REVIEW article
Impact of vaccines; health, economic and social perspectives.

- 1 Department of Zoology, University of Oxford, Oxford, United Kingdom
- 2 Department of Paediatric Infectious Diseases, St George’s University Hospitals NHS Foundation Trust, London, United Kingdom
- 3 Department of Pediatrics, University of Pennsylvania, Philadelphia, PA, United States
In the 20th century, the development, licensing and implementation of vaccines as part of large, systematic immunization programs started to address health inequities that existed globally. However, at the time of writing, access to vaccines that prevent life-threatening infectious diseases remains unequal to all infants, children and adults in the world. This is a problem that many individuals and agencies are working hard to address globally. As clinicians and biomedical scientists we often focus on the health benefits that vaccines provide, in the prevention of ill-health and death from infectious pathogens. Here we discuss the health, economic and social benefits of vaccines that have been identified and studied in recent years, impacting all regions and all age groups. After learning of the emergence of SARS-CoV-2 virus in December 2019, and its potential for global dissemination to cause COVID-19 disease was realized, there was an urgent need to develop vaccines at an unprecedented rate and scale. As we appreciate and quantify the health, economic and social benefits of vaccines and immunization programs to individuals and society, we should endeavor to communicate this to the public and policy makers, for the benefit of endemic, epidemic, and pandemic diseases.

Introduction
“The impact of vaccination on the health of the world’s peoples is hard to exaggerate. With the exception of safe water, no other modality has had such a major effect on mortality reduction and population growth” ( Plotkin and Mortimer, 1988 ).
The development of safe and efficacious vaccination against diseases that cause substantial morbidity and mortality has been one of the foremost scientific advances of the 21st century. Vaccination, along with sanitation and clean drinking water, are public health interventions that are undeniably responsible for improved health outcomes globally. It is estimated that vaccines have prevented 6 million deaths from vaccine-preventable diseases annually ( Ehreth, 2003 ). By 2055, the earth’s population is estimated to reach almost 10 billion ( United Nations Department of Economic and Social Affairs, 2019 ), a feat that in part is due to effective vaccines that prevent disease and prolong life expectancy across all continents. That said, there is still much to be done to ensure the financing, provision, distribution, and administration of vaccines to all populations, in particular those which are difficult to reach, including those skeptical about their protective value