Fluctuations in Nurses' Burnout
Add to collection, downloadable content.
- March 2, 2021
- Affiliation: School of Nursing
- Background: Burnout is the combination of feeling high levels of emotional exhaustion and depersonalization and low levels of personal accomplishment (Maslach & Jackson, 1981). Despite over 40 years of research on burnout, it persists in clinicians. Even before the current COVID-19 pandemic, approximately one third of nurses reported high levels of burnout (Aiken et al., 2001; Dyrbye et al., 2019; McHugh et al., 2011). The majority of previous studies on burnout have been based on cross-sectional data, therefore not exploring the movement of burnout over time. In this dissertation, two research questions were explored: 1) Does burnout fluctuate? and 2) Are job resources associated with daily burnout? Methods: This study was a secondary analysis of data from 136 acute care nurses in which their burnout levels were examined at the beginning and end of shift every shift they worked during a two week period. Burnout was measured by an abbreviated, three-item measure derived from the Maslach Burnout Inventory. The job resources included in the second research question were positive mood, measured by an abbreviated Positive and Negative Affect Scale, sleep quality, measured by an abbreviated Pittsburg Sleep Quality Index, and handoff quality, measured by a scale created for the parent study. Results: To examine burnout fluctuations within individuals, the intraclass correlation coefficient (ICC1) for each burnout dimension was calculated. It was found the percent of variance that was attributed to within-person differences was 70% for emotional exhaustion, 41% for depersonalization, and 66% for decreased personal accomplishment. To determine if any resources were associated with burnout, three path analyses were run --- one for emotional exhaustion, depersonalization, and decreased personal accomplishment. Each path model included job resources as the independent variables, the beginning of shift burnout dimension as the mediator, and the end of shift burnout dimension as the dependent variable. It was found that job resources had a significant, inverse relationship with at least one of the three dimensions of burnout. Conclusion: Each dimension of burnout fluctuated within individuals over time, although each dimension fluctuated differently. Job resources impacted burnout such that decreased resources led to higher levels of burnout.
- Fluctuations
- Experience Sampling Method
- Longitudinal
- Organizational behavior
- https://doi.org/10.17615/9gxg-6n42
- Dissertation
- Jones, Cheryl B
- Zimmer, Catherine
- Tonges, Mary C
- Christian, Michael
- Doctor of Philosophy
- University of North Carolina at Chapel Hill Graduate School
This work has no parents.

Select type of work
Master's papers.
Deposit your masters paper, project or other capstone work. Theses will be sent to the CDR automatically via ProQuest and do not need to be deposited.
Scholarly Articles and Book Chapters
Deposit a peer-reviewed article or book chapter. If you would like to deposit a poster, presentation, conference paper or white paper, use the “Scholarly Works” deposit form.
Undergraduate Honors Theses
Deposit your senior honors thesis.
Scholarly Journal, Newsletter or Book
Deposit a complete issue of a scholarly journal, newsletter or book. If you would like to deposit an article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
Deposit your dataset. Datasets may be associated with an article or deposited separately.
Deposit your 3D objects, audio, images or video.
Poster, Presentation, Protocol or Paper
Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
- Open access
- Published: 05 June 2020
Burnout in nursing: a theoretical review
- Chiara Dall’Ora 1 ,
- Jane Ball 2 ,
- Maria Reinius 2 &
- Peter Griffiths 1 , 2
Human Resources for Health volume 18 , Article number: 41 ( 2020 ) Cite this article
248k Accesses
301 Citations
321 Altmetric
Metrics details
Workforce studies often identify burnout as a nursing ‘outcome’. Yet, burnout itself—what constitutes it, what factors contribute to its development, and what the wider consequences are for individuals, organisations, or their patients—is rarely made explicit. We aimed to provide a comprehensive summary of research that examines theorised relationships between burnout and other variables, in order to determine what is known (and not known) about the causes and consequences of burnout in nursing, and how this relates to theories of burnout.
We searched MEDLINE, CINAHL, and PsycINFO. We included quantitative primary empirical studies (published in English) which examined associations between burnout and work-related factors in the nursing workforce.
Ninety-one papers were identified. The majority ( n = 87) were cross-sectional studies; 39 studies used all three subscales of the Maslach Burnout Inventory (MBI) Scale to measure burnout. As hypothesised by Maslach, we identified high workload, value incongruence, low control over the job, low decision latitude, poor social climate/social support, and low rewards as predictors of burnout. Maslach suggested that turnover, sickness absence, and general health were effects of burnout; however, we identified relationships only with general health and sickness absence. Other factors that were classified as predictors of burnout in the nursing literature were low/inadequate nurse staffing levels, ≥ 12-h shifts, low schedule flexibility, time pressure, high job and psychological demands, low task variety, role conflict, low autonomy, negative nurse-physician relationship, poor supervisor/leader support, poor leadership, negative team relationship, and job insecurity. Among the outcomes of burnout, we found reduced job performance, poor quality of care, poor patient safety, adverse events, patient negative experience, medication errors, infections, patient falls, and intention to leave.
Conclusions
The patterns identified by these studies consistently show that adverse job characteristics—high workload, low staffing levels, long shifts, and low control—are associated with burnout in nursing. The potential consequences for staff and patients are severe. The literature on burnout in nursing partly supports Maslach’s theory, but some areas are insufficiently tested, in particular, the association between burnout and turnover, and relationships were found for some MBI dimensions only.
Peer Review reports
Introduction
The past decades have seen a growing research and policy interest around how work organisation characteristics impact upon different outcomes in nursing. Several studies and reviews have considered relationships between work organisation variables and outcomes such as quality of care, patient safety, sickness absence, turnover, and job dissatisfaction [ 1 , 2 , 3 , 4 ]. Burnout is often identified as a nursing ‘outcome’ in workforce studies that seek to understand the effect of context and ‘inputs’ on outcomes in health care environments. Yet, burnout itself—what constitutes it, what factors contribute to its development, and what the wider consequences are for individuals, organisations, or their patients—is not always elucidated in these studies.
The term burnout was introduced by Freudenberger in 1974 when he observed a loss of motivation and reduced commitment among volunteers at a mental health clinic [ 5 ]. It was Maslach who developed a scale, the Maslach Burnout Inventory (MBI), which internationally is the most widely used instrument to measure burnout [ 6 ]. According to Maslach’s conceptualisation, burnout is a response to excessive stress at work, which is characterised by feelings of being emotionally drained and lacking emotional resources—Emotional Exhaustion; by a negative and detached response to other people and loss of idealism—Depersonalisation; and by a decline in feelings of competence and performance at work—reduced Personal Accomplishment [ 7 ].
Maslach theorised that burnout is a state, which occurs as a result of a prolonged mismatch between a person and at least one of the following six dimensions of work [ 7 , 8 , 9 ]:
Workload: excessive workload and demands, so that recovery cannot be achieved.
Control: employees do not have sufficient control over the resources needed to complete or accomplish their job.
Reward: lack of adequate reward for the job done. Rewards can be financial, social, and intrinsic (i.e. the pride one may experience when doing a job).
Community: employees do not perceive a sense of positive connections with their colleagues and managers, leading to frustration and reducing the likelihood of social support.
Fairness: a person perceiving unfairness at the workplace, including inequity of workload and pay.
Values: employees feeling constrained by their job to act against their own values and their aspiration or when they experience conflicts between the organisation’s values.
Maslach theorised these six work characteristics as factors causing burnout and placed deterioration in employees’ health and job performance as outcomes arising from burnout [ 7 ].
Subsequent models of burnout differ from Maslach’s in one of two ways: they do not conceptualise burnout as an exclusively work-related syndrome; they view burnout as a process rather than a state [ 10 ].
The job resources-demands model [ 11 ] builds on the view of burnout as a work-based mismatch but differs from Maslach’s model in that it posits that burnout develops via two separate pathways: excessive job demands leading to exhaustion, and insufficient job resources leading to disengagement. Along with Maslach and Schaufeli, this model sees burnout as the negative pole of a continuum of employee’s well-being, with ‘work engagement’ as the positive pole [ 12 ].
Among those who regard burnout as a process, Cherniss used a longitudinal approach to investigate the development of burnout in early career human services workers. Burnout is presented as a process characterised by negative changes in attitudes and behaviours towards clients that occur over time, often associated with workers’ disillusionment about the ideals that had led them to the job [ 13 ]. Gustavsson and colleagues used this model in examining longitudinal data on early career nurses and found that exhaustion was a first phase in the burnout process, proceeding further only if nurses present dysfunctional coping (i.e. cynicism and disengagement) [ 14 ].
Shirom and colleagues suggested that burnout occurs when individuals exhaust their resources due to long-term exposures to emotionally demanding circumstances in both work and life settings, suggesting that burnout is not exclusively an occupational syndrome [ 15 , 16 ].
This review aims to identify research that has examined theorised relationships with burnout, in order to determine what is known (and not known) about the factors associated with burnout in nursing and to determine the extent to which studies have been underpinned by, and/or have supported or refuted, theories of burnout.
This was a theoretical review conducted according to the methodology outlined by Campbell et al. and Pare et al. [ 17 , 18 ]. Theoretical reviews draw on empirical studies to understand a concept from a theoretical perspective and highlight knowledge gaps. Theoretical reviews are systematic in terms of searching and inclusion/exclusion criteria and do not include a formal appraisal of quality. They have been previously used in nursing, but not focussing on burnout [ 19 ]. While no reporting guideline for theoretical reviews currently exists, the PRISMA-ScR was deemed to be suitable, with some modifications, to enhance the transparency of reporting for the purposes of this review. The checklist, which can be found as Additional file 2 , has been modified as follows:
Checklist title has been modified to indicate that the checklist has been adapted for theoretical reviews.
Introduction (item 3) has been modified to reflect that the review questions lend themselves to a theoretical review approach.
Selection of sources of evidence (item 9) has been modified to state the process for selecting sources of evidence in the theoretical review.
Limitations (item 20) has been amended to discuss the limitations of the theoretical review process.
Funding (item 22) has been amended to describe sources of funding and the role of funders in the theoretical review.
All changes from the original version have been highlighted.
Literature search
A systematic search of empirical studies examining burnout in nursing published in journal articles since 1975 was performed in May 2019, using MEDLINE, CINAHL, and PsycINFO. The main search terms were ‘burnout’ and ‘nursing’, using both free-search terms and indexed terms, synonyms, and abbreviations. The full search and the total number of papers identified are in Additional file 1 .
We included papers written in English that measured the association between burnout and work-related factors or outcomes in all types of nurses or nursing assistants working in a healthcare setting, including hospitals, care homes, primary care, the community, and ambulance services. Because there are different theories of burnout, we did not restrict the definition of burnout according to any specific theory. Burnout is a work-related phenomenon [ 8 ], so we excluded studies focussing exclusively on personal factors (e.g. gender, age). Our aim was to identify theorised relationships; therefore, we excluded studies which were only comparing the levels of burnout among different settings (e.g. in cancer services vs emergency departments). We excluded literature reviews, commentaries, and editorials.
Data extraction and quality appraisal
The following data were extracted from included studies: country, setting, sample size, staff group, measure of burnout, variables the relationship with burnout was tested against, and findings against the hypothesised relationships. One reviewer (MEB) extracted data from all the studies, with CDO and JEB extracting 10 studies each to check for agreement in data extraction. In line with the theoretical review methodology, we did not formally assess the quality of studies [ 19 ]. However, in Additional file 3 , we have summarised the key aspects of quality for each study, covering generalisability (e.g. a multisite study with more than 500 participants); risk of bias from common methods variance (e.g. burnout and correlates assessed with the same survey. This bias arises when there is a shared (common) variance because of the common method rather than a true (causal) association between variables); evidence of clustering (e.g. nurses nested in wards, wards nested in hospitals); and evidence of statistical adjustment (e.g. the association between burnout and correlates has been adjusted to control for potentially influencing variables). It should be noted that cells are shaded in green when the above-mentioned quality standards have been met, and in red when they have not. In the ‘Discussion’ section, we offer a reflection on the common limitations of research in the field and present a graphic summary of the ‘strength of evidence’ in Fig. 1 .
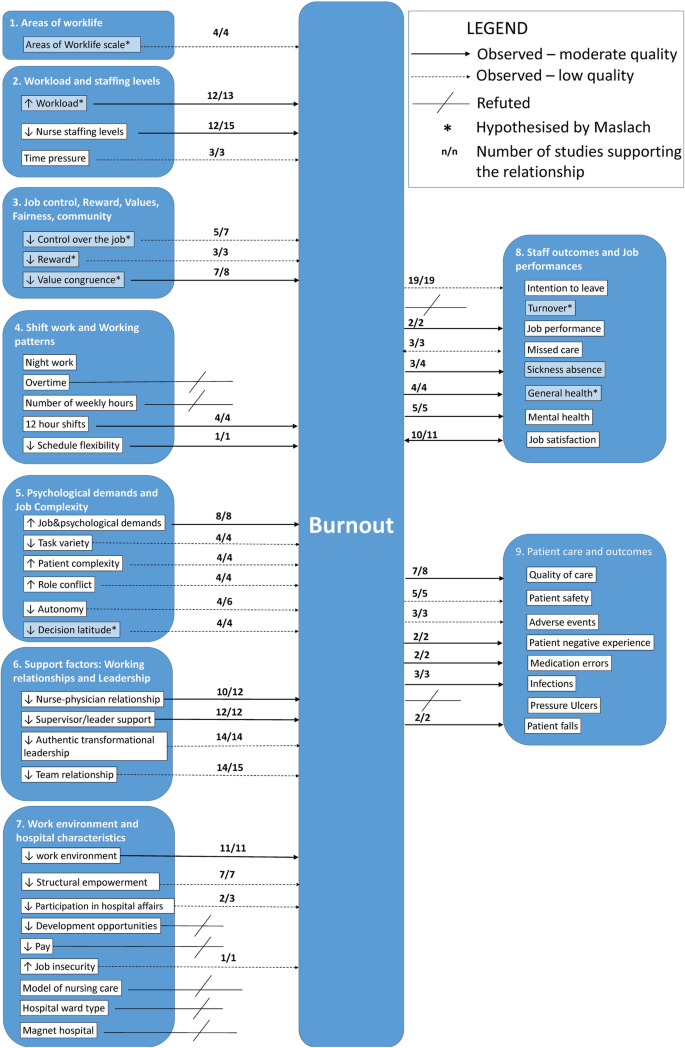
Graphical representation of strength of relationships with burnout
Data synthesis
Due to the breadth of the evidence, we summarised extracted data by identifying common categories through a coding frame. The starting point of the coding frame was the burnout multidimensional theory outlined by Maslach [ 7 ]. We then considered whether the studies’ variables fit into Maslach’s categorisation, and where they did not, we created new categories. We identified nine broad categories: (1) Areas of Worklife; (2) Workload and Staffing Levels; (3) Job Control, Reward, Values, Fairness, and Community; (4) Shift Work and Working Patterns; (5) Psychological Demands and Job Complexity; (6) Support Factors: Working Relationships and Leadership; (7) Work Environment and Hospital Characteristics; (8) Staff Outcomes and Job Performance; and (9) Patient Care and Outcomes. In the literature, categories 1–7 were treated as predictors of burnout and categories 8 and 9 as outcomes, with the exception of missed care and job satisfaction which were treated both as predictors and outcomes.
When the coding frame was finalised, CDO and MLR applied it to all studies. Where there was disagreement, a third reviewer (JEB) made the final decision.
The database search yielded 12 248 studies, of which 11 870 were rapidly excluded as either duplicates or titles and/or abstract not meeting the inclusion criteria. Of the 368 studies accessed in full text, 277 were excluded, and 91 studies were included in the review. Figure 2 presents a flow chart of the study selection.
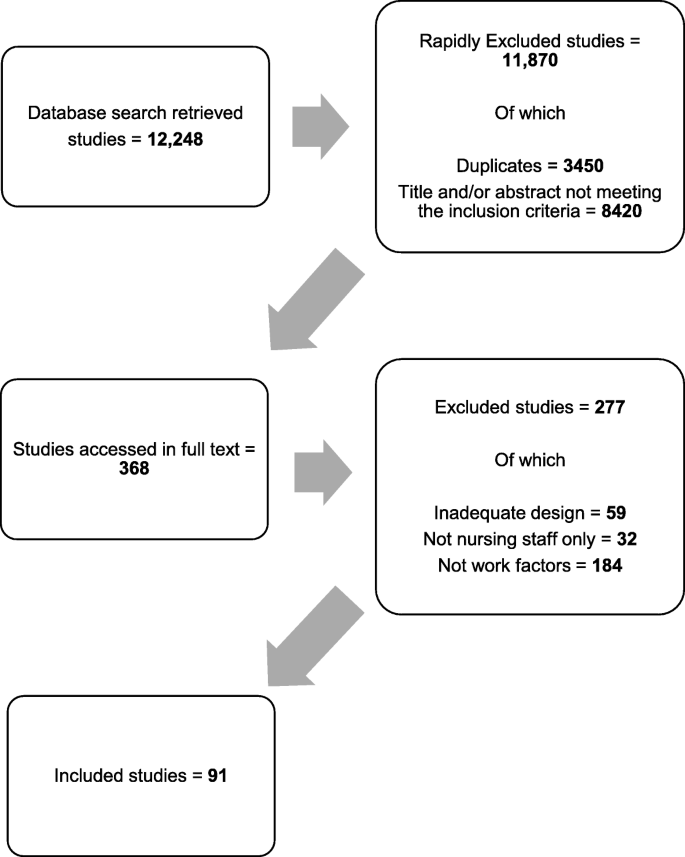
Study selection flow chart
The 91 studies identified covered 28 countries; four studies included multiple countries, and in one, the country was not reported. Most were from North America ( n = 35), Europe ( n = 28), and Asia ( n = 18).
