Essay on Smoking
500 words essay on smoking.
One of the most common problems we are facing in today’s world which is killing people is smoking. A lot of people pick up this habit because of stress , personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them. It has many ill-effects on the human body which we will go through in the essay on smoking.


Ill-Effects of Smoking
Tobacco can have a disastrous impact on our health. Nonetheless, people consume it daily for a long period of time till it’s too late. Nearly one billion people in the whole world smoke. It is a shocking figure as that 1 billion puts millions of people at risk along with themselves.
Cigarettes have a major impact on the lungs. Around a third of all cancer cases happen due to smoking. For instance, it can affect breathing and causes shortness of breath and coughing. Further, it also increases the risk of respiratory tract infection which ultimately reduces the quality of life.
In addition to these serious health consequences, smoking impacts the well-being of a person as well. It alters the sense of smell and taste. Further, it also reduces the ability to perform physical exercises.
It also hampers your physical appearances like giving yellow teeth and aged skin. You also get a greater risk of depression or anxiety . Smoking also affects our relationship with our family, friends and colleagues.
Most importantly, it is also an expensive habit. In other words, it entails heavy financial costs. Even though some people don’t have money to get by, they waste it on cigarettes because of their addiction.
How to Quit Smoking?
There are many ways through which one can quit smoking. The first one is preparing for the day when you will quit. It is not easy to quit a habit abruptly, so set a date to give yourself time to prepare mentally.
Further, you can also use NRTs for your nicotine dependence. They can reduce your craving and withdrawal symptoms. NRTs like skin patches, chewing gums, lozenges, nasal spray and inhalers can help greatly.
Moreover, you can also consider non-nicotine medications. They require a prescription so it is essential to talk to your doctor to get access to it. Most importantly, seek behavioural support. To tackle your dependence on nicotine, it is essential to get counselling services, self-materials or more to get through this phase.
One can also try alternative therapies if they want to try them. There is no harm in trying as long as you are determined to quit smoking. For instance, filters, smoking deterrents, e-cigarettes, acupuncture, cold laser therapy, yoga and more can work for some people.
Always remember that you cannot quit smoking instantly as it will be bad for you as well. Try cutting down on it and then slowly and steadily give it up altogether.
Get the huge list of more than 500 Essay Topics and Ideas
Conclusion of the Essay on Smoking
Thus, if anyone is a slave to cigarettes, it is essential for them to understand that it is never too late to stop smoking. With the help and a good action plan, anyone can quit it for good. Moreover, the benefits will be evident within a few days of quitting.
FAQ of Essay on Smoking
Question 1: What are the effects of smoking?
Answer 1: Smoking has major effects like cancer, heart disease, stroke, lung diseases, diabetes, and more. It also increases the risk for tuberculosis, certain eye diseases, and problems with the immune system .
Question 2: Why should we avoid smoking?
Answer 2: We must avoid smoking as it can lengthen your life expectancy. Moreover, by not smoking, you decrease your risk of disease which includes lung cancer, throat cancer, heart disease, high blood pressure, and more.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Tobacco, Nicotine, and E-Cigarettes Research Report What are the physical health consequences of tobacco use?
Cigarette smoking harms nearly every organ in the body, 1,44 and smoking is the leading preventable cause of premature death in the United States. Although rates of smoking have declined, it is estimated that it leads to about 480,000 deaths yearly. 1 Smokers aged 60 and older have a twofold increase in mortality compared with those who have never smoked, dying an estimated 6 years earlier. 45 Quitting smoking results in immediate health benefits, and some or all of the reduced life expectancy can be recovered depending on the age a person quits. 46
Although nicotine itself does not cause cancer, at least 69 chemicals in tobacco smoke are carcinogenic, 1 and cigarette smoking accounts for at least 30 percent of all cancer deaths. 22 The overall rates of death from cancer are twice as high among smokers as nonsmokers, with heavy smokers having a four times greater risk of death from cancer than nonsmokers. 1
Foremost among the cancers caused by tobacco use is lung cancer. Cigarette smoking has been linked to about 80 to 90 percent of all cases of lung cancer, the leading cause of cancer death for both men and women, and it is responsible for roughly 80 percent of deaths from this disease. 22,47 Smoking increases lung cancer risk five to tenfold, with greater risk among heavy smokers. 48 Smoking is also associated with cancers of the mouth, pharynx, larynx, esophagus, stomach, pancreas, cervix, kidney, and bladder, as well as acute myeloid. 1 Cigarette smoking is not the only form of tobacco use associated with cancers. Smokeless tobacco (see " Other Tobacco Products ") has been linked to cancer of the pharynx, esophagus, stomach, and lung, as well as to colorectal cancer. 49
In addition to cancer, smoking causes lung diseases such as chronic bronchitis and emphysema, and it has been found to exacerbate asthma symptoms in adults and children. Cigarette smoking is the most significant risk factor for chronic obstructive pulmonary disease (COPD). 50 Survival statistics indicate that quitting smoking results in repair to much of the smoking-induced lung damage over time. However, once COPD develops, it is irreversible; COPD-related lung damage is not repaired with time.
Smoking also substantially increases the risk of heart disease, including stroke, heart attack, vascular disease, and aneurysm. 51,52 Cardiovascular disease is responsible for 40 percent of all smoking-related deaths. 53 Smoking causes coronary heart disease, the leading cause of death in the United States. Smoking is also linked to many other major health conditions—including rheumatoid arthritis, inflammation, and impaired immune function. 1 Even young smokers aged 26 to 41 report reduced health-related quality of life compared with nonsmoking peers, according to a cross-sectional population study. 54 Recent animal research also identified a pathway between the pancreas and a part of the brain active in nicotine intake, potentially linking cigarette smoking to the risk of developing Type 2 Diabetes.
- Help & Support
- Quit Smoking
- Tobacco Facts
- Health Effects of Smoking and Tobacco Products
Health Effects of Smoking
Smoking is the number one cause of preventable disease and death worldwide. Smoking-related diseases claim more than 480,000 lives in the U.S. each year. Smoking costs the U.S. at least $289 billion each year, including at least $151 billion in lost productivity and $130 billion in direct healthcare expenditures. 1
Key Facts about Smoking
- Cigarette smoke contains more than 7,000 chemicals, at least 69 of which are known to cause cancer. 2 Smoking is directly responsible for approximately 90 percent of lung cancer deaths and approximately 80 percent of deaths caused by chronic obstructive pulmonary disease (COPD), including emphysema and chronic bronchitis. 1
- Among adults who have ever smoked daily, 78% had smoked their first cigarette by the time they were 18 years of age, and 94% had by age 21. 3
- Among current smokers, 73% of their diagnosed smoking-related conditions are chronic lung diseases. Even among smokers who have quit, chronic lung disease still accounts for 50% of smoking-related conditions. 4
- Smoking harms nearly every organ in the body, and is a main cause of lung cancer and COPD. It also is a cause of coronary heart disease, stroke and a host of other cancers and diseases. 1 See more of the health effects caused by smoking.
Smoking Rates among Adults & Youth
- In 2017, an estimated 34.3 million, or 14.0% of adults 18 years of age and older were current cigarette smokers. 5
- Men tend to smoke more than women. In 2017, 15.8% of men currently smoked cigarettes daily compared to 12.2% of women. 5
- Prevalence of current cigarette smoking in 2017 was highest among American Indians/Alaska Natives (24.6%), non-Hispanic whites (15.3%) and non-Hispanic blacks (15.1%), and was lowest among Hispanics (9.9%) and Asian-Americans (7.0%). 5
- In 2017, 7.6 % of high school students and 2.1% of middle school students were current cigarette users. 6
Facts about Quitting Smoking
- Nicotine is the chemical in cigarettes that causes addiction. Smokers not only become physically addicted to nicotine; they also link smoking with many social activities, making smoking an extremely difficult addiction to break. 7
- In 2017, an estimated 55.2 million adults were former smokers. Of the 34.3 million current adult smokers, 48.4% stopped smoking for a day or more in the preceding year because they were trying to quit smoking completely. 5
- Quitting smoking for good often requires multiple attempts. Using counseling or medication alone increases the chance of a quit attempt being successful; the combination of both is even more effective. 8
- There are seven medications approved by the U.S. Food and Drug Administration to aid in quitting smoking. Nicotine patches, nicotine gum and nicotine lozenges are available over the counter, and a nicotine nasal spray and inhaler are currently available by prescription. Bupropion SR (Zyban®) and varenicline (Chantix®) are non-nicotine pills. 8
- Individual, group and telephone counseling are effective. Telephone quitline counseling is available in all 50 states and is effective for many different groups of smokers. 8
Learn about the American Lung Association’s programs to help you or a loved one quit smoking , and join our advocacy efforts to reduce tobacco use and exposure to secondhand smoke. Visit Lung.org or call the Lung HelpLine at 1-800-LUNGUSA (1-800-586-4872).
The Health Effects of Smoking
U.S. Department of Health and Human Services. The Health Consequences of Smoking - 50 Years of Progress: A Report of the Surgeon General. 2014.
U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease A Report of the Surgeon General. 2010.
Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health, 2017. Analysis by the American Lung Association Epidemiology and Statistics Unit using SPSS software.
U.S. Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General, 2004.
Centers for Disease Control and Prevention. National Center for Health Statistics. National Health Interview Survey, 2015. Analysis performed by the American Lung Association Epidemiology and Statistics Unit using SPSS software.
Centers for Disease Control and Prevention. National Youth Tobacco Survey, 2017. Analysis by the American Lung Association Epidemiology and Statistics Unit using SPSS software.
National Institute on Drug Abuse. Tobacco/Nicotine Research Report: Is Nicotine Addictive? January 2018.
Fiore M, Jaen C, Baker T, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Vol 35. Rockville, MD; 2008.
Page last updated: May 2, 2024
A Breath of Fresh Air in Your Inbox
Join over 700,000 people who receive the latest news about lung health, including research, lung disease, air quality, quitting tobacco, inspiring stories and more!
You will now receive email updates from the American Lung Association.
Make a Donation
Your tax-deductible donation funds lung disease and lung cancer research, new treatments, lung health education, and more.
Become a Lung Health Insider
Thank you! You will now receive email updates from the American Lung Association.
Select Your Location
Select your location to view local American Lung Association events and news near you.
Change Language
Lung helpline.
Talk to our lung health experts at the American Lung Association. Our service is free and we are here to help you.
1-800-LUNG-USA
(1-800-586-4872)

Essay on Harmful Effects of Smoking
Students are often asked to write an essay on Harmful Effects of Smoking in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Harmful Effects of Smoking
Introduction.
Smoking is a dangerous habit that poses significant health risks. It’s not only harmful to smokers, but also to those around them.
Health Risks
Smoking can cause lung cancer, heart disease, and stroke. It damages nearly every organ in the body, leading to premature death.
Secondhand Smoke
Non-smokers exposed to secondhand smoke face similar health risks. They can develop respiratory problems and increased risk of heart disease.
Impact on Environment
Cigarette butts litter the environment and release toxic chemicals into the soil and water, harming wildlife.
Smoking is harmful for everyone. It’s important to stay away from this deadly habit.
250 Words Essay on Harmful Effects of Smoking
Smoking is a widespread habit, yet it is one of the most detrimental practices to human health. Despite the awareness campaigns and statutory warnings, many continue to smoke, oblivious of the damaging effects it has on their health and wellbeing.
Physical Health Risks
Primarily, smoking causes numerous fatal diseases. It is the leading cause of lung cancer, accounting for about 85% of all cases. It also significantly increases the risk of heart diseases and stroke. The harmful chemicals in cigarettes damage blood vessels, leading to atherosclerosis, which can result in heart attack or stroke.
Impact on Respiratory System
Moreover, smoking adversely affects the respiratory system. It leads to chronic bronchitis, emphysema, and other lung diseases. The smoke and toxins inhaled damage the airways and alveoli, the tiny air sacs in the lungs, causing chronic obstructive pulmonary disease (COPD).
Effect on Mental Health
Smoking also influences mental health. Nicotine addiction can lead to increased stress, anxiety, and depression. The temporary relief from stress that smoking provides is often mistaken for a stress reliever, while it is actually exacerbating the problem.
In conclusion, smoking is a harmful habit that poses significant threats to physical and mental health. The myriad diseases it causes, coupled with its addictive nature, make it a dangerous lifestyle choice. It is imperative to raise awareness about these harmful effects and encourage cessation to safeguard public health.
500 Words Essay on Harmful Effects of Smoking
Smoking is a prevalent habit, often started out of curiosity, peer pressure, or stress management. However, its harmful effects are well-documented, impacting nearly every organ in the human body. Despite the widespread knowledge of its adverse effects, smoking continues to be a significant public health concern.
The Impact on Physical Health
One of the most severe consequences of smoking is its impact on physical health. Smokers are at a higher risk of developing a plethora of diseases, including lung cancer, heart disease, stroke, and chronic obstructive pulmonary disease (COPD). These conditions are often fatal, leading to premature death. The toxins in cigarette smoke damage the lining of the lungs, making smokers more susceptible to infections like pneumonia.
Detrimental Effects on Mental Health
Smoking doesn’t just harm the physical body; it also has a profound effect on mental health. Nicotine, the addictive substance in tobacco, alters the brain chemistry, leading to dependence. This dependence can exacerbate mental health conditions such as anxiety and depression. Furthermore, the stress of addiction and the struggle to quit smoking can also take a toll on mental well-being.
Smoking and Second-hand Smoke
The harmful effects of smoking are not confined to the smoker alone. Second-hand smoke, also known as passive smoking, is a significant concern. Non-smokers exposed to second-hand smoke inhale the same dangerous chemicals as smokers. This exposure increases their risk of developing heart disease, lung cancer, and other respiratory conditions.
Societal Impact
Smoking also has societal implications. The economic burden of smoking is substantial, with healthcare costs for smoking-related illnesses reaching astronomical levels. Additionally, the loss of productivity due to illness or premature death contributes to economic strain.
In conclusion, the harmful effects of smoking are far-reaching, affecting not only the smoker but also those around them and society at large. The physical and mental health implications, coupled with the economic burden, make it a significant public health issue. Despite the addictive nature of smoking, quitting is possible with the right support and resources, leading to improved health outcomes and quality of life. Understanding the full scope of smoking’s harmful effects is crucial in motivating smokers to quit and preventing non-smokers from starting.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Effects of Smoking
- Essay on Dangers of Smoking
- Essay on Cyclone
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2012.

Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General.
1 introduction, summary, and conclusions.
- Introduction
Tobacco use is a global epidemic among young people. As with adults, it poses a serious health threat to youth and young adults in the United States and has significant implications for this nation’s public and economic health in the future ( Perry et al. 1994 ; Kessler 1995 ). The impact of cigarette smoking and other tobacco use on chronic disease, which accounts for 75% of American spending on health care ( Anderson 2010 ), is well-documented and undeniable. Although progress has been made since the first Surgeon General’s report on smoking and health in 1964 ( U.S. Department of Health, Education, and Welfare [USDHEW] 1964 ), nearly one in four high school seniors is a current smoker. Most young smokers become adult smokers. One-half of adult smokers die prematurely from tobacco-related diseases ( Fagerström 2002 ; Doll et al. 2004 ). Despite thousands of programs to reduce youth smoking and hundreds of thousands of media stories on the dangers of tobacco use, generation after generation continues to use these deadly products, and family after family continues to suffer the devastating consequences. Yet a robust science base exists on social, biological, and environmental factors that influence young people to use tobacco, the physiology of progression from experimentation to addiction, other health effects of tobacco use, the epidemiology of youth and young adult tobacco use, and evidence-based interventions that have proven effective at reducing both initiation and prevalence of tobacco use among young people. Those are precisely the issues examined in this report, which aims to support the application of this robust science base.
Nearly all tobacco use begins in childhood and adolescence ( U.S. Department of Health and Human Services [USDHHS] 1994 ). In all, 88% of adult smokers who smoke daily report that they started smoking by the age of 18 years (see Chapter 3 , “The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide”). This is a time in life of great vulnerability to social influences ( Steinberg 2004 ), such as those offered through the marketing of tobacco products and the modeling of smoking by attractive role models, as in movies ( Dalton et al. 2009 ), which have especially strong effects on the young. This is also a time in life of heightened sensitivity to normative influences: as tobacco use is less tolerated in public areas and there are fewer social or regular users of tobacco, use decreases among youth ( Alesci et al. 2003 ). And so, as we adults quit, we help protect our children.
Cigarettes are the only legal consumer products in the world that cause one-half of their long-term users to die prematurely ( Fagerström 2002 ; Doll et al. 2004 ). As this epidemic continues to take its toll in the United States, it is also increasing in low- and middle-income countries that are least able to afford the resulting health and economic consequences ( Peto and Lopez 2001 ; Reddy et al. 2006 ). It is past time to end this epidemic. To do so, primary prevention is required, for which our focus must be on youth and young adults. As noted in this report, we now have a set of proven tools and policies that can drastically lower youth initiation and use of tobacco products. Fully committing to using these tools and executing these policies consistently and aggressively is the most straight forward and effective to making future generations tobacco-free.
The 1994 Surgeon General’s Report
This Surgeon General’s report on tobacco is the second to focus solely on young people since these reports began in 1964. Its main purpose is to update the science of smoking among youth since the first comprehensive Surgeon General’s report on tobacco use by youth, Preventing Tobacco Use Among Young People , was published in 1994 ( USDHHS 1994 ). That report concluded that if young people can remain free of tobacco until 18 years of age, most will never start to smoke. The report documented the addiction process for young people and how the symptoms of addiction in youth are similar to those in adults. Tobacco was also presented as a gateway drug among young people, because its use generally precedes and increases the risk of using illicit drugs. Cigarette advertising and promotional activities were seen as a potent way to increase the risk of cigarette smoking among young people, while community-wide efforts were shown to have been successful in reducing tobacco use among youth. All of these conclusions remain important, relevant, and accurate, as documented in the current report, but there has been considerable research since 1994 that greatly expands our knowledge about tobacco use among youth, its prevention, and the dynamics of cessation among young people. Thus, there is a compelling need for the current report.
Tobacco Control Developments
Since 1994, multiple legal and scientific developments have altered the tobacco control environment and thus have affected smoking among youth. The states and the U.S. Department of Justice brought lawsuits against cigarette companies, with the result that many internal documents of the tobacco industry have been made public and have been analyzed and introduced into the science of tobacco control. Also, the 1998 Master Settlement Agreement with the tobacco companies resulted in the elimination of billboard and transit advertising as well as print advertising that directly targeted underage youth and limitations on the use of brand sponsorships ( National Association of Attorneys General [NAAG] 1998 ). This settlement also created the American Legacy Foundation, which implemented a nationwide antismoking campaign targeting youth. In 2009, the U.S. Congress passed a law that gave the U.S. Food and Drug Administration authority to regulate tobacco products in order to promote the public’s health ( Family Smoking Prevention and Tobacco Control Act 2009 ). Certain tobacco companies are now subject to regulations limiting their ability to market to young people. In addition, they have had to reimburse state governments (through agreements made with some states and the Master Settlement Agreement) for some health care costs. Due in part to these changes, there was a decrease in tobacco use among adults and among youth following the Master Settlement Agreement, which is documented in this current report.
Recent Surgeon General Reports Addressing Youth Issues
Other reports of the Surgeon General since 1994 have also included major conclusions that relate to tobacco use among youth ( Office of the Surgeon General 2010 ). In 1998, the report focused on tobacco use among U.S. racial/ethnic minority groups ( USDHHS 1998 ) and noted that cigarette smoking among Black and Hispanic youth increased in the 1990s following declines among all racial/ethnic groups in the 1980s; this was particularly notable among Black youth, and culturally appropriate interventions were suggested. In 2000, the report focused on reducing tobacco use ( USDHHS 2000b ). A major conclusion of that report was that school-based interventions, when implemented with community- and media-based activities, could reduce or postpone the onset of smoking among adolescents by 20–40%. That report also noted that effective regulation of tobacco advertising and promotional activities directed at young people would very likely reduce the prevalence and onset of smoking. In 2001, the Surgeon General’s report focused on women and smoking ( USDHHS 2001 ). Besides reinforcing much of what was discussed in earlier reports, this report documented that girls were more affected than boys by the desire to smoke for the purpose of weight control. Given the ongoing obesity epidemic ( Bonnie et al. 2007 ), the current report includes a more extensive review of research in this area.
