The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

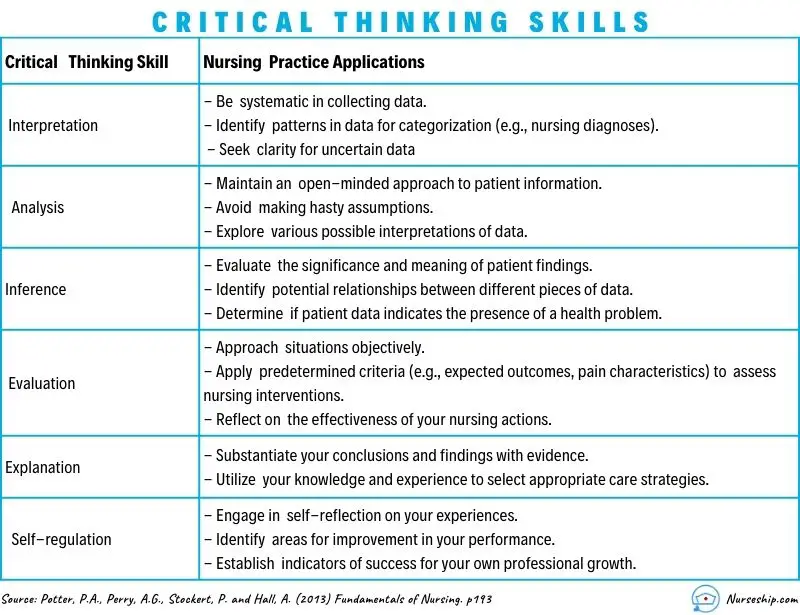
Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.

How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.
What Is Critical Thinking In Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?


An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Developing critical thinking skills for delivering optimal care
Scott IA, Hubbard RE, Crock C, et al. Developing critical thinking skills for delivering optimal care. Intern Med J. 2021;51(4):488-493. doi: 10.1111/imj.15272
Sound critical thinking skills can help clinicians avoid cognitive biases and diagnostic errors. This article describes three critical thinking skills essential to effective clinical care – clinical reasoning, evidence-informed decision-making, and systems thinking – and approaches to develop these skills during clinician training.
Medication use and cognitive impairment among residents of aged care facilities. June 23, 2021
COVID-19 pandemic and the tension between the need to act and the need to know. October 14, 2020
Choosing wisely in clinical practice: embracing critical thinking, striving for safer care. April 6, 2022
Scoping review of studies evaluating frailty and its association with medication harm. June 22, 2022
Countering cognitive biases in minimising low value care. June 7, 2017
'More than words' - interpersonal communication, cognitive bias and diagnostic errors. August 11, 2021
A partially structured postoperative handoff protocol improves communication in 2 mixed surgical intensive care units: findings from the Handoffs and Transitions in Critical Care (HATRICC) prospective cohort study. February 6, 2019
Enabling a learning healthcare system with automated computer protocols that produce replicable and personalized clinician actions. August 4, 2021
Analysis of lawsuits related to diagnostic errors from point-of-care ultrasound in internal medicine, paediatrics, family medicine and critical care in the USA. June 24, 2020
Developing and aligning a safety event taxonomy for inpatient psychiatry. July 13, 2022
Changes in unprofessional behaviour, teamwork, and co-operation among hospital staff during the COVID-19 pandemic. September 28, 2022
Pharmacists reducing medication risk in medical outpatient clinics: a retrospective study of 18 clinics. March 8, 2023
Prevalence and causes of diagnostic errors in hospitalized patients under investigation for COVID-19. April 12, 2023
Barriers to accessing nighttime supervisors: a national survey of internal medicine residents. March 17, 2021
Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016 March 3, 2017
Seroprevalence of SARS-CoV-2 among frontline health care personnel in a multistate hospital network--13 academic medical centers, April-June 2020. September 23, 2020
Transforming the medication regimen review process using telemedicine to prevent adverse events. December 16, 2020
The MedSafer study-electronic decision support for deprescribing in hospitalized older adults: a cluster randomized clinical trial. February 2, 2022
Perceived patient safety culture in a critical care transport program. July 31, 2013
Video-based communication assessment of physician error disclosure skills by crowdsourced laypeople and patient advocates who experienced medical harm: reliability assessment with generalizability theory. May 18, 2022
Implementation of the I-PASS handoff program in diverse clinical environments: a multicenter prospective effectiveness implementation study. November 16, 2022
Patient harm from cardiovascular medications. August 25, 2021
Delays in diagnosis, treatment, and surgery: root causes, actions taken, and recommendations for healthcare improvement. June 1, 2022
Influence of opioid prescription policy on overdoses and related adverse effects in a primary care population. May 19, 2021
Evaluation of a second victim peer support program on perceptions of second victim experiences and supportive resources in pediatric clinical specialties using the second victim experience and support tool (SVEST). November 3, 2021
Diagnostic errors in hospitalized adults who died or were transferred to intensive care. January 17, 2024
Estimation of breast cancer overdiagnosis in a U.S. breast screening cohort. March 16, 2022
Multiple meanings of resilience: health professionals' experiences of a dual element training intervention designed to help them prepare for coping with error. March 31, 2021
Care coordination strategies and barriers during medication safety incidents: a qualitative, cognitive task analysis. March 10, 2021
TRIAD IX: can a patient testimonial safely help ensure prehospital appropriate critical versus end-of-life care? September 15, 2021
An act of performance: exploring residents' decision-making processes to seek help. April 14, 2021
Preventing home medication administration errors. March 14, 2022
A randomized trial of a multifactorial strategy to prevent serious fall injuries. July 29, 2020
Clinical predictors for unsafe direct discharge home patients from intensive care units. October 21, 2020
Association between limiting the number of open records in a tele-critical care setting and retract-reorder errors. July 21, 2021
Standardized assessment of medication reconciliation in post-acute care. April 27, 2022
Estimating the economic cost of nurse sensitive adverse events amongst patients in medical and surgical settings. June 16, 2021
Survey of nurses' experiences applying The Joint Commission's medication management titration standards. November 3, 2021
Effectiveness of acute care remote triage systems: a systematic review. February 5, 2020
Physician task load and the risk of burnout among US physicians in a national survey. December 2, 2020
Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. September 23, 2020
Patient and physician perspectives of deprescribing potentially inappropriate medications in older adults with a history of falls: a qualitative study. May 5, 2021
We asked the experts: the WHO Surgical Safety Checklist and the COVID-19 pandemic: recommendations for content and implementation adaptations. March 17, 2021
Association between surgeon technical skills and patient outcomes. September 9, 2020
Influence of psychological safety and organizational support on the impact of humiliation on trainee well-being. June 8, 2022
Developing the Safer Dx Checklist of Ten Safety Recommendations for Health Care Organizations to address diagnostic errors. October 12, 2022
Comparison of health care worker satisfaction before vs after implementation of a communication and optimal resolution program in acute care hospitals. April 5, 2023
Not overstepping professional boundaries: the challenging role of nurses in simulated error disclosures. September 21, 2011
Temporal associations between EHR-derived workload, burnout, and errors: a prospective cohort study. July 20, 2022
Adherence to national guidelines for timeliness of test results communication to patients in the Veterans Affairs health care system. May 4, 2022
Deferral of care for serious non-COVID-19 conditions: a hidden harm of COVID-19. November 18, 2020
An observational study of postoperative handoff standardization failures. June 23, 2021
Content analysis of patient safety incident reports for older adult patient transfers, handovers, and discharges: do they serve organizations, staff, or patients? January 8, 2020
Exploring the impact of employee engagement and patient safety. September 14, 2022
Deprescribing for community-dwelling older adults: a systematic review and meta-analysis. September 16, 2020
The abrupt expansion of ambulatory telemedicine: implications for patient safety. February 9, 2022
Nurse's Achilles Heel: using big data to determine workload factors that impact near misses. April 14, 2021
A diagnostic time-out to improve differential diagnosis in pediatric abdominal pain. July 14, 2021
What safety events are reported for ambulatory care? Analysis of incident reports from a patient safety organization. October 21, 2020
Expert consensus on currently accepted measures of harm. September 9, 2020
The July Effect in podiatric medicine and surgery residency. July 14, 2021
The calm before the storm: utilizing in situ simulation to evaluate for preparedness of an alternative care hospital during COVID-19 pandemic. June 2, 2021
Missed nursing care in the critical care unit, before and during the COVID-19 pandemic: a comparative cross-sectional study. June 22, 2022
The association between nurse staffing and omissions in nursing care: a systematic review. July 11, 2018
Creating a learning health system for improving diagnostic safety: pragmatic insights from US health care organizations. June 22, 2022
Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. June 8, 2016
Impact of the initial response to COVID-19 on long-term care for people with intellectual disability: an interrupted time series analysis of incident reports. October 14, 2020
Pediatric surgical errors: a systematic scoping review. July 20, 2022
Racial bias in pulse oximetry measurement. December 20, 2020
Accuracy of practitioner estimates of probability of diagnosis before and after testing. May 5, 2021
Recommendations for the safe, effective use of adaptive CDS in the US healthcare system: an AMIA position paper. April 21, 2021
Impact of interoperability of smart infusion pumps and an electronic medical record in critical care. September 23, 2020
Decreased incidence of cesarean surgical site infection rate with hospital-wide perioperative bundle. September 29, 2021
Association of diagnostic stewardship for blood cultures in critically ill children with culture rates, antibiotic use, and patient outcomes: results of the Bright STAR Collaborative. May 18, 2022
Second victim experiences of nurses in obstetrics and gynaecology: a Second Victim Experience and Support Tool Survey December 23, 2020
Understanding the second victim experience among multidisciplinary providers in obstetrics and gynecology. May 19, 2021
eSIMPLER: a dynamic, electronic health record-integrated checklist for clinical decision support during PICU daily rounds. June 16, 2021
Treatment patterns and clinical outcomes after the introduction of the Medicare Sepsis Performance Measure (SEP-1). May 5, 2021
Organizational safety climate and job enjoyment in hospital surgical teams with and without crew resource management training, January 26, 2022
Evaluation of effectiveness and safety of pharmacist independent prescribers in care homes: cluster randomised controlled trial. March 1, 2023
The Critical Care Safety Study: the incidence and nature of adverse events and serious medical errors in intensive care. August 24, 2005
Safety II behavior in a pediatric intensive care unit. August 1, 2018
Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. October 21, 2020
The working hours of hospital staff nurses and patient safety. January 9, 2005
Effects of tall man lettering on the visual behaviour of critical care nurses while identifying syringe drug labels: a randomised in situ simulation. April 20, 2022
Family Input for Quality and Safety (FIQS): using mobile technology for in-hospital reporting from families and patients. March 2, 2022
Bundle interventions including nontechnical skills for surgeons can reduce operative time and improve patient safety. December 9, 2020
COVID-19: an emerging threat to antibiotic stewardship in the emergency department. October 21, 2020
Improving self-reported empathy and communication skills through harm in healthcare response training. January 26, 2022
Association between in-clinic opioid administration and discharge opioid prescription in urgent care: a retrospective cohort study. February 17, 2021
Predicting avoidable hospital events in Maryland. December 1, 2021
Specificity of computerized physician order entry has a significant effect on the efficiency of workflow for critically ill patients. April 21, 2005
Why do hospital prescribers continue antibiotics when it is safe to stop? Results of a choice experiment survey. September 2, 2020
COVID-19: patient safety and quality improvement skills to deploy during the surge. June 24, 2020
Patient safety skills in primary care: a national survey of GP educators. February 4, 2015
Implementing human factors in anaesthesia: guidance for clinicians, departments and hospitals: Guidelines from the Difficult Airway Society and the Association of Anaesthetists. March 1, 2023
Can an electronic prescribing system detect doctors who are more likely to make a serious prescribing error? June 8, 2011
Training in safe opioid prescribing and treatment of opioid use disorder in internal medicine residencies: a national survey of program directors. October 12, 2022
Diagnostic discordance, health information exchange, and inter-hospital transfer outcomes: a population study. June 20, 2018
Systematic review and meta-analysis of interventions for operating room to intensive care unit handoffs. March 10, 2021
Racial and ethnic harm in patient care is a patient safety issue. May 15, 2024
All in Her Head. The Truth and Lies Early Medicine Taught Us About Women's Bodies and Why It Matters Today. March 20, 2024
The racial disparities in maternal mortality and impact of structural racism and implicit racial bias on pregnant Black women: a review of the literature. December 6, 2023
A scoping review exploring the confidence of healthcare professionals in assessing all skin tones. October 4, 2023
Patient safety in palliative care at the end of life from the perspective of complex thinking. August 16, 2023
Only 1 in 5 people with opioid addiction get the medications to treat it, study finds. August 16, 2023
Factors influencing in-hospital prescribing errors: a systematic review. July 19, 2023
Introducing second-year medical students to diagnostic reasoning concepts and skills via a virtual curriculum. June 28, 2023
Context matters: toward a multilevel perspective on context in clinical reasoning and error. June 21, 2023
The good, the bad, and the ugly: operative staff perspectives of surgeon coping with intraoperative errors. June 14, 2023
Explicitly addressing implicit bias on inpatient rounds: student and faculty reflections. June 7, 2023
The time is now: addressing implicit bias in obstetrics and gynecology education. May 17, 2023
Listen to the whispers before they become screams: addressing Black maternal morbidity and mortality in the United States. May 3, 2023
Annual Perspective
Formalizing the hidden curriculum of performance enhancing errors. March 22, 2023
Implicit racial bias, health care provider attitudes, and perceptions of health care quality among African American college students in Georgia, USA. January 18, 2023
Structural racism and impact on sickle cell disease: sickle cell lives matter. January 11, 2023
The REPAIR Project: a prospectus for change toward racial justice in medical education and health sciences research: REPAIR project steering committee. January 11, 2023
Using the Assessment of Reasoning Tool to facilitate feedback about diagnostic reasoning. January 11, 2023
Exploring the intersection of structural racism and ageism in healthcare. December 7, 2022
Calibrate Dx: A Resource to Improve Diagnostic Decisions. October 19, 2022
Improved Diagnostic Accuracy Through Probability-Based Diagnosis. September 28, 2022
Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. September 21, 2022
A state-of-the-art review of speaking up in healthcare. August 24, 2022
Skin cancer is a risk no matter the skin tone. But it may be overlooked in people with dark skin. August 17, 2022
Oxford Professional Practice: Handbook of Patient Safety. July 27, 2022
Narrowing the mindware gap in medicine. July 20, 2022
From principles to practice: embedding clinical reasoning as a longitudinal curriculum theme in a medical school programme. June 15, 2022
A call to action: next steps to advance diagnosis education in the health professions. June 8, 2022
Does a suggested diagnosis in a general practitioners' referral question impact diagnostic reasoning: an experimental study. April 27, 2022

