Evidence-Based Reviews: Trends in Nephrology Nursing
Affiliations.
- 1 Nurse Practitioner, Hemodialysis, London Health Sciences Centre, London, Ontario, Canada.
- 2 Member of the ANNA Research Committee.
- 3 member of ANNA's MichigANNA Chapter.
- 4 Research Assistant, London Health Sciences Centre, London, Ontario, Canada.
- PMID: 31009191
Evidence-based practice (EBP) is one of the essential components of nephrology nursing. Reviews of such evidence are important as a means to synthesize research findings into one meaningful form of data. Publication trends of evidence reviews in nephrology nursing are unknown. The purpose of this systematic review was to identify trends in publications of evidence reviews in the Nephrology Nursing Journal. Titles of all publications in the Nephrology Nursing Journal from January 2003 to September/October 2018 were reviewed. A total of 23 evidence reviews were identified and formed the basis of this systematic review. Narrative analysis and concept mapping were used to synthesize data. There was a trend toward systematic reviews of quantitative studies, as well as evidence reviews that focused on the topics of quality of life and access to health services. The need for systematic rigorous reporting is recommended for EBP, as well as future reviews on identified priority areas of research.
Keywords: evidence-based practice; literature review; nursing research; systematic review.
Copyright© by the American Nephrology Nurses Association.

Publication types
- Systematic Review
- Evidence-Based Nursing*
- Nephrology Nursing / trends*
- Periodicals as Topic*
- Publications / trends*

Volume 17 Number 2
Sustaining the renal nursing workforce.
Kathy Hill, Kim Neylon, Kate Gunn, Shilpa Jesudason, Greg Sharplin, Anne Britton, Fiona Donnelly, Irene Atkins and Marion Eckert
Keywords Renal, workforce, nurse, nephrology
For referencing Hill K et al. Sustaining the renal nursing workforce. Renal Society of Australasia Journal 2021; 17(2):5-11.
DOI https://doi.org/10.33235/rsaj.17.2.5-11 Submitted 20 May 2021 Accepted 27 July 2021
Background The prevalence of kidney disease continues to increase, as does the acuity of kidney care. Patients with kidney failure are older, sicker and less mobile. Health systems are under more pressure to manage growing care needs and capacity constraints. This is likely to have an impact on nursing workforce experiences.
Aims The aim of this research was to examine nephrology nursing in South Australia to understand the impact of increasing acuity and organisational factors that may support and sustain the workforce.
Methods An exploratory semi-structured qualitative approach, facilitating eight focus groups with 36 nephrology nurses across six public metropolitan renal units was applied. Data were thematically analysed.
Findings Three central themes relating to nursing culture, patient acuity and organisational factors that impact the nursing workforce were identified. Sub-themes identified were pride and passion, teamwork and collegiality, increasing patient acuity and the lack of clinical rationalisation in kidney care, the value of a ‘flat’ hierarchy, and vulnerability during the COVID‑19 pandemic. Consequently, we identified a disconnect between institutional expectations and what the participants considered pragmatic reality. Participants reported sustained workplace pressure, a ‘triage’ approach to care, and a sense of work left undone.
Conclusion Nephrology nurses experience a gap between ‘supply and demand’ on their time, resources and workload. These findings highlight the need for further exploration of the root causes and the development of new systems to provide quality, safe and rewarding care for patients and to reduce the risk of workforce moral distress and burnout.
Introduction
The burden of chronic kidney disease (CKD) in Australia and New Zealand is high; it is estimated to affect one in 10 people over the age of 18 (Kidney Health Australia, 2020). As reported by the Australia and New Zealand Dialysis and Transplant Registry (ANZDATA, 2019), 26,746 Australian and New Zealanders received kidney replacement therapy (KRT) for kidney failure in 2019. The provision of KRT (haemodialysis, peritoneal dialysis and transplantation) nursing care is a highly specialised field (Wolfe, 2014).
However, limited research has been undertaken in the nephrology specific nursing workforce and the unmet workplace needs of nephrology nurses are not well reported (Brown et al., 2013).The shortage in the nephrology nursing workforce has largely been considered a “subset of overall supply” (Wolfe, 2014); however, with a significant number of vacancies in positions globally and increases in population level kidney failure, the nephrology nursing specialty is under additional pressure (Wolfe, 2014). Nurses in kidney care have a unique relationship with the people that they care for because of the lengthy and intensive context of care (Brown et al., 2013; Wolfe, 2014). Evidence suggests that the intensity of job burnout resulting from high stress environments is particularly high among dialysis nurses (Hayes, Douglas, & Bonner, 2015) and that job satisfaction and “organisational justice” is a critical factor that can ameliorate the negative effects of burnout (Hayes, Douglas, & Bonner, 2014; Kavurmacı, Cantekin, & Tan, 2014). Stress in nephrology nursing occurs due to increased pressure in the workplace without an associated increase in satisfaction with the job (Jones, 2014), the complexity of care, and unrealistic patient expectations (Dermody & Bennett, 2008). Inadequate staffing has been cited as a driver of stress and burnout and is correlated with nursing turnover. In turn, nursing turnover can disrupt care continuity and increase adverse events for patients (Gardner et al., 2007). Therefore, workforce renewal will be required to sustain this vitally important skilled nursing workforce and reduce turnover into the future.
The aim of this research was to examine nephrology nursing experiences in South Australia in order to understand the impact of increasing acuity on the workforce and on patients, and determine organisational factors that may support and sustain the nursing workforce.
Research methodology
This research used a qualitative focus group methodology with nephrology nurses in both acute and satellite care settings utilising a semi-structured method (Jayasekara, 2012). A focus group discussion guide (Figure 1) was used to explore how factors such as patient acuity, complex care, workplace culture, values, time, finances, shift work, overtime, and professional development opportunities affect decision making about and satisfaction with work, while also allowing participants to raise topics they considered most important. The focus group discussion guide was developed following an extensive review of the existing literature on this topic.
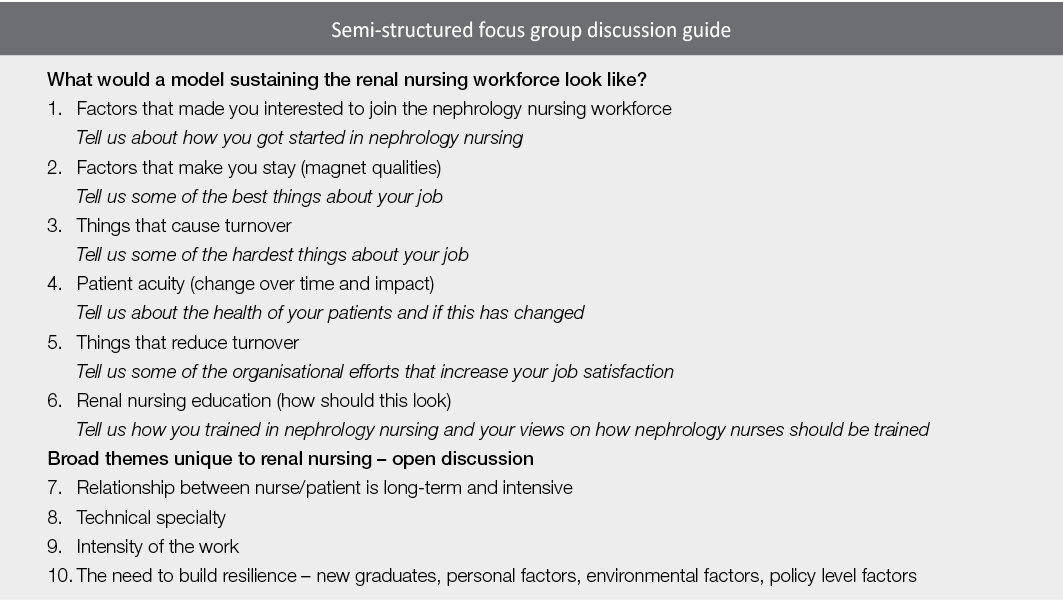
Figure 1. Semi-structured focus group discussion guide
The focus groups were conducted in six South Australian renal units; they were 1–2 hours in duration and audio-recorded, and field notes were also taken. A private room in the renal unit setting was booked ahead of time to allow participants to leave their workplace to participate. Two members of the research team facilitated the focus groups, one a senior renal nurse [KH PhD], the other a qualitative ethnographic researcher with no renal expertise [KN PhD]. The benefits of dual facilitators reduced perceived prior knowledge ‘leading’ the discussion.
Participants self-selected to participate by responding to a flyer advertising the research.
Data analysis
The audio recordings were de-identified and professionally transcribed verbatim; the researchers used NVivo 12™ to support coding trees and discourse analysis to code the data into common themes (Liamputtong, 2011). Discourse analysis uses not only the words in the transcripts but also the relationships seen between participants in the focus groups using the extensive field notes taken during the discussion. This analysis was conducted in the first instance independently by the focus group facilitators and then jointly examined for correlating themes. Data saturation was confirmed by the determination of several similar themes in all of the focus groups.
Ethical considerations
The research received approval from a human research ethics committee (CALHN HREC 12818) and all participants gave informed written consent. They were also assured of anonymity of both their identity and the specific renal unit in the reporting of the findings. Key findings in an abbreviated form were discussed with the units involved and all members of the research team before the analysis was finalised.
Thirty-six renal nurses participated in eight focus groups across six public metropolitan renal units, and included those working in leadership roles, haemodialysis, renal wards, peritoneal dialysis, transplantation and clinical trials. Participants had a range of experience in renal nursing from new graduates in their first year, mid-career nurses and those with over 30 years’ experience. Participants were predominantly female (97%, n=35).
Three broad themes were identified from the data: nursing culture, workforce education and professionalism; patient-related factors impacting on the workforce; and macroenvironmental factors impacting on the workforce.
Nursing culture, workforce education and professionalism
This theme explored the sustainability of the nephrology nursing workforce in relation to nursing culture, training modules and succession planning.
Experience versus recognised qualification: a false dichotomy in renal nurse training
There are currently two models of renal nurse education available to South Australian nursing clinicians. Trainees either undertake a university-accredited postgraduate qualification offered remotely from another state, or a hospital-based training program offered here in South Australia. Participants described fundamental flaws in this hybrid model that presents a false dichotomy:
That’s why nursing did go into the university sector to bring up the professionalism but often forgetting that it is a hands on role and we do a lot of our learning with our patients, you know, actually getting our hands dirty so to speak [FG 2].
Nurses also described the gradual and total erosion of renal specific in-place education opportunities in their units as patient numbers and acuity increased. No participants were able to describe any recent workplace-dedicated education sessions for nephrology nurses.
Training the future workforce in difficult working environments
In South Australia the three universities train a large number of undergraduate student nurses every year to address a predicted future workforce shortfall. This creates pressure on renal units already overwhelmed to find time to train the future workforce:
I could hear myself sometimes when say a student or someone would ask me something and I love teaching, I love working with students, I love working with the new grads, and I could hear this voice sometimes that was a bit snappy. I thought that’s not me, that’s awful [FG 4].
There was, however, a keen sense of the importance of developing early career nurses to sustain the renal nursing workforce, particularly given the increasing age of the nursing workforce overall.
Pride, enjoyment and passion
Nephrology nurses in South Australia consistently described themselves as proud of the work they do. They describe the capacity to “make a difference” and a passion for their specialty. Many of the more senior nurses described entering renal nursing almost by accident but “falling in love” with the specialty with very little intention of leaving:
I mean, it’s a fantastic area to work in. I didn’t know anything about renal at all before I came here. I love it. I’m passionate about renal. I love it. It’s very rewarding [FG 8].
Teamwork and collegiality
Whilst describing their challenges in an open way, participants also reported pride in their collegiality, teamwork and capacity to support each other:
Sometimes you just make yourself even later home by having a chat in the car park. Sometimes we stand in the wind and the rain and we don’t care [FG 3].
Supporting each other and working as a team is described as integral to a successful shift, especially after a challenging day. There was also consistent evidence of the extreme dedication that renal nurses have towards each other and towards their patients:
To be honest, even though I get annoyed about the staffing levels and whatever I get annoyed about that sort of side of it, it’s the patients you stay for and it’s the staff members that you stay for. Because we have got some beautiful patients and we’ve got some beautiful staff members [FG 8].
Patient-related factors impacting on the workforce
This theme explored the patient-related factors that supported the workforce culture or were a negative aspect of care.
The long-term trajectory of the patient/nurse relationship
A consistent theme raised by participants when discussing patient satisfaction was the longevity of patient/nurse relationships. Participants in all focus groups described how the long-term nature of the patient/nurse relationship generates a sense of closeness:
It’s like a family. In maintenance dialysis unit. The nurse/patient relationship is there but it’s more like a family. You’re caring like your family member [FG 2].
The nurses described continuity of care and emotional connection to their long-term patients in positive and endearing terms, often highlighting this as the most appealing aspect of renal nursing. While participants were saddened when seeing patients “at their worst” and witnessing the inevitable downward trajectory of their renal journey, their experience helping the patient and their families through that journey was often seen as a privilege and a highlight of their nursing careers. However, participants also indicated significant frustration and regret that increased patient acuity, ageing patients, and nurse/patient ratios limited their capacity to connect significantly with all patients.
Increased patient acuity, acute deterioration risk and safety
All participants reported experiencing a significant increase in patient acuity over the past few years, describing a much older, more frail dialysis population:
Patients are living longer. We have about four patients from nursing homes that come in, that you question why you even dialyse them. But the acuity of the patient is so much, is so different to what it used to be years ago. So different. They have so many more comorbidities. They yeah, they’re just more difficult. They have heart conditions that you can’t even dialyse them. You can’t even remove their fluid, so they’re in and out of hospital all the time [FG 5].
Many of the participants described patients that met medical emergency team (MET) criteria before dialysis treatment had even commenced. There was a strong sense that the units were struggling to find ways to manage these unwell patients, along with the rest of their patient group, and the use of the word ‘safe’ frequently occurred:
Just the increase in their acuity and all the comorbidities that they have and they’re getting sicker, they’re getting older, and we’re still in the process of finding ways to manage patient and staff safety and wellbeing [FG 3].
Participants also described a major change in the mobility of the patients, discussing the scene “ten or so years ago” when most people needing treatment walked into the unit and physically participated in their care. Participants remarked that this is simply no longer the case, with descriptions of lifting and carrying patients:
Three to four sling lifters, to chair lifters, it all takes time. So, let’s say we organise half an hour slots for putting on a (dialysis) patient, sometimes we might take 20 minutes to even get the stand lifters and get them into chair, let alone another 10 minutes to put on (dialysis) [FG 6].
Caseload pressure and limitations for patient care
Participants described a “conveyor belt” mentality in the dialysis units, with a sense of urgency to get people “in, on, and out” due to high caseloads. Staff described the pressing need for three shifts of patients per day and internal pressure to move patients through, and pressure on patients to rush the discharge; these factors reduced job satisfaction considerably:
I would say it was more stressful and I’d also say it impacts on your job satisfaction because you go home feeling like you haven’t done a good job even though you have and that you would have worked well within parameters. You go home and you think, on reflection, I don’t think you’re satisfied. I think you feel inept [FG 3].
Nurse/patient ratios in the setting of changing acuity
Renal nurses in South Australia accepted a standardised State-wide model for nurse-to-patient ratios several years ago that is still used to supply staff to renal units. Many of the focus group participants expressed regret regarding this agreement, as they believe it no longer reflects the actual nursing care hours needed due to the increased complexity of the people undergoing dialysis:
You do this many treatments therefore there’s this many staff and that is your barrier that you have to fight and prove that you require that extra staff member because why do you need that because you’ve only got this many patients, well that’s because this person is nearly dead and if I leave his side he’s going to be [FG 1].
Stress and responsibility
Participants overwhelmingly described a culture of chronic stress in the workplace. This was not just in dialysis units, but also in renal wards:
Like, it was so scary. Everybody was so sick and sometimes you had very little support and it was very intimidating looking after these very sick patients and sometimes you could be that second to most senior nurse as a graduate or the most senior on a night shift [FG 2].
On an afternoon shift, you never have a meal break, ever [FG 8].
Whilst all participants described nursing leadership support, they struggled to identify any organisational support for the difficulties and challenges centred within the specialty area. Participants across the board described having to source their own replacement staff to cover sick leave or work overtime, and at times the inability to support the team:
As a Shift Coordinator you just, you can see someone and you desperately want to help them but you’ve got 7 million other things you’re trying to deal with, it’s horrible, really, really horrible, it’s just like you spend a whole day trying to put out whatever fire is burning the most at that second and it’s awful [FG 4].
The patient as an expert
Renal nurses described the uniqueness of the renal patient and their “expertise”. This was genuinely viewed as a partnership for successful treatment. An ideal model of care was seen to involve an active patient:
A lot of, most of them are a knowledgeable group about their own healthcare so they can be quite strong advocates for themselves and are willing to question and I think the staff actually like that. We all like that these patients are questioning and challenging [FG 2].
However, participants also raised a downside to this, namely patient reliance on individual staff members, as long-term relationships facilitated trust or distrust in particular staff, particularly new staff members. Newly graduated nurses described being intimidated by patients that refused to allow them to perform tasks, for example to cannulate a fistula, because of a lack of trust in their ability:
Oh, who is this person, I’ve never seen you. Do you know how to needle? I don’t think you want to needle me [FG 6].
Overall, participants described the capacity to gain trust, and the sense that the patient as an active participant in managing their chronic condition was welcomed by the nursing staff.
Macroenvironmental factors impacting on the workforce
This theme explored factors that were impacting on the workforce that were organisational and external to the participants.
Lack of clinical rationalisation in kidney care impacting on nursing morale
A factor described as increasing the pressure on the nursing workforce was their perceived powerlessness when it comes to assessing a patient as “too unwell for dialysis” and the decision not being supported by the medical staff. Participants felt that, once a dialysis pathway is chosen, irrespective of the nurses’ beliefs about the patient’s capacity to cope with that treatment, there is pressure on the nursing staff from the medical team to find a way to complete the dialysis treatment:
We have patients here that, once upon a time, wouldn’t dialyse. They are so hypotensive, for example, and you’ll ring the renal registrar but the expectation in many cases is you dialyse them [FG 3].
Sentiments surrounded the way that the participants experienced the increasingly complex ageing population, the increasing burden of all that was expected from them with patients that they felt would have been considered too unwell previously. This theme described a despondent workforce that sometimes felt that they are unable to meet the needs of all deteriorating patients at all times.
A “flat hierarchy” and respect in the workplace
Several units described a “flat hierarchy” where nephrology nurses were respected and valued by the medical teams; this created a very positive workplace culture and increased job satisfaction:
And it’s always been strongly encouraged that if you’re not happy with something miss out the middle man, women, go straight to the consultant, and I think every renal nurse would have no qualms in, whether it’s the middle of the night if they felt something unsafe was happening, giving the consultant a call [FG 2].
Many nurses attributed this to the positive attitudes of doctors towards nurses and described close collegial relationships between the nursing and medical staff; this was celebrated as a positive aspect of nephrology nursing and care coordination.
The “old model for the new reality”: physical space constraints
There is a large degree of commonly felt dissatisfaction with the physical space provisions in renal units, described here as “the old model for a new reality”. Many units report simply having inadequate space and this relates to increased patient numbers, increased use of mobility aids, and increasing numbers of patients requiring dialysis, many of whom are so ill they are in a bed that is much larger than the space designed for the treatment. This was echoed in the units that had a central nursing station and patient stations placed in a circle around this, a model commonly seen in renal units:
And you’re now putting beds in there and sometimes it could look like a war zone [FG 7].
COVID‑19 and workforce vulnerability
This research was conducted in South Australia during the COVID‑19 pandemic which, whilst creating logistic difficulties in terms of research access and social distancing, brought additional insights into the pressure on the nephrology nursing workforce as participants considered the consequences of a potential outbreak in a dialysis facility:
I guess the difference is you can’t get someone else to come and cover from anywhere else. No one else can lend a hand [FG 3].
However, participants also described a common sense of purpose in upskilling as much of the nursing workforce as possible in preparation for the pandemic:
So, that’s where we’re concentrating because we had massive changes with the COVID happening and we had lots of people coming through upskilling. So, that was a major breakthrough for us in opening our eyes into saying, “Yes, we can do this. Yes, we can change things around” [FG 6].
The global COVID‑19 pandemic brought recognition to participants of their own strong commitment to nursing, but also a perceived increased recognition of the vulnerable position nurses put themselves in to help others in the wider community:
But COVID’s been the perfect example. Like we’ve been thanked so many times. I don’t think we’ve ever been thanked, well not as many times [FG 2].
This research found that nephrology nurse participants felt pride in their work, but often felt overwhelmed or “powerless” in the face of a rapidly changing renal patient population. Maintaining a professional identity is a strong predictor of personal accomplishment and the driving force “to keep going” (Georgios et al., 2017) and was expressed keenly by the participants of this research. However, increasing patient numbers, increasing patient acuity and physical space constraints led to the staff trying manage an old model of a dialysis unit based upon a smaller, younger and more independent cohort of patients around which renal units were designed, and not being able to successfully manage this. There is also evidence of sustained workplace pressure and a sense of work left “undone”, leading to increasing job dissatisfaction. White, Aiken and McHugh (2019) have previously discussed the interdependent concepts of working in an under-resourced setting creating stress and moral distress due to missed care in nursing (White et al., 2019), something which was evidenced in our focus group discussions.
In addition, Bong (2019) identified that the attrition rate for new graduates is a result of “moral distress”, a concept whereby the carer knows the right thing to do but is unable to do this due to institutional or resource constraints, and this is compelling enough to cause staff turnover. Whilst we spoke to graduates that were happy with their choice of specialty, senior staff indicated limitations in the training of graduates and students, particularly time restraints, that limited recruitment generally. This research also found that renal nurses wanted organisational acknowledgement, both of the new reality of renal care (compared to 20–30 years ago) and of their endeavours to combat structural constraints, to feel a sense of workplace achievement.
Hospital organisational culture has been found to be a dominant predictor of the quality of nursing care, and nurses, being a caring profession, are drawn to organisations that address “daily census” with appropriate staff patient ratios to increase the quality of care (Mudallal et al., 2017). Whilst intrinsic factors can reduce the impact of stress and burnout, critical to supporting nurses to cope with stress is addressing the macroenvironment with “adequate staffing, appropriate skill mix and support to manage extremely unwell patients” (Jones, 2014). Challenges were evident in participant experiences throughout the state, as they reported feelings of helplessness in the face of growing numbers, patient acuity and time constraints. This was most evident in concerns raised regarding patient safety and the pressure in maintaining visible composure in a chaotic environment. Nevertheless, participants overwhelmingly demonstrated pride in their work and a passion for renal care despite these structural constraints.
This research also provides evidence of a disconnect between the model of care utilised by hospitals and the increasing complexity of renal care. It highlights a need to consider alternative approaches to the delivery of renal care rather than a ‘business as usual’ service delivery that participants describe as inadequate and lowering both staff satisfaction and the quality of care for renal patients. This finding is particularly pertinent for renal staff here in South Australia, as the supply demand gap is widening, resulting in burnout and turnover (Halter et al., 2017). However, its impact could be applicable to renal nursing elsewhere where renal units may be experiencing the same increased acuity and structural constraints.
Whilst we acknowledge the inherent challenges of generalising from qualitative research, the four key findings from this research include:
- The renal nursing workforce has a strong internal supportive culture.
- The working environment and professional development opportunities need to be re-considered (larger spaces and increased training opportunities required).
- Changing patient acuity management requires modifications to the nurse/patient ratio model.
- Attracting nurses to the renal specialty is reliant on changes to the current education model and strategies to attract early career nurses to the speciality.
Limitations and strengths
We acknowledge a limitation of the focus group methodology is that participants self-selected, that senior and junior staff were interviewed together, and that being interviewed as teams could prioritise dominant voices and silence passive ones. Potentially the impact of COVID‑19 on the health system and staff could also confound some of the findings due to the contemporary pressures of the global pandemic. The strength of this research is participants from multiple sites with varying degrees of experience and the experienced facilitators.
In conclusion, the nephrology nurse focus groups undertaken across metropolitan South Australia found evidence of a dedicated and highly specialised nursing profession who described caring for a much larger and more complex cohort of patients under markedly different circumstances than the hospital renal unit structures and systems were designed to cope with. Consequently, a disconnect between institutional expectations and the pragmatic reality perceived by nurses caused these clinicians to feel unsupported and forced into what could be described as a ‘triage’ approach to care. Workplace culture was reported as particularly important with regard to the respect and recognition showed by senior staff both within the nursing teams, other staff such as doctors, other wards whose work intersected with renal, and the institution as a whole. This appeared to be crucial to job satisfaction and a sense of control and had an impact on their patient care. Overall, this research highlights the need for further study into the causes of changing workplace pressures and opportunities for organisations to explore and address key issues that are currently negatively impacting upon patient care and staff retention in this important nursing specialty.
Future work in this area
In addressing the nephrology nursing supply and demand issue that is emerging, research needs to focus on not just the current situation but in developing strategies to create solutions. This is vital to inform organisations how best to support the nephrology nursing workforce to ensure its sustainability. Phase 2 of our research will be investigating the sustainability of the nephrology nursing workforce using a discrete choice quantitative methodology (DCM) via a national workforce survey informed by the findings of this study. The themes developed in this qualitative work will guide the development of a DCM survey that will help us to work towards developing quantitative workforce models to understand and develop strategies to sustain the nephrology nursing workforce. Phase 2 is funded by Kidney Transplant Diabetes Research Australia and will be used to inform the National Strategic Action Plan on Kidney Disease.
Acknowledgements / Funding statement
The researchers would like to thank all of the renal nurses who participated in this study for their time, thoughts, ideas and expert opinions. This research was funded by a project specific grant from the Rosemary Bryant Foundation South Australia. Would also like to acknowledge the Rosemary Bryant AO Research Centre, University of South Australia for their support in progressing this research.
Conflict of interest
The authors declare no conflicts of interest.
Dr Kathy Hill PhD MPH Grad Cert (Neph) BN RN Lecturer in Nursing University of South Australia, SA, Australia
Dr Kim Neylon PhD University of South Australia, SA, Australia
Dr Kate Gunn PhD University of South Australia, SA, Australia
Dr Shilpa Jesudason MBBS, FRACP, PhD Central Northern Adelaide Renal Transplantation Service (CNARTS), SA, Australia
Greg Sharplin Mpsych (Org & HF) MSc (Epi) University of South Australia, SA, Australia
Anne Britton Clinical Practice Director, Central Northern Adelaide Renal Transplantation Service (CNARTS), SA, Australia Fiona Donnelly MNP Central Northern Adelaide Renal Transplantation Service (CNARTS), SA, Australia
Irene Atkins CNM Renal Unit FMC SALHN, SA, Australia
Professor Marion Eckert PhD University of South Australia, SA, Australia
Correspondence to Dr Kathy Hill, Lecturer in Nursing, School of Nursing and Midwifery City East Campus University of South Australia Email [email protected]
Australia and New Zealand Dialysis and Transplant Registry (ANZDATA). (2019). Annual report. South Australia: ANZDATA.
Bong, H. E. (2019). Understanding moral distress: How to decrease turnover rates of new graduate pediatric nurses. Pediatric Nursing, 45 , 109–114.
Brown, S., Bain, P., Broderick, P., & Sully, M. (2013). Emotional effort and perceived support in renal nursing: A comparative interview study. Journal of Renal Care, 39, 246–255.
Dermody, K., & Bennett, P. N. (2008). Nurse stress in hospital and satellite haemodialysis units. Journal of Renal Care, 34 (1), 28–32.
Gardner, J. K., Thomas-Hawkins, C., Fogg, L., & Latham, C. E. (2007). The relationships between nurses’ perceptions of the hemodialysis unit work environment and nurse turnover, patient satisfaction, and hospitalizations. Nephrology Nursing Journal, 34, 271–81.
Georgios, M., Theodora, K., Eugenia, M., Christos, T., Smaragdi, K., Athina, K., & Alexandra, D. (2017). Is self-esteem actually the protective factor of nursing burnout? International Journal of Caring Sciences, 10, 1348–1359.
Halter, M., Boiko, O., Pelone, F., Beighton, C., Harris, R., Gale, J., Gourlay, S., & Drennan, V. (2017). The determinants and consequences of adult nursing staff turnover: a systematic review of systematic reviews. BMC Health Services Research, 17, 824–824.
Hayes, B., Douglas, C., & Bonner, A. (2014). Predicting emotional exhaustion among haemodialysis nurses: A structural equation model using Kanter’s structural empowerment theory. Journal of Advanced Nursing, 70, 2897–2909.
Hayes, B., Douglas, C., & Bonner, A. (2015). Work environment, job satisfaction, stress and burnout among haemodialysis nurses. Journal of Nursing Management, 23, 588–598.
Jayasekara, R. S. (2012). Focus groups in nursing research: Methodological perspectives. Nursing Outlook, 60, 411–416.
Jones, C. (2014). Stress and coping strategies in renal staff. Nursing Times, 110, 22–25.
Kavurmacı, M., Cantekin, I., & Tan, M. (2014). Burnout levels of hemodialysis nurses. Renal Failure, 36, 1038–1042.
Kidney Health Australia. (2020). Chronic kidney disease management in primary care (4th ed). Melbourne: Kidney Health Australia.
Liamputtong, P. (2011). Focus group methodology: Principles and practice. London: Sage Publishing.
Mudallal, R. H., Saleh, M. Y. N., Al-Modallal, H. M., & Abdel-Rahman, R. Y. (2017). Quality of nursing care: The influence of work conditions, nurse characteristics and burnout. International Journal of Africa Nursing Sciences, 7, 24–30.
White, E. M., Aiken, L. H., & McHugh, M. D. (2019). Registered nurse burnout, job dissatisfaction, and missed care in nursing homes. Journal of the American Geriatric Society, 67, 2065–2071.
Wolfe, W. A. (2014). Are word-of-mouth communications contributing to a shortage of nephrology nurses? Nephrology Nursing Journal, 41, 371–378.
Previous Article
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 30 July 2020
The current and future landscape of dialysis
- Jonathan Himmelfarb ORCID: orcid.org/0000-0002-3319-1224 1 , 2 ,
- Raymond Vanholder ORCID: orcid.org/0000-0003-2633-1636 3 ,
- Rajnish Mehrotra ORCID: orcid.org/0000-0003-2833-067X 1 , 2 &
- Marcello Tonelli ORCID: orcid.org/0000-0002-0846-3187 4
Nature Reviews Nephrology volume 16 , pages 573–585 ( 2020 ) Cite this article
86k Accesses
258 Citations
130 Altmetric
Metrics details
- Haemodialysis
- Health care economics
- Health services
- Medical ethics
The development of dialysis by early pioneers such as Willem Kolff and Belding Scribner set in motion several dramatic changes in the epidemiology, economics and ethical frameworks for the treatment of kidney failure. However, despite a rapid expansion in the provision of dialysis — particularly haemodialysis and most notably in high-income countries (HICs) — the rate of true patient-centred innovation has slowed. Current trends are particularly concerning from a global perspective: current costs are not sustainable, even for HICs, and globally, most people who develop kidney failure forego treatment, resulting in millions of deaths every year. Thus, there is an urgent need to develop new approaches and dialysis modalities that are cost-effective, accessible and offer improved patient outcomes. Nephrology researchers are increasingly engaging with patients to determine their priorities for meaningful outcomes that should be used to measure progress. The overarching message from this engagement is that while patients value longevity, reducing symptom burden and achieving maximal functional and social rehabilitation are prioritized more highly. In response, patients, payors, regulators and health-care systems are increasingly demanding improved value, which can only come about through true patient-centred innovation that supports high-quality, high-value care. Substantial efforts are now underway to support requisite transformative changes. These efforts need to be catalysed, promoted and fostered through international collaboration and harmonization.
The global dialysis population is growing rapidly, especially in low-income and middle-income countries; however, worldwide, a substantial number of people lack access to kidney replacement therapy, and millions of people die of kidney failure each year, often without supportive care.
The costs of dialysis care are high and will likely continue to rise as a result of increased life expectancy and improved therapies for causes of kidney failure such as diabetes mellitus and cardiovascular disease.
Patients on dialysis continue to bear a high burden of disease, shortened life expectancy and report a high symptom burden and a low health-related quality of life.
Patient-focused research has identified fatigue, insomnia, cramps, depression, anxiety and frustration as key symptoms contributing to unsatisfactory outcomes for patients on dialysis.
Initiatives to transform dialysis outcomes for patients require both top-down efforts (that is, efforts that promote incentives based on systems level policy, regulations, macroeconomic and organizational changes) and bottom-up efforts (that is, patient-led and patient-centred advocacy efforts as well as efforts led by individual teams of innovators).
Patients, payors, regulators and health-care systems increasingly demand improved value in dialysis care, which can only come about through true patient-centred innovation that supports high-quality, high-value care.
Similar content being viewed by others