The majority had cross-sectional designs ( n = 87, 97%); of these, 84 were entirely survey-based. Three studies were longitudinal. Most studies were undertaken in hospitals ( n = 82). Eight studies surveyed nurses at a national level, regardless of their work setting.
Sample sizes ranged from hundreds of hospitals (max = 927) with hundreds of thousands of nurses (max = 326 750) [ 20 ] to small single-site studies with the smallest sample being 73 nurses [ 21 ] (see Additional file 3 ).
The relationships examined are summarised in Table 1 .
Measures of burnout
Most studies used the Maslach Burnout Inventory Scale ( n = 81), which comprises three subscales reflecting the theoretical model: Emotional Exhaustion, Depersonalisation, and reduced Personal Accomplishment. However, less than half (47%, n = 39) of the papers measured and reported results with all three subscales. Twenty-three papers used the Emotional Exhaustion subscale only, and 11 papers used the Emotional Exhaustion and Depersonalisation subscales. In nine studies, the three MBI subscales were summed up to provide a composite score of burnout, despite Maslach and colleagues advising against such an approach [ 22 ].
Five studies used the Copenhagen Burnout Inventory (CBI) [ 23 ]. This scale consists of three dimensions of burnout: personal, work-related, and client-related. Two studies used the Malach-Pines Scale [ 24 ], and one used the burnout subscale of the Professional Quality of Life Measure (ProQoL5) scale, which posits burnout as an element of compassion fatigue [ 25 ]. Two studies used idiosyncratic measures of burnout based on items from other instruments [ 20 , 26 ].
Factors examined in relation to burnout: an overview
The studies which tested the relationships between burnout and Maslach’s six areas of worklife—workload, control, reward, community, fairness, and values—typically supported Maslach’s theory that these areas are predictors of burnout. However, some evidence is based only on certain MBI dimensions. High scores on the Areas of Worklife Scale [ 27 ] (indicating a higher degree of congruence between the job and the respondent) were associated with less likelihood of burnout, either directly [ 28 , 29 ] or through high occupational coping self-efficacy [ 30 ] and presence of civility norms and co-worker incivility [ 31 ].
The majority of studies looking at job characteristics hypothesised by the Maslach model considered workload ( n = 31) and job control and reward ( n = 10). While only a few studies ( n = 9) explicitly examined the hypothesised relationships between burnout and community, fairness, or values, we identified 39 studies that covered ‘supportive factors’ including relationships with colleagues and leadership.
A large number of studies included factors that fall outside of the Maslach model. Six main areas were identified:
Working patterns and shifts working ( n = 15)
Features inherent in the job such as psychological demand and complexity ( n = 24)
Job support from working relationships and leadership ( n = 39)
Hospital or environmental characteristics ( n = 28)
Staff outcomes and job performance ( n = 33)
Patient outcomes ( n = 17)
Individual attributes (personal or professional) ( n = 16)
Workload and staffing levels
Workload and characteristics of jobs that contribute to workload, such as staffing levels, were the most frequently examined factor in relation to burnout. Thirty studies found an association between high workload and burnout.
Of these, 13 studies looked specifically at measures of workload as a predictor of burnout. Workload was associated with Emotional Exhaustion in five studies [ 32 , 33 , 34 , 35 , 36 ], with some studies also reporting a relationship with Depersonalisation, and others Cynicism. Janssen reported that ‘mental work overload’ predicted Emotional Exhaustion [ 37 ]. Three studies concluded that workload is associated with both Emotional Exhaustion and Depersonalisation [ 38 , 39 , 40 ]. Kitaoka-Higashiguchi tested a model of burnout and found that heavy workload predicted Emotional Exhaustion, which in turn predicted Cynicism [ 41 ]. This was also observed in a larger study by Greengrass et al. who found that high workload was associated with Emotional Exhaustion, which consequently predicted Cynicism [ 42 ]. One study reported no association between workload and burnout components [ 43 ], and one study found an association between manageable workload and a composite burnout score [ 44 ].
Further 15 studies looked specifically at nurse staffing levels, and most reported that when nurses were caring for a higher number of patients or were reporting staffing inadequacy, they were more likely to experience burnout. No studies found an association between better staffing levels and burnout.
While three studies did not find a significant association with staffing levels [ 32 , 45 , 46 ], three studies found that higher patient-to-nurse ratios were associated with Emotional Exhaustion [ 47 , 48 , 49 ], and in one study, higher patient-to-nurse-ratios were associated with Emotional Exhaustion, Depersonalisation, and Personal Accomplishment [ 50 ]. One study concluded that Emotional Exhaustion mediated the relationship between patient-to-nurse ratios and patient safety [ 51 ]. Akman and colleagues found that the lower the number of patients nurses were responsible for, the lower the burnout composite score [ 52 ]. Similar results were highlighted by Faller and colleagues [ 53 ]. Lower RN hours per patient day were associated with burnout in a study by Thompson [ 20 ].
When newly qualified RNs reported being short-staffed, they were more likely to report Emotional Exhaustion and Cynicism 1 year later [ 54 ]. In a further study, low staffing adequacy was associated with Emotional Exhaustion [ 55 ]. Similarly, Leineweber and colleagues found that poor staff adequacy was associated with Emotional Exhaustion, Depersonalisation, and Personal Accomplishment [ 56 ]. Leiter and Spence Laschinger explored the relationship between staffing adequacy and all MBI subscales and found that Emotional Exhaustion mediated the relationship between staffing adequacy and Depersonalisation [ 57 ]. Time pressure was investigated in three studies, which all concluded that reported time pressure was associated with Emotional Exhaustion [ 58 , 59 , 60 ].
In summary, there is evidence that high workload is associated with Emotional Exhaustion, nurse staffing levels are associated with burnout, and time pressure is associated with Emotional Exhaustion.
Job control, reward, values, fairness, and community
Having control over the job was examined in seven studies. Galletta et al. found that low job control was associated with all MBI subscales [ 40 ], as did Gandi et al. [ 61 ]. Leiter and Maslach found that control predicted fairness, reward, and community, and in turn, fairness predicted values, and values predicted all MBI subscales [ 35 ]. Low control predicted Emotional Exhaustion only for nurses working the day shift [ 62 ], and Emotional Exhaustion was significantly related to control over practice setting [ 63 ]; two studies reported no effect of job control on burnout [ 44 , 64 ].
Reward predicted Cynicism [ 35 ] and burnout on a composite score [ 44 ]. Shamian and colleagues found that a higher score in the effort and reward imbalance scale was associated with Emotional Exhaustion, and higher scores in the effort and reward imbalance scale were associated with burnout measured by the CBI [ 65 ].
Value congruence refers to a match between the requirements of the job and people’s personal principles [ 7 ]. Value conflicts were related with a composite score of burnout [ 44 ], and one study concluded that nurses with a high value congruence reported lower Emotional Exhaustion than those with a low value congruence, and nurses with a low value congruence experienced more severe Depersonalisation than nurses with a high value congruence [ 66 ]. Low value congruence was a predictor of all three MBI dimensions [ 35 ] and of burnout measured with the Malach-Pines Burnout Scale [ 67 ]. Two studies considered social capital, defined as a social structure that benefits its members including trust, reciprocity, and a set of shared values, and they both concluded that lower social capital in the hospital-predicted Emotional Exhaustion [ 33 , 36 ]. A single study showed fairness predicted values, which in turn predicted all MBI Scales [ 35 ]. Two studies looked at community, and one found that community predicts a composite score of burnout [ 44 ], while the other found no relationships [ 35 ].
While not directly expressed in the terms described by Maslach, other studies demonstrate associations with possible causal factors, many of which are reflected in Maslach’s theory.
In summary, there is evidence that control over the job is associated with reduced burnout, and value congruence is associated with reduced Emotional Exhaustion and Depersonalisation.
Working patterns and shift work
Shift work and working patterns variables were considered by 15 studies. Overall, there was mixed evidence on the relationship between night work, number of hours worked per week, and burnout, with more conclusive results regarding the association between long shifts and burnout, and the potential protective effect of schedule flexibility.
Working night shifts was associated with burnout (composite score) [ 68 ] and Emotional Exhaustion [ 62 ], but the relationship was not significant in two studies [ 69 , 70 ]. Working on permanent as opposed to rotating shift patterns did not impact burnout [ 71 ], but working irregular shifts did impact a composite burnout score [ 72 ]. When nurses reported working a higher number of shifts, they were more likely to report higher burnout composite scores [ 68 ], but results did not generalise in a further study [ 69 ]. One study found working that overtime was associated with composite MBI score [ 73 ]. On-call requirement was not significantly associated with any MBI dimensions [ 71 ].
The number of hours worked per week was not a significant predictor of burnout according to two studies [ 25 , 53 ], but having a higher number of weekly hours was associated with Emotional Exhaustion and Depersonalisation in one study [ 70 ]. Long shifts of 12 h or more were associated with all MBI subscales [ 74 ] and with Emotional Exhaustion [ 49 , 75 ]. A study using the ProQoL5 burnout scale found that shorter shifts were protective of burnout [ 25 ].
Having higher schedule flexibility was protective of Emotional Exhaustion [ 46 ], and so was the ability to schedule days off for a burnout composite score [ 76 ]. Having more than 8 days off per month was associated with lower burnout [ 69 ]. Stone et al. found that a positive scheduling climate was protective of Emotional Exhaustion only [ 77 ].
In summary, we found an association between ≥ 12-h shifts and Emotional Exhaustion and between schedule flexibility and reduced Emotional Exhaustion.
Psychological demands and job complexity
There is evidence from 24 studies that job demands and aspects intrinsic to the job, including role conflict, autonomy, and task variety, are associated with some burnout dimensions.
Eight studies considered psychological demands. The higher the psychological demands, the higher the likelihood of experiencing all burnout dimensions [ 72 ], and high psychological demands were associated with higher odds of Emotional Exhaustion [ 62 , 78 ]. Emotional demands, in terms of hindrances, had an effect on burnout [ 67 ]. One study reported that job demands, measured with the Effort-Reward Imbalance Questionnaire, were correlated with all burnout dimensions [ 79 ], and similarly, Garcia-Sierra et al. found that demands predict burnout, measured with a composite scale of Emotional Exhaustion and Cynicism [ 80 ]. According to one study, job demands were not associated with burnout [ 73 ], and Rouxel et al. concluded that the higher the job demands, the higher the impact on both Emotional Exhaustion and Depersonalisation [ 64 ].
Four studies looked at task nature and variety, quality of job content, in terms of skill variety, skill discretion, task identity, task significance, influenced Emotional Exhaustion through intrinsic work motivation [ 37 ]. Skill variety and task significance were related to Emotional Exhaustion; task significance was also related to Personal Accomplishment [ 60 ]. Having no administrative tasks in the job was associated with a reduced likelihood to experience Depersonalisation [ 71 ]. Higher task clarity was associated with reduced levels of Emotional Exhaustion and increased Personal Accomplishment [ 58 ].
Patient characteristics/requirements were investigated in four papers. When nurses were caring for suffering patients and patients who had multiple requirements, they were more likely to experience Emotional Exhaustion and Cynicism. Similarly, caring for a dying patient and having a high number of decisions to forego life-sustaining treatments were associated with a higher likelihood of burnout (measured with a composite score) [ 76 ]. Stress resulting from patient care was associated with a composite burnout score [ 73 ]. Patient violence also had an impact on burnout, measured with CBI [ 81 ], as did conflict with patients [ 76 ].
Role conflict is a situation in which contradictory, competing, or incompatible expectations are placed on an individual by two or more roles held at the same time. Role conflict predicted Emotional Exhaustion [ 41 ], and so it did in a study by Konstantinou et al., who found that role conflict was associated with Emotional Exhaustion and Depersonalisation [ 34 ]; Levert and colleagues reported that role conflict correlated with Emotional Exhaustion, Depersonalisation, and Personal Accomplishment. They also considered role ambiguity, which correlated with Emotional Exhaustion and Depersonalisation, but not Personal Accomplishment [ 39 ]. Andela et al. investigated the impact of emotional dissonance, defined as the mismatch between the emotions that are felt and the emotions required to be displayed by organisations. They reported that emotional dissonance is a mediator between job aspects (i.e. workload, patient characteristics, and team issues) and Emotional Exhaustion and Cynicism. Rouxel et al. found that perceived negative display rules were associated with Emotional Exhaustion [ 64 ].
Autonomy related to Emotional Exhaustion and Depersonalisation [ 60 ], and in another study, it only related to Depersonalisation [ 43 ]. Low autonomy impacted Emotional Exhaustion via organisational trust [ 82 ]. Autonomy correlated with burnout [ 67 ]. There was no effect of autonomy on burnout according to two studies [ 58 , 63 ]. Low decision-making at the ward level was associated with all MBI subscales [ 77 ]. Decision latitude impacted Personal Accomplishment only [ 36 ], and in one study, it was found to be related to Emotional Exhaustion [ 78 ]. High decision latitude was associated with Personal Accomplishment [ 41 ] and low Emotional Exhaustion [ 33 ].
Overall, high job and psychological demands were associated with Emotional Exhaustion, as was role conflict. Patient complexity was associated with burnout, while task variety, autonomy, and decision latitude were protective of burnout.
Working relationships and leadership
Overall, evidence from 39 studies supports that having positive support factors and working relationships in place, including positive relationships with physicians, support from the leader, positive leadership style, and teamwork, might play a protective role towards burnout.
The quality of the relationship with physicians was investigated by 12 studies. In two studies, having negative relationships with physicians was associated with all MBI dimensions [ 77 , 83 ]; quality of nurse-physician relationship was associated with Emotional Exhaustion and Depersonalisation, but not PA [ 50 ]. Two studies found an association with Emotional Exhaustion only [ 55 , 84 ], and one concluded that quality of relationship with physicians indirectly supported PA [ 36 ]. This was also found by Leiter and Laschinger, who found that positive nurse-physician collaborations predicted Personal Accomplishment [ 57 , 85 ]. When burnout was measured with composite scores of MBI and a not validated scale, two studies reported an association with nurse-physician relationship [ 20 , 76 ], and two studies found no associations [ 56 , 63 ].
Having support from the supervisor or leader was considered in 12 studies, which found relationships with different MBI dimensions. A relationship between low support from nurse managers and all MBI subscales was observed in one study [ 77 ], while two studies reported it is a protective factor from Emotional Exhaustion only [ 58 , 83 ], and one that it was also associated with Depersonalisation [ 86 ]. Kitaoka-Higashiguchi reported an association only with Cynicism [ 41 ], and Jansen et al. found it was only associated with Depersonalisation and Personal Accomplishment [ 60 ]. Van Bogaert and colleagues found that support from managers predicted low Emotional Exhaustion and high Personal Accomplishment [ 84 ], but in a later study, it only predicted high Personal Accomplishment [ 36 ]. Regarding the relationship with the manager, it had a direct effect on Depersonalisation, and it moderated the effect of time pressure on Emotional Exhaustion and Depersonalisation [ 59 ]; a protective effect of a quality relationship with the head nurse on a composite burnout score was also reported [ 76 ]. Two studies using different burnout scales found an association between manager support and reduced burnout [ 25 , 67 ]. Low trust in the leader showed a negative impact on burnout, measured with a composite score [ 87 ]. Two further studies focused on the perceived nurse manager’s ability: authors found that it was related to Emotional Exhaustion [ 46 ], and Emotional Exhaustion and Personal Accomplishment [ 50 ].
Fourteen studies looked at the leadership style and found that it affects burnout through different pathways and mechanisms. Boamah et al. found that authentic leadership—described as leaders who have high self-awareness, balanced processing, an internalised moral perspective, and transparency—predicted higher empowerment, which in turn predicted lower levels of Emotional Exhaustion and Cynicism a year later [ 54 ]. Authentic leadership had a negative direct effect on workplace bullying, which in turn had a direct positive effect on Emotional Exhaustion [ 88 ]. Effective leadership predicted staffing adequacy, which in turn predicted Emotional Exhaustion [ 57 , 85 ]. Authentic leadership predicted all areas of worklife, which in turn predicted all MBI dimensions of burnout [ 30 ], and a similar pathway was identified by Laschiner and Read, although authentic leadership impacted Emotional Exhaustion only and it was also through civility norms and co-worker incivility [ 31 ]. Emotional Exhaustion mediated the relationship between authentic leadership and intention to leave the job [ 89 ]. ‘Leader empowering behaviour’ had an indirect effect on Emotional Exhaustion through structural empowerment [ 29 ], and empowering leadership predicted trust in the leader, which in turn was associated with burnout composite score [ 87 ]. Active management-by-exception was beneficial for Depersonalisation and Personal Accomplishment, passive laissez-faire leadership negatively affected Emotional Exhaustion and Personal Accomplishment, and rewarding transformational leadership protected from Depersonalisation [ 90 ]. Contrary to this, Madathil et al. found that transformational leadership protected against Emotional Exhaustion, but not Depersonalisation, and promoted Personal Accomplishment [ 43 ]. Transformational leadership predicted positive work environments, which in turn predicted lower burnout (composite score) [ 44 ]. Positive leadership affected Emotional Exhaustion and Depersonalisation [ 56 ] and burnout measured with a non-validated scale [ 20 ].
