- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Overcoming Speech Impediment: Symptoms to Treatment
There are many causes and solutions for impaired speech
- Types and Symptoms
- Speech Therapy
- Building Confidence
Speech impediments are conditions that can cause a variety of symptoms, such as an inability to understand language or speak with a stable sense of tone, speed, or fluidity. There are many different types of speech impediments, and they can begin during childhood or develop during adulthood.
Common causes include physical trauma, neurological disorders, or anxiety. If you or your child is experiencing signs of a speech impediment, you need to know that these conditions can be diagnosed and treated with professional speech therapy.
This article will discuss what you can do if you are concerned about a speech impediment and what you can expect during your diagnostic process and therapy.
FG Trade / Getty Images
Types and Symptoms of Speech Impediment
People can have speech problems due to developmental conditions that begin to show symptoms during early childhood or as a result of conditions that may occur during adulthood.
The main classifications of speech impairment are aphasia (difficulty understanding or producing the correct words or phrases) or dysarthria (difficulty enunciating words).
Often, speech problems can be part of neurological or neurodevelopmental disorders that also cause other symptoms, such as multiple sclerosis (MS) or autism spectrum disorder .
There are several different symptoms of speech impediments, and you may experience one or more.
Can Symptoms Worsen?
Most speech disorders cause persistent symptoms and can temporarily get worse when you are tired, anxious, or sick.
Symptoms of dysarthria can include:
- Slurred speech
- Slow speech
- Choppy speech
- Hesitant speech
- Inability to control the volume of your speech
- Shaking or tremulous speech pattern
- Inability to pronounce certain sounds
Symptoms of aphasia may involve:
- Speech apraxia (difficulty coordinating speech)
- Difficulty understanding the meaning of what other people are saying
- Inability to use the correct words
- Inability to repeat words or phases
- Speech that has an irregular rhythm
You can have one or more of these speech patterns as part of your speech impediment, and their combination and frequency will help determine the type and cause of your speech problem.
Causes of Speech Impediment
The conditions that cause speech impediments can include developmental problems that are present from birth, neurological diseases such as Parkinson’s disease , or sudden neurological events, such as a stroke .
Some people can also experience temporary speech impairment due to anxiety, intoxication, medication side effects, postictal state (the time immediately after a seizure), or a change of consciousness.
Speech Impairment in Children
Children can have speech disorders associated with neurodevelopmental problems, which can interfere with speech development. Some childhood neurological or neurodevelopmental disorders may cause a regression (backsliding) of speech skills.
Common causes of childhood speech impediments include:
- Autism spectrum disorder : A neurodevelopmental disorder that affects social and interactive development
- Cerebral palsy : A congenital (from birth) disorder that affects learning and control of physical movement
- Hearing loss : Can affect the way children hear and imitate speech
- Rett syndrome : A genetic neurodevelopmental condition that causes regression of physical and social skills beginning during the early school-age years.
- Adrenoleukodystrophy : A genetic disorder that causes a decline in motor and cognitive skills beginning during early childhood
- Childhood metabolic disorders : A group of conditions that affects the way children break down nutrients, often resulting in toxic damage to organs
- Brain tumor : A growth that may damage areas of the brain, including those that control speech or language
- Encephalitis : Brain inflammation or infection that may affect the way regions in the brain function
- Hydrocephalus : Excess fluid within the skull, which may develop after brain surgery and can cause brain damage
Do Childhood Speech Disorders Persist?
Speech disorders during childhood can have persistent effects throughout life. Therapy can often help improve speech skills.
Speech Impairment in Adulthood
Adult speech disorders develop due to conditions that damage the speech areas of the brain.
Common causes of adult speech impairment include:
- Head trauma
- Nerve injury
- Throat tumor
- Stroke
- Parkinson’s disease
- Essential tremor
- Brain tumor
- Brain infection
Additionally, people may develop changes in speech with advancing age, even without a specific neurological cause. This can happen due to presbyphonia , which is a change in the volume and control of speech due to declining hormone levels and reduced elasticity and movement of the vocal cords.
Do Speech Disorders Resolve on Their Own?
Children and adults who have persistent speech disorders are unlikely to experience spontaneous improvement without therapy and should seek professional attention.
Steps to Treating Speech Impediment
If you or your child has a speech impediment, your healthcare providers will work to diagnose the type of speech impediment as well as the underlying condition that caused it. Defining the cause and type of speech impediment will help determine your prognosis and treatment plan.
Sometimes the cause is known before symptoms begin, as is the case with trauma or MS. Impaired speech may first be a symptom of a condition, such as a stroke that causes aphasia as the primary symptom.
The diagnosis will include a comprehensive medical history, physical examination, and a thorough evaluation of speech and language. Diagnostic testing is directed by the medical history and clinical evaluation.
Diagnostic testing may include:
- Brain imaging , such as brain computerized tomography (CT) or magnetic residence imaging (MRI), if there’s concern about a disease process in the brain
- Swallowing evaluation if there’s concern about dysfunction of the muscles in the throat
- Electromyography (EMG) and nerve conduction studies (aka nerve conduction velocity, or NCV) if there’s concern about nerve and muscle damage
- Blood tests, which can help in diagnosing inflammatory disorders or infections
Your diagnostic tests will help pinpoint the cause of your speech problem. Your treatment will include specific therapy to help improve your speech, as well as medication or other interventions to treat the underlying disorder.
For example, if you are diagnosed with MS, you would likely receive disease-modifying therapy to help prevent MS progression. And if you are diagnosed with a brain tumor, you may need surgery, chemotherapy, or radiation to treat the tumor.
Therapy to Address Speech Impediment
Therapy for speech impairment is interactive and directed by a specialist who is experienced in treating speech problems . Sometimes, children receive speech therapy as part of a specialized learning program at school.
The duration and frequency of your speech therapy program depend on the underlying cause of your impediment, your improvement, and approval from your health insurance.
If you or your child has a serious speech problem, you may qualify for speech therapy. Working with your therapist can help you build confidence, particularly as you begin to see improvement.
Exercises during speech therapy may include:
- Pronouncing individual sounds, such as la la la or da da da
- Practicing pronunciation of words that you have trouble pronouncing
- Adjusting the rate or volume of your speech
- Mouth exercises
- Practicing language skills by naming objects or repeating what the therapist is saying
These therapies are meant to help achieve more fluent and understandable speech as well as an increased comfort level with speech and language.
Building Confidence With Speech Problems
Some types of speech impairment might not qualify for therapy. If you have speech difficulties due to anxiety or a social phobia or if you don’t have access to therapy, you might benefit from activities that can help you practice your speech.
You might consider one or more of the following for you or your child:
- Joining a local theater group
- Volunteering in a school or community activity that involves interaction with the public
- Signing up for a class that requires a significant amount of class participation
- Joining a support group for people who have problems with speech
Activities that you do on your own to improve your confidence with speaking can be most beneficial when you are in a non-judgmental and safe space.
Many different types of speech problems can affect children and adults. Some of these are congenital (present from birth), while others are acquired due to health conditions, medication side effects, substances, or mood and anxiety disorders. Because there are so many different types of speech problems, seeking a medical diagnosis so you can get the right therapy for your specific disorder is crucial.
Centers for Disease Control and Prevention. Language and speech disorders in children .
Han C, Tang J, Tang B, et al. The effectiveness and safety of noninvasive brain stimulation technology combined with speech training on aphasia after stroke: a systematic review and meta-analysis . Medicine (Baltimore). 2024;103(2):e36880. doi:10.1097/MD.0000000000036880
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, language .
Mackey J, McCulloch H, Scheiner G, et al. Speech pathologists' perspectives on the use of augmentative and alternative communication devices with people with acquired brain injury and reflections from lived experience . Brain Impair. 2023;24(2):168-184. doi:10.1017/BrImp.2023.9
Allison KM, Doherty KM. Relation of speech-language profile and communication modality to participation of children with cerebral palsy . Am J Speech Lang Pathol . 2024:1-11. doi:10.1044/2023_AJSLP-23-00267
Saccente-Kennedy B, Gillies F, Desjardins M, et al. A systematic review of speech-language pathology interventions for presbyphonia using the rehabilitation treatment specification system . J Voice. 2024:S0892-1997(23)00396-X. doi:10.1016/j.jvoice.2023.12.010
By Heidi Moawad, MD Dr. Moawad is a neurologist and expert in brain health. She regularly writes and edits health content for medical books and publications.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Types of Speech Impediments
Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
:max_bytes(150000):strip_icc():format(webp)/SanjanaGupta-d217a6bfa3094955b3361e021f77fcca.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
Phynart Studio / Getty Images
Articulation Errors
Ankyloglossia, treating speech disorders.
A speech impediment, also known as a speech disorder , is a condition that can affect a person’s ability to form sounds and words, making their speech difficult to understand.
Speech disorders generally become evident in early childhood, as children start speaking and learning language. While many children initially have trouble with certain sounds and words, most are able to speak easily by the time they are five years old. However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders.
There are many different types of speech impediments, including:
- Articulation errors
This article explores the causes, symptoms, and treatment of the different types of speech disorders.
Speech impediments that break the flow of speech are known as disfluencies. Stuttering is the most common form of disfluency, however there are other types as well.
Symptoms and Characteristics of Disfluencies
These are some of the characteristics of disfluencies:
- Repeating certain phrases, words, or sounds after the age of 4 (For example: “O…orange,” “I like…like orange juice,” “I want…I want orange juice”)
- Adding in extra sounds or words into sentences (For example: “We…uh…went to buy…um…orange juice”)
- Elongating words (For example: Saying “orange joooose” instead of "orange juice")
- Replacing words (For example: “What…Where is the orange juice?”)
- Hesitating while speaking (For example: A long pause while thinking)
- Pausing mid-speech (For example: Stopping abruptly mid-speech, due to lack of airflow, causing no sounds to come out, leading to a tense pause)
In addition, someone with disfluencies may also experience the following symptoms while speaking:
- Vocal tension and strain
- Head jerking
- Eye blinking
- Lip trembling
Causes of Disfluencies
People with disfluencies tend to have neurological differences in areas of the brain that control language processing and coordinate speech, which may be caused by:
- Genetic factors
- Trauma or infection to the brain
- Environmental stressors that cause anxiety or emotional distress
- Neurodevelopmental conditions like attention-deficit hyperactivity disorder (ADHD)
Articulation disorders occur when a person has trouble placing their tongue in the correct position to form certain speech sounds. Lisping is the most common type of articulation disorder.
Symptoms and Characteristics of Articulation Errors
These are some of the characteristics of articulation disorders:
- Substituting one sound for another . People typically have trouble with ‘r’ and ‘l’ sounds. (For example: Being unable to say “rabbit” and saying “wabbit” instead)
- Lisping , which refers specifically to difficulty with ‘s’ and ‘z’ sounds. (For example: Saying “thugar” instead of “sugar” or producing a whistling sound while trying to pronounce these letters)
- Omitting sounds (For example: Saying “coo” instead of “school”)
- Adding sounds (For example: Saying “pinanio” instead of “piano”)
- Making other speech errors that can make it difficult to decipher what the person is saying. For instance, only family members may be able to understand what they’re trying to say.
Causes of Articulation Errors
Articulation errors may be caused by:
- Genetic factors, as it can run in families
- Hearing loss , as mishearing sounds can affect the person’s ability to reproduce the sound
- Changes in the bones or muscles that are needed for speech, including a cleft palate (a hole in the roof of the mouth) and tooth problems
- Damage to the nerves or parts of the brain that coordinate speech, caused by conditions such as cerebral palsy , for instance
Ankyloglossia, also known as tongue-tie, is a condition where the person’s tongue is attached to the bottom of their mouth. This can restrict the tongue’s movement and make it hard for the person to move their tongue.
Symptoms and Characteristics of Ankyloglossia
Ankyloglossia is characterized by difficulty pronouncing ‘d,’ ‘n,’ ‘s,’ ‘t,’ ‘th,’ and ‘z’ sounds that require the person’s tongue to touch the roof of their mouth or their upper teeth, as their tongue may not be able to reach there.
Apart from speech impediments, people with ankyloglossia may also experience other symptoms as a result of their tongue-tie. These symptoms include:
- Difficulty breastfeeding in newborns
- Trouble swallowing
- Limited ability to move the tongue from side to side or stick it out
- Difficulty with activities like playing wind instruments, licking ice cream, or kissing
- Mouth breathing
Causes of Ankyloglossia
Ankyloglossia is a congenital condition, which means it is present from birth. A tissue known as the lingual frenulum attaches the tongue to the base of the mouth. People with ankyloglossia have a shorter lingual frenulum, or it is attached further along their tongue than most people’s.
Dysarthria is a condition where people slur their words because they cannot control the muscles that are required for speech, due to brain, nerve, or organ damage.
Symptoms and Characteristics of Dysarthria
Dysarthria is characterized by:
- Slurred, choppy, or robotic speech
- Rapid, slow, or soft speech
- Breathy, hoarse, or nasal voice
Additionally, someone with dysarthria may also have other symptoms such as difficulty swallowing and inability to move their tongue, lips, or jaw easily.
Causes of Dysarthria
Dysarthria is caused by paralysis or weakness of the speech muscles. The causes of the weakness can vary depending on the type of dysarthria the person has:
- Central dysarthria is caused by brain damage. It may be the result of neuromuscular diseases, such as cerebral palsy, Huntington’s disease, multiple sclerosis, muscular dystrophy, Huntington’s disease, Parkinson’s disease, or Lou Gehrig’s disease. Central dysarthria may also be caused by injuries or illnesses that damage the brain, such as dementia, stroke, brain tumor, or traumatic brain injury .
- Peripheral dysarthria is caused by damage to the organs involved in speech. It may be caused by congenital structural problems, trauma to the mouth or face, or surgery to the tongue, mouth, head, neck, or voice box.
Apraxia, also known as dyspraxia, verbal apraxia, or apraxia of speech, is a neurological condition that can cause a person to have trouble moving the muscles they need to create sounds or words. The person’s brain knows what they want to say, but is unable to plan and sequence the words accordingly.
Symptoms and Characteristics of Apraxia
These are some of the characteristics of apraxia:
- Distorting sounds: The person may have trouble pronouncing certain sounds, particularly vowels, because they may be unable to move their tongue or jaw in the manner required to produce the right sound. Longer or more complex words may be especially harder to manage.
- Being inconsistent in their speech: For instance, the person may be able to pronounce a word correctly once, but may not be able to repeat it. Or, they may pronounce it correctly today and differently on another day.
- Grasping for words: The person may appear to be searching for the right word or sound, or attempt the pronunciation several times before getting it right.
- Making errors with the rhythm or tone of speech: The person may struggle with using tone and inflection to communicate meaning. For instance, they may not stress any of the words in a sentence, have trouble going from one syllable in a word to another, or pause at an inappropriate part of a sentence.
Causes of Apraxia
Apraxia occurs when nerve pathways in the brain are interrupted, which can make it difficult for the brain to send messages to the organs involved in speaking. The causes of these neurological disturbances can vary depending on the type of apraxia the person has:
- Childhood apraxia of speech (CAS): This condition is present from birth and is often hereditary. A person may be more likely to have it if a biological relative has a learning disability or communication disorder.
- Acquired apraxia of speech (AOS): This condition can occur in adults, due to brain damage as a result of a tumor, head injury , stroke, or other illness that affects the parts of the brain involved in speech.
If you have a speech impediment, or suspect your child might have one, it can be helpful to visit your healthcare provider. Your primary care physician can refer you to a speech-language pathologist, who can evaluate speech, diagnose speech disorders, and recommend treatment options.
The diagnostic process may involve a physical examination as well as psychological, neurological, or hearing tests, in order to confirm the diagnosis and rule out other causes.
Treatment for speech disorders often involves speech therapy, which can help you learn how to move your muscles and position your tongue correctly in order to create specific sounds. It can be quite effective in improving your speech.
Children often grow out of milder speech disorders; however, special education and speech therapy can help with more serious ones.
For ankyloglossia, or tongue-tie, a minor surgery known as a frenectomy can help detach the tongue from the bottom of the mouth.
A Word From Verywell
A speech impediment can make it difficult to pronounce certain sounds, speak clearly, or communicate fluently.
Living with a speech disorder can be frustrating because people may cut you off while you’re speaking, try to finish your sentences, or treat you differently. It can be helpful to talk to your healthcare providers about how to cope with these situations.
You may also benefit from joining a support group, where you can connect with others living with speech disorders.
National Library of Medicine. Speech disorders . Medline Plus.
Centers for Disease Control and Prevention. Language and speech disorders .
Cincinnati Children's Hospital. Stuttering .
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, and language .
Cleveland Clinic. Speech impediment .
Lee H, Sim H, Lee E, Choi D. Disfluency characteristics of children with attention-deficit/hyperactivity disorder symptoms . J Commun Disord . 2017;65:54-64. doi:10.1016/j.jcomdis.2016.12.001
Nemours Foundation. Speech problems .
Penn Medicine. Speech and language disorders .
Cleveland Clinic. Tongue-tie .
University of Rochester Medical Center. Ankyloglossia .
Cleveland Clinic. Dysarthria .
National Institute on Deafness and Other Communication Disorders. Apraxia of speech .
Cleveland Clinic. Childhood apraxia of speech .
Stanford Children’s Hospital. Speech sound disorders in children .
Abbastabar H, Alizadeh A, Darparesh M, Mohseni S, Roozbeh N. Spatial distribution and the prevalence of speech disorders in the provinces of Iran . J Med Life . 2015;8(Spec Iss 2):99-104.
By Sanjana Gupta Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.

An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.

On this page:
What is stuttering?
Who stutters, how is speech normally produced, what are the causes and types of stuttering, how is stuttering diagnosed, how is stuttering treated, what research is being conducted on stuttering, where can i find additional information about stuttering.
Stuttering is a speech disorder characterized by repetition of sounds, syllables, or words; prolongation of sounds; and interruptions in speech known as blocks. An individual who stutters exactly knows what he or she would like to say but has trouble producing a normal flow of speech. These speech disruptions may be accompanied by struggle behaviors, such as rapid eye blinks or tremors of the lips. Stuttering can make it difficult to communicate with other people, which often affects a person’s quality of life and interpersonal relationships. Stuttering can also negatively influence job performance and opportunities, and treatment can come at a high financial cost.
Symptoms of stuttering can vary significantly throughout a person’s day. In general, speaking before a group or talking on the telephone may make a person’s stuttering more severe, while singing, reading, or speaking in unison may temporarily reduce stuttering.
Stuttering is sometimes referred to as stammering and by a broader term, disfluent speech .
Roughly 3 million Americans stutter. Stuttering affects people of all ages. It occurs most often in children between the ages of 2 and 6 as they are developing their language skills. Approximately 5 to 10 percent of all children will stutter for some period in their life, lasting from a few weeks to several years. Boys are 2 to 3 times as likely to stutter as girls and as they get older this gender difference increases; the number of boys who continue to stutter is three to four times larger than the number of girls. Most children outgrow stuttering. Approximately 75 percent of children recover from stuttering. For the remaining 25 percent who continue to stutter, stuttering can persist as a lifelong communication disorder.
We make speech sounds through a series of precisely coordinated muscle movements involving breathing, phonation (voice production), and articulation (movement of the throat, palate, tongue, and lips). Muscle movements are controlled by the brain and monitored through our senses of hearing and touch.
The precise mechanisms that cause stuttering are not understood. Stuttering is commonly grouped into two types termed developmental and neurogenic.
Developmental stuttering
Developmental stuttering occurs in young children while they are still learning speech and language skills. It is the most common form of stuttering. Some scientists and clinicians believe that developmental stuttering occurs when children’s speech and language abilities are unable to meet the child’s verbal demands. Most scientists and clinicians believe that developmental stuttering stems from complex interactions of multiple factors. Recent brain imaging studies have shown consistent differences in those who stutter compared to nonstuttering peers. Developmental stuttering may also run in families and research has shown that genetic factors contribute to this type of stuttering. Starting in 2010, researchers at the National Institute on Deafness and Other Communication Disorders (NIDCD) have identified four different genes in which mutations are associated with stuttering. More information on the genetics of stuttering can be found in the research section of this fact sheet.
Neurogenic stuttering
Neurogenic stuttering may occur after a stroke, head trauma, or other type of brain injury. With neurogenic stuttering, the brain has difficulty coordinating the different brain regions involved in speaking, resulting in problems in production of clear, fluent speech.
At one time, all stuttering was believed to be psychogenic, caused by emotional trauma, but today we know that psychogenic stuttering is rare.
Stuttering is usually diagnosed by a speech-language pathologist, a health professional who is trained to test and treat individuals with voice, speech, and language disorders. The speech-language pathologist will consider a variety of factors, including the child’s case history (such as when the stuttering was first noticed and under what circumstances), an analysis of the child’s stuttering behaviors, and an evaluation of the child’s speech and language abilities and the impact of stuttering on his or her life.
When evaluating a young child for stuttering, a speech-language pathologist will try to determine if the child is likely to continue his or her stuttering behavior or outgrow it. To determine this difference, the speech-language pathologist will consider such factors as the family’s history of stuttering, whether the child’s stuttering has lasted 6 months or longer, and whether the child exhibits other speech or language problems.
Although there is currently no cure for stuttering, there are a variety of treatments available. The nature of the treatment will differ, based upon a person’s age, communication goals, and other factors. If you or your child stutters, it is important to work with a speech-language pathologist to determine the best treatment options.
Therapy for children
For very young children, early treatment may prevent developmental stuttering from becoming a lifelong problem. Certain strategies can help children learn to improve their speech fluency while developing positive attitudes toward communication. Health professionals generally recommend that a child be evaluated if he or she has stuttered for 3 to 6 months, exhibits struggle behaviors associated with stuttering, or has a family history of stuttering or related communication disorders. Some researchers recommend that a child be evaluated every 3 months to determine if the stuttering is increasing or decreasing. Treatment often involves teaching parents about ways to support their child’s production of fluent speech. Parents may be encouraged to:
- Provide a relaxed home environment that allows many opportunities for the child to speak. This includes setting aside time to talk to one another, especially when the child is excited and has a lot to say.
- Listen attentively when the child speaks and focus on the content of the message, rather than responding to how it is said or interruptng the child.
- Speak in a slightly slowed and relaxed manner. This can help reduce time pressures the child may be experiencing.
- Listen attentively when the child speaks and wait for him or her to say the intended word. Don't try to complete the child’s sentences. Also, help the child learn that a person can communicate successfully even when stuttering occurs.
- Talk openly and honestly to the child about stuttering if he or she brings up the subject. Let the child know that it is okay for some disruptions to occur.
Stuttering therapy
Many of the current therapies for teens and adults who stutter focus on helping them learn ways to minimize stuttering when they speak, such as by speaking more slowly, regulating their breathing, or gradually progressing from single-syllable responses to longer words and more complex sentences. Most of these therapies also help address the anxiety a person who stutters may feel in certain speaking situations.
Drug therapy
The U.S. Food and Drug Administration has not approved any drug for the treatment of stuttering. However, some drugs that are approved to treat other health problems—such as epilepsy, anxiety, or depression—have been used to treat stuttering. These drugs often have side effects that make them difficult to use over a long period of time.
Electronic devices
Some people who stutter use electronic devices to help control fluency. For example, one type of device fits into the ear canal, much like a hearing aid, and digitally replays a slightly altered version of the wearer’s voice into the ear so that it sounds as if he or she is speaking in unison with another person. In some people, electronic devices may help improve fluency in a relatively short period of time. Additional research is needed to determine how long such effects may last and whether people are able to easily use and benefit from these devices in real-world situations. For these reasons, researchers are continuing to study the long-term effectiveness of these devices.
Self-help groups
Many people find that they achieve their greatest success through a combination of self-study and therapy. Self-help groups provide a way for people who stutter to find resources and support as they face the challenges of stuttering.
Researchers around the world are exploring ways to improve the early identification and treatment of stuttering and to identify its causes. For example, scientists have been working to identify the possible genes responsible for stuttering that tend to run in families. NIDCD scientists have now identified variants in four such genes that account for some cases of stuttering in many populations around the world, including the United States and Europe. All of these genes encode proteins that direct traffic within cells, ensuring that various cell components get to their proper location within the cell. Such deficits in cellular trafficking are a newly recognized cause of many neurological disorders. Researchers are now studying how this defect in cellular trafficking leads to specific deficits in speech fluency.
Researchers are also working to help speech-language pathologists determine which children are most likely to outgrow their stuttering and which children are at risk for continuing to stutter into adulthood. In addition, researchers are examining ways to identify groups of individuals who exhibit similar stuttering patterns and behaviors that may be associated with a common cause.
Scientists are using brain imaging tools such as PET (positron emission tomography) and functional MRI (magnetic resonance imaging) scans to investigate brain activity in people who stutter. NIDCD-funded researchers are also using brain imaging to examine brain structure and functional changes that occur during childhood that differentiate children who continue to stutter from those who recover from stuttering. Brain imaging may be used in the future as a way to help treat people who stutter. Researchers are studying whether volunteer patients who stutter can learn to recognize, with the help of a computer program, specific speech patterns that are linked to stuttering and to avoid using those patterns when speaking.
The NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, taste, smell, voice, speech, and language.
Use the following keywords to help you find organizations that can answer questions and provide information on stuttering:
- Speech-language pathologists
- Physician/practitioner referrals
For more information, contact us at:
NIDCD Information Clearinghouse 1 Communication Avenue Bethesda, MD 20892-3456 Toll-free voice: (800) 241-1044 Toll-free TTY: (800) 241-1055 Email: [email protected]
NIH Pub. No. 97-4232 February 2016
* Note: PDF files require a viewer such as the free Adobe Reader .
- PRO Courses Guides New Tech Help Pro Expert Videos About wikiHow Pro Upgrade Sign In
- EDIT Edit this Article
- EXPLORE Tech Help Pro About Us Random Article Quizzes Request a New Article Community Dashboard This Or That Game Popular Categories Arts and Entertainment Artwork Books Movies Computers and Electronics Computers Phone Skills Technology Hacks Health Men's Health Mental Health Women's Health Relationships Dating Love Relationship Issues Hobbies and Crafts Crafts Drawing Games Education & Communication Communication Skills Personal Development Studying Personal Care and Style Fashion Hair Care Personal Hygiene Youth Personal Care School Stuff Dating All Categories Arts and Entertainment Finance and Business Home and Garden Relationship Quizzes Cars & Other Vehicles Food and Entertaining Personal Care and Style Sports and Fitness Computers and Electronics Health Pets and Animals Travel Education & Communication Hobbies and Crafts Philosophy and Religion Work World Family Life Holidays and Traditions Relationships Youth
- Browse Articles
- Learn Something New
- Quizzes Hot
- This Or That Game
- Train Your Brain
- Explore More
- Support wikiHow
- About wikiHow
- Log in / Sign up
- Education and Communications
- Communication Skills
- Speaking Skills
How to Get Rid of a Speech Disorder
Last Updated: December 4, 2023 Fact Checked
This article was co-authored by Devin Fisher, CCC-SLP . Devin Fisher is a Speech-Language Pathologist based in Las Vegas, Nevada. Devin specializes in speech and language therapy for individuals with aphasia, swallowing, voice, articulation, phonological social-pragmatic, motor speech, and fluency disorders. Furthermore, Devin treats cognitive-communication impairment, language delay, and Parkinson's Disease. He holds a BS and MS in Speech-Language Pathology from Fontbonne University. Devin also runs a related website and blog that offers speech-language therapy resources and information for clinicians and clients. There are 13 references cited in this article, which can be found at the bottom of the page. This article has been fact-checked, ensuring the accuracy of any cited facts and confirming the authority of its sources. This article has been viewed 330,690 times.
Many people feel insecure about their speech impediments, whether they're dealing with a lisp or an inability to articulate words. Although it may not seem like it—particularly if you have been dealing with this problem for years—you may be able to get rid of or improve your speech impediment with a few speech-training practices and some major confidence-boosters. And don't forget to seek out the professional opinion of a speech and language therapist/pathologist for more information.
Helping Yourself with a Speech Disorder

- One modern approach is to use technology. There are apps that can run on smartphones and tablets that listen to what you say and then give you feedback. For example, on Android there is the free app "Talking English." You can also find similar apps in the Apple App Store.

