
- Blood gases/acid-base
- Cardiac markers
- Coagulation/fibrinolysis
- Infection/sepsis
- Information management
- Kidneys/fluids
- Neonatology
- Point-of-care testing
- Process optimization
- Quality assurance
- Preanalytical phase
- Creatinine/urea
- Electrolytes
- Hemoglobins
- Natriuretic peptide
- About this site
- Journal scanner Explore selected articles curated by biochemist and journalist Chris Higgins
Sign up for our quarterly newsletter and get the newest articles from acutecaretesting.org

- Journal scans >
Printed from acutecaretesting.org

Severe diabetic ketoacidosis – a remarkable case study

Summarized from Van de Vyver C, Damen J, Haentjens C et al . An exceptional case of diabetic ketoacidosis. Case Reports in Emergency Medicine 2017.
Diabetic ketoacidosis (DKA) is a potentially life-threatening acute complication of type 1 diabetes caused by insulin deficiency. It is characterized by raised blood glucose (hyperglycemia), metabolic acidosis, and increased blood/urine ketones. Dehydration and electrolyte disturbance are common and affected patients may develop some degree of acute kidney injury (AKI) consequent on fluid loss (hypovolemia) due to osmotic diuresis associated with severe hyperglycemia. DKA evolves rapidly over a short time frame (hours rather than days) and can occur (rarely) in those with type 2 diabetes. This DKA case study is particularly noteworthy because of the severity of the hyperglycemia and acid-base disturbance, and the fact that the patient survived such profound metabolic disturbance and associated life-threatening hemodynamic changes. The case concerns a 33-year-old woman with ”brittle” type 1 diabetes treated with continuous subcutaneous insulin infusion (insulin pump). She had, in common with many brittle diabetics, a history of gastroparesis (delayed stomach emptying). Some 36 hours prior to emergency hospital admission she complained of abdominal pain and vomiting after attending a party. Her condition deteriorated before transfer to hospital. The ambulance team reported a rapid decline in Glasgow Coma Score (GCS) from 13 to 3 in only 10 minutes, sinus tachycardia, undetectable peripheral pulse, and hypotension (BP 99/52 mmHg).
Clinical examination revealed severe dehydration and respiratory distress (respiration rate 40 breaths/min). Urgent intubation was necessary and systolic blood pressure dropped further to 55 mmHg. Initial (fingerstick) blood glucose was above the upper detection limit of the analyzer and blood ketones were >8.0 mmol/L. Blood gas analysis revealed severe metabolic acidosis (pH 6.74, bicarbonate 5 mmol/L, p CO 2 39.9 mmHg (5.3 kPa) and hypoxemia ( p O 2 50.2 mmHg, 6.7 kPa). Among other abnormal laboratory test results, perhaps the most remarkable was serum glucose 107 mmol/L (1924 mg/dL). (Serum glucose >33 mmol/L (600 mg/dL) is rarely seen in patients with DKA.) White blood count (32.8x10 9 /L), C-reactive protein (789 nmol/L) and lactate (4.6 mmol/L) were also grossly elevated. Other laboratory testing revealed severe hyponatremia (sodium 113 mmol/L), severe hyperkalemia (6.7 mmol/L) and acute kidney failure (serum creatinine 332 µmol/L). Following presumptive diagnosis of DKA, sepsis and acute renal failure, the patient was treated with aggressive IV fluids, norepinephrine, bicarbonate, and insulin, IV bolus and drip. Intensive investigation for evidence of infection proved fruitless. With treatment, the patient’s condition improved over the following days and she was extubated. Normal renal function was restored after 2 days. In discussion of this case history, the authors briefly review the pathogenesis and treatment of DKA in general terms. They also highlight some interesting features of this case. One aspect discussed relates to the blood gas results on admission, in particular the curiously normal p CO 2 (39.9 mmHg, 5.3kPa).
Metabolic acidosis usually provokes compensatory hyperventilation and reduced p CO 2 . The authors propose plausible theories to explain the much higher than expected p CO 2 in this case. They also propose that the remarkably high blood glucose in this case is the result of the combined effect of reduced glucose elimination consequent on renal failure and the presence of gastroparesis.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info .

has a master's degree in medical biochemistry and he has twenty years experience of work in clinical laboratories.

Acute care testing handbook
Get the acute care testing handbook.
Your practical guide to critical parameters in acute care testing.

Scientific webinars
Check out the list of webinars.
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Sign up for the Acute Care Testing newsletter
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
On March 6th, 2019, Maria Fernandez, a 19-year-old female, presented to the Emergency Department with complaints of nausea, vomiting, abdominal pain, and lethargy. She reveals a recent diagnosis of type 1 diabetes but admits to noncompliance with treatment. At the time of admission, Maria’s vital signs were as follows: BP 87/50, HR 118, RR 28, O2 95% on room air, diffuse abdominal pain at a level of 5, on a verbal numeric 1-10 scale, with non-radiating pain beginning that morning. She was A&O x3, oriented to self, place, and situation, but sluggish. Upon assessment it is revealed that she is experiencing blurry vision, Kussmaul respirations, dry, flushed skin, poor skin turgor, weakness, and a fruity breath smell. Labs were drawn. During the first hour of admission, Maria requested water four times and urinated three times.
Code status: Full code
Medical hx : Type 1 Diabetes
Insurance : None
Allergies : NKA
Significant Lab Values
- Blood glucose 388
- ABGs: pH 7.25, Bicarb 12 mEq/L, paCO2 30 mm Hg, anion gap 20 mEq/L, paO2 94%
- Urinalysis: Ketones and acetone present, BUN 25 mL/dL, Cr 2.1 ml/dL
- Chemistry: sodium 111 mEq/L, potassium 5.5 mEq/L, chloride 90 mEq/L, phosphorus 2.5 mg/dL, Magnesium 2.0 mg/dL
- CBC: WBC 13,000 mcL, RBC 4.7 mcL, Hgb 12.6 g/dL , Hct 37% (Wolters Kluwer, 2018).
Diagnosis: Diabetes Ketoacidosis
- Oxygen administration by nasal cannula on 2L and airway management
- Establish IV access
- IV fluid administration with 0.9% NS; prepare to titrate to 0.45% normal saline as needed
- Monitor blood glucose levels
- Administer 0.1-0.15 unit/kg IV bolus of regular insulin
- IV drip infusion at 0.1 unit/kg/hr of regular insulin to hyperglycemia after bolus,
- Addition of Dextrose to 0.9% NS as glucose levels decreases to 250 mg/dL
- Monitor potassium levels
- Potassium replacement via IV when the potassium level is 5.0 mg/dL or less and urine output is adequate
- Assess for signs of hypokalemia or hyperkalemia
- Monitor vital signs and cardiac rhythm
- Q1-2hr fingerstick blood glucose checks initially, then q4-6hr once stabilized
- Monitor blood pH, I&O
- Assess level of consciousness; provide seizure and safety precautions (Henry et al., 2016)
- Notify MD of any critical changes
Maria Fernandez was then transferred to the ICU unit for close observation, maintenance of IV insulin drip, cardiac monitoring, fluid resuscitation, and correction for metabolic acidosis.
Upon discharge, Maria was reeducated on Type 1 Diabetes Mellitus through the use of preferred learning materials.
- What is the priority assessment data that supports DKA diagnosis?
- What education strategies would you consider implementing to improve treatment adherence after discharge?
- What considerations, services, or resources would you anticipate to be offered by case management or social services?
Henry, N.J., McMichael, M., Johnson, J., DiStasi, A., Ball, B.S., Holman, H.C., Elkins, C.B., Janowski, M.J., Hertel, R.A., Barlow, M.S., Leehy, P., & Lemon, T. (2016). RN adult medical surgical nursing: Review module (10 th ed.). Leawood, KS: Assessment Technologies Institute.
Wolters Kluwer. (2018). Lippincott Nursing Advisor (Version 4.1.0) [Mobile application software]. Retrieved from http://itunes.apple.com
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Diabetic Ketoacidosis (DKA)
- Pathophysiology |
- Symptoms and Signs |
- Diagnosis |
- Treatment |
- Prognosis |
- Key Points |
Diabetic ketoacidosis (DKA) is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis. Hyperglycemia causes an osmotic diuresis with significant fluid and electrolyte loss. DKA occurs mostly in type 1 diabetes mellitus. It causes nausea, vomiting, and abdominal pain and can progress to cerebral edema, coma, and death. DKA is diagnosed by detection of hyperketonemia and anion gap metabolic acidosis in the presence of hyperglycemia. Treatment involves volume expansion, insulin replacement, and prevention of hypokalemia.
(See also Diabetes Mellitus and Complications of Diabetes Mellitus .)
Diabetic ketoacidosis (DKA) occurs in patients with type 1 diabetes mellitus and is less common in those with type 2 diabetes. It develops when insulin levels are insufficient to meet the body’s basic metabolic requirements. DKA is the first manifestation of type 1 diabetes in a minority of patients. Insulin deficiency can be absolute (eg, during lapses in the administration of exogenous insulin ) or relative (eg, when usual insulin doses do not meet metabolic needs during physiologic stress).
Common physiologic stresses that can trigger DKA include
Acute infection (eg, pneumonia , urinary tract infection , COVID-19 )
Myocardial infarction
Pancreatitis
Missed insulin doses
Some medications implicated in causing DKA include
Corticosteroids
Thiazide diuretics
Sympathomimetics
Sodium-glucose co-transporter 2 (SGLT-2) inhibitors
DKA is less common in type 2 diabetes mellitus, but it may occur in situations of unusual physiologic stress. Ketosis-prone type 2 diabetes (also referred to as Flatbush diabetes) is a variant of type 2 diabetes, which sometimes occurs in patients with obesity, often those with African (including African American or Afro-Caribbean) ancestry. Patients with ketosis-prone diabetes can have significant impairment of beta-cell function with hyperglycemia, and are therefore more likely to develop DKA when significant hyperglycemia occurs.
SGLT-2 inhibitors have been implicated in causing DKA in both type 1 and type 2 diabetes. In pregnant patients and in patients taking SGLT2 inhibitors, DKA may occur at lower or even normal blood glucose levels.
Euglycemic DKA can also occur with alcohol overuse or cirrhosis.
Pathophysiology of DKA
Insulin deficiency and an increase in counterregulatory hormones ( glucagon , catecholamines, cortisol ) causes the body to metabolize triglycerides and amino acids instead of glucose for energy. Serum levels of glycerol and free fatty acids rise because of unrestrained lipolysis. Alanine levels rise because of muscle catabolism. Glycerol and alanine provide substrate for hepatic gluconeogenesis, which is stimulated by the excess of glucagon that accompanies insulin deficiency.
Glucagon also stimulates mitochondrial conversion of free fatty acids into ketones. Insulin normally blocks ketogenesis by inhibiting the transport of free fatty acid derivatives into the mitochondrial matrix, but ketogenesis proceeds in the absence of insulin . The major ketoacids produced, acetoacetic acid and beta-hydroxybutyric acid, are strong organic acids that create metabolic acidosis . Acetone derived from the metabolism of acetoacetic acid accumulates in serum and is slowly disposed of by respiration.
Hyperglycemia due to insulin deficiency causes an osmotic diuresis that leads to marked urinary losses of water and electrolytes. Urinary excretion of ketones obligates additional losses of sodium and potassium. Serum sodium may fall due to natriuresis or rise due to excretion of large volumes of free water.
Potassium is also lost in large quantities. Despite a significant total body deficit of potassium, initial serum potassium is typically normal or elevated because of the extracellular migration of potassium in response to acidosis. Potassium levels generally fall further during treatment as insulin therapy drives potassium into cells. If serum potassium is not monitored and replaced as needed, life-threatening hypokalemia may develop.
Symptoms and Signs of DKA
Symptoms and signs of diabetic ketoacidosis include symptoms of hyperglycemia with the addition of nausea, vomiting, and—particularly in children—abdominal pain. Lethargy and somnolence are symptoms of more severe decompensation. Patients may be hypotensive and tachycardic due to dehydration and acidosis; they may breathe rapidly and deeply to compensate for acidemia (Kussmaul respirations). They may also have fruity breath due to exhaled acetone. Fever is not a sign of DKA itself and, if present, signifies underlying infection. In the absence of timely treatment, DKA progresses to coma and death.
Acute cerebral edema, a complication in about 1% of DKA patients, occurs primarily in children and less often in adolescents and young adults. Headache and fluctuating level of consciousness herald this complication in some patients, but respiratory arrest is the initial manifestation in others. The cause is not well understood but may be related to too-rapid reductions in serum osmolality or to brain ischemia. It is most likely to occur in children < 5 years when DKA is the initial manifestation of diabetes mellitus . Children with the highest BUN (blood urea nitrogen) levels and lowest PaCO2 at presentation appear to be at greatest risk. Delays in correction of hyponatremia and the use of bicarbonate during DKA treatment are additional risk factors.
Diagnosis of DKA
Arterial pH
Serum ketones
Calculation of anion gap
In patients suspected of having diabetic ketoacidosis, serum electrolytes, blood urea nitrogen (BUN) and creatinine, glucose, ketones, and osmolarity should be measured. Urine should be tested for ketones. Patients who appear significantly ill and those with positive ketones should have arterial blood gas measurement.
DKA is diagnosed by an arterial pH < 7.30 with an anion gap > 12 and serum ketones. Guidelines differ on specific levels of hyperglycemia to be included in the diagnostic criteria for DKA. A blood glucose level > 200 (11.1 mmol/L) or > 250 mg/dL (13.8 mmol/L) is most often specified; however, because DKA can occur in patients with normal or mildly elevated glucose levels, some guidelines do not include a specific level ( 1, 2 ).
A presumptive diagnosis may be made when urine glucose and ketones are positive on urinalysis. Urine test strips and some assays for serum ketones may underestimate the degree of ketosis because they detect acetoacetic acid and not beta-hydroxybutyric acid, which is usually the predominant ketoacid.
Blood beta-hydroxybutyrate can be measured, or treatment can be initiated based on clinical suspicion and the presence of anion gap acidosis if serum or urine ketones are low.
Symptoms and signs of a triggering illness should be pursued with appropriate studies (eg, cultures, imaging studies). Adults should have an ECG to screen for acute myocardial infarction and to help determine the significance of abnormalities in serum potassium.
Other laboratory abnormalities include
Hyponatremia
Elevated serum creatinine
Elevated plasma osmolality
Hyperglycemia may cause dilutional hyponatremia, so measured serum sodium is corrected by adding 1.6 mEq/L (1.6 mmol/L) for each 100 mg/dL (5.6 mmol/L) elevation of serum glucose over 100 mg/dL (5.6 mmol/L).
To illustrate, for a patient with serum sodium of 124 mEq/L (124 mmol/L) and glucose of 600 mg/dL (33.3 mmol/L), add 1.6 ([600 − 100]/100) = 8 mEq/L (8 mmol/L) to 124 for a corrected serum sodium of 132 mEq/L (132 mmol/L).
As acidosis is corrected, serum potassium drops. An initial potassium level < 4.5 mEq/L (
Serum amylase and lipase are often elevated, even in the absence of pancreatitis (which may be present in patients with alcoholic ketoacidosis and in those with coexisting hypertriglyceridemia).
Diagnosis references
1. Buse JB, Wexler DJ, Tsapas A, et al : 2019 Update to: Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 43(2):487–493, 2020. doi: 10.2337/dci19-0066
2. Garber AJ, Handelsman Y, Grunberger G, et al : Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm--2020 executive summary. Endocrine Practice 26:107–139, 2020.
Treatment of DKA
IV 0.9% saline
Correction of hypokalemia
IV insulin (as long as serum potassium is ≥ 3.3 mEq/L [3.3 mmol/L])
< 7 after 1 hour of treatment)
The most urgent goals for treating diabetic ketoacidosis are rapid intravascular volume repletion, correction of hyperglycemia and acidosis, and prevention of hypokalemia ( 1, 2 ). Identification of precipitating factors is also important.
Treatment should occur in intensive care settings because clinical and laboratory assessments are initially needed every hour or every other hour with appropriate adjustments in treatment.
Volume repletion
Intravascular volume should be restored rapidly to raise blood pressure and ensure glomerular perfusion; once intravascular volume is restored, remaining total body water deficits are corrected more slowly, typically over about 24 hours. Initial volume repletion in adults is typically achieved with rapid IV infusion of 1 to 1.5 L of 0.9% saline solution in the first hour, followed by saline infusions at 250 to 500 mL/hour. Additional boluses or a faster rate of infusion may be needed to raise the blood pressure. Slower rates of infusion may be needed in patients with heart failure or in those at risk for volume overload. If the serum sodium level is normal or high, the normal saline is replaced by 0.45% saline after initial volume resuscitation. When plasma glucose falls to < 200 mg/dL ( <
For children, fluid deficits are estimated at 30 to 100 mL/kg body weight. Pediatric maintenance fluids < 300 mg/dL (16.7 mmol/L) and blood pressure is stable and urine output adequate. The remaining fluid deficit should be replaced over 24 to 48 hours, typically requiring a rate (including maintenance fluids) of about 2 to 5 mL/kg/hour, depending on the degree of dehydration.
Correction of hyperglycemia and acidosis
≥ 3.3 mEq/L ( ≥ 3.3 mmol/L) . Insulin adsorption onto IV tubing can lead to inconsistent effects, which can be minimized by preflushing the IV tubing with insulin solution. If plasma glucose does not fall by 50 to 75 mg/dL (2.8 to 4.2 mmol/L) in the first hour, insulin doses should be doubled. Children should be given a continuous IV insulin infusion of 0.1 unit/kg/hour or higher with or without a bolus.
Ketones should begin to clear within hours if insulin is given in sufficient doses. However, clearance of ketones may appear to lag because of conversion of beta-hydroxybutyrate to acetoacetate (which is the “ketone” measured in most hospital laboratories) as acidosis resolves.
Serum pH and bicarbonate levels should also quickly improve, but restoration of a normal serum bicarbonate level may take 24 hours. Bicarbonate should not be given routinely because it can lead to development of acute cerebral edema (primarily in children). If bicarbonate is used, it should be started only if the pH is < 7, and only modest pH elevation should be attempted with doses of 50 to 100 mEq (50 to 100 mmol) given over 2 hours, followed by repeat measurement of arterial pH and serum potassium.
When plasma glucose becomes < 200 mg/dL ( < insulin dose can be reduced to maintain glucose 150 to 200 mg/dL (8.3 to 11.1 mmol/L), but the continuous IV infusion of regular insulin should be maintained until the anion gap has narrowed on 2 consecutive blood tests and blood and urine are consistently negative for ketones. A longer duration of treatment with insulin
When the patient is stable and able to eat, a typical is begun. IV insulin should be continued for 2 hours after the initial dose of basal subcutaneous insulin is given. Children should continue to receive 0.05 unit/kg/hour insulin infusion until subcutaneous insulin is initiated and pH is > 7.3.
Hypokalemia prevention
Prevention of hypokalemia requires replacement of 20 to 30 mEq (20 to 30 mmol) potassium in each liter of IV fluid to keep serum potassium between 4 and 5 mEq/L (4 and 5 mmol/L). If serum potassium is < 3.3 mEq/L ( < 3.3 mmol/L), insulin should be withheld and potassium given at 40 mEq/hour until serum potassium is ≥ 3.3 mEq/L ( ≥ 3.3 mmol/L); if serum potassium is > 5 mEq/L ( > 5 mmol/L), potassium supplementation can be withheld.
Initially normal or elevated serum potassium measurements may reflect shifts from intracellular stores in response to acidemia and belie the true potassium deficits that almost all patients with DKA have. Insulin replacement rapidly shifts potassium into cells, so levels should be checked hourly or every other hour in the initial stages of treatment.
Other measures
Hypophosphatemia
Treatment references
1. Gosmanov AR, Gosmanova EO, Dillard-Cannon E : Management of adult diabetic ketoacidosis. Diabetes Metab Syndr Obes 7:255–264, 2014. doi:10.2147/DMSO.S50516
2. French EK, Donihi AC, Korytkowski MT : Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome: review of acute decompensated diabetes in adult patients. BMJ 365:l1114, 2019. doi: 10.1136/bmj.l1114
Prognosis for DKA
Overall mortality rates for diabetic ketoacidosis are 1, 2, 3 ). Another study had lower rates of persistent neurologic sequelae and death ( 4 ).
Prognosis references
1. Edge JA, Hawkins MM, Winter DL, Dunger DB : The risk and outcome of cerebral oedema developing during diabetic ketoacidosis. Arch Dis Child 85(1):16-22, 2001. doi:10.1136/adc.85.1.16
2. Marcin JP, Glaser N, Barnett P, et al : Factors associated with adverse outcomes in children with diabetic ketoacidosis-related cerebral edema. J Pediatr 141(6):793-797, 2002. doi:10.1067/mpd.2002.128888
3. Glaser N . Cerebral edema in children with diabetic ketoacidosis. Curr Diab Rep 2001;1(1):41-46. doi:10.1007/s11892-001-0009-7
4. Kuppermann N, Ghetti S, Schunk JE, et al . Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis. N Engl J Med 2018;378(24):2275-2287. doi:10.1056/NEJMoa1716816
Diabetic ketoacidosis (DKA) is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis.
DKA can occur when acute physiologic stressors (eg, infections, myocardial infarction) trigger acidosis, moderate glucose elevation, dehydration, and severe potassium loss in patients with type 1 diabetes.
Diagnose by an arterial pH < 7.30, with an anion gap > 12 and serum ketones in the presence of hyperglycemia.
Acidosis typically corrects with IV fluid and insulin ; consider bicarbonate only if marked acidosis (pH < 7) persists after 1 hour of therapy.
Withhold insulin until serum potassium is ≥ 3.3 mEq/L ( ≥ 3.3 mmol/L).
Acute cerebral edema is a rare (about 1%) but lethal complication, primarily in children and less often in adolescents and young adults.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Diabetic Ketoacidosis (DKA) Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Mr. Logan is a 32-year-old male with a history of DM Type I. He presented to the Emergency Department (ED) after being found by his family with decreased LOC, rapid heavy breathing, and fruity breath. His family reports flu-like symptoms for the last few days.

