- Privacy Policy

Home » Research Results Section – Writing Guide and Examples

Research Results Section – Writing Guide and Examples
Table of Contents

Research Results
Research results refer to the findings and conclusions derived from a systematic investigation or study conducted to answer a specific question or hypothesis. These results are typically presented in a written report or paper and can include various forms of data such as numerical data, qualitative data, statistics, charts, graphs, and visual aids.
Results Section in Research
The results section of the research paper presents the findings of the study. It is the part of the paper where the researcher reports the data collected during the study and analyzes it to draw conclusions.
In the results section, the researcher should describe the data that was collected, the statistical analysis performed, and the findings of the study. It is important to be objective and not interpret the data in this section. Instead, the researcher should report the data as accurately and objectively as possible.
Structure of Research Results Section
The structure of the research results section can vary depending on the type of research conducted, but in general, it should contain the following components:
- Introduction: The introduction should provide an overview of the study, its aims, and its research questions. It should also briefly explain the methodology used to conduct the study.
- Data presentation : This section presents the data collected during the study. It may include tables, graphs, or other visual aids to help readers better understand the data. The data presented should be organized in a logical and coherent way, with headings and subheadings used to help guide the reader.
- Data analysis: In this section, the data presented in the previous section are analyzed and interpreted. The statistical tests used to analyze the data should be clearly explained, and the results of the tests should be presented in a way that is easy to understand.
- Discussion of results : This section should provide an interpretation of the results of the study, including a discussion of any unexpected findings. The discussion should also address the study’s research questions and explain how the results contribute to the field of study.
- Limitations: This section should acknowledge any limitations of the study, such as sample size, data collection methods, or other factors that may have influenced the results.
- Conclusions: The conclusions should summarize the main findings of the study and provide a final interpretation of the results. The conclusions should also address the study’s research questions and explain how the results contribute to the field of study.
- Recommendations : This section may provide recommendations for future research based on the study’s findings. It may also suggest practical applications for the study’s results in real-world settings.
Outline of Research Results Section
The following is an outline of the key components typically included in the Results section:
I. Introduction
- A brief overview of the research objectives and hypotheses
- A statement of the research question
II. Descriptive statistics
- Summary statistics (e.g., mean, standard deviation) for each variable analyzed
- Frequencies and percentages for categorical variables
III. Inferential statistics
- Results of statistical analyses, including tests of hypotheses
- Tables or figures to display statistical results
IV. Effect sizes and confidence intervals
- Effect sizes (e.g., Cohen’s d, odds ratio) to quantify the strength of the relationship between variables
- Confidence intervals to estimate the range of plausible values for the effect size
V. Subgroup analyses
- Results of analyses that examined differences between subgroups (e.g., by gender, age, treatment group)
VI. Limitations and assumptions
- Discussion of any limitations of the study and potential sources of bias
- Assumptions made in the statistical analyses
VII. Conclusions
- A summary of the key findings and their implications
- A statement of whether the hypotheses were supported or not
- Suggestions for future research
Example of Research Results Section
An Example of a Research Results Section could be:
- This study sought to examine the relationship between sleep quality and academic performance in college students.
- Hypothesis : College students who report better sleep quality will have higher GPAs than those who report poor sleep quality.
- Methodology : Participants completed a survey about their sleep habits and academic performance.
II. Participants
- Participants were college students (N=200) from a mid-sized public university in the United States.
- The sample was evenly split by gender (50% female, 50% male) and predominantly white (85%).
- Participants were recruited through flyers and online advertisements.
III. Results
- Participants who reported better sleep quality had significantly higher GPAs (M=3.5, SD=0.5) than those who reported poor sleep quality (M=2.9, SD=0.6).
- See Table 1 for a summary of the results.
- Participants who reported consistent sleep schedules had higher GPAs than those with irregular sleep schedules.
IV. Discussion
- The results support the hypothesis that better sleep quality is associated with higher academic performance in college students.
- These findings have implications for college students, as prioritizing sleep could lead to better academic outcomes.
- Limitations of the study include self-reported data and the lack of control for other variables that could impact academic performance.
V. Conclusion
- College students who prioritize sleep may see a positive impact on their academic performance.
- These findings highlight the importance of sleep in academic success.
- Future research could explore interventions to improve sleep quality in college students.
Example of Research Results in Research Paper :
Our study aimed to compare the performance of three different machine learning algorithms (Random Forest, Support Vector Machine, and Neural Network) in predicting customer churn in a telecommunications company. We collected a dataset of 10,000 customer records, with 20 predictor variables and a binary churn outcome variable.
Our analysis revealed that all three algorithms performed well in predicting customer churn, with an overall accuracy of 85%. However, the Random Forest algorithm showed the highest accuracy (88%), followed by the Support Vector Machine (86%) and the Neural Network (84%).
Furthermore, we found that the most important predictor variables for customer churn were monthly charges, contract type, and tenure. Random Forest identified monthly charges as the most important variable, while Support Vector Machine and Neural Network identified contract type as the most important.
Overall, our results suggest that machine learning algorithms can be effective in predicting customer churn in a telecommunications company, and that Random Forest is the most accurate algorithm for this task.
Example 3 :
Title : The Impact of Social Media on Body Image and Self-Esteem
Abstract : This study aimed to investigate the relationship between social media use, body image, and self-esteem among young adults. A total of 200 participants were recruited from a university and completed self-report measures of social media use, body image satisfaction, and self-esteem.
Results: The results showed that social media use was significantly associated with body image dissatisfaction and lower self-esteem. Specifically, participants who reported spending more time on social media platforms had lower levels of body image satisfaction and self-esteem compared to those who reported less social media use. Moreover, the study found that comparing oneself to others on social media was a significant predictor of body image dissatisfaction and lower self-esteem.
Conclusion : These results suggest that social media use can have negative effects on body image satisfaction and self-esteem among young adults. It is important for individuals to be mindful of their social media use and to recognize the potential negative impact it can have on their mental health. Furthermore, interventions aimed at promoting positive body image and self-esteem should take into account the role of social media in shaping these attitudes and behaviors.
Importance of Research Results
Research results are important for several reasons, including:
- Advancing knowledge: Research results can contribute to the advancement of knowledge in a particular field, whether it be in science, technology, medicine, social sciences, or humanities.
- Developing theories: Research results can help to develop or modify existing theories and create new ones.
- Improving practices: Research results can inform and improve practices in various fields, such as education, healthcare, business, and public policy.
- Identifying problems and solutions: Research results can identify problems and provide solutions to complex issues in society, including issues related to health, environment, social justice, and economics.
- Validating claims : Research results can validate or refute claims made by individuals or groups in society, such as politicians, corporations, or activists.
- Providing evidence: Research results can provide evidence to support decision-making, policy-making, and resource allocation in various fields.
How to Write Results in A Research Paper
Here are some general guidelines on how to write results in a research paper:
- Organize the results section: Start by organizing the results section in a logical and coherent manner. Divide the section into subsections if necessary, based on the research questions or hypotheses.
- Present the findings: Present the findings in a clear and concise manner. Use tables, graphs, and figures to illustrate the data and make the presentation more engaging.
- Describe the data: Describe the data in detail, including the sample size, response rate, and any missing data. Provide relevant descriptive statistics such as means, standard deviations, and ranges.
- Interpret the findings: Interpret the findings in light of the research questions or hypotheses. Discuss the implications of the findings and the extent to which they support or contradict existing theories or previous research.
- Discuss the limitations : Discuss the limitations of the study, including any potential sources of bias or confounding factors that may have affected the results.
- Compare the results : Compare the results with those of previous studies or theoretical predictions. Discuss any similarities, differences, or inconsistencies.
- Avoid redundancy: Avoid repeating information that has already been presented in the introduction or methods sections. Instead, focus on presenting new and relevant information.
- Be objective: Be objective in presenting the results, avoiding any personal biases or interpretations.
When to Write Research Results
Here are situations When to Write Research Results”
- After conducting research on the chosen topic and obtaining relevant data, organize the findings in a structured format that accurately represents the information gathered.
- Once the data has been analyzed and interpreted, and conclusions have been drawn, begin the writing process.
- Before starting to write, ensure that the research results adhere to the guidelines and requirements of the intended audience, such as a scientific journal or academic conference.
- Begin by writing an abstract that briefly summarizes the research question, methodology, findings, and conclusions.
- Follow the abstract with an introduction that provides context for the research, explains its significance, and outlines the research question and objectives.
- The next section should be a literature review that provides an overview of existing research on the topic and highlights the gaps in knowledge that the current research seeks to address.
- The methodology section should provide a detailed explanation of the research design, including the sample size, data collection methods, and analytical techniques used.
- Present the research results in a clear and concise manner, using graphs, tables, and figures to illustrate the findings.
- Discuss the implications of the research results, including how they contribute to the existing body of knowledge on the topic and what further research is needed.
- Conclude the paper by summarizing the main findings, reiterating the significance of the research, and offering suggestions for future research.
Purpose of Research Results
The purposes of Research Results are as follows:
- Informing policy and practice: Research results can provide evidence-based information to inform policy decisions, such as in the fields of healthcare, education, and environmental regulation. They can also inform best practices in fields such as business, engineering, and social work.
- Addressing societal problems : Research results can be used to help address societal problems, such as reducing poverty, improving public health, and promoting social justice.
- Generating economic benefits : Research results can lead to the development of new products, services, and technologies that can create economic value and improve quality of life.
- Supporting academic and professional development : Research results can be used to support academic and professional development by providing opportunities for students, researchers, and practitioners to learn about new findings and methodologies in their field.
- Enhancing public understanding: Research results can help to educate the public about important issues and promote scientific literacy, leading to more informed decision-making and better public policy.
- Evaluating interventions: Research results can be used to evaluate the effectiveness of interventions, such as treatments, educational programs, and social policies. This can help to identify areas where improvements are needed and guide future interventions.
- Contributing to scientific progress: Research results can contribute to the advancement of science by providing new insights and discoveries that can lead to new theories, methods, and techniques.
- Informing decision-making : Research results can provide decision-makers with the information they need to make informed decisions. This can include decision-making at the individual, organizational, or governmental levels.
- Fostering collaboration : Research results can facilitate collaboration between researchers and practitioners, leading to new partnerships, interdisciplinary approaches, and innovative solutions to complex problems.
Advantages of Research Results
Some Advantages of Research Results are as follows:
- Improved decision-making: Research results can help inform decision-making in various fields, including medicine, business, and government. For example, research on the effectiveness of different treatments for a particular disease can help doctors make informed decisions about the best course of treatment for their patients.
- Innovation : Research results can lead to the development of new technologies, products, and services. For example, research on renewable energy sources can lead to the development of new and more efficient ways to harness renewable energy.
- Economic benefits: Research results can stimulate economic growth by providing new opportunities for businesses and entrepreneurs. For example, research on new materials or manufacturing techniques can lead to the development of new products and processes that can create new jobs and boost economic activity.
- Improved quality of life: Research results can contribute to improving the quality of life for individuals and society as a whole. For example, research on the causes of a particular disease can lead to the development of new treatments and cures, improving the health and well-being of millions of people.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

How to Cite Research Paper – All Formats and...

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...

Research Paper Format – Types, Examples and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples
When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
- How to Write Discussions and Conclusions

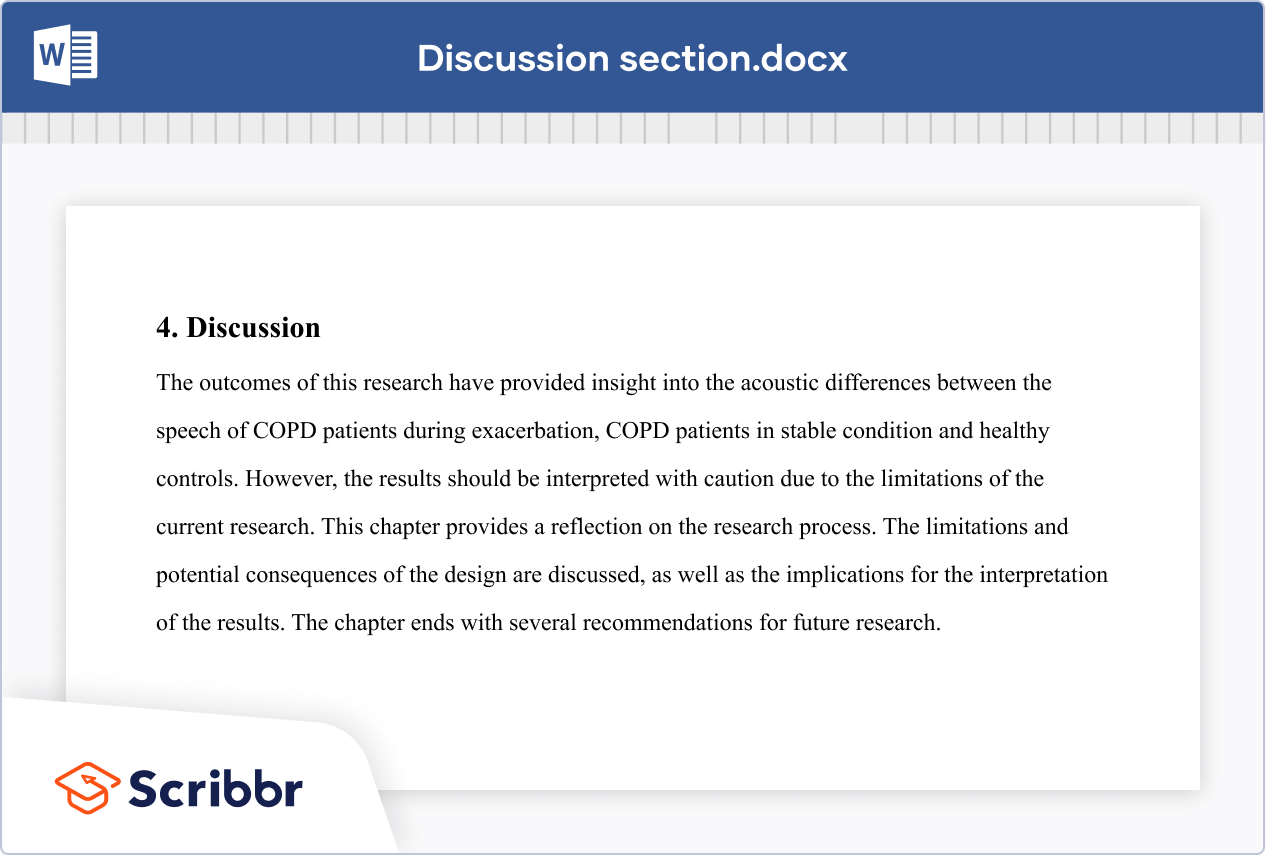
The discussion section contains the results and outcomes of a study. An effective discussion informs readers what can be learned from your experiment and provides context for the results.
What makes an effective discussion?
When you’re ready to write your discussion, you’ve already introduced the purpose of your study and provided an in-depth description of the methodology. The discussion informs readers about the larger implications of your study based on the results. Highlighting these implications while not overstating the findings can be challenging, especially when you’re submitting to a journal that selects articles based on novelty or potential impact. Regardless of what journal you are submitting to, the discussion section always serves the same purpose: concluding what your study results actually mean.
A successful discussion section puts your findings in context. It should include:
- the results of your research,
- a discussion of related research, and
- a comparison between your results and initial hypothesis.
Tip: Not all journals share the same naming conventions.
You can apply the advice in this article to the conclusion, results or discussion sections of your manuscript.
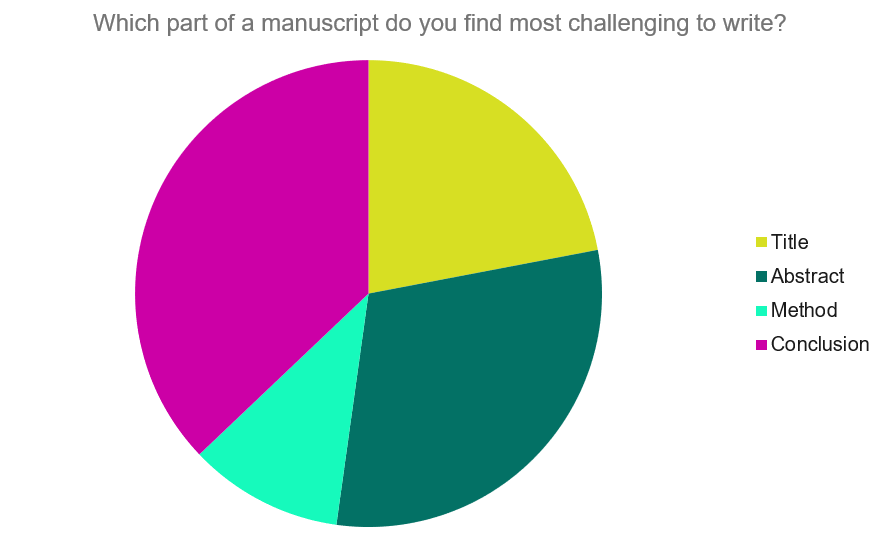
Our Early Career Researcher community tells us that the conclusion is often considered the most difficult aspect of a manuscript to write. To help, this guide provides questions to ask yourself, a basic structure to model your discussion off of and examples from published manuscripts.
Questions to ask yourself:
- Was my hypothesis correct?
- If my hypothesis is partially correct or entirely different, what can be learned from the results?
- How do the conclusions reshape or add onto the existing knowledge in the field? What does previous research say about the topic?
- Why are the results important or relevant to your audience? Do they add further evidence to a scientific consensus or disprove prior studies?
- How can future research build on these observations? What are the key experiments that must be done?
- What is the “take-home” message you want your reader to leave with?
How to structure a discussion
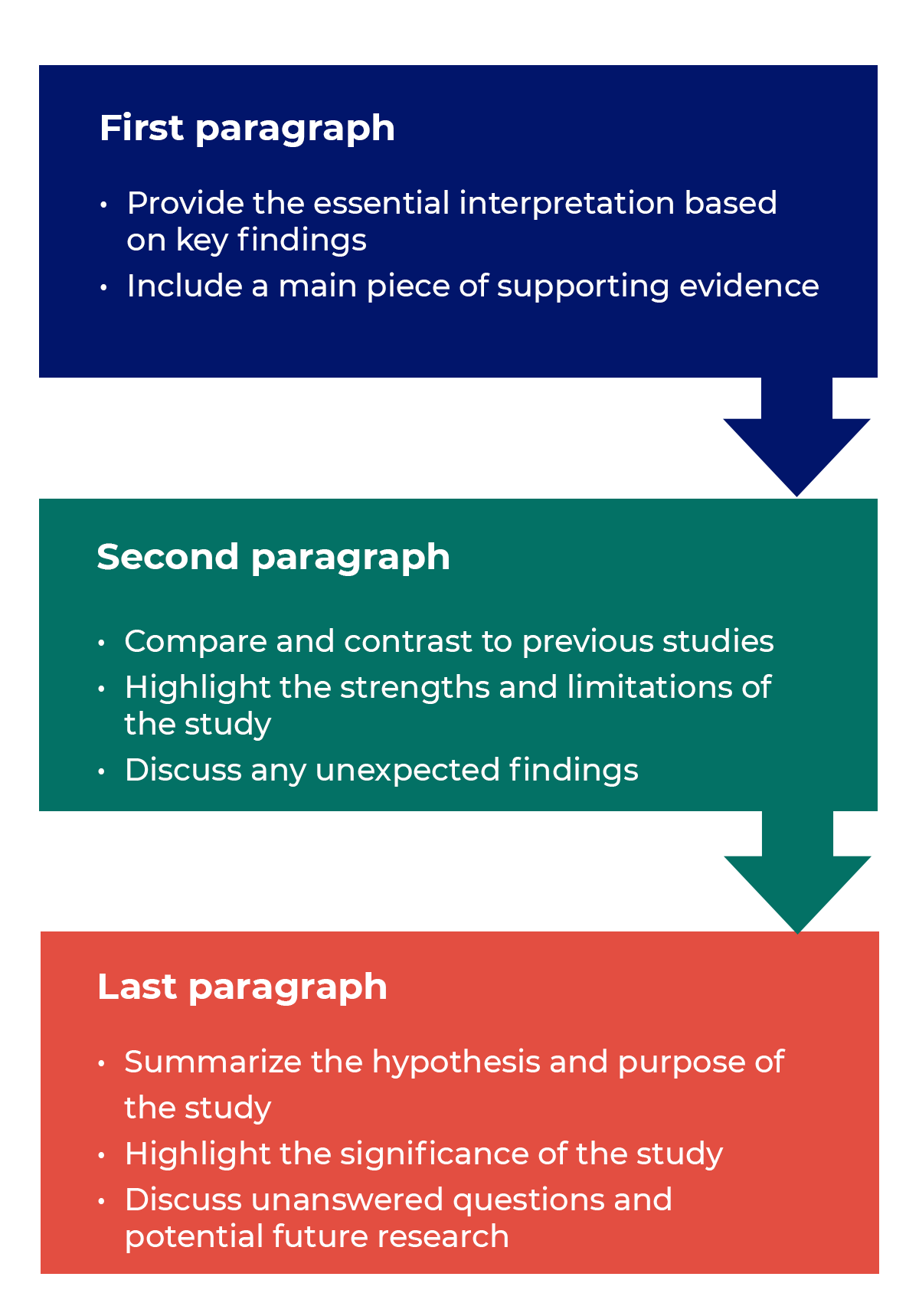
Trying to fit a complete discussion into a single paragraph can add unnecessary stress to the writing process. If possible, you’ll want to give yourself two or three paragraphs to give the reader a comprehensive understanding of your study as a whole. Here’s one way to structure an effective discussion:
Writing Tips
While the above sections can help you brainstorm and structure your discussion, there are many common mistakes that writers revert to when having difficulties with their paper. Writing a discussion can be a delicate balance between summarizing your results, providing proper context for your research and avoiding introducing new information. Remember that your paper should be both confident and honest about the results!

- Read the journal’s guidelines on the discussion and conclusion sections. If possible, learn about the guidelines before writing the discussion to ensure you’re writing to meet their expectations.
- Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion.
- Explain why the outcomes of your study are important to the reader. Discuss the implications of your findings realistically based on previous literature, highlighting both the strengths and limitations of the research.
- State whether the results prove or disprove your hypothesis. If your hypothesis was disproved, what might be the reasons?
- Introduce new or expanded ways to think about the research question. Indicate what next steps can be taken to further pursue any unresolved questions.
- If dealing with a contemporary or ongoing problem, such as climate change, discuss possible consequences if the problem is avoided.
- Be concise. Adding unnecessary detail can distract from the main findings.

Don’t
- Rewrite your abstract. Statements with “we investigated” or “we studied” generally do not belong in the discussion.
- Include new arguments or evidence not previously discussed. Necessary information and evidence should be introduced in the main body of the paper.
- Apologize. Even if your research contains significant limitations, don’t undermine your authority by including statements that doubt your methodology or execution.
- Shy away from speaking on limitations or negative results. Including limitations and negative results will give readers a complete understanding of the presented research. Potential limitations include sources of potential bias, threats to internal or external validity, barriers to implementing an intervention and other issues inherent to the study design.
- Overstate the importance of your findings. Making grand statements about how a study will fully resolve large questions can lead readers to doubt the success of the research.
Snippets of Effective Discussions:
Consumer-based actions to reduce plastic pollution in rivers: A multi-criteria decision analysis approach
Identifying reliable indicators of fitness in polar bears
- How to Write a Great Title
- How to Write an Abstract
- How to Write Your Methods
- How to Report Statistics
- How to Edit Your Work
The contents of the Peer Review Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
The contents of the Writing Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
There’s a lot to consider when deciding where to submit your work. Learn how to choose a journal that will help your study reach its audience, while reflecting your values as a researcher…
How To Write The Discussion Chapter
The what, why & how explained simply (with examples).
By: Jenna Crossley (PhD Cand). Reviewed By: Dr. Eunice Rautenbach | August 2021
If you’re reading this, chances are you’ve reached the discussion chapter of your thesis or dissertation and are looking for a bit of guidance. Well, you’ve come to the right place ! In this post, we’ll unpack and demystify the typical discussion chapter in straightforward, easy to understand language, with loads of examples .
Overview: Dissertation Discussion Chapter
- What (exactly) the discussion chapter is
- What to include in your discussion chapter
- How to write up your discussion chapter
- A few tips and tricks to help you along the way
What exactly is the discussion chapter?
The discussion chapter is where you interpret and explain your results within your thesis or dissertation. This contrasts with the results chapter, where you merely present and describe the analysis findings (whether qualitative or quantitative ). In the discussion chapter, you elaborate on and evaluate your research findings, and discuss the significance and implications of your results.
In this chapter, you’ll situate your research findings in terms of your research questions or hypotheses and tie them back to previous studies and literature (which you would have covered in your literature review chapter). You’ll also have a look at how relevant and/or significant your findings are to your field of research, and you’ll argue for the conclusions that you draw from your analysis. Simply put, the discussion chapter is there for you to interact with and explain your research findings in a thorough and coherent manner.

What should I include in the discussion chapter?
First things first: in some studies, the results and discussion chapter are combined into one chapter . This depends on the type of study you conducted (i.e., the nature of the study and methodology adopted), as well as the standards set by the university. So, check in with your university regarding their norms and expectations before getting started. In this post, we’ll treat the two chapters as separate, as this is most common.
Basically, your discussion chapter should analyse , explore the meaning and identify the importance of the data you presented in your results chapter. In the discussion chapter, you’ll give your results some form of meaning by evaluating and interpreting them. This will help answer your research questions, achieve your research aims and support your overall conclusion (s). Therefore, you discussion chapter should focus on findings that are directly connected to your research aims and questions. Don’t waste precious time and word count on findings that are not central to the purpose of your research project.
As this chapter is a reflection of your results chapter, it’s vital that you don’t report any new findings . In other words, you can’t present claims here if you didn’t present the relevant data in the results chapter first. So, make sure that for every discussion point you raise in this chapter, you’ve covered the respective data analysis in the results chapter. If you haven’t, you’ll need to go back and adjust your results chapter accordingly.
If you’re struggling to get started, try writing down a bullet point list everything you found in your results chapter. From this, you can make a list of everything you need to cover in your discussion chapter. Also, make sure you revisit your research questions or hypotheses and incorporate the relevant discussion to address these. This will also help you to see how you can structure your chapter logically.
Need a helping hand?
How to write the discussion chapter
Now that you’ve got a clear idea of what the discussion chapter is and what it needs to include, let’s look at how you can go about structuring this critically important chapter. Broadly speaking, there are six core components that need to be included, and these can be treated as steps in the chapter writing process.
Step 1: Restate your research problem and research questions
The first step in writing up your discussion chapter is to remind your reader of your research problem , as well as your research aim(s) and research questions . If you have hypotheses, you can also briefly mention these. This “reminder” is very important because, after reading dozens of pages, the reader may have forgotten the original point of your research or been swayed in another direction. It’s also likely that some readers skip straight to your discussion chapter from the introduction chapter , so make sure that your research aims and research questions are clear.
Step 2: Summarise your key findings
Next, you’ll want to summarise your key findings from your results chapter. This may look different for qualitative and quantitative research , where qualitative research may report on themes and relationships, whereas quantitative research may touch on correlations and causal relationships. Regardless of the methodology, in this section you need to highlight the overall key findings in relation to your research questions.
Typically, this section only requires one or two paragraphs , depending on how many research questions you have. Aim to be concise here, as you will unpack these findings in more detail later in the chapter. For now, a few lines that directly address your research questions are all that you need.
Some examples of the kind of language you’d use here include:
- The data suggest that…
- The data support/oppose the theory that…
- The analysis identifies…
These are purely examples. What you present here will be completely dependent on your original research questions, so make sure that you are led by them .

Step 3: Interpret your results
Once you’ve restated your research problem and research question(s) and briefly presented your key findings, you can unpack your findings by interpreting your results. Remember: only include what you reported in your results section – don’t introduce new information.
From a structural perspective, it can be a wise approach to follow a similar structure in this chapter as you did in your results chapter. This would help improve readability and make it easier for your reader to follow your arguments. For example, if you structured you results discussion by qualitative themes, it may make sense to do the same here.
Alternatively, you may structure this chapter by research questions, or based on an overarching theoretical framework that your study revolved around. Every study is different, so you’ll need to assess what structure works best for you.
When interpreting your results, you’ll want to assess how your findings compare to those of the existing research (from your literature review chapter). Even if your findings contrast with the existing research, you need to include these in your discussion. In fact, those contrasts are often the most interesting findings . In this case, you’d want to think about why you didn’t find what you were expecting in your data and what the significance of this contrast is.
Here are a few questions to help guide your discussion:
- How do your results relate with those of previous studies ?
- If you get results that differ from those of previous studies, why may this be the case?
- What do your results contribute to your field of research?
- What other explanations could there be for your findings?
When interpreting your findings, be careful not to draw conclusions that aren’t substantiated . Every claim you make needs to be backed up with evidence or findings from the data (and that data needs to be presented in the previous chapter – results). This can look different for different studies; qualitative data may require quotes as evidence, whereas quantitative data would use statistical methods and tests. Whatever the case, every claim you make needs to be strongly backed up.

Step 4: Acknowledge the limitations of your study
The fourth step in writing up your discussion chapter is to acknowledge the limitations of the study. These limitations can cover any part of your study , from the scope or theoretical basis to the analysis method(s) or sample. For example, you may find that you collected data from a very small sample with unique characteristics, which would mean that you are unable to generalise your results to the broader population.
For some students, discussing the limitations of their work can feel a little bit self-defeating . This is a misconception, as a core indicator of high-quality research is its ability to accurately identify its weaknesses. In other words, accurately stating the limitations of your work is a strength, not a weakness . All that said, be careful not to undermine your own research. Tell the reader what limitations exist and what improvements could be made, but also remind them of the value of your study despite its limitations.
Step 5: Make recommendations for implementation and future research
Now that you’ve unpacked your findings and acknowledge the limitations thereof, the next thing you’ll need to do is reflect on your study in terms of two factors:
- The practical application of your findings
- Suggestions for future research
The first thing to discuss is how your findings can be used in the real world – in other words, what contribution can they make to the field or industry? Where are these contributions applicable, how and why? For example, if your research is on communication in health settings, in what ways can your findings be applied to the context of a hospital or medical clinic? Make sure that you spell this out for your reader in practical terms, but also be realistic and make sure that any applications are feasible.
The next discussion point is the opportunity for future research . In other words, how can other studies build on what you’ve found and also improve the findings by overcoming some of the limitations in your study (which you discussed a little earlier). In doing this, you’ll want to investigate whether your results fit in with findings of previous research, and if not, why this may be the case. For example, are there any factors that you didn’t consider in your study? What future research can be done to remedy this? When you write up your suggestions, make sure that you don’t just say that more research is needed on the topic, also comment on how the research can build on your study.
Step 6: Provide a concluding summary
Finally, you’ve reached your final stretch. In this section, you’ll want to provide a brief recap of the key findings – in other words, the findings that directly address your research questions . Basically, your conclusion should tell the reader what your study has found, and what they need to take away from reading your report.
When writing up your concluding summary, bear in mind that some readers may skip straight to this section from the beginning of the chapter. So, make sure that this section flows well from and has a strong connection to the opening section of the chapter.
Tips and tricks for an A-grade discussion chapter
Now that you know what the discussion chapter is , what to include and exclude , and how to structure it , here are some tips and suggestions to help you craft a quality discussion chapter.
- When you write up your discussion chapter, make sure that you keep it consistent with your introduction chapter , as some readers will skip from the introduction chapter directly to the discussion chapter. Your discussion should use the same tense as your introduction, and it should also make use of the same key terms.
- Don’t make assumptions about your readers. As a writer, you have hands-on experience with the data and so it can be easy to present it in an over-simplified manner. Make sure that you spell out your findings and interpretations for the intelligent layman.
- Have a look at other theses and dissertations from your institution, especially the discussion sections. This will help you to understand the standards and conventions of your university, and you’ll also get a good idea of how others have structured their discussion chapters. You can also check out our chapter template .
- Avoid using absolute terms such as “These results prove that…”, rather make use of terms such as “suggest” or “indicate”, where you could say, “These results suggest that…” or “These results indicate…”. It is highly unlikely that a dissertation or thesis will scientifically prove something (due to a variety of resource constraints), so be humble in your language.
- Use well-structured and consistently formatted headings to ensure that your reader can easily navigate between sections, and so that your chapter flows logically and coherently.
If you have any questions or thoughts regarding this post, feel free to leave a comment below. Also, if you’re looking for one-on-one help with your discussion chapter (or thesis in general), consider booking a free consultation with one of our highly experienced Grad Coaches to discuss how we can help you.

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
You Might Also Like:

36 Comments
Thank you this is helpful!
This is very helpful to me… Thanks a lot for sharing this with us 😊
This has been very helpful indeed. Thank you.
This is actually really helpful, I just stumbled upon it. Very happy that I found it, thank you.
Me too! I was kinda lost on how to approach my discussion chapter. How helpful! Thanks a lot!
This is really good and explicit. Thanks
Thank you, this blog has been such a help.
Thank you. This is very helpful.
Dear sir/madame
Thanks a lot for this helpful blog. Really, it supported me in writing my discussion chapter while I was totally unaware about its structure and method of writing.
With regards
Syed Firoz Ahmad PhD, Research Scholar
I agree so much. This blog was god sent. It assisted me so much while I was totally clueless about the context and the know-how. Now I am fully aware of what I am to do and how I am to do it.
Thanks! This is helpful!
thanks alot for this informative website
Dear Sir/Madam,
Truly, your article was much benefited when i structured my discussion chapter.
Thank you very much!!!
This is helpful for me in writing my research discussion component. I have to copy this text on Microsoft word cause of my weakness that I cannot be able to read the text on screen a long time. So many thanks for this articles.
This was helpful
Thanks Jenna, well explained.
Thank you! This is super helpful.
Thanks very much. I have appreciated the six steps on writing the Discussion chapter which are (i) Restating the research problem and questions (ii) Summarising the key findings (iii) Interpreting the results linked to relating to previous results in positive and negative ways; explaining whay different or same and contribution to field of research and expalnation of findings (iv) Acknowledgeing limitations (v) Recommendations for implementation and future resaerch and finally (vi) Providing a conscluding summary
My two questions are: 1. On step 1 and 2 can it be the overall or you restate and sumamrise on each findings based on the reaerch question? 2. On 4 and 5 do you do the acknowlledgement , recommendations on each research finding or overall. This is not clear from your expalanattion.
Please respond.
This post is very useful. I’m wondering whether practical implications must be introduced in the Discussion section or in the Conclusion section?
Sigh, I never knew a 20 min video could have literally save my life like this. I found this at the right time!!!! Everything I need to know in one video thanks a mil ! OMGG and that 6 step!!!!!! was the cherry on top the cake!!!!!!!!!
Thanks alot.., I have gained much
This piece is very helpful on how to go about my discussion section. I can always recommend GradCoach research guides for colleagues.
Many thanks for this resource. It has been very helpful to me. I was finding it hard to even write the first sentence. Much appreciated.
Thanks so much. Very helpful to know what is included in the discussion section
this was a very helpful and useful information
This is very helpful. Very very helpful. Thanks for sharing this online!
it is very helpfull article, and i will recommend it to my fellow students. Thank you.
Superlative! More grease to your elbows.
Powerful, thank you for sharing.
Wow! Just wow! God bless the day I stumbled upon you guys’ YouTube videos! It’s been truly life changing and anxiety about my report that is due in less than a month has subsided significantly!
Simplified explanation. Well done.
The presentation is enlightening. Thank you very much.
Thanks for the support and guidance
This has been a great help to me and thank you do much
I second that “it is highly unlikely that a dissertation or thesis will scientifically prove something”; although, could you enlighten us on that comment and elaborate more please?
Sure, no problem.
Scientific proof is generally considered a very strong assertion that something is definitively and universally true. In most scientific disciplines, especially within the realms of natural and social sciences, absolute proof is very rare. Instead, researchers aim to provide evidence that supports or rejects hypotheses. This evidence increases or decreases the likelihood that a particular theory is correct, but it rarely proves something in the absolute sense.
Dissertations and theses, as substantial as they are, typically focus on exploring a specific question or problem within a larger field of study. They contribute to a broader conversation and body of knowledge. The aim is often to provide detailed insight, extend understanding, and suggest directions for further research rather than to offer definitive proof. These academic works are part of a cumulative process of knowledge building where each piece of research connects with others to gradually enhance our understanding of complex phenomena.
Furthermore, the rigorous nature of scientific inquiry involves continuous testing, validation, and potential refutation of ideas. What might be considered a “proof” at one point can later be challenged by new evidence or alternative interpretations. Therefore, the language of “proof” is cautiously used in academic circles to maintain scientific integrity and humility.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Qualitative Results and Discussion
- First Online: 20 August 2020
Cite this chapter