Stephanie Jeret
Cues and picture boards can help those with aphasia find words and express thoughts. For aphasia or trouble finding words, cues like the first sound can help jog your memory. Picture boards are great too, especially if speaking is very difficult. These tools allow people to communicate their needs and thoughts through other means.
Using Your Body to Improve Speech

- Shoulders relaxed
- Back straight
- Feet steady

- Sit comfortably and with an erect posture. Breathe in deeply through your nose. You should use your hand to feel your stomach expanding like a balloon being inflated. Hold the breath and then release it slowly, feeling your stomach deflating beneath your hand. Repeat this exercise before you have to speak publicly to relieve stress.

Getting Professional Help

- Speech therapy is helpful for correcting your impediment. The therapist will point out the part of speech where you're having problems, and will work with you to correct it. Private speech therapy sessions do not come cheap, although most insurance policies will fund services needed to treat speech disorders.
- There's no substitute for learning and practice when it comes to the proper and effective use of language. Take every opportunity to speak, to practice and brush up on the correct pronunciation and enunciation provided to you by a professional.

- Every time the dentist adjusts your braces (or even dentures), you need to train yourself to talk and to eat properly. It may be quite painful at first, but remember not to go too far, lest you end up with a mouth injury.
- Most braces are used for orthodontic purposes, although some braces can be used as decorations. Braces are rather expensive, and you may need to take out a dental plan or cash in on dental insurance to pay for them.
- Kids and teenagers don't like to wear braces because they're often teased as “metal mouths” or “railroad faces.” The fact is that braces are still the best way to correct a lisp caused by misaligned teeth.
Assessing Your Speech Disorder

- Cleft lips and palates were a major cause of speech impediments until surgery became affordable. Now, children born with clefts can have reconstructive surgery and a multidisciplinary team of providers that help with feeding and speech and language development. [14] X Research source
- Malocclusion is when the teeth do not have the proper normal bite. Malocclusions are usually corrected through braces, although orthodontic surgery is necessary in some cases. Individuals with this condition may talk with a lisp, make a whistle sound when certain words are spoken, or mumble.
- Neurological disorders caused by accidents or brain and nerve tumors can cause a speech disorder called dysprosody. Dysprosody involves difficulty in expressing the tonal and emotional qualities of speech such as inflection and emphasis.

Expert Q&A

- Welcome good speech. Look forward to it, and accept and celebrate even little improvements. Thanks Helpful 0 Not Helpful 0
- Try to slow down and pronounce each word properly, as this can also help when trying to overcome a speech problem. Thanks Helpful 0 Not Helpful 0

- See a Speech Pathologist who maintains their Certification of Clinical Competence from the American Speech and Hearing Association. These professionals are able to evaluate, diagnose and treat speech impairments. Nothing replaces sound medical advice from a specialist. Thanks Helpful 11 Not Helpful 14
You Might Also Like

- ↑ https://www.uts.edu.au/sites/default/files/2018-10/Camperdown%20Program%20Treatment%20Guide%20June%202018.pdf
- ↑ Devin Fisher, CCC-SLP. Speech Language Pathologist. Expert Interview. 15 January 2021.
- ↑ https://www.stutteringhelp.org/sites/default/files/Migrate/Book_0012_tenth_ed.pdf
- ↑ http://www.coli.uni-saarland.de/~steiner/publications/ISSP2014.pdf
- ↑ https://sps.columbia.edu/news/five-ways-improve-your-body-language-during-speech
- ↑ https://www.nhs.uk/mental-health/self-help/guides-tools-and-activities/breathing-exercises-for-stress/
- ↑ http://kidshealth.org/teen/diseases_conditions/sight/speech_disorders.html#
- ↑ https://www.nidcd.nih.gov/health/stuttering
- ↑ https://medlineplus.gov/ency/article/001058.htm
- ↑ http://www.asha.org/public/speech/disorders/CleftLip/
- ↑ https://www.cdc.gov/ncbddd/developmentaldisabilities/language-disorders.html
- ↑ https://www.stanfordchildrens.org/en/topic/default?id=stuttering-90-P02290
- ↑ https://raisingchildren.net.au/preschoolers/development/language-development/stuttering
About This Article

Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...
- Send fan mail to authors
Reader Success Stories
Bikash Pokharel
Apr 23, 2017
Did this article help you?

Mar 28, 2016
Manisha Singh
Feb 22, 2017

Featured Articles

Trending Articles

Watch Articles

- Terms of Use
- Privacy Policy
- Do Not Sell or Share My Info
- Not Selling Info
wikiHow Tech Help Pro:
Develop the tech skills you need for work and life
- Patient Care & Health Information
- Diseases & Conditions
- Childhood apraxia of speech
Childhood apraxia of speech (CAS) is a rare speech disorder. Children with this disorder have trouble controlling their lips, jaws and tongues when speaking.
In CAS , the brain has trouble planning for speech movement. The brain isn't able to properly direct the movements needed for speech. The speech muscles aren't weak, but the muscles don't form words the right way.
To speak correctly, the brain has to make plans that tell the speech muscles how to move the lips, jaw and tongue. The movements usually result in accurate sounds and words spoken at the proper speed and rhythm. CAS affects this process.
CAS is often treated with speech therapy. During speech therapy, a speech-language pathologist teaches the child to practice the correct way to say words, syllables and phrases.
Children with childhood apraxia of speech (CAS) may have a variety of speech symptoms. Symptoms vary depending on a child's age and the severity of the speech problems.
CAS can result in:
- Babbling less or making fewer vocal sounds than is typical between the ages of 7 to 12 months.
- Speaking first words late, typically after ages 12 to 18 months old.
- Using a limited number of consonants and vowels.
- Often leaving out sounds when speaking.
- Using speech that is hard to understand.
These symptoms are usually noticed between ages 18 months and 2 years. Symptoms at this age may indicate suspected CAS . Suspected CAS means a child may potentially have this speech disorder. The child's speech development should be watched to determine if therapy should begin.
Children usually produce more speech between ages 2 and 4. Signs that may indicate CAS include:
- Vowel and consonant distortions.
- Pauses between syllables or words.
- Voicing errors, such as "pie" sounding like "bye."
Many children with CAS have trouble getting their jaws, lips and tongues to the correct positions to make a sound. They also may have a hard time moving smoothly to the next sound.
Many children with CAS also have language problems, such as reduced vocabulary or trouble with word order.
Some symptoms may be unique to children with CAS , which helps to make a diagnosis. However, some symptoms of CAS are also symptoms of other types of speech or language disorders. It's hard to diagnose CAS if a child has only symptoms that are found both in CAS and in other disorders.
Some characteristics, sometimes called markers, help distinguish CAS from other types of speech disorders. Those associated with CAS include:
- Trouble moving smoothly from one sound, syllable or word to another.
- Groping movements with the jaw, lips or tongue to try to make the correct movement for speech sounds.
- Vowel distortions, such as trying to use the correct vowel but saying it incorrectly.
- Using the wrong stress in a word, such as pronouncing "banana" as "BUH-nan-uh" instead of "buh-NAN-uh."
- Using equal emphasis on all syllables, such as saying "BUH-NAN-UH."
- Separation of syllables, such as putting a pause or gap between syllables.
- Inconsistency, such as making different errors when trying to say the same word a second time.
- Having a hard time imitating simple words.
- Voicing errors, such as saying "down" instead of "town."
Other speech disorders sometimes confused with CAS
Some speech sound disorders often get confused with CAS because some of the symptoms may overlap. These speech sound disorders include articulation disorders, phonological disorders and dysarthria.
A child with an articulation or phonological disorder has trouble learning how to make and use specific sounds. Unlike in CAS , the child doesn't have trouble planning or coordinating the movements to speak. Articulation and phonological disorders are more common than CAS .
Articulation or phonological speech errors may include:
- Substituting sounds. The child might say "fum" instead of "thumb," "wabbit" instead of "rabbit" or "tup" instead of "cup."
- Leaving out final consonants. A child with CAS might say "duh" instead of "duck" or "uh" instead of "up."
- Stopping the airstream. The child might say "tun" instead of "sun" or "doo" instead of "zoo."
- Simplifying sound combinations. The child might say "ting" instead of "string" or "fog" instead of "frog."
Dysarthria is a speech disorder that occurs because the speech muscles are weak. Making speech sounds is hard because the speech muscles can't move as far, as quickly or as strongly as they do during typical speech. People with dysarthria may also have a hoarse, soft or even strained voice. Or they may have slurred or slow speech.
Dysarthria is often easier to identify than CAS . However, when dysarthria is caused by damage to areas of the brain that affect coordination, it can be hard to determine the differences between CAS and dysarthria.
Childhood apraxia of speech (CAS) has a number of possible causes. But often a cause can't be determined. There usually isn't an observable problem in the brain of a child with CAS .
However, CAS can be the result of brain conditions or injury. These may include a stroke, infections or traumatic brain injury.
CAS also may occur as a symptom of a genetic disorder, syndrome or metabolic condition.
CAS is sometimes referred to as developmental apraxia. But children with CAS don't make typical developmental sound errors and they don't grow out of CAS . This is unlike children with delayed speech or developmental disorders who typically follow patterns in speech and sounds development but at a slower pace than usual.
Risk factors
Changes in the FOXP2 gene appear to increase the risk of childhood apraxia of speech (CAS) and other speech and language disorders. The FOXP2 gene may be involved in how certain nerves and pathways in the brain develop. Researchers continue to study how changes in the FOXP2 gene may affect motor coordination and speech and language processing in the brain. Other genes also may impact motor speech development.
Complications
Many children with childhood apraxia of speech (CAS) have other problems that affect their ability to communicate. These problems aren't due to CAS , but they may be seen along with CAS .
Symptoms or problems that are often present along with CAS include:
- Delayed language. This may include trouble understanding speech, reduced vocabulary, or not using correct grammar when putting words together in a phrase or sentence.
- Delays in intellectual and motor development and problems with reading, spelling and writing.
- Trouble with gross and fine motor movement skills or coordination.
- Trouble using communication in social interactions.
Diagnosing and treating childhood apraxia of speech at an early stage may reduce the risk of long-term persistence of the problem. If your child experiences speech problems, have a speech-language pathologist evaluate your child as soon as you notice any speech problems.
Childhood apraxia of speech care at Mayo Clinic
- Jankovic J, et al., eds. Dysarthria and apraxia of speech. In: Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed April 6, 2023.
- Carter J, et al. Etiology of speech and language disorders in children. https://www.uptodate.com/contents/search. Accessed April 6, 2023.
- Childhood apraxia of speech. American Speech-Language-Hearing Association. https://www.asha.org/public/speech/disorders/childhood-apraxia-of-speech/. Accessed April 6, 2023.
- Apraxia of speech. National Institute on Deafness and Other Communication Disorders. http://www.nidcd.nih.gov/health/voice/pages/apraxia.aspx. Accessed April 6, 2023.
- Ng WL, et al. Predicting treatment of outcomes in rapid syllable transition treatment: An individual participant data meta-analysis. Journal of Speech, Language and Hearing Research. 2022; doi:10.1044/2022_JSLHR-21-00617.
- Speech sound disorders. American Speech-Language-Hearing Association. http://www.asha.org/public/speech/disorders/SpeechSoundDisorders/. Accessed April 6, 2023.
- Iuzzini-Seigel J. Prologue to the forum: Care of the whole child — Key considerations when working with children with childhood apraxia of speech. Language, Speech and Hearing Services in Schools. 2022; doi:10.1044/2022_LSHSS-22-00119.
- Namasivayam AK, et al. Speech sound disorders in children: An articulatory phonology perspective. 2020; doi:10.3389/fpsyg.2019.02998.
- Strand EA. Dynamic temporal and tactile cueing: A treatment strategy for childhood apraxia of speech. American Journal of Speech-Language Pathology. 2020; doi:10.1044/2019_AJSLP-19-0005.
- Ami TR. Allscripts EPSi. Mayo Clinic. March 13, 2023.
- Kliegman RM, et al. Language development and communication disorders. In: Nelson Textbook of Pediatrics. 21st ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed April 6, 2023.
- Adam MP, et al., eds. FOXP2-related speech and language disorder. In: GeneReviews. University of Washington, Seattle; 1993-2023. https://www.ncbi.nlm.nih.gov/books/NBK1116. Accessed April 6, 2023.
- How is CAS diagnosed? Childhood Apraxia of Speech Association of North America. https://www.apraxia-kids.org/apraxia_kids_library/how-is-cas-diagnosed/. Accessed April 13, 2023.
- Chenausky KV, et al. The importance of deep speech phenotyping for neurodevelopmental and genetic disorders: A conceptual review. Journal of Neurodevelopmental Disorders. 2022; doi:10.1186/s11689-022-09443-z.
- Strand EA. Dynamic temporal and tactile cueing: A treatment strategy for childhood apraxia of speech. American Journal of Speech Language Pathology. 2020; doi:10.1044/2019_AJSLP-19-0005.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Health Conditions
- Health Products
How to stop or reduce a stutter

Stuttering is a speech disorder. There are various ways to stop or reduce a stutter. These include mindfulness, avoiding triggering words, and speech therapy.
Stuttering affects more than 70 million people worldwide, including more than 3 million people in the United States. It is more common among men than women. Some people refer to stuttering as stammering or childhood onset fluency disorder.
People who stutter may repeat sounds, syllables, or words, or they may prolong sounds. There may also be interruptions to the typical flow of speech, known as blocks, along with unusual expressions or movements.
Approximately 5–10% of all children will stutter at some point in their lives, but most will typically outgrow this within a few months or years. Early intervention can help children overcome stuttering.
For 1 in 4 of these children, however, the problem will persist into adulthood and can become a lifelong communication disorder.
In this article, we describe strategies that people who stutter can use to try to reduce these speech disruptions. We also list ways in which parents and caregivers can help children overcome a stutter.
Quick tips for reducing stuttering

There is no instant cure for stuttering. However, certain situations — such as stress , fatigue , or pressure — can make stuttering worse. By managing these situations, as far as possible, people may be able to improve their flow of speech.
With this in mind, the following tips may be useful:
Practice speaking slowly
Speaking slowly and deliberately can reduce stress and the symptoms of a stutter. It can be helpful to practice speaking slowly every day.
For example, people could try reading aloud at a slow pace when they are on their own. Then, when they have mastered this, they can use this pace when speaking to others.
Another option is to add a brief pause between phrases and sentences to help slow down speech.
Avoid trigger words
People who stutter should not feel as though they have to stop using particular words if this is not their preference.
However, some people may wish to avoid specific words that tend to cause them to stammer. In this case, it might be helpful to make a list of these words and find alternatives to use.
Try mindfulness
Mindfulness is a proven way to reduce anxiety and stress. Research suggests that there is an overlap between the effects of mindfulness and the tools necessary for stuttering management, including:
- decreased use of avoidance strategies, such as speaking less
- improved emotional control
According to the authors of a 2018 case study , adding mindfulness meditation to a treatment program for stuttering may be beneficial for some people.
To practice mindfulness, consider joining a class, downloading a smartphone app, or watching videos online.
Long term treatments
Treatment usually works best when people begin to address stuttering at an early stage. The parents and caregivers of children who stutter should consider taking a child to see a speech therapist if:
- they have stuttered for 3–6 months
- they show signs of struggling with stuttering, such as lip tremors
- there is a family history of stuttering or other communication disorders
Although it may not stop stuttering completely, treatment at any age aims to improve speech fluency, build the person’s confidence, and help them participate in school, work, and social settings.
Treatments for stuttering include:
Speech therapy
A speech therapist can teach people to:
- slow down their rate of speech
- notice when they stutter
- manage situations in which stuttering gets worse
- work on a fluid speech pattern
Research suggests that speech therapy is the best treatment for both adults and children who stutter, with a large body of evidence supporting its efficacy.
Cognitive behavioral therapy (CBT)
CBT is a type of psychotherapy that helps people change how they think and alter their behavior accordingly. CBT for stuttering may involve:
- direct communication
- educating the person about stuttering
- problem solving
- exercises to extend the length of sounds
- relaxation techniques, including deep breathing
- challenging unhelpful thoughts
CBT may lead to positive changes in thoughts and attitudes around stuttering and reduce stuttering-related anxiety.
Electronic devices
Electronic devices are available to help people manage their speech and improve their fluency. Some of these devices work by assisting people in slowing down their speech. Others mimic speech so that it sounds as though the person is talking in unison with someone else.
According to the National Institute on Deafness and Other Communication Disorders , speaking in unison with someone else may temporarily reduce a person’s stuttering.
Some of the medications that doctors prescribe for stuttering include:
- alprazolam (Xanax), an anti-anxiety drug
- citalopram ( Celexa ), an antidepressant
- clomipramine (Anafranil), another antidepressant
However, The Stuttering Foundation advise that these drugs are not effective for the majority of people. Even when they do work, people report the improvements as being modest.
The National Stuttering Foundation suggest that medications may work best when people combine their use with speech therapy.
It is important that parents and caregivers support children who stutter. They can do this by:
- listening attentively and using appropriate eye contact
- refraining from completing words or phrases for a child
- avoiding interrupting, correcting, or criticizing a child
- avoiding focusing on the stutter and using phrases such as “slow down” or “take your time,” as these can make a child feel more self-conscious
- speaking slowly and deliberately to children who stutter, as they may mirror the adult’s pace when they speak
- minimizing stress in the home, as stress can make stuttering worse
- reducing a child’s exposure to situations in which they feel pressured or rushed and those that require them to speak in front of others
- speaking to a teacher if bullying is occurring in school as a result of a child’s stutter
Self-help groups
Connecting with others who stutter can be beneficial for many people. Self-help groups enable people to discover additional resources and supports for stuttering.
For more information, see the National Stuttering Association’s list of local chapters .
Stuttering causes
Researchers do not understand the exact cause of stuttering. Based on current knowledge, they typically class stuttering as one of the following types:
Developmental
Developmental stuttering is the most common type . It occurs in young children who are learning language skills. It is likely to be the result of multiple factors, including genetics.
Due to its genetic component, developmental stuttering can run in families. Approximately 60% of people who stutter have a family member who also stutters.
Neurogenic stuttering can occur due to brain trauma, such as that resulting from a stroke or head injury. The brain then struggles to coordinate the mechanisms that speech involves.
Psychogenic
In the past, scientists believed that all stuttering was psychogenic, meaning that it was due to emotional trauma. Now, they consider this type of stuttering to be rare .
Can a stutter be cured?
There is no cure for stuttering, although early treatment may stop childhood stuttering from persisting into adulthood.
A variety of treatments can help those with a lifelong stutter manage their speech and reduce the frequency and severity of stuttering.
Early intervention is important for children who stutter, most of whom will eventually outgrow it. About 25% will continue to experience stuttering throughout their adult lives, however.
While there is no cure for stuttering, speech therapy can be particularly effective in helping people gain control over their speech. CBT and mindfulness interventions may also help with some aspects of stuttering.
Researchers are continuing to explore the causes of stuttering and potential treatment options. In time, they may be able to identify the children who are more likely to continue stuttering in adulthood.
If scientists can understand the underlying cause of stuttering, they may be able to identify more effective medications or other treatments.
Last medically reviewed on September 9, 2019
- Pediatrics / Children's Health
- Psychology / Psychiatry
- Rehabilitation / Physical Therapy
How we reviewed this article:
- Bernstein Ratner, N. (2014). Stress & stuttering. https://www.stutteringhelp.org/stress-stuttering
- Blomgren, M. (2013). Behavioral treatments for children and adults who stutter: A review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3682852/
- Boyle, M. P. (2011). Mindfulness training in stuttering therapy: A tutorial for speech-language pathologists [Abstract]. https://www.ncbi.nlm.nih.gov/pubmed/21664530
- Brady, J. P., & Ali, Z. (2000). Alprazolam, citalopram, and clomipramine for stuttering. https://www.stutteringhelp.org/alprazolam-citalopram-and-clomipramine-stuttering
- Emge, G., & Pellowski, M. W. (2018). Incorporating a mindfulness meditation exercise into a stuttering treatment program [Abstract]. https://journals.sagepub.com/doi/abs/10.1177/1525740118783516?journalCode=cdqc
- F.A.Q.: Stuttering facts and information. (n.d.). https://www.stutteringhelp.org/faq
- Maguire, J. A. (n.d.). Pharmaceuticals for stuttering. https://westutter.org/what-is-stuttering/resources/pharmaceuticals-for-stuttering/
- Perez, H. R., & Stoeckle, J. H. (2016). Stuttering: Clinical and research update. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4907555/
- Reddy, R. P., et al. (2010). Cognitive behavior therapy for stuttering: A case series. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3137813/
- Stuttering. (2017). https://www.nidcd.nih.gov/health/stuttering
Share this article
Latest news
- Parkinson's: Caffeine may lower risk but doesn't slow progression
- Tattoos may increase blood cancer risk by 21%
- Flavonoid-rich foods and drinks tied to an up to 28% lower risk of type 2 diabetes
- In Conversation: What makes a diet truly heart-healthy?
- Nightmares, 'daymares' could be tell-tale signs of autoimmune disease
Related Coverage
Stuttering, or stammering, is a disruption in speech that causes people to repeat or prolong words, syllables, or phrases. Learn more here.
Even when hiccups last for just a few minutes, they can be annoying. If they last for over 48 hours, they are known as chronic hiccups. Chronic…
Speech therapy provides treatment and support for people with speech disorders and communication problems. Learn more here.
Eye twitching is very common and usually goes away on its own. Learn how to stop eye twitching more quickly and why it happens here.
What is face blindness? Read on to learn more about this neurological condition, including the different types, causes, symptoms, and management…
- For Parents
- For Educators
- Sitio para padres
- Parents Home
- General Health
- Growth & Development
- Diseases & Conditions
- Pregnancy & Baby
- Nutrition & Fitness
- Emotions & Behavior
- School & Family Life
- First Aid & Safety
- Doctors & Hospitals
- Expert Answers (Q&A)
- All Categories
- All Wellness Centers

- Sitio para niños
- How the Body Works
- Puberty & Growing Up
- Staying Healthy
- Staying Safe
- Health Problems
- Illnesses & Injuries
- Relax & Unwind
- People, Places & Things That Help

- Sitio para adolescentes
- Sexual Health
- Food & Fitness
- Drugs & Alcohol
- School & Jobs

Speech Problems
- Listen Play Stop Volume mp3 Settings Close Player
- Larger text size Large text size Regular text size
When you were younger and first began talking, you may have lisped, stuttered, or had a hard time pronouncing words. Maybe you were told that it was "cute," or not to worry because you would soon grow out of it. But if you're in your teens and still stuttering, you may not feel like it's so endearing.
You're not alone. More than 3 million Americans have the speech disorder known as stuttering (or stammering, as it's known in Britain). It's one of several conditions that can affect a person's ability to speak clearly.
Some Common Speech and Language Disorders
Stuttering is a problem that interferes with fluent (flowing and easy) speech. A person who stutters may repeat the first part of a word (as in wa-wa-wa-water ) or hold a single sound for a long time (as in caaaaaaake ). Some people who stutter have trouble getting sounds out altogether. Stuttering is complex, and it can affect speech in many different ways.
Articulation disorders involve a wide range of errors people can make when talking. Substituting a "w" for an "r" ("wabbit" for "rabbit"), omitting sounds ("cool" for "school"), or adding sounds to words ("pinanio" for "piano") are examples of articulation errors. Lisping refers to specific substitution involving the letters "s" and "z." A person who lisps replaces those sounds with "th" ("simple" sounds like "thimple").
Cluttering is another problem that makes a person's speech difficult to understand. Like stuttering, cluttering affects the fluency, or flow, of a person's speech. The difference is that stuttering is a speech disorder , while cluttering is a language disorder. People who stutter have trouble getting out what they want to say; those who clutter say what they're thinking, but it becomes disorganized as they're speaking. So, someone who clutters may speak in bursts or pause in unexpected places. The rhythm of cluttered speech may sound jerky, rather than smooth, and the speaker is often unaware of the problem.
Apraxia (also known as verbal apraxia or dyspraxia) is an oral-motor speech disorder. People with this problem have difficulty moving the muscles and structures needed to form speech sounds into words.
What Causes Speech Problems?
Normal speech might seem effortless, but it's actually a complex process that needs precise timing, and nerve and muscle control.
When we speak, we must coordinate many muscles from various body parts and systems, including the larynx, which contains the vocal cords; the teeth, lips, tongue, and mouth; and the respiratory system .
The ability to understand language and produce speech is coordinated by the brain. So a person with brain damage from an accident, stroke, or birth defect may have speech and language problems.
Some people with speech problems, particularly articulation disorders, may also have hearing problems. Even mild hearing loss can affect how people reproduce the sounds they hear. Certain birth defects, such as a cleft palate, can interfere with someone's ability to produce speech. People with a cleft palate have a hole in the roof of the mouth (which affects the movement of air through the oral and nasal passages), and also might have problems with other structures needed for speech, including the lips, teeth, and jaw.
Some speech problems, like stuttering, can run in families. But in some cases, no one knows exactly what causes a person to have speech problems.
How Are Speech Problems Treated?
The good news is that treatments like speech therapy can help people of any age overcome some speech problems.
If you are concerned about your speech, it's important to let your parents and doctor know. If hearing tests and physical exams don't reveal any problems, some doctors arrange a consultation with a speech-language pathologist (pronounced: puh-THOL-uh-jist).
A speech-language pathologist is trained to observe people as they speak and to identify their speech problems. Speech-language pathologists look for the type of problem (such as a lack of fluency, articulation, or motor skills) someone has. For example, if you stutter, the pathologist will examine how and when you do so.
Speech-language pathologists may evaluate their clients' speech either by recording them on audio or videotape or by listening during conversation. A few clinics that specialize in fluency disorders may use computerized analysis. By gathering as much information as possible about the way someone speaks, the pathologist can develop a treatment plan that meets each individual's needs. The plan will depend on things like a person's age and the type of speech disorder.
If you're being treated for a speech disorder, part of your treatment plan may include seeing a speech therapist , a person who is trained to treat speech disorders.
How often you have to see the speech therapist will vary — you'll probably start out seeing him or her fairly often at first, then your visits may decrease over time. Most treatment plans include breathing techniques, relaxation strategies that are designed to help you relax your muscles when you speak, posture control, and a type of voice exercise called oral-motor exercises . You'll probably have to do these exercises each day on your own to help make your treatment plan as successful as possible.
Dealing With a Speech Problem
People with speech problems know how frustrating they can be. People who stutter, for example, often complain that others try to finish their sentences or fill in words for them. Some feel like people treat them as if they're stupid, especially when a listener says things like "slow down" or "take it easy." (People who stutter are just as intelligent as people who don't.) People who stutter report that listeners often avoid eye contact and refuse to wait patiently for them to finish speaking. If you have a speech problem, it's fine to let others know how you like to be treated when speaking.
Some people look to their speech therapists for advice and resources on issues of stuttering. Your speech therapist might be able to connect you with others in similar situations, such as support groups in your area for teens who stutter.
If you have a speech problem, achieving and keeping control of your speech might be a lifelong process. Although speech therapy can help, you are sure to have ups and downs in your efforts to communicate. But the truth is that the way you speak is only a small part of who you are. Don't be embarrassed to make yourself heard!

