

FDA Approves New Vitiligo Treatment, Ruxolitinib (Opzelura)
The JAK inhibitor cream is the first medication that can restore pigment in people with this autoimmune disease.
On July 18, the U.S. Food and Drug Administration (FDA) approved ruxolitinib ( Opzelura ) cream 1.5 percent as a treatment for the most common form of vitiligo, according to a statement by Incyte, the manufacturer of the drug.
Vitiligo is a chronic autoimmune condition that causes patches of skin to lose pigment and turn milky white. The most prevalent form is nonsegmental (also known as generalized) vitiligo, in which white patches appear symmetrically on both sides of the body, such as on both hands or both knees, often covering large areas.
Ruxolitinib is the first medication that can restore pigment in patients with nonsegmental vitiligo. The FDA approved Incyte’s ruxolitinib cream for adults and children ages 12 and up.
“This approval is monumental,” says Daniel Gutierrez, MD , assistant professor of dermatology at NYU Grossman School of Medicine and dermatologist at NYU Langone Health in New York City, who was not involved in the drug development. “With Opzelura, we will have an FDA-approved pharmaceutical treatment option that can actually bring back color in patients who have vitiligo,” says Dr. Gutierrez.
He adds that prior to ruxolitinib, the only FDA-approved medication for vitiligo was monobenzyl ether of hydroquinone, a topical drug that removes pigment from skin to even out tones.
What Is Vitiligo?
Researchers estimate that between 1.9 and 2.8 million adults in the United States have vitiligo, with perhaps 40 percent of adults with vitiligo going undiagnosed.
Vitiligo causes immune cells to destroy melanocytes, the skin cells that produce pigment, according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases . “This makes vitiligo much more noticeable in patients of color — people whose skin is much more richly pigmented — because there is going to be much more of a contrast between the unaffected skin and the skin affected by the vitiligo,” says Gutierrez.
Vitiligo can occur at any age, but most people experience the initial symptoms before age 30.
About 50 Percent of People Using Ruxolitinib Had Significant Repigmentation After One Year
Ruxolitinib belongs to a class of drugs called Janus kinase (JAK) inhibitors. While doctors prescribe oral JAK inhibitors for diseases such as rheumatoid arthritis, ruxolitinib is the only topical JAK inhibitor approved in the United States.
The FDA previously approved ruxolitinib for mild to moderate atopic dermatitis (eczema) , in the fall of 2021.
JAK inhibitors work by decreasing the activity of the immune system, blocking certain enzymes that cause inflammation.
Patients using ruxolitinib apply the cream twice daily to the affected areas, covering up to 10 percent of their body’s surface area. It may take 24 weeks or more for people with vitiligo to see satisfactory results, according to Incyte.
The FDA based its approval on data from a clinical trial program that compared ruxolitinib to a placebo cream in more than 600 people (age 12 and older) with nonsegmental vitiligo. Investigators used the Vitiligo Area Scoring Index (VASI), a tool used to gauge disease severity and to measure improvements in face and body repigmentation.
In the two trials, by week 24 approximately 30 percent of people treated with ruxolitinib experienced significant improvements (at least 75 percent) as measured by VASI, which was the goal of the study. At one year, about 50 percent of those using the medication achieved that level of repigmentation.
“People using Opzelura had much more improvement in their vitiligo — very meaningful — compared to the placebo,” says Gutierrez.
The most common side effects seen in the trials were application-site acne, redness and itchiness, pharynx and nasal cavity inflammation, headache, urinary tract infection, and fever.
Ruxolitinib Comes With a Black Box Warning
The FDA added a black box warning to ruxolitinib, based on data showing that people taking oral JAK inhibitors faced a small increased risk of serious infections, major heart issues, clotting (thrombosis), cancer, and even death.
“However, in the clinical trials for people using ruxolitinib as a topical cream, the concentrations of the drug found in the blood were observed to be much lower compared to people who take ruxolitinib orally,” says Gutierrez. The same risks were not observed in the ruxolitinib trials, but the FDA is taking a “better safe than sorry” approach by including a warning on the box, he adds.
A conversation with your healthcare provider is the best way to determine whether the benefits of ruxolitinib outweigh the potential risks, as well as the need for any baseline and/or ongoing monitoring.
Patients Can Use Ruxolitinib on Their Face
Although dermatologists sometimes prescribe topical steroids off-label for vitiligo, there are risks when applying these medications to the face — the area where loss of pigment can impact appearance the most, says Gutierrez.
When used on the face, topical steroids can cause an acne-like rash that can persist for many months, called perioral dermatitis . Plus, “they can cause atrophy or dispigmentation, meaning you can have skin color changes. They can also thin the skin, cause stretch marks, and cause the growth of small blood vessels in the area,” Gutierrez says.
Ruxolitinib does not pose these risks, notes Gutierrez.
FDA Approval Means Better Access to Vitiligo Treatment
The FDA’s approval of ruxolitinib will definitely improve access to the drug by validating it as medically necessary. “Because vitiligo just creates a color change in the skin — there’s no itching or dermatitis under normal circumstances — sometimes it’s considered a cosmetic condition, meaning it’s not medically necessary to treat,” Gutierrez says. As a result, some insurers have declined to cover vitiligo treatments , according to the Vitiligo Research Foundation .
“However, this condition can dramatically impact how a patient sees themselves and how they present to the world. Vitiligo can cause significant psychological distress and negatively impact quality of life,” says Gutierrez.
“Vitiligo disproportionately impacts patients of color,” he adds. “This approval is an important step in improving a health disparity that does exist, and hopefully there will be more treatment options for vitiligo in the pipeline.”
How Much Will Ruxolitinib Cost?
The current Wholesale Acquisition Cost pricing is $1,950 for a 60 gram tube of Opzelura, according to Gabriella Greig, a spokesperson for Incyte. The actual cost to the consumer will vary depending on insurance coverage and how much of the cream is required for treatment.
“Incyte is committed to working with insurance providers in the U.S. to ensure eligible patients who can benefit from Incyte’s products have access to them,” says Greig. The company offers a copay savings card on its website for people with commercial insurance.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
July 21, 2022
FDA approves first topical treatment for vitiligo

The U.S. Food and Drug Administration has approved Opzelura (ruxolitinib) as the first topical treatment for vitiligo.
The 1.5 percent cream is approved for continuous topical use twice daily to affected areas of up to 10 percent of body surface area in patients aged 12 years and older. More than 24 weeks of treatment may be needed for satisfactory patient response.
The approval was based on results from the TRuE-V clinical trials , in which more than 600 patients were randomly assigned to Opzelura or placebo. At week 24, 30 percent of patients treated with Opzelura achieved ≥75 percent improvement from baseline in the facial Vitiligo Area Scoring Index (F-VASI75) versus 8 to 13 percent of patients treated with placebo. Approximately half of Opzelura-treated patients achieved F-VASI75 at week 52.
"There have been no FDA-approved therapies available to date and the approval of Opzelura therefore marks a significant milestone ," David Rosmarin, M.D., from Tufts Medical Center in Boston, said in a company press release. "I welcome a medical treatment that helps my patients with nonsegmental vitiligo who are interested in potentially reversing the depigmentation caused by their disease."
Approval was granted to Incyte.
Copyright © 2022 HealthDay . All rights reserved.
Explore further
Feedback to editors

Visual experiences unique to early infancy provide building blocks of human vision, study finds
6 hours ago

Study points to personalized treatment opportunities for glioblastoma
7 hours ago

Research team introduces new tool to boost battle against childhood undernutrition

How herpes hijacks a ride into cells
8 hours ago

How the brain is flexible enough for a complex world, without being thrown into chaos

Researchers create AI model to understand how brain activity relates to illness

Study reveals need to review temperature control measures in hospitals to manage Legionella

'What was that?' How brains convert sounds to actions
9 hours ago

ERR-gamma 'trains' stomach stem cells to become acid-producing cells

Scientists make progress on new charged particle therapy for cancer
10 hours ago
Related Stories

Topical cream shows promise in treatment of skin pigmentation disease, vitiligo
Jun 17, 2019

FDA approves first treatment for eosinophilic esophagitis
May 26, 2022

Atogepant prevents migraine in adults
Jun 15, 2022

FDA approves Skyrizi for moderately to severely active Crohn disease
Jun 20, 2022

FDA approves Rinvoq for treatment of atopic dermatitis
Jan 19, 2022

Skyrizi approved for psoriatic arthritis
Jan 26, 2022
Recommended for you

Analysis reveals new insights into global surge of Strep A infections
11 hours ago

New research traces the spread of HIV in and from Indonesia
15 hours ago

Collaboration uncovers an entirely new COVID-related syndrome
May 9, 2024

New drug reduces vascular leak and endothelial cell dysfunction in mice with sepsis
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 30 June 2020
- Correction 06 July 2020
Temprian Therapeutics: developing a gene-based treatment for vitiligo
- Charles Schmidt 0
Charles Schmidt is a freelance writer in Portland, Maine.
You can also search for this author in PubMed Google Scholar
Temprian Therapeutics is a spin-off from Northwestern University in Chicago, Illinois.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
doi: https://doi.org/10.1038/d41586-020-01808-5
This article is part of Nature Outlook: The Spinoff Prize 2020 , an editorially independent supplement produced with the financial support of third parties. About this content .
Updates & Corrections
Correction 06 July 2020 : An earlier version of this profile gave the wrong specialty for Caroline Le Poole and the wrong campus for Northwestern University.
Mosenson, J. A. et al. Sci. Transl. Med. 5 , 174ra28 (2013).
Article PubMed Google Scholar
Henning, S. W. et al. J. Invest. Dermatol. 138 , 2531–2539 (2018).
Download references
Related Articles

- Biotechnology
- Drug discovery
- Therapeutics

Vaccine-enhancing plant extract could be mass produced in yeast
News & Views 08 MAY 24

Computationally restoring the potency of a clinical antibody against Omicron
Article 08 MAY 24

Complete biosynthesis of QS-21 in engineered yeast
Accurate structure prediction of biomolecular interactions with AlphaFold 3

Major AlphaFold upgrade offers boost for drug discovery
News 08 MAY 24

Discovery of potent small-molecule inhibitors of lipoprotein(a) formation

Airway hillocks are injury-resistant reservoirs of unique plastic stem cells
Article 01 MAY 24

Cells destroy donated mitochondria to build blood vessels
News & Views 01 MAY 24

Rat neurons repair mouse brains — and restore sense of smell
News 25 APR 24
Southeast University Future Technology Institute Recruitment Notice
Professor openings in mechanical engineering, control science and engineering, and integrating emerging interdisciplinary majors
Nanjing, Jiangsu (CN)
Southeast University
Staff Scientist
A Staff Scientist position is available in the laboratory of Drs. Elliot and Glassberg to study translational aspects of lung injury, repair and fibro
Maywood, Illinois
Loyola University Chicago - Department of Medicine
W3-Professorship (with tenure) in Inorganic Chemistry
The Institute of Inorganic Chemistry in the Faculty of Mathematics and Natural Sciences at the University of Bonn invites applications for a W3-Pro...
53113, Zentrum (DE)
Rheinische Friedrich-Wilhelms-Universität
Principal Investigator Positions at the Chinese Institutes for Medical Research, Beijing
Studies of mechanisms of human diseases, drug discovery, biomedical engineering, public health and relevant interdisciplinary fields.
Beijing, China
The Chinese Institutes for Medical Research (CIMR), Beijing
Research Associate - Neural Development Disorders
Houston, Texas (US)
Baylor College of Medicine (BCM)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Updates and new medical treatments for vitiligo (Review)
Affiliations.
- 1 Department of Dermatology, Faculty of Medicine and University Hospital 'Dr. José Eleuterio González', Universidad Autónoma de Nuevo León, Monterrey, Nuevo León 64460, México.
- 2 Department of Biochemistry and Molecular Medicine, Faculty of Medicine and University Hospital 'Dr. José Eleuterio González', Universidad Autónoma de Nuevo León, Monterrey, Nuevo León 64460, México.
- 3 Department of Research, Faculty of Medicine Saltillo Unit, Universidad Autónoma de Coahuila, Saltillo 25000, México.
- 4 Department of Dermatology and Allergology and Skin Cancer Center, Städtisches Klinikum Dresden, D-01067 Dresden, Germany.
- 5 Department of Dermatology and Venereology, University of Rome G. Marconi, I-00193 Rome, Italy.
- 6 Department of Dermatology and Communicable Diseases, First Medical State University of Moscow I. M. Sechenev Ministry of Health, Moscow 119991, Russia.
- PMID: 34093753
- PMCID: PMC8170669
- DOI: 10.3892/etm.2021.10229
Vitiligo is a multifactorial disease characterized by the loss of skin pigment, which results in achromic macules and patches. There are currently several medical treatments available, which aim to arrest progression and induce skin repigmentation. These treatments alone or combined have exhibited varying degrees of pigmentation, and the majority are safe and effective. All therapies for vitiligo are limited, and no known treatment can consistently produce repigmentation in all patients. Individualized treatment is appropriate according to the location, clinical presentation and the presence of disease activity. The present review summarizes the medical treatments available for vitiligo: Systemic and topic pharmacological therapies, physical and depigmentation treatments. Several treatments are still underway and have not yet been approved. However, due to the promising preliminary results, these are also mentioned in the present review.
Keywords: combined modality therapy; immunosuppressive agents; phototherapy; skin lightening preparations; therapy; vitiligo.
Copyright: © Kubelis-López et al.
Publication types
Grants and funding.
The Vitiligo Research Foundation
Firmly committed to curing vitiligo, the VR Foundation is a 501(c)3 non-profit, focused research organization. Our mission is to accelerate the end of suffering for millions of people who live with vitiligo through research, support and education.
VR Foundation is a consultative member of the United Nations Economic and Social Council (UN ECOSOC).
Discover the World's First AI-Guide on Vitiligo, available in 50+ languages! Get insights on the latest research, natural remedies, nutrition, and mental health, all in user-friendly language.
Discover the World's First AI-Guide on Vitiligo, available in 50+ languages!
News All News
- 07 May `24 Understanding the Timeline for Vitiligo Treatment Treatment times can vary widely due to factors like health, genetic makeup, and where the spots appear. Here's what you need to know: Early Treatment is Key: Catching new spo... More
- 07 May `24 Update: Vitiligo Insurance Coverage Navigating the insurance maze for vitiligo treatments can be as unpredictable as the condition itself. Vitiligo, often misunderstood as merely a cosmetic issue, is in fact a ser... More
- 18 Apr `24 Beyond the Surface: New Frontiers in Dermatology Explored in Iași The Iași Dermatological Spring (PDI) conference is a cornerstone event for Europe's dermatology community. This year, it is set against the elegant backdrop of Hotel Internațio... More
Quick Links
Learn ABC`s of Vitiligo
Join our community
Watch cool videos on vitiligo
Vote the World Vitiligo Day
World Vitiligo Map
Find and connect with vitiligo researcher, doctor or support group nearby.
UMMS is focused on two things – the clinical diagnosis and treatment of patients with vitiligo, and the study of vitiligo with the goal of developing new treatments. The Director of the Center is Dr. John E. Harris, who sees patients with vitiligo in a weekly specialty clinic, and also directs a research laboratory focused on vitiligo. Dr. Dori Goldberg is a procedural dermatologist who is helping to bring procedural and surgical options for vitiligo patients to the Center. In addition, other dermatology faculty in the Dermatology Division at UMMS help to treat patients with vitiligo as well, with specialty training in pediatrics, analysis of skin biopsies, surgical removal of skin cancers, and the diagnosis of other diseases that may look like vitiligo.
55 Lake Avenue North, Worcester, MA 01545
+1 508 334 5979
www.umassmed.edu

What is Vitiligo?
Vitiligo is a long-term condition that causes pale, white patches to develop on the skin - in severe cases these cover the whole body. Vitiligo affects one in every hundred people and can strike anyone at any time, often leading to depression and isolation - especially amongst children.
Donate Today
Our work is entirely funded by private donations – we receive no money from government. Your money will help us continue funding research into vitiligo and supporting people affected by the condition.

