

FDA Approves New Vitiligo Treatment, Ruxolitinib (Opzelura)
The JAK inhibitor cream is the first medication that can restore pigment in people with this autoimmune disease.
On July 18, the U.S. Food and Drug Administration (FDA) approved ruxolitinib ( Opzelura ) cream 1.5 percent as a treatment for the most common form of vitiligo, according to a statement by Incyte, the manufacturer of the drug.
Vitiligo is a chronic autoimmune condition that causes patches of skin to lose pigment and turn milky white. The most prevalent form is nonsegmental (also known as generalized) vitiligo, in which white patches appear symmetrically on both sides of the body, such as on both hands or both knees, often covering large areas.
Ruxolitinib is the first medication that can restore pigment in patients with nonsegmental vitiligo. The FDA approved Incyte’s ruxolitinib cream for adults and children ages 12 and up.
“This approval is monumental,” says Daniel Gutierrez, MD , assistant professor of dermatology at NYU Grossman School of Medicine and dermatologist at NYU Langone Health in New York City, who was not involved in the drug development. “With Opzelura, we will have an FDA-approved pharmaceutical treatment option that can actually bring back color in patients who have vitiligo,” says Dr. Gutierrez.
He adds that prior to ruxolitinib, the only FDA-approved medication for vitiligo was monobenzyl ether of hydroquinone, a topical drug that removes pigment from skin to even out tones.
What Is Vitiligo?
Researchers estimate that between 1.9 and 2.8 million adults in the United States have vitiligo, with perhaps 40 percent of adults with vitiligo going undiagnosed.
Vitiligo causes immune cells to destroy melanocytes, the skin cells that produce pigment, according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases . “This makes vitiligo much more noticeable in patients of color — people whose skin is much more richly pigmented — because there is going to be much more of a contrast between the unaffected skin and the skin affected by the vitiligo,” says Gutierrez.
Vitiligo can occur at any age, but most people experience the initial symptoms before age 30.
About 50 Percent of People Using Ruxolitinib Had Significant Repigmentation After One Year
Ruxolitinib belongs to a class of drugs called Janus kinase (JAK) inhibitors. While doctors prescribe oral JAK inhibitors for diseases such as rheumatoid arthritis, ruxolitinib is the only topical JAK inhibitor approved in the United States.
The FDA previously approved ruxolitinib for mild to moderate atopic dermatitis (eczema) , in the fall of 2021.
JAK inhibitors work by decreasing the activity of the immune system, blocking certain enzymes that cause inflammation.
Patients using ruxolitinib apply the cream twice daily to the affected areas, covering up to 10 percent of their body’s surface area. It may take 24 weeks or more for people with vitiligo to see satisfactory results, according to Incyte.
The FDA based its approval on data from a clinical trial program that compared ruxolitinib to a placebo cream in more than 600 people (age 12 and older) with nonsegmental vitiligo. Investigators used the Vitiligo Area Scoring Index (VASI), a tool used to gauge disease severity and to measure improvements in face and body repigmentation.
In the two trials, by week 24 approximately 30 percent of people treated with ruxolitinib experienced significant improvements (at least 75 percent) as measured by VASI, which was the goal of the study. At one year, about 50 percent of those using the medication achieved that level of repigmentation.
“People using Opzelura had much more improvement in their vitiligo — very meaningful — compared to the placebo,” says Gutierrez.
The most common side effects seen in the trials were application-site acne, redness and itchiness, pharynx and nasal cavity inflammation, headache, urinary tract infection , and fever.
Ruxolitinib Comes With a Black Box Warning
The FDA added a black box warning to ruxolitinib, based on data showing that people taking oral JAK inhibitors faced a small increased risk of serious infections, major heart issues, clotting (thrombosis), cancer, and even death.
“However, in the clinical trials for people using ruxolitinib as a topical cream, the concentrations of the drug found in the blood were observed to be much lower compared to people who take ruxolitinib orally,” says Gutierrez. The same risks were not observed in the ruxolitinib trials, but the FDA is taking a “better safe than sorry” approach by including a warning on the box, he adds.
A conversation with your healthcare provider is the best way to determine whether the benefits of ruxolitinib outweigh the potential risks, as well as the need for any baseline and/or ongoing monitoring.
Patients Can Use Ruxolitinib on Their Face
Although dermatologists sometimes prescribe topical steroids off-label for vitiligo, there are risks when applying these medications to the face — the area where loss of pigment can impact appearance the most, says Gutierrez.
When used on the face, topical steroids can cause an acne-like rash that can persist for many months, called perioral dermatitis . Plus, “they can cause atrophy or dispigmentation, meaning you can have skin color changes. They can also thin the skin, cause stretch marks, and cause the growth of small blood vessels in the area,” Gutierrez says.
Ruxolitinib does not pose these risks, notes Gutierrez.
FDA Approval Means Better Access to Vitiligo Treatment
The FDA’s approval of ruxolitinib will definitely improve access to the drug by validating it as medically necessary. “Because vitiligo just creates a color change in the skin — there’s no itching or dermatitis under normal circumstances — sometimes it’s considered a cosmetic condition, meaning it’s not medically necessary to treat,” Gutierrez says. As a result, some insurers have declined to cover vitiligo treatments , according to the Vitiligo Research Foundation .
“However, this condition can dramatically impact how a patient sees themselves and how they present to the world. Vitiligo can cause significant psychological distress and negatively impact quality of life,” says Gutierrez.
“Vitiligo disproportionately impacts patients of color,” he adds. “This approval is an important step in improving a health disparity that does exist, and hopefully there will be more treatment options for vitiligo in the pipeline.”
How Much Will Ruxolitinib Cost?
The current Wholesale Acquisition Cost pricing is $1,950 for a 60 gram tube of Opzelura, according to Gabriella Greig, a spokesperson for Incyte. The actual cost to the consumer will vary depending on insurance coverage and how much of the cream is required for treatment.
“Incyte is committed to working with insurance providers in the U.S. to ensure eligible patients who can benefit from Incyte’s products have access to them,” says Greig. The company offers a copay savings card on its website for people with commercial insurance.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- News & Events for Human Drugs
FDA approves topical treatment addressing repigmentation in vitiligo in patients aged 12 and older
FDA has approved Opzelura (ruxolitinib) cream for the treatment of nonsegmental vitiligo in adult and pediatric patients 12 years of age and older. Opzelura is a topical Janus kinase (JAK) inhibitor currently approved for the topical short-term and non-continuous chronic treatment of mild to moderate atopic dermatitis in non-immunocompromised patients 12 years of age and older, whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable.
Opzelura is the first FDA-approved pharmacologic treatment to address repigmentation in vitiligo patients. Opzelura is applied twice a day to affected areas of up to 10% of the body’s surface area. Satisfactory patient response may require treatment with Opzelura for more than 24 weeks.
Disease or Condition
Nonsegmental vitiligo is the most common form of vitiligo. The condition involves loss of pigment (depigmentation) in patches of skin. Depigmentation may occur on the face, neck, and scalp, and around body openings such as the mouth and genitals, as well as areas that tend to experience rubbing or impact, such as the hands and arms.
Vitiligo is considered to be an autoimmune disorder. In people with vitiligo, the immune system appears to attack the pigment cells (melanocytes) in the skin. Many people with vitiligo are also affected by at least one other autoimmune disorder.
Effectiveness
Safety and effectiveness of Opzelura were demonstrated in two clinical trials, NCT04052425 and NCT04057573 . In both trials, subjects with nonsegmental vitiligo were randomized to treatment with Opzelura or placebo cream twice daily for 24 weeks, followed by an additional 28 weeks of treatment with Opzelura for all subjects. At the end of the 24-week treatment period, 30% of Opzelura patients had at least 75% improvement in the facial Vitiligo Area Scoring Index, compared with 10% of placebo patients.
Safety Information
The most common adverse reactions associated with Opzelura are application site acne, application site itching, common cold, headache, urinary tract infection, application site redness, and fever. Use of Opzelura in combination with therapeutic biologics, other JAK inhibitors, or potent immunosuppressants such as azathioprine or cyclosporine is not recommended.
Serious infections, mortality, malignancy, major adverse cardiovascular events, and thrombosis have been observed in patients treated with JAK inhibitors for inflammatory conditions.
See full prescribing information for additional information on risks associated with Opzelura.
Designation
Opzelura received priority review for this indication.
A new treatment is restoring skin coloration to some with vitiligo. It's giving patients hope.

- Vitiligo is an autoimmune disorder that leads to the loss of skin pigmentation.
- A recent study shows a medicated cream called ruxolitinib is extremely effective in about one-third of patients.
- The cream is giving patients hope that even if they don't benefit from the treatment there will soon be others.
Sarah Hayden owns a lot of turtlenecks. She also has chunky necklaces and tons of makeup – anything to cover up the blotchy white skin on her face, neck, hands and knees.
When she was about 23, Hayden was diagnosed with vitiligo, a noncontagious skin condition that leads to the loss of pigmentation. It struck first on the back of her neck and then, as with many people, slowly progressed under her eyes and across her face, before jumping down to her knees, elbows and fingertips.
Once, when she stepped into a hot tub, a woman made a comment about how people with skin conditions shouldn't be in hot tubs and paraded herself and her daughter out. Hayden pretended it didn't matter. That she still felt beautiful on the inside.
It was only when she joined a clinical trial for an experimental drug and her vitiligo began to recede that she "realized that having the skin condition affected me more than I thought it did," said Hayden, now 41, of Hood River, Oregon.
The medicated cream she used as part of that trial, ruxolitinib, was approved by the Food and Drug Administration this summer. Late Wednesday, The New England Journal of Medicine published a study showing ruxolitinib cream is extremely effective in about one-third of patients who use it for at least six months.
What is vitiligo and its treatment?
Somewhere between half a percent and 2% of people worldwide have vitiligo, which is now understood to be an autoimmune disorder, where the immune system attacks the cells in the skin that provide pigment.
Famous people with vitiligo include Michael Jackson, model Winnie Harlow, actor and director Jon Hamm, comedian Steve Martin, commentator and comedian Joe Rogan, and NFL player-turned coach Karl Dunbar.
The condition can be particularly distressing for people with naturally dark skin because the light blotches stand out even more.
Only one treatment has previously been approved by the FDA and it removes more coloration, to avoid blotchiness, rather than restoring the skin's natural color as ruxolitinib cream can sometimes do.
Right now, many patients are treated with steroids, which don't work well, or given controlled phototherapy sessions, which can be hard to access for people who live far from a center that offers it, said Dr. David Rosmarin, a lead author on the new study.
MORE: For patients with earliest stage of breast cancer, how much treatment is enough?
How ruxolitinib works
The use of ruxolitinib cream reflects a new understanding of vitiligo, Rosmarin said. It works by tamping down an overactive immune response. "We are now better at modulating, rebalancing" that arm of the immune system, Rosmarin said.
About 30% of the 450 people who received active treatment as part of two studies saw a dramatic improvement in facial pigmentation after six months. Up to half did after a year of treatment, indicating that the cream became more potent over time. More than 80% of people in both trials were white and only 3% to 5% were Black or Asian.
Formulated as a cream ruxolitinib does not affect the whole body, so side effects are relatively minor, usually just some acne where the cream is used, Rosmarin said.
Ruxolitinib cream seems to work best on the head and neck, with hands and feet the hardest to repigment, Rosmarin said. It's not yet known whether someone can take ruxolitinib for a period of time and then stop, or whether vitiligo will return without constant dosing.
Commercial insurers and Medicare have been covering ruxolitinib cream, Rosmarin said, now that there's "broad agreement in the medical community that it is a medical not cosmetic condition and treatment should be covered." One tube of the cream costs about $2,000 and can last anywhere from a few weeks to a few months, depending on how much skin needs to be covered.
The amount of time a patient had vitiligo didn't affect their likelihood of success.
People who had poliosis vitiligo, or a total loss of pigmentation leading to pure white hairs, did not improve on the drug, said Dr. Brett King, who was not directly involved in the study but consults for Incyte, the Delaware-based company that makes ruxolitinib cream and sells it under the brand name Opzelura.
Researchers are also developing other approaches to treating vitiligo for those who don't see much improvement with ruxolitinib cream, Rosmarin said.
The study and recent approval of ruxolitinib cream "sets a pathway for other treatments to hopefully move forward," he said. "This is just the start."
RESEARCH: These rats have human cells in their brains. They may help scientists understand autism and schizophrenia.
The origins of the new approach date to 2017 when King, an associate professor of dermatology at Yale University, decided to test a rheumatoid arthritis drug in a mouse that works in the same way as ruxolitinib. It seemed to help, so he gave it to a patient who had the condition "from nose to toes," he said. Her dramatic improvement "was our first clue" that his approach might work.
"When you have an observation, but in particular one anchored in science, not just in chance observation, it leads to paradigm shifts in how we think about disease and treat disease," King said.
The success with ruxolitinib will encourage other drug companies to develop vitiligo treatments, he said.
Because it takes so long to see a benefit from ruxolitinib cream, it would be useful to find a way of distinguishing patients who will respond well from those who won't, Dr. Liv Eidsmo wrote in an editorial accompanying the new study.
Eidsmo, a dermatologist and researcher at Karolinska University Hospital in Sweden, also pointed out that it's not clear what will happen if patients stop using the cream and raised concerns about the lack of diversity among trial participants, who were largely white.
Still, she wrote, thanks to ruxolitinib, "patients with vitiligo finally have the hope of efficient treatments."
WHAT DOCS WANT YOU TO KNOW: Study raises questions about colonoscopies
'It gave me back something I lost'
Hayden is one of those lucky patients.
The cream has returned about 90% of the pigment to her face. Even her hands, considered the hardest to reach for the drug, have mostly cleared up.
"It gave me back something I lost," said Hayden, who was wearing a V-neck shirt and a thin gold necklace on a recent video call. On weekends, she no longer insists on wearing makeup before leaving the house.
An instructional coach in her town's school district, Hayden had almost no side effects from the cream and didn't find it a burden to spread on her face, chest and hands twice a day during the two-year trial. "It was just part of my morning routine," she said, "and it was part of my bedtime routine after I brushed my teeth."
The treatment changed her relationship with the sun. Before, she would wear high SPF sunblock, a hat and long sleeves if she was in the sun for long periods. With vitiligo, she said "you are either normal or burnt," there was no such thing as a tan.
During the trial, she said, she was encouraged to get limited amounts of sun exposure to promote skin regeneration. "Now, I feel like when I'm in the sunlight, it's regenerative instead of harmful," she said. "I have to be careful, but it's not the same burden as it was."
Hayden said she's grateful to have been able to participate in the research to help others avoid some of the same challenges she's faced.
"That really kind of fueled my 'why' for engaging in the trial," she said. "Not just for my own hope and excitement – which it did 100% and I would do it again in a heartbeat – but also potentially having this available to other people living with vitiligo."
Contact Karen Weintraub at [email protected].
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input.
Ruxolitinib Cream 1.5%: A Review in Non-Segmental Vitiligo
- Adis Drug Evaluation
- Published: 16 April 2024
Cite this article
- Connie Kang 1
37 Accesses
Explore all metrics
Topical ruxolitinib 1.5% cream (Opzelura ® ), a Janus kinase (JAK) inhibitor, is the first treatment to be approved in several countries for use in patients aged ≥ 12 years with non-segmental vitiligo. In the identical phase III TRuE-V1 and TRuE-V2 trials, significantly more ruxolitinib cream recipients were able to achieve statistically significant and clinically meaningful facial and total body repigmentation, as well as reductions in vitiligo noticeability, compared with vehicle recipients. Efficacy was sustained in longer-term analyses to week 104 of treatment. Ruxolitinib 1.5% cream was generally tolerable in these trials; the most common treatment-related adverse events were acne, pruritus and exfoliation, all at the application site. As with orally administered JAK inhibitors, topical ruxolitinib carries boxed warnings in the USA for serious infections, mortality, malignancy, major adverse cardiovascular events (MACE) and thrombosis, although the incidences were low with topical application. Thus, topical ruxolitinib 1.5% cream is an effective and generally tolerable treatment option for patients aged ≥ 12 years with non-segmental vitiligo.
Plain Language Summary
Non-segmental vitiligo is a chronic autoimmune disease where the skin throughout the body loses its pigmentation, and is usually managed with topical therapies, light therapy or surgery. Topical ruxolitinib 1.5% cream (Opzelura ® ) is the first treatment approved in several countries for patients aged ≥ 12 years with non-segmental vitiligo. It inhibits Janus kinase (JAK) proteins, reducing the destruction of skin pigment-producing cells. In two clinical trials, significantly more ruxolitinib cream recipients achieved significant and meaningful skin repigmentation compared with patients who received a non-medicated cream; these results were sustained to week 104 of treatment. Ruxolitinib 1.5% cream was generally tolerable; the most common treatment-related adverse events were acne, itchiness and exfoliation, all at the application site. Topical ruxolitinib has special warnings in the USA for major adverse cardiovascular events (MACE), blood clots, serious infections, death and cancer (associated with the use of oral JAK inhibitors), although incidence rates for these adverse events were low in the clinical trials. Topical ruxolitinib 1.5% cream is an effective and generally tolerable treatment option for patients aged ≥ 12 years with non-segmental vitiligo.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
Manage vitiligo with a personalised approach: consider old and new treatments
Nicole L. France
Trifarotene: First Approval
Lesley J. Scott