- Speech Pathology Master’s Programs: Which is Right for You?
- What Can You Do with a Bachelor’s in Speech Pathology?
- Speech Pathology Doctoral Programs
- Online Masters in Speech Pathology at Emerson College (sponsored program)
- Online Masters in Speech Pathology at New York University (sponsored program)
- How to Become a Speech Pathologist: A Step-by-Step Guide
- Guide to Applying to Speech Pathology School
- How to Make a Career Change to Speech Pathology
- Is a Speech Pathology Degree Worth It?
- 10 Reasons to Love Being a Speech Pathologist
- What Is a CCC-SLP and Why It’s Important
- CCC-SLP Requirements: Become a CCC-SLP
- Guide to Applying for CCC-SLP Certification
- CCC-SLP Salary and Career Outlook
- The Guide to the ASHA Speech Pathology Certification Standards
- State-by-State Guide for Speech Pathology License Requirements
- 8 SLP Certifications that May Help Advance Your Career
- How to Become an Effective ASHA Clinical Fellowship Mentor
- How to Complete the ASHA Clinical Fellowship
- The Guide to Speech Pathology Job and Salary Negotiations
- What to Expect at Your First Speech Pathologist Job
- Bilingual Speech Pathologist Salary and Careers
- Child Speech Therapist Career and Salary Outlook
- Speech Pathology Assistant Careers and Salary Outlook
- How to Choose Your Speech Pathologist Career Setting
- Become a Speech Pathologist in a School Setting
- Become a Speech Pathologist in a Hospital Work Setting
- Opening a Speech Therapy Telepractice: What You Need to Know
- Speech Pathology Internships Guide
- Guide to Speech Therapy Volunteer Opportunities
- Choosing Between Speech Pathology or Occupational Therapy
- How to Become an Audiologist
- Scholarships
- Day in the Life of an SLP Student
- Speech Disorder Resources for College Students
- Common Speech Language Pathology Assessment Tools
- The SLP Guide to Evidence-Based Practice
- When to Take Your Bilingual Child to the Speech Pathologist
- When to Take Your Child to the SLP
Home / Resources
What are the Most Common Speech Disorders?
July 24, 2020
Speech disorders impact millions of people and their ability to communicate. The National Institute of Deafness and Other Communication Disorders estimates that 5% of children in the U.S. ages 3 to 17 have had a speech disorder in the past 12 months. Some speech disorders can be overcome, while others are lifelong conditions. In either case, therapy with a speech pathologist can help a person make the most of their speech capabilities and develop alternative methods of communication.
Speech pathologists or speech therapists complete a master’s program to be able to evaluate a person’s speech and communication, create a treatment plan and provide treatment to improve a person’s speech and other communication methods. Some speech pathologists’ careers deal with research and development treatment guidelines for various speech and language disorders.
What Is a Speech Disorder?
Speech is how people make sounds and words , according to the American Speech-Language-Hearing Association (ASHA). Speech problems can include the inability to make sounds clearly, having a raspy voice or stuttering (repeating sounds or pauses when speaking).
Language is not the same thing as speech; it is the words we use to share ideas. Problems with language can include difficulty understanding, talking, reading or writing.
According to ASHA, a speech disorder is an impairment of the articulation of sounds, fluency or voice. It is one of many types of communication disorders, which also include language and hearing disorders.
Types of Speech Disorders
There are three categories of speech disorders :
- Articulation disorders : An unusual production of speech sounds involving substitutions, omissions, additions or distortions that might interfere with whether the sounds are intelligible to others.
- Fluency disorders : Interruptions in the flow of a person’s speech, such as an uncommon rate, rhythm, or repetition of sounds, syllables, words or phrases.
- Voice disorders : An abnormal production or absence of vocal quality, pitch, volume, resonance or duration that’s inappropriate for the person’s age and sex.
Speech Disorder Causes
The medical community doesn’t know the cause of all speech disorders and, for many, the cause can vary. Potential causes for speech disorders include:
- Brain damage : Some speech and other communication disorders are due to a congenital condition. A child or adult who suffers a traumatic brain injury might sustain damage to a portion of the brain that impacts speech. Also, diseases and conditions such as stroke, dementia, Parkinson’s disease, ALS, Huntington’s disease, MS, cerebral palsy, muscular dystrophy, cancer and benign brain tumors can impact speech.
- Nervous system condition : A disorder that affects a person’s nervous system can affect the muscles in their mouth, jaw, lips, or tongue or their vocal folds (voice box).
- Nerve damage : Nerve damage in the voice box can impact the vocal folds and cause voice disorders, which are a type of speech disorder.
- Stress : In some cases, it’s believed that stress can trigger certain speech disorders.
10 Common Speech Disorders
1. childhood apraxia of speech.
To talk, messages from the brain tell the muscles around the mouth and throat to move. In childhood apraxia, the messages don’t get through to the muscles correctly, according to ASHA. The child’s muscles aren’t weak, but they can’t move their mouth or tongue the right way to make the necessary sounds. The severity of this condition can vary. In more severe cases, a child might not be able to talk much.
Childhood apraxia is not a developmental issue that a child can grow out of. With the help of a speech therapist, a child’s speech can improve. But ultimately, the way the child learns to make speech sounds won’t be typical of other children.
2. Adult Apraxia
Apraxia of speech in adults is also called acquired apraxia of speech, verbal apraxia and dyspraxia. Adults suffer from verbal apraxia because of brain damage, such as a stroke, oxygen deprivation or a traumatic brain injury.
Acquired apraxia in adults can affect their speech in various ways. A person might make a new sound, leave out sounds or say something the wrong way. They might not be able to make a sound the right way consistently. A person might have a hard time controlling their mouth, lips and tongue to make the right sounds. They might have to talk slowly. In severe cases, an adult might not be able to talk at all.
3. Dysarthria
Dysarthria is the result of muscle weakness due to brain damage. The severity of the condition can vary, and it can be accompanied by other conditions, like speech apraxia. People with dysarthria might slur their words, speak slowly or too fast, talk softly, sound robotic and not be able to move their mouth or tongue well. Some people’s voices sound different than before their injury.
4. Orofacial Myofunctional Disorders
People of any age can have an orofacial myofunctional disorder (OMD). An OMD might interfere with the development of the bones and muscles in a person’s face and mouth. This can impact a person’s ability to breathe, swallow, eat and talk. Various issues can cause an OMD, including anything that causes a person to rest their tongue in the right place or keep their lips together when at rest.
One type of OMC is called tongue thrusting, which involves children pushing their tongue out when they try to talk, drink or eat.
5. Speech Sound Disorders
A child who can’t correctly make speech sounds by 4 years old might have a speech sound disorder, also known as a phonological disorder or articulation disorder. Speech sound disorders are not only in children, though. Adults might have suffered from a disorder since childhood or acquired this disorder after sustaining brain damage.
With a speech sound disorder, a person might make one sound in place of another, add sounds, change a sound or leave a sound out. The changes can be severe enough to make it hard for others to understand them. It’s important to note that people with accents will do some of these things, like replace one sound with another. An accent or dialect is not a speech sound disorder.
6. Stuttering
A person who stutters might repeat whole words or sounds, stretch out sounds or have a hard time saying certain words. These are known as repetitions, prolongations and blocks, respectively. While everyone might stutter once in a while, stuttering becomes a speech disorder when it gets in the way of a person’s ability to communicate with others and is accompanied by negative feelings about talking.
There’s no specific cause for stuttering. It might be the result of differences in children’s brains. In many cases, there’s a family history of stuttering. Most children start to stutter between the ages of 2 and 6 years. If the stuttering lasts for more than 6 months, then treatment with a speech pathologist might be necessary.
7. Voice Disorders
Several conditions impact a person’s voice, and therefore, their ability to talk. These include:
Chronic cough : A cough that lasts more than four weeks in children and eight weeks in adults is considered chronic. It can alter the sound of a person’s voice or their ability to talk.
Paradoxical vocal fold movement : PVFM is when a person’s vocal folds (inside the voice box) close partly or all the way when they should open. This can cause breathing difficulties, change a person’s voice, or cause someone to lose their voice. PVFM can be triggered by acid reflux, stress, smoke, pollen, other allergens, exercise or breathing cold air, though no one knows the underlying cause.
Spasmodic dysphonia : With this long-term condition, a person’s vocal folds don’t move properly. A person with this disorder might not be able to speak all the time, though, at other times, their voice might sound normal. Their vocal folds might spasm or tighten when they talk, which can make them sound jerky or hoarse. A brain or nervous system disorder can cause this condition.
Vocal fold nodules and polyps : Growths on a person’s vocal folds can change their voice and cause discomfort and pain. This condition is usually caused by vocal abuse — typically long-term overuse or abuse.
Vocal fold paralysis : Vocal fold paralysis happens when one or both of your vocal folds can’t move. If they can’t come together, separate and vibrate, then a person doesn’t have a voice. It also causes issues with breathing and swallowing. When one fold is paralyzed, a person’s voice might be quiet. They might be limited in their pitch and tone and sound breathy. When two folds are paralyzed, the person might need a tracheotomy.
Aphasia is technically a language disorder caused by brain damage to the left side of the brain. People with aphasia might have a hard time understanding other people, speaking, reading or writing. For example, a person with aphasia might hear another person and understand them, but then have a difficult time responding with the correct speech sounds. Aphasia can cause people to not remember the right word, say the wrong word, make up words, have a hard time speaking in full sentences or have a hard time speaking coherent sentences.
9. Selective Mutism
Selective mutism is a childhood language disorder, often associated with a child being extremely shy, afraid of embarrassment, traumatized, wanting to be alone or having an anxiety disorder. A child might refuse to talk in certain situations, say in public or at school.
10. Childhood Speech Delays
A child who is significantly delayed in developing their language and speech skills might have a language disorder. These are called preschool language disorders. Delayed speech is also called alalia. Some children have a hard time with receptive language, which helps them follow directions, understand gestures and answer questions. Others have difficulties with expressive language, like asking questions, naming objects or putting words together for a sentence. Some children have trouble with both.
Speech Disorder Treatments
Many speech disorders cannot be cured, but by receiving speech and language therapy with a licensed speech pathologist, many children and adults can improve their speech or adapt to alternative communication methods.
Speech therapists can help individuals learn the correct way to make a sound, including when and how to move their mouth and tongue, practice saying certain sounds, learn to tell when a sound is correct or wrong and practice using sounds in longer sentences. Speech pathologists can give children and adults exercises to improve their speech. Additionally, depending on the type of speech disorder, other medical or mental health care might be necessary.
Speech disorders impact children and adults from all walks of life. But these disorders don’t have to stand in the way of their communication, education and careers. Licensed speech pathologists can help individuals improve their speaking, and when helpful, learn to use augmentative and alternative communication methods.
Information last updated June 2020
Sponsored online speech pathology programs

Online MS: Pursue SLP Certification. Study FT/PT
Speech@Emerson enables you to earn an MS online and pursue SLP certification in as few as 20 mos. Learn the same curriculum as the on-campus program. Study FT or PT.
- Prepares you to pursue certification as an SLP generalist
- In-person clinical placements at faculty-approved partner sites
- As few as 20 months to complete
info SPONSORED

Want to Become an SLP? Earn an MS Online at NYU
NYU Steinhardt’s online master of science program in Communicative Sciences and Disorders prepares aspiring speech-language pathologists with a comprehensive professional education.
- Prepares students to pursue SLP licensure
- Accredited by ASHA’s Council on Academic Accreditation
- As few as six terms to complete
- Full-time and part-time plans of study
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Committee on the Evaluation of the Supplemental Security Income (SSI) Disability Program for Children with Speech Disorders and Language Disorders; Board on the Health of Select Populations; Board on Children, Youth, and Families; Institute of Medicine; Division of Behavioral and Social Sciences and Education; National Academies of Sciences, Engineering, and Medicine; Rosenbaum S, Simon P, editors. Speech and Language Disorders in Children: Implications for the Social Security Administration's Supplemental Security Income Program. Washington (DC): National Academies Press (US); 2016 Apr 6.

Speech and Language Disorders in Children: Implications for the Social Security Administration's Supplemental Security Income Program.
- Hardcopy Version at National Academies Press
3 Treatment and Persistence of Speech and Language Disorders in Children
This chapter addresses three topics within the committee's charge: current standards of care for speech and language disorders in children; which of the disorders are amenable to treatment and the typical time course required for this treatment; and the persistence of these disorders in children. The discussion is limited to those childhood speech and language disorders that are most common in the Supplemental Security Income (SSI) population; it is not intended to be a comprehensive review of interventions for or the persistence of speech and language disorders. The chapter begins with an overview of the factors that influence treatment of speech and language disorders in children. This is followed by a summary of policies and guidelines that influence the provision of treatment services. Next is an age-based description of treatment approaches. The chapter ends with discussion of the persistence of childhood speech and language disorders and the committee's findings and conclusions.
Before beginning it is important to emphasize that treatment is considered to be essential for all children with speech and language disorders, but with few exceptions, it is most effective for less severe disorders. Nevertheless, even children with the most severe disorders can develop enhanced, functionally important communication skills that have a meaningful impact on their lives even though their speech and language disorders have not been completely resolved.
- FACTORS THAT INFLUENCE TREATMENT FOR SPEECH AND LANGUAGE DISORDERS
Speech and language treatment programs employ a variety of approaches that are dependent on the particular needs and circumstances of the child. Several important factors shape the appropriate intervention program for any given child. These include treatment objectives based on the severity of the disorder, the developmental level of the child, the individuals involved in the intervention (or “agents of change”), the setting in which treatment is provided, and certain key properties of speech and language. Each of these factors is described in turn below.
Objectives of Treatment Based on the Severity of the Disorder
For children with severe speech and language disorders, it often is not possible to alter underlying limitations in developmental processes and systems, partly because of the current state of knowledge in developmental and learning sciences. For some children, conventional means of communication are impossible given the child's level of development and severity of communication difficulties. In these cases, compensatory means of communication, such as picture cards or computer-based communication systems, are employed. Furthermore, parents of children with severe speech and language disorders often are in need of support as well ( Zebrowski and Schum, 1993 ).
Developmental Level of the Child
Treatment programs must be adapted to the child's current developmental status with respect to both speech and language skills and general social, emotional, and physical development. Treatment programs are, therefore, designed to build on the child's developmental level, regardless of the child's age ( Brown and Ferrara, 1999 ). Thus, for example, a 5-year-old child who is functioning at a 3-year-old level in language is unlikely to be able to acquire the language skills of a typical 5-year-old without having accumulated the intermediary skills normally acquired between ages 3 and 5.
Agent(s) of Change
Treatment programs for speech and language disorders nearly always require that someone, usually an adult, provide an environmental milieu that promotes speech and language growth ( Paul and Norbury, 2012 ). Some computer-based programs that require a minimum of adult interaction have been developed ( Tallal et al., 1996 ), but there is no consensus on their effectiveness ( Cohen et al., 2005 ; Gillam et al., 2008 ; Strong et al., 2011 ). Thus, speech and language therapy usually requires that the child be engaged with a partner (clinician, parent, peer) who is a competent speaker/listener of the language. This engagement becomes the means of producing learning and behavior change. Various types of individuals can be considered agents of change for and integral to speech and language treatment for children, including professionally trained and certified speech-language pathologists, parents, early childhood educators or teachers, and peers. In some cases, the role of the speech-language clinician may be as a consultant and educator for others who are the primary agents of change.
Treatment Setting
Treatment may occur in a number of settings or environments because speech and language skills develop within the context of a child's daily communication activities—for example, at home, in the neighborhood, and in school. Each setting provides opportunities for communication and interaction. In the past, speech and language therapy was provided almost exclusively in therapy rooms and classrooms where the speech-language clinician engineered the environment to promote learning ( McWilliam, 1995 ). In the past two decades, however, speech and language intervention has moved out of these special-purpose environments ( Peña and Quinn, 2003 ). This practice is predicated in part on the belief that treating in these natural settings will promote generalization of learning to these settings. For children younger than 3 years of age, services may be provided in the home ( Mahoney et al., 1999 ). Preschoolers may be served in an early childhood or daycare setting, while treatment programs for school-age children usually are integrated into the classroom.
Key Properties of Speech and Language
Chapter 2 describes language as involving several interrelated systems used together to accomplish communication. Box 3-1 briefly defines these systems, explaining how they make it possible to understand the meaning and intent of utterances spoken by others and to use words and sentences to express meaning and intent to others. What is heard and what is said can be thought of as the superficial manifestations of communication. Underlying these manifestations are complex knowledge systems stored in memory systems in the brain. This complex combination of knowledge and skills that must be acquired by a child is the common target of speech and language therapy.
Basic Systems and Subsystems That Enable Human Communication.
Speech and Language Knowledge Is Implicit
The typical child develops speech and language knowledge quickly and with little conscious effort and, importantly, with little intentional instruction by his or her parents ( Pinker, 1984 ). As an example, consider the following sentence: “The basketball player dribble ball.” Most native English-speaking adults would revise the sentence and automatically change “dribble ball” to “dribbles the ball.” Although these kinds of judgments of mature English speakers are common, many adults cannot explain why they make these judgments. This kind of knowledge is often called implicit knowledge —knowledge that is acquired through experience or exposure, rather than from explicit instruction—and much of a young child's speech and language learning develops through this implicit process ( Bock and Griffin, 2000 ; Conway et al., 2010 ). In this way, much of speech and language learning is akin to learning to tie a shoe or ride a bike—skills that can be acquired only by doing and, in fact, are difficult to explain without demonstrating. This type of learning requires repeated exposure or practice, and the resulting knowledge builds gradually.
Speech and Language Knowledge Is Abstract
The implicit knowledge that accumulates during speech and language development is abstract. Knowledge of grammar appears to require processing such notions as the subject of a sentence, which involves the role of a phrase in a sentence that governs certain grammatical features of the sentence. Words usually refer to classes of referents and phonemes (speech sounds) that comprise categories of specific speech sounds (phones). These abstract relations, roles, and categories allow language to express meanings in consistent but flexible ways. How these abstractions are acquired is a topic of considerable debate ( Bates and MacWhinney, 1987 ; Chomsky, 1986 ; St Clair et al., 2010 ). Although sentences involving such abstractions can be provided to a young child, the actual abstraction cannot; instead, the child must create it. Thus, the child can be given the raw material from which language is learned, but the abstract learning product must be generated through mental processes within the child. Unlike a physical therapist, who can physically change the state of a targeted tissue through manipulation, a speech-language clinician cannot make direct contact with these mental processes because they are dynamic learning processes within the brain.
Knowledge Allows for Creativity
Another important characteristic of speech and language knowledge is that it allows for considerable creativity and adaptability. A key feature of language is that what one says is often novel; that is, one can say things one has not heard before. This creative aspect of language can be used to adapt and adjust what one says to a particular situation. This adaptability also is seen in speech production and the ability to produce intelligible speech in a variety of ways. Thus, knowing a language is not simply imitating or storing away a collection of words or sentences to be called up when needed, but using rules or principles and abstract knowledge in flexible and creative ways. As a result, although treatment may target and change relatively specific aspects of speech and language, the child's ability to understand and produce novel utterances that are necessary for communication will be quite limited unless the treatment results in broader changes in underlying skills and knowledge.
- POLICIES AND GUIDELINES THAT INFLUENCE THE PROVISION OF SPEECH AND LANGUAGE SERVICES TO CHILDREN
Numerous factors influence the range of treatments and services received by children with speech and language disorders. Within the universe of children with such disorders who receive SSI benefits, several sets of policies might be expected to play an especially prominent role: the Individuals with Disabilities Education Act (IDEA); Medicaid and its special early and periodic screening, diagnosis, and treatment (EPSDT) benefit for children and adolescents up to age 21, to which all children receiving SSI are entitled; and policies established by the leading professional society in the area of speech and language treatment, which guide the provision of treatment under public programs.
Individuals with Disabilities Education Act
IDEA 1 requires that all children with disabilities—including speech and language disorders—be provided a free, appropriate public education in the least restrictive environment possible. Part B of this law applies this mandate to children aged 3-22, whereas Part C extends this mandate to children from birth to 3 years of age.
Within the United States, speech and language services for children usually are provided by school systems as part of special education services ( U.S. Bureau of Labor Statistics, 2014 ). However, speech and language services are not provided exclusively by public school systems; they also can be found in some community-based programs, such as Head Start. Payment for services both within and outside of the school system are covered by Medicaid. Children with speech and language disorders may also receive treatment and services through privately funded programs, such as those supported by Easter Seals or the Scottish Rite Language Clinics.
Medicaid Early and Periodic Screening, Diagnosis, and Treatment Program
Under the Medicaid EPSDT program, children under 21 who are enrolled in Medicaid must be provided appropriate preventive and specialty services for audiology and speech and language disorders ( CMS, n.d .). This includes “diagnostic, screening, preventive, or corrective services provided by or under the direction of a speech and language pathologist or audiologist.” 2 Specifically, the EPSDT benefit provides coverage for
- the identification of children with speech or language impairments;
- diagnosis and appraisal of specific speech or language impairments;
- referral for medical or other professional attention necessary for rehabilitation of speech or language impairment;
- provision of speech and language services; and
- counseling and guidance of parents, children, and teachers ( ASHA, n.d .).
American Speech-Language-Hearing Association
Services for children with speech and language disorders are also influenced by the American Speech-Language-Hearing Association (ASHA), which has issued practice guidelines for speech and language therapy:
Children receive intervention and/or consultation services when their ability to communicate effectively is impaired because of a communication disorder and when there is a reasonable expectation of benefit in body structure/function and/or activity/participation. Interventions that enhance activity and participation through modification of contextual factors may be warranted even if the prognosis for improved body structure/function is limited. ( ASHA, 2004 )
With regard to the duration of treatment, ASHA states,
Intervention extends long enough to accomplish stated objectives/predicted outcomes and ends when there is no expectation for further benefit during the current developmental stage. ( ASHA, 2004 )
In many cases, the duration of treatment can be protracted, given that throughout childhood, the functional requirements for language and communication continually increase and often outpace the child's growth (see Figure 3-1 ). Thus, a child with a speech and/or language disorder, although making progress, falls further behind his or her typically developing peers in the ability to meet functional communication expectations. As a result, and in keeping with the ASHA guidelines, treatment often is protracted, particularly for children with severe speech and language disorders.
Persistence of the disparity between growth in functional communica tion skills for typically developing children and for those with language disorders.
- TREATMENT FOR SPEECH AND LANGUAGE DISORDERS
The primary objective of treatment for speech and language disorders is to ameliorate a child's communication difficulties and thereby reduce or minimize the negative sequelae associated with these disorders. Optimal treatments would be those that resolved or cured the problem and thus resolved the disability. Indeed, some treatments for speech and language disorders may approach this level of efficacy for some children. Two examples are given here.
First, children born with clefts of the lip and palate are at considerable risk for poor speech intelligibility. Advances in early surgical management of clefts of the lip and/or palate have resulted in substantial improvements in the speech outcomes of affected children, often permitting normal levels of speech development ( Bzoch, 1997 ). Although surgery serves as an important treatment, surgery alone is not sufficient in the majority of instances to fully resolve the risk for speech impairment, and behavioral treatment (i.e., speech therapy) often is needed as well ( Hardin-Jones and Jones, 2005 ).
Similarly, children who are born deaf or hard of hearing have very high rates of speech and language impairment. During the past several decades, auditory prostheses such as hearing aids and cochlear implants, when paired with appropriate and intensive interventions, have been shown to lead to considerable improvements in the speech and language outcomes of these children ( Niparko et al., 2010 ; Tomblin et al., 2014b ). Yet despite the effectiveness of these prostheses, the risk of poor speech and language outcomes remains for some children.
Both surgery for cleft lip and palate and the provision of auditory prostheses are interventions directed at the fundamental cause of the speech/language disorder. Each reflects etiologies impacting peripheral systems for communication (anatomical structures for speech or sensory input) that are relatively amenable to direct intervention. For the vast majority of speech and language disorders, however, the cause is unknown or when known, involves developmental impairments of the brain (see Chapter 2 ). For these disorders, there currently are no interventions, such as a pharmacological or surgical treatment, that can resolve the cause of the problem and thus result in substantial resolution of the child's disability. Instead, the treatment of these pediatric speech and language disorders consists of behavioral approaches that improve function, and among more severely impaired children, treatment rarely results in resolution of the overall disability.
Early Intervention (Birth to Age 3) for Language and Speech Sound Disorders
Early intervention approaches.
The need for language intervention may be identified quite early in an infant's life, particularly when the child has comorbid disabilities that are known to be consequential for speech and language development (e.g., Down syndrome, cerebral palsy, fragile X syndrome, autism spectrum disorder, traumatic brain injury, being deaf or hard of hearing). In other cases, infants or young children fail to meet early language or speech milestones (e.g., development of meaningful speech, ability to produce or combine words by 24 months of age), which prompts enrollment in intervention. When children are quite young, language intervention typically is implemented through a family-centered approach. The intervention is carried out by the parents or caregivers, while the speech clinician takes on a support role, providing guidance that helps parents/caregivers develop the knowledge and skills needed to promote the child's development throughout everyday routines and interactions.
These approaches entail providing a context of emotional support for family members, who may be adjusting to the child's developmental challenges and the resulting impact on family life. In addition, family-centered practices recognize the influential role of caregivers and the home context in children's development. For example, a skilled clinician may provide early intervention for 1-2 hours per week, which represents only a fraction of a young child's nearly 100 hours weekly of awake and potential learning time ( Warren et al., 2006 ). The intent of family-centered, parent-implemented approaches is to support the ability of caregivers to promote the child's communicative development throughout everyday routines ( Rush and Shelden, 2008 ).
Very early research on talk to children ( Brown and Bellugi, 1964 ) revealed that parents sometimes rephrase things children say. For example, when a child says, “See doggy,” the parent may follow by saying, “Yes, see the doggy.” This form of parent behavior was termed “expansion” in that the parent provided a model of a grammatically well-formed sentence by expanding the child's utterance. A variant on expansion called “recasts” entails reformulation of a child's prior well-formed utterance to include additional and more advanced grammatical properties ( Nelson et al., 1973 ). Thus, the child might say, “The doggy is barking,” and the adult might follow by saying, “Yes, the doggy is barking very loudly, isn't he?” In one early study, children exposed to increased rates of expansion and recasts showed improved grammatical development ( Nelson et al., 1973 ). Subsequent research showed that children exposed to elevated rates of expansion have better language growth ( Cleave et al., 2015 ; Leonard et al., 2004 ; Nelson et al., 1996 ). Other examples of caregiver use of talk that encourages language development include “parallel talk” (e.g., describing in the moment what the child is doing or experiencing, such as “You are swinging so high.”) and open-ended questions whose answers are unknown to the caregiver (e.g., “What else do you want?”) ( Fey et al., 1999 ; Proctor-Williams et al., 2001 ; Szagun and Stumper, 2012 ).
In addition to supporting parents in using responsive language, it is important to reduce the use of caregiver styles that are overly directive and/or controlling of the child, such as leading the child's attention away from current interests, correcting grammar (“Say it this way, not that way.”), or withholding an object until the child speaks. Maternal directiveness has been negatively associated with subsequent child language outcomes ( Landry et al., 1997 , 2000 ; Rowe, 2008 ), which has led interventionists to provide caregivers with feedback and support that promote responsive rather than directive interactions.
Enhanced parental confidence is emphasized in interventions focused on caregiver promotion of language abilities throughout daily routines. Early interventionists seek to promote caregivers' self-efficacy in their roles in promoting the child's development, defined as the “expectations caregivers hold about their ability to parent successfully” ( Jones and Prinz, 2005 , p. 342). Caregivers with low levels of self-efficacy may find it difficult to persist when presented with challenges in parenting their child. In contrast, high levels of maternal self-efficacy have been linked to responsiveness to the child and the provision of stimulating interactions ( Coleman and Karraker, 2003 ).
Indeed, promoting caregiver responsiveness to the child and to the child's efforts to communicate is another primary goal of early intervention. This approach builds on decades of research showing that children exposed to conversational talk that is responsive have better rates of language development than those who are not ( Cross, 1978 ; Goldfield, 1987 ; Landry et al., 2006 ; Tamis-LeMonda et al., 1996 ). One form of this responsive communication occurs when the parent or clinician says something that builds on the meaning of the child's prior utterances—referred to as “semantic extensions” ( Cleave et al., 2015 ). The effectiveness of semantic extensions in promoting language growth was first shown by Cazden (1965) .
Interventions Focused on Promoting Language Growth in Young Children
The section above focuses on early intervention aimed at supporting caregivers in being responsive and employing qualitative features in their use of language that are known to promote children's linguistic development. Within the early intervention context, numerous intervention approaches have been developed to promote the child's growth along a developmental continuum. It is beyond the scope of this report to provide comprehensive coverage of the multiple goals, approaches, and techniques involved in child-focused interventions. However, commonly selected child targets in early language intervention and treatment goals for meeting those targets are summarized in Box 3-2 .
Selected Examples of Targets and Treatment Goals in Early Language Intervention (birth to age 3).
Interventions for Nonspeaking Children with Profound Hearing Loss
Some children are nonspeaking because of severe-to-profound deafness ( Brookhouser and Moeller, 1986 ). For these children, evidence points to two established options for improving communication skills: sign language and/or cochlear implants. Nonspeaking deaf children have been shown to be quite adept at acquiring sign language, which provides a rich means of communicating with members of the deaf community and others fluent in that form of communication ( Newport and Meier, 1985 ). In recent years, many of these children have been provided with cochlear implants, which have been shown for some to provide very good speech and language outcomes ( Niparko et al., 2010 ; Tomblin et al., 1999 ).
Efficacy of Early Interventions
Several meta-analyses in the early childhood special education literature demonstrate the impact of family-centered practices on caregiver abilities. One meta-analysis integrated 52 studies to estimate effect sizes in relation to specific family-centered practices ( Dunst et al., 2008 ). It examined the relationships between family-centered help giving and six categories of child and family outcomes (participant satisfaction, self-efficacy, program helpfulness, child functioning, parent–family functioning, and parenting behaviors). The relationships were significant in all six analyses, with average effect sizes ranging from 0.65 to 0.15 across the six outcomes. Overall, results suggest that family-centered practices have either direct effects on family and child functioning, indirect effects mediated through self-efficacy, or both. A more recent meta-analysis suggests that family-centered practices directly influence parental self-efficacy, and that indirect effects of these practices on parent–child interaction and child development are mediated by caregiver self-efficacy ( Trivette et al., 2010 ). The authors reviewed eight studies including 910 infants, toddlers, and preschoolers with and without developmental delays. Results, which were statistically significant, showed that family-centered help-giving practices and family-systems interventions directly influenced parental self-efficacy and well-being and that there were indirect effects on parent–child interaction and child development, mediated by caregiver self-efficacy and parental well-being.
Another meta-analysis focuses on 18 studies evaluating the effects of parent-implemented interventions for toddlers and preschoolers with language impairments ( Roberts and Kaiser, 2011 ). This analysis shows that parent-implemented language interventions have a positive impact on children's receptive and expressive language outcomes relative to a control group. Increasing parent–child turn taking in interactions and improving responsiveness to child communication also are associated with positive outcomes in child language. The effect sizes are statistically significant for receptive language and for expressive grammar. The authors note that the effect sizes for six of the seven language constructs measured are positive and significant. Increasing parent–child turn taking in interactions and improving responsiveness to child communication also are associated with positive outcomes in child language. Law and colleagues (2004) found a significant effect of expressive language intervention compared with no therapy. They also found that speech-language interventions administered to children by speech-language pathologists and interventions administered by parents trained by speech-language pathologists were comparable in effectiveness, suggesting that caregivers can become effective agents of change.
Because most of these studies involved parents of relatively high socioeconomic status, more research is needed to understand how these approaches are working or may need to be adapted with caregivers in circumstances of low income.
Preschool Intervention
The preschool period marks a time of transition for children. During this period, children begin to spend more time outside the home and in play-based settings with peers. By 3 years of age, many preschoolers can sit and attend for at least short intervals, and by the end of the preschool period, the typically developing child is expected to be capable of participating in group activities and attending to and following the instructions of an adult ( Paul and Norbury, 2012 ). For the preschooler with developmental disorders, the preschool years also mark a time when clinical services are likely to move out of the home and into centers and clinics. However, parent-based programs are common during these years. The following subsections summarize the treatment modalities that make up the typical standards of care for the preschool child with speech and/or language disorders and the evidence for their efficacy.
Treatment for Preschool-Age Children with Severe Language Disorders
Children with severe language disorders are likely to engage with others to accomplish a variety of communication acts, such as talking about things around them, asking questions, and expressing preferences (e.g., by saying “no”). Their language is likely to be characteristic of a younger child, with limited vocabulary and simple or immature sentences. Importantly, children with severe language disorders also are likely to understand things said to them at this lower level. If this gap in achievement persists into the early school years, these children are likely to enter school with language skills similar to those of children who are 3-4 years old. For these children, the goal of language treatment is to close this gap to the extent possible. To accomplish this goal, therapists need to promote growth in the child's implicit language knowledge base across a range of communication skills. The treatment programs for these preschool-age children (ages 3-5) are diverse and often tailored to the particular needs of the child, based on the factors described earlier in this chapter. The factors that influence language treatment programs for preschool children with language disorders fall into four general areas: (1) treatment goals, (2) mode of teaching, (3) learning context, and (4) parameters of service delivery. These factors are summarized in Box 3-3 and described in greater detail in the subsections that follow.
Selected Examples of Child-Focused Elements of Language Treatment Programs for Preschool-Age Children.
Treatment goals Several principles govern the selection of treatment goals. First, the goals are based on evidence of aspects of communication that are known to be vulnerable in children with language disorders. Second, the goals are selected to enhance the child's ability to participate in social interactions and develop precursor skills for school entry. Third, although treatment goals for children with severe language disorders may be itemized separately, they need to span comprehension, vocabulary, grammar, social communication/pragmatics, and preliteracy, and the treatment is likely to address several of these goals at once ( Paul and Norbury, 2012 ). Finally, specific treatment goals will be based on the child's developmental readiness for learning. For instance, Fey and colleagues (2003) suggest targeting grammatical forms that are used at low frequencies and thus likely emerging in the child's system. Readiness also can be indicated by evidence that the child is able to use a language form or function when supported by adults ( Schneider and Watkins, 1996 ).
Mode of teaching Two features are common to all of the teaching modes for preschool-age children with severe language disorders. First, an effort is made to increase the amount of language experience provided to the child. Learning theories in psychology often acknowledge that more trials in a learning task will result in better learning, and this principle also has been found to apply to language development ( Hart and Risley, 1995 ; Huttenlocher et al., 1991 ; Matthews et al., 2005 ; Moerk, 1983 ). Second, an effort is made to enhance the saliency or prominence of the language target being taught to the child by increasing emphasis on or control over the placement of the target in the utterance ( Dalal and Loeb, 2005 ; Weismer, 1997 ).
One instructional method, referred to as “modeling,” draws on the social learning theory that emphasizes observational learning ( Bandura, 1971 ). With this method, the child is provided an elevated number of exemplars of a language form. In some cases, this is done in the context of high-density exposures during focused treatment sessions, while in others, it is embedded in natural conversational interactions. In both kinds of settings, modeling has been found to result in gains in the targeted language forms ( Leonard et al., 2004 ; Nye et al., 1987 ; Vasilyeva et al., 2006 ; Weismer and Murray-Branch, 1989 ).
As was noted earlier, talk that encompasses semantic extensions, recasts, and expansions is also often used in preschool programs where clinicians are the agent of change. Several preschool language intervention programs emphasizing responsive language have shown evidence of effectiveness ( Bunce, 1991 ; Dale et al., 1996 ; Fey et al., 1993 ; Justice et al., 2008 ).
Common to all of the above teaching modes is the fact that the child is not taught directly to express the target language. In contrast, some treatment programs place a strong emphasis on a direct form of teaching through elicited imitation. In this case, the child is instructed to imitate a word or sentence and given feedback when he or she makes an imitative attempt. A substantial literature has shown that teaching through imitation can result in improved use of the targeted language forms ( Camarata et al., 1994 ; Connell, 1987 ; Connell and Stone, 1992 ; Nye et al., 1987 ). Yet while imitation is clearly effective in teaching specific targeted behaviors, generalization beyond these targets is often limited.
In summary, an array of basic patterns of language interactions with children can be used to promote language growth. For example, Law and colleagues (2004 , 2008 ) have performed meta-analyses on the effectiveness of language interventions and concluded that treatment programs are effective for improving vocabulary with a standardized mean difference of 0.89 and mixed evidence for improvement in expressive grammar. A recent meta-analysis on the effect of recasting on improvement in grammar found a mean standardized difference of 0.96 for gains in the targeted grammatical form measures and 0.76 for generalization to untreated grammatical forms ( Cleave et al., 2015 ). The evidence is strongest for those methods that include responsive interactions, although directive language engagement, particularly in limited amounts, can also be effective. Most language intervention programs combine several of these methods, along with a general emphasis on overall increments in the frequency of language use.
Learning context Most language intervention programs for preschool children use multiple modes of teaching. When these modes are combined, they can result in different types of learning contexts that may be clinician-centered, child-centered, or a mix of the two. The clinician-centered context is one in which the emphasis is on high rates of listening and speaking the targeted language forms within a highly structured drill-and-practice setting. The clinician controls what is said and what the child does. Paul and Norbury (2012) note that this approach has been advocated by several clinical investigators on the grounds that children with language disorders need the structure and intensity of this learning context. In contrast with clinician-centered approaches are those that are child-centered, in which the emphasis is on preserving the qualities of natural adult – child interactions, and in particular the pragmatics of conversation. The child is allowed to lead the interaction and thus the content, while the clinician follows. The hybrid approach represents a middle ground. One prominent example is incidental teaching ( Hart and Risley, 1975 ), in which the clinician arranges the play setting to provide for talk about the targets and motivations for talking. Interjected into the play are short intervals of focused teaching that involves more directive language. Many of these services are provided in school-based settings through IDEA.
Parameters of service delivery The ways in which speech and language services are provided vary along several parameters. One such parameter is the treatment “dose,” including such variables as the duration of the treatment session, the number of sessions, and the spacing of treatment. Although one might expect that more treatment is likely to be more effective, the evidence in this regard is not clear ( Schooling et al., 2010 ). Yoder and colleagues (2012) found that learner characteristics may interact with the influence of treatment dose and that dose effects are complex ( Yoder et al., 2012 ).
Another important parameter of service delivery is the agent of change. For preschool children, the principal agent of change may be a speech-language clinician, a preschool teacher, or the child's parents. Comparisons of parents and clinicians as agents have shown that outcomes are largely comparable ( Dale et al., 1996 ; Fey et al., 1993 , 1997 ; Schooling et al., 2010 ). Outcomes also are comparable whether services are provided in groups or individually, and in centers and clinics or the children's homes ( Schooling et al., 2010 ).
In summary, considerable evidence shows that clinical treatment for language disorders can improve preschool children's language abilities. However, the learning effects are greatest for those skills that are the target of intervention. The effects of treatment are less pronounced for those skills that reflect a widespread restructuring of the child's language system. As a result, the preschool child with a language disorder, particularly if the disorder is severe, is likely to continue to have the disorder by the time he or she enters school.
Treatment for Nonspeaking Preschool-Age Children
At the most extreme end of the continuum of severity of speech and language disorders are children who are nonspeaking. By 3 years of age, the absence of speech is indicative of some form of severe communication impairment ( Whitman and Schwartz, 1985 ).
The speech of one-third to one-half of children with cerebral palsy is so limited that it is not functionally intelligible ( Andersen et al., 2010 ; Himmelmann et al., 2013 ). Another group of children who fail to develop spoken communication are those with severe intellectual disability and/or autism. By 14 months of age, for example, most infants are able to draw the caregiver's attention to something by pointing and naming. This basic communication function is limited or absent in some children with severe intellectual disability or autism spectrum disorder. Provision of a basic functional communication system has been shown to reduce aggressive and self-injurious behavior in these children ( Kurtz et al., 2003 ).
Such systems—termed alternative and augmentative communication systems—can be organized into two groups: those that depend on alternative body systems, such as gestures or facial expressions (unaided communication systems), and those that require some tool or equipment (aided systems) ( Romski and Sevcik, 2005 ), ranging from a set of pictures or paper and pencil to computer-based speech-generating systems. For young children who are not literate, the most common options are those that do not require or use print. If such a child has good motor skills, an unaided system involving gesture or a picture-based system may be employed. A review of all of these systems is beyond the scope of this study, but given the focus of this report on young children with severe speech and language disorders, two systems used commonly with such children are described below.
One of the oldest alternative and augmentative communication systems entails the use of a set of pictures that are arranged on a board or placed on pages in a book ( Beukelman and Mirenda, 2005 ). The pictures often represent basic messages that the child needs or wishes to express. For children with very limited motor abilities, the communication board can be placed on a tray attached to the child's wheelchair. As the child progresses in the use of the device, it is usually necessary to alter its content to include new messages. Furthermore, as the child's capabilities with language, print, and mobility change, other alternative and augmentative communication systems may be appropriate.
For some nonspeaking children, the absence of spoken communication is due to their lack of understanding of communication functions such as informing a listener about basic needs. Such children need to be introduced to rudimentary communication activities in the hope of not only improving their functional communication skills but also enabling their overall further progress. A common treatment program for this purpose is the picture exchange communication system ( Bondy and Frost, 2001 ), in which the child is provided with pictures of desired objects and taught to use the pictures to request the objects from teachers or caregivers. Several studies have provided evidence that this treatment increases the number of communicative requests, although evidence that these skills generalize to other communication partners, to other communication functions, or to speech is limited at present ( Flippin et al., 2010 ; Preston and Carter, 2009 ).
Preschool children who are nonspeaking because of poor language ability are likely to have lifelong needs for support, particularly if their deficits reflect severe receptive language disorders and/or other neurodevelopmental disorders. If such children develop any spoken communication skills, those skills may be quite limited. In contrast, if the basis of the communication problem is largely a limitation in speech production, and receptive language abilities are relatively unaffected, computer-based electronic communication systems are likely to be effective, and these children have a good chance of entering into regular education and mainstream society.
It is important to emphasize that for many children with severe deficits, the use of alternative and augmentative communication systems may not result in levels of communication found in typically developing children. However, if such a system can increase the child's ability to communicate five or six messages rather than one or two, the resulting gains for communicating with parents, teachers, and others may be substantial, and may prevent or resolve aggressive and self-injurious behaviors. Because of the heterogeneity in the etiology of those disorders that necessitate the use of such systems, as well as in the cognitive ability and speech and language level of affected children, much of the research on these interventions has a single-case (single-subject) design ( Schlosser and Sigafoos, 2006 ). This literature indicates that children receiving these interventions improve in communication function, but with rare exceptions, they will not develop typical speaking ability and will continue to require alternative and augmentative systems as a primary means of communication.