Bookstore Other Books
This book is a practical, step-by-step guide for general practitioners. It contains a collection of protocols and tips regarding how to diagnose, treat and follow-up with vitiligo patients. Each of ten chapters features the experiences and opinions of vitiligo specialists from across the world – scientists, doctors and academics with vast experience and knowledge, who are all recognized as leaders in their field.
What does everyone need to know about vitiligo? Renowned author’s answer to this most difficult of questions uniquely combines the hard-won knowledge of traditional medicine with the stunning revelations of cutting-edge scientific research.
Subscribe to Vitiligo News
Events other events.
- Jun, 2024 24 Cali, Colombia 🇨🇴 World Vitiligo Day 2024 The World Vitiligo Day (WVD) Committee proudly announces the Cali, Colombia as the host for the global WVD 2024 celebrations. This momentous event will be held under the esteeme...
- Jun, 2024 19 Marriott Hotel Indianapolis, IN, USA 🇺🇸 World Vitiligo Day - USA 2024 The GVF and the Wonderfully Made Indianapolis Vitiligo Community are thrilled to announce a vibrant series of events celebrating World Vitiligo Day 2024 in Indianapolis, IN. Fi...
Answers To Frequently Asked Questions
I support the petition to designate June 25 as Vitiligo World Day and save millions of people worldwide from social isolation
FAQ Other Questions
There are so many different ways that people try and spell or even pronounce Vitiligo. Here are some common mis-spellings: bitiligo, vitigo, vitaligo, vitilago, vitiglio, vita...
Vitiligo can affect anyone, regardless of gender, age, or race. Vitiligo prevalence is between 0.76% and 1.11% of the U.S. population, including around 40% of those with the con...
Dead Sea climatotherapy has shown promising results in treating vitiligo in people of all ages. It is considered as the only treatment that’s safe for nearly all vitiligo patien...
Though it is not always easy to treat vitiligo, there is much to be gained by clearly understanding the diagnosis, the future implications, treatment options and their outcomes.
Many people deal with vitiligo while remaining in the public eye, maintaining a positive outlook, and having a successful career.
By taking a little time to fill in the anonymous questionnaire, you can help researchers better understand and fight vitiligo.
Project Background
The study of multifactorial diseases, such as vitiligo, requires analysis of complex interplay of symptoms, treatments and outcomes across a large number of people. Population surveys and biobanks are indispensable research tools, required for downstream therapy development. Even small collections of biosamples may be extremely precious for researcher in academic institution or biopharma company.
Until recently, vitiligo researchers were generally limited to conducting studies on patient samples they could acquire themselves. When the Foundation started there were no centralized biological database along with the pre-existing body of the clinical management or the historical study data, which is required in order to proceed with the development of specific therapies. We have run a special investigation study to determine whether VRF shall establish its own biobank.
Then the project's leadership crafted a careful strategy for vitiligo biobank development, with special attention paid to the security and confidentiality of the donor's information. 'Future proofing' involves collecting and processing samples to permit the widest possible range of scientific uses, while avoiding approaches that would impede possible future uses.
We have started the first Vitiligo Biobank with a 100+ sample collection from the completed research project in genetics in late January 2013. Three months later, it held approximately 1,000 biosamples and detailed clinical profiles. Our target number is 10,000 samples and we encourage patients to donate samples . The primary biorepository is located in Moscow (Russia) with networked locations in 11 countries.
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
New treatment could reverse hair loss caused by an autoimmune skin disease
Press contact :, media download.
*Terms of Use:
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."
Previous image Next image
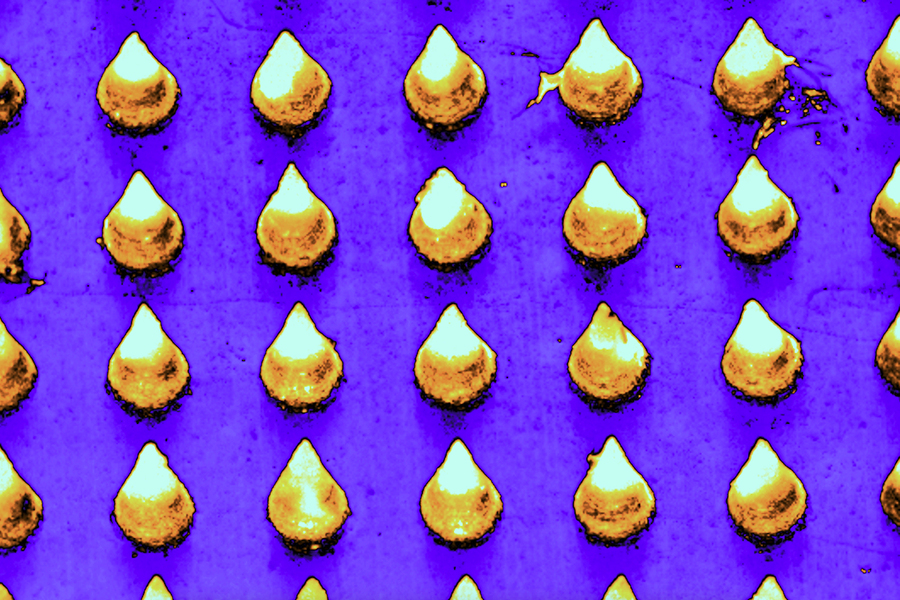
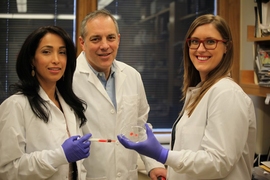
Researchers at MIT, Brigham and Women’s Hospital, and Harvard Medical School have developed a potential new treatment for alopecia areata, an autoimmune disorder that causes hair loss and affects people of all ages, including children.
For most patients with this type of hair loss, there is no effective treatment. The team developed a microneedle patch that can be painlessly applied to the scalp and releases drugs that help to rebalance the immune response at the site, halting the autoimmune attack.
In a study of mice, the researchers found that this treatment allowed hair to regrow and dramatically reduced inflammation at the treatment site, while avoiding systemic immune effects elsewhere in the body. This strategy could also be adapted to treat other autoimmune skin diseases such as vitiligo, atopic dermatitis, and psoriasis, the researchers say.
“This innovative approach marks a paradigm shift. Rather than suppressing the immune system, we’re now focusing on regulating it precisely at the site of antigen encounter to generate immune tolerance,” says Natalie Artzi, a principal research scientist in MIT’s Institute for Medical Engineering and Science, an associate professor of medicine at Harvard Medical School and Brigham and Women’s Hospital, and an associate faculty member at the Wyss Institute of Harvard University.
Artzi and Jamil R. Azzi, an associate professor of medicine at Harvard Medical School and Brigham and Women’s Hospital, are the senior authors of the new study , which appears in the journal Advanced Materials . Nour Younis, a Brigham and Women’s postdoc, and Nuria Puigmal, a Brigham and Women’s postdoc and former MIT research affiliate, are the lead authors of the paper.
The researchers are now working on launching a company to further develop the technology, led by Puigmal, who was recently awarded a Harvard Business School Blavatnik Fellowship.
Direct delivery
Alopecia areata, which affects more than 6 million Americans, occurs when the body’s own T cells attack hair follicles, leading the hair to fall out. The only treatment available to most patients — injections of immunosuppressant steroids into the scalp — is painful and patients often can’t tolerate it.
Some patients with alopecia areata and other autoimmune skin diseases can also be treated with immunosuppressant drugs that are given orally, but these drugs lead to widespread suppression of the immune system, which can have adverse side effects.
“This approach silences the entire immune system, offering relief from inflammation symptoms but leading to frequent recurrences. Moreover, it increases susceptibility to infections, cardiovascular diseases, and cancer,” Artzi says.
A few years ago, at a working group meeting in Washington, Artzi happened to be seated next to Azzi (the seating was alphabetical), an immunologist and transplant physican who was seeking new ways to deliver drugs directly to the skin to treat skin-related diseases.
Their conversation led to a new collaboration, and the two labs joined forces to work on a microneedle patch to deliver drugs to the skin. In 2021, they reported that such a patch can be used to prevent rejection following skin transplant. In the new study, they began applying this approach to autoimmune skin disorders.
“The skin is the only organ in our body that we can see and touch, and yet when it comes to drug delivery to the skin, we revert to systemic administration. We saw great potential in utilizing the microneedle patch to reprogram the immune system locally,” Azzi says.
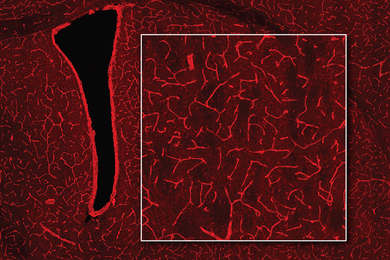
The microneedle patches used in this study are made from hyaluronic acid crosslinked with polyethylene glycol (PEG), both of which are biocompatible and commonly used in medical applications. With this delivery method, drugs can pass through the tough outer layer of the epidermis, which can’t be penetrated by creams applied to the skin.
“This polymer formulation allows us to create highly durable needles capable of effectively penetrating the skin. Additionally, it gives us the flexibility to incorporate any desired drug,” Artzi says. For this study, the researchers loaded the patches with a combination of the cytokines IL-2 and CCL-22. Together, these immune molecules help to recruit regulatory T cells, which proliferate and help to tamp down inflammation. These cells also help the immune system learn to recognize that hair follicles are not foreign antigens, so that it will stop attacking them.
Hair regrowth
The researchers found that mice treated with this patch every other day for three weeks had many more regulatory T cells present at the site, along with a reduction in inflammation. Hair was able to regrow at those sites, and this growth was maintained for several weeks after the treatment ended. In these mice, there were no changes in the levels of regulatory T cells in the spleen or lymph nodes, suggesting that the treatment affected only the site where the patch was applied.
In another set of experiments, the researchers grafted human skin onto mice with a humanized immune system. In these mice, the microneedle treatment also induced proliferation of regulatory T cells and a reduction in inflammation.
The researchers designed the microneedle patches so that after releasing their drug payload, they can also collect samples that could be used to monitor the progress of the treatment. Hyaluronic acid causes the needles to swell about tenfold after entering the skin, which allows them to absorb interstitial fluid containing biomolecules and immune cells from the skin.
Following patch removal, researchers can analyze samples to measure levels of regulatory T cells and inflammation markers. This could prove valuable for monitoring future patients who may undergo this treatment.
The researchers now plan to further develop this approach for treating alopecia, and to expand into other autoimmune skin diseases.
The research was funded by the Ignite Fund and Shark Tank Fund awards from the Department of Medicine at Brigham and Women’s Hospital.
Share this news article on:
Related links.
- Natalie Artzi
- Institute for Medical Engineering and Science
Related Topics
- Drug delivery
- Health sciences and technology
- Institute for Medical Engineering and Science (IMES)
Related Articles

A sprayable gel could make minimally invasive surgeries simpler and safer
Patch that delivers drug, gene, and light-based therapy to tumor sites shows promising results
MIT researchers design tailored tissue adhesives
Previous item Next item
More MIT News

The power of App Inventor: Democratizing possibilities for mobile applications
Read full story →
Using MRI, engineers have found a way to detect light deep in the brain
From steel engineering to ovarian tumor research
A better way to control shape-shifting soft robots

Professor Emeritus David Lanning, nuclear engineer and key contributor to the MIT Reactor, dies at 96

Discovering community and cultural connections
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
MINI REVIEW article
Advances in vitiligo: update on therapeutic targets.

