- Reference Manager
- Simple TEXT file

People also looked at
Perspective article, medical education through an invasion: insights from an elective programme for ukrainian medical students at the university of cambridge.

- 1 NHS Lothian, University of Edinburgh, Edinburgh, United Kingdom
- 2 School of Clinical Medicine, University of Cambridge, Cambridge, United Kingdom
Medical students in Ukraine have faced extraordinary disruption to their clinical studies with both the COVID-19 pandemic and subsequent Russian military invasion forcing a majority of their learning to be conducted remotely. Over the summer of 2022, the School of Clinical Medicine, University of Cambridge hosted 20 medical students from Kharkiv National Medical University for a seven-week intensive clinical elective programme. The aim was to provide an immersive clinical placement that would help students to attain the necessary knowledge and experience to become competent and confident practising doctors. This perspective piece aims to support the development of future equivalent exchanges through outlining the placement’s context, its planning and implementation, evidence of placement impact, and finally reflections and learning points.
1. Introduction
The wish to support our counterparts in Ukraine following the Russian invasion was a sentiment echoed across the UK and its medical schools. Dialogue between UK medical schools in March 2022 established what response would bring most value. While Ukrainian medical schools were delivering theoretical teaching online, the major educational omission was clinical placements, which were forced to be halted ( Figure 1 ). The hope therefore was for UK medical schools to help to bridge this gap by providing hospital placements to Ukrainian medical students.
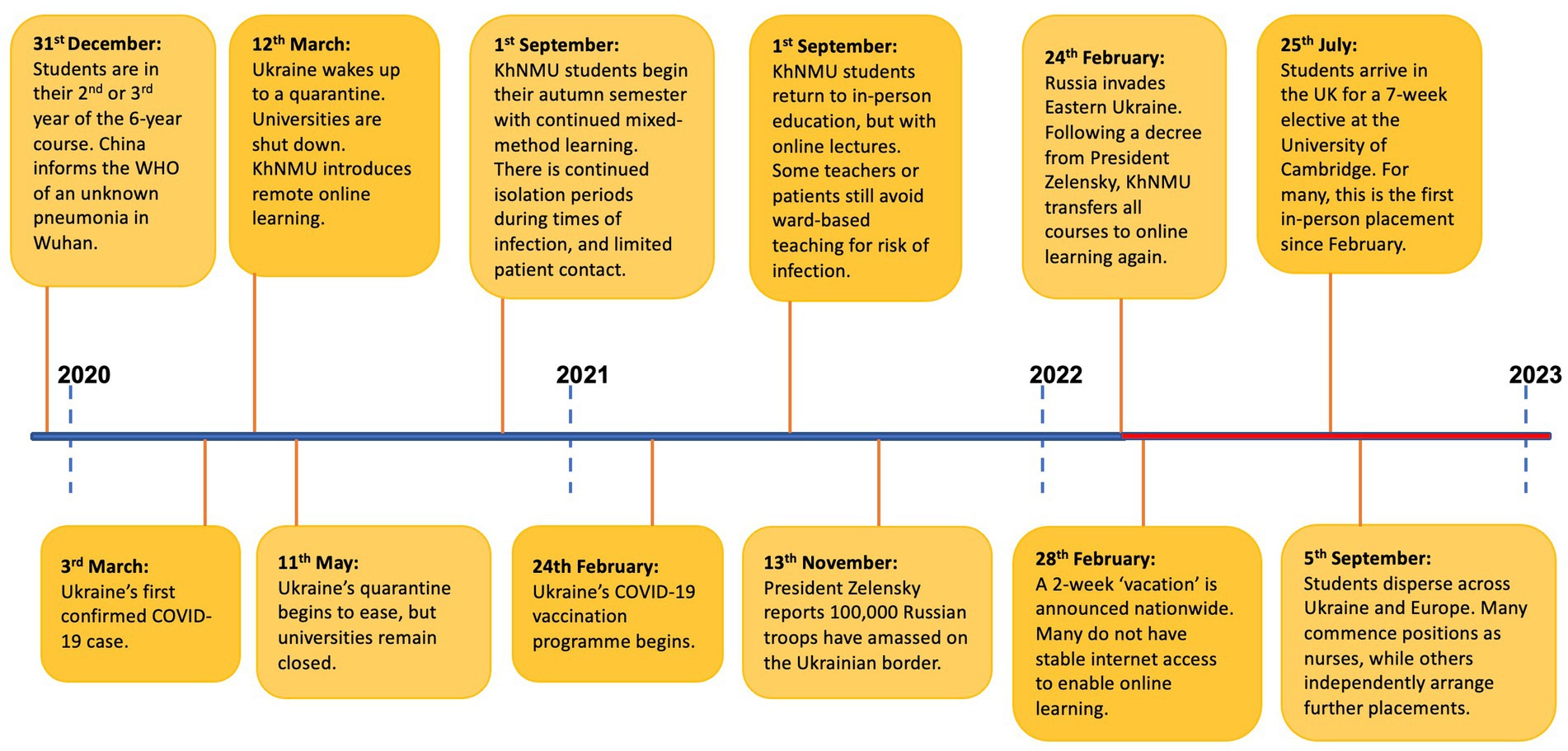
Figure 1 . Timeline outlining the disruption that students in the class of 2017 and 2018 at Kharkiv National Medical University have experienced over the course of the last 3 years ( 1 , 2 ).
A system of twinning was established between Ukrainian and UK medical schools. This would enable cohorts to remain together, facilitate administration, and allow placements to be tailored to redress each university’s most impacted curricular components. Thus, Cambridge School of Clinical Medicine and Kharkiv National Medical University (KhNMU), situated in Ukraine’s second city close to the frontline of the initial invasion, were paired. This process was facilitated by Cormack Consultancy Group ( 3 ) and the Medical Schools Council ( 1 ).
2. Placement arrangement and educational design
2.1. logistics.
It was agreed that placements would occur over the summer months. This timing facilitated the sourcing of supervisors, accommodation, and ensured minimal competition with local students for clinical opportunities. Weekly meetings between Cambridge University Hospitals (CUH), the Clinical School and colleagues at KhNMU drove placement development forward. Standing items included student selection, funding, visas, travel, accommodation, educational content, welfare, and communications. Smaller working groups reported back to weekly meetings which ran from late May–July 2022.
2.2. Selection of students
Electives were planned for up to 30 students. To be eligible, students were required to be Ukrainian Nationals proficient in the English language with CEFR scores of B2 or above. Change to Ukrainian Government Policy in June 2022 enabled male students to attend, following Government approval. Given the late timing of this decision, most students were female. Within these guidelines, KhNMU then invited students in their 4th and 5th years (at the time of selection) of their six-year medical degree to apply via means of an online application form. Students were subsequently ranked according to a combined score that was based upon their language proficiency, academic performance, and participation in scientific work, each with equal weighting.
2.3. Funding, hospitality and support
Funding for the programme was by virtue of two generous donations; one from Illumina ( 4 ), and another anonymous donation specifically to cover accommodation expenses. The total cost of the programme delivered to 20 students was £64,085. As such, the cost of visas, travel, accommodation, food, and other essentials were covered. Students resided in Homerton College, Cambridge, a 10-min walk from the hospital, with catering and kitchen facilities, and a library. Students additionally received a stipend of £500. For each of their three hospital placements, students were allocated a senior doctor working within the specialty to act as a supervisor. Junior doctor mentors, as outlined below, also provided guidance, particularly relating to the clinical environment. Students were encouraged to utilise KhNMU’s 24/7 mental health helpline should they require support. However, contact details for Cambridge Clinical School’s Welfare Officers were also provided.
2.4. Educational planning
To provide an educationally beneficial experience, the learning needs of the students were discussed with KhNMU. Situated clinical learning ( 5 ) was identified as the key aim. While KhNMU faculty had successfully delivered online teaching covering core topics relating to professional knowledge ( 6 ), students had not applied this through active participation within the clinical environment, nor received in-person clinical supervision. They therefore had not been able to consistently develop the professional skills expected of a medical graduate. The elective therefore comprised structured clinical placements based in Cambridge University Hospitals, the Royal Papworth Hospital, and the Ida Darwin Hospital.
2.5. Introductory week
The introductory week outlined the structure of the elective and incorporated mandatory NHS training and occupational health assessments ( Figure 2 ). Administrative tasks were nestled between clinical learning, including practical skills training and basic life support. Given the students’ lack of patient-facing experiences, a bespoke communications skills session was organised, based upon the Cambridge-Calgary Model ( 7 ) and incorporating simulated clinical encounters. Larger group sessions were arranged outlining the NHS structure and medical students’ professional responsibilities as per GMC guidance ( 8 ). Two half-day seminars took place: developing clinical reasoning skills and principles of palliative care.

