

Announcing 50 New Case-Based Questions in NEJM Knowledge+ Internal Medicine Board Review

At NEJM Knowledge+, we’re committed to ensuring that our products cover the breadth of knowledge that clinicians need for both clinical practice and Internal Medicine Board Exam preparation. NEJM Knowledge+ Internal Medicine Board Review already contains more than 1600 case-based questions on the most relevant and important topics in medicine today. We’re adding another 50 case-based questions now (and 50 more in December 2016) to further expand that knowledge base.
Most of the 50 new questions we’ve added relate to the following topics:
- Infectious Disease
- Dermatology
Each year, we plan to add at least 100 new questions to NEJM Knowledge+ Internal Medicine Board Review — this is in addition to continually updating our content when guidelines change and in response to user feedback. Our goal is to become increasingly comprehensive in the learning we provide while remaining as clinically relevant and up-to-date as possible.
Covering the ABIM Blueprint with New Learning Objectives
In June 2015, ABIM rolled out a revised blueprint for the Maintenance of Certification (MOC) exam that not only listed the topics and subtopics but also showed the likelihood of which aspects of the subtopic will be on the exam, such as diagnosis, testing, and treatment.
Our editorial team analyzed the new ABIM blueprint and are prioritizing development of new IM questions that map to topics in the blueprint that are highly likely to be on the MOC exam.
We have derived learning objectives from the topic/task combinations in the blueprint; for example, ABIM lists six subtopics under “ischemic heart disease”:
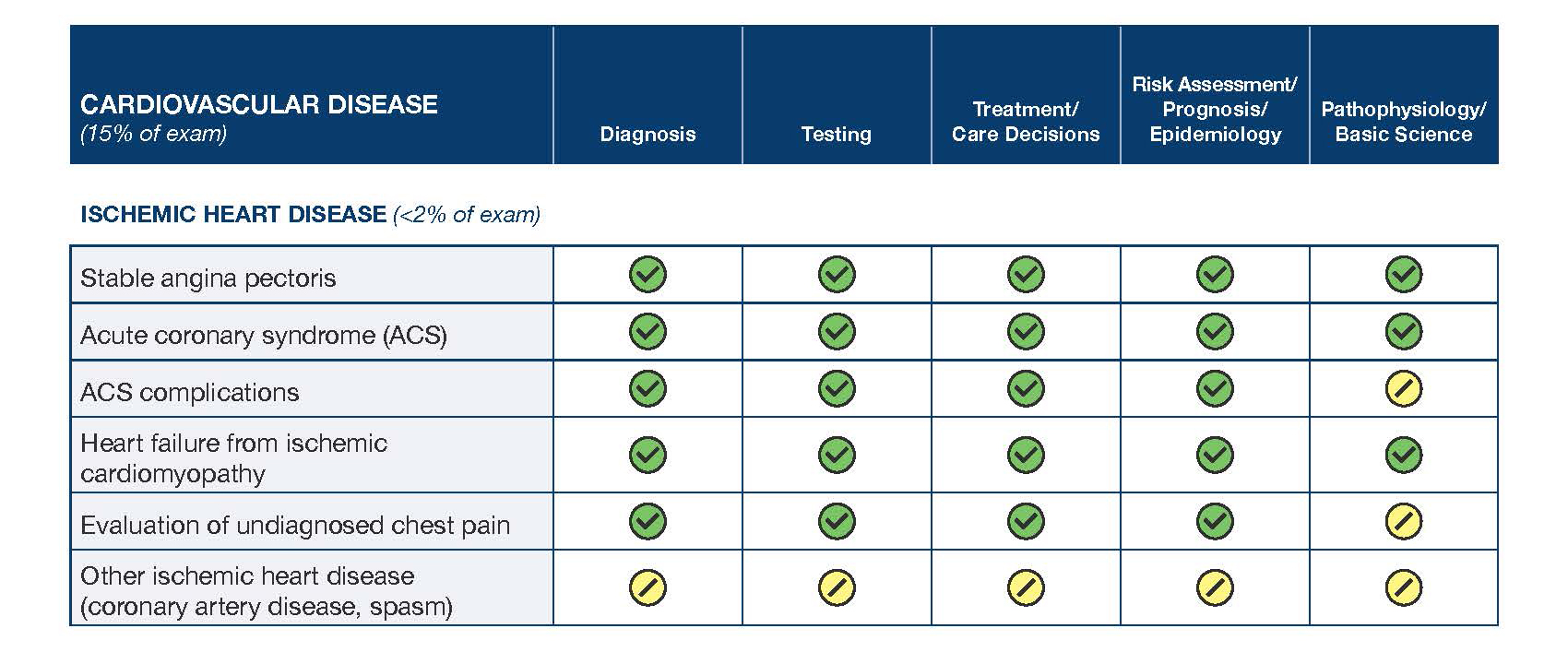
These subtopics mostly fall into the “highly likely to be on the exam” bucket (green), so we recruited physician experts to write case-based questions that test those learning objectives that we did not already have at least one question on in our question bank. Here are some examples of the learning objectives we just added to the IM question bank:
- Choose an optimal initial testing strategy for a patient with a prior acute anterior myocardial infarction who presents with a transient ischemic attack that has a suspected cardioembolic source.
- Choose an appropriate treatment for improving the likelihood of survival in a patient who has depressed left ventricular systolic function after an acute myocardial infarction.
- Choose appropriate evaluation for suspected heart failure with reduced ejection fraction.
- Choose the most appropriate pharmacologic management for a patient who has a recent diagnosis of heart failure with reduced ejection fraction and is already taking an angiotensin-converting enzyme inhibitor.
- Recognize heart failure with reduced left ventricular ejection fraction, secondary to ischemic cardiomyopathy.
Using this process for content development ensures that our question bank covers what you need to know for the board exam.
Case-Based Questions, Free from Outside Influence
All the questions we develop for NEJM Knowledge+ Internal Medicine Board Review meet the same high-quality standards you’ve come to expect from NEJM Group. The content was written by more than 300 clinicians from academic programs across the country and was subjected to a rigorous editorial process that included review by highly respected professional educators, leading specialists in their fields, generalists, PAs, and NEJM Group editors . You can be sure that what you’re learning in NEJM Knowledge+ is accurate, evidence-based, and relevant to your daily practice.
NEJM Knowledge+ offers a comprehensive question bank that reflects the breadth of primary care cases that physicians encounter in their practices today.
Personalized Learning, Tailored to You
NEJM Knowledge+ uses adaptive learning technology that tailors your learning to your needs. This adaptive learning technology continuously assesses the subjects you know and identifies the areas where you need reinforcement. It then delivers questions based on what you know already, what you need to study more, what you are struggling to master, what you think you know better than you do, and what you might be forgetting.
With the addition of these 50 new questions, NEJM Knowledge+ Internal Medicine Board Review now includes:
- more than 1680 case-based questions
- more than 4500 total questions tied to 2500 learning objectives
With the ability to earn:
- CME credits
- ABIM MOC points
All in all, we are strengthening one of the most comprehensive solutions available for continuous learning and board exam preparation.
More on NEJM Knowledge+ Content:
Roadmap to Great Content Work Less and Learn More: Here’s How in NEJM Knowledge+ Content Updates
Share This Post!
Having only a partial point of view of Cases Based Questins,I can see that you tried to do the best work in this section.I am totally sure, that the Clinical Cases presented will be carefully prepared.But, the problem that I see, in ER,Clinics-Hospitals-and in Home , it is that the patient, many times has not the Diagnostics written in his/her Chest.Many times, we have to do an intense work,trying to know what happen with the patients and trying to find(if we are in ER or Hospital) his/her medical record. Being agree with the way you prepared the questions,but I think that in Real Life,we have to face with patients, whose Diagnostics, we do not know,but we have to start with some measuresEx=relieving pain-giving IV solutions (if they are needed)-taking Exams, like Blood-Urina and others-XRay-CT Scan-Ultrasound and calling to others Physicians(Specialists=Cardiologists-Neurologists-Nephrologists etc-etc= so I suggest to add(if if is possible) some Complete Clinical Cases, where Students or Residents, must choose since the beginning the possible diagnostics-type of Blood-Urine -Bacteriologic Exams-Ultrasound-CT-Scan etcetcThis type of Questions(that NEJM sometimes present)are one of the best technique to know what the
Notify me by email with any comment
does anyone know of any journal/quis cme’s that are accepted for moc points in internal medicine? Also it seems like it varies from state to state. For example, JAMA articles/cme quizzes for some reason aren’t accepted in NY. I left my email if anyone should have any information. Thanks much
Comments are closed.
- McMaster University Health Sciences Library
Medicine - Undergraduate
- Case Scenarios
- Students from a Non-Science Background
- Anatomy & Physiology
- Clinical Skills
- Drugs & Natural Products
- EBM & JAMA Evidence
- PICO: writing a searchable question
- Black & Indigenous Health Resources
- Research Support - Book a Consult
- Landmark Papers
- Student Wellness

Case Studies & Scenarios

- Johns Hopkins Medicine- Case Studies
- Case Studies for Fellows (American Society of Hematology)
- LITFL Clinical Cases Dedicated to Emergency Medicine and Critical Care
- Emergency Medicine Cases Canadian medical education podcast
- NEJM Clinical Cases
- Springer Clinical Cases series A catalogue search
- << Previous: LMCC Prep
- Next: Anatomy & Physiology >>
- Last Updated: Feb 29, 2024 11:09 AM
- URL: https://hslmcmaster.libguides.com/medicine_UGM

Address Information
McMaster University 1280 Main Street West HSC 2B Hamilton, Ontario Canada L8S 4K1
Contact Information
Phone: (905) 525-9140 Ext. 22327
Email: [email protected]
Make A Suggestion
Website Feedback
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs
- Biochemistry
- Microbiology
- Neuroscience
- Pharmacology
- Anesthesiology
- Emergency Medicine
- Family Medicine
- Internal Medicine
- Clinical Neuroanatomy Cases
- Clinical Nutrition Cases
- Acid-Base Disturbance Cases
- Chest Imaging Cases
- Family Medicine Board Review
- Fluid/Electrolyte and Acid-Base Cases
- G&G Pharm Cases
- Harrison’s Visual Case Challenge
- Internal Medicine Cases
- Medical Microbiology Cases
- Pathophysiology Cases
- Principles of Rehabilitation Medicine Case-Based Board Review
- Browse by System
- Internal Medicine Med-Peds Pediatrics
- Browse by Curriculum

Case Files: Family Medicine, 5e
Author(s): Eugene C. Toy; Donald Briscoe; Bruce Britton; Joel J. Heidelbaugh
- 51 Diabetes Mellitus
- 59 Opioid Use Disorder and Chronic Pain Management
- 7 Tobacco Use and Cessation
- 20 Chest Pain
- 42 Palpitations
- 53 Acute Low Back Pain
- 3 Joint Pain
- 18 Geriatric Health Maintenance and End-of-Life Issues
- 49 Breast Diseases
- 47 Dyspepsia and Peptic Ulcer Disease
- 40 Irritable Bowel Syndrome
- 46 Jaundice
- 9 Anemia in the Geriatric Patient
- 45 HIV, AIDS, and Other Sexually Transmitted Infections
- 48 Fever and Rash
- 2 Dyspnea (Chronic Obstructive Pulmonary Disease)
- 24 Pneumonia
- 56 Wheezing and Asthma
- 21 Chronic Kidney Disease
- Acute Low Back Pain
- Anemia in the Geriatric Patient
- Breast Diseases
- Chronic Kidney Disease
- Diabetes Mellitus
- Dyspepsia and Peptic Ulcer Disease
- Dyspnea (Chronic Obstructive Pulmonary Disease)
- Fever and Rash
- Geriatric Health Maintenance and End-of-Life Issues
- HIV, AIDS, and Other Sexually Transmitted Infections
- Irritable Bowel Syndrome
- Opioid Use Disorder and Chronic Pain Management
- Palpitations
- Tobacco Use and Cessation
- Wheezing and Asthma

PICO: Form a Focused Clinical Question
- 1. Ask: PICO(T) Question
- 2. Align: Levels of Evidence
- 3a. Acquire: Resource Types
- 3b. Acquire: Searching
- 4. Appraise
- Primary vs. Secondary Sources
- Case Study Example
- Practice PICO
Formulate a Clinical Question from a Case Study
- Case: Hypertension
I: Intervention
C: comparison.
- PICO: Putting It Together
Clinical Scenario
A 68-year-old female patient has recently been diagnosed with high blood pressure. She is otherwise healthy and active. You need to decide whether to prescribe her a beta-blocker or an ACE inhibiter.

Image: "Blood pressure measuring. Doctor and patient. Health care." by agilemktg1 is marked with CC PDM 1.0
► Click on the P: Patient tab to proceed in developing a clinical question.
(Case study from EBM Librarian: Teaching Tools: Scenarios .)
Consider when choosing your patient/problem:
- What are the most important characteristics?
- Relevant demographic factors
- The setting
Patient: adult hypertensive female

Image: "Nurse measuring blood pressure of senior woman at home. Looking at camera, smiling.?" by agilemktg1 is marked with CC PDM 1.0
► Click on the I: Intervention tab to proceed in developing a clinical question.
Consider for your intervention:
- What is the main intervention, treatment, diagnostic test, procedure, or exposure?
- Think of dosage, frequency, duration, and mode of delivery
Intervention: beta-blocker

Image: "Atenolol Blood Pressure Tablets Image 4" by Doctor4U_UK is licensed under CC BY 2.0
► Click on the C: Comparison tab to proceed in developing a clinical question.
Consider for your comparison:
- Inactive control intervention: Placebo, standard care, no treatment
- Active control intervention: A different drug, dose, or kind of therapy
Comparison: ACE inhibiter

Image: "Ramipril Blood Pressure Capsules Image 5" by Doctor4U_UK is licensed under CC BY 2.0
► Click on the O: Outcome tab to proceed in developing a clinical question.
Consider for your outcome:
- Be specific and make it measurable
- It can be something objective or subjective
Outcome: relief of symptoms; controlled blood pressure

Image: "File:BP B6 Connect blood pressure monitor.png" by 百略醫學 is licensed under CC BY-SA 4.0
► Click on the PICO: Putting It Together tab to proceed in developing a clinical question.
Formulate a PICO Question
Answerable PICO Question: In middle-aged adult females with hypertension, are beta blockers more effective than ACE inhibiters in controlling blood pressure?

