- Open access
- Published: 05 August 2024

Co-creating community wellbeing initiatives: what is the evidence and how do they work?
- Nicholas Powell 1 ,
- Hazel Dalton 2 , 3 , 4 , 5 ,
- Joanne Lawrence-Bourne 1 &
- David Perkins 5
International Journal of Mental Health Systems volume 18 , Article number: 28 ( 2024 ) Cite this article
1463 Accesses
6 Altmetric
Metrics details
Addressing wellbeing at the community level, using a public health approach may build wellbeing and protective factors for all. A collaborative, community-owned approach can bring together experience, networks, local knowledge, and other resources to form a locally-driven, place-based initiative that can address complex issues effectively. Research on community empowerment, coalition functioning, health interventions and the use of local data provide evidence about what can be achieved in communities. There is less understanding about how communities can collaborate to bring about change, especially for mental health and wellbeing.
A comprehensive literature search was undertaken to identify community wellbeing initiatives that address mental health. After screening 8,972 titles, 745 abstracts and 188 full-texts, 12 exemplar initiatives were identified (39 related papers).
Eight key principles allowed these initiatives to become established and operate successfully. These principles related to implementation and outcome lessons that allowed these initiatives to contribute to the goal of increasing community mental health and wellbeing. A framework for community wellbeing initiatives addressing principles, development, implementation and sustainability was derived from this analysis, with processes mapped therein.
This framework provides evidence for communities seeking to address community wellbeing and avoid the pitfalls experienced by many well-meaning but short-lived initiatives.
Graphical Abstract

Despite large investments, rates of mental illness have risen for decades, particularly in western societies [ 1 ]. The reasons are varied and complex and have been the subject of intensive study [ 2 ]. Risk factors include loneliness, inequality, disempowerment, and multiple and compounding adversities, factors that have been amplified by the COVID-19 pandemic [ 3 ]. There is widespread recognition of the problem and broad agreement that policy changes are needed [ 4 , 5 ]. Recovery from the pandemic and an increased focus on mental health represent an opportunity to reinvent the way society invests in mental health and wellbeing. The question becomes where and how to intervene to improve population mental health and wellbeing.
Currently, most mental health expenditure occurs in the mental illness treatment system [ 4 ]. These individualised and medicalised approaches are effective for treating mental illness in some people [ 6 , 7 ], but do little to prevent declining population mental health, promote wellbeing, or improve the conditions that contribute to mental illness [ 8 ]. It is more expensive and difficult to treat advanced illness than to intervene early or prevent the illness in the first place, thus prevention and early intervention activities are key components within a comprehensive mental health system [ 9 ]. The concept of ‘mental health’ has become stigmatized, associated with mental illness and mental health problems in the public eye [ 10 ], thereby limiting its utility in the promotion of positive mental health. Thus for the purpose of this review, we have used the concept of eudemonic wellbeing to indicate positive mental health. This is a process of living well that supports positive psychological and physical wellness, underpinned by a theory of self-determination [ 11 ].
Since the 1960s programs have been developed to empower or share power with communities to create social and health change [ 12 ]. These include the Alma Ata Declaration [ 13 , 14 ], the Ottawa Charter [ 15 ], Healthy Cities [ 16 ], community empowerment projects [ 17 , 18 , 19 ], social capital promotion [ 20 , 21 ] and action on the social determinants of health [ 22 , 23 ], and have each made impacts on human wellbeing and informed the way that public and population health interventions are conducted [ 24 ]. Short political timeframes mean interventions in particular places are often abandoned, then replaced, this loss of continuity impairs trust and limits effectiveness [ 25 ]. Working through and with communities may be the most effective way to achieve long-term, independent and sustainable change, particularly when behaviour change is needed [ 26 ]. Initiatives to create vibrant and social communities may act at an appropriate level to improve mental health and wellbeing for all [ 27 ]. Working at the community level may also help to reframe the popular understanding of wellness so that poor wellbeing is seen less as a personal failing and more as a product of a pathogenic environment [ 28 ].
While there are many models of what community initiative can do to build wellbeing, there is little information on how they can accomplish these steps, or how factors change over time. For example, a review of community coalition-driven initiatives found beneficial changes in health outcomes and behaviours, however, there was insufficient process evidence on how the effects were mediated [ 12 ]. Previous research suggests that community level work should take a grassroots, bottom-up and codesigned, and collaborative approach (variously referred to as partnerships, coalitions, teams or working groups) that acknowledges complexity, power inequalities and shared priorities [ 29 ]. Community collaborative group-based social ecological approaches have been used for decades to facilitate ownership in a context-based and culturally sensitive manner through capacity building [ 30 ]. To help engage the community, there are framing and language recommendations so that needs and objectives are understood as opportunities, not problems or vulnerabilities [ 31 , 32 ]. Top-down and overly medicalised models have been seen to fail [ 33 ]. The collective and relational nature of problems/assets such as loneliness/social capital and various social determinants of mental health reinforce the utility of a broader community focus on mental health and wellbeing.
Community wellbeing initiatives
In this review, we examine the broader concept of community wellbeing initiatives by exploring the underlying sub-concepts. Wellbeing has become a catch-all term that is often used interchangeably or in partnership with mental and physical health, happiness, life satisfaction and others.
Whilst wellbeing is a more positive concept than mental health, it is a contested concept [ 34 ], used in communities, industry, policy and practice. Wellbeing has multiple aspects including: physical, mental, intellectual, social, emotional and spiritual components. As discussed above, in this review, we use the wellbeing definition as postulated in Ryan’s theory of self-determination, which stands in the positive mental health domain [ 11 ]. This distinguishes it from other community health and wellbeing reviews that focus on physical activity and dietary interventions.
In the context of public health and health policy, ‘community’ can be difficult to define. Two key approaches highlight geographical and functional communities [ 35 ]. This study uses the definition of “community to refer to a geographically bound group of people on a local scale who are subject to either direct or indirect interaction with each other” [ 36 ]. This is a setting where local place-based resources can be found and applied. Much policy focus has been applied to geographically bound areas, e.g. the UK government national approach is still deployed at the local government area level, where local context can be addressed [ 37 ]. Moreover, place is where things happen, such as natural disasters, acute economic insults such as the closure of local enterprises, and suicide clusters [ 3 ]. Place is where the context can be understood, challenges collectively felt and local strengths recognised and mobilised. Initiatives in these settings present an opportunity to deliver wellbeing and mental health promotion activities that are not provided by local health services, who focus overwhelmingly on the treatment of acute mental illness.
Community wellbeing concerns those factors that enable or hinder a citizen’s ability to build and maintain their wellbeing in a particular place [ 38 , 39 , 40 ]. For example, social capital, goods, infrastructure and service accessibility and cultural values influence individual wellbeing and can be built at the community level [ 41 ]. Community is where people live, it is the environment that shapes their wellbeing. In short, “community” concerns the level of analysis and “well-being” describes the scope of analysis [ 36 ].
In this paper, we analyse the literature on community-built wellbeing initiatives that have mental health and wellbeing as a stated objective or key outcome. For reasons discussed above, this paper focuses on initiatives that empower the community to create the change they wish to see in their area. The identified exemplars have been subjected to detailed analysis to create a common framework for the process factors associated with community wellbeing initiatives. The purpose of the study is to assist communities to build their own interventions to address mental health and wellbeing. The research questions are as follows:
Can community wellbeing initiatives, with wellbeing as a stated objective, be identified that have some implementation success as measured by (i) duration of existence (at least two years) and (ii) have published evidence regarding the initiative (e.g. peer-reviewed article)?
For the chosen community wellbeing initiatives:
What was the context for initiation?
Which stakeholders were involved and what were their roles in the successful implementation?
What was done to promote community wellbeing by these initiatives?
How was momentum sustained and progress measured?
What were the implementation and outcome lessons that may be used by other communities?
Search strategy
An initial scoping review of the field of community wellbeing [ 42 ], informed a structured search strategy, which was refined to remove false positives (excess unrelated papers). The search strategy focused on three factors: what were initiatives trying to achieve (what), the approach or philosophy they followed (how), and the area in which they worked (where). Results were limited to 2000–2019. The search strategy was developed in Medline and adapted for CINAHL, Web of Science, Psychinfo, Sociology Source and Cochrane library. The initial search strategy was deliberately broad to encapsulate the diversity of terms commonly used in this field. The search terms used, in Boolean structure of What AND How AND Where , were: ([wellbeing OR well-being OR mental health OR social determinant OR flourishing OR resilience OR social capital OR social cohesion OR salutogen* OR positive psychology] AND [ecological approach OR grassroot OR community driven OR capacity building OR empowerment OR engagement OR collective impact OR community development OR public health] AND [communit* OR local OR neighbo* OR city OR town]).
Inclusion and exclusion criteria
The inclusion and exclusion criteria were refined via reflective collaborative discussion. Evidence type was restricted to primary papers to enable a primary analysis of process themes for this review. This included process and outcome evaluations. Commentaries and secondary analysis or theoretical papers were excluded but reserved for consideration for inclusion in introduction and/or discussion. Community settings were included, whilst papers focused on more restrictive settings such as school, prisons and aged care were excluded. Initiatives required community involvement and a wellbeing focus. Papers were excluded if the focus was not wellbeing, if it was clearly top-down, externally applied or if there was insufficient detail to describe the initiative activities, processes and governance.
Data extraction, analysis and synthesis
Data extraction: All authors designed an analytical framework from which the data extraction tool was developed (Supplementary Table S1 ). Two authors (NP and JLB) reviewed each included paper using the data extraction tool to create a comprehensive dataset. Details of the initiatives were summarised and encompassed key details, formative and process factors.
A combination of content and thematic analysis [ 43 ] was used to identify themes and concepts within the dataset. The content analysis mapped to existing theories [ 17 , 44 , 45 , 46 ] of community health initiatives to develop themes on the factors that contributed to the functioning of the initiatives. The processes of the initiatives were thematically grouped, coded and discussed by the authors until a coding framework of eight themes was developed, with sub-coding within a matrix to illustrate developmental stages over time. This was developed iteratively with author discussion and regular comparison to the twelve exemplar initiatives and primary themes (NP, HD, DP). Each stage of the thematic analysis was conducted by at least two authors. NVivo was used to organise the themes and the included papers were reanalysed against the coding framework.
Search results
The search returned 8972 results without duplicates. Title and abstract screening excluded 8784 records. Following the search strategy (Fig. 1 ), two authors (NP and JLB) read half of the papers each and compared notes. Disagreements were resolved in discussions with a third author (HD). A total of 17 papers describing twelve separate initiatives were identified. Google Scholar was searched for all literature related to these twelve initiatives, with 26 additional papers found, primarily related to two initiatives.
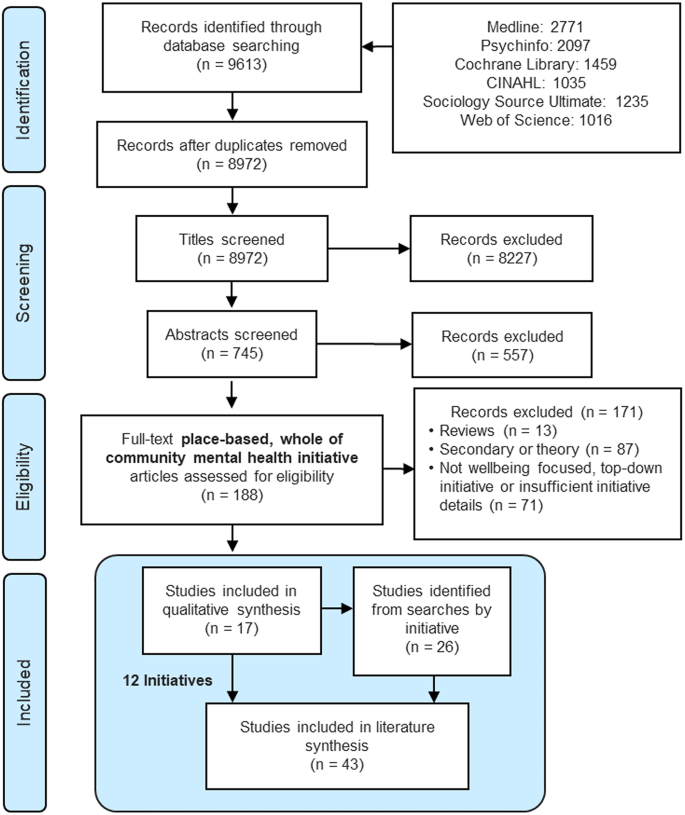
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) four-phase flow diagram
Context of the initiatives
The twelve exemplar initiatives employed different approaches and came from numerous countries – one each from New Zealand, Canada, Mexico, the United States of America (USA), two from Australia and six from the United Kingdom (UK). Key details of these initiatives are summarized in Table 1 .
Wellbeing approaches of the initiatives
To promote mental health and wellbeing, all initiatives encouraged the social dimensions of community, working to build social capital and many using community champions (initiatives # 3, 7, 11) and encouraging volunteerism (initiatives #2, 8, 9, 10). Typical health promotion activities were commonly used, including training (initiatives #3, 7, 9, 11, 12), raising awareness, de-stigmatising conversations, encouragement of self-reflection on what wellbeing and resilience meant to individuals, use of campaigns and tools such as ‘Five ways to wellbeing’ [ 86 ] (initiative #12) and providing opportunities for safe and social interactions (pop-up hubs, youth spaces, and community events). Others explicitly recognised the social and economic determinants of health and were also addressing those (initiatives #1, 2, 5, 10).
What assisted the initiatives to function?
We found eight key themes associated with successful community mental wellbeing initiatives (summarised under ‘principles’ in Fig. 2 ). The way that communities understood and exhibited each of these themes changed over time. For example, initial community engagement often focused on gathering community opinion and later developed into planning events and participation in working groups. The stages of the initiatives are iterative and there was no consistent developmental process – therefore these stages are more a set of component processes to be developed and monitored, rather than a definitive sequence. Each of these broad themes was found in at least eleven of the twelve initiatives and can be thought of as principles that underpinned the initiatives. Moreover, these principles were operationalised as different processes at different phases (‘initiation and planning’, ‘implementation’ and ‘continuation and sustainability’) and are summarised in Fig. 2 . The coding references for these principles and processes mapped against each initiative can be accessed in Supplementary Table S2 .
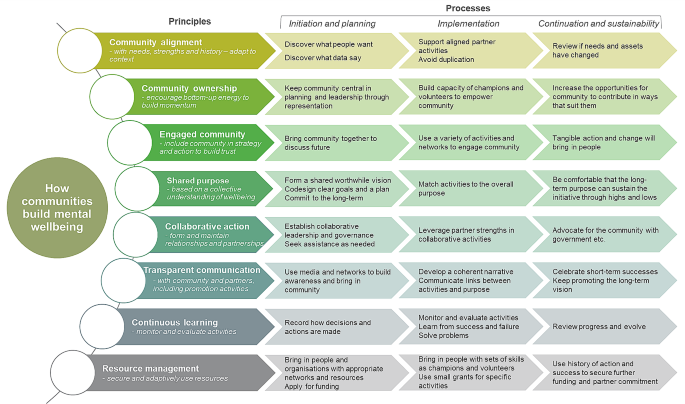
Framework for community wellbeing initiatives – key principles and processes
1. Community alignment – align with community needs, strengths, and history – adapt to context
The community initiatives included were sensitive to the context in which they operated. During initiation and planning, the collection of subjective and objective data enabled a contextual understanding of community need. The general community was asked what they wanted to change (10 of 12 initiatives), and publicly available community data was reviewed (9 of 12 initiatives), highlighting community assets and helping to prioritise needs. As some of the initiatives began to put this information into action, they took care to not duplicate existing activities (2 of 12 initiatives), which can cause wasted energy, community confusion and detract from the credibility of and support for the initiative. As the initiatives matured it was important to consult the community regularly (4 of 12 initiatives) to ensure that the initiative was adaptive and responsive to changes.
2. Community ownership – encourage bottom-up energy to build community ownership
The first step to generate community ownership, was to keep the community voice and vision as the anchor point for all planning and leadership (8 of 12 initiatives). This was achieved through community representation, but some initiatives navigated the concept of representation, with particular representatives having multiple roles. For example, if a professional member of the leadership group was appointed to represent their organisation, could they also be a resident representative? This raised considerations of conflicts of interest and how to handle them. Secondly, the ideas of empowerment and ownership are entwined. Capacity building of champions and volunteers were considered important steps to making their initiatives more acceptable and sustainable in the community (9 of 12 initiatives). Giving the community flexible opportunities to contribute to the initiative in ways that suit members was also important (8 of 12 initiatives). This allowed community members to “dial in and out” of the initiative depending on their interests and commitments.
3. Engaged community – include community in strategy and action to build trust
Five initiatives brought the community together to discuss the future, which was key to their planning and visioning, and may have played a role in engaging community members in leadership or working group positions. Diverse combinations of activities and networks were used to engage with a broad range of community members (11 of 12 initiatives). This is a recognition that not all community members can be reached through traditional networks and that not all activities will engage all community members. It was recognised that in the long term, tangible action and change in the community were key to engaging more people (3 of 12 initiatives).
4. Shared purpose – establish based on a collective understanding of wellbeing
A shared vision that reflected the community voice and aligned with the local context was an important factor in the organisation of initiatives (11 of 12 initiatives). Since wellbeing is a subjective term for individuals and communities, the visions were often based on a local understanding or definition. The desire to create an agreed community vision was undercut by concerns that many initiatives developed a vision based on influential, generally upper middle-class concerns of a subset of the community, rather than being truly representative. The shared visions were translated into specific goals or plans by at least nine of the initiatives. The importance of committing to the long term was raised, since the desired social change could not be achieved in the one to two years that were commonly funded (5 of 12 initiatives). To keep initiatives on track, the consistent linking of activities back to the overarching purpose helped get community involved and keep the leadership and working groups motivated (6 of 12 initiatives). Three initiatives recognised that the human value in the purpose of their initiative helped sustain the initiative through challenges.
5. Collaborative action – form and maintain relationships and partnerships
The selected initiatives had a locally based, collaborative leadership team (12 of 12 initiatives). The ways in which these teams arose differed, with some aided by an external organisation visiting the community and assisting in building a community leadership group (2 of 12 initiatives), others formed leadership groups as a result of local energy (3 of 12 initiatives), although they were assisted by external support to establish and legitimise their initiative.
Collaborative action was evident (11 of 12 initiatives). This included collaboration between community members, local council, health and mental health services, the education system, law enforcement, researchers, local businesses, and voluntary organisations. Many described the formation of a collaborative leadership and governance structure in the form of a steering committee (9 of 12 initiatives). The importance of partnering and supporting relevant community activities was outlined (6 of 12 initiatives). Assistance was sought for certain activities, including workshop facilitation, needs assessments, obtaining funding and evaluation (10 of 12 initiatives). Some of this external support also relied upon government intervention, especially on the issues that cannot be addressed by a community initiative. On these issues, some of the initiatives advocated to government, rather than assume responsibility for endemic issues (e.g., poor employment opportunities, housing or recreation space).
6. Transparent communication – openly communicate with community and partners, including promotion activities
Active communication between the initiative and the broader community was used to engage the community for initial discussion; to involve members as leaders, volunteers, or champions to advertise the purpose and vision of the initiative; to publicise the plan; to advertise sponsored or organised activities; and to list key community contacts for support or involvement (8 of 12 initiatives). This was achieved through promotion in traditional and new media (9 of 12 initiatives), through established networks and word of mouth. Communication between members of the initiative was important for cohesion and enabling democratic elements of decision making (8 of 12 initiatives). Development of a coherent narrative was key to the overall communication and engagement strategy (6 of 12 initiatives). Consistent explanation of the link between the activities of the initiative and the overall purpose was valued (8 of 12 initiatives). Celebrating short-term successes and promoting the long-term vision can illustrate that worthwhile change is possible and occurring (7 of 12 initiatives).
7. Continuous learning – monitor and evaluate activities
Each initiative adapted over time as they learned how to operate and be effective (12 of 12 initiatives). Continuous learning and improvement through monitoring and evaluating activities was described (11 of 12 initiatives). In the organisation stage, some made a point to record how decisions and actions were planned (4 of 12 initiatives). As the initiatives were implementing activities, solving problems and learning from success and failure were key parts of the initiative’s maturation (8 of 12 initiatives). To work towards sustainability in their community, progress reviews were central (11 of 12 initiatives) and helped initiatives to evolve as community needs and assets changed.
8. Resource management – secure and use resources flexibly
Several of the initiatives were described from the perspective of the funders, making it challenging to assess the financial resource dimension. Some initiatives were established only as funding was secured; others secured funding as they went along. Funding was often discussed, including receipt or application for funding and how relationships with funders were managed (7 of 12 initiatives). Small grants for very specific activities, often short term, were easier to obtain in some communities (5 of 12 initiatives). The gathering of non-fiscal resources was discussed by more initiatives than fiscal ones (10 of 12 initiatives). The importance of bringing in organisations and people with the networks and resources to support the initiative was identified, particularly in the early stages (9 of 12 initiatives). While networks and resources were particularly important in the planning stage, people with particular skills who could act as leaders, champions and volunteers were valuable in implementation and maturation. Finally, the importance of a history of action and success in securing new resources was discussed (2 of 12 initiatives). Grant applications were more successful if the initiative demonstrated a strong track record. Also, local organisations and individuals were more likely to contribute towards the initiative when they see that it is a realistic pathway to change.
In this study, we have sought to identify the principles and processes employed by successful community led initiatives to improve mental health and wellbeing. Success in this case was measured by duration of initiative (greater than two years) and supportive evidence of the initiative’s process development or outcomes in the literature. Twelve exemplar community-built wellbeing initiatives were identified. From these, detailed analysis yielded eight key themes (principles) associated with the factors that contributed to the functioning of the initiatives. These principles were community alignment, community ownership, community engagement, shared purpose, collaborative action, transparent communication, continuous learning, and resource management. These were expanded into a matrix to illustrate how the principles were enacted in practice (processes) over the developmental stages of initiation and planning, implementation, and continuation and sustainability. Thus, there is a matrix of component processes associated with how these initiatives were able to collaboratively address mental health and wellbeing in their communities in response to local need and with local ownership. These may be of interest and use for other collaborative initiatives aimed at addressing wellbeing.
Wellbeing is a complex phenomenon, which the twelve exemplar initiatives addressed multidimensionally, deliberately and contextually. The community alignment principle was exemplified by capturing community needs and strengths, both subjectively by listening to community members and objectively via public data sources, e.g. [ 80 ]. These included activities to enhance social connection, increase volunteering, access to support, access to leisure and hobbies, access to green and blue spaces and other social determinants of health that are supported in broader research [ 12 , 41 , 87 , 88 , 89 , 90 ]. Activities were chosen in response to community aspirations, the shared purpose, building both community ownership and engagement. Extensive community involvement in the initiatives was evident, providing information regarding need, collaborative planning and action, leveraging with partners and engaging with the wider community. This aligns with the weight of evidence which suggests that community codesign, empowerment or ownership are strongly linked to success, effectiveness and sustainability of health and behaviour change initiatives [ 91 ].
Community ownership was found to be a key principle; however, the evidence also suggested the importance of external support which could enable complex change in a community (bridging the principles of resource management and collaborative action). Therefore, some level of authority or decision-making power contributing top-down (outside-in) support in combination with bottom-up (inside-out) support and energy are essential for sustainability [ 92 , 93 ]. This raises an important point about power management within community initiatives [ 94 ]. The findings presented here support the broader literature, suggesting that the role of authority figures is to enable and aid the community to realise the codesigned vision [ 92 , 95 ]. The general recommendations from community public health initiatives are to enable a community to contribute and develop agency, that is, health interventions done with communities, not to communities [ 91 , 96 , 97 , 98 , 99 , 100 , 101 , 102 ]. As such, when the goals of an initiative are closely aligned with those of local government, cross sector collaboration flourishes (community alignment and collaborative action principles) [ 103 , 104 , 105 ].
Most of the community initiatives operated at a level between local government and the public. While power management was a consideration for most, the question of capacity and capabilities (resource management) was also relevant in deciding upon vision, goals, objectives, responsibilities and contributions [ 80 , 106 ]. Every community has local organisations with capacity to enact change at some level within the community. Whilst no single partner organisation might be essential for community initiatives, each partner opens new opportunities, and these partners may influence both ambitions and the ability to realise them (collaborative action). In order to understand community change, we must acknowledge that there are other networks, structures and systems that influence and can be leveraged to influence the overall outcome [ 107 , 108 ].
Transparent communication was a key principle, and was used by the included initiatives to traverse the developmentally vulnerable stage of initiation and planning [ 109 ]. Communication of short-term achievements and celebrations was used to build momentum, grassroots support and help reinforced a sense of realistic expectations. Active communication strategies can help build a coherent narrative and link activities to the shared purpose. However, for true change, the many factors that influence wellbeing in the community must be improved upon and be seen to be improving. There is evidence that citizens perceptions of their community and their pride in community are closely linked to the way they talk about their life satisfaction and mental wellbeing, and may be a key pragmatic measure for initiative success [ 78 , 110 , 111 ].
The challenges of evaluating the success of community-based initiatives persist [ 112 ], with attribution of causation especially difficult [ 113 , 114 ]. As noted earlier, a Cochrane review of community coalition-driven interventions [ 12 ] found evidence for positive benefit to individual health outcomes and behaviours, and care delivery systems. There was insufficient evidence on the workings of the coalitions themselves to explain how benefits were achieved, indicating a gap in process evidence. Whilst capturing both the process and the outcome is valued by the researcher, consideration should be given to the burden of documentation in a community-driven initiative should be given. There is a delicate balance between maintaining formal mechanisms and processes to track an initiative without intimidating or overpowering community voice and resourcefulness [ 114 , 115 ]. This study highlights that the documentation of initiative processes and activities supports three of the eight principles directly: the ability to share information and build the common narrative (transparent communication), to reflect and learn (continuous learning), and to leverage future funds with evidence of activity and impact (resource management). This may be a valuable strategy since short, fixed-term funding was identified as a key challenge for resource management and sustainability, which can lead to diminished trust for future initiatives [ 116 , 117 ]. By addressing documentation and evaluation of processes, activities and outcomes, further funds and resources may be secured, thus, providing the time needed to build and retain trust in the community wellbeing initiative. In recognition of the persistent challenge of short-term funding, contrasted with the acknowledged need for time to build trust and genuine collaborative action, policymakers and funders need to adjust to longer time spans. There are some relatively new philanthropic initiatives with explicitly longer time horizons of 10 or more years to address this and to genuinely work with communities for the duration of investment. These include the Hogg Foundation’s Collaborative Approaches to Well-Being in Rural Communities program in Texas [ 118 ], and the Fay Fuller Foundation’s Our Town program in South Australia [ 119 ]. These new funding approaches remain the exception, not the norm.
Strengths and limitations
Strengths: This study has focused on the processes of how community wellbeing initiatives develop and function, where most papers focus on short-term outcomes. It has covered a wide range of papers written by academics and others from a variety of disciplines using a variety of similar, overlapping, and distinct terminology. We have attempted to address temporal issues recognizing that needs for leadership, resources and engagement vary over time and due to changing circumstances. We have suggested a common language/framework which is accessible to communities, not just community development or other professionals.
Limitations: We could only analyse what has been published which is limited in many ways. Initiative processes are often poorly described or assumed, important components are missed out, and papers are written from particular perspectives or with partial perspectives. Our included initiatives had variable volumes of evidence with some having one paper, others many, and up to 14 papers for Well London. Some initiatives are not described or published and therefore there is likely a lot we don’t know. While considerable effort was made to find and select appropriate materials, we may have missed something. There is no common measurement of outcomes, although the variety of contexts may invalidate such comparisons [ 120 ]. Moreover, due to the varying reporting on outcomes, our criteria for selecting successful cases was limited to implementation success, as measured by (i) duration of existence (at least two years) and (ii) have published evidence regarding the initiative (e.g. peer-reviewed article). We also note that the initiatives included all come from Western democracies, predominantly English-speaking countries, and thus the process characteristics outlined here may not apply in other national and cultural contexts.
This review took a rigorous approach to finding twelve exemplar communities, which had successfully implemented community wellbeing initiatives. The focus on how the initiatives were implemented and sustained should aid interested communities to grow their own initiatives and may be used by other studies to design projects that can assess success and impact.
Data availability
Not applicable.
World Health Organization. Health Topics - Mental Health Burden Geneva2022 [ https://www.who.int/health-topics/mental-health#tab=tab_2 .