Treatment for School-Age Children with Language Disorders
As noted earlier, language demands increase substantially as children move from the home to the school setting. Throughout the formal educational process, learning occurs through language and communication. In the classroom, the content of language children hear, and later read, is often new. Classroom language also is “decontextualized”; that is, it refers to events occurring in other times and places ( Snow, 1991 ). Moreover, much of language in the classroom is no longer tailored or even directed to an individual child. In fact, in the primary grades, the majority of children in a classroom may not understand many of the important verbal concepts they encounter ( Boehm, 1991 ). Thus, even children with mild language disorders enter school at a high risk for academic difficulty.
Children with severe language disorders have a particularly high risk of learning problems during the elementary years. As discussed in Chapter 2 , children with severe and profound language disorders fall more than two standard deviations below the mean for their age group. Thus, a 6-year-old child may have language skills comparable to those of children 2 or more years younger. As a result, a large gap exists between the child's abilities and the array of language skills required to perform in school. As previously noted, speech and language treatments are not likely to resolve children's language difficulties completely, nor will they fully protect children from difficulties with school performance.
Researchers have recommended a curriculum-based model of treatment for school-age children with language disorders ( ASHA, 1999 ; Simon, 1987 ; Wallach, 2008 ). In this model, treatment goals are aligned with the school curriculum, and learning priorities involve skills linked directly to reading, writing, and mathematics. IDEA also plays a role in this curriculum focus by emphasizing that school-based speech and language services should focus on those skills that affect the child's educational performance. The past two decades have seen an increased emphasis on incorporating speech and language services into the classroom whenever possible instead of removing children from their classrooms for treatment. Evidence concerning the relative effectiveness of classroom-based and pull-out services for children with language impairments is mixed ( McGinty and Justice, 2006 ).
Curriculum-based treatment of speech and language disorders in school-age children emphasizes two related areas: (1) metalinguistics and (2) the language bases of reading and writing.
Metalinguistics
Reading and spelling require that a child think consciously about the sound composition of words and the meaning of words and whole narratives. This conscious knowledge of and talk about language itself is called metalinguistics ( Bialystok and Ryan, 1985 ). One of the most common metalinguistic treatment targets for school-age children with language disorders has been phonological awareness , a form of metalinguistic skill having to do with understanding and awareness of the sound components of words. Learning to read involves the identification of these sound elements and their mapping onto letters and sequences of letters. A number of systematic training programs are available for improving children's phonological awareness ( Adams et al., 1998 ; Blachman et al., 2000 ). In 2002, the National Reading Panel, commissioned by the U.S. Congress, identified 52 studies evaluating the effectiveness of phonological awareness training in improving reading and spelling ( Ehri et al., 2001 ), concluding that its effect was moderate. A more recent literature review by Snowling and Hulme (2011) yielded similar findings.
Language Bases of Reading and Writing
Several decades of research on reading and writing has led to an understanding that these abilities are highly linked to spoken language abilities ( Carroll and Snowling, 2004 ; Catts and Kamhi, 2005 ). A prominent model of reading comprehension by Hoover and Gough (1990) identifies two subcomponents that contribute to successful reading comprehension: word recognition and language comprehension. Oral language skills play an important role in each of these subprocesses, as shown in Figure 3-2 . This figure, from Scarborough (2001) , shows that children's word recognition entails phonological awareness, which is a common target of intervention for children with language disorders. In addition to being foundational for word reading, phonological awareness is important to spelling ( Caravolas et al., 2001 ). Understanding what is read also involves much of the same language knowledge (vocabulary, grammar, sentence meanings, understanding of story structure, and verbal reasoning such as inferencing) as that involved in understanding what has been spoken. This knowledge is a focal point of school-based language intervention as well. Many of the methods used to promote grammatical skills in school-age children are the same as those described in the section on preschool language interventions, although the goals for grammatical development are more likely to involve use and, in particular, comprehension of complex sentences, such as those with relative clauses.
A depiction of the bases of reading development. SOURCE: Used with permission by Guilford Press from the Handbook of Early Literacy , Figure 8.1, Scarborough's Rope, 2003.
Mezynski (1983) argues for a strong correlation between vocabulary and reading comprehension. Thus, a treatment program aimed at enhancing vocabulary could result in improvement in reading. More recently, Elleman and colleagues (2009) performed a meta-analysis of the literature on the effects of vocabulary intervention on reading comprehension. They found that children improved their reading comprehension only on measures that included the vocabulary they had been taught directly; their overall reading comprehension did not improve.
Other school-based treatment programs focus on the structure and content of stories and expository text ( Nippold et al., 2008 ; Roth et al., 1996 ), inference making, and metalinguistic knowledge about participation in classroom communication. In general, considerable evidence indicates that such language interventions can result in improvements in the targeted abilities; it is less likely that these treatment effects generalize broadly to effect widespread gains in academic function.
Treatment for Speech Sound Disorders
As with language disorders, the severity of speech disorders can range from relatively mild to quite severe, up to and including a complete inability to speak. Broadly, intervention for speech disorders can be completed at two levels. Mild to moderate speech disorders (e.g., speaking with a lisp; deleting or distorting the final sounds in words; deleting sounds and consonant clusters; or substituting one sound for another, such as “w” for “r”) often are treated with a focus on speech production accuracy for individual sounds (phonemes) ( Bernthal et al., 2012 ). In more severe speech disorders, the focus of intervention may be on improving global speech intelligibility , wherein whole word production rather than individual phonemes is targeted (see Camarata, 2010 ; Camarata et al., 2006 ; Levy et al., 2012 ; McLeod, 2006 ). When overall speech intelligibility is extremely limited, intervention includes augmentative and alternative communication prostheses, discussed earlier (see Costantino and Bonati, 2014 ). Generally, primary approaches to behavioral treatment of speech disorders, regardless of level or theoretical underpinnings, include practice moving and coordinating movements of oral structures such as the lips, tongue, and soft palate to improve speech production ( Williams et al., 2010 ).
Within the broad rubric of improving speech accuracy, there are a number of approaches, including articulation drill, motor learning, and phonological/lexical interventions. Examples of these approaches are briefly described below.
Articulation Drill and Motor Learning
Articulation drill approaches focused on motor placement and production of individual speech sounds (phonemes) often are a primary focus of intervention for speech disorders ( McLeod and Bleile, 2004 ). In essence, a child is taught directly how to move and coordinate the articulatory mechanism for producing individual speech sounds (phonemes). For example, a child with a mild speech disorder who says the word “rabbit” as “wabbit” is incorrectly pronouncing the phoneme “r” as a “w.” Intervention in this case would include direct instruction, motor practice, and drill on how to produce an “r” sound correctly. These drills often are completed on individual sounds in isolation as a preliminary step. After the child has learned to produce the phoneme correctly in isolation, syllabic productions are introduced (e.g., consonant-vowel syllables). Practice is then initiated until the target phoneme is produced correctly in this context as well. After the child has mastered production at the syllable level, word-level productions are initiated, with a transition to phrases and conversational speech to follow. This approach has long been a standard method in the field ( Nemoy and Davis, 1954 ; Swift, 1918 ) and remains a core feature of intervention for speech disorders in children ( Maas et al., 2014 ).
One key component of articulation drill is repeated motor practice of the tongue movements and coordination of the other articulators, such as lips and jaw, required for accurate pronunciation. Maas and colleagues (2014) review motor learning approaches as applied to speech disorders in children. Although treatment goals often focus on individual speech sounds (phonemes), the authors note that motor practice principles can include syllables, words, and even phrases: “The possible types of targets are numerous and diverse, and include isolated speech movements, speech sounds, syllables, phonetically modified words, real words, nonsense words, and phrases/sentences” (p. 199). In addition to these targets, the authors observe that motor learning can also be applied to intonation and stress patterns needed for accurate speech production (see also Shriberg et al., 1997 ).
Other variations on articulation drill focus on phonemes but introduce specific targets with the goal of generating broader systems change in speech production. For example, Gierut (1990) argues that in maximal contrast articulation drill, speech intervention will be more efficient if selected phonemic contrasts differ in terms of place of articulation in the mouth (e.g., lips, alveolar ridge, soft palate, larynx), voicing (voiced as in “b” versus voiceless as in “p”), and manner (vowel-like, frication, and so on). Gierut's model predicts that training in very different speech sounds (e.g., “p” versus “r”) will yield incidental learning of speech sounds with some of the features contained in the contrast (such as voicing and intermediate placement). Williams (2000) also hypothesizes that generalization will take place when training addresses contrasting speech targets, but that the generalization will be narrower than that proposed in maximal contrast treatment.
In a similar vein, some articulation drill intervention approaches focus on patterns of speech sound learning based on “phonological processes,” which are patterns of speech sound production rooted in linguistic feature classifications (e.g., Chomsky and Halle, 1968 ). In this model, the focus of intervention is on highlighting specific linguistic features that account for systematic errors in disordered speech. For example, it is not uncommon for children with speech disorders to produce the sounds “f,” “s,” and “th” as “p,” “t,” and “t,” respectively (saying pea for fee , tee for see , and bat for bath ). These errors indicate that sounds that should be produced with a turbulent airflow (fricatives such as “f,” “s,” and “th”) are instead being produced with complete occlusion of the oral cavity and an abrupt release (stops such as “p” and “t”). In phonological process intervention approaches, the substitution of stop consonants for fricative consonants is called “stopping” or “stopping of fricatives,” so that intervention is designed to highlight correct production of entire sound classes, such as fricatives, when these are produced incorrectly by substituting speech sounds from another class (see Hodson and Paden, 1981 ; Ingram, 1981 ; Shriberg and Kwiatkowski, 1980 ). Interventions based on phonological process analysis continue to be included in current intervention studies (e.g., Dodd, 2013 ).
Phonological/Lexical Approaches
Although articulation drill can be applied to words or even phrases, these levels are often generalization targets after motor planning and/or articulation practice on individual speech sounds has been completed (see Camarata, 1993 ). A different approach to treating speech disorders is rooted in considering speech sounds within the context of word productions (see Storkel, 2004 ). These interventions are designed to improve word-level production rather than starting at the motor learning or individual phoneme level. Some approaches focused on lexical-phonological learning do not include motor practice or articulation drill. For example, Camarata (1993) found that responsive-interaction intervention based on transactional learning was associated with improved speech production. Similarly, Yoder and colleagues (2005) found that “broad target recasts” improved speech production in children with comorbid speech and language disorders. In addition, Crosbie and colleagues (2005) found that word-level speech production improved speech disorders in children. These latter studies show that both speech accuracy and speech intelligibility can be improved using lexical-transactional intervention.
Efficacy of Treatment for Speech Sound Disorders
A number of studies have found treatment to be associated with significant gains in speech accuracy and intelligibility ( Almost and Rosenbaum, 1998 ; Baker and McCleod, 2011 ). However, there have been few long-term follow-up studies, and very few studies have been focused on children with severe speech disorders ( Baker and McCleod, 2011 ). Similarly, in a review of the literature on speech intervention in mild to moderate speech disorders, Bernthal and colleagues (2012) conclude that “when comparing groups receiving intervention to those receiving no treatment, the intervention group consistently perform better than the no treatment groups on outcome assessment measures. Thus, it would appear that intervention for speech sound disorders does make a difference; however, additional information is needed regarding the effectiveness of specific treatment methods” (p. 270).
As noted, the literature on severe speech disorders, such as dysarthria and childhood apraxia of speech, is highly limited ( Morgan and Vogel, 2008 ). Studies focus on populations such as children with Down syndrome and cerebral palsy as a means of evaluating treatment, and many of these studies are single-subject designs that provide evidence of individual short-term gains in speech intelligibility (as in Camarata et al., 2006 ). In general, randomized clinical trials that include children with severe speech disorders have been lacking. This is also the case for those children whose speech is so severely unintelligible that computerized speech devices are required. A recent meta-analysis of interventions using such devices ( Gevarter et al., 2013 ) found evidence for improvement in specific skills targeted by the treatment and improvement in the use of the devices, but it is difficult to determine whether such interventions result in long-term improvement in speech intelligibility.
In summary, as with language disorders, a substantial literature indicates that short-term improvements are observed following intervention for speech disorders. A majority of these studies focus on the mild-to-moderate range of severity. Evidence with regard to severe speech disorders is much more limited, and a great deal of this evidence is focused on short-term proximal gains demonstrated using single-subject designs.
Treatment for Stuttering
A wide range of treatments have been developed for stuttering over the past century. These include psychological-psychodynamic approaches, operant conditioning-behavioral approaches, and technology applications such as delayed auditory feedback devices. In addition, a limited number of pharmacological treatments have been studied, yielding some evidence that medication can be effective in improving symptomology.
Broadly, the treatment literature indicates that individual symptoms of stuttering, such as repetitions, intonation patterns, and timing disruptions, can be improved with a variety of treatments. However, Nye and colleagues (2013) conducted a meta-analysis of the stuttering treatment literature and found limited evidence that therapy improves stuttering symptomology. The literature also indicates that recovery rates are higher in preschool than in school-age children, but longitudinal randomized trials comparing treatment with untreated recovery are needed. Stuttering in children whose dysfluencies persist into school age and into early adolescence is most resistant to treatment ( Guitar, 2013 ).
- PERSISTENCE OF PEDIATRIC SPEECH AND LANGUAGE DISORDERS IN CHILDREN
Over the past three decades, several longitudinal studies have examined the persistence of early speech and language delays during later preschool years and well into the school years.
Persistence of Early Speech and Language Delays
The question of persistence requires that the age of onset of speech and language disorders be considered. As discussed in Chapter 2 , these disorders do not have a clear age of onset; rather, they emerge as a child begins to engage in spoken communication at around 2 years of age. This pattern of emergence results in a period of ambiguity with respect to when the diagnosis of a persistent disorder can be made. Early signs of delayed speech and language development become evident at approximately 2 years of age, when most children can understand and say a number of words. Several studies in the early 1990s analyzed parent reports of children's speech and language around this age. Parents were asked whether children who had very limited expressive language at around 2 years of age could be considered as having a persistent condition that warranted clinical intervention. Children in these studies who had very limited expressive language were categorized as “late talkers” ( Paul, 1993 ; Rescorla and Schwartz, 1990 ; Thal, 1991 ; Weismer et al., 1994 ). Usually, to be considered a late talker, the child had to be free of other developmental or sensory disorders; thus, being a late talker was viewed as a possible early manifestation of primary language disorder. Even though the diagnosis often emphasized expressive vocabulary, many of these children also were found to have poor speech sound production, reduced language comprehension, limited use of word combinations, and limited use of nonverbal gestures and symbolic play ( Desmarais et al., 2008 ). The investigators in these studies followed these late talkers longitudinally into the preschool years and in some cases into adolescence.
The language measures obtained during the preschool years for children who were late talkers as toddlers showed that, as a group, they continued to perform below their age mates on many language measures; however, their mean scores were also at the low end of the normal range ( Dale and Hayiou-Thomas, 2013 ). Thus, there was evidence of improvement among at least a subgroup of these children. It should be noted that, although late-talking children may also display speech disorders, longitudinal studies of this group have not systematically assessed speech skills during follow-up. Children who are late talkers are more likely to continue to manifest language development at the lower end of the normal range, often lagging behind their same-age peers ( Dollaghan, 2013 ; Thal et al., 2013 ).
An important feature of many of these studies is that the participants often were from socioeconomically advantaged homes. Paul and Weismer (2013) note that late talking can be viewed as one risk factor that, when combined with poverty, increases the risk that a child may have persistent problems. Many of the studies of late talkers also have identified other risk factors for persistence, such as poor language comprehension, limited engagement in communication, more severe language delay, and a family history of language and reading impairment (see also the discussion of risk factors in Chapter 2 ). Because most of the research on the persistence of late talking has focused on children with few other risk factors, further research is needed to determine the extent to which late talking in combination with other risk factors is predictive of the persistence of poor language skills.
Persistence of Language Disorders During the School Years
Although research on the persistence of early speech and language delay suggests that many children who are late to begin talking as toddlers show gains in language that eventually place them at the lower end of the normal range, a number of children who are late talkers as toddlers have persistent language disorders through the preschool years. Joining these children are those with normal language at 2 years of age who subsequently show declines in language skills ( Ukoumunne et al., 2011 ) and those who also display speech disorders.
Several studies have assessed the long-term persistence of speech and language disorders among children who are at the end of the preschool years. Beitchman and colleagues ( Johnson et al., 1999 ) followed a large sample of children with and without speech and language impairment at 5 years of age into adolescence and found that 71.4 percent had persisting language problems, compared with a rate of 5.5 percent in control children who had normal language in kindergarten. They also found that 10.9 percent of the speech-impaired group had persistent speech disorders at follow-up. These findings were similar to the statistically significant findings of Bishop and colleagues over a similar follow-up period: 90 percent of children with language impairment at 5 years of age continued to present with language impairment at 15 years of age ( Stothard et al., 1998 ). However, an earlier study by Stark and Tallal (1988) found that only 21 percent of the 6-year-olds in their cohort continued to have specific language impairment by 10 years of age. A 28-year follow-up of early-school-age children with and without speech disorders ( Felsenfeld et al., 1992 ) showed that performance on measures of both speech and expressive and receptive language in the speech-impaired group in adulthood was poorer than that of controls. Because the participants in this sample were initially identified using a speech measure only, their language ability at intake is unknown.
Subsequently, Tomblin and colleagues (2003) found that 51 percent of 6-year-old children who met criteria for language disorder continued to have impaired language 2 years later. A similar statistically significant rate of persistence (52 percent) was found 4 years later. Additional analyses of the language growth trajectories of these children with language impairment showed that they had very stable patterns of growth, and their language status at age 16 was highly predicted by their language status at age 6 ( Tomblin et al., 2014a ). Thus, although these children showed growth in language over the span of 10 years, there was little evidence of any recovery or resolution of their language impairment. In another recent examination of persistence of language impairment, Rice and Hoffman (2015) followed 519 children from age 2 to age 22 with regard to their vocabulary development. The authors found that children with language impairment had poorer rates of vocabulary growth than the controls throughout childhood. They found “minimal[ly], but statistically significant” male–female differences in this pattern of growth ( Rice and Hoffman, 2015 , p. 356). The results of these longitudinal studies strongly support the earlier conclusion drawn by Stothard and colleagues (1998) that “if a child's language difficulties are still present at age 5-6 prognosis is likely to be poor and the child will be at high risk of language, literacy, and educational difficulties throughout childhood and adolescence” (p. 417). This conclusion directly parallels what is seen in speech disorder. In a follow-up study of children with speech disorders, Shriberg and Kwiatkowski (1988) note that “findings indicate that a high percentage of children continued to have speech and language and other special educational needs as they neared middle school and beyond. Many children eventually required special class placements” (p. 144).
Persistence of Stuttering (Fluency Disorders)
As with mild to moderate speech disorders and mild to moderate language disorders, relatively minor dysfluencies of preschool children tend to resolve by the time children enter school or shortly thereafter. In a longitudinal study, for example, Kloth and colleagues (2000) found that 7 of 93 preschool children identified as at high risk for stuttering persisted as stutterers 6 years later. In contrast, in more severe cases and cases in which the onset of stuttering occurs later (i.e., after the child enters school), the disorder tends to persist and often is lifelong, although some improvement can be seen through the teenage years ( Howell and Davis, 2011 ; Yairi and Ambrose, 1999 ).
In summary, children who present with poor speech and language ability are likely to show long-term patterns of poor speech and language development throughout childhood. If deficits occur in early childhood and are not severe, the child's language outcomes may progress into the broad range of typical development by the end of the preschool years. However, deficits are likely to persist in young children with severe deficits and in those with other risk factors, such as other developmental disorders and challenging family environments. High rates of persistence become much more likely for children whose language deficits remain at the end of the preschool years. Thus, the determination of a persisting language disorder in early childhood is at best provisional.
- FINDINGS AND CONCLUSIONS
This chapter has reviewed the literature on current standards of care for speech and language disorders in children, which of these disorders are amenable to treatment and the typical time course required for this treatment, and the persistence of these disorders. Based on its review of the best available evidence, the committee reached the following findings and conclusions.
3-1. Few treatments exist that can alter the underlying cause of a speech or language disorder. 3-2. Alternative and augmentative communication treatment can provide nonspeech alternatives to speech that lead to functional gains in communication. 3-3. Speech and language therapy during the preschool years focuses on the promotion of implicit learning of an abstract system of principles and symbols. 3-4. In accordance with policies and practice guidelines, speech-language intervention often is conducted in the home and/or classroom and incorporates communication needs within the family and the educational curriculum. 3-5. Evidence indicates that speech and language therapy results in gains in the skills and behaviors targeted by the therapy.