Teamwork and social support were also explored. Co-worker cohesion was only related to Depersonalisation [ 58 ]; team collaboration problems predicted negative scores on all MBI subscales [ 38 ], and workplace support protected from Emotional Exhaustion [ 72 ]. Similarly, support received from peers had a protective effect on Emotional Exhaustion [ 60 ]. Collegial support was related to Emotional Exhaustion and Personal Accomplishment [ 39 ], and colleague support protected from burnout [ 67 ]. Interpersonal conflict affected Emotional Exhaustion through role conflict, but co-worker support had no effect on any burnout dimensions [ 41 ], and similarly, co-worker incivility predicted Emotional Exhaustion [ 31 ], and so did bullying [ 88 ]. Poor team communication was associated with all MBI dimensions [ 40 ], staff issues predicted burnout measured with a composite score [ 73 ], and so did verbal violence from colleagues [ 68 ]. One study found that seeking social support was not associated with any of the burnout dimensions, while another study found that low social support predicted Emotional Exhaustion [ 37 ], and social support was associated with lower Emotional Exhaustion and higher Personal Accomplishment [ 21 ]. Vidotti et al. found an association between low social support and all MBI dimensions [ 62 ].
Work environment and hospital characteristics
Eleven studies were considering the work environment measured with the PES-NWI scale [ 91 ], where higher scores indicate positive work environments. Five studies comprising diverse samples and settings concluded that the better rated the work environment, the lower the likelihood of experiencing Emotional Exhaustion [ 32 , 47 , 49 , 51 , 92 ], and four studies found the same relationship, but on both Emotional Exhaustion and Depersonalisation [ 50 , 66 , 93 , 94 ]; only one study concluded there is an association between work environment and all MBI dimensions [ 95 ]. Negative work environments affected burnout (measured with a composite score) via job dissatisfaction [ 96 ]. One study looked at organisational characteristics on a single scale and found that a higher rating of organisational characteristics predicted lower Emotional Exhaustion [ 82 ]. Environmental uncertainty was related to all MBI dimensions [ 86 ].
Structural empowerment was also considered in relation to burnout: high structural empowerment led to lower Emotional Exhaustion and Cynicism via staffing levels and worklife interference [ 54 ]; in a study using a similar methodology, structural empowerment affected Emotional Exhaustion via Areas of Worklife [ 29 ]. The relationship between Emotional Exhaustion and Cynicism was moderated by organisational empowerment [ 40 ], and organisational support had a protective effect on burnout [ 67 ]. Hospital management and organisational support had a direct effect on Emotional Exhaustion and Personal Accomplishment [ 84 ]. Trust in the organisation predicted lower levels of Emotional Exhaustion [ 82 ] and of burnout measured with a composite MBI score [ 87 ].
Three studies considered whether policy involvement had an effect on burnout. Two studies on the same sample found that having the opportunity to participate in policy decisions was associated with reduced burnout (all subscales) [ 57 , 85 ], and one study did not report results for the association [ 20 ]. Emotional Exhaustion mediated the relationship between nurses’ participation in hospital affairs and their intention to leave the job [ 97 ]; a further study did not found an association between participation in hospital affairs and Emotional Exhaustion, but only with Personal Accomplishment [ 50 ]. Lastly, one study investigated participation in research groups and concluded it was associated with reduced burnout measured with a composite score [ 76 ].
There was an association between opportunity for career advancement and all MBI dimensions [ 77 ]; however, another study found that having promotion opportunities was not related to burnout [ 79 ]. Moloney et al. found that professional development was not related to burnout [ 67 ]. Two studies considered pay. In one study, no effect was found on any MBI dimension [ 73 ], and a very small study ( n = 78 nurses) reported an effect of satisfaction with pay on Emotional Exhaustion and Depersonalisation [ 34 ]. Job insecurity predicted Depersonalisation and PA [ 79 ].
When the hospital adopted nursing models of care rather than medical models of care, nurses were more likely to report high levels of Personal Accomplishment [ 57 , 85 ]. However, another study found no significant relationship [ 20 ]. Regarding ward and hospital type, Aiken and Sloane found that RNs working in specialised AIDS units reported lower levels of Emotional Exhaustion [ 98 ]; however, ward type was not found to be significantly associated with burnout in a study on temporary nurses [ 53 ]. Working in different ward settings was not associated with burnout, but working in hospitals as opposed to in primary care was associated with lower Emotional Exhaustion [ 71 ]. Working in a small hospital was associated with a lower likelihood of Emotional Exhaustion, when compared to working in a community hospital [ 63 ]. Faller’s study also concluded that working in California was a significant predictor of reduced burnout.
When the hospitals’ investment in the quality of care was considered, one study found that having foundations for quality of care was associated with reduced Emotional Exhaustion only [ 50 ], but in another study, foundations for quality of care were associated with all MBI dimensions [ 83 ]. Working in a Magnet hospital was not associated with burnout [ 53 ].
In summary, having a positive work environment (generally work environments scoring higher on the PES-NWI scale) was associated with reduced Emotional Exhaustion, and so was higher structural empowerment. However, none of the organisational characteristics at the hospital level was consistently associated with burnout.
Staff outcomes and job performance
Nineteen studies considered the impact of burnout on intention to leave. Two studies found that Emotional Exhaustion and Cynicism had a direct effect on turnover intentions [ 28 , 99 ], and four studies reported that only Emotional Exhaustion affected intentions to leave the job [ 21 , 32 , 37 , 100 ], with one of these indicating that Emotional Exhaustion affected also intention to leave the organisation [ 32 ], but one study did not replicate such findings [ 101 ] and concluded that only Cynicism was associated with intention to leave the job and nursing. Similarly, one study found that Cynicism was directly related to intention to leave [ 35 ]. A further study found that Emotional Exhaustion affected turnover intentions via job satisfaction [ 88 ], and one article reported that Emotional Exhaustion mediated the effect of authentic leadership on intention to leave [ 89 ]. Emotional Exhaustion was a mediator between nurses’ involvement with decisions and intention to leave the organisation [ 97 ]. Burnout measured on a composite score was associated with a higher intention to leave [ 96 ]. Laeeque et al. reported that burnout, captured with CBI, related to intention to leave [ 81 ]; Estryn-Behar et al. used the same scale to measure burnout and found that high burnout was associated with higher intention to leave in all countries, except for Slovakia [ 102 ]. Burnout, measured with the Malach-Pines Scale, was associated with intention to quit, and stronger associations were found for nurses who had higher perceptions of organisational politics [ 103 ]. Burnout (Malach-Pines Scale) predicted both the intention to leave the job and nursing [ 67 ]. Three studies investigated the relationship between burnout and intention to leave; one of these aggregated all job outcomes in a single variable (i.e. job satisfaction, intention to leave the hospital, applied for another job, and intention to leave nursing) and reported that Depersonalisation and Personal Accomplishment predict job outcomes [ 84 ]; they replicated a similar approach and found the same associations [ 36 ]. They later found that all MBI dimensions were associated with leaving the nursing profession [ 104 ]. Only one study in a sample of 106 nurses from one hospital found an association between Depersonalisation and turnover within 2 years [ 105 ].
Two studies looked at the effect of burnout on job performance: one found a negative association between burnout (measured with CBI) and both task performance and contextual performance [ 106 ]. Only Emotional Exhaustion was associated with self-rated and supervisor-rated job performance of 73 RNs [ 21 ]. Missed care was investigated in three studies, and it was found to be both predictor of Emotional Exhaustion [ 32 ], an outcome of burnout [ 20 , 103 ].
Four studies considered sickness absence. When RNs had high levels of Emotional Exhaustion, they were more likely to experience short-term sickness absence (i.e. 1–10 days of absence), which was obtained from hospital administrative records. Similarly, Emotional Exhaustion was associated with seven or more days of absence in a longitudinal study [ 105 ]. Emotional Exhaustion was significantly associated with reported mental health absenteeism, but not reported physical health absenteeism, and sickness absence from administrative records [ 21 ]. One study did not find any meaningful relationships between burnout and absenteeism [ 107 ].
Emotional Exhaustion was a significant predictor of general health [ 73 ], and in a further study, both Emotional Exhaustion and Personal Accomplishment were associated with perceived health [ 70 ]. Final-year nursing students who experienced health issues were more likely to develop high burnout when entering the profession [ 26 ]. When quality of sleep was treated both as a predictor and outcome of burnout, relationships were found in both instances [ 106 ].
Focussing on mental health, one study found that burnout predicted mental health problems for newly qualified nurses [ 30 ], and Emotional Exhaustion and Cynicism predicted somatisation [ 42 ]. Depressive symptoms were predictive of Emotional Exhaustion and Depersonalisation, considering therefore depression as a predictor of burnout [ 108 ]. Rudman and Gustavsson also found that having depressive mood and depressive episodes were common features of newly qualified nurses who developed or got worse levels of burnout throughout their first years in the profession [ 26 ]. Tourigny et al. considered depression as a predictor and found it was significantly related to Emotional Exhaustion [ 107 ].
Eleven studies considered job satisfaction: of these, three treated job satisfaction as a predictor of burnout and concluded that higher levels of job satisfaction were associated with a lower level of composite burnout scores [ 52 , 96 ] and all MBI dimensions [ 94 ]. According to two studies, Emotional Exhaustion and Cynicism predicted job dissatisfaction [ 54 , 101 ], while four studies reported that Emotional Exhaustion only was associated with increased odds to report job dissatisfaction [ 73 , 82 , 88 , 100 ]; one study reported that Cynicism only was associated with job dissatisfaction [ 99 ]. Rouxel et al. did not find support in their hypothesised model that Emotional Exhaustion and Depersonalisation predicted job satisfaction [ 64 ].
In summary, considering 39 studies, there is conflicting evidence on the direction of the relationship between burnout and missed care, mental health, and job satisfaction. An association between burnout and intention to leave was found, although only one small study reported an association between burnout and turnover. A moderate relationship was found for the effect of burnout on sickness absence, job performance, and general health.
Patient care and outcomes
Among the patient outcomes of burnout, quality of care was investigated by eight studies. Two studies in diverse samples and settings reported that high Emotional Exhaustion, high Depersonalisation, and low Personal Accomplishment were associated with poor quality of care [ 109 , 110 ], but one study found that only Personal Accomplishment was related to better quality of care at the last shift [ 104 ]; Emotional Exhaustion and Cynicism predict low quality of care [ 54 ]; two articles reported that Emotional Exhaustion predicts poor nurse ratings of quality of care [ 82 , 84 ]. A high burnout composite score predicted poor nurse-assessed quality of care [ 96 ]. In one instance, no associations were found between any of the burnout dimensions and quality of care [ 36 ].
Five studies considered aspects of patient safety: burnout was correlated with negative patient safety climate [ 111 ]. Emotional Exhaustion and Depersonalisation were both associated with negative patient safety grades and safety perceptions [ 112 ], and burnout fully mediated the relationship between depression and individual-level safety perceptions and work area/unit level safety perceptions [ 108 ]. Emotional Exhaustion mediated the relationship between workload and patient safety [ 51 ], and a higher composite burnout score was associated with lower patient safety ratings [ 113 ].
Regarding adverse events, high DEP and low Personal Accomplishment predicted a higher rate of adverse events [ 85 ], but in another study, only Emotional Exhaustion predicted adverse events [ 51 ]. When nurses were experiencing high levels of Emotional Exhaustion, they were less likely to report near misses and adverse events, and when they were experiencing high levels of Depersonalisation, they were less likely to report near misses [ 112 ].
All three MBI dimensions predicted medication errors in one study [ 109 ], but Van Bogaert et al. found that only high levels of Depersonalisation were associated with medication errors [ 104 ]. High scores in Emotional Exhaustion and Depersonalisation predicted infections [ 109 ]. Cimiotti et al. found that Emotional Exhaustion was associated with catheter-associated urinary tract infections and surgical site infections [ 114 ], while in another study, Depersonalisation was associated with nosocomial infections [ 104 ]. Lastly, patient falls were also explored, and Depersonalisation and low Personal Accomplishment were significant predictors in one study [ 109 ], while in a further study, only Depersonalisation was associated with patient falls [ 104 ]. There was no association between burnout and hospital-acquired pressure ulcers [ 20 ].
Considering patient experience, Vahey et al. concluded that higher Emotional Exhaustion and low Personal Accomplishment levels were associated with patient dissatisfaction [ 93 ], and Van Bogaert et al. found that Emotional Exhaustion was related to patient and family verbal abuse, and Depersonalisation was related to both patient and family verbal abuse and patient and family complaints [ 104 ].
In summary, evidence deriving from 17 studies points to a negative effect of burnout on quality of care, patient safety, adverse events, error reporting, medication error, infections, patient falls, patient dissatisfaction, and family complaints, but not on pressure ulcers.
Individual characteristics
In total, 16 studies, which had examined work characteristics related to burnout, also considered the relationship between characteristics of the individual and burnout. Relationships were tested on demographic variables, including gender, age, and family status; on personality aspects; on work-life interference; and on professional attributes including length of experience and educational level. Because our focus on burnout is as a job-related phenomenon, we have not reported results of these studies into detail, but overall evidence on demographic and personality factors was inconclusive, and having family issues and high work-life interference was associated with different burnout dimensions. Being younger and not having a bachelor’s degree were found to be associated with a higher incidence of burnout.
This review aimed to identify research that had examined theorised relationships with burnout, in order to determine what is known (and not known) about the factors associated with burnout in nursing and to determine the extent to which studies have been underpinned by, and/or have supported or refuted, theories of burnout. We found that the associations hypothesised by Maslach’s theory between mismatches in areas of worklife and burnout were generally supported.
Research consistently found that adverse job characteristics—high workload, low staffing levels, long shifts, low control, low schedule flexibility, time pressure, high job and psychological demands, low task variety, role conflict, low autonomy, negative nurse-physician relationship, poor supervisor/leader support, poor leadership, negative team relationship, and job insecurity—were associated with burnout in nursing.
However few studies used all three MBI subscales in the way intended, and nine used different approaches to measuring burnout.
The field has been dominated by cross-sectional studies that seek to identify associations with one or two factors, rarely going beyond establishing correlation. Most studies were limited by their cross-sectional nature, the use of different or incorrectly applied burnout measures, the use of common methods (i.e. survey to capture both burnout and correlates), and omitted variables in the models. The 91 studies reviewed, while highlighting the importance of burnout as a feature affecting nurses and patient care, have generally lacked a theoretical approach, or identified mechanisms to test and develop a theory on the causes and consequences of burnout, but were limited in their testing of likely mechanisms due to cross-sectional and observational designs.
For example, 19 studies showed relationships between burnout and job satisfaction, missed care, and mental health. But while some studies treated these as predictors of burnout, others handled as outcomes of burnout. This highlights a further issue that characterises the burnout literature in nursing: the simultaneity bias, due to the cross-sectional nature of the evidence. The inability to establish a temporal link means limits the inference of causality [ 115 ]. Thus, a factor such as ‘missed care’ could lead to a growing sense of compromise and ‘crushed ideals’ in nurses [ 116 ], which causes burnout. Equally, it could be that job performance of nurses experiencing burnout is reduced, leading to increased levels of ‘missed care’. Both are plausible in relation to Maslach’s original theory of burnout, but research is insufficient to determine which is most likely, and thereby develop the theory.
To help address this, three areas of development within research are proposed. Future research adopting longitudinal designs that follow individuals over time would improve the potential to understand the direction of the relationships observed. Research using Maslach’s theory should use and report all three MBI dimensions; where only the Emotional Exhaustion subscale is used, this should be explicit and it should not be treated as being synonymous to burnout. Finally, to move our theoretical understanding of burnout forward, research needs to prioritise the use of empirical data on employee behaviours (such as absenteeism, turnover) rather than self-report intentions or predictions.
Addressing these gaps would provide better evidence of the nature of burnout in nursing, what causes it and its potential consequences, helping to develop evidence-based solutions and motivate work-place change. With better insight, health care organisations can set about reducing the negative consequences of having patient care provided by staff whose work has led them to become emotionally exhausted, detached, and less able to do the job, that is, burnout.
Limitations
Our theoretical review of the literature aimed to summarise information from a large quantity of studies; this meant that we had to report studies without describing their context in the text and also without providing estimates (i.e. ORs and 95% CIs). In appraising studies, we did not apply a formal quality appraisal instrument, although we noted key omissions of important details. However, the results of the review serve to illustrate the variety of factors that may influence/result from burnout and demonstrate where information is missing. We did not consider personality and other individual variables when extracting data from studies. However, Maslach and Leiter recently reiterated that although some connections have been made between burnout and personality characteristics, the evidence firmly points towards work characteristics as the primary drivers of burnout [ 8 ].