Burke S, Enticott J, Isaacs A, Meadows G, Rosenberg SP. Critical environmental and social determinants of mental health problems and their care. In: Meadows G, Farhall J, Fossey E, Happell B, McDermott F, Rosenberg S, et al. editors. Mental Health and Collaborative Community Practice. Australia: Oxford University Press; 2020. pp. 30–47.
Google Scholar
Lawrence-Bourne J, Dalton H, Perkins D, Farmer J, Luscombe G, Oelke N, et al. What is rural adversity, how does it affect wellbeing and what are the implications for action? Int J Environ Res Public Health. 2020;17:19.
Article Google Scholar
Productivity Commission. Mental Health, Report no. 95. Canberra2020.
National Mental Health Commission. Monitoring mental health and suicide prevention reform: National Report 2019. Sydney: NMHC; 2019.
Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391(10128):1357–66.
Article CAS PubMed PubMed Central Google Scholar
Bear HA, Edbrooke-Childs J, Norton S, Krause KR, Wolpert M. Systematic review and Meta-analysis: outcomes of routine specialist Mental Health Care for Young People with Depression and/or anxiety. J Am Acad Child Adolesc Psychiatry. 2020;59(7):810–41.
Article PubMed Google Scholar
Herrman H. The need for Mental Health Promotion. Aust N Z J Psychiatry. 2001;35(6):709–15.
Article CAS PubMed Google Scholar
Knapp M, McDaid D, Parsonage M. Mental health promotion and mental illness prevention: the economic case. London: Department of Health; 2011.
Donovan RJ, Henley N, Jalleh G, Silburn SR, Zubrick SR, Williams A. People’s beliefs about factors contributing to mental health: implications for mental health promotion. Health Promot J Austr. 2007;18(1):50–6.
Ryan RM, Huta V, Deci EL. Living well: a self-determination theory perspective on eudaimonia. J Happiness Stud. 2008;9:139–70.
Anderson LM, Adeney KL, Shinn C, Safranek S, Buckner-Brown J, Krause LK. Community coalition-driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst Rev. 2015(6):Cd009905.
International conference on. primary health care. Declaration of Alma-Ata. 1978.
No authorship i. Declaration of ALMA-ATA. Am J Public Health. 2015;105(6):1094–5.
World Health Organization. Ottawa charter for health promotion. Geneva; 1987.
World Health Organization. Healthy Cities Effective Approach to a Changing World. Geneva; 2020.
Laverack G. Improving health outcomes through community empowerment: a review of the literature. J Health Popul Nutr. 2006:113–20.
Marmot MG. Empowering communities. Am J Public Health. 2016;106(2):230–1.
Article PubMed PubMed Central Google Scholar
Douglas JA, Grills CT, Villanueva S, Subica AM. Empowerment Praxis: Community Organizing to redress systemic Health disparities. Am J Community Psychol. 2016;58(3–4):488–98.
Ehsan A, Klaas HS, Bastianen A, Spini D. Social capital and health: a systematic review of systematic reviews. SSM Popul Health. 2019;8:100425.
Ehsan AM, De Silva MJ. Social capital and common mental disorder: a systematic review. J Epidemiol Community Health. 2015;69(10):1021–8.
Marmot M. Universal health coverage and social determinants of health. Lancet. 2013;382(9900):1227–8.
Marmot M, Allen J, Bell R, Bloomer E, Goldblatt P. WHO European review of social determinants of health and the health divide. Lancet. 2012;380(9846):1011–29.
Stansfield J, South J, Mapplethorpe T. What are the elements of a whole system approach to community-centred public health? A qualitative study with public health leaders in England’s local authority areas. BMJ Open. 2020;10(8):e036044.
Boyle D. A history of community development. Linking the stories that connect community organisers across the world, from 1940–2020 [Essay]. Local Trust; 2021 [ https://longreads.localtrust.org.uk/2021/05/01/a-history-of-community-development/ .
Hystad P, Carpiano RM. Sense of community-belonging and health-behaviour change in Canada. J Epidemiol Commun Health. 2012;66(3):277–83.
Kearns A, Whitley E. Are housing and neighbourhood empowerment beneficial for mental health and wellbeing? Evidence from disadvantaged communities experiencing regeneration. SSM Popul Health. 2020;12:100645.
Dooris M, Farrier A, Froggett L. Wellbeing: the challenge of ‘operationalising’ an holistic concept within a reductionist public health programme. Perspect Public Health. 2018;138(2):93–9.
King C, Gillard S. Bringing together coproduction and community participatory research approaches: using first person reflective narrative to explore coproduction and community involvement in mental health research. Health Expect. 2019;22(4):701–8.
DiClemente RJ, Crosby RA, Kegler MC. Emerging theories in Health Promotion Practice and Research. San Francisco, CA: Jossey-Bass; 2009. p. 624.
Roy M, Levasseur M, Dore I, St-Hilaire F, Michallet B, Couturier Y, et al. Looking for capacities rather than vulnerabilities: the moderating effect of health assets on the associations between adverse social position and health. Prev Medicine: Int J Devoted Pract Theory. 2018;110:93–9.
Roy MJ. The assets-based approach: furthering a neoliberal agenda or rediscovering the old public health? A critical examination of practitioner discourses. Crit. 2017;27(4):455–64.
Perkins D, Farmer J, Salvador-Carulla L, Dalton H, Luscombe G. The Orange Declaration on rural and remote mental health. Aust J Rural Health. 2019;27(5):374–9.
Ereaut G, Whiting RA. What do we mean by ‘wellbeing’? and why might it matter? Department for Children, Schools and Families (DCSF); 2008. Report No.: ISBN 978 1 84775 271 0.
Fellin P. The community and the social worker. 3rd ed. Itasca, Ill.: F.E. Peacock; 2001.
Lee S, Kim Y. Searching for the meaning of Community Well-Being. In: Lee SJ, Kim Y, Phillips R, editors. Community Well-Being and Community Development SpringerBriefs in Well-Being and Quality of Life Research Cham. Springer International Publishing; 2015. pp. 9–23.
Lee SJ, Kim Y. Achieving community well-being through community participatory governance: the case of Saemaul Undong. Handbook of community well-being research. New York, NY: Springer Science + Business Media; US; 2017. pp. 115–28.
Bywater T, Berry V, Blower SL, Cohen J, Gridley N, Kiernan K, et al. Enhancing Social-Emotional Health and Wellbeing in the early years (E-SEE): a study protocol of a community-based randomised controlled trial with process and economic evaluations of the incredible years infant and toddler parenting programmes, delivered in a proportionate universal model. BMJ Open. 2018;8(12):e026906.
Cox D, Frere M, West S, Wiseman J. Developing and using local community wellbeing indicators: learning from the experience of community indicators Victoria. Australian J Social Issues (Australian Council Social Service). 2010;45(1):71–88.
Kim Y, Kee Y, Lee S. An analysis of the relative importance of components in Measuring Community Wellbeing: perspectives of Citizens, Public officials, and experts. Soc Indic Res. 2015;121(2):345–69.
Hunter BD, Neiger B, West J. The importance of addressing social determinants of health at the local level: the case for social capital. Health Soc Care Community. 2011;19(5):522–30.
Powell N, Dalton H, Perkins D, Review. A collaborative approach to community mental wellbeing. Orange NSW Centre for Rural and Remote Mental Health, University of Newcastle; 2018.
Ezzy D. Qualitative analysis: practice and innovation. Crows nest. New South Wales: Allen & Unwin; 2002.
Nutbeam D. What would the Ottawa Charter look like if it were written today? Crit. 2008;18(4):435–41.
Popay J, Attree P, Hornby D, Milton B, Whitehead M, French B et al. Community engagement in initiatives addressing the wider social determinants of health A rapid review of evidence on impact, experience and process. Social Determinants Eff Rev. 2007.
Atkinson S, Bagnall A, Corcoran R, South J. What is community wellbeing? Conceptual review. Leeds, UK: Leeds Beckett University; 2017.
Adams J, Witten K, Conway K. Community development as health promotion: evaluating a complex locality-based project in New Zealand. Community Dev J. 2009;44(2):140
Cheuy S, Fawcett L, Hutchinson K, Robertson T. A citizen-led approach to enhancing community well-being. Handbook of community well-being research. New York, NY: Springer Science + Business Media; US; 2017. p. 129–67.
Corbie-Smith G, Yaggy SD, Lyn M, Green M, Ornelas IJ, Simmons T, et al. Development of an Interinstitutional Collaboration to Support Community-Partnered Research Addressing the Health of Emerging Latino Populations. Acad Med. 2010;85(4):728–35.
Green MA, Perez G, Ornelas IJ, Tran AN, Blumenthal C, Lyn M, et al. Amigas Latinas Motivando el ALMA (ALMA): Development and Pilot Implementation of a Stress Reduction Promotora Intervention. Calif J Health Promot. 2012;10:52–64.
Perez G, Della Valle P, Paraghamian S, Page R, Ochoa J, Palomo F, et al. A community-engaged research approach to improve mental health among latina immigrants: ALMA Photovoice. Health Promot Pract. 2016;17(3):429–39.
Ryan D, Maurer S, Lengua L, Duran B, Ornelas IJ. Amigas Latinas Motivando el Alma (ALMA): an Evaluation of a Mindfulness Intervention to Promote Mental Health among Latina Immigrant Mothers. J Behav Health Serv Res. 2018;45(2):280–91.
Tran AN, Ornelas IJ, Kim M, Perez G, Green M, Lyn MJ, et al. Results from a pilot promotora program to reduce depression and stress among immigrant Latinas. Health Promot Pract. 2014;15(3):365–72.
Tran AN, Ornelas IJ, Perez G, Green MA, Lyn M, Corbie-Smith G. Evaluation of Amigas Latinas Motivando el Alma (ALMA): a pilot promotora intervention focused on stress and coping among immigrant Latinas. J Immigr Minor Health. 2014;16(2):280–9.
Draper A, Clow A, Lynch R, Jain S, Philips G, Petticrew M, et al. Building a logic model for a complex intervention: a worked example from the Well London CRCT. . In Population Health: Methods and Challenges, MRC Conference; Birmingham 2012.
Derges J, Lynch R, Clow A, Petticrew M, Draper A. Complaints about dog faeces as a symbolic representation of incivility in London, UK: a qualitative study. Crit. 2012;22(4):419–25.
Renton A, Phillips G, Daykin N, Yu G, Taylor K, Petticrew M. Think of your art-eries: arts participation, behavioural cardiovascular risk factors and mental well-being in deprived communities in London. Public Health. 2012;126 Suppl 1(5):S57–s64.
Phillips G, Renton A, Moore DG, Bottomley C, Schmidt E, Lais S, et al. The Well London program--a cluster randomized trial of community engagement for improving health behaviors and mental wellbeing: baseline survey results. Trials. 2012;13:105.
Derges J, Clow A, Lynch R, Jain S, Phillips G, Petticrew M, et al. 'Well London' and the benefits of participation: results of a qualitative study nested in a cluster randomised trial. BMJ Open. 2014;4(4):e003596.
Phillips G, Bottomley C, Schmidt E, Tobi P, Lais S, Ge Y, et al. Measures of exposure to the Well London Phase-1 intervention and their association with health well-being and social outcomes. J Epidemiol Community Health. 2014;68(7):597–605.
Phillips G, Bottomley C, Schmidt E, Tobi P, Lais S, Yu G, et al. Well London Phase-1: results among adults of a cluster-randomised trial of a community engagement approach to improving health behaviours and mental well-being in deprived inner-city neighbourhoods. J Epidemiol Community Health. 2014;68(7):606–14.
Sheridan K, Adams-Eaton F, Trimble A, Renton A, Bertotti M. Community engagement using World Café: The well London experience. Groupwork. 2010;20(3):32–50.
Wall M, Hayes R, Moore D, Petticrew M, Clow A, Schmidt E, et al. Evaluation of community level interventions to address social and structural determinants of health: a cluster randomised controlled trial. BMC Public Health. 2009;9:207.
Edmonds N. Well London: Mental well being impact assessment project report. 2009 [March, 20, 2022]. Available from: https://www.welllondon.org.uk/39/mental-well-being-impact-assessment.html .
Bertotti M, Adams-Eaton F, Sheridan K, Renton A. Key Barriers to Community Cohesion: Views from Residents of 20 London Deprived Neighbourhoods. Geo J. 2012;77(2):223–34.
Wittenberg R, Findlay G, Tobi P. Costs of the Well London programme. In: Unit PSSR, editor. Unit Costs of Health and Social Care 2016. Canterbury 2016. pp.12–6.
Frostick C, Watts P, Netuveli G, Renton A, Moore D. Well London: Results of a Community Engagement Approach to Improving Health Among Adolescents from Areas of Deprivation in London. J Com Prac. 2017;25(2):235–52.
Tobi P, Kemp P, Schmidt E. Cohort differences in exercise adherence among primary care patients referred for mental health versus physical health conditions. Pri Health Care Res Dev. 2017;18(5):463–71.
Giovannini M. Indigenous community enterprises in Chiapas: a vehicle for buen vivir? Community Dev J. 2015;50(1):71–87.
Giovannini M. Social enterprises for development as. J Enterpr Com: People Place Global Eco. 2012;6(3):284–99.
Haswell-Elkins M, Reilly L, Fagan R, Ypinazar V, Hunter E, Tsey K, et al. Listening, sharing understanding and facilitating consumer, family and community empowerment through a priority driven partnership in Far North Queensland. Australas Psychiatry. 2009;17 Suppl 1:S54–8.
Mantovani N, Pizzolati M, Gillard S. Engaging communities to improve mental health in African and African Caribbean groups: a qualitative study evaluating the role of community well-being champions. Health Soc Care Community. 2017;25(1):167–76.
Mantovani N, Pizzolati M, Gillard S. “Using my knowledge to support people”: A qualitative study of an early intervention adopting community wellbeing champions to improve the mental health and wellbeing of African and African Caribbean communities: St George’s University of London; 2014.
Lewis S, Bambra C, Barnes A, Collins M, Egan M, Halliday E, et al. Reframing ‘participation’ and ‘inclusion’ in public health policy and practice to address health inequalities: Evidence from a major resident-led neighbourhood improvement initiative. Health Soc Care Community. 2019;27(1):199–206.
McGowan VJ, Wistow J, Lewis SJ, Popay J, Bambra C. Pathways to mental health improvement in a community-led area-based empowerment initiative: evidence from the Big Local ‘Communities in Control’ study, England. J Public Health (Oxf). 2019;41(4):850–7.
Orton L, Ponsford R, Egan M, Halliday E, Whitehead M, Popay J. Capturing complexity in the evaluation of a major area-based initiative in community empowerment: what can a multi-site, multi team, ethnographic approach offer? Anthropol Med. 2019;26(1):48–64.
Saunders P, Campbell P, Webster M, Thawe M. Analysis of Small Area Environmental, Socioeconomic and Health Data in Collaboration with Local Communities to Target and Evaluate ‘Triple Win’ Interventions in a Deprived Community in Birmingham UK. Int J Environ Res Public Health. 2019;16(22).
Halliday E, Collins M, Egan M, Ponsford R, Scott C, Popay J. A ‘strategy of resistance’? How can a place-based empowerment programme influence local media portrayals of neighbourhoods and what are the implications for tackling health inequalities? Health Place. 2020;63:102353.
Ponsford R, Collins M, Egan M, Halliday E, Lewis S, Orton L, et al. Power, control, communities and health inequalities. Part II: measuring shifts in power. Health Promot Int. 2021;36(5):1290–9.
Powell N, Dalton H, Perkins D, Considine R, Hughes S, Osborne S, et al. Our healthy Clarence: A Community-Driven Wellbeing Initiative. Int J Environ Res Public Health. 2019;16(19):30.
Richardson J, Nichols A, Henry T. Do transition towns have the potential to promote health and well-being? A health impact assessment of a transition town initiative. Public Health. 2012;126(11):982–9.
Gui X, Nardi B, editors. Sustainability begins in the street: A story of Transition Town Totnes. EnviroInfo and ICT for Sustainability 2015; 2015: Atlantis Press.
Woodall J, White J, South J. Improving health and well-being through community health champions: a thematic evaluation of a programme in Yorkshire and Humber. Perspect Public Health. 2013;133(2):96–103.
White J, South J, Woodall J, Kinsella K. Altogether Better Thematic Evaluation - Community Health Champions and Empowerment. Leeds: Centre for Health Promotion Research, Leeds Metropolitan University; 2010.
Zeidler M, Zeidler L, Lee B. Positive psychology at a city scale. The Routledge international handbook of critical positive psychology. Routledge international handbooks. New York, NY, US: Routledge/Taylor & Francis Group; 2018. p. 523–31.
Aked J, Marks N, Cordon C, Thompson S. Five ways to wellbeing. UK; 2008. p. 22.
Perez E, Braen C, Boyer G, Mercille G, Rehany E, Deslauriers V et al. Neighbourhood community life and health: a systematic review of reviews. Health Place. 2019:102238.
Raphael D, Renwick R, Brown I, Steinmetz B, Sehdev H, Phillips S. Making the links between community structure and individual well-being: community quality of life in Riverdale, Toronto, Canada. Health Place. 2001;7(3):179–96.
Houlden V, Weich S, Porto de Albuquerque J, Jarvis S, Rees K. The relationship between greenspace and the mental wellbeing of adults: a systematic review. PLoS ONE. 2018;13(9):e0203000.
Kahana E, Bhatta T, Lovegreen LD, Kahana B, Midlarsky E. Altruism, helping, and volunteering: pathways to well-being in late life. J Aging Health. 2013;25(1):159–87.
O’Mara-Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, Thomas J. The effectiveness of community engagement in public health interventions for disadvantaged groups: a meta-analysis. BMC Public Health. 2015;15:129.
Baum F. Cracking the nut of health equity: top down and bottom up pressure for action on the social determinants of health. Promot Educ. 2007;14(2):90–5.
Singer J, Bennett-Levy J, Rotumah D. You didn’t just consult community, you involved us: transformation of a ‘top-down’ Aboriginal mental health project into a ‘bottom-up’ community-driven process. Australas. 2015;23(6):614–9.
Wolff T, Minkler M, Wolfe SM, Berkowitz B, Bowen L, Butterfoss FD et al. Collaborating for equity and justice: moving beyond collective impact. Nonprofit Q. 2017:42–53.
Cooper LA, Purnell TS, Showell NN, Ibe CA, Crews DC, Gaskin DJ, et al. Progress on Major Public Health challenges: the importance of equity. Public Health Rep. 2018;133(1suppl):S15–9.
Pfefferbaum B, Pfefferbaum RL, Van Horn RL. Community resilience interventions: participatory, assessment-based, action-oriented processes. Am Behav Sci. 2015;59(2):238–53.
Bromley E, Figueroa C, Castillo EG, Kadkhoda F, Chung B, Miranda J, et al. Community Partnering for Behavioral Health Equity: Public Agency and Community leaders’ views of its Promise and Challenge. Ethn Dis. 2018;28(Suppl 2):397–406.
Holden K, Akintobi T, Hopkins J, Belton A, McGregor B, Blanks S et al. Community Engaged Leadership to Advance Health Equity and Build healthier communities. Soc Sci (Basel). 2016;5(1).
Pastor M, Terriquez V, May L. How Community Organizing Promotes Health Equity, and how Health Equity affects Organizing. Health Aff (Millwood). 2018;37(3):358–63.
Reid A, Abraczinskas M, Scott V, Stanzler M, Parry G, Scaccia J, et al. Using Collaborative Coalition Processes to Advance Community Health, Well-Being, and equity: a multiple-case study analysis from a National Community Transformation Initiative. Health Educ Behav. 2019;46(1suppl):S100–9.
Torres S, Labonte R, Spitzer DL, Andrew C, Amaratunga C. Improving health equity: the promising role of community health workers in Canada. Healthc Policy. 2014;10(1):73–85.
PubMed PubMed Central Google Scholar
Davis EJ. Collaborative processes and connection to Community Wellbeing. Eugene, Oregon: University of Oregon; 2021.
Rosen J, O’Neill M, Hutson M. The important role of government in Comprehensive Community initiatives: a Case Study Analysis of the Building Healthy communities Initiative. J Plann Educ Res. 2022;42(3):350–64.
Turner D, Martin S. Social Entrepreneurs and social inclusion: building local capacity or delivering National priorities? Int J Public Adm. 2005;28(9/10):797–806.
Gratzer D, Goldbloom D. ThriveNYC is ambitious—lessons from the International Experience with Mental Health Reform can make it successful. Am J Public Health. 2019;109:S166–7.
Hacker K, Tendulkar SA, Rideout C, Bhuiya N, Trinh-Shevrin C, Savage CP, et al. Community capacity building and sustainability: outcomes of community-based participatory research. Prog Community Health Partnersh. 2012;6(3):349–60.
Hargreaves MB, Pecora PJ, Williamson G. Aligning Community Capacity, Networks, and solutions to address adverse childhood experiences and increase resilience. Acad Pediatr. 2017;17(7S):S7–8.
Hargreaves MB, Verbitsky-Savitz N, Coffee-Borden B, Perreras L, White CR, Pecora PJ, et al. Advancing the measurement of collective community capacity to address adverse childhood experiences and resilience. Child Youth Serv Rev. 2017;76:142–53.
Butterfoss FD. Coalitions and partnerships in community health. San Francisco, CA, US: Jossey-Bass; 2007. xxv, 579-xxv, p.
Halliday E, Popay J, Anderson de Cuevas R, Wheeler P. The elephant in the room? Why spatial stigma does not receive the public health attention it deserves. J Public Health (Oxf). 2018;42(1):38–43.
Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55(1):125–39.
Todd H, editor. The Partners in Action Evaluation Project: A learning journey in building the evaluation capacity and evaluative culture of a local community coalition2015.
Flores EC, Fuhr DC, Bayer AM, Lescano AG, Thorogood N, Simms V. Mental health impact of social capital interventions: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2018;53(2):107–19.
Kadushin C, Lindholm M, Ryan D, Brodsky A, Saxe L. Why it is so difficult to Form Effective Community coalitions. City Community. 2005;4:255–75.
Muenchberger H, Kendall E, Rushton C. Pressure to perform: a content analysis of critical considerations in health coalition development. Leadersh Health Serv. 2012;25(3):186–202.
Hayes A, Freestone M, Day J, Dalton H, Perkins D. Collective impact approaches to promoting community health and wellbeing in a regional township: learnings for integrated care. Int J Integr Care. 2021;21(2).
Miller WD, Pollack CE, Williams DR. Healthy homes and communities: putting the pieces together. Am J Prev Med. 2011;40(1 Suppl 1):S48–57.
Hogg Foundation for Mental Health. Collaborative Approaches to Well-Being in Rural Communities [ https://hogg.utexas.edu/initiatives/collaborative-approaches-well-being-rural-communities .
Fay Fuller Foundation. Our Town [ https://www.fayfullerfoundation.com.au/focus/our-town .
Salvador-Carulla L, Lukersmith S, Sullivan W. From the EBM pyramid to the Greek temple: a new conceptual approach to guidelines as implementation tools in mental health. Epidemiol Psychiatr Sci. 2017;26(2):105–14.
Download references
Acknowledgements
We thank Ms Debbie Booth, University of Newcastle Library, for her professional support to develop and refine our literature search strategy. We thank Centre for Rural and Remote Mental Health staff Rosie Dunnett, Corinna West, Joanna Joseph, Naomi Ruming and A/Prof Peter Simmons for providing critical and constructive feedback on the presentation of the thematic summaries in figure format. We thank the Global Leadership Exchange (GLE) – Rural Behavioral Health Collaborative for bringing new long-term funded initiatives mentioned in the discussion to our attention.
We acknowledge seed funding for the scoping review which formed the foundational concepts of this paper was provided by the NSW Mental Health Commission. From 2018 to 2021, NP, HD, JLB and DP were employed by the University of Newcastle Centre for Rural and Remote Mental Health, with core funding support from NSW Health, Mental Health Branch. HD acknowledges support for completing and publishing this paper via a grant from the Commonwealth of Australia, represented by the Department of Health (Grant Activity 4-DGEJZ1O/4-CW7UT14).
Author information
Authors and affiliations.
Independent researcher. Formerly Centre for Rural and Remote Mental Health, University of Newcastle, Orange, NSW, Australia
Nicholas Powell & Joanne Lawrence-Bourne
Rural Health Research Institute, Charles Sturt University, Orange, NSW, Australia
Hazel Dalton
School of Medicine and Public Health, University of Newcastle, Callaghan, NSW, Australia
Healthy Minds Research Program, Hunter Medical Research Institute, Newcastle, NSW, Australia
Mental Health Policy Unit, Health Services Research Institute, University of Canberra, Canberra, ACT, Australia
Hazel Dalton & David Perkins
You can also search for this author in PubMed Google Scholar
Contributions
NP: conceptualization; search strategy; analysis strategy; formal analysis; draft and revised thematic summary; writing-original draft; writing-review & editing. HD: conceptualization; analysis strategy; revised thematic summary; figure preparation; writing-review & editing. JLB: formal analysis; draft thematic summary; review & editing. DP: funding acquisition; conceptualization; revised thematic summary; writing-review & editing.
Corresponding author
Correspondence to Hazel Dalton .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Powell, N., Dalton, H., Lawrence-Bourne, J. et al. Co-creating community wellbeing initiatives: what is the evidence and how do they work?. Int J Ment Health Syst 18 , 28 (2024). https://doi.org/10.1186/s13033-024-00645-7
Download citation
Received : 05 October 2023
Accepted : 09 July 2024
Published : 05 August 2024
DOI : https://doi.org/10.1186/s13033-024-00645-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Capacity building
- Collaborative
International Journal of Mental Health Systems
ISSN: 1752-4458
- Submission enquiries: [email protected]

Community Mental Health Journal
Community Mental Health Journal is devoted to the evaluation and improvement of public sector mental health services for people affected by severe mental disorders, serious emotional disturbances and/or addictions.
- Coverage includes nationally representative epidemiologic projects, intervention research involving benefit and risk comparisons between service programs, and methodology, such as instrumentation, where particularly pertinent to public sector behavioral health evaluation or research.
- *Please note: All studies must be approved by human subjects committees (also known as institutional review boards). At the end of the Methods section, authors must state which human subject committee (IRB) approved the study.
This is a transformative journal , you may have access to funding.
- Sandra Steingard
Societies and partnerships
Latest issue
Volume 60, Issue 7
Latest articles
Bridging the gap of inequity in implementation science: adaptations of group ebps for those with serious mental illness in the public sector.
- Erika R. Carr
Programmatic and Organizational Barriers and Facilitators to Addressing High-Risk Issues in Supportive Housing and Housing First Programs
- Nick Kerman
- Timothy de Pass
- Vicky Stergiopoulos
Peer Support Workers in Mental Health Services: A Qualitative Exploration of Emotional Burden, Moral Distress and Strategies to Reduce the Risk of Mental Health Crisis
- Justyna Klingemann
- Halina Sienkiewicz-Jarosz
- Piotr Świtaj
Taking what you get or Getting what you Need: A Qualitative Study on Experiences with Mental Health and Welfare Services in Long-Term Recovery in First-Episode Psychosis
- Hanne Haavind
- Carmen Simonsen

Addressing Hispanic Veterans that Live in Rural Area’s Needs to Improve Suicide Prevention Efforts
- I. Magaly Freytes
- Nathaniel Eliazar-Macke
- Constance Uphold
Journal updates
Supporting the sustainable developmental goals.
New Article Type: Fresh Focus
Community Mental Health Journal is introducing a new article type, focusing on emerging topics of discussion within community psychiatry. The new article type, Fresh Focus, spans several possible formats and focus topics listed here.
Journal information
- Current Contents/Social & Behavioral Sciences
- Google Scholar
- Japanese Science and Technology Agency (JST)
- Norwegian Register for Scientific Journals and Series
- OCLC WorldCat Discovery Service
- Semantic Scholar
- Social Science Citation Index
- TD Net Discovery Service
- UGC-CARE List (India)
Rights and permissions
Editorial policies
© Springer Science+Business Media, LLC, part of Springer Nature
- Find a journal
- Publish with us
- Track your research
Community Psychology and Community Mental Health: A Call for Reengagement
Affiliations.
- 1 Department of Psychology, Portland State University, Portland, OR, USA.
- 2 Department of Psychology, DePaul University, Chicago, IL, USA.
- 3 Center for Research on Educational and Community Services, University of Ottawa, Ottawa, ON, Canada.
