Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 16 June 2020

COVID-19 impact on research, lessons learned from COVID-19 research, implications for pediatric research
- Debra L. Weiner 1 , 2 ,
- Vivek Balasubramaniam 3 ,
- Shetal I. Shah 4 &
- Joyce R. Javier 5 , 6
on behalf of the Pediatric Policy Council
Pediatric Research volume 88 , pages 148–150 ( 2020 ) Cite this article
147k Accesses
81 Citations
19 Altmetric
Metrics details
The COVID-19 pandemic has resulted in unprecedented research worldwide. The impact on research in progress at the time of the pandemic, the importance and challenges of real-time pandemic research, and the importance of a pediatrician-scientist workforce are all highlighted by this epic pandemic. As we navigate through and beyond this pandemic, which will have a long-lasting impact on our world, including research and the biomedical research enterprise, it is important to recognize and address opportunities and strategies for, and challenges of research and strengthening the pediatrician-scientist workforce.
The first cases of what is now recognized as SARS-CoV-2 infection, termed COVID-19, were reported in Wuhan, China in December 2019 as cases of fatal pneumonia. By February 26, 2020, COVID-19 had been reported on all continents except Antarctica. As of May 4, 2020, 3.53 million cases and 248,169 deaths have been reported from 210 countries. 1
Impact of COVID-19 on ongoing research
The impact on research in progress prior to COVID-19 was rapid, dramatic, and no doubt will be long term. The pandemic curtailed most academic, industry, and government basic science and clinical research, or redirected research to COVID-19. Most clinical trials, except those testing life-saving therapies, have been paused, and most continuing trials are now closed to new enrollment. Ongoing clinical trials have been modified to enable home administration of treatment and virtual monitoring to minimize participant risk of COVID-19 infection, and to avoid diverting healthcare resources from pandemic response. In addition to short- and long-term patient impact, these research disruptions threaten the careers of physician-scientists, many of whom have had to shift efforts from research to patient care. To protect research in progress, as well as physician-scientist careers and the research workforce, ongoing support is critical. NIH ( https://grants.nih.gov/policy/natural-disasters/corona-virus.htm ), PCORI ( https://www.pcori.org/funding-opportunities/applicant-and-awardee-faqs-related-covid-19 ), and other funders acted swiftly to provide guidance on proposal submission and award management, and implement allowances that enable grant personnel to be paid and time lines to be relaxed. Research institutions have also implemented strategies to mitigate the long-term impact of research disruptions. Support throughout and beyond the pandemic to retain currently well-trained research personnel and research support teams, and to accommodate loss of research assets, including laboratory supplies and study participants, will be required to complete disrupted research and ultimately enable new research.
In the long term, it is likely that the pandemic will force reallocation of research dollars at the expense of research areas funded prior to the pandemic. It will be more important than ever for the pediatric research community to engage in discussion and decisions regarding prioritization of funding goals for dedicated pediatric research and meaningful inclusion of children in studies. The recently released 2020 National Institute of Child Health and Development (NICHD) strategic plan that engaged stakeholders, including scientists and patients, to shape the goals of the Institute, will require modification to best chart a path toward restoring normalcy within pediatric science.
COVID-19 research
This global pandemic once again highlights the importance of research, stable research infrastructure, and funding for public health emergency (PHE)/disaster preparedness, response, and resiliency. The stakes in this worldwide pandemic have never been higher as lives are lost, economies falter, and life has radically changed. Ultimate COVID-19 mitigation and crisis resolution is dependent on high-quality research aligned with top priority societal goals that yields trustworthy data and actionable information. While the highest priority goals are treatment and prevention, biomedical research also provides data critical to manage and restore economic and social welfare.
Scientific and technological knowledge and resources have never been greater and have been leveraged globally to perform COVID-19 research at warp speed. The number of studies related to COVID-19 increases daily, the scope and magnitude of engagement is stunning, and the extent of global collaboration unprecedented. On January 5, 2020, just weeks after the first cases of illness were reported, the genetic sequence, which identified the pathogen as a novel coronavirus, SARS-CoV-2, was released, providing information essential for identifying and developing treatments, vaccines, and diagnostics. As of May 3, 2020 1133 COVID-19 studies, including 148 related to hydroxychloroquine, 13 to remdesivir, 50 to vaccines, and 100 to diagnostic testing, were registered on ClinicalTrials.gov, and 980 different studies on the World Health Organization’s International Clinical Trials Registry Platform (WHO ICTRP), made possible, at least in part, by use of data libraries to inform development of antivirals, immunomodulators, antibody-based biologics, and vaccines. On April 7, 2020, the FDA launched the Coronavirus Treatment Acceleration Program (CTAP) ( https://www.fda.gov/drugs/coronavirus-covid-19-drugs/coronavirus-treatment-acceleration-program-ctap ). On April 17, 2020, NIH announced a partnership with industry to expedite vaccine development ( https://www.nih.gov/news-events/news-releases/nih-launch-public-private-partnership-speed-covid-19-vaccine-treatment-options ). As of May 1, 2020, remdesivir (Gilead), granted FDA emergency use authorization, is the only approved therapeutic for COVID-19. 2
The pandemic has intensified research challenges. In a rush for data already thousands of manuscripts, news reports, and blogs have been published, but to date, there is limited scientifically robust data. Some studies do not meet published clinical trial standards, which now include FDA’s COVID-19-specific standards, 3 , 4 , 5 and/or are published without peer review. Misinformation from studies diverts resources from development and testing of more promising therapeutic candidates and has endangered lives. Ibuprofen, initially reported as unsafe for patients with COVID-19, resulted in a shortage of acetaminophen, endangering individuals for whom ibuprofen is contraindicated. Hydroxychloroquine initially reported as potentially effective for treatment of COVID-19 resulted in shortages for patients with autoimmune diseases. Remdesivir, in rigorous trials, showed decrease in duration of COVID-19, with greater effect given early. 6 Given the limited availability and safety data, the use outside clinical trials is currently approved only for severe disease. Vaccines typically take 10–15 years to develop. As of May 3, 2020, of nearly 100 vaccines in development, 8 are in trial. Several vaccines are projected to have emergency approval within 12–18 months, possibly as early as the end of the year, 7 still an eternity for this pandemic, yet too soon for long-term effectiveness and safety data. Antibody testing, necessary for diagnosis, therapeutics, and vaccine testing, has presented some of the greatest research challenges, including validation, timing, availability and prioritization of testing, interpretation of test results, and appropriate patient and societal actions based on results. 8 Relaxing physical distancing without data regarding test validity, duration, and strength of immunity to different strains of COVID-19 could have catastrophic results. Understanding population differences and disparities, which have been further exposed during this pandemic, is critical for response and long-term pandemic recovery. The “Equitable Data Collection and Disclosure on COVID-19 Act” calls for the CDC (Centers for Disease Control and Prevention) and other HHS (United States Department of Health & Human Services) agencies to publicly release racial and demographic information ( https://bass.house.gov/sites/bass.house.gov/files/Equitable%20Data%20Collection%20and%20Dislosure%20on%20COVID19%20Act_FINAL.pdf )
Trusted sources of up-to-date, easily accessible information must be identified (e.g., WHO https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov , CDC https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html , and for children AAP (American Academy of Pediatrics) https://www.aappublications.org/cc/covid-19 ) and should comment on quality of data and provide strategies and crisis standards to guide clinical practice.
Long-term, lessons learned from research during this pandemic could benefit the research enterprise worldwide beyond the pandemic and during other PHE/disasters with strategies for balancing multiple novel approaches and high-quality, time-efficient, cost-effective research. This challenge, at least in part, can be met by appropriate study design, collaboration, patient registries, automated data collection, artificial intelligence, data sharing, and ongoing consideration of appropriate regulatory approval processes. In addition, research to develop and evaluate innovative strategies and technologies to improve access to care, management of health and disease, and quality, safety, and cost effectiveness of care could revolutionize healthcare and healthcare systems. During PHE/disasters, crisis standards for research should be considered along with ongoing and just-in-time PHE/disaster training for researchers willing to share information that could be leveraged at time of crisis. A dedicated funded core workforce of PHE/disaster researchers and funded infrastructure should be considered, potentially as a consortium of networks, that includes physician-scientists, basic scientists, social scientists, mental health providers, global health experts, epidemiologists, public health experts, engineers, information technology experts, economists and educators to strategize, consult, review, monitor, interpret studies, guide appropriate clinical use of data, and inform decisions regarding effective use of resources for PHE/disaster research.
Differences between adult and pediatric COVID-19, the need for pediatric research
As reported by the CDC, from February 12 to April 2, 2020, of 149,760 cases of confirmed COVID-19 in the United States, 2572 (1.7%) were children aged <18 years, similar to published rates in China. 9 Severe illness has been rare. Of 749 children for whom hospitalization data is available, 147 (20%) required hospitalization (5.7% of total children), and 15 of 147 required ICU care (2.0%, 0.58% of total). Of the 95 children aged <1 year, 59 (62%) were hospitalized, and 5 (5.3%) required ICU admission. Among children there were three deaths. Despite children being relatively spared by COVID-19, spread of disease by children, and consequences for their health and pediatric healthcare are potentially profound with immediate and long-term impact on all of society.
We have long been aware of the importance and value of pediatric research on children, and society. COVID-19 is no exception and highlights the imperative need for a pediatrician-scientist workforce. Understanding differences in epidemiology, susceptibility, manifestations, and treatment of COVID-19 in children can provide insights into this pathogen, pathogen–host interactions, pathophysiology, and host response for the entire population. Pediatric clinical registries of COVID-infected, COVID-exposed children can provide data and specimens for immediate and long-term research. Of the 1133 COVID-19 studies on ClinicalTrials.gov, 202 include children aged ≤17 years. Sixty-one of the 681 interventional trials include children. With less diagnostic testing and less pediatric research, we not only endanger children, but also adults by not identifying infected children and limiting spread by children.
Pediatric considerations and challenges related to treatment and vaccine research for COVID-19 include appropriate dosing, pediatric formulation, and pediatric specific short- and long-term effectiveness and safety. Typically, initial clinical trials exclude children until safety has been established in adults. But with time of the essence, deferring pediatric research risks the health of children, particularly those with special needs. Considerations specific to pregnant women, fetuses, and neonates must also be addressed. Childhood mental health in this demographic, already struggling with a mental health pandemic prior to COVID-19, is now further challenged by social disruption, food and housing insecurity, loss of loved ones, isolation from friends and family, and exposure to an infodemic of pandemic-related information. Interestingly, at present mental health visits along with all visits to pediatric emergency departments across the United States are dramatically decreased. Understanding factors that mitigate and worsen psychiatric symptoms should be a focus of research, and ideally will result in strategies for prevention and management in the long term, including beyond this pandemic. Social well-being of children must also be studied. Experts note that the pandemic is a perfect storm for child maltreatment given that vulnerable families are now socially isolated, facing unemployment, and stressed, and that children are not under the watch of mandated reporters in schools, daycare, and primary care. 10 Many states have observed a decrease in child abuse reports and an increase in severity of emergency department abuse cases. In the short term and long term, it will be important to study the impact of access to care, missed care, and disrupted education during COVID-19 on physical and cognitive development.
Training and supporting pediatrician-scientists, such as through NIH physician-scientist research training and career development programs ( https://researchtraining.nih.gov/infographics/physician-scientist ) at all stages of career, as well as fostering research for fellows, residents, and medical students willing to dedicate their research career to, or at least understand implications of their research for, PHE/disasters is important for having an ongoing, as well as a just-in-time surge pediatric-focused PHE/disaster workforce. In addition to including pediatric experts in collaborations and consortiums with broader population focus, consideration should be given to pediatric-focused multi-institutional, academic, industry, and/or government consortiums with infrastructure and ongoing funding for virtual training programs, research teams, and multidisciplinary oversight.
The impact of the COVID-19 pandemic on research and research in response to the pandemic once again highlights the importance of research, challenges of research particularly during PHE/disasters, and opportunities and resources for making research more efficient and cost effective. New paradigms and models for research will hopefully emerge from this pandemic. The importance of building sustained PHE/disaster research infrastructure and a research workforce that includes training and funding for pediatrician-scientists and integrates the pediatrician research workforce into high-quality research across demographics, supports the pediatrician-scientist workforce and pipeline, and benefits society.
Johns Hopkins Coronavirus Resource Center. Covid-19 Case Tracker. Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html (2020).
US Food and Drug Administration. Coronavirus (COVID-19) update: FDA issues emergency use authorization for potential COVID-19 treatment. FDA News Release . https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-emergency-use-authorization-potential-covid-19-treatment (2020).
Evans, S. R. Fundamentals of clinical trial design. J. Exp. Stroke Transl. Med. 3 , 19–27 (2010).
Article Google Scholar
Antman, E. M. & Bierer, B. E. Standards for clinical research: keeping pace with the technology of the future. Circulation 133 , 823–825 (2016).
Food and Drug Administration. FDA guidance on conduct of clinical trials of medical products during COVID-19 public health emergency. Guidance for Industry, Investigators and Institutional Review Boards . https://www.fda.gov/regulatory-information/search-fda-guidance-documents/fda-guidance-conduct-clinical-trials-medical-products-during-covid-19-public-health-emergency (2020).
National Institutes of Health. NIH clinical trials shows remdesivir accelerates recovery from advanced COVID-19. NIH New Releases . https://www.nih.gov/news-events/news-releases/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19#.XrIX75ZmQeQ.email (2020).
Radcliffe, S. Here’s exactly where we are with vaccines and treatments for COVID-19. Health News . https://www.healthline.com/health-news/heres-exactly-where-were-at-with-vaccines-and-treatments-for-covid-19 (2020).
Abbasi, J. The promise and peril of antibody testing for COVID-19. JAMA . https://doi.org/10.1001/jama.2020.6170 (2020).
CDC COVID-19 Response Team. Coronavirus disease 2019 in children—United States, February 12–April 2, 2020. Morb. Mortal Wkly Rep . 69 , 422–426 (2020).
Agarwal, N. Opinion: the coronavirus could cause a child abuse epidemic. The New York Times . https://www.nytimes.com/2020/04/07/opinion/coronavirus-child-abuse.html (2020).
Download references
Author information
Authors and affiliations.
Department of Pediatrics, Division of Emergency Medicine, Boston Children’s Hospital, Boston, MA, USA
Debra L. Weiner
Harvard Medical School, Boston, MA, USA
Department of Pediatrics, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA
Vivek Balasubramaniam
Department of Pediatrics and Division of Neonatology, Maria Fareri Children’s Hospital at Westchester Medical Center, New York Medical College, Valhalla, NY, USA
Shetal I. Shah
Division of General Pediatrics, Children’s Hospital Los Angeles, Los Angeles, CA, USA
Joyce R. Javier
Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
You can also search for this author in PubMed Google Scholar
Contributions
All authors made substantial contributions to conception and design, data acquisition and interpretation, drafting the manuscript, and providing critical revisions. All authors approve this final version of the manuscript.
Pediatric Policy Council
Scott C. Denne, MD, Chair, Pediatric Policy Council; Mona Patel, MD, Representative to the PPC from the Academic Pediatric Association; Jean L. Raphael, MD, MPH, Representative to the PPC from the Academic Pediatric Association; Jonathan Davis, MD, Representative to the PPC from the American Pediatric Society; DeWayne Pursley, MD, MPH, Representative to the PPC from the American Pediatric Society; Tina Cheng, MD, MPH, Representative to the PPC from the Association of Medical School Pediatric Department Chairs; Michael Artman, MD, Representative to the PPC from the Association of Medical School Pediatric Department Chairs; Shetal Shah, MD, Representative to the PPC from the Society for Pediatric Research; Joyce Javier, MD, MPH, MS, Representative to the PPC from the Society for Pediatric Research.
Corresponding author
Correspondence to Debra L. Weiner .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Pediatric Policy Council are listed below Author contributions.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Weiner, D.L., Balasubramaniam, V., Shah, S.I. et al. COVID-19 impact on research, lessons learned from COVID-19 research, implications for pediatric research. Pediatr Res 88 , 148–150 (2020). https://doi.org/10.1038/s41390-020-1006-3
Download citation
Received : 07 May 2020
Accepted : 21 May 2020
Published : 16 June 2020
Issue Date : August 2020
DOI : https://doi.org/10.1038/s41390-020-1006-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Catalysing global surgery: a meta-research study on factors affecting surgical research collaborations with africa.
- Thomas O. Kirengo
- Hussein Dossajee
- Nchafatso G. Obonyo
Systematic Reviews (2024)
Lessons learnt while designing and conducting a longitudinal study from the first Italian COVID-19 pandemic wave up to 3 years
- Alvisa Palese
- Stefania Chiappinotto
- Carlo Tascini
Health Research Policy and Systems (2023)
Pediatric Research and COVID-19: the changed landscape
- E. J. Molloy
- C. B. Bearer
Pediatric Research (2022)
Cancer gene therapy 2020: highlights from a challenging year
- Georgios Giamas
- Teresa Gagliano
Cancer Gene Therapy (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Research article
- Open access
- Published: 04 June 2021
Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews
- Israel Júnior Borges do Nascimento 1 , 2 ,
- Dónal P. O’Mathúna 3 , 4 ,
- Thilo Caspar von Groote 5 ,
- Hebatullah Mohamed Abdulazeem 6 ,
- Ishanka Weerasekara 7 , 8 ,
- Ana Marusic 9 ,
- Livia Puljak ORCID: orcid.org/0000-0002-8467-6061 10 ,
- Vinicius Tassoni Civile 11 ,
- Irena Zakarija-Grkovic 9 ,
- Tina Poklepovic Pericic 9 ,
- Alvaro Nagib Atallah 11 ,
- Santino Filoso 12 ,
- Nicola Luigi Bragazzi 13 &
- Milena Soriano Marcolino 1
On behalf of the International Network of Coronavirus Disease 2019 (InterNetCOVID-19)
BMC Infectious Diseases volume 21 , Article number: 525 ( 2021 ) Cite this article
16k Accesses
29 Citations
13 Altmetric
Metrics details
Navigating the rapidly growing body of scientific literature on the SARS-CoV-2 pandemic is challenging, and ongoing critical appraisal of this output is essential. We aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Nine databases (Medline, EMBASE, Cochrane Library, CINAHL, Web of Sciences, PDQ-Evidence, WHO’s Global Research, LILACS, and Epistemonikos) were searched from December 1, 2019, to March 24, 2020. Systematic reviews analyzing primary studies of COVID-19 were included. Two authors independently undertook screening, selection, extraction (data on clinical symptoms, prevalence, pharmacological and non-pharmacological interventions, diagnostic test assessment, laboratory, and radiological findings), and quality assessment (AMSTAR 2). A meta-analysis was performed of the prevalence of clinical outcomes.
Eighteen systematic reviews were included; one was empty (did not identify any relevant study). Using AMSTAR 2, confidence in the results of all 18 reviews was rated as “critically low”. Identified symptoms of COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%) and gastrointestinal complaints (5–9%). Severe symptoms were more common in men. Elevated C-reactive protein and lactate dehydrogenase, and slightly elevated aspartate and alanine aminotransferase, were commonly described. Thrombocytopenia and elevated levels of procalcitonin and cardiac troponin I were associated with severe disease. A frequent finding on chest imaging was uni- or bilateral multilobar ground-glass opacity. A single review investigated the impact of medication (chloroquine) but found no verifiable clinical data. All-cause mortality ranged from 0.3 to 13.9%.
Conclusions
In this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic were of questionable usefulness. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards.
Peer Review reports
The spread of the “Severe Acute Respiratory Coronavirus 2” (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [ 1 ]. The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [ 2 ], causing massive economic strain, and escalating healthcare and public health expenses [ 3 , 4 ].
The research community has responded by publishing an impressive number of scientific reports related to COVID-19. The world was alerted to the new disease at the beginning of 2020 [ 1 ], and by mid-March 2020, more than 2000 articles had been published on COVID-19 in scholarly journals, with 25% of them containing original data [ 5 ]. The living map of COVID-19 evidence, curated by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), contained more than 40,000 records by February 2021 [ 6 ]. More than 100,000 records on PubMed were labeled as “SARS-CoV-2 literature, sequence, and clinical content” by February 2021 [ 7 ].
Due to publication speed, the research community has voiced concerns regarding the quality and reproducibility of evidence produced during the COVID-19 pandemic, warning of the potential damaging approach of “publish first, retract later” [ 8 ]. It appears that these concerns are not unfounded, as it has been reported that COVID-19 articles were overrepresented in the pool of retracted articles in 2020 [ 9 ]. These concerns about inadequate evidence are of major importance because they can lead to poor clinical practice and inappropriate policies [ 10 ].
Systematic reviews are a cornerstone of today’s evidence-informed decision-making. By synthesizing all relevant evidence regarding a particular topic, systematic reviews reflect the current scientific knowledge. Systematic reviews are considered to be at the highest level in the hierarchy of evidence and should be used to make informed decisions. However, with high numbers of systematic reviews of different scope and methodological quality being published, overviews of multiple systematic reviews that assess their methodological quality are essential [ 11 , 12 , 13 ]. An overview of systematic reviews helps identify and organize the literature and highlights areas of priority in decision-making.
In this overview of systematic reviews, we aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Methodology
Research question.
This overview’s primary objective was to summarize and critically appraise systematic reviews that assessed any type of primary clinical data from patients infected with SARS-CoV-2. Our research question was purposefully broad because we wanted to analyze as many systematic reviews as possible that were available early following the COVID-19 outbreak.
Study design
We conducted an overview of systematic reviews. The idea for this overview originated in a protocol for a systematic review submitted to PROSPERO (CRD42020170623), which indicated a plan to conduct an overview.
Overviews of systematic reviews use explicit and systematic methods for searching and identifying multiple systematic reviews addressing related research questions in the same field to extract and analyze evidence across important outcomes. Overviews of systematic reviews are in principle similar to systematic reviews of interventions, but the unit of analysis is a systematic review [ 14 , 15 , 16 ].
We used the overview methodology instead of other evidence synthesis methods to allow us to collate and appraise multiple systematic reviews on this topic, and to extract and analyze their results across relevant topics [ 17 ]. The overview and meta-analysis of systematic reviews allowed us to investigate the methodological quality of included studies, summarize results, and identify specific areas of available or limited evidence, thereby strengthening the current understanding of this novel disease and guiding future research [ 13 ].
A reporting guideline for overviews of reviews is currently under development, i.e., Preferred Reporting Items for Overviews of Reviews (PRIOR) [ 18 ]. As the PRIOR checklist is still not published, this study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 statement [ 19 ]. The methodology used in this review was adapted from the Cochrane Handbook for Systematic Reviews of Interventions and also followed established methodological considerations for analyzing existing systematic reviews [ 14 ].
Approval of a research ethics committee was not necessary as the study analyzed only publicly available articles.
Eligibility criteria
Systematic reviews were included if they analyzed primary data from patients infected with SARS-CoV-2 as confirmed by RT-PCR or another pre-specified diagnostic technique. Eligible reviews covered all topics related to COVID-19 including, but not limited to, those that reported clinical symptoms, diagnostic methods, therapeutic interventions, laboratory findings, or radiological results. Both full manuscripts and abbreviated versions, such as letters, were eligible.
No restrictions were imposed on the design of the primary studies included within the systematic reviews, the last search date, whether the review included meta-analyses or language. Reviews related to SARS-CoV-2 and other coronaviruses were eligible, but from those reviews, we analyzed only data related to SARS-CoV-2.
No consensus definition exists for a systematic review [ 20 ], and debates continue about the defining characteristics of a systematic review [ 21 ]. Cochrane’s guidance for overviews of reviews recommends setting pre-established criteria for making decisions around inclusion [ 14 ]. That is supported by a recent scoping review about guidance for overviews of systematic reviews [ 22 ].
Thus, for this study, we defined a systematic review as a research report which searched for primary research studies on a specific topic using an explicit search strategy, had a detailed description of the methods with explicit inclusion criteria provided, and provided a summary of the included studies either in narrative or quantitative format (such as a meta-analysis). Cochrane and non-Cochrane systematic reviews were considered eligible for inclusion, with or without meta-analysis, and regardless of the study design, language restriction and methodology of the included primary studies. To be eligible for inclusion, reviews had to be clearly analyzing data related to SARS-CoV-2 (associated or not with other viruses). We excluded narrative reviews without those characteristics as these are less likely to be replicable and are more prone to bias.
Scoping reviews and rapid reviews were eligible for inclusion in this overview if they met our pre-defined inclusion criteria noted above. We included reviews that addressed SARS-CoV-2 and other coronaviruses if they reported separate data regarding SARS-CoV-2.
Information sources
Nine databases were searched for eligible records published between December 1, 2019, and March 24, 2020: Cochrane Database of Systematic Reviews via Cochrane Library, PubMed, EMBASE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Web of Sciences, LILACS (Latin American and Caribbean Health Sciences Literature), PDQ-Evidence, WHO’s Global Research on Coronavirus Disease (COVID-19), and Epistemonikos.
The comprehensive search strategy for each database is provided in Additional file 1 and was designed and conducted in collaboration with an information specialist. All retrieved records were primarily processed in EndNote, where duplicates were removed, and records were then imported into the Covidence platform [ 23 ]. In addition to database searches, we screened reference lists of reviews included after screening records retrieved via databases.
Study selection
All searches, screening of titles and abstracts, and record selection, were performed independently by two investigators using the Covidence platform [ 23 ]. Articles deemed potentially eligible were retrieved for full-text screening carried out independently by two investigators. Discrepancies at all stages were resolved by consensus. During the screening, records published in languages other than English were translated by a native/fluent speaker.
Data collection process
We custom designed a data extraction table for this study, which was piloted by two authors independently. Data extraction was performed independently by two authors. Conflicts were resolved by consensus or by consulting a third researcher.
We extracted the following data: article identification data (authors’ name and journal of publication), search period, number of databases searched, population or settings considered, main results and outcomes observed, and number of participants. From Web of Science (Clarivate Analytics, Philadelphia, PA, USA), we extracted journal rank (quartile) and Journal Impact Factor (JIF).
We categorized the following as primary outcomes: all-cause mortality, need for and length of mechanical ventilation, length of hospitalization (in days), admission to intensive care unit (yes/no), and length of stay in the intensive care unit.
The following outcomes were categorized as exploratory: diagnostic methods used for detection of the virus, male to female ratio, clinical symptoms, pharmacological and non-pharmacological interventions, laboratory findings (full blood count, liver enzymes, C-reactive protein, d-dimer, albumin, lipid profile, serum electrolytes, blood vitamin levels, glucose levels, and any other important biomarkers), and radiological findings (using radiography, computed tomography, magnetic resonance imaging or ultrasound).
We also collected data on reporting guidelines and requirements for the publication of systematic reviews and meta-analyses from journal websites where included reviews were published.
Quality assessment in individual reviews
Two researchers independently assessed the reviews’ quality using the “A MeaSurement Tool to Assess Systematic Reviews 2 (AMSTAR 2)”. We acknowledge that the AMSTAR 2 was created as “a critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both” [ 24 ]. However, since AMSTAR 2 was designed for systematic reviews of intervention trials, and we included additional types of systematic reviews, we adjusted some AMSTAR 2 ratings and reported these in Additional file 2 .
Adherence to each item was rated as follows: yes, partial yes, no, or not applicable (such as when a meta-analysis was not conducted). The overall confidence in the results of the review is rated as “critically low”, “low”, “moderate” or “high”, according to the AMSTAR 2 guidance based on seven critical domains, which are items 2, 4, 7, 9, 11, 13, 15 as defined by AMSTAR 2 authors [ 24 ]. We reported our adherence ratings for transparency of our decision with accompanying explanations, for each item, in each included review.
One of the included systematic reviews was conducted by some members of this author team [ 25 ]. This review was initially assessed independently by two authors who were not co-authors of that review to prevent the risk of bias in assessing this study.
Synthesis of results
For data synthesis, we prepared a table summarizing each systematic review. Graphs illustrating the mortality rate and clinical symptoms were created. We then prepared a narrative summary of the methods, findings, study strengths, and limitations.
For analysis of the prevalence of clinical outcomes, we extracted data on the number of events and the total number of patients to perform proportional meta-analysis using RStudio© software, with the “meta” package (version 4.9–6), using the “metaprop” function for reviews that did not perform a meta-analysis, excluding case studies because of the absence of variance. For reviews that did not perform a meta-analysis, we presented pooled results of proportions with their respective confidence intervals (95%) by the inverse variance method with a random-effects model, using the DerSimonian-Laird estimator for τ 2 . We adjusted data using Freeman-Tukey double arcosen transformation. Confidence intervals were calculated using the Clopper-Pearson method for individual studies. We created forest plots using the RStudio© software, with the “metafor” package (version 2.1–0) and “forest” function.
Managing overlapping systematic reviews
Some of the included systematic reviews that address the same or similar research questions may include the same primary studies in overviews. Including such overlapping reviews may introduce bias when outcome data from the same primary study are included in the analyses of an overview multiple times. Thus, in summaries of evidence, multiple-counting of the same outcome data will give data from some primary studies too much influence [ 14 ]. In this overview, we did not exclude overlapping systematic reviews because, according to Cochrane’s guidance, it may be appropriate to include all relevant reviews’ results if the purpose of the overview is to present and describe the current body of evidence on a topic [ 14 ]. To avoid any bias in summary estimates associated with overlapping reviews, we generated forest plots showing data from individual systematic reviews, but the results were not pooled because some primary studies were included in multiple reviews.
Our search retrieved 1063 publications, of which 175 were duplicates. Most publications were excluded after the title and abstract analysis ( n = 860). Among the 28 studies selected for full-text screening, 10 were excluded for the reasons described in Additional file 3 , and 18 were included in the final analysis (Fig. 1 ) [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Reference list screening did not retrieve any additional systematic reviews.

PRISMA flow diagram
Characteristics of included reviews
Summary features of 18 systematic reviews are presented in Table 1 . They were published in 14 different journals. Only four of these journals had specific requirements for systematic reviews (with or without meta-analysis): European Journal of Internal Medicine, Journal of Clinical Medicine, Ultrasound in Obstetrics and Gynecology, and Clinical Research in Cardiology . Two journals reported that they published only invited reviews ( Journal of Medical Virology and Clinica Chimica Acta ). Three systematic reviews in our study were published as letters; one was labeled as a scoping review and another as a rapid review (Table 2 ).
All reviews were published in English, in first quartile (Q1) journals, with JIF ranging from 1.692 to 6.062. One review was empty, meaning that its search did not identify any relevant studies; i.e., no primary studies were included [ 36 ]. The remaining 17 reviews included 269 unique studies; the majority ( N = 211; 78%) were included in only a single review included in our study (range: 1 to 12). Primary studies included in the reviews were published between December 2019 and March 18, 2020, and comprised case reports, case series, cohorts, and other observational studies. We found only one review that included randomized clinical trials [ 38 ]. In the included reviews, systematic literature searches were performed from 2019 (entire year) up to March 9, 2020. Ten systematic reviews included meta-analyses. The list of primary studies found in the included systematic reviews is shown in Additional file 4 , as well as the number of reviews in which each primary study was included.
Population and study designs
Most of the reviews analyzed data from patients with COVID-19 who developed pneumonia, acute respiratory distress syndrome (ARDS), or any other correlated complication. One review aimed to evaluate the effectiveness of using surgical masks on preventing transmission of the virus [ 36 ], one review was focused on pediatric patients [ 34 ], and one review investigated COVID-19 in pregnant women [ 37 ]. Most reviews assessed clinical symptoms, laboratory findings, or radiological results.
Systematic review findings
The summary of findings from individual reviews is shown in Table 2 . Overall, all-cause mortality ranged from 0.3 to 13.9% (Fig. 2 ).

A meta-analysis of the prevalence of mortality
Clinical symptoms
Seven reviews described the main clinical manifestations of COVID-19 [ 26 , 28 , 29 , 34 , 35 , 39 , 41 ]. Three of them provided only a narrative discussion of symptoms [ 26 , 34 , 35 ]. In the reviews that performed a statistical analysis of the incidence of different clinical symptoms, symptoms in patients with COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%), gastrointestinal disorders, such as diarrhea, nausea or vomiting (5.0–9.0%), and others (including, in one study only: dizziness 12.1%) (Figs. 3 , 4 , 5 , 6 , 7 , 8 and 9 ). Three reviews assessed cough with and without sputum together; only one review assessed sputum production itself (28.5%).

A meta-analysis of the prevalence of fever

A meta-analysis of the prevalence of cough

A meta-analysis of the prevalence of dyspnea

A meta-analysis of the prevalence of fatigue or myalgia

A meta-analysis of the prevalence of headache

A meta-analysis of the prevalence of gastrointestinal disorders

A meta-analysis of the prevalence of sore throat
Diagnostic aspects
Three reviews described methodologies, protocols, and tools used for establishing the diagnosis of COVID-19 [ 26 , 34 , 38 ]. The use of respiratory swabs (nasal or pharyngeal) or blood specimens to assess the presence of SARS-CoV-2 nucleic acid using RT-PCR assays was the most commonly used diagnostic method mentioned in the included studies. These diagnostic tests have been widely used, but their precise sensitivity and specificity remain unknown. One review included a Chinese study with clinical diagnosis with no confirmation of SARS-CoV-2 infection (patients were diagnosed with COVID-19 if they presented with at least two symptoms suggestive of COVID-19, together with laboratory and chest radiography abnormalities) [ 34 ].
Therapeutic possibilities
Pharmacological and non-pharmacological interventions (supportive therapies) used in treating patients with COVID-19 were reported in five reviews [ 25 , 27 , 34 , 35 , 38 ]. Antivirals used empirically for COVID-19 treatment were reported in seven reviews [ 25 , 27 , 34 , 35 , 37 , 38 , 41 ]; most commonly used were protease inhibitors (lopinavir, ritonavir, darunavir), nucleoside reverse transcriptase inhibitor (tenofovir), nucleotide analogs (remdesivir, galidesivir, ganciclovir), and neuraminidase inhibitors (oseltamivir). Umifenovir, a membrane fusion inhibitor, was investigated in two studies [ 25 , 35 ]. Possible supportive interventions analyzed were different types of oxygen supplementation and breathing support (invasive or non-invasive ventilation) [ 25 ]. The use of antibiotics, both empirically and to treat secondary pneumonia, was reported in six studies [ 25 , 26 , 27 , 34 , 35 , 38 ]. One review specifically assessed evidence on the efficacy and safety of the anti-malaria drug chloroquine [ 27 ]. It identified 23 ongoing trials investigating the potential of chloroquine as a therapeutic option for COVID-19, but no verifiable clinical outcomes data. The use of mesenchymal stem cells, antifungals, and glucocorticoids were described in four reviews [ 25 , 34 , 35 , 38 ].
Laboratory and radiological findings
Of the 18 reviews included in this overview, eight analyzed laboratory parameters in patients with COVID-19 [ 25 , 29 , 30 , 32 , 33 , 34 , 35 , 39 ]; elevated C-reactive protein levels, associated with lymphocytopenia, elevated lactate dehydrogenase, as well as slightly elevated aspartate and alanine aminotransferase (AST, ALT) were commonly described in those eight reviews. Lippi et al. assessed cardiac troponin I (cTnI) [ 25 ], procalcitonin [ 32 ], and platelet count [ 33 ] in COVID-19 patients. Elevated levels of procalcitonin [ 32 ] and cTnI [ 30 ] were more likely to be associated with a severe disease course (requiring intensive care unit admission and intubation). Furthermore, thrombocytopenia was frequently observed in patients with complicated COVID-19 infections [ 33 ].
Chest imaging (chest radiography and/or computed tomography) features were assessed in six reviews, all of which described a frequent pattern of local or bilateral multilobar ground-glass opacity [ 25 , 34 , 35 , 39 , 40 , 41 ]. Those six reviews showed that septal thickening, bronchiectasis, pleural and cardiac effusions, halo signs, and pneumothorax were observed in patients suffering from COVID-19.
Quality of evidence in individual systematic reviews
Table 3 shows the detailed results of the quality assessment of 18 systematic reviews, including the assessment of individual items and summary assessment. A detailed explanation for each decision in each review is available in Additional file 5 .
Using AMSTAR 2 criteria, confidence in the results of all 18 reviews was rated as “critically low” (Table 3 ). Common methodological drawbacks were: omission of prospective protocol submission or publication; use of inappropriate search strategy: lack of independent and dual literature screening and data-extraction (or methodology unclear); absence of an explanation for heterogeneity among the studies included; lack of reasons for study exclusion (or rationale unclear).
Risk of bias assessment, based on a reported methodological tool, and quality of evidence appraisal, in line with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method, were reported only in one review [ 25 ]. Five reviews presented a table summarizing bias, using various risk of bias tools [ 25 , 29 , 39 , 40 , 41 ]. One review analyzed “study quality” [ 37 ]. One review mentioned the risk of bias assessment in the methodology but did not provide any related analysis [ 28 ].
This overview of systematic reviews analyzed the first 18 systematic reviews published after the onset of the COVID-19 pandemic, up to March 24, 2020, with primary studies involving more than 60,000 patients. Using AMSTAR-2, we judged that our confidence in all those reviews was “critically low”. Ten reviews included meta-analyses. The reviews presented data on clinical manifestations, laboratory and radiological findings, and interventions. We found no systematic reviews on the utility of diagnostic tests.
Symptoms were reported in seven reviews; most of the patients had a fever, cough, dyspnea, myalgia or muscle fatigue, and gastrointestinal disorders such as diarrhea, nausea, or vomiting. Olfactory dysfunction (anosmia or dysosmia) has been described in patients infected with COVID-19 [ 43 ]; however, this was not reported in any of the reviews included in this overview. During the SARS outbreak in 2002, there were reports of impairment of the sense of smell associated with the disease [ 44 , 45 ].
The reported mortality rates ranged from 0.3 to 14% in the included reviews. Mortality estimates are influenced by the transmissibility rate (basic reproduction number), availability of diagnostic tools, notification policies, asymptomatic presentations of the disease, resources for disease prevention and control, and treatment facilities; variability in the mortality rate fits the pattern of emerging infectious diseases [ 46 ]. Furthermore, the reported cases did not consider asymptomatic cases, mild cases where individuals have not sought medical treatment, and the fact that many countries had limited access to diagnostic tests or have implemented testing policies later than the others. Considering the lack of reviews assessing diagnostic testing (sensitivity, specificity, and predictive values of RT-PCT or immunoglobulin tests), and the preponderance of studies that assessed only symptomatic individuals, considerable imprecision around the calculated mortality rates existed in the early stage of the COVID-19 pandemic.
Few reviews included treatment data. Those reviews described studies considered to be at a very low level of evidence: usually small, retrospective studies with very heterogeneous populations. Seven reviews analyzed laboratory parameters; those reviews could have been useful for clinicians who attend patients suspected of COVID-19 in emergency services worldwide, such as assessing which patients need to be reassessed more frequently.
All systematic reviews scored poorly on the AMSTAR 2 critical appraisal tool for systematic reviews. Most of the original studies included in the reviews were case series and case reports, impacting the quality of evidence. Such evidence has major implications for clinical practice and the use of these reviews in evidence-based practice and policy. Clinicians, patients, and policymakers can only have the highest confidence in systematic review findings if high-quality systematic review methodologies are employed. The urgent need for information during a pandemic does not justify poor quality reporting.
