Featured Topics
Featured series.
A series of random questions answered by Harvard experts.

Explore the Gazette
Read the latest.
A molecular ‘warhead’ against disease

Asking the internet about birth control

‘Harvard Thinking’: Facing death with dignity
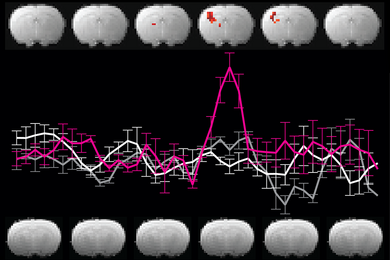
‘Dramatic’ inroads against aggressive brain cancer
Cutting-edge therapy shrinks tumors in early glioblastoma trial
Haley Bridger
Mass General Communications
A collaborative project to bring the promise of cell therapy to patients with a deadly form of brain cancer has shown dramatic results among the first patients to receive the novel treatment.
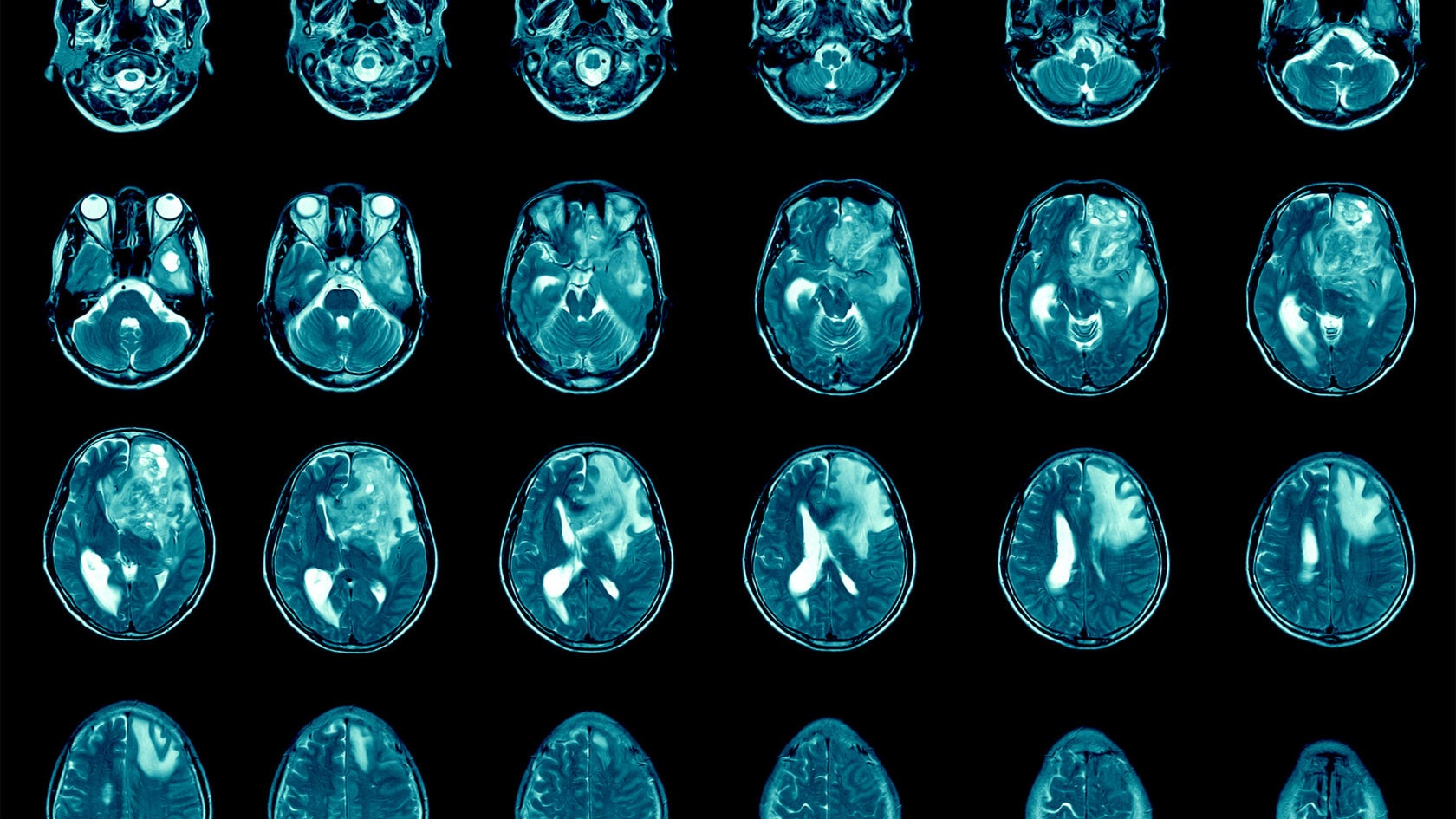
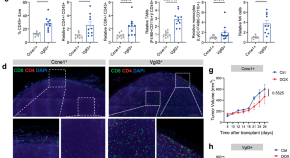
In a paper published Wednesday in The New England Journal of Medicine, researchers from Mass General Cancer Center shared the results for the first three patient cases from a Phase 1 clinical trial evaluating a new approach to CAR-T therapy for glioblastoma.
Just days after a single treatment, patients experienced dramatic reductions in their tumors, with one patient achieving near-complete tumor regression. In time, the researchers observed tumor progression in these patients, but given the strategy’s promising preliminary results, the team will pursue strategies to extend the durability of response.
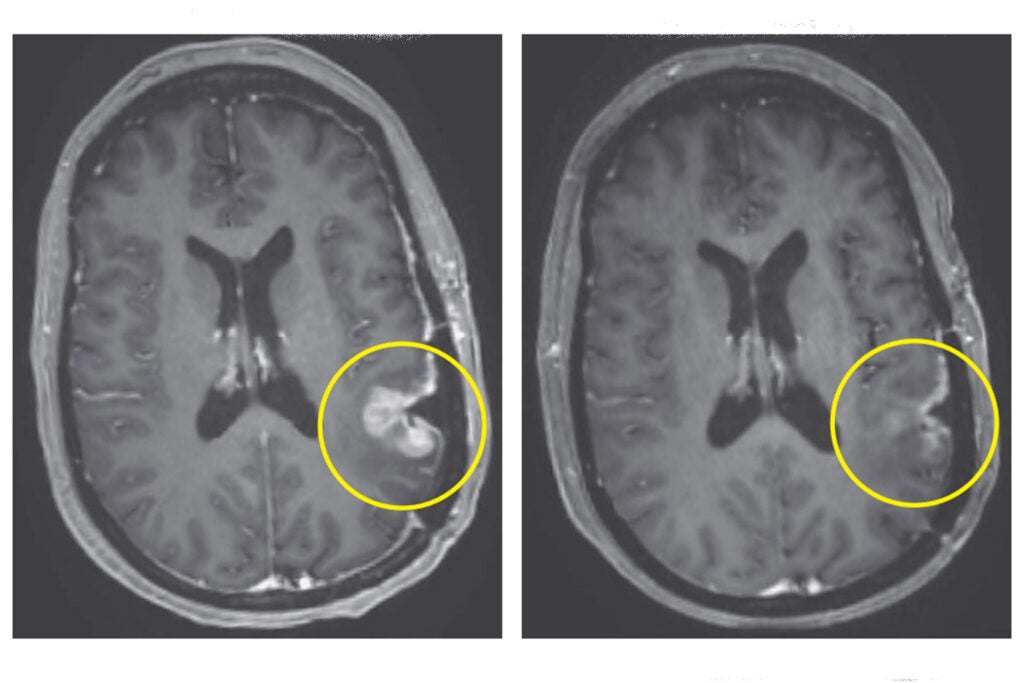
Left: MRI in Participant 3 before infusion. Right: After infusion on day five.
Image courtesy of The New England Journal of Medicine
“This is a story of bench-to-bedside therapy, with a novel cell therapy designed in the laboratories of Massachusetts General Hospital and translated for patient use within five years, to meet an urgent need,” said co-author Bryan Choi , a neurosurgeon at Harvard-affiliated Mass General and an assistant professor at Harvard Medical School. “The CAR-T platform has revolutionized how we think about treating patients with cancer, but solid tumors like glioblastoma have remained challenging to treat because not all cancer cells are exactly alike and cells within the tumor vary. Our approach combines two forms of therapy, allowing us to treat glioblastoma in a broader, potentially more effective way.”
The new approach is a result of years of collaboration and innovation springing from the lab of Marcela Maus , director of the Cellular Immunotherapy Program and an associate professor at the Medical School. Maus’ lab has set up a team of collaborating scientists and expert personnel to rapidly bring next-generation genetically modified T cells from the bench to clinical trials in patients with cancer.
“We’ve made an investment in developing the team to enable translation of our innovations in immunotherapy from our lab to the clinic, to transform care for patients with cancer,” said Maus. “These results are exciting, but they are also just the beginning — they tell us that we are on the right track in pursuing a therapy that has the potential to change the outlook for this intractable disease. We haven’t cured patients yet, but that is our audacious goal.”
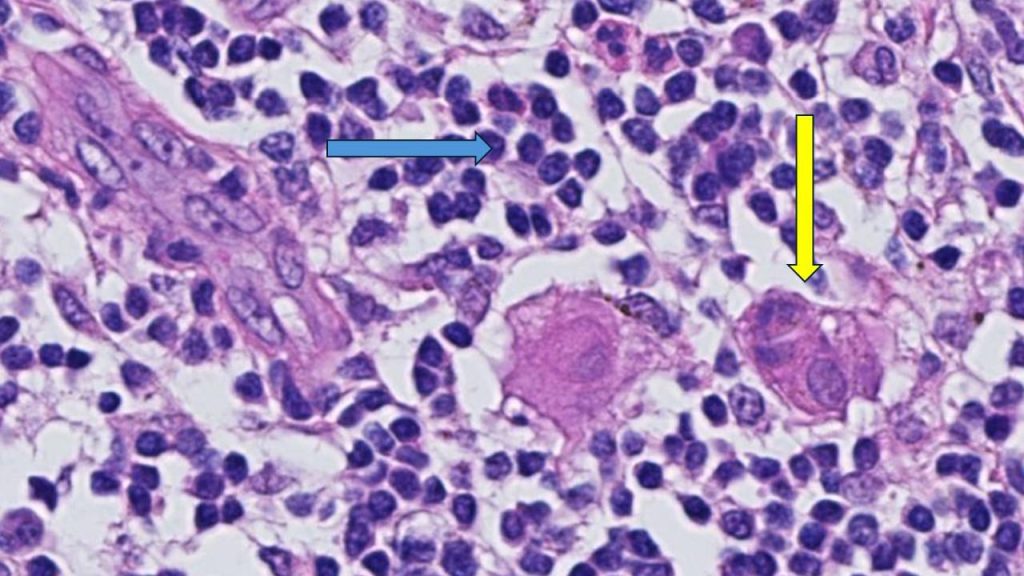
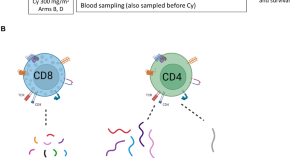
CAR-T (chimeric antigen receptor T-cell) therapy works by using a patient’s own cells to fight cancer — it is known as the most personalized way to treat the disease. A patient’s cells are extracted, modified to produce proteins on their surface called chimeric antigen receptors, and then injected back into the body to target the tumor directly. Cells used in this study were manufactured by the Connell and O’Reilly Families Cell Manipulation Core Facility of the Dana-Farber/Harvard Cancer Center.
CAR-T therapies have been approved for the treatment of blood cancers, but the therapy’s use for solid tumors is limited. Solid tumors contain mixed populations of cells, allowing some malignant cells to continue to evade the immune system’s detection even after treatment with CAR-T. Maus’ team is working to overcome this challenge by combining two previously separate strategies: CAR-T and bispecific antibodies, known as T-cell engaging antibody molecules. The version of CAR-TEAM for glioblastoma is designed to be directly injected into a patient’s brain.
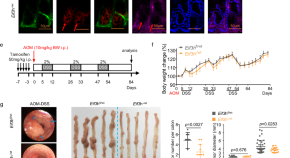
In the new study, the three patients’ T cells were collected and transformed into the new version of CAR-TEAM cells, which were then infused back into each patient. Patients were monitored for toxicity throughout the duration of the study. All patients had been treated with standard-of-care radiation and temozolomide chemotherapy and were enrolled in the trial after disease recurrence.
- A 74-year-old man had his tumor regress rapidly but transiently after a single infusion of the new CAR-TEAM cells.
- A 72-year-old man was treated with a single infusion of CAR-TEAM cells. Two days after receiving the cells, an MRI showed a decrease in the tumor’s size by 18 percent. By day 69, the tumor had decreased by 60 percent, and the response was sustained for more than six months.
- A 57-year-old woman was treated with CAR-TEAM cells. An MRI five days after the infusion showed near-complete tumor regression.
The authors note that despite the remarkable responses among the first three patients, they observed eventual tumor progression in all the cases, though in one case, there was no progression for over six months. Progression corresponded in part with the limited persistence of the CAR-TEAM cells over the weeks following infusion. As a next step, the team is considering serial infusions or preconditioning with chemotherapy to prolong the response.
“We report a dramatic and rapid response in these three patients. Our work to date shows signs that we are making progress, but there is more to do,” said co-author Elizabeth Gerstner, a Mass General neuro-oncologist.
In addition to Choi, Maus, and Gerstner, other authors are Matthew J. Frigault, Mark B. Leick. Christopher W. Mount, Leonora Balaj, Sarah Nikiforow, Bob S. Carter, William T. Curry, and Kathleen Gallagher.
The study was supported in part by the National Gene Vector Biorepository at Indiana University, which is funded under a National Cancer Institute contract.
Share this article
You might like.
Approach attacks errant proteins at their roots

Only a fraction of it will come from an expert, researchers say

In podcast episode, a chaplain, a bioethicist, and a doctor talk about end-of-life care
Forget ‘doomers.’ Warming can be stopped, top climate scientist says
Michael Mann points to prehistoric catastrophes, modern environmental victories
Yes, it’s exciting. Just don’t look at the sun.
Lab, telescope specialist details Harvard eclipse-viewing party, offers safety tips
Navigating Harvard with a non-apparent disability
4 students with conditions ranging from diabetes to narcolepsy describe daily challenges that may not be obvious to their classmates and professors
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Gastroenterol Surg
- v.5(4); 2021 Jul

Recent developments in cancer research: Expectations for a new remedy
1 Department of Surgery and Science, Kyushu University, Fukuoka Japan
Qingjiang Hu
Yuta kasagi, masaki mori.
Cancer research has made remarkable progress and new discoveries are beginning to be made. For example, the discovery of immune checkpoint inhibition mechanisms in cancer cells has led to the development of immune checkpoint inhibitors that have benefited many cancer patients. In this review, we will introduce and describe the latest novel areas of cancer research: exosomes, microbiome, immunotherapy. and organoids. Exosomes research will lead to further understanding of the mechanisms governing cancer proliferation, invasion, and metastasis, as well as the development of cancer detection and therapeutic methods. Microbiome are important in understanding the disease. Immunotherapy is the fourth treatment in cancer therapy. Organoid biology will further develop with a goal of translating the research into personalized therapy. These research areas may result in the creation of new cancer treatments in the future.
Cancer research has made remarkable progress and new discoveries are beginning to be made. In this review, we will introduce and describe the latest novel areas of cancer research: exosomes, microbiomes, immunotherapy, and organoids.