Real-World Use of Ruxolitinib Cream: Safety Analysis at 1 Year
Wilson Hu, Michele Thornton & Robert A. Livingston
Böhm M, Schunter JA, Fritz K, et al. S1 guideline: diagnosis and therapy of vitiligo. J Dtsch Dermatol Ges. 2022;20(3):365–78.
PubMed Google Scholar
van Geel N, Speeckaert R, Taïeb A, et al. Worldwide expert recommendations for the diagnosis and management of vitiligo: position statement from the International Vitiligo Task Force part 1: towards a new management algorithm. J Eur Acad Dermatol Venereol. 2023;37(11):2173–84.
Article PubMed Google Scholar
AL-smadi K, Imran M, Leite-Silva VR, et al. Vitiligo: a review of aetiology, pathogenesis, treatment, and psychosocial impact. Cosmetics. 2023;10(3):84.
Article CAS Google Scholar
Bibeau K, Ezzedine K, Harris JE, et al. Mental health and psychosocial quality-of-life burden among patients with vitiligo: findings from the global VALIANT study. JAMA Dermatol. 2023;159(10):1124–8.
Article PubMed PubMed Central Google Scholar
Seneschal J, Speeckaert R, Taïeb A, et al. Worldwide expert recommendations for the diagnosis and management of vitiligo: position statement from the international Vitiligo Task Force part 2: specific treatment recommendations. J Eur Dermatol Venerol. 2023;37(11):2185–95.
Article Google Scholar
Martins C, Migayron L, Drullion C, et al. Vitiligo skin T cells are prone to produce type 1 and type 2 cytokines to induce melanocyte dysfunction and epidermal inflammatory response through Jak signaling. J Investig Dermatol. 2022;142(4):1194-205.e7.
Article CAS PubMed Google Scholar
Incyte Biosciences Distribution B.V. Opzelura 15 mg/g cream: EU summary of product characteristics. 2023. https://www.ema.europa.eu . Accessed 20 Mar 2024.
Incyte Biosciences UK Ltd. Opzelura 15mg/g cream: UK summary of product characteristics. 2023. https://products.mhra.gov.uk . Accessed 20 Mar 2024.
Incyte Corporation. OPZELURA™ (ruxolitinib) cream, for topical use: US prescribing information. 2022. https://dailymed.nlm.nih.gov . Accessed 20 Mar 2024.
Hoy SM. Ruxolitinib cream 1.5%: a review in mild to moderate atopic dermatitis. Am J Clin Dermatol. 2023;24(1):143–51.
Fridman JS, Scherle PA, Collins R, et al. Preclinical evaluation of local JAK1 and JAK2 inhibition in cutaneous inflammation. J Investig Dermatol. 2011;131(9):1838–44.
Persaud I, Diamond S, Pan R, et al. Plasma pharmacokinetics and distribution of ruxolitinib into skin following oral and topical administration in minipigs. Int J Pharm. 2020;590(119889):1–6.
Google Scholar
Rothstein B, Joshipura D, Saraiya A, et al. Treatment of vitiligo with the topical Janus kinase inhibitor ruxolitinib. J Am Acad Dermatol. 2017;76(6):1054-60.e1.
Rosmarin D, Pandya AG, Lebwohl M, et al. Ruxolitinib cream for treatment of vitiligo: a randomised, controlled, phase 2 trial. Lancet. 2020;396(10244):110–20.
Harris JE, Pandya AG, Lebwohl M, et al. Safety and efficacy of ruxolitinib cream for the treatment of vitiligo: 156-week data from a phase II study [abstract no. P96 plus poster]. Br J Dermatol. 2022;187(Suppl. 1):80–1.
Rosmarin D, Passeron T, Pandya AG, et al. Two phase 3, randomized, controlled trials of ruxolitinib cream for vitiligo. N Engl J Med. 2022;387(16):1445–55.
Rosmarin D, Ezzedine K, Desai S. Efficacy and safety of ruxolitinib cream for the treatment of vitiligo by patient demographics and baseline clinical characteristics: pooled subgroup analysis from two randomized phase 3 studies [abstract no. 35187 plus poster]. J Am Acad Dermatol. 2022;87(3):AB50.
Rosmarin D, Ezzedine K, Md P, et al. Efficacy and safety of ruxolitinib cream for the treatment of vitiligo: week 24 pooled analysis of the TRuE-V phase 3 studies [abstract no. 34789 plus poster]. J Am Acad Dermatol. 2022;87(3):AB51.
Ezzedine K, van Geel N, Butler K, et al. Subgroup analysis of quality of life and treatment satisfaction by disease duration and use of prior treatment: pooled results from two randomized phase 3 studies of ruxolitinib cream for the treatment of vitiligo [abstract no. CO108 plus poster]. Value Health. 2022;25(7 Suppl.):S324.
Pandya AG, van Geel N, Butler K, et al. Subgroup analysis of quality of life and treatment satisfaction by baseline patient characteristics: pooled results from two randomized phase 3 studies of ruxolitinib cream for the treatment of vitiligo [abstract no. CO96 plus poster]. Value Health. 2022;25(7 Suppl.):S321–2.
Harris JE, Rosmarin D, Seneschal J, et al. Facial vitiligo area scoring index response maintenance or shift during 52 weeks of ruxolitinib cream treatment for vitiligo: pooled analysis of the TRuE-V phase 3 studies [abstract no. 43912 plus poster]. In: American Academy of Dermatology (AAD) Annual Meeting. 2023.
Rosmarin D, Harris JE, Wolkerstorfer A, et al. Total vitiligo area scoring index response maintenance or shift during 52 weeks of ruxolitinib cream treatment for vitiligo: pooled analysis of the TRuE-V phase 3 studies [abstract no. 43938 plus poster]. In: American Academy of Dermatology (AAD) Annual Meeting. 2023.
Ezzedine K, Passeron T, Rosmarin D, et al. Vitiligo noticeability scale score maintenance or shift during 52 weeks of ruxolitinib cream treatment for vitiligo: pooled analysis of the TRuE-V phase 3 studies [abstract no. 43959 plus poster]. In: American Academy of Dermatology (AAD) Annual Meeting. 2023.
Seneschal J, Wolkerstorfer A, Desai SR, et al. Efficacy and safety of ruxolitinib cream for the treatment of vitiligo by patient demographics and baseline clinical characteristics: week 52 pooled subgroup analysis from two randomized phase 3 studies [abstract no. 555 plus poster P1383]. In: 31st European Academy of Dermatology and Venereology (EADV) Congress. 2022.
Seneschal J, Grimes P, Desai SR, et al. Efficacy and safety of ruxolitinib cream in adolescent patients with vitiligo: pooled analysis of the 52-week TRuE-V phase 3 studies. In: Society for Pediatric Dermatology 47th Annual Meeting. 2022.
Seneschal J, Wolkerstorfer A, Ezzedine K, et al. Efficacy and safety of ruxolitinib cream through week 104 in patients with vitiligo: subgroup analysis of the TRuE-V long-term extension phase 3 study [abstract no. 927 plus poster P2229]. In: 32nd European Academy of Dermatology and Venereology (EADV) Congress. 2023.
Rosmarin D, Sebastian M, Amster M, et al. Facial and total vitiligo area scoring index response shift during 104 weeks of ruxolitinib cream treatment for vitiligo: results from the open-label arm of the TRuEV long-term extension phase 3 study [abstract plus presentation]. In: American Academy of Dermatology (AAD) Annual Meeting. 2023.
Pandya AG, Ezzedine K, Rosmarin D, et al. Treatment-emergent adverse events of interest for janus kinase inhibitors: pooled analysis of the 52-week TRuE-V phase 3 studies of ruxolitinib cream treatment for vitiligo [abstract no. 43978 plus poster]. In: American Academy of Dermatology (AAD) Annual Meeting. 2023.
Hu W, Thornton M, Livingston RA. Real-world use of ruxolitinib cream: safety analysis at 1 year. Am J Clin Dermatol. 2024;25(2):327–32.
Eleftheriadou V, Atkar R, Batchelor J, et al. British Association of Dermatologists guidelines for the management of people with vitiligo 2021. Br J Dermatol. 2021;186(1):18–29.
Kitchen H, Wyrwich KW, Carmichael C, et al. Meaningful changes in what matters to individuals with vitiligo: content validity and meaningful change thresholds of the Vitiligo Area Scoring Index (VASI). Dermatol Ther (Heidelb). 2022;12(7):1623–37.
Ehsan M, Rehman AU, Ayyan M, et al. Efficacy and safety of topical ruxolitinib cream for the treatment of vitiligo: a systematic review and meta-analysis of randomized controlled trials. J Cosmet Dermatol. 2023;31(1):350–3.
Download references
Acknowledgements
During the peer review process, the manufacturer of ruxolitinib cream was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and affiliations.
Springer Nature, Private Bag 65901, Mairangi Bay, Auckland, 0754, New Zealand
Connie Kang
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Connie Kang .
Ethics declarations
The preparation of this review was not supported by any external funding.
Authorship and Conflict of interest
Connie Kang is a salaried employee of Adis International Ltd/Springer Nature, and declares no relevant conflicts of interest. All authors contributed to this article and are responsible for its content.
Ethics approval, Consent to participate, Consent to publish, Availability of data and material, Code availability
Not applicable.
Additional information
The manuscript was reviewed by : D. Ioannidis , 1st Department of Dermatology, Aristotle University School of Medicine, Thessaloniki, Greece; M.Y. Wang , Department of Dermatology, Peking University First Hospital, Beijing, China.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PDF 219 KB)
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Kang, C. Ruxolitinib Cream 1.5%: A Review in Non-Segmental Vitiligo. Drugs (2024). https://doi.org/10.1007/s40265-024-02027-2
Download citation
Accepted : 19 March 2024
Published : 16 April 2024
DOI : https://doi.org/10.1007/s40265-024-02027-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Vitiligo articles from across Nature Portfolio
Vitiligo is a skin disease that is characterized by loss of pigmentation caused by death or dysfunction of melanocytes, which are pigment producing cells. Autoimmune processes, oxidative stress, genetic factors and environmental triggers all have been implicated in the pathogenesis of the disease.
Latest Research and Reviews

Sexual dimorphism in melanocyte stem cell behavior reveals combinational therapeutic strategies for cutaneous repigmentation
Vitiligo is an autoimmune condition that results in skin depigmentation due to melanocyte loss, but the root causes are not well understood. Here they identify sexual dimorphism in melanocyte stem cells behavior arising from distinct skin inflammatory responses, and propose Prostaglandin E2 as a potential therapy for depigmentation conditions.
- Andrew C. White

Based on network pharmacology and bioinformatics to analyze the mechanism of action of Astragalus membranaceus in the treatment of vitiligo and COVID-19
- Yaojun Wang
Associations between serum levels of brain-derived neurotrophic factor, corticotropin releasing hormone and mental distress in vitiligo patients
- Assiya Kussainova
- Laura Kassym
- Yuliya Semenova

Vitiligo-specific soluble biomarkers as early indicators of response to immune checkpoint inhibitors in metastatic melanoma patients
- Maria Luigia Carbone
- Gabriele Madonna
- Cristina Maria Failla
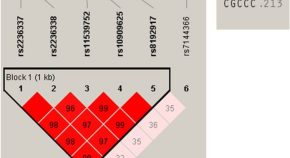
Association of GZMB polymorphisms and susceptibility to non-segmental vitiligo in a Korean population
- Ki-Heon Jeong
- Su Kang Kim
- Mu-Hyoung Lee
Association of multiple sclerosis with vitiligo: a systematic review and meta-analysis
- Meng-Han Shen
- Chau Yee Ng
- Ching-Chi Chi
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
On this page
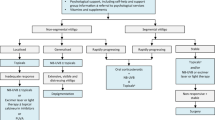
Alternative medicine, coping and support, preparing for your appointment.
Your health care provider will ask about your medical history and examine your skin, possibly with a special lamp. The evaluation might also include a skin biopsy and blood tests.
More Information
- Antinuclear antibody (ANA) test
- Complete blood count (CBC)
- Skin biopsy
The choice of treatment depends on your age, how much skin is involved and where, how quickly the disease is progressing, and how it's affecting your life.
Medications and light-based therapies are available to help restore skin color or even out skin tone, though results vary and are unpredictable. And some treatments have serious side effects. So your health care provider might suggest that you first try changing the appearance of your skin by applying a self-tanning product or makeup.
If you and your health care provider decide to treat your condition with a drug, surgery or therapy, the process may take many months to judge its effectiveness. And you may have to try more than one approach or a combination of approaches before you find the treatment that works best for you.
Even if treatment is successful for a while, the results may not last or new patches may appear. Your health care provider might recommend a medication applied to the skin as maintenance therapy to help prevent relapse.
Medications
No drug can stop the process of vitiligo — the loss of pigment cells (melanocytes). But some drugs, used alone, in combination or with light therapy, can help restore some color.
Drugs that control inflammation. Applying a corticosteroid cream to affected skin might return color. This is most effective when vitiligo is still in its early stages. This type of cream is effective and easy to use, but you might not see changes in your skin's color for several months. Possible side effects include skin thinning or the appearance of streaks or lines on your skin.
Milder forms of the drug may be prescribed for children and for people who have large areas of discolored skin.
Corticosteroid pills or injections might be an option for people whose condition is progressing rapidly.
- Medications that affect the immune system. Calcineurin inhibitor ointments, such as tacrolimus (Protopic) or pimecrolimus (Elidel) might be effective for people with small areas of depigmentation, especially on the face and neck. The U.S. Food and Drug Administration (FDA) has warned about a possible link between these drugs and lymphoma and skin cancer.
Light therapy. Phototherapy with narrow band ultraviolet B (UVB) has been shown to stop or slow the progression of active vitiligo. It might be more effective when used with corticosteroids or calcineurin inhibitors. You'll need therapy two to three times a week. It could take 1 to 3 months before you notice any change, and it could take 6 months or longer to get the full effect.
Given the Food and Drug Administration (FDA) warning regarding possible risk of skin cancer with use of calcineurin inhibitors, talk with your health care provider about the risks and benefits of using these drugs with phototherapy.
For people who can't go to a clinic for treatment, smaller portable or handheld devices for narrow band ultraviolet B therapy are available for home use. Talk with your health care provider about this option as well if needed.
Possible side effects of narrow band ultraviolet B therapy include redness, itching and burning. These side effects usually clear up within a few hours after treatment.
- Combining psoralen and light therapy. This treatment combines a plant-derived substance called psoralen with light therapy (photochemotherapy) to return color to the light patches. After you take psoralen by mouth or apply it to the affected skin, you're exposed to ultraviolet A (UVA) light. This approach, while effective, is more difficult to administer and has been replaced in many practices by narrow band ultraviolet B (UVB) therapy.
Removing the remaining color (depigmentation). This therapy may be an option if your vitiligo is widespread and other treatments haven't worked. A depigmenting agent is applied to unaffected areas of skin. This gradually lightens the skin so that it blends with the discolored areas. The therapy is done once or twice a day for nine months or longer.
Side effects can include redness, swelling, itching and very dry skin. Depigmentation is permanent.
If light therapy and medications haven't worked, some people with stable disease may be candidates for surgery. The following techniques are intended to even out skin tone by restoring color:
Skin grafting. In this procedure, your doctor transfers very small sections of your healthy, pigmented skin to areas that have lost pigment. This procedure is sometimes used if you have small patches of vitiligo.
Possible risks include infection, scarring, a cobblestone appearance, spotty color and failure of the area to recolor.
Blister grafting. In this procedure, your doctor creates blisters on your pigmented skin, usually with suction, and then transplants the tops of the blisters to discolored skin.
Possible risks include scarring, a cobblestone appearance and failure of the area to recolor. And the skin damage caused by suctioning may trigger another patch of vitiligo.
Cellular suspension transplant. In this procedure, your doctor takes some tissue on your pigmented skin, puts the cells into a solution and then transplants them onto the prepared affected area. The results of this repigmentation procedure start showing up within four weeks.
Possible risks include scarring, infection and uneven skin tone.
Potential future treatments
Treatments being studied include:
- A drug to stimulate color-producing cells (melanocytes). Called afamelanotide, this potential treatment is implanted under the skin to promote the growth of melanocytes.
- A drug that helps control melanoctyes. Prostaglandin E2 is being tested as a way to restore skin color in people with vitiligo that isn't widespread or spreading. It's applied to the skin as a gel.
If you have vitiligo, the following self-care tactics may help you care for your skin and improve its appearance:
Protect your skin from the sun and artificial sources of UV light. Use a broad-spectrum, water-resistant sunscreen with an SPF of at least 30. Apply sunscreen generously and reapply every two hours — or more often if you're swimming or sweating.
You can also seek shade and wear clothing that shields your skin from the sun. Don't use tanning beds and sunlamps.
Protecting your skin from the sun helps prevent sunburn of the discolored skin. Sunscreen also minimizes tanning, which accentuates the vitiligo patches.
- Conceal affected skin. Makeup and self-tanning products can help minimize the differences in skin color. You may need to try several brands of makeup or self-tanners to find one that blends well with your normal skin tone. The coloring of self-tanning products doesn't wash off, but it gradually fades over several days. If you use a self-tanner, select one that contains dihydroxyacetone, as it is approved by the U.S. Food and Drug Administration.
- Don't get a tattoo. Damage to your skin, such as that caused by a tattoo, may cause a new patch of vitiligo to appear within two weeks.
Limited studies show that the herb Ginkgo biloba may return skin color in people with vitiligo. Other small studies show that alpha-lipoic acid, folic acid, vitamin C and vitamin B-12 plus phototherapy may restore skin color for some people.
As with any nonprescription treatment, check with your health care provider before trying alternative medicine therapies to be sure they won't interfere with other treatments you're using.
The change in your appearance caused by vitiligo might make you feel stressed, self-conscious or sad. These self-care approaches can help you cope with vitiligo:
- Make a good connection. Find a doctor who knows a lot about the condition. A dermatologist is a doctor who specializes in the care of skin.
- Learn about your condition. Find out as much as you can about vitiligo and your treatment options so that you can help decide what steps to take.
- Communicate your feelings. Let your health care provider know if you're feeling depressed. You might benefit from a referral to a mental health provider who specializes in helping people with depression.
- Talk with others. Ask your health care provider about psychotherapy or support groups in your area for people with vitiligo.
- Confide in loved ones. Seek understanding and support from your family and friends.
You're likely to start by seeing your primary care provider. You may then be referred to a specialist in skin disorders (dermatologist).
Here's some information to help you prepare for your appointment.
What you can do
- Review your family medical history. Find out if anyone in your family has vitiligo, a thyroid condition or a disease in which the immune system attacks healthy tissues in the body (autoimmune disease).
- List relevant personal information, such as recent major stressful events, life changes, sunburns and rashes.
- List any medications, vitamins and supplements you're taking, including doses.
- Make note of questions you'd like to ask your health care provider, which will help you make the most of your limited time together.
Some basic questions to consider include:
- What's the most likely cause of my symptoms?
- What are other possible causes?
- Do I need any tests?
- Is this condition temporary or long lasting?
- What treatments are available, and which do you recommend?
- What side effects can I expect from treatment?
- Can I do anything to help, such as avoid the sun at certain times or wear a specific sunscreen?
- Can you recommend a product to conceal the discolored patches?
- Do you have brochures or other printed material I can take home? What websites do you recommend?
What to expect from your doctor
Your health care provider is likely to ask you a few questions, such as:
- When did you begin noticing light patches on your skin?
- Did you have a sunburn or skin rash before you noticed the patches?
- Are you sensitive to the sun?
- Do the discolored patches itch or cause any other symptoms?
- Have you ever had this type of skin change before?
- Does anyone in your family have vitiligo, a thyroid condition or an autoimmune disease?
- What is your occupation, and what are your hobbies? Are you exposed to any harsh chemicals in either?
- Does this condition affect your quality of life?
- Are you taking any medications or supplements?
What you can do in the meantime
While you're waiting to see your health care provider, limit your sun exposure and use a broad-spectrum sunscreen with an SPF of at least 30. If you're feeling self-conscious about the changes in your skin, use makeup or a self-tanning product to cover the affected areas.
Nov 10, 2022
- AskMayoExpert. Vitiligo. Mayo Clinic; 2019.
- Grimes PE. Vitiligo: Management and prognosis. https://www.uptodate.com/contents/search. Accessed Dec. 23, 2019.
- Grimes PE. Vitiligo: Pathogenesis, clinical features, and diagnosis. https://www.uptodate.com/contents/search. Accessed Dec. 23, 2019.
- Lebwohl MG, et al. Vitiligo. In: Treatment of Skin Disease: Comprehensive Therapeutic Strategies. 5th ed. Elsevier; 2018. https://www.clinicalkey.com. Accessed Dec. 23, 2019.
- Felsten LM, et al. Vitiligo: A comprehensive overview. Journal of the American Academy of Dermatology. 2011; doi:10.1016/j.jaad.2010.10.043.
- Whitton ME, et al. Interventions for vitiligo (review). Cochrane Database of Systematic Reviews. http://www.thecochranelibrary.com/view/0/index.html for link to abstract online. Accessed Dec. 23, 2019.
- Bae JM, et al. Phototherapy for vitiligo: A systematic review and meta-analysis. JAMA Dermatology. 2017; doi:10.1001/jamadermatology.2017.0002.
- Lee JH, et al. Treatment outcomes of topical calcineurin inhibitor therapy for patients with vitiligo: A systematic review and meta-analysis. JAMA Dermatology. 2019; doi:10.1001/jamadermatol.2019.0696.
- Thakur V, et al. Efficacy of transplantation of combination of noncultured dermal and epidermal cell suspension vs epidermal ell suspension alone in vitiligo: A randomized clinical trial. 2019; doi:10.1001/jamadermatol.2018.4919.
- Vitiligo. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/vitiligo. Accessed Dec. 23, 2019.
- Patient education: Vitiligo (The basics). https://www.uptodate.com/contents/search. Accessed Dec. 30, 2019.
- Vitiligo: Tips for managing. American Academy of Dermatology. https://www.aad.org/diseases/a-z/vitiligo-self-care. Accessed Dec. 30, 2019.
- Gibson LE (expert opinion). Mayo Clinic. Jan. 20, 2020.
- Symptoms & causes
- Doctors & departments
- Diseases & Conditions
- Vitiligo diagnosis & treatment
Associated Procedures
Products & services.
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
CON-XXXXXXXX
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Janus kinase inhibitors and the changing landscape of vitiligo management: a scoping review
Affiliations.
- 1 Department of Pharmacy, National Skin Centre, Singapore, Singapore.
- 2 Department of Dermatology, National Skin Centre, Singapore, Singapore.
- PMID: 38610078
- DOI: 10.1111/ijd.17157
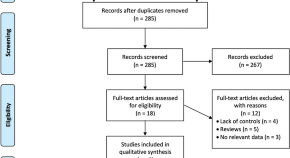
Vitiligo is a chronic skin condition caused by an autoimmune response that results in the progressive loss of melanocytes and recent studies have suggested that Janus kinase inhibitors (JAKi) are emerging as a promising new treatment modality. Therefore, to assess and understand the extent of knowledge in the emerging field of JAKi use in vitiligo, a scoping review of the literature was undertaken. The reviewed articles explored a wide variety of JAKi administered either orally or topically for vitiligo. There were no injectable JAKi studied. Tofacitinib was the most commonly studied oral JAKi in 16 of the 35 studies selected for review, followed by baricitinib (n = 3), and one study each with ritlecitinib, ruxolitinib, and upadacitinib. Ruxolitinib (n = 6) and tofacitinib (n = 6) were the most often studied topical JAKi, followed by delgocitinib (n = 1). Potential benefits may vary between JAKi based on their receptor selectivity profile and coexistent autoimmune diseases. A topical JAKi would be advantageous in limited body area involvement and in adolescents. Concurrent use of JAKi with phototherapy or sun exposure appears beneficial. Most studies permitted the use of other topical agents. Acne-related events, though frequent yet mild, were reported with both oral and topical JAKi. Nasopharyngitis, upper respiratory tract infections, and headaches were the most common adverse effects seen in the larger trials with JAKi. No serious or clinically meaningful hematology or thromboembolic events were detected. Treatment of vitiligo with oral or topical JAKi seems to be promising and the growing evidence shows a favorable risk-benefit profile.
Keywords: JAK inhibitor; JAK/STAT; Janus kinase inhibitor; hypomelanosis; hypopigmentation; interferon gamma; macule; melanocyte; patch; vitiligo management; vitiligo treatment.
© 2024 The Authors. International Journal of Dermatology published by Wiley Periodicals LLC on behalf of the International Society of Dermatology.
Publication types
News - 04 Feb `24 Vitiligo Treatment News at IMCAS 2024
Our youtube channels.
The IMCAS Congress in Paris recently emerged as a pivotal gathering for nearly 20,000 skin specialists worldwide.
Thanks to an educational grant from IMCAS and a sponsored booth (K203), Prof. Torello Lotti and I engaged directly with attendees interested in vitiligo. Our activities included distributing World Vitiligo Day 2024 leaflets, discussing World Health Academy's Publishing House initiatives, and introducing our innovative AI-Guide on Vitiligo, which generated significant interest. Additionally, I was thrilled to present the hard copy of the second edition of my book, " A No-Nonsense Guide On Vitiligo ," fresh off the press.
The vitiligo session on February 1st at the Palais des Congrès de Paris featured two hours of in-depth discussions. Prof. Thierry Passeron opened the session with updates on vitiligo treatment and future directions, followed by Prof. Manal Bosseila, who elaborated on dermoscopic criteria for distinguishing vitiligo from other skin conditions. Dr. Albert Wolkerstorfer, Dr. Reinhart Speeckaert, and others continued with insights on current and emerging treatments, such as JAK inhibitors and photodynamic therapy, demonstrating the field's innovative progress.
A roundtable discussion, led by Dr. Wolkerstorfer with Prof. Lotti and distinguished colleagues, provided a dynamic forum for exchanging vitiligo case studies, underscoring the congress's collaborative ethos and its role in enhancing patient care.
Dr. Gabriel Serrano, President of World Vitiligo Day 2024 , initiated this year's campaign from the Dominican Republic, alongside an organizational meeting with Sesderma, the event's Platinum sponsor.
The congress also unveiled three new home phototherapy UVB 308 nm devices by Mediderma, offering enhanced treatment accessibility and adherence. These robust, battery-operated LED lamps, pending regulatory approval, are set to revolutionize treatment compliance.
Moreover, the significant interest in AI's role in dermatology, including tools like ChatGPT, signaled AI's firm establishment in skincare practices. This enthusiasm has solidified our plans to launch the weekly AI-News On Vitiligo .
This congress, sometimes overlooked by vitiligo specialists, has proven essential for connecting with a wide array of skincare professionals dealing with vitiligo. We are immensely grateful to IMCAS and Dr. Huges Cartier for their steadfast support of our efforts.
Room: Room 143 - Level 1 Date: Thursday 1 February 2024 at 13:30 to 15:30 Format: FOCUS SESSION
13:30 Prof Thierry PASSERON. Vitiligo treatment: what’s new and what’s coming next? 13:41 Prof Manal BOSSEILA. Validity and reliability of dermoscopic criteria used to differentiate vitiligo from other hyperpigmented skin lesions 13:52 Dr Albert WOLKERSTORFER. Current vitiligo treatments 14:03 Dr Reinhart SPEECKAERT. Emerging treatments for vitiligo 14:14 Prof Laila BENZEKRI Role of VZV in segmental vitiligo pathogenesis 14:25 Dr Amr RATEB. Vitiligo: PUVA, laser, or JAK inhibitors? 14:36 Dr Pierre Andre BECHEREL. JAK inhibitors for vitiligo 14:47 Prof Antonio A G MASSA. PDL in vitiligo treatment 14:58 Dr Cheryl M BURGESS. Treatment of segmental vitiligo with topical ruxolitinib and 308 nm monochromatic excimer light 15:09 Prof Torello M LOTTI. Vitiligo Research Foundation 15:10 Dr Albert WOLKERSTORFER. Moderator and panelist: roundtable on vitiligo cases 15:10 Prof Torello M LOTTI. Roundtable panelist on vitiligo cases 15:10 Prof Laila BENZEKRI. Roundtable panelist on vitiligo cases 15:10 Dr Reinhart SPEECKAERT. Roundtable panelist on vitiligo cases
FAQ Other Questions
People have used herbs and natural remedies to treat skin conditions for centuries. Vitiligo is an auto-immune condition that causes white patches of skin to develop and expand...
It’s important to remember there are multiple factors involved in vitiligo onset, including genetic predisposition, living and working environments, and exposure to certain chem...
Vitiligo can be puzzling for a child because a person who has it isn't "ill" in a common sense. To choose the right words to explain vitiligo diagnosis to a child, first consi...
Donate Today
Our work is entirely funded by private donations – we receive no money from government. Your money will help us continue funding research into vitiligo and supporting people affected by the condition.
Though it is not always easy to treat vitiligo, there is much to be gained by clearly understanding the diagnosis, the future implications, treatment options and their outcomes.
Many people deal with vitiligo while remaining in the public eye, maintaining a positive outlook, and having a successful career.
By taking a little time to fill in the anonymous questionnaire, you can help researchers better understand and fight vitiligo.
Project Background
The study of multifactorial diseases, such as vitiligo, requires analysis of complex interplay of symptoms, treatments and outcomes across a large number of people. Population surveys and biobanks are indispensable research tools, required for downstream therapy development. Even small collections of biosamples may be extremely precious for researcher in academic institution or biopharma company.
Until recently, vitiligo researchers were generally limited to conducting studies on patient samples they could acquire themselves. When the Foundation started there were no centralized biological database along with the pre-existing body of the clinical management or the historical study data, which is required in order to proceed with the development of specific therapies. We have run a special investigation study to determine whether VRF shall establish its own biobank.
Then the project's leadership crafted a careful strategy for vitiligo biobank development, with special attention paid to the security and confidentiality of the donor's information. 'Future proofing' involves collecting and processing samples to permit the widest possible range of scientific uses, while avoiding approaches that would impede possible future uses.
We have started the first Vitiligo Biobank with a 100+ sample collection from the completed research project in genetics in late January 2013. Three months later, it held approximately 1,000 biosamples and detailed clinical profiles. Our target number is 10,000 samples and we encourage patients to donate samples . The primary biorepository is located in Moscow (Russia) with networked locations in 11 countries.
- Patient Portal
- Physician Referral
- Medical & Surgical Dermatology
- Mohs Surgery
- Medical Aesthetics
- Specials & Referral Program
- Forever Young BBL
- Neuromodulators
- Dermal Fillers
- HALO™ Laser
- CoolSculpting® Elite
- PDO Lifting Threads
- SkinPen Microneedling
- HydraFacial™
- Optima Research
- Current & Recruiting Dermatology Studies
- Physicians & Providers
- Request Appointment
- Covid-19 Protocols
- Find a Location
- Book Appointment
Optima Dermatology on New Day Cleveland – Vitiligo
Vitiligo is am autoimmune disease that affects 70 million people worldwide. While there’s no one cure for Vitiligo, a dermatologist can offer treatment plans to help restore a person’s natural skin tone and reduce vitiligo from spreading to other areas. Board-certified dermatologist, Dr. Gregory Delost recently sat down with New Day Cleveland to discuss the commonality of Vitiligo, the different types, and newly available treatment options, including Ruxolitinib Cream with results shown in the photos to the right. If you have vitiligo, it’s important to seek treatment with a dermatologist sooner rather than later! Check out the full interview to learn more from Dr. Delost.