Before even gathering further information - what do you think is going on? Why?
Diabetic Ketoacidosis – he is a Type I Diabetic with heavy breathing (Kussmaul Respirations) and fruity breath. These are classic signs. It’s important to recognize them and immediately begin anticipating the patient’s needs.
What diagnostic or lab tests would you expect the provider to order?
- Complete metabolic panel to check serum glucose, anion gap, potassium, etc.
- Arterial Blood Gas to assess for acidosis
- Urinalysis to look for ketones
The nurse draws a Complete Metabolic Panel and notifies the Respiratory Therapist to obtain an Arterial Blood Gas. Upon further assessment, the patient is oriented x 2 and drowsy. He is breathing heavily. Lungs are clear to auscultation, S1/S2 present, bowel sounds active, pulses present and palpable x 4 extremities. A POC glucose reads >450 (meter max).
Vital signs are as follows: HR 87 RR 32 BP 123/77 SpO 2 96%
Mr. Logan’s labs result and show the following: Glucose 804 mg/dL K 6.1 mEq/L BUN 39 mg/dL pH 7.12 Cr 1.9 mg/dL pCO 2 30 Anion Gap 29 mEq/L HCO 3 – 17 Urine = Positive for Ketones
Using these lab results, explain what is going on physiologically with Mr. Logan.
- His glucose is extremely high and he is positive for ketones, which says that his body is having to break down fatty acids to make energy
- His anion gap is high, meaning there are other “ions” in the system besides the electrolytes – in this case, the extra acids are creating this ‘gap’
- He is in metabolic acidosis because of the ketoacids – this is what’s causing the Kussmaul respirations – his body is trying to breathe off CO2 to bring his pH up
- His potassium is high because the body will kick potassium out of the cells to compensate for an acidotic state. This way instead of having H+ (acids) in the blood stream, we have K+ – this protects many tissues, but puts our heart at risk
- His BUN/Cr are elevated because of the dehydration caused by osmotic diuresis (caused by hyperglycemia and hyperosmolarity)
What is the #1 priority for Mr. Logan at this time?
- The #1 priority for DKA is to get the blood sugar down and get insulin into the system. Getting insulin into the system allows the gluconeogenesis to STOP (so that the body will STOP making ketoacids and start using the glucose it has).
- The #2 priority is fluid replacement due to severe dehydration from osmotic diuresis
The provider writes an order for an Insulin Lispro infusion IV, titrating to decrease blood glucose per protocol, 1L NS bolus NOW, and a continuous infusion of Normal Saline IV at 250 mL/hr, and to change the fluids to D5 ½ NS at 125 mL/hr once the blood glucose level falls below 250 mg/dL.
What is the first action you should take after receiving these orders?
Remind the provider that the only insulin that can be given IV is Regular Insulin and request that he change the order. Call the Pharmacist if you have to
- **Note – most facilities have a computerized ordering that prevents something like this from happening, but it’s important that you know this!!
The provider adjusts the order to Regular Insulin IV infusion. Orders are also written for hourly POC glucose checks and a q2h BMP.
Why is it important to check a BMP frequently? What are we monitoring for?
- Frequent BMP’s are important to confirm the blood glucose when the POC meter is just reading MAX.
- It’s also important to monitor the Anion Gap to see when it “closes” – indicating resolution of the acidosis
- We are also monitoring potassium levels. They will start elevated, but insulin drives potassium into the cells – causing it to decrease rapidly.
After 4 hours and another 1L bolus of NS, Mr. Logan’s blood glucose level has dropped to 174 mg/dL, but his anion gap is still 19. The nurse changes his fluids to D5 ½ NS per the order and continues the insulin infusion. The most recent BMP showed a K of 3.7, down from 6.1, so the provider orders to give 40 mEq of KCl PO.
Why is the insulin continued even after the blood glucose decreases?
- The goal is to stop gluconeogenesis and reverse the acidosis. The glucose may fall rapidly while there are still ketoacids being made.
- By giving D5 ½ NS infusion with the insulin, we can continue to bring down the acidosis process while maintaining safe blood sugars.
After another 4 hours, Mr. Logan’s anion gap is now 12, a repeat ABG shows a pH of 7.36 with normal CO 2 and HCO 3 – levels. The nurse begins to transition Mr. Logan off of the IV infusion to SubQ insulin per protocol. He is feeling much better and says he’s embarrassed that he had to be brought to the hospital.
What education can you provide Mr. Logan to help him understand why this happened and how to prevent it from recurring in the future?
- When you are ill, you should check your blood sugar more often as sometimes the body’s healing processes and stress response can make your sugar go higher than normal
- Notify your provider if you’re ill, they may recommend increasing your long-acting insulin
- Notify your provider or go to the ED at the FIRST indication of DKA – fruity breath, heavy breathing, feeling dry and hot, excessive urination, blurry vision, or a blood glucose over 400 mg/dL or over your meter MAX.
- If you have an insulin pump, make sure it is working appropriately – if not, notify your provider or turn the pump OFF and switch to SubQ insulin until the pump can be fixed
- **Note – if a patient comes in with an insulin pump, it should always be turned OFF – we will manage their sugars with SubQ insulin and don’t want them to receive a double dose.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Daily Do Lesson Plans
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning
MyNSTA Community
- My Collections
Diabetic Ketoacidosis Upon Diagnosis
A Biochemistry Case Study
By Ali Chaari, Aisha Kafoud
Share Start a Discussion

This directed case study is designed to help students integrate biochemical and physiological concepts with clinical aspects of disease. The case tells the story of a little girl who experiences diabetic ketoacidosis and is diagnosed with type 1 diabetes mellitus (T1DM). The story is based on an actual patient and the presented data are authentic. The case can be delivered as an individual assignment by using the case study handout or displayed in class with optional role play by using the PowerPoint presentation (see Supplemental Materials). Both versions of the case cover the same basic content, but the questions are somewhat different. Upon successful completion of the case, students should understand the basics of metabolic acidosis in T1DM, differences between T1DM and T2DM, and the behavior of the blood buffer equilibrium in response to physiological change. The case was originally written for an intermediate biochemistry course, but it could also be used in a physiology or an advanced biology course.
Download Case
Date Posted
- Discuss the basics of metabolic acidosis in T1DM.
- Distinguish T1DM from T2DM.
- Predict the behavior of the blood buffer equilibrium in response to a physiological change.
- Use Winter’s formula to perform calculations with real patient data.
- Correlate real clinical data with biochemical tests.
- Explain the role of insulin and how ketoacidosis can occur due to insulin insufficiency.
Diabetes; type 1 diabetes; T1DM; ketoacidosis; blood buffer; acidosis; Winter’s formula; insulin insufficiency
Subject Headings
EDUCATIONAL LEVEL
Undergraduate lower division, Undergraduate upper division, Clinical education
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials.
The PowerPoint presentation below offers an alternative way to deliver the case in class.
- PowerPoint Presentation (~3.9 MB)
You may also like
Web Seminar
Join us on Thursday, June 13, 2024, from 7:00 PM to 8:00 PM ET, to learn about the science and technology of firefighting. Wildfires have become an e...
Join us on Thursday, October 10, 2024, from 7:00 to 8:00 PM ET, for a Science Update web seminar presented by NOAA about climate science and marine sa...
Secondary Pre-service Teachers! Join us on Monday, October 21, 2024, from 7:00 to 8:15 PM ET to learn about safety considerations for the science labo...
Diabetic ketoacidosis
On this page, preparing for your appointment.
A physical exam and blood tests can help diagnose diabetic ketoacidosis. In some cases, other tests may be needed to help find what caused the diabetic ketoacidosis.
Blood tests
Blood tests used in the diagnosis of diabetic ketoacidosis will measure:
- Blood sugar level. If there isn't enough insulin in the body to allow sugar to enter cells, the blood sugar level will rise. This is known as hyperglycemia. As the body breaks down fat and protein for energy, the blood sugar level will keep rising.
- Ketone level. When the body breaks down fat and protein for energy, acids known as ketones enter the bloodstream.
- Blood acidity. A too-high blood ketone level will cause the blood to become acidic. This can change how organs throughout the body work.
Other tests
Tests that can help find health problems that might have contributed to diabetic ketoacidosis and check for complications might include:
- Blood electrolyte tests
- Chest X-ray
- A recording of the electrical activity of the heart, also known as an electrocardiogram
More Information
- Chest X-rays
- Electrocardiogram (ECG or EKG)
If you're diagnosed with diabetic ketoacidosis, you might be treated in the emergency room or admitted to the hospital. Treatment usually involves:
- Fluids. Fluids replace those lost through too much urinating. They also thin out the blood sugar. Fluids can be given by mouth or through a vein. When given through a vein, they're called IV fluids.
- Electrolyte replacement. Electrolytes are minerals in the blood, such as sodium, potassium and chloride, that carry an electric charge. Too little insulin can lower the level of several electrolytes in the blood. IV electrolytes are given to help keep the heart, muscles and nerve cells working as they should.
- Insulin therapy. Insulin reverses diabetic ketoacidosis. In addition to fluids and electrolytes, insulin is given, usually through a vein. A return to regular insulin therapy may be possible when the blood sugar level falls to about 200 mg/dL (11.1 mmol/L) and the blood is no longer acidic.
Diabetic ketoacidosis is life-threatening. If you develop mild symptoms, contact your health care provider immediately.
Call 911 or your local emergency number if:
- You can't reach your care provider
- Your symptoms are getting worse
- Your symptoms are already very bad
A health care provider who sees you for possible diabetic ketoacidosis needs answers to these questions as quickly as possible:
- What are your symptoms?
- When did your symptoms develop? Are they getting worse?
- Have you been diagnosed with diabetes?
- Have you recently checked your blood sugar level?
- Have you recently checked your ketone level?
- Have you lost your appetite?
- Can you keep fluids down?
- Are you having trouble breathing?
- Do you have chest pain?
- Have you had a recent illness or infection?
- Have you had recent stress or trauma?
- Have you recently used alcohol or recreational drugs?
- How closely have you been following your diabetes treatment plan?
- How well have you been managing your diabetes just before these symptoms started?
Oct 06, 2022
- DKA (ketoacidosis) and ketones. American Diabetes Association. https://diabetes.org/diabetes/dka-ketoacidosis-ketones. Accessed Sept. 17, 2022.
- Diabetic ketoacidosis (DKA). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetic-ketoacidosis-dka?query=Diabetic ketoacidosis (DKA). Accessed Sept. 17, 2022.
- Hirsch IB, et al. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Clinical features, evaluation, and diagnosis. https://www.uptodate.com/contents/search. Accessed Sept. 17, 2022.
- Hirsch IB, et al. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Treatment. https://www.uptodate.com/contents/search. Accessed Sept. 17, 2022.
- Ferri FF. Diabetic ketoacidosis. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Sept. 17, 2022.
- Evans K. Diabetic ketoacidosis: Update on management. Clinical Medicine. 2019; doi:10.7861/clinmed.2019-0284.
- Symptoms & causes
- Doctors & departments
- Diseases & Conditions
- Diabetic ketoacidosis diagnosis & treatment
Associated Procedures
Products & services.
- A Book: The Essential Diabetes Book
- Assortment of Health Products from Mayo Clinic Store
CON-XXXXXXXX
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