While we used a reproducible search strategy searching MEDLINE, CINAHL, and PsycINFO, it is possible that there are studies indexed elsewhere and we did not identify them, and we did not include grey literature. It seems unlikely that these exist in sufficient quantity to substantively change our conclusions.
Patterns identified across 91 studies consistently show that adverse job characteristics are associated with burnout in nursing. The potential consequences for staff and patients are severe. Maslach’s theory offers a plausible mechanism to explain the associations observed. However incomplete measurement of burnout and limited research on some relationships means that the causes and consequences of burnout cannot be reliably identified and distinguished, which makes it difficult to use the evidence to design interventions to reduce burnout.
Availability of data and materials
Not applicable
Abbreviations
- Maslach Burnout Inventory
Copenhagen Burnout Inventory
Professional Quality of Life Measure
Dall’Ora C, Ball J, Recio-Saucedo A, Griffiths P. Characteristics of shift work and their impact on employee performance and wellbeing: a literature review. Int J Nurs Stud. 2016;57:12–27.
Article PubMed Google Scholar
Griffiths P, Ball J, Drennan J, Dall’Ora C, Jones J, Maruotti A, et al. Nurse staffing and patient outcomes: Strengths and limitations of the evidence to inform policy and practice. A review and discussion paper based on evidence reviewed for the National Institute for Health and Care Excellence Safe Staffing guideline development. Int J Nurs Stud. 2016;63:213–25.
Cummings GG, MacGregor T, Davey M, Lee H, Wong CA, Lo E, et al. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Stud. 2010;47(3):363–85.
Rafferty AM, Ball J, Aiken LH. Are teamwork and professional autonomy compatible, and do they result in improved hospital care? Qual Health Care. 2001;10(suppl 2):ii32-iii7.
Freudenberger HJ. Staff burn-out. J Soc Issues. 1974;30(1):159–65.
Article Google Scholar
Maslach C, Jackson SE. The measurement of experienced burnout. J Occup Behav. 1981;2(2):99–113.
Maslach C. A Multidimensional theory of burnout. In: Cooper CL, editor. Theories of Organizational Stress Oxford University Press Inc.; 1999.
Maslach C, Leiter M. Burnout. Fink G, editor. London, UK: Academic Press; 2016. 351-7 p.
Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52(1):397–422.
Article CAS PubMed Google Scholar
Ekstedt M. Burnout and sleep: Institutionen för folkhälsovetenskap/Department of Public Health Sciences; 2005.
Google Scholar
Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499.
Schaufeli WB, Leiter MP, Maslach C. Burnout: 35 years of research and practice. Career Dev Int. 2009;14(2-3):204–20.
Cherniss C. Burnout in new professionals: a long-term follow-up study. J Health Hum Resour Adm. 1989;12(1):11–24.
Gustavsson JP, Hallsten L, Rudman A. Early career burnout among nurses: modelling a hypothesized process using an item response approach. Int J Nurs Stud. 2010;47(7):864–75.
Shirom A. Job-related burnout: a review. Handbook of occupational health psychology. Washington, DC, US: American Psychological Association; 2003. p. 245-264.
Melamed S, Kushnir T, Shirom A. Burnout and risk factors for cardiovascular diseases. Behav Med. 1992;18(2):53–60.
Campbell M, Egan M, Lorenc T, Bond L, Popham F, Fenton C, et al. Considering methodological options for reviews of theory: illustrated by a review of theories linking income and health. Syst Rev. 2014;3(1):114.
Article PubMed PubMed Central Google Scholar
Pare G, Trudel MC, Jaana M, Kitsiou S. Synthesizing information systems knowledge: a typology of literature reviews. Inf Manag. 2015;52(2):183–99.
Lavoie P, Michaud C, Bélisle M, Boyer L, Gosselin É, Grondin M, et al. Learning theories and tools for the assessment of core nursing competencies in simulation: a theoretical review. J Adv Nurs. 2018;74(2):239–50.
Thompson D. The examination of practice environment, burnout, and missed care on pressure ulcer prevalence rates using a complexity science framework: University of Kansas; 2014.
Parker PA, Kulik JA. Burnout, self- and supervisor-rated job performance, and absenteeism among nurses. J Behav Med. 1995;18(6):581–99.
Maslach C, Jackson SE, Leiter M. Maslach burnout inventory manual. 3rd ed. ed: Mind Garden, Inc.; 2010.
Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress. 2005;19(3):192–207.
Malach-Pines A. The burnout measure, short version. Int J Stress Manag. 2005;12(1):78–88.
Hunsaker S, Chen HC, Maughan D, Heaston S. Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. J Nurs Scholarsh. 2015;47(2):186–94.
Rudman A, Gustavsson JP. Early-career burnout among new graduate nurses: a prospective observational study of intra-individual change trajectories. Int J Nurs Stud. 2011;48(3):292–306.
Leiter MP, Maslach C. Areas of worklife survey manual. Centre for Organizational Research and Development, Acadia University, Wolfville. 2006.
Boamah SA, Laschinger H. The influence of areas of worklife fit and work-life interference on burnout and turnover intentions among new graduate nurses. J Nurs Manag. 2016;24(2):E164–74.
Greco P, Laschinger HK, Wong C. Leader empowering behaviours, staff nurse empowerment and work engagement/burnout. Nurs Leadersh (Tor Ont). 2006;19(4):41–56.
Laschinger HK, Borgogni L, Consiglio C, Read E. The effects of authentic leadership, six areas of worklife, and occupational coping self-efficacy on new graduate nurses’ burnout and mental health: a cross-sectional study. Int J Nurs Stud. 2015;52(6):1080–9.
Laschinger HK, Read EA. The effect of authentic leadership, person-job fit, and civility norms on new graduate nurses’ experiences of coworker incivility and burnout. J Nurs Adm. 2016;46(11):574–80.
Flynn L, Thomas-Hawkins C, Clarke SP. Organizational traits, care processes, and burnout among chronic hemodialysis nurses. West J Nurs Res. 2009;31(5):569–82.
Kowalski C, Ommen O, Driller E, Ernstmann N, Wirtz MA, Kohler T, et al. Burnout in nurses - the relationship between social capital in hospitals and emotional exhaustion. J Clin Nurs. 2010;19(11-12):1654–63.
Konstantinou AK, Bonotis K, Sokratous M, Siokas V, Dardiotis E. Burnout evaluation and potential predictors in a Greek cohort of mental health nurses. Arch Psychiatr Nurs. 2018;32(3):449–56.
Leiter MP, Maslach C. Nurse turnover: the mediating role of burnout. J Nurs Manag. 2009;17(3):331–9.
Van Bogaert P, Kowalski C, Weeks SM, Van Heusden D, Clarke SP. The relationship between nurse practice environment, nurse work characteristics, burnout and job outcome and quality of nursing care: a cross-sectional survey. Int J Nurs Stud. 2013;50(12):1667–77.
Janssen PP, Jonge JD, Bakker AB. Specific determinants of intrinsic work motivation, burnout and turnover intentions: a study among nurses. J Adv Nurs. 1999;29(6):1360–9.
Andela M, Truchot D, Van der Doef M. Job stressors and burnout in hospitals: the mediating role of emotional dissonance. Int J Stress Manag. 2016;23(3):298–317.
Levert T, Lucas M, Ortlepp K. Burnout in psychiatric nurses: contributions of the work environment and a Sense of Coherence. S Afr J Psychol. 2000;30(2):36–43.
Galletta M, Portoghese I, Ciuffi M, Sancassiani F, Aloja E, Campagna M. Working and environmental factors on job burnout: a cross-sectional study among nurses. Clin Pract Epidemiol Ment Health. 2016;12:132–41.
Kitaoka-Higashiguchi K. Burnout as a developmental process among Japanese nurses: investigation of Leiter’s model. Jpn J Nurs Sci. 2005;2(1):9–16.
Greenglass ER, Burke RJ, Fiksenbaum L. Workload and burnout in nurses. J Community Appl Soc Psychol. 2001;11(3):211–5.
Madathil R, Heck NC, Schuldberg D. Burnout in psychiatric nursing: examining the interplay of autonomy, leadership style, and depressive symptoms. Arch Psychiatr Nurs. 2014;28(3):160–6.
Lewis HS, Cunningham CJ. Linking nurse leadership and work characteristics to nurse burnout and engagement. Nurs Res. 2016;65(1):13–23.
Lu M, Ruan H, Xing W, Hu Y. Nurse burnout in China: a questionnaire survey on staffing, job satisfaction, and quality of care. J Nurs Manag. 2015;23(4):440–7.
Dhaini SR, Denhaerynck K, Bachnick S, Schwendimann R, Schubert M, De Geest S, et al. Work schedule flexibility is associated with emotional exhaustion among registered nurses in Swiss hospitals: a cross-sectional study. Int J Nurs Stud. 2018;82:99–105.
Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;38(5):223–9.
Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93.
Zhou W, He G, Wang H, He Y, Yuan Q, Liu D. Job dissatisfaction and burnout of nurses in Hunan, China: A cross-sectional survey. Nurs Health Sci. 2015;17(4):444–50.
Hanrahan NP, Aiken LH, McClaine L, Hanlon AL. Relationship between psychiatric nurse work environments and nurse burnout in acute care general hospitals. Issues Ment Health Nurs. 2010;31(3):198–207.
Liu X, Zheng J, Liu K, Baggs JG, Liu J, Wu Y, et al. Hospital nursing organizational factors, nursing care left undone, and nurse burnout as predictors of patient safety: a structural equation modeling analysis. Int J Nurs Stud. 2018;86:82–9.
Akman O, Ozturk C, Bektas M, Ayar D, Armstrong MA. Job satisfaction and burnout among paediatric nurses. J Nurs Manag. 2016;24(7):923–33.
Faller MS, Gates MG, Georges JM, Connelly CD. Work-related burnout, job satisfaction, intent to leave, and nurse-assessed quality of care among travel nurses. J Nurs Adm. 2011;41(2):71–7.
Boamah SA, Read EA, Spence Laschinger HK. Factors influencing new graduate nurse burnout development, job satisfaction and patient care quality: a time-lagged study. J Adv Nurs. 2017;73(5):1182–95.
Kanai-Pak M, Aiken LH, Sloane DM, Poghosyan L. Poor work environments and nurse inexperience are associated with burnout, job dissatisfaction and quality deficits in Japanese hospitals. J Clin Nurs. 2008;17(24):3324–9.
Leineweber C, Westerlund H, Chungkham HS, Lindqvist R, Runesdotter S, Tishelman C. Nurses’ practice environment and work-family conflict in relation to burn out: a multilevel modelling approach. PLoS One. 2014;9(5):e96991.
Article PubMed PubMed Central CAS Google Scholar
Leiter MP, Spence Laschinger HK. Relationships of work and practice environment to professional burnout: testing a causal model. Nurs Res. 2006;55(2):137–46.
Adali E, Priami M, Evagelou H, Mougia V, Ifanti M, Alevizopoulos G. Burnout in psychiatric nursing personnel in Greek hospitals. European Journal of Psychiatry. 2003;17(3):173–81.
Cao X, Naruse T. Effect of time pressure on the burnout of home-visiting nurses: the moderating role of relational coordination with nursing managers. Jpn J Nurs Sci. 2019;16(2):221–31.
Jansen PG, Kerkstra A, Abu-Saad HH, van der Zee J. The effects of job characteristics and individual characteristics on job satisfaction and burnout in community nursing. Int J Nurs Stud. 1996;33(4):407–21.
Gandi JC, Wai PS, Karick H, Dagona ZK. The role of stress and level of burnout in job performance among nurses. Ment Health Fam Med. 2011;8(3):181–94.
PubMed PubMed Central Google Scholar
Vidotti V, Ribeiro RP, Galdino MJQ, Martins JT. Burnout syndrome and shift work among the nursing staff. Rev Lat Am Enfermagem. 2018;26:e3022.
Shamian J, Kerr MS, Laschinger HK, Thomson D. A hospital-level analysis of the work environment and workforce health indicators for registered nurses in Ontario’s acute-care hospitals. Can J Nurs Res. 2002;33(4):35–50.
CAS PubMed Google Scholar
Rouxel G, Michinov E, Dodeler V. The influence of work characteristics, emotional display rules and affectivity on burnout and job satisfaction: a survey among geriatric care workers. Int J Nurs Stud. 2016;62:81–9.
Colindres CV, Bryce E, Coral-Rosero P, Ramos-Soto RM, Bonilla F, Yassi A. Effect of effort-reward imbalance and burnout on infection control among Ecuadorian nurses. Int Nurs Rev. 2018;65(2):190–9.
Shao J, Tang L, Wang X, Qiu R, Zhang Y, Jia Y, et al. Nursing work environment, value congruence and their relationships with nurses’ work outcomes. J Nurs Manag. 2018;26(8):1091–9.
Moloney W, Boxall P, Parsons M, Cheung G. Factors predicting registered nurses’ intentions to leave their organization and profession: a job demands-resources framework. J Adv Nurs. 2018;74(4):864–75.
Anwar MM, Elareed HR. Burnout among Egyptian nurses. Journal of Public Health-Heidelberg. 2017;25(6):693–7.
Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, Uaphanthasath R, Wiwatanadate P. Shift work and burnout among health care workers. Occup Med (Lond). 2014;64(4):279–86.
Article CAS Google Scholar
Ilhan MN, Durukan E, Taner E, Maral I, Bumin MA. Burnout and its correlates among nursing staff: questionnaire survey. J Adv Nurs. 2008;61(1):100–6.
Canadas-De la Fuente GA, Vargas C, San Luis C, Garcia I, Canadas GR, De la Fuente EI. Risk factors and prevalence of burnout syndrome in the nursing profession. Int J Nurs Stud. 2015;52(1):240–9.
Bagheri Hosseinabadi M, Ebrahimi MH, Khanjani N, Biganeh J, Mohammadi S, Abdolahfard M. The effects of amplitude and stability of circadian rhythm and occupational stress on burnout syndrome and job dissatisfaction among irregular shift working nurses. J Clin Nurs. 2019;28(9-10):1868–78.
Khamisa N, Peltzer K, Ilic D, Oldenburg B. Work related stress, burnout, job satisfaction and general health of nurses: a follow-up study. Int J Nurs Pract. 2016;22(6):538–45.
Dall’Ora C, Griffiths P, Ball J, Simon M, Aiken LH. Association of 12 h shifts and nurses’ job satisfaction, burnout and intention to leave: findings from a cross-sectional study of 12 European countries. BMJ Open. 2015;5(9):e008331.
Stimpfel AW, Sloane DM, Aiken LH. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Aff (Millwood). 2012;31(11):2501–9.
Poncet MC, Toullic P, Papazian L, Kentish-Barnes N, Timsit JF, Pochard F, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175(7):698–704.
Stone PW, Du Y, Gershon RR. Organizational climate and occupational health outcomes in hospital nurses. J Occup Environ Med. 2007;49(1):50–8.
Bourbonnais R, Comeau M, Vezina M, Dion G. Job strain, psychological distress, and burnout in nurses. Am J Ind Med. 1998;34(1):20–8.
Basinska BA, Wilczek-Ruzyczka E. The role of rewards and demands in burnout among surgical nurses. Int J Occup Med Environ Health. 2013;26(4):593–604.
Garcia-Sierra R, Fernandez-Castro J, Martinez-Zaragoza F. Relationship between job demand and burnout in nurses: does it depend on work engagement? J Nurs Manag. 2016;24(6):780–8.
Laeeque SH, Bilal A, Babar S, Khan Z, Rahman SU. How patient-perpetrated workplace violence leads to turnover intention among nurses: the mediating mechanism of occupational stress and burnout. J Aggress Maltreat Trauma. 2018;27(1):96–118.
Laschinger HKS, Shamian J, Thomson D. Impact of magnet hospital characteristics on nurses’ perceptions of trust, burnout, quality of care, and work satisfaction. Nurs Econ. 2001;19(5):209–19.
Li B, Bruyneel L, Sermeus W, Van den Heede K, Matawie K, Aiken L, et al. Group-level impact of work environment dimensions on burnout experiences among nurses: a multivariate multilevel probit model. Int J Nurs Stud. 2013;50(2):281–91.
Van Bogaert P, Meulemans H, Clarke S, Vermeyen K, Van de Heyning P. Hospital nurse practice environment, burnout, job outcomes and quality of care: test of a structural equation model. J Adv Nurs. 2009;65(10):2175–85.
Laschinger HKS, Leiter MP. The impact of nursing work environments on patient safety outcomes - the mediating role of burnout/engagement. J Nurs Adm. 2006;36(5):259–67.
Garrett DK, McDaniel AM. A new look at nurse burnout: the effects of environmental uncertainty and social climate. J Nurs Adm. 2001;31(2):91–6.
Bobbio A, Bellan M, Manganelli AM. Empowering leadership, perceived organizational support, trust, and job burnout for nurses: a study in an Italian general hospital. Health Care Manag Rev. 2012;37(1):77–87.
Spence Laschinger HK, Wong CA, Grau AL. The influence of authentic leadership on newly graduated nurses’ experiences of workplace bullying, burnout and retention outcomes: a cross-sectional study. Int J Nurs Stud. 2012;49(10):1266–76.