- New Castle County
- Sussex County
- Kent County
- Health care
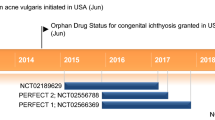
Incyte announces skin disease treatment venture with Chinese company
Incyte and China Medical System Holdings Limited reached an agreement whereby Incyte and CMS, through a wholly-owned dermatology medical aesthetic subsidiary of CMS (CMS Skinhealth), for the development and commercialization of povorcitinib.
The agreement calls for research, development, registration, and commercialization of the product in Mainland China, Hong Kong, Macao, Taiwan Region, and eleven Southeast Asian countries, and receive a non-exclusive license to manufacture the product in CMS’ Territory.
Under the agreement, CMS will pay Incyte an upfront payment. Incyte is eligible to receive additional potential development, commercial milestones, and royalties on the licensed product’s net sales in CMS’ territory.
CMS will receive an exclusive license to develop and commercialize and a non-exclusive license to manufacture povorcitinib in autoimmune and inflammatory dermatologic diseases, including non-segmental vitiligo and asthma for patients in mainland China and other nations in Asia. Patients suffering from non-segmental vitiligo lose skin pigment in white patches.
“We are excited to announce the addition of this collaboration for povorcitinib, expanding our relationship with CMS in the Dermatology space beyond ruxolitinib cream, to include two products with the potential to help patients with limited treatment options,” said Hervé Hoppenot, CEO of Incyte. “There remains a significant need for new, innovative treatment for vitiligo and other immune-mediated dermatologic conditions, and we look forward to working together with the CMS team to bringing these products to market in China.”
Huang Anjun, the general manager of CMS Skinhealth, stated that, “We expect that this collaboration will enhance CMS Skinhealth’s portfolio of potential treatments for vitiligo that, if approved, will provide differentiated treatment options for vitiligo patients in China.”
Earlier, Incyte reported promising results from a drug trial for patients suffering from a painful skin condition.
Incyte is based near Wilmington and has nearly 1,500 employees in the area.
RELATED ARTICLES MORE FROM AUTHOR

Highway Safety office announces distracted driving enforcement effort in April

Energize Delaware’s commercial property clean energy program gets boost

Avelo notes: Passenger boardings in Wilmington; UConn championship fare promotion
- Privacy Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Mol Sci

Current Status of Cell-Based Therapies for Vitiligo
Anna domaszewska-szostek.
1 Department of Human Epigenetics, Mossakowski Medical Research Institute, PAS, 02-106 Warsaw, Poland
Agnieszka Polak
2 Faculty of Biology, University of Cambridge, Cambridge CD2 1TN, UK
Monika Słupecka-Ziemilska
Marta krzyżanowska.
3 Division of Ophthalmology and Optometry, Department of Ophthalmology, Collegium Medicum, Nicolaus Copernicus University in Toruń, 85-168 Bydgoszcz, Poland
Monika Puzianowska-Kuźnicka
4 Department of Geriatrics and Gerontology, Medical Centre of Postgraduate Education, 01-813 Warsaw, Poland
Associated Data
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Vitiligo is a chronic pigmentary disease with complex etiology, the signs of which are caused by the destruction of melanocytes in the epidermis, leading to the lack of melanin pigment responsible for skin coloration. The treatment of vitiligo, which aims at repigmentation, depends both on the clinical characteristics of the disease as well as on molecular markers that may predict the response to treatment. The aim of this review is to provide an overview of the clinical evidence for vitiligo cell-based therapies taking into account the required procedures and equipment necessary to carry them out as well as their effectiveness in repigmentation, assessed using the percentage of repigmentation of the treated area. This review was conducted by assessing 55 primary clinical studies published in PubMed and ClinicalTrails.gov between 2000 and 2022. This review concludes that the extent of repigmentation, regardless of the treatment method, is highest in stable localized vitiligo patients. Moreover, therapies that combine more than one cell type, such as melanocytes and keratinocytes, or more than one method of treatment, such as the addition of NV-UVB to another treatment, increase the chances of >90% repigmentation. Lastly, this review concludes that various body parts respond differently to all treatments.
1. Background
Vitiligo is a chronic pigmentary disease that affects approximately 1% of the world’s population. This dermatological condition affects skin and hair and manifests itself by characteristic white macules and patches. The disease can be segmental, localized in one area of the body, or generalized, affecting a broader area. It can also be stable or unstable, depending on the appearance of new decoloration. Non-segmental vitiligo is prone to reactivation but, as in many of the studies, patients are required to have stable vitiligo, those with the segmental type of the disease are more likely to be selected for treatment. The loss of skin pigmentation is caused by the destruction of melanocytes in the epidermis, leading to the lack of melanin pigment responsible for skin coloration [ 1 , 2 ]. The published data suggest that the causes of melanin deficiency are multifactorial; mostly, it has an autoimmune origin with an underlying genetic tendency [ 3 , 4 ].
The disease has vast deleterious consequences beyond the aesthetical aspect, negatively affecting the patient’s emotional well-being and self-esteem. It is reported that around 75% of vitiligo patients have a psychological disorder [ 5 ], and female vitiligo patients experience significantly more significant impairment of general and psychological health, intimate relationships, and sexual function compared to healthy women [ 6 ].
The standard treatment for vitiligo varies based on the patient’s tolerance and consists of topical steroid therapy, immunosuppressant, sun protection, phototherapy, vitamin D, or narrow-band ultraviolet B (UVB) phototherapy ( Figure 1 ). While these treatment options can be successful for certain patients, for others, they do not bring satisfactory results [ 7 ]. Moreover, some patients are resistant to conventional medical treatments [ 8 ], probably due to polymorphisms in the genes involved in the immune response and melanogenesis [ 9 ], which motivates the search for novel combination therapy.

Standard and cell-based therapies for vitiligo. The figure was created with Biorender.com, accessed on 3 November 2022.
Therefore, there is a great interest in introducing other novel therapies that are effective and safe for vitiligo patients ( Figure 1 ).
This narrative literature review aims to bring a comprehensive knowledge of cell-based therapies in the treatment of vitiligo. In the present study, we discuss the development of these methods in recent years and point out various technical aspects affecting the effectiveness of the given methods for a better understanding of which procedure could be recommended, taking into account the characteristics of vitiligo and the patient’s age as well as facilities available in the clinic. Different transplantation approaches using keratinocytes and melanocytes or both cell types are presented with a description of the most applicable techniques such as hair follicle cell transplantation, the ReCell system, the Jodhpur Technique, and an approach where cell transplantations are combined with narrowband ultraviolet B (NB-UVB) or autologous platelet-rich plasma.
This literature review aims to bring knowledge of cell-based therapies by assessing 55 of the most effective primary clinical studies published in PubMed ( https://pubmed.ncbi.nlm.nih.gov/ , accessed on 20 November 2022) [ 10 ] and ClinicalTrails.gov ( https://clinicaltrials.gov , accessed on 20 November 2022) [ 11 ] between 2000 and 2022 with the oldest studies being discussed for historical relevance. Moreover, this review aims to give an indication of the therapies depending on the vitiligo type and location. Only human-based clinical studies and case reports were included in this review.
This review is divided into five sections, each considering a different cell-based therapy, its background, studies, and effects. It should be stated that the studies presented here have been conducted on several different ethnic groups. It is known that people of varying skin colors respond differently to vitiligo treatment; thus, this must be kept in mind when analyzing the results of clinical trials.
2. Melanocytes and Keratinocytes as the Targets for Vitiligo Therapy
Neural crest cell-derived melanocytes are the melanin-producing cells of the skin; several melanocyte cell death mechanisms have been proposed to explain the origin of vitiligo. As such, the transplantation of healthy cells shows great promise for treating vitiligo patients. Several methods for the delivery of non-cultured melanocytes into the affected skin areas of patients have been attempted [ 12 , 13 , 14 ], including transplantation onto dermabraded or laser-abraded areas. In this approach, the skin sample is shortly incubated with trypsin and centrifuged before spreading on the recipient area. As the number of melanocytes in this method is not increased in culture, its efficacy might be lower compared to cultured melanocyte transplantation. This is suggested by the relatively low (57.4%) number of patients achieving >50% repigmentation in the study by Ghorbani et al. [ 14 ]. Melanocytes only account for up to 10% of skin cells and thus should be amplified in vitro prior to transplantation to maximize the chances of success [ 15 ].
Therefore, there are numerous approaches for transplanting pure cultured melanocytes [ 13 , 16 , 17 , 18 ]. For example, in the Chen et al. study [ 16 ], 25 segmental vitiligo patients were treated with cultured autologous melanocytes. The cells were transplanted into laser-denuded areas at a density of 70,000 to 100,000 melanocytes per cm 2 . Complete repigmentation was seen in most patients in less than one month, although in some cases, a thin vitiliginous line at the junction between normal skin and the transplant was visible. Hair follicles, the outer root sheath, are rich in melanocytes with potential proliferative ability. Thus, this offers a potential donor site for autologous cell transplants and was recently explored in several studies [ 19 , 20 , 21 , 22 , 23 ]. In the study by Shi et al. [ 23 ], the occipital area was used to obtain a scalp specimen containing at least 15 hair follicles. Following the removal of adipose tissue, the remaining hair follicles and dermal papillae were incubated, and a single-cell suspension was created. The sterilized recipient area was then abraded superficially using a motorized dermabrader or a CO 2 laser and covered with the cell suspension and a hyaluronic acid dressing. In the nine months following treatment, 22 of the 26 patients achieved >75% repigmentation, and of those, 9 individuals achieved >90% repigmentation. Moreover, hair follicle transplantation using the hair follicular unit transplantation (FUT) technique is a cheap, simple method requiring minimal infrastructure, which makes it suitable for small stable lesions affecting hairy body parts [ 24 ].
Melanocytes can also be transplanted using dermarolling treatment, which involves microneedles piercing the epidermis for cell delivery. Melanocytes can be obtained with superficial shaving of scalp skin, as this is another area known to be particularly rich in these cells. Following incubation in a trypsin solution, the epidermis can easily be separated from the dermis using forceps. The epidermis is then centrifuged, the supernatant removed, and the pellet suspended in plasma. Following cleaning with an antiseptic spray, the recipient site can be dermarolled to deliver the melanocytes. Benzekri and Gauthier [ 25 ] have shown that after 24 h, nearly all holes had closed up without signs of infection, and melanocytes had been observed in the basal layer of the epidermis. After six months, 40% of the patients had an excellent response (76–100%) to the treatment. Autologous melanocytes can also be obtained from the thigh or buttock areas with normal skin color, which was explored in generalized vitiligo patients. The autologous material was incubated with trypsin then mixed with patients’ serum and centrifuged. The cell suspension mixed with hyaluronic acid was then evenly spread on recipient areas, previously injected with lidocaine, and shaved with a curate device. The success of the treatment was highly dependent on the recipient area, with the highest proportion of excellent and good results achieved in various areas of the face (57.4% on the face compared to the overall success of 50%) [ 14 ]. Using eyelid skin to harvest melanocytes and subsequent transplantation of the autologous melanocytes yielded similar results, with >80% repigmentation in 56% of the cases. The high success rate could be in part due to the selective growth of melanocytes while inhibiting fibroblasts and keratinocyte cells, as their faster growth and high proportion prevent the growth of melanocytes. The best results and even coloration were achieved in the legs, trunk, and face, and it was observed that sunlight could promote pigment production of transplanted cells [ 26 ]. Even though the results of the three latter studies are satisfactory, using hair root melanocytes appears to be the most effective solution. Moreover, it is clear that the choice of melanocyte donor area for melanocytes should be influenced by the recipient area affected by vitiligo, as the different methods showed varying success in various locations on the body [ 27 ]. Interestingly, Zhu et al. [ 26 ] found a higher level of anti-melanocyte antibodies in the vitiligo patients’ serum, indicating that humoral immunological mechanisms could play a role in the development of the disease.
The clinical characteristic of vitiligo is another important aspect determining the effectiveness of transplantation. One hundred and twenty cases of vitiligo patients were studied, and it was investigated whether stable localized vitiligo, stable generalized vitiligo, and active generalized vitiligo show different outcomes after cultured autologous pure melanocytes transplantation. In this study, similar to previous work of this group [ 16 ], 60,000 to 100,000 melanocytes/cm 2 were applied on the skin after carbon dioxide laser abrasion of the vitiligous areas. The best outcome was observed in the stable localized vitiligo group, where 84% of patients achieved 90% to 100% repigmentation. An excellent percentage of coverage was shown in 54% of patients in the stable generalized vitiligo group and none in patients suffering from active generalized vitiligo. This study proved the validity of the treatment of stable vitiligo with cultured autologous pure melanocytes [ 28 ]. The clinical applications of melanocyte cell transplantation in vitiligo are summarized in Table 1 and Figure 2 . However, most clinical trials attempt to transplant keratinocytes in co-culture with melanocytes [ 29 , 30 ].