Long-term kidney outcomes of semaglutide in obesity and cardiovascular disease in the SELECT trial

Acute kidney injury

An overview of clinical decision support systems: benefits, risks, and strategies for success
Introduction.
Haemodialysis as a treatment for irreversible kidney failure arose from the pioneering efforts of Willem Kolff and Belding Scribner, who together received the 2002 Albert Lasker Clinical Medical Research Award for this accomplishment. Kolff treated his first patient with an artificial kidney in 1943 — a young woman who was dialysed 12 times successfully but ultimately died because of vascular access failure. By 1945, Kolff had dialysed 15 more patients who did not survive, when Sofia Schafstadt — a 67-year-old woman who had developed acute kidney injury — recovered, becoming the first long-term survivor after receipt of dialysis. In 1960, Belding Scribner, Wayne Quinton and colleagues at the University of Washington, WA, USA, designed shunted cannulas, which prevented the destruction of blood vessels and enabled repeated haemodialysis sessions. The first patient who received long-term treatment (named Clyde Shields) lived a further 11 years on haemodialysis. In their writings, both Kolff and Scribner eloquently described being motivated by their perception of helplessness as physicians who had little to offer for the care of young patients who were dying of uraemia and stated that the goal of dialysis was to achieve full rehabilitation to an enjoyable life 1 .
The potential to scale the use of dialysis to treat large numbers of patients with kidney failure created great excitement. At the 1960 meeting of the American Society for Artificial Internal Organs (ASAIO), Scribner introduced Clyde Shields to physicians interested in dialysis, and Quinton demonstrated fabrication of the shunt. The following decade saw rapid gains in our understanding of kidney failure, including the discovery of uraemia-associated atherogenesis and metabolic bone disease, and in virtually every aspect of haemodialysis, including improvements in dialyser technology, dialysate composition, materials for haemocompatibility and water purification systems. The Scribner–Quinton shunt rapidly became an historical artefact once Brescia and colleagues developed the endogenous arteriovenous fistula in 1966 (ref. 2 ), and prosthetic subcutaneous interpositional ‘bridge’ grafts were developed shortly thereafter. Concomitant with these pioneering efforts, in 1959, peritoneal dialysis (PD) was first used successfully to sustain life for 6 months. Within 2 years a long-term PD programme was established in Seattle, WA, USA, and within 3 years the first automated PD cycler was developed 3 .
In 1964, Scribner’s presidential address to the ASAIO described emerging ethical issues related to dialysis, including considerations for patient selection, patient self-termination of treatment as a form of suicide, approaches to ensure death with dignity and selection criteria for transplantation 4 . Indeed, the process of selecting who would receive dialysis contributed to the emergence of the field of bioethics. The early success of dialysis paradoxically created social tensions, as access to this life-sustaining therapy was rationed by its availability and the ‘suitability’ of patients. In the early 1970s, haemodialysis remained a highly specialized therapy, available to ~10,000 individuals, almost exclusively in North America and Europe, with a high frequency of patients on home haemodialysis. In a portentous moment, Shep Glazer, an unemployed salesman, was dialysed in a live demonstration in front of the US Congress House Ways and Means Committee. Soon thereafter, in October 1972, an amendment to the Social Security Act creating Medicare entitlement for end-stage renal disease (now known as kidney failure), for both dialysis and kidney transplantation, was passed by Congress and signed into law by President Nixon.
The resulting expansion of dialysis, previously described as “from miracle to mainstream” 5 , set in motion dramatic changes 6 , including the development of a for-profit outpatient dialysis provider industry; relaxation of stringent patient selection for dialysis eligibility in most HICs; a move away from home towards in-centre dialysis; efforts on the part of single payors such as Medicare in the USA to restrain per-patient costs through the introduction of bundled payments and the setting of composite rates; the development of quality indicators — such as adequate urea clearance per treatment — that were readily achievable but are primarily process rather than outcome measures; consolidation of the dialysis industry, particularly in the USA owing to economies of scale, eventually resulting in a duopoly of dialysis providers; the development of joint ventures and other forms of partnerships between dialysis providers and nephrologists; the globalization of dialysis, which is now available, albeit not necessarily accessible or affordable in many low-income and middle-income countries (LMICs); and finally, a dramatic slowing in the rate of true patient-centred innovation, with incremental gains in dialysis safety and efficiency replacing the pioneering spirit of the early innovators.
The population of patients receiving dialysis continues to grow rapidly, especially in LMICs, as a result of an increase in the availability of dialysis, population ageing, increased prevalence of hypertension and diabetes mellitus, and toxic environmental exposures. However, despite the global expansion of dialysis, notable regional differences exist in the prevalence of different dialysis modalities and in its accessibility. Worldwide, a substantial number of people do not have access to kidney replacement therapy (KRT), resulting in millions of deaths from kidney failure each year. Among populations with access to dialysis, mortality remains high and outcomes suboptimal, with high rates of comorbidities and poor health-related quality of life. These shortcomings highlight the urgent need for innovations in the dialysis space to increase accessibility and improve outcomes, with a focus on those that are a priority to patients. This Review describes the current landscape of dialysis therapy from an epidemiological, economic, ethical and patient-centred framework, and provides examples of initiatives that are aimed at stimulating innovations in dialysis and transform the field to one that supports high-quality, high-value care.
Epidemiology of dialysis
Kidney failure is defined by a glomerular filtration rate <15 ml/min/1.73 m 2 (ref. 7 ) and may be treated using KRT (which refers to either dialysis or transplantation) or with supportive care 8 . The global prevalence of kidney failure is uncertain, but was estimated to be 0.07%, or approximately 5.3 million people in 2017 (ref. 9 ), with other estimates ranging as high as 9.7 million. Worldwide, millions of people die of kidney failure each year owing to a lack of access to KRT 10 , often without supportive care. Haemodialysis is costly, and current recommendations therefore suggest that haemodialysis should be the lowest priority for LMICs seeking to establish kidney care programmes. Rather, these programmes should prioritize other approaches, including treatments to prevent or delay kidney failure, conservative care, living donor kidney transplantation and PD 11 . Nonetheless, haemodialysis is the most commonly offered form of KRT in LMICs, as well as in high-income countries (HICs) 12 , and continued increases in the uptake of haemodialysis are expected worldwide in the coming decades. Here, we review the basic epidemiology of kidney failure treated with long-term dialysis and discuss some of the key epidemiological challenges of the future (Fig. 1a ).
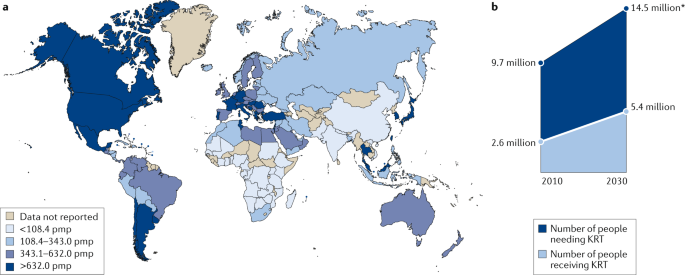
Growth is continuously outpacing the capacity of kidney replacement therapy (KRT), defined as maintenance dialysis or kidney transplant, especially in low-income and middle-income countries. a | Global prevalence of chronic dialysis. b | Estimated worldwide need and projected capacity for KRT by 2030. pmp, per million population. Adapted with permission from the ISN Global Kidney Health Atlas 2019.
Prevalence of dialysis use
Prevalence of haemodialysis.
Worldwide, approximately 89% of patients on dialysis receive haemodialysis; the majority (>90%) of patients on haemodialysis live in HICs or the so-called upper middle-income countries such as Brazil and South Africa 12 , 13 . The apparent prevalence of long-term dialysis varies widely by region but correlates strongly with national income 14 . This variation in prevalence in part reflects true differences in dialysis use 12 , 15 but also reflects the fact that wealthier countries are more likely than lower income countries to have comprehensive dialysis registries. Of note, the prevalence of haemodialysis is increasing more rapidly in Latin America (at a rate of ~4% per year) than in Europe or the USA (both ~2% per year), although considerable variation between territories exists in all three of these regions, which again correlates primarily (but not exclusively) with wealth 16 , 17 . The prevalence of haemodialysis varies widely across South Asia, with relatively high prevalence (and rapid growth) in India and lower prevalence in Afghanistan and Bangladesh 18 . Limited data are available on the prevalence of dialysis therapies in sub-Saharan Africa 19 . A 2017 report suggests that haemodialysis services were available in at least 34 African countries as of 2017, although haemodialysis was not affordable or accessible to the large majority of resident candidates 13 .
Prevalence of peritoneal dialysis
Worldwide, PD is less widely available than haemodialysis. In a 2017 survey of 125 countries, PD was reportedly available in 75% of countries whereas haemodialysis was available in 96% 20 . In 2018, an estimated 11% of patients receiving long-term dialysis worldwide were treated with PD; a little over half of these patients were living in China, Mexico, the USA and Thailand 21 .
Large variation exists between territories in the relative use of PD for treating kidney failure; in Hong Kong for example, >80% of patients on dialysis receive PD, whereas in Japan this proportion is <5% 22 . This variation is, in part, determined by governmental policies and the density of haemodialysis facilities 23 . In some countries such as the USA, rates of PD utilization also vary by ethnicity with African Americans and Hispanics being much less likely than white Americans to receive PD 24 . Disparate secular trends in PD use are also evident, with rapid growth in the use of PD in some regions such as the USA, China and Thailand and declining or unchanging levels of PD use in other regions, for example, within Western Europe 22 . As for haemodialysis, access to PD is poor in many LMICs for a variety of reasons, as comprehensively discussed elsewhere 25 .
Incidence of dialysis use
Following a rapid increase in dialysis use over a period of approximately two decades, the incidence of dialysis initiation in most HICs reached a peak in the early 2000s and has remained stable or slightly decreased since then 22 , 26 , 27 . Extrapolation of prevalence data from LMICs suggests that the incidence of dialysis initiation seems to be steadily increasing in LMICs 10 , 28 , 29 , 30 , with further increases expected over the coming decades. However, incidence data in LMICs are less robust than prevalence data, although neither reflect the true demand for KRT given the lack of reporting.
Of note, the incidence of dialysis initiation in HICs is consistently 1.2-fold to 1.4-fold higher for men than for women, despite an apparently higher risk of chronic kidney disease (CKD) in women 31 . Whether this finding reflects physician or health system bias, different preferences with regard to KRT, disparities in the competing risk of death, variation in rates of kidney function loss in women versus men, or other reasons is unknown and requires further study. Few data describe the incidence of haemodialysis by sex in LMICs.
Dialysis outcomes
Mortality is very high among patients on dialysis, especially in the first 3 months following initiation of haemodialysis treatment. Approximately one-quarter of patients on haemodialysis die within a year of initiating therapy in HICs, and this proportion is even higher in LMICs 32 , 33 , 34 . Over the past two decades, reductions in the relative and absolute risk of mortality have seemingly been achieved for patients on haemodialysis. Data suggest that relative gains in survival may be greater for younger than for older individuals; however, absolute gains seem to be similar across age groups 35 . Although controversial, improvements in mortality risk seem to have been more rapid among patients on dialysis than for the general population 36 , suggesting that better care of patients receiving dialysis treatments rather than overall health gains might be at least partially responsible for these secular trends. The factors responsible for these apparent trends have not been confirmed, but could include better management of comorbidities, improvements in the prevention or treatment of dialysis-related complications such as infection, and/or better care prior to the initiation of dialysis (which may translate into better health following dialysis initiation). Historically, although short-term mortality was lower for patients treated with PD than for those treated with haemodialysis, the long-term mortality risk was higher with PD 37 , 38 . In the past two decades, the reduction in mortality risk has been greater for patients treated with PD than with haemodialysis, such that in most regions the long-term survival of patients treated with PD and haemodialysis are now similar 39 , 40 , 41 .
Despite these improvements, mortality remains unacceptably high among patients on dialysis and is driven by cardiovascular events and infection. For example, a 2019 study showed that cardiovascular mortality among young adults aged 22–29 years with incident kidney failure was 143–500-fold higher than that of otherwise comparable individuals without kidney failure, owing to a very high burden of cardiovascular risk factors 42 . The risk of infection is also markedly greater among patients on dialysis than in the general population, in part driven by access-related infections in patients on haemodialysis with central venous catheters and peritonitis-related infections in patients on PD 43 , 44 , 45 , 46 , 47 . Hence, strategies to reduce the risk of infection associated with dialysis access should continue to be a high clinical priority.
The risk of mortality among patients on dialysis seems to be influenced by race. In the USA, adjusted mortality is lower for African American patients than for white patients on dialysis, although there is a significant interaction with age such that this observation held only among older adults, and the converse is actually true among younger African American patients aged 18 to 30 years 48 . A similar survival advantage is observed among Black patients compared with white patients or patients of Asian heritage on haemodialysis in the Netherlands 49 . In Canada, dialysis patients of indigenous descent have higher adjusted mortality, and patients of South Asian or East Asian ethnicity have lower adjusted mortality than that of white patients. In addition, between-region comparisons indicate that mortality among incident dialysis patients is substantially lower for Japan than for other HICs. Whether this difference is due to ethnic origin, differences in health system practices, a combination of these factors or other, unrelated factors is unknown 30 . No consistent evidence exists to suggest that mortality among incident adult dialysis patients varies significantly by sex 50 , 51 , 52 .
Other outcomes
Hospitalization, inability to work and loss of independent living are all markedly more common among patients on dialysis than in the general population 53 , 54 , 55 . In contrast to the modest secular improvements in mortality achieved for patients on dialysis, health-related quality of life has remained unchanged for the past two decades and is substantially lower than that of the general population, due in part to high symptom burden 56 , 57 , 58 , 59 . Depression is also frequent among patients on dialysis 60 , and factors such as high pill burden 61 , the need to travel to dialysis sessions and pain associated with vascular access puncture all affect quality of life 62 .
Future epidemiological challenges
The changing epidemiology of kidney failure is likely to present several challenges for the optimal management of these patients. For example, the ageing global population together with continuing increases in the prevalence of key risk factors for the development of kidney disease, such as diabetes mellitus and hypertension, mean that the incidence, prevalence and costs of kidney failure will continue to rise for the foreseeable future. This increased demand for KRT will undoubtedly lead to an increase in the uptake of haemodialysis, which will pose substantial economic challenges for health systems worldwide. Moreover, as growth in demand seems to be outpacing increases in KRT capacity, the number of deaths as a result of kidney failure is expected to rise dramatically (Fig. 1b ).
The same risk factors that drive the development of kidney disease will also increase the prevalence of multimorbidities within the dialysis population. These comorbidities will in turn require effective management in addition to the management of kidney failure per se 63 and will require technical innovations of dialysis procedures, as well as better evidence to guide the management of comorbidities in the dialysis population.
Finally, the particularly rapid increases in the incidence and prevalence of kidney failure among populations in LMICs will place considerable strain on the health systems of these countries. The associated increases in mortality resulting from a lack of access to KRT will create difficult choices for decision makers. Although LMIC should prioritize forms of KRT other than haemodialysis, some haemodialysis capacity will be required 11 , for example, to manage patients with hypercatabolic acute kidney injury or refractory PD-associated peritonitis, which, once available, will inevitably increase the use of this modality.
Health economy-related considerations
The cost of dialysis (especially in-centre or in-hospital dialysis) is high 64 , and the cost per quality-adjusted life-year associated with haemodialysis treatment is often considered to be the threshold value that differentiates whether a particular medical intervention is cost-effective or not 65 . Total dialysis costs across the population will probably continue to rise, owing to increases in life expectancy of the general population and the availability of improved therapeutics for causes of kidney failure such as diabetes mellitus, which have increased the lifespan of these patients and probably will also increase their lifespan on dialysis. KRT absorbs up to 5–7% of total health-care budgets, despite the fact that kidney failure affects only 0.1–0.2% of the general population in most regions 66 . Although societal costs for out-of-centre dialysis (for example, home or self-care haemodialysis, or PD) are in general lower than that of in-centre haemodialysis in many HICs, these options are often underutilized 67 , adding to the rising costs of dialysis.
Reimbursement for haemodialysis correlates with the economic strength of each region 68 , but in part also reflects willingness to pay . In most regions, the correlation curve for PD or reimbursement with respect to gross domestic product projects below that of in-centre haemodialysis, which in part reflects the lower labour costs associated with PD 68 . Unfortunately, little clarity exists with regard to the aggregated cost of single items that are required to produce dialysis equipment for both PD and haemodialysis and the labour costs involved in delivering haemodialysis 69 , which makes it difficult for governments to reimburse the real costs of haemodialysis.
Although increasing reimbursement of home dialysis strategies would seem to be an appropriate strategy to stimulate uptake of these modalities, evidence from regions that offer high reimbursement rates for PD suggests that the success of this strategy is variable 23 , 68 . However, financial incentives may work. In the USA, reimbursement for in-centre and home dialysis (PD or home haemodialysis) has for a long time been identical. The introduction of the expanded prospective payment system in 2011 further enhanced the financial incentives for PD for dialysis providers, which led to a doubling in both the absolute number of patients and the proportion of patients with kidney failure treated with PD 70 , 71 , 72 , 73 .
Although in countries with a low gross domestic product, dialysis consumes less in absolute amounts, it absorbs a higher fraction of the global health budget 68 , likely at the expense of other, potentially more cost-effective interventions, such as prevention or transplantation. Although society carries most of the costs associated with KRT in most HICs, some costs such as co-payment for drugs or consultations are borne by the individual, and these often increase as CKD progresses. In other regions, costs are covered largely or entirely by the patient’s family, leading to premature death when resources are exhausted 74 . In addition, costs are not limited to KRT but also include the costs of medication, hospitalizations and interventions linked to kidney disease or its complications (that is, indirect costs), as well as non-health-care-related costs such as those linked to transportation or loss of productivity.
Dialysis also has an intrinsic economic impact. Patients on dialysis are often unemployed. In the USA, >75% of patients are unemployed at the start of dialysis, compared with <20% in the general population 53 . Unemployment affects purchasing power but also lifestyle, self-image and mental health. Moreover, loss of productivity owing to unemployment and/or the premature death of workers with kidney failure also has economic consequences for society 75 . Therefore, continued efforts to prevent kidney failure and develop KRT strategies that are less time consuming for the patient and allow more flexibility should be an urgent priority. Concomitantly, employers must also provide the resources needed to support employees with kidney failure.
Hence, a pressing need exists to rethink the current economic model of dialysis and the policies that direct the choice of different treatment options. The cost of dialysis (especially that of in-centre haemodialysis) is considerable and will continue to rise as the dialysis population increases. Maintaining the status quo will prevent timely access to optimal treatment for many patients, especially for those living in extreme poverty and with a low level of education and for patients living in LMICs.
Ethical aspects
A 2020 review by a panel of nephrologists and ethicists appointed by three large nephrology societies outlined the main ethical concerns associated with kidney care 76 . With regard to management of kidney failure (Box 1 ), equitable access to appropriate treatment is probably the most important ethical issue and is relevant not only in the context of haemodialysis but also for the other modalities of kidney care (including transplantation, PD and comprehensive conservative care) 76 . Of note, conservative care is not equivalent to the withdrawal of treatment, but rather implies active management excluding KRT.
As mentioned previously, access to such care is limited in many countries 10 , 77 . Inequities in access to dialysis at the individual level are largely dependent on factors such as health literacy, education and socio-economic status, but also on the wealth and organization of the region in which the individual lives. Even when dialysis itself is reimbursed, a lack of individual financial resources can limit access to care. Moreover, elements such as gender, race or ethnicity and citizenship status 78 , 79 can influence an individual’s ability to access dialysis 80 . These factors impose a risk that patients who are most vulnerable are subject to further discrimination. In addition, without necessarily being perceived as such, dialysis delivery may be biased by the financial interests of dialysis providers or nephrologists, for example, by influencing whether a patient receives in-centre versus home dialysis, or resulting in the non-referral of patients on dialysis for transplantation or conservative care 81 , 82 .
A potential reason for the high utilization of in-centre haemodialysis worldwide is a lack of patient awareness regarding the alternatives. When surveyed, a considerable proportion of patients with kidney failure reported that information about options for KRT was inadequate 83 , 84 . Patient education and decision support could be strengthened and its quality benchmarked, with specific attention to low health literacy, which is frequent among patients on dialysis 85 . Inadequate patient education might result from a lack of familiarity with home dialysis (including PD) and candidacy bias among treating physicians and nurses. Appropriate education and training of medical professionals could help to solve this problem. However, the first step to increase uptake of home dialysis modalities is likely policy action undertaken by administrations, but stimulated by advocacy by patients and the nephrology community, as suggested by the higher prevalence of PD at a lower societal cost of regions that already have a PD-first policy in place 68 .
Although the provision of appropriate dialysis at the lowest possible cost to the individual is essential if access is to be improved 86 , approaches that unduly compromise the quality of care should be minimized or avoided. General frameworks to deal with this challenge can be provided by the nephrology community, but trade-offs between cost and quality may be necessary and will require consultation between authorities, medical professionals and patient representatives. Consideration must also be given to whether the societal and individual impact of providing dialysis would be greater than managing other societal health priorities (for example, malaria or tuberculosis) or investing in other sectors to improve health (for example, access to clean drinking water or improving road safety).
The most favourable approach in deciding the most appropriate course of action for an individual is shared decision-making 87 , which provides evidence-based information to patients and families about all available therapeutic options in the context of the local situation. Providing accurate and unbiased information to support such decision-making is especially relevant for conservative care, to avoid the perception that this approach is being recommended to save resources rather than to pursue optimal patient comfort. Properly done, shared decision-making should avoid coercion, manipulation, conflicts of interest and the provision of ‘futile dialysis’ to a patient for whom the harm outweighs the benefits, life expectancy is low or the financial burden is high 88 . However, the views of care providers do not always necessarily align with those of patients and their families, especially in multicultural environments 89 . Medical professionals are often not well prepared for shared decision-making, and thus proper training is essential 90 . Policy action is also required to create the proper ethical consensus and evidence-based frameworks at institutional and government levels 91 to guide decision-making in the context of dialysis care that can be adapted to meet local needs.
Box 1 Main ethical issues in dialysis
Equity in access to long-term dialysis
Inequities in the ability to access kidney replacement therapy exist worldwide; however, if dialysis is available, the ability to transition between different dialysis modalities should be facilitated as much as possible. Specific attention should be paid to the factors that most prominently influence access to dialysis, such as gender, ethnicity, citizenship status and socio-economic status
Impact of financial interests on dialysis delivery
Financial interests of dialysis providers or nephrologists should in no way influence the choice of dialysis modality and/or result in the non-referral of patients for transplantation or conservative care
Cost considerations
Local adaptations are needed to ensure that the costs of dialysis provision are as low as possible without compromising quality of care
The high cost of dialysis means that consideration must be given to whether the benefits obtained by dialysis outweigh those obtained by addressing other health-care priorities, such as malaria or tuberculosis
Shared decision-making
Shared decision-making, involving the patient and their family, is recommended as an approach to allow an informed choice of the most appropriate course to follow
Approaches to shared decision-making must be evidence based and adapted to local circumstances
Futile dialysis should be avoided
Proper training is required to prepare physicians for shared decision-making
Clinical outcomes to measure progress
Over the past six decades, the availability of long-term dialysis has prolonged the lives of millions of people worldwide, often by serving as a bridge to kidney transplantation. Yet, patients on dialysis continue to bear a high burden of disease, both from multimorbidity and owing to the fact that current dialysis modalities only partially replace the function of the native kidney, resulting in continued uraemia and its consequences. Thus, although dialysis prevents death from kidney failure, life expectancy is often poor, hospitalizations (particularly for cardiovascular events and infection) are frequent, symptom burden is high and health-related quality of life is low 22 , 92 , 93 .
Given the multitude of health challenges faced by patients on dialysis, it is necessary to develop a priority list of issues. For much of the past three decades, most of this prioritization was performed by nephrology researchers with the most effort to date focusing on approaches to reducing all-cause mortality and the risk of fatal and non-fatal cardiovascular events. However, despite the many interventions that have been tested, including increasing the dose of dialysis (in the HEMO and ADEMEX trials 94 , 95 ), increasing dialyser flux (in the HEMO trial and MPO trial 94 , 96 ), increasing haemodialysis frequency (for example, the FHN Daily and FHN Nocturnal trials 97 , 98 ), use of haemodiafiltration (the CONTRAST 99 , ESHOL 100 and TURKISH-OL-HDF trials 101 ), increasing the haemoglobin target (for example, the Normal Haematocrit Trial 102 ), use of non-calcium-based phosphate binders (for example, the DCOR trial 103 ), or lowering of the serum cholesterol level (for example, the 4D, AURORA and SHARP trials 104 , 105 , 106 ), none of these or other interventions has clearly reduced all-cause or cardiovascular mortality for patients on dialysis. These disappointments notwithstanding, it is important that the nephrology community perseveres in finding ways to improve patient outcomes.
In the past 5 years, nephrology researchers have increasingly engaged with patients to understand their priorities for meaningful outcomes that should be used to measure progress. The overarching message from this engagement is that although longevity is valued, many patients would prefer to reduce symptom burden and achieve maximal functional and social rehabilitation. This insight highlights the high symptom burden experienced by patients receiving long-term dialysis 92 , 93 , 96 , 107 . These symptoms arise as a consequence of the uraemic syndrome. Some of these symptoms, such as anorexia, nausea, vomiting, shortness of breath and confusion or encephalopathy, improve with dialysis initiation 108 , 109 , 110 , but many other symptoms, such as depression, anxiety and insomnia do not. Moreover, other symptoms, such as post-dialysis fatigue, appear after initiation of haemodialysis.
Of note, many symptoms of uraemic syndrome might relate to the persistence of protein-bound uraemic toxins and small peptides (so-called middle molecules) that are not effectively removed by the current dialysis modalities. The development of methods to improve the removal of those compounds is one promising approach to improving outcomes and quality of life for patients on dialysis, as discussed by other articles in this issue.
Patients on dialysis report an average of 9–12 symptoms at any given time 92 , 93 , 107 . To determine which of these should be prioritized for intervention, the Kidney Health Initiative used a two-step patient-focused process involving focus groups and an online survey to identify six symptoms that should be prioritized by the research community for intervention. These include three physical symptoms (fatigue, insomnia and cramps) and three mood symptoms (depression, anxiety and frustration) 111 . Parallel to these efforts, the Standardizing Outcomes in Nephrology Group (SONG) workgroup for haemodialysis ( SONG-HD ) has identified several tiers of outcomes that are important to patients, caregivers and health-care providers. Fatigue was identified as one of the four core outcomes, whereas depression, pain and feeling washed out after haemodialysis were identified as middle-tier outcomes 112 , 113 , 114 . Along these same lines, the SONG workgroup for PD ( SONG-PD ) identified the symptoms of fatigue, PD pain and sleep as important middle-tier outcomes 115 , 116 . Despite the importance of these symptoms to patients on dialysis, only a few studies have assessed the efficacy of behavioural and pharmacological treatments on depression 117 , 118 , 119 , 120 , 121 . Even more sobering is the observation that very few, if any, published studies have rigorously tested interventions for fatigue or any of the other symptoms. The nephrology community must now develop standardized and psychometrically robust measures that accurately capture symptoms and outcomes that are important to patients and ensure that these are captured in future clinical trials 122 , 123 .
Approaches to maximizing functional and social rehabilitation are also important to patients with kidney failure. In addition to the above-mentioned symptoms, SONG-HD identified ability to travel, ability to work, dialysis-free time, impact of dialysis on family and/or friends and mobility as important middle-tier outcomes 112 , 113 , 114 . SONG-PD identified life participation as one of five core outcomes, and impact on family and/or friends and mobility as other outcomes that are important to patients 115 , 116 . Given the importance of these outcomes to stakeholders, including patients, it is imperative that nephrology researchers develop tools to enable valid and consistent measurement of these outcomes and identify interventions that favourably modify these outcomes.
Fostering innovation
As described above, the status quo of dialysis care is suboptimal. Residual symptom burden, morbidity and mortality, and economic cost are all unacceptable, which begs the question of what steps are needed to change the established patterns of care. Patients are currently unable to live full and productive lives owing to the emotional and physical toll of dialysis, its intermittent treatment schedule, the dietary and fluid limitations, and their highly restricted mobility during treatment. Current technology requires most patients to travel to a dialysis centre, and current modalities are non-physiological, resulting in ‘washout’, which is defined as extensive fatigue, nausea and other adverse effects, caused by the build-up of uraemic toxins between treatments and the rapid removal of these solutes and fluids over 4-h sessions in the context of haemodialysis. LMICs face additional difficulties in the provision of dialysis owing to infrastructural requirements, the high cost of this treatment, the need for a constant power supply and the requirement for high volumes of purified water. For LMICs, innovations that focus on home-based, low-cost therapies that promote rehabilitation would be especially beneficial.
We contend that initiatives to transform dialysis outcomes for patients require both top-down efforts (for example, those that involve systems changes at the policy, regulatory, macroeconomic and organizational levels) and bottom-up efforts (for example, patient-led and patient-centred advocacy and individual teams of innovators). Top-down efforts are required to support, facilitate and de-risk the work of innovators. Conversely, patient-led advocacy is essential for influencing governmental and organizational policy change. Here, by considering how selected programmes are attempting to transform dialysis outcomes through innovation in support of high-value, high-quality care, we describe how top-down and bottom-up efforts can work synergistically to change the existing ecosystem of dialysis care (Fig. 2 ). The efforts described below are not an exhaustive list; rather, this discussion is intended to provide a representative overview of how the dialysis landscape is changing. Additional articles in this issue describe in more detail some of the bottom-up efforts of innovators to create wearable 124 , portable 125 , more environmentally friendly 126 and more physiological dialysis systems 127 , 128 , priorities from the patients’ perspective 129 , and the role of regulators in supporting innovation in the dialysis space 130 .
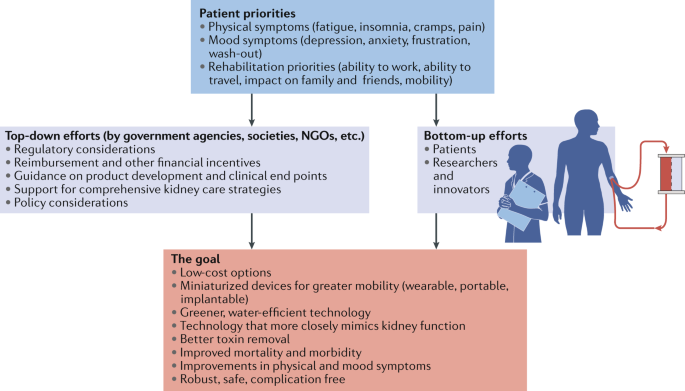
Initiatives to transform dialysis outcomes for patients require both top-down efforts (for example, those that involve systems-level changes at the policy, regulatory, macroeconomic and organizational level) and bottom-up efforts (for example, patient-led and patient-centred advocacy efforts and efforts from individual teams of innovators). Both of these efforts need to be guided by priorities identified by patients. Such an approach, focused on patient-centred innovation, has the potential to result in meaningful innovations that support high-quality, high-value care. NGOs, non-governmental organizations.
The Kidney Health Initiative