Image: "Dagstuhl 2008-02-01 - 37" by Nic's events is licensed under CC BY-SA 2.0
Suggested MeSH Terms: Adrenergic beta-Antagonists/therapeutic use; Angiotensin-Converting Enzyme Inhibitors/therapeutic use; hypertension/drug therapy
Tip: Incorporating sex into the search may not be necessary unless there is a significant difference between males and females in relevant studies.
Click "Next" below to practice formulating clinical questions using PICO format.
- << Previous: Primary vs. Secondary Sources
- Next: Practice PICO >>
- Last Updated: Oct 5, 2023 2:35 PM
- URL: https://med-fsu.libguides.com/pico
Maguire Medical Library Florida State University College of Medicine 1115 W. Call St., Tallahassee, FL 32306 Call 850-644-3883 (voicemail) or Text 850-724-4987 Questions? Ask us .

- Advanced Life Support
- Endocrinology
- Gastroenterology
- Infectious disease
- Intensive care
- Palliative Care
- Respiratory
- Rheumatology
- Haematology
- Endocrine surgery
- General surgery
- Neurosurgery
- Ophthalmology
- Plastic surgery
- Vascular surgery
- Abdo examination
- Cardio examination
- Neurolo examination
- Resp examination
- Rheum examination
- Vasc exacmination
- Other examinations
- Clinical Cases
- Communication skills
- Prescribing

ABG Examples (ABG exam questions for medical students and PACES)

ABG Examples (ABG exam questions for medical students OSCEs and MRCP PACES)
Below are some brief clinical scenarios with ABG results. Try to interpret each ABG and formulate a differential diagnosis before looking at the answer.
Question 1.
You are called to see a 54 year old lady on the ward. She is three days post-cholecystectomy and has been complaining of shortness of breath. Her ABG is as follows:
- pH: 7.49 (7.35-7.45)
- pO2: 7.5 (10–14)
- pCO2: 3.9 (4.5–6.0)
- HCO3: 22 (22-26)
- BE: -1 (-2 to +2)
- Other values within normal range
- This is type 1 respiratory failure. The PO2 is low with a low CO2.
- The accompanying alkalosis is a response, due to the patient blowing off CO2 due to her likely high respiratory rate.
What is the differential diagnosis?
- Pulmonary embolus (PE)
- Pulmonary oedema
- Pneumothorax
- Severe atelectasis
What would you do?
- Acutely unwell: ABCDE and call for help
- All of these conditions can may you tachypnoeic and tachycardic. Wheeze will predominate in asthma. Pyrexia points more towards pneumonia (but PE can give a mild pyrexia). Pulmonary embolus will be the only condition that will likely be normal on auscultation.
- Sudden onset: more likely PE
- Purulent cough: more likely pneumonia
- Raised JVP, ankle swelling, fine basal creps: more likely oedema
- Cultures if pyrexial
- PE : Heparinisation or thrombolysis if unstable. Remember this patient is post-op so it is a complex decision.
- Pneumonia : Antibiotics for hospital acquired pneumonia
- Asthma : Salbutamol, ipatropium and steroid in the first instance
- Pulmonary oedema : Sit patient up, furosemide, consider catheter
Question 2.
A 75 year old gentleman living in the community is being assessed for home oxygen. His ABG is as follows:
- pH: 7.36 (7.35-7.45)
- pO2: 8.0 (10–14)
- pCO2: 7.6 (4.5–6.0)
- HCO3: 31 (22-26)
- BE: +5 (-2 to +2)
- This does not represent acute pathology.
- Rather it reflects a compensation for a chronic respiratory acidosis secondary to chronic pulmonary disease.
- Note this is an acidosis, not an acidaemia (pH normal, but only due to compensatory mechanisms: the high bicarbonate).
- Lifestyle advice and smoking cessation of necessary.
- PaO 2 less than 7.3 kPa when stable.
- Secondary polycythaemia
- Peripheral oedema
- Nocturnal hypoxaemia
- Pulmonary hypertension
Question 3.
A 64 year old gentleman with a history of COPD presents with worsening shortness of breath and increased sputum production .
- pH: 7.21 (7.35-7.45)
- pO2: 7.2 (10–14)
- pCO2: 8.5 (4.5–6.0)
- HCO3: 29 (22-26)
- BE: +4 (-2 to +2)
- Note that the HCO3 is raised in this patient despite the abnormal pH.
- With the above history this is likely to represent an acute on chronic respiratory acidosis.
- This would indicate that the patient normally retains CO2 and has a chronically raised HCO3.
- The drop in pH represents the normal mechanisms of compensation being over whelmed.
- This is one of the cases where having an old ABG from a previous admission can be useful.
How much oxygen would you give this man?
- Oxygen administration in this group is a complicated issue. 100% oxygen makes subsets of COPD patients retain CO2, decreasing respiratory drive and worsening hypoxia and hypercapnia.
- More information can be found on this page: Prescribing oxygen in COPD patients
- The British Thoracic Society have produced guidelines which give a helpful overview and can be found here.
Question 4.
A 21 year-old woman presents feeling acutely lightheaded and short of breath. She has her final university exams next week.
- pH: 7.48 (7.35-7.45)
- pO2: 13.9 (10–14)
- pCO2: 3.5 (4.5–6.0)
- HCO3: 22 (22-26)
- BE: +2 (-2 to +2)
- This is a respiratory alkalaemia
- Pulmonary disease
- Hypermetabolic states (e.g. infection or fever)
- Anxiety hyperventilation
What's the most likely diagnosis?
- Based on the history, anxiety hyperventilation is the most likely cause here. However, it is very important to have considered the other options, in particular and to have ruled out a primary respiratory pathology or infection.
- In the anxious patient who is short of breath and persistently tachycardic have you thought of PE?
Question 5.
A 32 year-old man presents to the emergency department having been found collapsed by his girlfriend.
- pH: 7.25 (7.35-7.45)
- pO2: 11.1 (10–14)
- pCO2: 3.2 (4.5–6.0)
- HCO3: 11 (22-26)
- BE: -15 (-2 to +2)
- Potassium: 4.5
- Sodium: 135
- Chloride: 100
- Anion gap = ([Na + ] + [K + ]) − ([Cl − ] + [HCO 3 − ])
- Reference range usually 7–16 mEq/L (but varies between hospitals, some using 3-11)
- Anion gap = [Na + ] − ([Cl – ] + [HCO 3 − ])
What is the anion gap in this case?
- N.B. Some analysers won’t include potassium in their calculations therefore for them >15 constitutes a raised anion gap.
- Either way, this is a raised anion gap metabolic acidosis.
What is the differential diagnosis for a metabolic acidosis with raised anion gap? The traditional mnemonic for the causes of a metabolic acidosis with raised anion gap is ‘MUDPILES’:
- D iabetic ketoacidosis (and alcoholic/starvation ketoacidosis)
- P ropylene glycol
- E thylene glycol
- S alicylates
However, another way is to think about the mechanism of acidosis:
- DKA, lactic acidosis (produced by poorly perfused tissues)
- Methanol, ethanol, ethylene glycol
- Renal failure
[/toggle title="What is the differential diagnosis for a metabolic acidosis with normal or decreased anion gap?" active="false"]
- From the GI tract (diarrhoea or high-output stoma)
- From the kidneys ( renal tubular acidosis )
Question 6.
A 67 year-old man with a history of peptic ulcer disease presents with persistent vomiting.
- pH: 7.56 (7.35-7.45)
- pO2: 10.7 (10–14)
- pCO2: 5.0 (4.5–6.0)
- HCO3: 31 (22-26)
- BE: +5 (-2 to +2)
- This is metabolic alkalaemia
[/toggle title="What' s the differential diagnosis of this ABG picture?" active="false"]
Differential diagnosis of a metabolic alkalosis or alkalaemia:
- E.g. gastric outlet obstruction (the classic example is pyloric stenosis in a baby)
- Hyperaldosteronaemia
- Diuretic use
- Milk alkali syndrome
- Massive transfusion
Question 7.
A seventeen year-old girl presents to the emergency department after an argument with her boyfriend. He says that she took lots of tablets. She denies this. You persuade her to let you do an ABG:
- pH: 7.46 (7.35-7.45)
- pO2: 12.5 (10–14)
- BE: +1 (-2 to +2)
A few hours later she says she feels increasingly unwell and is complaining of ringing in her ears. A repeat gas shows:
- pH: 7.15 (7.35-7.45)
- pO2: 11.0 (10–14)
- HCO3: 9 (22-26)
- BE: -18 (-2 to +2)
- This is the classic picture of aspirin overdose.
- There is an initial respiratory alkalosis due to central respiratory centre stimulation causing increased respiratory drive.
- In the later stages a metabolic acidosis develops along side the respiratory alkalosis as a result of direct effect of the metabolite salicylic acid and more complex disruption of normal cellular metabolism.
How would you manage this patient?
How do you manage an aspirin overdose?
Presentation of aspirin overdose
- Hyperventilation
- Nausea & vomiting
- Epigastric pain
- ARDS (rare)
- Hypoglycaemia (children in particular)
Investigations in aspirin overdose
- Plasma salicylate concentration (initial and repeats)
- Paracetamol levels (always check in any case of poisoning by anything)
- Renal failure (rare) sometimes other electrolyte imbalances
- If dropping sats or any suspicion of ARDS (non-cardiogenic pulmonary oedema)
Management of aspirin overdose
- ABCDE and supportive care
- Gastric lavage within 1h of ingestion (although no evidence for mortality reduction)
- Activated charcoal
- Correct electrolyte abnormalities
- Give 225ml of 8.4% bicarbonate solution over 1hr
- Bicarbonate will increase any pre-existing hypokalaemia – so don’t let it happen
- N.B. Acidosis increases salicylate transfer across the blood brain barrier
- Monitor U+Es regularly
- Haemodialysis
Prognosis in aspirin overdose
- Generally good with treatment.
Question 8.
A normally fit and well 11 year-old boy presents with diarrhoea and vomiting. He is complaining of non-specific abdominal pain. A venous blood gas shows :
- pH: 7.12 (7.35-7.45)
- pO2: 11.5 (10–14)
- BE: -17 (-2 to +2)
- Lactate: 4.0
- Potassium: 5.5
- Glucose: 22 mmol/L (395 mg/dL)
- This is diabetic ketoacidosis (DKA) .
What are you going to do?
- Priorities for management include fluid resuscitation, insulin administration and careful management of potassium levels. Click here for a page detailing this, and click here for DKA questions
Question 9.
A 22 year-old lady with a known history of asthma presents to the emergency department with difficulty in breathing. Her initial ABG on 15 litres of oxygen shows:
- pH: 7.54 (7.35-7.45)
- pO2: 10.0 (10–14)
- HCO3: 24 (22-26)
- BE: +0 (-2 to +2)
After initial treatment the nurse in resus calls you to review the patient. The nurse says that although the patient’s respiratory rate has come down slightly she is looking more unwell. Her repeat gas shows:
- pO2: 9.8 (10–14)
- BE: -2 (-2 to +2)
- This patient has asthma, ongoing difficulty in breathing and a rising CO2 (the fact that it is in the normal range is irrelevant) .
- This is an extremely worrying sign as it shows that the patient is tiring.
- This patient should be managed in a high dependency area and closely monitored for further deterioration.
Question 10.
A 62 year-old woman with a history of diabetes and a long smoking history presents to the emergency department with worsening shortness of breath. On auscultation of the chest there are widespread crackles and you notice moderate ankle oedema. ABG shows:
- pH: 7.20 (7.35-7.45)
- pO2: 8.9 (10–14)
- pCO2: 6.3 (4.5–6.0)
- HCO3: 17 (22-26)
- BE: -8 (-2 to +2)
- Note that despite the low pH the pCO2 is also high.
- This is a picture of a mixed respiratory and metabolic acidosis.
- Given the history of diabetes and ankle swelling, renal failure is a unifying diagnosis with pulmonary oedema contributing to a respiratory acidosis whilst the failure to clear acids causes a metabolic acidosis.
Click here for further questions on ABGs
…and click here to learn the best way to interpret abgs.
Perfect revision for MRCP PACES, OSCES and medical student finals
- Off-Campus Access
- Find Resources
- Research Support
- Reserve Space
- --> X
- YouTube
- HSHSL Updates RSS Feed
- Connective Issues Newsletter

601 West Lombard Street Baltimore MD 21201-1512 Reference: 410-706-7996 Circulation: 410-706-7928
Evidence-Based Practice Tutorial: Asking Clinical Questions
- Asking Clinical Questions
- Acquiring the Evidence
- Appraising the Evidence
- Applying the Results
- Assessing the Outcome
- Practicing Evidence-Based Medicine
- Additional Resources
Using PICO to Create a Well-Built Clinical Question
It is important to be purposeful about creating a well-built clinical question so that you will be able to find the most relevant results possible. A well-built question will address four important items: P atient or Problem, I ntervention, C omparison, and O utcome. To help you remember this, you can use the mnemonic PICO. When you are designing your clinical question, here are some topics to take into consideration.
P= Patient or Problem:
How would you describe a group of patients similar to yours? What are the most important characteristics of the patient? This may include the primary problem, disease, or co-existing conditions. Sometimes the gender, age or race of a patient might be relevant to the diagnosis or treatment of a disease.
I= Intervention:
Which main intervention, prognostic factor, or exposure are you considering? What do you want to do for the patient? Prescribe a drug? Order a test? Order surgery? Or what factor may influence the prognosis of the patient - age, co-existing problems, or previous exposure?
C= Comparison:
What is the main alternative to compare with the intervention? Are you trying to decide between two drugs, a drug and no medication or placebo, or two diagnostic tests? Your clinical question may not always have a specific comparison.
O= Outcome:
What can you hope to accomplish, measure, improve or affect? What are you trying to do for the patient? Relieve or eliminate the symptoms? Reduce the number of adverse events? Improve function or test scores?
PICO Example
Using our clinical scenario, we will use PICO to develop a clinical question.
Question: In patients with type 2 diabetes and obesity, does bariatric surgery promote the management of diabetes and weight loss as compared to standard medical care?
Categories of Clinical Questions
Different types of clinical questions have certain kinds of studies that best answer them. The chart below lists the categories of clinical questions and the studies you should look for to answer them.