CT-cell therapy. The highest percentage of repigmentation depending on the cell-based therapy used (based on papers presented in Table 1 ).
3. Melanocyte–Keratinocyte Cell Transplantation (MKCT)
It should be clarified that MKCT is the complete clinical grafting procedure which includes harvesting epithelium from the donor site, preparing the recipient site, and applying the suspension and dressing the wound, whereas non-cultured epidermal suspension (NCES) refers to a prepared cell suspension used in MKCT. The first introduction of non-cultured epidermal cellular grafting in the treatment of stable vitiligo took place in 1992 [ 31 ] after several successful attempts under experimental conditions on piebald guinea pig skin [ 32 ]. In this treatment, both melanocytes and keratinocytes are transferred, as melanocytes grow better in the presence of keratinocytes and produce better repigmentation. For instance, Phillips et al. [ 33 ] demonstrated the significance of improving the method of maintaining melanocyte numbers by introducing a feeder layer. The use of a hyaluronic acid-enriched cellular graft gave a repigmentation rate of over 70% in the vitiligous areas in 77% of patients after 12 months compared to a placebo in a double-blind study [ 1 ]. For a change, Khodadadi et al. [ 34 ] replenished the missing melanocytes and keratinocytes using a different route of their administration: the cell suspension was injected intraepidermally into vitiligous lesions. In the 6-month follow-up, 4 out of 10 patients had achieved moderate repigmentation (76–100%) and one patient’s patch was fully repigmented. The authors found no correlation between the number of transplanted cells and the outcome. Further development of this technique gave a repigmentation rate of over 50% in 32.2% of treated patches, whereas acquired repigmentation remained stable in 79.3% of treated patches during the 30-month-long follow-up period. Observing 300 patients, the first pigmentation loss in treated patches started around 9 months post-transplantation and mostly occurred during the first year (68.5%, n = 150) after treatment [ 35 ]. It is worth mentioning the results of the study by Budania et al. [ 34 ] and Bao et al. [ 36 ] which compared the NCES method with suction blister epidermal grafting (SPEG) and showed a better extent of repigmentation after NCES. Interestingly, in the study by Budania et al. [ 37 ], no melanocyte culture media, trypsin inhibitor, or hyaluronic acid was used, and only simple syringe-base suction was applied. Moreover, a comparison between an autologous non-cultured extracted hair follicle outer root sheath cell suspension (NCORSHFS) and NCES showed comparable efficacy in repigmentation [ 38 , 39 ], although, patients in the NCES group were significantly more satisfied than the patients in the NCORSHFS group [ 38 ]. However, there is also a study that suggests that cultured melanocyte transplantation (CMT) may give better repigmentation as compared with NCES in the case of stable generalized and segmental vitiligo [ 40 ]. Interestingly, a superior repigmentation to NCES or NCORSHFS alone was achieved when those two techniques were combined. The authors suggested that this approach may be a good alternative for the more resistant-to-treatment acral vitiligo [ 41 ].
The MKCT grafting procedure was also substantially developed since its discovery by Olsson and Juhlin in 1998 [ 42 ]. Initially, the sample of superficial skin was removed, and cells were isolated, separated, and cultured in a melanocyte growth medium. To carry out this procedure in one day, the next step was to apply the melanocyte-enriched epidermal cell suspension directly on dermabraded depigmented skin. Some of the changes proposed by Mulekar [ 43 ] concern the use of Dulbecco’s Modified Eagle’s Medium (DMEM) and Ham’s F-12 Nutrient Mixture for cell separation procedure and CO 2 incubator substitution with an ordinary incubator. The CO 2 incubator helps to maintain the pH in the cell cultures; however, it makes the procedure more expensive. Currently, melanocyte–keratinocyte cell transplantation (MKCT) involves obtaining a skin biopsy from the donor site one-tenth of the recipient area size. This is followed by soaking it in trypsin-EDTA solution, separating the dermis from the epidermis, and disposing of the dermis. The sample is then centrifuged, and the stratum corneum is discarded. Finally, the cell suspension is transplanted onto the deep epidermis of the dermabraded recipient area, which is then covered with a dry collagen sheet. The whole treatment can be conducted as a 2 to 4 h outpatient procedure [ 44 ].
In this technique, repigmentation can be seen between 2 weeks and 2 months after surgery [ 45 ]. Many patients show hyperpigmentation, but it usually blends with the surrounding skin in 6 to 8 months, and the likelihood increases when patients expose the transplanted areas to sunlight [ 43 ]. This method is most effective in segmental and focal vitiligo patients, for whom a scarring or cobblestone appearance is unlikely. Interestingly, the only post-operative pain that can be observed is in the feet and ankles [ 43 ]. Six months following the surgery, 84% of the patients showed good to excellent repigmentation, and in the long term, six years after the surgery, the treatment results remained positive for patients with segmental, stable vitiligo with the absence of fingertip involvement [ 46 ]. Mulekar et al. [ 47 ] also evaluated the effects of this treatment in 49 patients with segmental vitiligo and 15 patients with focal vitiligo who were followed up for up to 5 years. Overall, 95% to 100% of repigmentation was achieved in 84% of patients with segmental vitiligo and 73% of those with focal vitiligo, while a poor outcome was observed in 10% and 20%, respectively. Another study using MKCT reported that in the 12 to 72 months post-treatment, good to excellent repigmentation remained in 71% and 54% of patients with stable and non-stable vitiligo, respectively, confirming the success of this treatment for stable vitiligo patients. Interestingly, at 12 months, 62% of patients showed additional repigmentation that was not present before, and only 26% showed partial or complete regression. It was noted that improvement peaked at 10 months post-surgery and stabilized by up to a year, plateauing at around 18–24 months [ 44 ]. In another paper by Mulekar et al. [ 48 ], 142 patients were followed up to 6 years after autologous, non-cultured melanocyte-keratinocyte cell transplantation. Complete repigmentation was shown in 56% of patients, while poor pigmentation was observed in 24%. Another group [ 49 ] presented data concerning three cases of patients with stable genital vitiligo. A 26-year-old male with the loss of pigmentation on the penis glans and neck, and 24- and 39-year-old males with depigmentation of the glans and shaft of the penis, all of whom were treated with autologous, non-cultured MKCT. All of the patients achieved almost complete repigmentation. In another study [ 50 ], patients with stable vitiligo were treated using the same method as Mulekar and co-workers [ 43 ]. The outcome of the treatment of eight vitiligous patches treated with autologous non-cultured melanocyte–keratinocyte transplantation was compared to six control lesions, which were only dermabraded. The results were evaluated after 4 months. Over 95% repigmentation was observed in 50% and 0% to 24% repigmentation in 37% of patients treated with MKT. Five out of six control patches failed to show repigmentation, and one patch resulted in hyperpigmentation following inflammation.
Vazques-Martinez et al. [ 51 ] and Quezada et al. [ 52 ] compared the efficacy of the transplantation of melanocyte and keratinocyte (MKCT) cell suspension after dermabrasion (DA) or with dermabrasion only. In the 12-month follow-up period in Vazquez-Martinez’s study [ 51 ], there was no statistically significant difference between MKCT + DA and DA alone in the area of depigmentation but clinically MKCT + DA showed slightly better results. Quezada et al. [ 52 ] analyzed the results 3 months after transplantation and observed no significant differences between the treatments. It should be noted that the two latter studies indicate that MKCT + DA and DA alone are similar in terms of efficacy, whereas Mulekar and co-workers have found MKCT to be significantly better. This highlights the differences between methods and samples used in different studies even when, in principle, the technique used is the same.
Huggins et al. [ 53 ] performed 29 MKCT procedures in 23 patients with focal, generalized, or segmental vitiligo with no control group. Overall, 52% of the vitiligous lesions were localized on the extremities. Patients were evaluated monthly between the 3rd and 6th month after the procedure. Excellent repigmentation was achieved in 17% and poor in 41% of patients. The presence of vitiligo on the face/neck was associated with a better response to the treatment, with 19% of patients showing excellent repigmentation and 50% good.
Ebadi et al. [ 54 ] conducted a study where patients with stable generalized vitiligo, with a total of 39 patches, were divided into four groups. Nine patches were treated with MKCT alone, ten patches with MKCT and excimer laser, ten patches with excimer laser alone, and ten patches served as controls and did not receive any treatment. The authors reported that excimer laser combined with non-cultured MKCT improves the repigmentation rate, with an average of 41.9% reduction in the depigmented area surface. For comparison, it was only 4.7% for patients treated with excimer laser alone, 15.9% for those treated with MKCT alone, and 0.1% for the control group.
Lastly, it has been observed that the ethnicity of patients must be considered in the choice of MKCT treatment, for instance, Asian patients are more prone to hypertrophic scarring [ 30 ]. Even though vitiligo affects all ethnic groups similarly, it may be more noticeable in people with darker skin, and some treatments may show varying efficacy between the different groups.
It is worth mentioning that the response to NCES treatment may depend on the location of the lesions. The best results were observed in face and neck lesions (88% of satisfactory responses) and the worst in the extremity lesions (33% of satisfactory responses). However, based on their results, Mulekar et al. [ 55 ] concluded that the concept of a “difficult-to-treat site” is a relative term and depends upon the technique used. The non-cultured MKCT seems to be favorable as this technique does not require special precautions to treat these anatomical sites. According to some authors, using a higher density of melanocytes in the suspension [ 56 ], a strict immobilization procedure for the treated areas, and post-operative phototherapy in the form of sun exposure might improve the results in such a “difficult-to-treat site” [ 57 ]. Others reported that a better response was achieved in segmental vitiligo patients compared to non-segmental ones (84% compared to 63%) [ 58 ]. Moreover, NCES was also successfully used in the repigmentation of leucotrichia in vitiliginous patches. The proposed mechanism of this process is a retrograde migration of transplanted melanocytes or interfollicular epidermal stem cells to the hair bulb and/or their production of cytokines, which stimulates melanogenesis in the follicular bulbs [ 59 ]. It should also be mentioned that skin grafting may be considered to treat localized vitiligo in children [ 60 , 61 ]. In this group of patients, an MKTP is favorable as it does not require a long surgical time, and there is no need for absolute immobility and any special precautions to treat ‘‘difficult-to-treat’’ sites. The clinical applications of MKCT in vitiligo are summarized in Table 1 and Figure 2 .
4. ReCell System in Vitiligo Therapy
ReCell is a robust point-of-care autologous therapy designed to treat skin defects such as small and large thermal burn wounds using a patient’s regenerative cells. The ReCell system enables the harvesting of autologous cells, processing them, and delivering them using a spray applicator. Three clinical trials analyzed the results of treating patients with stable vitiligo with ReCell (a cell suspension with keratinocytes, melanocytes, dermal papillary fibroblasts, and Langerhans cells sprayed over the wound) [ 62 ]. Mulekar et al. [ 63 ] compared the efficacy of the ReCell system and melanocyte–keratinocyte transplantation 4 months after the procedure. In both methods, the cell suspension was spread to previously dermabraded areas, and the results of the treatments were comparable.
Due to efficacy, time, and cost, surfaces that can be covered with cultured melanocytes are larger than those that can be covered with non-cultured cells. Cervelli et al. [ 62 ] treated 15 patients, and 12 of them (80%) achieved more than 75% repigmentation. The authors observed an excellent color match in 66% of patients.
In 2010, the same group [ 64 ] presented a case report of a 30-year-old man suffering from stable vitiligo on his hands. Before undergoing ReCell therapy, he had vitamin A, C, E, and UVB therapy, none of which were beneficial. Treatment with the ReCell system gave excellent results, both in the extent of repigmentation and the skin color match. The clinical applications of the ReCell system in vitiligo are summarized in Table 1 and Figure 2 .

5. Autologous Non-Cultured, Non-Trypsinized Epidermal Cell Grafting
This method is also known as the Jodhpur Technique (JT) (the first time was carried out in the Medical College in Jodhpur in India) and is a modification of the autologous non-cultured, non-trypsinized keratinocyte–melanocyte cellular graft technique. The grafting material is rich in melanocytes and is obtained following the dermabrasion of the donor area. The epidermal particles fragmented during dermabrasion become entangled in an ointment, and a paste-like material is obtained. This material is laid out over the recipient lesion area using a graft spreader. This technique is very low-cost and does not need any sophisticated equipment.
The study by Tyagi et al. [ 65 ] with the use of the JT technique revealed that in both epidermal cell suspension and epidermal curettes, over 75% repigmentation was achieved in 60% of lesions. Moreover, the color matching with surrounding skin and yield of grafts was not significantly different between these techniques. Even better results were presented in the study by Lamoria et al. [ 24 ], where excellent repigmentation (>75%) was observed in 70% of lesions. In terms of the repigmentation rate, side effects, patient satisfaction, and dermatology life quality index reduction, this method was superior to FUT. The clinical applications of non-cultured epidermal cell grafting in vitiligo are summarized in Table 1 and Figure 2 .
6. Cell Transplantations in Combination Therapy with a Narrowband Ultraviolet B (NB-UVB) or Autologous Platelet-Rich Plasma
Narrowband ultraviolet B (NB-UVB) is one of the treatment options for patients suffering from active vitiligo [ 66 ]. It promotes the proliferation and migration of cultured melanocytes. Zhang et al. [ 67 ] collected a group of 473 patients and investigated the effect of NB-UVB in combination with autologous melanocyte transplantation. The patients were divided into four groups: group 1 underwent NB-UVB sessions before melanocyte transplantation, group 2 was NB-UVB treated after transplantation, group 3 received NB-UVB before and after transplantation, while group 4 did not undergo NB-UVB sessions and received only transplantation. The best results were observed in group 3, where ≥90% repigmentation was achieved in 81% of patients, which suggests that NB-UVB given before and after transplantation of the melanocytes gives the best chance of repigmentation in active vitiligo patients. Interestingly, Yao et al. demonstrated more than 90% repigmentation at the 1-year follow-up in all patients treated with low-density cultured autologous melanocytes combined with NB-UVB treatment after cell transplantation [ 68 ]. Excellent repigmentation (85–100%) was also achieved in the small four-patient study where the non-cultured autologous melanocytes and keratinocytes transplantation was combined with UVA or UVB therapy after grafting [ 69 ].
Platelet-rich plasma (PRP) originates from the collection of venous blood, which is then centrifuged in the presence of anticoagulants. After centrifugation, autologous platelets are suspended in a small amount of plasma. Topical application using an intradermal injection of PRP through the secretion of platelet’s alpha granules increases the release of growth factors (especially basic fibroblast growth factor, bFGF), adhesion molecules, and chemokines, which, by interacting with the local environment, stimulate melanocyte migration along with the stimulation of keratinocyte and fibroblast proliferation. Moreover, PRP promotes the release of inflammatory mediators and modulators through the release of numerous anti-inflammatory cytokines, such as interleukins (IL-4, IL-10, IL-13), IL-1 receptor antagonist (IL-1ra), soluble tumor necrosis factor (TNF) receptor (sTNF-R) I, and interferon-gamma (IFN-γ). Although intralesional injection of PRP alone did not induce repigmentation, a combination of PRP with NB-UVB induced statistically significant repigmentation in a series of 60 patients from Egypt [ 70 ]. An interesting and promising study was performed with NCES suspended in PRP. Parambath et al. [ 71 ] compared the extent of repigmentation achieved using the transplantation of NCES in PRP and NCES in phosphate-buffered saline (PBS) in 21 patients with stable vitiligo. After 6 months, the repigmentation was 75.6% after NCES in PRP and 65% after NCES and PBS treatment ( p = 0.0036). Moreover, the suspension in PRP was better assessed by patients in the visual analog scale. The clinical applications of combination therapy for vitiligo are summarized in Table 1 and Figure 2 .
7. Are Cell-Based Therapies Appropriate for All Vitiligo Patients? Limitations and Challenges
Although vitiligo cell-based therapy is safe, well-tolerated, and effective at repigmentation with matching color and texture in appropriate candidates, it is still an underperformed treatment. There are several reasons for this: a limited number of practitioners know the technique details, a lack of awareness on the part of physicians, and a lack of insurance coverage for vitiligo because many consider it a cosmetic disease. Moreover, not all patients are willing to undergo this type of therapy. Parambath et al. [ 71 ] found that 11 out of 38 patients screened for the study were not willing to undergo surgery. When asked about the reasons for refusal, patients indicated the desire to receive a trial of medical therapy from a tertiary care center, fear of surgery, unwillingness for follow-up visits, and high costs. It should also be noted that not every vitiligo patient is eligible for surgical therapy. Depending on the clinical practice, most patients must have clinically stable vitiligo for 6 months to one year to qualify [ 45 , 58 ]. Clinically stable vitiligo is determined by the non-appearance of new lesions and by the absence of changes in the existing ones. Patients with segmental or focal vitiligo are better candidates because they tend to achieve greater repigmentation than those with generalized disease. Higher rates of repigmentation were also reported in young patients compared to older ones [ 72 ].
It is also very important to note that it is difficult to estimate the overall percentage of people who have recovered from vitiligo, as only a fraction of them undergo treatment. Moreover, even though combination therapy is more effective than monotherapy, recurrence affects up to 40% of patients [ 73 ].
Patients are excluded from surgery if they had a history of koebnerization, hypertrophic scarring, keloids, or are susceptible to poor wound healing. According to Ramos et al., isolated scalp leukotrichia is an adverse prognostic sign, and the presence of significant distal fingertip, periorificial, or acrofacial involvement is also an exclusion criterion because these disease variants typically respond poorly to the melanocyte–keratinocyte transplantation procedure [ 45 ]. However, as we discuss below, patients with leucotrichia in vitiliginous patches may also have a chance for successful treatment [ 59 ]. Recently, molecular markers were suggested for better predictions of vitiligo diagnosis and response to treatment. The RNA sequencing in vitiligo patients showed differences in expression levels of 470 genes between the skin specimens of responder versus non-responder patients. Two hundred sixty-nine upregulated genes were involved in processes, such as fatty acid omega oxidation, whereas down-regulated genes (two hundred and one) were related to PPAR and estrogen signaling pathways [ 74 ].
8. Conclusions
In conclusion, cell therapies undergo continuous improvements both toward better re-pigmentation effects and simplifying the methods, making them more accessible to dermatological clinics [ 75 ]. Modifications of procedures involving simplifying cell collection, ensuring their good transplantation potential, as well as using less sophisticated laboratory equipment, reduce the cost of the procedure and make it more accessible to patients. Another important factor when considering cell-based vitiligo treatment is the selection of appropriate candidates. In the meta-regression analyses by Ju et al. [ 75 ], the successful outcome (>90% repigmentation) was associated with younger age, segmental vitiligo, and a non-acral area.
It should also be mentioned that repigmentation after cell therapy progresses gradually and may continue beyond 12 months following the procedure. Thus, there is a great need for more extended follow-up studies (minimum 6 months) for evaluation of the effectiveness and real cost that the patients must undertake on their way along the treatment of vitiligo.
The clinical applications of melanocyte transplantation, melanocyte–keratinocyte cell transplantation, ReCell, non-cultured epidermal cell grafting, and combination therapy for vitiligo.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, A.D.-S. and M.S.-Z.; writing—original draft preparation, A.D.-S., A.P., M.S.-Z., M.K. and M.P.-K.; writing—review and editing, A.D.-S., A.P., M.S.-Z., M.K. and M.P.-K.; visualization, A.D.-S. and M.S.-Z.; supervision, A.D.-S., M.S.-Z. and M.P.-K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My Portfolio
- Stock Market
- Biden Economy
- Stocks: Most Actives
- Stocks: Gainers
- Stocks: Losers
- Trending Tickers
- World Indices
- US Treasury Bonds
- Top Mutual Funds
- Highest Open Interest
- Highest Implied Volatility
- Stock Comparison
- Advanced Charts
- Currency Converter
- Basic Materials
- Communication Services
- Consumer Cyclical
- Consumer Defensive
- Financial Services
- Industrials
- Real Estate
- Mutual Funds
- Credit Cards
- Balance transfer cards
- Cash-back cards
- Rewards cards
- Travel cards
- Personal Loans
- Student Loans
- Car Insurance
- Options 101
- Good Buy or Goodbye
- Options Pit
- Yahoo Finance Invest
- EV Deep Dive
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
Yahoo Finance
Cybin announces publication of research manuscript in the journal of medicinal chemistry.
- Publication explores structure-activity relationships ("SAR") of a broad range of 2C-X analogs -
- Innovative research led to the discovery of CYB210010, a potent and long-acting serotonin 5-HT 2 receptor agonist with favorable pharmacokinetic properties -
TORONTO, April 18, 2024 --( BUSINESS WIRE )-- Cybin Inc. (NYSE American:CYBN) (Cboe CA:CYBN) (" Cybin " or the " Company "), a clinical-stage biopharmaceutical company committed to revolutionizing mental healthcare by developing new and innovative next-generation psychedelic-based treatment options, today announced that its research manuscript, entitled "Synthesis and Structure-Activity Relationships of 2,5-dimethoxy-4-substituted phenethylamines and the discovery of CYB210010: A potent, orally bioavailable and long-acting serotonin 5-HT 2 receptor agonist," has been published in the Journal of Medicinal Chemistry , a prestigious bi-weekly peer-reviewed publication.
"We are delighted that our research on phenethylamine serotonin 5-HT 2 receptor agonists was published in this important journal," said Doug Drysdale, Chief Executive Officer of Cybin. "This study is an example of our expanding scope of innovative development work beyond our clinical tryptamine programs. This publication is a testament not only to our scientific leadership in the field of 5-HT 2 receptor agonists, the receptor family believed to mediate the therapeutic effects of classic psychedelics, but also to the depth and breadth of our expertise as we continue to advance the study of the role of next-generation psychedelic-based treatment options for mental health and neurological disorders."
"In the past decade, there has been a revival of interest in serotonin (5-HT)-based psychedelics as pharmacotherapeutics for neuropsychiatric disorders," said Geoff Varty, Ph.D., Head of R&D of Cybin. "Given the clinical potential of 2C-X phenethylamines, our studies explored the SARs of a broad range of 2C-X analogs, focusing on 4-thio derivatives, to identify novel 5-HT 2 receptor ligands with unique pharmacodynamic ("PD") and pharmacokinetic ("PK") properties. We synthesized 39 proprietary 4-substituted-2,5-dimethoxyphenethylamines and these phenethylamines were profiled for their ability to interact with the serotonin system and to induce psychedelic-like effects in preclinical models. This research led to the discovery of CYB210010, a potent and long-acting serotonin 5-HT 2 receptor agonist with favorable PK and PD properties," concluded Dr. Varty.
Future investigations will focus on the development of CYB210010 and related molecules as novel therapeutics for psychiatric and neurological disorders with unmet needs.
Click here to view the full publication.
Title: Synthesis and Structure-Activity Relationships of 2,5-dimethoxy-4-substituted phenethylamines and the discovery of CYB210010: A potent, orally bioavailable and long-acting serotonin 5-HT2 receptor agonist
Authors: Geoff Varty, Clint Canal, Tina Mueller, Josh Hartsel, Richa Tyagi, Ken Avery, Mike Morgan, Amy Reichelt, Pradip Pathare, Erik Stang, Mike Palfreyman, Alex Nivorozhkin
About Cybin
Cybin is a clinical-stage biopharmaceutical company on a mission to create safe and effective psychedelic-based therapeutics to address the large unmet need for new and innovative treatment options for people who suffer from mental health conditions.
Cybin’s goal of revolutionizing mental healthcare is supported by a network of world-class partners and internationally recognized scientists aimed at progressing proprietary drug discovery platforms, innovative drug delivery systems, and novel formulation approaches and treatment regimens. The Company is currently developing CYB003, a proprietary deuterated psilocybin analog for the treatment of major depressive disorder and CYB004, a proprietary deuterated DMT molecule for generalized anxiety disorder and has a research pipeline of investigational psychedelic-based compounds.
Headquartered in Canada and founded in 2019, Cybin is operational in Canada, the United States, the United Kingdom, the Netherlands and Ireland. For company updates and to learn more about Cybin, visit www.cybin.com or follow the team on X, LinkedIn, YouTube and Instagram.
Cautionary Notes and Forward-Looking Statements
Certain statements in this news release relating to the Company are forward-looking statements and are prospective in nature. Forward-looking statements are not based on historical facts, but rather on current expectations and projections about future events and are therefore subject to risks and uncertainties which could cause actual results to differ materially from the future results expressed or implied by the forward-looking statements. These statements generally can be identified by the use of forward-looking words such as "may", "should", "could", "intend", "estimate", "plan", "anticipate", "expect", "believe" or "continue", or the negative thereof or similar variations. Forward-looking statements in this news release include statements regarding the development of CYB210010; and the Company’s proprietary drug discovery platforms, innovative drug delivery systems, novel formulation approaches and treatment regimens for mental health conditions.
These forward-looking statements are based on reasonable assumptions and estimates of management of the Company at the time such statements were made. Actual future results may differ materially as forward-looking statements involve known and unknown risks, uncertainties, and other factors which may cause the actual results, performance, or achievements of the Company to materially differ from any future results, performance, or achievements expressed or implied by such forward-looking statements. Such factors, among other things, include: fluctuations in general macroeconomic conditions; fluctuations in securities markets; expectations regarding the size of the psychedelics market; the ability of the Company to successfully achieve its business objectives; plans for growth; political, social and environmental uncertainties; employee relations; the presence of laws and regulations that may impose restrictions in the markets where the Company operates; implications of disease outbreaks on the Company's operations; and the risk factors set out in each of the Company's management's discussion and analysis for the three and nine month periods ended December 31, 2023 and the Company’s annual information form for the year ended March 31, 2023, which are available under the Company's profile on www.sedarplus.ca and with the U.S. Securities and Exchange Commission on EDGAR at www.sec.gov . Although the forward-looking statements contained in this news release are based upon what management of the Company believes, or believed at the time, to be reasonable assumptions, the Company cannot assure shareholders that actual results will be consistent with such forward-looking statements, as there may be other factors that cause results not to be as anticipated, estimated or intended. Readers should not place undue reliance on the forward-looking statements and information contained in this news release. The Company assumes no obligation to update the forward-looking statements of beliefs, opinions, projections, or other factors, should they change, except as required by law.
Cybin makes no medical, treatment or health benefit claims about Cybin’s proposed products. The U.S. Food and Drug Administration, Health Canada or other similar regulatory authorities have not evaluated claims regarding psilocybin, psychedelic tryptamine, tryptamine derivatives or other psychedelic compounds. The efficacy of such products has not been confirmed by approved research. There is no assurance that the use of psilocybin, psychedelic tryptamine, tryptamine derivatives or other psychedelic compounds can diagnose, treat, cure or prevent any disease or condition. Rigorous scientific research and clinical trials are needed. Cybin has not conducted clinical trials for the use of its proposed products. Any references to quality, consistency, efficacy and safety of potential products do not imply that Cybin verified such in clinical trials or that Cybin will complete such trials. If Cybin cannot obtain the approvals or research necessary to commercialize its business, it may have a material adverse effect on Cybin’s performance and operations.
Neither the Cboe Canada, nor the NYSE American LLC stock exchange have approved or disapproved the contents of this news release and are not responsible for the adequacy and accuracy of the contents herein.
View source version on businesswire.com: https://www.businesswire.com/news/home/20240418413250/en/
Investors & Media: Gabriel Fahel Chief Legal Officer Cybin Inc. 1-866-292-4601 [email protected] – or – [email protected]
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
After 40 years of smoking, she survived lung cancer thanks to new treatments

Yuki Noguchi

Denise Lee on her last day of chemo. In addition to chemo and surgery, she was treated with immunotherapy. She's currently in remission. Denise Lee hide caption
Denise Lee on her last day of chemo. In addition to chemo and surgery, she was treated with immunotherapy. She's currently in remission.
Denise Lee grew up in Detroit in the mid-1970s and went to an all-girls Catholic high school. She smoked her first cigarette at age 14 at school, where cigarettes were a popular way of trying to lose weight.
Instead, her nicotine addiction lasted four decades until she quit in her mid-50s.
"At some point it got up as high as 2.5 packs a day," Lee, 62, recalls.
Yet she didn't think about lung cancer risk — until she saw a billboard urging former smokers to get screened. Lee, a retired lawyer living in Fremont, Calif., used to drive past it on her way to work.
"The thing that caught my attention was the fact that it was an African American female on the front," she recalls.