1. INTRODUCTION
The cancer research field has developed significantly through use of new equipment and technology. One example of new technology is Next‐Generation Sequencing (NGS). Also known as high‐throughput sequencing, NGS is the catch‐all term used to describe a number of different modern nucleic acid sequencing technologies. These methods allow for much quicker and cheaper sequencing of DNA and RNA compared with the previously used Sanger sequencing, and as such have revolutionized the study of genomics and molecular biology. NGS also allows for easier detection of mutations in cancer samples, leading to development of many new agents that can be used to treat patients. For example, if the RAS gene status is detected as wild type in a colorectal cancer patient, then an anti‐EGFR antibody, such as cetuximab or panitumumab, can be used for treatment.
A liquid biopsy, also known as fluid biopsy or fluid phase biopsy, is the sampling and analysis of non‐solid biological tissue, primarily blood. 1 It is being used as a novel way to detect cancer. Like a traditional biopsy, this type of technique is mainly used as a diagnostic and monitoring tool for diseases, and also has the added benefit of being largely noninvasive. Therefore, liquid biopsies can be performed more frequently, allowing for better tracking of tumors and mutations over a duration of time. This technique may also be used to validate the effectiveness of a cancer treatment drug by taking multiple liquid biopsy samples in the span of a few weeks. It may also prove to be beneficial for monitoring relapse in patients after treatment.
Novel devices and drugs have also been developed and used for cancer treatment. For surgery procedures, robotic‐assisted laparoscopic surgery has evolved and made it possible to visualize the fine movement of the forceps in three dimensions. This method is now used in esophageal, gastric, and rectal cancer surgeries in Japan. 2 , 3 , 4
Recently, immunotherapy became an additional method for treating cancer patients. The discovery of the immune checkpoint by Dr Honjo led to the development of immune checkpoint inhibitors. 5 Despite these developments, gastrointestinal cancers are still a major problem in need of new treatment methods. In this review, we introduce and describe four new areas of cancer research that may contribute to cancer treatment in the future: exosomes, microbiome, immunotherapy, and organoids.
2. AN APPLICATION OF EXOSOME RESEARCH IN CANCER THERAPY
An exosome is a small particle that is secreted by cells. Its size can range from 50 to 150 nm and has a surface consisting of proteins and lipids that originate from the cell membrane. Additionally, proteins and nucleic acids, such as DNA, microRNAs, and mRNAs, can be found inside the exosome as its “cargo.” 6 Recently, many researchers have discovered that exosomes are involved in the mechanisms of various diseases. As mentioned above, various functional compounds, such as microRNAs, mRNAs, and proteins, can be contained within exosomes. 7 , 8 Many cells use secretion of exosomes to communicate with one another, and these exosomes can even reach distant cells. Cancer cells can also secrete exosomes that contain molecules beneficial to cancer growth. For example, microRNAs found in cancer exosomes can modulate gene expression to induce angiogenesis in the tumor microenvironment, which supports metastasis. 9 Exosomes released from cancer cells can also reportedly break the blood‐brain barrier, which makes it contribute to brain metastasis. 10 , 11 Cancer cells themselves are similarly affected by the exosomes secreted by the surrounding normal cells. 12 In one case, the exosomes secreted by bone marrow‐delivered mesenchymal stem cells can force cancer cells into a dormant state. 13 These dormant cancer cells become resistant to chemotherapy and are involved in long‐term disease recurrence. Thus, exosomes are deeply involved in cancer proliferation, invasion, and metastasis, as well as in the formation of the tumor microenvironment and pre‐metastatic niche. 13 Further research on cancer‐related exosomes is ongoing.
Knowledge of exosomes can be applied to cancer treatment. If the secretion of exosomes from cancer cells can be prevented, then signal transduction supporting the formation of the tumor microenvironment and pre‐metastatic niche can be blocked. Work focusing on the removal of cancer exosomes is now ongoing. 14
Exosomes can also be utilized for cancer diagnosis. Exosomes secreted by many cell types are found in various body fluids, such as blood and urine. Capturing and analyzing exosomes from cancer cells can be used to detect the presence of disease. 15 Obtaining blood or urine from patients is not very invasive or painful. Since many molecules, such as various proteins, DNA, and microRNAs, can be found in exosomes from normal cells, it is important to distinguish them from cancer‐related ones. If exosomes are to be used for cancer diagnosis, then specific biomarkers need to be discovered. Additionally, the development of a method to detect these exosomes must be done. Currently, exosome detection methods for exosomes abundantly found in the serum of colorectal and pancreatic cancer patients, as well as exosomes found in the urine of bladder cancer patients, are being developed. 16 , 17 Thus, further understanding of the mechanisms governing cancer proliferation, invasion, and metastasis, as well as the development of cancer detection and therapeutic methods, is significantly affected by exosome research.
3. MICROBIOME IN CANCER RESEARCH
A large number of microorganisms inhabit the human body. These microorganisms include bacteria, viruses, and fungi. Among them, bacteria have the most important relationship with the human body. Bacteria can live anywhere within the human body, including the digestive tract, respiratory system, and oral cavity. 18 , 19 , 20 In particular, bacteria in the digestive tract are rich in type and number, 21 with possibly 1000 types and more than 100 trillion individual bacterial cells present. 22 , 23 The overall population of various bacteria found in the human intestine is referred to as the “intestinal flora.” Recently, the terms “microbiota” or “microbiome” have also been widely used.
Recent advancements with NGS have led to a much more precise understanding of the intestinal microbiome. 24 The bacteria in the human microbiome mainly belong to four phyla: Firmicutes, Bacteroidetes, Proteobacteria, and Actinobacteri. Of these, Firmicutes and Bacteroidetes are the most dominant species. It is reported that microbiome vary depending on age and race. 25 , 26 Dysbiosis is a condition in which the diversity of the microbiome is reduced. Dysbiosis is reportedly involved in various diseases such as inflammatory bowel disease, colorectal cancer, obesity, diabetes, and allergic diseases. 27 , 28 , 29 For example, bacteria such as Atopobium parvulum and Actinomyces odontolyticus increase in number during the early stages of colorectal cancer (adenomas or intramucosal cancers) and decrease in number during cancer progression. 30 This suggests that a specific microbiome is associated with early stages of colorectal cancer development, which may be useful knowledge for early cancer detection.
Various studies have also been conducted to elucidate the relationship between the microbiome and the human immune system. 31 The IgA antibody, which is one of the most important elements in the intestinal immune system, is believed to play a role in the elimination of pathogens and maintenance of the intestinal environment. The IgA antibody recognizes, eliminates, and neutralizes pathogenic bacteria and toxins. It also maintains a symbiotic relationship by recognizing and binding to the normal microbiome of the host. 32 Mice lacking a microbiome have reduced production of the IgA antibody. A microbiome is required for IgA antibody differentiation. Recent studies have identified W27IgA antibodies that have the ability to bind to various bacteria. 33 Oral administration of a W27IgA antibody to enteritis model mice suppressed enteritis by altering the microbiome. This W27IgA antibody can recognize a part of the amino acid sequence of serine hydroxymethyl transferase, which is a metabolic enzyme involved in bacterial growth. The W27IgA antibody can suppress the growth of E coli by binding to them. However, the W27IgA antibody does not bind to bacteria that suppress enteritis, such as bifidobacteria and lactic acid bacteria. 33 Thus, the microbiome is deeply involved in human intestinal immunity. Recently, it is having been established that the microbiome is not only involved in intestinal immunity, but also in the systemic immune system.
As the analysis of the microbiome progresses, the pathophysiology of various diseases, such as cancers, and its relationship with the regulatory function of the human immune system will be further elucidated. It has been demonstrated that F nucleatum plays a role in the development and progression of colon adenomas and colorectal cancer. It is also related to lymph node metastases and distant metastasis. 34 , 35 Also, microbiome is associated with hepatocellular carcinoma. 36 Studying microbiome will give us some clue in the development and remedy for gastrointestinal cancers (Table 1 ).
Gastrointestinal cancer and their related microbiome
4. THE RISE OF IMMUNOTHERAPY IN CANCER TREATMENT
For many years, surgery, chemotherapy, and radiation therapy were the main methods of cancer treatment. In addition to these therapies, immunotherapy has recently attracted great attention worldwide (Table 2 ). 37 , 38 Under normal circumstances, a cancer antigen will activate the patient's immune system to attack the cancer cells. However, sometimes the immune system does not recognize the cancer cells as non‐self, or it simply fails to attack them. This can result in the development and progression of cancer.
Immune checkpoint inhibitors
Although therapies that activate the immune system against cancer cells have been studied for a long time, the use of the patient's own immune system for cancer treatment was not established. Recently, the effectiveness of both immune checkpoint inhibition therapy and chimeric antigen receptor (CAR)‐T cell therapy has proved to be promising. 39 , 40 Immunotherapy has moved to the forefront of cancer treatment strategies.
There are two major reasons why proving the efficacy of cancer immunotherapies was difficult for some time. First, cancer immunity is strongly suppressed. Signal transduction from immune checkpoint compounds, such as PD‐1 and CTLA4, strongly inhibits cytotoxic T cells (CTLs). 38 This checkpoint mechanism can prevent the immune system from attacking cancer cells. The development of immune checkpoint inhibitors has arisen from the discovery of this mechanism. Inhibition of immune checkpoint molecules with neutralizing antibodies can release the suppression of cancer‐specific CTLs, activate immunity, and promote cancer elimination. The effectiveness of immune checkpoint antibodies has been confirmed and clinically applied to many solid cancers such as melanoma, 41 lung cancer, 42 urothelial cancer, 43 gastric cancer, 44 and esophageal cancer. 45 In addition to PD‐1 and CTLA4, new immune checkpoint molecules, such as LAG3, TIGIT, and SIRPA, are also being actively studied. 46 , 47 , 48 Although this therapy is promising, the cancer cases who respond to these therapies are limited. This is because use of this therapy requires the presence of cancer‐specific CTLs in the patient's body. To maximize the therapeutic effect, it is desirable to select appropriate cases and develop useful biomarkers.
The second difficulty for immunotherapy is that T cells do not recognize specific cancer cell antigens and immune accelerators are too weak. One goal of CAR‐T cell therapy is to strengthen the immune accelerator by administering CTLs to the patient's body that recognize specific cancer cell‐specific antigens. A CAR is prepared by fusing a single chain Fv (scFv), derived from a monoclonal antibody that recognizes a specific antigen expressed by cancer cells, with CD3z and costimulatory molecules (CD28, 4‐1BB, and others). Next, the CAR is introduced to the T cells obtained from a cancer patient and CAR‐T cells are made. CAR‐T cells recognize the specific antigen of the cancer cells and are activated to damage these cells. CAR‐T cells recognize cancer‐specific antigens with high antibody specificity and attack the respective cancer cells with strong cytotoxic activity and high proliferative activity. CAR‐T therapy is effective in blood cancers such as B‐cell acute lymphoblastic leukemia and myeloma. 49 , 50 While CAR‐T cell therapy has a high therapeutic effect, a frequent and serious adverse event called cytokine release syndrome has been observed in some patients. 51 , 52 The development of a technique for suppressing the occurrence of cytokine release syndrome is anticipated. In addition, the development of CAR‐T cell therapies for solid tumors is ongoing.
Recently, there was new progress made in treating gastrointestinal cancer patients. For MSI‐H colorectal cancer, the combination therapy with nivolumab and ipilimumab was approved. From the nivolumab plus ipilimumab cohort of CheckMate‐142, progression‐free survival rates were 76% (9 months) and 71% (12 months); respective overall survival rates were 87% and 85% which were quite high. This new treatment will benefit MSI‐H colorectal cancer patients. 53
Thus, it is expected that further understanding of cancer immune mechanisms and the development of various immunotherapies will contribute to great progress in cancer treatment.
One problem for immunotherapy is that there is no certain predictive biomarker. It was thought that the expression of PD‐1 or PD‐L1 would predict the effect. However, this was not the case. To find a new biomarker, we assessed the cytolytic activity (CYT) score. The CYT score is a new index of cancer immunity calculated from the mRNA expression levels of GZMA and PRF1. We are now evaluating CYT score in gastric cancer patients (data not published). The development in the biomarker search will benefit many gastrointestinal cancer patients.
5. ADVANTAGES FOR USING ORGANOIDS IN CANCER RESEARCH
The three‐dimensional (3D) organoid system is a cell culture‐based, novel, and physiologically relevant biologic platform. 54 An organoid is a miniaturized and simplified version of an organ that is produced in vitro in 3D and shows realistic microanatomy. With only one to a few cells isolated from tissue or cultured cells as the starting material, organoids are grown and passaged in a basement membrane matrix, which contributes to their self‐renewal and differentiation capacities. 54 , 55 The technique used for growing organoids has rapidly improved since the early 2010s with the advent of the field of stem cell biology. The characteristics of stem, embryonic stem cells (ES cells), or induced pluripotent stem cells (iPS cells) that allow them to form an organoid in vitro are also found in multiple types of carcinoma tissues and cells. Therefore, cancer researchers have applied ES cells or iPS cells in their field. 56 , 57 , 58
Organoid formation generally requires culturing stem cells or their progenitor cells in 3D. 54 , 55 The morphological and functional characteristics of various types of carcinoma tissue have been recapitulated in organoids that were generated from single‐cell suspensions or cell aggregates. These suspensions or aggregates were isolated from murine and human tissues or cultured cells, as well as from cancer stem cells propagated in culture. The structures of the organoids show the potential of cancer stem cell self‐renewal, proliferation, and differentiation abilities, and also provide insights into the roles of molecular pathways and niche factors that are essential in cancer tissues. 56 , 57 , 59 , 60 , 61 , 62 The organoid system also has been utilized for studying multiple biological processes, including motility, stress response, cell‐cell communications, and cellular interactions that involve a variety of cell types such as fibroblasts, endothelial cells, and inflammatory cells. These interactions are mediated via cell surface molecules, extracellular matrix proteins, and receptors in the microenvironment under homeostatic and pathologic conditions.
Although the organoid system is a complex and not effortless procedure that requires specific media, supplements, and many tricky techniques, 58 , 63 application of this system has been extended to a variety of cell types from different carcinomas (colorectal, pancreatic, prostate, breast, ovary, and esophageal cancers). 56 , 57 , 59 , 60 , 61 An organoid is generally induced within a few days to weeks, and is faster and less costly than the murine xenograft assay. Furthermore, applying novel genetic manipulations (e.g. CRISPR‐Cas9) can be carried out in the organoid system. 64 , 65
Kasagi et al modified keratinocyte serum‐free medium to grow 3D organoids from endoscopic esophageal biopsies, immortalized human esophageal epithelial cells, and murine esophagi. Esophageal 3D organoids serve as a novel platform to investigate regulatory mechanisms in squamous epithelial homeostasis in the context of esophageal cancers. 64
We anticipate that many experimental results that utilize the organoid system will be published in the future.
The 3D organoid system has emerged in the past several years as a robust tool in basic research with the potential to be used for personalized medicine. 66 By passaging dissociated primary structures to generate secondary 3D organoids, this system can be performed using live tissue pieces obtained from biopsies, operative‐resected specimens, or even frozen tissues. This method has the potential to transform personalized therapy. For example, in the case of cancer recurrence, an effective chemotherapy can be selected by testing the chemotherapeutic sensitivity of cancer‐derived organoids from an individual patient's tissue stocks. In many cases, a patient's organoid accumulation is helpful for testing the sensitivity of novel therapeutic agents for treating carcinoma. 66 Hence, it appears that organoid biology will further develop with a goal of translating the research into personalized therapy.
6. SUMMARY AND FUTURE DIRECTIONS
This review describes four new cancer‐related studies: exosomes, microbiome, immunotherapy, and organoids (Figure 1 ).

The summary of the four cancer research areas. In this figure the summary of the four cancer research areas is shown: exosome, microbiome, immunotherapy, and organoid research
Since exosomes are released in blood or urine, if the capturing system is established, it will be a less invasive test to diagnose cancer. In the present, the presence of circulating tumor DNA (ctDNA) is one of the tools to detect the minimal residual disease. However, since ctDNA is only DNA, it is difficult to spread to cancer research. In that respect, as exosomes include not only DNA but also other nucleic acids and proteins, this will be a new tool for cancer research such as the diagnosis of early cancer.
Microbiome may lead to improved cancer diagnosis and treatment. Detecting a specific microbiome in a gastrointestinal tract may predict a specific cancer. And changing microbiome in some way may result in preventing cancer development.
Organoids may help address the problem of drug resistance, and also lead to the development of personalized therapy. However, producing organoids takes time and testing the drug resistance may take more time. If we could overcome these problems, the research into organoids can contribute to overcoming cancer.
As shown in Table 3 , many new studies and findings are reported into this field of research. These four novel cancer research areas will make many contributions to the diagnosis and treatment of cancer.
Recent studies on exosome, microbiome, immunotherapy, and organoids
Conflict of Interest: All the authors have no conflict of interest to disclose.
ACKNOWLEDGMENTS
We thank Dr Hirofumi Hasuda and Dr Naomichi Koga for their help in preparing this manuscript. We also thank J. Iacona, PhD, from Edanz Group for editing a draft of this manuscript.
Ando K, Hu Q, Kasagi Y, Oki E, Mori M. Recent developments in cancer research: Expectations for a new remedy . Ann Gastroenterol Surg . 2021; 5 :419–426. 10.1002/ags3.12440 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]

- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

Cancer research highlights from 2023
Share this:.
By Mayo Clinic staff
Researchers at Mayo Clinic Comprehensive Cancer Center spent 2023 studying the biology of cancer and new ways to predict, prevent, diagnose and treat the disease. Their discoveries are creating hope and transforming the quality of life for people with cancer today and in the future. Here are some highlights from their research over the past year:
Mayo Clinic researchers link ovarian cancer to bacteria colonization in the microbiome.
A specific colonization of microbes in the reproductive tract is commonly found in people with ovarian cancer, according to a study from the Mayo Clinic Center for Individualized Medicine . Published in Scientific Reports and led by Marina Walther-Antonio, Ph.D. , a Mayo Clinic researcher, and Abigail Asangba, Ph.D., the discovery strengthens the evidence that the bacterial component of the microbiome — a community of microorganisms that also consists of viruses, yeasts and fungi — is an important indicator for early detection, diagnosis and prognosis of ovarian cancer . The study also suggests that a higher accumulation of pathogenic microbes plays a role in treatment outcomes and could be a potential indicator for predicting a patient's prognosis and response to therapy. Read more .
Artificial intelligence is forging a new future for colorectal cancer and other digestive system diseases.
Colonoscopy remains the gold standard in detecting and preventing colorectal cancer , but the procedure has limitations. Some studies suggest that more than half of post-colonoscopy colon cancer cases arise from lesions missed at patients' previous colonoscopies. In 2022, Michael Wallace, M.D. , a Mayo Clinic gastroenterologist, published the results of an international, multicenter study testing the impact of adding artificial intelligence (AI) to routine colonoscopies. His team, including James East, M.D. , a Mayo Clinic gastroenterologist, and other researchers from the U.S., the U.K., Italy, Germany and Ireland, found that incorporating AI into colonoscopies reduced the risk of missing polyps by 50%. Read more .
A big step forward: Bringing DNA sequencing data to routine patient care.
The Tapestry study , an extensive genomic sequencing clinical research study, aims to complete exome sequencing (sequencing the protein-coding regions of a genome) for 100,000 Mayo Clinic patients. The results will be integrated into patients’ electronic health records for three hereditary conditions, and the amassed data will contribute to a research dataset stored within the Mayo Clinic Cloud on the Omics Data Platform. The overall hope of Tapestry is to accelerate discoveries in individualized medicine to tailor prevention, diagnosis and treatment to a patient's unique genetic makeup. It is poised to advance evidence that exome sequencing, when applied to a diverse and comprehensive general population, can proficiently identify carriers of genetic variants that put them at higher risk for a disease, allowing them to take preventive measures. Read more .
Patients with multiple tumors in one breast may not need a mastectomy.
Patients who have multiple tumors in one breast may be able to avoid a mastectomy if surgeons can remove the tumors while leaving enough breast tissue, according to research led by the Alliance in Clinical Trials in Oncology and Mayo Clinic Comprehensive Cancer Center . Patients would receive breast-conserving therapy — a lumpectomy followed by whole-breast radiation therapy — rather than mastectomy . The study is published in the Journal of Clinical Oncology . Historically, women with multiple tumors in one breast have been advised to have a mastectomy. Now, patients can be offered a less invasive option with faster recovery, resulting in better patient satisfaction and cosmetic outcomes, says Judy Boughey, M.D. , lead author, Mayo Clinic breast surgical oncologist and the W.H. Odell Professor of Individualized Medicine. Read more .
Staging pancreatic cancer early with minimally invasive surgery shows positive results in patient prognosis.
A study published in the Journal of the American College of Surgeons reveals that performing a minor surgical procedure on patients newly diagnosed with pancreatic cancer helps to identify cancer spread early and determine the stage of cancer. The researchers add that the surgery ideally should be performed before the patient begins chemotherapy. "This is an important study because it supports that staging laparoscopy may help determine a patient's prognosis and better inform treatment so that patients avoid unhelpful or potentially harmful surgical therapy," says Mark Truty, M.D. , a Mayo Clinic surgical oncologist who led the research. Read more .
Mayo Clinic study reveals proton beam therapy may shorten breast cancer treatment.
In a trial published in The Lancet Oncology , Mayo Clinic Comprehensive Cancer Center researchers uncovered evidence supporting a shorter treatment time for people with breast cancer . The study compared two separate dosing schedules of pencil-beam scanning proton therapy , known for its precision in targeting cancer cells while preserving healthy tissue to reduce the risk of side effects. The investigators found that both 25-day and 15-day proton therapy schedules resulted in excellent cancer control while sparing surrounding non-cancerous tissue. Further, complication rates were comparable between the two study groups. "We can now consider the option of 15 days of therapy for patients based on the similar treatment outcomes observed," says Robert Mutter, M.D. , a Mayo Clinic radiation oncologist and physician-scientist. Read more .
Harnessing the immune system to fight ovarian cancer.
Mayo Clinic research is biomanufacturing an experimental, cell-based ovarian cancer vaccine and combining it with immunotherapy to study a "one-two punch" approach to halting ovarian cancer progression. This research begins with a blood draw from people with advanced ovarian cancer whose tumors have returned after standard surgery and chemotherapy. White blood cells are extracted from the blood, biomanufactured to become dendritic cells and returned to the patient. Dendritic cells act as crusaders that march through the body, triggering the immune system to recognize and fight cancer. "We're building on an earlier phase 1 clinical trial that showed promising results in terms of survival after the dendritic cell-based vaccine," says Matthew Block, M.D., Ph.D. , co-principal investigator and Mayo Clinic medical oncologist. "Of the 18 evaluable patients in the phase 1 study, 11 had cancer return, but seven of them — 40% — have been cancer-free for almost 10 years. We typically expect 90% of patients in this condition to have the cancer return." Read more .
New gene markers detect Lynch syndrome-associated colorectal cancer.
Researchers from Mayo Clinic Comprehensive Cancer Center and Mayo Clinic Center for Individualized Medicine have discovered new genetic markers to identify Lynch syndrome-associated colorectal cancer with high accuracy. Studies are underway to determine if these genetic markers are in stool samples and, if so, how this could lead to a non-invasive screening option for people with Lynch syndrome . The research was published in Cancer Prevention Research , a journal of the American Association for Cancer Research. "This is an exciting finding that brings us closer to the reality that clinicians may soon be able to offer a non-invasive cancer screening option to patients with the highest risk of getting cancer," says Jewel Samadder, M.D. , co-lead author of the paper and a Mayo Clinic gastroenterologist. Read more .
Mayo Clinic prepares to biomanufacture a new CAR-T cell therapy for B-cell blood cancers.
Mayo Clinic research has developed a new type of chimeric antigen receptor-T cell therapy (CAR-T cell therapy) aimed at killing B-cell blood cancers that have returned and are no longer responding to treatment. This pioneering technology, designed and developed in the lab of Hong Qin, M.D., Ph.D. , a Mayo Clinic cancer researcher, killed B-cell tumors grown in the laboratory and tumors implanted in mouse models. The preclinical findings are published in Cancer Immunology, Immunotherapy . "This study shows our experimental CAR-T cell therapy targets several blood cancers, specifically chronic lymphocytic leukemia," says Dr. Qin. "Currently, there are six different CAR-T cell therapies approved for treatment of relapsed blood cancers. While the results are impressive, not everyone responds to this treatment. Our goal is to provide novel cell therapies shaped to each patient's individual need." Read more .
Related Posts

Richard Vile, Ph.D., is leading research into genetically engineered viruses called oncolytic viruses for cancer treatment at Mayo Clinic.

After receiving CAR-T cell therapy at Mayo Clinic, Welsh-born John Cadwallader achieved remission and found new hope. He now receives care in the U.K. and is monitored by Mayo in the U.S. and London.