- Department of Dermatology, Jiangsu Province People’s Hospital and Nanjing Medical University First Affiliated Hospital, Nanjing, China
Vitiligo, whose treatment remains a serious concern and challenge, is an autoimmune skin disease characterized by patches of depigmentation. The increasing application of molecular-targeted therapy in skin diseases, such as psoriasis and systemic lupus erythematosus, has dramatically improved their condition. Besides, there is a favorable effect of repigmentation in the treatment of the above diseases combined with vitiligo, implying that molecular-targeted therapy may also have utility in vitiligo treatment. Recently, the role of cytokine and signaling pathways in vitiligo pathogenesis are increasingly recognized. Thus, investigations are underway targeting the molecules described above. In this paper, we present a synopsis of current practices in vitiligo treatment and introduce the improvement in identifying new molecular targets and applying molecular-targeted therapies, including those under development in vitiligo treatment, providing valuable insight into establishing further precision medicine for vitiligo patients.
1 Introduction
Vitiligo is a primary, circumscribed, or generalized depigmentation of the skin and mucosa, related to genetic factors, self-destruction of melanocytes, cytokines, autoimmunity, and oxidative stress ( 1 ). While the detailed molecular mechanisms still require further investigation. In recent years, various studies have showed that the IFN-γ-CXCL9/10-CXCR3 axis appears to be important in vitiligo, via inhibiting melanogenesis, inducing apoptosis of melanocytes, and further recruiting T cells to the skin. These are all involved in the JAK/STAT pathway. In addition, cytokine, including HSP70i, IL-15, IL-17/23, TNF as well as wnt signaling pathway, Tregs, miRNAs have also been proved to be involved in the pathogenesis of vitiligo.
Vitiligo can be treated by different modalities of phototherapy, surgical procedures, and topical therapies, such as glucocorticosteroids, immunosuppressive agents, calcineurin inhibitors, and vitamin D. However, current treatments for vitiligo remain suboptimal, which may not be equally effective in all vitiligo patients, and it would be inconvenient for patients to visit clinics for phototherapy. Targeted therapies, such as biologics targeting cytokines and small-molecule inhibitors targeting intracellular signaling molecules, are recently emerging as promising therapeutics for autoimmune diseases. Their applications also promote our understanding of the detailed molecular mechanism of vitiligo and are essential for guiding a more precise vitiligo treatment. In this article, details of the roles that related cytokines and pathways play as well as the efficacy of targeted therapy have been described.
2 Current treatment
Topical, systemic treatment, and phototherapy are useful for stabilization and repigmentation of vitiligo. Treatment modalities are chosen in the individual patient, based on disease severity, disease activity (stable versus progressive disease), patient preference (including cost and accessibility), and response evaluation. For rapidly progressive disease, low-dose oral glucocorticoids and phototherapy are useful in stabilizing the disease. Therapeutic options for stable, segmental vitiligo include topical therapies (eg, topical corticosteroids, topical calcineurin inhibitors), targeted phototherapy, and surgical therapy (tissue grafts and cellular grafts) ( Table 1 ) ( 14 ). In recent years, attempts have been made to improve the repigmentation of vitiligo phototherapy by combination therapies, including NB-UVB with glucocorticoids ( 15 ), and topical calcineurin inhibitors ( 16 ). While their positive results were not confirmed in all studies. However, the method of treatment described, which were nonspecific, general, off-label, non-targeted with modest efficacy led to the problem of recurrence after stopping treatment. Therefore, efforts should be made to achieve a more comprehensive understanding of vitiligo pathogenesis to develop novel effective therapies ( Table 2 ).
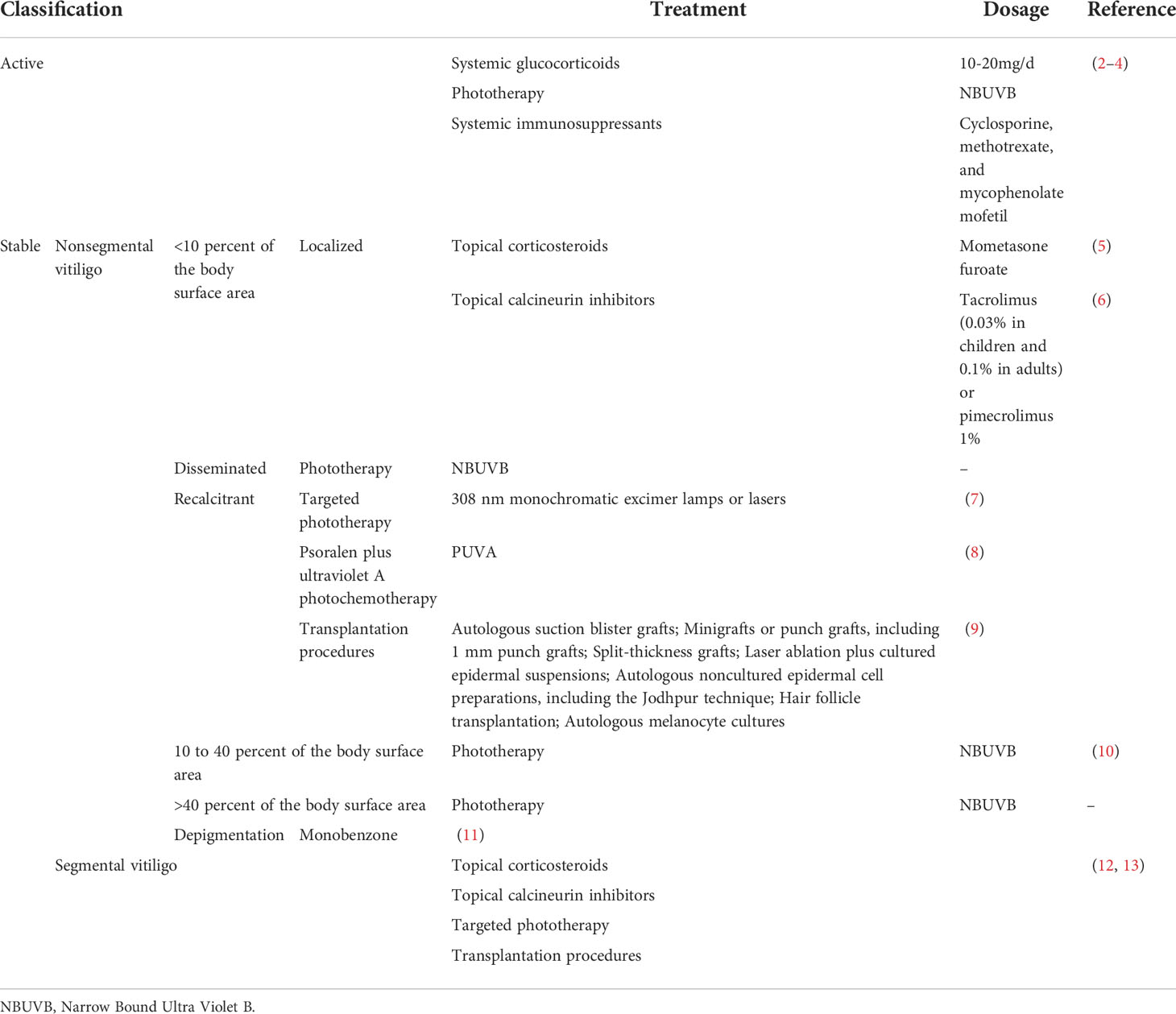
Table 1 Current treatment modalities for vitiligo.
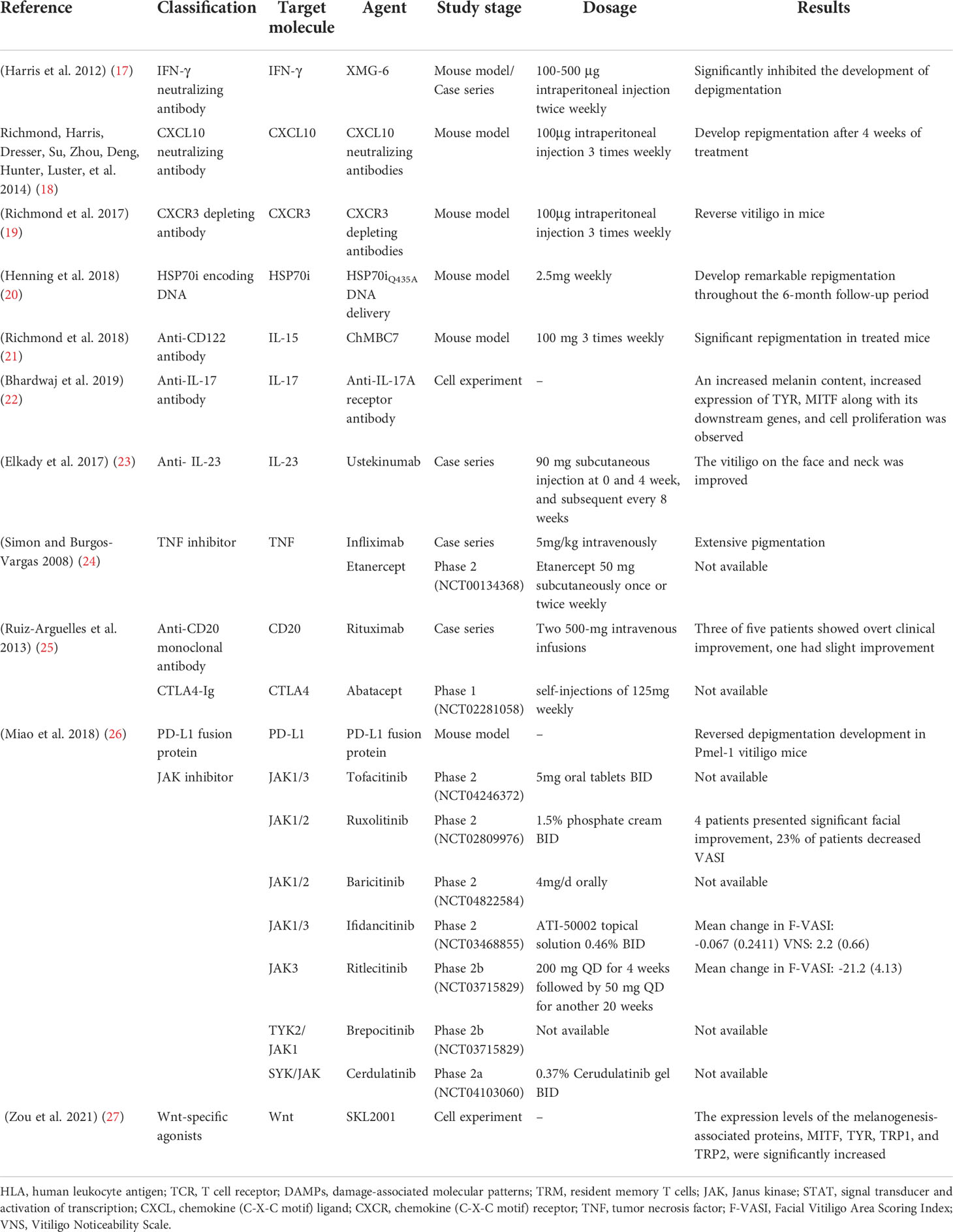
Table 2 Molecular-targeted therapies for the treatment of vitiligo.
3 Small molecules
3.1 emerging therapeutics targeting janus-activated kinase (jak) signaling.
The Janus kinases family consists of JAK1, JAK2, JAK3, and TYK2, which is engaged in the important JAK/STAT pathway, exhibiting pleiotropic effects on transducing multiple extracellular signals involved in regulating proliferative signaling, differentiation, migration, and apoptotic properties ( 28 ).
There are no licensed JAK/STAT inhibitors available against dermatological problems, however, some of them (ruxolitinib and tofacitinib) are used to treat other conditions such as myelofibrosis and RA. However, off-label usage of these medications in the treatment of vitiligo has shown promising outcomes.
JAK-STAT inhibitors promote Sonic Hedgehog and Wnt signaling in epidermal pigmentation, with the former inducing the migration, proliferation, and differentiation of melanocyte ( 29 ). Expanding our knowledge of these medications’ efficacy and safety profiles, as well as their use in dermatological conditions, is critical for establishing their risk-benefit ratio.
3.1.1 Tofacitinib
Tofacitinib is an FDA-cleared JAK1/3 inhibitor for treating RA, PsA, and active ulcerative colitis.
Tofacitinib 5-10 mg QD/BID has demonstrated superior efficacy against vitiligo, with improvement ratios of 5.4% in 5/10 patients with sun-exposed areas or areas treated only with phototherapy ( 30 ), and a reduced rate in vitiligo area scoring index (VASI) score of 4.68 at baseline to 3.95 at 5 months in another trial ( 31 ). In addition, a decline in the number of CD8 + T cells and chemokines, such as CXCL9 and CXCL10 has been observed after tofacitinib treatment, but no variations were observed for the percentage of melanocyte-specific T cells ( 30 ).
Unfortunately, this oral medication is associated with a host of systemic side effects, including infections, malignancies, and cytopenia. Thus, topical JAK inhibitors may be more preferred. 11 vitiligo patients treated with 2% tofacitinib cream twice a day in conjunction with NB-UVB therapy thrice-weekly demonstrated a mean improvement of 70% in facial VASI. There was also a significant difference between facial and non-facial lesions (P=0.022) ( 32 ).
3.1.2 Ruxolitinib
Ruxolitinib, the first Jakinib to get FDA approval, is a JAK1/2 inhibitor designed to deal with polycythemia vera and intermediate- and high-risk primary myelofibrosis ( 33 ).
Studies have shown that except for JAK inhibition, ruxolitinib also inhibited the differentiation and migration of DCs in vitiligo, increasing CD8 + cytotoxic T cell responses ( 34 ). In a double-blind phase 2 trial, 157 recruited vitiligo patients were randomized, in a 1:1:1:1:1 ratio, to receive topical ruxolitinib cream 1.5% BID, 1.5% QD, 0.5% QD, 0.15% QD, or a vehicle for 24 weeks, with the result showing considerably decreased CXCL9 and CXCL10 expression in 1.5% BID and 1.5% QD groups, and more individuals in groups receiving ruxolitinib cream 1.5% BID, 1.5% QD and 0.5% QD achieving F-VASI50, during which 1.5% BID group produced the highest responses in F-VASI50 (58%), F-VASI75 (52%), and F-VASI90 (33%). Besides, three positive responsive groups demonstrated significant repigmentation of vitiligo lesions and acceptable tolerability with a follow-up period of 52 weeks ( 35 ). Vitiligo on the face appears to respond more vigorously to therapy than non-facial lesions, reinforced by a 20-week, open-label trial in which patients with significant facial involvement experienced a 76% improvement in facial VASI scores ( 36 ). Furthermore, better repigmentation rates could be achieved both in oral and topical ruxolitinib treatment combined with phototherapy ( 37 ).
3.1.3 Baricitinib
Baricitinib is a selective JAK1/2 inhibitor that inhibits signal transduction of numerous proinflammatory cytokines ( 38 ), approved for the treatment of RA. To our knowledge, there was only one case report describing repigmentation in vitiligo patients with baricitinib 4 mg daily for the treatment of RA. Besides, an ongoing phase 2 trial (NCT04822584) in which patients received a combination therapy of baricitinib 4mg/d and phototherapy is being performed.
3.1.4 Ifidancitinib (ATI-50002)
Ifidancitinib is another dual JAK1/3 inhibitor for alopecia areata treatment, which is now undergoing phase II clinical trials for its application in vitiligo treatment. Patients with facial NSV(NCT03468855) receiving topical ATI-50002 BID for 24 weeks presented with an improved F-VASI and the Vitiligo Noticeability Scale (VNS) ( 39 ).
3.1.5 Ritlecitinib (PF-06651600) and Brepocitinib (PF-06700841)
Ritlecitinib, an irreversible inhibitor of JAK3 and tyrosine kinase applicable to the treatment of moderate-to-severe RA ( 40 ) and Brepocitinib, a TYK2/JAK1 inhibitor, are currently undergoing evaluation of their efficacy and safety profile in active NSV in combination with phototherapy (NCT03715829) ( 41 ).
3.1.6 Cerdulatinib (PRT062070)
Cerdulatinib, an SYK/JAK dual kinase inhibitor ( 42 ), has been assessed (NCT04103060) for its safety and tolerability for vitiligo treatment in topical formation (0.37% cerudulatinib gel BID).
However, additional studies are needed to determine the best-suited drug regimen and recommended dosage forms and doses to attain the optimum curative effect and minimal toxicity. As the occurrence of depigmentation after the withdrawal of JAK inhibitors, the mechanisms underlying need further exploration, and more work need to be done to corroborate the effectiveness in combination with other therapies.
3.2 Wnt signaling and its agonists
It has been shown that Wnt/β-catenin signaling plays a pivotal role in the proliferation, migration, and differentiation of melanocytes in vitiligo patients ( 29 ), which could be inhibited by oxidative stress ( 43 ). In addition, the Wnt/β-catenin pathway participates in the activation of MITF and its downstream enzymes ( 44 ). Intradermal injection of IWR-1 (inhibitor of Wnt response 1), a chemical inhibitor of β-catenin activation, and small interfering RNA (siRNA) against Wnt7α suppressed the number of epidermal melanocytes ( 45 ). This evidence suggested that stimulation of Wnt signaling may be an adjuvant therapy for vitiligo treatment. Micro-injury ( 46 ) as well as some phenanthridine-derived Wnt-specific agonists binding with the Axin protein have been proved to promote melanogenesis ( 47 ) and induce repigmentation.
3.3 Emerging therapeutics targeting microRNAs (miRNAs)
MiRNAs, which are a highly conservative small class of non-coding RNA molecules, participate in mRNA expression regulation via degradation or repression of mRNA translation ( 48 ). Previous studies have demonstrated that miRNAs were associated with genetic polymorphisms (e.g., miR-196a-2 rs11614913), immune response (e.g., miR-133b, miR-224-3p, miR-4712-3p, miR-3940-5p, miR-21−5p), oxidative stress (e.g., miR-135a, miR-9, miR-34a, miR-183, miR-184, miR-1, miR-25, miR-211, miR-383, miR-577, miR-421) and melanocyte functions (e.g., miR-434-5p, miR-330-5p, miR-137, miR-148, miR-145, miR-155, miR-203, miR-125, miR-377, miR-2909, miR-200c, hsa-miR-149-5p) ( 49 – 54 ), participating in pathological mechanism of vitiligo. These findings suggest that miRNAs may be involved in vitiligo pathogenesis via the modulation of vital genes expression in melanocytes and serve as novel therapeutic targets for vitiligo therapy.
There are two strategies for the therapeutic application of miRNAs: 1) anti-miRNAs, locked-nucleic acids (LNA), or antagomiRs ( 55 ) can be used to counteract the over-activation of miRNA. Short tandem target mimic (STTM)- miR-508-3p has been validated to upregulate SOX6 expression, leading to increased expression of key melanogenic genes CREB, MITF, TYR, and TYRP1/2 with increased melanogenesis ( 56 ). Besides, STTM-miR-143-5p also upregulates the expression of MYO5A, leading to an increase in the level of MITF, TYR, TYRP1, melanin, and Rab27a ( 57 ). 2) miRNA replacement, involving the reintroduction of a gene-suppressor miRNA mimic or AAV (adeno-associated virus)-mediated miRNA gain-of-function to modulate gene expression ( 55 ). A study demonstrated that the migratory capacity of melanocytes was altered by the application of miR-211 mimic through the p53-TRPM1/miR-211-MMP9 axis ( 58 ).
3.4 Emerging therapeutics targeting regulatory T-cells (Tregs)
Tregs are a suppressive CD4 + T cell subset that possesses a capacity to suppress self-reactive T cell activation and expansion ( 59 ). A clear decrease in Treg cells was observed in vitiligo skin within lesional, non-lesional, and perilesional sections ( 60 ), indicating that increasing the number of Tregs with normal function might be an important therapeutic intervention for vitiligo treatment.
Infusing purified populations of Tregs is the most direct way for the supply of Tregs. The current methods mainly include polyclonally-expanded Tregs, antigen-specific Tregs, and engineered Treg cells. In a mouse model of vitiligo, adoptive transfer of polyclonal Tregs may be effective in the short-term ( 61 ), which might however impart systemic immunosuppression ( 62 ). Besides, a TCR transgenic mouse with spontaneous vitiligo, receiving CAR Tregs treatment, developed a significant delay in depigmentation ( 63 ).
However, a limitation of infusing purified populations of Tregs might be the technical difficulty for therapeutic agent delivery to specific cells. A topical application of Tregs or the combination with CCR4 Treg homing receptor ligand CCL22 ( 64 ) by local needle-free jet injection of DNA ( 20 ) or CCL22-encoding plasmid DNA ( 64 ) may help resolve that issue. Besides, various strategies have been applied towards the modulation of Tregs function by targeting Treg-intrinsic pathways and functional modulators for Tregs. HO-1, a functional modulator of Tregs, was decreased in vitiligo Tregs. Treatment with Hemin, an agonist of HO-1, was found to enhance HO-1-induced restoration of Tregs function by up-regulating IL-10 expression ( 65 ). In addition, therapeutic method for microbiota modulation, such as neomycin treatment can significantly delay depigmentation in vitiligo mice and promote the infiltration of Tregs to the skin ( 66 ). Rapamycin, an inhibitor of PI3Kakt-mTORC1 signaling ( 67 ), efficiently halts the depigmentation process by increasing the abundance of Treg in h3TA2 mice, which effect lasted till 6 weeks after treatment ( 61 ). At present, a phase 2 clinical trial(NCT05342519) is underway for assessing the efficacy of the application of 0.1% topical rapamycin ( 68 ) (2022). In addition, nanoparticles containing rapamycin and autoantigen HEL46-61(NPHEL46-61/Rapa) were synthesized, the administration of which halted the disease progression ( 69 ). Also, the calcium-NFATc1-signaling pathway may be involved in defective Tregs function, indicating a potential therapeutic target for vitiligo treatment ( 70 ).
4 Cytokine-targeted therapies
Multiple monoclonal antibodies are available for vitiligo treatment, targeting IFN-γ, CXCL10, CXCR3, HSP70i, IL-15, IL-17/23, and TNF. In addition to full-size immunoglobulin, affibodies and nanobodies, composed of considerably smaller proteins, are currently being developed, which have higher bioavailability as well as affinity and specificity to the targeted molecules.
4.1 IFN-γ and the inhibitors
The IFN-γ-CXCL9/10-CXCR3 axis may be crucial for vitiligo pathogenesis, contributing to disease progression by inhibiting melanogenesis, inducing apoptosis of melanocytes, and further recruiting T cells to the skin ( Figure 1 ) ( 71 ). A study showed a higher expression of IFN-γ mRNA in non-lesional and perilesional skin, especially in active vitiligo ( 72 ), which is associated with disease activity ( 73 ).
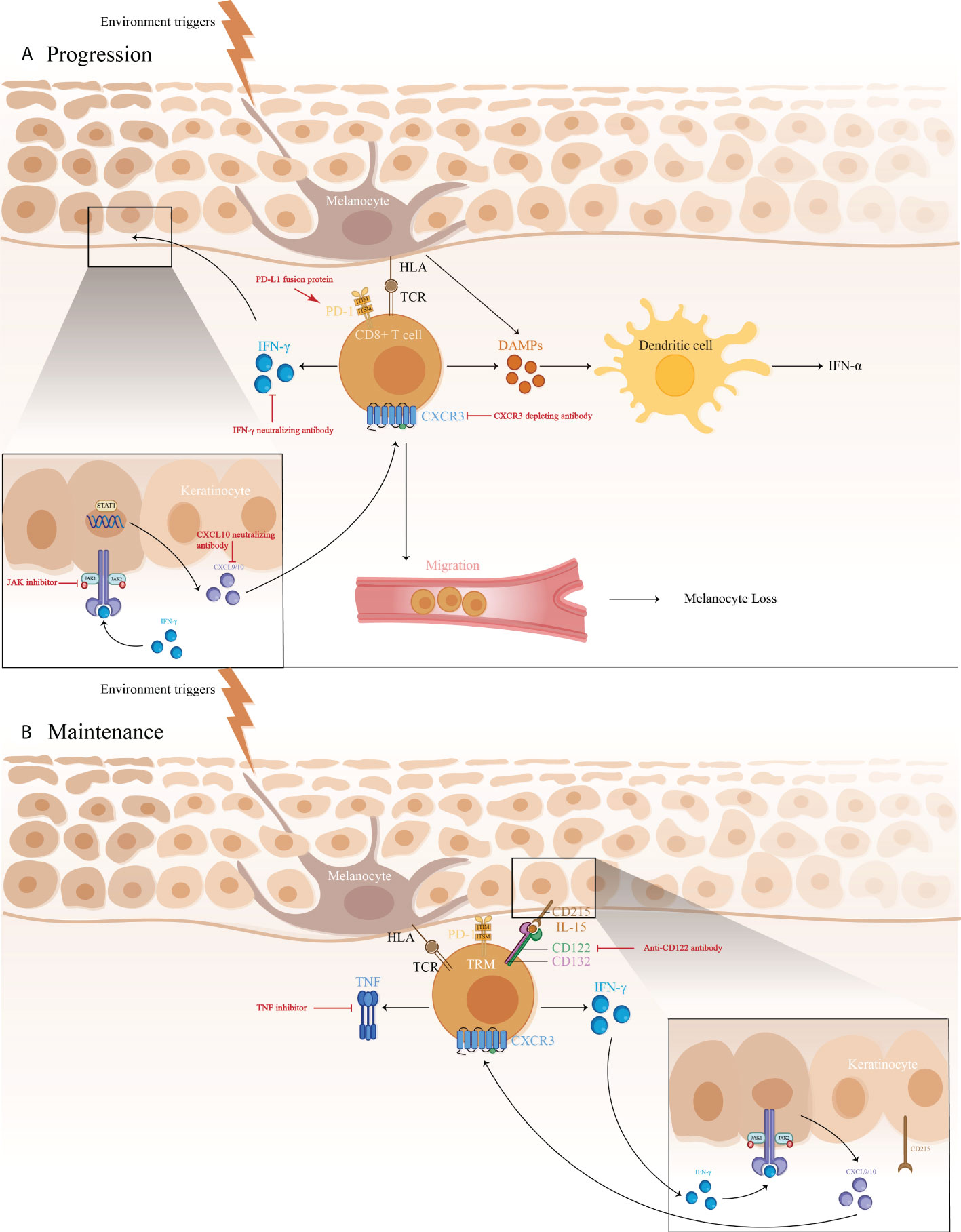
Figure 1 1) The immune pathogenesis of vitiligo: (A) CD8 + T cell expression of IFN-γ in vitiligo lesions activated the JAK/STAT pathway after binding to IFN-γ receptor, thus facilitating the release of CXCL9/10. The binding of CXCL9/10 to CXCR3 increased CXCR3+ T cells recruitment; (B) Maintenance of vitiligo lesions was influenced by the function of IL-15-dependent TRM cells, which produce IFN-γ and TNF-α. 2)Targeted therapeutic interventions in vitiligo mainly include therapies targeting IFN-γ-CXCL9/10-CXCR3 axis (IFN-γ neutralizing antibody, CXCL10 neutralizing antibody, and CXCR3 depleting antibody, as well as JAK inhibitors), anti-CD122 antibody (IL-15 receptor subunit) to decrease IFN-γ production and deplete autoreactive CD8 + TRM cells, TNF inhibitor to inhibit autoantibody production, and PD-L1 fusion protein to reduce the numbers of melanocyte-reactive T cells.
Anti-IFN-γ can have been proved to be effective in rheumatoid arthritis (RA), multiple sclerosis (MS), prevention of corneal rejection, autoimmune skin diseases, and others. In a recent study, vitiligo induction mice, treated with intraperitoneal injection with IFN-γ neutralizing antibody (XMG-6) at a dose of 100-500 μg twice a week, presented with significant improvement of depigmentation ( 17 ), with the same trend observed in vitiligo patients. Four patients who received intradermal perilesional injections presented with repigmentation of the treated area and boundary retreat ( 74 ). More research is warranted to be initiated for further definition of the role that IFN-γ plays in vitiligo and to examine whether IFN-γ neutralization would be more viable in reversing skin depigmentation.