Figure 2 . Students from Kharkiv National Medical University are welcomed to Cambridge School of Clinical Medicine and begin a week of inductions prior to commencing their 6-week clinical placement. Permissions: University of Cambridge.
2.6. Clinical rotations
Students were subsequently divided into three groups and entered two-week clinical rotations in medicine, surgery, and a student selected component (SSC). There were no pre-requisite selection criteria for the 12 available SCC options, and all students received their first-choice SSC placement.
Weekly hourly seminars were delivered by faculty and covered common clinical scenarios. Aside from this, didactic teaching was minimised, given its suitability for remote formats. Instead, weekly one-hour, near-peer small-group bedside teaching was delivered by junior doctors recruited from CUH. Bedside teaching focused upon adult medical and surgical history and examinations, diagnostic reasoning, interpretation of investigations and management planning, addressing core intended learning outcomes including GMC outcomes 10, 11, 12 and 14 around interpersonal skills, diagnosis and medical management ( 6 ). The neer-peer sessions were structured so that the junior doctors met the same 5–6 students each week, and thus could tailor sessions to meet students’ specific learning objectives. They were guided to cover adult medical and surgical assessment routines using a thematic approach with cardiovascular, respiratory, abdominal (medical/surgical), neurological and musculoskeletal focus to the sessions over the 6 weeks. Generally, these sessions took place at the bedside, on the wards of CUH, with review of assessment routines, confirmation of clinical signs and discussion of relevant clinical reasoning (including diagnosis, investigations, management, etc.). Furthermore, the junior doctors undertook a teaching-to-teach training session prior to the elective that included briefing on the details of the programme, an overview of the Kharkiv curriculum, the intended learning outcome for the weekly sessions and the support processes that were in place. One-to-one debriefs with each student took place in the final week to reflect upon student’s developing professional knowledge, skills and behaviours. Pro-forma similar to that used for University of Cambridge medical students aided reflection. These debriefs provided formative feedback that was included in the student’s learning portfolio.
2.7. Student feedback
Students completed end-of-placement feedback, to review the impact of the programme. Thirteen of the twenty students completed the paper form that was distributed to students on conclusion of the placement. An informal group interview was also conducted with students. Additionally, one student and one consultant clinical supervisor were interviewed individually. Upon conclusion of the programme, the Institute of the Quality of Education at KhNMU developed a short paper questionnaire to further measure placement impact. The above evidence underpins the following programme reflections and discussion.
3. Student satisfaction and placement reflections
3.1. clinical communication skills (ccs).
“It’s been hard, as online we’ve had minimal practise. My Kharkiv study group has the best academic marks but we struggle with patient interaction. After this workshop, my fear is gone.”
Simulated communication stations, a mainstay of medical education in the UK, have not been a component of the curriculum at KhNMU. Feedback resoundingly affirmed the inclusion of these sessions. Timing the workshops towards the beginning of the seven-weeks enabled students to further hone their skills. Interestingly, students spoke of the differences in communication styles between medical professionals in the United Kingdom and Ukraine. In particular, students were impressed by the culture of shared-decision making between doctors and patients in the NHS, and it was evident that they had reflected upon the distinct benefits and challenges of the differing cultures of communication. Encouragingly, students planned to adopt the format of the session and establish a student-led communications skills workshop to share their learning points with KhNMU peers. KhNMU faculty members have subsequently expressed enthusiasm for adopting such sessions.
3.2. Varied learning opportunities
“Some people know from childhood that they want to be a surgeon, but I never did so I would say ‘I’m not a surgical person’. I never had the chance to observe in Theatre but when I finally watched open heart surgery I thought ‘yes, I could do this’.”
The inclusion of a SSC was a highlight for students. Varied specialty options were available. These ranged from child and adolescent psychiatry to transplant surgery. KhNMU’s curriculum had necessarily honed upon core topics, and the chance to explore interests was limited. Surgery was particularly popular amongst students, many of whom had never had the chance to scrub into Theatre. Indeed, one consultant ENT surgeon shared that “the eagerness of the Ukrainian students to learn put our UK medical students to shame.”
Outside of SSCs, students were welcoming of the flexibility in their schedules, and of the chance to pursue their interests. Although importantly a small number of students expressed concerns of feeling “lost”, unaccustomed to independently seeking learning opportunities. The inclusion of junior doctor led bedside teaching was well received, ensuring continuity as well as allowing pastoral support alongside teaching delivery. Student feedback referenced increased confidence in their clinical skills.
3.3. CUH healthcare infrastructure
“We have similar [IT] in Ukraine, but it’s nowhere near as good. It’s amazing to have patient’s records accessible at your fingertips.”
Without doubt it was “EPIC”, CUH’s clinical software, that elicited the most rejoicing amongst students. Students expressed their desire to push towards the future development of improved IT programmes in Ukraine.
Another clear highlight was access to the Deakin Centre, a 24/7 simulated clinical learning environment where students could practise cannulation and catheterisation to their hearts’ content. Such practical elements were understandingly popular given the obvious limitations of online learning environments.
3.4. Student concerns
The timing of the placement during summer months conferred the drawback of coinciding with periods of staff annual leave. This meant that on occasion students received less support from the senior clinicians who were assigned to supervise their placements, and some teaching opportunities did not materialise. Students emphasised that on such occasions, healthcare staff endeavored to provide them with alternative opportunities, but the usefulness was variable.
Importantly, one student raised concerns regarding sexism on placement, particularly highlighting Theatre as a rife environment with only male students actively involved and encouraged to assist on some occasions. Their experiences point towards an ongoing need for active initiatives to tackle sexism within the NHS and echo experiences of UK female surgeons ( 9 ).
3.5. Contrasting healthcare systems
“In Ukraine surgeons are ‘Gods’ and you are expected to know everything. But in the UK we could ask simple questions. They were on our side.”
It was encouraging to hear students reflect, with great insight, into the UK’s healthcare delivery. Students were grateful for the openness of staff to their queries, and for the safe learning environment that was fostered. One student recalled the humility that UK doctors demonstrated, greatly impressed by a consultant offering that they did not know the answer to a question.
Students also considered the benefit to patients of Ukraine’s more accessible primary care system, with GPs contactable over text at any time of day, while valuing the UK’s emphasis on promoting doctors’ work-life balance. Indeed, students spoke of the aspects of their education in Ukraine that were “definitely better” and sung praises of KhNMU.
Finally, it is worthy of note that the programme has had the supplementary benefit of furthering the English language skills of students, as noted by KhNMU faculty. This is a particular advantage given the need for many to continue their studies overseas.
4. Discussion
Medical students studying in Ukraine have faced an unthinkable level of disruption to their studies. As may be seen in the above timeline, some students have had only a few months of their studies unencumbered from the COVID-19 pandemic and the war in Ukraine. In our current era much may be gained from online learning. Yet it is without question that one cannot become a safe, competent, and confident doctor without in-person experiential learning. The aim of the placement therefore was to provide students with a seven-week period in which they could immerse themselves in the clinical environment, free from the toll of wartime, financial burdens, or the administrative challenges of seeking out educational opportunities. In the following discussion we consider the overall impact of the placement, and explore how future placements at UK medical schools might build upon our experiences.
4.1. Placement impact
“The pandemic, the war, and endless online learning had left me close to burnout. This summer’s placement came at just the right time and prevented this. I now can’t wait to become a doctor.”
Student feedback was unanimous in the view that the seven weeks had strengthened their communication skills, practical and examination skills, and clinical acumen. Indeed, KhNMU faculty have been impressed by students’ tangible academic progress, enabling them to be signed off for specific components of their curriculum. The enthusiasm expressed by KhNMU faculty to incorporate elements of the elective, notably the CCS components, is testament to its beneficial impact for students, many of whom continue to have minimal patient interactions.
Due to the ongoing conflict, after the placement, students returned to Ukraine, and across Europe. There they commenced their 5th and 6th years of their degree, comprising a combination of KhNMU-led distance learning and time spent either in temporary employment as a nurse, or in self-organised and self-funded placements. Whilst the elective placement has clearly bolstered students’ clinical education, it would be naïve to suggest that a seven-week elective can make amends for verging on three years of educational disruption. As such, no students have yet been granted an early graduation from KhNMU, although we hope that their experience will be formally recognised and facilitate their timely progression to working as doctors in Ukraine.
4.2. Shaping career paths
In contrast to the United Kingdom, upon graduation from medical school in Ukraine, students must choose a speciality to pursue. For many students involved in the exchange, their experience of clinical medicine has been limited to a few specialities. The prospect of their career paths being sculpted by such limited exposure is understandably daunting. The programme has undoubtedly broadened their clinical experience, particularly in the area of surgery. Future programmes should continue to prioritise flexibility and student choice within their structure so as to capture this valuable element.
4.3. Strengthening Ukraine’s medical workforce
“I really want to return to Ukraine and contribute what I have learnt. I think if the war stops, 90% of students will go back as soon as possible. It is home.”
Electives have long been a core component of UK medical courses, with good reason. The chance to encounter varied healthcare delivery confers cross-cultural learning. Students’ perceptive feedback demonstrated that this knowledge exchange had indeed taken place. As organisers of the exchange, we reflected upon the potential consequence of students being encouraged to pursue careers elsewhere than Ukraine. However, this was resoundingly not the case. The NHS was by no means a utopia in their eyes. Overwhelmingly, students echoed a desire to return “home” with haste, and to contribute to the rebuilding of their nation post-conflict.
4.4. Learning points
There were numerous logistical hurdles to the development of placements at relatively short notice. Crucially, the programme did not occur without significant investment, and was reliant upon the generosity of donors. We are mindful that continued financial backing is a prerequisite to future initiatives. Furthermore, the administrative time in arranging the programme was substantial, and it would be appropriate to fund the creation of a specific administrative post.
A barrier was represented by the requirement for students to obtain visas, which was made challenging by the absence of a British consulate in Ukraine. It would be sensible to create an exchange waiting list, to maximise the number of attending students should visa issues arise. Future initiatives should factor in delays in obtaining visas into timelines, as well as advise students of visa application processes.
Occupational health assessment, specifically TB screening, was problematic for students, some of whom were required to undergo multiple screenings at different international borders. Again, a waiting list might be wise, given the possibility of students testing positive. Consideration of ways to minimise such bureaucratic and financial burden students forced to cross multiple borders should occur.
Although the faculty teams in Kharkiv and Cambridge worked together closely, to ensure that the programme developed met the needs of the Kharkiv students, the intended learning outcomes of the programme and the framework developed was based on the outcomes and curriculum used in Cambridge and mapped to the GMC outcomes for graduates. There was an exchange of information, across both faculty teams, to ensure that the programme that was developed explicitly linked with prior student learning (delivered by the Kharkiv faculty). However, for future programmes and to support educational quality assurance processes, it would be worthwhile more explicitly aligning the intended outcomes of the programme with those of the overall Kharkiv programme, since this would allow students and faculty (in both institutions) to review student learning from the programme and map the learning to future assessment processes ( 10 , 11 ).
Feedback from students has focussed our attention upon the difficulty that reduced hospital staffing levels in summer presents. The timing of the placement was considered carefully, and it was deemed infeasible to accommodate the students during the academic year. In future, the roles and expectations for senior clinical supervisors should be made clear in advance of volunteering. Additionally, enlisting a larger volunteer pool, to cover unexpected absences, would be prudent. Notably, the inclusion of near-peer teaching with junior doctors helped to provide students with continuity and mentorship and acted as an antidote to some of the aforementioned difficulties. We would encourage the incorporation of this element into future programmes, as it was greatly valued.
Finally, whilst Cambridge stipulated some eligibility criteria, KhNMU selected academically higher achieving students. The aim of the programme was to help ameliorate some of the disruption to training imposed by the pandemic and war, and this distinction does not necessarily align with the objective. Given the level of financial support provided, the need to instead prioritise students from lower-income backgrounds should be considered since they may not otherwise be afforded overseas placements. As such, we need to think carefully about future selection criteria.
4.5. Future directions
There is a mutual wish to repeat the programme, and ongoing dialogue to arrange an exchange in summer 2023. This commitment is regardless of the exact political context, as medical students will undoubtedly still benefit from additional clinical exposure, given the continued disruptions. We also hope to increase the intake by 50%, up to a total of 30 students. Impetus is needed to secure funding, which represents the main obstacle.
Our aim, ultimately, is that this placement could enable students to begin their working careers sooner, so as to bolster Ukraine’s medical workforce (as has occurred in the NHS during the COVID-19 pandemic). As the current cohort progresses through their training, it remains to be seen whether this will be possible, and we await further impact statements from KhNMU.
Future programmes should consider the changing needs of students as the war, and thus medical education, in Ukraine evolves. The focus and content of placements, and specialities experienced, may need to be adapted, as new cohorts progress through training with varying curricular gaps. We recognise our role to primarily be that of hosts and facilitators, and as such are keen to be guided by KhNMU faculty and Ukraine’s medical student body in this regard.
Multiple UK-Ukraine Medical School twinnings took place in 2022, and several other medical schools have supported Ukrainian students by means of clinical placement, or have expressed an interest in doing so. Ukraine has 45 medical schools accredited by the World Health Organisation (WHO) and UNESCO ( 12 ) and the conflict shows no sign of imminent resolution. As such, we are eager to share our learnings, with the aspiration to support the establishment of equivalent programmes. We are mindful to recognise that many medical students across the globe are impacted by ongoing conflicts, and other such barriers to their education. While our donors specifically gifted funds for Ukraine, we hope that the positive impact of this exchange will encourage support for medical students who are facing adversity across the globe.
5. Conclusion
The positive experience of the Ukrainian medical students is testament to the effectiveness of institutional collaboration, and highlights ways in which UK medical schools may support our peers in Ukraine. We asked students if there was anything that they might want readers to take away from this article. Without hesitation their response was simply that of thanks to those who have facilitated the programme.
The fortitude of the Ukrainian students, who display such drive to continue their medical education, must be acknowledged. These are a cohort of medical students who have, and continue, to study under circumstances that are unimaginably challenging for many. Their dedication and enthusiasm to further their education concurrent to the ongoing conflict is admirable. We are hopeful that the exchange has offered some reprieve from the disruption to their studies and respite from the grave weight of wartime.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JF, PW, and ML contributed to the development and running of the elective programme along with Cambridge University Hospitals and Cambridge School of Clinical Medicine staff. JH and JF contributed to the conception of the manuscript structure and content. JH wrote the draft of the manuscript, conducted interviews with students, and produced figures. PW contributed to writing the introduction while ML contributed to writing the educational planning, introductory week, and clinical rotations. SB facilitated student interviews and provided figures. TS contributed to the development of the timeline figure. VC contributed to the student perspective quotes used in the manuscript. Further drafts, revisions and edits of the manuscript were conducted by JH and JF. All authors contributed to the article and approved the submitted version.
The authors declare that the elective programme received funding from Illumina Biotechnology Company and a donor. Funding was used solely for the cost of running the seven-week elective programme. This included aspects such as travel, accommodation, visas and student stipends, as well as delivery of the educational programme. The authors declare that this perspective piece received no funding from Illumina Biotechnology Company or other donors. The funders were not involved in the article design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Acknowledgments
We wish to thank the Ukrainian students for their candid feedback and insightful reflections. Cassandra Mura, Sarah Monamy, Philippa Moore were also integral to the delivery of the programme and we are grateful for their hard work. For their friendly welcome and support of the programme, we would like to thank Homerton College, Cambridge. There is no doubt that the programme would not have been feasible in its existing format without such financial backing. As such, we extend our utmost thanks to our donors. Finally, we wish to thank Dr. Isobel Fitzgerald O’Connor for her impetus in helping the development of the programme, her work to obtain funding, and for her ongoing commitment to widening access to medical training for medical students from across the globe.
Conflict of interest
JH is an alumnus of the Cambridge School of Clinical Medicine. TS and VC are current students at Kharkiv National Medical University and took part in the 2022 exchange. JF, SB, ML, and PW work at Cambridge School of Clinical Medicine and are employed by the University of Cambridge.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kyiv Post. Timeline of Ukraine’s response to coronavirus pandemic. Available at: https://www.kyivpost.com/post/10406 (Accessed April 8, 2023).
Google Scholar
2. House of Commons Library. Research briefing. Conflict in Ukraine: a timeline. Available at: https://researchbriefings.files.parliament.uk/documents/CBP-9476/CBP-9476.pdf (Accessed April 8, 2023).
3. Medical Schools Council. Available at: https://www.medschools.ac.uk/ (Accessed April 8, 2023).
4. Cormack Consultancy Group. Available at: https://www.consultcormack.com/ (Accessed April 8, 2023).
5. Illumina. Available at: https://www.illumina.com/ (Accessed April 8, 2023).
6. Lave, J, and Wenger, E. Situated learning: legitimate peripheral participation . Cambridge: Cambridge University Press (1991).
7. General Medical Council. Outcomes for graduates . Available at: https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates (Accessed June 22, 2023).
8. Silverman, J, Kurtz, S, and Draper, J. Skills for communicating with patients (3rd edition) . Boca Raton, FL: CRC Press (2013).
9. General Medical Council. Good medical practice. Available at: https://www.gmc-uk.org/-/media/documents/good-medical-practice---english-20200128_pdf-51527435.pdf (Accessed April 8, 2023).
10. The Times. Sexual assault, crude banter – What it’s like to be a female surgeon. Available at: https://www.thetimes.co.uk/article/sexism-assault-female-surgeons-nhs-times-health-commission-lnqbm2kjp (Accessed April 8, 2023).
11. Harden, RM. AMEE guide no. 21: curriculum mapping: a tool for transparent and authentic teaching and learning. Med Teach . (2001) 23:123–37. doi: 10.1080/01421590120036547
PubMed Abstract | CrossRef Full Text | Google Scholar
12. Biggs, J. Enhancing teaching through constructive alignment. High Educ . (1996) 32:347–64. doi: 10.1007/BF00138871
13. Times Higher Education. The US should admit Ukrainian medical students to help them rebuild their country. Available at: https://www.timeshighereducation.com/campus/us-should-admit-ukrainian-medical-students-help-them-rebuild-their-country (Accessed April 8, 2023).
Keywords: Ukraine, Kharkiv, Cambridge, medical, student, war, placement, elective
Citation: Hodkinson J, Lillicrap M, Wilkinson P, Bevan S, Shenheliia T, Chupina V and Fuld J (2023) Medical education through an invasion: insights from an elective programme for Ukrainian medical students at the University of Cambridge. Front. Med . 10:1211526. doi: 10.3389/fmed.2023.1211526
Received: 24 April 2023; Accepted: 06 September 2023; Published: 28 September 2023.
Reviewed by:
Copyright © 2023 Hodkinson, Lillicrap, Wilkinson, Bevan, Shenheliia, Chupina and Fuld. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joy Hodkinson, [email protected]
- April 2024 20th Apr 2024