After undergoing genetic screening as part of a research study, Tammy LeDoux learned she had Lynch syndrome, which put her at high risk of cancer.
- Português Br
- Journalist Pass
New study finds triple-negative breast cancer tumors with an increase in immune cells have lower risk of recurrence after surgery
Kelley Luckstein
Share this:

ROCHESTER, Minn. — A new multicenter, international study suggests that people who have early-stage triple-negative breast cancer (TNBC) and high levels of immune cells within their tumors may have a lower risk of recurrence and better survival rates even when not treated with chemotherapy. The study was published today in the Journal of American Medical Association (JAMA).
TNBC is a breast cancer subtype that does not respond to drugs that target the estrogen receptor or the HER2 protein. It grows rapidly, is more likely to spread beyond the breast before diagnosis and is more likely to recur than other breast cancers. TNBC represents about 15% of all breast cancers and is more common in younger people and in women of African American, Hispanic and Indian descent. Immune cells, also known as tumor-infiltrating lymphocytes, or TILs, are naturally existing immune system cells that can move from the bloodstream into a tumor and can recognize and destroy cancer cells.
"This is an important finding because it highlights that the abundance of TILs in breast tissue is a prognostic biomarker in people with early-stage triple-negative breast cancer, even when chemotherapy is not administered," says Roberto Leon-Ferre, M.D. , a breast medical oncologist at Mayo Clinic Comprehensive Cancer Center and first author of the study. "The study's findings may inspire future clinical trials to explore whether patients with a favorable prognosis (high TILs) can avoid intensive chemotherapy regimens."
"This meta-analysis confirms robustly the prognostic value of TILs that we have previously reported in TNBC patients treated with chemotherapy and expands it to patients treated without chemotherapy," says Sarah Flora Jonas, Ph.D., a statistician at Gustave Roussy and co-first author of the study. "Future studies may allow the use of this biomarker along with standard clinicopathological factors to inform treatment decisions in TNBC patients."
"Of interest, the first report suggesting that an increased number of immune cells being associated with better prognosis in breast cancer patients was described by doctors at Mayo Clinic more than 100 years ago," says Roberto Salgado, M.D., co-chair of the International Immuno-Oncology Biomarker Working Group; co-lead of the study; and pathologist from the Peter MacCallum Cancer Centre, Melbourne, Australia, and ZAS Hospitals, Antwerp, Belgium. "It took a global effort and a century later to reexamine this biomarker and bring it closer to application in patient care."
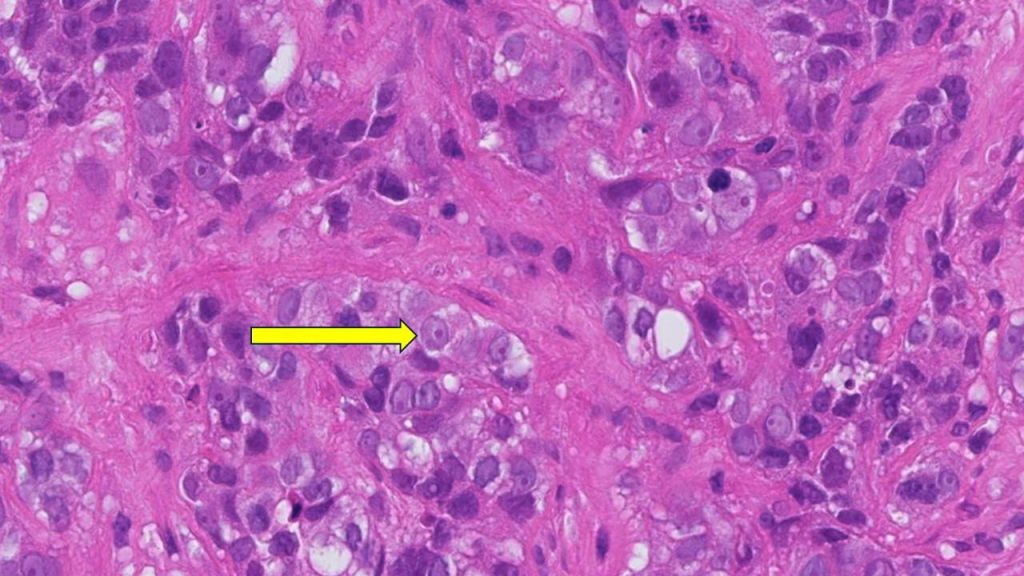
"TILs are not currently measured or reported in the routine examination of tissue samples of breast cancer," says co-senior author, Matthew Goetz, M.D. , a medical oncologist at Mayo Clinic Comprehensive Cancer Center and the Erivan K. Haub Family Professor of Cancer Research Honoring Richard F. Emslander, M.D. "While prior studies have focused on measuring TILs in people treated with chemotherapy, this is the largest study to comprehensively demonstrate that the presence of TILs influences the natural behavior of breast cancer in people who have surgery and/or radiation with no additional medical treatment."
For this study, Mayo Clinic and Gustave Roussy researchers, in collaboration with the International Immuno-Oncology Biomarker Working Group, led 11 additional groups to collect data on 1,966 participants with early-stage TNBC who only underwent surgery with or without radiation therapy but did not receive chemotherapy. The participants had been followed for a median of 18 years. The results showed that higher levels of TILs in breast cancer tissue were associated with lower recurrence rates among participants with early-stage TNBC.
"Five years after surgery, 95% of participants with small tumors, stage 1 TNBC, and whose tumors had high TILs were alive, compared to 82% of patients whose tumors had low TILs. Importantly, the breast cancer recurrence rate was significantly lower among patients whose tumors had high TILs," says co-senior author, Stefan Michiels, Ph.D. , head of Oncostat team, Gustave Roussy, Inserm U1018, University Paris-Saclay. "With nearly 2,000 participants involved in the study, we have now assembled the largest international cohort across three continents of people with TNBC in which the primary treatment was surgery without chemotherapy."
"The results of this study could lead to a recommendation to include TILs in the pathology reports of early-stage TNBC worldwide, as it has the potential to inform clinicians and patients when they discuss treatment options," says Dr. Salgado.
Furthermore, this biomarker would only require a visual evaluation by a pathologist looking through a microscope, meaning there are no additional costs associated with identifying the presence of immune cells. This could be particularly beneficial to regions with limited resources, adds Dr. Leon-Ferre.
Most people with early-stage TNBC undergo chemotherapy either before or after surgery, including people with stage 1 breast cancer. Most people receive multiple chemotherapy drugs in combination, which can cause significant side effects. Currently, the main factors taken into consideration to determine the course of chemotherapy treatment for each person are the tumor size and the presence of lymph node metastases. However, the authors identified that the number of TILs further influences the risk of future recurrence.
The researchers plan to evaluate TILs as biomarkers in prospective clinical trials evaluating chemotherapy selection based on TIL levels. Ongoing efforts to conduct additional research with other potential biomarkers are underway.
For a complete list of authors, disclosures and funding, see the full paper here .
About Mayo Clinic Comprehensive Cancer Center Designated as a comprehensive cancer center by the National Cancer Institute , Mayo Clinic Comprehensive Cancer Center is defining new boundaries in possibility, focusing on patient-centered care, developing novel treatments, training future generations of cancer experts and bringing cancer research to communities. At Mayo Clinic Comprehensive Cancer Center, a culture of innovation and collaboration is driving research breakthroughs that are changing approaches to cancer prevention, screening and treatment, and improving the lives of cancer survivors.
About Mayo Clinic Mayo Clinic is a nonprofit organization committed to innovation in clinical practice, education and research, and providing compassion, expertise and answers to everyone who needs healing. Visit the Mayo Clinic News Network for additional Mayo Clinic news.
About Gustave Roussy Ranked as the leading French and European Cancer Centre and fourth in the world, Gustave Roussy is a centre with comprehensive expertise and is devoted entirely to patients suffering with cancer. The Institute is a founding member of the Paris Saclay Cancer Cluster. It is a source of diagnostic and therapeutic advances. It caters for almost 50,000 patients per year and its approach is one that integrates research, patient care and teaching. It is specialized in the treatment of rare cancers and complex tumors and it treats all cancers in patients of any age. Its care is personalized and combines the most advanced medical methods with an appreciation of the patient’s human requirements. In addition to the quality of treatment offered, the physical, psychological and social aspects of the patient’s life are respected. 4,100 professionals work on its two campuses: Villejuif and Chevilly-Larue. Gustave Roussy brings together the skills, which are essential for the highest quality research in oncology: 40% of patients treated are included in clinical studies. For further information: www.gustaveroussy.fr/en , Twitter , Facebook , LinkedIn , Instagram
Media contact:
- Kelley Luckstein, Mayo Clinic Communications, [email protected]
- CAR-T cell therapy helps man continue community advocacy Protect those eyes on the sky
Related Articles

- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
News Release
Monday, June 4, 2018
NCI-MATCH precision medicine clinical trial releases new findings, strengthens path forward for targeted cancer therapies

The National Cancer Institute’s Molecular Analysis for Therapy Choice (NCI-MATCH) trial, the largest precision medicine trial of its kind, has achieved a milestone with the release of results from several treatment arms, or sub-studies, of the trial. The new results offer findings of interest for future cancer research that could ultimately play a role in bringing targeted treatments to patients with certain gene abnormalities, regardless of their cancer type.
Findings from three arms were released at this year’s American Society of Clinical Oncology (ASCO) annual meeting in Chicago, adding to findings from one arm released in November 2017 . The study was co-developed by NCI, part of the National Institutes of Health, and the ECOG-ACRIN Cancer Research Group, part of the NCI-sponsored National Clinical Trials Network (NCTN). ECOG-ACRIN and NCI are co-leading the trial.
“The outcomes data being released today from this groundbreaking precision medicine trial are an exciting step for NCI-MATCH,” said Lyndsay Harris, M.D., of NCI’s Cancer Diagnosis Program and NCI study chair. “These findings represent a large collection of data in populations of patients who may not have been studied in conventional clinical trials, and they will have important implications for future precision medicine trials.”
NCI-MATCH, a phase 2 clinical trial, seeks to determine whether targeted therapies for people whose tumors have certain gene mutations will be effective regardless of their cancer type. Researchers use a DNA sequencing test to identify gene mutations in patients’ tumors. The test looks for mutations in 143 genes associated with cancer that can be targeted by one of the drugs being studied in the trial. The trial launched in August 2015 and has nearly 40 treatment arms, each of which aims to enroll at least 35 patients whose tumors have a specific genetic change. As the first findings are released at ASCO, many other arms are still enrolling patients and several additional arms are in development for possible opening later in 2018.
“NCI-MATCH represents the first attempt to systematically leverage next-generation sequencing to explore so many therapies in parallel,” said ECOG-ACRIN study chair Keith T. Flaherty, M.D., a medical oncologist at Massachusetts General Hospital Cancer Center in Boston. “By focusing our investigational effort on new biomarker-guided therapies in understudied cancer types, we have accelerated the opportunity to find signals of efficacy.”
The study is a signal-finding trial, meaning that treatments that show promise can advance to larger, more definitive studies outside of the trial. NCI-MATCH is for adults who have solid tumors, lymphoma, or myeloma that have progressed on standard treatment or rare cancers for which there is no standard treatment. A goal of the study was for about 25 percent of patients in the trial to have rare cancers. Surprisingly, 62.5 percent of the first 6,000 patients enrolled in NCI-MATCH had tumors other than the four most common cancers (breast, colorectal, non-small cell lung, and prostate), providing more opportunities for less common and rare tumors than expected based on initial estimates.
The first arm for which results were released (Arm Z1D), in November 2017 at the Society for Immunotherapy of Cancer annual meeting, showed that the drug nivolumab has promising activity in mismatch repair–deficient non-colorectal cancers.
Highlights from the findings from the three arms announced at ASCO include:
- Arm I studied the drug taselisib in 65 patients with mutations in the PIK3CA gene. There were no objective responses to the drug, meaning the tumors did not shrink substantially. However, 24 percent of the patients had progression-free survival — or prolonged stable disease — of greater than six months. This prolonged stable disease was seen even in patients with aggressive cancer types, including lung cancer and cholangiocarcinoma (bile duct) cancer. The observation of prolonged disease control in these cancer types suggests the drug warrants further research.
- In Arm Q, the drug ado-trastuzumab emtansine (T-DM1) was studied in patients with HER2-overexpressing tumors, excluding breast and gastric/gastroesophageal junction cancers. Partial responses (at least 30 percent shrinkage of the tumor) were seen in three of the 37 patients, each of whom had a rare cancer: mucoepidermoid carcinoma of the parotid gland, squamous cell cancer of the parotid gland, and extramammary Paget disease of the scrotum. In addition, 46 percent of the patients had stable disease, including patients with ovarian, uterine, and colorectal cancers. The researchers concluded that the findings warrant further study, particularly in certain rare cancers.
- Arm W tested the drug AZD4547 in 50 patients with mutations in the FGFR pathway. Ten percent of patients had a partial response. Among four patients who had a partial response, whose tumors all had different sites of origin, two had point mutations in the FGFR2/3 gene and the other two had FGFR3 gene fusions, in which part of the FGFR gene is joined to part of another gene. This suggests that these mutations may be particularly sensitive to the drug, warranting further studies in tumors harboring these fusions.
Many of the patients in these three arms had been treated with more than three lines of therapy before entering the trial (Arm I: 37 percent, Arm Q: 33 percent, Arm W: 50 percent), so the results are particularly encouraging. It suggests that future studies in populations with earlier-stage disease could potentially see more responses.
Results of additional treatment arms that have completed accrual will be released on a rolling basis as their data mature. The trial is ongoing and enrolling patients at more than 1,100 cancer centers and community hospitals in every state, the District of Columbia, and Puerto Rico. All trial sites are either members of the research groups in the NCTN that focus on adult cancers — the Alliance for Clinical Trials in Oncology, ECOG-ACRIN Cancer Research Group, NRG Oncology, and SWOG — or are members of the NCI Community Oncology Research Program (NCORP).
Genentech, a member of the Roche group, provided the study drugs for Arms I and Q, and AstraZeneca provided the drug for Arm W.
About the National Cancer Institute (NCI): NCI leads the National Cancer Program and NIH’s efforts to dramatically reduce the prevalence of cancer and improve the lives of cancer patients and their families, through research into prevention and cancer biology, the development of new interventions, and the training and mentoring of new researchers. For more information about cancer, please visit the NCI website at cancer.gov or call NCI’s Contact Center (formerly known as the Cancer Information Service) at 1-800-4-CANCER (1-800-422-6237).
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Connect with Us
- More Social Media from NIH
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
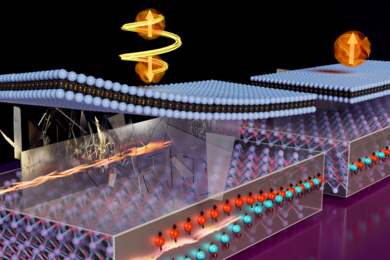
Scientists develop a rapid gene-editing screen to find effects of cancer mutations
Press contact :, media download.

*Terms of Use:
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."

Previous image Next image
Tumors can carry mutations in hundreds of different genes, and each of those genes may be mutated in different ways — some mutations simply replace one DNA nucleotide with another, while others insert or delete larger sections of DNA.
Until now, there has been no way to quickly and easily screen each of those mutations in their natural setting to see what role they may play in the development, progression, and treatment response of a tumor. Using a variant of CRISPR genome-editing known as prime editing, MIT researchers have now come up with a way to screen those mutations much more easily.
The researchers demonstrated their technique by screening cells with more than 1,000 different mutations of the tumor suppressor gene p53, all of which have been seen in cancer patients. This method, which is easier and faster than any existing approach, and edits the genome rather than introducing an artificial version of the mutant gene, revealed that some p53 mutations are more harmful than previously thought.
This technique could also be applied to many other cancer genes, the researchers say, and could eventually be used for precision medicine, to determine how an individual patient’s tumor will respond to a particular treatment.
“In one experiment, you can generate thousands of genotypes that are seen in cancer patients, and immediately test whether one or more of those genotypes are sensitive or resistant to any type of therapy that you’re interested in using,” says Francisco Sanchez-Rivera, an MIT assistant professor of biology, a member of the Koch Institute for Integrative Cancer Research, and the senior author of the study.
MIT graduate student Samuel Gould is the lead author of the paper , which appears today in Nature Biotechnology .
Editing cells
The new technique builds on research that Sanchez-Rivera began 10 years ago as an MIT graduate student. At that time, working with Tyler Jacks, the David H. Koch Professor of Biology, and then-postdoc Thales Papagiannakopoulos, Sanchez-Rivera developed a way to use CRISPR genome-editing to introduce into mice genetic mutations linked to lung cancer.
In that study, the researchers showed that they could delete genes that are often lost in lung tumor cells, and the resulting tumors were similar to naturally arising tumors with those mutations. However, this technique did not allow for the creation of point mutations (substitutions of one nucleotide for another) or insertions.
“While some cancer patients have deletions in certain genes, the vast majority of mutations that cancer patients have in their tumors also include point mutations or small insertions,” Sanchez-Rivera says.
Since then, David Liu, a professor in the Harvard University Department of Chemistry and Chemical Biology and a core institute member of the Broad Institute, has developed new CRISPR-based genome editing technologies that can generate additional types of mutations more easily. With base editing, developed in 2016, researchers can engineer point mutations, but not all possible point mutations. In 2019, Liu, who is also an author of the Nature Biotechnology study, developed a technique called prime editing, which enables any kind of point mutation to be introduced, as well as insertions and deletions.
“Prime editing in theory solves one of the major challenges with earlier forms of CRISPR-based editing, which is that it allows you to engineer virtually any type of mutation,” Sanchez-Rivera says.
When they began working on this project, Sanchez-Rivera and Gould calculated that if performed successfully, prime editing could be used to generate more than 99 percent of all small mutations seen in cancer patients.
However, to achieve that, they needed to find a way to optimize the editing efficiency of the CRISPR-based system. The prime editing guide RNAs (pegRNAs) used to direct CRISPR enzymes to cut the genome in certain spots have varying levels of efficiency, which leads to “noise” in the data from pegRNAs that simply aren’t generating the correct target mutation. The MIT team devised a way to reduce that noise by using synthetic target sites to help them calculate how efficiently each guide RNA that they tested was working.
“We can design multiple prime-editing guide RNAs with different design properties, and then we get an empirical measurement of how efficient each of those pegRNAs is. It tells us what percentage of the time each pegRNA is actually introducing the correct edit,” Gould says.
Analyzing mutations
The researchers demonstrated their technique using p53, a gene that is mutated in more than half of all cancer patients. From a dataset that includes sequencing information from more than 40,000 patients, the researchers identified more than 1,000 different mutations that can occur in p53.
“We wanted to focus on p53 because it’s the most commonly mutated gene in human cancers, but only the most frequent variants in p53 have really been deeply studied. There are many variants in p53 that remain understudied,” Gould says.
Using their new method, the researchers introduced p53 mutations in human lung adenocarcinoma cells, then measured the survival rates of these cells, allowing them to determine each mutation’s effect on cell fitness.
Among their findings, they showed that some p53 mutations promoted cell growth more than had been previously thought. These mutations, which prevent the p53 protein from forming a tetramer — an assembly of four p53 proteins — had been studied before, using a technique that involves inserting artificial copies of a mutated p53 gene into a cell.
Those studies found that these mutations did not confer any survival advantage to cancer cells. However, when the MIT team introduced those same mutations using the new prime editing technique, they found that the mutation prevented the tetramer from forming, allowing the cells to survive. Based on the studies done using overexpression of artificial p53 DNA, those mutations would have been classified as benign, while the new work shows that under more natural circumstances, they are not.
“This is a case where you could only observe these variant-induced phenotypes if you're engineering the variants in their natural context and not with these more artificial systems,” Gould says. “This is just one example, but it speaks to a broader principle that we’re going to be able to access novel biology using these new genome-editing technologies.”
Because it is difficult to reactivate tumor suppressor genes, there are few drugs that target p53, but the researchers now plan to investigate mutations found in other cancer-linked genes, in hopes of discovering potential cancer therapies that could target those mutations. They also hope that the technique could one day enable personalized approaches to treating tumors.
“With the advent of sequencing technologies in the clinic, we'll be able to use this genetic information to tailor therapies for patients suffering from tumors that have a defined genetic makeup,” Sanchez-Rivera says. “This approach based on prime editing has the potential to change everything.”
The research was funded, in part, by the National Institute of General Medical Sciences, an MIT School of Science Fellowship in Cancer Research, a Howard Hughes Medical Institute Hanna Gray Fellowship, the V Foundation for Cancer Research, a National Cancer Institute Cancer Center Support Grant, the Ludwig Center at MIT, the Koch Institute Frontier Research Program via the Casey and Family Foundation Cancer Research Fund, Upstage Lung Cancer, and the Michael (1957) and Inara Erdei Cancer Research Fund, and the MIT Research Support Committee.
Share this news article on:
Related links.
- Francisco Sanchez-Rivera
- Koch Institute
- Department of Biology
Related Topics
- Broad Institute
Related Articles
Gene-editing technique could speed up study of cancer mutations
Fast modeling of cancer mutations
Previous item Next item
More MIT News

For Julie Greenberg, a career of research, mentoring, and advocacy
Read full story →
Reevaluating an approach to functional brain imaging
Propelling atomically layered magnets toward green computers

Q&A: Tips for viewing the 2024 solar eclipse
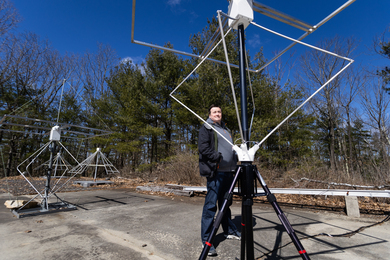
MIT Haystack scientists prepare a constellation of instruments to observe the solar eclipse’s effects

Drinking from a firehose — on stage
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Collection 01 July 2020
Cancer at Nature Portfolio
The Nature Portfolio editors who handle cancer primary research, methods, protocols and reviews bring you the latest articles, covering all aspects from disease mechanisms to therapeutic approaches. Collected here you will also find specially curated content, such as collections, focus issues and animations, all ready to be used in presentations and educational materials. You can also find out about the editors handling cancer content, and the journals at Nature Portfolio that publish articles on this topic and how to submit to them.