We acknowledge that there are numerous challenges associated with analyzing COVID-19 data during a pandemic [ 47 ]. High-quality evidence syntheses are needed for decision-making, but each type of evidence syntheses is associated with its inherent challenges.
The creation of classic systematic reviews requires considerable time and effort; with massive research output, they quickly become outdated, and preparing updated versions also requires considerable time. A recent study showed that updates of non-Cochrane systematic reviews are published a median of 5 years after the publication of the previous version [ 48 ].
Authors may register a review and then abandon it [ 49 ], but the existence of a public record that is not updated may lead other authors to believe that the review is still ongoing. A quarter of Cochrane review protocols remains unpublished as completed systematic reviews 8 years after protocol publication [ 50 ].
Rapid reviews can be used to summarize the evidence, but they involve methodological sacrifices and simplifications to produce information promptly, with inconsistent methodological approaches [ 51 ]. However, rapid reviews are justified in times of public health emergencies, and even Cochrane has resorted to publishing rapid reviews in response to the COVID-19 crisis [ 52 ]. Rapid reviews were eligible for inclusion in this overview, but only one of the 18 reviews included in this study was labeled as a rapid review.
Ideally, COVID-19 evidence would be continually summarized in a series of high-quality living systematic reviews, types of evidence synthesis defined as “ a systematic review which is continually updated, incorporating relevant new evidence as it becomes available ” [ 53 ]. However, conducting living systematic reviews requires considerable resources, calling into question the sustainability of such evidence synthesis over long periods [ 54 ].
Research reports about COVID-19 will contribute to research waste if they are poorly designed, poorly reported, or simply not necessary. In principle, systematic reviews should help reduce research waste as they usually provide recommendations for further research that is needed or may advise that sufficient evidence exists on a particular topic [ 55 ]. However, systematic reviews can also contribute to growing research waste when they are not needed, or poorly conducted and reported. Our present study clearly shows that most of the systematic reviews that were published early on in the COVID-19 pandemic could be categorized as research waste, as our confidence in their results is critically low.
Our study has some limitations. One is that for AMSTAR 2 assessment we relied on information available in publications; we did not attempt to contact study authors for clarifications or additional data. In three reviews, the methodological quality appraisal was challenging because they were published as letters, or labeled as rapid communications. As a result, various details about their review process were not included, leading to AMSTAR 2 questions being answered as “not reported”, resulting in low confidence scores. Full manuscripts might have provided additional information that could have led to higher confidence in the results. In other words, low scores could reflect incomplete reporting, not necessarily low-quality review methods. To make their review available more rapidly and more concisely, the authors may have omitted methodological details. A general issue during a crisis is that speed and completeness must be balanced. However, maintaining high standards requires proper resourcing and commitment to ensure that the users of systematic reviews can have high confidence in the results.
Furthermore, we used adjusted AMSTAR 2 scoring, as the tool was designed for critical appraisal of reviews of interventions. Some reviews may have received lower scores than actually warranted in spite of these adjustments.
Another limitation of our study may be the inclusion of multiple overlapping reviews, as some included reviews included the same primary studies. According to the Cochrane Handbook, including overlapping reviews may be appropriate when the review’s aim is “ to present and describe the current body of systematic review evidence on a topic ” [ 12 ], which was our aim. To avoid bias with summarizing evidence from overlapping reviews, we presented the forest plots without summary estimates. The forest plots serve to inform readers about the effect sizes for outcomes that were reported in each review.
Several authors from this study have contributed to one of the reviews identified [ 25 ]. To reduce the risk of any bias, two authors who did not co-author the review in question initially assessed its quality and limitations.
Finally, we note that the systematic reviews included in our overview may have had issues that our analysis did not identify because we did not analyze their primary studies to verify the accuracy of the data and information they presented. We give two examples to substantiate this possibility. Lovato et al. wrote a commentary on the review of Sun et al. [ 41 ], in which they criticized the authors’ conclusion that sore throat is rare in COVID-19 patients [ 56 ]. Lovato et al. highlighted that multiple studies included in Sun et al. did not accurately describe participants’ clinical presentations, warning that only three studies clearly reported data on sore throat [ 56 ].
In another example, Leung [ 57 ] warned about the review of Li, L.Q. et al. [ 29 ]: “ it is possible that this statistic was computed using overlapped samples, therefore some patients were double counted ”. Li et al. responded to Leung that it is uncertain whether the data overlapped, as they used data from published articles and did not have access to the original data; they also reported that they requested original data and that they plan to re-do their analyses once they receive them; they also urged readers to treat the data with caution [ 58 ]. This points to the evolving nature of evidence during a crisis.
Our study’s strength is that this overview adds to the current knowledge by providing a comprehensive summary of all the evidence synthesis about COVID-19 available early after the onset of the pandemic. This overview followed strict methodological criteria, including a comprehensive and sensitive search strategy and a standard tool for methodological appraisal of systematic reviews.
In conclusion, in this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all the reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic could be categorized as research waste. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards to provide patients, clinicians, and decision-makers trustworthy evidence.
Availability of data and materials
All data collected and analyzed within this study are available from the corresponding author on reasonable request.
World Health Organization. Timeline - COVID-19: Available at: https://www.who.int/news/item/29-06-2020-covidtimeline . Accessed 1 June 2021.
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available at: https://coronavirus.jhu.edu/map.html . Accessed 1 June 2021.
Anzai A, Kobayashi T, Linton NM, Kinoshita R, Hayashi K, Suzuki A, et al. Assessing the Impact of Reduced Travel on Exportation Dynamics of Novel Coronavirus Infection (COVID-19). J Clin Med. 2020;9(2):601.
Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. https://doi.org/10.1126/science.aba9757 .
Article CAS PubMed PubMed Central Google Scholar
Fidahic M, Nujic D, Runjic R, Civljak M, Markotic F, Lovric Makaric Z, et al. Research methodology and characteristics of journal articles with original data, preprint articles and registered clinical trial protocols about COVID-19. BMC Med Res Methodol. 2020;20(1):161. https://doi.org/10.1186/s12874-020-01047-2 .
EPPI Centre . COVID-19: a living systematic map of the evidence. Available at: http://eppi.ioe.ac.uk/cms/Projects/DepartmentofHealthandSocialCare/Publishedreviews/COVID-19Livingsystematicmapoftheevidence/tabid/3765/Default.aspx . Accessed 1 June 2021.
NCBI SARS-CoV-2 Resources. Available at: https://www.ncbi.nlm.nih.gov/sars-cov-2/ . Accessed 1 June 2021.
Gustot T. Quality and reproducibility during the COVID-19 pandemic. JHEP Rep. 2020;2(4):100141. https://doi.org/10.1016/j.jhepr.2020.100141 .
Article PubMed PubMed Central Google Scholar
Kodvanj, I., et al., Publishing of COVID-19 Preprints in Peer-reviewed Journals, Preprinting Trends, Public Discussion and Quality Issues. Preprint article. bioRxiv 2020.11.23.394577; doi: https://doi.org/10.1101/2020.11.23.394577 .
Dobler CC. Poor quality research and clinical practice during COVID-19. Breathe (Sheff). 2020;16(2):200112. https://doi.org/10.1183/20734735.0112-2020 .
Article Google Scholar
Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. 2010;7(9):e1000326. https://doi.org/10.1371/journal.pmed.1000326 .
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231. https://doi.org/10.1186/s13643-017-0617-1 .
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane. 2020. Available from www.training.cochrane.org/handbook .
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane. 2020; Available from www.training.cochrane.org/handbook .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18. https://doi.org/10.1186/s13643-018-0914-3 .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):29. https://doi.org/10.1186/s13643-018-0768-8 .
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39. https://doi.org/10.1186/s13643-018-0695-8 .
Pollock M, Fernandes RM, Pieper D, Tricco AC, Gates M, Gates A, et al. Preferred reporting items for overviews of reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):335. https://doi.org/10.1186/s13643-019-1252-9 .
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009;3(3):e123–30.
Krnic Martinic M, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol. 2019;19(1):203. https://doi.org/10.1186/s12874-019-0855-0 .
Puljak L. If there is only one author or only one database was searched, a study should not be called a systematic review. J Clin Epidemiol. 2017;91:4–5. https://doi.org/10.1016/j.jclinepi.2017.08.002 .
Article PubMed Google Scholar
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254. https://doi.org/10.1186/s13643-020-01509-0 .
Covidence - systematic review software. Available at: https://www.covidence.org/ . Accessed 1 June 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Borges do Nascimento IJ, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med. 2020;9(4):941.
Article PubMed Central Google Scholar
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. https://doi.org/10.1186/s40249-020-00646-x .
Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279–83. https://doi.org/10.1016/j.jcrc.2020.03.005 .
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–8. https://doi.org/10.1007/s00392-020-01626-9 .
Article CAS PubMed Google Scholar
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577–83. https://doi.org/10.1002/jmv.25757 .
Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63(3):390–1. https://doi.org/10.1016/j.pcad.2020.03.001 .
Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med. 2020;75:107–8. https://doi.org/10.1016/j.ejim.2020.03.014 .
Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020;505:190–1. https://doi.org/10.1016/j.cca.2020.03.004 .
Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–8. https://doi.org/10.1016/j.cca.2020.03.022 .
Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–95. https://doi.org/10.1111/apa.15270 .
Lupia T, Scabini S, Mornese Pinna S, di Perri G, de Rosa FG, Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J Glob Antimicrob Resist. 2020;21:22–7. https://doi.org/10.1016/j.jgar.2020.02.021 .
Marasinghe, K.M., A systematic review investigating the effectiveness of face mask use in limiting the spread of COVID-19 among medically not diagnosed individuals: shedding light on current recommendations provided to individuals not medically diagnosed with COVID-19. Research Square. Preprint article. doi : https://doi.org/10.21203/rs.3.rs-16701/v1 . 2020 .
Mullins E, Evans D, Viner RM, O’Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586–92. https://doi.org/10.1002/uog.22014 .
Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JIP, et al. Potential Rapid Diagnostics, Vaccine and Therapeutics for 2019 Novel coronavirus (2019-nCoV): a systematic review. J Clin Med. 2020;9(3):623.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. https://doi.org/10.1016/j.tmaid.2020.101623 .
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. https://doi.org/10.2214/AJR.20.23034 .
Sun P, Qie S, Liu Z, Ren J, Li K, Xi J. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis. J Med Virol. 2020;92(6):612–7. https://doi.org/10.1002/jmv.25735 .
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. https://doi.org/10.1016/j.ijid.2020.03.017 .
Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Investig. 2020;50(3):e13209. https://doi.org/10.1111/eci.13209 .
Article CAS Google Scholar
Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwanica. 2006;15(1):26–8.
Google Scholar
Suzuki M, Saito K, Min WP, Vladau C, Toida K, Itoh H, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope. 2007;117(2):272–7. https://doi.org/10.1097/01.mlg.0000249922.37381.1e .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7. https://doi.org/10.1016/S1473-3099(20)30244-9 .
Wolkewitz M, Puljak L. Methodological challenges of analysing COVID-19 data during the pandemic. BMC Med Res Methodol. 2020;20(1):81. https://doi.org/10.1186/s12874-020-00972-6 .
Rombey T, Lochner V, Puljak L, Könsgen N, Mathes T, Pieper D. Epidemiology and reporting characteristics of non-Cochrane updates of systematic reviews: a cross-sectional study. Res Synth Methods. 2020;11(3):471–83. https://doi.org/10.1002/jrsm.1409 .
Runjic E, Rombey T, Pieper D, Puljak L. Half of systematic reviews about pain registered in PROSPERO were not published and the majority had inaccurate status. J Clin Epidemiol. 2019;116:114–21. https://doi.org/10.1016/j.jclinepi.2019.08.010 .
Runjic E, Behmen D, Pieper D, Mathes T, Tricco AC, Moher D, et al. Following Cochrane review protocols to completion 10 years later: a retrospective cohort study and author survey. J Clin Epidemiol. 2019;111:41–8. https://doi.org/10.1016/j.jclinepi.2019.03.006 .
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. 2015;13(1):224. https://doi.org/10.1186/s12916-015-0465-6 .
COVID-19 Rapid Reviews: Cochrane’s response so far. Available at: https://training.cochrane.org/resource/covid-19-rapid-reviews-cochrane-response-so-far . Accessed 1 June 2021.
Cochrane. Living systematic reviews. Available at: https://community.cochrane.org/review-production/production-resources/living-systematic-reviews . Accessed 1 June 2021.
Millard T, Synnot A, Elliott J, Green S, McDonald S, Turner T. Feasibility and acceptability of living systematic reviews: results from a mixed-methods evaluation. Syst Rev. 2019;8(1):325. https://doi.org/10.1186/s13643-019-1248-5 .
Babic A, Poklepovic Pericic T, Pieper D, Puljak L. How to decide whether a systematic review is stable and not in need of updating: analysis of Cochrane reviews. Res Synth Methods. 2020;11(6):884–90. https://doi.org/10.1002/jrsm.1451 .
Lovato A, Rossettini G, de Filippis C. Sore throat in COVID-19: comment on “clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis”. J Med Virol. 2020;92(7):714–5. https://doi.org/10.1002/jmv.25815 .
Leung C. Comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1431–2. https://doi.org/10.1002/jmv.25912 .
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. Response to Char’s comment: comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1433. https://doi.org/10.1002/jmv.25924 .
Download references
Acknowledgments
We thank Catherine Henderson DPhil from Swanscoe Communications for pro bono medical writing and editing support. We acknowledge support from the Covidence Team, specifically Anneliese Arno. We thank the whole International Network of Coronavirus Disease 2019 (InterNetCOVID-19) for their commitment and involvement. Members of the InterNetCOVID-19 are listed in Additional file 6 . We thank Pavel Cerny and Roger Crosthwaite for guiding the team supervisor (IJBN) on human resources management.
This research received no external funding.
Author information
Authors and affiliations.
University Hospital and School of Medicine, Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
Israel Júnior Borges do Nascimento & Milena Soriano Marcolino
Medical College of Wisconsin, Milwaukee, WI, USA
Israel Júnior Borges do Nascimento
Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare, College of Nursing, The Ohio State University, Columbus, OH, USA
Dónal P. O’Mathúna
School of Nursing, Psychotherapy and Community Health, Dublin City University, Dublin, Ireland
Department of Anesthesiology, Intensive Care and Pain Medicine, University of Münster, Münster, Germany
Thilo Caspar von Groote
Department of Sport and Health Science, Technische Universität München, Munich, Germany
Hebatullah Mohamed Abdulazeem
School of Health Sciences, Faculty of Health and Medicine, The University of Newcastle, Callaghan, Australia
Ishanka Weerasekara
Department of Physiotherapy, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka
Cochrane Croatia, University of Split, School of Medicine, Split, Croatia
Ana Marusic, Irena Zakarija-Grkovic & Tina Poklepovic Pericic
Center for Evidence-Based Medicine and Health Care, Catholic University of Croatia, Ilica 242, 10000, Zagreb, Croatia
Livia Puljak
Cochrane Brazil, Evidence-Based Health Program, Universidade Federal de São Paulo, São Paulo, Brazil
Vinicius Tassoni Civile & Alvaro Nagib Atallah
Yorkville University, Fredericton, New Brunswick, Canada
Santino Filoso
Laboratory for Industrial and Applied Mathematics (LIAM), Department of Mathematics and Statistics, York University, Toronto, Ontario, Canada
Nicola Luigi Bragazzi
You can also search for this author in PubMed Google Scholar
Contributions
IJBN conceived the research idea and worked as a project coordinator. DPOM, TCVG, HMA, IW, AM, LP, VTC, IZG, TPP, ANA, SF, NLB and MSM were involved in data curation, formal analysis, investigation, methodology, and initial draft writing. All authors revised the manuscript critically for the content. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Livia Puljak .
Ethics declarations
Ethics approval and consent to participate.
Not required as data was based on published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Search strategies used in the study.
Additional file 2: Appendix 2.
Adjusted scoring of AMSTAR 2 used in this study for systematic reviews of studies that did not analyze interventions.
Additional file 3: Appendix 3.
List of excluded studies, with reasons.
Additional file 4: Appendix 4.
Table of overlapping studies, containing the list of primary studies included, their visual overlap in individual systematic reviews, and the number in how many reviews each primary study was included.
Additional file 5: Appendix 5.
A detailed explanation of AMSTAR scoring for each item in each review.
Additional file 6: Appendix 6.
List of members and affiliates of International Network of Coronavirus Disease 2019 (InterNetCOVID-19).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Borges do Nascimento, I.J., O’Mathúna, D.P., von Groote, T.C. et al. Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect Dis 21 , 525 (2021). https://doi.org/10.1186/s12879-021-06214-4
Download citation
Received : 12 April 2020
Accepted : 19 May 2021
Published : 04 June 2021
DOI : https://doi.org/10.1186/s12879-021-06214-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Coronavirus
- Evidence-based medicine
- Infectious diseases
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
- Coronavirus (COVID-19)
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Just 20% of the public views the coronavirus as a major threat to the health of the U.S. population and only 10% are very concerned about getting a serious case themselves. In addition, a relatively small share of U.S. adults (28%) say they’ve received an updated COVID-19 vaccine since last fall.
How the Pandemic Has Affected Attendance at U.S. Religious Services
During the pandemic, a stable share of U.S. adults have been participating in religious services in some way – either virtually or in person – but in-person attendance is slightly lower than it was before COVID-19. Among Americans surveyed across several years, the vast majority described their attendance habits in roughly the same way in both 2019 and 2022.
Mental health and the pandemic: What U.S. surveys have found
Here’s a look at what surveys by Pew Research Center and other organizations have found about Americans’ mental health during the pandemic.
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Just 20% of the public views the coronavirus as a major threat to the health of the U.S. population and only 10% are very concerned about getting a serious case themselves. In addition, a relatively small share of U.S. adults (28%) say they’ve received an updated COVID-19 vaccine since last fall.
Online Religious Services Appeal to Many Americans, but Going in Person Remains More Popular
About a quarter of U.S. adults regularly watch religious services online or on TV, and most of them are highly satisfied with the experience. About two-in-ten Americans (21%) use apps or websites to help with reading scripture.
About a third of U.S. workers who can work from home now do so all the time
About a third of workers with jobs that can be done remotely are working from home all the time, according to a new Pew Research Center survey.
Economy Remains the Public’s Top Policy Priority; COVID-19 Concerns Decline Again
Americans now see reducing the budget deficit as a higher priority for the president and Congress to address than in recent years. But strengthening the economy continues to be the public’s top policy priority.
At least four-in-ten U.S. adults have faced high levels of psychological distress during COVID-19 pandemic
58% of those ages 18 to 29 have experienced high levels of psychological distress at least once between March 2020 and September 2022.
Key findings about COVID-19 restrictions that affected religious groups around the world in 2020
Our study analyzes 198 countries and territories and is based on policies and events in 2020, the most recent year for which data is available.
How COVID-19 Restrictions Affected Religious Groups Around the World in 2020
Nearly a quarter of countries used force to prevent religious gatherings during the pandemic; other government restrictions and social hostilities related to religion remained fairly stable.
What Makes Someone a Good Member of Society?
Most in advanced economies say voting, taking steps to reduce climate change and getting a COVID-19 vaccine are ways to be a good member of society; fewer say this about attending religious services.
REFINE YOUR SELECTION
Research teams.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
The impact of the COVID-19 pandemic on scientific research in the life sciences
Roles Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing
Affiliation AXES, IMT School for Advanced Studies Lucca, Lucca, Italy
Roles Conceptualization, Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Chair of Systems Design D-MTEC, ETH Zürich, Zurich, Switzerland
- Massimo Riccaboni,
- Luca Verginer

- Published: February 9, 2022
- https://doi.org/10.1371/journal.pone.0263001
- Reader Comments
The COVID-19 outbreak has posed an unprecedented challenge to humanity and science. On the one side, public and private incentives have been put in place to promptly allocate resources toward research areas strictly related to the COVID-19 emergency. However, research in many fields not directly related to the pandemic has been displaced. In this paper, we assess the impact of COVID-19 on world scientific production in the life sciences and find indications that the usage of medical subject headings (MeSH) has changed following the outbreak. We estimate through a difference-in-differences approach the impact of the start of the COVID-19 pandemic on scientific production using the PubMed database (3.6 Million research papers). We find that COVID-19-related MeSH terms have experienced a 6.5 fold increase in output on average, while publications on unrelated MeSH terms dropped by 10 to 12%. The publication weighted impact has an even more pronounced negative effect (-16% to -19%). Moreover, COVID-19 has displaced clinical trial publications (-24%) and diverted grants from research areas not closely related to COVID-19. Note that since COVID-19 publications may have been fast-tracked, the sudden surge in COVID-19 publications might be driven by editorial policy.
Citation: Riccaboni M, Verginer L (2022) The impact of the COVID-19 pandemic on scientific research in the life sciences. PLoS ONE 17(2): e0263001. https://doi.org/10.1371/journal.pone.0263001
Editor: Florian Naudet, University of Rennes 1, FRANCE
Received: April 28, 2021; Accepted: January 10, 2022; Published: February 9, 2022
Copyright: © 2022 Riccaboni, Verginer. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The processed data, instructions on how to process the raw PubMed dataset as well as all code are available via Zenodo at https://doi.org/10.5281/zenodo.5121216 .
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The COVID-19 pandemic has mobilized the world scientific community in 2020, especially in the life sciences [ 1 , 2 ]. In the first three months after the pandemic, the number of scientific papers about COVID-19 was fivefold the number of articles on H1N1 swine influenza [ 3 ]. Similarly, the number of clinical trials related to COVID-19 prophylaxis and treatments skyrocketed [ 4 ]. Thanks to the rapid mobilization of the world scientific community, COVID-19 vaccines have been developed in record time. Despite this undeniable success, there is a rising concern about the negative consequences of COVID-19 on clinical trial research, with many projects being postponed [ 5 – 7 ]. According to Evaluate Pharma, clinical trials were one of the pandemic’s first casualties, with a record number of 160 studies suspended for reasons related to COVID-19 in April 2020 [ 8 , 9 ] reporting a total of 1,200 trials suspended as of July 2020. As a consequence, clinical researchers have been impaired by reduced access to healthcare research infrastructures. Particularly, the COVID-19 outbreak took a tall on women and early-career scientists [ 10 – 13 ]. On a different ground, Shan and colleagues found that non-COVID-19-related articles decreased as COVID-19-related articles increased in top clinical research journals [ 14 ]. Fraser and coworker found that COVID-19 preprints received more attention and citations than non-COVID-19 preprints [ 1 ]. More recently, Hook and Porter have found some early evidence of ‘covidisation’ of academic research, with research grants and output diverted to COVID-19 research in 2020 [ 15 ]. How much should scientists switch their efforts toward SARS-CoV-2 prevention, treatment, or mitigation? There is a growing consensus that the current level of ‘covidisation’ of research can be wasteful [ 4 , 5 , 16 ].
Against this background, in this paper, we investigate if the COVID-19 pandemic has induced a shift in biomedical publications toward COVID-19-related scientific production. The objective of the study is to show that scientific articles listing covid-related Medical Subject Headings (MeSH) when compared against covid-unrelated MeSH have been partially displaced. Specifically, we look at several indicators of scientific production in the life sciences before and after the start of the COVID-19 pandemic: (1) number of papers published, (2) impact factor weighted number of papers, (3) opens access, (4) number of publications related to clinical trials, (5) number of papers listing grants, (6) number of papers listing grants existing before the pandemic. Through a natural experiment approach, we analyze the impact of the pandemic on scientific production in the life sciences. We consider COVID-19 an unexpected and unprecedented exogenous source of variation with heterogeneous effects across biomedical research fields (i.e., MeSH terms).
Based on the difference in difference results, we document the displacement effect that the pandemic has had on several aspects of scientific publishing. The overall picture that emerges from this analysis is that there has been a profound realignment of priorities and research efforts. This shift has displaced biomedical research in fields not related to COVID-19.
The rest of the paper is structured as follows. First, we describe the data and our measure of relatedness to COVID-19. Next, we illustrate the difference-in-differences specification we rely on to identify the impact of the pandemic on scientific output. In the results section, we present the results of the difference-in-differences and network analyses. We document the sudden shift in publications, grants and trials towards COVID-19-related MeSH terms. Finally, we discuss the findings and highlight several policy implications.
Materials and methods
The present analysis is based primarily on PubMed and the Medical Subject Headings (MeSH) terminology. This data is used to estimate the effect of the start of the COVID 19 pandemic via a difference in difference approach. This section is structured as follows. We first introduce the data and then the econometric methodology. This analysis is not based on a pre-registered protocol.
Selection of biomedical publications.
We rely on PubMed, a repository with more than 34 million biomedical citations, for the analysis. Specifically, we analyze the daily updated files up to 31/06/2021, extracting all publications of type ‘Journal Article’. For the principal analysis, we consider 3,638,584 papers published from January 2019 to December 2020. We also analyze 11,122,017 papers published from 2010 onwards to identify the earliest usage of a grant and infer if it was new in 2020. We use the SCImago journal ranking statistics to compute the impact factor weighted number (IFWN) of papers in a given field of research. To assign the publication date, we use the ‘electronically published’ dates and, if missing, the ‘print published’ dates.
Medical subject headings.
We rely on the Medical Subject Headings (MeSH) terminology to approximate narrowly defined biomedical research fields. This terminology is a curated medical vocabulary, which is manually added to papers in the PubMed corpus. The fact that MeSH terms are manually annotated makes this terminology ideal for classification purposes. However, there is a delay between publication and annotation, on the order of several months. To address this delay and have the most recent classification, we search for all 28 425 MeSH terms using PubMed’s ESearch utility and classify paper by the results. The specific API endpoint is https://eutils.ncbi.nlm.nih.gov/entrez/eutils/esearch.fcgi , the relevant scripts are available with the code. For example, we assign the term ‘Ageusia’ (MeSH ID D000370) to all papers listed in the results of the ESearch API. We apply this method to the whole period (January 2019—December 2020) and obtain a mapping from papers to the MeSH terms. For every MeSH term, we keep track of the year they have been established. For instance, COVID-19 terms were established in 2020 (see Table 1 ): in January 2020, the WHO recommended 2019-nCoV and 2019-nCoV acute respiratory disease as provisional names for the virus and disease. The WHO issued the official terms COVID-19 and SARS-CoV-2 at the beginning of February 2020. By manually annotating publications, all publications referring to COVID-19 and SARS-CoV-2 since January 2020 have been labelled with the related MeSH terms. Other MeSH terms related to COVID-19, such as coronavirus, for instance, have been established years before the pandemic (see Table 2 ). We proxy MeSH term usage via search terms using the PubMed EUtilities API; this means that we are not using the hand-labelled MeSH terms but rather the PubMed search results. This means that the accuracy of the MeSH term we assign to a given paper is not perfect. In practice, this means that we have assigned more MeSH terms to a given term than a human annotator would have.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0263001.t001
The list contains only terms with at least 100 publications in 2020.
https://doi.org/10.1371/journal.pone.0263001.t002
Clinical trials and publication types.
We classify publications using PubMed’s ‘PublicationType’ field in the XML baseline files (There are 187 publication types, see https://www.nlm.nih.gov/mesh/pubtypes.html ). We consider a publication to be related to a clinical trial if it lists any of the following descriptors:
- D016430: Clinical Trial
- D017426: Clinical Trial, Phase I
- D017427: Clinical Trial, Phase II
- D017428: Clinical Trial, Phase III
- D017429: Clinical Trial, Phase IV
- D018848: Controlled Clinical Trial
- D065007: Pragmatic Clinical Trial
- D000076362: Adaptive Clinical Trial
- D000077522: Clinical Trial, Veterinary
In our analysis of the impact of COVID-19 on publications related to clinical trials, we only consider MeSH terms that are associated at least once with a clinical trial publication over the two years. We apply this restriction to filter out MeSH terms that are very unlikely to be relevant for clinical trial types of research.
Open access.
We proxy the availability of a journal article to the public, i.e., open access, if it is available from PubMed Central. PubMed Central archives full-text journal articles and provides free access to the public. Note that the copyright license may vary across participating publishers. However, the text of the paper is for all effects and purposes freely available without requiring subscriptions or special affiliation.
We infer if a publication has been funded by checking if it lists any grants. We classify grants as either ‘old’, i.e. existed before 2019, or ‘new’, i.e. first observed afterwards. To do so, we collect all grant IDs for 11,122,017 papers from 2010 on-wards and record their first appearance. This procedure is an indirect inference of the year the grant has been granted. The basic assumption is that if a grant number has not been listed in any publication since 2010, it is very likely a new grant. Specifically, an old grant is a grant listed since 2019 observed at least once from 2010 to 2018.
Note that this procedure is only approximate and has a few shortcomings. Mistyped grant numbers (e.g. ‘1234-M JPN’ and ‘1234-M-JPN’) could appear as new grants, even though they existed before, or new grants might be classified as old grants if they have a common ID (e.g. ‘Grant 1’). Unfortunately, there is no central repository of grant numbers and the associated metadata; however, there are plans to assign DOI numbers to grants to alleviate this problem (See https://gitlab.com/crossref/open_funder_registry for the project).
Impact factor weighted publication numbers (IFWN).
In our analysis, we consider two measures of scientific output. First, we simply count the number of publications by MeSH term. However, since journals vary considerably in terms of impact factor, we also weigh the number of publications by the impact factor of the venue (e.g., journal) where it was published. Specifically, we use the SCImago journal ranking statistics to weigh a paper by the impact factor of the journal it appears in. We use the ‘citation per document in the past two years’ for 45,230 ISSNs. Note that a journal may and often has more than one ISSN, i.e., one for the printed edition and one for the online edition. SCImago applies the same score for a venue across linked ISSNs.
For the impact factor weighted number (IFWN) of publication per MeSH terms, this means that all publications are replaced by the impact score of the journal they appear in and summed up.
COVID-19-relatedness.
To measure how closely related to COVID-19 is a MeSH term, we introduce an index of relatedness to COVID-19. First, we identify the focal COVID-19 terms, which appeared in the literature in 2020 (see Table 1 ). Next, for all other pre-existing MeSH terms, we measure how closely related to COVID-19 they end up being.
Our aim is to show that MeSH terms that existed before and are related have experienced a sudden increase in the number of (impact factor weighted) papers.
Intuitively we can read this measure as: what is the probability in 2020 that a COVID-19 MeSH term is present given that we chose a paper with MeSH term i ? For example, given that in 2020 we choose a paper dealing with “Ageusia” (i.e., Complete or severe loss of the subjective sense of taste), there is a 96% probability that this paper also lists COVID-19, see Table 1 .
Note that a paper listing a related MeSH term does not imply that that paper is doing COVID-19 research, but it implies that one of the MeSH terms listed is often used in COVID-19 research.
In sum, in our analysis, we use the following variables:
- Papers: Number of papers by MeSH term;
- Impact: Impact factor weighted number of papers by MeSH term;
- PMC: Papers listed in PubMed central by MeSH term, as a measure of Open Access publications;
- Trials: number of publications of type “Clinical Trial” by MeSH term;
- Grants: number of papers with at least one grant by MeSH term;
- Old Grants: number of papers listing a grant that has been observed between 2010 and 2018, by MeSH term;
Difference-in-differences
The difference-in-differences (DiD) method is an econometric technique to imitate an experimental research design from observation data, sometimes referred to as a quasi-experimental setup. In a randomized controlled trial, subjects are randomly assigned either to the treated or the control group. Analogously, in this natural experiment, we assume that medical subject headings (MeSH) have been randomly assigned to be either treated (related) or not treated (unrelated) by the pandemic crisis.
Before the COVID, for a future health crisis, the set of potentially impacted medical knowledge was not predictable since it depended on the specifics of the emergency. For instance, ageusia (loss of taste), a medical concept existing since 1991, became known to be a specific symptom of COVID-19 only after the pandemic.
Specifically, we exploit the COVID-19 as an unpredictable and exogenous shock that has deeply affected the publication priorities for biomedical scientific production, as compared to the situation before the pandemic. In this setting, COVID-19 is the treatment, and the identification of this new human coronavirus is the event. We claim that treated MeSH terms, i.e., MeSH terms related to COVID-19, have experienced a sudden increase in terms of scientific production and attention. In contrast, research on untreated MeSH terms, i.e., MeSH terms not related to COVID-19, has been displaced by COVID-19. Our analysis compares the scientific output of COVID-19 related and unrelated MeSH terms before and after January 2020.
In our case, some of the terms turn out to be related to COVID-19 in 2020, whereas most of the MeSH terms are not closely related to COVID-19.
Thus β 1 identifies the overall effect on the control group after the event, β 2 the difference across treated and control groups before the event (i.e. the first difference in DiD) and finally the effect on the treated group after the event, net of the first difference, β 3 . This last parameter identifies the treatment effect on the treated group netting out the pre-treatment difference.
For the DiD to have a causal interpretation, it must be noted that pre-event, the trends of the two groups should be parallel, i.e., the common trend assumption (CTA) must be satisfied. We will show that the CTA holds in the results section.
To specify the DiD model, we need to define a period before and after the event and assign a treatment status or level of exposure to each term.
Before and after.
The pre-treatment period is defined as January 2019 to December 2019. The post-treatment period is defined as the months from January 2020 to December 2020. We argue that the state of biomedical research was similar in those two years, apart from the effect of the pandemic.
Treatment status and exposure.
The treatment is determined by the COVID-19 relatedness index σ i introduced earlier. Specifically, this number indicates the likelihood that COVID-19 will be a listed MeSH term, given that we observe the focal MeSH term i . To show that the effect becomes even stronger the closer related the subject is, and for ease of interpretation, we also discretize the relatedness value into three levels of treatment. Namely, we group MeSH terms with a σ between, 0% to 20%, 20% to 80% and 80% to 100%. The choice of alternative grouping strategies does not significantly affect our results. Results for alternative thresholds of relatedness can be computed using the available source code. We complement the dichotomized analysis by using the treatment intensity (relatedness measure σ ) to show that the result persists.
Panel regression.
In this work, we estimate a random effects panel regression where the units of analysis are 28 318 biomedical research fields (i.e. MeSH terms) observed over time before and after the COVID-19 pandemic. The time resolution is at the monthly level, meaning that for each MeSH term, we have 24 observations from January 2019 to December 2020.
The outcome variable Y it identifies the outcome at time t (i.e., month), for MeSH term i . As before, P t identifies the period with P t = 0 if the month is before January 2020 and P t = 1 if it is on or after this date. In (3) , the treatment level is measure by the relatedness to COVID-19 ( σ i ), where again the γ 1 identifies pre-trend (constant) differences and δ 1 the overall effect.
In total, we estimate six coefficients. As before, the δ l coefficient identifies the DiD effect.
Verifying the Common Trend Assumption (CTA).
We show that the CTA holds for this model by comparing the pre-event trends of the control group to the treated groups (COVID-19 related MeSH terms). Namely, we show that the pre-event trends of the control group are the same as the pre-event trends of the treated group.
Co-occurrence analysis
To investigate if the pandemic has caused a reconfiguration of research priorities, we look at the MeSH term co-occurrence network. Precisely, we extract the co-occurrence network of all 28,318 MeSH terms as they appear in the 3.3 million papers. We considered the co-occurrence networks of 2018, 2019 and 2020. Each node represents a MeSH term in these networks, and a link between them indicates that they have been observed at least once together. The weight of the edge between the MeSH terms is given by the number of times those terms have been jointly observed in the same publications.
Medical language is hugely complicated, and this simple representation does not capture the intricacies, subtle nuances and, in fact, meaning of the terms. Therefore, we do not claim that we can identify how the actual usage of MeSH terms has changed from this object, but rather that it has. Nevertheless, the co-occurrence graph captures rudimentary relations between concepts. We argue that absent a shock to the system, their basic usage patterns, change in importance (within the network) would essentially be the same from year to year. However, if we find that the importance of terms changes more than expected in 2020, it stands to reason that there have been some significant changes.
To show that that MeSH usage has been affected, we compute for each term in the years 2018, 2019 and 2020 their PageRank centrality [ 17 ]. The PageRank centrality tells us how likely a random walker traversing a network would be found at a given node if she follows the weights of the empirical edges (i.e., co-usage probability). Specifically, for the case of the MeSH co-occurrence network, this number represents how often an annotator at the National Library of Medicine would assign that MeSH term following the observed general usage patterns. It is a simplistic measure to capture the complexities of biomedical research. Nevertheless, it captures far-reaching interdependence across MeSH terms as the measure uses the whole network to determine the centrality of every MeSH term. A sudden change in the rankings and thus the position of MeSH terms in this network suggests that a given research subject has risen as it is used more often with other important MeSH terms (or vice versa).
We then compare the growth for each MeSH i term in g i (2019), i.e. before the the COVID-19 pandemic, with the growth after the event ( g i (2020)).
Publication growth
Changes in output and COVID-19 relatedness
Before we show the regression results, we provide descriptive evidence that publications from 2019 to 2020 have drastically increased. By showing that this growth correlates strongly with a MeSH term’s COVID-19 relatedness ( σ ), we demonstrate that (1) σ captures an essential aspect of the growth dynamics and (2) highlight the meteoric rise of highly related terms.
We look at the year over year growth in the number of the impact weighted number of publications per MeSH term from 2018 to 2019 and 2019 to 2020 as defined in the methods section.
Fig 1 shows the yearly growth of the impact weighted number of publications per MeSH term. By comparing the growth of the number of publications from the years 2018, 2019 and 2020, we find that the impact factor weighted number of publications has increased by up to a factor of 100 compared to the previous year for Betacoronavirus, one of the most closely related to COVID-19 MeSH term.
Each dot represents, a MeSH term. The y axis (growth) is in symmetric log scale. The x axis shows the COVID-19 relatedness, σ . Note that the position of the dots on the x-axis is the same in the two plots. Below: MeSH term importance gain (PageRank) and their COVID-19 relatedness.
https://doi.org/10.1371/journal.pone.0263001.g001
Fig 1 , first row, reveals how strongly correlated the growth in the IFWN of publication is to the term’s COVID-19 relatedness. For instance, we see that the term ‘Betacoronavirus’ skyrocketed from 2019 to 2020, which is expected given that SARS-CoV-2 is a species of the genus. Conversely, the term ‘Alphacoronavirus’ has not experienced any growth given that it is twin a genus of the Coronaviridae family, but SARS-CoV-2 is not one of its species. Note also the fast growth in the number of publications dealing with ‘Quarantine’. Moreover, MeSH terms that grew significantly from 2018 to 2019 and were not closely related to COVID-19, like ‘Vaping’, slowed down in 2020. From the graph, the picture emerges that publication growth is correlated with COVID-19 relatedness σ and that the growth for less related terms slowed down.
To show that the usage pattern of MeSH terms has changed following the pandemic, we compute the PageRank centrality using graph-tool [ 18 ] as discussed in the Methods section.
Fig 1 , second row, shows the change in the PageRank centrality of the MeSH terms after the pandemic (2019 to 2020, right plot) and before (2018 to 2019, left plot). If there were no change in the general usage pattern, we would expect the variance in PageRank changes to be narrow across the two periods, see (left plot). However, PageRank scores changed significantly more from 2019 to 2020 than from 2018 to 2019, suggesting that there has been a reconfiguration of the network.
To further support this argument, we carry out a DiD regression analysis.