- Company Profile
- Our Mission
- Academic Advisors
- Local Support – Armenia
- Local Support – Georgia
- Local Support – Ukraine
- Local Support –Serbia
- Local Support – Romania
- Local Support – Bulgaria
- Corporate News
- Our Articles
- Graduate Entry
- Costs & Fees
- Our Offices
- Partner Universities
Authorised Recruiters
- Our Distinguished Supporters
- Our Students
- Entry Exams
- Networking Events
- Social Events
- Undergraduate Entry
- Commonwealth University
- University of Health Sciences Antigua
- Victoria University of Barbados
- Saint James School of Medicine
- National and Kapodistrian University of Athens
- Aristotle University of Thessaloniki
- University of Crete
- “Grigore T. Popa” University of Medicine and Pharmacy – Iasi
- “Vasile Goldis” Western University of Arad
- Sofia University “St Kliment Ohridski”
- Trakia University – Stara Zagora
- Burgas University “Prof. Dr. Asen Zlatarov”
- Sofia Medical University
- Plovdiv Medical University
- Varna Medical University
- Pleven Medical University
- University of Belgrade
- University of Traditional Medicine
- East West Teaching University
- New Vision University
- Caucasus International University
- Georgian National University
- Ivane Javakhishvili Tbilisi State University
- Trakia University – Stara Zagora
- Forestry University – Sofia
- Join Our Open Days & Win A Scholarship
- Sofia University ‘St Kliment Ohridski’
- Trakia University Stara Zagora
- Forestry University Sofia
- Student Loans
- Scholarships
- Student Loans for Medical Studies in Europe
- Medical School Scholarships in Europe
- Study in Armenia
- Medical Education in Armenia
- Medical School Programme
- Dental School Programme
- Medical Postgraduate Study
- Tuition Fees in Armenia
- Medical University Requirements
- Application Deadlines
- Application Documents
- Medical School Acceptance Letter
- Medical Student Transfer
- Medical School Accreditation
- Living Costs in Armenia
- Student Accommodation
- Student Loans in Armenia
- Armenian Student Visa
- Student Residence Permit
- Medical Insurance
- Medical Student Life
- Weather Conditions
- Transportation in Armenia
- Safety and Security in Armenia
- Study in Georgia
- Medical Education in Georgia
- Tuition Fees in Georgia
- Living Costs in Georgia
- Scholarships in Georgia
- Student Loans in Georgia
- Georgian Student Visa
- Transportation in Georgia
- Safety and Security in Georgia
- Study in Serbia
- Medical Education in Serbia
- Tuition Fees in Serbia
- Living Costs in Serbia
- Scholarships in Serbia
- Student Loans in Serbia
- Serbian Student Visa
- Transportation in Serbia
- Safety and Security in Serbia
- Study in Romania
- Medical Education in Romania
- Veterinary School Programme
- Tuition Fees in Romania
- Living Costs in Romania
- Scholarships for Romania
- Student Loans in Romania
- Romanian Student Visa
- Transportation in Romania
- Safety and Security in Romania
- Study in Bulgaria
- Medical Education in Bulgaria
- Postgraduate Medical Study
- Tuition Fees in Bulgaria
- Living Costs in Bulgaria
- Scholarships in Bulgaria
- Student Loans in Bulgaria
- Bulgarian Student Visa
- Transportation in Bulgaria
- Safety and Security in Bulgaria
- Getting There
- Ongoing Support
- 24/7 Information Availability
- Academic Advice & Skills Assessment
- Complete Information Packages
- Official University Representatives
- Docs Legalization & Translation
- In-Person Application Submission
- Application Tracking & Reports
- Entry Tests Prep Courses & Materials
- Information and Support from Day 1
- Online Lessons, Notes & Sample Tests
- Scholarships & Bursaries
- Student Loans & Grants
- Student Visa Issuance (If applicable)
- Arrival Services, Escorting & Lodging
- Annual Open Days (Pre-departure)
- Orientation, Support Meetups Abroad
- Finding Accommodation & Amenities
- Residence Permit
- University Course registration
- Open a Local Bank Account
- Emergency Support Until Graduation
- Ongoing Academic Support
- Online Tutoring
- Bi-Monthly Follow Ups
- Postgraduate Support Webinars
- Clinical Work Experience in the UK/USA
- License to Practice in the UK
- License to Practice in the USA
- Job Seeking Support
- Career Fairs with UK/USA Employers
- Belgrade University
- Pleven University
- Trakia University
Kiev Medical University
- Pleven Medical university


Click here to view
Scholarships requirements.
- Real Success Stories
Click to view
Our real success stories.
- New Student
- Current Student

- March Intake
- September Intake

Our Partner Universities

Authorised recruiters for Kiev Medical University, Ukraine
In the photograph (from right to left): Prof. Borys Ivnyev, Rector of the University; Mr. Aris Grigoriou, Student Recruitment Manager of Study Medicine Europe.