The 2004 Surgeon General’s report on the health consequences of smoking ( USDHHS 2004 ) concluded that there is sufficient evidence to infer that a causal relationship exists between active smoking and (a) impaired lung growth during childhood and adolescence; (b) early onset of decline in lung function during late adolescence and early adulthood; (c) respiratory signs and symptoms in children and adolescents, including coughing, phlegm, wheezing, and dyspnea; and (d) asthma-related symptoms (e.g., wheezing) in childhood and adolescence. The 2004 Surgeon General’s report further provided evidence that cigarette smoking in young people is associated with the development of atherosclerosis.
The 2010 Surgeon General’s report on the biology of tobacco focused on the understanding of biological and behavioral mechanisms that might underlie the pathogenicity of tobacco smoke ( USDHHS 2010 ). Although there are no specific conclusions in that report regarding adolescent addiction, it does describe evidence indicating that adolescents can become dependent at even low levels of consumption. Two studies ( Adriani et al. 2003 ; Schochet et al. 2005 ) referenced in that report suggest that because the adolescent brain is still developing, it may be more susceptible and receptive to nicotine than the adult brain.
Scientific Reviews
Since 1994, several scientific reviews related to one or more aspects of tobacco use among youth have been undertaken that also serve as a foundation for the current report. The Institute of Medicine (IOM) ( Lynch and Bonnie 1994 ) released Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youths, a report that provided policy recommendations based on research to that date. In 1998, IOM provided a white paper, Taking Action to Reduce Tobacco Use, on strategies to reduce the increasing prevalence (at that time) of smoking among young people and adults. More recently, IOM ( Bonnie et al. 2007 ) released a comprehensive report entitled Ending the Tobacco Problem: A Blueprint for the Nation . Although that report covered multiple potential approaches to tobacco control, not just those focused on youth, it characterized the overarching goal of reducing smoking as involving three distinct steps: “reducing the rate of initiation of smoking among youth (IOM [ Lynch and Bonnie] 1994 ), reducing involuntary tobacco smoke exposure ( National Research Council 1986 ), and helping people quit smoking” (p. 3). Thus, reducing onset was seen as one of the primary goals of tobacco control.
As part of USDHHS continuing efforts to assess the health of the nation, prevent disease, and promote health, the department released, in 2000, Healthy People 2010 and, in 2010, Healthy People 2020 ( USDHHS 2000a , 2011 ). Healthy People provides science-based, 10-year national objectives for improving the health of all Americans. For 3 decades, Healthy People has established benchmarks and monitored progress over time in order to encourage collaborations across sectors, guide individuals toward making informed health decisions, and measure the impact of prevention activities. Each iteration of Healthy People serves as the nation’s disease prevention and health promotion roadmap for the decade. Both Healthy People 2010 and Healthy People 2020 highlight “Tobacco Use” as one of the nation’s “Leading Health Indicators,” feature “Tobacco Use” as one of its topic areas, and identify specific measurable tobacco-related objectives and targets for the nation to strive for. Healthy People 2010 and Healthy People 2020 provide tobacco objectives based on the most current science and detailed population-based data to drive action, assess tobacco use among young people, and identify racial and ethnic disparities. Additionally, many of the Healthy People 2010 and 2020 tobacco objectives address reductions of tobacco use among youth and target decreases in tobacco advertising in venues most often influencing young people. A complete list of the healthy people 2020 objectives can be found on their Web site ( USDHHS 2011 ).
In addition, the National Cancer Institute (NCI) of the National Institutes of Health has published monographs pertinent to the topic of tobacco use among youth. In 2001, NCI published Monograph 14, Changing Adolescent Smoking Prevalence , which reviewed data on smoking among youth in the 1990s, highlighted important statewide intervention programs, presented data on the influence of marketing by the tobacco industry and the pricing of cigarettes, and examined differences in smoking by racial/ethnic subgroup ( NCI 2001 ). In 2008, NCI published Monograph 19, The Role of the Media in Promoting and Reducing Tobacco Use ( NCI 2008 ). Although young people were not the sole focus of this Monograph, the causal relationship between tobacco advertising and promotion and increased tobacco use, the impact on youth of depictions of smoking in movies, and the success of media campaigns in reducing youth tobacco use were highlighted as major conclusions of the report.
The Community Preventive Services Task Force (2011) provides evidence-based recommendations about community preventive services, programs, and policies on a range of topics including tobacco use prevention and cessation ( Task Force on Community Preventive Services 2001 , 2005 ). Evidence reviews addressing interventions to reduce tobacco use initiation and restricting minors’ access to tobacco products were cited and used to inform the reviews in the current report. The Cochrane Collaboration (2010) has also substantially contributed to the review literature on youth and tobacco use by producing relevant systematic assessments of health-related programs and interventions. Relevant to this Surgeon General’s report are Cochrane reviews on interventions using mass media ( Sowden 1998 ), community interventions to prevent smoking ( Sowden and Stead 2003 ), the effects of advertising and promotional activities on smoking among youth ( Lovato et al. 2003 , 2011 ), preventing tobacco sales to minors ( Stead and Lancaster 2005 ), school-based programs ( Thomas and Perara 2006 ), programs for young people to quit using tobacco ( Grimshaw and Stanton 2006 ), and family programs for preventing smoking by youth ( Thomas et al. 2007 ). These reviews have been cited throughout the current report when appropriate.
In summary, substantial new research has added to our knowledge and understanding of tobacco use and control as it relates to youth since the 1994 Surgeon General’s report, including updates and new data in subsequent Surgeon General’s reports, in IOM reports, in NCI Monographs, and in Cochrane Collaboration reviews, in addition to hundreds of peer-reviewed publications, book chapters, policy reports, and systematic reviews. Although this report is a follow-up to the 1994 report, other important reviews have been undertaken in the past 18 years and have served to fill the gap during an especially active and important time in research on tobacco control among youth.
- Focus of the Report
Young People
This report focuses on “young people.” In general, work was reviewed on the health consequences, epidemiology, etiology, reduction, and prevention of tobacco use for those in the young adolescent (11–14 years of age), adolescent (15–17 years of age), and young adult (18–25 years of age) age groups. When possible, an effort was made to be specific about the age group to which a particular analysis, study, or conclusion applies. Because hundreds of articles, books, and reports were reviewed, however, there are, unavoidably, inconsistencies in the terminology used. “Adolescents,” “children,” and “youth” are used mostly interchangeably throughout this report. In general, this group encompasses those 11–17 years of age, although “children” is a more general term that will include those younger than 11 years of age. Generally, those who are 18–25 years old are considered young adults (even though, developmentally, the period between 18–20 years of age is often labeled late adolescence), and those 26 years of age or older are considered adults.
In addition, it is important to note that the report is concerned with active smoking or use of smokeless tobacco on the part of the young person. The report does not consider young people’s exposure to secondhand smoke, also referred to as involuntary or passive smoking, which was discussed in the 2006 report of the Surgeon General ( USDHHS 2006 ). Additionally, the report does not discuss research on children younger than 11 years old; there is very little evidence of tobacco use in the United States by children younger than 11 years of age, and although there may be some predictors of later tobacco use in those younger years, the research on active tobacco use among youth has been focused on those 11 years of age and older.
Tobacco Use
Although cigarette smoking is the most common form of tobacco use in the United States, this report focuses on other forms as well, such as using smokeless tobacco (including chew and snuff) and smoking a product other than a cigarette, such as a pipe, cigar, or bidi (tobacco wrapped in tendu leaves). Because for young people the use of one form of tobacco has been associated with use of other tobacco products, it is particularly important to monitor all forms of tobacco use in this age group. The term “tobacco use” in this report indicates use of any tobacco product. When the word “smoking” is used alone, it refers to cigarette smoking.
- Organization of the Report
This chapter begins by providing a short synopsis of other reports that have addressed smoking among youth and, after listing the major conclusions of this report, will end by presenting conclusions specific to each chapter. Chapter 2 of this report (“The Health Consequences of Tobacco Use Among Young People”) focuses on the diseases caused by early tobacco use, the addiction process, the relation of body weight to smoking, respiratory and pulmonary problems associated with tobacco use, and cardiovascular effects. Chapter 3 (“The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide”) provides recent and long-term cross-sectional and longitudinal data on cigarette smoking, use of smokeless tobacco, and the use of other tobacco products by young people, by racial/ethnic group and gender, primarily in the United States, but including some worldwide data as well. Chapter 4 (“Social, Environmental, Cognitive, and Genetic Influences on the Use of Tobacco Among Youth”) identifies the primary risk factors associated with tobacco use among youth at four levels, including the larger social and physical environments, smaller social groups, cognitive factors, and genetics and neurobiology. Chapter 5 (“The Tobacco Industry’s Influences on the Use of Tobacco Among Youth”) includes data on marketing expenditures for the tobacco industry over time and by category, the effects of cigarette advertising and promotional activities on young people’s smoking, the effects of price and packaging on use, the use of the Internet and movies to market tobacco products, and an evaluation of efforts by the tobacco industry to prevent tobacco use among young people. Chapter 6 (“Efforts to Prevent and Reduce Tobacco Use Among Young People”) provides evidence on the effectiveness of family-based, clinic-based, and school-based programs, mass media campaigns, regulatory and legislative approaches, increased cigarette prices, and community and statewide efforts in the fight against tobacco use among youth. Chapter 7 (“A Vision for Ending the Tobacco Epidemic”) points to next steps in preventing and reducing tobacco use among young people.
- Preparation of the Report
This report of the Surgeon General was prepared by the Office on Smoking and Health (OSH), National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention (CDC), USDHHS. In 2008, 18 external independent scientists reviewed the 1994 report and suggested areas to be added and updated. These scientists also suggested chapter editors and a senior scientific editor, who were contacted by OSH. Each chapter editor named external scientists who could contribute, and 33 content experts prepared draft sections. The draft sections were consolidated into chapters by the chapter editors and then reviewed by the senior scientific editor, with technical editing performed by CDC. The chapters were sent individually to 34 peer reviewers who are experts in the areas covered and who reviewed the chapters for scientific accuracy and comprehensiveness. The entire manuscript was then sent to more than 25 external senior scientists who reviewed the science of the entire document. After each review cycle, the drafts were revised by the chapter and senior scientific editor on the basis of the experts’ comments. Subsequently, the report was reviewed by various agencies within USDHHS. Publication lags prevent up-to-the-minute inclusion of all recently published articles and data, and so some more recent publications may not be cited in this report.
- Evaluation of the Evidence
Since the first Surgeon General’s report in 1964 on smoking and health ( USDHEW 1964 ), major conclusions concerning the conditions and diseases caused by cigarette smoking and the use of smokeless tobacco have been based on explicit criteria for causal inference ( USDHHS 2004 ). Although a number of different criteria have been proposed for causal inference since the 1960s, this report focuses on the five commonly accepted criteria that were used in the original 1964 report and that are discussed in greater detail in the 2004 report on the health consequences of smoking ( USDHHS 2004 ). The five criteria refer to the examination of the association between two variables, such as a risk factor (e.g., smoking) and an outcome (e.g., lung cancer). Causal inference between these variables is based on (1) the consistency of the association across multiple studies; this is the persistent finding of an association in different persons, places, circumstances, and times; (2) the degree of the strength of association, that is, the magnitude and statistical significance of the association in multiple studies; (3) the specificity of the association to clearly demonstrate that tobacco use is robustly associated with the condition, even if tobacco use has multiple effects and multiple causes exist for the condition; (4) the temporal relationship of the association so that tobacco use precedes disease onset; and (5) the coherence of the association, that is, the argument that the association makes scientific sense, given data from other sources and understanding of biological and psychosocial mechanisms ( USDHHS 2004 ). Since the 2004 Surgeon General’s report, The Health Consequences of Smoking , a four-level hierarchy ( Table 1.1 ) has been used to assess the research data on associations discussed in these reports ( USDHHS 2004 ). In general, this assessment was done by the chapter editors and then reviewed as appropriate by peer reviewers, senior scientists, and the scientific editors. For a relationship to be considered sufficient to be characterized as causal, multiple studies over time provided evidence in support of each criteria.
Four-level hierarchy for classifying the strength of causal inferences based on available evidence.
When a causal association is presented in the chapter conclusions in this report, these four levels are used to describe the strength of the evidence of the association, from causal (1) to not causal (4). Within the report, other terms are used to discuss the evidence to date (i.e., mixed, limited, and equivocal evidence), which generally represent an inadequacy of data to inform a conclusion.
However, an assessment of a casual relationship is not utilized in presenting all of the report’s conclusions. The major conclusions are written to be important summary statements that are easily understood by those reading the report. Some conclusions, particularly those found in Chapter 3 (epidemiology), provide observations and data related to tobacco use among young people, and are generally not examinations of causal relationships. For those conclusions that are written using the hierarchy above, a careful and extensive review of the literature has been undertaken for this report, based on the accepted causal criteria ( USDHHS 2004 ). Evidence that was characterized as Level 1 or Level 2 was prioritized for inclusion as chapter conclusions.
In additional to causal inferences, statistical estimation and hypothesis testing of associations are presented. For example, confidence intervals have been added to the tables in the chapter on the epidemiology of youth tobacco use (see Chapter 3 ), and statistical testing has been conducted for that chapter when appropriate. The chapter on efforts to prevent tobacco use discusses the relative improvement in tobacco use rates when implementing one type of program (or policy) versus a control program. Statistical methods, including meta-analytic methods and longitudinal trajectory analyses, are also presented to ensure that the methods of evaluating data are up to date with the current cutting-edge research that has been reviewed. Regardless of the methods used to assess significance, the five causal criteria discussed above were applied in developing the conclusions of each chapter and the report.
- Major Conclusions
- Cigarette smoking by youth and young adults has immediate adverse health consequences, including addiction, and accelerates the development of chronic diseases across the full life course.
- Prevention efforts must focus on both adolescents and young adults because among adults who become daily smokers, nearly all first use of cigarettes occurs by 18 years of age (88%), with 99% of first use by 26 years of age.
- Advertising and promotional activities by tobacco companies have been shown to cause the onset and continuation of smoking among adolescents and young adults.
- After years of steady progress, declines in the use of tobacco by youth and young adults have slowed for cigarette smoking and stalled for smokeless tobacco use.
- Coordinated, multicomponent interventions that combine mass media campaigns, price increases including those that result from tax increases, school-based policies and programs, and statewide or community-wide changes in smoke-free policies and norms are effective in reducing the initiation, prevalence, and intensity of smoking among youth and young adults.
- Chapter Conclusions
The following are the conclusions presented in the substantive chapters of this report.
Chapter 2. The Health Consequences of Tobacco Use Among Young People
- The evidence is sufficient to conclude that there is a causal relationship between smoking and addiction to nicotine, beginning in adolescence and young adulthood.
- The evidence is suggestive but not sufficient to conclude that smoking contributes to future use of marijuana and other illicit drugs.
- The evidence is suggestive but not sufficient to conclude that smoking by adolescents and young adults is not associated with significant weight loss, contrary to young people’s beliefs.
- The evidence is sufficient to conclude that there is a causal relationship between active smoking and both reduced lung function and impaired lung growth during childhood and adolescence.
- The evidence is sufficient to conclude that there is a causal relationship between active smoking and wheezing severe enough to be diagnosed as asthma in susceptible child and adolescent populations.
- The evidence is sufficient to conclude that there is a causal relationship between smoking in adolescence and young adulthood and early abdominal aortic atherosclerosis in young adults.
- The evidence is suggestive but not sufficient to conclude that there is a causal relationship between smoking in adolescence and young adulthood and coronary artery atherosclerosis in adulthood.
Chapter 3. The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide
- Among adults who become daily smokers, nearly all first use of cigarettes occurs by 18 years of age (88%), with 99% of first use by 26 years of age.
- Almost one in four high school seniors is a current (in the past 30 days) cigarette smoker, compared with one in three young adults and one in five adults. About 1 in 10 high school senior males is a current smokeless tobacco user, and about 1 in 5 high school senior males is a current cigar smoker.
- Among adolescents and young adults, cigarette smoking declined from the late 1990s, particularly after the Master Settlement Agreement in 1998. This decline has slowed in recent years, however.
- Significant disparities in tobacco use remain among young people nationwide. The prevalence of cigarette smoking is highest among American Indians and Alaska Natives, followed by Whites and Hispanics, and then Asians and Blacks. The prevalence of cigarette smoking is also highest among lower socioeconomic status youth.
- Use of smokeless tobacco and cigars declined in the late 1990s, but the declines appear to have stalled in the last 5 years. The latest data show the use of smokeless tobacco is increasing among White high school males, and cigar smoking may be increasing among Black high school females.
- Concurrent use of multiple tobacco products is prevalent among youth. Among those who use tobacco, nearly one-third of high school females and more than one-half of high school males report using more than one tobacco product in the last 30 days.
- Rates of tobacco use remain low among girls relative to boys in many developing countries, however, the gender gap between adolescent females and males is narrow in many countries around the globe.
Chapter 4. Social, Environmental, Cognitive, and Genetic Influences on the Use of Tobacco Among Youth
- Given their developmental stage, adolescents and young adults are uniquely susceptible to social and environmental influences to use tobacco.
- Socioeconomic factors and educational attainment influence the development of youth smoking behavior. The adolescents most likely to begin to use tobacco and progress to regular use are those who have lower academic achievement.
- The evidence is sufficient to conclude that there is a causal relationship between peer group social influences and the initiation and maintenance of smoking behaviors during adolescence.
- Affective processes play an important role in youth smoking behavior, with a strong association between youth smoking and negative affect.
- The evidence is suggestive that tobacco use is a heritable trait, more so for regular use than for onset. The expression of genetic risk for smoking among young people may be moderated by small-group and larger social-environmental factors.
Chapter 5. The Tobacco Industry’s Influences on the Use of Tobacco Among Youth
- In 2008, tobacco companies spent $9.94 billion on the marketing of cigarettes and $547 million on the marketing of smokeless tobacco. Spending on cigarette marketing is 48% higher than in 1998, the year of the Master Settlement Agreement. Expenditures for marketing smokeless tobacco are 277% higher than in 1998.
- Tobacco company expenditures have become increasingly concentrated on marketing efforts that reduce the prices of targeted tobacco products. Such expenditures accounted for approximately 84% of cigarette marketing and more than 77% of the marketing of smokeless tobacco products in 2008.
- The evidence is sufficient to conclude that there is a causal relationship between advertising and promotional efforts of the tobacco companies and the initiation and progression of tobacco use among young people.
- The evidence is suggestive but not sufficient to conclude that tobacco companies have changed the packaging and design of their products in ways that have increased these products’ appeal to adolescents and young adults.
- The tobacco companies’ activities and programs for the prevention of youth smoking have not demonstrated an impact on the initiation or prevalence of smoking among young people.
- The evidence is sufficient to conclude that there is a causal relationship between depictions of smoking in the movies and the initiation of smoking among young people.
Chapter 6. Efforts to Prevent and Reduce Tobacco Use Among Young People
- The evidence is sufficient to conclude that mass media campaigns, comprehensive community programs, and comprehensive statewide tobacco control programs can prevent the initiation of tobacco use and reduce its prevalence among youth.
- The evidence is sufficient to conclude that increases in cigarette prices reduce the initiation, prevalence, and intensity of smoking among youth and young adults.
- The evidence is sufficient to conclude that school-based programs with evidence of effectiveness, containing specific components, can produce at least short-term effects and reduce the prevalence of tobacco use among school-aged youth.
- Adriani W, Spijker S, Deroche-Gamonet V, Laviola G, Le Moal M, Smit AB, Piazza PV. Evidence for enhanced neurobehavioral vulnerability to nicotine during peri-adolescence in rats. Journal of Neuroscience. 2003; 23 (11):4712–6. [ PMC free article : PMC6740776 ] [ PubMed : 12805310 ]
- Alesci NL, Forster JL, Blaine T. Smoking visibility, perceived acceptability, and frequency in various locations among youth and adults. Preventive Medicine. 2003; 36 (3):272–81. [ PubMed : 12634018 ]
- Anderson G. Chronic Care: Making the Case for Ongoing Care. Princeton (NJ): Robert Wood Johnson Foundation; 2010. [accessed: November 30, 2011]. < http://www .rwjf.org/files /research/50968chronic .care.chartbook.pdf >.
- Bonnie RJ, Stratton K, Wallace RB, editors. Ending the Tobacco Problem: A Blueprint for the Nation. Washington: National Academies Press; 2007.
- Cochrane Collaboration. Home page. 2010. [accessed: November 30, 2010]. < http://www .cochrane.org/ >.
- Community Preventive Services Task Force. First Annual Report to Congress and to Agencies Related to the Work of the Task Force. Community Preventive Services Task Force. 2011. [accessed: January 9, 2012]. < http://www .thecommunityguide .org/library /ARC2011/congress-report-full.pdf >.