- Peijian Paul Sun 2
302 Accesses
This chapter presents the results and discussion in line with the five research questions of the present study based on the qualitative data collected from the focus groups and semi-structured interviews. A total of 7 focus groups and 10 semi-structured interviews were conducted to explore the research questions from a more in-depth qualitative perspective. Two types of interviews were utilized in order to bring different lines of insights together to ensure that more profound and appropriate understandings of the research questions could be facilitated. This chapter starts with an introduction to the background information of the participants and the coding system. The qualitative findings in relation to each research question are presented sequentially followed by a summary and discussion.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Alrabai, Fakieh. 2015. The Influence of Teachers’ Anxiety-Reducing Strategies on Learners’ Foreign Language Anxiety. Innovation in Language Learning and Teaching 9 (2): 128–163. https://doi.org/10.1080/17501229.2014.890203 .
Article Google Scholar
Amiryousefi, Mohammad. 2018. Willingness to Communicate, Interest, Motives to Communicate with the Instructor, and L2 Speaking: A Focus on the Role of Age and Gender. Innovation in Language Learning and Teaching 12 (3): 221–234. https://doi.org/10.1080/17501229.2016.1170838 .
Armon-Lotem, Sharon, Susan Joffe, Hadar Abutbul-Oz, Carmit Altman, and Joel Walters. 2014. Language Exposure, Ethnolinguistic Identity and Attitudes in the Acquisition of Hebrew as a Second Language among Bilingual Preschool Children from Russian- and English-Speaking Backgrounds. In Input and Experience in Bilingual Development , edited by Theres Grüter and Johanne Paradis, 77–98. Amsterdam, Netherlands: John Benjamins.
Google Scholar
Bright, Peter, Julia Ouzia, and Roberto Filippi. 2019. Multilingualism and Metacognitive Processing. In The Handbook of the Neuroscience of Multilingualism , ed. John W. Schwieter, 355–371. Chichester, UK: Wiley. https://doi.org/10.1002/9781119387725.ch17 .
Caprara, Gian Vittorio, Michele Vecchione, Guido Alessandri, Maria Gerbino, and Claudio Barbaranelli. 2011. The Contribution of Personality Traits and Self-Efficacy Beliefs to Academic Achievement: A Longitudinal Study. British Journal of Educational Psychology 81 (1): 78–96. https://doi.org/10.1348/2044-8279.002004 .
Cenoz, Jasone, and Durk Gorter. 2019. Multilingualism, Translanguaging, and Minority Languages in SLA. The Modern Language Journal 103: 130–135. https://doi.org/10.1111/modl.12529 .
Clément, Richard, Susuan C. Baker, and Peter D. MacIntyre. 2003. Willingness to Communicate in a Second Language: The Effect of Context, Norms, and Vitality. Journal of Language and Social Psychology 22: 190–209.
Dörnyei, Zoltán. 2005. The Psychology of the Language Learner: Individual Differences in Second Language Acquisition . Mahwah, NJ: Lawrence Erlbaum.
Dörnyei, Zoltán. 2009. The L2 Motivational Self System. In Motivation, Language Identity and the L2 Self , edited by Zoltán Dörnyei and Ema Ushioda, 9–42. Bristol, UK: Multilingual Matters.
Effiong, Okon. 2016. Getting Them Speaking: Classroom Social Factors and Foreign Language Anxiety. TESOL Journal 7 (1): 132–161. https://doi.org/10.1002/tesj.194 .
Florack, Arnd, Anette Rohmann, Johanna Palcu, and Agostino Mazziotta. 2014. How Initial Cross-Group Friendships Prepare for Intercultural Communication: The Importance of Anxiety Reduction and Self-Confidence in Communication. International Journal of Intercultural Relations 43, Part B (0): 278–288. https://doi.org///dx.doi.org/10.1016/j.ijintrel.2014.09.004 .
Ghorbani, Mohammad Reza, and Seyyed Ehsan Golparvar. 2019. Modeling the Relationship between Socioeconomic Status, Self-Initiated, Technology-Enhanced Language Learning, and Language Outcome. Computer Assisted Language Learning 1–21. https://doi.org/10.1080/09588221.2019.1585374 .
Hernández, Todd A. 2006. Integrative Motivation as a Predictor of Success in the Intermediate Foreign Language Classroom. Foreign Language Annals 22: 30–37.
Hu, Hsueh-chao Marcella, and Hossein Nassaji. 2014. Lexical Inferencing Strategies: The Case of Successful versus Less Successful Inferencers. System 45 (1): 27–38. https://doi.org/10.1016/j.system.2014.04.004 .
Huang, Becky, Yung-Hsiang Shawn Chang, Luping Niu, and Mingxia Zhi. 2018. Examining the Effects of Socio-Economic Status and Language Input on Adolescent English Learners’ Speech Production Outcomes. System 73: 27–36. https://doi.org/10.1016/j.system.2017.07.004 .
Hyland, Ken. 1993. Culture and Learning: A Study of the Learning Style Preferences of Japanese Students. RELC Journal 24 (2): 69–87. https://doi.org/10.1177/003368829302400204 .
Kang, Su-Ja. 2005. Dynamic Emergence of Situational Willingness to Communicate in a Second Language. System 33 (2): 277–292. https://doi.org/10.1016/j.system.2004.10.004 .
Khajavy, Gholam Hassan, Peter D. MacIntyre, and Elyas Barabadi. 2018. Role of the Emotions and Classroom Environment in Willingness to Communicate: Applying Doubly Latent Multilevel Analysis in Second Language Acquisition Research. Studies in Second Language Acquisition 40 (3): 605–624. https://doi.org/10.1017/S0272263117000304 .
Kim, Tae-Young, and Yoon-Kyoung Kim. 2014. A Structural Model for Perceptual Learning Styles, the Ideal L2 Self, Motivated Behavior, and English Proficiency. System 46 (0): 14–27. https://doi.org///dx.doi.org/10.1016/j.system.2014.07.007 .
Kırkgöz, Yasemin. 2018. Fostering Young Learners’ Listening and Speaking Skills. In The Routledge Handbook of Teaching English to Young Learners , ed. Sue Carton and Fiona Copland, 171–187. Routledge.
Krashen, Stephen D. 1982. Principles and Practice in Second Language Acquisition . Oxford, UK: Pergamon.
Liu, Meihua, and Wenhong Huang. 2011. An Exploration of Foreign Language Anxiety and English Learning Motivation. Education Research International 12: 1–8.
MacIntyre, Peter D. 2007. Willingness to Communicate in the Second Language: Understanding the Decision to Speak as a Volitional Process. The Modern Language Journal 91 (4): 564–576. https://doi.org/10.1111/j.1540-4781.2007.00623.x .
MacIntyre, Peter D., Zoltán Dörnyei, Richard Clément, and Kimberly A. Noels. 1998. Conceptualizing Willingness to Communicate in a L2: A Situational Model of L2 Confidence and Affiliation. The Modern Language Journal 82 (4): 545–62. https://doi.org/10.1111/j.1540-4781.1998.tb05543.x .
Magogwe, Joel Mokuedi, and Rhonda Oliver. 2007. The Relationship Between Language Learning Strategies, Proficiency, Age and Self-Efficacy Beliefs: A Study of Language Learners in Botswana. System 35 (3): 338–352. https://doi.org/10.1016/j.system.2007.01.003 .
Mahmoodzadeh, Masoud. 2012. Investigating Foreign Language Speaking Anxiety within the EFL Learner’s Interlanguage System: The Case of Iranian Learners. Journal of Language Teaching and Research 3 (3): 466–476. https://doi.org/10.4304/jltr.3.3.466-476 .
Minagawa, Harumi, Dallas Nesbitt, Masayoshi Ogino, Junji Kawai, and Ryoko de Burgh-Hirabe. 2019. Why I Am Studying Japanese: A National Survey Revealing the Voices of New Zealand Tertiary Students. Japanese Studies. https://doi.org/10.1080/10371397.2019.1678365 .
Nakatani, Yasuo. 2006. Developing an Oral Communication Strategy Inventory. The Modern Language Journal 90 (2): 151–168. https://doi.org/10.1111/j.1540-4781.2006.00390.x .
Nakatani, Yasuo, and Christine Goh. 2007. A Review of Oral Communication Strategies: Focus on Interactionist and Psycholinguistic Perspectives. In Language Learner Strategies: Thirty Years of Research and Practice , ed. Andrew D. Cohen and Ernesto Macaro, 207–227. Oxford, UK: Oxford University Press.
Naserieh, Farid, and Mohammad Reza Anani Sarab. 2013. Perceptual Learning Style Preferences among Iranian Graduate Students. System 41 (1): 122–133. https://doi.org/10.1016/j.system.2013.01.018 .
Nicolson, Margaret, and Helga Adams. 2008. Travelling in Space and Encounters of the Third Kind: Distance Language Learner Negotiation of Speaking Activities. Innovation in Language Learning and Teaching 2 (2): 105–116. https://doi.org/10.1080/17501220802158859 .
Nomura, Kazuyuki, and Rui Yuan. 2019. Long-Term Motivations for L2 Learning: A Biographical Study from a Situated Learning Perspective. Journal of Multilingual and Multicultural Development 40 (2): 164–178. https://doi.org/10.1080/01434632.2018.1497041 .
Oxford, Rebecca L. 1990. Language Learning Strategies: What Every Teacher Should Know . Boston, MA: Heinle and Heinle.
Peacock, Matthew. 2001. Match or Mismatch? Learning Styles and Teaching Styles in EFL. International Journal of Applied Linguistics 11 (1): 1–20. https://doi.org/10.1111/1473-4192.00001 .
Peng, Jian-E. 2019. The Roles of Multimodal Pedagogic Effects and Classroom Environment in Willingness to Communicate in English. System 82: 161–173. https://doi.org/10.1016/j.system.2019.04.006 .
Phongsa, Manivone, Shaik Abdul Malik Mohamed Ismail, and Hui Min Low. 2018. Multilingual Effects on EFL Learning: A Comparison of Foreign Language Anxiety Experienced by Monolingual and Bilingual Tertiary Students in the Lao PDR. Journal of Multilingual and Multicultural Development 39 (3): 271–282. https://doi.org/10.1080/01434632.2017.1371723 .
Psaltou-Joycey, Angeliki, and Zoe Gavriilidou. 2018. Language Learning Strategies of Greek EFL Primary and Secondary School Learners: How Individual Characteristics Affect Strategy Use. In Language Learning Strategies and Individual Learner Characteristics: Situating Strategy Use in Diverse Contexts , ed. Rebecca L. Oxford and Carmen M. Amerstorfer, 167–187. London, UK: Bloomsbury.
Ryan, Richard M., and Edward L. Deci. 2000. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. American Psychologist 55 (1): 68–78. https://doi.org/10.1037/0003-066X.55.1.68 .
Saito, Kazuya, Masatoshi Sato, and Roy Lyster. 2013. Oral Corrective Feedback in Second Language Classrooms. Language Teaching 46 (2): 1–40.
Sauer, Luzia, and Rod Ellis. 2019. The Social Lives of Adolescent Study Abroad Learners and Their L2 Development. The Modern Language Journal 103 (4): 739–762. https://doi.org/10.1111/modl.12589 .
Schauer, Gila A. 2006. The Development of ESL Learners’ Pragmatic Competence: A Longitudinal Investigation of Awareness and Production. In Pragmatics and Language Learning Volume 11 , edited by Kathleen Bardovi-Harlig, César Félix-Brasdefer, and Alwiya S. Omar, 135–64. Mānoa, HI: University of Hawaii Press.
Scovel, Thomas. 1978. The Effect of Affect on Foreign Language Learning: A Review of the Anxiety Research. Language Learning 28 (1): 129–142. https://doi.org/10.1111/j.1467-1770.1978.tb00309.x .
Segalowitz, Norman. 2010. Cognitive Bases of Second Language Fluency . New York, NY: Routledge.
Shaikholeslami, Razieh, and Mohammad Khayyer. 2006. Intrinsic Motivation, Extrinsic Motivation, and Learning English as a Foreign Language. Psychological Reports 99 (3): 813–818.
Stewart, David W, and Prem N Shamdasani. 2015. Focus Groups: Theory and Practice . 3rd ed. Thousand Oaks, CA: Sage.
Taguchi, Naoko, Feng Xiao, and Shuai Li. 2016. Effects of Intercultural Competence and Social Contact on Speech Act Production in a Chinese Study Abroad Context. Modern Language Journal 100 (4): 775–796. https://doi.org/10.1111/modl.12349 .
Tarone, Elaine. 1981. Some Thoughts on the Notion of Communication Strategy. TESOL Quarterly 15 (3): 285–95. https://doi.org/10.2307/3586754 .
Download references
Author information
Authors and affiliations.
Department of Linguistics, Zhejiang University, Hangzhou, China
Peijian Paul Sun
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Peijian Paul Sun .
Rights and permissions
Reprints and permissions
Copyright information
© 2020 The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Sun, P.P. (2020). Qualitative Results and Discussion. In: Chinese as a Second Language Multilinguals’ Speech Competence and Speech Performance. Springer, Singapore. https://doi.org/10.1007/978-981-15-6941-8_7
Download citation
DOI : https://doi.org/10.1007/978-981-15-6941-8_7
Published : 20 August 2020
Publisher Name : Springer, Singapore
Print ISBN : 978-981-15-6940-1
Online ISBN : 978-981-15-6941-8
eBook Packages : Education Education (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

- LEARNING SKILLS
- Writing a Dissertation or Thesis
- Results and Discussion
Search SkillsYouNeed:
Learning Skills:
- A - Z List of Learning Skills
- What is Learning?
- Learning Approaches
- Learning Styles
- 8 Types of Learning Styles
- Understanding Your Preferences to Aid Learning
- Lifelong Learning
- Decisions to Make Before Applying to University
- Top Tips for Surviving Student Life
- Living Online: Education and Learning
- 8 Ways to Embrace Technology-Based Learning Approaches
- Critical Thinking Skills
- Critical Thinking and Fake News
- Understanding and Addressing Conspiracy Theories
- Critical Analysis
- Study Skills
- Exam Skills
- How to Write a Research Proposal
- Ethical Issues in Research
- Dissertation: The Introduction
- Researching and Writing a Literature Review
- Writing your Methodology
- Dissertation: Results and Discussion
- Dissertation: Conclusions and Extras
Writing Your Dissertation or Thesis eBook

Part of the Skills You Need Guide for Students .
- Research Methods
- Teaching, Coaching, Mentoring and Counselling
- Employability Skills for Graduates
Subscribe to our FREE newsletter and start improving your life in just 5 minutes a day.
You'll get our 5 free 'One Minute Life Skills' and our weekly newsletter.
We'll never share your email address and you can unsubscribe at any time.
Writing your Dissertation: Results and Discussion
When writing a dissertation or thesis, the results and discussion sections can be both the most interesting as well as the most challenging sections to write.
You may choose to write these sections separately, or combine them into a single chapter, depending on your university’s guidelines and your own preferences.
There are advantages to both approaches.
Writing the results and discussion as separate sections allows you to focus first on what results you obtained and set out clearly what happened in your experiments and/or investigations without worrying about their implications.This can focus your mind on what the results actually show and help you to sort them in your head.
However, many people find it easier to combine the results with their implications as the two are closely connected.
Check your university’s requirements carefully before combining the results and discussions sections as some specify that they must be kept separate.
Results Section
The Results section should set out your key experimental results, including any statistical analysis and whether or not the results of these are significant.
You should cover any literature supporting your interpretation of significance. It does not have to include everything you did, particularly for a doctorate dissertation. However, for an undergraduate or master's thesis, you will probably find that you need to include most of your work.
You should write your results section in the past tense: you are describing what you have done in the past.
Every result included MUST have a method set out in the methods section. Check back to make sure that you have included all the relevant methods.
Conversely, every method should also have some results given so, if you choose to exclude certain experiments from the results, make sure that you remove mention of the method as well.
If you are unsure whether to include certain results, go back to your research questions and decide whether the results are relevant to them. It doesn’t matter whether they are supportive or not, it’s about relevance. If they are relevant, you should include them.
Having decided what to include, next decide what order to use. You could choose chronological, which should follow the methods, or in order from most to least important in the answering of your research questions, or by research question and/or hypothesis.
You also need to consider how best to present your results: tables, figures, graphs, or text. Try to use a variety of different methods of presentation, and consider your reader: 20 pages of dense tables are hard to understand, as are five pages of graphs, but a single table and well-chosen graph that illustrate your overall findings will make things much clearer.
Make sure that each table and figure has a number and a title. Number tables and figures in separate lists, but consecutively by the order in which you mention them in the text. If you have more than about two or three, it’s often helpful to provide lists of tables and figures alongside the table of contents at the start of your dissertation.
Summarise your results in the text, drawing on the figures and tables to illustrate your points.
The text and figures should be complementary, not repeat the same information. You should refer to every table or figure in the text. Any that you don’t feel the need to refer to can safely be moved to an appendix, or even removed.
Make sure that you including information about the size and direction of any changes, including percentage change if appropriate. Statistical tests should include details of p values or confidence intervals and limits.
While you don’t need to include all your primary evidence in this section, you should as a matter of good practice make it available in an appendix, to which you should refer at the relevant point.
For example:
Details of all the interview participants can be found in Appendix A, with transcripts of each interview in Appendix B.
You will, almost inevitably, find that you need to include some slight discussion of your results during this section. This discussion should evaluate the quality of the results and their reliability, but not stray too far into discussion of how far your results support your hypothesis and/or answer your research questions, as that is for the discussion section.
See our pages: Analysing Qualitative Data and Simple Statistical Analysis for more information on analysing your results.
Discussion Section
This section has four purposes, it should:
- Interpret and explain your results
- Answer your research question
- Justify your approach
- Critically evaluate your study
The discussion section therefore needs to review your findings in the context of the literature and the existing knowledge about the subject.
You also need to demonstrate that you understand the limitations of your research and the implications of your findings for policy and practice. This section should be written in the present tense.
The Discussion section needs to follow from your results and relate back to your literature review . Make sure that everything you discuss is covered in the results section.
Some universities require a separate section on recommendations for policy and practice and/or for future research, while others allow you to include this in your discussion, so check the guidelines carefully.
Starting the Task
Most people are likely to write this section best by preparing an outline, setting out the broad thrust of the argument, and how your results support it.
You may find techniques like mind mapping are helpful in making a first outline; check out our page: Creative Thinking for some ideas about how to think through your ideas. You should start by referring back to your research questions, discuss your results, then set them into the context of the literature, and then into broader theory.
This is likely to be one of the longest sections of your dissertation, and it’s a good idea to break it down into chunks with sub-headings to help your reader to navigate through the detail.
Fleshing Out the Detail
Once you have your outline in front of you, you can start to map out how your results fit into the outline.
This will help you to see whether your results are over-focused in one area, which is why writing up your research as you go along can be a helpful process. For each theme or area, you should discuss how the results help to answer your research question, and whether the results are consistent with your expectations and the literature.
The Importance of Understanding Differences
If your results are controversial and/or unexpected, you should set them fully in context and explain why you think that you obtained them.
Your explanations may include issues such as a non-representative sample for convenience purposes, a response rate skewed towards those with a particular experience, or your own involvement as a participant for sociological research.
You do not need to be apologetic about these, because you made a choice about them, which you should have justified in the methodology section. However, you do need to evaluate your own results against others’ findings, especially if they are different. A full understanding of the limitations of your research is part of a good discussion section.
At this stage, you may want to revisit your literature review, unless you submitted it as a separate submission earlier, and revise it to draw out those studies which have proven more relevant.
Conclude by summarising the implications of your findings in brief, and explain why they are important for researchers and in practice, and provide some suggestions for further work.
You may also wish to make some recommendations for practice. As before, this may be a separate section, or included in your discussion.
The results and discussion, including conclusion and recommendations, are probably the most substantial sections of your dissertation. Once completed, you can begin to relax slightly: you are on to the last stages of writing!
Continue to: Dissertation: Conclusion and Extras Writing your Methodology
See also: Writing a Literature Review Writing a Research Proposal Academic Referencing What Is the Importance of Using a Plagiarism Checker to Check Your Thesis?
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Dissertation
- How to Write a Discussion Section | Tips & Examples
How to Write a Discussion Section | Tips & Examples
Published on 21 August 2022 by Shona McCombes . Revised on 25 October 2022.

The discussion section is where you delve into the meaning, importance, and relevance of your results .
It should focus on explaining and evaluating what you found, showing how it relates to your literature review , and making an argument in support of your overall conclusion . It should not be a second results section .
There are different ways to write this section, but you can focus your writing around these key elements:
- Summary: A brief recap of your key results
- Interpretations: What do your results mean?
- Implications: Why do your results matter?
- Limitations: What can’t your results tell us?
- Recommendations: Avenues for further studies or analyses
Instantly correct all language mistakes in your text
Be assured that you'll submit flawless writing. Upload your document to correct all your mistakes.

Table of contents
What not to include in your discussion section, step 1: summarise your key findings, step 2: give your interpretations, step 3: discuss the implications, step 4: acknowledge the limitations, step 5: share your recommendations, discussion section example.
There are a few common mistakes to avoid when writing the discussion section of your paper.
- Don’t introduce new results: You should only discuss the data that you have already reported in your results section .
- Don’t make inflated claims: Avoid overinterpretation and speculation that isn’t directly supported by your data.
- Don’t undermine your research: The discussion of limitations should aim to strengthen your credibility, not emphasise weaknesses or failures.
The only proofreading tool specialized in correcting academic writing
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Correct my document today
Start this section by reiterating your research problem and concisely summarising your major findings. Don’t just repeat all the data you have already reported – aim for a clear statement of the overall result that directly answers your main research question . This should be no more than one paragraph.
Many students struggle with the differences between a discussion section and a results section . The crux of the matter is that your results sections should present your results, and your discussion section should subjectively evaluate them. Try not to blend elements of these two sections, in order to keep your paper sharp.
- The results indicate that …
- The study demonstrates a correlation between …
- This analysis supports the theory that …
- The data suggest that …
The meaning of your results may seem obvious to you, but it’s important to spell out their significance for your reader, showing exactly how they answer your research question.
The form of your interpretations will depend on the type of research, but some typical approaches to interpreting the data include:
- Identifying correlations , patterns, and relationships among the data
- Discussing whether the results met your expectations or supported your hypotheses
- Contextualising your findings within previous research and theory
- Explaining unexpected results and evaluating their significance
- Considering possible alternative explanations and making an argument for your position
You can organise your discussion around key themes, hypotheses, or research questions, following the same structure as your results section. Alternatively, you can also begin by highlighting the most significant or unexpected results.
- In line with the hypothesis …
- Contrary to the hypothesised association …
- The results contradict the claims of Smith (2007) that …
- The results might suggest that x . However, based on the findings of similar studies, a more plausible explanation is x .
As well as giving your own interpretations, make sure to relate your results back to the scholarly work that you surveyed in the literature review . The discussion should show how your findings fit with existing knowledge, what new insights they contribute, and what consequences they have for theory or practice.
Ask yourself these questions:
- Do your results support or challenge existing theories? If they support existing theories, what new information do they contribute? If they challenge existing theories, why do you think that is?
- Are there any practical implications?
Your overall aim is to show the reader exactly what your research has contributed, and why they should care.
- These results build on existing evidence of …
- The results do not fit with the theory that …
- The experiment provides a new insight into the relationship between …
- These results should be taken into account when considering how to …
- The data contribute a clearer understanding of …
- While previous research has focused on x , these results demonstrate that y .
Even the best research has its limitations. Acknowledging these is important to demonstrate your credibility. Limitations aren’t about listing your errors, but about providing an accurate picture of what can and cannot be concluded from your study.
Limitations might be due to your overall research design, specific methodological choices , or unanticipated obstacles that emerged during your research process.
Here are a few common possibilities:
- If your sample size was small or limited to a specific group of people, explain how generalisability is limited.
- If you encountered problems when gathering or analysing data, explain how these influenced the results.
- If there are potential confounding variables that you were unable to control, acknowledge the effect these may have had.
After noting the limitations, you can reiterate why the results are nonetheless valid for the purpose of answering your research question.
- The generalisability of the results is limited by …
- The reliability of these data is impacted by …
- Due to the lack of data on x , the results cannot confirm …
- The methodological choices were constrained by …
- It is beyond the scope of this study to …
Based on the discussion of your results, you can make recommendations for practical implementation or further research. Sometimes, the recommendations are saved for the conclusion .
Suggestions for further research can lead directly from the limitations. Don’t just state that more studies should be done – give concrete ideas for how future work can build on areas that your own research was unable to address.
- Further research is needed to establish …
- Future studies should take into account …
- Avenues for future research include …
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
McCombes, S. (2022, October 25). How to Write a Discussion Section | Tips & Examples. Scribbr. Retrieved 29 April 2024, from https://www.scribbr.co.uk/thesis-dissertation/discussion/
Is this article helpful?
Shona McCombes
Other students also liked, how to write a results section | tips & examples, research paper appendix | example & templates, how to write a thesis or dissertation introduction.
- Open access
- Published: 29 April 2024
Pathways and identity: toward qualitative research careers in child and adolescent psychiatry
- Andrés Martin 1 , 2 , 3 ,
- Madeline DiGiovanni 1 , 2 , 3 ,
- Amber Acquaye 1 , 2 , 3 ,
- Matthew Ponticiello 1 , 2 , 3 ,
- Débora Tseng Chou 2 , 3 , 4 ,
- Emilio Abelama Neto 2 , 3 , 4 ,
- Alexandre Michel 2 , 3 , 5 ,
- Jordan Sibeoni 2 , 3 , 5 ,
- Marie-Aude Piot 2 , 3 , 5 ,
- Michel Spodenkiewicz 2 , 3 , 6 &
- Laelia Benoit 1 , 2 , 3
Child and Adolescent Psychiatry and Mental Health volume 18 , Article number: 49 ( 2024 ) Cite this article
11 Accesses
Metrics details
Qualitative research methods are based on the analysis of words rather than numbers; they encourage self-reflection on the investigator’s part; they are attuned to social interaction and nuance; and they incorporate their subjects’ thoughts and feelings as primary sources. Despite appearing well suited for research in child and adolescent psychiatry (CAP), qualitative methods have had relatively minor uptake in the discipline. We conducted a qualitative study of CAPs involved in qualitative research to learn about these investigators’ lived experiences, and to identify modifiable factors to promote qualitative methods within the field of youth mental health.
We conducted individual, semi-structured 1-h long interviews through Zoom. Using purposive sample, we selected 23 participants drawn from the US (n = 12) and from France (n = 11), and equally divided in each country across seniority level. All participants were current or aspiring CAPs and had published at least one peer-reviewed qualitative article. Ten participants were women (44%). We recorded all interviews digitally and transcribed them for analysis. We coded the transcripts according to the principles of thematic analysis and approached data analysis, interpretation, and conceptualization informed by an interpersonal phenomenological analysis (IPA) framework.
Through iterative thematic analysis we developed a conceptual model consisting of three domains: (1) Becoming a qualitativist: embracing a different way of knowing (in turn divided into the three themes of priming factors/personal fit; discovering qualitative research; and transitioning in); (2) Being a qualitativist: immersing oneself in a different kind of research (in turn divided into quality: doing qualitative research well; and community: mentors, mentees, and teams); and (3) Nurturing : toward a higher quality future in CAP (in turn divided into current state of qualitative methods in CAP; and advocating for qualitative methods in CAP). For each domain, we go on to propose specific strategies to enhance entry into qualitative careers and research in CAP: (1) Becoming: personalizing the investigator’s research focus; balancing inward and outward views; and leveraging practical advantages; (2) Being: seeking epistemological flexibility; moving beyond bibliometrics; and the potential and risks of mixing methods; and (3) Nurturing : invigorating a quality pipeline; and building communities.
Conclusions
We have identified factors that can support or impede entry into qualitative research among CAPs. Based on these modifiable findings, we propose possible solutions to enhance entry into qualitative methods in CAP ( pathways ), and to foster longer-term commitment to this type of research ( identity ).
…we must reckon that numbers can say only so much, and that we need to better listen and better represent the voices of those under our care, especially of those who have been unheard or disenfranchised for far too long. We believe that less quantity and more quality can help us meet those aspirations [ 1 ], p.3.
Qualitative methods of research favor the analysis of words over that of numbers, which are in turn the main focus of quantitative approaches. With its preference for thoughts, ideas, feelings, and other aspects of internal life, qualitative inquiry is particularly well suited for psychiatry [ 2 ]. Moreover, with child and adolescent psychiatry’s (CAP’s) interest in exploring the interactions between groups of individuals and their role as interconnected social actors, qualitative methods are especially well suited for the discipline. The link between CAP as a subject matter and qualitative methods as a favored research approach would appear to be a natural one.
If only it were. Qualitative studies in CAP are in fact scant. For example, a search for the terms “qualitative” AND “child OR adolescent” AND “psychiatry” using Google Scholar (date of access: December 1, 2023) returned 2,588 entries, in contrast to a comparable search yielding 75,196 entries when substituting the first term with “quantitative,” representing a 29-fold difference favoring quantitative over qualitative publications. Stratifying the same analysis across decades reveals a more telling pattern: the fraction of qualitative studies from among all those published in CAP during the decade ending in 2013 was 2% (359/18,154); by the following decade, the proportion had doubled, to 4% (2,229/54,454). The number of qualitative studies increased sixfold from one decade to the next, compared to a threefold change for quantitative studies. In short, these trends reflect how even if the absolute number of qualitative studies in CAP has remained low, there has been a proportional increment in their publication, reflecting growing interest in qualitative methods in CAP research.
Glancing at the table of contents of scholarly outlets suggests yet another story. Specifically, it is not uncommon for leading CAP journals to publish no qualitative studies for years on end—when at all. Qualitative science often finds its way into different periodicals, some without any mental health focus. The point here is how spliced qualitative science remains from the more “mainstream” science and publications of CAP, which remain almost exclusively focused on quantitative methods [ 3 ]. Conferring a “second class science” status to qualitative methods [ 4 ] has implications not just for scholarship, but for patient care, including to “contribute voice to advance equity in health [ 5 ].” CAP has been slow in the uptake of qualitative methods seen in other specialties (including oncology, primary care, and medical education), in which there has been a movement toward a more collaborative person-centered approach, one with more consideration for the lived experience of patients and their caregivers [ 6 ].
Partly at the root of this tension is what has been termed epistemological unconsciousness or positivist orthodoxy [ 7 ], a worldview prevalent in medicine and the sciences that has a built-in preference for objectivist (i.e., quantitative) rather than constructivist (i.e., qualitative) views. The rise of the evidence-based movement, which continues to prioritize quantitative research, has introduced further challenges to the qualitative community [ 8 ]. Moreover, the relative scarcity of qualitative studies in CAP may not be entirely coincidental. Falissard et al. [ 1 ] have posited three likely contributors. First, a focus on children, the research agenda of whom is commonly overtaken by that of adults. Despite higher returns on earlier life stage investments, decisions on funding allocations—from education to healthcare to research—rarely prioritize children. Considered through the lens of childism [ 9 ], the systematic societal prejudice against children, CAP research priorities are commonly overshadowed by those of general psychiatry and medicine more broadly, much as qualitative methods can become lost under a quantitative hegemon.
Second, the focus of CAP on mental health has become almost interchangeable with a focus on brain disease and the particular tools for its “proper” study: genetics, brain imaging, clinical trials, and other “objective” instruments. Despite the advances in these areas, laboratory tools cannot access important aspects of mental health function, such as mind and relationships. The “decade of the brain” has left limited room for the mind, and in so doing, contributed to reifying the “brainlessness and mindlessness” that Leon Eisenberg warned against in the late 1980s [ 10 ]. A disillusionment with biomedicine and its tools has introduced an epistemological malaise into medicine, which those working under a qualitative framework are striving to address.
Finally, qualitative research’s connection to psychoanalysis may have proved a burden to its application in psychiatry, particularly CAP. With its interest in words, thoughts, feelings, and deep reflection, psychoanalysis would appear a natural precursor to qualitative methods. Psychoanalytic literature can have an uncanny resemblance to qualitative papers, such as biographical or narrative studies. Despite the similarities and shared roots in sociology, anthropology, and literature, qualitative methods in mental health research have suffered under the shortcomings of analysis, including its insularity and exclusive focus on the individual. In the end, two disciplines rooted in interpretivism drifted apart; the methodological shortcomings [ 11 ] and stigma of psychoanalysis cast a shadow on the promise of the fledgling qualitative field.
Provocative as these hypotheses are, they are speculative and not based on actual data. To our knowledge, there are no studies that have empirically investigated the reasons propelling or impeding research careers in qualitative methods, and certainly none in the field of CAP. Faced with this gap in the literature, and through what may be considered a "meta" approach, we used qualitative methods to interview CAPs actively involved in different stages of qualitative research . The overall goal of our effort was to identify factors, particularly modifiable ones, that could enhance the number and methodological rigor of this type of research in CAP, and to help enrich the pipeline of future investigators dedicated to the intersection of the two disciplines: in short, to help grow quality CAP research and those dedicated to it.
Participants and individual interviews
We conducted individual, semi-structured interviews organized around a guide consisting of 23 sensitizing questions (Additional file 1 : Appendix S1). Each of the interviews was 1 h long and conducted thorough videoconferencing using Zoom (San Jose, CA). Semi-structured interviewing is a flexible, commonly used method in qualitative research in healthcare that uses a prepared list of questions to guide researchers and participants to “co-create meaning” through an exploration of thoughts, feelings, and opinions, especially those around potentially sensitive or personal topics [ 12 , 13 ]. Interviewees were not necessarily asked all of the sensitizing questions. Using convenience and purposive sampling [ 14 ], we selected 23 participants drawn from the US (n = 12) and from France (n = 11), and equally divided in each country across seniority level. All participants had published at least one peer-reviewed qualitative article, and were classified as junior if having 5 or fewer years of post-doctoral experience; those with 6 or more years were considered senior. Ten participants were women (44%).
Data collection, qualitative analysis, theoretical framework, and reflexivity
We recorded all interviews digitally and transcribed them for analysis using Deepgram (deepgram.com, San Francisco, CA). We uploaded the collection of transcripts into software for qualitative analysis (NVivo version 12; QSR International, Melbourne, Australia). We coded the transcripts according to the principles of thematic analysis, a qualitative approach involving the active construction of overarching patterns and meaning across a dataset [ 15 , 16 ]. Thematic analysis allows the flexible and atheoretical exploration of rich text data to construct themes that “reframe, reinterpret, and/or connect elements of the data” without developing a final theory. We approached analysis, interpretation, and conceptualization informed by interpretative phenomenological analysis (IPA), an approach based in psychology that attends to participants’ inner realities [ 17 , 18 ]. We adopted an inductive approach, with our research questions evolving beyond the initial sensitizing questions.
Three authors coded independently throughout the study span in an iterative manner, with coding and interviewing interdigitated to allow for the inductive approach to inform subsequent interviews. They then combined and triangulated codes, and established the final codebook to eliminate redundancies, clarify domains, themes, and subthemes. In this way we ensured theoretical sufficiency [ 19 ]. Each final code was supported by quotes from more than one participant.
All authors were interviewed and took part as study participants; five authors served as interviewers, and four as data coders. We were attentive to positionality, with no instance of a hierarchical or working relationship between interviewers and interviewees. The closeness between all authors/study participants, the fact that as CAPs they were looking into their own guild and in some way into themselves, and the subject matter of the study itself, all required careful attention to everyone’s reflexivity [ 20 ] during the discussion and write-up process. The dual role as researchers and participants provided broader insights, as the resonance between the views of non-researcher-participants and those of researcher-participants improved the triangulation and comprehension of the gained insights [ 21 ]. This view is aligned with the “patient-as-partner” approach to health care, education and research, in which participants are not limited to just providing feedback on results. Instead, they are included as participants from the very beginning of the conceptualization of the project and until its end, e.g., the in-depth review of its ensuing manuscript [ 22 ]. Through involvement not only as investigators but as beneficiaries, stakeholders, and participants, our group effort exemplified the principles of Participatory Action Research (PAR) [ 23 , 24 ].
Ethics approval
We obtained ethics approval from the Yale Human Investigation Committee (Protocol # 2000035118), which considered the study exempt under 45CFR46.104 (2) (ii). We informed participants about the goals and methods of the study and provided a copy of the consent form. The form noted that participation was entirely voluntary and optional; it described in detail the study procedures and potential risks, including discomfort during the interview and a small risk of loss of confidentiality, minimized by encryption consistent with institutional policies. We recorded each participant’s consent before starting their interview. In writing our findings, we adhered to best practices in qualitative research, as articulated in the COREQ guidelines [ 25 ].
Through iterative thematic analysis we developed a conceptual model, depicted in Fig. 1 , consisting of three domains: (1) Becoming a qualitativist: embracing a different way of knowing; (2) Being a qualitativist: immersing oneself in a different kind of research; and (3) Nurturing: toward a higher quality future in CAP. We go on to describe each domain in the three subsections and corresponding tables that follow. We organized the tables following a similar rubric: (a) definition of each domain; (b) division into underlying themes and subthemes; and (c) support of constructs through representative quotations.