Lee HF, Chiang HY, Kuo HT. Relationship between authentic leadership and nurses’ intent to leave: the mediating role of work environment and burnout. J Nurs Manag. 2019;27(1):52–65.
Kanste O, Kyngas H, Nikkila J. The relationship between multidimensional leadership and burnout among nursing staff. J Nurs Manag. 2007;15(7):731–9.
Lake ET. Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–88.
Nantsupawat A, Kunaviktikul W, Nantsupawat R, Wichaikhum OA, Thienthong H, Poghosyan L. Effects of nurse work environment on job dissatisfaction, burnout, intention to leave. Int Nurs Rev. 2017;64(1):91–8.
Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Med Care. 2004;42(2 Suppl):II57–66.
Klopper HC, Coetzee SK, Pretorius R, Bester P. Practice environment, job satisfaction and burnout of critical care nurses in South Africa. J Nurs Manag. 2012;20(5):685–95.
Zhang LF, You LM, Liu K, Zheng J, Fang JB, Lu MM, et al. The association of Chinese hospital work environment with nurse burnout, job satisfaction, and intention to leave. Nurs Outlook. 2014;62(2):128–37.
Liu Y, Aungsuroch Y. Factors influencing nurse-assessed quality nursing care: a cross-sectional study in hospitals. J Adv Nurs. 2018;74(4):935–45.
Marques-Pinto A, Jesus EH, Mendes A, Fronteira I, Roberto MS. Nurses’ intention to leave the organization: a mediation study of professional burnout and engagement. Span J Psychol. 2018;21:E32.
Aiken LH, Sloane DM. Effects of organizational innovations in AIDS care on burnout among urban hospital nurses. Work Occup. 1997;24(4):453–77.
Spence Laschinger HK, Leiter M, Day A, Gilin D. Workplace empowerment, incivility, and burnout: impact on staff nurse recruitment and retention outcomes. J Nurs Manag. 2009;17(3):302–11.
Dutra HS, Cimiotti JP, Guirardello EB. Nurse work environment and job-related outcomes in Brazilian hospitals. Appl Nurs Res. 2018;41:68–72.
Laschinger HK. Job and career satisfaction and turnover intentions of newly graduated nurses. J Nurs Manag. 2012;20(4):472–84.
Estryn-Behar M, Van der Heijden BI, Oginska H, Camerino D, Le Nezet O, Conway PM, et al. The impact of social work environment, teamwork characteristics, burnout, and personal factors upon intent to leave among European nurses. Med Care. 2007;45(10):939–50.
Basar U, Basim N. A cross-sectional survey on consequences of nurses’ burnout: moderating role of organizational politics. J Adv Nurs. 2016;72(8):1838–50.
Van Bogaert P, Timmermans O, Weeks SM, van Heusden D, Wouters K, Franck E. Nursing unit teams matter: impact of unit-level nurse practice environment, nurse work characteristics, and burnout on nurse reported job outcomes, and quality of care, and patient adverse events--a cross-sectional survey. Int J Nurs Stud. 2014;51(8):1123–34.
Firth H, Britton P. Burnout, absence and turnover amongst British nursing staff. J Occup Psychol. 1989;62(1):55–9.
Giorgi F, Mattei A, Notarnicola I, Petrucci C, Lancia L. Can sleep quality and burnout affect the job performance of shift-work nurses? A hospital cross-sectional study. J Adv Nurs. 2018;74(3):698–708.
Tourigny L, Baba VV, Wang XY. Burnout and depression among nurses in Japan and China: the moderating effects of job satisfaction and absence. Int J Hum Resour Manag. 2010;21(15):2741–61.
Johnson J, Louch G, Dunning A, Johnson O, Grange A, Reynolds C, et al. Burnout mediates the association between depression and patient safety perceptions: a cross-sectional study in hospital nurses. J Adv Nurs. 2017;73(7):1667–80.
Nantsupawat A, Nantsupawat R, Kunaviktikul W, Turale S, Poghosyan L. Nurse burnout, nurse-reported quality of care, and patient outcomes in Thai hospitals. J Nurs Scholarsh. 2016;48(1):83–90.
Poghosyan L, Clarke SP, Finlayson M, Aiken LH. Nurse burnout and quality of care: cross-national investigation in six countries. Res Nurs Health. 2010;33(4):288–98.
Zarei E, Khakzad N, Reniers G, Akbari R. On the relationship between safety climate and occupational burnout in healthcare organizations. Saf Sci. 2016;89:1–10.
Halbesleben JR, Wakefield BJ, Wakefield DS, Cooper LB. Nurse burnout and patient safety outcomes: nurse safety perception versus reporting behavior. West J Nurs Res. 2008;30(5):560–77.
Teng CI, Shyu YI, Chiou WK, Fan HC, Lam SM. Interactive effects of nurse-experienced time pressure and burnout on patient safety: a cross-sectional survey. Int J Nurs Stud. 2010;47(11):1442–50.
Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40(6):486–90.
Antonakis J, Bendahan S, Jacquart P, Lalive R. On making causal claims: a review and recommendations. Leadersh Q. 2010;21(6):1086–120.
Maben J, Latter S, Clark JM. The sustainability of ideals, values and the nursing mandate: evidence from a longitudinal qualitative study. Nurs Inq. 2007;14(2):99–113.
Download references
Acknowledgements
We would like to thank Jane Lawless who performed the second screening of the provisionally included papers.
Author information
Authors and affiliations.
School of Health Sciences, and Applied Research Collaboration Wessex, Highfield Campus, University of Southampton, Southampton, SO17 1BJ, UK
Chiara Dall’Ora & Peter Griffiths
Department of Learning, Informatics, Management and Ethics, Karolinska Institutet, Tomtebodavägen 18a, 17177, Solna, Sweden
Jane Ball, Maria Reinius & Peter Griffiths
You can also search for this author in PubMed Google Scholar
Contributions
CDO led the paper write-up at all stages, designed and conducted the search strategy, completed the initial screening of papers, co-developed the coding frame, and applied the coding frame to all studies. JB conceived the review, co-developed the coding frame, applied the coding frame to all studies, and contributed substantially to drafting the paper at various stages. MR extracted all the data from studies and produced evidence tables. PG conceived the review and contributed substantially to the drafting of the paper at various stages. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Chiara Dall’Ora .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:.
MEDLINE via OVID, CINAHL with full text via EBSCO, and PsycINFO via EBSCO.

Additional file 2:
PRISMA-ScR Checklist.
Additional file 3:
Studies’ settings, sample sizes, burnout and correlates measurement, and appraisal of quality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dall’Ora, C., Ball, J., Reinius, M. et al. Burnout in nursing: a theoretical review. Hum Resour Health 18 , 41 (2020). https://doi.org/10.1186/s12960-020-00469-9
Download citation
Received : 04 December 2019
Accepted : 24 March 2020
Published : 05 June 2020
DOI : https://doi.org/10.1186/s12960-020-00469-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Job demands
- Practice environment
Human Resources for Health
ISSN: 1478-4491
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Burnout in nursing: a theoretical review
Affiliations.
- 1 School of Health Sciences, and Applied Research Collaboration Wessex, Highfield Campus, University of Southampton, Southampton, SO17 1BJ, UK. [email protected].
- 2 Department of Learning, Informatics, Management and Ethics, Karolinska Institutet, Tomtebodavägen 18a, 17177, Solna, Sweden.
- 3 School of Health Sciences, and Applied Research Collaboration Wessex, Highfield Campus, University of Southampton, Southampton, SO17 1BJ, UK.
- PMID: 32503559
- PMCID: PMC7273381
- DOI: 10.1186/s12960-020-00469-9
Background: Workforce studies often identify burnout as a nursing 'outcome'. Yet, burnout itself-what constitutes it, what factors contribute to its development, and what the wider consequences are for individuals, organisations, or their patients-is rarely made explicit. We aimed to provide a comprehensive summary of research that examines theorised relationships between burnout and other variables, in order to determine what is known (and not known) about the causes and consequences of burnout in nursing, and how this relates to theories of burnout.
Methods: We searched MEDLINE, CINAHL, and PsycINFO. We included quantitative primary empirical studies (published in English) which examined associations between burnout and work-related factors in the nursing workforce.
Results: Ninety-one papers were identified. The majority (n = 87) were cross-sectional studies; 39 studies used all three subscales of the Maslach Burnout Inventory (MBI) Scale to measure burnout. As hypothesised by Maslach, we identified high workload, value incongruence, low control over the job, low decision latitude, poor social climate/social support, and low rewards as predictors of burnout. Maslach suggested that turnover, sickness absence, and general health were effects of burnout; however, we identified relationships only with general health and sickness absence. Other factors that were classified as predictors of burnout in the nursing literature were low/inadequate nurse staffing levels, ≥ 12-h shifts, low schedule flexibility, time pressure, high job and psychological demands, low task variety, role conflict, low autonomy, negative nurse-physician relationship, poor supervisor/leader support, poor leadership, negative team relationship, and job insecurity. Among the outcomes of burnout, we found reduced job performance, poor quality of care, poor patient safety, adverse events, patient negative experience, medication errors, infections, patient falls, and intention to leave.
Conclusions: The patterns identified by these studies consistently show that adverse job characteristics-high workload, low staffing levels, long shifts, and low control-are associated with burnout in nursing. The potential consequences for staff and patients are severe. The literature on burnout in nursing partly supports Maslach's theory, but some areas are insufficiently tested, in particular, the association between burnout and turnover, and relationships were found for some MBI dimensions only.
Keywords: Burnout; Job demands; Maslach Burnout Inventory; Nursing; Practice environment.
Publication types
- Systematic Review
- Burnout, Professional / epidemiology*
- Health Status
- Internal-External Control
- Job Satisfaction
- Nurse's Role / psychology
- Nurses / psychology*
- Nurses / statistics & numerical data*
- Patient Safety
- Personnel Turnover / statistics & numerical data
- Quality of Health Care
- Sick Leave / statistics & numerical data
- Time Factors
- Workload / psychology
- Workplace / psychology*
- Introduction
- Conclusions
- Article Information
Data are from the 2018 National Sample Survey of Registered Nurses.
eTable. Top 5 Reasons for Leaving Job and Considering Leaving Job by Respondents, 2018 National Sample Survey of Registered Nurses
- Error in Sample Sizes JAMA Network Open Correction March 16, 2021
- Error in Funding/Support JAMA Network Open Correction April 25, 2023
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Shah MK , Gandrakota N , Cimiotti JP , Ghose N , Moore M , Ali MK. Prevalence of and Factors Associated With Nurse Burnout in the US. JAMA Netw Open. 2021;4(2):e2036469. doi:10.1001/jamanetworkopen.2020.36469
Manage citations:
© 2024
- Permissions
Prevalence of and Factors Associated With Nurse Burnout in the US
- 1 Department of Family and Preventive Medicine, Emory University School of Medicine, Atlanta, Georgia
- 2 Nell Hodgson Woodruff School of Nursing, Emory University, Atlanta, Georgia
- 3 Department of Global Health, Rollins School of Public Health, Emory University, Atlanta, Georgia
- Correction Error in Sample Sizes JAMA Network Open
- Correction Error in Funding/Support JAMA Network Open
Question What were the most recent US national estimates of nurse burnout and associated factors that may put nurses at risk for burnout?
Findings This secondary analysis of cross-sectional survey data from more than 50 000 US registered nurses (representing more than 3.9 million nurses nationally) found that among nurses who reported leaving their current employment (9.5% of sample), 31.5% reported leaving because of burnout in 2018. The hospital setting and working more than 20 hours per week were associated with greater odds of burnout.
Meaning With increasing demands placed on frontline nurses during the coronavirus disease 2019 pandemic, these findings suggest an urgent need for solutions to address burnout among nurses.
Importance Clinician burnout is a major risk to the health of the US. Nurses make up most of the health care workforce, and estimating nursing burnout and associated factors is vital for addressing the causes of burnout.
Objective To measure rates of nurse burnout and examine factors associated with leaving or considering leaving employment owing to burnout.
Design, Setting, and Participants This secondary analysis used cross-sectional survey data collected from April 30 to October 12, 2018, in the National Sample Survey of Registered Nurses in the US. All nurses who responded were included (N = 50 273). Data were analyzed from June 5 to October 1, 2020.
Exposures Age, sex, race and ethnicity categorized by self-reported survey question, household income, and geographic region. Data were stratified by workplace setting, hours worked, and dominant function (direct patient care, other function, no dominant function) at work.
Main Outcomes and Measures The primary outcomes were the likelihood of leaving employment in the last year owing to burnout or considering leaving employment owing to burnout.
Results The weighted sample of 50 273 respondents (representing 3 957 661 nurses nationally) was predominantly female (90.4%) and White (80.7%); the mean (SD) age was 48.7 (0.04) years. Among nurses who reported leaving their job in 2017 (n = 418 769), 31.5% reported burnout as a reason, with lower proportions of nurses reporting burnout in the West (16.6%) and higher proportions in the Southeast (30.0%). Compared with working less than 20 h/wk, nurses who worked more than 40 h/wk had a higher likelihood identifying burnout as a reason they left their job (odds ratio, 3.28; 95% CI, 1.61-6.67). Respondents who reported leaving or considering leaving their job owing to burnout reported a stressful work environment (68.6% and 59.5%, respectively) and inadequate staffing (63.0% and 60.9%, respectively).
Conclusions and Relevance These findings suggest that burnout is a significant problem among US nurses who leave their job or consider leaving their job. Health systems should focus on implementing known strategies to alleviate burnout, including adequate nurse staffing and limiting the number of hours worked per shift.
Clinician burnout is a threat to US health and health care. 1 At more than 6 million in 2019, 2 nurses are the largest segment of our health care workforce, making up nearly 30% of hospital employment nationwide. 3 Nurses are a critical group of clinicians with diverse skills, such as health promotion, disease prevention, and direct treatment. As the workloads on health care systems and clinicians have grown, so have the demands placed on nurses, negatively affecting the nursing work environment. When combined with the ever-growing stress associated with the coronavirus disease 2019 (COVID-19) pandemic, this situation could leave the US with an unstable nurse workforce for years to come. Given their far-ranging skill set, importance in the care team, and proportion of the health care workforce, it is imperative that we better understand job-related outcomes and the factors that contribute to burnout in nurses nationwide.
Demanding workloads and aspects of the work environment, such as poor staffing ratios, lack of communication between physicians and nurses, and lack of organizational leadership within working environments for nurses, are known to be associated with burnout in nurses. 4 , 5 However, few, if any, recent national estimates of nurse burnout and contributing factors exist. We used the most recent nationally representative nurse survey data to characterize burnout in the nurse workforce before COVID-19. Specifically, we examined to what extent aspects of the work environment resulted in nurses leaving the workforce and the factors associated with nurses’ intention to leave their jobs and the nursing profession.
We used data from the 2018 US Department of Health and Human Services’ Health Resources and Service Administration National Sample Survey of Registered Nurses (NSSRN), a nationally representative anonymous sample of registered nurses in the US. The weighted response rate for the 2018 NNRSN is estimated at 49.0%. 6 Details on sampling frame, selection, and noninterview adjustments are described elsewhere. 7 Weighted estimates generalize to state and national nursing populations. 6 The American Association for Public Opinion Research Response Rate 3 method was used to calculate the NSSRN response rate. 6 This study of deidentified publicly available data was determined to be exempt from approval and informed consent by the institutional review board of Emory University. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline for cross-sectional studies. Data were collected from April 30 to October 12, 2018.
We generated demographic characteristics from questions about years worked in the profession, primary and secondary nursing positions, and work environment. We included the work environment variables of primary employment setting and full-time or part-time status. We grouped responses to a question on dominant nursing tasks as direct patient care, other, and no dominant task. We included 3 categories of educational attainment (diploma/ADN, BSN, or MSN/PhD/DNP degrees) and whether the respondent was internationally educated. Other variables included change in employment setting in the last year, hours worked per week, and reasons for employment change.
We categorized employment setting as (1) hospital (not mental health), (2) other inpatient setting, (3) clinic or ambulatory care, and (4) other types of setting. Workforce stability was defined as the percentage of nurses with less than 5 years of experience in the nursing profession.
We used 2 questions to assess burnout and other reasons for leaving or planning to leave a nursing position. Nurses who had left the position they held on December 31, 2017, were asked to identify the reasons contributing to their decision to leave their prior position. Nurses who were still employed in the position they held on December 31, 2017, and answered yes to the question “Have you ever considered leaving the primary nursing position you held on December 31, 2017?” were asked “Which of the following reasons would contribute to your decision to leave your primary nursing position?”
Data were analyzed from June 5 to October 1, 2020. We used descriptive statistics to characterize nurse survey responses. For continuous variables, we reported means and SDs and for categorical variables, frequencies (number [percentage]). Further, we examined the overlap of the proportions who reported leaving or considered leaving their job owing to burnout and other factors. We then fit 2 separate logistic regression models to estimate the odds that aspects of the work environment, hours, and tasks were associated with the following outcomes related to burnout: (1) left job owing to burnout and (2) considered leaving their job owing to burnout. We controlled for nurse demographic characteristics of age, sex, race, household income, and geographic region and reported odds ratios (ORs) and 95% CIs. Two separate sensitivity analyses were performed: (1) we used a broader theme of burnout defined as a response of burnout, inadequate staffing, or stressful work environment for the regression models; and (2) we stratified the regression models by respondents younger than 45 years and 45 years or older to examine difference by age.