- Dalton MA, Beach ML, Adachi-Mejia AM, Longacre MR, Matzkin AL, Sargent JD, Heatherton TF, Titus-Ernstoff L. Early exposure to movie smoking predicts established smoking by older teens and young adults. Pediatrics. 2009; 123 (4):e551–e558. [ PMC free article : PMC2758519 ] [ PubMed : 19336346 ]
- Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ (British Medical Journal). 2004; 32 :1519. [ PMC free article : PMC437139 ] [ PubMed : 15213107 ] [ CrossRef ]
- Fagerström K. The epidemiology of smoking: health consequences and benefits of cessation. Drugs. 2002; 62 (Suppl 2):1–9. [ PubMed : 12109931 ]
- Family Smoking Prevention and Tobacco Control Act, Public Law 111-31, 123 U.S. Statutes at Large 1776 (2009)
- Grimshaw G, Stanton A. Tobacco cessation interventions for young people. Cochrane Database of Systematic Reviews. 2006;(4):CD003289. [ PubMed : 17054164 ] [ CrossRef ]
- Kessler DA. Nicotine addiction in young people. New England Journal of Medicine. 1995; 333 (3):186–9. [ PubMed : 7791824 ]
- Lovato C, Linn G, Stead LF, Best A. Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours. Cochrane Database of Systematic Reviews. 2003;(4):CD003439. [ PubMed : 14583977 ] [ CrossRef ]
- Lovato C, Watts A, Stead LF. Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours. Cochrane Database of Systematic Reviews. 2011;(10):CD003439. [ PMC free article : PMC7173757 ] [ PubMed : 21975739 ] [ CrossRef ]
- Lynch BS, Bonnie RJ, editors. Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youths. Washington: National Academies Press; 1994. [ PubMed : 25144107 ]
- National Association of Attorneys General. Master Settlement Agreement. 1998. [accessed: June 9, 2011]. < http://www .naag.org/back-pages /naag/tobacco /msa/msa-pdf/MSA%20with %20Sig%20Pages%20and%20Exhibits .pdf/file_view >.
- National Cancer Institute. Changing Adolescent Smoking Prevalence. Bethesda (MD): U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 2001. Smoking and Tobacco Control Monograph No. 14. NIH Publication. No. 02-5086.
- National Cancer Institute. The Role of the Media in Promoting and Reducing Tobacco Use. Bethesda (MD): U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2008. Tobacco Control Monograph No. 19. NIH Publication No. 07-6242.
- National Research Council. Environmental Tobacco Smoke: Measuring Exposures and Assessing Health Effects. Washington: National Academy Press; 1986. [ PubMed : 25032469 ]
- Office of the Surgeon General Reports of the Surgeon General, U.S. Public Health Service. 2010. [accessed: November 30, 2010]. < http://www .surgeongeneral .gov/library/reports/index.html >.
- Perry CL, Eriksen M, Giovino G. Tobacco use: a pediatric epidemic [editorial] Tobacco Control. 1994; 3 (2):97–8.
- Peto R, Lopez AD. Future worldwide health effects of current smoking patterns. In: Koop CE, Pearson CE, Schwarz MR, editors. Critical Issues in Global Health. San Francisco: Wiley (Jossey-Bass); 2001. pp. 154–61.
- Reddy KS, Perry CL, Stigler MH, Arora M. Differences in tobacco use among young people in urban India by sex, socioeconomic status, age, and school grade: assessment of baseline survey data. Lancet. 2006; 367 (9510):589–94. [ PubMed : 16488802 ]
- Schochet TL, Kelley AE, Landry CF. Differential expression of arc mRNA and other plasticity-related genes induced by nicotine in adolescent rat forebrain. Neuroscience. 2005; 135 (1):285–97. [ PMC free article : PMC1599838 ] [ PubMed : 16084664 ]
- Sowden AJ. Mass media interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews. 1998;(4):CD001006. [ PubMed : 10796581 ] [ CrossRef ]
- Sowden AJ, Stead LF. Community interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews. 2003;(1):CD001291. [ PubMed : 12535406 ] [ CrossRef ]
- Stead LF, Lancaster T. Interventions for preventing tobacco sales to minors. Cochrane Database of Systematic Reviews. 2005;(1):CD001497. [ PubMed : 15674880 ] [ CrossRef ]
- Steinberg L. Risk taking in adolescence: what changes, and why? Annals of the New York Academy of Sciences. 2004; 1021 :51–8. [ PubMed : 15251873 ]
- Task Force on Community Preventive Services. Recommendations regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. American Journal of Preventive Medicine. 2001; 20 (2 Suppl):S10–S15. [ PubMed : 11173214 ]
- Task Force on Community Preventive Services. Tobacco. In: Zaza S, Briss PA, Harris KW, editors. The Guide to Preventive Services: What Works to Promote Health? New York: Oxford University Press; 2005. pp. 3–79. < http://www .thecommunityguide .org/tobacco/Tobacco.pdf >.
- Thomas RE, Baker PRA, Lorenzetti D. Family-based programmes for preventing smoking by children and adolescents. Cochrane Database of Systematic Reviews. 2007;(1):CD004493. [ PubMed : 17253511 ] [ CrossRef ]
- Thomas RE, Perera R. School-based programmes for preventing smoking. Cochrane Database of Systematic Reviews. 2006;(3):CD001293. [ PubMed : 16855966 ] [ CrossRef ]
- US Department of Health and Human Services. Preventing Tobacco Use Among Young People A Report of the Surgeon General. Atlanta (GA): US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994.
- US Department of Health and Human Services. Tobacco Use Among US Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998.
- U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington: U.S. Government Printing Office; 2000.
- US Department of Health and Human Services. Reducing Tobacco Use: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000.
- US Department of Health and Human Services. Women and Smoking A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2001.
- US Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004.
- US Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [ PubMed : 20669524 ]
- US Department of Health and Human Services. How Tobacco Smoke Causes Disease—The Biology and Behavioral Basis for Tobacco-Attributable Disease: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [ PubMed : 21452462 ]
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020. 2011. [accessed: November 1, 2011]. < http://www .healthypeople .gov/2020/default.aspx >.
- US Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Center for Disease Control; 1964. PHS Publication No. 1103.
- Cite this Page National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2012. 1, Introduction, Summary, and Conclusions.
- PDF version of this title (18M)
In this Page
Other titles in these collections.
- Reports of the Surgeon General
- Health Services/Technology Assessment Text (HSTAT)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Introduction, Summary, and Conclusions - Preventing Tobacco Use Among Youth and ... Introduction, Summary, and Conclusions - Preventing Tobacco Use Among Youth and Young Adults
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Health Effects of Cigarette Smoking
- Secondhand Smoke
- E-cigarettes (Vapes)
- Menthol Tobacco Products
- Morbidity and Mortality Weekly Reports (MMWR)
- About Surveys
- Other Tobacco Products
- Smoking and Tobacco Use Features
- Patient Care Settings and Smoking Cessation
- Patient Care
- Funding Opportunity Announcements
- State and Community Work
- National and State Tobacco Control Program
- Multimedia and Tools
- Tobacco - Health Equity
- Tobacco - Surgeon General's Reports
- State Tobacco Activities Tracking and Evaluation (STATE) System
- Global Tobacco Control
Health Effects of Cigarettes: Cardiovascular Disease
At a glance.
- Smoking is a major cause of cardiovascular disease (CVD) and is responsible for one in every four deaths from CVD.
- Secondhand smoke exposure causes heart disease and stroke.
- Quitting smoking can protect people from cardiovascular disease and death. People who already have heart disease also benefit from quitting smoking.

Cardiovascular disease overview
Cardiovascular diseases (CVDs) are diseases of the heart and blood vessels. CVDs include heart disease , stroke , and peripheral artery disease . 1
Heart disease includes several types of heart conditions. In the United States, the most common type of heart disease is coronary heart disease (CHD). CHD is also known as coronary artery disease. CHD is caused by plaque buildup in the walls of the arteries that carry blood to the heart. 2 3 Plaque is made up of deposits of cholesterol and other substances. It can cause the arteries to narrow over time. This process is called atherosclerosis. CHD can cause:
- Chest pain 2
- Heart attack (when blood flow to the heart becomes blocked and a section of the heart muscle is damaged or dies) 2 4
- Heart failure (when the heart cannot pump enough blood and oxygen to support other organs) 2 5
- Arrhythmia (when the heart beats too fast, too slow, or irregularly) 2 6
A stroke occurs when there is a blockage to the blood supply to the brain or when a blood vessel in the brain bursts. This causes parts of the brain to become damaged or die. 7 Stroke can cause disability such as paralysis (loss of muscle movement), muscle weakness, trouble speaking, and memory loss. 7 It can also cause death. 7
Peripheral artery disease (PAD) is the narrowing or blocking of peripheral arteries. These arteries carry blood from the heart to other parts of the body. 8 9 Similar to CHD, plaque in the arteries can cause this narrowing or blockage. PAD most commonly affects the legs and lower body. But it can also occur in the arms and upper body. Symptoms of PAD can include:
- Muscle pain during physical activity, like walking, that quickly gets better after resting.
- Feelings of weakness or numbness in the legs that make it feel harder to walk.
- Having one arm or leg feel colder than the other.
Smoking and cardiovascular disease
Smoking is a major cause of CVD, causing one in every four deaths from CVD. 10
Smoking can: 11
- Raise triglycerides (a type of fat in your blood)
- Lower "good" cholesterol (HDL)
- Make blood sticky and more likely to clot, which can block blood flow to the heart and brain
- Damage cells that line the blood vessels
- Increase the buildup of plaque in blood vessels
- Cause thickening and narrowing of blood vessels
Smoking increases the risk of many CVDs including: 10 11
- Atherosclerosis
- Coronary heart disease (CHD), including heart attack and sudden cardiac death
- Peripheral arterial disease (PAD)
- Abdominal aortic aneurysm
Secondhand smoke exposure and cardiovascular disease
Secondhand smoke is the smoke from burning tobacco products like cigarettes, cigars, pipes, or hookahs. Secondhand smoke exposure occurs when people breathe in smoke from burning tobacco products. Exposure also occurs when people breathe in smoke breathed out by a person smoking. 10 11 12 13 Exposure to secondhand smoke increases the risk for coronary heart disease and stroke. 10 11 12 13 14
- Each year in the United States, secondhand smoke causes nearly 34,000 deaths from coronary heart disease among people who do not smoke. It also causes more than 8,000 deaths from stroke among people who do not smoke.
- People who do not smoke but breathe secondhand smoke at home or at work increase their risk of developing heart disease by 25%–30%.
- Secondhand smoke increases the risk for stroke by 20%−30%.
- Breathing secondhand smoke, even for a short time, can damage blood vessels and cause blood to become stickier. These changes can increase the risk of having a heart attack.
Quitting smoking can protect people from cardiovascular disease
Quitting smoking is one of the most important actions people who smoke can take to reduce their risk for cardiovascular disease and death. This is true for all people who smoke, regardless of age or how long or how much someone has smoked. 14
Quitting smoking: 14
- Reduces markers of inflammation and hypercoagulability (a condition where blood is more likely to form blood clots)
- Improves "good" cholesterol (HDL)
- Reduces the development and progression of atherosclerosis
- Reduces the risk of coronary heart disease A
- Reduces the risk of stroke A
- Reduces the risk of abdominal aortic aneurysm A
Research also suggests that quitting smoking may reduce the risk of:
- Atrial fibrillation
- Sudden cardiac death
- Heart failure
- Venous thromboembolism
- Peripheral arterial disease
People who already have coronary heart disease also benefit from quitting smoking. Quitting smoking can lower the risk of having another heart attack and the risk of dying from heart disease. 14
After quitting smoking, the risk of cardiovascular disease drops rapidly and then continues to decrease over time: 14
- 1 to 2 years after quitting, risk of heart attack drops sharply
- 3 to 6 years after quitting, added risk of coronary heart disease drops by half
- 5 to 10 years after quitting, risk of stroke decreases
- 15 years after quitting, risk of coronary heart disease drops to close to that of someone who does not smoke

Continue reading
- CDC.gov/quit
- About Heart Disease
- About Stroke
- Smoking and Heart Disease and Stroke
- Million Hearts ® Tobacco Use
- Heart Disease Resources for Health Care Professionals
- Tobacco Use and Cessation Resources Health Care Providers
- Reduced risk refers to quitting smoking in comparison to continued smoking.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: What It Means to You. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2004. Accessed April 24, 2024. https://stacks.cdc.gov/view/cdc/11987
- Centers for Disease Control and Prevention. About Heart Disease . Accessed April 24, 2024. https://www.cdc.gov/heartdisease/about.htm
- U.S. National Library of Medicine. Coronary Heart Disease . Accessed April 24, 2024. https://medlineplus.gov/ency/article/007115.htm
- Centers for Disease Control and Prevention. Heart Attack . Accessed April 24, 2024. https://www.cdc.gov/heartdisease/heart_attack.htm
- Centers for Disease Control and Prevention . Heart Failure Fact Sheet . Accessed April 24, 2024. https://www.cdc.gov/heartdisease/heart_failure.htm
- National Heart, Lung, and Blood Institute. What is an Arrhythmia? Accessed April 24, 2024. https://www.nhlbi.nih.gov/health-topics/arrhythmia
- Centers for Disease Control and Prevention. About Stroke . Accessed April 24, 2024. https://www.cdc.gov/stroke/about.htm
- Centers for Disease Control and Prevention. Peripheral Arterial Disease (PAD). Accessed April 24, 2024. https://www.cdc.gov/heartdisease/PAD.htm
- National Heart, Lung, and Blood Institute. Peripheral Artery Disease - What Is Peripheral Artery Disease? Accessed April 24, 2024. https://www.nhlbi.nih.gov/health/peripheral-artery-disease
- U.S. Department of Health and Human Services . The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014. Accessed April 24, 2024. https://www.ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf
- U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2010. Accessed April 24, 2024. https://www.ncbi.nlm.nih.gov/books/NBK53017/
- Institute of Medicine. Secondhand Smoke Exposure and Cardiovascular Effects: Making Sense of the Evidence. Washington: National Academy of Sciences, Institute of Medicine, 2009. Accessed April 24, 2024. https://www.ncbi.nlm.nih.gov/books/NBK219565/pdf/Bookshelf_NBK219565.pdf
- National Toxicology Program. Report on Carcinogens, Fourteenth Edition . Research Triangle Park (NC): U.S. Department of Health and Human Services, Public Health Service, 2016. Sense of the Evidence. Washington: National Academy of Sciences, Institute of Medicine, 2009. Accessed April 24, 2024. https://ntp.niehs.nih.gov/pubhealth/roc/index-1.html
- U.S. Department of Health and Human Services. Smoking Cessation: A Report of the Surgeon General . Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2020. Accessed April 24, 2024. https://www.hhs.gov/sites/default/files/2020-cessation-sgr-full-report.pdf
Smoking and Tobacco Use
Commercial tobacco use is the leading cause of preventable disease, disability, and death in the United States.
For Everyone
Health care providers, public health.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 24 March 2022
Tobacco and nicotine use
- Bernard Le Foll 1 , 2 ,
- Megan E. Piper 3 , 4 ,
- Christie D. Fowler 5 ,
- Serena Tonstad 6 ,
- Laura Bierut 7 ,
- Lin Lu ORCID: orcid.org/0000-0003-0742-9072 8 , 9 ,
- Prabhat Jha 10 &
- Wayne D. Hall 11 , 12
Nature Reviews Disease Primers volume 8 , Article number: 19 ( 2022 ) Cite this article
34k Accesses
69 Citations
96 Altmetric
Metrics details
- Disease genetics
- Experimental models of disease
- Preventive medicine
Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will die prematurely from tobacco-related complications. In addition, people who smoke have a significant reduction in their quality of life. Neurobiological findings have identified the mechanisms by which nicotine in tobacco affects the brain reward system and causes addiction. These brain changes contribute to the maintenance of nicotine or tobacco use despite knowledge of its negative consequences, a hallmark of addiction. Effective approaches to screen, prevent and treat tobacco use can be widely implemented to limit tobacco’s effect on individuals and society. The effectiveness of psychosocial and pharmacological interventions in helping people quit smoking has been demonstrated. As the majority of people who smoke ultimately relapse, it is important to enhance the reach of available interventions and to continue to develop novel interventions. These efforts associated with innovative policy regulations (aimed at reducing nicotine content or eliminating tobacco products) have the potential to reduce the prevalence of tobacco and nicotine use and their enormous adverse impact on population health.
Similar content being viewed by others

Associations between classic psychedelics and nicotine dependence in a nationally representative sample
Use of electronic cigarettes and heated tobacco products during the covid-19 pandemic.

Smoking cessation behaviors and reasons for use of electronic cigarettes and heated tobacco products among Romanian adults
Introduction.
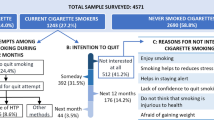
Tobacco is the second most commonly used psychoactive substance worldwide, with more than one billion smokers globally 1 . Although smoking prevalence has reduced in many high-income countries (HICs), tobacco use is still very prevalent in low-income and middle-income countries (LMICs). The majority of smokers are addicted to nicotine delivered by cigarettes (defined as tobacco dependence in the International Classification of Diseases, Tenth Revision (ICD-10) or tobacco use disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)). As a result of the neuro-adaptations and psychological mechanisms caused by repeated exposure to nicotine delivered rapidly by cigarettes, cessation can also lead to a well-characterized withdrawal syndrome, typically manifesting as irritability, anxiety, low mood, difficulty concentrating, increased appetite, insomnia and restlessness, that contributes to the difficulty in quitting tobacco use 2 , 3 , 4 .
Historically, tobacco was used in some cultures as part of traditional ceremonies, but its use was infrequent and not widely disseminated in the population. However, since the early twentieth century, the use of commercial cigarettes has increased dramatically 5 because of automated manufacturing practices that enable large-scale production of inexpensive products that are heavily promoted by media and advertising. Tobacco use became highly prevalent in the past century and was followed by substantial increases in the prevalence of tobacco-induced diseases decades later 5 . It took decades to establish the relationship between tobacco use and associated health effects 6 , 7 and to discover the addictive role of nicotine in maintaining tobacco smoking 8 , 9 , and also to educate people about these effects. It should be noted that the tobacco industry disputed this evidence to allow continuing tobacco sales 10 . The expansion of public health campaigns to reduce smoking has gradually decreased the use of tobacco in HICs, with marked increases in adult cessation, but less progress has been achieved in LMICs 1 .
Nicotine is the addictive compound in tobacco and is responsible for continued use of tobacco despite harms and a desire to quit, but nicotine is not directly responsible for the harmful effects of using tobacco products (Box 1 ). Other components in tobacco may modulate the addictive potential of tobacco (for example, flavours and non-nicotine compounds) 11 . The major harms related to tobacco use, which are well covered elsewhere 5 , are linked to a multitude of compounds present in tobacco smoke (such as carcinogens, toxicants, particulate matter and carbon monoxide). In adults, adverse health outcomes of tobacco use include cancer in virtually all peripheral organs exposed to tobacco smoke and chronic diseases such as eye disease, periodontal disease, cardiovascular diseases, chronic obstructive pulmonary disease, stroke, diabetes mellitus, rheumatoid arthritis and disorders affecting immune function 5 . Moreover, smoking during pregnancy can increase the risk of adverse reproductive effects, such as ectopic pregnancy, low birthweight and preterm birth 5 . Exposure to secondhand cigarette smoke in children has been linked to sudden infant death syndrome, impaired lung function and respiratory illnesses, in addition to cognitive and behavioural impairments 5 . The long-term developmental effects of nicotine are probably due to structural and functional changes in the brain during this early developmental period 12 , 13 .
Nicotine administered alone in various nicotine replacement formulations (such as patches, gum and lozenges) is safe and effective as an evidence-based smoking cessation aid. Novel forms of nicotine delivery systems have also emerged (called electronic nicotine delivery systems (ENDS) or e-cigarettes), which can potentially reduce the harmful effects of tobacco smoking for those who switch completely from combustible to e-cigarettes 14 , 15 .
This Primer focuses on the determinants of nicotine and tobacco use, and reviews the neurobiology of nicotine effects on the brain reward circuitry and the functioning of brain networks in ways that contribute to the difficulty in stopping smoking. This Primer also discusses how to prevent tobacco use, screen for smoking, and offer people who smoke tobacco psychosocial and pharmacological interventions to assist in quitting. Moreover, this Primer presents emerging pharmacological and novel brain interventions that could improve rates of successful smoking cessation, in addition to public health approaches that could be beneficial.
