Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic

RELATED TOPICS
INTRODUCTION
This topic will provide an overview of major issues related to breech presentation, including choosing the best route for delivery. Techniques for breech delivery, with a focus on the technique for vaginal breech delivery, are discussed separately. (See "Delivery of the singleton fetus in breech presentation" .)
TYPES OF BREECH PRESENTATION
● Frank breech – Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term.
● Complete breech – Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
When viewing this topic in a different language, you may notice some differences in the way the content is structured, but it still reflects the latest evidence-based guidance.
Breech presentation
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Breech presentation in pregnancy occurs when a baby presents with the buttocks or feet rather than the head first (cephalic presentation) and is associated with increased morbidity and mortality for both the mother and the baby. [1] Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997. [2] Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002. There is good current evidence regarding effective management of breech presentation in late pregnancy using external cephalic version and/or planned cesarean section.
History and exam
Key diagnostic factors.
- buttocks or feet as the presenting part
- fetal head under costal margin
- fetal heartbeat above the maternal umbilicus
Other diagnostic factors
- subcostal tenderness
- pelvic or bladder pain
Risk factors
- premature fetus
- small for gestational age fetus
- nulliparity
- fetal congenital anomalies
- previous breech delivery
- uterine abnormalities
- abnormal amniotic fluid volume
- placental abnormalities
- female fetus
Diagnostic investigations
1st investigations to order.
- transabdominal/transvaginal ultrasound
Treatment algorithm
<37 weeks' gestation, ≥37 weeks' gestation not in labor, ≥37 weeks' gestation in labor: no imminent delivery, ≥37 weeks' gestation in labor: imminent delivery, contributors, natasha nassar, phd.
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Disclosures
NN has received salary support from Australian National Health and a Medical Research Council Career Development Fellowship; she is an author of a number of references cited in this topic.
Christine L. Roberts, MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
CLR declares that she has no competing interests.
Jonathan Morris, MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
JM declares that he has no competing interests.
Peer reviewers
John w. bachman, md.
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
JWB declares that he has no competing interests.
Rhona Hughes, MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
RH declares that she has no competing interests.
Brian Peat, MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
BP declares that he has no competing interests.
Lelia Duley, MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
LD declares that she has no competing interests.
Justus Hofmeyr, MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa
JH is an author of a number of references cited in this topic.
Differentials
- Transverse lie
- Antenatal corticosteroids to reduce neonatal morbidity and mortality
- Caesarean birth
Use of this content is subject to our disclaimer
Help us improve BMJ Best Practice
Please complete all fields.
I have some feedback on:
We will respond to all feedback.
For any urgent enquiries please contact our customer services team who are ready to help with any problems.
Phone: +44 (0) 207 111 1105
Email: [email protected]
Your feedback has been submitted successfully.
Advertisement

A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case–control study
- Maternal-Fetal Medicine
- Open access
- Published: 18 November 2019
- Volume 301 , pages 393–403, ( 2020 )
Cite this article
You have full access to this open access article

- Anna E. Toijonen ORCID: orcid.org/0000-0002-4812-2766 1 , 3 ,
- Seppo T. Heinonen 1 ,
- Mika V. M. Gissler 2 &
- Georg Macharey 1
9920 Accesses
28 Citations
1 Altmetric
Explore all metrics
To determine if the common risks for breech presentation at term labor are also eligible in preterm labor.
A Finnish cross-sectional study included 737,788 singleton births (24–42 gestational weeks) during 2004–2014. A multivariable logistic regression analysis was used to calculate the risks of breech presentation.
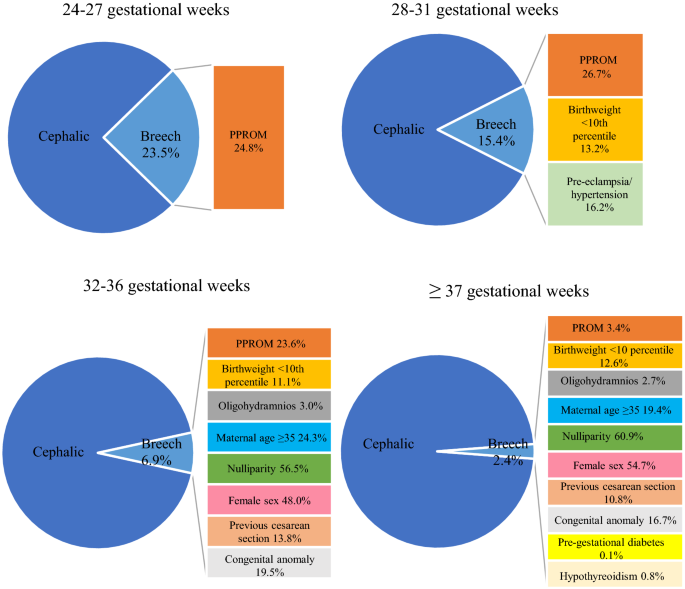
The incidence of breech presentation at delivery decreased from 23.5% in pregnancy weeks 24–27 to 2.5% in term pregnancies. In gestational weeks 24–27, preterm premature rupture of membranes was associated with breech presentation. In 28–31 gestational weeks, breech presentation was associated with maternal pre-eclampsia/hypertension, preterm premature rupture of membranes, and fetal birth weight below the tenth percentile. In gestational weeks 32–36, the risks were advanced maternal age, nulliparity, previous cesarean section, preterm premature rupture of membranes, oligohydramnios, birth weight below the tenth percentile, female sex, and congenital anomaly. In term pregnancies, breech presentation was associated with advanced maternal age, nulliparity, maternal hypothyroidism, pre-gestational diabetes, placenta praevia, premature rupture of membranes, oligohydramnios, congenital anomaly, female sex, and birth weight below the tenth percentile.