In 2012, the American Society of Nephrology (ASN) and the FDA established the KHI as an umbrella organization through which the kidney community can work collaboratively to remove barriers to the development of innovative drugs, devices, biologics and food products, in order to improve outcomes for people living with kidney diseases. To advance its mission, KHI has initiated a number of projects composed of multidisciplinary workgroups. A major accomplishment for the KHI was the establishment of a precompetitive environment to promote innovation while ensuring patient safety.
The KHI is the largest consortium in the kidney community, with over 100 member organizations including patient groups, health professional organizations, dialysis organizations, pharmaceutical and device companies, and government agencies. During the first 7 years of its existence, the KHI has launched and in many cases completed projects that have facilitated the development of new therapeutic options for dialysis patients (Box 2 ), as well as published position papers on topics relevant to innovation in haemodialysis care, including innovations in fluid management 131 and symptom management 132 in patients on haemodialysis, recommendations for clinical trial end points for vascular access 133 , perspectives on pragmatic trials in the haemodialysis population 134 and regulatory considerations for the use of haemodiafiltration 135 .
Box 2 Kidney Heath Initiative Projects that Support Dialysis Innovation
Patient and Family Partnership Council
Since 2015, the Kidney Health Initiative (KHI) Patient and Family Partnership Council (PFPC) has helped KHI stakeholders to engage and network with patients and patient organizations. The PFPC also advises industry and research partners of patient needs and preferences as new products are planned and developed. The PFPC continually emphasizes that innovation will only be successful if built around the needs of people with kidney disease and focused on improving their quality of life.
ESRD Data Standard Project
The aim of this project is to create a harmonized common data standard for kidney failure. The availability of a uniform data standard could accelerate the pace of scientific discovery, facilitate the creation of scientific registries for epidemiological surveillance and allow the development of common metrics for value-based health care.
Building Capacity to Incorporate Patient Preferences into the Development of Innovative Alternatives to kidney replacement therapy (KRT)
This project, which is supported by a 3-year contract with the FDA, is based on the premise that access to scientifically valid patient preference information could positively inform the decisions of industry and regulators as they design and review new devices for individuals with kidney failure. This project will collect patients’ preference information and also address a stated goal of the Advancing American Kidney Health (AAKH) initiative, which instructs the FDA to “develop a new survey to gain insight into patient preferences for new kidney failure treatments” 137 .
Clinical Trial Design to Support Innovative Approaches to KRT
This project is intended to facilitate coordinated efforts between regulators and the nephrology community to streamline the clinical development pathway. The primary objectives of the project are to define terminology for future KRT products (for example, wearable, portable, implantable and artificial kidney) and identify the most appropriate trial designs and end points for a variety of KRT products.
Advancing American Kidney Health
In July 2019, President Donald Trump signed an Executive Order on Advancing American Kidney Health (AAKH) 136 , which promises to fundamentally change the clinical care of kidney disease in general and kidney failure in particular. Components of the AAKH that are relevant to dialysis care include a directive for education and support programmes to promote awareness of kidney disease; a shift in the focus of reimbursement initiatives from in-centre haemodialysis to home therapies, transplantation and upstream CKD care; a system that rewards clinicians and dialysis facilities for providing a range of treatments for kidney failure, with the aim of increasing uptake of home dialysis and transplantation; and incentives for nephrology care teams to focus on reducing costs and improving outcomes by providing longitudinal care of patients with kidney disease.
Finally, and perhaps most radically, the AAKH calls on the US Department of Health and Human Services to support premarket approval of wearable and implantable artificial kidneys and welcomes other strategies to facilitate transformative innovation in dialysis devices. The AAKH directive specifically identifies the KidneyX programme (described below) as the vehicle with which to drive this innovation. The AAKH is the most ambitious US policy initiative ever undertaken to transform the care of patients with advanced kidney disease. Its agenda is still being shaped by the federal governmental agencies, with input from professional societies and other kidney community stakeholders, but this initiative provides a framework and support for transformative innovation in dialysis care.
The KHI Technology Roadmap and KidneyX
The KHI Technology Roadmap for Innovative Approaches to KRT, published in 2019 (ref. 137 ), is aimed at supporting the development of innovative dialysis devices by providing guidance on technical criteria, patient preferences, assessment of patient risk tolerances and regulatory, reimbursement and marketing considerations. Key strengths of the Roadmap include its patient-centred focus and the description of multiple solution pathways for different technologies (for example, portable, wearable and implantable devices that may be purely mechanical, cell-based or hybrid systems), each with appropriate timeline projections.
The KRT Roadmap was designed to be complementary to the Kidney Innovation Accelerator (also known as KidneyX). KidneyX is a public–private partnership between the Department of Health and Human Services and the ASN, and is aimed at accelerating the development of drugs, devices, biologics and other therapies across the spectrum of kidney care. The current major focus of KidneyX is to catalyse the fundamental redesign of dialysis, supported by a series of competitions. Phase I prizes focused on innovations in biomaterials, novel biosensors and safety monitors used for haemodialysis, as well as approaches for improved vascular access and the development of novel technologies that replicate kidney function more precisely than conventional dialysis. Phase II focuses on strategies to build and test prototype solutions or components of solutions that can replicate normal kidney function or improve haemodialysis access. KidneyX has also awarded a series of Patient Innovator Challenge prizes to patients who have proposed innovative solutions to problems emanating from their everyday experiences with kidney disease, including approaches to monitoring blood electrolyte levels and increasing the accessibility of patient education resources.
Dutch Kidney Foundation and Neokidney
The Dutch Kidney Foundation (DKF; or Nierstichting Nederland ) was founded in 1968. It supports research into the causes, prevention and treatment of kidney failure. Furthermore, it works to improve the quality of dialysis treatment and increase the number of kidney transplants. All projects are planned and organized with considerable patient involvement. The DKF also offers financial support to kidney research projects by large Dutch multi-centric consortia. These projects not only promote innovation in the Netherlands but also support trans-national European Union (EU)-supported projects with Dutch participation or leadership, such as Horizon 2020 and Horizon Europe.
Neokidney is a partnership between the DKF and several companies that specialize in miniaturization of dialysis equipment (including dialysis pumps) and sorbent technology for dialysate regeneration. This partnership is aimed at developing a small, portable haemodialysis device that will enable more frequent dialysis sessions, permit more flexibility for patients and improve patient quality of life, as well as reduce health-care costs. The first prototype is currently undergoing preclinical testing and is expected to be tested in humans soon, with the aim of demonstrating proof-of-concept for the first portable haemodialysis machine for daily use, requiring only a limited volume of dialysate. In addition to the development of miniaturization technologies, the partnership is also investigating the use of polymer membranes that permit combined filtration and absorption to achieve more effective haemodialysis 138 .
Nephrologists Transforming Hemodialysis Safety
Nephrologists Transforming Hemodialysis Safety (NTDS) is a collaborative initiative of the ASN and Centers for Disease Control and Prevention (CDC) that is aimed at addressing a specific complication inherent to contemporary dialysis — infection. In 2016, the CDC observed that 10% of dialysis patients in the USA died each year as the result of infections — most of which were preventable. The aim of NTDS is to develop and deploy innovations to achieve zero preventable infections in dialysis facilities across the USA. To reach this goal, NTDS uses a multi-pronged approach. For example, education strategies via publications 139 , 140 , 141 , 142 , 143 and webinars that address various aspects of infection prevention and standards of care, use of social media, development of an interactive chapter for trainees and clinicians, and invited lectures are aimed at ensuring that nephrologists, nurses, dialysis administrators and other professionals understand the risk of dialysis-related infections and evidence-based best working practices.
NTDS also interacts with experts in infection detection, prevention and treatment within federal, state and local health departments who can provide advice and assistance that is independent of the regulatory and potentially punitive arms of health departments. NTDS promotes the appropriate use of these experts in settings where expert advice is needed.
To promote leadership among physicians and nurses, NTDS is sponsoring a leadership academy to ensure that knowledge pertaining to evidence-based best working practices is applied to improve workflows in clinical practice. Effective leadership is a requirement, particularly in complex settings, to ensure that patient safety is prioritized and to motivate staff to use best practices.
NTDS are also collaborating with human factors engineers to study the workflows used in haemodialysis facilities and help to define ways of avoiding errors that lead to infection. As a first step in this process, NTDS and human factors engineers have spent time in various haemodialysis facilities to obtain information about the complex processes of care within those facilities, particularly with regard to the use of haemodialysis catheters and approaches to hand hygiene, injection safety and disinfection. Better understanding of current processes may lead to better workflow design.
Finally, based on lessons learned during the Ebola Crisis of 2014, an NTDS work group has designed processes to anticipate and respond to unexpected health-care crises. At the time of writing this Review, the NTDS team is working with CDC and haemodialysis organizations to anticipate and respond to the COVID-19 epidemic and its effect on dialysis care.
The Affordable Dialysis Prize
As discussed earlier, kidney failure remains a death sentence for many residents of LMICs owing to a lack of access to dialysis. In response to the pressing need for cost-effective dialysis options, the International Society of Nephrology in collaboration with the George Institute for Global Health and the Asian Pacific Society of Nephrology launched the Affordable Dialysis Prize in 2017 with the objective of facilitating the design of a dialysis system that would cost less than US $1,000, and provide treatment for less than $5 a day, yet be as safe and effective as existing dialysis systems. The prize was awarded to an engineer for a system that runs off solar power and includes a miniature distiller for producing pure water from any source via steam distillation. The purified water can then be mixed with electrolytes in empty PD bags to produce cheap, homemade dialysis solutions. This strategy identifies the lack of cheap, high-quality water as a major impediment to dialysis in LMICs and LICs. The system will ideally fit into a small suitcase 144 . This device remains under development with the goal of initiating clinical trials and ultimately commercializing the technology.
Empowered in-centre haemodialysis
For some patients with kidney failure, maintenance in-centre haemodialysis will always be the preferred treatment, and despite incentivizing policy levers, they will not be interested in pursuing home dialysis or kidney transplantation. In-centre self-dialysis (also referred to as empowered haemodialysis) originated in Sweden, when a young engineer named Christian Farman returned to haemodialysis in 2010 after a failed transplant. Farman began negotiating with his nurses to perform his own dialysis treatments with staff supervision and caught the attention of other patients 145 . Eventually, the process of self-dialysis within this centre — whereby coaches in the dialysis unit train people to take over control of their own treatments and health — grew so popular that a new unit was built at the hospital for self-dialysis patients only, with patient input into the design of the unit. Since then, self-care units were installed in several haemodialysis units in Europe and the USA, offering patients the autonomy and flexibility of home haemodialysis within the safety of a controlled environment. This approach to empowering patients has not been widely used to date, but deserves rigorous study and evaluation 146 .
Remote monitoring to support self-care
Telemedicine is defined as the electronic exchange of medical information between sites with the aim of improving a patient’s health. Telehealth encompasses a broader set of services such as the provision of educational content. New technologies have broadened the scope of telemedicine and telehealth applications and services, making these tools more accessible and useful in the care of patients who live remotely or have difficulty visiting a clinic. The range of services that can be delivered by telehealth now includes two-way interactive video, device data programming, asynchronous messaging , sensors for remote monitoring and portals to enable patients to access electronic health records. Although relatively understudied in haemodialysis patients to date, telehealth has the potential to increase the acceptance of home dialysis and improve patient satisfaction, while potentially decreasing costs and improving outcomes.
Telehealth and the remote monitoring of dialysis patients has become more commonplace in the past decade, particularly in Australia, where telehealth is used widely for patients receiving home dialysis. Telemedicine is also considered a support tool for kidney care in disaster situations such as earthquakes where many individuals in remote locations can be affected. Telemedicine has also been used for distance monitoring of patients receiving PD 147 , 148 . In the USA, the Bipartisan Budget Act of 2018 included provisions to expand telehealth coverage to include patients on home dialysis. This legislation allows patients on home dialysis to choose to have their monthly care-provider visits take place via telehealth, without geographic restrictions. The ongoing COVID-19 pandemic has also resulted in an unprecedented and rapid expansion in the use of telemedicine for providing health care in many regions worldwide, including for the care of patients undergoing in-centre haemodialysis. The experience gained during this pandemic has the potential to permanently embed telemedicine in health-care delivery in many health-care systems.
Although telehealth has considerable promise for the care of dialysis patients, the implementation of telehealth in clinical practice can be challenging 149 . Telehealth-guided digital interactions have the potential to improve outcomes through the provision of activities such as individualized patient-centred education, remote communication and data exchange, in-home clinical guidance and monitoring, assessment of prescription and/or treatment efficacy and adherence, real-time modification of treatments and early alerts for problems that require intervention, although all of these interventions need to be rigorously tested 150 .
The European Kidney Health Alliance
The European Kidney Health Alliance (EKHA) is a non-governmental organization based in Brussels, Belgium, which advocates for kidney patients and the nephrology community at relevant bodies of the EU and also at European national organizations. The EKHA represents all of the major stakeholders in kidney care, including physicians, patients, nurses and foundations. The actions of the EKHA are supported by a dedicated group of Members of European Parliament. Of note, according to the treaty of Lisbon 151 , health-care systems are the responsibility of the national authorities of EU countries, which limits the role of the European Commission to one of complementing national policies and fostering cooperation. The EKHA has undertaken several initiatives in the area of kidney care, mainly focusing on measures to decrease the costs of kidney care while maintaining quality of care and access for all appropriate candidates, and to reduce demand for dialysis by promoting efforts to prevent the progression of kidney disease, and encouraging kidney transplantation as the KRT of choice 66 , 152 . In 2021, the EKHA will focus on reimbursement strategies and access to KRT, especially home haemodialysis.
The Nephrology and Public Policy Committee is a similar initiative created by the European Renal Association–European Dialysis and Transplant Association (ERA–EDTA). This committee aims to translate important kidney-related clinical topics into public policy, including the search for novel biomarkers of CKD, improving transition between paediatric and adult nephrology, and improving collaboration between the ERA-EDTA Registry and the guidance body of the ERA-EDTA, European Renal Best Practice 153 .
Beating Kidney Disease
Together with the Dutch Federation for Nephrology and the Dutch Kidney Patients Association, the DKF has initiated a strategic agenda for research and innovation in the Netherlands. This initiative, called Beating Kidney Disease (Nierziekte de Baas) will promote four specific research areas 154 : prevention of kidney failure, including root causes such as other chronic diseases; personalized medicine including genome and big data analyses, and studies of rare diseases; patient-centred outcomes and quality of life, transplantation and home haemodialysis; and regenerative medicine including bio-artificial kidneys. In collaboration with the EKHA, the Beating Kidney Disease initiative will be proposed as a framework for future initiatives at the Directorate General for Health and Food Safety of the European Commission, and the European Commissioner of Health. Similar to European initiatives that have promoted transplantation 152 , 155 , 156 , these efforts will emphasize shifts in policy action to strengthen institutional frameworks, improve education, training and information, optimize registries, and ensure appropriate benchmarking in nephrology.
Conclusions
The past 50 years have seen rapid changes in how and to whom dialysis is provided. From a global perspective, the escalating numbers of patients who require dialysis mean that even current costs are not sustainable, and yet most people who develop kidney failure forego treatment owing to a lack of access, with millions of lives lost every year as a consequence. Also important, the limitations of current dialysis treatment in alleviating patient suffering, morbidity and mortality are now viewed as unacceptable. Consequently, patients, payors, regulators and health-care systems are increasingly demanding improved value, which can only come about through true patient-centred innovation that supports high-quality, high-value care. Substantial efforts are now underway to support requisite transformative changes. These efforts need to be catalysed, promoted and fostered through international collaboration and harmonization to ensure that in the future, people living with kidney failure have more and better treatment options than exist today.
Peitzman, S. J. Chronic dialysis and dialysis doctors in the United States: a nephrologist-historian’s perspective. Semin. Dial. 14 , 200–208 (2001).
Article CAS PubMed Google Scholar
Brescia, M. J., Cimino, J. E., Appel, K. & Hurwich, B. J. Chronic hemodialysis using venipuncture and a surgically created arteriovenous fistula. N. Engl. J. Med. 275 , 1089–1092 (1966).
Blagg, C. R. The early history of dialysis for chronic renal failure in the United States: a view from Seattle. Am. J. Kidney Dis. 49 , 482–496 (2007).
Article PubMed Google Scholar
Scribner, B. H. Ethical problems of using artificial organs to sustain human life. Trans. Am. Soc. Artif. Intern. Organs 10 , 209–212 (1964).
CAS PubMed Google Scholar
Blagg, D. C. R. From Miracle to Mainstream: Creating the World’s First Dialysis Organization (Northwest Kidney Centers, 2017).
Himmelfarb, J., Berns, A., Szczech, L. & Wesson, D. Cost, quality, and value: the changing political economy of dialysis care. J. Am. Soc. Nephrol. 18 , 2021–2027 (2007).
KDIGO. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 3 , 163 (2013).
Google Scholar
Hole, B. et al. Supportive care for end-stage kidney disease: an integral part of kidney services across a range of income settings around the world. Kidney Int. Suppl. 10 , e86–e94 (2020).
Article Google Scholar
Bikbov, B. et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 395 , 709–733 (2020).
Liyanage, T. et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet 385 , 1975–1982 (2015).
Tonelli, M. et al. Framework for establishing integrated kidney care programs in low- and middle-income countries. Kidney Int. Suppl. 10 , e19–e23 (2020).
Pecoits-Filho, R. et al. Capturing and monitoring global differences in untreated and treated end-stage kidney disease, kidney replacement therapy modality, and outcomes. Kidney Int. Suppl. 10 , e3–e9 (2020).
Bello A. K. L. et al. Global Kidney Health Atlas: a report by the International Society of Nephrology on the current state of organization and structures for kidney care across the globe. https://www.kidneycareuk.org/documents/52/ISN_Global_kidney_health_atlas.pdf (2017).
White, S. et al. How can we achieve global equity in provision of renal replacement therapy? Bull. World Health Organ. 86 , 229–237 (2008).
Article PubMed PubMed Central Google Scholar
Bello, A. K. et al. Status of care for end stage kidney disease in countries and regions worldwide: international cross sectional survey. BMJ 367 , l5873 (2019).
Luxardo, R. et al. The epidemiology of renal replacement therapy in two different parts of the world: the Latin American Dialysis and Transplant Registry versus the European Renal Association-European Dialysis and Transplant Association Registry. Rev. Panam. Salud Publica 42 , e87 (2018).
United States Renal Data System. Volume 2: ESRD in the United States https://www.usrds.org/2018/download/2018_Volume_2_ESRD_in_the_US.pdf (2018).
Jha, V. et al. The state of nephrology in South Asia. Kidney Int. 95 , 31–37 (2019).
Barsoum, R. S., Khalil, S. S. & Arogundade, F. A. Fifty years of dialysis in Africa: challenges and progress. Am. J. Kidney Dis. 65 , 502–512 (2015).
Bello, A. K. et al. Assessment of Global Kidney Health Care Status. JAMA 317 , 1864–1881 (2017).
Fresenius Medical Care. Annual Report 2018: Care and Live. https://www.freseniusmedicalcare.com/fileadmin/data/com/pdf/Media_Center/Publications/Annual_Reports/FME_Annual-Report_2018.pdf (2018).
United States Renal Data System. US Renal Data System 2019 Annual Data Report: epidemiology of kidney disease in the United States. https://www.usrds.org/2019/view/USRDS_2019_ES_final.pdf (2019).
Liu, F. X. et al. A global overview of the impact of peritoneal dialysis first or favored policies: an opinion. Perit. Dial. Int. 35 , 406–420 (2015).
Article CAS PubMed PubMed Central Google Scholar
Mehrotra, R. et al. Racial and ethnic disparities in use of and outcomes with home dialysis in the United States. J. Am. Soc. Nephrol. 27 , 2123–2134 (2016).
Li, P. K.-T. et al. Changes in the worldwide epidemiology of peritoneal dialysis. Nat. Rev. Nephrol. 13 , 90–103 (2017).
ANZDATA Registry. ANZDATA 42nd Annual Report 2019. https://www.anzdata.org.au/report/anzdata-42nd-annual-report-2019/ (2019).
Kramer, A. et al. The European Renal Association - European Dialysis and Transplant Association (ERA-EDTA) Registry annual report 2015: a summary. Clin. Kidney J. 11 , 108–122 (2018).
Anand, S., Bitton, A. & Gaziano, T. The gap between estimated incidence of end-stage renal disease and use of therapy. PLoS ONE 8 , e72860 (2013).
Modi, G. K. & Jha, V. The incidence of end-stage renal disease in India: a population-based study. Kidney Int. 70 , 2131–2133 (2006).
Robinson, B. M. et al. Factors affecting outcomes in patients reaching end-stage kidney disease worldwide: differences in access to renal replacement therapy, modality use, and haemodialysis practices. Lancet 388 , 294–306 (2016).
Antlanger, M. et al. Sex differences in kidney replacement therapy initiation and maintenance. Clin. J. Am. Soc. Nephrol. 14 , 1616 (2019).
Chan, K. E. et al. Early outcomes among those initiating chronic dialysis in the United States. Clin. J. Am. Soc. Nephro 6 , 2642–2649 (2011).
Article CAS Google Scholar
Thamer, M. et al. Predicting early death among elderly dialysis patients: development and validation of a risk score to assist shared decision making for dialysis initiation. Am. J. Kidney Dis. 66 , 1024–1032 (2015).
Garcia-Garcia, G. et al. Survival among patients with kidney failure in Jalisco, Mexico. J. Am. Soc. Nephrol. 18 , 1922–1927 (2007).
Foster, B. J., Mitsnefes, M. M., Dahhou, M., Zhang, X. & Laskin, B. L. Changes in excess mortality from end stage renal disease in the United States from 1995 to 2013. Clin. J. Am. Soc. Nephrol. 13 , 91–99 (2018).
Storey, B. C. et al. Declining comorbidity-adjusted mortality rates in English patients receiving maintenance renal replacement therapy. Kidney Int. 93 , 1165–1174 (2018).
Fenton, S. S. et al. Hemodialysis versus peritoneal dialysis: a comparison of adjusted mortality rates. Am. J. Kidney Dis. 30 , 334–342 (1997).
Vonesh, E. F., Snyder, J. J., Foley, R. N. & Collins, A. J. The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney Int. 66 , 2389–2401 (2004).
Mehrotra, R., Chiu, Y. W., Kalantar-Zadeh, K., Bargman, J. & Vonesh, E. Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Arch. Intern. Med. 171 , 110–118 (2011).
Mehrotra, R., Devuyst, O., Davies, S. J. & Johnson, D. W. The current state of peritoneal dialysis. J. Am. Soc. Nephrol. 27 , 3238–3252 (2016).
Mehrotra, R. et al. Chronic peritoneal dialysis in the United States: declining utilization despite improving outcomes. J. Am. Soc. Nephrol. 18 , 2781–2788 (2007).
Modi, Z. J. et al. Risk of cardiovascular disease and mortality in young adults with end-stage renal disease: an analysis of the us renal data system. JAMA Cardiol. 4 , 353–362 (2019).
Wetmore, J. B. et al. Insights from the 2016 peer kidney care initiative report: still a ways to go to improve care for dialysis patients. Am. J. Kidney Dis. 71 , 123–132 (2018).
Skov Dalgaard, L. et al. Risk and prognosis of bloodstream infections among patients on chronic hemodialysis: a population-based cohort study. PLoS One 10 , e0124547 (2015).
Article PubMed PubMed Central CAS Google Scholar
Nelveg-Kristensen, K. E., Laier, G. H. & Heaf, J. G. Risk of death after first-time blood stream infection in incident dialysis patients with specific consideration on vascular access and comorbidity. BMC Infect. Dis. 18 , 688 (2018).
Chaudry, M. S. et al. Risk of infective endocarditis in patients with end stage renal disease. Clin. J. Am. Soc. Nephrol. 12 , 1814–1822 (2017).
Pruthi, R., Steenkamp, R. & Feest, T. UK renal registry 16th annual report: chapter 8 survival and cause of death of UK adult patients on renal replacement therapy in 2012: national and centre-specific analyses. Nephron. Clin. Pract. 125 , 139–169 (2013).
Kucirka, L. M. et al. Association of race and age with survival among patients undergoing dialysis. JAMA 306 , 620–626 (2011).
CAS PubMed PubMed Central Google Scholar
van den Beukel, T. O. et al. The role of psychosocial factors in ethnic differences in survival on dialysis in The Netherlands. Nephrol. Dial. Transpl. 27 , 2472–2479 (2012).
Depner, T. et al. Dialysis dose and the effect of gender and body size on outcome in the HEMO study. Kidney Ing. 65 , 1386–1394 (2004).
Villar, E., Remontet, L., Labeeuw, M. & Ecochard, R. Effect of age, gender, and diabetes on excess death in end-stage renal failure. J. Am. Soc. Nephrol. 18 , 2125–2134 (2007).
Hecking, M. et al. Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: the dialysis outcomes and practice patterns study (DOPPS). PLoS Med. 11 , e1001750 (2014).
Erickson, K. F., Zhao, B., Ho, V. & Winkelmayer, W. C. Employment among patients starting dialysis in the United States. Clin. J. Am. Soc. Nephrol. 13 , 265–273 (2018).
Kurella Tamura, M. et al. Functional status of elderly adults before and after initiation of dialysis. N. Eng. J. Med. 361 , 1539–1547 (2009).
Daratha, K. B. et al. Risks of subsequent hospitalization and death in patients with kidney disease. Clin. J. Am. Soc. Nephrol. 7 , 409–416 (2012).
Davison, S. N. & Jhangri, G. S. Impact of pain and symptom burden on the health-related quality of life of hemodialysis patients. J. Pain. Symptom Manage. 39 , 477–485 (2010).
Eneanya, N. D. et al. Longitudinal patterns of health-related quality of life and dialysis modality: a national cohort study. BMC Nephrol. 20 , 7 (2019).
Ju, A. et al. Patient-reported outcome measures for fatigue in patients on hemodialysis: a systematic review. Am. J. Kidney Dis. 71 , 327–343 (2018).
Rhee, E. P. et al. Prevalence and persistence of uremic symptoms in incident dialysis patients. Kidney360 1 , 86–92 (2020).
Kimmel, P. L. & Peterson, R. A. Depression in patients with end-stage renal disease treated with dialysis: has the time to treat arrived? Clin. J. Am. Soc. Nephrol. 1 , 349–352 (2006).
Burnier, M., Pruijm, M., Wuerzner, G. & Santschi, V. Drug adherence in chronic kidney diseases and dialysis. Nephrol. Dial. Transpl. 30 , 39–44 (2015).
Viecelli, A. K. et al. Identifying critically important vascular access outcomes for trials in haemodialysis: an international survey with patients, caregivers and health professionals. Nephrol. Dial. Transpl. 35 , 657–668 (2020).
Ceretta, M. L. et al. Changes in co-morbidity pattern in patients starting renal replacement therapy in Europe-data from the ERA-EDTA registry. Nephrol. Dial. Transpl. 33 , 1794–1804 (2018).
Vanholder, R. et al. Reimbursement of dialysis: a comparison of seven countries. J. Am. Soc. Nephrol. 23 , 1291–1298 (2012).
Winkelmayer, W. C., Weinstein, M. C., Mittleman, M. A., Glynn, R. J. & Pliskin, J. S. Health economic evaluations: the special case of end-stage renal disease treatment. Med. Decis. Mak. 22 , 417–430 (2002).
Vanholder, R. et al. Reducing the costs of chronic kidney disease while delivering quality health care: a call to action. Nat. Rev. Nephrol. 13 , 393–409 (2017).
Klarenbach, S. & Manns, B. Economic evaluation of dialysis therapies. Semin. Nephrol. 29 , 524–532 (2009).
van der Tol, A., Lameire, N., Morton, R. L., Van Biesen, W. & Vanholder, R. An international analysis of dialysis services reimbursement. Clin. J. Am. Soc. Nephrol. 14 , 84–93 (2019).
Beaudry, A. et al. Cost of dialysis therapy by modality in Manitoba. Clin. J. Am. Soc. Nephrol. 13 , 1197–1203 (2018).
Golper, T. A. The possible impact of the US prospective payment system (“bundle”) on the growth of peritoneal dialysis. Perit. Dial. Int. 33 , 596–599 (2013).
Lin, E. et al. Home dialysis in the prospective payment system era. J. Am. Soc. Nephrol. 28 , 2993–3004 (2017).
Shen, J. I. et al. Expanded prospective payment system and use of and outcomes with home dialysis by race and ethnicity in the United States. Clin. J. Am. Soc. Nephrol. 14 , 1200–1212 (2019).
Wang, V. et al. Medicare’s new prospective payment system on facility provision of peritoneal dialysis. Clin. J. Am. Soc. Nephrol. 13 , 1833–1841 (2018).
Swanepoel, C. R., Wearne, N. & Okpechi, I. G. Nephrology in Africa–not yet uhuru. Nat. Rev. Nephrol. 9 , 610–622 (2013).
Wang, V., Vilme, H., Maciejewski, M. L. & Boulware, L. E. The economic burden of chronic kidney disease and end-stage renal disease. Semin. Nephrol. 36 , 319–330 (2016).
Martin, D. E. et al. A call for professional collaboration to address ethical challenges in nephrology. Nat Rev Nephrol. https://doi.org/10.1038/s41581-020-0295-4 (2020).
Harris, D. C. H. et al. Increasing access to integrated ESKD care as part of universal health coverage. Kidney Int. 95 , S1–S33 (2019).
Rodriguez, R. A. Dialysis for undocumented immigrants in the United States. Adv. Chronic Kidney Dis. 22 , 60–65 (2015).
Saunders, M. R., Lee, H., Maene, C., Schuble, T. & Cagney, K. A. Proximity does not equal access: racial disparities in access to high quality dialysis facilities. J. Racial Ethn. Health Disparities 1 , 291–299 (2014).
Shaikh, M. et al. Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int. 94 , 440–445 (2018).
Ladin, K. & Smith, A. K. Active medical management for patients with advanced kidney disease. JAMA Intern. Med. 179 , 313–315 (2019).
Boulware, L. E., Wang, V. & Powe, N. R. Improving access to kidney transplantation: business as usual or new ways of doing business? JAMA 322 , 931–933 (2019).
Van Biesen, W., van der Veer, S. N., Murphey, M., Loblova, O. & Davies, S. Patients’ perceptions of information and education for renal replacement therapy: an independent survey by the European Kidney Patients’ Federation on information and support on renal replacement therapy. PLoS ONE 9 , e103914 (2014).
Mehrotra, R., Marsh, D., Vonesh, E., Peters, V. & Nissenson, A. Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. Kidney Int. 68 , 378–390 (2005).
Taylor, D. M. et al. A systematic review of the prevalence and associations of limited health literacy in CKD. Clin. J. Am. Soc. Nephrol. 12 , 1070–1084 (2017).
Vanholder, R., Van Biesen, W. & Lameire, N. Renal replacement therapy: how can we contain the costs? Lancet 383 , 1783–1785 (2014).
Moss, A. H. Revised dialysis clinical practice guideline promotes more informed decision-making. Clin. J. Am. Soc. Nephrol. 5 , 2380–2383 (2010).
Williams, A. W. et al. Critical and honest conversations: the evidence behind the “Choosing Wisely” campaign recommendations by the American Society of Nephrology. Clin. J. Am. Soc. Nephrol. 7 , 1664–1672 (2012).
Rinehart, A. Beyond the futility argument: the fair process approach and time-limited trials for managing dialysis conflict. Clin. J. Am. Soc. Nephrol. 8 , 2000–2006 (2013).
Ladin, K. et al. Characterizing approaches to dialysis decision making with older adults: a qualitative study of nephrologists. Clin. J. Am. Soc. Nephrol. 13 , 1188–1196 (2018).
Luyckx, V. A. et al. Developing the ethical framework of end-stage kidney disease care: from practice to policy. Kidney Int. Suppl. 10 , e72–e77 (2020).
Davison, S. N., Jhangri, G. S. & Johnson, J. A. Cross-sectional validity of a modified Edmonton symptom assessment system in dialysis patients: a simple assessment of symptom burden. Kidney Int. 69 , 1621–1625 (2006).
Weisbord, S. D. et al. Renal provider recognition of symptoms in patients on maintenance hemodialysis. Clin. J. Am. Soc. Nephrol. 2 , 960–967 (2007).
Eknoyan, G. et al. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N. Engl. J. Med. 347 , 2010–2019 (2002).
Paniagua, R. et al. Effects of increased peritoneal clearances on mortality rates in peritoneal dialysis: ADEMEX, a prospective, randomized, controlled trial. J. Am. Soc. Nephrol. 13 , 1307–1320 (2002).
Locatelli, F. et al. Effect of membrane permeability on survival of hemodialysis patients. J. Am. Soc. Nephrol. 20 , 645–654 (2009).
Group, F. H. N. T. et al. In-center hemodialysis six times per week versus three times per week. N. Engl. J. Med. 363 , 2287–2300 (2010).
Rocco, M. V. et al. The effects of frequent nocturnal home hemodialysis: the frequent hemodialysis network nocturnal trial. Kidney Int. 80 , 1080–1091 (2011).
Grooteman, M. P. C. et al. Effect of online hemodiafiltration on all-cause mortality and cardiovascular outcomes. J. Am. Soc. Nephrol. 23 , 1087 (2012).
Farrington, K. & Davenport, A. The ESHOL study: hemodiafiltration improves survival - but how? Kidney Int. 83 , 979–981 (2013).
Maduell, F. et al. High-efficiency postdilution online hemodiafiltration reduces all-cause mortality in hemodialysis patients. J. Am. Soc. Nephrol. 24 , 487 (2013).
Besarab, A. et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N. Engl. J. Med. 339 , 584–590 (1998).
Suki, W. N. et al. Effects of sevelamer and calcium-based phosphate binders on mortality in hemodialysis patients. Kidney Int. 72 , 1130–1137 (2007).
Wanner, C. et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N. Engl. J. Med. 353 , 238–248 (2005).
Fellstrom, B. C. et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N. Engl. J. Med. 360 , 1395–1407 (2009).
Baigent, C. et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet 377 , 2181–2192 (2011).
Abdel-Kader, K., Unruh, M. L. & Weisbord, S. D. Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin. J. Am. Soc. Nephrol. 4 , 1057–1064 (2009).
Mehrotra, R., Berman, N., Alistwani, A. & Kopple, J. D. Improvement of nutritional status after initiation of maintenance hemodialysis. Am. J. Kidney Dis. 40 , 133–142 (2002).
Pupim, L. B. et al. Improvement in nutritional parameters after initiation of chronic hemodialysis. Am. J. Kidney Dis. 40 , 143–151 (2002).
Rivara, M. B. et al. Changes in symptom burden and physical performance with initiation of dialysis in patients with chronic kidney disease. Hemodial. Int. 19 , 147–150 (2015).
Flythe, J. E. et al. Symptom prioritization among adults receiving in-center hemodialysis: a mixed methods study. Clin. J. Am. Soc. Nephrol. 13 , 735–745 (2018).
Tong, A. et al. Establishing core outcome domains in hemodialysis: report of the standardized outcomes in nephrology-hemodialysis (SONG-HD) consensus workshop. Am. J. Kidney Dis. 69 , 97–107 (2017).
Evangelidis, N. et al. Developing a set of core outcomes for trials in hemodialysis: an international Delphi survey. Am. J. Kidney Dis. 70 , 464–475 (2017).