Box 1 Tobacco products
Conventional tobacco products include combustible products that produce inhaled smoke (most commonly cigarettes, bidis (small domestically manufactured cigarettes used in South Asia) or cigars) and those that deliver nicotine without using combustion (chewing or dipping tobacco and snuff). Newer alternative products that do not involve combustion include nicotine-containing e-cigarettes and heat-not-burn tobacco devices. Although non-combustion and alternative products may constitute a lesser risk than burned ones 14 , 15 , 194 , no form of tobacco is entirely risk-free.
Epidemiology
Prevalence and burden of disease.
The Global Burden of Disease Project (GBDP) estimated that around 1.14 billion people smoked in 2019, worldwide, increasing from just under a billion in 1990 (ref. 1 ). Of note, the prevalence of smoking decreased significantly between 1990 and 2019, but increases in the adult population meant that the total number of global smokers increased. One smoking-associated death occurs for approximately every 0.8–1.1 million cigarettes smoked 16 , suggesting that the estimated worldwide consumption of about 7.4 trillion cigarettes in 2019 has led to around 7 million deaths 1 .
In most populations, smoking prevalence is much higher among groups with lower levels of education or income 17 and among those with mental health disorders and other co-addictions 18 , 19 . Smoking is also more frequent among men than women (Figs 1 – 3 ). Sexual and/or gender minority individuals have disproportionately high rates of smoking and other addictions 17 , 20 . In addition, the prevalence of smoking varies substantially between regions and ethnicities; smoking rates are high in some regions of Asia, such as China and India, but are lower in North America and Australia. Of note, the prevalence of mental health disorders and other co-addictions is higher in individuals who smoke compared with non-smokers 18 , 19 , 21 . For example, the odds of smoking in people with any substance use disorder is more than five times higher than the odds in people without a substance use disorder 19 . Similarly, the odds of smoking in people with any psychiatric disorder is more than three times higher than the odds of smoking in those without a psychiatric diagnosis 22 . In a study in the USA, compared with a population of smokers with no psychiatric diagnosis, subjects with anxiety, depression and phobia showed an approximately twofold higher prevalence of smoking, and subjects with agoraphobia, mania or hypomania, psychosis and antisocial personality or conduct disorders showed at least a threefold higher prevalence of smoking 22 . Comorbid disorders are also associated with higher rates of smoking 22 , 23 .
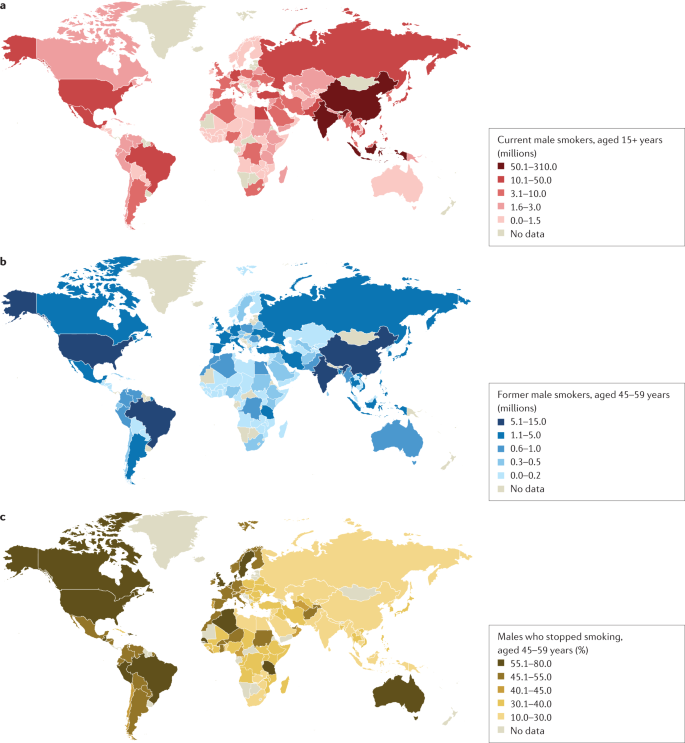
a | Number of current male smokers aged 15 years or older per country expressed in millions. b | Former male smokers aged 45–59 years per country expressed in millions. c | Former male smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for male smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among males is less variable than among females. Data from ref. 1 .
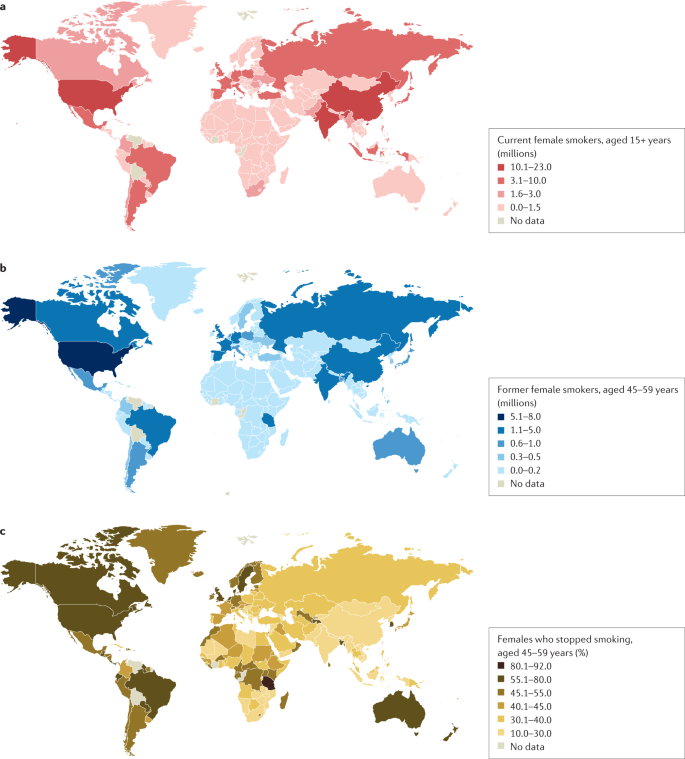
a | Number of current female smokers aged 15 years or older per country expressed in millions. b | Former female smokers aged 45–59 years per country expressed in millions. c | Former female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for female smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among females is much lower in East and South Asia than in Latin America or Eastern Europe. Data from ref. 1 .
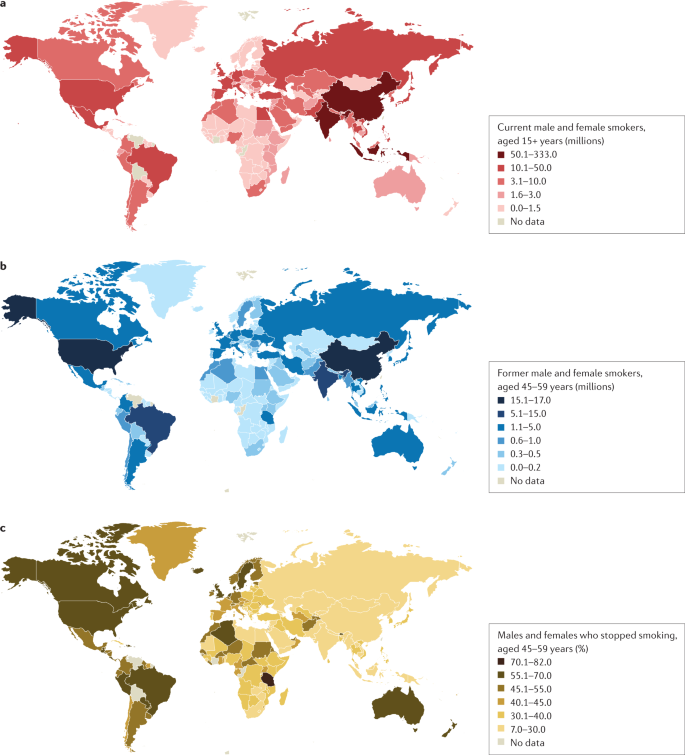
a | Number of current male and female smokers aged 15 years or older per country expressed in millions. b | Former male and female smokers aged 45–59 years per country expressed in millions. c | Former male and female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for the period 2015–2019 from countries with direct smoking surveys. Cessation rates are higher in high-income countries, but also notably high in Brazil. Cessation is far less common in South and East Asia and Russia and other Eastern European countries, and also low in South Africa. Data from ref. 1 .
Age at onset
Most smokers start smoking during adolescence, with almost 90% of smokers beginning between 15 and 25 years of age 24 . The prevalence of tobacco smoking among youths substantially declined in multiple HICs between 1990 and 2019 (ref. 25 ). More recently, the widespread uptake of ENDS in some regions such as Canada and the USA has raised concerns about the long-term effects of prolonged nicotine use among adolescents, including the possible notion that ENDS will increase the use of combustible smoking products 25 , 26 (although some studies have not found much aggregate effect at the population level) 27 .
Smoking that commences in early adolescence or young adulthood and persists throughout life has a more severe effect on health than smoking that starts later in life and/or that is not persistent 16 , 28 , 29 . Over 640 million adults under 30 years of age smoke in 22 jurisdictions alone (including 27 countries in the European Union where central efforts to reduce tobacco dependence might be possible) 30 . In those younger than 30 years of age, at least 320 million smoking-related deaths will occur unless they quit smoking 31 . The actual number of smoking-related deaths might be greater than one in two, and perhaps as high as two in three, long-term smokers 5 , 16 , 29 , 32 , 33 . At least half of these deaths are likely to occur in middle age (30–69 years) 16 , 29 , leading to a loss of two or more decades of life. People who smoke can expect to lose an average of at least a decade of life versus otherwise similar non-smokers 16 , 28 , 29 .
Direct epidemiological studies in several countries paired with model-based estimates have estimated that smoking tobacco accounted for 7.7 million deaths globally in 2020, of which 80% were in men and 87% were current smokers 1 . In HICs, the major causes of tobacco deaths are lung cancer, emphysema, heart attack, stroke, cancer of the upper aerodigestive areas and bladder cancer 28 , 29 . In some lower income countries, tuberculosis is an additional important cause of tobacco-related death 29 , 34 , which could be related to, for example, increased prevalence of infection, more severe tuberculosis/mortality and higher prevalence of treatment-resistant tuberculosis in smokers than in non-smokers in low-income countries 35 , 36 .
Despite substantial reductions in the prevalence of smoking, there were 34 million smokers in the USA, 7 million in the UK and 5 million in Canada in 2017 (ref. 16 ), and cigarette smoking remains the largest cause of premature death before 70 years of age in much of Europe and North America 1 , 16 , 28 , 29 . Smoking-associated diseases accounted for around 41 million deaths in the USA, UK and Canada from 1960 to 2020 (ref. 16 ). Moreover, as smoking-associated diseases are more prevalent among groups with lower levels of education and income, smoking accounts for at least half of the difference in overall mortality between these social groups 37 . Any reduction in smoking prevalence reduces the absolute mortality gap between these groups 38 .
Smoking cessation has become common in HICs with good tobacco control interventions. For example, in France, the number of ex-smokers is four times the number of current smokers among those aged 50 years or more 30 . By contrast, smoking cessation in LMICs remains uncommon before smokers develop tobacco-related diseases 39 . Smoking cessation greatly reduces the risks of smoking-related diseases. Indeed, smokers who quit smoking before 40 years of age avoid nearly all the increased mortality risks 31 , 33 . Moreover, individuals who quit smoking by 50 years of age reduce the risk of death from lung cancer by about two-thirds 40 . More modest hazards persist for deaths from lung cancer and emphysema 16 , 28 ; however, the risks among former smokers are an order of magnitude lower than among those who continue to smoke 33 .
Mechanisms/pathophysiology
Nicotine is the main psychoactive agent in tobacco and e-cigarettes. Nicotine acts as an agonist at nicotinic acetylcholine receptors (nAChRs), which are localized throughout the brain and peripheral nervous system 41 . nAChRs are pentameric ion channels that consist of varying combinations of α 2 –α 7 and β 2 –β 4 subunits, and for which acetylcholine (ACh) is the endogenous ligand 42 , 43 , 44 . When activated by nicotine binding, nAChR undergoes a conformational change that opens the internal pore, allowing an influx of sodium and calcium ions 45 . At postsynaptic membranes, nAChR activation can lead to action potential firing and downstream modulation of gene expression through calcium-mediated second messenger systems 46 . nAChRs are also localized to presynaptic membranes, where they modulate neurotransmitter release 47 . nAChRs become desensitized after activation, during which ligand binding will not open the channel 45 .
nAChRs with varying combinations of α-subunits and β-subunits have differences in nicotine binding affinity, efficacy and desensitization rate, and have differential expression depending on the brain region and cell type 48 , 49 , 50 . For instance, at nicotine concentrations found in human smokers, β 2 -containing nAChRs desensitize relatively quickly after activation, whereas α 7 -containing nAChRs have a slower desensitization profile 48 . Chronic nicotine exposure in experimental animal models or in humans induces an increase in cortical expression of α 4 β 2 -containing nAChRs 51 , 52 , 53 , 54 , 55 , but also increases the expression of β 3 and β 4 nAChR subunits in the medial habenula (MHb)–interpeduncular nucleus (IPN) pathway 56 , 57 . It is clear that both the brain localization and the type of nAChR are critical elements in mediating the various effects of nicotine, but other factors such as rate of nicotine delivery may also modulate addictive effects of nicotine 58 .
Neurocircuitry of nicotine addiction
Nicotine has both rewarding effects (such as a ‘buzz’ or ‘high’) and aversive effects (such as nausea and dizziness), with the net outcome dependent on dose and others factors such as interindividual sensitivity and presence of tolerance 59 . Thus, the addictive properties of nicotine involve integration of contrasting signals from multiple brain regions that process reward and aversion (Fig. 4 ).
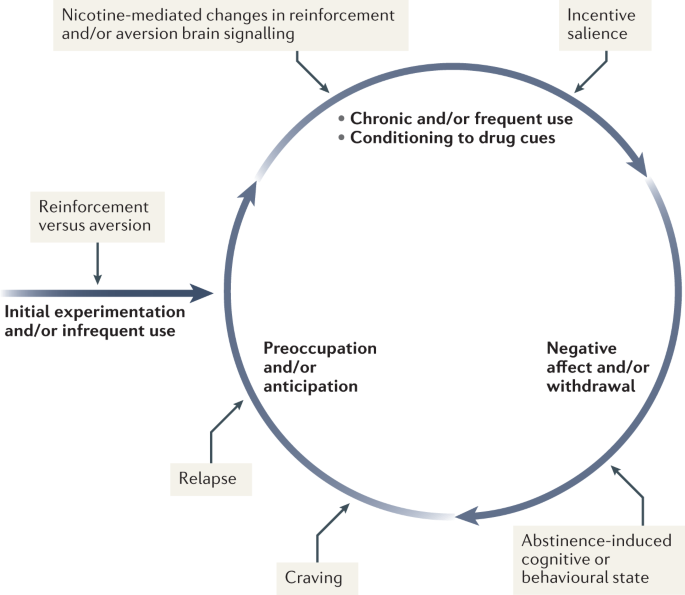
During initial use, nicotine exerts both reinforcing and aversive effects, which together determine the likelihood of continued use. As the individual transitions to more frequent patterns of chronic use, nicotine induces pharmacodynamic changes in brain circuits, which is thought to lead to a reduction in sensitivity to the aversive properties of the drug. Nicotine is also a powerful reinforcer that leads to the conditioning of secondary cues associated with the drug-taking experience (such as cigarette pack, sensory properties of cigarette smoke and feel of the cigarette in the hand or mouth), which serves to enhance the incentive salience of these environmental factors and drive further drug intake. When the individual enters into states of abstinence (such as daily during sleep at night or during quit attempts), withdrawal symptomology is experienced, which may include irritability, restlessness, learning or memory deficits, difficulty concentrating, anxiety and hunger. These negative affective and cognitive symptoms lead to an intensification of the individual’s preoccupation to obtain and use the tobacco/nicotine product, and subsequently such intense craving can lead to relapse.
The rewarding actions of nicotine have largely been attributed to the mesolimbic pathway, which consists of dopaminergic neurons in the ventral tegmental area (VTA) that project to the nucleus accumbens and prefrontal cortex 60 , 61 , 62 (Fig. 5 ). VTA integrating circuits and projection regions express several nAChR subtypes on dopaminergic, GABAergic, and glutamatergic neurons 63 , 64 . Ultimately, administration of nicotine increases dopamine levels through increased dopaminergic neuron firing in striatal and extrastriatal areas (such as the ventral pallidum) 65 (Fig. 6 ). This effect is involved in reward and is believed to be primarily mediated by the action of nicotine on α 4 -containing and β 2 -containing nAChRs in the VTA 66 , 67 .
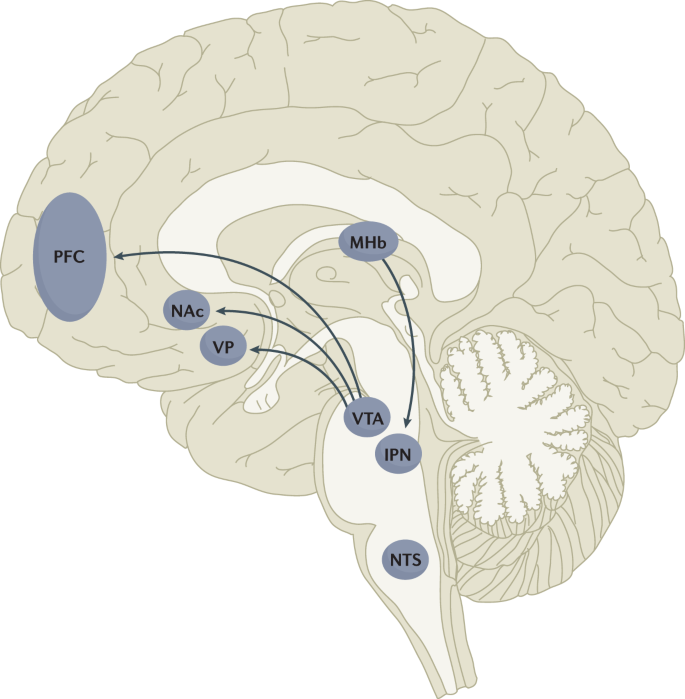
Multiple lines of research have demonstrated that nicotine reinforcement is mainly controlled by two brain pathways, which relay predominantly reward-related or aversion-related signals. The rewarding properties of nicotine that promote drug intake involve the mesolimbic dopamine projection from the ventral tegmental area (VTA) to the nucleus accumbens (NAc). By contrast, the aversive properties of nicotine that limit drug intake and mitigate withdrawal symptoms involve the fasciculus retroflexus projection from the medial habenula (MHb) to the interpeduncular nucleus (IPN). Additional brain regions have also been implicated in various aspects of nicotine dependence, such as the prefrontal cortex (PFC), ventral pallidum (VP), nucleus tractus solitarius (NTS) and insula (not shown here for clarity). All of these brain regions are directly or indirectly interconnected as integrative circuits to drive drug-seeking and drug-taking behaviours.
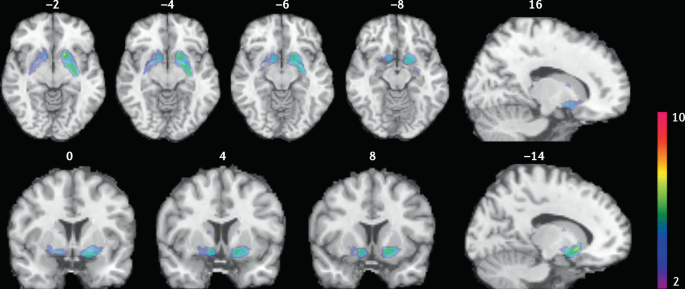
Smokers received brain PET scans with [ 11 C]PHNO, a dopamine D 2/3 PET tracer that has high sensitivity in detecting fluctuations of dopamine. PET scans were performed during abstinence or after smoking a cigarette. Reduced binding potential (BP ND ) was observed after smoking, indicating increased dopamine levels in the ventral striatum and in the area that corresponds to the ventral pallidum. The images show clusters with statistically significant decreases of [ 11 C]PHNO BP ND after smoking a cigarette versus abstinence condition. Those clusters have been superimposed on structural T1 MRI images of the brain. Reprinted from ref. 65 , Springer Nature Limited.