Why Study Medicine in English at Kiev Medical University in Ukraine?
No Entry Exams
$4,000 /year
Not Available
Up to the last 3 years
- The most prestigious medical education institution in Kiev, Kiev Medical University (KMU) is one of the best medical universities in Ukraine.
- The university boasts excellent teaching standards and stays up-to-date with the ongoing international developments in medical education.
- Medical students are offered many opportunities to engage in international exchange programs, conferences and scientific projects.
- The university features many extracurricular activities and sports activities to encourage students to remain fit and active.
- Centrally located in the vibrant city of Kiev, this university is an attractive option for students.
- The programme is available in English, Russian and Ukrainian.
- It is 6 years in duration and each year is split into two semesters.
- The university has devised the curriculum in accordance to EU rules.
- The first three years are dedicated to pre-clinical subjects while the final three years focus on clinical subjects.
- The course is taught through a variety of formats including: lectures, class-based learning, labs, workshops, seminars and consultations.
- The faculty members are dynamic, experienced, versatile and fluent in English. They strive to incorporate all the latest methods into their teaching.
- As per Paragraph 3 of Order, No 1541 of the Ministry of Education and Science of Ukraine , online learning is prohibited. Therefore any student who wishes to study medicine at a local Ukrainian medical university must be present at the university.
- In Ukraine, graduate entry is not permitted as local medical universities refuse to acknowledge non-Ukrainian Bachelor’s degrees because of contrasts between the study programmes of the medicine courses and the non-Ukrainian BSc degrees. So, Ukrainian medical transcripts cannot include subjects that have been studied in a BSc degree.
- An application which includes the following details: bio, education history and course for which you are applying.
- A copy of your secondary education results with subjects studied.
- Documents from your home country confirming that you are authorised to study in Ukraine.
- Two small photos of 4-5cm.
- Many of the world’s Medical Councils require that the Medical School that awarded the Doctor of Medicine degree (MD) be listed on the World Directory of Medical Schools (WDMS).
- Additionally, each region has its own requirements:
- The General Medical Council (GMC) expects a medical degree to have a minimum 5,500 Clock Hours over a minimum period of three years.
- The Educational Commission For Foreign Medical Graduates (ECFMG) requires a medical degree to have a minimum duration of four years.
- The Australian Medical Council (AMC) maintains an additional database of Recognised Medical Schools.
- It also requires a medical degree to have a minimum duration of four years.
- The historic fifth century city of Kiev features a rich culture, stunning architecture and beautiful scenery.
- Kiev is famous for its unique food culture and is an excellent spot for gourmands with top-quality food available at very affordable prices.
- The city boasts an abundance of parks and is located near to a beach.
- It offers a variety of inexpensive public transport options including a metro, buses and trams.
- With its low cost of living and wealth of things to do, Kiev is a highly attractive prospect for students with a taste for adventure.
- The country of Ukraine is one of Europe’s biggest countries and has a wealth of diverse cultures.
- A nature-lover’s haven, Ukraine has 20 natural reserves and is renowned for its beautiful landscapes which include breathtaking mountains, deep lakes and dense forests.
- Ukrainians are well-known for their openness and hospitality.

Subscribe to Our Newsletters
Sme referral programme, check out our brochure, excellent reviews.

- Privacy Policy
- Cookies Notice
- Cookie Policy (EU)
- Cookie Policy (UK)
- Cookie Policy (CA)
- Cookie Policy (AU)
- Opt-out preferences

Fill in your details:
Join our open days, 20th april 2024.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Glob Health
- v.88(1); 2022