4.2 CXCL10 and the inhibitors
Recent studies report a Th1/IFN-γ immune response in both human and a mouse model of vitiligo that involves elevated CXCL9, 10, and 11 productions, among which CXCL10 participated in the targeted migration of T cells ( 18 ), triggering an immune cell infiltration at the early stage ( 72 ), and involved in the downregulation of keratinocyte glycoprotein non-metastatic melanoma protein B (GPNMB) ( 75 ). A study showed that mice receiving CXCL10 neutralizing antibodies developed more repigmentation after 4 weeks’ treatment, which continued for an additional 4 weeks ( 18 ), thereby supporting CXCL10 suppression as a great therapeutic strategy.
4.3 CXCR3 antibodies
CXCR3 has been proved to be expressed in skin lesions, autoreactive T cells ( 18 ), and the vast majority of skin infiltrating CD8 + resident memory T cells (TRM), which stimulate the secretion of IFN-γ and TNF-α ( 76 ).
In a study, vitiligo mice with >75% depigmentation on their tails are treated with CXCR3 depleting antibodies for 7-8 weeks, which significantly reversed the clinical disease in a perifollicular pattern and a diminution of PMEL in the epidermis, with slightly reduced host CD8 + T cell numbers ( 19 ) compared to neutralizing antibody treatment ( 18 ). Although these results are preliminary, they may provide justification for further studies in targeting CXCR3 in vitiligo ( 19 ), which proposes the use of a depleting Ab to create a greater clinical efficacy by removing autoreactive cells rather than modulating their migration phenotype.
4.4 Inducible HSP70 (HSP70i) DNA
Indeed, HSP70i is the core participant in vitiligo predominantly through HSP70i-plasmacytoid dendritic cells (pDCs)-IFN-α-CXCL9 and CXCL10-cytotoxic T lymphocyte (CTL) axis. Pmel-1 mice vaccinated with HSP70i encoding DNA exhibited significant depigmentation, rarely seen in models knockout for HSP70i, indicating that elevated HSP70i expression alone would be enough to induce depigmentation in vitiligo prone animals ( 77 ). A study revealed that the expression of HSP-70 mRNA in skin lesions of active vitiligo patients was much higher ( 78 ), correlated with the disease activity.
Blocking HSP70i activity might have the potential to reverse vitiligo development. A recent study showed that a Sinclair swine, receiving HSP70iQ435A-encoding DNA treatment, showed remarkable repigmentation with an initial influx of T cells and increased CD4/CD8 ratios ( 20 ), which was also detected in mice with HSP70i Q435A -encoding DNA treatment, resulting in 76% restoration of skin pigmentation. Furthermore, the treatment halted T cells accumulation and transition to T cell phenotype in mice and human skin, engaging HSP70i Q435A DNA delivery as a potent effective therapeutic intervention for vitiligo ( 79 ).
4.5 IL-15 and the inhibitors
It has been established that IL-15 seems to participate in IL-17 regulation and maintenance of TRM signals ( 80 ), with the latter responsible for long-term maintenance and potential relapse of vitiligo ( 81 ). The study has demonstrated a higher serum level of IL-15 in vitiligo patients than in controls, highly associated with epidermal H 2 O 2 content and the disease activity ( 82 , 83 ).
In vitiligo mice, an anti-CD122 antibody that targets IL-15 signaling was reported to effectively reverse depigmentation. Anti-CD122 therapy, either systemically or locally, decreases TRM-induced IFN-γ production and results in long-term repigmentation. These findings consider CD122-targeted drugs as a valid therapy method, which results in effective and long-lasting responses in vitiligo and other tissue-specific autoimmune disorders involving TRM ( 21 ).
4.6 PD-1/PD-L1 pathway
Involvement of the PD-1/PD-L1 pathway has been shown in many autoimmune diseases, including RA, MS, and vitiligo. PD-L1 expression was found limited in normal skin, and only expressed on dermal T cells, and increased in primary melanocytes and fibroblasts after exposure to IFN-γ. No such effect was seen in vitiligo patients, indicating the absence of self-protection ability for melanocytes against T-cell attack during vitiligo pathogenesis. In agreement with this, treatment with PD-L1 fusion protein reduced the numbers of melanocyte-reactive T cells, inhibited the activation of Vβ12-expressing T cells, and increased Tregs numbers, reversing depigmentation in a Pmel-1 T-cell receptor transgenic vitiligo mouse model ( 26 ). However, PD-L1 treatment may still call for extended phototherapy treatment, especially NB-UVB therapy, which likely upregulates PD-L1 expression in an NF-κB-dependent manner ( 84 ), indicating a combination use of local PD-1/PD-L1 agonistic treatment and NB-UVB therapy as a promising option.
4.7 Other cytokine-targeted therapies under investigation
4.7.1 il-17/23 and the inhibitors.
Studies on the effect of IL-17/23 in vitiligo resulted in contradictory findings. On one hand, Th17 cells and IL-17 in vitiligo patients may inhibit function-related factors, repress melanogenesis, and dramatically induct other Th17 type cytokines as well as IL-1β production from dermal fibroblasts and keratinocytes ( 85 ). Elevated Th17 cells and IL-17/23 levels in skin lesions and serum of vitiligo patients, were positively correlated with disease activity ( 86 , 87 ), and decreased after narrowband ultraviolet B (NBUVB) treatment ( 88 ). Primary melanocyte culture showed an increased expression of MITF and its downstream genes, increased melanin pigment, and cell proliferation after blockade with anti-IL-17RA ( 22 ). Besides, incidences of repigmentation have been documented in ustekinumab treatment of vitiligo ( 23 ). However, secukinumab treatment in patients with active non‐segmental vitiligo (NSV) contributed to disease progression in 7/8 patients with no general reduction in CXCL9/10, sCD25/27, Th1 cells, or cytotoxic cells, resulting in early termination of study ( 89 ). There are also reports of ustekinumab-induced new-onset vitiligo and alopecia areata. The above studies showed IL-17/23 signal may not play a direct role in vitiligo pathogenesis, which needs further investigation to confirm this conjecture.
4.7.2 TNF and the inhibitors
As an anti-inflammatory mediator, TNF-α is considered to play a role in vitiligo, which may promote apoptosis in melanocytes, induce B-cell activation, increase autoantibody production, and inhibit melanogenesis ( 90 ). Recent data has shown a significantly higher expression of TNF-α in vitiligo skin. TNF inhibitors are beneficial in the treatment of plaque-type psoriasis, psoriatic arthritis (PsA), RA, and inflammatory bowel disease (IBD), arousing growing interest in their use in vitiligo.
Infliximab is a chimeric anti-TNF-α monoclonal antibody specifically binding to both soluble and membrane-bound TNF ( 91 , 92 ). Intravenous infliximab is widely licensed in the treatment of RA, psoriasis, ankylosing spondylitis (AS), IBD, uveitis, and Behcet’s disease. A 24-year-old patient with ankylosing spondylitis and refractory vitiligo improved significantly following six months of infliximab therapy at a dose of 5mg/kg intravenously in weeks 0, 2, and 6, and then every eight weeks for ten months ( 24 ). Besides, Etanercept is a monoclonal antibody targeted against TNF-α ( 93 ), which has been approved for the treatment of RA, juvenile RA, AS, psoriasis, and PsA. Treatment with etanercept 50 mg subcutaneously once or twice weekly for at least 2 months has shown a great curative effect on established vitiligo ( 94 ).
However, it has been shown that anti‐TNF‐α agents, especially adalimumab and infliximab ( 95 ), may exacerbate established vitiligo and induce new-onset vitiligo during treatment of other autoimmune diseases, including AS ( 96 ), Crohn’s disease ( 97 ), ulcerative colitis ( 98 ), psoriasis ( 99 ), and RA ( 100 ). The mechanism responsible for the TNF-α inhibitors-induced vitiligo is not fully understood. On the one hand, TNF-α inhibitors may increase the nucleosome-mediated autoantibody formation, interfere with the cytotoxic T-cell suppression of autoreactive B cells, and decrease Treg synthesis and activation. Additionally, infliximab increases pDC-produced IFN-γ, participating in further T cells recruiting. Although very rare, new-onset or exacerbations of vitiligo can occur in the anti‐TNF‐α treatment of other autoimmune diseases, the risk of which must not be ignored.
4.7.3 Rituximab
Rituximab has specific affinity for the B-lymphocyte transmembrane protein, CD20, which is expressed on B cells ( 101 ), participating in the activation of the CD8 + T cells and the ensuing autoreactive reaction ( 102 ). Rituximab is licensed for the treatment of lymphomas, leukemias, transplant rejection crisis, and a series of autoimmune diseases ( 103 , 104 ). An intravenous infusion of Rituximab was administered to five active disseminated vitiligo patients, the three of whom exhibited a considerable improvement in both the disease’s symptoms and histology ( 25 ).
4.7.4 Abatacept
Abatacept, a fusion protein consisting of IgG1 coupled to the extracellular domain of CTLA-4 via the immunoglobulin’s Fc region, was licensed for treating moderate to severe RA. Ten eligible patients with active vitiligo have been included to receive self-injections of 125mg abatacept weekly from week 0 to week 24. Secondary endpoints will be evaluated during a 32-week follow-up visit ( 105 ).
5 Future therapeutic prospects
As a future direction, new therapeutic approaches should be developed to reduce vitiligo progression. Among the new approaches being developed, the strategy of targeting the IFN-γ-CXCL9/10-CXCR3 axis has been clinically tested. OPZELURA has been indicated for the topical treatment of nonsegmental vitiligo in adult and pediatric patients 12 years of age and older. MiRNA-based therapeutics are also in development. However, the absence of organ or tissue selectivity may also lead to off-target side effects, which must be considered and excluded in the process of miRNA-based therapeutics development. Besides, a suitable vector system, as well as the assurance of chemical and biological stability should also be taken into account. Adoptive Treg cell therapy has also been the research hotspot in recent years. However, it has always been a difficult point for reassurance for safety and the development of the delivery system.
Treating vitiligo remains a challenge. As is presented in this paper, a greater variety of precision treatments is currently being studied. With a better understanding and further validation of these therapeutic targets, patients can be stratified to achieve individualized treatment.
6 Conclusion
Current models of treatment for vitiligo are often nonspecific and general. Various therapy options are available for active vitiligo patients, including systemic glucocorticoids, phototherapy, and systemic immunosuppressants. While stable vitiligo patients may benefit from topical corticosteroids, topical calcineurin inhibitors, phototherapy, as well as transplantation procedures. Recently, a better understanding of the pathophysiological processes of vitiligo led to the advent of novel targeted therapies. To date, JAK inhibitors are the only category that has been proved to have a good tolerability profile and functional outcomes in vitiligo treatment, even though the risk of activation of latent infection and systemic side effects still existed, like other immunosuppressive agents. Research is in progress to investigate the important cytokines involved in the pathogenesis of vitiligo, including IFN-γ, CXCL10, CXCR3, HSP70i, IL-15, IL-17/23, and TNF, the blockade of which has undergone preliminary attempts in animal models and some patients. In addition, studies on miRNA-based therapeutics as well as adoptive Treg cell therapy are still primary, and more studies are necessary.
Author contributions
YFF and YL contributed to the conceptual design, writing, editing, and generation of figures for this manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ezzedine K, Eleftheriadou V, Whitton M, van Geel N. Vitiligo. Lancet (London England) (20159988) 386:74–84. doi: 10.1016/S0140-6736(14)60763-7
CrossRef Full Text | Google Scholar
2. Bishnoi A, Vinay K, Kumaran MS, Parsad D. “Oral mycophenolate mofetil as a stabilizing treatment for progressive non-segmental vitiligo: results from a prospective, randomized, investigator-blinded pilot study”. Arch Dermatol Res (2021) 313(5):357–65. doi: 10.1007/s00403-020-02108-8
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Garza-Mayers AC, Kroshinsky D. “Low-dose methotrexate for vitiligo”. Drugs Dermatol (2017) 16(7):705–6.
Google Scholar
4. Singh H, Kumaran MS, Bains A, Parsad D. A randomized comparative study of oral corticosteroid minipulse and low-dose oral methotrexate in the treatment of unstable vitiligo. Dermatology (2015) 231(3):286–90. doi: 10.1159/000433424
5. Taieb A, Alomar A, Bohm M, Dell'anna ML, De Pase A, Eleftheriadou V, et al. Guidelines for the management of vitiligo: The European dermatology forum consensus. Br J Dermatol (2013) 168(1):5–19. doi: 10.1111/j.1365-2133.2012.11197.x
6. Lee JiH, Kwon HS, Jung HMi, Lee H, Kim GM, Yim HW, et al. Treatment outcomes of topical calcineurin inhibitor therapy for patients with vitiligo: A systematic review and meta-analysis. JAMA Dermatol (2019) 155(8):929–38. doi: 10.1001/jamadermatol.2019.0696
7. Lopes C, Trevisani VF, Melnik T. Efficacy and safety of 308-nm monochromatic excimer lamp versus other phototherapy devices for vitiligo: A systematic review with meta-analysis. Am J Clin Dermatol (2016) 17(1):23–32. doi: 10.1007/s40257-015-0164-2
8. Zubair R, Hamzavi IH. Phototherapy for vitiligo. Dermatol Clinics (2020) 38(1):55–62. doi: 10.1016/j.det.2019.08.005
9. Mohammad TF, Hamzavi IH. Surgical therapies for vitiligo. Dermatol Clinics (2017) 35(2):193–203. doi: 10.1016/j.det.2016.11.009
10. Mohammad TF, Al-Jamal M, Hamzavi IH, Harris JE, Leone G, Cabrera R, et al. The vitiligo working group recommendations for narrowband ultraviolet b light phototherapy treatment of vitiligo. J Am Acad Dermatol (2017) 76(5):879–88. doi: 10.1016/j.jaad.2016.12.041
11. Grimes PE, Nashawati R. Depigmentation therapies for vitiligo. Dermatol Clinics (2017) 35(2):219.
12. Mulekar SV, Al Eisa A, Delvi MB, Al Issa A, Al Saeed AH. Childhood vitiligo: A long-term study of localized vitiligo treated by noncultured cellular grafting. Pediatr Dermatol (2010) 27(2):132–6. doi: 10.1111/j.1525-1470.2009.00978.x
13. Mulekar SV. Long-term follow-up study of segmental and focal vitiligo treated by autologous, noncultured melanocyte-keratinocyte cell transplantation. Arch Dermatol (2004) 140(10):1211–5. doi: 10.1001/archderm.140.10.1211
14. Bohm M, Schunter JA, Fritz K, Salavastru C, Dargatz S, Augustin M, et al. S1 guideline: Diagnosis and therapy of vitiligo. J Dtsch Dermatol Ges (2022) 20(3):365–78. doi: 10.1111/ddg.14713
15. Batchelor JM, Thomas KS, Akram P, Azad J, Bewley A, Chalmers JR, et al. Home-based narrowband UVB, topical corticosteroid or combination for children and adults with vitiligo: HI-light vitiligo three-arm RCT. Health Technol Assess (2020) 24(64):1–128. doi: 10.3310/hta24640
16. Li R, Qiao M, Wang X, Zhao X, Sun Q. Effect of narrow band ultraviolet b phototherapy as monotherapy or combination therapy for vitiligo: A meta-analysis. Photodermatol Photoimmunol Photomed (2017) 33(1):22–31. doi: 10.1111/phpp.12277
17. Harris JE, Harris TH, Weninger W, Wherry EJ, Hunter CA, Turka LA. A mouse model of vitiligo with focused epidermal depigmentation requires IFN-gamma for autoreactive CD8(+) T-cell accumulation in the skin. J Invest Dermatol (2012) 132(7):1869–76. doi: 10.1038/jid.2011.463
18. Rashighi M, Agarwal P, Richmond JM, Harris TH, Dresser K, Su M-W, et al. CXCL10 is critical for the progression and maintenance of depigmentation in a mouse model of vitiligo. Sci Trans Med (2014) 6(223):223ra23. doi: 10.1126/scitranslmed.3007811
19. Richmond JM, Masterjohn E, Chu R, Tedstone J, Youd ME, Harris JE. CXCR3 depleting antibodies prevent and reverse vitiligo in mice. J Invest Dermatol (2017) 137(4):982–5. doi: 10.1016/j.jid.2016.10.048
20. Henning SW, Fernandez MF, Mahon JP, Duff R, Azarafrooz F, Guevara-Patino JA, et al. HSP70iQ435A-encoding DNA repigments vitiligo lesions in Sinclair swine. J Invest Dermatol (2018) 138(12):2531–9. doi: 10.1016/j.jid.2018.06.186
21. Richmond JM, Strassner JP, Zapata L, Garg M, Riding RL, Refat MA, et al. Antibody blockade of IL-15 signaling has the potential to durably reverse vitiligo. Sci Trans Med (2018) 10(450):eaam7710. doi: 10.1126/scitranslmed.aam7710
22. Bhardwaj S, Bhatia A, Kumaran MS, Parsad D. Role of IL-17A receptor blocking in melanocyte survival: A strategic intervention against vitiligo. Exp Dermatol (2019) 28(6):682–9. doi: 10.1111/exd.13773
23. Elkady A, Bonomo L, Amir Y, Vekaria AS, Guttman-Yassky E. Effective use of ustekinumab in a patient with concomitant psoriasis, vitiligo, and alopecia areata. JAAD Case Rep (2017) 3(6):477–9. doi: 10.1016/j.jdcr.2017.07.009
24. Simon JA, Burgos-Vargas R. Vitiligo improvement in a patient with ankylosing spondylitis treated with infliximab. Dermatology (2008) 216(3):234–5. doi: 10.1159/000112932
25. Ruiz-Arguelles A, Garcia-Carrasco M, Jimenez-Brito G, Sanchez-Sosa S, Perez-Romano B, Garces-Eisele J, et al. Treatment of vitiligo with a chimeric monoclonal antibody to CD20: A pilot study. Clin Exp Immunol (2013) 174(2):229–36. doi: 10.1111/cei.12168