The aversive properties of nicotine are mediated by neurons in the MHb, which project to the IPN. Studies in rodents using genetic knockdown and knockout strategies demonstrated that the α 5 -containing, α 3 -containing and β 4 -containing nAChRs in the MHb–IPN pathway mediate the aversive properties of nicotine that limit drug intake, especially when animals are given the opportunity to consume higher nicotine doses 68 , 69 , 70 , 71 , 72 . In addition to nAChRs, other signalling factors acting on the MHb terminals in the IPN also regulate the actions of nicotine. For instance, under conditions of chronic nicotine exposure or with optogenetic activation of IPN neurons, a subtype of IPN neurons co-expressing Chrna5 (encoding the α 5 nAChR subunit) and Amigo1 (encoding adhesion molecule with immunoglobulin-like domain 1) release nitric oxide from the cell body that retrogradely inhibits MHb axon terminals 70 . In addition, nicotine activates α 5 -containing nAChR-expressing neurons that project from the nucleus tractus solitarius to the IPN, leading to release of glucagon-like peptide-1 that binds to GLP receptors on habenular axon terminals, which subsequently increases IPN neuron activation and decreases nicotine self-administration 73 . Taken together, these findings suggest a dynamic signalling process at MHb axonal terminals in the IPN, which regulates the addictive properties of nicotine and determines the amount of nicotine that is self-administered.
Nicotine withdrawal in animal models can be assessed by examining somatic signs (such as shaking, scratching, head nods and chewing) and affective signs (such as increased anxiety-related behaviours and conditioned place aversion). Interestingly, few nicotine withdrawal somatic signs are found in mice with genetic knockout of the α 2 , α 5 or β 4 nAChR subunits 74 , 75 . By contrast, β 2 nAChR-knockout mice have fewer anxiety-related behaviours during nicotine withdrawal, with no differences in somatic symptoms compared with wild-type mice 74 , 76 .
In addition to the VTA (mediating reward) and the MHb–IPN pathway (mediating aversion), other brain areas are involved in nicotine addiction (Fig. 5 ). In animals, the insular cortex controls nicotine taking and nicotine seeking 77 . Moreover, humans with lesions of the insular cortex can quit smoking easily without relapse 78 . This finding led to the development of a novel therapeutic intervention modulating insula function (see Management, below) 79 , 80 . Various brain areas (shell of nucleus accumbens, basolateral amygdala and prelimbic cortex) expressing cannabinoid CB 1 receptors are also critical in controlling rewarding effects and relapse 81 , 82 . The α 1 -adrenergic receptor expressed in the cortex also control these effects, probably through glutamatergic afferents to the nucleus accumbens 83 .
Individual differences in nicotine addiction risk
Vulnerability to nicotine dependence varies between individuals, and the reasons for these differences are multidimensional. Many social factors (such as education level and income) play a role 84 . Broad psychological and social factors also modulate this risk. For example, peer smoking status, knowledge on effect of tobacco, expectation on social acceptance, exposure to passive smoking modulate the risk of initiating tobacco use 85 , 86 .
Genetic factors have a role in smoking initiation, the development of nicotine addiction and the likelihood of smoking cessation. Indeed, heritability has been estimated to contribute to approximatively half of the variability in nicotine dependence 87 , 88 , 89 , 90 . Important advances in our understanding of such genetic contributions have evolved with large-scale genome-wide association studies of smokers and non-smokers. One of the most striking findings has been that allelic variation in the CHRNA5 – CHRNA3 – CHRNB4 gene cluster, which encodes α 5 , α 3 and β 4 nAChR subunits, correlates with an increased vulnerability for nicotine addiction, indicated by a higher likelihood of becoming dependent on nicotine and smoking a greater number of cigarettes per day 91 , 92 , 93 , 94 , 95 . The most significant effect has been found for a single-nucleotide polymorphism in CHRNA5 (rs16969968), which results in an amino acid change and reduced function of α 5 -containing nAChRs 92 .
Allelic variation in CYP2A6 (encoding the CYP2A6 enzyme, which metabolizes nicotine) has also been associated with differential vulnerability to nicotine dependence 96 , 97 , 98 . CYP2A6 is highly polymorphic, resulting in variable enzymatic activity 96 , 99 , 100 . Individuals with allelic variation that results in slow nicotine metabolism consume less nicotine per day, experience less-severe withdrawal symptoms and are more successful at quitting smoking than individuals with normal or fast metabolism 101 , 102 , 103 , 104 . Moreover, individuals with slow nicotine metabolism have lower dopaminergic receptor expression in the dopamine D2 regions of the associative striatum and sensorimotor striatum in PET studies 105 and take fewer puffs of nicotine-containing cigarettes (compared with de-nicotinized cigarettes) in a forced choice task 106 . Slower nicotine metabolism is thought to increase the duration of action of nicotine, allowing nicotine levels to accumulate over time, therefore enabling lower levels of intake to sustain activation of nAChRs 107 .
Large-scale genetic studies have identified hundreds of other genetic loci that influence smoking initiation, age of smoking initiation, cigarettes smoked per day and successful smoking cessation 108 . The strongest genetic contributions to smoking through the nicotinic receptors and nicotine metabolism are among the strongest genetic contributors to lung cancer 109 . Other genetic variations (such as those related to cannabinoid, dopamine receptors or other neurotransmitters) may affect certain phenotypes related to smoking (such as nicotine preference and cue-reactivity) 110 , 111 , 112 , 113 , 114 , 115 .
Diagnosis, screening and prevention
Screening for cigarette smoking.
Screening for cigarette smoking should happen at every doctor’s visit 116 . In this regard, a simple and direct question about a person’s tobacco use can provide an opportunity to offer information about its potential risks and treatments to assist in quitting. All smokers should be offered assistance in quitting because even low levels of smoking present a significant health risk 33 , 117 , 118 . Smoking status can be assessed by self-categorization or self-reported assessment of smoking behaviour (Table 1 ). In people who smoke, smoking frequency can be assessed 119 and a combined quantity frequency measure such as pack-year history (that is, average number of cigarettes smoked per day multiplied by the number of years, divided by 20), can be used to estimate cumulative risk of adverse health outcomes. The Association for the Treatment of Tobacco Use and Dependence recommends that all electronic health records should document smoking status using the self-report categories listed in Table 1 .
Owing to the advent of e-cigarettes and heat-not-burn products, and the popularity of little cigars in the US that mimic combustible cigarettes, people who use tobacco may use multiple products concurrently 120 , 121 . Thus, screening for other nicotine and tobacco product use is important in clinical practice. The self-categorization approach can also be used to describe the use of these other products.
Traditionally tobacco use has been classified according to whether the smoker meets criteria for nicotine dependence in one of the two main diagnostic classifications: the DSM 122 (tobacco use disorder) and the ICD (tobacco dependence) 123 . The diagnosis of tobacco use disorder according to DSM-5 criteria requires the presence of at least 2 of 11 symptoms that have produced marked clinical impairment or distress within a 12-month period (Box 2 ). Of note, these symptoms are similar for all substance use disorder diagnoses and may not all be relevant to tobacco use disorder (such as failure to complete life roles). In the ICD-10, codes allow the identification of specific tobacco products used (cigarettes, chewing tobacco and other tobacco products).
Dependence can also be assessed as a continuous construct associated with higher levels of use, greater withdrawal and reduced likelihood of quitting. The level of dependence can be assessed with the Fagerström Test for Nicotine Dependence, a short questionnaire comprising six questions 124 (Box 2 ). A score of ≥4 indicates moderate to high dependence. As very limited time may be available in clinical consultations, the Heaviness of Smoking Index (HSI) was developed, which comprises two questions on the number of cigarettes smoked per day and how soon after waking the first cigarette is smoked 125 . The HSI can guide dosing for nicotine replacement therapy (NRT).
Other measures of cigarette dependence have been developed but are not used in the clinical setting, such as the Cigarette Dependence Scale 126 , Hooked on Nicotine Checklist 127 , Nicotine Dependence Syndrome Scale 128 , the Wisconsin Inventory of Smoking Dependence Motives (Brief) 129 and the Penn State Cigarette Dependence Index 130 . However, in practice, these are not often used, as the most important aspect is to screen for smoking and encourage all smokers to quit smoking regardless of their dependence status.
Box 2 DSM-5 criteria for tobacco use disorder and items of the Fagerström Test for nicotine dependence
DSM-5 (ref. 122 )
Taxonomic and diagnostic tool for tobacco use disorder published by the American Psychiatric Association.
A problematic pattern of tobacco use leading to clinically significant impairment or distress as manifested by at least two of the following, occurring within a 12-month period.
Tobacco often used in larger amounts or over a longer period of time than intended
A persistent desire or unsuccessful efforts to reduce or control tobacco use
A great deal of time spent in activities necessary to obtain or use tobacco
Craving, or a strong desire or urge to use tobacco
Recurrent tobacco use resulting in a failure to fulfil major role obligations at work, school or home
Continued tobacco use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of tobacco (for example, arguments with others about tobacco use)
Important social, occupational or recreational activities given up or reduced because of tobacco use
Recurrent tobacco use in hazardous situations (such as smoking in bed)
Tobacco use continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by tobacco use
Tolerance, defined by either of the following.
A need for markedly increased amounts of tobacco to achieve the desired effect
A markedly diminished effect with continued use of the same amount of tobacco
Withdrawal, manifesting as either of the following.
Withdrawal syndrome for tobacco
Tobacco (or a closely related substance, such as nicotine) taken to relieve or avoid withdrawal symptoms
Fagerström Test for Nicotine Dependence 124
A standard instrument for assessing the intensity of physical addiction to nicotine.
How soon after you wake up do you smoke your first cigarette?
Within 5 min (scores 3 points)
5 to 30 min (scores 2 points)
31 to 60 min (scores 1 point)
After 60 min (scores 0 points)
Do you find it difficult not to smoke in places where you should not, such as in church or school, in a movie, at the library, on a bus, in court or in a hospital?
Yes (scores 1 point)
No (scores 0 points)
Which cigarette would you most hate to give up; which cigarette do you treasure the most?
The first one in the morning (scores 1 point)
Any other one (scores 0 points)
How many cigarettes do you smoke each day?
10 or fewer (scores 0 points)
11 to 20 (scores 1 point)
21 to 30 (scores 2 points)
31 or more (scores 3 points)
Do you smoke more during the first few hours after waking up than during the rest of the day?
Do you still smoke if you are so sick that you are in bed most of the day or if you have a cold or the flu and have trouble breathing?
A score of 7–10 points is classified as highly dependent; 4–6 points is classified as moderately dependent; <4 points is classified as minimally dependent.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Young people who do not start smoking cigarettes between 15 and 25 years of age have a very low risk of ever smoking 24 , 131 , 132 . This age group provides a critical opportunity to prevent cigarette smoking using effective, evidence-based strategies to prevent smoking initiation and reduce escalation from experimentation to regular use 131 , 132 , 133 , 134 , 135 .
Effective prevention of cigarette uptake requires a comprehensive package of cost-effective policies 134 , 136 , 137 to synergistically reduce the population prevalence of cigarette smoking 131 , 135 . These policies include high rates of tobacco taxation 30 , 134 , 137 , 138 , widespread and rigorously enforced smoke-free policies 139 , bans on tobacco advertising and promotions 140 , use of plain packaging and graphic warnings about the health risks of smoking 135 , 141 , mass media and peer-based education programmes to discourage smoking, and enforcement of laws against the sale of cigarettes to young people below the minimum legal purchase age 131 , 135 . These policies make cigarettes less available and affordable to young people. Moreover, these policies make it more difficult for young people to purchase cigarettes and make smoking a much less socially acceptable practice. Of note, these policies are typically mostly enacted in HICs, which may be related to the declining prevalence of smoking in these countries, compared with the prevalence in LMICs.
Pharmacotherapy
Three evidence-based classes of pharmacotherapy are available for smoking cessation: NRT (using nicotine-based patches, gum, lozenges, mini-lozenges, nasal sprays and inhalers), varenicline (a nAChR partial agonist), and bupropion (a noradrenaline/dopamine reuptake inhibitor that also inhibits nAChR function and is also used as an antidepressant). These FDA-approved and EMA-approved pharmacotherapies are cost-effective smoking cessation treatments that double or triple successful abstinence rates compared with no treatment or placebo controls 116 , 142 .
Combinations of pharmacotherapies are also effective for smoking cessation 116 , 142 . For example, combining NRTs (such as the steady-state nicotine patch and as-needed NRT such as gum or mini-lozenge) is more effective than a single form of NRT 116 , 142 , 143 . Combining NRT and varenicline is the most effective smoking cessation pharmacotherapy 116 , 142 , 143 . Combining FDA-approved pharmacotherapy with behavioural counselling further increases the likelihood of successful cessation 142 . Second-line pharmacotherapies (for example, nortriptyline) have some potential for smoking cessation, but their use is limited due to their tolerability profile.
All smokers should receive pharmacotherapy to help them quit smoking, except those in whom pharmacotherapy has insufficient evidence of effectiveness (among adolescents, smokeless tobacco users, pregnant women or light smokers) or those in whom pharmacotherapy is medically contraindicated 144 . Table 2 provides specific information regarding dosing and duration for each FDA-approved pharmacotherapy. Extended use of pharmacotherapy beyond the standard 12-week regimen after cessation is effective and should be considered 116 . Moreover, preloading pharmacotherapy (that is, initiating cessation medication in advance of a quit attempt), especially with the nicotine patch, is a promising treatment, although further studies are required to confirm efficacy.
Cytisine has been used for smoking cessation in Eastern Europe for a long time and is available in some countries (such as Canada) without prescription 145 . Cytisine is a partial agonist of nAChRs and its structure was the precursor for the development of varenicline 145 . Cytisine is at least as effective as some approved pharmacotherapies for smoking cessation, such as NRT 146 , 147 , 148 , and the role of cytisine in smoking cessation is likely to expand in the future, notably owing to its much lower cost than traditional pharmacotherapies. E-cigarettes also have the potential to be useful as smoking cessation devices 149 , 150 . The 2020 US Surgeon General’s Report concluded that there was insufficient evidence to promote cytisine or e-cigarettes as effective smoking cessation treatments, but in the UK its use is recommended for smoking cessation (see ref. 15 for regularly updated review).
Counselling and behavioural treatments
Psychosocial counselling significantly increases the likelihood of successful cessation, especially when combined with pharmacotherapy. Even a counselling session lasting only 3 minutes can help smokers quit 116 , although the 2008 US Public Health Service guidelines and the Preventive Services Task Force 151 each concluded that more intensive counselling (≥20 min per session) is more effective than less intensive counselling (<20 min per session). Higher smoking cessation rates are obtained by using behavioural change techniques that target associative and self-regulatory processes 152 . In addition, behavioural change techniques that will favour commitment, social reward and identity associated with changed behaviour seems associated with higher success rates 152 . Evidence-based counselling focuses on providing social support during treatment, building skills to cope with withdrawal and cessation, and problem-solving in challenging situations 116 , 153 . Effective counselling can be delivered by diverse providers (such as physicians, nurses, pharmacists, social workers, psychologists and certified tobacco treatment specialists) 116 .
Counselling can be delivered in a variety of modalities. In-person individual and group counselling are effective, as is telephone counselling (quit lines) 142 . Internet and text-based intervention seem to be effective in smoking cessation, especially when they are interactive and tailored to a smoker’s specific circumstances 142 . Over the past several years, the number of smoking cessation smartphone apps has increased, but there the evidence that the use of these apps significantly increases smoking cessation rates is not sufficient.
Contingency management (providing financial incentives for abstinence or engagement in treatment) has shown promising results 154 , 155 but its effects are not sustained once the contingencies are removed 155 , 156 . Other treatments such as hypnosis, acupuncture and laser treatment have not been shown to improve smoking cessation rates compared with placebo treatments 116 . Moreover, no solid evidence supports the use of conventional transcranial magnetic stimulation (TMS) for long-term smoking cessation 157 , 158 .
Although a variety of empirically supported smoking cessation interventions are available, more than two-thirds of adult smokers who made quit attempts in the USA during the past year did not use an evidence-based treatment and the rate is likely to be lower in many other countries 142 . This speaks to the need to increase awareness of, and access to, effective cessation aids among all smokers.
Brain stimulation
The insula (part of the frontal cortex) is a critical brain structure involved in cigarette craving and relapse 78 , 79 . The activity of the insula can be modulated using an innovative approach called deep insula/prefrontal cortex TMS (deep TMS), which is effective in helping people quit smoking 80 , 159 . This approach has now been approved by the FDA as an effective smoking cessation intervention 80 . However, although this intervention was developed and is effective for smoking cessation, the number of people with access to it is limited owing to the limited number of sites equipped and with trained personnel, and the cost of this intervention.
Quality of life
Generic instruments (such as the Short-Form (SF-36) Health Survey) can be used to evaluate quality of life (QOL) in smokers. People who smoke rate their QOL lower than people who do not smoke both before and after they become smokers 160 , 161 . QOL improves when smokers quit 162 . Mental health may also improve on quitting smoking 163 . Moreover, QOL is much poorer in smokers with tobacco-related diseases, such as chronic respiratory diseases and cancers, than in individuals without tobacco-related diseases 161 , 164 . The dimensions of QOL that show the largest decrements in people who smoke are those related to physical health, day-to-day activities and mental health such as depression 160 . Smoking also increases the risk of diabetes mellitus 165 , 166 , which is a major determinant of poor QOL for a wide range of conditions.
The high toll of premature death from cigarette smoking can obscure the fact that many of the diseases that cause these deaths also produce substantial disability in the years before death 1 . Indeed, death in smokers is typically preceded by several years of living with the serious disability and impairment of everyday activities caused by chronic respiratory disease, heart disease and cancer 2 . Smokers’ QOL in these years may also be adversely affected by the adverse effects of the medical treatments that they receive for these smoking-related diseases (such as major surgery and radiotherapy).
Expanding cessation worldwide
The major global challenge is to consider individual and population-based strategies that could increase the substantially low rates of adult cessation in most LMICs and indeed strategies to ensure that even in HICs, cessation continues to increase. In general, the most effective tools recommended by WHO to expand cessation are the same tools that can prevent smoking initiation, notably higher tobacco taxes, bans on advertising and promotion, prominent warning labels or plain packaging, bans on public smoking, and mass media and educational efforts 29 , 167 . The effective use of these policies, particularly taxation, lags behind in most LMICs compared with most HICs, with important exceptions such as Brazil 167 . Access to effective pharmacotherapies and counselling as well as support for co-existing mental health conditions would also be required to accelerate cessation in LMICs. This is particularly important as smokers living in LMICs often have no access to the full range of effective treatment options.
Regulating access to e-cigarettes
How e-cigarettes should be used is debated within the tobacco control field. In some countries (for example, the UK), the use of e-cigarettes as a cigarette smoking cessation aid and as a harm reduction strategy is supported, based on the idea that e-cigarette use will lead to much less exposure to toxic compounds than tobacco use, therefore reducing global harm. In other countries (for example, the USA), there is more concern with preventing the increased use of e-cigarettes by youths that may subsequently lead to smoking 25 , 26 . Regulating e-cigarettes in nuanced ways that enable smokers to access those products whilst preventing their uptake among youths is critical.
Regulating nicotine content in tobacco products
Reducing the nicotine content of cigarettes could potentially produce less addictive products that would allow a gradual reduction in the population prevalence of smoking. Some clinical studies have found no compensatory increase in smoking whilst providing access to low nicotine tobacco 168 . Future regulation may be implemented to gradually decrease the nicotine content of combustible tobacco and other nicotine products 169 , 170 , 171 .
Tobacco end games
Some individuals have proposed getting rid of commercial tobacco products this century or using the major economic disruption arising from the COVID-19 pandemic to accelerate the demise of the tobacco industry 172 , 173 . Some tobacco producers have even proposed this strategy as an internal goal, with the idea of switching to nicotine delivery systems that are less harmful ( Philip Morris International ). Some countries are moving towards such an objective; for example, in New Zealand, the goal that fewer than 5% of New Zealanders will be smokers in 2025 has been set (ref. 174 ). The tobacco end-game approach would overall be the best approach to reduce the burden of tobacco use on society, but it would require coordination of multiple countries and strong public and private consensus on the strategy to avoid a major expansion of the existing illicit market in tobacco products in some countries.
Innovative interventions
The COVID-19 pandemic has shown that large-scale investment in research can lead to rapid development of successful therapeutic interventions. By contrast, smoking cessation has been underfunded compared with the contribution that it makes to the global burden of disease. In addition, there is limited coordination between research teams and most studies are small-scale and often underpowered 79 . It is time to fund an ambitious, coordinated programme of research to test the most promising therapies based on an increased understanding of the neurobiological basis of smoking and nicotine addiction (Table 3 ). Many of those ideas have not yet been tested properly and this could be carried out by a coordinated programme of research at the international level.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 397 , 2337–2360 (2021). This study summarizes the burden of disease induced by tobacco worldwide .