In our clinical scenario, we are want to determine whether or not bariatric surgery will benefit the patient, so this is a therapy question. As such, we will want to find randomized control trials to answer our question. If we found numerous RCTs on this topic, we might want to consider searching for a systematic review that synthesizes the results of these trials.
Hierarchy of Evidence
The strength of the evidence produced varies among the different types of studies. Filtered sources like systematic reviews and meta-analyses provide stronger evidence because they evaluate and compare a number of original studies. The image below demonstrates the relative strengths of the study types - generally, the higher up on the pyramid you go, the more rigorous the study design and the lesser likelihood of bias or systematic error.
Types of Studies
Types of studies we are going to cover all fall under one of two categories - primary sources or secondary sources. Primary sources are those that report original research and secondary sources are those that compile and evaluate original studies.
Primary Sources
Randomized Controlled Trials are studies in which subjects are randomly assigned to two or more groups; one group receives a particular treatment while the other receives an alternative treatment (or placebo). Patients and investigators are "blinded", that is, they do not know which patient has received which treatment. This is done in order to reduce bias.
Cohort Studies are cause-and-effect observational studies in which two or more populations are compared, often over time. These studies are not randomized.
Case Control Studies study a population of patients with a particular condition and compare it with a population that does not have the condition. It looks the exposures that those with the condition might have had that those in the other group did not.
Cross-Sectional Studies look at diseases and other factors at a particular point in time, instead of longitudinally. These are studies are descriptive only, not relational or causal. A particular type of cross-sectional study, called a Prospective, Blind Comparison to a Gold Standard, is a controlled trial that allows a research to compare a new test to the "gold standard" test to determine whether or not the new test will be useful.
Case Studies are usually single patient cases.
Secondary Sources
Systematic Reviews are studies in which the authors ask a specific clinical question, perform a comprehensive literature search, eliminate poorly done studies, and attempt to make practice recommendations based on the well-done studies.
Meta-Analyses are systematic reviews that combine the results of select studies into a single statistical analysis of the results.
Practice Guidelines are systematically developed statements used to assist practitioners and patients in making healthcare decisions.
- << Previous: Steps in the Evidence-Based Practice Process
- Next: Acquiring the Evidence >>
- Last Updated: Nov 22, 2022 3:19 PM
- URL: https://guides.hshsl.umaryland.edu/ebptutorial
Projects Maintained by the HSHSL
- Alumni & Associates
- Congenital Heart Disease
- Corporate Services
- Embracing mHealth
- Faith Community Nursing
- Project SHARE Curriculum
- Citizen Science: Gearing Up For Discovery (edX)
- UMB Digital Archive
- Weise Gallery
University of Maryland Schools
- School of Dentistry
- Graduate School
- School of Law
- School of Medicine
- School of Nursing
- School of Pharmacy
- School of Social Work
Connective Issues E-Newsletter
Read Our Latest Issue
Join our subscribers!
Contact Us | Hours | Directions | Privacy Policy | Disclaimers | Supporting the Library | Suggestion Box | HSHSL Building Work Order | Web Accessibility | Diversity Statement
601 W. Lombard Street | Baltimore, Maryland 21201-1512 | 410-706-7995

The Graduate Health & Life Sciences Research Library at Georgetown University Medical Center
Evidence-based medicine resource guide.
- Defining EBM
Types of Clinical Questions
Formulating a well built clinical question, type of clinical question and study design.
- Point-of-Care Tools
- Databases for Clinical Research
- Drug Information
- Books & eBooks
- EBM Journals
- EBM Organizations & Centers
- Health Sciences: The Research Process
Resources and Types of Clinical Question
Background questions are best answered by medical textbooks, point-of-care tools such as DynaMed Plus and Essential Evidence Plus, and narrative reviews.
Foreground questions are best answered by consulting medical databases such as MEDLINE (via PubMed or Ovid), Embase, Cochrane Database of Systematic Reviews and ACP Journal Club.
DML's Clinical Quick Reference page is a great place to locate EBM resources. Each resource has been labeled background and/or foreground, for you!
Clinical questions may be categorized as either background or foreground. Why is this important?
Determining the type of question will help you to select the best resource to consult for your answer.
Background questions ask for general knowledge about an illness, disease, condition, process or thing. These types of questions typically ask who, what, where, when, how & why about things like a disorder, test, or treatment, etc.
For example
- How overweight is a woman to be considered slightly obese?
- What are the clinical manifestations of menopause?
- What causes migraines?
Foreground questions ask for specific knowledge to inform clinical decisions. These questions typically concern a specific patient or particular population. Foreground questions tend to be more specific and complex compared to background questions. Quite often, foreground questions investigate comparisons, such as two drugs, two treatments, two diagnostic tests, etc. Foreground questions may be further categorized into one of 4 major types: treatment/therapy, diagnosis, prognosis, or etiology/harm.
- Is Crixivan effective when compared with placebo in slowing the rate of functional impairment in a 45 year old male patient with Lou Gehrig's Disease?
- In pediatric patients with Allergic Rhinitis, are Intranasal steroids more effective than antihistamines in the management of Allergic Rhinitis symptoms?
According to the Centre for Evidence Based Medicine (CEBM) , "one of the fundamental skills required for practising EBM is the asking of well-built clinical questions. To benefit patients and clinicians, such questions need to be both directly relevant to patients' problems and phrased in ways that direct your search to relevant and precise answers."
A well-built clinical foreground question should have all four components. The PICO model is a helpful tool that assists you in organizing and focusing your foreground question into a searchable query. Dividing into the PICO elements helps identify search terms/concepts to use in your search of the literature.
P = Patient, Problem, Population (How would you describe a group of patients similar to you? What are the most important characteristics of the patient?)
I = Intervention, Prognostic Factor, Exposure (What main intervention are you considering? What do you want to do with this patient?)
C = Comparison (What are you hoping to compare with the intervention: another treatment, drug, placebo, a different diagnostic test, etc.? It's important to include this element and to be as specific as possible.)
O = Outcome (What are you trying to accomplish, measure, improve or affect? Outcomes may be disease-oriented or patient-oriented.)

Small collection. Updated monthly.
Two additional important elements of the well-built clinical question to consider are the type of foreground question and the type of study (methodology) . This information can be helpful in focusing the question and determining the most appropriate type of evidence.
Foreground questions can be further divided into questions that relate to therapy, diagnosis, prognosis, etiology/harm
- Therapy: Questions of treatment in order to achieve some outcome. May include drugs, surgical intervention, change in diet, counseling, etc.
- Diagnosis: Questions of identification of a disorder in a patient presenting with specific symptoms.
- Prognosis: Questions of progression of a disease or likelihood of a disease occurring.
- Etiology/Harm: Questions of negative impact from an intervention or other exposure.

Meta-analysis: A statistical technique that summarizes the results of several studies in a single weighted estimate, in which more weight is given to results of studies with more events and sometimes to studies of higher quality.
Systematic Review: a review in which specified and appropriate methods have been used to identify, appraise, and summarize studies addressing a defined question. (It can, but need not, involve meta-analysis). In Clinical Evidence, the term systematic review refers to a systematic review of RCTs unless specified otherwise.
Randomized Controlled Trial: a trial in which participants are randomly assigned to two or more groups: at least one (the experimental group) receiving an intervention that is being tested and another (the comparison or control group) receiving an alternative treatment or placebo. This design allows assessment of the relative effects of interventions.
Controlled Clinical Trial: a trial in which participants are assigned to two or more different treatment groups. In Clinical Evidence, we use the term to refer to controlled trials in which treatment is assigned by a method other than random allocation. When the method of allocation is by random selection, the study is referred to as a randomized controlled trial (RCT). Non-randomized controlled trials are more likely to suffer from bias than RCTs.
Cohort Study: a non-experimental study design that follows a group of people (a cohort), and then looks at how events differ among people within the group. A study that examines a cohort, which differs in respect to exposure to some suspected risk factor (e.g. smoking), is useful for trying to ascertain whether exposure is likely to cause specified events (e.g. lung cancer). Prospective cohort studies (which track participants forward in time) are more reliable than retrospective cohort studies.
Case control study: a study design that examines a group of people who have experienced an event (usually an adverse event) and a group of people who have not experienced the same event, and looks at how exposure to suspect (usually noxious) agents differed between the two groups. This type of study design is most useful for trying to ascertain the cause of rare events, such as rare cancers.
Case Series: analysis of series of people with the disease (there is no comparison group in case series).
- << Previous: Defining EBM
- Next: Point-of-Care Tools >>
- Last Updated: Apr 11, 2024 8:45 AM
- URL: https://guides.dml.georgetown.edu/ebm
The Responsible Use of Electronic Resources policy governs the use of resources provided on these guides. © Dahlgren Memorial Library, Georgetown University Medical Center. Unless otherwise stated, these guides may be used for educational or academic purposes as long as proper attribution is given. Please seek permission for any modifications, adaptations, or for commercial purposes. Email [email protected] to request permission. Proper attribution includes: Written by or adapted from, Dahlgren Memorial Library, URL.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Case study: 33-year-old female presents with chronic sob and cough.
Sandeep Sharma ; Muhammad F. Hashmi ; Deepa Rawat .
Affiliations
Last Update: February 20, 2023 .
- Case Presentation
History of Present Illness: A 33-year-old white female presents after admission to the general medical/surgical hospital ward with a chief complaint of shortness of breath on exertion. She reports that she was seen for similar symptoms previously at her primary care physician’s office six months ago. At that time, she was diagnosed with acute bronchitis and treated with bronchodilators, empiric antibiotics, and a short course oral steroid taper. This management did not improve her symptoms, and she has gradually worsened over six months. She reports a 20-pound (9 kg) intentional weight loss over the past year. She denies camping, spelunking, or hunting activities. She denies any sick contacts. A brief review of systems is negative for fever, night sweats, palpitations, chest pain, nausea, vomiting, diarrhea, constipation, abdominal pain, neural sensation changes, muscular changes, and increased bruising or bleeding. She admits a cough, shortness of breath, and shortness of breath on exertion.
Social History: Her tobacco use is 33 pack-years; however, she quit smoking shortly prior to the onset of symptoms, six months ago. She denies alcohol and illicit drug use. She is in a married, monogamous relationship and has three children aged 15 months to 5 years. She is employed in a cookie bakery. She has two pet doves. She traveled to Mexico for a one-week vacation one year ago.
Allergies: No known medicine, food, or environmental allergies.
Past Medical History: Hypertension
Past Surgical History: Cholecystectomy
Medications: Lisinopril 10 mg by mouth every day
Physical Exam:
Vitals: Temperature, 97.8 F; heart rate 88; respiratory rate, 22; blood pressure 130/86; body mass index, 28
General: She is well appearing but anxious, a pleasant female lying on a hospital stretcher. She is conversing freely, with respiratory distress causing her to stop mid-sentence.
Respiratory: She has diffuse rales and mild wheezing; tachypneic.
Cardiovascular: She has a regular rate and rhythm with no murmurs, rubs, or gallops.
Gastrointestinal: Bowel sounds X4. No bruits or pulsatile mass.
- Initial Evaluation
Laboratory Studies: Initial work-up from the emergency department revealed pancytopenia with a platelet count of 74,000 per mm3; hemoglobin, 8.3 g per and mild transaminase elevation, AST 90 and ALT 112. Blood cultures were drawn and currently negative for bacterial growth or Gram staining.
Chest X-ray
Impression: Mild interstitial pneumonitis
- Differential Diagnosis
- Aspiration pneumonitis and pneumonia
- Bacterial pneumonia
- Immunodeficiency state and Pneumocystis jiroveci pneumonia
- Carcinoid lung tumors
- Tuberculosis
- Viral pneumonia
- Chlamydial pneumonia
- Coccidioidomycosis and valley fever
- Recurrent Legionella pneumonia
- Mediastinal cysts
- Mediastinal lymphoma
- Recurrent mycoplasma infection
- Pancoast syndrome
- Pneumococcal infection
- Sarcoidosis
- Small cell lung cancer
- Aspergillosis
- Blastomycosis
- Histoplasmosis
- Actinomycosis
- Confirmatory Evaluation
CT of the chest was performed to further the pulmonary diagnosis; it showed a diffuse centrilobular micronodular pattern without focal consolidation.
On finding pulmonary consolidation on the CT of the chest, a pulmonary consultation was obtained. Further history was taken, which revealed that she has two pet doves. As this was her third day of broad-spectrum antibiotics for a bacterial infection and she was not getting better, it was decided to perform diagnostic bronchoscopy of the lungs with bronchoalveolar lavage to look for any atypical or rare infections and to rule out malignancy (Image 1).
Bronchoalveolar lavage returned with a fluid that was cloudy and muddy in appearance. There was no bleeding. Cytology showed Histoplasma capsulatum .
Based on the bronchoscopic findings, a diagnosis of acute pulmonary histoplasmosis in an immunocompetent patient was made.
Pulmonary histoplasmosis in asymptomatic patients is self-resolving and requires no treatment. However, once symptoms develop, such as in our above patient, a decision to treat needs to be made. In mild, tolerable cases, no treatment other than close monitoring is necessary. However, once symptoms progress to moderate or severe, or if they are prolonged for greater than four weeks, treatment with itraconazole is indicated. The anticipated duration is 6 to 12 weeks total. The response should be monitored with a chest x-ray. Furthermore, observation for recurrence is necessary for several years following the diagnosis. If the illness is determined to be severe or does not respond to itraconazole, amphotericin B should be initiated for a minimum of 2 weeks, but up to 1 year. Cotreatment with methylprednisolone is indicated to improve pulmonary compliance and reduce inflammation, thus improving work of respiration. [1] [2] [3]
Histoplasmosis, also known as Darling disease, Ohio valley disease, reticuloendotheliosis, caver's disease, and spelunker's lung, is a disease caused by the dimorphic fungi Histoplasma capsulatum native to the Ohio, Missouri, and Mississippi River valleys of the United States. The two phases of Histoplasma are the mycelial phase and the yeast phase.
Etiology/Pathophysiology
Histoplasmosis is caused by inhaling the microconidia of Histoplasma spp. fungus into the lungs. The mycelial phase is present at ambient temperature in the environment, and upon exposure to 37 C, such as in a host’s lungs, it changes into budding yeast cells. This transition is an important determinant in the establishment of infection. Inhalation from soil is a major route of transmission leading to infection. Human-to-human transmission has not been reported. Infected individuals may harbor many yeast-forming colonies chronically, which remain viable for years after initial inoculation. The finding that individuals who have moved or traveled from endemic to non-endemic areas may exhibit a reactivated infection after many months to years supports this long-term viability. However, the precise mechanism of reactivation in chronic carriers remains unknown.
Infection ranges from an asymptomatic illness to a life-threatening disease, depending on the host’s immunological status, fungal inoculum size, and other factors. Histoplasma spp. have grown particularly well in organic matter enriched with bird or bat excrement, leading to the association that spelunking in bat-feces-rich caves increases the risk of infection. Likewise, ownership of pet birds increases the rate of inoculation. In our case, the patient did travel outside of Nebraska within the last year and owned two birds; these are her primary increased risk factors. [4]
Non-immunocompromised patients present with a self-limited respiratory infection. However, the infection in immunocompromised hosts disseminated histoplasmosis progresses very aggressively. Within a few days, histoplasmosis can reach a fatality rate of 100% if not treated aggressively and appropriately. Pulmonary histoplasmosis may progress to a systemic infection. Like its pulmonary counterpart, the disseminated infection is related to exposure to soil containing infectious yeast. The disseminated disease progresses more slowly in immunocompetent hosts compared to immunocompromised hosts. However, if the infection is not treated, fatality rates are similar. The pathophysiology for disseminated disease is that once inhaled, Histoplasma yeast are ingested by macrophages. The macrophages travel into the lymphatic system where the disease, if not contained, spreads to different organs in a linear fashion following the lymphatic system and ultimately into the systemic circulation. Once this occurs, a full spectrum of disease is possible. Inside the macrophage, this fungus is contained in a phagosome. It requires thiamine for continued development and growth and will consume systemic thiamine. In immunocompetent hosts, strong cellular immunity, including macrophages, epithelial, and lymphocytes, surround the yeast buds to keep infection localized. Eventually, it will become calcified as granulomatous tissue. In immunocompromised hosts, the organisms disseminate to the reticuloendothelial system, leading to progressive disseminated histoplasmosis. [5] [6]
Symptoms of infection typically begin to show within three to17 days. Immunocompetent individuals often have clinically silent manifestations with no apparent ill effects. The acute phase of infection presents as nonspecific respiratory symptoms, including cough and flu. A chest x-ray is read as normal in 40% to 70% of cases. Chronic infection can resemble tuberculosis with granulomatous changes or cavitation. The disseminated illness can lead to hepatosplenomegaly, adrenal enlargement, and lymphadenopathy. The infected sites usually calcify as they heal. Histoplasmosis is one of the most common causes of mediastinitis. Presentation of the disease may vary as any other organ in the body may be affected by the disseminated infection. [7]
The clinical presentation of the disease has a wide-spectrum presentation which makes diagnosis difficult. The mild pulmonary illness may appear as a flu-like illness. The severe form includes chronic pulmonary manifestation, which may occur in the presence of underlying lung disease. The disseminated form is characterized by the spread of the organism to extrapulmonary sites with proportional findings on imaging or laboratory studies. The Gold standard for establishing the diagnosis of histoplasmosis is through culturing the organism. However, diagnosis can be established by histological analysis of samples containing the organism taken from infected organs. It can be diagnosed by antigen detection in blood or urine, PCR, or enzyme-linked immunosorbent assay. The diagnosis also can be made by testing for antibodies again the fungus. [8]
Pulmonary histoplasmosis in asymptomatic patients is self-resolving and requires no treatment. However, once symptoms develop, such as in our above patient, a decision to treat needs to be made. In mild, tolerable cases, no treatment other than close monitoring is necessary. However, once symptoms progress to moderate or severe or if they are prolonged for greater than four weeks, treatment with itraconazole is indicated. The anticipated duration is 6 to 12 weeks. The patient's response should be monitored with a chest x-ray. Furthermore, observation for recurrence is necessary for several years following the diagnosis. If the illness is determined to be severe or does not respond to itraconazole, amphotericin B should be initiated for a minimum of 2 weeks, but up to 1 year. Cotreatment with methylprednisolone is indicated to improve pulmonary compliance and reduce inflammation, thus improving the work of respiration.
The disseminated disease requires similar systemic antifungal therapy to pulmonary infection. Additionally, procedural intervention may be necessary, depending on the site of dissemination, to include thoracentesis, pericardiocentesis, or abdominocentesis. Ocular involvement requires steroid treatment additions and necessitates ophthalmology consultation. In pericarditis patients, antifungals are contraindicated because the subsequent inflammatory reaction from therapy would worsen pericarditis.
Patients may necessitate intensive care unit placement dependent on their respiratory status, as they may pose a risk for rapid decompensation. Should this occur, respiratory support is necessary, including non-invasive BiPAP or invasive mechanical intubation. Surgical interventions are rarely warranted; however, bronchoscopy is useful as both a diagnostic measure to collect sputum samples from the lung and therapeutic to clear excess secretions from the alveoli. Patients are at risk for developing a coexistent bacterial infection, and appropriate antibiotics should be considered after 2 to 4 months of known infection if symptoms are still present. [9]
Prognosis
If not treated appropriately and in a timely fashion, the disease can be fatal, and complications will arise, such as recurrent pneumonia leading to respiratory failure, superior vena cava syndrome, fibrosing mediastinitis, pulmonary vessel obstruction leading to pulmonary hypertension and right-sided heart failure, and progressive fibrosis of lymph nodes. Acute pulmonary histoplasmosis usually has a good outcome on symptomatic therapy alone, with 90% of patients being asymptomatic. Disseminated histoplasmosis, if untreated, results in death within 2 to 24 months. Overall, there is a relapse rate of 50% in acute disseminated histoplasmosis. In chronic treatment, however, this relapse rate decreases to 10% to 20%. Death is imminent without treatment.
- Pearls of Wisdom
While illnesses such as pneumonia are more prevalent, it is important to keep in mind that more rare diseases are always possible. Keeping in mind that every infiltrates on a chest X-ray or chest CT is not guaranteed to be simple pneumonia. Key information to remember is that if the patient is not improving under optimal therapy for a condition, the working diagnosis is either wrong or the treatment modality chosen by the physician is wrong and should be adjusted. When this occurs, it is essential to collect a more detailed history and refer the patient for appropriate consultation with a pulmonologist or infectious disease specialist. Doing so, in this case, yielded workup with bronchoalveolar lavage and microscopic evaluation. Microscopy is invaluable for definitively diagnosing a pulmonary consolidation as exemplified here where the results showed small, budding, intracellular yeast in tissue sized 2 to 5 microns that were readily apparent on hematoxylin and eosin staining and minimal, normal flora bacterial growth.
- Enhancing Healthcare Team Outcomes
This case demonstrates how all interprofessional healthcare team members need to be involved in arriving at a correct diagnosis. Clinicians, specialists, nurses, pharmacists, laboratory technicians all bear responsibility for carrying out the duties pertaining to their particular discipline and sharing any findings with all team members. An incorrect diagnosis will almost inevitably lead to incorrect treatment, so coordinated activity, open communication, and empowerment to voice concerns are all part of the dynamic that needs to drive such cases so patients will attain the best possible outcomes.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Histoplasma Contributed by Sandeep Sharma, MD
Disclosure: Sandeep Sharma declares no relevant financial relationships with ineligible companies.
Disclosure: Muhammad Hashmi declares no relevant financial relationships with ineligible companies.
Disclosure: Deepa Rawat declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Sharma S, Hashmi MF, Rawat D. Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough. [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Palliative Chemotherapy: Does It Only Provide False Hope? The Role of Palliative Care in a Young Patient With Newly Diagnosed Metastatic Adenocarcinoma. [J Adv Pract Oncol. 2017] Review Palliative Chemotherapy: Does It Only Provide False Hope? The Role of Palliative Care in a Young Patient With Newly Diagnosed Metastatic Adenocarcinoma. Doverspike L, Kurtz S, Selvaggi K. J Adv Pract Oncol. 2017 May-Jun; 8(4):382-386. Epub 2017 May 1.
- Review Breathlessness with pulmonary metastases: a multimodal approach. [J Adv Pract Oncol. 2013] Review Breathlessness with pulmonary metastases: a multimodal approach. Brant JM. J Adv Pract Oncol. 2013 Nov; 4(6):415-22.
- A 50-Year Old Woman With Recurrent Right-Sided Chest Pain. [Chest. 2022] A 50-Year Old Woman With Recurrent Right-Sided Chest Pain. Saha BK, Bonnier A, Chong WH, Chenna P. Chest. 2022 Feb; 161(2):e85-e89.
- Suicidal Ideation. [StatPearls. 2024] Suicidal Ideation. Harmer B, Lee S, Duong TVH, Saadabadi A. StatPearls. 2024 Jan
- Review Domperidone. [Drugs and Lactation Database (...] Review Domperidone. . Drugs and Lactation Database (LactMed®). 2006
Recent Activity
- Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough - StatPearls Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Top 100 Ultrasound
Litfl 100+ ultrasound quiz.
Clinical cases and self assessment problems from the Ultrasound library to enhance interpretation skills through Ultrasound problems. Preparation for examinations.
Each case presents a clinical scenario; a series of questions; clinical images and finally some pearls to highlight the key learning points. We trust that you will find a few clinical pearls or reminders that you could apply to your patients that you care for in your emergency department or other health setting
Search by keywords; disease process; condition; eponym or clinical features…
LITFL Top 100 Self Assessment Quizzes
ULTRASOUND LIBRARY
POCUS, eFAST and basic principles