We used SAS, version 9.4 (SAS Institute, Inc), with statistical significance set at 2-sided α = .05. We used sample weights to account for the differential selection probabilities and nonresponse bias.
Of the 50 273 nurse respondents (representing 3 957 661 nurses nationally), respondents in 2018 were mostly female (90.4%) and White (80.7%). The mean (weighted SD) age of nurse respondents was 48.7 (0.04) years, and 95.3% were US graduates. The percentage of nurses with a BSN degree was 45.8%; with an MSN, PhD, or DNP degree, 16.3%; and 49.5% of nurses reported that they worked in a hospital. The mean (weighted SD) age of nurses who left their job due to burnout was 42.0 (0.6) years; for those considering leaving their job due to burnout, 43.7 (0.3) years ( Table 1 ).
Of the total weighted sample of nurses (N = 3 957 661), 9.5% reported leaving their most recent position (n = 418 769), and of those, 31.5% reported burnout as a reason contributing to their decision to leave their job (3.3% of the total sample) (eTable in the Supplement ). For nurses who had considered leaving their position (n = 676 122), 43.4% identified burnout as a reason that would contribute to their decision to leave their current job. Additional factors in these decisions were a stressful work environment (34.4% as the reason for leaving and 41.6% as the reason for considering leaving), inadequate staffing (30.0% as the reason for leaving and 42.6% as the reason for considering leaving), lack of good management or leadership (33.9% as the reason for leaving and 39.6% as the reason for considering leaving), and better pay and/or benefits (26.5% as the reason for leaving and 50.4% as the reason for considering leaving). By geographic regions of the US, lower proportions of nurses reported burnout in the West (16.6%), and higher proportions reported burnout in the Southeast (30.0%) ( Figure 1 and Figure 2 ). Figure 3 shows the overlap between leaving or considering leaving their position owing to burnout and other reasons. For both outcomes, the highest overlap response with burnout was for stressful work environment (68.6% of those who left their job and 63.0% of those who considered leaving their job due to burnout).
The adjusted regression models estimating the odds of nurses indicating burnout as a reason for leaving their positions or considering leaving their position revealed statistically significant associations between workplace settings and hours worked per week, but not for tasks performed, and burnout ( Table 2 ). For nurses who had left their jobs, compared with nurses working in a clinic setting, nurses working in a hospital setting had more than twice higher odds of identifying burnout as a reason for leaving their position (OR, 2.10; 95% CI, 1.41-3.13); nurses working in other inpatient settings had an OR of 2.26 (95% CI, 1.39-3.68). Compared with working less than 20 h/wk, nurses who worked more than 40 h/wk had an OR of 3.28 (95% CI, 1.61-6.67) for identifying burnout as a reason they left their position.
For nurses who reported ever considering leaving their job, working in a hospital setting was associated with 80% higher odds of burnout as the reason than for nurses working in a clinic setting (OR, 1.80; 95% CI, 1.55-2.08), whereas among nurses who worked in other inpatient settings, burnout was associated with a 35% higher odds that nurses intended to leave their job (OR, 1.35; 95% CI, 1.05-1.73). Compared with working less than 20 h/wk, the odds of identifying burnout as a reason for considering leaving their position increased with working 20 to 30 h/wk (OR, 2.56; 95% CI, 1.85-3.55), 31 to 40 h/wk, (OR, 2.98; 95% CI, 2.24-3.98), and more than 40 h/wk, (OR, 3.64; 95% CI, 2.73-4.85).
The sensitivity analysis results in which a broader classification of burnout was used showed a similar relationship between odds of burnout and working more than 40 h/wk (OR, 3.86; 95% CI, 2.27-6.59) for those who left their job (OR, 2.66; 95% CI, 2.13-3.31). Stratification by those younger than 45 years and 45 years or older did not significantly change the findings. Figure 3 shows the overlap in nurses who reported burnout and other reasons for leaving their current position or considering leaving their current positions. The greatest overlap occurred in responses of burnout and stressful work environment (68.6% of those who reported leaving and 59.5% of those who considered leaving) and inadequate staffing (63.0% of those who reported leaving and 60.9% of those who considered leaving).
Our findings from the 2018 NSSRN show that among those nurses who reported leaving their jobs in 2017, high proportions of US nurses reported leaving owing to burnout. Hospital setting was associated with greater odds of identifying burnout in decisions to leave or to consider leaving a nursing position, and there was no difference by dominant work function.
Health care professionals are generally considered to be in one of the highest-risk groups for experience of burnout, given the emotional strain and stressful work environment of providing care to sick or dying patients. 8 , 9 Previous studies demonstrate that 35% to 54% of clinicians in the US experience burnout symptoms. 10 - 13 The recent National Academy of Medicine report, “Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being,” recommended health care organizations routinely measure and monitor clinician burnout and hold leaders accountable for the health of their organization’s work environment in an effort to reduce burnout and promote well-being. 1
Moreover, it appears the numbers have increased over time. Data from the 2008 NSSRN showed that approximately 17% of nurses who left their position in 2007 cited burnout as the reason for leaving, 14 and our data show that 31.5% of nurses cited burnout as the reason for leaving their job in the last year (2017-2018). Despite this evidence, little has changed in health care delivery and the role of registered nurses. The COVID-19 pandemic has further complicated matters; for example, understaffing of nurses in New York and Illinois was associated with increased odds of burnout amidst high patient volumes and pandemic-related anxiety. 15
Our findings show that among nurses who reported leaving their job owning to burnout, a high proportion reported a stressful work environment. Substantial evidence documents that aspects of the work environment are associated with nurse burnout. Increased workloads, lack of support from leadership, and lack of collaboration among nurses and physicians have been cited as factors that contribute to nurse burnout. 4 , 16 Magnet hospitals and other hospitals with a reputation for high-quality nursing care have shown that transforming features of the work environment, including support for education, positive physician-nurse relationships, nurse autonomy, and nurse manager support, outside of increasing the number of nurses, can lead to improvements in job satisfaction and lower burnout among nurses. 17 - 19 The qualities of Magnet hospitals not only attract and retain nurses and result in better nurse outcomes, based on features of the work environment, but also improvements in the overall quality of patient care. 17 - 19
Self-reported regional variation in burnout deserves attention. The lower reported rates of nurse burnout in California and Massachusetts could be attributed to legislation in these states regulating nurse staffing ratios; California has the most extensive nurse staffing legislation in the US. 20 The high rates of reported burnout in the Southeast and the overlap of burnout and inadequate staffing in our findings could be driven by shortages of nurses in the states in this area, particularly South Carolina and Georgia. 15 Geographic distribution, nurse staffing, and its association with self-reported burnout warrant further exploration.
Our data show that the number of hours worked per week by nurses, but not the dominant function at work, was positively associated with identifying burnout as a reason for leaving their position or considering leaving their position. Research suggests nurses who work longer shifts and who experience sleep deprivation are likely to develop burnout. 21 - 23 Others have reported a strong correlation between sleep deprivation and errors in the delivery of patient care. 22 , 24 Emotional exhaustion has been identified as a major component of burnout; such exhaustion is likely exacerbated by excessive work hours and inadequate sleep. 25 , 26
The nurse workforce represents most current frontline workers providing care during the COVID-19 pandemic. Literature from past epidemics (eg, H1N1 influenza, severe acute respiratory syndrome, Ebola) suggest that nurses experience significant stress, anxiety, and physical effects related to their work. 27 These factors will most certainly be amplified during the current pandemic, placing the nurse workforce at risk of increased strain. Recent reports suggest that nurses are leaving the bedside owing to COVID-19 at a time when multiple states are reporting a severe nursing shortage. 28 - 31 Furthermore, given that the nurse workforce is predominantly female and married, the child rearing and domestic responsibilities of current lockdowns and quarantines can only increase their burden and risk of burnout. Our results demonstrate that the mean age at which nurses who have left or considered leaving their current jobs is younger than 45 years. In the present context, our results forewarn of major effects to the frontline nurse workforce. Further studies are needed to elucidate the effect of the current pandemic on the nurse workforce, particularly among younger nurses of color, who are underrepresented in these data. Policy makers and health systems should also focus on aspects of the work environment known to improve job satisfaction, including staffing ratios, continued nursing education, and support for interdisciplinary teamwork.
Our study has some limitations. First, our findings are from cross-sectional data and limit causal inference; however, these data represent the most recent and, to our knowledge, the only national survey with data on nurse burnout. Second, our burnout measure is crude, and more extensive measures of burnout are needed. Third, 4 states did not have enough respondents to release data (Montana, Wyoming, North Dakota, and South Dakota). However, these data were weighted, and they represent the most comprehensive data available on the registered nurse workforce. Fourth, nonresponse analyses of these data reveal underestimation of certain races/ethnicities, specifically Hispanic nurses, and small sample sizes limited analyses of burnout by race/ethnicity. Fifth, the public use file of the NSSRN does not disaggregate the MSN, PhD, and DNP degrees in nursing practice categories. Given that these job tasks can vary, we addressed this limitation by examining dominant function at work. Last, the response rate was modest at 49.0% (weighted). Despite these limitations, this analysis is most likely the first to provide an updated overview of registered nurse burnout across the US.
Burnout continues to be reported by registered nurses across a variety of practice settings nationwide. How the COVID-19 pandemic will affect burnout rates owing to unprecedented demands on the workforce is yet to be determined. Legislation that supports adequate staffing ratios is a key part of a multitiered solution. Solutions must come through system-level efforts in which we reimagine and innovate workflow, human resources, and workplace wellness to reduce or eliminate burnout among frontline nurses and work toward healthier clinicians, better health, better care, and lower costs. 32
Accepted for Publication: December 16, 2020.
Published: February 4, 2021. doi:10.1001/jamanetworkopen.2020.36469
Correction: This article was corrected on March 16, 2021, to clarify that the given sample sizes were weighted values based on a smaller number of survey responses; changes have been made to the sample sizes in the Key Points, Abstract, Results section, and Table 1. The Supplement was corrected on April 7, 2021, to clarify in the eTable that the sample sizes are weighted values. The article was corrected on April 25, 2023, to add a previously missing grant awarded to Dr Cimiotti to the Funding/Support section.
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2021 Shah MK et al. JAMA Network Open .
Corresponding Author: Megha K. Shah, MD, MSc, Department of Family and Preventive Medicine, Emory University School of Medicine, 4500 N Shallowford Rd, Dunwoody, GA 30338 ( [email protected] ).
Author Contributions: Drs Shah and Gandrakota had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Shah, Cimiotti, Ghose, Moore, Ali.
Acquisition, analysis, or interpretation of data: Shah, Gandrakota, Cimiotti, Moore.
Drafting of the manuscript: Shah, Gandrakota, Cimiotti, Moore.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Gandrakota, Cimiotti, Moore.
Obtained funding: Shah.
Administrative, technical, or material support: Shah, Gandrakota, Ghose.
Supervision: Ali.
Conflict of Interest Disclosures: Dr Ali reported receiving grants from Merck & Co outside the submitted work. No other disclosures were reported.
Funding/Support: This study was supported by grant K23 MD015088-01 from the National Institute on Minority Health and Health Disparities (Dr Shah), grant R01HS026232 from the Agency for Healthcare Research and Quality (Dr Cimiotti), and in part by the Georgia Center for Diabetes Translation Research, funded by grant P30DK111024 from the National Institute of Diabetes and Digestive and Kidney Diseases (Dr Ali).
Role of the Funder/Sponsor: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 29 April 2024
Exploring the relationships between resilience, burnout, work engagement, and intention to leave among nurses in the context of the COVID-19 pandemic: a cross-sectional study
- Apiradee Nantsupawat 1 ,
- Ann Kutney-Lee 2 ,
- Kulwadee Abhicharttibutra 1 ,
- Orn-Anong Wichaikhum 1 &
- Lusine Poghosyan 3
BMC Nursing volume 23 , Article number: 290 ( 2024 ) Cite this article
192 Accesses
Metrics details
Nurses have faced significant personal and professional stressors during the COVID-19 pandemic that have contributed to increased rates of burnout, intention to leave, and poorer work engagement. Resilience has been identified as a critical factor influencing job outcomes; however, the dynamics of this association have not yet been investigated within the context of the Thai workforce. The study objective was to determine the associations between resilience and job outcomes, including burnout, intention to leave, and work engagement among nurses working in Thailand during the COVID-19 pandemic.
This cross-sectional study gathered data from a sample of 394 registered nurses employed across 12 hospitals. The research instruments comprised the Connor–Davidson Resilience Scale (CD-RISC), the Maslach Burnout Inventory-Health Services Survey (MBI-HSS), a questionnaire assessing the intention to leave the job, and the Utrecht Work Engagement Scale (UWES). To determine the associations among the measured variables, multivariate logistic regression analyses were conducted.
One-third of nurses experienced emotional exhaustion and depersonalization, and about half experienced reduced personal accomplishment; one-tenth of nurses intended to leave their job. Nurses who exhibited higher levels of resilience were found to have a significantly reduced likelihood of experiencing high emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment. Conversely, these nurses were more likely to report higher levels of work engagement than their less resilience.
The COVID-19 pandemic offers important lessons learned about promoting the well-being of the nursing workforce and protecting against adverse job outcomes. While we identified resilience as a significant predictor of several nurse outcomes, other work environment factors should be considered. Government and hospital administrations should allocate resources for individual and organizational-level interventions to promote resilience among frontline nurses so that hospitals will be better prepared for the next public health emergency and patient and nurse outcomes can be optimized.
Peer Review reports
Since the coronavirus disease 2019 (COVID-19) global health emergency was declared in January 2020 [ 6 ], nurses working on the frontlines have faced substantial professional and personal stress. Especially during the early phases of the pandemic, nurses working in hospitals experienced staffing shortages and worked long hours with limited medical supplies and resources, all while placing their personal health and well-being at risk [ 3 ]. Three years later, the pandemic has eased due to effective vaccines and treatments; however, the pandemic’s impact on the nursing workforce is still being felt. The adverse effects of working during the pandemic on nurses’ physical (e.g., fatigue, sleeplessness) and psychosocial (e.g., post-traumatic stress disorder, depression) well-being have been well-documented [ 7 ]. Taken together, these stressors are increasingly acknowledged as significant contributors to increasing rates of burnout and intention to leave and lower levels of work engagement among nurses, all of which may negatively affect patient safety [ 21 ].
Numerous international studies, including systematic reviews and meta-analyses, have documented higher rates of burnout [ 15 ] and intention to leave [ 41 ] among nursing professionals in the period of the COVID-19 pandemic. Burnout is defined as a syndrome emerging from a context of unmanaged chronic workplace stress. Burnout is characterized by three core dimensions: a sustained sense of exhaustion and energy loss, a growing detachment or a cynical attitude toward one’s job, and a perceived decline in professional efficacy and accomplishment [ 44 ]. Employing the three distinct subscales of the MBI—a widely recognized tool for assessing burnout—Galanis et al. [ 15 ] found that 34.1% exhibited substantial emotional exhaustion in their global analysis of nurses. Additionally, 12.6% demonstrated significant levels of depersonalization, while 15.2% reported a profound lack of personal accomplishment.
Similarly, nurses also had high rates of intention to leave, referred to as one’s plan to leave their current job, and is strongly related to actual turnover [ 17 ]. The construct of ‘intention to leave’ is widely utilized as a predictive indicator of the potential attrition within the nursing workforce, which has significant implications for maintaining safe workplace environments and ensuring the quality of patient care [ 23 ]. A recent systematic review and meta-analysis to evaluate the prevalence of turnover intentions among nurses throughout the COVID-19 pandemic revealed that approximately 31.7% of nurses were considering leaving their positions during the outbreak [ 41 ]. Moreover, turnover intentions were higher than before COVID-19 [ 33 ].
Work engagement among nurses has also been impacted by the pandemic [ 2 , 10 ]. Work engagement is commonly conceptualized as a positive and fulfilling work-related state of mind that is manifested by three key elements: vigor, dedication, and absorption [ 37 ]. Vigor is defined as the propensity to expend persistent effort in one’s occupational tasks; dedication encompasses the degree of personal involvement in one’s professional role; and absorption pertains to the depth of concentration and engrossment in work-related activities. Nurses with high levels of engagement can work in extraordinarily stressful conditions and handle undesirable consequences while continuing to contribute to work-related creativity, productivity, and job performance. Past research has demonstrated that a workforce composed of highly engaged nurses is associated with high-quality patient care [ 34 , 39 ]. Research on work engagement among nurses internationally during the COVID-19 pandemic has yielded inconsistent results. Some studies have identified low to moderate levels of work engagement among frontline nurses during the pandemic [ 10 , 16 , 28 ], whereas other studies report high levels of engagement [ 2 , 26 ]. Differences in work engagement among nurses have been attributed to differences in resilience, which may be influenced by both personal attributes and the environment in which nurses work [ 35 ].