Overseas Medical Students in Ukraine and War-Related Interruption in Education: Global Health Considerations from India
Shubhajeet roy.
1 Faculty of Medicine, King George’s Medical University, Lucknow, India
2 St. John’s Medical College, Bangalore, India
Ahmad Ozair
Background:.
The Russian invasion of Ukraine in 2022 has caused a humanitarian crisis impacting millions of individuals within Ukraine and globally. While war-related healthcare delivery has been discussed in both the academic biomedical literature and in non-peer-reviewed sources, little academic attention has been paid to overseas medical students who have had to abandon their education. These constitute nearly a third of the 80,000 international students in Ukraine and represent a valuable part of the global healthcare workforce.
This article utilizes the illustrative case of the over 18,000 Indian-origin medical students enrolled in Ukraine to review the state of overseas medical students in Ukraine and war-related interruption in education.
Literature, both academic and non-academic, published up until October 1, 2022, pertaining to the conflict, the impact on students, the demands of various stakeholders, and the proposed solutions, was reviewed through the use of appropriate keyword-based searches.
Factors influencing the decision to pursue education in Ukraine and their pre-crisis pathway to home practice are first discussed. Indian-origin students have historically gone on to Ukraine after securing insufficiently competitive ranks in the national medical school entrance exam, thus preventing them from getting a heavily subsidized education at publicly funded institutions in India. In the 2022 Russo-Ukrainian conflict, these students have faced not only actual and potential challenges related to their safety, shelter, food, and home return, they have been considerably impacted by the uncertainty regarding their educational prospects back home. The article then delineates the nuances and challenges in attempting to reintegrate a large potential healthcare workforce in the home country, and discusses possible solutions, especially those being implemented by the government.
Conclusion:
Urgent need exists for the involvement of all stakeholders and careful consensus-building before the proposed reintegration from an equity-based perspective.
Introduction
The Russian invasion of Ukraine that began on 24 th February 2022 has impacted millions across the world. While conflict between the two countries had been occurring for almost a decade, this large-scale, unprecedented incursion has caused a humanitarian crisis. 20,000–50,000 casualties have been reported, and over five million residents of Ukraine have had to flee since the start of the conflict [ 1 , 2 , 3 , 4 ].
The war has had an overarching impact on populations worldwide, as evident in the global challenges related to the supply of oil/gasoline and cereal grains [ 1 , 2 , 3 , 4 ]. While all Ukrainian communities have suffered a large number of deaths, students in Ukraine in particular have additionally suffered a loss of future skill development and have had livelihood prospects impaired. The population-level impact of disturbed career prospects of a large cohort of future working professionals, including physicians-in-training, is likely sizable [ 5 ]. While war-related healthcare delivery has been discussed in both the academic biomedical literature and in non-peer-reviewed sources [ 6 , 7 ], little academic attention has been paid to the thousands of overseas medical students who have had to abandon their education in Ukraine. In particular, the complex nuances behind their pursuit of foreign medical education and the challenges of reintegration in their home countries remain undiscussed, even though some brief calls to help trainees have been published in the literature [ 6 , 7 , 8 , 9 , 10 , 11 ].
This article aims to utilize the illustrative case of the over 18,000 Indian-origin medical students enrolled in Ukraine to review the state of overseas medical students in Ukraine and war-related interruption in education. Literature, both academic and non-academic, published up until October 1, 2022, pertaining to the conflict, the impact on students, the demands of various stakeholders, and the proposed solutions, was reviewed through the use of appropriate keyword-based searches.
Overseas Medical Students in Ukraine
The 2022 conflict, by disrupting medical education in Ukraine, has impacted healthcare workforce development, not only in the country but on a global scale. To recognize this, it is essential to note that a large number of overseas individuals, including from India, had historically been part of Ukraine’s populace [ 12 ]. Before the crisis, a Ukrainian Ministry of Education report had indicated that over 80,000 students from over 150 countries had been enrolled in Ukraine [ 5 ]. Of these, nearly half were in professional education related to healthcare, with over 26,000 students from overseas enrolled in Ukrainian medical schools. Many of these schools often had more than 50% of their class strength constituted by overseas students. In particular, estimates from India state that almost 18,000 Indians were enrolled in medical schools across Ukraine before the war [ 13 , 14 ]. These students were among the first to be affected by the invasion since several Ukrainian medical schools with Indian students were in the eastern part of Ukraine, which was the first region to be invaded by Russia [ 15 ]. Similarly affected were the thousands of Pakistani-origin students enrolled with them as well [ 16 ].
The multidimensional impact on these students carries implications for the healthcare workforce, not just in South Asia where most of these physicians-in-training return to practice, but across the world. For instance, in the United States (US), a 2021 report by the Federation of State Medical Boards (FSMB) indicated that international medical graduates (IMGs) constitute over a fifth of all licensed US physicians [ 17 ]. Similarly, the General Medical Council (GMC) of the United Kingdom (UK) reported that more individuals (IMGs) from outside the UK and Europe joined the UK medical workforce in 2020 than those from the UK and Europe combined [ 18 ].
The majority of these overseas students have been evacuated by their respective governments, with India having had a particularly high rate of successful evacuations [ 19 , 20 ]. However, given that they cannot continue their medical education in Ukraine for the foreseeable future, significant concerns remain. Discussed below is the impact thereof and challenges behind the educational reintegration of overseas candidates of Ukrainian medical education, in particular from India. As of October 1, 2022, relevant national administrative organizations in India have not decided favorably regarding their reintegration into Indian medical schools. Hence, we also highlight potential solutions to the challenge of reintegration.
Medical Education in Ukraine
A comprehensive understanding of why there are over 18,000 Indian students enrolled in Ukrainian medical schools may be obtained by examination of the pre-crisis state of medical education in Ukraine and India. Recognition of this historical context is also critical in appreciating the nuances of and the potential challenges against reintegration, particularly from financial and ethical perspectives.
Medical school in Ukraine begins straight after high school, similar to the arrangement in India, Pakistan, Bangladesh, and Sri Lanka, along with the majority of spots in the UK and Europe, amongst others. This is a five-and-a-half-year course, after which the students are awarded the Bachelor of Medicine & Bachelor of Surgery (MBBS) degree. The course includes one year of a compulsory rotatory internship, wherein MBBS candidates work in major clinical departments with a provisional medical license, but under senior supervision and with a limited scope of practice.
India’s National Medical Commission (NMC), the erstwhile Medical Council of India (MCI), currently recognizes MBBS degrees from 45 medical schools in Ukraine for practice in India. For these foreign medical graduates (FMGs) to obtain licensure to practice, they must complete their internship in that foreign country and then clear the MCI Screening Test. This criterion-referenced test, now widely known as the Foreign Medical Graduates Examination (FMGE), was started in 2002 and has historically had dismal pass rates [ 21 , 22 ]. Held biannually, it is anecdotally known that those failing to clear it attempt it several times. After passing FMGE, FMGs may either practice as general physicians or attempt to get selected for residency training in India.
Medical Education in India
Given the rapidly evolving nature of events, the terminology related to medical school admissions is described below. The country has over 550 NMC-accredited medical schools which offer over 80,000 positions annually for a five-and-a-half-year-long undergraduate MBBS program. Unlike several other countries that utilize a holistic application system, such as the US, UK, Canada, and Australia, the Indian system continues to depend only on an annually held, standardized, norm-referenced test.
Admission to medical school is thus based solely on the test-day performance on a single examination, called the National Entrance cum Eligibility Test – Undergraduates (NEET-UG). Candidates obtaining a score higher than a set threshold, which is determined by the National Testing Agency (NTA) of the Government of India, are said to have ‘qualified’ NEET-UG. This, by no means, is a guarantee of a position, as over 50% of the test-takers qualify [ 23 ]. It merely indicates that the candidate is suitable for proceeding with medical education either in India or abroad since all students going overseas must necessarily ‘qualify’ NEET-UG [ 24 ]. In addition to their score, each examinee receives an all-India rank (AIR), as well as a ‘category rank’.
Private medical schools are permitted to offer all their seats to ‘general category’ candidates, that is, they are permitted to not have affirmative action policies. Meanwhile, the system offers, in the case of publicly funded schools, nearly half the spots for the general category, and reserves the other half for candidates from historically marginalized groups. Major reserved categories include Scheduled Castes (SC), having 15% of these spots reserved, Scheduled Tribes (ST) having 7.5% spots reserved, and Other-Backward Classes belonging to Non-Creamy Layer (OBC-NCL), having 27% reservation [ 25 ]. This represents a formal fulfillment of an affirmative action policy, given that these groups are considerably under-represented in medicine. This system of reservation has also contributed to considerable hostility amidst candidates not belonging to reserved categories, a fact that is of consideration in the overseas education issue [ 26 ].
Post-examination, multiple rounds of a process called ‘counseling’ occur wherein the candidate digitally submits a rank order list of preferred schools and the system allots their best possible choice of the institution based on their AIR, category rank, and the number of positions remaining – the process repeating several times until all spots have been filled. Thus, the first ranker has access to all spots in the country, while somebody having an AIR of 10,000, would expect to obtain a spot that may not be at the top of their list, more so if they belong to the general category. Notably, the competitiveness and the processes associated with NEET-UG are quite similar to the annually held exam used for residency selection, known as the NEET-Post-Graduate (NEET-PG).
Two financial tiers of undergraduate medical education exist in India, one having heavily subsidized spots, and the other having fully self-funded ones, with some differences in quality and extreme differences in cost between the two. Typically, the subsidized education is through (1) all spots at publicly funded medical schools, more commonly known in India as Government Medical Colleges (GMCs), or (2) some spots in select private institutions where the provincial government has asked for earmarking of subsidized seats. The remaining seats, typically always in private institutions, require the candidate to submit typically a few orders of magnitude higher tuition fees than subsidized spots. This is further compounded by publicly funded medical schools having a generally higher quality of clinical training [ 27 ], as reflected in both national hospital rankings published annually by the Government of India [ 28 ] and in medical school rankings of external agencies [ 29 ]. For instance, one major private ranking system ranked only publicly funded schools as the top ten in India [ 30 ].
Factors Driving Pursuit of Overseas Medical Education in Ukraine
Popular destinations for Indian students who move abroad for medical training include Russia, Ukraine, the Philippines, Germany, Kazakhstan, and China [ 31 ]. Among these, several factors have come together to make Ukraine a highly preferred destination for Indian students, with the chief factors being (1) a mismatch between the number of applicants and the number of subsidized medical school seats in India, (2) the cost of non-subsidized medical education in India, compared to Ukraine, and (3) quality and recognition of education in Ukraine compared with other overseas alternatives.
(1) Supply-Demand Mismatch
The primary factor which drives students to pursue medical education is the extremely competitive nature of medical school admissions in India. In 2021, over 1.6 million candidates registered for the NEET-UG, while the total number of available medical school spots was 83,075, resulting in a supply-demand mismatch of 20 times [ 32 ]. Of these spots, those at publicly funded schools are more competitive, stemming not just from the better clinical education, but also their affordability compared to privately funded schools.
This mismatch is supposedly worsened for ‘general category’ candidates because half the seats in government-funded medical schools are reserved for certain communities [ 33 ]. As further described below, private schools in India frequently cost more than foreign medical schools. Hence, many candidates, particularly from lower- and lower-middle-class families seek opportunities abroad if unable to secure a spot in India.
Meanwhile, admission to Ukrainian medical schools has historically been far less competitive. Their self-stated primary admission requirement has typically been that candidates must have scored at least 50% in their high school final examinations. that is, the ‘10+2 board examination’ in the home country, with no additional test-taking required.
(2) Lower Attendance Costs at Ukrainian Medical Schools
Tuition fees in Indian privately funded schools can be as high as 13.3 million INR (almost 180,000 USD) for the entire course – an expenditure that is typically out of reach for the average Indian aspirant [ 9 ]. Meanwhile, tuition fees in most Ukrainian medical schools are known to be much more affordable, costing around 30,000 USD for the entire course [ 34 , 35 ]. Additionally, attendance costs in Ukraine are lower than in most other popular foreign destinations for Indian medical students. For example, in Russia, Kyrgyzstan, and Poland, attendance costs for the entire MBBS course are approximately around 41,000, 36,000, and 72,000 USD respectively. Finally, the cost of living in Ukraine is comparatively low, travel to Ukraine is relatively cheap, and travel within Ukraine is subsidized for medical students [ 35 , 36 ].
(3) Quality and Recognition of Ukrainian Education over Alternatives
Several factors related to the quality and the international recognition of the coursework have made Ukraine a more attractive choice. First, in most of the popular locations for overseas medical education, the country’s national language is the typical medium of instruction. For example, in China, as of 2021, only 45 medical schools out of over 420 had English as the primary medium of instruction. Similarly, in Russia, only 25 out of 70 medical schools utilize English instruction [ 37 , 38 ]. In Ukraine, however, English has uniformly been the medium of instruction.
Second, for Indian students who may wish to return to their home country, trends in the biannually held FMGE are a major factor of consideration. The national pass rates of graduates from Ukraine are higher than those of other countries. Official data spanning from 2015–2018 report that 16% of Ukrainian graduates passed the FMGE, compared to a global pass rate of 14%, and pass rates of 12% and 13% among graduates from China and Russia respectively [ 39 ]. Further, recognizing the needs of these Indian students, numerous private institutes have opened in Ukraine offering classes for the FMGE. Pre-crisis, the Ukrainian Government, through its official reports, had also indicated support for the home return of overseas candidates [ 5 ]. Notably, no academic literature exists regarding the outcomes of those failing the FMGE, especially concerning the mean number of attempts required, how many FMGs finally practice in India, and how many emigrate.
Third, MBBS degrees awarded in Ukraine are recognized in India, the US, Canada, the UK, and most countries in Europe, ensuring that candidates can return home or go elsewhere for further training or general practice. The vast majority of Ukrainian medical schools are listed in the World Directory of Medical Schools (WDOMS) – a database maintained by the World Federation for Medical Education (WFME) and the Foundation for Advancement of International Medical Education and Research (FAIMER) [ 40 ]. Thus, these schools are recognized by the Educational Commission for Foreign Medical Graduates (ECFMG), an organization headquartered in the United States (US), but responsible for primary source verification (PSV) for medical regulators in the US, Canada, UK, Australia, and so on. For comparison, at the time of writing, from China, only 162 medical schools, out of over 420, are listed as operational on WDOMS [ 41 ]. However, the authors of this work do note that the WDOMS/WFME accreditation process is now changing – it is moving from the listing of individual schools in different countries to the accreditation of the national body overseeing schools in the country [ 40 ]. Further, Ukraine is part of the European Higher Education Area (EHEA), and follows the Bologna process for the standardization of European higher education, unlike China, Russia, and the Philippines, for instance [ 42 , 43 , 44 ]. Additionally, Ukrainian medical school degrees are recognized by the UK’s General Medical Council. This means that graduates have the opportunities available for training and practice in the high-income countries of North America or Western Europe, should they wish to do so.