Shots - Health News
The american cancer society says more people should get screened for lung cancer.
She eventually got the low-dose CT scan recommended for current and former smokers. When doctors found an early, but dangerous, tumor, Lee cried and panicked. Her mother had cared for her father, who'd died of prostate cancer. "My biggest concern was telling my mom," she says.
But that was six years ago, and Lee is cancer free today. Surgery removed the 2-inch tumor in her lung, then new treatments also boosted her immune system, fighting off any recurrence.
Lung cancer remains the most lethal form of the disease, killing about 135,000 Americans a year – more than breast, prostate and colon cancer combined – which is why many people still think of a diagnosis as synonymous with a death sentence. But with new treatments and technology, the survival rates from lung cancer are dramatically improving, allowing some patients with relatively late-stage cancers to live for years longer.
"If you're gonna have lung cancer, now is a good time," Lee says of the advances that saved her.

Denise Lee has been cancer-free for six years. She says she's grateful she got screened and caught her lung cancer early enough that treatment has been effective. Denise Lee hide caption
Denise Lee has been cancer-free for six years. She says she's grateful she got screened and caught her lung cancer early enough that treatment has been effective.
The key breakthrough, says Robert Winn, a lung cancer specialist at Virginia Commonwealth University, is the ability to better pinpoint the mutations of a patient's particular form of cancer. In the past, treatments were blunt tools that caused lots of collateral damage to healthy parts of the body while treating cancer.
"We've gone from that to molecular characterization of your lung cancer, and it has been a game changer," Winn says. "This is where science and innovation has an impact."
One of those game-changing treatments is called targeted therapy . Scientists identify genetic biomarkers in the mutated cancer cells to target and then deliver drugs that attack those targets, shrinking tumors.

CRISPR gene-editing may boost cancer immunotherapy, new study finds
Another is immunotherapy, usually taken as a pill, which stimulates the body's own defense system to identify foreign cells, then uses the immune system's own power to fight the cancer as if it were a virus.
As scientists identify new cancer genes, they're creating an ever-broader array of these drugs.
Combined, these treatments have helped increase national survival rates by 22% in the past five years – a rapid improvement over a relatively short time, despite the fact that screening rates are very slow to increase. Winn says as these treatments get cheaper and readily available, the benefits are even reaching rural and Black populations with historic challenges accessing health care.
The most remarkable thing about the drugs is their ability to, in some cases, reverse late-stage cancers. Chi-Fu Jeffrey Yang, a thoracic surgeon at Massachusetts General Hospital and faculty at Harvard Medical School, recalls seeing scans where large dark shadows of tumor would disappear: "It was remarkable to see the lung cancer completely melting away."
To Yang, such progress feels personal. He lost his beloved grandfather to the disease when Yang was in college. If he were diagnosed today, he might still be alive.
"Helping to take care of him was a big reason why I wanted to be a doctor," Yang says.
But the work of combating lung cancer is far from over; further progress in lung cancer survival hinges largely on getting more people screened.
Low-dose CT scans are recommended annually for those over 50 who smoked the equivalent of a pack a day for 20 years. But nationally, only 4.5% of those eligible get those scans , compared to rates of more than 75% for mammograms.
Andrea McKee, a radiation oncologist and spokesperson for the American Lung Association, says part of the problem is that lung cancer is associated with the stigma of smoking. Patients often blame themselves for the disease, saying: "'I know I did this to myself. And so I don't I don't think I deserve to get screened.'"
McKee says that's a challenge unique to lung cancer. "And it just boggles my mind when I hear that, because, of course, nobody deserves to die of lung cancer."
Denise Lee acknowledges that fear. "I was afraid of what they would find," she admits. But she urges friends and family to get yearly scans, anyway.
"I'm just so grateful that my diagnosis was early because then I had options," she says. "I could have surgery, I could have chemotherapy, I could be a part of a clinical trial."
And all of that saved her life.
- lung cancer screening
- immunotherapy
- lung cancer
MINI REVIEW article
Advances in vitiligo: update on therapeutic targets.

