Brought to you by:


Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management
By: Richard M. Kesner
This case considers the process of organizational transformation undertaken by Partners Healthcare System (PHS) since the 1990s as their hospital and affiliated ambulatory medical practices have…
- Length: 15 page(s)
- Publication Date: Feb 26, 2010
- Discipline: Information Technology
- Product #: 909E23-PDF-ENG
What's included:
- Teaching Note
- Educator Copy
$4.95 per student
degree granting course
$8.95 per student
non-degree granting course
Get access to this material, plus much more with a free Educator Account:
- Access to world-famous HBS cases
- Up to 60% off materials for your students
- Resources for teaching online
- Tips and reviews from other Educators
Already registered? Sign in
- Student Registration
- Non-Academic Registration
- Included Materials
This case considers the process of organizational transformation undertaken by Partners Healthcare System (PHS) since the 1990s as their hospital and affiliated ambulatory medical practices have adopted both EMR and CPOE systems. Encompassing a strategic investment in information technologies, wide-spread process change, and the pervasive use of institutional clinical decision support and knowledge management systems, this story has been 15 years in the making, culminating in 2009 with the network-wide use of EMR and CPOE by all PHS doctors. These developments in turn opened the door to the redefinition of services delivery and to the replacement of established therapies through the leveraging of the knowledge residing in 4.6 million now-digitized PHS patient records. As such, the PHS experience serves as a window into how one organization strove to address the daunting challenges of 21st century health care services information management, as a template for success in the implementation of large-scale information systems among research-based hospitals across the United States, and more broadly as a learning platform for industry executives in their efforts to transform health care delivery through data and knowledge management.
Learning Objectives
This case has a number of useful teaching applications. First and foremost, the PHS case describes the transformation of a health care services organization, enabled by the deployment of major medical informatics systems. This story serves as an example and even a model for similar courses of action across the health care services industry in the coming decade. From this perspective, the instructors and students who use this case study may explore the professional, ethical and business drivers behind the efforts by Partners HealthCare System to implement its version of the EMR, the Longitudinal Medical Record (LMR) system, and the CPOE system. Second and in a broader context, the PHS case is a study in organizational innovation and change in which a strategic investment in information systems aligned with the transformation of core clinical processes to improve the ways PHS delivers health care services. The resultant information technology platform both enabled day-to-day improvements in health care delivery and patient safety and afforded a rich knowledge base to inform best practices and innovation. Here too, students may consider the implications of change management at PHS. Lastly, the PHS case may serve as the basis for various learning exercises for management information systems (MIS) and computer science (CS) classes, where the story may be viewed through the lens of the system development or project management life cycle. In this approach, the instructor may decide to work with the class to address the related themes of successfully deploying enterprise resource planning (ERP), a decision support system (DSS) and a knowledge management system (KMS).
Feb 26, 2010
Discipline:
Information Technology
Geographies:
United States
Industries:
Healthcare service industry
Ivey Publishing
909E23-PDF-ENG
We use cookies to understand how you use our site and to improve your experience, including personalizing content. Learn More . By continuing to use our site, you accept our use of cookies and revised Privacy Policy .

Product details

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Sci Rep
- v.4(4); 2021 Dec
Improving primary health care through partnerships: Key insights from a cross‐case analysis of multi‐stakeholder partnerships in two Canadian provinces
Ekaterina loban.
1 St. Mary's Research Centre, Montreal Quebec, Canada
2 Department of Family Medicine, McGill University, Montreal Quebec, Canada
Catherine Scott
3 Department of Community Health Sciences, University of Calgary, Calgary Alberta, Canada
Virginia Lewis
4 Australian Institute for Primary Care & Ageing, La Trobe University, Melbourne Victoria, Australia
5 Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto Ontario, Canada
Jeannie Haggerty
Associated data.
The raw data are not publicly available due to privacy restrictions given the small sample and the qualitative nature of inquiry.
Background and Aims
Multi‐stakeholder partnerships offer strategic advantages in addressing multi‐faceted issues in complex, fast‐paced, and rapidly‐evolving community health contexts. Synergistic partnerships mobilize partners' complementary financial and nonfinancial resources, resulting in improved outcomes beyond that achievable through individual efforts. Our objectives were to explore the manifestations of synergy in partnerships involving stakeholders from different organizations with an interest in implementing organizational solutions that enhance access to primary health care (PHC) for vulnerable populations, and to describe structures and processes that facilitated the work of these partnerships.
This was a longitudinal case study in two Canadian provinces of two collaborative partnerships involving decision makers, academic representatives, clinicians, health system administrators, patient partners, and representatives of health and social service organizations providing services to vulnerable populations. Document review, nonparticipant observation of partnerships' meetings (n = 14) and semi‐structured in‐depth interviews (n = 16) were conducted between 2016 and 2018. Data analysis involved a cross‐case synthesis to compare the cases and framework analysis to identify prominent themes.
Four major themes emerged from the data. Partnership synergy manifested itself in the following: (a) the integration of resources, (b) partnership atmosphere, (c) perceived stakeholder benefits, and (d) capacity for adaptation to context. Synergy developed before the intended PHC access outcomes could be assessed and acted both as a dynamic indicator of the health of the partnership and a source of energy fuelling partnership improvement and vitality. Synergistic action among multiple stakeholders was achieved through enabling processes at interpersonal, operational, and system levels.
Conclusions
The partnership synergy framework is useful in assessing the intermediate outcomes of ongoing partnerships when it is too early to evaluate the achievement of long‐term intended outcomes. Enabling processes require attention as part of routine partnership assessment.
1. INTRODUCTION
In the environment of increasing demands and limited resources, rapid technological change, and an aging and progressively complex patient population, partnerships involving multiple stakeholders from different sectors offer a meaningful way of tackling complex health care system problems. 1 , 2 , 3 , 4 Multi‐stakeholder partnerships including community members and representatives of academic institutions are prevalent across multiple disciplines and spheres. 5 To a certain extent, this can be attributed to the role of governments and funding agencies that mandate partnerships as an essential element of the programs and initiatives that they support. 4 , 5 For example, the Canadian Government has promoted collaboration as a means of improving the quality of health care provided to the Canadian population. 6 The partnership approach to health care system change and service redesign has also enjoyed widespread endorsement in other countries, particularly within the context of health and welfare services. 4 , 7
Partnership benefits have been studied from a diverse range of perspectives, disciplines, and communities of practice. 8 , 9 Academic literature outlines what constitutes an effective partnership and describes approaches and strategies to enhance partnership processes and to increase partnership effectiveness. 5 , 10 , 11 , 12 , 13 , 14 , 15 In theory, effective partnerships can be useful for overcoming organizational fragmentation and traditional divisions of power, improving communication and access to information, optimizing resource utilization, and helping to avoid a wasteful duplication of effort. 16 In addition, there is evidence to suggest that effective partnerships contribute to more comprehensive interventions, help to contextualize policy, and support the feasibility and relevance of research through direct involvement of knowledge users. 1 , 16 , 17 In primary health care (PHC), cross‐sector partnerships have been used to ensure integrated service delivery. 18 Reported facilitating processes include capitalizing on the diverse perspectives of partners, pooling of resources, promoting a common understanding of issues, forging common action plans, ensuring joint accountability and evaluation of progress, and employing appropriate forms of leadership and coordinating activities to ensure the alignment of efforts. 3 , 19
In practice, however, partnerships are frequently unable to generate effective collaborative advantage and achieve the intended change in systems and/or health outcomes. 19 , 20 Many crumble under challenges such as insufficient resources, significant time commitments, conflicting interests, problems with governance and leadership, lack of necessary skills, insufficient recognition, and lack of buy‐in from key stakeholders. 2 , 5 , 19 , 21 Considering these challenges, there is a growing need for evidence demonstrating the link between the implementation of processes and approaches that are claimed to enhance partnership effectiveness and the achievement of intended outcomes.
The notion of “partnership synergy” has been proposed as a marker or a “proximal outcome” of partnership functioning. 4 (p182) Partnerships are said to be synergistic when they combine resources successfully and mobilize the complementary knowledge and expertise of all the partners. 22 Synergy is reached when the combined efforts of partners enhance the outcomes beyond what could be achieved independently by each stakeholder/stakeholder group working toward the same goals, 23 namely that the whole becomes greater than the sum of the parts. 4 Synergy could manifest itself through creative and holistic ways of thinking, the ability to carry out more comprehensive interventions aimed at target populations, the relationships between partners and relationships of partnerships with the broader community. 4 Lasker et al identified a number of elements of partnership functioning that are likely to influence partnership synergy (Table 1 ) and suggested looking at synergy as a predictor of an effective partnership. 4 Subsequent research conceptualized synergy as being both a process and a product of partnership, and highlighted the dynamic and cumulative nature of partnership synergy demonstrating its capacity to build over time and its role as an evolving indicator of effectiveness and sustainability. 23 , 24 , 25
Determinants of partnership synergy (adapted from Reference 4 )
This study adopted partnership synergy as an umbrella framework for looking at the functioning of two multi‐stakeholder partnerships in two Canadian provinces involving stakeholders from different organizations and constituent groups with an interest in implementing organizational solutions to enhance access to appropriate PHC for vulnerable populations. The overall aim of our study was to gain an in‐depth understanding of the effectiveness of multi‐stakeholder partnerships in addressing complex issues in PHC. PHC is conceptualized here as an approach to health that encompasses continuous and comprehensive care across diverse curative, preventative, education, and rehabilitation services, with a person (micro), community (meso), and population (macro) orientation. 26 , 27 , 28 For the purposes of this paper, we conceptualize “partnership effectiveness” in relation to both the processes and outcomes of partnerships: the quality of the processes and relationships between partners and the health of the partnership on the one hand, and the realization of intended outcomes on the other. We define a multi‐stakeholder partnership as a complex human system based on voluntary collaborative relationships among stakeholders who agree to work together to achieve a common purpose and to share competencies, resources, responsibilities, risks, and benefits (adapted from Reference 29 ). We focused on partnerships involving representatives of different organizations—each bringing their unique perspectives, competencies, organizational mandates, interests and weaknesses, working toward a common goal of transforming PHC service delivery. The main research questions that this study attempted to address were as follows: (a) How does partnership synergy manifest itself in multi‐stakeholder partnerships? and (b) What structures and processes are required to build synergistic action among actors from different sectors?
2.1. Study context
This study was undertaken within a Canada‐Australia research program entitled “Innovative Models Promoting Access‐to‐Care Transformation” (IMPACT) conducted between 2013 and 2018. 30 The aim of this program was to design, implement, and evaluate, through a network of local partnerships, organizational interventions to improve access to appropriate PHC for vulnerable populations in three Australian states (Victoria, South Australia, and New South Wales) and three Canadian provinces (Quebec, Ontario, and Alberta). 30 Each of the six projects entailed identifying, in consultation with a broader set of local stakeholders, PHC access needs, and selecting, adapting, and implementing coordinated actions to best address these needs, within available resources. This study focused on two of the Canadian IMPACT local partnerships, namely the Primary Care Connection Partnership (PCCP) and the Community Health Resources Partnership (CHRP) (Table 2 ).
Overview of interventions in two Canadian IMPACT local partnerships (adapted from References 30 , 31 , 32 )
Abbreviation: PHC ‐ primary health care.
The stakeholders within each partnership included a mix of decision makers, clinicians, health system administrators, service providers, academic members—composed of academic investigators, including principal investigators and co‐investigators, and research coordinators, and, in some cases, members of vulnerable populations. 30 Vulnerable populations were “community members whose demographic, geographic, economic and/or cultural characteristics impeded or compromised their access to PHC.” 30 (p4)
2.2. Study design
This longitudinal case study 33 , 34 involved document review, nonparticipant observation 35 of partnerships' meetings, and semi‐structured in‐depth interviews 36 with a sample of study stakeholders in two partnerships. The study was conducted between August 2016 and September 2018. The rationale for studying both cases longitudinally was to follow their development over time, to understand the evolution of processes, to trace any changes that affected the partnerships, and identify how the partnerships responded to these changes. Consolidated criteria for reporting qualitative research ( COREQ ) were used in the reporting of this study. 37
2.3. Sampling and recruitment
The PCCP stakeholders represented two administrative jurisdictions covered by two regional health networks, two local general practice divisions, community development organizations serving the two neighborhoods, and two universities. The CHRP included stakeholders from one health authority, a university, community and home care services, social and public health services, community health centers, information resources, primary care, and the community.
Interview candidates were selected using purposive sampling with the aim to achieve maximum variation within the sample. 38 The goal of the sampling strategy was to include representatives of each stakeholder group, who varied in seniority in the partnership and nature of engagement. The PCCP interview candidates were identified by the first author based on meeting observations; the CHRP candidates were identified by the CHRP principal investigator.
2.4. Data collection
Preliminary documents reviewed (between August 2016 and May 2017) were minutes of meetings, protocols, and reports produced by the IMPACT program and the two partnerships. The first author subsequently observed (between January 2017 and September 2018) 11 PCCP and three CHRP meetings—all available meetings that took place during this time frame. The document review and observations provided data on the operational elements, contextual factors, participants' roles and responsibilities, the common agenda of each initiative, and how this common agenda and the involvement of different stakeholders evolved since the start of the IMPACT research program in 2013. The first author then conducted (between July 2017 and March 2018) nine interviews with PCCP stakeholders and seven with CHRP stakeholders. Interview candidates were initially invited to participate via e‐mails that were sent by PCCP and CHRP research coordinators. Follow‐up contact by the first author was in person, at the end of partnership meetings, and via e‐mails sent directly to each candidate. The interviews lasted approximately 1 hour, were conducted either in‐person or over the telephone, and were audio‐recorded.
The interview guide (Appendix A ) was developed with reference to the literature on partnership synergy. 4 , 25 Synergy dimensions explored included the organization of partnerships, work sharing, decision‐making/problem‐solving, complementarity of skills, outcomes, and experience. The guide was pilot tested, in both English and French, prior to administration.
2.5. Ethics
Ethics approval for the study was obtained from the St Mary's Hospital Centre Research Ethics Committee (No. SMHC‐13‐30C). Authorization to conduct research was obtained from the second participating institution. All participants were provided with written information about the study and consent was obtained prior to data collection.
2.6. Data analysis
Nonparticipant observations (which entailed observing participants without actively participating in their meetings) were recorded as field notes. All interviews were transcribed verbatim, in the original language, with subsequent translation from French into English for quotation purposes. Our analysis of notes and transcripts reflected the dual‐level inquiry of the study: it involved a cross‐case synthesis to describe the cases and generate insights 34 and framework analysis. 39 The strategy used for data analysis involved a hybrid deductive‐inductive approach, 39 , 40 involving assigning data into predefined themes based on the partnership synergy framework, revising themes based on nuances within the data, and identifying new themes arising from the data. The data were coded iteratively, going back and forth from text to themes. NVivo 12 software was used to support data management and analysis. The material was analyzed by the first author. Coding was verified with another co‐author. Emerging findings were discussed at regular team meetings. The final codes were grouped along the dimensions of partnership synergy and six categories of factors likely to foster synergy: structure; partner characteristics; partnership characteristics; relationships among partners; resources; and external environment.
3. FINDINGS
The following paragraphs detail the key findings from this study. Section 3.1 presents the characteristics of the sample. Section 3.2 summarizes the key findings and refers to descriptive cross‐case synthesis (presented in Appendix B ) that is based on observations and accounts of interview respondents. In Section 3.3 we elaborate on four themes that emerged from our data where partnership synergy was apparent, namely resource integration, partnership atmosphere, reported benefits, and partnership's capacity for adaptation to context. Finally, Section 3.4 describes partnership collaborative processes that enabled stakeholders from different organizations to achieve synergistic action.
3.1. Study participants
Interview participants represented a range of organizational expertise (Table 3 ). Academic representatives and decision makers constituted the largest two groups (n = 10, 63%). Participants (n = 16) were predominantly female (n = 13, 81%).
Study sample characteristics (n = 16)
3.2. Cross‐case synthesis
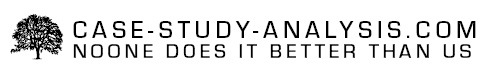
Our key findings are summarized in Figure 1 . It portrays human and material resources as the building blocks of partnerships. These resources are then activated via interpersonal, operational, and system‐level processes to produce partnership synergy. Partnership synergy manifests itself in different ways: in the integration of resources, partnership atmosphere, perceived stakeholder benefits, and the capacity for adaptation to context. It acts as both a dynamic indicator of the health of the partnership, highlighting the likelihood of achieving partnership effectiveness, and as the source of energy fuelling partnership improvement and vitality. The boundaries of the partnership are permeable, reflecting the exchange of influence between the partnership and its context. Appendix B displays how the cases align against the partnership synergy framework and describes how the two partnerships were resourced and structured.