War-Related Impact on Returning Medical Students
Prior studies from medical students in other war-torn countries provide some indications regarding the possible current mental status of returned students. These studies reported heightened levels of anxiety, depression, and suicidal ideation in their participants [ 45 ]. Besides fearing for their well-being, shelter, food, and transport, affected students reported significant uncertainty regarding their clinical competence and career prospects, with this uncertainty being a contributory factor to poor mental health [ 46 , 47 ]. Similar parallels may be drawn regarding the students from Ukraine. Likely, the destruction of their second home and the deaths of its people have had a significant impact on the students that have safely escaped. All this comes in the background of the COVID-19 pandemic, where medical students particularly have already had their education compromised, and education-related stress heightened [ 48 , 49 ].
Continued education in Ukrainian medical schools is uncertain, with a low likelihood of return for these overseas students. Some schools have resumed online classes for these students and declared that they will hold exams later in the year, in safer parts of the country [ 50 ]. However, detailed instructions are sparse.
For students who wish to continue their education in India, their prospects are just as unclear. Individuals at different stages of their six-year medical school program face different challenges. Candidates early in their medical training may be concerned about the prospect of preparing for NEET-UG once again, having already spent significant time and effort to obtain a medical training spot abroad. Preparing for this exam, which is based on high school subjects and requires focused preparation for several years, will be more difficult with each year of medical training completed. Meanwhile, senior medical students may face concerns about whether their years of training, almost to completion, will need to be repeated. Notably, FMGs have historically had to complete the internship year in the overseas country for becoming eligible to take the FMGE. Without being eligible to take the FMGE, an exam for which there has never been a mass exemption granted, overseas students may potentially never be able to practice in India.
Protests and Demands of Returning Students
Since their return to India, returning students have struggled, initially with uncertain directions from authorities, and later, with an outright refusal of support from national organizations. After their return in February-March 2022, aggrieved students filed several public interest litigations (PILs), that is, ‘litigations undertaken to secure public interest and demonstrate the availability of justice to socially disadvantaged parties’, in the Indian Supreme Court, as well as the New Delhi High Court seeking clarifications regarding their continued education. Their plea to the Supreme Court also sought for the Indian government to provide an orientation program for potential admission to Indian medical schools [ 51 ]. The Indian Medical Association (IMA), the pan-national body of Indian physicians, wrote a formal letter to the Prime Minister in support of these students [ 52 ].
Primarily, these students have demanded reintegration into publicly funded Indian medical schools through direct lateral entry, the same ones described above as being the most competitive institutions for obtaining admissions through the NEET-UG. On May 15, 2022, overseas students hailing from the state of Tamil Nadu, staged a large protest in the state’s capital Chennai, requesting the state and Central governments to look into their concerns [ 53 ]. Similarly, on May 17, 2022, a group of these students from the state of Uttar Pradesh (UP), met the state’s Chief Minister, asking for a continuation of their education in any of the state medical schools [ 54 ]. Additionally, parents of overseas medical students formed a body to have their demands better heard, named the ‘Parents’ Association of Ukraine MBBS Students’. The latter held a major press conference on June 23, 2022, expressing their concerns about their children’s academic losses, and seeking urgent federal intervention to accommodate their children at the local medical colleges as a one-time measure [ 55 ]. On June 25, 2022, a large group of students and their parents from multiple states, staged a demonstration outside the NMC office in New Delhi, the country’s capital, reiterating their demands [ 56 ]. June 26, 2022, saw another group of students start a hunger strike in the nation’s capital, in the hopes of prompting urgent national action [ 57 ].
Multi-Dimensional Challenges to Reintegration
Significant challenges hinder the reintegration of overseas medical students into established Indian medical schools. In addition to ethical challenges to equity and justice, there are numerous logistical barriers to potential solutions, including but not limited to the admissions process, medical school capacity, and academic overburden on clinical faculty. Importantly, the Government of India has no legal obligation to ensure the completion of these students’ medical training, even though arguments may be made regarding a moral obligation [ 58 ]. Furthermore, while these individuals may be seen as a potentially useful future healthcare workforce, their current status as students requires a considerable investment of public and private resources, thus preventing the enforcement of a moral obligation for non-home countries to help in the reintegration process.
The decision to reintegrate carries ethical concerns of equity and justice. It must be understood that while competition is significant for any publicly funded medical school spot in India, it is vastly more intense for the top-ranked colleges. It is widely known across the country that pre-medical students in India, who have secured sufficiently high ranks in the NEET-UG, had historically begun preparations for the exam at the start of high school at the latest and frequently even earlier. Given the pre-existing supply-demand mismatch, there exist several individuals who, because of their rank, had to opt for an institution that they did not originally want, because that was the spot available to them, or had to join private schools at significant cost. For these individuals, who obtained better ranks than the Ukrainian students and are studying in India, the reintegration of lower-ranked overseas candidates into schools ranked better than their current ones would be unjust and would go against the principle of equity. This concern is further aggravated when one considers the case of low-income Indian high school students. Often, students from resource-limited families see the publicly funded medical school spots as their primary source of upwards mobility, given that they would be unable to pay the fees for education either in private institutions in India or in Ukraine. While relevant academic literature is limited, it is widely known in India that there is not an insignificant number of contemporary students who could not obtain a publicly funded medical school spot and had to take a year off to prepare again for the annual examination. Thus, permitting the returned students to join local medical schools would potentially be a violation of the merit-based system that is the fundamental basis of NEET-UG.
Consider the complex scenario where these students are permitted to enter Indian medical education. With over 550 medical schools in India, it is hypothetically possible to accommodate the vast majority of these students. Historically, ranks of medical schools have driven applicant choice, with the schools themselves lacking any say in selecting candidates. The top rankers in the NEET-UG uniformly choose the top-ranked colleges [ 59 ]. Thus, these students’ demand for publicly funded medical spots has an unclear basis, given that most students studying in Ukraine had not secured a high enough rank to secure a publicly funded spot, driving their pursuit of overseas education [ 60 , 61 ]. This point is best highlighted by the case of allotting a Ukrainian return student an additional spot at the All India Institute of Medical Sciences (AIIMS), New Delhi. For a general category student to gain admission to the historically consistent number one medical school choice opted for after NEET-UG, they must typically score among the top 100 students in the >1.6 million test takers annually. Those obtaining admission to AIIMS New Delhi, receive cultural adulation in a manner, akin to hero worship, that may be challenging to fully comprehend for non-Indian residents [ 62 , 63 , 64 , 65 , 66 , 67 ]. Thus, the allotment of such a prized spot to a Ukrainian may lead to considerable discontentment amongst previous test-takers, and may likely lead to widespread protests.
Additionally, several logistical questions come to the fore. Should the students be assigned only publicly funded schools, given that they are under the purview of the government; or should privately-funded schools also be asked to help with the reintegration? What determines the number of students allotted to each Indian institution – should it be based on the existing number of approved seats, for instance, a 20% additional capacity for accommodating Ukrainian students per institution? Should medical schools themselves have a say in this new allotment? Given the intensely ranked-choice nature of medical school selection in India, what factor basis should drive the assignment of overseas students to Indian schools? Given the differences between Indian and Ukrainian curricula, how much credit should be transferred? Consider, for instance, third-year Ukrainian medical students requesting the maximal amount of their education be considered for credit back – two years – are those two years of Ukrainian education sufficient for Indian standards, given the new vertically integrated NMC 2019 curricula? Such questions remain unclear.
Finally, questions regarding the baseline and the final competency of these candidates have been raised, the former being more justified than the latter. With regards to their baseline competency, these candidates typically scored much lower on the NEET-UG than their counterparts training in medical schools in India, forcing them to move to foreign medical schools [ 68 , 69 ]. However, given the lack of literature, it is unclear as to what level of baseline competency in NEET-UG is an appropriate predictor, if at all, of being a safe and competent physician. With regards to competency after medical school, the dismal pass percentages in the FMGE, typically between 10–20% overall per year, have raised warranted questions about the quality of medical training in foreign schools [ 39 , 68 ]. While these questions regarding the possession of required competencies by graduating students are justified, it should also be considered that medical graduates from India currently do not give any sort of exit exam. It may well be possible that not dissimilar pass rates may be seen for Indian medical school graduates upon being mandated to take the same exit exam. Notably, a national exit exam (NEXT) is planned for the future, which is currently planned as an annually held test to be taken by all Indian and foreign graduates, whose passage will provide a license to practice and scores on which will provide ranks for residency selection [ 70 , 71 ]. Thus, the purposes served by FMGE and NEET-PG for foreign graduates will be served together by NEXT in the future.
Potential Benefits of Reintegration
Despite these barriers, these students are Indian citizens and physicians-in-training, many hoping to contribute to the country’s overburdened healthcare system. The country has a significant deficit of trained healthcare workers, having far fewer physicians than the World Health Organization’s (WHO) recommendation of 10 doctors per 10,000 people [ 70 ]. While estimates vary, an analysis of labor databases managed by the National Sample Survey Office (NSSO) of the Government of India, had reported that the number of active, adequately qualified physicians was only 5 per 10,000 people in 2018 [ 72 ]. Data published in 2019 by the WHO itself indicated a ratio of 7.4 physicians per 10,000 people [ 71 ].
Rural areas bear the brunt of physician shortage due to heterogeneous distribution and clustering. Physicians typically prefer to practice in urban areas, with commonly cited reasons being better infrastructure along with greater opportunities for career progression and family support in these areas [ 73 ]. In 2015, it was reported that almost 10% of primary healthcare centers – the first point of contact between village residents and a physician – did not have a single doctor. In community health centers (CHCs), the next tier of rural healthcare, the situation was even direr. CHCs are officially recommended to have one physician, one surgeon, one pediatrician, and one gynecologist, yet in 2015, there were shortages of around 80% for each specialist [ 74 , 75 ]. Unfortunately, projections for the future have predicted little improvement. The analysis of NSSO data projected that the density of skilled healthcare workers would remain largely unchanged in 2030, while a slightly older analysis of the MCI’s database of registered doctors projected that India would have around 1 million active physicians in 2030, compared to a requirement of 1.5 million physicians [ 72 , 73 , 76 ].
From an ethical perspective, it may be argued that India strongly needs a much larger physician workforce, but provides limited training opportunities, leading to aspirants seeking the best possible alternatives. The country also suffers from considerable emigration, with a 2017 analysis reporting that over 90,000 Indian medical graduates were in active practice overseas [ 76 ].
From a financial standpoint, allowing these students’ training to be passively wasted would be a significant loss, given that state and federal governments in India spend a significant amount per year of publicly funded medical education [ 77 , 78 ]. The total amount for educating an MBBS student at AIIMS was estimated to be close to 17 million INR, as per a formal estimation using traditional costing methodology, that was published in 2013. Data collection for this estimate was carried out over thirteen years ago, so the cost has likely increased considerably since then [ 79 ]. Thus, the Indian government could save a significant amount by building on the partial training obtained by students in Ukraine. Graduating these students rapidly for entering into residency training may potentially provide India’s healthcare system with a vital injection of manpower and also add considerable economic value.
One potential nuance to this issue is having reintegration at the juncture of preclinical and clinical education in medical school. Compared to clinical training, preclinical education in medical schools across countries is more standardized, has curricular similarities, and shares common reference textbooks. While courses across countries may be structured differently, some disciplines – anatomy, physiology, pathophysiology, pharmacology, biochemistry, microbiology, immunology, genetics, molecular biology, and neuroscience – typically form the core of preclinical education worldwide. Meanwhile, undergraduate clinical education, given its focus on learning patient-centered care, is more tailored to local requirements and curricula. Most clinical subjects require students to have mastered communication in the predominant language of the patients coming to the affiliated hospital of their medical school, even though the medium of instruction may be different. Thus, assessing competency in preclinical subjects and thereafter transferring requisite credits may be done more reliably. In India, the rigid curriculum set by the NMC mandates the primary teaching of preclinical subjects must occur in the first two years, with minimal curricular flexibility permitted to individual medical schools, allowing for high levels of standardization. Thus, returning students who have completed their preclinical education in Ukraine may be reliably given transfer credits for two years of medical school in India.
While no formal economic analyses regarding the benefit of reintegration in this case have been published, we provide below a brief estimation that is based on several major assumptions. Let us assume that of the 18,000 Indian medical students in Ukraine, nearly 80% (N = 15,000) are rescued safely, a figure more conservative than official estimates, and wish to continue to continue their education and all of them apply for formal reintegration into government medical schools. Further, assuming that these students are uniformly distributed through different years of medical school, the current median education of a current student comes out to be year three. Given that the student has completed competency-related exams for two years, it may be reasonable to provide two years of transfer credits. Thus, in total, India will gain 2*15,000 person-years of completed training. If the traditional costing data from AIIMS of 3,131,000 INR per student per year is used, an expected total savings of 93,930,000,000 INR (93.93 billion INR or 1.15 billion USD) may be potentially made. While this number may be adjusted downwards given that educating a student at the most competitive medical school in India is likely to be amongst the costliest, consideration could also be made for adjusting upwards inflation, since data for the costing was reportedly collected during 2007–08 [ 79 ]. Unfortunately, we must acknowledge one glaring limitation to this estimate – to the best of our knowledge and literature search, there exist no newer Indian data regarding costs, be it from AIIMS or other medical schools. Usage of the AIIMS-estimated cost per student per year requires a high level of caution, given that its reporting article has major limitations and non-financial conflicts of interest – two of its authors were the founding editors-in-chief of the same journal, of which it was the first research article in the journal’s first published volume [ 79 ].