- Department of Dermatology, Jiangsu Province People’s Hospital and Nanjing Medical University First Affiliated Hospital, Nanjing, China
Vitiligo, whose treatment remains a serious concern and challenge, is an autoimmune skin disease characterized by patches of depigmentation. The increasing application of molecular-targeted therapy in skin diseases, such as psoriasis and systemic lupus erythematosus, has dramatically improved their condition. Besides, there is a favorable effect of repigmentation in the treatment of the above diseases combined with vitiligo, implying that molecular-targeted therapy may also have utility in vitiligo treatment. Recently, the role of cytokine and signaling pathways in vitiligo pathogenesis are increasingly recognized. Thus, investigations are underway targeting the molecules described above. In this paper, we present a synopsis of current practices in vitiligo treatment and introduce the improvement in identifying new molecular targets and applying molecular-targeted therapies, including those under development in vitiligo treatment, providing valuable insight into establishing further precision medicine for vitiligo patients.
1 Introduction
Vitiligo is a primary, circumscribed, or generalized depigmentation of the skin and mucosa, related to genetic factors, self-destruction of melanocytes, cytokines, autoimmunity, and oxidative stress ( 1 ). While the detailed molecular mechanisms still require further investigation. In recent years, various studies have showed that the IFN-γ-CXCL9/10-CXCR3 axis appears to be important in vitiligo, via inhibiting melanogenesis, inducing apoptosis of melanocytes, and further recruiting T cells to the skin. These are all involved in the JAK/STAT pathway. In addition, cytokine, including HSP70i, IL-15, IL-17/23, TNF as well as wnt signaling pathway, Tregs, miRNAs have also been proved to be involved in the pathogenesis of vitiligo.
Vitiligo can be treated by different modalities of phototherapy, surgical procedures, and topical therapies, such as glucocorticosteroids, immunosuppressive agents, calcineurin inhibitors, and vitamin D. However, current treatments for vitiligo remain suboptimal, which may not be equally effective in all vitiligo patients, and it would be inconvenient for patients to visit clinics for phototherapy. Targeted therapies, such as biologics targeting cytokines and small-molecule inhibitors targeting intracellular signaling molecules, are recently emerging as promising therapeutics for autoimmune diseases. Their applications also promote our understanding of the detailed molecular mechanism of vitiligo and are essential for guiding a more precise vitiligo treatment. In this article, details of the roles that related cytokines and pathways play as well as the efficacy of targeted therapy have been described.
2 Current treatment
Topical, systemic treatment, and phototherapy are useful for stabilization and repigmentation of vitiligo. Treatment modalities are chosen in the individual patient, based on disease severity, disease activity (stable versus progressive disease), patient preference (including cost and accessibility), and response evaluation. For rapidly progressive disease, low-dose oral glucocorticoids and phototherapy are useful in stabilizing the disease. Therapeutic options for stable, segmental vitiligo include topical therapies (eg, topical corticosteroids, topical calcineurin inhibitors), targeted phototherapy, and surgical therapy (tissue grafts and cellular grafts) ( Table 1 ) ( 14 ). In recent years, attempts have been made to improve the repigmentation of vitiligo phototherapy by combination therapies, including NB-UVB with glucocorticoids ( 15 ), and topical calcineurin inhibitors ( 16 ). While their positive results were not confirmed in all studies. However, the method of treatment described, which were nonspecific, general, off-label, non-targeted with modest efficacy led to the problem of recurrence after stopping treatment. Therefore, efforts should be made to achieve a more comprehensive understanding of vitiligo pathogenesis to develop novel effective therapies ( Table 2 ).
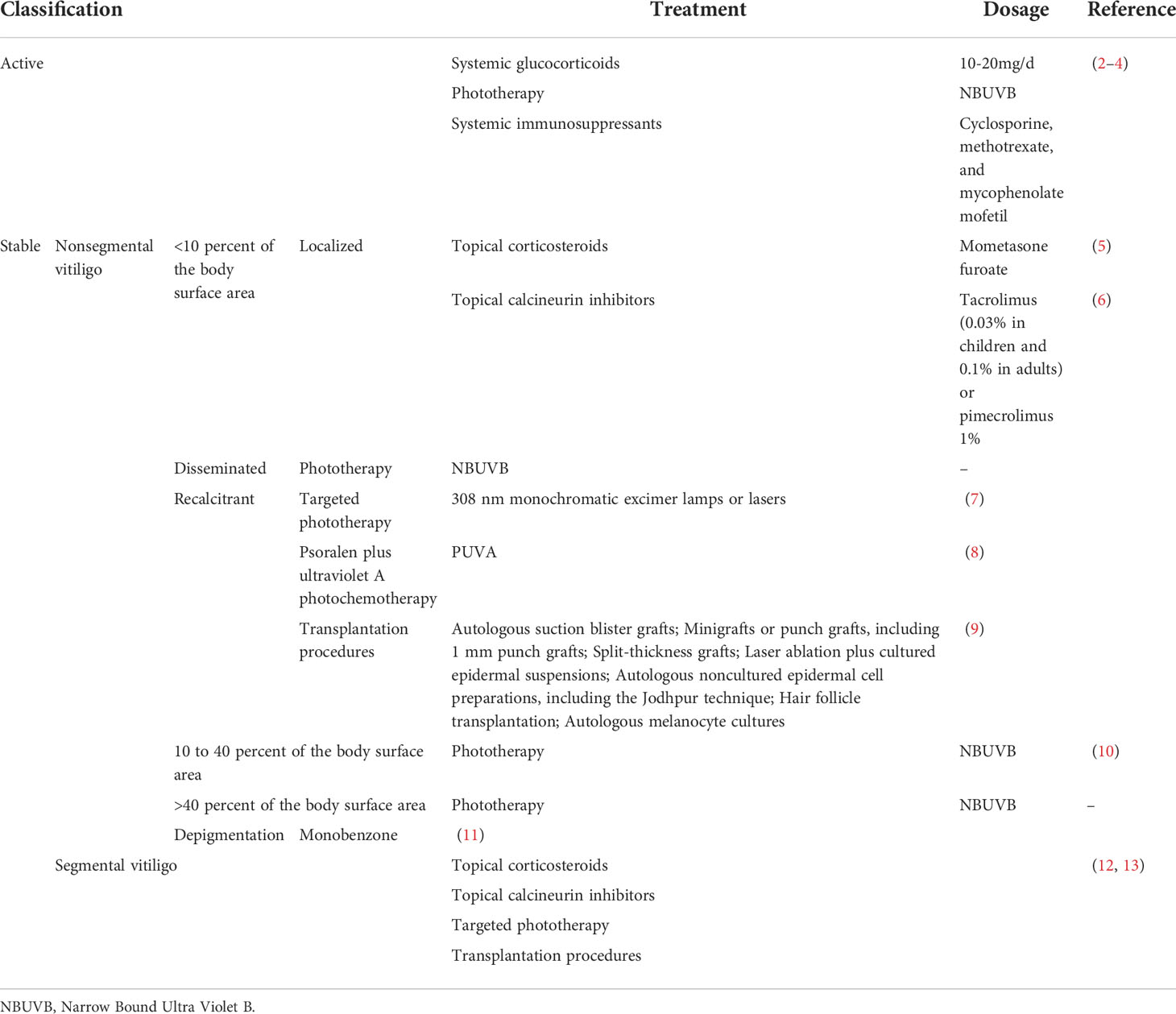
Table 1 Current treatment modalities for vitiligo.
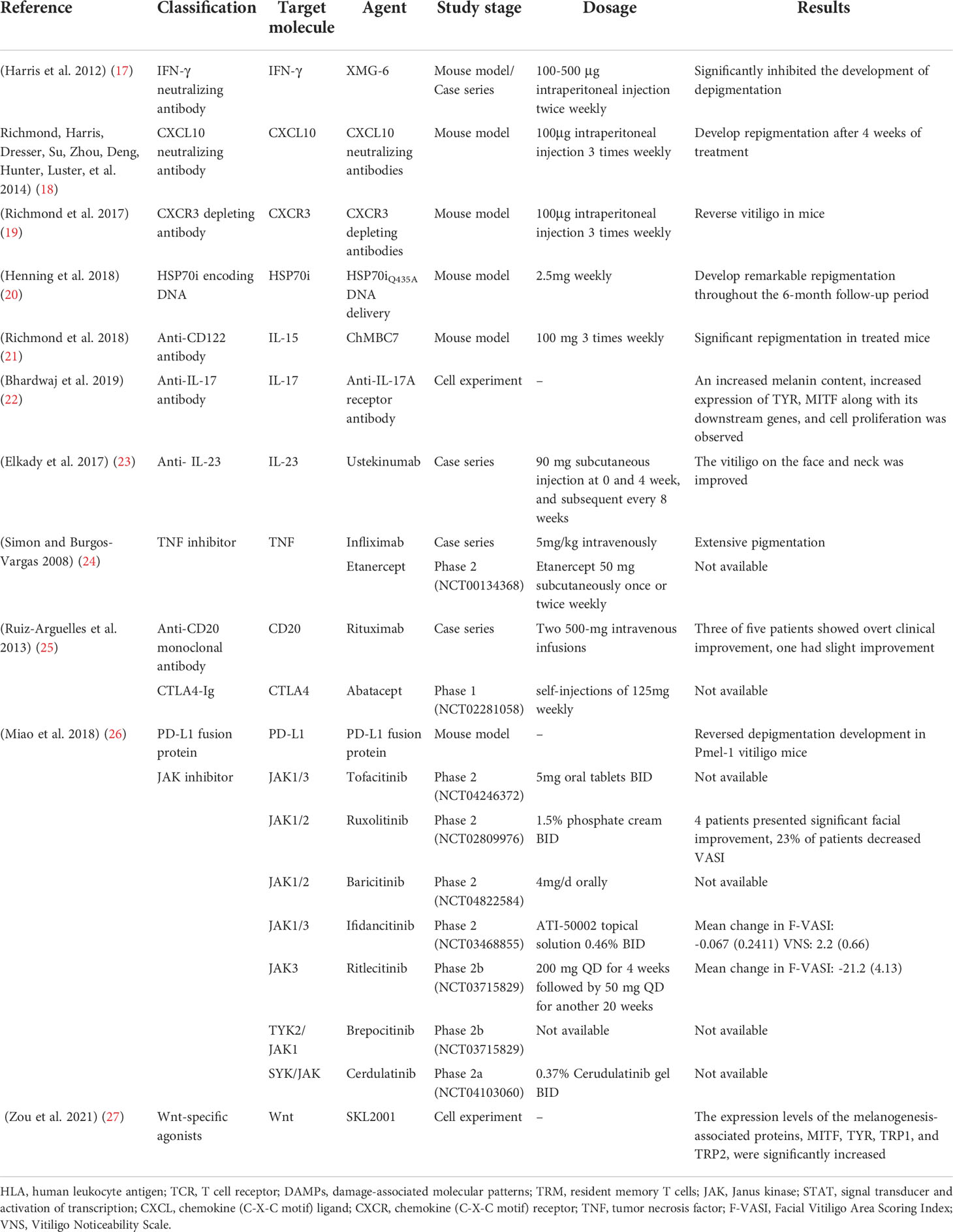
Table 2 Molecular-targeted therapies for the treatment of vitiligo.
3 Small molecules
3.1 emerging therapeutics targeting janus-activated kinase (jak) signaling.
The Janus kinases family consists of JAK1, JAK2, JAK3, and TYK2, which is engaged in the important JAK/STAT pathway, exhibiting pleiotropic effects on transducing multiple extracellular signals involved in regulating proliferative signaling, differentiation, migration, and apoptotic properties ( 28 ).
There are no licensed JAK/STAT inhibitors available against dermatological problems, however, some of them (ruxolitinib and tofacitinib) are used to treat other conditions such as myelofibrosis and RA. However, off-label usage of these medications in the treatment of vitiligo has shown promising outcomes.
JAK-STAT inhibitors promote Sonic Hedgehog and Wnt signaling in epidermal pigmentation, with the former inducing the migration, proliferation, and differentiation of melanocyte ( 29 ). Expanding our knowledge of these medications’ efficacy and safety profiles, as well as their use in dermatological conditions, is critical for establishing their risk-benefit ratio.
3.1.1 Tofacitinib
Tofacitinib is an FDA-cleared JAK1/3 inhibitor for treating RA, PsA, and active ulcerative colitis.
Tofacitinib 5-10 mg QD/BID has demonstrated superior efficacy against vitiligo, with improvement ratios of 5.4% in 5/10 patients with sun-exposed areas or areas treated only with phototherapy ( 30 ), and a reduced rate in vitiligo area scoring index (VASI) score of 4.68 at baseline to 3.95 at 5 months in another trial ( 31 ). In addition, a decline in the number of CD8 + T cells and chemokines, such as CXCL9 and CXCL10 has been observed after tofacitinib treatment, but no variations were observed for the percentage of melanocyte-specific T cells ( 30 ).
Unfortunately, this oral medication is associated with a host of systemic side effects, including infections, malignancies, and cytopenia. Thus, topical JAK inhibitors may be more preferred. 11 vitiligo patients treated with 2% tofacitinib cream twice a day in conjunction with NB-UVB therapy thrice-weekly demonstrated a mean improvement of 70% in facial VASI. There was also a significant difference between facial and non-facial lesions (P=0.022) ( 32 ).
3.1.2 Ruxolitinib
Ruxolitinib, the first Jakinib to get FDA approval, is a JAK1/2 inhibitor designed to deal with polycythemia vera and intermediate- and high-risk primary myelofibrosis ( 33 ).
Studies have shown that except for JAK inhibition, ruxolitinib also inhibited the differentiation and migration of DCs in vitiligo, increasing CD8 + cytotoxic T cell responses ( 34 ). In a double-blind phase 2 trial, 157 recruited vitiligo patients were randomized, in a 1:1:1:1:1 ratio, to receive topical ruxolitinib cream 1.5% BID, 1.5% QD, 0.5% QD, 0.15% QD, or a vehicle for 24 weeks, with the result showing considerably decreased CXCL9 and CXCL10 expression in 1.5% BID and 1.5% QD groups, and more individuals in groups receiving ruxolitinib cream 1.5% BID, 1.5% QD and 0.5% QD achieving F-VASI50, during which 1.5% BID group produced the highest responses in F-VASI50 (58%), F-VASI75 (52%), and F-VASI90 (33%). Besides, three positive responsive groups demonstrated significant repigmentation of vitiligo lesions and acceptable tolerability with a follow-up period of 52 weeks ( 35 ). Vitiligo on the face appears to respond more vigorously to therapy than non-facial lesions, reinforced by a 20-week, open-label trial in which patients with significant facial involvement experienced a 76% improvement in facial VASI scores ( 36 ). Furthermore, better repigmentation rates could be achieved both in oral and topical ruxolitinib treatment combined with phototherapy ( 37 ).
3.1.3 Baricitinib
Baricitinib is a selective JAK1/2 inhibitor that inhibits signal transduction of numerous proinflammatory cytokines ( 38 ), approved for the treatment of RA. To our knowledge, there was only one case report describing repigmentation in vitiligo patients with baricitinib 4 mg daily for the treatment of RA. Besides, an ongoing phase 2 trial (NCT04822584) in which patients received a combination therapy of baricitinib 4mg/d and phototherapy is being performed.
3.1.4 Ifidancitinib (ATI-50002)
Ifidancitinib is another dual JAK1/3 inhibitor for alopecia areata treatment, which is now undergoing phase II clinical trials for its application in vitiligo treatment. Patients with facial NSV(NCT03468855) receiving topical ATI-50002 BID for 24 weeks presented with an improved F-VASI and the Vitiligo Noticeability Scale (VNS) ( 39 ).
3.1.5 Ritlecitinib (PF-06651600) and Brepocitinib (PF-06700841)
Ritlecitinib, an irreversible inhibitor of JAK3 and tyrosine kinase applicable to the treatment of moderate-to-severe RA ( 40 ) and Brepocitinib, a TYK2/JAK1 inhibitor, are currently undergoing evaluation of their efficacy and safety profile in active NSV in combination with phototherapy (NCT03715829) ( 41 ).
3.1.6 Cerdulatinib (PRT062070)
Cerdulatinib, an SYK/JAK dual kinase inhibitor ( 42 ), has been assessed (NCT04103060) for its safety and tolerability for vitiligo treatment in topical formation (0.37% cerudulatinib gel BID).
However, additional studies are needed to determine the best-suited drug regimen and recommended dosage forms and doses to attain the optimum curative effect and minimal toxicity. As the occurrence of depigmentation after the withdrawal of JAK inhibitors, the mechanisms underlying need further exploration, and more work need to be done to corroborate the effectiveness in combination with other therapies.
3.2 Wnt signaling and its agonists
It has been shown that Wnt/β-catenin signaling plays a pivotal role in the proliferation, migration, and differentiation of melanocytes in vitiligo patients ( 29 ), which could be inhibited by oxidative stress ( 43 ). In addition, the Wnt/β-catenin pathway participates in the activation of MITF and its downstream enzymes ( 44 ). Intradermal injection of IWR-1 (inhibitor of Wnt response 1), a chemical inhibitor of β-catenin activation, and small interfering RNA (siRNA) against Wnt7α suppressed the number of epidermal melanocytes ( 45 ). This evidence suggested that stimulation of Wnt signaling may be an adjuvant therapy for vitiligo treatment. Micro-injury ( 46 ) as well as some phenanthridine-derived Wnt-specific agonists binding with the Axin protein have been proved to promote melanogenesis ( 47 ) and induce repigmentation.
3.3 Emerging therapeutics targeting microRNAs (miRNAs)
MiRNAs, which are a highly conservative small class of non-coding RNA molecules, participate in mRNA expression regulation via degradation or repression of mRNA translation ( 48 ). Previous studies have demonstrated that miRNAs were associated with genetic polymorphisms (e.g., miR-196a-2 rs11614913), immune response (e.g., miR-133b, miR-224-3p, miR-4712-3p, miR-3940-5p, miR-21−5p), oxidative stress (e.g., miR-135a, miR-9, miR-34a, miR-183, miR-184, miR-1, miR-25, miR-211, miR-383, miR-577, miR-421) and melanocyte functions (e.g., miR-434-5p, miR-330-5p, miR-137, miR-148, miR-145, miR-155, miR-203, miR-125, miR-377, miR-2909, miR-200c, hsa-miR-149-5p) ( 49 – 54 ), participating in pathological mechanism of vitiligo. These findings suggest that miRNAs may be involved in vitiligo pathogenesis via the modulation of vital genes expression in melanocytes and serve as novel therapeutic targets for vitiligo therapy.
There are two strategies for the therapeutic application of miRNAs: 1) anti-miRNAs, locked-nucleic acids (LNA), or antagomiRs ( 55 ) can be used to counteract the over-activation of miRNA. Short tandem target mimic (STTM)- miR-508-3p has been validated to upregulate SOX6 expression, leading to increased expression of key melanogenic genes CREB, MITF, TYR, and TYRP1/2 with increased melanogenesis ( 56 ). Besides, STTM-miR-143-5p also upregulates the expression of MYO5A, leading to an increase in the level of MITF, TYR, TYRP1, melanin, and Rab27a ( 57 ). 2) miRNA replacement, involving the reintroduction of a gene-suppressor miRNA mimic or AAV (adeno-associated virus)-mediated miRNA gain-of-function to modulate gene expression ( 55 ). A study demonstrated that the migratory capacity of melanocytes was altered by the application of miR-211 mimic through the p53-TRPM1/miR-211-MMP9 axis ( 58 ).
3.4 Emerging therapeutics targeting regulatory T-cells (Tregs)
Tregs are a suppressive CD4 + T cell subset that possesses a capacity to suppress self-reactive T cell activation and expansion ( 59 ). A clear decrease in Treg cells was observed in vitiligo skin within lesional, non-lesional, and perilesional sections ( 60 ), indicating that increasing the number of Tregs with normal function might be an important therapeutic intervention for vitiligo treatment.
Infusing purified populations of Tregs is the most direct way for the supply of Tregs. The current methods mainly include polyclonally-expanded Tregs, antigen-specific Tregs, and engineered Treg cells. In a mouse model of vitiligo, adoptive transfer of polyclonal Tregs may be effective in the short-term ( 61 ), which might however impart systemic immunosuppression ( 62 ). Besides, a TCR transgenic mouse with spontaneous vitiligo, receiving CAR Tregs treatment, developed a significant delay in depigmentation ( 63 ).
However, a limitation of infusing purified populations of Tregs might be the technical difficulty for therapeutic agent delivery to specific cells. A topical application of Tregs or the combination with CCR4 Treg homing receptor ligand CCL22 ( 64 ) by local needle-free jet injection of DNA ( 20 ) or CCL22-encoding plasmid DNA ( 64 ) may help resolve that issue. Besides, various strategies have been applied towards the modulation of Tregs function by targeting Treg-intrinsic pathways and functional modulators for Tregs. HO-1, a functional modulator of Tregs, was decreased in vitiligo Tregs. Treatment with Hemin, an agonist of HO-1, was found to enhance HO-1-induced restoration of Tregs function by up-regulating IL-10 expression ( 65 ). In addition, therapeutic method for microbiota modulation, such as neomycin treatment can significantly delay depigmentation in vitiligo mice and promote the infiltration of Tregs to the skin ( 66 ). Rapamycin, an inhibitor of PI3Kakt-mTORC1 signaling ( 67 ), efficiently halts the depigmentation process by increasing the abundance of Treg in h3TA2 mice, which effect lasted till 6 weeks after treatment ( 61 ). At present, a phase 2 clinical trial(NCT05342519) is underway for assessing the efficacy of the application of 0.1% topical rapamycin ( 68 ) (2022). In addition, nanoparticles containing rapamycin and autoantigen HEL46-61(NPHEL46-61/Rapa) were synthesized, the administration of which halted the disease progression ( 69 ). Also, the calcium-NFATc1-signaling pathway may be involved in defective Tregs function, indicating a potential therapeutic target for vitiligo treatment ( 70 ).
4 Cytokine-targeted therapies
Multiple monoclonal antibodies are available for vitiligo treatment, targeting IFN-γ, CXCL10, CXCR3, HSP70i, IL-15, IL-17/23, and TNF. In addition to full-size immunoglobulin, affibodies and nanobodies, composed of considerably smaller proteins, are currently being developed, which have higher bioavailability as well as affinity and specificity to the targeted molecules.
4.1 IFN-γ and the inhibitors
The IFN-γ-CXCL9/10-CXCR3 axis may be crucial for vitiligo pathogenesis, contributing to disease progression by inhibiting melanogenesis, inducing apoptosis of melanocytes, and further recruiting T cells to the skin ( Figure 1 ) ( 71 ). A study showed a higher expression of IFN-γ mRNA in non-lesional and perilesional skin, especially in active vitiligo ( 72 ), which is associated with disease activity ( 73 ).
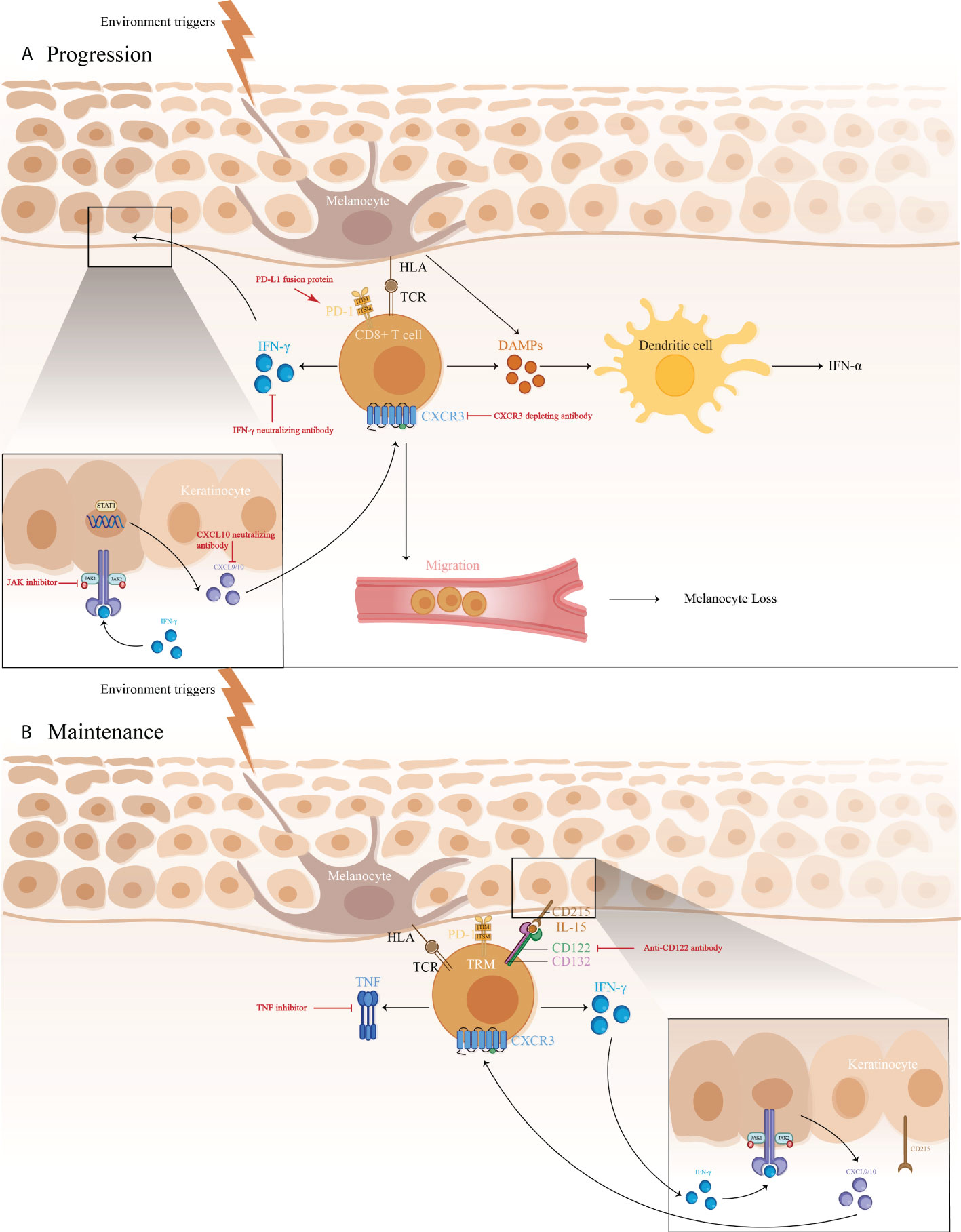
Figure 1 1) The immune pathogenesis of vitiligo: (A) CD8 + T cell expression of IFN-γ in vitiligo lesions activated the JAK/STAT pathway after binding to IFN-γ receptor, thus facilitating the release of CXCL9/10. The binding of CXCL9/10 to CXCR3 increased CXCR3+ T cells recruitment; (B) Maintenance of vitiligo lesions was influenced by the function of IL-15-dependent TRM cells, which produce IFN-γ and TNF-α. 2)Targeted therapeutic interventions in vitiligo mainly include therapies targeting IFN-γ-CXCL9/10-CXCR3 axis (IFN-γ neutralizing antibody, CXCL10 neutralizing antibody, and CXCR3 depleting antibody, as well as JAK inhibitors), anti-CD122 antibody (IL-15 receptor subunit) to decrease IFN-γ production and deplete autoreactive CD8 + TRM cells, TNF inhibitor to inhibit autoantibody production, and PD-L1 fusion protein to reduce the numbers of melanocyte-reactive T cells.
Anti-IFN-γ can have been proved to be effective in rheumatoid arthritis (RA), multiple sclerosis (MS), prevention of corneal rejection, autoimmune skin diseases, and others. In a recent study, vitiligo induction mice, treated with intraperitoneal injection with IFN-γ neutralizing antibody (XMG-6) at a dose of 100-500 μg twice a week, presented with significant improvement of depigmentation ( 17 ), with the same trend observed in vitiligo patients. Four patients who received intradermal perilesional injections presented with repigmentation of the treated area and boundary retreat ( 74 ). More research is warranted to be initiated for further definition of the role that IFN-γ plays in vitiligo and to examine whether IFN-γ neutralization would be more viable in reversing skin depigmentation.
4.2 CXCL10 and the inhibitors
Recent studies report a Th1/IFN-γ immune response in both human and a mouse model of vitiligo that involves elevated CXCL9, 10, and 11 productions, among which CXCL10 participated in the targeted migration of T cells ( 18 ), triggering an immune cell infiltration at the early stage ( 72 ), and involved in the downregulation of keratinocyte glycoprotein non-metastatic melanoma protein B (GPNMB) ( 75 ). A study showed that mice receiving CXCL10 neutralizing antibodies developed more repigmentation after 4 weeks’ treatment, which continued for an additional 4 weeks ( 18 ), thereby supporting CXCL10 suppression as a great therapeutic strategy.
4.3 CXCR3 antibodies
CXCR3 has been proved to be expressed in skin lesions, autoreactive T cells ( 18 ), and the vast majority of skin infiltrating CD8 + resident memory T cells (TRM), which stimulate the secretion of IFN-γ and TNF-α ( 76 ).
In a study, vitiligo mice with >75% depigmentation on their tails are treated with CXCR3 depleting antibodies for 7-8 weeks, which significantly reversed the clinical disease in a perifollicular pattern and a diminution of PMEL in the epidermis, with slightly reduced host CD8 + T cell numbers ( 19 ) compared to neutralizing antibody treatment ( 18 ). Although these results are preliminary, they may provide justification for further studies in targeting CXCR3 in vitiligo ( 19 ), which proposes the use of a depleting Ab to create a greater clinical efficacy by removing autoreactive cells rather than modulating their migration phenotype.
4.4 Inducible HSP70 (HSP70i) DNA
Indeed, HSP70i is the core participant in vitiligo predominantly through HSP70i-plasmacytoid dendritic cells (pDCs)-IFN-α-CXCL9 and CXCL10-cytotoxic T lymphocyte (CTL) axis. Pmel-1 mice vaccinated with HSP70i encoding DNA exhibited significant depigmentation, rarely seen in models knockout for HSP70i, indicating that elevated HSP70i expression alone would be enough to induce depigmentation in vitiligo prone animals ( 77 ). A study revealed that the expression of HSP-70 mRNA in skin lesions of active vitiligo patients was much higher ( 78 ), correlated with the disease activity.
Blocking HSP70i activity might have the potential to reverse vitiligo development. A recent study showed that a Sinclair swine, receiving HSP70iQ435A-encoding DNA treatment, showed remarkable repigmentation with an initial influx of T cells and increased CD4/CD8 ratios ( 20 ), which was also detected in mice with HSP70i Q435A -encoding DNA treatment, resulting in 76% restoration of skin pigmentation. Furthermore, the treatment halted T cells accumulation and transition to T cell phenotype in mice and human skin, engaging HSP70i Q435A DNA delivery as a potent effective therapeutic intervention for vitiligo ( 79 ).
4.5 IL-15 and the inhibitors
It has been established that IL-15 seems to participate in IL-17 regulation and maintenance of TRM signals ( 80 ), with the latter responsible for long-term maintenance and potential relapse of vitiligo ( 81 ). The study has demonstrated a higher serum level of IL-15 in vitiligo patients than in controls, highly associated with epidermal H 2 O 2 content and the disease activity ( 82 , 83 ).
In vitiligo mice, an anti-CD122 antibody that targets IL-15 signaling was reported to effectively reverse depigmentation. Anti-CD122 therapy, either systemically or locally, decreases TRM-induced IFN-γ production and results in long-term repigmentation. These findings consider CD122-targeted drugs as a valid therapy method, which results in effective and long-lasting responses in vitiligo and other tissue-specific autoimmune disorders involving TRM ( 21 ).
4.6 PD-1/PD-L1 pathway
Involvement of the PD-1/PD-L1 pathway has been shown in many autoimmune diseases, including RA, MS, and vitiligo. PD-L1 expression was found limited in normal skin, and only expressed on dermal T cells, and increased in primary melanocytes and fibroblasts after exposure to IFN-γ. No such effect was seen in vitiligo patients, indicating the absence of self-protection ability for melanocytes against T-cell attack during vitiligo pathogenesis. In agreement with this, treatment with PD-L1 fusion protein reduced the numbers of melanocyte-reactive T cells, inhibited the activation of Vβ12-expressing T cells, and increased Tregs numbers, reversing depigmentation in a Pmel-1 T-cell receptor transgenic vitiligo mouse model ( 26 ). However, PD-L1 treatment may still call for extended phototherapy treatment, especially NB-UVB therapy, which likely upregulates PD-L1 expression in an NF-κB-dependent manner ( 84 ), indicating a combination use of local PD-1/PD-L1 agonistic treatment and NB-UVB therapy as a promising option.
4.7 Other cytokine-targeted therapies under investigation
4.7.1 il-17/23 and the inhibitors.
Studies on the effect of IL-17/23 in vitiligo resulted in contradictory findings. On one hand, Th17 cells and IL-17 in vitiligo patients may inhibit function-related factors, repress melanogenesis, and dramatically induct other Th17 type cytokines as well as IL-1β production from dermal fibroblasts and keratinocytes ( 85 ). Elevated Th17 cells and IL-17/23 levels in skin lesions and serum of vitiligo patients, were positively correlated with disease activity ( 86 , 87 ), and decreased after narrowband ultraviolet B (NBUVB) treatment ( 88 ). Primary melanocyte culture showed an increased expression of MITF and its downstream genes, increased melanin pigment, and cell proliferation after blockade with anti-IL-17RA ( 22 ). Besides, incidences of repigmentation have been documented in ustekinumab treatment of vitiligo ( 23 ). However, secukinumab treatment in patients with active non‐segmental vitiligo (NSV) contributed to disease progression in 7/8 patients with no general reduction in CXCL9/10, sCD25/27, Th1 cells, or cytotoxic cells, resulting in early termination of study ( 89 ). There are also reports of ustekinumab-induced new-onset vitiligo and alopecia areata. The above studies showed IL-17/23 signal may not play a direct role in vitiligo pathogenesis, which needs further investigation to confirm this conjecture.
4.7.2 TNF and the inhibitors
As an anti-inflammatory mediator, TNF-α is considered to play a role in vitiligo, which may promote apoptosis in melanocytes, induce B-cell activation, increase autoantibody production, and inhibit melanogenesis ( 90 ). Recent data has shown a significantly higher expression of TNF-α in vitiligo skin. TNF inhibitors are beneficial in the treatment of plaque-type psoriasis, psoriatic arthritis (PsA), RA, and inflammatory bowel disease (IBD), arousing growing interest in their use in vitiligo.
Infliximab is a chimeric anti-TNF-α monoclonal antibody specifically binding to both soluble and membrane-bound TNF ( 91 , 92 ). Intravenous infliximab is widely licensed in the treatment of RA, psoriasis, ankylosing spondylitis (AS), IBD, uveitis, and Behcet’s disease. A 24-year-old patient with ankylosing spondylitis and refractory vitiligo improved significantly following six months of infliximab therapy at a dose of 5mg/kg intravenously in weeks 0, 2, and 6, and then every eight weeks for ten months ( 24 ). Besides, Etanercept is a monoclonal antibody targeted against TNF-α ( 93 ), which has been approved for the treatment of RA, juvenile RA, AS, psoriasis, and PsA. Treatment with etanercept 50 mg subcutaneously once or twice weekly for at least 2 months has shown a great curative effect on established vitiligo ( 94 ).
However, it has been shown that anti‐TNF‐α agents, especially adalimumab and infliximab ( 95 ), may exacerbate established vitiligo and induce new-onset vitiligo during treatment of other autoimmune diseases, including AS ( 96 ), Crohn’s disease ( 97 ), ulcerative colitis ( 98 ), psoriasis ( 99 ), and RA ( 100 ). The mechanism responsible for the TNF-α inhibitors-induced vitiligo is not fully understood. On the one hand, TNF-α inhibitors may increase the nucleosome-mediated autoantibody formation, interfere with the cytotoxic T-cell suppression of autoreactive B cells, and decrease Treg synthesis and activation. Additionally, infliximab increases pDC-produced IFN-γ, participating in further T cells recruiting. Although very rare, new-onset or exacerbations of vitiligo can occur in the anti‐TNF‐α treatment of other autoimmune diseases, the risk of which must not be ignored.
4.7.3 Rituximab
Rituximab has specific affinity for the B-lymphocyte transmembrane protein, CD20, which is expressed on B cells ( 101 ), participating in the activation of the CD8 + T cells and the ensuing autoreactive reaction ( 102 ). Rituximab is licensed for the treatment of lymphomas, leukemias, transplant rejection crisis, and a series of autoimmune diseases ( 103 , 104 ). An intravenous infusion of Rituximab was administered to five active disseminated vitiligo patients, the three of whom exhibited a considerable improvement in both the disease’s symptoms and histology ( 25 ).
4.7.4 Abatacept
Abatacept, a fusion protein consisting of IgG1 coupled to the extracellular domain of CTLA-4 via the immunoglobulin’s Fc region, was licensed for treating moderate to severe RA. Ten eligible patients with active vitiligo have been included to receive self-injections of 125mg abatacept weekly from week 0 to week 24. Secondary endpoints will be evaluated during a 32-week follow-up visit ( 105 ).
5 Future therapeutic prospects
As a future direction, new therapeutic approaches should be developed to reduce vitiligo progression. Among the new approaches being developed, the strategy of targeting the IFN-γ-CXCL9/10-CXCR3 axis has been clinically tested. OPZELURA has been indicated for the topical treatment of nonsegmental vitiligo in adult and pediatric patients 12 years of age and older. MiRNA-based therapeutics are also in development. However, the absence of organ or tissue selectivity may also lead to off-target side effects, which must be considered and excluded in the process of miRNA-based therapeutics development. Besides, a suitable vector system, as well as the assurance of chemical and biological stability should also be taken into account. Adoptive Treg cell therapy has also been the research hotspot in recent years. However, it has always been a difficult point for reassurance for safety and the development of the delivery system.
Treating vitiligo remains a challenge. As is presented in this paper, a greater variety of precision treatments is currently being studied. With a better understanding and further validation of these therapeutic targets, patients can be stratified to achieve individualized treatment.
6 Conclusion
Current models of treatment for vitiligo are often nonspecific and general. Various therapy options are available for active vitiligo patients, including systemic glucocorticoids, phototherapy, and systemic immunosuppressants. While stable vitiligo patients may benefit from topical corticosteroids, topical calcineurin inhibitors, phototherapy, as well as transplantation procedures. Recently, a better understanding of the pathophysiological processes of vitiligo led to the advent of novel targeted therapies. To date, JAK inhibitors are the only category that has been proved to have a good tolerability profile and functional outcomes in vitiligo treatment, even though the risk of activation of latent infection and systemic side effects still existed, like other immunosuppressive agents. Research is in progress to investigate the important cytokines involved in the pathogenesis of vitiligo, including IFN-γ, CXCL10, CXCR3, HSP70i, IL-15, IL-17/23, and TNF, the blockade of which has undergone preliminary attempts in animal models and some patients. In addition, studies on miRNA-based therapeutics as well as adoptive Treg cell therapy are still primary, and more studies are necessary.
Author contributions
YFF and YL contributed to the conceptual design, writing, editing, and generation of figures for this manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ezzedine K, Eleftheriadou V, Whitton M, van Geel N. Vitiligo. Lancet (London England) (20159988) 386:74–84. doi: 10.1016/S0140-6736(14)60763-7
CrossRef Full Text | Google Scholar
2. Bishnoi A, Vinay K, Kumaran MS, Parsad D. “Oral mycophenolate mofetil as a stabilizing treatment for progressive non-segmental vitiligo: results from a prospective, randomized, investigator-blinded pilot study”. Arch Dermatol Res (2021) 313(5):357–65. doi: 10.1007/s00403-020-02108-8
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Garza-Mayers AC, Kroshinsky D. “Low-dose methotrexate for vitiligo”. Drugs Dermatol (2017) 16(7):705–6.
Google Scholar
4. Singh H, Kumaran MS, Bains A, Parsad D. A randomized comparative study of oral corticosteroid minipulse and low-dose oral methotrexate in the treatment of unstable vitiligo. Dermatology (2015) 231(3):286–90. doi: 10.1159/000433424
5. Taieb A, Alomar A, Bohm M, Dell'anna ML, De Pase A, Eleftheriadou V, et al. Guidelines for the management of vitiligo: The European dermatology forum consensus. Br J Dermatol (2013) 168(1):5–19. doi: 10.1111/j.1365-2133.2012.11197.x
6. Lee JiH, Kwon HS, Jung HMi, Lee H, Kim GM, Yim HW, et al. Treatment outcomes of topical calcineurin inhibitor therapy for patients with vitiligo: A systematic review and meta-analysis. JAMA Dermatol (2019) 155(8):929–38. doi: 10.1001/jamadermatol.2019.0696
7. Lopes C, Trevisani VF, Melnik T. Efficacy and safety of 308-nm monochromatic excimer lamp versus other phototherapy devices for vitiligo: A systematic review with meta-analysis. Am J Clin Dermatol (2016) 17(1):23–32. doi: 10.1007/s40257-015-0164-2
8. Zubair R, Hamzavi IH. Phototherapy for vitiligo. Dermatol Clinics (2020) 38(1):55–62. doi: 10.1016/j.det.2019.08.005
9. Mohammad TF, Hamzavi IH. Surgical therapies for vitiligo. Dermatol Clinics (2017) 35(2):193–203. doi: 10.1016/j.det.2016.11.009
10. Mohammad TF, Al-Jamal M, Hamzavi IH, Harris JE, Leone G, Cabrera R, et al. The vitiligo working group recommendations for narrowband ultraviolet b light phototherapy treatment of vitiligo. J Am Acad Dermatol (2017) 76(5):879–88. doi: 10.1016/j.jaad.2016.12.041
11. Grimes PE, Nashawati R. Depigmentation therapies for vitiligo. Dermatol Clinics (2017) 35(2):219.
12. Mulekar SV, Al Eisa A, Delvi MB, Al Issa A, Al Saeed AH. Childhood vitiligo: A long-term study of localized vitiligo treated by noncultured cellular grafting. Pediatr Dermatol (2010) 27(2):132–6. doi: 10.1111/j.1525-1470.2009.00978.x
13. Mulekar SV. Long-term follow-up study of segmental and focal vitiligo treated by autologous, noncultured melanocyte-keratinocyte cell transplantation. Arch Dermatol (2004) 140(10):1211–5. doi: 10.1001/archderm.140.10.1211
14. Bohm M, Schunter JA, Fritz K, Salavastru C, Dargatz S, Augustin M, et al. S1 guideline: Diagnosis and therapy of vitiligo. J Dtsch Dermatol Ges (2022) 20(3):365–78. doi: 10.1111/ddg.14713
15. Batchelor JM, Thomas KS, Akram P, Azad J, Bewley A, Chalmers JR, et al. Home-based narrowband UVB, topical corticosteroid or combination for children and adults with vitiligo: HI-light vitiligo three-arm RCT. Health Technol Assess (2020) 24(64):1–128. doi: 10.3310/hta24640
16. Li R, Qiao M, Wang X, Zhao X, Sun Q. Effect of narrow band ultraviolet b phototherapy as monotherapy or combination therapy for vitiligo: A meta-analysis. Photodermatol Photoimmunol Photomed (2017) 33(1):22–31. doi: 10.1111/phpp.12277
17. Harris JE, Harris TH, Weninger W, Wherry EJ, Hunter CA, Turka LA. A mouse model of vitiligo with focused epidermal depigmentation requires IFN-gamma for autoreactive CD8(+) T-cell accumulation in the skin. J Invest Dermatol (2012) 132(7):1869–76. doi: 10.1038/jid.2011.463
18. Rashighi M, Agarwal P, Richmond JM, Harris TH, Dresser K, Su M-W, et al. CXCL10 is critical for the progression and maintenance of depigmentation in a mouse model of vitiligo. Sci Trans Med (2014) 6(223):223ra23. doi: 10.1126/scitranslmed.3007811
19. Richmond JM, Masterjohn E, Chu R, Tedstone J, Youd ME, Harris JE. CXCR3 depleting antibodies prevent and reverse vitiligo in mice. J Invest Dermatol (2017) 137(4):982–5. doi: 10.1016/j.jid.2016.10.048
20. Henning SW, Fernandez MF, Mahon JP, Duff R, Azarafrooz F, Guevara-Patino JA, et al. HSP70iQ435A-encoding DNA repigments vitiligo lesions in Sinclair swine. J Invest Dermatol (2018) 138(12):2531–9. doi: 10.1016/j.jid.2018.06.186
21. Richmond JM, Strassner JP, Zapata L, Garg M, Riding RL, Refat MA, et al. Antibody blockade of IL-15 signaling has the potential to durably reverse vitiligo. Sci Trans Med (2018) 10(450):eaam7710. doi: 10.1126/scitranslmed.aam7710
22. Bhardwaj S, Bhatia A, Kumaran MS, Parsad D. Role of IL-17A receptor blocking in melanocyte survival: A strategic intervention against vitiligo. Exp Dermatol (2019) 28(6):682–9. doi: 10.1111/exd.13773
23. Elkady A, Bonomo L, Amir Y, Vekaria AS, Guttman-Yassky E. Effective use of ustekinumab in a patient with concomitant psoriasis, vitiligo, and alopecia areata. JAAD Case Rep (2017) 3(6):477–9. doi: 10.1016/j.jdcr.2017.07.009
24. Simon JA, Burgos-Vargas R. Vitiligo improvement in a patient with ankylosing spondylitis treated with infliximab. Dermatology (2008) 216(3):234–5. doi: 10.1159/000112932
25. Ruiz-Arguelles A, Garcia-Carrasco M, Jimenez-Brito G, Sanchez-Sosa S, Perez-Romano B, Garces-Eisele J, et al. Treatment of vitiligo with a chimeric monoclonal antibody to CD20: A pilot study. Clin Exp Immunol (2013) 174(2):229–36. doi: 10.1111/cei.12168
26. Miao X, Xu R, Fan B, Chen J, Li X, Mao W, et al. PD-L1 reverses depigmentation in pmel-1 vitiligo mice by increasing the abundance of tregs in the skin. Sci Rep (2018) 8(1):1605. doi: 10.1038/s41598-018-19407-w
27. Zou DP, Chen YM, Zhang LZ, Yuan XH, Zhang YJ, Inggawati A, et al. SFRP5 inhibits melanin synthesis of melanocytes in vitiligo by suppressing the wnt/beta-catenin signaling. Genes Dis (2021) 8(5):677–88. doi: 10.1016/j.gendis.2020.06.003
28. Rawlings JS, Rosler KM, Harrison DA. The JAK/STAT signaling pathway. J Cell Sci (2004) 117(Pt 8):1281–3. doi: 10.1242/jcs.00963
29. Birlea SA, Costin GE, Roop DR, Norris DA. Trends in regenerative medicine: Repigmentation in vitiligo through melanocyte stem cell mobilization. Med Res Rev (2017) 37(4):907–35. doi: 10.1002/med.21426
30. Liu LY, Strassner JP, Refat MA, Harris JE, King BA. Repigmentation in vitiligo using the janus kinase inhibitor tofacitinib may require concomitant light exposure. J Am Acad Dermatol (2017) 77(4):675–82.e1. doi: 10.1016/j.jaad.2017.05.043
31. Vu M, Heyes C, Robertson SJ, Varigos GA, Ross G. Oral tofacitinib: A promising treatment in atopic dermatitis, alopecia areata and vitiligo. Clin Exp Dermatol (2017) 42(8):942–4. doi: 10.1111/ced.13290
32. Mobasher P, Guerra R, Li SJ, Frangos J, Ganesan AK, Huang V. Open-label pilot study of tofacitinib 2% for the treatment of refractory vitiligo. Br J Dermatol (2020) 182(4):1047–9. doi: 10.1111/bjd.18606
33. Deisseroth A, Kaminskas E, Grillo J, Chen W, Saber H, Lu HL, et al. U.S. food and drug administration approval: ruxolitinib for the treatment of patients with intermediate and high-risk myelofibrosis. Clin Cancer Res (2012) 18(12):3212–7. doi: 10.1158/1078-0432.CCR-12-0653
34. Heine A, Held SA, Daecke SN, Wallner S, Yajnanarayana SP, Kurts C, et al. The JAK-inhibitor ruxolitinib impairs dendritic cell function in vitro and in vivo . Blood (2013) 122(7):1192–202. doi: 10.1182/blood-2013-03-484642
35. Rosmarin D, Pandya AG, Lebwohl M, Grimes P, Hamzavi I, Gottlieb AB, et al. Ruxolitinib cream for treatment of vitiligo: A randomised, controlled, phase 2 trial. Lancet (2020) 396(10244):110–20. doi: 10.1016/S0140-6736(20)30609-7
36. Rothstein B, Joshipura D, Saraiya A, Abdat R, Ashkar H, Turkowski Y, et al. Treatment of vitiligo with the topical janus kinase inhibitor ruxolitinib. J Am Acad Dermatol (2017) 76(6):1054–60.e1. doi: 10.1016/j.jaad.2017.02.049
37. Gianfaldoni S, Tchernev G, Wollina U, Roccia MG, Fioranelli M, Lotti J, et al. Micro - focused phototherapy associated to janus kinase inhibitor: A promising valid therapeutic option for patients with localized vitiligo. Open Access Maced J Med Sci (2018) 6(1):46–8. doi: 10.3889/oamjms.2018.042
38. Norman P. Selective JAK inhibitors in development for rheumatoid arthritis. Expert Opin Investig Drugs (2014) 23(8):1067–77. doi: 10.1517/13543784.2014.918604
39. A study of ATI-50002 topical solution for the treatment of vitiligo (2018). Available at: https://clinicaltrials.gov/ct2/show/NCT03468855 .
40. Robinson MF, Damjanov N, Stamenkovic B, Radunovic G, Kivitz A, Cox L, et al. Efficacy and safety of PF-06651600 (Ritlecitinib), a novel JAK3/TEC inhibitor, in patients with moderate-to-Severe rheumatoid arthritis and an inadequate response to methotrexate. Arthritis Rheumatol (2020) 72(10):1621–31. doi: 10.1002/art.41316
41. A phase 2b study to evaluate the efficacy and safety profile of PF-06651600 and PF-06700841 in active non-segmental vitiligo subjects (2018). Available at: https://clinicaltrials.gov/ct2/show/NCT03715829 .
42. Coffey G, Betz A, DeGuzman F, Pak Y, Inagaki M, Baker DC, et al. The novel kinase inhibitor PRT062070 (Cerdulatinib) demonstrates efficacy in models of autoimmunity and b-cell cancer. J Pharmacol Exp Ther (2014) 351(3):538–48. doi: 10.1124/jpet.114.218164
43. Regazzetti C, Joly F, Marty C, Rivier M, Mehul B, Reiniche P, et al. Transcriptional analysis of vitiligo skin reveals the alteration of WNT pathway: A promising target for repigmenting vitiligo patients. J Invest Dermatol (2015) 135(12):3105–14. doi: 10.1038/jid.2015.335
44. Harris JE. Melanocyte regeneration in vitiligo requires WNT beneath their wings. J Invest Dermatol (2015) 135(12):2921–3. doi: 10.1038/jid.2015.372
45. Yamada T, Hasegawa S, Inoue Y, Date Y, Yamamoto N, Mizutani H, et al. Wnt/beta-catenin and kit signaling sequentially regulate melanocyte stem cell differentiation in UVB-induced epidermal pigmentation. J Invest Dermatol (2013) 133(12):2753–62. doi: 10.1038/jid.2013.235
46. Han X, Chang Li, Qiu Z, Lin M, Wang Y, Liu D, et al. Micro-injury induces hair regeneration and vitiligo repigmentation through wnt/β-catenin pathway. Stem Cells Dev (2022) 31(5-6):111–8. doi: 10.1089/scd.2021.0276
47. Yang BJ, Fan SR, Zhang XF, Cai JY, Ruan T, Xiang ZR, et al. Design, synthesis and structure-activity relationship optimization of phenanthridine derivatives as new anti-vitiligo compounds. Bioorg Chem (2022) 119:105582. doi: 10.1016/j.bioorg.2021.105582
48. Baek D, Villen J, Shin C, Camargo FD, Gygi SP, Bartel DP. The impact of microRNAs on protein output. Nature (2008) 455(7209):64–71. doi: 10.1038/nature07242
49. Li L. The role of MicroRNAs in vitiligo: Regulators and therapeutic targets. Ann Dermatol (2020) 32(6):441–51. doi: 10.5021/ad.2020.32.6.441
50. Huo J, Liu T, Li F, Song X, Hou X. MicroRNA215p protects melanocytes via targeting STAT3 and modulating Treg/Teff balance to alleviate vitiligo. Mol Med Rep (2021) 23(1):51. doi: 10.3892/mmr.2020.11689
51. Vaish U, Kumar AA, Varshney S, Ghosh S, Sengupta S, Sood C, et al. Micro RNAs upregulated in vitiligo skin play an important role in its aetiopathogenesis by altering TRP1 expression and keratinocyte-melanocytes cross-talk. Sci Rep (2019) 9(1):10079. doi: 10.1038/s41598-019-46529-6
52. Zhao C, Wang D, Wang X, Mao Y, Xu Z, Sun Y, et al. Down-regulation of exosomal miR-200c derived from keratinocytes in vitiligo lesions suppresses melanogenesis. J Cell Mol Med (2020) 24(20):12164–75. doi: 10.1111/jcmm.15864
53. Li L, Xie Z, Qian X, Wang T, Jiang M, Qin J, et al. Identification of a potentially functional circRNA-miRNA-mRNA regulatory network in melanocytes for investigating pathogenesis of vitiligo. Front Genet (2021) 12:663091. doi: 10.3389/fgene.2021.663091
54. Shang Z, Li H. Altered expression of four miRNA (miR-1238-3p, miR-202-3p, miR-630 and miR-766-3p) and their potential targets in peripheral blood from vitiligo patients. J Dermatol (2017) 44(10):1138–44. doi: 10.1111/1346-8138.13886
55. Kwekkeboom RF, Lei Z, Doevendans PA, Musters RJ, Sluijter JP. Targeted delivery of miRNA therapeutics for cardiovascular diseases: opportunities and challenges. Clin Sci (Lond) (2014) 127(6):351–65. doi: 10.1042/CS20140005
56. Liu B, Zhang J, Yang S, Ji K, Liu X, Du B, et al. Effect of silencing microRNA-508 by STTM on melanogenesis in alpaca (Vicugna pacos). Gene (2018) 678:343–8. doi: 10.1016/j.gene.2018.08.011
57. Qi S, Liu B, Zhang J, Liu X, Dong C, Fan R. Knockdown of microRNA1435p by STTM technology affects eumelanin and pheomelanin production in melanocytes. Mol Med Rep (2019) 20(3):2649–56. doi: 10.3892/mmr.2019.10492
58. Su M, Miao F, Jiang S, Shi Y, Luo L, He X, et al. Role of the p53−TRPM1/miR−211−MMP9 axis in UVB−induced human melanocyte migration and its potential in repigmentation. Int J Mol Med (2020) 45(4):1017–26. doi: 10.3892/ijmm.2020.4478
59. Levings MK, Sangregorio R, Roncarolo MG. Human cd25(+)cd4(+) t regulatory cells suppress naive and memory T cell proliferation and can be expanded in vitro without loss of function. J Exp Med (2001) 193(11):1295–302.
PubMed Abstract | Google Scholar
60. Klarquist J, Denman CJ, Hernandez C, Wainwright DA, Strickland FM, Overbeck A, et al. Reduced skin homing by functional treg in vitiligo. Pigment Cell Melanoma Res (2010) 23(2):276–86. doi: 10.1111/j.1755-148X.2010.00688.x
61. Chatterjee S, Eby JM, Al-Khami AA, Soloshchenko M, Kang HK, Kaur N, et al. A quantitative increase in regulatory T cells controls development of vitiligo. J Invest Dermatol (2014) 134(5):1285–94. doi: 10.1038/jid.2013.540
62. Alzhrani A, Bottomley M, Wood K, Hester J, Issa F. Identification, selection, and expansion of non-gene modified alloantigen-reactive tregs for clinical therapeutic use. Cell Immunol (2020) 357:104214. doi: 10.1016/j.cellimm.2020.104214
63. Mukhatayev Z, Dellacecca ER, Cosgrove C, Shivde R, Jaishankar D, Pontarolo-Maag K, et al. Antigen specificity enhances disease control by tregs in vitiligo. Front Immunol (2020) 11:581433. doi: 10.3389/fimmu.2020.581433
64. Eby JM, Kang HK, Tully ST, Bindeman WE, Peiffer DS, Chatterjee S, et al. CCL22 to activate treg migration and suppress depigmentation in vitiligo. J Invest Dermatol (2015) 135(6):1574–80. doi: 10.1038/jid.2015.26
65. Zhang Q, Cui T, Chang Y, Zhang W, Li S, He Y, et al. HO-1 regulates the function of treg: Association with the immune intolerance in vitiligo. J Cell Mol Med (2018) 22(9):4335–43. doi: 10.1111/jcmm.13723
66. Dellacecca ER, Cosgrove C, Mukhatayev Z, Akhtar S, Engelhard VH, Rademaker AW, et al. Antibiotics drive microbial imbalance and vitiligo development in mice. J Invest Dermatol (2020) 140(3):676–687 e6. doi: 10.1016/j.jid.2019.08.435
67. Powell JD, Delgoffe GM. The mammalian target of rapamycin: linking T cell differentiation, function, and metabolism. Immunity (2010) 33(3):301–11. doi: 10.1016/j.immuni.2010.09.002
68. Daily topical rapamycin for vitiligo (2022). Available at: https://clinicaltrials.gov/ct2/show/NCT05342519 .
69. Zhang X, Liu D, He M, Lin M, Tu C, Zhang B. Polymeric nanoparticles containing rapamycin and autoantigen induce antigen-specific immunological tolerance for preventing vitiligo in mice. Hum Vaccin Immunother (2021) 17(7):1923–9. doi: 10.1080/21645515.2021.1872342
70. Giri PS, Bharti AH, Begum R, Dwivedi M. Calcium controlled NFATc1 activation enhances suppressive capacity of regulatory T cells isolated from generalized vitiligo patients. Immunology (2022). doi: 10.1111/imm.13538
71. Yang L, Wei Y, Sun Y, Shi W, Yang J, Zhu L, et al. Interferon-gamma inhibits melanogenesis and induces apoptosis in melanocytes: A pivotal role of CD8+ cytotoxic T lymphocytes in vitiligo. Acta Derm Venereol (2015) 95(6):664–70. doi: 10.2340/00015555-2080
72. Maouia A, Sormani L, Youssef M, Helal AN, Kassab A, Passeron T. Differential expression of CXCL9, CXCL10, and IFN-gamma in vitiligo and alopecia areata patients. Pigment Cell Melanoma Res (2017) 30(2):259–61. doi: 10.1111/pcmr.12559
73. Shi F, Erf GF. IFN-gamma, IL-21, and IL-10 co-expression in evolving autoimmune vitiligo lesions of smyth line chickens. J Invest Dermatol (2012) 132(3 Pt 1):642–9. doi: 10.1038/jid.2011.377
74. Skurkovich S, Skurkovich B, Kelly J. Anticytokine therapy, particularly anti-IFN-gamma, in Th1-mediated autoimmune diseases. Expert Rev Clin Immunol (2005) 1(1):11–25. doi: 10.1586/1744666X.1.1.11
75. Biswas KB, Takahashi A, Mizutani Y, Takayama S, Ishitsuka A, Yang L, et al. GPNMB is expressed in human epidermal keratinocytes but disappears in the vitiligo lesional skin. Sci Rep (2020) 10(1):4930. doi: 10.1038/s41598-020-61931-1
76. Boniface K, Jacquemin Clément, Darrigade A-S, Dessarthe Benoît, Martins C, Boukhedouni N, et al. Vitiligo skin is imprinted with resident memory CD8 T cells expressing CXCR3. J Invest Dermatol (2018) 138(2):355–64. doi: 10.1016/j.jid.2017.08.038
77. Mosenson JA, Zloza A, Klarquist J, Barfuss AJ, Guevara-Patino JA, Poole ICLe. HSP70i is a critical component of the immune response leading to vitiligo. Pigment Cell melanoma Res (2012) 25(1):88–98. doi: 10.1111/j.1755-148X.2011.00916.x
78. Doss RW, El-Rifaie AA, Abdel-Wahab AM, Gohary YM, Rashed LA. Heat shock protein-70 expression in vitiligo and its relation to the disease activity. Indian J Dermatol (2016) 61(4):408–12. doi: 10.4103/0019-5154.185704
79. Mosenson JA, Zloza A, Nieland JD, Garrett-Mayer E, Eby JM, Huelsmann EJ, et al. Mutant HSP70 reverses autoimmune depigmentation in vitiligo. Sci Transl Med (2013) 5(174):174ra28. doi: 10.1126/scitranslmed.3005127
80. Tokura Y, Phadungsaksawasdi P, Kurihara K, Fujiyama T, Honda T. Pathophysiology of skin resident memory T cells. Front Immunol (2020) 11:618897. doi: 10.3389/fimmu.2020.618897
81. Richmond JM, Strassner JP, Rashighi M, Agarwal P, Garg M, Essien KI, et al. Resident memory and recirculating memory T cells cooperate to maintain disease in a mouse model of vitiligo. J Invest Dermatol (2019) 139(4):769–78. doi: 10.1016/j.jid.2018.10.032
82. Chen X, Guo W, Chang Y, Chen J, Kang P, Yi X, et al. Oxidative stress-induced IL-15 trans-presentation in keratinocytes contributes to CD8(+) T cells activation via JAK-STAT pathway in vitiligo. Free Radic Biol Med (2019) 139:80–91. doi: 10.1016/j.freeradbiomed.2019.05.011
83. Atwa MA, Ali SMM, Youssef N, Mahmoud Marie RE. Elevated serum level of interleukin-15 in vitiligo patients and its correlation with disease severity but not activity. J Cosmet Dermatol (2021) 20(8):2640–4. doi: 10.1111/jocd.13908
84. Wang W, Chapman NM, Zhang B, Li M, Fan M, Laribee RN, et al. Upregulation of PD-L1 via HMGB1-activated IRF3 and NF-kappaB contributes to UV radiation-induced immune suppression. Cancer Res (2019) 79(11):2909–22. doi: 10.1158/0008-5472.CAN-18-3134
85. Kotobuki Y, Tanemura A, Yang L, Itoi S, Wataya-Kaneda M, Murota H, et al. Dysregulation of melanocyte function by Th17-related cytokines: significance of Th17 cell infiltration in autoimmune vitiligo vulgaris. Pigment Cell Melanoma Res (2012) 25(2):219–30. doi: 10.1111/j.1755-148X.2011.00945.x
86. Bassiouny DA, Shaker O. Role of interleukin-17 in the pathogenesis of vitiligo. Clin Exp Dermatol (2011) 36(3):292–7. doi: 10.1111/j.1365-2230.2010.03972.x
87. Vaccaro M, Cannavo SP, Imbesi S, Cristani M, Barbuzza O, Tigano V, et al. Increased serum levels of interleukin-23 circulating in patients with non-segmental generalized vitiligo. Int J Dermatol (2015) 54(6):672–4. doi: 10.1111/ijd.12392
88. Hegazy RA, Fawzy MM, Gawdat HI, Samir N, Rashed LA. T helper 17 and tregs: A novel proposed mechanism for NB-UVB in vitiligo. Exp Dermatol (2014) 23(4):283–6. doi: 10.1111/exd.12369
89. Speeckaert R, Mylle S, van Geel N. IL-17A is not a treatment target in progressive vitiligo. Pigment Cell melanoma Res (2019) 32(6):842–7. doi: 10.1111/pcmr.12789
90. Birol A, Kisa U, Kurtipek GS, Kara F, Kocak M, Erkek E, et al. Increased tumor necrosis factor alpha (TNF-alpha) and interleukin 1 alpha (IL1-alpha) levels in the lesional skin of patients with nonsegmental vitiligo. Int J Dermatol (2006) 45(8):992–3. doi: 10.1111/j.1365-4632.2006.02744.x
91. Chan AC, Carter PJ. Therapeutic antibodies for autoimmunity and inflammation. Nat Rev Immunol (2010) 10(5):301–16.
92. Horiuchi T. Transmembrane TNF-α: structure, function and interaction with anti-TNF agents. Rheumatology (2010) 49(7):1215–28.
93. Spencer-Green and G. Etanercept (Enbrel): update on therapeutic use. Ann Rheum Dis (2000) 59 Suppl 1(90001):i46–9.
94. Webb KC, Tung R, Winterfield LS, Gottlieb AB, Eby JM, Henning SW, et al. Tumour necrosis factor-α inhibition can stabilize disease in progressive vitiligo. Br J Dermatol (2015) 173(3):641–50. doi: 10.1111/bjd.14016
95. Bae JM, Kim M, Lee HH, Kim KJ, Shin H, Ju HJ, et al. Increased risk of vitiligo following anti-tumor necrosis factor therapy: A 10-year population-based cohort study. J Invest Dermatol (2018) 138(4):768–74. doi: 10.1016/j.jid.2017.11.012
96. Toussirot E, Salard D, Algros MP, Aubin F. [Occurrence of vitiligo in a patient with ankylosing spondylitis receiving adalimumab]. Ann Dermatol Venereol (2013) 140(12):801–2. doi: 10.1016/j.annder.2013.09.158
97. Jung JM, Lee YJ, Won CH, Chang SE, Lee MW, Choi JH, et al. Development of vitiligo during treatment with adalimumab: A plausible or paradoxical response?". Ann Dermatol (2015) 27(5):620–1. doi: 10.5021/ad.2015.27.5.620
98. Ryu TH, Lee DW, Choi JE, Ahn HH, Kye YC, Seo SH. A type II segmental vitiligo developed under infliximab treatment for ulcerative colitis. Ann Dermatol (2017) 29(6):826–7. doi: 10.5021/ad.2017.29.6.826
99. Smith DI, Heffernan MP. Vitiligo after the resolution of psoriatic plaques during treatment with adalimumab. J Am Acad Dermatol (2008) 58(2 Suppl):S50–2. doi: 10.1016/j.jaad.2006.05.035
100. Carvalho CLDB, Ortigosa LCM. Segmental vitiligo after infliximab use for rheumatoid arthritis–a case report. Anais bras dermatol (2014) 89(1):154–6. doi: 10.1590/abd1806-4841.20142887
101. Banchereau J, Rousset F. Human b lymphocytes: phenotype, proliferation, and differentiation. Adv Immunol (1992) 52:125–262. doi: 10.1016/s0065-2776(08)60876-7
102. Lin X, Tian H, Xianmin M. Possible roles of b lymphocyte activating factor of the tumour necrosis factor family in vitiligo autoimmunity. Med Hypotheses (2011) 76(3):339–42. doi: 10.1016/j.mehy.2010.10.034
103. Eisenberg R, Albert D. B-cell targeted therapies in rheumatoid arthritis and systemic lupus erythematosus. Nat Clin Pract Rheumatol (2006) 2(1):20–7. doi: 10.1038/ncprheum0042
104. Ioannou Y, Isenberg DA. Current concepts for the management of systemic lupus erythematosus in adults: A therapeutic challenge. Postgrad Med J (2002) 78(924):599–606. doi: 10.1136/pmj.78.924.599
105. Open-label pilot study of abatacept for the treatment of vitiligo . Available at: https://clinicaltrials.gov/ct2/show/NCT02281058 .
Keywords: vitiligo, targeted therapy, JAK inhibitors, biological, treatment, miRNA - microRNA, Treg
Citation: Feng Y and Lu Y (2022) Advances in vitiligo: Update on therapeutic targets. Front. Immunol. 13:986918. doi: 10.3389/fimmu.2022.986918
Received: 05 July 2022; Accepted: 04 August 2022; Published: 31 August 2022.
Reviewed by:
Copyright © 2022 Feng and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Lu, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 19, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Dietary treatment found to be more effective than medicines in irritable bowel syndrome
by University of Gothenburg