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
Critical thinking in nursing clinical practice, education and research: From attitudes to virtue
Affiliations.
- 1 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, Consolidated Research Group Quantitative Psychology (2017-SGR-269), University of Barcelona, Barcelona, Spain.
- 2 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, Consolidated Research Group on Gender, Identity and Diversity (2017-SGR-1091), University of Barcelona, Barcelona, Spain.
- 3 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, University of Barcelona, Barcelona, Spain.
- 4 Multidisciplinary Nursing Research Group, Vall d'Hebron Research Institute (VHIR), Vall d'Hebron Hospital, Barcelona, Spain.
- PMID: 33029860
- DOI: 10.1111/nup.12332
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing profession. In this context, the ethics of virtue is a theoretical framework that becomes essential for analyse the critical thinking concept in nursing care and nursing science. Because the ethics of virtue consider how cultivating virtues are necessary to understand and justify the decisions and guide the actions. Based on selective analysis of the descriptive and empirical literature that addresses conceptual review of critical thinking, we conducted an analysis of this topic in the settings of clinical practice, training and research from the virtue ethical framework. Following JBI critical appraisal checklist for text and opinion papers, we argue the need for critical thinking as an essential element for true excellence in care and that it should be encouraged among professionals. The importance of developing critical thinking skills in education is well substantiated; however, greater efforts are required to implement educational strategies directed at developing critical thinking in students and professionals undergoing training, along with measures that demonstrate their success. Lastly, we show that critical thinking constitutes a fundamental component in the research process, and can improve research competencies in nursing. We conclude that future research and actions must go further in the search for new evidence and open new horizons, to ensure a positive effect on clinical practice, patient health, student education and the growth of nursing science.
Keywords: critical thinking; critical thinking attitudes; nurse education; nursing care; nursing research.
© 2020 John Wiley & Sons Ltd.
- Attitude of Health Personnel*
- Education, Nursing / methods
- Nursing Process
- Nursing Research / methods
Grants and funding
- PREI-19-007-B/School of Nursing. Faculty of Medicine and Health Sciences. University of Barcelona
Critical Thinking in Medicine and Health
- First Online: 01 March 2020
Cite this chapter
- Louise Cummings 2
741 Accesses
1 Citations
This chapter addresses why there is a need for experts and lay people to think critically about medicine and health. It will be argued that illogical, misleading, and contradictory information in medicine and health can have pernicious consequences, including patient harm and poor compliance with health recommendations. Our cognitive resources are our only bulwark to the misinformation and faulty logic that exists in medicine and health. One resource in particular—reasoning—can counter the flawed thinking that pervades many medical and health issues. This chapter examines how concepts such as reasoning, logic and argument must be conceptualised somewhat differently (namely, in non-deductive terms) to accommodate the rationality of the informal fallacies. It also addresses the relevance of the informal fallacies to medicine and health and considers how these apparently defective arguments are a source of new analytical possibilities in both domains.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Albano, J. D., Ward, E., Jemal, A., Anderson, R., Cokkinides, V. E., Murray, T., et al. (2007). Cancer mortality in the United States by education level and race. Journal of the National Cancer Institute, 99 (18), 1384–1394.
Article Google Scholar
Coxon, J., & Rees, J. (2015). Avoiding medical errors in general practice. Trends in Urology & Men’s Health, 6 (4), 13–17.
Google Scholar
Croskerry, P. (2003). The importance of cognitive errors in diagnosis and strategies to minimize them. Academic Medicine, 78 (8), 775–780.
Cummings, L. (2002). Reasoning under uncertainty: The role of two informal fallacies in an emerging scientific inquiry. Informal Logic, 22 (2), 113–136.
Cummings, L. (2004). Analogical reasoning as a tool of epidemiological investigation. Argumentation, 18 (4), 427–444.
Cummings, L. (2009). Emerging infectious diseases: Coping with uncertainty. Argumentation, 23 (2), 171–188.
Cummings, L. (2010). Rethinking the BSE crisis: A study of scientific reasoning under uncertainty . Dordrecht: Springer.
Book Google Scholar
Cummings, L. (2011). Considering risk assessment up close: The case of bovine spongiform encephalopathy. Health, Risk & Society, 13 (3), 255–275.
Cummings, L. (2012a). Scaring the public: Fear appeal arguments in public health reasoning. Informal Logic, 32 (1), 25–50.
Cummings, L. (2012b). The public health scientist as informal logician. International Journal of Public Health, 57 (3), 649–650.
Cummings, L. (2013a). Public health reasoning: Much more than deduction. Archives of Public Health, 71 (1), 25.
Cummings, L. (2013b). Circular reasoning in public health. Cogency, 5 (2), 35–76.
Cummings, L. (2014a). Informal fallacies as cognitive heuristics in public health reasoning. Informal Logic, 34 (1), 1–37.
Cummings, L. (2014b). The ‘trust’ heuristic: Arguments from authority in public health. Health Communication, 29 (10), 1043–1056.
Cummings, L. (2014c). Coping with uncertainty in public health: The use of heuristics. Public Health, 128 (4), 391–394.
Cummings, L. (2014d). Circles and analogies in public health reasoning. Inquiry, 29 (2), 35–59.
Cummings, L. (2014e). Analogical reasoning in public health. Journal of Argumentation in Context, 3 (2), 169–197.
Cummings, L. (2015). Reasoning and public health: New ways of coping with uncertainty . Cham, Switzerland: Springer.
Fowler, F. J., Jr., Levin, C. A., & Sepucha, K. R. (2011). Informing and involving patients to improve the quality of medical decisions. Health Affairs, 30 (4), 699–706.
Graber, M. L., Franklin, N., & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165 (13), 1493–1499.
Hamblin, C. L. (1970). Fallacies . London: Methuen.
Johnson, R. H. (2011). Informal logic and deductivism. Studies in Logic, 4 (1), 17–37.
Kahane, H. (1971). Logic and contemporary rhetoric: The use of reason in everyday life . Belmont, CA: Wadsworth Publishing Company.
Loucks, E. B., Buka, S. L., Rogers, M. L., Liu, T., Kawachi, I., Kubzansky, L. D., et al. (2012). Education and coronary heart disease risk associations may be affected by early life common prior causes: A propensity matching analysis. Annals of Epidemiology, 22 (4), 221–232.
Saposnik, G., Redelmeier, D., Ruff, C. C., & Tobler, P. N. (2016). Cognitive biases associated with medical decisions: A systematic review. BMC Medical Informatics and Decision Making, 16, 138. https://doi.org/10.1186/s12911-016-0377-1 .
Trowbridge, R. L. (2008). Twelve tips for teaching avoidance of diagnostic errors. Medical Teacher, 30, 496–500.
Walton, D. N. (1985a). Are circular arguments necessarily vicious? American Philosophical Quarterly, 22 (4), 263–274.
Walton, D. N. (1985b). Arguer’s Position . Westport, CT: Greenwood Press.
Walton, D. N. (1987). The ad hominem argument as an informal fallacy. Argumentation, 1 (3), 317–331.
Walton, D. N. (1991). Begging the question: Circular reasoning as a tactic of argumentation . New York: Greenwood Press.
Walton, D. N. (1992). Plausible argument in everyday conversation . Albany: SUNY Press.
Walton, D. N. (1996). Argumentation schemes for presumptive reasoning . Mahwah, NJ: Erlbaum.
Walton, D. N. (2010). Why fallacies appear to be better arguments than they are. Informal Logic, 30 (2), 159–184.
Weingart, S. N., Wilson, R. M., Gibberd, R. W., & Harrison, B. (2000). Epidemiology of medical error. Western Journal of Medicine, 172 (6), 390–393.
Woods, J. (1995). Appeal to force. In H. V. Hansen & R. C. Pinto (Eds.), Fallacies: Classical and contemporary readings (pp. 240–250). University Park: The Pennsylvania State University Press.
Woods, J. (2004). The death of argument: Fallacies in agent-based reasoning . Dordrecht: Kluwer Academic.
Woods, J. (2007). Lightening up on the ad hominem. Informal Logic, 27 (1), 109–134.
Woods, J. (2008). Begging the question is not a fallacy. In C. Dégremont, L. Keiff, & H. Rükert (Eds.), Dialogues, logics and other strange things: Essays in honour of Shahid Rahman (pp. 523–544). London: College Publications.
Download references
Author information
Authors and affiliations.
Department of English, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong
Louise Cummings
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Louise Cummings .
Chapter Summary
Medicine and health have tended to be overlooked in the critical thinking literature . And yet robust critical thinking skills are needed to evaluate the large number and range of health messages that we are exposed to on a daily basis.
An ability to think critically helps us to make better personal health choices and to uncover biases and errors in health messages and other information. An ability to think critically allows us to make informed decisions about medical treatments and is vital to efforts to reduce medical diagnostic errors.
A key element in critical thinking is the ability to distinguish strong or valid reasoning from weak or invalid reasoning. When an argument is weak or invalid, it is called a ‘fallacy’ or a ‘fallacious argument’.
The informal fallacies are so-called on account of the presence of epistemic and dialectical flaws that cannot be captured by formal logic . They have been discussed by many generations of philosophers and logicians , beginning with Aristotle .
Historically, philosophers and logicians have taken a pejorative view of the informal fallacies. Much of the criticism of these arguments is related to a latent deductivism in logic , the notion that arguments should be evaluated according to deductive standards of validity and soundness . Against deductive standards and norms, many reasonable arguments are judged to be fallacies.
Developments in logic , particularly the teaching of logic, forced a reconsideration of the prominence afforded to deductive logic in the evaluation of arguments. New criteria based on presumptive reasoning and plausible argument started to emerge. Against this backdrop, non-fallacious variants of most of the informal fallacies began to be described for the first time.
Today, some argument analysts characterize non-fallacious variants of the informal fallacies in terms of cognitive heuristics . During reasoning , these heuristics function as mental shortcuts, allowing us to bypass knowledge and come to judgement about complex health problems.
Suggestions for Further Reading
Sharples, J. M., Oxman, A. D., Mahtani, K. R., Chalmers, I., Oliver, S., Collins, K., Austvoll-Dahlgren, A., & Hoffmann, T. (2017). Critical thinking in healthcare and education. British Medical Journal, 357 : j2234. https://doi.org/10.1136/bmj.j2234 .
The authors examine the role of critical thinking in medicine and healthcare, arguing that critical thinking skills are essential for doctors and patients. They describe an international project that involves collaboration between education and health. Its aim is to develop a curriculum and learning resources for critical thinking about any action that is claimed to improve health.
Hitchcock, D. (2017). On reasoning and argument: Essays in informal logic and on critical thinking . Cham: Switzerland: Springer.
This collection of essays provides more advanced reading on several of the topics addressed in this chapter, including the fallacies, informal logic , and the teaching of critical thinking . Chapter 25 considers if fallacies have a place in the teaching of critical thinking and reasoning skills.
Hansen, H. V., & Pinto, R. C. (Eds.). (1995). Fallacies: Classical and contemporary readings . University Park: The Pennsylvania State University Press.
This edited collection of 24 chapters contains historical selections on the fallacies, contemporary theory and criticism, and analyses of specific fallacies. It also examines fallacies and teaching. There are chapters on four of the fallacies that will be examined in this book: appeal to force; appeal to ignorance ; appeal to authority; and post hoc ergo propter hoc .
Diagnostic errors are a significant cause of death and serious injury in patients. Many of these errors are related to cognitive factors. Trowbridge ( 2008 ) has devised twelve tips to familiarize medical students and physician trainees with the cognitive underpinnings of diagnostic errors. One of these tips is to explicitly describe heuristics and how they affect clinical reasoning . These heuristics include the following:
Representativeness —a patient’s presentation is compared to a ‘typical’ case of specific diagnoses.
Availability —physicians arrive at a diagnosis based on what is easily accessible in their minds, rather than what is actually most probable.
Anchoring —physicians may settle on a diagnosis early in the diagnostic process and subsequently become ‘anchored’ in that diagnosis.
Confirmation bias —as a result of anchoring, physicians may discount information discordant with the original diagnosis and accept only that which supports the diagnosis.
Using the above information, identify any heuristics and biases that occur in the following scenarios:
Scenario 1: A 60-year-old man has epigastric pain and nausea. He is sitting forward clutching his abdomen. He has a history of several bouts of alcoholic pancreatitis. He states that he felt similar during these bouts to what he is currently feeling. The patient states that he has had no alcohol in many years. He has normal blood levels of pancreatic enzymes. He is given a diagnosis of acute pancreatitis. It is eventually discovered that he has had acute myocardial infarction.
Scenario 2: A 20-year-old, healthy man presents with sudden onset of severe, sharp chest pain and back pain. Based on these symptoms, he is suspected of having a dissecting thoracic aortic aneurysm. (In an aortic dissection, there is a separation of the layers within the wall of the aorta, the large blood vessel branching off the heart.) He is eventually diagnosed with pleuritis (inflammation of the pleura, the thin, transparent, two-layered membrane that covers the lungs).
Many of the logical terms that were introduced in this chapter also have non-logical uses in everyday language. Below are several examples of the use of these terms. For each example, indicate if the word in italics has a logical or a non - logical meaning or use:
University ‘safe spaces’ are a dangerous fallacy —they do not exist in the real world ( The Telegraph , 13 February 2017).
The MRI findings beg the question as to whether a careful ultrasound examination might have yielded some of the same information on haemorrhages ( British Medical Journal: Fetal & Neonatal , 2011).
The youth justice system is a slippery slope of failure ( The Sydney Morning Herald , 26 July 2016).
The EU countered with its own gastronomic analogy , saying that “cherry picking” the best bits of the EU would not be tolerated ( BBC News , 28 July 2017).
As Ebola spreads, so have several fallacies ( The New York Times , 23 October 2014).
Removing the statue of Confederacy Army General Robert E. Lee no more puts us on a slippery slope towards ousting far more nuanced figures from the public square than building the statue in the first place put us on a slippery slope toward, say, putting up statues of Hitler outside of Holocaust museums or of Ho Chi Minh at Vietnam War memorials ( Chicago Tribune , 16 August 2017).
We can expand the analogy a bit and think of a culture as something akin to a society’s immune system—it works best when it is exposed to as many foreign bodies as possible ( New Zealand Herald , 4 May 2010).
The Josh Norman Bowl begs the question : What’s an elite cornerback worth? ( The Washington Post , 17 December 2016).
The intuition behind these analogies is simple: As a homeowner, I generally have the right to exclude whoever I want from my property. I don’t even have to have a good justification for the exclusion. I can choose to bar you from my home for virtually any reason I want, or even just no reason at all. Similarly, a nation has the right to bar foreigners from its land for almost any reason it wants, or perhaps even no reason at all ( The Washington Post , 6 August 2017).
Legalising assisted suicide is a slippery slope toward widespread killing of the sick, Members of Parliament and peers were told yesterday ( Mail Online , 9 July 2014).
In the Special Topic ‘What’s in a name?’, an example of a question-begging argument from the author’s recent personal experience was used. How would you reconstruct the argument in this case to illustrate the presence of a fallacy?
On 9 July 2017, the effect of coconut oil on health was also discussed in an article in The Guardian entitled ‘Coconut oil: Are the health benefits a big fat lie?’ The following extract is taken from that article. (a) What type of reasoning is the author using in this extract? In your response, you should reconstruct the argument by presenting its premises and conclusion . Also, is this argument valid or fallacious in this particular context?
When it comes to superfoods, coconut oil presses all the buttons: it’s natural, it’s enticingly exotic, it’s surrounded by health claims and at up to £8 for a 500 ml pot at Tesco, it’s suitably pricey. But where this latest superfood differs from benign rivals such as blueberries, goji berries, kale and avocado is that a diet rich in coconut oil may actually be bad for us.
The article in The Guardian also makes extensive use of expert opinion. Two such opinions are shown below. (b) What three linguistic devices does the author use to confer expertise or authority on the individuals who advance these opinions?
Christine Williams, professor of human nutrition at the University of Reading, states: “There is very limited evidence of beneficial health effects of this oil”.
Tom Sanders, emeritus professor of nutrition and dietetics at King’s College London, says: “It is a poor source of vitamin E compared with other vegetable oils”.
The author of the article in The Guardian went on to summarize the findings of a study by two researchers that was published in the British Nutrition Foundation’s Nutrition Bulletin. The author’s summary included the following statement: There is no good evidence that coconut oil helps boost mental performance or prevent Alzheimer’s disease . (c) In what type of informal fallacy might this statement be a premise ?
Scenario 1: An anchoring error has occurred in which the patient is given a diagnosis of acute pancreatitis early in the diagnostic process. The clinician becomes anchored in this diagnosis, with the result that he overlooks two pieces of information that would have allowed this diagnosis to be disconfirmed—the fact that the patient has reported no alcohol use in many years and the presence of normal blood levels of pancreatic enzymes. By dismissing this information, the clinician is also showing a confirmation bias —he attends only to information that confirms his original diagnosis.
Scenario 2: A representativeness error has occurred. The patient’s presentation is typical of aortic dissection. However, this condition can be dismissed in favour of conditions like pleuritis or pneumothorax on account of the fact that aortic dissection is exceptionally rare in 20-year-olds.
(2) (a) non-logical; (b) non-logical; (c) non-logical; (d) non-logical; (e) non-logical; (f) logical; (g) logical; (h) non-logical; (i) logical; (j) logical
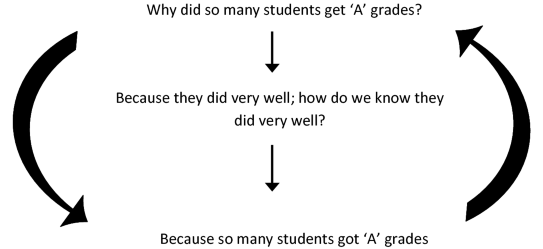
(3) The fallacy can be illustrated as follows. The head of department asks the question ‘Why did so many of these students get ‘A’ grades’? He receives the reply ‘Because they did very well’. But someone might reasonably ask ‘How do we know that they did very well?’ To which the reply is ‘Because so many students got ‘A’ grades’. The reasoning can be reconstructed in diagram form as follows:
The author is using an analogical argument , which has the following form:
P1: Blueberries, goji berries, kale, avocado and coconut oil are natural, exotic, pricey and surrounded by health claims.
P2: Blueberries, goji berries, kale and avocado have health benefits.
C: Coconut oil has health benefits.
This is a false analogy , or a fallacious analogical argument , because coconut oil does not share with these other superfoods the property or attribute < has health benefits >.
The author uses academic rank, field of specialization, and university affiliation to confer authority or expertise on individuals who advance expert opinions.
This statement could be a premise in an argument from ignorance .
Rights and permissions
Reprints and permissions
Copyright information
© 2020 The Author(s)
About this chapter
Cummings, L. (2020). Critical Thinking in Medicine and Health. In: Fallacies in Medicine and Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-28513-5_1
Download citation
DOI : https://doi.org/10.1007/978-3-030-28513-5_1
Published : 01 March 2020
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-28512-8
Online ISBN : 978-3-030-28513-5
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