Common trends assumption
As discussed in the Methods section, we need to show that the CTA assumption holds for the DiD to be defined appropriately. We do this by estimating for each month the number of publications and comparing it across treatment groups. This exercise also serves the purpose of a placebo test. By assuming that each month could have potentially been the event’s timing (i.e., the outbreak), we show that January 2020 is the most likely timing of the event. The regression table, as noted earlier, contains over 70 estimated coefficients, hence for ease of reading, we will only show the predicted outcome per month by group (see Fig 2 ). The full regression table with all coefficients is available in the S1 Table .
The y axis is in log scale. The dashed vertical line identifies January 2020. The dashed horizontal line shows the publications in January 2019 for the 0–20% group before the event. This line highlights that the drop happens after the event. The bands around the lines indicate the 95% confidence interval of the predicted values. The results are the output of the Stata margins command.
https://doi.org/10.1371/journal.pone.0263001.g002
Fig 2 shows the predicted number per outcome variable obtained from the panel regression model. These predictions correspond to the predicted value per relatedness group using the regression parameters estimated via the linear panel regression. The bands around the curves are the 95% confidence intervals.
All outcome measures depict a similar trend per month. Before the event (i.e., January 2020), there is a common trend across all groups. In contrast, after the event, we observe a sudden rise for the outcomes of the COVID-19 related treated groups (green and red lines) and a decline in the outcomes for the unrelated group (blue line). Therefore, we can conclude that the CTA assumption holds.
Regression results
Table 3 shows the DiD regression results (see Eq (3) ) for the selected outcome measures: number of publications (Papers), impact factor weighted number of publications (Impact), open access (OA) publications, clinical trial related publications, and publications with existing grants.
https://doi.org/10.1371/journal.pone.0263001.t003
Table 3 shows results for the discrete treatment level version of the DiD model (see Eq (4) ).
Note that the outcome variable is in natural log scale; hence to get the effect of the independent variable, we need to exponentiate the coefficient. For values close to 0, the effect is well approximated by the percentage change of that magnitude.
In both specifications we see that the least related group, drops in the number of publications between 10% and 13%, respectively (first row of Tables 3 and 4 , exp(−0.102) ≈ 0.87). In line with our expectations, the increase in the number of papers published by MeSH term is positively affected by the relatedness to COVID-19. In the discrete model (row 2), we note that the number of documents with MeSH terms with a COVID-19 relatedness between 20 and 80% grows by 18% and highly related terms by a factor of approximately 6.6 (exp(1.88)). The same general pattern can be observed for the impact weighted publication number, i.e., Model (2). Note, however, that the drop in the impact factor weighted output is more significant, reaching -19% for COVID-19 unrelated publications, and related publications growing by a factor of 8.7. This difference suggests that there might be a bias to publish papers on COVID-19 related subjects in high impact factor journals.
https://doi.org/10.1371/journal.pone.0263001.t004
By looking at the number of open access publications (PMC), we note that the least related group has not been affected negatively by the pandemic. However, the number of COVID-19 related publications has drastically increased for the most COVID-19 related group by a factor of 6.2. Note that the substantial increase in the number of papers available through open access is in large part due to journal and editorial policies to make preferentially COVID research immediately available to the public.
Regarding the number of clinical trial publications, we note that the least related group has been affected negatively, with the number of publications on clinical trials dropping by a staggering 24%. At the same time, publications on clinical trials for COVID-19-related MeSH have increased by a factor of 2.1. Note, however, that the effect on clinical trials is not significant in the continuous regression. The discrepancy across Tables 3 and 4 highlights that, especially for trials, the effect is not linear, where only the publications on clinical trials closely related to COVID-19 experiencing a boost.
It has been reported [ 19 ] that while the number of clinical trials registered to treat or prevent COVID-19 has surged with 179 new registrations in the second week of April 2020 alone. Only a few of these have led to publishable results in the 12 months since [ 20 ]. On the other hand, we find that clinical trial publications, considering related MeSH (but not COVID-19 directly), have had significant growth from the beginning of the pandemic. These results are not contradictory. Indeed counting the number of clinical trial publications listing the exact COVID-19 MeSH term (D000086382), we find 212 publications. While this might seem like a small number, consider that in 2020 only 8,485 publications were classified as clinical trials; thus, targeted trials still made up 2.5% of all clinical trials in 2020 . So while one might doubt the effectiveness of these research efforts, it is still the case that by sheer number, they represent a significant proportion of all publications on clinical trials in 2020. Moreover, COVID-19 specific Clinical trial publications in 2020, being a delayed signal of the actual trials, are a lower bound estimate on the true number of such clinical trials being conducted. This is because COVID-19 studies could only have commenced in 2020, whereas other studies had a head start. Thus our reported estimates are conservative, meaning that the true effect on actual clinical trials is likely larger, not smaller.
Research funding, as proxied by the number of publications with grants, follows a similar pattern, but notably, COVID-19-related MeSH terms list the same proportion of grants established before 2019 as other unrelated MeSH terms, suggesting that grants which were not designated for COVID-19 research have been used to support COVID-19 related research. Overall, the number of publications listing a grant has dropped. Note that this should be because the number of publications overall in the unrelated group has dropped. However, we note that the drop in publications is 10% while the decline in publications with at least one grant is 15%. This difference suggests that publications listing grants, which should have more funding, are disproportionately COVID-19 related papers. To further investigate this aspect, we look at whether the grant was old (pre-2019) or appeared for the first time in or after 2019. It stands to reason that an old grant (pre-2019) would not have been granted for a project dealing with the pandemic. Hence we would expect that COVID-19 related MeSH terms to have a lower proportion of old grants than the unrelated group. In models (6) in Table 4 we show that the number of old grants for the unrelated group drops by 13%. At the same time, the number of papers listing old grants (i.e., pre-2019) among the most related group increased by a factor of 3.1. Overall, these results suggest that COVID-19 related research has been funded largely by pre-existing grants, even though a specific mandate tied to the grants for this use is unlikely.
The scientific community has swiftly reallocated research efforts to cope with the COVID-19 pandemic, mobilizing knowledge across disciplines to find innovative solutions in record time. We document this both in terms of changing trends in the biomedical scientific output and the usage of MeSH terms by the scientific community. The flip side of this sudden and energetic prioritization of effort to fight COVID-19 has been a sudden contraction of scientific production in other relevant research areas. All in all, we find strong support to the hypotheses that the COVID-19 crisis has induced a sudden increase of research output in COVID-19 related areas of biomedical research. Conversely, research in areas not related to COVID-19 has experienced a significant drop in overall publishing rates and funding.
Our paper contributes to the literature on the impact of COVID-19 on scientific research: we corroborate previous findings about the surge of COVID-19 related publications [ 1 – 3 ], partially displacing research in COVID-19 unrelated fields of research [ 4 , 14 ], particularly research related to clinical trials [ 5 – 7 ]. The drop in trial research might have severe consequences for patients affected by life-threatening diseases since it will delay access to new and better treatments. We also confirm the impact of COVID-19 on open access publication output [ 1 ]; also, this is milder than traditional outlets. On top of this, we provide more robust evidence on the impact weighted effect of COVID-19 and grant financed research, highlighting the strong displacement effect of COVID-19 on the allocation of financial resources [ 15 ]. We document a substantial change in the usage patterns of MeSH terms, suggesting that there has been a reconfiguration in the way research terms are being combined. MeSH terms highly related to COVID-19 were peripheral in the MeSH usage networks before the pandemic but have become central since 2020. We conclude that the usage patterns have changed, with COVID-19 related MeSH terms occupying a much more prominent role in 2020 than they did in the previous years.
We also contribute to the literature by estimating the effect of COVID-19 on biomedical research in a natural experiment framework, isolating the specific effects of the COVID-19 pandemic on the biomedical scientific landscape. This is crucial to identify areas of public intervention to sustain areas of biomedical research which have been neglected during the COVID-19 crisis. Moreover, the exploratory analysis on the changes in usage patterns of MeSH terms, points to an increase in the importance of covid-related topics in the broader biomedical research landscape.
Our results provide compelling evidence that research related to COVID-19 has indeed displaced scientific production in other biomedical fields of research not related to COVID-19, with a significant drop in (impact weighted) scientific output related to non-COVID-19 and a marked reduction of financial support for publications not related to COVID-19 [ 4 , 5 , 16 ]. The displacement effect is persistent to the end of 2020. As vaccination progresses, we highlight the urgent need for science policy to re-balance support for research activity that was put on pause because of the COVID-19 pandemic.
We find that COVID-19 dramatically impacted clinical research. Reactivation of clinical trials activities that have been postponed or suspended for reasons related to COVID-19 is a priority that should be considered in the national vaccination plans. Moreover, since grants have been diverted and financial incentives have been targeted to sustain COVID-19 research leading to an excessive entry in COVID-19-related clinical trials and the ‘covidisation’ of research, there is a need to reorient incentives to basic research and otherwise neglected or temporally abandoned areas of biomedical research. Without dedicated support in the recovery plans for neglected research of the COVID-19 era, there is a risk that more medical needs will be unmet in the future, possibly exacerbating the shortage of scientific research for orphan and neglected diseases, which do not belong to COVID-19-related research areas.
Limitations
Our empirical approach has some limits. First, we proxy MeSH term usage via search terms using the PubMed EUtilities API. This means that the accuracy of the MeSH term we assign to a given paper is not fully validated. More time is needed for the completion of manually annotated MeSH terms. Second, the timing of publication is not the moment the research has been carried out. There is a lead time between inception, analysis, write-up, review, revision, and final publication. This delay varies across disciplines. Nevertheless, given that the surge in publications happens around the alleged event date, January 2020, we are confident that the publication date is a reasonable yet imperfect estimate of the timing of the research. Third, several journals have publicly declared to fast-track COVID-19 research. This discrepancy in the speed of publication of COVID-19 related research and other research could affect our results. Specifically, a surge or displacement could be overestimated due to a lag in the publication of COVID-19 unrelated research. We alleviate this bias by estimating the effect considering a considerable time after the event (January 2020 to December 2020). Forth, on the one hand, clinical Trials may lead to multiple publications. Therefore we might overestimate the impact of COVID-19 on the number of clinical trials. On the other hand, COVID-19 publications on clinical trials lag behind, so the number of papers related COVID-19 trials is likely underestimated. Therefore, we note that the focus of this paper is scientific publications on clinical trials rather than on actual clinical trials. Fifth, regarding grants, unfortunately, there is no unique centralized repository mapping grant numbers to years, so we have to proxy old grants with grants that appeared in publications from 2010 to 2018. Besides, grant numbers are free-form entries, meaning that PubMed has no validation step to disambiguate or verify that the grant number has been entered correctly. This has the effect of classifying a grant as new even though it has appeared under a different name. We mitigate this problem by using a long period to collect grant numbers and catch many spellings of the same grant, thereby reducing the likelihood of miss-identifying a grant as new when it existed before. Still, unless unique identifiers are widely used, there is no way to verify this.
So far, there is no conclusive evidence on whether entry into COVID-19 has been excessive. However, there is a growing consensus that COVID-19 has displaced, at least temporally, scientific research in COVID-19 unrelated biomedical research areas. Even though it is certainly expected that more attention will be devoted to the emergency during a pandemic, the displacement of biomedical research in other fields is concerning. Future research is needed to investigate the long-run structural consequences of the COVID-19 crisis on biomedical research.
Supporting information
S1 table. common trend assumption (cta) regression table..
Full regression table with all controls and interactions.
https://doi.org/10.1371/journal.pone.0263001.s001
- View Article
- Google Scholar
- PubMed/NCBI
- 8. Brown A, Edwin E, Fagg J. Evaluate Pharma 2021 Preview; 2020. https://www.evaluate.com/thought-leadership/vantage/evaluate-vantage-2021-preview .
- 15. Hook D, Porter S. The COVID Brain Drain; 2020. https://www.natureindex.com/news-blog/covid-brain-drain-scientific-research .
- 17. Page L, Brin S, Motwani R, Winograd T. The PageRank citation ranking: Bringing order to the web. Stanford InfoLab; 1999.
- Current Students
New study differentiates perinatal risks of COVID-19 infection from pandemic era societal changes
California preterm births declined during pandemic
- 2 min. read ▪ Published May 9
- Share on LinkedIn
- Share on Facebook
- Share on X (Twitter)
A new study has disentangled the risks to infants and birth parents from infection with SARS-CoV-2—the virus that causes COVID-19— from risks related to broader societal changes during the pandemic period.
Led by Dr. Shelley Jung , a UC Berkeley School of Public Health researcher, and published today in JAMA Network Open , the article shows that COVID-19 infection was associated with increased risk of preterm birth, hypertension, and severe maternal morbidity—which the CDC defines as “unexpected outcomes of labor and delivery that result in significant short- or long-term consequences to a woman’s health.” Interestingly, the pandemic period itself was associated with a lower risk of preterm birth, but a higher risk of hypertension and gestational diabetes.
This is the first study to separate the infant and birth parent risks linked to the pre-pandemic period, the societal changes of the pandemic period, and individual COVID-19 infection. “As far as we know, ours is the first within one coherent set of data to pull these three groups apart,” said Dr. Jennifer Ahern , a UC Berkeley epidemiology professor and the paper’s senior author.
The societal changes that may have affected health included differential access to care, economic strain, physical inactivity, and other stressors.
“It was an extremely stressful time for people for a variety of reasons,” said Ahern. “There were the economic impacts, which were pretty substantial, people losing jobs and sources of income.”
Jung noted that while COVID-19 infections had negative effects, the pandemic did also bring some positive impact.
“You’ve got maybe less commute stress, less physical stress during pregnancy,” she said. “It’s just a very complex set of changes that all coincided. It was exciting to dig into the net effect of the period on the people of California.” This study examined statewide California data, individually linking all birth and hospital discharge records for 2019 to 2020. “We linked the birth records to the hospital records,” Jung said. “Then we looked nine months back at the birth parent’s pregnancy and looked at all the hospital visits during those nine months.”
Ahern praised the state of California for coordinating data sources and making them available through a rigorous process that she said allows for valuable research while also protecting patient privacy.
The team will move on to look not just at the overall effect of the COVID pandemic period on the population, but how COVID may affect health disparities.
Additional authors include: Emily F. Liu, Mahasin S. Mujahid, and William H. Dow of UC Berkeley School of Public Health and Dana E. Goin and Kara E. Rudolph of Mailman School of Public Health at Columbia University.
This project was funded by grants from the National Institutes of Health.
People of BPH found in this article include:
- Jennifer Ahern Professor, Epidemiology
- William Dow Professor, Health Policy and Management
- Mahasin Mujahid Chair, Epidemiology Division
More in category “Research Highlights”:
Timing of puberty varies by up to 14 months among asian youth, surgery in a hospital doesn’t necessarily lead to better outcomes than surgery in a surgical center, collaboration is key to pioneering research with youth experiencing homelessness, exposure to wildfire smoke during pregnancy increases risk of preterm birth.
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Mortality in Patients Hospitalized for COVID-19 vs Influenza in Fall-Winter 2023-2024
- 1 Clinical Epidemiology Center, VA St Louis Health Care System, St Louis, Missouri
In the first year of the COVID-19 pandemic, risk of death in people hospitalized for COVID-19 was substantially higher than in people hospitalized for seasonal influenza. 1 , 2 The risk of death due to COVID-19 has since declined. In fall-winter 2022-2023, people hospitalized for COVID-19 had a 60% higher risk of death compared with those hospitalized for seasonal influenza. 3 New variants of SARS-CoV-2 have continued to appear, including the emergence of JN.1, the predominant variant in the US since December 24, 2023. 4 This study evaluated the risk of death in a cohort of people hospitalized for COVID-19 or seasonal influenza in fall-winter 2023-2024.
Read More About
Xie Y , Choi T , Al-Aly Z. Mortality in Patients Hospitalized for COVID-19 vs Influenza in Fall-Winter 2023-2024. JAMA. Published online May 15, 2024. doi:10.1001/jama.2024.7395
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
The independent source for health policy research, polling, and news.
COVID-19 Cases and Deaths by Race/Ethnicity: Current Data and Changes Over Time
Latoya Hill and Samantha Artiga Published: Aug 22, 2022
Over the course of the COVID-19 pandemic, analyses of federal, state, and local data have shown that people of color have experienced a disproportionate burden of cases and deaths. This brief examines racial disparities in COVID-19 cases and deaths and how they have changed over time based on KFF analysis of data on COVID-19 infections and deaths from CDC. It updates a February 2022 analysis to reflect data through mid-2022, amid the ongoing surge associated with the Omicron variant. It finds:
- Total cumulative data show Black, Hispanic, American Indian or Alaska Native (AIAN), and Native Hawaiian or Other Pacific Islander (NHOPI) people have experienced higher rates of COVID-19 cases and deaths compared to White people when data are adjusted to account for differences in age by race and ethnicity.
- Disparities in infections and deaths have both widened and narrowed at various times over the course of the pandemic, with disparities generally widening during periods in which the virus has surged and narrowing when overall infection rates fall. In data that has not been adjusted for age, there were some periods when death rates for White people were higher than or similar to some groups of color. However, in the age-adjusted data, White people have lower death rates than AIAN, Black, and Hispanic people over most of the course of the pandemic and disparities are larger for AIAN, Black, and Hispanic people, reflecting an older White population and higher rates of death across all age groups among people of color compared to White people.
Continuing to assess COVID-19 health impacts by race/ethnicity is important for both identifying and addressing disparities and preventing against further widening of disparities in health going forward. While disparities in cases and deaths have narrowed and widened over time, the underlying structural inequities in health and health care and social and economic factors that placed people of color at increased risk at the outset of the pandemic remain. As such, they may remain at increased risk as the pandemic continues to evolve and for future health threats, such as the Monkeypox virus, for which early data show similar disparities emerging.
Disparities in Total COVID-19 Cases and Deaths
As of August 5, 2022, the Centers for Disease Control and Prevention (CDC) reported a total of over 84 million cases, for which race/ethnicity was known for 65% or over 55 million, and a total of over 880,000 deaths, for which race/ethnicity was known for 85% or over 750,000. These estimates are based on a subset of data for which case-level demographic information has been reported to CDC by state health departments, so they differ from those reported elsewhere. For example, CDC reports a total of over 1 million deaths from COVID as of August 5, 2022. Data on cases also are likely significantly underreported as they do not reflect individuals who test positive on home tests and do not report findings to their public health agency.
Total cumulative data show that Black, Hispanic, AIAN, and NHOPI people have experienced higher rates of COVID-19 cases and deaths than White people when data are adjusted to account for differences in age by race and ethnicity. Age-standardized data show that that NHOPI, Hispanic, and AIAN people are at about one and a half times greater risk of COVID-19 infection than White people, and AIAN, Hispanic, NHOPI, and Black people are about twice as likely to die from COVID-19 as their White counterparts (Figure 1). The CDC also reports large disparities in COVID-19 hospitalizations for AIAN, Black, and Hispanic people. (CDC data does not include separate reporting for NHOPI people.) Adjusting for age when comparing groups on health measures is important because risk of infection, illness, and death can vary by age, and age distribution differs by racial and ethnic group. Age adjustment allows for direct comparison between groups on health measures independent of the age distribution differences. For example, unadjusted rates underestimate racial disparities for COVID-19 deaths, since the White population is older compared to populations of color and COVID-19 death rates have been higher among older individuals. Age adjustment has limited impact on case rates by race and ethnicity, suggesting that age plays a more limited role in risk of infection.
Disparities in Cases and Deaths Over Time
Analysis of monthly data on COVID-19 infections from CDC and deaths from NCHS shows disparities in infections and deaths have both widened and narrowed over the course of the pandemic. During periods in which the virus has surged, disparities have generally widened, while they have narrowed when overall infection rates fall. However, over the course of the pandemic, specific patterns of disparities have varied by race and ethnicity and between cases and deaths.
Trends in Cases
Figure 2 shows age-adjusted monthly data on cases by race and ethnicity between April 2020 and July 2022. There were no notable differences in patterns of disparities between unadjusted and age-adjusted data for reported cases. The data show that during periods of resurgence, disparities have generally widened for people of color compared to White people, while they have narrowed when overall infection rates fall.
- Early in the pandemic Hispanic, AIAN, and Black people had higher rates of COVID-19 cases compared to their White counterparts, with a particularly high rate among Hispanic people. Asian people had the lowest monthly infection rate.
- Case rates increased through Winter 2021, spiking in December 2021, and disparities further widened for Hispanic and AIAN people. Following the spike in December 2021, monthly infection rates fell across all groups. By June 2021, gaps between groups narrowed.
- By August 2021, infection rates rose again across groups, reflecting the spread of the Delta variant, with higher rates for Black and AIAN people compared to White people during this resurgence.
- During January 2022, infections sharply rose again across all groups amidst the spread of the Omicron variant, resulting in the highest case rates recorded since the start of the pandemic. Rates were higher for all groups of color compared to White people, with AIAN people having the highest infection rate during this surge, followed closely by Hispanic people. This surge was also the first time since early in the pandemic that the infection rate for Asian people was comparable to other groups of color. By February 2022, infection rates had fallen sharply, and disparities once again narrowed.
- Between Winter 2022 and June 2022 case rates have fallen across groups. In April, Asian people had the highest infection rate and Black, AIAN and Hispanic people had the lowest infection rate, marking the first time these patterns were observed since the start of the pandemic. More research is needed to understand the factors that contributed to this recent shift in trends. However, by June 2022, this pattern began to reverse with White people having the lowest infection rate, and Hispanic people at highest risk of infection in June and July.
Trends in deaths
Figure 3 presents age-adjusted monthly data on COVID-19 deaths by race and ethnicity between April 2020 and May 2022. Both the unadjusted and age-adjusted data show large disparities in death rates for people of color during surges in the pandemic, with the highest rates among AIAN people for most of the pandemic. In unadjusted data, there were some periods when death rates for White people were higher than or similar to some groups of color. However, in the age-adjusted data, White people have lower death rates than AIAN, Black, and Hispanic people over most of the course of the pandemic and disparities are larger for AIAN, Black, and Hispanic people, reflecting an older White population and higher rates of death across all age groups among people of color compared to White people.
- During the initial surge in summer 2020, AIAN, Hispanic, and Black people experienced higher rates of death than White people. As of July 2020, Hispanic people were five times more likely to die than White people, while AIAN and Black people were roughly four and three times as likely to die than White people, respectively. Asian people were at a similar risk of death as White people.
- Deaths peaked in December 2020 and January 2021 across groups. AIAN and Hispanic people had the highest rates of death, and all groups of color had a higher death rate than White people as of January 2021. Following that surge, death rates fell across all racial and ethnic groups and disparities narrowed by early summer 2021.
- Moving into late summer 2021, amid the rise of the Delta variant, death rates rose and were highest among AIAN people. Black and Hispanic people had higher death rates than White people, while Asian people had the lowest rate of death Following the Delta surge, monthly deaths declined slightly across groups with higher rates of death for AIAN people persisting before climbing again across groups in late 2021 with the arrival of the Omicron variant.
- As of January 2022, during the Omicron surge, Black, AIAN, and Hispanic people experienced the highest rates of death (36.5, 33.1, and 29.4 per 100,000 population, respectively). Following the spike in early 2022, monthly death rates fell across all groups and gaps between groups narrowed with similar rates of death across all groups (2.4 per 100,000 for AIAN and White people, 2.0 per 100,000 for Black people, 1.5 per 100,000 for Hispanic people, and 1.4 per 100,000 for Asian people.)
In sum, these data show that, overall, Black, Hispanic, and AIAN people have experienced higher rates of COVID-19 infection and death compared to White people when accounting for age differences across racial and ethnic groups. The age-adjusted data also suggest that while these disparities have narrowed at times over the course of the pandemic, people of color are disproportionately impacted by surges caused by new variants, with disparities widening during these periods.
The higher rates of infection among people of color likely reflect increased exposure risk due to working, living, and transportation situations, including being more likely to work in jobs that cannot be done remotely, to live in larger households, and to rely on public transportation. Black, Hispanic, and AIAN people have experienced the highest age-adjusted death rates amid each resurgence period, reflecting higher rates of death across all age groups among people of color compared to White people and an older White population. Overall, death rates have decreased across groups over the course of the pandemic as vaccination rates have increased and vaccination – particularly with boosters – continues to be highly effective at reducing the risk of hospitalization and death. Early disparities in vaccination rates by race and ethnicity have also narrowed over time. However, data suggest potential disparities in access to COVID-19 treatments , which will be important to monitor going forward.
Looking ahead, continuing to assess COVID-19 health impacts by race/ethnicity is important for both identifying and addressing disparities and preventing against further widening of disparities in health going forward. While disparities in cases and deaths have narrowed and widened during different periods over time, the underlying structural inequities in health and health care and social and economic factors that placed people of color at increased risk at the outset of the pandemic remain. As such, they may remain at increased risk as the pandemic continues to evolve and for future health threats, such as the Monkeypox virus, for which early data show similar disparities emerging.
This analysis uses data from multiple sources including the Centers for Disease Control and Prevention (CDC) COVID Data Tracker, the Centers for Disease Control and Prevention COVID-19 Response. COVID-19 Case Surveillance Data, the National Center for Health Statistics (NCHS) Provisional COVID-19 Deaths, and the Census Bureau Annual Estimates of the Resident Population. Unless otherwise noted, race/ethnicity was categorized by non-Hispanic White (White), non-Hispanic Black (Black), Hispanic, non-Hispanic American Indian and Alaska Native (AIAN), non-Hispanic Asian (Asian), and non-Hispanic Native Hawaiian or Other Pacific Islander (NHOPI).
Data on COVID-19 infections includes reported cases as of August 1, 2022 and data on COVID-19 deaths includes provisional deaths as of July 30, 2022 where race/ethnicity was available. Age-adjusted infection and death rates were standardized to the 2019 U.S. Census Bureau Annual Estimates of the Resident Population using the direct method of standardization. The direct method of age standardization is calculated by multiplying the age specific crude rates for each population by the appropriate weight in standard population and summing them to produce an age-standardized rate. Data for monthly age adjusted NHOPI cases and deaths not shown due to small number of observations. Age standardization allows for direct comparison of groups on health measures independent of differences in age distribution that may influence the measure being examined.
- Coronavirus (COVID-19)
- Racial Equity and Health Policy
- Race/Ethnicity
- Coronavirus
Also of Interest
- Latest Data on COVID-19 Vaccinations by Race/Ethnicity
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Coronavirus disease 2019 (COVID-19): A literature review
Harapan harapan.
a Medical Research Unit, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia
b Tropical Disease Centre, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia
c Department of Microbiology, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia
d Division of Infectious Diseases, AichiCancer Center Hospital, Chikusa-ku Nagoya, Japan

Amanda Yufika
e Department of Family Medicine, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia
Wira Winardi
f Department of Pulmonology and Respiratory Medicine, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia
g School of Medicine, The University of Western Australia, Perth, Australia
Haypheng Te
h Siem Reap Provincial Health Department, Ministry of Health, Siem Reap, Cambodia
Dewi Megawati
i Department of Microbiology and Parasitology, Faculty of Medicine and Health Sciences, Warmadewa University, Denpasar, Indonesia
j Department of Medical Microbiology and Immunology, University of California, Davis, CA, USA
Zinatul Hayati
k Department of Clinical Microbiology, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia
Abram L. Wagner
l Department of Epidemiology, University of Michigan, Ann Arbor, Michigan, MI 48109, USA
Mudatsir Mudatsir
In early December 2019, an outbreak of coronavirus disease 2019 (COVID-19), caused by a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), occurred in Wuhan City, Hubei Province, China. On January 30, 2020 the World Health Organization declared the outbreak as a Public Health Emergency of International Concern. As of February 14, 2020, 49,053 laboratory-confirmed and 1,381 deaths have been reported globally. Perceived risk of acquiring disease has led many governments to institute a variety of control measures. We conducted a literature review of publicly available information to summarize knowledge about the pathogen and the current epidemic. In this literature review, the causative agent, pathogenesis and immune responses, epidemiology, diagnosis, treatment and management of the disease, control and preventions strategies are all reviewed.
On December 31, 2019, the China Health Authority alerted the World Health Organization (WHO) to several cases of pneumonia of unknown aetiology in Wuhan City in Hubei Province in central China. The cases had been reported since December 8, 2019, and many patients worked at or lived around the local Huanan Seafood Wholesale Market although other early cases had no exposure to this market [1] . On January 7, a novel coronavirus, originally abbreviated as 2019-nCoV by WHO, was identified from the throat swab sample of a patient [2] . This pathogen was later renamed as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the Coronavirus Study Group [3] and the disease was named coronavirus disease 2019 (COVID-19) by the WHO. As of January 30, 7736 confirmed and 12,167 suspected cases had been reported in China and 82 confirmed cases had been detected in 18 other countries [4] . In the same day, WHO declared the SARS-CoV-2 outbreak as a Public Health Emergency of International Concern (PHEIC) [4] .
According to the National Health Commission of China, the mortality rate among confirmed cased in China was 2.1% as of February 4 [5] and the mortality rate was 0.2% among cases outside China [6] . Among patients admitted to hospitals, the mortality rate ranged between 11% and 15% [7] , [8] . COVID-19 is moderately infectious with a relatively high mortality rate, but the information available in public reports and published literature is rapidly increasing. The aim of this review is to summarize the current understanding of COVID-19 including causative agent, pathogenesis of the disease, diagnosis and treatment of the cases, as well as control and prevention strategies.
The virus: classification and origin
SARS-CoV-2 is a member of the family Coronaviridae and order Nidovirales. The family consists of two subfamilies, Coronavirinae and Torovirinae and members of the subfamily Coronavirinae are subdivided into four genera: (a) Alphacoronavirus contains the human coronavirus (HCoV)-229E and HCoV-NL63; (b) Betacoronavirus includes HCoV-OC43, Severe Acute Respiratory Syndrome human coronavirus (SARS-HCoV), HCoV-HKU1, and Middle Eastern respiratory syndrome coronavirus (MERS-CoV); (c) Gammacoronavirus includes viruses of whales and birds and; (d) Deltacoronavirus includes viruses isolated from pigs and birds [9] . SARS-CoV-2 belongs to Betacoronavirus together with two highly pathogenic viruses, SARS-CoV and MERS-CoV. SARS-CoV-2 is an enveloped and positive-sense single-stranded RNA (+ssRNA) virus [16] .
SARS-CoV-2 is considered a novel human-infecting Betacoronavirus [10] . Phylogenetic analysis of the SARS-CoV-2 genome indicates that the virus is closely related (with 88% identity) to two bat-derived SARS-like coronaviruses collected in 2018 in eastern China (bat-SL-CoVZC45 and bat-SL-CoVZXC21) and genetically distinct from SARS-CoV (with about 79% similarity) and MERS-CoV [10] . Using the genome sequences of SARS-CoV-2, RaTG13, and SARS-CoV [11] , a further study found that the virus is more related to BatCoV RaTG13, a bat coronavirus that was previously detected in Rhinolophus affinis from Yunnan Province, with 96.2% overall genome sequence identity [11] . A study found that no evidence of recombination events detected in the genome of SARS-CoV-2 from other viruses originating from bats such as BatCoV RaTG13, SARS-CoV and SARSr-CoVs [11] . Altogether, these findings suggest that bats might be the original host of this virus [10] , [11] .
However, a study is needed to elucidate whether any intermediate hosts have facilitated the transmission of the virus to humans. Bats are unlikely to be the animal that is directly responsible for transmission of the virus to humans for several reasons [10] : (1) there were various non-aquatic animals (including mammals) available for purchase in Huanan Seafood Wholesale Market but no bats were sold or found; (2) SARS-CoV-2 and its close relatives, bat-SL-CoVZC45 and bat-SL-CoVZXC21, have a relatively long branch (sequence identity of less than 90%), suggesting those viruses are not direct ancestors of SARS-CoV-2; and (3) in other coronaviruses where bat is the natural reservoir such as SARS-CoV and MERS-CoV, other animals have acted as the intermediate host (civets and possibly camels, respectively). Nevertheless, bats do not always need an intermediary host to transmit viruses to humans. For example, Nipah virus in Bangladesh is transmitted through bats shedding into raw date palm sap [12] .
Transmission
The role of the Huanan Seafood Wholesale Market in propagating disease is unclear. Many initial COVID-19 cases were linked to this market suggesting that SARS-CoV-2 was transmitted from animals to humans [13] . However, a genomic study has provided evidence that the virus was introduced from another, yet unknown location, into the market where it spread more rapidly, although human-to-human transmission may have occurred earlier [14] . Clusters of infected family members and medical workers have confirmed the presence of person-to-person transmission [15] . After January 1, less than 10% of patients had market exposure and more than 70% patients had no exposure to the market [13] . Person-to-person transmission is thought to occur among close contacts mainly via respiratory droplets produced when an infected person coughs or sneezes. Fomites may be a large source of transmission, as SARS-CoV has been found to persist on surfaces up to 96 h [16] and other coronaviruses for up to 9 days [17] .
Whether or not there is asymptomatic transmission of disease is controversial. One initial study published on January 30 reported asymptomatic transmission [18] , but later it was found that the researchers had not directly interviewed the patient, who did in fact have symptoms prior to transmitting disease [19] . A more recent study published on February 21 also purported asymptomatic transmission [20] , but any such study could be limited by errors in self-reported symptoms or contact with other cases and fomites.
Findings about disease characteristics are rapidly changing and subject to selection bias. A study indicated the mean incubation period was 5.2 days (95% confidence interval [95%CI]: 4.1–7.0) [13] . The incubation period has been found to be as long as 19 or 24 days [21] , [22] , although case definitions typically rely on a 14 day window [23] .
The basic reproductive number ( R 0 ) has been estimated with varying results and interpretations. R 0 measures the average number of infections that could result from one infected individual in a fully susceptible population [24] . Studies from previous outbreaks found R 0 to be 2.7 for SARS [25] and 2.4 for 2009 pandemic H1N1 influenza [26] . One study estimated that that basic reproductive number ( R 0 ) was 2.2 (95% CI: 1.4–3.9) [13] . However, later in a further analysis of 12 available studies found that R 0 was 3.28 [27] . Because R 0 represents an average value it is also important to consider the role of super spreaders, who may be hugely responsible for outbreaks within large clusters but who would not largely influence the value of R 0 [28] . During the acute phase of an outbreak or prepandemic, R 0 may be unstable [24] .
In pregnancy, a study of nine pregnancy women who developed COVID-19 in late pregnancy suggested COVID-19 did not lead to substantially worse symptoms than in nonpregnant persons and there is no evidence for intrauterine infection caused by vertical transmission [29] .
In hospital setting, a study involving 138 COVID-19 suggested that hospital-associated transmission of SARS-CoV-2 occurred in 41% of patients [30] . Moreover, another study on 425 patients found that the proportion of cases in health care workers gradually increased by time [13] . These cases likely reflect exposure to a higher concentration of virus from sustained contact in close quarters.
Outside China, as of February 12, 2020, there were 441 confirmed COVID-19 cases reported in 24 countries [6] of which the first imported case was reported in Thailand on January 13, 2020 [6] , [31] . Among those countries, 11 countries have reported local transmission with the highest number of cases reported in Singapore with 47 confirmed cases [6] .
Risk factors
The incidence of SARS-CoV-2 infection is seen most often in adult male patients with the median age of the patients was between 34 and 59 years [20] , [30] , [7] , [32] . SARS-CoV-2 is also more likely to infect people with chronic comorbidities such as cardiovascular and cerebrovascular diseases and diabetes [8] . The highest proportion of severe cases occurs in adults ≥60 years of age, and in those with certain underlying conditions, such as cardiovascular and cerebrovascular diseases and diabetes [20] , [30] . Severe manifestations maybe also associated with coinfections of bacteria and fungi [8] .
Fewer COVID-19 cases have been reported in children less than 15 years [20] , [30] , [7] , [32] . In a study of 425 COVID-19 patients in Wuhan, published on January 29, there were no cases in children under 15 years of age [13] , [33] . Nevertheless, 28 paediatric patients have been reported by January 2020 [34] . The clinical features of infected paediatric patients vary, but most have had mild symptoms with no fever or pneumonia, and have a good prognosis [34] . Another study found that although a child had radiological ground-glass lung opacities, the patient was asymptomatic [35] . In summary, children might be less likely to be infected or, if infected, present milder manifestations than adults; therefore, it is possible that their parents will not seek out treatment leading to underestimates of COVID-19 incidence in this age group.
Pathogenesis and immune response
Like most other members of the coronavirus family, Betacoronavirus exhibit high species specificity, but subtle genetic changes can significantly alter their tissue tropism, host range, and pathogenicity. A striking example of the adaptability of these viruses is the emergence of deadly zoonotic diseases in human history caused by SARS-CoV [36] and MERS-CoV [37] . In both viruses, bats served as the natural reservoir and humans were the terminal host, with the palm civet and dromedary camel the intermediary host for SARS-CoV and MERS-CoV, respectively [38] , [39] . Intermediate hosts clearly play a critical role in cross species transmission as they can facilitate increased contact between a virus and a new host and enable further adaptation necessary for an effective replication in the new host [40] . Because of the pandemic potential of SARS-CoV-2, careful surveillance is immensely important to monitor its future host adaptation, viral evolution, infectivity, transmissibility, and pathogenicity.
The host range of a virus is governed by multiple molecular interactions, including receptor interaction. The envelope spike (S) protein receptor binding domain of SARS-CoV-2 was shown structurally similar to that of SARS-CoV, despite amino acid variation at some key residues [10] . Further extensive structural analysis strongly suggests that SARS-CoV-2 may use host receptor angiotensin-converting enzyme 2 (ACE2) to enter the cells [41] , the same receptor facilitating SARS-CoV to infect the airway epithelium and alveolar type 2 (AT2) pneumocytes, pulmonary cells that synthesize pulmonary surfactant [42] . In general, the spike protein of coronavirus is divided into the S1 and S2 domain, in which S1 is responsible for receptor binding and S2 domain is responsible for cell membrane fusion [10] . The S1 domain of SARS-CoV and SARS-CoV-2 share around 50 conserved amino acids, whereas most of the bat-derived viruses showed more variation [10] . In addition, identification of several key residues (Gln493 and Asn501) that govern the binding of SARS-CoV-2 receptor binding domain with ACE2 further support that SARS-CoV-2 has acquired capacity for person-to-person transmission [41] . Although, the spike protein sequence of receptor binding SARS-CoV-2 is more similar to that of SARS-CoV, at the whole genome level SARS-CoV-2 is more closely related to bat-SL-CoVZC45 and bat-SL-CoVZXC21 [10] .
However, receptor recognition is not the only determinant of species specificity. Immediately after binding to their receptive receptor, SARS-CoV-2 enters host cells where they encounter the innate immune response. In order to productively infect the new host, SARS-CoV-2 must be able to inhibit or evade host innate immune signalling. However, it is largely unknown how SARS-CoV-2 manages to evade immune response and drive pathogenesis. Given that COVID-19 and SARS have similar clinical features [7] , SARS-CoV-2 may have a similar pathogenesis mechanism as SARS-CoV. In response to SARS-CoV infections, the type I interferon (IFN) system induces the expression of IFN-stimulated genes (ISGs) to inhibit viral replication. To overcome this antiviral activity, SARS-CoV encodes at least 8 viral antagonists that modulate induction of IFN and cytokines and evade ISG effector function [43] .