Concept map: domains and themes toward qualitative research careers in child and adolescent psychiatry
Becoming a qualitativist: embracing a different way of knowing
Priming factors, personal fit.
We identified four commonalities in personal and professional characteristics among most study participants. Specifically, shared traits included ways of approaching scientific inquiry and knowledge creation, as well as struggle and unease with prevailing medical models of research (Table 1 ).
Comfort with uncertainty
Whether stating it explicitly or not, virtually all participants demonstrated an ability or interest to navigate gray zones of uncertainty. They embraced a “less rigid form of creativity,” one in which their mental pliability and freedom to be playful in solving problems were valued skills:
I found that qualitative research both fosters and demands a certain level of intellectual flexibility, like mental gymnastics, which quantitative research is not as conducive to. (French female, FF)
Participants reported feeling more at ease with relative, rather than purportedly absolute truths. They valued scientists who pursued “indeterminate spaces,” seen as role models who favored salient questions over predetermined methods: “those who go to where the science needs to go.” Participants did not decry qualitative methods and their underlying philosophy (positivism), so much as thrive under the opportunities afforded by a complementary approach (qualitative) and philosophy (constructivism).
Our societies are not only modern societies. They are also postmodern societies. And with postmodernity you are allowed to consider that universalism does not exist. Singularity exists. Identities exist. (French male, FM)
Whether established or fledgling, this group of qualitativists welcomed opportunities to change their minds and reevaluate intellectual preconceptions. They sought ways to complement their uncertain understanding of reality by entering the “narrative truths” of their subjects.
Interest in narrative and subjectivity
With qualitative methods being as reliant on words as they are, it is only natural that the approach exerts a strong pull on physicians and scientists who are drawn to the humanities, literature in particular. A plurality of participants described qualitative methods using terms not common in the sciences: “applied literature,” “humanities-adjacent,” “bridging medicine and science with humanities and art.” One participant described the qualitative interview and subsequent analysis as “capturing, curating, and sharing life stories; as if reading, rather than writing, life experiences needing to be shared.” (American male, AM).
Some participants experienced traditional medical research as too confining and prescriptive of what it valued as “real (i.e., objective.)” They felt limited by an approach that was too simplistic, linear, basic, and formulaic for their sensibilities. By contrast, in qualitative methods, they found a venue to explore political and social determinants of health more adequately, to think about philosophical principles and their applications. Participants considered their own views, however biased they may be, as also relevant and informative, partly because as full participants in the research endeavor, they saw the interdependence between the perceiver and the perceived, the revealing exchange between themselves and their subjects, for
as Merleau-Ponty puts it, in “The Flesh of the Real”: I discovered the world from the fact that I myself am in it. (FM).
From early on in their experience, several participants described a natural inclination to “think about thinking” and an appreciation for the relativity of psychological truths. For them, the qualitative approach was more than a methodology; it proved a veritable way of approaching and making sense of the world, of moving between “reality” and overarching philosophical conceptualizations:
What I liked about qualitative research was that it was a way to think about philosophical ideas from an imaginative and interpretive angle–but always based on real-life data. (American female, AF)
For a minority of participants, the road to qualitative methods could be considered escapist: less a pull towards it than a push away from quantitative approaches. For some of them, a dislike of lab work, a sense of overly delayed gratification, or a feeling of abstraction to the point of irrelevance were considerable motivators away from quantitative methods. In one or two instances, the avoidance of “real, i.e., quantitative” research fortuitously led them to qualitative research, which they perceived as “more human, more nuanced, more forgiving, and more welcoming and indeed encouraging of subjective experiences.” (FF).
Experiences with deconstruction and reconstruction
Qualitative methods are inherently deconstructive: by exploring the connections and assumptions between text and meaning, particularly by attending to the inner workings of language. Transcripts—fragments of a life transcribed—are the most common building block for the deconstruction performed by qualitative studies. More precisely, qualitative research is an intellectual endeavor of construction and deconstruction:
It’s like Penelope waiting for Ulysses: weave, reweave, unweave...it doesn’t matter that it’s iterative or that there are changes as you go along. In fact, that’s precisely where the action is. (FM)
Among over half of participants, it was not just texts that were being deconstructed: They thought of their own formative experiences source material for deconstruction. This was particularly the case for those participants who experienced themselves as “outsiders,” whether through immigration, language or culture, social disconnection, or distance from the house of medicine, “as if fighting for the legitimacy of our field.” (AM) These members saw a link between their personal experiences reconciling dualities with their academic draw to qualitative methods, to sense-making work. Qualitative deconstruction and reconstruction proved a way of putting to use their experiences navigating more than one world at once, of unlocking realities taken for granted by others. The joys of qualitative research were at times described as a paradigm shift that allowed for the “unlocking” of new and singular realities:
Quantitative methods by their very nature simplify data; every time you take an analytic step in order to find commonalities, you lose something about the subjects as individuals. In qualitative, by contrast, you highlight their uniqueness, you bring them into sharper relief. (AF)
Struggles with identity as a medical researcher
Throughout professional development, many participants had struggled to reconcile their medical or clinical selves with their research interests. After negative experiences or feeling disconnected from projects, several had gone on to avoid or become uninterested in traditional medical research. When first exposed to qualitative methods, several participants were surprised: of their existence, their relevance, and their role within medicine, where “I didn’t know that I, as an MD, was allowed in; it was something for social scientists, not for me.” (FF).
Research had meant statistics. During this time, no one ever told me there was an alternative approach. I was already reading sociology, philosophy, social science, but more as something that I was interested in than as something you could use in medical research. This is how they would do research in the humanities, good for them, but this was not research for physicians. (FF)
Quantitative methods were described by some as distant, manipulated, or divorced from real meaning; as dry and reductionistic. Perhaps more than anything, participants sensed a tension between patient-proximal vs patient-distal approaches, admiring the ability of qualitative methods to access and reveal people’s lives through the specific details and richness of shared stories. Early experiences often took novice researchers aback, with “the granularity of the qualitative stories being so intense that you cannot but pay attention.” (AM) One participant described relief on learning there was a place for their preferred aspects of research, as “qualitative is like a place where valuable and meaningful things end, things that otherwise would not have gone anywhere else.” Placing similar sentiments into a broader context of medicine within society, another participant described hope in a renewed sense of patient-centered care, one in keeping with qualitative approaches:
As we find that medicine gets more impersonal, cold, and distant, and that the doctor doesn’t know their patient, maybe that's part of the re-invigoration of qualitative approaches: To say that as physicians we care, we really care about story. About your story. (AF)
It is worth noting that over half of participants had conducted and published mixed-methods research, yet only one or two mentioned the approach during their interviews, perhaps reflecting an internalized dichotomy of two methods often seen at odds with each other. And yet, this quote captured a sentiment that would likely be endorsed by most subjects:
I think that there is a role for both. There’s a role for numerical research and I still do some of it and, you know, it's great but it’s different. And I have a very small list of mixed methods papers, and I would like over time to have more of those, because I think that when you bring the two approaches together, the science is particularly rich. (FM)
Discovering qualitative research
Participants’ first acquaintance with qualitative methods was often indirect, unexpected, or serendipitous: an encounter by virtue of relevant non-medical experiences. Several participants found themselves in qualitative territory only once immersed in a field they hadn’t realized they had fully entered. Once into qualitative methodology, several described experiences of rejuvenation, recalibration, or veritable professional reinvention.
Learning through other, non-medical fields
Most study participants reported having very limited exposure to qualitative methods or research during medical school. As such, their entry into the field was only rarely influenced by having been exposed to seminal qualitative papers or influential talks. Instead, common pathways in were through personal experiences in psychotherapy, or by a rekindling of early experiences with disciplines “outside” of medicine: anthropology, sociology, literature, or occasionally through “medicine-humanities” hybrid disciplines like medical education, history of medicine, or global health.
Interest in psychotherapy and psychoanalysis, both in theory as in personal experience, led some participants to question whether there was a potentially important crosstalk between the disciplines:
I started talking to my supervisor about philosophy of science, anthropology, and the problems I saw with psychoanalysis. I wondered if there was something good in psychoanalysis that we could salvage? That’s what we were talking about, and that’s what first led to my interest in qualitative. (FM)
Classic papers in the psychoanalytic literature, with their thick descriptions, held an immediate appeal, activating an entreaty to reinvigorate contemporary approaches to medical research and writing that appeared currently dry and untextured:
We've jettisoned our whole case report culture in medicine, and maybe our qualitative research now supplants or overlaps that empty space to an extent. (AM)
A common sentiment among many was that the biopsychosocial model of medicine had given short shrift to the social component, “the last of the three, and not by coincidence.” That unintentional omission compounded the mothballing of social science skills that participants feared during their socialization as physicians. As a result, social content and skills became relegated to atrophy and disuse. By contrast, what often first opened the doors to qualitative methods was approaching social- and language-based questions in medicine, particularly in the context of knowledgeable and supportive mentors:
He told me “You are really asking yourself sociological questions; this is really good, because you think like sociologists do.” I was not shamed nor made to feel a dilettante; I was encouraged to keep trying, and I did. (FF)
Stumbling in, not knowing what it was
For some, a serendipitous path into qualitative methods occurred through a chance encounter with a mentor or research team, or through peers who identified interests and skills well suited to the methodological approach. A few others, focused and self-driven, found the path intentionally. For yet others, qualitative was more of an incidental find than an active search. “Someone names it for you. Meeting an informant or guide (a friend, a colleague), who unexpectedly tells you about qualitative research—and that you may already be in the midst of it. Unsuspecting you”:
It's almost like in Molière’s Le Bourgeois Gentilhomme , in which Monsieur Jourdain speaks in prose without knowing it’s prose. This is a little bit of what I experienced: “You’re already doing it, but don’t know that you’re doing it.” (FM)
Drawn in, reinvigorated
No matter how one first enters the qualitative field, novices soon find a qualitativist peer—someone with similar ways of thinking about clinical phenomena and research. It is a discovery of a team, as much as of a method; of a social as much as of a scientific direction. People get enmeshed through the encouragement and referrals of others, and qualitative methods are social in a unique way: the research cannot be done in isolation, as.
Two people cannot triangulate, certainly not one person: you need three. That summarizes for me the inherent team-based nature of qualitative work. Being invited into a team got me started. I have not looked back since. (AF)
About half of the senior participants described arriving late in their professional careers to qualitative methods. For all of them, the new approach, the new colleagues, the new of seeing their work, was described in terms such as “reinvigoration,” “recalibration,” “renovation,” “reinvention,” or “getting me out of a career hole.” A few without prior qualitative background described the turning point as “nothing short of a mid-career renaissance.” Two participants used the word “love” in describing the experience:
I don’t regret anything. It would have been very nice to discover this back in medical school, but I eventually discovered it and it’s fine. I’ve had a very interesting, fun career, and in some ways I’m glad that I'm finding it late on because now I have like this brand new love affair with medicine. (AM)
Transitioning in
A common sentiment on entering the field was around stigma, the notion that qualitative research was somehow “less than,” that it could perhaps even hurt career prospects. This internalized bias could manifest as fear of irrelevance, of engaging in lower-quality research perhaps not worth doing, of being relegated to lower-impact journals. Some described worries about their efforts being irrelevant or self-indulgent. For those who found a home in qualitative work, its meaningfulness outweighed those considerations, even if deemed “risky” to their training or career prospects:
It's awful to say this, but there’s a certain utilitarianism, certain things that you need to do to progress in the academic ladder. Traditional approaches were okay only for a while, before I saw that those questions were not important enough to keep me going. (FM)
On finding a group of peers invested in qualitative methods, the challenge moved away from devaluation into misrepresentation: how to make others understand the role and the value of as different a way of approaching medical research. How to defend the approach confidently to others, to uphold its legitimacy, and to explain its basic tenets. One participant put it in gendered terms:
“There seems to be a gendered aspect to the type of research: qualitative research (soft/feminine) not considered as legitimate as quantitative (hard/male). It is a jaundiced view, of course, but may explain a skew to women participating in qualitative, as if there was some kind of feminization of empathy.” (AM)
A gradual settling in followed for most, through the external validation from mentors, peers, and role models, and after presenting and publishing their work. These externalities led to internal acceptance, to letting go of what had been expected as necessary to conduct “real” research (one participant stated how they had been socialized to believe how “if you don’t suffer, it’s not real research”). (FF) The more comfortable in their new qualitative selves, the more insecurities were dropped, and the focus shifted to meaning rather than external standards.
The tension between qualitative and quantitative approaches was certainly not a Manichean one. Several participants spoke of the power of mixing the two approaches; of how questions could be enhanced by combining the approaches into mixed methods designs. For some, the advantages proved not only scientific, but fiscal as well: Funding agencies looked favorably upon (when not outright expecting) a qualitative component to otherwise traditional grants. But in the final analysis, personal meaning was of utmost importance:
I'm just trying to do something that’s important and meaningful to me. I'm not going to commit to a research career that is merely strategic: “If I do x, then I'll get funding y; rinse and repeat...” I would be betraying myself. For the past ten years, I’ve become consistent with my inner compass. Qualitative research has been central to that. (AF)
Being a qualititavist: immersing oneself into a different kind of research
Quality: doing qualitative research well.
Once into the fold of qualitative methodologies and research, participants reflected on two broad areas of importance: 1) Selecting particular methodologies most suitable to their background, personality, and specific research questions; and 2) Finding and fostering a community of peers committed to qualitative work (Table 2 ).
Selecting the right methodology
In settling on the right types of methodologies for their work, participants described three general stages they had experienced or seen in others.
The first was common at the outset: learning by doing rather than through explicit teaching; practice over theory, as through an emphasis on coding. “Learning by doing” is what pulled in many novices at the outset, the ability to start coding and analyzing from the get-go, without lengthy prerequisites necessary. In this early phase of exhilarated discovery, software and small samples could make the work appear deceptively simple. The use of software could result in a pause in critical thinking, a sense that “coding is like coloring by numbers,” of simply sorting and filing away. However initially attractive, this phase represented a shortcut that participants had to unlearn with experience as their coding became more nuanced. Small samples were also appealing, both in the efficiency of data collection and in their make-up: children, families, patients, human lives in their full richness. Although these subjects were often the very reason that made qualitative methods of interest in the first place, the richness of qualitative samples could lead to getting lost in details and hyper-specificities, especially when considering the large amount of data created during qualitative analysis.
A qualitative study could theoretically require one person’s story, because one person is an entire universe within themselves. One person being enough: so much richness in the singular. (AM)
A second stage indicated growing knowledge about and ease with specific methods. For some, it required “unlearning traditional quantitative approaches,” although most participants recognized that their original skills, including around scientific rigor, collaboration, and experience with scholarly writing, transferred and generalized. Turning from quantitative to qualitative (and particularly mixed) methods was described more as supplementing and enriching research skills than as supplanting an original skillset with a newer one. Learning to do qualitative research well and gaining comfort with its specific methods reinforced interest and eased joining a new community and way of thinking. The transition had its challenges, as when navigating the degree of structure vs freedom in research, and of dealing with “hard” vs “soft” findings.
It's nice that there aren’t specific statistical tests that you have to apply based on a given dataset. No correct answers. Instead, there are many correct ways. It’s nice to have that freedom. Freeing, but also terrifying. (AF)
In selecting the methodologies of their choice, some participants identified a cautionary tale in the “overdoing” they had seen in other colleagues, even in themselves. In such instances, methodological fetishization could prevail over pragmatism and derail original goals. An over-emphasis on the right methodology could result in a tree-for-forest problem, a focus away from a project’s central question.
If I could use my magic wand, I would make a qualitative world where there are fewer “methodological churches,” but rather different ways to work, a respect for how we work with the same finality of helping kids. And in that world, every clinician would be a little bit of a researcher, and every researcher would be a little bit of a clinician, or at least know what the other one does, and take interest. We must fix this if we want to consolidate the field. (FM)
Reflexivity and triangulation
Reflexivity can be conceptualized as the awareness and incorporation of the role of oneself in a research project. It is a central feature of qualitative research, and one that distinguishes it from the “selfless” and “ego-neutral” tenets of its quantitative counterpart. Through reflexivity, personal thoughts, feelings, past history, even prejudices become a filter through which to see and conceptualize research findings; in quantitative methods, these same elements would be dismissed as bias. As a result, qualitativists engage in interpretative, reflective work as a matter of course. The ensuing challenges include being able to balance the “dose of oneself,” of being deeply reflective and attuned to one’s role in the project, while remaining able to go against personal prejudices and beliefs, of remaining humble by “being able to think against yourself.” Psychiatrists and mental health professionals may be particularly attuned to this approach: On the one hand, with few procedures or objective laboratory findings to rely on, we often practice with little more than ourselves as the tool of diagnosis and healing; on the other, our work is largely one of reflection, of thinking about others, about understanding another’s subjectivity through our own, of doing so while not centering the experience on ourselves.
The qualitative approach makes it possible to think about both the object perceived and the object that perceives it and tries to explain the structures of perception and how they can influence the result of this perception. In other words, an approach that aims to make subjectivity explicit, to make explicit the consciousness that perceives and assumes it, and to put it to work. (FF)
A cautionary note regarding over-thinking in qualitative work is warranted: Participants warned that the potential to over-interpret and pathologize can be a barrier. Psychoanalytic thinking in particular can be as helpful as it can lead astray. Reading too much theory or searching for the perfect theoretical framework can prevent the researcher from listening to the participants’ experience. Psychologizing can be a challenge for early qualitativists, “a shortcut blunting their own formulations and creativity.”
I used to “psychologize” much more. And progressively, I found a way not to fall into this psychologization or sociologization trap and remain at an experiential level and at a phenomenological descriptive level. But I think it wasn’t easy, and it’s very tempting at the beginning to also put your clinical intuition, and defense mechanisms and all of this, and it's only with time that you can clean that and really respect the qualitative methodology as it should be. (FM)
For many participants, triangulation offers the remedy for potential solipsistic thinking. Triangulation is a principal tenet of qualitative rigor, requiring confirmation between at least three sources (e.g., coders, texts, timepoints) before accepting a proposed finding. By comparing codes in an iterative fashion, and by casting light on the interview, coding, analysis, and writing stages, investigators can retain the transparency of their findings. They can also hold personal views and biases in check. Similar to clinical work, the subjective “truth” is approached only by crossing diverse subjective experiences. Qualitative work cannot be done in a social vacuum: Qualitative work is necessarily teamwork.
We already have a dimension of mutual surveillance. I don’t mean that in a bad way, but in a good way, i.e., we watch each other’s work. And that’s why I think this research is so enriching. (AF)
Community: mentors, mentees, and teams
Mentorship, supervision, and guidance were among the most fulfilling aspects of entering qualitative research—and among the most frustrating. In terms of frustration, some experienced abandonment early on, as when mentors encouraged participants to write a manuscript but then failed to follow through in email exchanges, or when participants were blindly congratulated for great teamwork despite feeling lost in a project. Some mentors had felt let down or used by students who upon graduation vanished and abandoned a paper without publishing it. In the list of discontents, there was a common theme agreed on by all: the shortage of highly skilled and knowledgeable mentors with a proven track record. Development could be stunted by the lack of senior experts available. Navigating qualitative methods without mentors could be unfulfilling, unsatisfying, even lead to premature departure from the field. For mid-career qualitativists, a lack of senior mentors had forced some to “grow up” ahead of schedule, placing them in a vulnerable position as they tried to keep developing while also breaking down barriers, leading, and carrying others on their proverbial backs. They may not have been strong enough at that stage of their careers to carry themselves and others at once.
The problem with qualitative research is that you're not always properly supervised. I think it’s sufficiently new in psychiatric research that people with little experience are put in as trainers. When I was a young researcher, I was asked to be the advisor of a resident doing qualitative research, even though I wasn’t really ready. (FF)
Notwithstanding the small number of qualitative mentors available, particularly in CAP, virtually all participants had found at least once such mentor during their professional development. Meetings had been either fortuitous (as when preassigned to someone) or by active choice, often after meeting with several candidates. Those choices were based on relational fit (or in the evocative French term, by “la resonance,” or “echo”). The “echolocation” could work as well for individuals as for groups. Indeed, group-wide mentorship, typically comprising members of different backgrounds and levels of seniority, was highly valued and sought after. People are drawn to another’s work and actively create community with them; they enjoy and benefit from diversity among reviewers and their perspectives:
We've got people doing phenomenology, grounded theory, sociology…The idea is precisely to show that everyone can work together and get around the table to move a question forward, whatever the method of the paper. Which is different, I think, from the old ways of doing research, when it was really about either being with us or against us. (FF)
Nurturing: toward a higher quality future in child and adolescent psychiatry (CAP)
Current state of qualitative methods in cap.
Participants envisioned a larger role for qualitative methods in the future of CAP, and for the contribution they could make in getting the fields to more frequently and more seamlessly come together (Table 3 ).
Advantages and opportunities
By virtue of being so inherently part of the research—through their reflexivity, subjectivity, interpretation, or contextualization—many participants conveyed a sense of ease within the qualitative realm. From an epistemological perspective, they considered the possible research questions and the specific qualitative methods as getting closer to the truth; and if not to the elusive truth, at least to meaningful moments of discovery that said something new or described new phenomena.
You get to bring yourself as the investigator, you get to bring your true self. You don’t have to hide behind anything. You bring whatever, you know, blips, limitations, liabilities, blind spots, and whatever. It’s all good. (AM) It helped me find an “ecological niche,” a term that I've taken from this work. A niche where I feel I want to be, where I feel like I fit and belong. And my existing skills, interests, and strengths naturally fit with it as well. (AF)
For some, qualitative methods permitted a view at the cracks in traditional, accepted forms of research. But rather than offering just a perch to see those limitations, it allowed entry through different ways: a range of variety, novelty, and puzzles not typically a part of medicine, and a framework through which to synthesize a range of different inputs and interests. The work led to more “existential relevance,” more resonance with personal values, to a wider lens into the world. Indeed, work with marginalized and historically excluded voices seemed especially well suited for qualitative methods, giving “the appropriate tools for this work of community epistemological justice,” all the more during this “DEI moment.”
Qualitative methods held an appeal for investigators with a more social and interpersonal approach, when interviewing different actors such as children, parents, teachers, and social workers in the case of CAP. The approach also proved a good fit for international work and collaborations, insofar as much of the work (whether international or not) had migrated to videoconferencing platforms. The low costs and high quality to interview and transcribe leveled the research playing field, making qualitative studies affordable at a distance and in resource-constrained settings. Aside from its social dimension, qualitative methods proved consistent with clinical interview skills and the refinement of reflective and empathic skills:
I sometimes try to do my clinical interviews as if they were qualitative interviews. I have learned so many things that are different from the usual stuff, from the diagnostic criteria and what not. And so, qualitative methods sanitized me to the fact that we’re far from done and have so many more things to know. (AF)
Participants also valued qualitative skills in answering the entreaty to be more spontaneous in our clinical actions:
Something that sticks out to me about child and adolescent psychiatry and about qualitative research is just how playful both of them are.
Disadvantages and limitations
Several participants described having been made to feel like second-class researchers, yet unsure how much their counterparts understood qualitative methods and their role within medicine. This sentiment was especially biting for psychiatrists, who had invariably been made to feel like “stepchildren” of medicine with a yearning to be welcome as full-fledged, legitimate doctors. One participant described the “dual stigma” compounding their identities as a CAP and as a qualitativist. Both stigmas, it needs to be said, are internalized forms of bias, the internalization of other individuals’ and communities’ negative perceptions.
A very different and very concrete disadvantage had to with funding. The ability to fund a long-term career in qualitative methods was challenging. Even if the costs are generally low, funding one’s time can be challenging, particularly through traditional federal sources. Participants shared experiences with funding through private foundations, but were generally frustrated in their attempts at larger grants. Some felt the need to include a qualitative component in proposals “as a hook to get reviewers’ attention, or to reassure them that we know how to conduct research.” Alternatively, others described a sense of “tokenization” when asked to include a (small) qualitative component as part of a larger grant.
Advocating for qualitative methods in CAP
Several of the characteristics of qualitative research make it particularly well fitting for early career researchers, regardless of specialty: Small samples and low budgets are usually sufficient, and projects can be completed in a relatively short period of time. In the case of child psychiatry, additional advantages include the interest in subjectivity and on family and social dynamics. In all instances, qualitative work resonates with clinical work in a patient-centered way that is less abstract than quantitativist research. In brief, it deepens the clinical work, and at its best can be a form of citizen science that involves patients and families in the design and interpretation of the studies, for
All qualitative research in some ways is participatory action research. Both of us are being researched as we speak. You are part of the exchange. We will honor your words as we present them, before we send the paper for publication, we will want to send it to you to make sure that we got things right, or not. That's part of the beauty of qualitative work. (AM)
Given its many advantages and the richness of its findings, a common sentiment was still having to justify qualitative methods to others as “real” science, of addressing its existence in medicine (rather than in the humanities). As member of a methodological minority, one participant stated how.
This is what they call a “minority burden.” Always explaining, justifying, “why, how?” Having to tell your story many more times than others do. (AF)
On select occasions, some were able to pivot from justifying to teaching: from having their peers ostracize the method to becoming intrigued by it. Some participants went on to implement introductory or advanced courses in qualitative methods, exposing peers to the new epistemology earlier in their professional trajectory. Regardless of its initial specialty focus, the growth of qualitative methods in a medical center or university stands to benefit all disciplines: through incorporation into curricula, research opportunities, availability of mentors, or exposure to different methodologies. In the final analysis, it may well be that.
The job of the quantitative paper is to restore meaning...but meaning runs through all qualitative research because it's based on real encounters and on clinical questions that matter. (AM)
Based on the qualitative analysis of individual interviews of CAP clinician-investigators at different stages of professional development and hailing from two different countries, we have identified pathways facilitating or impeding their interest in qualitative research. We organized our overall framework along a temporal sequence, from priming and discovery to transitioning into the field ( Becoming ); through doing, connecting, and belonging ( Being ); and into innovating, refining, mentoring others, and advocating for the discipline ( Nurturing ). We arrange the section that follows along the same three temporal domains, and complemented by the perspectives of the individual investigator (internal factors), the qualitative discipline and the scientific environment (external), and the future development of qualitative research in CAP. Along the way, we emphasize those modifiable factors that may strengthen a quality pipeline: one with more dedicated researchers and greater quality of research.
Becoming a qualitativist: the investigator
We view the transformation of a prospective scientist into a qualitative researcher as subsumed under three categories: grounding, de/centering, and practicalities.
By grounding we refer to the personalizing of the investigator’s research focus in such a way that does not jettison prior strengths and interests. To the contrary, investigators, either fledgling or seasoned, can incorporate those priors in a meaningful way. Specifically, previous interest or knowledge in the humanities and social sciences (HSS) provides a template for comfort with uncertainty, concrete tools for textual analysis and deconstruction, and an example for learning from other fields of inquiry.
An emerging literature in medical education, as well as changing practices in medical school admissions committees, suggest the benefits of HSS to medical practice beyond qualitative research. Medical students with HSS premedical education perform on par with peers on more traditional tracks [ 26 ]. The Humanities and Medicine Program (HuMed) at the Mount Sinai School of Medicine replicated the finding and found an additional trend toward residency careers in psychiatry and primary care [ 27 ]. As an added benefit, humanistic factors taken into account for admission into medical school have been found to promote the selection of physicians with stronger communication skills [ 28 ]. Supporting–and indeed encouraging—the application of students from “nontraditional” (i.e. HSS) backgrounds stands to strengthen the medical workforce [ 29 ]. A shift in the hidden curriculum (i.e., from scientific exclusivity) toward one of “epistemological inclusion” [ 29 ] (i.e. to welcoming HSS) stands to benefit child psychiatry in general, and its qualitative research portfolio in particular.
By de/centering we refer to the balance that every qualitative researcher must have between their outer and inner views. At its best, qualitative research relies on “polyocular sampling,” [ 30 ] in which multiple viewpoints are incorporated. The outward-facing view—decentering—is particularly relevant in CAP research, where the voices of children need to be incorporated together with those of their caretakers and relevant others. The compelling nature of young lives can be a major research draw, and one that needs to be carefully and ethically balanced by the precondition to conduct research “ with, rather than on children.” [ 31 ]. But the inward-facing view—centering—needs to be just as strong. Less experienced investigators may consider this posture self-serving or narcissistic, before coming to realize the centrality of their personal narrative, identity struggles, and overall reflexivity in conducting qualitative work. The degree of inward-facing view can range from minimal hovering (e.g., baseline awareness of relevant conflict), all the way to complete centering on one’s personal experience, as in the case of autoethnography [ 32 ].
In contrast to traditional quantitative studies such as randomized control trials, or in brain imaging, epidemiology, or genetics, the practicalities of conducting qualitative research are generally facilitators rather than impediments, particularly to new investigators: First, data collection can be completed in a relatively short time (weeks or months, not years); second, given the non-interventional nature of most qualitative studies, institutional review approval usually falls under expedited or exempt categories (whether involving minors or not, respectively); third, synchronized videoconferencing makes interviews and data collection simple, even at geographic remove; fourth, costs are low, additionally so since the advent of AI-supported transcription with platforms such as in Deepgram; finally, analytic methods such as thematic analysis (TA) are accessible and require a modest learning curve–as opposed to grounded theory and other more demanding approaches.
Being a qualitativist: the discipline and the scientific environment
Medicine and psychiatry at times do not welcome—and often do not understand—qualitative methods or the role they can play in advancing their respective fields. This seeming misalignment in views and scientific priorities can make for a disorienting entry into the qualitative field. Likewise, the lack of common and visible templates and role models, as well of the high flexibility and uncertainty that are inherent to the field [ 33 ], all need to be reconciled and overcome. Finding academic lodging within groups and institutions that espouse scientific openness is one way to do so: epistemological flexibility —the ability to use the right methodology for a given task, as opposed to embracing preconceived scientific notions—is not only to be sought and embraced, but indeed developed and fostered by maturing investigators and educators.
The principles of narrative medicine (NM) [ 34 ] can provide a useful bridge, particularly at a time of high patient unease and physician discontent: “Clinical practice fortified by narrative competence —the capacity to recognize, absorb, metabolize, interpret, and be moved by stories of illness” [ 35 ]—can help close the gaps between patients and providers. In the case of psychiatry, it can help close its gap with medicine; to bring mind and body closer in line. Qualitative methods can further and complement the goals of NM through scholarly work and research. Like NM, qualitative methods—beginning with their interviews and focus groups—harness the fact that we are storytelling beings eager to tell our own stories and listen to the ones of those we are interested in learning from—and with. The revitalizing force of storytelling in psychiatry is far from new and has continued to change organically with the technologies of the times, as exemplified by the Multimedia Digital Storytelling in Psychiatry project [ 36 ].
Albert Einstein is credited with saying that “not everything that can be counted counts, and not everything that counts can be counted.” The possibly apocryphal line is relevant in the context of qualitative research in medicine and psychiatry, areas in which citation numbers and impact factors are consistently low for qualitative when compared to quantitative science. Despite optimistic prognostications [ 37 ] of greater acceptance and assimilation of qualitative methods into the “medical model,” the divisive current state of publication affairs is unlikely to change anytime soon, as journals compete for higher ratings, and a wider array of alternative outlets become available. Stated differently: a coming together under the banner of epistemological flexibility remains aspirational. Submissions will continue to go to separate and more specialized journals, with only a few periodicals able to straddle the field (or interested in doing so). Once again, the narrative perspective (like Einstein's words) may provide an important salve: “Before psychiatry rushes in to ‘save’ its bioscientific self, however, it seems this moment offers an opportunity for self-reflection and deeper understanding of the process of psychiatric meaning-making…The implication of narrative for psychiatry is that there are many ways to tell the story of mental health problems—not just one right way and many other wrong ways [ 38 ].”
Among the challenges identified toward the integration of qualitative methods into the medical scientific mainstream is the fact that journals and funders commonly use evaluation criteria that are incongruent with qualitative methods and constructivist epistemology. Ungar [ 30 ] offered four different proposals to address this chasm through, and which can be construed either as creative solutions or as self-defeating concessions: (i) Dressing up, in which a qualitativist is incorporated into a larger project (and funded by it), but where their contribution is seen as supplemental to the “real work” under way, invariably culminating with the quantitative analysis of a large-sample dataset; (ii) Sleeping with the elephant, which involves a practical path to funding by creating mixed-method designs that leave all parties satisfied. The challenge in mixed-method designs is to reach a detente between researchers from different paradigms; (iii) Seek but never find: accepting one’s role as a qualitativist, but only en route to a “real” yet at times elusive (quantitative) study; and (iv) Table scraps. Be satisfied with small funding requests, especially if aligned with service delivery rather than research. As noted above, table scraps may be sufficient to support a qualitative research project. Universities and foundations are commonly able to fund seed grants of smaller dollar amount; however, the longer-term challenge is that they will rarely provide salary support (Table 4 ).
Nurturing quality: the future
In our view, the longer-term success of qualitativists in CAP—their movement from pathways into identity—hinges on two main factors: Capacity building, the invigoration of a quality pipeline through education and early exposure; and Joining, the strengthening and commitment through an enduring community.
With respect to education, one of our study participants wondered why it is that the word “epistemology” is never used in the context of learning about quantitative methods: “Isn’t an objectivist epistemology just as important as a constructivist one?” The observation was telling: Qualitative methods (and their underlying epistemology) are usually defined not by themselves, but rather in contrast to quantitative methods and their underlying epistemology. These observations, which usually animate first introductory lessons, invite the question over the optimal way, timing, and curricular placement of how and when best to introduce qualitative methodology into medical and psychiatric education. As noted, qualitative methodologies are often at odds with the objectivist epistemology deeply embedded in medical school settings. The success of a qualitativist in medicine will depend on being knowledgeable about their methods, but also of being “better prepared to successfully negotiate the politics of science, the politics of evidence, and the politics of funding within their home institutions [ 39 ].”
One way of addressing the politics of “methodological conservativism” [ 40 ] is through the deliberate and organized teaching of alternative approaches to “traditional” science, such as qualitative methods within a medical context. In addition to foundational concepts such as sampling, questionnaire development, or data collection and analysis, some qualitative concepts may be hard to grasp for someone socialized under traditional medical mores. As such, additional emphasis on topics such as reflexivity (as opposed to bias), or transferability (as opposed to external validity), will be important pedagogic investments to any successful course addressing qualitative methods within medicine [ 41 ]. There is by now a broadening literature and expertise on incorporating qualitative methods into medical education [ 42 ], and specifically into mental health, where they remain underutilized [ 37 ]. Adaptations to medical science include important lessons from nursing science as well. For example, interpretive description (ID) is a qualitative approach first developed by nursing that has deliberately practical, applied, here-and-now goals [ 43 ]. Aimed at circulating research findings quickly back “to the bedside,” ID incorporates quality improvement and practical aspects at a timescale and applicability relevant to medicine and nursing in ways very different from those of sociology or anthropology, examples of two foundational sciences behind qualitative methodology.
A community of practice (CoP) is a group of like-minded individuals who share a specific interest or area of expertise. First described outside of the realm of medicine [ 44 ], the CoP construct has proven fruitful in it [ 45 , 46 ]. Medical CoPs have been organized around particular specialties, emerging areas of interest, or the refining of evolving technical skills. CoPs have the added function of bringing together different cohorts, which in turn helps with the intergenerational transmission, refinement, and preservation of skills and knowledge. CoPs provide an entry point for novice learners—being more welcoming, personalized, and less diffuse and overwhelming than large society meetings tend to be.
CoPs can be a prime way to launch into a first study accompanied, feeling support and guidance at such a critical career juncture. Education is necessary but not sufficient in pursuit of qualitative competence; Theory and learning need to come alive in practice. Members of a CoP may propose ideas, or invite a new member to participate in an ongoing project. In that spirit, we formed a qualitative CoP in 2022. Through the binational partnership between the Yale Child Study Center in the US, and the Centre de Recherche en Épidémiologie et Santé des Populations in France, we developed in 2022 Qua Lab , the Qualitative and Mixed Methods Lab. Our group has since grown to include members from Canada, Brazil, and the Dominican Republic. As a group, we meet twice monthly to review protocols and manuscripts under preparation. We welcome, and indeed encourage the participation of medical students along senior faculty, and are committed to the growth and generational transmission of qualitative methods. One way of fomenting such growth is through peer-near support, in which junior participants guide more recent or inexperienced members. Critically, as young mentors, they are in turn provided with senior support to assuages worries and prevent them from feeling “farmed out,” or of carrying others on their (junior) backs. In this way, our effort has resulted in a virtual cycle of qualitative development [ 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 ]. We hope others will join us and create their own CoPs to support quality growth in CAP.
Limitations
We acknowledge several limitations. First, we did not interview CAP researchers with a predominant or exclusive quantitative focus. Such extreme sampling could have been informative and “kept us honest” regarding our conclusions about their research and their world views. We would also have learned about their perceptions, as “outsiders,” of qualitative work. Second, we recognize than in a polarized view of epistemologies, we failed to incorporate mixed methods research in a meaningful way. Several of the authors have conducted and published mixed methods research; some of them mentioned it during their interviews. However, the approach was difficult to isolate for analysis in this study; it may become a fruitful subject for future research. Third, through an exclusive focus on CAP clinician-investigators, we missed insights that others could provide, starting with psychiatrists, pediatricians, and physicians more broadly, as well as social workers, nurses, psychologists, and other allied professionals.
A final and noteworthy omission is worth pointing out: During their interviews, not a single one of the study participants mentioned large language models (LLMs, such as ChatGPT) and the disruption they are sure to bring into qualitative methodologies [ 56 , 57 ]. The omission could be related to a lack of knowledge (e.g., about LLMs), to a failure of imagination (e.g., of their possible applications), or perhaps even to an existential threat (e.g., “will we become the tools of our tools?”). It is clear that we are at the dawn of a methodological revolution: in an exponential way, LLMs will save time, reduce costs, and increase the throughput of coded materials. But gathering rich data through interviews, and planning and interpreting results will still require emotionally competent human researchers. LLM-assisted qualitative research may become faster and stronger, but the accuracy, novelty, and relevance of its results will still depend on humans: We shall not become obsolete.
Availability of data and materials
Supporting data will be provided by the corresponding author upon reasonable request.
Falissard B, Benoit L, Martin A. Qualitative methods in child and adolescent psychiatry: the time has come. Eur Child Adolesc Psychiatry. 2022;0123456789:1–4. https://doi.org/10.1007/s00787-022-01978-9 .
Article Google Scholar
Falissard B, Révah A, Yang S, Fagot-Largeault A. The place of words and numbers in psychiatric research. Philos Ethics Humanit Med. 2013;8(1):1–9.
Greenhalgh T, Annandale E, Ashcroft R, et al. An open letter to the BMJ editors on qualitative research. BMJ. 2016;352(2):1–4. https://doi.org/10.1136/bmj.i563 .
Shuval K, Harker K, Roudsari B, et al. Is qualitative research second class science? A quantitative longitudinal examination of qualitative research in medical journals. PLoS ONE. 2011;6(2):1–6. https://doi.org/10.1371/journal.pone.0016937 .
Article CAS Google Scholar
Daniels K, Loewenson R, George A, et al. Fair publication of qualitative research in health systems: a call by health policy and systems researchers. Int J Equity Health. 2016;15(1):1–9. https://doi.org/10.1186/s12939-016-0368-y .
Truog RD. Patients and doctors-evolution of a relationship. N Engl J Med. 2012;366(7):581–5. https://doi.org/10.1056/NEJMp1110848 .
Article CAS PubMed Google Scholar
Steinmetz G, editor. The politics of method in human sciences: positivism and its epistemological others. Durham: Duke University Press; 2005.
Google Scholar
Malterud K. The art and science of clinical knowledge: evidence beyond measures and numbers. Lancet. 2001;358(9279):397–400. https://doi.org/10.1016/S0140-6736(01)05548-9 .
Young-Bruehl E. Childism: confronting prejudice against children. New Haven: Yale University Press; 2012.
Eisenberg L. Mindlessness and brainlessness in psychiatry. Br J Psychiatry. 1986;148(5):497–508.
Kvale S. The psychoanalytic interview as qualitative research. Qual Inq. 1999;5(1):87–113. https://doi.org/10.1177/107780049900500105 .
Barriball L, While A. Collecting data using a semi-structured interview: a discussion paper. J Adv Nurs. 1994;19(2):328–35. https://doi.org/10.1111/j.1365-2648.1994.tb01088.x .
DiCicco-Bloom B, Crabtree BF. The qualitative research interview. Med Educ. 2006;40(4):314–21. https://doi.org/10.1111/j.1365-2929.2006.02418.x .
Article PubMed Google Scholar
Emmel N. Theoretical or purposive sampling. In: Sampling and choosing cases in qualitative research: a realist approach. London: SAGE Publications Ltd; 2013.
Chapter Google Scholar
Kiger ME, Varpio L. Thematic analysis of qualitative data: AMEE Guide. Med Teach. 2020. https://doi.org/10.1080/0142159X.2020.1755030 .
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Smith J, Flowers P, Larkin M. Interpretative phenomenological analysis: theory, research, practice. London: SAGE; 2009.
Harper D, Thompson AR. Interpretative phenomenological analysis. In: Qualitative research methods in mental health and psychotherapy: a guide for students and practitioners. Wiley; 2011. p. 101–16. https://doi.org/10.1002/9781119973249 .
Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907. https://doi.org/10.1007/s11135-017-0574-8 .
Finlay L. Negotiating the swamp: the opportunity and challenge of reflexivity in research practice. Qual Res. 2002;2(2):209–30. https://doi.org/10.1177/146879410200200205 .
Shaw VN. Research with participants in problem experience: challenges and strategies. Qual Health Res. 2005;15(6):841–54. https://doi.org/10.1177/1049732305275639 .
Karazivan P, Dumez V, Flora L, et al. The patient-as-partner approach in health care: a conceptual framework for a necessary transition. Acad Med. 2015;90(4):437–41. https://doi.org/10.1097/ACM.0000000000000603 .
Bergold J, Thomas S. Participatory research methods: a methodological approach in motion. Hist Soc Res. 2012;37(4):191–222. https://doi.org/10.17169/fqs-13.1.1801 .
Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health. 2006;60(10):854–7. https://doi.org/10.1136/jech.2004.028662 .
Article PubMed PubMed Central Google Scholar
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Heal Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042 .
Hall JN, Woods N, Hanson MD. Is social sciences and humanities (SSH) premedical education marginalized in the medical school admission process? A review and contextualization of the literature. Acad Med. 2014;89(7):1075–86. https://doi.org/10.1097/ACM.0000000000000284 .
Muller D, Kase N. Challenging traditional premedical requirements as predictors of success in medical school: the Mount Sinai School of Medicine humanities and medicine program. Acad Med. 2010;85(8):1378–83. https://doi.org/10.1097/ACM.0b013e3181dbf22a .
Hirshfield LE, Yudkowsky R, Park YS. Pre-medical majors in the humanities and social sciences: impact on communication skills and specialty choice. Med Educ. 2019;53(4):408–16. https://doi.org/10.1111/medu.13774 .
Lam JTH, Hanson MD, Martimianakis MAT. Exploring the socialization experiences of medical students from social science and humanities backgrounds. Acad Med. 2020;95(3):401–10.
Ungar M. ‘Too ambitious’: what happens when funders misunderstand the strengths of qualitative research design. Qual Soc Work. 2006;5(2):261–77. https://doi.org/10.1177/1473325006064262 .
Grover S. Why won’t they listen to us? On giving power and voice to children participating in social research. Childhood. 2004;11(1):81–93.
Haeffner M, Hames F, Barbour MM, Reeves JM, Platell G, Grover S. Expanding collaborative autoethnography into the world of natural science for transdisciplinary teams. One Earth. 2022;5(2):157–67. https://doi.org/10.1016/j.oneear.2022.01.002 .
Bassett R. Time to catch up... Qualitative research in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2010;19(1):2.
PubMed PubMed Central Google Scholar
Charon R, Dasgupta S, Hermann N, et al. The principles and practice of narrative medicine. Oxford: Oxford University Press; 2016.
Book Google Scholar
Charon R. What to do with stories: the sciences of narrative medicine. Can Fam Physician. 2007;53(7):1265–7. https://doi.org/10.1055/s-0039-1696844 .
Zaretsky A, Rodney H, Morassaei S, et al. The Out of Darkness Project: innovative multimedia digital storytelling in psychiatry. Acad Psychiatry. 2022;46(5):644–9. https://doi.org/10.1007/s40596-022-01637-w .
Joseph S, Beer C, Clarke D, et al. Qualitative research into mental health: reflections on epistemology. Ment Heal Rev J. 2009;14(1):36–42. https://doi.org/10.1108/13619322200900006 .
Lewis B. The art of medicine: taking a narrative turn in psychiatry. Lancet. 2014;383(9911):22–3. https://doi.org/10.1016/S0140-6736(13)62722-1 .
Staller KM. Epistemological boot camp: the politics of science and what every qualitative researcher needs to know to survive in the academy. Qual Soc Work. 2013;12(4):395–413. https://doi.org/10.1177/1473325012450483 .
Lincoln YS, Cannella GS. Dangerous discourses: methodological conservatism and governmental regimes of truth. Qual Inq. 2004;10(1):5–14. https://doi.org/10.1177/1077800403259717 .
Hanson JL, Balmer DF, Giardino AP. Qualitative research methods for medical educators. Acad Pediatr. 2011;11(5):375–86. https://doi.org/10.1016/j.acap.2011.05.001 .