Google Scholar
West, R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol. Health 32 , 1018–1036 (2017).
PubMed PubMed Central Google Scholar
West, R. The multiple facets of cigarette addiction and what they mean for encouraging and helping smokers to stop. COPD 6 , 277–283 (2009).
PubMed Google Scholar
Fagerström, K. Determinants of tobacco use and renaming the FTND to the Fagerström test for cigarette dependence. Nicotine Tob. Res. 14 , 75–78 (2012).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Doll, R. & Hill, A. B. Smoking and carcinoma of the lung; preliminary report. Br. Med. J. 2 , 739–748 (1950).
CAS PubMed PubMed Central Google Scholar
Royal College of Physicians. Smoking and health. Summary of a report of the Royal College of Physicians of London on smoking in relation to cancer of the lung and other diseases (Pitman Medical Publishing, 1962).
Henningfield, J. E., Smith, T. T., Kleykamp, B. A., Fant, R. V. & Donny, E. C. Nicotine self-administration research: the legacy of Steven R. Goldberg and implications for regulation, health policy, and research. Psychopharmacology 233 , 3829–3848 (2016).
Le Foll, B. & Goldberg, S. R. Effects of nicotine in experimental animals and humans: an update on addictive properties. Hand. Exp. Pharmacol. https://doi.org/10.1007/978-3-540-69248-5_12 (2009).
Article Google Scholar
Proctor, R. N. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll. Tob. Control. 21 , 87–91 (2012).
Hall, B. J. et al. Differential effects of non-nicotine tobacco constituent compounds on nicotine self-administration in rats. Pharmacol. Biochem. Behav. 120 , 103–108 (2014).
Musso, F. et al. Smoking impacts on prefrontal attentional network function in young adult brains. Psychopharmacology 191 , 159–169 (2007).
CAS PubMed Google Scholar
Goriounova, N. A. & Mansvelder, H. D. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb. Perspect. Med. 2 , a012120 (2012).
Fagerström, K. O. & Bridgman, K. Tobacco harm reduction: the need for new products that can compete with cigarettes. Addictive Behav. 39 , 507–511 (2014).
Hartmann-Boyce, J. et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 9 , CD010216 (2021).
Jha, P. The hazards of smoking and the benefits of cessation: a critical summation of the epidemiological evidence in high-income countries. eLife https://doi.org/10.7554/eLife.49979 (2020).
Article PubMed PubMed Central Google Scholar
Palipudi, K. M. et al. Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. PLoS ONE 7 , e33466 (2012).
Goodwin, R. D., Pagura, J., Spiwak, R., Lemeshow, A. R. & Sareen, J. Predictors of persistent nicotine dependence among adults in the United States. Drug Alcohol. Depend. 118 , 127–133 (2011).
Weinberger, A. H. et al. Cigarette use is increasing among people with illicit substance use disorders in the United States, 2002-14: emerging disparities in vulnerable populations. Addiction 113 , 719–728 (2018).
Evans-Polce, R. J., Kcomt, L., Veliz, P. T., Boyd, C. J. & McCabe, S. E. Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates. Am. J. Psychiatry 177 , 1073–1081 (2020).
Hassan, A. N. & Le Foll, B. Survival probabilities and predictors of major depressive episode incidence among individuals with various types of substance use disorders. J. Clin. Psychiatry https://doi.org/10.4088/JCP.20m13637 (2021).
Article PubMed Google Scholar
Smith, P. H., Mazure, C. M. & McKee, S. A. Smoking and mental illness in the U.S. population. Tob. Control. 23 , e147–e153 (2014).
Bourgault, Z., Rubin-Kahana, D. S., Hassan, A. N., Sanches, M. & Le Foll, B. Multiple substance use disorders and self-reported cognitive function in U.S. adults: associations and sex-differences in a nationally representative sample. Front. Psychiatry https://doi.org/10.3389/fpsyt.2021.797578 (2022).
Reitsma, M. B. et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990-2019. Lancet Public Health 6 , e472–e481 (2021).
Warner, K. E. How to think–not feel–about tobacco harm reduction. Nicotine Tob. Res. 21 , 1299–1309 (2019).
Soneji, S. et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 171 , 788–797 (2017).
Levy, D. T. et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob. Control. 28 , 629–635 (2019).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking — 50 years of progress: a report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Jha, P. & Peto, R. Global effects of smoking, of quitting, and of taxing tobacco. N. Engl. J. Med. 370 , 60–68 (2014). This review covers the impact of tobacco, of quitting smoking and the importance of taxation to impact prevalence of smoking .
Jha, P. & Peto., R. in Tobacco Tax Reform: At the Crossroads of Health and Development . (eds Marquez, P. V. & Moreno-Dodson, B.) 55–72 (World Bank Group, 2017).
Jha, P. et al. 21st-century hazards of smoking and benefits of cessation in the United States. N. Engl. J. Med. 368 , 341–350 (2013).
Banks, E. et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 13 , 38 (2015).
Pirie, K. et al. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 381 , 133–141 (2013).
Jha, P. et al. A nationally representative case-control study of smoking and death in India. N. Engl. J. Med. 358 , 1137–1147 (2008).
Chan, E. D. et al. Tobacco exposure and susceptibility to tuberculosis: is there a smoking gun? Tuberculosis 94 , 544–550 (2014).
Wang, M. G. et al. Association between tobacco smoking and drug-resistant tuberculosis. Infect. Drug Resist. 11 , 873–887 (2018).
Jha, P. et al. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 368 , 367–370 (2006).
Jha, P., Gelband, H, Irving, H. & Mishra, S. in Reducing Social Inequalities in Cancer: Evidence and Priorities for Research (eds Vaccarella, S et al.) 161–166 (IARC, 2018).
Jha, P. Expanding smoking cessation world-wide. Addiction 113 , 1392–1393 (2018).
Jha, P. Avoidable global cancer deaths and total deaths from smoking. Nat. Rev. Cancer 9 , 655–664 (2009).
Wittenberg, R. E., Wolfman, S. L., De Biasi, M. & Dani, J. A. Nicotinic acetylcholine receptors and nicotine addiction: a brief introduction. Neuropharmacology 177 , 108256 (2020).
Boulter, J. et al. Functional expression of two neuronal nicotinic acetylcholine receptors from cDNA clones identifies a gene family. Proc. Natl Acad. Sci. USA 84 , 7763–7767 (1987).
Couturier, S. et al. A neuronal nicotinic acetylcholine receptor subunit (α7) is developmentally regulated and forms a homo-oligomeric channel blocked by α-BTX. Neuron 5 , 847–856 (1990).
Picciotto, M. R., Addy, N. A., Mineur, Y. S. & Brunzell, D. H. It is not “either/or”: activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog. Neurobiol. 84 , 329–342 (2008).
Changeux, J. P. Structural identification of the nicotinic receptor ion channel. Trends Neurosci. 41 , 67–70 (2018).
McKay, B. E., Placzek, A. N. & Dani, J. A. Regulation of synaptic transmission and plasticity by neuronal nicotinic acetylcholine receptors. Biochem. Pharmacol. 74 , 1120–1133 (2007).
Wonnacott, S. Presynaptic nicotinic ACh receptors. Trends Neurosci. 20 , 92–98 (1997).
Wooltorton, J. R., Pidoplichko, V. I., Broide, R. S. & Dani, J. A. Differential desensitization and distribution of nicotinic acetylcholine receptor subtypes in midbrain dopamine areas. J. Neurosci. 23 , 3176–3185 (2003).
Gipson, C. D. & Fowler, C. D. Nicotinic receptors underlying nicotine dependence: evidence from transgenic mouse models. Curr. Top. Behav. Neurosci. 45 , 101–121 (2020).
Hamouda, A. K. et al. Potentiation of (α4)2(β2)3, but not (α4)3(β2)2, nicotinic acetylcholine receptors reduces nicotine self-administration and withdrawal symptoms. Neuropharmacology 190 , 108568 (2021).
Lallai, V. et al. Nicotine acts on cholinergic signaling mechanisms to directly modulate choroid plexus function. eNeuro https://doi.org/10.1523/ENEURO.0051-19.2019 (2019).
Benwell, M. E., Balfour, D. J. & Anderson, J. M. Evidence that tobacco smoking increases the density of (-)-[3H]nicotine binding sites in human brain. J. Neurochem. 50 , 1243–1247 (1988).
Perry, D. C., Davila-Garcia, M. I., Stockmeier, C. A. & Kellar, K. J. Increased nicotinic receptors in brains from smokers: membrane binding and autoradiography studies. J. Pharmacol. Exp. Ther. 289 , 1545–1552 (1999).
Marks, M. J. et al. Nicotine binding and nicotinic receptor subunit RNA after chronic nicotine treatment. J. Neurosci. 12 , 2765–2784 (1992).
Le Foll, B. et al. Impact of short access nicotine self-administration on expression of α4β2* nicotinic acetylcholine receptors in non-human primates. Psychopharmacology 233 , 1829–1835 (2016).
Meyers, E. E., Loetz, E. C. & Marks, M. J. Differential expression of the beta4 neuronal nicotinic receptor subunit affects tolerance development and nicotinic binding sites following chronic nicotine treatment. Pharmacol. Biochem. Behav. 130 , 1–8 (2015).
Zhao-Shea, R., Liu, L., Pang, X., Gardner, P. D. & Tapper, A. R. Activation of GABAergic neurons in the interpeduncular nucleus triggers physical nicotine withdrawal symptoms. Curr. Biol. 23 , 2327–2335 (2013).
Jensen, K. P., Valentine, G., Gueorguieva, R. & Sofuoglu, M. Differential effects of nicotine delivery rate on subjective drug effects, urges to smoke, heart rate and blood pressure in tobacco smokers. Psychopharmacology 237 , 1359–1369 (2020).
Villanueva, H. F., James, J. R. & Rosecrans, J. A. Evidence of pharmacological tolerance to nicotine. NIDA Res. Monogr. 95 , 349–350 (1989).
Corrigall, W. A., Coen, K. M. & Adamson, K. L. Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res. 653 , 278–284 (1994).
Nisell, M., Nomikos, G. G., Hertel, P., Panagis, G. & Svensson, T. H. Condition-independent sensitization of locomotor stimulation and mesocortical dopamine release following chronic nicotine treatment in the rat. Synapse 22 , 369–381 (1996).
Rice, M. E. & Cragg, S. J. Nicotine amplifies reward-related dopamine signals in striatum. Nat. Neurosci. 7 , 583–584 (2004).
Mameli-Engvall, M. et al. Hierarchical control of dopamine neuron-firing patterns by nicotinic receptors. Neuron 50 , 911–921 (2006).
Picciotto, M. R., Higley, M. J. & Mineur, Y. S. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron 76 , 116–129 (2012).
Le Foll, B. et al. Elevation of dopamine induced by cigarette smoking: novel insights from a [11C]-+-PHNO PET study in humans. Neuropsychopharmacology 39 , 415–424 (2014). This brain imaging study identified the brain areas in which smoking elevates dopamine levels .
Maskos, U. et al. Nicotine reinforcement and cognition restored by targeted expression of nicotinic receptors. Nature 436 , 103–107 (2005). This article discusses the implication of the β 2 - containing nAChRs in the VTA in mammalian cognitive function .
Picciotto, M. R. et al. Acetylcholine receptors containing the beta2 subunit are involved in the reinforcing properties of nicotine. Nature 391 , 173–177 (1998). This article discusses the implication of the β 2 - containing nAChRs in addictive effects of nicotine .
Fowler, C. D., Lu, Q., Johnson, P. M., Marks, M. J. & Kenny, P. J. Habenular alpha5 nicotinic receptor subunit signalling controls nicotine intake. Nature 471 , 597–601 (2011). This article discusses the implication of the α5 nicotinic receptor located in the MHb in a mechanism mediating the aversive effects of nicotine .
Elayouby, K. S. et al. α3* Nicotinic acetylcholine receptors in the habenula-interpeduncular nucleus circuit regulate nicotine intake. J. Neurosci. https://doi.org/10.1523/JNEUROSCI.0127-19.2020 (2020).
Ables, J. L. et al. Retrograde inhibition by a specific subset of interpeduncular α5 nicotinic neurons regulates nicotine preference. Proc. Natl Acad. Sci. USA 114 , 13012–13017 (2017).
Frahm, S. et al. Aversion to nicotine is regulated by the balanced activity of β4 and α5 nicotinic receptor subunits in the medial habenula. Neuron 70 , 522–535 (2011).
Jackson, K. J. et al. Role of α5 nicotinic acetylcholine receptors in pharmacological and behavioral effects of nicotine in mice. J. Pharmacol. Exp. Ther. 334 , 137–146 (2010).
Tuesta, L. M. et al. GLP-1 acts on habenular avoidance circuits to control nicotine intake. Nat. Neurosci. 20 , 708–716 (2017).
Salas, R., Pieri, F. & De Biasi, M. Decreased signs of nicotine withdrawal in mice null for the β4 nicotinic acetylcholine receptor subunit. J. Neurosci. 24 , 10035–10039 (2004).
Salas, R., Sturm, R., Boulter, J. & De Biasi, M. Nicotinic receptors in the habenulo-interpeduncular system are necessary for nicotine withdrawal in mice. J. Neurosci. 29 , 3014–3018 (2009).
Jackson, K. J., Martin, B. R., Changeux, J. P. & Damaj, M. I. Differential role of nicotinic acetylcholine receptor subunits in physical and affective nicotine withdrawal signs. J. Pharmacol. Exp. Ther. 325 , 302–312 (2008).
Le Foll, B. et al. Translational strategies for therapeutic development in nicotine addiction: rethinking the conventional bench to bedside approach. Prog. Neuropsychopharmacol. Biol. Psychiatry 52 , 86–93 (2014).
Naqvi, N. H., Rudrauf, D., Damasio, H. & Bechara, A. Damage to the insula disrupts addiction to cigarette smoking. Science 315 , 531–534 (2007). This article discusses the implication of the insular cortex in tobacco addiction .
Ibrahim, C. et al. The insula: a brain stimulation target for the treatment of addiction. Front. Pharmacol. 10 , 720 (2019).
Zangen, A. et al. Repetitive transcranial magnetic stimulation for smoking cessation: a pivotal multicenter double-blind randomized controlled trial. World Psychiatry 20 , 397–404 (2021). This study validated the utility of deep insula/prefrontal cortex rTMS for smoking cessation .
Le Foll, B., Forget, B., Aubin, H. J. & Goldberg, S. R. Blocking cannabinoid CB1 receptors for the treatment of nicotine dependence: insights from pre-clinical and clinical studies. Addict. Biol. 13 , 239–252 (2008).
Kodas, E., Cohen, C., Louis, C. & Griebel, G. Cortico-limbic circuitry for conditioned nicotine-seeking behavior in rats involves endocannabinoid signaling. Psychopharmacology 194 , 161–171 (2007).
Forget, B. et al. Noradrenergic α1 receptors as a novel target for the treatment of nicotine addiction. Neuropsychopharmacology 35 , 1751–1760 (2010).
Garrett, B. E., Dube, S. R., Babb, S. & McAfee, T. Addressing the social determinants of health to reduce tobacco-related disparities. Nicotine Tob. Res. 17 , 892–897 (2015).
Polanska, K., Znyk, M. & Kaleta, D. Susceptibility to tobacco use and associated factors among youth in five central and eastern European countries. BMC Public Health 22 , 72 (2022).
Volkow, N. D. Personalizing the treatment of substance use disorders. Am. J. Psychiatry 177 , 113–116 (2020).
Li, M. D., Cheng, R., Ma, J. Z. & Swan, G. E. A meta-analysis of estimated genetic and environmental effects on smoking behavior in male and female adult twins. Addiction 98 , 23–31 (2003).
Carmelli, D., Swan, G. E., Robinette, D. & Fabsitz, R. Genetic influence on smoking–a study of male twins. N. Engl. J. Med. 327 , 829–833 (1992).
Broms, U., Silventoinen, K., Madden, P. A. F., Heath, A. C. & Kaprio, J. Genetic architecture of smoking behavior: a study of Finnish adult twins. Twin Res. Hum. Genet. 9 , 64–72 (2006).
Kendler, K. S., Thornton, L. M. & Pedersen, N. L. Tobacco consumption in Swedish twins reared apart and reared together. Arch. Gen. Psychiat 57 , 886–892 (2000).
Saccone, N. L. et al. The CHRNA5-CHRNA3-CHRNB4 nicotinic receptor subunit gene cluster affects risk for nicotine dependence in African-Americans and in European-Americans. Cancer Res. 69 , 6848–6856 (2009).
Bierut, L. J. et al. Variants in nicotinic receptors and risk for nicotine dependence. Am. J. Psychiatry 165 , 1163–1171 (2008). This study demonstrates that nAChR gene variants are important in nicotine addiction .
Bierut, L. J. et al. Novel genes identified in a high-density genome wide association study for nicotine dependence. Hum. Mol. Genet. 16 , 24–35 (2007).
Berrettini, W. et al. α-5/α-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol. Psychiatry 13 , 368–373 (2008).
Sherva, R. et al. Association of a single nucleotide polymorphism in neuronal acetylcholine receptor subunit alpha 5 (CHRNA5) with smoking status and with ‘pleasurable buzz’ during early experimentation with smoking. Addiction 103 , 1544–1552 (2008).
Thorgeirsson, T. E. et al. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat. Genet. 42 , 448–453 (2010).
Ray, R., Tyndale, R. F. & Lerman, C. Nicotine dependence pharmacogenetics: role of genetic variation in nicotine-metabolizing enzymes. J. Neurogenet. 23 , 252–261 (2009).
Bergen, A. W. et al. Drug metabolizing enzyme and transporter gene variation, nicotine metabolism, prospective abstinence, and cigarette consumption. PLoS ONE 10 , e0126113 (2015).
Mwenifumbo, J. C. et al. Identification of novel CYP2A6*1B variants: the CYP2A6*1B allele is associated with faster in vivo nicotine metabolism. Clin. Pharmacol. Ther. 83 , 115–121 (2008).
Raunio, H. & Rahnasto-Rilla, M. CYP2A6: genetics, structure, regulation, and function. Drug Metab. Drug Interact. 27 , 73–88 (2012).
CAS Google Scholar
Patterson, F. et al. Toward personalized therapy for smoking cessation: a randomized placebo-controlled trial of bupropion. Clin. Pharmacol. Ther. 84 , 320–325 (2008).
Rodriguez, S. et al. Combined analysis of CHRNA5, CHRNA3 and CYP2A6 in relation to adolescent smoking behaviour. J. Psychopharmacol. 25 , 915–923 (2011).
Strasser, A. A., Malaiyandi, V., Hoffmann, E., Tyndale, R. F. & Lerman, C. An association of CYP2A6 genotype and smoking topography. Nicotine Tob. Res. 9 , 511–518 (2007).
Liakoni, E. et al. Effects of nicotine metabolic rate on withdrawal symptoms and response to cigarette smoking after abstinence. Clin. Pharmacol. Ther. 105 , 641–651 (2019).
Di Ciano, P. et al. Influence of nicotine metabolism ratio on [11C]-(+)-PHNO PET binding in tobacco smokers. Int. J. Neuropsychopharmacol. 21 , 503–512 (2018).
Butler, K. et al. Impact of Cyp2a6 activity on nicotine reinforcement and cue-reactivity in daily smokers. Nicotine Tob. Res. https://doi.org/10.1093/ntr/ntab064 (2021).
Benowitz, N. L., Swan, G. E., Jacob, P. 3rd, Lessov-Schlaggar, C. N. & Tyndale, R. F. CYP2A6 genotype and the metabolism and disposition kinetics of nicotine. Clin. Pharmacol. Ther. 80 , 457–467 (2006).
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51 , 237–244 (2019).
McKay, J. D. et al. Large-scale association analysis identifies new lung cancer susceptibility loci and heterogeneity in genetic susceptibility across histological subtypes. Nat. Genet. 49 , 1126–1132 (2017).
Chukwueke, C. C. et al. The CB1R rs2023239 receptor gene variant significantly affects the reinforcing effects of nicotine, but not cue reactivity, in human smokers. Brain Behav. 11 , e01982 (2021).
Ahrens, S. et al. Modulation of nicotine effects on selective attention by DRD2 and CHRNA4 gene polymorphisms. Psychopharmacology 232 , 2323–2331 (2015).
Harrell, P. T. et al. Dopaminergic genetic variation moderates the effect of nicotine on cigarette reward. Psychopharmacology 233 , 351–360 (2016).