- PMID: 29315707
- DOI: 10.1002/ajcp.12225
Community psychology is rooted in community mental health research and practice and has made important contributions to this field. Yet, in the decades since its inception, community psychology has reduced its focus on promoting mental health, well-being, and liberation of individuals with serious mental illnesses. This special issue endeavors to highlight current efforts in community mental health from our field and related disciplines and point to future directions for reengagement in this area. The issue includes 12 articles authored by diverse stakeholder groups. Following a review of the state of community mental health scholarship in the field's two primary journals since 1973, the remaining articles center on four thematic areas: (a) the community experience of individuals with serious mental illness; (b) the utility of a participatory and cross-cultural lens in our engagement with community mental health; (c) Housing First implementation, evaluation, and dissemination; and (d) emerging or under-examined topics. In reflection, we conclude with a series of challenges for community psychologists involved in future, transformative, movements in community mental health.
Keywords: Community mental health; Community psychology; Serious mental illness; Transformative change.
© Society for Community Research and Action 2018.
Publication types
- Introductory Journal Article
- Research Support, Non-U.S. Gov't
- Community Mental Health Services
- Community Networks*
- Mental Health*
- Psychology, Social
- Severity of Illness Index
REVIEW article
Current insights of community mental healthcare for people with severe mental illness: a scoping review.

- 1 School of Social and Behavioral Sciences, Tranzo Scientific Center for Care and Wellbeing, Tilburg University, Tilburg, Netherlands
- 2 Kwintes Housing and Rehabilitation Services, Zeist, Netherlands
- 3 Trimbos Institute, Dutch Institute of Mental Health and Addiction, Utrecht, Netherlands
- 4 HVO-Querido, Amsterdam, Netherlands
- 5 Faculty of Social Sciences – HIVA, University of Leuven, Leuven, Belgium
Background: For the last four decades, there has been a shift in mental healthcare toward more rehabilitation and following a more humanistic and comprehensive vision on recovery for persons with severe mental illness (SMI). Consequently, many community-based mental healthcare programs and services have been developed internationally. Currently, community mental healthcare is still under development, with a focus on further inclusion of persons with enduring mental health problems. In this review, we aim to provide a comprehensive overview of existing and upcoming community mental healthcare approaches to discover the current vision on the ingredients of community mental healthcare.
Methods: We conducted a scoping review by systematically searching four databases, supplemented with the results of Research Rabbit, a hand-search in reference lists and 10 volumes of two leading journals. We included studies on adults with SMI focusing on stimulating independent living, integrated care, recovery, and social inclusion published in English between January 2011 and December 2022 in peer-reviewed journals.
Results: The search resulted in 56 papers that met the inclusion criteria. Thematic analysis revealed ingredients in 12 areas: multidisciplinary teams; collaboration within and outside the organization; attention to several aspects of health; supporting full citizenship; attention to the recovery of daily life; collaboration with the social network; tailored support; well-trained staff; using digital technologies; housing and living environment; sustainable policies and funding; and reciprocity in relationships.
Conclusion: We found 12 areas of ingredients, including some innovative topics about reciprocity and sustainable policies and funding. There is much attention to individual ingredients for good community-based mental healthcare, but very little is known about their integration and implementation in contemporary, fragmented mental healthcare services. For future studies, we recommend more empirical research on community mental healthcare, as well as further investigation(s) from the social service perspective, and solid research on general terminology about SMI and outpatient support.
1. Introduction
For the last three decades, there has been a shift in mental healthcare from a biomedical model to a more biopsychosocial model with a focus on rehabilitation, strengths, all areas of recovery, citizenship, empowerment, autonomy, and shared decision-making as leading principles ( 1–5 ). Still, the “social aspect” of the biopsychosocial model has long remained neglected ( 6 ). In 2007, human rights for people with disabilities were covered in the convention ( 7 ), and several community-based mental healthcare programs and services have been developed in Europe for these groups, enhanced by peer-to-peer initiatives and recovery colleges ( 8 ). Over the past few years, concepts such as social inclusion, citizenship, and participation have become the heart of the deinstitutionalization movement. Additionally, more and more people with mental healthcare issues receive outreach support. An indication of the development of intensive outpatient care for people with severe mental illness (SMI) is the development of (flexible) assertive community treatment ((F)ACT) teams. For example, in Netherlands in 2020, there were an estimated 400 FACT teams ( 9 ) and about 30% of people with SMI in England receive support from a specialist mental health floating outreach service ( 10 ).
In general, the definition of SMI consists of three criteria: a psychiatric diagnosis according to Diagnostic and Statistical Manual of Mental Disorders, illness duration of more than 2 years, and disability in functioning ( 11 ). A subgroup of people with SMI needs intensive care and support in daily living and receives residential care, supported housing in a 24/7 facility, or floating outreach ( 12 ). Most people with SMI who live in residential supported housing facilities have a strong preference to live independently in the community with flexible support with a view to a meaningful and fulfilling life ( 13 ). Nowadays, there are several community-based support services for these people who want to live independently, such as Housing First (HF). HF is an evidence-based housing intervention in the social domain that combats homelessness ( 14 ). It combines rapid access to permanent, nonabstinence-contingent ordinary housing and recovery-oriented mental health support teams ( 15 ). Individuals with SMI are at a higher risk of homelessness, and a high proportion of individuals experiencing homelessness are also living with mental illness ( 16 ). Therefore, measures should be available to prevent those who do not make use of, or leave, supported housing from becoming homeless.
Different services for mental health conditions have traditionally been separate from other services such as physical healthcare and social services. However, there is increasing emphasis internationally on developing a whole-system approach to improve the integration of these services to maximize an individual’s quality of life and social inclusion by encouraging their skills, promoting independence and autonomy to give them hope for the future. That leads to successful community living through appropriate support, with particular focus on patient-centered development and delivery ( 17–19 ). Furthermore, following the rehabilitation and recovery movement, care should involve all areas of living ( 20 ), and community-based mental healthcare thus should be a more integrated package of services. Many studies have appeared on the development and impact of multidisciplinary teams in mental healthcare ( 21 , 22 ). A lot less research is available on supported housing services, including accommodation-based and floating outreach services, leading to a lack of evidence on what works in this area ( 23 , 24 ).
In this literature review, we focus on all services for persons with SMI which are living independently in the community. These services aim to support these people in their daily life. This includes services initiated by treatment organizations, such as ambulatory interdisciplinary teams, as well as by welfare and supported housing organizations. Following McPherson et al. ( 25 ), who developed the simple taxonomy for supported accommodation (STAX-SA) to capture the defining features of different supported accommodation models, in this study we focus on supported housing services meant for persons moving forward from a hospital admission or a full-time staffed housing accommodation in a congregate setting with high support, toward more individual accommodation with no staff on-site. These services can be low or might need to be medium or intensive to support independent living for all ( 25 ).
Currently, there is a lack of research about what is needed to successfully provide this type of intensive support for people with SMI, and especially about how this support can be organized as an integrated community-based mental healthcare approach, including housing, rehabilitation, citizenship, all areas of recovery, empowerment, autonomy, and decision-making power. We aim to provide a comprehensive overview of existing and upcoming community mental healthcare approaches to discover the current vision and empirical findings on the ingredients of community mental healthcare. To do so, we will look in this review for both empirical evidence, as well as leading concepts in this research topic. The findings of this study contribute to the further development of community-based mental healthcare for persons with SMI and high-volume healthcare needs. This paper will address the following question: What are the current insights (both leading concepts and empirical findings) regarding a community mental healthcare system to support all persons with SMI in their independent living and recovery, and stimulate further social inclusion?
This review follows the PRISMA guidelines for scoping reviews ( 26 ). The completed PRISMA checklist is available on request from the authors.
2.1. Study design
We performed a scoping review, following the steps of the framework of Arksey and O’Malley ( 27 ): (a) identify the research question; (b) identify relevant studies; (c) select the studies; (d) chart the data; and (e) collate, summarize and report the results. A scoping review contributes to mapping rapidly the key concepts underpinning a research area and the main sources and types of evidence available ( 28 ).
2.2. Eligibility criteria
2.2.1. inclusion criteria.
We included papers published in English from January 2011 to December 2022 in peer-reviewed journals, aimed at 18 years and older adults with severe mental illness, focusing on stimulating independent living, integrated care, recovery, and social inclusion. For reasons of comparability, and fit in Western healthcare systems, studies were included if they were conducted in Western countries only (i.e., United States of America, Canada, countries in Western Europe, Australia, New Zealand, and Japan). Finally, all study designs were included, and we also included papers about interventions related to collaboration.
2.2.2. Exclusion criteria
Studies were excluded if (a) they primarily focused on treatment without support or care, (b) social inclusion or recovery was not the aim, (c) they focused on interventions that concentrated on one area of life and did not provide an integrated offering, or (d) if they focused on psychometric or physical diseases.
2.3. Search strategy
To find the right search terms for our search, we used the program Research Rabbit. This program helps to explore the literature of a research topic and links authors and papers on the same topic to each other. Before conducting the search, the research team determined the eight most relevant papers on this topic and added them to the program. With the function “similar work,” we added another eight relevant papers. Figure 1 shows these 16 relevant papers with the biggest bullets and shows that some papers have more in common with each other than others. The most common keywords from the 16 papers were the basis for our search terms.
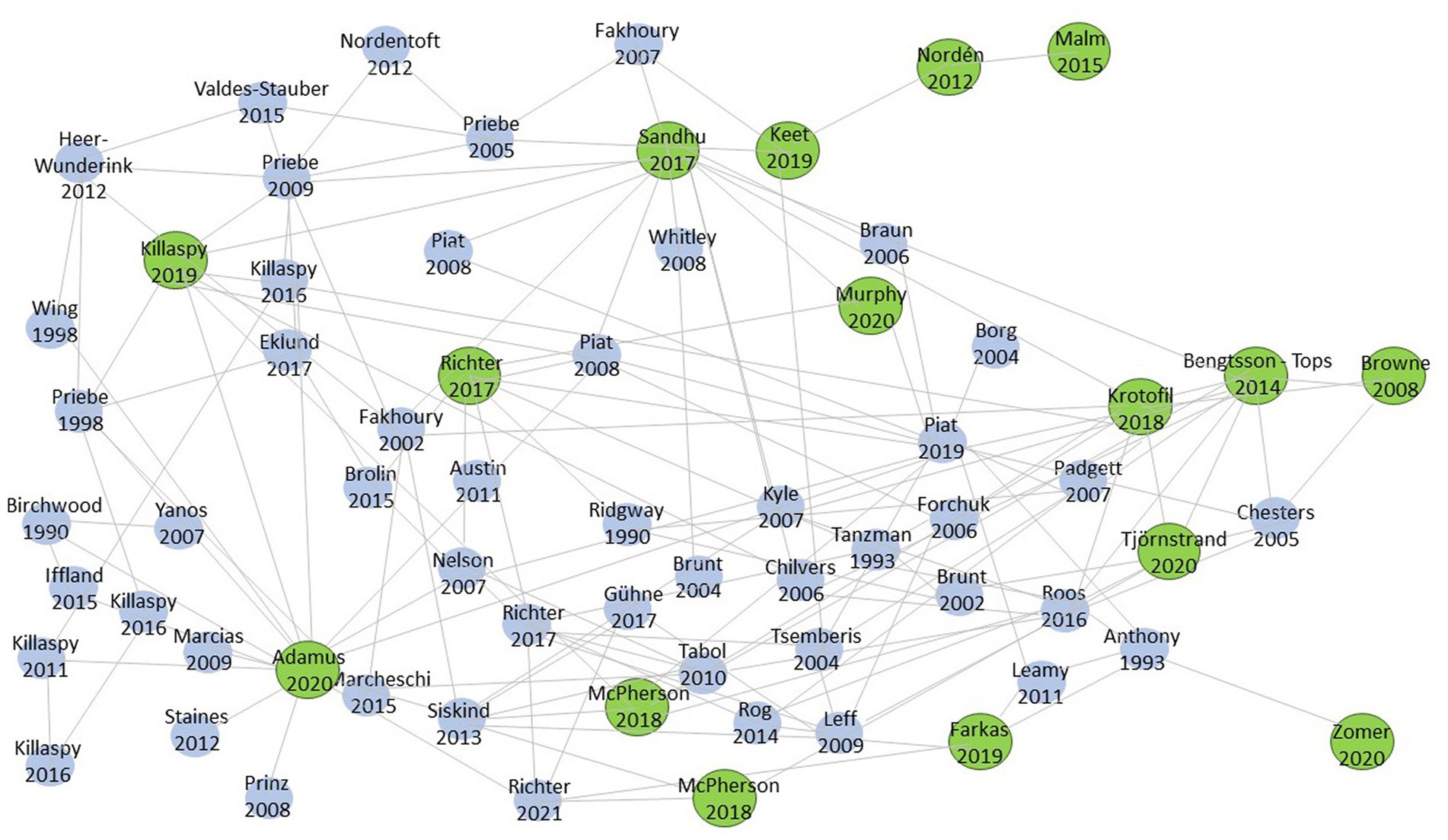
Figure 1 . Research Rabbit.
We formulated and combined search terms concerning: (a) population (Serious Mental Illness* OR Severe Mental Illness* OR SMI OR Mental Illness OR Psychiatric Disabilities); (b) the setting (Community Mental Health* OR Supported Housing OR Supportive Housing OR Supported Accommodation OR Community-based mental healthcare OR Independent Living OR Independent Housing); (c) outcomes (Recovery OR Psychiatric Rehabilitation OR Rehabilitation OR Participation OR Social Inclusion OR Empowerment); and (d) contemporary paradigm (Deinstitutionali* OR De-Institutionali* OR Community Living OR Integrated Care). To reduce the number of irrelevant studies, exclusion terms based on the eligibility criteria were added to the search strategy (e.g., somatic disease, dementia, and COVID-19).
We systematically searched the following electronic databases: PubMed, PsycInfo, Medline, and Cinahl (September 2021, updated in December 2021 and December 2022). These databases were chosen to cover medical (PubMed and Medline), psychological (PsycInfo), and nursing (Cinahl) literature. After the database search, we reviewed the reference lists from papers included by title and abstract to find missing important papers, and additionally, the volumes of the Journal of Integrated Care and the Community Mental Health Journal published in the same period (2011–2021) were reviewed. Finally, we added several papers manually in consensus with our research group that were found lacking in the results, but which did meet the inclusion criteria.
2.4. Study selection process
After the removal of duplicate papers by the first author, the papers were screened in three rounds. In the title, abstract, full-text screenings phase, and thematic analysis, the first author screened all the hits and the second and third authors screened a random sample of 5% to ensure, and reach consensus on, fidelity to the inclusion criteria.
2.5. Data analysis
A qualitative synthesis of included studies was performed using the method of thematic analysis. All papers were screened on elements of relevance (or ingredients needed) for current community mental healthcare with the aim to support persons with SMI in their independent living, recovery, and to stimulate further social inclusion. All papers were coded, and codes were synthesized into areas of ingredients.
First, we present the descriptives in a PRISMA flow diagram, and a summary of the characteristics and quality of the studies included. Second, we present the results of our qualitative synthesis using thematic analysis.
3.1. Flowchart and summary of studies found
After the removal of duplicates and screening all papers on the title, abstract, and full text, the final sample consisted of 56 papers. Figure 2 shows the PRISMA flow diagram of the search.
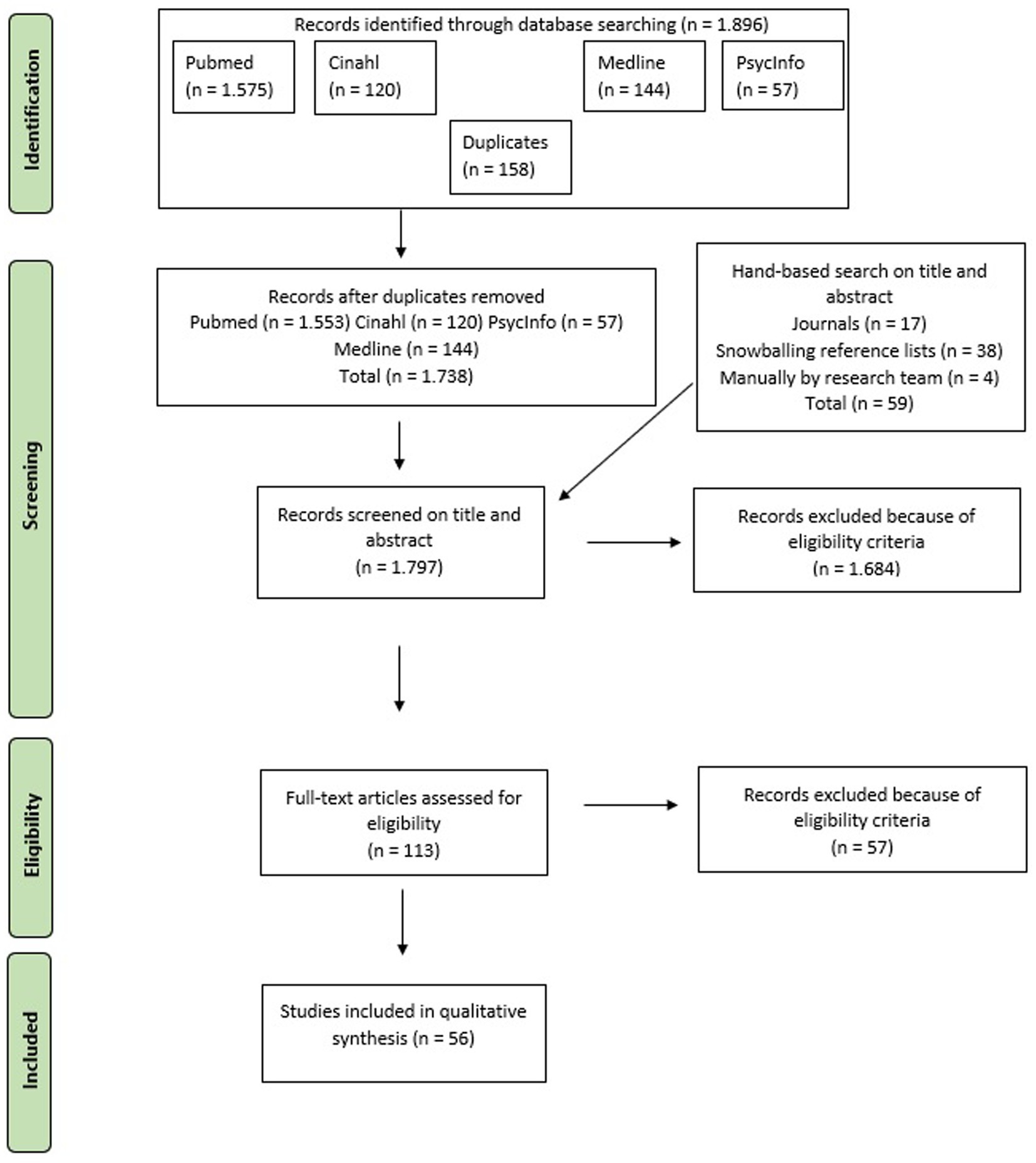
Figure 2 . PRISMA flowchart.
The 56 papers were published spread throughout our time frame, but by far the most papers were conducted in 2018 ( n = 8), 2020 ( n = 7), and 2021 ( n = 9). Most of the papers were conducted in the United States ( n = 17). Twenty-seven of the included papers were conducted primarily in Europe; the majority in the United Kingdom ( n = 7), Netherlands ( n = 5), and Sweden ( n = 5). Four papers compared the situations in two countries: Australia and England, England and Italy, England and North Macedonia, and Canada and the United States. Other regions are Canada ( n = 3) and Australia ( n = 3). Four papers did not report their country, because they did not focus their research specifically on a country. We included 12 reviews, including three scoping reviews and four systematic reviews. In addition, we included 19 quantitative papers, including five RCTs and seven papers with a longitudinal design. We included 20 papers with a qualitative design, of which six were evaluative papers, seven opinion papers and seven descriptive papers. Finally, we included three mixed-methods studies and five expert papers. Table 1 shows the main information from the 56 papers found.
Table 1 . Summary of papers included in the scoping review.
3.2. Thematic analysis
We found ingredients of community-based mental healthcare for persons with SMI in 12 areas: 1. multidisciplinary teams; 2. collaboration within and outside the organization; 3. attention to several aspects of health; 4. supporting full citizenship; 5. attention to the recovery of daily life; 6. collaboration with the social network; 7. tailored support; 8. well-trained staff; 9. using digital technologies; 10. housing and living environment; 11. sustainable policies and funding; and 12. reciprocity in relationships. The subcategories were indicated in the results in bold. Table 2 shows which ingredients were found in which papers, arranged by study design. All papers were classified into nine categories of study designs. The first category contains all types of reviews, including one systematic meta-analysis. The quantitative papers were divided into three categories: RCTs, cross-sectional, and longitudinal. The qualitative papers were also divided into three categories: evaluative (papers in which respondents shared their experiences with the researchers); opinion (in which participants are asked for their opinions about a phenomenon); and descriptive (papers describing a phenomenon). The remaining two categories are mixed-method and expert papers (papers without empirical research but with the opinion of the authors).
Table 2 . Results of the thematic analysis.
3.2.1. Multidisciplinary teams
Multidisciplinary teams came up as important in twenty-five of the included papers. Five were reviews, three were RCTs, one was a quantitative cross-sectional paper, five were quantitative longitudinal papers and one a mixed-method paper. Additionally, two were qualitative evaluative papers, three were qualitative opinion papers, three were qualitative descriptive papers and two were expert papers.
Five papers recommend close involvement within different disciplines in multidisciplinary teams. Of these, three were qualitative papers ( 46 , 47 , 49 ), one expert paper ( 52 ), and one review ( 29 ). Therefore, one RCT finds positive results with regard to the health benefits for individuals for having received nurse practitioner services in a mental health setting to address primary care needs ( 34 ). In addition, two papers with a qualitative design emphasize adding an occupational therapist to a multidisciplinary team ( 44 , 50 ). Finally, seven papers show the value of peer support to multidisciplinary teams; of which these seven papers, there are three reviews ( 29–31 ), three qualitative papers ( 47 , 48 , 51 ), and one expert paper ( 53 ).
An example of working in multidisciplinary teams is the (flexible) assertive community treatment ((F)ACT) teams. We found mainly empirical studies about the implementation and efficacy of (F)ACT and collaboration with (F)ACT teams. Of these, we found two reviews ( 32 , 33 ), one RCT with positive results ( 35 ), and one RCT without significant results ( 36 ). In addition, six quantitative papers ( 37–42 ), one mixed-method paper ( 43 ), and two qualitative papers ( 44 , 45 ) report on (F)ACT. Lastly, we found one review about the history of assertive community treatment (ACT) ( 32 ).
3.2.2. Collaboration within and outside the organization
Collaboration inside and outside the mental healthcare organization was studied in 20 of the included papers. Three were reviews, two were qualitative longitudinal studies, one was a quantitative longitudinal paper, three were qualitative evaluative papers, three were qualitative opinion papers, two were qualitative descriptive papers, two were mixed-method papers, and four were expert papers.
Intersectoral collaboration is often mentioned in the literature found. The collaboration between mental healthcare, physical care, and social service sectors was found in four qualitative papers ( 45 , 46 , 48 , 49 ) and in one scoping review ( 54 ). In addition, collaboration between the government and the mental health sector was found in three qualitative studies ( 45 , 59 , 60 ) and one quantitative paper ( 40 ). Furthermore, we found three expert papers about collaboration in an integrated care system ( 3 , 53 , 63 ). Therefore, one systematic metareview ( 31 ), one mixed-method paper ( 57 ), one quantitative study ( 55 ), and one opinion paper ( 52 ) recommend an integrated care system with the integration of primary care in mental healthcare, and one descriptive paper shows an integrated mental health information system ( 62 ).
Growing evidence shows that integrative care is the new standard of care for people with mental illnesses, with the necessity of continuity of care from the emergency department to community mental health services. Continuity of care was found in two scoping reviews ( 29 , 54 ), one quantitative longitudinal paper ( 56 ), and one qualitative paper ( 61 ).
Finally, two qualitative papers ( 59 , 61 ) and one mixed-method paper ( 58 ) show the facilitators and barriers to intensive, intersectoral collaboration in community mental healthcare, such as cultural differences between the sectors as a barrier and face-to-face communication as a facilitator.
3.2.3. Attention to several aspects of health
Several aspects of health were studied in 18 of the included papers. Of these 15 papers, one was a systematic-meta review, two were quantitative longitudinal papers, one was a cross-sectional paper, eight were qualitative opinion papers, two were mixed-method papers, and four were expert papers.
Eight papers mention the focus on physical health in mental healthcare. Three qualitative, one mixed-method, and one quantitative paper report on the integration of physical health in mental healthcare ( 46 , 55 , 57 , 65 , 66 ). According to one expert paper, healthcare services need to recognize the far lower life expectancy among people with mental disorders and develop and evaluate new methods to reduce this health disparity ( 63 ). Respondents of a qualitative, opinion study stated that their main preoccupation and motivation was to be mentally well but they also recognized that many things that improve physical health also improved their mental health ( 67 ). In addition, one paper with a mixed-method design found that there is growing interest in models integrating physical healthcare delivery, management, or coordination into specialty mental health programs in the United States ( 58 ). One expert paper indicates the same ( 70 ). Finally, one systematic review found that this integration improves rates of immunization and screening for medical disorders, accompanied by positive effects on physical health, as well as improving general medical outcomes ( 31 ).
Another important aspect of health is cognitive functioning, which was found in two papers. One qualitative study mentioned that cognitive and physical health conditions might impact individuals’ ability to function in their daily lives during and after homelessness ( 48 ). In addition, one cross-sectional paper found that homebodies reported significantly poorer cognitive function than venturers ( 64 ).
In addition, we found two papers on psychosocial health. One quantitative study indicates that investment by teams to improve a patient’s psychosocial situation can lead to improvements in substance problems ( 41 ) and one expert paper aligns the importance of addressing social determinants of health within integrated care models for people with SMI ( 70 ).
Also, three qualitative papers ( 62 , 68 , 69 ) and one expert paper ( 52 ) emphasize the importance of positive health. The focus in positive healthis on the strengths, preferences, needs, and wishes of the service user, families, and communities that contribute to recovery.
Finally, two expert papers emphasize public health as actions seek to achieve equity between groups and a state of population-level health ( 52 , 53 ).One expert paper shows the role of mental and public health promotion and prevention, taking the needs of the entire population into account ( 53 ).
3.2.4. Promoting full citizenship
Promoting full citizenship was a topic of relevance in 14 of the included papers. Three were reviews, two were RCTs, two were qualitative evaluative papers, one was a qualitative opinion paper, two were qualitative descriptive papers, and four were expert papers.
Human rights and destigmatization contribute to promoting full citizenship and are addressed in six papers ( 3 , 29 , 48 , 53 , 63 , 82 ). One quantitative paper found that staffing intensity was negatively associated with human rights ( 82 ). One expert paper reports that historically the protection of human rights is one of the drivers for deinstitutionalization. Additionally, people with SMI experience more violations than others and suffer from stigma and discrimination ( 53 ). With this in mind, another expert paper states that mental health services should provide specific modules to reduce stigma and discrimination experienced by people with SMI ( 63 ). The same paper also states that some programs to reduce stigma and discrimination are presently active at the local level. They now need to be coordinated at the national level and adequately financed ( 63 ). In addition, providing training and coaching to health and social care staff on recovery and rights can reduce human rights violations that occur in the context of mental health services ( 53 ). One scoping review ( 29 ) found that there were an overwhelming number of anti-stigma campaigns from 1995 to 2015, but with a lowering trend of publication year over year on this topic.
In addition, several papers describe the Resource Group methodology that also promotes citizenship because the main feature of this methodology is that ownership and direction lie with the client. Of the included studies, there were two RCTs ( 73 , 74 ) with positive results, one meta-analysis ( 71 ), one review ( 72 ), and one qualitative paper ( 75 ). Finally, we found some papers on self-reliance. Two qualitative papers describe that a recovery-oriented system of care should give a holistic view of a person’s strengths and build on the strengths and resiliencies of individuals, families, and communities ( 62 , 69 ). One qualitative evaluative paper finds that FACT may support citizenship by relating to service users as whole people, facilitating empowerment and involvement ( 60 ).One expert paper states that signpost ways are needed for people to self-care, make useful contributions to society ( 52 ), and to be able to feel a fully-fledged citizen.

3.2.5. Attention to the recovery of daily life
Recovery of daily life was studied in 12 of the included papers. Of these 10 papers, one was a quantitative cross-sectional paper, one was a qualitative opinion paper, four were qualitative descriptive papers and four were expert papers.