Ng SL, Baker L, Cristancho S, Kennedy TJ, Lingard L. Qualitative research in medical education: methodologies and methods. In: Understanding medical education: evidence, theory, and practice. John Wiley & Sons Ltd; 2018. p. 427–41. https://doi.org/10.1002/9781119373780.ch29 .
Thompson Burdine J, Thorne S, Sandhu G. Interpretive description: a flexible qualitative methodology for medical education research. Med Educ. 2021;55(3):336–43. https://doi.org/10.1111/medu.14380 .
Wenger E. Communities of practice: learning, meaning, and identity. Cambridge: Cambridge University Press; 1998.
Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185–91. https://doi.org/10.1097/ACM.0000000000001826 .
de Carvalho-Filho MA, Tio RA, Steinert Y. Twelve tips for implementing a community of practice for faculty development. Med Teach. 2018. https://doi.org/10.1080/0142159X.2018.1552782 .
Chou D, Abelama Neto E, Thomas I, Martin A, Benoit L. Climate awareness, anxiety, and actions among youth: a qualitative study in a middle-income country. Braz J Psychiatry. 2023;45(00):258–67. https://doi.org/10.47626/1516-4446-2022-2890 .
Thomas I, Benoit L, Duvivier R, Antonio M, Filho DC, Martin A. Family dyads, emotional labor, and holding environments in the simulated encounter: co-constructive patient simulation as a reflective tool in child and adolescent psychiatry training. Child Adolesc Psychiatry Ment Health. 2023;2:1–15.
DiGiovanni MJ, Weller I, Martin A. Pivoting in the pandemic: a qualitative study of child and adolescent psychiatrists in the times of COVID-19. Child Adolesc Psychiatry Ment Health. 2021;15(32):1–18. https://doi.org/10.1016/j.jaac.2020.08.421 .
Herrington OD, Clayton A, Benoit L, et al. Viral time capsule: a global photo-elicitation study of child and adolescent mental health professionals during COVID-19. Child Adolesc Psychiatry Ment Health. 2021;15(1):1–18. https://doi.org/10.1186/s13034-021-00359-5 .
Stone LA, Benoit L, Martin A, Hafler J. Barriers to identifying learning disabilities: a qualitative study of clinicians and educators. Acad Pediatr. 2023;23(6):1166–74. https://doi.org/10.1016/j.acap.2022.12.008 .
Asuzu K, Ijeli C, Cardona L, et al. Perceptions of racism in a children’s psychiatric inpatient unit: a qualitative study of entrenching and uprooting factors. J Psychiatr Ment Health Nurs. 2022;30:501–14. https://doi.org/10.1111/jpm.12885 .
Benoit L, Thomas I, Martin A. Ecological awareness, anxiety, and actions among youth and their parents: a qualitative study of newspaper narratives. Child Adolesc Ment Health. 2021. https://doi.org/10.1111/camh.12514 .
Calhoun A, Herrington OD, Leckman JF, Martin A. Supporting clinician-scientist development in child psychiatry: a four-domain model for individual or programmatic self-reflection. Front Psychiatry. 2021;12(March):1–16. https://doi.org/10.3389/fpsyt.2021.651722 .
Martin A, Weller I, Amsalem D, et al. From learning psychiatry to becoming psychiatrists: a qualitative study of co-constructive patient simulation. Front Psychiatry. 2021;11(616239):1–15.
Safranek CW, Sidamon-Eristoff AE, Gilson A, Chartash D. The role of large language models in medical education: applications and implications. JMIR Med Educ. 2023;9:1–12. https://doi.org/10.2196/50945 .
Thirunavukarasu AJ, Ting DSJ, Elangovan K, Gutierrez L, Tan TF, Ting DSW. Large language models in medicine. Nat Med. 2023;29(8):1930–40. https://doi.org/10.1038/s41591-023-02448-8 .
Download references
Acknowledgements
The authors are grateful to each of the study participants for their engaged and candid participation. They also thank other members of the QuaLab for their enthusiasm and collaboration.
Supported by the Riva Ariella Ritvo Endowment at the Yale Child Study Center.
Author information
Authors and affiliations.
Child Study Center, Yale School of Medicine, New Haven, CT, USA
Andrés Martin, Madeline DiGiovanni, Amber Acquaye, Matthew Ponticiello & Laelia Benoit
QUALab, Qualitative and Mixed Methods Lab, a collaboration between the Yale Child Study Center, 230 South Frontage Road, New Haven, CT, 06520, USA
Andrés Martin, Madeline DiGiovanni, Amber Acquaye, Matthew Ponticiello, Débora Tseng Chou, Emilio Abelama Neto, Alexandre Michel, Jordan Sibeoni, Marie-Aude Piot, Michel Spodenkiewicz & Laelia Benoit
CESP, The Centre de Recherche en Épidémiologie et Santé des Populations, Paris, France
Departamento de Psiquiatria da Faculdade de Medicina da, Universidade de São Paulo, São Paulo, Brazil
Débora Tseng Chou & Emilio Abelama Neto
Inserm U1018, CESP, Team DevPsy, Paris-Saclay University, Villejuif, France
Alexandre Michel, Jordan Sibeoni & Marie-Aude Piot
Department of Psychiatry, McGill University Faculty of Medicine, Montréal, QC, Canada
Michel Spodenkiewicz
You can also search for this author in PubMed Google Scholar
Contributions
Each of the eleven authors made substantial contributions to the conception of the work, and to the analysis or interpretation of the data. Each author took an active part in drafting and substantively revising the manuscript and approved the submitted version. Each author agreed to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Correspondence to Andrés Martin .
Ethics declarations
Ethics approval and consent to participate.
We obtained ethics approval from the Yale Human Investigation Committee (Protocol # 2000035118), which considered the study exempt under 45CFR46.104 (2) (ii). We informed participants about the goals and methods of the study and provided a copy of the consent form. We recorded each participant’s consent before starting their interview.
Consent for publication
All study participants and all authors consented publication of the final draft version and submitted manuscript.
Competing interests
The authors have no disclosures or potential conflicts to declare.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
INTERVIEW GUIDE - Sensitizing questions.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Martin, A., DiGiovanni, M., Acquaye, A. et al. Pathways and identity: toward qualitative research careers in child and adolescent psychiatry. Child Adolesc Psychiatry Ment Health 18 , 49 (2024). https://doi.org/10.1186/s13034-024-00738-8
Download citation
Received : 21 January 2024
Accepted : 28 March 2024
Published : 29 April 2024
DOI : https://doi.org/10.1186/s13034-024-00738-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Child and Adolescent Psychiatry and Mental Health
ISSN: 1753-2000
- Submission enquiries: [email protected]
- Open access
- Published: 27 April 2024
Exploring health care providers’ engagement in prevention and management of multidrug resistant Tuberculosis and its factors in Hadiya Zone health care facilities: qualitative study
- Bereket Aberham Lajore 1 na1 nAff5 ,
- Yitagesu Habtu Aweke 2 na1 nAff6 ,
- Samuel Yohannes Ayanto 3 na1 nAff7 &
- Menen Ayele 4 nAff5
BMC Health Services Research volume 24 , Article number: 542 ( 2024 ) Cite this article
88 Accesses
Metrics details
Engagement of healthcare providers is one of the World Health Organization strategies devised for prevention and provision of patient centered care for multidrug resistant tuberculosis. The need for current research question rose because of the gaps in evidence on health professional’s engagement and its factors in multidrug resistant tuberculosis service delivery as per the protocol in the prevention and management of multidrug resistant tuberculosis.
The purpose of this study was to explore the level of health care providers’ engagement in multidrug resistant tuberculosis prevention and management and influencing factors in Hadiya Zone health facilities, Southern Ethiopia.
Descriptive phenomenological qualitative study design was employed between 02 May and 09 May, 2019. We conducted a key informant interview and focus group discussions using purposely selected healthcare experts working as directly observed treatment short course providers in multidrug resistant tuberculosis treatment initiation centers, program managers, and focal persons. Verbatim transcripts were translated to English and exported to open code 4.02 for line-by-line coding and categorization of meanings into same emergent themes. Thematic analysis was conducted based on predefined themes for multidrug resistant tuberculosis prevention and management and core findings under each theme were supported by domain summaries in our final interpretation of the results. To maintain the rigors, Lincoln and Guba’s parallel quality criteria of trustworthiness was used particularly, credibility, dependability, transferability, confirmability and reflexivity.
Total of 26 service providers, program managers, and focal persons were participated through four focus group discussion and five key informant interviews. The study explored factors for engagement of health care providers in the prevention and management of multidrug resistant tuberculosis in five emergent themes such as patients’ causes, perceived susceptibility, seeking support, professional incompetence and poor linkage of the health care facilities. Our findings also suggest that service providers require additional training, particularly in programmatic management of drug-resistant tuberculosis.
The study explored five emergent themes: patient’s underlying causes, seeking support, perceived susceptibility, professionals’ incompetence and health facilities poor linkage. Community awareness creation to avoid fear of discrimination through provision of support for those with multidrug resistant tuberculosis is expected from health care providers using social behavioral change communication strategies. Furthermore, program managers need to follow the recommendations of World Health Organization for engaging healthcare professionals in the prevention and management of multidrug resistant tuberculosis and cascade trainings in clinical programmatic management of the disease for healthcare professionals.
Peer Review reports
Introduction
Mycobacterium tuberculosis, the infectious agent that causes multi-drug resistant tuberculosis (MDR-TB), is resistant to at least rifampicin and isoniazid. Direct infection can cause the disease to spread, or it can develop secondary to improper management of tuberculosis among drug susceptible tuberculosis cases and associated poor adherence [ 1 ].
Multidrug-resistant strains of mycobacterium tuberculosis have recently emerged, which makes achieving “End TB Strategy” more difficult [ 2 ]. Multi drug resistant tuberculosis (MDR-TB) has been found to increasingly pose a serious threat to global and Ethiopian public health sector. Despite the fact that a number of risk factors for MDR-TB have been identified through various research designs, the epidemiology of this disease is complex, contextual, and multifaceted [ 1 ]. Quantitative studies demonstrate that prior treatment history [ 3 , 4 , 5 , 6 , 7 ], interrupted drug supply [ 8 ], inappropriate treatments and poor patient compliance [ 3 , 7 , 9 ], poor quality directly observed treatment short course (DOTS), poor treatment adherence [ 10 ], age [ 5 ], and malnutrition [ 11 ] were factors associated with multi drug resistant TB.
Globally, an estimated 20% of previously treated cases and 3.3% of new cases are thought to have MDR-TB; these levels have essentially not changed in recent years. Globally, 160,684 cases of multidrug-resistant TB and rifampicin-resistant TB (MDR/RR-TB) were notified in 2017, and 139,114 cases were enrolled into treatment in 2017 [ 12 ]. A systematic review in Ethiopia reported 2% prevalence of MDR-TB [ 3 ] that is higher than what is observed in Sub-Saharan Africa, 1.5% [ 13 ]. The prevalence of MDR-TB, according to the national drug-resistant tuberculosis (DR-TB) sentinel report, was 2.3% among newly diagnosed cases of TB and 17.8% among cases of TB who had already received treatment,. This suggests a rising trend in the prevalence of TB drug resistance compared to the results of the initial drug-resistant TB survey carried out in Ethiopia from 2003 to 2005 [ 14 ].
Ethiopia has placed strategies into place that emphasize political commitment, case finding, appropriate treatment, a continuous supply of second-line anti-TB medications of high quality, and a recording system. Due to other competing health priorities, the nation is having difficulty accelerating the scale-up of the detection, enrollment and treatment of drug-resistant TB patients [ 15 , 16 ]. To address these issues, the nation switched from a hospital-based to a clinic-based ambulatory model of care, which has allowed MDR-TB services to quickly decentralize and become more accessible. Accordingly, the nation has set up health facilities to act as either treatment initiating centers (TIC) or treatment follow-up centers (TFC) or both for improved referral and communication methods [ 15 ].
One of the key components of the “End TB strategy” is engagement of health care professionals in the prevention and management of multidrug resistant tuberculosis [ 17 ]. Inadequate engagement of healthcare providers is one aspect of the healthcare system that negatively influences MDR-TB prevention and control efforts [ 17 ]. This may be manifested in a number of ways, including inadequate understanding of drug-resistant tuberculosis, improper case identification, failure to initiate treatment again, placement of the wrong regimens, improper management of side effects and poor infection prevention [ 1 ]. These contributing factors are currently being observed in Ethiopia [ 18 ], Nigeria [ 7 , 19 , 20 ] and other countries [ 21 , 22 ]. According to a study conducted in Ethiopia, MDR-TB was linked to drug side effects from first-line treatments, being not directly observed, stopping treatment for at least a day, and retreating with a category II regimen [ 17 ].
This may be the result of a synergy between previously investigated and other contextual factors that have not yet been fully explored, such as professional engagement, beliefs, and poor preventive practices. The engagement of health professionals in MDR-TB prevention and control is assessed using a number of composite indicators. Health professionals may interact primarily inside the healthcare facilities. Typically, they play a significant role in connecting healthcare services with neighborhood-based activities [ 17 ]. One of the main research areas that have not sufficiently addressed is evidence indicating the status of healthcare professionals’ engagement and contextual factors in MDR-TB prevention and management.
It is increasingly urgent to identify additional and existing factors operating in a particular context that contribute to the development of the disease in light of the epidemic of drug resistance, including multi-drug resistance (MDR-TB) and extensively drug resistant TB (XDR-TB) in both new and previously treated cases of the disease [ 23 ]. In order to develop and implement control measures, it is therefore essential to operationally identify a number of contextual factors operating at the individual, community, and health system level.
Therefore, the overall purpose of this study was to explore the level of engagement of health care providers and contextual factors hindering/enabling the prevention and provision of patient-centered care for MDR-TB in health facilities, DOTS services centers and MDR-TB treatment initiation center [TIC], in Hadiya Zone, Southern Ethiopia.
Qualitative approach and research paradigm
Descriptive phenomenological qualitative study design was employed to explore factors influencing engagement of health professionals in MDR-TB prevention and management and thematic technique was employed for the analysis of the data.
Researchers’ characteristics and reflexivity
Three Principal investigators conducted this study. Two of them had Masters of public health in Epidemiology and Reproductive health and PhD candidates and the third one had Bachelor’s degree in public health with clinical experience in the area of Tuberculosis prevention and management and MPH in Biostatistics. The principal investigators have research experience with published articles in different reputable journals. There were no prior contacts between researchers and participants before the study whereas researchers have built positive rapport with study participants during data collection to foster open communication and trust and had no any assumptions and presuppositions about the research topic and result.
Context/ study setting and period
The study was conducted between 2 and 9 May, 2019 in Hadiya Zone with more than 1.7 million people residing in the Zone. There are 300 health posts, 63 health centers, 3 functional primary hospitals and 1 comprehensive specialized hospital in the Zone. Also, there are more than 350 private clinics and 1 private hospital in the Zone. All of the public health facilities and some private health facilities provide directly observed short course treatment (DOTS) service for tuberculosis patients. There are more than eight treatment initiation centers (TICs) for MDR-TB patients in Hadiya Zone. MDR-TB (Multidrug-resistant tuberculosis) treatment initiation centers are specialized facilities that provide comprehensive care, diagnosis and treatment initiation, psychosocial support, and follow up services to individuals with MDR-TB. The linkage between MDR-TB treatment initiation centers and other healthcare facilities lies in the coordination of care, referral pathways, and collaboration to ensure comprehensive and integrated care for individuals with MDR-TB. Overall, healthcare providers play a crucial role in the management of MDR-TB by providing specialized care, ensuring treatment adherence, monitoring progress and outcomes, and supporting individuals in achieving successful treatment outcomes and improved health.
Units of study and sampling strategy
Our study participants were health care professionals working in MDR-TB TICs in both private and public health facilities, and providing DOTS services, MDR-TB program leaders in treatment initiation centers, as well as TB focal persons, disease prevention and health promotion focal person, and project partners from district health offices. The study involved four focus group discussion (FGDs) and five key informants’ interview (KII) with a total of 26 participants to gather the necessary information. Expert purposive sampling technique was employed and sample size was determined based on the saturation of idea required during data collection process.
Data collection methods and instruments
Focus group discussion and face to face key informants’ interviews were employed to collect the data. We conducted a total of four FGD and five key informants’ interviews with participants chosen from DOTS providing health facilities and MDR-TB program leaders in treatment initiation centers, as well as TB focal persons and project partners from district health offices and disease prevention and health promotion focal person. One of the FGDs was conducted among health professionals from the public MDR-TB treatment initiation centers. Three FGDs were conducted among disease prevention and health promotion focal persons, TB focal persons and DOTS providers in public health facilities (health centers).
An observation checklist was developed to assess the general infection prevention and control measures used by specific healthcare facilities in the study area. We used unstructured FGD guide, key informant interview guide, observation checklist and audio recorders to collect primary data and it was collected using local language called Amharic. Prior to data collection, three people who are not among principal investigators with at least a master’s degree in public health and prior experience with qualitative research were trained by principal investigators. Three of them acts as a tape recorder, a moderator, and as a note taker alternatively. The length of FGD ranged from 58 to 82 min and that of key informants’ interview lasted from 38 to 56 min.
Data processing and data analysis
Memos were written immediately after interviews followed by initial analysis. Transcription of audio records was performed by principal investigators. The audio recordings and notes were refined, cleaned and matched at the end of each data collection day to check for inconsistencies, correct errors, and modify the procedures in response to evolving study findings for subsequent data collection. Transcribed interviews, memos, and notes from investigator’s observation were translated to English and imported to Open Code 4.02 [ 2 ] for line by line coding of data, and categorizing important codes (sub theming). The pre-defined themes for MDR-TB prevention and control engagement were used to thematize the line-by-line codes, categories, and meanings using thematic analysis. Finally, the phenomenon being studied was explained by emerging categories and themes. Explanations in themes were substantiated by participants’ direct quotations when necessary.
Trustworthiness
Phone calls and face to face briefing were requested from study participants when some expressions in the audio seems confusing while transcripts were performed. To ensure the credibility of the study, prolonged engagement was conducted, including peer debriefing with colleagues of similar status during data analysis and inviting available study participants to review findings to ensure as it is in line with their view or not. Memos of interviews and observation were crosschecked while investigator was transcribing to ensure credibility of data as well as to triangulate investigator’s categorizing and theming procedures. For transferability, clear outlines of research design and processes were provided, along with a detailed study context for reader judgment. Dependability was ensured through careful recording and transcription of verbal and non-verbal data, and to minimize personal bias, scientific procedures were followed in all research stages. Conformability was maintained by conducting data transcription, translation, and interpretation using scientific methods. Researchers did all the best to show a range of realities, fairly and faithfully. Finally, an expert was invited to put sample of codes and categories to emerged corresponding categories and themes respectively.
Demographic characteristics of study participants
Four focus group discussions and five key informants’ interviews were conducted successfully. There were 26 participants in four focus group discussions, and key informants’ interview. Ages of participants ranges from 20 to 50 years with an average age of 33.4 ± 6.24 SD years. Participants have five to ten years of professional experience with DOTS services (Table 1 ).
Emergent themes and subthemes
The study explored how health care providers’ engagement in MDR-TB prevention and management was influenced. The investigation uncovered five major themes. These themes were the patient’s underlying causes, seeking support, perceived susceptibility, healthcare providers’ incompetence, and poor linkage between health facilities. Weak community TB prevention, health system support, and support from colleagues were identified subthemes in the search for help by health professionals whereas socioeconomic constraints, lack of awareness, and fear of discrimination were subthemes under patients underlying factors (Fig. 1 ).
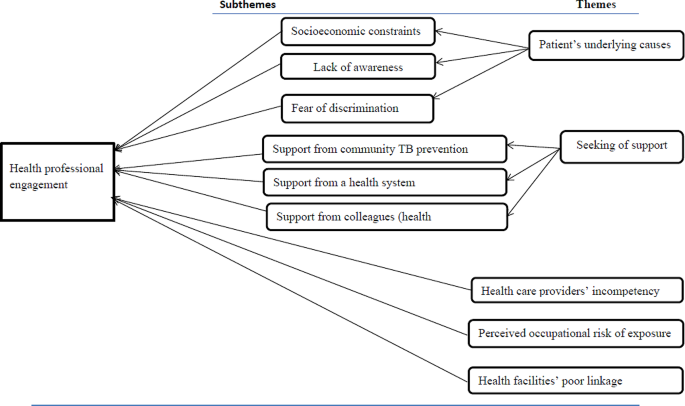
Themes and subthemes emerged from the analysis of health professionals’ engagement in MDR-TB prevention and management study in Hadiya zone’s health facilities, 2019
The patient’s underlying causes
This revealed why TB/MDR-TB treatment providers believe health professionals are unable to provide standard MDR-TB services. The subthemes include TB/MDR-TB awareness, fear of discrimination, and patients’ socioeconomic constraints.
Socioeconomic constraints
According to our research, the majority of healthcare professionals who provided directly observed short-course treatment services mentioned socioeconomic constraints as barriers to engage per standard and provide MDR-TB prevention and management service. More than half of the participants stated that patients’ primary reasons include lack of money for house rental close to the treatment centers, inability to afford food and other expenses, and financial constraints to cover transportation costs.
In addition to this, patients might have additional responsibilities to provide food and cover other costs for their families’ need. The majority of health care professionals thought that these restrictions led to their poor engagement in MDR-TB prevention and management. One of the focus groups’ discussants provided description of the scenario in the following way:
“…. I have many conversations with my TB/MDR-TB patients. They fail to complete DOTS or treatment intensive care primarily as a result of the requirement of prolonged family separation. They might provide most of the family needs, including food and other expenses” (FGD-P01).
Lack of awareness about MDR-TB
This subtheme explains how MDR-TB patients’ knowledge of the illness can make it more difficult for health professionals to provide DOTS or TICs services. The majority of DOTS providers stated that few TB or MDR-TB patients were aware of how MDR-TB spreads, how it is treated, and how much medication is required. Additionally, despite the fact that they had been educated for the disease, majority of patients did not want to stop contact with their families or caregivers. A health care provider stated,
“…. I provided health education for MDR-TB patients on how the disease is transmitted and how they should care for their family members. They don’t care; however, give a damn about their families .” (FGD-P05).
Some healthcare professionals reported that some patients thought that MDR-TB could not be cured by modern medication. One medical professional described the circumstance as follows:
“…. I noticed an MDR-TB patient who was unwilling to be screened. He concluded that modern medication is not effective and he went to spiritual and traditional healers” (FGD-P02).
As a result, almost all participants agreed on the extent to which patient knowledge of TB and MDR-TB can influence a provider’s engagement to MDR-TB services. The majority suggested that in order to improve treatment outcomes and preventive measures, the media, community leaders, health development armies, one-to-five networks, non-governmental organizations, treatment supporters, and other bodies with access to information need to put a lot of efforts.
Fear of discrimination
According to our research, about a quarter of healthcare professionals recognized that patients’ fear of discrimination prevents them from offering MDR-TB patients the DOTS services they need, including counseling index cases and tracing contact histories.
HEWs, HDAs, and 1-to-5 network members allegedly failed to monitor and counsel the index cases after their immediate return to their homes, according to the opinions from eight out of twenty-six healthcare professionals. The patients began to engage in routine social and political activities with neighbors while hiding their disease status. A healthcare professional described this situation as follows:
“…. I understood from my MDR-TB patient’s words that he kept to himself and avoided social interaction. He made this decision as a result of stigmatization by locals, including health extension workers. As a result, the patient can’t attend social gatherings. …. In addition, medical professionals exclude MDR-TB patients due to fear of exposures. As a result, patients are unwilling to undergo early screening” (FGD-P04).
Professionals’ perceived risk of occupational exposure
This theme highlights the anxiety that healthcare workers experience because of MDR-TB exposure when providing patient care. Our research shows that the majority of health professionals viewed participation as “taking coupons of death.” They believed that regardless of how and where they engaged in most healthcare facilities, the risk of exposure would remain the same. According to our discussion and interview, lack of health facility’s readiness takes paramount shares for the providers’ risk of exposures and their susceptibility.
According to the opinion from the majority of FGD discussants and in-depth interviewees, participants’ self-judgment score and our observation, the majority of healthcare facilities that offer DOTS for DS-TB and MDR-TB did not create or uphold standards in infection prevention in the way that could promote better engagement. These include poor maintenance of care facilities, lack of personal protective equipment, unsuitable facility design for service provision, lack of patient knowledge regarding the method of MDR-TB transmission, and lack of dedication on the part of health care staff.
As one of our key informant interviewees [District Disease Prevention Head], described health professionals’ low engagement has been due to fear of perceived susceptibility. He shared with us what he learned from a community forum he moderated.
Community forum participant stated that “… There was a moment a health professional run-away from the TB unit when MDR-TB patient arrived. At least they must provide the necessary service, even though they are not willing to demonstrate respectful, compassionate, or caring attitude to MDR-TB patients” (KII-P01). Besides , one of the FGD discussants described the circumstance as follows:
“…. Emm…. Because most health facilities or MDR-TB TIC are not standardized, I am concerned about the risk of transmission. They are crammed together and poor ventilation is evident as well as their configuration is improper. Other medical services are causing the TICs to become overcrowded. Most patients and some medical professionals are unconcerned with disease prevention ” (FGD-P19).
Participants’ general fear of susceptibility may be a normal psychological reaction and may serve as a motivation for taking preventative actions. However, almost all participants were concerned that the main reasons for their fear were brought up by the improper application of programmatic management and MDR-TB treatment standards and infection prevention protocols in healthcare facilities.
Health care providers’ incompetence
This theme illustrates how professionalism and dedication impact participation in MDR-TB prevention and management. The use of DS-TB prevention and management by health professionals was also taken into account because it is a major factor in the development of MDR-TB. This theme includes the participants’ perspectives towards other healthcare workers involved in and connected to MDR-TB.
Nearly all of the participants were aware of the causes and danger signs of MDR-TB. The majority of the defined participants fit to the current guidelines. However, participants in focus groups and key informant interviews have brought up shortcomings in MDR-TB service delivery practice and attitude. We looked at gaps among healthcare professionals’ knowledge, how they use the national recommendations for programmatic management and prevention of MDR-TB, prevent infections, take part in community MDR-TB screenings, and collaborate with other healthcare professionals for better engagement.
More than half of the participants voiced concerns about their attitudes and skill sets when using MDR-TB prevention and management guideline. When asked about his prior experiences, one of the focus group participants said:
“…. Ok, let me tell you my experience, I was new before I attended a training on MDR-TB. I was unfamiliar with the MDR-TB definition given in the recommendations. When I was hired, the health center’s director assigned me in the TB unit. I faced difficulties until I received training” (FGD-P24). Furthermore , one of the key informant interview participants shared a story: “…. In my experience, the majority of newly graduated health professionals lack the required skill. I propose that pre-service education curricula to include TB/MDR-TB prevention and management guideline trainings” (KII-P01).
The majority of participants mentioned the skill gap that was seen among health extension workers and laboratory technicians in the majority of healthcare facilities. Some of the participants in the in-depth interviews and FGD described the gaps as follows:
“…. According to repeated quality assurance feedbacks, there are many discordant cases in our [ District TB Focal Person ] case. Laboratory technicians who received a discrepant result (KII-P01) are not given training which is augmented by shared story from FGD discussants, “According to the quality assurance system, laboratory technicians lack skill and inconsistent results are typical necessitating training for newly joining laboratory technicians” (FGD-P20).
Through our discussions, we explored the level of DOTS providers’ adherence to the current TB/MDR-TB guideline. As a result, the majority of participants pointed out ineffective anti-TB management and follow-up care. One of the participants remembered her practical experience as follows:
“…. In my experience, the majority of health professionals fail to inform patients about the drug’s side effects, follow-up procedures, and other techniques for managing the burden of treatment. Only the anti-TB drug is provided, and the patient is left alone. The national treatment recommendation is not properly implemented by them” (FGD-P04).
Many barriers have been cited as reasons that might have hindered competencies for better engagement of health professionals. Training shortage is one of the major reasons mentioned by many of the study participants. One of discussants from private health facility described the problem as
“…. We are incompetent, in my opinion. Considering that we don’t attend update trainings. Many patients who were diagnosed negative at private medical facilities turned out to be positive, and vice versa which would be risky for drug resistance” (FGD-P14) which was supported by idea from a participant in our in-depth interview: “…. We [Program managers] are running short of training for our health care providers at different health centers and revealed that four out of every five healthcare professionals who work in various health centers are unaware of the TB/MDR-TB new guideline” (KII-P02).
Seeking support
This theme focuses on the significance and effects of workplace support in the engagement of MDR-TB prevention and control. This also explains the enabling and impeding elements in the engagement condition of health professionals. Three elements make up the theme: coworkers (other health professionals) in the workplace, support from community TB prevention actors, and a healthcare system.
Support from community TB prevention actors
This subtheme includes the assistance provided to study participants by important parties such as community leaders, the health development army, and other stakeholders who were involved in a community-based TB case notification, treatment adherence, and improved patient outcomes.
Many of the study participants reported that health extension workers have been poorly participating in MDR-TB and TB-related community-based activities like contact tracing, defaulter tracing, community forums, health promotion, and treatment support. One study participant described their gap as follows:
“…. I understood that people in the community were unaware of MDR-TB. The majority of health extension workers do not prioritize raising community awareness of MDR-TB” (FGD-P13). This was supported by idea from a district disease prevention head and stated as: “…. There is no active system for contacts tracing. Health educators send us information if they find suspected cases. However, some patients might not show up as expected. We have data on three family members who tested positive for MDR-TB” (KII-P3).
Support from a health system
The prime focus of this subtheme is on the enabling elements that DOTS providers require assistance from the current healthcare system for better engagement. All study participants expressed at least two needs to be met from the health system in order for them to effectively participate in MDR-TB prevention, treatment, and management. All study participants agreed that issues with the health system had a negative impact on their engagement in the prevention, treatment, diagnosis, and management of MDR-TB in almost all healthcare facilities. Poor conditions in infrastructure, resources (supplies, equipment, guidelines, and other logistics), capacity building (training), supportive supervision, establishment of public-private partnerships, and assignment of motivated and trained health professionals are some of the barriers that needs to be worked out in order to make them engage better. One of the participants pronounces supplies and logistics problems as:
“…. The health center I worked in is listed as a DOTS provider. However, it lacks constant electricity, a working microscope, lab supplies, medications, etc, and we refer suspected cases to nearby health centers or district hospitals for AFB-examination and, “Sometimes we use a single kit for many patients and wait for the medication supply for three or more weeks and patients stops a course of therapy that might induce drug resistance” (FGD-PI04) which was augmented by statement from FGD participant who works at a treatment initiation center: “…. We faced critical shortage of supplies and hospital administrators don’t care about funding essential supplies for patient care. For instance, this hospital (the hospital in which this FGD was conducted) can easily handle N-95 masks. Why then they (hospital administrators working in some TIC) can’t do it?” (FGD-P18).”
Regarding in-service training on MDR-TB, almost all participants pointed out shortage of on-job training mechanisms. One of our FGD participants said:
“…. I missed the new training on MDRTB programmatic management guidelines. I’ve heard that new updates are available. I still work using the old standard” (FGD-PI05). A health professional working in private clinic heightens the severity of training shortage as: “…. We have not participated in TB/MDR-TB guidelines training. You know, most of for-profit healthcare facilities do not provide any training for their staff. I’m not sure if I’m following the (TB/MDR-TB) guideline” (FGD-P14). One of our key informant interview participants; MDR-TB center focal person suggested the need for training as: “…. I’ve received training on the MDR-TB services and public-private partnership strategy. It was crucial in my opinion for better engagement. It is provided for our staff [MDRTB center focal person]. However, this has not yet been expanded to other health facilities” (KII-P04).
Concerning infrastructures, transportation problem was one of the frequently mentioned obstacles by many participants that hinder engagement in MDR-TB/TB service. This factor had a negative impact to both sides (health professionals and patients). One of discussants said:
“…. I face obstacles such as transport cost to perform effective TB/MDR-TB outreach activities like health education, tracing family contacts and defaulters and community mobilization. Rural kebeles are far apart from each other. How can I support 6 rural Kebeles?” (FGD-P01). One of the participants; MDR-TB treatment centers supervisor/program partner seconded the above idea as: “…. I suggest government must establish a system to support health professionals working in remote health care facilities in addition to MDR-TB centers. I guess there are more than 30 government health centers and additional private clinics. We can’t reach them all due to transportation challenges” (KII-P05). One of the participants , a district disease prevention head added: “…. Our laboratory technicians take sample from MDR-TB suspects to the post office and then, the post office sends to MDR-TB site. Sometimes, feedback may not reach timely. There is no any system to cover transportation cost. That would make case detection challenging” (FGD-P02).
Support from colleagues
Study participants stated the importance of having coworker with whom they could interconnect. However, eight participants reported that they were discriminated by their workmates for various reasons, such as their perceived fear of exposure to infection and their perception as if health professionals working in TB/MDR-TB unit get more training opportunities and other incentives. One of the focus group discussants said:
“…. My colleagues [health professional working out of MDR-TB TICs] stigmatize us only due to our work assignment in MDR-TB clinic. I remember that one of my friends who borrowed my headscarf preferred to throw it through a window than handing-over it back safely. Look, how much other health professionals are scared of working in MDR-TB unit. This makes me very upset. I am asking myself that why have I received such training on MDR-TB?” (FGD-P04).
Some of the participants also perceived that, health professionals working in MDR-TB/TB unit are the only responsible experts regarding MDR-TB care and treatment. Because, other health professionals consider training as if it is an incentive to work in such units. One of the FGD discussants described:
“… Health professionals who work in other service units are not volunteer to provide DOTS if TB focal person/previously trained staffs are not available. Patients wait for longer time” (FGD-P11).
Health facilities’ poor linkage
This theme demonstrates how various healthcare facilities, including private and public healthcare facilities such as, health posts, health care centers and hospitals, and healthcare professionals working at various levels of the healthcare system in relation to TB/MDR-TB service, are inter-linked or communicating with one another.
Many study participants noted a lack of coordination between higher referral hospitals, TB clinics, health posts, and health centers. Additionally, the majority of the assigned healthcare professionals had trouble communicating with patients and their coworkers. A focus group discussant also supported this idea as
“…. There is a lack of communication between us [DOTS providers at treatment initiation centers] and health posts, health centers, and private clinics. We are expected to support about 30 public health facilities. It’s of too much number, you know. They are out of our reach. We only took action when a problem arose” (FGD-P16).
Significant number of participants had raised the problem of poor communication between health facilities and treatment initiation centers. One of the interviewees [program manager] said:
“…. I see that one of our challenges is the weak referral connections between treatment initiation centers and health centers. As a result, improper sample transfer to Gene- Xpert sites and irregular postal delivery are frequent” . “Our; DOTS staff at the MDR-TB center, DOTS staff at the health center, and health extension workers are not well connected to one another. Many patients I encountered came to this center [MDR-TB center] after bypassing both health post and health center. Poor linkage and communication, in my opinion, could be one of the causes. The same holds true for medical facilities that are both public and private ” (KII-P02).
Engagement of individual healthcare providers is one of the peculiar interventions to achieve the goal of universal access to drug resistance tuberculosis care and services [ 17 ]. Healthcare providers engagement in detecting cases, treating and caring for multidrug resistant tuberculosis (MDR-TB) may be influenced by various intrinsic (individual provider factors) and extrinsic (peer, health system, political and other factors) [ 15 ]. Our study explored engagement of individual DOTS providers and factors that influence their engagement in MDR-TB prevention and management service. This is addressed through five emergent themes and subthemes as clearly specified in our results section.
The findings showed patients’ socioeconomic constraints were important challenges that influence health professionals’ engagement, and provision of MDR-TB prevention and management services. Although approaches differ, studies in Ethiopia [ 24 ], South Africa [ 25 ] and India [ 26 , 27 ] documented that such factors influence health providers’ engagement in the prevention and management of multi drug resistant tuberculosis. Again, the alleviation of these factors demands the effort from patients, stakeholders working on TB, others sectors, and the healthcare system so that healthcare providers can deliver the service more effectively in their day-to-day activities and will be more receptive to the other key factors.
We explored participants’ experiences on how patients’ awareness about drug sensitive or multi drug resistant tuberculosis influenced their engagement. Accordingly, participants encountered numerous gaps that restricted their interactions with TB/MDR-TB patients. In fact, our study design and purposes vary, studies [ 28 , 29 , 30 ] indicated that patients awareness influenced providers decision in relation to MDR-TB services and patients’ awareness status is among factors influencing healthcare providers’ decision making about the care the MDR-TB patient receives. As to our knowledge, patients’ perceived fear of discrimination was not documented whether it had direct negative impact on reducing providers’ engagement. Therefore, patients’ awareness creation is an important responsibility that needs to be addressed by the community health development army, health extension workers, all other healthcare providers and stakeholder for better MDR-TB services and patient outcomes.
Our study indicates that healthcare providers perceived that they would be exposed to MDR-TB while they are engaged. Some of the participants were more concerned about the disadvantages of engagement in providing care to MDR-TB patients which were predominantly psychological and physical pressure. In this context, the participants emphasized that engagement in MDR-TB patient care is “always being at risk” and expressed a negative attitude. This finding is similar to what has been demonstrated in a cross-sectional study conducted in South Africa in which majority of healthcare providers believed their engagement in MDR-TB services would risk their health [ 21 ].
However, majority of the healthcare providers demonstrated perceived fear of exposures mainly due to poor infection prevention practices and substandard organization of work environment in most TB/MDR-TB units. This is essentially reasonable fear, and needs urgent intervention to protect healthcare providers from worsening/reducing their effective engagement in MDR-TB patient care. On the other side of the coin, perceived risk of occupational exposure to infection could be source for taking care of oneself to combat the spread of the infection.
In our study, healthcare provider’s capability (competence) also had an impact on their ability to engage in prevention and management of MDR-TB. Here, participants had frequently raised their and other healthcare providers’ experience regarding skill gaps, negative attitude towards the service unit they were working in, ineffective use of MDR-TB guideline, poor infection prevention practices and commitment. In addition, many health professionals report serious problems regarding case identification and screening, drug administration, and side effect management. These findings were supported by other studies in Ethiopia [ 7 ] and in Nigeria [ 19 , 20 ]. This implies an urgent need for training of health care worker on how to engage in prevention and management of multidrug resistant TB.
Moreover, our findings provide insights into the role of community TB prevention actors, currently functioning health system, and colleagues and other stakeholders’ regarding healthcare providers’ engagement. Participants emphasized that support from community TB prevention actors is a key motivation to effectively engage on management and prevention roles towards MDR-TB. Evidence shows that community TB prevention is one of the prominent interventions that study participants would expect in DOTS provision as community is the closest source of information regarding the patients [ 31 , 32 ].
Similarly, all participants had pointed out the importance of support from a health system directly or indirectly influence their engagement in the prevention, diagnosis, treatment, and management of MDR-TB. Researches indicated that health system supports are enabling factors for healthcare providers in decision making regarding TB/MDR-TB prevention and treatment [ 33 ]. This problem is documented by the study done in Ethiopia [ 22 ]. In addition, support from colleagues and other stakeholders was also a felt need to engage in MDR-TB which was supported by the World Health Organization guideline which put engagement in preventing MDR-TB and providing patients centered care needs collaborative endeavor among healthcare providers, patients, and other stakeholders [ 17 ].
Participants showed that there were poor linkage among/within DOTS providers working in health post (extension workers), health centers, hospitals and MDRTB treatment initiation centers. Our finding is consistent with a research in South Africa which shows poor health care attitude is linked to poor treatment adherence [ 34 ]. Our study implies the need for further familiarization especially on clinical programmatic management of drug resistant tuberculosis. Moreover, program managers need to follow health professionals’ engagement approaches recommended by the World Health Organization: End TB strategy [ 17 ].
Limitations of the study
There are some limitations that must be explicitly acknowledged. First, participants from private health facilities were very few, which might have restricted the acquisition and incorporation of perspectives from health care providers from private health care facilities. Second, healthcare providers’ engagement was not measured from patient side given that factors for engagement may differ from what has been said by the healthcare provides. Third, power relationships especially among focus group discussant in MDR-TB treatment initiation centers might have influenced open disclosures of some sensitive issues.
The study showed how healthcare provider’s engagement in MDR-TB management and prevention was influenced. Accordingly, patient’s underlying causes, seeking support, perceived occupational exposure, healthcare provider’s incompetence and health facilities poor linkage were identified from the analysis. Weak community TB prevention efforts, poor health system support and support from colleagues, health care providers’ incompetence and health facilities poor linkage were among identified factors influencing engagement in MDR – TB prevention and management. Therefore, measures need to be in place that avert the observed obstacles to health professionals’ engagement including further quantitative studies to determine the effects of the identified reasons and potential factors in their engagement status.
Furthermore, our findings pointed out the need for additional training of service providers, particularly in clinical programmatic management of drug-resistant tuberculosis. Besides, program managers must adhere to the World Health Organization’s recommendations for health professional engagement. Higher officials in the health sector needs to strengthen the linkage between health facilities and service providers at different levels. Community awareness creation to avoid fear of discrimination including provision of support for those with MDR-TB is expected from health experts through implementation of social behavioral change communication activities.
Abbreviations
Directly observed treatment short-course
Drug susceptible tuberculosis
Millennium development goals
Multidrug resistant tuberculosis
Sustainable development goals
Tuberculosis
Treatment initiation center
World Health Organization
Extensively drug resistant TB
WHO. Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. WHO; Geneva, Switherland. 2014.
WHO. Implementing the end TB Strategy: The Essentials. WHO, Geneva. Switherland; 2015.
Eshetie S, Gizaw M, Dagnew M, Kumera G, Woldie H, Fikadu A. et.al. Multidrug-resistant tuberculosis in Ethiopian settings and its association with previous history of anti-tuberculosis treatment: a systematic review and meta-analysis Ethiopia: efforts to expand diagnostic services, treatment and care. BMC Antimicrobial Resist Infect Control. 2014;3:31.
Biadglegne F, Sack U, Rodloff AC. Multidrug-resistant tuberculosis in Ethiopia: efforts to expand diagnostic services, treatment and care. BMC Antimicro Resist Infect Control. 2014;3:31.
Lema NA, Majigo M, Mbelele PM, Abade AMIM. Risk factors associated with multidrug resistant tuberculosis among patients referred to Kibong’oto Infectious Disease Hospital in northern Tanzania. Tanzania J Health Res. 2016;18:4.
Mekonnen F, Tessema B, Moges F, Gelaw A, Eshetie S. G. K. Multidrug resistant tuberculosis: prevalence and risk factors in districts of metema and west armachiho, Northwest Ethiopia. BMC Infect Dis. 2015;15:461.
Selamawit H, Girmay M, Belaineh G, Muluken M, Alemayehu M, et al. PS. Determinants of multidrug-resistant tuberculosis in patients who underwent first-line treatment in Addis Ababa: a case control study. BMC Public Health 2013. 2013;13:782.
Google Scholar
Safwat TM, Elmasry AA, Mohamed A. Prevalence of multi-drug resistant tuberculosis in abbassia Chest hospital from july 2006 to december 2009. Egyptian J Bronchol. 2011;5(2):124–30.
World Health Organization. WHO Global tuberculosis report 2015. Geneva: WHO. 2015.
Rifat M, Hall J, Oldmeadow C, Husain A, Hinderaker SG. AH. M. Factors related to previous tuberculosis treatment of patients with multidrug resistant tuberculosis in Bangladesh. BMJ Open. 2015;5.
Gupta KB, Gupta R, Atreja A, Verma MSV. Tuberculosis and nutrition. Lung India: Offic Organ of Indian Chest Soc. 2009;26(1):9–16. https://doi.org/10.4103/0970-2113.45198 . 2009.
World Health Organization. WHO Global tuberculosis report 2018. Geneva: WHO. 2018.
Deus L, Willy S, Kenneth M, George WK, Frank JCMJ. et al. Variation and risk factors of drug resistant tuberculosis in sub-Saharan Africa: a systematic review and meta-analysis. BMC Public Health 2015;15.
Federal Ministry of Health. Guidelines for Clinical and Programmatic Management of TB, TB/HIV and Leprosy in Ethiopia. Fifth Edition. Addis Ababa. March, 2013.
FDRE/MOH. Guidelines on programmatic management of drug resistant tuberculosis in Ethiopia. 2ND ED.2014 ADDIS ABABA. 2014.
CSIS. Center for Strategic and International Studies. As Ethiopia moves toward tuberculosis elimination, success requires higher investment: A report of CSIS global health policy center. CSIS, Washinton DC, America. 2016.
World Health organization. Framework for the engagement of all health care providers in the management of drug resistant tuberculosis. Geneva; Switherland. WHO 2015.
Vries G, Tsolova S, Anderson LF, Gebhard AC, Helda E, Hollo V. Health system factors influencing management of multidrug-resistant tuberculosis in four European Union countries - learning from country experiences. BMC Public Health. 2017;17:334.
Isara AR, Akpodiete A. Concerns about the knowledge and attitude of multidrug resistant tuberculosis among health care workers and patients in Delta State, Nigeria. Nigerian J Clin Pract. 2015;18:5.
Luka MI, Idris SH, Patrick N, Ndadilnasiya EW, Moses OA, Phillip P., et al. Health care workers’ knowledge and attitude towards TB patients under Direct Observation of Treatment in Plateau state Nigeria, 2011. Pan Afr Med J. 2014;18 (Supp1):8.
Malangu N, Adebanjo OD. Knowledge and practices about multidrug-resistant tuberculosis amongst healthcare workers in Maseru. Afr J Prm Health Care Fam Med. 2015;7:1.
Molla Y, Jerene D, Jema I, Nigussie G, Kebede T, Kassie Y. et.al. The experience of scaling up a decentralized, ambulatory model of care for management of multidrug-resistant tuberculosis in two regions of Ethiopia. J Clinic Tubercul Other Mycobacter Dis. 2017;7:28–33.
Merza MA, Farnia P, Tabarsi P, Khazampour M, Masjedi MR. AA. V. Anti-tuberculosis drug resistance and associated risk factors in a tertiary level TB centre in Iran: a retrospective analysis. J Infect Dev Ctries. 2011;5(7):511–19.
Gebremariam MK, Bjune GA. FJ. Barriers and facilitators of adherence to TB treatment in patients on concomitant TB and HIV treatment: a qualitative study. BMC Public Health. 2010;10:651.
Suri AGK. S. C. Voices from the Field: Perspectives from Community Health Workers on Health Care Delivery in Rural KwaZulu-Natal, South Africa. J Infect Dis. 2007;196:S505–11.
Deshmukh RD, Dhande DJ, Sachdeva KS, Sreenivas AN, Kumar AMV. M. P. Social support a key factor for adherence to multidrug-resistant tuberculosis treatment. Indian J Tubercul. 2017.
Samuel B, Volkmann T, Cornelius S, Mukhopadhay S, Mitra K, Kumar AM., et al. Relationship between Nutritional Support and Tuberculosis Treatment Outcomes in West Bengal, India. J Tuberc Res. 2016;4(4):213–19.
NC. E. The making of a public health problem: multi-drug resistant tuberculosis in India. Health Policy Plan 2013;28:375–85.
Gler MT, Podewils LJ, Munez N, Galipot M, Quelapio MID, Tupasi TE. Impact of patient and program factors on default during treatment of multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2012;16(7):955–60. https://doi.org/10.5588/ijtld.11.0502 .
Article CAS Google Scholar
Horter S, Stringer B, Greig J, Amangeldiev A, Tillashaikhov MN, Parpieva N., et al. Where there is hope: a qualitative study examining patients’ adherence to multidrug resistant tuberculosis treatment in Karakalpakstan, Uzbekistan. BMC Infect Dis. 2016;16:362.
Naidoo P, Niekerk MV, Toit ED, Beyers N, Leon N. Pathways to multidrug-resistant tuberculosis diagnosis and treatment initiation: a qualitative comparison of patients’ experiences in the era of rapid molecular diagnostic tests. BMC Health Serv Res. 2015;15:488.
WHO. ENGAGE-TB. Training of community health workers and community volunteers. Integrating community-based tuberculosis activities into the work of nongovernmental and other civil society organizations. 2015.
Gerard de Vries S, Tsolova FL, Anderson AC, Gebhard E, Heldal et al. Health system factors influencing management of multidrug-resistant tuberculosis in four European Union countries - learning from country experiences BMC Public Health. 2017;17:334. https://doi.org/10.1186/s12889-017-4216-9 .
Finlay A, Lancaster JHT, Weyer K, Miranda A. M. W. Patient- and Provider level risk factors associated with default from tuberculosis treatment, South Africa: a case control study. BMC Publich Health. 2012;12:56.
Download references
Acknowledgements
We would like to acknowledge Hosanna College of Health Sciences Research and community service directorate for providing us the opportunity and necessary fund to conduct this research. Our appreciation also goes to heads of various health centers, hospitals, district health and Hadiya Zone Health office for unreserved cooperation throughout data collection.
The authors declare that this study received funding from Hosanna College of Health Sciences. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.