- Collection content
- Collections
- PrimeViews and posters
Research Articles

Polygenic risk score for ulcerative colitis predicts immune checkpoint inhibitor-mediated colitis
Colitis is one of the most common immune-related adverse events in patients with cancer treated with immune checkpoint inhibitors. Here the authors show that a polygenic risk score for ulcerative colitis can predict immune checkpoint inhibitor-mediated colitis in patients with cancer.
- Pooja Middha
- Rohit Thummalapalli
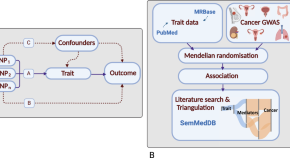
Phenome-wide Mendelian randomisation analysis of 378,142 cases reveals risk factors for eight common cancers
Mendelian randomisation can identify potential risk factors from large populations. Here, the authors analyse 3000 traits across multiple cancer types to search for potential risk factors and molecular biomarkers.
- Richard Houlston
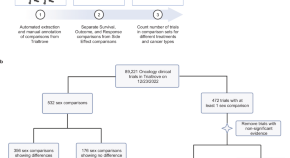
Outcome differences by sex in oncology clinical trials
The role of sex differences in response to cancer therapy remains unclear but this could be improved by reporting sex comparisons of outcomes in clinical trials. Here, the authors characterise the sex outcome comparisons in 89,221 interventional trials, finding that while comparisons were rare, important insights could be obtained.
- Ashwin V. Kammula
- Alejandro A. Schäffer
- Eytan Ruppin
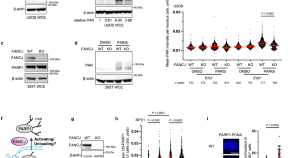
FANCJ promotes PARP1 activity during DNA replication that is essential in BRCA1 deficient cells
Here the authors show that PARPi efficacy along with the fitness of BRCA1 deficient cells relies on FANCJ, which maintains S-phase PARP1 activity by preventing its sequestration with MSH2 on G-quadruplexes.
- Nathan MacGilvary
- Sharon B. Cantor

Threonine fuels glioblastoma through YRDC-mediated codon-biased translational reprogramming
Rich and colleagues show that glioblastoma stem cells have increased global protein translation, which is achieved via the tRNA modifier YRDC. They show that targeting it or reducing its substrate threonine suppresses tumor growth.
- Huairui Yuan
- Jeremy N. Rich

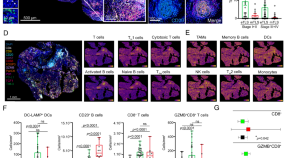
Cancer cell genetics shaping of the tumor microenvironment reveals myeloid cell-centric exploitable vulnerabilities in hepatocellular carcinoma
Distinct genetic mutations can shape the tumor immune microenvironment. Here the authors generate preclinical mouse models of hepatocellular carcinoma bearing clinically-relevant oncogenic driver combinations, identifying myeloid cell-centric exploitable therapeutic vulnerabilities.
- Christel F. A. Ramirez
- Daniel Taranto
- Leila Akkari
Multipeptide vaccines for melanoma in the adjuvant setting: long-term survival outcomes and post-hoc analysis of a randomized phase II trial
Peptide-based cancer vaccines require epitopes for both CD8+ and CD4+ T cells. Here the authors report the long-term outcomes of a randomized phase II trial (NCT00118274) in patients with melanoma designed to evaluate a class I MHC-restricted peptide vaccine plus one of two “helper” peptide preparations to stimulate CD4+ T cells, either non-specific help or melanoma-specific help.
- Emily K. Ninmer
- Craig L. Slingluff Jr

BET inhibitors drive Natural Killer activation in non-small cell lung cancer via BRD4 and SMAD3
Combination of BET inhibitors (BETi) with immunotherapy has been reported to be synergic for the treatment of non-small cell lung carcinoma (NSCLC). Here, the authors show that BETi-induced epigenetic reprogramming downregulates the expression of NK cell inhibitory receptors on NK cells, increasing their activation and cytotoxicity against NSCLC.
- Francesca Reggiani
- Giovanna Talarico
- Valentina Sancisi
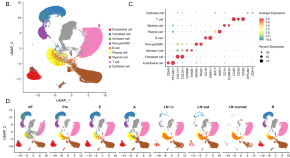
Single cell deciphering of progression trajectories of the tumor ecosystem in head and neck cancer
Head and neck squamous cell carcinoma (HNSCC) is characterised with high heterogeneity and unfavourable prognosis. Here, the authors perform single cell transcriptomics to investigate the tumour microenvironment features of HNSCC initiation, progression, lymph node metastasis and recurrence.
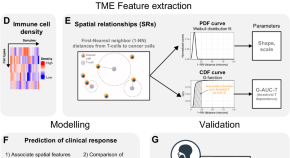
Spatial relationships in the urothelial and head and neck tumor microenvironment predict response to combination immune checkpoint inhibitors
Spatial positioning of cells within the tumour microenvironment may have a function in the success of immune checkpoint immunotherapy (ICI). Here the authors analyse spatial relationships from immunohistochemistry samples prior to ICI therapy and show that CD8 T cell or macrophage proximity to cancer cells is associated with better responses.
- Alberto Gil-Jimenez
- Nick van Dijk
- Lodewyk F. A. Wessels
The EIF3H-HAX1 axis increases RAF-MEK-ERK signaling activity to promote colorectal cancer progression
Eukaryotic initiation translation factor 3 subunit h (EIF3H) possesses an alternative “moonlighting” function of deubiquitinase, while its role in colorectal carcinogenesis remains to be explored. Here the authors show that EIF3H deubiquitinates and stabilizes HAX1, which enhances RAF-MEK-ERK signaling to promote colorectal tumor growth and metastasis.
- Xiaoling Huang
- Mong-Hong Lee
Tertiary lymphoid structures and B cells determine clinically relevant T cell phenotypes in ovarian cancer
Intratumoral tertiary lymphoid structure (TLS) density has been associated with better prognosis in several cancer types. Here the authors provide a comprehensive characterization of TLSs in patients with high-grade serous ovarian carcinoma.
- Lenka Kasikova
- Jana Rakova
- Jitka Fucikova

Aberrant non-canonical NF-κB signalling reprograms the epigenome landscape to drive oncogenic transcriptomes in multiple myeloma
The downstream molecular mechanisms following the activation of the NF-κB pathway in multiple myeloma (MM) remain to be characterised. Here, it is shown that aberrant non-canonical NF-κB signalling causes epigenomic reprogramming leading to transcriptional changes that favour MM progression.
- Daniel A. Ang
- Jean-Michel Carter
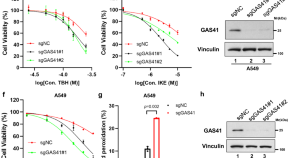
GAS41 modulates ferroptosis by anchoring NRF2 on chromatin
GAS41 is recognized as a histone reader and oncogene, but the mechanism by which GAS41 contributes to tumorigenesis is not well understood. Here, the authors discover that GAS41 is a ferroptosis repressor that anchors NRF2 to chromatin, promoting tumor growth.
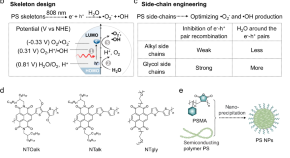
Oxygen-independent organic photosensitizer with ultralow-power NIR photoexcitation for tumor-specific photodynamic therapy
Conventional photodynamic therapy (PDT) is hindered by oxygen-dependent photosensitization pathways and high-power-density photoexcitation. Here, the authors develop polymer-based organic photosensitizers (PSs) through PS skeleton design and side-chain engineering to allow tumor-specific PDT under oxygen-free conditions using ultralow-power 808 nm photoexcitation.
- Yuanyuan Li

PIEZO1 mechanically regulates the antitumour cytotoxicity of T lymphocytes
Blocking the mechanical sensor PIEZO1 in cytotoxic T lymphocytes strengthens their traction forces and augments their cytotoxicity against tumour cells.
- Ruiyang Pang

Generation of synthetic whole-slide image tiles of tumours from RNA-sequencing data via cascaded diffusion models
Cascaded diffusion models can be used to synthesize realistic whole-slide image tiles from latent representations of RNA-sequencing data from human tumours.
- Francisco Carrillo-Perez
- Marija Pizurica
- Olivier Gevaert
Metabolic targeting of cancer associated fibroblasts overcomes T-cell exclusion and chemoresistance in soft-tissue sarcomas
Cancer associated fibroblasts can shape the tumor microenvironment (TME) and modulate immune infiltration. Here the authors characterize the TME in preclinical models of softtissue sarcomas, identifying a subset of “glycolytic” cancer-associated fibroblasts that inhibit cytotoxic T cell infiltration into the tumor parenchyma.
- Marina T. Broz
- Emily Y. Ko
- Jlenia Guarnerio

Reciprocal inhibition between TP63 and STAT1 regulates anti-tumor immune response through interferon-γ signaling in squamous cancer
TP63 is a master regulator transcription factor in squamous cell carcinomas (SCCs). Here the authors report that TP63 suppresses IFNγ signaling in SCC tumors and that its inhibition is associated with enhanced anti-tumor immunity and response to anti-PD1.
- Yueyuan Zheng
- Yan-Yi Jiang

Combined KRAS-MAPK pathway inhibitors and HER2-directed drug conjugate is efficacious in pancreatic cancer
The MAPK pathway is an important therapeutic target in pancreatic ductal adenocarcinoma (PDAC), but success is limited by pathway reactivation, which drives resistance. Here, the authors investigate the mechanism underlying HER2-reactivation post KRAS-MAPK inhibition, identifying combination of MAPK and HER2 inhibition as a therapeutic strategy.
- Ashenafi Bulle
- Kian-Huat Lim
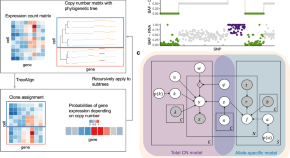
Allele-specific transcriptional effects of subclonal copy number alterations enable genotype-phenotype mapping in cancer cells
Quantifying the impact of copy-number alterations (CNAs) on gene expression at the subclone level in cancer remains a challenge. Here, the authors develop TreeAlign, a method that integrates sample-matched single-cell DNA and RNA sequencing data to infer the impact of CNAs on subclonal gene expression.
- Marc J. Williams
- Sohrab P. Shah
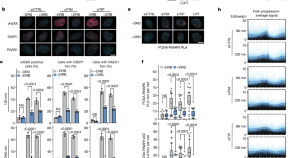
Transcription–replication conflicts underlie sensitivity to PARP inhibitors
Poly(ADP-ribose) polymerase 1 (PARP1) functions together with TIMELESS and TIPIN to protect the replisome in early S phase from transcription–replication conflicts, and inhibiting PARP1 enzymatic activity may suffice for treatment efficacy in homologous recombination-deficient settings.
- Michalis Petropoulos
- Angeliki Karamichali
- Thanos D. Halazonetis
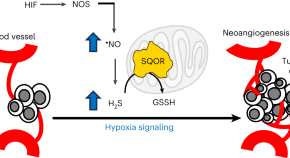
Sulfide oxidation promotes hypoxic angiogenesis and neovascularization
Hypoxia induces ·NO-dependent hydrogen sulfide (H 2 S) biogenesis by inhibiting the transsulfuration pathway. H 2 S oxidation promotes endothelial cell proliferation to support neovascularization in tissue injury and tumor xenograft models.
- Roshan Kumar
- Victor Vitvitsky
- Ruma Banerjee

A distinct Fusobacterium nucleatum clade dominates the colorectal cancer niche
A study reveals that Fusobacterium nucleatum subspecies animalis is bifurcated into two distinct clades, and shows that only one of these dominates the colorectal cancer niche, probably through increased colonization of the human gastrointestinal tract.
- Martha Zepeda-Rivera
- Samuel S. Minot
- Christopher D. Johnston

The pleiotropic functions of reactive oxygen species in cancer
Papagiannakopoulos and colleagues discuss the roles of reactive oxygen species in cancer and the ways in which redox mechanisms may be exploited for cancer therapy.
- Katherine Wu
- Ahmed Ezat El Zowalaty
- Thales Papagiannakopoulos
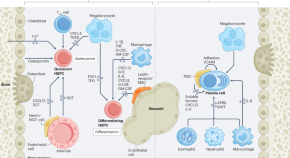
Bone marrow inflammation in haematological malignancies
Haematological malignancies are associated with inflammation in the bone marrow. In this Review, the authors discuss how tumour-associated inflammation affects the normal functions of the bone marrow and supports the outgrowth and survival of malignant cells. Moreover, they describe how the inflammatory changes in the bone marrow differ in myeloid and lymphoid malignancies.
- Madelon M. E. de Jong
- Lanpeng Chen
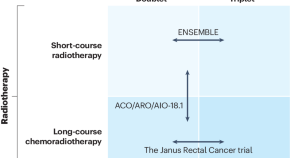
Future direction of total neoadjuvant therapy for locally advanced rectal cancer
In this article, the authors discuss the use of total neoadjuvant therapy for locally advanced rectal cancer. They highlight ongoing trials and discuss future treatment options, including the potential use of multi-omics and artificial intelligence to facilitate treatment selection and prediction of response.
- Yoshinori Kagawa
- J. Joshua Smith
- Takayuki Yoshino

Targeting cuproplasia and cuproptosis in cancer
Copper is an essential trace element with inherent redox properties and fundamental roles in a diverse range of biological processes; therefore, maintaining copper homeostasis is crucial. In this Review, the authors discuss new insights into the mechanisms by which disrupted copper homeostasis contributes to tumour initiation and development, including the recently defined concepts of cuproplasia (copper-dependent cell growth and proliferation) and cuproptosis (a mitochondrial pathway of cell death triggered by excessive copper exposure). They also discuss potential strategies to exploit cuproplasia and cuproptosis for the treatment of cancer.
- Daolin Tang
- Guido Kroemer

Immunogenic cell death in cancer: targeting necroptosis to induce antitumour immunity
In this Review, Meier et al. discuss the molecular mechanisms of necroptosis, delineate how this form of immunogenic cell death activates antitumour immune responses and explore the opportunities and limitations of targeting necroptosis for anticancer therapy.
- Pascal Meier
- Arnaud J. Legrand
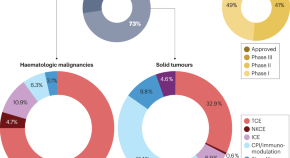
The present and future of bispecific antibodies for cancer therapy
Bispecific antibodies (bsAbs) can mediate therapeutic effects beyond those of natural monospecific antibodies. This Review provides an overview of recent developments in the field of bsAbs for cancer therapy and an outlook into next-generation bsAbs in earlier stages of development.
- Christian Klein
- Ulrich Brinkmann
- Roland E. Kontermann
Fungi in cancer
In this Viewpoint article, we asked three scientists working on the cancer mycobiome to provide their opinions on advancements and challenges and what the future holds for this exciting field of cancer research.
- Jessica Galloway-Peña
- Iliyan D. Iliev
- Florencia McAllister
Cancer burden in low-income and middle-income countries
In this Viewpoint, we asked four experts to discuss the increasing burden of cancer in low- and middle-income countries; they explore the changes that are necessary to improve cancer diagnosis, prevention and treatment within these nations.
- Sharmila Anandasabapathy
- Chite Asirwa
- Chemtai Mungo
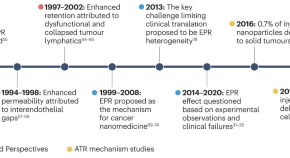
The mechanisms of nanoparticle delivery to solid tumours
The mechanisms of nanoparticle delivery to solid tumours guide the engineering of nanoparticles for cancer applications. This Review discusses two contrasting nanoparticle delivery mechanisms, the enhanced permeability and retention effect and the active transport and retention principle, and their implications for the design of cancer nanomedicines.
- Luan N. M. Nguyen
- Warren C. W. Chan

Dendritic cells as orchestrators of anticancer immunity and immunotherapy
Dendritic cells (DCs) are antigen-presenting cells that function at the interface between innate and adaptive immunity, thereby acting as key mediators of antitumour immune responses and immunotherapy efficacy. In this Review, the authors outline the emerging complexity of intratumoural DC states that is being revealed through single-cell analyses as well as the contributions of different DC subsets to anticancer immunity and the activity of immune-checkpoint inhibitors. The authors also discuss advances in the development of DC-based cancer therapies and considerations for their potential combination with other anticancer therapies.
- Ignacio Heras-Murillo
- Irene Adán-Barrientos
- David Sancho

Molecular profile of bladder cancer progression to clinically aggressive subtypes
In this Review, the authors describe the molecular profile of bladder cancer progression associated with the subtypes of this disease and comment on their potential diagnostic, prognostic and therapeutic importance.
- Charles C. Guo
- Sangkyou Lee
- Bogdan Czerniak

Multiplex protein imaging in tumour biology
In this Review, de Souza et al. discuss how advances in the ability to image protein markers at high-plex, at single-cell and even subcellular resolution, are expanding our understanding of tumour biology and clinical outcomes, and outline the future promise of combining such multiplex protein imaging methods with other forms of spatial omics.
- Natalie de Souza
- Bernd Bodenmiller

The yin and yang of chromosomal instability in prostate cancer
Chromosomal instability is a hallmark of advanced prostate cancer. In this Review, the authors discuss the biological causes and paradoxical consequences of chromosomal instability, its potential clinical role in the stratification of prostate cancer aggressiveness and the development of novel treatment strategies.
- Marc Carceles-Cordon
- Jacob J. Orme
- Veronica Rodriguez-Bravo
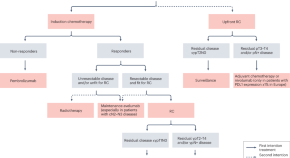
Management of patients with muscle-invasive bladder cancer with clinical evidence of pelvic lymph node metastases
Muscle-invasive bladder cancer with clinically positive pelvic lymph nodes is a particular situation at the interface between localized and metastatic disease. In this Review, the authors discuss the advances and challenges of currently available strategies for the diagnosis and treatment of patients with muscle-invasive bladder cancer with clinically positive pelvic lymph nodes.
- Elisabeth Grobet-Jeandin
- Louis Lenfant
- Thomas Seisen
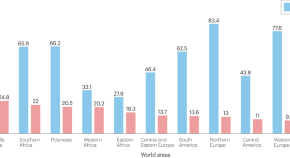
The complex interplay of modifiable risk factors affecting prostate cancer disparities in African American men
African American men are disproportionately affected by prostate cancer in the USA. In this Review, the authors discuss the complex interplay of modifiable risk factors that might underlie the glaring prostate cancer disparities observed.
- Jabril R. Johnson
- Nicole Mavingire
- Rick A. Kittles

Extrachromosomal DNA in cancer
Extrachromosomal DNA (ecDNA) is now accepted as a major contributor to cancer pathogenesis. In this Review, Yan, Mischel and Chang highlight the recent advancements in ecDNA research, providing new insights into the biogenesis and maintenance of ecDNA, as well as its role in altering gene expression and promoting tumour heterogeneity.
- Xiaowei Yan
- Paul Mischel
- Howard Chang
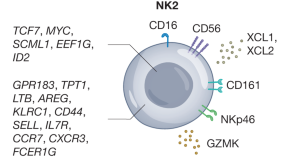
Natural killer cell therapies
This Review explores in detail the complexity of NK cell biology in humans and highlights the role of these cells in cancer immunity.
- Eric Vivier
- Lucas Rebuffet
- Valeria R. Fantin

Clinical and translational attributes of immune-related adverse events
Suijkerbuijk et al. summarize the clinical manifestation and classification of immune-related adverse events, discuss the immunopathogenesis of immune-related adverse events and provide key insights into their management and future therapeutic directions.
- Karijn P. M. Suijkerbuijk
- Mick J. M. van Eijs
- Alexander M. M. Eggermont

Translating p53-based therapies for cancer into the clinic
Although p53 was once considered undruggable, in this Review, Peuget et al. discuss the progress made in targeting p53 as a form of cancer therapy with approaches ranging from restoration of mutant p53 function to inhibition of the negative regulator of p53, MDM2, as well as newer strategies, including p53-based mRNA vaccines and antibodies.
- Sylvain Peuget
- Xiaolei Zhou
- Galina Selivanova
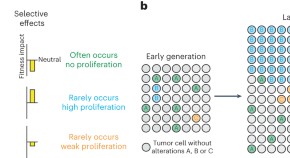
Aneuploidy and complex genomic rearrangements in cancer evolution
Van Loo and colleagues review the mechanistic underpinnings of large genomic alterations and their roles in tumor development and evolution.
- Toby M. Baker
- Peter Van Loo

FLIP(C1orf112)-FIGNL1 complex regulates RAD51 chromatin association to promote viability after replication stress
Recombination is essential for life. Here, the authors characterize FLIP as a novel regulator of the key recombination protein RAD51’s functions. FLIP loss caused marked sensitivity to DNA damage, increased DNA breakage and defective replication.
- Jessica D. Tischler
- Hiroshi Tsuchida
- Richard O. Adeyemi