Privacy Overview
Medicine Cases Quiz

General level. Note that cases are simulated cases for learning purposes and not known patients. Just enter your name and enjoy the quiz.
A 70 years old man who has been smoking for 40 years was observed to be losing weight,having occasional seizures and coughing for 3 weeks. Three months to presentation he was noted during a clinic visit to be depressed and having memory impairment.Which is the most likely diagnosis?
Small cell Lung Cancer
Squamous Cell Cancer
Mesothelioma
Pulmonary Tuberculosis
Rate this question:
A 60 years old baker was diagnosed of a Primary Brain tumor. He was placed on oral dexamethasone 16 mg daily in divided dose by the managing Oncologist. The primary rationale for such action is
To reduce intracranial pressure from edema associated with the tumor
To aid the shrinking of tumor
To inhibit tumor markers produced by the tumor
To aid subsequent surgical resection of tumor
A 80 years old retired military man was diagnosed of glial tumor after recurrent episodes of seizures. Which is the most likely neuroimaging modality that was used?
Cranial MRI with gandolium contrast adminstration
Skull X-ray
Cranial MRI
Cranial CT scan
A patient presented to the hospital and was subsequently diagnosed of High grade glial malignant tumor. Which of the following is not likely to be a presenting feature?
Visual field deficit
Hemiparaesis
After extensive investigation a patient was diagnosed of Meningioma. Which is not likely to be presenting features when he presented to the hospital?
Quiz Review Timeline +
Our quizzes are rigorously reviewed, monitored and continuously updated by our expert board to maintain accuracy, relevance, and timeliness.
- Current Version
- Mar 21, 2023 Quiz Edited by ProProfs Editorial Team
- Dec 31, 2014 Quiz Created by Ceolado
Related Topics
- Health Care
- Herbal Medicine
Recent Quizzes
Featured Quizzes
Popular Topics
- Abdomen Quizzes
- Addiction Quizzes
- Aging Quizzes
- Arthritis Quizzes
- Beauty Quizzes
- Blood Quizzes
- Body Quizzes
- Bone Quizzes
- Brain Quizzes
- Child Health Quizzes
- Dermatology Quizzes
- Digestive System Quizzes
- Disease Quizzes
- Fertility Quizzes
- First Aid Quizzes
- Hair care Quizzes
- Health And Nutrition Quizzes
- Health And Wellness Quizzes
- Health Policy Quizzes
- Health Psychology Quizzes
- Health Worldwide Quizzes
- Hearing Quizzes
- Heart Quizzes
- Hospital Quizzes
- Illness Quizzes
- Injury Quizzes
- Kidney Quizzes
- Liver Quizzes
- Lung Quizzes
- Medical Quizzes
- Mental Health Quizzes
- Nose Quizzes
- Nutrition Quizzes
- Obesity Quizzes
- Ophthalmology Quizzes
- Patient Quizzes
- Patient care Quizzes
- Pharmacy Quizzes
- Pregnancy Quizzes
- Puberty Quizzes
- Public Health Quizzes
- Respiratory System Quizzes
- Sleep Quizzes
- Stress Quizzes
- Surgery Quizzes
- Surgical Instruments Quizzes
- Throat Quizzes
- Weight Quizzes
- Wellness Quizzes

Related Quizzes
Wait! Here's an interesting quiz for you.
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- April 2024 | Volume 109, I...
- Understanding Surgical CPT...
Understanding Surgical CPT Coding Essentials Will Help Ensure Proper Reimbursement
Megan McNally, MD, FACS, Jayme Lieberman, MD, FACS, and Jan Nagle, MS
April 10, 2024
Numerous Current Procedural Terminology (CPT)* coding questions raised during ACS coding courses and received via the ACS Coding Hotline underscore the need to explain key coding concepts in order to ensure accurate coding.
This article examines crucial coding concepts through fictional cases that should be familiar to general surgeons and related surgical specialties.
Laparoscopic Liver Biopsy
Case: While performing a laparoscopic appendectomy for appendiceal carcinoma, the surgeon also performs a liver biopsy of a suspicious lesion. Reportable codes include the following: 44970, Laparoscopy, surgical, appendectomy, and 47379, Unlisted laparoscopic procedure, liver.
Concept: It would not be appropriate to report add-on code 47001, Biopsy of liver, needle; when done for indicated purpose at time of other major procedure (List separately in addition to code for primary procedure), for the biopsy procedure. The intent of code 47001 has always been for a liver biopsy at the time of an open procedure as discussed in the AMA CPT Assistant 1992 Code Update (Winter 1991) after code 47001 was established. Additional CPT Assistant articles have reinforced that 47001 may only be reported for a liver biopsy via an open approach. Therefore, code 47379 should be reported when a liver biopsy is performed via a laparoscopic approach in addition to a laparoscopic primary procedure and add-on code 47001 should be used as a “proxy” for charges. This information supersedes guidance that was provided in the October 2018 ACS Bulletin column “CPT Coding for Hepatobiliary Surgery.”
Case: A patient with hepatocellular carcinoma underwent an exploratory laparoscopy to obtain a liver biopsy and assess the peritoneal cavity to exclude advance disease. The reportable code is 47379, Unlisted laparoscopic procedure, liver.
Concept: It would not be appropriate to report 49321, Laparoscopy, surgical; with biopsy (single or multiple) if the biopsy is the only laparoscopic procedure performed as this code is in the Abdomen, Peritoneum, and Omentum subsection of CPT and not the Liver subsection. For this clinical scenario, code 47379 should be reported and code 49321 should be used as a “proxy” for charges. This information supersedes guidance that was provided in the October 2018 ACS Bulletin column “CPT Coding for Hepatobiliary Surgery.”
Laparoscopic Appendectomy for Perforation
Case: A patient undergoes a laparoscopic appendectomy for perforated appendicitis requiring significantly more work than a typical laparoscopic appendectomy. The reportable code is 44970, Laparoscopy, surgical, appendectomy.
Concept: Although there are separate codes to differentiate an open appendectomy without rupture (44950) and with rupture (44960), there is only one code for a laparoscopic appendectomy (44970), and it is used to report a laparoscopic appendectomy for either scenario; with rupture or without rupture. It would not be correct to report 44979, Unlisted laparoscopy procedure, appendix for a laparoscopic appendectomy for perforation with abscess and peritonitis and use the open code 44960, Appendectomy; for ruptured appendix with abscess or generalized peritonitis as a “proxy” for charges. However, depending on the amount of extra time and/or work effort required when compared to a laparoscopic appendectomy without rupture, it may be appropriate to append modifier 22, Increased procedural services. Documentation must support the substantial additional work and the reason for the additional work (i.e., increased intensity, time, technical difficulty of procedure, severity of patient’s condition, physical and mental effort required).
Adjacent Tissue Transfer after Breast Surgery
Case: Immediately following a lumpectomy, the surgeon performs reconstructive tissue rearrangement including dissection through the breast parenchyma in order to create a pedicled flap of breast tissue that is then transposed into the defect to improve the contour of the breast. Reportable codes include the following: 19301, Mastectomy, partial (e.g., lumpectomy, tylectomy, quadrantectomy, segmentectomy) and code(s) for adjacent tissue transfer as appropriate (14000-14041, 14301-14302).
Concept: Reporting adjacent tissue transfer for immediate, partial breast reconstruction following lumpectomy is possible, although it requires the specific criteria for reporting adjacent tissue transfer. In addition to a description of the defect, it requires full documentation of the incisions required to create the pedicled flap of breast tissue, preservation of vascularity, the dimensions of the tissue mobilized, and the technique for transfer of the tissue into the defect. Undermining of the breast tissue off the pectoralis major muscle alone or undermining tissue within the breast parenchyma to advance tissue for primary repair is not considered adjacent tissue transfer and is bundled with the partial mastectomy code and not separately reportable.
Endocrine Surgery
Ca se: A patient underwent a right thyroid lobectomy years ago. It is now necessary to go back and remove the rest of the right lobe and also remove the left lobe (previously untouched). Reportable codes include the following: 60260-RT, Thyroidectomy, removal of all remaining thyroid tissue following previous removal of a portion of thyroid, and 60220-LT-59, Total thyroid lobectomy, unilateral; with or without isthmusectomy.
Concept: This reporting is based on the fact that 60260 is considered a bilateral procedure and since the left lobe was previously untouched, it would be incorrect to report a code for removal of remaining tissue when a total lobectomy is performed.
Case: A patient had a left lobectomy on March 1. On March 14, the patient is taken back to surgery by the same surgeon for a right thyroid lobectomy after pathology showed a malignancy in the right thyroid lobe. Reportable code for the first operation: 60220-LT, Total thyroid lobectomy, unilateral; with or without isthmusectomy. Reportable code for the subsequent operation: 60220-RT-58.
Concept: Modifier 58 is appended to the second operation because it was a “staged or related procedure or service by the same physician or other qualified healthcare professional during the postoperative period.”
The ACS collaborates with KZA, Inc. on courses that provide the tools necessary to increase revenue and decrease compliance risk. These courses are an opportunity to sharpen your coding skills. You also will be provided online access to the KZA alumni website, where you will find additional resources and other FAQs about correct coding. Information about the courses can be accessed on the KZA website .
In addition, as part of the College’s ongoing efforts to help members and their practices submit clean claims and receive proper reimbursement, a coding consultation service—the ACS Coding Hotline—has been established for coding and billing questions. ACS members are offered five free consultation units (CUs) per calendar year. One CU is a period of up to 10 minutes of coding services time. Access the ACS Coding Hotline website today .
Dr. Megan McNally is a surgical oncologist at Saint Luke’s Health System in Kansas City, Missouri, and assistant clinical professor in the Department of Surgery at the University of Missouri-Kansas City School of Medicine. She also is a member of the ACS General Surgery Coding and Reimbursement Committee and an ACS advisor to the AMA CPT Editorial Panel.
*All specific references to CPT codes and descriptions are ©2023 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association.
Related Pages