Urquhart-Secord, R. et al. Patient and caregiver priorities for outcomes in hemodialysis: an international nominal group technique study. Am. J. Kidney Dis. 68 , 444–454 (2016).
Manera, K. E. et al. Patient and caregiver priorities for outcomes in peritoneal dialysis: multinational nominal group technique study. Clin. J. Am. Soc. Nephrol. 14 , 74–83 (2019).
Manera, K. E. et al. An international Delphi survey helped develop consensus-based core outcome domains for trials in peritoneal dialysis. Kidney Int. 96 , 699–710 (2019).
Duarte, P. S., Miyazaki, M. C., Blay, S. L. & Sesso, R. Cognitive-behavioral group therapy is an effective treatment for major depression in hemodialysis patients. Kidney Int. 76 , 414–421 (2009).
Taraz, M. et al. Sertraline decreases serum level of interleukin-6 (IL-6) in hemodialysis patients with depression: results of a randomized double-blind, placebo-controlled clinical trial. Int. Immunopharmacol. 17 , 917–923 (2013).
Cukor, D. et al. Psychosocial intervention improves depression, quality of life, and fluid adherence in hemodialysis. J. Am. Soc. Nephrol. 25 , 196–206 (2014).
Friedli, K. et al. Sertraline versus placebo in patients with major depressive disorder undergoing hemodialysis: a randomized, controlled feasibility trial. Clin. J. Am. Soc. Nephrol. 12 , 280–286 (2017).
Mehrotra, R. et al. Comparative efficacy of therapies for treatment of depression for patients undergoing maintenance hemodialysis: a randomized clinical trial. Ann. Intern. Med. 170 , 369–379 (2019).
Mendu, M. L. et al. Measuring quality in kidney care: an evaluation of existing quality metrics and approach to facilitating improvements in care delivery. J. Am. Soc. Nephrol. 31 , 602–614 (2020).
Nair, D. & Wilson, F. P. Patient-reported outcome measures for adults with kidney disease: current measures, ongoing initiatives, and future opportunities for incorporation into patient-centered kidney care. Am. J. Kidney Dis. 74 , 791–802 (2019).
Himmelfarb, J. & Ratner, B. Wearable artificial kidney: problems, progress and prospects. Nat. Rev. Nephrol. in press [doi to be supplied]
Foo, M. W. Y. & Htay, H. Innovations in peritoneal dialysis. Nat. Rev. Nephrol. https://doi.org/10.1038/s41581-020-0283-8 (2020).
Agar, J. W. M. & Barraclough, K. A. Water use in dialysis: environmental considerations. Nat. Rev. Nephrol. https://doi.org/10.1038/s41581-020-0296-3 (2020).
Masereeuw, R. & Verhaar, M. C. Innovations in approaches to remove uraemic toxins. Nat. Rev. Nephrol. https://doi.org/10.1038/s41581-020-0299-0 (2020).
Geremia, I. & Stamatialis, D. Innovations in dialysis membranes for improved kidney replacement therapy. Nat. Rev. Nephrol. https://doi.org/10.1038/s41581-020-0293-6 (2020).
Gedney, N., Sipma, W. & Søndergaard, H. Innovations in dialysis: the user’s perspective. Nat. Rev. Nephrol. https://doi.org/10.1038/s41581-020-0292-7 (2020).
Wieringa, F. P., Sheldon, M. I. & Hidalgo-Simon, A. Regulatory approaches to stimulate innovative renal replacement therapies. Nat. Rev. Nephrol. https://doi.org/10.1038/s41581-020-0275-8 (2020).
Kidney Health Initiatve. Fostering Innovation in Fluid Management. https://khi.asn-online.org/uploads/KHI_InnovationsInFluidManagement.pdf (2019).
Flythe, J. E. et al. Fostering innovation in symptom management among hemodialysis patients. Clin. J. Am. Soc. Nephrol. 14 , 150 (2019).
Shenoy, S. et al. Clinical trial end points for hemodialysis vascular access. Clin. J. Am. Soc. Nephrol. 13 , 490 (2018).
Dember, L. M. et al. Pragmatic trials in maintenance dialysis: perspectives from the kidney health initiative. J. Am. Soc. Nephrol. 27 , 2955 (2016).
Canaud, B., Vienken, J., Ash, S. & Ward, R. A. Hemodiafiltration to address unmet medical needs ESKD patients. Clin. J. Am. Soc. Nephrol. 13 , 1435 (2018).
Trump, D. J. Executive Order on Advancing American Kidney Health. The White House https://www.whitehouse.gov/presidential-actions/executive-order-advancing-american-kidney-health/ (2019).
Kidney Health Initiative. Technology Roadmap for Innovative Approaches to Renal Replacement Therapy. https://www.asn-online.org/g/blast/files/KHI_RRT_Roadmap1.0_FINAL_102318_web.pdf (2018).
Tijink, M. S. L. et al. Mixed matrix membranes: a new asset for blood purification therapies. Blood Purif. 37 , 1–3 (2014).
Vijayan, A. & Boyce, J. M. 100% use of infection control procedures in hemodialysis facilities: call to action. Clin. J. Am. Soc. Nephrol. 13 , 671–673 (2018).
Wong, L. P. Achieving dialysis safety: the critical role of higher-functioning teams. Semin. Dial. 32 , 266–273 (2019).
Kliger, A. S. & Collins, A. J. Long overdue need to reduce infections with hemodialysis. Clin. J. Am. Soc. Nephrol. 12 , 1728–1729 (2017).
Kliger, A. S. Targeting zero infections in dialysis: new devices, yes, but also guidelines, checklists, and a culture of safety. J. Am. Soc. Nephrol. 29 , 1083–1084 (2018).
Collins, A. J. & Kliger, A. S. Urgent: stop preventable infections now. Clin. J. Am. Soc. Nephrol. 13 , 663–665 (2018).
The George Institute. World’s first affordable dialysis machine a finalist in 2017 Eureka Awards. https://www.georgeinstitute.org.au/media-releases/worlds-first-affordable-dialysis-machine-a-finalist-in-2017-eureka-awards (2017).
Institute for Healthcare Improvement. A patient directs his own care. http://www.ihi.org/resources/Pages/ImprovementStories/APatientDirectsHisOwnCareFarmanSelfDialysis.aspx (2020).
Shinkman, R. Is “empowered dialysis” the key to better outcomes? NEJM Catalyst Carryover https://doi.org/10.1056/CAT.18.0232 (2018).
Nayak, K. S., Ronco, C., Karopadi, A. N. & Rosner, M. H. Telemedicine and remote monitoring: supporting the patient on peritoneal dialysis. Perit. Dial. Int. 36 , 362–366 (2016).
Rohatgi, R., Ross, M. J. & Majoni, S. W. Telenephrology: current perspectives and future directions. Kidney Int. 92 , 1328–1333 (2017).
Lew, S. Q. & Sikka, N. Operationalizing telehealth for home dialysis patients in the United States. Am. J. Kidney Dis. 74 , 95–100 (2019).
Bieber, S. D. & Gadegbeku, C. A. A call to action for the kidney community: nephrologists’ perspective on advancing American kidney health. Clin. J. Am. Soc. Nephrol. 14 , 1799–1801 (2019).
Foundation for EU democracy. Consolidated Reader-Friendly Edition of the Treaty on European Union (TEU) and the Treaty on the Functioning of the European Union (TFEU) as amended by the Treaty of Lisbon (2007) Third edition. http://en.euabc.com/upload/books/lisbon-treaty-3edition.pdf (2009).
European Kidney Health Alliance. Thematic Network on Improving Organ Donation and Transplantation in the EU 2019. http://ekha.eu/wp-content/uploads/FINAL_Joint-Statement-of-the-Thematic-Network-on-Organ-Donation-and-Transplantation.pdf (2019).
Massy, Z. A. et al. Nephrology and public policy committee propositions to stimulate research collaboration in adults and children in Europe. Nephrol. Dial. Transpl. 34 , 1469–1480 (2019).
Beating kidney disease. A joint agenda for research and innovation. https://www.nierstichting.nl/media/filer_public/4d/6d/4d6d6b4e-ce56-4a4b-8ba2-f5ac957d0df8/beating_kidney_disease_-_joint_agenda_for_ri_june_2018.pdf (2018).
Matesanz, R., Marazuela, R., Coll, E., Mahillo, B. & Dominguez-Gil, B. About the Opt-Out system, live transplantation, and information to the public on organ donation in Spain… Y ole! Am. J. Transpl. 17 , 1695–1696 (2017).
Zivcic-Cosic, S. et al. Development of the Croatian model of organ donation and transplantation. Croat. Med. J. 54 , 65–70 (2013).
Download references
Author information
Authors and affiliations.
Kidney Research Institute, Seattle, WA, USA
Jonathan Himmelfarb & Rajnish Mehrotra
Division of Nephrology, Department of Medicine, University of Washington, Seattle, WA, USA
Nephrology Section, Department of Internal Medicine and Pediatrics, University Hospital, Ghent, Belgium and European Kidney Health Alliance (EKHA), Brussels, Belgium
Raymond Vanholder
Division of Nephrology, Department of Medicine, University of Calgary, Calgary, Alberta, Canada
Marcello Tonelli
You can also search for this author in PubMed Google Scholar
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Correspondence to Jonathan Himmelfarb .
Ethics declarations
Competing interests.
J.H. declares that The Kidney Research Institute and the Center for Dialysis Innovation at the University of Washington, which he directs, has received gift and grant support from the Northwest Kidney Centers, a not-for-profit dialysis provider. The Center for Dialysis Innovation has also received a Phase I prize from KidneyX, and a grant from the Veterans Administration. J.H. is also a founder and holds equity in AKTIV-X Technologies, Inc. R.V. has consulted for Baxter Healthcare, B. Braun and Neokidney. R.M. has received an honorarium from Baxter Healthcare and serves as a member of the Board of Trustees of the Northwest Kidney Centers. M.T. has received a lecture fee from B. Braun, which was donated to charity.
Additional information
Peer review information.
Nature Reviews Nephrology thanks M. Verhaar, who co-reviewed with M. van Gelder, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Affordable Dialysis Prize: https://www.dialysisprize.org/
Dutch Kidney Foundation: https://www.narcis.nl/organisation/RecordID/ORG1238896/Language/en
ESRD Data Standard Project: https://khi.asn-online.org/projects/project.aspx?ID=78
European Kidney Health Alliance: http://ekha.eu/
Kidney Health Initiative: https://khi.asn-online.org/
KidneyX: https://www.kidneyx.org/
Neokidney: https://www.nextkidney.com/
Nephrologists Transforming Hemodialysis Safety: https://www.asn-online.org/ntds/
Nephrology and Public Policy Committee: https://www.era-edta.org/en/nppc/
Nierstichting Nederland: https://nierstichting.nl/
Patient and Family Partnership Council: https://khi.asn-online.org/pages/?ID=1
SONG-HD: https://songinitiative.org/projects/song-hd/
SONG-PD : https://songinitiative.org/projects/song-pd/
Standardizing Outcomes in Nephrology Group (SONG): https://songinitiative.org/
The total ‘real’ price of a given treatment, including the amount paid by the individual and the amount paid by society.
The ratio of the cost of the intervention compared with a relevant measure of its effect.
The share of treatment cost paid by society; that is, by government or insurers.
Money paid by governments or insurers to health-care providers for money spent on treatment.
The value of everything produced in that country at the prices prevailing in that country, usually expressed as gross domestic product.
The maximum price at or below which a society is prepared to buy a product.
The monetary value of all finished goods and services made within a country during a specific period.
Total amount of money spent by government on health care.
Engineers who design systems, devices, software and tools to fit human capabilities and limitations.
A communication method where the message is placed in a queue, and can be processed at a later time point.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Himmelfarb, J., Vanholder, R., Mehrotra, R. et al. The current and future landscape of dialysis. Nat Rev Nephrol 16 , 573–585 (2020). https://doi.org/10.1038/s41581-020-0315-4
Download citation
Accepted : 19 June 2020
Published : 30 July 2020
Issue Date : October 2020
DOI : https://doi.org/10.1038/s41581-020-0315-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Lipid parameters, adipose tissue distribution and prognosis prediction in chronic kidney disease patients.
- Hui-fen Chen
- Bing-jie Xiao
Lipids in Health and Disease (2024)
Renal rehabilitation learning in Japanese physical therapy schools: a fact-finding study
- Toshiki Kutsuna
- Yuhei Otobe
- Ryota Matsuzawa
Renal Replacement Therapy (2024)
The disruptor of telomeric silencing 1-like (DOT1L) promotes peritoneal fibrosis through the upregulation and activation of protein tyrosine kinases
- Yingfeng Shi
Molecular Biomedicine (2024)
The Intersectoral Coordination Unit for the Sustainable Intensification of Peritoneal Dialysis in Schleswig–Holstein (SKIP-SH) cohort study
- Hauke S. Wülfrath
- Thorben Schrumpf
- Benedikt Kolbrink
BMC Nephrology (2024)
Quality of life and nutritional status in peritoneal dialysis patients: a cross-sectional study from Palestine
- Dania Haddad
- Inad Nawajah
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 21 May 2024
Exploring the factors influencing evidence-based approaches to advanced chronic kidney disease: a qualitative study involving nurses and physicians
- Elena Pintado-Outumuro 1 , 4 ,
- Victoria Morin-Fraile 2 , 5 ,
- Betlem Salvador-González 3 , 4 ,
- Llúcia Benito 6 , 7 ,
- Maricel Julve-Ibáñez 8 ,
- M.-Pilar Sancho-Campos 9 ,
- Carolina Alves-Tafur 10 &
- Iris Lumillo-Gutiérrez 2 , 4 , 5 , 11
BMC Primary Care volume 25 , Article number: 177 ( 2024 ) Cite this article
255 Accesses
1 Altmetric
Metrics details
Advanced chronic kidney disease (ACKD) is associated with a high risk of adverse cardiovascular and renal events and has a significant impact on quality of life and life expectancy. Several studies have identified areas for improvement in their management in primary care. Some professional and environmental factors can act as key barriers to appropriate care.
To analyse attitudes, subjective norms, and perceived behavioural control among primary care professionals related to the implementation of an evidence-based approach for individuals with ACKD in primary care.
Methodology
This was a qualitative study using an interpretative phenomenological approach based on the theory of planned behaviour. Two aspects of the evidence-based approach were explored: the implementation of clinical practice guidelines and the utilisation of electronic kidney disease records within the scope of this study. Primary care nurses and physicians participated in a previous pilot interview and five focus groups. Subsequently, a thematic analysis of the gathered data was conducted.
Thirty-three primary care professionals participated. The emerging themes included: experiences in the management of ACKD (highlighting a distinct profile of older, frail patients with comorbidities masking CKD and a CKD follow-up primarily focused on analytical monitoring and drug adjustment); factors in the professional environment influencing the use of scientific evidence (such as time constraints, excessive electronic health records, and unfamiliar reference guidelines); attitudes towards the application of recommendations on ACKD (recognising limitations of computer systems despite considering them as guidance); and capacities to implement evidence-based recommendations (acknowledging formative needs and challenges in coordinating care with nephrology services).
Conclusions
Several psychological elements identified through the TBP hinder the adequate implementation of an evidence-based approach for individuals with CKD. Attitudes have been identified as factors modulating the use of standardised electronic records. Instead, subjective norms (influences from the professional environment) and perceived behavioral control (perception of capabilities) acted as barriers to the proper application of clinical practice guidelines and standardised records.
Implications for practice
Strategies aimed at optimising the management of people with ACKD should focus not only on training but also on improving attitudes, organisational structures, IT systems and coordination between primary care and nephrology.
Peer Review reports
Chronic kidney disease (CKD) is a major public health problem. The global prevalence of CKD is estimated to be 13% [ 1 ]. Advanced chronic kidney disease (ACKD) comprises individuals with an estimated glomerular filtration rate less than 30 ml/min/1.63 m2 and includes stages G4 and G5 [ 2 ]. It accounts for < 5% of all CKD cases but is associated with a very high risk of adverse cardiovascular and renal events and has a significant impact on quality of life and life expectancy [ 1 , 3 ]. The global mission of the Kidney Disease Improving Global Outcomes (KDIGO) Initiative is to improve the care and health outcomes of people with CKD by promoting coordination, collaboration, and integration of initiatives, while the goals of the International Society of Nephrology are to raise awareness, promote preventive measures, educate professionals in CKD screening, and reduce risk [ 4 ]. These guidelines are the framework of care used by local nephrology societies to promote clinical recommendations to patients in primary care [ 5 , 6 , 7 ]. Currently, the management of ACKD is predominantly performed in the hospital setting. The prevalence of CKD is increasing in association with obesity, diabetes mellitus and aging [ 8 ], and consequently, the number of patients with ACKD will also increase. ACKD is frequently associated with high comorbidity, complexity, and frailty, and approximately one-third of ACKD patients who reach the G5 stage in primary care are not treated with renal replacement therapy [ 9 ]. This percentage is even greater for older individuals. Therefore, the expected increase in the number of ACKD patients will require greater involvement of primary care in its management [ 8 ]. Primary care professionals are in a privileged position to provide care from the earliest to the most advanced stages, especially in the group of elderly people without renal replacement therapy. However, the primary care approach still has room for improvement [ 7 , 10 , 11 , 12 , 13 ]. CKD management, including diagnosis, prognosis evaluation, monitoring, and risk factor control, can improve [ 14 ]. Although the prevalence of CKD is considerable, a large percentage of people with CKD who have improved are unaware that they have CKD, possibly due to a lack of awareness and limited capacity of primary care professionals to adequately identify and treat people with CKD [ 15 ].
Context-specific implementation strategies are necessary to optimise the utilisation of scientific evidence. Moreover, research highlights the need to develop standardised care programmes to improve the quality of care for people with ACKD. Indeed, integration into a model comparable to that of people with other diseases would bring similar benefits [ 10 ]. Standardised follow-up programs could support the clinical practice of primary care professionals [ 12 ] and enhance their evidence base [ 16 ]. However, the literature suggests that standardised records are not widely used [ 17 ], mainly because of barriers in the care setting [ 18 , 19 ]. The attitudes of professionals play a key role in the development of actions and therefore in the use of this evidence [ 20 ]. However, the implementation of clinical practice guideline recommendations and standardised monitoring systems is a complex process that goes beyond the attitudes of professionals [ 21 ]. Some scholars view a lack of knowledge and skills or organisational factors as barriers to implementation [ 22 ]. In fact, the Global Kidney Health Atlas notes that some of the barriers to achieving optimal kidney care include factors related to knowledge, attitudes, professional environment factors, and low disease awareness [ 23 ]. As such, knowledge, skills, and aspects of work organisation could be seen as shapers of the social norms and perceived behavioural control described by some psychological theories, such as the theory of planned behaviour (TPB) [ 20 ]. The TPB is among the most suitable for elucidating and forecasting human behaviour because it pertains to decision-making. According to this theory, behaviour is shaped by a behavioural intention, which, in turn, is influenced by an individual’s attitude towards the behaviour, subjective norms, and perceived behavioural control. Attitude refers to the evaluative belief regarding the outcomes of engaging in a particular behaviour. Subjective norms represent the social pressure to conform to a specific course of action, while behavioural control encompasses one's capability to execute the perceived behaviour, influenced by preidentified obstacles and impediments [ 24 ]. As a general guideline, the more favourable the attitude and subjective norm are, and the greater the perceived behavioural control is, the stronger an individual's inclination to enact the contemplated behaviour [ 20 ].
Following this line of argument, to gain a deeper understanding of the factors that condition the evidence-based management of people with ACKD in primary care, we performed a qualitative study to explore the psychosocial elements that modulate such management according to the TPB. The aim of this study was to specifically analyse the attitudes, subjective norms, and perceived behavioural control of primary care professionals in managing individuals with ACKD within the primary care setting.
General description
This qualitative study was part of an exploratory mixed-methods study that will form the basis for the implementation of interventions to improve the management of people with ACKD in the Atenció Primària Metropolitana Sud, a primary care setting south of Barcelona. This area provides care to 1,370,709 people and has 9,196 professionals working in 61 primary care centres.
We used an interpretative phenomenological approach [ 25 , 26 ] in which experiences are investigated from the perspective of the individual [ 27 ]. Focus group accounts were collected from professionals regarding their attitudes, subjective norms, and behavioural control [ 20 ] in the management of people with ACKD. The recommended consolidated criteria for reporting qualitative research were followed [ 28 ].
The study was approved by the reference primary care Fundació Institut Universitari per la Recerca a l'Atenció Primària de Salut Jordi Gol i Gurina (IDIAPJGol) Clinical Research Ethics Committee (22/092-P).
Study participants
Participants were purposively selected from among nurses and physicians in the field. The project was presented at a general management meeting, and subsequently, an email was sent with further information. A meeting was arranged at those primary care centers that agreed to participate, and all professionals were invited to participate. The criteria for homogeneity were nurses and physicians working in the Atenció Primària Metropolitana Sud area. The criteria for heterogeneity included sex, professional profile, and level of clinical experience in the management of people with ACKD. We aimed to include various primary care professionals, including nurses and physicians, working in different capacities related to their experience in managing ACKD. This includes roles such as primary care consultation, chronicity profiles, or case manager nurses.
Data collection
The data were gathered between 1 October 2022 and 31 April 2023 from distinct focus groups of physicians and nurses and from mixed focus groups, aiming to acquire more comprehensive, pertinent, and diverse information relevant to the research query. We initially worked with the professional groups separately to extract maximum information regarding the specific interventions within their daily practice, as well as to identify the specific barriers unique to each profession. This approach aligns with phenomenological principles, wherein the central focus of the study is on the phenomena under examination [ 29 , 30 ]. Furthermore, standardised follow-up is more commonly conducted by nurses, while physicians tend to rely more on clinical practice guidelines. The mixed group aimed for heterogeneity according to discipline but homogeneity in terms of greater expertise in managing people with advanced chronic diseases. It consisted of physicians specialising in chronicity and nurses specialising in case management. These professionals dedicate more time to treating this profile of patients, and here, the aim was to complement experiences and opinions through the exchange of interventions and barriers and facilitators. We used a script outlining thematic areas derived from the theoretical constructs of the TBP to explore attitudes, subjective norms, and perceived behavioural control regarding the management of individuals with ACKD, as well as the implementation of evidence-based guidelines and standardised electronic records (Additional file 1). Narratives (EPO, ILG, VMF, and MJI) were audio-recorded and subsequently transcribed. Field notes were used during and after the interviews. The interviews, conducted either in Catalan or Spanish depending on the interviewee's preferred language at the time, were transcribed in their respective languages and subsequently translated by a certified translation company. The authors subsequently compared these translations to ensure the semantic accuracy of each phrase. The data were anonymised by assigning them a numerical code.
Data analysis
The interview data were analysed using thematic analysis procedures [ 31 ].
Initially, to obtain a condensed view of the information, the raw data were transformed into usable data by breaking down texts and establishing units of semantic meaning. Relevant data pertaining to the research question were systematically coded. Once all the data had been encoded and the entire dataset had been coded, the codes were grouped into potential subthemes. These subthemes were then integrated within the main themes identified in accordance with the TBP [ 20 ]. Subsequently, a review was conducted to assess the coherence of the themes with the coded extracts, ensuring sufficient and relevant data to demonstrate the prevalence of each theme related to the conditioning factors in the approach and use of scientific evidence on ACKD. This process was facilitated by a thematic map, aiding in understanding the relationships between the main themes, subthemes, and codes while applying criteria for internal homogeneity within each theme and external heterogeneity between themes [ 32 ]. Finally, the final themes and subthemes were defined and refined, and the report was prepared for thematic analysis of the data [ 31 ]. The coding and analysis were conducted by two researchers (ILG and EPO), who developed the thematic map, codebook, subtopics, and topics. A third researcher (VMF) was consulted during the analysis process to resolve any discrepancies in data interpretation [ 31 ]. The average interview duration was 55.3 min. The analysis was conducted concurrently with the interviews and continued until thematic saturation. The transcripts were returned to the participants for correction, and no comments were made. All the transcripts were entered into the qualitative analysis software Atlas.ti Web to assist with the data management and analysis. The authors did not employ generative artificial intelligence or AI-assisted technologies in any phase of this research or in its composition. The authors did not employ generative artificial intelligence or AI-assisted technologies in any phase of this research or in its composition.
Characteristics of the participants
Thirty-three primary care professionals (7 primary care nurse case managers, 14 primary care nurses, 6 family physicians, and 6 family physicians with expertise in complex chronicity) were interviewed in a pilot interview and 5 focus groups in four urban areas and one rural area until information saturation was reached. The average age and average years of professional experience were 46.8 and 19.6 years, respectively (Table 1 ). Different codes, subtopics ( n = 11) and topics ( n = 4) were obtained (Table 2 ). The topics were experiences in the management of ACKD (topic 1), factors in the professional environment that influence the use of evidence-based action recommendations (topic 2), attitudes toward the use of recommendations (topic 3), and perceived capacities to implement recommendations (topic 4).
Experiences in the management of ACKD
Profile of patients with ackd seen in primary care.
In primary care, the predominant profile of people with ACKD corresponds to elderly individuals with comorbidities. The most frequently mentioned were cardiovascular diseases, diabetes and hypertension. Furthermore, in all the focus groups, the associations between frailty and these comorbidities were highlighted.
“ What I normally see are old, fragile, complex patient s.” G01.2 Primary Care Nurse
Although less common, another profile of people with ACKD was identified—those who were younger and without frailty—who were mainly followed by hospital nephrology and were more disengaged from primary care for this reason.
“These filtration values ( < 30) do not pass through primary care because patients already spend enough time on their disease while on dialysis and have enough time to come for follow-up in primary care.” G02.8 Case Manager Nurse in Primary Care
A feature repeatedly mentioned is that people most commonly seen in primary care tend to have limited knowledge of their ACKD diagnosis, as opposed to those who require renal replacement therapy.
“In many cases, it may be our own fault for not having trained it well .” G04.3 Primary care nurse.
“They are not aware of advanced kidney disease (…). When they become aware, they make changes, if necessary at that point of the disease, in their lifestyles, diet,… ” G02.3 Case Manager Nurse in Primary Care.
Masked disease in primary care
In three of the five focus groups, we found stories highlighting that ACKD, both in its diagnosis and in its management in primary care, was masked by other diseases whose follow-up was prioritised over CKD.
“ However, this condition is not considered important for diabetes, hypertension or other (frequent) pathologies. In addition, it should be .” G01.2. Primary care nurse.
Therefore, the first step is to become aware of the disease they present, both professionals and patients and their families.
“ All of us have experienced the disease less, and therefore probably also convey this message less to patients. ” G02.9 Family physician with expertise in chronicity.
“ I also thought until now that the (ACKD patient) went (only) to the hospital. I swear.” G04.6 Primary care nurse.
The presence of comorbidities could play a dual role, acting as both a barrier and a facilitator.
On the one hand, three focus groups indicated that when there were numerous comorbidities, they prioritised other diseases over ACKD, which proved to be an obstacle. On the other hand, at times, it serves as a facilitator, as the disease or its progression is frequently detected during the follow-up of other comorbidities. The need to involve nursing input in the proactive follow-up of this population is met.
“ I think that in general, chronic kidney disease is seen as a consequence of other diseases and rarely occurs as an individual entity. ” G02.9 Family physician with expertise in chronicity.
“ I also believe that on many occasions, with the primary care structure, it is very clear to us that we have to attend to the hypertensive patient, the diabetic patient, the patient such as…and we treat it as such. However, we do not treat (for patients with CKD), we do not perform a blood test, or we do not provide specialised care if it is just kidney failure. It rarely appears in the consultation if you only have kidney failure. It may be difficult to find.” G04.3. Primary care nurse.
Clinical practices according to professional profile
In relation to the management of ACKD, the most important elements identified included the control of cardiovascular risk factors, regular blood and urine test follow-up, review and adjustment of prescribed medication, management of dietary habits and controls, social support and, in the final stages, decision making to ‘stop doing’, i.e., to reduce medical interventions and prioritise quality of life. However, the implementation barriers discussed throughout the study were also reported.
In terms of the nursing approach, health education predominated over lifestyle modification, suggesting on several occasions the importance of a low-sodium diet and strict water restriction, as well as interventions to measure anthropometric variables, vital signs and medication review (in all nursing focus groups). Caregiver support and intervention in the socioeconomic dimension also appeared, in contrast to the findings for the groups treated by physicians only. In terms of the approach taken by primary care physicians, in all of the focus groups reported, the main focus was on the review of nephrotoxic drugs, follow-up tests and the detection of complications. In contrast, in more specialised chronicity roles (G03.2, G03.5, G02.3, G02.6, and G02.7), such as case managers and chronicity physicians, aspects such as shared decision making, anticipation of possible complications arising from disease progression and 'stop doing' interventions predominated.
“The patient is the one who has to make decisions, right? It is a disease that will progress, and there will come a time when they will have to make important decisions such as dialysis, whether to do it or not, and I think that sometimes it is difficult to reach this point of view, whether they are primary care professionals, specialists, or the patient him/herself ” . G02.7 Case Manager Nurse in Primary Care.
Patient contextual factors
The common presence of multiple comorbidities often poses a challenge for professionals, hindering adherence to recommendations regarding medication, diet, and other lifestyle factors. For example, long lists of medicines can trigger adverse effects and poor adherence. In addition, older age, according to the perceptions of professionals, is a barrier to lifestyle change. Another difficulty that was strongly emphasised was the socioeconomic conditions that are undermined by the increased overall frailty of people with ACKD. These findings were evident in all the focus groups.
“ I mean, it is very difficult. When you see lists of medications and see the amount of things they cannot eat… Well, I do not know, it would be difficult for me. ” G06.3 Family physician.
“ They are chronic patients, and they are tired of their illness, so for a while they do it (the change of habits), but then you have to insist because…” G05.3 Primary care nurse.
Factors in the professional environment that influence the use of scientific evidence
Pressure from the care environment.
Limited time was identified as the primary barrier to seeking and implementing the recommended guidelines. Some professionals across four focus groups addressed this challenge by implementing time optimisation strategies and fostering teamwork. Specifically, physicians employed a wider range of strategies regarding clinical guidelines (e.g., consulting with colleagues G01.3 by storing reference guides in folders readily accessible for daily practice G03.5), while nurses concentrated on standardised electronic records (prioritising the disease with the poorest control, G05.8). Both groups observed that collaborative working helped alleviate pressure barriers in the work environment.
Another obstacle to the utilisation of specific CKD systematic records lies in the annual incentives for accessing general electronic records. These incentives encourage all primary care professionals to record other patient clinical variables that are not specific to ACKD. This resulted in family physicians (G01.3, G06.2, G06.3, G06,5) prioritising the recording of those nonspecific ACKD variables within a limited timeframe rather than the typical standardised monitoring variables that should be applied to CKD patients. Consequently, professionals reported recording variables that were not the most crucial and thus failed to deliver the care considered a priority.
“ They look at you; they take (data) pictures of things that are not important. (…) But, instead of focusing on significant matters, something different arises after taking the photo. ” G06.2 Family physician.
Excessive electronic records on a day-to-day basis
In the nursing focus groups (G04, G05, and the nurse case managers from G02), standardised care plans were seen to create surplus documentation when caring for individuals with multiple conditions, as each plan is tailored to address specific needs. This means that the clinical care of the individual requires the implementation of several plans, multiplying the records. This aspect was identified as a barrier to implementation. In fact, nurses who try to implement the care plan together with other plans for other diseases describe the recording situation as complicated, attributed to its terms such as "surviving" (G05.8) or "juggling" (G05.9) , due to the limited time available during the consultation with the patient.
“ The perception I have when we do things like this is that then it is like a mental breakdown of having to fill it all in. In addition, then you lose a little bit of focus, so if you look at it as something structural, it is fine because it will help me to control it, it will not slip away; I will keep an eye on it. However, the reality is that there are many more things because that is what it is: heart failure, I do not know what, I don't know how many… so I have the feeling that I lose the sense of direction a little bit between all the little things. ” G06.3 Family physician.
“ Yes, I understand that the objective is that everyone, all patients with advanced kidney disease receive quality care. But if we look at quality care for this, then I think we fall a little short. Obviously, this should be possible in some way, right? But… medicine and nursing are not data. There is data… ” G06.2 Family physician.
Implementation of clinical recommendations: poorly accessible and poorly known CKD clinical practice guidelines
It was often considered that there is more knowledge of other diseases that are more prevalent in primary care with respect to the reference guidelines of the hospital and primary care settings; therefore, they are applied with a certain cohesion between professionals in both settings. However, in relation to CKD and, specifically, ACKD, none of the participants in the study clearly identified the reference guidelines. Although some professionals were aware of some of the recommendations, they doubted that they were the same as those given by the reference nephrology services and therefore doubted whether a unified message was being given from the two areas.
“ There is no clear algorithm that gives you clear instructions. ” G04.4 Primary care nurse. “I don't see any pathway. I don't see anything, I mean, the feeling is that we are here in primary care and we are all out of date, and you are looking for a life with your colleagues because no one from there will come to give you any sessions ” G05.8 Primary Care nurse. “ There are many things that we do have, but kidney disease, as far as I know, no, there is none. ” G01.2 Primary care nurse case manager