A study conducted at the University of Gothenburg found that with dietary adjustments, more than 7 out of 10 irritable bowel syndrome (IBS) patients had significantly reduced symptoms, compared with medications. The work is published in The Lancet Gastroenterology & Hepatology journal.
IBS is a common diagnosis that causes abdominal pain , gas and abdominal bloating, diarrhea, and constipation, in various combinations and with varying degrees of severity.
Treatment often consists of dietary advice such as eating small and frequent meals and avoiding excessive intake of food triggers such as coffee, alcohol and fizzy drinks. Patients may also be given medications to improve specific symptoms, such as gas or constipation, diarrhea, bloating or abdominal pain. Antidepressants are sometimes used to improve symptoms in IBS.
The study compared three treatments: two dietary and one based on use of medications. The participants were adult patients with severe or moderate IBS symptoms at Sahlgrenska University Hospital in Gothenburg.
More symptom relief after dietary adjustment
The first group was given traditional IBS dietary advice, focusing on eating behavior combined with low intake of fermentable carbohydrates, known as FODMAPs. These include products with lactose, legumes, onions, and grains, which ferment in the colon and can cause pain in IBS.
The second group received a dietary treatment low in carbohydrates and proportionally high in protein and fat. In the third group, the best possible medication was given based on the patient's most troublesome IBS symptoms.
Each group included around 100 participants and the treatment periods lasted four weeks. When the researchers then examined how well the participants responded to the treatments, using an established IBS symptom scoring scale, the results were clear.
Of those who received traditional IBS dietary advice and low content of FODMAPs, 76% had significantly reduced symptoms. In the group receiving low carbohydrates and high protein and fat, the proportion was 71%, and in the medication group 58%.
All groups reported significantly better quality of life, fewer physical symptoms and fewer symptoms of anxiety and depression.
The importance of personalization
At a six-month follow-up, when participants in the dietary groups had partially returned to their previous eating habits, a large proportion still had clinically significant symptom relief; 68% in the traditional dietary advice and low FODMAP group, and 60% in the low-carbohydrate diet group.
The study was led by Sanna Nybacka, Researcher and Dietician, Stine Störsrud, Associate Professor, and Magnus Simrén, Professor and Senior Consultant, all at Sahlgrenska Academy, University of Gothenburg.
"With this study, we can show that diet plays a central role in the treatment of IBS, but that there are several alternative treatments that are effective," says Sanna Nybacka.
"We need more knowledge about how to best personalize the treatment of IBS in the future and we will further investigate whether there are certain factors that can predict whether individuals will respond better to different treatment options," she concludes.
Explore further
Feedback to editors