Breech presentation in preterm labor is associated with obstetric risk factors compared to cephalic presentation. These risks decrease linearly with the gestational age. In moderate to late preterm delivery, breech presentation is a high-risk state and some obstetric risk factors are yet visible in early preterm delivery. Breech presentation in extremely preterm deliveries has, with the exception of preterm premature rupture of membranes, similar clinical risk profiles as in cephalic presentation.
Similar content being viewed by others
Risk factors associated with adverse perinatal outcome in planned vaginal breech labors at term: a retrospective population-based case-control study, breech presentation at term and associated obstetric risks factors—a nationwide population based cohort study.
Risk factors for adverse outcomes in vaginal preterm breech labor
Avoid common mistakes on your manuscript.
Introduction
The prevalence of breech presentation at delivery decreases with increasing gestational age. At 28 pregnancy weeks, every fifth fetus lies in the breech presentation and in term pregnancies, less than 4% of all singleton fetuses are in breech presentation at delivery [ 1 , 2 ]. Most likely this is due to a lack of fetal movements [ 3 ] or an incomplete fetal rotation, since the possibility of a spontaneous rotation declines with increasing gestational age. Consequently, preterm labor itself is often associated with breech presentation at delivery, since the fetus was not yet able to rotate [ 4 , 5 , 6 , 7 , 8 , 9 ]. This fact makes preterm labor as one of the strongest risk factors for breech presentation.
Vaginal breech delivery in term pregnancies is not only associated with poorer perinatal outcomes compared to vaginal delivery with a fetus in cephalic presentation [ 6 , 10 , 11 ], but also it is debated whether the cause of breech presentation itself is a risk for adverse peri- and neonatal outcomes [ 3 , 12 , 13 ]. Several fetal and maternal features, such as fetal growth restriction, congenital anomaly, oligohydramnios, gestational diabetes, and previous cesarean section, are linked to a higher risk of breech presentation at term, and, furthermore, are associated with an increased risk for adverse perinatal outcomes [ 3 , 4 , 5 , 8 , 9 , 14 , 15 , 16 , 17 ].
The literature lacks studies on the risk factors of breech presentation in preterm pregnancies. It remains unclear whether breech presentation at preterm labor is only caused by the incomplete fetal rotation, or whether breech presentation in preterm labor is also associated with other obstetric risk factors. Most of the studies reviewing risk factors for breech presentation focus on term pregnancies. Our hypothesis is that breech presentation in preterm deliveries is, besides preterm pregnancy itself, associated with other risk factors similar to breech presentation at term. We aim to compare the risks of preterm breech presentation to those in cephalic presentation by gestational age. Such information would be valuable in the risk stratification of breech deliveries by gestational age.
Materials and methods
We conducted a retrospective population-based cross-sectional study. The population included all the singleton preterm and term births, from January 2004 to December 2014 in Finland. The data were collected from the national medical birth register and the hospital discharge register, maintained by the National Institute for Health and Welfare. All Finnish maternity hospitals are obligated to contribute clinical data on births from 22 weeks or birth weight of 500 g to the register. All newborn infants are examined by a pediatrician and given a personal identification number that can be traced in the case of perinatal mortality or morbidity. The hospital discharge register contains information on all surgical procedures and diagnoses (International Statistical Classification of Diseases and Related Health Problems 10th Revision, ICD-10) in all inpatient care and outpatient care in public hospitals.
Authorization to use the data was obtained from the National Institute for Health and Welfare as required by the national data protection law in Finland (reference number THL/652/5.05.00/2017).
The study population included all the women with a singleton fetus in breech presentation at the time of delivery. The control group included all the women with a singleton fetus in cephalic presentation at delivery. Other presentations were excluded from the study ( N = 1671) (Fig. 1 ). Gestational age was determined according to early ultrasonographic measurement which is routinely performed in Finland and it encompasses over 95% of the mothers, or if not available, to the last menstrual period. We excluded neonates delivered before 24 weeks of gestation and birth weight of less than 500 g, because the lower viability may have influenced the mode of the delivery or the outcome. The study population was divided into four categories according to the World Health Organization (WHO) definitions of preterm and term deliveries. WHO defines preterm birth as a fetus born alive before 37 completed weeks of pregnancy. WHO recommends sub-categories of preterm birth, based on gestational age, as extremely preterm (less than 28 pregnancy weeks), very preterm (28–32 pregnancy weeks), and moderate to late preterm (32–37 pregnancy weeks).