The host immune system response to viral infection by mediating inflammation and cellular antiviral activity is critical to inhibit viral replication and dissemination. However, excessive immune responses together with lytic effects of the virus on host cells will result in pathogenesis. Studies have shown patients suffering from severe pneumonia, with fever and dry cough as common symptoms at onset of illness [7] , [8] . Some patients progressed rapidly with Acute Respiratory Stress Syndrome (ARDS) and septic shock, which was eventually followed by multiple organ failure and about 10% of patients have died [8] . ARDS progression and extensive lung damage in COVID-19 are further indications that ACE2 might be a route of entry for the SARS-CoV-2 as ACE2 is known abundantly present on ciliated cells of the airway epithelium and alveolar type II (cells (pulmonary cells that synthesize pulmonary surfactant) in humans [44] .
Patients with SARS and COVID-19 have similar patterns of inflammatory damage. In serum from patients diagnosed with SARS, there is increased levels of proinflammatory cytokines (e.g. interleukin (IL)-1, IL6, IL12, interferon gamma (IFNγ), IFN-γ-induced protein 10 (IP10), macrophage inflammatory proteins 1A (MIP1A) and monocyte chemoattractant protein-1 (MCP1)), which are associated with pulmonary inflammation and severe lung damage [45] . Likewise, patients infected with SARS-CoV-2 are reported to have higher plasma levels of proinflammatory cytokines including IL1β, IL-2, IL7, TNF-α, GSCF, MCP1 than healthy adults [7] . Importantly, patients in the intensive care unit (ICU) have a significantly higher level of GSCF, IP10, MCP1, and TNF-α than those non-ICU patients, suggesting that a cytokine storm might be an underlying cause of disease severity [7] . Unexpectedly, anti-inflammatory cytokines such as IL10 and IL4 were also increased in those patients [7] , which was uncommon phenomenon for an acute phase viral infection. Another interesting finding, as explained before, was that SARS-CoV-2 has shown to preferentially infect older adult males with rare cases reported in children [7] , [8] . The same trend was observed in primate models of SARS-CoV where the virus was found more likely to infect aged Cynomolgus macaque than young adults [46] . Further studies are necessary to identify the virulence factors and the host genes of SARS-CoV-2 that allows the virus to cross the species-specific barrier and cause lethal disease in humans.
Clinical manifestations
Clinical manifestations of 2019-nCoV infection have similarities with SARS-CoV where the most common symptoms include fever, dry cough, dyspnoea, chest pain, fatigue and myalgia [7] , [30] , [47] . Less common symptoms include headache, dizziness, abdominal pain, diarrhoea, nausea, and vomiting [7] , [30] . Based on the report of the first 425 confirmed cases in Wuhan, the common symptoms include fever, dry cough, myalgia and fatigue with less common are sputum production, headache, haemoptysis, abdominal pain, and diarrhoea [13] . Approximately 75% patients had bilateral pneumonia [8] . Different from SARS-CoV and MERS-CoV infections, however, is that very few COVID-19 patients show prominent upper respiratory tract signs and symptoms such as rhinorrhoea, sneezing, or sore throat, suggesting that the virus might have greater preference for infecting the lower respiratory tract [7] . Pregnant and non-pregnant women have similar characteristics [48] . The common clinical presentation of 2019-nCoV infection are presented in Table 1 .
Clinical symptoms of patients with 2019-nCoV infection.
Severe complications such as hypoxaemia, acute ARDS, arrythmia, shock, acute cardiac injury, and acute kidney injury have been reported among COVID-19 patients [7] , [8] . A study among 99 patients found that approximately 17% patients developed ARDS and, among them, 11% died of multiple organ failure [8] . The median duration from first symptoms to ARDS was 8 days [30] .
Efforts to control spread of COVID-19, institute quarantine and isolation measures, and appropriately clinically manage patients all require useful screening and diagnostic tools. While SARS-CoV-2 is spreading, other respiratory infections may be more common in a local community. The WHO has released a guideline on case surveillance of COVID-19 on January 31, 2020 [23] . For a person who meets certain criteria, WHO recommends to first screen for more common causes of respiratory illness given the season and location. If a negative result is found, the sample should be sent to referral laboratory for SARS-CoV-2 detection.
Case definitions can vary by country and will evolve over time as the epidemiological circumstances change in a given location. In China, a confirmed case from January 15, 2020 required an epidemiological linkage to Wuhan within 2 weeks and clinical features such as fever, pneumonia, and low white blood cell count. On January 18, 2020 the epidemiological criterion was expanded to include contact with anyone who had been in Wuhan in the past 2 weeks [50] . Later, the case definitions removed the epidemiological linkage.
The WHO has put forward case definitions [23] . Suspected cases of COVID-19 are persons (a) with severe acute respiratory infections (history of fever and cough requiring admission to hospital) and with no other aetiology that fully explains the clinical presentation and a history of travel to or residence in China during the 14 days prior to symptom onset; or (b) a patient with any acute respiratory illness and at least one of the following during the 14 days prior to symptom onset: contact with a confirmed or probable case of SARS-CoV-2 infection or worked in or attended a health care facility where patients with confirmed or probable SARS-CoV-2 acute respiratory disease patients were being treated. Probable cases are those for whom testing for SARS-CoV-2 is inconclusive or who test positive using a pan-coronavirus assay and without laboratory evidence of other respiratory pathogens. A confirmed case is one with a laboratory confirmation of SARS-CoV-2 infection, irrespective of clinical signs and symptoms.
For patients who meet diagnostic criteria for SARS-CoV-2 testing, the CDC recommends collection of specimens from the upper respiratory tract (nasopharyngeal and oropharyngeal swab) and, if possible, the lower respiratory tract (sputum, tracheal aspirate, or bronchoalveolar lavage) [51] . In each country, the tests are performed by laboratories designated by the government.
Laboratory findings
Among COVID-19 patients, common laboratory abnormalities include lymphopenia [8] , [20] , [30] , prolonged prothrombin time, and elevated lactate dehydrogenase [30] . ICU-admitted patients had more laboratory abnormalities compared with non-ICU patients [30] , [7] . Some patients had elevated aspartate aminotransferase, creatine kinase, creatinine, and C-reactive protein [20] , [7] , [35] . Most patients have shown normal serum procalcitonin levels [20] , [30] , [7] .
COVID-19 patients have high level of IL1β, IFN-γ, IP10, and MCP1 [7] . ICU-admitted patients tend to have higher concentration of granulocyte-colony stimulating factor (GCSF), IP10, MCP1A, MIP1A, and TNF-α [7] .
Radiology findings
Radiology finding may vary with patients age, disease progression, immunity status, comorbidity, and initial medical intervention [52] . In a study describing 41 of the initial cases of 2019-nCoV infection, all 41 patients had pneumonia with abnormal findings on chest computed tomography (CT-scan) [7] . Abnormalities on chest CT-scan were also seen in another study of 6 cases, in which all of them showed multifocal patchy ground-glass opacities notably nearby the peripheral sections of the lungs [35] . Data from studies indicate that the typical of chest CT-scan findings are bilateral pulmonary parenchymal ground-glass and consolidative pulmonary opacities [7] , [8] , [20] , [30] , [32] , [53] . The consolidated lung lesions among patients five or more days from disease onset and those 50 years old or older compared to 4 or fewer days and those 50 years or younger, respectively [47] .
As the disease course continue, mild to moderate progression of disease were noted in some cases which manifested by extension and increasing density of lung opacities [49] . Bilateral multiple lobular and subsegmental areas of consolidation are typical findings on chest CT-scan of ICU-admitted patients [7] . A study among 99 patients, one patient had pneumothorax in an imaging examination [8] .
Similar to MERS-CoV and SARS-CoV, there is still no specific antiviral treatment for COVID-19 [54] . Isolation and supportive care including oxygen therapy, fluid management, and antibiotics treatment for secondary bacterial infections is recommended [55] . Some COVID-19 patients progressed rapidly to ARDS and septic shock, which was eventually followed by multiple organ failure [7] , [8] . Therefore, the effort on initial management of COVID-19 must be addressed to the early recognition of the suspect and contain the disease spread by immediate isolation and infection control measures [56] .
Currently, no vaccination is available, but even if one was available, uptake might be suboptimal. A study of intention to vaccinate during the H1N1 pandemic in the United States was around 50% at the start of the pandemic in May 2009 but had decreased to 16% by January 2010 [57] .
Neither is a treatment available. Therefore, the management of the disease has been mostly supportive referring to the disease severity which has been introduced by WHO. If sepsis is identified, empiric antibiotic should be administered based on clinical diagnosis and local epidemiology and susceptibility information. Routine glucocorticoids administration are not recommended to use unless there are another indication [58] . Clinical evidence also does not support corticosteroid treatment [59] . Use of intravenous immunoglobulin might help for severely ill patients [8] .
Drugs are being evaluated in line with past investigations into therapeutic treatments for SARS and MERS [60] . Overall, there is not robust evidence that these antivirals can significantly improve clinical outcomes A. Antiviral drugs such as oseltamivir combined with empirical antibiotic treatment have also been used to treat COVID-19 patients [7] . Remdesivir which was developed for Ebola virus, has been used to treat imported COVID-19 cases in US [61] . A brief report of treatment combination of Lopinavir/Ritonavir, Arbidol, and Shufeng Jiedu Capsule (SFJDC), a traditional Chinese medicine, showed a clinical benefit to three of four COVID-19 patients [62] . There is an ongoing clinical trial evaluating the safety and efficacy of lopinavir-ritonavir and interferon-α 2b in patients with COVID-19 [55] . Ramsedivir, a broad spectrum antivirus has demonstrated in vitro and in vivo efficacy against SARS-CoV-2 and has also initiated its clinical trial [63] , [64] . In addition, other potential drugs from existing antiviral agent have also been proposed [65] , [66] .
Control and prevention strategies
COVID-19 is clearly a serious disease of international concern. By some estimates it has a higher reproductive number than SARS [27] , and more people have been reported to have been infected or died from it than SARS [67] . Similar to SARS-CoV and MERS-CoV, disrupting the chain of transmission is considered key to stopping the spread of disease [68] . Different strategies should be implemented in health care settings and at the local and global levels.
Health care settings can unfortunately be an important source of viral transmission. As shown in the model for SARS, applying triage, following correct infection control measures, isolating the cases and contact tracing are key to limit the further spreading of the virus in clinics and hospitals [68] . Suspected cases presenting at healthcare facilities with symptoms of respiratory infections (e.g. runny nose, fever and cough) must wear a face mask to contain the virus and strictly adhere triage procedure. They should not be permitted to wait with other patients seeking medical care at the facilities. They should be placed in a separated, fully ventilated room and approximately 2 m away from other patients with convenient access to respiratory hygiene supplies [69] . In addition, if a confirmed COVID-19 case require hospitalization, they must be placed in a single patient room with negative air pressure – a minimum of six air changes per hour. Exhausted air has to be filtered through high efficiency particulate air (HEPA) and medical personnel entering the room should wear personal protective equipment (PPE) such as gloves, gown, disposable N95, and eye protection. Once the cases are recovered and discharged, the room should be decontaminated or disinfected and personnel entering the room need to wear PPE particularly facemask, gown, eye protection [69] .
In a community setting, isolating infected people are the primary measure to interrupt the transmission. For example, immediate actions taken by Chinese health authorities included isolating the infected people and quarantining of suspected people and their close contacts [70] . Also, as there are still conflicting assumptions regarding the animal origins of the virus (i.e. some studies linked the virus to bat [71] , [72] while others associated the virus with snake [73] ), contacts with these animal fluids or tissues or consumption of wild caught animal meet should be avoided. Moreover, educating the public to recognize unusual symptoms such as chronic cough or shortness of breath is essential therefore that they could seek medical care for early detection of the virus. If large-scale community transmission occurs, mitigating social gatherings, temporary school closure, home isolation, close monitoring of symptomatic individual, provision of life supports (e.g. oxygen supply, mechanical ventilator), personal hand hygiene, and wearing personal protective equipment such as facemask should also be enforced [74] .
In global setting, locking down Wuhan city was one of the immediate measure taken by Chinese authorities and hence had slowed the global spread of COVID-19 [74] . Air travel should be limited for the cases unless severe medical attentions are required. Setting up temperature check or scanning is mandatory at airport and border to identify the suspected cases. Continued research into the virus is critical to trace the source of the outbreak and provide evidence for future outbreak [74] .
Conclusions
The current COVID-19 pandemic is clearly an international public health problem. There have been rapid advances in what we know about the pathogen, how it infects cells and causes disease, and clinical characteristics of disease. Due to rapid transmission, countries around the world should increase attention into disease surveillance systems and scale up country readiness and response operations including establishing rapid response teams and improving the capacity of the national laboratory system.
Competing interests
The authors declare that they have no competing interests.
Ethical approval
Not required.
Managing boundaries for well-being: a study of work-nonwork balance crafting during the COVID-19 pandemic
- Open access
- Published: 17 May 2024
Cite this article
You have full access to this open access article

- Sophie E. Brogle 1 ,
- Philipp Kerksieck ORCID: orcid.org/0000-0001-5327-3668 1 ,
- Georg F. Bauer ORCID: orcid.org/0000-0003-0232-8141 1 &
- Anja I. Morstatt ORCID: orcid.org/0000-0001-6223-9939 1
126 Accesses
Explore all metrics
In the wake of the COVID-19 pandemic, the boundaries between the work and nonwork domain have rapidly blurred, presenting employees with new challenges and potentially heightening interference of the work with the nonwork domain (work-home interference, WHI) and vice versa (home-work interference, HWI). To counteract these interferences, employees can apply work-nonwork balance crafting (WNBC), referring to proactive efforts for balancing both life domains by targeting the permeability of the boundary between them. Employees may focus their crafting on the boundary toward the work domain (WNBC-work) or the non-work domain (WNBC-nonwork), e.g., shielding each domain from negative spillover from the other. This study aims to investigate the longitudinal associations of WNBC with health outcomes during the COVID-19 pandemic. We hypothesized that individuals who exhibited more such crafting behaviors at the onset of the pandemic would experience higher mental well-being and work engagement at later points in the COVID-19 pandemic, mediated by lower WHI and HWI. We surveyed N = 2,171 German-speaking employees from Germany, Austria, and Switzerland at three time points during 2020. Structural equation model results indicate that only WNBC-work is longitudinally negatively associated with reduced HWI and positively associated with mental well-being and work engagement. Further, in our sample, only HWI is longitudinally associated with lower mental well-being. No indirect effect reaches significance. Our results underline the importance of WNBC in the work domain in the early phases of the COVID-19 pandemic. Future research should explore the nature of the direct links between WNBC and mental well-being and work engagement and consider alternative mediating processes, such as gain spirals. Lastly, our study underscores that supporting employees in crafting boundaries for well-being can be crucial, particularly during times of crisis.
Avoid common mistakes on your manuscript.
Introduction
The world was hit by the COVID-19 pandemic in March 2020, and governments worldwide aimed to contain the virus and prevent its spreading by inaugurating various measures, e.g., school closures, remote work, nationwide lockdowns (Hale et al., 2021 ; Rudolph et al., 2021 ). Since then, life for many employees has changed drastically, and the boundaries between work and nonwork have blurred increasingly (Cho, 2020 ; Vaziri et al., 2020 ). For many, their life domains clashed literally, as they were forced to work remotely, through which private and professional life occurred in the same physical space (Kaltiainen & Hakanen, 2023 ; Kniffin et al., 2021 ). For others, e.g., health workers or supermarket staff, a drastic increase in workload and increasingly straining mental and physical work conditions might have interfered with their capacities to deal with nonwork demands (Benfante et al., 2020 ). Such life domain conflicts are associated with adverse health consequences such as exhaustion (Reinke & Gerlach, 2022 ), but also reduced work engagement (Karatepe & Karadas, 2016 ) and impaired mental health (Yucel & Fan, 2019 ). For the time of the pandemic, a large study in the UK covering only a time frame until May 2020 indicated that mental health was negatively affected in this early phase (O’Connor et al., 2021 ). Thus, more knowledge on how life domain conflicts and impaired health unfolded throughout the pandemic is needed. Further, employees might have experienced the pandemic differentially, likely depending on their proactive and agentic efforts to deal with the pandemic (Demerouti & Bakker, 2022 ). Thus, the present study aims to examine how employees’ proactive crafting of the boundaries between work and non-work life domains is related to employee health during the COVID-19 crisis. We hypothesized that exhibiting more WNBC at the start of the pandemic would be associated with higher mental well-being and work engagement 8 months later, mediated by lower WHI and HWI.
Proactive behaviors, e.g., job crafting (Tims et al., 2012 ; Tims & Bakker, 2010 ; Wrzesniewski & Dutton, 2001 ), have been shown to play a relevant role in changing situations, e.g., organizational changes, and in maintaining work engagement (Petrou et al., 2018 ). Further, job crafting has been identified as a buffer to life domain conflicts (Lyu & Fan, 2022 ). However, the single life domain focus for crafting lacks breadth in understanding proactivity. The concept of job crafting has recently been transferred to the off-job domain (see literature on off-job crafting; Kujanpää et al., 2022 ) and further to the idea that the boundaries between life domains and, therefore, a balance between them can also be actively crafted (work nonwork balance crafting; WNBC) (Kerksieck et al., 2022 ). Due to the above-described shifting and blurring of work-nonwork boundaries during the COVID-19 crisis, WNBC, as a targeted, proactive strategy, is well suited to study how employees dealt with the clashing of life domains and how this is related to mental well-being and work engagement of employees during the first year of the global health crisis. Recent research indicates that there may be associations between crafting in different life domains, and that crafting is not limited to specific life domains but can also span across life domains (de Bloom et al., 2020 ; Demerouti et al., 2020 ). Consequently, WNBC itself focuses on the proactive crafting of said boundary and not, as other types of crafting, on crafting specific life domain characteristics with a focus on a single domain. We used a cross-lagged panel model approach with three waves, covering a period of 8 months during 2020. For the analysis, a structural equation model was specified, and the hypotheses were tested using path estimates. Our research model is depicted in Fig. 1 .
Our study makes two main contributions to research on the COVID-19 pandemic and crafting in general. First, our study captures a significant part of the first pandemic year and can shed light on long-term associations of proactive behaviors early in the pandemic. The beginning of the pandemic was a difficult time for most people. In many cases, workers faced a completely new situation, e.g., when affected by home office regulations (Tušl et al., 2021 ). However, by forming new routines and adapting behaviors to the novel needs caused by the pandemic and lockdown measures, people had a chance to influence their future experience of the pandemic (Chankasingh et al., 2022 ). By reviewing how WNBC at the pandemic onset is longitudinally linked with life domain conflicts and well-being, we provide knowledge on how to design early interventions supporting employees in their own crafting during future emergencies. For policymakers as well as organizations, this can increase future crisis preparedness.
Second, we add knowledge to WNBC research and, more specifically, whether life domain conflicts mediate between WNBC and well-being in both life domains, more specifically with mental well-being and work engagement. Previously, it was already demonstrated that WNBC is longitudinally linked with family role and job performance, job and life satisfaction, and work engagement (Kerksieck et al., 2022 ). However, the mechanisms still need to be clarified. Further, we closely examine domain-specific associations, which aids in understanding which domain focus might be more relevant in maintaining well-being over time. Those insights are highly significant for a more informed crisis management and can help organizations in supporting their employees to use bottom-up self-management crafting strategies to their benefit. This is important, since research on life-role interference during the pandemic has indicated the urgent need for proactive adjustments of roles employees fulfill at work and at home (Syrek et al., 2022 ). Furthermore, this knowledge about the role of WNBC will become ever more important even outside of the pandemic context, as the future of work will increasingly require the ability to deal with demands from the continuously intertwined work and nonwork domains (Caringal-Go et al., 2022 ; Mäkikangas et al., 2024 ; Rudolph et al., 2021 ).
Work-nonwork balance crafting as a buffer to life domain conflicts
Crafting generally describes self-initiated behaviors people undertake to shape or mold certain aspects of their lives according to their individual needs or preferences (Wrzesniewski & Dutton, 2001 ). Specifically, WNBC (Kerksieck et al., 2022 ) builds on this conceptualization and refers to proactive behaviors aiming to craft the boundaries between work and nonwork life according to individual needs (de Bloom et al., 2020 ). Other forms of crafting, e.g., job crafting (Tims et al., 2012 ; Wrzesniewski & Dutton, 2001 ) or off-job crafting (Kujanpää et al., 2022 ) show negative associations with stress experience (Ingusci et al., 2021 ) and burnout (Pijpker et al., 2022 ), among others.
WNBC efforts can focus on different life domains, resp. dimensions. For example, if someone tries hard to make time to take care of their remotely schooled children (due to the lockdown) while being strongly demanded by their work tasks, they focus on their private life and proactively ensure that they can meet their family obligations. Employees might be proactively setting clear time boundaries for work-related requests. In this way, the caring responsibilities in the nonwork life domain are prioritized. Work-related demands are dealt with after caring duties have been completed. In this way, crafting efforts are directed towards the employee’s nonwork life domain (WNBC-nonwork). On the other hand, employees might also proactively regulate a bad mood due to non-work reasons, e.g., increasingly demanding and stressful caring responsibilities due to COVID-19 measures, so that their work life is not affected. Their crafting efforts are then focused on the work life domain (WNBC-work). These two behaviors – protecting the work domain from the nonwork domain and vice versa – are not mutually exclusive and can take place simultaneously. Additionally, WNBC can occur as physical, relational, or cognitive crafting (Kerksieck et al., 2022 ). While theories on segmentation and integration are already well studied (Ashforth et al., 2000 ), they lack a nuanced perspective of how the boundary between life domains is created. WNBC suggests an active process whereby employees build their boundary from both sides: When guarding the work domain, they may prevent spillover from the non-work domain to the work domain, while still allowing a spillover from work to non-work, and vice versa. Therefore, WNBC offers a more comprehensive perspective that also allows for the prioritization of one domain. To summarize, WNBC refers to proactive behaviors aimed at balancing life domains – or managing life domain conflicts – and can be focused on the work or the nonwork domain.
Intensified life domain conflicts as consequence of pandemic working conditions
At the beginning of the pandemic, forced teleworking, increasing strain at work, and, for many, also increased care duties rapidly aggravated life domain conflicts. Both work-home interference (WHI) and home-work interference (HWI) (Kopelman et al., 1983 ) are indicators of a disturbed life domain balance, resulting in, i.e., life domain conflicts. When experiencing high WHI, an individual might not be able to fully enjoy the company of their family and friends because they worry about their work, which might be more demanding than usual due to the changed work form and workplace uncertainty during the pandemic. Whereas when experiencing high HWI, an individual might have issues focusing on work because they are preoccupied with worries about one of their family members being ill or struggling during the pandemic. Although the two constructs are conceptually separated due to the different directions of influence, they are related and can co-occur (Frone et al., 1992 ).
During the pivotal pandemic phase when first containment measures were put in place, we assume that the adoption and extent of WNBC practices varied among individuals and that WNBC potentially acted as a buffer against the escalation of life domain conflicts. Especially the beginning of the pandemic has been a crucial phase that set how employees experienced the subsequent course of the pandemic (Chankasingh et al., 2022 ). When crafting for the boundaries between the work and nonwork life, potentially a work-nonwork balance is created (Gravador & Teng-Calleja, 2018 ) and accompanied by lower conflicts between the two domains (both WHI and HWI), depending on the domain focus of the crafting.
Relationships between WNBC and life domain conflicts
We assume a life domain congruence in the association between WNBC and the life domain conflicts, such that WNBC with a focus on the nonwork domain is negatively associated with WHI, and WNBC with a focus on the work domain is negatively associated with HWI. Previous research found that high work demands, e.g., a high workload, predict WHI and high demands in the private domain predict HWI (Demerouti et al., 2004 ). In general, employees employing WNBC use different behaviors to prevent the potential for conflict between their work and private life domains. Employees focusing on WNBC in the nonwork domain, e.g., strategically distribute their work hours, thereby creating pockets of dedicated quality time with their family or partner. By orchestrating such intentional compartmentalization, WNBC minimizes the permeation of work-related stressors into the nonwork domain. Similarly, employees focus WNBC on the work domain, e.g., craft clashing domains, by actively planning their working days and fitting small time pockets to complete necessary private chores while ensuring that their work receives sufficient attention. Further, WNBC also captures employees’ behaviors to prevent negative affect spillover in the work or the nonwork domain to protect their resources and maintain their functioning in both life domains. This should in the long run reduce life domain conflicts as well.
Drawing a specific lens on the unfolding of the pandemic, we suggest that individuals who embraced WNBC strategies during the initial stages of the crisis were able to mitigate the aggravation of life domain conflicts. This proactive stance towards WNBC might have acted as a buffer against the rising challenges imposed by the pandemic. Consequently, as the pandemic unfolded, individuals who had actively engaged in higher levels of WNBC might have been better positioned to navigate subsequent challenges, leading to a diminished prevalence of life domain conflicts in their ongoing experiences compared to those who had engaged in comparatively less WNBC practices.
Based on the above literature review, we derive the following hypotheses:
H1.1: WNBC-nonwork at the pandemic onset (t1) is negatively associated with WHI in the middle of 2020 (t2).
H1.2: WNBC-work at the pandemic onset (t1) is negatively associated with HWI in the middle of 2020 (t2).
Life domain conflicts and impaired long-term mental well-being and work engagement
Experiencing life domain conflicts impairs health and well-being both in the short and long run (e.g., Karatepe & Karadas, 2016 ; Yucel & Fan, 2019 ). According to the Work-Home Resources Model (ten Brummelhuis & Bakker, 2012 ), chronic demands or life domain conflicts lead to a person having to constantly invest resources, which can lead to a depletion process over time. This continuous resource depletion (termed “loss spiral” in the Conservation of Resources Theory (COR; Hobfoll, 1989 ) is associated with negative consequences (e.g., Brosschot et al., 2006 ), including reduced work engagement (Halbesleben, 2010 ; Xanthopoulou et al., 2009 ).
Thus, we suggest that also during the COVID-19 pandemic, both types of life domain conflicts are negatively associated with subsequent mental well-being and work engagement, the health indicators of our study. Whether in pre-pandemic times or since the onset of the pandemic, whenever employees experience life domain conflicts, they need to invest resources to maintain their usual level of performance and to deal with the demands of their work and nonwork life, which further drains their resources and impairs their health.
First, we study how life domain conflicts are linked with mental well-being. The WHO defines mental well-being as a state ‘which allows individuals to realize their abilities, cope with the normal stresses of life, work productively and fruitfully, and make a contribution to their community’ (World Health Organization, 2001 , p. 1). It captures both aspects of satisfaction, positive affect, and psychological functioning (Ryan & Deci, 2001 ). As life domain conflicts have been linked with higher stress (Chapman et al., 1994 ), lower life satisfaction (Adams et al., 1996 ), and reduced general well-being (Grant-Vallone & Donaldson, 2001 ), we suggest that they predict reduced mental well-being as well.
H2.1: (a) HWI and (b) WHI in the middle of 2020 (t2) are negatively related to mental well-being at the end of 2020 (t3).
Second, we study how life domain conflicts are linked with work engagement. Work engagement can be defined as a positive, fulfilling state in which employees strive to actively use their personal resources to accomplish the work tasks at hand and perform well in the process (Schaufeli & Greenglass, 2001 ). Previous research has shown that life domain conflicts in both directions are negatively associated with work engagement (Karatepe & Karadas, 2016 ), both before and during the pandemic (Galanti et al., 2021 ). When private life interferes with work, e.g., due to additional care duties for stay-at-home children who had remote classes during the pandemic (Rieth & Hagemann, 2021 ), employees might have a more challenging time focusing on work, thereby limiting the experience of work engagement. However, work might also interfere with private life, e.g., due to forced teleworking, which might call employees to invest additional resources to maintain performance, increasing exhaustion in the long run. Accordingly, Kaltiainen and Hakaken ( 2023 ) report an indirect link between increased telework due to the pandemic and decreased work engagement via WHI. To conclude, we suggest that both types of life domain conflicts are associated with lower work engagement:
H2.2: (a) HWI and (b) WHI in the middle of 2020 (t2) are negatively related to work engagement at the end of 2020 (t3).
WNBC and subsequent mental well-being and work engagement
Finally, in this study, we also aim to study the long-term association between WNBC and both mental well-being and work engagement via reduced life domain conflicts. This adds depth to our understanding of how proactive behaviors early in the pandemic could be connected to long-term health and well-being. Notably, the direct link between WNBC and heightened work engagement has been substantiated in existing literature (Kerksieck et al., 2022 ). Our study examines a potential mechanism explaining this association by reviewing the life domain conflicts as mediators. Therefore, we link WNBC as a proactive and preventive strategy to the loss spiral between life domain conflicts and health and well-being. By its proactive nature, WNBC might preempt and neutralize potential conflicts that may arise in the context of the COVID-19 pandemic’s unique demands. In doing so, WNBC may counter the loss spiral and prevent the gradual depletion of personal resources occasioned by unaddressed life domain conflicts. In turn, WNBC potentially aids in preserving and potentially augmenting precious personal resources and maintaining health and well-being.
To conclude, we suggest the following hypotheses:
H3.1: WNBC-nonwork at the pandemic onset (t1) is indirectly positively related to (a) work engagement and (b) mental well-being at the end of 2020 (t3), mediated by WHI in the middle of 2020 (t2).
H3.2: WNBC-work at the pandemic onset (t1) is indirectly positively related to (a) work engagement and (b) mental well-being at the end of 2020 (t3), mediated by HWI in the middle of 2020 (t2).
Data collection and sample
For our study, we refer to three time points from a more extensive longitudinal panel data collection. The three survey waves cover the period from April 2020 to December 2020 (see Fig. 1 ). Participants were recruited via the market research provider Bilendi (formerly respondi; www.bilendi.de ). Inclusion criteria were a weekly working time of at least 20 h per week and being employed. The age ranged from 17 to 66 years ( M = 46.9, SD = 11.23), with 45.78% of the sample identifying as female. Participants came from Germany, Austria, or Switzerland. Sample sizes were 2,130 (wave 1), 1,633 (wave 2), and 1,178 (wave 3). In total, adjusted data points from 2,171 participants are available between waves 1 and 3, whereby participants who only took part in one wave were also included.
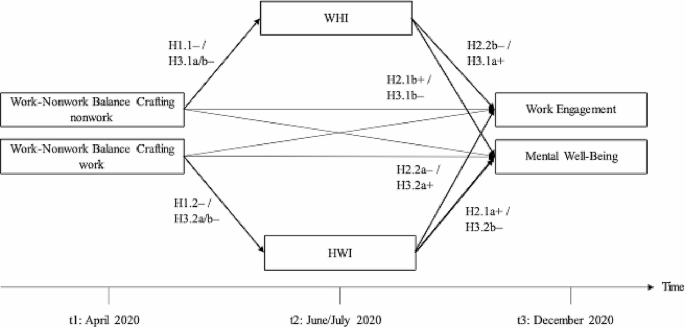
Research model. Note . H3.1 and H3.2 are mediation hypotheses whose sub-paths are shown in the model. For the constructs at t2 and t3, stability was controlled by including an autoregressive path from the previous wave, though not shown in the model. The nationwide Swiss lockdown due to the COVID-19 pandemic began on March 16 th , 2020 (Lockdown, 2021 )
Dropout analyses of those participants who only participated in wave 1 and not in waves 2 and 3 were performed (dropout: N = 497). Mean differences in age ( M continuers = 47.71 years vs. M dropout = 44.02 years; t (764.15) = 6.1501, p < .001) and life domain conflicts (WHI: M continuers = 1.85 vs. M dropout = 1.92; t (778.56) = -2.482, p = .013; HWI: M continuers = 1.55 vs. M dropout = 1.62; t (778.32) = -2.684, p = .007) were significant, indicating that the participants who dropped out after wave 1 were slightly younger and experienced higher life domain conflicts than the people who kept on participating in wave 2 and/or 3. In both cases, the group means were close to each other. There was no significant difference for gender and WNBC.
All measures were presented in German. In Table 1 , descriptive statistics and correlations between measures are presented.
- Work-nonwork balance crafting
WNBC was measured at wave 1 with 16 items of the Work-Nonwork Balance Crafting Scale (Kerksieck et al., 2022 ). The construct consists of two factors – crafting in the work and the nonwork domain. In the original scale, both factors contain all three crafting behaviors established (physical, relational, and cognitive/emotional). Example items are: ‘ If I must get personal chores done during working time, I make sure that my work won’t be negatively affected. ’ (WNBC-work) and ‘ I try hard to meet my private obligations, even if I’m demanded strongly by my work. ’ (WNBC-nonwork). The response format corresponds to a 5-point Likert scale (1 = ‘strongly disagree’ to 5 = ‘strongly agree’). Thus, a higher score indicated that respondents craft a less permeable boundary toward the focused domain, e.g., the work domain. In such a case, employees inhibit a spillover from, for example, negative emotions experienced outside of work to the work domain. The items were asked concerning the last four weeks. The original WNBC construct as a two-factor solution had a poor model fit (χ 2 (76) = 2055.731, p < .001, CFI = 0.669, TLI = 0.602, RMSEA = 0.111, SRMR = 0.092). We suggest that the scale in its complete form is not fully applicable to participants’ situations at the onset of the pandemic. Therefore, the scale was shortened via an iterative, theory-based process based on the consensus of two raters (First and last author), and all authors agreed to the shortened version. We removed items referring to, e.g., physical crafting, vacations, and work goals, as during the pandemic, many employees worked from home, vacations were not possible, and we argue that work goals might not have been a priority in such uncertain times. For example, Kossek et al. ( 2021 ) identified in a qualitative study on women working in STEM jobs that they experienced substantial role demands associated with work and nonwork role sacrifice during the pandemic. Thus, adapting the original WNBC scale to represent the challenging and unique time more adequately at the onset of the pandemic resulted in a shortened scale of 8 items, four mirroring items for each of the two factors (see Appendix Table 3 ). Since each of the items that belong to a different crafting domain (e.g., work) share variance through a common crafting dimension (e.g., relational), four residual covariances for each of the mirroring items were added, resulting in a satisfactory model fit (χ 2 (15) = 99.859, p < .001, CFI = 0.970, TLI = 0.944, RMSEA = 0.052, SRMR = 0.029). In allowing such residual covariances, we follow the approach taken by (Kerksieck et al., 2022 ) for the initial scale.
Home-work-interaction and work-home-interaction
HWI and WHI (Kopelman et al., 1983 ) were assessed at wave 1 (stability control) and wave 2 (mediators in research model) with four and eight items from the Survey Work-Home Interaction – NijmeGen (Geurts et al., 2005 ). Items were anchored on a 4-point Likert scale (0 = ‘never’ to 3 = ‘always’). An example item for HWI is: ‘ How often does it occur that problems with your spouse/family/friends affect your job performance? ’ and for WHI, an example item is: ‘ How often does it occur that you are irritable at home because your work is demanding? ’. The higher the score, the more respondents experienced an interference between the work and home life domains.
Mental well-being and work engagement
Mental well-being was assessed at wave 2 (stability control) and wave 3 (outcome in research model) with seven items from the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS; Tennant et al., 2007 ). The items refer to the last two weeks. An example item is: ‘ I felt optimistic about the future ’. The 5-point Likert scale ranges from 1 = ‘none of the time’ to 5 = ‘all of the time’, whereby a higher score indicated more mental well-being.
Work engagement was assessed at wave 2 (stability control) and wave 3 (outcome in research model) with nine items from the Utrecht Work Engagement Scale (UWES-9; Schaufeli et al., 2006 ). These include the three dimensions of vitality, dedication, and absorbedness. An example item is: ‘ At my work, I feel bursting with energy. ’ (dedication). The 7-point Likert scale ranges from 0 = ‘never’ to 6 = ‘always’, whereby a higher score reflects more work engagement.
Data analysis strategy
The data was prepared and analyzed with the open-source statistical program R Project (R Core Team, 2020 ) and the R package lavaan (Rosseel, 2012 ). First, the data was processed and checked to see if any cases needed to be excluded, e.g., due to unemployment at the time of the survey. Because four constructs were included in the model from two points, measurement invariance was analyzed for these constructs using confirmatory factor analyses (CFA) and following the common recommendations for longitudinal analyses (Putnick & Bornstein, 2016 ). As a minimum requirement, metric measurement invariance (equal factor structure and factor loadings) referring to equal factor loadings across time should hold in longitudinal models (Putnick & Bornstein, 2016 ). Model fit indices were accepted if close to recommended cut-off criteria, e.g., Root Mean Square Error of Approximation (RMSEA < 0.06) or Comparative Fit-Index (CFI ≥ 0.95) (Hu & Bentler, 1999 ). Furthermore, model comparison tests between the proposed measurement models against one-factor models were conducted for each wave. In the next step, the structural equation model was specified, and the hypotheses were tested using path estimates. Hypotheses 3.1a, 3.1b, 3.2a, and 3.2b, which predict a mediation effect, were also tested. Bootstrapping with 2,000 bootstraps was used as the calculation method, which, according to Hayes and Scharkow ( 2013 ), is the most suitable procedure for indirect effects. For missing values, the full information maximum likelihood method was used (Arbuckle et al., 1996 ). After the results of the hypothesized associations, post hoc analyses were conducted to investigate hypotheses that did not turn out as expected.
Before specifying the full research model, we examined whether assumptions of measurement invariance hold for those constructs for which we control for stability in the model. For WHI together with HWI, the model with metric measurement invariance indicated a good model fit (χ 2 (244) = 1238.667, p < .001, CFI = 0.955, TLI = 0.949, RMSEA = 0.044, SRMR = 0.040). For mental well-being and work engagement, the models with residual measurement invariance (additionally equal item intercepts and residual variances) fit the data well and superior to less strict assumptions (mental well-being: χ 2 (75) = 831.135, p < .001, CFI = 0.940, TLI = 0.927, RMSEA = 0.078, SRMR = 0.046; work engagement: χ 2 (151) = 705.050, p < .001, CFI = 0.982, TLI = 0.982, RMSEA = 0.047, SRMR = 0.020). Our final model reaches a good fit as well (χ 2 (1955) = 9421.085, p < .001, CFI = 0.897, TLI = 0.894, RMSEA = 0.042, SRMR = 0.076).
The direct and indirect effects of the research model are presented in Table 2 . First, we review the associations from WNBC to the life domain conflicts. The link between WNBC-work and HWI is significant ( b = -0.047, SE = 0.021, p = .024), but the link between WNBC-nonwork and WHI is not significant at a = 0.05 ( b = 0.018, SE = 0.025, p = .465). Therefore, our results support H1.2, but not H1.1. Next, we review the associations of HWI and WHI with work engagement and mental well-being. Only the link between HWI and mental well-being is significant ( b = -0.154, SE = 0.066, p = .018), but all other hypothesized links are not significant (WHI to mental well-being: b = 0.002, SE = 0.045, p = .959; HWI to work engagement: b = -0.181, SE = 0.113, p = .109; WHI to work engagement: b = -0.096, SE = 0.083, p = .250). Therefore, our results support H2.1a, but not H2.1b, H2.2a, or H2.2b. Lastly, we specified indirect effects from WNBC-work and -nonwork to work engagement and mental well-being via life domain conflicts. We obtained these results by bootstrapping our research model (no. of bootstraps = 2000). No significant indirect effects emerged as all 95% confidence intervals include zero (see Table 2 for full results). Therefore, our results do not support the hypotheses H3.1a, H3.1b, H3.2a, or H3.2b.