26. Miao X, Xu R, Fan B, Chen J, Li X, Mao W, et al. PD-L1 reverses depigmentation in pmel-1 vitiligo mice by increasing the abundance of tregs in the skin. Sci Rep (2018) 8(1):1605. doi: 10.1038/s41598-018-19407-w
27. Zou DP, Chen YM, Zhang LZ, Yuan XH, Zhang YJ, Inggawati A, et al. SFRP5 inhibits melanin synthesis of melanocytes in vitiligo by suppressing the wnt/beta-catenin signaling. Genes Dis (2021) 8(5):677–88. doi: 10.1016/j.gendis.2020.06.003
28. Rawlings JS, Rosler KM, Harrison DA. The JAK/STAT signaling pathway. J Cell Sci (2004) 117(Pt 8):1281–3. doi: 10.1242/jcs.00963
29. Birlea SA, Costin GE, Roop DR, Norris DA. Trends in regenerative medicine: Repigmentation in vitiligo through melanocyte stem cell mobilization. Med Res Rev (2017) 37(4):907–35. doi: 10.1002/med.21426
30. Liu LY, Strassner JP, Refat MA, Harris JE, King BA. Repigmentation in vitiligo using the janus kinase inhibitor tofacitinib may require concomitant light exposure. J Am Acad Dermatol (2017) 77(4):675–82.e1. doi: 10.1016/j.jaad.2017.05.043
31. Vu M, Heyes C, Robertson SJ, Varigos GA, Ross G. Oral tofacitinib: A promising treatment in atopic dermatitis, alopecia areata and vitiligo. Clin Exp Dermatol (2017) 42(8):942–4. doi: 10.1111/ced.13290
32. Mobasher P, Guerra R, Li SJ, Frangos J, Ganesan AK, Huang V. Open-label pilot study of tofacitinib 2% for the treatment of refractory vitiligo. Br J Dermatol (2020) 182(4):1047–9. doi: 10.1111/bjd.18606
33. Deisseroth A, Kaminskas E, Grillo J, Chen W, Saber H, Lu HL, et al. U.S. food and drug administration approval: ruxolitinib for the treatment of patients with intermediate and high-risk myelofibrosis. Clin Cancer Res (2012) 18(12):3212–7. doi: 10.1158/1078-0432.CCR-12-0653
34. Heine A, Held SA, Daecke SN, Wallner S, Yajnanarayana SP, Kurts C, et al. The JAK-inhibitor ruxolitinib impairs dendritic cell function in vitro and in vivo . Blood (2013) 122(7):1192–202. doi: 10.1182/blood-2013-03-484642
35. Rosmarin D, Pandya AG, Lebwohl M, Grimes P, Hamzavi I, Gottlieb AB, et al. Ruxolitinib cream for treatment of vitiligo: A randomised, controlled, phase 2 trial. Lancet (2020) 396(10244):110–20. doi: 10.1016/S0140-6736(20)30609-7
36. Rothstein B, Joshipura D, Saraiya A, Abdat R, Ashkar H, Turkowski Y, et al. Treatment of vitiligo with the topical janus kinase inhibitor ruxolitinib. J Am Acad Dermatol (2017) 76(6):1054–60.e1. doi: 10.1016/j.jaad.2017.02.049
37. Gianfaldoni S, Tchernev G, Wollina U, Roccia MG, Fioranelli M, Lotti J, et al. Micro - focused phototherapy associated to janus kinase inhibitor: A promising valid therapeutic option for patients with localized vitiligo. Open Access Maced J Med Sci (2018) 6(1):46–8. doi: 10.3889/oamjms.2018.042
38. Norman P. Selective JAK inhibitors in development for rheumatoid arthritis. Expert Opin Investig Drugs (2014) 23(8):1067–77. doi: 10.1517/13543784.2014.918604
39. A study of ATI-50002 topical solution for the treatment of vitiligo (2018). Available at: https://clinicaltrials.gov/ct2/show/NCT03468855 .
40. Robinson MF, Damjanov N, Stamenkovic B, Radunovic G, Kivitz A, Cox L, et al. Efficacy and safety of PF-06651600 (Ritlecitinib), a novel JAK3/TEC inhibitor, in patients with moderate-to-Severe rheumatoid arthritis and an inadequate response to methotrexate. Arthritis Rheumatol (2020) 72(10):1621–31. doi: 10.1002/art.41316
41. A phase 2b study to evaluate the efficacy and safety profile of PF-06651600 and PF-06700841 in active non-segmental vitiligo subjects (2018). Available at: https://clinicaltrials.gov/ct2/show/NCT03715829 .
42. Coffey G, Betz A, DeGuzman F, Pak Y, Inagaki M, Baker DC, et al. The novel kinase inhibitor PRT062070 (Cerdulatinib) demonstrates efficacy in models of autoimmunity and b-cell cancer. J Pharmacol Exp Ther (2014) 351(3):538–48. doi: 10.1124/jpet.114.218164
43. Regazzetti C, Joly F, Marty C, Rivier M, Mehul B, Reiniche P, et al. Transcriptional analysis of vitiligo skin reveals the alteration of WNT pathway: A promising target for repigmenting vitiligo patients. J Invest Dermatol (2015) 135(12):3105–14. doi: 10.1038/jid.2015.335
44. Harris JE. Melanocyte regeneration in vitiligo requires WNT beneath their wings. J Invest Dermatol (2015) 135(12):2921–3. doi: 10.1038/jid.2015.372
45. Yamada T, Hasegawa S, Inoue Y, Date Y, Yamamoto N, Mizutani H, et al. Wnt/beta-catenin and kit signaling sequentially regulate melanocyte stem cell differentiation in UVB-induced epidermal pigmentation. J Invest Dermatol (2013) 133(12):2753–62. doi: 10.1038/jid.2013.235
46. Han X, Chang Li, Qiu Z, Lin M, Wang Y, Liu D, et al. Micro-injury induces hair regeneration and vitiligo repigmentation through wnt/β-catenin pathway. Stem Cells Dev (2022) 31(5-6):111–8. doi: 10.1089/scd.2021.0276
47. Yang BJ, Fan SR, Zhang XF, Cai JY, Ruan T, Xiang ZR, et al. Design, synthesis and structure-activity relationship optimization of phenanthridine derivatives as new anti-vitiligo compounds. Bioorg Chem (2022) 119:105582. doi: 10.1016/j.bioorg.2021.105582
48. Baek D, Villen J, Shin C, Camargo FD, Gygi SP, Bartel DP. The impact of microRNAs on protein output. Nature (2008) 455(7209):64–71. doi: 10.1038/nature07242
49. Li L. The role of MicroRNAs in vitiligo: Regulators and therapeutic targets. Ann Dermatol (2020) 32(6):441–51. doi: 10.5021/ad.2020.32.6.441
50. Huo J, Liu T, Li F, Song X, Hou X. MicroRNA215p protects melanocytes via targeting STAT3 and modulating Treg/Teff balance to alleviate vitiligo. Mol Med Rep (2021) 23(1):51. doi: 10.3892/mmr.2020.11689
51. Vaish U, Kumar AA, Varshney S, Ghosh S, Sengupta S, Sood C, et al. Micro RNAs upregulated in vitiligo skin play an important role in its aetiopathogenesis by altering TRP1 expression and keratinocyte-melanocytes cross-talk. Sci Rep (2019) 9(1):10079. doi: 10.1038/s41598-019-46529-6
52. Zhao C, Wang D, Wang X, Mao Y, Xu Z, Sun Y, et al. Down-regulation of exosomal miR-200c derived from keratinocytes in vitiligo lesions suppresses melanogenesis. J Cell Mol Med (2020) 24(20):12164–75. doi: 10.1111/jcmm.15864
53. Li L, Xie Z, Qian X, Wang T, Jiang M, Qin J, et al. Identification of a potentially functional circRNA-miRNA-mRNA regulatory network in melanocytes for investigating pathogenesis of vitiligo. Front Genet (2021) 12:663091. doi: 10.3389/fgene.2021.663091
54. Shang Z, Li H. Altered expression of four miRNA (miR-1238-3p, miR-202-3p, miR-630 and miR-766-3p) and their potential targets in peripheral blood from vitiligo patients. J Dermatol (2017) 44(10):1138–44. doi: 10.1111/1346-8138.13886
55. Kwekkeboom RF, Lei Z, Doevendans PA, Musters RJ, Sluijter JP. Targeted delivery of miRNA therapeutics for cardiovascular diseases: opportunities and challenges. Clin Sci (Lond) (2014) 127(6):351–65. doi: 10.1042/CS20140005
56. Liu B, Zhang J, Yang S, Ji K, Liu X, Du B, et al. Effect of silencing microRNA-508 by STTM on melanogenesis in alpaca (Vicugna pacos). Gene (2018) 678:343–8. doi: 10.1016/j.gene.2018.08.011
57. Qi S, Liu B, Zhang J, Liu X, Dong C, Fan R. Knockdown of microRNA1435p by STTM technology affects eumelanin and pheomelanin production in melanocytes. Mol Med Rep (2019) 20(3):2649–56. doi: 10.3892/mmr.2019.10492
58. Su M, Miao F, Jiang S, Shi Y, Luo L, He X, et al. Role of the p53−TRPM1/miR−211−MMP9 axis in UVB−induced human melanocyte migration and its potential in repigmentation. Int J Mol Med (2020) 45(4):1017–26. doi: 10.3892/ijmm.2020.4478
59. Levings MK, Sangregorio R, Roncarolo MG. Human cd25(+)cd4(+) t regulatory cells suppress naive and memory T cell proliferation and can be expanded in vitro without loss of function. J Exp Med (2001) 193(11):1295–302.
PubMed Abstract | Google Scholar
60. Klarquist J, Denman CJ, Hernandez C, Wainwright DA, Strickland FM, Overbeck A, et al. Reduced skin homing by functional treg in vitiligo. Pigment Cell Melanoma Res (2010) 23(2):276–86. doi: 10.1111/j.1755-148X.2010.00688.x
61. Chatterjee S, Eby JM, Al-Khami AA, Soloshchenko M, Kang HK, Kaur N, et al. A quantitative increase in regulatory T cells controls development of vitiligo. J Invest Dermatol (2014) 134(5):1285–94. doi: 10.1038/jid.2013.540
62. Alzhrani A, Bottomley M, Wood K, Hester J, Issa F. Identification, selection, and expansion of non-gene modified alloantigen-reactive tregs for clinical therapeutic use. Cell Immunol (2020) 357:104214. doi: 10.1016/j.cellimm.2020.104214
63. Mukhatayev Z, Dellacecca ER, Cosgrove C, Shivde R, Jaishankar D, Pontarolo-Maag K, et al. Antigen specificity enhances disease control by tregs in vitiligo. Front Immunol (2020) 11:581433. doi: 10.3389/fimmu.2020.581433
64. Eby JM, Kang HK, Tully ST, Bindeman WE, Peiffer DS, Chatterjee S, et al. CCL22 to activate treg migration and suppress depigmentation in vitiligo. J Invest Dermatol (2015) 135(6):1574–80. doi: 10.1038/jid.2015.26
65. Zhang Q, Cui T, Chang Y, Zhang W, Li S, He Y, et al. HO-1 regulates the function of treg: Association with the immune intolerance in vitiligo. J Cell Mol Med (2018) 22(9):4335–43. doi: 10.1111/jcmm.13723
66. Dellacecca ER, Cosgrove C, Mukhatayev Z, Akhtar S, Engelhard VH, Rademaker AW, et al. Antibiotics drive microbial imbalance and vitiligo development in mice. J Invest Dermatol (2020) 140(3):676–687 e6. doi: 10.1016/j.jid.2019.08.435
67. Powell JD, Delgoffe GM. The mammalian target of rapamycin: linking T cell differentiation, function, and metabolism. Immunity (2010) 33(3):301–11. doi: 10.1016/j.immuni.2010.09.002
68. Daily topical rapamycin for vitiligo (2022). Available at: https://clinicaltrials.gov/ct2/show/NCT05342519 .
69. Zhang X, Liu D, He M, Lin M, Tu C, Zhang B. Polymeric nanoparticles containing rapamycin and autoantigen induce antigen-specific immunological tolerance for preventing vitiligo in mice. Hum Vaccin Immunother (2021) 17(7):1923–9. doi: 10.1080/21645515.2021.1872342
70. Giri PS, Bharti AH, Begum R, Dwivedi M. Calcium controlled NFATc1 activation enhances suppressive capacity of regulatory T cells isolated from generalized vitiligo patients. Immunology (2022). doi: 10.1111/imm.13538
71. Yang L, Wei Y, Sun Y, Shi W, Yang J, Zhu L, et al. Interferon-gamma inhibits melanogenesis and induces apoptosis in melanocytes: A pivotal role of CD8+ cytotoxic T lymphocytes in vitiligo. Acta Derm Venereol (2015) 95(6):664–70. doi: 10.2340/00015555-2080
72. Maouia A, Sormani L, Youssef M, Helal AN, Kassab A, Passeron T. Differential expression of CXCL9, CXCL10, and IFN-gamma in vitiligo and alopecia areata patients. Pigment Cell Melanoma Res (2017) 30(2):259–61. doi: 10.1111/pcmr.12559
73. Shi F, Erf GF. IFN-gamma, IL-21, and IL-10 co-expression in evolving autoimmune vitiligo lesions of smyth line chickens. J Invest Dermatol (2012) 132(3 Pt 1):642–9. doi: 10.1038/jid.2011.377
74. Skurkovich S, Skurkovich B, Kelly J. Anticytokine therapy, particularly anti-IFN-gamma, in Th1-mediated autoimmune diseases. Expert Rev Clin Immunol (2005) 1(1):11–25. doi: 10.1586/1744666X.1.1.11
75. Biswas KB, Takahashi A, Mizutani Y, Takayama S, Ishitsuka A, Yang L, et al. GPNMB is expressed in human epidermal keratinocytes but disappears in the vitiligo lesional skin. Sci Rep (2020) 10(1):4930. doi: 10.1038/s41598-020-61931-1
76. Boniface K, Jacquemin Clément, Darrigade A-S, Dessarthe Benoît, Martins C, Boukhedouni N, et al. Vitiligo skin is imprinted with resident memory CD8 T cells expressing CXCR3. J Invest Dermatol (2018) 138(2):355–64. doi: 10.1016/j.jid.2017.08.038
77. Mosenson JA, Zloza A, Klarquist J, Barfuss AJ, Guevara-Patino JA, Poole ICLe. HSP70i is a critical component of the immune response leading to vitiligo. Pigment Cell melanoma Res (2012) 25(1):88–98. doi: 10.1111/j.1755-148X.2011.00916.x
78. Doss RW, El-Rifaie AA, Abdel-Wahab AM, Gohary YM, Rashed LA. Heat shock protein-70 expression in vitiligo and its relation to the disease activity. Indian J Dermatol (2016) 61(4):408–12. doi: 10.4103/0019-5154.185704
79. Mosenson JA, Zloza A, Nieland JD, Garrett-Mayer E, Eby JM, Huelsmann EJ, et al. Mutant HSP70 reverses autoimmune depigmentation in vitiligo. Sci Transl Med (2013) 5(174):174ra28. doi: 10.1126/scitranslmed.3005127
80. Tokura Y, Phadungsaksawasdi P, Kurihara K, Fujiyama T, Honda T. Pathophysiology of skin resident memory T cells. Front Immunol (2020) 11:618897. doi: 10.3389/fimmu.2020.618897
81. Richmond JM, Strassner JP, Rashighi M, Agarwal P, Garg M, Essien KI, et al. Resident memory and recirculating memory T cells cooperate to maintain disease in a mouse model of vitiligo. J Invest Dermatol (2019) 139(4):769–78. doi: 10.1016/j.jid.2018.10.032
82. Chen X, Guo W, Chang Y, Chen J, Kang P, Yi X, et al. Oxidative stress-induced IL-15 trans-presentation in keratinocytes contributes to CD8(+) T cells activation via JAK-STAT pathway in vitiligo. Free Radic Biol Med (2019) 139:80–91. doi: 10.1016/j.freeradbiomed.2019.05.011
83. Atwa MA, Ali SMM, Youssef N, Mahmoud Marie RE. Elevated serum level of interleukin-15 in vitiligo patients and its correlation with disease severity but not activity. J Cosmet Dermatol (2021) 20(8):2640–4. doi: 10.1111/jocd.13908
84. Wang W, Chapman NM, Zhang B, Li M, Fan M, Laribee RN, et al. Upregulation of PD-L1 via HMGB1-activated IRF3 and NF-kappaB contributes to UV radiation-induced immune suppression. Cancer Res (2019) 79(11):2909–22. doi: 10.1158/0008-5472.CAN-18-3134
85. Kotobuki Y, Tanemura A, Yang L, Itoi S, Wataya-Kaneda M, Murota H, et al. Dysregulation of melanocyte function by Th17-related cytokines: significance of Th17 cell infiltration in autoimmune vitiligo vulgaris. Pigment Cell Melanoma Res (2012) 25(2):219–30. doi: 10.1111/j.1755-148X.2011.00945.x
86. Bassiouny DA, Shaker O. Role of interleukin-17 in the pathogenesis of vitiligo. Clin Exp Dermatol (2011) 36(3):292–7. doi: 10.1111/j.1365-2230.2010.03972.x
87. Vaccaro M, Cannavo SP, Imbesi S, Cristani M, Barbuzza O, Tigano V, et al. Increased serum levels of interleukin-23 circulating in patients with non-segmental generalized vitiligo. Int J Dermatol (2015) 54(6):672–4. doi: 10.1111/ijd.12392
88. Hegazy RA, Fawzy MM, Gawdat HI, Samir N, Rashed LA. T helper 17 and tregs: A novel proposed mechanism for NB-UVB in vitiligo. Exp Dermatol (2014) 23(4):283–6. doi: 10.1111/exd.12369
89. Speeckaert R, Mylle S, van Geel N. IL-17A is not a treatment target in progressive vitiligo. Pigment Cell melanoma Res (2019) 32(6):842–7. doi: 10.1111/pcmr.12789
90. Birol A, Kisa U, Kurtipek GS, Kara F, Kocak M, Erkek E, et al. Increased tumor necrosis factor alpha (TNF-alpha) and interleukin 1 alpha (IL1-alpha) levels in the lesional skin of patients with nonsegmental vitiligo. Int J Dermatol (2006) 45(8):992–3. doi: 10.1111/j.1365-4632.2006.02744.x
91. Chan AC, Carter PJ. Therapeutic antibodies for autoimmunity and inflammation. Nat Rev Immunol (2010) 10(5):301–16.
92. Horiuchi T. Transmembrane TNF-α: structure, function and interaction with anti-TNF agents. Rheumatology (2010) 49(7):1215–28.
93. Spencer-Green and G. Etanercept (Enbrel): update on therapeutic use. Ann Rheum Dis (2000) 59 Suppl 1(90001):i46–9.
94. Webb KC, Tung R, Winterfield LS, Gottlieb AB, Eby JM, Henning SW, et al. Tumour necrosis factor-α inhibition can stabilize disease in progressive vitiligo. Br J Dermatol (2015) 173(3):641–50. doi: 10.1111/bjd.14016
95. Bae JM, Kim M, Lee HH, Kim KJ, Shin H, Ju HJ, et al. Increased risk of vitiligo following anti-tumor necrosis factor therapy: A 10-year population-based cohort study. J Invest Dermatol (2018) 138(4):768–74. doi: 10.1016/j.jid.2017.11.012
96. Toussirot E, Salard D, Algros MP, Aubin F. [Occurrence of vitiligo in a patient with ankylosing spondylitis receiving adalimumab]. Ann Dermatol Venereol (2013) 140(12):801–2. doi: 10.1016/j.annder.2013.09.158
97. Jung JM, Lee YJ, Won CH, Chang SE, Lee MW, Choi JH, et al. Development of vitiligo during treatment with adalimumab: A plausible or paradoxical response?". Ann Dermatol (2015) 27(5):620–1. doi: 10.5021/ad.2015.27.5.620
98. Ryu TH, Lee DW, Choi JE, Ahn HH, Kye YC, Seo SH. A type II segmental vitiligo developed under infliximab treatment for ulcerative colitis. Ann Dermatol (2017) 29(6):826–7. doi: 10.5021/ad.2017.29.6.826
99. Smith DI, Heffernan MP. Vitiligo after the resolution of psoriatic plaques during treatment with adalimumab. J Am Acad Dermatol (2008) 58(2 Suppl):S50–2. doi: 10.1016/j.jaad.2006.05.035
100. Carvalho CLDB, Ortigosa LCM. Segmental vitiligo after infliximab use for rheumatoid arthritis–a case report. Anais bras dermatol (2014) 89(1):154–6. doi: 10.1590/abd1806-4841.20142887
101. Banchereau J, Rousset F. Human b lymphocytes: phenotype, proliferation, and differentiation. Adv Immunol (1992) 52:125–262. doi: 10.1016/s0065-2776(08)60876-7
102. Lin X, Tian H, Xianmin M. Possible roles of b lymphocyte activating factor of the tumour necrosis factor family in vitiligo autoimmunity. Med Hypotheses (2011) 76(3):339–42. doi: 10.1016/j.mehy.2010.10.034
103. Eisenberg R, Albert D. B-cell targeted therapies in rheumatoid arthritis and systemic lupus erythematosus. Nat Clin Pract Rheumatol (2006) 2(1):20–7. doi: 10.1038/ncprheum0042
104. Ioannou Y, Isenberg DA. Current concepts for the management of systemic lupus erythematosus in adults: A therapeutic challenge. Postgrad Med J (2002) 78(924):599–606. doi: 10.1136/pmj.78.924.599
105. Open-label pilot study of abatacept for the treatment of vitiligo . Available at: https://clinicaltrials.gov/ct2/show/NCT02281058 .
Keywords: vitiligo, targeted therapy, JAK inhibitors, biological, treatment, miRNA - microRNA, Treg
Citation: Feng Y and Lu Y (2022) Advances in vitiligo: Update on therapeutic targets. Front. Immunol. 13:986918. doi: 10.3389/fimmu.2022.986918
Received: 05 July 2022; Accepted: 04 August 2022; Published: 31 August 2022.
Reviewed by:
Copyright © 2022 Feng and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Lu, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