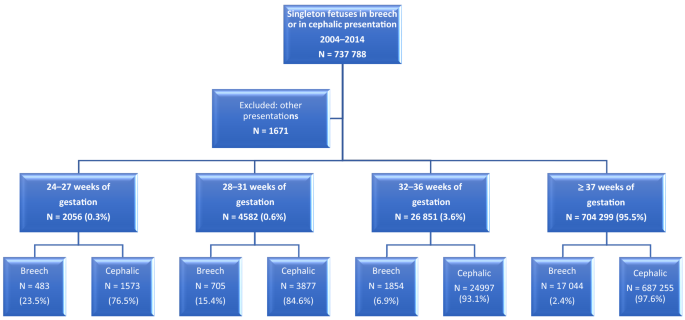
Breech presentation for singleton pregnancies during the period of 2004–2014 in Finland
In our study, we assessed four factors that may be associated with breech presentation based on prior reports [ 3 , 4 , 5 , 14 , 17 , 18 , 19 , 20 ]. These factors were: maternal age below 25 and 35 years or more, smoking, pre-pregnancy body mass index (BMI) over 30, and in vitro fertilization. The following factors were also analyzed: nulliparity, more than three previous deliveries, and history of cesarean section. The obstetric risk factors including maternal hypo- or hyperthyroidism (ICD-10 E03, E05), gestational diabetes (ICD-10 O24.4) and other diabetes treated with insulin (ICD-10 O24.0), arterial hypertension or pre-eclampsia (ICD-10 O13, O14), and maternal care for (suspected) damage to fetus by alcohol or drugs (ICD-10 O35.4, O35.5) were assessed in the analysis. The variables that were also included in the analysis were: oligohydramnios (ICD-10 O41.0), placenta praevia (ICD-10 O44), placental abruption (ICD-10 O45), preterm premature rupture of membranes (PPROM) (ICD-10 O42), infant sex, fetal birth weight below the tenth percentile, fetuses with birth weight above the 97th percentile, and fetal congenital anomalies as defined in the register of congenital malformations.
The babies born in breech presentation from the four study groups were compared with the babies born in cephalic presentation with the equal gestational age, according to WHO classification. The calculations were performed using SPSS 19. Statistical differences in categorical variables were evaluated with the Chi-squared test or Fisher’s exact test when appropriate. We calculated odds ratios (ORs) with corresponding 95% confidence intervals (CIs) using binary logistic regression. Each study group was separately adjusted, according to gestational age at delivery, defined by WHO. The adjustment for the risk factors was done by multivariable logistic regression model for all variables. Differences were deemed to be statistically significant with P value < 0.05.
This analysis includes 737,788 singleton births, from these 20,086 were in breech presentation at the time of delivery. Out of all deliveries, 33,489 infants were born preterm. The prevalence of breech presentation at delivery decreased with the increase of the gestational age: 23.5% in extremely preterm delivery, 15.4% very preterm deliveries, and 6.7% in moderate to late preterm deliveries. At term, the prevalence of breech presentation at delivery was 2.5% (Fig. 1 ).
From all deliveries, 2056 fetuses were born extremely preterm (24 + 0 to 27 + 6 gestational weeks). The differences in the possible risk factors for breech presentation at delivery were higher odds of PPROM (aOR 1.39, 95% CI 1.08–1.79, P = 0.010) and a lower risk of placental abruption (aOR 0.59, 95% CI 0.36–0.98, P = 0.040). No statistically significant differences were observed for the other factors (Table 1 , Figs. 1 , 2 , 3 , 4 ).
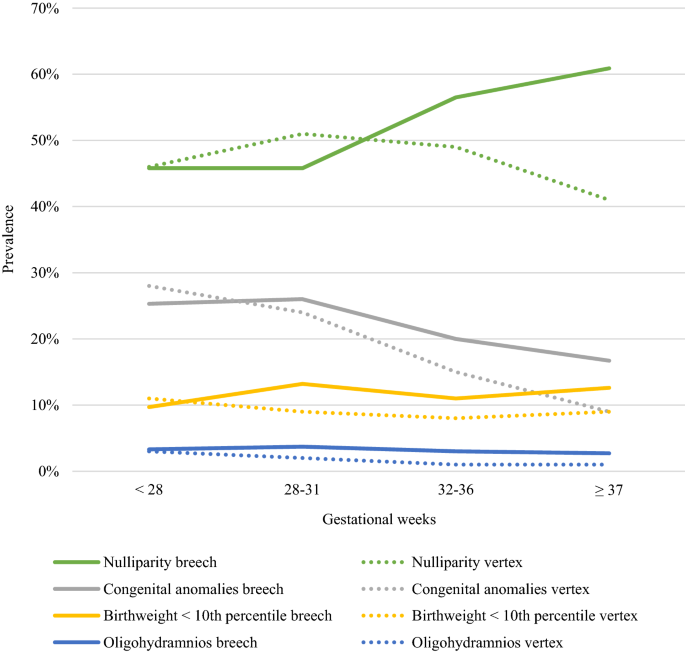
Prevalence of obstetric risk factors for breech presentation compared to cephalic by gestational age. PPROM preterm premature rupture of membranes, PROM premature rupture of membranes
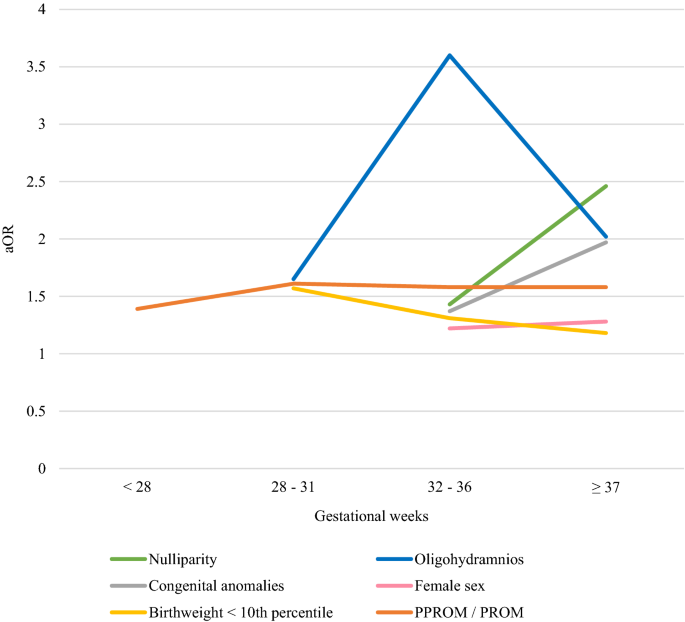
Obstetric risk factors for breech presentation with adjusted odds ratios by gestational age. PPROM preterm premature rupture of membranes, PROM premature rupture of membranes, aOR adjusted odds ratio
The determinants of breech presentation by gestational age. PPROM preterm premature rupture of membranes, PROM premature rupture of membranes
The group of very preterm deliveries (28 + 0 to 31 + 6 gestational weeks) included 4582 singleton newborns. Breech presentation at delivery was associated with PPROM (aOR 1.61, 95% CI 1.32–1.96, P < 0.001), oligohydramnios (aOR 1.65, 95% CI 1.03–2.64, P = 0.038), fetal birth weight below the tenth percentile (aOR 1.57, 95% CI 1.19–2.08, P = 0.002), and maternal pre-eclampsia and arterial hypertension (aOR 1.31, 95% CI 1.04–1.66, P = 0.023). Details of risk factors in very preterm breech deliveries are described in Table 2 . The risk of placenta praevia as well as having a birth weight above the 97th percentile was lower in pregnancies with fetuses in breech rather than in cephalic presentation (Table 2 , Figs. 2 , 3 , 4 ).