and those living in civil disruption. Agencies including the World Health Organization (WHO), United Nations Children’s Fund (UNICEF), Gavi, the Vaccine Alliance, The Bill & Melinda Gates Foundation, and the Coalition for Epidemic Preparedness Initiative (CEPI), with their multiple funding streams have been instrumental in expanding vaccine benefits to all. These importance of these organizations in global co-operation and participation was essential in the setting of the 2019 global pandemic of SARS-CoV-2, in light of the health and economic impact of COVID-19 on societies in high-, middle- and low-income countries. This review will highlight the benefits of vaccinations to society from the perspectives of health, economy, and social fabric ( Figure 1 ), which need to be considered in the overall assessment of impact to ensure that vaccines are prioritized by those making funding decisions.
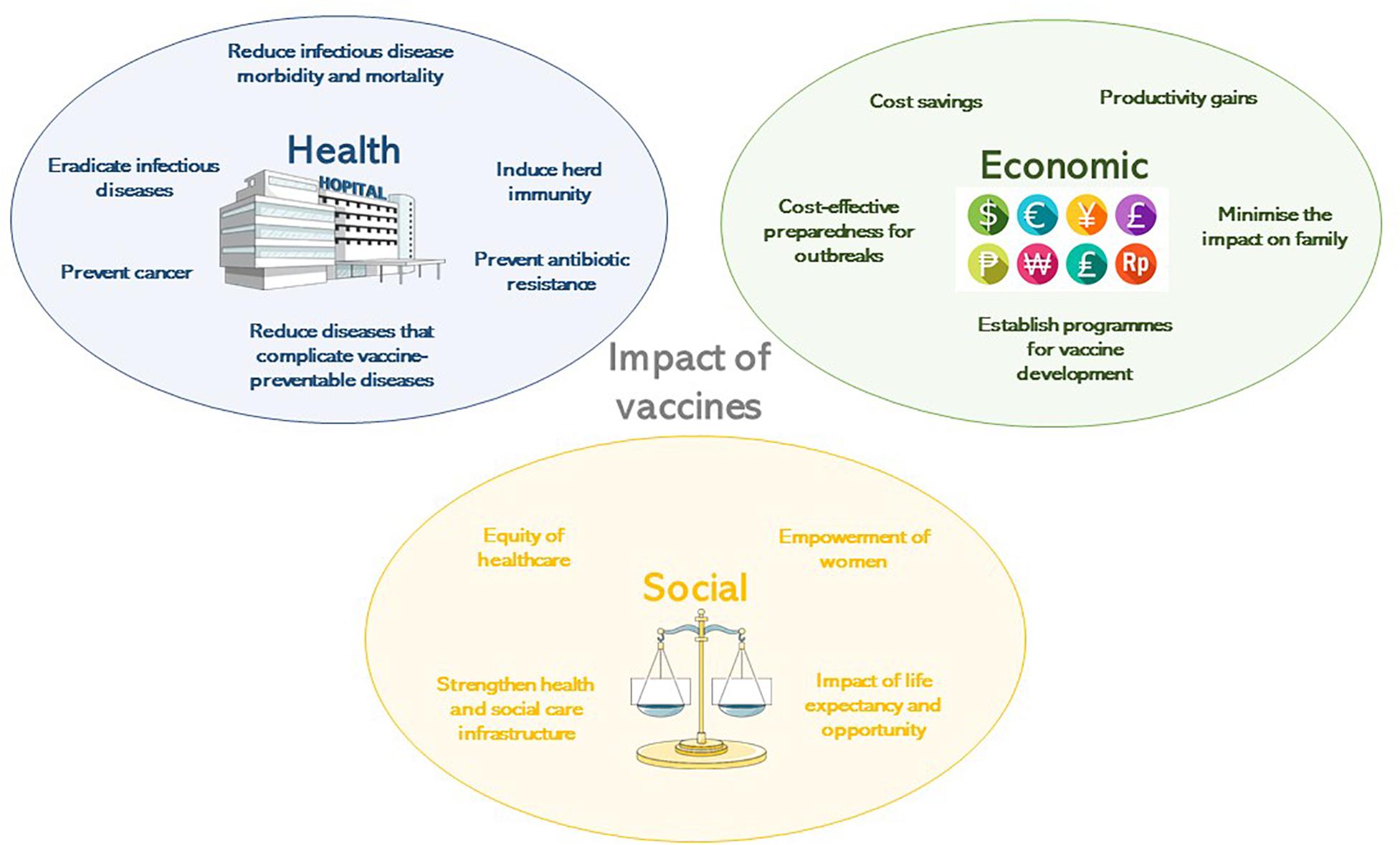
Figure 1. The impact of vaccines according to their health, economic or social benefit.
Brief History of Vaccine Development
Human use of preparations to prevent specific infections have been described since 1500 AD, beginning in China ( Needham, 2000 ) where smallpox was prevented by variolation, which is the introduction of material from scabs into the skin. In 1796 in the United Kingdom, Edward Jenner observed the immunity to smallpox of milkmaids having previously had natural infection with cowpox ( Jenner, 1798 ). He determined that inoculating small amounts of pus from the lesions of cowpox, presumably containing a virus related to vaccinia, into susceptible hosts rendered them immune to smallpox. The vaccine against smallpox was developed in 1798. The next phase of scientific developments involving the manipulation of infectious agents to extract suitable vaccine antigens took almost a century of research. Louis Pasteur’s work with attenuation by oxygen or heat led to live-attenuated chicken cholera, inactivated anthrax and live-attenuated rabies vaccines at the turn of the 20th century ( Pasteur, 1880 , 1881 , 1885 ). Alternative methods of attenuation using serial passage of Mycobacterium bovis led to the live Bacille Calmette-Guerin (BCG) ( Calmette, 1927 ) vaccine, still in use today for the prevention of tuberculosis. Serial passage was also used in the development of yellow fever vaccines ( Theiler and Smith, 1937a ) which are grown in chicken embryo tissues ( Theiler and Smith, 1937b ). Whole cell killed bacterial vaccines were developed when methods to treat and kill bacteria through heat or chemicals were established and whole cell typhoid, cholera and pertussis vaccines resulted at the end of the 19th Century. In 1923, Alexander Glenny and Barbara Hopkins developed methods to inactivate bacterial toxins with formaldehyde, leading to the diphtheria and tetanus toxoid vaccines ( Glenny and Hopkins, 1923 ).