We found several aspects of community-based support that contribute to recovery. According to one qualitative paper ( 68 ) and two expert papers ( 53 , 63 ), mental health services should develop dedicated programs for recovery. Also, three qualitative papers ( 48 , 49 , 77 ) focus on gaining and regaining skills for more independent living in vivo . Moreover, two expert papers mention that signpost self-care options ( 52 ) and recovery colleges can contribute to the recovery of daily life ( 3 ). Besides that, one expert paper states that evidence-based, psychosocial interventions should be deployed to support individuals to achieve both personal recovery and increased independence ( 3 ). In addition, one qualitative study reports that occupational therapists should support clients in their recovery to find their best self ( 50 ). Lastly, one cross-sectional paper states that most of their respondents (64.8%) were not employed, but those who were working presented higher levels of functional capacity than those who were not ( 76 ).
3.2.6. Collaboration with the social network
Collaboration with the social network of the client was studied in 10 of the included papers. Of these 10 papers, three were reviews, two were RCTs, one was a qualitative evaluative paper, three were qualitative descriptive papers and one was an expert paper.
Many papers mention several models in which it is important to involve the clients and their social network in the recovery process. We found the collaboration with the social network papers applying the Resource Group methodology in two RCTs ( 73 , 74 ), one meta-analysis ( 71 ), one review ( 72 ), and one qualitative paper ( 75 ). In addition, we found two qualitative descriptive papers that described approaches that place collaboration with the social network at the center of the client’s recovery process: namely, the Peer-Supported Open Dialogue ( 51 ), and the Active Recovery Triad (ART) model ( 68 ). Also, one expert paper and one qualitative paper mention that actively supporting the ability to empower and involve users and their families is important in community mental healthcare ( 3 , 49 ). Finally, one scoping review suggests that network size is not consistently associated with reported loneliness, social support, recovery, or quality of life. A deep relationship with at least one supportive person may be more or equally valuable than a larger network ( 78 ).
3.2.7. Tailored support
Tailored support came up as important in eight of the included papers. Of these eight papers, one was a review, two were qualitative evaluative papers, three were qualitative descriptive papers, and two were expert papers.
Two expert papers and three qualitative papers state that mental healthcare should provide care that service users (and their family members) find accessible and acceptable ( 3 , 60 , 63 , 80 ) and 24/7 available ( 77 ). In addition, one qualitative paper states that recovery-oriented care should be more effective when combined with support when required ( 49 ).One review found that support must also be flexible and user-driven ( 79 ). Therefore, one qualitative paper states that care should always be started with a Care Planning Meeting ( 68 ) and, according to one expert paper ( 63 ) and one qualitative paper ( 77 ), individualized care plans should be made through shared-decision making. Also, one expert paper states that care should be independent of location ( 63 ). Finally, we found two descriptive papers that describe that deinstitutionalization today means positive risk-taking and serious rethinking of questions in terms of distance, power, and language ( 77 ) and it provides new approaches to opportunity and safety ( 49 ).
3.2.8. Well-trained staff
Well-trained staff came up as important in eight of the included papers. Of these papers, there were two reviews, one quantitative cross-sectional paper, two qualitative descriptive papers, one mixed-method study, and two expert papers.
Two papers reported on education for mental healthcare staff. One review found that education for staff regarding identifying and responding to comorbidity is important ( 54 ).One qualitative descriptive paper states that peer-support open-dialogue teams should be trained in family systems ( 51 ). Furthermore, we found two expert papers and one qualitative paper that recommend the knowledge and use of evidence-based interventions and treatment by caregivers to provide social inclusion and recovery ( 49 , 53 , 63 ). In addition, one quantitative paper found that service teams should be of moderate size with adequate staffing to support service users in gaining and regaining skills for more independent living ( 82 ).One systematic review identified characteristics of well-trained staff, with practices that included routine monitoring and evaluation, good communication, equality between team members, and clear documentation practices ( 81 ). On the other hand, one mixed-method paper found difficulty in recruiting and retaining qualified staff ( 58 ).
3.2.9. Using digital technologies
Using digital technologies was studied in seven of the included papers. Of these seven papers, three were reviews, one was a qualitative descriptive paper, one was a mixed-method study, and two were expert papers.
One scoping review ( 29 ) found that digital platforms have an important role in improving the reach, scale, and accessibility of community-based support. Additionally, digital platforms add addressing public health issues and peer-led interventions are achieved effectively through the utilization of social media tools ( 29 ). Therefore, the same scoping review found that eHealth tools are becoming prevalent in the processes of promotion, prevention, and treatment in mental healthcare. In addition, the increased use of these eHealth tools continues to shape the future of community mental healthcare, particularly in low-access areas and areas where certain local expertise is lacking ( 29 ). Also, one expert paper states that the use of digital technologies should encourage self-care ( 52 ). Besides that, one mixed-method study and one systematic meta-review recommended the use of digital technology in electronic health records to enhance care coordination and promote integrated care ( 31 , 58 ). Finally, one systematic review ( 81 ), one qualitative paper ( 63 ), and one expert paper ( 49 ) state that digital monitoring through technology may improve practices and patient outcomes.
3.2.10. Housing and living environment
Housing and living environment came up as important in five of the included papers. Two were reviews, one was a quantitative cross-sectional paper, one was a qualitative descriptive paper, and one was an expert paper.
One review ( 79 ) describes the principles of the supportive housing approach in the United States. In addition, one systematic review ( 24 ) found positive results with regard to supported accommodation on several outcomes and the importance of connection to, and affiliation with, the living environment.
Furthermore, one expert paper ( 52 ) and one quantitative paper ( 82 ) state that writing live manuals tailored to local needs helps to stimulate a grand alliance for health. Also, one qualitative paper ( 77 ) describes the cornerstones of the Trieste Model. Two of the cornerstones are actively working on the environment and the social fabric, and service accountability toward the community.
3.2.11. Sustainable policies and funding
Sustainable policies and funding came up as important in four of the included papers. Of these four papers, one was a scoping review, one was a qualitative descriptive paper, and two were expert papers.
One expert paper states that the integration of community mental healthcare services, sectors, and collaboration with the social network of the service user can be hindered by a financing system that favors institutional care. Therefore, it is recommended to create a flexible financing system that allows incentives for different services that address the relevant life domains of people with SMI in the community ( 53 ). Another expert paper states that financial barriers are also encountered when integrating general practitioner care and mental healthcare ( 70 ). In addition, one qualitative paper describes a successful financial model that was developed in Italy. The personal health budget includes all economic, professional, and human resources needed to trigger a process aimed at restoring a person – through an individual rehabilitation process – to an acceptable level of social functioning ( 49 ). Finally, one review found that improved reforms on national mental health policies and deinstitutionalization are important for community mental healthcare ( 29 ).
3.2.12. Reciprocity in relationships
Reciprocity in relationships is a topic of interest in three of the included papers. Of these three papers, one was a qualitative opinion paper, one was a qualitative descriptive paper, and one was an expert paper.
This topic is about the reciprocity in relationships between clients and caregivers, but also in contributions to society by all people. One qualitative paper shows the importance of establishing and maintaining contact between the caregiver with the service user, by building a mutual relationship of trust ( 68 ). Therefore, one expert paper found that all people, with or without mental health problems, should make useful contributions to society, including paid and voluntary work that helps strengthen the local community, appreciate those around them and increase their webs of trusted relationships ( 52 ). Finally, to promote reciprocity, one qualitative opinion study states that the use of person-centered strategies is important. This focus on a person’s interests and goals was frequently indicated to foster relationships, gain trust, and develop self-efficacy ( 46 ).
4. Discussion
4.1. summary of main findings.
With this scoping review, we aimed to give a comprehensive overview of existing and upcoming community mental healthcare approaches to discover the current vision explained in areas of ingredients. To our knowledge, there are still a few publications that attempt to combine all the necessary elements for community mental health ( 53 , 83 , 84 ). We found 56 papers that met the inclusion criteria. Thematic analysis resulted in 12 areas of ingredients for community mental healthcare. In this section, we answer our research questions and show what was striking in the found literature. Finally, we present the strengths and limitations of our scoping review and our conclusions.
We aimed to give an overview of the existing and upcoming insights on community mental healthcare for people with SMI. Based on the number of papers found, most attention is paid to several aspects of health, multidisciplinary teams, collaboration within and outside the organization, collaboration with the social network, and supporting full citizenship. However, empirical evidence from quantitative studies was found in only four of the 12 areas based on our included papers: multidisciplinary teams; collaboration with the social network; collaboration within and outside the organization; and supporting full citizenship. Nevertheless, the other areas that are not yet supported by evidence in this scoping review are no less important for community mental healthcare. Although no empirical research has yet been done on these topics, they are being addressed in several papers. This shows that there is increasing attention to them in the field.
Notably, given the low number of included empirical studies from the welfare or supported housing sector, we can conclude that little empirical research has been done on community mental healthcare in these sectors for this target group. The few empirical studies we from the mental health care sector and were primarily about (F)ACT and the Resource Group methodology. Even though (F)ACT has been around for a few decades, this shows that for the last 10 years (F)ACT has remained an important model within community mental healthcare for this target group to achieve recovery. Additionally, given the number of papers reporting on it and the evidence provided, collaborative mental healthcare within teams, organizations, and clients and their social network has been seen as important over the past decade.
In addition to the topics found that received attention for more than 10 years within community mental healthcare, such as recovery, tailored support, and multidisciplinary teams, we found several papers that are about more recent and innovative areas. Such as, reciprocity in relationships; sustainable policy and funding; using digital technologies; and supporting full citizenship. The results from this scoping review show that in recent years new shifts are taking place in the field of mental healthcare, whereby there is more attention paid to full citizenship, but empirical research is still lacking. Further, the more innovative areas were published in more recent literature, but frequently in expert papers. Due to the few RCTs found, we cannot conclude that these areas are also the most important, but we could say that these areas can form the basis for further research in community-based mental healthcare to provide social inclusion and recovery in the future.
Recovery was one of our research terms and we expected recovery to be an important part of our scoping review because more and more studies have been conducted on the areas of recovery. Ten included papers reported on the recovery of daily life, but no empirical studies were found on that topic. This is probably due to the exclusion of intervention studies that focus on a single life domain and did not seek collaboration, which is often the case in studies of recovery and all aspects of health. The upcoming attention to recovery-based care for persons with SMI is also shown in recent scoping reviews. Bitter et al. ( 85 ), in their review on recovery interventions for supported housing and clinical settings, found 53 papers, of which about a quarter of recovery interventions showed added value based on RCTs and half of them had initial promising results based on case studies and follow-up designs without a control group. Additionally, van Weeghel and colleagues ( 86 ) reviewed the conceptualization of recovery, showing that personal recovery is conceptualized as complementary to clinical recovery and represents processes rather than outcomes. They state that a broad framework of recovery is required, and more research is needed into the working mechanisms of personal recovery processes. Our search and the previous scoping reviews show that recovery is still a guiding concept for people with SMI that needs to be paid attention to both in today’s and future community-based mental healthcare, but more empirical research is necessary to find the working mechanisms that contribute to recovery.
Further, we found many papers concerning multidisciplinary teams. Peer supporters ( 29 , 30 , 47 , 48 , 51 , 53 ), occupational therapists ( 44 , 50 ), and nurses ( 34 ) are frequently mentioned as important disciplines in a multidisciplinary team, besides the regular disciplines of psychologists, psychiatrists, and social psychiatric care workers. Peer supporters have been a part of the (F)ACT teams for more than our searched 10 years ( 87 ). Adding peer supporters to multidisciplinary teams is found in seven papers, including three reviews. Because of this, there is much evidence that peer support adds value to multidisciplinary teams.
Additionally, intersectoral collaboration appears regularly in the literature. First, several papers studied the collaboration with primary care to provide the physical health of people with SMI and the importance of attention being paid to clients’ physical health in mental healthcare. This builds on previous research that shows that people with SMI experience premature mortality of around 15–20 years earlier than the general population ( 88 ), have a high prevalence of substance use disorder ( 89 ), and are at risk of the development of often preventable secondary health conditions ( 90 , 91 ). Second, collaboration with the municipalities is recommended in the literature. The importance of collaboration between mental healthcare and community services is lacking in the papers. Currently, the mental healthcare sector seems the most important party in the found literature to support this target group. The collaboration between mental healthcare and municipal services is most often mentioned in papers about (F)ACT from Scandinavian countries ( 40 , 45 , 59 , 60 , 72 ). This is an enhancement of the multidisciplinarity, used in the (F)ACT program, that has been practiced and recommended for the last decades.
Intersectoral collaboration is often recommended in the literature found, but, notably, the literature found does not elaborate on what integrated collaboration should look like in practice. Possibly that is because other literature confirms that this collaboration is not easy to achieve ( 92 ). Integration can be defined as the search to connect the healthcare system (acute, primary medical, and skilled) with other human service systems (e.g., long-term care, education, and vocational and housing services) to improve outcomes (clinical, satisfaction, and efficiency). Leutz places full integration into the larger context of good human service practices by integrating services through linkage and coordination ( 92 ). Accordingly, we should not set full integration as the goal for community mental healthcare, rather, good connections and collaboration are more achievable.
In recent years, citizenship for people with (severe) mental health problems is a topic that has received increasing attention ( 93–95 ). Citizenship concerns one’s connections to the responsibilities, rights, roles, relationships, and resources offered to people in society ( 96 ). There have also been an increasing number of empirical studies, such as the cross-sectional study by Nesse and colleagues ( 97 ). This study suggests that citizenship and occupational meaningfulness may have positive implications for recovery. Additionally, Rowe and Davidson presented “recovering citizenship” as a concept and metaphor to capture the individual recovery process within the context and goal of a life in the community that the citizenship framework supports ( 98 ), and which is also about social inclusion and the full participation of individuals with mental illness in society ( 99 ).
Worthy of note is that just a few papers come from the leading journals on integrated community mental healthcare, which we explicitly searched, including the International Journal of Integrated Care and Community Mental Health Journal . Remarkably, the term “SMI” appears just once in the titles and abstracts of the volumes of 2011–2021 of the first journal. Moreover, in the Community Mental Health Journal we found several papers about community care, but only a few in combination with SMI. This confirms the idea that little research has been done on this topic. Besides that, many papers also seem to be written from the point of view of the mental healthcare sector. Loneliness, debts, and poverty are important topics in community care, but there does not yet seem to be much published about these main topics in social services because they did not show up in the results of the papers found. In addition, research in the shelter and supported housing sector is still limited ( 23 , 24 ). We also noticed that social work as a distinct support sector alongside the mental healthcare sector that includes supported housing receives little attention in the literature found. It is recommended that there should be more attention paid in future research to mental healthcare from the community perspective in which the municipalities and social services play a larger role.
In this scoping review, we have chosen to exclude papers on interventions that focus on a specific area of life and do not provide an integrated offering for people with SMI only, because of the risk of investigating too broad a scope. In the last decade, some interventions have become an important and innovative part of community care but would be too much information to present in one scoping review. Consequently, we did not include papers about (returning to) work, and papers primarily focused on recovery. Nevertheless, interventions are the important link between theory and practice and are worth mentioning. The literature proves their importance because of the many available interventions for this target group to improve, for example, lifestyle ( 100 , 101 ), internalized stigma ( 102 ), housing ( 103 ), employment ( 104 , 105 ), cognition ( 106 ), social skills ( 107 ), and self-management ( 108 ). Therefore, the focus on psycho-social aspects of support for people with SMI in the included papers is limited. This may also be due to our focus on the broader literature and not on interventions that address these aspects more specifically.
Finally, it was difficult to compare the papers. One example is the difficulty of comparison in the context of national differences in legal frameworks and public policies. Not every recommendation could be implied in all societies. We tried to take this into account to some extent by including only Western literature. In addition, for both the target group and the outpatient setting, a very varied vocabulary is used in the various papers and the general terms do not mean the same in every article. First, the term “supported housing” is used for support to people in a 24/7 aggregated setting, but also with regard to clients who live independently in the community with 24/7 available support, which is what we were looking for. Second, the term “SMI” is interpreted differently. Some papers are limited to clients with schizophrenia and bipolar disorder, while other papers focus more on autism and anxiety. Other requirements for SMI are also handled differently. Several papers seem to focus more on common mental illnesses rather than SMI. This makes it hard to compare and generalize the different papers on this topic. Previous research has already indicated that varying terminology is used internationally to describe the different housing settings and approaches to the provision of housing and support ( 13 ). Further research is necessary to create general terminology with clear definitions of the outpatient setting.
4.2. Strengths and limitations
The main strength of our review is the broad and systematic search. We used several search strategies, including database search, hand-searching the reference lists and leading journals to find as complete an overview as possible of all papers on our topic. We have done everything possible to find all relevant papers from the past 10 years. To ensure that we did not miss innovative topics, we did not choose certain study designs as inclusion criteria. This also has the advantage that we could find enough papers. As a result, there are large differences between the study designs in the papers. This creates more difficulties when comparing the papers and ingredients. It is hard to conclude which ingredient is more important for community-based mental healthcare than another. Nevertheless, to the best of our knowledge, this is the first scoping review on all developments in community mental healthcare and gives a good overview of the current relevant topics. Notably, less than half of the included papers are empirical studies, and a large part of the included papers was composed of descriptive or opinion papers. More empirical research is needed on this subject.
Conducting a scoping review provides a broad view of the literature, but it also has some limitations. One of these includes the search terms. With these search terms, it was not possible to find everything in the field through database search due to the variation in terminology, and in recent years the main focus of the research has been on individual interventions. Despite all efforts, including the Research Rabbit software and hand-search, there is still the possibility that we missed some relevant papers. The second limitation of our study is the generalizability of the conclusions. We did not use search terms in our search strategy to find specific themes, such as citizenship and social work, but these themes are related to our search terms recovery, participation, social inclusion, and empowerment. The final limitation concerns citizenship. Despite the increasing attention being paid to citizenship in the scientific literature, we included only a few citizenship papers. Due to the target population of our broader study, we only included papers on adults with SMI while the citizenship papers focus on (common) mental illness. Nevertheless, the focus on citizenship is a relevant development that deserves attention in this scoping review.
5. Conclusion
This scoping review aimed to give a comprehensive overview of existing and upcoming community mental healthcare approaches to discover the current vision in the areas of ingredients. We found 12 areas of ingredients, including some innovative topics about reciprocity and sustainable policies and funding. There is much attention paid to individual ingredients for good community-based mental healthcare, but very little is known about their integration and implementation in contemporary, fragmented mental healthcare services. No earlier, international study has connected all the current elements of good community mental healthcare together. Thus, our research contributes to the existing research and adds value to future research on community-based mental healthcare. For future studies, we recommend more empirical research on community mental healthcare, as well as further investigation(s) from the social service perspective, and solid research on general terminology about SMI and outpatient support.
Author contributions
CvG contributed to the development of the search question and strategies, screening papers and analysis, and to the main part of the manuscript. DR and MvV participated in the development of the search question and strategies, participated in screening papers, the thematic analysis, and writing the manuscript. JvW and TvR participated in the development of the search question, strategies, and supervised advancement of the project. All authors contributed to the article and approved the submitted version.
This scoping review belongs to a broader project which received ethical approval from the Ethics Review Board Tilburg School of Social and Behavioral Sciences and was funded by three organizations for supported housing and shelter in Netherlands: Kwintes, Leviaan, and HVO Querido.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Anthony, W. Recovery from mental illness. The guiding vision of the mental health service system in the 1990s. Psychosocial Rehabil J . (1993) 16:11–23. doi: 10.1037/h0095655
CrossRef Full Text | Google Scholar
2. van Regenmortel, T. Empowerment en Maatzorg. Een krachtgerichte psychologische kijk op armoede Armoede en Social Uitsluiting, Jaarboek 2002 . Leuven/Leusden: Acco; (2002). p. 71–84.
Google Scholar
3. Killaspy, H, McPherson, P, Samele, C, Keet, R, and Caldas de Almeida, J. EU compass for action on mental health and well-being. Providing community-based mental health services. Position Paper. (2018).
4. Pieters, G, Ruud, T, van Weeghel, J, Bahler, M, Murphy, B, Shields-Zeeman, L, et al. Recovery for all in the community. Learning from eachother. Consensus paper on fundamental principles and key elements of community based mental health care. BMC Psychiatry . (2017) 19:174. doi: 10.1186/s12888-019-2162-z
5. Stupak, R, and Dobroczyński, B. From mental health industry to humane care. Suggestions for an alternative systemic approach to distress. Int J Environ Res Public Health . (2021) 18:6625. doi: 10.3390/ijerph18126625
6. Johnson, S. Social interventionals in mental health. A call to action. Social Psychiatry Psychiatric Epidemiol . (2017) 52:245–7. doi: 10.1007/s00127-017-1360-6
7. UN General Assembly. Convention on the rights of persons with disabilities: resolution/adopted by the general assembly. Sixty-First Session UN General Assembly (2007).
8. Perkins, R, Repper, J, Rinaldi, M, and Brown, H. Recovery colleges: Centre for Mental Health NHS Confederation Mental Health Network. (2012).
9. van Vugt, M. Implementatie van FACT: Stand van zaken o.b.v. auditdata. Webinar CCAF. (2020).
10. Killaspy, H, and Priebe, S. Research into mental health supported accommodation – desperately needed but challenging to deliver. Br J Psychiatry . (2021) 218:179–81. doi: 10.1192/bjp.2020.74
PubMed Abstract | CrossRef Full Text | Google Scholar
11. World Health Organization. International classification of functioning, disability, and health . Geneva: WHO (2001).
12. Priebe, S, Saidi, M, Want, A, Mangalore, R, and Knapp, M. Housing services for people with mental disorders in England: patient characteristics, care provision and costs. Soc Psychiatry Psychiatr Epidemiol . (2009) 44:805–14. doi: 10.1007/s00127-009-0001-0
13. Richter, D, and Hoffmann, H. Preference for independent housing of persons with mental disorders: systematic review and meta-analysis. Admin Pol Ment Health . (2017) 44:817–23. doi: 10.1007/s10488-017-0791-4
14. Tsemberis, S. Housing first: the pathways model to end homelessness for people with mental illness and addiction manual. Eur J Homelessness . (2011):5.
15. Hwang, S, and Burns, T. Health interventions for people who are homeless. Lancet . (2014) 384:1541–7. doi: 10.1016/S0140-6736(14)61133-8
16. Fazel, S, Khosla, V, Doll, H, and Geddes, J. The prevalence of mental disorders among the homeless in Western countries: systematic review and meta-regression analysis. PLoS Med . (2008) 5:1670–81. doi: 10.1371/journal.pmed.0050225
17. Croze, C. Healthcare integration in the era of the affordable care act. In: Wellness AfBHa, editor. Washington, DC: Association for Behavioral Health and Wellness. (2015).
18. Social Care Local Government and Care Partnership Directorate. Closing the gap: priorities for essential change in mental health. In: Health Do. (London: Department of Health) (2014).
19. Killaspy, H. Contemporary mental health rehabilitation. East Asian Arch Psychiatr . (2014) 24:89–94. doi: 10.1017/S2045796018000318
20. Westen, K, Boyle, P, and Kroon, H. An observational comparison of FACT and ACT in the Netherlands and the US. BMC Psychiatry . (2022) 22:311. doi: 10.1186/s12888-022-03927-x
21. Bond, G, Drake, R, Mueser, K, and Latimer, E. Assertive community treatment for people with severe mental illness, critical ingredients and impact on patients. Dis Manage Health Outcomes . (2001) 9:141–59. doi: 10.2165/00115677-200109030-00003
22. van Veldhuizen, J, and Bahler, M. Manual: Flexible assertive community treatment: Vision, model, practice and organization . Groningen: CCAF (2013).
23. Chilvers, R, Macdonald, G, and Hayes, A. Supported housing for people with severe mental disorders. Cochrane Database Syst Rev . (2006) 2006:CD000453. doi: 10.1002/14651858.CD000453.pub2
24. McPherson, P, Krotofil, J, and Killaspy, H. Mental health supported accommodation services: a systematic review of mental health and psychosocial outcomes. BMC Psychiatry . (2018) 18:128. doi: 10.1186/s12888-018-1725-8
25. McPherson, P, Krotofil, J, and Killaspy, H. What Works? Toward a new classification system for mental health supported accommodation services: the simple taxonomy for supported accommodation (STAX-SA). Int J Environ Res Public Health . (2018) 15:190. doi: 10.3390/ijerph15020190
26. Tricco, A, Lillie, E, O'Brien, K, Colquhoun, H, Levac, D, Moher, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med . (2018) 169:467–73. doi: 10.7326/M18-0850
27. Arksey, H, and O'Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol . (2005) 8:19–32. doi: 10.1080/1364557032000119616
28. Mays, N, Roberts, E, and Popaj, J. Synthesising research evidence. Studying the organisation and delivery of health services: research methods . London: Routledge (2001).