Lerman, C. et al. Role of functional genetic variation in the dopamine D2 receptor (DRD2) in response to bupropion and nicotine replacement therapy for tobacco dependence: results of two randomized clinical trials. Neuropsychopharmacology 31 , 231–242 (2006).
Le Foll, B., Gallo, A., Le Strat, Y., Lu, L. & Gorwood, P. Genetics of dopamine receptors and drug addiction: a comprehensive review. Behav. Pharmacol. 20 , 1–17 (2009).
Chukwueke, C. C. et al. Exploring the role of the Ser9Gly (rs6280) dopamine D3 receptor polymorphism in nicotine reinforcement and cue-elicited craving. Sci. Rep. 10 , 4085 (2020).
The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff A clinical practice guideline for treating tobacco use and dependence: 2008 update: a U.S. Public Health Service report. Am. J. Prev. Med. 35 , 158–176 (2008).
Hackshaw, A., Morris, J. K., Boniface, S., Tang, J. L. & Milenković, D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ 360 , j5855 (2018).
Qin, W. et al. Light cigarette smoking increases risk of all-cause and cause-specific mortality: findings from the NHIS cohort study. Int. J. Env. Res. Public Health https://doi.org/10.3390/ijerph17145122 (2020).
Rodu, B. & Plurphanswat, N. Mortality among male smokers and smokeless tobacco users in the USA. Harm Reduct. J. 16 , 50 (2019).
Kasza, K. A. et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med. 376 , 342–353 (2017).
Richardson, A., Xiao, H. & Vallone, D. M. Primary and dual users of cigars and cigarettes: profiles, tobacco use patterns and relevance to policy. Nicotine Tob. Res. 14 , 927–932 (2012).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental disorders 5th edn (American Psychiatric Association, 2013).
World Health Organization. Tobacco fact sheet. WHO https://www.who.int/news-room/fact-sheets/detail/tobacco (2021).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C. & Fagerström, K. O. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br. J. Addict. 86 , 1119–1127 (1991).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., Rickert, W. & Robinson, J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 84 , 791–799 (1989).
Etter, J. F., Le Houezec, J. & Perneger, T. V. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology 28 , 359–370 (2003).
DiFranza, J. R. et al. Measuring the loss of autonomy over nicotine use in adolescents: the DANDY (Development and Assessment of Nicotine Dependence in Youths) study. Arch. Pediatr. Adolesc. Med. 156 , 397–403 (2002).
Shiffman, S., Waters, A. & Hickcox, M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob. Res. 6 , 327–348 (2004).
Smith, S. S. et al. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nicotine Tob. Res. 12 , 489–499 (2010).
Foulds, J. et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking E-cigarette users. Nicotine Tob. Res. 17 , 186–192 (2015).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing tobacco use among youth and young adults: a report of the Surgeon General (Centers for Disease Control and Prevention, 2012).
World Health Organization. Tobacco control to improve child health and development. Thematic brief (WHO, 2021).
Lantz, P. M. et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tob. Control. 9 , 47–63 (2000).
Leão, T., Kunst, A. E. & Perelman, J. Cost-effectiveness of tobacco control policies and programmes targeting adolescents: a systematic review. Eur. J. Public Health 28 , 39–43 (2018).
Royal College of Physicians. Smoking and health 2021: a coming of age for tobacco control? (RCP, 2021).
Higashi, H. et al. Cost effectiveness of tobacco control policies in Vietnam: the case of population-level interventions. Appl. Health Econ. Health Policy 9 , 183–196 (2011).
Ranson, M. K., Jha, P., Chaloupka, F. J. & Nguyen, S. N. Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine Tob. Res. 4 , 311–319 (2002).
International Agency for Research on Cancer. I ARC Handbooks of Cancer Prevention: Tobacco control Vol. 14 (IARC, 2011).
Frazer, K. et al. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2 , CD005992 (2016).
Hoffman, S. J. & Tan, C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health 15 , 744 (2015).
McNeill, A. et al. Tobacco packaging design for reducing tobacco use. Cochrane Database Syst. Rev. 4 , CD011244 (2017).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General (Department of Health and Human Services, 2020).
Lindson, N. et al. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 4 , CD013308 (2019).
Krist, A. H. et al. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force recommendation statement. JAMA 325 , 265–279 (2021).
Tutka, P. & Zatonski, W. Cytisine for the treatment of nicotine addiction: from a molecule to therapeutic efficacy. Pharmacol. Rep. 58 , 777–798 (2006).
Courtney, R. J. et al. Effect of cytisine vs varenicline on smoking cessation: a randomized clinical trial. JAMA 326 , 56–64 (2021).
Walker, N. et al. Cytisine versus nicotine for smoking cessation. N. Engl. J. Med. 371 , 2353–2362 (2014). This study validated the utility of cytisine for smoking cessation .
West, R. et al. Placebo-controlled trial of cytisine for smoking cessation. N. Engl. J. Med. 365 , 1193–1200 (2011).
Hajek, P. et al. E-cigarettes compared with nicotine replacement therapy within the UK Stop Smoking Services: the TEC RCT. Health Technol. Assess. 23 , 1–82 (2019).
Walker, N. et al. Nicotine patches used in combination with e-cigarettes (with and without nicotine) for smoking cessation: a pragmatic, randomised trial. Lancet Respir. Med. 8 , 54–64 (2020).
Siu, A. L., U.S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 163 , 622–634 (2015).
Black, N. et al. Behaviour change techniques associated with smoking cessation in intervention and comparator groups of randomized controlled trials: a systematic review and meta-regression. Addiction 115 , 2008–2020 (2020).
Center for Substance Abuse and Treatment. Detoxification and Substance Abuse Treatment (Center for Substance Abuse and Treatment, 2006).
Cahill, K., Hartmann-Boyce, J. & Perera, R. Incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub5 (2015).
Secades-Villa, R., Aonso-Diego, G., García-Pérez, Á. & González-Roz, A. Effectiveness of contingency management for smoking cessation in substance users: a systematic review and meta-analysis. J. Consult. Clin. Psychol. 88 , 951–964 (2020).
Cahill, K. & Perera, R. Competitions and incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub4 (2011).
Trojak, B. et al. Transcranial magnetic stimulation combined with nicotine replacement therapy for smoking cessation: a randomized controlled trial. Brain Stimul. 8 , 1168–1174 (2015).
Wing, V. C. et al. Brain stimulation methods to treat tobacco addiction. Brain Stimul. 6 , 221–230 (2013).
Dinur-Klein, L. et al. Smoking cessation induced by deep repetitive transcranial magnetic stimulation of the prefrontal and insular cortices: a prospective, randomized controlled trial. Biol. Psychiatry 76 , 742–749 (2014).
Goldenberg, M., Danovitch, I. & IsHak, W. W. Quality of life and smoking. Am. J. Addict. 23 , 540–562 (2014).
Heikkinen, H., Jallinoja, P., Saarni, S. I. & Patja, K. The impact of smoking on health-related and overall quality of life: a general population survey in Finland. Nicotine Tob. Res. 10 , 1199–1207 (2008).
Moayeri, F., Hsueh, Y. A., Dunt, D. & Clarke, P. Smoking cessation and quality of life: insights from analysis of longitudinal Australian data, an application for economic evaluations. Value Health 24 , 724–732 (2021).
Taylor, G. M. et al. Smoking cessation for improving mental health. Cochrane Database Syst. Rev. 3 , CD013522 (2021).
López-Nicolás, Á., Trapero-Bertran, M. & Muñoz, C. Smoking, health-related quality of life and economic evaluation. Eur. J. Health Econ. 19 , 747–756 (2018).
Morris, A. Linking nicotine addiction and T2DM. Nat. Rev. Endocrinol. 16 , 6 (2020).
Willi, C., Bodenmann, P., Ghali, W. A., Faris, P. D. & Cornuz, J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. Jama 298 , 2654–2664 (2007).
World Health Organization. WHO report on the global tobacco epidemic (WHO, 2019).
Donny, E. C. et al. Randomized trial of reduced-nicotine standards for cigarettes. N. Engl. J. Med. 373 , 1340–1349 (2015). This study tested the impact of reducing the quantity of nicotine present in cigarettes on smoking .
Benowitz, N. L. & Henningfield, J. E. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N. Engl. J. Med. 331 , 123–125 (1994).
Benowitz, N. L. & Henningfield, J. E. Reducing the nicotine content to make cigarettes less addictive. Tob. Control. 22 , i14–i17 (2013).
Gottlieb, S. & Zeller, M. A nicotine-focused framework for public health. N. Engl. J. Med. 377 , 1111–1114 (2017).
Hall, W. & West, R. Thinking about the unthinkable: a de facto prohibition on smoked tobacco products. Addiction 103 , 873–874 (2008).
Ioannidis, J. P. A. & Jha, P. Does the COVID-19 pandemic provide an opportunity to eliminate the tobacco industry? Lancet Glob. Health 9 , e12–e13 (2021).
Smokefree. Smokefree 2025. Smokefree https://www.smokefree.org.nz/smokefree-in-action/smokefree-aotearoa-2025 (2021).
Morgan, C. J., Das, R. K., Joye, A., Curran, H. V. & Kamboj, S. K. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict. Behav. 38 , 2433–2436 (2013).
Elsaid, S., Kloiber, S. & Le Foll, B. Effects of cannabidiol (CBD) in neuropsychiatric disorders: a review of pre-clinical and clinical findings. Prog. Mol. Biol. Transl. Sci. 167 , 25–75 (2019).
Butler, K. & Le Foll, B. Novel therapeutic and drug development strategies for tobacco use disorder: endocannabinoid modulation. Expert Opin. Drug Discov. 15 , 1065–1080 (2020).
D’Souza, D. C. et al. Efficacy and safety of a fatty acid amide hydrolase inhibitor (PF-04457845) in the treatment of cannabis withdrawal and dependence in men: a double-blind, placebo-controlled, parallel group, phase 2a single-site randomised controlled trial. Lancet Psychiatry 6 , 35–45 (2019).
Robinson, J. D. et al. Pooled analysis of three randomized, double-blind, placebo controlled trials with rimonabant for smoking cessation. Addict. Biol. 23 , 291–303 (2018).
Gueye, A. B. et al. The CB1 neutral antagonist AM4113 retains the therapeutic efficacy of the inverse agonist rimonabant for nicotine dependence and weight loss with better psychiatric tolerability. Int. J. Neuropsychopharmacol. https://doi.org/10.1093/ijnp/pyw068 (2016).
Yammine, L. et al. Exenatide adjunct to nicotine patch facilitates smoking cessation and may reduce post-cessation weight gain: a pilot randomized controlled trial. Nicotine Tob. Res. 23 , 1682–1690 (2021).
Eren-Yazicioglu, C. Y., Yigit, A., Dogruoz, R. E. & Yapici-Eser, H. Can GLP-1 be a target for reward system related disorders? A qualitative synthesis and systematic review analysis of studies on palatable food, drugs of abuse, and alcohol. Front. Behav. Neurosci. 14 , 614884 (2020).
Vanderkam, P. et al. Effectiveness of drugs acting on adrenergic receptors in the treatment for tobacco or alcohol use disorders: systematic review and meta-analysis. Addiction 116 , 1011–1020 (2021).
Sokoloff, P. & Le Foll, B. The dopamine D3 receptor, a quarter century later. Eur. J. Neurosci. 45 , 2–19 (2017).
David, S. P., Lancaster, T., Stead, L. F., Evins, A. E. & Prochaska, J. J. Opioid antagonists for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003086.pub3 (2013).
Ray, L. A. et al. Efficacy of combining varenicline and naltrexone for smoking cessation and drinking reduction: a randomized clinical trial. Am. J. Psychiatry 178 , 818–828 (2021).
Mooney, M. E. et al. Bupropion and naltrexone for smoking cessation: a double-blind randomized placebo-controlled clinical trial. Clin. Pharmacol. Ther. 100 , 344–352 (2016).
Justinova, Z., Le Foll, B., Redhi, G. H., Markou, A. & Goldberg, S. R. Differential effects of the metabotropic glutamate 2/3 receptor agonist LY379268 on nicotine versus cocaine self-administration and relapse in squirrel monkeys. Psychopharmacology 233 , 1791–1800 (2016).
Le Foll, B., Wertheim, C. E. & Goldberg, S. R. Effects of baclofen on conditioned rewarding and discriminative stimulus effects of nicotine in rats. Neurosci. Lett. 443 , 236–240 (2008).
Franklin, T. R. et al. The GABA B agonist baclofen reduces cigarette consumption in a preliminary double-blind placebo-controlled smoking reduction study. Drug Alcohol. Depend. 103 , 30–36 (2009).
Lotfy, N., Elsawah, H. & Hassan, M. Topiramate for smoking cessation: systematic review and meta-analysis. Tob. Prev. Cessat. 6 , 14 (2020).
Shanahan, W. R., Rose, J. E., Glicklich, A., Stubbe, S. & Sanchez-Kam, M. Lorcaserin for smoking cessation and associated weight gain: a randomized 12-week clinical trial. Nicotine Tob. Res. 19 , 944–951 (2017).
Higgins, G. A., Fletcher, P. J. & Shanahan, W. R. Lorcaserin: a review of its preclinical and clinical pharmacology and therapeutic potential. Pharmacol. Ther. 205 , 107417 (2020).
Stead, L. F. & Lancaster, T. Interventions to reduce harm from continued tobacco use. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD005231.pub2 (2007).
Download references
Acknowledgements
B.Le F. is supported by a clinician-scientist award from the Department of Family and Community Medicine at the University of Toronto and the Addiction Psychiatry Chair from the University of Toronto. The funding bodies had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. The authors thank H. Fu (University of Toronto) for assistance with Figs 1–3.
Author information
Authors and affiliations.
Translational Addiction Research Laboratory, Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, University of Toronto, Toronto, Ontario, Canada
Bernard Le Foll
Departments of Family and Community Medicine, Psychiatry, Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada
Department of Medicine, University of Wisconsin, Madison, WI, USA
Megan E. Piper
University of Wisconsin Center for Tobacco Research and Intervention, Madison, WI, USA
Department of Neurobiology and Behaviour, University of California Irvine, Irvine, CA, USA
Christie D. Fowler
Section for Preventive Cardiology, Department of Endocrinology, Morbid Obesity and Preventive Medicine, Oslo University Hospital, Oslo, Norway
Serena Tonstad
Department of Psychiatry, Washington University School of Medicine, St. Louis, MO, USA
Laura Bierut
Institute of Mental Health, Peking University Sixth Hospital, Peking University, Beijing, China
National Institute on Drug Dependence, Peking University Health Science Center, Beijing, China
Centre for Global Health Research, Unity Health Toronto, University of Toronto, Toronto, Ontario, Canada
- Prabhat Jha
National Centre for Youth Substance Use Research, The University of Queensland, St Lucia, Queensland, Australia
Wayne D. Hall
Queensland Alliance for Environmental Health Sciences, The University of Queensland, Woolloongabba, Queensland, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (B.Le F.); Epidemiology (P.J. and W.D.H.); Mechanisms/pathophysiology (C.D.F., L.B., L.L. and B.Le F.); Diagnosis, screening and prevention (P.J., M.E.P., S.T. and B.Le F.); Management (M.E.P., S.T., W.D.H., L.L. and B.Le F.); Quality of life (P.J. and W.D.H.); Outlook (all); Conclusions (all). All authors contributed substantially to the review and editing of the manuscript.
Corresponding author
Correspondence to Bernard Le Foll .
Ethics declarations
Competing interests.
B.Le F. has obtained funding from Pfizer (GRAND Awards, including salary support) for investigator-initiated projects. B.Le F. has received some in-kind donations of cannabis product from Aurora and medication donation from Pfizer and Bioprojet and was provided a coil for TMS study from Brainsway. B.Le F. has obtained industry funding from Canopy (through research grants handled by CAMH or the University of Toronto), Bioprojet, ACS, Indivior and Alkermes. B.Le F. has received in-kind donations of nabiximols from GW Pharma for past studies funded by CIHR and NIH. B.Le F. has been an advisor to Shinoghi. S.T. has received honoraria from Pfizer the manufacturer of varenicline for lectures and advice. All other authors declare no competing interests.
Peer review
Peer reviewer information.
Nature Reviews Disease Primers thanks Jamie Brown, Elisardo Iglesias and Ming Li for their contribution to the peer review of this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
CTRI website: https://d3futrf33lk36a.cloudfront.net/wp-content/uploads/sites/240/2019/04/Meds-Chart.pdf
Philip Morris International: https://www.pmi.com/
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Le Foll, B., Piper, M.E., Fowler, C.D. et al. Tobacco and nicotine use. Nat Rev Dis Primers 8 , 19 (2022). https://doi.org/10.1038/s41572-022-00346-w
Download citation
Accepted : 07 February 2022
Published : 24 March 2022
DOI : https://doi.org/10.1038/s41572-022-00346-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Integrated mrna- and mirna-sequencing analyses unveil the underlying mechanism of tobacco pollutant-induced developmental toxicity in zebrafish embryos.
- Jiasheng Chen
- Xiaoping Zhong
Journal of Translational Medicine (2024)
Influence of substance use on male reproductive health and offspring outcomes
- Jamie O. Lo
- Jason C. Hedges
- Charles A. Easley
Nature Reviews Urology (2024)
Reductions in smoking due to ratification of the Framework Convention for Tobacco Control in 171 countries
- Guillermo Paraje
- Mauricio Flores Muñoz
Nature Medicine (2024)
Nicotinic regulation of microglia: potential contributions to addiction
- Alexa R. Soares
- Marina R. Picciotto
Journal of Neural Transmission (2024)
When smoke meets gut: deciphering the interactions between tobacco smoking and gut microbiota in disease development
- Guangyi Zeng
- Changtao Jiang
Science China Life Sciences (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Home — Essay Samples — Nursing & Health — Nursing — Argumentative Essay On Smoking Cigarettes
Argumentative Essay on Smoking Cigarettes
- Categories: Nursing
About this sample

Words: 507 |
Published: Mar 13, 2024
Words: 507 | Page: 1 | 3 min read
Table of contents
Health effects of smoking, economic implications, impact on non-smokers, the case for regulation, references:.
- Centers for Disease Control and Prevention. (2020). Smoking & Tobacco Use. Retrieved from https://www.cdc.gov/tobacco/data_statistics/index.htm

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 872 words
1 pages / 599 words
2 pages / 988 words
4 pages / 2141 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Nursing
When driving around Miami, FL there are a copious number of billboards that I see advertising for people to become nurses throughout the city. When doing research, I’ve only come across a couple of news articles, advertising on [...]
In the ever-evolving landscape of healthcare, the resilient nurse stands as a beacon of unwavering dedication and adaptability. The key phrase, "pinnacle of nursing strength," captures the image of a nurse who has honed their [...]
Clinical learning experiences hold a paramount role in nursing education, serving as a bridge between theoretical knowledge and practical application. This essay explores the essential role of clinical placements in developing [...]
Gagnon, K., & Sabus, C. (2015). Professionalism in a Digital Age: Opportunities and Considerations for Using Social Media in Health Care. Physical Therapy, 95(3), 406–414.Nayak, S. G. (2018). Time Management in Nursing -- Hour [...]
Postpartum hemorrhage is a significant risk in the postpartum period, requiring prompt recognition, assessment, prevention, and management. Nursing care plays a pivotal role in ensuring the well-being of women experiencing [...]
Are you passionate about the field of nursing but have faced obstacles in your journey to becoming a nurse? In this appeal letter essay, we will explore the challenges and setbacks that aspiring nurses may encounter, and the [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center
Essay: Causes and Effects of Smoking Among Students

Smoking is one of the most dangerous widespread phenomena that threaten lives of a huge number of people worldwide. It starts as a way of having fun, but ends as an addiction that is therefore so difficult to give up. Today, we often hear of “smoking among students”. So why do students smoke and what are the effects that smoking has on them?
Related Papers
The Journal of Contemporary Issues in Business and Government
Tabssum Naz
Introduction: The World Health Organisation has declared that smoking is the biggest health problem, since over four million people die because of it every year and it causes much harm. The assumption that all over the world, including Turkey, about 45% of the population over 15 years old has a smoking habit on a very serious scale reveals how important the problem is for the young population. Material and Method: This study was carried out to determine the smoking status of the final grade students at Atatürk University in the 2003-2004 academic year. A questionnaire form developed by the researchers was used as the data gathering tool. Results: It was found that 42.0% of the participants had smoked (continuous and occasional smoking). The age of onset of smoking was mainly between 14 and 21 years. There was a statistically strong association between duration of smoking, starting time, and smoking amount (p<0.001), including the association between age of onset and smoking status of the students (p<0.05). Of the students, 22.1% stated that they did not know why they started smoking. Their main answers were; 56.5% of them stated they smoked to relieve their stress feelings, 24.6% stated they smoked for pleasure. Conclusion: Cigarette are widely used by university students. The reason why the students started smoking was mostly fellowship environment, and the reason for continuing to smoke was mostly to relieve stress. (Tur Toraks Der 2008;9:93-8) Key words: Smoking, university student, Erzurum, Turkey.