Author information
Bereket Aberham Lajore & Menen Ayele
Present address: Hossana College of Health Sciences, Hosanna, SNNPR, Ethiopia
Yitagesu Habtu Aweke
Present address: College of Health Sciences, School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia
Samuel Yohannes Ayanto
Present address: College of Health Sciences, Institute of Public Health, Department of -Population and Family Health, Jimma University, Jimma, Ethiopia
Bereket Aberham Lajore, Yitagesu Habtu Aweke and Samuel Yohannes Ayanto contributed equally to this work.
Authors and Affiliations
Department of Family Health, Hossana College of health sciences, Hossana, Ethiopia
Bereket Aberham Lajore
Department of Health informatics, Hossana College of Health Sciences, Hossana, Ethiopia
Department of Midwifery, Hossana College of Health Sciences, Hossana, Ethiopia
Department of Clinical Nursing, Hossana College of Health Sciences, Hossana, Ethiopia
Menen Ayele
You can also search for this author in PubMed Google Scholar
Contributions
Bereket Aberham Lajore, Yitagesu Habtu Aweke, and Samuel Yohannes Ayanto conceived the idea and wrote the proposal, participated in data management, analyzed the data and drafted the paper and revised the analysis and subsequent draft of the paper. Menen Ayele revised and approved the proposal, revised the analysis and subsequent draft of the paper. Yitagesu Habtu and Bereket Aberham Lajore wrote the main manuscript text and prepared all tables. All authors reviewed and approved the final manuscript.
Corresponding author
Correspondence to Bereket Aberham Lajore .
Ethics declarations
All methods and report contents were performed in accordance with the standards for reporting qualitative research.
Ethics approval and consent to participate
Ethical approval was obtained from Institutional review board [IRB] of Hossana College of health sciences after reviewing the protocol for ethical issues and provided a formal letter of permission to concerned bodies in the health system. Accordingly, permission to conduct this study was granted by respective health facilities in Hadiya zone. Confidentiality of the information was assured and participants’ autonomy not to participate or to opt-out at any stage of the interview were addressed. Finally, informed consent was obtained from the study participants after detailed information.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lajore, B.A., Aweke, Y.H., Ayanto, S.Y. et al. Exploring health care providers’ engagement in prevention and management of multidrug resistant Tuberculosis and its factors in Hadiya Zone health care facilities: qualitative study. BMC Health Serv Res 24 , 542 (2024). https://doi.org/10.1186/s12913-024-10911-6
Download citation
Received : 27 February 2023
Accepted : 27 March 2024
Published : 27 April 2024
DOI : https://doi.org/10.1186/s12913-024-10911-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Healthcare providers
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 17 April 2024
Breaking down barriers to mental healthcare access in prison: a qualitative interview study with incarcerated males in Norway
- Line Elisabeth Solbakken 1 , 2 ,
- Svein Bergvik 3 &
- Rolf Wynn 1 , 4
BMC Psychiatry volume 24 , Article number: 292 ( 2024 ) Cite this article
456 Accesses
Metrics details
Mental health problems are highly prevalent in prison populations. Incarcerated persons generally come from disadvantaged backgrounds and are living under extraordinary conditions while in prison. Their healthcare needs are complex compared to the general population. Studies have found that incarcerated individuals are reluctant to seek help and that they experience challenges in accessing mental healthcare services. To some extent, seeking treatment depends on the degree of fit between potential users and health services, and actual use might be a better indication of accessibility than the fact that services are available. This study aimed to explore individual and systemic facilitators and barriers to accessing mental healthcare in a prison context.
An analytical approach drawing on elements of constructivist Grounded theory was the methodological basis of this study. Fifteen male participants were recruited from three prisons in Northern Norway. Data was collected through in-depth interviews on topics such as help-seeking experiences, perceived access to services and availability of health information.
We found that distrust in the system, challenges with the referral routines, worries about negative consequences, and perceived limited access to mental healthcare were barriers to help-seeking among incarcerated individuals. How prison officers, and healthcare personnel respond to incarcerated persons reporting mental distress could also be critical for their future willingness to seek help. Providing information about mental health and available services, initiating outreaching mental health services, and integrating mental health interventions into treatment programs are examples of efforts that might reduce barriers to accessing services.
Conclusions
Facilitating access to mental health services is crucial to accommodate the mental health needs of those incarcerated. This study provides insights into the complex interplay of individual, social and systemic factors that may contribute to the utilization of mental health care among incarcerated persons. We suggest that correctional and healthcare systems review their practices to facilitate access to healthcare for people in prison.
Peer Review reports
Mental health of people in prison
The rates of mental disorders are considerably higher among incarcerated individuals than in the general population [ 1 , 2 , 3 , 4 ]. Co-morbidities are common, and around 20% of incarcerated individuals have concurrent mental and substance use disorders [ 5 ]. They are at increased risk for all-cause mortality, self-harm, violence, and victimization, and suicide rates are about 3–6 times higher among incarcerated males relative to males in the broader population [ 6 ]. Adverse life experiences and disadvantaged living conditions from an early age may explain the observed accumulation of mental health problems in prison populations worldwide [ 7 , 8 ]. Genetic predispositions combined with environmental stressors are implicated in the development of mental disorders [ 9 , 10 ]. People in prison generally experience low educational achievements, low income, and unstable housing. Thus, the poor mental health of prison populations is caused by a complex interplay of social, environmental, and genetic factors [ 7 , 11 ]. In addition to the pre-existing burdens, incarcerated individuals are facing prison–specific challenges such as loss of autonomy, social isolation, bullying and violence that may exacerbate mental health issues [ 12 , 13 , 14 , 15 ]. Considering the elevated rates of mental health problems in prison, facilitating access to mental health services is crucial to accommodate the needs of those incarcerated.
Access to mental health services
The treatment gap refers to the proportion of individuals with mental health problems within a specific community that require treatment without receiving it [ 16 ]. Variable access to mental healthcare and high levels of unmet mental health needs are universal challenges in communities across the world [ 17 , 18 ]. Even when health services are available, individual and systemic barriers may hinder their use. In a narrow sense, access to healthcare may be considered equivalent to available services. However, some argue that a more meaningful way to define access is the “degree of fit” between the potential users and health services [ 19 ]. For instance, if services are accessible in terms of transportation and treatment costs and whether they are compatible with potential users’ personal attitudes, beliefs and preferences. “Having access” can be understood as the potential for using available mental health services. “Gaining access”, is the individual process of choosing to use those services [ 20 ]. Within this frame of reference, access to services is more precisely defined by the actual use of services.
Mental health help-seeking
Across settings and populations, the majority of those suffering from mental health problems do not seek treatment [ 21 , 22 , 23 ]. The literature on help-seeking gives insight into the intrapersonal factors involved in accessing mental health care. Within this context, help-seeking has been defined as: " an adaptive coping process that is the attempt to obtain external assistance to deal with a mental health concern” [ 24 ]. The process of seeking help involves becoming aware of a mental health problem that may require intervention; articulating the psychological challenges in a way that can be understood by others; awareness of help sources that are available and accessible; and a willingness to talk about the mental health problem to available help sources [ 25 ]. Throughout the help-seeking process, personal thoughts and feelings become increasingly interpersonal as an individual confides in and seeks support from others. It is not uncommon to share mental health concerns with informal sources of support such as friends and family prior to, or even instead of, seeking professional help [ 26 ]. Moreover, informal networks are found to facilitate but may also discourage professional formal help-seeking for mental health problems [ 27 , 28 ].
The theory of planned behavior (TPB), a well-known model within behavior change research, may also provide a framework for understanding how personal attitudes and social influences are implicated in accessing healthcare. Subjective norms, attitudes, and perceived behavioral control are elements of TPB that are particularly important for understanding the help-seeking process [ 29 ]. In this context, subjective norms refer to a person’s beliefs about other peoples’ practice or approval of help-seeking and are related to expectations of social support in pursuing professional help. Attitudes refer to appraisals of seeking professional mental help as beneficial or harmful and a judgement of whether help-seeking would be constructive compared to alternative behaviors. Perceived behavioral control can be divided into self-efficacy (the confidence that one can seek help), and controllability (the extent of personal control in the help-seeking process). A recent review found that attitudes and perceived behavioral control predict help-seeking intentions across different population groups and cultures [ 30 ].
Access to mental health services in prison
Equity is essential in healthcare to ensure that the health system meets the needs of different groups of people and individuals [ 20 ]. “The principle of equivalence” is a widely endorsed standard for healthcare in correctional settings [ 31 ]. This principle is laid down in the United Nations´ Nelson Mandela Rules. Rule number 24 states that: “Prisoners should enjoy the same standards of health care that are available in the community, and should have access to necessary health-care services free of charge without discrimination on the grounds of their legal status” [ 32 ] (p.8) However, some argue that equal standards are not sufficient to meet the complex needs of incarcerated individuals and that mental healthcare in prison must be more intensive and integrative than services provided in the community [ 33 , 34 , 35 ]. In reality there are several reports of shortcomings in the delivery of mental healthcare in prison in many countries across the world, as mental disorders in incarcerated persons are underdiagnosed and undertreated [ 6 , 34 ]. Studies from Canada, the US, and the UK indicate that a significant proportion of incarcerated people with mental health problems have not received adequate treatment [ 36 , 37 , 38 , 39 ]. Suggested explanations for unmet needs are underfunding, failure in screening procedures and quality at reception, demand for more mental health knowledge among prison staff, and possible underrating of the severity of mental health problems by the prison administrations to reduce treatment costs [ 36 , 37 , 38 , 39 , 40 ]. Taken together these reports suggest that mental health services do not fit the complex needs of incarcerated persons in high-income countries. There is less knowledge about the situation in low- and middle-income countries. However, the elevated rates of mental disorders in these countries suggest that unmet needs among incarcerated persons are a widespread challenge [ 1 ].
Mental health help-seeking in prison
Evidence suggests that the immense burden of mental disorders among people in prison is not matched by a proportional use of mental healthcare [ 41 ]. Several reports from various correctional settings have documented that incarcerated persons are reluctant to seek help for mental health problems [ 41 ]. Among the reported barriers to help-seeking in prison are confidentiality concerns [ 42 ], fear of stigma associated with a diagnosis [ 43 ], a preference for self-management or informal support [ 44 ], lack of knowledge of psychological services [ 42 , 44 ] and distrust in the system [ 45 ]. In addition, systemic factors may influence access to healthcare in prison. The culture in all-male prisons typically demands that those imprisoned mask their vulnerabilities by adopting a tough and dominant demeanor [ 46 ]. Experiencing mental illness and receiving professional mental health treatment is also associated with an increased risk of victimization in incarcerated individuals [ 47 ].
Mental health literacy (MHL) is a concept that includes the knowledge and attitudes that influence how people manage their mental health needs [ 48 ]. Having sufficient knowledge and access to information about mental health and mental health services can be a prerequisite for seeking professional help [ 49 ]. For people living in the community, seeking online information and advice is an important strategy for gaining knowledge about how to cope with mental health challenges [ 50 , 51 , 52 ]. For security reasons, access to the Internet is typically severely limited for those imprisoned [ 53 , 54 ]. Hence, this essential mental health information source is largely unavailable to them. Accordingly, incarcerated individuals are reliant on finding mental health information through information pamphlets, books, TV programs, newspapers or consulting healthcare professionals [ 55 ]. Some argue that limited access to online information and digital health services may have consequences for the well-being and successful rehabilitation of those incarcerated [ 53 , 56 , 57 ]. Thus, there are reasons to believe that restricted access to mental health information may also affect help-seeking and access to healthcare for incarcerated individuals.
The rationale for the current study
Fostering health-promoting environments and adequate access to mental healthcare within prisons is a public health imperative increasingly acknowledged in the literature [ 33 ]. Moreover, the mental health of incarcerated persons is a matter of public safety since untreated severe mental disorders are associated with a higher risk of recidivism [ 58 , 59 ]. People in prison retain their right to health services, and in principle, incarcerated persons have access to mental health services. A vital question, however, is how incarcerated persons experience gaining access and how this affects their actual use of services. Existing research on the provision of mental healthcare in prisons, particularly within a Scandinavian context, is sparse, leaving significant knowledge gaps. The question of access to health information for incarcerated persons is similarly understudied. This study aimed to investigate how incarcerated persons experience individual and systemic factors that facilitate or impede access to mental healthcare in prison.
The Helsinki Declaration of Medical Research involving human subjects and services laid the basis of the ethical considerations of this study [ 60 ]. The study was approved by the Data Protection Officer of the University Hospital of North Norway (No. 02415). The Norwegian Correctional system, which is responsible for the welfare of incarcerated individuals, approved of the study (Ref. 200900463-347). The Regional Health Research Ethics Committee concluded that the project was outside their mandate (Ref. 40,701).
The principles of voluntariness and informed consent are central to human subject research. Individuals in prison are considered vulnerable due to their restricted freedom and autonomy, poor health status, higher incidence of learning disabilities, and lower literacy levels. Consequently, additional precautions are required to ensure that research with incarcerated participants is conducted ethically [ 61 ]. User participation in designing research that includes vulnerable groups is crucial to achieving this objective [ 61 , 62 ]. Measures in accordance with recommendations were taken to ensure consent information that is complete, relevant, and understandable [ 63 ]. A user representative from Way-Back, an organization that supports incarcerated persons with reentry to their communities, contributed to the project’s planning. The user representative provided input on information about the study, research questions, the interview guide and how to conduct the interviews. The input was used to tailor information and for conducting the interviews in accordance with the constraints of the prison contexts and the needs of the incarcerated individuals. The choice of whether to reimburse participants in prison studies is debated. Because of the relative deprivation of prison life, some argue that even small incentives could potentially result in undue influence for participation in research [ 64 ]. For this reason, we chose to abstain from offering reimbursement for the participants in this study.
Study context
At any given time, about 3000 persons are serving a sentence in Norway, of which 5.6% are women and 26.2% are non-Norwegian citizens [ 65 ]. A recent study found that almost 60% of incarcerated persons in Norway had a diagnosed mental disorder, together with a 33% rise in the one-year prevalence of mental disorders between the years 2010–2019 [ 66 ]. Thus, the proportion of people with mental disorders entering prison has been increasing. In Norway, access to necessary healthcare is considered a basic human right and is legislated in the Patient’s Rights Act section 2 [ 67 ]. Healthcare is primarily tax-funded, with a nominal service fee and a relatively low cap on yearly individual costs [ 68 ]. Norway has committed to “the principle of equivalence” meaning that those imprisoned retain their right to healthcare equal to that of the general population [ 31 ]. Prison health services serve incarcerated persons with milder mental health problems and are accessible by self-referral through a paper-based request system. The prison health services can refer those who experience moderate to severe mental disorders to specialist mental health services, and treatment is often provided in prison by mental health professionals from local hospitals For people imprisoned in Norway, healthcare and medications are free of charge [ 69 ], eliminating one significant barrier to mental healthcare access [ 70 ]. Furthermore, as the municipalities and local hospitals provide health services - the importation of services promotes equity and that services are independent of the correctional system, thereby strengthening the rights of people in prison [ 71 ].
A study found that incarcerated persons in Norway were reluctant to seek help for mental health problems from prison health services unless they had concurrent sleep or substance use problems [ 72 ]. A survey by Bjørngaard et al. [ 73 ] found lower patient satisfaction with prison health services compared to people using community health services and that those with mental health problems were less satisfied compared to incarcerated patients with other health challenges. A survey representative of the Norwegian prison population found that 20% of incarcerated males sample reported that they had received mental health services, while 25% reported that they had been in need of mental health services in prison but had not received any [ 11 ]. More recent reports suggest that mental health services are insufficient to meet the needs of those imprisoned in Norway and that incarcerated individuals referred due to their severe mental illness may not be admitted to specialist services for in-patient assessment and treatment [ 74 , 75 ]. These reports indicate that mental health services do not fit the complex needs of incarcerated persons in Norway and that there are potential obstacles in their access to mental healthcare.
Study design
This study was underpinned by relativist epistemology which is based on the assumption of multiple individual realities that allow for different understandings of the same phenomenon [ 76 ]. The study design was suitable for exploring and explaining commonly experienced individual, social, cultural and structural factors that influence help-seeking and access to mental healthcare for incarcerated individuals. The study incorporates vital Grounded Theory (GT) components, including initial coding, categorizing data, constant comparative methods involving inductive and abductive reasoning, and memoing [ 77 ]. The use of theoretical sampling, which is rare in prison research due to ethical and practical constraints [ 78 ], was not employed in this study. Data collection concluded once additional data no longer contributed new insights or further elaborated the developed categories.
Preconceptions
The first author, a clinical community psychologist and a PhD student, worked part-time as a prison officer for two years during her psychology education. This experience gave her an insider’s view of the correctional system, inevitably influencing her initial perceptions. Before conducting the interviews, she held a somewhat optimistic view of the correctional system’s capacity to support and enhance the mental health of those incarcerated. However, this perspective was challenged through the narratives of the study participants, who conveyed powerful personal accounts that highlighted substantial barriers to obtaining mental health services within the prison environment. The other two authors, serving as supervisors, are also researchers and mental health professionals with considerable clinical experience. Their diverse backgrounds contributed to a supervisory dynamic that adresssed the research topic’s complexities. Throughout the study, the authors engaged in a process of collaborative reflection, concerned with maintaining a balance between engaging with participant stories and sustaining a critical stance towards the data. These discussions were essential in helping the first author navigate an empathetic understanding of the participant’s experiences with the necessary analytical objectivity required for rigorous qualitative research.
Participants and study settings
Fifteen males serving a prison sentence were recruited from three prisons in Northern Norway. Thirteen of the participants served a sentence at a high security level, while two served at lower security. The participants’ age ranged from the early twenties to the late sixties (M: 43.6 years). Two participants had other nationalities, while the rest were Norwegian citizens. Further details about the participants must be withheld to preserve their privacy. When citing individual participants, they are anonymized by using pseudonyms.
Recruitment
Participants were recruited through posters in the prison ward that conveyed basic information, including the fact that the interviews were confidential and would be recorded. The posters encouraged those interested in participating to approach a contact person for more information. A prison officer, a social worker or a reintegration coordinator were assigned the role as contact persons in the selected prisons. Those who actively approached the contact person were given more comprehensive written information about the study. Requiring an active choice by incarcerated individuals was done to enhance their experience of self-determination and autonomy in their decision to participate. The contact person scheduled appointments with the participants, and the interviewer had no prior knowledge of the participants other than what they presented in the interviews. One potential participant cancelled the interview appointment due to health issues on the interview day and withdrew from the study.
The first author conducted face-to-face, in-depth interviews. The interviews took place in prison visitation rooms or in an office in the health wards. Before the interview, the participants were given information about the study and their rights as research participants and signed a written consent form. The interviewer was alone with the participants during the interview and had a personal alarm as a safety precaution. The interview guide covered topics on knowledge of mental health and available services, help-seeking experiences, and access to mental health information (sample questions provided in Table 1 ). The participants were asked open-ended questions and were invited to speak freely on these topics. Thus, the order and framing of questions varied depending on where they fit into the participants’ narratives. This allowed for following up on the participants’ experiences and may have given the participants an increased sense of control in the interview. The first author who conducted the interviews was attentive to signs of emotional discomfort in participants and avoided pressure on sensitive topics. After the interviews, the participants were encouraged to ask questions and comment on their experience and reminded of their right to withdraw from the study. Nearly all the participants expressed that the experience of participating in the study was positive and that they appreciated the chance to contribute to the research project.
The first author transcribed the audio-recorded interviews in Norwegian, ensuring a verbatim account of the participants’ narratives. The initial eight interviews were transcribed before initiating data analysis. This early examination of the data facilitated a refinement of the interview guide, which was then applied to the subsequent seven interviews to deepen the inquiry. Data collection and analysis were concurrent as the study progressed from the ninth interview, which allowed for immediate integration of new data into the evolving analytical framework. The data was examined using the NVivo 12 software, which supported the systematic organization and analysis of the data. The data was analyzed line-by-line, searching for incidents in the form of recurring beliefs, actions, experiences, and explanations [ 79 ]. The constant comparison method was applied throughout the analysis. In the initial coding phase, incidents were compared to incidents, and through this process underlying recurring concepts and similarities were identified and assigned codes. Subsequently, codes were then compared to codes, and related codes were organized into conceptual categories, reflecting both common features and divergent viewpoints [ 77 ]. In the intermediate coding phase, the data was abstracted into categories which were compared to each other, and relationships between categories were developed and refined. The authors engaged in a collaborative and reflective dialogue throughout this process, meeting regularly to deliberate on preconceptions, the emerging categories and their interpretations. This dynamic exchange was informed by memos that captured analytical decisions, insights, and evolving interpretations, thus guiding the reflective process. In the last stage, advanced coding, a core category which binds the other categories and sub-categories together was developed. Through a collaborative process the categories were substantiated with representative quotes, which, upon completion of the analysis, were translated from Norwegian to English for inclusion in the report. This resulted in a nuanced understanding grounded in the participants’ experiences and the researchers’ interpretative lens.
The data analysis yielded four main categories illustrating the participants’ active engagement in identifying challenges and facilitators for mental healthcare access within the prison environment. The first category, “Mental health awareness,” captures how beliefs and knowledge concerning mental health were influenced by the experiences and constraints inherent to prison life, potentially affecting the pursuit of help and access to healthcare services. The second main category reveals how systemic sub-cultural values can obstruct healthcare access, whereas, on a personal level, fellow inmates served as vital support for obtaining mental health services. The third main category, “Access to mental health care,” examines how organizational and systemic barriers impede access to mental healthcare. The final main category, “Enhancing access to services,” delineates factors that lowered the bar for mental healthcare access. The core category, “Breaking down barriers,” encapsulates the dynamic interplay between incarcerated individuals and the contextual factors that influenced their ability and willingness to access mental healthcare in prison. This central theme also recognizes the collaborative effort between participants and researchers in identifying problem areas and solutions to mental healthcare access, thereby “breaking down barriers”. An outline of these categories is presented in Table 2 .
Mental health awareness
An information void.
Seeking information can be an essential first step for recognizing symptoms of mental illness that may require intervention. Prior to imprisonment, visiting their general practitioner or using online search engines were the preferred methods for finding health information for the participants in this study. In prison, however, access to the Internet is severely limited:
Where can we get information? We do not have access to computers or anything. So, I would have to call someone on the outside to get them to print articles and send them to me by post. So, no. We don’t know our rights, we don’t know about the services available to us, as a matter of fact we know very little. There’s an information void. Stuart
A few of the participants referred to the prison library as a source of information. Some also said that they could talk to health care professionals, correctional officers, or other staff members like the priest, to get mental health information. Fellow incarcerated individuals who had experienced mental health problems and received health services were also mentioned by some participants. The common thread in all suggestions was a dependency on others to access information about mental health. Only a couple of participants had tried to find mental health information during their time in prison. However, they found it difficult to obtain:
The only choice I have is to ask the prison officers to print it [mental health information], but sometimes they don’t want to do it because they think it’s bad. And I have tried to search for psychosis and such in school [in prison], but then the teachers ask why I would seek out such a gloomy subject. It feels a bit complicated to obtain information. Larry
Participants from all three prisons also pointed out the need for more information about mental healthcare in prison:
We have a notice board on the ward (…). The information should be hung there for people to see, that there is a psychologist here, and that you can talk to her. ‘cause I’ve seen little of that sort in here. Liam
One participant underscored that information about available mental health services is particularly important for those with no experience from such services prior to imprisonment:
It [information] must tell you about your opportunities. To normalize it [seeking help] in a way. And the threshold must be low. I think many experience that it is too high. If I hadn’t been in contact with mental health services before I came here, the threshold for seeking help would have been sky high for me as well. Neil
Awareness of mental health issues
Factors in the prison context were fundamental to the participants’ explanations of mental health problems. Many participants attributed the onset or worsening of mental health problems to the shock of imprisonment and to the continuous hardships of prison life. Understanding symptoms as primarily caused by external stressors such as prison hardship may have influenced their appraisals about the need to seek help. As Frank stated:
I’ve always had good mental health. Until I came here, inside these walls. Frank
Frank reported considerable symptoms of post-traumatic stress. Understanding his symptoms as something triggered by the prison living conditions, he did not see how seeking professional help could benefit him. Like many other participants, he insisted that the correctional system needed to change and had lost hope that he could improve his own situation.
In contrast, other participants who attributed their mental health problems to external stressors concluded that they indeed needed help to cope. The suffering they experienced during their first weeks in prison motivated them to seek formal help:
I asked to talk to a psychologist in here. ‘Cause, I felt that I needed to. ‘Cause in the beginning when I came here, it all seemed dark. No matter how hard I tried to do the right thing, there was some sort of dark force that was just pushing on, and the obstacles were piling up. Travis
For some, their main motivation for seeking help was to receive professional validation from healthcare personnel regarding the negative health consequences of their prison experiences. Some also hoped that healthcare professionals could advocate for better living conditions:
And it is good that others [psychologists] can take part in these things. So that it is manifested what prisons actually do to people. Jack
Social influences on help-seeking
Prison culture and mental health stigma.
The participants described how the culture within prison influenced their willingness to talk about mental health issues. The importance of appearing strong and dominant within the prison setting was emphasized by many. According to several participants, the talk at the wards was characterized by attempts to one-up the others’ stories about criminal activities to appear tough. Many also explained that hiding vulnerabilities was critical in the prison community, and some also underlined the potential for victimization for those who were not able to conform to the prison norms:
You are wearing a prison mask. You cannot show weakness. ‘Cause then you’ll soon be a victim, a sitting duck. I have experienced inmates that have, eh mostly stayed in their cells. They have been harassed so badly that they are sitting there crying. The prison milieu can be tough. Neil
Choosing to confide in and seek advice from peers can also have negative consequences. Several of the participants said that it was wise to be careful with who you chose to share mental health related issues with:
Let’s say you talk about your personal feelings, and about your sentence and stuff, right. They can be very nice to you there and then, before they stab you in the back later on, spreading everything you’ve said to destroy you. It is a cynical game. Bobby
Bobby went on to explain that a fellow incarcerated individual could use personal information for harassing, blackmailing and threatening the family of someone who has confided in them, if a conflict should arise. Some of the participants also addressed directly how the prison climate may influence willingness to seek mental health treatment:
They do not want to go to a psychologist and talk. Because then they are seen as weak and not able to cope. Because in prison everyone should be tough. Drug lords and such. But, on the inside they are not like that. Nicky
The role of peers in accessing mental health services
Despite the clear barriers, fellow incarcerated appeared to be an important informal help source for mental health problems. Many of the participants had observed signs of emotional distress among their incarcerated peers and described how they had given them advice and encouragement. According to several participants, those imprisoned also had an essential role in recognizing mental health problems in their peers:
There is no-one who talks to us regularly to check on how we are doing. That’s not a priority here. So, unless some of the inmates take on the role of an officer or a psychologist, then there’s no-one who reports concern (…) There are many inmates who are taking on a role as a social worker, but it’s kinda wrong. They are neither paid for it, nor qualified. They do it because no-one else does. Stuart
Although none of the participants said that they themselves had been prompted to seek help by peers, they told stories of how they had pushed their peers to seek formal help:
A fellow inmate. I could tell he was struggling because he talked to me as the only person. In a way, I was his psychologist. The days when he was down in the dumps, I tried to talk to him (…) And I said, listen up. It’s for your own good. I will write a request form, and we will arrange contact with a psychologist (…) and it will help. Nicky
Experiencing fellow incarcerated people in distress appeared to be common, and participants also explained how they reported to prison officers their concerns about peers with self-harm and suicide plans:
There was a fella’ who told me that he knew exactly how to take his own life (…). “I’ll just do it like this and this and this”. And, uhm. Then he said he was going to do it. And I thought that I would have to report it, and I did. Roy
Roy went on to describe in detail how his reported concern led to a prison officer interrupting the suicide attempt by the fellow incarcerated, thereby saving his life. Several other participants shared similar stories, indicating that peers played a significant role in recognizing and getting help for mental health related problems in prison.
Access to mental healthcare
Self-referral and disempowerment.
In order to access prison healthcare, those imprisoned must write and deliver a paper-based request form. All the participants in this study were aware that this is the way to contact prison healthcare, and most of them knew that the general practitioner working at the prison could refer them to a psychologist or to a psychiatric hospital. Unfortunately, the request form system seemed to amplify the participants’ perceptions of disempowerment. Rather than seeing themselves as agents taking charge of their own situation and health, they were left passively waiting to be contacted after filling out the forms:
You are pacified when you must write a request form to talk to someone. Then you don’t know when they are coming to talk to you. And then it’s like, the problem may be swept under the rug when they finally get to you. Tommy
According to the participants, many of these request forms seemed to disappear, and it could take an exceedingly long time before they got any response to their request:
Many times, when you write a request form it disappears. Nothing happens. Those request forms are worthless most of the time. Keith
There were also several participants who voiced concern over the confidentiality of the request forms even when the forms were delivered in closed envelopes:
We can see for ourselves that they [prison officers] open and read, uhm, confidential information, [lowers his voice] and to put it mildly, uhm, breaches in confidentiality are all too common. It is alarming! Neil
One of the informants also explained that incarcerated persons who had mother tongues other than Norwegian could have problems with understanding and filling out request forms to health, and that forms that were not filled out correctly were of no value. According to Roy and other participants, the correctional system did not give sufficient information and guidance about the request forms:
They might not know how to write, or understand what it [the form] says, you know? Potentially it is severe for that guy, right. It’s garbage! Garbage, that request form. They haven’t received any request from him. Roy
The perceived availability of mental healthcare
The perceptions of accessibility of mental health care varied between the participants. A few of the participants were in active treatment with a psychologist at the time of the interviews, and they had experienced the access as unproblematic. Common for some of these participants was that they had been in treatment before they entered prison:
From sending my request and to receiving an acceptance letter it took one and a half weeks. Less than three weeks later I was in treatment. It was efficient. Much quicker than I’ve ever experienced before. Neil
However, many participants said that they could not access secondary mental health services. There were two notable sub-groups among the participants who perceived that access to specialized psychological treatment was limited. The first group shared stories about living unstructured lives at the edge of society. They seemed to have little confidence in health care and correctional services, and were less hopeful of their own potential of being rehabilitated:
I have tried for several years now, but I didn’t get help. They can say whatever they want about how easy it is to access a psychologist and prison healthcare and everything, but it is not true. Ronny
Two of the participants explained how they would have to take drastic measures such as performing violent acts or acting weird to get help for their mental health problems When Marlon was asked how he could access mental health services he responded:
You would have to either hurt yourself, or someone else, so that they end up in hospital. Marlon
The interviewer asked if it was possible to access mental health services by using less drastic measures, Marlon answered:
Uhm. Naaah. I don’t know. I do not think so. Not from my experience. Marlon
Another sub-group having difficulties accessing mental health services was those in prison for the first time. Most had led more typical lives with stable employment and housing conditions before imprisonment. When they sought mental health services, they were told that these adjustment problems were normal in prison:
I’ve been struggling for several periods here and have said that I wanted to talk to a nurse or a psychologist. And then I was referred to a psychologist. And the psychologist assessed me, and said that: “Nothing’s wrong with you, you are just having a hard time, I cannot help you”. So, you do not get anyone to talk to, unless you- I don’t know what you must have really, but I sure ain’t got it. The nurses say that they haven’t got the time, and the psychologist says that I am not ill. And then I am left to feel bad. In my case, there is no service really. Stuart
Prison officers’ role in mental healthcare and accessing services
Several participants stated that mental health problems and well-being were not high on the prison agenda. Many would have appreciated it if correctional officers on a more regular basis had asked how they were doing and believed that this would have facilitated them to open up and talk about mental health issues.
In my opinion, mental health is forgotten here in a way. Physical activity, movement, workouts, yes. Since I arrived here some months ago, only twice I’ve been asked: “Hi, how are you? Is there something you want to talk about?” Travis
Some also said that they knew people in prison who were unaware of their own need for mental health care or unable to access help, and argued that the correctional system should do more to help these people to access care:
You have the type where people do not get help because they themselves are not able to request help from the prison health services and the prison officers do not see to that they get the help they need. Neil
Some were concerned about how acute health problems were handled in the weekends and evenings when prison health services were unavailable. In these situations, prison officers were left to decide whether or not to contact emergency healthcare services. Several of the participants were not satisfied by this arrangement:
(…) they think that they can make a doctor’s judgement. That they can decide that it is not that important. It is rude. It is trespassing norms. Jack
Some participants told stories of how their peers in prison did not seem to get the help they needed even though it was apparent that they were in a bad state mentally:
I have reported concern about people, before they started cutting themselves and f***ing themselves up. But what worries me, is that even though I voiced my concern to both prison health services and prison officers, no measures were taken. Before it was too late. Stuart
Asking for help from correctional officers could also have consequences. Ronny served at a lower security level. He experienced that his requests to see a psychologist were met by suggestions of transferring him to a higher security level:
I have written request forms: “I need to speak to a psychologist. Immediately”. And then they [the prison officers] are threatening me by saying that they are going to transfer me to a higher security level. They ask if I am going to hurt myself. No, I tell them. I’m not going to hurt myself. I just need to talk to a psychologist. Ronny
Another participant described how he had sometimes cut himself by shards from plates and drinking glass to suppress mental suffering. He explained how he on one occasion used the intercom to notify the officers that they needed to come and pick up a glass that was triggering an urge to self-harm. The participant said that initially a single officer came to his cell to pick up the glass:
A few minutes later there were four officers, and they unlocked the cell door, and there were a lot of questions. I guess they were worried about my mental state, and I said that I appreciated the concern. Then I reminded them that I had asked them to pick up the glass so I would NOT cut myself, so if they were to use that against me, it would be unfair. Tommy
He reassured that the situation had been resolved with the conversation. However, he had the impression that disclosing mental distress to officers could increase the risk for being transferred to a higher security level, or to a security cell.
Enhancing access to services