29. Bajraktarov, S, Kalpak, G, and Jovanovic, N. Community mental healthcare: new developments and innovative strategies. Curr Opin Psychiatry . (2020) 33:491–500. doi: 10.1097/YCO.0000000000000629
30. Gaiser, M, Buche, J, Wayment, C, Schoebel, V, Smith, J, Chapman, S, et al. A systematic review of the roles and contributions of peer providers in the behavioral health workforce. Am J Prev Med . (2021) 61:e203–10. doi: 10.1016/j.amepre.2021.03.025
31. Gaebel, W, Kerst, A, Janssen, B, Becker, T, Musalek, M, Rössler, W, et al. EPA guidance on the quality of mental health services: a systematic meta-review and update of recommendations focusing on care coordination. Eur Psychiatry . (2020) 63:e75. doi: 10.1192/j.eurpsy.2020.75
32. Rochefort, D. Innovation and its discontents: pathways and barriers in the diffusion of assertive community treatment. Milbank Q . (2019) 97:1151–99. doi: 10.1111/1468-0009.12429
33. Wright-Berryman, J, McGuire, A, and Salyers, M. A review of consumer-provided services on assertive community treatment and intensive case management teams: implications for future research and practice. J Am Psychiatr Nurses Assoc . (2011) 17:37–44. doi: 10.1177/1078390310393283
34. Rogers, E, Maru, M, Kash-MacDonald, M, Archer-Williams, M, Hashemi, L, and Boardman, J. A randomized clinical trial investigating the effect of a healthcare access model for individuals with severe psychiatric disabilities. Community Ment Health J . (2016) 52:667–74. doi: 10.1007/s10597-016-0009-3
35. Nielsen, C, Hjorthoj, C, Killaspy, H, and Nordentoft, M. The effect of flexible assertive community treatment in Denmark: a quasi-experimental controlled study. Lancet Psychiatry . (2021) 8:27–35. doi: 10.1016/S2215-0366(20)30424-7
36. Mueller-Stierlin, A, Helmbrecht, M, Herder, K, Prinz, S, Rosenfeld, N, Walendzik, J, et al. Does one size really fit all? The effectiveness of a non-diagnosis-specific integrated mental health care program in Germany in a prospective, parallel-group controlled multi-Centre trial. BMC Psychiatry . (2017) 17:283. doi: 10.1186/s12888-017-1441-9
37. Harvey, C, Killaspy, H, Martino, S, White, S, Priebe, S, Wright, C, et al. A comparison of the implementation of assertive community treatment in Melbourne, Australia and London, England. Epidemiol Psychiatric Sci . (2011) 20:151–61. doi: 10.1017/S2045796011000230
38. Firn, M, Hindhaugh, K, Hubbeling, D, Davies, G, Jones, B, and White, S. A dismantling study of assertive outreach services: comparing activity and outcomes following replacement with the FACT model. Soc Psychiatry Psychiatr Epidemiol . (2013) 48:997–1003. doi: 10.1007/s00127-012-0602-x
39. Nugter, A, Engelsbel, F, Bahler, M, Keet, R, and van Veldhuizen, R. Outcomes of FLEXIBLE assertive community treatment (FACT) implementation: a prospective real life study. Community Ment Health J . (2016) 52:898–907. doi: 10.1007/s10597-015-9831-2
40. Svensson, B, Hansson, L, and Lexen, A. Outcomes of clients in need of intensive team care in flexible assertive community treatment in Sweden. Nord J Psychiatry . (2018) 72:226–31. doi: 10.1080/08039488.2018.1430168
41. van Vugt, M, Kroon, H, Delespaul, P, and Mulder, C. Assertive community treatment and associations with substance abuse problems. Community Ment Health J . (2014) 50:460–5. doi: 10.1007/s10597-013-9626-2
42. Young, M, Barrett, B, Engelhardt, M, and Moore, K. Six-month outcomes of an integrated assertive community treatment team serving adults with complex behavioral health and housing needs. Community Ment Health J . (2014) 50:474–9. doi: 10.1007/s10597-013-9692-5
43. LeFebvre, A, Dare, B, Farrell, S, and Cuddeback, G. Transitions from assertive community treatment among urban and rural teams: identifying barriers, service options, and strategies. Community Ment Health J . (2018) 54:469–79. doi: 10.1007/s10597-017-0162-3
44. Milbourn, B, McNamara, B, and Buchanan, A. A qualitative study of occupational well-being for people with severe mental illness. Scand J Occup Ther . (2017) 24:269–80. doi: 10.1080/11038128.2016.1241824
45. Trane, K, Aasbrenn, K, Rønningen, M, Odden, S, Lexén, A, and Landheim, A. Flexible assertive community treatment teams can change complex and fragmented service systems: experiences of service providers. Int J Ment Health Syst . (2021) 15:38. doi: 10.1186/s13033-021-00463-1
46. Meyer-Kalos, P, Lee, M, Studer, L, Line, T, and Fisher, C. Opportunities for integrating physical health within assertive community treatment teams: results from practitioner focus groups. Community Ment Health J . (2017) 53:306–15. doi: 10.1007/s10597-016-0043-1
47. Asad, S, and Chreim, S. Peer support providers’ role experiences on Interprofessional mental health care teams: a qualitative study. Community Ment Health J . (2016) 52:767–74. doi: 10.1007/s10597-015-9970-5
48. Marshall, C, Cooke, A, Gewurtz, R, Barbic, S, Roy, L, Ross, C, et al. Bridging the transition from homelessness: developing an occupational therapy framework. Scand J Occup Ther . (2021) 1-17:1–17. doi: 10.1080/11038128.2021.1962970
49. Ridente, P, and Mezzina, R. From residential facilities to supported housing: the personal health budget model as a form of coproduction. Int J Ment Health . (2016) 45:59–70. doi: 10.1080/00207411.2016.1146510
50. Lama, T, Fu, Y, and Davis, J. Exploring the ideal practice for occupational therapists on assertive community treatment teams. Br J Occup Ther . (2021) 84:582–90. doi: 10.1177/03080226211026558
51. Razzaque, R, and Stockmann, T. An introduction to peer-supported open dialogue in mental healthcare. BJPsych Advances . (2016) 22:348–56. doi: 10.1192/apt.bp.115.015230
52. Gupta, S, Jenkins, R, Spicer, J, Marks, M, Mathers, N, Hertel, L, et al. How primary care can contribute to good mental health in adults. London J Prim Care (Abingdon) . (2018) 10:3–7. doi: 10.1080/17571472.2017.1410043
53. Keet, R, de Vetten-Mc, MM, Shields-Zeeman, L, Ruud, T, van Weeghel, J, Bahler, M, et al. Recovery for all in the community; position paper on principles and key elements of community-based mental health care. BMC Psychiatry . (2019) 19:174. doi: 10.1186/s12888-019-2162-z
54. Lee, S, Crowther, E, Keating, C, and Kulkarni, J. What is needed to deliver collaborative care to address comorbidity more effectively for adults with a severe mental illness? Aust NZ J Psychiatry . (2013) 47:333–46. doi: 10.1177/0004867412463975
55. Brar, J, Maise, A, Schake, P, Bills, L, Washington, L, Nikolajski, C, et al. Implementing a learning collaborative for population-based physical and behavioral health integration. Community Ment Health J . (2021) 57:1361–73. doi: 10.1007/s10597-020-00769-3
56. Zubritsky, C, Rothbard, AB, Dettwyler, S, Kramer, S, and Chhatre, S. Evaluating the effectiveness of an integrated community continuum of care program for individuals with serious mental illness. J Ment Health . (2013) 22:12–21. doi: 10.3109/09638237.2012.670882
57. Fisher, K, Weissinger, G, O'Rorke, R, Edwards, E, and Diamond, G. Consumers with serious mental illness perspectives on care integration: preparation for integration. J Am Psychiatr Nurses Assoc . (2022) 28:193–202. doi: 10.1177/10783903221091974
58. Scharf, D, Eberhart, N, Schmidt, N, Vaughan, C, Dutta, T, Pincus, H, et al. Integrating primary care into community behavioral health settings: programs and early implementation experiences. Psychiatr Serv . (2013) 64:660–5. doi: 10.1176/appi.ps.201200269
59. Davidsen, A, Davidsen, J, Jønsson, A, Nielsen, M, Kjellberg, P, and Reventlow, S. Experiences of barriers to trans-sectoral treatment of patients with severe mental illness. A qualitative study. Int J Ment Heal Syst . (2020) 14:87. doi: 10.1186/s13033-020-00419-x
60. Brekke, E, Clausen, HK, Brodahl, M, Lexén, A, Keet, R, Mulder, CL, et al. Service user experiences of how flexible assertive community treatment may support or inhibit citizenship: a qualitative study. Front Psychol . (2021) 12:727013. doi: 10.3389/fpsyg.2021.727013
61. Belling, R, Whittock, M, McLaren, S, Burns, T, Catty, J, Jones, IR, et al. Achieving continuity of care: facilitators and barriers in community mental health teams. Implement Sci . (2011) 6:23. doi: 10.1186/1748-5908-6-23
62. Hirdes, J, van Everdingen, C, Ferris, J, Franco-Martin, M, Fries, B, Heikkilä, J, et al. The interRAI suite of mental health assessment instruments: an integrated system for the continuum of care. Front Psych . (2020) 10:926. doi: 10.3389/fpsyt.2019.00926
63. Thornicroft, G, and Tansella, M. Community mental health care in the future: nine proposals. J Nerv Ment Dis . (2014) 202:507–12. doi: 10.1097/NMD.0000000000000151
64. McCormick, B, Brusilovskiy, E, Snethen, G, Klein, L, Townley, G, and Salzer, M. Getting out of the house: the relationship of venturing into the community and neurocognition among adults with serious mental illness. Psychiatr Rehabil J . (2022) 45:18–25. doi: 10.1037/prj0000483
65. Huck, G, Morrison, B, Finnicum, C, Kaseroff, A, and Umucu, E. Consumer perspectives on physical activity interventions within assertive community treatment programs. Psychiatr Rehabil J . (2018) 41:312–8. doi: 10.1037/prj0000311
66. Shattell, M, Donnelly, N, Scheyett, A, and Cuddeback, G. Assertive community treatment and the physical health needs of persons with severe mental illness: issues around integration of mental health and physical health. J Am Psychiatr Nurses Assoc . (2011) 17:57–63. doi: 10.1177/1078390310393737
67. Edmondson, A, Borthwick, R, Hughes, E, and Lucock, M. Using photovoice to understand and improve healthy lifestyles of people diagnosed with serious mental illness. J Psychiatr Ment Health Nurs . (2022) 29:676–87. doi: 10.1111/jpm.12863
68. Zomer, L, Voskes, Y, van Weeghel, J, Widdershoven, G, van Mierlo, T, Berkvens, B, et al. The active recovery triad model: a new approach in Dutch long-term mental health care. Frontiers Psychiatry . (2020) 11:11. doi: 10.3389/fpsyt.2020.592228
69. DiClemente, C, Norwood, A, Gregory, W, Travaglini, L, Graydon, M, and Corno, C. Consumer-centered, collaborative, and comprehensive care: the Core essentials of recovery-oriented system of care. J Addict Nurs . (2016) 27:94–100. doi: 10.1097/JAN.0000000000000120
70. McGinty, E, Presskreischer, R, Breslau, J, Brown, JD, Domino, ME, Druss, BG, et al. Improving physical health among people with serious mental illness: the role of the specialty mental health sector. Psychiatr Serv . (2021) 72:1301–10. doi: 10.1176/appi.ps.202000768
71. Norden, T, Malm, U, and Norlander, T. Resource group assertive community treatment (RACT) as a tool of Empowerment for clients with severe mental illness: a meta-analysis. Clin Pract Epidemiol Ment Health . (2012) 8:144–51. doi: 10.2174/1745017901208010144
72. Malm, U, Lundin, L, Rydell, P, Nordén, T, and Norlander, T. Resource group ACT (RACT) – a review of an integrative approach to psychoeducation of individual families involving the patient. Int J Ment Health . (2015) 44:269–76. doi: 10.1080/00207411.2015.1076290
73. Malm, U, Ivarsson, B, and Allebeck, P. Durability of the efficacy of integrated Care in Schizophrenia: a five-year randomized controlled study. Psychiatr Serv . (2014) 65:1054–7. doi: 10.1176/appi.ps.201300164
74. Tjaden, C, Mulder, CL, den Hollander, W, Castelein, S, Delespaul, P, Keet, R, et al. Effectiveness of resource groups for improving empowerment, quality of life, and functioning of people with severe mental illness: a randomized clinical trial. JAMA Psychiat . (2021) 78:1309–18. doi: 10.1001/jamapsychiatry.2021.2880
75. Norden, T, Eriksson, A, Kjellgren, A, and Norlander, T. Involving clients and their relatives and friends in the psychiatric case. Case managers' experiences of training in resource group assertive community treatment. Psych Journal . (2012) 1:15–27. doi: 10.1002/pchj.1
76. Ciampa, M, Roca, M, and Lysaght, R. Work patterns and support needs of people with serious mental illness. Community Ment Health J . (2022) 58:1207–13. doi: 10.1007/s10597-021-00930-6
77. Mezzina, R. Community mental health care in Trieste and beyond: an "open door-no restraint" system of care for recovery and citizenship. J Nerv Ment Dis . (2014) 202:440–5. doi: 10.1097/NMD.0000000000000142
78. Meyer, MS, Agner, J, Botero, A, and Cha, T. Mapping community: a scoping review of clubhouse members' social networks and their impact on recovery in mental illness. Psychiatr Rehabil J . (2022) 1–15. doi: 10.1037/prj0000520
79. Farkas, M, and Coe, S. From residential care to supportive housing for people with psychiatric disabilities: past, present, and future. Front Psych . (2019) 10:862. doi: 10.3389/fpsyt.2019.00862
80. Wusinich, C, Lindy, D, Russell, D, Pessin, N, and Friesen, P. Experiences of parachute NYC: an integration of open dialogue and intentional peer support. Community Ment Health J . (2020) 56:1033–43. doi: 10.1007/s10597-020-00556-0
81. Woody, C, Baxter, A, Harris, M, Siskind, D, and Whiteford, H. Identifying characteristics and practices of multidisciplinary team reviews for patients with severemental illness: a systematic review. Australas Psychiatry . (2018) 26:267–75. doi: 10.1177/1039856217751783
82. Dalton-Locke, C, Attard, R, Killaspy, H, and White, S. Predictors of quality of care in mental health supported accommodation services in England: a multiple regression modelling study. BMC Psychiatry . (2018) 18:344. doi: 10.1186/s12888-018-1912-7
83. Baumgardt, J, Schwarz, J, Bechdolf, A, Nikolaidis, K, Heinze, M, Hamann, J, et al. Implementation, efficacy, costs and processes of inpatient equivalent home-treatment in German mental health care (AKtiV): protocol of a mixed-method, participatory, quasi-experimental trial. BMC Psychiatry . (2021) 21:173. doi: 10.1186/s12888-021-03163-9
84. van Weeghel, J, van Audenhove, C, Colucci, M, Garanis-Papadatos, T, Liégeois, A, McCulloch, A, et al. The components of good community care for people with severe mental illnesses: views of stakeholders in five European countries. Psychiatr Rehabil J . (2005) 28:274–81. doi: 10.2975/28.2005.274.281
85. Bitter, N, Roeg, D, van Nieuwenhuizen, C, and van Weeghel, J. Recovery in supported accommodations: a scoping review and synthesis of interventions for people with severe mental illness. Community Ment Health J . (2020) 56:1053–76. doi: 10.1007/s10597-020-00561-3
86. van Weeghel, J, van Zelst, C, Boertien, D, and Hasson-Ohayon, I. Conceptualizations, assessments, and implications of personal recovery in mental illness: a scoping review of systematic reviews and meta-analysis. Psychiatr Rehabil J . (2019) 42:169–81. doi: 10.1037/prj0000356
87. van Veldhuizen, J, and Bähler, M. Flexible assertive community treatment. Vision, model, practice and organisation. (2013) doi: 10.13140/RG.2.1.3925.1683
88. Ribe, A, Laursen, T, Sandbaek, A, Charles, M, Nordentoft, M, and Vestergaard, M. Long-term mortality of persons with severe mental illness and diabetes: a population-based cohort study in Denmark. Psychol Med . (2014) 44:3097–107. doi: 10.1017/S0033291714000634
89. McGovern, M, Xie, H, Segal, S, Siembab, L, and Drake, R. Addiction treatment services and co-occurring disorders. J Subst Abus Treat . (2006) 31:267–75. doi: 10.1016/j.jsat.2006.05.003
90. Gardner-Sood, P, Lally, J, Smith, S, Atakan, Z, Ismail, K, Greenwood, K, et al. Cardiovascular risk factors and metabolic syndrome in people with established psychotic illnesses: baseline data form the IMPaCT randomized controlled trial. Psychol Med . (2015) 45:2619–29. doi: 10.1017/S0033291715000562
91. Schoepf, D, Uppal, H, Potluri, R, and Heun, R. Physical comorbidity and its relevance on mortality in schizophrenia: a naturalistic 12-year follow-up in general hospital admissions. Eur Arch Psychiatry Clin Neurosci . (2014) 264:3–28. doi: 10.1007/s00406-013-0436-x
92. Leutz, W. Five laws for integrating medical and social services: lessons from the United States and the United Kingdom. Milbank Q . (1999) 77:77–110. doi: 10.1111/1468-0009.00125
93. Reis, G, Bromage, B, Rowe, M, Restrepo-Toro, ME, Bellamy, C, Costa, M, et al. Citizenship, social justice and collective empowerment: living outside mental illness. Psychiatry Q . (2022) 93:537–46. doi: 10.1007/s11126-021-09968-x
94. Carr, E, and Ponce, A. Supporting mental health recovery, citizenship, and social justice. Community Ment Health J . (2021) 58:11–9. doi: 10.1007/s10597-021-00900-y
95. Harper, A, Kriegel, L, Morris, C, Hamer, H, and Gambino, M. Finding citizenship: what works? Am J Psychiatr Rehabil . (2017) 20:200–17. doi: 10.1080/15487768.2017.1338036
96. Ponce, A, and Rowe, M. Citizenship and community mental health care. Am J Community Psychol . (2018) 61:22–31. doi: 10.1002/ajcp.12218
97. Nesse, L, Aamodt, G, Gonzalez, M, Rowe, M, and Raanaas, R. The role of occupational meaningfulness and citizenship as mediators between occupational status and recovery: a cross-sectional study among residents with co-occurring problems. Adv Dual Diagn . (2021) 14:99–118. doi: 10.1108/ADD-08-2020-0018
98. Rowe, M, and Davidson, L. Recovering citizenship. Isr J Psychiatry Relat Sci . (2016) 53:14–20.
99. Quinn, N, Bromage, B, and Rowe, M. Collective citizenship: from citizenship and mental health to citizenship and solidarity. Soc Policy Adm . (2020) 54:361–74. doi: 10.1111/spol.12551
100. Weinstein, L, Chilton, M, Turchi, R, Klassen, A, LaNoue, M, Lamar, S, et al. Reaching for a healthier lifestyle: a Photovoice investigation of healthy living in people with serious mental illness. Prog Community Health Partnersh . (2019) 13:371–83. doi: 10.1353/cpr.2019.0061
101. Koomen, L, van der Horst, M, Deenik, J, and Cahn, W. Lifestyle interventions for people with a severe mental illness living in supported housing: a systematic review and meta-analysis. Front Psych . (2022) 13:966029. doi: 10.3389/fpsyt.2022.966029
102. González-Domínguez, S, González-Sanguino, C, and Munoz, M. Efficacy of a combined intervention program for the reduction of internalized stigma in people with severe mental illness. Schizophr Res . (2019) 211:56–62. doi: 10.1016/j.schres.2019.07.010
103. Brown, M, Jason, L, Malone, D, Srebnick, D, and Sylla, L. Housing first as an effective model for community stabilization among vulnerable individuals with chronic and nonchronic homelessness histories. J Community Psychol . (2016) 44:384–90. doi: 10.1002/jcop.21763
104. Drake, R, Bond, G, and Becker, D. Individual placement and support: an evidence-based approach to supported employment . New York: Oxford University Press (2013).
105. Roeg, D, de Winter, L, Bergmans, C, Couwenbergh, C, McPherson, P, Killaspy, H, et al. IPS in supported housing: Fidelity and employment outcomes over a 4 year period. Front Psych . (2021) 11:11. doi: 10.3389/fpsyt.2020.622061
106. van Duin, D, de Winter, L, Oud, M, Kroon, H, Veling, W, and van Weeghel, J. The effect of rehabilitation combined with cognitive remediation on functioning in persons with severe mental illness: systematic review and meta-analysis. Psychol Med . (2019) 49:1414–25. doi: 10.1017/S003329171800418X
107. Killaspy, H, Harvey, C, Brasier, C, Brophy, L, Ennals, P, Fletcher, J, et al. Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry . (2022) 21:96–123. doi: 10.1002/wps.20940
108. Strong, S, and Letts, L. Personal narratives of learning self-management: lessons for practice based on experiences of people with serious mental illness. Aust Occup Ther J . (2021) 68:395–406. doi: 10.1111/1440-1630.12748
Keywords: severe mental illness, community care, recovery, social inclusion, scoping review, current insights, human rights, independent living
Citation: van Genk C, Roeg D, van Vugt M, van Weeghel J and Van Regenmortel T (2023) Current insights of community mental healthcare for people with severe mental illness: A scoping review. Front. Psychiatry 14:1156235. doi: 10.3389/fpsyt.2023.1156235
Received: 01 February 2023; Accepted: 23 March 2023; Published: 18 April 2023.
Reviewed by:
Copyright © 2023 van Genk, Roeg, van Vugt, van Weeghel and Van Regenmortel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Caroline van Genk, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 10 May 2023
Mental health awareness: uniting advocacy and research
Nature Mental Health volume 1 , pages 295–296 ( 2023 ) Cite this article
4591 Accesses
16 Altmetric
Metrics details
Mental Health Month has been observed to reduce the stigma that is associated with mental illness and to educate the public and encourage individuals to make their mental health and wellbeing a priority. It is an important moment to bring the strengths of advocacy groups and researchers together to promote mental health awareness and to improve equity.
Observances have become a popular tool to garner media and notice for topics deserving attention, from medical conditions to public health concerns, commemoration of notable events, or celebration of cultural groups. Codifying the scope and needs connected to an issue or illness through awareness campaigns can provide opportunities for imparting useful information, reducing stigma and marshalling support for policy change. The impact of awareness campaigns can be difficult to measure beyond tallying social media mentions or news stories. Effective advocacy, however, extends beyond traffic and paves the way for the creation of knowledge and partnerships among allies and with those whose interests are being represented. When the magnitude of an issue and the potential for improvement are great and are matched by broad involvement and recognition by stakeholders, the possibility for impact is also great.

Held annually in May, Mental Health Month , also called Mental Health Awareness Month, is an observance with such reach, resonating with many people. Nearly everyone has experience with the challenges that are associated with mental health, either first-hand or through loved ones or in their community. There is a need for education, support and initiative to improve our understanding of the causes of mental health disorders and to increase the availability of resources for prevention and treatment. Mental Health Month also offers the possibility of bringing together groups who often work in parallel, such as mental health advocates and mental health research organizations, that can mutually benefit from each other’s functions and expertise.
Mental Health Month was first established in the US in 1949 by the National Mental Health Association, now known as Mental Health America . At a time more often associated with the outset of the Cold War and Marshall Plan than setting an agenda for domestic mental health and wellbeing advocacy, in the more than 70 years since, Mental Health Month has grown into an international event designed to reduce exclusion, stigma and discrimination against people with mental health conditions or disorders. Mental Health America are joined by other prominent mental health advocacy groups to sponsor related observances: Mental Health Awareness Week Canada (1–7 May, 2023) and Europe (22–28 May, 2023); and federal agencies such as the Substance Use Abuse and Mental Health Services Administration ( SAMSHA ) in the US, promoting related public education platforms, including National Prevention Week (7–13 May, 2023).
Observances and awareness campaigns also provide occasions to put mental health in context. Increasing acknowledgment of the role of social determinants, for example, as mechanisms that can increase vulnerability for developing disorders and that drive disparities in mental health are an important framework to underscore as part of promoting mental health awareness. Given the complex and broad scope of people, disorders, conditions and issues under the umbrella of mental health, observances also give us the chance to focus more closely on specific problems or experiences. The theme for Mental Health Month in 2023 is ‘Look Around, Look Within’, which emphasizes the interdependence of mental health and wellness with an individual’s internal and external experiences and environments.
“The ‘Look Around, Look Within’ theme builds on the growing recognition that all humans have mental health needs and that our available resources to build resilience and heal come in many forms — including in the natural world,” explains Jennifer Bright, Mental Health America Board Chair and President of Momentum Health Strategies. “Mental Health America’s strategic plan, focused on NextGen Prevention, carries a similar theme — that the social factors supporting mental health are essential building blocks. These encompass basic needs like healthy food, stable housing, and access to treatment and supports, but they also include spirituality, connection with peers with lived experience, and safe and natural spaces.”
Overlapping with Mental Health Month, Mental Health Foundation sponsors Mental Health Week in the UK (15–21 May, 2023), dedicating this year to raising awareness around anxiety. It shares an individual-centered approach to advocacy. In addition to providing toolkits and resources that point to how prevalent stress and anxiety can be to reduce stigma, it also promotes the accessibility of coping strategies for managing anxiety. As part of the Mental Health Awareness Week campaign, Mental Health Foundation and others use the international symbol of wearing a green ribbon or clothing to physically raise awareness around mental health. Nature Mental Health also incorporates the symbol of the green ribbon on the cover of this month’s issue and as our journal theme color. Green evokes the ideas of vitality, growth, new beginnings and hope — powerful imagery in mental health awareness.
Alongside stories, sponsorships and social media resources, mental health advocacy toolkits and strategy documents include fact sheets and messaging that are shaped and informed by research. Yet, there is often a perception that a divide exists between the mental health advocacy and research spaces, but observances such as Mental Health Month can bridge the two.
According to Lea Milligan, Chief Executive Officer of MQ: Transforming Mental Health , an international mental health research organization, there are complementary approaches and priorities in advocacy and research: “Mental health research can be used to bolster awareness by providing evidence-based information and resources that can help individuals and communities better understand mental health and the factors that contribute to mental health problems. This can include information on risk factors, prevention strategies, and available treatments.”
In addition, increased efforts to involve people with lived experience of mental illness in the research enterprise is a goal that is well-served through connection with advocacy. “While MQ is primarily focused on promoting mental health research, it also recognizes the importance of advocacy in advancing the mental health agenda” suggests Milligan. “MQ advocates for increased funding and support for mental health research, as well as policies that promote mental health and wellbeing. Additionally, MQ seeks to empower individuals with lived experience of mental health conditions to be involved in research and advocacy efforts, and to have their voices heard in the development of policies and programs that affect their lives. MQ provides resources and support for individuals with lived experience who wish to be involved in research or advocacy efforts, including training programs, research grants, and opportunities to participate in research studies.”
Involvement or engagement is certainly one of the most important metrics of advocacy. By strengthening collaboration between advocacy and research organizations and identifying the mutual areas of benefit, such as engagement and increased funding, we may find new ways to green light mental health awareness and action toward mental health equity.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Mental health awareness: uniting advocacy and research. Nat. Mental Health 1 , 295–296 (2023). https://doi.org/10.1038/s44220-023-00072-6
Download citation
Published : 10 May 2023
Issue Date : May 2023
DOI : https://doi.org/10.1038/s44220-023-00072-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Please note: This website has recently moved from www.health.gov to odphp.health.gov. www.health.gov is now the official website of ODPHP’s parent organization, the Office of the Assistant Secretary for Health (OASH). Please update your bookmarks for easy access to all our resources.
Social Determinants of Health
What are social determinants of health.
Social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.
SDOH can be grouped into 5 domains:
Suggested citation
Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Retrieved [date graphic was accessed], from https://odphp.health.gov/healthypeople/objectives-and-data/social-determinants-health
Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life. Examples of SDOH include:
- Safe housing, transportation, and neighborhoods
- Racism, discrimination, and violence
- Education, job opportunities, and income
- Access to nutritious foods and physical activity opportunities
- Polluted air and water
- Language and literacy skills
SDOH also contribute to wide health disparities and inequities. For example, people who don't have access to grocery stores with healthy foods are less likely to have good nutrition. That raises their risk of health conditions like heart disease, diabetes, and obesity — and even lowers life expectancy relative to people who do have access to healthy foods.
Just promoting healthy choices won't eliminate these and other health disparities. Instead, public health organizations and their partners in sectors like education, transportation, and housing need to take action to improve the conditions in people's environments.
That's why Healthy People 2030 has an increased and overarching focus on SDOH.
How Does Healthy People 2030 Address SDOH?
One of Healthy People 2030’s 5 overarching goals is specifically related to SDOH: “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”
In line with this goal, Healthy People 2030 features many objectives related to SDOH. These objectives highlight the importance of "upstream" factors — usually unrelated to health care delivery — in improving health and reducing health disparities.
More than a dozen workgroups made up of subject matter experts with different backgrounds and areas of expertise developed these objectives. One of these groups, the Social Determinants of Health Workgroup , focuses solely on SDOH.
Explore Research Related to SDOH
Social determinants of health affect nearly everyone in one way or another. Our literature summaries provide a snapshot of the latest research related to specific SDOH.
View SDOH Infographics
Each SDOH infographic represents a single example from each of the 5 domains of the social determinants of health. You can download them, print them, and share them with your networks.
Learn How SDOH Affect Older Adults
SDOH have a big impact on our chances of staying healthy as we age. Healthy People’s actionable scenarios highlight ways professionals can support older adults’ health and well-being.
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Disaster mental health preparedness in the community: A systematic review study
Juliet roudini, hamid reza khankeh, evelin witruk.
- Author information
- Article notes
- Copyright and License information
Hamid Reza Khankeh, Emergency and Disaster Health Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. Email: [email protected]
Collection date 2017 Jan-Jun.
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 License ( http://www.creativecommons.org/licenses/by-nc/4.0/ ) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access page ( https://us.sagepub.com/en-us/nam/open-access-at-sage ).
The objective of this study was to perform a systematic review of articles that cover aspects of disaster mental health preparedness. This assessment was done by a thorough review and summary of the available studies which provided a considerable background and amplified the gaps in knowledge about community mental health preparedness. By this systematic review, we tried to identify available concept of community mental health preparedness and related tools that communities and individuals will need to prepare for natural disasters. We found there is a lack of mental health preparedness in the majority of countries; valid and reliable tools and context-bound programs should be developed based on the experiences and perceptions of the community.
Keywords: community preparedness, disaster, mental health, systematic review
Introduction
Many natural disasters such as earthquakes, cyclones, floods, droughts, and tsunami happen in just few seconds. Disasters are stressful events not only for individuals who suffer from personal loss but also for the community at large ( Khankeh et al., 2011 ; Norris et al., 1999 ). During the past two decades, natural hazards have affected more than 3 million families around the world and from an economical perspective. The occurrence and human consequences of disasters have been increasing due to the increasing population ( McFarlane and Williams, 2012 ). According to the report of the Annual Disaster Statistical Review from 2013, natural hazards killed a noteworthy number of individuals (21,610) but fortunately mostly below the annual average report between 2003 and 2012 (106,654) ( Guha-Sapir et al., 2014 ).
In the Middle East, there are countries with major natural disasters such as Iran. Iran is the one of the most afflicted countries in the world for earthquakes in terms of frequency, intensity, and the number of victims (BBC reported). The city of Bam in southeast Iran was devastated completely by an earthquake in 2003: around 43,000 people were killed and more than 30,000 were injured ( Fialko et al., 2005 ).
A growing body of evidence demonstrates that major depressive disorder, post-traumatic stress disorder (PTSD), depression, and anxiety undesirably and forcefully influence quality of life and functioning ( Fergusson et al., 2014 ; Kessler et al., 1995 ; Simmons et al., 2008 ). It is not entirely unexpected that the comorbidity of these disorders is great; around 50 percent of PTSD patients also meet the criteria for major depressive disorder ( Goenjian et al., 2000 ; Kessler et al., 1995 ). Research also indicates that earlier substance abuse problems may relapse or be exacerbated ( Keyes et al., 2011 ; North et al., 2011 ). Moreover, the research indicates that individuals with poor mental health are at a high risk ( Clay et al., 2014 ). The experience of dealing with hazards such as tsunami has demonstrated that psychosocial characteristics and mental health are vital in disaster preparedness and management. Natural disaster funding also needs to include psychosocial retrieval, which is a crucial component of restoring individuals’ and communities’ well-being and mental health ( Burke, 2014 ; Reser and Morrissey, 2009 ).