Summary of key findings—relationships among partnership synergy, partnership resources, enabling partnership processes and outcomes
3.3. Partnership synergy
3.3.1. theme 1: resource integration.
There was evidence of partnership synergy in the integration of nonfinancial and financial resources. Nonfinancial resources included the time, knowledge, expertise, and connections that the stakeholders contributed, as well as the relationships and learning that transpired in the course of partnership work. The partnerships demonstrated capacity to recruit stakeholders with a range of perspectives, skills, information, and connections to a broader set of stakeholders and health systems exerting influence over the partnerships. These unique perspectives and insights (Table 4 ) were deemed to be complementary in that they allowed the group to explore the issues of access from various angles, to obtain timely information from different sectors in order to adapt interventions, and to enhance the relevance of interventions: “ I think it ' s a really good mix of people, and you can hear it in the discussion . The very different points of view and they all complement each other very well .” (016, CHRP).
Stakeholder perspectives within two Canadian IMPACT local partnerships
Abbreviation: IMPACT—Innovative Models Promoting Access‐to‐Care Transformation.
I honestly don't think that there's any other way to do it, because it's in primary care and primary care is incredibly complex, there are so many players involved […]. If we didn't have those other people at the table how would we know what's going on. (013, CHRP).
In both cases, the nucleus of the partnership, including the research team and a number of key nonacademic stakeholders, remained consistent over time, while new members were invited to join based on project evolution and the need to attract additional expertise and resources. This heterogeneity and fluidity in the composition of the partnerships reflected the complexity and scope of the tasks at hand, the dynamic nature of the projects and organizational and policy changes in the external context that took place over the years. These composition dynamics, however, necessitated a significant investment of coordination resources and time on the part of the research teams and ongoing attention to and management of stakeholder engagement dynamics.
The CHRP was larger, reflecting a broader array of stakeholders and language groups. Some CHRP interview participants felt that the size of the partnership (23 stakeholders) was too large, potentially inhibiting contribution from some members. The PCCP was smaller (13 members) but had the complexity of involving two independent health authorities, with different organizational cultures and authority structures, with one interview participant describing the partnership's initiative as “ one research project […] with two different speeds ” (011, PCCP). Despite the differences between cases in size and diversity, the mix of stakeholders in both was perceived by interviewees to be optimal for achieving project goals. The composition was described by stakeholders as an “ excellent mixture of people […] from diverse sectors ” (016, CHRP) and as “ driven by the research team, but nourished by the practitioners in the field ” (014, PCCP).
The partnerships demonstrated the ability to effectively combine their nonfinancial resources. In both cases, the level of engagement was deemed by most interview respondents to be appropriate for the stated project objectives and the function of the partnership. All stakeholders had clarity regarding their own roles and what was expected of them. Several participants referred to the alignment of efforts of partners and the richness and integrative nature of collaboration: “ These [partnership] tables are an example of integration . […] We become more integrated and stronger, and there is a certain level of coherence between us .” (020, PCCP); “ It is very rich . […] Not everyone has the same reality, and we inspire each other . In understanding the point of view of the other, we advance the discussion .” (014, PCCP).
Partnership synergy was also apparent in the ways partners leveraged financial resources and sustained partnership activities and interventions despite contextual challenges and funding gaps. The IMPACT research grant included funding for the coordinating infrastructure/research support, including the partnership coordinator position in each site, as well as the evaluation of interventions. There was no funding for intervention implementation, and stakeholders other than research coordinators were not remunerated for participation in partnership activities. Consequently, the successful implementation and sustainability of interventions relied entirely on the local players' capacity to commit to them, provide adequate resources, and maintain them beyond the life of the IMPACT research funding. Both partnerships devised low‐cost lay navigator models to address the needs of the target populations. Both worked toward integrating the interventions into existing health system organizational structures, aligning the proposed models with health system priorities. In the process, the CHRP relied on additional research funding that was secured early on in the project to support a randomized controlled trial to test the effectiveness of the developed navigator model.
3.3.2. Theme 2: Partnership atmosphere
Partnership synergy was apparent in the quality of stakeholder relationships, in the perceived value of the initiative, and the general partnership atmosphere, which was described as “ positive ” (011, 018, CHRP), “ dynamic ” (017, CHRP), “ respectful ” (019, CHRP), “ open ” (013, PCCP), “ friendly ” (015, CHRP), “ collaborative ,” “ energising ” and “ engaging ” (013, CHRP): “ Everybody seems to be happy to be involved .” (018, CHRP); “ I usually see it as we all come together, sort of . I don ' t feel a sense of that there ' s some difference between anyone […] . I feel like they do treat me as an equal .” (019, CHRP).
The exchanges are very open. That is to say, when we […] put forth a proposal or a possible solution, it is always well received … not necessarily always accepted, but well received. Lots of openness. That, I find that interesting. (013, PCCP).
These positive collaborative relationships benefitted the partnerships by enabling more open conversations, faster and effective decision‐making, and enhanced project ownership: “ The commitment to the project is higher when you have built it together . […] When you have done it in collaboration, it is closer to your heart and I think that this is one of the advantages .” (012, PCCP).
The synergy in relationships blossomed with time; as the work progressed, participants felt that they could speak more openly, including voicing concerns and disagreement:
I have the impression that we are less afraid of losing our partners, we walk less on eggshells, we are more open […] the partnership is a little more solid and we are more capable of […] exposing a little, being less artificial in our meetings. (011, PCCP).
Participants highlighted the importance of face‐to‐face meetings and having signed letters of understanding with institutions at the start of the project. Despite the fact that membership fluctuated, these letters underscored the credibility of the project and facilitated trust‐building with new members.
3.3.3. Theme 3: Reported benefits
Members in both cases reported a variety of anticipated and actual benefits stemming from their participation in the project, reflecting a core component of partnership synergy. Participants described more professional than personal benefits. Benefits included, but were not limited to the following: learning about the work of other organizations and sectors; understanding how the services in one's organization complement services and approaches in others; learning about how a well‐organized meeting unfolds; devising more effective ways of addressing an issue that the organization had been grappling with; and ensuring system‐wide benefits if the project can demonstrate that the approach that is pursued works. In addition, respondents highlighted the benefits of the partnership approach to delivery of project goals, stating that “ there is no other way to approach it ” (013, PCCP). A number of indirect benefits were also reported, including enhanced visibility of one's own organization and opportunities for face‐to‐face exchange with other key stakeholders under the same organizational umbrella. Partnership members who were early career researchers were less positive about the benefits, citing high demands of participation for limited academic outputs. However, some of them remained committed to the partnership due to the strength of relationships with other stakeholders. While for most members participation in the project had been mandated by their respective organizations, the majority participated willingly, looked forward to meetings and saw a direct fit between the project's objectives and the priorities of the entities they represented. According to most interview respondents, the benefits of participation outweighed the drawbacks, effectively demonstrating positive partnership synergy.
The mutually beneficial nature of the partnerships was apparent as participants described mutual and personal learning and satisfaction with their involvement in the projects:
So to be able to be part of the project […] I think that they had a great idea, it's really smart, and I felt really glad to be part of that. You know because I feel like that's a good project […] very helpful, this is a very […] significant issue for people. And to be able to be part of maybe, you know, exploring why it's a problem and offering my insights, I'm very excited to be able to do that. (019, CHRP).
3.3.4. Theme 4: Capacity for adaptation to context
Partnership activities were unfolding within the context of health care system reforms in both provinces. Both partnerships had to make adaptations to the interventions to respond to evolving contextual opportunities and threats, but the extent of contextual impact and adaptation was far greater in the case of the PCCP, which demonstrated synergy in its ability to adapt to its changing context. During the implementation period, the province's health care system underwent a major reform, 41 , 42 leading to a number of policy changes. In the process, the partnership lost most of its nonacademic members, had to re‐develop relationships with new stakeholders, and had to modify the intervention several times to accommodate new system priorities. Academic partnership participants revealed that the impact of changes was so profound that they feared a complete dissolution of the partnership and termination of the project. These developments reflected weakened partnership synergy. However, the momentum generated through synergy in other areas, namely trust, partnership credibility, and organizational buy‐in, contributed to keeping the project alive:
[…] even though everyone around the table had changed, we have managed to keep representatives roughly the same from each of the organizations that were with us since the beginning. What made it easier was that we had the commitment of people pretty high up in those organizations […] In addition, we managed to establish a climate of trust. So even though the people around the table changed, they knew that the organizations had been there for a while and it was going well. (011, PCCP).
Given that contextual changes were frequent topics of conversation during face‐to‐face PCCP meetings, there were no reported differences in stakeholders' appreciation of the impact of context depending on their roles in the partnership.
The CHRP stakeholders described the context as “ chaotic ” (018, CHRP), with a well‐integrated hospital and specialist sector, poorly organized community health services, and fragmented primary care. At the time of project activities, the province underwent significant changes in its health care system, with services being integrated sub‐regionally based on geographical utilization patterns, within the framework of tight budgets, contract negotiations, and increasing demands on the system. It was felt that the project was timely in terms of addressing some of these challenges posed by changes in the context. The main concern voiced related to the possibility of the intervention duplicating existing services. The research team proactively addressed this concern by incorporating at the start of some partnership meetings a description of how the navigator model was different from and complementary to other services, and by allocating time for dialogue around it. At a closer, organizational, level the CHRP experienced a gap of 1.5 years between partner meetings due to delays in ethics protocols approvals. However, similar to the PCCP, the partnership synergy generated earlier, evidenced in the quality of stakeholder relationships and the importance attributed to the initiative, contributed to sustained stakeholder participation. Overall, the stakeholders' appreciation of the impact of external context on the project and partnership varied depending on their role in the partnership. Decision makers provided a more in‐depth assessment of the context and how it affected the intervention. Most stakeholders felt that contextual changes were inevitable, and the partnership just had to adapt to them: “[…] coping with the environment, the environment is what it is, it ' s a changing environment and you have to adapt ” (018, CHRP).
Interviewees also noted the influence of the partnerships and the interventions on their organizations and the broader context. Decision makers in particular referred to acquiring and sharing within their respective organizations a deeper understanding of the plight of vulnerable populations in relation to access issues. Members of community‐based service organizations referred to generating insights into how to improve their organizations' services, whereas family physicians became more aware of existing services that patients could be referred to.
3.4. Synergy enabling processes
Both partnerships employed specific processes to facilitate the work of the partnerships. The following main categories of processes emerged from our data: (a) interpersonal processes, (b) operational processes, and (c) system‐level processes (Figure 1 ).
3.4.1. Interpersonal processes
At the interpersonal level, participants highlighted the importance of communication processes, relationship building and maintenance, and learning loops. Both partnerships had open and multidirectional channels of communication, mostly confined to regular partnership face‐to‐face meetings and electronic means, to communicate internally with stakeholders within the partnership. Learning loops involved soliciting feedback during meetings around issues related to the project and being transparent about how this input was subsequently incorporated. External communication aimed at increasing the support for interventions, recruiting medical practices, and disseminating information about partnership activities and achievements to wider audiences. While some stakeholders had a history of working together, relationships with other stakeholders had to be built and nurtured. Face‐to‐face meetings were identified as being key to developing relationships.
3.4.2. Operational processes
At the operational level, the processes involved resource management, leadership, administration and management, and decision‐making. Both partnerships utilized a variety of ways to engage respective stakeholders. The partnerships organized deliberative fora involving a broad range of stakeholders, to learn about unmet health care needs of vulnerable populations, relevant community organizations, and available resources to support interventions. The PCCP subsequently involved stakeholders in various aspects of the research process, with a number of nonacademic stakeholders fulfilling tasks outside the partnership meetings. Conversely, the CHRP adopted a research advisory approach to working with stakeholders, with limited contribution of nonacademic stakeholders outside face‐to‐face meetings. Both partnerships used regular meetings to discuss project progress and to engage in collaborative learning. Participants emphasized the added value of acquiring relevant knowledge, having space to exchange with other partners, reflect and innovate (which was not always possible within the stakeholders' respective organizational contexts), as well as educational and capacity‐building opportunities.
The partnerships were largely driven by the research teams responsible for the overall management of the projects, providing strategic direction and facilitating the development of interventions at the local level, through continuous dialogue and learning, as well as sharing of information. The research teams capitalized upon the various strengths and perspectives of stakeholders, by providing sufficient time to discuss pressing issues, soliciting input from all stakeholders, offering stakeholders different mechanisms to contribute, and tailoring tasks to stakeholders' availabilities and interest. The PCCP leveraged the power of leadership distributed among academic and nonacademic stakeholders, while in the CHRP, the leadership was centralized within the research team. However, the CHRP interview participants reported that the research team seemed genuinely interested in hearing from all stakeholders and made efforts to check in with various groups around the partnership table.
A number of leadership processes were common to both cases. Both partnerships had formal and informal academic leaders knowledgeable about the context and skilled at mobilizing the various perspectives of partners. The leaders did not possess all of the required partnership‐related knowledge and skills at the outset, but made intentional efforts to learn from experience and best practices in partnership literature and to acquire additional skills through training. Moreover, as the partnerships evolved and the level of trust within teams increased, the leaders were more transparent about their own gaps in knowledge surrounding the interventions and eagerly welcomed input from different stakeholders. This demonstration of vulnerability contributed to creating further trust.
The PCCP stakeholders reported that the decision‐making process was inclusive and transparent, which was particularly useful in relation to adapting the intervention to its evolving context. Conversely, consistent with the advisory nature of the partnership, the CHRP decision‐making power was centralized within the research team.
3.4.3. System‐level processes
At the system level, participants described processes geared toward making ongoing adaptations to the evolving context. In both cases, responsiveness to external stimuli involved adaptations to the interventions' structure, implementation strategy, and personnel resources. Participants reported that processes such as conducting extensive fieldwork to gather information, having around the table a variety of key stakeholders with medium to high level of decision‐making power in their respective organizations, open dialogue about the evolving context, and, in the case of the PCCP, transparent processes of decision‐making, contributed to the ability of the partnerships to adapt interventions to rapidly changing policy contexts. The situational analysis involved leveraging the knowledge of multiple partners. The active engagement in the partnerships of decision makers and health system planners was critical in this respect, as it contributed to an in‐depth understanding of health system priorities.
4. DISCUSSION
This study illustrated the multidimensional, dynamic nature of partnership synergy and its role not only as a proximal outcome of partnership functioning but also as a facilitator of multi‐stakeholder partnerships in two geographical settings, in the context of tackling challenges in the delivery of high‐quality PHC to vulnerable populations. The study also provided insights into the structures and processes to sustain these partnerships. These two key findings are discussed in more detail below. Although there is a substantial number of quantitative and review studies that have incorporated concepts from the partnership synergy framework, 10 , 22 , 23 , 43 , 44 , 45 , 46 , 47 to our knowledge, empirical studies applying these concepts to frame qualitative research findings are rare, with Brush et al 24 and Corbin and Mittelmark 48 being two examples of such studies, which also proposed synergy models. Employing the partnership synergy lens allowed us to systematically assess its manifestations and to acquire a deeper understanding of this phenomenon. Taking into consideration that the partnerships were in the implementation stage of their interventions, we could not comprehensively assess the intended partnership outcomes. Our data contained preliminary evidence of the positive impacts of the interventions in both cases. However, the sustainability of interventions and partnerships beyond the life of the IMPACT grant was, according to our interview respondents, questionable.
This study will be followed by a quantitative study involving all six IMPACT partnerships that will attempt to measure whether (and how) the partnerships have achieved partnership synergy and whether certain partnership processes contributed to more strategic advantages. The results pertaining to the outcomes of the developed IMPACT interventions will be reported elsewhere. 49
4.1. Partnership synergy
Our first key finding relates to the multidimensional nature of partnership synergy. Our data indicate that partnership synergy manifests itself in different ways. We identified the following four areas where partnership synergy was apparent: (a) the integration of nonfinancial and financial resources, (b) partnership atmosphere, (c) reported benefits, and (d) capacity for adaptation to context. Our analysis revealed the complex interactions among the four areas. The composition that reflected the diversity and complexity of the presenting problem allowed for faster adaptations to contextual stimuli. The generated benefits were critical to the sustained level of stakeholder commitment. The quality of collaborative relationships and positive partnership atmosphere facilitated additional stakeholder recruitment and allowed to maintain momentum. These inter‐connections suggest that synergy components are neither static nor independent; similar to a hologram, 50 they allow us to obtain a more intense picture of partnership synergy. Given the highly contingent nature of partnerships, there will arguably be other areas where synergy might manifest itself, depending on a partnership's objectives and internal and external influences. The original Lasker and Weiss's model (2001), viewing partnership synergy as an outcome, for example, placed more emphasis on outcome elements, such as the ability of developed strategies to address the needs of target populations.
Second, our findings highlight the dynamic nature of partnership synergy. As partnerships progressed, partnership synergy in both partnerships fluctuated. Both partnerships evolved from a group of individuals with common interests (low synergy) into entities with a requisite degree of openness, inter‐dependence, and enhanced understanding of presenting issues (higher synergy)—all of which contributed to deeper decision‐making and effective adaptations to intervention models. Conversely, partnership synergy could weaken, as was illustrated with an example of the profound impact on the PCCP of its volatile context. This finding is broadly consistent with prior research that suggested that synergy was a dynamic health indicator of a collaborative process 24 and that it was more likely to accrue during the formation stage of the partnership but subsequently decrease during the implementation stage. 51
The third characteristic of partnership synergy revealed in our analysis is the contribution of partnership synergy to sustaining partnerships. The composite strength of partnership synergy in the PCCP was sufficient to offset the impact of the destructive contextual circumstances and allowed the partnership to regenerate itself. Analogous to the body's immune system, partnership synergy appeared to provoke a protective response allowing the partnership to persevere in the face of adversity. In addition, partnership synergy contributed to partnership improvement. Given that working in partnership required skills that were different from those employed in the typical running of research studies, the partnerships made strategic financial investments into acquiring these new skills. Instead of outsourcing certain partnership‐related tasks, the partnerships built capacity in‐house through training partnership coordinators in group process facilitation techniques and then providing them with opportunities to facilitate partnership meetings. This investment was not only part of building capacity within the partnership; the coordinators used the training as a springboard for subsequent process improvements and self‐organization that benefitted the partnerships directly, strengthening them and contributing to synergy. The return on this investment was high and contributed to lower effort on the part of academic investigators to facilitate partnership activities.
4.2. Structures and processes
This study adds depth to understanding of partnership resource requirements and demonstrates the centrality of enabling processes at the interpersonal, organizational and system levels to achieve synergistic action among multiple stakeholders. Due to the organizational structure and type of the IMPACT program funding, the two partnerships under investigation were largely driven by the research teams that initiated the partnerships—a finding that is consistent with the literature on collaborative health research partnerships. 17 These research teams and a number of key nonacademic stakeholders constituted a relatively consistent continuous core in each partnership, effectively acting as “champions” keeping the collaboration going. 52 Other members were selected strategically, to attract specific expertise, perspectives, and additional resources. This was supplemented by more organic selection based on emerging needs as the projects unfolded. The dynamic composition allowed for fluidity, complementarity, and heterogeneity that reflected the critical dimensions of the problem to be addressed and of the changing context. Having stakeholders around the table with medium to high level of authority in their respective organizations allowed for timely adaptations to interventions.
The CHRP was larger than the PCCP, reflected more linguistic diversity, and had more permeable organizational boundaries due to receiving additional funding for the second phase of the research project. This independent funding added complexity by broadening the scope of the project and requiring the involvement of additional expertise. The partnership's size necessitated a higher degree of formalization, which was evidenced in the structured ways of organizing meetings and soliciting input from stakeholders. This finding is consistent with the argument from organizational theory that larger organizations tend to require more formalized behavior and more developed administrative components. 53 Different stakeholders were brought in as the needs of the partnership evolved, with relatively consistent representation from the target population. The partnership adopted a research advisory approach, with the decision‐making power centralized with the research team, and a limited contribution of nonacademic stakeholders outside the face‐to‐face meetings. Overall, the project undertaken by the CHRP was deemed by interview respondents to be meaningful and timely.
The PCCP was smaller, with more defined boundaries, but had a higher degree of internal complexity due to working with two local health authorities, each with different organizational cultures and processes. The PCCP exhibited elements of horizontal decentralization 53 and holographic organization, 50 with the diffusion of leadership and decision‐making power among academic and nonacademic stakeholders. All stakeholders participated actively in the co‐construction of the various aspects of the project, and some nonacademic stakeholders fulfilled tasks outside the partnership meetings. The small size and decentralization of power allowed the PCCP to remain nimble and responsive to change. These findings are aligned with organizational theory that states that more complex and dynamic environments necessitate more organic and decentralized structures and decision‐making power. 53
We identified a number of collaborative processes driving the synergy of the two partnerships, at interpersonal, operational, and system levels, each a critical piece of the synergy puzzle, but also a source of potential problems if misaligned with the needs or context. For example, the decentralized form of leadership that contributed to partnership synergy in one partnership may have been counterproductive in the other. In practice, however, the key contributor or threat to partnership synergy cannot be isolated due to the inherent complexity of partnerships within their local contexts. “Because an element in a group can affect other elements, any element or combination of elements could be contributing to the group's ineffectiveness.” 54 Our study demonstrated how contextual adaptation in the case of the PCCP necessitated certain decision‐making processes, appropriate forms of communication, and specific actions from the team that fulfilled the “backbone” 3 coordinating support to the partnership. This interaction of process variables is not confined to the partnership itself, for partnerships are subject to the influences of their constituent organizations and larger contexts. When partnerships experience decreased synergy, our evolving model of synergy (as depicted in Figure 1 ) can support the diagnostic task of identifying the sources of the problem and the task of devising solutions to address it, paying particular attention to the interplay of variables.
The optimal configurations of these processes and their interaction with partnership resources and context can be highly variable, depending on the specifics of each partnership. 43 Indeed, as the IMPACT program progressed, each of the partnerships under our investigation evolved in different ways, based upon the specific context within which it was developing, the local access need that the partnership tried to address, tailored processes and requirements to meet this need, and the relationships that formed to move the work forward. In participatory research terms, the PCCP stakeholder participation exhibited elements of “co‐construction” or “co‐governance,” whereas in the CHRP it was more aligned with “consultation.” 55 Each of these configurations fit the objectives and the needs of the respective partnerships. Our findings support prior research that highlights that partnership as a form of multi‐organizational working relationship is a variable concept and works differently under different circumstances. 56 , 57
It is important to note that an in‐depth exploration of the challenges of partnering was beyond the scope of this study. The main challenges reported by our study participants included the following: considerable time commitments, insufficient credit for investing energy into the partnership, challenges with bridging organizational divides, and difficulties optimizing the involvement of knowledge users (the people affected by the partnership's work). These obstacles affected some stakeholders' motivation, their level of participation, and, subsequently, partnership synergy. These findings indicate the importance of devoting attention to the balance of costs and benefits and recognizing and responding to perceived and actual disengagement throughout the life of the partnership.
4.3. Implications for practice and future research
The partnership synergy framework 4 is useful in assessing the intermediate outcomes of ongoing partnerships when it is too early to evaluate the achievement of long‐term intended outcomes. It should be incorporated into routine partnership evaluation, starting with a baseline assessment. The list of variables offered by the framework allows partnership practitioners and evaluators to select those relevant to a particular partnership, identify the levers of change, and calibrate inputs accordingly in an attempt to increase partnership synergy. Future research should focus on identifying other manifestations of partnership synergy and documenting conditions under which these manifestations emerge. The ultimate objective would be to determine if partnership synergy could indeed become a source of “renewable energy” for a partnership. It would equally be important to document instances of negative partnership synergy or antagony 48 and identify “tipping point” scenarios where the composite partnership synergy no longer offers its protective effect.
4.4. Limitations
This section outlines the limitations of this study and how these limitations were mitigated. First, the study of the partnership aspects was largely conducted by one member of the research team (the first author). Individual biases may have affected the coding and interpretation of data. However, the first author is experienced in qualitative data gathering, coding, and analysis. In addition to being exposed to the partnership phenomena over a prolonged period of time, the following strategies were employed to reduce the effect of investigator bias: (a) triangulation from multiple sources of evidence, and (b) keeping an “audit trail” to document decisions made throughout the research process. 58 Moreover, the coding frames and analytic plan were developed and validated with other members of the research team. Second, participants may have provided a more favorable assessment of the partnerships, given the voluntary nature of engagement and the stage of the partnerships by which those who did not see value in participating would have resigned. We attempted to minimize this limitation through the use of purposive sampling, which enabled the selection for interviews of a mix of seasoned and new partnership participants and those demonstrating high and low levels of participation. In addition, the semi‐structured interview format allowed the interviewer to explore negative cases. Third, this study analyzed only two of the six IMPACT local partnerships and just some of the partnership manifestations. Some important aspects of partnership functioning may not have been captured. The two partnerships were chosen in light of feasibility considerations, and the partnership dimensions were selected in alignment with the chosen theoretical framework. This study will be followed by a quantitative study involving all six IMPACT partnerships. Finally, the study unfolded within the context of a funded program of research with a targeted scope to improve accessibility to PHC for vulnerable populations. Caution is warranted when transferring these results to different, less resourced contexts. Rich contextual descriptions were provided for each of the two IMPACT local partnerships allowing other scholars and practitioners to determine whether and how the results may be applicable in different contexts.
This research would not have been possible without the support of the IMPACT program's funders. IMPACT—Improving Models Promoting Access‐to‐Care Transformation program was funded by the Canadian Institutes of Health Research (TTF‐130729) Signature Initiative in Community‐Based Primary Healthcare, the Fonds de recherche du Québec ‐ Santé and the Australian Primary Health Care Research Institute, which was supported by a grant from the Australian Government Department of Health, under the Primary Health Care Research, Evaluation and Development Strategy. Ekaterina Loban would like to acknowledge funding of a doctoral stipend through the IMPACT research program (2015‐2018). The funding bodies played no role in the study design, data collection, analysis, interpretation, or writing of the manuscript.
CONFLICT OF INTEREST
The authors of this paper have no conflict of interest to declare.
AUTHOR CONTRIBUTIONS
Conceptualization: Ekaterina Loban, Catherine Scott, Virginia Lewis, Susan Law, Jeannie Haggerty.
Data Curation: Ekaterina Loban.
Formal Analysis: Ekaterina Loban.
Funding Acquisition: Catherine Scott, Virginia Lewis, Jeannie Haggerty.
Investigation: Ekaterina Loban.
Methodology: Ekaterina Loban.
Project Administration: Ekaterina Loban.
Resources: Catherine Scott, Virginia Lewis, Jeannie Haggerty.
Supervision: Catherine Scott, Jeannie Haggerty.
Validation: Ekaterina Loban, Catherine Scott, Virginia Lewis, Susan Law, Jeannie Haggerty.
Writing–Original Draft Preparation: Ekaterina Loban.
Writing—Review and Editing: Ekaterina Loban, Catherine Scott, Virginia Lewis, Susan Law, Jeannie Haggerty.
All authors agreed on the order in which their names are listed in the article.
I, Ekaterina Loban (the corresponding author), confirm that I had full access to all of the data in the study and take complete responsibility for the integrity of the data and the accuracy of the data analysis.
TRANSPARENCY STATEMENT
We confirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
ACKNOWLEDGEMENTS
This research would not have been possible without the support of the IMPACT program research team and all stakeholders who were involved in this study. We also acknowledge the contribution of the following supporting partners: the Department of Family Medicine of McGill University, St. Mary's Research Centre, Université de Sherbrooke, Bruyère Research Institute, PolicyWise for Children & Families, Monash University, La Trobe University, the University of Adelaide, the Bureau of Health Information, and the University of New South Wales.
APPENDIX A. INTERVIEW PROTOCOL
As you are aware, each IMPACT site has established a local innovation partnership (LIP)—partenariat d'innovation local (PLI). These look slightly different in each of the six sites. The first couple of questions are just to get an initial picture or overview of “what” it is and how you are involved.
- When you say “your LIP” or “the LIP” what are you referring to?
- How long have you been involved with your LIP?
Work sharing:
- How is the work divided among the different partners?
- How would you describe the roles of members? How do they contribute?
Decision‐making/problem‐solving:
- 4 Can you name 2 to 3 significant decisions that were made in the past year?
- 5 How are decisions made? How are decisions communicated? (prompts: committee process; voting/consensus; transparency).
- 6 How are challenges resolved/ conflict dealt with?
- 7 Can you name 2 to 3 significant problems encountered in the past year? How were they resolved? (if appropriate: What were the consequences of conflict or efforts to resolve problems [benefits, risks]?)
Complementarity of skills:
- What facilitates member contributions?
- What limits member contributions (barriers)?
- 9 How is the partnership including the views and priorities of the people affected by the partnership's work?
- 10 Has there been any change over time in terms of how team members contribute?
Benefits/value added:
- How do you benefit (professionally/personally)?
- How does your organization benefit (policy/practice/service delivery)?
- 12 How do you perceive that others are benefitting from their participation?
- 13 What sorts of benefits do you perceive that are above and beyond what might have been expected as a result of working in this partnership, as opposed to working independently? If yes, could you provide a few examples? If no, are there any limitations that you can think of?
- 14 What is the LIP trying to achieve?
- 15 Does it seem as if everyone understands and supports these goals (ie, Is everyone headed in the same direction)?
- 16 How would you describe the LIP's progress toward these goals to date?
Experience:
- 17 How would you describe your overall experience of being part of this LIP?
- 18 What has been the most positive aspect of your involvement?
- 19 What has been the most negative aspect of your involvement?
- 20 Do you look forward to the meetings of the LIP? Why or why not?
- 21 What words would you use to describe the general atmosphere of the LIP (eg, level of energy surrounding the LIP)
Synergy‐promoting strategies (enablers and barriers to partnership):
- 22 Describe the processes and approaches that have been used to facilitate the work of the LIP.
- 23 What's working well? How do you know (are there any indicators of success)?
- 24 From your perspective, what might be improved? And how? What would make your LIP more effective?
- 25 Is there anything else that you would like to mention?
APPENDIX B. CROSS‐CASE SYNTHESIS HIGHLIGHTING FACTORS FOSTERING/HINDERING PARTNERSHIP SYNERGY, INCLUDING ILLUSTRATIVE QUOTATIONS
Abbreviation: IMPACT ‐ Innovative Models Promoting Access‐to‐Care Transformation.
Loban E, Scott C, Lewis V, Law S, Haggerty J. Improving primary health care through partnerships: Key insights from a cross‐case analysis of multi‐stakeholder partnerships in two Canadian provinces . Health Sci Rep . 2021; 4 :e397. doi: 10.1002/hsr2.397 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Funding information Canadian Institutes of Health Research, Grant/Award Number: TTF‐130729; Fonds de recherche du Québec ‐ Santé; Australian Primary Health Care Research Institute
DATA AVAILABILITY STATEMENT