What is Critical Thinking in Nursing? (Explained W/ Examples)
Last updated on August 23rd, 2023
Critical thinking is a foundational skill applicable across various domains, including education, problem-solving, decision-making, and professional fields such as science, business, healthcare, and more.
It plays a crucial role in promoting logical and rational thinking, fostering informed decision-making, and enabling individuals to navigate complex and rapidly changing environments.
In this article, we will look at what is critical thinking in nursing practice, its importance, and how it enables nurses to excel in their roles while also positively impacting patient outcomes.
What is Critical Thinking?
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
It’s a mental activity that goes beyond simple memorization or acceptance of information at face value.
Critical thinking involves careful, reflective, and logical thinking to understand complex problems, consider various perspectives, and arrive at well-reasoned conclusions or solutions.
Key aspects of critical thinking include:
- Analysis: Critical thinking begins with the thorough examination of information, ideas, or situations. It involves breaking down complex concepts into smaller parts to better understand their components and relationships.
- Evaluation: Critical thinkers assess the quality and reliability of information or arguments. They weigh evidence, identify strengths and weaknesses, and determine the credibility of sources.
- Synthesis: Critical thinking involves combining different pieces of information or ideas to create a new understanding or perspective. This involves connecting the dots between various sources and integrating them into a coherent whole.
- Inference: Critical thinkers draw logical and well-supported conclusions based on the information and evidence available. They use reasoning to make educated guesses about situations where complete information might be lacking.
- Problem-Solving: Critical thinking is essential in solving complex problems. It allows individuals to identify and define problems, generate potential solutions, evaluate the pros and cons of each solution, and choose the most appropriate course of action.
- Creativity: Critical thinking involves thinking outside the box and considering alternative viewpoints or approaches. It encourages the exploration of new ideas and solutions beyond conventional thinking.
- Reflection: Critical thinkers engage in self-assessment and reflection on their thought processes. They consider their own biases, assumptions, and potential errors in reasoning, aiming to improve their thinking skills over time.
- Open-Mindedness: Critical thinkers approach ideas and information with an open mind, willing to consider different viewpoints and perspectives even if they challenge their own beliefs.
- Effective Communication: Critical thinkers can articulate their thoughts and reasoning clearly and persuasively to others. They can express complex ideas in a coherent and understandable manner.
- Continuous Learning: Critical thinking encourages a commitment to ongoing learning and intellectual growth. It involves seeking out new knowledge, refining thinking skills, and staying receptive to new information.
Definition of Critical Thinking
Critical thinking is an intellectual process of analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
What is Critical Thinking in Nursing?
Critical thinking in nursing is a vital cognitive skill that involves analyzing, evaluating, and making reasoned decisions about patient care.
It’s an essential aspect of a nurse’s professional practice as it enables them to provide safe and effective care to patients.
Critical thinking involves a careful and deliberate thought process to gather and assess information, consider alternative solutions, and make informed decisions based on evidence and sound judgment.
This skill helps nurses to:
- Assess Information: Critical thinking allows nurses to thoroughly assess patient information, including medical history, symptoms, and test results. By analyzing this data, nurses can identify patterns, discrepancies, and potential issues that may require further investigation.
- Diagnose: Nurses use critical thinking to analyze patient data and collaboratively work with other healthcare professionals to formulate accurate nursing diagnoses. This is crucial for developing appropriate care plans that address the unique needs of each patient.
- Plan and Implement Care: Once a nursing diagnosis is established, critical thinking helps nurses develop effective care plans. They consider various interventions and treatment options, considering the patient’s preferences, medical history, and evidence-based practices.
- Evaluate Outcomes: After implementing interventions, critical thinking enables nurses to evaluate the outcomes of their actions. If the desired outcomes are not achieved, nurses can adapt their approach and make necessary changes to the care plan.
- Prioritize Care: In busy healthcare environments, nurses often face situations where they must prioritize patient care. Critical thinking helps them determine which patients require immediate attention and which interventions are most essential.
- Communicate Effectively: Critical thinking skills allow nurses to communicate clearly and confidently with patients, their families, and other members of the healthcare team. They can explain complex medical information and treatment plans in a way that is easily understood by all parties involved.
- Identify Problems: Nurses use critical thinking to identify potential complications or problems in a patient’s condition. This early recognition can lead to timely interventions and prevent further deterioration.
- Collaborate: Healthcare is a collaborative effort involving various professionals. Critical thinking enables nurses to actively participate in interdisciplinary discussions, share their insights, and contribute to holistic patient care.
- Ethical Decision-Making: Critical thinking helps nurses navigate ethical dilemmas that can arise in patient care. They can analyze different perspectives, consider ethical principles, and make morally sound decisions.
- Continual Learning: Critical thinking encourages nurses to seek out new knowledge, stay up-to-date with the latest research and medical advancements, and incorporate evidence-based practices into their care.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed.
It’s a dynamic process that enhances clinical reasoning , problem-solving, and overall patient outcomes.
What are the Levels of Critical Thinking in Nursing?
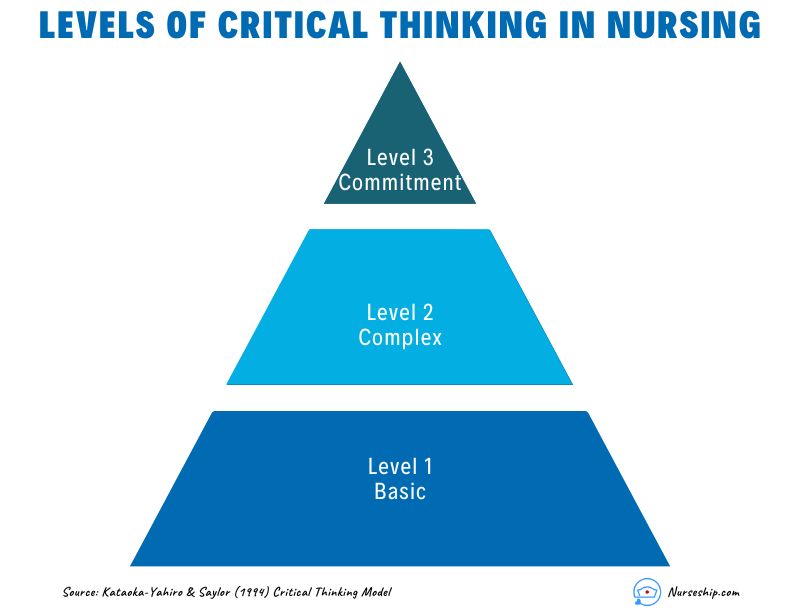
The development of critical thinking in nursing practice involves progressing through three levels: basic, complex, and commitment.
The Kataoka-Yahiro and Saylor model outlines this progression.
1. Basic Critical Thinking:
At this level, learners trust experts for solutions. Thinking is based on rules and principles. For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted.
2. Complex Critical Thinking:
Learners start to analyze choices independently and think creatively. They recognize conflicting solutions and weigh benefits and risks. Thinking becomes innovative, with a willingness to consider various approaches in complex situations.
3. Commitment:
At this level, individuals anticipate decision points without external help and take responsibility for their choices. They choose actions or beliefs based on available alternatives, considering consequences and accountability.
As nurses gain knowledge and experience, their critical thinking evolves from relying on experts to independent analysis and decision-making, ultimately leading to committed and accountable choices in patient care.
Why Critical Thinking is Important in Nursing?
Critical thinking is important in nursing for several crucial reasons:
Patient Safety:
Nursing decisions directly impact patient well-being. Critical thinking helps nurses identify potential risks, make informed choices, and prevent errors.
Clinical Judgment:
Nursing decisions often involve evaluating information from various sources, such as patient history, lab results, and medical literature.
Critical thinking assists nurses in critically appraising this information, distinguishing credible sources, and making rational judgments that align with evidence-based practices.
Enhances Decision-Making:
In nursing, critical thinking allows nurses to gather relevant patient information, assess it objectively, and weigh different options based on evidence and analysis.
This process empowers them to make informed decisions about patient care, treatment plans, and interventions, ultimately leading to better outcomes.
Promotes Problem-Solving:
Nurses encounter complex patient issues that require effective problem-solving.
Critical thinking equips them to break down problems into manageable parts, analyze root causes, and explore creative solutions that consider the unique needs of each patient.
Drives Creativity:
Nursing care is not always straightforward. Critical thinking encourages nurses to think creatively and explore innovative approaches to challenges, especially when standard protocols might not suffice for unique patient situations.
Fosters Effective Communication:
Communication is central to nursing. Critical thinking enables nurses to clearly express their thoughts, provide logical explanations for their decisions, and engage in meaningful dialogues with patients, families, and other healthcare professionals.
Aids Learning:
Nursing is a field of continuous learning. Critical thinking encourages nurses to engage in ongoing self-directed education, seeking out new knowledge, embracing new techniques, and staying current with the latest research and developments.
Improves Relationships:
Open-mindedness and empathy are essential in nursing relationships.
Critical thinking encourages nurses to consider diverse viewpoints, understand patients’ perspectives, and communicate compassionately, leading to stronger therapeutic relationships.
Empowers Independence:
Nursing often requires autonomous decision-making. Critical thinking empowers nurses to analyze situations independently, make judgments without undue influence, and take responsibility for their actions.
Facilitates Adaptability:
Healthcare environments are ever-changing. Critical thinking equips nurses with the ability to quickly assess new information, adjust care plans, and navigate unexpected situations while maintaining patient safety and well-being.
Strengthens Critical Analysis:
In the era of vast information, nurses must discern reliable data from misinformation.
Critical thinking helps them scrutinize sources, question assumptions, and make well-founded choices based on credible information.
How to Apply Critical Thinking in Nursing? (With Examples)
Here are some examples of how nurses can apply critical thinking.
Assess Patient Data:
Critical Thinking Action: Carefully review patient history, symptoms, and test results.
Example: A nurse notices a change in a diabetic patient’s blood sugar levels. Instead of just administering insulin, the nurse considers recent dietary changes, activity levels, and possible medication interactions before adjusting the treatment plan.
Diagnose Patient Needs:
Critical Thinking Action: Analyze patient data to identify potential nursing diagnoses.
Example: After reviewing a patient’s lab results, vital signs, and observations, a nurse identifies “ Risk for Impaired Skin Integrity ” due to the patient’s limited mobility.
Plan and Implement Care:
Critical Thinking Action: Develop a care plan based on patient needs and evidence-based practices.
Example: For a patient at risk of falls, the nurse plans interventions such as hourly rounding, non-slip footwear, and bed alarms to ensure patient safety.
Evaluate Interventions:
Critical Thinking Action: Assess the effectiveness of interventions and modify the care plan as needed.
Example: After administering pain medication, the nurse evaluates its impact on the patient’s comfort level and considers adjusting the dosage or trying an alternative pain management approach.
Prioritize Care:
Critical Thinking Action: Determine the order of interventions based on patient acuity and needs.
Example: In a busy emergency department, the nurse triages patients by considering the severity of their conditions, ensuring that critical cases receive immediate attention.
Collaborate with the Healthcare Team:
Critical Thinking Action: Participate in interdisciplinary discussions and share insights.
Example: During rounds, a nurse provides input on a patient’s response to treatment, which prompts the team to adjust the care plan for better outcomes.
Ethical Decision-Making:
Critical Thinking Action: Analyze ethical dilemmas and make morally sound choices.
Example: When a terminally ill patient expresses a desire to stop treatment, the nurse engages in ethical discussions, respecting the patient’s autonomy and ensuring proper end-of-life care.
Patient Education:
Critical Thinking Action: Tailor patient education to individual needs and comprehension levels.
Example: A nurse uses visual aids and simplified language to explain medication administration to a patient with limited literacy skills.
Adapt to Changes:
Critical Thinking Action: Quickly adjust care plans when patient conditions change.
Example: During post-operative recovery, a nurse notices signs of infection and promptly informs the healthcare team to initiate appropriate treatment adjustments.
Critical Analysis of Information:
Critical Thinking Action: Evaluate information sources for reliability and relevance.
Example: When presented with conflicting research studies, a nurse critically examines the methodologies and sample sizes to determine which study is more credible.
Making Sense of Critical Thinking Skills
What is the purpose of critical thinking in nursing.
The purpose of critical thinking in nursing is to enable nurses to effectively analyze, interpret, and evaluate patient information, make informed clinical judgments, develop appropriate care plans, prioritize interventions, and adapt their approaches as needed, thereby ensuring safe, evidence-based, and patient-centered care.
Why critical thinking is important in nursing?
Critical thinking is important in nursing because it promotes safe decision-making, accurate clinical judgment, problem-solving, evidence-based practice, holistic patient care, ethical reasoning, collaboration, and adapting to dynamic healthcare environments.
Critical thinking skill also enhances patient safety, improves outcomes, and supports nurses’ professional growth.
How is critical thinking used in the nursing process?
Critical thinking is integral to the nursing process as it guides nurses through the systematic approach of assessing, diagnosing, planning, implementing, and evaluating patient care. It involves:
- Assessment: Critical thinking enables nurses to gather and interpret patient data accurately, recognizing relevant patterns and cues.
- Diagnosis: Nurses use critical thinking to analyze patient data, identify nursing diagnoses, and differentiate actual issues from potential complications.
- Planning: Critical thinking helps nurses develop tailored care plans, selecting appropriate interventions based on patient needs and evidence.
- Implementation: Nurses make informed decisions during interventions, considering patient responses and adjusting plans as needed.
- Evaluation: Critical thinking supports the assessment of patient outcomes, determining the effectiveness of intervention, and adapting care accordingly.
Throughout the nursing process , critical thinking ensures comprehensive, patient-centered care and fosters continuous improvement in clinical judgment and decision-making.
What is an example of the critical thinking attitude of independent thinking in nursing practice?
An example of the critical thinking attitude of independent thinking in nursing practice could be:
A nurse is caring for a patient with a complex medical history who is experiencing a new set of symptoms. The nurse carefully reviews the patient’s history, recent test results, and medication list.
While discussing the case with the healthcare team, the nurse realizes that the current treatment plan might not be addressing all aspects of the patient’s condition.
Instead of simply following the established protocol, the nurse independently considers alternative approaches based on their assessment.
The nurse proposes a modification to the treatment plan, citing the rationale and evidence supporting the change.
This demonstrates independent thinking by critically evaluating the situation, challenging assumptions, and advocating for a more personalized and effective patient care approach.
How to use Costa’s level of questioning for critical thinking in nursing?
Costa’s levels of questioning can be applied in nursing to facilitate critical thinking and stimulate a deeper understanding of patient situations. The levels of questioning are as follows:
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
- Nursing Concept Map (FREE Template)
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
Critical thinking in nursing is the foundation that underpins safe, effective, and patient-centered care.
Critical thinking skills empower nurses to navigate the complexities of their profession while consistently providing high-quality care to diverse patient populations.
Reading Recommendation
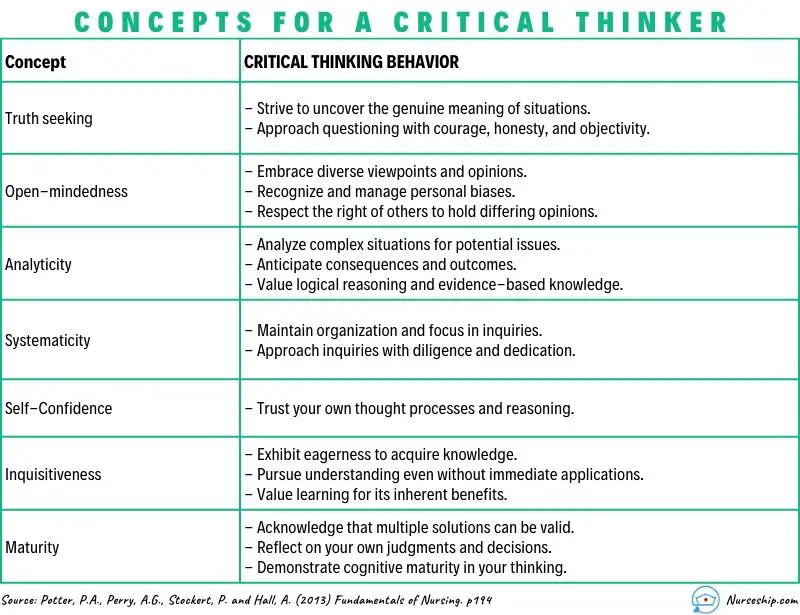
Potter, P.A., Perry, A.G., Stockert, P. and Hall, A. (2013) Fundamentals of Nursing
Comments are closed.

Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.
You are using an outdated browser
Unfortunately Ausmed.com does not support your browser. Please upgrade your browser to continue.
Cultivating Critical Thinking in Healthcare
Published: 06 January 2019

Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).
Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught , assessed and integrated into the design and development of staff and nurse education and training programs (Papp et al. 2014).
So, what exactly is critical thinking and how can healthcare educators cultivate it amongst their staff?
What is Critical Thinking?
In general terms, ‘ critical thinking ’ is often used, and perhaps confused, with problem-solving and clinical decision-making skills .
In practice, however, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and critiquing solutions .
Several formal definitions of critical thinking can be found in literature, but in the view of Kahlke and Eva (2018), most of these definitions have limitations. That said, Papp et al. (2014) offer a useful starting point, suggesting that critical thinking is:
‘The ability to apply higher order cognitive skills and the disposition to be deliberate about thinking that leads to action that is logical and appropriate.’
The Foundation for Critical Thinking (2017) expands on this and suggests that:
‘Critical thinking is that mode of thinking, about any subject, content, or problem, in which the thinker improves the quality of his or her thinking by skillfully analysing, assessing, and reconstructing it.’
They go on to suggest that critical thinking is:
- Self-directed
- Self-disciplined
- Self-monitored
- Self-corrective.

Key Qualities and Characteristics of a Critical Thinker
Given that critical thinking is a process that encompasses conceptualisation , application , analysis , synthesis , evaluation and reflection , what qualities should be expected from a critical thinker?
In answering this question, Fortepiani (2018) suggests that critical thinkers should be able to:
- Formulate clear and precise questions
- Gather, assess and interpret relevant information
- Reach relevant well-reasoned conclusions and solutions
- Think open-mindedly, recognising their own assumptions
- Communicate effectively with others on solutions to complex problems.
All of these qualities are important, however, good communication skills are generally considered to be the bedrock of critical thinking. Why? Because they help to create a dialogue that invites questions, reflections and an open-minded approach, as well as generating a positive learning environment needed to support all forms of communication.
Lippincott Solutions (2018) outlines a broad spectrum of characteristics attributed to strong critical thinkers. They include:
- Inquisitiveness with regard to a wide range of issues
- A concern to become and remain well-informed
- Alertness to opportunities to use critical thinking
- Self-confidence in one’s own abilities to reason
- Open mindedness regarding divergent world views
- Flexibility in considering alternatives and opinions
- Understanding the opinions of other people
- Fair-mindedness in appraising reasoning
- Honesty in facing one’s own biases, prejudices, stereotypes or egocentric tendencies
- A willingness to reconsider and revise views where honest reflection suggests that change is warranted.
Papp et al. (2014) also helpfully suggest that the following five milestones can be used as a guide to help develop competency in critical thinking:
Stage 1: Unreflective Thinker
At this stage, the unreflective thinker can’t examine their own actions and cognitive processes and is unaware of different approaches to thinking.
Stage 2: Beginning Critical Thinker
Here, the learner begins to think critically and starts to recognise cognitive differences in other people. However, external motivation is needed to sustain reflection on the learners’ own thought processes.
Stage 3: Practicing Critical Thinker
By now, the learner is familiar with their own thinking processes and makes a conscious effort to practice critical thinking.
Stage 4: Advanced Critical Thinker
As an advanced critical thinker, the learner is able to identify different cognitive processes and consciously uses critical thinking skills.
Stage 5: Accomplished Critical Thinker
At this stage, the skilled critical thinker can take charge of their thinking and habitually monitors, revises and rethinks approaches for continual improvement of their cognitive strategies.
Facilitating Critical Thinking in Healthcare
A common challenge for many educators and facilitators in healthcare is encouraging students to move away from passive learning towards active learning situations that require critical thinking skills.
Just as there are similarities among the definitions of critical thinking across subject areas and levels, there are also several generally recognised hallmarks of teaching for critical thinking . These include:
- Promoting interaction among students as they learn
- Asking open ended questions that do not assume one right answer
- Allowing sufficient time to reflect on the questions asked or problems posed
- Teaching for transfer - helping learners to see how a newly acquired skill can apply to other situations and experiences.
(Lippincott Solutions 2018)
Snyder and Snyder (2008) also make the point that it’s helpful for educators and facilitators to be aware of any initial resistance that learners may have and try to guide them through the process. They should aim to create a learning environment where learners can feel comfortable thinking through an answer rather than simply having an answer given to them.
Examples include using peer coaching techniques , mentoring or preceptorship to engage students in active learning and critical thinking skills, or integrating project-based learning activities that require students to apply their knowledge in a realistic healthcare environment.
Carvalhoa et al. (2017) also advocate problem-based learning as a widely used and successful way of stimulating critical thinking skills in the learner. This view is echoed by Tsui-Mei (2015), who notes that critical thinking, systematic analysis and curiosity significantly improve after practice-based learning .
Integrating Critical Thinking Skills Into Curriculum Design
Most educators agree that critical thinking can’t easily be developed if the program curriculum is not designed to support it. This means that a deep understanding of the nature and value of critical thinking skills needs to be present from the outset of the curriculum design process , and not just bolted on as an afterthought.
In the view of Fortepiani (2018), critical thinking skills can be summarised by the statement that 'thinking is driven by questions', which means that teaching materials need to be designed in such a way as to encourage students to expand their learning by asking questions that generate further questions and stimulate the thinking process. Ideal questions are those that:
- Embrace complexity
- Challenge assumptions and points of view
- Question the source of information
- Explore variable interpretations and potential implications of information.
To put it another way, asking questions with limiting, thought-stopping answers inhibits the development of critical thinking. This means that educators must ideally be critical thinkers themselves .
Drawing these threads together, The Foundation for Critical Thinking (2017) offers us a simple reminder that even though it’s human nature to be ‘thinking’ most of the time, most thoughts, if not guided and structured, tend to be biased, distorted, partial, uninformed or even prejudiced.
They also note that the quality of work depends precisely on the quality of the practitioners’ thought processes. Given that practitioners are being asked to meet the challenge of ever more complex care, the importance of cultivating critical thinking skills, alongside advanced problem-solving skills , seems to be taking on new importance.
Additional Resources
- The Emotionally Intelligent Nurse | Ausmed Article
- Refining Competency-Based Assessment | Ausmed Article
- Socratic Questioning in Healthcare | Ausmed Article
- Carvalhoa, D P S R P et al. 2017, 'Strategies Used for the Promotion of Critical Thinking in Nursing Undergraduate Education: A Systematic Review', Nurse Education Today , vol. 57, pp. 103-10, viewed 7 December 2018, https://www.sciencedirect.com/science/article/abs/pii/S0260691717301715
- Fortepiani, L A 2017, 'Critical Thinking or Traditional Teaching For Health Professionals', PECOP Blog , 16 January, viewed 7 December 2018, https://blog.lifescitrc.org/pecop/2017/01/16/critical-thinking-or-traditional-teaching-for-health-professions/
- Jacob, E, Duffield, C & Jacob, D 2017, 'A Protocol For the Development of a Critical Thinking Assessment Tool for Nurses Using a Delphi Technique', Journal of Advanced Nursing, vol. 73, no. 8, pp. 1982-1988, viewed 7 December 2018, https://onlinelibrary.wiley.com/doi/10.1111/jan.13306
- Kahlke, R & Eva, K 2018, 'Constructing Critical Thinking in Health Professional Education', Perspectives on Medical Education , vol. 7, no. 3, pp. 156-165, viewed 7 December 2018, https://link.springer.com/article/10.1007/s40037-018-0415-z
- Lippincott Solutions 2018, 'Turning New Nurses Into Critical Thinkers', Lippincott Solutions , viewed 10 December 2018, https://www.wolterskluwer.com/en/expert-insights/turning-new-nurses-into-critical-thinkers
- Papp, K K 2014, 'Milestones of Critical Thinking: A Developmental Model for Medicine and Nursing', Academic Medicine , vol. 89, no. 5, pp. 715-720, https://journals.lww.com/academicmedicine/Fulltext/2014/05000/Milestones_of_Critical_Thinking___A_Developmental.14.aspx
- Snyder, L G & Snyder, M J 2008, 'Teaching Critical Thinking and Problem Solving Skills', The Delta Pi Epsilon Journal , vol. L, no. 2, pp. 90-99, viewed 7 December 2018, https://dme.childrenshospital.org/wp-content/uploads/2019/02/Optional-_Teaching-Critical-Thinking-and-Problem-Solving-Skills.pdf
- The Foundation for Critical Thinking 2017, Defining Critical Thinking , The Foundation for Critical Thinking, viewed 7 December 2018, https://www.criticalthinking.org/pages/our-conception-of-critical-thinking/411
- Tsui-Mei, H, Lee-Chun, H & Chen-Ju MSN, K 2015, 'How Mental Health Nurses Improve Their Critical Thinking Through Problem-Based Learning', Journal for Nurses in Professional Development , vol. 31, no. 3, pp. 170-175, viewed 7 December 2018, https://journals.lww.com/jnsdonline/Abstract/2015/05000/How_Mental_Health_Nurses_Improve_Their_Critical.8.aspx
Anne Watkins View profile
Help and feedback, publications.
Ausmed Education is a Trusted Information Partner of Healthdirect Australia. Verify here .
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Critical thinking: what it is and why it counts. 2020. https://tinyurl.com/ybz73bnx (accessed 27 April 2021)
Faculty of Intensive Care Medicine. Curriculum for training for advanced critical care practitioners: syllabus (part III). version 1.1. 2018. https://www.ficm.ac.uk/accps/curriculum (accessed 27 April 2021)
Guerrero AP. Mechanistic case diagramming: a tool for problem-based learning. Acad Med.. 2001; 76:(4)385-9 https://doi.org/10.1097/00001888-200104000-00020
Harasym PH, Tsai TC, Hemmati P. Current trends in developing medical students' critical thinking abilities. Kaohsiung J Med Sci.. 2008; 24:(7)341-55 https://doi.org/10.1016/S1607-551X(08)70131-1
Hayes MM, Chatterjee S, Schwartzstein RM. Critical thinking in critical care: five strategies to improve teaching and learning in the intensive care unit. Ann Am Thorac Soc.. 2017; 14:(4)569-575 https://doi.org/10.1513/AnnalsATS.201612-1009AS
Health Education England. Multi-professional framework for advanced clinical practice in England. 2017. https://www.hee.nhs.uk/sites/default/files/documents/multi-professionalframeworkforadvancedclinicalpracticeinengland.pdf (accessed 27 April 2021)
Health Education England, NHS England/NHS Improvement, Skills for Health. Core capabilities framework for advanced clinical practice (nurses) working in general practice/primary care in England. 2020. https://www.skillsforhealth.org.uk/images/services/cstf/ACP%20Primary%20Care%20Nurse%20Fwk%202020.pdf (accessed 27 April 2021)
Health Education England. Advanced practice mental health curriculum and capabilities framework. 2020. https://www.hee.nhs.uk/sites/default/files/documents/AP-MH%20Curriculum%20and%20Capabilities%20Framework%201.2.pdf (accessed 27 April 2021)
Jacob E, Duffield C, Jacob D. A protocol for the development of a critical thinking assessment tool for nurses using a Delphi technique. J Adv Nurs.. 2017; 73:(8)1982-1988 https://doi.org/10.1111/jan.13306
Kohn MA. Understanding evidence-based diagnosis. Diagnosis (Berl).. 2014; 1:(1)39-42 https://doi.org/10.1515/dx-2013-0003
Clinical reasoning—a guide to improving teaching and practice. 2012. https://www.racgp.org.au/afp/201201/45593
McGee S. Evidence-based physical diagnosis, 4th edn. Philadelphia PA: Elsevier; 2018
Norman GR, Monteiro SD, Sherbino J, Ilgen JS, Schmidt HG, Mamede S. The causes of errors in clinical reasoning: cognitive biases, knowledge deficits, and dual process thinking. Acad Med.. 2017; 92:(1)23-30 https://doi.org/10.1097/ACM.0000000000001421
Papp KK, Huang GC, Lauzon Clabo LM Milestones of critical thinking: a developmental model for medicine and nursing. Acad Med.. 2014; 89:(5)715-20 https://doi.org/10.1097/acm.0000000000000220
Rencic J, Lambert WT, Schuwirth L., Durning SJ. Clinical reasoning performance assessment: using situated cognition theory as a conceptual framework. Diagnosis.. 2020; 7:(3)177-179 https://doi.org/10.1515/dx-2019-0051
Examining critical thinking skills in family medicine residents. 2016. https://www.stfm.org/FamilyMedicine/Vol48Issue2/Ross121
Royal College of Emergency Medicine. Emergency care advanced clinical practitioner—curriculum and assessment, adult and paediatric. version 2.0. 2019. https://tinyurl.com/eps3p37r (accessed 27 April 2021)
Young ME, Thomas A, Lubarsky S. Mapping clinical reasoning literature across the health professions: a scoping review. BMC Med Educ.. 2020; 20 https://doi.org/10.1186/s12909-020-02012-9
Advanced practice: critical thinking and clinical reasoning
Sadie Diamond-Fox
Senior Lecturer in Advanced Critical Care Practice, Northumbria University, Advanced Critical Care Practitioner, Newcastle upon Tyne Hospitals NHS Foundation Trust, and Co-Lead, Advanced Critical/Clinical Care Practitioners Academic Network (ACCPAN)
View articles
Advanced Critical Care Practitioner, South Tees Hospitals NHS Foundation Trust