Interestingly, the autoregressive paths of both WHI ( b = 0.824, SE = 0.019, p < .001) and HWI ( b = 0.797, SE = 0.023, p < .001) were relatively stable between the two waves, as were the autoregressive paths of mental well-being ( b = 0.766, SE = 0.028, p < .001) and work engagement ( b = 0.784, SE = 0.022, p < .001). The discussion examines how this high stability, especially of life domain conflicts, could help explain the results.
Furthermore, although no hypotheses were formulated for the direct association between the WNBC facets and the outcomes, the paths were also specified in the structural equation model. Direct paths between WNBC-work at wave 1, mental well-being at wave 3, and work engagement at wave 3, resp. WNBC-nonwork at wave 1, mental well-being at wave 3, and work engagement at wave 3 were specified. Results show a significant positive association between WNBC-work and work engagement ( b = 0.371, SE = 0.148, p = .012) and WNBC-work and mental well-being ( b = 0.145, SE = 0.061, p = .018). No significant associations were found for WNBC-nonwork and work engagement ( b = -0.037, SE = 0.124, p = .763), nor WNBC-nonwork and mental well-being ( b = -0.013, SE = 0.059, p = .828).
We aimed to explore the role of WNBC during the COVID-19 pandemic and its longitudinal associations with mental well-being and work engagement via WHI and HWI. For our study, we referred to survey data that captured a significant part of 2020, where the onset of the pandemic and two lockdowns had major implications for the lives of many employees. Therefore, our study provides valuable information on how behavior early in the pandemic is associated with long-term health and well-being. This section discusses our main findings concerning their theoretical and practical contributions.
WNBC and life domain conflicts during the COVID-19 pandemic
We hypothesized that WNBC-work is negatively associated with HWI and WNBC-nonwork with WHI, but our results only support the first relationship (support for H1.2, but not H1.1). Considering the unique context of the pandemic, mandatory work reductions or increased workload were previously found to be associated with a perceived negative impact of the pandemic on work-life (Tušl et al., 2021 ), which might have overshadowed and impaired individual efforts. This shows that to address WHI, individual efforts were not enough, and employees were in high need of support from organizations, e.g., through more flexibility. On the other hand, individual efforts to protect the work domain prevented HWI, highlighting that employees can effectively support themselves in this area.
Further, we discuss two additional aspects that might have played a role in these findings. First, we note the relatively high stability of the life domain conflicts that emerged in our analyses. WHI and HWI turned out to be more stable than expected between wave 1 and wave 2, meaning that people’s perceived life domain conflicts between April and June/July hardly changed. This leaves little room for individual efforts such as crafting to explain remaining variance. Considering shorter timeframes to investigate the association between WNBC and life domain conflicts might be useful. Potentially, individual crafting has a more nuanced effect on life domain conflicts on a shorter, weekly to monthly basis, whereas, in more extended periods, more stable trends occur. Indeed, previous research points to short-term fluctuations in life domain conflicts, predicted by, e.g., daily workload (Ilies et al., 2007 ), but higher mean stability over mid- to long-term time frames (Smith et al., 2022 ). Similar stabilities have been reported when comparing pre-pandemic and pandemic levels of work-family conflict (Bernhardt et al., 2023 ; Reimann et al., 2022 ). Thus, we suggest that future research on the association of WNBC and life domain conflicts also considers shorter time frames.
Within our study, we used a shortened 8-item version of the WNBC-scale that better fits the context of the pandemic than the original full scale. During the iterative, theory-driven, and two-person consensus-based process, aspects of the initial scale were dropped, e.g., the aspect of crafting a physical boundary. The original scale incorporated physical WNBC as, e.g., an earlier or later start to work if needed due to obligations outside of work (Kerksieck et al., 2022 ). During the pandemic, employees may have adopted other crafting strategies, such as going grocery shopping during working hours to avoid big crowds and, therefore, limit the spread of covid viruses. Furthermore, some of the items that were omitted for the shortened scale included strategies that were thought to be deprioritized due to the crisis. For example, one item describes a cognitive/emotional strategy in which employees temporarily emphasize their work (e.g., work more before vacations to get things done; Kerksieck et al., 2022 ). Since the pandemic and its lockdown measures caused a shift in focus and impeded travelling plans, vacations were not a well-suited example during this time of crisis. In modern working times, such behaviors and possible scenarios should also be considered and captured by a revised WNBC scale.
The shortened WNBC scale focuses mainly on cognitive crafting. Therefore, we can also interpret our findings regarding the specific aspects of crafting retained in the scale: To prevent HWI, aspects of cognitive crafting are quite important. However, more action-oriented or social crafting strategies, such as communicating with others, might play a more vital role in preventing WHI. As these aspects are not reflected in our shortened scale, this might explain the absence of a link between WNBC-nonwork and WHI. However, communicating with others to secure boundaries between work and nonwork was reported as the least often used strategy by parents working from home in a study by Allen et al. ( 2021 ). Considering that the pandemic likely had lasting impacts on the accelerated new work movement, a revised balance crafting scale could be helpful to represent better the post-pandemic work context (Kniffin et al., 2021 ; Rudolph et al., 2021 ). Lastly, future use of our shortened scale would provide more information on its validity and reliability measures (Clark & Watson, 2016 ).
Life domain conflicts, work engagement, and mental well-being
Partly in line with previous findings (e.g., Karatepe & Karadas, 2016 ), we only found a significant association between HWI and mental well-being (supporting H2.1a, but not H2.1b, H2.2a, or H2.2b). Therefore, employees who experienced high levels of HWI in the middle of 2020 reported lower mental well-being at the end of 2020, highlighting them as an at-risk group in need of further support. For those employees whose life outside of work was affecting their work life, organizational support might be highly relevant, e.g., by providing appropriate flexibility and autonomy or reviewing projects and workload (Kossek et al., 2021 ). However, work engagement was not longitudinally associated with HWI, and neither was WHI with the health outcomes we reviewed. The unique context of the pandemic needs to be considered and might provide possible explanations. Research highlighted that compared to pre-pandemic states, life domain conflicts, and other stressors increased (Reimann et al., 2022 ). The WHO reported that from the onset of the pandemic onwards, the prevalence of mental health issues (e.g., anxiety) rose, yet at the same time also the awareness of mental health issues (World Health Organization, 2022 ). In milder cases, the open discussion of risk factors such as life domain conflicts and stressors might have equipped employees with more coping tools (Pfefferbaum & North, 2020 ), therefore limiting the effect of life domain conflicts on work engagement and mental well-being. Accordingly, research also found a growing resilience in mental health of the population in response to the pandemic (Daly & Robinson, 2021 ).
WNBC and long-term health and well-being during the pandemic
Lastly, we assumed a longitudinal link between WNBC, work engagement, and mental well-being via life domain conflicts. Our results do not support such an indirect effect (H3.1a, H3.1b, H3.2a, H3.2b), but we found direct significant links between WNBC-work and both outcomes. Considering the complex, differentiated associations between WNBC with the life domain conflicts and the life domain conflicts with the health outcomes, it is unsurprising that we did not find an indirect effect. The significant relationship between WNBC-work and work engagement over eight months is in line with a previous finding, which showed the same association for a three-month period (Kerksieck et al., 2022 ). Thus, we corroborate the longitudinal association, but the effect is not mediated by life domain conflicts, as was assumed in the hypotheses of this study. It is unknown whether this finding might be caused by a lagged or a cumulative effect or if interpersonal differences in traits, such as identification with one’s job, are responsible for this association between eight months. Identification with one’s job could explain why those employees who emphasized protecting their work domain also report higher work engagement, as for both the proactive behavior and high work engagement, a high priority of work might be a driver. Future research should corroborate this finding using different time lags and investigate potential third-variable explanations.
Further, as we could not shed light on a longitudinal mechanism explaining the association between WNBC and health outcomes, we suggest that future research dives into alternative mediating processes, reviewing gain spirals instead of a loss spiral, as we did in our research. Like the loss spiral, the gain spiral can be derived from the COR theory (Hobfoll, 1989 ). It describes a process where an initial resource gain enables further resource gains, leading to an upward spiral (Hobfoll, 2002 ). If, for example, a person can save time by working from home (because they do not have to commute), they can then use that time to gain other resources, such as energetic resources through recovery. Tims et al. ( 2015 ) have found that through job crafting, employees can improve their well-being (e.g., more work engagement, more job satisfaction, less burnout) through increased social job resources. Therefore, this relationship might apply to WNBC because persons who actively craft their boundaries between the work and the nonwork domains can improve their outcomes through increased resources (e.g., measured by work-home enrichment instead of interference; Kopelman et al., 1983 ). Thus, looking at WNBC and its association with the gain spiral instead of the loss spiral could be a promising next step to understanding the WNBC construct from a resource perspective.
Strengths and limitations
The research of this paper contributes to the existing literature in three main ways: First, it extends the literature by looking at a relatively new crafting construct that still offers a high research potential. We demonstrate here that a shortened version of the WNBC provides a good fit with the unique context of the pandemic, yet also that the structure of WNBC could be subject to revision in future research. Second, our study shows that WNBC partly played a role in reducing life domain conflicts at the beginning of the pandemic, which points to a strategy that could be taken up by early interventions in future times of crisis, as well as the limits of individual proactive behaviors. For the work domain, individual efforts should be coupled with organizational support to reduce life domain conflicts. Third, our study adds knowledge on the longitudinal association between life domain conflicts and health outcomes, showing that contrary to earlier findings, only HWI was associated with lower mental well-being in our study. This opens a field for new research in which the unique context of the pandemic and specific developments could be reviewed. For example, the overall more open conversation about struggles might have aided in buffering the effects of life domain conflicts on health (Bu et al., 2021 ).
Besides these strengths, the study has several limitations. The first limitation that needs to be addressed is the inability to use the full scale for WNBC due to its low fit. As outlined earlier, we attempted to increase fit in terms of both content validity to the pandemic context and statistical fit. Our shortened scale highlights those generalizable parts of WNBC that also fit the unique context of the COVID-19 pandemic, but we note that other parts still need to be included. To address this, further research is required to corroborate the shortened scale or revise the original scale to fit newer developments in working life.
Second, our study solely relies on data collected in 2020, and our findings cannot be lightly generalized to other non-pandemic periods or populations. Contrary to previous research, we did not find a link between WHI and studied health outcomes. We discussed earlier that this could be due to the unique context of the pandemic, in which the increased collective awareness about the daily struggles employees faced might have also increased awareness and individual ways of coping. To shed more light on this assumption, these findings should be corroborated in other (milder) times of crisis, e.g., financial crises or severe organizational changes, and outside of exceptional circumstances. Further, our sample consists solely of German-speaking employees from Germany, Austria, and Switzerland. Our findings may not be generalizable to other cultural contexts, e.g., more feminine cultures such as Finland (Hofstede, 2016 ). For the original WNBC scale, a cross-cultural validation has been conducted, which also showed a longitudinal correlation between WNBC-nonwork and work engagement in Finland, likely due to the restoration and spillover of relevant resources (Kerksieck et al., 2022 ). In similar fashion, future research should investigate further cultural differences in the associations between WNBC, life domain conflicts, and employee well-being.
Lastly, we note that in the dropout analysis, a significant difference was found for life domain conflicts, meaning that out of all participants participating in wave 1, those that did not participate in waves 2 and 3 reported significantly more life domain conflicts, likely because they had less time or energy for study participation. However, the remaining sample should still be representative, and severely biased results are not expected because of this dropout, especially since missing values were treated with the reliable full information maximum likelihood method in which the parameters are estimated using the available data in the sample (Newman, 2014 ).
Practical implications
We can derive two main practical implications from our findings, primarily concerning political and organizational institutions. First, we have found that WNBC focusing on the work domain is longitudinally associated with lower HWI, higher work engagement, and mental well-being. In times of crisis, organizations can support their employees in crafting by disseminating information about how proactive crafting can aid them in maintaining their own well-being. On top of that, organizations should enable employees to use these strategies for their own benefit. In any case, employees can proactively enact crafting efforts to improve their work and nonwork lives. Taking advantage of this bottom-up self-management strategy is what makes crafting a convincing concept in theory and practice since its early outlines (Wrzesniewski & Dutton, 2001 ) to a concept with obvious relevance during the COVID-19 pandemic and for the future of work (Bakker et al., 2023 ; Tims et al., 2022 ).
Second, our results also point to the limits of individual crafting. WNBC might not have enough force to reduce WHI, which could instead be addressed through support in organizing work and granting flexibility and autonomy. Other forms of crafting interventions, e.g., targeted toward job crafting (van den Heuvel et al., 2015 ; van Wingerden et al., 2017 ) or off-job/needs crafting (Kosenkranius et al., 2023 ; Laporte et al., 2022 ), as well as targeted organizational support for employees, should be considered to complement pandemic or crisis mitigation plans.
We aimed to study the role of WNBC for long-term health and well-being during the COVID-19 pandemic. Using a shortened version of the WNBC scale to fit the context of the pandemic, our results point to complex associations between WNBC and life domain conflicts, work engagement, and mental well-being. We found a direct positive association between WNBC-work and work engagement and mental well-being and a negative association between WNBC-work and HWI, yet no indirect association between WNBC-work and WNBC-nonwork with work engagement and mental well-being via life domain conflicts. We conclude that engaging in WNBC early in times of crisis is associated with better long-term health. This urges companies to take responsibility and support their workers by providing a crafting-friendly environment and helping reduce their life domain conflicts. Our findings are not only relevant during future crises but also to support employees in the future of work.
Data availability
The data that support the findings of this study are available from the authors upon reasonable request. Study participants were asked to give consent to use the data for research and within research publication, but not for open public access.
Adams, G. A., King, L. A., & King, D. W. (1996). Relationships of job and family involvement, family social support, and work–family conflict with job and life satisfaction. Journal of Applied Psychology, 81 (4), 411–420. https://doi.org/10.1037/0021-9010.81.4.411 .
Article Google Scholar
Allen, T. D., Merlo, K., Lawrence, R. C., Slutsky, J., & Gray, C. E. (2021). Boundary management and work-nonwork balance while working from home. Applied Psychology, 70 (1), 60–84. https://doi.org/10.1111/apps.12300 .
Arbuckle, J. L., Marcoulides, G. A., & Schumacker, R. E. (1996). Full information estimation in the presence of incomplete data. In G. A. Marcoulides, & R. E. Schumacker (Eds.), Advanced structural equation modeling: Issues and techniques (pp. 243–277). Lawrence Erlbaum Associates, Inc.
Google Scholar
Ashforth, B. E., Kreiner, G. E., & Fugate, M. (2000). All in a day’s work: Boundaries and micro role transitions. The Academy of Management Review, 25 (3), 472–491. https://doi.org/10.2307/259305
Bakker, A. B., Demerouti, E., & Sanz-Vergel, A. (2023). Job Demands-Resources theory: Ten years later . https://doi.org/10.1146/annurev-orgpsych-120920 .
Benfante, A., Di Tella, M., Romeo, A., & Castelli, L. (2020). Traumatic stress in healthcare workers during COVID-19 pandemic: A review of the immediate impact. Frontiers in Psychology, 11 . https://doi.org/10.3389/fpsyg.2020.569935 .
Bernhardt, J., Recksiedler, C., & Linberg, A. (2023). Work from home and parenting: Examining the role of work-family conflict and gender during the COVID-19 pandemic. Journal of Social Issues, 79 (3), 935–970. https://doi.org/10.1111/josi.12509 .
Brosschot, J. F., Gerin, W., & Thayer, J. F. (2006). The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research, 60 (2), 113–124. https://doi.org/10.1016/j.jpsychores.2005.06.074 .
Bu, F., Mak, H. W., & Fancourt, D. (2021). Rates and predictors of uptake of mental health support during the COVID-19 pandemic: An analysis of 26,720 adults in the UK in lockdown. Social Psychiatry and Psychiatric Epidemiology, 56 (12), 2287–2297. https://doi.org/10.1007/s00127-021-02105-w .
Article PubMed PubMed Central Google Scholar
Caringal-Go, J. F., Teng-Calleja, M., Bertulfo, D. J., & Manaois, J. O. (2022). Work-life balance crafting during COVID-19: Exploring strategies of telecommuting employees in the Philippines. Community Work and Family, 25 (1), 112–131. https://doi.org/10.1080/13668803.2021.1956880 .
Chankasingh, K., Booth, A., Albert, A., Kaida, A., Smith, L. W., Racey, C. S., Gottschlich, A., Murray, M. C. M., Sadarangani, M., Ogilvie, G. S., Galea, L. A. M., & Brotto, L. A. (2022). Coping during the COVID-19 pandemic: A mixed methods approach to understand how social factors influence coping ability. Heliyon, 8 (10). https://doi.org/10.1016/j.heliyon.2022.e10880 .
Chapman, N. J., Ingersoll-Dayton, B., & Neal, M. B. (1994). Balancing the multiple roles of work and caregiving for children, adults, and elders. In Job stress in a changing workforce: Investigating gender, diversity, and family issues (pp. 283–300). American Psychological Association. https://doi.org/10.1037/10165-018 .
Cho, E. (2020). Examining boundaries to understand the impact of COVID-19 on vocational behaviors. Journal of Vocational Behavior, 119 . https://doi.org/10.1016/j.jvb.2020.103437 .
Clark, L. A., & Watson, D. (2016). Constructing validity: Basic issues in objective scale development. Methodological issues and strategies in clinical research (4th ed., pp. 187–203). American Psychological Association. https://doi.org/10.1037/14805-012 .
Daly, M., & Robinson, E. (2021). Psychological distress and adaptation to the COVID-19 crisis in the United States. Journal of Psychiatric Research, 136 , 603–609. https://doi.org/10.1016/j.jpsychires.2020.10.035 .
de Bloom, J., Vaziri, H., Tay, L., & Kujanpää, M. (2020). An identity-based integrative needs model of crafting: Crafting within and across life domains. Journal of Applied Psychology, 105 (12), 1423–1446. https://doi.org/10.1037/apl0000495 .
Article PubMed Google Scholar
Demerouti, E., & Bakker, A. B. (2022). Job demands-resources theory in times of crises: New propositions. Organizational Psychology Review, 204138662211350. https://doi.org/10.1177/20413866221135022 .
Demerouti, E., Geurts, S. A. E., & Kompier, M. (2004). Positive and negative work-home interaction: Prevalence and correlates. Equal Opportunities International, 23 (1/2), 6–35. https://doi.org/10.1108/02610150410787837 .
Demerouti, E., Hewett, R., Haun, V., de Gieter, S., Rodríguez-Sánchez, A., & Skakon, J. (2020). From job crafting to home crafting: A daily diary study among six European countries. Human Relations, 73 (7), 1010–1035. https://doi.org/10.1177/0018726719848809
Frone, M. R., Russell, M., & Cooper, M. L. (1992). Antecedents and outcomes of work-family conflict: Testing a model of the work-family interface. Journal of Applied Psychology, 77 (1), 65–78. https://doi.org/10.1037/0021-9010.77.1.65 .
Galanti, T., Guidetti, G., Mazzei, E., Zappalà, S., & Toscano, F. (2021). Work from home during the COVID-19 outbreak: The impact on employees’ remote work productivity, engagement, and stress. Journal of Occupational & Environmental Medicine, 63 (7), e426–e432. https://doi.org/10.1097/JOM.0000000000002236 .
Geurts, S. A. E., Taris, T. W., Kompier, M. A. J., Dikkers, J. S. E., Van Hooff, M. L. M., & Kinnunen, U. M. (2005). Work-home interaction from a work psychological perspective: Development and validation of a new questionnaire, the SWING. Work and Stress, 19 (4), 319–339. https://doi.org/10.1080/02678370500410208 .
Grant-Vallone, E. J., & Donaldson, S. I. (2001). Consequences of work-family conflict on employee well-being over time. Work and Stress, 15 (3), 214–226. https://doi.org/10.1080/02678370110066544 .
Gravador, L. N., & Teng-Calleja, M. (2018). Work-life balance crafting behaviors: An empirical study. Personnel Review, 47 (4), 786–804. https://doi.org/10.1108/PR-05-2016-0112 .
Halbesleben, J. R. B. (2010). A meta-analysis of work engagement: Relationships with burnout, demands, resources, and consequences. In A. B. Bakker, & M. P. Leiter (Eds.), Work engagement: A handbook of essential theory and research (pp. 102–117). Psychology.
Hale, T., Angrist, N., Goldszmidt, R., Kira, B., Petherick, A., Phillips, T., Webster, S., Cameron-Blake, E., Hallas, L., Majumdar, S., & Tatlow, H. (2021). A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nature Human Behaviour, 5 (4), 529–538. https://doi.org/10.1038/s41562-021-01079-8 .
Hayes, A. F., & Scharkow, M. (2013). The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: Does method really matter? Psychological Science, 24 (10), 1918–1927. https://doi.org/10.1177/0956797613480187 .
Hobfoll, S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44 (3), 513–524.
Hobfoll, S. E. (2002). Social and psychological resources and adaptation. Review of General Psychology, 6 (4), 307–324. https://doi.org/10.1037/1089-2680.6.4.307 .
Hofstede, G. (2016). Masculinity at the national cultural level. In Y. J. Wong & S. R. Wester (Eds.), APA handbook of men and masculinities (pp. 173–186). American Psychological Association. https://doi.org/10.1037/14594-008 .
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6 (1), 1–55. https://doi.org/10.1080/10705519909540118 .
Ilies, R., Schwind, K. M., Wagner, D. T., Johnson, M. D., DeRue, D. S., & Ilgen, D. R. (2007). When can employees have a family life? The effects of daily workload and affect on work-family conflict and social behaviors at home. Journal of Applied Psychology, 92 (5), 1368–1379. https://doi.org/10.1037/0021-9010.92.5.1368 .
Ingusci, E., Signore, F., Giancaspro, M. L., Manuti, A., Molino, M., Russo, V., Zito, M., & Cortese, C. G. (2021). Workload, techno overload, and behavioral stress during COVID-19 emergency: The role of job crafting in remote workers. Frontiers in Psychology, 12 . https://doi.org/10.3389/fpsyg.2021.655148 .
Kaltiainen, J., & Hakanen, J. J. (2023). Why increase in telework may have affected employee well-being during the COVID-19 pandemic? The role of work and non-work life domains. Current Psychology . https://doi.org/10.1007/s12144-023-04250-8 .
Karatepe, O. M., & Karadas, G. (2016). Service employees’ fit, work-family conflict, and work engagement. Journal of Services Marketing, 30 (5), 554–566. https://doi.org/10.1108/JSM-02-2015-0066 .
Kerksieck, P., Brauchli, R., de Bloom, J., Shimazu, A., Kujanpää, M., Lanz, M., & Bauer, G. F. (2022). Crafting work-nonwork balance involving life domain boundaries: Development and validation of a novel scale across five countries. Frontiers in Psychology, 13 . https://doi.org/10.3389/fpsyg.2022.892120 .
Kniffin, K. M., Narayanan, J., Anseel, F., Antonakis, J., Ashford, S. P., Bakker, A. B., Bamberger, P., Bapuji, H., Bhave, D. P., Choi, V. K., Creary, S. J., Demerouti, E., Flynn, F. J., Gelfand, M. J., Greer, L. L., Johns, G., Kesebir, S., Klein, P. G., Lee, S. Y., & van Vugt, M. (2021). COVID-19 and the workplace: Implications, issues, and insights for future research and action. American Psychologist, 76 (1), 63–77. https://doi.org/10.1037/amp0000716 .
Kopelman, R. E., Greenhaus, J. H., & Connolly, T. F. (1983). A model of work, family, and interrole conflict: A construct validation study. Organizational Behavior and Human Performance, 32 (2), 198–215. https://doi.org/10.1016/0030-5073(83)90147-2 .
Kosenkranius, M., Rink, F., Weigelt, O., Van den Heuvel, M., & De Bloom, J. (2023). The effectiveness of a hybrid off-job crafting intervention on employees: Psychological needs satisfaction and well-being. Scandinavian Journal of Work and Organizational Psychology, 8 (1), 6. https://doi.org/10.16993/sjwop.181 .
Kossek, E. E., Dumas, T. L., Piszczek, M. M., & Allen, T. D. (2021). Pushing the boundaries: A qualitative study of how stem women adapted to disrupted work–nonwork boundaries during the COVID-19 pandemic. Journal of Applied Psychology, 106 (11), 1615–1629. https://doi.org/10.1037/apl0000982 .
Kujanpää, M., Syrek, C., Tay, L., Kinnunen, U., Mäkikangas, A., Shimazu, A., Wiese, C. W., Brauchli, R., Bauer, G. F., Kerksieck, P., Toyama, H., & de Bloom, J. (2022). Needs-based off-job crafting across different life domains and contexts: Testing a novel conceptual and measurement approach. Frontiers in Psychology, 13 . https://doi.org/10.3389/fpsyg.2022.959296 .
Laporte, N., van den Bogaard, D., Brenning, K., Soenens, B., & Vansteenkiste, M. (2022). Testing an online program to foster need crafting during the COVID-19 pandemic. Current Psychology, 0123456789 . https://doi.org/10.1007/s12144-022-03012-2 .
Lockdown: Vor einem Jahr hat Der Bundesrat die Schweiz abgeriegelt . (2021). SWI Swissinfo.Ch.. https://www.swissinfo.ch/ger/lockdown--vor-einem-jahr-hat-der-bundesrat-die-schweiz-abgeriegelt/46451438 .
Lyu, X., & Fan, Y. (2022). Research on the relationship of work family conflict, work engagement and job crafting: A gender perspective. Current Psychology, 41 (4), 1767–1777. https://doi.org/10.1007/s12144-020-00705-4 .
Mäkikangas, A., de Bloom, J., Kerksieck, P., & Kujanpää, M. (2024). Sustainable work through crafting. In P. Kruyen, S. André, & van der B. Heijden (Eds.), New horizons in management. Maintaining a sustainable work-life balance: An interdisciplinary path to a better future (pp. 213–220). Edward Elgar.
Newman, D. A. (2014). Missing data: Five practical guidelines. Organizational Research Methods, 17 (4), 372–411. https://doi.org/10.1177/1094428114548590 .
O’Connor, R. C., Wetherall, K., Cleare, S., McClelland, H., Melson, A. J., Niedzwiedz, C. L., O’Carroll, R. E., O’Connor, D. B., Platt, S., Scowcroft, E., Watson, B., Zortea, T., Ferguson, E., & Robb, K. A. (2021). Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. British Journal of Psychiatry, 218 (6), 326–333. https://doi.org/10.1192/bjp.2020.212 .
Petrou, P., Demerouti, E., & Schaufeli, W. B. (2018). Crafting the change: The role of employee job crafting behaviors for successful organizational change. Journal of Management, 44 (5), 1766–1792. https://doi.org/10.1177/0149206315624961 .
Pfefferbaum, B., & North, C. S. (2020). Mental health and the COVID-19 pandemic. New England Journal of Medicine, 383 (6), 510–512. https://doi.org/10.1056/NEJMp2008017 .
Pijpker, R., Kerksieck, P., Tušl, M., de Bloom, J., Brauchli, R., & Bauer, G. F. (2022). The role of off-job crafting in burnout prevention during COVID-19 crisis: A longitudinal study. International Journal of Environmental Research and Public Health, 19 (4), 2146. https://doi.org/10.3390/ijerph19042146 .
Putnick, D. L., & Bornstein, M. H. (2016). Measurement invariance conventions and reporting: The state of the art and future directions for psychological research. Developmental Review, 41 , 71–90. https://doi.org/10.1016/j.dr.2016.06.004 .
R Core Team. (2020). R: A language and environment for statistical computing . R Foundation for Statistical Computing.
Reimann, M., Peters, E., & Diewald, M. (2022). COVID-19 and work–family conflicts in Germany: Risks and chances across gender and parenthood. Frontiers in Sociology, 6 . https://doi.org/10.3389/fsoc.2021.780740 .
Reinke, K., & Gerlach, G. I. (2022). Linking availability expectations, bidirectional boundary management behavior and preferences, and employee well-being: An integrative study approach. Journal of Business and Psychology, 37 (4), 695–715. https://doi.org/10.1007/s10869-021-09768-x .
Rieth, M., & Hagemann, V. (2021). The impact of telework and closure of educational and childcare facilities on working people during COVID-19. Zeitschrift Fur Arbeits- Und Organisationspsychologie, 65 (4), 202–214. https://doi.org/10.1026/0932-4089/a000370 .
Rosseel, Y. (2012). Lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48 (2). https://doi.org/10.18637/jss.v048.i02 .
Rudolph, C. W., Allan, B., Clark, M., Hertel, G., Hirschi, A., Kunze, F., Shockley, K., Shoss, M., Sonnentag, S., & Zacher, H. (2021). Pandemics: Implications for research and practice in industrial and organizational psychology. Industrial and Organizational Psychology, 14 (1–2), 1–35. https://doi.org/10.1017/iop.2020.48 .
Ryan, R. M., & Deci, E. L. (2001). On happiness and human potentials: A review of research on hedonic and eudaimonic well-being. Annual Review of Psychology, 52 (1), 141–166. https://doi.org/10.1146/annurev.psych.52.1.141 .
Schaufeli, W. B., Bakker, A. B., & Salanova, M. (2006). The measurement of work engagement with a short questionnaire. Educational and Psychological Measurement, 66 (4), 701–716. https://doi.org/10.1177/0013164405282471 .
Schaufeli, W. B., & Greenglass, E. R. (2001). Introduction to special issue on burnout and health. Psychology & Health, 16 (5), 501–510. https://doi.org/10.1080/08870440108405523 .
Smith, C. E., Wayne, J. H., Matthews, R. A., Lance, C. E., Griggs, T. L., & Pattie, M. W. (2022). Stability and change in levels of work–family conflict: A multi-study, longitudinal investigation. Journal of Occupational and Organizational Psychology, 95 (1), 1–35. https://doi.org/10.1111/joop.12372 .
Syrek, C., Kühnel, J., Vahle-Hinz, T., & de Bloom, J. (2022). Being an accountant, cook, entertainer and teacher—all at the same time: Changes in employees’ work and work-related well-being during the coronavirus (COVID-19) pandemic. International Journal of Psychology, 57 (1), 20–32. https://doi.org/10.1002/ijop.12761
ten Brummelhuis, L. L., & Bakker, A. B. (2012). A resource perspective on the work-home interface: The work-home resources model. American Psychologist, 67 (7), 545–556. https://doi.org/10.1037/a0027974 .
Tennant, R., Hiller, L., Fishwick, R., Platt, S., Joseph, S., Weich, S., Parkinson, J., Secker, J., & Stewart-Brown, S. (2007). The Warwick-Dinburgh mental well-being scale (WEMWBS): Development and UK validation. Health and Quality of Life Outcomes, 5 . https://doi.org/10.1186/1477-7525-5-63 .
Tims, M., & Bakker, A. B. (2010). Job crafting: Towards a new model of individual job redesign. SA Journal of Industrial Psychology, 36 (2), 1–9. https://doi.org/10.4102/sajip.v36i2.841 .
Tims, M., Bakker, A. B., & Derks, D. (2012). Development and validation of the job crafting scale. Journal of Vocational Behavior, 80 (1), 173–186. https://doi.org/10.1016/j.jvb.2011.05.009 .
Tims, M., Bakker, A. B., & Derks, D. (2015). Job crafting and job performance: A longitudinal study. European Journal of Work and Organizational Psychology, 24 (6), 914–928. https://doi.org/10.1080/1359432X.2014.969245 .
Tims, M., Twemlow, M., & Fong, C. Y. M. (2022). A state-of-the-art overview of job-crafting research: Current trends and future research directions. Career Development International, 27 (1), 54–78. https://doi.org/10.1108/CDI-08-2021-0216 .
Tušl, M., Brauchli, R., Kerksieck, P., & Bauer, G. F. (2021). Impact of the COVID-19 crisis on work and private life, mental well-being and self-rated health in German and Swiss employees: A cross-sectional online survey. Bmc Public Health, 21 (1), 741. https://doi.org/10.1186/s12889-021-10788-8 .
van den Heuvel, M., Demerouti, E., & Peeters, M. C. W. (2015). The job crafting intervention: Effects on job resources, self-efficacy, and affective well-being. Journal of Occupational and Organizational Psychology, 88 (3), 511–532. https://doi.org/10.1111/joop.12128 .
van Wingerden, J., Bakker, A. B., & Derks, D. (2017). The longitudinal impact of a job crafting intervention. European Journal of Work and Organizational Psychology, 26 (1), 107–119. https://doi.org/10.1080/1359432X.2016.1224233 .
Vaziri, H., Casper, W. J., Wayne, J. H., & Matthews, R. A. (2020). Changes to the work–family interface during the COVID-19 pandemic: Examining predictors and implications using latent transition analysis. Journal of Applied Psychology, 105 (10), 1073–1087. https://doi.org/10.1037/apl0000819 .
World Health Organization. (2001). Strengthening mental health promotion . World Health Organization.
World Health Organization. (2022). Mental health and COVID-19: Scientific brief. WHO/2019-nCoV/Sci_Brief/Mental_health/2022.1
Wrzesniewski, A., & Dutton, J. E. (2001). Crafting a job: Revisioning employees as active crafters of their work. Academy of Management Review, 26 (2), 179–201.
Xanthopoulou, D., Bakker, A. B., Demerouti, E., & Schaufeli, W. B. (2009). Reciprocal relationships between job resources, personal resources, and work engagement. Journal of Vocational Behavior, 74 (3), 235–244. https://doi.org/10.1016/j.jvb.2008.11.003 .
Yucel, D., & Fan, W. (2019). Work–family conflict and well-being among German couples: A longitudinal and dyadic approach. Journal of Health and Social Behavior, 60 (3), 377–395. https://doi.org/10.1177/0022146519870535 .
Download references
Open access funding provided by University of Zurich. The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Swiss National Foundation (SNF) [grant number 100019M_201113].
Author information
Authors and affiliations.
Public and Organizational Health / Center of Salutogenesis, Institute of Epidemiology, Biostatistics, and Prevention, University of Zurich, Zurich, Switzerland
Sophie E. Brogle, Philipp Kerksieck, Georg F. Bauer & Anja I. Morstatt
You can also search for this author in PubMed Google Scholar
Contributions
SB: Conceptualization, Project administration, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review and editing. PK: Conceptualization, Data curation, Supervision, Writing – review and editing. GB: Conceptualization, Data curation, Funding Acquisition, Supervision, Writing – review and editing. AM: Conceptualization, Project administration, Formal analysis, Methodology, Supervision, Visualization, Writing – review and editing.
Corresponding author
Correspondence to Anja I. Morstatt .
Ethics declarations
Informed consent.
Informed consent was given by study participants upon starting the surveys.
Ethical approval
For this study, no ethical approval based on the author’s institute’s regulations in accordance with Switzerland’s Federal Act on Research Involving Human Beings (Human Research Act, HRA) was required (further information are available: https://www.uzh.ch/en/researchinnovation/ethics/humanresearch.html ). This observational study collected anonymized data through a panel provider and did not assess any health-related data. Further, the data collection did not present any psychological distress to participants or use any form of experimental manipulation.
Conflicts of interest
All authors declare no conflicts of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Brogle, S.E., Kerksieck, P., Bauer, G.F. et al. Managing boundaries for well-being: a study of work-nonwork balance crafting during the COVID-19 pandemic. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-06118-x
Download citation
Accepted : 07 May 2024
Published : 17 May 2024
DOI : https://doi.org/10.1007/s12144-024-06118-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Crafting behaviors
- Work-home resources model
- Life domain conflicts
- Work engagement
- Work-related burnout
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 14 May 2024
Rain, rain, go away, come again another day: do climate variations enhance the spread of COVID-19?
- Masha Menhat 1 ,
- Effi Helmy Ariffin ORCID: orcid.org/0000-0002-8534-0113 2 ,
- Wan Shiao Dong 3 ,
- Junainah Zakaria 2 ,
- Aminah Ismailluddin 3 ,
- Hayrol Azril Mohamed Shafril 4 ,
- Mahazan Muhammad 5 ,
- Ahmad Rosli Othman 6 ,
- Thavamaran Kanesan 7 ,
- Suzana Pil Ramli 8 ,
- Mohd Fadzil Akhir 2 &
- Amila Sandaruwan Ratnayake 9
Globalization and Health volume 20 , Article number: 43 ( 2024 ) Cite this article
315 Accesses
3 Altmetric
Metrics details
The spread of infectious diseases was further promoted due to busy cities, increased travel, and climate change, which led to outbreaks, epidemics, and even pandemics. The world experienced the severity of the 125 nm virus called the coronavirus disease 2019 (COVID-19), a pandemic declared by the World Health Organization (WHO) in 2019. Many investigations revealed a strong correlation between humidity and temperature relative to the kinetics of the virus’s spread into the hosts. This study aimed to solve the riddle of the correlation between environmental factors and COVID-19 by applying RepOrting standards for Systematic Evidence Syntheses (ROSES) with the designed research question. Five temperature and humidity-related themes were deduced via the review processes, namely 1) The link between solar activity and pandemic outbreaks, 2) Regional area, 3) Climate and weather, 4) Relationship between temperature and humidity, and 5) the Governmental disinfection actions and guidelines. A significant relationship between solar activities and pandemic outbreaks was reported throughout the review of past studies. The grand solar minima (1450-1830) and solar minima (1975-2020) coincided with the global pandemic. Meanwhile, the cooler, lower humidity, and low wind movement environment reported higher severity of cases. Moreover, COVID-19 confirmed cases and death cases were higher in countries located within the Northern Hemisphere. The Blackbox of COVID-19 was revealed through the work conducted in this paper that the virus thrives in cooler and low-humidity environments, with emphasis on potential treatments and government measures relative to temperature and humidity.
• The coronavirus disease 2019 (COIVD-19) is spreading faster in low temperatures and humid area.
• Weather and climate serve as environmental drivers in propagating COVID-19.
• Solar radiation influences the spreading of COVID-19.
• The correlation between weather and population as the factor in spreading of COVID-19.
Graphical abstract
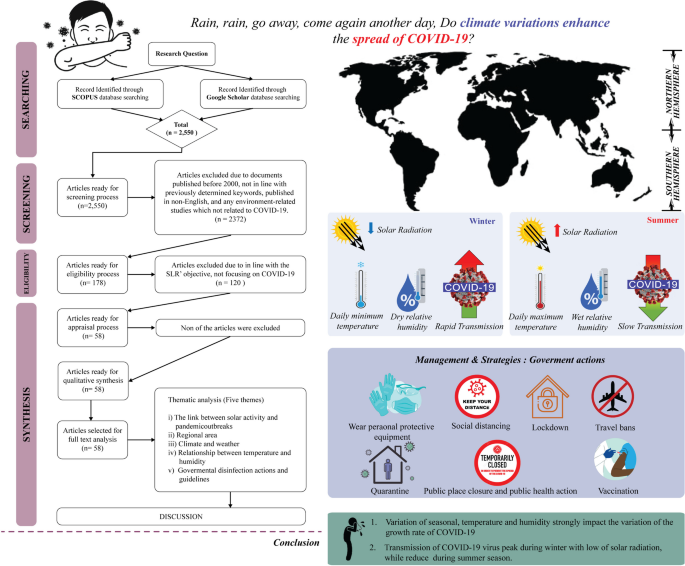
Introduction
The revolution and rotation of the Earth and the Sun supply heat and create differential heating on earth. The movements and the 23.5° inclination of the Earth [ 1 ] separate the oblate-ellipsoid-shaped earth into northern and southern hemispheres. Consequently, the division results in various climatic zones at different latitudes and dissimilar local temperatures (see Fig. 1 ) and affects the seasons and length of a day and night in a particular region [ 2 ]. Global differential heating and climate variability occur due to varying solar radiation received by each region [ 3 ]. According to Trenberth and Fasullo [ 4 ] and Hauschild et al. [ 5 ] the new perspective on the issue of climate change can be affected relative to the changes in solar radiation patterns. Since the study by Trenberth and Fasullo [ 4 ] focused on climate model changes from 1950 to 2100, it was found that the role of changing clouds and trapped sunlight can lead to an opening of the aperture for solar radiation.