The perceived advantages of seeking professional help.
There were some commonly experienced benefits of seeking mental healthcare among the participants. Coming off drugs and living under stable conditions in prison provided some participants an opportunity to reflect on their lives and to gather motivation to work on their addiction and mental health problems:
I have been thinking a lot about treatment in an institution. I know how it went the last few times I got out [of prison]. Within half an hour I was sitting there with the needle. And if I don’t do anything before I get out, the same will happen again. I’m trying to prevent it (…) I’ve had treatment for drug and alcohol use before. And back then there was a psychologist who said that, once you’ve been clean for a year, then the brain is back to normal. I can feel it, like, my mindset is already changing . Kurt
For about half of the participants, seeking professional help was related to their motivation for living a law-abiding life after prison. The participants linked substance use to both mental health problems and a criminal lifestyle, and getting treatment was seen as essential for preventing recidivism:
I have lived a rough life, and I have no-one, NO-ONE. How long am I going to live? One doesn’t know. But I’ll be fifty soon. So, I must make it now. I really have to make it now [his voice bursts]. And it depends on many psychological factors. So, I’m choosing to use all the things that I have access to in prison, like treatment for drug addiction. Roy
Although many had previous experience of treatment for their substance use, they still had hopes that treatment could help them. Liam had previously experienced that consultations with a psychologist brought up subjects that was difficult for him to talk about:
I regret that I quit, because it could have done me good. But I guess it got too personal, and it stirred up things. Liam
He also explained that at the time he was more interested in doing drugs than going to therapy. However, he still believed that treatment could help him:
I will probably contact a psychologist, now that I’m about to get treatment for my addictions. It is easier to open up when there are no substances involved. Liam
In summary, seeking professional help for mental health problems was perceived to promote in-prison coping, rehabilitation, and preparation for life outside of prison for most of the participants.
Lowering the bar for accessing mental health services .
Many of the participants expressed skepticism towards ‘the system’. They described how they had been let down and disappointed by the child welfare services, the criminal justice system, and healthcare professionals. Experiences from childhood to adult life had led to a lack of confidence that healthcare personnel and the correctional system and society had their best interest at heart. For them, it was important that healthcare professionals were perceived as genuine and “on their side”:
The experience of being believed and listened to… They do not have to relate, to say that they understand so damn much, ‘cause that’s not really important. Marlon
Several participants said that barriers for talking about mental health were reduced when healthcare personnel reached out in the prison ward. One of the prisoners described two nurses who used to visit the prison wing every day at lunch-hour. He appreciated that it was possible to request a private conversation in the cell, and that he was taken seriously:
They were highly skilled. And they listened. They listened to what you had to say, and they understood you. Tommy
Having previous positive experiences of mental health treatment and knowledge of what to expect from mental health services also seemed to reduce barriers for in-prison help-seeking from some of the participants:
I saw a psychologist on a regular basis, once a week (…). And after six consultations I was past the worst in some sense. I was provided with the tools I needed to cope. Bobby .
This participant had experience with psychological treatment outside of prison and had tried to access mental health services for months in prison. However, he believed his challenges were too mild to get help from a psychologist. He emphasized the need for available low-threshold services for those who suffer from milder mental health problems:
It should be available for everyone who wants it. It should not be embarrassing, it should not be taboo, it should be… A natural part of it, really. Bobby
In addition, when services were provided as standard procedure and a natural part of rehabilitation, they were perceived as less stigmatizing. Nicky described how he was placed on a prison ward that was specialized in substance use treatment:
And when you are placed in that ward, then you are automatically assigned to a psychologist from the substance use clinic, that you can have weekly consultations with. Nicky .
Some also suggested that the systematic screening and assessment of health and social problems also could facilitate access to mental health services and this was suggested as an integral part of healthcare and rehabilitation in prison by some of the participants. Ronny underscored the importance of proper assessment:
What is this person’s problem? Why did he come back? Is there something happening to him on the outside? Could he need help with anything? Maybe someone should ask him? Ronny
Ronny went on describing the nice brochures of the correctional system, with promises of assessment of strengths and needs of individuals, but he claimed that this did not happen in reality. This view was shared by several of the other participants, as they called for more assessment to benefit the mental health and rehabilitation of incarcerated individuals.
Mental health support from different sources
The participants had different preferences regarding where to get help. Support from friends and family was seen as important for most of the participants. However, health professionals could sometimes be preferred over informal or semi-formal sources because of their role in advocating for better living conditions in prison:
I get visits from my family, but I’d like to talk to someone here in prison, so that they could gain awareness of the actual problem. If I’m spitting venom to some random lady that is here as a volunteer with the Red Cross, it’s useless, I think. If I talk to a nurse who works here at this establishment, she could perhaps do something about some of our challenges. Stuart
The cultural competency of health care personnel could also be a key factor in promoting help-seeking and forming a therapeutic alliance with people in prison. Many incarcerated individuals have lived on the edge of society, while most health care personnel, and particularly doctors and psychologists, are from the upper middle class. These cultural differences may form an abyss between the incarcerated individuals and mental healthcare personnel:
A psychologist does not have a criminal record. Now I’m generalizing. But they have performed well in school. Have passed through the system. Highly educated. Their lives have been smooth sailing (…) They have not experienced the shadow side of life. Tommy
This participant had one prior positive experience with a psychologist, but his general impression of psychologists was that they were of no help. He did not feel a connection with any of the others and had written them off completely. He preferred talking to a representative from a user organization who have led a similar life to himself:
I know that they know exactly how I’m feeling. They have served a prison sentence. And they… They have lived experience, and then it’s much easier to listen to what they have to say, because I know it’s not knowledge that they have acquired through reading. Tommy
Prison officers can also be of help to incarcerated people who experience mental health problems. Nicky said that while he was at a lower security level, he had been to a sports event outside prison with an officer and some fellow incarcerated. He had a panic attack because of all the people who kept arriving at the venue and he had to go outside for some fresh air. The prison officer followed him and was understanding, and told Nicky that he had seen many incarcerated people with similar reactions:
He was understanding and said: It will be OK. After that day at the match, coincidently, he ended up being my primary contact officer. And to socialize me back to society he fixed it so that every weekend he was working we could go to a shopping mall, to try. Little by little, by little. (…) It helped. It did. Yes. Nicky
Although Nicky had no plan to seek help for his anxiety symptoms, he appreciated the support he received from his primary contact officer.
Bobby, on the other hand, had some informal support from fellow incarcerated and had also talked with a priest. He said that he often ruminated when he had time alone in his cell and emphasized his need for sharing his thoughts with others and receiving advice. He explained why he preferred to get help from formal sources:
So, to have someone who is an outsider. Who’s not an inmate. Who has got a sensible outlook on life, that can guide you– I think that’s important. (…) Because when you talk to a fellow inmate, then… It can go in the opposite direction, right. Because many have been through major crises, they have lost friends, they have lost family, maybe they have lost their girlfriend and wife, their children won’t speak to them, right? Bobby
Most participants also held the prison priests in high regard and appreciated the availability of the service. However, talking with a priest was not seen as a replacement for a consultation with a psychologist:
It was peculiar, when I asked for someone to talk with, the priest was offered first. For me it is alright, I go to church. But I’m thinking, if someone is not a Christian. I’m like: a priest? Or if you’re not religious. A session with the priest is more like a consultation towards God and his will. He can be a good listener [the priest], but you might not get the help you need in a mental sense. So, a psychologist, a “talking person” in prison is necessary. That could check on you sometimes.
This study’s findings demonstrate that many of the factors deciding access to mental healthcare are firmly rooted at the organizational level of the correctional and healthcare systems. Prisons in the Scandinavian countries, including Norway, are presumptuously humane compared to harsher correctional settings in other parts of the world. One could assume that these favorable conditions would be more conducive to mental healthcare access. However, the systemic barriers we found largely overlapped with challenges reported in other countries [ 42 , 43 , 44 ]. In addition, we found that individual beliefs, attitudes and aspirations also influence willingness to seek mental healthcare. Interestingly, most of these intrapersonal factors are tightly interwoven with the participant’s appraisals of how the prison conditions influence their mental health. This study also addresses an important knowledge gap in the literature, namely how restrictions on access to mental health information could influence mental health help-seeking for people in prison. The identified core category, “Breaking down barriers”, reflects an overarching focus on solutions to improving mental healthcare access based on the experiences of the participants in this study.
Access to health information
Knowledge of available services and how to access them is a prerequisite for mental health help-seeking [ 80 ]. The participants in our study claimed that information about mental health services was unsatisfactory, and lack of such information has also been noted as a barrier to help-seeking in other prison-based studies [ 44 ]. Moreover, sufficient levels of mental health literacy are positively associated with increased intentions for help-seeking from both informal and formal sources [ 81 ]. The participants in our study reported severely restricted access to their preferred sources of health information and a dependency on others to obtain such information. Since information seeking may occur before individuals are ready to share their health concerns with others, having to rely on others for accessing information is a potential barrier for recognizing mental health problems [ 25 ]. Thus, it is likely that the limited access to mental health information negatively impacts incarcerated persons capacity to manage their own mental health needs. The potential consequences of restrictions on access to health information among people in prison need more research attention. However, findings from other populations suggest that closing the apparent health information gap could be an important intervention for improving help-seeking for mental health problems [ 82 , 83 ].
The social influences on accessing mental healthcare
The participants reported that prison culture reduced their willingness to seek support from fellow incarcerated and the use of professional help for mental health problems. The TBP element “subjective norms” posits that beliefs about the opinions of others may influence the willingness to seek help [ 29 ]. Attributing mental health problems to personal weakness may reflect a stereotyped attitude involved in stigmatizing mental disorders [ 84 ]. Stigma may lead to concerns about what others might think if one were to seek help, and may delay or hinder help-seeking efforts [ 80 , 85 ]. It also seemed to be an important constraint to mental healthcare access in our study. This corresponds with findings from other studies [ 45 , 46 , 47 ] and suggests that fear of appearing weak is also a significant barrier to help-seeking in a Scandinavian prison context. Based on our findings and recommendations, we advise that focus on health education and normalization of mental health problems are measures that could decrease stigma [ 86 ], and increase willingness to seek mental health support and treatment among people in prison.
Although the culture among those incarcerated was perceived to discourage seeking support for mental health problems, fellow incarcerated also played a key role in supporting those who experienced mental health problems. They were more available than other help sources and had lived experience with distress related to imprisonment. Since information about available services was insufficient, fellow incarcerated were also perceived as an important source of information. Thus, naturally occurring peer support seemed to normalize mental health problems, possibly reducing stigma and lowering the threshold for mental health help-seeking. From the literature, we know that peer-based health interventions is effective in correctional settings [ 87 ], and formalizing peer-based health information and support could be beneficial in interventions aiming to increase the use of mental health services.
Beliefs and motivations for help-seeking
The prison environment was embedded in the participants’ beliefs: attributing the onset and worsening of mental health problems to the prison conditions was common among the participants. According to the Theory of Planned Behavior (TPB), attitudes about the potential benefits of help-seeking and alignment with individual goals affect the readiness and willingness to seek professional help [ 29 ]. Our data supported this notion. Some participants abstained from seeking professional help as they did not see how it might benefit them in their goal of improving their living conditions. For others, a prominent motive for seeking professional help was to receive validation and help managing their challenging life situations and the everyday stressors of prison life. A few participants also framed mental health help-seeking as a mission to document the consequences of imprisonment. By sharing their experiences with professionals, they hoped healthcare personnel could help them advocate for better conditions in prison. Obtaining sufficient knowledge about essential aspects of prison life is essential for health professionals working in a prison setting [ 88 ]. Based on our findings we propose that the ability of healthcare staff to communicate their understanding of the influence of prison living conditions on mental health is crucial for gaining trust and building an alliance with their incarcerated patients.
Another important motivator for many participants seeking help was their aspirations to live a law-abiding life after being released. It has been increasingly recognized that the relationship between mental disorders and criminal activity is complex and that integrated treatment that addresses both criminogenic factors (i.e. antisocial attitudes and behavior, substance use, criminal network, family issues and low educational/vocational engagement) and mental health issues is a must to prevent recidivism [ 89 ]. This view corresponds with the beliefs and preferences for rehabilitation and healthcare of several participants in our study. They were worried about their reintegration into society, which motivated them to seek professional help. Substance use treatment, in particular, was seen as essential to attaining rehabilitative goals. However, some participants who had served multiple sentences were less positive towards help-seeking. They had more negative experiences and seemed less hopeful that mental healthcare could improve their situation. Their low expectations for potential gain combined with a perceived lack of personal control in the help-seeking process, appeared to stall help-seeking for these participants. We suggest that implementing health services with a concurrent focus on addressing both criminogenic needs and mental disorders could be especially important for fostering healthcare utilization for people with a history of reoffending.
Organizational barriers to accessing mental healthcare
The perceived challenges with the paper-based request system were considered a significant barrier to healthcare access. TPB postulates that behavioral control and self-efficacy are important in help-seeking [ 29 ]. In a system where autonomy is limited, one could assume that a self-referral system can be empowering for those seeking help. However, the participants seemed to experience the opposite as they were left passively waiting for an answer to their request. Some also expressed confidentiality concerns, as they believed that prison officers read the request notes. Thus, the process of accessing health services seemed to diminish, rather than enhance their notions of control and self-efficacy. Improving the reliability of responses to requests and ensuring confidentiality could increase the experience of control in the self-referral process and may also empower imprisoned persons to seek help.
A barrier rooted in the interactions between the individual and the helping services was found in various expressions of skepticism towards “the system” by many participants. Earlier studies have also reported distrust in the system as a barrier to help-seeking [ 41 , 44 ]. Our results elaborate on these findings as the participants spoke of how suicides and severe self-harm by fellow incarcerated people contributed to diminished faith in the system. Some had voiced concern over the health and welfare of peers and had experienced that they were not listened to by the prison officers. According to the participants, many of their fellow incarcerated people had more severe symptoms of mental health problems and did not seem to have access to the help they needed. This confirmed their beliefs that the system took little interest in their mental health, and for some of them this led to a growing feeling of hopelessness and resentment. In addition, the high prevalence of mental disorders in prison implies that incarcerated persons witness people in severe distress regularly and for prolonged periods. This issue is largely unexplored and unrecognized in prison research, and the impact of these experiences on mental well-being and recovery should be investigated further.
Participants who experienced mental distress and adjustment problems had difficulties in accessing mental health services. They needed someone to talk to about their situation that could give them advice on how to cope, however they did not fulfil the criteria for secondary mental health services. Minor mental health problems in Norwegian prisons are to be handled by the prison healthcare services. However, according to the participants their capacity is very limited. This finding corresponds to other studies [ 90 ] documenting that access to integrated mental health services was limited for those with milder mental health problems. In the community, the establishment of low threshold services for people with mental health problems has been an important commitment as early intervention can prevent the development of more serious conditions. This may be even more important for those imprisoned, since coping strategies such as physical activity and seeking social support are less accessible [ 91 ].
Prison officer’s influence on access to mental healthcare
Prison officers were perceived to have a key role as gatekeepers to healthcare. Officers can facilitate access to healthcare by encouraging help-seeking or directly contacting healthcare services based on observations and conversations with incarcerated individuals [ 39 , 41 , 92 ]. The participants in our study pointed out the need for prison officers to take their health concerns more seriously, and that the threshold for contacting healthcare services by their request was too high. In addition, being asked directly about their psychological state by staff members was seen to ease talks about mental health by the participants. Our results support the notion that prison officers that are responsive to the mental healthcare needs of incarcerated persons could build confidence that these needs would be attended to when required [ 92 ]. Thus, ensuring sufficient mental health knowledge and awareness among prison officers of their role in mental healthcare access is an essential task for correctional systems.
Previous studies have found that the correctional systems´ procedures for managing suicidal risk is a potential obstacle for help-seeking. The fear of being moved or placed in a safety cell without personal belongings was identified as a barrier to disclosing suicidal thoughts [ 39 , 93 ]. In Norway, the risk of self-harm and suicide is ideally handled by increasing social contact, activities, monitoring and healthcare. However, in the face of acute mental crisis and severe suicide risk, placing persons in solitary confinement is not an uncommon practice [ 94 ]. Challenges with having incarcerated persons admitted and treated in specialized health care institutions, understaffing, and a lack of central guidelines for handling suicide risk may contribute to the use of solitary confinement for incarcerated persons in acute mental distress in the Norwegian correctional system [ 94 ]. The Norwegian Parliamentary Ombudsman reports that fear of solitary confinement and being placed in a security cell is a barrier to seeking help for suicidal ideations and plans [ 95 ]. In our study, participants who had asked for help when they were in acute distress experienced that the officers assumed that they intended to harm themselves. They were faced with the potential of being transferred to a higher security level or being placed in solitary confinement. Thus, how prison officers respond to incarcerated persons’ reports of acute mental distress could be of critical importance for their willingness to seek help for mental health issues in the future. However, more research on the perceived and actual consequences of disclosing mental distress and suicidal ideations in prison is needed to inform interventions to promote help-seeking.
Enhancing access to mental healthcare in prison
The participants underscore some conditions that may lower the bar mental healthcare utilization. Earlier positive experiences with mental healthcare in the community was mentioned by participants as important for their willingness to seek such services in prison, which also corresponds with findings in earlier studies [ 42 , 96 ]. In addition, the participants saw mental health services that were outreaching and integrated as positive. A few participants also highlighted mental health screening at reception to discover mental disorders that may need intervention. Screening at intake, and outreaching and integrated services are also recommended in the prison research literature [ 88 ]. Our findings show that these recommended measures may also make intuitive sense to incarcerated persons - common for all of them are that they seem to reduce stigma related to utilizing mental healthcare.
Our results indicate that incarcerated persons with both milder and more severe mental disorders experience barriers to accessing mental healthcare. These results are in line with studies from other correctional settings reporting unmet needs due to challenges with access and delivery of mental healthcare [ 37 , 38 , 39 ]. The underutilization of mental health services by incarcerated persons suggests that the ‘degree of fit’ between their needs and the available mental healthcare requires improvement. The World Health Organization (WHO) advocates for correctional systems with health and well-being as an integrated part of their core business and culture [ 33 ]. Along these lines, we found that participants called for a correctional system with mental health higher on the agenda. Some also preferred to seek help for mental health problems from other sources than mental health professionals. This finding supports the recommendation of the WHO that it is important to build mental health competency in all staff members in contact with those imprisoned. As many of the barriers to mental healthcare utilization are rooted in the wider correctional setting, we also suggest that the correctional and healthcare systems, in collaboration, should review their practices to enhance perceived efficacy in accessing healthcare.
Limitations
The data in this study are based on interviews with fifteen participants from three prisons. The participants were self-selected and may have had more knowledge, interest, and willingness to talk about mental health issues than the average person in prison. We cannot claim that the results represent a complete account of access to mental healthcare and help-seeking among incarcerated persons in Norway. However, our findings were consistent with findings from other studies from Norway and correctional settings in some other countries. We have presented details about the participants, method, data, and context to allow others to consider the potential transferability of the results. We hope our findings encourage further research on access to mental healthcare for people in prison.
Mental healthcare that is outreaching and integrated is perceived to facilitate access and decrease stigma. The correctional system should address access to health information, the referral system, and their responses to incarcerated persons who disclose distress to facilitate access to healthcare. Our results also indicate that mental healthcare extends beyond the scope of health services, suggesting that sufficient mental health knowledge and agency is needed at all levels of the correctional system.
Data availability
The data produced in the course of this research is not openly accessible owing to considerations regarding privacy. However, they can be obtained from the corresponding author upon a reasonable request.
Abbreviations
Theory of planned behavior
Mental health literacy
Baranyi G, Scholl C, Fazel S, Patel V, Priebe S, Mundt AP. Severe mental illness and substance use disorders in prisoners in low-income and middle-income countries: a systematic review and meta-analysis of prevalence studies. Lancet Glob Health. 2019;7(4):e461–71.
Article PubMed PubMed Central Google Scholar
Butler T, Andrews G, Allnutt S, Sakashita C, Smith NE, Basson J. Mental disorders in Australian prisoners: a comparison with a community sample. Aust N Z J Psychiatry. 2006;40(3):272–6.
Article PubMed Google Scholar
Cramer V. The prevalence of mental disorders among convicted inmates in Norwegian prisons. 2014.
Sirdifield C, Gojkovic D, Brooker C, Ferriter M. A systematic review of research on the epidemiology of mental health disorders in prison populations: a summary of findings. J Forensic Psychiatry Psychol. 2009;20(sup1):S78–101.
Article Google Scholar
Baranyi G, Fazel S, Langerfeldt SD, Mundt AP. The prevalence of comorbid serious mental illnesses and substance use disorders in prison populations: a systematic review and meta-analysis. Lancet Public Health. 2022;7(6):e557–68.
Fazel S, Hayes AJ, Bartellas K, Clerici M, Trestman R. Mental health of prisoners: prevalence, adverse outcomes, and interventions. Lancet Psychiatry. 2016;3(9):871–81.
Ford K, Bellis MA, Hughes K, Barton ER, Newbury A. Adverse childhood experiences: a retrospective study to understand their associations with lifetime mental health diagnosis, self-harm or suicide attempt, and current low mental wellbeing in a male Welsh prison population. Health Justice. 2020;8(1):13.
Schnittker J, Massoglia M, Uggen C. Out and down: Incarceration and Psychiatric disorders. J Health Soc Behav. 2012;53(4):448–64.
Mahgoub M, Monteggia LM. Epigenetics Psychiatry Neurother. 2013;10(4):734–41.
CAS Google Scholar
Ray M, Wallace MK, Grayson SC, Cummings MH, Davis JA, Scott J, et al. Epigenomic Links between Social Determinants of Health and symptoms: a scoping review. Biol Res Nurs. 2023;25(3):404–16.
Revold MK. Innsattes levekår 2014 Før, under Og etter soning. Oslo-Kongsvinger: Statistics Norway; 2015. Report No. 47.
Google Scholar
De Viggiani N. Unhealthy prisons: exploring structural determinants of prison health. Sociol Health Illn. 2007;29:115–35.
Goomany A, Dickinson T. The influence of prison climate on the mental health of adult prisoners: a literature review. J Psychiatr Ment Health Nurs. 2015;22(6):413–22.
Article CAS PubMed Google Scholar
Nurse J, Woodcock P, Ormsby J. Influence of environmental factors on mental health within prisons: focus group study. BMJ. 2003;327(7413):480.
Solbakken LE, Bergvik S, Wynn R. Beliefs about mental health in incarcerated males: a qualitative interview study. Front Psychiatry [Internet]. 2023;14. https://www.frontiersin.org/articles/ https://doi.org/10.3389/fpsyt.2023.1242756
Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82(11):858–66.
PubMed PubMed Central Google Scholar
Pathare S, Brazinova A, Levav I. Care gap: a comprehensive measure to quantify unmet needs in mental health. Epidemiol Psychiatr Sci. 2018;27(5):463–7.
Article CAS PubMed PubMed Central Google Scholar
Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370(9590):841–50.
Penchansky R, Thomas JW. The Concept of Access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–40.
Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, Beech R, et al. What does ‘access to health care’ mean? J Health Serv Res Policy. 2002;7(3):186–8.
Alonso J, Liu Z, Evans-Lacko S, Sadikova E, Sampson N, Chatterji S, et al. Treatment gap for anxiety disorders is global: results of the World Mental Health Surveys in 21 countries. Depress Anxiety. 2018;35(3):195–208.
Doll CM, Michel C, Rosen M, Osman N, Schimmelmann BG, Schultze-Lutter F. Predictors of help-seeking behaviour in people with mental health problems: a 3-year prospective community study. BMC Psychiatry. 2021;21(1):432.
Thornicroft G. Most people with mental illness are not treated. Lancet. 2007;370(9590):807–8.
Rickwood D, Thomas K. Conceptual measurement framework for help-seeking for mental health problems. Psychol Res Behav Manag. 2012;5:173–83.
Rickwood D, Deane FP, Wilson CJ, Ciarrochi J. Young people’s help-seeking for mental health problems. Aust E-J Adv Ment Health. 2005;4(3):218–51.
Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. 2012;67(3):231–43.
Lui JC, Sagar-Ouriaghli I, Brown JSL. Barriers and facilitators to help-seeking for common mental disorders among university students: a systematic review. J Am Coll Health. 2022;1–9.
Lynch L, Moorhead A, Long M, Hawthorne-Steele I. The role of Informal sources of help in Young people’s Access to, Engagement with, and maintenance in Professional Mental Health Care—A Scoping Review. J Child Fam Stud. 2023;32(11):3350–65.
Tomczyk S, Schomerus G, Stolzenburg S, Muehlan H, Schmidt S, Ready. Willing and able? An investigation of the theory of Planned Behaviour in help-seeking for a community sample with current untreated depressive symptoms. Prev Sci. 2020;21(6):749–60.
Adams C, Gringart E, Strobel N. Explaining adults’ mental health help-seeking through the lens of the theory of planned behavior: a scoping review. Syst Rev. 2022;11(1):160.
Niveau G. Relevance and limits of the principle of ‘equivalence of care’ in prison medicine. J Med Ethics. 2007;33(10):610–3.
The United Nations Standard Minimum Rules for the Treatment of Prisoners [Internet]. United Nations Office On Drugs and Crime. 2015. https://www.unodc.org/documents/justice-and-prison-reform/Nelson_Mandela_Rules-E-ebook.pdf
Durcan G, Zwemstra JCZ. Mental health in prison. In: Enggist S, Møller L, Gauden G, Udesen C, editors. Prisons and Health [Internet]. Geneva: World Health Organization; 2014. pp. 87–94. https://www.euro.who.int/__data/assets/pdf_file/0005/249188/Prisons-and-Health.pdf
Forrester A, Till A, Simpson A, Shaw J. Mental illness and the provision of mental health services in prisons. Br Med Bull. 2018;127(1):101–9.
Lines R. From equivalence of standards to equivalence of objectives: the entitlement of prisoners to health care standards higher than those outside prisons. Int J Prison Health. 2006;2(4):269–80.
Simpson AIF, McMaster JJ, Cohen SN. Challenges for Canada in meeting the needs of persons with serious mental illness in prison. J Am Acad Psychiatry Law. 2013;41(4):501–9.
PubMed Google Scholar
Reingle Gonzalez JM, Connell NM. Mental Health of prisoners: identifying barriers to Mental Health Treatment and Medication Continuity. Am J Public Health. 2014;104(12):2328–33.
Patel R, Harvey J, Forrester A. Systemic limitations in the delivery of mental health care in prisons in England. Int J Law Psychiatry. 2018;60:17–25.
Gilling McIntosh L, Rees C, Kelly C, Howitt S, Thomson LDG. Understanding the mental health needs of Scotland’s prison population: a health needs assessment. Front Psychiatry [Internet]. 2023 [cited 2023 Dec 27];14. https://www.frontiersin.org/articles/ https://doi.org/10.3389/fpsyt.2023.1119228
Wright N, Jordan M, Kane E. Mental health/illness and prisons as place: Frontline clinicians׳ perspectives of mental health work in a penal setting. Health Place. 2014;29:179–85.
Byrne E, Bradshaw D, Kerin M, Pepe I. A social identity approach to mental health help-seeking behaviour in prisoners: A systematic review. J Community Appl Soc Psychol. 2023;casp.2727.
Morgan RD, Steffan J, Shaw LB, Wilson S. Needs for and Barriers to Correctional Mental Health Services: inmate perceptions. Psychiatr Serv. 2007;58(9):1181–6.
Howerton A, Byng R, Campbell J, Hess D, Owens C, Aitken P. Understanding help seeking behaviour among male offenders: qualitative interview study. BMJ. 2007;334(7588):303.
Mitchell J, Latchford G. Prisoner perspectives on mental health problems and help-seeking. J Forensic Psychiatry Psychol. 2010;21(5):773–88.
Kupers TA. Toxic masculinity as a barrier to mental health treatment in prison. J Clin Psychol. 2005;61(6):713–24.
De Viggiani N. Trying to be something you are not: masculine performances within a prison setting. Men Masculinities. 2012;15(3):271–91.
Daquin JC, Daigle LE. Mental disorder and victimisation in prison: examining the role of mental health treatment: Mental Disorder, treatment, and victimisation. Crim Behav Ment Health. 2018;28(2):141–51.
Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Mental health literacy: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. 1997;166(4).
Picco L, Abdin E, Pang S, Vaingankar JA, Jeyagurunathan A, Chong SA, et al. Association between recognition and help-seeking preferences and stigma towards people with mental illness. Epidemiol Psychiatr Sci. 2018;27(1):84–93.
Marco-Ruiz L, Wynn R, Oyeyemi SO, Budrionis A, Yigzaw KY, Bellika JG. Impact of illness on Electronic Health Use (the Seventh Tromsø Study - Part 2): Population-based Questionnaire Study. J Med Internet Res. 2020;22(3):e13116.
Pretorius C, Chambers D, Coyle D. Young people’s Online help-seeking and Mental Health difficulties: systematic narrative review. J Med Internet Res. 2019;21(11):e13873.
Reavley NJ, Cvetkovski S, Jorm AF. Sources of information about mental health and links to help seeking: findings from the 2007 Australian National Survey of Mental Health and Wellbeing. Soc Psychiatry Psychiatr Epidemiol. 2011;46(12):1267–74.
Rantanen T, Järveläinen E, Leppälahti T. Prisoners as Users of Digital Health Care and Social Welfare Services: a Finnish attitude survey. Int J Environ Res Public Health. 2021;18(11):5528.
Smith PS. Imprisonment and Internet-Access; Human rights, the Principle of normalization and the question of prisoners Access to Digital Communications Technology. Nord J Hum Rights. 2013;30(04):454–82.
Novisky MA, Schnellinger RP, Adams RE, Williams B. Health Information seeking behaviors in prison: results from the U.S. PIAAC Survey. J Correct Health Care. 2022;28(2):90–9.
Toreld EM, Haugli KO, Svalastog AL. Maintaining normality when serving a prison sentence in the digital society. Croat Med J. 2018;59(6):335–9.
Zivanai E, Mahlangu G. Digital prison rehabilitation and successful re-entry into a digital society: a systematic literature review on the new reality on prison rehabilitation. Cogent Soc Sci. 2022;8(1):2116809.
Baillargeon J, Contreras S, Grady JJ, Black SA, Murray O. Compliance with antidepressant medication among prison inmates with depressive disorders. Psychiatr Serv. 2000;51(11):1444–6.
Wallace D, Wang X. Does in-prison physical and mental health impact recidivism? SSM -. Popul Health. 2020;11:100569.
The World Medical Association-WMA Declaration of Helsinki– Ethical Principles for Medical Research Involving Human Subjects [Internet]. 2018 [cited 2022 Mar 14]. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
Gostin LO, Vanchieri C, Pope A, editors. Ethical Considerations for Research Involving Prisoners. [Internet]. Washington (DC): Institute of Medicine (US) Committee on Ethical Considerations for Revisions to DHHS Regulations for Protection of Prisoners Involved in Research; 2007. https://www.ncbi.nlm.nih.gov/books/NBK19882/
Moore LW, Miller M. Initiating research with doubly vulnerable populations. J Adv Nurs. 1999;30(5):1034–40.
Sacristán JA, Aguarón A, Avendaño-Solá C, Garrido P, Carrión J, Gutiérrez A, et al. Patient involvement in clinical research: why, when, and how. Patient Prefer Adherence. 2016;10:631–40.
Christopher PP, Garcia-Sampson LG, Stein M, Johnson J, Rich J, Lidz C. Enrolling in Clinical Research while incarcerated: what influences participants’ decisions? Hastings Cent Rep. 2017;47(2):21–9.
Norway| World Prison Brief [Internet]. 2024 [cited 2024 Mar 15]. https://www.prisonstudies.org/country/norway
Bukten A, Virtanen S, Hesse M, Chang Z, Kvamme TL, Thylstrup B, et al. The prevalence and comorbidity of mental health and substance use disorders in scandinavian prisons 2010–2019: a multi-national register study. BMC Psychiatry. 2024;24:95.
Lov om pasient- og brukerrettigheter [Internet]. Section 2, LOV-1999-07-02-63 1997. https://lovdata.no/dokument/NL/lov/1999-07-02-63/KAPITTEL_2#%C2%A72-5a
Saunes IS. International Health Care System Profiles: Norway [Internet]. New York: The Commonwealth Fund; 2020 Dec. https://www.commonwealthfund.org/international-health-policy-center/countries/norway
Helsedirektoratet. Helse- og omsorgstjenester til innsatte i fengsel [Internet]. 2013 [cited 2023 Nov 24]. https://www.helsedirektoratet.no/veiledere/helse-og-omsorgstjenester-til-innsatte-i-fengsel/Helse-%20og%20omsorgstjenester%20til%20innsatte%20i%20fengsel%20%E2%80%93%20Veileder.pdf/_/attachment/inline/54b7b100-9415-4bc0-993e-66175a4cd4c1:5537f215b0ba85ca4a0159612413ab7450b23467/Helse-%20og%20omsorgstjenester%20til%20innsatte%20i%20fengsel%20%E2%80%93%20Veileder.pdf
World Health Organization. World mental health report: Transforming mental health for all [Internet]. Geneva. 2022. Available from: https://www.who.int/publications/i/item/9789240049338
Pont J, Enggist S, Stöver H, Williams B, Greifinger R, Wolff H. Prison Health Care Governance: guaranteeing clinical independence. Am J Public Health. 2018;108(4):472–6.
Nesset M, Rustad ÅB, Kjelsberg E, Almvik R, Bjørngaard J. Health care help seeking behaviour among prisoners in Norway. BMC Health Serv Res. 2011.
Bjørngaard JH, Rustad ÅB, Kjelsberg E. The prisoner as patient - a health services satisfaction survey. BMC Health Serv Res. 2009;9(1):176.
Magnussen SF, Tingvold L. Kartlegging av helse- og omsorgsbehov blant innsatte i fengsel [Internet]. Gjøvik: Senter for omsorgsforskning, øst; 2022 [cited 2023 Aug 8]. Report No.: 1. https://omsorgsforskning.brage.unit.no/omsorgsforskning-xmlui/bitstream/handle/11250/2992945/Kartlegging_innsatte.pdf?sequence=1&isAllowed=y
Kriminalomsorgen K. Årsrapport 2020 [Internet]. Kriminalomsorgsdirektoratet; 2021 Feb. https://www.regjeringen.no/contentassets/b04b5cf8bb32490c990a82fd90fa05a0/arsrapport_kdi_2020.pdf
Appleton J, King L. Journeying from the philosophical contemplation of constructivism to the methodological pragmatics of health service research. J Adv Nurs. 2003;40:641–8.
Birks M, Hoare K, Mills J. Grounded Theory: The FAQs. Int J Qual Methods [Internet]. 2019 Jan 1 [cited 2023 Aug 16];18. http://journals.sagepub.com/doi/10.1177/1609406919882535
Abbott P, DiGiacomo M, Magin P, Hu W. A Scoping Review of Qualitative Research Methods Used With People in Prison. Int J Qual Methods [Internet]. 2018 Dec 1 [cited 2023 Aug 16];17(1). http://journals.sagepub.com/doi/ https://doi.org/10.1177/1609406918803824
Birks M, Mills J, Grounded Theory. A practical guide. 3rd ed. SAGE Publications, Ltd.; 2023.
Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113.
Waldmann T, Staiger T, Oexle N, Rüsch N. Mental health literacy and help-seeking among unemployed people with mental health problems. J Ment Health Abingdon Engl. 2020;29(3):270–6.
Rüsch N, Evans-Lacko SE, Henderson C, Flach C, Thornicroft G. Knowledge and attitudes as predictors of intentions to seek help for and disclose a Mental illness. Psychiatr Serv. 2011;62(6):675–8.
Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust [Internet]. 2007 Oct [cited 2024 Mar 19];187(S7). https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.5694/j.1326-5377.2007.tb01332.x
Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16–20.
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11–27.
Thornicroft G, Sunkel C, Alikhon Aliev A, Baker S, Brohan E, El Chammay R, et al. The Lancet Commission on ending stigma and discrimination in mental health. Lancet Lond Engl. 2022;400(10361):1438–80.
Bagnall AM, South J, Hulme C, Woodall J, Vinall-Collier K, Raine G, et al. A systematic review of the effectiveness and cost-effectiveness of peer education and peer support in prisons. BMC Public Health. 2015;15(1):290.
Fovet T, Mundt AP, Fazel S et al. Psychiatry in Prisons and Corrections. In: Tasman A, Riba MB, Alarcón RD, Alfonso CA, Kanba S, Ndetei DM, editors. Tasman’s Psychiatry [Internet]. Cham: Springer International Publishing; 2020 [cited 2024 Feb 22]. pp. 1–28. https://doi.org/10.1007/978-3-030-42825-9_103-1
Morgan RD, Scanlon F, Van Horn SA. Criminogenic risk and mental health: a complicated relationship. CNS Spectr. 2020;25(2):237–44.
Durcan G. The future of prison mental health care in England: A national consultation and review [Internet]. London: Centre for Mental Health; 2021. https://www.centreformentalhealth.org.uk/wp-content/uploads/2021/06/CentreforMentalHealth_TheFutureofPrisonMentalHealthCare_0.pdf
Solbakken LE, Wynn R. Barriers and opportunities to accessing social support in the transition from community to prison: a qualitative interview study with incarcerated individuals in Northern Norway. BMC Psychol. 2022;10(1):185.
Ross MW, Liebling A, Tait S. The Relationships of Prison Climate to Health Service in Correctional environments: Inmate Health Care Measurement, satisfaction and Access in prisons. Howard J Crim Justice. 2011;50(3):262–74.
Skogstad P, Deane FP, Spicer J. Barriers to Helpseeking among New Zealand prison inmates. J Offender Rehabil. 2005;42(2):1–24.
Norwegian Parliamentary Ombudsman. Special report to the Storting on solitary confinement and lack of human contact in Norwegian prisons [Internet]. Oslo: Norwegian Parliamentary Ombudsman. 2019. (4:3). https://www.sivilombudet.no/wp-content/uploads/2019/08/SOM_Særskilt-melding_ENG_WEB.pdf
Sivilombudet. Selvmord og selvmordsforsøk i fengsel. En undersøkelse under OPCAT-mandatet [Internet]. Oslo: Sivilombudet; 2023. https://www.sivilombudet.no/wp-content/uploads/2023/03/Rapport_Selvmord_i_fengsel.pdf
Skogstad P, Deane FP, Spicer J. Social-cognitive determinants of help-seeking for mental health problems among prison inmates. Crim Behav Ment Health CBMH. 2006;16(1):43–59.
Download references
Acknowledgements
The authors thank the study participants and the correctional facilities for their cooperation.
Open access funding provided by UiT The Arctic University of Norway (incl University Hospital of North Norway). The study was supported by a grant from the North Norway Regional Health Authority (Helse Nord RHF). The funding body had no role in study design, data collection, analysis, or writing of the manuscript. The study was supported by the Publication Fund of UiT The Arctic University of Norway.
Open access funding provided by UiT The Arctic University of Norway (incl University Hospital of North Norway)
Author information
Authors and affiliations.
Department of Clinical Medicine, UiT The Arctic University of Norway, Tromsø, N-9038, Norway
Line Elisabeth Solbakken & Rolf Wynn
Division of Mental Health and Substance Use, University Hospital of North, Tromsø, Norway
Line Elisabeth Solbakken
Department of Psychology, UiT The Arctic University of Norway, Tromsø, Norway
Svein Bergvik
Department of Education, ICT and Learning, Østfold University College, Tromsø, Norway
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the conception and design of the study. LES conducted the interviews and their transcription. All authors analyzed the data. LES drafted the manuscript. All authors participated in revising the manuscript and approved the final version.