As a proposal to improve this aspect, they reported that territorial care processes could contribute to improving and updating practices through recommendations in the guidelines (focus groups G03, G05, G06). This approach would make it easier to work in a more unified way at the territorial level, i.e., in primary and hospital care settings.
“ Yes, I think it is necessary to review and reinforce pathways to work all in the same direction” G05.2. Primary care nurse.
The lack of updating of care pathways, according to professionals, has contributed to the dilution of guidelines and pathways over time, resulting in a lack of knowledge about them. Integration into the computerised medical records platform was advocated, as had been done in the past for other pathologies. In a primary care context with significant variability in the reasons for consultation and care pressure, they considered that it is necessary to activate digital resources that facilitate access to the best available evidence in a simple way.
“ I think are not so easily accessible” G03.2. Family physician with expertise in chronicity.
Attitudes toward the implementation of the CKD recommendations
Standardised care plans for ckd that provide guidance for practice.
Some participating nurses highlighted that the use of these standardised electronic records in primary care carries controversial implications within the same team. While some nurses perceive them as burdensome and disconnected from day-to-day usefulness (G02.8, G04.6, G06.2), others view them as practical guidelines that establish the foundation for standardised care among professionals who utilise them, aiding in enhancing knowledge about the disease and its management (G01.2, G02.6, G04.5, G05.3, G06.5).
“ Sometimes, it's a tool (standardised plans) that, when I've used it and seen it over time, is fantastic because it provides access to a multitude of links that offer a wealth of information. However, the issue arises when this information often doesn’t have enough time to be conveyed to the patient. (…) There simply isn't enough time to accomplish all of that. But if you have the time, it's remarkable .”G05.7 Primary Care nurse. “ It would help to learn more about advanced chronic kidney disease ” G05.3 Primary care nurse.
Unhelpful standardised electronic care plans
There was an attitudinal barrier related to the belief that standardised care plans were not useful for sharing health information among colleagues. The professionals argued for two technical reasons. First, this information tended to be met with resistance from professionals who use and review it (G03,2, G02.8), primarily because of its format within the patient's medical records. It is often described as lacking clarity or personalisation to the patient's specific circumstances (G02,3, G02,7, G02.8).
“ I would say that I am now indignant because I think that the clinical assessment is detracting, because that is precisely what I am not interested in seeing (with this type of language). It is the least interesting for a patient with complex or advanced chronicity, it is the least informative for colleagues, and it also takes up space and time that makes no sense at all.” G02.8 Primary care nurse case manager.
The second reason they perceived standardised electronic records as being of little use was because, at present, in the shared medical records—accessed electronically from other healthcare settings and providers, such as hospitals—only some clinical follow-up data from primary care is visible, not all, as is the case with electronic records for conditions such as CKD. These are only accessible in the primary care setting and not in other hospital settings (G04,6, G02.4, G02.5, G02.6). Therefore, healthcare professionals opt to use alternative clinical records that are visible in shared medical records, even though they are not standardised electronic records for CKD patients. Knowing that important follow-up data entered into electronic CKD records will not be seen by other hospital colleagues who are involved in the care of these patients, such as nephrologists, leads professionals to choose other types of clinical records. This approach is relevant because, on many occasions, clinical information of interest to both parties is shared.
“ If you enter through the standardised care plan, no one else sees it, that is, we see it here in the centre, but not in the hospital ” G04.6 Primary care nurse
“ I’m following it but they cannot see the follow-up that we do, it is clear, it is as if it was not followed at all ” G02.5 Case Manager Nurse in Primary Care.
Capacities to implement evidence-based recommendations
Lack of training to implement the recommendations in practice.
Practitioners reported that the CKD care plan improves safety and guides practice. However, to optimise its use, they underlined the need to implement specific training strategies to enable its correct application. Team sessions on various clinical management topics are recognised as an important element in keeping professionals up to date and cohesive in the management of the population with chronic health conditions. However, in line with the masking of CKD with other diseases, this dynamic is also reflected in primary care team sessions (G02.3, G06.4) and nonexisting face-to-face consultations with nephrology professionals in the hospital setting (G03.2, G03.5), considering that nephrology services are distant from primary care (G02.4, G02.9, G06.3).
“I think that the nephrologist is a specialist far removed from primary care. Others do (face-to-face) consultations, endocrinologists, I don't know, and nephrologists are inaccessible. ” G02.4 Case Manager Nurse in Primary Care.
Another aspect related to the capacity for a specific approach to this disease is that, thus far, the primary care nurse has not been fully and proactively engaged in the overall follow-up of this patient profile. This lack of involvement does not allow for the teamwork that is essential for jointly addressing ACKD, as indicated in the recommendations.
“ Kidney failure at the nursing level is hardly followed up, if at all ” G02.6 Case Manager Nurse in Primary Care
Shared management and counselling in the follow-up of ACKD patients
A frequently encountered situation identified was the lack of professional meetings with specialists from the referral service, as well as the lack of two-way communication channels with them. This aspect, which was repeatedly mentioned in the focus groups, has been considered an important factor associated with the implementation of the recommendations. The potential to exchange viewpoints and treatments is considered crucial, as it enhances understanding and boosts confidence in their application. Professionals emphasised that collaborative follow-up (G01.2, G03.3), based on the same evidence-backed guidelines, would contribute to enhancing care for this particular group.
“ That would make it much easier? to follow these guidelines, because it is much more natural, it would give more consistency to the person's case management and it would be easier and better for them. ” G03.3. Family physician with expertise in chronicity.
“ There is a lack of communication between the different levels and between the different systems. ” G05.9 Primary Care Nurse
Virtual consultations have become the standard method for discussing clinical management between primary care providers and hospitals. However, they are one-sided, which hinders the effective exchange of information among professionals in both settings (G06,2, G06.3, G06.4, G03.2, G03.4, G03.5). Professionals advocated for interactions that create opportunities for interdisciplinary and transdisciplinary care (G01.2, G03.3, G04.2, G04.3). While primary care providers seek guidance from the nephrology department, professionals also highlight that primary care providers possess a deeper understanding of the patient's sociofamilial context. Hence, deferred teleconsultation does not entirely resolve this issue, as collaborative work between both services is necessary. Participants reported that this collaboration should consider all perspectives to enable genuine shared decision-making.
“ The advantage we have is that you go to the patient's home and see their environment, which is very different from when the patient goes to the nephrology department with dialysis; you don't see the day-to-day reality and we can see that. ” G03.2 Family physician with expertise in chronicity.
In this qualitative study, we specifically identified attitudinal, environmental, and behavioural control elements as outlined in the Theory of Planned Behaviour concerning ACKD management within a population of primary care nurses and physicians.
Although qualitative studies on practitioners' views on the management of ACKD exist [ 12 ], to our knowledge, this is the first study to use the conceptual components of this theory to study factors associated with practitioners' implementation of practice-based management of ACKD. To contextualise the elements of the theory studied, we investigated the characteristics of the people with ACKD most frequently seen in primary care from the perspective of professionals. First, the usual profile is that of an elderly person with global frailty and comorbidities. These findings are supported by the literature, in which CKD has strong links with chronic diseases [ 2 , 33 ], and their accumulation occurs with age and leads to frailty [ 34 ]. In the present study, the context of comorbidity and its consequences was recognised as a barrier to the application of evidence-based clinical recommendations. Furthermore, Squires et al. [ 35 ] In a 2019 study on contextual attributes for practitioners' use of evidence, patient context was one of the most frequently cited attributes more than 90% of the time [ 35 ]. Indeed, Kim et al. [ 36 ] reported that uncertainty and social support (which were also identified in our study population) were important factors associated with adherence in CKD patients [ 36 ]. Another barrier identified in the present study was educational barriers in terms of patients’ lack of knowledge about their disease and even lack of disease awareness. This finding has also been echoed in other studies, which estimate that 90% of kidney patients are unaware of their diagnosis [ 15 ]. In our study, professionals acknowledged that they do not play a prominent role in informing patients about this pathology, a situation that has also been observed in other primary care settings related to CKD [ 37 ]. Indeed, a systematic review on barriers to and facilitators of CKD treatment in primary care highlighted a deficiency in resources for patient education [ 38 ]. With regard to the approach to treating ACKD in primary care, another relevant finding of the study was that this disease is neglected in relation to other active pathologies, as the interventions recommended in the clinical practice guidelines were not given the same weight. The causes were diverse and included issues such as time constraints, limited accessibility, lack of familiarity with reference clinical guidelines, and inadequate professional training. In this regard, the results were consistent with multiple studies that have shown CKD to be a significant clinical problem with lower priority [ 38 ]. Additionally, a worldwide study revealed that professional barriers, such as low knowledge, negative attitudes, and limited professional awareness, were prevalent in more than 80% of the surveyed countries [ 39 ]. One possible explanation for this could be the examination of the perspectives of family physicians involved in CKD care, highlighting issues such as a lack of confidence and limited experience in follow-up care, among other factors [ 12 ].
Although several authors have investigated the approach and limitations of family physicians in primary care for patients with ACKD, few studies have explored this aspect in nurses. In our study, most nurses expressed the belief that ACKD was addressed only in the hospital and that it was not proactively and comprehensively followed up in primary care for this reason. This indicated that nurses have not fully developed their contribution to the care of people with ACKD in primary care and that the same standards applied in other pathologies are not used. The work of primary care nurses in the care of people with ACKD requires the systematisation of evidence-based care, as indicated in the healthcare context in which this study was carried out [ 40 ]. In addition, our study revealed the need to involve nurses, especially since patients were identified as having little knowledge of self-management of ACKD, which implies significant educational needs. To promote self-care, primary care nurses, as experts in health education, need to include people with ACKD in global and proactive follow-up, as indicated by multidisciplinary models of care [ 41 ]. One study highlighted the need to improve the accessibility of educational interventions for patients with ACKD among nephrology nurses [ 13 ]. It is therefore reasonable that nurses in this primary care setting should be able to develop educational interventions to optimise patient self-care. Enhancing the role of nurses within the multidisciplinary care model for people with ACKD would contribute to slowing disease progression, decreasing mortality and reducing the annual costs of the disease [ 41 ].
To investigate the subjective norms that influence the application of ACKD management guidelines, we examined factors in the professional environment in a universal health primary care setting. The pressure of care was identified at two levels: limited time and the excessive burden of electronic records. Historically, time constraints in patient consultations have been recognised as barriers to the implementation of evidence-based practices [ 16 ]. However, it is important to consider the excessive electronic record-keeping demands placed on professionals. In the context of our study, implementing standardised plans and evidence-based clinical recommendations was not an easy task, as the participants assured that it requires updated knowledge and skills for their integration into everyday life [ 16 ]. This scenario has prompted a sense of resistance towards electronic records, attributed to the sheer volume that professionals are required to manage when addressing comprehensive patient care, encompassing all their comorbidities. In a systematic review examining barriers to and facilitators of e-health implementation, while mismatch with daily clinical practice was acknowledged, this particular issue was not explicitly pinpointed [ 42 ]. This could be due to the desire to integrate all dimensions of health and the profile of patients in primary care. Another subjective standard identified was the accessibility of clinical practice guidelines in the work environment. In our study, this issue was evident in all the focus groups, where reference Clinical Practice Guidelines for CKD were reported to be unfamiliar to practitioners and perceived as inaccessible. Although accessibility has improved dramatically through internet search engines, keeping up to date with the literature, they reported that this improvement was difficult due to the wide variety of studies and information available. Selecting the best evidence and in cohesion with the rest of the providers requires efforts on the part of health care companies to implement these strategies in the context and organisation [ 43 ].
In exploring further attitudes toward the application of evidence-based practices, subtopics related to standardised electronic CKD plans emerged. On the one hand, and in line with other studies, these findings can guide practice and contribute to professional knowledge of ACKD. This is because standardised electronic records have the potential to enhance the quality and coordination of care for individuals with multiple chronic diseases [ 44 ]. They incorporate recommendations for patient follow-up, with technological support being identified as the most common facilitator [ 38 ]. On the other hand, a barrier to their use was that they were considered not very useful for recording and interprofessional communication. This remains a major barrier to the management of CKD [ 38 ]. Some research identifies the quality of electronic records as a challenge, and proposals focus on improving the functionality of the software and improving multidisciplinary cooperation [ 45 ]. Similarly, in our study, standardised records were also seen as hindering communication and diminishing the recognition of the nurse's role, as they are primarily responsible for implementing this type of documentation within our study’s context.
In exploring the elements of perceived behavioural control specifically, two interrelated subtopics emerged. On the one hand, training to implement the recommendations is lacking.
This can be explained by three related factors: dissatisfaction with the guidelines to be followed, perceived lack of knowledge, and a lack of awareness of support resources [ 38 ]. The present study revealed that the implementation of standardised care plans, in addition to overcoming the aforementioned environmental barriers, must be complemented by specific training strategies within the primary care team. In addition, consulting with nephrology providers could improve this approach to incorporate the recommendations into practice. Finally, aligning with findings from other studies, enhancing the collaborative relationship between primary care and nephrology professionals was suggested as a factor to increase perceived behavioural control [ 12 , 13 , 38 , 46 ]. In the context of our study, professionals perceived the necessity of establishing bidirectional communication channels to enable the shared follow-up of people with ACKD.
Limitations
This study has several limitations. First, professionals who agreed to participate were recruited through the primary care centres. Afterwards, nurses and physicians from the participating centres were summoned and invited to attend on an agreed-upon day and time. To reach a wider audience, the focus groups were conducted in the workplace. However, it is possible that we may have gathered results on the attitudes, subjective norms, and behavioural control of professionals most involved in the care of individuals with this condition, potentially overlooking the barriers faced by those less familiar with the disease. This was an aspect we could not control in the research field. Additionally, another aspect beyond our control was the age of the participants. The studied sample had an average age of 46 years, meaning that we may have omitted elements of the TPB related to younger ages, for instance, concerning the implementation of standardised electronic records. Second, we sought to analyse the three main elements described in the TPB, which are the conditioning factors for following evidence-based recommendations. When guiding research based on this theory, we have not explored other elements that could influence it, such as moral norms, an extension of the TPB, which should be considered to fully understand the psychological factors associated with evidence-based approaches to ACKD. The moral norm is understood as a person's perception of the appropriateness of certain behaviours [ 24 ]. The authors of the TPB argue that moral a reliable predictor of behaviour in situations where strong social pressures exist, as in the case of the present study. Therefore, the fact that some beliefs and experiences analysed in this study are linked to social pressure suggests that the values and beliefs studied alongside the moral norm could play a significant role in analysing the use of evidence-based practice. In essence, further investigation is needed to comprehend why key guidelines for treating ERCA have not been implemented, even when they are known or if the environment supports them positively. Perhaps exploring this aspect through moral standards is necessary. Additionally, by examining the three elements of the TPB, we may have overlooked other facets related to the application of the TBP or the context in which it is studied, as indicated by Squires et al. [ 35 ] in a study on different contextual attributes that influence the application of evidence-based practice. Finally, our results are based on self-reported practices, and we do not know to what extent self-reported practices and other contextual factors reflect reality and how patients perceive this care. In future research, it would be useful to analyse the influence of the abovementioned aspects that may help to gain a deeper understanding of the factors behind evidence-based practices in the management of people with ACKD.
The clinical, social, and healthcare context of CKD patients presented challenges in implementing an evidence-based team approach. This approach has impacted the application of clinical practice guidelines and standardised care plans. Several psychological elements identified through the TBP make it challenging to adequately implement an evidence-based approach for people with ACKD. Attitudes have been recognised as factors that modulate the use of standardised electronic records. Professionals suggested enhancing information technology systems and effectively integrating them into shared medical records. However, subjective norms (influences from the professional environment) and perceived behavioural control (perception of capabilities) acted as barriers to the appropriate application of clinical practice guidelines and standardised records. Professionals advocated overcoming these barriers through team clinical sessions, collaborative teamwork involving nurses in active ACKD monitoring, and cooperation with referring nephrology services.
This study aimed to specifically understand the attitudes, subjective norms, and behavioural control underlying the use of the evidence-based approach for people with ACKD in primary care. The TBP aided in identifying the psychological elements underlying an evidence-based approach for individuals with ACKD. On the one hand, standardised electronic ACKD records face significant limitations in terms of attitudes, subjective norms, and behavioural monitoring. In the short term, to address this issue, strategies should focus on enhancing positive attitudes, which guide professional practice, and counteracting negative attitudes, thus improving their utility to enhance work and the visibility of interventions. In the long term, improving subjective norms would involve reducing the overall demand for records in primary care, while enhancing perceived behavioural control would involve promoting the use and sharing of records among all team members.
On the other hand, the implementation of CKD clinical practice guidelines identified barriers related to subjective norms and behavioural control. In the short term, strategies to address this issue should aim to integrate these guidelines into workplace information systems so that they are readily accessible and can be shared by colleagues in team sessions, enabling continuous updating. This strategy lays the groundwork for improving perceived behavioural control, with longer-term strategies including the development of new communication channels for advice and shared management of patients between primary care and nephrology professionals.
Availability of data and materials
The datasets used, generated or analyzed during this study are available from corresponding author on reasonable request.
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease- a systematic review and meta-analysis. PLoS One. 2016;11:1–18. https://doi.org/10.1371/journal.pone.0158765 .
Article CAS Google Scholar
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150.
Google Scholar
Gorostidi M, Sánchez-Martínez M, Ruilope LM, Graciani A, de la Cruz JJ, Santamaría R, et al. Prevalencia de enfermedad renal crónica en España: impacto de la acumulación de factores de riesgo cardiovascular. Nefrologia. 2018;38:606–15. https://doi.org/10.1016/J.NEFRO.2018.04.004 .
Article PubMed Google Scholar
World Kidney Day. Brussels. 2023. https://www.worldkidneyday.org/ . Accessed 16 April 2024.
García-Maset R, Bover J, de la Morena JS, GoicoecheaDiezhandino M, del Hoyo JC, San Martín JE, et al. Documento de información y consenso para la detección y manejo de la enfermedad renal crónica. Nefrología. 2022;42:233–64. https://doi.org/10.1016/J.NEFRO.2021.07.010 .
Hernández-Sanahuja Anquera JM, Mundet Tudurí X, Cegri Lombardo F, Giménez Pérez E, Salvador González B, Segura Anducas A, et al. Consens català sobre atenció a la malaltia renal crònica. Societat Catalana de Medicina Familiar i Comunitària (CAMFiC), Societat Catalana de Nefrologia (SCN), Societat Catalana d'Hipertensió Arterial (SCHTA), Associació Catalana de Diabetis (ACD), Associació d'Infermeria Familiar i Comunitària de Catalunya (AIFiCC). Barcelona; 2023.
Díaz JM, Otero S, Quintela M, Riba F, Vidal A, Franco M, et al. Consens interdisciplinari sobre l’abordatge de la persona amb malaltia renal crònica avançada: pla operatiu de la malaltia renal crònica. Barcelona: Direcció General de Planificació i Recerca en Salut; 2023.
Bikbov B, Purcell CA, Levey AS, Smith M, Abdoli A, Abebe M, et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–33. https://doi.org/10.1016/S0140-6736(20)30045-3 .
Article Google Scholar
Bundó D, Cunillera O, Arbiol-Roca A, Cobo-Guerrero S, Romano J, Gil-Terron N, et al. Final stage of chronic kidney disease with conservative kidney management or renal replacement therapy: a primary-care population study. J Clin Med. 2023;12:4602. https://doi.org/10.3390/JCM12144602 .
Article PubMed PubMed Central Google Scholar
Van Gelder VA, Scherpbier-De Haan ND, De Grauw WJC, Vervoort GMM, Van Weel C, Biermans MCJ, et al. Quality of chronic kidney disease management in primary care: a retrospective study. Scand J Prim Health Care. 2016;34:73–80. https://doi.org/10.3109/02813432.2015.1132885 .
Greer RC, Ameling JM, Cavanaugh KL, Jaar BG, Grubbs V, Andrews CE, et al. Specialist and primary care physicians’ views on barriers to adequate preparation of patients for renal replacement therapy: a qualitative study. BMC Nephrol. 2015;16. https://doi.org/10.1186/S12882-015-0020-X .
Tonkin-Crine S, Santer M, Leydon GM, Murtagh FEM, Farrington K, Caskey F, et al. GPs’ views on managing advanced chronic kidney disease in primary care: a qualitative study. Br J Gen Pract. 2015;65:e469–77. https://doi.org/10.3399/BJGP15X685693 .
Lo C, Ilic D, Teede H, Fulcher G, Gallagher M, Kerr PG, et al. Primary and tertiary health professionals’ views on the health-care of patients with co-morbid diabetes and chronic kidney disease - A qualitative study. BMC Nephrol. 2016;17:1–12. https://doi.org/10.1186/S12882-016-0262-2/FIGURES/1 .
Eckardt KU, Delgado C, Heerspink HJL, Pecoits-Filho R, Ricardo AC, Stengel B, et al. Trends and perspectives for improving quality of chronic kidney disease care: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2023;104:888–903. https://doi.org/10.1016/J.KINT.2023.05.013 .
Bello AK, Johnson DW. Educating primary healthcare providers about kidney disease. Nat Rev Nephrol. 2022;18:133. https://doi.org/10.1038/S41581-021-00527-Y .
Zipkin DA, Greenblatt L, Kushinka JT. Evidence-based medicine and primary care: keeping up is hard to do. Mt Sinai J Med. 2012;79:545–54. https://doi.org/10.1002/MSJ.21337 .
Falck L, Zoller M, Rosemann T, Martínez-González NA, Chmiel C. Toward standardized monitoring of patients with chronic diseases in primary care using electronic medical records: systematic review. JMIR Med Inform. 2019;7. https://doi.org/10.2196/10879 .
De Rosis S, Seghieri C. Basic ICT adoption and use by general practitioners: an analysis of primary care systems in 31 European countries. BMC Med Inform Decis Mak. 2015;15. https://doi.org/10.1186/S12911-015-0185-Z .
Harahap NC, Handayani PW, Hidayanto AN. Functionalities and issues in the implementation of personal health records: systematic review. J Med Internet Res. 2021;23. https://doi.org/10.2196/26236 .
Ajzen I. The theory of planned behavior. Organ behav hum decis process. 1991;50:179–211. https://doi.org/10.47985/dcidj.475 .
Øvretveit J, Scott T, Rundall TG, Shortell SM, Brommels M. Improving quality through effective implementation of information technology in healthcare. Int J Qual Health Care. 2007;19:259–66. https://doi.org/10.1093/INTQHC/MZM031 .
Majid S, Foo S, Luyt B, Zhang X, Theng YL, Chang YK, et al. Adopting evidence-based practice in clinical decision making: nurses’ perceptions, knowledge, and barriers. J Med Libr Assoc. 2011;99:229–36. https://doi.org/10.3163/1536-5050.99.3.010 .
Bello A, Levin A, Tonelli M, Okpechi I, Feehally J, Harris D, et al. Global kidney health Atlas: a report by the International Society of Nephrology on the current state of organization and structures for kidney care across the globe. Brussels: Belgium; 2017.
Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. J Appl Soc Psychol. 2002;32:665–83. https://doi.org/10.1111/J.1559-1816.2002.TB00236.X .
Soto Núñez CA, Vargas Celis IE. La Fenomenología de Husserl y Heidegger. Cultur de Los Cuidados. 2017;21:43–50 10.14198/cuid.2017.48.05.
Heidegger M. The phenomenology of religious life. 1st ed. Bloomington, Indiana: Indiana University Press; 2010.
Tenny S, Brannan JM, Brannan GD. Qualitative Study. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470395/ .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. https://doi.org/10.1093/intqhc/mzm042 .
Grove SK, Gray JR. Investigación en enfermería. Desarrollo de la práctica enfermera basada en la evidencia. 7th ed. Barcelona: Elsevier; 2019
Clarke V, Braun V. Successful qualitative research: a practical guide for beginners. 1st ed. Los Angeles (CA): SAGE; 2013.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. https://doi.org/10.1191/1478088706QP063OA .
Quinn Patton M. Qualitative research & evaluation methods. 4th ed. Newbury Park (CA): SAGE; 2014.
Salvador-González B, Gil-Terrón N, Cerain-Herrero MJ, Subirana I, Güell-Miró R, Rodríguez-Latre LM, et al. Estimated glomerular filtration rate, cardiovascular events and mortality across age groups among individuals older than 60 years in Southern Europe. Rev Esp Cardiol (Engl Ed). 2018;71:450–7. https://doi.org/10.1016/J.REC.2017.09.010 .
Observatorio de la Atención al Paciente. Informe 2021. 2021. https://www.plataformadepacientes.org/sites/default/files/informe2021_oap_vf_2.pdf .
Squires JE, Aloisio LD, Grimshaw JM, Bashir K, Dorrance K, Coughlin M, et al. Attributes of context relevant to healthcare professionals’ use of research evidence in clinical practice: a multi-study analysis. Implement Sci. 2019;14. https://doi.org/10.1186/S13012-019-0900-8 .
Kim B, Kim J. Influence of uncertainty, depression, and social support on self-care compliance in hemodialysis patients. Ther Clin Risk Manag. 2019;15:1243. https://doi.org/10.2147/TCRM.S218934 .
Blakeman T, Protheroe J, Chew-Graham C, Rogers A, Kennedy A. Understanding the management of early-stage chronic kidney disease in primary care: a qualitative study. Br J Gen Pract. 2012;62. https://doi.org/10.3399/BJGP12X636056 .
Neale EP, Middleton J, Lambert K. Barriers and enablers to detection and management of chronic kidney disease in primary healthcare: a systematic review. BMC Nephrol 2020;21. https://doi.org/10.1186/S12882-020-01731-X .
Bello AK, Okpechi IG, Levin A, Ye F, Saad S, Zaidi D, et al. ISN–Global Kidney Health Atlas: A report by the International Society of Nephrology: An Assessment of Global Kidney Health Care Status focussing on Capacity, Availability, Accessibility, Affordability and Outcomes of Kidney Disease. Brussels: International Society of Nephrology; 2023.
Grup d’Infermeres Clíniques Territorials del Programa Ares-AP. Plans de cures estandarditzats per a persones ateses en atenció primària. Barcelona: Institut Català de la Salut; 2021.
Hsu HT, Chiang YC, Lai YH, Lin LY, Hsieh HF, Chen JL. Effectiveness of multidisciplinary care for chronic kidney disease: a systematic review. Worldviews Evid Based Nurs. 2021;18:33–41. https://doi.org/10.1111/WVN.12483 .
Ross J, Stevenson F, Lau R, Murray E. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implement Sci. 2016;11. https://doi.org/10.1186/S13012-016-0510-7 .
Fernández-Salazar S, Ramos-Morcillo AJ, Leal-Costa C, García-González J, Hernández-Méndez S, Ruzafa-Martínez M. Evidence-based practice competency and associated factors among primary care nurses in Spain. Aten Primaria. 2021;53. https://doi.org/10.1016/J.APRIM.2021.102050 .
Norton JM, Ip A, Ruggiano N, Abidogun T, Camara DS, Fu H, et al. Assessing progress toward the vision of a comprehensive, shared electronic care plan: scoping review. J Med Internet Res. 2022;24:e36569. https://doi.org/10.2196/36569 .
Ni K, Chu H, Zeng L, Li N, Zhao Y. Barriers and facilitators to data quality of electronic health records used for clinical research in China: a qualitative study. BMJ Open. 2019;9. https://doi.org/10.1136/BMJOPEN-2019-029314 .
Haase A, Stracke S, Chenot JF, Weckmann G. Nephrologists’ perspectives on ambulatory care of patients with non-dialysis chronic kidney disease - A qualitative study. Health Soc Care Community. 2019;27:e438–48. https://doi.org/10.1111/HSC.12744 .
Download references
Acknowledgements
Thanks to the generosity and personal effort of all the nurses and family physicians from the Primary Care Centers Montclar, El Castell, Unitat d'Atenció a la Cronicitat i Complexitat del Servei d'Atenció Primària Alt Penedès Garraf i Baix Llobregat Nord, i Baix Llobregat Centre, who contributed their professional experience by participating in the study.
This study is part of a broader research project funded by the Department of Health of the Government of Catalonia through the Strategic Plan for Health Research and Innovation (PERIS-5th call SLT021), with file number SLT021/21/000031. The funding from this project supported the analysis and compilation of qualitative data in this study.
Author information
Authors and affiliations.
Primary Care Center El Pla. Servei d’Atenció Primària Baix Llobregat Centre, Atenció Primària Metropolitana Sud, Institut Català de la Salut, Sant Feliu de Llobregat, Barcelona, 08980, Spain
Elena Pintado-Outumuro
Department of Public Health, Mental Health and Maternal and Child Health Nursing. Faculty of Nursing, University of Barcelona. Pavelló de Govern, 3Rd Floor, L’Hospitalet de Llobregat, Barcelona, 08907, Spain
Victoria Morin-Fraile & Iris Lumillo-Gutiérrez
Unitat de Suport a la Recerca Metropolitana Sud, Fundació Institut Universitari per a la recerca a l’Atenció Primària de Salut Jordi Gol i Gurina (IDIAPJGol), L’Hospitalet de Llobregat, Barcelona, 08907, Spain
Betlem Salvador-González
Research Group On Disease, Cardiovascular Risk and Lifestyles in Primary Care, Institut Universitari d’Investigació en Atenció Primària (IDIAP) Jordi Gol, Barcelona, 08007, Spain
Elena Pintado-Outumuro, Betlem Salvador-González & Iris Lumillo-Gutiérrez
Research Group On Environments and Materials for Learning, Universitat de Barcelona, Barcelona, Spain
Fundamental and Clinic Nursing Department, Faculty of Nursing, University of Barcelona, Pavelló de Govern, 3Rd Floor, L’Hospitalet de Llobregat, Barcelona, 08907, Spain
Llúcia Benito
IDIBELL, Bellvitge Biomedical Research Institute, Avinguda de la Gran Via, 199, L’Hospitalet de Llobregat, Barcelona, 08908, Spain
Primary Care Center El Castell, Servei d’Atenció Primària Delta del Llobregat, Atenció Primària Metropolitana Sud, Institut Català de la Salut, Castelldefels, 08860, Barcelona, Spain
Maricel Julve-Ibáñez
Primary Care Center Sant Ildefons. Servei d’Atenció Primària Baix Llobregat Centre, Atenció Primària Metropolitana Sud, Institut Català de la Salut, Cornellà de Llobregat, Barcelona, 08940, Spain
M.-Pilar Sancho-Campos
Primary Care Center Montclar and Primary Care Center Camps Blancs. Servei d’Atenció Primària Baix Llobregat Centre, Atenció Primària Metropolitana Sud, Institut Català de la Salut, Sant Boi de Llobregat, Barcelona, 08830, Spain
Carolina Alves-Tafur
Chronicity and Complexity Care Unit (UTACC) Baix Llobregat Centre, Atenció Primària Metropolitana Sud, Institut Català de la Salut, Cornellà de Llobregat, 08940, Spain
Iris Lumillo-Gutiérrez
You can also search for this author in PubMed Google Scholar
Contributions
Betlem Salvador, Iris Lumillo, Elena Pintado, Pilar Sancho, and Carolina Alves participated in project design and literature review. Iris Lumillo, Elena Pintado, Victoria Morin, and Maricel Julvé participated in pre-interviews, expert consultation, recruitment, informed consent, interviews, and data collation. Iris Lumillo, Llúcia Benito, Betlem Salvador, Victoria Morin, and Elena Pintado participated in the comprehensive manuscript review and preparation.
Corresponding author
Correspondence to Iris Lumillo-Gutiérrez .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in accordance with the principles of the Declaration of Helsinki. The study was approved by the Ethics Committees at the primary care and hospital reference centers:
Comitè Ètic d’Investigació amb medicaments (CEIm) of the IDIAP Jordi Gol (22/092-P).
Comitè d’Ètica de la Investigació de l’Hospital Universitari de Bellvitge (PR292/22).
All participants were informed of the research objectives, interview topics, and data usage, explained the confidentiality criteria, were anonymous, and were right to withdraw from the study. Each participant was provided with an informed consent form, giving them the choice to participate. By signing this form, they voluntarily confirmed their participation and agreed to the anonymous use of their data for communications and scientific publications. Participants were informed of their rights regarding access, rectification, erasure, objection, processing restrictions, and data portability. These rights could be exercised by contacting the study's principal investigator. Participants also had the right to lodge a complaint with the Catalan Data Protection Authority if they felt that their rights were violated by any actions of the Department of Health. The study personnel processed and utilised the data while maintaining strict confidentiality, adhering to the guidelines outlined in Organic Law 3/2018, dated December 5, regarding personal data protection and digital rights guarantees, and the subsequent Regulation (EU) 2016/679 General Data Protection Regulation.
Consent for publication
Not applicable.

Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pintado-Outumuro, E., Morin-Fraile, V., Salvador-González, B. et al. Exploring the factors influencing evidence-based approaches to advanced chronic kidney disease: a qualitative study involving nurses and physicians. BMC Prim. Care 25 , 177 (2024). https://doi.org/10.1186/s12875-024-02418-0
Download citation
Received : 29 December 2023
Accepted : 06 May 2024
Published : 21 May 2024
DOI : https://doi.org/10.1186/s12875-024-02418-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Advanced chronic kidney disease
- Primary health care
- Theory of planned behaviour
- Attitudes of health personnel
- Qualitative research
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
Nephrology Nursing Research Paper Topics

Nephrology nursing research paper topics are incredibly diverse and integral to the medical world. Nephrology nursing involves the care of patients with kidney disease and encompasses a variety of topics from the pathophysiology of kidney disease, to the management of kidney failure, requiring dialysis or transplantation. This field is constantly evolving with the advent of new technologies and treatments. As such, it is important for nursing students and professionals to be up-to-date with the latest research and trends in nephrology nursing. This article will provide a comprehensive list of research paper topics, a detailed discussion on the significance of nephrology nursing, an introduction to iResearchNet’s writing services, and a compelling call-to-action.
100 Nephrology Nursing Research Paper Topics
Nephrology nursing is a specialized area of nursing dedicated to individuals with kidney disease or kidney-related issues. It plays a vital role in managing the various stages of kidney diseases, from early detection and intervention to the management of advanced kidney failure. Research in this field is of paramount importance as it leads to the development of new treatments, management strategies, and preventive measures. The nephrology nursing research paper topics encompass a wide range of areas such as Acute Kidney Injury, Chronic Kidney Disease, Dialysis, Kidney Transplantation, and many more. Exploring these topics will not only enhance the knowledge of nursing students but also contribute to the betterment of patient care. List of 100 nephrology nursing research paper topics:
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
Acute Kidney Injury:
- The role of nursing in the management of acute kidney injury.
- Early detection and prevention of acute kidney injury.
- The impact of hydration status on the development of acute kidney injury.
- Pharmacological interventions in acute kidney injury.
- Acute kidney injury in critically ill patients.
- The relationship between sepsis and acute kidney injury.
- Biomarkers for early detection of acute kidney injury.
- The role of renal replacement therapy in acute kidney injury.
- Strategies to prevent contrast-induced acute kidney injury.
- The impact of acute kidney injury on long-term kidney function.
Chronic Kidney Disease:
- The role of nephrology nursing in the management of chronic kidney disease.
- Strategies for early detection of chronic kidney disease.
- The impact of dietary management on the progression of chronic kidney disease.
- Exercise and its impact on chronic kidney disease progression.
- The role of blood pressure control in the management of chronic kidney disease.
- Management of anemia in chronic kidney disease.
- The relationship between diabetes and chronic kidney disease.
- Strategies to slow the progression of chronic kidney disease.
- The impact of chronic kidney disease on cardiovascular health.
- The role of patient education in the management of chronic kidney disease.
- Best practices in hemodialysis care.
- The role of peritoneal dialysis in kidney failure management.
- Strategies to prevent infections in dialysis patients.
- The impact of dialysis on quality of life.
- Strategies to improve vascular access in hemodialysis patients.
- The role of nursing in the management of dialysis-related complications.
- Strategies to optimize fluid management in dialysis patients.
- The impact of dialysis frequency on patient outcomes.
- Nutritional management in dialysis patients.
- The role of psychological support in the management of dialysis patients.
Kidney Transplantation:
- Strategies to improve kidney transplantation outcomes.
- The role of immunosuppressive therapy in kidney transplantation.
- The impact of donor-recipient matching on kidney transplantation outcomes.
- Strategies to prevent rejection in kidney transplant recipients.
- The role of nursing in the post-transplant care of kidney transplant recipients.
- Management of infections in kidney transplant recipients.
- The impact of kidney transplantation on quality of life.
- Strategies to prevent cardiovascular disease in kidney transplant recipients.
- The role of patient education in the post-transplant period.
- The impact of kidney transplantation on mental health.
Glomerular Diseases:
- The role of nursing in the management of glomerular diseases.
- Strategies for early detection of glomerular diseases.
- The impact of immunosuppressive therapy on glomerular diseases.
- Management of nephrotic syndrome.
- Strategies to prevent progression of glomerular diseases.
- The role of dietary management in glomerular diseases.
- The impact of glomerular diseases on cardiovascular health.
- Strategies to manage hypertension in patients with glomerular diseases.
- The role of patient education in the management of glomerular diseases.
- The impact of glomerular diseases on quality of life.
Tubulointerstitial Diseases:
- The role of nursing in the management of tubulointerstitial diseases.
- Strategies for early detection of tubulointerstitial diseases.
- The impact of pharmacological interventions on tubulointerstitial diseases.
- Management of acute interstitial nephritis.
- Strategies to prevent progression of tubulointerstitial diseases.
- The role of dietary management in tubulointerstitial diseases.
- The impact of tubulointerstitial diseases on kidney function.
- Strategies to manage electrolyte abnormalities in tubulointerstitial diseases.
- The role of patient education in the management of tubulointerstitial diseases.
- The impact of tubulointerstitial diseases on quality of life.
Genetic Disorders Affecting the Kidneys:
- The role of nursing in the management of genetic disorders affecting the kidneys.
- Strategies for early detection of genetic disorders affecting the kidneys.
- The impact of genetic counseling on the management of genetic disorders affecting the kidneys.
- Management of polycystic kidney disease.
- Strategies to prevent progression of genetic disorders affecting the kidneys.
- The role of dietary management in genetic disorders affecting the kidneys.
- The impact of genetic disorders affecting the kidneys on cardiovascular health.
- Strategies to manage hypertension in patients with genetic disorders affecting the kidneys.
- The role of patient education in the management of genetic disorders affecting the kidneys.
- The impact of genetic disorders affecting the kidneys on quality of life.
Hypertension and the Kidneys:
- The role of nursing in the management of hypertension and the kidneys.
- Strategies for early detection of hypertension-related kidney disease.
- The impact of antihypertensive therapy on kidney function.
- Management of hypertensive nephropathy.
- Strategies to prevent progression of hypertension-related kidney disease.
- The role of dietary management in hypertension and the kidneys.
- The impact of hypertension on cardiovascular health.
- Strategies to manage electrolyte abnormalities in hypertension-related kidney disease.
- The role of patient education in the management of hypertension and the kidneys.
- The impact of hypertension on quality of life.
Diabetic Nephropathy:
- The role of nursing in the management of diabetic nephropathy.
- Strategies for early detection of diabetic nephropathy.
- The impact of glycemic control on the progression of diabetic nephropathy.
- Management of diabetic kidney disease.
- Strategies to prevent progression of diabetic nephropathy.
- The role of dietary management in diabetic nephropathy.
- The impact of diabetic nephropathy on cardiovascular health.
- Strategies to manage hypertension in patients with diabetic nephropathy.
- The role of patient education in the management of diabetic nephropathy.
- The impact of diabetic nephropathy on quality of life.
Pediatric Nephrology:
- The role of nursing in the management of pediatric nephrology.
- Strategies for early detection of kidney disease in children.
- The impact of congenital kidney anomalies on pediatric kidney function.
- Management of pediatric acute kidney injury.
- Strategies to prevent progression of kidney disease in children.
- The role of dietary management in pediatric nephrology.
- The impact of pediatric kidney disease on growth and development.
- Strategies to manage hypertension in children with kidney disease.
- The role of patient and parent education in pediatric nephrology.
- The impact of pediatric kidney disease on quality of life.
The aforementioned list of nephrology nursing research paper topics covers a wide spectrum of issues related to kidney health and its management. Nephrology nursing is an essential and dynamic field, constantly adapting to the evolving medical landscape. It is crucial for students and professionals in the nursing field to delve into research topics that contribute to a better understanding of kidney diseases, improve patient outcomes, and enhance the quality of life for individuals with kidney-related health issues. This comprehensive list aims to facilitate the exploration of essential topics in nephrology nursing and contribute to the development of innovative strategies and interventions in kidney care.
The Range of Nephrology Nursing Research Paper Topics
Nephrology nursing is a critical and specialized area within the broader nursing discipline, focusing on the care of patients with kidney disease or kidney-related issues. It encompasses a wide range of activities, from early detection and management of kidney diseases to the care of patients undergoing dialysis or kidney transplantation. The significance of nephrology nursing cannot be understated, given the increasing prevalence of kidney diseases worldwide. This article will discuss the importance of nephrology nursing and various aspects of it, such as acute kidney injury, chronic kidney disease, and dialysis, which are all crucial nephrology nursing research paper topics.
Significance of Nephrology Nursing
The kidney is a vital organ responsible for various functions, including filtering waste products from the blood, regulating blood pressure, and maintaining electrolyte balance. Any dysfunction or disease affecting the kidney can have a significant impact on an individual’s overall health and quality of life. Nephrology nurses play a crucial role in the management of patients with kidney diseases, providing specialized care that can help manage symptoms, slow disease progression, and improve outcomes.
Nephrology nurses are trained to manage various aspects of kidney care, including administering medications, managing fluid and electrolyte balance, providing dialysis treatments, and educating patients and their families about kidney disease and its management. They also play a crucial role in the early detection of kidney diseases, as early intervention can often prevent or delay the progression of the disease.
Acute Kidney Injury
Acute kidney injury (AKI) is a sudden decline in kidney function that can occur due to various reasons, such as decreased blood flow to the kidneys, exposure to toxic substances, or an inflammatory process affecting the kidneys. AKI is a common condition associated with high morbidity and mortality rates, particularly among hospitalized patients. It is one of the essential nephrology nursing research paper topics as timely and appropriate management of AKI can significantly affect its outcome.
Nephrology nurses play a vital role in the management of patients with AKI. They are involved in the early detection of AKI by monitoring patients’ urine output, serum creatinine levels, and other relevant indicators. They also play a crucial role in the management of AKI by administering medications, managing fluid and electrolyte balance, and providing supportive care to patients.
Chronic Kidney Disease
Chronic kidney disease (CKD) is a long-term condition characterized by a gradual loss of kidney function over time. It is a common condition that affects millions of people worldwide and is associated with an increased risk of cardiovascular disease and other comorbidities. Managing CKD effectively is crucial to prevent its progression to end-stage kidney disease (ESKD), which requires dialysis or kidney transplantation.
Nephrology nurses play a vital role in the management of patients with CKD. They are involved in the early detection and monitoring of CKD by assessing patients’ kidney function and other relevant indicators regularly. They also play a crucial role in the management of CKD by administering medications, managing fluid and electrolyte balance, providing dietary counseling, and educating patients about the disease and its management.
Dialysis is a life-saving treatment that replaces the function of the kidneys in patients with ESKD. There are two main types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis involves filtering the blood through a machine, while peritoneal dialysis involves filtering the blood through the lining of the abdomen. Both types of dialysis require specialized care and management to ensure their effectiveness and minimize complications.
Nephrology nurses play a crucial role in the care of patients undergoing dialysis. They are involved in the preparation and management of the dialysis procedure, monitoring patients during dialysis, managing complications, and providing education and support to patients and their families. Nephrology nursing research paper topics related to dialysis include strategies to prevent infections, improve vascular access, optimize fluid management, and enhance patients’ quality of life.
In summary, nephrology nursing is a specialized area of nursing that plays a crucial role in the management of patients with kidney diseases. Nephrology nurses are involved in various aspects of kidney care, including the early detection and management of acute kidney injury and chronic kidney disease, and the care of patients undergoing dialysis. These are all essential nephrology nursing research paper topics that contribute to the improvement of patient outcomes and the advancement of the field. It is crucial for nursing students and professionals to explore these topics in-depth to develop a comprehensive understanding of nephrology nursing and contribute to the betterment of patient care.
iResearchNet’s Custom Writing Services
Are you a nursing student assigned to write a research paper on nephrology nursing? If so, you understand the importance of choosing a relevant and impactful topic. Nephrology nursing involves specialized care for patients with kidney diseases, from early detection and management to dialysis and transplantation. With the increasing prevalence of kidney diseases worldwide, it is crucial for nursing students and professionals to develop a comprehensive understanding of this field. At iResearchNet, we offer students the opportunity to order a custom nephrology nursing research paper on any topic. Our writing services are designed to help you produce a high-quality research paper that contributes to your academic success and the advancement of nephrology nursing.
- Expert degree-holding writers : Our team of writers holds advanced degrees in nursing and related fields. They have extensive experience in writing research papers on various nephrology nursing research paper topics. You can be confident that your paper will be written by an expert with a deep understanding of the subject matter.
- Custom written works : Every research paper we produce is custom written to your specific requirements. We do not reuse or recycle previously written papers. Your paper will be unique and tailored to your needs.
- In-depth research : Our writers conduct thorough research on your chosen topic using the latest and most relevant sources. We ensure that your paper is well-researched, evidence-based, and reflects the current state of knowledge in the field of nephrology nursing.
- Custom formatting : We format your paper according to your preferred citation style. Our writers are familiar with all major citation styles and will ensure that your paper is properly formatted and referenced.
- Top quality : We pride ourselves on the quality of our work. Every paper we produce is carefully reviewed and edited to ensure it meets our high-quality standards. You can be confident that your paper will be well-written, well-organized, and free of errors.
- Customized solutions : We understand that every student has unique needs and requirements. We offer customized solutions to meet your specific needs. Whether you need a full research paper, a literature review, or help with any part of your paper, we are here to help.
- Flexible pricing : We offer flexible pricing options to suit your budget. Our pricing is transparent and straightforward, with no hidden fees. You can choose the level of service that fits your needs and budget.
- Short deadlines : We understand that sometimes you may need your paper urgently. We offer short deadlines up to 3 hours for urgent orders. Our writers are experienced and efficient, and we will make every effort to deliver your paper on time.
- Timely delivery : We know how important it is for you to submit your paper on time. We make every effort to deliver your paper by the deadline you specify. In most cases, we deliver the paper ahead of time to give you a chance to review it before submission.
- 24/7 support : Our customer support team is available 24/7 to answer your questions and address your concerns. You can contact us via phone, email, or live chat at any time.
- Absolute privacy : We take your privacy very seriously. Your personal information will never be shared with any third party. All transactions are confidential and secure.
- Easy order tracking : Once you place your order, you can easily track its progress online. You will receive regular updates on the status of your order, and you can communicate with your writer directly if you have any questions or concerns.
- Money-back guarantee : Your satisfaction is our top priority. If you are not satisfied with the final paper, we offer a money-back guarantee. We will refund your money if we are unable to meet your requirements.
In conclusion, iResearchNet offers a comprehensive range of writing services to help you produce a high-quality nephrology nursing research paper. Our expert degree-holding writers, custom written works, in-depth research, and customized solutions are designed to meet your specific needs and contribute to your academic success. We offer flexible pricing, short deadlines, timely delivery, 24/7 support, absolute privacy, easy order tracking, and a money-back guarantee to ensure your satisfaction. We encourage you to utilize our services for your research paper needs and contribute to the advancement of nephrology nursing.
Secure Your Academic Success with iResearchNet!
As a nursing student, you are well aware of the critical role that nephrology nurses play in healthcare. They specialize in the care of patients with kidney diseases and disorders, a field that is both challenging and rewarding. A research paper in this area not only contributes to your academic success but also to the broader knowledge base of this essential nursing specialty. At iResearchNet, we are committed to supporting your academic journey by offering you the opportunity to order a custom nephrology nursing research paper on any topic of your choice.
We understand the challenges you face as a student – the pressure to perform well academically, the tight deadlines, and the multiple responsibilities you have to juggle. That’s why we offer a comprehensive and customized solution to meet your needs. Our expert degree-holding writers will conduct in-depth research and craft a well-organized, evidence-based paper that reflects the current state of knowledge in nephrology nursing. With flexible pricing options, the ability to track your order online, and a money-back guarantee, you can be confident in your decision to choose iResearchNet.
Your academic success is essential for your future career as a nurse, and submitting a high-quality research paper is a crucial part of that journey. At iResearchNet, we are dedicated to helping you achieve that success. With our customized solutions, expert writers, and commitment to quality, we provide a service that is unmatched. Don’t miss the opportunity to submit a research paper that stands out and reflects your dedication to excellence in nephrology nursing.
Take the first step towards securing your academic success. Order a custom nephrology nursing research paper from iResearchNet today and contribute to the advancement of this critical field of nursing. Your future patients and your professional development will thank you!
ORDER HIGH QUALITY CUSTOM PAPER