Journal of emerging technologies and innovative research
Dr. Manjur Hossain
IJHASS Journal
International Journal of Public Health Science (IJPHS)
Smoking is the main cause of morbidity and mortality in the world and is estimated to kill 5 million people each year worldwide. If current patterns of tobacco consumption continue, smoking will kill more than 8 million people each year globally by the year 2030, with 80% of these deaths in the developing countries. This study aimed to determine the prevalence and associated factors of cigarette smoking among male university students in Muzaffarabad, Pakistan. A descriptive cross-sectional study was conducted among 542 male students at University of Azad Jammu & Kashmir in Muzaffarabad from July to December 2015. The socio-demographic characteristics and cigarette smoking behavior of the students were measured by using a standardized pre-tested self-administrated validated questionnaire in English. The overall prevalence of cigarette smoking among students was found to be 49.4%. The mean age of starting cigarette smoking was 19.2 2.73 years. Age, marital status and education were found significantly associted with cigarette smoking behavior (p-value<0.05). The most common reason for cigarette smoking was stress alleviation (35.0%) followed by peer pressure (24.5%). As cigarette smoking is considerably higher among students. There is a need to develop effective tobacco control measures among university students in Muzaffarabad.
Mubarak Hussain
Aija Zobena
Despite the detrimental impact of smoking to health, its prevalence remains high. Most students who smoke start to do so regularly around the age of 16-18. Although the proportion of smokers in Latvia is decreasing, the share of electronic cigarette users among young people is growing prematurely, which indicates a change of habits among young people. The aim of the study is to investigate the motives for starting smoking, the factors that contribute to smoking initiation and how high school students become “regular smokers” from “trying” tobacco products. In February 2019, two focus group discussions were organized to obtain information on young people's smoking experience. In each of them, high school students (aged over 18) and students took part. The participants of the focus group discussion were chosen by the “snowball” method. Social factors and the social and psychological characteristics of adolescents have a major impact on the transition from the first cigarette smoke...
Journal of Tropical Pediatrics
Shubhadeep Das
Turk J Med Sci
Sevgi ONCEL
Journal of King Abdulaziz University-Medical Sciences
Samar Alsaggaf
RELATED PAPERS
BMJ Global Health
Theresa Diaz
Chemical Science
Sergiy Rosokha
harsha raju
Archives of Clinical Neuropsychology
Marina Rodríguez Pérez
Aneta Wierzbicka
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology
Endocrinology & metabolic syndrome
Butheinah al-Sharafi
4th International Scientific Conference on Civil Engineering 13, May 16-17, Jelgava, Latvia
Patricia Kara De Maeijer
TasAnyamanPlastik
Jual Tas Anyaman Plastik Hajatan Samarinda
Computers in Biology and Medicine
Mohammed M Elmogy
Agustina Sosa
Vladimir Socor
Letícia Tessarini
alex karagrigoriou
Physical Review C
Isao Tanihata
Estudios Internacionales
Ismael Khalil
Angel De La Torre
Jurnal Pendidikan Indonesia
amandus hutasoit
Pain Physician
Kim Nhu Phan Nguyen
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Persuasive Essay Guide
Persuasive Essay About Smoking
Persuasive Essay About Smoking - Making a Powerful Argument with Examples

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
How to Write a Persuasive Essay About Covid19 | Examples & Tips
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Are you wondering how to write your next persuasive essay about smoking?
Smoking has been one of the most controversial topics in our society for years. It is associated with many health risks and can be seen as a danger to both individuals and communities.
Writing an effective persuasive essay about smoking can help sway public opinion. It can also encourage people to make healthier choices and stop smoking.
But where do you begin?
In this blog, we’ll provide some examples to get you started. So read on to get inspired!
- 1. What You Need To Know About Persuasive Essay
- 2. Persuasive Essay Examples About Smoking
- 3. Argumentative Essay About Smoking Examples
- 4. Tips for Writing a Persuasive Essay About Smoking
What You Need To Know About Persuasive Essay
A persuasive essay is a type of writing that aims to convince its readers to take a certain stance or action. It often uses logical arguments and evidence to back up its argument in order to persuade readers.
It also utilizes rhetorical techniques such as ethos, pathos, and logos to make the argument more convincing. In other words, persuasive essays use facts and evidence as well as emotion to make their points.
A persuasive essay about smoking would use these techniques to convince its readers about any point about smoking. Check out an example below:
Simple persuasive essay about smoking
Tough Essay Due? Hire Tough Writers!
Persuasive Essay Examples About Smoking
Smoking is one of the leading causes of preventable death in the world. It leads to adverse health effects, including lung cancer, heart disease, and damage to the respiratory tract. However, the number of people who smoke cigarettes has been on the rise globally.
A lot has been written on topics related to the effects of smoking. Reading essays about it can help you get an idea of what makes a good persuasive essay.
Here are some sample persuasive essays about smoking that you can use as inspiration for your own writing:
Persuasive speech on smoking outline
Persuasive essay about smoking should be banned
Persuasive essay about smoking pdf
Persuasive essay about smoking cannot relieve stress
Persuasive essay about smoking in public places
Speech about smoking is dangerous
Persuasive Essay About Smoking Introduction
Persuasive Essay About Stop Smoking
Short Persuasive Essay About Smoking
Stop Smoking Persuasive Speech
Check out some more persuasive essay examples on various other topics.
Argumentative Essay About Smoking Examples
An argumentative essay is a type of essay that uses facts and logical arguments to back up a point. It is similar to a persuasive essay but differs in that it utilizes more evidence than emotion.
If you’re looking to write an argumentative essay about smoking, here are some examples to get you started on the arguments of why you should not smoke.
Argumentative essay about smoking pdf
Argumentative essay about smoking in public places
Argumentative essay about smoking introduction
Check out the video below to find useful arguments against smoking:
Tips for Writing a Persuasive Essay About Smoking
You have read some examples of persuasive and argumentative essays about smoking. Now here are some tips that will help you craft a powerful essay on this topic.
Choose a Specific Angle
Select a particular perspective on the issue that you can use to form your argument. When talking about smoking, you can focus on any aspect such as the health risks, economic costs, or environmental impact.
Think about how you want to approach the topic. For instance, you could write about why smoking should be banned.
Check out the list of persuasive essay topics to help you while you are thinking of an angle to choose!
Research the Facts
Before writing your essay, make sure to research the facts about smoking. This will give you reliable information to use in your arguments and evidence for why people should avoid smoking.
You can find and use credible data and information from reputable sources such as government websites, health organizations, and scientific studies.
For instance, you should gather facts about health issues and negative effects of tobacco if arguing against smoking. Moreover, you should use and cite sources carefully.
Paper Due? Why Suffer? That's our Job!
Make an Outline
The next step is to create an outline for your essay. This will help you organize your thoughts and make sure that all the points in your essay flow together logically.
Your outline should include the introduction, body paragraphs, and conclusion. This will help ensure that your essay has a clear structure and argument.
Use Persuasive Language
When writing your essay, make sure to use persuasive language such as “it is necessary” or “people must be aware”. This will help you convey your message more effectively and emphasize the importance of your point.
Also, don’t forget to use rhetorical devices such as ethos, pathos, and logos to make your arguments more convincing. That is, you should incorporate emotion, personal experience, and logic into your arguments.
Introduce Opposing Arguments
Another important tip when writing a persuasive essay on smoking is to introduce opposing arguments. It will show that you are aware of the counterarguments and can provide evidence to refute them. This will help you strengthen your argument.
By doing this, your essay will come off as more balanced and objective, making it more convincing.
Finish Strong
Finally, make sure to finish your essay with a powerful conclusion. This will help you leave a lasting impression on your readers and reinforce the main points of your argument. You can end by summarizing the key points or giving some advice to the reader.
A powerful conclusion could either include food for thought or a call to action. So be sure to use persuasive language and make your conclusion strong.
To conclude,
By following these tips, you can write an effective and persuasive essay on smoking. Remember to research the facts, make an outline, and use persuasive language.
However, don't stress if you need expert help to write your essay! Our professional essay writing service is here for you!
Our persuasive essay writing service is fast, affordable, and trustworthy.
Try it out today!

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading

Smoking and Its Negative Effects on Human Beings Research Paper
Smoking is one of the most common negative habits that people indulge in. Many health experts have warned that smoking is unhealthy and dangerous to the human health. This essay will discuss the negative effects of smoking on human beings.
Smoking cigarette is addictive that is why many smokers have difficulties in giving up the habit. Cigarettes are produced of tobacco with a large percent of other additives, which account for the largest number of preventable deaths in the world. People who smoke commonly face different health problems, which are caused by tobacco consumption. Therefore, smoking has negative health consequences for smokers and people who live with them and become passive smokers as a result.
The WHO and other health organisations have sensitised people on the dangers of smoking. There are many health conditions which smokers are likely to suffer from (Pampel 61). Their bodies absorb harmful toxins which cigarettes contain which are dangerous to their health.
Smoking is a major health risk which results in heart attacks, strokes, bronchitis, and other respiratory diseases. The accumulation of tobacco and other toxins in the respiratory tract of a smoker makes a person suffer from respiratory health conditions.
Smokers, therefore, are likely to incur huge medical bills when they seek for treatment for these diseases. Many governments spend a lot of money on treating smoking related diseases, which increases the cost of healthcare. Pampel argues that smokers can succumb to such illnesses unless they stop smoking (64).
Tobacco consumption causes dental problems which are difficult to reverse. Smokers are likely to have bad breath, stained teeth and smelly gums. Toxic elements, which cigarettes contain, for instance, tar, have dangerous impacts on human health. These substances cause smokers to have poor dents and even lose their teeth (Peate 362).
Smokers are likely to suffer emotionally and psychologically because poor health and unattractive appearance, caused, for example, by stained or broken teeth, make a person lose his/her own self-esteem. Smokers are likely to be shunned by people close to them because of fetid breath, bad body odour and poor outward appearance. Therefore, people need to be made aware of dental and other health problems they are likely to experience as a result of smoking.
Tobacco consumption causes a lot of deaths in developing countries. These countries have weak laws which do not effectively regulate cigarette selling and consumption. Advertisement implicit messages encourage the young to become smokers. Tobacco advertising in many developed countries has been prohibited. However, some third world countries still allow tobacco advertising, which encourages more people to acquire this bad habit.
The images of sophistication, bravery and glamour which are carried by tobacco adverts easily persuade the young to become smokers. Peate reveals that tobacco companies target adolescents and women to increase their sales (363). These people are easily influenced by what they see in the media. People who begin smoking at early age are likely to be addicted for a longer period than those who develop the habit at mature age (Cox).
Smokers are exposed to various carcinogens in cigarettes. These carcinogens cause cancer and negatively affect human health. Lung, throat, brain, bladder, cervical cancer as well as other forms are caused by smoking. The symptoms are often detected at the time when the smoker’s health condition is already chronic.
Cancer is one of the leading causes of death world wide. A significant number of cancer patients have a history of smoking and tobacco consumption (Peate 365). If people get exposed to exhaled smoke, they are likely to be affected by it. They breathe in toxic components of the exhaled smoke that deposit in their lungs and other respiratory organs. These people can suffer from respiratory illnesses as well.
Women, who smoke during pregnancy, are likely to expose their unborn babies to toxic substances contained in cigarettes. The tar that is present in cigarettes is likely to be embedded in the DNA of a mother, who may pass it on to the child in her womb. These toxic components inhibit the normal growth of a baby in the fetus, which results in death and still births. Cox reveals that if the pregnancy proceeds to full term, the delivered child can have severe brain disorders.
Such children are very slow at learning because their cognitive functions are impaired. Female smokers are likely to become infertile or their reproductive abilities are limited. Nicotine restricts the ability of the female reproductive system to generate estrogen. Many physiological and reproductive functions in women depend on estrogen.
Nicotine is a substance found in cigarettes which is very addictive. People who try to give up smoking experience severe withdrawal symptoms, which restrict their ability to function effectively. They are likely to experience several episodes of depression.
This is because their bodies are used to the intake of nicotine and have difficulties in performing its functions without it (Cox). Nicotine stimulates the human mind just like any other drug, which increases the risk of high blood pressure in a smoker. From the above mentioned, it is easy to conclude that smoking has negative effects on people’s health.
Works Cited
Cox, Jack. “ The Lesser Known Harmful Effects of Smoking .” The Register . 2012. Orange Country Register News . Web.
Pampel, Fred C. Tobacco Industry and Smoking . New York: Infobase Publishing, 2009. Print.
Peate, Ian. “The Effects of Smoking on the Reproductive Health of Men”. British Journal of Nursing 14.7 (2005): 362–366. Print.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, June 18). Smoking and Its Negative Effects on Human Beings. https://ivypanda.com/essays/smoking-effects/
"Smoking and Its Negative Effects on Human Beings." IvyPanda , 18 June 2018, ivypanda.com/essays/smoking-effects/.
IvyPanda . (2018) 'Smoking and Its Negative Effects on Human Beings'. 18 June.
IvyPanda . 2018. "Smoking and Its Negative Effects on Human Beings." June 18, 2018. https://ivypanda.com/essays/smoking-effects/.
1. IvyPanda . "Smoking and Its Negative Effects on Human Beings." June 18, 2018. https://ivypanda.com/essays/smoking-effects/.
Bibliography
IvyPanda . "Smoking and Its Negative Effects on Human Beings." June 18, 2018. https://ivypanda.com/essays/smoking-effects/.
- Nicotine: E-Cigarettes and Tobacco Use
- How Smoking Cigarettes Effects Your Health
- Pharmacology of Nicotine: Absorption and Distribution
- Langley Park: Public Health Services
- Importance of Nutrition and Exercise in the Society
- A Major Health Issue in our Society
- Fatigue in workplace
- Problems of Everyday Addictions in Society

IMAGES
VIDEO
COMMENTS
Smoking is the practice of inhaling smoke from burning plant material. Nicotine works on your brain to create a relaxing, pleasurable feeling that makes it tough to quit. But smoking tobacco puts you at risk for cancer, stroke, heart attack, lung disease and other health issues. Nicotine replacements and lifestyle changes may help you quit.
Introduction. Tobacco use, including smoking, has become a universally recognized issue that endangers the health of the population of our entire planet through both active and second-hand smoking. Pro-tobacco arguments are next to non-existent, while its harm is well-documented and proven through past and contemporary studies (Jha et al., 2013).
500 Words Essay On Smoking. One of the most common problems we are facing in today's world which is killing people is smoking. A lot of people pick up this habit because of stress, personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them.
Smoking: Causes and Effects Essay. Among numerous bad habits of modern society smoking seems to be of the greatest importance. Not only does it affect the person who smokes, but also those who are around him. Many people argue about the appropriate definition of smoking, whether it is a disease or just a bad habit.
Smoking affects the lungs and respiratory organs causing such terrible diseases as cancer. Among the most wider spread diseases are peptic ulcers, cancer of the larynx, kidney, pancreas, and other major organs. The resins from the smoke enter the blood and ruin cells. This process is inevitable if a person smokes for years.
Foremost among the cancers caused by tobacco use is lung cancer. Cigarette smoking has been linked to about 80 to 90 percent of all cases of lung cancer, the leading cause of cancer death for both men and women, and it is responsible for roughly 80 percent of deaths from this disease. 22,47 Smoking increases lung cancer risk five to tenfold ...
Tobacco kills more than 8 million people each year, including an estimated 1.3 million non-smokers who are exposed to second-hand smoke (4). Around 80% of the world's 1.3 billion tobacco users live in low- and middle-income countries. In 2020, 22.3% of the world's population used tobacco: 36.7% of men and 7.8% of women.
Smoking can affect a person's health in many other ways as well, harming nearly every organ in the body. Here are a few examples of other ways smoking tobacco can affect your health: Increased risk of gum disease and tooth loss. Lowered immune system function. Increased risk of type 2 diabetes.
Smoking causes about 90% (or 9 out of 10) of all lung cancer deaths. 1,2 More women die from lung cancer each year than from breast cancer. 5. Smoking causes about 80% (or 8 out of 10) of all deaths from chronic obstructive pulmonary disease (COPD). 1. Cigarette smoking increases risk for death from all causes in men and women. 1.
Even among smokers who have quit, chronic lung disease still accounts for 50% of smoking-related conditions. 4. Smoking harms nearly every organ in the body, and is a main cause of lung cancer and COPD. It also is a cause of coronary heart disease, stroke and a host of other cancers and diseases. 1See more of the health effects caused by smoking.
Health Effects. Smoking leads to disease and disability and harms nearly every organ of the body. More than 16 million Americans are living with a disease caused by smoking. For every person who dies because of smoking, at least 30 people live with a serious smoking-related illness. Smoking causes cancer, heart disease, stroke, lung diseases ...
This damages the blood vessels. Smoking can result in stroke and heart attacks since it hinders blood flow, interrupting oxygen to various parts of the body, such as feet and hands. Introduction of cigarettes with low tar does not reduce these effects since smokers often prefer deeper puffs and hold the smoke in lungs for a long period.
The net result of the broad spectrum of short-term and long-term deleterious health effects caused by cigarette smoking and the substantial prevalence of smoking is that cigarette smoking is the single most important cause of preventable disease and premature mortality in the United States and in many other high-income nations (Thun et al., 2012).
Health impact of smoking. Table Table1 1 lists the main causes of death from smoking. Tobacco smoking is estimated to lead to the premature death of approximately 6 million people worldwide and 96,000 in the UK each year (Action on Smoking and Health, 2016b; World Health Organization, 2013).A 'premature death from smoking' is defined as a death from a smoking-related disease in an ...
500 Words Essay on Harmful Effects of Smoking Introduction. Smoking is a prevalent habit, often started out of curiosity, peer pressure, or stress management. However, its harmful effects are well-documented, impacting nearly every organ in the human body. Despite the widespread knowledge of its adverse effects, smoking continues to be a ...
Introduction. Tobacco use is a global epidemic among young people. As with adults, it poses a serious health threat to youth and young adults in the United States and has significant implications for this nation's public and economic health in the future (Perry et al. 1994; Kessler 1995).The impact of cigarette smoking and other tobacco use on chronic disease, which accounts for 75% of ...
Smoking and cardiovascular disease. Smoking is a major cause of CVD, causing one in every four deaths from CVD. 10. Smoking can: 11. Raise triglycerides (a type of fat in your blood) Lower "good" cholesterol (HDL) Make blood sticky and more likely to clot, which can block blood flow to the heart and brain.
Smoking is associated with various adverse effects. For instance, smoking of tobacco is known to cause gum diseases, yellowing of teeth as well as teeth decay. Similarly, the tar that is contained in tobacco is very dangerous. The tar is known to cause discoursing of teeth as well as triggering throat cancer.
Abstract. Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will ...
The dangers of smoking cigarettes have been well-documented, yet millions of people continue to engage in this harmful habit. The debate over the impact of smoking on public health is ongoing, with some arguing for stricter regulations and others advocating for personal freedom. In this essay, we will explore the various arguments surrounding smoking cigarettes and ultimately make the case for ...
Smoking causes cancer. As a result, the addict students would suffer from health problems that end in death. Another effect is that after certain years, the addict would develop respiratory problems and will face a lot of problems in running without losing breath. So, asthma and bronchitis are always a lingering threat.
Smoking is also known to contribute to other health conditions. According to Graham (2010), smoking has been confirmed to be the leading cause of some forms of cancer. The above scholar says that smoking always increases the chances of one developing such cancers as cancer of the throat and mouth. Cancer is a medical condition that has been ...
Persuasive Essay Examples About Smoking. Smoking is one of the leading causes of preventable death in the world. It leads to adverse health effects, including lung cancer, heart disease, and damage to the respiratory tract. However, the number of people who smoke cigarettes has been on the rise globally. A lot has been written on topics related ...
Smokers are exposed to various carcinogens in cigarettes. These carcinogens cause cancer and negatively affect human health. Lung, throat, brain, bladder, cervical cancer as well as other forms are caused by smoking. The symptoms are often detected at the time when the smoker's health condition is already chronic.