg, 25 mg, or 50 mg once daily or ...
Still being run through clinical trials at UW Medicine, the procedure called burst wave lithotripsy uses an ultrasound wand and soundwaves to break apart the kidney stone. Ultrasonic propulsion is ...
Kidney Stones. Researchers in the Department of Urology are investigating all facets of kidney stones, including why they form, how they damage the kidneys and potential new treatment options to add to the existing options of extracorporeal shock wave lithotripsy (ESWL), ureteroscopy with laser fragmentation of stones, and percutaneous nephrolithotomy.
Several years ago, Cima and Brian Eisner, who co-directs the Kidney Stone Program at MGH and is also an author of the paper, began thinking about ways to improve the treatment of kidney stones. While some larger stones require surgery, the usual treatment plan is simply to wait for the stones to pass, which takes an average of 10 days.
90 genes related to Monogenic Stone Disease will be determined via DNA analysis by the Mayo Rare Kidney Stone Consortium (RKSC) research staff. ... confirmed PH3 and relatively intact renal function and to explore the potential relationship between Uox and new stone formation. This is a natural history study of adults, adolescents, and children ...
In addition, new stone formation that was detected by imaging and restricted mean time to relapse (time to new stone formation) were similar — 1338.8±104.0 days in the treatment group and 1381. ...
Calcium-based kidney stone disease is a highly prevalent and morbid condition, with an often complicated and multifactorial aetiology. An abundance of research on the role of specific vitamins (B6 ...
In their recent research, summarized in Nature Reviews Urology, the researchers primarily used GeoBioCell to study growing calcium oxalate crystals, which account for about 70 percent of kidney ...
In the new work, the research team -- brought together by the Mayo Clinic and Illinois Alliance for Technology-Based Healthcare -- describes in detail the multiple phases kidney stones go through ...
Kidney stone disease, also known as nephrolithiasis or urolithiasis, is a disorder in which urinary solutes precipitate to form aggregates of crystalline material in the urinary space. The incidence of nephrolithiasis has been increasing, and the demographics have been evolving. Once viewed as a limited disease with intermittent exacerbations that are simply managed by urologists ...
Credit: Microbiome (2023). DOI: 10.1186/s40168-023-01703-x. A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the ...
According to the National Kidney Foundation, it is estimated that 1 in 10 people will have a kidney stone at some time in their lives. "We hope to transform the surgical care of kidney stone patients," said co-principal investigator Nicholas Kavoussi, MD, assistant professor of Urology at Vanderbilt University Medical Center.
Calcium-based kidney stone disease is a highly prevalent and morbid condition, with an often complicated and multifactorial aetiology. An abundance of research on the role of specific vitamins (B 6, C and D) in stone formation exists, but no consensus has been reached on how these vitamins influence stone disease.As a consequence of emerging research on the role of the gut microbiota in ...
In the new study, the researchers tested the burst wave technique in 19 patients who were undergoing kidney stone treatment with a procedure called ureteroscopy.It involves threading a thin scope ...
New tech gives kidney stone patients options. Using high-frequency waves, the new treatment pushes smaller stones from the bottom of the kidney toward the ureter. October 25, 2021. Media Contact: Barbara Clements - 253-740-5043, [email protected]. Getty Images New handheld technology lets doctors maneuver small stones to the ureter, so they can be ...
Kidney stone disease is a crystal concretion formed usually within the kidneys. It is an increasing urological disorder of human health, affecting about 12% of the world population. ... Thus, further understanding of the pathophysiology of kidney stone formation is a research area to manage urolithiasis using new drugs. Therefore, this review ...
Kidney stones are common, painful, and frequently recur. Although precise estimates of the incidence of symptomatic kidney stones for the entire US are unavailable, a Minnesota population-based study reported that between 1984 and 2012, the incidence of symptomatic kidney stones that required treatment increased from 51 to 217 per 100 000 person-years in women and from 145 to 299 per 100 000 ...
With funding from Kidney Research UK, the National Institute for Health Research and the Wellcome Trust, Dr Sarah Howles and her team used data from the UK Biobank - a collection of health and genetic information from around 500,000 participants - to investigate the link between fat and kidney stone disease.
In the United States, an estimated 1 in 11 people have kidney stones. They affect more men than women; more than 10 percent of men develop them, compared with 7.1 percent of women. Though ...
Second, when evaluating the effectiveness of new laser technology, the real-life application should be leading as laboratory settings cannot always be reproduced bedside. Finally, Prof. Traxer presented a useful rule of thumb for the audience: for kidney stones, work from surface to centre and always use 20-25W or less.
Lawson Health Research Institute Summary: A new study has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones. ... "Kidney stone disease ...
People with a history of kidney stones should drink enough fluids to pass about 80 oz (2.5 liters) of urine every day. This is the most effective therapy available to prevent future kidney stones. Your healthcare team may ask you to measure your urine output to ensure you drink enough water. Eat fewer oxalate-rich foods.
New drugs that boost weight loss and treat type 2 diabetes could also help to prevent or reduce stress on the kidneys, but these, too, are too expensive for many people in need.
Kidney stones that are too large to pass on their own or cause bleeding, kidney damage or ongoing urinary tract infections may require more-extensive treatment. ... You will also receive emails from Mayo Clinic on the latest health news, research, and care. If you don't receive our email within 5 minutes, check your SPAM folder, then contact ...
The research team adjusted the odds of developing kidney stones per year during the trial for a range of factors including gender, age, race or ethnicity, relative income and body mass index (BMI).
Purpose: This study investigates gender-based disparities in health-related quality of life (HRQOL) outcomes among kidney stone patients and explores potential contributing factors. Methods: A retrospective review of medical records at the University of Rochester Medical Center was conducted on 2199 new urolithiasis patients who completed the Wisconsin Stone Quality of Life Questionnaire ...
Kidney stones are hard masses that can form in the kidneys and cause pain. While evidence notes that smoking is a risk factor, no research suggests cannabis increases the risk of kidney stones.
Acute kidney injury (AKI), also known as Acute Renal Failure, is a sudden episode of kidney failure or kidney damage that happens within a few hours or a few days. AKI causes a build-up of waste products in your blood and makes it hard for your kidneys to keep the right balance of fluid in your body. AKI can also affect other organs such as the brain, heart, and lungs.
New Password. Too Short Weak Medium Strong Very Strong Too Long ... Biomedical Research; Biotechnology and Regenerative Medicine; Medicine and Surgery; ... ChatGPT for Patient Counseling in Kidney Stone Clinic: Comment. Authors: Dr. hinpetch daungsupawong and Prof. viroj wiwanitkit Authors Info & Affiliations.