ACS Cancer Conference Highlights Quality Efforts, Current Complexities in Cancer Care
Sessions highlighted new information on standards and data collection, and offered insights into the new pediatric accreditation standards.

Trauma Meeting Spotlights New Image-Focused STOP THE BLEED Course
A Special Session at the COT Annual Meeting provided an overview of the new version of the STOP THE BLEED course.

ACS Statement Guides Surgeons in Telehealth Practices
The ACS Board of Regents approved a new policy statement on telehealth at its February 2023 meeting.

JACS Highlights
Read capsule summaries of articles appearing in the April 2024 issue of the Journal of the American College of Surgeons.

Engineering Surgical Innovation Is a Joint Effort
The Annual Surgeons and Engineers meeting hosted its first DIY simulator/model competition and provided a platform for innovative collaboration.
In Memoriam: Dr. Edward (Ted) Copeland, ACS Past-President
Renowned breast cancer surgeon and ACS Past-President Dr. Edward Copeland passed away March 31, 2024, at the age of 86.
Member News April 2024
Learn more about ACS members who have been recognized for noteworthy achievements.

ACS’s Advocacy Achievements
Dr. Turner addresses the importance of surgeon advocacy and details some recent successes.
Are Antibiotics the Answer to Treating Appendicitis?
Discover new perspectives on operative versus nonoperative approaches to managing uncomplicated acute appendicitis.
For Optimal Outcomes, Surgeons Should Tap into “Collective Surgical Consciousness”
Learn about the role of AI in medical imaging and its potential impact on patient decision-making.

New Technologies, Approaches Help Surgeons Maximize the Use of Transplant Organs
Read about innovative advancements that help recover, preserve, and rehabilitate donor organs in an effort to streamline the allocation process.
Physician Workforce Data Suggest Epochal Change
Gain new perspectives on current and future surgeon workforce supply culled from the AAMC’s US Physician Workforce Data Dashboard.

Artificial Intelligence: The Future Is Now
Surgeons are encouraged to take an active role in the adoption of AI to ensure the quality of care and safety of our patients.

Artificial Intelligence: The Future Is What We Make It
Members of the ACS Health Information Technology Committee respond to Dr. James Elsey's insights on AI in healthcare.
FDA Authorizes COVID Drug Pemgarda for High-Risk Patients
BY CARRIE MACMILLAN April 5, 2024

The Food and Drug Administration (FDA) granted an emergency use authorization (EUA) to a medicine meant to protect certain immunocompromised people against COVID-19 .
The medicine, pemivibart (brand name Pemgarda™), is for people who are at least 12 years of age, weigh more than 88 pounds, and are moderately to severely immunocompromised.
An EUA is a tool the FDA uses to expedite the availability of drugs, vaccines , and other products during a public health emergency. While the public health emergency for COVID officially expired in May 2023, the FDA can still issue EUAs related to it.
“This medication provides important protection for the immunocompromised, a population that is more likely to have serious COVID illness and a higher mortality rate,” says Scott Roberts, MD , a Yale Medicine infectious diseases specialist.
Being immunocompromised means your immune system doesn’t work as well as it should to protect against infection because of a medical condition, such as cancer , that weakens immune function or because you receive medicines or treatments, such as immunotherapy , that suppress the immune system.
“The population identified as moderately to severely immunocompromised includes solid organ transplant recipients, stem cell transplant recipients, and those who are on chemotherapy for cancers such as lymphoma and leukemia, among many others,” Dr. Roberts explains. (The Centers for Disease Control and Prevention (CDC) provides a more detailed list .) Approximately 3% of adults in the United States are immunocompromised.
“This group is also less likely to build enough protection against COVID after vaccination. For these patients, the pandemic is not over,” says Dr. Roberts. “Hopefully, this new treatment will help the vulnerable feel safer.”
Below, we talk more about Pemgarda with Dr. Roberts.
Why isn’t COVID vaccination as effective in immunocompromised individuals?
Those who are not immunocompromised most likely have a strong mix of “hybrid” immunity to COVID at this point, both from vaccination and natural infection, Dr. Roberts explains.
“Most people should not be concerned when a new COVID variant arises because even if it bypasses some of their protection, it's not going to bypass all of it,” Dr. Roberts says. “But some immunocompromised people do not have that luxury. Any COVID infection is going to hit them the hardest. And vaccination is still the best tool we have to offer for the prevention of severe COVID.”
However, this drug is a new tool that can help immunocompromised patients feel safe going about daily activities as many other people do at this phase of the pandemic, he adds.
How does Pemgarda work?
Pemgarda is a type of medicine called pre-exposure prophylaxis (PrEP), which is taken to prevent COVID infection. Anyone with COVID—or who has a known recent exposure to someone with a COVID infection—cannot take Pemgarda.
Paxlovid and Remdesivir, conversely, are meant to be taken after a known COVID infection and are for anyone deemed high-risk for serious illness, including those who are immunocompromised.
Pemgarda is a type of monoclonal antibody (mAb), a drug therapy that uses antibodies made in a laboratory. These antibodies attach to the spike protein of SARS-CoV-2, the virus that causes COVID-19, and prevent the virus from entering the body’s cells.
“Despite vaccination, many immunocompromised patients are still unable to generate the antibodies necessary to block this entry; Pemgarda serves as a tool to increase SARS-CoV-2-specific antibodies to levels seen in nonimmunocompromised individuals after vaccination,” says Dr. Roberts.
It is given as an infusion in a medical setting and takes about an hour to complete. Patients can get a dose of the medication as often as every three months.
Is this the first preventive drug for COVID?
A previous mAb treatment, Evusheld™, was authorized by the FDA in 2021 to prevent COVID in immunocompromised patients. However, the medication proved ineffective against newer COVID variants and was taken off the market in January 2023.
Pemgarda is the only COVID PrEP drug on the market.
How effective is Pemgarda against COVID?
Pemgarda was granted an EUA based on data from an ongoing Phase 3 CANOPY clinical trial, as well as efficacy data from previous clinical trials of adintrevimab, the parent mAb for pemivibart, and other monoclonal antibody products.
In trials, adintrevimab was associated with an approximate 70% risk reduction of developing symptomatic COVID-19 compared to a placebo, according to Invivyd , the company that makes the drug. The CANOPY studies were done when the JN.1 subvariant was circulating. JN.1 is still the predominant coronavirus subvariant.
Is Pemgarda safe?
In the trial, 623 participants received at least one dose of the drug. The most common side effects included skin reactions at the infusion site, cold and flu-like illness, headache, fatigue, and nausea. Four people experienced anaphylaxis (a severe allergic reaction).
“For patients who are worried about the trade-off, I think it requires a risk-benefit analysis,” says Dr. Roberts. “I think in most cases the benefit is going to outweigh the risk of anaphylaxis, especially if doctors can mitigate it by having medications such as an Epi-pen there in case a patient does have a severe allergic reaction.”
Where and when can patients get Pemgarda?
Immunocompromised people who are interested in taking Pemgarda should talk to their doctor. “It might be better for some patients to talk to a specialist first—for instance, if an individual has cancer, it might be best for them to talk to their oncologist about whether this drug is right for them,” Dr. Roberts advises.
The medication is expected to be available in April. The price has not yet been set, but Medicare and private insurance plans are expected to cover it, according to news reports.
More news from Yale Medicine

This paper is in the following e-collection/theme issue:
Published on 11.4.2024 in Vol 26 (2024)
Patients’ Experiences With Digitalization in the Health Care System: Qualitative Interview Study
Authors of this article:

Original Paper
- Christian Gybel Jensen 1 * , MA ;
- Frederik Gybel Jensen 1 * , MA ;
- Mia Ingerslev Loft 1, 2 * , MSc, PhD
1 Department of Neurology, Rigshospitalet, Copenhagen, Denmark
2 Institute for People and Technology, Roskilde University, Roskilde, Denmark
*all authors contributed equally
Corresponding Author:
Mia Ingerslev Loft, MSc, PhD
Department of Neurology
Rigshospitalet
Inge Lehmanns Vej 8
Phone: 45 35457076
Email: [email protected]
Background: The digitalization of public and health sectors worldwide is fundamentally changing health systems. With the implementation of digital health services in health institutions, a focus on digital health literacy and the use of digital health services have become more evident. In Denmark, public institutions use digital tools for different purposes, aiming to create a universal public digital sector for everyone. However, this digitalization risks reducing equity in health and further marginalizing citizens who are disadvantaged. Therefore, more knowledge is needed regarding patients’ digital practices and experiences with digital health services.
Objective: This study aims to examine digital practices and experiences with public digital health services and digital tools from the perspective of patients in the neurology field and address the following research questions: (1) How do patients use digital services and digital tools? (2) How do they experience them?
Methods: We used a qualitative design with a hermeneutic approach. We conducted 31 semistructured interviews with patients who were hospitalized or formerly hospitalized at the department of neurology in a hospital in Denmark. The interviews were audio recorded and subsequently transcribed. The text from each transcribed interview was analyzed using manifest content analysis.
Results: The analysis provided insights into 4 different categories regarding digital practices and experiences of using digital tools and services in health care systems: social resources as a digital lifeline, possessing the necessary capabilities, big feelings as facilitators or barriers, and life without digital tools. Our findings show that digital tools were experienced differently, and specific conditions were important for the possibility of engaging in digital practices, including having access to social resources; possessing physical, cognitive, and communicative capabilities; and feeling motivated, secure, and comfortable. These prerequisites were necessary for participants to have positive experiences using digital tools in the health care system. Those who did not have these prerequisites experienced challenges and, in some cases, felt left out.
Conclusions: Experiences with digital practices and digital health services are complex and multifaceted. Engagement in digital practices for the examined population requires access to continuous assistance from their social network. If patients do not meet requirements, digital health services can be experienced as exclusionary and a source of concern. Physical, cognitive, and communicative difficulties might make it impossible to use digital tools or create more challenges. To ensure that digitalization does not create inequities in health, it is necessary for developers and institutions to be aware of the differences in digital health literacy, focus on simplifying communication with patients and next of kin, and find flexible solutions for citizens who are disadvantaged.
Introduction
In 2022, the fourth most googled question in Denmark was, “Why does MitID not work?” [ 1 ]. MitID (My ID) is a digital access tool that Danes use to enter several different private and public digital services, from bank accounts to mail from their municipality or the state. MitID is a part of many Danish citizens’ everyday lives because the public sector in Denmark is digitalized in many areas. In recent decades, digitalization has changed how governments and people interact and has demonstrated the potential to change the core functions of public sectors and delivery of public policies and services [ 2 ]. When public sectors worldwide become increasingly digitalized, this transformation extends to the public health sectors as well, and some studies argue that we are moving toward a “digital public health era” that is already impacting the health systems and will fundamentally change the future of health systems [ 3 ]. While health systems are becoming more digitalized, it is important that both patients and digitalized systems adapt to changes in accordance with each other. Digital practices of people can be understood as what people do with and through digital technologies and how people relate to technology [ 4 ]. Therefore, it is relevant to investigate digital practices and how patients perceive and experience their own use of digital tools and services, especially in relation to existing digital health services. In our study, we highlight a broad perspective on experiences with digital practices and particularly add insight into the challenges with digital practices faced by patients who have acute or chronic illness, with some of them also experiencing physical, communicative, or cognitive difficulties.
An international Organization for Economic Cooperation and Development report indicates that countries are digitalized to different extents and in different ways; however, this does not mean that countries do not share common challenges and insights into the implementation of digital services [ 2 ].
In its global Digital Government Index, Denmark is presented as one of the leading countries when it comes to public digitalization [ 2 ]. Recent statistics indicate that approximately 97% of Danish families have access to the internet at home [ 5 ]. The Danish health sector already offers many different digital services, including web-based delivery of medicine, e-consultations, patient-related outcome questionnaires, and seeking one’s own health journal or getting test results through; “Sundhed” [ 6 ] (the national health portal) and “Sundhedsjournalen” (the electronic patient record); or the apps “Medicinkortet” (the shared medication record), “Minlæge” (My Doctor, consisting of, eg, communication with the general practitioner), or “MinSP” (My Health Platform, consisting of, eg, communication with health care staff in hospitals) [ 6 - 8 ].
The Danish Digital Health Strategy from 2018 aims to create a coherent and user-friendly digital public sector for everyone [ 9 ], but statistics indicate that certain groups in society are not as digitalized as others. In particular, the older population uses digital services the least, with 5% of people aged 65 to 75 years and 18% of those aged 75 to 89 years having never used the internet in 2020 [ 5 ]. In parts of the literature, it has been problematized how the digitalization of the welfare state is related to the marginalization of older citizens who are socially disadvantaged [ 10 ]. However, statistics also indicate that the probability of using digital tools increases significantly as a person’s experience of using digital tools increases, regardless of their age or education level [ 5 ].
Understanding the digital practices of patients is important because they can use digital tools to engage with the health system and follow their own health course. Researching experiences with digital practices can be a way to better understand potential possibilities and barriers when patients use digital health services. With patients becoming more involved in their own health course and treatment, the importance of patients’ health literacy is being increasingly recognized [ 11 ]. The World Health Organization defines health literacy as the “achievement of a level of knowledge, personal skills and confidence to take action to improve personal and community health by changing personal lifestyles and living conditions” [ 12 ]. Furthermore, health literacy can be described as “a person’s knowledge and competencies to meet complex demands of health in modern society, ” and it is viewed as a critical step toward patient empowerment [ 11 , 12 ]. In a digitalized health care system, this also includes the knowledge, capabilities, and resources that individuals require to use and benefit from eHealth services, that is, “digital health literacy (eHealth literacy)” [ 13 ]. An eHealth literacy framework created by Norgaard et al [ 13 ] identified that different aspects, for example, the ability to process information and actively engage with digital services, can be viewed as important facets of digital health literacy. This argument is supported by studies that demonstrate how patients with cognitive and communicative challenges experience barriers to the use of digital tools and require different approaches in the design of digital solutions in the health sector [ 14 , 15 ]. Access to digital services and digital literacy is becoming increasingly important determinants of health, as people with digital literacy and access to digital services can facilitate improvement of health and involvement in their own health course [ 16 ].
The need for a better understanding of eHealth literacy and patients’ capabilities to meet public digital services’ demands as well as engage in their own health calls for a deeper investigation into digital practices and the use of digital tools and services from the perspective of patients with varying digital capabilities. Important focus areas to better understand digital practices and related challenges have already been highlighted in various studies. They indicate that social support, assessment of value in digital services, and systemic assessment of digital capabilities are important in the use and implementation of digital tools, and they call for better insight into complex experiences with digital services [ 13 , 17 , 18 ]. Therefore, we aimed to examine digital practices and experiences with public digital health services and digital tools from the perspective of patients, addressing the following research questions: how do patients use digital services and digital tools, and how do they experience them?
We aimed to investigate digital practices and experiences with digital health services and digital tools; therefore, we used a qualitative design and adopted a hermeneutic approach as the point of departure, which means including preexisting knowledge of digital practices but also providing room for new comprehension [ 19 ]. Our interpretive approach is underpinned by the philosophical hermeneutic approach by Gadamer et al [ 19 ], in which they described the interpretation process as a “hermeneutic circle,” where the researcher enters the interpretation process with an open mind and historical awareness of a phenomenon (preknowledge). We conducted semistructured interviews using an interview guide. This study followed the COREQ (Consolidated Criteria for Reporting Qualitative Research) checklist [ 20 ].
Setting and Participants
To gain a broad understanding of experiences with public digital health services, a purposive sampling strategy was used. All 31 participants were hospitalized or formerly hospitalized patients in a large neurological department in the capital of Denmark ( Table 1 ). We assessed whether including patients from the neurological field would give us a broad insight into the experiences of digital practices from different perspectives. The department consisted of, among others, 8 inpatient units covering, for example, acute neurology and stroke units, from which the patients were recruited. Patients admitted to a neurological department can have both acute and transient neurological diseases, such as infections in the brain, stroke, or blood clot in the brain from which they can recover completely or have persistent physical and mental difficulties, or experience chronic neurological and progressive disorders such as Parkinson disease and dementia. Some patients hospitalized in neurological care will have communicative and cognitive difficulties because of their neurological disorders. Nursing staff from the respective units helped the researchers (CGJ, FGJ, and MIL) identify patients who differed in terms of gender, age, and severity of neurological illness. Some patients (6/31, 19%) had language difficulties; however, a speech therapist assessed them as suitable participants. We excluded patients with severe cognitive difficulties and those who were not able to speak the Danish language. Including patients from the field of neurology provided an opportunity to study the experience of digital health practice from various perspectives. Hence, the sampling strategy enabled the identification and selection of information-rich participants relevant to this study [ 21 ], which is the aim of qualitative research. The participants were invited to participate by either the first (CGJ) or last author (MIL), and all invited participants (31/31, 100%) chose to participate.
All 31 participants were aged between 40 to 99 years, with an average age of 71.75 years ( Table 1 ). Out of the 31 participants, 10 (32%) had physical disabilities or had cognitive or communicative difficulties due to sequela in relation to neurological illness or other physical conditions.
Data Collection
The 31 patient interviews were conducted over a 2-month period between September and November 2022. Of the 31 patients, 20 (65%) were interviewed face-to-face at the hospital in their patient room upon admission and 11 (35%) were interviewed on the phone after being discharged. The interviews had a mean length of 20.48 minutes.
We developed a semistructured interview guide ( Table 2 ). The interview questions were developed based on the research aim, findings from our preliminary covering of literature in the field presented in the Introduction section, and identified gaps that we needed to elaborate on to be able to answer our research question [ 22 ]. The semistructured interview guide was designed to support the development of a trusting relationship and ensure the relevance of the interviews’ content [ 22 ]. The questions served as a prompt for the participants and were further supported by questions such as “please tell me more” and “please elaborate” throughout the interview, both to heighten the level of detail and to verify our understanding of the issues at play. If the participant had cognitive or communicative difficulties, communication was supported using a method called Supported Communication for Adults with Aphasia [ 23 ] during the interview.
The interviews were performed by all authors (CGJ, FGJ, and MIL individually), who were skilled in conducting interviews and qualitative research. The interviewers are not part of daily clinical practice but are employed in the department of neurology from where the patients were recruited. All interviews were audio recorded and subsequently transcribed verbatim by all 3 authors individually.
a PRO: patient-related outcome.
Data Analysis
The text from each transcribed interview was analyzed using manifest content analysis, as described by Graneheim and Lundman [ 24 ]. Content analysis is a method of analyzing written, verbal, and visual communication in a systematic way [ 25 ]. Qualitative content analysis is a structured but nonlinear process that requires researchers to move back and forth between the original text and parts of the text during the analysis. Manifest analysis is the descriptive level at which the surface structure of the text central to the phenomenon and the research question is described. The analysis was conducted as a collaborative effort between the first (CGJ) and last authors (MIL); hence, in this inductive circular process, to achieve consistency in the interpretation of the text, there was continued discussion and reflection between the researchers. The transcriptions were initially read several times to gain a sense of the whole context, and we analyzed each interview. The text was initially divided into domains that reflected the lowest degree of interpretation, as a rough structure was created in which the text had a specific area in common. The structure roughly reflected the interview guide’s themes, as guided by Graneheim and Lundman [ 24 ]. Thereafter, the text was divided into meaning units, condensed into text-near descriptions, and then abstracted and labeled further with codes. The codes were categorized based on similarities and differences. During this process, we discussed the findings to reach a consensus on the content, resulting in the final 4 categories presented in this paper.
Ethical Considerations
The interviewees received oral and written information about the study and its voluntary nature before the interviews. Written informed consent was obtained from all participants. Participants were able to opt of the study at any time. Data were anonymized and stored electronically on locked and secured servers. The Ethics Committee of the Capitol Region in Denmark was contacted before the start of the study. This study was registered and approved by the ethics committee and registered under the Danish Data Protection Agency (number P2021-839). Furthermore, the ethical principles of the Declaration of Helsinki were followed for this study.
The analysis provided insights into 4 different categories regarding digital practices and experiences of using digital tools and services in health care systems: social resources as a digital lifeline, possessing the necessary capabilities, big feelings as facilitators or barriers, and life without digital tools.
Social Resources as a Digital Lifeline
Throughout the analysis, it became evident that access to both material and social resources was of great importance when using digital tools. Most participants already possessed and had easy access to a computer, smartphone, or tablet. The few participants who did not own the necessary digital tools told us that they did not have the skills needed to use these tools. For these participants, the lack of material resources was tied particularly to a lack of knowledge and know-how, as they expressed that they would not know where to start after buying a computer—how to set it up, connect it to the internet, and use its many systems.
However, possessing the necessary material resources did not mean that the participants possessed the knowledge and skill to use digital tools. Furthermore, access to material resources was also a question of having access to assistance when needed. Some participants who had access to a computer, smartphone, and tablet and knew how to use these tools still had to obtain help when setting up hardware, updating software, or getting a new device. These participants were confident in their own ability to use digital devices but also relied on family, friends, and neighbors in their everyday use of these tools. Certain participants were explicitly aware of their own use of social resources when expressing their thoughts on digital services in health care systems:
I think it is a blessing and a curse. I think it is both. I would say that if I did not have someone around me in my family who was almost born into the digital world, then I think I would be in trouble. But I feel sorry for those who do not have that opportunity, and I know quite a few who do not. They get upset, and it’s really frustrating. [Woman, age 82 years]
The participants’ use of social resources indicates that learning skills and using digital tools are not solely individual tasks but rather continuously involve engagement with other people, particularly whenever a new unforeseen problem arises or when the participants want a deeper understanding of the tools they are using:
If tomorrow I have to get a new ipad...and it was like that when I got this one, then I had to get XXX to come and help me move stuff and he was sweet to help with all the practical stuff. I think I would have cursed a couple of times (if he hadn’t been there), but he is always helpful, but at the same time he is also pedagogic so I hope that next time he showed me something I will be able to do it. [Man, age 71 years]
For some participants, obtaining assistance from a more experienced family member was experienced as an opportunity to learn, whereas for other participants, their use of public digital services was even tied directly to assistance from a spouse or family member:
My wife, she has access to mine, so if something comes up, she can just go in and read, and we can talk about it afterwards what (it is). [Man, age 85 years]
The participants used social resources to navigate digital systems and understand and interpret communication from the health care system through digital devices. Another example of this was the participants who needed assistance to find, answer, and understand questionnaires from the health care department. Furthermore, social resources were viewed as a support system that made participants feel more comfortable and safer when operating digital tools. The social resources were particularly important when overcoming unforeseen and new challenges and when learning new skills related to the use of digital tools. Participants with physical, cognitive, and communicative challenges also explained how social resources were of great importance in their ability to use digital tools.
Possessing the Necessary Capabilities
The findings indicated that possessing the desire and knowing how to use digital tools are not always enough to engage with digital services successfully. Different health issues can carry consequences for motor skills and mobility. Some of these consequences were visibly affecting how our participants interacted with digital devices, and these challenges were somewhat easy to discover. However, our participants revealed hidden challenges that posed difficulties. In some specific cases, cognitive and communicative inabilities can make it difficult to use digital tools, and this might not always be clear until the individual tries to use a device’s more complex functions. An example of this is that some participants found it easy to turn on a computer and use it to write but difficult to go through security measures on digital services or interpret and understand digital language. Remembering passwords and logging on to systems created challenges, particularly for those experiencing health issues that directly affect memory and cognitive abilities, who expressed concerns about what they were able to do through digital tools:
I think it is very challenging because I would like to use it how I used to before my stroke; (I) wish that everything (digital skills) was transferred, but it just isn’t. [Man, age 80 years]
Despite these challenges, the participants demonstrated great interest in using digital tools, particularly regarding health care services and their own well-being. However, sometimes, the challenges that they experienced could not be conquered merely by motivation and good intentions. Another aspect of these challenges was the amount of extra time and energy that the participants had to spend on digital services. A patient diagnosed with Parkinson disease described how her symptoms created challenges that changed her digital practices:
Well it could for example be something like following a line in the device. And right now it is very limited what I can do with this (iPhone). Now I am almost only using it as a phone, and that is a little sad because I also like to text and stuff, but I also find that difficult (...) I think it is difficult to get an overview. [Woman, age 62 years]
Some participants said that after they were discharged from the hospital, they did not use the computer anymore because it was too difficult and too exhausting , which contributed to them giving up . Using digital tools already demanded a certain amount of concentration and awareness, and some diseases and health conditions affected these abilities further.
Big Feelings as Facilitators or Barriers
The findings revealed a wide range of digital practices in which digital tools were used as a communication device, as an entertainment device, and as a practical and informative tool for ordering medicine, booking consultations, asking health-related questions, or receiving email from public institutions. Despite these different digital practices, repeating patterns and arguments appeared when the participants were asked why they learned to use digital tools or wanted to improve their skills. A repeating argument was that they wanted to “follow the times, ” or as a participant who was still not satisfied with her digital skills stated:
We should not go against the future. [Woman, age 89 years]
The participants expressed a positive view of the technological developments and possibilities that digital devices offered, and they wanted to improve their knowledge and skills related to digital practice. For some participants, this was challenging, and they expressed frustration over how technological developments “moved too fast ,” but some participants interpreted these challenges as a way to “keep their mind sharp. ”
Another recurring pattern was that the participants expressed great interest in using digital services related to the health care system and other public institutions. The importance of being able to navigate digital services was explicitly clear when talking about finding test answers, written electronic messages, and questionnaires from the hospital or other public institutions. Keeping up with developments, communicating with public institutions, and taking an interest in their own health and well-being were described as good reasons to learn to use digital tools.
However, other aspects also affected these learning facilitators. Some participants felt alienated while using digital tools and described the practice as something related to feelings of anxiety, fear, and stupidity as well as something that demanded “a certain amount of courage. ” Some participants felt frustrated with the digital challenges they experienced, especially when the challenges were difficult to overcome because of their physical conditions:
I get sad because of it (digital challenges) and I get very frustrated and it takes a lot of time because I have difficulty seeing when I look away from the computer and have to turn back again to find out where I was and continue there (...) It pains me that I have to use so much time on it. [Man, age 71 years]
Fear of making mistakes, particularly when communicating with public institutions, for example, the health care system, was a common pattern. Another pattern was the fear of misinterpreting the sender and the need to ensure that the written electronic messages were actually from the described sender. Some participants felt that they were forced to learn about digital tools because they cared a lot about the services. Furthermore, fears of digital services replacing human interaction were a recurring concern among the participants. Despite these initial and recurring feelings, some participants learned how to navigate the digital services that they deemed relevant. Another recurring pattern in this learning process was repetition, the practice of digital skills, and consistent assistance from other people. One participant expressed the need to use the services often to remember the necessary skills:
Now I can figure it out because now I’ve had it shown 10 times. But then three months still pass... and then I think...how was it now? Then I get sweat on my forehead (feel nervous) and think; I’m not an idiot. [Woman, age 82 years]
For some participants, learning how to use digital tools demanded time and patience, as challenges had to be overcome more than once because they reappeared until the use of digital tools was more automatized into their everyday lives. Using digital tools and health services was viewed as easier and less stressful when part of everyday routines.
Life Without Digital Tools: Not a Free Choice
Even though some participants used digital tools daily, other participants expressed that it was “too late for them.” These participants did not view it as a free choice but as something they had to accept that they could not do. They wished that they could have learned it earlier in life but did not view it as a possibility in the future. Furthermore, they saw potential in digital services, including digital health care services, but they did not know exactly what services they were missing out on. Despite this lack of knowledge, they still felt sad about the position they were in. One participant expressed what she thought regarding the use of digital tools in public institutions:
Well, I feel alright about it, but it is very, very difficult for those of us who do not have it. Sometimes you can feel left out—outside of society. And when you do not have one of those (computers)...A reference is always made to w and w (www.) and then you can read on. But you cannot do that. [Woman, age 94 years]
The feeling of being left out of society was consistent among the participants who did not use digital tools. To them, digital systems seemed to provide unfair treatment based on something outside of their own power. Participants who were heavily affected by their medical conditions and could not use digital services also felt left out because they saw the advantages of using digital tools. Furthermore, a participant described the feelings connected to the use of digital tools in public institutions:
It is more annoying that it does not seem to work out in my favour. [Woman, age 62 years]
These statements indicated that it is possible for individuals to want to use digital tools and simultaneously find them too challenging. These participants were aware that there are consequences of not using digital tools, and that saddens them, as they feel like they are not receiving the same treatment as other people in society and the health care system.
Principal Findings
The insights from our findings demonstrated that our participants had different digital practices and different experiences with digital tools and services; however, the analysis also highlighted patterns related to how digital services and tools were used. Specific conditions were important for the possibility of digital practice, including having access to social resources; possessing the necessary capabilities; and feeling motivated, secure, and comfortable . These prerequisites were necessary to have positive experiences using digital tools in the health care system, although some participants who lived up to these prerequisites were still skeptical toward digital solutions. Others who did not live up to these prerequisites experienced challenges and even though they were aware of opportunities, this awareness made them feel left out. A few participants even viewed the digital tools as a threat to their participation in society. This supports the notion of Norgaard et al [ 13 ] that the attention paid to digital capability demands from eHealth systems is very important. Furthermore, our findings supported the argument of Hjeltholt and Papazu [ 17 ] that it is important to better understand experiences related to digital services. In our study, we accommodate this request and bring forth a broad perspective on experiences with digital practices; we particularly add insight into the challenges with digital practices for patients who also have acute or chronic illness, with some of them also experiencing physical, communicative, and cognitive difficulties. To our knowledge, there is limited existing literature focusing on digital practices that do not have a limited scope, for example, a focus on perspectives on eHealth literacy in the use of apps [ 26 ] or intervention studies with a focus on experiences with digital solutions, for example, telemedicine during the COVID-19 pandemic [ 27 ]. As mentioned by Hjeltholt et al [ 10 ], certain citizens are dependent on their own social networks in the process of using and learning digital tools. Rasi et al [ 28 ] and Airola et al [ 29 ] argued that digital health literacy is situated and should include the capabilities of the individual’s social network. Our findings support these arguments that access to social resources is an important condition; however, the findings also highlight that these resources can be particularly crucial in the use of digital health services, for example, when interpreting and understanding digital and written electronic messages related to one’s own health course or when dealing with physical, cognitive, and communicative disadvantages. Therefore, we argue that the awareness of the disadvantages is important if we want to understand patients’ digital capabilities, and the inclusion of the next of kin can be evident in unveiling challenges that are unknown and not easily visible or when trying to reach patients with digital challenges through digital means.
Studies by Kayser et al [ 30 ] and Kanoe et al [ 31 ] indicated that patients’ abilities to interpret and understand digital health–related services and their benefits are important for the successful implementation of eHealth services—an argument that our findings support. Health literacy in both digital and physical contexts is important if we want to understand how to better design and implement services. Our participants’ statements support the argument that communication through digital means cannot be viewed as similar to face-to-face communication and that an emphasis on digital health literacy demonstrates how health systems are demanding different capabilities from the patients [ 13 ]. We argue that it is important to communicate the purposes of digital services so that both the patient and their next of kin know why they participate and how it can benefit them. Therefore, it is important to make it as clear as possible that digital health services can benefit the patient and that these services are developed to support information, communication, and dialogue between patients and health professionals. However, our findings suggest that even after interpreting and understanding the purposes of digital health services, some patients may still experience challenges when using digital tools.
Therefore, it is important to understand how and why patients learn digital skills, particularly because both experience with digital devices and estimation of the value of digital tools have been highlighted as key factors for digital practices [ 5 , 18 ]. Our findings indicate that a combination of these factors is important, as recognizing the value of digital tools was not enough to facilitate the necessary learning process for some of our participants. Instead, our participants described the use of digital tools as complex and continuous processes in which automation of skills, assistance from others, and time to relearn forgotten knowledge were necessary and important facilitators for learning and understanding digital tools as well as becoming more comfortable and confident in the use of digital health services. This was particularly important, as it was more encouraging for our participants to learn digital tools when they felt secure, instead of feeling afraid and anxious, a point that Bailey et al [ 18 ] also highlighted. The value of digital solutions and the will to learn were greater when challenges were viewed as something to overcome and learn from instead of something that created a feeling of being stupid. This calls for attention on how to simplify and explain digital tools and services so that users do not feel alienated. Our findings also support the argument that digital health literacy should take into account emotional well-being related to digital practice [ 32 ].
The various perspectives that our participants provided regarding the use of digital tools in the health care system indicate that patients are affected by the use of digital health services and their own capabilities to use digital tools. Murray et al [ 33 ] argued that the use of digital tools in health sectors has the potential to improve health and health delivery by improving efficacy, efficiency, accessibility, safety, and personalization, and our participants also highlighted these positive aspects. However, different studies found that some patients, particularly older adults considered socially vulnerable, have lower digital health literacy [ 10 , 34 , 35 ], which is an important determinant of health and may widen disparities and inequity in health care [ 16 ]. Studies on older adult populations’ adaptation to information and communication technology show that engaging with this technology can be limited by the usability of technology, feelings of anxiety and concern, self-perception of technology use, and the need for assistance and inclusive design [ 36 ]. Our participants’ experiences with digital practices support the importance of these focus areas, especially when primarily older patients are admitted to hospitals. Furthermore, our findings indicate that some older patients who used to view themselves as being engaged in their own health care felt more distanced from the health care system because of digital services, and some who did not have the capabilities to use digital tools felt that they were treated differently compared to the rest of society. They did not necessarily view themselves as vulnerable but felt vulnerable in the specific experience of trying to use digital services because they wished that they were more capable. Moreover, this was the case for patients with physical and cognitive difficulties, as they were not necessarily aware of the challenges before experiencing them. Drawing on the phenomenological and feministic approach by Ahmed [ 37 ], these challenges that make patients feel vulnerable are not necessarily visible to others but can instead be viewed as invisible institutional “walls” that do not present themselves before the patient runs into them. Some participants had to experience how their physical, cognitive, or communicative difficulties affected their digital practice to realize that they were not as digitally capable as they once were or as others in society. Furthermore, viewed from this perspective, our findings could be used to argue that digital capabilities should be viewed as a privilege tied to users’ physical bodies and that digital services in the health care system are indirectly making patients without this privilege vulnerable. This calls for more attention to the inequities that digital tools and services create in health care systems and awareness that those who do not use digital tools are not necessarily indifferent about the consequences. Particularly, in a context such as the Danish one, in which the digital strategy is to create an intertwined and user-friendly public digital sector for everyone, it needs to be understood that patients have different digital capabilities and needs. Although some have not yet had a challenging experience that made them feel vulnerable, others are very aware that they receive different treatment and feel that they are on their own or that the rest of the society does not care about them. Inequities in digital health care, such as these, can and should be mitigated or prevented, and our investigation into the experiences with digital practices can help to show that we are creating standards and infrastructures that deliberately exclude the perspectives of those who are most in need of the services offered by the digital health care system [ 8 ]. Therefore, our findings support the notions that flexibility is important in the implementation of universal public digital services [ 17 ]; that it is important to adjust systems in accordance with patients’ eHealth literacy and not only improve the capabilities of individuals [ 38 ]; and that the development and improvement of digital health literacy are not solely an individual responsibility but are also tied to ways in which institutions organize, design, and implement digital tools and services [ 39 ].
Limitations
This qualitative study provided novel insights into the experiences with public digital health services from the perspective of patients in the Danish context, enabling a deeper understanding of how digital health services and digital tools are experienced and used. This helps build a solid foundation for future interventions aimed at digital health literacy and digital health interventions. However, this study has some limitations. First, the study was conducted in a country where digitalization is progressing quickly, and people, therefore, are accustomed to this pace. Therefore, readers must be aware of this. Second, the study included patients with different neurological conditions; some of their digital challenges were caused or worsened by these neurological conditions and are, therefore, not applicable to all patients in the health system. However, the findings provided insights into the patients’ digital practices before their conditions and other challenges not connected to neurological conditions shared by patients. Third, the study was broad, and although a large number of informants was included, from a qualitative research perspective, we would recommend additional research in this field to develop interventions that target digital health literacy and the use of digital health services.
Conclusions
Experiences with digital tools and digital health services are complex and multifaceted. The advantages in communication, finding information, or navigating through one’s own health course work as facilitators for engaging with digital tools and digital health services. However, this is not enough on its own. Furthermore, feeling secure and motivated and having time to relearn and practice skills are important facilitators. Engagement in digital practices for the examined population requires access to continuous assistance from their social network. If patients do not meet requirements, digital health services can be experienced as exclusionary and a source of concern. Physical, cognitive, and communicative difficulties might make it impossible to use digital tools or create more challenges that require assistance. Digitalization of the health care system means that patients do not have the choice to opt out of using digital services without having consequences, resulting in them receiving a different treatment than others. To ensure digitalization does not create inequities in health, it is necessary for developers and the health institutions that create, design, and implement digital services to be aware of differences in digital health literacy and to focus on simplifying communication with patients and next of kin through and about digital services. It is important to focus on helping individuals meet the necessary conditions and finding flexible solutions for those who do not have the same privileges as others if the public digital sector is to work for everyone.
Acknowledgments
The authors would like to thank all the people who gave their time to be interviewed for the study, the clinical nurse specialists who facilitated interviewing patients, and the other nurses on shift who assisted in recruiting participants.
Conflicts of Interest
None declared.
- Year in search 2022. Google Trends. URL: https://trends.google.com/trends/yis/2022/DK/ [accessed 2024-04-02]
- Digital government index: 2019. Organisation for Economic Cooperation and Development. URL: https://www.oecd-ilibrary.org/content/paper/4de9f5bb-en [accessed 2024-04-02]
- Azzopardi-Muscat N, Sørensen K. Towards an equitable digital public health era: promoting equity through a health literacy perspective. Eur J Public Health. Oct 01, 2019;29(Supplement_3):13-17. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Digital practices. Umeå University. URL: https://www.umu.se/en/humlab/research/digital-practice/ [accessed 2024-04-02]
- It-anvendelse i befolkningen 2020. Danmarks Statistik. URL: https://www.dst.dk/da/Statistik/nyheder-analyser-publ/Publikationer/VisPub?cid=29450 [accessed 2024-04-02]
- Sundhed.dk homepage. Sundhed.dk. URL: https://www.sundhed.dk/borger/ [accessed 2024-04-02]
- Nøhr C, Bertelsen P, Vingtoft S, Andersen SK. Digitalisering af Det Danske Sundhedsvæsen. Odense, Denmark. Syddansk Universitetsforlag; 2019.
- Eriksen J, Ebbesen M, Eriksen KT, Hjermitslev C, Knudsen C, Bertelsen P, et al. Equity in digital healthcare - the case of Denmark. Front Public Health. Sep 6, 2023;11:1225222. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Digital health strategy. Sundhedsdatastyrelsen. URL: https://sundhedsdatastyrelsen.dk/da/english/digital_health_solutions/digital_health_strategy [accessed 2024-04-02]
- Hjelholt M, Schou J, Bojsen LB, Yndigegn SL. Digital marginalisering af udsatte ældre: arbejdsrapport 2. IT-Universitetet i København. 2018. URL: https://egv.dk/images/Projekter/Projekter_2018/EGV_arbejdsrapport_2.pdf [accessed 2024-04-02]
- Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. Jan 25, 2012;12(1):80. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Improving health literacy. World Health Organization. URL: https://www.who.int/activities/improving-health-literacy [accessed 2024-04-02]
- Norgaard O, Furstrand D, Klokker L, Karnoe KA, Batterham R, Kayser L, et al. The e-health literacy framework: a conceptual framework for characterizing e-health users and their interaction with e-health systems. Knowl Manag E Learn. 2015;7(4). [ CrossRef ]
- Kramer JM, Schwartz A. Reducing barriers to patient-reported outcome measures for people with cognitive impairments. Arch Phys Med Rehabil. Aug 2017;98(8):1705-1715. [ CrossRef ] [ Medline ]
- Menger F, Morris J, Salis C. Aphasia in an internet age: wider perspectives on digital inclusion. Aphasiology. 2016;30(2-3):112-132. [ CrossRef ]
- Richardson S, Lawrence K, Schoenthaler AM, Mann D. A framework for digital health equity. NPJ Digit Med. Aug 18, 2022;5(1):119. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hjelholt M, Papazu I. "De har fået NemID, men det er ikke nemt for mig” - Digital rum(me)lighed i den danske velfærdsstat. Social Kritik. 2021;2021-2(163). [ FREE Full text ]
- Bailey C, Sheehan C. Technology, older persons’ perspectives and the anthropological ethnographic lens. Alter. 2009;3(2):96-109. [ CrossRef ]
- Gadamer HG, Weinsheimer HG, Marshall DG. Truth and Method. New York, NY. Crossroad Publishing Company; 1991.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. Dec 16, 2007;19(6):349-357. [ CrossRef ] [ Medline ]
- Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. Philadelphia, PA. Lippincott Williams & Wilkins, Inc; 2012.
- Kvale S, Brinkmann S. InterViews: Learning the Craft of Qualitative Research Interviewing. Thousand Oaks, CA. SAGE Publications; 2009.
- Kagan A. Supported conversation for adults with aphasia: methods and resources for training conversation partners. Aphasiology. Sep 1998;12(9):816-830. [ CrossRef ]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. Feb 2004;24(2):105-112. [ CrossRef ] [ Medline ]
- Krippendorff K. Content Analysis: An Introduction to Its Methodology. Thousand Oaks, CA. SAGE Publications; 1980.
- Klösch M, Sari-Kundt F, Reibnitz C, Osterbrink J. Patients' attitudes toward their health literacy and the use of digital apps in health and disease management. Br J Nurs. Nov 25, 2021;30(21):1242-1249. [ CrossRef ] [ Medline ]
- Datta P, Eiland L, Samson K, Donovan A, Anzalone AJ, McAdam-Marx C. Telemedicine and health access inequalities during the COVID-19 pandemic. J Glob Health. Dec 03, 2022;12:05051. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rasi P, Lindberg J, Airola E. Older service users’ experiences of learning to use eHealth applications in sparsely populated healthcare settings in Northern Sweden and Finland. Educ Gerontol. Nov 24, 2020;47(1):25-35. [ CrossRef ]
- Airola E, Rasi P, Outila M. Older people as users and non-users of a video conferencing service for promoting social connectedness and well-being – a case study from Finnish Lapland. Educ Gerontol. Mar 29, 2020;46(5):258-269. [ CrossRef ]
- Kayser L, Kushniruk A, Osborne RH, Norgaard O, Turner P. Enhancing the effectiveness of consumer-focused health information technology systems through eHealth literacy: a framework for understanding users' needs. JMIR Hum Factors. May 20, 2015;2(1):e9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Karnoe A, Furstrand D, Christensen KB, Norgaard O, Kayser L. Assessing competencies needed to engage with digital health services: development of the ehealth literacy assessment toolkit. J Med Internet Res. May 10, 2018;20(5):e178. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nielsen AS, Hanna L, Larsen BF, Appel CW, Osborne RH, Kayser L. Readiness, acceptance and use of digital patient reported outcome in an outpatient clinic. Health Informatics J. Jun 03, 2022;28(2):14604582221106000. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Murray E, Hekler EB, Andersson G, Collins LM, Doherty A, Hollis C, et al. Evaluating digital health interventions: key questions and approaches. Am J Prev Med. Nov 2016;51(5):843-851. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chesser A, Burke A, Reyes J, Rohrberg T. Navigating the digital divide: a systematic review of eHealth literacy in underserved populations in the United States. Inform Health Soc Care. Feb 24, 2016;41(1):1-19. [ CrossRef ] [ Medline ]
- Chesser AK, Keene Woods N, Smothers K, Rogers N. Health literacy and older adults: a systematic review. Gerontol Geriatr Med. Mar 15, 2016;2:2333721416630492. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mitra S, Singh A, Rajendran Deepam S, Asthana MK. Information and communication technology adoption among the older people: a qualitative approach. Health Soc Care Community. Nov 21, 2022;30(6):e6428-e6437. [ CrossRef ] [ Medline ]
- Ahmed S. How not to do things with words. Wagadu. 2016. URL: https://sites.cortland.edu/wagadu/wp-content/uploads/sites/3/2017/02/v16-how-not-to-do-ahmed.pdf [accessed 2024-04-02]
- Monkman H, Kushniruk AW. eHealth literacy issues, constructs, models, and methods for health information technology design and evaluation. Knowl Manag E Learn. 2015;7(4). [ CrossRef ]
- Brørs G, Norman CD, Norekvål TM. Accelerated importance of eHealth literacy in the COVID-19 outbreak and beyond. Eur J Cardiovasc Nurs. Aug 15, 2020;19(6):458-461. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 14.03.23; peer-reviewed by G Myreteg, J Eriksen, M Siermann; comments to author 18.09.23; revised version received 09.10.23; accepted 27.02.24; published 11.04.24.
©Christian Gybel Jensen, Frederik Gybel Jensen, Mia Ingerslev Loft. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 11.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
- Find a Lawyer
- Ask a Lawyer
- Research the Law
- Law Schools
- Laws & Regs
- Newsletters
- Justia Connect
- Pro Membership
- Basic Membership
- Justia Lawyer Directory
- Platinum Placements
- Gold Placements
- Justia Elevate
- Justia Amplify
- PPC Management
- Google Business Profile
- Social Media
- Justia Onward Blog
Q: Can I sue a large hospital for dropping the ball about 4 times before I got help for a severe case of sepsis
I think it first started with the placement of my pacemaker in January of 2022. I told the nurse I had a serious sinus infection and should we not wait? I was ignored. Then on February 28, 2022 I finally succumbed to a severe case of sepsis and ended up in the hospital where I almost died. I was there about 3 months in a coma, then almost 3 months of rehabilitation after that. What I'm complaining about are the numerous attempts I made to get help leading up to that horrible evening on 2-28-23 Visits to my primary care, visits to the ER, I finally had to Google my symptoms but by then it was too late and I couldn't get anyone at the ER to believe me. I am now permanently damaged, my face and neck are scarred and the skin is loose and saggy, my mind and brain were affected, my heart, I how have stage 3b kidney disease, my bladder is shot to hell, my diabetes worsened, I can barely walk, my back pain increased by leaps and bounds , I jerk, I shake, have trembles, don't sleep well