Corresponding author
Correspondence to Rolf Wynn .
Ethics declarations
Ethics approval and consent to participate.
The study was performed in accordance with the Declaration of Helsinki. All relevant guidelines and regulations were followed. All participants gave written informed consent. The study was approved by the Data Protection Officer of the University Hospital of North Norway. The Norwegian Correctional System, Region North, also approved the study. The study was submitted to and deemed outside the mandate of the Regional Health Research Ethics Committee of Northern Norway.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Solbakken, L.E., Bergvik, S. & Wynn, R. Breaking down barriers to mental healthcare access in prison: a qualitative interview study with incarcerated males in Norway. BMC Psychiatry 24 , 292 (2024). https://doi.org/10.1186/s12888-024-05736-w
Download citation
Received : 01 January 2024
Accepted : 03 April 2024
Published : 17 April 2024
DOI : https://doi.org/10.1186/s12888-024-05736-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Incarcerated
- Correctional
- Mental health
- Help-seeking
- Utilization
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 30 April 2024
Explaining the barriers faced by veterinarians against preventing antimicrobial resistance: an innovative interdisciplinary qualitative study
- Razie Toghroli 1 ,
- Laleh Hassani 1 ,
- Teamur Aghamolaei 1 ,
- Manoj Sharma 2 ,
- Hamid Sharifi 3 , 5 &
- Maziar Jajarmi 4
BMC Infectious Diseases volume 24 , Article number: 455 ( 2024 ) Cite this article
Metrics details
Considering the significance of increased antimicrobial resistance (AMR) and its adverse effects on individual and social health and the important and effective role that veterinarians play in controlling this growing issue worldwide, it is essential to have effective preventive control programs. To this aim, the first step is to identify the factors behind the prevalence of AMR in Iran and the barriers veterinarians face to controlling this problem. Thus, the present study was conducted to explain the barriers veterinarians faced in the prevention of AMR from an Iranian veterinarian’s perspective.
The present research was done in three cities in Iran in 2021. The data were collected through in-depth interviews with 18 veterinarians selected through purposive and snowball sampling and analyzed using conventional qualitative content analysis.
The data analysis results were classified into 4 main categories and 44 subcategories. The former included: educational factors, administrative/legal factors, client-related factors, and veterinarian-related factors.
Conclusions
The increased AMR can be approached from multiple aspects. Considering the different factors that affect the increased AMR, it is necessary to consider them all through effective planning and policy-making at multi-level and multidisciplinary dimensions. There is special attention needed to scientific and practical interventions at the individual, interpersonal, social, and even political levels. At the same time, measures should be taken to rehabilitate and maintain the health of society to strengthen supervision and attract the full participation of interested organizations.
Peer Review reports
Introduction
Antimicrobial resistance (AMR) refers to the reduced effectiveness of antimicrobial agents, such as antibiotics, antivirals, antifungals, and antiparasitics, against infections caused by bacteria, viruses, fungi, and parasites [ 1 ]. This phenomenon makes infections harder to treat and increases the risk of disease spread, severe illness, and death. Misuse and overuse of these agents in humans, animals, and plants are key contributors to the development of AMR. AMR is a natural process that occurs gradually over time through genetic changes in microorganisms, but human activities, particularly the improper use of antimicrobials, significantly speed up this process. Veterinarians play a vital role in managing AMR, as they frequently prescribe antimicrobials to protect animal health. However, overprescription and misuse of antimicrobials in veterinary practice contribute to the development of AMR in humans. AMR presents a substantial challenge to global public health and economic stability. If left unchecked, AMR will lead to increased healthcare costs, decreased productivity, and potentially millions of avoidable deaths annually. To combat AMR, governments, healthcare providers, and researchers must collaborate to implement policies promoting judicious antimicrobial use, invest in innovative therapies, and foster educational initiatives to empower individuals to understand the importance of responsible antimicrobial stewardship [ 2 ].
AMR is an increasingly global issue that needs to be settled cooperatively. Resistant organisms exist in animals, humans, the environment, the food, and the main cause of this, is antimicrobial usage. AMR will become a leading cause of mortality in the world in the near future. As reported by some studies, by 2050, AMR will be the main cause of death on a global scale, which surpasses cancer deaths [ 3 , 4 ].
The mortality rate caused by microbial resistance is higher than the total number of deaths induced by cancer worldwide. Yet, the former has been largely neglected and, instead, issues such as cancer and how to treat it have been addressed more [ 5 , 6 , 7 ].
Unintentional antibiotic ingestion occurs frequently due to the widespread use of antibiotics in society. According to a report from 2010, approximately 10 pills, capsules, or teaspoons of antibiotics are taken annually by every person on Earth, which suggests a high degree of accidental consumption. Healthy individuals who consume significant amounts of antibiotics unintentionally may experience negative impacts on their health, particularly concerning the disturbance of the normal microbiome. This disturbance can lead to long-term complications, such as an increased risk of developing conditions like type 1 and 2 diabetes, inflammatory bowel diseases, celiac disease, allergies, and asthma [ 8 ]. Additionally, antibiotic exposure can contribute to the emergence of antibiotic-resistant strains, posing a challenge to public health. It is essential to note that antibiotics are necessary and lifesaving medicines when used appropriately under medical supervision. However, excessive or unnecessary use of antibiotics can pose risks to individual and population health [ 9 , 10 ].
According to the report of the World Health Organization, half of the antibiotics produced in the world are used in medicine and the other half in veterinary, agriculture and aquaculture [ 11 ]. In general, there is no difference between antibiotics used in veterinary medicine and antibiotics used in medicine. These drugs are used to prevent and treat diseases and promote growth in animal farms (pigs and poultry), unfortunately, the use of antibiotics in veterinary medicine leads to leaving residues in meat, milk and eggs [ 12 ]. Drug residues in food have adverse effects such as antibiotic resistance in humans, allergies, and inhibition of bacterial starter cultures used in dairy fermentation industries [ 13 ]. Despite the beneficial effects of antibiotics on the treatment of livestock infectious diseases, the presence of their residues in milk and animal meat, as well as their transfer to the human body have adverse effects on health, industry, and economics. As reported by the National Center for Rational Prescription of Antibiotics, consuming antibiotics in Iran is 16 times as high as the global standard. Some researchers believe that the spread of microbial resistance to antibiotics results not only from the unnecessary prescription and use of these compounds in humans but also from the widespread use of antimicrobial drugs in veterinary medicine. It has caused the transfer of such pathogenic bacteria from animals to human pathogens. The main difference between microbial resistance to antimicrobial drugs in humans and animals is that microbial resistance in humans affects the individual, whereas microbial resistance in livestock affects a large population due to the consumption of raw animal products by humans. Exposure to both resistant bacteria and antibiotic compounds prescribed for the treatment of infectious diseases for livestock through transmission causes the accumulation of drugs and drug residues in raw livestock products. It seems that attempts to prevent the occurrence of microbial resistance in livestock and its consequences for humans are effective and can be implemented efficiently by veterinarians and those active in this domain. What veterinarians can do with this respect is wide-ranging.
Most of the studies conducted in Iran in the field of antimicrobial resistance were in the medical and human fields, and the studies conducted in the veterinary field were mostly quantitative. A systematic review and meta-analysis showed a high level of antibiotic resistance in Staphylococcus aureus bovine mastitis in Iran. This pathogen is the common and main cause of bovine bacterial mastitis, which leads to high economic losses and can easily lead to the transmission of these treatment-resistant bacteria to humans [ 14 ]. In a qualitative study, which is one of the few qualitative and phenomenological studies conducted in Iran in the field of AMR, the lived experience of livestock breeders, their role and views in this field has been investigated. The results of this study have confirmed the importance of antibiotic resistance in Iran and the lack of existing research in this field, especially with a qualitative approach [ 15 ]. In another study that was conducted with semi-structured interviews with key stakeholders in Iran, including managers of the Ministry of Health, Iran Veterinary Organization, national professional associations and researchers through thematic analysis, the international enabling and predisposing factors related to It identified the control of AMR in Iran. The enabling factors that have been highlighted in this review were discussed in general, and more attention was paid to political factors such as formulation and implementation processes, and AMR surveillance, and challenges such as the smuggling of infected animals and antimicrobial drugs and livestock from neighboring countries and the impact of imposed sanctions. The review emphasizes the global nature of AMR as a challenge that requires consensus and international cooperation to effectively deal with this issue, but it does not specifically and specifically deal with why and analyze how AMR occurs and examine ways to prevent it, and only generally with the approaches Emphasizes political, including health diplomacy, to strengthen national efforts in the fight against AMR [ 16 ]. However, the present study, in an interdisciplinary manner, has specifically addressed one of the most important fields involved in the occurrence of AMR in human societies, and a field similar to it has received less attention before.
Yet, it is hard to make interventions with veterinarians directly involved because they are not easily available for research; therefore, veterinary students are the best and closest population for interventional studies. If this population adequately understand the principles of prescribing antibiotics, this successful learning will be productive in practice too [ 17 ].
Overcoming this problem will be possible with an One health approach, taking into account humans, animals, and environmental health altogether [ 18 , 19 , 20 ].
Today, AMR occurs in humans, wildlife, domestic animals, plants, and our environment directly by using antibiotics, and there is a risk on a much larger and more significant scale in animal-source foods consumed by humans indirectly. So it is logical to take a multidisciplinary health approach to solve this problem by eliminating the inappropriate use of antibiotics [ 21 , 22 ].
In the medical domain, extensive research has been done to examine physicians’ beliefs about prescribing antibiotics [ 23 ]. Many interventions have been made to reduce physicians’ over-prescription. The various aspects of antibiotic prescription have been extensively investigated so far in medical and clinical sciences. However, these interventions alone have not managed to prevent the occurrence of this important event. Thus, resolving this problem needs a multidimensional approach [ 24 ] .
Moreover, veterinarians prescribing drugs without using paraclinical services and selling over-the-counter (OTC) drugs are very common in several countries including Iran. In many stockbreeding industries, antibiotics are widely used not only for medical purposes but also as growth stimulants. There has been a serious lack of effective monitoring of these patterns of use. Similarly, there has scarcely been any strict preventive rule for this. Thus, it is likely that the AMR incidence rate is high in countries such as Iran [ 25 , 26 ].
A vast majority of research so far on the effect of AMR has only addressed this issue in human health [ 16 , 24 ]. In veterinary medicine, the body of existing literature has been limited to laboratory research and animal health. Veterinarians’ role in integrated health, especially AMR has not been adequately addressed. Therefore, there is no complete and clear understanding of veterinarians’ mental patterns and perceived social barriers to their decisions during diagnosis and treatment [ 27 ].
The over-prescribing of drugs is very common in animal products and animal-source foods (to be consumed by humans) in Iran. Moreover, each of these foods contains antimicrobial residues. Thus, it can be conjectured that people ingest significant amounts of antibiotics every day unintentionally without suffering from any infectious disease. Therefore, veterinarians must pay adequate attention to AMR in human health [ 28 ].
Overall, the world is faced with increasing availability and misuse of antibiotics in veterinary medicine, which threatens public health. There is a significant increase in AMR on a global scale, and there is a threat of increasing infections that do not respond well to treatment. It is essential to take appropriate measures and plan to prevent the over-prescription of antibiotics by veterinarians. There is an increasing need for education and empowerment policies, all deemed impossible unless the barriers facing veterinarians are recognized in appropriate prescribing. In other words, to deal with the AMR issue, the first step is to identify the causes and underlying contributing factors to this event in veterinary medicine and the disastrous conditions veterinarians face in Iran and the world. It is not possible to adequately approach what veterinarians go through and how they perceive the existing context only through quantitative research. A qualitative approach is needed to explore all aspects of this problem. Therefore, the present study employed this approach to explore the Iranian veterinarians’ perceptions of barriers to AMR prevention. We hope that the results generated from this study will help promote programs to curb slow down and the development of AMR in Iran and the world. The present findings can be used to make new social, economic, and even political decisions.
Materials and methods
Research design.
This research was conducted with a qualitative approach and qualitative content analysis method from three cities of Iran: Kerman (with a large population of large and small livestock), Bandar Abbas (a fishing and aquaculture hub), and Tehran (with a large population of pets and industrial poultry). The present qualitative study used semi-structured interviews with veterinarians who had experience in treating and prescribing antibiotics or office work in veterinary medicine, or those with sufficient experience and knowledge of issues in veterinary diagnosis and treatment. The interviews were held face-to-face from May 3, 2021 to August 13, 2021. In this study, theme analysis was used, which is a common type of qualitative content analysis. It seeks a deep understanding of the complexity, details, and embedded context of a given phenomenon. In this type of analysis, interviews with individuals provide a better understanding and richer information about participants’ experiences and perspectives. This research approach allows for an in-depth and rich exploration of participants’ experiences.
The panel of experts offering advice on research questions and reviewing the transcripts for reliability consisted of one epidemiologist, three health education and health promotion specialists, and two veterinary professors collaborating with three organizations: (Hormozgan University of Medical Sciences, Veterinary Department of Kerman University and Iranian Veterinary Organization). The present participants were selected through maximum variation and snowball sampling.
Participants
The research population consisted of veterinarians from three cities (Tehran, Kerman, and Bandar Abbas) in Iran, all dealing with a large population of livestock, poultry, and aquatic animals in 2021. The inclusion criteria were: veterinary work experience at least three years, the experience of therapeutic clinical work or working as a veterinary administrative and supervisory staff, willingness to participate (in the research), and ability to answer the questions. The exclusion criteria were unwillingness to participate and withdrawal from the interview. Purposive sampling was used with maximum variation (in terms of the province of work, age, sex, the field of work in a clinic or pharmacy, and affiliation with the public or private sector) at first steps and snowball sampling methods In the following. That means some veterinarians were concerned about expressing their opinions or reporting any illegal case they had dealt with. Therefore, they had to be selected through snowball sampling. After reaching the first participant and holding the interview, s/he was asked to suggest the next veterinarian who was aware of or was experienced in prescribing antibiotics against paraclinical rules. Therefore, each participant connected and introduced us to the next participant. Interviews were held in a public place at the interviewee’s convenience. In some cases, the interview was held in the clinic, and in others in the interviewee’s office. The data were collected and analyzed simultaneously. The interviews continued until the data were saturated (i.e. when no new information was obtained) and until all the extracted themes were sufficiently supported by the data. After the 17th interview, no new data were collected, but to be on the safe side, another interview was also conducted, and after the interview with the 18th participant, the sampling was stopped.
Data collection
Guided questions and semi-structured interviews were used for data collection. The interviews were held face-to-face and video calls. When required, a trained research assistant conducted a qualitative interview to increase the accuracy and speed of data collection. The interview questions were derived from a review of the existing literature on AMR with a focus on the underlying causes and also the comments made by a panel of experts. At the beginning of the interview, the purpose of the study was revealed to the participants and they were assured of the confidentiality of the information they provided and the anonymity of their responses. The interviewees were ensured they could withdraw from the study upon their will. Then, an informed letter of consent was signed. The required permission was gained to record all the conversations. The main focus of the questions included:
What are the barriers to veterinarians’ prevention of increased AMR? Explain.
What do you know about the causes and precursors of AMR occurrence in Iran?
What are the determinants of prescribing and using antibiotics in veterinary medicine in Iran in your opinion? Explain.
What are the determinants of the increased AMR in your opinion as a veterinarian?
Based on the participants’ previous answers, more exploratory questions were asked and, as a result, we extracted the main reasons why veterinarians over-prescribed drugs and why antibiotics were overconsumed in the animal source food industry. The sample size was determined by the theoretical data saturation criterion. In other words, during the data collection, when we concluded that more interviews and observations could not add any new information and only led to repeated findings, we stopped the data collection. Therefore, 18 active veterinarians in clinical, medical, educational and administrative fields were interviewed in Tehran, Kerman and Hormozgan (provinces). Individual interviews lasted between 42 and 57 min.
Data analysis
The process of data analysis was done using Granheim and Lundman method [ 29 , 30 ] and with the help of MAXQDA-2010 software by the first and second authors of the article. The first and second authors listened to recorded interviews and transcribed them into a written format in Word 2017 software immediately after every interview and on the same day with the help of other research colleagues. In the second step, the text of the interviews was read by the researchers very carefully to get a general view of their text. In the third stage, all the texts of the interviews were read line by line and very carefully, and the initial codes were started.
In the fourth step, the researchers placed the codes that were similar in terms of meaning and concept and were placed in a category in a subcategory and determined the relationship between them. In the fifth step, the codes and categories were placed in the main categories, which were conceptually more comprehensive and abstract [ 31 ]. Finally, in a joint meeting, the entire process of data analysis was shared and conflicting opinions on the content of a topic were discussed by a research team with two qualitative health researchers and two veterinarians.
Guba and Lincoln evaluation criteria [ 32 ] were used to check the trustworthiness of the findings. To substantiate the validity of the findings, the researcher’s self-review technique was used in data collection and analysis as well as a peer check during which the codes were provided to two participants to resolve misunderstandings. To substantiate the reliability of findings, intra- and inter-rater reliability tests were used. To this aim, the recorded and transcribed conversations were given to several experts for review. After analyzing the data, they were re-analyzed by colleagues. The next step was documentation to test the accuracy and comprehensibility of the procedures, and the underlying mechanisms of errors.
Ethical considerations
This research was approved by the Ethics Committee of Hormozgan University of Medical Sciences (IR.HUMS.REC.1400.207). In the interviews, the researcher, by introducing herself and also explaining the purposes of the study, tried to create an amicable atmosphere for the interview. The participants were also ensured of the confidentiality of the information they provided, the anonymity of recorded conversations, and also why they were selected. They consented to their voice being recorded. The participants were free to withdraw or leave the interview any time they requested.
The present study was conducted as interviews with 18 veterinarian participants in Tehran, Kerman, and Hormozgan provinces. Both sexes were included. There were 11 male and 7 female participants whose ages ranged between 27 and 58, with an average age of 42.5 years. The participants’ work experience ranged between 3 and 27 years, with an average of 15 years. The demographic information is summarized in Table 1 .
The data analysis led to the extraction of 4 main categories and 44 subcategories (see Table 2 ), each examined separately.
Educational factors
The first determinant of the increased AMR deals with academic issues in university. Among the most important issues are those concerning students, clients’ lacking awareness and knowledge of AMR in animals, and its transmission to humans (from animal source foods).
Unsystematic internship
During the summer holidays of the final 2–3 academic years of veterinary students, they are required to take the internship. Yet, some participants complained about the unsystematic and inefficiency of this internship.
“During our student days, we took up the internship, but we did not learn anything special at all”. (Participant #13)
Unadjusted curricula
The majority of participants agreed that during their studies, only in the bacteriology course, they learn about AMR (only superficially) and that in the university curriculum, this subject was not adequately included.
“All faculty members should teach something about AMR, not just the bacteriology professor. Also, do we not prescribe antibiotics once we diagnose viral diseases in clinical sciences and the like? If so, then why are we not taught what AMR actually is”? (Participant # 9)
Outdated education
As the participants described, it was essential to teach new things about AMR and to develop strict, principled, written instructions on this subject. The participants recommended following effective and efficient exemplar instructions (in foreign countries) to strengthen the educational system not also at university but in food and drug administrative organizations. It is essential to update basic and clinical sciences curricula and add AMR to all courses, as most participants agreed.
“We should keep up with the global community in this regard so that we can be fully aware of the new knowledge and instructions, and can create new instructions based on the preexisting ones”. (Participant #2) ”I think one thing that can definitely help is to see how successful projects in developed countries proceed. Let us follow their example”. (Participant #13) ”They still teach the way they did a hundred years ago. The subject matter should be changed. It seems as if discussing AMR does not matter at all”. (Participant #9)
Lack of specialized training courses
A key determinant of AMR prevention was the need for useful and effective training courses for all those somehow affected or affected by the AMR, including vets, the health staff, medics, therapists, as well as the livestock and poultry breeders, and the like.
“It is essential to hold relevant and useful training courses for ranchers, poultry farmers, pharmacists, as well as veterinarians, veterinary staff who perform inspection and monitoring work for others. So, everyone is expected to cooperate”. (Participant #2). “Farmers should know that adhering to the (medical) interval helps decrease antibiotic concentration in the animal being treated. Thus, the farmer or breeder needs to postpone the slaughter time. Or he is advised not to consume animal source foods while they are being medically treated”. (Participant #7).
Low specialized study index
As in many other sciences, gaining up-to-date knowledge requires studying the most recent research findings.
“We should not only encourage those who influence drug resistance to study about this subject, but universities should also encourage professors to study more about the specialized topic. If a professor fails to have updated knowledge, s/he cannot teach students well. Thus, how can we expect the students to act efficiently in near future”? (Participant #5)
Lack of empowering educational system
Some participants expressed concerns that the educational system did not adequately prepare students for accurate diagnosis and prescription in near future.
“At university, nothing matters more than studying and getting good marks. The educational system does not actually prepare students for the work market. In other words, it does not simulate real conditions before students leave academic life and enter the work market”. (Participant #9)
Lacking cooperation of all medical sectors affiliated with the university
In the present study, participants, all veterinary graduates or instructors, raised the question why discussing AMR was limited to the bacteriology course and not included in clinical and practical courses.
“Why is medical resistance only limited to bacteriology? All other basic and clinical sciences sectors at university are talking about diagnosis and treatment, and are prescribing drugs. But, when they come to medical resistance, they only refer to bacteriologists and the bacteriology labs”. (Participant #9)
Administrative and legal factors
There are issues about the rules/regulations and policies on veterinarians’ practice and that of all people somehow concerned with animal source foods, which can add to the existing problems. Here are the categories and the relevant excerpts:
Problems with rules and regulations
As the participants pinpointed, there is a strong need for food safety rules and regulations especially in terms of AMR. Adherence to these rules and regulations should be closely monitored too.
“Though there are rules, you can never be sure they are abided by fully. No one is afraid of not following the rules. Even I myself, who is doing clinical work, am not sure whether there is any prohibitory rule for this or not!” (Participant #8) . “Breeders who administer drugs themselves or those who slaughter animals being medically treated should be fined or prosecuted because they threaten public health. But, in reality there is no way to stop them”. (Participant #5)
Poor monitoring and administration
A number of participants acknowledged that even if there are rules and regulations, they are not fully observed. There has not been any efficient monitoring over how rules and regulations are followed. That is why rules have been ineffective.
“ All these are just instructions. In practice, there is no veterinary body monitoring how things are done. The rules are ineffective“(Participant #7) .
Selling over-the-counter (OTC) drugs or those without laboratory-based approval
Selling all kinds of drugs, including antibiotics without prescription, without laboratory approval and freely in Iran has caused serious trouble.
“ You can get any medicine you want from any pharmacy at any time. Actually, the main customers of pharmacies are those who buy drugs arbitrarily”. (Participant# 11) ” In my opinion, pharmacies should not sell every kind of drug especially antibiotics unless they receive a laboratory approval for the antibiogram test. Likewise, a vet should not prescribe antibiotics unless s/he receives the lab test result first”. (Participant #2) ” In my opinion, the sale of medicine, especially antibiotics, should be subject to laboratory approval. That is, a person should not be allowed to buy medicine until the laboratory has determined the type of disease or at least the effective antibiotic, even if the vet has prescribed it”. (Participant #9)
Inadequate advocacy
As some participants commented, gaining the full support of international, national and regional communities was a great issue.
“ We need the help of international and national organizations to solve this global issue. When a problem is global, the solution will definitely be achieved with the cooperation of international organizations”. (Participant #2)
Lack of interdisciplinary cooperative approach
According to some participants, to achieve an optimal solution to this problem, all administrative, supervisory, diagnostic, and medical sectors should cooperate.
“ Solving this problem is not what only one organization can do. Universities should teach students in the right way; veterinary administrative organizations should do their job efficiently; the private sector (e.g., clinics and pharmacies) should obey the rules. Most importantly, there should be strict rules made and abided by with all sectors cooperating”. (Participant #4) ” Our clients should be aware of the importance of AMR and also aware of how the drugs are cycled among the environment, animals, and humans. The Environment and Veterinary Organization, public health and agriculture, and the like should all take serious actions. If one ring is missing from this chain, the whole chain is broken. All efforts will end up fruitless”. (Participant #6).
Problems with the production and use of electronic health records (EHRs)
Developing systems such as the integrated prescription system and the use of EHRs can significantly help to prevent AMR occurrence.
“ If the EHR system was used, things would be better now. No pharmacy could then sell OTC drugs. Thus, no customer could buy antibiotics arbitrarily”. (Participant #14)
Slaughtering medically treated livestock
According to some participants, a stock not responding to an antibiotic treatment does not need any lab test. Neither does it need any abstinence interval. It can easily gain slaughter permission even in emergency cases.
“Here, an animal that is taking medicine and is not becoming well or is getting worse is sent for emergency slaughter. Is there any organization in charge here? Only if a buyer comes to know that an animal shows symptoms of a disease, he may buy it at a lower price”. “Before the slaughter, the antibiotic residues are controlled in poultry but not in macro-livestock (e.g., cattle, sheep and goat)”. (Participant #12)
Non-compulsory training courses before issuing a license for animal husbandry
Some participants insisted that the government should make it compulsory for applicants (for stockbreeding or husbandry) to complete AMR training courses before issuing a license for stock breeding. Here are some comments.
“ Certainly, people seeking for an establishment and operation license for livestock, poultry, fish ponds, and in short, any kind of livestock, must be obliged by the relevant governmental body to first pass a series of training courses and then get a license”. (Participant# 2)
Lacking coordination between medical and veterinary organizations
Due to the lack of the required infrastructure in veterinary medicine, this organization needs to cooperate with the Ministry of Health (for service provision), and medical and laboratory sectors especially to perform laboratory tests.
“ We can say that great concern is that veterinary medicine and medical sciences are affiliated with two different ministries. The former is deprived of the facilities provided by the ministry of health. Even for simple antibiogram tests, we should visit veterinary labs provincial centers, or big cities”. (Participant #11)
Lacking attention to micro-industries and micro-breeders
With the expansion and development of livestock, poultry, and aquaculture industries, the main attention has been focused on this group (of industries), and domestic and micro-breeders have been neglected.
“ If there are any rules and regulations, they are mostly about industries such as macro-level poultry breeding or husbandries. Yet, in practice, the national livestock is to a great extent bred by domestic and micro-level breeders that are largely neglected”. (Participant #3)
Limited facilities in small towns
The lack of diagnostic facilities such as laboratories equipped with antibiogram testing for cases sent from veterinary clinics have caused serious problems for clients and veterinarians.
“ For a simple antibiogram test, we have to refer to the provincial center, and this is both time-consuming and costly. More importantly, most of our livestock population is in small towns, not in provincial centers”! (Participant #1)
Client-related factors
Another determinant of the increased AMR as perceived by Iranian veterinarians is the factors related to livestock/poultry breeding and animal owners (termed here as “clients”). The clients’ choices, decisions, and behaviors will have significant effects on increasing AMR.
Quick response : Among the reasons for an emergent antibiotic prescription without any diagnostic test are: concerns about high mortality rate if the drug is not used immediately, the breeder’s referral at the onset or peak of a disease spread, or substantial losses in the herd, or the referral rush to improve conditions.
“ Mostly, livestock farmers especially poultry farmers or any other breeder with a significant number of livestock, poultry, or aquatic animals, insist on getting a strong antibiotic immediately so that the mortality rate does not rise any further. They cannot even wait for the antibiogram test result. If we do not prescribe antibiotics for them, they go get it from somewhere else, and even if they go for the antibiogram test, they may not be patient enough to receive the test result and, thus, arbitrarily begin other antibiotics”. (Participant #6)
Customer satisfaction
Some clients have used several specific drugs for years and found them effective. Thus, they have no faith in the lab diagnostic test result. Besides, some clinicians and especially vets are sometimes subject to too many demands, which can be tempting. They might occasionally be tempted to violate the existing rules and, upon a client’s persistence, they may neglect the protocols and easily give in.
“ For our clients, the drug manufacturing company even matters. Sometimes, they carry the former drug vial to show us and insist that the same drug be prescribed”. (Participant #3) ” Even when the required facilities were available, I faced too many suggestions. Some guys came to tell us to take it easy and let them get away with it (by granting or renewing their permit)”. (Participant #16)
Low purchasing power
As there is no drug and treatment insurance for animals in veterinary medicine in Iran, the cost of treatment or the price of drugs was found as another determinant of antibiotic prescription, as mentioned by the present veterinarian participants.
“ Sometimes prescriptions are written out according to the customer’s affordance. Sometimes, customers ask us to prescribe something they can afford to buy. As there is no insurance coverage for veterinary medicine, the price matters, and it significantly affects the act of prescription”. (Participant #7)
Social learning
An effective factor in antibiotic self-medication or arbitrary use of antibiotics is to learn about it. There are often others living in the same place (city or village) where the clients live, who used a certain drug and found it effective. Now the clients tend to follow their steps. Besides, self-medication cuts down on the diagnostic and therapeutic costs too.
“A farmer might come to us and insist on buying the same drug that his neighbor has already bought. He does not consider that the diseases might be different. Overall, clients are more influenced by neighbors than us”!
Pharmaceutical determinants
In some cases, what causes the clients to insist on our prescribing OTC drugs is the price and effectiveness of the drug (as perceived by the clients) and even the drug manufacturing company.
“ Some clients insist on buying a certain antibiotic because either they have already used and found it effective. Thus, they may ignore what the vet’s diagnosis is”. (Participant #11)
Unawareness of antibiotic residues and abstinence interval
While using antibiotics, the livestock, poultry, and aquaculture breeders should be aware of the animal source food abstinence interval. But in reality, they are mostly unaware of that.
“Many clients are not adequately aware of the abstinence interval after taking antibiotics, and this issue makes them send the animal products into the food cycle during the treatment period”. (Participant # 11)
Drug replacement or early cessation
When seemingly the symptoms of the disease are gone, some breeders ignore the medical instructions and cease the drug sooner than they should.
“For example, a drug should be taken for not shorter than a week. But when a client takes the drug for two days and feels the disease is gone, he stops administering the drug. He does not care about the medical resistance and how it occurs. He ignores them all”. (Participant # 5) ”A client may purchase an antibiotic (either prescribed or self-medicated) and begin the treatment. After one or two days, when there is no sign of recovery, he replaces the drug easily”. (Participant #8)
Antibiotics use as a growth stimulant
Antibiotics have long been used as growth stimulants on a large scale by breeders of raw animal products in Iran.
“ In large breeding industries such as livestock and poultry farming, antibiotics are used as a growth stimulant, and this is very common”. (Participant #4)
Self-medication or arbitrary use of drugs
As the participants mentioned, many clients take some therapeutic measures before visiting a veterinary diagnostic and medical center. They have already begun taking several antibiotics or have quit the treatment half in the way.
“ Sometimes a farmer arbitrarily buys and consumes several drugs before going to any veterinary, diagnostic or medical center”. (Participant #5) ” Some ranchers already take many antibiotics. When we ask them why they say they had it refrigerated since the last time they ever purchased and consumed the drug. They intended to use the remains of the drug and visit a clinic only if their self-medication did not prove effective”. (Participant #8)
The unconventionality of the antibiogram test
As perceived by the present participants, antibiogram testing is a new thing that has not been yet received well by many clients. Not many participants welcome or even prioritize this test. They think doing this test is not compulsory and, thus, they do not feel obliged to take it at all.
“Unless the customer is obliged to, he does not go for the test to a laboratory at all. Thus, it needs to be mandatory; yet in reality, it is not”! (Participant #15) ” When we tell a client that he should take a sample for an antibiogram test and wait until then, he is surprised. It seems as if he has never heard of such a thing. He wonders why none of his fellow breeders were already sent for such a test when they faced the same problem”. (Participant #18) ”Nobody cares about AMR in the future. They laugh at us and wonder what the consequences are”. (Participant #2)
Clients’ preference for over-prescribing vets
As perceived by the present participants, any veterinarian or clinician who prescribes more drugs to treat animals is more popular.
“ If you do not prescribe any drug, the client prefers to go to another vet. He will not wait at all for you to tell him about the importance of drug resistance. Now every doctor who prescribes more drugs becomes more popular and he is perceived as a better doctor”. (Participant #18)
Clients’ lacking foresight
Some participants acknowledged that the AMR problem is unthinkable in the future and far-fetched to many clients.
“ People do not really know what will happen in the future and people will suffer from drug resistance. No one can even imagine what will happen in the future. It is not tangible to them”. (Participant #2)
Rejection of paraclinical costs
Some clients, as the participants’ accounts, revealed, do not bear costs higher than those of the visit, including the cost of a laboratory.
“ Our clients are mostly reluctant to pay much, especially when the cost of the treatment is higher than that of, for example, a domestic chicken that they bring here for treatment”. (Participant #18)
Materialistic view
Many ranchers ignore many important things and are just concerned with more production and productivity, and gaining as much money as they can. So, they do things that are sometimes unethical and illegal but just cost-effective.
“I don’t think it matters how you make money. You just need to be smart and know when to do what. For example, I know a guy who drugs his chickens the day before slaughter but keeps some of them apart for his own family’s use. He sends one of the undrugged chickens to the laboratory so that he gets a negative lab test result. This way, if there is any loss, it will happen to the undrugged chickens and not the whole poultry”. (Participant #9) “Sometimes they breed a few chickens apart from others only to send them later on to the laboratory. The lab also cooperates with them and hides things in the actual report”. (Participant #13)
Veterinarian-related factors
In addition to the above-mentioned factors, veterinarians also sometimes cause an increase in AMR. Here we see how their characteristics affect their decisions on AMR development.
Inadequate job security
The current job market for veterinarians in Iran is not very prosperous and any factor that endangers the current position of activists in this field will fail.
“If you cannot keep the customer satisfied with yourself in the job market right now and put extra costs on the customer, he will quickly go to another clinic and another vet”. (Participant #14)
Lacking experience in the correct act of prescription
As perceived by the participants, many veterinarians who have just entered the work market lack any experience in prescribing drugs. Thus, they significantly account for the increased AMR.
“ As novice veterinarians do not have much experience in prescribing medicine, they prescribe several antibiotics together, with the hope that one of them works”. (Participant #13)
Prescription based on prior experience
Prescribing drugs based solely on diagnostic experience is common practice in more experienced veterinarians.
“ As soon as most colleagues see cases similar to what they have already faced and treated, they begin to write out the same prescription. It is generally well-established that certain drugs are always prescribed for respiratory infections, some for gastrointestinal infections, and so on”. (Participant #14)
The unconventionality of diagnostic tests among veterinarians
Many veterinarians have diagnosed diseases and prescribed them mainly based on their own experience. Antibiogram testing is a new therapeutic measure that has not been welcomed warmly by vets.
“There are very few vets who wait for the antibiogram test before writing out any prescription. Actually, antibiogram tests are still very uncommon”. (Participant #9)
Being labeled as inexperienced if dependent on laboratory diagnosis
As our participants described, a veterinarian who does not make a diagnosis or give treatment immediately and independently (from lab tests) and hinders it until the paraclinical test results are labeled as inexperienced.
“We have no problem sending the client to the lab, but unfortunately it seems as if we were unable to make a diagnosis ourselves and we were inexperienced and because of that we got help from the lab”. (Participant #12)
Fear of losing clients
Some veterinarians acknowledged if they delayed the diagnosis to a later time (to receive the lab test result), they could easily lose many customers.