Persistence
3-6. Toddlers who are late talkers often make developmental gains; however, these gains may be less likely in children whose condition is severe and who have other neurodevelopmental and socioeconomic risk factors. 3-7. Children with language disorders at the age of 5 or 6 are likely to have persistent language problems throughout childhood.
Conclusions
3-1. Severe speech and language disorders are likely to persist throughout childhood. 3-2. Speech and language therapy does not substantially alter the course of these disorders and thus is not curative; however, it provides improved function in those areas that are targeted. 3-3. Although there is a large literature on treatment effects, data are lacking on the effect of treatment on more general quality-of-life outcomes, particularly among children with severe disorders and those living in poverty.
- Adams MJ, Foorman BR, Lundberg I, Beeler T. Phonemic awareness in young children: A classroom curriculum. Baltimore, MD: Paul H. Brookes Publishing Co.; 1998.
- Almost D, Rosenbaum P. Effectiveness of speech intervention for phonological disorders: A randomized controlled trial. Developmental Medicine and Child Neurology. 1998; 40 (5):319–325. [ PubMed : 9630259 ]
- Andersen G, Mjøen TR, Vik T. Prevalence of speech problems and the use of augmentative and alternative communication in children with cerebral palsy: A registry-based study in Norway. SIG 12 Perspectives on Augmentative and Alternative Communication. 2010; 19 (1):12–20.
- ASHA (American Speech-Language-Hearing Association). The guidelines for the roles and responsibilities of the school-based speech-language pathologist. Rockville, MD: ASHA; 1999.
- ASHA. Preferred practice patterns for the profession of speech-language pathology. 2004. [September 29, 2015]. http://www .asha.org/policy/PP2004-00191 .htm .
- ASHA. Federal Medicaid requirements speech, language, and hearing benefits. n.d. [October 26, 2015]. http://www .asha.org/practice /reimbursement /medicaid/medicaid_intro.htm .
- Baker E, S. McLeod S. Evidence-based practice for children with speech sound disorders. Part 1: Narrative review. Language, Speech, and Hearing Services in Schools. 2011; 42 (2):102–139. [ PubMed : 20844274 ]
- Bandura A. Psychological modeling. New York: Lieber-Antherton; 1971.
- Barnes S, Gutfreund M, Satterly D, Wells G. Characteristics of adult speech which predicts children's language development. Journal of Child Language. 1983; 10 (1):65–84. [ PubMed : 6841502 ]
- Bates E. Language and context. New York: Academic Press; 1976. (Studies in the acquisition of pragmatics).
- Bates E, MacWhinney B. Mechanisms of language acquisition. MacWhinney B, editor. Hillsdale, NJ: Lawrence Erlbaum Associates; 1987. pp. 157–193. (Competition, variation, and language learning).
- Bernthal JE, Bankson NW, Flipsen P. Articulation and phonological disorders: Speech sound disorders in children. New York: Pearson Higher Education; 2012.
- Beukelman D, Mirenda P. Augmentative and alternative communication. Baltimore, MD: Paul H. Brookes Publishing Co.; 2005.
- Bialystok E, Ryan EB. Toward a definition of metalinguistic skill. Merrill-Palmer Quarterly. 1985; 31 (3):229–251.
- Blachman BA, Ball EW, Black R, Tangel DM. Road to the code: A phonological awareness program for young children. Baltimore, MD: Paul H. Brookes Publishing Co.; 2000.
- Bock K, Griffin ZM. The persistence of structural priming: Transient activation or implicit learning? Journal of Experimental Psychology: General. 2000; 129 (2):177. [ PubMed : 10868333 ]
- Boehm A. The psychoeducational assessment of preschool children. 2nd ed. Bracken BA, editor. Boston, MA: Allyn and Bacon; 1991. pp. 86–106. (Assessment of basic relational concepts).
- Bondy A, Frost L. The picture exchange communication system. Behavior Modification. 2001; 25 (5):725–744. [ PubMed : 11573337 ]
- Boyle J, McCartney E, Forbes J, O'Hare A. A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment. Health Technology Assessment (Winchester, England). 2007; 11 (25):iii–iv. xi-xii, 1-139. [ PubMed : 17610807 ]
- Bradshaw ML, Hoffman PR, Norris JA. Efficacy of expansions and cloze procedures in the development of interpretations by preschool children exhibiting delayed language development. Language, Speech, and Hearing Services in Schools. 1998; 29 (2):85–95. [ PubMed : 27764430 ]
- Brookhouser PE, Moeller MP. Choosing the appropriate habilitative track for the newly identified hearing-impaired child. Annals of Otology, Rhinology & Laryngology. 1986; 95 (1):51–59. [ PubMed : 3511829 ]
- Brown A, Ferrara RA. Diagnosing zones of proximal development. In. Lloyd P, Vygotsky L, editors. New York: Routledge; Critical assessments: The zone of proximal development. 1999; III :225–256.
- Brown R, Bellugi U. Three processes in the child's acquisition of syntax. Harvard Educational Review. 1964; 34 (2):133–151.
- Bunce BH. Referential communication skills: Guidelines for therapy. Language, Speech, and Hearing Services in Schools. 1991; 22 (1):296–301.
- Byrne-Saricks MC. Human communication and its disorders. Winitz H, editor. Norwood, NJ: Ablex Publishing Corp.; 1987. pp. 167–201. (Treatment of language disorders in children: A review of experimental studies).
- Bzoch KR. Communicative disorders related to cleft lip and palate. Austin, TX: PRO-ED, Inc; 1997.
- Camarata SM. The application of naturalistic conversation training to speech production in children with speech disabilities. Journal of Applied Behavior Analysis. 1993; 26 (2):173–182. [ PMC free article : PMC1297736 ] [ PubMed : 8331014 ]
- Camarata SM. Phonological intervention in children. Williams L, McCloud S, McCauley R, editors. Baltimore, MD: Paul H. Brookes Publishing Co.; 2010. pp. 381–406. (Word based phonological intervention: Issues and evidence).
- Camarata SM, Nelson KE, Camarata MN. Comparison of conversational-recasting and imitative procedures for training grammatical structures in children with specific language impairment. Journal of Speech, Language, and Hearing Research. 1994; 37 (6):1414–1423. [ PubMed : 7877298 ]
- Camarata SM, Yoder P, Camarata MN. Simultaneous treatment of grammatical and speech-comprehensibility deficits in children with Down syndrome. Down Syndrome Research and Practice. 2006; 11 (1):9–17. [ PubMed : 17048805 ]
- Caravolas M, Hulme C, Snowling MJ. The foundations of spelling ability: Evidence from a 3-year longitudinal study. Journal of Memory and Language. 2001; 45 (4):751–774.
- Carroll JM, Snowling MJ. Language and phonological skills in children at high risk of reading difficulties. Journal of Child Psychology and Psychiatry. 2004; 45 (3):631–640. [ PubMed : 15055381 ]
- Catts HW, Kamhi AG. The connections between language and reading disabilities. Mahwah, NJ: Lawrence Erlbaum Associates; 2005.
- Cazden CB. Environmental assistance to the child's acquisition of grammar. Cambridge, MA: Harvard University; 1965.
- Chomsky N. Knowledge of language: Its nature origins and use. Westport, CT: Greenwood Publishing Group; 1986.
- Chomsky N, Halle M. The sound pattern of English. Cambridge, MA: MIT Press; 1968.
- Cleave PL, Becker SD, Curran MK, Van Horne AJO, Fey ME. The efficacy of recasts in language intervention: A systematic review and meta-analysis. American Journal of Speech-Language Pathology. 2015; 24 (2):237–255. [ PMC free article : PMC4450887 ] [ PubMed : 25654306 ]
- CMS (Centers for Medicare & Medicaid Services). Early and periodic screening, diagnostic, and treatment. n.d. [October 26, 2015]. http://www .medicaid.gov /Medicaid-CHIP-Program-Information /ByTopics /Benefits/Early-and-Periodic-Screening-Diagnostic-and-Treatment.html .
- Cohen W, Hodson A, O'Hare A, Boyle J, Durrani T, McCartney E, Mattey M, Naftalin L, Watson J. Effects of computer-based intervention through acoustically modified speech (Fast ForWord) in severe mixed receptive-expressive language impairment: Outcomes from a randomized controlled trial. Journal of Speech, Language, and Hearing Research. 2005; 48 (3):715–729. [ PubMed : 16197283 ]
- Coleman PK, Karraker KH. Maternal self-efficacy beliefs, competence in parenting, and toddlers' behavior and developmental status. Infant Mental Health Journal. 2003; 24 (2):126–148.
- Connell PJ. An effect of modeling and imitation teaching procedures on children with and without specific language impairment. Journal of Speech Language and Hearing Research. 1987; 30 (1):105–113. [ PubMed : 3560888 ]
- Connell PJ, Stone CA. Morpheme learning of children with specific language impairment under controlled instructional conditions. Journal of Speech and Hearing Research. 1992; 35 (4):844–852. [ PubMed : 1383608 ]
- Conway CM, Bauernschmidt A, Huang SS, Pisoni DB. Implicit statistical learning in language processing: Word predictability is the key. Cognition. 2010; 114 (3):356–371. [ PMC free article : PMC2823831 ] [ PubMed : 19922909 ]
- Costantino MA, Bonati M. A scoping review of interventions to supplement spoken communication for children with limited speech or language skills. PLoS ONE. 2014; 9 (3):e90744. [ PMC free article : PMC3953121 ] [ PubMed : 24625465 ]
- Crosbie S, Holm A, Dodd B. Intervention for children with severe speech disorder: A comparison of two approaches. International Journal of Language & Communication Disorders. 2005; 40 (4):467–491. [ PubMed : 16195201 ]
- Cross T. The development of communication. Waterso N, Snow C, editors. Chichester, England: Wiley & Sons; 1978. pp. 199–216. (Mother's speech and its association with rate of linguistic development in young children).
- Dalal RH, Loeb DF. Imitative production of regular past tense-ed by English-speaking children with specific language impairment. International Journal of Language & Communication Disorders. 2005; 40 (1):67–82. [ PubMed : 15832526 ]
- Dale PS, Hayiou-Thomas ME. Late talkers: Language development, interventions and outcomes. Dale PS, Rescorla L, editors. Baltimore, MD: Paul H. Brookes Publishing Co.; 2013. pp. 241–257. (Outcomes for late talkers: A twin study).
- Dale PS, Crain-Thoreson C, Notari-Syverson A, Cole K. Parent-child book reading as an intervention technique for young children with language delays. Topics in Early Childhood Special Education. 1996; 16 (2):213–235.
- Desmarais C, Sylvestre A, Meyer F, Bairati I, Rouleau N. Systematic review of the literature on characteristics of late-talking toddlers. International Journal of Language & Communication Disorders/Royal College of Speech & Language Therapists. 2008; 43 (4):361–389. [ PubMed : 17885825 ]
- Dodd B. Differential diagnosis and treatment of children with speech disorder. New York: John Wiley & Sons; 2013.
- Dollaghan C. Late talkers: Language development, interventions and outcomes. Rescorla L, Dale PS, editors. Baltimore, MD: Paul H. Brookes Publishing Co.; 2013. pp. 91–112. (Late talker as a clinical category).
- Dunst CJ, Trivette CM, Hamby DW. Research synthesis and meta-analysis of studies of family-centered practices. Asheville, NC: Winterberry Press; 2008. [ PubMed : 17979208 ]
- Ehri LC, Nunes SR, Willows DM, Schuster BV, Yaghoub-Zadeh Z, Shanahan T. Phonemic awareness instruction helps children learn to read: Evidence from the National Reading Panel's meta-analysis. Reading Research Quarterly. 2001; 36 (3):250–287.
- Elleman AM, Lindo EJ, Morphy P, Compton DL. The impact of vocabulary instruction on passage-level comprehension of school-age children: A meta-analysis. Journal of Research on Educational Effectiveness. 2009; 2 (1):1–44.
- Felsenfeld S, Broen PA, McGue M. A 28-year follow-up of adults with a history of moderate phonological disorder: Linguistic and personality results. Journal of Speech and Hearing Research. 1992; 35 (5):1114–1125. [ PubMed : 1280310 ]
- Fey ME, Cleave PL, Long SH, Hughes DL. Two approaches to the facilitation of grammar in children with language impairment: An experimental evaluation. Journal of Speech, Language, and Hearing Research. 1993; 36 (1):141–157. [ PubMed : 7680731 ]
- Fey ME, Cleave PL, Long SH. Two models of grammar facilitation in children with language impairments: Phase 2. Journal of Speech, Language, and Hearing Research. 1997; 40 (1):5–19. [ PubMed : 9113855 ]
- Fey ME, Krulik TE, Loeb DF, Proctor-Williams K. Sentence recast use by parents of children with typical language and children with specific language impairment. American Journal of Speech-Language Pathology. 1999; 8 (3):273.
- Fey ME, Long SH, Finestack LH. Ten principles of grammar facilitation for children with specific language impairments. American Journal of Speech-Language Pathology. 2003; 12 (1):3–15. [ PubMed : 12680809 ]
- Fey ME, Warren SF, Fairchild M, Sokol S, Yoder PJ. Early effects of responsivity education/prelinguistic milieu teaching for children with developmental delays and their parents. Journal of Speech, Language, and Hearing Research. 2006; 49 (3):526–547. [ PubMed : 16787894 ]
- Finestack LH, Fey ME. Late talkers: Language development, interventions, and outcomes. Rescorla LA, Dale PS, editors. Baltimore, MD: Paul H. Brookes Publishing Co.; 2013. pp. 283–302. (Evidence-based language intervention approaches for young late talkers).
- Flippin M, Reszka S, Watson LR. Effectiveness of the Picture Exchange Communication System (PECS) on communication and speech for children with autism spectrum disorders: A meta-analysis. American Journal of Speech-Language Pathology. 2010; 19 (2):178–195. [ PubMed : 20181849 ]
- Gevarter C, O'Reilly MF, Rojeski L, Sammarco N, Lang R, Lancioni GE, Sigafoos J. Comparisons of intervention components within augmentative and alternative communication systems for individuals with developmental disabilities: A review of the literature. Research in Developmental Disabilities. 2013; 34 (12):4404–4414. [ PubMed : 24139716 ]
- Gierut JA. Differential learning of phonological oppositions. Journal of Speech, Language, and Hearing Research. 1990; 33 (3):540–549. [ PubMed : 2232772 ]
- Gillam RB, Loeb DF, Hoffman LM, Bohman T, Champlin CA, Thibodeau L, Widen J, Brandel J, Friel-Patti S. The efficacy of Fast ForWord language intervention in school-age children with language impairment: A randomized controlled trial. Journal of Speech, Language, and Hearing Research. 2008; 51 (1):97–119. [ PMC free article : PMC2361096 ] [ PubMed : 18230858 ]
- Girolametto L, Verbey M, Tannock R. Improving joint engagement in parent-child interaction: An intervention study. Journal of Early Intervention. 1994; 18 (2):155–167.
- Girolametto L, Weitzman E, Clements-Baartman J. Vocabulary intervention for children with Down syndrome: Parent training using focused stimulation. Infant-Toddler Intervention: The Transdisciplinary Journal. 1998; 8 (2):109–125.
- Goldfield BA. The contributions of child and caregiver to referential and expressive language. Applied Psycholinguistics. 1987; 8 (3):267–280.
- Guitar B. Stuttering: An integrated approach to its nature and treatment. Philadelphia, PA: Lippincott Williams & Wilkins; 2013.
- Hadley PA. Approaching early grammatical intervention from a sentence-focused framework. Language, Speech, and Hearing Services in Schools. 2014; 45 (2):110–116. [ PubMed : 24788641 ]
- Hardin-Jones MA, Jones DL. Speech production of preschoolers with cleft palate. The Cleft Palate-Craniofacial Journal. 2005; 42 (1):7–13. [ PubMed : 15643919 ]
- Hart B, Risley TR. Incidental teaching of language in the preschool. Journal of Applied Behavior Analysis. 1975; 8 (4):411–420. [ PMC free article : PMC1311874 ] [ PubMed : 16795506 ]
- Hart B, Risley TR. Meaning differences in the everyday experiences of young American children. Baltimore, MD: Paul H. Brookes Publishing Co.; 1995.
- Hemmeter ML, Kaiser AP. Enhanced milieu teaching effects of parent-implemented language intervention. Journal of Early Intervention. 1994; 18 (3):269–289.
- Himmelmann K, Lindh K, Hidecker MJC. Communication ability in cerebral palsy: A study from the CP register of western Sweden. European Journal of Paediatric Neurology. 2013; 17 (6):568–574. [ PubMed : 23672835 ]
- Hodson BW, Paden EP. Phonological processes which characterize unintelligible and intelligible speech in early childhood. Journal of Speech and Hearing Disorders. 1981; 46 (4):369–373.
- Hoover WA, Gough PB. The simple view of reading. Reading and Writing. 1990; 2 (2):127–160.
- Howell P, Davis S. Predicting persistence of and recovery from stuttering by the teenage years based on information gathered at age 8 years. Journal of Developmental & Behavioral Pediatrics. 2011; 32 (3):196–205. [ PubMed : 21336144 ]
- Huttenlocher J, Haight W, Bryk A, Seltzer M, Lyons T. Early vocabulary growth: Relation to language input and gender. Developmental Psychology. 1991; 27 (2):236–248.
- Ingersoll B, Lalonde K. The impact of object and gesture imitation training on language use in children with autism spectrum disorder. Journal of Speech, Language, and Hearing Research. 2010; 53 (4):1040–1051. [ PMC free article : PMC3671906 ] [ PubMed : 20631228 ]
- Ingram D. Procedures for the phonological analysis of children's language. Baltimore, MD: University Park Press; 1981.
- Johnson CJ, Beitchman J, Young A, Escobar MD, Atkinson L, Wilson B, Brownlie EB, Douglas L, Taback N, Lam I, Wang M. Fourteen-year follow-up of children with and without speech/language impairments: Speech/language stability and outcomes. Journal of Speech-Language-Hearing Research. 1999; 42 (3):744–760. [ PubMed : 10391637 ]
- Jones TL, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: A review. Clinical Psychology Review. 2005; 25 (3):341–363. [ PubMed : 15792853 ]
- Justice LM, Ezell HK. Enhancing children's print and word awareness through home-based parent intervention. American Journal of Speech-Language Pathology. 2000; 9 (3):257–269.
- Justice LM, Kaderavek JN. Embedded-explicit emergent literacy intervention. I: Background and description of approach. Language, Speech, and Hearing Services in Schools. 2004; 35 (3):201–211. [ PubMed : 15248791 ]
- Justice LM, Mashburn A, Pence KL, Wiggins A. Experimental evaluation of a preschool language curriculum: Influence on children's expressive language skills. Journal of Speech, Language, and Hearing Research. 2008; 51 (4):983–1001. [ PubMed : 18658066 ]
- Kasari C, Gulsrud AC, Wong C, Kwon S, Locke J. Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. Journal of Autism and Developmental Disorders. 2010; 40 (9):1045–1056. [ PMC free article : PMC2922697 ] [ PubMed : 20145986 ]
- Kloth SAM, Kraaimaat FW, Janssen P, Brutten GJ. Persistence and remission of incipient stuttering among high-risk children. Journal of Fluency Disorders. 2000; 24 (4):253–265.
- Kouri TA. Lexical training through modeling and elicitation procedures with late talkers who have specific language impairment and developmental delays. Journal of Speech, Language, and Hearing Research. 2005; 48 (1):157–171. [ PubMed : 15934450 ]
- Kurtz PF, Chin MD, Huete JM, Tarbox RS, O'Connor JT, Paclawskyj TR, Rush KS. Functional analysis and treatment of self-injurious behavior in young children: A summary of 30 cases. Journal of Applied Behavior Analysis. 2003; 36 (2):205–219. [ PMC free article : PMC1284433 ] [ PubMed : 12858985 ]
- Landry SH, Smith KE, Miller-Loncar CL, Swank PR. Predicting cognitive-language and social growth curves from early maternal behaviors in children at varying degrees of biological risk. Developmental Psychology. 1997; 33 (6):1040. [ PubMed : 9383626 ]
- Landry SH, Smith KE, Swank PR, Miller-Loncar CL. Early maternal and child influences on children's later independent cognitive and social functioning. Child Development. 2000; 71 (2):358–375. [ PubMed : 10834470 ]
- Landry SH, Smith KE, Swank PR, Assel MA, Vellet S. Does early responsive parenting have a special importance for children's development or is consistency across early childhood necessary? Developmental Psychology. 2001; 37 (3):387. [ PubMed : 11370914 ]
- Landry SH, Smith KE, Swank PR. Responsive parenting: Establishing early foundations for social, communication, and independent problem-solving skills. Developmental Psychology. 2006; 42 (4):627. [ PubMed : 16802896 ]
- Law J, Conti-Ramsden G. Treating children with speech and language impairments: Six hours of therapy is not enough. British Medical Journal. 2000; 321 (7266):908. [ PMC free article : PMC1118716 ] [ PubMed : 11030659 ]
- Law J, Garrett Z, Nye C. The efficacy of treatment for children with developmental speech and language delay/disorder: A meta-analysis. Journal of Speech, Language, and Hearing Research. 2004; 47 (4):924–943. [ PubMed : 15324296 ]
- Law J, Garrett Z, Nye C. Speech and language therapy interventions for children with primary speech and language delay or disorder. The Cochrane Collaboration. 2008; 1 :1–62.
- Leonard LB. Facilitating linguistic skills in children with specific language impairment. Applied Psycholinguistics. 1981; 2 :8118.
- Leonard LB, Schwartz RG, Chapman K, Rowan LE, Prelock PA, Terrell B, Weiss AL, Messick C. Early lexical acquisition in children with specific language impairment. Journal of Speech, Language, and Hearing Research. 1982; 25 (4):554–564. [ PubMed : 7162156 ]
- Leonard LB, Camarata SM, Brown B, Camarata MN. Tense and agreement in the speech of children with specific language impairment patterns of generalization through intervention. Journal of Speech, Language, and Hearing Research. 2004; 47 (6):1363–1379. [ PubMed : 15842016 ]
- Levy ES, Ramig LO, Camarata SM. The effects of two speech interventions on speech function in pediatric dysarthria. Journal of Medical Speech-Language Pathology. 2012; 20 (4):82–87.
- Lonigan CJ, Whitehurst GJ. Relative efficacy of parent and teacher involvement in a shared-reading intervention for preschool children from low-income backgrounds. Early Childhood Research Quarterly. 1998; 13 (2):263–290.
- Lovelace S, Stewart SR. Increasing print awareness in preschoolers with language impairment using non-evocative print referencing. Language, Speech, and Hearing Services in Schools. 2007; 38 (1):16–30. [ PubMed : 17218533 ]
- Maas E, Gildersleeve-Neumann CE, Jakielski KJ, Stoeckel R. Motor-based intervention protocols in treatment of childhood apraxia of speech (CAS). Current Developmental Disorders Reports. 2014; 1 (3):197–206. [ PMC free article : PMC4192721 ] [ PubMed : 25313348 ]
- Mahoney G, Kaiser A, Girolametto L, MacDonald J, Robinson C, Safford P, Spiker D. Parent education in early intervention: A call for a renewed focus. Topics in Early Childhood Special Education. 1999; 19 (3):131–140.
- Marton K, Abramoff B, Rosenzweig S. Social cognition and language in children with specific language impairment (SLI). Journal of Communication Disorders. 2005; 38 (2):143–162. [ PubMed : 15571714 ]
- Marulis LM, Neuman SB. The effects of vocabulary intervention on young children's word learning: A meta-analysis. Review of Educational Research. 2010; 80 (3):300–335.
- Matthews D, Lieven E, Theakston A, Tomasello M. The role of frequency in the acquisition of English word order. Cognitive Development. 2005; 20 (1):121–136.
- McGinty A, Justice L. Classroom-based versus pullout interventions: A review of the experimental evidence. EBP Briefs. 2006; 1 (1):3–25.
- McLeod S. An holistic view of a child with unintelligible speech: Insights from the ICF and ICF-CY. International Journal of Speech-Language Pathology. 2006; 8 (3):293–315.
- McLeod S, Bleile K. The ICF: A framework for setting goals for children with speech impairment. Child Language Teaching and Therapy. 2004; 20 (3):199–219.
- McWilliam R. Integration of therapy and consultative special education: A continuum in early intervention. Infants & Young Children. 1995; 7 (4):29–38.
- Mezynski K. Issues concerning the acquisition of knowledge: Effects of vocabulary training on reading comprehension. Review of Educational Research. 1983; 53 (2):253–279.
- Moerk EL. A behavioral analysis of controversial topics in first language acquisition: Reinforcements, corrections, modeling, input frequencies, and the three-term contingency pattern. Journal of Psycholinguistic Research. 1983; 12 (2):129–155.
- Morgan AT, Vogel AP. Intervention for childhood apraxia of speech. The Cochrane Database of Systematic Reviews. 2008; 16 (3) [ PubMed : 18646142 ]
- Nelson K, Gruendel J. Event knowledge: Structure and function in development. Mahwah, NJ: Lawrence Erlbaum Associates; 1986.
- Nelson KE, Carskaddon G, Bonvillian JD. Syntax acquisition: Impact of experimental variation in adult verbal interaction with the child. Child Development. 1973; 44 (3):497–504.
- Nelson KE, Camarata SM, Welsh J, Butkovsky L, Camarata M. Effects of imitative and conversational recasting treatment on the acquisition of grammar in children with specific language impairment and younger language-normal children. Journal of Speech, Language, and Hearing Research. 1996; 39 (4):850–859. [ PubMed : 8844564 ]
- Nemoy E, Davis S. The correction of defective consonant sounds. Magnolia, MA: The Expression Company; 1954.
- Newport EL, Meier RP. The acquisition of American Sign Language. Hillsdale, NJ: Lawrence Erlbaum Associates; 1985.
- Niparko JK, Tobey EA, Thal DJ, Eisenberg LS, Wang NY, Quittner AL, Fink NE. Spoken language development in children following cochlear implantation. Journal of the American Medical Association. 2010; 303 (15):1498–1506. [ PMC free article : PMC3073449 ] [ PubMed : 20407059 ]
- Nippold MA, Mansfield TC, Billow JL, Tomblin JB. Expository discourse in adolescents with language impairments: Examining syntactic developments. American Journal of Speech-Language Pathology. 2008; 17 :356–366. [ PubMed : 18840698 ]
- Nye C, Foster SH, Seaman D. Effectiveness of language intervention with the language/learning disabled. Journal of Speech and Hearing Disorders. 1987; 52 (4):348–357. [ PubMed : 3669632 ]
- Nye C, Vanryckeghem M, Schwartz JB, Herder C, Turner HM, Howard C. Behavioral stuttering interventions for children and adolescents: A systematic review and meta-analysis. Journal of Speech, Language, and Hearing Research. 2013; 56 (3):921–932. [ PubMed : 23275413 ]
- Owens RE Jr. Language disorders: A functional approach to assessment and intervention. New York: Pearson Higher Ed; 2013.
- Paul R. Patterns of development in late talkers: Preschool years. Communication Disorders Quarterly. 1993; 15 (1):7–14.
- Paul R, Norbury C. Language disorders from infancy through adolescence: Listening, speaking, reading, writing, and communicating. St. Louis, MO: Elsevier Mosby; 2012.
- Paul R, Weismer SE. Late talkers: Language development, interventions and outcomes. Dale PS, Rescorla L, editors. Baltimore, MD: Paul H. Brookes Publishing Co.; 2013. pp. 203–218. (Late talking in contex: The clinicial implications of delayed language development).
- Peña ED, Quinn R. developing effective collaboration teams in speech-language pathology: A case study. Communication Disorders Quarterly. 2003; 24 (2):53–63.
- Pinker S. Language learnability and language development. Cambridge, MA: Harvard University Press; 1984.
- Plante E, Ogilvie T, Vance R, Aguilar JM, Dailey NS, Meyers C, Lieser AM, Burton R. Variability in the language input to children enhances learning in a treatment context. American Journal of Speech-Language Pathology. 2014; 23 (4):530–545. [ PubMed : 24700145 ]