- Medical Malpractice Lawyer
- Las Vegas, NV
- (800) 894-2889
- Email Lawyer
- View Website
A: Yes you may have a case. Medical malpractice means that a doctor violated the standard of care. A bad outcome is not enough. Another doctor would be needed to evaluate what the doctors did.
Justia Ask a Lawyer is a forum for consumers to get answers to basic legal questions. Any information sent through Justia Ask a Lawyer is not secure and is done so on a non-confidential basis only.
The use of this website to ask questions or receive answers does not create an attorney–client relationship between you and Justia, or between you and any attorney who receives your information or responds to your questions, nor is it intended to create such a relationship. Additionally, no responses on this forum constitute legal advice, which must be tailored to the specific circumstances of each case. You should not act upon information provided in Justia Ask a Lawyer without seeking professional counsel from an attorney admitted or authorized to practice in your jurisdiction. Justia assumes no responsibility to any person who relies on information contained on or received through this site and disclaims all liability in respect to such information.
Justia cannot guarantee that the information on this website (including any legal information provided by an attorney through this service) is accurate, complete, or up-to-date. While we intend to make every attempt to keep the information on this site current, the owners of and contributors to this site make no claims, promises or guarantees about the accuracy, completeness or adequacy of the information contained in or linked to from this site.
- Bankruptcy Lawyers
- Business Lawyers
- Criminal Lawyers
- Employment Lawyers
- Estate Planning Lawyers
- Family Lawyers
- Personal Injury Lawyers
- Estate Planning
- Personal Injury
- Business Formation
- Business Operations
- Intellectual Property
- International Trade
- Real Estate
- Financial Aid
- Course Outlines
- Law Journals
- US Constitution
- Regulations
- Supreme Court
- Circuit Courts
- District Courts
- Dockets & Filings
- State Constitutions
- State Codes
- State Case Law
- Legal Blogs
- Business Forms
- Product Recalls
- Justia Connect Membership
- Justia Premium Placements
- Justia Elevate (SEO, Websites)
- Justia Amplify (PPC, GBP)
- Testimonials