Disaster mental health preparedness is a significant reduction method to protect individuals from detrimental psychological effects arising from unexpected natural disasters.
Results of investigation by E.W. show that people with a strong belief in a just world believe the hazards to be a result of human failure, and this belief is an important factor when dealing with natural disasters ( Witruk et al., 2014 ).
Psychological attitudes play a constitutional and an essential part in disaster research, particularly with regard to disaster response in trauma management to the people who are affected by natural disasters and also providing counseling and therapy services. It has only been in the past 50 years that psychologists have become more active as researchers and specialists in this field ( Zulch et al., 2012 ). In addition, the need for mental health services is significant before and after the disaster. The research of H.R.K. revealed the essential basic needs that should be taken into consideration to deliver comprehensive recovery facilities. One of the basic needs includes the requirement of continuous mental health care in the community ( Khankeh et al., 2013 ).
Considerable research on the mental consequences of disaster has been undertaken in several countries. Nevertheless, the existing investigations about disaster mental health preparedness are few in number. Since vulnerable countries from around the world are at high risk of natural catastrophe, disaster mental health preparedness plays a vital role. The research of Clay and his colleagues demonstrated a positive connection between disaster preparedness and mental health, and probability of the mental disorder following disasters is due to an absence of preparedness.
Psychological preparedness can help people to think logically and wisely, which in turn may decrease the risk of severe injury and loss of life. Therefore, individuals and communities need to prepare psychologically for confronting a disaster. People are not fully aware of disasters and the mental effects on human’s health, so natural disaster mental health preparedness is frequently unnoticed due to the more immediate and basic physical needs in disaster situations. Therefore, additional research is needed to improve the concept of the mental preparedness for disaster based on international experience ( Barron, 2004 ; Zulch et al., 2012 ). The main concern involved in the community mental health preparedness investigations is the lack of context-bound tools to evaluate this important issue based on a clear conceptual definition. Because of the above-mentioned reasons, we are going to explore different evidence regarding concept of community mental health preparedness, related tools, and its different aspects. This assessment was done by a thorough review and summary of the available studies which provided a considerable background and amplified the gaps in knowledge about community mental health preparedness.
Eligibility criteria and search strategies
Search strategy.
This systematic review research was done according to the Preferred Reporting Item for Systematic Reviews and Meta-analyses (PRISMA) standard ( Moher et al., 2009 ). A literature search was conducted in May 2015 to identify peer-reviewed, English-language literature providing evidence of community disaster mental health preparedness. We used an extensive collection of search methods in the literature review. The search plan was to use varied electronic databases and publications with a combination of subject titles and free text searching such as natural disasters, community mental health, mental health concepts and evidence, mental disorders, and community mental health services. Most of the investigations were to be found in MEDLINE through PubMed (196 citations), Psych INFO (350 citations), PILOTS (120 citations), Academic Search Premier (30 citations), Cochrane Database of Systematic Reviews (zero citations), and Google Scholar (114 citations). Additional literature was gathered through various institutional reports, books, and theses. The search yielded around 810 single articles. In the final analysis, after evaluation of all documents, 14 full text sources were selected. Figure 1 indicates the search strategy and process. The main limitation of the review was that only English-language documents are included. Therefore, we lost some of the related studies which were not in English.
PRISMA Flow Diagram
Inclusion criteria
The protocol for this review was registered with the International Prospective Register of Systematic Reviews (PROSPERO; registration number CRD42016026844). We have included papers that described the concept of community mental health preparedness in natural disasters, the existing tools that were utilized to measure it, and the problems experienced regarding the lack of community mental health preparedness in different contexts.
This systematic search has been retrieved from articles published between 1940 and 2016. The term mental health appeared first in a paper that was published in the 1940s.
Exclusion criteria
Papers were excluded if the focus was unrelated to the purpose of our systematic review for the following reasons:
The analytical and interventional studies were not included because in this review, we are not considering the outcomes and the effects of exposure and intervention. In contrast, we explored the meaning, the measurement, and the related problems of community mental health preparedness in natural disaster.
Some articles which were considered as unreliable were also excluded from the final list either by the research team or according to the PRISMA model.
Web-based sources are not included in the review.
Selection of articles and analysis
In the beginning, articles were evaluated based on their titles and later based on their abstracts to eliminate the articles which did not meet the inclusion criteria. The related studies were reviewed completely and the articles without the inclusion criteria were omitted. In this systematic review, the information is derived from both quantitative and qualitative studies. The quantitative studies were discussed in terms of the total bias related to the different strategies with respect to the main research attention. The summary of the results, study design, and demographics were reviewed by the co-authors. Since one of our aims was to determine what had been written about community mental health preparedness and how mental preparedness in disaster was conceptualized in the literature, the primary search plan was to cast as widely as possible. In this way, free text searches using the terms “mental preparedness concepts” and “community preparedness meanings” were conducted in a variety of the mentioned databanks. Free text searches are an appropriate approach when the term is first-hand and perhaps has not yet been added to a dictionary.
Data extraction and management
Data on authors, year of publication, method, target group, study design, study setting, study focus, and assessment tools used were extracted by the authors. Results from the selected papers were extracted and gathered in a summary. Included papers were grouped by subject, and fields were determined once the data were completely collected. All papers were appraised using the PRISMA guideline, and J.R., H.R.K., and E.W. agreed the amplitude by consensus.
A total of 810 relevant articles were identified through the search strategy. After further review of papers and abstracts, 525 articles were excluded due to the exclusion criteria or lack of coverage of evidence and concepts of disaster related to mental health and duplications. The concentrations of these research works were mostly on the influence of mental disorders and theories rather than community mental health preparedness concepts and context-bound programs. Many papers (450 papers) had another approach or were not focused on mental health preparedness. In the last phase, 65 articles out of 75 papers during data extraction were omitted due to not being available in full or not directly related to mental health preparedness. These articles were classified by the emphasis of the article on disaster mental health concepts and valid and reliable tools and context-bound programs and categorized by type (review, commentary, opinion, original research, and reports). In the last stage, 14 unique articles on disaster mental health preparedness were included in this review ( Figure 1 )
Tables 1 and 2 indicate a summary of the features of the involved papers. From 14 selected original articles, 6 of the documents (42%) used quantitative methods, 3 articles (21%) were qualitative studies dealing with mental health preparedness, 1 paper (9%) used mixed methods, and, finally, 4 review papers (28%) dealing with the effects of disaster on mental health were also involved. In Table 2 , for characteristics of disasters, all types of disaster events such as earthquakes, tsunamis, and hurricanes are also investigated.
Type of Selected methods.
Characteristic of the disasters.
In total, 9 out of the 14 studies (64%) were conducted in developed countries, 5 of the 14 papers (35%) were focused on developing countries, and 2 papers (14%) were done on an international level (See Table 3 ). Regarding the demographics of the papers, 20 percent focused on children and adolescents, 74 percent on adults, and 6 percent of papers focused on women.
Research sources.
After a full reading of the papers, the descriptive analysis is designated in Table 4 to deliver a summary of the characteristics of the studies involved. The articles nominated for the systematic review were verified by title of publication, the year of publication within the period 1940–2015, methods, target group, research sources, the summary of results of all selected studies, and the conclusion.
Included studies for final analysis.
PTSD: post-traumatic stress disorder.
Discussions
The main purpose of this review is to identify available concept and tools that communities and individuals will need to prepare themselves for natural disasters. The main study’s results also show that there are currently no clear and comprehensive concept of community mental health preparedness and related tools to evaluate community mental health preparedness. This assessment carried out by means of a thorough review and summary of the studies provided considerable background and highlighted the gaps in knowledge about community mental health preparedness. In line with the research of Hannah R Zulch et al. (2012) , and after a widespread review of the literature, an effective definition for mental health preparedness is suggested. In the context of a threatening situation, mental health preparedness should be a state of awareness and expectation of an individual’s psychological reactions to the disaster warning. Furthermore, mental health preparedness will significantly support the ability to identify particular stress-related emotions and thoughts. Consequently, this also contains the perception, appraisal, and understanding of threatening events and the risk communication.
Primarily, most research shows that disaster mental health consequences and disorders have been taken into consideration in many countries. However, the available studies about disaster mental health preparedness are few and the number of the documents related to mental health preparedness programs, models, or tools have not increased significantly in recent years, especially in those countries that they are at high risk of natural disasters. According to the above-mentioned studies, many countries will experience a high number of disasters in the future and the impact of the psychological effect will become more critical. Providing only financial and medical help immediately after a disaster cannot stop the long-term psychological effects of disasters on human life. Therefore, individuals and communities need to prepare psychologically for confronting a disaster.
The review of the articles suggested that natural disasters have a potentially negative impact on mental health, with increasing levels of PTSD, depression, anxiety, and use of psychotropic medications ( McCabe et al., 2014 ; Malkina-Pykh and Pykh, 2013 ; Mangelsdorff, 1985 ; Panyayong, 2006; Zulch et al., 2012 ). According to the research, the central components of preparedness are very similar, even though dissimilar disasters need different reactions depending on the context, type of hazards, requirements, and magnitude of preparedness. The effect of natural disasters on mental health is similar in both developing and developed countries ( Barron, 2004 ). However, there can be cultural differences related to the manifestation of reactions and expression of emotions. In some reviews, we have found some important research gaps and insufficient attention being paid to helping a disaster-struck community according to its own cultural standards and methods. These studies showed that there is a need to develop a more context-bound tool to evaluate the mental health preparedness of the community. Reser’s research indicated that mental health readiness contains some intertwined factors within individual abilities and developments such as awareness, knowledge, anticipation, concern, thinking, feeling, experienced stress, motivation, intentions, and decision-making, and management of, or coping with, one’s thoughts, feelings, and actions ( Reser and Morrissey, 2009 ).
Also, the review showed that the majority of the studies considered that more research needed to be done into the psychological effects of natural disasters and mental health preparedness.
The term mental health preparedness has been referred to in the disaster literature in the last few years; however, only a few efforts have been made recently to operationalize mental health. Moreover, an investigation from 30 years ago ( Mangelsdorff, 1985 ) shows the necessity of developing community disaster preparedness plans for establishing, training mental health teams, and coordinating with government departments and policy makers. The local mental health agencies should develop operational disaster intervention techniques for community mental health preparedness. Individuals in the community need to be informed of their role responsibilities in a disaster. They should be informed about their possible reactions regarding casualties and victims which are normal in a disaster situation.
Research in Bangladesh and India indicated that no committee or special team had been created for the organization of disaster-related psychosocial problems for the community, particularly for women and children. The reaction of the majority of women shows they are poorly prepared with some gaps in their awareness and preparedness. However, it showed that a large number of the aforementioned women are interested to take part in disaster preparedness training provided by the public authorities ( Sharma et al., 2015 ). The most significant finding in study from Bangladesh shows that children and women were more psychologically troubled than adult men due to the practical limitations of the situation or due to a lack of awareness of disaster mental health ( Choudhury et al., 2006 ). Preparedness efforts have to put emphasis on recognizing and addressing the mental health problems of children, and their anxieties should be a part of all phases of mitigations, preparedness planning, response, and recovery.
A study in Australia examined the assessing of the efficiency of psychological preparedness guidance in community cyclone preparation training. The research delivers persuasive support for the efficiency of the modified stress inoculation intervention in a real cyclone threat situation. The aim of the research was to test, evaluate, and improve a pioneering natural disaster public training and information intervention, concentrating on tropical cyclone training and reaction. The material for this preparation was derived from “Stress Inoculation Theory.” The research outcomes show that avoidance coping, previous traumatic experience, anxiousness, and stress were significantly interacting in a mental health condition in a disaster situation. Psychological factors and procedures during this threat period are important for effective coping and adaptive reacting. Therefore, the pre-disaster plans are a critically significant factor for prevention and mitigation ( Morrissey and Reser, 2003 ).
The results of the developed and validated measure of psychological preparedness, known as the Psychological Preparedness for Disaster Threat Scale (PPDTS), demonstrated that a much more precise meaning of psychological preparedness along with a reliable and valid measure of psychological preparedness has been developed ( Zulch et al., 2012 ).
Psychological First Aid (PFA) as a disaster intervention tool has also demonstrated a positive effect on mental health preparedness in disaster conditions ( Fox et al., 2012 ). According to this study, people should be provided with the information about the probable responses they might have. This information comprises how they can receive help from the community, what is their own capability to help themselves (coping strategies), and where and how to obtain additional assistance if required.
A few Asian countries like Thailand and Myanmar have established a national instruction program for mental health interventions after the 2004 tsunami, both as a tool and strategy for improving preparedness in disasters and for enhanced protection of property, life, environment, improved community safety, physical well-being, mental health, and the ability to sustain the well-being. Their consideration facilitated the creation of a significant community mental health structure which served the immediate as well as the long-term needs of the community, and it was intended to become a part of the standard health care delivery system in these countries.
Community mental health preparedness plays a crucial role in responding to public health emergencies in every country. Although governmental organizations and assistance agencies have a significant responsibility, mental health preparedness is not adequately included in the government’s responsibilities. Indeed, individuals and families continue to organize prearranged efforts with the help of governmental and non-governmental support ( US Department of Health and Human Services Centers for Disease Control and Prevention, 2011 ).
There is also an absence of research using qualitative methods which are the recommended approaches to exploring the meaning of experiences and perceptions. In review of Table 1 , we have recognized only four studies and they were conducted in the United States, Australia, Myanmar, and Thailand. Moreover, the use of mixed methods improves the conclusions and leads to a depth of understanding of the community mental health preparedness. This review showed that there are some restrictions in the published qualitative studies, such as a lack of discussion on the philosophical basis of the research, because the belief structure of the researcher influences the interpretation of the research. Therefore, it is essential to discuss the philosophy underpinning the research, the role of the investigators and their relationship with contributors, any potential biases or assumptions of the researchers, and the sampling procedure. Regarding responses and feedback about the used methods and programs, there is limited evidence regarding their effectiveness or impact and a lack of monitoring of the system. Some of this research addresses the effectiveness of mental health interventions to reduce the impact of disasters. They reached the same conclusion: more effort is required to evaluate the efficiency of these interventions. It also emphasized the limitations of mental health experts, insufficient knowledge, and practices concerning mental health preparedness in Asia. Therefore, an advance study is necessary on the topic of mental health preparedness for disasters. The experience of dealing with the 2004 Indian Ocean tsunami emphasized the fact that disaster preparedness strategies must meet the mental health and psychosocial needs of the community.
Finally, we found a lack of information on vulnerable groups such as children, women, people living with disabilities, and the elderly. Assessment efforts for mental health preparedness training in general and those related to vulnerable populations such as children, women, and elderly people in particular should be encouraged ( Choudhury et al., 2006 ; Morrissey and Reser, 2003 ; Sharma et al., 2015 ; Udomratn, 2008 ). These efforts confirm that an evidence-based guidance health system needs to strengthen intra- and inter-sector collaboration and coordination, information management systems, and community-based initiatives for disaster preparedness. It is also necessary to pay more attention to disaster risk reduction while increasing the reaction capacity. Investing in related research would contribute to the future decision-making in the field of disaster health supervision. Specialists and health system administrators should pay attention to the physical and mental health of their team and workers, and they should assign strategies to develop the quality of emergency medical care ( Khankeh et al., 2011 ; Panyayong, 2006).
Through the assessment of the gaps across research investigations, some overall themes have appeared. First, we note an absence of policy and planning for people experiencing economic difficulty, individuals with mental disorders, and specific population groups like children, women, and elderly people. In addition, standard training exercises for general and specific populations are required. Collaborative efforts between government organizations and NGOs (non-governmental organizations) are insufficient. The study’s results also show that there are currently no comprehensive concepts or tools to evaluate community mental health preparedness. Based on the articles archived and selected, and similar programs, tools and models are more frequently used in developed and developing countries, where there is little evidence regarding mental health preparedness. Consequently, health care systems in a community need reliable evaluation tools which are established using expert knowledge and authenticated through the procedure of psychometric evaluation. Mental health services should be developed so that there is a community mental health structure that can provide immediate support and then be part of the routine health care system. As regards the improvement in successful education, training, and informational resources, it is important to involve all of these organizations, agencies, and individuals. This has to be considered due to climate change and the increasing percentage of the population who are young, especially in Asia countries; natural disasters like tsunami, earthquake, and floods are going to be more frequent. Therefore, having evidence of the influence of disasters on the mental health of individuals at any age is important.
Further investigations are required to document the effectiveness of the most common methods and to develop psychological mental health as well as household disaster preparedness. Community mental health preparedness is important to discover the most appropriate tool to enable a suitable response when facing disasters. Given the weaknesses or lack of the current community mental health preparedness tools, further qualitative studies and mixed methods are desirable to explore and clarify the concept of community mental health preparedness. Developed comprehensive context-bound tools, based on a concept of definition and analysis, are highly desired. These tools will facilitate the assessment of the functional features of mental health preparedness.
Acknowledgments
In this study, because we are not assessing the outcome of an intervention, bias is not an issue. However, two review authors independently assessed the risk of bias in the included studies by categorizing the papers by type of study. The quantitative and qualitative studies were reviewed in terms of their research consistency and of the utility of the results.
Author contribution: All authors contributed to the development of the study. H.R.K. and J.R. contributed to the conception and design of the study. J.R. conducted the search, reviewed the literature, organized and wrote the initial article, and conceptualized and compiled figures and tables. H.R.K. and E.W. critically revised the article, contributed to the writing and the structure, and were consulted on the general structure and direction the article should take. All authors participated in preparing, reading, and approving the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
- Barron RA. (2004) International disaster mental health. The Psychiatric Clinics of North America 27(3): 505–519. [ DOI ] [ PubMed ] [ Google Scholar ]
- Burke S. (2014) A response by the Australian psychological society to the draft report of the productivity commission inquiry into natural disaster funding. Australian Psychological Society. Available at: https://www.psychology.org.au/Assets/Files/APS%20Response%20to%20Draft%20Productivity%20Commission%20report%20on%20natural%20disaster%20funding.pdf
- Choudhury WA, Quraishi FA, Haque Z. (2006) Mental health and psychosocial aspects of disaster preparedness in Bangladesh. International Review of Psychiatry Journal 18(6): 529–535. [ DOI ] [ PubMed ] [ Google Scholar ]
- Clay LA, Goetschius JB, Papas MA, et al. (2014) Influence of mental health on disaster preparedness: Findings from the behavioral risk factor surveillance system, 2007–2009. Journal of Homeland Security and Emergency Management 11(3): 375–392. [ Google Scholar ]
- Fergusson DM, Horwood LJ, Boden JM, et al. (2014) Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry 71(9): 1025–1031. [ DOI ] [ PubMed ] [ Google Scholar ]
- Fialko Y, Sandwell D, Simons M, et al. (2005) Three-dimensional deformation caused by the Bam, Iran, earthquake and the origin of shallow slip deficit. Nature 435(7040): 295–299. [ DOI ] [ PubMed ] [ Google Scholar ]
- Fox JH, Burkle FM, Bass J, et al. (2012) The effectiveness of psychological first aid as a disaster intervention tool: Research analysis of peer-reviewed literature from 1990–2010. Disaster Medicine and Public Health Preparedness 6: 247–252. [ DOI ] [ PubMed ] [ Google Scholar ]
- Goenjian AK, Steinberg AM, Najarian LM, et al. (2000) Prospective study of posttraumatic stress, anxiety, and depressive reactions after earthquake and political violence. The American Journal of Psychiatry 157(6): 911–916. [ DOI ] [ PubMed ] [ Google Scholar ]
- Guha-Sapir D, Hoyois P, Below R. (2014) Annual Disaster Statistical Review 2013: The Numbers and Trends. Brussels: CRED. [ Google Scholar ]
- Kessler RC, Sonnega A, Bromet E, et al. (1995) Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry 52: 1048–1060. [ DOI ] [ PubMed ] [ Google Scholar ]
- Keyes KM, Hatzenbuehler ML, Hasin DS. (2011) Stressful life experiences, alcohol consumption, and alcohol use disorders: The epidemiologic evidence for four main types of stressors. Psychopharmacology 218(1): 1–17. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Khankeh HR, Khorasani-Zavareh D, Johanson E, et al. (2011) Disaster health-related challenges and requirements: A grounded theory study in Iran. Prehospital and Disaster Medicine 26(3): 151–158. [ DOI ] [ PubMed ] [ Google Scholar ]
- Khankeh HR, Nakhaei M, Masoumi G, et al. (2013) Life recovery after disasters: A qualitative study in the Iranian context. Prehospital and Disaster Medicine 28(6): 573–579. [ DOI ] [ PubMed ] [ Google Scholar ]
- McCabe OL, Semon NL, Lating JM, et al. (2014) An academic-government-faith partnership to build disaster mental health preparedness and community resilience. Public Health Reports 129(Suppl. 4): 96–106. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4187312&;tool=pmcentrez&rendertype=abstract [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McFarlane AC, Williams R. (2012) Mental health services required after disasters: Learning from the lasting effects of disasters. Depression Research and Treatment 2012: 970194. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Malkina-Pykh IG, Pykh YA. (2013) An integrated model of psychological preparedness for threat and impacts of climate change disasters. WIT Transactions on the Built Environment 133: 121–132. [ Google Scholar ]
- Mangelsdorff AD. (1985) Lessons learned and forgotten: The need for prevention and mental health interventions in disaster preparedness. Journal of Community Psychology 13(3): 239–257. [ DOI ] [ PubMed ] [ Google Scholar ]
- Moher D, Liberati A, Tetzlaff J, et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine 151: 264–269. [ DOI ] [ PubMed ] [ Google Scholar ]
- Morrissey SA, Reser JP. (2003) Evaluating the effectiveness of psychological preparedness advice in community cyclone preparedness materials. The Australian Journal of Emergency Management 18(2): 46–61. [ Google Scholar ]
- Norris FH, Perilla JL, Riad JK, et al. (1999) Stability and change in stress, resources, and psychological distress following natural disaster: Findings from hurricane Andrew. Anxiety, Stress & Coping 12(4): 363–396. [ DOI ] [ PubMed ] [ Google Scholar ]
- North CS, Ringwalt CL, Downs D, et al. (2011) Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Archives of General Psychiatry 68(2): 173. [ DOI ] [ PubMed ] [ Google Scholar ]
- Perry RW, Lindell MK. (1978) The psychological consequences of natural disaster: A review of research on American communities. Mass Emergencies 3: 105–115. [ Google Scholar ]
- Panyayong B, Pengjunter W. (2006) Mental health and psychosocial aspects of disaster preparedness in Bangladesh. International review of psychiatry 18(6): 529–535. [ DOI ] [ PubMed ] [ Google Scholar ]
- Reser J, Morrissey S. (2009) The crucial role of psychological preparedness for disasters. InPsych: The Bulletin of the Australian Psychological Society 31(2): 14–15. [ Google Scholar ]
- Schonfeld DJ, Gurwitch RH. (2009) Addressing disaster mental health needs of children: Practical guidance for pediatric emergency health care providers. Clinical Pediatric Emergency Medicine 10(3): 208–215. [ Google Scholar ]
- Sharma R, Kumar V, Raja D. (2015) Disaster preparedness amongst women, the invisible force of resilience: A study from Delhi, India. International Journal of Health System & Disaster Management 3(3): 163–168. [ Google Scholar ]
- Simmons AN, Paulus MP, Thorp SR, et al. (2008) Functional activation and neural networks in women with posttraumatic stress disorder related to intimate partner violence. Biological Psychiatry 64(8): 681–690. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Udomratn P. (2008) Mental health and the psychosocial consequences of natural disasters in Asia. International Review of Psychiatry 20(5): 441–444. [ DOI ] [ PubMed ] [ Google Scholar ]
- US Department of Health and Human Services Centers for Disease Control and Prevention (2011) Public health preparedness capabilities: National standards for state and local planning. Available at: https://www.cdc.gov/phpr/readiness/capabilities.htm
- Witruk E, Lee Y, Otto K. (2014) Dealing with earthquake disaster on Java 2006: A comparison of affected and non-affected people. Indonesian Psychological Journal 29(3): 121–135. [ Google Scholar ]
- Zulch HR, Reser JP, Creed P. (2012) Psychological preparedness for natural disasters. In: Proceedings of the first international conference on urban sustainability and resilience, UCL, London, 5–6 November [ Google Scholar ]
- View on publisher site
- PDF (512.1 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Vitamin D and Depression: Where is all the Sunshine?
Sue penckofer , phd, rn, joanne kouba , phd, rd, mary byrn , bsn, rn, carol estwing ferrans , phd, rn, faan.
- Author information
- Copyright and License information
Address correspondence to Sue Penckofer, Loyola University—Chicago, School of Nursing, 2160 S. First Avenue, Maywood, IL 60153. [email protected]
Depression in its own right is a disabling condition impairing all aspects of human function. In persons with a chronic medical disease, depression often makes the management of chronic illness more difficult. Recently, vitamin D has been reported in the scientific and lay press as an important factor that may have significant health benefits in the prevention and the treatment of many chronic illnesses. Most individuals in this country have insufficient levels of vitamin D. This is also true for persons with depression as well as other mental disorders. Whether this is due to insufficient dietary intake, lifestyle (e.g., little outdoor exposure to sunshine), or other factors is addressed in this paper. In addition, groups at risk and suggested treatment for inadequate vitamin D levels are addressed. Effective detection and treatment of inadequate vitamin D levels in persons with depression and other mental disorders may be an easy and cost-effective therapy which could improve patients’ long-term health outcomes as well as their quality of life.
Depression is the leading cause of disability worldwide, affecting about 121 million people ( World Health Organization [WHO], 2008 ). In the United States, 14.8 million (or about 6.7%) adults have depression. Depression is the leading cause of disability for Americans between the ages of 15 and 44 ( National Institutes of Mental Health [NIMH], 2008 ). Currently, the WHO has determined that depression is ranked fourth on the global burden of disease list. The rates of depression continue to increase and the WHO predicts that it will be the second most common global burden of disease by the year 2020. Depression costs $36.6 billion and 225 million lost workdays each year in the United States ( NIMH, 2006 ).
DEPRESSION TREATMENT CONSIDERATIONS
Common treatments for depression include antidepressant medication and psychotherapy. Treatment for depression has been found to be successful 60 to 80% of the time; however, fewer than 25% of people with depression receive treatment ( WHO, 2008 ). When treatment is not successful, it is usually related to non-compliance with medication. Patients discontinue their medication due to unwanted side effects, financial reasons, fear of addiction, and the belief that the medication is no longer necessary. It has been reported that 42.4% of patients discontinue medication within 30 days of initiating treatment and 52.1% of patients discontinue medication within 60 days ( Olfson, Marcus, Tedeschi, & Wan, 2006 ).
Depression is considered a chronic or recurrent condition. People with a history of three prior episodes of major depression have a relapse rate of 70 to 80% and people with no prior history have a relapse rate of 20 to 30% ( Segal, Pearson, & Thase, 2003 ). In addition, persons who have less than an 85% adherence to the recommended medication treatment plan are at great risk for relapse ( Thase, 2003 ). Due to the high rate of patient medication discontinuation as well as the high rates of relapse, it is important to consider other factors that can be targeted to treat depression. One important factor needing examination is nutrition, particularly dietary supplements.
Evidence-based nutritional recommendations for persons with depression and other mental disorders have not been determined. Recently, Lakhan and Vieria (2008) reported on proposed nutritional deficiencies and treatments for persons with major depression, bipolar disorder, schizophrenia, and obsessive compulsive disorder ( Table 1 ). Others have reported on the association between depression and inadequate intakes of some selected nutrients such as folate ( Murakami et al., 2008 ; Payne et al., 2008 ), vitamin B12 ( Sanchez-Villegas et al., 2009 ), as well as selenium, iron, and zinc ( Bodnar & Wisner, 2005 ). In addition, intake of certain fatty acids suggests a possible beneficial effect on some mental disorders ( Sanchez-Villegas et al., 2007 ), and for treatment of depressive symptoms in middle-aged women ( Lucas, Asselin, Merette, Poulin & Dodin, 2009 ). Although vitamin D has recently gained widespread interest, little information relative to its impact on mental disorders is available.
Mental Disorders and Alternative Treatments
Note : Adapted with permission from Lakhan, S. E., & Viera, K.F. (2008) . Nutritional therapies for mental disorders. Nutrition Journal , 7(2): doi:10.1186/1475-2891-7-2.