Research is needed to understand factors that reduce burnout and intention to leave and increase work engagement among nurses to promote workforce retention and maintain quality of care throughout the pandemic and beyond. Such evidence is critically important for healthcare administrators and policymakers to invest efforts to support the nursing workforce in critical times. With innovative policies supporting nurses’ well-being, patients may experience better care. During the COVID-19 pandemic, studying nurse resilience has emerged as an increasingly studied characteristic of nurses that may be essential to these outcomes. Resilience is defined as the capacity to recover from difficulties or adapt to challenging and adverse circumstances [ 13 ]. An individual demonstrating resilience actively endeavors to progress constructively, drawing upon the insights and knowledge gained from confronting adverse experiences. Indeed, several studies among healthcare workers and nurses during the pandemic have found associations between resilience and lower levels of burnout [ 4 , 20 , 25 , 42 ], intention to leave [ 29 , 40 ] and a higher level of work engagement [ 9 , 26 ]. However, these studies have been limited to the United States, Australia, China, Brazil, and Spain. Furthermore, many of these studies focused on resilience without adequate emphasis on significant contextual factors necessary for safe nursing care.
Thailand was recognized as the first country to confirm cases of COVID-19 beyond the borders of the People’s Republic of China. The preliminary measures enacted by the Thai Ministry of Public Health to mitigate the spread of the pandemic were centered on enhancing personal and communal hygiene practices [ 45 ]. Following the proclamation of an emergency decree, the Thai government implemented stringent control measures to curtail the spread of COVID-19. These measures included the imposition of travel restrictions, the prohibition of public gatherings, the enforcement of physical distancing, the strategic lockdown of areas deemed high-risk for transmission, the suspension of all international flights into Thailand, and mandatory government-managed quarantine for individuals returning from abroad for 14 days (Department of Disease Control, 2020). When this study was conducted in 2022, a cumulative total of 4.7 million COVID-19 cases had been confirmed in Thailand. During the height of the pandemic, however, resources to support nurses and other healthcare professionals in the delivery of patient care were under severe constraints [ 24 ]. As such, nurses in Thailand have experienced burnout, depression, and post-traumatic stress disorder [ 8 ] at rates similar to those documented in other countries [ 15 ]. However, to our knowledge, studies have yet to be conducted on nurse resilience and its relationships with nurse job outcomes in Thailand. This study examined the associations between resilience and job outcomes, including burnout, intention to leave, and work engagement among nurses working in Thailand during the COVID-19 pandemic.
Participants and procedures
The sample size was determined using the Yamane formula (1973), with a 95% confidence level and p = 0.05. Including an allowance of approximately 20% for potential loss, 477 questionnaires were distributed to nurses who were required to possess a minimum of one year of experience at general hospitals, providing direct nursing care to patients during the COVID-19 pandemic. A multistage sampling method was conducted to enroll participants from 12 general hospitals with 200–500 beds nationwide located in six of the country’s twelve health regions. This investigation constitutes a segment of a study examining nurses’ perceptions of job-related outcomes amidst the COVID-19 pandemic in Thailand’s general hospitals. For further details regarding the sample selection, please look at a prior study [ 32 ].
Before starting data collection, ethical approval was obtained from the Research Ethics Review Committee of the Faculty of Nursing under the reference number EXP:055-2022 and by the hospital administrators of the participating hospitals. Then the researcher convened with coordinators who were hospital staff designated by the hospital administrators to collect the data and to explain data collection procedures. Invitations and questionnaires were sent to nurses. Nurses who indicated a willingness to participate were issued invitations detailing the study’s objectives, the methodologies employed in data collection, the estimated time commitment required for questionnaire completion, the potential risks and benefits associated with the study, and guarantees of participant confidentiality. Participants were instructed to return the completed questionnaires and signed informed consent documents in separate, sealed envelopes to a designated collection point. Hospital coordinators were responsible for forwarding all collected materials to the principal investigator via postal service. Of the 477 questionnaires distributed to nurses who met the inclusion criteria, 394 were completed and returned, yielding a response rate of 82.6%.
Instruments
The questionnaire included demographic items and measures of resilience, burnout, intent to leave, and work engagement. Demographic items included age, gender, education, marital status, years working on their current unit, years in professional nursing, the number of children, and family members.
We used the CD-RISC-10, a 10-item instrument, to measure resilience. The items were scored on a 5-point Likert scale ranging from 0 (never) to 4 (almost always), with higher scores reflecting greater resilience [ 11 ]. The Cronbach’s alpha coefficient for the instrument was calculated to be 0.92 in the current study.
Burnout : We used the Maslach Burnout Inventory-Health Services Survey (MBI-HSS) [ 27 ] to measure burnout. The three subscales of the MBI-HSS include Emotional Exhaustion (EE), Depersonalization (DPER), and Personal Accomplishments (PAC) and consist of nine items, five items, and eight items, respectively. Responses are evaluated using a 7-point Likert scale ranging from 0, indicating ‘never’, to 6, signifying ‘every day’. The following criteria can characterize burnout: achieving a score of 27 or higher on the Emotional Exhaustion (EE) subscale, attaining a score of 10 or higher on the Depersonalization (DPER) subscale, and scoring below 33 on the Personal Accomplishment (PAC) subscale. We have obtained the permission to use this scale. The MBI-HSS has been translated into Thai and was utilized in a prior study conducted in Thailand. The Cronbach’s alpha for the three MBI-HSS subscales were 0.89, 0.79, and 0.87, respectively [ 31 ].
- Intention to leave
On the questionnaire, respondents were asked if they intended to leave their current position in the next year. Responses included leaving the job within 6 or 12 months and without intention to leave. The intention of nurses to leave has been demonstrated to serve as a predictor for the subsequent decision to leave the position, and it can also serve as an early indicator of potential turnover [ 14 ].
- Work engagement
We used the UWES-9, a 9-item instrument with three subscales, vigor, dedication, and absorption, to measure work engagement. The instrument is scored on a 7-point Likert-type scale ranging from never (1) to always (7) [ 37 ]. A higher score indicates better work engagement. Following the scoring guidance provided by Schaufeli and Bakker [ 37 ], nurses with a UWES-9 score equal to or above the 75th percentile were defined as having “high work engagement.” In the current study, the internal consistency of the UWES-9 was assessed using Cronbach’s alpha, yielding a coefficient of 0.92, which indicates excellent reliability within our sample.
Data analysis
Descriptive statistics were calculated to examine the characteristics of nurses and key variables of interest, including resilience, burnout, intention to leave, and work engagement. Logistic regressions were applied to explore the association of resilience with work engagement, burnout, and intention to leave. These associations were estimated unadjusted and then adjusted for nurse characteristics including age, gender, education, marital status, years worked as a RN, and the number of family members. We used the Huber-White sandwich estimator to adjust for the clustering of nurses within hospitals. All tests were performed using 0.05 levels of significance. Data analyses were performed using STATA software, version 14 (StataCorp, 2015).
Table 1 presents the characteristics of nurses in the sample. Nurses were 37 years of age on average, while most were female (95.18%) and held a bachelor’s degree (90.61%). Over half of the sample (52.28%) were married, and over 76.84% had at least one child. Over half (51.52%) of the participants lived with more than three family members. On average, nurses had worked for nearly 14 years as registered nurses and nine years in their current unit. The mean resilience score among nurses in the sample was 28.07 (S.D.= 7.20). The assessment of burnout using the three MBI-HSS subscales yielded the following results: 35.79% of nurses reported high levels of emotional exhaustion, 29.95% reported high levels of depersonalization, and 48.22% reported diminished personal accomplishment. Nearly one in ten nurses (9.14%) indicated an intention to leave their current job within 6 or 12 months, and over one-quarter (27.41%) reported a high level of work engagement.
Table 2 displays the results of the unadjusted and adjusted logistic regression models indicating the effect of a one-unit increase in the resilience score on the odds of burnout (as indicated by high emotional exhaustion, high depersonalization, and reduced personal accomplishment), intention to leave, and work engagement. In the unadjusted models, higher levels of resilience demonstrated statistically significant associations with all five outcomes. In the adjusted models that accounted for individual differences in age, gender, highest education, years worked as RNs, marital status, and the number of family numbers, a one-unit increase in the resilience score was associated with lower odds of high emotional exhaustion (odds ratio [OR] 0.98, 95% confidence interval [CI]: 0.97–0.99), high depersonalization (OR 0.97, 95% CI: 0.96–0.98), reduced personal accomplishment (OR 0.98, 95% CI: 0.98–0.99). A one-unit increase in the resilience score was associated with a 4% increase in the odds of reporting high work engagement (OR 1.04, 95% CI: 1.03–1.05). The association between higher resilience and intention to leave became statistically insignificant in the adjusted models ( p = 0.081).
In this study of Thai nurses conducted during the COVID-19 pandemic, we observed a significant association between resilience and nurse job outcomes related to retention and patient safety. These relationships were observed even after accounting for several individual characteristics, such as age and experience, that could be associated with job outcomes. While the observed level of emotional exhaustion (35.8%) among Thai nurses was similar to the estimated 34.1% reported by Galanis and colleagues [ 15 ] in a recent meta-analysis of international studies, levels of high depersonalization and reduced personal accomplishment among nurses in Thailand were markedly higher than other countries (29.6% vs. 12.6% for high depersonalization; 48.2% vs. 15.2% for reduced personal accomplishment). Compared to other countries, the study sample had a higher resilience score than nurses in the Regional Health Service in Spain [ 36 ], nurses at the Japanese Red Cross Medical Center in Japan [ 5 ], and frontline nurses in Wuhan, China [ 19 ]. Higher resilience among Thai nurses may be attributable to growing up in close-knit families and having strong community ties that provided additional emotional and social support through this time of added stress and adversity. In our study, one-tenth of Thai nurses intended to leave their job which was lower compared to other countries where researchers have found that about one-third of nurses intended to leave their job during the COVID-19 pandemic [ 41 ]. Although previous studies were undertaken at varying stages of the pandemic, the present research augments the global body of knowledge by providing preliminary comparative data on the resilience and occupational outcomes among nurses in Thailand throughout the COVID-19 crisis.
The results of the current study indicated that higher levels of resilience were associated with lower levels of emotional exhaustion, depersonalization, and diminished personal accomplishment among nurses working in Thailand during the pandemic period. The findings largely confirm previous studies where higher resilience has been linked to lower emotional exhaustion, depersonalization, and reduced personal accomplishment among nurses working in public hospitals in Madrid, Spain [ 20 ], nurse managers in tertiary public hospitals in China [ 25 ], nurses and nursing students from a college and a state nursing association in Pennsylvania, USA [ 18 ], nurses in Brazil [ 42 ], and hospital staff in Australia [ 4 ].
Our adjusted models did not observe a statistically significant association between resilience and intention to leave. The current findings diverge from those of earlier studies, which demonstrated that an elevated level of resilience among nurses correlated with a reduced propensity to leave their positions. This was particularly evident in studies of nurses employed within a multi-hospital system in the southeastern United States during the COVID-19 pandemic [ 22 ] and amongst nurse leaders based in Birmingham, Alabama, USA [ 29 ].
A systematic review examining the determinants of turnover intentions among nursing personnel during the COVID-19 pandemic found that resilience could mitigate negative associations with turnover intention [ 40 ]. Since our survey was conducted two years into the pandemic, it is possible that nurses who completed the survey were those with higher levels of resilience who persevered through the surges of the pandemic and remained committed to their job.
Nurses with higher resilience may have a well-developed adaptive process to deal with trauma, adversity, tragedy, and stressors [ 39 ]. As such, they can embrace problem-solving, cope with emotional avoidance, and pursue social support to persevere through crises. These positive personal characteristics may contribute to nurses being able to work effectively in a traumatic crisis such as COVID-19 [ 12 ]. While these nurses may have been exhausted and fatigued during the height of the pandemic, their higher levels of resilience allowed them to cope effectively and, therefore, have lower feelings of burnout.
Finally, our study found that higher levels of resilience were associated with reporting high work engagement. Our findings are similar to previous international studies, which demonstrated that nurses who worked during the pandemic with higher resilience had higher work engagement, including emergency department nurses in Midwestern and Southwestern US states [ 9 ] and frontline nurses in 6 provinces of China [ 26 ]. Our findings suggest that nurses with resilient personalities working during the pandemic were better positioned to recover from adverse work-related situations. Through an adaptive process, building resilience may have allowed nurses to overcome the crisis due to personal strength, positive psychological adjustment, and the ability to maintain function [ 39 ]. Therefore, even though working in stressful events, nurses with higher levels of resilience can continue to be involved at work accompanied by feelings of energy, enthusiasm, and significance.
Although personal characteristics partially determine the development of resilience, the characteristics of the work environment are also recognized as a significant contributing factor [ 35 ]. Indeed, nurses across the globe have been practicing in challenging work environments during the COVID-19 pandemic. A preceding study recently established that nurses employed in hospitals characterized by better work environments before the pandemic have reported markedly improved patient care quality and enhanced well-being among clinicians throughout the pandemic [ 1 ]. Further, a robust body of evidence from Thailand shows that hospital nurses working in poor work environments are likelier to leave their jobs [ 30 ].
Implications
Even though our study was conducted in one country, our findings have implications for health policies internationally. The COVID-19 pandemic was a global phenomenon, and all frontline nurses have been experiencing similar challenges. Our findings suggest that interventions to build nurse resilience may improve nurse well-being and work engagement, which have been linked to better patient care. At the individual level, the allocation of time for emotional recharge, the availability of peer support, and the encouragement of open communication can facilitate the development and enhancement of an individual’s inherent adaptive systems, thereby fostering resilience [ 46 ]. However, other research suggests that resilience training interventions alone may not significantly impact nurse outcomes if not coupled with organizational policies to improve the nurse work environment [ 43 ]. In terms of organizational-level actions, hospital and nurse administrators can foster the development of work environments that provide adequate resources and support, promote nurse involvement in organizational decision-making, and promote collegial relationships between nurses and physicians. Further, hospital-based programs that provide positive reinforcement and recognition, coping strategies [ 38 ], and training on resilience [ 46 ] may also be considered. Such organizational strategies are essential for everyday nursing care but are even more critical during crises such as the COVID-19 pandemic.
Limitations
Some limitations of the study should be considered while interpreting the results. This study collected data between August 2022 and October 2022, after the COVID-19 pandemic peaked in Thailand; this may influence nurses’ reported levels of resilience. Furthermore, unmeasured confounding variables, such as the quality of the work environment, could introduce bias into our estimates. Future work on resilience and nurse outcomes should incorporate work environment measures. Finally, the potential for same source bias exists in our study as the same nurses provided data for the independent and dependent variables.
The COVID-19 pandemic has exerted a sustained and profound effect on healthcare systems worldwide for three years. As frontline healthcare professionals during this time, nurses are at high risk for burnout, intention to leave their job, and poor work engagement, which can negatively impact nurse retention and quality of care. Our study is one of the pioneering investigations to examine nurses working during the pandemic in Thailand. We found that higher levels of resilience were a protective factor against burnout and intention to leave and were positively associated with higher work engagement. Nevertheless, resilience should not be considered the only factor necessary for the well-being of nurses. The COVID-19 pandemic offers important lessons learned about many factors that should be improved, including the work environment, to promote the well-being of the nursing workforce and protect against adverse job outcomes. Government and hospital administrations should allocate financial support and resources to develop individual and organizational-level interventions to promote resilience among frontline nurses so that hospitals will be better prepared for the next public health emergency and patient and nurse outcomes can be optimized.
Data availability
All data supporting the findings of this study are available within the paper and its Supplementary Information including study instruments such as the Connor-Davison Resilience Scale-10 (CD-RISC-10) and the Utrecht Work Engagement Scale-9 (UWES-9).
Abbreviations
Connor–Davidson Resilience Scale
Maslach Burnout Inventory–Health Services Survey
Utrecht Work Engagement Scale
Coronavirus Disease 2019
Emotional Exhaustion
Depersonalization
Personal Accomplishments
Aiken LH, Sloane DM, McHugh MD, Pogue CA, Lasater KB. A repeated cross-sectional study of nurses immediately before and during the COVID-19 pandemic: implications for action. Nurs Outlook. 2023;71(1):101903.
Article PubMed Google Scholar
Allande-Cussó R, García-Iglesias JJ, Ruiz-Frutos C, Domínguez-Salas S, Rodríguez-Domínguez C, Gómez-Salgado J. Work Engagement in nurses during the Covid-19 pandemic: a cross-sectional study. Healthc (Basel). 2021;9(3):253.
Google Scholar
Al Thobaity A, Alshammari F. Nurses on the Frontline against the COVID-19 pandemic: an integrative review. Dubai Med J. 2020;3:87–92.
Article Google Scholar
Armstrong SJ, Porter JE, Larkins JA, Mesagno C. Burnout, stress and resilience of an Australian regional hospital during COVID-19: a longitudinal study. BMC Health serv res. 2022;22:1115.
Article PubMed PubMed Central Google Scholar
Awano N, Oyama N, Akiyama K, Inomata M, Kuse N, Tone M, Takada K, Muto Y, Fujimoto K, Akagi Y, Mawatari M, Ueda A, Kawakami J, Komatsu J, Izumo T. Anxiety, Depression, and Resilience of Healthcare Workers in Japan during the Coronavirus Disease 2019 Outbreak. Intern Med. 2020;59(21):2693–9.