Mental wellbeing of patients who have Vitiligo: Tips, tricks, ways to motivate patients
V itiligo is a skin condition that causes white patches to appear on the skin due to loss of pigmentation and has a significant impact on the mental well-being of an affected individual because coming to terms with the changes in appearance, daily social ostracization, non-inclusion and the resulting sense of isolation can be emotionally draining for vitiligo patients. It is essential to acknowledge that these challenges stem from ignorance and stigma and that collective action is essential to remedy the situation.
In an interview with HT Lifestyle, Dr Vikram Vora, Medical Director at Indian Subcontinent – International SOS, shared, “There are numerous strategies to help promote self-acceptance and foster resilience in those impacted by this condition. However, these need to be credible, comprehensive and coordinated. Due to prior experiences, vitiligo sufferers may have a lesser degree of faith in people. Building trust and empathy with the affected individuals, demonstrating a genuine understanding of their experiences and acknowledging the emotional impact of living with vitiligo is a good start. Many vitiligo sufferers may have developed self-stigma about their condition and educating them is crucial to help manage their mental well-being effectively. Accurate information about causes, symptoms and available management options, along with clearing any misconceptions about the condition can alleviate their anxiety. With increased awareness and knowledge, these individuals can develop a better understanding of their condition and feel more in control.”
He highlighted, “As vitiligo impacts one’s self-esteem and body image, the development of a positive self-image can be achieved by helping them focus on their strengths and talents rather than solely their appearance. Psychologists suggest that self-compassion and reducing negative self-talk can assist in building a more realistic and positive self-perception. Acceptance of the condition can be achieved by encouraging overall well-being rather than a singular focus on physical appearance. Regular exercise, healthy eating, and engaging in hobbies or creative pursuits are self-care strategies that definitely help. Encouraging adoption of relaxation techniques and the practice of mindfulness reduces stress and anxiety and helps to challenge and counter negative thought patterns.”
According to him, having a robust support network comprising of family, friends, colleagues and managers provides a sense of belonging and support, through experience-sharing. Dr Vikram Vora revealed, “ This support can be in-person or even online via multiple available forums. Local support groups, counselling services in the community and EAPs at the workplace can also offer ways for patients to share their stories, gain insights, develop adaptive coping mechanisms and receive validation of their efforts. Empathy can create a safe space for expressing emotions and begin the healing process. Addressing the mental well-being challenges of those who have vitiligo requires an honest and empathetic approach. Keeping them away from normal social discourse and interactions is something that should not and cannot be accepted in today’s world. All sections of society need to work together, towards promoting a society that embraces diversity and inclusion. For those impacted, self-acceptance, resilience, and a positive self-image that ensures a fulfilling life, can only happen when we make this effort.”
Adding to the list of few simple methods to motivate patients with vitiligo, Dr Sushil Tahiliani, Consultant Dermatologist at PD Hinduja Hospital and Medical Research Centre in Mumbai, suggested, “Post-diagnosis, it is extremely important to normalise the disease as only the loss of colour from the body. It is crucial to establish that their bodies are healthy and because it does not affect their health, if they don't get bogged down psychologically, they can achieve goals which a lot of vitiligo patients have achieved in their life because they did not look at vitiligo as a very serious disease which should finish their aspersions and aspirations in life but rather continues to follow and achieve them. The second most important thing that I have definitely incorporated in my practice is examining the patients without gloves if not required. By touching the lesions and trying to win their confidence and reassure them about the non-contagious nature of this condition.”
He explained, “By also sharing statistics and success stories of patients being affected by vitiligo would create a sense of confidence in the patients. Translating that into figures to tell them that at least 28 million Indians must be having vitiligo - would help in reducing the feeling of being the odd one out. Additionally, inform them about the modern ways of treating vitiligo and give them guarded optimism because in good 60% odd cases, you can re-pigment them. While they are being re-pigmented, they are also given options of using camouflage creams on the open areas of the body, because it goes a long way in building confidence because when they look at the world, they can discuss what they've gone to discuss, they can study what they're going to study and the topic doesn't get diverted to vitiligo, which can be an irritant and harm the self-confidence.”
He concluded, “While also highlighting to them that in case the medicines don't work in some of the stable vitiligo cases, especially the segmental vitiligo cases, we have surgical options which work very well. And in those cases where everything fails, and they got two colours, and about 40, or 50% of the body turns white, I give them the option of removing the balance pigmentation to give them a uniform colour. Added-on tips would include protecting their skin against excessive sun exposure because they don't have melanin to protect their skin, and thus will be at a higher risk of skin ageing. The challenge is bigger if we have a child as a patient because we had to do hand holding and counselling for the parents first so that they don't cry in front of the child and they don't have drop jaws and sad faces. It's very important for the child to have encouragement and support from the parents and for the parents to keep the child happy and give the child a lot of confidence that does half the job done. The more you normalise the disease, the better it would be for those affected.”
Read more news like this on HindustanTimes.com