Advances in virus culture in vitro allowed viral pathogens to be studied in greater detail and attenuation methods due to cultivation in artificial conditions led to the live oral polio, measles, rubella, mumps and varicella virus vaccines. In the 1960’s at the Walter Reed Army Institute of Research, vaccines were developed using capsular polysaccharides ( Gold and Artenstein, 1971 ; Artenstein, 1975 ), of encapsulated organisms including meningococci and later pneumococci ( Austrian, 1989 ) and Haemophilus influenzae type b (Hib) ( Anderson et al., 1972 ). To protect against multiple serotype variants of polysaccharide capsules, polyvalent vaccines were developed and later conjugated to carrier proteins to enhance their efficacy in infants in particular by recruiting T-cell mediated help to induce memory B-cells ( Schneerson et al., 1980 ). Vaccines made solely from proteins were rare, with the exception of the toxoid vaccines, but the acellular pertussis vaccine containing five protein antigens, was developed to mitigate the unwanted effects of the whole cell vaccine ( Sato and Sato, 1999 ).
The end of the 20th century marked a revolution in molecular biology and provided insights into microbiology and immunology allowing a greater understanding of pathogen epitopes and host responses to vaccination. Molecular genetics and genome sequencing has enabled the development of vaccines against RNA viruses possessing multiple variants of epitopes, such as the live and inactivated influenza vaccines ( Maassab and DeBorde, 1985 ) and live rotavirus vaccines ( Clark et al., 2006 ). DNA manipulation and excision allowed the use of surface antigen for hepatitis B viral vectors ( Plotkin, 2014 ). The human papilloma virus (HPV) vaccine benefits from enhanced immunogenicity due to the formation of virus-like particles by the L1 antigen of each virus contained in the vaccine ( Kirnbauer et al., 1992 ). Bacterial genome sequencing has provided in depth analysis of meningococcal antigens, to identify potential proteins for meningococcal B vaccines ( Serruto et al., 2012 ).
Vaccine development was tested in 2020 when a novel coronavirus, SARS-CoV-2, emerged from China causing a severe acute respiratory illness, which subsequently spread globally. Within 5 months of the discovery of this virus (7th January 2020) ( Zhu et al., 2020 ) and person-person transmission ( Chan et al., 2020 ), 5,697,334 cases had been identified, with orders of magnitude likely not measured and almost no country escaped the pandemic. Owing to the previous advances in vaccinology, by 8th April 2020, there were 73 vaccine candidates under pre-clinical investigation ( Thanh Le et al., 2020 ). Of these, six were in Phase 1 or 1/2 trials and one was in Phase 2/3 trials by 28th May 2020. The rapidity of this response demonstrated the ability to harness existing technologies including: RNA vaccine platforms (NCT04283461), DNA vaccine platforms (NCT04336410), recombinant vector vaccines (NCT04313127, NCT04324606) and adjuvants. The regulation, manufacturer and distribution of these vaccines will require expedition given the global public health need, from a period of many years to a matter of months. The efficacy and health impact of these vaccines is yet to be established, but if they are effective, then vaccines need to be made available for all global regions affected by SARS-CoV-2. The funding of this endeavor will prove challenging in a global context of national social and economic lockdown and massive government borrowing, but the justification for this provision will be through the multiple benefits to society that will need healthy citizens to rebuild economies in the decades post-COVID-19.
The history of vaccination is not complete without describing the public health intervention that led to the routine use of these vaccines for children globally. The Expanded Program of Immunization (EPI) was founded by WHO in 1974 with the aim of providing routine vaccines to all children by 1990 ( World Health Assembly, 1974 ). In 1977, global policies for immunization against diphtheria, pertussis, tetanus, measles, polio, and tuberculosis were set out. The EPI includes hepatitis B, Hib, and pneumococcal vaccines in many areas and by 2017, 85% of the world’s children (12–23 months of age) received diphtheria, pertussis, tetanus, and measles vaccines ( World Bank, 2019 ).
Health Benefits of Vaccination
Reduction in infectious diseases morbidity and mortality.
The most significant impact of vaccines has been to prevent morbidity and mortality from serious infections that disproportionately affect children. Vaccines are estimated to prevent almost six million deaths/year and to save 386 million life years and 96 million disability-adjusted life years (DALYs) globally ( Ehreth, 2003 ). The traditional measures of vaccine impact include: vaccine efficacy, the direct protection offered to a vaccinated group under optimal conditions e.g., trial settings; or vaccine effectiveness, the direct and indirect effect of vaccines on the population in a real-life setting ( Wilder-Smith et al., 2017 ). Providing a numerical measure of vaccine impact therefore involves estimating the extent of morbidity and mortality prevented. In the United States in 2009, amongst an annual birth cohort vaccinated against 13 diseases it was estimated that nearly 20 million cases of disease and ∼42,000 deaths were prevented ( Zhou et al., 2009 ). Infectious diseases that accounted for major mortality and morbidity in the early 20th century in the United States all showed over a 90% decline in incidence by 2017 from the pre-vaccine peak incidence ( Roush and Murphy, 2007 ), due to high vaccine uptake of over 90% for the DTaP (diphtheria, tetanus, and acellular pertussis), MMR (measles, mumps, and rubella) and polio vaccines ( World Health Organisation, 2019a ; Table 1 ). A similar pattern of infectious diseases reduction was seen across other high-income countries, demonstrating the efficacy of vaccines when available and accessible.