Partners Healthcare System Case Solution & Answer
Home » Case Study Analysis Solutions » Partners Healthcare System
Partners Healthcare System Case Study Analysis
PARTNERS HEALTHCARE SYSTEM (PHS): TRANSFORMING HEALTH CARE SERVICES DELIVERY THROUGH INFORMATION MANAGEMENT
The Partners Healthcare System (PHS) faced a lot of obstacles in implementing the ERP system whose sole responsibility was to make the current processes as efficient as possible. In addition to this, once this information system is along with Computerized Patient Order Entry (CPOE) system then it would help the health care professionals in accessing patient complete profile from the scratch that is the patients’ first visit to the health practitioner. However, there was a lot of resistance regarding the system from the doctors. It is reported that two-third of the doctors had prior links to the hospitals and were hesitant to adopt the latest technology. In addition to this, the same number of doctors who had affiliations with the PHS hospital also met their patients at some other venues.
The already established workforce lacked in its ability to use the advanced technology and was reluctant to this type of system. As they were trained to write prescriptions manually, hence they were not accepting this new mode of data reposition. In addition to a lack in ability to apt the latest technology, they also lacked the basic infrastructure or resources to finance this implementation. Moreover, if the technology gets implemented then the lack for support and after implementation maintenance was another problem. This further declined their ability to pursue new treatment techniques and methods, or prescribe new drugs that would be of great help to the patient rather than giving the traditional prescriptions. As these practitioners were not at all technology savvy, hence, another reason to be concerned was their ability to type and see and the customer. This reflects the practitioner’s inability to be multi-tasker.
In addition, last but not the least is the cost of implementing the module. As calculated through the case study, the cost to implement such ERP coupled with CPOE was $40,000 per doctor, hence, making it hard for a primary physician to afford its integration. Moreover, the existing practitioners found it a threat to the current practices that hurt their profits later. Traditionally, the authority was assumed to be the central figure but after this, implementation was assumed to be decentralized.
Question 02
From a project management perspective, the system deployment factors that appear to be present in case of Partners Healthcare System (PHS) includes value added service to the patient on one hand and on the other hand it would increase the experience of the doctor or practitioner himself. Equipped with the full details of the history of the patient at disposal, the complete description of the patient’s medication and the performance evaluation of the drug on the patient during the treatment through the notes would add value to the doctor’s experience as well. In addition to this, another important factor that was assessed in the implementation of the system is that doctors get advice on the new drugs and the compatibility with the disease being cured that makes the process more helpful for him. The system is updated on a regular basis to incorporate the addition of the new drugs and the subtraction of the obsolete ones from the market that makes the process more efficient.
This system would help the doctor diagnose the disease and the cure in a more technologically updated fashion rather going through the manual process and enhancing their knowledge base for the cost effectiveness of the new therapies. This would also help them in serving the cost related issue of the patients who are unable to afford the expensive therapies. The system would generate the best optimal solution and the therapy for the patient according the patient budget, which is a true reflection of an intelligent system.
This would help the heath care centers speed up the process of data reposition and making the system develop sets of recognized and recommended therapies. This hassle free process, of automation of the health care system was best to become cost effective as it would help boost the patients’ diagnosis and treatment within a few seconds. It would help extraordinary implications in a shorter time frame and help elevate success path for those, who support the change in the organization.
Along with the fringe benefits of this technology, system deployment factors appear to be absent in the implementation that include lack of financial incentives for those who are a part and parcel of the organization for a relatively longer period of time. The Partners Healthcare System (PHS) was a decentralized one, therefore, the change needed to be done to the organization that was centralized in the past. In addition to this, the power to implement the system lies in the hands of the medical practitioner; therefore, before implementing the system it was a pre-requisite to make the management accept the change, which would be the ultimate success of the implementation…………………..
This is just a sample partical work. Please place the order on the website to get your own originally done case solution.
Related Case Solutions:

LOOK FOR A FREE CASE STUDY SOLUTION
- Harvard Business School →
- Faculty & Research →
- August 2005 (Revised May 2007)
- HBS Case Collection
Partners Healthcare
- Format: Print
- | Pages: 14
About The Author
Joshua D. Coval
More from the author.
- February 2023
- Faculty Research
Success Academy Charter Schools
- December 2022
Managing Pain in the Midst of an Opioid Epidemic
- Success Academy Charter Schools By: Robin Greenwood, Joshua D. Coval, Denise Han, Ruth Page and Dave Habeeb
- Success Academy Charter Schools By: Robin Greenwood, Joshua Coval and Denise Han
- Managing Pain in the Midst of an Opioid Epidemic By: Joshua D. Coval, Richard S. Ruback and Christopher Diak
Information Management Strategy: PHS Clinic Case Study
Before the introduction of the LMR and the CPOE systems into the company’s framework, the PHS Clinic was an exact representation of a company, whose decision-making process was based on the principles of a traditional, non-computerized approach to data management, which caused numerous issues in data accuracy and patient safety.
The incorporation of the LMR and the CPOE approaches allowed for designing an entirely different strategy for information management, In other words, the latest information technology innovations could be incorporated into the framework of the organization so that the process of information transfer could become easier and safer.
The investment, which the company’s leadership had to make into the process of enhancing the quality of the service delivery and increasing the rates of patient satisfaction, allowed the company to propel itself into a new stage of development, which involved digital communication.
The fact that the organization managed to allocate its costs in a proper manner and, therefore, make a reasonable investment into the further progress, can be viewed as the key factor promoting the further redesign of the information system.
The formalities related to the staff’s affiliation to the PHS management style, the use of out-of-hospital offices by the latter, the absence of the relevant technology and skills among the local doctors, the reluctance of the staff to learn new skills, and a comparatively high cost of the overall change can be viewed as the key impediments to the change.
The transformation in question allowed for making impressive changes in the design of the organization and the attitude of the staff towards technology. Specifically, the incorporation of the IT architectural framework, which helped the staff get accustomed to the alterations, the design of a specific code for the staff to collaborate efficiently, the design of the governing systems, and the integration of quality assurance tools deserve to be mentioned.
Improving the process of data management on an enterprise-wide level is fraught with a range of issues, including the problem of training the staff and making sure that every single member has been made aware of the specifics of the new information management approach.
The process of establishing the decision support system in the specified environment, however, is associated with a range of difficulties, the need for creating the corresponding tools, to design a new approach towards establishing the patient-therapist relationships, and the introduction of the new information management principle into the framework, to name a few.
The integration of an information management platform can definitely be viewed as a major success factor. However, the fact that the staff will have to adapt to significant changes and, therefore, make mistakes in the process, is a huge downgrade.
The elimination of the key risks, which the architectural design allows for, can be explained by the fact that the specified approach helps not only locate the key variable, but also identify the relationships between them instantly.
Reducing the key costs spent on the design of the solutions for addressing specific issues within a community, research and development centres fully justify their existence.
The PHS management will have to locate the ways of promoting change among the reluctant staff. The healthcare practitioners will need to incorporate entirely new approaches into their practice, thus, facing the risk of delivering poor services, while the allied agencies interacting with the PHS may be liable in case the latter fail. Thus, the TCO implications can be considered rather high.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, April 14). Information Management Strategy: PHS Clinic. https://ivypanda.com/essays/partners-healthcare-a-case-study-analysis/
"Information Management Strategy: PHS Clinic." IvyPanda , 14 Apr. 2022, ivypanda.com/essays/partners-healthcare-a-case-study-analysis/.
IvyPanda . (2022) 'Information Management Strategy: PHS Clinic'. 14 April.
IvyPanda . 2022. "Information Management Strategy: PHS Clinic." April 14, 2022. https://ivypanda.com/essays/partners-healthcare-a-case-study-analysis/.
1. IvyPanda . "Information Management Strategy: PHS Clinic." April 14, 2022. https://ivypanda.com/essays/partners-healthcare-a-case-study-analysis/.
Bibliography
IvyPanda . "Information Management Strategy: PHS Clinic." April 14, 2022. https://ivypanda.com/essays/partners-healthcare-a-case-study-analysis/.
- Usability of Computerizes Provider Order Entry Systems
- Safety Score Improvement Plan for St. Vincent Rehabilitation Center
- Paper-Based Methods and E-prescription: Evaluation Project
- The Mitochondria and Autism - Results and Main Function
- Debates on Euthanasia - Opposes the Use
- The Function of Kinase Inhibitor Staurosporine in Healthy and Disease States
- Ways of Improving the Communication Process in Health and Social Care Setting
- Barriers to the Use of Technology to Support Users of Health and Social Care
- Search Search Search …
- Search Search …
Partners HealthCare System Inc. (A)
Subjects Covered Capacity planning Competition Mergers Operating systems Organizational change
by Gary P. Pisano, Maryam Golnaraghi
Source: Harvard Business School
23 pages. Publication Date: Feb 16, 1996. Prod. #: 696062-PDF-ENG
Partners HealthCare System, Inc. (A) Harvard Case Study Solution and HBR and HBS Case Analysis
Related Posts