GABA = gamma-aminobutyric, SAM = S-adenosylmethionine
It has been estimated that over one billion people have either vitamin D insufficiency or deficiency ( Holick, 2007 ). The best assessment of vitamin D is by a serum 25-hyroxyvitamin D (25-OH D) level ( Holick, 2006 ). Vitamin D deficiency is defined as a level less than 20 ng/mL and vitamin D insufficiency is a level less than 30 ng/mL ( Holick, 2007 ). The impact that vitamin D may have on disorders such as cancer, osteoporosis, cardiovascular disease, and, more recently, diabetes has been reported ( Holick, 2007 ; Lee, O’Keefe, Bell, Hensrud, & Holick, 2008 ; Penckofer, Kouba, Wallis, & Emanuele, 2008 ; Pittas, Lau, Hu, & Dawson-Hughes, 2007 ; Wallis, Penckofer, & Sizemore, 2008 ). Berk et al. (2007) reported that vitamin D deficiency may play a role in depression and possibly other mental disorders. In addition, they suggested that it could play a role in the supplementary treatment of depression. Another recent report summarized studies on vitamin D and mood disorders in women, suggesting that vitamin D may be an important nutrient for women’s physical and mental well being ( Murphy & Wagner, 2008 ).
RELATIONSHIPS BETWEEN VITAMIN D AND DEPRESSION AND OTHER MENTAL HEALTH DISORDERS
There has been research examining the relationship of vitamin D to seasonal affective disorder (SAD), schizophrenia, and depression. Several studies have examined whether light therapy improved mood. Partonen, Vakkuri, Lamberg-Allardt, and Lonnqvist (1996) randomized 29 patients (16 with SAD and 13 controls) in a parallel fashion to either one hour or 15 minutes of light therapy in the morning for two weeks in the winter. One hour of light therapy significantly decreased depressive symptoms more so in the group with SAD than the control group ( p = .003). Gloth, Alam, and Hollis (1999) randomized 15 participants with SAD to either 100,000 IU of vitamin D (one time dose) ( n = 8) or phototherapy ( n = 7). They reported that depression (assessed with the Hamilton Depression Scale) decreased in persons who received vitamin D (from 10.9 to 6.2, p = .040) as compared to those who received phototherapy (from 12.6 to 11.3, p = ns). There were no untoward side effects from the dose of vitamin D; however, a limitation of the study was the one time dose.
Studies have examined the relationship of vitamin D to other psychiatric disorders. In a prospective birth cohort that studied the intake of vitamin D supplements in the first year of life, it was noted that an intake of 2,000 IU or more per day was associated with a reduced risk of developing schizophrenia (RR = 0.23, CI = .06–.95) for males. The limitations of the study were that although there was a large sample (over 9,114 persons), the number of individuals with schizophrenia was small ( n = 79) ( McGrath et al., 2004 ). In addition, exposure to vitamin D was based on the mother’s self-report in the first year of life. Lower levels of vitamin D have been noted with other mental disorders. Schneider, Weber, Frensch, Stein, and Fritze (2000) reported that vitamin D levels were lower in persons with schizophrenia (Mean = 35.1 pg/ml) and major depression (37.3) when compared to healthy controls (45.9). However, the difference was lower only for those with schizophrenia when compared to the controls ( p < .02).
For other groups, the relationship of vitamin D and mood has been explored. In a cross sectional study of 80 older adults (40 mild Alzheimer and 40 nondemented), aged 60 to 92, more than half (58%) were noted to have vitamin D levels that were abnormally low. In addition, vitamin D deficiency was associated with the presence of an active mood disorder as assessed by the depressive symptoms inventory (Odds ratio: 11.69, p = .022) ( Wilkins, Sheline, Roe, Birge, & Morris, 2006 ). Interestingly, vitamin D category (sufficient, insufficient, and deficient) was not predictive of Alzheimer disease. For persons with the chronic illness of fibromyalgia ( n = 75), 69% were noted to have deficient or insufficient levels of vitamin D. Depression was higher (assessed with the Hospital and Anxiety Depression Scale [HADS] Median = 31) for those individuals with vitamin D deficiency when compared to those with insufficient (HADS = 22.5) or normal (HADS = 23.5) levels of vitamin D ( Armstrong et al., 2007 ). Finally, it has been reported that for persons with secondary hyperparathyroidism ( n = 21), lower serum vitamin D was significantly related to higher scores on the Beck Depression Inventory when compared to controls ( n = 63, p <.05) ( Jorde, Waterloo, Saleh, Haug, & Svartberg, 2006 ).
Recently, Hoogendijk et al. (2008) reported in a population-based cohort study of over 1,200 persons aged 65 and older, that levels of 25 (OH) D were 14% lower in persons with minor depression and 14% lower in persons with major depressive disorder when compared to controls ( p < .001). The Center for Epidemiologic Studies-Depression (CES-D) scale was used to assess for depression, and persons also had a psychiatric evaluation using the Diagnostic Interview Schedule to verify their mental status. Depression severity was associated with low serum 25 (OH) D ( p < .001), even after adjustment for age, sex, body mass index, smoking status, and the number of chronic conditions ( p = .01).
The mechanism whereby vitamin D may be associated with mental disorders is not clearly understood. It has been reported that there are vitamin D receptors in the hypothalamus, which may be important in neuroendocrine functioning ( Eyles, Smith, Kinobe, Hewison, & McGrath, 2005 ). Some investigators have reported that vitamin D is important for brain development ( Eyles, Brown, Mackay-Sim, McGrath, & Feron, 2003 ; McCann & Ames, 2008 ). Eyles et al. (2003) reported that when rats were born to vitamin D deficient mothers, this negatively affected the development of their brain in terms gross morphology, cellular proliferation, and growth factor signaling. They also had decreased expression of nerve growth factor. Although these types of changes have been noted in the brains of persons with schizophrenia-like disorders, they cautioned against drawing a strong inference since more research is needed to examine the long term consequences of vitamin D depletion on the brain.
EFFECTS OF VITAMIN D SUPPLEMENTATION ON MENTAL AND PHYSICAL WELL BEING
The use of vitamin D supplementation has been examined for its effects on mood outcomes, particularly in healthy persons. In one study ( Harris & Dawson-Hughes, 1993 ), 250 healthy women were randomized to daily vitamin D (400 IU) or a placebo for a period of one year. Both groups received supplemental calcium during the trial. Findings indicated no difference in mood scores (Profile of Mood States) between the two groups. In addition, changes in vitamin D levels were not correlated to changes in mood scores. Results suggested that the dose of vitamin D may have been insufficient to cause a significant treatment difference between groups. Lansdowne and Provost (1998) randomly assigned 44 healthy persons to varying doses of vitamin A plus one of the following: 400 IU of vitamin D/day or 800 IU of vitamin D/day, or a placebo for a period of five days. The Positive and Negative Affect Scale was used to assess mood at the end of the five days. Results showed enhanced positive affect for the vitamin D treatment groups when compared to the placebo group ( p < .001). In addition, although both vitamin D treatment groups experienced a reduction in negative affect when compared to the placebo group, it was not statistically significant. Although the study demonstrated positive benefits in persons who were healthy, the effect on persons with depression or mood problems was not explored.
Kenny, Biskup, Robbins, Marcella, and Burleson (2003) used a randomized trial to determine the benefit of cholecalciferol (1000 IU of D 3 ) or a placebo in elderly men (65 to 87). All patients received supplemental calcium. Results indicated that there was no effect on general, physical, and mental health outcomes. However, men who participated in the study were in excellent health and did not have vitamin D deficiency. Therefore, this may have affected the ability to detect a significant treatment effect. However, a relationship between vitamin D levels and mental health outcomes was found (r = 0.30, p = .025). Vieth, Kimball, Hu, and Walfish (2004) conducted a randomized trial that examined the effect of vitamin D supplementation on well being. Well being was measured using a brief questionnaire based on conventional depression screening tools. One group of patients ( n = 33) received 600 IU per day while the other group ( n = 33) received 4000 IU per day for three months. A significant improvement in well being over time in both groups was noted following treatment (December to February) ( p < .012). Although the group receiving the higher dose had a greater response than the lower dose group, the difference was not statistically significant.
More recently, the effect of vitamin D supplementation on symptoms of depression in overweight and obese persons was studied ( Jorde, Sneve, Figenschau, Svartberg, & Waterloo, 2008 ). For participants who participated in this clinical trial, they were randomized into one of three groups where vitamin D (20,000 IU cholecalciferol) was given twice per week, once per week, or not at all (placebo) for one year. All participants also received calcium supplementation (500 mg daily). Findings indicated that for the two groups that received vitamin D, there was a significant improvement in depression (using the Beck Depression Inventory) which was more pronounced in those with higher depression at baseline. Limitations of the study were that only overweight and obese adults were included, and participants did not have to have depression at baseline to participate.
Research indicates that vitamin D may improve many health outcomes, particularly cancer and osteoporosis ( Bischoff-Ferrari, 2007 ; Bouillon et al., 2006 ; Holick, 2007 ). A meta-analysis of randomized, controlled trials for vitamin D noted that intake of ordinary supplemental doses of vitamin D (from 300 IU to 2000 IU) was associated with a reduced risk of mortality (RR = 0.93, CI = 0.87–0.99) ( Autier & Gandini, 2007 ). However, a recent report by the Agency for Healthcare Research and Quality (2009) , which included 165 primary articles and 11 systematic reviews, reported that because of significant differences in the quality of the studies conducted, findings regarding vitamin D, calcium, or both nutrients on various health outcomes were inconsistent, and determining a dose-response relationship was difficult. For that reason, future placebo-controlled randomized trials will need to be conducted to examine the benefit of vitamin D supplementation on health outcomes targeted at life stages.
THE IMPACT OF SUNLIGHT ON VITAMIN D STATUS
Assessment of vitamin D status will need consideration of other factors, such as light therapy and sun exposure. Exposure to sunlight accounts for over 90% of the vitamin D requirement for most individuals ( Holick, 2004 ). Amount of exposure to ultraviolet B radiation is affected by latitude, season, and time of the day. It has been reported that sun exposure is greatest in spring to early fall and during sunlight hours ( Holick, 2004 ). Although places closer to the equator have greater sun exposure (Hawaii, Arizona, Florida), recently it has been reported that in even in these areas vitamin D insufficiency persists ( Binkley et al., 2007 ; Jacobs et al., 2008 ; Levis et al., 2005 ). Since it is possible that persons who are outdoors may be more physically active, it is important to consider whether sunshine alone or in combination with physical activity is related to improved mood.
Light therapy and exercise are two well known alternative treatments to depression. However, there are few studies that demonstrate a benefit from combining the two together. In one study, 98 participants were randomized to one of three groups: (a) aerobic training program in bright light, (b) aerobic training program in normal light, or (c) stretching/relaxation program in bright light ( Leppamaki, Partonen, Hurme, Haukka, & Lonnqvist, 2002 ). There was an improvement in depression scores ( p = .05) and atypical symptoms of depression (carbohydrate craving, weight gain, social avoidance, increased appetite, fatigue, afternoon slump, and increased need for sleep) ( p = .02) for those exposed to bright light. Although people who exercised in normal light had an improvement in depression ( p = .02), there was no significant improvement in the atypical symptoms of depression. Therefore, the bright light may be important for improvement of atypical depression symptoms.
It may be beneficial to exercise outdoors with increased exposure to natural sunlight. A tri-modal intervention (LEVITY) which targeted mood and included (1) a brisk 20-minute outdoor walk five days per week, (2) increased light exposure, and (3) a special vitamin regimen (thiamine, pyroxidine, riboflavin, folic acid, selenium, and vitamin D), was tested in healthy women, aged 19 to 78, who reported mild to moderate depressive symptoms (scores between 11 and 29 on the CES-D) ( Brown, Goldstein-Shirley, Robinson, & Casey, 2001 ; Brown & Shirley, 2005 ). Women were randomized to the treatment group ( n = 53) or the control group (who only received placebo vitamins) ( n = 51) and received the intervention for eight weeks. Both groups improved over time on all measures. Although the control group scores were worse at baseline despite the randomization, after controlling for baseline differences, the improvement in mood, overall well being, self esteem, happiness, and depression was significantly greater in the group that received the tri-modal intervention.
Mind, a charity group in the United Kingdom, has recommend Ecotherapy as a treatment to depression. Ecotherapy involves exercising outdoors instead of inside a facility. A research study was done with 20 people each walked outside and at an indoor shopping center ( Mind, 2007 ). Participants then rated their feelings of self-esteem, depression, and tension after both walks. Improvements were greater when walking outdoors as compared to walking indoors (self-esteem: 90% vs. 17%, depression: 71% vs. 45%, and tension: 71% vs. 28%, respectively) ( Mind, 2007 ). Lack of information regarding specific measurements and methods used for data collection are significant limitations of this report.
Exercise involving exposure to natural sunlight is a new development in alternative treatment to depression. Combining exercise and light therapy can easily be accomplished by encouraging people to exercise outdoors during daylight hours. However, the benefit of exercise with natural sunlight exposure needs to be weighed against the risk of skin cancer if sun exposure is significant. Therefore, additional research is needed in this area.
IMPACT OF OTHER FACTORS ON VITAMIN D STATUS
Individuals obtain vitamin D either exogenously, from dietary sources, or endogenously, from activation of a subcutaneous vitamin D precursor by ultraviolet rays ( Holick, 2006 ). Dietary sources can be obtained through (a) naturally-occurring vitamin D in foods, (b) fortification of foods with vitamin D, and (c) a vitamin D supplement. As vitamin D is a fat-soluble nutrient, metabolism requires normal digestion and absorption of fat. Subcutaneous synthesis is stimulated by exposure to sunlight though this effect varies based on the amount and duration of exposure, latitude, season, and race ( Centers for Disease Control and Prevention [CDC], 2008 ).
Optimal vitamin D status is hampered by several factors. The limited number of naturally rich foods with this nutrient causes some groups to be at risk for inadequacy ( Whiting & Calvo, 2006 ). The optimal daily requirement for various age groups is under scientific debate ( CDC, 2008 ). The current Adequate Intake (AI), which is part of the Dietary Reference Intakes (DRIs), is 200 IU/day for both women and men from infancy to age 50; 400 IU/day for those between 51–70 years; and 600 IU/day for those >70 years ( Otten, Hellwig, & Meyers, 2006 ). Recently, the American Academy of Pediatrics recommended increasing the daily intake of vitamin D to 400 IU/day for all infants, children, and adolescents ( Wagner, Green, & the Section on Breast Feeding and Committee on Nutrition, 2008 ).
Effective methods to ensure adequate nutrient delivery for all age groups are an issue. Vieth (1999) has suggested a range of 800–1,000 IU/day for elderly individuals and possibly even as high as 4,000 IU/day for some. Heaney (2000) recommends 1,000 IU/day routinely for elderly patients seen in an osteoporosis clinic. Other reports have suggested that optimal oral D 3 intake be in the range of 400–1,600 IU/day with individual variation possibly due to adipose mass and other metabolic conditions ( Arunabh, Pollack, Yes, & Aloia, 2003 ; Dawson-Hughes et al., 2005 ; Heaney, 2000 ; Wortsman, Matsuoka, Chen, Lu, & Holick, 2000 ). The Institute of Medicine (2009) has appointed a committee to make recommendations related to revised vitamin D DRIs. This is important as current recommendations are based on the amount needed to prevent rickets ( Cashman, 2007 ; Cashman et al., 2008 ; Vieth et al., 2007 ; Whiting & Calvo, 2005 ).
ASSESSMENT AND GROUPS AT RISK FOR LOW VITAMIN D
The signs and symptoms of vitamin D deficiency vary depending on the age and severity. For children, there has been a reappearance of rickets from vitamin D deficiency. Symptoms of rickets can vary and may include bone pain, delayed tooth eruption, and poor growth ( Misra et al., 2008 ). Deficient adults may experience muscle weakness, bone pain, difficulty walking, and frequent falls ( Holick 2007 ; Powell & Greenberg, 2006 ). Persons more at risk for vitamin D include those with malabsorption syndromes such as inflammatory bowel disease, celiac disease, and chronic diarrhea ( Wallis, Penckofer, & Sizemore, 2008 ).
Other factors may influence the availability and metabolism of this nutrient. Thus, various population groups have been identified as high risk for vitamin D insufficiency or deficiency. Those with limited sun exposure, due to being homebound, living in latitudes >34° north or south, and/or clothing that covers most of the body, are at risk for vitamin D deficiency ( Office of Dietary Supplements [ODS], 2009 ). Similarly, older adults are often at risk of vitamin D inadequacy. This is due to reduced subcutaneous production and intestinal absorption ( Whiting & Calvo, 2005 ). When coupled with limited sun exposure, which is the case for many older adults, the risk increases ( Heaney, 2006 ).
Findings from the National Health and Nutrition Examination Survey (NHANES-III, 1988–1994), which included more than 15,000 adults, indicated significantly lower levels of vitamin D for female than male participants. In addition, vitamin D levels were highest in whites, followed by Hispanics and then African Americans ( Zadshir, Tareen Pan, Norris, Martins, 2005 ). More recent findings from NHANES (2001–2004) have indicated that these differences race continue to exist for vitamin D insufficiency ( Ginde, Liu, & Camargo, 2009 ). For individuals who have darker skin, decreased vitamin D is more common. Due to higher melanin levels, dark-skinned individuals experience reduced subcutaneous vitamin D synthesis compared to those with lighter pigmentation, making them another high risk group for vitamin D deficiency ( Harris, 2006 ).
For infants, breast feeding is highly recommended; however, human milk is a poor source of vitamin D, making deficiency a concern for breast-fed infants. The American Academy of Pediatrics recommends that infants who are solely or partially breast-fed receive 400 IU/day of vitamin D within the first few days until consuming adequate amounts of another vitamin D fortified formula or whole milk ( Wagner et al., 2008 ).
In healthy adolescents, vitamin D deficiency has been noted as a common finding in the United States and abroad ( Das, Crocombe, McGrath & Mughal, 2006 ; Gordon, DePeter, Feldman, Grace, & Emans, 2004 ). Similar to findings for adults, African American adolescents and girls experience a higher prevalence of vitamin D deficiency than white or Asian adolescents and boys ( Gordon et al., 2004 ). Dietary habits inversely related to vitamin D deficiency were consumption of milk and ready-to-eat cereals; whereas soda, juice, and iced tea intake were positively correlated to vitamin D deficiency ( Gordon et al., 2004 ). Adolescents also may be prone to vitamin D deficiency because of obesity.
Obesity has been found to be inversely related to vitamin D level ( Arunabh et al., 2003 ; McGill, Stewart, Lithander, Strik & Poppitt, 2008 ; Wortsman, Matsuoka, Chen, Lu, & Holick, 2000 ). This may be due to excess adipose tissue that sequesters vitamin D thereby altering its release into circulation ( Wortsman et al., 2000 ). Body image concerns may also cause obese individuals to avoid skin exposure to the sun resulting in inadequate vitamin D levels ( McGill et al., 2008 ). Obesity is associated with insulin resistance, and there is evidence to suggest that vitamin D may be important in the prevention of diabetes ( Pittas, Lau, Hu, & Dawson-Hughes, 2007 ). There is also evidence to suggest that vitamin D may be important in the treatment and prevention of complications associated with diabetes ( Penckofer et al., 2008 ).
TREATMENT AND PRACTICE IMPLICATIONS FOR INADEQUATE VITAMIN D
Sunshine has been suggested as an approach to maintain healthy vitamin D levels. Holick (2004) reported that sun exposure to the arms and legs for five to ten minutes, two or three times per week, may be beneficial for maintaining vitamin D sufficiency. However, because the time of day, season, and latitude influence sunlight absorption and thus, the amount of vitamin D produced, it becomes difficult to make universal recommendations. In addition, because the risk of skin cancer is associated with unprotected sun exposure, it is usually not recommended for treatment of inadequate vitamin D levels.
Nutritional sources of vitamin D are limited. Two forms of vitamin D are found in foods naturally ( Holick, 2007 ). Certain fatty fish, fish oils, and eggs are some of the richest sources of Vitamin D 3 , or cholecalciferol without fortification. Vitamin D 2 , or ergocalciferol, is found in some mushrooms. Vitamin D content of foods is lacking in commonly used databases ( Holden & Lemar, 2008 ). The USDA Nutrient Data Laboratory is currently collaborating with experts to update existing information including evaluation of optimal analytical methods ( Holden, 2008 ). Table 2 summarizes both naturally-occurring and fortified food sources of vitamin D based on currently available information. It is anticipated that these resources will be expanded in the near future.
Vitamin D Content of Selected Foods
Based on a Daily Value = 400 IU for adults and children older than 4 years old. Food labels are not required to list vitamin D content unless fortified.
Examples of ready-to-eat cereals fortified with vitamin D include: Corn Chex ® , Cherrios ® , Wheaties ® , Special K ® , Product 19 ® , and Corn Flakes ® . Many others are available and identified by reading the nutrition facts labels on food packages.
General Mills product information retrieved February 4, 2009, from http://www.generalmills.com/corporate/brands/brand.aspx?catID = 50amp;groupID = 19412
Kellogg product information retrieved February 2, 2009, from http://www2.kelloggs.com/Product/FoodCategory.aspx?id = cereal
United States Department of Agriculture. National Nutrient Database for Standard Reference, Release 21 (2008). Retrieved February 4, 2009, from http://www.nal.usda.gov/fnic/foodcomp/cgi-bin/nut_search_new.pl
Weihrauch, J. L., & Tamaki, J., (1999, March). Provisional table on the vitamin D content of foods, United Stated Department of Agriculture, Human Nutrition Information Service, HNIS/PT-108.
Yoplait product information retrieved February 4, 2009, from http://www.yoplait.com/products_original.aspx mcg = microgram, IU = International Unit, 1 mcg = 40 IU
In the United States, vitamin D fortification is required for nonfat dry and evaporated milk, and is optional, but common, for fluid milk at a maximum level of 400 IU/quart ( Rover & O’Brien, 2008 ). Other foods with optional fortification status and that are commonly available are many ready-to-eat cereals, and some juices, yogurt, farina, pastas, and margarines ( Rover & O’Brien, 2008 ). Because only some foods are fortified with vitamin D, and since food manufacturers frequently change product formulations, including vitamin fortification, patients should be encouraged to read the nutrition facts label on a regular basis in making food choices. The success of food fortification in treating other diseases, namely pellagra with niacin and neural tube defects with folate, has lead to consideration of enhanced vitamin D food fortification. This might include expanded optional and/or mandatory fortification (similar to folate in grain products) ( Vieth et al., 2007 ; Whiting & Calvo, 2006 ). Since cheese is commonly used in foods prepared at and away from home, food scientists are in the process of developing ways to use this popular food as a new source of vitamin D fortification ( Johnson et al., 2005 ). While interesting options for food fortification are being investigated, the most effective or acceptable strategies have not been determined.
For many persons, sunshine or diet alone will not be sufficient in providing adequate amounts of vitamin D. There is evidence to suggest that supplementation may be necessary. Supplemental doses that provide the AI (400–600 IU vitamin D/day) result in small increases in serum 25 (OH) D levels but may not be adequate to correct deficiency in a timely manner or optimize vitamin D nutrition ( Talwar, Aloia, Pollack, & Yeh, 2007 ; Vieth et al., 2007 ). Holick recommends a standard supplementation protocol for non-pregnant adults to treat vitamin D deficiency using a two-phase protocol. The initial phase is a single 50,000 IU vitamin D 2 capsule weekly, for eight weeks ( Holick, 2007 ). After the initial phase, serum 25 (OH) D levels should be evaluated and ideally be >30 ng/ml. If this minimal serum level has not been achieved, then the initial phase may need to be repeated. The second phase is a 50,000 IU vitamin D 2 capsule every one to four weeks ongoing.
In African American post-menopausal women, Talwar et al. (2007) developed an algorithm of vitamin D 3 supplementation to achieve optimal serum concentrations. They suggested a dose of 2,800 IU/d if serum 25 (OH) D was >18 ng/ml or 4,000 IU/d if serum 25 (OH) D was <18 ng/ml. Correction of deficiency may vary in those with malabsorption and/or nephrotic syndromes, obesity, or medication use that activates steriod or xenobiotic receptors ( Holick, 2007 ). Hyperparathyroidism or granulomatous disorders also require special consideration in treating vitamin D deficiency. Specific vitamin D recommendations for those with diabetes, with or without vitamin D deficiency, have yet to be determined ( Pittas et al., 2007 ).
Discussions of revised recommendations are often accompanied by cautionary words related to prevention of toxicity ( Heaney, 2000 ). Clinical manifestations of vitamin D toxicity include nonspecific symptoms of nausea, vomiting, poor appetite, constipation, and weakness ( ODS, 2009 ). Vitamin D toxicity is an elevated vitamin D level greater than 150 ng/dl. The normal upper limit has been considered to be 55 to 60 ng/ml, but is being re-evaluated as levels up to 125 ng/dl have been reported without adverse effects ( Holick, 2006 ). Serum calcium levels should be monitored with administration of vitamin D as toxicity is associated with hypercalcemia which may cause mental status changes and irregular heart rhythms ( ODS, 2009 ). Therefore, treatment of deficiency and supplementation should be coupled with appropriate medical supervision and monitoring.
As previously discussed, those groups who are at risk for vitamin D deficiency include the elderly, adolescents, obese individuals, and those with chronic illnesses (e.g., diabetes). Interestingly, it is these same groups that have also been reported to be at risk for depression ( CDC, 2009 ; Lemstra et al., 2008 ; Lustman, Penckofer, & Clouse, 2008 ; Strine et al., 2008 ). The role that vitamin D supplementation could play in the prevention and treatment of depression has not been studied and should be an important area of future research. If exercising outdoors in the sunshine, eating foods rich in vitamin D, and/or taking dietary supplements to improve vitamin D deficiency could improve one’s mental well being, it would be a simple and cost-effective solution for many who are at risk for depression and possibly other mental disorders.
Acknowledgments
Funding for this article was provided by Loyola University School of Nursing Research Funds, NINR/NIH (NR009240), & NIDDK/NIH-sponsored DRTC at the University of Chicago.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Contributor Information
Sue Penckofer, Loyola University Chicago, School of Nursing, Maywood, Illinois, USA.
Joanne Kouba, Loyola University Chicago, School of Nursing, Maywood, Illinois, USA.
Mary Byrn, Loyola University Chicago, School of Nursing, Maywood, Illinois, USA.
Carol Estwing Ferrans, University of Illinois Chicago, College of Nursing, Chicago, Illinois, USA.
- Agency for Healthcare Research and Quality. Vitamin D and Calcium: Systematic review of health outcomes. 2009 Evidence Report (AHRQ Publication No. 09-E015). Retrieved August 27, 2009, from www.ahrq.gov/tp/vitacaltp.htm .
- Armstrong DJ, Meenagh GK, Bickle I, Lee ASH, Curran ES, Finch MB. Vitamin D deficiency is associated with anxiety and depression in fibromyalgia. Clinical Rheumatology. 2007;26:551–554. doi: 10.1007/s10067-006-0348-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- Arunabh S, Pollack S, Yes J, Aloia JF. Body fat content and 25-hydroxvitamin D levels in healthy women. Journal of Clinical Endocrinology & Metabolism. 2003;88:157–161. doi: 10.1210/jc.2002-020978. [ DOI ] [ PubMed ] [ Google Scholar ]
- Autier P, Gandini S. Vitamin D supplementation and total mortality: A meta-analysis of randomized controlled trials. Archives of Internal Medicine. 2007;167:1730–1737. doi: 10.1001/archinte.167.16.1730. [ DOI ] [ PubMed ] [ Google Scholar ]
- Berk M, Sanders KM, Pasco JA, Jacka FN, Williams LJ, Hayles AL, Dodd S. Vitamin D deficiency may play a role in depression. Medical Hypotheses. 2007;69:1316–1319. doi: 10.1016/j.mehy.2007.04.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- Binkley N, Novotny R, Krueger D, Kawahara T, Daida YG, Lensmeyer B, Hollis BW, Drezner MK. Low vitamin D status despite abundant sun exposure. Journal of Clinical Endocrinology & Metabolism. 2007;92(6):2130–2135. doi: 10.1210/jc.2006-2250. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bischoff-Ferrari HA. The 25-hydroxyvitamin D threshold for better health. Journal of Steroid Biochemistry & Molecular Biology. 2007;103:614–619. doi: 10.1016/j.jsbmb.2006.12.016. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bodnar LM, Wisner KL. Nutrition and depression: Implications for improving mental health among childbearing-aged women. Biological Psychiatry. 2005;58:679–685. doi: 10.1016/j.biopsych.2005.05.009. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bouillon R, Eelen G, Verlinden L, Mathieu C, Carmeliet G, Verstuyf A. Vitamin D and cancer. Journal of Steroid Biochemistry & Molecular Biology. 2006;102:156–162. doi: 10.1016/j.jsbmb.2006.09.014. [ DOI ] [ PubMed ] [ Google Scholar ]
- Brown M, Goldstein-Shirley J, Robinson J, Casey S. The effects of a multi-modal intervention trial of light, exercise, and vitamins on women’s mood. Women & Health. 2001;34(3):93–112. doi: 10.1300/J013v34n03_06. [ DOI ] [ PubMed ] [ Google Scholar ]
- Brown MA, Shirley JL. Enhancing women’s mood and energy: A research-based program for subthreshold depression using light, exercise, and vitamins. Holistic Nursing Practice. 2005;19(6):278–284. doi: 10.1097/00004650-200511000-00009. [ DOI ] [ PubMed ] [ Google Scholar ]
- Cashman KD. Vitamin D in childhood and adolescence. Postgraduate Medicine. 2007;83:230–235. doi: 10.1136/pgmj.2006.052787. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cashman KD, Hill TR, Lucey AJ, Taylor N, Seamans KM, Muldowney S, FitzGerald AP, Flynn A, Barnes MS, Horigan G, Bonham MP, Duffy EM, Strain JJ, Wallace JMW, Kiely M. Estimation of the dietary requirement for vitamin D in healthy adults. American Journal of Clinical Nutrition. 2008;88(6):1535–1542. doi: 10.3945/ajcn.2008.26594. [ DOI ] [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention. National report on biochemical indicators of diet and nutrition in the U.S. population 1999–2002. 2008 Retrieved September 12, 2008, from http://www.cdc.gov/nutritionreport .