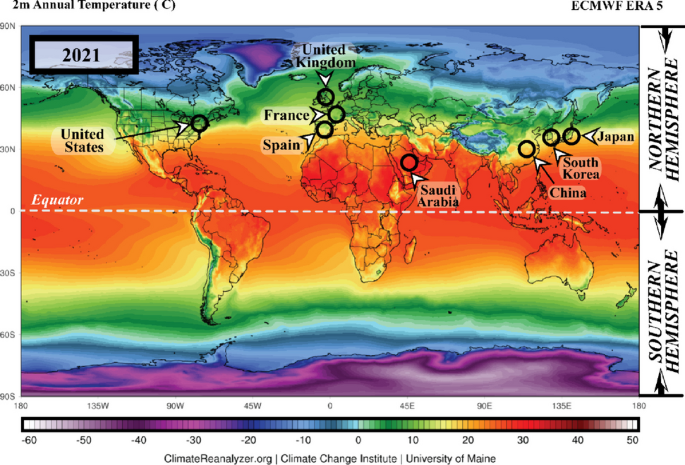
The annual average temperature data for 2021 in the northern and southern hemispheres ( Source: meteoblue.com ). Note: The black circles mark countries with high Coronavirus disease 2019 (COVID-19) infections
Furthermore, the heat from sunlight is essential to humans; several organisms could not survive without it. Conversely, the spread of any disease-carrying virus tends to increase with less sunlight exposure [ 6 ]. Historically, disease outbreaks that led to epidemic and pandemic eruptions were correlated to atmospheric changes. Pandemic diseases, such as the flu (1918), Asian flu (1956–1958), Hong Kong flu (1968), and recently, the coronavirus disease 2019 (COVID-19) (2019), recorded over a million death toll each during the winter season or minimum temperature conditions [ 7 ]. The total number of COVID-19 cases is illustrated in Fig. 2 .
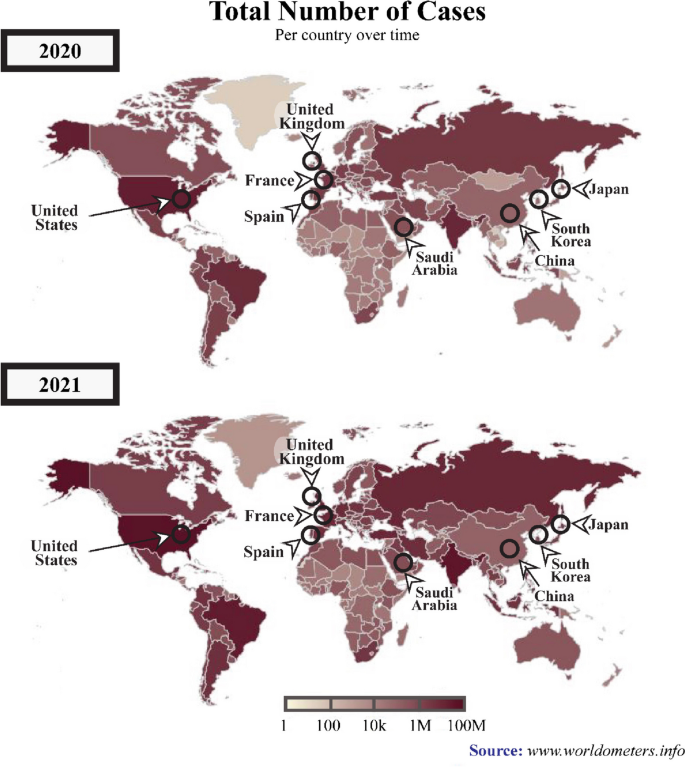
A graphical representation of the total number of COVID-19 cases across various periods between 2020 and 2021. ( Source : www.worldometers.info ). Note: The black circles indicate countries with high numbers COVID-19-infections
In several previous outbreaks, investigations revealed a significant association between temperature and humidity with a particular focus on the transmission dynamics of the infection from the virus into the hosts [ 8 , 9 , 10 ]. Moreover, disease outbreaks tended to heighten in cold temperatures and low humidity [ 11 ]. Optimal temperature and sufficient relative humidity during evaporation are necessary for cloud formation, resulting in the precipitated liquid falling to the ground as rain, snow, or hail due to the activity of solar radiation balancing [ 4 ].
Consequently, the radiation balancing processes in the atmosphere are directly linked to the living beings on the earth, including plants and animals, and as well as viruses and bacterias. According to Carvalho et al. [ 12 ]‘s study, the survival rate of the Coronaviridae Family can decrease during summer seasons. Nevertheless, numerous diseases were also developed from specific viruses, such as influenza, malaria, and rubella, and in November 2019, a severe health threat originated from a 125 nm size of coronavirus, had resulted in numerous deaths worldwide.
Transmission and symptoms of COVID-19
The COVID-19, or severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is an infectious disease caused by a newly discovered pathogenic virus from the coronavirus family, the novel coronavirus (2019-nCoV) [ 13 ]. The first case was recorded in Wuhan, China, in December 2019 [ 14 ]. The pathogenic virus is transmitted among humans when they breathe in air contaminated with droplets and tiny airborne particles containing the virus [ 14 , 15 , 16 , 17 , 18 ].
According to the World Health Organization (WHO), the most common symptoms of COVID-19 infection include fever, dry cough, and tiredness. Nevertheless, older people and individuals with underlying health problems (lung and heart problems, high blood pressure, diabetes, or cancer) are at higher risk of becoming seriously ill and developing difficulty breathing [ 19 ]. The COVID-19 was initially only predominant in China but rapidly spread to other countries globally. The remarkably swift acceleration of the number of infections and mortality forced WHO to declare COVID-19 a global public health emergency on the 30th of January 2020, which was later declared as a pandemic on the 11th of March 2020 [ 20 ].
Since no vaccine was available then, WHO introduced the COVID-19 preventative measures to reduce the chances of virus transmission. The guideline for individual preventative included practising hand and respiratory hygiene by regularly cleaning hands with soap and water or alcohol-based sanitisers, wear a facemask and always maintaining at least a one-meter physical distance [ 21 ]. Nevertheless, the worldwide transmission of COVID-19 has resulted in fear and forced numerous countries to impose restrictions rules, such as lockdown, travel bans, closed country borders, restrictions on shipping activities, and movement limitations, to diminish the spread of COVID-19 [ 22 ].
According to WHO, by the 2nd of December 2020, 63,379,338 confirmed cases and 1,476,676 mortalities were recorded globally. On the 3rd of December 2021, 263,655,612 confirmed cases and deaths were recorded, reflecting increased COVID-19 infections compared to the previous year. The American and European regions documented the highest COVID-19 patients with 97,341,769 and 88,248,591 cases, respectively (see Fig. 2 ), followed by Southeast Asia with 44,607,287, Eastern Mediterranean accounted 16,822,791, Western Pacific recorded 6,322,034, and Africa reported the lowest number of cases at 6,322,034 [ 19 ].
Recently, an increasing number of studies are investigating the association between environmental factors (temperature and humidity) and the viability, transmission, and survival of the coronavirus [ 23 , 24 , 25 , 26 ]. The results primarily demonstrated that temperature was more significantly associated with the transmission of COVID-19 [ 27 , 28 , 29 ] and its survival period on the surfaces of objects [ 30 ]. Consequently, the disease was predominant in countries with low temperature and humidity [ 31 ], which was also proven by Diao et al. [ 32 ]‘s study demonstrating higher rates of COVID-19 transmission in China, England, Germany, and Japan.
A comprehensive systematic literature review (SLR) is still lacking despite numerous research on environmental factors linked to coronavirus. Accordingly, this article aimed to fill the gap in understanding and identifying the correlation between environmental factors and COVID-19 by analysing existing reports. Systematically reviewing existing literature is essential to contribute to the body of knowledge and provide beneficial information for public health policymakers.
Methodology
The present study reviewed the protocols, formulation of research questions, selection of studies, appraisal of quality, and data abstraction and analysis.
The protocol review
The present SLR was performed according to the reporting standards for systematic evidence syntheses (ROSES) and followed or adapted the guidelines as closely as possible. Thus, in this study, a systematic literature review was guided by the ROSES review protocol (Fig. 3 ). Compared to preferred reporting items for systematic review and meta-analysis (PRISMA), ROSES is a review protocol specifically designed for a systematic review in the conservation or environment management fields [ 33 ]. Compared to PRISMA, ROSES offers several advantages, as it is tailored to environmental systematic review, which reduces emphasis on quantitative synthesis (e.g. meta-analysis etc.) that is only reliable when used with appropriate data [ 34 ].
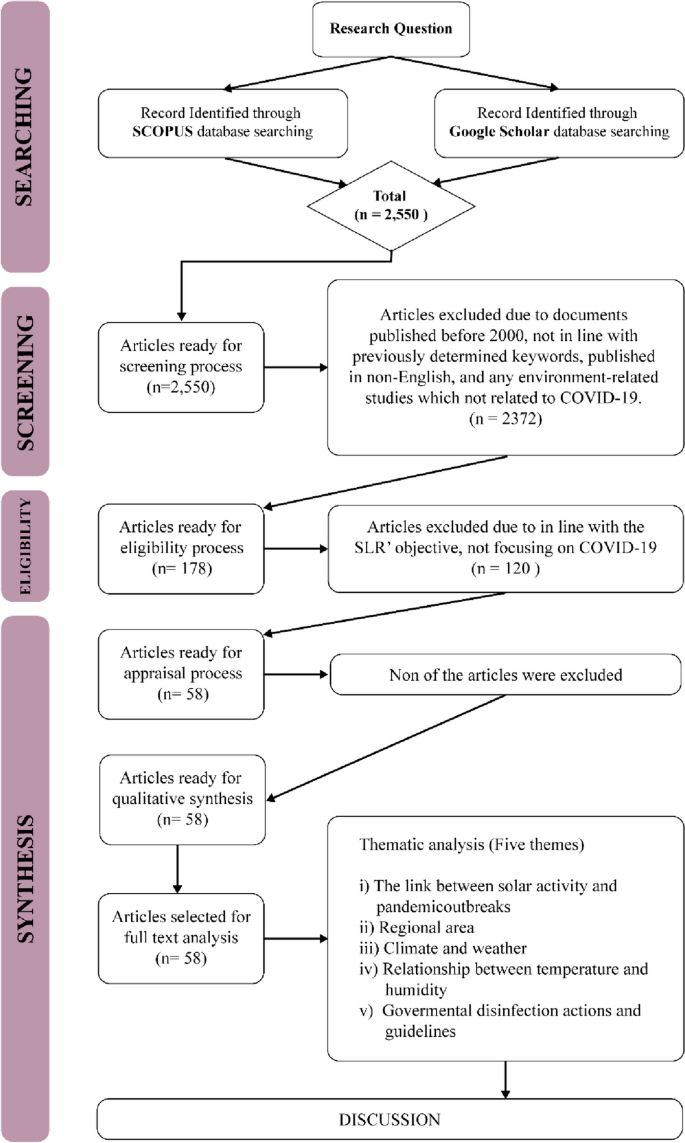
The flow diagram guide by ROSES protocol and Thematical Analysis
The current SLR started by determining the appropriate research questions, followed by the selection criteria, including the review, specifically on the keywords employed and the selection of journals database. Subsequently, the appraisal quality process and data abstraction and analysis were conducted.
Formulation of research questions
The entire process of this SLR was guided by the specific research questions, while sources to be reviewed and data abstraction and analysis were in line with the determined research question [ 35 , 36 ]. In the present article, a total of five research questions were formed, namely:
What the link between solar activity and COVID-19 pandemic outbreaks?
Which regions were more prone to COVID-19?
What were the temporal and spatial variabilities of high temperature and humidity during the spread of COVID-19?
What is the relationship between temperature and humidity in propagating COVID-19?
How did the government’s disinfection actions and guidelines can be reducing the spread of COVID-19?
Systematic searching strategies
Selection of studies.
In this stage of the study, the appropriate keywords to be employed in the searching process were determined. After referring to existing literature, six main keywords were chosen for the searching process, namely COVID-19, coronavirus, temperature, humidity, solar radiation and population density. The current study also utilised the boolean operators (OR, AND, AND NOT) and phrase searching.
Scopus was employed as the main database during the searching process, in line with the suggestion by Gusenbauer and Haddaway [ 37 ], who noted the strength of the database in terms of quality control and search and filtering functions. Furthermore, Google Scholar was selected as the supporting database. Although Halevi et al. [ 38 ] expressed concerns about its quality, Haddaway et al. [ 39 ] reported that due to its quantity, Google Scholar was suitable as a supporting database in SLR studies.
In the first stage of the search, 2550 articles were retrieved, which were then screened. The suitable criteria were also determined to control the quality of the articles reviewed [ 40 ]. The criteria are: any documents published between 2000 to 2022, documents that consist previously determined keywords, published in English, and any environment-related studies that focused on COVID-19. Based on these criteria, 2372 articles were excluded and 178 articles were proceeded to the next step namely eligibility. In the eligibility process, the title and the abstract of the articles were examined to ensure its relevancy to the SLR and in this process a total of 120 articles were excluded and only 58 articles were processed in the next stage.
Appraisal of the quality
The study ensured the rigor of the chosen articles based on best evidence synthesis. In the process, predefined inclusion criteria for the review were appraised by the systematic review team based on previously established guidelines and the studies were then judged as being scientifically admissible or not [ 40 ]. Hence, by controlling the quality based on the best evidence synthesis, the present SLR controls its quality by including articles that are in line with the inclusion criteria. It means that any article published within the timeline (in the year 2000 and above), composed of predetermined keywords, in English medium, and environment-related investigations focusing on COVID-19 are included in the review. Based on this process, all 58 articles fulfilled all the inclusion criteria and are considered of good quality and included in the review.
Data abstraction and analysis
The data abstraction process in this study was performed based on five research questions (please refer to 2.2, formulation of research questions). The data that was able to answer the questions were abstracted and placed in a table to ease the data analysis process. The primary data analysis technique employed in the current study was qualitative and relied on thematic analysis.
The thematic technique is a descriptive method that combines data flexibly with other information evaluation methods [ 41 ], aiming to identify the patterns in studies. Any similarities and relationships within the abstracted data emerge as patterns. Subsequently, suitable themes and sub-themes would be developed based on obtained patterns [ 42 ]. Following the thematic process, five themes were selected in this study.
Background of the selected articles
The current study selected 58 articles for the SLR. Five themes were developed based on the thematic analysis from the predetermined research questions: the link between solar activity and pandemic outbreaks, regional area, climate and weather, the relationship between temperature and humidity, and government disinfection action guidelines. Among the articles retrieved between 2000 and 2022; two were published in 2010, one in 2011, four in 2013, three in 2014, two in 2015, six in 2016 and 2017, respectively, one in 2018, six in 2019, twelve in 2020, eight in 2021, and seven in 2022.
Temperature- and humidity-related themes
The link between solar activity and pandemic outbreaks.
Numerous scientists have investigated the relationship between solar activities and pandemic outbreaks over the years ([ 43 ]; A [ 27 , 44 , 45 ].). Nuclear fusions from solar activities have resulted in minimum and maximum solar sunspots. Maximum solar activities are characterised by a high number of sunspots and elevated solar flare frequency and coronal mass injections. Minimum solar sunspot occurrences are identified by low interplanetary magnetic field values entering the earth [ 1 ].
A diminished magnetic field was suggested to be conducive for viruses and bacteria to mutate, hence the onset of pandemics. Nonetheless, Hoyle and Wickramasinghe [ 46 ] reported that the link between solar activity and pandemic outbreaks is only speculative. The literature noted that the data recorded between 1930 and 1970 demonstrated that virus transmissions and pandemic occurrences were coincidental. Moreover, no pandemic cases were reported in 1979, when minimum solar activity was recorded [ 47 ].
Chandra Wickramasinghe et al. [ 48 ] suggested a significant relationship between pandemic outbreaks and solar activities as several grand solar minima, including Sporer (1450–1550 AD), Mounder (1650–1700 AD), and Dalton (1800–1830) minimums, were recorded coinciding with global pandemics of diseases, such as smallpox, the English sweat, plague, and cholera pandemics. Furthermore, since the Dalton minimum, which recorded minimum sunspots, studies from 2002 to 2015 have documented the reappearance of previous pandemics. For example, influenza subtype H1N1 1918/1919 episodically returned in 2009, especially in India, China, and other Asian countries. Zika virus, which first appeared in 1950, flared and became endemic in 2015, transmitted sporadically, specifically in African countries. Similarly, SARS-CoV was first recorded in China in 2002 and emerged as an outbreak, MERS-CoV, in middle east countries a decade later, in 2012.
In 2020, the World Data Centre Sunspot Index and Long-term Solar Observations ( http://sidc.be ) confirmed that a new solar activity was initiated in December 2019, during which a novel coronavirus pandemic also occurred, and present a same as the previous hypothesis. Nevertheless, a higher number of pandemic outbreaks were documented during low minimum solar activities, including Ebola (1976), H5N1 (Nipah) (1967–1968), H1N1 (2009), and COVID-19 (2019–current). Furthermore, Wickramasinghe and Qu [ 49 ] reported that since 1918 or 1919, more devastating and recurrent pandemics tend to occur, particularly after a century. Consequently, within 100 years, a sudden surge of influenza was recorded, and novel influenza was hypothesised to emerge.
Figure 4 demonstrates that low minimum solar activity significantly reduced before 2020, hence substantiating the claim that pandemic events are closely related to solar activities. Moreover, numerous studies (i.e. [ 43 ], Chandra [ 46 , 47 , 48 ]) reported that during solar minimums, new viruses could penetrate the surfaces of the earth and high solar radiation would result in lower infection rates, supporting the hypothesis mentioned above.
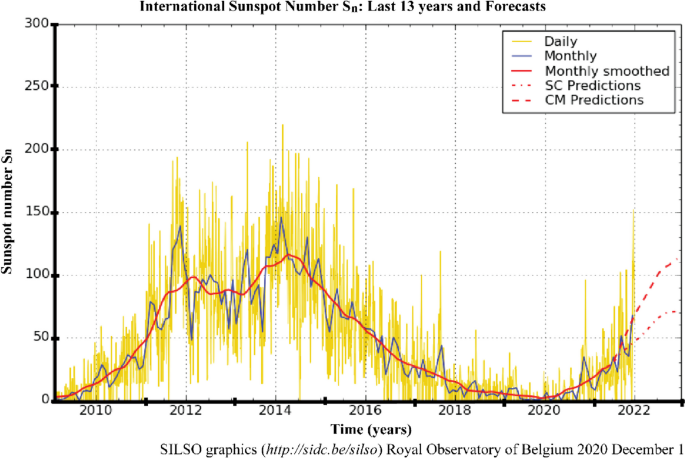
The number of sunspots in the last 13 years. Note : The yellow curve indicates the daily sunspot number and the 2010–2021 delineated curve illustrates the minimum solar activity recorded (source: http://sidc.be/silso )
Regional area
In early December 2019, Wuhan, China, was reported as the centre of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak [ 50 ]. Chinese health authorities immediately investigated and controlled the spread of the disease. Nevertheless, by late January 2020, the WHO announced that COVID-19 was a global public health emergency. The upgrade was due to the rapid rise in confirmed cases, which were no longer limited to Wuhan [ 28 ]. The disease had spread to 24 other countries, which were mainly in the northern hemisphere, particularly the European and Western Pacific regions, such as France, United Kingdom, Spain, South Korea, Japan, Malaysia, and Indonesia [ 51 , 52 ]. The migration or movement of humans was the leading agent in the spread of COVID-19, resulting in an almost worldwide COVID-19 pandemic [ 53 ].
The first hotspots of the epidemic outspread introduced by the Asian and Western Pacific regions possessed similar winter climates with an average temperature and humidity rate of 5–11 °C and 47–79%. Consequently, several publications reviewed in the current study associated the COVID-19 outbreak with regional climates (i.e. [ 1 , 29 , 54 , 55 ]) instead of its close connection to China. This review also discussed the effects of a range of specific climatological variables on the transmission and epidemiology of COVID-19 in regional climatic conditions.
America and Europe documented the highest COVID-19 cases, outnumbering the number reported in Asia [ 19 ] and on the 2nd of December 2020, the United States of America (USA) reported the highest number of confirmed COVID-19 infections, with over 13,234,551 cases and 264,808 mortalities (Da S [ 56 ].). The cases in the USA began emerging in March 2020 and peaked in late November 2020, during the wintertime in the northern hemisphere (December to March) [ 53 ]. Figure 5 demonstrates the evolution of the COVID-19 pandemic in several country which represent comparison two phase of summer and one phase of winter. Most of these countries tend to increase of COVID cases close to winter season. Then, it can be worsening on phase two of summer due to do not under control of human movement although the normal trend it is presenting during winter phase.
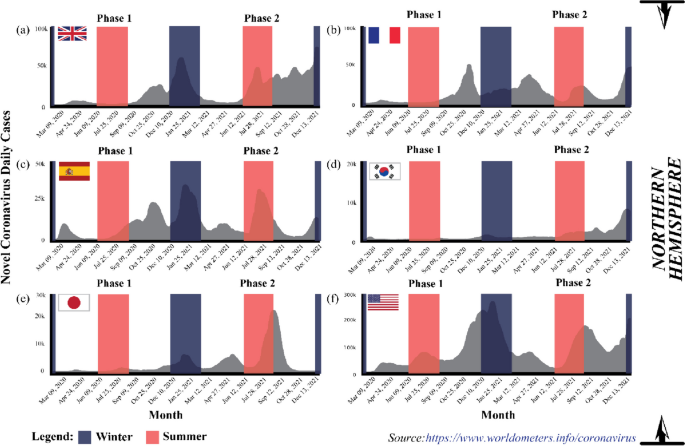
The evolution of the COVID-19 pandemic from the 15th of February 2020 to the 2nd of December 2020 ( Source: https://www.worldometers.info/coronavirus )
The coronavirus spread aggressively across the European region, which recorded the second highest COVID-19 confirmed cases after America. At the end of 2020, WHO reported 19,071,275 Covid-19 cases in the area, where France documented 2,183,275 cases, the European country with the highest number of confirmed cases, followed by the United Kingdom (1,629,661 cases) and Spain (1,652,801 cases) [ 19 ]. Europe is also located in the northern hemisphere and possesses a temperate climate.
The spatial and temporal transmission patterns of coronavirus infection in the European region were similar to America and the Eastern Mediterranean, where the winter season increased COVID-19 cases. Typically, winter in Europe occurs at the beginning of October and ends in March. Hardy et al. [ 57 ] also stated that temperature commonly drops below freezing (approximately − 1 °C) when snow accumulates between December to mid-March, resulting in an extreme environment. Figure 5 indicates that COVID-19 cases peaked in October when the temperature became colder [ 21 ]. Similarly, the cases were the highest in the middle of the year in Australia and South Asian countries, such as India, that experience winter and monsoon, respectively, during the period.
In African regions, the outbreak of COVID-19 escalated rapidly from June to October before falling from October to March, as summer in South Africa generally occurs from November to March, while winter from June to August. Nevertheless, heavy rainfall generally transpires during summer, hence the warm and humid conditions in South Africa and Namibia during summer, while the opposite happens during winter (cold and dry). Consequently, the outbreak in the region recorded an increasing trend during winter and subsided during the summer, supporting the report by Gunthe et al. [ 58 ]. Novel coronavirus disease presents unique and grave challenges in Africa, as it has for the rest of the world. However, the infrastructure and resources have limitations for Africa countries facing COVID-19 pandemic and the threat of other diseases [ 59 ].
Conclusively, seasonal and regional climate patterns were associated with COVID-19 outbreaks globally. According to Kraemer et al. [ 60 ], they used real-time mobility data in Wuhan and early measurement presented a positive correlation between human mobility and spread of COVID-19 cases. However, after the implementation of control measures, this correlation dropped and growth rates became negative in most locations, although shifts in the demographics of reported cases were still indicative of local chains of transmission outside of Wuhan.
Climate and weather
The term “weather” represents the changes in the environment that occur daily and in a short period, while “climate” is defined as atmospheric changes happening over a long time (over 3 months) in specific regions. Consequently, different locations would experience varying climates. Numerous reports suggested climate and weather variabilities as the main drivers that sped or slowed the transmission of SARS-CoV-2 worldwide [ 44 , 61 , 62 , 63 ].
From a meteorological perspective, a favourable environment has led to the continued existence of the COVID-19 virus in the atmosphere [ 64 ]. Studies demonstrated that various meteorological conditions, such as the rate of relative humidity (i.e. [ 28 ]), precipitation (i.e. [ 65 ]), temperature (i.e. [ 66 ]), and wind speed factors (i.e. [ 54 ]), were the crucial components that contributed to the dynamic response of the pandemic, influencing either the mitigation or exacerbation of novel coronavirus transmission. In other words, the environment was considered the medium for spreading the disease when other health considerations were put aside. Consequently, new opinions, knowledge, and findings are published and shared to increase awareness, thus encouraging preventive measures within the public.
The coronavirus could survive in temperatures under 30 °C with a relative humidity of less than 80% [ 67 ], suggesting that high temperatures and lower relative humidity contributed to the elicitation of COVID-19 cases [ 18 , 51 , 58 , 68 ]. Lagtayi et al. [ 7 ] highlighted temperature as a critical factor, evidently from the increased transmission rate of MERS-Cov in African states with a warm and dry climate. Similarly, the highest COVID-19 cases were recorded in dry temperate regions, especially in western Europe (France and Spain), China, and the USA, while the countries nearer to the equator were less affected. Nevertheless, the temperature factor relative to viral infections depends on the protein available in the viruses. According to Chen and Shakhnovich [ 69 ], there is a good correlation between decreasing temperature and the growth of proteins in virus. Consequently, preventive measures that take advantage of conducive environments for specific viruses are challenging.
Precipitation also correlates with influenza [ 43 ]. A report demonstrated that regions with at least 150 mm of monthly precipitation threshold level experienced fewer cases than regions with lower precipitation rates. According to Martins et al. [ 70 ], influenza and COVID-19 can be affected by climate, where virus can be spread through the respiratory especially during rainfall season. The daily spread of Covid-19 cases in tropical countries, which receive high precipitation levels, are far less than in temperate countries [ 27 ]. Likewise, high cases of COVID-19 were reported during the monsoon season (mid-year) in India during which high rainfall is recorded [ 71 ]. Moreover, the majority of the population in these regions has lower vitamin D levels, which may contribute to weakened immune responses during certain seasons [ 27 ].
Rainfall increases the relative atmospheric humidity, which is unfavourable to the coronaviruses as its transmission requires dry and cold weather. Moreover, several reports hypothesised that rain could wash away viruses on object surfaces, which is still questioned. Most people prefer staying home on rainy days, allowing less transmission or close contact. Conversely, [ 72 ] exhibited that precipitation did not significantly impact COVID-19 infectiousness in Oslo, Norway due the location in northern hemisphere which are during winter season presenting so cold.
Coşkun et al. [ 54 ] and Wu et al. [ 29 ] claimed that wind could strongly correlate with the rate of COVID-19 transmission. Atmospheric instability (turbulent occurrences) leads to increased wind speed and reduces the dispersion of particulate matter (PM 2.5 and PM 10 ) in the environment and among humans. An investigation performed in 55 cities in Italy during the COVID-19 outbreak proved that the areas with low wind movement (stable atmospheric conditions) possessed a higher correlation coefficient and exceeded the threshold value of the safe level of PM 2.5 and PM 10 . Resultantly, more individuals were recorded infected with the disease in the regions. As mentioned in Martins et al. [ 70 ] the COVID-19 can be affected by climate and the virus can be spread through respiratory which is the virus moving in the wind movement.
The relationship between temperature and humidity
Climatic parameters, such as temperature and humidity, were investigated as the crucial factors in the epidemiology of the respiratory virus survival and transmission of COVID-19 ([ 61 ]; S [ 73 , 74 ].). The rising number of confirmed cases indicated the strong transmission ability of COVID-19 and was related to meteorological parameters. Furthermore, several studies found that the disease transmission was associated with the temperature and humidity of the environment [ 55 , 64 , 68 , 75 ], while other investigations have examined and reviewed environmental factors that could influence the epidemiological aspects of Covid-19.
Generally, increased COVID-19 cases and deaths corresponded with temperature, humidity, and viral transmission and mortality. Various studies reported that colder and dryer environments favoured COVID-19 epidemiologically [ 45 , 76 , 77 ]. As example tropical region, the observations indicated that the summer (middle of year) and rainy seasons (end of the year) could effectively diminish the transmission and mortality from COVID-19. High precipitation statistically increases relative air humidity, which is unfavourable for the survival of coronavirus, which prefers dry and cold conditions [ 32 , 34 , 78 , 79 ]. Consequently, warmer conditions could reduce COVID-19 transmission. A 1 °C increase in the temperature recorded a decrease in confirmed cases by 8% increase [ 45 ].
Several reports established that the minimum, maximum, and average temperature and humidity correlated with COVID-19 occurrence and mortality [ 55 , 80 , 81 ]. The lowest and highest temperatures of 24 and 27.3 °C and a humidity between 76 and 91% were conducive to spreading the virulence agents. The propagation of the disease peaked at the average temperature of 26 °C and humidity of 55% before gradually decreasing with elevated temperature and humidity [ 78 ].
Researchers are still divided on the effects of temperature and humidity on coronavirus transmission. Xu et al. [ 26 ] confirmed that COVID-19 cases gradually increased with higher temperature and lower humidity, indicating that the virus was actively transmitted in warm and dry conditions. Nevertheless, several reports stated that the spread of COVID-19 was negatively correlated with temperature and humidity [ 10 , 29 , 63 ]. The conflicting findings require further investigation. Moreover, other factors, such as population density, elderly population, cultural aspects, and health interventions, might potentially influence the epidemiology of the disease and necessitate research.
Governmental disinfection actions and guidelines
The COVID-19 is a severe health threat that is still spreading worldwide. The epidemiology of the SAR-CoV-2 virus might be affected by several factors, including meteorological conditions (temperature and humidity), population density, and healthcare quality, that permit it to spread rapidly [ 16 , 17 ]. Nevertheless, in 2020, no effective pharmaceutical interventions or vaccines were available for the diagnosis, treatment, and epidemic prevention against COVID-19 [ 73 , 82 ]. Consequently, after 2020 the governments globally have designed and executed non-pharmacological public health measures, such as lockdown, travel bans, social distancing, quarantine, public place closure, and public health actions, to curb the spread of COVID-19 infections and several studies have reported on the effects of these plans [ 13 , 83 ].
The COVID-19 is mainly spread via respiratory droplets from an infected person’s mouth or nose to another in close contact [ 84 ]. Accordingly, WHO and most governments worldwide have recommended wearing facemasks in public areas to curb the transmission of COVID-19. The facemasks would prevent individuals from breathing COVID-19-contaminated air [ 85 ]. Furthermore, the masks could hinder the transmission of the virus from an infected person as the exhaled air is trapped in droplets collected on the masks, suspending it in the atmosphere for longer. The WHO also recommended adopting a proper hand hygiene routine to prevent transmission and employing protective equipment, such as gloves and body covers, especially for health workers [ 86 ].
Besides wearing protective equipment, social distancing was also employed to control the Covid-19 outbreak [ 74 , 87 ]. Social distancing hinders the human-to-human transmission of the coronavirus in the form of droplets from the mouth and nose, as evidenced by the report from Sun and Zhai [ 88 ]. Conversely, Nair & Selvaraj [ 89 ] demonstrated that social distancing was less effective in communities and cultures where gatherings are the norm. Nonetheless, the issue could be addressed by educating the public and implementing social distancing policies, such as working from home and any form of plague treatment.
Infected persons, individuals who had contact with confirmed or suspected COVID-19 patients, and persons living in areas with high transmission rates were recommended to undergo quarantine by WHO. The quarantine could be implemented voluntarily or legally enforced by authorities and applicable to individuals, groups, or communities (community containment) [ 90 ]. A person under mandatory quarantine must stay in a place for a recommended 14-day period, based on the estimated incubation period of the SARS-CoV-2 [ 19 , 91 ]. According to Stasi et al. [ 92 ], 14-days period for mandatory quarantine it is presenting a clinical improvement after they found 5-day group and 10-day group can be decrease number of patient whose getting effect of COVID-19 from 64 to 54% respectively. This also proven by Ahmadi et al. [ 43 ] and Foad et al. [ 93 ], quarantining could reduce the transmission of COVID-19.
Lockdown and travel bans, especially in China, the centre of the coronavirus outbreak, reduced the infection rate and the correlation of domestic air traffic with COVID-19 cases [ 17 ]. The observations were supported by Sun & Zhai [ 88 ] and Sun et al. [ 94 ], who noted that travel restrictions diminished the number of COVID-19 reports by 75.70% compared to baseline scenarios without restrictions. Furthermore, example in Malaysia, lockdowns improved the air quality of polluted areas especially in primarily at main cities [ 95 ]. As additional, Martins et al. [ 70 ] measure the Human Development Index (HDI) with the specific of socio-economic variables as income, education and health. In their study, the income and education levels are the main relevant factors that affect the socio-economic.
A mandatory lockdown is an area under movement control as a preventive measure to stop the coronavirus from spreading to other areas. Numerous governments worldwide enforced the policy to restrict public movements outside their homes during the pandemic. Resultantly, human-to-human transmission of the virus was effectively reduced. The lockdown and movement control order were also suggested for individuals aged 80 and above or with low or compromised immunities, as these groups possess a higher risk of contracting the disease [ 44 ].
Governments still enforced movement orders even after the introduction of vaccines by Pfizer, Moderna, and Sinovac, as the vaccines only protect high-risk individuals from the worst effects of COVID-19. Consequently, in most countries, after receiving the first vaccine dose, individuals were allowed to resume life as normal but were still required to follow the standard operating procedures (SOP) outlined by the government.
The government attempted to balance preventing COVID-19 spread and recovering economic activities, for example, local businesses, maritime traders, shipping activities, oil and gas production and economic trades [ 22 , 96 ]. Nonetheless, the COVID-19 cases demonstrated an increasing trend during the summer due to the higher number of people travelling and on vacation, primarily to alleviate stress from lockdowns. Several new variants were discovered, including the Delta and Omicron strains, which spread in countries such as the USA and the United Kingdom. The high number of COVID-19 cases prompted the WHO to suggest booster doses to ensure full protection.
As mentioned in this manuscript, the COVID-19 still uncertain for any kind factors that can be affected on spreading of this virus. However, regarding many sources of COVID-19 study, the further assessment on this factor need to be continue to be sure, that we ready to facing probably in 10 years projection of solar minimum phase can be held in same situation for another pandemic.
The sun has an eleven-year cycle known as the solar cycle, related to its magnetic field, which controls the activities on its surface through sunspots. When the magnetic fields are active, numerous sunspots are formed on its surface, hence the sun produces more radiation energy emitted to the earth. The condition is termed solar maximum (see Fig. 6 , denoted by the yellow boxes). Alternatively, as the magnetic field of the sun weakens, the number of sunspots decreases, resulting in less radiation energy being emitted to the earth. The phenomenon is known as the solar minimum (see Fig. 6 , represented by the blue boxes).
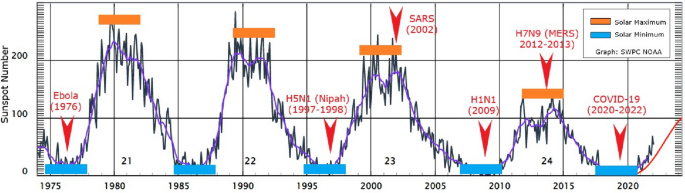
The emergence and recurrence of pandemics every 5 years in relation to solar activities ( Source: www.swpc.noaa.gov/ ). Note: The yellow boxes indicate the solar maximum, while the blue boxes represent the solar minimum
The magnetic field of the sun protects the earth from cosmic or galactic cosmic rays emitted by supernova explosions, stars, and gamma-ray bursts [ 97 ]. Nevertheless, galactic cosmic rays could still reach the earth during the solar minimum, the least solar radiation energy period. In the 20th and early 21st centuries, several outbreaks of viral diseases that affected the respiratory system (pneumonia or influenza), namely the Spanish (1918–1919), Asian (1957–1958) and Hong Kong (1968) flu, were documented. Interestingly, the diseases that claimed numerous lives worldwide occurred at the peak of the solar maximum.
Figure 6 illustrates the correlation between the number of sunspots and disease outbreaks from 1975 to 2021, including COVID-19, that began to escalate in December 2019. Under the solar minimum conditions, the spread of Ebola (1976), H5N1 (1997–1998), H1N1 (2009), and COVID-19 (2019-2020) were documented, while the solar maximum phenomenon recorded SARS (2002) and H7N9 (2012–2013) or MERS outbreaks. Nonetheless, solar activity through the production of solar sunspots began to decline since the 22nd solar cycle. Accordingly, further studies are necessary to investigate the influence such solar variations could impart or not on pandemic development.
Despite the findings mentioned above, the sun and cosmic radiations could influence the distribution or outspread of disease-spreading viruses. The rays could kill the viruses via DNA destruction or influence their genetic mutations, which encourage growth and viral evolution. Nevertheless, the connection between radiation and the evolutionary process requires further study by specialists in the field it is become true or not.
The spread of viral diseases transpires naturally in our surroundings and occurs unnoticed by humans. According to records, the spread of pandemic diseases, including the Black Death (fourteenth century) and the Spanish flu (1919), was significantly influenced by the decline and peak of solar activities. Furthermore, in the past 20 years, various diseases related to the influenza virus have been recorded. According to the pattern observed, if all diseases were related to the solar cycle (solar maximum and minimum), the viral diseases would reoccur every 5 to 6 years since they first appeared between 1995 and 2020. Accordingly, the next pandemic might occur around 2024 or 2025 and need to have a proper study for prove these statements. Nonetheless, the activities on the surface of the sun have been weakening since the 23rd solar cycle and it can be proven later after the proper study can be make it.
The beginning of the COVID-19 spread, only several countries with the same winter climate with an average temperature of 5–11 °C and an average humidity rate of 47–79% located at latitudes 30–50 N reported cases. The areas included Wuhan distribution centres in China, the United Kingdom, France, Spain, South Korea, Japan, and the USA (see Fig. 5 ). Other than biological aspects, the higher number of confirmed cases recorded in colder environments was due to the human body secreting less lymphoproliferative hormone, leading to decreased immunogenicity effects and increased risk of infection [ 24 ]. Consequently, the virus could attack and rapidly infect humans during the period [ 1 , 54 ].
The lymphoproliferative response is a protective immune response that plays a vital role in protecting and eradicating infections and diseases. On the other hand, staying in warm conditions or being exposed to more sunlight would lower the risks of infection. According to Asyary and Veruswati [ 98 ], sunlight triggers vitamin D, which increases immunity and increases the recovery rates of infected individuals.