BRAF — a tumour-agnostic drug target with lineage-specific dependencies
Various BRAF alterations are found and function as oncogenic drivers across diverse cancer types. BRAF inhibitor-based therapy has improved outcomes for patients with cancers harbouring BRAF V600 mutations, although resistance develops in most, and the current inhibitors are not effective against other types of BRAF alterations. In this Review, the authors describe the mechanisms underlying oncogenic BRAF signalling, as well as pan-cancer and lineage-specific mechanisms of intrinsic, adaptive and acquired resistance to BRAF inhibitors. They also discuss novel RAF inhibitors and drug combinations designed to overcome these resistance mechanisms and/or expand the applicability of molecularly targeted therapy to a broader range of BRAF -mutant cancers.
- Aphrothiti J. Hanrahan
- David B. Solit
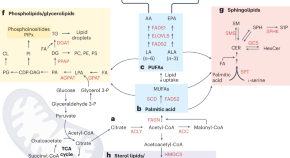
Lipids as mediators of cancer progression and metastasis
Schulze and colleagues discuss the latest advances in understanding the role of lipids in cancer progression and metastasis and reflect on opportunities to target lipid metabolism in tumors.
- Felix C. E. Vogel
- Adriano B. Chaves-Filho
- Almut Schulze

New immune cell engagers for cancer immunotherapy
Immune cell engagers — antibody-based molecules engineered to direct immune effector cells to recognize and kill cancer cells — represent a rapidly expanding approach in cancer therapy. Here, the authors bring us up to date with the targets, challenges and opportunities for harnessing the anticancer activities of T cells, natural killer cells and myeloid cells with immune cell engagers.
- Aurore Fenis
- Olivier Demaria
- Emilie Narni-Mancinelli
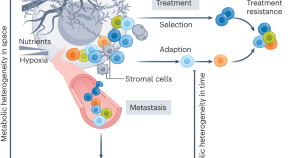
Metabolic heterogeneity in cancer
Demicco, Liu et al. discuss how metabolic adaptations in cancer contribute to tumour progression. These adaptations entail high spatial and temporal metabolic heterogeneity, based on local adaptations in different regions of the tumour microenvironment, as well as metabolic evolution over time as the tumour progresses and metastasizes.
- Margherita Demicco
- Xiao-Zheng Liu
- Sarah-Maria Fendt
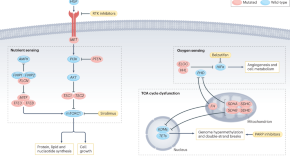
Metabolic alterations in hereditary and sporadic renal cell carcinoma
Renal cell carcinoma is a metabolic disease linked to a variety of alterations in genes that regulate cellular metabolism. Here, the authors examine cell-intrinsic metabolic alterations in hereditary and sporadic renal cell carcinoma, and how they can be exploited to develop novel therapeutic interventions.
- Nathan J. Coffey
- M. Celeste Simon
News & Commentary

The death gaze of MEDUSA
Chemogenetic profiling can reveal genetic determinants that coordinate phenotypic responses to therapeutics, along with predicting potential pathways of resistance. A new analytical method for evaluating chemogenetic profiles reveals contributions from death-regulatory genes.
- Jesse D. Gelles
- Jerry Edward Chipuk
Mirvetuximab soravtansine has activity in platinum-sensitive epithelial ovarian cancer
- Diana Romero
Enhancing diagnostic precision in liver lesion analysis using a deep learning-based system: opportunities and challenges
A recent study reported the development and validation of the Liver Artificial Intelligence Diagnosis System (LiAIDS), a fully automated system that integrates deep learning for the diagnosis of liver lesions on the basis of contrast-enhanced CT scans and clinical information. This tool improved diagnostic precision, surpassed the accuracy of junior radiologists (and equalled that of senior radiologists) and streamlined patient triage. These advances underscore the potential of artificial intelligence to enhance hepatology care, although challenges to widespread clinical implementation remain.
- Jeong Min Lee
- Jae Seok Bae
IL-13Rα2-targeted CAR T cells show promise in patients with recurrent high-grade gliomas
- David Killock
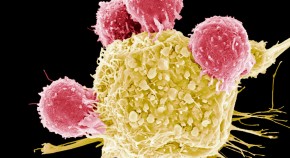
Cutting-edge CAR-T cancer therapy is now made in India — at one-tenth the cost
The treatment, called NexCAR19, raises hopes that this transformative class of medicine will become more readily available in low- and middle-income countries.
- Smriti Mallapaty
A new standard of care for advanced-stage urothelial carcinoma
- Peter Sidaway
Identification of dynamic microbiota signatures in patients with melanoma receiving ICIs: opportunities and challenges
The composition of the gut microbiota has emerged as a tumour-extrinsic factor that modulates response to immune-checkpoint inhibitors (ICIs), although the lack of consistency in microbiota signatures across studies has limited their value as reliable biomarkers. Herein, we discuss a recent study in which longitudinal microbiome profiling identified several taxa that are persistently enriched in patients with melanoma and a favourable response to ICIs.
- Saman Maleki Vareki
- Diwakar Davar

‘Woah, this is affecting me’: why I’m fighting racial inequality in prostate-cancer research
Olugbenga Samuel Oyeniyi sought a career with a stronger public-health focus after learning that Black men are twice as likely as white men to get prostate cancer.
- Jacqui Thornton
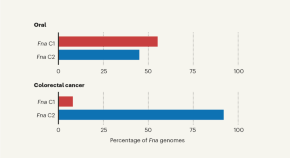
Whittling down the bacterial subspecies that might drive colon cancer
Understanding the factors that drive formation of particular types of cancer can aid efforts to develop better diagnostics or treatments. The identification of a bacterial subspecies with a connection to colon cancer has clinical relevance.
- Cynthia L. Sears
- Jessica Queen
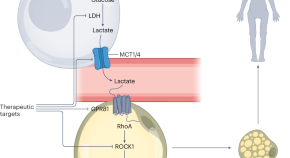
A waste product’s unexpected role in wasting
The mechanisms that drive cancer cachexia are unclear. Adipocyte activation of GPR81 by high levels of lactate is now shown to drive adipose tissue browning, thermogenesis and a loss of body weight in mouse models of cancer.
- Jack D. Sanford
- Marcus D. Goncalves

Why are so many young people getting cancer? What the data say
Clues to a modern mystery could be lurking in information collected generations ago.
- Heidi Ledford
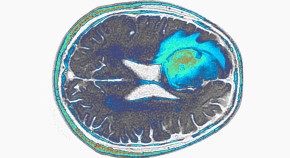
Deadly brain cancer shrinks after CAR-T therapy — but for how long is unclear
Early studies with engineered immune cells show drastic but often short-lived results in glioblastoma, the most aggressive brain cancer.
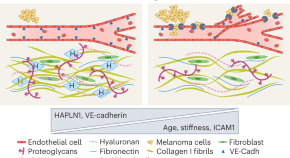
Mechanisms of melanoma aggressiveness with age
The extracellular matrix is an essential component of the tumor microenvironment and affects cancer progression. Weeraratna and colleagues have now uncovered that age-related reductions in the level of hyaluronan and proteoglycan link protein 1 (HAPLN1) stimulate neoangiogenesis and compromise the vascular integrity of intratumoral blood vessels. These biological modifications converge to fuel distant melanoma metastasis.
- Corine Bertolotto

Engineered T cells call for back-up
- M. Teresa Villanueva


New pathogen on the block
Fu et al. provide data indicating a pathogenic role for Streptococcus anginosus in gastric cancer.
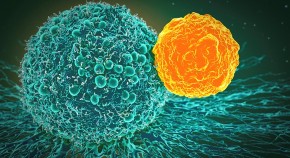
MEGA CRISPR rejuvenates exhausted CAR T cells
MEGA is a new CRISPR-based RNA-editing platform with the ability to enhance the fitness of CAR T cells; it may also overcome certain limitations of conventional DNA-targeting CRISPR–Cas9 systems.
- Karen O’Leary
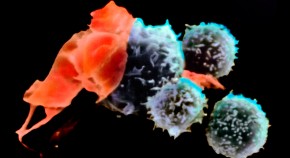
First cell therapy for solid tumours heads to the clinic: what it means for cancer treatment
Therapy built on tumour-infiltrating lymphocytes is now being prepared for at least 20 people in the United States with advanced melanoma.
- Sara Reardon
FIRSTMAPPP prospectively charts the efficacy of sunitinib for phaeochromocytoma and paraganglioma

Enabling comparative gene regulatory network analysis on single-cell data with SCORPION
We present SCORPION, a computational tool to model gene regulatory networks based on single-cell transcriptomic data and prior knowledge of gene regulation. SCORPION networks can be modeled for specific cell types in individual samples, and are therefore suitable for conducting comparisons between experimental groups.

Improved identification of cancer mutational processes
Mutational signatures help to deconvolve the different processes that shape cancer genomes. A new tool now alleviates some of the persistent challenges in the field.
- Tom L. Kaufmann
- Roland F. Schwarz
Non-inferiority of simple versus radical hysterectomy in low-risk cervical cancer
Personalized cancer care can’t rely on molecular testing alone.
- James Larkin
- Chloe Beland
- Alexander R. Lyon
The future of precision cancer therapy might be to try everything
Researchers are blasting patients’ cancer cells with dozens of drugs in the hope of finding the right treatment.
- Elie Dolgin

Repurposing the dopamine transporter antagonist vanoxerine to treat colorectal cancer
Self-renewing cancer stem cells drive tumor initiation and progression and represent a major target for therapeutic development. A study now shows that vanoxerine, a dopamine transporter antagonist, precisely inhibits this cell population in colorectal cancer, which leads to attenuation of tumor initiation and increased infiltration by immune cells.
- Winnie Chen
Low risk of CAR T cells going rogue
- Maria Papatriantafyllou
Rare CTR9 variants and myeloid malignancies
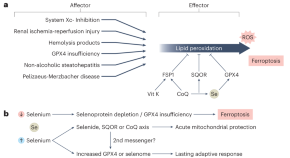
Selenium abandons selenoproteins to inhibit ferroptosis rapidly
Selenium is usually incorporated into selenoproteins, with important functions in redox regulation. A new study in Nature Metabolism reveals a previously unappreciated role for selenium-based chemical species as direct electron donors to reduce ubiquinone, thus contributing to redox homeostasis by preventing lipid peroxidation.
- Ian G. Chambers
- Rajiv R. Ratan

Melanoma leverages local cues to promote liver-specific metastasis
Using CRISPR–Cas9 screens, we found that cancer-cell-intrinsic loss of Pip4k2c conferred liver-metastatic organotropism in melanoma through hypersensitization to insulin-mediated PI3K–AKT signaling via co-optation of distinct hepatic metabolic cues. Additionally, we showed that combinatorial therapies that abolished physiological and drug-induced changes in glucose and insulin levels specifically reduced liver metastasis.
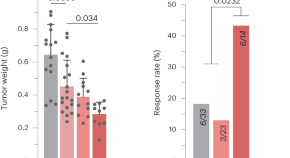
Mitochondrial DNA mutation enhances sensitivity to immunotherapy in melanoma
Mitochondrial DNA mutations are present in over 50% of all cancers, and truncating mutations in several genes encoding components of complex I of the respiratory chain are most recurrent. We found that these mutations are a source of Warburg-like metabolic shifts that promote a pro-inflammatory immunological state, enhancing sensitivity to checkpoint blockade.

Why we need to rethink how we talk about cancer
Naming metastatic cancers after parts of the body could be holding up research and preventing people from accessing the best treatment
- Lucy Odling-Smee

PD-L2 expression in senescent cancer cells limits tumor clearance after chemotherapy
Senescent cancer cells, which are characteristically present in tumors after genotoxic therapies, upregulate the immune checkpoint ligand programmed cell death 1 ligand 2 (PD-L2). We show that genetic or pharmacological ablation of PD-L2 prevents the accumulation of intratumoral senescent cells, reducing the recruitment of immunosuppressive myeloid cells and facilitating tumor clearance by T cells.
Methods & Protocols

Engineering megabase-sized genomic deletions with MACHETE (Molecular Alteration of Chromosomes with Engineered Tandem Elements)
The authors introduce MACHETE (molecular alteration of chromosomes with engineered tandem elements), a clustered regularly interspaced short palindromic repeats directed Cas9-based system for the efficient deletion of megabase-sized genomic regions.
- Francisco M. Barriga
- Scott W. Lowe
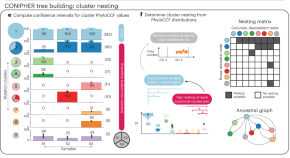
CONIPHER: a computational framework for scalable phylogenetic reconstruction with error correction
CONIPHER is a computational framework for accurately inferring subclonal structure and the phylogenetic tree from multisample tumor sequencing, accounting for both copy number alterations and mutation errors.
- Kristiana Grigoriadis
- Ariana Huebner
- Nicholas McGranahan

Robust scoring of selective drug responses for patient-tailored therapy selection
This protocol presents a computational approach to scoring drug sensitivity that integrates multiple dose–response parameters into a single response metric and identifies differences in drug-response patterns between cancer cells and healthy control cells.
- Yingjia Chen
- Tero Aittokallio

INVADEseq to identify cell-adherent or invasive bacteria and the associated host transcriptome at single-cell-level resolution
Invasion–adhesion-directed expression sequencing adapts the 10x Genomics 5′ single-cell RNA sequencing protocol to enable generation of bacterial and eukaryotic DNA libraries to identify adherent or invasive bacteria and the associated host transcriptome at a single-cell level.
- Jorge Luis Galeano Niño
- Susan Bullman
Genome-wide pooled CRISPR screening in neurospheres
The authors present a protocol for genome-wide clustered regularly interspaced short palindromic repeat screening of three-dimensional neurospheres.
- Amy B. Goodale
- David E. Root
Newly diagnosed AML: quizartinib improves OS

Promising results for antisense RNA therapy in mouse models of diffuse midline glioma
- Caroline Barranco
Serum tumour markers for testicular cancer recurrence
The current serum tumour markers α-fetoprotein, human chorionic gonadotrophin, and lactate dehydrogenase show limited value for testicular cancer relapse detection. A recent study highlights that false-positive elevations in follow-up monitoring are common and, conversely, many patients do not have elevations despite proven relapse. These findings highlight the potential for circulating microRNAs to be used as improved biomarkers for relapse detection.
- Matthew J. Murray
- Cinzia G. Scarpini
- Nicholas Coleman

Stress response in tumor-infiltrating T cells is linked to immunotherapy resistance
A newly composed single-cell transcriptomic atlas of tumor-infiltrating T cells across 16 cancer types revealed previously undescribed T cell states and heterogeneity. A unique T cell stress response state, T STR , was linked to immunotherapy resistance. Our high-resolution T cell reference maps, web portal, and annotation tool can assist efforts to develop T cell therapies.

CD4 + CAR T cells — more than helpers
Therapeutic products containing CD8 + and CD4 + T cells expressing CARs are effective at inducing remission in patients with cancer. How CD4 + CAR T cells contribute to the anti-tumor response has not been well established. A study uses syngeneic models and in vivo imaging to glean mechanistic insights into how CD4 + T cells target tumors.
- M. Eric Kohler
- Terry J. Fry
Venetoclax–obinutuzumab combinations are effective in fit patients with CLL

Taking the temperature of lung cancer antigens
Antigen presentation is fundamental to anti-tumor immunity, but our understanding of the physiological and molecular inputs to the process in different contexts remains limited. Two new studies explore the contribution of cell-intrinsic proteolytic mechanisms and cell-extrinsic hot and cold tumor microenvironments in shaping the antigenic landscape in lung cancer.
- Paul A. Stewart
- Alex M. Jaeger
A skull bone marrow niche for antitumour neutrophils in glioblastoma
A preprint by Lad et al. shows that tumour-associated neutrophils in glioblastoma originate from skull bone marrow and acquire an antigen-presenting cell phenotype intratumorally in the presence of local T cells.
- Austeja Baleviciute
Impaired RNA clearance
In this study, Insco et al. find patient-specific CDK13 mutations to impede RNA surveillance, leading to the accumulation and translation of prematurely terminated RNAs that drive malignancy in melanoma models.
- Gabrielle Brewer
Peptide-mediated CRISPR engineering of cells
An article in Nature Biomedical Engineering reports a simple and hardware-independent peptide-mediated delivery method for the CRISPR-mediated engineering of T cells.
- Nesma El-Sayed Ibrahim
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Our top 5 cancer research breakthroughs of 2022
15th December 2022
2022 has likely been your first full year back to ‘normal’ since the COVID-19 pandemic, and that’s no different for cancer researchers. Back into full swing in the lab, Worldwide Cancer Research scientists have been busy making exciting new discoveries about cancer. Here are the top five cancer research breakthroughs made by our scientists in 2022.
1. Stopping the spread of breast cancer
Our scientists in Italy discovered a previously unknown way that breast cancer cells survive treatment . They found that breast cancer cells hiding in places like the lungs seem to rely on specific antioxidants to survive there. This could be a new way to wipe out breast cancer cells that have escaped treatment.
Click here to read more about this incredible discovery, or find out what other ground-breaking work we're funding .
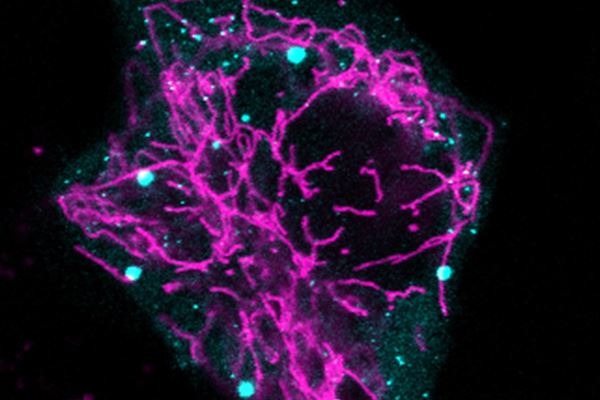
Our hope is that these findings can be translated into a real drug treatment that can kill “sleeping” cancer cells before they awake into full-blown metastases.
2. Stool samples can reveal pancreatic cancer sooner
Our researchers in Spain, led by Dr Núria Malats, have found a new way to spot if someone is at higher risk of pancreatic cancer, and even diagnose patients at an early stage of the disease . Specific microorganisms in a stool sample could signal that there is a problem in a rapid, non-invasive, and affordable way.
Read the full story here , or find out what else our scientists have discovered about pancreatic cancer this year.

This new breakthrough builds on the growing evidence that the microbiome is linked to the development of cancer. Early detection and diagnosis are just as important an approach to starting new cancer cures as developing treatments.
Become a Curestarter today and join us in supporting pioneering cancer research breakthroughs like these in 2023.
3. targeting cancer’s energy supply.
Our scientists in Germany discovered they could prevent head and neck cancer spreading by stopping it getting the extra energy it needs to do so. If they prevented a change happening in the RNA of mitochondria (the powerhouse of the cell), the cancer didn’t spread as much.
Click here to learn more about this breakthrough, or learn how your donations are used to start cancer cures .

The funding from Worldwide Cancer Research helped us to get a step closer to succeeding in fighting cancer metastasis, the leading cause of cancer death.
4. Making radiotherapy work for more patients
Our researchers in Spain made a breakthrough that could help treat people with cancer that has spread to the brain . In the future, a blood test could reveal if patients will respond to radiotherapy or if the cancer will resist it, then a drug called a RAGE inhibitor could make radiotherapy work better for those that would resist it.
Learn more about this important discovery , or read Anne and Cathrin's personal story.

We are very excited about the findings of this study and specifically the drug we have found. We really hope that what we have discovered will lead to a new way to personalise the use of radiotherapy that maximises the benefits for each patient.
5. Engineering immune cells to hunt down cancer
Our researchers in Italy have made a breakthrough that could lead to better, more effective immunotherapy options for cancer patients . They discovered how to engineer a specific type of immune cell to target and kill cancer cells, then boost its cancer-killing ability using a drug delivered with nanotechnology.
Find out the full story , or see how we've contributed to the discovery of new immunotherapies .

We hope we have laid the foundations for an innovative approach of adoptive cell therapy of cancer, hopefully more efficient than the current ones.

Breakthroughs of the future: 2023!
And finally, we were delighted to commit to funding £5.3 million to 25 new research projects that will start in 2023! It is incredibly important to continue supporting ground-breaking discovery cancer research if we hope to end the suffering caused by cancer.
Breakthroughs like these are vital if we hope to end the suffering caused by cancer. Unfortunately, funding for discovery research has dropped by ~25% in recent years.
Become a Curestarter today and you can help start new cancer cures.