IMAGES
VIDEO
COMMENTS
Clincal Case Practice Question 1. A 24-year-old woman presents with a fever and myalgias. She experienced brief, self-limited diarrhea 24 hours after attending a barbecue two weeks earlier. She remained asymptomatic until the day prior to presentation when she developed a fever of 39.4 C (103 F), conjunctivitis, and severe muscle pain.
The LITFL Clinical Case Collection includes over 250 Q&A style clinical cases to assist ' Just-in-Time Learning ' and ' Life-Long Learning '. Cases are categorized by specialty and can be interrogated by keyword from the Clinical Case searchable database. Search by keywords; disease process; condition; eponym or clinical features….
Hyperglycaemia case study with questions and answers - for doctors and medical students exams, finals and OSCEs.
Our Family Medicine Board Review Questions Help You Learn. The NEJM Knowledge+ Question of the Week provides an excellent way to test your core knowledge of family medicine topics. We draw from our bank of thousands of case-based questions across a range of diagnoses, settings, and patient demographics and aim to ensure that our questions are ...
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more. Download the Access App here: iOS and Android. Learn more here! Below is a limited selection of Case Files content on AccessMedicine. Click here to browse the full set of Case Files on Case Files Collection, which ...
Pinterest: ezmedlearning - Easy illustrations and flashcards. Practice clinical case scenario for medical, nursing, and healthcare students, as well as USMLE, NCLEX, board exam preparation and studies. Step-by-step report of the case presentation, diagnostic work up, differential diagnosis, management, and treatment.
Each scenario allows you to work through history taking, investigations, diagnosis and management. You might also be interested in our bank of 1000+ OSCE Stations. A collection of interactive medical and surgical OSCE cases (clinical case scenarios) to put your history, examination, investigation, diagnostic and management skills to the test.
NEJM Knowledge+ Internal Medicine Board Review already contains more than 1600 case-based questions on the most relevant and important topics in medicine today. We're adding another 50 case-based questions now (and 50 more in December 2016) to further expand that knowledge base. Most of the 50 new questions we've added relate to the ...
AccessMedicine Case Files Collection This link opens in a new window AccessMedicine's Case Files Collection from McGraw-Hill Education offers the best-selling Case Files content in an interactive format. Updated regularly, this comprehensive case collection helps students learn and apply basic science and clinical medicine concepts in the context of realistic patient cases.
Read full-text medical journal articles from Medscape's Internal Medicine Cases & Quizzes. News & Perspective Drugs & Diseases CME & Education Academy Video Decision Point Specialty: ...
On examination, the temperature was 36.4°C, the heart rate 103 beats per minute, the blood pressure 79/51 mm Hg, the respiratory rate 30 breaths per minute, and the oxygen saturation 99% while ...
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more. Download the Access App here: iOS and Android. Learn more here! Below is a limited selection of Case Files content on AccessMedicine. Click here to browse the full set of Case Files on Case Files Collection, which ...
(Case study from EBM Librarian: Teaching Tools: Scenarios.) ... Click "Next" below to practice formulating clinical questions using PICO format. << Previous: Primary vs. Secondary ... Maguire Medical Library Florida State University College of Medicine 1115 W. Call St., Tallahassee, FL 32306 Call 850-644-3883 (voicemail) or Text 850-724-4987 ...
ABG Examples (ABG exam questions for medical students OSCEs and MRCP PACES) Below are some brief clinical scenarios with ABG results. Try to interpret each ABG and formulate a differential diagnosis before looking at the answer. Question 1. You are called to see a 54 year old lady on the ward.
It is best to simply tell the story and let the outcome speak for itself. With these points in mind, let's begin the process of writing the case study: Title page: Title: The title page will contain the full title of the article. Remember that many people may find our article by searching on the internet.
Case Studies are usually single patient cases. Secondary Sources. Systematic Reviews are studies in which the authors ask a specific clinical question, perform a comprehensive literature search, eliminate poorly done studies, and attempt to make practice recommendations based on the well-done studies.
Background questions are best answered by medical textbooks, point-of-care tools such as DynaMed Plus and Essential Evidence Plus, and narrative reviews. ... Case control study: a study design that examines a group of people who have experienced an event (usually an adverse event) and a group of people who have not experienced the same event ...
A 68-year-old man was admitted to the hospital with fever, shortness of breath, and acute kidney injury. Testing of a nasopharyngeal swab for SARS-CoV-2 RNA was positive. Respiratory failure and hy...
Case Presentation. History of Present Illness: A 33-year-old white female presents after admission to the general medical/surgical hospital ward with a chief complaint of shortness of breath on exertion.She reports that she was seen for similar symptoms previously at her primary care physician's office six months ago.
LITFL 100+ Ultrasound quiz. Clinical cases and self assessment problems from the Ultrasound library to enhance interpretation skills through Ultrasound problems. Preparation for examinations. Each case presents a clinical scenario; a series of questions; clinical images and finally some pearls to highlight the key learning points.
Case Study Set 3: The patient arrives at the doctor's office complaining go pain in his left side. Upon palpation, the doctor determines that the patient has an ABNORMALLY LARGE SPLEEN which is known medically as _____. The doctor orders a blood test the results of which show AN ABNORMALLY RESULTED NUMBER OF PLATELETS IN THE SAMPLE OF BLOOD that was drawn for analysis.
2 0. 2. A 60 years old baker was diagnosed of a Primary Brain tumor. He was placed on oral dexamethasone 16 mg daily in divided dose by the managing Oncologist. The primary rationale for such action is. A. To reduce intracranial pressure from edema associated with the tumor. B. To aid the shrinking of tumor.
An 82-year-old woman was admitted because of difficulty walking, falls, and cognitive decline. Light touch of the right hand, right knee, and both feet caused pain. A diagnosis was made.
This information supersedes guidance that was provided in the October 2018 ACS Bulletin column "CPT Coding for Hepatobiliary Surgery.". Case: A patient with hepatocellular carcinoma underwent an exploratory laparoscopy to obtain a liver biopsy and assess the peritoneal cavity to exclude advance disease. The reportable code is 47379 ...
RADIOLOGY.AND NUCLEAR MEDICINE 869 Wyinr {arnia PRACTICAL APPLICATIONS CASE STUDY: MELANOMA FOLLOW-UP Rill ¢ Bill Smith, a 51-year-old sales representative, was initially diagnosed with stage II1 melanoma 4 years ago 3-month follow-up CT. 1. lswers to the questions are found on page 876 He underwent surgery and received interferon treatment at ...
The random and representative nature of the case-cohort design enables its application to future outcome studies [Citation 20]. The study was rigorously conducted with regular external quality monitoring. GA was established in all participants using ultrasound before 14 weeks' gestation, minimizing the risk of misclassifying PTB and term births.
The Food and Drug Administration (FDA) granted an emergency use authorization (EUA) to a medicine meant to protect certain immunocompromised people against COVID-19. The medicine, pemivibart (brand name Pemgarda™), is for people who are at least 12 years of age, weigh more than 88 pounds, and are moderately to severely immunocompromised.
Background: The digitalization of public and health sectors worldwide is fundamentally changing health systems. With the implementation of digital health services in health institutions, a focus on digital health literacy and the use of digital health services have become more evident. In Denmark, public institutions use digital tools for different purposes, aiming to create a universal public ...
Read 1 Answer from lawyers to Can I sue a large hospital for dropping the ball about 4 times before I got help for a severe case of sepsis - Tennessee Medical Malpractice Questions & Answers - Justia Ask a Lawyer