- Centers for Disease Control and Prevention. Health information for older adults. 2009 Retrieved February 10, 2009, from http://www.cdc.gov/aging/info.htm.
- Das G, Crocombe S, McGrath M, Berry JL, Mughal MZ. Hypovitaminosis D among healthy adolescent girls attending an inner city school. Archives of Disease in Childhood. 2006;91:569–572. doi: 10.1136/adc.2005.077974. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R. Estimates of optimal vitamin D status. Osteoporosis International. 2005;16:713–716. doi: 10.1007/s00198-005-1867-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- Eyles D, Brown J, Mackay-Sim A, McGrath J, Feron F. Vitamin D3 and brain development. Neuroscience. 2003;118:641–653. doi: 10.1016/s0306-4522(03)00040-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Eyles DW, Smith S, Kinobe R, Hewison M, McGrath JJ. Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. Journal of Chemical Neuroanatomy. 2005;29:21–30. doi: 10.1016/j.jchemneu.2004.08.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ginde AA, Liu MC, Camargo CA. Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Archives of Internal Medicine. 2009;169:626–632. doi: 10.1001/archinternmed.2008.604. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gloth FM, Alam W, Hollis B. Vitamin D vs broad spectrum phototherapy in the treatment of seasonal affective disorder. Journal of Nutrition, Health, & Aging. 1999;3(1):5–7. [ PubMed ] [ Google Scholar ]
- Gordon CM, DePeter KC, Feldman HA, Grace E, Emans J. Prevalence of vitamin D deficiency among health adolescents. Archives of Pediatric & Adolescent Medicine. 2004;158:531–537. doi: 10.1001/archpedi.158.6.531. [ DOI ] [ PubMed ] [ Google Scholar ]
- Harris S. Vitamin D and African Americans. Journal of Nutrition. 2006;136:1126–1129. doi: 10.1093/jn/136.4.1126. [ DOI ] [ PubMed ] [ Google Scholar ]
- Harris S, Dawson-Hughes B. Seasonal mood changes in 250 normal women. Psychiatry Research. 1993;49:77–87. doi: 10.1016/0165-1781(93)90031-b. [ DOI ] [ PubMed ] [ Google Scholar ]
- Heaney RP. Vitamin D: How much do we need, and how much is too much? Osteoporosis International. 2000;11:553–555. doi: 10.1007/s001980070074. [ DOI ] [ PubMed ] [ Google Scholar ]
- Heaney RP. Barriers to optimizing vitamin D3 intake for the elderly. Journal of Nutrition. 2006;136:1123–1125. doi: 10.1093/jn/136.4.1123. [ DOI ] [ PubMed ] [ Google Scholar ]
- Holden JM, Lemar LE. Assessing vitamin D contents in foods and supplements: Challenges and needs. American Journal of Clinical Nutrition. 2008;88(2):551S–553S. doi: 10.1093/ajcn/88.2.551S. [ DOI ] [ PubMed ] [ Google Scholar ]
- Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune disease, cancers, and cardiovascular disease. American Journal of Clinical Nutrition. 2004;80(S):1678S–1688S. doi: 10.1093/ajcn/80.6.1678S. [ DOI ] [ PubMed ] [ Google Scholar ]
- Holick MF. Chapter 20: Vitamin D. In: Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ, editors. Modern nutrition in health and disease. 10th ed. Baltimore, MD: Lippincott Williams and Wilkins; 2006. pp. 376–395. [ Google Scholar ]
- Holick MF. Vitamin D deficiency. The New England Journal of Medicine. 2007;357:266–281. doi: 10.1056/NEJMra070553. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hoogendijk WJG, Lips P, Dik MG, Deeg DJH, Beekman ATF, Penninx BWJH. Depression is associated with decreased 25-hydroxyvitamin D and increased parathyroid hormone levels in older adults. Archives of General Psychiatry. 2008;65(5):508–512. doi: 10.1001/archpsyc.65.5.508. [ DOI ] [ PubMed ] [ Google Scholar ]
- Institute of Medicine. Projects: dietary reference intakes for vitamin D and calcium. 2009. Retrieved February 11, 2009, from http://www.iom.edu/CMS/3788/61170.aspx . [ Google Scholar ]
- Jacobs ET, Alberts DS, Foote JA, Green SB, Hollis BW, Yu Z, Martinez ME. Vitamin D deficiency in southern Arizona. American Journal of Clinical Nutrition. 2008;87(3):608–613. doi: 10.1093/ajcn/87.3.608. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Johnson JL, Mistry VV, Vukovich MD, Hogle-Lorenzen T, Hollis BW, Specker BL. Bioavailability of vitamin D from fortified process cheese and effects on vitamin D status in the elderly. Journal of Dairy Science. 2005;88:2295–2301. doi: 10.3168/jds.S0022-0302(05)72907-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- Jorde R, Sneve M, Figenschau Y, Svartberg J, Waterloo K. Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: Randomized double blind trial. Journal of Internal Medicine. 2008;264:599–609. doi: 10.1111/j.1365-2796.2008.02008.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Jorde R, Waterloo K, Saleh F, Haug E, Svartberg J. Neuropsychological function in relation to serum parathyroid hormone and serum 25-hydroxvitamin D levels: The Tromso Study. Journal of Neurology. 2006;253:464–470. doi: 10.1007/s00415-005-0027-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kenny AM, Biskup B, Robbins B, Marcella G, Burleson JA. Effects of vitamin D supplementation on strength, physical function, and health perception in older, community-welling men. Journal of the American Geriatrics Society. 2003;51:1762–1767. doi: 10.1046/j.1532-5415.2003.51561.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lakhan SE, Viera KF. Nutritional therapies for mental disorders. Nutrition Journal. 2008;7(2) doi: 10.1186/1475-2891-7-2. doi:10.1186/1475-2891-7-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Landsdowne ATG, Provost SC. Vitamin D3 enhances mood in healthy subjects during winter. Psychopharmacology. 1998;135:319–323. doi: 10.1007/s002130050517. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lee JH, O’Keefe JH, Bell D, Hensrud DD, Holick MF. Vitamin D deficiency: And important, common, and easily treatable cardiovascular risk factor? Journal of the American College of Cardiology. 2008;52:1949–1956. doi: 10.1016/j.jacc.2008.08.050. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lemstra M, Neudorf C, D’Arcy C, Kunst A, Warren LM, Bennett NR. A systematic review of depressed mood and anxiety by SES in youth aged 10–15 years. Canadian Journal of Public Health. 2008;99(2):125–129. doi: 10.1007/BF03405459. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Leppamaki S, Partonen T, Hurme J, Haukka J, Lonnqvist J. Randomized trial of the efficacy of bright-light exposure and aerobic exercise on depressive symptoms and serum lipids. Journal of Clinical Psychiatry. 2002;63(4):316–321. [ PubMed ] [ Google Scholar ]
- Levis S, Gomez A, Jimenez C, Veras L, Ma F, Lai S, Hollis B, Roos BA. Vitamin D deficiency and seasonal variation in an adult south Florida population. The Journal of Endocrinology & Metabolism. 2005;90(3):1557–1562. doi: 10.1210/jc.2004-0746. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lucas M, Asselin G, Merette C, Poulin M-J, Dodin S. Ethyleicosapentaenoic acid for the treatment of psychological distress and depressive symptoms in middle-aged women: A double-blind placebo-controlled, randomized trial. American Journal of Clinical Nutrition. 2009;89:641–651. doi: 10.3945/ajcn.2008.26749. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lustman P, Penckofer S, Clouse R. Recent advances in understanding depression adults with diabetes? Current Diabetes Report. 2008;7:114–122. doi: 10.1007/s11892-007-0020-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McCann JC, Ames BN. Is there convincing biological or behavioral evidence linking vitamin D deficiency to brain dysfunction? FASEB Journal. 2008;22:982–1001. doi: 10.1096/fj.07-9326rev. [ DOI ] [ PubMed ] [ Google Scholar ]
- McGill AT, Stewart JM, Lithander FE, Strik CM, Poppitt SD. Relationships of low serum vitamin D3 with anthropometry and markers of the metabolic syndrome and diabetes in overweight and obesity. Nutrition Journal. 2008;7(4) doi: 10.1186/1475-2891-7-4. doi: 10.1186/1475–2891-7–4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McGrath J, Saari K, Hakko H, Jokelainen J, Jones P, Jarvelin MR, Chant D, Isohanni M. Vitamin D supplementation during the first year of life and risk of schizophrenia: A Finnish birth cohort study. Schizophrenia Research. 2004;67(3):237–245. doi: 10.1016/j.schres.2003.08.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- Mind Ecotherapy: The green agenda for mental health. 2007 Retrieved September 2, 2008, from www.mind.org.uk/mindweek . [ Google Scholar ]
- Misra M, Pacaud D, Petryk A, Collett-Solberg P, Kappy M. Vitamin D deficiency in children and its management: Review of current knowledge and recommendations. Pediatrics. 2008;122(2):398–417. doi: 10.1542/peds.2007-1894. [ DOI ] [ PubMed ] [ Google Scholar ]
- Murakami K, Mizoue T, Sasaki S, Ohta M, Sato M, Matusushita Y, Mishima N. Dietary intake of folate, other B vitamins, and omega-3 polyunsaturated fatty acids in relation to depressive symptoms in Japanese adults. Nutrition. 2008;24(2):140–147. doi: 10.1016/j.nut.2007.10.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- Murphy PK, Wagner CL. Vitamin D and mood disorders among women: An integrative review. Journal of Midwifery & Women’s Health. 2008;53(5):440–446. doi: 10.1016/j.jmwh.2008.04.014. [ DOI ] [ PubMed ] [ Google Scholar ]
- National Institute of Mental Health. Bipolar disorder exacts twice depression’s toll in workplace, productivity lags even after mood lifts. 2006 Retrieved July 29, 2008, from http://www.nimh.nih.gov/science-news/2006/bipolar-disorder-exacts-twice-depressions-toll-in-workplace-productivity-lags-even-after-mood-lifts.shtml .
- National Institute of Mental Health. The numbers count: Mental disorders in America. 2008 Retrieved July 29, 2008, from http://www.nimh.nih.gov/health/publications/the-numbers-count-mental-disorders-in-america/index.shtml .
- Office of Dietary Supplements. Dietary supplement fact sheet: Vitamin D (Updated 9/11/2009) Retrieved October 20, 2009, from http://ods.od.nih.gov/factsheets/VitaminD_pf.asp .
- Olfson M, Marcus SC, Tedeschi M, Wan GJ. Continuity of antidepressant treatment for adults with depression in the United States. American Journal of Psychiatry. 2006;163:101–108. doi: 10.1176/appi.ajp.163.1.101. [ DOI ] [ PubMed ] [ Google Scholar ]
- Otten JJ, Hellwig JP, Meyers LD, editors. Dietary reference intakes: The essential guide to nutrient requirements. Washington, DC: National Academies Press; 2006. [ Google Scholar ]
- Partonen T, Vakkuri O, Lamberg-Allardt C, Lonnqvist J. Effects of bright light on sleepiness, melatonin, and 25-hydroxyvitamin D3 in winter seasonal affective disorder. Biological Psychiatry. 1996;39:865–872. doi: 10.1016/0006-3223(95)00294-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- Payne ME, Jamerson BD, Potocky CF, Ashley-Koch AE, Speer MC, Steffens DC. Natural food folate and late-life depression. Journal of American Dietetic Association. 2008;108(9):A35. doi: 10.1080/01639360903417181. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Penckofer S, Kouba J, Wallis DE, Emanuele MA. Vitamin D and diabetes: Let the sunshine in. Diabetes Educator. 2008;34(6):939–954. doi: 10.1177/0145721708326764. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pittas AG, Lau J, Hu FB, Dawson-Hughes B. Review: The role of vitamin D and calcium in Type 2 diabetes. A systematic review and meta-analysis. Journal of Clinical Endocrinology & Metabolism. 2007;92:2017–2029. doi: 10.1210/jc.2007-0298. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Powell HS, Greenberg D. Tackling vitamin D deficiency. Post-graduate Medicine. 2006;119:25–30. doi: 10.3810/pgm.2006.06.1637. [ DOI ] [ PubMed ] [ Google Scholar ]
- Rover AJ, O’Brien KO. Hypovitaminosis D among healthy children in the United States. Archives of Pediatric & Adolescent Medicine. 2008;162(6):513–519. doi: 10.1001/archpedi.162.6.513. [ DOI ] [ PubMed ] [ Google Scholar ]
- Sanchez-Villegas A, Doreste J, Schlatter J, Pla J, Bes-Rastrollo M, Martinez-Gonzalez MA. Association between folate, vitamin B (6), and vitamin B (12) intake and depression in the SUN cohort study. Journal of Human Nutrition & Dietetics. 2009;22(2):122–133. doi: 10.1111/j.1365-277X.2008.00931.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Sanchez-Villegas A, Henriquez P, Figueiras A, Ortuno F, Lahortiga F, Martinez-Gonzalez MA. Long chain omega-3 fatty acids intake, fish consumption and mental disorders in the SUN cohort. European Journal of Nutrition. 2007;46:337–346. doi: 10.1007/s00394-007-0671-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Schneider B, Weber B, Frensch A, Stein J, Fritze J. Vitamin D in schizophrenia, major depression and alcoholism. Journal of Neural Transmission. 2000;107:839–842. doi: 10.1007/s007020070063. [ DOI ] [ PubMed ] [ Google Scholar ]
- Segal Z, Pearson J, Thase M. Challenges in preventing relapse in major depression: Report of a National Institute of Mental Health workshop on state of the science of relapse prevention in major depression. Journal of Affective Disorders. 2003;77(2):97–108. doi: 10.1016/s0165-0327(02)00112-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- Strine TW, Mokdad AH, Dube SR, Balluz LS, Gonzalez O, Berry JT, Manderscheid R, Kroenke K. The association of depression and anxiety with obesity and unhealthy behaviors across community dwelling US adults. General Hospital Psychiatry. 2008;30:127–137. doi: 10.1016/j.genhosppsych.2007.12.008. [ DOI ] [ PubMed ] [ Google Scholar ]
- Talwar SA, Aloia JF, Pollack S, Yeh JK. Does response to vitamin D supplementation among postmenopausal African American women. American Journal of Clinical Nutrition. 2007;86:1657–1662. doi: 10.1093/ajcn/86.5.1657. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thase M. Achieving remission and managing relapse in depression. Journal of Clinical Psychiatry. 2003;64(suppl 18):3–7. [ PubMed ] [ Google Scholar ]
- Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. American Journal of Clinical Nutrition. 1999;69:842–856. doi: 10.1093/ajcn/69.5.842. [ DOI ] [ PubMed ] [ Google Scholar ]
- Vieth R, Bischoff-Ferrari H, Boucher BJ, Dawson-Hughes B, Garland CF, Heaney RP, Holick MF, Hollis BW, Lamberg-Allardt C, McGrath JJ, Norman AW, Scragg R, Shiting SJ, Willett WC, Zittermann A. The urgent need to recommend an intake of vitamin D that is effective. American Journal of Clinical Nutrition. 2007;85:649–650. doi: 10.1093/ajcn/85.3.649. [ DOI ] [ PubMed ] [ Google Scholar ]
- Vieth R, Kimball S, Hu A, Walfish PG. Randomized comparison of the effects of the vitamin D3 adequate intake versus 100 mcg (4000 IU) per day on biochemical responses and the well being of patients. Nutrition Journal. 2004;3(8) doi: 10.1186/1475-2891-3-8. doi: 10.1186/1475-2891-3-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wagner CL, Greer FR the Section on Breastfeeding and Committee on Nutrition. Prevention of Rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142–1152. doi: 10.1542/peds.2008-1862. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wallis DE, Penckofer S, Sizemore GW. The “sunshine deficit” and cardiovascular disease. Circulation. 2008;118:1476–1485. doi: 10.1161/CIRCULATIONAHA.107.713339. [ DOI ] [ PubMed ] [ Google Scholar ]
- Whiting SJ, Calvo MS. Dietary recommendations to meet both endocrine and autocrine needs of vitamin D. Journal of Steroid Biochemistry & Molecular Biology. 2005;97:7–12. doi: 10.1016/j.jsbmb.2005.06.022. [ DOI ] [ PubMed ] [ Google Scholar ]
- Whiting SJ, Calvo MS. Optimizing vitamin D intake for populations with special needs: Barriers to effective food fortification and supplementation. Journal of Nutrition. 2006;136:1114–1116. doi: 10.1093/jn/136.4.1114. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wilkins CH, Sheline YI, Roe CM, Birge SJ, Morris JC. Vitamin D deficiency is associated with low mood and worse cognitive performance in older adults. American Journal of Geriatric Psychiatry. 2006;14(12):1032–1040. doi: 10.1097/01.JGP.0000240986.74642.7c. [ DOI ] [ PubMed ] [ Google Scholar ]
- World Health Organization. Depression. 2008 Retrieved July 29, 2008, from http://www.who.int/mental_health/management/depression/definition/en/print.html .
- Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. American Journal of Clinical Nutrition. 2000;72:690–693. doi: 10.1093/ajcn/72.3.690. [ DOI ] [ PubMed ] [ Google Scholar ]
- Zadshir A, Tareen N, Pan D, Norris K, Martins D. The prevalence of hypovitaminosis D among US adults: Data from the NHANES III. Ethnicity & Disease. 2005;15(suppl. 5):S5-97–S5-101. [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (65.1 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
research@BSPH
The School’s research endeavors aim to improve the public’s health in the U.S. and throughout the world.
- Funding Opportunities and Support
- Faculty Innovation Award Winners
Conducting Research That Addresses Public Health Issues Worldwide
Systematic and rigorous inquiry allows us to discover the fundamental mechanisms and causes of disease and disparities. At our Office of Research ( research@BSPH), we translate that knowledge to develop, evaluate, and disseminate treatment and prevention strategies and inform public health practice. Research along this entire spectrum represents a fundamental mission of the Johns Hopkins Bloomberg School of Public Health.
From laboratories at Baltimore’s Wolfe Street building, to Bangladesh maternity wards in densely packed neighborhoods, to field studies in rural Botswana, Bloomberg School faculty lead research that directly addresses the most critical public health issues worldwide. Research spans from molecules to societies and relies on methodologies as diverse as bench science and epidemiology. That research is translated into impact, from discovering ways to eliminate malaria, increase healthy behavior, reduce the toll of chronic disease, improve the health of mothers and infants, or change the biology of aging.
120+ countries
engaged in research activity by BSPH faculty and teams.
of all federal grants and contracts awarded to schools of public health are awarded to BSPH.
citations on publications where BSPH was listed in the authors' affiliation in 2019-2023.
publications where BSPH was listed in the authors' affiliation in 2019-2023.
Departments
Our 10 departments offer faculty and students the flexibility to focus on a variety of public health disciplines
Centers and Institutes Directory
Our 80+ Centers and Institutes provide a unique combination of breadth and depth, and rich opportunities for collaboration
Institutional Review Board (IRB)
The Institutional Review Board (IRB) oversees two IRBs registered with the U.S. Office of Human Research Protections, IRB X and IRB FC, which meet weekly to review human subjects research applications for Bloomberg School faculty and students
Generosity helps our community think outside the traditional boundaries of public health, working across disciplines and industries, to translate research into innovative health interventions and practices
Introducing the research@BSPH Ecosystem
The research@BSPH ecosystem aims to foster an interdependent sense of community among faculty researchers, their research teams, administration, and staff that leverages knowledge and develops shared responses to challenges. The ultimate goal is to work collectively to reduce administrative and bureaucratic barriers related to conducting experiments, recruiting participants, analyzing data, hiring staff, and more, so that faculty can focus on their core academic pursuits.
Research at the Bloomberg School is a team sport.
In order to provide extensive guidance, infrastructure, and support in pursuit of its research mission, research@BSPH employs three core areas: strategy and development, implementation and impact, and integrity and oversight. Our exceptional research teams comprised of faculty, postdoctoral fellows, students, and committed staff are united in our collaborative, collegial, and entrepreneurial approach to problem solving. T he Bloomberg School ensures that our research is accomplished according to the highest ethical standards and complies with all regulatory requirements. In addition to our institutional review board (IRB) which provides oversight for human subjects research, basic science studies employee techniques to ensure the reproducibility of research.
Research@BSPH in the News
Four bloomberg school faculty elected to national academy of medicine.
Considered one of the highest honors in the fields of health and medicine, NAM membership recognizes outstanding professional achievements and commitment to service.
The Maryland Maternal Health Innovation Program Grant Renewed with Johns Hopkins
Lerner center for public health advocacy announces inaugural sommer klag advocacy impact award winners.
Bloomberg School faculty Nadia Akseer and Cass Crifasi selected winners at Advocacy Impact Awards Pitch Competition

COMMENTS
A vast body of multidisciplinary research supports the idea that there is a relationship between where people live and their mental health. More specifically, there is evidence that people who live in relatively disadvantaged or "resource-scarce" neighborhoods have worse mental health than those who live in neighborhoods that are advantaged or "resource-abundant" (Cruwys et al., 2022a ...
This paper is part of a series describing the development of community mental health care in regions around the world (see 1,2), produced by a Task Force appointed by the WPA as part of its Action Plan 2008-2011 3,4.The WPA Guidance on Steps, Obstacles and Mistakes to Avoid in the Implementation of Community Mental Health Care, developed by this Task Force, has been previously published in the ...
Background Addressing wellbeing at the community level, using a public health approach may build wellbeing and protective factors for all. A collaborative, community-owned approach can bring together experience, networks, local knowledge, and other resources to form a locally-driven, place-based initiative that can address complex issues effectively. Research on community empowerment ...
Worthy of note is that just a few papers come from the leading journals on integrated community mental healthcare, which we explicitly searched, including the International Journal of Integrated Care and Community Mental Health Journal. Remarkably, the term "SMI" appears just once in the titles and abstracts of the volumes of 2011-2021 of ...
This journal publishes research on public sector mental health services for people with severe mental disorders, serious emotional disturbances and/or addictions. It is a hybrid journal, meaning that some articles are open access and some are not, and it has an impact factor of 2.7.
Research that helps identify methods of protecting community members' mental health and well-being whilst maintaining social cohesion is thus imperative (O'Connor et al., 2020; Van Bavel et al., 2020). However, whilst the pandemic has created an urgent need for people to find opportunities for social connection to support their mental health ...
The most frequent topic area was community mental health centers and services (n = 49), but the past three decades demonstrate a clear shift away from mental health service provision to address pressing social issues that impact community mental health, particularly homelessness (n = 42) and community integration of adults with serious mental ...
Community psychology is rooted in community mental health research and practice and has made important contributions to this field. Yet, in the decades since its inception, community psychology has reduced its focus on promoting mental health, well-being, and liberation of individuals with serious m …
After the database search, we reviewed the reference lists from papers included by title and abstract to find missing important papers, and additionally, the volumes of the Journal of Integrated Care and the Community Mental Health Journal published in the same period (2011-2021) were reviewed. Finally, we added several papers manually in ...
Aims. This study objects to explore the role of social support in the development of, experience of, and recovery from mental health problems. The main aims of this article are to map and explore existing literature regarding (a) the associations between social support, mental health and recovery, and (b) explore the key features of community mental health services that integrate social ...
Results. Among the total 420 study participants (197,46.9%) of them had an overall unfavorable attitude towards mental illness. The majority (153,36.4%) of the study participants agreed on avoidance of anyone who has mental health problems and (150,35.7%) participants described marrying a person with a mental health problem or recovered from the problem is foolishness.
Not only the WHO but also various authors and research papers have developed instruments, innovations and programmes for improving access to healthcare and the quality of mental healthcare services ... Hence the shortage of community mental health resources and psychiatric rehabilitation services (Ali & Agyapong, 2016; ...
This article reviews the current state of homelessness in the U.S. and the psychological research and interventions to address it. It also introduces a special issue of Psychological Services that features new and innovative approaches to understand and end homelessness.
The paper includes a discussion of the concept of transference, including a case example of the adoption of the concept of mental health recovery in different countries.
The two most often researched mental health consequences of mass actions, riots, and social unrest are depression and PTSD. 15, [20] [21][22] Notably, the frequency of depression and PTSD after ...
In Ontario, wait times of 6 months to 1 year are common. 14 In 2017, in Ontario alone, 12,000 children and youth were reported to be waiting up to 2.5 years for services, with an average wait time for intensive treatment of 92 days. 10 An underfunding of community-based mental health services and a reliance on high-cost services like the ED or ...
Similarly, a review of research on the mental health impact of a devastating earthquake in Japan in 2011 found long-term negative mental health impact for the population affected (Ando et al. 2017). While posttraumatic stress symptoms tended to decline over time, and initial increases in suicide decreased two years after the quake, elevated ...
The World Health Organization defines mental well-being as an individual's ability to develop their potential, work productively and creatively, build strong and positive relationships with others and contribute to their community. 1 This view distinguishes subjective happiness or life satisfaction (hedonic well-being) from positive psychological functioning (eudaimonic well-being).
Promoting mental health awareness and education can lead to improved mental health outcomes and foster more informed and supportive attitudes within the community. Perceptions of mental health disorders shape societal understanding and responses, with stigma being a deeply ingrained challenge . Negative labels lead to discrimination and hinder ...
Mental Health America are joined by other prominent mental health advocacy groups to sponsor related observances: Mental Health Awareness Week Canada (1-7 May, 2023) and Europe (22-28 May ...
When it comes to health, it matters where people live, learn, work, play, and age. That's why Healthy People 2030 has an increased focus on how social, economic, and environmental factors can impact people's health. ... Social and Community Context. Image. Download SDOH graphic (141.23 KB) ... Our literature summaries provide a snapshot of ...
The term mental health appeared first in a paper that was published in the 1940s. ... Reser's research indicated that mental health readiness contains some intertwined factors within individual abilities and developments such as ... Community mental health preparedness plays a crucial role in responding to public health emergencies in every ...
This document calls attention to the growing concerns about the effects of social media on youth mental health and offers recommendations for action. It explores the current evidence on the positive and negative impacts of social media on children and adolescents, some of the primary areas for mental health and well-being concerns, and opportunities for additional research.
RELATIONSHIPS BETWEEN VITAMIN D AND DEPRESSION AND OTHER MENTAL HEALTH DISORDERS. There has been research examining the relationship of vitamin D to seasonal affective disorder (SAD), schizophrenia, and depression. ... Effects of vitamin D supplementation on strength, physical function, and health perception in older, community-welling men ...
Learn how decent work can protect and promote mental health, and how poor working environments can pose a risk to mental health. Find out the key facts, risks, actions and interventions to prevent and support mental health conditions at work.
The Bloomberg School conducts research that addresses public health issues worldwide, from molecules to societies. It has 10 departments, 80+ centers and institutes, and a strong IRB to ensure ethical and reproducible research.
It's a simple, low-cost way of improving your mental health. ... Try it on paper first. Writing with pen and paper helps you process your feelings better. It's also easier to add drawings to ...