“If you keep the client waiting or send him to a lab to fetch the test results, he will for sure prefer to visit another vet”. (Participant #5)
Diminishing ethical values
Another determining factor raised by the participants was the need to have a working conscience and commitment to livestock/poultry breeders, laboratories, and those having contracts with labs. In other words, the vets should rely on the lab test results.
“When I used to work on a poultry farm, I saw a separate hall for raising chickens with no antibiotics. The sample sent to the lab was taken from this hall. Or the chickens were slaughtered for the farmer’s own family. The other (drugged) chickens were sent to the slaughterhouse for public use”. (Participant #10) “Some colleagues are not committed enough to their job and do not feel it on their conscience. Similarly, the test results coming from some labs are not reliable either. So, the negative antibiotic results we receive from them might be false”. (Participant #5)
Lacking foresight
AMR is not familiar to many people in society. They do not adequately know what AMR is, which can affect their practice.
“Veterinarians cannot even imagine how dangerous AMR can be to human health in the future. When they have no idea what AMR is and can be, how can we expect them to be worried about it”? (Participant #8)
The insignificance of AMR
The AMR issue is not very important for some veterinarians in diagnosis, treatment, and monitoring.
“Rarely does veterinarian care about drug resistance. I do not think it is even their last priority to consider”! (Participant #10)
Lack of self-efficacy in overcoming barriers
A few interviewees admitted that they or some colleagues have a specific drug classification for most diseases according to which they act spontaneously. It means that they do not take different therapeutic measures when faced with different cases.
“Some clinicians do not consider that everyone can have his disease. I mean, they treat all patients the same way and prescribe strong broad-spectrum antibiotics for 90% of cases”. (Participant #5)
Competitive drug market
Many veterinarians are not required to sell drugs on a prescription, and selling without a prescription is a legal and common task. So active veterinarians in the field compete with each other for selling drugs and evidently for more income.
“Everyone likes to open up a pharmacy because he can easily earn money with no trouble with diagnostic and surgical measures. It is much better if you can persuade customers to buy more”. (Participant #8)
Apparent issues with prescriptions
The last subcategory of veterinarian-related factors was the appearance of prescriptions. The present prescriptions encourage vets to prescribe more drugs.
“The size and shape of prescriptions are such that the vet is encouraged to prescribe more drugs. The prescriptions should be refined in shape to allow for one or two drugs only and no more”. (Participant #5)
The present study aimed to explore the barriers faced by Irainian veterinarians against preventing Antimicrobial resistance. A few qualitative studies have been conducted on AMR, which dealt with the causes of progress and the obstacles faced by those involved in this problem, especially in the veterinary profession [ 33 , 34 ]. The results showed that different educational, legal/administrative and veterinarian-related factors account for the increased AMR in Iranian society. The first category included factors related to the educational system, such as the lack of any specialized training course for veterinary students, those in charge of monitoring veterinary practice, veterinary departments, and ranchers struggling with educational problems who may all be implicated in increasing AMR. In Iran, various educational initiatives have been implemented, such as the publication of a book on rational prescription principles, academic papers, and reports from the National Committee on Prescribing and Rational Drug Use. Despite these efforts, there are numerous educational obstacles in veterinary colleges in Iran when it comes to instructing students on prescription fundamentals and the rational utilization of medications.
The required material has been also developed; training and retraining programs have been planned based on eclectic drug use criteria; workshops, conferences, and seminars have been held too. A prescription can simply be representative of a whole nation’s sociocultural values and medical conditions. Many studies have been conducted worldwide to improve rational drug prescription and consumption [ 35 ]. The effects of educational interventions on the improved prescription pattern have been reported in Iranians and other studies too [ 36 , 37 ]. Continued training on rational drug prescription and pharmacy education has been recommended to doctors in the existing literature [ 38 , 39 ].
In Zareh’s study, the most commonly prescribed drugs were injections and antibiotics. The research findings showed that, after the training, there was an increase in the rational prescriptions for most prescribed drugs [ 40 ]. As for teaching strategies, the WHO has published The Guide to Good Prescribing for medical students. This guidebook contains six rational steps that can significantly reduce the irrational prescription of drugs: 1- defining the patient’s problem 2- defining the goals of treatment 3- ensuring that the treatment is appropriate for the patient. 4 – initiating the therapeutic measure 5 - providing information, instructions and warnings (if any) 6 - monitoring and ceasing the treatment [ 41 ]. Outdated education was a sub-category found in this study. Different studies showed that dentists often, due to a lack of knowledge about the side effects of improper prescribing of antibiotics, tend to over-prescribe them [ 42 , 43 ].
Veterinarians also are central to antimicrobial stewardship on farms, with their prescribing decisions significantly impacting AMR.A study on Canadian dairy cattle veterinarians’ revealed factors influencing their antimicrobial prescribing, attitudes towards reducing antimicrobial use, awareness of AMR, and perceived barriers to improving stewardship [ 44 ]. In addition educational resources have been developed to enhance veterinarians’ understanding of AMR and promote rational antimicrobial use. Online courses such as “Antimicrobial stewardship in veterinary practice” and “Farmed Animal Antimicrobial Stewardship Initiative” aim to educate veterinarians on responsible antimicrobial use [ 45 , 46 ].
What we need is a high-quality time management element added to the existing curricula so that students can be well-equipped with whatever they need to act professionally. Excessive imitation of medical sciences in specialized courses can only lower the efficiency of a vet’s profession. Rather, there is a need for incorporating courses on different animal species both at the general practitioner’s level and the specialized doctorate degrees [ 47 ].
There is also the issue of time management in the curriculum. Decreasing the quantity of content and increasing the quality (by adding more useful content) can better reform the veterinary curriculum. Goal-setting in veterinary sciences has already been revolutionized, and veterinary universities cannot ignore it. Thus, it is essential to consider the present and future needs in defining the required specialties to handle the existing national health issues, each of which can impose a loss of millions of dollars nationally. For many years, curricula have been developed in the European Union to achieve the necessary specializations by the existing needs, at least in the cattle breeding industry [ 48 ]. A deficient educational system is one factor that increases the overuse of antibiotics. Therefore, it is necessary to take basic measures based on the macro-planning of students’ knowledge and increase the quality of internships. In a study by Wushouer et al. in China, it was observed that an increasing awareness was followed by a decreasing rate of antibiotic administration [ 49 ]. Therefore, it is necessary to increase knowledge through a different approach in the educational system. Most experts believe that education in medical sciences should follow a different approach than other fields of study because knowledge construction in these fields of study (i.e., medicine, veterinary medicine) affects the content that students receive and the experiences they gain [ 50 ].
Failure to hold training courses for producers of raw animal products and unsystematic student internships can significantly lower the quality of education. Raising the study index in AMR and modeling on successful examples can be considered in curriculum design. Moreover, all departments of the veterinary faculties should cooperate and the heavy burden of teaching AMR should be removed from the bacteriology department only, and be shared by all basic sciences and clinical courses. Only then can we hope to see improved practice in students’ learning experiences and professional life in the near future.
The present findings showed that currently in our country, the educational system needs to be seriously reformed by appropriate training programs and pre-employment awareness-raising programs for veterinarians and ranchers [ 51 ]. People working in this field should be more empowered, better aware, and skilled enough at a correct diagnosis or proper functioning [ 52 ]. Only then we can hope that their self-efficacy is increased and they can learn to act more responsibly. These can help to prevent the occurrence of AMR and to begin to resolve it rather than worsening the issue.
The second category of the determinants of increased AMR was administrative and legal factors. Problems with the law, monitoring, and selling OTC drugs are important issues that can increase the costs of treatment too. This finding is consistent with several studies. For example, it is estimated that about 100,000 people in the United States die every year from the adverse effects of drugs [ 53 ]. In the United Kingdom, problems in 11% of prescriptions cost over € 400 million in loss, and about 16% of these problems harm patients [ 54 ]. Most of these errors are preventable, including drugs prescribed heedless of contraindications, those taken incorrectly, or those not having been properly monitored. The WHO, along with other relevant international organizations, proposed certain criteria to evaluate the quality of prescriptions to prevent the occurrence of problems and lower treatment costs [ 55 , 56 ]. A useful way of evaluating the prescription pattern in a country is to evaluate the doctors’ prescriptions. A simple prescription can represent the current state of medical education in a country, how laws and regulations affect the medical community, socio-cultural beliefs, and the medical condition [ 36 ]. Based on WHO guidelines use of medically important antimicrobials in food-producing animals, any level of restriction in antibiotic prescription should be considered, including a complete cessation of the use of one or more antibiotics. Examples of restrictions that WHO considered are: any prohibition on the use of antibiotics, such as but not limited to the prohibited use for specific indications (e.g., for prophylaxis of disease or growth promotion), the requirement of a prescription by a veterinarian for the use of antibiotics, voluntary restrictions on farms or organic interventions [ 55 ]. Drugs that need confirmation from a specially qualified person or organization should not be sold over the counter. Prescribed drugs are regulated by the US Food and Drug Administration (FDA). Having a federal license with a medical leaflet is a prerequisite for the packing of any drug. A medical leaflet usually consists of four parts: indications, contraindications, warnings, and dosage [ 57 ]. He who writes out a prescription decides who can consume the drug. A pharmacist can buy drugs, but he should sell them only to those authorized by a legally qualified person. Thus, a prescribed drug has 3 parts [ 58 ]: (1) The doctor’s prescription, (2) The pharmacist’s written prescription while delivering the drug, and (3) the drug package with a label on it. That is why officials are expected to always think about formulating new and public policies to implement correct and new strategies for the use of antibiotics [ 59 ]. Educational and political interventions, establishing and implementing laws regarding AMR stewardship may be effective and acceptable either before or during the livestock and poultry breeding programs, even for pet owners [ 60 ]. Success in the coordinated implementation of related laws is not possible without the advocacy of various stakeholders, including policymakers, veterinarians and ranchers, pet owners, public sector employees, farmers, and consumers [ 51 ]. It seems that the use of effective legislation, contractual requirements, professional obligations and the distribution of suitable facilities in more distant areas makes the implementation of this plan possible [ 21 , 22 ].
The third category was the client-related factors. Quick response and arbitrary drug use were among the sub-categories. With the expansion of public access to the internet system, people may want to refer less to vets and, instead, self-medicate or they may expect a quick response and begin to use antibiotics. In their research, Hofmeister et al. investigated veterinary visitors and found the internet connection speed as the third most important source of retrieving pet health information after GPs and specialized vets and before family and friends and other mass media [ 61 ]. Kogan et al. maintained that internet-based sources are considered an extra source of information about pet health for pet owners besides visiting vets for consultation [ 62 ]. Volk et al. reckoned that the internet and online health information could replace veterinarians and lead to fewer pet owners visiting veterinary clinics [ 63 ]. Thus, since some clients do not want to pay the visit and para clinic fees, by searching on the Internet and cyberspace, or based on their previous experience or else, they prescribe and take antibiotics arbitrarily before any visit to vets. If they do not find some proper treatment, they try other antibiotics, which leads to the problem of changing or stopping the antibiotics early before the end of the treatment period.
Some other poultry or aquatic breeders who have farms of several thousand pieces are very worried about the loss of their livestock, poultry and the aquatic population at the beginning of the disease. Since there may be a large population of their herd while waiting for the antibiogram test, they prefer to use a broad-spectrum and preferably cheaper antibiotic (for large-scale use for a large herd) to begin with and prevent their economic loss to a large extent [ 60 ]. Therefore, both in the producers and breeders of animal-origin food and in the owners of pets, the customer’s demand needs quick response and the customer’s demand should be prioritized [ 22 ].
In addition, a person who once used a broad-spectrum antibiotic without a prescription and got a response, suggests that to his/her colleagues or other breeders, and by promoting social learning, this behavior promotes the progress of antimicrobial resistance. In addition, many of these people are unaware of antibiotic residues and abstinence intervals, and currently do not feel threatened about the future of antimicrobial resistance. When they go to the vet, they prefer to go to a vet who prescribes some antibiotics to return home without any drug prescribed [ 33 ].
Another subcategory extracted from the present findings was the use of antibiotics as growth stimulants by poultry farmers. The use of antibiotics, both as a treatment in humans and as a therapeutic measure or growth stimulant in animals, has a great effect on the microbial flora of the intestine and also induces resistant strains in these animals [ 64 ]. When used as a growth stimulant, antibiotics can have adverse effects on humans and animals [ 65 ].
The fourth category was the veterinarian-related factors. The lack of an inter-sectoral approach was one subcategory extracted from the findings. Foreign studies mentioned a multi-sectoral approach and knowledge sharing in educational environments [ 66 ]. There seems to be a need for all institutions to have the required knowledge about the use of antibiotics through shared efforts between universities, the government, and the various professions. One subcategory was the insignificance of antimicrobial resistance to veterinarians. Antibiotic-containing products have harmful effects and there is a significant increase in the resistance of different types of infectious bacteria [ 67 ] besides the important role that antibiotic-containing animal products play in this process. Thus, global efforts are needed to reduce antibiotic use and attempt to control it. More control is needed over veterinary drugs and their use in livestock and poultry farms [ 68 ].
In line with the qualitative study in the UK, this study showed various behavioral and contextual factors involved in the participants’ beliefs about AMR stewardship and their responsibilities in the right direction [ 33 ]. One of these issues is the lack of experience in writing correct prescriptions among novice vets who prescribe several antibiotics at the same time in the hope that at least one works. This finding is in line with some studies that acknowledged that, when uncertain, most new clinicians tend to over-treat with antimicrobial drugs instead of refraining from treatment [ 1 , 69 , 70 , 71 ]. They prescribe several antibiotics in the hope that one works. The other extreme case is also possible when experienced veterinarians prescribe drugs based on their long-held experience. These clinicians have more faith in a series of antibiotics. On the other hand, the diagnosis of the disease and the prescription are dependent n each other. When they are told about the laboratory evidence, they react as if their credibility has been damaged. Therefore, they provide waves of unprincipled recommendations and increase antimicrobial resistance. If a veterinarian intends to prescribe antibiotics based on the principles and guidelines, s/he will face other problems, including the fear of losing clients because, as mentioned earlier, if the prescription is not in accordance with the client’s wishes or the urgency of responding to it, the client will prefer to go to another vet, and this issue will endanger the job security even more.
Another sub-category is lacking self-efficacy in dealing with different visits.In other words, the approach of veterinarians to prescribing antibiotics is to a great extent pre-established and classified. For example, oxytetracycline is the preferred antibiotic for most respiratory diseases. Any cause of disease that requires more attention to the self-efficacy of veterinarians and clinicians can be improved by training methods and participation in appropriate courses. Diminishing moral values becomes important in cases where full-time monitoring of antibiotic residues in animal products and their transfer to society and the environment is not possible, and where the government and regulatory agencies fail due to poor enforcement of laws. The regulatory forces cannot monitor and take care of the veterinary private sector employees and breeders. We can only hope that the vets will feel committed enough in their acts of diagnosis and prescription and the resultant effect on antimicrobial resistance. In the end, it is possible to recommend the modification of the appearance of prescriptions as a solution, because most of the headers of the veterinarians’ prescriptions in Iran are designed in a large way, which encourages the person to fill most of the prescription with writing the unnecessary drugs, so maybe it is recommended to design and implement a single protocol in limiting the written space of the prescriptions, we can take a step in reducing the obstacles facing the control of antimicrobial resistance.
Limitations, strengths and future directions
There were certain limitations in this study. As the interviews were face-to-face, participants might have been tempted to provide socially acceptable answers. Also, some veterinarians showed concerns about the illegal cases they were aware of and reported. So, they were selected through snowball sampling. In addition, selecting interviewees with work experience and an adequate understanding of the relevant problems and interviewing them in a private place were somehow difficult.
As in other qualitative studies, researchers’ beliefs may have influenced the study procedure from conceptualization to interaction with participants and data interpretation [ 72 ].There were chances that the interviewees’ comments did not cover all factors possibly because of the limited sample size. Sampling in qualitative studies continues until the saturation happens. Thus, in this study also the interviews continued until the data were saturated (i.e., when no new information was obtained) and until all the extracted themes were sufficiently supported by the data. No formula was included.
It is possible that besides the factors mentioned by the present participants, other experiences are gained in other parts of the country that cannot be subsumed under the present categories.
Despite the potential limitations, the present study has several strengths. The first is the sampling method with maximum variation (in terms of the province of work, age, sex, and work in the clinic or drug supply or employed in public and private sectors). The next strength is that during the interviews, some participants were dissatisfied with the current conditions, and this study provided an opportunity for them to find solutions. Moreover, there has been extensive research on AMR, but the vast majority of them are quantitative. Few have explored AMR determinants in society. The present study goes beyond the laboratory work, and with the One Health approach, using numerous interviews, it gains a deep understanding of work experience, and comprehensive and valid data to solve the AMR issue. The authors of this study intend to use the data from this study or at least part of the data for future educational interventions. A focus on the categories extracted from these studies helps to plan effective multidimensional interventions. This study can also guide future lines of research.
The results showed that AMR in veterinary medicine induced by veterinarians active in the clinical field occurs under the influence of different factors. To increase AMR stewardship, in the first step, the barriers facing all people involved should be deeply studied and identified. Appropriate plans and policies should be made to deal with the underlying factors. Educational, administrative and legal, client-related factors, and veterinarian-related factors should be considered as the determinants of the increased AMR. It is essential to reform the education system and strengthhen the interdisciplinary relationships, especially among universities and between the university and regulatory organizations. Removing the barriers these people face and reducing the consequent trouble can make the widespread emergence of AMR more evident. Its adverse effects on society will become a crisis which increases the causes of mortality due to the resistance produced to the antibiotics prescribed to patients.
Data availability
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding authors.
Abbreviations
Antimicrobial Resistance
over-the-counter
Prestinaci F et al. Antimicrobial resistance: a global multifaceted phenomenon 2015. 109(7): pp. 309–318.
Kovačević Z et al. Veterinary practitioners’ standpoints and comprehension towards antimicrobial use—are there opportunities for antimicrobial stewardship improvement? 2022. 11(7): p. 867.
Boucher HW. Bad bugs, no drugs 2002–2020: progress, challenges, and call to action. Trans Am Clin Climatol Assoc. 2020;131:65.
PubMed PubMed Central Google Scholar
Ghanbarpour R, et al. Domestic and game pigeons as reservoirs for Escherichia coli harbouring antimicrobial resistance genes. J Global Antimicrob Resist. 2020;22:571–7.
Article Google Scholar
Mahmoudi R, Golchin A, Farhoodi A. A Review on Antibiotic Residues in Animal-derived Foods in Iran over the Last Thirty Years 2014. 24(119): pp. 213–222.
Aidara-Kane A et al. World Health Organization (WHO) guidelines on use of medically important antimicrobials in food-producing animals 2018. 7: pp. 1–8.
Barlow JJ. Antimicrobial resistance and the use of antibiotics in the dairy industry: Facing consumer perceptions and producer realities 2011. 23: pp. 47–58.
Organization WH. Antimicrobial resistance: global report on surveillance. World Health Organization; 2014.
Kadri S. S.J.C.c.m., Key takeaways from the US CDC’s 2019 antibiotic resistance threats report for frontline providers 2020. 48(7): pp. 939–945.
Kuehn BJJ. Antibiotic Resist Threat Grows. 2019;322(24):2376–2376.
Google Scholar
Organization WHO. Use of antimicrobials outside human medicine 2001.
AL Wabel, N. The pharmacokinetics and milk residual behaviour of tylosin in lactating Najdi ewes 2008.
Nisha AJVw. Antibiotic residues-a Global Health Hazard. 2008;1(12):375.
Sharifi A, Sobhani K, Mahmoudi P. A systematic review and meta-analysis revealed a high-level antibiotic resistance of bovine mastitis Staphylococcus aureus in Iran 2023.
Toghroli R et al. Determinants of antimicrobial resistance occurrence in animal-based food, perceived by livestock farmers: a qualitative phenomenological study. 2023. 6(3): p. e1160.
Mehtarpour M et al. Control of antimicrobial resistance in Iran: The role of international factors 2020. 20: pp. 1–10.
Hassani L et al. An intervention to improve antibiotic prescription behavior in veterinary students: A protocol based on the multi-theory model to tackle antimicrobial resistance 2024. 7(2): p. e1886.
Laxminarayan R, et al. Antibiotic resistance—the need for global solutions. Lancet Infect Dis. 2013;13(12):1057–98.
Article PubMed Google Scholar
O’Neill J. Review on antimicrobial resistance: tackling drug-resistant infections globally: final report and recommendations Review on antimicrobial resistance: tackling drug-resistant infections globally: final report and recommendations., 2016.
Aenishaenslin C, et al. Evidence needed for antimicrobial resistance surveillance systems. Bull World Health Organ. 2019;97(4):283.
Article PubMed PubMed Central Google Scholar
Samuels R, Qekwana DN, Oguttu JW. Antibiotic prescription practices and attitudes towards the use of antimicrobials among veterinarians in the City of Tshwane, South Africa. PeerJ. 2021;9:e10144.
Van Boeckel TP, et al. Global trends in antimicrobial use in food animals. Proc Natl Acad Sci. 2015;112(18):p5649–5654.
Tonkin-Crine S, Yardley L, Little P. Antibiotic prescribing for acute respiratory tract infections in primary care: a systematic review and meta-ethnography. J Antimicrob Chemother. 2011;66(10):2215–23.
Article CAS PubMed Google Scholar
Drekonja DM, et al. Antimicrobial stewardship in outpatient settings: a systematic review. Infect Control Hosp Epidemiol. 2015;36(2):142–52.
van Dijk L, et al. Participatory policy making by dairy producers to reduce anti-microbial use on farms. Zoonoses Public Health. 2017;64(6):476–84.
Speksnijder DC, et al. Effect of structural animal health planning on antimicrobial use and animal health variables in conventional dairy farming in the Netherlands. J Dairy Sci. 2017;100(6):4903–13.
Sazmand A, et al. Assessment of knowledge, attitudes and practices relating to parasitic diseases and anthelmintic resistance among livestock farmers in Hamedan. Iran. 2020;7:584323.
Odetokun IA et al. Knowledge of antimicrobial resistance among veterinary students and their personal antibiotic use practices: a national cross-sectional survey. 2019. 8(4): p. 243.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Toghroli R, et al. Explaining the determinants of Pediculosis Control and Prevention: a qualitative study in Southern Iran. INQUIRY: J Health Care Organ Provis Financing. 2022;59:00469580221086369.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Lincoln YS, Lynham SA, Guba EG. Paradigmatic controversies, contradictions, and emerging confluences, revisited. Sage Handb Qualitative Res. 2011;4(2):97–128.
Golding SE, Ogden J, Higgins HM. Shared goals, different barriers: a qualitative study of UK veterinarians’ and farmers’ beliefs about antimicrobial resistance and stewardship. Front Veterinary Sci. 2019;6:132.
Doidge C, et al. Farmers’ perceptions of preventing antibiotic resistance on sheep and beef farms: risk, responsibility, and action. Front Veterinary Sci. 2020;7:524.
Irshaid YM, et al. A pharmacoepidemiological study of prescription pattern in outpatient clinics in Southwestern Saudi Arabia. Saudi Med J. 2004;25(12):1864–70.
PubMed Google Scholar
Mohagheghi M, et al. Community-based outpatient practice of antibiotics use in Tehran. Pharmacoepidemiol Drug Saf. 2005;14(2):135–8.
Madridejos-Mora R, Amado-Guirado E, Pérez-Rodríguez MT. Effectiveness of the combination of feedback and educational recommendations for improving drug prescription in general practice Medical care, 2004: pp. 643–648.
Chaturvedi V, Mathur A, Anand A. Rational drug use–As common as common sense? Med J Armed Forces India. 2012;68(3):206.
Article CAS PubMed PubMed Central Google Scholar
Rashmi S, Chaman L, Bhuvneshwar K. Antibacterial resistance: current problems and possible solutions. Indian J Med Sci. 2005;59:120–9.
Zare N et al. Effectiveness of the feedback and recalling education on quality of prescription by general practitioners in Shiraz 2008.
De Vries T, et al. Impact of a short course in pharmacotherapy for undergraduate medical students: an international randomised controlled study. Lancet. 1995;346(8988):1454–7.
Dar-Odeh NS et al. Antibiotic prescribing practices by dentists: a review Therapeutics and clinical risk management, 2010. 6: p. 301.
Öcek Z, et al. Development of a rational antibiotic usage course for dentists. Eur J Dent Educ. 2008;12(1):41–7.
Cobo-Angel C, Roche SM, LeBlanc SJJPo. Understanding the role of veterinarians in antimicrobial stewardship on Canadian dairy farms: a mixed-methods study. 2023. 18(7): p. e0289415.
Lloyd DH. S.W.J.A.r.i.b.f.l. Page, and c. animals, Antimicrobial stewardship in veterinary medicine 2018: pp. 675–697.
Allerton F, Russell JJJ-AR. Antimicrob Stewardship Veterinary Medicine: Rev Online Resour. 2023;5(3):dlad058.
Espinosa G-S, Román J et al. Veterinary Education and Training on Non-Traditional Companion Animals, Exotic, Zoo, and Wild Animals: Concepts Review and Challenging Perspective on Zoological Medicine 2023. 10(5): p. 357.
Barret D. Training and evaluation of the european cattle specialist of the future . in Proceeding of 24th World Buiatrics Congress . 2006.
Wushouer H et al. The impact of physicians’ knowledge on outpatient antibiotic use: Evidence from China’s county hospitals. Medicine, 2020. 99(3).
Holopainen A, Hakulinen-Viitanen T, Tossavainen K. Nurse teacherhood: systematic descriptive review and content analysis. Int J Nurs Stud. 2007;44(4):611–23.
Moradi G, et al. National action plan of the Islamic Republic of Iran for combating antimicrobial resistance during 2016–2021. Med J Islamic Repub Iran. 2018;32:82.
Organization WH. Strategic framework for collaboration on antimicrobial resistance: together for one health. Food & Agriculture Org; 2022.
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279(15):1200–5.
FitzGerald RJ. Medication errors: the importance of an accurate drug history. Br J Clin Pharmacol. 2009;67(6):671–5.
Organization WH. WHO guidelines on use of medically important antimicrobials in food-producing animals: web annex A: evidence base. World Health Organization; 2017.
Yimenu DK, et al. Assessment of antibiotic prescribing patterns at outpatient pharmacy using world health organization prescribing indicators. J Prim Care Community Health. 2019;10:2150132719886942.
Watson KT, Barash PG. The new Food and Drug Administration drug package insert: implications for patient safety and clinical care. Anesth Analgesia. 2009;108(1):211–8.
Wynn R, Meiller T, Crossley H. Drug information handbook for dentistry: oral medicine for medically-compromised patients & specific oral conditions. Lexi-Comp, US; 2000.
Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. Pharm Ther. 2015;40(4):277.
Butcher A, Cañada JA, Sariola S. How to make noncoherent problems more productive: towards an AMR management plan for low resource livestock sectors. Humanit Social Sci Commun. 2021;8(1):1–10.
Hofmeister EH, et al. Validity and client use of information from the world wide web regarding veterinary anesthesia in dogs. J Am Vet Med Assoc. 2008;233(12):1860–4.
Kogan LR, Schoenfeld-Tacher R, Viera AR. The internet and health information: differences in pet owners based on age, gender, and education. J Med Libr Association: JMLA. 2012;100(3):197.
Volk JO, et al. Executive summary of the Bayer veterinary care usage study. J Am Vet Med Assoc. 2011;238(10):1275–82.
Price LB, et al. Elevated risk of carrying gentamicin-resistant Escherichia coli among US poultry workers. Environ Health Perspect. 2007;115(12):1738–42.
Awosanya EJ, Akande H. Animal health care seeking behavior of pets or livestock owners and knowledge and awareness on zoonoses in a university community. Veterinary World. 2015;8(7):841.
Santosh S, Panda S. Sharing of knowledge among faculty in a mega open university. Open Praxis. 2016;8(3):247–64.
Adib N, et al. Antibiotic resistance profile and virulence genes of uropathogenic Escherichia coli isolates in relation to phylogeny. Trop Biomed. 2014;31(1):17–25.
CAS PubMed Google Scholar
Kim H, Xie B. Health literacy in the eHealth era: a systematic review of the literature. Patient Educ Couns. 2017;100(6):1073–82.
Blaser MJJS. Antibiotic use and its consequences for the normal microbiome 2016. 352(6285): pp. 544–545.
Organization WH. World Health Organization Antimicrobial Resistance: Global Report on Surveillance. 2014 . 2014.
Weiner LM, et al. Vital signs: preventing antibiotic-resistant infections in hospitals—United States, 2014. Elsevier; 2016. pp. 2224–30.
Yeh CJ, Inman AG. Qualitative data analysis and interpretation in counseling psychology: strategies for best practices. Couns Psychol. 2007;35(3):369–403.
Download references
Acknowledgements
The authors would like to acknowledge all participants for their participation who patiently participated in this study.
This study received funding from Hormozgan University of Medical Sciences. The funder was not involved in the research design, collection, interpretation of data, analysis, the writing of the article or the decision to submit it for publication.
Author information
Authors and affiliations.
Social Determinants in Health Promotion Research Center, Hormozgan Health Institute, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
Razie Toghroli, Laleh Hassani & Teamur Aghamolaei
Department of Social and Behavioral Health, School of Public Health, University of Nevada, Las Vegas (UNLV), Las Vegas, NV, 89119, USA
Manoj Sharma
HIV/STI Surveillance Research Center, and WHO Collaborating Center for HIV Surveillance, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
Hamid Sharifi
Department of Pathobiology, Faculty of Veterinary Medicine, Shahid Bahonar University of Kerman, Kerman, Iran
Maziar Jajarmi
Institute for Global Health Sciences, University of California, San Francisco, CA, USA
You can also search for this author in PubMed Google Scholar
Contributions
RT, LH, TA and M-SH designed the study. MJ and RT conducted the laboratory analyses. RT, MJ collected the specimens. H-SH conducted the data analysis. RT, LH and M-SH wrote the main manuscript text. All authors reviewed and approved the manuscript.
Corresponding author
Correspondence to Laleh Hassani .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Research Ethics Committee of Hormozgan University of Medical Sciences (IR.HUMS.REC.1400.207). A written informed consent was obtained from all the study participants. All methods were performed in accordance with the relevant guidelines and regulations by including a statement in the declarations.
Consent for publication
Not applicable.
Competing interests
All the authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Note: Here, what we mean by “Livestock” is all animals, including cattle, sheep, goats, camels, poultry, and aquatic animals bred and consumed by humans and consumed as animal-origin food.
By “stockbreeder”, “breeder” and “client”, we mean all those who own livestock and pet. AMR represents antimicrobial resistance.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Toghroli, R., Hassani, L., Aghamolaei, T. et al. Explaining the barriers faced by veterinarians against preventing antimicrobial resistance: an innovative interdisciplinary qualitative study. BMC Infect Dis 24 , 455 (2024). https://doi.org/10.1186/s12879-024-09352-7
Download citation
Received : 13 July 2023
Accepted : 25 April 2024
Published : 30 April 2024
DOI : https://doi.org/10.1186/s12879-024-09352-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Antimicrobial resistance (AMR)
- Food Safety
- Veterinarian
- Qualitative research
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Discussion section example. Here is an example of how you can introduce your discussion section. Note that it includes everything mentioned above: notably research outcomes, limitations, interpretations, and avenues for future research. ... In qualitative research, results and discussion are sometimes combined.
The results section of a research paper tells the reader what you found, while the discussion section tells the reader what your findings mean. The results section should present the facts in an academic and unbiased manner, avoiding any attempt at analyzing or interpreting the data. Think of the results section as setting the stage for the ...
1. Begin by discussing the research question and talking about whether it was answered in the research paper based on the results. 2. Highlight any unexpected and/or exciting results and link them to the research question. 3. Point out some previous studies and draw comparisons on how your study is different. 4.
Research results refer to the findings and conclusions derived from a systematic investigation or study conducted to answer a specific question or hypothesis. These results are typically presented in a written report or paper and can include various forms of data such as numerical data, qualitative data, statistics, charts, graphs, and visual aids.
The results chapter in a dissertation or thesis (or any formal academic research piece) is where you objectively and neutrally present the findings of your qualitative analysis (or analyses if you used multiple qualitative analysis methods ). This chapter can sometimes be combined with the discussion chapter (where you interpret the data and ...
Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion. Explain why the outcomes of your study are important to the reader. Discuss the implications of your findings realistically based on previous literature, highlighting both the strengths and ...
Chapters 4 through 7 consider the typical sections of a qualitative research paper— the introductory sections, Method, Results, and Discussion. These chapters emphasize aspects of reporting that are unique to qualitative research. They describe the general elements that should be reported in qualitative papers and can assist authors in devel-
What exactly is the discussion chapter? The discussion chapter is where you interpret and explain your results within your thesis or dissertation. This contrasts with the results chapter, where you merely present and describe the analysis findings (whether qualitative or quantitative).In the discussion chapter, you elaborate on and evaluate your research findings, and discuss the significance ...
It also discusses methods for reviewers to assess the rigour, quality, and usefulness of qualitative research. Examples of different ways to present data from interviews, observations, and focus groups are included. ... It is common practice to include some discussion within the results section of qualitative research and follow with a ...
Abstract. This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions ...
Tips to Write the Results Section. Direct the reader to the research data and explain the meaning of the data. Avoid using a repetitive sentence structure to explain a new set of data. Write and highlight important findings in your results. Use the same order as the subheadings of the methods section.
Results and discussion: Provide summaries and interpretations of the data (e.g., themes, conceptual models) and select illustrative quotes. ... For example, qualitative research could contribute to the study of health care providers and systems with the goal of optimizing our health care delivery models. Given the increasing diversity of the ...
The qualitative findings in relation to each research question are presented sequentially followed by a summary and discussion. This chapter presents the results and discussion in line with the five research questions of the present study based on the qualitative data collected from the focus groups and semi-structured interviews. A total of 7 ...
This handout was created to accompany the Writing in the Sciences video series. The purpose of the Results is to prepare readers for the discussion section by presenting the data in manageable chunks, in an order that corresponds with the research questions or objectives. The purpose of the Discussion section is used to contain analysis and ...
IMRaD Results Discussion. Results and Discussion Sections in Scientific Research Reports (IMRaD) After introducing the study and describing its methodology, an IMRaD* report presents and discusses the main findings of the study. In the results section, writers systematically report their findings, and in discussion, they interpret these findings.
Summarise your results in the text, drawing on the figures and tables to illustrate your points. The text and figures should be complementary, not repeat the same information. You should refer to every table or figure in the text. Any that you don't feel the need to refer to can safely be moved to an appendix, or even removed.
Table of contents. What not to include in your discussion section. Step 1: Summarise your key findings. Step 2: Give your interpretations. Step 3: Discuss the implications. Step 4: Acknowledge the limitations. Step 5: Share your recommendations. Discussion section example.
Curriculum is the only thing that appears on the time table and if the curriculum is not monitored, defining and communicating the vision and goals fails. 3. Monitoring and providing feedback on the teaching and learning process. They argued that monitoring and providing feedback is imperative for effective learning.
Results and Discussions. Presented in this chapter is the result of the data analysi s. Discussions are also provided to give a comprehensive explanation of the themes that were generated in response to the objectives set in this study. First subheading, based on first Research Objectives Effect of Poor Internet Connection
QUALITATIVE RESEARCH PAPER 45 population sample, so your study is limited by the number of participants, or that you used a convenience sample. Summary Then the author would wrap up the chapter with the summarization of the chapter and a transition to the next chapter as described above. Notice that this section started with a
Objective Qualitative research methods are based on the analysis of words rather than numbers; they encourage self-reflection on the investigator's part; they are attuned to social interaction and nuance; and they incorporate their subjects' thoughts and feelings as primary sources. Despite appearing well suited for research in child and adolescent psychiatry (CAP), qualitative methods ...
The research results on walking as well as on mindfulness-based interventions in BC patients illustrate the effectiveness and relevance of both types of ... A limitation might be the sample of interviewed women: The interviewees had to have participated in at least 6 from 8 group dates, the participants who rarely came to the intervention dates ...
For example, children with ... RB, SS, and TT) entered the abstraction phase of the inductive content analysis. Through collaborative discussion, the research team re-reviewed the data, code list, and categories and described themes. Together, the research team discussed different approaches to understanding and describing the themes that ...
The sample was prepared in a 10 mL volumetric flask using 0.1 mL of ethanolic cherry leaf extract ... Results and Discussion 3.1. Qualitative and Quantitative Composition of the Phenolic Compounds of Sour Cherry (Prunus cerasus L.) Leaves ... The obtained research results could be potentially valuable for using the plant raw material of cherry ...
The results chapter or section simply and objectively reports what you found, without speculating on why you found these results. The discussion interprets the meaning of the results, puts them in context, and explains why they matter. In qualitative research, results and discussion are sometimes combined. But in quantitative research, it's ...
Engagement of healthcare providers is one of the World Health Organization strategies devised for prevention and provision of patient centered care for multidrug resistant tuberculosis. The need for current research question rose because of the gaps in evidence on health professional's engagement and its factors in multidrug resistant tuberculosis service delivery as per the protocol in the ...
These discussions were essential in helping the first author navigate an empathetic understanding of the participant's experiences with the necessary analytical objectivity required for rigorous qualitative research. Participants and study settings. Fifteen males serving a prison sentence were recruited from three prisons in Northern Norway.
The present research was done in three cities in Iran in 2021. The data were collected through in-depth interviews with 18 veterinarians selected through purposive and snowball sampling and analyzed using conventional qualitative content analysis. The data analysis results were classified into 4 main categories and 44 subcategories.