- Previous Article
- Next Article
Case Presentation
Clinical pearls, article information, a case of euglycemic diabetic ketoacidosis triggered by a ketogenic diet in a patient with type 2 diabetes using a sodium–glucose cotransporter 2 inhibitor.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Paola Sanchez Garay , Gabriela Zuniga , Robert Lichtenberg; A Case of Euglycemic Diabetic Ketoacidosis Triggered by a Ketogenic Diet in a Patient With Type 2 Diabetes Using a Sodium–Glucose Cotransporter 2 Inhibitor. Clin Diabetes 1 April 2020; 38 (2): 204–207. https://doi.org/10.2337/cd19-0055
Download citation file:
- Ris (Zotero)
- Reference Manager
Sodium–glucose cotransporter 2 (SGLT2) inhibitors are one of the newest classes of antihyperglycemic medications now available for the treatment of type 2 diabetes ( 1 ). Clinical guidelines recommend this type of medication as one of various possible approaches for pharmacological therapy after failure of or intolerance to metformin ( 1 ).
SGLT2 inhibitors are the first class of medications that act on the kidneys to optimize glycemic control; they prevent the reabsorption of glucose in the proximal renal tubules by targeting the action of the protein SGLT2 ( 2 ). As glucose is excreted through the urine, plasma glucose levels fall, leading to an improvement in glycemia ( 1 ).
The most common adverse side effects attributed to SGLT2 inhibitors are genital and urinary infections. Because of osmotic diuresis induced by the glucosuria resulting from SGLT2 inhibition, volume depletion is also a possibility ( 3 ). Recently, episodes of diabetic ketoacidosis (DKA) have been identified as a rare side effect ( 2 ).
As a consequence of the glucosuria induced by SGLT2 inhibition, the majority of reported DKA episodes have been associated with a mild to moderate increased glycemia ( 4 ).
R.F., a 44-year-old man with a history of type 2 diabetes, presented to the hospital emergency department with complaints of malaise, fatigue, heartburn, and decreased exercise capacity. He had been taking the dipeptidyl peptidase 4 inhibitor sitagliptin 100 mg, the SGLT2 inhibitor empagliflozin 25 mg, and metformin 1,000 mg twice daily for the past 2 years. He said his symptoms started 4 days earlier. The only change he could identify in his lifestyle was that he had switched to a ketogenic diet and was restricting carbohydrates, which he had been doing for 7 days before coming to the hospital.
R.F.’s heart rate was 120 bpm, his blood pressure was 120/80 mmHg, and his temperature was 97.8°F. On physical exam, he was found to be uncomfortable and in mild distress, and he exhibited tenderness to palpation over the epigastric area. Initial laboratory test values were sodium 132 mmol/L (normal 134–148), potassium 5.5 mmol/L (normal 3.5–5.5), serum bicarbonate 9 mmol/L (normal 22–32), anion gap 24 mmol/L (normal 7–14), serum glucose 199 mmol/L (normal 70–100), and β-hydroxybutyrate 8.89 mmol/L (normal 0.02–0.27). Urine tests revealed ketones 150 mg/dL (normal negative) and urine glucose 1,000 mmol/L (normal negative). Arterial blood gases taken on 2 L of oxygen supplementation by nasal cannula were significant for a pH 7.11 (normal 7.35–7.45), partial pressure of carbon dioxide <19 mmHg (normal 35–45), partial pressure of oxygen 105 mmHg (normal 80–100), and bicarbonate 8.2 mmol/L (normal 22–26).
R.F.’s acidosis was thought to be the result of euglycemic DKA, likely triggered by his ketogenic diet; other etiologies, including infection and lactic acidosis secondary to metformin use, were ruled out with further testing, which revealed a lactic acid level of 1.8 mmol/L (normal 0–2), an ethanol level <10 mg/dL, and a negative salicylate level. Chest X-ray showed no signs of pneumonia, and results of a urinalysis were unremarkable.
R.F. was admitted to the intensive care unit for suspicion of euglycemic DKA. He was started on an insulin drip and intravenous (IV) fluids per DKA protocol. The main difference in therapy for euglycemic DKA versus ordinary DKA was the type of IV fluids provided and the insulin dosage administered. Based on his blood glucose level, he was started on D5/0.45% sodium chloride with 20 mEq potassium chloride at 250 mL/hour instead of normal saline. The initial standard regular insulin dosage of the drip was decreased from 0.14 to 0.07 units/kg/hour based on glycemia. No additional potassium supplementation was required based on his admission potassium level.
The patient was kept on an insulin drip for 16 hours while progressively decreasing the IV fluids rate and monitoring blood glucose hourly to avoid hypoglycemia. Once his bicarbonate level was >18 mmol/L and the anion gap had closed, he was transitioned to weight-based basal and premeal insulin and then transferred to the medical floor.
At discharge, it was recommended that he continue on metformin and sitagliptin and discontinue empagliflozin. He was encouraged to follow up with endocrinology as an outpatient.
What is the relationship between SGLT2 inhibitors and euglycemic DKA?
What are the precipitating factors for euglycemic DKA with the use of an SGLT2 inhibitor?
What are the potential mechanisms by which the combination of an SGLT2 inhibitor and a ketogenic diet can cause euglycemic DKA?
What considerations are specific to the management of euglycemic DKA induced by an SGLT2 inhibitor?
DKA is a severe complication of diabetes that can be lethal ( 2 ). It can result from a severe lack of insulin action in the body ( 2 ). It can be defined as a triad that includes metabolic acidosis, hyperglycemia, and increased ketone bodies in the blood and urine; however, it can also be seen in the setting of normal or slightly elevated glycemia ( 2 , 5 ). This latter form of DKA is known as euglycemic or normoglycemic DKA and was initially characterized by blood glucose values <300 mg/dL. In 2015, the American Association of Clinical Endocrinologists and the American College of Endocrinology recommended calling this form of DKA “DKA with lower-than-anticipated levels of glucose” instead of “euglycemic DKA,” because the majority of 80 DKA cases reviewed were found to have a blood glucose level >250 mg/dL ( 6 ).
In May 2015, the U.S. Food and Drug Administration (FDA) issued a warning regarding the risk of DKA with the use of SGLT2 inhibitors. The FDA performed a review of its system database from March 2013 to May 2015 and identified 73 reported cases of DKA in patients treated with SGLT2 inhibitors. The warning mentioned that, in many of these cases, DKA was not immediately recognized because of the presence of low to normal blood glucose levels ( 7 ). All SGLT2 inhibitors currently approved by the FDA for the management of type 2 diabetes have been associated with DKA, leading the FDA to require a warning on their package labels ( 7 , 8 ).
Burke et al. ( 9 ) performed a systematic review investigating the relationship between SGLT2 inhibitors and DKA in patients with diabetes. They found 34 case reports of patients with type 1 or type 2 diabetes who developed DKA while receiving an SGLT2 inhibitor. Of these cases, 26 involved canagliflozin, 5 involved dapagliflozin, 2 involved empagliflozin, and 1 involved ipragliflozin, which is an SGLT2 inhibitor approved in Japan ( 9 ).
Similar to our patient, the two cases involving empagliflozin that were previously described in the literature presented as euglycemic DKA. One case was reported in a 64-year-old woman with type 2 diabetes using the glucagon-like peptide 1 receptor agonist liraglutide, who developed DKA 5 days after initiating empagliflozin ( 10 ). The second case was in a 53-year-old man with type 2 diabetes who was admitted to the hospital with acute pancreatitis; he had been taking empagliflozin for 3 years and was found to have euglycemic DKA ( 11 ).
Metabolic stress has been the unifying theme among the reported cases of DKA involving SGLT2 inhibitors ( 7 , 9 ). SGLT2 inhibitors are thought to increase the risk of euglycemic DKA by two potential mechanisms. The first is an increase in urinary glucose excretion, which in turn leads to a decrease in glycemic levels, resulting in the reduction of endogenous insulin secretion and increased production of free fatty acids (FFAs), which are later converted into ketone bodies ( 6 , 9 ). The second mechanism is the decrease in blood glucose levels induced by SGLT2 inhibition, which leads to reduced insulin production from pancreatic β-cells and increased stimulation of α-cells, which in turn increases plasma glucagon concentrations ( 9 ). In addition, SGLT2 inhibitors act independently on pancreatic α-cells, promoting an increase in plasma glucagon levels ( 9 , 12 ).
The two mechanisms described above cause a decrease in the insulin-to-glucagon ratio, which stimulates lipolysis, augmenting delivery of FFAs to the liver and resulting in mild stimulation of ketogenesis. If insulin deficiency is more profound, as can happen in patients with type 1 diabetes, or if carbohydrate availability is drastically restricted, as with adherence to a ketogenic diet, this mild ketosis can evolve into DKA ( 12 ).
The unique presentation of euglycemic DKA induced by SGLT2 inhibitors makes both its diagnosis and management challenging. At presentation, patients may be normoglycemic, so health care providers should carefully consider which type of IV fluids should be given based on serum potassium levels and glycemia ( 13 ). Relatively lower amounts of IV insulin should be initiated to avoid hypoglycemia. It has also been observed that low to normal serum potassium levels may be present, and patients might require earlier replacement ( 13 ).
Several risk factors have been associated with the development of DKA with SLGT2 inhibitor use. These include a decrease in insulin or secretagogue dose, starvation or decrease in carbohydrate intake, acute illness, pregnancy, and alcohol intake ( 14 ).
A change in diet, notably decreased carbohydrate intake, shifts metabolism to the use of fat for energy, which promotes ketone production and may contribute to the eventual development of DKA under stressful conditions ( 6 ). The ketogenic diet is characterized by a reduction in carbohydrate intake (usually to <50 g/day) while maintaining a sufficient protein intake and consuming >70% of daily calories from fatty foods ( 15 , 16 ).
Although the ketogenic diet has become popular as a weight loss approach, its long-term side effects and sustainability have yet to be studied in depth. In the case of patients with type 2 diabetes who are under treatment with an SGLT2 inhibitor, it is contraindicated because it can cause euglycemic DKA ( 12 , 17 ).
Euglycemic DKA is an underdiagnosed medical emergency that can develop in patients who are taking an SGLT2 inhibitor. A nonspecific clinical presentation and near-normal blood glucose levels are likely the main reasons this diagnosis is often missed.
The interaction between diet and SGLT2 inhibition has not been fully studied. It is particularly important to note new side effects in patients who have started a ketogenic diet while on one of these medications.
Given the difficulty of diagnosing this syndrome, we encourage health care providers prescribing these medications to counsel their patients about possible complications and side effects.
By understanding the etiology and precipitating factors of DKA with the use of SGLT2 inhibitors, clinicians can take the necessary precautions to reduce such events.
We recommend that patients with type 2 diabetes avoid changing their diet without consulting a physician or dietitian.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
P.S.G. and G.Z. researched the data and wrote the manuscript. R.L. reviewed and edited the manuscript. P.S.G. is the guarantor of this work and, as such, had full access to all the data presented and takes responsibility for the integrity of the data and the accuracy of the case report.
Email alerts
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
COVID-19 and diabetic ketoacidosis: A case series at an urban district hospital in South Africa
Affiliation.
- 1 Department of Family Medicine, Northdale Hospital, Pietermaritzburg, South Africa; and, Department of Family Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban. [email protected].
- PMID: 36226949
- PMCID: PMC9557943
- DOI: 10.4102/safp.v64i1.5590
Background: Coronavirus disease 2019 (COVID-19) is associated with an increased prevalence and mortality from diabetic ketoacidosis (DKA) globally. With limited access to specialised care, most patients with DKA in South Africa are managed at district hospital level. This study describes the profile of patients admitted to a district hospital in South Africa with DKA and COVID-19 and examines associated risk factors encountered.
Methods: This was a case series of all patients presenting to a district hospital with DKA and COVID-19 infection between July 2020 and July 2021. Data extracted included patients' demographic profiles, biochemical results, comorbidities and clinical outcomes.
Results: The median age of the 10 patients admitted during the study period was 39 years old (±12), six of whom were male. The hemoglobin A1c (HbA1c) values on admission ranged from 9.7 to 13.8. Five of the patients had pre-existing type 2 diabetes mellitus (DM). Four of the known DM patients were on metformin only, and one was on biphasic insulin. Three patients had other pre-existing comorbidities, two patients with hypertension and one with human immunodeficiency virus (HIV). Three patients demised, two of whom were hypoxic on admission.
Conclusion: Diabetic ketoacidosis appears more commonly in COVID-19 infected patients with type 2 DM and at a young age. Suboptimal glycaemic control was associated with DKA, and hypoxia was a strong predictor for mortality. Treatment inertia was evident in the known DM group, who were on monotherapy despite persistent hyperglycaemia. Greater vigilance is required to detect ketosis in type 2 DM and intensify therapy to improve glycaemic control.
Keywords: COVID-19; HbA1c; diabetes; diabetic ketoacidosis; district hospital.
- Biphasic Insulins / therapeutic use
- COVID-19* / complications
- COVID-19* / epidemiology
- Diabetes Mellitus, Type 2* / complications
- Diabetes Mellitus, Type 2* / drug therapy
- Diabetes Mellitus, Type 2* / epidemiology
- Diabetic Ketoacidosis* / diagnosis
- Diabetic Ketoacidosis* / epidemiology
- Diabetic Ketoacidosis* / therapy
- Glycated Hemoglobin / analysis
- Glycated Hemoglobin / therapeutic use
- Hospitals, District
- Metformin* / therapeutic use
- Retrospective Studies
- South Africa / epidemiology
- Biphasic Insulins
- Glycated Hemoglobin A
- ALiEM Library
- ALiEMU: Be Free To Learn
- Bridge to EM: Senior Medical Student Curriculum
- Chief Resident Incubator: Legacy Edition
- EM Bound: Medical student newsletter
- EM Match Advice Series
- Faculty Incubator
- GroundED in EM: A Third-Year Student Curriculum
- How I Educate Series
- IDEA Series
- The Leader’s Library
- MEdIC series
- How I Podcast Smarter Series
- How I Stay Healthy Series
- How I Work Smarter Series
- Social Media & Tech
- 60-Second Soapbox
- EM Pharm Pearls
- Lab It Up Library
- SAEM Clinical Images
- SplintER Series
- Tricks of the Trade
- Ultrasound for the Win
- Meet the Team
- Culture Book
- Disclaimer / Privacy / Copyright
EM ReSCu Peds 5: Diabetic Ketoacidosis
Play this case online for free with Full Code
Presentation
Brief narrative description of case.
The patient’s parents brought her in for vomiting, and “tiredness.” The whole family has had the flu for the past week and all three children were home from school with fever, myalgias, diarrhea. She had a negative COVID-19 swab at a community testing site yesterday. Her siblings seem to be feeling better, but she hasn’t improved yet. She is somnolent, ill-appearing, and severely dehydrated. She is in early hypotensive shock with poor perfusion. Intravenous access attempts will be minimally effective (22g only x 1). She is hyperglycemic, and there is difficulty obtaining additional vascular access. She is hypokalemic (DKA plus diarrhea) and acidotic, which should prompt recognition of DKA with complications.
Management will require IV access (IO), appropriate fluid resuscitation, insulin drip, potassium replacement and admission/transfer.
Download the Case Summary
- What are case summaries? [PDF]
- Quick reference guide for the case [PDF]
Primary Learning Objectives
At the end of this simulation, participants should be able to:
Describe signs/symptoms of shock in a child (comprehension)
Demonstrate early evaluation of a critically ill patient (application).
- Interpret signs/symptoms of DKA including hyperglycemia and acidosis (evaluation)
Construct and implement an initial management plan for a child in DKA (application)
Consider risks of aggressive fluid administration in the setting of dka such as cerebral edema (evaluation).
- Manage hypokalemia and hyperglycemia in the setting of insulin administration (application)
Demonstrate focused history taking from a caregiver (application)
Effectively communicate diagnosis and management to caregivers and respond appropriately to their concerns (synthesis), demonstrate teamwork and closed loop communication (application), critical actions.
- Assign/assume team roles
- Obtain brief history from parent
- Place patient on continuous cardiac monitor
- Obtain a point of care glucose
- Establish vascular access – consider IO or ultrasound guided peripheral IV (USGPIV)
- Obtain a venous/capillary blood gas to establish electrolytes/pH level
- Perform focused physical exam/primary survey
- Verbalize diagnosis of DKA
- Initiate appropriate fluid resuscitation for severe DKA
- Initiate appropriate medications (insulin, potassium)
- Communicate effectively with PICU +/- Endocrine consultants
- Explain diagnosis to parent(s) and how it relates to the patient’s presentation
- Effectively manage anxious family members
Case Creators
- Kimberly Schertzer, MD, FACEP
- Melissa Hersh, MD
- Ilana Bank, MDCM, FRCPC, FAAP
- Rebekah Burns, MD
- Sherri Rudlinsky, MD
- Josh Davis, MD, NASM-CPT
- Myto Duong, MD
Updated March 29, 2023
Chief complaint: Vomiting and lethargy Patient age: 8 years old Weight: 30 kg
Recommended Supplies
- Manikin : Any model to reflect age of patient (8 years old)
- Moulage: None
- Resources: PALS card and/or length-based tape (e.g., Broselow), local DKA pathways/procedures, if applicable
- Manikin set up : IV line available x 1 in place with drainage bag
- Point of care tester (for glucose/VBG/K+)
- Intraosseous equipment including E-Z IO, needle, stabilizer, and connectors; saline flushes
- ECG machine
- Cardiac monitor
- Continuous oximeter
- Simple facemask
- Non-rebreather
- Nasal cannula
- Oxygen tubing
- Medications: Normal saline, IV insulin, sodium bicarbonate, mannitol, hypertonic saline, ondansetron (ODT or IV), D10 1⁄2 NS (optional)
Supporting Files
- Point-of-care labs (VBG/CBG, glucose, electrolytes)
- First ECG showing sinus tachycardia with signs of hypokalemia
- Second ECG (if insulin started without checking/giving potassium) showing Torsades de Pointes
Participants/Roles
- Team Leader
- Airway Manager
- Survey Physician
- Medication Preparer
- Medication Giver
- +/- Family Liaison
- Consultant (PICU or Endocrine)
- Embedded participants can play a nurse, respiratory therapist, or tech.
- Standardized patient (actor or faculty) to play patient’s parent
Team roles may need to be adjusted in order to suit local practices and norms
Prerequisite Knowledge
- PALS protocols
- General knowledge of emergency medicine
- Simulation implementation and debriefing experience
- Any stage of training (PGY-1,2 for basic case, PGY3+ advanced case)
- Completed PALS certification