- General Dermatology
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Psoriatic Arthritis
- Atopic Dermatitis
- Skin Cancer
- Hidradenitis Suppurativa
- Pigmentary Disorders
- Pediatric Dermatology
- Practice Management
Striving for Melanoma Advancements With the Melanoma Research Alliance
Marc Hurlbert, PhD, discusses how the Melanoma Research Alliance works with dermatology clinicians to provide fundings and resources for melanoma research.
“The Melanoma Research Alliance works closely with dermatologists, oncologists, surgeons, and other experts to advance melanoma research. For dermatologists specifically, we have a few award mechanisms where we support advanced research that dermatologists are conducting... Starting this year, we have a new award mechanism called the Dermatology Career Development award, which is to help new dermatologists as they enter their first faculty appointment,” said Marc Hurlbert, PhD, the chief executive officer of the Melanoma Research Alliance.
Hurlbert recently spoke to Dermatology Times to dive into the Melanoma Research Alliance , its mission, and how it supports dermatology clinicians with funding and resources for melanoma research.
The Melanoma Research Alliance was founded in 2007 and is the world’s largest non-profit funder of melanoma research. Overall, the organization has invested over $150 million through 415 grant awards toward scientific research. 1
May is Melanoma and Skin Cancer Awareness Month and an important time for dermatology clinicians to promote skin cancer education and prevention, emphasize the importance of regular skin checks for their patients, and share their latest updates in melanoma research.
“The Melanoma Research Alliance has useful information for anyone about preventing and detecting melanoma. But more specifically, we also have a deep interest in rare melanoma subtypes which could affect all of your populations from any background, race, or ethnicity. We have some literature around acral melanoma and mucosal melanoma, which are often more common in populations from skin of color communities,” said Hurlbert.