Join our monthly newsletter
Keep up to date with all our latest news, events, groundbreaking research discoveries and much more!
You're now a Curestarter!
Our newsletter usually drops towards the end of each month
Thanks for subscribing
- The Information Commons
- Shifting the Research Paradigm
- The Cancer Commons Difference
- Our Approach
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Colorectal Cancer
- Diffuse Midline Glioma
- Esophageal Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Uterine Cancer
- Facing Advanced Cancer
- Meet the Team that Cares
- Our Partners
- Support Our Services
- Financial Documents
- All Testimonials
- Many Ways to Give
- What Your Support Makes Possible
New Cancer Research & Perspectives
From new clinical trial findings to remarkable patient stories, our expert team and distinguished guest contributors curate and report on the latest, most important developments in cancer care. We hope these stories provide valuable insights for people on their own cancer journey.
Treating Pancreatic Cancer: Could Metabolism—Not Genomics—Be the Key?
April 2, 2024 Thomas N. Seyfried, PhD Derek Lee, MS Tomás Duraj, MD, PhD Curious Dr. George
- Treatment Options
Protean BioDiagnostics: One Way to Access Full-Service Precision Oncology Testing
March 10, 2024 Anthony M. Magliocco, MD Curious Dr. George
- All Cancers
How Would a Harvard Oncologist Manage His Own Metastatic Kidney Cancer?
March 5, 2024 David J. Einstein, MD Curious Dr. George
How an Expert Would Manage His Own Stage 4 Pancreatic Cancer: An Update
February 21, 2024 John H. Strickler, MD Curious Dr. George
How Would a Northwestern Professor Manage His Own Liver Cancer?
February 13, 2024 Al B. Benson III, MD, FACP, FACCC, FASCO Curious Dr. George
Successful Control of High Blood Pressure, a Major Cancer Comorbidity
December 7, 2023 Robert E. Matthews Curious Dr. George
- Diffuse Midline Glioma (DMG/DIPG)
10 new breakthroughs in the fight against cancer

Medical advances are continuing to help the world fight cancer. Image: Unsplash/National Cancer Institute
.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Victoria Masterson
Madeleine north.

.chakra .wef-9dduvl{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-9dduvl{font-size:1.125rem;}} Explore and monitor how .chakra .wef-15eoq1r{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;color:#F7DB5E;}@media screen and (min-width:56.5rem){.chakra .wef-15eoq1r{font-size:1.125rem;}} Global Health is affecting economies, industries and global issues

.chakra .wef-1nk5u5d{margin-top:16px;margin-bottom:16px;line-height:1.388;color:#2846F8;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-1nk5u5d{font-size:1.125rem;}} Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:, global health.
Listen to the article
This article was originally published in May 2022, and most recently updated in January 2024 .
- Cancer is one of the world’s biggest killers, with around 10 million deaths per year due to the disease.
- Scientists are using artificial intelligence, DNA sequencing, precision oncology and other technologies to improve treatment and diagnosis.
- The Centre for the Fourth Industrial Revolution India, a collaboration with the World Economic Forum, hopes to accelerate 18 cancer interventions.
Cancer kills around 10 million people a year and is a leading cause of death globally, according to the World Health Organization.
Breast, lung and colon cancer are among the most common. Death rates from cancer were falling before the pandemic . But COVID-19 caused a big backlog in diagnosis and treatment .
There is some good news, however. Medical advances are accelerating the battle against cancer. Here are 10 recent developments.
Test to identify 18 early-stage cancers
Researchers in the US have developed a test they say can identify 18 early-stage cancers. Instead of the usual invasive and costly methods, Novelna's test works by analyzing a patient's blood protein. In a screening of 440 people already diagnosed with cancer, the test correctly identified 93% of stage 1 cancers in men and 84% in women. The researchers believe the findings "pave the way for a cost-effective, highly accurate, multi-cancer screening test that can be implemented on a population-wide scale". It's early days, however. With such a small sample screening and a lack of information on co-existing conditions, the test is currently more of "a starting point for developing a new generation of screening tests for the early detection of cancer".
The seven-minute cancer treatment jab
England's National Health Service (NHS) is to be the first in the world to make use of a cancer treatment injection , which takes just seven minutes to administer, rather than the current time of up to an hour to have the same drug via intravenous infusion. This will not only speed up the treatment process for patients, but also free up time for medical professionals. The drug, Atezolizumab or Tecentriq, treats cancers including lung and breast, and it's expected most of the 3,600 NHS patients in England currently receiving it intravenously will now switch to the jab.
Precision oncology
Precision oncology is the “ best new weapon to defeat cancer ”, the chief executive of Genetron Health, Sizhen Wang, says in a blog for the World Economic Forum. This involves studying the genetic makeup and molecular characteristics of cancer tumours in individual patients. The precision oncology approach identifies changes in cells that might be causing the cancer to grow and spread. Personalized treatments can then be developed. The 100,000 Genomes Project, a National Health Service initiative, studied more than 13,000 tumour samples from UK cancer patients , successfully integrating genomic data to more accurately pin-point effective treatment. Because precision oncology treatments are targeted – as opposed to general treatments like chemotherapy – it can mean less harm to healthy cells and fewer side effects as a result.
Artificial intelligence fights cancer
In India, World Economic Forum partners are using emerging technologies like artificial intelligence (AI) and machine learning to transform cancer care. For example, AI-based risk profiling can help screen for common cancers like breast cancer, leading to early diagnosis. AI technology can also be used to analyze X-rays to identify cancers in places where imaging experts might not be available. These are two of 18 cancer interventions that The Centre for the Fourth Industrial Revolution India, a collaboration with the Forum , hopes to accelerate.

Greater prediction capabilities
Lung cancer kills more people in the US yearly than the next three deadliest cancers combined. It's notoriously hard to detect the early stages of the disease with X-rays and scans alone. However, MIT scientists have developed an AI learning model to predict a person's likelihood of developing lung cancer up to six years in advance via a low-dose CT scan. Trained using complex imaging data, 'Sybil' can forecast both short- and long-term lung cancer risk, according to a recent study. "We found that while we as humans couldn't quite see where the cancer was, the model could still have some predictive power as to which lung would eventually develop cancer," said co-author Jeremy Wohlwend.
Clues in the DNA of cancer
At Cambridge University Hospitals in England, the DNA of cancer tumours from 12,000 patients is revealing new clues about the causes of cancer, scientists say. By analyzing genomic data, oncologists are identifying different mutations that have contributed to each person’s cancer. For example, exposure to smoking or UV light, or internal malfunctions in cells. These are like “fingerprints in a crime scene”, the scientists say – and more of them are being found. “We uncovered 58 new mutational signatures and broadened our knowledge of cancer,” says study author Dr Andrea Degasperi, from Cambridge’s Department of Oncology.
Liquid and synthetic biopsies
Biopsies are the main way doctors diagnose cancer – but the process is invasive and involves removing a section of tissue from the body, sometimes surgically, so it can be examined in a laboratory. Liquid biopsies are an easier and less invasive solution where blood samples can be tested for signs of cancer. Synthetic biopsies are another innovation that can force cancer cells to reveal themselves during the earliest stages of the disease.
The application of “precision medicine” to save and improve lives relies on good-quality, easily-accessible data on everything from our DNA to lifestyle and environmental factors. The opposite to a one-size-fits-all healthcare system, it has vast, untapped potential to transform the treatment and prediction of rare diseases—and disease in general.
But there is no global governance framework for such data and no common data portal. This is a problem that contributes to the premature deaths of hundreds of millions of rare-disease patients worldwide.
The World Economic Forum’s Breaking Barriers to Health Data Governance initiative is focused on creating, testing and growing a framework to support effective and responsible access – across borders – to sensitive health data for the treatment and diagnosis of rare diseases.
The data will be shared via a “federated data system”: a decentralized approach that allows different institutions to access each other’s data without that data ever leaving the organization it originated from. This is done via an application programming interface and strikes a balance between simply pooling data (posing security concerns) and limiting access completely.
The project is a collaboration between entities in the UK (Genomics England), Australia (Australian Genomics Health Alliance), Canada (Genomics4RD), and the US (Intermountain Healthcare).
CAR-T-cell therapy
A treatment that makes immune cells hunt down and kill cancer cells was recently declared a success for leukaemia patients. The treatment, called CAR-T-cell therapy, involves removing and genetically altering immune cells, called T cells, from cancer patients. The altered cells then produce proteins called chimeric antigen receptors (CARs). These recognize and can destroy cancer cells. In the journal Nature, scientists at the University of Pennsylvania announced that two of the first people treated with CAR-T-cell therapy were still in remission 12 years on.
Fighting pancreatic cancer
Pancreatic cancer is one of the deadliest cancers. It is rarely diagnosed before it starts to spread and has a survival rate of less than 5% over five years. At the University of California San Diego School of Medicine, scientists developed a test that identified 95% of early pancreatic cancers in a study. The research, published in Nature Communications Medicine , explains how biomarkers in extracellular vesicles – particles that regulate communication between cells – were used to detect pancreatic, ovarian and bladder cancer at stages I and II.
Have you read?
Cancer: how to stop the next global health crisis, how to improve access to cancer medicines in low and middle-income countries, why is cancer becoming more common among millennials, a tablet to cut breast cancer risk.
A drug that could halve the chance of women developing breast cancer is being tested out by England's National Health Service (NHS). It will be made available to almost 300,000 women seen as being at most risk of developing breast cancer, which is the most common type of cancer in the UK . The drug, named anastrozole, cuts the level of oestrogen women produce by blocking the enzyme aromatase . It has already been used for many years as a breast cancer treatment but has now been repurposed as a preventive medicine. “This is the first drug to be repurposed through a world-leading new programme to help us realize the full potential of existing medicines in new uses to save and improve more lives on the NHS," says NHS Chief Executive Amanda Pritchard.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Related topics:
The agenda .chakra .wef-n7bacu{margin-top:16px;margin-bottom:16px;line-height:1.388;font-weight:400;} weekly.
A weekly update of the most important issues driving the global agenda
.chakra .wef-1dtnjt5{display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;} More on Global Health .chakra .wef-nr1rr4{display:-webkit-inline-box;display:-webkit-inline-flex;display:-ms-inline-flexbox;display:inline-flex;white-space:normal;vertical-align:middle;text-transform:uppercase;font-size:0.75rem;border-radius:0.25rem;font-weight:700;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;line-height:1.2;-webkit-letter-spacing:1.25px;-moz-letter-spacing:1.25px;-ms-letter-spacing:1.25px;letter-spacing:1.25px;background:none;padding:0px;color:#B3B3B3;-webkit-box-decoration-break:clone;box-decoration-break:clone;-webkit-box-decoration-break:clone;}@media screen and (min-width:37.5rem){.chakra .wef-nr1rr4{font-size:0.875rem;}}@media screen and (min-width:56.5rem){.chakra .wef-nr1rr4{font-size:1rem;}} See all

Could private provision be the key to delivering universal health coverage?
Gijs Walraven
April 7, 2024

A generation adrift: Why young people are less happy and what we can do about it
Andrew Moose and Ruma Bhargava
April 5, 2024
This gene-editing technology lets scientists cut HIV out of cells

Child deaths have reached a historic low – but there's still much more to do
Amira Ghouaibi
April 2, 2024

Call for action on rising cholera cases, and other health stories
Shyam Bishen
March 28, 2024

Here’s how scientists are studying Parkinson’s disease using robots

In A New Clinical Trial, Researchers Tested A Novel Cancer Vaccine Formulation That May Significantly Reduce Melanoma Fatalities Among Men
A n innovative vaccine could significantly reduce skin cancer fatalities among men, according to promising findings from a recent clinical trial.
This groundbreaking research, conducted by scientists at the University of Virginia, focuses on a multi-peptide vaccine designed to combat melanoma, one of the most aggressive types of skin cancer. The trial showed substantial progress in extending the survival of high-risk melanoma patients.
Central to this study is a deep dive into the intricate workings of the immune system, with a spotlight on T cells’ pivotal role in combating cancer.
Historically, cancer vaccines have mainly aimed at activating cytotoxic CD8+ T cells, which directly target cancer cells. Yet, this strategy tends to ignore the vital supportive functions of CD4+ helper T cells.
These cells are key orchestrators of a robust immune defense, assisting in the maturation of additional immune cells and delivering essential signals that enable CD8+ T cells to operate effectively.
So, the study evaluated two different vaccine formulations aimed at engaging key elements of the immune response. One formulation adhered to the traditional method, activating CD8+ T cells using a sequence of melanoma-specific peptides.
The alternative formulation adopted a novel strategy, incorporating peptides that target CD8+ T cells along with extra peptides crafted to stimulate CD4+ helper T cells.
For almost 15 years, the research team monitored the participants for survival rates and recurrence of the disease. Findings showed that those who received the vaccine containing CD4+ helper peptides had significantly extended survival rates.
This advantage was predominantly observed in male patients, suggesting possible biological variances between genders that may affect how immunotherapies work.
Sign up for Chip Chick’s newsletter and get stories like this delivered to your inbox.
“These findings support the promise of this second-generate melanoma vaccine for prolonging survival of patients after surgery for high-risk melanoma,” said Craig L. Slingluff, a surgical oncologist and translational immunologist at the University of Virginia School of Medicine and UVA Health.
“We hope that we can make this available to patients in addition to other effective immune therapies so that they may have even greater benefit than either treatment alone.”
The study also explored administering cyclophosphamide, a chemotherapy agent, prior to the vaccine as a strategy to potentially boost its efficacy.
Cyclophosphamide was thought to decrease the population of regulatory T cells that typically hinder the immune system’s ability to fight tumors, thereby making the vaccine more effective.
Although the impact of cyclophosphamide was minimal on the whole study group, further examination indicated that it could greatly benefit certain subgroups, especially when used in conjunction with the vaccine designed to activate both CD8+ and CD4+ T cells.
Now, the team’s findings have significant implications. Primarily, they underscore the concept that effectively fighting melanoma, and potentially other types of cancer, demands a comprehensive approach that engages the entire range of the body’s immune defenses.
Furthermore, they pave the way for innovative treatment combinations, including vaccines and checkpoint inhibitors, which have proven effective against various cancer forms.
The only remaining question is why this new cancer vaccine doesn’t offer the same advantages to women.
“The differences in benefit based on age and biologic [gender] highlight the need to understand reasons for those differences so that we can provide the same benefit for all patients,” concluded Slingluff.
“We are excited to build on these exciting findings.”
To read the study’s complete findings, which have since been published in Nature Communications , visit the link here .

New findings on the link between CRISPR gene-editing and mutated cancer cells
A protein that protects cells from DNA damage, p53, is activated during gene editing using the CRISPR technique. Consequently, cells with mutated p53 have a survival advantage, which can cause cancer. Researchers at Karolinska Institutet in Sweden have found new links between CRISPR, p53 and other cancer genes that could prevent the accumulation of mutated cells without compromising the gene scissors' effectiveness. The study, published in Cancer Research , can contribute to tomorrow's precision medicine.
Much hope is being pinned on the potential of gene editing using the CRISPR (gene scissors) method as a crucial part in the precision medicine of the future. However, before the method can become hospital routine, several hurdles need to be overcome.
One of these challenges is associated with how cells behave when subjected to DNA damage, which CRISPR gene editing causes in a controlled fashion. Damage to cells activates the protein p53, which acts as the cell's "first aid" response to DNA damage.
It is already known that the technique is less effective when p53 is active; at the same time, however, a lack of p53 can allow cells to start growing uncontrollably and become cancerous. In over half of all cancers the gene for p53 is mutated and thus unable to protect against uncontrolled cell division. It is therefore important to avoid the enrichment (accumulation) of such mutated cells.
Researchers at Karolinska Institutet have now shown that cells with inactivating mutations of the p53 gene gain a survival advantage when subjected to CRISPR and can thus accumulate in a mixed cell population.
The researchers have also identified a network of linked genes with mutations that have a similar effect to p53 mutations, and shown that the transient inhibition of p53 is a possible pharmaceutical strategy for preventing the enrichment of cells with such mutations.
"It can seem contradictory to inhibit p53 in a CRISPR context," says the study's first author Long Jiang, doctoral student at the Department of Medicine, Karolinska Institutet (Solna). "However, some of the literature supports the idea that p53 inhibition can make CRISPR more effective. In our study we show that this can also counteract the enrichment of cells with mutations in p53 and a group of associated genes."
The research has a contributory potential to the future clinical implementation of CRISPR in having identified a network of possible candidate genes that should be carefully controlled for mutations when cells are subjected to the CRISPR technique. Another possible conclusion is that the transient inhibition of p53 could prove a strategy for reducing the enrichment of mutated cells.
The researchers have also studied the DNA-damage response as a possible marker in the development of more precise guide RNA sequences, which are used to show CRISPR where a DNA sequence is to be altered.
"We believe that the up-regulation of genes involved in the DNA damage response can be a sensitive marker for how much unspecific ('off-target') activity a guide RNA has, and can thus help in the selection of 'safer' guide RNAs," says the study's last author Fredrik Wermeling, researcher at the Department of Medicine, Karolinska Institutet (Solna).
The study is largely based on CRISPR, CRISPR screening experiments on isolated cells and analyses of the DepMap database.
The next step of the research is to understand how relevant the described mechanisms are.
"In cell cultures, we see a rapid and pronounced enrichment of cells with p53 mutations when we subject the cells to CRISPR, provided, however, that cells with mutations are there from the start," says Dr. Wermeling. "So we can show that the mechanism exists and factors that affect it, but don't currently know at what level this is a genuine problem, and that's something we want to explore further in more clinic-centered tests."
The study was conducted in collaboration with David P. Lane's group (MTC) and financed by the Swedish Research Council, the Swedish Cancer Society, Karolinska Institutet, the Magnus Bergvall Foundation, the China Scholarship Council and the Nanyang Technological University-Karolinska Institutet Joint PhD Program (VSI).
- Brain Tumor
- CRISPR Gene Editing
- Biotechnology and Bioengineering
- Biotechnology
- Gene therapy
- Prostate cancer
- Chemotherapy
- Immune system
Story Source:
Materials provided by Karolinska Institutet . Note: Content may be edited for style and length.
Journal Reference :
- Long Jiang, Katrine Ingelshed, Yunbing Shen, Sanjaykumar V Boddul, Vaishnavi Srinivasan Iyer, Zsolt Kasza, Saikiran Sedimbi, David P Lane, Fredrik Wermeling. CRISPR/Cas9-induced DNA damage enriches for mutations in a p53-linked interactome: implications for CRISPR-based therapies. . Cancer Research , 2021; canres.1692.2021 DOI: 10.1158/0008-5472.CAN-21-1692
Cite This Page :
Explore More
- Drug Development Made Easier
- RNA That Doesn't Age
- 'Rainbow' Detected On an Exoplanet
- Spears and Throwing Sticks 300,000 Years Old
- High Carbon Impact of Tourism at Yellowstone
- Extreme Starburst Galaxy
- Asthma: Disease May Be Stoppable
- Stellar Collisions and Zombie-Like Survivors
- Tiny Robot Swarms Inspired by Herd Mentality
- How the Brain Regulates Emotions
Trending Topics
Strange & offbeat.