Clinical reasoning is a multi-faceted and complex construct, the understanding of which has emerged from multiple fields outside of healthcare literature, primarily the psychological and behavioural sciences. The application of clinical reasoning is central to the advanced non-medical practitioner (ANMP) role, as complex patient caseloads with undifferentiated and undiagnosed diseases are now a regular feature in healthcare practice. This article explores some of the key concepts and terminology that have evolved over the last four decades and have led to our modern day understanding of this topic. It also considers how clinical reasoning is vital for improving evidence-based diagnosis and subsequent effective care planning. A comprehensive guide to applying diagnostic reasoning on a body systems basis will be explored later in this series.
The Multi-professional Framework for Advanced Clinical Practice highlights clinical reasoning as one of the core clinical capabilities for advanced clinical practice in England ( Health Education England (HEE), 2017 ). This is also identified in other specialist core capability frameworks and training syllabuses for advanced clinical practitioner (ACP) roles ( Faculty of Intensive Care Medicine, 2018 ; Royal College of Emergency Medicine, 2019 ; HEE, 2020 ; HEE et al, 2020 ).
Rencic et al (2020) defined clinical reasoning as ‘a complex ability, requiring both declarative and procedural knowledge, such as physical examination and communication skills’. A plethora of literature exists surrounding this topic, with a recent systematic review identifying 625 papers, spanning 47 years, across the health professions ( Young et al, 2020 ). A diverse range of terms are used to refer to clinical reasoning within the healthcare literature ( Table 1 ), which can make defining their influence on their use within the clinical practice and educational arenas somewhat challenging.
The concept of clinical reasoning has changed dramatically over the past four decades. What was once thought to be a process-dependent task is now considered to present a more dynamic state of practice, which is affected by ‘complex, non-linear interactions between the clinician, patient, and the environment’ ( Rencic et al, 2020 ).
Cognitive and meta-cognitive processes
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting. Facione (2020) described critical thinking as ‘purposeful reflective judgement’ that consists of six discrete cognitive skills: analysis, inference, interpretation, explanation, synthesis and self–regulation. Ross et al (2016) identified that critical thinking positively correlates with academic success, professionalism, clinical decision-making, wider reasoning and problem-solving capabilities. Jacob et al (2017) also identified that patient outcomes and safety are directly linked to critical thinking skills.
Harasym et al (2008) listed nine discrete cognitive steps that may be applied to the process of critical thinking, which integrates both cognitive and meta-cognitive processes:
- Gather relevant information
- Formulate clearly defined questions and problems
- Evaluate relevant information
- Utilise and interpret abstract ideas effectively
- Infer well-reasoned conclusions and solutions
- Pilot outcomes against relevant criteria and standards
- Use alternative thought processes if needed
- Consider all assumptions, implications, and practical consequences
- Communicate effectively with others to solve complex problems.
There are a number of widely used strategies to develop critical thinking and evidence-based diagnosis. These include simulated problem-based learning platforms, high-fidelity simulation scenarios, case-based discussion forums, reflective journals as part of continuing professional development (CPD) portfolios and journal clubs.
Dual process theory and cognitive bias in diagnostic reasoning
A lack of understanding of the interrelationship between critical thinking and clinical reasoning can result in cognitive bias, which can in turn lead to diagnostic errors ( Hayes et al, 2017 ). Embedded within our understanding of how diagnostic errors occur is dual process theory—system 1 and system 2 thinking. The characteristics of these are described in Table 2 . Although much of the literature in this area regards dual process theory as a valid representation of clinical reasoning, the exact causes of diagnostic errors remain unclear and require further research ( Norman et al, 2017 ). The most effective way in which to teach critical thinking skills in healthcare education also remains unclear; however, Hayes et al (2017) proposed five strategies, based on well-known educational theory and principles, that they have found to be effective for teaching and learning critical thinking within the ‘high-octane’ and ‘high-stakes’ environment of the intensive care unit ( Table 3 ). This is arguably a setting that does not always present an ideal environment for learning given its fast pace and constant sensory stimulation. However, it may be argued that if a model has proven to be effective in this setting, it could be extrapolated to other busy clinical environments and may even provide a useful aide memoire for self-assessment and reflective practices.
Integrating the clinical reasoning process into the clinical consultation
Linn et al (2012) described the clinical consultation as ‘the practical embodiment of the clinical reasoning process by which data are gathered, considered, challenged and integrated to form a diagnosis that can lead to appropriate management’. The application of the previously mentioned psychological and behavioural science theories is intertwined throughout the clinical consultation via the following discrete processes:
- The clinical history generates an initial hypothesis regarding diagnosis, and said hypothesis is then tested through skilled and specific questioning
- The clinician formulates a primary diagnosis and differential diagnoses in order of likelihood
- Physical examination is carried out, aimed at gathering further data necessary to confirm or refute the hypotheses
- A selection of appropriate investigations, using an evidence-based approach, may be ordered to gather additional data
- The clinician (in partnership with the patient) then implements a targeted and rationalised management plan, based on best-available clinical evidence.
Linn et al (2012) also provided a very useful framework of how the above methods can be applied when teaching consultation with a focus on clinical reasoning (see Table 4 ). This framework may also prove useful to those new to the process of undertaking the clinical consultation process.
Evidence-based diagnosis and diagnostic accuracy
The principles of clinical reasoning are embedded within the practices of formulating an evidence-based diagnosis (EBD). According to Kohn (2014) EBD quantifies the probability of the presence of a disease through the use of diagnostic tests. He described three pertinent questions to consider in this respect:
- ‘How likely is the patient to have a particular disease?’
- ‘How good is this test for the disease in question?’
- ‘Is the test worth performing to guide treatment?’
EBD gives a statistical discriminatory weighting to update the probability of a disease to either support or refute the working and differential diagnoses, which can then determine the appropriate course of further diagnostic testing and treatments.
Diagnostic accuracy refers to how positive or negative findings change the probability of the presence of disease. In order to understand diagnostic accuracy, we must begin to understand the underlying principles and related statistical calculations concerning sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios.
The construction of a two-by-two square (2 x 2) table ( Figure 1 ) allows the calculation of several statistical weightings for pertinent points of the history-taking exercise, a finding/sign on physical examination, or a test result. From this construct we can then determine the aforementioned statistical calculations as follows ( McGee, 2018 ):
- Sensitivity , the proportion of patients with the diagnosis who have the physical sign or a positive test result = A ÷ (A + C)
- Specificity , the proportion of patients without the diagnosis who lack the physical sign or have a negative test result = D ÷ (B + D)
- Positive predictive value , the proportion of patients with disease who have a physical sign divided by the proportion of patients without disease who also have the same sign = A ÷ (A + B)
- Negative predictive value , proportion of patients with disease lacking a physical sign divided by the proportion of patients without disease also lacking the sign = D ÷ (C + D)
- Likelihood ratio , a finding/sign/test results sensitivity divided by the false-positive rate. A test of no value has an LR of 1. Therefore the test would have no impact upon the patient's odds of disease
- Positive likelihood ratio = proportion of patients with disease who have a positive finding/sign/test, divided by proportion of patients without disease who have a positive finding/sign/test OR (A ÷ N1) ÷ (B÷ N2), or sensitivity ÷ (1 – specificity) The more positive an LR (the further above 1), the more the finding/sign/test result raises a patient's probability of disease. Thresholds of ≥ 4 are often considered to be significant when focusing a clinician's interest on the most pertinent positive findings, clinical signs or tests
- Negative likelihood ratio = proportion of patients with disease who have a negative finding/sign/test result, divided by the proportion of patients without disease who have a positive finding/sign/test OR (C ÷ N1) ÷ (D÷N1) or (1 – sensitivity) ÷ specificity The more negative an LR (the closer to 0), the more the finding/sign/test result lowers a patient's probability of disease. Thresholds <0.4 are often considered to be significant when focusing clinician's interest on the most pertinent negative findings, clinical signs or tests.
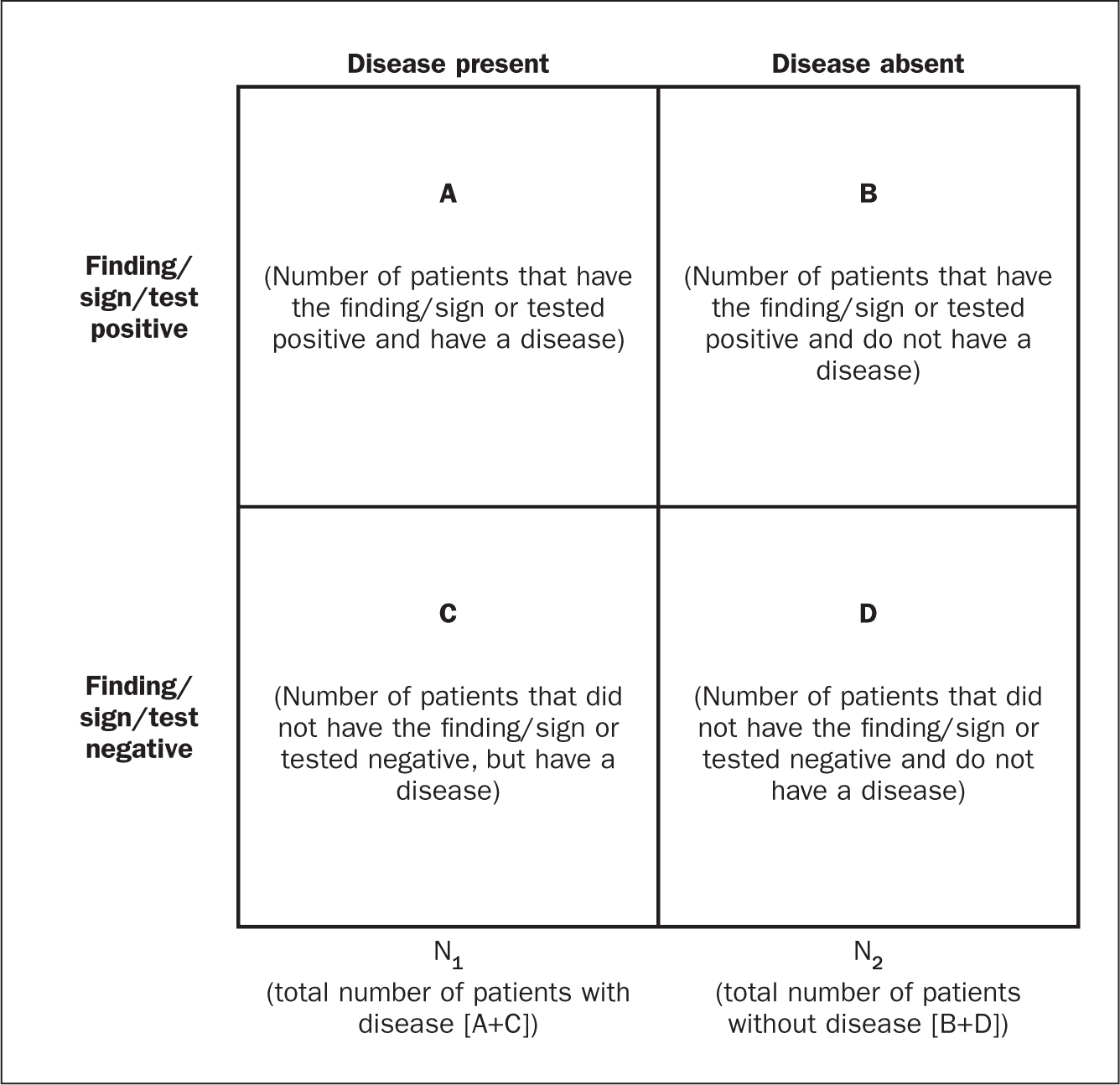
There are various online statistical calculators that can aid in the above calculations, such as the BMJ Best Practice statistical calculators, which may used as a guide (https://bestpractice.bmj.com/info/toolkit/ebm-toolbox/statistics-calculators/).
Clinical scoring systems
Evidence-based literature supports the practice of determining clinical pretest probability of certain diseases prior to proceeding with a diagnostic test. There are numerous validated pretest clinical scoring systems and clinical prediction tools that can be used in this context and accessed via various online platforms such as MDCalc (https://www.mdcalc.com/#all). Such clinical prediction tools include:
- 4Ts score for heparin-induced thrombocytopenia
- ABCD² score for transient ischaemic attack (TIA)
- CHADS₂ score for atrial fibrillation stroke risk
- Aortic Dissection Detection Risk Score (ADD-RS).
Conclusions
Critical thinking and clinical reasoning are fundamental skills of the advanced non-medical practitioner (ANMP) role. They are complex processes and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories. There are multiple constructs to guide these processes, not all of which will be suitable for the vast array of specialist areas in which ANMPs practice. There are multiple opportunities throughout the clinical consultation process in which ANMPs can employ the principles of critical thinking and clinical reasoning in order to improve patient outcomes. There are also multiple online toolkits that may be used to guide the ANMP in this complex process.
- Much like consultation and clinical assessment, the process of the application of clinical reasoning was once seen as solely the duty of a doctor, however the advanced non-medical practitioner (ANMP) role crosses those traditional boundaries
- Critical thinking and clinical reasoning are fundamental skills of the ANMP role
- The processes underlying clinical reasoning are complex and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories
- Through the use of the principles underlying critical thinking and clinical reasoning, there is potential to make a significant contribution to diagnostic accuracy, treatment options and overall patient outcomes
CPD reflective questions
- What assessment instruments exist for the measurement of cognitive bias?
- Think of an example of when cognitive bias may have impacted on your own clinical reasoning and decision making
- What resources exist to aid you in developing into the ‘advanced critical thinker’?
- What resources exist to aid you in understanding the statistical terminology surrounding evidence-based diagnosis?

The Importance of Critical Thinking in Nursing

An American Association of Nurse Practitioners (AANP) survey found that a majority of nurse practitioners saw three or more patients per hour. Nurse practitioners see patients of all ages with a broad spectrum of potential ailments. Critical thinking skills in nursing improve patient outcomes by enabling evidence-based decision-making.
Nurse practitioners gather considerable amounts of patient data through evaluations, tests and conversations. Each patient's information can be interpreted and analyzed to determine the best courses of action for their health. A growing emphasis on critical thinking in nursing stems from the increasing importance of nurse practitioners in primary care.
Earn Your MSN-FNP Part-Time For Less than $30k
Growing need for critical thinking in nursing.
There is a significant shortage of primary care services throughout the United States. GoodRx identified 80% of counties as "health care deserts" or locations without easy access to necessary services. This data includes the following categories relevant to family nurse practitioners:
- 9% of counties lack enough primary care providers to serve the local population
- Residents in 20% of counties are at least 30 minutes away from hospitals
- Residents in 45% of counties are at least 20 minutes away from community health centers
"Health care deserts" are worsening because of a shortage of primary care physicians. The Association of American Medical Colleges ( AAMC ) estimates up to 48,000 more primary care providers are needed to meet patient care needs by 2034. This shortfall translates to a lack of preventive care and increased reliance on emergency care facilities.
The U.S. Bureau of Labor Statistics ( BLS ) projects a 52% growth in nurse practitioner roles by 2030. This growth is fueled not only by "health care deserts" but an aging population and public health threats like COVID-19. Critical thinking by nurse practitioners can overcome these challenges even with limited resources and stressful situations.
The Critical Thinking Process
The first step in incorporating critical thinking into patient care is understanding the critical thinking process. The National League for Nursing Accreditation Commission ( NLNAC ) defines critical thinking as:
"the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief based."
Critical thinking in nursing does not move in a straight line because each patient is unique. There isn't a one-size-fits-all diagnosis for patients because there isn't a single type of patient. Nurse practitioners can apply the following steps in the Clinical Reasoning Cycle as they evaluate patient care decisions.
Consider the Situation
First impressions of new patients can distract from effective evaluations. Personal experiences and assumptions may lead to hasty conclusions about patient needs. The first step to critical thinking in nursing involves a dispassionate consideration of the facts.
Nurse practitioners often have the basic facts about their patients' conditions before stepping into exam rooms. A simple repetition of the patient's age and reported illness counters assumptions that can negatively impact patient care.
Collect Information
Critical thinking requires the synthesis of existing and new information for effective analysis. Nurse practitioners can pull useful details from patient charts and histories when they are available. An evaluation of visual appearance, speech, blood pressure and other metrics builds on this previous work.
Skilled practitioners automatically apply their knowledge of physiology, pharmacology and other areas during the collection process. They also keep best practices, cultural competence and ethics in mind while working with patients. This recall makes it easier to process information during diagnosis.
Process Information
There is a multi-step process for turning raw information into useful insights for patient care. Nurse practitioners effectively process patient data by:
- Analyzing information within the context of normal and abnormal ranges
- Separating relevant and irrelevant data while finding information gaps
- Focus on relationships between symptoms and cues
- Deduce potential causes of health problems
- Compare similar situations between current and past patients
- Predict potential outcomes and complications from treatment
Nurse practitioners are ready to diagnose patient conditions following this process. Depending on symptoms, they'll have considered and eliminated multiple diagnoses based on careful consideration of the facts. This step also takes into consideration risks for other health issues without treatment.
Set Goals and Act
A patient's course of treatment should follow the SMART model for goal-setting. The best treatment plans are Specific, Measurable, Achievable, Realistic and Timely to support the measurement of their efficacy. This model creates a repeatable process that is effective across patient demographics and conditions.
Critical thinking in nursing produces clear goals that are essential to patient adherence to treatment. Treatment plans may include prescribed medications, therapies and visits with specialists. Nurse practitioners collaborate with their patients and colleagues on supportive frameworks for effective treatment.
Evaluate and Reflect
Follow-up appointments provide opportunities for evaluation of treatment plans. Nurse practitioners compare past and present metrics when determining improvements in patient conditions. A useful method for evaluating success is whether the following rights of clinical reasoning were applied:
- Right patient
- Right action
- Right reason
Frequent reflection on this process is essential for improvement as a nurse practitioner. Self-directed explorations of what should have been done and what could have happened in each case sharpen critical thinking skills. An understanding of what was learned in each case creates points of comparison for future patients.
Improving Your Critical Thinking
Critical thinking in nursing improves through thoughtful deliberation and frequent use. Nurse practitioners should speak with their colleagues and mentors about their applications of critical thinking. Frequent collaboration on patient care also places the focus on evidence-based care rather than personal assumptions.
Updated knowledge of nursing resources and tools makes it easier to implement critical thinking in nursing. Medical journals and continuing education courses reinforce what nurse practitioners have learned throughout their careers. Carson-Newman University provides a strong foundation for improved critical thinking through its Online MSN-FNP.
Preparing for Clinical Decisions at Carson-Newman
Carson-Newman's innovative program prepares BSN & MSN-educated nurses for future roles as family nurse practitioners (FNPs). The in-person requirements for this 100% online degree are clinical placements and a three-day campus residency. Students can complete the Online MSN-FNP in as little as 32 months.
Every course in the program is taught by an experienced nurse educator who also practices in their community. Carson-Newman reinforces the importance of critical thinking in nursing with courses on topics including:
- Advanced Health Assessment
- Advanced Pathophysiology
- Advanced Primary Care Nursing for Adults
FNP students receive full support from Carson-Newman to identify clinical placements in their communities. They also receive one-on-one guidance from Student Success Advisors throughout their time at the University. This commitment to nursing education helped Carson-Newman reach the top third of graduate nursing programs in U.S. News & World Report's rankings.
Contact an enrollment advisor today to learn how Carson-Newman can prepare you for a role as an FNP.
Request Your Free Program Brochure

Jon Rappoport
Critical thinking: the confounding variable.