The moderate to late preterm delivery group (32 + 0 to 36 + 6 gestational weeks) included 26,851 deliveries. Breech presentation in moderate to late preterm deliveries was associated with older maternal age (maternal age 35 years or more aOR 1.24, 95% CI 1.10–1.39, P < 0.001), nullipara (aOR 1.43, 95% CI 1.27–1.60, P < 0.001), maternal BMI less than 25 (maternal BMI ≥ 25 aOR 0.75, 95% CI 0.62–0.91, P = 0.004), previous cesarean section (aOR 1.31, 95% CI 1.12–1.53, P < 0.001), female sex (aOR 1.22, 95% CI 1.11–1.34, P < 0.001), congenital anomaly (aOR 1.37, 95% CI 1.22–1.55, P < 0.001), fetal birth weight below the tenth percentile (aOR 1.31, 95% CI 1.10–1.56, P = 0.003), oligohydramnios (aOR 3.60, 95% CI 2.63–4.92, P < 0.001), and PPROM (aOR 1.58, 95% CI 1.41–1.78, P < 0.001). Breech presentation decreased the odds of having a fetus with birth weight above the 97th percentile (aOR 0.60, 95% CI 0.42–0.85, P = 0.004) (Table 3 , Figs. 2 , 3 , 4 ).
The term and post-term group included 704,299 deliveries, among them 17,044 fetuses in breech presentation. The factors associated with breech presentation amongst these were: maternal age of 35 years or more (aOR 1.24, 95% CI 1.19–1.29, P < 0.001), nullipara (aOR 2.46, 95% CI 2.37–2.55, P < 0.001), maternal BMI less than 25 (BMI ≥ 25 aOR 0.90, 95% CI 0.85–0.96, P < 0.001), maternal hypothyroidism (aOR 1.53, 95% CI 1.28–1.82, P < 0.001), pre-gestational diabetes treated with insulin (aOR 1.24, 95% CI 1.00–1.53, P = 0.049), placenta praevia (aOR 1.45, 95% CI 1.11–1.91, P = 0.007), premature rupture of membranes (PROM) (aOR 1.58, 95% CI 1.45–1.72, P < 0.001), oligohydramnios (aOR 2.02, 95% CI 1.83–2.22, P < 0.001), congenital anomaly (aOR 1.97, 95% CI 1.89–2.06, P < 0.001), female sex (aOR 1.28, 95% CI 1.24–1.32, P < 0.001), and birth weight below the tenth percentile (aOR 1.18, 95% CI 1.12–1.24, P < 0.001) Table 4 includes details for risk factors of term and post-term group (Figs. 2 , 3 , 4 ).
The main novel finding of our study was that the risk associations increase with each gestational age group after 28 weeks of gestation. With the exception of PPROM, the extremely preterm breech deliveries have similar clinical risk profiles as in cephalic presentation when matched for gestational age. However, as gestation proceeds, the risks start to cluster. In moderate to late preterm pregnancies as in term pregnancies, the breech presentation is a high-risk state being associated with several risk factors: PPROM, oligohydramnios, advanced maternal age, nulliparity, previous cesarean section, fetal birth weight below the tenth percentile, female sex, and fetal congenital anomalies. These are in line with the findings of previous studies [ 3 , 5 , 7 , 8 ], that associated breech presentation at term with obstetric risk factors. The prevalence of breech presentation was negatively correlated with the gestational age with a decline from 23.5% in extremely preterm pregnancies to 2.5% at term. The prevalence of breech presentation in preterm pregnancies observed in our trial is similar to that of comparable studies [ 1 , 2 ].