- Preston D, Carter M. A review of the efficacy of the picture exchange communication system intervention. Journal of Autism and Developmental Disorders. 2009; 39 (10):1471–1486. [ PubMed : 19495952 ]
- Proctor-Williams K, Fey ME, Loeb DF. Parental recasts and production of copulas and articles by children with specific language impairment and typical language. American Journal of Speech-Language Pathology. 2001; 10 (2):155–168.
- Rescorla L, Schwartz E. Outcome of toddlers with specific expressive language delay. Applied Psycholinguistics. 1990; 11 (4):393–407.
- Rescorla L, Mirak J, Singh L. Vocabulary growth in late talkers: Lexical development from 2; 0 to 3; 0. Journal of Child Language. 2000; 27 (2):293–311. [ PubMed : 10967889 ]
- Rice ML, Hoffman L. Predicting vocabulary growth in children with and without specific language impairment: a longitudinal study from 2; 6 to 21 years of age. Journal of Speech, Language, and Hearing Research. 2015; 58 (2):345–359. [ PMC free article : PMC4398600 ] [ PubMed : 25611623 ]
- Rice ML, Warren SF, Betz SK. Language symptoms of developmental language disorders: An overview of autism, Down syndrome, fragile X, specific language impairment, and Williams syndrome. Applied Psycholinguistics. 2005; 26 (1):7–27.
- Roberts MY, Kaiser AP. The effectiveness of parent-implemented language interventions: A meta-analysis. American Journal of Speech-Language Pathology. 2011; 20 (3):180–199. [ PubMed : 21478280 ]
- Robertson SB, Weismer SE. Effects of treatment on linguistic and social skills in toddlers with delayed language development. Journal of Speech, Language, and Hearing Research. 1999; 42 (5):1234–1248. [ PubMed : 10515518 ]
- Romski M, Sevcik RA. Augmentative communication and early intervention: Myths and realities. Infants & Young Children. 2005; 18 (3):174–185.
- Roth FP, Speece DL, Cooper DH, De La Paz S. Unresolved mysteries: How do metalinguistic and narrative skills connect with early reading? Journal of Special Education. 1996; 30 (3):257–277.
- Rowe ML. Child-directed speech: relation to socioeconomic status, knowledge of child development and child vocabulary skill. Journal of Child Language. 2008; 35 (1):185–205. [ PubMed : 18300434 ]
- Rush DD, Shelden ML. Tips and techniques for effective coaching interactions. Brief Case. 2008; 1 (2):1–4.
- Scarborough H. Handbook for research in early literacy. Neuman S, Dickinson D, editors. New York: Guilford Press; 2001. pp. 97–110. (Connecting early language and literacy to later reading (dis)abilities: Evidence, theory, and practice).
- Schank RC, Ableson RP. Scripts, plans, goals, and understanding. Hillsdale, NJ: Lawrence Earlbaum Associates; 1977.
- Schlosser RW, Sigafoos J. Augmentative and alternative communication interventions for persons with developmental disabilities: Narrative review of comparative single-subject experimental studies. Research in Developmental Disabilities. 2006; 27 (1):1–29. [ PubMed : 16360073 ]
- Schneider P, Watkins RV. Applying Vygotskian developmental theory to language intervention. Language, Speech, and Hearing Services in Schools. 1996; 27 (2):157–170.
- Schooling T, Venediktov R, Leech H. Evidence-based systematic review: Effects of service delivery on the speech and language skills of children from birth to 5 years of age. Rockville, MD: ASHA; 2010.
- Schuele CM, Tolbert L. Omissions of obligatory relative markers in children with specific language impairment. Clinical Linguistics & Phonetics. 2001; 15 (4):257–274.
- Shriberg LD, Kwiatkowski J. Natural process analysis (NPA). Hoboken, NJ: John Wiley & Sons; 1980.
- Shriberg LD, Kwiatkowski J. A follow-up study of children with phonologic disorders of unknown origin. Journal of Speech & Hearing Disorders. 1988; 53 (2):144–155. [ PubMed : 3361857 ]
- Shriberg LD, Aram DM, Kwiatkowski J. Developmental Apraxia of Speech III. A Subtype Marked by Inappropriate Stress. Journal of Speech, Language, and Hearing Research. 1997; 40 (2):313–337. [ PubMed : 9130201 ]
- Simon CS. Out of the broom closet and into the classroom: The emerging SLP. Communication Disorders Quarterly. 1987; 11 (1):41–66.
- Snow CE. The theoretical basis for relationships between language and literacy in development. Journal of Research in Childhood Education. 1991; 6 (1):5–10.
- Snowling MJ, Hulme C. Evidence-based interventions for reading and language difficulties: Creating a virtuous circle. British Journal of Educational Psychology. 2011; 81 (1):1–23. [ PubMed : 21391960 ]
- St Clair MC, Monaghan P, Christiansen MH. Learning grammatical categories from distributional cues: Flexible frames for language acquisition. Cognition. 2010; 116 (3):341–360. [ PubMed : 20674613 ]
- Stark RE, Tallal P. Language, speech, and reading disorders in children. Boston, MA: Little, Brown and Co.; 1988.
- Storkel HL. The emerging lexicon of children with phonological delays: Phonotactic constraints and probability in acquisition. Journal of Speech, Language, and Hearing Research. 2004; 47 (5):1194–1212. [ PubMed : 15603471 ]
- Stothard SE, Snowling MJ, Bishop DVM, Chipchase BB, Kaplan CA. Language-impaired preschoolers: A follow-up into adolescence. Journal of Speech Language and Hearing Research. 1998; 41 (2):407–418. [ PubMed : 9570592 ]
- Strong GK, Torgerson CJ, Torgerson D, Hulme C. A systematic meta-analytic review of evidence for the effectiveness of the “Fast ForWord” language intervention program. Journal of Child Psychology and Psychiatry. 2011; 52 (3):224–235. [ PMC free article : PMC3061204 ] [ PubMed : 20950285 ]
- Swift W. Speech defects in school age children. Boston, MA: Houghton Mifflin Harcourt; 1918.
- Szagun G, Stumper B. Age or experience? The influence of age at implantation, social and linguistic environment on language development in children with cochlear implants. Journal of Speech Language and Hearing Research. 2012; 55 (6):1640–1654. [ PubMed : 22490622 ]
- Tallal P, Miller SL, Bedi G, Byma G, Wang X, Nagarajan SS, Schreiner C, Jenkins WM, Merzenich MM. Language comprehension in language-learning impaired children improved with acoustically modified speech. Science. 1996; 271 (5245):81–84. [ PubMed : 8539604 ]
- Tamis-LeMonda CS, Bornstein MH, Baumwell L, Melstein Damast A. Responsive parenting in the second year: Specific influences on children's language and play. Early Development and Parenting. 1996; 5 (4):173–183.
- Thal D. Language and cognition in normal and late-talking toddlers. Topics in Language Disorders. 1991; 11 (4):33–42.
- Thal D, Marchman V, Tomblin JB. Late talkers: Language development, interventions, and outcomes. Dale PS, Rescorla L, editors. Baltimore, MD: Paul H. Brookes Publishing Co.; 2013. pp. 169–202. (Late-talking toddlers: Characterization and prediction continued delay).
- Tomblin JB, Spencer L, Flock S, Tyler R, Gantz B. A comparison of language achievement in children with cochlear implants and children using hearing aids. Journal of Speech Language and Hearing Research. 1999; 42 (2):497–509. [ PMC free article : PMC3210571 ] [ PubMed : 10229463 ]
- Tomblin JB, Zhang X, Buckwalter P, O'Brien M. The stability of primary language disorder: Four years after kindergarten diagnosis. Journal of Speech Language and Hearing Research. 2003; 46 (6):1283–1296. [ PubMed : 14700355 ]
- Tomblin JB, Nippold MA, Fey M. Understanding individual differences in language development across the school years. Tomblin JB, Nippold MA, editors. New York: Psychological Press; 2014a. pp. 47–78. (The character and course of individual differences in spoken language).
- Tomblin JB, Oleson JJ, Ambrose SE, Walker E, Moeller M. The influence of hearing aids on the speech and language development of children with hearing loss. JAMA Otolaryngology—Head & Neck Surgery. 2014b; 140 (5):403–409. [ PMC free article : PMC4066968 ] [ PubMed : 24700303 ]
- Trivette CM, Dunst CJ, Hamby DW. Influences of family-systems intervention practices on parent-child interactions and child development. Topics in Early Childhood Special Education. 2010; 30 (1):3–19.
- Ukoumunne OC, Wake M, Carlin J, Bavin EL, Lum J, Skeat J, Williams J, Conway L, Cini E, Reilly S. Profiles of language development in pre-school children: A longitudinal latent class analysis of data from the Early Language in Victoria Study. Child: Care, Health and Development. 2011; 38 (3):341–349. [ PubMed : 21434972 ]
- U.S. Bureau of Labor Statistics. Occupational outlook handbook. 2014. [July 17, 2015]. http://www .bls.gov/ooh .
- van Kleeck A, Vander Woude J, Hammett L. Fostering literal and inferential language skills in Head Start preschoolers with language impairment using scripted book-sharing discussions. American Journal of Speech-Language Pathology. 2006; 15 (1):85–95. [ PubMed : 16533095 ]
- Vasilyeva M, Huttenlocher J, Waterfall H. Effects of language intervention on syntactic skill levels in preschoolers. Developmental Psychology. 2006; 42 (1):164. [ PubMed : 16420126 ]
- Wallach GP. Language intervention for school-age students: Setting goals for academic success. St. Louis, MO: Elsevier Health Sciences; 2008.
- Warren SF, Bredin-Oja SL, Fairchild M, Finestack LH, Fey ME, Brady NC, McCauley RJ. Treatment of language disorders in children. McCauley RJ, Fey MD, editors. Baltimore, MD: Paul H. Brookes Publishing Co.; 2006. pp. 47–75. (Responsivity education/prelinguistic milieu teaching).
- Warren SF, Fey ME, Finestack LH, Brady NC, Bredin-Oja SL, Fleming KK. A randomized trial of longitudinal effects of low-intensity responsivity education/prelinguistic milieu teaching. Journal of Speech, Language, and Hearing Research. 2008; 51 (2):451–470. [ PubMed : 18367689 ]
- Weismer SE. The role of stress in language processing and intervention. Topics in Language Disorders. 1997; 17 (4):41–52.
- Weismer SE, Murray-Branch J. Modeling versus modeling plus evoked production training: A comparison of two language intervention methods. Journal of Speech and Hearing Disorders. 1989; 54 (2):269–281. [ PubMed : 2709845 ]
- Weismer SE, Murray-Branch J, Miller J. A prospective longitudinal study of language development in late talkers. Journal of Speech and Hearing Research. 1994; 37 (4):852–867. [ PubMed : 7967571 ]
- Whitehurst GJ, Arnold DS, Epstein JN, Angell AL, Smith M, Fischel JE. A picture book reading intervention in day care and home for children from low-income families. Developmental Psychology. 1994; 30 (5):679.
- Whitman RL, Schwartz ER. The pediatrician's approach to the preschool child with language delay. Clinical Pediatrics. 1985; 24 (1):26–31. [ PubMed : 3965228 ]
- Williams AL. Multiple oppositions theoretical foundations for an alternative contrastive intervention approach. American Journal of Speech-Language Pathology. 2000; 9 (4):282–288.
- Williams AL, McLeod S, McCauley RJ. Interventions for speech sound disorders in children. Baltimore, MD: Paul H. Brookes Publishing Co.; 2010.
- Yairi E, Ambrose NG. Early childhood stuttering. I: Persistency and recovery rates. Journal of Speech, Language, and Hearing Research. 1999; 42 (5):1097–1112. [ PubMed : 10515508 ]
- Yoder PJ, Warren SF. Maternal responsivity predicts the prelinguistic communication intervention that facilitates generalized intentional communication. Journal of Speech, Language, and Hearing Research. 1998; 41 (5):1207–1219. [ PubMed : 9771641 ]
- Yoder PJ, Warren SF. Relative treatment effects of two prelinguistic communication interventions on language development in toddlers with developmental delays vary by maternal characteristics. Journal of Speech, Language, and Hearing Research. 2001; 44 (1):224–237. [ PubMed : 11218105 ]
- Yoder PJ, Warren SF. Effects of prelinguistic milieu teaching and parent responsivity education on dyads involving children with intellectual disabilities. Journal of Speech, Language, and Hearing Research. 2002; 45 (6):1158–1174. [ PubMed : 12546485 ]
- Yoder P, Camarata S, Gardner E. Treatment effects on speech intelligibility and length of utterance in children with specific language and intelligibility impairments. Journal of Early Intervention. 2005; 28 (1):34–49.
- Yoder P, Fey ME, Warren SF. Studying the impact of intensity is important but complicated. International Journal of Speech-Language Pathology. 2012; 14 (5):410–413. [ PMC free article : PMC4048952 ] [ PubMed : 22646316 ]
- Zebrowski PM, Schum RL. Counseling parents of children who stutter. American Journal of Speech-Language Pathology. 1993; 2 (2):65–73.
Individuals with Disabilities Education Act of 2004, Public Law 108-446, 108th Cong. (December 3, 2004).
42 C.F.R. § 440.110(c).
- Cite this Page Committee on the Evaluation of the Supplemental Security Income (SSI) Disability Program for Children with Speech Disorders and Language Disorders; Board on the Health of Select Populations; Board on Children, Youth, and Families; Institute of Medicine; Division of Behavioral and Social Sciences and Education; National Academies of Sciences, Engineering, and Medicine; Rosenbaum S, Simon P, editors. Speech and Language Disorders in Children: Implications for the Social Security Administration's Supplemental Security Income Program. Washington (DC): National Academies Press (US); 2016 Apr 6. 3, Treatment and Persistence of Speech and Language Disorders in Children.
- PDF version of this title (5.7M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Treatment and Persistence of Speech and Language Disorders in Children - Speech ... Treatment and Persistence of Speech and Language Disorders in Children - Speech and Language Disorders in Children
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Skip to content
Childhood Apraxia of Speech
Center for childhood communication, what is childhood apraxia of speech.
Childhood apraxia of speech (CAS) is a speech disorder where your child's mouth cannot make the quick movements needed to speak, even after their brain tells their mouth what to do. There is usually no muscle weakness. If your child has CAS, it may be difficult for them to plan and complete the quick mouth movements needed to make sounds into syllables, words and sentences (motor planning). CAS is also sometimes called verbal apraxia, developmental apraxia of speech or verbal dyspraxia.
Causes of childhood apraxia of speech
In most cases the cause of CAS is unknown. Here at Children’s Hospital of Philadelphia (CHOP), we are always working to find out more about why this condition occurs in some children. We know it is a rare disorder. It only affects about 3 to 5% of all preschoolers with diagnosed speech disorders. It is more common for children to have other developmental speech disorders. CAS is sometimes seen with other conditions like genetic, neurological or developmental disorders. But sometimes there are no other conditions present.
Symptoms of childhood apraxia of speech
The American Speech-Language-Hearing Association lists three features as the most common you may notice if your child has CAS:
- Your child says the same word differently each time they say it.
- Your child has difficulty starting or transitioning between sounds or words, making their speech sound disconnected or “choppy”.
- Your child finds the timing, rhythm and flow of speech challenging.
A child with CAS is often hard to understand. In addition to the three symptoms above, your child may:
- Produce vowel sound errors
- Have a slow rate of speech
- Have stress or voicing errors
- Have a tough time starting oral movements to say something
- Have multiple sound errors that do not follow the patterns expected in young children
- Use a limited variety of consonant and vowel sounds
- Have difficulty with longer words
- Use extra mouth movements when trying to make speech sounds
- Say a word or words with an additional sound
- Say a word once perfectly but not be able to say it again
- Say automatic words (like “hi” and “thank you”) more easily than less routine words
- Switch sounds in words or add sounds or syllables to words
- Have differences in the quality of the voice that come from sound vibrations in the throat, mouth and nose (resonance or nasality differences)
- Have a history of late development of first words and sounds
Testing and diagnosis for childhood apraxia of speech
Here at CHOP, we have a dedicated team of licensed speech-language pathologists (SLP) who can diagnose whether your child has CAS. Your child may be referred to our SLPs for evaluation by their pediatrician, neurologist or developmental pediatrician. Our SLP will first do a speech and language evaluation.
During the speech and language evaluation, our SLP will review your child’s birth, medical and developmental histories. They will evaluate your child’s ability to:
- Understand and use language
- Communicate using speech, sign language and/or gestures
- Produce consonant and vowel sounds, syllables, words and phrases
- Speak with appropriate timing, rhythm and flow of speech
- Move parts of their mouth, including tongue, lips and jaw
- Play and interact with others
Our SLP will look for signs of CAS by asking your child to say certain sounds, words and phrases. It is harder to diagnose CAS in very young children and children with limited language skills. Our SLP may not be able to diagnose or rule out CAS on the first visit. They may recommend therapy, teach you language-building activities to do with your child at home, or ask you to come back in a few months to check your child’s progress.
Treatment for childhood apraxia of speech
Our SLP will create goals to support your child’s ability to be understood by others. The therapy approach will depend on your child’s specific needs. Goals may include learning how to say speech sounds, syllables, words and phrases.
If your child has a limited number of words in their vocabulary, therapy will start with improving their functional communication skills. This may include having your child practice with word approximations, picture communication systems, and speech-generating devices. To reduce frustration, some children with CAS may use one of these methods to express themselves while their speech develops. As your child’s speech improves, these systems may no longer be needed.
Speech-language therapy sessions will involve you, your child, their other caregiver(s) and our SLP. Sessions may be play-based or structured with tabletop activities. This will depend on your child’s needs and abilities. Sessions will also include your child's interests and your family's culture. This leads to better engagement, relevance, learning and fun.
At CHOP, our goal is to identify and treat CAS so your child can have the best communication outcomes.
Frequently asked questions
How long will speech therapy last.
Children improve at different rates. In general, if your child has CAS, they may be in speech therapy longer than children with other speech disorders. The length of therapy depends on the severity of your child’s CAS (mild, moderate or severe), but intensive therapy may last several years.
Speech therapy may occur in your home, at your child’s school and/or with a private SLP. As your child’s speech gets clearer and their sentences become longer, therapy intensity may be gradually reduced. Children with milder forms of CAS and young children (younger than age two) may require therapy less often. If your child has no other language, cognitive or behavioral concerns, they will usually make faster progress. If you have concerns about your child’s language, cognitive or behavioral development, it is important to address those concerns as well.
What will my child do in speech therapy?
It is important for therapy to be motivating and rewarding. Activities may include games, play and drill-work, along with engaging in strategies like repetition, feedback, cues (visual, touch and/or verbal) and imitation.
Our SLP may focus on developing a core vocabulary or “power words” with your child, like their name, age, names of family members and pets, “help”, “open”, “yes”, “no” and “all done.” These words and phrases will improve your child’s overall communication and decrease their frustration. Gestures, sign language, picture boards and electronic devices may also be introduced to support your child’s verbal communication.
Will my child need to do oral motor exercises?
In general, your child must practice talking. All practice with mouth movements should relate to a specific sound or word that your child is practicing. For example, our SLP may ask your child to, “Round your lips” for the “w” sound in “want”, when asking for a toy. Rounding lips to blow bubbles or a whistle will not directly improve your child’s speech production skills.
What can I do for my child at home?
Your child’s SLP will teach you how to help your child practice and communicate at home. If your child has CAS, they will need to practice speech outside of the therapy room. We recommend practicing for a few minutes, a few times each day. This tends to be more effective than practicing once per week for a longer amount of time. Your practice activities at home should include things that your child can do easily and well. This makes home practice fun and successful and builds your child’s confidence when speaking.
Does a child with CAS often have needs other than speech therapy?
Children with CAS often have difficulties with language skills, as well. Your child may need help with learning to speak in sentences, using correct grammar and communicating during social interactions and play. As children with CAS get older, they may have additional learning difficulties (like reading skills). Some children with CAS may have gross motor or fine motor issues requiring occupational or physical therapy.
Reviewed by Arielle Berne, MA, CCC-SLP
Health Library Speech Disorders
What is a speech disorder.
Many children will experience a temporary delay in speech and language development. Most will eventually catch up. Others will continue to have difficulty with communication development. Communication disorders include speech disorders and language disorders. Speech disorders are discussed in this article and some general guidelines are also given. This will help you decide if your child needs to be tested by a speech-language pathologist.
A child with a speech disorder may have difficulty with speech sound production, voice, resonance or fluency (the flow of speech).
Speech Sound Disorders
A child with a speech sound disorder is unable to say all of the speech sounds in words. This can make the child’s speech hard to understand. People may not understand the child in everyday situations. For most children, the cause of the speech sound disorder is unknown. Other speech sound disorders can be linked to things such as a cleft palate, problems with the teeth, hearing loss, or difficulty controlling the movements of the mouth.
Reasons for Concern
- The child doesn't babble using consonant sounds (particularly b, d, m, and n) by age 8 or 9 months.
- The child uses mostly vowel sounds or gestures to communicate after 18 months.
- The child’s speech cannot be understood by many people at age 3.
- The child’s speech is difficult to understand at age 4 or older.
Voice Disorders
The voice is produced as air from the lungs moves up through and vibrates the vocal folds. This is called phonation. With voice disorders, the voice may be harsh, hoarse, raspy, cut in and out, or show sudden changes in pitch. Voice disorders can be due to vocal nodules, cysts, papillomas, paralysis or weakness of the vocal folds.
- The voice is hoarse, harsh or breathy.
- The voice is always too loud or too soft.
- The pitch is inappropriate for the child's age or gender.
- The voice often "breaks" or suddenly changes pitch.
- Frequent loss of voice
Resonance Disorders
Resonance is the overall quality of the voice. A resonance disorder is when the quality of the voice changes as it travels through the different-shaped spaces of the throat, nose and mouth. Resonance disorders include the following:
Hyponasality (Denasality): This is when not enough sound comes through the nose, making the child sound “stopped up.” This might be caused by a blockage in the nose or by allergies.
Hypernasality : This happens when the movable, soft part of the palate (the velum) does not completely close off the nose from the back of the throat during speech. Because of this, too much sound escapes through the nose. This can be due to a history of cleft palate, a submucous cleft, a short palate, a wide nasopharynx, the removal of too much tissue during an adenoidectomy, or poor movement of the soft palate.
Cul-de-Sac Resonance: This is when there is a blockage of sound in the nose, mouth or throat. The voice sounds muffled or quiet as a result.
Reasons for Concern:
- Speech sounds hyponasal or hypernasal
- Air is heard coming out of the nose during speech
Fluency Disorders (Stuttering)
Fluency is the natural “flow” or forward movement of speech. Stuttering is the most common type of fluency disorder. Stuttering happens when there are an abnormal number of repetitions , hesitations, prolongations, or blocks in this rhythm or flow of speech. Tension may also be seen in the face, neck, shoulders or fists. There are many theories about why children stutter. At present, the cause is most likely linked to underlying neurological differences in speech and language processing. Internal reactions from the person talking, and external reactions from other listeners, may impact stuttering, but they do not cause stuttering.
- The parents are concerned about stuttering.
- The child has an abnormal number of repetitions, hesitations, prolongations or blocks in the natural flow of speech.
- The child exhibits tension during speech.
- The child avoids speaking due to a fear of stuttering.
- The child considers themselves to be someone who stutters.
Treatment for Speech Disorders
Early intervention is very important for children with communication disorders. Treatment is best started during the toddler or preschool years. These years are a critical period of normal language learning. The early skills needed for normal speech and language development can be tested even in infants. At that age, the speech-language pathologist works with the parents on stimulating speech and language development in the home. Active treatment in the form of individual therapy usually starts between the ages of 2 and 4 years.
If you have concerns about your child’s communication skills, discuss them with your child’s doctor. The doctor will likely refer the child to a speech-language pathologist for evaluation and treatment.
All children with speech and language disorders should also have their hearing tested.
Helping Your Child
Children learn speech and language skills by listening to the speech of others, and practicing as they talk to others. Parents are the most important teachers for their child in their early years.
They can help the child by giving lots of opportunities to listen to speech and to talk. This can be done by frequently pointing out and naming important people, places, and things. They can also read and talk to the child throughout the day, especially during daily routines, interactive plays, and favorite activities. Parents can give the child models of words and sentences to repeat.
Parents can also set up opportunities for the child to answer questions and talk. Listening to music, singing songs and sharing nursery rhymes are also great ways to build speech and language skills while having fun with your child.
Last Updated 12/2023
Connect With Us
3333 Burnet Avenue, Cincinnati, Ohio 45229-3026
© 1999-2024 Cincinnati Children's Hospital Medical Center. All rights reserved.