- News Releases
Mass General Cancer Center researchers present key findings at AACR
Mass General Brigham
Leaders from the Mass General Cancer Center, a member of the Mass General Brigham healthcare system, will present research discoveries and outcomes from clinical trials in cancer at the 2024 American Association for Cancer Research (AACR) Annual Meeting, held April 5-10, in San Diego.
AACR brings together leading experts in cancer research to share the latest breakthroughs in cancer science and medicine. Presentations from Mass General Cancer Center investigators will cover a wide range of topics, from clinical studies to cancer biology, screening and early detection, treatment and more.
Below are a few highlights from this year’s presentations. All times are in EST. View a full list of Mass General Cancer Center presentations here .
Rapid on-site nucleic acid detection using CRISPR and digital signal processing for portable and integrated cervical cancer screening in low resource settings
When : April 9, 2024, 4:30-8 p.m.
Who : Cesar Castro, MD
What : Addressing the global disparity in cancer care necessitates the development of rapid and affordable nucleic acid (NA) testing technologies. This need is particularly critical for cervical cancer. Molecular detection of human papillomavirus (HPV) has emerged as a highly accurate screening method, surpassing traditional Pap smears. However, implementing this transition in low- and middle-income countries has been challenging due to the high costs and centralized facilities required for current NA tests. Here, Dr. Castro and team present CreDiT (CRISPR Enhanced Digital Testing), an advanced diagnostic system for rapid, on-site NA detection. CreDiT integrates two major technical breakthroughs: 1) a one-pot CRISPR strategy that simultaneously amplifies both target NAs and analytical signals; and 2) a robust fluorescent detection method based on digital communication (encoding/decoding) technology. The team adapted CreDiT for point-of-care HPV screening by designing probes for high-risk HPV genes and oncoprotein mRNAs and developing a portable CreDiT device capable of processing 12 samples. CreDiT demonstrated sensitive detection of cell-derived HPV DNA targets down to single copies and accurately identified HPV types in every clinical cervical brushing specimen (n = 121) we tested. This technology has the potential to facilitate prompt and reliable triaging of high-risk HPV, overcoming pathology bottlenecks and circumventing geographical and socioeconomic barriers to effective cervical cancer screening in resource-limited regions. This work has spearheaded recent screening research efforts in Uganda and Ghana.
KRYSTAL-1: Pooled phase 1/2 efficacy and safety of adagrasib (MRTX849) in combination with cetuximab in patients with metastatic colorectal cancer (CRC) harboring a KRASG12C mutation
When : April 8, 2024, 2:10-2:25 p.m.
Who : Samuel Klempner, MD
What : The abstract for this presentation is embargoed until 11:30am on Monday, April 8.
Improving CAR T cell efficacy in pancreatic cancer using an in vivo CRISPR Cas9 screen
When : April 7, 2024, 4:30-8 p.m. Who : Marcela Maus, MD, PhD
What : Chimeric antigen receptor (CAR) T cell therapy has demonstrated remarkable success in the treatment of certain hematologic malignancies. However, efficacy against solid tumors has remained limited and is associated with relatively low T cell persistence. Here, the team performed an in vivo CAR T cell CRISPR screen in pancreatic adenocarcinoma using a curated guide library to identify genes that enhance CAR T cell persistence in vivo. The transcription factor, GATA3, was consistently identified as the most enriched hit across two donor T cells when Mario-CART was recovered at the 2-week timepoint. When compared to control or a depleted hit, GATA3 KO CAR showed early improvements in tumor clearance in vivo. However, relapse occurred at similar timepoints across groups. Findings highlight the dynamic nature of CAR T-tumor interactions. Gene knockouts that confer enhancements may change over time with varying context (such as in vitro vs in vivo conditions). It may be difficult to identify single gene knockouts that enhance CAR-T cell functions across different conditions and over time, but rather it may be necessary to exert more dynamic functional control of CAR T cells to enhance their function in different settings.
TOP1 mutations mediate cross resistance to ADCs in metastatic breast cancer
When : April 8, 2024, 6:05-6:20 p.m.
Who : Rachel Occhiogrosso Abelman, MD
What : Antibody-drug conjugates (ADCs) have improved survival for patients with metastatic breast cancer (MBC). In patients with HER2 negative MBC, two ADCs have FDA approval: sacituzumab govitecan (SG) and trastuzumab deruxtecan (T-DXd), both with topoisomerase-I (topo-I) inhibitor payloads. Given the many other ADCs in development, there is great interest in using ADC after ADC to maximize treatment benefit for patients. However, there is limited understanding regarding resistance mechanisms to ADCs and impact on ADC sequencing. The team conducted a translational study to report the incidence of TOP1 mutations and clinical impact on ADC sequencing. Based on comprehensive plasma-based genotyping, the team identified four distinct TOP1 mutations: S57C, R364H, W401C, G359E, at a frequency of 6.0% (4/67) at the time of disease progression on ADC compared to a frequency of 0.5% described in primary breast cancer in TCGA. Two of the amino acids found to be mutated are known to form direct interactions with the DNA backbone (G359) or the topoisomerase inhibitor itself (R364). This is the first report describing emergence of TOP1 mutations under selective pressure from ADCs and the impact on mediating cross-resistance to ADC after ADC with topo-I inhibitor payloads. Novel ADCs with alternative payloads may potentially be more effective when used sequentially after an ADC with a topo-I inhibitor. Further biomarker research is needed to optimize ADC sequencing for patients with TOP1 mutant MBC.
Analysis of biomarker and outcomes data: 7-year update from COLUMBUS
When : April 9, 2024, 12-3:30 p.m.
Who : Keith Flaherty, MD
What : In the randomized, two-part, phase 3 COLUMBUS study (NCT01909453), encorafenib (enco) + binimetinib (bini)—an approved regimen in the US, EU, and other countries—improved seven-year progression-free survival (PFS) and overall survival (OS) vs vemurafenib (vemu) in patients with BRAF V600E/K-mutant locally advanced unresectable or metastatic melanoma. The team investigated genetic and transcriptional correlates of outcomes in an exploratory biomarker analysis of COLUMBUS Parts 1 and 2. They found that enco + bini showed benefit across molecular subtypes in BRAF V600E/K-mutant melanoma. The contribution of bini was most pronounced in the immune-high cluster. Improved outcomes in this cluster support ongoing trials of combinations with immune checkpoint inhibitors, such as STARBOARD and PORTSIDE.
Dissecting and quantifying pancreatic cancer plasticity using single-cell multiomics, lineage tracing and functional genomics reveals novel mediators of therapy resistance
When : April 9, 2024, 1:39-1:57 p.m.
Who : Arnav Mehta, MD, PhD
What : Pancreatic cancer (PDAC) is a lethal disease in part because tumor cells exist in distinct transcriptional states (e.g. basal/mesenchymal vs. classical/epithelial) with unique phenotypic properties that contribute to tumor growth and treatment resistance. Amongst the most well-described forms of plasticity in human development and cancer is epithelial-mesenchymal plasticity (EMP), which includes epithelial to mesenchymal transition (EMT) and mesenchymal to epithelial transition (MET). To better understand and quantify the role of EMP in driving treatment resistance of human PDAC, we have developed single-cell multiomic, functional genomic and computational methods applied to patient-derived models and clinical biopsies. Our efforts define a robust experimental and quantitative framework for studying tumor cell plasticity in patient-derived model systems with validation in human patient samples using single-cell and spatial transcriptomics. Collectively, we nominate several regulators that alter the propensity of EMP in PDAC, thus posing a paradigm whereby perturbations may be used to homogenize tumor populations towards treatment-sensitive phenotypes for combination therapy.
About Mass General Brigham
Mass General Brigham is an integrated academic health care system, uniting great minds to solve the hardest problems in medicine for our communities and the world. Mass General Brigham connects a full continuum of care across a system of academic medical centers, community and specialty hospitals, a health insurance plan, physician networks, community health centers, home care, and long-term care services. Mass General Brigham is a nonprofit organization committed to patient care, research, teaching, and service to the community. In addition, Mass General Brigham is one of the nation’s leading biomedical research organizations with several Harvard Medical School teaching hospitals. For more information, please visit www.massgeneralbrigham.org .
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.
Cancer cases could increase 77% as global population balloons. These types are most common.

The release of 2022 cancer data gives the latest look into which types of cancer are most prevalent around the world as population growth expects to drive global cases as much as 77% by 2050.
There were nearly 20 million new cancer cases and 9.7 million deaths from cancer in 2022, said the study published Thursday in the journal CA: A Cancer Journal for Clinicians , part of the American Cancer Society Journals. Findings were also disclosed by the World Health Organization in February.
Those numbers indicate that an estimated one in five people will be diagnosed with cancer in their life, and that will lead to death in one in nine men and one in 12 women, according to the report. Keeping the rates the same and projecting into the future with population growth and aging, the study says new cancer cases will increase 77% to 35 million by the year 2050.
"The overall scale of cancer and the diversity of cancer profiles by world region and human development level reemphasize the need for a global escalation of targeted cancer control measures ," the study concludes. "Investments in prevention, including the targeting of key risk factors for cancer...can avert millions of future cancer diagnoses and save many lives worldwide."
Americans have 40% chance of cancer: Who's most at risk and how can you prevent it?
Publication reveals most common types of cancer
The publication utilized the GLOBOCAN database to study 36 types of cancer in 185 countries in 2022. The following are the overall most common types of cancer for both sexes combined, though within the sexes there are notable differences. For example, breast cancer amongst females is more common than lung cancer, a flip from the general population ranking.
- Lung cancer - 12.4%
- Female breast cancer - 11.6%
- Colorectum - 9.6%
- Prostate - 7.3%
- Stomach - 4.9%
The 10 leading cancer types account for approximately two thirds of the total cases globally. Liver, thyroid, cervix uteri, bladder and non-Hodgkin lymphoma make up the rest of the top 10 leading cancer types amongst both sexes.
Likelihood of cancer changes based on where you live
The prevalence of cancer, mortality rates and leading cancer types change country by country. Here is the breakdown by geographic region, according to the study:
- Asia - 49.2% of new cases, 56.1% of deaths
- Africa - 5.9% of new cases, 7.8% of deaths
- Oceania - 1.4% of cases, 0.8% of deaths
- Europe - 22.4% of cases, 20.4% of deaths
- Americas - 21.1% of cases, 14.9% of deaths
A country's economic and societal development also changes the likelihood someone will be diagnosed with cancer. The higher a country's Human Development Index (HDI) level, which is measured by human health, longevity and standards of living, the more likely its residents are to develop cancer, the report states.
Cancer to increase 77% by 2050 globally
The report says that the world's growing population will be the biggest driver in cancer cases, and countries with high HDIs will see a large increase in actual numbers. But low HDI countries stand to see a remarkable relative increase of new cases, 142%, by 2050.
Lung cancer, already the leading cause of cancer mortality globally, could further increase in occurrence rate among less developed countries. The report attributes this to the "stage of the tobacco epidemic" in any given country and its link to lung cancer rates. For example, the lung cancer rates in the U.K. and the U.S. declined after prevalence of smoking waned in those countries, but not until 20-25 years later. But in countries undergoing economic transition and seeing a greater uptake of smoking, the lung cancer rates are likely to continue to climb for the next few decades without mitigation.
The study concludes that targeting risk factors, including smoking, obesity and infections is needed to not only save lives, but provide economic and societal benefits.
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Many cancer drugs remain unproven 5 years after accelerated approval, a study finds
FILE - A sign for the Food and Drug Administration is displayed outside their offices in Silver Spring, Md., on Dec. 10, 2020. According to research published Sunday, April 7, 2024, in the Journal of the American Medical Association, most cancer drugs granted accelerated approval by the FDA, meant to give patients early access to promising drugs, do not demonstrate such benefits within five years. (AP Photo/Manuel Balce Ceneta, File)
- Copy Link copied
The U.S. Food and Drug Administration’s accelerated approval program is meant to give patients early access to promising drugs. But how often do these drugs actually improve or extend patients’ lives?
In a new study, researchers found that most cancer drugs granted accelerated approval do not demonstrate such benefits within five years.
“Five years after the initial accelerated approval, you should have a definitive answer,” said Dr. Ezekiel Emanuel, a cancer specialist and bioethicist at the University of Pennsylvania who was not involved in the research. “Thousands of people are getting those drugs. That seems a mistake if we don’t know whether they work or not.”
The program was created in 1992 to speed access to HIV drugs. Today, 85% of accelerated approvals go to cancer drugs.
It allows the FDA to grant early approval to drugs that show promising initial results for treating debilitating or fatal diseases. In exchange, drug companies are expected to do rigorous testing and produce better evidence before gaining full approval.
Patients get access to drugs earlier, but the tradeoff means some of the medications don’t pan out. It’s up to the FDA or the drugmaker to withdraw disappointing drugs, and sometimes the FDA has decided that less definitive evidence is good enough for a full approval.
The new study found that between 2013 and 2017, there were 46 cancer drugs granted accelerated approval. Of those, 63% were converted to regular approval even though only 43% demonstrated a clinical benefit in confirmatory trials.
The research was published in the Journal of the American Medical Association and discussed at the American Association for Cancer Research annual meeting in San Diego on Sunday.
It’s unclear how much cancer patients understand about drugs with accelerated approval, said study co-author Dr. Edward Cliff of Harvard Medical School.
“We raise the question: Is that uncertainty being conveyed to patients?” Cliff said.
Drugs that got accelerated approval may be the only option for patients with rare or advanced cancers, said Dr. Jennifer Litton of MD Anderson Cancer Center in Houston, who was not involved in the study.
It’s important for doctors to carefully explain the evidence, Litton said.
“It might be shrinking of tumor. It might be how long the tumor stays stable,” Litton said. “You can provide the data you have, but you shouldn’t overpromise.”
Congress recently updated the program, giving the FDA more authority and streamlining the process for withdrawing drugs when companies don’t meet their commitments.
The changes allow the agency “to withdraw approval for a drug approved under accelerated approval, when appropriate, more quickly,” FDA spokesperson Cherie Duvall-Jones wrote in an email. The FDA can now require that a confirmatory trial be underway when it grants preliminary approval, which speeds up the process of verifying whether a drug works, she said.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 5, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
More than 25% of cancer survivors report significant levels of disability after cancer diagnosis, according to new study
by Dana-Farber Cancer Institute

A survey of nearly 50,000 cancer survivors has found that more than a quarter had a physical disability that impaired their mobility and almost 10% had a disability affecting self-care, Dana-Farber Cancer Institute researchers report in a new study, published in the Journal of Clinical Oncology . Both rates are sharply higher than those for adults who have not had cancer.
If the findings are extended to the estimated 18.1 million cancer survivors in the U.S., they suggest that more than 5 million survivors have a mobility disability and 1.3 million have a self-care disability, according to the study authors. The impact of such disabilities falls especially heavily on members of racial and ethnic minorities, underserved groups, and individuals with unhealthy lifestyles or other medical conditions.
The study findings underscore the importance of developing ways to limit the long-term side effects of cancer treatment, and of the benefits of exercise, both during and after treatment, to preserve physical function and ward off disability, researchers say.
"The effects of cancer and its treatment can lead to a variety of physical limitations that impair people's quality of life and ability to care for themselves," says Chao Cao, Ph.D., MPH, first author of the study.
"Even as the number of cancer survivors has grown, the prevalence and patterns of physical disabilities in this group have received little scientific attention. Our study is one of the first to examine this issue."
Data for the study came from the Behavioral Risk Factor Surveillance System, a nationwide, telephone-based survey by the U.S. Centers for Disease Control and Prevention that collected data on health-related risk behaviors and chronic medical conditions among U.S. adults. Researchers focused on data from 47,768 cancer survivors and 2.4 million adults without a history of cancer who participated in the survey.
After adjusting for demographic and lifestyle factors and health conditions, the researchers found that 27.9% of cancer survivors had a mobility disability—difficulty walking or climbing stairs, for example—compared to 13.4% among non-cancer adults. And 7.4% of survivors had a disability in self-care activities such as dressing or bathing, compared to 3.8% of non-cancer adults.
Investigators also found different rates of disability within different groups of survivors. Female survivors, for example, were significantly more likely to report mobility problems than male survivors were. Mobility-related disabilities were also more common in non-Hispanic Blacks, Native Americans, and Hispanics than in non-Hispanic whites.
Low educational attainment, low family annual income, being unmarried, having obesity, current smoking, being physically inactive, and having a chronic condition, were also associated with a higher prevalence of mobility disability among cancer survivors.
"These results point to the need for prevention efforts targeted at groups more likely to experience cancer-related disability," says study senior author, Jennifer Ligibel, MD, of Dana-Farber.
Explore further
Feedback to editors

Stopping aspirin 1 month after coronary stenting significantly reduces bleeding complications in heart attack patients

Oral vaccine for UTI is potential alternative to antibiotics, finds 9-year study
19 hours ago

Study: Epilepsy patients benefit from structured 'seizure action plans'
Apr 6, 2024

Screening with a PSA test has a small impact on prostate cancer deaths but leads to overdiagnosis, finds study

Clinical trial: First cardiac bioimplants for treatment of myocardial infarction using umbilical cord stem cells
Apr 5, 2024

Research team builds first tandem repeat expansions genetic reference maps

Human neuron model paves the way for new Alzheimer's therapies

A deep dive into the genetics of alcohol consumption

First atlas of the human ovary with cell-level resolution is a step toward artificial ovary

Pig hearts kept alive outside the body for more than 24 hours offers hope for many humans needing a transplant
Related stories.

Psychological distress may lead to more care and high medical costs for adolescent and young adult cancer survivors
Jan 10, 2022

Lesbian, gay, and bisexual survivors of adolescent and young adult cancers often have chronic health conditions: Study
Dec 4, 2023

Substance use disorders on the rise for survivors of specific cancers
Jan 15, 2024

How did the early COVID-19 pandemic affect cancer survivors?
Aug 22, 2022

Poor physical function persists in childhood cancer survivors
Nov 21, 2023

More than half of cancer survivors have underlying medical conditions associated with severe COVID-19
Feb 3, 2021
Recommended for you

Radiation before mastectomy found to cut time delays for reconstructive surgery in breast cancer patients

The architectural role of p53: Early 3D chromatin remodeling to trigger cellular stress response

Researchers discuss the unseen community effects of COVID-19 stay-at-home orders

Molecular subtypes of advanced kidney cancer matter for treatment response

How do wildfires affect mental health? A new study examines the connection
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

University of Cincinnati researchers present at national conference
New basic science findings on potential drugs, targets highlight aacr abstracts.