In extremely preterm deliveries, PPROM was the only risk factor for breech presentation and it stayed as a risk for breech presentation through the gestational weeks. This finding is comparable to the previous literature suggesting that PPROM occurs more often at earlier gestational age in pregnancies with the fetus in breech presentation compared with cephalic [ 21 , 22 ]. PPROM might prevent the fetus to change into cephalic presentation. Furthermore, Goodman and colleagues (2013) reported that in pregnancies with a fetus in a presentation other than cephalic had more complications such as oligohydramnios, infections, placental abruption, and even stillbirths. In our study, surprisingly, placental abruption seemed to have a negative correlation with breech presentation among extremely preterm deliveries. This inconsistency between our results and the literature might be due to the small number of cases. Many of the obstetric complications, for example gestational diabetes, late pre-eclampsia, and late intrauterine growth restriction develop during the second or the third trimester of the pregnancy which explains partially why the risk factors for breech presentation are rarer in extremely preterm deliveries.
In very preterm delivery, breech presentation was associated with PPROM, pre-eclampsia, and fetal birth weight below the tenth percentile. Fetal growth restriction is a known risk factor for breech presentation at term, since it is associated with reduced fetal movements due to diminished resources [ 23 , 24 , 25 ]. Furthermore, fetal growth restriction is known to be the single largest factor for stillbirth and neonatal mortality [ 26 , 27 , 28 , 29 , 30 ]. Maternal arterial hypertension disturbs placental function which might cause low birth weight [ 31 , 32 ]. Arterial hypertension and pre-eclampsia increased the risk for breech presentation in very preterm births, but not in earlier or later preterm pregnancies. This finding may be due to the bias that pre-eclampsia is a well-described risk factor for PPROM, fetal growth restriction, and preterm deliveries which are also independent markers for breech presentation itself [ 4 , 5 , 31 , 33 , 34 ]. The severity of early pre-eclampsia might affect the fetal wellbeing, reduce fetal movements and growth, which might reduce the spontaneous fetal rotation to the cephalic position [ 35 ]. In addition, the most severe cases might not reach older gestational age before the delivery.
The risk factor for breech presentation in moderate to late preterm breech delivery was PPROM, oligohydramnios, advanced maternal age, nulliparity, previous cesarean section, fetal birth weight below the tenth percentile, female sex, and fetal congenital anomalies. Oligohydramnios is a known significant risk factor for term breech pregnancies [ 25 ] and it is linked to the reduced fetal movements partly due to a restricted intrauterine space [ 24 , 35 ] and nuchal cords [ 35 ]. Additionally, oligohydramnios is associated with placental dysfunction, which might reduce fetal resources and thus has a progressive effect on the fetal movements and prevent the fetus from turning into cephalic presentation [ 3 , 4 , 18 ]. Fetal female sex in moderate to late preterm breech pregnancies remained as a risk factor, as identified previously for term pregnancies [ 3 , 4 , 5 ]. It has been debated whether this risk is due to a smaller fetal size or that female fetuses tend to move less [ 9 , 20 ]. The mothers of infants born in breech presentation in moderate to late preterm and term and post-term pregnancies seemed to be older and had an increased risk of having a fetus with a congenital anomaly. The advanced maternal age is associated with negative effects on vascular health, which may have an influence on the developing fetus and increase the incidence of congenital anomalies [ 19 , 34 , 36 ]. Furthermore, congenital anomalies may have a negative influence on fetal movements [ 19 , 35 ]. Whereas, the low birth weight was found as a risk for breech presentation, a birth weight above the 97th percentile was, coherently a protective factor for breech presentation in very to term and post-term pregnancies.
We found that in term pregnancies, breech presentation was associated with advanced maternal age, nulliparity, maternal hypothyroidism, pre-gestational diabetes, placenta praevia, PROM, oligohydramnios, fetal congenital anomaly, female sex of the fetus, and birth weight below the tenth percentile. A previous cesarean section is known to be positively related to the odds of having a fetus in breech presentation at term [ 5 , 14 ], and in our study, this risk factor started to show already in moderate to late preterm pregnancies. Instead of the scar being the cause of breech presentation, it is more likely that the women with a history of breech cesarean section have, during subsequent pregnancies, a fetus in breech presentation again or have a cesarean section for another reason [ 3 , 5 , 37 ]. Our data suggest that the advanced maternal age and nulliparity are the risks for breech presentation at term, but as well as in moderate to late preterm pregnancies. The tight wall of the abdomen and the uterus of nulliparous women might inhibit the fetus from rotating to cephalic presentation [ 9 ]. In a meta-analysis from 2017, older maternal age has been considered to increase the risk of placental dysfunction such as pre-eclampsia and preterm birth [ 36 ] that are also common risk factors for breech presentation [ 4 , 5 ]. Bearing the first child in older maternal age and giving birth by cesarean section may affect the decision not to have another child and might explain the higher rate of nulliparity among moderate to late preterm and term deliveries [ 1 ]. Our study found correlation between maternal hypothyroidism and breech presentation at term. Some studies have demonstrated an association between maternal thyroid hypofunction and adverse pregnancy outcomes such as pre-eclampsia and low birth weight which are, furthermore, risks for breech presentation and may explain partly the higher prevalence of maternal hypothyroidism in term breech deliveries [ 38 , 39 , 40 ]. However, the absence of screening of, for example, thyroid diseases may cause bias in the diagnoses.
Our study demonstrated that as gestation proceeds, more obstetric risk factors can be found associating with breech presentation. In the earlier gestation and excluding PPROM, breech deliveries did not differ in obstetric risk factors compared to cephalic. The risk factors in 32 weeks of gestational age are comparable to those in term pregnancy, and several of these factors, such as low birth weight, congenital anomalies and history of cesarean section, are associated with adverse fetal outcomes [ 1 , 4 , 5 , 8 , 14 , 17 ] and must be taken into account when treating breech pregnancies. Risk factors should be evaluated prior to offering a patient an external cephalic version, as the presence of some of these risks may increase the change of failed version or fetal intolerance of the procedure. This study had adequate power to show differences between the risk profiles of breech and cephalic presentations in different gestational phase. Further research, however, is needed for improving the identification of patients at risk for preterm breech labor and elucidating the optimal route for delivery in preterm breech pregnancies.