Case Alternatives
- If residents fail to recognize DKA within 5 minutes of the case (e.g., gives normal saline boluses, +/- administers antibiotics, +/- gives pressors), the patient will become more lethargic (cerebral edema) and will need emergent airway management.
- If intubation is performed, the patient will become more acidotic and hypotensive.
- For advanced learners, the initial ECG will show u-waves and a wide QRS. If this is not recognized, the patient will develop torsades (and ultimately ventricular tachycardia if not recognized). (See Stage 2 )
Virtual Resus Room
This simulation case can be run virtually using Google Slides and Zoom from the Virtual Resus Room (Peds DKA) page.
PC1. Emergency Stabilization PC2. Performance of Focused History & Physical Exam PC3. Diagnostic Studies PC4. Differential Diagnoses and Management PC5. Pharmacotherapy PC9. General Approach to Procedures PC14 . Vascular Access PC15. Medical Knowledge ICS1. Patient Centered Communication ICS2. Team Management
- Kuppermann N, Ghetti S, Schunk JE, et al. Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis. N Engl J Med. 2018;378:2275-2287. PMID 29897851
- Wolfsdorf J, Glaser N, Sperling MA. Diabetic ketoacidosis in infants, children, and adolescents: A consensus statement from the American Diabetes Association. Diabetes Care. 2006;29:1150-1159. PMID 16644656
- Wolfsdorf J, Craig ME, Daneman D, et al. Diabetic ketoacidosis. Pediatr Diabetes. 2007;8(1):28-43. PMID 17341289
- Glaser NS, Stoner MJ, Garro A, et al.; Pediatric Emergency Care Applied Research Network (PECARN) DKA FLUID Study Group. Serum Sodium Concentration and Mental Status in Children With Diabetic Ketoacidosis. Pediatrics. 2021 Sep;148(3):e2021050243. doi: 10.1542/peds.2021-050243. Epub 2021 Aug 9. PMID: 34373322 .
- Kuppermann N. Pediatric DKA: Don’t Fear the Fluids! EMRA Cast, 2020.
- Glaser N, Kuppermann N. A Sweet New Year to All – DKA . PEM Podcast, 2020.
- Woods J, Bukowski J. PEM Pearls: Treatment of Pediatric Diabetic Ketoacidosis and the Two-Bag Method . Acad Life in Emerg Med, 2017. .
Hyperglycemia
Evaluation to identification of DKA
- Team leader assigns tasks
- Obtains brief history from parent
- Performs primary survey
- Request patient placement on continuous cardiac monitor
- Performs focused physical exam
- Verbalizes recognition of shock
- Obtains point-of-care glucose (high)
- Obtains vascular access
- IO or ultrasound-guided peripheral IV preferred, if peripheral access is unsuccessful
- Verbalizes recognition of hyperglycemia
- Obtains point-of-care VBG/CBG and electrolytes (abnormal)- if extended electrolytes are ordered (Mg+, PO4-, they are not available during case)
- Verbalizes hypokalemia on POC testing OR obtains ECG showing hypokalemia-related changes
- Discusses progress/plan of care with the family
* Unbolded items may be excluded depending on local practices and norms
Physical Exam
Instructor notes: changes and case branch points, dka stabilization.
Identification of DKA through start of insulin drip and IV fluids
- Verbalize recognition of DKA, complicated by hypokalemia
- Administer 10 mL/kg normal saline for moderate dehydration
- Reassess perfusion status following initial bolus
- Reassess mental status following initial bolus
- Reassess glucose level following initial bolus
- Begins IV insulin AFTER saline bolus is completed (0.05-0.1 units/kg/hour)
- Begins IV potassium for K<3.5 mEq/L (0.5 mEq/kg over 1 hour) – can be given peripherally as bolus
Case Conclusion and Disposition
Time 1 hour after arrival through reassessment (physical exam and labs)
- Verbalize need for repeat neuro checks for cerebral edema evaluation
- Verbalize need for q 2 hour electrolyte/glucose monitoring
- Orders VBG + electrolytes STAT if worse in any way
- Explains diagnosis to parent and how it relates to the patient presentation
- Consults PICU and/or Endocrine for admission (if not done in Stage 2)
TIME ADVANCE:
Instructors: please state “time has advanced 1 hour since the patient arrived at the ED.”
Shock is the state where blood flow to tissues/organs flow does not adequately meet the demand. Children are more susceptible to cardiovascular compromise from shock because of both physiologic differences (compared with adults) and their limited reserve.
- In general, hypotension is a late finding in pediatric shock. Assessment of perfusion status (e.g., capillary refill) may give an early indication: delayed capillary refill suggests “cold shock” (cardiovascular or hypovolemic source) and very brisk capillary refill suggests “warm shock” (e.g., anaphylactic or distributive etiology)
- Another early sign of shock in children is tachycardia and decreased capillary refill, compared to a low blood pressure.
In general, the evaluation of a critically ill child requires quick assessment of the pediatric triangle (appearance, breathing, color) in conjunction with the primary survey with an emphasis on the clinical status
- Appearance: Mental status, level of arousal, and changes in speech/cry
- Work of breathing: Note presence of abnormal breath sounds, retractions, nasal flaring, grunting, apnea
- Circulation to skin: Note presence of pallor, delayed capillary refill, mottling, cyanosis
Primary survey:
- Airway: Does the patient have a patent airway?
- Breathing: Auscultate for bilateral breath sounds
- Circulation: Assess for presence/absence of pulses and degree of peripheral perfusion, cardiac sounds, liver distension
- Disability: Report Glasgow Coma Scale, examine pupils, D * for dextrose
- Exposure: Allow for adequate visualization of the patient
Interpret signs/symptoms and laboratory changes of DKA including hyperglycemia and acidosis (evaluation)
- Hyperglycemia >200 mg/dL
- Acidosis: Venous pH <7.3 or HCO 3 – <15 mEq/L
- Mild DKA (pH: 7.2-7.3) (HCO 3 -: 10-14 mEq/L)
- Moderate DKA (pH: 7.1-7.2) (HCO 3 : 5-9 mEq/L)
- Severe DKA (pH: <7.1) (HCO 3 -: <5 mEq/L)
- The initial step in DKA treatment is assessment of dehydration status, weight, and mental status.
- Blood glucose level
- Blood beta-hydroxybutyrate (may not be available POC in all locations)
- Urine ketones (may be found on urine dipstick)
- Blood glucose level (for more accurate values)
- Serum electrolytes (including bicarbonate – allows for anion gap calculation)
- BUN/creatinine
- Complete blood count
- Calcium, phosphorous, magnesium
- Saline (see detailed discussion below)
- +/- Potassium
- Avoidance of bicarbonate (lack of benefit and potential for harm)
Cerebral injury (or cerebral edema) is rare. Its clinically significant incidence is between 0.3-0.9% of episodes in children with DKA. (Many or most others with DKA will have subclinical cerebral edema without neurological signs). It is more common in children with DKA than adults, and those with the most severe DKA are at highest risk for the cerebral complications. It may be present prior to DKA treatment or during it (between 3-12 hours after treatment begins). The cause is not completely understood. Early work thought it may be the rate of fluid administration but this is being challenged with current lines of research.
– “Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis”: June 14, 2018 — N Engl J Med 2018; 378:2275-2287 (DOI: 10.1056/NEJMoa1716816 )
- Severely acidotic on original presentation
- High BUN on presentation (suggests greater hypovolemia)
- Insufficient rise of sodium level when DKA treatment starts
- Younger age (<3-5 yrs old) on presentation (because diagnosis is often delayed)
- Abnormal verbal or motor response to pain
- Posturing (decorticate or decerebrate)
- Double vision or cranial nerve palsy (III, IV, VI)
- Abnormal respiratory pattern (Cheyne-Stokes, apnea, grunting, tachypnea)
- Age-inappropriate incontinence
- Abnormal, fluctuating or declining mental status after therapy begins (including agitation)
- Abnormal heart rate sowing (declining by more than 20 beats) that is not explained by sleep or improved intravascular volume status
- Lethargy or irritability*
- Elevated blood pressure (e.g., diastolic BP >90 mmHg)
- *Especially if begins/resumes after DKA treatment initiated
- 1 major plus 1 minor criteria (if age <5 years old)
- Avoid drugs that increase ICP
- Elevate head of the bed 30 degrees
- Hyperosmolar therapy:
- First line treatment: Mannitol 0.5-1g/kg IV over 10-15 minutes. May repeat in 30 minutes.
- Second line treatment: Hypertonic saline 2.5-5 mL/ kg over 30 minutes
- Neurosurgery consult for possible ICP measuring
- IV saline to improve intravascular compromise
- 10-20 mL/kg normal saline or lactated ringers
- Ensure adequate airway and assist ventilation as needed
- Supplemental oxygen as needed to maintain a normal O 2 level
- Avoid intubation if possible
- If intubation is necessary, hyperventilate to maintain the pCO 2 they had before they decompensated. Reduce this over several hours.
Manage hypokalemia and hyperglycemia with potential of hypoglycemia in the setting of insulin administration (application)
Patients in severe DKA may also need supplemental IV potassium. Since the goal of insulin administration is closure of the anion gap, supplemental dextrose may be needed when the serum glucose level falls below 250.
When adding dextrose for glucose <250 mg/dL, you may use the “2- bag method”.
- 4 mL/kg/hr for the first 10 kg body weight
- 2 mL/kg/hr for the second 10 kg body weight
- 1 mL/kg/hr for the remaining weight
- In this case (pt weighs 30 kg): 70 mL/hr
- In this case: 105 mL/hour
- Finally, determine which percentage of which bag to give.
Two-Bag Method of IV Fluids in Hypoglycemia
- 1 bag normal saline
- 1 bag D10NS
- 1 bag D12.5 NS
- PRN dextrose
Hypokalemia in the setting of DKA
Hypokalemia on presentation signifies a profound total potassium deficit. Caution with IV insulin and bicarbonate therapy is warranted, because it could further drop the potassium levels. Davis et al. 2016 presented a case of profound hypokalemia associated with DKA (Pediatr Diabetes Feb; 17 (1): 61-65). In this case, the patient’s potassium level was 1.3 mEq/L. 0.3 mEq/kg KCI over 1 hour was initiated and insulin held until potassium level was 2.7 mEq/L.They reported that their institution had a policy which prevented them from giving a more aggressive replenishment of 0.5 mEq/kg over an hour potassium via a peripheral line. They opted to avoid risks associated with central line placements. Additionally, 30 mEq/L potassium acetate and 30 mEq/L potassium phosphate were given at 1.5x maintenance.
PFCCS (Pediatric Fundamental Critical Care Support) recommends a conservative IV potassium replacements regimen:
- If K+ 3.0-3.5 mEq/L, administer 0.25 mEq/kg KCL over 1 hour.
- If K+ 2.5-3.0 mEq/L, administer 0.5 mEq/kg over 2 hours.
- If K+ <2.5 mEq/L, administer 0.75 mEq/kg over 3 hours, with checking of the K level half-way through this infusion.
Evaluation of a critically ill child should include obtaining a history from all possible sources including EMS, old records (if time), and especially caregivers. Paying attention to details such as trauma or recent illness may give hints toward identifying the underlying pathophysiology. A history of polyuria, polydipsia, increased hunger and weight loss may suggest undiagnosed diabetes. Children may present with DKA after a mild illness so a review of systems should also include evaluation for infection symptoms.
Compassionate, understandable communication with caregivers is critical, as they are strong partners in the treatment of their children. This should not impede lifesaving treatment, but if at all possible, a member of the treatment staff should be assigned to help communicate with parents. Failure to provide a communication liaison may result in anxious parents that may obstruct care. When not actively resuscitating (as in this case), the physician should be able to communicate with patients throughout the child’s care. For complicated concepts, like DKA, it is important to ensure the caregivers understand the explanations being given to them.
Teams may use different frameworks to improve team dynamics and communication. Below are a few definitions that may be helpful to discuss, adapted from the AHRQ TeamSTEPPS Pocket Guide .
- Brief : Short session prior to start of encounter to share the plan, discuss team formation, assign roles and responsibilities, establish expectations and climate, anticipate outcomes and likely contingencies
- Huddle : Ad hoc team discussion to re-establish Situation Awareness; designed to reinforce plans already in place and assess the need to adjust the plan
- Callout: A strategy used to communicate critical information during an emergent event. Helps the team prepare for vital next steps in patient care. (Example: Leader- “Airway status?”; Surveying provider- “Airway clear”; Leader- “Breath sounds?”; Surveying provider- “Breath sounds decreased on right”)
- Check-back: A closed-loop communication strategy that requires a verification of information ensuring that information conveyed by the sender is understood by the receiver as intended. The sender initiates the message; the receiver accepts it and restates the message. In return, the sender verifies that the re-statement of the original message is correct or amends if not. (Example: Leader- “Give diphenhydramine 25 mg IV push”; Med Prep- “Diphenhydramine 25 mg IV push”; Leader- “That’s correct”)
- S = Situation (What is going on with the patient?)
- B = Background (What is the clinical background or context?)
- A = Assessment (What do I think the problem is?)
- R = Recommendation (What would I do to correct it?)
- Situation monitoring: The process of continually scanning and assessing a situation to gain and maintain an understanding of what is going on around you.
- Situation awareness: The state of “knowing what’s going on around you.”
- Shared mental model: Result of each team member maintaining situation awareness and ensures that all team members are “on the same page.” An organizing knowledge structure of relevant facts and relationships about a task or situation that are commonly held by team members.
- STEP: A tool for monitoring situations during complex situations. A systematic method to review S tatus of patient, T eam members’ performance and status, E nvironment, and P rogress towards goal.
- Cross-monitoring: A harm error reduction strategy that involves 1. Monitoring actions of other team members 2. Providing a safety net within the team. 3. Ensuring that mistakes or oversights are caught quickly and easily. 4. “Watching each other’s back.”
- CUS: Signal phrases that denote “I am C oncerned,” “I am U ncomfortable,” and “This is a S afety Issue.” When spoken, all team members should understand clearly not only the issue but also the magnitude of the issue.

Download Case 5 supporting files
- ECG 1 interpretation: ECG with signs of hypokalemia. Image from Dr. Ilana Bank.
- ECG 2 interpretation: ECG with torsades de pointes. Image from Dr. Ilana Bank.
For the embedded participants playing the role of the patient and mother
Case Background Information
You are bringing your daughter to the ED for vomiting and “tiredness.”
Over the past week the whole family has had the “flu,” with intermittent fevers, myalgias and fevers. Her 3 siblings, however, are all feeling better – but she doesn’t seem to be back to herself. Additionally, for the last 2 days she has been complaining of stomach aches with “too many to count” episodes of vomiting (NB/NB). You took her to an urgent care earlier in the day and they told you that some children take longer to recover from illnesses than others. You’re not satisfied with that response.
Who are the Learners?
Emergency medicine residents
This case is specifically aimed at first and second year residents who should have experience in gathering information from patients and families, and standard medical treatments and procedures. They may be less familiar with escalating medical therapies when first measures are not successful.
Standardized Patient Information
Mother: Your demeanor is overall anxious and concerned. You are a nervous parent with limited medical acumen. Interrupt the doctors often with questions – but do not be belligerent or aggressive. You are especially concerned about her stomach-ache and really want to know if she will need surgery. If given space, tell the team about your friend’s daughter who has a stomach-ache and then needed surgery, and then ask repeatedly “is this the same thing?” Her nausea is making you very anxious and want it managed quickly. Something is VERY wrong with your child and you know it. You keep giving her Motrin and Robitussin, but it is not making her any better.
Patient: She doesn’t contribute much. She is awake, tired appearing, not moving a lot on the bed, but intermittently rubs her stomach, clutches her vomit bag (if offered one) and talks about feeling like she might throw up. When examined, she cannot specifically tell them where your pain is – “it’s everywhere.” She is alert and oriented if asked. She is also thirsty if asked.
Patient Information
(Please remember not to offer any of this information, but when asked please respond while remaining in character.)
- CHIEF COMPLAINT: “My stomach hurts.”
- AGE: 8 years old
- ADDITIONAL HISTORY : “I had a cold last week, my whole body hurt and since then I feel crummy.”
- PAST MEDICAL HISTORY : None
- SOCIAL HISTORY: None, no recent travel. They have never left California.
- FAMILY HISTORY : Grandma has trouble with sugars – offer only if specifically asked
- PAST SURGICAL HISTORY : None
- MEDICATIONS: None
- ALLERGIES: No known drug allergies
- IMMUNIZATIONS: Up-to-date
- BIRTH HISTORY : Unremarkable. She was born full term, no medical complications (patient is 8 years old, ok if they don’t ask about birth history)
Potential Dialogue
IMPORTANT: Do not offer unsolicited information. Please allow the learners to ask questions. Do not offer information unless they ask you.
Things Mom could say without being asked:
- “All the vomiting has made her lose weight. She keeps eating but is so skinny. I think it’s the vomiting.”
- “Everyone else got better, why isn’t she getting better?”
- “She is such a healthy child, she is never sick and never complains. I know something is wrong.”
Things you might say triggered by events in the scenario:
The learners enter the room to find a patient who is dry, uncomfortable, and tired appearing – she is mildly somnolent but fully arousable. They immediately place the patient on a bedside monitor and recognize that the patient is in early hypovolemic shock. Access needs to be obtained and might be difficult; the residents can place an IO and an IV fluid bolus should be ordered. Initial blood work should also be ordered at this time – including point of care glucose – the result of which should immediately prompt the residents to move down the DKA management pathway.
After completing a physical examination and obtaining an appropriate history, the learners should note that the patient appears to be worsening – her blood pressure has decreased slightly and remains tachycardic. At this point they discuss the risk of cerebral edema with aggressive fluid management. Patient’s perfusion status remains stable and BP is still above 5% for her age range so conservative management should continue. Insulin is ordered and potassium is measured. Potassium returns 3.1 mEq/L, which should prompt the learners to recognize the need to give potassium (either as a bolus or incorporated into maintenance fluid) prior to the initiation of the insulin drip (regardless of whether they additional IVF). Patient remains stable and starts to hemodynamically improve as the second bolus starts.
No signs of cerebral edema are noted on 1 hr neurologic check. She is admitted to ICU, and the endocrine team is consulted, who will follow the patient in the unit. Prior to the end of the case, DKA diagnosis is explained to the patient and her mother, and DKA education is started.
Anticipated Management Mistakes
- Inadequate IV access: Learners may be hesitant to perform IO/ ultrasound-guided peripheral IV (USGPIV) access. Some may be unfamiliar with it or may be concerned that it is painful or frightening for parents to watch. However, with need for IVF, IV insulin, and potassium, access is critical. Furthermore, in critically ill patients, anticipating a need for access is crucial. While IO access and USGPIV are becoming more mainstream, it may be helpful to have a nurse prompt with “we do this all the time”. If learners fail to recognize how ill the child is, a nurse may prompt with “she seems pretty sick, I worry she may get worse quickly.”
- Intubation of a patient in DKA: It would be unlikely in a patient with a fairly normal mental status for intubation to be considered. However, some learners may bring an element of simulation artifact (“it is sim so this is going to go downhill fast”) to the case. In this scenario, intubation leads to worsening acidosis, and PEA requiring CPR and epinephrine. If the conversation heads toward intubation, it may be helpful to discuss the risk/benefit of intubation in an acidotic patient who is relying on respiratory compensation. It is actually quite dangerous to intubate a patient such as this unless the patient is severely obtunded and not maintaining respiratory effort or protecting their airway. It is very hard to be able to compensate as well as the patient can with a ventilator.
- Excessive fluid resuscitation: Some of our learners may provide aggressive fluid resuscitation in an attempt to normalize heart rate and blood pressure. Concerns for cerebral edema increase with aggressive fluid management. This however, is controversial. Please refer to the Kuppermann et al. trial as a point of discussion.
Return to the EM ReSCu Peds curriculum home page
Please complete our brief survey describing your experience.
Learner (scan or click on QR code)

Facilitator (click or scan QR code)

- Latest Posts

Michelle Lin, MD
Latest posts by michelle lin, md ( see all ).
- EM Match Advice 42: Mid Interview Season Check-In - January 5, 2024
- EM Match Advice 41: The 2024 ERAS Application – New and Improved - July 24, 2023
- EM Match Advice 40: Program Directors Reflect on the 2023 Match - May 17, 2023
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Clin Diagn Res
- v.9(6); 2015 Jun
Clinical Profile of Diabetic Ketoacidosis: A Prospective Study in a Tertiary Care Hospital
Pankaj seth.
1 Assistant Professor, Department of Emergency Medicine, Dayanand Medical College and Hospital, Ludhiana, India.
Harpreet Kaur
2 Assistant Professor, Department of Emergency Medicine, Dayanand Medical College and Hospital, Ludhiana, India.
Maneet Kaur
3 Assistant Professor, Department of Emergency Medicine, Dayanand Medical College and Hospital, Ludhiana, India.
Diabetic ketoacidosis, a well-known and major acute metabolic complication classically occurs in young patients with type 1 diabetes. However, it may occur in patients with type 2 Diabetes Mellitus too.
Aim of this study was to look into the clinical profile, precipitating factors and clinical outcome in the patients presenting with Diabetic ketoacidosis in the Emergency of a Tertiary care hospital.
The study was a prospective study conducted over a period of two years in Kasturba Medical College, Manipal Karnataka, India.
Materials and Methods
Clinical profile of 60 diabetic patients admitted in the Emergency with the diagnosis of Diabetic ketoacidosis were analysed.
Out of 60 patients, 12 were of Type 1 and 48 were Type 2 Diabetes Mellitus. Mean duration of diabetes was 8.65 years. Only 14 (23.3%) patients were taking regular treatment for Diabetes Mellitus whereas 32 (53.33%) patients were on irregular treatment and eight (13.33%) were not on any treatment at all. Among 12 Type 1 Diabetic patients, six patients were freshly diagnosed to be diabetic when they presented with Diabetic ketoacidosis complication. Nausea and vomiting (63.33%) were the most common symptoms of these patients. Infections (73.33%) were the most common precipitating factor for Diabetic ketoacidosis. Mean fluid requirement on first day of therapy was 3.51 liters. Mortality of 10% was seen.
Diabetic ketoacidosis is a fatal acute metabolic complication of Diabetes Mellitus with heterogeneous clinical presentation. Early diagnosis and treatment can avoid morbidity & mortality.
Introduction
Diabetic Ketoacidosis (DKA) is the most serious hyperglycaemic emergency in patients with type 1 and type 2 Diabetes Mellitus (DM) and is associated with significant morbidity and mortality [ 1 ]. DKA is responsible for more than 500,000 hospital days per year [ 2 , 3 ]. It is conceptualized that DKA occurs most often in patients with Type 1 diabetes but this is not true. DKA is also reported in type 2 diabetes; however, it rarely occurs without a precipitating event [ 4 - 6 ]. National Centre for health statistics showed that most patients with DKA were between the ages of 18 and 44 years (56%) and 45 and 65 years (24%), with only 18% of patients <20 years of age. Two-thirds of DKA patients were considered to have type 1 diabetes and 34% to have type 2 diabetes; 50% were female and 45% were nonwhite [ 2 ]. Another previous study by Adhikari et al., also showed predominance of type 2 diabetes mellitus (62.8%) as compared to type 1 diabetes mellitus (37.8%) who presented with DKA [ 7 ].
DKA consists of the triad of hyperglycaemia, ketosis, and acidemia. An arterial pH of less than 7.35, a Serum Bicarbonate (HCO3-) value of less than 15 mEq/L, and a blood glucose level of greater than 250 mg/dl with a moderate degree of ketonaemia and/or ketonuria (as determined by nitroprusside method) are necessary for the diagnosis of DKA [ 8 ].
Pathophysiology of DKA involves reduction of the effective insulin concentrations in the body which are not able to match the glycaemic overload either due to high intake or increased concentrations of counter-regulatory hormones (catecholamines, cortisol, glucagon, and growth hormone). This imbalance leads to hyperglycaemia and ketosis. Hyperglycaemia can be due to increased gluconeogenesis, accelerated glycogenolysis, or impaired glucose utilization by peripheral tissues [ Table/Fig-1 ][ 9 ]. DKA is a catabolic state and there is an alteration of protein, carbohydrate and lipid metabolism. The anion gap is increased from normal (8-12 mmol/L) in DKA. It has heterogeneous clinical presentation. Increased mortality and fatal complications are seen in untreated patients.