Researchers believe that viruses could survive in the environment for up to 3 to 4 years or even longer. The survival rate of the microorganisms is relatively high, which is related to their biological structures, adaptability on any surfaces, and transmission medium to spread diseases. Viruses possess simple protein structures, namely the spike, membrane, and envelope protein; therefore, when they enter living organisms (such as through the respiratory system), the viruses are easily transmitted.
Once they have entered a host, the viruses duplicate exponentially and swarm the lungs. Subsequently, after the targeted organs, such as the lungs, are invaded, the viruses attack the immune system and create confusion in protective cells to destroy healthy cells. The situation is still considered safe in younger and healthy individuals as their immune systems could differentiate and counter-attack the viruses, curing them. Nonetheless, in elders and individuals with several chronic diseases, most of their protective cells are dead, hence their immune system is forced to work hard to overcome the infection. Pneumonia and death tend to occur when the situation is overwhelming [ 85 ]. Consequently, the viruses are harmful to humans as they could multiply in a short period, enter the blood, and overrun the body.
The coronavirus could attach to surfaces without a host, including door knobs and steel and plastic materials. The microorganisms could survive alone, but virologists have yet to determine how long. If someone touches any surface with the virus, the individual would then be infected. The situation would worsen if the infected person contacted numerous people and became a super spreader. A super spreader does not exhibit any symptoms and continuously transmits the virus without realising it. An infected individual transmits the coronavirus via droplets from coughs or sneezes. Nevertheless, scientists have yet to determine if coronavirus is spread via airborne or droplets, hence requiring thorough evaluation [ 99 ].
The COVID-19 virus mutates over time, and it can be changing any times. Mutations alter the behaviour and genetic structure of the virus, resulting in a new strain. Numerous research have been conducted to procure vaccines and anti-viral medications, but mutations have led to evolutionary disadvantages. The novel strains are more infectious than the original ones. As of November 2020, approximately six new coronavirus strains have been detected, each displaying different transmission behaviours [ 100 ].
Recent studies demonstrated that the mutated viruses exhibit little variability, allowing scientists to produce viable vaccines [ 71 ]. Furthermore, different types of vaccines are manufactured by different countries, which could be advantageous. Currently, most countries also recommend booster doses to attain extra protection after receiving the mandatory two vaccine doses. In same time, the social and physical interactions between humans also necessitate to be aware.
The COVID-19 virus is primarily transmitted through droplets produced by an infected person. Accordingly, physical distancing, a one-metre minimum distance between individuals [ 19 ], and following the SOP might prevent or avoid spreading the disease. Moreover, self-quarantine, school closures, working from home, cancelling large events, limiting gatherings, and avoiding spending long periods in crowded places are essential strategies in enforcing physical distancing at a community level. The policies are essential precautions that could reduce the further spreading of coronavirus and break the chain of transmission.
Government support also need to control the spread of COVID-19 with the strict SOP. The SOP enforcement in public places would enhance adherence to the new practice among the public and the community, aiding in curbing disease transmission. Practising limited meetings and social gatherings, avoiding crowded places, workplace distancing, preventing non-necessary travels of high-risk family members, especially those with chronic disease, and adhering to the recommended SOP could reduce coronavirus outbreaks. Nonetheless, individual awareness is also necessary to achieve COVID-19 spread prevention.
Many researchers are focused on identifying the primary drivers of pandemic outbreaks. Seasonal, temperature, and humidity differences significantly impacted COVID-19 growth rate variations. It is crucial to highlight the potential link between the recurrence of pandemics every 5 years and solar activities, which can influence temperature and humidity variations. Notable variations in COVID-19 mortality rates were observed between northern and southern hemisphere countries, with the former having higher rates. One hypothesis suggests that populations in the northern hemisphere may receive insufficient sunlight to maintain optimal vitamin D levels during winter, possibly leading to higher mortality rates.
The first COVID-19 case was detected in Wuhan, China, which is in the northern hemisphere. The number of cases rapidly propagated in December during the winter season. At the time, the temperature in Wuhan was recorded at 13–18 °C. Accordingly, one theory proposes that the survival and transmission of the coronavirus were due to meteorological conditions, namely temperatures between 13 and 18 °C and 50–80% humidity.
Daily rainfall directly impacts humidity levels. The coronavirus exhibited superior survival rates in cold and dry conditions. Furthermore, transmissible gastroenteritis (TGEV) suspensions and possibly other coronaviruses remain viable longer in their airborne states, which are more reliably collected in low relative humidity than in high humidity. Consequently, summer rains would effectively reduce COVID-19 transmission in southern hemisphere regions.
In southern hemisphere regions, the summer seasons are accompanied by a high average temperature at the end and beginning of the year. Countries with temperatures exceeding 24 °C reported fewer infections. As temperatures rise from winter to summer, virus transmission is expected to decline. Nonetheless, the activities and transmission of the virus were expected to decrease during winter to summer transitions, when the countries would be warmer. The peak intensity of infections strongly depends on the level of seasonal transmissions.
Social distancing plays a critical role in preventing the overload of healthcare systems. Many respiratory pathogens, including those causing mild common cold-like syndromes, show seasonal fluctuations, often peaking in winter. This trend can be attributed to increased indoor crowding, school reopening, and climatic changes during autumn.
The spread of COVID-19 to neighbouring regions can be attributed to population interactions. Migration patterns, such as the movement from northern to southern regions during the warmer months, have significant epidemiological impacts. This trend mirrors the behavior of influenza pandemics where minor outbreaks in spring or summer are often followed by major waves in autumn or winter.
Availability of data and materials
Not applicable.
Abbreviations
Novel coronavirus
Coronavirus disease 2019
Deoxyribonucleic acid
Swine influenza
Influenza A virus subtype H5N1
Asian Lineage Avian Influenza A(H7N9) Virus
Middle East respiratory syndrome
Middle East respiratory syndrome Coronavirus
Particulate matter
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
RepOrting standards for Systematic Evidence Syntheses
Severe Acute Respiratory Syndrome
Severe Acute Respiratory Syndrome Coronavirus
Syndrome coronavirus 2
Systematic literature review
Standard operating procedure
Transmissible gastroenteritis Virus
United States of America
World Health Organization
Apanovich I. Climate and man. Opposition or natural stage of the earth’s evolution? Norwegian journal of development of the international. Science. 2019;26(25):12–27.
Google Scholar
Borah P, Singh MK, Mahapatra S. Estimation of degree-days for different climatic zones of north-East India. Sustain Cities Soc. 2015;14(1):70–81.
Article Google Scholar
Chen D, Chen HW. Using the Köppen classification to quantify climate variation and change: an example for 1901-2010. Environmental Development. 2013;6(1):69–79.
Trenberth KE, Fasullo JT. Global warming due to increasing absorbed solar radiation. Geophys Res Lett. 2009;36
Hauschild MZ, Huijbregts MAJ, Guinée L, Lane J, Fantke P, Zelm v R, et al. Life Cycle Impact Assessment – The Complete World of Life Cycle Assessment; 2015. p. 345.
Book Google Scholar
Nakada LYK, Urban RC. COVID-19 pandemic: environmental and social factors influencing the spread of SARS-CoV-2 in São Paulo. Brazil Environmental Science and Pollution Research. 2021;28(30):40322–8.
Article CAS PubMed Google Scholar
Lagtayi, R., Lairgi, L., Daya, A., & Khouya, A. (2021). The impact of the average temperature, humidity, wind speed, altitude and population density on daily COVID-19 infections’ evolution. January, 9094.
Majumder MS, Liu D, Poirier C, Mandl KD, Lipsitch M, The MS. The role of absolute humidity on transmission rates of the COVID-19 outbreak; 2020.
Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review. JAMA - Journal of the American Medical Association. 2020;324(8):782–93.
Zhang X, Maggioni V, Houser P, Xue Y, Mei Y. The impact of weather condition and social activity on COVID-19 transmission in the United States. J Environ Manag. 2022;302:114085.
Article CAS Google Scholar
Mäkinen TM, Juvonen R, Jokelainen J, Harju TH, Peitso A, Bloigu A, et al. Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respir Med. 2009;103(3):456–62.
Article PubMed Google Scholar
Carvalho FRS, Henriques DV, Correia O, Schmalwieser AW. Potential of solar UV radiation for inactivation of Coronaviridae family. Photochem Photobiol. 2021;97:213–20.
Ali I, Alharbi OM. COVID-19: disease, management, treatment, and social impact. Sci Total Environ. 2020;728:138861.
Article CAS PubMed PubMed Central Google Scholar
Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, epidemiology, pathogenesis, and control of covid-19. Viruses. 2020;12(4):1–17.
Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World health organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–6.
Article PubMed PubMed Central Google Scholar
Wang J, Tang K, Feng K, Lv W. High temperature and high humidity reduce the transmission of COVID-19; 2020a.
Wang L, Duan Y, Zhang W, Liang J, Xu J, Zhang Y, et al. Epidemiologic and clinical characteristics of 26 cases of covid-19 arising from patient-to-patient transmission in Liaocheng, China. Clinical Epidemiology. 2020b;12:387–91.
Xie J, Zhu Y. Science of the Total environment association between ambient temperature and COVID-19 infection in 122 cities from China. Sci Total Environ. 2020;724:138201.
World Health Organization. (2020a). Director-General’s opening remarks at the media briefing on COVID-19-10April 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—10- april-2020.
Bostock B. South Korea is testing 200,000 members of a doomsday church linked to more than 60% of its coronavirus cases; 2020.
World Health Organization. (2020b). Health topics/coronavirus. https://www.who.int/health-topics/coronavirus#tab=tab_1.
Menhat M, Mohd Zaideen IM, Yusuf Y, Salleh NHM, Zamri MA, Jeevan J. The impact of Covid-19 pandemic: A review on maritime sectors in Malaysia. Ocean Coast Manag. 2021;209:105638.
Byun WS, Heo SW, Jo G, Kim JW, Kim S, Lee S, et al. Is coronavirus disease (COVID-19) seasonal? A critical analysis of empirical and epidemiological studies at global and local scales. Environ Res. 2021;196:110972.
Dhakal P, Pokhrel P, B. Seasonal variation and COVID-19 pandemic in Nepal. Nepal Medical Journal. 2020;3(2):77–80.
Mehmet Ş. Science of the Total environment impact of weather on COVID-19 pandemic in Turkey. 728; 2020.
Xu H, Yan C, Fu Q, Xiao K, Yu Y, Han D, et al. Science of the Total environment possible environmental effects on the spread of COVID-19 in China. Sci Total Environ. 2020;731:139211.
Rosario DKA, Mutz YS, Bernardes PC, Conte-Junior CA. Relationship between COVID-19 and weather: case study in a tropical country. Int J Hyg Environ Health. 2020;229:113587.
Wang J, Tang K, Feng K, Lin X, Lv W, Chen K, et al. Impact of temperature and relative humidity on the transmission of COVID-19: A modelling study in China and the United States. BMJ Open. 2021;11(2):1–16.
Wu Y, Jing W, Liu J, Ma Q, Yuan J, Wang Y, et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci Total Environ. 2020;729:1–7.
Casanova LM, Jeon S, Rutala WA, Weber DJ, Sobsey MD. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl Environ Microbiol. 2010;76(9):2712–7.
Islam N, Bukhari Q, Jameel Y, Shabnam S, Erzurumluoglu AM, Siddique MA, et al. COVID-19 and climatic factors: A global analysis. Environ Res. 2021;193:110355.
Diao Y, Kodera S, Anzai D, Gomez-Tames J, Rashed EA, Hirata A. Influence of population density, temperature, and absolute humidity on spread and decay durations of COVID-19: A comparative study of scenarios in China, England, Germany, and Japan. One Health. 2021;12:100203.
Haddaway NR, Macura B, Whaley P, Pullin AS. ROSES reporting standards for systematic evidence syntheses: pro forma, flow-diagram and descriptive summary of the plan and conduct of environmental systematic reviews and systematic maps. Environ Evid. 2018;7(1):4–11.
Sharif N, Dey SK. Impact of population density and weather on COVID-19 pandemic and SARS-CoV-2 mutation frequency in Bangladesh. Epidemiol Infect. 2021:1–10.
Kraus S, Breier Dasí-Rodríguez S. El arte de elaborar una revisión bibliográfica sistemática en la investigación sobre el espíritu empresarial. Int Entrep Manag J. 2020;16:1023–42.
Xiao Y, Watson M. Guidance on conducting a systematic literature review. J Plan Educ Res. 2019;39(1):93–112.
Gusenbauer M, Haddaway NR. Which academic search systems are suitable for systematic reviews or meta-analyses? Evaluating retrieval qualities of Google scholar, PubMed, and 26 other resources. Res Synth Methods. 2020;11(2):181–217.
Halevi G, Moed H, Bar-Ilan J. Suitability of Google scholar as a source of scientific information and as a source of data for scientific evaluation—review of the literature. Journal of Informetrics. 2017;11(3):823–34.
Haddaway NR, Collins AM, Coughlin D, Kirk S. The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS One. 2015;10(9):1–17.
Littlewood C, Chance-Larsen K, McLean S. Quality appraisal as a part of the systematic review. International Journal of Physiotherapy and Rehabilitation. 2010;1(1):53–8.
Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Ahmadi M, Sharifi A, Dorosti S, Jafarzadeh Ghoushchi S, Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci Total Environ. 2020;729
Gupta A, Banerjee S, Das S. Significance of geographical factors to the COVID-19 outbreak in India. Modeling Earth Systems and Environment. 2020;6(4):2645–53.
Pequeno P, Mendel B, Rosa C, Bosholn M, Souza JL, Baccaro F, et al. Air transportation, population density and temperature predict the spread of COVID-19 in Brazil. PeerJ. 2020;2020(6):1–15.
Hoyle F, Wickramasinghe NC. Sunspots and influenza [6]. Nature. 1990;343(6256):304.
Wickramasinghe NC, Rocca MC, Tokoro G, Temple R. Journal of infectious diseases. Scienctific Research and Community. 2020;1(4):1–10.
Wickramasinghe NC, Steele EJ, Wainwright M, Tokoro G, Fernando M, Qu J. Sunspot cycle minima and pandemics : A case for vigilance at the present time. Journal of Astrobiology & Outreach. 2017;5:2332–519.
Wickramasinghe NC, Qu J. Are we approaching a new influenza pandemic. Virol Curr Res. 2018;2(107):2.
Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Disease 2019 in China; 2020.
Bashir MF, Ma B, Bilal K, Bashir MA, Tan D, Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci Total Environ. 2020;728:138835.
Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–60.
PubMed PubMed Central Google Scholar
Lin C, Lau AKH, Fung JCH, Guo C, Chan JWM, Yeung DW, et al. A mechanism-based parameterisation scheme to investigate the association between transmission rate of COVID-19 and meteorological factors on plains in China. Sci Total Environ. 2020;737:140348.
Coşkun H, Yıldırım N, Gündüz S. The spread of COVID-19 virus through population density and wind in Turkey cities. Sci Total Environ. 2021;751
Yang HY, Lee JKW. The impact of temperature on the risk of covid-19: A multinational study. Int J Environ Res Public Health. 2021;18(8)
Candido DD, Watts A, Abade L, Kraemer MUG, Pybus OG, Croda J, et al. Routes for COVID-19 importation in Brazil. Journal of Travel Medicine. 2020;27(3):1–3.
Hardy JP, Groffman PM, Fitzhugh RD, Henry KS, Welman AT, Demers JD, et al. Snow depth manipulation and its influence on soil frost and water dynamics in a northern hardwood forest. Biogeochemistry. 2001;56(2):151–74.
Gunthe SS, Swain B, Patra SS, Amte A. On the global trends and spread of the COVID-19 outbreak: preliminary assessment of the potential relation between location-specific temperature and UV index. Journal of Public Health (Germany). 2020:1–10.
Rosenthal PJ, et al. COVID-19: shining the light on Africa. Am J Trop Med Hyg. 2020;102(6):1145–8.
Kraemer MUG, et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–7.
Dalziel BD, Kissler S, Gog JR, Viboud C, Bjørnstad ON, Metcalf CJE, et al. Urbanization and humidity shape the intensity of influenza epidemics in U.S. cities. Science. 2018;362:75–9.
Sahoo PK, Powell MA, Mittal S, Garg VK. Is the transmission of novel coronavirus disease (COVID-19) weather dependent? J Air Waste Manage Assoc. 2020;70(11):1061–4.
Selcuk M, Gormus S, Guven M. Impact of weather parameters and population density on the COVID-19 transmission: evidence from 81 provinces of Turkey. Earth Syst Environ. 2021;5(1):87–100.
Abraham J, Turville C, Dowling K, Florentine S. Does climate play any role in covid-19 spreading?—an Australian perspective. Int J Environ Res Public Health. 2021;18(17)
Sehra ST, Salciccioli JD, Wiebe DJ, Fundin S, Baker JF. Maximum daily temperature, precipitation, ultraviolet light, and rates of transmission of severe acute respiratory syndrome coronavirus 2 in the United States. Clin Infect Dis. 2020;71(9):2482–7.
CAS PubMed Google Scholar
Rubin D, Huang J, Fisher BT, Gasparrini A, Tam V, Song L, et al. Association of Social Distancing, population density, and temperature with the instantaneous reproduction number of SARS-CoV-2 in counties across the United States. JAMA Netw Open. 2020;3(7):1–12.
Comunian S, Dongo D, Milani C, Palestini P. Air pollution and covid-19: The role of particulate matter in the spread and increase of covid-19’s morbidity and mortality. Int J Environ Res Public Health. 2020;17(12):1–22.
Tosepu R, Gunawan J, Effendy DS, Ahmad LOAI, Lestari H, Bahar H, et al. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci Total Environ. 2020;725
Chen and Shakhnovich. Thermal adaptation of viruses and Bacteria. Biophys J. 2010;98:1109–18.
Martins LD, da Silva I, Batista WV, Andrade MF, Freitas ED, Jorge Alberto Martins JA. How socio-economic and atmospheric variables impact COVID-19 and influenza outbreaks in tropical and subtropical regions of Brazil. Environ Res. 2020;191:110184.
Kulkarni H, Khandait H, Narlawar UW, Rathod P, Mamtani M. Independent association of meteorological characteristics with initial spread of Covid-19 in India. Sci Total Environ. 2021;764:142801.
Menebo MM. Science of the Total environment temperature and precipitation associate with Covid-19 new daily cases : A correlation study between weather and Covid-19 pandemic in. Sci Total Environ. 2020;737:139659.
Gupta S, Patel KK. Global Epidemiology of First 90 Days into COVID-19 Pandemic :Disease Incidence , Prevalence , Case Fatality Population Density, Urbanisation. J Health Manag. 2020;22(2):117–28.
Haque SE, Rahman M. Association between temperature, humidity, and COVID-19 outbreaks in Bangladesh. Environ Sci Pol. 2020;114:253–5.
Sharma P, Singh AK, Agrawal B, Sharma A. Correlation between weather and COVID-19 pandemic in India: an empirical investigation. J Public Aff. 2020;20(4)
Fu S, Wang B, Zhou J, Xu X, Liu J, Ma Y, et al. Meteorological factors, governmental responses and COVID-19: evidence from four European countries. Environ Res. 2021;194:110596.
Mecenas P, Bastos RT, Vallinoto AC, Normando D. Effects of temperature and humidity on the spread of COVID-19: A systematic review. PLoS One. 2020;15:1–21.
Malki Z, Atlam ES, Hassanien AE, Dagnew G, Elhosseini MA, Gad I. Association between weather data and COVID-19 pandemic predicting mortality rate: machine learning approaches. Chaos, Solitons Fractals. 2020;138:110137.
Sasikumar K, Nath D, Nath R, Chen W. Impact of extreme hot climate on COVID-19 outbreak in India. GeoHealth. 2020;4(12)
Kodera S, Rashed EA, Hirata A. Correlation between COVID-19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity. Int J Environ Res Public Health. 2020;17(15):1–14.
Sobral MFF, Duarte GB, da Penha Sobral AIG, Marinho MLM, de Souza Melo A. Association between climate variables and global transmission oF SARS-CoV-2. Sci Total Environ. 2020;729:138997.
Patel SK, Pathak M, Tiwari R, Yatoo MI, Malik YS. A vaccine is not too far for COVID-19 coronavirus pandemic A vaccine is not too far for COVID-19. May; 2020.
Nicola M, Neill NO, Sohrabi C, Khan M, Agha M, Agha R. Evidence based management guideline for the COVID-19 pandemic - review article. Int J Surg. 2020;77:206–16.
Atangana E, Atangana A. Facemasks simple but powerful weapons to protect against COVID-19 spread: can they have sides effects? Results in Physics. 2020;19:103425.
Sarmadi M, Moghanddam VK, Dickerson AS, Martelletti L. Association of COVID-19 distribution with air quality, sociodemographic factors, and comorbidities: an ecological study of US states. Air Qual Atmos Health. 2021;14(4):455–65.
Chung CJ, Nazif TM, Wolbinski M, Hakemi E, Lebehn M, Brandwein R, et al. The restructuring of structural heart disease practice during The Covid-19 pandemic. J Am Coll Cardiol. 2020; InPress
Bukhari Q, Massaro JM, D’agostino RB, Khan S. Effects of weather on coronavirus pandemic. Int J Environ Res Public Health. 2020;17(15):1–12.
Sun C, Zhai Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain Cities Soc. 2020;62:102390.
Nair N, Selvaraj P. Using a cultural and social identity lens to understand pandemic responses in the US and India. Int J Cross-cult Manag. 2021;21(3):545–68.
Cetron M, Landwirth J. Public health and ethical considerations in planning for quarantine. Yale J Biol Med. 2005;78(5):325–30.
Jernigan DB. Update: public health response to the coronavirus disease 2019 outbreak—United States, February 24, 2020. MMWR. Morbidity and mortality weekly report, 69. 2020.
Stasi C, Fallani S, Voller F, Silvestri C. Treatment for COVID-19: an overview. Eur J Pharmacol. 2020;889:173644.
Foad CAKK, Xun N, Pejman J, Nataraj RC. Nonlinear dynamic analysis of an epidemiological model for COVID-19 including public behavior and government action. Nonlinear Dynamics. 2020;101(3):1545–59.
Sun Z, Zhang H, Yang Y, Wan H, Wang Y. Science of the Total environment impacts of geographic factors and population density on the COVID-19 spreading under the lockdown policies of China. Sci Total Environ. 2020;746(666):141347.
Abdullah S, Mansor AA, Napi NNLM, Mansor WNW, Ahmed AN, Ismail M, et al. Air quality status during 2020 Malaysia movement control order (MCO) due to 2019 novel coronavirus (2019-nCoV) pandemic. Sci Total Environ. 2020;729:139022.
Menhat M, Yusuf Y. Factors influencing the choice of performance measures for the oil and gas supply chain - exploratory study. IOP Conference Series: Materials Science and Engineering. 2018;342(1)
Ćirkovića MM, Vukotića B. Long-term prospects: mitigation of supernova and gamma-ray burst threat to intelligent beings. Acta Astronautica. 2016;129:438–46.
Asyary A, Veruswati M. Science of the Total environment sunlight exposure increased Covid-19 recovery rates : A study in the central pandemic area of Indonesia. Sci Total Environ. 2020;729:139016.
Jayaweeraa M, Pererab H, Gunawardanaa B, Manatungea J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ Res. 2020;188:1–18.
Leung K, Shum MHH, Leung GM, Lam TTY, Wu JT. Early transmissibility assessment of the N501Y mutant strains of SARS-CoV-2 in the United Kingdom, October to November 2020. Euro Surveill. 2020;26(1)
Download references
Acknowledgements
The authors would also like to acknowledge the Editors and an anonymous reviewer, who contributed immensely to improving the quality of this publication and a special thanks to Muhammad Hafiy Nauwal Effi Helmy, that contributed an excellent idea through singing during the COVID-19 lockdown period.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Faculty of Maritime Studies, Universiti Malaysia Terengganu, 21030, Kuala Nerus, Terengganu, Malaysia
Masha Menhat
Institute of Oceanography and Environment, Universiti Malaysia Terengganu, 21030, Kuala Nerus, Terengganu, Malaysia
Effi Helmy Ariffin, Junainah Zakaria & Mohd Fadzil Akhir
Faculty of Science and Marine Environment, Universiti Malaysia Terengganu, 21030, Kuala Nerus, Terengganu, Malaysia
Wan Shiao Dong & Aminah Ismailluddin
Institute for Social Science Studies, Universiti Putra Malaysia, 43400, Serdang, Selangor, Malaysia
Hayrol Azril Mohamed Shafril
Social, Environmental and Developmental Sustainability Research Center, Faculty of Social Sciences and Humanities, Universiti Kebangsaan Malaysia, 43600, Bangi, Selangor, Malaysia
Mahazan Muhammad
Institute of Geology Malaysia, Board of Geologists, 62100, Putrajaya, Malaysia
Ahmad Rosli Othman
Executive Office, Proofreading By A UK PhD, 51-1, Biz Avenue II, 63000, Cyberjaya, Malaysia
Thavamaran Kanesan
Faculty of Engineering, Universiti Malaya, 50603, Kuala Lumpur, Malaysia
Suzana Pil Ramli
Faculty of Applied Sciences, Uva Wellassa University, Badulla, 90000, Sri Lanka
Amila Sandaruwan Ratnayake
You can also search for this author in PubMed Google Scholar
Contributions
All authors have been involved in writing this editorial and contributing to the review of the manuscript. MM and EHA contribute to conceptualization. IA and ARO have made the figure.
Corresponding author
Correspondence to Effi Helmy Ariffin .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Menhat, M., Ariffin, E.H., Dong, W.S. et al. Rain, rain, go away, come again another day: do climate variations enhance the spread of COVID-19?. Global Health 20 , 43 (2024). https://doi.org/10.1186/s12992-024-01044-w
Download citation
Received : 27 July 2023
Accepted : 22 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12992-024-01044-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Coronavirus
- Solar radiation
- Temperature
- Social distancing
Globalization and Health
ISSN: 1744-8603
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 13 May 2024
“ We might not have been in hospital, but we were frontline workers in the community ”: a qualitative study exploring unmet need and local community-based responses for marginalised groups in Greater Manchester during the COVID-19 pandemic
- Stephanie Gillibrand 1 ,
- Ruth Watkinson 2 ,
- Melissa Surgey 2 ,
- Basma Issa 3 &
- Caroline Sanders 2 , 4
BMC Health Services Research volume 24 , Article number: 621 ( 2024 ) Cite this article
135 Accesses
2 Altmetric
Metrics details
The response to the COVID-19 pandemic saw a significant increase in demand for the voluntary, community, faith and social enterprise (VCFSE) sector to provide support to local communities. In Greater Manchester (GM), the VCFSE sector and informal networks provided health and wellbeing support in multiple ways, culminating in its crucial supportive role in the provision of the COVID-19 vaccination rollout across the GM city region. However, the support provided by the VCFSE sector during the pandemic remains under-recognised. The aims of the study were to: understand the views and experiences of marginalised communities in GM during the COVID-19 pandemic; explore how community engagement initiatives played a role during the pandemic and vaccine rollout; assess what can be learnt from the work of key stakeholders (community members, VCFSEs, health-system stakeholders) for future health research and service delivery.
The co-designed study utilised a participatory approach throughout and was co-produced with a Community Research Advisory Group (CRAG). Focus groups and semi-structured interviews were conducted remotely between September-November 2021, with 35 participants from local marginalised communities, health and care system stakeholders and VCFSE representatives. Thematic framework analysis was used to analyse the data.
Local communities in GM were not supported sufficiently by mainstream services during the course of the COVID-19 pandemic, resulting in increased pressure onto the VCFSE sector to respond to local communities’ need. Community-based approaches were deemed crucial to the success of the vaccination drive and in providing support to local communities more generally during the pandemic, whereby such approaches were in a unique position to reach members of diverse communities to boost uptake of the vaccine. Despite this, the support delivered by the VCFSE sector remains under-recognised and under-valued by the health system and decision-makers.
Conclusions
A number of challenges associated with collaborative working were experienced by the VSCE sector and health system in delivering the vaccination programme in partnership with the VCFSE sector. There is a need to create a broader, more inclusive health system which allows and promotes inter-sectoral working. Flexibility and adaptability in ongoing and future service delivery should be championed for greater cross-sector working.
Peer Review reports
The response to the COVID-19 pandemic saw a significant increase in demand for the voluntary, community, faith and social enterprise (VCFSE) sector to provide support to local communities [ 1 , 2 ]. The role of communities was seen as crucial to supporting the pandemic response, to better mobilise public health pandemic responses and supportive health services [ 3 ]. VCFSE organisations nationally had to quickly mobilise to adapt their service offer to meet increased demand, new gaps in service provision and deliver services in different ways to address the challenges faced by local communities. These included loss of income and financial hardship, closure of schools and childcare, increased social isolation, digital exclusion, and increased mental health issues [ 4 ]. However, previous research has concluded that support provided by the voluntary sector during the pandemic has been under-recognised [ 5 ]. Some authors have explored the role that VCFSEs played at the national level, in supporting communities during the pandemic [ 4 , 5 , 6 ]. Yet, whilst it is well-known that tens of thousands of UK volunteers supported local vaccine delivery [ 7 ], no existing academic literature has explored the role of VCFSEs in supporting the vaccination rollout.
We focus on Greater Manchester (GM), where increased support from VCFSE organisations, including smaller, community-based networks, responded to increased demand from local communities and the NHS to provide key health and wellbeing-related services, including food and care packages for clinically vulnerable households, food bank services, support for people experiencing homelessness, mental health and domestic violence services and support to local community organisations [ 8 ]. This support culminated in the sector’s supportive role in the delivery of the COVID-19 vaccination rollout, in response to the need for mass immunisation across the region.
Over the last decade, the English health and care system has been evolving to integrate health and social care. A key focus is building closer working relationships between the NHS, local authorities and other providers– including the VCFSE sector– to deliver joined up care for communities [ 9 , 10 ]. To aid integration, a new model for organising health and care on different geographical footprints has been developed: Integrated Care Systems (ICSs), place-based partnerships and neighbourhood models. These collaborative partnerships bring together existing health and care organisations to coordinate health and care planning and delivery in a more integrated way and include councils, NHS provider trusts, Primary Care Networks, GP federations and health and care commissioners [ 11 ]. These new geographically-based partnerships have an emphasis on collaborative working beyond traditional health and care partners. This includes acknowledging the role that VCFSE organisations can have in supporting wider population wellbeing, particularly as part of multi-disciplinary neighbourhood teams embedded in local communities [ 12 ]. National guidance on the development of ICSs and place-based partnerships strongly encourages health and care leaders to include VCFSE organisations in partnership arrangements and embed them into service delivery [ 12 ]. In GM, the partnership working approach pre-dates the formal mandating of ICSs, with a combined authority which brings together the ten local authorities and an association of Clinical Commissioning Groups (CCGs) which represented health commissioners, and a VCFSE umbrella group which also operates as a joint venture to represent the sector’s interests at a GM level Footnote 1 . However, reorganisation to the ICS system may present new local challenges for the VCFSE sector to find a meaningful ‘seat at the table’. That withstanding, the COVID-19 pandemic coincided with the development of ICSs and place-based partnerships as arguably one of the earliest and most intense tests of partnership working across health and care organisations within the current policy landscape.
Here, we present findings from a co-designed qualitative research project, drawing on insights from 35 participants, including members of diverse communities in GM, VCFSE participants, and key decision-making health and care system stakeholders. The aims of the study were to: understand the views and experiences of marginalised communities in GM during the COVID-19 pandemic; explore how community engagement initiatives played a role during the pandemic and vaccine rollout; assess what can be learnt from the work of key stakeholders (including community members, VCFSEs, health and care system stakeholders) for future health research and service delivery. The rationale for the study developed from a related piece of work assessing inequalities in the COVID-19 vaccine uptake in GM [ 13 ]. At that time, there was little research on the experiences of under-served communities during the pandemic. As such, the public and stakeholder engagement for the related project identified a need for a qualitative workstream to explore more fully the drivers behind and context surrounding the vaccination programme in GM, centring also local communities’ experiences during the pandemic (explored in a related paper [ 14 ]).
In this paper, we examine the role the VCFSE sector played in supporting unmet needs for marginalised groups in GM during the COVID-19 pandemic and as part of the rapid rollout of the COVID-19 vaccination programme. We consider the opportunities and barriers that may influence the full integration of the VCFSE sector into health and care services in the future. This paper provides additional evidence around the role of local community-led support in the context of identified unmet needs from marginalised local communities. Whilst focused on GM, it provides an exemplar of the role of VCFSEs and community networks during the pandemic, with relevant learning for other regions and international settings with place-based partnerships.
Study design
The study utilised a participatory approach throughout and was co-designed and co-produced with a diverse Community Research Advisory Group (CRAG). The CRAG were members of local community groups who were disproportionately impacted by the COVID-19 pandemic, including one member who is a co-author on this paper. This included members of three VCFSE organisations working with specific ethnic minority communities including Caribbean and African, South Asian and Syrian communities.
CRAG members acted as champions for the research, supporting design of appropriate information and fostering connections for recruitment via their existing community networks. The strong partnerships built through our approach were crucial to enabling a sense of trust and legitimacy for the research amongst underserved communities invited to participate.
Interviews and focus groups took place between September-November 2021 and sought to explore: the context surrounding the rollout of the vaccination programme; key aspects of support delivered as part of the vaccination programme; the use of localised approaches to support vaccine delivery including engagement initiatives, as well as broader community-level responses to the COVID-19 pandemic; perceptions around barriers to vaccine uptake Footnote 2 ; experiences of local communities (including healthcare) during the pandemic Footnote 3 . During the data collection period, national pandemic restrictions were largely lifted with no restrictions on social distancing or limits to gatherings, and all public venues reopened. A self-isolation period of 10 days after a positive COVID-19 test remained a legal requirement, but self-isolation after contact with a positive case was not required if fully vaccinated [ 15 ]. By July 2021, every UK adult had been offered their first dose of the COVID-19 vaccine, with every adult offered both doses by mid-September 2021 [ 16 ]. By early September 2021, more than 92 million doses had been administered in the UK [ 15 ].
Interviews and focus groups were conducted by one member of the research team (SG) and were conducted remotely due to the pandemic, via Zoom and telephone calls. The limitations of undertaking remote qualitative research interviews are acknowledged in academic literature, including potential restrictions to expressing compassion and assessing the participant’s environment [ 17 , 18 ]. However, given the remaining prevalence of COVID-19 at the time of interview, it was judged that the ensuing risk posed by COVID-19 to both researchers and participants outweighed the potential drawbacks. Nevertheless, participants were offered face-to-face options if they were unable to participate remotely to maximise inclusion (although no participants chose to participate face-to-face).
Interviews and focus groups were audio recorded with an encrypted recorder and transcribed by a professional transcription service. Informed written consent to participate was taken prior to the interviews and focus groups. The average length of the interviews was 34 min and average length of the focus groups was 99 min. Two focus groups were co-facilitated by a CRAG member, a member of the local community who works for a mental health charity that supports local South Asian communities, who also provided translation support. In respect to authors positionality, coauthors SG, RW, MS and CS are university researchers in academic roles and had prior links to the CRAG members via a wider community forum (co-ordinated by the NIHR funded Applied Research Collaboration for Greater Manchester). The wider group met regularly to discuss and share learning regarding community experiences, community action and related research during the pandemic. BI is a member of the CRAG and a member of a local Syrian community.
Sampling & recruitment
The sampling strategy for community participants centred around groups that had been disproportionately affected by the COVID-19 pandemic in England, including ethnic minority groups, young adults, and those with long-term physical and mental health conditions. VCFSE participants included community and religious leaders, members of local community VCFSE organisations and smaller, informal community networks and groups from local communities. Health and care system stakeholders included local council workers and health and care system stakeholders (e.g. those organising the vaccination response in CCGs and GP Federations). Characteristics of the sample are provided in Table 1 . Overall, the study achieved a diverse sample of participants on the basis of gender and ethnicity.
A combination of purposive and snowballing sampling was used to recruit via pre-established links and connections to community networks and stakeholders to ensure the inclusion of specific seldom-heard groups. For example, members of African and Caribbean communities were recruited via a charity which supports the health of these groups, and members of South Asian communities were recruited via a mental health charity.
Quotes are described by respondent type (community member, VCFSE participant, health and care system stakeholder) and participant identifier number to maintain anonymity whilst providing important contextual detail.
Data analysis
We analysed the data using an adapted framework approach [ 19 ]. We adopted a framework approach to analysis as this is viewed as a helpful method when working within large multidisciplinary teams or when not all members of the team have experience of qualitative data analysis, as was the case within our team. This structured thematic approach is also considered valuable when handling large volumes of data [ 20 , 21 ] and was found to be a helpful way to present, discuss and refine the themes within the research team and CRAG meetings. We created an initial list of themes from coding four transcripts, and discussions with CRAG members: personal or family experiences/stories; work/education experiences; racism and racialised experiences; trust and mistrust; fear and anxiety; value of community/community approaches; access to services including healthcare; operational and logistical factors around vaccine rollout; communication and (mis)information. We used this set of themes and sub themes to code the remaining transcripts, including further inductively generated codes as analysis progressed, regularly discussing within the team.
We shared transcript coding amongst the study team, with one team member responsible for collating coded transcripts into a charting framework of themes/subthemes with illustrative transcript extracts. The themes were refined throughout the analysis period (November 2021-March 2022) with the research team and CRAG and were sense-checked with CRAG members and the wider study team, to synthesise a final iteration of the themes and sub-themes (see supplementary material). We present findings related to five overarching themes: (1) unmet needs of local communities during the pandemic: inaccessible care and distrust; (2) community-led approaches: social support and leadership to support services; (3) community led support to COVID-19 vaccination delivery; (4) operational and logistical barriers to community-based pandemic responses: challenges faced by the voluntary and community sector; (5) learning from the pandemic response in GM: trust building and harnessing community assets. Themes are discussed in more detail below.
Ethical approval
This study was approved by University of Manchester Ethics Committee (Proportionate University Research Ethics Committee) 24/06/21. Ref 2021-11646-19665.
Unmet needs of local communities during the pandemic: inaccessible care and distrust
The COVID-19 pandemic brought an unprecedented shift in the way NHS services could function due to social distancing and lockdown measures. Pressures included unprecedented demand on hospital capacity and infection control measures (within hospitals and across the NHS) which reduced workforce capacity. There were also staff shortages due to high levels of COVID-19 infection amongst NHS staff, and shortages in non-acute capacity due to staff re-deployment [ 22 , 23 ]. In an effort to reduce pressure on the NHS, the policy mantra “Protect the NHS” was coined as a keynote slogan from the early stages of the pandemic [ 24 ].
It is within this context that many community participants raised (spontaneously) that there was a general inability to access health services during the pandemic, including GP and specialist services.
when I tried to contact my doctor’s surgery I was on the call for over an hour, number 20, number 15. Then by the time I’m under ten I get cut off. And it happened continuously. I just couldn’t get through and I just gave up really…now it’s like a phone consultation before you can even go and see someone, and even for that you’re waiting two, three weeks. (1029, VCFSE participant)
This resulted in frustration amongst some community participants, who questioned the logic of “protecting the NHS”, seemingly at the expense of their health-related needs. This led to sentiments that other health needs were de-prioritised by decision-makers during the pandemic. It was felt that this logic was counter-productive and fell short of the principles of protecting the most vulnerable.