Our study is unique since it is the first study, to our knowledge, that compares the risks for breech presentation in preterm and term deliveries. The analysis is based on a large nationwide population, which is the major strength of our study. The study population included nearly 34,000 preterm births over 11 years in Finland and 737,788 deliveries overall. The medical treatment of pregnancies is homogenous, since there are no private hospitals treating deliveries. A further strength relates to the important information on the characteristics of the mother, for example smoking during pregnancy and pre-pregnancy body mass index. The retrospective approach is a limitation of the study, another one is the design as a record linkage study, due to which the variables were restricted to the data availability. Therefore, we were not able to assess, for example uterine anomalies or previous breech deliveries to the analysis.
Our results show that the factors associated with breech presentation in very late preterm breech deliveries resemble those in term pregnancies. However, breech presentation in extremely preterm breech birth has similar clinical risk profiles as in cephalic presentation.
Abbreviations
International Statistical Classification of Diseases and Related Health Problems 10th Revision
World Health Organization; BMI, body mass index
Preterm premature rupture of membranes
Crude odds ratio
Confidence interval
Adjusted odds ratio
Premature rupture of membranes
Albrechtsen S, Rasmussen S, Dalaker K, Irgens LM (1998) The occurrence of breech presentation in Norway 1967–1994. Acta Obstet Gynecol Scand 77:410–415
Article CAS Google Scholar
Hickok D, Gordon DC, Milberg JA, Williams MA, Daling JR (1992) The frequency of breech presentation by gestational age at birth: a large population-based study. Am J Obstet Gynecol 166:851–852
Macharey G, Gissler M, Rahkonen L, Ulander VM, Väisänen-Tommiska M, Nuutila M et al (2017) Breech presentation at term and associated obstetric risks factors—a nationwide population based cohort study. Arch Gynecol Obstet 295(4):833–838
Article Google Scholar
Zsirai L, Csákány GM, Vargha P, Fülöp V, Tabák ÁG (2016) Breech presentation: its predictors and consequences. An analysis of the Hungarian Tauffer Obstetric Database (1996–2011). Acta Obstet Gynecol Scand 95(3):347–354
Cammu H, Dony N, Martens G, Colman R (2014) Common determinants of breech presentation at birth in singletons: a population-based study. Eur J Obstet Gynecol Reprod Biol 177:106–109
Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR (2000) Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Lancet 356(9239):1375–1383
Rayl J, Gibson PJ, Hickok DE (1996) A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol 174:28–32
Fruscalzo A, Londero AP, Salvador S, Bertozzi S, Biasioli A, Della Martina M et al (2014) New and old predictive factors for breech presentation: our experience in 14 433 singleton pregnancies and a literature review. J Matern Neonatal Med 27(2):167–172
Macharey G. Breech presentation and delivery in singleton term pregnancies in Finland [Internet]. Vol. 1, Medical Faculty of the University of Helsinki. 2018. 1–179 p. Available from: urn:ISBN:978–951–51–4023–4
Whyte H, Hannah ME, Saigal S, Hannah WJ, Hewson S, Amankwah K et al (2004) Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obst Gynecol 191(3):864–871
Bjellmo S, Andersen GL, Martinussen MP, Romundstad PR, Hjelle S, Moster D et al (2017) Is vaginal breech delivery associated with higher risk for perinatal death and cerebral palsy compared with vaginal cephalic birth? Registry-based cohort study in Norway. BMJ Open 7:4
Krebs L, Topp M, Langhoff-Roos J (1999) The relation of breech presentation at term to cerebral palsy. Br J Obstet Gynaecol 106(9):943–947
Krebs L, Langhoff-Roos J (2006) The relation of breech presentation at term to epilepsy in childhood. Eur J Obstet Gynecol Reprod Biol 127(1):26–28
Bin YS, Roberts CL, Nicholl MC, Nassar N, Ford JB (2016) Contribution of changing risk factors to the trend in breech presentation at term. Aust New Zeal J Obstet Gynaecol 56(6):564–570
Sekulić SR, Mikov A, Petrovi DS (2010) Probability of breech presentation and its significance. J Maternal-Fetal Neonatal Med 23(10):1160–1164
Madden JV, Flatley CJ, Kumar S (2018) Term small-for-gestational-age infants from low-risk women are at significantly greater risk of adverse neonatal outcomes. Am J Obstet Gynecol 218(5):525
Berhan Y, Haileamlak A (2016) The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies. BJOG 123(1):49–57
Demol S, Bashiri A, Furman B, Maymon E, Shoham-Vardi I, Mazor M (2000) Breech presentation is a risk factor for intrapartum and neonatal death in preterm delivery. Eur J Obstet Gynecol Reprod Biol 93(1):47–51
Mostello D, Chang JJ, Bai F, Wang J, Guild C, Stamps K et al (2014) Breech presentation at delivery: a marker for congenital anomaly? J Perinatol 34(1):11–15
Roberts CL, Algert CS, Peat B, Henderson-Smart D (1999) Small fetal size: a risk factor for breech birth at term. Int J Gynecol Obstet 67(1):1–8