You hear it many times: “Correlation doesn’t equal causation.”
Example: 30 people in a town fall ill. The CDC, correlating these people with COVID symptoms—“fever, fatigue, cough, and elevated temperature”—declare them COVID cases. COVID is the cause of their health issues.
But there is a confounding variable. Meaning an element that confounds (disrupts, contradicts) this analysis. A sudden release of noxious air from a nearby factory.
Therefore, correlation didn’t point to the inevitable “COVID” cause.
But how about this? In a city, in various clinics and drug stores, 30 people get COVID shots on the same day, and they all immediately fall ill. Very ill. That’s a correlation. A very convincing one.
It certainly seems to indicate the cause: the vaccinations.
There is no pure logic to consult, to come up with a conclusion.
Critical thinking involves common sense.
Yes, it’s theoretically possible that some unknown cause(s) was a confounding factor, and the vaccine wasn’t the cause of illness. But the circumstances of the situation, and common sense, dictate how to apply critical thinking.
In that situation, you’re going to say correlation DOES equal causation.
So…you have to take things on a case by case basis.
Sometimes correlation does and sometimes it doesn’t equal causation.
This also shows you that logic and critical thinking aren’t always the same thing. Meaning there isn’t always an overriding hard and fast rule you can follow.
When I was writing AIDS INC. in 1987, I had reached the conclusion that HIV didn’t cause AIDS. It would be years before I realized there was no proof viruses existed.
A person challenged my conclusion about HIV. He said, “Research teams have been doing antibody tests for HIV all over Africa and the tests are coming up positive for HIV.”
He was pointing to thousands of people who had what were called AIDS symptoms, and the correlation between those people and the antibody tests they’d been given—which were positive for HIV.
So I looked for a confounding factor. Eventually, I found it:
This post is for paid subscribers
- Augsburg.edu
- Inside Augsburg
Search Strommen Center for Meaningful Work
- Faculty & Staff
- Graduate Students
- First Generation
- International
- Students With Disabilities
- Undocumented
- Business & Finance
- Culture and Language
- Environmental Sustainability
- Government, Law & Policy
- Health Professions
- Human & Social Services
- Information Technology & Data
- Marketing, Media & Communications
- Resumes and Cover Letters
- Expand Your Network / Mentor
- Explore Your Interests / Self Assessment
- Negotiate an Offer
- Prepare for an Interview
- Prepare for Graduate School
- Search for a Job / Internship
- Job Fair Preparation
- Start Your Internship
- Choosing a Major
- Career Collaborative
- Travelers EDGE
- Meet the Team
Critical Thinking: A Simple Guide and Why It’s Important
- Share This: Share Critical Thinking: A Simple Guide and Why It’s Important on Facebook Share Critical Thinking: A Simple Guide and Why It’s Important on LinkedIn Share Critical Thinking: A Simple Guide and Why It’s Important on X
Critical Thinking: A Simple Guide and Why It’s Important was originally published on Ivy Exec .
Strong critical thinking skills are crucial for career success, regardless of educational background. It embodies the ability to engage in astute and effective decision-making, lending invaluable dimensions to professional growth.
At its essence, critical thinking is the ability to analyze, evaluate, and synthesize information in a logical and reasoned manner. It’s not merely about accumulating knowledge but harnessing it effectively to make informed decisions and solve complex problems. In the dynamic landscape of modern careers, honing this skill is paramount.
The Impact of Critical Thinking on Your Career
☑ problem-solving mastery.
Visualize critical thinking as the Sherlock Holmes of your career journey. It facilitates swift problem resolution akin to a detective unraveling a mystery. By methodically analyzing situations and deconstructing complexities, critical thinkers emerge as adept problem solvers, rendering them invaluable assets in the workplace.
☑ Refined Decision-Making
Navigating dilemmas in your career path resembles traversing uncertain terrain. Critical thinking acts as a dependable GPS, steering you toward informed decisions. It involves weighing options, evaluating potential outcomes, and confidently choosing the most favorable path forward.
☑ Enhanced Teamwork Dynamics
Within collaborative settings, critical thinkers stand out as proactive contributors. They engage in scrutinizing ideas, proposing enhancements, and fostering meaningful contributions. Consequently, the team evolves into a dynamic hub of ideas, with the critical thinker recognized as the architect behind its success.
☑ Communication Prowess
Effective communication is the cornerstone of professional interactions. Critical thinking enriches communication skills, enabling the clear and logical articulation of ideas. Whether in emails, presentations, or casual conversations, individuals adept in critical thinking exude clarity, earning appreciation for their ability to convey thoughts seamlessly.
☑ Adaptability and Resilience
Perceptive individuals adept in critical thinking display resilience in the face of unforeseen challenges. Instead of succumbing to panic, they assess situations, recalibrate their approaches, and persist in moving forward despite adversity.
☑ Fostering Innovation
Innovation is the lifeblood of progressive organizations, and critical thinking serves as its catalyst. Proficient critical thinkers possess the ability to identify overlooked opportunities, propose inventive solutions, and streamline processes, thereby positioning their organizations at the forefront of innovation.
☑ Confidence Amplification
Critical thinkers exude confidence derived from honing their analytical skills. This self-assurance radiates during job interviews, presentations, and daily interactions, catching the attention of superiors and propelling career advancement.
So, how can one cultivate and harness this invaluable skill?
✅ developing curiosity and inquisitiveness:.
Embrace a curious mindset by questioning the status quo and exploring topics beyond your immediate scope. Cultivate an inquisitive approach to everyday situations. Encourage a habit of asking “why” and “how” to deepen understanding. Curiosity fuels the desire to seek information and alternative perspectives.
✅ Practice Reflection and Self-Awareness:
Engage in reflective thinking by assessing your thoughts, actions, and decisions. Regularly introspect to understand your biases, assumptions, and cognitive processes. Cultivate self-awareness to recognize personal prejudices or cognitive biases that might influence your thinking. This allows for a more objective analysis of situations.
✅ Strengthening Analytical Skills:
Practice breaking down complex problems into manageable components. Analyze each part systematically to understand the whole picture. Develop skills in data analysis, statistics, and logical reasoning. This includes understanding correlation versus causation, interpreting graphs, and evaluating statistical significance.
✅ Engaging in Active Listening and Observation:
Actively listen to diverse viewpoints without immediately forming judgments. Allow others to express their ideas fully before responding. Observe situations attentively, noticing details that others might overlook. This habit enhances your ability to analyze problems more comprehensively.
✅ Encouraging Intellectual Humility and Open-Mindedness:
Foster intellectual humility by acknowledging that you don’t know everything. Be open to learning from others, regardless of their position or expertise. Cultivate open-mindedness by actively seeking out perspectives different from your own. Engage in discussions with people holding diverse opinions to broaden your understanding.
✅ Practicing Problem-Solving and Decision-Making:
Engage in regular problem-solving exercises that challenge you to think creatively and analytically. This can include puzzles, riddles, or real-world scenarios. When making decisions, consciously evaluate available information, consider various alternatives, and anticipate potential outcomes before reaching a conclusion.
✅ Continuous Learning and Exposure to Varied Content:
Read extensively across diverse subjects and formats, exposing yourself to different viewpoints, cultures, and ways of thinking. Engage in courses, workshops, or seminars that stimulate critical thinking skills. Seek out opportunities for learning that challenge your existing beliefs.
✅ Engage in Constructive Disagreement and Debate:
Encourage healthy debates and discussions where differing opinions are respectfully debated.
This practice fosters the ability to defend your viewpoints logically while also being open to changing your perspective based on valid arguments. Embrace disagreement as an opportunity to learn rather than a conflict to win. Engaging in constructive debate sharpens your ability to evaluate and counter-arguments effectively.
✅ Utilize Problem-Based Learning and Real-World Applications:
Engage in problem-based learning activities that simulate real-world challenges. Work on projects or scenarios that require critical thinking skills to develop practical problem-solving approaches. Apply critical thinking in real-life situations whenever possible.
This could involve analyzing news articles, evaluating product reviews, or dissecting marketing strategies to understand their underlying rationale.
In conclusion, critical thinking is the linchpin of a successful career journey. It empowers individuals to navigate complexities, make informed decisions, and innovate in their respective domains. Embracing and honing this skill isn’t just an advantage; it’s a necessity in a world where adaptability and sound judgment reign supreme.
So, as you traverse your career path, remember that the ability to think critically is not just an asset but the differentiator that propels you toward excellence.

How nursing is changing in the age of AI
T he healthcare industry has gone through a lot of transformation in the past century. But what has always remained unchanged, or has been the heart of this profession, is the care provided by nurses â anywhere in the world.Â
Artificial Intelligence (AI) has been the buzzword since 2023. Experts predict sweeping changes in the way the world functions going ahead. The nursing profession will also see a lot of changes.Â
But at its heart, nurses are the first point of contact when a patient is admitted to a hospital, and the last contact when a patient is discharged. The bond that nurses share with their patients will remain unchanged.
NURSING IN THE AGE OF AI
What AI is going to change, and the process has already started, are healthcare delivery methods, and the incorporation of AI-based solutions into clinical care. Nurses are trained to adapt quickly to any changing environment.
We saw that when a pandemic affected the world. Nurses, all around the world, rose to the challenge and conquered it with not just their medical expertise but their empathy and humanity. What AI will do is ease the burden of daily tasks of nurses by redefining some old positions, while improving patient care results.
AI-driven technologies like EHRs, clinical decision support systems, and predictive analytics help simplify administrative tasks, improve productivity, and lessen the manual documentation workload for nurses.Â
Automating routine tasks allows nurses to focus more on providing direct patient care, critical thinking, and making complex decisions.
AI-powered tools are also enabling nurses to provide patients with more customised care and changing the landscape of preventive healthcare too.Â
HOW IS AI MAKING NURSING BETTER?
Machine learning algorithms review extensive patient data, such as medical history, diagnostic tests and treatment results to pinpoint patterns and risk factors. This allows nurses to predict patient needs, act proactively, and customise care plans based on personal preferences and situations.
The field of nursing education and training will also see positive changes. Virtual simulation technology and immersive educational opportunities can replicate real-life situations, giving nursing students the chance to improve clinical abilities, boost critical thinking, and build self-assurance.Â
AI could also enhance nurses' ability to conduct research - natural language, processing algorithms, analyse large amounts of scientific literature, extract important insights, combine evidence, and recognise top strategies.Â
The future of nursing in India looks bright and promising. AI will continue to evolve, and it has the potential to redefine nursing not just as a profession but as a cornerstone of innovative, patient-centred healthcare.
However, nursing, at its core, comes from the heart. As legendary American poet May Angelou once said, "As a nurse, we have the opportunity to heal the mind, soul, heart, and body of our patients. They may forget your name, but they will never forget how you made them feel."
(Disclaimer: This is an authored article. The views and opinions expressed by the doctors and experts are their independent professional judgement, and we do not take any responsibility for the accuracy of their views.)

- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Re: Critical thinking in healthcare and education
Rapid response to:
Critical thinking in healthcare and education
- Related content
- Article metrics
- Rapid responses
Rapid Response:
Walker (2003) highlighted that many individuals believe that the tendency to think critically must be nurtured. We have seen educated healthcare professionals in healthcare facilities but does that mean that they have critical thinking skills? I agree with Jonathan Sharples et al in the article, “Critical thinking in healthcare and education”arguing about the importance for clinicians and patients to learn to think critically and that the teaching and learning of these skills to be explicitly considered.
Critical thinking includes “analysis, inference, interpretation, explanation, synthesis and self –regulation” (Facione, 2011). The healthcare team should be able to utilize their critical thinking skills as they come in contact with their patients daily. Critical thinking has been well documented in nursing but the evidence in medicine is limited (Batool, 2010; Iranfar, Sepahi, Khoshay, Rezaei, Matin, Keshavarzi, & Bashiri, 2012; Mahmoodabad, Nadrian, & Nahangi, 2012; Maudsley & Strivens, 2000). Are nurses the only group of health professionals taking care of patients? Certainly not, other members of the healthcare team work collaboratively with each other to ensure optimal patient care. Thus critical thinking is essential among healthcare professionals.
Critical thinking is integral in caring for patients and before one can teach patients to think critically, he or she needs to model the behavior but how can one model what they do not know? Riddel (2007) emphasized that critical thinking is a complex process and not a single way of thinking. Cottrell (2011) concurred with Riddel and added that critical thinking includes identification of the views of individuals, evaluation of evidence to explore alternate views, being unbiased in weighing the evidence and opposing arguments.
However, Romeo (2010) defines critical thinking as an attribute that strengthens the decision making and problem solving skills of an individual. In order for students to develop critical thinking skills and depositions, the faculty needs to reconsider their philosophy of teaching and implement critical thinking in the curricula (Billings & Halstead, 2012). Educators can design their teaching plans to facilitate critical thinking disposition and critical learning. If students in healthcare professions are taught critical thinking early in their programs, they will be able to develop the skill and will be able to utilize same effectively in their practice.
The healthcare system is evolving and emphasis should be placed on healthcare professionals to develop creative and critical thinking skills so that they can administer optimal patient care and be able to teach their patients how to think critically.
References Batool, T. (2010). Hyposkillia and critical thinking: Lost skills of doctors.APS Journal of case reports, 1(1), 9. Billings, D. M., & Halstead, J. A. (2012). Teaching in nursing: A guide for faculty (4th ed.). St. Louis: Elsevier Health Sciences. Cottrell, S. (2011). Critical thinking skills: Developing effective analysis and argument. Palgrave Macmillan. Facione, P. A. (2011). Critical thinking: What it is and why it counts. Insight Assessment, 2007(1), 1-23. Iranfar, S., Sepahi, V., Khoshay, A., Rezaei, M., Matin, B. K., Keshavarzi, F., & Bashiri, H. (2012). Critical thinking disposition among medical students of Kermanshah University of Medical Sciences. ducational Research in Medical Sciences Journal, 1(2), 63-68. Mahmoodabad, S. S. M., Nadrian, H., & Nahangi, H. (2012). Critical thinking ability and its associated factors among preclinical students in Yazd Shaheed Sadoughi University of Medical Sciences (Iran). Medical Journal of the Islamic Republic of Iran, 26(2), 50. Maudsley, G., & Strivens, J. (2000). ‘Science’,‘critical thinking’and ‘competence’ for tomorrow’s doctors. A review of terms and concepts.Medical Education, 34(1), 53-60. Riddell, T. (2007). Critical assumptions: Thinking critically about critical thinking. Journal of Nursing Education, 46(3). Romeo, E. M. (2010). Quantitative research on critical thinking and predicting nursing students’ NCLEX-RN performance. Journal of Nursing Education, 49(7), 378-386. Walker, S. E. (2003). Active learning strategies to promote critical thinking. Journal of athletic training, 38(3), 263.
Competing interests: No competing interests
Main navigation
- Our Articles
- Dr. Joe's Books
- Media and Press
- Our History
- Public Lectures
- Past Newsletters
Subscribe to the OSS Weekly Newsletter!
Register for the oss 25th anniversary event, twisting facts about cancer.