Article CAS PubMed PubMed Central Google Scholar
Dhar Chowdhury S, Oommen AM. Epidemiology of COVID-19. J Dig Endoscopy. 2020;11(1):3–7.
Chemali S, Mari-Sáez A, El Bcheraoui C, Weishaar H. Health care workers’ experiences during the COVID-19 pandemic: a scoping review. Hum Resour Health. 2022;20(1):27.
Chinvararak C, Kerdcharoen N, Pruttithavorn W, Polruamngern N, Asawaroekwisoot T, Munsukpol W, et al. Mental health among healthcare workers during COVID-19 pandemic in Thailand. PLoS ONE. 2022;17(5):e0268704.
Clark P, Hulse B, Polivka BJ, Resilience. Moral Distress, and job satisfaction driving Engagement in Emergency Department nurses: a qualitative analysis. J Nurs Adm. 2022;52(2):112–7.
Courson S, Breen K, Smith J, Flynn A, Evans J, Moffitt R, Staake C, McPherson S. Impact of COVID-19 on the level of Work Engagement of nurses at a small, rural hospital. J Contin Educ Nurs. 2022;53(4):157–64.
Davidson JR. Connor-Davidson Resilience Scale (CD-RISC) manual; 2018. http://www.cd-risc.com . Accessed May 2022.
Davis M, Batcheller J. Managing Moral Distress in the Workplace:: creating a Resiliency Bundle. Nurse Lead. 2020;18(6):604–8.
Fletcher D, Sarkar M. Psychological resilience: a review and critique of definitions, concepts and theory. Eur Psychol. 2013;18(1):12–23.
Flinkman M, Leino-Kilpi H, Salanterä S. Nurses’ intention to leave the profession: integrative review. J Adv Nurs. 2010;66(7):1422–34.
Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3286–302.
Giménez-Espert MDC, Prado-Gascó V, Soto-Rubio A, Psychosocial, Risks. Work Engagement, and job satisfaction of nurses during COVID-19 pandemic. Front Public Health. 2020;8:566896.
Hayes LJ, O’Brien-Pallas L, Duffield C, Shamian J, Buchan J, Hughes F, et al. Nurse turnover: a literature review. Int J Nurs Stud. 2006;43(2):237–63.
Hetzel-Riggin MD, Swords BA, Tuang HL, Deck JM, Spurgeon NS. Work Engagement and Resiliency Impact the relationship between nursing stress and burnout. Psychol Rep. 2020;123(5):1835–53.
Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMedicine. 2020;24:100424.
Jiménez-Fernández R, Corral-Liria I, Trevissón-Redondo B, Lopez-Lopez D, Losa-Iglesias M, Becerro-de-Bengoa-Vallejo R, et al. Burnout, resilience and psychological flexibility in frontline nurses during the acute phase of the COVID-19 pandemic (2020) in Madrid, Spain. J Nurs Manag. 2022;30(7):2549–56.
Kakemam E, Chegini Z, Rouhi A, Ahmadi F, Majidi S. Burnout and its relationship to self-reported quality of patient care and adverse events during COVID-19: a cross-sectional online survey among nurses. J Nurs Manag. 2021;29(7):1974–82.
Kleier JA, Lawrence C, Cavanaugh G, Schivinski E, Holland S, Bruewer J. Professional commitment, resilience and intent to leave the profession among nurses during the COVID-19 pandemic - a descriptive study. J Nurs Manag. 2022;30(7):2577–84.
Koch P, Zilezinski M, Schulte K, Strametz R, Nienhaus A, Raspe M. How perceived quality of care and job satisfaction are Associated with Intention to leave the Profession in Young Nurses and Physicians. Int J Environ Res Public Health. 2020;17(8):2714.
Komwong D, Prasanthanakul J, Phanasathit M, Wongwan T. Prevalence of mental health problems and associated factors of Thai healthcare workers during the first wave of COVID-19 pandemic. J Public Hlth Dev. 2022;20(1):106–19.
Luo D, Song Y, Cai X, Li R, Bai Y, Chen B, Liu Y. Nurse managers’ burnout and organizational support: the serial mediating role of leadership and resilience. J Nurs Manag. 2022;30(8):4251–61.
Lyu H, Yao M, Zhang D, Liu X. The Relationship among Organizational Identity, Psychological Resilience and Work Engagement of the First-Line nurses in the Prevention and Control of COVID-19 based on structural equation Model. Risk Manag Healthc Policy. 2020;13:2379–86.
Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Mountain View: CPP, Inc.; 1996.
Mohamed SA, Hendy A, Ezzat Mahmoud O, Mohamed Mohamed S. Mattering perception, work engagement and its relation to burnout amongst nurses during coronavirus outbreak. Nurs Open. 2022;9(1):377–84.
Montgomery AP, Patrician PA. Work environment, resilience, burnout, intent to leave during COVID pandemic among nurse leaders: a cross-sectional study. J Nurs Manag. 2022;30(8):4015–23.
Nantsupawat A, Kunaviktikul W, Nantsupawat R, Wichaikhum OA, Thienthong H, Poghosyan L. Effects of nurse work environment on job dissatisfaction, burnout, intention to leave. Int Nurs Rev. 2017;64(1):91–8.
Article CAS PubMed Google Scholar
Nantsupawat A, Srisuphan W, Kunaviktikul W, Wichaikhum OA, Aungsuroch Y, Aiken LH. Impact of nurse work environment and staffing on hospital nurse and quality of care in Thailand. J Nurs Scholarsh. 2011;43(4):426–32.
Nantsupawat A, Wichaikhum OA, Abhicharttibutra K, Sadarangani T, Poghosyan L. The relationship between nurse burnout, missed nursing care, and care quality following COVID-19 pandemic. J Clin Nurs. 2023;32(15–16):5076–83.
Nashwan AJ, Abujaber AA, Villar RC, Nazarene A, Al-Jabry MM, Fradelos EC. Comparing the impact of COVID-19 on nurses’ turnover intentions before and during the pandemic in Qatar. J Pers Med. 2021;11(6):456.
Parr JM, Teo S, Koziol-McLain J. A quest for quality care: exploration of a model of leadership relationships, work engagement, and patient outcomes. J Adv Nurs. 2021;77(1):207–20.
Park K, Jang A. Factors affecting the resilience of New nurses in their Working Environment. Int J Environ Res Public Health. 2022;19(9):5158.
Rivas N, López M, Castro MJ, Luis-Vian S, Fernández-Castro M, Cao MJ, et al. Analysis of Burnout Syndrome and Resilience in nurses throughout the COVID-19 pandemic: a cross-sectional study. Int J Environ Res Public Health. 2021;18(19):10470.
Schaufeli W, Bakker A, UWES Utrecht Work Engagement Scale Preliminary Manual. Occupational Health Psychology Unit Utrecht University, Utrecht; 2004. https://www.wilmarschaufeli.nl/publications/Schaufeli/Test%20Manuals/Test_manual_UWES_English.pdf . Accessed March 2022.
Sierra-García E, Sosa-Palanca EM, Saus-Ortega C, Ruiz-Hontangas A, Juárez-Vela R, Gea-Caballero V. Modulating elements of nurse resilience in Population Care during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(8):4452.
Slåtten T, Lien G, Mutonyi BR. Precursors and outcomes of work engagement among nursing professionals-a cross-sectional study. BMC Health Serv Res. 2022;22(1):21.
Tolksdorf KH, Tischler U, Heinrichs K. Correlates of turnover intention among nursing staff in the COVID-19 pandemic: a systematic review. BMC Nurs. 2022;21(1):174.
Ulupınar F, Erden Y. Intention to leave among nurses during the COVID-19 outbreak: a rapid systematic review and Meta-analysis. J Clin Nurs. 2022; 1–11.
Vieira LS, Machado WL, Dal Pai D, Magnago TSBS, Azzolin KO, Tavares JP. Burnout and resilience in intensive care nursing professionals in the face of COVID-19: a multicenter study. Rev Lat Am Enfermagem. 2022;30:e3589.
PubMed PubMed Central Google Scholar
World Health Organization Alliance for Patient. World Alliance for Patient Safety. Geneva: World health Organization; 2008.
World Health Organization. Burnout an, World Health Organization. occupational phenomenon: International classification of diseases. 2019. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-internationalclassification-of-diseases . Accessed May 2023.
World Health Organization Thailand. The situation report on COVID19 from WHO Thailand. 2023. https://www.who.int/thailand/news/detail/25-04-2023-the-situation-report-on-covid19 . Accessed May 2023.
Zenani NE, Gause G, Sehularo L. Strategies to enhance resilience to cope with workplace adversities post-COVID-19 among ICU nurses. Curationis. 2022;45(1):e1–8.
Download references
Acknowledgements
The authors would like to thank all nurses who participate in the study.
This research received funding from Faculty of Nursing, Chiang Mai University.
Author information
Authors and affiliations.
Faculty of Nursing, Chiang Mai University, Chiang Mai, Thailand
Apiradee Nantsupawat, Kulwadee Abhicharttibutra & Orn-Anong Wichaikhum
Center for Health Outcomes and Policy Research, University of Pennsylvania School of Nursing, Philadelphia, USA
Ann Kutney-Lee
Columbia University School of Nursing, New York, USA
Lusine Poghosyan
You can also search for this author in PubMed Google Scholar
Contributions
AN, KA, OW designed the research, collected and analyzed the data. AN, AKL, LP wrote the main manuscript and prepared Tables 1-2. All authors reviewed the manuscript
Corresponding author
Correspondence to Apiradee Nantsupawat .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Research Ethics Review Committee of Faculty of Nursing, Chiang Mai University, Thailand (EXP:055-2022). The study methodologies were executed following the guidelines outlined by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) initiative and adhered to the ethical principles of the Declaration of Helsinki. Informed consent was obtained from all participants involved in this study.
Consent for publication
No applicable.
Competing interests
No conflict of interest has been declared by the authors.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nantsupawat, A., Kutney-Lee, A., Abhicharttibutra, K. et al. Exploring the relationships between resilience, burnout, work engagement, and intention to leave among nurses in the context of the COVID-19 pandemic: a cross-sectional study. BMC Nurs 23 , 290 (2024). https://doi.org/10.1186/s12912-024-01958-1
Download citation
Received : 11 December 2023
Accepted : 21 April 2024
Published : 29 April 2024
DOI : https://doi.org/10.1186/s12912-024-01958-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- COVID-19 pandemic
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

IMAGES
COMMENTS
This thesis analyzed and defined nurse burnout, explored the determinants of nurse burnout, and proposed personal and administrative recommendations to lower the rates of nurse burnout. In this thesis, recommendations for best practice were derived from evidence-based research articles that address nurse burnout, including interventions and ...
In Michigan, 42% of nurses reported wanting to quit the nursing profession after one to 10 more years according to a 2013 survey by the Mich- igan Center for Nursing (National Nurses United 2015). Burnout is a problem in nursing. These studies and others indicate the prevalence of burnout in the nursing profession.
Community nursing is associated with stress and burnout, which can impact heavily on the individuals and organizations. These impacts can be both economically and also the negatives effects on the quality of patient care. The purpose of this thesis is to provide evidence based information about prevention of burnout among nurses. This thesis ...
These free-text data responses provided insights into. how the pandemics impacted ER nurses' sense of stress and burnout. This study is the first to specifically assess the relationship of personal coping. strategies, social support sources, and counseling resources on levels of burnout in United. States ER nurses.
Methods: This study was a secondary analysis of data from 136 acute care nurses in which their burnout levels were examined at the beginning and end of shift every shift they worked during a two week period. Burnout was measured by an abbreviated, three-item measure derived from the Maslach Burnout Inventory.
The literature on burnout in nursing partly supports Maslach's theory, but some areas are insufficiently tested, in particular, the association between burnout and turnover, and relationships were found for some MBI dimensions only. Keywords: Burnout, Nursing, Maslach Burnout Inventory, Job demands, Practice environment.
The organizational-related outcomes associated with nurse burnout were (1) patient safety, (2) quality of care, (3) nurses' organizational commitment, (4) nurse productivity, and (5) patient satisfaction. For these themes, nurse burnout was consistently inversely associated with outcome measures. Conclusions: Nurse burnout is an occupational ...
1. Introduction. Burnout has been studied extensively among nurses across the United States (US), and previous estimates have shown that between 35% and 45% of the US nursing workforce is burned out [1,2,3].The World Health Organization (WHO) defines burnout as an occupational phenomenon, noting its inherent relationship to the workplace, and describes it as feeling emotionally exhausted ...
Introduction. Clinician burnout is a threat to US health and health care. 1 At more than 6 million in 2019, 2 nurses are the largest segment of our health care workforce, making up nearly 30% of hospital employment nationwide. 3 Nurses are a critical group of clinicians with diverse skills, such as health promotion, disease prevention, and direct treatment.
Background Workforce studies often identify burnout as a nursing 'outcome'. Yet, burnout itself—what constitutes it, what factors contribute to its development, and what the wider consequences are for individuals, organisations, or their patients—is rarely made explicit. We aimed to provide a comprehensive summary of research that examines theorised relationships between burnout and ...
Nursing Name of thesis NURSE BURNOUT: Prevention and Recovery Instructor MARIA BJÖRKMARK Pages 34+ 2 Supervisor ANITA HOLLANTI The purpose of this study was to explore the protective measures of nurses burnout. The aim was to provide information on how nurses can prevent and recover from burnout. This study will be useful
Conclusions: The patterns identified by these studies consistently show that adverse job characteristics-high workload, low staffing levels, long shifts, and low control-are associated with burnout in nursing. The potential consequences for staff and patients are severe. The literature on burnout in nursing partly supports Maslach's theory, but ...
The Assessment of Burnout and Resiliency Among Nurse Practitioners survey developer completed Institutional Review Board (IRB) approval through North Dakota State University (NDSU) prior to beginning this study. The project was granted approval on April 16th, 2020 (See Appendix A). Timeline of Project Phases.
NURS 4500: Nursing Research and Thesis Dr. Patricia Harris April 27, 2022 . NURSE BURNOUT AS A RESULT OF THE PANDEMIC AND WAYS FOR NURSES TO IMPROVE THEIR MENTAL WELL-BEING 2. Acknowledgements. To my family and friends who have given me all the support and love throughout my ... NURSE BURNOUT AS A RESULT OF THE PANDEMIC AND WAYS FOR NURSES TO
Key Points. Question What were the most recent US national estimates of nurse burnout and associated factors that may put nurses at risk for burnout?. Findings This secondary analysis of cross-sectional survey data from more than 50 000 US registered nurses (representing more than 3.9 million nurses nationally) found that among nurses who reported leaving their current employment (9.5% of ...
1.1. Background. Burnout syndrome is the continuous exposure to work-stress associated with poor working conditions, in which pleasure and work performance decrease [4, 5].In view of this, it is considered a multi-causal pathology, as it is related to excessive exposure to prolonged stress; it has identified aspects related to several stressors in the work environment that imply the commitment ...
A 2010 study at the University of Pennsylvania, showed 29% of nurses in California experienced high burnout, compared to 34% of nurses in. New Jersey and 36% of nurses in Pennsylvania, states without minimum staffing ratios during. the period of research.
The findings of this research can inform. the provision of appropriate education for nurse managers, leading to reduced burnout in. staff nurses, a reduction in the nursing shortage, and improved quality of patient care. The burnout information least known by nurse managers is evidence-based knowledge.
According to a national nursing engagement report released in April 2019, of the 2,000+ health care partners responding to the survey, 15.6% of all nurses self -reported feelings of burnout, with emergency room nurses being at a higher risk.3. Findings from another 2019 survey reveal that burnout is among the leading patient safety and quality
NURS 4500 Nursing Research & Thesis Patricia Harris November 20, 2022. NURSING BURNOUT AND PREVENTATIVE MEASURES 2 . ... Some of the major causes of nursing burnout include the effects of the work environment, emotional strain, and lack of sleep. Several nurses have stated that some environmental factors related to work that is causing
Nurse burnout is a widespread phenomenon characterized by a reduction in nurses' energy that manifests in emotional exhaustion, lack of motivation, and feelings of frustration and may lead to reductions in work efficacy. This study was conducted to assess the level of burnout among Jordanian nurses and to investigate the influence of leader ...
low nurse well-being scores that were impacted by the stress and emotional exhaustion experienced by nursing staff. Cross-national research findings from studies in the United States, Canada, and the United Kingdom have identified that approximately 33% to 54% of hospital nurses exhibited burnout (i.e., emotional exhaustion as measured by the
3. Results. We identified 906 studies and seven were selected (Figure 1).All articles conducted research on 1006 healthcare workers with a diagnosis of Burnout Syndrome and investigated the efficacy of coping strategies (Table 1).In particular, the first article highlighted those medical residents who reported low depersonalization, high personal accomplishment, high satisfaction with medicine ...
Background Nurses have faced significant personal and professional stressors during the COVID-19 pandemic that have contributed to increased rates of burnout, intention to leave, and poorer work engagement. Resilience has been identified as a critical factor influencing job outcomes; however, the dynamics of this association have not yet been investigated within the context of the Thai ...