Watskin clothing | Image credit: © Watskin

The Melanoma Research Alliance has partners in the community and large academic/medical center levels to advance melanoma research. Hurlbert encourages all dermatology clinicians to reach out to the Melanoma Research Alliance to work toward the common goal to end melanoma.
Hurlbert mentioned that one of the Melanoma Research Alliance’s important partners is the Watskin UPF clothing brand . Watskin’s outdoor clothing is designed with UPF 50+ material to block harmful UV rays. For patients who love the outdoors but need increased sun protection, dermatology clinicians can recommend sun-protective clothing.
Marc Hurlbert, PhD : Hi, I'm Marc Hurlburt, the chief executive officer of the Melanoma Research Alliance.
Dermatology Times : Can you please provide an overview of the Melanoma Research Alliance and its goals?
Hurlbert: The Melanoma Research Alliance is the world's largest nonprofit funder of melanoma research. Our mission is to end melanoma by advancing the world's most promising research. The Melanoma Research Alliance, or MRA, for short, has invested more than $160 million in melanoma researcher since we were founded just more than 15 years ago.
Dermatology Times : What is your role with the Melanoma Research Alliance?
Hurlbert : At MRA, I serve as the chief executive officer, however, my background is as a scientist by training. I was MRA's chief science officer for about 5 years and just recently stepped up to become CEO. In my role, I get to work very closely with patients and families touched by melanoma, as well as dermatologists, oncologists, and laboratory researchers studying melanoma all over the world trying to advance new treatments and new ways to detect and prevent melanoma.
Dermatology Times : How does the Melanoma Research Alliance support dermatology clinicians regarding providing patient information or educational resources to share?
Hurlbert : The Melanoma Research Alliance works closely with dermatologists, oncologists, surgeons, and other experts to advance melanoma research. For dermatologists specifically, we have a few award mechanisms where we support advanced research that dermatologists are conducting. We recently ended a program that we had where we funded dermatology fellowships. These were derm residents in their final year or 2 of dermatology residency. We invested in 45 of those since 2019. And starting this year, we have a new award mechanism called the Dermatology Career Development award, which is to help new dermatologists as they enter their first faculty appointment. Also, MRA has a lot of educational resources. The audience can visit us at Curemelanoma.org and download or contact us to get any flyers or informational brochures. The Melanoma Research Alliance has useful information for anyone about preventing and detecting melanoma. But more specifically, we also have a deep interest in rare melanoma subtypes which could affect all of your populations from any background, race, or ethnicity. And specifically, we have some literature around acral melanoma and mucosal melanoma, which are often more common in populations from skin of color communities.
Dermatology Times : Can dermatology clinicians work with or be involved with the Melanoma Research Alliance?
Hurlbert : We encourage all dermatologists to reach out to us. We love to partner, whether you're at a big academic center or community derm practice. We love to be engaged with dermatologists. The Melanoma Research Alliance partners both at the community level as well as at the large city academic medical center level to help advance melanoma research. So, reach out to us, you can reach out to myself or any of the staff at Curemelanoma.org , which has all of our contact information, email, cell phones, and we'd love to partner with you if you're interested in helping advance melanoma research.
Dermatology Times : What does Melanoma and Skin Cancer Awareness Month mean to the Melanoma Research Alliance?
Hurlbert : May is Skin Cancer and Melanoma Awareness Month. And this is really critical we believe at the Melanoma Research Alliance, because it's sort of the first month when people really begin to think of transitioning from spring to summer, people might be planning their upcoming Memorial Day or summer vacations. And it's a great month to remind people to wear sunscreen and UPF protective clothing year-round, but especially we'd like to remind people during the month of May. For us at MRA, Melanoma Awareness Month is a critical time to raise visibility about the importance of sun protection. Melanoma is a relatively rare skin cancer, only about 100,000 cases in the United States each year. However, it is the deadliest form of skin cancer with about 8000 people that will die from the disease this year. So it's important as we enter the month of May and throughout the year to practice sun safety and I'm happy to share some tips.
Dermatology Times : What challenges do you still see in melanoma and skin cancer education, prevention, or treatment?
Hurlbert : The biggest challenges that we see in melanoma prevention as well as treatment are a few fold. One, a lot of people think of melanoma as just a simple skin cancer, you cut it out and you're cured. And sadly, that's not the case for 1000s and 1000s of people each year. They need surgery as well as follow-up treatments. We've made great progress, in part with MRA research funding. There have been 17 new drugs approved in the last roughly decade and a half to help treat advanced cases of melanoma. And this is turning patients' stories with an advanced melanoma from a story of struggle and not having a good outcome, to potentially a story of survival. But even these latest treatments only cure about half of patients with advanced melanoma. So, we still have a lot of work to do. And the MRA is committed to doubling down and investing in more research until we ultimately can cure and prevent melanoma.
Dermatology Times : What do you want dermatology clinicians to know about the Watskin sun protection clothing brand?
Hurlbert : At the MRA, we believe that everyone should practice sun safety throughout the year. We believe that includes starting with sunblock. You should always look for broad-spectrum sun protection that protects against UVA and UVB radiation. We believe in recommending an SPF factor of 30 or higher. I personally use SPF 50 every day. If I'm going to be outdoors all day, then I'll use a mineral sunscreen which has ingredients like zinc oxide on my face and exposed skin. And if I'm going to be indoors, I'll use more of a chemical sunscreen, one that rubs in a little bit nicer and doesn't leave a white cast so much if I'm indoors. But every day you need to apply it and reapply it every 2 hours or so. We believe that Watskin and ultraviolet protective clothing (UPF) is really critical in our fight at preventing more skin cancers and more melanomas. Watskin is an amazing brand. The founder, Lois Robbins, had her own diagnosis with skin cancer and then launched a brand in 2018, after her own diagnosis and really trying to understand how to implement the most sun-protective clothing in her day-to-day life.
We find Watskin is one of our favorite partners; it's really stylish and if you'll have it, a sexy brand, great swimwear and sun safety clothing for women and children. Just this spring they launched their latest collection for moms and daughters. So, if you haven't visited and checked it out, I encourage everyone to visit it. It really is an amazing stylish UPF clothing line that you can wear year-round. But importantly we like to encourage people to use it when they're going outdoors during May and during the summer months but it's a great brand whether you're skiing in the winter, or whether you're coming out of the pool or the beach in the summer. The Watskin is a really fabulous up if clothing brand that my own family members are our customers and an aunt and a niece who are avid outdoors people down in Florida love it and wear it wear routinely throughout the year.
Dermatology Times : Do you have any closing thoughts regarding Melanoma and Skin Cancer Awareness Month?
Hurlbert : I think in closing I really would like to remind the audience that everyone can get melanoma, no matter. your race or ethnicity or background. Yes, having paler skin and red hair and blue eyes like I have you know is a risk factor for melanoma among lighter skin populations, but anyone, any race or ethnicity, can get melanoma. Specifically for their dermatologists please be mindful of acral melanoma, acral lentiginous, which can occur on the palms of the hands or the soul that feet, and these are proportionately more common in populations of color. We see these rare melanomas more often in patients with Black, Hispanic, or Asian ancestry. And so just encourage and remind the dermatology audience that any patient can get melanoma and to do the proper skin checks
[Transcript lightly edited for space and clarity]
- About MRA. The Melanoma Research Alliance. Accessed May 6, 2024. https://www.curemelanoma.org/mra-overview/mra-overview

The Cutaneous Connection: A Reminder of Patient Impact

Skin Cancer Awareness Month: Resources to Share With Your Patients

The Cutaneous Connection: Make Data-Driven Decisions For Personalized AD Treatment

VYNE Therapeutics Provides Updates on VYN201 for Nonsegmental Vitiligo and VYN202 for Inflammatory Diseases

A Combination of Surgical and Non-Surgical Approaches May Prove Beneficial in Treatment of Facial Acne Scars
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

IMAGES
VIDEO
COMMENTS
On July 18, the U.S. Food and Drug Administration (FDA) approved ruxolitinib ( Opzelura) cream 1.5 percent as a treatment for the most common form of vitiligo, according to a statement by Incyte ...
Vitiligo Advancements and Discoveries. There has been an increase in the amount of research being undertaken in vitiligo over recent years and dermatologists have an improved understanding of the natural history and different types of the condition. Here you will find a brief summary of research into several areas, with references to the ...
1. Introduction. Vitiligo is the most common disorder of depigmentation, and in 2012 its worldwide prevalence ranged from 0.06-2.28% (1,2).It is characterized by the absence of pigment in the skin, secondary to the loss of melanocytes (1,3).Melanocytes are found in several tissues in the skin, hair follicles, eyes, inner ear, bones, heart and brain ().
Vitiligo is a chronic autoimmune disease that results in skin depigmentation 1,2 and reduced quality of life. 3,4 Quality-of-life burden is affected by a high prevalence of psychosocial coexisting ...
Vitiligo affects 0.5 to 2% of the population worldwide. This chronic autoimmune disease manifests as pale skin patches, caused by local death of pigment-producing melanocytes. The extent and percei...
Latest Research and Reviews. ... Vitiligo is an autoimmune condition that results in skin depigmentation due to melanocyte loss, but the root causes are not well understood. Here they identify ...
The U.S. Food and Drug Administration has approved Opzelura (ruxolitinib) as the first topical treatment for vitiligo. The 1.5 percent cream is approved for continuous topical use twice daily to ...
Vitiligo is an acquired depigmentation of the skin, which affects approximately 1% of the population worldwide. The condition can profoundly affect the wellbeing and the social, sexual, and professional lives of affected individuals and thus induces a strong therapeutic demand.1 Actual treatments rely on the use of topical steroids or topical calcineurin inhibitors, and are better combined ...
Phase 3 vitiligo clinical trial results to test topical ruxolitinib as a new treatment. I've recently received many requests for an update on the new ruxolitinib cream to treat vitiligo. To remind everyone, we initially reported that oral ruxolitinib, a Janus Kinase inhibitor initially approved to treat a type of blood cancer, reversed ...
Temprian Therapeutics is a spin-off from Northwestern University in Chicago, Illinois. Vitiligo is an autoimmune disease that affects an estimated 50 million people worldwide. It isn't life ...
More research is warranted to be initiated for further definition of the role that IFN-γ plays in vitiligo and to examine whether IFN-γ neutralization would be more viable in reversing skin depigmentation. ... There are also reports of ustekinumab-induced new-onset vitiligo and alopecia areata. The above studies showed IL-17/23 signal may not ...
Vitiligo is a multifactorial disease characterized by the loss of skin pigment, which results in achromic macules and patches. ... Updates and new medical treatments for vitiligo (Review) Exp Ther Med. 2021 Aug;22(2) :797. ... 3 Department of Research, Faculty of Medicine Saltillo Unit, Universidad Autónoma de Coahuila, ...
Vitiligo is a common autoimmune-related depigmenting disease resulting from epidermal melanocyte loss. It is characterized by white patches in the skin or mucous, affecting around 0.1-2% of the ... Treatment update for vitiligo based on autoimmune inhibition and melanocyte protection: Expert Opinion on Therapeutic Targets: Vol 27 , No 3 - Get ...
Vitiligo is a chronic pigmentary disease that affects approximately 1% of the world's population. This dermatological condition affects skin and hair and manifests itself by characteristic white macules and patches. The disease can be segmental, localized in one area of the body, or generalized, affecting a broader area.
This study highlights the need for standardised epidemiological data collection globally to inform public health policies and improve vitiligo diagnosis and management. Emphasis on the impact on individuals with darker skin tones is crucial to reducing stigma and improving quality of life. Furthermore, our study highlights the need to conduct more research in regions and populations that have ...
The autoimmune condition vitiligo, characterized by skin depigmentation, presents challenges for effective treatment design, with Janus kinase (JAK) inhibitors and other repurposed drugs offering a promising strategy for symptom management. This review explores advantages and shortcomings of current therapies, while presenting the urgent need for further innovative approaches. We emphasize the ...
Lego Launches New Vitiligo Minifigure; Maybe it's NOT vitiligo! New NIH Grant Awarded to Create the Vitiligo Center of Research Translation; Opzelura, the first FDA-approved drug to treat vitiligo! Our new research study in Science Translational Medicine describes a new treatment that may have long-term benefit in vitiligo patients; Patterns ...
Guest Writer for Treatments and Research. Ritlecitinib (under the commercial name LITFULO by Pfizer) is an anti-inflammatory and immunosuppressive drug that was recently approved for treatment of severe alopecia areata in the USA and Japan. The drug is being tested for treatment of vitiligo, ulcerative colitis, and Crohn's disease, all of ...
Abigail Hurrell. We're delighted to announce that the videos of talks from our 2022 Research Summit are now available to view on our YouTube Channel .This was the biggest event of the vitiligo calendar, and a fantastic opportunity to hear from leading experts who have extensive knowledge in vitiligo research, current & future treatment options.
Vitiligo, a common depigmenting cutaneous condition, is thought to affect 0.5%-2% of the world's population. During this condition, melanocytes are selectively lost, resulting in non-scaly, chalky-white macules. Achromic macules and patches are side effects of the multifaceted disease vitiligo, defined as the absence of epidermal pigmentation.
The Vitiligo Research Foundation. Firmly committed to curing vitiligo, the VR Foundation is a 501(c)3 non-profit, focused research organization. ... Get insights on the latest research, natural remedies, nutrition, and mental health, all in user-friendly language. Discover the World's First AI-Guide on Vitiligo, available in 50+ languages!
This strategy could also be adapted to treat other autoimmune skin diseases such as vitiligo, atopic dermatitis, and psoriasis, the researchers say. ... a principal research scientist in MIT's Institute for Medical Engineering and Science, an associate professor of medicine at Harvard Medical School and Brigham and Women's Hospital, and an ...
Background/Objectives: There is currently no guidance on how to interpret the global degrees of activity (worsening) and repigmentation (improvement) in vitiligo. Stratification into global degrees can be completed for static evaluations (e.g., visible disease activity signs) and dynamic assessments (e.g., evolution over time). For the latter, the Vitiligo Disease Activity Score (VDAS15&60 ...
Among the new approaches being developed, the strategy of targeting the IFN-γ-CXCL9/10-CXCR3 axis has been clinically tested. OPZELURA has been indicated for the topical treatment of nonsegmental vitiligo in adult and pediatric patients 12 years of age and older. MiRNA-based therapeutics are also in development.
Vitiligo is associated with reduced risks of BCC and SCC, as well as internal malignancies, which are consistent across different subgroups of patients, including male gender, ages more than 40 years, and those receiving long-term systemic disease-modifying antirheumatic drugs and phototherapies.
Adding to the list of few simple methods to motivate patients with vitiligo, Dr Sushil Tahiliani, Consultant Dermatologist at PD Hinduja Hospital and Medical Research Centre in Mumbai, suggested ...
Introduction. Vitiligo is a chronic inflammatory autoimmune disease that results in skin depigmentation due to the loss of melanocytes [1-3].Lesions can appear at any age, but onset usually occurs at ≤ 30 years of age [2, 4, 5].Global prevalence is approximately 0.5-2.0% and varies geographically [].Similar prevalence rates have been reported for adult populations as well as children and ...
Research and development expenses decreased by $0.3 million to $1.2 million for the three months ended March 31, 2024 compared to $1.5 million for the same period last year primarily due to ...
Hurlbert: The Melanoma Research Alliance is the world's largest nonprofit funder of melanoma research. Our mission is to end melanoma by advancing the world's most promising research. The Melanoma Research Alliance, or MRA, for short, has invested more than $160 million in melanoma researcher since we were founded just more than 15 years ago.
A New Era of Vitiligo Research and Treatment. This is a very exciting phase of vitiligo research in which vitiligo is being tackled by multipronged attacks in the form of advancement in basic research, genetics and treatment including surgical management. In order to achieve the ultimate goal of total stability and complete repigmentation ...