Pathogenesis of DKA and HHS: stress, infection, or insufficient insulin
DKA usually presents with symptoms like nausea, vomiting, pain abdomen. They may also have increased thirst and polyuria. On examination usually a fruity odour can be smelled and the breathing is typical of DKA, rapid shallow kussmaul breathing. Severe cases may present with hypotension, altered sensorium. Features of the precipitating cause may also be present. A study was done by Munro et al., who noticed the frequency of nausea and vomiting (86%), pain abdomen (27%), polyuria/polydipsia in 24% of patients [ 10 ]. Umpierrez et al., did a study and found abdominal pain in 46% of patients with DKA [ 11 ]. Adhikari et al., noticed vomiting and abdominal pain in 34.9% of patients, altered sensorium in 47%, kussmaul breathing in 28% and hypotension in 46% of patients with DKA [ 7 ].
DKA can be the initial presentation of diabetes mellitus or precipitated in known patients with diabetes mellitus by many factors, most commonly infection [ 12 ]. Other precipitating factors include acute myocardial infarction, any cerebrovascular accident or any postoperative stress. Adhikari et al., found infection as a precipitating factor for DKA in 58% of patients [ 7 ]. Studies of Vignati et al., emphasized the importance of infection as a precipitating cause occurring in up to 50% of patients [ 13 ]. Matoo et al., and Westphal found an incidence of infection in 30% and 40% of patients respectively [ 14 , 15 ]. Noncompliance is also one major precipitating factor for DKA. Matoo et al., found that incidence of non-compliance to treatment was 20% and while Westphal found it 16% [ 14 , 15 ]. Often more than factors may be present in a patient or rarely no obvious factor can be identified. A study conducted by Umpierrz et al., found no obvious factor of DKA in 2-10% of cases [ 16 ].
The management of diabetic ketoacidosis is complex and involves many aspects [ 17 ]. These include:
1. A careful clinical evaluation of the patient and identification of all the metabolic abnormalities and their correction.
2. Meanwhile all efforts should be made for identification of precipitating and co-morbid conditions and its treatment.
3. Once acute phase is over, a comprehensive approach should be made for appropriate long-term treatment of diabetes, and plans to prevent recurrence.
Another most important aspect of management is patient education so as to ensure compliance to treatment as non-compliance may lead to DKA in patients with DM [ 14 , 15 ].
DKA is the most common acute complication in children and adolescents with Type 1 Diabetes which leads to high mortality. It accounts for almost 50% mortality in diabetic patients younger than 24 years of age [ 18 ]. Though the overall mortality is rare in adults with DKA; a higher mortality rates occur in the elderly and in patients with co-morbidities [ 19 , 20 ]. Underlying precipitating illness is the major cause of death in these patients than hyperglycaemia or ketoacidosis [ 7 , 21 ].
This study was conducted to study the clinical profile of DKA patients. The mortality from DKA varies from 3-13%, therefore it is important to recognize DKA at an earlier stage as early recognition of DKA, leads to less complications and is associated with increased incidence of successful recovery.
Study design This study was a prospective study conducted in a Tertiary care Hospital taking a total of 60 patients of Type 1 and 2 Diabetes Mellitus admitted in the Emergency who were diagnosed to have DKA on the basis of following criteria:
Diagnostic Criteria for Diabetic Ketoacidosis (DKA) [ 8 ]
• Blood glucose (mg/dl) > 250
• Arterial pH <7.3
• Serum bicarbonate (mEq/l) <15
• Moderate degree of ketonaemia and ketonuria (As determined by nitroprusside method)
Patients on steroids and other Endocrine disorders like Cushing’s syndrome, Acromegaly which can also cause Hyperglycaemia were excluded from the study.
The clinical profile, precipitating factors and clinical outcome was analysed.
Ethics: This study was conducted in accordance with the ethical standards of the responsible committee on human experimentation of the institution.
Statistical Analysis
Statistical analysis was done just by calculating percentages. No other statistical test was required in this study.
Out of 60 patients, 12 (20%) patients belong to type 1 diabetes mellitus and 48 (80%) patients belong to Type 2 DM. Among them, 34 (56.66%) were males and 26 (43.33%) were females. The male: female ratio was 1.3:1. Our study showed that only 14 (23.3%) patients were on regular treatment while 32 patients (53.33%) were on irregular treatment and eight patients (13.33%) were not taking any treatment for Diabetes. In six (10%) patients Diabetic status was detected only when they presented with DKA complication. Age and sex distribution of the patients is stated in [ Table/Fig-2 ].
[Table/Fig-2]:
Age and sex distribution in patients with diabetic ketoacidosis
Clinical presentation was analysed and it was found that nausea and vomiting were present in maximum number of patients (63.33%). Symptoms related to precipitating cause were also present in a large number of patients (60%). Pain abdomen was present in (43.33%) of patients, while altered sensorium and polyuria/ polydipsia were present in 30% and 26.66% of cases respectively. Twenty (33.33%) patients were dehydrated. Weakness was present in ten (16.66%) of patients. Kussmaul breathing was present in ten (16.66%) patients. Only eight (13.33%) patients had hypotension [ Table/Fig-3 ].
[Table/Fig-3]:
Symptomatology in patients with diabetic ketoacidosis
The most common precipitating factor was found to be infection (73.33%), followed by non-compliance to treatment (66.66%), and followed by stressful conditions (26.66%). In six (10%) patients diabetic status was detected only when they presented with DKA complication and all the six patients belong to Type 1 DM [ Table/Fig-4 ].
[Table/Fig-4]:
Precipitating factors of diabetic ketoacidosis
Since out of 60 patients of DKA, 44 (73.33%) patients had evidence of infection, types of infections were further analysed. Most common infection was found to be of pneumonia (18 patients, 40.90%). Four (9.09%) patients had sputum AFB positive pulmonary tuberculosis. Urinary tract infection was the precipitating cause of DKA in 12 patients (27.27%). Among them, two patients had emphysematous pyelonephritis. four patients (9.09%) had diabetic foot and two patients (4.54%) had gastrointestinal tract infection.
Four patients (9.09%) had mixed infection like two patients had pneumonia and urinary tract infection and the other two had diabetic foot and urinary tract infection [ Table/Fig-5 ].
[Table/Fig-5]:
Infections precipitating diabetic ketoacidosis
Mean blood glucose at admission was 535.6 mg/dl in Type 1 and 380.07 mg/dl in Type 2 DM patients. Mean serum potassium (4.55mEq/l), arterial pH (7.23) & bicarbonate level (12.46 mmol/l) were calculated. In our study severe acidosis with arterial pH <7.0 was found mainly in Type 1 Diabetic patients with DKA.
Mean fluid requirement on first day of therapy was 3.51 litres. Mean insulin dosage required for clearance of urinary ketones was 115 units while mean time taken for clearance of urinary ketones was 36.20 hours. However, 6 patients expired before clearance of urinary ketones.
In our study, a total of 60 patients presenting to the emergency with diagnosis of diabetic ketoacidosis were taken, out of which 12 (20%) patients belong to Type 1 DM and 48 (80%) patients belong to Type 2 DM. It is because prevalence of Type 2 DM is much higher than Type 1 DM. Moreover, in a developing country like India, due to poor socio-economic status, many patients with type 2 DM tend to have poor compliance and poor control of blood sugar levels so any precipitating factor tends to land them in a state of DKA. National Centre for health statistics and study by Adhikari et al., also showed the same [ 2 , 7 ]. A recent study evaluating 138 consecutive admissions for DKA at a large academic center observed that 21.7% had type 2 diabetes [ 22 ]. In a study conducted in Taiwan, the patients attacked with DKA were predominant type 2 DM (98 vs. 39 patients) [ 23 ]. Nearly 70% of the admissions involved discontinuation of medications, and almost half had an identifiable infection when an intensive search was undertaken. S Mishra has reviewed the pathophysiology of ketosis prone type 2 diabetes in his recent article and shown that DKA is not just the feature restricted to Type 1 diabetes but can also be a complication of type 2 diabetes usually with a precipitating factor and in some races even without precipitating cause [ 5 , 24 ].
Mean age of patients in our study group was 51.46 years which also points in favour of type 2 diabetes to be causing DKA more than type 1 diabetes. Many studies support this finding. In the study by Adhikari et al., the mean age was 44.78 years [ 7 ]. Faich et al., and Kreisberg et al., studies reported that the mean age of patients admitted for DKA was between 40-50 years [ 25 , 26 ]. Beigelman et al., study reported 47 years as the mean age of presentation for DKA [ 27 ].
The percentage of freshly diagnosed diabetes has been variably reported. Our study result matches with Kretz AJ et al., which also found that 10% patients were freshly diagnosed [ 28 ]. Casteels and Mathieu found DKA was the presenting illness in 20-25% of newly diagnosed patients with type 1 diabetes [ 29 ]. Westphal found ketosis onset diabetes in 27% of patients [ 15 ].
Nausea and vomiting were the most common symptoms (63.33%) of DKA patients in our study, followed by pain abdomen (43.33%). One third (33.33%) of patients were dehydrated. Altered sensorium was seen in 30% of patients. 26.66% of patients were complaining of polyuria and polydipsia. Only 16.66% of patients had kussmaul breathing and 13.33% had hypotension. Symptoms related to precipitating cause were present in 60% of patients. A similar incidence of symptoms has been reported in previous studies by Munro et al., Umpierrez et al., and Adhikari et al., [ 7 , 10 , 11 ].
In our study many patients had more than one precipitating factor like patients who were non-compliant to treatment also had infection and associated stressful situations like acute myocardial infarction, cerebrovascular accident, postoperative stress etc. Thus, it is seen that presence of non-compliance to treatment is an important precipitating factor which indicates that prevalence of DKA can be reduced by proper education of patients about their illness and harm of non-compliance. Welch et al., did a case study on patients with type 2 diabetes presenting with DKA and found that some precipitating factor is required in a type 2 diabetic patient to land up in DKA as similar to our study [ 4 ].
Present study showed pneumonia as the most common infection precipitating DKA in 40.90% of patients. Sputum AFB positive Pulmonary Tuberculosis was present in 9.09% patients. Urinary Tract Infection was the precipitating infection in 27.27% of cases, among them, one patient had Emphysematous Pyelonephritis. 9.09% patients had diabetic foot and gastrointestinal tract infection in 4.54% of patients. Mixed infection was the causative factor in 9.09% of patients. Several factors including hyperglycaemia, leucocyte dysfunction, macrovascular disease and acidosis predispose the diabetic with ketoacidosis to common and rare infections. This is in accordance with previous studies which also showed that infection of any site is an important precipitating factor in causing DKA [ 13 - 16 ]. Adhikari et al., showed diabetic foot as the infection precipitating DKA in 30.23% of patients [ 7 ].
The overall mortality in our study was 10% which is quite similar to other studies. Westphal found mortality of 5.1% [ 15 ], while Beigelman and Faich et al., found mortality rate of 9% [ 25 , 27 ]. Adhikari et al., found mortality of 16.3% and Matoo et al., study showed mortality of 23.7% [ 7 , 14 ]. Estimated mortality rate for DKA is between 4-10% showed by Chaisson et al., [ 30 ]. This shows that DKA in patients with type-2 DM is a more severe disease with worse outcomes compared with type-1 DM. A comparative study in patients presenting with DKA also showed that type 2 DM patients who present in DKA have significantly severe presentation and worse outcome than those who have Type 1 DM [ 31 ]. Indian studies still report mortality figures in the range of 20-30%, and hence, may constitute preventable mortality. Delayed presentation and poor socio-economic conditions which influenced the selection of better antibiotics were contributory. This study shows that the clinical profile of patients with diabetic ketoacidosis is similar to that reported from West and other Indian studies. Delay in hospitalization, severity of acidosis and peripheral vascular insufficiency appeared to be a major risk factor for the higher mortality rate.
An active measure should be taken stressfully to rule out DKA in any diabetic and comatose patient to prevent complications and mortality, as the mortality mainly depends on the general condition of the patient, as well as the coexistent medical illness and time of onset of therapy. Therefore, education of a diabetic patient about warning symptoms of ketosis such as weakness, abdominal pain, vomiting and drowsiness are mandatory for early diagnosis and treatment.
Financial or Other Competing Interests
- Search the site GO Please fill out this field.
- Newsletters
- Health Conditions A-Z
- Endocrine Diseases
- Type 1 Diabetes
Signs and Symptoms of Diabetic Ketoacidosis (DKA)
:max_bytes(150000):strip_icc():format(webp)/SB-headshot-Dotdash-9969efdd9a684f1ea4ff441ca264ce97.jpeg)
Mayur Kakade / Getty Images
Diabetic ketoacidosis (DKA) is a dangerous buildup of acids called ketones in your blood. Ketones are produced when your body doesn’t have enough insulin to convert sugar into energy. As a result, your liver begins breaking down fat cells instead. This breakdown of fat often happens much too quickly, turning your blood acidic and making you feel sick.
DKA is common in people with type 1 diabetes. It can also occur with type 2 diabetes, but it’s not as common and is usually not as severe. Early symptoms include extreme thirst and frequent urination. Symptoms can quickly progress to more serious, potentially life-threatening symptoms like rapid breathing, dehydration, and vomiting.
It’s important to be aware of diabetic ketoacidosis symptoms if you have diabetes so you can seek prompt medical attention. Most people who receive treatment recover from DKA, but it can be fatal if left untreated.
Early Symptoms
Diabetic ketoacidosis occurs when your body doesn’t make enough insulin to process the glucose in your blood. This leads to very high blood glucose levels , which can cause many complications.
DKA sometimes leads people with previously undiagnosed type 1 diabetes to get medical care: they seek treatment for their symptoms and are diagnosed with diabetes. DKA can also develop if a person with type 1 diabetes isn’t managing their condition well or becomes sick with another infection.
Polyuria and polydipsia are two physical symptoms that may occur in the early stages of DKA:
- Polyuria: High blood glucose levels can cause glucose to build up in your urine, forcing your kidneys to produce more urine to flush it out. This results in polyuria, or frequent urination.
- Polydipsia : It’s easy to become dehydrated during or before DKA due to increased urination. One of the most obvious signs of dehydration is extreme thirst, or an increased urge to keep drinking, also known as polydipsia. You may also have an excessively dry mouth.
Testing Blood Glucose and Ketones at Home
If you have already been diagnosed with diabetes , you may be able to test your blood glucose levels and even your ketones at home. One or both levels will likely be elevated if you have diabetic ketoacidosis.
You can use a blood sugar monitor or meter to check your glucose levels if you think you may have DKA. Your healthcare provider can tell you your optimal glucose range. You should generally check for ketones if your blood sugar level is greater than 240 milligrams per deciliter (mg/dL). You can use a simple urine test strip kit.
Progressive Symptoms
Without prompt medical attention, diabetic ketoacidosis can cause additional symptoms that may become severe. These symptoms include:
- Gastrointestinal illness: Nausea , vomiting, and stomach pain are common symptoms of DKA. This is due to your sodium levels becoming depleted with frequent urination as well as the buildup of ketones in your blood.
- Respiratory problems: Difficulty breathing or deep, rapid breathing are signs of DKA. Decreasing electrolytes (minerals your body needs to function) can cause severe muscle weakness that affects breathing. This deep, rapid breathing—similar to hyperventilation—is usually called Kussmaul breathing or Kussmaul respiration. It's common in conditions that cause high blood acid levels.
- Flu-like symptoms: You may feel generally unwell as your body tries to get rid of excess ketones. Possible symptoms include fatigue , weakness, muscle aches, headache, and flushed skin.
- Confusion: Symptoms like dehydration and difficulty breathing can cause you to feel less alert or have difficulty concentrating. Extreme confusion, or delirium, could be a sign of cerebral edema (brain swelling)—a rare but often fatal complication of DKA.
- Fruity-smelling breath: Acetone is one of the ketones produced by the body during DKA. It can give your breath a fruity smell.
Symptoms in Children
Diabetic ketoacidosis symptoms in children are the same as symptoms in adults. However, it can be harder to differentiate between DKA and other common childhood illnesses (like the flu or a stomach virus ), especially if your child hasn’t been previously diagnosed with type 1 diabetes.
As many as 30% of children with type 1 diabetes are diagnosed because they experience an episode of DKA. About 6-8% of children diagnosed with type 1 diabetes will experience DKA at some point because of illness or poor diabetes management .
Diabetic ketoacidosis in children is quite serious. It’s the most common cause of hospitalization and death in children with type 1 diabetes. Cerebral edema is rare in adults, but it occurs in up to 1% of pediatric patients with DKA. Seek medical attention if your child shows any symptoms of DKA—whether or not they have a type 1 diabetes diagnosis.
When to Contact a Healthcare Provider
Any diabetic ketoacidosis symptoms, whether early or progressive, require immediate medical care. If your regular healthcare provider is available by phone, you can contact them first for the next steps. If they aren’t available, go to the nearest emergency room or urgent care facility.
Questions To Ask Your Provider
When seeking emergency medical care for symptoms of DKA, ask your provider the following questions:
- What is my blood glucose level? Can you perform a urine test for ketones?
- What needs to be done to get my blood glucose levels back to normal?
- Will I need to be admitted to the hospital to manage my symptoms? If so, how long can I expect to stay there?
- What possible complications can occur during treatment?
- Once recovered, how can I prevent DKA from happening again?
A Quick Review