You may also like

Congo River Basin Project: Role for Dr. Beni
Subjects Covered Decision making Nongovernmental organizations Nonprofit organizations Social enterprise Tradeoff analysis by Kathleen L. McGinn, Deborah M. Kolb, Cailin B. Hammer, […]

Financing Entrepreneurial Ventures Business Fundamentals Series
Subjects Covered Business plans Development stage enterprises Entrepreneurial management Venture capital by William A. Sahlman, Howard H. Stevenson, Amar V. Bhide, James […]

Hewlett-Packard: Manufacturing Productivity Division (D) Glossary
Subjects Covered Applications Interdepartmental relations Product development Product lines R&D by Benson P. Shapiro Source: Harvard Business School 2 pages. Publication Date: […]

Kirk Stone (B)
Subjects Covered Career planning Personal strategy & style Values by Vijay V. Sathe, Robert Mueller Jr. Source: Harvard Business School 3 pages. […]

- Predictive Analytics Workshops
- Corporate Strategy Workshops
- Advanced Excel for MBA
- Powerpoint Workshops
- Digital Transformation
- Competing on Business Analytics
- Aligning Analytics with Strategy
- Building & Sustaining Competitive Advantages
- Corporate Strategy
- Aligning Strategy & Sales
- Digital Marketing
- Hypothesis Testing
- Time Series Analysis
- Regression Analysis
- Machine Learning
- Marketing Strategy
- Branding & Advertising
- Risk Management
- Hedging Strategies
- Network Plotting
- Bar Charts & Time Series
- Technical Analysis of Stocks MACD
- NPV Worksheet
- ABC Analysis Worksheet
- WACC Worksheet
- Porter 5 Forces
- Porter Value Chain
- Amazing Charts
- Garnett Chart
- HBR Case Solution
- 4P Analysis
- 5C Analysis
- NPV Analysis
- SWOT Analysis
- PESTEL Analysis
- Cost Optimization
Partners HealthCare System, Inc. (A)
- Technology & Operations / MBA EMBA Resources
Next Case Study Solutions
- American Medical Association-Sunbeam Deal (B): The Deal Collapses Case Study Solution
- Hospital Clinic de Barcelona Case Study Solution
- Patient Flow at Brigham and Women's Hospital (B) Case Study Solution
- Paperless Healthcare: Progress and Challenges of an IT-Enabled Healthcare System Case Study Solution
- Customers in Health Care Case Study Solution
Previous Case Solutions
- Connectivity in Health Care Case Study Solution
- Healthware S.p.A. - From an Underdeveloped Region of Italy - Can it be a Global Firm? Case Study Solution
- Raiser Senior Services--The Stratford (B) Case Study Solution
- Deaconess-Glover Hospital (D) Case Study Solution
- Hopital de Pontoise Case Study Solution

Predictive Analytics
May 16, 2024

Popular Tags
Case study solutions.

Case Study Solution | Assignment Help | Case Help
Partners healthcare system, inc. (a) description.
Focuses on the decision confronting senior administrators at the Brigham and Women's Hospital: whether to enter into an affiliation with the Massachusetts General Hospital. Requires students to analyze the complex institutional changes in the health environment and to determine how the proposed affiliation might influence the hospital's chances for successfully carrying out its core missions.
Case Description Partners HealthCare System, Inc. (A)
Strategic managment tools used in case study analysis of partners healthcare system, inc. (a), step 1. problem identification in partners healthcare system, inc. (a) case study, step 2. external environment analysis - pestel / pest / step analysis of partners healthcare system, inc. (a) case study, step 3. industry specific / porter five forces analysis of partners healthcare system, inc. (a) case study, step 4. evaluating alternatives / swot analysis of partners healthcare system, inc. (a) case study, step 5. porter value chain analysis / vrio / vrin analysis partners healthcare system, inc. (a) case study, step 6. recommendations partners healthcare system, inc. (a) case study, step 7. basis of recommendations for partners healthcare system, inc. (a) case study, quality & on time delivery.
100% money back guarantee if the quality doesn't match the promise
100% Plagiarism Free
If the work we produce contain plagiarism then we payback 1000 USD
Paypal Secure
All your payments are secure with Paypal security.
300 Words per Page
We provide 300 words per page unlike competitors' 250 or 275
Free Title Page, Citation Page, References, Exhibits, Revision, Charts
Case study solutions are career defining. Order your custom solution now.
Case Analysis of Partners HealthCare System, Inc. (A)
Partners HealthCare System, Inc. (A) is a Harvard Business (HBR) Case Study on Technology & Operations , Texas Business School provides HBR case study assignment help for just $9. Texas Business School(TBS) case study solution is based on HBR Case Study Method framework, TBS expertise & global insights. Partners HealthCare System, Inc. (A) is designed and drafted in a manner to allow the HBR case study reader to analyze a real-world problem by putting reader into the position of the decision maker. Partners HealthCare System, Inc. (A) case study will help professionals, MBA, EMBA, and leaders to develop a broad and clear understanding of casecategory challenges. Partners HealthCare System, Inc. (A) will also provide insight into areas such as – wordlist , strategy, leadership, sales and marketing, and negotiations.
Case Study Solutions Background Work
Partners HealthCare System, Inc. (A) case study solution is focused on solving the strategic and operational challenges the protagonist of the case is facing. The challenges involve – evaluation of strategic options, key role of Technology & Operations, leadership qualities of the protagonist, and dynamics of the external environment. The challenge in front of the protagonist, of Partners HealthCare System, Inc. (A), is to not only build a competitive position of the organization but also to sustain it over a period of time.
Strategic Management Tools Used in Case Study Solution
The Partners HealthCare System, Inc. (A) case study solution requires the MBA, EMBA, executive, professional to have a deep understanding of various strategic management tools such as SWOT Analysis, PESTEL Analysis / PEST Analysis / STEP Analysis, Porter Five Forces Analysis, Go To Market Strategy, BCG Matrix Analysis, Porter Value Chain Analysis, Ansoff Matrix Analysis, VRIO / VRIN and Marketing Mix Analysis.
Texas Business School Approach to Technology & Operations Solutions
In the Texas Business School, Partners HealthCare System, Inc. (A) case study solution – following strategic tools are used - SWOT Analysis, PESTEL Analysis / PEST Analysis / STEP Analysis, Porter Five Forces Analysis, Go To Market Strategy, BCG Matrix Analysis, Porter Value Chain Analysis, Ansoff Matrix Analysis, VRIO / VRIN and Marketing Mix Analysis. We have additionally used the concept of supply chain management and leadership framework to build a comprehensive case study solution for the case – Partners HealthCare System, Inc. (A)
Step 1 – Problem Identification of Partners HealthCare System, Inc. (A) - Harvard Business School Case Study
The first step to solve HBR Partners HealthCare System, Inc. (A) case study solution is to identify the problem present in the case. The problem statement of the case is provided in the beginning of the case where the protagonist is contemplating various options in the face of numerous challenges that Affiliation Hospital is facing right now. Even though the problem statement is essentially – “Technology & Operations” challenge but it has impacted by others factors such as communication in the organization, uncertainty in the external environment, leadership in Affiliation Hospital, style of leadership and organization structure, marketing and sales, organizational behavior, strategy, internal politics, stakeholders priorities and more.
Step 2 – External Environment Analysis
Texas Business School approach of case study analysis – Conclusion, Reasons, Evidences - provides a framework to analyze every HBR case study. It requires conducting robust external environmental analysis to decipher evidences for the reasons presented in the Partners HealthCare System, Inc. (A). The external environment analysis of Partners HealthCare System, Inc. (A) will ensure that we are keeping a tab on the macro-environment factors that are directly and indirectly impacting the business of the firm.
What is PESTEL Analysis? Briefly Explained
PESTEL stands for political, economic, social, technological, environmental and legal factors that impact the external environment of firm in Partners HealthCare System, Inc. (A) case study. PESTEL analysis of " Partners HealthCare System, Inc. (A)" can help us understand why the organization is performing badly, what are the factors in the external environment that are impacting the performance of the organization, and how the organization can either manage or mitigate the impact of these external factors.
How to do PESTEL / PEST / STEP Analysis? What are the components of PESTEL Analysis?
As mentioned above PESTEL Analysis has six elements – political, economic, social, technological, environmental, and legal. All the six elements are explained in context with Partners HealthCare System, Inc. (A) macro-environment and how it impacts the businesses of the firm.
How to do PESTEL Analysis for Partners HealthCare System, Inc. (A)
To do comprehensive PESTEL analysis of case study – Partners HealthCare System, Inc. (A) , we have researched numerous components under the six factors of PESTEL analysis.
Political Factors that Impact Partners HealthCare System, Inc. (A)
Political factors impact seven key decision making areas – economic environment, socio-cultural environment, rate of innovation & investment in research & development, environmental laws, legal requirements, and acceptance of new technologies.
Government policies have significant impact on the business environment of any country. The firm in “ Partners HealthCare System, Inc. (A) ” needs to navigate these policy decisions to create either an edge for itself or reduce the negative impact of the policy as far as possible.
Data safety laws – The countries in which Affiliation Hospital is operating, firms are required to store customer data within the premises of the country. Affiliation Hospital needs to restructure its IT policies to accommodate these changes. In the EU countries, firms are required to make special provision for privacy issues and other laws.
Competition Regulations – Numerous countries have strong competition laws both regarding the monopoly conditions and day to day fair business practices. Partners HealthCare System, Inc. (A) has numerous instances where the competition regulations aspects can be scrutinized.
Import restrictions on products – Before entering the new market, Affiliation Hospital in case study Partners HealthCare System, Inc. (A)" should look into the import restrictions that may be present in the prospective market.
Export restrictions on products – Apart from direct product export restrictions in field of technology and agriculture, a number of countries also have capital controls. Affiliation Hospital in case study “ Partners HealthCare System, Inc. (A) ” should look into these export restrictions policies.
Foreign Direct Investment Policies – Government policies favors local companies over international policies, Affiliation Hospital in case study “ Partners HealthCare System, Inc. (A) ” should understand in minute details regarding the Foreign Direct Investment policies of the prospective market.
Corporate Taxes – The rate of taxes is often used by governments to lure foreign direct investments or increase domestic investment in a certain sector. Corporate taxation can be divided into two categories – taxes on profits and taxes on operations. Taxes on profits number is important for companies that already have a sustainable business model, while taxes on operations is far more significant for companies that are looking to set up new plants or operations.
Tariffs – Chekout how much tariffs the firm needs to pay in the “ Partners HealthCare System, Inc. (A) ” case study. The level of tariffs will determine the viability of the business model that the firm is contemplating. If the tariffs are high then it will be extremely difficult to compete with the local competitors. But if the tariffs are between 5-10% then Affiliation Hospital can compete against other competitors.
Research and Development Subsidies and Policies – Governments often provide tax breaks and other incentives for companies to innovate in various sectors of priority. Managers at Partners HealthCare System, Inc. (A) case study have to assess whether their business can benefit from such government assistance and subsidies.
Consumer protection – Different countries have different consumer protection laws. Managers need to clarify not only the consumer protection laws in advance but also legal implications if the firm fails to meet any of them.
Political System and Its Implications – Different political systems have different approach to free market and entrepreneurship. Managers need to assess these factors even before entering the market.
Freedom of Press is critical for fair trade and transparency. Countries where freedom of press is not prevalent there are high chances of both political and commercial corruption.
Corruption level – Affiliation Hospital needs to assess the level of corruptions both at the official level and at the market level, even before entering a new market. To tackle the menace of corruption – a firm should have a clear SOP that provides managers at each level what to do when they encounter instances of either systematic corruption or bureaucrats looking to take bribes from the firm.
Independence of judiciary – It is critical for fair business practices. If a country doesn’t have independent judiciary then there is no point entry into such a country for business.
Government attitude towards trade unions – Different political systems and government have different attitude towards trade unions and collective bargaining. The firm needs to assess – its comfort dealing with the unions and regulations regarding unions in a given market or industry. If both are on the same page then it makes sense to enter, otherwise it doesn’t.
Economic Factors that Impact Partners HealthCare System, Inc. (A)
Social factors that impact partners healthcare system, inc. (a), technological factors that impact partners healthcare system, inc. (a), environmental factors that impact partners healthcare system, inc. (a), legal factors that impact partners healthcare system, inc. (a), step 3 – industry specific analysis, what is porter five forces analysis, step 4 – swot analysis / internal environment analysis, step 5 – porter value chain / vrio / vrin analysis, step 6 – evaluating alternatives & recommendations, step 7 – basis for recommendations, references :: partners healthcare system, inc. (a) case study solution.
- sales & marketing ,
- leadership ,
- corporate governance ,
- Advertising & Branding ,
- Corporate Social Responsibility (CSR) ,
Amanda Watson
Leave your thought here

© 2019 Texas Business School. All Rights Reserved
USEFUL LINKS
Follow us on.
Subscribe to our newsletter to receive news on update.


Dark Brown Leather Watch
$200.00 $180.00

Dining Chair
$300.00 $220.00

Creative Wooden Stand
$100.00 $80.00
2 x $180.00
2 x $220.00
Subtotal: $200.00
Free Shipping on All Orders Over $100!