Nevertheless, while our figures are highly preliminary, these data do warrant grounds-level formal costing by the NMC and/or the Ministry of Health and Family Welfare (MoHFW), given that no national data could be found. A grounds-level costing may not only help the federal government estimate the public benefit of reintegration, but it may also help them in notifying all public medical schools to charge overseas returning students the same (or higher) annual fees that the costing provides. Meanwhile, the standard students enrolled through routine NEET-UG admissions would be charged the routine, highly subsidized fees. In this way, the medical education of these students remains self-funded, initially for two years in Ukraine and later in India. Thus, it would potentially not burden the economy, while helping add to the country’s healthcare workforce.
Current State of Government Support for Reintegration
Currently, there exists little formal support for reintegration in Indian medical schools, particularly amongst the national authorities, despite several large-scale protest marches [ 80 , 81 ]. While no academic literature exists on this evolving subject, potential reasons behind the denial of the demand for reintegration are manifold, including those stated by the Government itself, as described below along with the evolving response of national authorities.
The Union Minister of State for the Ministry of Health and Family Welfare (MoHFW), Government of India had declared on July 22, 2022, that there were no legal provisions to accommodate these students in Indian medical schools. The National Medical Commission (NMC) had a similar stance of opposition to either accommodation in India or transfer elsewhere [ 80 , 81 ]. However, on August 3, 2022, the Committee on External Affairs (2021–22), in a report to the Indian Parliament, stated that the Ministry of External Affairs had recommended the MoHFW to allow these students to be enrolled in private Indian medical schools on a one-time exemption basis. As per the report, the committee believed that this was the only solution to the problem of these students and the only way they can complete their courses [ 80 , 81 ].
The Supreme Court, starting on August 26, 2022, then heard the case of seven petitions by affected students, who requested an appropriate solution given the recommendation of the Ministry of External Affairs. Here, the Court initially commented that these students were ‘not meritorious students in India’. In response to opposition from the students’ representative, who stated that these students had indeed cleared the NEET-UG, but could not afford privately funded medical schools, the Court retorted that regardless of their actual merit, these students had voluntarily chosen to go to Ukraine. This notwithstanding, their representative pointed out that the current situation was an extraordinary one and sought for the Supreme Court to direct the Central Government to act on the Ministry’s recommendation. He argued that the Government could exercise extraordinary powers under Section 45 of the NMC Act 2019 and direct the NMC to make an exception for these students. Additionally, the bench was made aware of the fact that students from other foreign countries, who had completed their MBBS studies, but not their internship due to the pandemic, had been permitted by the NMC to do the same in India. While Ukraine-returned interns had been given the same exception, provided they clear the FMGE, this would not apply to all the Ukraine returnees, as many of them had not reached internship yet [ 82 , 83 , 84 ]. The hearing was concluded by issuing notice on September 5, 2022.
The Solicitor General of India, representing the NMC, requested the Supreme Court for adjournment, in order for the NMC to deliberate [ 84 ]. The court agreed to adjourn the case till September 15. 2022. At this juncture, the NMC, in a reversal from its opposition [ 81 ], released a statement that it had no objection to any ‘academic mobility programs’ (AMP), that is, programs implemented privately, that allowed students to continue their education in countries other than Ukraine or India. However, the NMC clarified that the final MBBS degree must be awarded only by the original Ukrainian university and that these students were still required to pass the FMGE if they wished to return to India [ 85 , 86 , 87 ]. Meanwhile, several foreign medical schools, sensing an opportunity through the AMP, hiked fees from a maximum of 5000 USD/semester to 7000 USD/semester [ 85 , 86 , 87 ].
On September 15, 2022, the Central Government informed the Supreme Court that these students cannot be accommodated in Indian medical schools due to the absence of any such provision in the NMC act. Here, they stated their opposition to reintegration in India on the following grounds: (A) measures allowing such students might hamper the standard of medical education in India (B) these students went to Ukraine for two main reasons – low scores in NEET and affordability. Allowing students with poor merit in premier medical colleges in India could lead to further litigation. (C) These students wouldn’t be able to afford the fee structure in these private Indian colleges. Additionally, the Central Government, along with the NMC, professed their support for the official implementation of an AMP. However, the petitioners objected that there were not enough spots available in this program to accommodate all of them [ 85 , 86 , 87 ]. In response to this, the very next day, on September 16, the Supreme Court asked the Central Government to consider creating a web portal with details of foreign medical schools, where Ukraine-returned students could apply to complete their courses under the approved AMP [ 89 ]. On September 22, the NMC declared three medical schools in Georgia approved under the AMP [ 87 ], and on September 23, the Central Government officially informed the Supreme Court that the concerned federal organizations were working on creating the portal as requested [ 90 ]. However, they clarified that this program could not be used as a ‘backdoor entry’ to Indian colleges [ 88 ].
Along with the three major reasons stated by the Central government in its affidavit opposing reintegration, another major barrier to federal support is the likely fallout expected amongst large parts of the national populace if reintegration into publicly funded institutions is done. The NEET-UG and/or its predecessor (called AIPMT) have held historically high levels of socio-cultural significance [ 62 , 63 , 64 , 65 , 66 , 67 ]. NEET-UG is widely perceived as an engine of upward mobility and a pathway to generational success, similar to China’s National College Entrance Examination (NCEE), GaoKao [ 91 , 92 , 93 , 94 ]. The NEET-UG is administered by the National Testing Agency (NTA) of the Indian government itself, unlike most standardized tests worldwide such as MCAT, SAT, ACT, GRE, TOEFL, and OET, which are administered by private organizations. Notably, concerns have been raised regarding the supposed ‘non-profit’ classification of these administering organizations, which grants them tax deductions, but also permits them to charge significant fees for the exam and related preparation material [ 95 , 96 , 97 , 98 ]. NEET-UG must strictly adhere to curricula and textbooks developed by the National Council of Educational Research and Training (NCERT), an organization under the Government of India. All core textbooks, the material of which NEET-UG questions have to be framed material, are freely available online, while their hard copies are sold without profit to the government [ 99 , 100 ]. All of this has served to democratize access to and preparation for NEET-UG, for which students start preparing typically from grade 11 (two years of preparation), less commonly from grade 8 (four years of preparation), and rarely in grade 6 (six years of preparation) [ 94 , 9 ]. Affordable offline and online learning programs exist, including free classes on YouTube, where students learn material beyond their current grades in order to become ready for the NEET-UG, a praxis also performed by all authors of this review. A culture has thus long existed where NEET-UG aspirants and their parents believe that years of hard work will prove to be the deciding factor in scoring well and thus putting them on an upward trajectory, similar to the ‘Gaokao’ [ 62 , 63 , 64 , 65 , 66 , 67 , 91 , 92 , 93 , 94 ]. An attempt at reintegration is likely to be perceived to be against the decades of meritocracy that has been espoused culturally, and may incite mass public unrest. Therefore, the NMC and the Central Government have been hostile to the idea of reintegration, and no permissions have been granted at a national level from either of the legislative, the executive or the judiciary. In response, student protests across the country have continued.
Some state governments have extended support to these students, while the Supreme Court deliberates on the issue [ 14 , 17 ]. The government of the state of West Bengal permitted 412 students hailing from the state to continue training in the state’s publicly funded colleges. While initially appointed as observers, they were later allowed to attend lectures and practical classes. Of these, 78 students who had taken the same year’s NEET-UG were allowed to undergo counseling for ‘management quota seats’, typically the most expensive spots in private medical schools [ 101 ]. In March 2022, the health minister of the state of Karnataka had announced that around 700 returned medical students would be accommodated in around 60 different medical schools in the state. However, this announcement has not come to fruition. Similarly, in July 2022, the Chief Minister of the state of Tamil Nadu reiterated the state’s support for these students and requested that they be accommodated, in response to the central government’s statement to the Supreme Court [ 102 ].
Possible Alternatives
There exists a need to examine all possible solutions to this issue and achieve consensus in consultation with several stakeholders, given that ‘direct reintegration into publicly funded medical schools’ represents a highly contentious option. Compared to this solution where consensus would be difficult, these alternatives may carry fewer socio-cultural and/or legal barriers, which may lead to potentially faster implementation. This is important given that these students were in the midst of their education, and the break in education may impact their future competency as physicians, given that interruptions in in-person clinical education from the now-receding COVID-19 pandemic still linger [ 103 ]. Additionally, if the pathway chosen is contentious, it may lead to further delays secondary to legal disputes, appeals, challenges in higher courts, retrials, appointments of task forces, and the like. Amidst this, the less privileged returning students will most suffer, given that inequity and disparities in medical education in India continue to rise [ 104 ].
One option, which is well-supported by current Indian medical students, is the retaking of NEET-UG in the next cycle by concerned candidates. While it fully complies with existing admission guidelines of NMC, it does raise questions of deliberate waste of resources and harsh decision-making for candidates afflicted by extraordinary events ( force majeure ). It is being estimated, informally, that nearly a third of returning students from Ukraine did take the NEET-UG [ 105 ]. Other than students in their internship year in Ukraine, students in all other years have been concerned about the prospect of performing well in the NEET-UG, having already spent significant time, money, and effort in obtaining medical education overseas. Preparing for NEET-UG, which requires standardized test-taking practice along with knowledge of physics, chemistry and biology, will be more difficult with more time invested in medical education. However, it does satisfy the harsh criteria of norm-referenced testing and meritocracy in a country granting these attributes socio-cultural sanctity [ 62 , 63 , 64 , 65 , 66 , 67 ], notwithstanding their inherent limitations.
Another potential solution is the transfer of these candidates to other foreign medical schools, with governmental and/or non-government-organizational support, as evident in the AMP. This avenue has been utilized by a few overseas students to continue their education in Georgia, Kazakhstan, and Kyrgyzstan, among others, being possible mainly through existing tie-ups between these schools and Ukrainian schools. While this system had been in place pre-crisis, albeit not as a governmental initiative, it had two main issues: (1) until recently, it had no official support, and (2) it was highly dependent on the whims of these schools, as well as middlemen, who often exploited these students to earn greater commissions [ 81 , 85 , 86 ]. There have been allegations of Ukrainian universities and the agents common between the Ukrainian universities and universities in other countries, of not releasing their marksheets and other educational documents, in an effort by the universities to hold on to their students [ 81 ]. Some Ukrainian universities have asked their students to come to the still-war torn country and pay their full due fees and collect their documents. However, with the recent announcement of support from the government and the NMC, it is likely that a fair, non-exploitative system can be created. As it stands today, the inclusion of more participating schools is needed, but it represents an ethically gracious and equitable solution to these sufferers of extraordinary events. Foreign medical schools need to roll out detailed transfer pathways and associated policies, specifically for Ukraine-evacuated students, in a timely, transparent manner. This solution is formally supported by the authors of this review, even though it requires significant logistical maneuvering, including governmental efforts from India as well as the recipient country.
Meanwhile, returning students have themselves been searching for options. Education consultants have reported that medical schools in Bangladesh, Nepal, and Kyrgyzstan have received significant interest [ 106 ]. Russia has announced that these students may continue their education there, with some universities even offering discounts on tuition and accommodation fees [ 107 ]. However, given their status as primary aggressors in this conflict, many students have expressed opposition to this [ 108 ]. Given the concerning status of all individuals leaving Ukraine, it may be argued that there exists some degree of moral imperative for high-income countries to incorporate these students into their own medical schools. The counterargument is that these returning students are distinct from Ukrainian refugees, who have been defined by the 1951 Refugee Convention to be ‘someone who is unable or unwilling to return to their country of origin owing to a well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group, or political opinion’ [ 109 ]. For HICs, these Indian-origin students are potentially immigrants, and likely no ethical obligation exists for integrating students. Similar to India, considerable public discontentment may potentially occur in HICs as well if medical school spots were provided to non-Ukrainian immigrants.
Another solution, fully discussed for the first time in this article, is to reintegrate all returning students through a one-time mandated expanded enrolment by 10–20%, at all medical schools in India, both public and private, a capacity expansion size that would avoid significant overburdening. While this solution requires considerable legal support and faces the challenge of fair allotment of medical school spots, it is, however, ethically appropriate. The difficulty would be in deciding on a merit list based on which a round of counseling may be carried out. Creating a new rank list may be done in several ways – (A) using the original NEET-UG percentiles of returning candidates, a method that is fair, equitable, and feasible; (B) using students’ performance in the Ukrainian medical schools, which may have problems related to transcript verification, and difficult logistics of merging different grading schemas into one standardized measure through manual assessment; or (C) using a new norm-referenced examination, testing knowledge of basic sciences, held solely for Ukrainian medical students, which is fair but faces financial and logistical barriers to designing and conducting a national examination.
Each solution to this complex issue carries its limitations. However, given that over six months have passed since the return of the students, additional delays may decrease the utility of this large future workforce and may lead to further unrest. A lack of public clarity and transparency regarding newly proposed regulations related to FMGE and foreign medical schools has led to systemic uncertainty [ 110 ]. National advocacy and urgent decision-making are required to ensure the maximum benefit to the currently involved students, future enrollees in foreign medical schools, and the country’s healthcare workforce.
Conclusions
Urgent attention is needed to address the educational status of 18,000 Indian medical students, who await clarity following their return from Ukraine more than six months ago ( Figure 1 ). Potential challenges to their reintegration into the Indian medical system include ethical and sociocultural concerns surrounding their meritocracy, as well as significant logistical hurdles. These challenges have been reflected in the less-than-favorable decisions by key legislative and executive authorities. However, given the extraordinary circumstances, the potential economic benefits to their integration, as well as the dire need for trained physicians in India, a measured approach allowing their integration could be of significant value to the country. Potential solutions, for which federal support may help, include academic mobility involving other foreign medical schools; or retaking of the medical school entrance examination by returning students; or their reintegration with credit transfer into Indian medical schools through a one-time enrollment expansion. The latter may be done using their original standardized test percentiles, or performance in Ukrainian medical schools, or new national assessment. While the involvement of all stakeholders and careful consensus-building is warranted, urgent decision-making is critical to prevent resource wastage.