Goodman JR, Lambert AE, Peck JD, Sutton KM, Deschamps DR (2013) Outcomes in cephalic vs noncephalic presentation in the setting of preterm premature rupture of membranes. Am J Obst Gynecol 208(3):231
Joy S (2014) Impact of fetal presentation on pregnancy outcome in preterm premature rupture of membranes. J Clin Diagn Res 8(11):3–6
Google Scholar
Zeitlin J, El Ayoubi M, Jarreau P-H, Draper ES, Blondel B, Künzel W et al (2010) Impact of fetal growth restriction on mortality and morbidity in a very preterm birth cohort. J Pediatr 157(5):733–739
Harrington K, Thompson O, Jordan L, Page J, Carpenter RG, Campbell S (1998) Obstetric outcome in women who present with a reduction in fetal movements in the third trimester of pregnancy. J Perinat Med 26(2):77–82
Macharey G, Gissler M, Ulander VM, Rahkonen L, Väisänen-Tommiska M, Nuutila M et al (2017) Risk factors associated with adverse perinatal outcome in planned vaginal breech labors at term: a retrospective population-based case–control study. BMC Pregnancy Childbirth 17(1):93
Gardosi J, Madurasinghe V, Williams M, Malik A, Francis A (2013) Maternal and fetal risk factors for stillbirth: population based study. Obst Gynecol Surv 346:108
Fretts R (2010) Stillbirth epidemiology, risk factors, and opportunities for stillbirth prevention. Clin Obst Gynecol 53(3):588–596
Newtonraj A, Kaur M, Gupta M, Kumar R (2017) Level, causes, and risk factors of stillbirth: a population-based case control study from Chandigarh. India. BMC Pregnancy Childbirth 17:371
Figueras F, Caradeux J, Crispi F, Eixarch E, Peguero A, Gratacos E (2018) Diagnosis and surveillance of late-onset fetal growth restriction. Am J Obst Gynecol 218(2S):S790–S802
Hinnenberg P, Toijonen A, Gissler M, Heinonen S, Macharey G (2019) Outcome of small for gestational age-fetuses in breech presentation at term according to mode of delivery: a nationwide, population-based record linkage study. Arch Gynecol Obstet 299(4):969–974
Ryan RM, McCarthy FP (2018) Hypertension in pregnancy. Obst Gynaecol Reprod Med. 28:141–147
Berger H, Gagnon R, Sermer M, Basso M, Bos H, Brown RN et al (2016) Diabetes in pregnancy. J Obstet Gynaecol Canada. 38:667–679
Yang X, Hsu-Hage B, Zhang H, Zhang C, Zhang Y, Zhang C (2002) Women with impaired glucose tolerance during pregnancy have significantly poor pregnancy outcomes. Diabetes Care 25(9):1619–1624
Gordon A, Raynes-Greenow C, McGeechan K, Morris J, Jeffery H (2013) Risk factors for antepartum stillbirth and the influence of maternal age in New South Wales Australia: a population based study. BMC Pregnancy Childbirth 13:12
Olesen AG, Svare JA (2004) Decreased fetal movements: background, assessment, and clinical management. Acta Obst Gynecol Scand 83(9):818–826
Lean SC, Derricott H, Jones RL, Heazell AEP (2017) Advanced maternal age and adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS ONE 12(10):e0186287
Hehir MP, Ananth CV, Siddiq Z, Flood K, Friedman AM, D’Alton ME (2018) Cesarean delivery in the United States 2005 through 2014: a population-based analysis using the Robson 10-Group Classification System. Am J Obstet Gynecol 219(1):105
Maraka S, Ospina NMS, Okeeffe DT, Espinosa de Ycaza AE, Gionfriddo MR, Erwin PJ, et al. Subclinical hypothyroidism in pregnancy: a systematic review and meta-analysis. Thyroid. 2016; 26(4):580–90.
Cleary-Goldman J, Malone FD, Lambert-Messerlian G, Sullivan L, Canick J, Porter TF et al (2008) Maternal thyroid hypofunction and pregnancy outcome. Obstet Gynecol 112(1):85–92
Nazarpour S, Tehrani FR, Simbar M, Azizi F (2015) Thyroid dysfunction and pregnancy outcomes. Iran J Reprod Med 13(7):387–396
PubMed PubMed Central Google Scholar
Download references
Acknowledgements
Open access funding provided by University of Helsinki including Helsinki University Central Hospital.
This study was supported by Helsinki University Hospital Research Grants. Authorization to use of the data was obtained from the National Institute for Health and Welfare as required by the national data protection legislation in Finland (reference number THL/652/5.05.00/2017).
Author information
Authors and affiliations.
Department of Obstetrics and Gynecology, University Hospital (HUS), University of Helsinki, Haartmaninkatu 2, 00290, Helsinki, Finland
Anna E. Toijonen, Seppo T. Heinonen & Georg Macharey
National Institute for Health and Welfare (THL), Helsinki, Finland
Mika V. M. Gissler
School of Medicine, University of Helsinki, Helsinki, Finland
Anna E. Toijonen
You can also search for this author in PubMed Google Scholar
Contributions
AT: Project development, manuscript writing. SH: Project development. MG: Data collection and analysis, manuscript editing. GM: Project development, manuscript editing.
Corresponding author
Correspondence to Anna E. Toijonen .
Ethics declarations
Conflict of interest.
We declare that we have no conflict of interest.
Informed consent statement
For this type of study, formal consent is not required. The National Institute for Health and Welfare authorized to use the data (reference number THL/652/5.05.00/2017).