Wooden round table
$360.00 $300.00
Hurley Dry-Fit Chino Short. Men's chino short. Outseam Length: 19 Dri-FIT Technology helps keep you dry and comfortable. Made with sweat-wicking fabric. Fitted waist with belt loops. Button waist with zip fly provides a classic look and feel .
- Open access
- Published: 15 May 2024
Learning together for better health using an evidence-based Learning Health System framework: a case study in stroke
- Helena Teede 1 , 2 na1 ,
- Dominique A. Cadilhac 3 , 4 na1 ,
- Tara Purvis 3 ,
- Monique F. Kilkenny 3 , 4 ,
- Bruce C.V. Campbell 4 , 5 , 6 ,
- Coralie English 7 ,
- Alison Johnson 2 ,
- Emily Callander 1 ,
- Rohan S. Grimley 8 , 9 ,
- Christopher Levi 10 ,
- Sandy Middleton 11 , 12 ,
- Kelvin Hill 13 &
- Joanne Enticott ORCID: orcid.org/0000-0002-4480-5690 1
BMC Medicine volume 22 , Article number: 198 ( 2024 ) Cite this article
Metrics details
In the context of expanding digital health tools, the health system is ready for Learning Health System (LHS) models. These models, with proper governance and stakeholder engagement, enable the integration of digital infrastructure to provide feedback to all relevant parties including clinicians and consumers on performance against best practice standards, as well as fostering innovation and aligning healthcare with patient needs. The LHS literature primarily includes opinion or consensus-based frameworks and lacks validation or evidence of benefit. Our aim was to outline a rigorously codesigned, evidence-based LHS framework and present a national case study of an LHS-aligned national stroke program that has delivered clinical benefit.
Current core components of a LHS involve capturing evidence from communities and stakeholders (quadrant 1), integrating evidence from research findings (quadrant 2), leveraging evidence from data and practice (quadrant 3), and generating evidence from implementation (quadrant 4) for iterative system-level improvement. The Australian Stroke program was selected as the case study as it provides an exemplar of how an iterative LHS works in practice at a national level encompassing and integrating evidence from all four LHS quadrants. Using this case study, we demonstrate how to apply evidence-based processes to healthcare improvement and embed real-world research for optimising healthcare improvement. We emphasize the transition from research as an endpoint, to research as an enabler and a solution for impact in healthcare improvement.
Conclusions
The Australian Stroke program has nationally improved stroke care since 2007, showcasing the value of integrated LHS-aligned approaches for tangible impact on outcomes. This LHS case study is a practical example for other health conditions and settings to follow suit.
Peer Review reports
Internationally, health systems are facing a crisis, driven by an ageing population, increasing complexity, multi-morbidity, rapidly advancing health technology and rising costs that threaten sustainability and mandate transformation and improvement [ 1 , 2 ]. Although research has generated solutions to healthcare challenges, and the advent of big data and digital health holds great promise, entrenched siloes and poor integration of knowledge generation, knowledge implementation and healthcare delivery between stakeholders, curtails momentum towards, and consistent attainment of, evidence-and value-based care [ 3 ]. This is compounded by the short supply of research and innovation leadership within the healthcare sector, and poorly integrated and often inaccessible health data systems, which have crippled the potential to deliver on digital-driven innovation [ 4 ]. Current approaches to healthcare improvement are also often isolated with limited sustainability, scale-up and impact [ 5 ].
Evidence suggests that integration and partnership across academic and healthcare delivery stakeholders are key to progress, including those with lived experience and their families (referred to here as consumers and community), diverse disciplines (both research and clinical), policy makers and funders. Utilization of evidence from research and evidence from practice including data from routine care, supported by implementation research, are key to sustainably embedding improvement and optimising health care and outcomes. A strategy to achieve this integration is through the Learning Health System (LHS) (Fig. 1 ) [ 2 , 6 , 7 , 8 ]. Although there are numerous publications on LHS approaches [ 9 , 10 , 11 , 12 ], many focus on research perspectives and data, most do not demonstrate tangible healthcare improvement or better health outcomes. [ 6 ]
Monash Learning Health System: The Learn Together for Better Health Framework developed by Monash Partners and Monash University (from Enticott et al. 2021 [ 7 ]). Four evidence quadrants: Q1 (orange) is evidence from stakeholders; Q2 (green) is evidence from research; Q3 (light blue) is evidence from data; and, Q4 (dark blue) is evidence from implementation and healthcare improvement
In developed nations, it has been estimated that 60% of care provided aligns with the evidence base, 30% is low value and 10% is potentially harmful [ 13 ]. In some areas, clinical advances have been rapid and research and evidence have paved the way for dramatic improvement in outcomes, mandating rapid implementation of evidence into healthcare (e.g. polio and COVID-19 vaccines). However, healthcare improvement is challenging and slow [ 5 ]. Health systems are highly complex in their design, networks and interacting components, and change is difficult to enact, sustain and scale up. [ 3 ] New effective strategies are needed to meet community needs and deliver evidence-based and value-based care, which reorients care from serving the provider, services and system, towards serving community needs, based on evidence and quality. It goes beyond cost to encompass patient and provider experience, quality care and outcomes, efficiency and sustainability [ 2 , 6 ].
The costs of stroke care are expected to rise rapidly in the next decades, unless improvements in stroke care to reduce the disabling effects of strokes can be successfully developed and implemented [ 14 ]. Here, we briefly describe the Monash LHS framework (Fig. 1 ) [ 2 , 6 , 7 ] and outline an exemplar case in order to demonstrate how to apply evidence-based processes to healthcare improvement and embed real-world research for optimising healthcare. The Australian LHS exemplar in stroke care has driven nationwide improvement in stroke care since 2007.
An evidence-based Learning Health System framework
In Australia, members of this author group (HT, AJ, JE) have rigorously co-developed an evidence-based LHS framework, known simply as the Monash LHS [ 7 ]. The Monash LHS was designed to support sustainable, iterative and continuous robust benefit of improved clinical outcomes. It was created with national engagement in order to be applicable to Australian settings. Through this rigorous approach, core LHS principles and components have been established (Fig. 1 ). Evidence shows that people/workforce, culture, standards, governance and resources were all key to an effective LHS [ 2 , 6 ]. Culture is vital including trust, transparency, partnership and co-design. Key processes include legally compliant data sharing, linkage and governance, resources, and infrastructure [ 4 ]. The Monash LHS integrates disparate and often siloed stakeholders, infrastructure and expertise to ‘Learn Together for Better Health’ [ 7 ] (Fig. 1 ). This integrates (i) evidence from community and stakeholders including priority areas and outcomes; (ii) evidence from research and guidelines; (iii) evidence from practice (from data) with advanced analytics and benchmarking; and (iv) evidence from implementation science and health economics. Importantly, it starts with the problem and priorities of key stakeholders including the community, health professionals and services and creates an iterative learning system to address these. The following case study was chosen as it is an exemplar of how a Monash LHS-aligned national stroke program has delivered clinical benefit.
Australian Stroke Learning Health System
Internationally, the application of LHS approaches in stroke has resulted in improved stroke care and outcomes [ 12 ]. For example, in Canada a sustained decrease in 30-day in-hospital mortality has been found commensurate with an increase in resources to establish the multifactorial stroke system intervention for stroke treatment and prevention [ 15 ]. Arguably, with rapid advances in evidence and in the context of an ageing population with high cost and care burden and substantive impacts on quality of life, stroke is an area with a need for rapid research translation into evidence-based and value-based healthcare improvement. However, a recent systematic review found that the existing literature had few comprehensive examples of LHS adoption [ 12 ]. Although healthcare improvement systems and approaches were described, less is known about patient-clinician and stakeholder engagement, governance and culture, or embedding of data informatics into everyday practice to inform and drive improvement [ 12 ]. For example, in a recent review of quality improvement collaborations, it was found that although clinical processes in stroke care are improved, their short-term nature means there is uncertainty about sustainability and impacts on patient outcomes [ 16 ]. Table 1 provides the main features of the Australian Stroke LHS based on the four core domains and eight elements of the Learning Together for Better Health Framework described in Fig. 1 . The features are further expanded on in the following sections.
Evidence from stakeholders (LHS quadrant 1, Fig. 1 )
Engagement, partners and priorities.
Within the stroke field, there have been various support mechanisms to facilitate an LHS approach including partnership and broad stakeholder engagement that includes clinical networks and policy makers from different jurisdictions. Since 2008, the Australian Stroke Coalition has been co-led by the Stroke Foundation, a charitable consumer advocacy organisation, and Stroke Society of Australasia a professional society with membership covering academics and multidisciplinary clinician networks, that are collectively working to improve stroke care ( https://australianstrokecoalition.org.au/ ). Surveys, focus groups and workshops have been used for identifying priorities from stakeholders. Recent agreed priorities have been to improve stroke care and strengthen the voice for stroke care at a national ( https://strokefoundation.org.au/ ) and international level ( https://www.world-stroke.org/news-and-blog/news/world-stroke-organization-tackle-gaps-in-access-to-quality-stroke-care ), as well as reduce duplication amongst stakeholders. This activity is built on a foundation and culture of research and innovation embedded within the stroke ‘community of practice’. Consumers, as people with lived experience of stroke are important members of the Australian Stroke Coalition, as well as representatives from different clinical colleges. Consumers also provide critical input to a range of LHS activities via the Stroke Foundation Consumer Council, Stroke Living Guidelines committees, and the Australian Stroke Clinical Registry (AuSCR) Steering Committee (described below).
Evidence from research (LHS quadrant 2, Fig. 1 )
Advancement of the evidence for stroke interventions and synthesis into clinical guidelines.
To implement best practice, it is crucial to distil the large volume of scientific and trial literature into actionable recommendations for clinicians to use in practice [ 24 ]. The first Australian clinical guidelines for acute stroke were produced in 2003 following the increasing evidence emerging for prevention interventions (e.g. carotid endarterectomy, blood pressure lowering), acute medical treatments (intravenous thrombolysis, aspirin within 48 h of ischemic stroke), and optimised hospital management (care in dedicated stroke units by a specialised and coordinated multidisciplinary team) [ 25 ]. Importantly, a number of the innovations were developed, researched and proven effective by key opinion leaders embedded in the Australian stroke care community. In 2005, the clinical guidelines for Stroke Rehabilitation and Recovery [ 26 ] were produced, with subsequent merged guidelines periodically updated. However, the traditional process of periodic guideline updates is challenging for end users when new research can render recommendations redundant and this lack of currency erodes stakeholder trust [ 27 ]. In response to this challenge the Stroke Foundation and Cochrane Australia entered a pioneering project to produce the first electronic ‘living’ guidelines globally [ 20 ]. Major shifts in the evidence for reperfusion therapies (e.g. extended time-window intravenous thrombolysis and endovascular clot retrieval), among other advances, were able to be converted into new recommendations, approved by the Australian National Health and Medical Research Council within a few months of publication. Feedback on this process confirmed the increased use and trust in the guidelines by clinicians. The process informed other living guidelines programs, including the successful COVID-19 clinical guidelines [ 28 ].
However, best practice clinical guideline recommendations are necessary but insufficient for healthcare improvement and nesting these within an LHS with stakeholder partnership, enables implementation via a range of proven methods, including audit and feedback strategies [ 29 ].
Evidence from data and practice (LHS quadrant 3, Fig. 1 )
Data systems and benchmarking : revealing the disparities in care between health services. A national system for standardized stroke data collection was established as the National Stroke Audit program in 2007 by the Stroke Foundation [ 30 ] following various state-level programs (e.g. New South Wales Audit) [ 31 ] to identify evidence-practice gaps and prioritise improvement efforts to increase access to stroke units and other acute treatments [ 32 ]. The Audit program alternates each year between acute (commencing in 2007) and rehabilitation in-patient services (commencing in 2008). The Audit program provides a ‘deep dive’ on the majority of recommendations in the clinical guidelines whereby participating hospitals provide audits of up to 40 consecutive patient medical records and respond to a survey about organizational resources to manage stroke. In 2009, the AuSCR was established to provide information on patients managed in acute hospitals based on a small subset of quality processes of care linked to benchmarked reports of performance (Fig. 2 ) [ 33 ]. In this way, the continuous collection of high-priority processes of stroke care could be regularly collected and reviewed to guide improvement to care [ 34 ]. Plus clinical quality registry programs within Australia have shown a meaningful return on investment attributed to enhanced survival, improvements in quality of life and avoided costs of treatment or hospital stay [ 35 ].
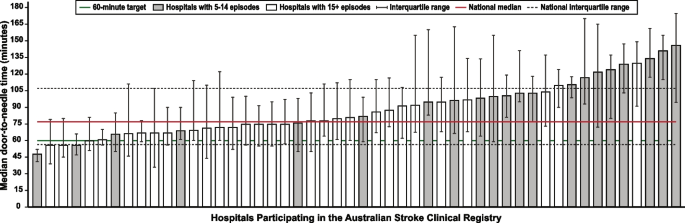
Example performance report from the Australian Stroke Clinical Registry: average door-to-needle time in providing intravenous thrombolysis by different hospitals in 2021 [ 36 ]. Each bar in the figure represents a single hospital
The Australian Stroke Coalition endorsed the creation of an integrated technological solution for collecting data through a single portal for multiple programs in 2013. In 2015, the Stroke Foundation, AuSCR consortium, and other relevant groups cooperated to design an integrated data management platform (the Australian Stroke Data Tool) to reduce duplication of effort for hospital staff in the collection of overlapping variables in the same patients [ 19 ]. Importantly, a national data dictionary then provided the common data definitions to facilitate standardized data capture. Another important feature of AuSCR is the collection of patient-reported outcome surveys between 90 and 180 days after stroke, and annual linkage with national death records to ascertain survival status [ 33 ]. To support a LHS approach, hospitals that participate in AuSCR have access to a range of real-time performance reports. In efforts to minimize the burden of data collection in the AuSCR, interoperability approaches to import data directly from hospital or state-level managed stroke databases have been established (Fig. 3 ); however, the application has been variable and 41% of hospitals still manually enter all their data.
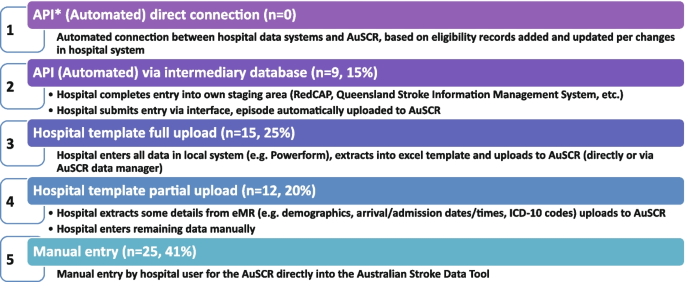
Current status of automated data importing solutions in the Australian Stroke Clinical Registry, 2022, with ‘ n ’ representing the number of hospitals. AuSCR, Australian Stroke Clinical Registry; AuSDaT, Australian Stroke Data Tool; API, Application Programming Interface; ICD, International Classification of Diseases; RedCAP, Research Electronic Data Capture; eMR, electronic medical records
For acute stroke care, the Australian Commission on Quality and Safety in Health Care facilitated the co-design (clinicians, academics, consumers) and publication of the national Acute Stroke Clinical Care Standard in 2015 [ 17 ], and subsequent review [ 18 ]. The indicator set for the Acute Stroke Standard then informed the expansion of the minimum dataset for AuSCR so that hospitals could routinely track their performance. The national Audit program enabled hospitals not involved in the AuSCR to assess their performance every two years against the Acute Stroke Standard. Complementing these efforts, the Stroke Foundation, working with the sector, developed the Acute and Rehabilitation Stroke Services Frameworks to outline the principles, essential elements, models of care and staffing recommendations for stroke services ( https://informme.org.au/guidelines/national-stroke-services-frameworks ). The Frameworks are intended to guide where stroke services should be developed, and monitor their uptake with the organizational survey component of the Audit program.
Evidence from implementation and healthcare improvement (LHS quadrant 4, Fig. 1 )
Research to better utilize and augment data from registries through linkage [ 37 , 38 , 39 , 40 ] and to ensure presentation of hospital or service level data are understood by clinicians has ensured advancement in the field for the Australian Stroke LHS [ 41 ]. Importantly, greater insights into whole patient journeys, before and after a stroke, can now enable exploration of value-based care. The LHS and stroke data platform have enabled focused and time-limited projects to create a better understanding of the quality of care in acute or rehabilitation settings [ 22 , 42 , 43 ]. Within stroke, all the elements of an LHS culminate into the ready availability of benchmarked performance data and support for implementation of strategies to address gaps in care.
Implementation research to grow the evidence base for effective improvement interventions has also been a key pillar in the Australian context. These include multi-component implementation interventions to achieve behaviour change for particular aspects of stroke care, [ 22 , 23 , 44 , 45 ] and real-world approaches to augmenting access to hyperacute interventions in stroke through the use of technology and telehealth [ 46 , 47 , 48 , 49 ]. The evidence from these studies feeds into the living guidelines program and the data collection systems, such as the Audit program or AuSCR, which are then amended to ensure data aligns to recommended care. For example, the use of ‘hyperacute aspirin within the first 48 h of ischemic stroke’ was modified to be ‘hyperacute antiplatelet…’ to incorporate new evidence that other medications or combinations are appropriate to use. Additionally, new datasets have been developed to align with evidence such as the Fever, Sugar, and Swallow variables [ 42 ]. Evidence on improvements in access to best practice care from the acute Audit program [ 50 ] and AuSCR is emerging [ 36 ]. For example, between 2007 and 2017, the odds of receiving intravenous thrombolysis after ischemic stroke increased by 16% 9OR 1.06 95% CI 1.13–1.18) and being managed in a stroke unit by 18% (OR 1.18 95% CI 1.17–1.20). Over this period, the median length of hospital stay for all patients decreased from 6.3 days in 2007 to 5.0 days in 2017 [ 51 ]. When considering the number of additional patients who would receive treatment in 2017 in comparison to 2007 it was estimated that without this additional treatment, over 17,000 healthy years of life would be lost in 2017 (17,786 disability-adjusted life years) [ 51 ]. There is evidence on the cost-effectiveness of different system-focussed strategies to augment treatment access for acute ischemic stroke (e.g. Victorian Stroke Telemedicine program [ 52 ] and Melbourne Mobile Stroke Unit ambulance [ 53 ]). Reciprocally, evidence from the national Rehabilitation Audit, where the LHS approach has been less complete or embedded, has shown fewer areas of healthcare improvement over time [ 51 , 54 ].
Within the field of stroke in Australia, there is indirect evidence that the collective efforts that align to establishing the components of a LHS have had an impact. Overall, the age-standardised rate of stroke events has reduced by 27% between 2001 and 2020, from 169 to 124 events per 100,000 population. Substantial declines in mortality rates have been reported since 1980. Commensurate with national clinical guidelines being updated in 2007 and the first National Stroke Audit being undertaken in 2007, the mortality rates for men (37.4 deaths per 100,000) and women (36.1 deaths per 100,0000 has declined to 23.8 and 23.9 per 100,000, respectively in 2021 [ 55 ].
Underpinning the LHS with the integration of the four quadrants of evidence from stakeholders, research and guidelines, practice and implementation, and core LHS principles have been addressed. Leadership and governance have been important, and programs have been established to augment workforce training and capacity building in best practice professional development. Medical practitioners are able to undertake courses and mentoring through the Australasian Stroke Academy ( http://www.strokeacademy.com.au/ ) while nurses (and other health professionals) can access teaching modules in stroke care from the Acute Stroke Nurses Education Network ( https://asnen.org/ ). The Association of Neurovascular Clinicians offers distance-accessible education and certification to develop stroke expertise for interdisciplinary professionals, including advanced stroke co-ordinator certification ( www.anvc.org ). Consumer initiative interventions are also used in the design of the AuSCR Public Summary Annual reports (available at https://auscr.com.au/about/annual-reports/ ) and consumer-related resources related to the Living Guidelines ( https://enableme.org.au/resources ).
The important success factors and lessons from stroke as a national exemplar LHS in Australia include leadership, culture, workforce and resources integrated with (1) established and broad partnerships across the academic-clinical sector divide and stakeholder engagement; (2) the living guidelines program; (3) national data infrastructure, including a national data dictionary that provides the common data framework to support standardized data capture; (4) various implementation strategies including benchmarking and feedback as well as engagement strategies targeting different levels of the health system; and (5) implementation and improvement research to advance stroke systems of care and reduce unwarranted variation in practice (Fig. 1 ). Priority opportunities now include the advancement of interoperability with electronic medical records as an area all clinical quality registry’s programs needs to be addressed, as well as providing more dynamic and interactive data dashboards tailored to the need of clinicians and health service executives.
There is a clear mandate to optimise healthcare improvement with big data offering major opportunities for change. However, we have lacked the approaches to capture evidence from the community and stakeholders, to integrate evidence from research, to capture and leverage data or evidence from practice and to generate and build on evidence from implementation using iterative system-level improvement. The LHS provides this opportunity and is shown to deliver impact. Here, we have outlined the process applied to generate an evidence-based LHS and provide a leading exemplar in stroke care. This highlights the value of moving from single-focus isolated approaches/initiatives to healthcare improvement and the benefit of integration to deliver demonstrable outcomes for our funders and key stakeholders — our community. This work provides insight into strategies that can both apply evidence-based processes to healthcare improvement as well as implementing evidence-based practices into care, moving beyond research as an endpoint, to research as an enabler, underpinning delivery of better healthcare.
Availability of data and materials
Not applicable
Abbreviations
Australian Stroke Clinical Registry
Confidence interval
- Learning Health System
World Health Organization. Delivering quality health services . OECD Publishing; 2018.
Enticott J, Braaf S, Johnson A, Jones A, Teede HJ. Leaders’ perspectives on learning health systems: A qualitative study. BMC Health Serv Res. 2020;20:1087.
Article PubMed PubMed Central Google Scholar
Melder A, Robinson T, McLoughlin I, Iedema R, Teede H. An overview of healthcare improvement: Unpacking the complexity for clinicians and managers in a learning health system. Intern Med J. 2020;50:1174–84.