Diabetic ketoacidosis (DKA) is a complication of type 1 diabetes that occurs when acids called ketones build up in your blood. It is a dangerous and potentially life-threatening condition that requires urgent medical care.
Early symptoms of DKA include increased thirst and frequent urination. Progressive symptoms include nausea, vomiting, lethargy , muscle weakness, difficulty breathing and hyperventilation, and a fruity odor to your breath. Seek immediate medical attention if you or someone in your care has any potential DKA symptoms.
Frequently Asked Questions
There’s no official blood glucose level associated with DKA. Most experts agree that ketones are likely to be reaching dangerous levels when blood glucose is 200-250 mg/dL.
Ketoacidosis is a serious and potentially fatal condition that requires emergency medical care.
Untreated DKA can cause a diabetic coma and, in severe cases, death.
Centers for Disease Control and Prevention. Diabetic ketoacidosis .
American Diabetes Association. Diabetes & DKA (ketoacidosis) .
MedlinePlus. Diabetic ketoacidosis .
JDRF. Diabetic Ketoacidosis (DKA): Symptoms and Prevention .
Lizzo JM, Goyal A, Gupta V. Adult diabetic ketoacidosis . In: StatPearls . StatPearls Publishing; 2024.
JDRF. Frequent urination (polyuria) and type 1 diabetes .
JDRF. Excessive thirst (polydipsia) and type 1 diabetes .
Centers for Disease Control and Prevention. Monitoring your blood sugar .
Takai T, Okada Y, Takebe R, Nakamura T. Vomiting and hyperkalemia are novel clues for emergency room diagnosis of type 1 diabetic ketoacidosis: a retrospective comparison between diabetes types . Diabetol Int . 2021;13(1):272-279. doi:10.1007/s13340-021-00539-w
MedlinePlus. Electrolytes .
Gallo de Moraes A, Surani S. Effects of diabetic ketoacidosis in the respiratory system . World Journal of Diabetes . 2019;10(1):16-22. doi:10.4239/wjd.v10.i1.16
Whited L, Hashmi MF, Graham DD. Abnormal respirations . In: StatPearls . StatPearls Publishing; 2024.
JDRF. The serious side of the flu for people with T1D .
Namatame K, Igarashi Y, Nakae R, et al. Cerebral edema associated with diabetic ketoacidosis: Two case reports . Acute Medicine & Surgery . 2023;10(1):e860. doi:10.1002/ams2.860
Reinhart J. Early detection of diabetic ketoacidosis by breathalyzer in a sailor reporting for duty . Military Medicine . 2019;184(11-12):e951-e952. doi:10.1093/milmed/usz127
EL-Mohandes N, Yee G, Bhutta BS, Huecker MR. Pediatric diabetic ketoacidosis . In: StatPearls . StatPearls Publishing; 2024.
Tzimenatos L, Nigrovic LE. Managing diabetic ketoacidosis in children . Ann Emerg Med . 2021;78(3):340-345. doi:10.1016/j.annemergmed.2021.02.028
Related Articles
- Open access
- Published: 09 April 2024
Knowledge, attitude, and practice of insulin among diabetic patients and pharmacists in Egypt: “cross-sectional observational study”
- Alaa H. Mohamed 1 ,
- Maggie M. Abbassi 1 &
- Nirmeen A. Sabry 1
BMC Medical Education volume 24 , Article number: 390 ( 2024 ) Cite this article
90 Accesses
Metrics details
Diabetes recently has been identified as a growing epidemic. Although insulin’s vital role in both types of diabetes, it is considered one of the harmful medications if used incorrectly. In Egypt, effective usage of insulin remains a challenge due to insufficient knowledge of insulin and diabetes management, leading to errors in insulin therapy. As pharmacists are experts in pharmacological knowledge, they are uniquely situated to assess adherence to treatment regimens, the effect of drug therapy, or potential alterations in drug therapy to meet patient goals. To provide effective patient education and counseling, community pharmacists in Egypt should be efficiently knowledgeable about diabetes and insulin.
To identify the knowledge, attitude, and practice of pharmacists and patients about insulin. To identify pharmacists’ educational preparedness and confidence in counseling diabetic patients.
A descriptive, cross-sectional study was conducted with two knowledge, attitude, and practice surveys. This study was carried out from September 2016 to February 2023. Face-to-face interviews were conducted with patients, and a paper-based questionnaire was administered to pharmacists. The two questionnaires were adapted from previous studies.
A total of 492 patients and 465 pharmacists participated in this study. The mean knowledge score of correct answers among patients and pharmacists was 10.67 ± 1.9 and 15 ± 3.6. Most of the patients and pharmacists had a positive attitude regarding insulin’s role in improving health and to better control blood glucose. On the negative side, around half of the patients reported that they believe that regular use of insulin leads to addiction, while only 14.5% of the pharmacists believed that insulin could cause addiction. Self-confidence scores for pharmacists differed statistically with sex, years of experience, and pharmacist’s direct exposure to diabetic patients.
Conclusions
This study uncovers considerable deficiencies in patients’ and pharmacists’ knowledge about insulin therapy. This study also strongly recommends higher education and a more structured pharmacist training schedule.
Peer Review reports
Introduction
Diabetes mellitus (DM) is a heterogeneous disorder of metabolism characterized by chronic high blood glucose levels resulting from either deficiency in insulin secretion or insensitivity of tissues to insulin or both [ 1 ]. Diabetes recently has been identified as a growing epidemic due to its significant increase over the past 10 years. Egypt is listed as the 9th among the top 10 countries with diabetes, and the number of adult diabetic patients was 8,850,400 in early 2020, predicted to double to 16.9 million by 2045 [ 2 ]. Although insulin plays a vital role in both types of DM, it is considered one of the most harmful medications if used incorrectly. For this reason, it is recognized as one of the five “high alert” medications that have the highest hazard of inducing harm to patients due to medication errors [ 3 ].
In developing countries, such as Egypt, the effective use of insulin in the management of DM remains a challenge due to several factors. An important one is insufficient knowledge of insulin and diabetes management on the part of healthcare providers and patients, leading to errors in insulin therapy [ 4 ]. Consequently, preventable, and life-threatening complications, such as hyperglycemia and hypoglycemia, may occur [ 5 ]. El-Khawaga et al. [ 6 ] and Soliman et al., [ 7 ] reported that among the most common insulin misuses in Egyptian diabetic patients are managing hypoglycemic symptoms and the proper way of mixing insulin, where only 24.1% knew the conditions leading to hypoglycemia and only 13.0% knew the proper way of mixing insulin, disposal of the sharp syringes, needles, and lancets. Another study [ 8 ] identified some major errors in the self-administration of insulin among diabetic patients such as not removing air bubbles from the syringe before injecting, injection on the scar leading to lipodystrophy, not rotating the injection site, using insulin while it is cold that can result in increasing pain during injection, and unsafe disposal of used needles or syringes. Therefore, the assessment of diabetes knowledge, attitude, and practice (KAP) has become essential for the development of control programs and techniques for effective health education and patient counseling. This aids in ensuring that each diabetic patient has satisfactory information and is interested in leading a better life [ 9 ]. Various KAP studies have been conducted worldwide on patients receiving insulin [ 10 , 11 , 12 , 13 ]. Various Egyptian studies have emphasized diabetes epidemiology [ 2 , 14 , 15 ], but no study was conducted in Egypt regarding KAP in diabetic patients on insulin.
Pharmacists have a potential role in identifying and preventing medication misuse among diabetic patients in Egypt [ 16 ]. As they are experts in pharmacological knowledge, pharmacists are uniquely situated to assess adherence to treatment regimens, the effect of drug therapy, or potential alterations in drug therapy to meet patient goals [ 17 ]. With prolonged working hours and commonly no appointment needed for service, resulting in easier accessibility and lower cost, therefore Egyptian patients seek immediate health advice from community pharmacists rather than physicians [ 18 ]. Pharmacists who have good knowledge and are well-educated could implement group education for diabetic patients, thus making the load on primary health care centers easier and giving participants the time they need. To provide effective patient education and counseling, community pharmacists in Egypt should be efficiently knowledgeable about diabetes and insulin. Therefore, there is a need to survey whether community pharmacists in Egypt possess adequate knowledge and attitudes to deliver proper patient education services.
This study aims to assess the knowledge, attitude, and practice of pharmacists and patients about insulin, assess pharmacists’ educational preparedness and confidence in counseling diabetic patients, and measure patients’ satisfaction with their diabetes care.
Study design
This descriptive cross-sectional study was conducted in Greater Cairo (Giza and Cairo), Egypt, using a KAP survey regarding insulin therapy among pharmacists and diabetic patients, between September 2016 and February 2023.
Study population
The inclusion criteria for this study were diabetic patients > 18 years old, patients on insulin treatment, and those willing to participate in the study.
The exclusion criteria were the inability to be interviewed and patients taking only oral hypoglycemic drugs for diabetes mellitus.
- Pharmacists
The inclusion criteria for this study were as follows:
Fully licensed pharmacists working at community or hospital pharmacies.
Sample size
In Greater Cairo, it was estimated that there were 60,000 registered pharmacists and 63,000 licensed community pharmacies at the general pharmacy syndicate until 2016 [ 19 ]. Yellow pages were used to help the author determine the actual number of pharmacies in each district so that the author can be able to determine the percentage of pharmacists that should be recruited from each district in Cairo and Giza [ 20 ], and the number of pharmacies to be visited in each district was calculated by cross-multiplication of the sample size, the number of pharmacies in each district, and the total number of pharmacies. After calculating the number of pharmacies to be visited in each district, the researcher randomly visited the pharmacies. Another study performed in Egypt, in addition to the International Diabetes Federation reports were used to determine the approximate total number of diabetic patients in Egypt [ 14 , 21 ].
The sample size was calculated using Raosoft sample size calculation software, in which the population size (the number of pharmacists was 60,000 and the number of diabetic patients was 8 million), response distribution was 50%, and margin of error and confidence interval were set at 5 and 95%, respectively [ 22 ]. A minimum sample size of 382 pharmacists and 385 patients was calculated.
Study sites
Patients were recruited from public hospitals in great Cairo, which is affiliated with the Ministry of Health and Population and the Ministry of Higher Education.
Ethics approval
The study protocol was approved by the Research and Ethics Committee for Experimental and Clinical Studies of the Faculty of Pharmacy, Cairo University. Approval has been valid since May 2016.
Consent to participate
The Research Ethics Committee for Experimental and Clinical Studies at the Faculty of Pharmacy, Cairo University waived the requirement for the use of the standard written informed consent. Instead, written informed consent was replaced by verbal consent. Both questionnaires included an introductory cover letter asking candidates’ permission to participate after providing a brief description of the topic, the objectives of the research, and the duration needed to complete the questionnaire. Confidentiality of data was assured by the anonymity of the questionnaire. Acceptance of the interview was considered consent to participate in the study.
Questionnaires development and validation
Preliminary questionnaire development.
Questionnaires were used to evaluate pharmacists’ and patients’ knowledge, attitudes, and practices toward insulin use. The two questionnaires were adapted from previously published studies in English [ 5 , 10 , 23 ]. The final validated form of the pharmacists’ questionnaire was in English language where pharmacy education in Egypt is in English. The patients’ questionnaire was developed in English and translated into Arabic (the official language in Egypt) by a professional English/Arabic language translator.
Pilot testing and questionnaire validation
Content validity was tested by distributing the questionnaire to staff members of the Clinical Pharmacy Department at Cairo University. They were asked to complete the questionnaire and provide comments on both structure and content accuracy. Their comments were used to improve language and/or content. A few modifications were made.
Face validity was then assured by carrying out a pilot study on 50 pharmacists and 50 patients. Relevant modifications were instituted before the commencement of actual data collection. The data collected from the pilot study were not included in the results. Age question was changed to an open-ended question (continuous data), and the “do not know” option was added to both questionnaires. Regarding the pharmacists’ questionnaire, three open-ended questions were deleted to decrease the length and time needed to complete the questionnaire, and the “one or multiple answers” word was added to questions 18,19, 24, and 30. Four questions were deleted from the attitude section of the pharmacists’ questionnaire. Regarding the patients’ questionnaire, the attitude scale was changed from 5 points to a 3-point Likert-scale for ease of understanding the difference between scales in the patients’ category.
Reliability of patients’ questionnaire
The patient’s attitude scale was meant to be a formative construct, where each item contributes a unique aspect to the construct, and items do not necessarily correlate with each other. This is because each item represents a different dimension that forms or contributes to the overall construct, and changes in one item do not necessarily imply changes in the others. Indeed, the correlation between the attitude items did not exceed 0.25 for any pair of items.
This contrasts with reflective constructs, where all items are expected to correlate highly with each other as they reflect the same underlying construct. Indeed, the items included in the attitude scale were meant to assess the satisfaction of patients with the different aspects of insulin therapy such as cost, ease of use, associated pain, and perceived glycemic control. These items are not correlated with each other. Thus, calculating Cronbach’s alpha is not applicable in such a case. This contrasts with reflective constructs (e.g. experience with physician), where all items are expected to correlate highly with each other as they reflect the same underlying construct which permits the calculation of indices such as Cronbach’s alpha. For the “experience with the physician” which was a reflective construct. The reliability was 0.8 and 0.77 for the pilot and main studies, respectively.
Reliability of the pharmacists’ questionnaire
The attitude of the pharmacists towards was also regarded as a formative rather than a reflective measure which makes Cronbach’s alpha not suitable. Thus, reliability was only calculated for the confidence scale , which was 0.88 and 0.85, for the pilot and main studies, respectively.
The final form of the questionnaire
Patients’ questionnaire.
The final patient questionnaire (Additional file 1 ) was divided into 3 parts. The first part (nine questions) covered demographics and other patient characteristics, including age, sex, occupation, education level, residence, monitoring blood glucose at home, method of insulin administration (needle/syringe or pen), and duration of insulin use. The second part was designed to assess the patients’ KAP regarding insulin. It consists of 36 questions grouped into three sections. Section I included 15 questions (10 (Yes/No) questions, 3 close-ended (multiple choice), and 2 open-ended) about knowledge regarding insulin, covering the timing of short insulin administration, insulin route of administration, mixing of insulin different types, injection process, and insulin side effects. Section II included 15 questions based on a Likert scale of three levels (disagree/neutral/agree) to evaluate the attitude of patients towards insulin (benefits, fears about side effects, effectiveness, compliance, and cost). Section III assessed the patients’ practice of insulin self-injection using a 6-step checklist. The third part was composed of three questions assessing patients’ satisfaction with diabetes care, based on a Likert scale of 3 levels and two questions about reasons for dissatisfaction.
Pharmacist’s questionnaire
This was composed of three parts. The first part (8 questions) covered the demographic data of pharmacists (age, sex, year of graduation, years of practice as a pharmacist, education level (postgraduate studies), graduating university, and direct exposure to patients on insulin during practice). The second part assessed pharmacists’ knowledge and attitudes regarding DM and insulin. It was composed of 38 questions, grouped into two sections. Section I (Knowledge) was composed of 27 questions (1 open-ended question, 15 Yes/No, and 11 multiple-choice questions) related to pharmacists’ knowledge about the nature of insulin, from where insulin is secreted, which patients require insulin, insulin storage, insulin use in pregnancy, switching between different types of insulin, side effects and contraindications of insulin, hypoglycemia, diabetic ketoacidosis, insulin injection sites, decreasing pain during injection, and preparation of insulin injection. Section II (11 questions) was designed to assess pharmacists’ attitudes towards insulin (benefits, side effects, effectiveness, compliance, cost), using a 5-point scale from strongly disagree to strongly agree. The third part (7 questions) covered questions about the pharmacists’ confidence in their therapeutic knowledge regarding insulin using a 5-point scale ranging from “poor” to “excellent” (Additional file 2 ).
Questionnaires distribution
A face-to-face interview was used with the patient’s category. The interview was conducted in a single session of 10–15 minutes and filled at once.
For this sector, a paper-based questionnaire was distributed by the investigator to be self-filled by the participants in their pharmacies. The completion time of the survey was designed to be 12 minutes but, in some instances, it took more than that according to the pharmacist’s spare time. Some pharmacists asked to finish the survey in a few days to complete it in their spare time. Surveys returned entirely blank were counted as non-responders and were not used in the analysis.
Scoring system