University of Cincinnati Cancer Center researchers will present abstracts at the American Association for Cancer Research annual meeting 2024, April 5-10 in San Diego, California.
Drug increases radiation effectiveness in preclinical study
Advanced stage non-small cell lung cancer often spreads to the brain, and the National Institutes of Health reports patients with these brain metastases have a median survival rate of about 12 months.
Radiation therapy is an important component of the current standard of care to treat the brain metastases, but challenges to this treatment include significant side effects and overcoming radiation resistance.
A research team led by Debanjan Bhattacharya, PhD, and Soma Sengupta, MD, PhD, tested whether administering a brain-permeable drug called AM-101 with radiation treatment improves the effectiveness of radiation.
The drug is designed to activate GABA(A) receptors in the brain, which have been found to weaken non-small cell lung cancer cells. For the first time, the researchers found the drug sensitizes the brain metastatic tumors to radiation and significantly improves survival in a preclinical animal model.
“In patients receiving radiotherapy, GABA(A) receptor activation may improve tumor control while allowing radiation dose de-intensification to reduce the toxicity of radiation treatment,” said Bhattacharya, research instructor in the Department of Neurology and Rehabilitation Medicine in UC’s College of Medicine.
Bhattacharya said the study also found the specific mechanism that weakens the cancer cells, as the drug activating the GABA(A) receptors triggers a domino effect of dysregulation in mitochondria, the cell’s power source, which induces autophagy, the cell’s recycling process. Activation of a selective autophagy function increased the effectiveness of radiation treatment and improved tumor control in the animal model.
Moving forward, Bhattacharya said these results pave the way to begin clinical trials in the near future testing AM-101 combined with whole brain radiation treatment for lung brain metastatic patients.
“The therapeutic effect of this combination has promise that can lead to improved survival compared to stand-alone whole brain radiation therapy, which in a majority of cases is palliative and has responses which are not durable,” he said.
Researchers examine different ways fibroblasts aid melanoma drug resistance
Bruna da Silva Soley, PhD. Photo provided.
Researchers in the lab of Yuhang Zhang, PhD, study the role of cancer-associated fibroblasts (CAF), a type of cell often found in the area around melanoma cells within the tumor microenvironment. While normal fibroblasts provide structural support, CAFs change their behavior in response to signals from the cancer cells around them.
“CAFs are known to play diverse roles in cancer progression, including promoting tumor growth, invasion, metastasis, the formation of new blood vessels and therapeutic resistance,” said Bruna da Silva Soley, PhD, abstract first author and a postdoctoral fellow in Zhang’s lab in the College of Pharmacy.
Previous research found that one of the most common drugs used to treat melanoma, called BRAF inhibitors, boost the CAF’s activity.
“It is as if CAFs are giving the cancer cells a way to resist the treatment designed to fight them,” Soley said.
The researchers found BRAF inhibitors specifically cause an accumulation of a certain protein within CAFs that helps activate the processes that aid cancer cells in escaping treatment. In contrast, two other common melanoma treatments did not lead to the same protein accumulating within CAFs.
Additionally, the team learned that targeting this protein within fibroblasts can suppress melanoma progression in animal models. Moving forward, the team will aim to learn more about this mechanism in order to develop new therapies to be combined with other targeted therapies and immunotherapy drugs.
“Unraveling the biology of CAFs in melanoma holds promise for developing innovative therapeutic strategies that target both the tumor cells and their microenvironment,” Soley said. “That could mean more effective treatments and better outcomes for patients.”
Yao Xiao. Photo provided.
Another research team in Zhang’s lab took a different angle to examine how CAFs influence melanoma drug sensitivity.
“Melanoma stands out as one of the most aggressive forms of skin cancer in the United States, with many patients developing drug resistance relatively quickly,” said Yao Xiao, abstract first author and a research assistant in Zhang’s lab. “This phenomenon occurs because melanoma cells possess the ability to adapt and evade targeted therapies, making it crucial to identify alternative avenues for treatment.”
The team focused on the role of a protein called YAP1 that has been previously found to play a critical role in regulating melanoma progression and protecting the cancer cells from treatment through its function in CAFs. In the most recent study, they additionally identified another protein, PRMT1, that binds with YAP1 to reinforce drug resistance.
When CAFs were treated with BRAF inhibitors, they underwent significant changes that helped bolster drug resistance. But when YAP1 and PRMT1 were blocked, this process was suppressed, leading to less drug resistance.
Xiao said PRMT1 is a potential additional target within CAFs to improve melanoma treatment.
Researchers identify protein as potential target for subset of breast cancer
Wasim Feroz. Photo provided.
Another team of researchers in Garrett’s lab studied the role of a protein called NMIIA in driving cancer growth in a subset of breast cancers with a specific genetic mutation called PIK3CA.
Abstract first author Wasim Feroz said lab member Samar Alanazi, PhD, found that NMIIA interacts with the HER3 protein that promotes cancer growth, and this interaction is increased when the tumors are treated with drugs that target the HER family of proteins. Additionally, higher levels of NMIIA were associated with worse survival outcomes for patients with the PIK3CA mutation compared to those with low levels of NMIIA.
“Loss of NMIIA reduced HER3 protein levels and downstream signaling, suggesting that NMIIA may be a crucial factor in promoting cancer growth in these types of breast cancers,” said Feroz, a graduate assistant in Garrett’s lab.
Moving forward, Feroz said the team plans to further study the interaction between NMIIA and HER3, as well as whether inhibiting NMIAA can increase the effectiveness of other therapies that target HER3 and PIK3.
“This research holds promise for identifying new therapeutic targets and improving treatment outcomes for breast cancer patients, particularly those with HER2-positive tumors or mutations in the PIK3CA gene,” Feroz said. “By understanding the underlying mechanisms driving cancer growth and resistance to current therapies, the findings from this study could ultimately lead to the development of more effective treatments and better management of breast cancer in the clinic.”
Targeting multiple mutations controls tumor growth in cell lines, patient samples
Approximately 53,000 Americans died of colorectal cancer (CRC) in 2023, and many colorectal tumors have one or more gene mutations that contribute to their growth.
First author Mary Kate Kilroy said a team of researchers in the lab of Joan Garrett, PhD, is studying the co-occurrence of two mutations, called KRAS and HER3, in CRCs. About 41% of all colorectal tumors contain a KRAS mutation, about 6% of all tumors contain a HER3 mutation and both mutations can help the tumors grow unchecked at an accelerated rate.
After an analysis of publicly available data, the research team found there was a significant co-occurrence of HER3 and KRAS mutations in colorectal cancer.
“We were looking to see if co-targeting HER3 along with mutant KRAS would inhibit tumor growth in colorectal cancer,” said Kilroy, a doctoral candidate in Garrett’s lab in UC’s James L. Winkle College of Pharmacy.
The researchers found that a drug that targets the KRAS G12D mutation (which accounts for 29% of KRAS mutations in CRCs) led to an increase in HER3 activation in cell lines and patient-derived samples. However, when the KRAS-targeting drug was combined with several different drugs that inhibit the HER family of proteins, there was a decrease in tumor cell growth.
“In the future, we are hoping to test an antibody drug conjugate targeting HER3 itself in combination with KRAS inhibitors and observe if there is an effect on tumor proliferation,” Kilroy said. “Our lab is very excited about this project and I am looking forward to moving it forward.”
Impact Lives Here
The University of Cincinnati is leading public urban universities into a new era of innovation and impact. Our faculty, staff and students are saving lives, changing outcomes and bending the future in our city's direction. Next Lives Here.
UC involvement at the AACR annual meeting includes:
- Bhattacharya presenting the poster "GABA(A) receptor activation drives GABARAP-Nix mediated autophagy to radiosensitize primary and metastatic lung adenocarcinoma tumors" April 7 at 1:30 p.m.
- Soley presenting the poster "BRAFi-induced ROCK-mediated non-canonical nuclear β-catenin shuttling drives a phenotypic switch in cancer-associated fibroblasts" April 7 at 1:30 p.m.
- Aniruddha Sunil Karve presenting the poster "Translational research to facilitate development of novel therapeutic combinations of letrozole for the treatment of glioblastoma" April 8 at 9 a.m.
- Xiao presenting the poster "BRAFi-induced epigenetic switch drives the reprogramming of resistant cancer-associated fibroblasts" April 8 at 1:30 p.m.
- Feroz presenting the poster "Non-muscle myosin IIA as a promising therapeutic target in breast cancer" April 9 at 1:30 p.m.
- Kilroy presenting the poster "Molecular insights into the oncogenic influence between mutant HER3, mutant KRAS, and their synergistic interplay in colorectal cancer pathogenesis" April 10 at 9 a.m.
Featured photo at top of Debanjan Bhattacharya working in the lab. Photo/Joseph Fuqua II/UC Marketing + Brand.
- Faculty Staff
- College of Pharmacy
- College of Medicine
- Neurology & Rehabilitation Medicine
- UC Cancer Institute
Related Stories
A potential new treatment for brain tumors.
September 23, 2022
The University of Cincinnati's Pankaj Desai, PhD, has received a $1.19 million grant from the National Institutes of Health/National Institute of Neurological Disorders and Stroke to continue research into the use of a drug called letrozole to treat glioblastomas, the most deadly form of brain tumors.
Collaborative University of Cincinnati Cancer Center team opens Phase 2 brain tumor trial
March 26, 2024
A multidisciplinary team of University of Cincinnati Cancer Center researchers have opened a Phase 2 clinical trial to test a new combination treatment for glioblastomas, the most deadly form of brain tumors.
April 4, 2024
Advances in Pancreatic Cancer Research
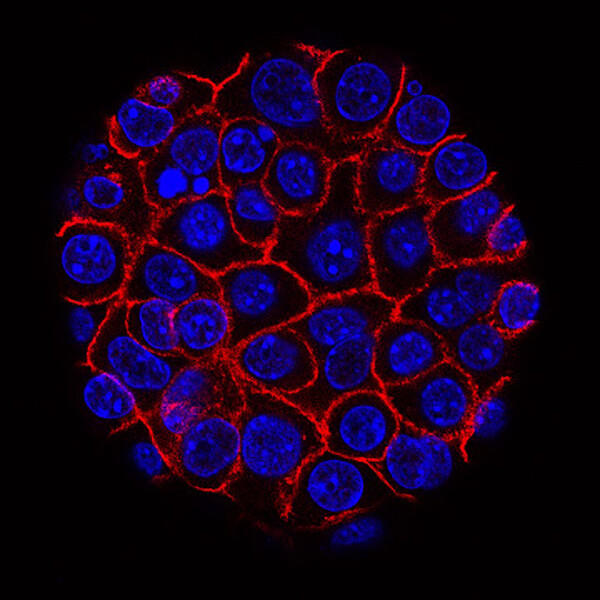
Pancreatic cancer cells (blue) growing as a sphere encased in membranes (red).
NCI-funded researchers are working to advance our understanding of how to prevent, detect, and treat pancreatic cancer, which includes pancreatic ductal adenocarcinoma (PDAC) and pancreatic neuroendocrine tumors (PNET). PNET is much less common than PDAC and has a better prognosis .
This page highlights some of the latest research in pancreatic adenocarcinoma, including clinical advances that may soon translate into improved care, NCI-supported programs that are fueling progress, and research findings from recent studies.
Early Detection of Pancreatic Cancer
Currently, no screening tests exist that can catch pancreatic cancer early, before symptoms develop. NCI is now funding several large research projects that are working to develop such an early-detection tool.
One known risk factor for developing pancreatic cancer is a new diagnosis of diabetes, sometimes called new-onset diabetes . About 1 in 100 people with new onset diabetes are diagnosed with pancreatic cancer within 3 years after learning they have diabetes. And 1 in 4 people who get pancreatic cancer had already been diagnosed with diabetes.
The NCI-funded New Onset Diabetes (NOD) Study , which is scheduled to run through 2025, is currently enrolling 10,000 people with new-onset diabetes or hyperglycemia (also known as prediabetes). The NOD researchers hope to develop a blood test that can identify the few individuals with a new diabetes diagnosis who may need further testing for pancreatic cancer.
Other NCI-funded teams, coordinated through the Pancreatic Cancer Detection Consortium (PCDC) , are trying to create a blood test that could pick up early pancreatic cancer in the general population. PCDC researchers are also working to improve imaging of the pancreas, by developing methods that may be able to pick up tiny deposits of tumor cells.
Pancreatic Cancer Treatment
Pancreatic cancer can be hard to treat surgically due to the location of the organ, and because the disease has often spread in the body by the time it is diagnosed.
Standard treatment for pancreatic cancer usually consists of surgery , chemotherapy , radiation , or combinations of each, depending on the cancer’s stage. Beyond these standard treatments, NCI scientists continue to look for ways to treat pancreatic cancer more effectively. Researchers are looking at the potential of new drugs, ways to combine standard drugs, and new modalities (such as immunotherapy ) to give to patients.
Patients with pancreatic cancer are generally recommended to have both biomarker testing and testing for inherited genetic changes. Both types of testing can help suggest possible treatments and can indicate with a patient’s family members might have an increased risk for pancreatic cancer or other types of cancer.
Testing treatments for early-stage pancreatic cancer
Therapies for early-stage disease that are being tested in clinical trials right now include
- new adjuvant chemotherapy drug combinations Some of these postsurgical drug combinations are already known to extend the lives of patients with metastatic disease, but it's not clear if they are better at killing cancer cells left behind after surgery than standard treatments.
- neoadjuvant chemotherapy This form of chemotherapy is given before surgery, with the goal of improving outcomes by shrinking the tumor before it’s removed. Pre-surgical chemotherapy also may help by killing cancer cells that have escaped from the tumor that would continue to grow as the patient recovers from surgery.
Testing treatments for advanced pancreatic cancer
New treatments for metastatic pancreatic cancer that are being investigated in clinical trials include immunotherapy and targeted therapy . Immunotherapy uses substances to stimulate or suppress the immune system to help the body fight cancer. Targeted therapy uses drugs or other substances to target specific molecules that cancer cells need to survive and spread.
Drug Targets Common Mutation in Pancreatic Cancer
In mice, experimental drug MRTX1133 shrank pancreatic tumors with KRAS G12D mutations.
- Ras-directed therapies . The RAS gene s makes proteins that take part in signaling pathways that control cell growth. Altered forms of these genes are found in more than 90% of pancreatic cancers. Drugs that target mutant forms of RAS are now being tested. One example is a drug that targets a form of RAS that has a mutation called G12C and another drug that targets a more common mutation, G12D.
- olaparib . Olaparib (Lynparza) is used as maintenance therapy in adults with metastatic cancer that has not progressed after platinum chemotherapy and has certain mutations in the BRCA1 or BRCA2 gene.
- pembrolizumab . In rare cases, people with pancreatic cancer have mutations in their tumor that cause high microsatellite instability (MSI) . Pembrolizumab (Keytruda) is an immune checkpoint inhibitor approved for patients with pancreatic cancer that has high MSI.
- novel immune checkpoint inhibitors and combinations . Using one drug for immunotherapy treatment has not been effective for most people with pancreatic cancer. Therefore, researchers are combining several immunotherapies that can act on different parts of the immune system.
- combinations of immunotherapy drugs with other treatments . These include radiation therapy, stromal modifying agents, and other targeted drugs.
- cell therapies . Researchers are exploring the use of cell-based therapies for pancreatic cancer. These therapies use immune cells such as T cells and natural killer cells that are altered in the lab to kill cancer cells.
- the stroma is the fibrous tissue around a tumor that does not contain cancer cells. It is mostly made up of connective tissue , blood vessels , lymphatic vessels , and nerves . Some of these components can help to support cancer cells and/ or prevent the immune system from recognizing cancer cells.
- pancreatic cancers have much denser stroma than most tumors. Agents that help break down or remodel this stroma may help more chemotherapy drugs reach cancer cells. Or they may help reduce cancer cell resistance to killing by other agents.
For a list of specific drugs, see Drugs Approved for Pancreatic Cancer .
Clinical Trials
Because of the complex nature of pancreatic cancer, many experts believe it’s important for all patients to join a clinical trial , even if they have early-stage disease. NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Trials are available for pancreatic cancer treatment .
NCI-Supported Research Programs
Many NCI-funded researchers at the NIH campus, and across the United States and world, are seeking ways to address pancreatic cancer more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer and the social factors that affect cancer risk. And some is more clinical, seeking to translate this basic information into improved patient outcomes. The programs listed below are a small sampling of NCI’s research efforts in pancreatic cancer.
- The Pancreatic Cancer Cohort Consortium consists of more than a dozen prospective epidemiologic cohort studies that investigate the causes and natural history of pancreatic cancer. This includes the launching of a genome-wide association study (GWAS) known as PanScan .
- The Pancreatic Cancer Detection Consortium (PCDC) develops and tests biomarkers to detect early stage pancreatic cancer and identify individuals at high risk for the disease.
- The Pancreatic Ductal Adenocarcinoma (PDAC) Stromal Reprogramming Consortium (PSRC) is a multidisciplinary community of PDAC researchers that will bridge biological research with preclinical/translational research. The goal is to identify and evaluate elements in the tumor microenvironment that drive PDAC progression and response to therapy.
- The Pancreatic Specialized Programs of Research Excellence (Pancreatic SPOREs) are designed to quickly move basic scientific findings into clinical settings. The Pancreatic SPORE grants support new and diverse approaches to the prevention, early detection, diagnosis, and treatment of pancreatic cancer. Two of NCI's Gastrointestinal (GI) SPOREs also conduct research in pancreatic cancer.
- The RAS Initiative looks to understand mutations in RAS genes to ultimately create effective, new therapies for RAS -related cancers. More than 90% of pancreatic cancers are caused by mutations in the RAS family of genes.
Pancreatic Cancer Research Results
The following are some of our latest news articles on pancreatic cancer research:
- No Glucose? Pancreatic Cancer May Have a Ready Energy Alternative
- In Mouse Study, KRAS-Targeted Drug Shows Potential against Pancreatic Cancer
- Abnormal Collagen May Be Weak Spot for Pancreatic Cancer
- Belzutifan Approved to Treat Tumors Linked to Inherited Disorder VHL
- Could A Diabetes Diagnosis Help Detect Pancreatic Cancer Early?
- Boosting Dendritic Cells Helps the Immune System Find Pancreatic Cancer
View the full list of Pancreatic Cancer Research Results and Study Updates .

IMAGES
COMMENTS
March 14, 2024 5 min read. A collaborative project to bring the promise of cell therapy to patients with a deadly form of brain cancer has shown dramatic results among the first patients to receive the novel treatment. In a paper published Wednesday in The New England Journal of Medicine, researchers from Mass General Cancer Center shared the ...
Find research articles on cancer treatment, including news stories, clinical trials, ... New research suggests that fungi in the gut may affect how tumors respond to cancer treatments. ... New findings from a clinical trial suggest that a single dose of radiation therapy may control painful bone metastases as effectively as multiple lower doses ...
In this review, we introduce and describe four new areas of cancer research that may contribute to cancer treatment in the future: exosomes, microbiome, immunotherapy, and organoids. 2. ... As shown in Table 3, many new studies and findings are reported into this field of research. These four novel cancer research areas will make many ...
Immunotherapy is a promising strategy to treat cancer by stimulating the body's own immune system to destroy tumor cells, but it only works for a handful of cancers. MIT researchers have now discovered a new way to jump-start the immune system to attack tumors, which they hope could allow immunotherapy to be used against more types of cancer.
Mar. 20, 2024 — There is a surprising dearth of research about how breast cancer cells can go dormant, spread and then resurface years or even decades later, according to a new review of in ...
Cancer research highlights from 2023. Researchers at Mayo Clinic Comprehensive Cancer Center spent 2023 studying the biology of cancer and new ways to predict, prevent, diagnose and treat the disease. Their discoveries are creating hope and transforming the quality of life for people with cancer today and in the future.
New research suggests that people who have early-stage triple-negative breast cancer and high levels of immune cells within their tumors may have a lower risk of recurrence and better survival rates. ... "The study's findings may inspire future clinical trials to explore whether patients with a favorable prognosis (high TILs) can avoid ...
The new results offer findings of interest for future cancer research that could ultimately play a role in bringing targeted treatments to patients with certain gene abnormalities, regardless of their cancer type. Findings from three arms were released at this year's American Society of Clinical Oncology (ASCO) annual meeting in Chicago ...
Using their new method, the researchers introduced p53 mutations in human lung adenocarcinoma cells, then measured the survival rates of these cells, allowing them to determine each mutation's effect on cell fitness. Among their findings, they showed that some p53 mutations promoted cell growth more than had been previously thought.
The Nature Portfolio editors who handle cancer primary research, methods, protocols and reviews bring you the latest articles, covering all aspects from disease mechanisms to therapeutic ...
The latest cancer news from the US government's principal agency for cancer research, plus resources designed for science writers and ... that predict cancer risk in the general population may also predict elevated risk of new cancers among childhood cancer survivors. Findings could potentially inform screening and long-term follow-up of those ...
CLOSE. ATLANTA, April 4, 2024 — The American Cancer Society (ACS) today released Global Cancer Statistics, 2024, the organization's report on global cancer facts and trends. According to the findings, an estimated 20 million cancer cases were newly diagnosed in 2022 and 9.7 million people died from the disease worldwide.
Back into full swing in the lab, Worldwide Cancer Research scientists have been busy making exciting new discoveries about cancer. Here are the top five cancer research breakthroughs made by our scientists in 2022. 1. Stopping the spread of breast cancer. Our scientists in Italy discovered a previously unknown way that breast cancer cells ...
New Cancer Research & Perspectives. From new clinical trial findings to remarkable patient stories, our expert team and distinguished guest contributors curate and report on the latest, most important developments in cancer care. We hope these stories provide valuable insights for people on their own cancer journey.
Researchers at Memorial Sloan Kettering Cancer Center (MSK) continued to make strides against cancer in 2023. Laboratory research teams across the institution investigated many fundamental biological questions to advance the global understanding of cancer and the development of new therapies. "MSK is known for providing unparalleled care to ...
Precision oncology is the "best new weapon to defeat cancer", the chief executive of Genetron Health, Sizhen Wang, says in a blog for the World Economic Forum. This involves studying the genetic makeup and molecular characteristics of cancer tumours in individual patients. The precision oncology approach identifies changes in cells that might be causing the cancer to grow and spread.
An innovative vaccine could significantly reduce skin cancer fatalities among men, according to promising findings from a recent clinical trial. This groundbreaking research, conducted by ...
ATLANTA, October 12, 2023 — Reversing historical patterns, new findings led by researchers at the American Cancer Society (ACS) show higher lung cancer incidence in women than in men has not only continued in adults younger than 50 years, but now extends to women 50 to 54 years of age in the United States. The findings are published today in the Journal of the American Medical Association ...
The Breast Specialized Programs of Research Excellence (Breast SPOREs) are designed to quickly move basic scientific findings into clinical settings. The Breast SPOREs support the development of new therapies and technologies, and studies to better understand tumor resistance, diagnosis, prognosis, screening, prevention, and treatment of breast ...
Researchers from Fred Hutchinson Cancer Center, the American Cancer Society Cancer Action Network and peer institutions released new findings in the Journal of Clinical Oncology showing that when ...
Breast cancer treatment. New kinds of treatments for breast cancer are always being studied. For example, in recent years, several new targeted drugs have been approved to treat breast cancer. But more and better treatment options are needed, especially for cancers like triple-negative breast cancer, where chemotherapy is the main option.
New findings on the link between CRISPR gene-editing and mutated cancer cells. ScienceDaily . Retrieved April 1, 2024 from www.sciencedaily.com / releases / 2021 / 11 / 211118061556.htm
Leaders from the Mass General Cancer Center, a member of the Mass General Brigham healthcare system, will present research discoveries and outcomes from clinical trials in cancer at the 2024 ...
Female breast cancer - 11.6%. Colorectum - 9.6%. Prostate - 7.3%. Stomach - 4.9%. The 10 leading cancer types account for approximately two thirds of the total cases globally. Liver, thyroid ...
FILE - A sign for the Food and Drug Administration is displayed outside their offices in Silver Spring, Md., on Dec. 10, 2020. According to research published Sunday, April 7, 2024, in the Journal of the American Medical Association, most cancer drugs granted accelerated approval by the FDA, meant to give patients early access to promising drugs, do not demonstrate such benefits within five years.
Kinase inhibitors: A class of targeted drugs known as kinase inhibitors may help treat thyroid cancer cells with mutations in certain genes, such as BRAF and RET/PTC. Many of these drugs also affect tumor blood vessel growth. In many papillary thyroid cancers, the cells have changes in the BRAF gene, which helps them grow.
If the findings are extended to the estimated 18.1 million cancer survivors in the U.S., they suggest that more than 5 million survivors have a mobility disability and 1.3 million have a self-care ...
More patients these days are taking part in cancer research, a new study finds. At least one in five people with cancer (22%) participate in some form of clinical research. ... The findings of a ...
University of Cincinnati Cancer Center researchers will present abstracts at the American Association for Cancer Research annual meeting 2024, April 5-10 in San Diego, California. ... New basic science findings on potential drugs, targets highlight AACR abstracts ... "This research holds promise for identifying new therapeutic targets and ...
Find what's new in pancreatic cancer research, including current progress in treatment with stroma modifying drugs and immunotherapy. Selected NCI-supported programs that address pancreatic cancer are also described. ... NCI-supported programs that are fueling progress, and research findings from recent studies. On This Page. Early Detection ...