Article PubMed Google Scholar
Alberto IRI, Alberto NRI, Ghosh AK, Jain B, Jayakumar S, Martinez-Martin N, et al. The impact of commercial health datasets on medical research and health-care algorithms. Lancet Digit Health. 2023;5:e288–94.
Article CAS PubMed PubMed Central Google Scholar
Dixon-Woods M. How to improve healthcare improvement—an essay by Mary Dixon-Woods. BMJ. 2019;367: l5514.
Enticott J, Johnson A, Teede H. Learning health systems using data to drive healthcare improvement and impact: A systematic review. BMC Health Serv Res. 2021;21:200.
Enticott JC, Melder A, Johnson A, Jones A, Shaw T, Keech W, et al. A learning health system framework to operationalize health data to improve quality care: An Australian perspective. Front Med (Lausanne). 2021;8:730021.
Dammery G, Ellis LA, Churruca K, Mahadeva J, Lopez F, Carrigan A, et al. The journey to a learning health system in primary care: A qualitative case study utilising an embedded research approach. BMC Prim Care. 2023;24:22.
Foley T, Horwitz L, Zahran R. The learning healthcare project: Realising the potential of learning health systems. 2021. Available from https://learninghealthcareproject.org/wp-content/uploads/2021/05/LHS2021report.pdf . Accessed Jan 2024.
Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Washington: The National Academies Press; 2013.
Google Scholar
Zurynski Y, Smith CL, Vedovi A, Ellis LA, Knaggs G, Meulenbroeks I, et al. Mapping the learning health system: A scoping review of current evidence - a white paper. 2020:63
Cadilhac DA, Bravata DM, Bettger J, Mikulik R, Norrving B, Uvere E, et al. Stroke learning health systems: A topical narrative review with case examples. Stroke. 2023;54:1148–59.
Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: The 60–30-10 challenge. BMC Med. 2020;18:1–8.
Article Google Scholar
King D, Wittenberg R, Patel A, Quayyum Z, Berdunov V, Knapp M. The future incidence, prevalence and costs of stroke in the UK. Age Ageing. 2020;49:277–82.
Ganesh A, Lindsay P, Fang J, Kapral MK, Cote R, Joiner I, et al. Integrated systems of stroke care and reduction in 30-day mortality: A retrospective analysis. Neurology. 2016;86:898–904.
Lowther HJ, Harrison J, Hill JE, Gaskins NJ, Lazo KC, Clegg AJ, et al. The effectiveness of quality improvement collaboratives in improving stroke care and the facilitators and barriers to their implementation: A systematic review. Implement Sci. 2021;16:16.
Australian Commission on Safety and Quality in Health Care. Acute stroke clinical care standard. 2015. Available from https://www.safetyandquality.gov.au/our-work/clinical-care-standards/acute-stroke-clinical-care-standard . Accessed Jan 2024.
Australian Commission on Safety and Quality in Health Care. Acute stroke clinical care standard. Sydney: ACSQHC; 2019. Available from https://www.safetyandquality.gov.au/publications-and-resources/resource-library/acute-stroke-clinical-care-standard-evidence-sources . Accessed Jan 2024.
Ryan O, Ghuliani J, Grabsch B, Hill K, G CC, Breen S, et al. Development, implementation, and evaluation of the Australian Stroke Data Tool (AuSDaT): Comprehensive data capturing for multiple uses. Health Inf Manag. 2022:18333583221117184.
English C, Bayley M, Hill K, Langhorne P, Molag M, Ranta A, et al. Bringing stroke clinical guidelines to life. Int J Stroke. 2019;14:337–9.
English C, Hill K, Cadilhac DA, Hackett ML, Lannin NA, Middleton S, et al. Living clinical guidelines for stroke: Updates, challenges and opportunities. Med J Aust. 2022;216:510–4.
Cadilhac DA, Grimley R, Kilkenny MF, Andrew NE, Lannin NA, Hill K, et al. Multicenter, prospective, controlled, before-and-after, quality improvement study (Stroke123) of acute stroke care. Stroke. 2019;50:1525–30.
Cadilhac DA, Marion V, Andrew NE, Breen SJ, Grabsch B, Purvis T, et al. A stepped-wedge cluster-randomized trial to improve adherence to evidence-based practices for acute stroke management. Jt Comm J Qual Patient Saf. 2022.
Elliott J, Lawrence R, Minx JC, Oladapo OT, Ravaud P, Jeppesen BT, et al. Decision makers need constantly updated evidence synthesis. Nature. 2021;600:383–5.
Article CAS PubMed Google Scholar
National Stroke Foundation. National guidelines for acute stroke management. Melbourne: National Stroke Foundation; 2003.
National Stroke Foundation. Clinical guidelines for stroke rehabilitation and recovery. Melbourne: National Stroke Foundation; 2005.
Phan TG, Thrift A, Cadilhac D, Srikanth V. A plea for the use of systematic review methodology when writing guidelines and timely publication of guidelines. Intern Med J . 2012;42:1369–1371; author reply 1371–1362
Tendal B, Vogel JP, McDonald S, Norris S, Cumpston M, White H, et al. Weekly updates of national living evidence-based guidelines: Methods for the Australian living guidelines for care of people with COVID-19. J Clin Epidemiol. 2021;131:11–21.
Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7:50.
Harris D, Cadilhac D, Hankey GJ, Hillier S, Kilkenny M, Lalor E. National stroke audit: The Australian experience. Clin Audit. 2010;2:25–31.
Cadilhac DA, Purvis T, Kilkenny MF, Longworth M, Mohr K, Pollack M, et al. Evaluation of rural stroke services: Does implementation of coordinators and pathways improve care in rural hospitals? Stroke. 2013;44:2848–53.
Cadilhac DA, Moss KM, Price CJ, Lannin NA, Lim JY, Anderson CS. Pathways to enhancing the quality of stroke care through national data monitoring systems for hospitals. Med J Aust. 2013;199:650–1.
Cadilhac DA, Lannin NA, Anderson CS, Levi CR, Faux S, Price C, et al. Protocol and pilot data for establishing the Australian Stroke Clinical Registry. Int J Stroke. 2010;5:217–26.
Ivers N, Jamtvedt G, Flottorp S, Young J, Odgaard-Jensen J, French S, et al. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev . 2012
Australian Commission on Safety and Quality in Health Care. Economic evaluation of clinical quality registries. Final report. . 2016:79
Cadilhac DA, Dalli LL, Morrison J, Lester M, Paice K, Moss K, et al. The Australian Stroke Clinical Registry annual report 2021. Melbourne; 2022. Available from https://auscr.com.au/about/annual-reports/ . Accessed 6 May 2024.
Kilkenny MF, Kim J, Andrew NE, Sundararajan V, Thrift AG, Katzenellenbogen JM, et al. Maximising data value and avoiding data waste: A validation study in stroke research. Med J Aust. 2019;210:27–31.
Eliakundu AL, Smith K, Kilkenny MF, Kim J, Bagot KL, Andrew E, et al. Linking data from the Australian Stroke Clinical Registry with ambulance and emergency administrative data in Victoria. Inquiry. 2022;59:469580221102200.
PubMed Google Scholar
Andrew NE, Kim J, Cadilhac DA, Sundararajan V, Thrift AG, Churilov L, et al. Protocol for evaluation of enhanced models of primary care in the management of stroke and other chronic disease (PRECISE): A data linkage healthcare evaluation study. Int J Popul Data Sci. 2019;4:1097.
CAS PubMed PubMed Central Google Scholar
Mosalski S, Shiner CT, Lannin NA, Cadilhac DA, Faux SG, Kim J, et al. Increased relative functional gain and improved stroke outcomes: A linked registry study of the impact of rehabilitation. J Stroke Cerebrovasc Dis. 2021;30: 106015.
Ryan OF, Hancock SL, Marion V, Kelly P, Kilkenny MF, Clissold B, et al. Feedback of aggregate patient-reported outcomes (PROs) data to clinicians and hospital end users: Findings from an Australian codesign workshop process. BMJ Open. 2022;12:e055999.
Grimley RS, Rosbergen IC, Gustafsson L, Horton E, Green T, Cadigan G, et al. Dose and setting of rehabilitation received after stroke in Queensland, Australia: A prospective cohort study. Clin Rehabil. 2020;34:812–23.
Purvis T, Middleton S, Craig LE, Kilkenny MF, Dale S, Hill K, et al. Inclusion of a care bundle for fever, hyperglycaemia and swallow management in a national audit for acute stroke: Evidence of upscale and spread. Implement Sci. 2019;14:87.
Middleton S, McElduff P, Ward J, Grimshaw JM, Dale S, D’Este C, et al. Implementation of evidence-based treatment protocols to manage fever, hyperglycaemia, and swallowing dysfunction in acute stroke (QASC): A cluster randomised controlled trial. Lancet. 2011;378:1699–706.
Middleton S, Dale S, Cheung NW, Cadilhac DA, Grimshaw JM, Levi C, et al. Nurse-initiated acute stroke care in emergency departments. Stroke. 2019:STROKEAHA118020701.
Hood RJ, Maltby S, Keynes A, Kluge MG, Nalivaiko E, Ryan A, et al. Development and pilot implementation of TACTICS VR: A virtual reality-based stroke management workflow training application and training framework. Front Neurol. 2021;12:665808.
Bladin CF, Kim J, Bagot KL, Vu M, Moloczij N, Denisenko S, et al. Improving acute stroke care in regional hospitals: Clinical evaluation of the Victorian Stroke Telemedicine program. Med J Aust. 2020;212:371–7.
Bladin CF, Bagot KL, Vu M, Kim J, Bernard S, Smith K, et al. Real-world, feasibility study to investigate the use of a multidisciplinary app (Pulsara) to improve prehospital communication and timelines for acute stroke/STEMI care. BMJ Open. 2022;12:e052332.
Zhao H, Coote S, Easton D, Langenberg F, Stephenson M, Smith K, et al. Melbourne mobile stroke unit and reperfusion therapy: Greater clinical impact of thrombectomy than thrombolysis. Stroke. 2020;51:922–30.
Purvis T, Cadilhac DA, Hill K, Reyneke M, Olaiya MT, Dalli LL, et al. Twenty years of monitoring acute stroke care in Australia from the national stroke audit program (1999–2019): Achievements and areas of future focus. J Health Serv Res Policy. 2023.
Cadilhac DA, Purvis T, Reyneke M, Dalli LL, Kim J, Kilkenny MF. Evaluation of the national stroke audit program: 20-year report. Melbourne; 2019.
Kim J, Tan E, Gao L, Moodie M, Dewey HM, Bagot KL, et al. Cost-effectiveness of the Victorian Stroke Telemedicine program. Aust Health Rev. 2022;46:294–301.
Kim J, Easton D, Zhao H, Coote S, Sookram G, Smith K, et al. Economic evaluation of the Melbourne mobile stroke unit. Int J Stroke. 2021;16:466–75.
Stroke Foundation. National stroke audit – rehabilitation services report 2020. Melbourne; 2020.
Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. 2023. Webpage https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts/contents/about (accessed Jan 2024).
Download references
Acknowledgements
The following authors hold National Health and Medical Research Council Research Fellowships: HT (#2009326), DAC (#1154273), SM (#1196352), MFK Future Leader Research Fellowship (National Heart Foundation #105737). The Funders of this work did not have any direct role in the design of the study, its execution, analyses, interpretation of the data, or decision to submit results for publication.
Author information
Helena Teede and Dominique A. Cadilhac contributed equally.
Authors and Affiliations
Monash Centre for Health Research and Implementation, 43-51 Kanooka Grove, Clayton, VIC, Australia
Helena Teede, Emily Callander & Joanne Enticott
Monash Partners Academic Health Science Centre, 43-51 Kanooka Grove, Clayton, VIC, Australia
Helena Teede & Alison Johnson
Stroke and Ageing Research, Department of Medicine, School of Clinical Sciences at Monash Health, Monash University, Level 2 Monash University Research, Victorian Heart Hospital, 631 Blackburn Rd, Clayton, VIC, Australia
Dominique A. Cadilhac, Tara Purvis & Monique F. Kilkenny
Stroke Theme, The Florey Institute of Neuroscience and Mental Health, University of Melbourne, Heidelberg, VIC, Australia
Dominique A. Cadilhac, Monique F. Kilkenny & Bruce C.V. Campbell
Department of Neurology, Melbourne Brain Centre, Royal Melbourne Hospital, Parkville, VIC, Australia
Bruce C.V. Campbell
Department of Medicine, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia
School of Health Sciences, Heart and Stroke Program, University of Newcastle, Hunter Medical Research Institute, University Drive, Callaghan, NSW, Australia
Coralie English
School of Medicine and Dentistry, Griffith University, Birtinya, QLD, Australia
Rohan S. Grimley
Clinical Excellence Division, Queensland Health, Brisbane, Australia
John Hunter Hospital, Hunter New England Local Health District and University of Newcastle, Sydney, NSW, Australia
Christopher Levi
School of Nursing, Midwifery and Paramedicine, Australian Catholic University, Sydney, NSW, Australia
Sandy Middleton
Nursing Research Institute, St Vincent’s Health Network Sydney and and Australian Catholic University, Sydney, NSW, Australia
Stroke Foundation, Level 7, 461 Bourke St, Melbourne, VIC, Australia
Kelvin Hill
You can also search for this author in PubMed Google Scholar
Contributions
HT: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. DAC: conception, design and initial draft, provided essential literature and case study examples, approved the submitted version. TP: revised the manuscript critically for important intellectual content, approved the submitted version. MFK: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. BC: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. CE: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. AJ: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. EC: revised the manuscript critically for important intellectual content, approved the submitted version. RSG: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. CL: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. SM: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. KH: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. JE: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. All authors read and approved the final manuscript.
Authors’ Twitter handles
@HelenaTeede
@DominiqueCad
@Coralie_English
@EmilyCallander
@EnticottJo
Corresponding authors
Correspondence to Helena Teede or Dominique A. Cadilhac .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Teede, H., Cadilhac, D.A., Purvis, T. et al. Learning together for better health using an evidence-based Learning Health System framework: a case study in stroke. BMC Med 22 , 198 (2024). https://doi.org/10.1186/s12916-024-03416-w
Download citation
Received : 23 July 2023
Accepted : 30 April 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12916-024-03416-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Evidence-based medicine
- Person-centred care
- Models of care
- Healthcare improvement
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Fern Fort University
Partners healthcare system (phs): transforming health care services delivery through information management case study analysis & solution, harvard business case studies solutions - assignment help.
Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management is a Harvard Business (HBR) Case Study on Technology & Operations , Fern Fort University provides HBR case study assignment help for just $11. Our case solution is based on Case Study Method expertise & our global insights.
Technology & Operations Case Study | Authors :: Richard M. Kesner
Case study description.
This case considers the process of organizational transformation undertaken by Partners Healthcare System (PHS) since the 1990s as their hospital and affiliated ambulatory medical practices have adopted both EMR and CPOE systems. Encompassing a strategic investment in information technologies, wide-spread process change, and the pervasive use of institutional clinical decision support and knowledge management systems, this story has been 15 years in the making, culminating in 2009 with the network-wide use of EMR and CPOE by all PHS doctors. These developments in turn opened the door to the redefinition of services delivery and to the replacement of established therapies through the leveraging of the knowledge residing in 4.6 million now-digitized PHS patient records. As such, the PHS experience serves as a window into how one organization strove to address the daunting challenges of 21st century health care services information management, as a template for success in the implementation of large-scale information systems among research-based hospitals across the United States, and more broadly as a learning platform for industry executives in their efforts to transform health care delivery through data and knowledge management.
Order a Technology & Operations case study solution now
To Search More HBR Case Studies Solution Go to Fern Fort University Search Page
[10 Steps] Case Study Analysis & Solution
Step 1 - reading up harvard business review fundamentals on the technology & operations.
Even before you start reading a business case study just make sure that you have brushed up the Harvard Business Review (HBR) fundamentals on the Technology & Operations. Brushing up HBR fundamentals will provide a strong base for investigative reading. Often readers scan through the business case study without having a clear map in mind. This leads to unstructured learning process resulting in missed details and at worse wrong conclusions. Reading up the HBR fundamentals helps in sketching out business case study analysis and solution roadmap even before you start reading the case study. It also provides starting ideas as fundamentals often provide insight into some of the aspects that may not be covered in the business case study itself.
Step 2 - Reading the Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management HBR Case Study
To write an emphatic case study analysis and provide pragmatic and actionable solutions, you must have a strong grasps of the facts and the central problem of the HBR case study. Begin slowly - underline the details and sketch out the business case study description map. In some cases you will able to find the central problem in the beginning itself while in others it may be in the end in form of questions. Business case study paragraph by paragraph mapping will help you in organizing the information correctly and provide a clear guide to go back to the case study if you need further information. My case study strategy involves -
- Marking out the protagonist and key players in the case study from the very start.
- Drawing a motivation chart of the key players and their priorities from the case study description.
- Refine the central problem the protagonist is facing in the case and how it relates to the HBR fundamentals on the topic.
- Evaluate each detail in the case study in light of the HBR case study analysis core ideas.
Step 3 - Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management Case Study Analysis
Once you are comfortable with the details and objective of the business case study proceed forward to put some details into the analysis template. You can do business case study analysis by following Fern Fort University step by step instructions -
- Company history is provided in the first half of the case. You can use this history to draw a growth path and illustrate vision, mission and strategic objectives of the organization. Often history is provided in the case not only to provide a background to the problem but also provide the scope of the solution that you can write for the case study.
- HBR case studies provide anecdotal instances from managers and employees in the organization to give a feel of real situation on the ground. Use these instances and opinions to mark out the organization's culture, its people priorities & inhibitions.
- Make a time line of the events and issues in the case study. Time line can provide the clue for the next step in organization's journey. Time line also provides an insight into the progressive challenges the company is facing in the case study.
Step 4 - SWOT Analysis of Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management
Once you finished the case analysis, time line of the events and other critical details. Focus on the following -
- Zero down on the central problem and two to five related problems in the case study.
- Do the SWOT analysis of the Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management . SWOT analysis is a strategic tool to map out the strengths, weakness, opportunities and threats that a firm is facing.
- SWOT analysis and SWOT Matrix will help you to clearly mark out - Strengths Weakness Opportunities & Threats that the organization or manager is facing in the Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management
- SWOT analysis will also provide a priority list of problem to be solved.
- You can also do a weighted SWOT analysis of Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management HBR case study.
Step 5 - Porter 5 Forces / Strategic Analysis of Industry Analysis Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management
In our live classes we often come across business managers who pinpoint one problem in the case and build a case study analysis and solution around that singular point. Business environments are often complex and require holistic solutions. You should try to understand not only the organization but also the industry which the business operates in. Porter Five Forces is a strategic analysis tool that will help you in understanding the relative powers of the key players in the business case study and what sort of pragmatic and actionable case study solution is viable in the light of given facts.
Step 6 - PESTEL, PEST / STEP Analysis of Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management
Another way of understanding the external environment of the firm in Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management is to do a PESTEL - Political, Economic, Social, Technological, Environmental & Legal analysis of the environment the firm operates in. You should make a list of factors that have significant impact on the organization and factors that drive growth in the industry. You can even identify the source of firm's competitive advantage based on PESTEL analysis and Organization's Core Competencies.
Step 7 - Organizing & Prioritizing the Analysis into Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management Case Study Solution
Once you have developed multipronged approach and work out various suggestions based on the strategic tools. The next step is organizing the solution based on the requirement of the case. You can use the following strategy to organize the findings and suggestions.
- Build a corporate level strategy - organizing your findings and recommendations in a way to answer the larger strategic objective of the firm. It include using the analysis to answer the company's vision, mission and key objectives , and how your suggestions will take the company to next level in achieving those goals.
- Business Unit Level Solution - The case study may put you in a position of a marketing manager of a small brand. So instead of providing recommendations for overall company you need to specify the marketing objectives of that particular brand. You have to recommend business unit level recommendations. The scope of the recommendations will be limited to the particular unit but you have to take care of the fact that your recommendations are don't directly contradict the company's overall strategy. For example you can recommend a low cost strategy but the company core competency is design differentiation.
- Case study solutions can also provide recommendation for the business manager or leader described in the business case study.
Step 8 -Implementation Framework
The goal of the business case study is not only to identify problems and recommend solutions but also to provide a framework to implement those case study solutions. Implementation framework differentiates good case study solutions from great case study solutions. If you able to provide a detailed implementation framework then you have successfully achieved the following objectives -
- Detailed understanding of the case,
- Clarity of HBR case study fundamentals,
- Analyzed case details based on those fundamentals and
- Developed an ability to prioritize recommendations based on probability of their successful implementation.
Implementation framework helps in weeding out non actionable recommendations, resulting in awesome Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management case study solution.
Step 9 - Take a Break
Once you finished the case study implementation framework. Take a small break, grab a cup of coffee or whatever you like, go for a walk or just shoot some hoops.
Step 10 - Critically Examine Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management case study solution
After refreshing your mind, read your case study solution critically. When we are writing case study solution we often have details on our screen as well as in our head. This leads to either missing details or poor sentence structures. Once refreshed go through the case solution again - improve sentence structures and grammar, double check the numbers provided in your analysis and question your recommendations. Be very slow with this process as rushing through it leads to missing key details. Once done it is time to hit the attach button.
Previous 5 HBR Case Study Solution
- We've Got Rhythm! Medtronic Corp.'s Cardiac Pacemaker Business Case Study Solution
- Duke Heart Failure Program Case Study Solution
- Istituto Clinico Humanitas (A) Case Study Solution
- CareGroup Case Study Solution
- Pharmacy Service Improvement at CVS (A) Case Study Solution
Next 5 HBR Case Study Solution
- Electronic Medical Records System Implementation at Stanford Hospital and Clinics Case Study Solution
- Six Sigma at Academic Medical Hospital (A) Case Study Solution
- Mount Auburn Hospital: Physician Order Entry Case Study Solution
- Disruptive Technology a Heartbeat Away: Ecton, Inc. Case Study Solution
- Hospital Equipment Corp. Case Study Solution
Special Offers