Summary of major aspects related to the Indian-origin medical students who were enrolled in Ukrainian medical schools and had their education interrupted.
Competing Interests
The authors have no competing interests to declare.
Author Contributions
Shubhajeet Roy, Vivek Bhat and Ahmad Ozair authors contributed equally.
Medical education and war in Ukraine
Affiliations.
- 1 Richard is a GP and Public Health Specialty Registrar, and Honorary Assistant Professor at the University of Nottingham's Academic Unit of Population and Lifespan Sciences. At the time of writing he was providing primary care to internally displaced people in the east of Ukraine. Email: [email protected]@drricharmitage.
- 2 Mariia is a Medical Student at the Poltava State Medical University, Poltava, Ukraine. [email protected].
- PMID: 35902249
- PMCID: PMC9343034
- DOI: 10.3399/bjgp22X720329
Publication types
- Historical Article
- Education, Medical*
- History, 20th Century
- Military Medicine*

IMAGES
COMMENTS
Medical education in Ukraine is an integral part of national educational and health care system. It is considered to be one of the best in the world, despite of the Soviet Union breakup, and therefore it attracts thousands of foreign students each year. Graduates of Ukrainian medical universities are of high demand for their fundamental ...
Medical education in Ukraine is considered to be one of the best in the world. It attracts tens of thousands of foreign students each year. Graduates of Ukrainian medical universities are in high demand for their advanced knowledge and excellent practical skills. Based on the latest data, the educational potential of Ukraine has allowed it to enter the group of the top ten countries in the ...
Background As Ukraine struggles with the education of healthcare professionals due to the war, we aimed to identify the specific effects of the war on medical education, the resulting needs, and ...
Zaporizhzhia State Medical University (ZSMU) is a leader in the field of medical education and innovation in Ukraine. This 6-years undergraduate entry programme is highly competitive and aligns with European Union standards. The university has a prestigious English-language medical programme which is fully-accredited and globally-recognised.
In keeping with that in most other countries, medical education in Ukraine was deeply disrupted by COVID-19. For substantial portions of 2020 and 2021, direct patient contact and bedside clinical teaching was suspended, student instruction was delivered virtually, and summative assessments were largely conducted online. 4 The harmful impacts of ...
About TNMU. I. Horbachevsky Ternopil National Medical University of the Ministry of Health of Ukraine is a leading higher medical education institution in Ukraine, which has been training highly qualified healthcare professionals for over 65 years. Since its establishment, the University has trained more than 25,000 specialists in the fields of ...
Mariia is a Medical Student at the Poltava State Medical University, Poltava, Ukraine. moc.liamg@89oknelvapom. The Ukrainian system of medical education is considered to be both one of the highest quality and relative affordability in the world, and therefore attracts thousands of native and foreign medical students each year. 1 Medical ...
Historically, our University was the top medical educational institution in Ukraine. The Degree of MBBS (MD - General Medicine, BDS - Dentistry, Pharmacy, Nursing) of Kharkov National Medical University is prestigious and it is recognized all over the world. International students may study medicine in English or Russian optionally.
Medical education in Ukraine is an integral part of national education system. Even after the collapse of the Soviet Union,medical education in Ukraine was considered one of world's best and its reputation was still strong enough to attract thousands of foreign students each year. Its students, graduates and academics have been known and ...
Follow the complete guide to studying medicine in Britain. The number of years to study medicine in Ukraine varies by major: General Medicine (Doctor's Certificate) - 6 years. Dentistry (certificate of a dentist) - 5 years. Pediatrics (Doctor's Certificate) - 6 years. Pharmacy (Bachelor's degree in Pharmacy) - 5 years.
The Ministry of Health of Ukraine has developed the Medical Education Strategy as an integral part of the transformation of the national healthcare system. The Strategy sets the vision for the next ten years. It is essential to enable Ukrainian health practitioners to become knowledgeable and engaged professionals who provide high quality services focusing on the patient and the individual's ...
Accordingly, medical trainees and institutions must adapt to a high degree of uncertainty and turmoil. The first medical school in Ukraine was the Collegium Medicum founded in 1773 in Lviv. With the fall of the Soviet Union in 1991, Ukraine had 14 medical institutes within its borders aimed at teaching students medical and pharmaceutical ...
The author presents the concept of the study of medical education in Ukraine, which is characterized by systemic integrity and procedural continuity in the organic unity of general, special, specific and personally oriented components. The emphasis is on the world and European trends in higher education. The article analyzes the main contexts of reforming the medical education in Ukraine ...
Ukraine has over the years become a popular student-friendly destination for medical education. Its age-old academic experiences, availability of infrastructure and provision of easily accessible value-for-money educational opportunities helped it achieve the status of a global educational hub.
Medical students in Ukraine have faced extraordinary disruption to their clinical studies with both the COVID-19 pandemic and subsequent Russian military invasion forcing a majority of their learning to be conducted remotely. Over the summer of 2022, the School of Clinical Medicine, University of Cambridge hosted 20 medical students from Kharkiv National Medical University for a seven-week ...
The most prestigious medical education institution in Kiev, Kiev Medical University (KMU) is one of the best medical universities in Ukraine. The university boasts excellent teaching standards and stays up-to-date with the ongoing international developments in medical education.
Medical students in Ukraine have faced extraordinary disruption to their clinical studies with both the COVID-19 pandemic and subsequent Russian military invasion forcing a majority of their ...
2. Methods. Our university was one of the first in Ukraine to adapt to the new reality and to evaluate the quality of online learning during the COVID-19 pandemic. The current sociological study involved 169 fourth-year-students enrolled into the online studying in "Kyiv Medical University" (KMU).
Medical education and war in Ukraine Richard Armitage a Academic Unit of Population and Lifespan Sciences, School of Medicine, University of Nottingham, Nottingham, UK Correspondence [email protected]
As the Russia-Ukraine war enters its third week, the United Nations has estimated that over 2 million people have fled Ukraine,1 including international medical students studying in the country. According to the Ukrainian government, there are over 76 0002 international students enrolled in its universities. While most have chosen to leave, some have decided to remain.
Findings: Factors influencing the decision to pursue education in Ukraine and their pre-crisis pathway to home practice are first discussed. Indian-origin students have historically gone on to Ukraine after securing insufficiently competitive ranks in the national medical school entrance exam, thus preventing them from getting a heavily subsidized education at publicly funded institutions in ...
Affiliations. 1 Richard is a GP and Public Health Specialty Registrar, and Honorary Assistant Professor at the University of Nottingham's Academic Unit of Population and Lifespan Sciences. At the time of writing he was providing primary care to internally displaced people in the east of Ukraine. Email: [email protected]@drricharmitage.
In keeping with that in most other countries, medical education in Ukraine was deeply disrupted by COVID-19. For substantial portions of 2020 and 2021, direct patient contact and bedside clinical teaching was suspended, student instruction was delivered virtually, and summative assessments were largely conducted online.4 The harmful impacts of ...
The highest proportion of foreign medical students in Ukraine are from India. Sonia Sarkar reports on their experiences fleeing the invasion—and the uncertainty they have found on returning home Shreyoshree Sheel, a first year student at Ukraine's Ternopil National Medical University, loved the "academic discipline" of her university, which required her to take a test almost every day.
In our series taking you to meet medical students from across the globe from the comfort of your own home, BMJ student spoke to a medical student who has made a truly international curriculum for herself and her peers in the wake of war and destruction in her home country You have just set off from home to attend your placement or to meet your friends for a cocktail or a cup of coffee. Life ...