- Add to calendar
- Tweet Widget
Let’s start with some facts. Antiperspirants, cell phones, root canals or wired bras do not cause cancer. Sugar or dairy products do not “feed” the disease. You cannot cure cancer with an alkaline diet, crystals, juices, shark cartilage, apricot pits, magnets, mistletoe, soursop, chlorella, black walnuts, coconut oil, cesium chloride, reiki, psychic surgery, baking soda, antineoplastons, bioresonance machines, orgone accumulators, Rife frequency generators or coffee enemas.
All of this comes to mind now because I was forwarded a link to a document entitled “Everyday Products Linked to Cancer” which also offers solutions to the problem. So, I clicked. I quickly learned that the discoverer of “the missing link” to “conquering cancer” is identified as a “natural health researcher and certified holistic cancer coach.” That immediately set my alarm bells ringing. This is not terminology that would ever be used to describe a legitimate scientist. And those bells really started to clamor when I encountered phrases like “groundbreaking,” “unveil cancer care known only to a few,” “challenge the one-sided, conventional understanding and offer more effective ways to conquer cancer,” “discover the proven protocols that have helped hundreds of thousands of people prevent and conquer cancer,” and “discover why many cancer treatments and prevention protocols fail.”
It seems Nathan Crane, also described as a “plant-based athlete,” has found the secret that has eluded thousands and thousands of researchers around the globe and is now equipped to “pave the way for future generations to live cancer free.” A search for this sage’s educational background reveals only that he went to Belgrade High School in Montana.
What is the key to living cancer-free? Staying away from “toxic household and personal care products” and “turning to nature” for replacements. Of course, we also need to fortify our body against toxins. How? By making use of “the power of nature’s detoxifiers.” Let me point out that the term “detoxify” is generally indicative of pseudoscience since the toxins being removed are never identified nor is the mechanism by which they are eliminated elucidated.
There is nothing novel in this “Conquering Cancer” manuscript. The Internet and bookstores brim with articles and books about purported carcinogens in everyday products and secret cures hidden by “Big Pharma” for fear of losing profits from the sale of ineffective, toxic chemotherapeutic agents. The idea of secret cures is nonsense, but when it comes to chemicals found in consumer products, there are some legitimate issues. However, fear-mongering documents, such as this one, generally smack of an ignorance of dose-response relationships and claim to have greater knowledge of the impact of these chemicals on health than what actually exists. Suppositions are presented as facts.
Some personal care products and cleaning agents contain chemicals that can be classified as endocrine disruptors or carcinogens. Furthermore, some of these can be detected in our bloodstream and urine. But it is critical to understand that the presence of a chemical cannot be equated to the presence of risk. Labeling a substance as an endocrine disruptor or carcinogen is in general based on cell culture or animal studies that use amounts far greater than what humans can possibly encounter. This does not mean that concerns about the likes of phthalates, bisphenol A, dioxane and nonylphenol ethoxylates should be swept under the carpet, but proclamations that “we’re poisoning ourselves” by using products that contain traces of these substances magnify whatever risk they may pose in an unrealistic fashion.
While reducing our use of products that contain chemicals that have the shadow of carcinogen or endocrine disruptor hanging over them has merit, the claim that turmeric, ginger, cayenne pepper, cinnamon, frankincense, Camu Camu or blueberries are “nature’s detoxifiers” and protect us from cancer is not evidence-based.
However, my biggest problem with this publication is the simplistic view it presents about preventing cancer. This is a very complex disease in which genetics, diet, infections, overweight, smoking, alcohol consumption, certain chemicals, exposure to ionizing radiation, changes in hormone levels, physical activity and age can all play roles. Suggestions that cancer risk can be significantly reduced by adding turmeric to the diet or replacing a commercial cleaning agent with vinegar, or switching from store-bought shampoo to a homemade concoction of aloe vera gel, coconut milk and castile soap, are naïve.
Something else is bothersome about this publication. The talk about “dangerous” everyday products and the use of herbs to “bolster our natural defenses” seems to be just bait to hook people to click on a link to a docuseries about “Conquering Cancer.” We are asked if we are “ready to explore the hidden cause of cancer that has eluded experts for years” and told that we will discover “how to starve your cancer cells without chemo, radiation or surgery.” The latter is a hallmark of quackery.
I did not take the bait because I follow cancer research closely and know that there are no hidden causes or magical cures. Certainly not any that have been discovered by a “certified holistic cancer coach.” I also suspect that if I were to click on the link for a “free ticket” to the series that promises to reveal “how natural, proven methods have helped over 591,753 people prevent and treat this life-threatening disease,” I might at some point be prompted to dig out my credit card for some over-hyped dietary supplement or a book with an assortment of twisted facts. But that’s just a guess.
@JoeSchwarcz
What to read next
Processed foods have many faces 17 may 2024.

Reports of the Death of Dental Cavities Are Greatly Exaggerated 17 May 2024

Methylene Chloride Can Strip Paint but Can Also Strip Years Off Your Life 15 May 2024

No, Eating French Fries is Not the Same as Smoking Cigarettes 10 May 2024

Navigating the Twisted World of Varicose Veins 10 May 2024
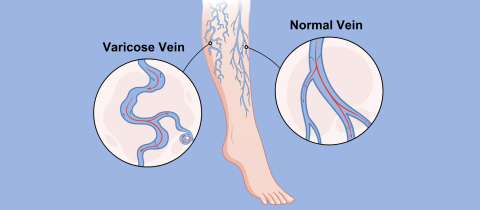
Pass on the Salt: Should We Ask for Potassium Chloride at the Dinner Table Instead? 17 May 2024

Department and University Information
Office for science and society.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Am Thorac Soc
Critical Thinking in Critical Care: Five Strategies to Improve Teaching and Learning in the Intensive Care Unit
Margaret m. hayes.
1 Division of Pulmonary, Critical Care and Sleep Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts
2 Shapiro Institute for Education and Research at Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, Massachusetts; and
Souvik Chatterjee
3 Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda, Massachusetts
Richard M. Schwartzstein
Associated data.
Critical thinking, the capacity to be deliberate about thinking, is increasingly the focus of undergraduate medical education, but is not commonly addressed in graduate medical education. Without critical thinking, physicians, and particularly residents, are prone to cognitive errors, which can lead to diagnostic errors, especially in a high-stakes environment such as the intensive care unit. Although challenging, critical thinking skills can be taught. At this time, there is a paucity of data to support an educational gold standard for teaching critical thinking, but we believe that five strategies, routed in cognitive theory and our personal teaching experiences, provide an effective framework to teach critical thinking in the intensive care unit. The five strategies are: make the thinking process explicit by helping learners understand that the brain uses two cognitive processes: type 1, an intuitive pattern-recognizing process, and type 2, an analytic process; discuss cognitive biases, such as premature closure, and teach residents to minimize biases by expressing uncertainty and keeping differentials broad; model and teach inductive reasoning by utilizing concept and mechanism maps and explicitly teach how this reasoning differs from the more commonly used hypothetico-deductive reasoning; use questions to stimulate critical thinking: “how” or “why” questions can be used to coach trainees and to uncover their thought processes; and assess and provide feedback on learner’s critical thinking. We believe these five strategies provide practical approaches for teaching critical thinking in the intensive care unit.
Critical thinking, the capacity to be deliberate about thinking and actively assess and regulate one’s cognition ( 1 – 4 ), is an essential skill for all physicians. Absent critical thinking, one typically relies on heuristics, a quick method or shortcut for problem solving, and can fall victim to cognitive biases ( 5 ). Cognitive biases can lead to diagnostic errors, which result in increased patient morbidity and mortality ( 6 ).
Diagnostic errors are the number one cause of medical malpractice claims ( 7 ) and are thought to account for approximately 10% of in-hospital deaths ( 8 ). Many factors contribute to diagnostic errors, including cognitive problems and systems issues ( 9 ), but it has been shown that cognitive errors are an important source of diagnostic error in almost 75% of cases ( 10 ). In addition, a recent report from the Risk Management Foundation, the research arm of the malpractice insurer for the Harvard Medical School hospitals, labeled more than half of the malpractice cases they evaluated as “assessment failures,” which included “narrow diagnostic focus, failure to establish a differential diagnosis, [and] reliance on a chronic condition of previous diagnosis ( 11 ).” In light of these data and the Institute of Medicine’s 2015 recommendation to “enhance health care professional education and training in the diagnostic process ( 8 ),” we present this framework as a practical approach to teaching critical thinking skills in the intensive care unit (ICU).
The process of critical thinking can be taught ( 3 ); however, methods of instruction are challenging ( 12 ), and there is no consensus on the most effective teaching model ( 13 , 14 ). Explicit teaching about reasoning, metacognition, cognitive biases, and debiasing strategies may help avoid cognitive errors ( 3 , 15 , 16 ) and enhance critical thinking ( 17 ), but empirical evidence to inform best educational practices is lacking. Assessment of critical thinking is also difficult ( 18 ). However, because it is of paramount importance to providing high-quality, safe, and effective patient care, we believe critical thinking should be both explicitly taught and explicitly assessed ( 12 , 18 ).
Critical thinking is particularly important in the fast-paced, high-acuity environment of the ICU, where medical errors can lead to serious harm ( 19 ). Despite the paucity of data to support an educational gold standard in this field, we propose five strategies, based on educational principles, we have found effective in teaching critical thinking in the ICU ( Figure 1 ). These strategies are not dependent on one another and often overlap. Using the following case scenario as an example for discussion, we provide a detailed explanation, as well as practical tips on how to employ these strategies.
A 45-year-old man with a history of hypertension presents to the emergency department with fatigue, sore throat, low-grade fever, and mild shortness of breath. On arrival to the emergency department, his heart rate is 110 and his blood pressure is 90/50 mm Hg. He is given 2 L fluids, but his blood pressure continues to fall, and norepinephrine is started. Physical examination is normal with the exception of dry mucous membranes. Laboratory studies performed on blood samples obtained before administration of intravenous fluid show: white blood cell count, 6.0 K/uL; hematocrit, 35%; lactate, 0.8 mmol/L; blood urea nitrogen, 40 mg/dL; and creatinine, 1.1 mg/dL. A chest radiograph shows no infiltrates. He is admitted to the medical intensive care unit. Attending: What is your assessment of this patient? Resident: This is a 45-year-old male with a history of hypertension who was sent to us from the emergency department with sepsis. Attending: That is interesting. I am puzzled: What is the source of infection? And how do you account for the low hematocrit in an essentially healthy man whom you believe to be volume depleted? Resident: Well, maybe pneumonia will appear on the X-ray in the next 24 hours. With respect to the hematocrit...I’m not really sure.

Five strategies to teach critical thinking skills in a critical care environment.
Strategy 1: Make the “Thinking Process” Explicit
In the ICU, many attendings are satisfied with the trainee simply putting forth an assessment and plan. In the case presented here, the resident’s assessment that the patient has sepsis is likely based on the resident remembering a few facts about sepsis (i.e., hypotension is not responsive to fluids) and recognizing a pattern (history of possible infection + fever + hypotension = sepsis). With this information, we may determine that the learner is operating at the lowest level of Bloom’s taxonomy: remembering ( 20 ) ( Figure 2 ), in this case, she seems to be using reflexive or automatic thought. In a busy ICU, it is tempting for the attending to simply overlook the response and proceed with one’s own plan, but we should be expecting more. As indicated in the attending’s response, we should make the thinking process explicit and push the resident up Bloom’s taxonomy: to describe, explain, apply, analyze, evaluate, and ultimately create ( 20 ) ( Figure 2 ).