How myeloid cell replacement could help treat autoimmune encephalomyelitis
13 minutes ago

Engineered peptides open new avenue for immunotherapy drug development
3 hours ago

Signs of multiple sclerosis show up in blood years before symptoms, study finds

Study of cancer-induced liver inflammation finds a promising therapeutic target

Researchers discover new therapeutic target for non-small cell lung cancer
16 hours ago

Immune cells carry a long-lasting 'memory' of early-life pain

Cannabis legalization and rising sales have not contributed to increase in substance abuse, study finds

No negative impact from prolonged eye patching on child's development or family stress levels

COVID-19 booster immunity lasts much longer than primary series alone, study shows
17 hours ago

Study finds that human neuron signals flow in one direction
18 hours ago
Related Stories

FODMAP diet beats general dietary advice for IBS
Nov 30, 2017

Why am I bloated? Here are some possibilities to consider
Nov 15, 2022

Study first to report benefits and safety of FODMAP diet in children
Sep 24, 2019

Q&A: Irritable bowel syndrome and lifestyle modifications
Jul 14, 2022

Mediterranean diet could help people with irritable bowel symptoms
Mar 19, 2024
Mayo Clinic Q and A: Irritable bowel syndrome and lifestyle modifications
May 20, 2022
Recommended for you

Researchers discover how gut muscle can be vital for growth, repair and treatments
Apr 17, 2024

Researchers find evidence a natural juice can help gut health

Microplastics make their way from the gut to other organs, researchers find
Apr 15, 2024

Carbon beads help restore healthy gut microbiome and reduce liver disease progression, researchers find
Apr 14, 2024

Inflammation discovery advances the fight against chronic liver disease
Apr 12, 2024

Study lays the basis for new perspectives on gastrointestinal diseases
Apr 11, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
On July 18, the U.S. Food and Drug Administration (FDA) approved ruxolitinib ( Opzelura) cream 1.5 percent as a treatment for the most common form of vitiligo, according to a statement by Incyte ...
On July 18, the US Food and Drug Administration (FDA) based on clinical trials approved topical Ruxolitinib (Opzelura) 1.5% in patients 12 years of age or older for the treatment of non-segmental vitiligo [].Vitiligo is a chronic autoimmune condition that causes white macules of the skin due to an acquired lack of functional melanocytes with highly obvious, disfiguring lesions [].
FDA has approved Opzelura (ruxolitinib) cream for the treatment of nonsegmental vitiligo in adult and pediatric patients 12 years of age and older. Opzelura is a topical Janus kinase (JAK ...
1. Introduction. Vitiligo is the most common disorder of depigmentation, and in 2012 its worldwide prevalence ranged from 0.06-2.28% (1,2).It is characterized by the absence of pigment in the skin, secondary to the loss of melanocytes (1,3).Melanocytes are found in several tissues in the skin, hair follicles, eyes, inner ear, bones, heart and brain ().
The U.S. Food and Drug Administration has approved Opzelura (ruxolitinib) as the first topical treatment for vitiligo. The 1.5 percent cream is approved for continuous topical use twice daily to ...
Vitiligo is a chronic autoimmune disease that results in skin depigmentation 1,2 and reduced quality of life. 3,4 Quality-of-life burden is affected by a high prevalence of psychosocial coexisting ...
USA TODAY. 0:00. 3:02. Vitiligo is an autoimmune disorder that leads to the loss of skin pigmentation. A recent study shows a medicated cream called ruxolitinib is extremely effective in about one ...
Vitiligo is an acquired depigmentation of the skin, which affects approximately 1% of the population worldwide. The condition can profoundly affect the wellbeing and the social, sexual, and professional lives of affected individuals and thus induces a strong therapeutic demand.1 Actual treatments rely on the use of topical steroids or topical calcineurin inhibitors, and are better combined ...
Vitiligo affects 0.5 to 2% of the population worldwide. This chronic autoimmune disease manifests as pale skin patches, caused by local death of pigment-producing melanocytes. The extent and percei...
Temprian Therapeutics is a spin-off from Northwestern University in Chicago, Illinois. Vitiligo is an autoimmune disease that affects an estimated 50 million people worldwide. It isn't life ...
Topical ruxolitinib 1.5% cream (Opzelura®), a Janus kinase (JAK) inhibitor, is the first treatment to be approved in several countries for use in patients aged ≥ 12 years with non-segmental vitiligo. In the identical phase III TRuE-V1 and TRuE-V2 trials, significantly more ruxolitinib cream recipients were able to achieve statistically significant and clinically meaningful facial and total ...
Vitiligo is a skin disease that is characterized by loss of pigmentation caused by death or dysfunction of melanocytes, which are pigment producing cells. Autoimmune processes, oxidative stress ...
Phase 3 vitiligo clinical trial results to test topical ruxolitinib as a new treatment. I've recently received many requests for an update on the new ruxolitinib cream to treat vitiligo. To remind everyone, we initially reported that oral ruxolitinib, a Janus Kinase inhibitor initially approved to treat a type of blood cancer, reversed ...
Among the new approaches being developed, the strategy of targeting the IFN-γ-CXCL9/10-CXCR3 axis has been clinically tested. OPZELURA has been indicated for the topical treatment of nonsegmental vitiligo in adult and pediatric patients 12 years of age and older. MiRNA-based therapeutics are also in development.
New Research: Half of New Vitiligo Cases Go Untreated. A new study highlighted in Springer Link reveals that within the first year of being diagnosed with vitiligo, a skin condition marked by loss of pigment, a surprisingly large number of patients are not receiving any treatment. Additionally, those ... 2023-11-03.
Medications. No drug can stop the process of vitiligo — the loss of pigment cells (melanocytes). But some drugs, used alone, in combination or with light therapy, can help restore some color. Drugs that control inflammation. Applying a corticosteroid cream to affected skin might return color.
The treatment of vitiligo remains challenging due to the complexity of its pathogenesis, influenced by genetic factors, oxidative stress and abnormal cell adhesion that collectively impact melanocyte survival and trigger immune system attacks, resulting in melanocyte death. ... The activation of melanocyte stem cells is a promising research ...
When Dr. Anand K. Ganesan started a vitiligo specialty practice in 2018 at the UCI Health Beckman Laser Institute & Medical Clinic, it was to find new therapies to reverse the disfiguring skin disorder.. Vitiligo — pronounced vit-ill-EYE-go — causes white patches, often on the face and hands, the result of the immune system destroying the skin's pigment-producing cells.
Vitiligo is a chronic skin condition caused by an autoimmune response that results in the progressive loss of melanocytes and recent studies have suggested that Janus kinase inhibitors (JAKi) are emerging as a promising new treatment modality. Therefore, to assess and understand the extent of knowle …
Vitiligo Treatment News at IMCAS 2024. The IMCAS Congress in Paris recently emerged as a pivotal gathering for nearly 20,000 skin specialists worldwide. Thanks to an educational grant from IMCAS and a sponsored booth (K203), Prof. Torello Lotti and I engaged directly with attendees interested in vitiligo. Our activities included distributing ...
Outcomes included all-cause and vitiligo-related costs (2021 dollars) and all-cause HCRU, including mental health-related HCRU. Patients with vitiligo incurred significantly higher all-cause costs ...
Board-certified dermatologist, Dr. Gregory Delost recently sat down with New Day Cleveland to discuss the commonality of Vitiligo, the different types, and newly available treatment options, including Ruxolitinib Cream with results shown in the photos to the right.
The agreement calls for research, development, registration, and commercialization of the product in Mainland China, Hong Kong, Macao, Taiwan Region, and eleven Southeast Asian countries, and receive a non-exclusive license to manufacture the product in CMS' Territory. ... "There remains a significant need for new, innovative treatment for ...
The treatment of vitiligo, which aims at repigmentation, depends both on the clinical characteristics of the disease as well as on molecular markers that may predict the response to treatment. ... affecting a broader area. It can also be stable or unstable, depending on the appearance of new decoloration. Non-segmental vitiligo is prone to ...
Bay Area Lyme Foundation, a national organization committed to making Lyme disease easy to diagnose and simple to cure, is the leading public not-for-profit sponsor of innovative Lyme disease ...
TORONTO, April 18, 2024--Cybin Inc. (NYSE American:CYBN) (Cboe CA:CYBN) ("Cybin" or the "Company"), a clinical-stage biopharmaceutical company committed to revolutionizing mental healthcare by ...
More than 25 million adults in the U.S. have tinnitus, a condition that causes ringing or buzzing in the ears. An FDA approved device that stimulates the tongue, helped 84% of people who tried it.
Scientific advances in immunotherapy and new targeted therapies have increased survival rates. But screening among former and current smokers still needs to improve to save more lives.
Among the new approaches being developed, the strategy of targeting the IFN-γ-CXCL9/10-CXCR3 axis has been clinically tested. OPZELURA has been indicated for the topical treatment of nonsegmental vitiligo in adult and pediatric patients 12 years of age and older. MiRNA-based therapeutics are also in development.
A study conducted at the University of Gothenburg found that with dietary adjustments, more than 7 out of 10 irritable bowel syndrome (IBS) patients had significantly reduced symptoms, compared ...