Spasmodic Dysphonia Treatment: Addressing a Shaky Voice

Struggling to express yourself verbally, with your voice breaking or trembling uncontrollably, can lead to frustration and embarrassment. This is the reality for those living with spasmodic dysphonia, a chronic voice disorder that can significantly impact daily life.
The good news is that with accurate diagnosis and effective spasmodic dysphonia treatment, many individuals can manage their symptoms and maintain their quality of life.
Key Points:
Spasmodic dysphonia is a chronic voice disorder characterized by involuntary spasms of the vocal cords, leading to disrupted speech.
Effective treatments for managing symptoms include botulinum toxin injections to relax vocal muscles and voice therapy to improve speech quality.
Early diagnosis and ongoing care from specialized healthcare providers are crucial for individuals to manage their condition effectively.
Understanding Types of Spasmodic Dysphonia
Living with a shaky voice: symptoms, impact, and the power of early action, identifying the root causes, how is spasmodic dysphonia diagnosed, treatment options for spasmodic dysphonia, living with spasmodic dysphonia: tips and support, frequently asked questions, how connected speech pathology can help.

Spasmodic dysphonia (SD) is a lifelong condition characterized by involuntary spasms of the vocal folds within the voice box, causing voice breaks and vocal tremors that may worsen over time.
Voice characteristics include voice breaks, tremors, and strain, creating an often choppy, breathy, or shaky quality.
This voice problem typically occurs in individuals between the ages of 30 and 50 and is more prevalent in women than men.
There are three types of spasmodic dysphonia: abductor, adductor, and mixed, each with its own set of symptoms and characteristics.
Abductor Spasmodic Dysphonia
Abductor spasmodic dysphonia is marked by vocal fold spasms that cause the cords to open too wide, resulting in a weak, breathy voice. This occurs when the muscles responsible for opening the vocal cords during speech are affected, leading to sudden breathy or whispering voice breaks when the voice sounds breathy.
The primary cause of abductor spasmodic dysphonia is spasms that force the vocal folds to stay open, preventing them from vibrating correctly.
Adductor Spasmodic Dysphonia
Adductor spasmodic dysphonia, on the other hand, is characterized by spasms that cause the vocal cords to close too tightly, leading to a strained, strangled voice.
This type results from spasms in the vocal folds that cause them to close tightly, affecting the muscles responsible for closing the vocal cords and making it difficult for them to vibrate correctly. Adductor spasmodic dysphonia affects approximately 3.5-7.0 per 100,000 individuals.
Mixed Spasmodic Dysphonia
Mixed SD involves both abductor and adductor spasms, causing a combination of voice symptoms . The manifestations of mixed spasmodic dysphonia include speech sounds that are weak, quiet, and breathy, as well as a strained, tight, or breathy voice.
The precise origin of mixed spasmodic dysphonia is yet to be determined. Still, it is speculated to be a disorder of the central nervous system originating from an issue in the basal ganglia of the brain.
Spasmodic Dysphonia (SD) throws your voice for a loop, causing involuntary muscle spasms that disrupt speech and confidence. But understanding the symptoms and their impact, along with the importance of early diagnosis and treatment, can empower you to regain control.
Spasmodic Dysphonia Symptoms
Shaky, strained, or breathy voice: This hallmark symptom can sound like choppiness, breaks, or involuntary pitch changes.
Difficulty starting or sustaining words: Muscle spasms may make certain sounds or syllables challenging to pronounce.
Increased effort while speaking: The struggle to control your voice can become draining and tiring.
Variations in severity: Symptoms may worsen with stress, fatigue, or certain speaking situations.
Impact on Daily Life
Limited communication: Difficulty speaking clearly can hinder meaningful interactions at work, school, and social settings.
Isolation and anxiety: Frustration and embarrassment around your voice can lead to social withdrawal and emotional distress.
Reduced job opportunities: Communication is crucial for many careers, and SD can create barriers to professional success.
Impact on mental health: Chronic challenges with communication can affect self-esteem and overall well-being.
Spasmodic dysphonia isn't just one factor; it's a complex mix of potential culprits, each playing a unique role in this "shaky voice" disorder. One key player is how our brains handle voice production. Misfiring signals can lead to uncontrollable muscle spasms in the vocal cords, causing vocal tremors.
Research suggests abnormal brain activity sends "glitchy" messages to the vocal folds, making them vibrate abnormally and causing the voice to tremble. Additionally, genes appear to hold a hand in this disorder. Some people inherit a "spasmodic dysphonia susceptibility gene," increasing their risk. Understanding these genetic links helps us see how nature and nurture work together in this condition.
Another facet is physical injury. Damage to the delicate voice muscles can cause "breaks," tightness, and strain, making spasms more likely. Whether from direct injury or overuse, compromised vocal cords become vulnerable to spasmodic dysphonia.
Stress and anxiety , unfortunately, also play a part. Feeling overwhelmed can worsen the frequency and intensity of spasms, making the condition more challenging to manage. This connection between mental stress and the body's vocal response highlights the importance of emotional well-being for vocal health.

Accurate diagnosis of spasmodic dysphonia is fundamental for effective treatment. The diagnostic procedure consists of fiberoptic nasolaryngoscopy, a detailed medical history review, and a neurological evaluation.
SD is strongly linked to neurological issues, with abnormal brain signals potentially triggering muscle spasms. Many other voice disorders have different causes, such as vocal misuse (muscle tension dysphonia), structural issues (vocal nodules), or nerve damage (vocal fold paralysis).
Fiberoptic Nasolaryngoscopy
The fiberoptic nasolaryngoscopy procedure allows for a detailed examination of the vocal cords, while the medical history and neurological evaluation help identify any underlying neurological problems or other potential causes of voice issues.
Fiberoptic nasolaryngoscopy is a diagnostic procedure that utilizes a camera inserted through the nose to examine the vocal cords. During the process, a small flexible telescope is passed through the nose and into the throat to inspect the nose, throat, and airway. Visualization of the vocal folds is made as the vocal cords vibrate. The procedure can be completed in a doctor's office within 5 to 10 minutes and carries some potential risks, including:
Mucosal tearing and bleeding
Epistaxis (nosebleeds)
Breathing difficulties
Medical History and Neurological Evaluation
A detailed medical history and neurological assessment by otolaryngologists (ENTs) and speech-language pathologists (SLPs) are essential to accurately identifying any underlying neurological conditions or other potential causes of voice disturbances. The medical history typically yields information such as:
Patient symptoms
Duration and progression of symptoms
Voice triggers
Medical and family history
Medications and treatments
Impact on daily life
Neurological examinations, perceptual analysis, acoustic analysis, aerodynamic analysis, and electromyographic analysis are typically conducted.

There are multiple treatment options for spasmodic dysphonia, including:
Botulinum toxin injections
Voice therapy
Oral medications
Surgical treatments
These treatments aim to lessen symptoms and enhance voice quality, including voice sounds, to support patients in maintaining their quality of life.
The effectiveness of each treatment varies, and a combination of treatments may be necessary for some individuals.
Botulinum Toxin Injections
Botulinum toxin injections are a popular treatment option for spasmodic dysphonia, as they temporarily weaken the affected vocal cord muscles, resulting in improved speech clarity and requiring repeat injections every few months.
The initial side effects of botulinum toxin injections may include a temporarily weak, breathy voice and occasional swallowing difficulty. Still, they typically provide a three to four-month improvement in the voice.
Botulinum toxin injections are not as effective in treating abductor spasmodic dysphonia compared to adductor spasmodic dysphonia. Other treatment options may be better suited for this type of dysphonia.
Voice Therapy
Voice therapy can help patients manage their symptoms and improve their voice quality, alone or in combination with other treatments. A speech-language pathologist provides voice therapy and management strategies to address compromised speech and voice symptoms.
Voice therapy can help patients with spasmodic dysphonia by:
Developing better control and coordination of their respiratory muscles
Improving breath support during speech
Reducing tension and muscle spasms in the laryngeal area.
Oral Medications
Oral medications may help alleviate symptoms of spasmodic dysphonia, although they are typically less effective than botulinum toxin injections. Commonly prescribed oral medications for spasmodic dysphonia include benzodiazepines, anticholinergics, and dopamine antagonists.
The potential side effects of oral medications used for treating spasmodic dysphonia may include:
Temporarily weak and breathy voice
Occasional swallowing difficulties
Potential adverse events such as excessive sleepiness, depression, and cognitive impairment.
Surgical Treatments
Surgical treatments, such as nerve surgery, may be considered for some patients with spasmodic dysphonia, particularly if other treatments have not been effective. Although surgery cannot cure the disease, it can help patients manage their symptoms.
Surgical treatments can be effective, but the individual results will differ. Positive outcomes have been demonstrated as a whole.

While living with spasmodic dysphonia can pose challenges, there are methods to manage the disorder and sustain a high quality of life. Some strategies include:
Counseling, which can provide emotional support and validation
Support groups, where individuals can connect with others facing similar challenges and share coping strategies
Communication aids, such as speech therapy or assistive devices, can help improve communication and daily living
These methods can help individuals with spasmodic dysphonia manage their symptoms and enhance their overall well-being.
Participating in support groups can also help individuals feel less isolated and more empowered in their journey with spasmodic dysphonia.
Finding the Right Specialist
Finding an appropriate specialist, like a laryngologist or speech-language pathologist , is vital for precise diagnosis and effective treatment of spasmodic dysphonia. Professionals with experience in diagnosing and treating vocal cord injuries, including spasmodic dysphonia, will be better equipped to provide the appropriate care and management strategies.
To find a reputable specialist, consider asking for recommendations from:
your primary care physician
local hospitals or medical centers
support groups
organizations dedicated to spasmodic dysphonia

1. What triggers spasmodic dysphonia?
Spasmodic dysphonia is caused by a trigger in the brain and nervous system that can affect the voice and, in some cases, psychological stress.
2. What is the most effective treatment option for spasmodic dysphonia?
The most effective treatment option for spasmodic dysphonia is the injection of very small amounts of botulinum toxin directly into the affected muscles of the larynx (voice box). This helps reduce vocal tremors by blocking abnormal nerve impulses from reaching the muscle, which alters the person's voice.
3. How do you treat spasmodic dysphonia naturally?
Unfortunately, there's no scientifically proven "natural" cure for spasmodic dysphonia. However, specific lifestyle changes and vocal hygiene practices, like reducing stress, getting enough sleep, and avoiding vocal strain, can sometimes show mild improvements in symptom management.
Consulting a speech-language pathologist for personalized strategies remains crucial for effectively managing the condition.
4. Is spasmodic dysphonia a central nervous system disorder?
While the exact cause is unknown, SD is strongly linked to central nervous system dysfunction, with abnormal brain signals potentially triggering muscle spasms in the vocal cords. Research suggests specific areas involved in controlling voice movement and coordination may be affected.
5. Is SD a movement disorder?
SD can be considered a movement disorder as it involves involuntary muscle spasms in the vocal cords, a key structure for producing sound. However, it is not the same as other movement disorders like Parkinson's, as it specifically affects spoken communication rather than overall motor function.

If spasmodic dysphonia (SD) disrupts your voice and confidence, Connected Speech Pathology offers expert support to empower you on your journey to clearer communication. We understand the challenges of living with SD, and our specialized speech-language pathologists use evidence-based approaches to help you:
Reduce involuntary muscle spasms : Through targeted vocal exercises and relaxation techniques, we can help manage the physical aspects of SD and improve vocal control.
Find alternative communication strategies : We explore communication aids and augmentative techniques to ensure your voice is always heard, boosting your confidence and social interaction.
Navigate emotional impact : We provide psychological support and counseling to manage the frustration and anxiety associated with SD, aiding your overall well-being.
Connected Speech Pathology:
Offers flexible scheduling and telehealth options for convenient care.
Collaborates closely with you and your support network for a personalized approach.
Utilizes cutting-edge techniques and stays abreast of current research.
Don't let SD silence your voice. Take the first step towards clearer communication and regain control. Contact Connected Speech Pathology today!
In conclusion, spasmodic dysphonia is a complex and chronic voice disorder that can significantly impact an individual's daily life. Accurate diagnosis and effective treatment are essential for managing symptoms and maintaining quality of life.
By understanding the condition, exploring available treatment options, and finding the right specialist, individuals with spasmodic dysphonia can take control of their voices and continue to live fulfilling lives.

About the Author
Allison Geller is a speech-language pathologist (SLP) and the owner of Connected Speech Pathology. She obtained her Bachelor’s and Master’s degrees from the University of Florida in Speech-Language Pathology. Allison has practiced speech therapy in a number of settings including telepractice, acute care, outpatient rehabilitation, and private practice. She has worked extensively with individuals across the lifespan including toddlers, preschoolers, school-aged children, and adults. She specializes in the evaluation, diagnosis, and treatment of a variety of communication disorders including receptive/expressive language disorders, articulation disorders, voice disorders, fluency disorders, brain injury, and swallowing disorders.
Allison served as the clinical coordinator of research in aphasia in the Neurological Institute at Columbia University Medical Center in New York. She is on the Board of Directors for the Corporate Speech Pathology Network (CORSPAN), a Lee Silverman Voice Treatment ( LSVT ) certified clinician, and a proud Family Empowerment Scholarship/Step-Up For Students provider. Allison is passionate about delivering high quality-effective treatment remotely because it’s convenient and easy to access. What sets us apart from other online speech therapy options is—Allison takes great care to hire the very best SLPs from all over the country.
Why Do People Have Lisps and How They Affect Speech
Effective strategies in resonant voice therapy.
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Study reveals brain mechanisms behind speech impairment in Parkinson’s
Most Parkinson’s disease patients struggle with speech problems. New research by Stanford Medicine scientists uncovers the brain connections that could be essential to preserving speech.
May 28, 2024 - By Nina Bai

Research by Stanford Medicine scientists may explain why some treatments for Parkinson’s — developed mainly to target motor symptoms — can improve speech impairments while other treatments make them worse. Lightspring /Shutterstock.com
Parkinson’s disease is most well-known and well-studied for its motor impairments — tremors, stiffness and slowness of movement. But less visible symptoms such as trouble with memory, attention and language, which also can profoundly impact a person’s quality of life, are less understood. A new study by Stanford Medicine researchers reveals the brain mechanisms behind one of the most prevalent, yet often overlooked, symptoms of the disease — speech impairment.
Based on brain imaging from Parkinson’s patients, the researchers identified specific connections in the brain that may determine the extent of speech difficulties.
The findings , reported May 20 in the Proceedings of the National Academy of Sciences , could help explain why some treatments for Parkinson’s — developed mainly to target motor symptoms — can improve speech impairments while other treatments make them worse.
More than a motor disorder
“Parkinson’s disease is a very common neurological disorder, but it’s mostly considered a motor disorder,” said Weidong Cai , PhD, clinical associate professor of psychiatry and behavioral sciences and the lead author of the new study. “There’s been lots of research on how treatments such as medications and deep brain stimulation can help improve motor function in patients, but there was limited understanding about how these treatments affect cognitive function and speech.”
Over 90% of people with Parkinson’s experience difficulties with speech, an intricate neurological process that requires motor and cognitive control. Patients may struggle with a weak voice, slurring, mumbling and stuttering.
“Speech is a complex process that involves multiple cognitive functions, such as receiving auditory feedback, organizing thoughts and producing the final vocal output,” Cai said.
The senior author of the study is Vinod Menon , PhD, professor of psychiatry and behavioral sciences and director of the Stanford Cognitive and Systems Neuroscience Laboratory .
The researchers set out to study how levodopa, a common Parkinson’s drug that replaces the dopamine lost from the disease, affects overall cognitive function. They focused on the subthalamic nucleus, a small, pumpkin-seed-shaped region deep within the brain.

Weidong Cai
The subthalamic nucleus is known for its role in inhibiting motor activity, but there are clues to its involvement in other functions. For example, deep brain stimulation, which uses implanted electrodes to stimulate the subthalamic nucleus, has proven to be a powerful way to relieve motor symptoms for Parkinson’s patients — but a common side effect is worsened speech impairment.
Same test, different scores
In the new study, 27 participants with Parkinson’s disease and 43 healthy controls, all older than 60, took standard tests of motor and cognitive functioning. The participants with Parkinson’s took the tests while on and off their medication.
As expected, the medication improved motor functioning in the patients, with those having the most severe symptoms improving the most.
The test for cognitive functioning offered a surprise. The test, known as the Symbol Digit Modalities Test, is given in two forms — oral and written. Patients are provided with nine symbols, each matched with a number — a plus sign for the number 7, for example. They are then asked to translate a string of symbols into numbers, either speaking or writing down their answers, depending on the version of the test.
As a group, the patients’ performance on both versions of the cognitive test was little affected by medication. But taking a closer look, the researchers noticed that the subset of patients who performed particularly poorly on the spoken version of the test without medication improved their spoken performance on the medication. Their written test scores did not change significantly.
“It was quite interesting to find this dissociation between the written and oral version of the same test,” Cai said.
The dissociation suggested that the medication was not enhancing general cognitive functions such as attention and working memory, but it was selectively improving speech.
“Our research unveiled a previously unrecognized impact of dopaminergic drugs on the speech function of Parkinson’s patients,” Menon said.
Uncovering connections
Next, the researchers analyzed fMRI brain scans of the participants, looking at how the subthalamic nucleus interacted with brain networks dedicated to various functions, including hearing, vision, language and executive control.

Vinod Menon
They found that different parts of the subthalamic nucleus interacted with different networks.
In particular, they discovered that improvements on the oral version of the test correlated with better functional connectivity between the right side of the subthalamic nucleus and the brain’s language network.
Using a statistical model, they could even predict a patient’s improvement on the oral test based on changes in their brain’s functional connectivity.
“Here we’re not talking about an anatomical connection,” Cai explained. Rather, functional connectivity between brain regions means the activity in these regions is closely coordinated, as if they are talking to each other.
“We discovered that these medications influence speech by altering the functional connectivity between the subthalamic nucleus and crucial language networks,” Menon said. “This insight opens new avenues for therapeutic interventions tailored specifically to improve speech without deteriorating other cognitive abilities.”
This newly identified interaction between the subthalamic nucleus and the language network could serve as a biological indicator of speech behavior — in Parkinson’s as well as other speech disorders like stuttering.
Such a biomarker could be used to monitor treatment outcomes and inspire new therapies. “Of course, you can directly observe the outcome of a medication by observing behavior, but I think to have a biomarker in the brain will provide more useful information for the future development of drugs,” Cai said.
The findings also provide a detailed map of the subthalamic nucleus, which could guide neurosurgeons performing deep brain stimulation in avoiding damage to an area critical to speech function. “By identifying key neural maps and connections that predict speech improvement, we can craft more effective treatment plans that are both precise and personalized for Parkinson’s disease patients,” Menon said.
The study received funding from the National Institutes of Health (grants P50 AG047366, P30 AG066515, RF1 NS086085, R21 DC017950-S1, R01 NS115114, R01 MH121069 and K99 AG071837) and the Alzheimer’s Association.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Hope amid crisis
Psychiatry’s new frontiers

- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 29, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Study reveals brain mechanisms behind speech impairment in Parkinson's
by Nina Bai, Stanford University
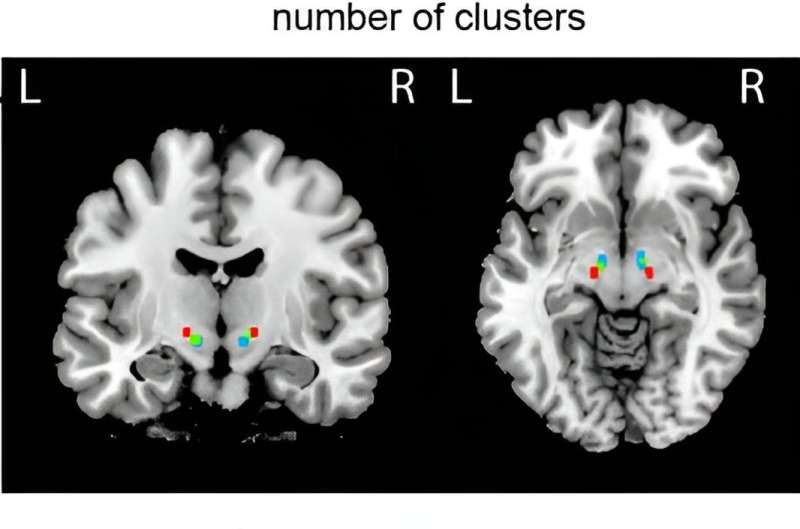
Parkinson's disease is most well-known and well-studied for its motor impairments—tremors, stiffness and slowness of movement. But less visible symptoms such as trouble with memory, attention and language, which can also profoundly impact a person's quality of life, are less understood.
A new study by Stanford Medicine researchers reveals the brain mechanisms behind one of the most prevalent, yet often overlooked, symptoms of the disease— speech impairment. Based on brain imaging from Parkinson's patients, the researchers identified specific connections in the brain that may determine the extent of speech difficulties.
The findings , reported May 20 in the Proceedings of the National Academy of Sciences , could help explain why some treatments for Parkinson's—developed mainly to target motor symptoms—can improve speech impairments while other treatments make them worse.
More than a motor disorder
"Parkinson's disease is a very common neurological disorder, but it's mostly considered a motor disorder," said Weidong Cai, Ph.D., clinical associate professor of psychiatry and behavioral sciences and the lead author of the new study.
"There's been lots of research on how treatments such as medications and deep brain stimulation can help improve motor function in patients, but there was limited understanding about how these treatments affect cognitive function and speech."
More than 90% of people with Parkinson's experience difficulties with speech, an intricate neurological process that requires motor and cognitive control. Patients may struggle with a weak voice, slurring, mumbling and stuttering.
"Speech is a complex process that involves multiple cognitive functions, such as receiving auditory feedback, organizing thoughts and producing the final vocal output," Cai said.
The senior author of the study is Vinod Menon, Ph.D., professor of psychiatry and behavioral sciences and director of the Stanford Cognitive and Systems Neuroscience Laboratory.
The researchers set out to study how levodopa, a common Parkinson's drug that replaces the dopamine lost from the disease, affects overall cognitive function. They focused on the subthalamic nucleus, a small, pumpkin-seed-shaped region deep within the brain.
The subthalamic nucleus is known for its role in inhibiting motor activity, but there are clues to its involvement in other functions. For example, deep brain stimulation, which uses implanted electrodes to stimulate the subthalamic nucleus, has proven to be a powerful way to relieve motor symptoms for Parkinson's patients—but a common side effect is worsened speech impairment.
Same test, different scores
In the new study, 27 participants with Parkinson's disease and 43 healthy controls, all older than 60, took standard tests of motor and cognitive functioning. The participants with Parkinson's took the tests while on and off their medication.
As expected, the medication improved motor functioning in the patients, with those having the most severe symptoms improving the most.
The test for cognitive functioning offered a surprise. The test, known as the Symbol Digit Modalities Test, is given in two forms—oral and written. Patients are provided with nine symbols, each matched with a number—a plus sign for the number 7, for example. They are then asked to translate a string of symbols into numbers, either speaking or writing down their answers, depending on the version of the test.
As a group, the patients' performance on both versions of the cognitive test was little affected by medication. But taking a closer look, the researchers noticed that the subset of patients who performed particularly poorly on the spoken version of the test without medication improved their spoken performance on the medication. Their written test scores did not change significantly.
"It was quite interesting to find this dissociation between the written and oral version of the same test," Cai said.
The dissociation suggested that the medication was not enhancing general cognitive functions such as attention and working memory, but it was selectively improving speech.
"Our research unveiled a previously unrecognized impact of dopaminergic drugs on the speech function of Parkinson's patients," Menon said.
Uncovering connections
Next, the researchers analyzed fMRI brain scans of the participants, looking at how the subthalamic nucleus interacted with brain networks dedicated to various functions, including hearing, vision, language and executive control.
They found that different parts of the subthalamic nucleus interacted with different networks.
In particular, they discovered that improvements on the oral version of the test correlated with better functional connectivity between the right side of the subthalamic nucleus and the brain's language network.
Using a statistical model , they could even predict a patient's improvement on the oral test based on changes in their brain's functional connectivity.
"Here we're not talking about an anatomical connection," Cai explained. Rather, functional connectivity between brain regions means the activity in these regions is closely coordinated, as if they are talking to each other.
"We discovered that these medications influence speech by altering the functional connectivity between the subthalamic nucleus and crucial language networks," Menon said. "This insight opens new avenues for therapeutic interventions tailored specifically to improve speech without deteriorating other cognitive abilities."
This newly identified interaction between the subthalamic nucleus and the language network could serve as a biological indicator of speech behavior—in Parkinson's as well as other speech disorders like stuttering.
Such a biomarker could be used to monitor treatment outcomes and inspire new therapies. "Of course, you can directly observe the outcome of a medication by observing behavior, but I think to have a biomarker in the brain will provide more useful information for the future development of drugs," Cai said.
The findings also provide a detailed map of the subthalamic nucleus , which could guide neurosurgeons performing deep brain stimulation in avoiding damage to an area critical to speech function.
"By identifying key neural maps and connections that predict speech improvement, we can craft more effective treatment plans that are both precise and personalized for Parkinson's disease patients," Menon said.
Explore further
Feedback to editors

Eye-tracking techniques could help primary care providers diagnose autism sooner, more accurately
5 hours ago

This self-powered sensor could make MRIs more efficient
6 hours ago

Not eating can hinder weight loss, study in fruit flies suggests
7 hours ago

Neuroscience research suggests ketones can enhance cognitive function and protect brain networks
8 hours ago