Regarding the knowledge section, a score of one was given for correct answers and a zero for incorrect, and “do not know” answers. The grading of participants’ knowledge according to their total score was as follows: adequate knowledge > 75%, moderately adequate knowledge 51–75%, and inadequate knowledge< 50% [ 24 ]. Regarding the attitude and practice sections, the data were expressed as frequencies and percentages. For the self-confidence part of the pharmacists’ questionnaire, scoring was performed as follows: a score from 1 to 5 was given to responses from poor to excellent (< 10 points for poor self-confidence, 10–20 points for good self-confidence, and > 20 points for excellent self-confidence).
Statistical analysis
Statistical analyses were performed using Statistical Packages for Social Science (SPSS) version 23. The figures were produced using Microsoft Excel 2010. Nonparametric tests (Mann–Whitney U test and Kruskal-Wallis test) were performed to relate knowledge scores and demographic variables. Statistical significance was set at P < 0.05. The data collected using the preliminary questionnaire were not used in the final analysis.
A total of 492 patients were included in the study, of whom 369(75%) were female with an age range of 51–60 years (175(35.6%)). More than half of the respondents, 277(56.3%) were uneducated. Unemployed patients, 363(73.8%) were the highest proportion. Patients’ demographics are shown in Table 1 .
Most patients 325(66.1%) used syringes, and 164(33.3%) used pen devices to administer insulin. Most of the respondents (281(57.1%)) had been on insulin treatment for a period between 1 and 10 years, 76(15.2%) had used insulin for less than 1 year, and 132(26.8%) had used insulin for more than 10 years.
Knowledge, attitude, and practice of patients towards insulin
Of the 15 questions related to insulin knowledge, the mean score of correct answers was 10.67 ± 1.9, compared to the maximum score of 16, and 458(93.1%) showed moderately adequate knowledge. The frequency distribution of the responses regarding knowledge is presented in Table 2 .
The findings of this study revealed that knowledge differed significantly with sex ( p = 0.002), and female patients were more knowledgeable. In addition, knowledge differed with the duration of insulin use ( p = 0.021), with those who had been using insulin for > 30 years having the highest scores, while those who had an insulin treatment history of less than 6 months scored the lowest. Knowledge of insulin use was not associated with age, education, employment, or residence (Table 3 ).
Approximately half of the patients (251(52.7%)) thought that the pen device would be easier to use, while 48(10.1%) did not agree. Most patients, 461(96.8%) perceived that insulin was initiated due to worsened DM. A summary of patients’ attitudes and perceptions is presented in Fig. 1 .
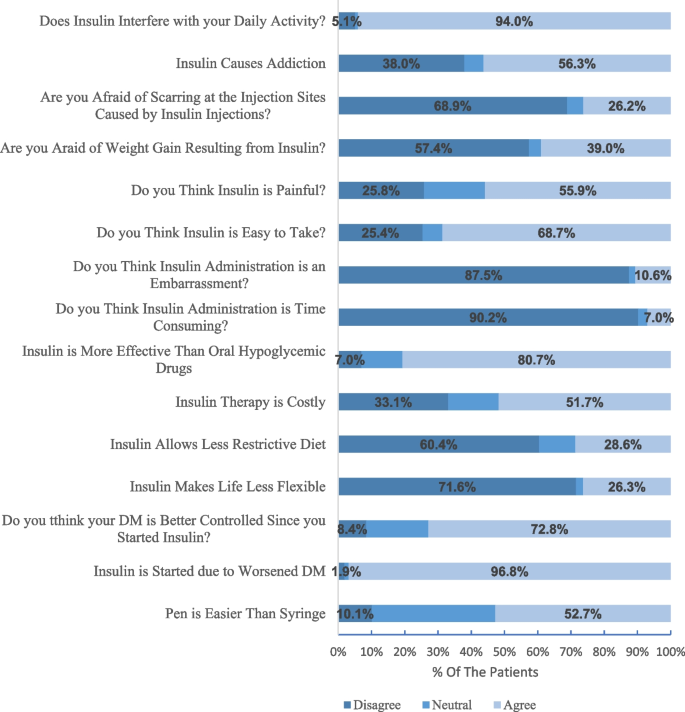
Perception of patients towards insulin use and administration
The differences in the perceptions of patients regarding insulin regimen stratified by age, sex, education status, employment, and method of insulin administration are shown in Table 4 .
There were 260(52.8%) patients who had good insulin administration practice. The mean score of correct practice was 2.61 ± 1.1 compared to the maximum score of 5 (Table 5 ).
When asking patients if they were satisfied with their doctors, most of the patients, 304(61.8%), were satisfied while 115(23.4%) patients were not satisfied with diabetic care. The satisfaction of patients with physician-patient interactions is shown in Table 6 . Of the 115 dissatisfied patients, 88 preferred to visit another diabetes clinic.
When asking patients about the causes of dissatisfaction with their physicians, 109(35.9%) and 107(35.2%) were dissatisfied because there was not enough time for consultation and no follow-up, respectively.
Of the 10 hospitals visited, 7 offered patient education sessions for their patients. The present study showed a statistical difference between the knowledge scores of patients recruited from hospitals that offered educational courses and those recruited from hospitals that did not ( P = 0.015). Mann-Whitney U test was used, as shown in Table 7 .
An analysis of the sample demographics and descriptive statistics is presented in Table 8 . Most respondents were females, 279(60.1%). The mean age was 28.4 ± 7.7. Only 62(13.3%) pharmacists held postgraduate degrees.
Knowledge and attitude of pharmacists towards insulin
The knowledge assessment revealed that 97(21%) of the pharmacists had inadequate knowledge,309(66.5%) had moderately adequate knowledge, and only 59(12.7%) had adequate knowledge. The overall mean score percentage of knowledge was 61.22 ± 12.9%. The response distribution to the questions about pharmacists’ knowledge regarding insulin use is shown in Table 9 .
When pharmacists were asked about the most preferred method for continued learning about DM and insulin, 180(41.5%) pharmacists considered online courses to be the most preferred method, 135(31.1%) preferred workshops, and 197(45.4%) considered brochures distributed to the pharmacy as a good way to continue learning about diabetes. Other options mentioned by 29(6.7%) pharmacists were campaigns, lectures, and short message services on their mobile phones, while the remaining pharmacists were not interested in continuing to learn about DM and insulin.
Two out of every five pharmacists (40%) agreed that DM was better controlled once insulin was started, and 188(44.7%) thought that insulin was more effective than oral hypoglycemic drugs. In contrast, 210(50%) pharmacists agreed that insulin therapy is costly and 160(38%) thought that insulin is painful. A summary of pharmacist’s attitudes is shown in Fig. 2 .
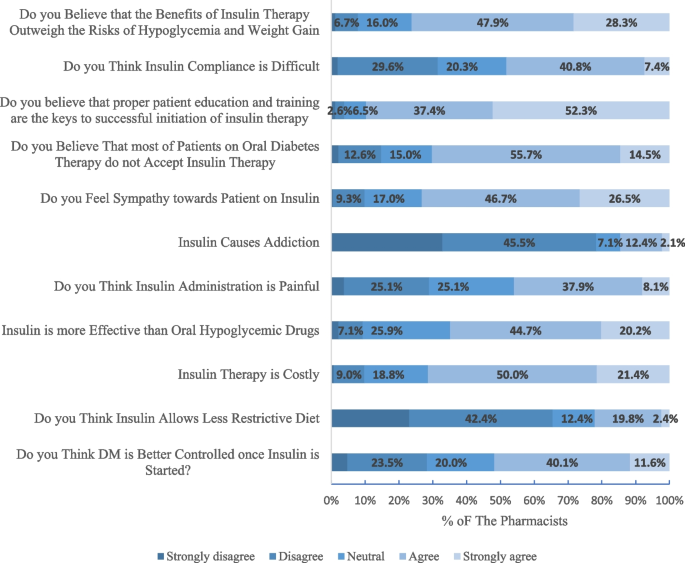
Pharmacists’ attitudes towards insulin use
Differences in perceptions of pharmacists regarding insulin regimen stratified by age, gender, postgraduate studies, type of postgraduate studies, and years of practice as a pharmacist are shown in Table 10 .
The mean score for self-confidence was 25.37 ± 6.4, with a minimum score of 3 and a maximum score of 35. Only 13(2.8%) pharmacists had poor self-confidence, 63(13.5%) had good knowledge, while 341(73.3%) had excellent self-confidence. Table 11 shows the self-perceived confidence of pharmacists in counseling patients on insulin.
Further analyses were conducted to investigate the influence of the pharmacists’ characteristics on their self-assessed confidence. Self-confidence scores differed statistically with sex ( P = 0.018), where female patients’ scores were higher than males, years of experience ( P = 0.000), and pharmacist’s direct exposure to diabetic patients ( P = 0.007). However, the self-confidence scores of pharmacists were not influenced by age, university of graduation, or postgraduate studies. It is being found that self-confidence significantly increases as knowledge increases (Spearman’s rho = 0.367, P value = 0.000).
To ensure that the long period of the study did not affect the results of the questionnaire, a comprehensive analysis comparing data from two distinct cohorts: pre-COVID and post-COVID was conducted. Our findings revealed that the knowledge scores between the pre-COVID and post-COVID cohorts were remarkably consistent, with a minimal average difference of approximately 3% observed. Similarly, attitude scores across both cohorts showed negligible variance, with a difference of merely 0.3 points. Furthermore, an examination of socio-demographic characteristics and most other variables considered in our study demonstrated no significant differences between the cohorts. These results suggest that the temporal context of the COVID-19 pandemic had a limited effect on the primary outcomes of our research.
Insulin is frequently used in the management of both type 1 and type 2 diabetes mellitus. However, insufficient knowledge and malpractice on insulin self-administration could result in poor disease prognosis and insulin-related complications [ 13 ]. Pharmacists help control diabetes and enhance the quality of life by providing pharmaceutical care and prescription management services [ 25 ]. This is the first Egyptian cross-sectional study of insulin injection knowledge, attitude, and practice among pharmacists and patients in different healthcare settings across Cairo and Giza. The study uncovers certain areas of deficiencies in both pharmacists’ and patients’ knowledge. The study also reveals practice deficiencies among patients that can be addressed to improve their practices and thus diabetes care.
More than half of the patients in the current study were females, 75% of patients with a mean age of 52.4 ± 12.4. This could be because recruiting the patients was usually between 9 am and 2 pm in the hospital clinics so most of the patients were either female or older patients who were not working. This is quite similar to studies conducted in Egypt as 78.8% of patients were female with a median age of 52 years [ 26 ]. Most of the patients were using needles and syringes for insulin administration. This can be attributed to the fact that insulin syringes are provided free of charge through public hospitals, while pens should be paid for in some hospitals.
Although the American Diabetic Association has legislative recommendations for self-monitoring blood glucose levels using glucometer in all diabetic patients on insulin for better disease management and quality of life [ 27 ], 61.8% of our patients did not have access to glucometers despite being on insulin therapy for fairly long periods. This could be due to the low-income level among our patients and the inability to buy a glucometer. Also, it could be due to the illiteracy level among the patients and the inability to use the device. Other studies from developing countries like Kenya (59%) and Iraq (44%) also have reported low utilization of glucometers and adherence to self-monitoring [ 28 , 29 ]. Given the importance of self-monitoring in improving glycemic control, there is a need to afford those low-income diabetic patients with glucometers and appropriate education on its use.
Regarding the level of knowledge among the study patients, only 2.6% of them had adequate knowledge, and 93.1% had moderately adequate knowledge. The overall knowledge percentage was 67.61%. This percentage was higher than the study conducted in India [ 30 ] and in line with a study conducted in Ethiopia [ 13 ] where the overall knowledge score was 46.9% and 63.4% respectively. The prime reason for good knowledge in the study patients may be because of better health facilities and accessibility in the study sites (Cairo and Giza). Regarding the pharmacists, knowledge assessment revealed that about 66.5% of the participants had moderately adequate knowledge, and only 59(12.7%) had adequate knowledge. The overall mean score among pharmacists was 61.2% which was higher than the overall mean score (49%) of pharmacists in the United Kingdom [ 31 ].
Our study found that female patients were more knowledgeable about insulin than males ( P = 0.002). We also found that patients who have been on insulin treatment for a longer period are more likely to have better knowledge ( P = 0.030). This could be attributed to the higher chances of exposure to information which helps the patients to obtain the knowledge.
Two main findings should be of concern both for pharmacists and patients. First, cloudy insulin must be mechanically resuspended so that it goes back into solution before injection [ 32 ]. Vigorous shaking should be avoided because this produces bubbles that will affect correct dosing [ 32 ]. However, in our study 38.2 and 12.2% of patients did it inappropriately (vigorous shaking) or did not know how to do this, respectively. These percentages were higher than in an Ethiopian study where 33.7% did not know that shaking insulin vials can make insulin more likely to clump [ 24 ]. Among the pharmacists, only (31.8%) of participants knew that insulin could be resuspended by either gentle mixing or rotating. Other pharmacists did not know the proper ways for resuspension. This poor knowledge may be due to inadequate training among pharmacists and not being up to date about current guidelines on diabetes management. Second, an interesting defect in knowledge was related to injecting insulin while it was cold, more than half (63.4%) of the patients did not know that injecting insulin while it was cold could increase the pain during injection. On the other hand, more than half (55%) of the pharmacists knew that insulin should not be injected while it’s cold. This could be translated as inadequate pharmacists’ counseling regarding the ways to minimize the pain during insulin injections.
Most of the patients (72.8%) had a positive attitude regarding insulin’s role in improving health and better controlling blood glucose, this was higher than studies conducted in Trinidad and Baghdad where only 43.6% and 34.5% thought that their glucose levels would be better controlled on insulin respectively [ 10 , 33 ]. Regarding the pharmacists, half of them believed that diabetes is better controlled once insulin is started, so they can convince the patients who refuse to take insulin and those who believe that insulin has no privilege over oral hypoglycemic drugs.
Most of the patients and the pharmacists agreed that insulin therapy was more beneficial in regulating blood glucose levels in comparison with oral antidiabetic drugs; however, insulin injection was painful in 55.9% and 46.1% of the patients and pharmacists respectively. Most of them (60.4% of patients and 65.5% of pharmacists) did not agree with the fact that following the administration of insulin, a healthy diet was not needed to maintain blood glucose levels, same results were reported in a study conducted in Eastern India [ 34 ]. On the negative side, around half of the patients reported that they believe that regular use of insulin leads to addiction as they associate needles with drug abuse, and when they stop using insulin, they experience discomfort. This was similar to a Turkish study [ 35 ] and higher than a study conducted in Ethiopia [ 36 ], where half of the patients and only 7.3% reported that they believe that regular use of insulin leads to addiction respectively. On the other hand, only 14.5% of the pharmacists believed that insulin could cause addiction. So, pharmacists should educate patients that this is just a myth, and that insulin is a natural substance needed by the body and cannot get addicted to it.
Most of the patients (87.5%) felt self-conscious about taking injections in a public place while 10.6% felt that insulin administration is an embarrassment and 73.2% of pharmacists reported sympathy towards patients on insulin.
In the current study, 94% of the patients found that insulin therapy interfered with their daily activities and their social lives. This result might be a consequence of some factors. First, inadequate knowledge of appropriate storage conditions such as opened insulin vials could be stored at room temperature. Therefore, some patients when they go outside their home, they could skip their doses as they neither want to take nor have ice bags for insulin storage, and this could lead to insulin non-adherence. For that reason, 48.2% of the pharmacists agreed that insulin compliance is difficult as they thought that insulin therapy impacts lifestyle. Second, some of the patients (25.4%) believed that insulin is not easy to take and were dependent on others (pharmacists, family members, and neighbors) for injections, which may be a barrier to multiple daily insulin injections. Furthermore, the people who assist with injections may not always be available and this may lead to skipping insulin injections. A similar picture was observed in a Nigerian study, in which 28.2% did not inject themselves [ 37 ]. This finding further emphasizes the pharmacists’ role.
Although some aspects of practice were correctly followed by patients, all surveyed patients were making at least one insulin injection technique error. The three most common incorrect steps were skipping washing hands, not pressing on the skin for 5 seconds after pulling out the needle, and not checking for bleeding after injection. It is recommended to lift the skin as pinching up the skin decreases the chance of intramuscular injection [ 38 ], and most of the study subjects reported lifting the skinfold correctly. The most common correct practice observed in more than 89.2% of patients reported inserting the needle into the skin. This is an important step as insulin should be injected into the subcutaneous fat layer for better absorption while intradermal injections result in therapeutic ineffectiveness due to failure of delivering insulin at this site and increase the risk of local complications [ 39 ]. The ideal practice of keeping the needles under the skin for 5 seconds or longer after injecting was followed by 39.2% of the subjects in this study. Not leaving the needle after injection is found to be related to a higher frequency of insulin leakage from the site of injection [ 40 ].
Our study has several strengths. Our study patients were recruited from different hospitals located in Cairo and Giza, the two largest cities in Egypt that include different sociodemographic levels of the patients. The study ensured good representation of pharmacists as it included pharmacists from different sectors in Cairo and Giza districts including districts with different socioeconomic levels and distant agricultural and rural districts.
Despite these strengths, our study has several limitations. One study limitation is that the researcher almost visited the pharmacies in the time between 9 am and 9 pm. No data was obtained from the 9 pm to 9 am shift. Replication of the study in different parts of Egypt is recommended to test the generalizability of our findings. Another limitation of the study is that some pharmacists asked to finish the survey in a few days to complete it in their spare time which could affect the data collected in the knowledge section. The study has additional limitations, such as no random selection for patients, cross-sectional design, and social desirability bias for attitude.
This study recommends improving patients’ knowledge about diabetes management in several ways as continuous audio and video display when the patients are waiting in the clinics, a flyer with illustrations could be given to the patient that contains information on different types of insulin with their color code, sites of insulin administration, techniques of insulin administration, storage of insulin, signs of hypoglycemia and hyperglycemia, complications of insulin and its management [ 41 ].
This study identifies considerable gaps in patients’ and pharmacists’ knowledge about insulin therapy. The vital part of comprehensive diabetes care is the information and education which leads to improvement in knowledge, attitude, and practice. The findings of this study could be useful for policy or decision makers, healthcare providers, and patient support groups who may need to design interventions to improve the health outcomes of patients with diabetes. This might help the patients to have a better understanding of the self-administration of insulin and improve their practice skills. This study also strongly recommends higher education and a more structured pharmacist training schedule. It also shows a willingness among most pharmacists to attend workshops dealing with insulin therapy. Different learning strategies may be of interest to pharmacists who regularly assist diabetic patients but cannot attend such workshops.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Diabetes mellitus