Order custom Harvard Business Case Study Analysis & Solution. Starting just $19
Amazing Business Data Maps. Send your data or let us do the research. We make the greatest data maps.
We make beautiful, dynamic charts, heatmaps, co-relation plots, 3D plots & more.
Buy Professional PPT templates to impress your boss
Nobody get fired for buying our Business Reports Templates. They are just awesome.
- More Services
Feel free to drop us an email
- fernfortuniversity[@]gmail.com
- (000) 000-0000
Don't have an account? Sign up now
Already have an account login, get 10% off on your next order.
Subscribe now to get your discount coupon *Only correct email will be accepted
(Approximately ~ 0.0 Page)
Total Price
Thank you for your email subscription. Check your email to get Coupon Code.
Partners HealthCare System Inc A Case Analysis and Case Solution
Posted by Peter Williams on Aug-09-2018
Introduction of Partners HealthCare System Inc A Case Solution
The Partners HealthCare System Inc A case study is a Harvard Business Review case study, which presents a simulated practical experience to the reader allowing them to learn about real life problems in the business world. The Partners HealthCare System Inc A case consisted of a central issue to the organization, which had to be identified, analysed and creative solutions had to be drawn to tackle the issue. This paper presents the solved Partners HealthCare System Inc A case analysis and case solution. The method through which the analysis is done is mentioned, followed by the relevant tools used in finding the solution.
The case solution first identifies the central issue to the Partners HealthCare System Inc A case study, and the relevant stakeholders affected by this issue. This is known as the problem identification stage. After this, the relevant tools and models are used, which help in the case study analysis and case study solution. The tools used in identifying the solution consist of the SWOT Analysis, Porter Five Forces Analysis, PESTEL Analysis, VRIO analysis, Value Chain Analysis, BCG Matrix analysis, Ansoff Matrix analysis, and the Marketing Mix analysis. The solution consists of recommended strategies to overcome this central issue. It is a good idea to also propose alternative case study solutions, because if the main solution is not found feasible, then the alternative solutions could be implemented. Lastly, a good case study solution also includes an implementation plan for the recommendation strategies. This shows how through a step-by-step procedure as to how the central issue can be resolved.
Problem Identification of Partners HealthCare System Inc A Case Solution
Harvard Business Review cases involve a central problem that is being faced by the organization and these problems affect a number of stakeholders. In the problem identification stage, the problem faced by Partners HealthCare System Inc A is identified through reading of the case. This could be mentioned at the start of the reading, the middle or the end. At times in a case analysis, the problem may be clearly evident in the reading of the HBR case. At other times, finding the issue is the job of the person analysing the case. It is also important to understand what stakeholders are affected by the problem and how. The goals of the stakeholders and are the organization are also identified to ensure that the case study analysis are consistent with these.
Analysis of the Partners HealthCare System Inc A HBR Case Study
The objective of the case should be focused on. This is doing the Partners HealthCare System Inc A Case Solution. This analysis can be proceeded in a step-by-step procedure to ensure that effective solutions are found.
- In the first step, a growth path of the company can be formulated that lays down its vision, mission and strategic aims. These can usually be developed using the company history is provided in the case. Company history is helpful in a Business Case study as it helps one understand what the scope of the solutions will be for the case study.
- The next step is of understanding the company; its people, their priorities and the overall culture. This can be done by using company history. It can also be done by looking at anecdotal instances of managers or employees that are usually included in an HBR case study description to give the reader a real feel of the situation.
- Lastly, a timeline of the issues and events in the case needs to be made. Arranging events in a timeline allows one to predict the next few events that are likely to take place. It also helps one in developing the case study solutions. The timeline also helps in understanding the continuous challenges that are being faced by the organisation.
SWOT analysis of Partners HealthCare System Inc A
An important tool that helps in addressing the central issue of the case and coming up with Partners HealthCare System Inc A HBR case solution is the SWOT analysis.
- The SWOT analysis is a strategic management tool that lists down in the form of a matrix, an organisation's internal strengths and weaknesses, and external opportunities and threats. It helps in the strategic analysis of Partners HealthCare System Inc A.
- Once this listing has been done, a clearer picture can be developed in regards to how strategies will be formed to address the main problem. For example, strengths will be used as an advantage in solving the issue.
Therefore, the SWOT analysis is a helpful tool in coming up with the Partners HealthCare System Inc A Case Study answers. One does not need to remain restricted to using the traditional SWOT analysis, but the advanced TOWS matrix or weighted average SWOT analysis can also be used.
Porter Five Forces Analysis for Partners HealthCare System Inc A
Another helpful tool in finding the case solutions is of Porter's Five Forces analysis. This is also a strategic tool that is used to analyse the competitive environment of the industry in which Partners HealthCare System Inc A operates in. Analysis of the industry is important as businesses do not work in isolation in real life, but are affected by the business environment of the industry that they operate in. Harvard Business case studies represent real-life situations, and therefore, an analysis of the industry's competitive environment needs to be carried out to come up with more holistic case study solutions. In Porter's Five Forces analysis, the industry is analysed along 5 dimensions.
- These are the threats that the industry faces due to new entrants.
- It includes the threat of substitute products.
- It includes the bargaining power of buyers in the industry.
- It includes the bargaining power of suppliers in an industry.
- Lastly, the overall rivalry or competition within the industry is analysed.
This tool helps one understand the relative powers of the major players in the industry and its overall competitive dynamics. Actionable and practical solutions can then be developed by keeping these factors into perspective.
PESTEL Analysis of Partners HealthCare System Inc A
Another helpful tool that should be used in finding the case study solutions is the PESTEL analysis. This also looks at the external business environment of the organisation helps in finding case study Analysis to real-life business issues as in HBR cases.
- The PESTEL analysis particularly looks at the macro environmental factors that affect the industry. These are the political, environmental, social, technological, environmental and legal (regulatory) factors affecting the industry.
- Factors within each of these 6 should be listed down, and analysis should be made as to how these affect the organisation under question.
- These factors are also responsible for the future growth and challenges within the industry. Hence, they should be taken into consideration when coming up with the Partners HealthCare System Inc A case solution.
VRIO Analysis of Partners HealthCare System Inc A
This is an analysis carried out to know about the internal strengths and capabilities of Partners HealthCare System Inc A. Under the VRIO analysis, the following steps are carried out:
- The internal resources of Partners HealthCare System Inc A are listed down.
- Each of these resources are assessed in terms of the value it brings to the organization.
- Each resource is assessed in terms of how rare it is. A rare resource is one that is not commonly used by competitors.
- Each resource is assessed whether it could be imitated by competition easily or not.
- Lastly, each resource is assessed in terms of whether the organization can use it to an advantage or not.
The analysis done on the 4 dimensions; Value, Rareness, Imitability, and Organization. If a resource is high on all of these 4, then it brings long-term competitive advantage. If a resource is high on Value, Rareness, and Imitability, then it brings an unused competitive advantage. If a resource is high on Value and Rareness, then it only brings temporary competitive advantage. If a resource is only valuable, then it’s a competitive parity. If it’s none, then it can be regarded as a competitive disadvantage.
Value Chain Analysis of Partners HealthCare System Inc A
The Value chain analysis of Partners HealthCare System Inc A helps in identifying the activities of an organization, and how these add value in terms of cost reduction and differentiation. This tool is used in the case study analysis as follows:
- The firm’s primary and support activities are listed down.
- Identifying the importance of these activities in the cost of the product and the differentiation they produce.
- Lastly, differentiation or cost reduction strategies are to be used for each of these activities to increase the overall value provided by these activities.
Recognizing value creating activities and enhancing the value that they create allow Partners HealthCare System Inc A to increase its competitive advantage.
BCG Matrix of Partners HealthCare System Inc A
The BCG Matrix is an important tool in deciding whether an organization should invest or divest in its strategic business units. The matrix involves placing the strategic business units of a business in one of four categories; question marks, stars, dogs and cash cows. The placement in these categories depends on the relative market share of the organization and the market growth of these strategic business units. The steps to be followed in this analysis is as follows:
- Identify the relative market share of each strategic business unit.
- Identify the market growth of each strategic business unit.
- Place these strategic business units in one of four categories. Question Marks are those strategic business units with high market share and low market growth rate. Stars are those strategic business units with high market share and high market growth rate. Cash Cows are those strategic business units with high market share and low market growth rate. Dogs are those strategic business units with low market share and low growth rate.
- Relevant strategies should be implemented for each strategic business unit depending on its position in the matrix.
The strategies identified from the Partners HealthCare System Inc A BCG matrix and included in the case pdf. These are either to further develop the product, penetrate the market, develop the market, diversification, investing or divesting.
Ansoff Matrix of Partners HealthCare System Inc A
Ansoff Matrix is an important strategic tool to come up with future strategies for Partners HealthCare System Inc A in the case solution. It helps decide whether an organization should pursue future expansion in new markets and products or should it focus on existing markets and products.
- The organization can penetrate into existing markets with its existing products. This is known as market penetration strategy.
- The organization can develop new products for the existing market. This is known as product development strategy.
- The organization can enter new markets with its existing products. This is known as market development strategy.
- The organization can enter into new markets with new products. This is known as a diversification strategy.
The choice of strategy depends on the analysis of the previous tools used and the level of risk the organization is willing to take.
Marketing Mix of Partners HealthCare System Inc A
Partners HealthCare System Inc A needs to bring out certain responses from the market that it targets. To do so, it will need to use the marketing mix, which serves as a tool in helping bring out responses from the market. The 4 elements of the marketing mix are Product, Price, Place and Promotions. The following steps are required to carry out a marketing mix analysis and include this in the case study analysis.
- Analyse the company’s products and devise strategies to improve the product offering of the company.
- Analyse the company’s price points and devise strategies that could be based on competition, value or cost.
- Analyse the company’s promotion mix. This includes the advertisement, public relations, personal selling, sales promotion, and direct marketing. Strategies will be devised which makes use of a few or all of these elements.
- Analyse the company’s distribution and reach. Strategies can be devised to improve the availability of the company’s products.
Partners HealthCare System Inc A Blue Ocean Strategy
The strategies devised and included in the Partners HealthCare System Inc A case memo should have a blue ocean strategy. A blue ocean strategy is a strategy that involves firms seeking uncontested market spaces, which makes the competition of the company irrelevant. It involves coming up with new and unique products or ideas through innovation. This gives the organization a competitive advantage over other firms, unlike a red ocean strategy.
Competitors analysis of Partners HealthCare System Inc A
The PESTEL analysis discussed previously looked at the macro environmental factors affecting business, but not the microenvironmental factors. One of the microenvironmental factors are competitors, which are addressed by a competitor analysis. The Competitors analysis of Partners HealthCare System Inc A looks at the direct and indirect competitors within the industry that it operates in.
- This involves a detailed analysis of their actions and how these would affect the future strategies of Partners HealthCare System Inc A.
- It involves looking at the current market share of the company and its competitors.
- It should compare the marketing mix elements of competitors, their supply chain, human resources, financial strength etc.
- It also should look at the potential opportunities and threats that these competitors pose on the company.
Organisation of the Analysis into Partners HealthCare System Inc A Case Study Solution
Once various tools have been used to analyse the case, the findings of this analysis need to be incorporated into practical and actionable solutions. These solutions will also be the Partners HealthCare System Inc A case answers. These are usually in the form of strategies that the organisation can adopt. The following step-by-step procedure can be used to organise the Harvard Business case solution and recommendations:
- The first step of the solution is to come up with a corporate level strategy for the organisation. This part consists of solutions that address issues faced by the organisation on a strategic level. This could include suggestions, changes or recommendations to the company's vision, mission and its strategic objectives. It can include recommendations on how the organisation can work towards achieving these strategic objectives. Furthermore, it needs to be explained how the stated recommendations will help in solving the main issue mentioned in the case and where the company will stand in the future as a result of these.
- The second step of the solution is to come up with a business level strategy. The HBR case studies may present issues faced by a part of the organisation. For example, the issues may be stated for marketing and the role of a marketing manager needs to be assumed. So, recommendations and suggestions need to address the strategy of the marketing department in this case. Therefore, the strategic objectives of this business unit (Marketing) will be laid down in the solutions and recommendations will be made as to how to achieve these objectives. Similar would be the case for any other business unit or department such as human resources, finance, IT etc. The important thing to note here is that the business level strategy needs to be aligned with the overall corporate strategy of the organisation. For example, if one suggests the organisation to focus on differentiation for competitive advantage as a corporate level strategy, then it can't be recommended for the Partners HealthCare System Inc A Case Study Solution that the business unit should focus on costs.
- The third step is not compulsory but depends from case to case. In some HBR case studies, one may be required to analyse an issue at a department. This issue may be analysed for a manager or employee as well. In these cases, recommendations need to be made for these people. The solution may state that objectives that these people need to achieve and how these objectives would be achieved.
The case study analysis and solution, and Partners HealthCare System Inc A case answers should be written down in the Partners HealthCare System Inc A case memo, clearly identifying which part shows what. The Partners HealthCare System Inc A case should be in a professional format, presenting points clearly that are well understood by the reader.
Alternate solution to the Partners HealthCare System Inc A HBR case study
It is important to have more than one solution to the case study. This is the alternate solution that would be implemented if the original proposed solution is found infeasible or impossible due to a change in circumstances. The alternate solution for Partners HealthCare System Inc A is presented in the same way as the original solution, where it consists of a corporate level strategy, business level strategy and other recommendations.
Implementation of Partners HealthCare System Inc A Case Solution
The case study does not end at just providing recommendations to the issues at hand. One is also required to provide how these recommendations would be implemented. This is shown through a proper implementation framework. A detailed implementation framework helps in distinguishing between an average and an above average case study answer. A good implementation framework shows the proposed plan and how the organisations' resources would be used to achieve the objectives. It also lays down the changes needed to be made as well as the assumptions in the process.
- A proper implementation framework shows that one has clearly understood the case study and the main issue within it.
- It shows that one has been clarified with the HBR fundamentals on the topic.
- It shows that the details provided in the case have been properly analysed.
- It shows that one has developed an ability to prioritise recommendations and how these could be successfully implemented.
- The implementation framework also helps by removing out any recommendations that are not practical or actionable as these could not be implemented. Therefore, the implementation framework ensures that the solution to the Partners HealthCare System Inc A Harvard case is complete and properly answered.
Recommendations and Action Plan for Partners HealthCare System Inc A case analysis
For Partners HealthCare System Inc A, based on the SWOT Analysis, Porter Five Forces Analysis, PESTEL Analysis, VRIO analysis, Value Chain Analysis, BCG Matrix analysis, Ansoff Matrix analysis, and the Marketing Mix analysis, the recommendations and action plan are as follows:
- Partners HealthCare System Inc A should focus on making use of its strengths identified from the VRIO analysis to make the most of the opportunities identified from the PESTEL.
- Partners HealthCare System Inc A should enhance the value creating activities within its value chain.
- Partners HealthCare System Inc A should invest in its stars and cash cows, while getting rid of the dogs identified from the BCG Matrix analysis.
- To achieve its overall corporate and business level objectives, it should make use of the marketing mix tools to obtain desired results from its target market.
Baron, E. (2015). How They Teach the Case Method At Harvard Business School. Retrieved from https://poetsandquants.com/2015/09/29/how-they-teach-the-case-method-at-harvard-business-school/
Bartol. K, & Martin, D. (1998). Management, 3rd edition. Boston: Irwin McGrawHill.
Free Management E-Books. (2013a). PESTLE Analysis. Retrieved from http://www.free-management-ebooks.com/dldebk-pdf/fme-pestle-analysis.pdf
Gupta, A. (2013). Environment & PEST analysis: an approach to the external business environment. International Journal of Modern Social Sciences, 2(1), 34-43.
Hambrick, D. C., MacMillan, I. C., & Day, D. L. (1982). Strategic attributes and performance in the BCG matrix—A PIMS-based analysis of industrial product businesses. Academy of Management Journal, 25(3), 510-531.
Hill, C., & Jones, G. (2010). Strategic Management Theory: An Integrated Approach, Ninth Ed. Mason, OH: South-Western, Cengage Learning.
Hussain, S., Khattak, J., Rizwan, A., & Latif, M. A. (2013). ANSOFF matrix, environment, and growth-an interactive triangle. Management and Administrative Sciences Review, 2(2), 196-206.
IIBMS. (2015). 7 Effective Steps to Solve Case Study. Retrieved from http://www.iibms.org/c-7-effective-steps-to-solve-case-study/
Kim, W. C., & Mauborgne, R. (2004). Blue ocean strategy. If you read nothing else on strategy, read thesebest-selling articles., 71.
Kotler, P., & Armstrong, G. (2010). Principles of marketing. Pearson education.
Kulkarni, N. (2018). 8 Tips to Help You Prepare for the Case Method. Retrieved from https://www.hbs.edu/mba/blog/post/8-tips-to-help-you-prepare-for-the-case-method
Lin, C., Tsai, H. L., Wu, Y. J., & Kiang, M. (2012). A fuzzy quantitative VRIO-based framework for evaluating organizational activities. Management Decision, 50(8), 1396-1411.
Nixon, J., & Helms, M. M. (2010). Exploring SWOT analysis – where are we now?: A review of academic research from the last decade. Journal of Strategy and Management, 3(3), 215-251.
Panagiotou, G. (2003). Bringing SWOT into Focus. Business Strategy Review, 14(2), 8-10.
Pickton, D. W., & Wright, S. (1998). What's swot in strategic analysis? Strategic Change, 7(2), 101-109.
Porter, M. E. (2001). The value chain and competitive advantage. Understanding Business Processes, 50-66.
Porter, M. E. (1985). Competitive advantage: creating and sustaining superior performance (Vol. 2). New York: Free Press.
Porter, M.E. (1979, March). Harvard Business Review: Strategic Planning, How Competitive Forces Shape Strategy. Retrieved July 7, 2016, from https://hbr.org/1979/03/how-competitive-forces-shape-strategy
Rastogi, N., & Trivedi, M. K. (2016). PESTLE Technique–a Tool to Identify External Risks in Construction Projects. International Research Journal of Engineering and Technology (IRJET), 3(1), 384-388.
Rauch, P. (2007). SWOT analyses and SWOT strategy formulation for forest owner cooperations in Austria. European Journal of Forest Research, 126(3), 413-420.
Warning! This article is only an example and cannot be used for research or reference purposes. If you need help with something similar, please submit your details here .
9414 Students can’t be wrong
PhD Experts
Colton Brian
I was doubtful and assuming maybe you people will make the poor assignment but after proofreading I knew that it’s right. Thank you thank you sooo much!
Carter Angus
The content looked superb. The structure of the project was satisfactory and I contained a good paper.
Ameena Nasir
This firm is worth a try because it has a very professional turnaround and distinctive features that don’t let students think for any other service.
Katalin Oliver
They provided me promptly formulated paper with open-line communication. Thanks a lot!
Calculate the Price
(approx ~ 0.0 page), total price $0, next articles.
- American Medical Association Sunbeam Deal (B): The Deal Collapses Case Analysis
- Hospital Clinic De Barcelona Case Analysis
- Patient Flow At Brigham And Women's Hospital (B) Case Analysis
- Paperless Healthcare: Progress And Challenges Of An IT Enabled Healthcare System Case Analysis
- Customers In Health Care Case Analysis
- Deaconess Glover Hospital (C) Case Analysis
- President And The Power Of The Purchaser: Consumer Protection And Managed Care In The United States Case Analysis
- Deaconess Glover Hospital (E) Case Analysis
- Shared Decision Making Case Analysis
- Innovative Healthcare Delivery Case Analysis
Previous Articles
- Connectivity In Health Care Case Analysis
- Healthware S.p.A. From An Underdeveloped Region Of Italy Can It Be A Global Firm? Case Analysis
- Raiser Senior Services The Stratford (B) Case Analysis
- Deaconess Glover Hospital (D) Case Analysis
- Hopital De Pontoise Case Analysis
- Patient Flow At Brigham And Women's Hospital (A) Case Analysis
- American Medical Association Sunbeam Deal (C): The Denouement Case Analysis
- The Brave New World Of Valuing Life Sciences And Healthcare Enterprises Case Analysis
- The Promises And Constraints Of Consumer Directed Healthcare Case Analysis
- British Columbia's Pharmanet Project Case Analysis
Be a great writer or hire a greater one!
Academic writing has no room for errors and mistakes. If you have BIG dreams to score BIG, think out of the box and hire Case48 with BIG enough reputation.