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Toijonen, A.E., Heinonen, S.T., Gissler, M.V.M. et al. A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case–control study. Arch Gynecol Obstet 301 , 393–403 (2020). https://doi.org/10.1007/s00404-019-05385-5
Download citation
Received : 05 July 2019
Accepted : 09 November 2019
Published : 18 November 2019
Issue Date : February 2020
DOI : https://doi.org/10.1007/s00404-019-05385-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breech presentation
- Risk factor
- Preterm delivery
- Preterm labor
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
P03.0 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2024 edition of ICD-10-CM P03.0 became effective on October 1, 2023. This is the American ICD-10-CM version of P03.0 - other international versions of ICD-10 P03.0 may differ. ICD-10-CM Coding Rules.
Screening ultrasound is clinically indicated for infants born with breech presentation ... If there were a family history of dysplasia, that too would be supportive of the reason for screening. The guidelines indicate that hip dysplasia is often found later in infancy and is a developmental condition so code V79.3 may be applicable for follow ...
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
Newborn affected by other complications of labor and delivery. ( P03) P03.0 is a billable diagnosis code used to specify a medical diagnosis of newborn affected by breech delivery and extraction. The code is valid during the current fiscal year for the submission of HIPAA-covered transactions from October 01, 2023 through September 30, 2024.
The ICD code P030 is used to code Breech birth. A breech birth is the birth of a baby from a breech presentation, in which the baby exits the pelvis with the buttocks or feet first as opposed to the normal head-first presentation. In breech presentation, fetal heart sounds are heard just above the umbilicus.
ICD-10-CM Code for Newborn affected by breech delivery and extraction P03.0 ICD-10 code P03.0 for Newborn affected by breech delivery and extraction is a medical classification as listed by WHO under the range - Certain conditions originating in the perinatal period . ... Patient was born breech presentation via C-Section. Normal Hip Exam ...
Summary. Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal ...
Z87.898 is a billable diagnosis code used to specify a medical diagnosis of personal history of other specified conditions. The code is valid during the current fiscal year for the submission of HIPAA-covered transactions from October 01, 2023 through September 30, 2024. The code is exempt from present on admission (POA) reporting for inpatient ...
O32.1XX0 is a billable diagnosis code used to specify maternal care for breech presentation, unsp. Synonyms: abnormal delivery, breech deeply engaged, breech ... The approximate mapping means there is not an exact match between the ICD-10 and ICD-9 codes and the mapped code is not a precise ... Code History. FY 2024 - No Change, effective from ...
ICD-10. ICD-10-CM Codes. Pregnancy, childbirth and the puerperium. Maternal care related to the fetus and amniotic cavity and possible delivery problems. Maternal care for malpresentation of fetus (O32) Maternal care for breech presentation (O32.1) O32.0XX9.
Search All ICD-10 Toggle Dropdown. Search All ICD-10; ICD-10-CM Diagnosis Codes; ICD-10-PCS Procedure Codes; ICD-10-CM Diagnosis Index; ICD-10-CM External Causes Index; ICD-10-CM Table of Drugs; ICD-10-CM Table of Neoplasms; HCPCS Codes; ICD-9-CM Diagnosis Codes; ICD-9-Vol-3 Procedure Code; Search All Data
The incidence of breech presentation at term is around 3%-4% [1-3], and fewer than 10% of foetuses who are breech at term revert spontaneously to a vertex presentation . Although breech presentation is easy to detect through ultrasound screening, many women go into labour with an undetected breech presentation . The majority of these women ...
Breech presentation of the fetus appears in around 2% to 4% of all births. 7 At delivery, breech presentation is a known marker for adverse neonatal outcomes. Previous studies have shown an association between breech presentation at delivery and congenital anomalies. 7 - 11 However, these studies are limited by study size and the lack of ...
Abstract Introduction Breech presentation is linked to abnormal pregnancy outcomes. However, the causality of this association is unknown. ... 1 230 227 (96.7%) were cephalic presentations and 41 796 (3.3%) were breech presentations. Maternal medical history was recorded by the treating physician at the time of delivery and it included the ...
P01.7 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2024 edition of ICD-10-CM P01.7 became effective on October 1, 2023. This is the American ICD-10-CM version of P01.7 - other international versions of ICD-10 P01.7 may differ. ICD-10-CM Coding Rules.
Introduction. The prevalence of breech presentation at delivery decreases with increasing gestational age. At 28 pregnancy weeks, every fifth fetus lies in the breech presentation and in term pregnancies, less than 4% of all singleton fetuses are in breech presentation at delivery [1, 2].Most likely this is due to a lack of fetal movements [] or an incomplete fetal rotation, since the ...
Z87.59 is a billable diagnosis code used to specify a medical diagnosis of personal history of other complications of pregnancy, childbirth and the puerperium. The code is valid during the current fiscal year for the submission of HIPAA-covered transactions from October 01, 2023 through September 30, 2024.
The prevalence of breech presentation at delivery decreases with increasing gestational age. At 28 pregnancy weeks, every fifth fetus lies in the breech presentation and in term pregnancies, less than 4% of all singleton fetuses are in breech presentation at delivery [1, 2].Most likely this is due to a lack of fetal movements [] or an incomplete fetal rotation, since the possibility of a ...
O32.1XX3 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2024 edition of ICD-10-CM O32.1XX3 became effective on October 1, 2023. This is the American ICD-10-CM version of O32.1XX3 - other international versions of ICD-10 O32.1XX3 may differ. O32.1XX3 is applicable to maternity ...