- Frontiers in Physiology
- Renal Physiology and Pathophysiology
- Research Topics
Renal Function in Acute and Chronic Kidney Diseases
Total Downloads
Total Views and Downloads
About this Research Topic
Acute and chronic kidney diseases have devastating consequences on human health. Renal vascular function, glomerular filtration, and epithelial transport are required for water and electrolyte homeostasis. Nephrotoxicity and diseases such as hypertension, diabetes and metabolic syndrome contribute ...
Keywords : kidney disease, acute kidney injury, chronic kidney diseases, renal vascular, renal epithelia
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Medicine (Baltimore)
- v.101(3); 2022 Jan 21
The most influential articles on kidney transplantation
Heungman jun.
a Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Republic of Korea
Ji Woong Hwang
b Department of Surgery, Chung-Ang University Gwangmyeong Hospital, Chung-Ang University, Gwangmyeong, Republic of Korea.
Associated Data
Background:.
Kidney transplantation (KT) has become common in the treatment of end-stage renal disease. However, to date, there have been no bibliometric analyses of KT research to identify the most influential articles. The purpose of this research is to identify and characterize the 100 most cited articles that focus on KT and to clarify the trends in the accomplishments in this field.
We searched the Thomson Reuters Web of Science citation indexing database and used keyword mapping of VOSviewer. The top 100 most cited manuscripts were analyzed based on their titles, authors, institutions, countries of origin, years of publication, and topics.
The New England Journal of Medicine has published the most manuscripts on kidney transplantation (n = 26) and is the most cited journal (n = 15,642). The United States has the highest number of publications (n = 61). Kashika is the corresponding author with the most published papers (n = 5; 2892 citations). The most common topics of publication are immunosuppressant (n = 34), clinical outcome (n = 26), and pathology (n = 22). Keywords related to immunosuppressant are the most common in keyword mapping with VOSviewer.
Conclusions:
This bibliometric analysis of KT research provides the research characteristics and publication trends of this topic. In KT research, immunosuppressants and post-transplant clinical outcomes have been important topics.
1. Introduction
Kidney transplantation (KT) has become common as an alternative treatment in patients with end-stage renal disease. [ 1 ] KT, which was implemented approximately 50 years ago, has improved long-term results with the development of immunosuppressants. [ 2 ] Donors, including living and deceased, are needed for KT. Immunosuppressants have been developed for graft survival, and pathology has been further developed for the diagnosis of kidney grafts sensitive to immune conditions. In particular, research on KT is focused on rejection, pathology, and immunosuppressants.
Bibliometric analysis is used to identify publication trends, including authorships, years of publication, countries, and topics in a particular field. [ 3 ] It aims to determine research themes that have been most influential in developing the understanding and management of a field. The degree of intellectual impact of a publication can be identified through the list of citation rankings. [ 4 ] Using citation ranking, many medical researchers have identified and analyzed the most influential articles in various medical fields, such as orthopedic surgery, [ 5 ] plastic surgery, [ 6 ] and oncology. [ 7 ] However, to date, there have been no bibliometric analyses of KT research to identify the most influential articles. The purpose of this research is to identify and characterize the 100 most cited articles (T100) that focus on KT and clarify the trends in the accomplishments in this field.
The Institutional Review Board approved the review of medical articles using a publicly available database (Ilsan Paik Hospital Institutional Review Board No. 2021-04-030). A search of the Thomson Reuters Web of Science (WoS) citation indexing database was completed (1983–2019) using the following search terms: “kidney transplant∗,” “renal transplant∗,” “kidney allograft∗,” “renal allograft∗,” “kidney graft∗,” and “renal graft∗.” The search was conducted on a single day, April 20, 2020, to prevent changes in the number of citations as much as possible. Articles other than original or review articles were excluded, and only articles written in English were included. All articles were sorted by the number of citations, based on a method initially developed by Paladugu et al [ 8 ] ; the title and abstract of each article were thoroughly read and evaluated for inclusion by 2 independent reviewers (JWH and HJ) to ensure their relevance to KT. Because only the characteristics of KT needed to be analyzed, studies involving other transplantations, such as liver and pancreas transplantation, were excluded, even though KT was included. Animal studies were also included if the study was performed for renal allografts.
The selected T100 were then evaluated further according to the following parameters: year of publication, country of origin, institution, authorship, journal, number of citations, and article topic. Since a potential bias in this type of study is that older manuscripts have had more time to be cited, the citation rate was analyzed by dividing the number of citations by the number of years since publication. If the number of publications was the same, the ranking was determined based on the total number of citations.
All articles were analyzed according to their topic: immunosuppressant, clinical outcome, pathology, graft outcome, and donor. The “clinical outcome” group included post-transplant diabetes, infection, cancer, quality of life, medication adherence, and practice guideline. The “pathology” group included pathologic, immunologic, and molecular studies about post-transplant allograft nephropathy and included the diagnostic classification such as Banff. The “graft outcome” group included graft survival, graft rejection, and graft function. The “donor” group included management of living and deceased donors and operative graft perfusion in KT.
VOSviewer version 1.6.15 software (Leiden University, Leiden, Netherlands) was used to analyze the relationship between the keywords to generate a map and cluster visualization. [ 9 ] In the network visualization, each circle represented a keyword, and the size of circles represented the frequency of occurrence. Larger circles indicate that the keywords appear more frequently. The circle color on the map indicates the cluster to which the keyword belongs. The line between each circle indicates that the keywords are connected, and the length of the line represents the degree of the relationship. Overlay visualization reveals a changing trend of keywords as time progresses by representing the color of each circle. [ 10 ] The blue color represents that the timing of keyword appearance is earlier, and the red color represents that the timing is later. Before performing the analysis, keywords were manually standardized by the authors because different expressions of the same keywords may lead to errors in the results. [ 11 ]
The WoS database search returned 93,167 full manuscript publications. Table S1, Supplemental Digital Content lists the T100. The number of citations ranged from 2418 for Racusen et al (“The Banff 97 working classification of renal allograft pathology”) [ 12 ] to 363 for Colvin et al (“Antibody-mediated renal allograft rejection: Diagnosis and pathogenesis”). [ 13 ] The mean number of citations for all articles was 586.4 ± 284.9. The citation rate was the highest for the article “Banff 07 classification of renal allograft pathology: Updates and future directions” by Solez et al. [ 14 ] Although the citation rate was applied to prevent time bias, the citation rate of each article was not quite different from its citation numbers, as shown in Table S1, Supplemental Digital Content.
The T100 are published between 1983 and 2013. The years with the highest number of publications are 1999 and 2000, with a total of 10 papers. The oldest article on the T100, which discusses the Epstein−Barr virus-induced B-cell lymphoproliferative disease after KT, was published in 1983. [ 15 ] The most recent article, “Complement-binding anti-HLA antibodies and kidney-allograft survival” was published in 2013. [ 16 ]
The T100 are published in 15 journals (Table (Table1). 1 ). The New England Journal of Medicine has published the highest number of articles (n = 26; 15,642 citations), followed by Transplantation (n = 24; 12,883 citations). Half of the T100 are published in the 2 aforementioned journals.
Journals with 5 or more articles in the top 100.
The highest number of contributions comes from the United States (n = 61), followed by Canada (n = 11) and France (n = 5) (Fig. (Fig.1). 1 ). Although the United States has published more than half of the T100, the institution that has published the highest number of articles is University Alberta in Canada (Table (Table2). 2 ). Seven corresponding authors have more than 3 papers on the T100. Kasiske and Meier−Kriesche have the highest number of articles on the T100 (n = 5) (Table (Table3 3 ).

Countries that have contributed to the 100 most cited articles on kidney transplantation.
Institutions with 3 or more articles in the top 100.
Corresponding authors with 3 or more articles in the top 100.
The primary subject matter of the articles is categorized as follows: immunosuppressant, clinical outcome, pathology, graft outcome, and donor (Fig. (Fig.2). 2 ). The most studied topic in publications on KT is “Immunosuppressant” (n = 31), followed by “Clinical outcome” (n = 25) and “Pathology” (n = 20). Throughout the period, the topic of “Clinical outcome” has been continuously studied. Studies on “Pathology” have increased since 1991, and the studies of “Immunosuppressant” have increased significantly since 1996. Figure Figure2 2 shows the topical trend of the T100 over a 5-year period from 1981 to 2015.

The topical trend of the 100 most cited articles on kidney transplantation by 5-year periods.
Author-selected keywords of the T100 were analyzed through a co-occurrence network analysis tool using VOSviewer. A total of 106 keywords were extracted from the T100, with a total frequency of 137 (Table S2, Supplemental Digital Content). In the network visualization, the highest frequency of occurrence is kidney transplantation (n = 8), followed by graft survival (n = 6) and antibody-mediated rejection (n = 4). Figure Figure3A 3 A is a network formed by 106 keywords and 898 links; it is divided into 5 clusters: red, green, blue, yellow, and purple. The red cluster is the largest, consisting of 32 keywords, including kidney, transplantation, mycophenolate-mofetil, tacrolimus, sirolimus, and cyclosporine. The green cluster includes 20 keywords, mainly related to kidney transplantation, graft survival, waiting list, and era effect. The blue cluster consists of 18 keywords, mainly antibody-mediated rejection, kidney transplants, dialysis, end-stage renal disease, nonadherence, and donor-specific antibody. The yellow cluster includes 16 keywords, mainly malignancies, immunosuppression, and cardiovascular disease. The purple cluster is the smallest cluster with 15 keywords, mainly about acute rejection, Banff, acute allograft rejection, and acute cellular rejection.

Keyword co-occurrence analysis of the 100 most cited articles on kidney transplantation. (A) Keyword co-occurrence network visualization of the 100 most cited articles. Each circle represents a keyword, and the size of the circles represents the frequency of occurrence. Larger circles indicate that the keyword appears more frequently. Keywords included in the same cluster are displayed in the same color. The distance between the 2 circles shows the degree of the relationship. (B) Keyword co-occurrence overlay visualization. The color of the circle represents the average year of publication, from blue (distant year) to red (last year).
In the overlay visualization, keywords related to transplantation (average published year, 2000) or graft survival (average published year; 2004) in the T100 appear in the early phase (Fig. (Fig.3B). 3 B). However, recently, keywords related to immunosuppression (average published year, 2009) or antibody-mediated rejection (average published year, 2010) have appeared. Notably, keywords of transplantation-related diseases, such as malignancies or cardiovascular disease have appeared in recent years.
4. Discussion
Bibliometric analysis is used to identify publication trends and has been used in various fields. [ 3 ] Only in the field of solid organ transplantation, the bibliometric analyses of overall transplantation, [ 17 ] liver transplantation (LT), [ 18 ] and heart transplantation [ 19 ] have been sequentially published since 2014. Unfortunately, there have been no previous bibliometric studies on KT fields. To the best of our knowledge, this is the first bibliometric study to evaluate the subspecialty of KT. In the research topics, there are differences between LT and KT. In the T100 on LT, there are many studies on donors, including allocation, and surgery, including preservation and size mismatching. [ 18 ] The T100 on KT are mainly focused on immunology and clinical aspects rather than surgery. Robotic KT has become more common in KT surgery, and research on robotic KT is also being active. [ 20 ]
An important theme in the history of KT is the introduction of innovative surgery and the development of immunosuppressants. The first human KT was performed with a deceased donor in 1933 by Voronoy. Although the result of the graft was not good, it is a pioneer surgery in the history of clinical KT. This historical event is first reported in a Spanish journal in 1936. [ 21 ] A successful KT was reported in identical twins in 1955 by Murray, which won him the Nobel Prize in 1990. [ 22 ] In 1962, the first useful immunosuppressants including azathioprine and 6-mercaptopurine were used in a KT from a deceased donor. [ 23 ] Since then, the combination of azathioprine and corticosteroid has become the standard immunosuppressant treatment. [ 24 ] Antilymphocyte globulin, consisting of polyclonal antibodies obtained from various animals, is used as an adjuvant. [ 25 ] In the 1980s, the combinations of cyclosporine improved the results of KTs. [ 26 ] FK 506, discovered in 1984, is now widely used as a standard immunosuppressant in KT. [ 27 ] Since then, various immunosuppressants have been introduced more rapidly, thus improving KT results. Recently, due to the shortage of kidney allografts, interest in and research on expanded criteria donors, including elderly deceased and high Kidney Donor Risk Index donors, has increased. [ 28 ] For the best preservation of kidney allografts, many studies such as hypothermic machine perfusion and donor pretreatment are being conducted. [ 29 ]
VOSviewer analyzes large-scale bibliographic data and the relationships between keywords selected by authors in their own publications and cluster publications based on direct citation relations. [ 30 ] It also shows the time trend of keyword changes to inform the progress of the research field. In a recent bibliometric analysis, trend analysis was diversified through the keyword mapping methods of VOSviewer. [ 31 ] The keywords presented in the T100 on KT are mainly distributed in 5 clusters: transplantation, graft survival, immunosuppressant, rejection, and post-transplant clinical outcome. Interestingly, keyword analysis through VOSviewer shows that keywords such as “malignancy” or “cardiovascular diseases,” which are complications that can occur after KT, have emerged relatively recently, along with the long history of KT. Expanded criteria donor, graft preservation, and immune tolerance, which have recently been increasing interest in transplantation, were not included as keywords. Although there are many topics related to transplantation, it is difficult to clearly classify them as studies on KT. The authors thought that the artificial classification by the authors could induce another bias.
As in many previous bibliometric analyses, our study has some limitations. First, only 1 database was used in our study as a reference source. This can result in the omission of articles not recognized by WoS, although it is the largest bibliometric database currently available. Second, influential recent articles were rarely included in our study because they might need the time to accumulate citations. [ 32 ] Lastly, although a significant portion of the literature was not written in English, articles in languages other than English were not included in our database.
5. Conclusions
This bibliometric analysis of KT research provides the research characteristics and publication trends of this topic. In KT research, immunosuppressants and posttransplant clinical outcomes have been important topics.
Author contributions
Conceptualization: Ji Woong Hwang.
Data curation: Heungman Jun, Ji Woong Hwang.
Formal analysis: Heungman Jun.
Visualization: Ji Woong Hwang.
Writing – original draft: Heungman Jun, Ji Woong Hwang.
Writing – review & editing: Heungman Jun, Ji Woong Hwang.
Supplementary Material
Abbreviations: KT = kidney transplantation, LT = liver transplantation, T100 = 100 most cited articles, WoS = Web of Science.
How to cite this article: Jun H, Hwang JW. The most influential articles on kidney transplantation: a PRISMA-compliant bibliometric and visualized analysis. Medicine . 2022;101:3(e28614).
The authors have no funding and conflicts of interests to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
- Login / Register

‘These three individuals will leave very big shoes to fill’
STEVE FORD, EDITOR
Explore this zone to keep up with what’s happening in renal nursing. You will find relevant clinical articles, including must-read recommendations, Self-assessment and Journal Club articles for CPD, and related news and opinion.
Latest clinical articles

Seven findings that could save the NHS money and improve care

Renal system 4: causes, diagnosis and treatment of chronic kidney disease

Indwelling urinary catheter insertion 2: procedure for adults

Renal system 3: categorising, assessing and managing acute kidney injury

Indwelling urinary catheter insertion 1: children and young people

Renal system 2: acute kidney injury and other types of kidney dysfunction

Renal system 1: the anatomy and physiology of the kidneys

Providing home haemodialysis for a young adult with learning disabilities

Have a question about nursing? Ask Nursing Times is here to help you. Our new AI search engine gives instant answers exclusively from the Nursing Times content you know you can rely on. Nursing Times is trusted by healthcare organisations and education bodies around the UK. Click here to find out more.
Have a question about nursing? Ask Nursing Times is here to help you. Our new AI search engine gives instant answers exclusively from the Nursing Times content you know you can rely on. Nursing Times is trusted by healthcare organisations and education bodies around the UK. Click here to try now.

Dialysis nurse to take on Silverstone pit crew to boost renal awareness

NHS 75: Nurses reflect on history of the health service

Experienced nurse takes up deputy mayor post in Greenwich

Transplant nurse becomes Bradford’s first living donor co-ordinator

Type of diabetes drug ‘may protect against serious kidney problems’
‘practice-changing’ trial finds post-op chemo cuts return of rare cancer, drug ‘reduces’ risk of kidney failure for type 2 diabetes patients.

‘Avoidable’ hip operation death sparks changes at Lancs trust
From our sponsors.

The environmental footprint of catheters
In reality, studies show that the usage of a urinary catheter which is made from more sustainable material, could reduce the user’s carbon footprint by 20 kg CO2e annually.
Webinar series: Continence care – essential skills
▶ watch: assessment of bladder function and the continence pathway, ▶ watch: management of bowel incontinence, ▶ watch: assessment and management of continence problems in acute care, ▶ watch: incontinence associated dermatitis, bitesize learning: management and prevention of leg ulcers, ▶ video 1: immediate and necessary care, ▶ video 2: leg ulcer assessment, ▶ video 3: vascular assessment, ▶ video 4: wound cleansing and wound-bed preparation, ▶ workforce strategy: recruitment (domestic and international), ▶ ensuring safe staffing: a crucial step towards quality care, ▶ workforce strategy: retention, wellbeing, cpd and edi, ▶ workforce strategy: education and preceptorship.
- Academic Clinician Track
- Nephrology / Critical Care Medicine Track
- Nephrology / Palliative Care Medicine Track
- Research Track
- Advanced Transplant Nephrology Track
- Customizing Your Education
- Current Fellows and Graduate Information
- Diversity & Inclusion in Yale Nephrology
- Patient Care
- August 2023
Inherited Diseases of the Kidney
Glomerular disease, acute kidney injury, interventional data science, kidney transport and stone disease, interstitial nephritis, kidney transplantation, kidney tubule bioengineering, clinical trials.
- Summer Research
- Research Faculty
- Current Fellows
- Support Staff
- Animal Physiology and Phenotyping Core
- Disease Models and Mechanisms Core
- Human Genetics and Clinical Research Core
- Past Events
- Administrative Resources
- American Society of Nephrology (ASN) Conferences
INFORMATION FOR
- Residents & Fellows
- Researchers
Research Areas
The research activities of our faculty cover a broad range of topics in renal physiology and nephrology from laboratory bench to patient oriented investigation. Current areas of research focus include studies of the mechanisms of acute kidney injury and repair, molecular genetics of polycystic kidney disease and other cilia related disorders, renal tubular electrolyte transport and acid base regulation, renal epithelial cell biology and morphogenesis, and biomarkers in acute kidney injury and other kidney diseases.
In addition to a large spectrum of research projects supported by individual NIH research grants, the Yale Section of Nephrology is home to two NIH-funded centers of kidney disease research excellence, the George M. O’Brien Kidney Center at Yale and the Yale Center for the Study of Polycystic Kidney Disease.
The Clinical and Translational Research Accelerator recruits scientists and trains students in methods of translational research and offers access to a large biorepository of samples and national databases for research projects.
Yale Summer Undergraduate Medical Research
Hot Topics in Kidney Health
Join us as we highlight the latest in kidney research, dispel myths, bring you up-to-date news in kidney care, and answer questions from patients to help them live well with kidney disease or a transplant.
Subscribe on Apple Podcasts
Subscribe on spotify.
Power lifechanging research, education and advocacy to ensure that every person facing kidney disease gets the chance to thrive—not simply survive. Give today and help us provide FREE resources, support, and hope for patients, loved ones and healthcare heroes.
Unfiltered Story: Next steps after losing a transplant
Losing a kidney transplant can feel very overwhelming. Today we're here with Anthony Tuggle, a former NKF board member, to hear how he's coping with losing a transplant and learn what's next for him.
Coping with losing a transplant
Everyone loves to talk about kidney transplant success stories but rarely do we talk about what happens if a transplant fails. On today's episode Dori Muench, a post transplant social worker, and Sue George, a kidney warrior with experience losing a transplant, are here to discuss the impact of losing a kidney and how to cope.
Artificial Kidneys
When will the artificial kidney be ready for human use? Learn more about the progress of the artificial kidney and how it will affect someone's quality of life from expert Shuvo Roy, Ph.D.
What is a high KDPI kidney?
When a kidney from a deceased donor becomes available, it is scored on a system called the Kidney Donor Profile Index (KDPI). How accurate is it at predicting possible transplant survival? On this episode, we speak with experts to get the facts
Fad diets and kidney diets
It’s hard to keep up with all the new fad diets out there. Do you know which ones are right for you and your kidney health? On this episode, you will hear from experts on finding the diet that's right for you and how to stick to it.
Superfoods for people with kidney disease
You may have heard the buzzword superfoods but what are they and do they have special qualities? Board-certified renal dietitian, Jen Hernadez is here to break it down.
What do clinical end points and trials mean for CKD research?
Clinical trials exist to help prevent, screen for, diagnose, or treat diseases and other health problems. Without them, we would not have new treatments or other advances in health and medicine. But how are the clinical trial endpoints, or the preferred outcomes of these trials determined? Today, Anthony Gucciardo NKF’s Senior Vice President of Strategic Partnerships, Dr. Joseph Vassalotti, NKF’s Chief Medical Officer, and Kent Bressler, a Patient advocate and FSGS patient, discuss this and more.
Mindfulness meditation for kidney patients
You may have heard the term mindfulness before but what does it mean, what are the benefits, and how can you integrate mindfulness into your life? On today’s episode Gary Petingola a Social Worker certified to teach Mindfulness-Based Stress Reductionexplains all this and more.
Transplants for All
At the National Kidney Foundation, we believe that everyone who needs a kidney should get a kidney. To make this dream a reality, we’ve launched the Transplants for All Initiative. What is this initiative and how will it make a difference in the lives of people with kidney disease? In today’s episode special guests Morgan Reid, NKF’s Transplant Policy & Strategy Director and Haley Jenson, NKF’s Transplant Programs Director explain this and more.
BONUS: Sexuality and kidney disease
Sexual dysfunction is incredibly common in patients with kidney disease. In today's bonus episode, you'll learn about why it is so prevalent, the different treatment options, and how to improve communication around this important but often neglected aspect of health.
LGBTQ+ advocacy in healthcare
Over 50% of LGBTQIA-plus people have experienced some form of healthcare discrimination and over 25% of transgender people reported being denied care due to their transgender status. Not having proper health care or avoiding health care due to discrimination, can result in dire consequences, including an increased risk of health problems like kidney disease. What is this discrimination, and how can you advocate for yourself and LGBTQIA+ rights? In today’s episode Dr. Joshua Wilder, a podiatrist, and Representative Jeff Currey, two kidney transplant recipients and members of the LGBTQIA+ community, discuss this and more.
NKF Innovation Fund: developing new treatments for kidney patients
For far too long treatments for CKD haven’t changed. Launched in 2021, the NKF Innovation Fund works to accelerate funding, and development of therapies that kidney patients deserve. On this episode, you will hear from NKF CEO Kevin Longino interviews Kathleen St. Jean, Chief Commercial Officer of 34 Lives, one of the first recipients of a significant investment from NKF’s Innovation Fund to help further develop a new technology to rehabilitate donated kidneys for transplantation.
Living donors and mental health
Donating a kidney is one of the most selfless gifts one person can give to another. But what is that experience like for the donor before and after the transplant surgery? Today, we'll hear from Jessica Kolansky, a living kidney donor, and Alexandra Catalyst, a transplant coordinator, about the post transplant experience and what resources are available to donors after the surgery.
Laughter therapy for kidney patients
Is laughter really the best medicine? On today’s episode we’ll discuss an exciting new coping strategy for dialysis patients called guided group laughing therapy. What is it and how does it help? Dr. Paul Bennet who ran a study on the benefits of laughing therapy and Kimberly Super-Harrigan, a dialysis patient, are here to break it down.
BMI and weight management for kidney patients and living donors
Obesity is one of the major risk factors for developing kidney disease, which is measured through the body mass index or BMI. This measurement factors into the process for both living donors and transplant recipients. On today’s episode, you’ll learn how to measure your BMI and hear from both kidney patients on how managing their weight affected their kidney health.
Access to reproductive care for kidney patients
In 2022, the US Supreme Court overturned precedent established by Roe v Wade, eliminating the constitutional right to abortion. Family planning decisions can be difficult and complex for kidney patients. On today’s episode, we’ll discuss how this impacts kidney patients and disadvantaged patients with limited access to healthcare.
Game Changers: Treating CKD earlier
Did you know that 40% of chronic kidney disease progression may be preventable with earlier diagnosis and treatment? On this episode, you will hear the facts around treating CKD earlier from Dr. Joe Vassalotti, NKF’s Chief Medical Officer. You will also hear from Jane DeMeis on her journey with kidney disease.
Exercise and bone health: what CKD patients should know
Keeping your body and bones strong are important when you have kidney disease. Do you know what types of exercise are good for kidney patients? What about for transplant recipients or people on dialysis? In this episode, we sat down with experts to discuss the benefits and recommendations of managing an exercise routine.
Managing fluid intake as a CKD patient
It is important that certain individuals with CKD limit their fluid intake, but many don’t understand why or where to begin. On today’s episode, we sat down with experts to discuss fluid restriction, such as why it’s important, the negative effects of consuming too much, and ways to manage a fluid-restricted diet.
Treatment options for undocumented people with kidney disease
Undocumented people face increased barriers to accessing health coverage and care, including treatment for kidney disease. In this episode, our guest experts discuss what treatment options are currently available for undocumented people and what kind of advocacy efforts are being made to improve their access to health care.
Breaking Down New Medicare Coverage for Immunosuppressant Drugs
The Medicare coverage for immunosuppressive drugs for kidney transplant patients has recently been expanded. But what does this new benefit cover and who is eligible? in this podcast, Cynthia Nichols-Jackson, a registered nurse and a program coordinator for the National Kidney Foundation, and Troy Zimmerman, a special projects director for the National Kidney Foundation, discuss how this new policy will affect the future for kidney transplants.
Should You Follow A Special Diet After Transplant?
How potassium affects kidney patients
One of the jobs your kidneys is to manage your body’s levels of potassium, which keeps your heartbeat regular and your muscles working right. Many kidney patients need to watch what they eat to ensure that their potassium levels don’t become too high and cause dangerous health risks. On today’s episode, you’ll hear how to best manage your potassium levels to protect yourself.
How kidney patients should protect themselves from COVID-19 in 2022
While many people feel like the world is headed back to normal, many kidney patients can feel left behind. COVID-19 is still top of mind for those who are immunocompromised and we're here to offer resources and support. On today's episode, our guests will answer your questions about how COVID-19 affects transplant, dialysis, and early stage CKD patients.
What is basic science research and why is it important?
When we hear the word research, most of us think of innovative breakthrough treatments and technologies. But applied clinical research could not be possible without another type of research called basic science research in which scientists study the fundamental processes of the human body. In this episode, we’ll learn what basic science research is and how it applies to the area of kidneys and kidney disease.
Working with your clinician to make shared decisions for your care
Shared decision making can play a vital role in the treatment of kidney disease. When physicians involve patients in their care, they may be able to help slow progression and improve outcomes. In this episode, we discussed how patients and their physicians can achieve this and hear stories from patients who have been there.
How kidney disease affects your mental health
People with chronic conditions like kidney disease face mental health struggles such as depression or anxiety. In many kidney patients those challenges often go overlooked or undertreated. In this episode, we sat down with a mentor and mentee from NKF Peers to discuss their experiences and the importance of talking to someone who knows what you've been through.
Tips for finding a living donor
If you are in need of a kidney transplant, finding a living donor can sound scary and overwhelming. Where should you start and what’s the best way to share your story with the world? In this episode, you will hear from transplant recipients who once stood in your shoes.
Pig kidneys in humans? Xenotransplantation explained.
From the invention of the dialysis machine to the first successful kidney transplant, science has come a long way in extending life for kidney patients. Is transplantation between humans and animals the next step? In this episode, you will hear from a doctor behind the first successful transplant of a human receiving a pig kidney and where the science can take us from here.
Deciding to become a living donor
Pregnancy and kidney disease
Pregnancy can be an exciting time for most people, but what does it look like if you are a kidney patient? What does pregnancy look like if they have kidney disease, are on dialysis, or have received a transplant? In this episode, we’ll hear useful facts and tips from transplant nephrologist Dr. Mariana Markell, as well as personal stories from Cari Maxwell and Katie Reed, two mothers living with kidney disease.
What are SGLT2 Inhibitors and are they the right drug for you?
You might have heard about drugs called SGLT2 inhibitors used in treatment of kidney disease, but, just like many other kidney patients, you might not know if they’re right for you. On this episode, we explain how different SGLT2 inhibitors are from other kidney disease medications, discuss side effects, cost, and the ongoing research around this category of drugs.
How much sodium is safe for kidney patients?
Most patients on dialysis need to limit the amount of sodium in their diets. But how much sodium is safe and what are some ways to add flavor to your diet? On today‘s episode, our experts cover examples of high sodium foods, recommendations for low sodium substitutes, and how much sodium people with kidney disease should have as a part of a healthy diet.
What do changes to eGFR calculation mean for patients?
Tips for overcoming financial hardship for kidney patients
Many kidney disease patients often face financial hardships, such as having to leave a job or struggling to pay for medications. We sat down with physician and a postdoctoral research fellow Dr. Issac Acquah to talk about his recent research into the financial impact on people with chronic kidney disease.
How to become an advocate for kidney health
Over the past year, NKF advocates have won a number of policy campaigns both in Congress and state capitals across the country - but we're not done yet. In this episode, we discussed some recent wins and our upcoming challenges for the kidney advocate community with Jeff Currey, a Connecticut State Representative and kidney transplant recipient, and Armand Halter, an NKF patient advocate who helped lead NKF’s efforts to pass the Connecticut version of the Living Donor Protection Act.
A major worry for many people right now is the Delta variant, a highly contagious strain of COVID-19 which is making headlines across the United States. The FDA has just authorized a third dose of the COVID-19 vaccine so that immune compromised patients can better protecting themselves from the virus. What does this mean for CKD, dialysis, and transplant patients? We spoke with Dr. Joseph Vassalotti, NKF Chief Medical Officer, in a recent Facebook Live to share the facts about the Delta variant, COVID-19 booster shots, and other concerns facing kidney patients.
Coping with depression & anxiety during a global pandemic
ASN's Mission
To create a world without kidney diseases, the ASN Alliance for Kidney Health elevates care by educating and informing, driving breakthroughs and innovation, and advocating for policies that create transformative changes in kidney medicine throughout the world.
Contact ASN
1401 H St, NW, Ste 900, Washington, DC 20005
202-640-4660
The Latest on X
- Excellence in Patient Care
- Kidney Health Initiative
- Communities