New research finds antidepressants may help deliver other drugs into the brain

Mediterranean diet tied to one-fifth lower risk of death in women
9 hours ago

Scientists find new method to enhance efficacy of bispecific antibodies for solid tumors

Cardiomyocytes study discovers new way to regenerate damaged heart cells

Study: The route into the cell influences the outcome of SARS-CoV-2 infection

Prenatal testing offers a window for finding a mother's cancer risk
10 hours ago
Related Stories

Researchers identify brain region involved in control of attention
Apr 15, 2024

Neural circuit location of strong sense of discomfort found
Nov 6, 2023

Researchers confirm brain region's role in mind-body communication
Jul 26, 2022

Effects of deep brain stimulation in patients with Parkinson's disease
Aug 29, 2018

Electrophysiological signals identify Parkinson's disease subtypes
Aug 23, 2018

Quality of life outcomes stable with neurostimulation in Parkinson disease: Study
Jan 22, 2024
Recommended for you

Researchers identify a genetic cause of intellectual disability affecting tens of thousands

New avenues to developing personalized treatments for schizophrenia
May 30, 2024

How does the word 'not' affect what we understand? Scientists find negation mitigates our interpretation of phrases

In the brain at rest, study indicates neurons rehearse future experience
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Researchers have located the brain network responsible for stuttering
An international research group led by researchers from the University of Turku and Turku University Hospital in Finland has succeeded in identifying the probable origin of stuttering in the brain.
Stuttering is a speech rhythm disorder characterised by involuntary repetitions, prolongations or pauses in speech that prevent typical speech production. Approximately 5-10% of young children stutter, and an estimated 1% continue to stutter into adulthood. A severe stutter can have a profound negative impact on the life of the individual affected.
"Stuttering was once considered a psychological disorder. However, with further research, it is now understood to be a brain disorder related to the regulation of speech production," says Professor of Neurology Juho Joutsa from the University of Turku.
Stuttering may also be acquired as a result of certain neurological diseases, such as Parkinson's disease or a stroke. However, the neurobiological mechanisms of stuttering are not yet fully understood, and where it originates in the brain remains uncertain. The findings from brain imaging studies are partly contradictory, and it is challenging to determine which changes are the root cause of stuttering and which are merely associated phenomena.
Stuttering localised in the same brain network regardless of its cause
Researchers from Finland, New Zealand, the United States and Canada developed a new research design that could provide a solution to this problem. The study included individuals who had suffered a stroke, some of whom developed a stutter immediately after it. The researchers discovered that although the strokes were located in different parts of the brain, they all localised to the same brain network, unlike the strokes that did not cause stuttering.
In addition to people who had suffered a stroke, the researchers used magnetic resonance imaging (MRI) to scan the brains of 20 individuals with developmental stuttering. In these individuals, the stuttering was associated with structural changes in the nodes of the brain network originally identified in relation to causal stroke lesions -- the greater the changes, the more severe the stuttering. This finding suggests that stuttering is caused by a common brain network, regardless of the aetiology (developmental or neurological).
The key nodes of the network identified by the researchers were putamen, amygdala and claustrum located deep within the brain, and the connections between them.
"These findings explain well-known features of stuttering, such as the motor difficulties in speech production and the significant variability in stuttering severity across emotional states. As major nuclei in the brain, the putamen regulates motor function and the amygdala regulates emotions. The claustrum, in turn, acts as a node for several brain networks and relays information between them," explains Joutsa.
The results of the study provide a unique insight into the neurobiological basis of stuttering. Locating stuttering in the brain opens up new possibilities for medical treatment. Researchers hope that in the future, stuttering could be effectively treated, for example, with brain stimulation that can be targeted specifically to the now identified brain network.
- Brain Tumor
- Nervous System
- Psychology Research
- Medical Devices
- Language Acquisition
- Brain Injury
- Child Development
- Brain-Computer Interfaces
- Positron emission tomography
- Child prodigy
- Brain damage
- Vaccination
- Psycholinguistics
Story Source:
Materials provided by University of Turku . Note: Content may be edited for style and length.
Journal References :
- Catherine Theys, Elina Jaakkola, Tracy R Melzer, Luc F De Nil, Frank H Guenther, Alexander L Cohen, Michael D Fox, Juho Joutsa. Localization of stuttering based on causal brain lesions . Brain , 2024; DOI: 10.1093/brain/awae059
Cite This Page :
Explore More
- Resting Brain: Neurons Rehearse for Future
- Observing Single Molecules
- A Greener, More Effective Way to Kill Termites
- One Bright Spot Among Melting Glaciers
- Martian Meteorites Inform Red Planet's Structure
- Volcanic Events On Jupiter's Moon Io: High Res
- What Negative Adjectives Mean to Your Brain
- 'Living Bioelectronics' Can Sense and Heal Skin
- Extinct Saber-Toothed Cat On Texas Coast
- Some Black Holes Survive in Globular Clusters
Trending Topics
Strange & offbeat.
Two-time NBA champion Bill Walton dead at 71
Two-time NBA champion Bill Walton, who dominated the hard court during a 13-year pro basketball career and later excelled as a broadcaster who both delighted and dismayed sports fans with his sometimes zany color commentary, died after a "prolonged battle with cancer," the league announced Monday.
Walton, who was 71, was with his family when he died, NBA spokesperson Mark Broussard said in a statement.

"Bill Walton was truly one of a kind," NBA Commissioner Adam Silver said in a statement. "As a Hall of Fame player, he redefined the center position."
Walton led the Portland Trail Blazers to an NBA championship in 1977 and won a second NBA title as a member of the Boston Celtics in 1986.
And after a 13-year career on the hardwood, Walton "translated his infectious enthusiasm and love for the game to broadcasting, where he delivered insightful and colorful commentary which entertained generations of basketball fans," Silver said.
Born Nov. 5, 1952, in La Mesa, California, Walton was a 6-11 high school basketball phenom before he went to play for coach John Wooden and the UCLA Bruins.
There, Walton won three consecutive National College Player of the Year awards from 1972 to 1974 and helped lead the Bruins to NCAA championships in 1972 and 1973.
More Sports from NBC News
- Mike Tyson is 'doing great' after health scare on flight
- Nadal loses to Zverev in the first round of what could be his final French Open
- Dallas crowd boos Travis Kelce at NBA playoff game with Patrick and Brittany Mahomes
- U.S. Olympic break dancers ready to show off the sport's community and culture at Paris Games
Walton was selected for the 1972 U.S. Olympic basketball team but opted not to play.
Off the court, Walton became one of the most polarizing athletes in the country with his outspoken opposition to the Vietnam War , the Nixon administration and the FBI. He was even arrested at a war protest during his junior year.
Walton also broke the mold for what a college athlete should look like with his shock of flame red hair and flannel shirts. He declared himself a vegetarian, practiced meditation and became a lifelong fan of The Grateful Dead.
“Your generation has screwed up the world,” he said in a statement after his arrest. “My generation is trying to straighten it out. Money doesn’t mean anything to me. It can’t buy happiness, and I just want to be happy.”
Being happy to Walton meant pursuing an NBA career.
Selected as the first overall pick in the 1974 NBA draft, he led the Trail Blazers to a championship three years later and also won the NBA Finals Most Valuable Player award.

In 1978, Walton won the NBA's Most Valuable Player award.
But starting in high school and for the rest of his career, Walton was dogged by foot and leg injuries that forced him to play through the pain. He missed three seasons because of injuries that required some three dozen operations to correct.
At age 34, Walton retired after having played just 10 games of the 1986-87 season.
In his autobiography , he wrote that his biggest regret was playing hurt.
“I didn’t let pain be my guide,” Walton wrote. “I didn’t say, ‘If it hurt a lot, don’t play.'"
But he was not done with basketball.
A stutterer, Walton overcame his speech impediment to become one of the country's best-known — and sometimes controversial — basketball commentators.
Walton called games for NBC, ABC, CBS, Fox, ESPN, Turner Sports and, most recently, ESPN broadcasts of Pac-12 basketball. In 2001, he received an Emmy for best live sports television broadcast.
Along the way, he built a collection of outlandish quips , some of which were compiled online by an outfit called Awful Announcing.
"Come on, that was no foul," Walton once declared midgame. "It may be a violation of all the basic rules of human decency, but it’s not a foul."
Walton once likened a player to a mosquito.
“If you ever think you’re too small to make a difference, you’ve never spent a night in bed with a mosquito or you’ve never played basketball against Taylor from Utah — No. 11 in your program, No. 1 in your heart.”
Walton could also go over the top with praise. For example:
“John Stockton is one of the true marvels, not just of basketball or in America, but in the history of Western civilization!”
While doing a live broadcast of another college game in 2015, Walton posed a head-scratching question: "Have you ever been milked?"
He is survived by his second wife, Lori, and his sons from his first marriage: Adam, Luke, Nate and Chris, according to the NBA.
Corky Siemaszko is a senior reporter for NBC News Digital.

Joe Biden Mocked by Critics After West Point Speech Gaffe
P resident Joe Biden was mocked by his critics on social media after he seemed to have lost his train of thought during a speech to West Point cadets graduating from the United States Military Academy in New York on Saturday.
Biden talked about current conflicts that the world is facing, including the ongoing Russia-Ukraine war. He mentioned the various missions that service members are conducting in Ukraine to help the war-torn nation in the conflict.
"We are standing strong with Ukraine and we will stand with them. We are standing against a man who I have known well for many years, a brutal tyrant, and we will not walk away," the president said.
When talking about how Russian President Vladimir Putin had launched a full-scale invasion of Ukraine in February 2022, starting a war that is now over two years old, Biden seemed to trail off.
"Putin was certain that NATO [North Atlantic Treaty Organization] would fracture. I met with him right after being elected president before, right after I was sworn in, and we talked about this very issue. The fall, he attacked that fall—he decided to, look, I shouldn't get into this probably. It gets me a little excited," Biden said.
He continued: "Putin was certain that NATO would fracture. I said to him in Switzerland, if you want to Finlandization of Ukraine, you're going to get the Finlandization, you're going to get the NATO-ization of Europe. He had a brazen vision which we stepped up and stopped. Instead, today, the greatest defense alliance in the history of the world, stronger than ever."
Finlandization is a term used in diplomatic discourse that refers to Finland's neutral stance during the Cold War. In 1948, Finland signed a treaty with the Soviet Union. As part of the treaty, Finland could not join Western security and defense organizations. The treaty dissolved in 1992 and Finland ultimately joined NATO in April 2023.
RNC Research, an account on X, formerly Twitter , managed by the Republican National Committee (RNC), posted a clip of Biden's speech gaffe on Saturday, writing that Biden was "confused again."
X user @TiffMoodNukes, who has amassed 179,700 followers, wrote: "Joe Biden is finished."
"Breaking News: Joe Biden couldn't give his speech at West Point," X user Wendy Patterson, who has 174,700 followers, posted.
X user @JannaPart2, who identifies as part of former President Donald Trump 's MAGA (Make America Great Again) movement and has 108,700 followers, jokingly wrote , "Is this dude smokin' crack ???" and attached a meme of Biden that read: "If You're Thinking Of Voting For Me, Don't."
Newsweek reached out to the White House and Biden's campaign via email for comment.
Biden, the Democratic incumbent, and Trump, the presumptive GOP presidential nominee, have faced criticism for various speech gaffes as they campaign for November's presidential election. At a rally in Wildwood, New Jersey, last week, Trump made a series of bizarre comments , calling Hannibal Lecter, the serial killer protagonist from The Silence of the Lambs , "a wonderful man." He also accidentally called former President Jimmy Carter "Jimmy Connors."
With Biden being 81 years old and Trump nearing 78, mental fitness has been a major talking point of this campaign cycle .
According to a Pew Research Center poll from last month, 47 percent of registered voters are not at all confident that Biden has the mental fitness needed for the job and 35 percent said the same for Trump. The poll was conducted from April 8 to 14 and surveyed 7,166 registered voters. The margin of error for the poll was plus or minus 1.6 percentage points.
Related Articles
- Justice Samuel Alito's 'Dumb' Flag Flying Rebuked by Federal Judge
- Mary Trump's Warning About Samuel Alito and Clarence Thomas
- Pete Buttigieg Ridiculed for Joe Biden's $7.5 Billion 'Massive Failure'
- Marjorie Taylor Greene Wants to Invest in Democratic Stronghold
Start your unlimited Newsweek trial

- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Trump tries to move past his guilty verdict by attacking the criminal justice system
A day after a New York jury delivered a historic guilty verdict in Donald Trump’s criminal hush money trial, the presumptive Republican presidential nominee again railed against a “rigged trial” during remarks at Trump Tower.

Donald Trump’s conviction on 34 felony counts marks the end of his historic hush money trial but the fight over the case is far from over.

Donald Trump attacked the judge and the star witness in his criminal hush money trial and again tried to undermine New York’s criminal justice system on Friday while seeking to turn his conviction on 34 felony charges into fuel — and not an impediment — to his bid to return to the White House.

President Joe Biden says Donald Trump was found guilty in his hush money trial and called it “reckless...dangerous” and “irresponsible” for anyone to claim the process was “rigged.”
Former President Donald Trump speaks during a news conference at Trump Tower, Friday, May 31, 2024, in New York. A day after a New York jury found Donald Trump guilty of 34 felony charges, the presumptive Republican presidential nominee addressed the conviction and likely attempt to cast his campaign in a new light. (AP Photo/Julia Nikhinson)
- Copy Link copied
Former President Donald Trump walks out of court and toward the media following the verdict in his hush money trial, in New York, Thursday, May 30, 2024. (Mark Peterson/New York Magazine via AP, Pool)
A crowd gathers across the street from Trump Tower, Friday, May 31, 2024, in New York. A day after a New York jury found Donald Trump guilty of 34 felony charges, the presumptive Republican presidential nominee will address the conviction and likely attempt to cast his campaign in a new light. (AP Photo/Julia Nikhinson)
The White House in Washington is seen past the security fence on Thursday, May 30, 2024. Former President Donald Trump became the first former president to be convicted of felony crimes as a New York jury found him guilty of 34 felony counts of falsifying business records in a scheme to illegally influence the 2016 election through hush money payments to a porn actor who said the two had sex. (AP Photo/Pablo Martinez Monsivais)
The White House in Washington on Thursday, May 30, 2024. Former President Donald Trump became the first former president to be convicted of felony crimes as a New York jury found him guilty of 34 felony counts of falsifying business records in a scheme to illegally influence the 2016 election through hush money payments to a porn actor who said the two had sex. (AP Photo/Pablo Martinez Monsivais)
Donald Trump, far left, watches as jury foreperson #1 delivers guilty verdicts with judge Juan Merchan listening on the bench in Manhattan Criminal Court, Thursday, May 30, 2024, in New York. Donald Trump became the first former president to be convicted of felony crimes as a New York jury found him guilty of 34 felony counts of falsifying business records in a scheme to illegally influence the 2016 election through hush money payments to a porn actor who said the two had sex. (Elizabeth Williams via AP)
A crowd gathers across the street from Trump Tower after the guilty verdict announced against Donald Trump, Thursday, May 30, 2024, in New York. Donald Trump became the first former president to be convicted of felony crimes as a New York jury found him guilty of 34 felony counts of falsifying business records in a scheme to illegally influence the 2016 election through hush money payments to a porn actor who said the two had sex. (AP Photo/Julia Nikhinson)
NEW YORK (AP) — Donald Trump sought to move past his historic criminal conviction on Friday and build momentum for his bid to return to the White House with fierce attacks on the judge who oversaw the case, the prosecution’s star witness and the criminal justice system as a whole.
Speaking from his namesake tower in Manhattan in a symbolic return to the campaign trail, the presumptive Republican presidential nominee delivered a message aimed squarely at his most loyal supporters. Defiant as ever, he insisted without evidence that the verdict was “rigged” and driven by politics.
Donald Trump’s conviction on 34 felony counts marks the end of his historic hush money trial. But the fight is far from over. Here’s what to know.
- How did Trump respond? Trump falsely blasted a ‘rigged trial’ and attacked star witness in a speech on Friday. Follow the AP’s live coverage .
- When is the sentencing? July 11, just days before Republicans are set to pick Trump as the 2024 nominee.
- Can Trump vote? He may be convicted and reside in Florida, but can still vote as long as he stays out of prison in New York state.
- Will this impact the election? It’s unclear whether Trump’s once-imaginable status as a person convicted of a felony will have any impact at all on voters.
“We’re going to fight,” Trump said from the atrium of Trump Tower, where he descended a golden escalator to announce his 2016 campaign nine years ago next month. The machinations during the final, dramatic weeks of that campaign ultimately led to the charges that made Trump the first former president and presumptive presidential nominee of a major party to be convicted of a crime, exposing him to potential prison time.
While the guilty verdict has energized Trump’s base, fueling millions of dollars in new campaign contributions, it’s unclear how the conviction and his rambling response will resonate with the kinds of voters who are likely to decide what is expected to be an extremely close November election. They include suburban women, independents, and voters turned off by both candidates.
Speaking before dozens of reporters and cameras that carried his remarks live, Trump cast himself as a martyr, suggesting that if this could happen to him, “They can do this to anyone.”
“I’m willing to do whatever I have to do to save our country and save our Constitution. I don’t mind,” he said, as he traded the aging lower Manhattan courthouse where he spent much of the last two months for a backdrop of American flags, rose marble and brass.

“It’s a very unpleasant thing, to be honest,” he added. “But it’s a great, great honor.”
President Joe Biden, responding to the verdict at the White House, said Trump “was given every opportunity to defend himself” and blasted his rhetoric.
“It’s reckless, it’s dangerous, it’s irresponsible for anyone to say this is rigged just because they don’t like the verdict,” Biden said.
Trump has made his legal woes the centerpiece of his campaign message as he has argued, without evidence, that Biden orchestrated the four indictments against him to hobble his campaign. The hush money case was filed by local prosecutors in Manhattan who don’t work for the Justice Department or any White House office.
A Manhattan jury on Thursday found Trump guilty of 34 charges in a scheme to illegally influence the 2016 election through a hush money payment to a porn actor who said the two had sex.
Despite the historic ruling, a convicted Trump sounded much the same as a pre-convicted Trump, as he delivered what amounted to a truncated version of his usual rally speech. He argued the verdict was illegitimate and driven by politics and sought to downplay the facts underlying the case. He said he would appeal.
What to know about the 2024 Election
- Democracy: American democracy has overcome big stress tests since 2020. More challenges lie ahead in 2024.
- AP’s Role: The Associated Press is the most trusted source of information on election night, with a history of accuracy dating to 1848. Learn more.
- Read the latest: Follow AP’s complete coverage of this year’s election.
“It’s not hush money. It’s a nondisclosure agreement,” he said. “Totally legal, totally common.”
When Trump emerged from the courtroom immediately after the verdict Thursday, he had appeared tense and deeply angry, his words pointed and clipped. But by Friday, he seemed more relaxed — if a little congested — especially as he moved on to other topics. He did not take questions from reporters, marching off as supporters assembled in the lobby cheered.
His lawyer, Todd Blanche, who was with him at Trump Tower but didn’t speak, said in an interview later Friday that he had been “shocked” by how well Trump took the verdict.
“He’s not happy about it, but there’s no defendant in the history of our justice system who’s happy about a conviction the day after,” he said. “But I think he knows there’s a lot of fight left and there’s a lot of opportunity to fix this and that’s what we’re going to try to do.”
Trump has portrayed himself as a passionate supporter of law enforcement and has even talked favorably of officers handling suspects roughly. But he has spent the last two years attacking parts of the criminal justice system as it applies to him and raising questions about the honesty and motives of agents and prosecutors.
In his disjointed remarks, Trump attacked Biden’s immigration and tax policies before pivoting to his case, growling that he was threatened with jail time if he violated a gag order . He cast intricate parts of the case and trial proceedings as unfair, making false statements and misrepresentations as he went.
Trump said he had wanted to testify in his trial, a right that he opted not to exercise. Doing so would have allowed prosecutors to cross-examine him under oath. He raised the specter on Friday of being charged with perjury for a verbal misstep, saying, “The theory is you never testify because as soon as you testify — anybody, if it were George Washington — don’t testify because they’ll get you on something that you said slightly wrong.”
Testing the limits of the gag order that continues to prohibit him from publicly critiquing witnesses including Michael Cohen, Trump called his former fixer, the star prosecution witness in the case, “a sleazebag,” without referencing him by name.
He also blasted the judge in the case, saying his side’s chief witness had been “literally crucified by this man who looks like an angel, but he’s really a devil.”
He also circled back to some of the same authoritarian themes he has repeatedly focused on in speeches and rallies, painting the U.S. under Biden as a “corrupt” and “fascist” nation.
His son Eric Trump and daughter-in-law, Lara Trump, joined him, but his wife, Melania Trump, who has been publicly silent since the verdict, was not seen.
Outside, on Manhattan’s Fifth Avenue, supporters gathered across the street flew a giant red “TRUMP OR DEATH” sign that flapped in front of a high-end boutique. A small group of protesters held signs saying “Guilty” and “Justice matters.”
Trump’s campaign announced Friday evening it had raised $52.8 million in the 24 hours after the verdict. The campaign said one-third of those donors had not previously given to him.
Trump and his campaign had been preparing for a guilty verdict for days, even as they held out hope for a hung jury. On Tuesday, Trump railed that not even Mother Teresa, the nun and saint, could beat the charges, which he repeatedly labeled as “rigged.”
His top aides on Wednesday released a memo in which they insisted a verdict would have no impact on the election, whether Trump was convicted or acquitted.
The news nonetheless landed with a jolt. Trump listened as the jury delivered a guilty verdict on every count. Trump sat stone-faced while the verdict was read.
His campaign fired off a flurry of fundraising appeals, and GOP allies rallied to his side. One text message called him a “political prisoner,” even though he hasn’t yet found out if he will be sentenced to prison. The campaign also began selling black “Make America Great Again” caps, instead of the usual red, to reflect a “dark day in history.”
Aides reported an immediate rush of contributions so intense that WinRed, the platform the campaign uses for fundraising, crashed.
In the next two months, Trump is set to have his first debate with Biden, announce a running mate and formally accept his party’s nomination at the Republican National Convention. But before he goes to Milwaukee for the RNC, Trump will have to return to court on July 11 for sentencing. He could face penalties ranging from a fine or probation up to prison time.
Associated Press writers Adriana Gomez Licon in Miami, Meg Kinnard in Columbia, South Carolina, Gary Fields in Washington and Ali Swenson and Michael R. Sisak in New York contributed to this report.


IMAGES
VIDEO
COMMENTS
A speech impediment, or speech disorder, is a condition that makes it hard for you to communicate. There are many types of speech impediments, and anyone can develop one. In some cases, children are born with conditions that affect speech. Other times, people have conditions or injuries that affect speech. Speech therapy can help.
Common causes of childhood speech impediments include: Autism spectrum disorder: A neurodevelopmental disorder that affects social and interactive development. Cerebral palsy: A congenital (from birth) disorder that affects learning and control of physical movement. Hearing loss: Can affect the way children hear and imitate speech.
Speech disorders affect a person's ability to produce sounds that create words, and they can make verbal communication more difficult. Types of speech disorder include stuttering, apraxia, and ...
Diagnosis. Stuttering is diagnosed by a healthcare professional trained to evaluate and treat children and adults who have a problem with speech and language. This professional is called a speech-language pathologist. The speech-language pathologist listens and talks with the adult or child in different types of situations.
However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders. There are many different types of speech impediments, including: Disfluency. Articulation errors. Ankyloglossia. Dysarthria. Apraxia. This article explores the causes, symptoms, and treatment of the different ...
Home Remedies to Help Lisps. Whether or not your child sees a speech-language pathologist, there are things you can do at home to help your child's lisp, including: Treat allergies and sinus ...
Stuttering is a speech disorder characterized by repetition of sounds, syllables, or words; prolongation of sounds; and interruptions in speech known as blocks. An individual who stutters exactly knows what he or she would like to say but has trouble producing a normal flow of speech. These speech disruptions may be accompanied by struggle ...
Dysarthria symptoms include: Slurred speech or mumbling when you talk. Speaking too quickly or more slowly than intended. Speaking quieter or louder than intended. Sounding hoarse, harsh, strained, breathy, nasal, robotic or monotone. Speaking in short, choppy bursts with several pauses, instead of in complete sentences.
3. Practice diaphragmatic breathing. Sometimes, impediments in speech, like stuttering, grow from nerves and anxiety. Before you have to speak in front of a group, go through a deep breathing activity to calm your nerves, relax your body, and get you in the right mental state for proper speech.
Childhood apraxia of speech (CAS) is a rare speech disorder. Children with this disorder have trouble controlling their lips, jaws and tongues when speaking. In CAS, the brain has trouble planning for speech movement. The brain isn't able to properly direct the movements needed for speech. The speech muscles aren't weak, but the muscles don't ...
With this in mind, the following tips may be useful: Practice speaking slowly. Speaking slowly and deliberately can reduce stress and the symptoms of a stutter. It can be helpful to practice ...
A person who lisps replaces those sounds with "th" ("simple" sounds like "thimple"). Cluttering is another problem that makes a person's speech difficult to understand. Like stuttering, cluttering affects the fluency, or flow, of a person's speech. The difference is that stuttering is a speech disorder, while cluttering is a language disorder.
Speech disorders, impairments, or impediments, are a type of communication disorder in which normal speech is disrupted. This can mean fluency disorders like stuttering, cluttering or lisps.Someone who is unable to speak due to a speech disorder is considered mute. Speech skills are vital to social relationships and learning, and delays or disorders that relate to developing these skills can ...
Speech disorders impact millions of people and their ability to communicate. The National Institute of Deafness and Other Communication Disorders estimates that 5% of children in the U.S. ages 3 to 17 have had a speech disorder in the past 12 months. Some speech disorders can be overcome, while others are lifelong conditions.
This chapter addresses three topics within the committee's charge: current standards of care for speech and language disorders in children; which of the disorders are amenable to treatment and the typical time course required for this treatment; and the persistence of these disorders in children. The discussion is limited to those childhood speech and language disorders that are most common in ...
Childhood apraxia of speech (CAS) is a speech disorder where your child's mouth cannot make the quick movements needed to speak, even after their brain tells their mouth what to do. There is usually no muscle weakness. If your child has CAS, it may be difficult for them to plan and complete the quick mouth movements needed to make sounds into ...
A child with a speech disorder may have difficulty with speech sound production, voice, resonance or fluency (the flow of speech). Speech Sound Disorders. A child with a speech sound disorder is unable to say all of the speech sounds in words. This can make the child's speech hard to understand. People may not understand the child in everyday ...
The most effective treatment option for spasmodic dysphonia is the injection of very small amounts of botulinum toxin directly into the affected muscles of the larynx (voice box). This helps reduce vocal tremors by blocking abnormal nerve impulses from reaching the muscle, which alters the person's voice. 3.
The subthalamic nucleus is known for its role in inhibiting motor activity, but there are clues to its involvement in other functions. For example, deep brain stimulation, which uses implanted electrodes to stimulate the subthalamic nucleus, has proven to be a powerful way to relieve motor symptoms for Parkinson's patients — but a common side effect is worsened speech impairment.
This discovery could lead to novel treatments of this speech disorder. Understanding Stuttering as a Brain Disorder. Stuttering affects about 5-10% of young children, with roughly 1% continuing ...
A new study by Stanford Medicine researchers reveals the brain mechanisms behind one of the most prevalent, yet often overlooked, symptoms of the disease— speech impairment. Based on brain ...
Stuttering is a speech rhythm disorder characterised by involuntary repetitions, prolongations or pauses in speech that prevent typical speech production. Approximately 5-10% of young children ...
A stutterer, Walton overcame his speech impediment to become one of the country's best-known — and sometimes controversial — basketball commentators. Walton called games for NBC, ABC, CBS, Fox ...
President was mocked by his critics on social media after he seemed to have lost his train of thought during a speech to West Point cadets graduating from the United States Military Academy in New ...
By MICHELLE L. PRICE and JILL COLVIN. Updated 10:01 AM PDT, May 31, 2024. NEW YORK (AP) — Donald Trump launched into attacks on the judge in his criminal trial and continued to undermine New York's criminal justice system Friday as he tried to repackage his conviction on 34 felony charges as fuel, not an impediment, to his latest White ...