Knowledge, attitude, and practice
Statistical packages for social science
Subcutaneous
Degree of freedom
American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care. 2017;40(Supplement_1):S11–24. https://doi.org/10.2337/dc17-S005 .
Article Google Scholar
Abouzid MR, Ali K, Elkhawas I, et al. An overview of diabetes mellitus in Egypt and the significance of integrating preventive cardiology in diabetes management. Cureus. 2022;14(7):e27066. https://doi.org/10.7759/cureus.27066 .
Gerensea H, Moges A, Shumiyee B. Type one diabetic patients’ knowledge and attitude on Insulin self-administration in Mekele Tigray, Ethiopia. J Diabet Complicat Med. 2016;1(1):1–6. https://doi.org/10.4172/JDCM.1000.104 .
Halawa M, Shelbaya S, Nasr M. The management of care of Egyptian patients with diabetes: a report from the international diabetes management practices study wave 7. The Medical Journal of Cairo University. 2020;88:1413–21.
Jasper US, Opara MC, Pyiki EB, et al. Knowledge of insulin use and its determinants among Nigerian insulin requiring diabetes patients. J Diabetes Metab Disord. 2014;13(1):1–8. https://doi.org/10.1186/2251-6581-13-10 .
El-Khawaga G, Abdel-Wahab F. Knowledge, attitudes, practice, and compliance of diabetic patients in Dakahlia, Egypt. Euro J Res Med Sci. 2015;3(1)
Soliman HM, Abdou MH, Fetohy EM, Hussein MF. Assessment of knowledge, attitude, and practice of diabetic patients regarding sharps disposal. p. 107–17.
Atalla HR. Effectiveness of nursing intervention regarding self-insulin administration among diabetic patients. Clin Nurs Stud. 2016;4(2):57–66.
Google Scholar
Reddy PA, Saravanan K, Madhukar A. To assess and compare the knowledge, attitude, and practice of patients with diabetes in control and intervention groups. Biol Pharm Bull. 2023;46(4):586–91. https://doi.org/10.1248/bpb.b22-00699 .
Beneby N, Isaacs C, King L, et al. Knowledge, attitudes, and perceptions of patients towards insulin therapy at primary care centers in Trinidad. J Community Med Public Health Care. 2015;2(4) https://doi.org/10.24966/CMPH-1978/100004 .
Getachew F, Solomon D. Knowledge, attitude, practice, and associated factors towards self-insulin administration among diabetic patients in Hawassa referral hospital, Southern Ethiopia. RRMED. 2019;1(1):10–7. https://doi.org/10.33702/rremd.2019.1.1.3 .
Ngo TKC, Vo TH, Le C. Knowledge, attitude, and practice concerning hypoglycemia, insulin use, and insulin pens in Vietnamese diabetic outpatients: Prevalence and impact on safety and disease control. J Eval Clin Pract. 2020;27(2):404–13. https://doi.org/10.1111/jep.13454 .
Nasir BB, Buseir MS, Muhammed OS. Knowledge, attitude and practice towards insulin self-administration and associated factors among diabetic patients at Zewditu Memorial Hospital, Ethiopia. PLoS One. 2021;16(2):e0246741. https://doi.org/10.1371/journal.pone.0246741 .
Hegazi R, El-Gamal M, Abdel-Hady N, Hamdy O. Epidemiology of and risk factors for type 2 diabetes in Egypt. Ann Glob Health. 2015;81(6):814–20. https://doi.org/10.1016/j.aogh.2015.12.011 .
Assaad Khalil SH, Megallaa MH, Rohoma KH, et al. Prevalence of type 2 diabetes mellitus in a sample of the adult population of Alexandria. Egypt. Diabetes Res Clin Pract. 2018;144:63–73. https://doi.org/10.1016/j.diabres.2018.07.025 .
Amin MEK, Chewning B. Community pharmacists’ knowledge of diabetes management during Ramadan in Egypt. Int J Clin Pharm. 2014;36(6):1213–21. https://doi.org/10.1007/s11096-014-0019-6 .
Sisson E, Kuhn C. Pharmacist roles in the management of patients with type 2 diabetes. J Am Pharm Assoc. 2009;49(5):S41–5. https://doi.org/10.1331/JAPhA.2009.09075 .
Abdelaziz AI, Tawfik AG, Rabie KA, et al. Quality of community pharmacy practice in antibiotic self-medication encounters: a simulated patient study in upper Egypt. Antibiotics. 2019;8(2):35. https://doi.org/10.3390/antibiotics8020035 .
Abdel-Latif MM, Sabra K. Clinical pharmacy practice in Egyptian hospitals. Am J Health-Syst Pharm. 2016;73(1):e63–6. https://doi.org/10.2146/ajhp150250 .
Yellow Pages. 2016. https://www.yellowpages.com.eg/ar/ Accessed 20 Jan 2017.
Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes research and clinical practice. 2011;94(3):311–21.
Raosoft. 2004. An Online Sample Size Calculator. http://www.raosoft.com/samplesize.html Accessed 10 Apr 2016.
Weeraratne CL, de Abrew WK, Kuruppumullage RP. Knowledge on insulin therapy among healthcare professionals. J Ceylon Coll Physicians. 2011;41:67–71.
Netere AK, Ashete E, Gebreyohannes EA, Belachew SA. Evaluations of knowledge, skills and practices of insulin storage and injection handling techniques of diabetic patients in Ethiopian primary hospitals. BMC Public Health. 2020;20:1.
Arif R, Khan AZ, Hammad M, et al. Current practices, and perceived role of community pharmacists in type 2 diabetes services in Pakistan. Cureus. 2023;15(4):e37311. https://doi.org/10.7759/cureus.37311 .
Azzam MM, Ibrahim AA, Abd El-Ghany MI. Factors affecting glycemic control among Egyptian people with diabetes attending primary health care facilities in Mansoura District. Egypt J Intern Med. 2021;33(1):1–10. https://doi.org/10.1186/s43162-021-00065-w .
Elsayed NA, Aleppo G, Aroda VR, et al. 7. Diabetes technology: standards of care in diabetes—2023. Diabetes Care. 2023;46(supp):S111–27. https://doi.org/10.2337/dc23-S007 .
Charity KW, Kumar AMV, Hinderaker SG, et al. Do diabetes mellitus patients adhere to self-monitoring of blood glucose (SMBG) and is this associated with glycemic control? Experiences from a SMBG program in western Kenya. Diabetes Res Clin Pract. 2016;112:37–43. https://doi.org/10.1016/j.diabres.2015.11.006 .
Ebrahim SM, Jassim UT, Baji DM. A study to assess the attitude and practice of diabetic patient towards self-administration of insulin in Basra city, Iraq. Int J Gen Med. 2014;3(4):65–74.
Surendranath A, Nagaraju B, Padmavathi G, et al. A study to assess the knowledge and practice of insulin self-administration among patients with diabetes mellitus. Asian J Pharm Clin Res. 2012;5(1):63–6.
Bain A, Kavanagh S, McCarthy S, et al. Assessment of insulin-related knowledge among healthcare professionals in a large teaching hospital in the United Kingdom. Pharmacy. 2019;7(1):16.
Bahendeka S, Kaushik R, Swai AB, et al. EADSG guidelines: insulin storage and optimization of injection technique in diabetes management. Diabetes Ther. 2019;10(2):341–66. https://doi.org/10.1007/s13300-019-0574-x .
Zidane RN, Hussein WA. Barriers for insulin therapy initiation among type 2 diabetic patients attending the specialized center for endocrinology and diabetes/Baghdad 2019. IPMJ. 2021;20(2):186–92. https://doi.org/10.52573/IPMJ.2020.168628 .
Das AK, Sannigrahi P, Mukherjee M, et al. Assessment of knowledge, attitude, and practice regarding insulin use and its adverse effects in adult diabetic population in a tertiary care hospital. Majmaah J Heal Sci. 2023;11(2):91. https://doi.org/10.5455/mjhs.2023.02.009 .
Soylar P, Kadioglu B, Kilic K. Investigation of the barriers about insulin therapy in patients with type 2 diabetes. Niger J Clin Pract. 2020;23(1):98–102. https://doi.org/10.4103/njcp.njcp_138_19 .
Gurmu AE, Teni FS. Knowledge, attitude, and practice among diabetic patients on insulin therapy towards the disease and their medication at a university hospital in Northwestern Ethiopia: a cross-sectional study. Int J Pharma Sci Res. 2014;5(10):685–92.
Olamoyegun MA, Akinlade AT, Ala OA. Audit of insulin prescription patterns and associated burden among diabetics in a tertiary health institution in Nigeria. Afr Health Sci. 2018;18(4):852–64. https://doi.org/10.4314/ahs.v18i4.3 .
Kalra S, Mithal A, Sahay R, John M, et al. Indian injection technique study: population characteristics and injection practices. Diabetes Therapy. 2017;8:637–57. https://doi.org/10.1007/s13300-017-0243-x .
Kamrul-Hasan AB, Paul AK, Amin MN, et al. Insulin injection practice and injection complications–results from the Bangladesh insulin injection technique survey. Eur Endocrinol. 2020;16(1):41. https://doi.org/10.17925/EE.2020.16.1.41 .
Tandon N, Kalra S, Balhara YP, et al. Forum for injection technique and therapy expert recommendations, India: The Indian recommendations for best practice in insulin injection technique. Indian J Endocrinol Metab. 2017;21(4):600. https://doi.org/10.4103/ijem.IJEM_97_17 .
Venkataraman AP, Kamath L, Shankar S. Knowledge, attitude, and practice of insulin use of diabetic patients in India. Pharmacol Clin Pharm Res. 2020;5(1):23–32. https://doi.org/10.15416/pcpr.v4i3.26564 .
Download references
Acknowledgements
The author would like to thank Dr. Ahmed Mohamed Sayed, lecturer of the clinical pharmacy department, Cairo University, for his outstanding efforts in data analysis .
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and affiliations.
Department of Clinical Pharmacy, Faculty of Pharmacy, Cairo University, Kasr El-Aini St, P.O. Box: 11562, Cairo, Egypt
Alaa H. Mohamed, Maggie M. Abbassi & Nirmeen A. Sabry
You can also search for this author in PubMed Google Scholar
Contributions
A.H.M, M.M.A, N.A.S: conception and design of the study. A.H.M: performing of the research, collection of data, and drafting the manuscript. All authors (A.H.M, M.M.A, N.A.S) contributed to the analysis, review, and interpretation of data. M.M.A and N.A.S: revision of the manuscript. A.H.M, M.M.A, N.A.S approved the final version of the manuscript, including the authorship list.
Corresponding author
Correspondence to Alaa H. Mohamed .
Ethics declarations
Ethics approval and consent to participate.
The study protocol was approved by the Research and Ethics Committee for Experimental and Clinical Studies of the Faculty of Pharmacy, Cairo University. A cover letter replaced the informed consent form to invite the participants to participate in the study. Acceptance of the interview was considered a consent form to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mohamed, A.H., Abbassi, M.M. & Sabry, N.A. Knowledge, attitude, and practice of insulin among diabetic patients and pharmacists in Egypt: “cross-sectional observational study”. BMC Med Educ 24 , 390 (2024). https://doi.org/10.1186/s12909-024-05367-5
Download citation
Received : 01 November 2023
Accepted : 28 March 2024
Published : 09 April 2024
DOI : https://doi.org/10.1186/s12909-024-05367-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Self-confidence
- Diabetic patient
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Diabetic ketoacidosis (DKA) is a cardinal feature of type 1 diabetes. However, there is a strong, almost dogmatic, errant perception by physicians that DKA ... Case Study: Diabetic Ketoacidosis in Type 2 Diabetes: "Look Under the Sheets" Brian J. Welch, MD; Brian J. Welch, MD Search for other works by this author on:
Diabetic ketoacidosis is characterized by the blood sugar above 250 mg/dl (American Diabetic Association, 2019), so the complete blood test is done to see the blood sugar level for this patient. ... Case Study Of A Patient With Diabetes Mellitus Nursing Essay. Patient Mr. NCS is a 53 year old Chinese man with the height of 1.72m, and weighs ...
Case Reports in Emergency Medicine 2017. Diabetic ketoacidosis (DKA) is a potentially life-threatening acute complication of type 1 diabetes caused by insulin deficiency. It is characterized by raised blood glucose (hyperglycemia), metabolic acidosis, and increased blood/urine ketones. Dehydration and electrolyte disturbance are common and ...
We presented a case of new-onset diabetes presenting as DKA precipitated by COVID-19 infection. The relationship between DKA and COVID-19 has been explored sparingly thus far in the literature. In a study by Li et al., that included 658 hospitalized patients with confirmed COVID-19 infection, 42 of them presented with ketosis on admission.
Diabetic ketoacidosis (DKA) is an acute complication of uncontrolled diabetes mellitus that is associated with increased morbidity and mortality. ... Original articles, consensus statements, professional guidelines, systematic and nonsystematic reviews, meta-analysis, case-control studies, cohort studies, case series and case reports published ...
Diabetic Ketoacidosis commonly presents with hyponatremia, but hypernatremia is a rare entity. We report a unique case of a 50-year-old woman admitted with altered sensorium with blood glucose 979 milligrams/deciliter, serum osmolarity 363 mOsm/kilograms, and serum sodium 144 milliequivalents/liter.
Severe hypertriglyceridemia (HTG) is a rare complication of insulin resistance. Its presentation with diabetic ketoacidosis (DKA) has been reported in a few cases, where most patients have type-1 diabetes mellitus (DM). Our case represents a unique presentation of DKA associated with severe HTG above 10,000 mg/dL in an adult with type-2 DM.
Diabetic Ketoacidosis Upon Diagnosis: A Biochemistry Case Study. Diabetes mellitus is a metabolic disorder characterised by hyperglycemia. The two main types of diabetes mellitus are type 1 diabetes mellitus (T1DM) and type 2 (T2DM), which exhibit similar symptoms while having two very difer-ent pathophysiologies (Alam et al., 2014).
On March 6th, 2019, Maria Fernandez, a 19-year-old female, presented to the Emergency Department with complaints of nausea, vomiting, abdominal pain, and lethargy. She reveals a recent diagnosis of type 1 diabetes but admits to noncompliance with treatment. At the time of admission, Maria's vital signs were as follows: BP 87/50, HR 118, RR 28 ...
** The data in Tables 1 and 2 (following page) and the description of the patient's condition and treatment have been modified from a case reported by A.N. Cebeci and A. G. Üven ("Delirium in Diabetic Ketoacidosis: A Case Report," The Journal of Clinical Research in Pediatric Endo-crinology . 4(1): 39-41, 2012).
Diabetic ketoacidosis (DKA) is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis. Hyperglycemia causes an osmotic diuresis with significant fluid and electrolyte loss. DKA occurs mostly in type 1 diabetes mellitus. It causes nausea, vomiting, and abdominal pain and can progress to ...
In a multicenter, case-controlled, retrospective study involving pediatric patients with diabetic ketoacidosis, Glaser et al. 45 observed that the risk of cerebral edema was significantly ...
Diabetic ketoacidosis, or DKA for short, is a life-threatening complication of diabetes mellitus characterized by a severe insulin deficiency and glucagon excess. It typically but not exclusively occurs in the setting of type 1 diabetes, with common triggers that include illness or infection, as well as known diabetes with suboptimal glycemic control or interruption in therapy.
The nurse draws a Complete Metabolic Panel and notifies the Respiratory Therapist to obtain an Arterial Blood Gas. Upon further assessment, the patient is oriented x 2 and drowsy. He is breathing heavily. Lungs are clear to auscultation, S1/S2 present, bowel sounds active, pulses present and palpable x 4 extremities.
The prevalence of onset of diabetic ketoacidosis among type 1 diabetes mellitus was found to be 26.3% in one of the studies . ... We present a case of diabetic ketoacidosis in a child with type 1 diabetic mellitus. It is a life threatening complications if timely intervention is not done. Timely management with fluid therapy along with insulin ...
Diabetic ketoacidosis (DKA) is the leading cause of death before the age of 30 in people with type 1 diabetes, therefore prompt diagnosis and treatment is vital. This article provides some clinical case studies to illustrate how the presentation of DKA can
Diabetes-related ketoacidosis (DKA) is a serious and life-threatening condition, so acting fast if you're experiencing symptoms is very important. It's much easier to treat diabetes-related ketoacidosis in its early phase than it is once symptoms become more severe. Be sure to call your healthcare provider if you experience symptoms.
This directed case study is designed to help students integrate biochemical and physiological concepts with clinical aspects of disease. The case tells the story of a little girl who experiences diabetic ketoacidosis and is diagnosed with type 1 diabetes mellitus (T1DM). The story is based on an actual patient and the presented data are authentic.
Treatment. If you're diagnosed with diabetic ketoacidosis, you might be treated in the emergency room or admitted to the hospital. Treatment usually involves: Fluids. Fluids replace those lost through too much urinating. They also thin out the blood sugar. Fluids can be given by mouth or through a vein. When given through a vein, they're called ...
R.F.'s acidosis was thought to be the result of euglycemic DKA, likely triggered by his ketogenic diet; other etiologies, including infection and lactic acidosis secondary to metformin use, were ruled out with further testing, which revealed a lactic acid level of 1.8 mmol/L (normal 0-2), an ethanol level <10 mg/dL, and a negative salicylate level.
Diabetic ketoacidosis occurs primarily in people who have type 1 diabetes, although one-third of cases occur in those with type 2 diabetes. 2 In 30% to 40% of pediatric cases and 15% to 20% of adult cases, DKA is the initial presentation of diabetes. 2 It's the most common hyperglycemic condition among people with diabetes and its prevalence ...
In people with type 1 diabetes, we assessed for psychopathology in those with and without recurrent diabetic ketoacidosis (DKA). Method: The design was a case-control study. Cases were defined as people with two or more DKA episodes in a 12-month period (recurrent DKA). Cases and controls were matched for gender and age.
Background: Coronavirus disease 2019 (COVID-19) is associated with an increased prevalence and mortality from diabetic ketoacidosis (DKA) globally. With limited access to specialised care, most patients with DKA in South Africa are managed at district hospital level. This study describes the profile of patients admitted to a district hospital in South Africa with DKA and COVID-19 and examines ...
Obtain a venous/capillary blood gas to establish electrolytes/pH level. Perform focused physical exam/primary survey. Verbalize diagnosis of DKA. Initiate appropriate fluid resuscitation for severe DKA. Initiate appropriate medications (insulin, potassium) Communicate effectively with PICU +/- Endocrine consultants.
Diabetic ketoacidosis, a well-known and major acute metabolic complication classically occurs in young patients with type 1 diabetes. However, it may occur in patients with type 2 Diabetes Mellitus too. ... Case Study: Diabetes Ketoacidosis in Type 2 Diabetes: "Look Under the Sheets" Clinical Diabetes. 2004; 22 (4):198-200. doi: 10.2337 ...
Diabetic ketoacidosis (DKA) is a complication of type 1 diabetes that occurs when acids called ketones build up in your blood. It is a dangerous and potentially life-threatening condition that ...
The findings of this study revealed that knowledge differed significantly with sex (p = 0.002), and female patients were more knowledgeable.In addition, knowledge differed with the duration of insulin use (p = 0.021), with those who had been using insulin for > 30 years having the highest scores, while those who had an insulin treatment history of less than 6 months scored the lowest.