The revised Bloom’s taxonomy. This schematic, first created in 1956, depicts six levels of the cognitive domain. Remembering is the lowest level; creating is the highest level. Adapted from Anderson and Krathwol ( 20 ).
Faculty members should probe the thought process used to arrive at the assessment and encourage the resident to think about her thinking; that is, to engage in the process of metacognition. We recommend doing this in real time as the trainee is presenting the case by asking “how” and “why” questions (see strategy 4).
Attending: Why do you think he has sepsis? Resident: Well, he came in with infectious symptoms. Also, his blood pressure is quite low, and it only improved slightly with fluids in the emergency department. Attending: Okay, but how is blood pressure generated? How could you explain hypotension using other data in the case, such as the low hematocrit?
If the trainee is encouraged to think about her thinking, she may conclude that she was trying to force a “pattern” of sepsis, perhaps because she frequently sees patients with sepsis and because the emergency department framed the case in that way. It is possible that she does not have enough experience in the ICU or specific knowledge about sepsis to accurately assess this patient; in the actual case, a third-year resident with significant ICU experience ultimately admitted to defaulting to pattern recognition.
One way to push learners up Bloom’s taxonomy is to help them understand dual-process theory: the idea that the brain uses two thinking processes, type 1 and type 2 (alternately known as system 1 and system 2). Type 1 thinking is the more intuitive process of decision making; type 2 is an analytical process ( 17 , 21 , 22 ). Type 1 thinking is immediate and unconscious, and the hallmark is pattern recognition; type 2 is deliberate and effortful ( 17 ).
Critical thinkers understand and recognize the dual processes ( 21 ) and the fact that type I thinking is common in their daily lives. Furthermore, they acknowledge that type 1 reasoning, which is often automatic and unconscious, can be prone to error. There is a paucity of data linking cognitive errors to the particular type of thinking ( 14 ), but many of these studies are plagued by the fact that they do not test the atypical pattern. As a consequence, they do not truly test the hypothesis that type 2 reasoning will reduce error in more complex cases. It has been shown that combining type 1 and type 2 thinking improves diagnostic accuracy compared with just using one method versus another ( 23 ). We believe that helping learners understand how their minds work will help them recognize when they may be falling into pattern recognition and when this will be problematic (e.g., when there are discordant data, or one can only quickly think of one diagnosis). By expecting more from our learners, by compelling them to understand, analyze, and evaluate, we must provide constant feedback and coaching to help them develop, and we must ask the right questions (see strategy 4) to guide them.
Strategy 2: Discuss Cognitive Biases and De-Biasing Strategies
Cognitive biases are thought patterns that deviate from the typical way of decision making or judging ( 24 ). These occur commonly when we are under stress or time constrained when making decisions. At this time, there are more than 100 described cognitive biases, some of which are more common in medicine than others ( 25 ). We believe that the six outlined in Table 1 are particularly prevalent in the ICU.
Six common biases frequently used in the intensive care unit
The definitions of these biases are based on their application and use in clinical medicine. Table adapted from Croskerry ( 6 ), Croskerry ( 27 ), and Hogarth ( 37 ).
Although there are many proponents of teaching cognitive biases ( 6 ), there are no studies showing that teaching these to trainees improves their clinical decision making ( 14 ), again recognizing that research in this area has often not focused on the scenarios in which cognitive bias is likely to lead to error. Most cognitive biases are quiescent until the right scenario presents itself ( 26 ), which makes them difficult to study in the clinical context. Imagine an overworked, tired resident in a busy ICU or one who received an incomplete sign-out or felt pressure from the system to make a quick decision to move along patient care. These scenarios occur daily in the ICU; as a consequence, we believe that teaching residents how to recognize biases and giving them strategies to debias is important.
The resident in the clinical scenario outlined here is falling prey to many biases in her assessment that the patient has sepsis. First, it is likely that on her ICU rotation she has seen many patients with sepsis, and thus sepsis is a diagnosis that is easily available to her mind (availability bias). Next, she is falling victim to confirmation bias: The presence of hypotension supports a diagnosis of sepsis and is disproportionately appreciated by the trainee compared with a white blood cell count of 6,000, which does not easily fit with the diagnosis and is ignored. Next, she anchors and prematurely closes on the diagnosis of sepsis and does not look for other possible explanations of hypotension. The resident does not realize that she is subject to these biases; explicitly discussing them will help her understand her thinking process, enable her to recognize when she may be jumping to conclusions, and help her identify when she must switch to type 2 thinking.
Attending: Why do you think he has sepsis? Resident: Well, he came in with infectious symptoms. Also, his blood pressure is quite low, and it did not improve with fluids in the emergency department. This is similar to the other patient with sepsis. Attending: I can see why sepsis easily comes to your mind, as we have recently admitted three other patients with sepsis. These patients had similar features to this patient, so your mind is jumping to that conclusion, but if we stop and think together about what pieces of the case don’t fit with sepsis, we may come up with a different diagnosis. Resident: Well, the lack of leukocytosis doesn’t make sense. Attending: Yes! I agree, that is a bit odd. Let’s broaden our differential and not anchor on sepsis. What else could this be?
Cognitive forcing strategies ( 16 ), the process of making trainees aware of their cognitive biases and then developing strategies to overcome the bias, may help this resident. Studies show that debiasing can be taught to emergency medicine trainees ( 27 ), and we believe it can also be taught to critical care trainees, who experience a similar fast-paced and high-stakes learning environment. Proposed debiasing strategies include encouraging trainees to consider alternative diagnoses ( 3 , 6 , 27 , 28 ) and promoting broad differentials. In particular, they need to be able to rethink cases when confronted with information that is not consistent with the working diagnosis; for example, leukocytosis, as above. They should be allowed to communicate their level of uncertainty, and we should not think less of them if they do not have a single final answer with a targeted plan ( 29 ). When we do not discuss inconsistent information, we essentially give trainees permission to ignore it.
Attending: In addition to the white blood cell count not fitting, I’m also struggling with the hematocrit: How is it 35% in the setting of presumed decreased intravascular volume? Resident: Hmm.... I’m actually not sure. You’re right, though, it doesn’t make sense. Attending: I agree. Let’s pause and think about how we are thinking about this case .
To a large degree, recognition of cognitive bias requires metacognition, defined as thinking about one’s thinking ( 3 , 16 , 27 ). This process is optimized with a familiarity with how the mind works; that is, a basic understanding of dual-process theory and cognitive biases. In the ICU, we find it easiest to engage in a group metacognition exercise. The attending asks, “How are we thinking about this case?” This allows both the attending and the team to reflect together on how and why the diagnosis has been made. This can provide insight into the tendency to prematurely close or limit considerations, which has been shown to be the most common cause of inaccurate clinical synthesis ( 10 ).
Other debiasing strategies include accountability ( 6 ) and feedback ( 25 , 30 ). Giving specific and in-the-moment feedback can help residents understand their decisions ( 25 ). It is our job as attendings to provide this feedback, and it is thought that this is one of the most effective debiasing strategies ( 25 ).
Strategy 3: Model and Teach Inductive Reasoning
In medicine, we classically teach clinical reasoning via the hypothetico-deductive strategy ( 31 ) and rarely discuss inductive reasoning. To date, there are no data proving the advantages of one strategy over another, but we believe that modeling inductive reasoning is an important part of critical thinking, especially when type 1 thinking provides limited answers. In hypothetico-deductive reasoning, physicians make a cognitive jump from a few facts to hypotheses framed as a differential diagnosis from which one then deduces characteristics that are matched to the patient ( 32 ). Because this way of thinking relies on memory and pattern recognition, we find that it is more subject to cognitive biases, including premature closure, than inductive reasoning.
In our case, the presence of hypotension leads the trainee to come up with a differential based primarily on that single observation; the resident thinks of diagnoses such as sepsis or cardiogenic shock. Contrast this way of thinking with inductive reasoning, which proceeds in an orderly way from multiple facts to hypotheses ( 32 ). In our case, putting together the facts of hypotension, decreased hematocrit, and elevated blood urea nitrogen/creatinine would lead to a broader list of possible explanations or hypotheses that would include bleeding (see Figure 3 to compare and contrast inductive and deductive reasoning). We propose that this way of thinking is grounded more deeply in pathophysiology, and we believe it leads to broader thinking, because trainees do not have to rely on memory, pattern recognition, or heuristics; rather, they can reason their way through the problem via an understanding of basic mechanisms of health and disease.

Schematic representations of deductive ( 1 ) and inductive ( 2 ) reasoning apropos to the clinical case. In deductive reasoning, one fact ( F ; hypotension ) is used to generated multiple hypotheses ( H ), and then facts that pertain to each are retrofitted ( red F* ; fever ). In inductive reasoning, facts are grouped and used to generate hypotheses. Adapted from Pottier ( 32 ).
Inductive reasoning can be practiced using both mechanism and concept maps. Mechanism maps are a visual representation of how the pathophysiology of disease leads to the clinical symptoms ( 33 ), whereas concept maps graphically represent relationships between multiple concepts ( 33 ) and make links explicit. Both types reinforce mechanistic thinking and can be used as tools to avoid cognitive biases. Using our case as an example, if the resident started with the hypotension and made a mechanism ( Figure 4A ) or concept ( Figure 4B ) map, she would be less likely to anchor on the diagnosis of sepsis. This process gives trainees a strategy to broaden their differential and a way to think about the case when they do not know what is going on.

( A ) A mechanism map of a 45-year-old man presenting with cough, shortness of breath. Found to have an increased BUN/Cr ration, a decreased hematocrit, and a normal white blood cell count. ( B ) A concept map of the clinical case. AFib = atrial fibrillation; BUN/Cr = blood urea nitrogen to creatinine ratio; CAD = coronary artery disease; CO/Q = cardiac output; CVP = central venous pressure; CXR = chest X-ray; GI = gastrointestinal; HR = heart rate; Hx HTN = history of hypertension; MAP = mean arterial pressure; RV = right ventricle; SV = stroke volume; SVR = systemic vascular resistance; WBC = white blood cell.
Although critics contend that these maps take time and do not have a place in the ICU, we find that quickly sketching a mechanism map on rounds while the case is being presented only takes 1–2 minutes and is a powerful way of making your method of clinical reasoning explicit to the learner. This can also be done later as a way to review pathophysiology. We hold monthly concept mapping sessions for our students ( 34 ) to improve their clinical reasoning skills, but find that in the ICU with residents, doing this quickly in real time with a mechanism map is more effective.
Strategy 4: Use Questions to Stimulate Critical Thinking
Questions can be used to engage the learners and inspire them to think critically. When questioning trainees, it is important to avoid the “quiz show” type questions that just test whether a trainee can recall a fact (e.g., “What is the most common cause of X”?). In our current advanced technological age, answers to this type of question reveal less about thinking abilities than how adept one is at searching the internet. These questions do not provide insight into the trainee’s understanding but can, we fear, subtly emphasize that the practice of medicine is about memorization, rather than thinking. In addition, this type of question is often perceived by the trainee as “pimping.” This can belittle the trainee while securing the attending physician’s place of power ( 35 ) and create a hostile learning environment.
Attending: Why do you think this patient is hypotensive? Attending: How does the BUN/creatinine ratio relate to the hypotension? Attending: How would you expect the intravascular volume depletion to affect his hematocrit?
Questions like these allow the trainee to elaborate on her knowledge, which feels much safer to the learner and provides the attending insight into her thinking.
Resident: If my theory of sepsis were correct, I would think the patient would be intravascularly dry and have a higher hematocrit. The fact that it is only 35% and that his BUN/creatinine ratio is consistent with a prerenal picture is making me worried that maybe the hypotension is not from sepsis but, rather, from bleeding. I think we need to evaluate for gastrointestinal bleeding.
When the right questions are used to coach the resident, her thought processes are uncovered and she can be guided to the correct diagnosis. Although experience and domain-specific knowledge are important, data indicate that in the majority of malpractice cases involving diagnostic error, the problem is not that the doctor did not know the diagnosis; rather, she did not think of it. Reasoning, rather than knowledge, is key to avoiding mistakes in cases with confounding data.
Strategy 5: Assess Your Learner’s Critical Thinking
It is difficult, but necessary for trainee development, to assess critical thinking ( 18 ). Milestones, ranging from challenged and unreflective thinkers to accomplished critical thinkers, have been proposed ( 18 ). This approach is helpful not only for providing feedback to trainees on their critical thinking but also to give the trainees a framework to guide reflection on how they are thinking (see Table 2 for a description of the milestones).
Milestones of critical thinking and the descriptions of each stage
Note that “Challenged thinker” is in italics because any thinker can be challenged as a result of environmental pressures or time constraints. Adapted from Papp ( 18 ).
It is important to note that anyone, even accomplished critical thinkers, can become “challenged critical thinkers” when the environment precludes critical thinking. This is particularly relevant in critical care. In a busy ICU, one is often faced with time pressure, which contributes to premature closure. In our case presented earlier, perhaps the resident had limited time to admit this patient, and thus settled on the diagnosis of sepsis. It is our hope that teaching trainees to recognize this risk will lead to fewer cognitive biases. Imagine a different exchange between faculty and resident:
Attending: How are you doing with the new admission? How are you thinking about the case? Resident: I’m concerned this is sepsis, but there are few pieces that don’t fit. However, given the two other admissions and the cardiac arrest on the floor who is heading our way, I haven’t been able to give this case as much thought as I would like to. Attending: Okay, do you want to work through the case together? Or could I help with some other tasks so you have more time to think about this?
This type of response reflects a practicing critical thinker: one who is aware of her limitations and thinking processes. This can only occur, however, if the attending creates an environment in which critical thinking is valued by making a safe space and asking the right questions.
Conclusions
The ICU is a high-acuity, fast-paced, and high-stakes environment in which critical thinking is imperative. Despite the limited empirical evidence to guide faculty on best teaching practices for enhancing reasoning skills, it is our hope that these strategies will provide practical approaches for teaching this topic in the ICU. Given how fast medical knowledge grows and how rapidly technology allows us to find factual information, it is important to teach enduring principles, such as how to think.
Our job in the ICU, where literal life-and-death decisions are made daily, is to teach trainees to focus on how we actually think about problems and to uncover cognitive biases that cause flawed thinking and may lead to diagnostic error. The focus of the preclerkship curriculum at the undergraduate level is increasingly moving away from transfer of content to application of knowledge ( 36 ). When teaching residents and fellows, faculty should also emphasize thinking skills by making the thinking process explicit, discussing cognitive biases, and debiasing strategies, modeling and teaching inductive reasoning, using questions to stimulate curiosity, and assessing critical thinking skills.
As Albert Einstein said, “Education... is not the learning of facts, but the training of the mind to think...” ( 38 ).
Supplementary Material
Author Contributions : M.M.H. contributed to manuscript drafting, figure creation, and editing; S.C. contributed to figure creation, critical review, and editing; and R.M.S. contributed to figure creation, critical review, and editing.
Author disclosures are available with the text of this article at www.atsjournals.org .

IMAGES
VIDEO
COMMENTS
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient's sex and age, and you begin to think about what ...
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
The development of critical thinking skills in healthcare is somewhat unique. In chess, students can start playing using the same tools employed by the experts (the chess board); however, in healthcare, allowing students to make medical decisions is ethically inappropriate and irresponsible. Simulations centers allow students to gain needed ...
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. ... Critical Thinking. Nursing education has emphasized critical thinking as an essential nursing skill for more than 50 years. 1 The definitions of critical thinking have evolved over the years ...
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
Sound critical thinking skills can help clinicians avoid cognitive biases and diagnostic errors. This article describes three critical thinking skills essential to effective clinical care - clinical reasoning, evidence-informed decision-making, and systems thinking - and approaches to develop these skills during clinician training.
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered.
Nurses are critical thinkers. The characteristic that distinguishes a professional nurse is cognitive rather than psychomotor ability. Nursing practice demands that practitioners display sound judgement and decision-making skills as critical thinking and clinical decision making is an essential component of nursing practice.
Critical thinking skills are also a vital resource for the medical and health professionals who deliver our healthcare. Notwithstanding significant improvements in the standard of patient care in hospitals, it remains the case that medical errors are alarmingly common, and can result in death and significant patient harm.
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information to make reasoned and informed decisions. It's a mental activity that goes beyond simple memorization or acceptance of information at face value. Critical thinking involves careful, reflective, and logical thinking to understand complex ...
Abstract Healthcare systems across the world are challenged with problems of misdiagnosis, non-beneficial care, unwarranted practice variation and inefficient or unsafe practice. ... Three critical thinking skills underpin effective care: clinical reasoning, evidence-informed decision-making and systems thinking. It is important to define these ...
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from ...
Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).. Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught, assessed and integrated into the design and development of staff and nurse education and training ...
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting.
Critical thinking skills in nursing improve patient outcomes by enabling evidence-based decision-making. Nurse practitioners gather considerable amounts of patient data through evaluations, tests and conversations. Each patient's information can be interpreted and analyzed to determine the best courses of action for their health.
Critical thinking is the ability to effectively analyze information and form a judgment. To think critically, you must be aware of your own biases and assumptions when encountering information, and apply consistent standards when evaluating sources. Critical thinking skills help you to: Identify credible sources. Evaluate and respond to arguments.
Critical thinking is connected to a broader idea of what 'good thinking'—and, by extension, the 'good professional'—looks like for each educator [ 38] within a given context or community. These observations lead one to speculate about what purpose fluidity in conceptions of critical thinking might serve.
Critical thinking involves common sense. Yes, it's theoretically possible that some unknown cause(s) was a confounding factor, and the vaccine wasn't the cause of illness. But the circumstances of the situation, and common sense, dictate how to apply critical thinking. In that situation, you're going to say correlation DOES equal causation.
Health Expectations is a health and social care journal promoting critical thinking and debate around patient and public engagement in health services & policy. Abstract Background Disability is often an essentialised and oversimplified concept.
Habilidades de pensamiento crítico para enfermeras en la era de la tecnología sanitaria. La tecnología ha revolucionado la práctica de la enfermería y los sistemas sanitarios. Ya sea la mayor prestación de atención virtual, la conectividad de los registros de los pacientes o la implementación de planes de tratamiento personalizados ...
Apply critical thinking in real-life situations whenever possible. This could involve analyzing news articles, evaluating product reviews, or dissecting marketing strategies to understand their underlying rationale. In conclusion, critical thinking is the linchpin of a successful career journey.
Critical thinking is the ability to analyze facts logically and objectively to form a clear and informed judgment. In the context of education and professional development, writing is one of the key tools for deepening and strengthening critical thinking. It is an active form of learning that requires one to fully immerse oneself in the subject ...
Background and Purpose. The purpose of this systematic review is to determine if critical-thinking skills in health care professional students change as a result of participating in a health care professional education program, and to assess the quality of the evidence evaluating this change.. Method/Model Description and Evaluation.
The nursing profession will also see a lot of changes.Â. But at its heart, nurses are the first point of contact when a patient is admitted to a hospital, and the last contact when a patient is ...
Critical thinking includes "analysis, inference, interpretation, explanation, synthesis and self -regulation" (Facione, 2011). The healthcare team should be able to utilize their critical thinking skills as they come in contact with their patients daily. Critical thinking has been well documented in nursing but the evidence in medicine is ...
Suppositions are presented as facts. Some personal care products and cleaning agents contain chemicals that can be classified as endocrine disruptors or carcinogens. Furthermore, some of these can be detected in our bloodstream and urine. But it is critical to understand that the presence of a chemical cannot be equated to the presence of risk.
Critical thinking, the capacity to be deliberate about thinking, is increasingly the focus of undergraduate medical education, but is not commonly addressed in graduate medical education. Without critical thinking, physicians, and particularly residents, ...