Our Guarantees
Zero plagiarism, best quality, qualified writers, absolute privacy, timely delivery.
Interesting Fact
Most recent surveys suggest that around 76 % students try professional academic writing services at least once in their lifetime!
Allow Our Skilled Essay Writers to Proficiently Finish Your Paper.
We are here to help. Chat with us on WhatsApp for any queries.
Customer Representative

- Order Status
- Testimonials
- What Makes Us Different
Partners Healthcare Harvard Case Solution & Analysis
Home >> Harvard Case Study Analysis Solutions >> Partners Healthcare

Partners Healthcare Case Solution
Problem Identification
It is expected that many different investment pools have been established by the management of the company, which includes both short term and long term investment pools . The management of the hospital invests the funds in order to generate desired expected return by minimizing the overall risk of the portfolio. It is expected that short term investment pools are considered as a risk free investment among the overall portfolio as it generates high quality fixed return.
However, the long term investment pool generates greater return as compared to the short term investment pool but it also carries highest risk therefore, the investment committee of the Partners Healthcare is trying to identify an optimal portfolio mix which could provide greater return by minimizing the risk.
The structure of the Partners Healthcare system comprises of all the physicians who could invest in the investment pool of the Partners Healthcare.The detailed structure of the organization is as follows:
On the other hand, long term investment pools are considered as risky pools, which mostly comprise of various type of equities.
It is expected that the risk profile of each hospital is different, therefore the Partners Healthcare managed its investment pools according to the desired returns and expected risk tolerance level of each hospital. The maturity period and expected return from the short term investment pool is low and it provides low risk free return to its holders.
It is expected that long term investment pools are considered as risky assets with greater return and greater maturity period as compared to the short term investment pools. Moreover, the risk appetite of each hospital is different, therefore each hospital investment is as per its risk appetite in order to generate greater return by minimizing overall risk of the portfolio.
It is expected that each hospital of the Partners Healthcare provides various healthcare services across England, therefore investment returns are more critical for each hospital as it provides funds in order to satisfy the need of each hospital in a timely manner.Thus, the financial strategy with respect to managing investment pools is more important as each hospital is considered as a non for profit organization and it involves greater number of stakeholder and beneficiaries. Moreover, investing in financial instruments is also considered as more risky as they get affected majorly in case of financial crisis and in economic downturn hence, the investment committee of the Partners Healthcare should formulate financial strategies with respect to the investment pools as return from these investment pools satisfy the need of community at greater level.
Motives behind the addition of Real Assetsto LTP
It is expected that the investment committee of the Partners Healthcare introduced real assets in the long term investment pools of the organization...................
This is just a sample partial case solution. Please place the order on the website to order your own originally done case solution.
Related Case Solutions & Analyses:

Hire us for Originally Written Case Solution/ Analysis
Like us and get updates:.
Harvard Case Solutions
Search Case Solutions
- Accounting Case Solutions
- Auditing Case Studies
- Business Case Studies
- Economics Case Solutions
- Finance Case Studies Analysis
- Harvard Case Study Analysis Solutions
- Human Resource Cases
- Ivey Case Solutions
- Management Case Studies
- Marketing HBS Case Solutions
- Operations Management Case Studies
- Supply Chain Management Cases
- Taxation Case Studies
More From Harvard Case Study Analysis Solutions
- PetroChina: International Corporate Governance with Chinese Characteristics
- Fundamental Enterprise Valuation: Return on Invested Capital (ROIC)
- EAZY'S GARAGE - Confidential Instructions for the Counsel of Dr. Susan Garfield, Psychiatrist
- IVEY (London Grand Bend Bicycle Tour)
- Benetton Factory Tour--Ponzano Italy Video
- IntellectExchange Inc.
- Ashland Oil, Inc.: Trouble at Floreffe (A)
Contact us:
Check Order Status

How Does it Work?
Why TheCaseSolutions.com?


IMAGES
VIDEO
COMMENTS
This case considers the process of organizational transformation undertaken by Partners Healthcare System (PHS) since the 1990s as their hospital and affiliated ambulatory medical practices have adopted both EMR and CPOE systems. Encompassing a strategic investment in information technologies, wide-spread process change, and the pervasive use of institutional clinical decision support and ...
Please place the order on the website to order your own originally done case solution. Partners Healthcare Case Solution. This case deals with the process of organizational transformation undertaken by Partners Healthcare System (PHS) in 1990 at their hospital and affiliated outpatient practice accepted as EMR and CPOE systems.
Limitations: While most Partners Community HealthCare physicians are not employed by Partners HealthCare, they are clinically and financially integrated within the system. Further, providers in the Boston marketplace tend to be more organized than in other areas of the country, with a substantial percentage of physicians coming together in ...
The report will provide a recommendation on how Manning should proceed with the analysis, including both the size and composition of the real portfolio segment to improve the risk/return profile of the long-term pool of Partner's Healthcare System. Introduction Partners Healthcare is a network of numerous nonprofit health care services.
As such, the PHS experience serves as a window into how one organization strove to address the daunting challenges of 21st century health care services information management, as a template for success in the implementation of large-scale information systems among research-based hospitals across the United States, and more broadly as a learning ...
Methods. This was a longitudinal case study in two Canadian provinces of two collaborative partnerships involving decision makers, academic representatives, clinicians, health system administrators, patient partners, and representatives of health and social service organizations providing services to vulnerable populations.
The Partners Healthcare System (PHS) was a decentralized one, therefore, the change needed to be done to the organization that was centralized in the past. In addition to this, the power to implement the system lies in the hands of the medical practitioner; therefore, before implementing the system it was a pre-requisite to make the management ...
Focuses on the decision confronting senior administrators at the Brigham and Women's Hospital: whether to enter into an affiliation with the Massachusetts General Hospital. Requires students to analyze the complex institutional changes in the health environment and to determine how the proposed affiliation might influence the hospital's chances ...
Subjects Covered Capacity planning Competition Mergers Operating systems Organizational change. by Gary P. Pisano, Maryam Golnaraghi. Source: Harvard Business School. 23 pages. Publication Date: Apr 05, 1996. Prod. #: 696063-PDF-ENG. Partners HealthCare System, Inc. (B): Cardiac Care Improvement Harvard Case Study Solution and HBR and HBS Case Analysis
Subjects Covered Change management Information systems. by Richard M. Kesner. Source: Richard Ivey School of Business Foundation. 15 pages. Publication Date: Feb 26, 2010. Prod. #: 909E23-PDF-ENG. Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management Harvard Case Study Solution and HBR and HBS Case Analysis
Partners Healthcare. By: Joshua D. Coval. Format: Print ... Provides a setting to study portfolio theory, including mean-variance analysis, the capital market line, and the efficient frontier. ... Decisions; Health Industry. Citation. Coval, Joshua D. "Partners Healthcare." Harvard Business School Case 206-005, August 2005. (Revised May 2007 ...
Case Analysis by Sarang Ananda Rao, Jeff Behm, Mike Bauer from the University of Cincinnati. Business. 1 of 11. Download now. Download to read offline. Partners Healthcare Case Analysis - Download as a PDF or view online for free.
Information Management Strategy: PHS Clinic Case Study. Before the introduction of the LMR and the CPOE systems into the company's framework, the PHS Clinic was an exact representation of a company, whose decision-making process was based on the principles of a traditional, non-computerized approach to data management, which caused numerous ...
Step 2 - Reading the Partners HealthCare System, Inc. (A) HBR Case Study. To write an emphatic case study analysis and provide pragmatic and actionable solutions, you must have a strong grasps of the facts and the central problem of the HBR case study. Begin slowly - underline the details and sketch out the business case study description map.
Partners Healthcare System Case Study Solution. Health Care practitioners and allied agencies (such as insurance companies and state and federal agencies) who must interact with PHS. The major barrier for Partners Healthcare System (PHS) was the lack of sufficient financing in the information technology within the office.
Partners Health Care System case study - Management Information Systems. Case Study. University Northeastern University. Course. Management Information Systems (MISM 2301) 151 Documents. ... Pepsi Americas Case Analysis; Session 5 - Bay State Realty Case Study Homework; Session 4 - Progressive Case Homework ...
Partners HealthCare System Inc. (A) case analysis, Partners HealthCare System Inc. (A) case study solution, Partners HealthCare System Inc. (A) xls file, Partners HealthCare System Inc. (A) excel file, Subjects Covered Capacity planning Competition Mergers Operating systems Organizational change by Gary P. Pisano, Maryam Golnaraghi Source: Harvard
Introduction The Partners Healthcare system is the largest health-care network by providing a range of healthcare services for patients mainly in Eastern Massachusetts. Partners Healthcare were founded by two famous acute-care hospitals, the Massachusetts General Hospital and the Brigham & Women's Hospital, and then joined by four suburban hospitals and many physician organizations in the ...
Case Analysis of Partners HealthCare System, Inc. (A) ... Affiliation Hospital in case study Partners HealthCare System, Inc. (A)" should look into the import restrictions that may be present in the prospective market. Export restrictions on products - Apart from direct product export restrictions in field of technology and agriculture, a ...
Internationally, health systems are facing a crisis, driven by an ageing population, increasing complexity, multi-morbidity, rapidly advancing health technology and rising costs that threaten sustainability and mandate transformation and improvement [1, 2].Although research has generated solutions to healthcare challenges, and the advent of big data and digital health holds great promise ...
Step 5 - Porter 5 Forces / Strategic Analysis of Industry Analysis Partners Healthcare System (PHS): Transforming Health Care Services Delivery Through Information Management. In our live classes we often come across business managers who pinpoint one problem in the case and build a case study analysis and solution around that singular point.
The method through which the analysis is done is mentioned, followed by the relevant tools used in finding the solution. The case solution first identifies the central issue to the Partners HealthCare System Inc A case study, and the relevant stakeholders affected by this issue. This is known as the problem identification stage.
Partners HealthCare System Inc. (A) Case Solution,Partners HealthCare System Inc. (A) Case Analysis, Partners HealthCare System Inc. (A) Case Study Solution, Focused on the decision faced by senior administrators at Brigham and Women's Hospital: whether to enter into a relationship with Massachusetts General
Partners Healthcare Case Solution. Problem Identification It is expected that many different investment pools have been established by the management of the company, which includes both short term and long term investment pools.The management of the hospital invests the funds in order to generate desired expected return by minimizing the overall risk of the portfolio.