Kidney Week
Kidney week 2024: highlights.
- Thursday, October 24: David C. Rhew, MD, Global Chief Medical Officer, Microsoft , "Accelerating Health Care Innovation in Nephrology with AI"
- Friday, October 25: Sekar Kathiresan, MD, CEO, Verve Therapeutics , "From Reading the Genome for Risk to Rewriting It for Cardiovascular Health"
- Saturday, October 26: Melissa H. Little, PhD, Chief Scientist, Murdoch Children's Research Institute , "Understanding, Improving, and Applying Human Pluripotent Stem Cell-Derived Kidney Tissues"
- Sunday, October 27: Michael R. DeBaun, MD, MPH, Director for Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Vanderbilt University , "The Curative Therapy for Sickle Cell Disease: The Good, The Bad, and The Future"
Late-Breaking Clinical Trials
ASN welcomes randomized trials (Phase 2, 3, 4) that will have significant impact on clinical practice on all topics touching kidney diseases including AKI, CKD, Diabetes, Dialysis, Genetic Diseases, Glomerular Diseases, Hypertension, Kidney Stones, Pediatrics, Transplantation, and more. The submission period opens on Wednesday, July 17, and closes on Wednesday, September 4, at 2:00 p.m. EDT.
Why Submit to Kidney Week?
- Reach a global audience: More than 12,000 leading nephrologists, researchers, industry professionals, and others attend this largest kidney meeting in the world.
- Gain immediate recognition: Attract media attention and scientific interest. All main stage podium presentations will be invited to present at a press-embargoed session.
What's New?
- Multiple late-breaking oral sessions.
- More presentation time for high-impact research.
- Increased collaboration with JASN, JAMA, and NEJM.
Early Programs on Wednesday, October 23
- Acid-Base, Fluid, and Electrolyte Balance Disorders 2024: Challenging Issues for Clinicians
- Advances in Research Conference - Genome Engineering and RNA-Based Therapeutics: From Bench to Potentially Curative Medicines
- Between a Rock and a Hard Place: Practical Updates in Kidney Stone Prevention and Management
- Critical Care Nephrology: 2024 Update
- Glomerular Diseases: 2024 Update
- Onconephrology: Cancer, Its Treatments, and the Kidneys
- Point-of-Care Ultrasound in Nephrology
Welcome Reception on Thursday, October 24, 6:00-7:00 p.m.
All Kidney Week participants are invited to this reception in the exhibit hall. Join us for food, drinks, and networking.
The webpage has been translated to .
Translate This Page
The ASN website can be translated into a number of different languages. For more information view the disclaimer .
This site requires javascript, which you do not appear to have enabled. In order for everything to function properly, please enable javascript .

40+ Research Topics on Renal Nursing: An Extensive Guide for Nursing Students
- Carla Johnson
- August 29, 2023
- Nursing Topics and Ideas
Renal nursing holds a pivotal position in the realm of healthcare, catering to patients with kidney-related ailments. For nursing students, comprehending the nuances of renal nursing is paramount. This article delves deep into the research topics on renal nursing, presenting several resources, project concepts, and research questions to assist nursing students in mastering this specialized arena.
Introduction to Renal Nursing
Renal nursing also recognized as nephrology nursing, encompasses the care of individuals afflicted with kidney disorders. It encompasses various dimensions including prevention, assessment, intervention, and patient education. Renal nurses collaborate closely with patients spanning all age groups who are afflicted by kidney diseases, renal failure, and related conditions. They work in harmony with interdisciplinary teams to provide holistic care, manage treatments such as dialysis, and enlighten patients about disease management.
Exploring PICOT Questions in Renal Nursing
- P: Pediatric patients undergoing kidney transplant surgery; I: Integration of play therapy and distraction techniques; C: Traditional preoperative preparation; O: Decrease in preoperative anxiety and stress; T: Before kidney transplant surgery. In pediatric renal transplant cases, can the integration of play therapy and distraction techniques prior to surgery substantially reduce preoperative anxiety and stress compared to conventional preoperative preparation methods?
- P: Elderly patients on hemodialysis; I: Introduction of personalized exercise regimens; C: Standard care devoid of exercise programs; O: Enhancement in physical function and quality of life; T: Over a span of 3 months. Among elderly patients undergoing hemodialysis, can the introduction of individualized exercise regimens result in noticeable improvements in physical function and overall quality of life in contrast to the standard care without exercise interventions, over a period of 3 months?
- P: Adult patients with chronic kidney disease ; I: Deployment of telehealth monitoring; C: In-person clinic visits; O: Enhanced disease management and decrease in hospital admissions; T: Over a period of 1 year. For adults grappling with chronic kidney disease, does the implementation of telehealth monitoring lead to improved disease management, as evidenced by a decelerated disease progression and reduced hospital admissions, when juxtaposed with conventional in-person clinic visits over the course of 1 year?
- P: Patients undergoing peritoneal dialysis; I: Adoption of aseptic technique training; C: Conventional technique instruction; O: Marked reduction in peritonitis rates; T: Monitored over 6 months. In patients undergoing peritoneal dialysis, can the provision of aseptic technique training lead to a substantial decrease in peritonitis rates as compared to the standard technique instruction, observed over a monitoring period of 6 months?
- P: Renal transplant recipients; I: Introduction of mindfulness meditation; C: Standard post-transplant care; O: Reduction in stress, anxiety, and enhanced immune function; T: Assessed up to 1 year post-transplant. In the case of renal transplant recipients, can incorporating mindfulness meditation into the post-transplant care regimen bring about a noteworthy reduction in stress and anxiety, along with an improved immune function, within the first year following the transplant?
- P: Patients with end-stage renal disease ; I: Implementing a patient-centric education program; C: Traditional patient education practices; O: Augmented adherence to treatment regimens and improved self-management; T: Evaluated over 9 months. For individuals diagnosed with end-stage renal disease, does implementing a patient-centric education program result in enhanced adherence to treatment regimens and improved self-management compared to conventional patient education practices, over a period of 9 months?
- P: Diabetic patients with comorbid chronic kidney disease; I: Adoption of interdisciplinary collaboration; C: Disconnected care between diabetes and nephrology teams; O: Enhanced glycemic control and slower kidney function decline; T: Studied over a span of 2 years. Among diabetic patients concurrently grappling with chronic kidney disease, does an approach of interdisciplinary collaboration in care lead to improved glycemic control and a decelerated pace of kidney function decline compared to care lacking coordination between diabetes and nephrology teams, over a span of 2 years?
- P: Patients undergoing continuous renal replacement therapy in the ICU; I: Early initiation of nutrition support; C: Delayed nutrition intervention; O: Improved nutritional status and reduced ICU stay; T: Assessed during the ICU stay. In patients undergoing continuous renal replacement therapy in the intensive care unit, does the early initiation of nutrition support result in improved nutritional status and a shortened ICU stay in comparison to delayed nutrition intervention, measured throughout the ICU stay?
- P: Patients with polycystic kidney disease; I: Implementation of genetic counseling services; C: Absence of genetic counseling; O: Informed decision-making regarding family planning and disease management; T: Evaluated immediately following genetic counseling session. For patients diagnosed with polycystic kidney disease, does the utilization of genetic counseling services lead to informed decision-making regarding family planning options and disease management compared to those without genetic counseling, immediately after the counseling session?
- P: Renal transplant candidates; I: Introduction of pre-transplant psychosocial assessments; C: Conventional transplant evaluation process; O: Improved patient selection and post-transplant psychological adjustment; T: Monitored from pre-transplant assessment to 1 year post-transplant. In renal transplant candidates, can the inclusion of pre-transplant psychosocial assessments result in enhanced patient selection and improved psychological adjustment post-transplant, in comparison to the standard transplant evaluation process, studied from pre-transplant assessment through 1 year post-transplant?
Resources for Evidence-Based Practice Projects
- Investigating the influence of exercise on the psychological well-being of patients undergoing dialysis.
- Analyzing the efficacy of educational interventions in ameliorating dietary adherence among individuals with chronic kidney disease.
- Evaluating the utilization of telehealth platforms to monitor renal transplant recipients’ medication adherence .
- Assessing the impact of early intervention in preventing infections related to catheters in patients on peritoneal dialysis.
- Exploring the consequences of nurse-led programs for smoking cessation on outcomes of renal transplants.
Nursing Capstone Project Concepts
- Developing a comprehensive educational toolkit for patients transitioning from peritoneal dialysis to hemodialysis.
- Designing a peer support initiative for teenagers with kidney transplant s to address psychological and social challenges.
- Formulating guidelines for renal nurses to identify and manage interactions between medications in patients with multiple comorbidities.
- Implementing an initiative for quality enhancement to reduce the incidence of infections stemming from bloodstream in hemodialysis patients.
- Designing and evaluating a patient education program on renal health that is culturally sensitive for a specific ethnic community.
Nursing Research Paper Topics
- Analyzing the effects of chronic kidney disease on caregiver burden and family dynamics.
- Investigating the correlation between social determinants of health and the progression of renal diseases.
- Examining the efficiency of strategies for pain management in patients undergoing renal surgeries.
- Exploring the psychosocial challenges faced by living kidney donors after transplantation.
- Scrutinizing the ethical ramifications of policies for organ allocation in renal transplantation.
Renal Nursing Research Questions
- How does the incorporation of music therapy affect the emotional well-being of pediatric patients undergoing dialysis?
- What are the factors that hinder or facilitate adherence to medications among elderly patients with chronic kidney disease?
- How do telehealth interventions impact self-management behaviors in individuals on peritoneal dialysis?
- What is the effect of renal-specific mindfulness-based interventions on the quality of life of patients on hemodialysis?
- How does the nurse-patient relationship impact adherence to treatment in adolescent patients with kidney transplants?
Essay Topics and Examples
- The Role of Renal Nurses in Advancing Patient Education and Self-Care.
- Ethical Predicaments in Renal Transplantation: Striking a Balance Between Equity and Patient Outcomes.
- Cultural Considerations in Renal Nursing: Delivering Care that is Culturally Competent.
- The Influence of Psychosocial Support on the Quality of Life of Recipients of Renal Transplants.
- Investigating the Interplay Between Chronic Kidney Disease and Mental Health: A Comprehensive Approach.
Aspiring nursing professionals embarking on their careers must fully embrace the realm of renal nursing. The PICOT questions, resources, and project ideas in this article pave the way for a journey toward mastery in this specialized discipline. By immersing yourselves in these subjects and pursuing evidence-based practice, capstone projects, and research papers, you contribute to the advancement of renal nursing and play an integral role in elevating patient care and outcomes. Take your step into renal nursing with confidence. Consider contacting our writing services to receive expert guidance and support in crafting impeccable assignments and essays. Our accomplished team of writers is committed to assisting nursing students in excelling within their academic pursuits. Contact us today to unlock your full potential as a future renal nurse.
Frequently Asked Questions (FAQs)
- Why is renal nursing important? Renal nursing is vital as it focuses on patients with kidney-related conditions, ensuring proper care, treatment, and education to enhance their quality of life and overall well-being.
- What is the role of a nurse in renal function tests? Nurses play a critical role in renal function tests by administering tests, monitoring patients’ kidney function , explaining procedures, and providing support and education throughout the testing process.
- What does renal stand for? “Renal” is derived from the Latin word “ren,” meaning kidney. Thus, “renal” pertains to anything related to the kidneys.
- What are the key responsibilities of a dialysis nurse? Dialysis nurses are responsible for administering dialysis treatments, monitoring patients’ vital signs, assessing their well-being during and after the procedure, ensuring proper equipment operation, and offering patient education on kidney health and self-care.
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, worried about your paper we can help, frequently asked questions.
When you pay us, you are paying for a near perfect paper and the time convenience.
Upon completion, we will send the paper to via email and in the format you prefer (word, pdf or ppt).
Yes, we have an unlimited revision policy. If you need a comma removed, we will do that for you in less than 6 hours.
As you Share your instructions with us, there’s a section that allows you to attach as any files.
Yes, through email and messages, we will keep you updated on the progress of your paper.
Start by filling this short order form thestudycorp.com/order
And then follow the progressive flow.
Having an issue, chat with us here
Dr. James Logan – Admin msnstudy.com
Popular Posts
- Academic Writing Guides
- Nursing Care Plan
- Nursing Theory
- Writing Guides for MSN students
Important Links
Knowledge base, utilize our guides & services for flawless nursing papers: custom samples available.
MSNSTUDY.com helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
We Accept:

Best Nursing Research Topics for Students
What is a nursing research paper.
- What They Include
- Choosing a Topic
- Best Nursing Research Topics
- Research Paper Writing Tips

Writing a research paper is a massive task that involves careful organization, critical analysis, and a lot of time. Some nursing students are natural writers, while others struggle to select a nursing research topic, let alone write about it.
If you're a nursing student who dreads writing research papers, this article may help ease your anxiety. We'll cover everything you need to know about writing nursing school research papers and the top topics for nursing research.
Continue reading to make your paper-writing jitters a thing of the past.
A nursing research paper is a work of academic writing composed by a nurse or nursing student. The paper may present information on a specific topic or answer a question.
During LPN/LVN and RN programs, most papers you write focus on learning to use research databases, evaluate appropriate resources, and format your writing with APA style. You'll then synthesize your research information to answer a question or analyze a topic.
BSN , MSN , Ph.D., and DNP programs also write nursing research papers. Students in these programs may also participate in conducting original research studies.
Writing papers during your academic program improves and develops many skills, including the ability to:
- Select nursing topics for research
- Conduct effective research
- Analyze published academic literature
- Format and cite sources
- Synthesize data
- Organize and articulate findings
About Nursing Research Papers
When do nursing students write research papers.
You may need to write a research paper for any of the nursing courses you take. Research papers help develop critical thinking and communication skills. They allow you to learn how to conduct research and critically review publications.
That said, not every class will require in-depth, 10-20-page papers. The more advanced your degree path, the more you can expect to write and conduct research. If you're in an associate or bachelor's program, you'll probably write a few papers each semester or term.
Do Nursing Students Conduct Original Research?
Most of the time, you won't be designing, conducting, and evaluating new research. Instead, your projects will focus on learning the research process and the scientific method. You'll achieve these objectives by evaluating existing nursing literature and sources and defending a thesis.
However, many nursing faculty members do conduct original research. So, you may get opportunities to participate in, and publish, research articles.
Example Research Project Scenario:
In your maternal child nursing class, the professor assigns the class a research paper regarding developmentally appropriate nursing interventions for the pediatric population. While that may sound specific, you have almost endless opportunities to narrow down the focus of your writing.
You could choose pain intervention measures in toddlers. Conversely, you can research the effects of prolonged hospitalization on adolescents' social-emotional development.
What Does a Nursing Research Paper Include?
Your professor should provide a thorough guideline of the scope of the paper. In general, an undergraduate nursing research paper will consist of:
Introduction : A brief overview of the research question/thesis statement your paper will discuss. You can include why the topic is relevant.
Body : This section presents your research findings and allows you to synthesize the information and data you collected. You'll have a chance to articulate your evaluation and answer your research question. The length of this section depends on your assignment.
Conclusion : A brief review of the information and analysis you presented throughout the body of the paper. This section is a recap of your paper and another chance to reassert your thesis.
The best advice is to follow your instructor's rubric and guidelines. Remember to ask for help whenever needed, and avoid overcomplicating the assignment!
How to Choose a Nursing Research Topic
The sheer volume of prospective nursing research topics can become overwhelming for students. Additionally, you may get the misconception that all the 'good' research ideas are exhausted. However, a personal approach may help you narrow down a research topic and find a unique angle.
Writing your research paper about a topic you value or connect with makes the task easier. Additionally, you should consider the material's breadth. Topics with plenty of existing literature will make developing a research question and thesis smoother.
Finally, feel free to shift gears if necessary, especially if you're still early in the research process. If you start down one path and have trouble finding published information, ask your professor if you can choose another topic.
The Best Research Topics for Nursing Students
You have endless subject choices for nursing research papers. This non-exhaustive list just scratches the surface of some of the best nursing research topics.
1. Clinical Nursing Research Topics
- Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties.
- Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings.
- Explore the effectiveness of pain management protocols in pediatric patients.
2. Community Health Nursing Research Topics
- Assess the impact of nurse-led diabetes education in Type II Diabetics.
- Analyze the relationship between socioeconomic status and access to healthcare services.
3. Nurse Education Research Topics
- Review the effectiveness of simulation-based learning to improve nursing students' clinical skills.
- Identify methods that best prepare pre-licensure students for clinical practice.
- Investigate factors that influence nurses to pursue advanced degrees.
- Evaluate education methods that enhance cultural competence among nurses.
- Describe the role of mindfulness interventions in reducing stress and burnout among nurses.
4. Mental Health Nursing Research Topics
- Explore patient outcomes related to nurse staffing levels in acute behavioral health settings.
- Assess the effectiveness of mental health education among emergency room nurses .
- Explore de-escalation techniques that result in improved patient outcomes.
- Review the effectiveness of therapeutic communication in improving patient outcomes.
5. Pediatric Nursing Research Topics
- Assess the impact of parental involvement in pediatric asthma treatment adherence.
- Explore challenges related to chronic illness management in pediatric patients.
- Review the role of play therapy and other therapeutic interventions that alleviate anxiety among hospitalized children.
6. The Nursing Profession Research Topics
- Analyze the effects of short staffing on nurse burnout .
- Evaluate factors that facilitate resiliency among nursing professionals.
- Examine predictors of nurse dissatisfaction and burnout.
- Posit how nursing theories influence modern nursing practice.
Tips for Writing a Nursing Research Paper
The best nursing research advice we can provide is to follow your professor's rubric and instructions. However, here are a few study tips for nursing students to make paper writing less painful:
Avoid procrastination: Everyone says it, but few follow this advice. You can significantly lower your stress levels if you avoid procrastinating and start working on your project immediately.
Plan Ahead: Break down the writing process into smaller sections, especially if it seems overwhelming. Give yourself time for each step in the process.
Research: Use your resources and ask for help from the librarian or instructor. The rest should come together quickly once you find high-quality studies to analyze.
Outline: Create an outline to help you organize your thoughts. Then, you can plug in information throughout the research process.
Clear Language: Use plain language as much as possible to get your point across. Jargon is inevitable when writing academic nursing papers, but keep it to a minimum.
Cite Properly: Accurately cite all sources using the appropriate citation style. Nursing research papers will almost always implement APA style. Check out the resources below for some excellent reference management options.
Revise and Edit: Once you finish your first draft, put it away for one to two hours or, preferably, a whole day. Once you've placed some space between you and your paper, read through and edit for clarity, coherence, and grammatical errors. Reading your essay out loud is an excellent way to check for the 'flow' of the paper.
Helpful Nursing Research Writing Resources:
Purdue OWL (Online writing lab) has a robust APA guide covering everything you need about APA style and rules.
Grammarly helps you edit grammar, spelling, and punctuation. Upgrading to a paid plan will get you plagiarism detection, formatting, and engagement suggestions. This tool is excellent to help you simplify complicated sentences.
Mendeley is a free reference management software. It stores, organizes, and cites references. It has a Microsoft plug-in that inserts and correctly formats APA citations.
Don't let nursing research papers scare you away from starting nursing school or furthering your education. Their purpose is to develop skills you'll need to be an effective nurse: critical thinking, communication, and the ability to review published information critically.
Choose a great topic and follow your teacher's instructions; you'll finish that paper in no time.

Joleen Sams is a certified Family Nurse Practitioner based in the Kansas City metro area. During her 10-year RN career, Joleen worked in NICU, inpatient pediatrics, and regulatory compliance. Since graduating with her MSN-FNP in 2019, she has worked in urgent care and nursing administration. Connect with Joleen on LinkedIn or see more of her writing on her website.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

IMAGES
VIDEO
COMMENTS
Evidence-based practice (EBP) is one of the essential components of nephrology nursing. Reviews of such evidence are important as a means to synthesize research findings into one meaningful form of data. Publication trends of evidence reviews in nephrology nursing are unknown. The purpose of this systematic review was to identify trends in ...
Despite notable progress in basic, clinical and translational nephrology research in the past 50 years, many challenges remain. In this Review, the authors provide an overview of the current ...
INTRODUCTION. Nephrology nursing is an evolving specialisation of nursing practice, providing care for patients experiencing kidney failure. Chronic kidney disease (CKD) is a complex disease that affects approximately 800 million people globally (Kovesdy, 2022).As kidney disease progresses to kidney failure, kidney replacement therapy (dialysis or kidney transplantation) is required to sustain ...
1 article. An innovative journal in the expanding area of experimental and clinical nephrology. It advances understanding of kidney and renal diseases, diagnosis and treatment - ultimately leading to better o...
Abstract. Four peer-reviewed nephrology nursing society journal publications from 2010 to 2015 were analysed. Journal articles (n=638) were categorised into type, treatment cohort, specific topic ...
The renal nursing workforce has a strong internal supportive culture. The working environment and professional development opportunities need to be re-considered (larger spaces and increased training opportunities required). Changing patient acuity management requires modifications to the nurse/patient ratio model.
Kidney failure is defined by a glomerular filtration rate <15 ml/min/1.73 m 2 (ref. 7) and may be treated using KRT (which refers to either dialysis or transplantation) or with supportive care 8 ...
Now in its fifth edition, Renal Nursing continues to be the essential evidence-based guide to nephrology and kidney care for nurses and allied health care professionals. This comprehensive text examines the stages of chronic kidney disease, pre-dialysis care, acute kidney injury, renal replacement therapy, renal nutrition, renal care in children and young people and more. Offers thorough ...
In relation to nursing research, as well as executing a qualitative phenomenological study as advocated above, this topic of the continuing care of the renal patient would also benefit from further quantitative studies that use appropriate sampling techniques to generate random samples and produce results that can be generalized. More ...
Keywords: Nephrology, chronic kidney diseases, new advances, kideny function, renal diseases . Important Note: All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements.Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer ...
Objectives: to develop a protocol for Nursing Process operationalization in approaching older adults with vulnerability to chronic kidney disease in Primary Health Care, based on Neuman's stressors. Methods: a methodological study, carried out in two stages: 1) synthesis of evidence using an inductive strategy (mixed method study) and 2 ...
Chronic kidney disease (CKD) is a major public health problem. The global prevalence of CKD is estimated to be 13% [].Advanced chronic kidney disease (ACKD) comprises individuals with an estimated glomerular filtration rate less than 30 ml/min/1.63 m2 and includes stages G4 and G5 [].It accounts for < 5% of all CKD cases but is associated with a very high risk of adverse cardiovascular and ...
Research in this field is of paramount importance as it leads to the development of new treatments, management strategies, and preventive measures. The nephrology nursing research paper topics encompass a wide range of areas such as Acute Kidney Injury, Chronic Kidney Disease, Dialysis, Kidney Transplantation, and many more.
Keywords: kidney disease, acute kidney injury, chronic kidney diseases, renal vascular, renal epithelia . Important Note: All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements.Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any ...
A collection of Nephrology information, resources and CME activities on Medscape.
1. Introduction. Chronic renal failure [] is secondary to the continuous progression of various chronic kidney diseases and is characterized by renal insufficiency, metabolite retention, dysregulation of the internal environment, and functional imbalance of systems.Clinical statistics show that the annual incidence of chronic renal failure is about 0.3%, which exhibits an increasing trend in ...
Research Topics. SHARE A A. Research Topics. Kidney disease is complex. There are several sub-categories of kidney disease with various causes, symptoms, treatments and outcomes. BC kidney care professionals - and patient partners who are increasingly part of research teams - address a number of research and quality improvement questions.
The T100 are published in 15 journals (Table. . 1 ). The New England Journal of Medicine has published the highest number of articles (n = 26; 15,642 citations), followed by Transplantation (n = 24; 12,883 citations). Half of the T100 are published in the 2 aforementioned journals.
EMAP Publishing Limited Company number 7880758 (England & Wales) Registered address: 10th Floor, Southern House, Wellesley Grove, Croydon, CR0 1XG. x. Visit the Nursing Times renal zone for latest news, peer-reviewed clinical research articles, and material for CPD and practice innovation.
Coping with chronic kidney disease (CKD) is challenging for many people, since symptoms often don't appear until the disease is advanced and the patient is close to requiring dialysis. This two-part article aims to provide nurses with the basic information necessary to assess and manage patients with CKD. Part 1, which appeared last month, offered an overview of the disease, described ...
Research Areas. The research activities of our faculty cover a broad range of topics in renal physiology and nephrology from laboratory bench to patient oriented investigation. Current areas of research focus include studies of the mechanisms of acute kidney injury and repair, molecular genetics of polycystic kidney disease and other cilia ...
Hot Topics in Kidney Health. Join us as we highlight the latest in kidney research, dispel myths, bring you up-to-date news in kidney care, and answer questions from patients to help them live well with kidney disease or a transplant.
ASN welcomes randomized trials (Phase 2, 3, 4) that will have significant impact on clinical practice on all topics touching kidney diseases including AKI, CKD, Diabetes, Dialysis, Genetic Diseases, Glomerular Diseases, Hypertension, Kidney Stones, Pediatrics, Transplantation, and more. The submission period opens on Wednesday, July 17, and ...
Nursing Research Paper Topics. Analyzing the effects of chronic kidney disease on caregiver burden and family dynamics. Investigating the correlation between social determinants of health and the progression of renal diseases. Examining the efficiency of strategies for pain management in patients undergoing renal surgeries.
1. Clinical Nursing Research Topics. Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties. Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings. Explore the effectiveness of pain management protocols in pediatric patients. 2.
World-renowned physicians and researchers from City of Hope ® will present new data and offer expert perspectives on leading-edge cancer research and treatments in development at the 2024 ASCO Annual Meeting, which will take place in Chicago from May 31 to June 4. Highlights include the following: About 40,000 oncology professionals will ...
A Swedish study has found a potential link between tattoos and a type of cancer called malignant lymphoma, but it ultimately calls for more research on the topic, and cancer experts say the ...
The 16 fellows in the 2024 cohort of the Betty Irene Moore Fellowship for Nurse Leaders and Innovators. The competitive fellowship program selects early- to mid-career nursing scholars and innovators and provides $450,000 in funding over three years for an innovative project or study plus $50,000 for their home institution.
Based on nursing data and experiences, "Everybody's Work" delves into the intricate issue of structural racism in nursing by focusing on personal narratives. Through the voices of nurses, educators, leaders and advocates nationwide, the documentary sheds light on their efforts amid challenges.