We were like it just didn’t matter, it could have been much more serious than just a cough or a cold, [] but the help was just not there” (1028, community participant). what about people who actually need to see a doctor so the very vulnerable ones that we’re supposed to be protecting. Yes, we’re protecting the NHS, I understand that, I said, but we’ve also got to protect all those vulnerable people that are out there that are actually isolated (1011, community participant).
Community participants described their fear of accessing healthcare service because of potential risks of catching the virus in these settings, and fear of insufficient care due to well-publicised pressures in NHS settings. Some VCFSE participants noted that the widely publicised pressures faced by the NHS, and heightened media and political attention around COVID-19 cases in health settings led to fear and anxiety Footnote 4 .
I didn’t go to the hospital because I was scared shitless whether I was going to come out alive from hospital.” (1023, community participant). …the number of people who didn’t access services when they should have done… They were either terrified they were going to go into hospital and catch COVID straightaway and die, or they were terrified that they were taking [the hospital space] away from someone else (2003, VCFSE participant).
Overall, this led to a strong sense that mainstream services were not supporting the needs of local communities. This was especially felt for those requiring specialist services (e.g. mental health or secondary services), and for those who had faced intersecting inequalities, such as health issues, language and digital/IT barriers, and newly settled refugees and immigrants.
Community-led approaches: social support and leadership to support services
As a consequence of this unmet need, VCFSE and community participants identified that local communities themselves increased activities to provide community support. Participants felt strongly that this increased support provided by the VCFSE sector and community networks remains under-recognised and under-valued by the health system and wider public.
BAME organisations were going around door to door, giving hand sanitisers, giving masks to everybody [ ]. And it was the BAME community that was the most active during COVID delivering medication, delivering food to houses, doing the shopping. [ ] Nobody gave credit to that. Nobody talks about the good work that the BAME community has done. (1020, community participant)
A number of community and VCFSE sector participants highlighted the work done at the community level, by either themselves or other networks to support local communities. This included providing support packages, running errands for vulnerable community members, cooking and food shopping services, a helpline and communication networks for local communities, and online wellbeing and support groups.
We might not have been in hospital, but we were frontline workers in the community. (1028, community participant)
Support was provided by formal VCFSE organisations and by smaller, sometimes informal, community networks and channels, in which support mechanisms included mental health support and wellbeing focused communications to combat loneliness and boost wellbeing. This was often focused around outreach and the provision of community-based support to the most marginalised and vulnerable groups that had been disproportionately impacted during the pandemic, e.g. recently settled refugees and asylum seekers, older individuals.
We have an Iranian group in Salford…And one of them spotted this young woman in the queue and she thought she looked Iranian, you know….anyway she started a conversation, and this person had been an asylum seeker at the beginning of the pandemic and had been in a detention centre during the pandemic. And then, finally got their leave to remain and then were just basically dumped in Salford. [ ] just having that friendly face and someone was trying to start that conversation, she was able to be linked into this group of women who support other refugees and asylum seekers from the Middle East. (2014, VCFSE participant)
Community led support to COVID-19 vaccination delivery
The VCFSE sector and community networks also played a crucial part in supporting the COVID-19 vaccine delivery. Community, VCFSE and system-sector participants recognised the unique role that the VCFSE sector had played in reaching diverse communities and sections of communities not reached by the mainstream vaccination programme. For example, VCFSE groups aided vaccine delivery by helping run vaccine ‘pop-up’ sites in community spaces including mosques and other religious sites, children’s centres, and local specialist charities (e.g.: refugee and sex worker charities).
The use of community ‘champions’ and community ‘connectors’ to convey messaging around the vaccination drive were deemed especially vital in this regard. Trusted members of communities (e.g. community leaders) who had crucial pre-existing communication channels were able to effectively interact with different parts of communities to advocate for the vaccine and address misinformation. Situated within communities themselves, these ‘champions’ held established trust within communities, allowing conversations surrounding the vaccine to be held on the basis of shared experiences, honesty, openness, compassion and understanding.
So, as with any ethnic minority community, unless you’re part of it, it’s almost impossible to completely dig out all its norms and its very, very fine distinctions…[ ] what is acceptable, what is not acceptable[ ]? Unless you’re part of it, or you’ve really immersed yourself in the culture for decades, it’s almost impossible to get it (2015, VCFSE participant) One of the strongest approaches that you can take to increase uptake in any community, whether it be pregnant women or a faith group or a geographical area or a cultural group, is that if you’ve got a representative from that community leading on and advocating for the vaccine, you’re going to have the best impact (2011, health and care system stakeholder participant). unless Imams or significant people in the community were coming out for them and saying, it’s absolutely fine, it’s safe, and culturally it’s the right thing to do, there was a bit of uncertainty there (2010, health and care system stakeholder participant).
Health and care system stakeholders also emphasised the importance of “community ownership” of vaccination approaches, and of system responsiveness to identified needs and priorities at the community level. Health and care system stakeholders recognised that they were able to utilise community links to have better on-the-ground knowledge, provided in real time, to supplement locally held data to inform targeted efforts to boost uptake. This included council led initiatives including door-knocking with council staff, local health improvement practitioners, and VCFSE representatives working together to provide information about vaccine clinics and register people for vaccine appointments.
if messages went out and they didn’t land right they [the VCFSE sector] could be the first people [that] would hear about that and they could feed that back to us. [ ]….we were able to regularly go to them and say, look from a geographical perspective we can see these key areas…[ ] the people aren’t coming for vaccinations, [ ] what more can you tell us. Or, we can say, from these ethnicities in this area we’re not getting the numbers, what more can you tell us. And when we’ve fed them that intelligence then they could then use that to go and gain further insight for us, so they were a kind of, key mechanism (2010, health and care system participant).
Operational and logistical barriers to community-based pandemic responses: challenges faced by the voluntary and community sector
VCFSE sector and health and care system stakeholder participants reported significant logistical barriers to partnership working to support communities during the pandemic. Barriers included red tape and bureaucracy, which delayed responses to communities’ health and wellbeing needs.
whilst we were buying masks and hand sanitisers and going door to door, [ ] the council were still getting their paperwork in order, their policies in order, it was meeting after meeting. It took them seven to eight weeks for them to say [ ] we’ve got masks, would you like to help dish them out. (1029, VCFSE participant)
VCFSE and health and care system participants also raised challenges with respect to the VCFSE sector supporting the vaccination programme. This resulted in frustration amongst both VCFSE and health and care system participants who recognised the value of these community-based approaches.
The time that trickles through to the council and the time that the council turn around and say all right, we’ll actually let you do it was weeks later, and the community is turning round to us and saying to us well, what’s going on? We don’t like being messed around like this… (2008, VCFSE participant).
Participants highlighted the numerous health-related bodies with various roles which comprise a complex system for VCFSE partners to navigate, in part due to organisational and cultural clashes. Frustration was felt by both VCFSE and health and care system stakeholder participants (from local councils) in this respect. One VCFSE participant discussing the vaccine rollout noted:
We hit dead end after dead end within the council and there was literally very little response….You’ve got so many departments within this massive organisation called the council…[ ].it’s very difficult to navigate all that and deal with all that bureaucracy… (2008, VCFSE participant).
Broader institutional and organisational barriers to VCFSE support were identified, where cultural clashes between differing values and ways of working emerged, including ethos surrounding risk aversion and the system-level commitment to privilege value-for-money during the vaccination rollout. More practical issues around information governance and training were also raised as barriers to collaborative working.
I don’t think that they understand the power of community and the way community works. I don’t think that at a governmental level they understand what it means to penetrate into a community and actually understand what needs to be done to help a community…[ ] If they did and they had better links and ties into understanding that and helping that then we likely wouldn’t have had so many hurdles to get through (2008, VCFSE participant). ….in terms of public money, this is a public programme, we need to get value for the public pound. So we’re saying to [VCFSE organisation], how much is it going to cost? And [VCFSE organisation] are like, well, we don’t really know, until we deliver it. And we’re like, well, we can’t really approve it, until we know what it’s going to cost…. (2006, health and care system stakeholder participant)
Overall, these issues surmounted to difficulties of power-sharing between public sector organisations and VCFSEs during a time of rapid response to a public health crisis, political, institutional, and other external pressures. This was echoed amongst VCFSE and health and care system stakeholder participants, where frustration towards this was felt from both sides.
the public sector [ ] need to get better at letting go of some of the control. So even still, after I said, so many times, [VCFSE organisation] are delivering this, [VCFSE organisation] are doing everything, [ ] I still got the comms team going, are we doing a leaflet? No, [VCFSE organisation] are doing it, this is a [VCFSE organisation] programme, this isn’t a Council programme. (2006, local authority participant) it is difficult sometimes working with organisations, I find myself very much stuck in the middle sometimes [ ] I engage with [community groups] and ask them how best we do it and then we put things in place that they’ve asked for, and then they’ve told us it’s not working why have you done it like that. [ ] I think it’s acknowledgement to do it right, it takes time, and it takes effort, it takes resource. (2010, local authority participant)
Health and care system stakeholders also highlighted the importance of accessibility and localised vaccination hubs to reach different parts of diverse local communities e.g. sites in local mosques and sites near local supermarkets to reach different demographics. For instance, having mobile vaccination sites to reduce accessibility barriers, alongside dialogue-based initiatives to answer questions and respond to concerns from local communities about the vaccine, with the view to building trust without explicit pressure to receive the vaccine. Describing their efforts to engage with a member of the local community over the vaccine, two local health and care system stakeholders detailed the following example of how localised, communication-based approaches were deemed successful:
She came to the clinic and there were a lot of tears. It was very emotional. She’d been through a very difficult journey and had got pregnant by IVF, so it was a big decision for her, a big risk that she thought she was taking. Whether she took the vaccine or not, it felt like a risk to her, [ ] we were able to sit down and talk to her. We had some peers there. So we had other pregnant women there who’d had the vaccine, that were able to give her some confidence. We had the specialist multicultural midwife there, [ ] And we literally just sat and drank coffee with her and let her talk and she ended up agreeing to have the vaccine [ ] (2011, system-level stakeholder). …And the feedback from that lady was amazing. A couple of weeks ago I contacted her to make sure she was going to come down for her booster and she was just so grateful. [ ] she’d had backlash from her family and people within her community for taking up the vaccine and they still thought it was a massive risk. But she had no doubts that she’d done absolutely the right thing… (2012, system-level stakeholder).
Learning from the pandemic response in GM: trust building and harnessing community assets
Taking these findings from health and care system stakeholders, community and VCFSE participants, several learning points were identified.
In terms of vaccine delivery, some health and care system stakeholder participants reflected the need for more joined-up ways of working, across existing services and amongst VCFSE partners, to ensure efficiency and maximise uptake by embedding the vaccination programmes into other health services. For example, offering vaccination through health visiting or health checks, or offering COVID-19 vaccine boosters and flu vaccinations in single visits at care homes. These settings could also provide opportunities for dialogue with local communities where there is pushback against vaccination. Another health and care system stakeholder identified the need for greater joined up delivery of services; utilising the VCFSE sector to deliver multiple services simultaneously, including the vaccine, to improve vaccine uptake and access to other healthcare services:
the sex worker clinic is a good example of that. [ ] People were coming in for another reason, to get their health check and to get their support from the advisors there at that voluntary organisation, [ ]…if there’s a multiple purpose at the site, for people to attend, you can start to engage them in the conversation and then take the opportunity and vaccinate them. So I’m really interested in looking at that a little bit more, about how that can help to increase uptake. (2011, health and care system stakeholder participant)
A VCFSE participant suggested using educational settings such as schools as a channel to disseminate public health and vaccine-related information, as trusted settings which have wide-reach to many different communities.
A number of health and care system stakeholders, VCFSE and community participants noted that long-term, continuous, meaningful engagement is crucial to build longer-term trust between institutions and communities, and to improve the efficacy of public health measures. It was felt that more concentrated efforts were required from the NHS and other statutory organisations to reach the most marginalised and minoritised communities, for example through door-knocking and welfare calls. Participants highlighted that this was required not solely at times of public health crises, but as part of continued engagement efforts, in order to adequately engage with the most marginalised groups and effectively build long-term trust. This may be done most effectively by building on existing links to marginalised communities, for example using education liaison staff to understand traveller communities’ perspectives on the vaccine.
proactive engagement with communities both locally and nationally to say, [the health system] are looking at this, what’s people’s thoughts, views, you know, is there any issues with this, what more can we do, what do you need to know to make an informed decision. This is what we were thinking of, how would this land…I think we could learn by, [ ] doing that insight work, spending more time working with communities at a kind of, national, regional, and local level (2010, health and care system stakeholder participant). [the health system] could have engaged better with communities, I think bringing them in at the beginning. So, having them sat around the table, representatives from different groups, understanding how to engage with them from the very beginning…I think they could have used the data very very early on to inform who were engaging. We didn’t quite get it right at the beginning, we didn’t link the public health data teams with the comms and engagement teams (2013, health and care system stakeholder participant).
The tone of communications was also seen to be important. One health and care system stakeholder participant noted that the strategy of pushing communications and public health messaging aimed at behavioural change did not achieve the desired effect as these did not engage effectively with the communities to alleviate or address key concerns about the vaccine. These were deemed less successful than starting from a place of understanding and openness to generate constructive dialogue which could foster trust and respect.
There was also more specific learning identified in terms of collaboration between public sector institutions, VCFSEs and community links, with this seen as vital to build strong, long-term relationships between sectors based on trust and mutual respect. This should also involve working to share knowledge between sectors in real-time.
Health and care system stakeholder and VCFSE participants both suggested a failure to further develop partnerships fostered during the pandemic would be a lost opportunity that could potentially create distrust and additional barriers between communities, VCFSEs and public organisations, perhaps further marginalising seldom-heard groups.
we need to find ways which we have ongoing engagement, and I think it needs to be more informal. People don’t want to be just constantly asked and asked and asked (2010, health and care system stakeholder participant). a network of just sharing information and insight, rather than just engaging when you’ve got something specific to engage about. (2010, health and care system stakeholder participant) We were then thinking to ourselves, well, maybe we shouldn’t be doing this. If it’s going to cause us damage, if the council can’t work with us properly maybe we just shouldn’t do it. We’ve got to weigh up. We don’t want to lose our trust within the community (2008, VCFSE participant).
In terms of dynamics and working arrangements between sectors, participants thought it important to allow community organisations and VCFSEs to lead on their areas of speciality, e.g.: community organisations leading on outreach and communications within and to communities. This relates to the identified need of pursuing adaptable and flexible approaches to vaccine delivery. Moreover, there is a need to allow more joined-up decision-making between the health system and VCFSEs to ensure better use of local intelligence and improved planning.
Discussion & policy implications
Unmet need and the role of communities during the pandemic.
Our findings clearly demonstrate that local communities were not supported sufficiently by mainstream services during the COVID-19 pandemic. This in turn led to frustration, fear and loss of faith in the healthcare system as a whole, evidenced also in responses to the COVID-19 vaccination programme in which distrust results from wider experiences of historical marginalisation and structural inequalities [ 14 ]. In the absence of mainstream service support, our findings demonstrate how VCFSE organisations and community networks mobilised to support local communities to fulfil unmet health, social care, and wellbeing needs. This supports emerging evidence from across England which finds that the VCFSE sector played a key role in supporting communities during the pandemic [ 6 , 8 , 25 ].
The importance of community-based, localised approaches, community-led and community owned initiatives, ‘community champions’ and community connectors’ were also highlighted as crucial to the success of the COVID-19 vaccination drive. Participants noted that community-led approaches were uniquely positioned to reach some communities when mainstream approaches were unsuccessful. This is echoed in existing literature, where the role of localised community responses was deemed important to reach marginalised groups, as part of the wider pandemic response [ 26 ].
Operational and logistical barriers
Operational and logistical barriers created dissonance between communities and the system. These barriers included difficulties with decision-making and power-sharing between VCFSE and commissioning or clinical organisations, organisational cultural clashes, red-tape and bureaucracy, and complex systems and power structures to navigate. This builds on existing evidence of barriers to partnership working during the pandemic, including cultural clashes and bureaucracy/red tape [ 5 , 27 ]. The VCFSE sector also suffered from the closure of services, and reduced funding and resources due to increased demand for services and needing to adapt service provision [ 8 ].
These factors hindered collaborative working and created risk for VCFSEs, including putting tension on relationships with local communities resulting from delays implementing services. In most VCFSE-health system partnerships, participants noted that power is generally held by the health system partner, but reputational risk and additional resource-based costs lie with VCFSE partners. Supporting capacity building and workforce resource within the voluntary sector will strengthen this [ 28 ].
Inadequate processes to establish collaborative working enhance distrust between the health system and VCFSE sector, which in turn enhances difficulties for collaborative working. Trust is an important factor in how the system interacts with VCFSEs, with a lack of trust leading to further bottlenecks in VCFSE activities [ 29 ]. Alongside this, is the need for greater health system appreciation for the VCFSE sector, with VSCE partners reporting they faced greater scrutiny and more arduous administrative processes than private sector partners [ 2 , 29 ].
Learning from the pandemic: service prioritisation
All sectors of the health and care system face pressures from resource shortages, internal and external targets [ 30 , 31 ]. This is often linked to drives to increase the value-for-money of services, but key questions remain as to how to assimilate the goals of achieving health equity within value-for-money objectives [ 32 ]. To this end, prioritising value-for-money may come at odds with reducing health inequities. For example, during the rollout of the vaccination programme, additional resources and innovative approaches were required to reach marginalised communities [ 33 , 34 ]. This is supported by emerging evidence from England and internationally that efforts to drive vaccination uptake and reduce inequities in uptake amongst marginalised populations require significant resources and a breadth of approaches to maximise uptake [ 34 ]. Our findings suggest that changes in vaccine uptake were smaller and slower to be realised in these populations, resulting in a “slow burn” in terms of demonstrating quantifiable outcomes. Given the NHS principles of equity [ 10 , 35 ], reaching these groups should remain a public health priority, and failure to prioritise these groups may incur greater long-term financial costs resulting from greater health service needs. Our findings support that challenging entrenched attitudes and frameworks for how success is measured and adapting structures to better incentivise targeted interventions for marginalised or high-risk groups is essential to prioritising addressing unmet needs amongst marginalised communities.
The changing commissioning landscape
The development of ICSs and place-based partnerships has changed how health and care services are commissioned. National guidance encourages health and care leaders to include VCFSE organisations in partnership arrangements and embed them into service delivery [ 12 ], with ‘alliance models’ between ICSs and the VCFSE sector [ 36 ] established in certain regions (see for example [ 37 ]. However, this rests on “a partnership of the willing” [ 37 ] between ICS partners and VCFSE sector players, and concrete guidance for achieving collaborative working in practice, is lacking. As the findings in this paper point to, evolving decision-making processes may add to resource burdens for VCFSE organisations. Traditional health and care partners such as the NHS and local authorities should consider how their ways of working may need to change to foster full VCFSE inclusion on an equal standing, otherwise only the VCFSE stakeholders with sufficient capacity and resource may be able to be meaningfully involved.
Creating a VCFSE-accessible health and care system
In terms of fostering relationships between different sectors, participants acknowledged that pre-pandemic efforts to engage communities and community networks and VCFSEs were insufficient, with more meaningful, well-resourced engagement required going forward. It was also identified by participants the importance of avoiding tokenistic involvement of the VCFSE sector, which may be counter-productive for developing meaningful long-term partnerships. More equal relationships between statutory and VCFSE sectors are needed to foster improved collaborative working [ 5 , 38 ], and this is identified already at the GM level [ 28 ]. Central to this is actioned principles of co-design, including power-sharing, community ownership and trust. In order for co-design strategies to be successful, recognition of the role of the VCFSE sector and their ownership of approaches must be championed within co-design strategies and the enactment of co-designed activities.
Relatedly, greater trust of the VCFSE sector to deliver services effectively and efficiently is needed from health and social care decision-makers to ensure that funding compliance measures and processes are proportionate and not overly burdensome, to avoid funding bottlenecks which in turn impact service delivery [ 2 ]. Currently at the national level, VCFSE applicants typically only become aware of funding through existing networks, leaving less-connected organisations to find out ‘by chance’, thereby limiting reach amongst other organisations [ 2 ]. This may be especially true for smaller or ad-hoc VCFSE networks and groups. Our findings support that bottlenecks to applying for funding should be removed, and more streamlined processes for accessing funding championed [ 2 ].
Our findings also suggest that health systems should engage with the full breadth of the VCFSE sector, creating space for the involvement of smaller scale and less formal organisations as partners. Sharing of best practice and advice for adapting to local contexts should be promoted, alongside evaluation of collaborative models.
Finally, the pandemic period saw unprecedented state-sponsored investment into the VCFSE sector [ 29 ]. Within the GM context, this funding enabled VCFSEs to develop organisational capacity and systems, develop new partnerships, and better respond to the (unmet) needs of local communities [ 39 ]. Currently there are no clear plans to maintain this investment, but sustained inter-sector partnership working will require continued investment in the VCFSE sector.
Strengths & limitations
There are two main limitations to this study. Firstly, whilst the study achieved diversity in its sample, we could not achieve representation across all marginalised communities and therefore could not cover the experiences of all marginalised communities in-depth. As such, whilst the analyses provides valuable insights, such insights may not be transferrable and do not reflect all communities in GM. Secondly, whilst other studies focused on multiple city-regions or areas, our study is limited to the city region of GM. However, this focus provides an in-depth analysis on one region, and, as we discuss in the framing of the paper, we contend that the analysis presented in this paper serves as an exemplar to explore further at the national and international level. It should also be noted that co-design approaches are inevitably time and resource-heavy, and this was challenging in the context of this study, as local stakeholders wanted timely insights to inform the vaccination programme. However, one of the key strengths of our participatory approach was that this enabled a direct connection with the experiences of communities as relevant to the research, in order to shape the research questions, as well as the design and conduct of the study.
Overall, the contribution of the VCFSE sector during the pandemic is clear, with significant support provided in respect to community health and wellbeing and vaccination delivery. Nevertheless, there remains much to learn from the pandemic period, with the potential to harness capacity to tackle inequalities and build trust through shared learning and greater collaborative working. Maintaining an environment in which VCFSE partners are under-recognised, under-valued, and seemingly face further bureaucratic barriers will only exacerbate issues to collaborative working. There are also significant questions around systemic issues and sustainability, which must be addressed to overcome existing barriers to collaborative working between sectors. For instance, our findings identify the importance of flexibility and adaptability, in ongoing and future service delivery. Where this is not pursued this may not only impact service delivery but also create roadblocks to collaboration between sectors, creating divisions between entities whilst ultimately trying to effect change on similar goals (i.e. improved population health). ICS–VCFSE Alliances and community connectors may be a mechanism to promote this, but clear, actionable guidance will be required to translate rhetoric to real-world progress.
Data availability
Data for this research data will not be made publicly available as individual privacy could be compromised. Please contact Stephanie Gillibrand ([email protected]) for further information.
10 GM is an umbrella group which seeks to represent the VCSE sector in GM. More information is available here: https://10gm.org.uk/ .
These themes are explored in a related paper by Gillibrand et al. [ 14 ].
Topic guides are provided as supplementary material.
Distrust was also raised in relation to fear and anxiety in NHS settings, and this is discussed in detail in a related paper from this study by Gillibrand et al. [ 14 ].
Abbreviations
Clinical Commissioning Groups
Community Research Advisory Group
Greater Manchester
Integrated Care Systems
Voluntary, Community and Social Enterprise
Craston MRB. Susan Mackay, Daniel Cameron, Rebecca Writer-Davies, Dylan Spielman. Impact Evaluation of the Coronavirus Community Support Fund. 2021.
NatCen Social Research. Evaluation of VCSE COVID-19 Emergency Funding Package. Department for Digital, Culture, Media & Sport (DCMS); 2022. 27 April 2022.
Marston CRA, Miles S. Community participation is crucial in a pandemic. Lancet. 2020;395(10238):1676–8.
Article CAS PubMed PubMed Central Google Scholar
Frost S, Rippon S, Gamsu M, Southby K, Bharadwa M, Chapman J. Space to Connect Keeping in Touch sessions: A summary write up (unpublished). Leeds: Leeds Beckett University; 2021 2021.
Pilkington G, Southby K, Gamsu M, Bagnall AM, Bharadwa M, Chapman J, Freeman C. Through different eyes: How different stakeholders have understood the contribution of the voluntary sector to connecting and supporting people in the pandemic.; 2021.
Dayson CaW A. Capacity through crisis: The role and contribution of the VCSE Sector in Sheffield during the COVID-19 pandemic; 2021.
Timmins B. The COVID-19 vaccination programme: trials, tribulations and successes. The Kings Fund; 2022.
Howarth M, Martin P, Hepburn P, Sheriff G, Witkam R. A Realist evaluation of the state of the Greater Manchester Voluntary, Community and Social Enterprise Sector 2021. GMCVO/University of Salford; 2021.
NHS England. Five Year Forward View. Leeds. 2014 October 2014.
NHS England. The NHS Long Term Plan. NHS England. 2019 January 2019.
Surgey M. With great power: Taking responsibility for integrated care. 2022.
NHS England. Integrating care: next steps to building strong and effective integrated care systems across England. Leeds: NHS England; 2020.
Google Scholar
RE W. Ethnic inequalities in COVID-19 vaccine uptake and comparison to seasonal influenza vaccine uptake in Greater Manchester, UK: a cohort study. PLoS Med. 2022;19(3).
Gillibrand S, Kapadia D, Watkinson R, Issa B, Kwaku-Odoi C, Sanders C. Marginalisation and distrust in the context of the COVID-19 vaccination programme: experiences of communities in a northern UK city region. BMC Public Health. 2024;24(1):853.
Article PubMed PubMed Central Google Scholar
Cabinet Office. COVID-19 response: autumn and Winter Plan 2021. Guidance: GOV.UK; 2021.
Department of Health and Social Care. Every adult in UK offered COVID-19 vaccine [press release]. GOV.UK, 19 July 2021 2021.
Irani E. The Use of Videoconferencing for qualitative interviewing: opportunities, challenges, and considerations. Clin Nurs Res. 2019;28(1):3–8.
Article PubMed Google Scholar
Seitz S. Pixilated partnerships, overcoming obstacles in qualitative interviews via Skype: a research note. Qualitative Res. 2016;16(2):229–35.
Article Google Scholar
Gale NK. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):1–8.
Castleberry A, Nolen A. Thematic analysis of qualitative research data: is it as easy as it sounds? Curr Pharm Teach Learn. 2018;10(6):807–15.
Braun V, Clarke V. Thematic analysis. APA handbook of research methods in psychology, Vol 2: Research designs: Quantitative, qualitative, neuropsychological, and biological2012. pp. 57–71.
Burn S, Propper C, Stoye G, Warner M, Aylin P, Bottle A. What happened to English NHS hospital activity during the COVID-19 pandemic? Brief Note IFS; 2021 13th May 2021.
NHS. COVID-19: Deploying our people safely. 2020 [updated 30th April 2020. https://www.england.nhs.uk/coronavirus/documents/COVID-19-deploying-our-people-safely/ .
Department of Health and Social Care. New TV advert urges public to stay at home to protect the NHS and save lives. [press release]. Department of Health and Social Care, 21st. January 2021 2021.
McCabe A, Wilson M, Macmillian R. Stronger than anyone thought: communities responding to COVID-19. Local Trust. Sheffieldn Hallam University. TSRC.; 2020.
McCabe A, Afridi A, Langdale E. Community responses to COVID-19: connecting communities? How relationships have mattered in community responses to COVID-19 Local Trust. TSRC, Sheffield Hallam University; 2022. January 2022.
Carpenter J. Exploring lessons from Covid-19 for the role of the voluntary sector in Integrated Care Systems. July 2021. Oxford Brookes University; 2021.
Greater Manchester Combined Authority. GM VCSE Accord Agreement. 2021 [ https://www.greatermanchester-ca.gov.uk/media/5207/gm-vcse-accord-2021-2026-final-signed-october-2021-for-publication.pdf .
Department for Digital, Culture, Media & Sport. Financial support for voluntary, community and social enterprise (VCSE) organisations to respond to coronavirus (COVID-19).: Department for Digital, Culture, Media & Sport and Office for Civil Society. 2020 [updated 20th may 2020. https://www.gov.uk/guidance/financial-support-for-voluntary-community-and-social-enterprise-vcse-organisations-to-respond-to-coronavirus-COVID-19 .
Smee C. Improving value for money in the United Kingdom National Health Service: performance measurement and improvement in a centralised system. Measuring Up: Improving Health Systems Performance in OECD Countries; 2002.
McCann L, Granter E, Hassard J, Hyde P. You can’t do both—something will give: limitations of the targets culture in managing UK health care workforces. Hum Resour Manag. 2015;54(5):773–91.
Smith P. Measuring value for money in healthcare: concepts and tools. London: Centre for Health Economics, University of York. The Health Foundation; 2009 September 2009.
Ekezie W, Awwad S, Krauchenberg A, Karara N, Dembiński Ł, Grossman Z, et al. Access to Vaccination among Disadvantaged, isolated and difficult-to-Reach communities in the WHO European Region: a systematic review. Vaccines. 2022;10(7):1038.
British Academy. Vaccine equity in Multicultural Urban settings: a comparative analysis of local government and community action, contextualised political economies and moral frameworks in Marseille and London. London: The British Academy; 2022.
England NHS. Core20PLUS5 (adults)– an approach to reducing healthcare inequalities 2023. https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/core20plus5/ .
NHS England. Building strong integrated care systems everywhere 2021. Available from here: https://www.england.nhs.uk/wp-content/uploads/2021/06/B0664-ics-clinical-and-care-professional-leadership.pdf .
Anfilogoff T, Marovitch J. Who Creates Health in Herts and West Essex? Presentation to NHS Confederation Seminar: Who Creates Health? 8 November 2022. 2022.
Bergen JWS. Pandemic pressures: how Greater Manchester equalities organisations have responded to the needs of older people during the covid-19 crisis. GMCVO; 2021.
Graham M. Learning from Covid-19 pandemic grant programmes lessons for funders and support agencies. May 2022. GMCVO; 2022.
Download references
Acknowledgements
The research team would like to thank ARC-GM PCIE team (Sue Wood, Aneela McAvoy, & Joanna Ferguson) and the Caribbean and African Health Network for their support in this study. We would also like to thank the Advisory Group members: Nasrine Akhtar, Basma Issa and Charles Kwaku-Odoi for their dedicated time, commitment, and valuable inputs into this research project and to partners who contributed to the early inception of this work, including members of the ARC-GM PCIE Panel & Forum & Nick Filer. We would also like to extend our thanks to the study participants for their participation in this research.
The project was funded by an internal University of Manchester grant and supported by the National Institute for Health and Care (NIHR) Applied Research Collaboration for Greater Manchester. Melissa Surgey’s doctoral fellowship is funded by the Applied Research Collaboration for Greater Manchester. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
Author information
Authors and affiliations.
Centre for Primary Care and Health Services Research, University of Manchester, Greater Manchester, England, UK
Stephanie Gillibrand
NIHR Applied Research Collaboration for Greater Manchester, Greater Manchester, England, UK
Ruth Watkinson, Melissa Surgey & Caroline Sanders
Independent (public contributor), Greater Manchester, England, UK
Greater Manchester Patient Safety Research Centre, University of Manchester, Greater Manchester, England, UK
Caroline Sanders
You can also search for this author in PubMed Google Scholar
Contributions
SG, lead writer/editor, design of the work, RW, design of the work, drafting of article, review and revise suggestionsMS, draft of the article, review and revise suggestionsBI, design of the work, review and revise suggestionsCS, design of the work, draft of the article, review and revise suggestionsAll authors read and approved the final manuscript.
Corresponding author
Correspondence to Stephanie Gillibrand .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by University of Manchester Ethics Committee (Proportionate UREC) 24/06/21. Ref 2021-11646-19665. Informed consent to participate in the research was taken from all research participants ahead of their participation in the study. Consent to participate in the study was taken from each participant by a member of the research team. All experiments were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, supplementary material 5, supplementary material 6, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gillibrand, S., Watkinson, R., Surgey, M. et al. “ We might not have been in hospital, but we were frontline workers in the community ”: a qualitative study exploring unmet need and local community-based responses for marginalised groups in Greater Manchester during the COVID-19 pandemic. BMC Health Serv Res 24 , 621 (2024). https://doi.org/10.1186/s12913-024-10921-4
Download citation
Received : 10 November 2023
Accepted : 28 March 2024
Published : 13 May 2024
DOI : https://doi.org/10.1186/s12913-024-10921-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Marginalised groups
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

IMAGES
COMMENTS
The impact on research in progress prior to COVID-19 was rapid, dramatic, and no doubt will be long term. The pandemic curtailed most academic, industry, and government basic science and clinical ...
The spread of the "Severe Acute Respiratory Coronavirus 2" (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [].The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [], causing massive economic strain ...
Global research on coronavirus disease (COVID-19) WHO is bringing the world's scientists and global health professionals together to accelerate the research and development process, and develop new norms and standards to contain the spread of the coronavirus pandemic and help care for those affected. The R&D Blueprint has been activated to ...
Yet well into the fourth year of the Covid-19 pandemic, intense political and scientific debates about its origins continue. The two major hypotheses are a natural zoonotic spillover, most likely ...
Research and data on Coronavirus (COVID-19) from Pew Research Center Numbers, Facts and Trends Shaping Your World ... At least four-in-ten U.S. adults have faced high levels of psychological distress during COVID-19 pandemic. ... Our study analyzes 198 countries and territories and is based on policies and events in 2020, the most recent year ...
Find COVID-19 datasets, data tools, and publications to use in research. EXPLORE COVID-19 DATA. Learn how NIH is supporting research in COVID-19 testing, treatments, and vaccines.
Further research and more complete global data on national adherence to non-pharmaceutical interventions might help identify the other specific pathways by which government and interpersonal trust have affected COVID-19 outcomes, particularly for the first 10 months of the pandemic before vaccines were widely available.
Conducting such research has its challenges. The objective of this chapter is to review the impact of SARS-CoV-2 on ongoing and new pregnancy research during the pandemic, describe the challenges encountered and summarize the key strategies necessary for a successful research environment. Keywords: COVID-19, Pregnancy, Research, Pandemic.
For instance, in May 2020, shortly after the pandemic outbreak, 1,221 COVID studies were declared in the international clinical trial registry ... The impact of the COVID-19 pandemic on research. Trans Perioper Pain Med. 2021; 8:312-314. [Google Scholar] Atkinson C (2009) The backchannel: How audiences are using Twitter and social media and ...
A high prevalence of adverse psychiatric symptoms was reported in most studies. The COVID-19 pandemic represents an unprecedented threat to mental health in high, middle, and low-income countries. ... A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.069.
1. The COVID-19 pandemic has mobilised researchers worldwide on a scale and timeframe that have never been seen before for one specific disease. In hopes of rapid discovery of therapeutics, vaccines, and diagnostics for COVID-19, a substantial amount of money is being invested towards clinical research. Despite the sheer volume of research and ...
The conducted qualitative research was aimed at capturing the biggest challenges related to the beginning of the COVID-19 pandemic. The interviews were carried out in March-June (five stages of the research) and in October (the 6th stage of the research). A total of 115 in-depth individual interviews were conducted online with 20 respondents, in 6 stages. The results of the analysis showed ...
The COVID-19 outbreak has posed an unprecedented challenge to humanity and science. On the one side, public and private incentives have been put in place to promptly allocate resources toward research areas strictly related to the COVID-19 emergency. However, research in many fields not directly related to the pandemic has been displaced. In this paper, we assess the impact of COVID-19 on ...
Noah Deitrick and Adam Streff provided excellent research assistance. All errors that remain are ... In order to understand the impact of the COVID-19 pandemic on higher education, we surveyed ... One quarter of students increased their study time by more than 4 hours per week due to COVID-19, while another quarter decreased their study time by ...
The COVID-19 pandemic has affected a variety of researchers, students and academics. As institutions of higher education have limited in-person activities, research and training have been disrupted. Many graduate students have faced new barriers as a result (Chenneville and Schwartz-Mette, 2020; Thompson, 2020).
Mental health is a focus of NIH research during the COVID-19 pandemic. Researchers at NIH and supported by NIH are creating and studying tools and strategies to understand, diagnose, and prevent mental illnesses or disorders and improve mental health care for those in need. ... a five-year research study called RECOUP-NY to promote the mental ...
SARS-CoV-2 infection has physiologic effects on pregnancy that influence perinatal health, including immune and inflammatory responses that affect placental function. 1 To date, connections of COVID-19 with adverse perinatal outcomes have been documented in large population studies and meta-analyses, 2 but research separating individual SARS-CoV-2 infection from other changing risks during the ...
Interestingly, the pandemic period itself was associated with a lower risk of preterm birth, but a higher risk of hypertension and gestational diabetes. This is the first study to separate the infant and birth parent risks linked to the pre-pandemic period, the societal changes of the pandemic period, and individual COVID-19 infection.
In the first year of the COVID-19 pandemic, risk of death in people hospitalized for COVID-19 was substantially higher than in people hospitalized for seasonal influenza. 1,2 The risk of death due to COVID-19 has since declined. In fall-winter 2022-2023, people hospitalized for COVID-19 had a 60% higher risk of death compared with those hospitalized for seasonal influenza. 3 New variants of ...
Disparities in Total COVID-19 Cases and Deaths. As of August 5, 2022, the Centers for Disease Control and Prevention (CDC) reported a total of over 84 million cases, for which race/ethnicity was ...
In a study of 425 COVID-19 patients in Wuhan, ... Continued research into the virus is critical to trace the source of the outbreak and provide evidence for future outbreak . Conclusions. The current COVID-19 pandemic is clearly an international public health problem. There have been rapid advances in what we know about the pathogen, how it ...
This study aims to investigate the longitudinal associations of WNBC with health outcomes during the COVID-19 pandemic. We hypothesized that individuals who exhibited more such crafting behaviors at the onset of the pandemic would experience higher mental well-being and work engagement at later points in the COVID-19 pandemic, mediated by lower ...
The world experienced the severity of the 125 nm virus called the coronavirus disease 2019 (COVID-19), a pandemic declared by the World Health Organization (WHO) in 2019. ... The present study reviewed the protocols, formulation of research questions, selection of studies, appraisal of quality, and data abstraction and analysis. ...
The COVID-19 pandemic in the spring dramatically shifted the way children were being educated. From May 28 to June 2, when many school districts across the country are normally in session, 80% of people living with children distance learning reported the children were using online resources. About 20% were using paper materials sent home by the ...
The research project was supported by the Hellenic Foundation for Research and Innovation (H.F.R.I.) under the 4th Call for Action "Science and Society"- Emblematic Action - "Interventions to address the economic and social effects of the COVID-19 pandemic" (Project Number: 04958)
The COVID-19 pandemic has profoundly reshaped life across the globe, significantly influencing the future of housing. The enactment and densification of diverse activities within one place have resulted in varying degrees of conflict between the built and social environment. This conflict is directly related to the degree of housing adaptability to new life, work, and leisure conditions.
The response to the COVID-19 pandemic saw a significant increase in demand for the voluntary, community, faith and social enterprise (VCFSE) sector to provide support to local communities. In Greater Manchester (GM), the VCFSE sector and informal networks provided health and wellbeing support in multiple ways, culminating in its crucial supportive role in the provision of the COVID-19 ...