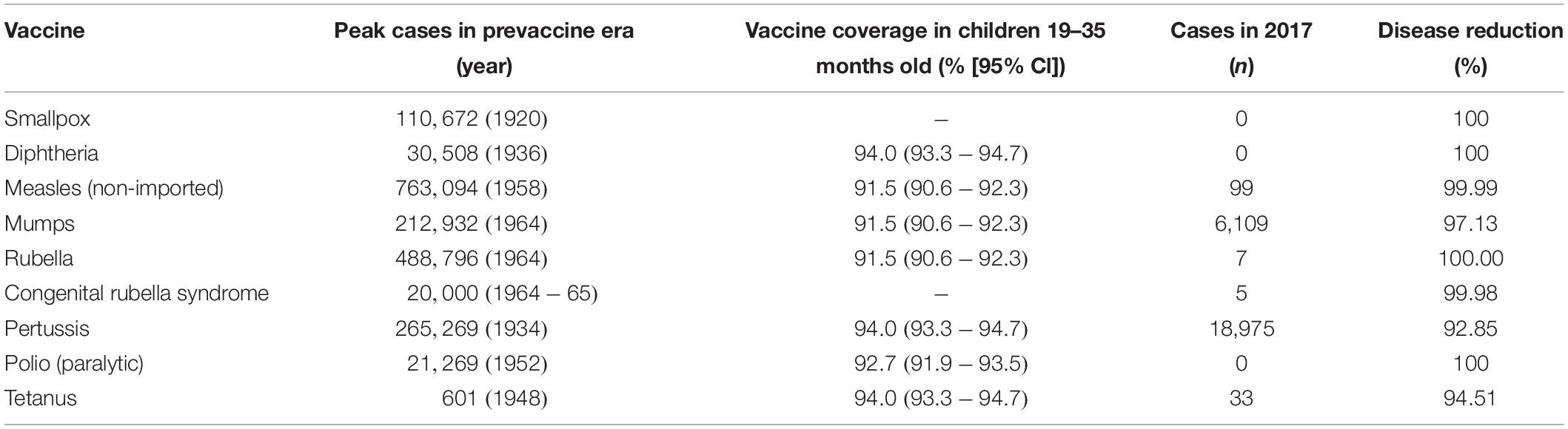
Table 1. Vaccine impact in United States comparing the incidence of diseases prior to the implementation of vaccine ( Roush and Murphy, 2007 ), described as the pre-vaccine era and the vaccine coverage ( Hill et al., 2017 ) and disease incidence ( Centers for Disease Control and Prevention, 2017 ) in 2017, as reported by the Centers for Disease Control and Prevention.
Globally, the provision of vaccines is more challenging in many low- and middle- income countries (LMIC), as evidenced by the failure to make the EPI vaccines available to every child by 1990, irrespective of setting ( Keja et al., 1988 ). Central to this is limited financial resources, but other barriers to vaccine introduction include: underappreciation of the value of vaccines locally/regionally though insufficient relevant data on disease burden, vaccine efficacy, or cost-effectiveness; inadequate healthcare infrastructure for vaccine handling, storage, programmatic management, and disease surveillance; and lack of global, regional or local policy-making and leadership ( Munira and Fritzen, 2007 ; Hajjeh, 2011 ). In 2018, the global uptake of three doses of DTaP reached 86% which corresponded to 116,300,000 infants ( World Health Organisation, 2019a ). The vaccine coverage is, however, variable between low-, middle- and high-income countries because of a combination of economic and political circumstances as well as variable access to non-governmental support from Gavi, the Vaccine Alliance ( Turner et al., 2018 ; Figure 2 ). Nevertheless, there has been a decrease in the global burden of diseases caused by vaccine-preventable pathogens ( Figure 3 ) enabling healthier lives for many millions of children. A further benefit following vaccination, is the evidence that although vaccines may not always prevent an infection, for example VZV or pertussis, a milder disease course may follow ( Andre et al., 2008 ; Bonanni et al., 2015 ).
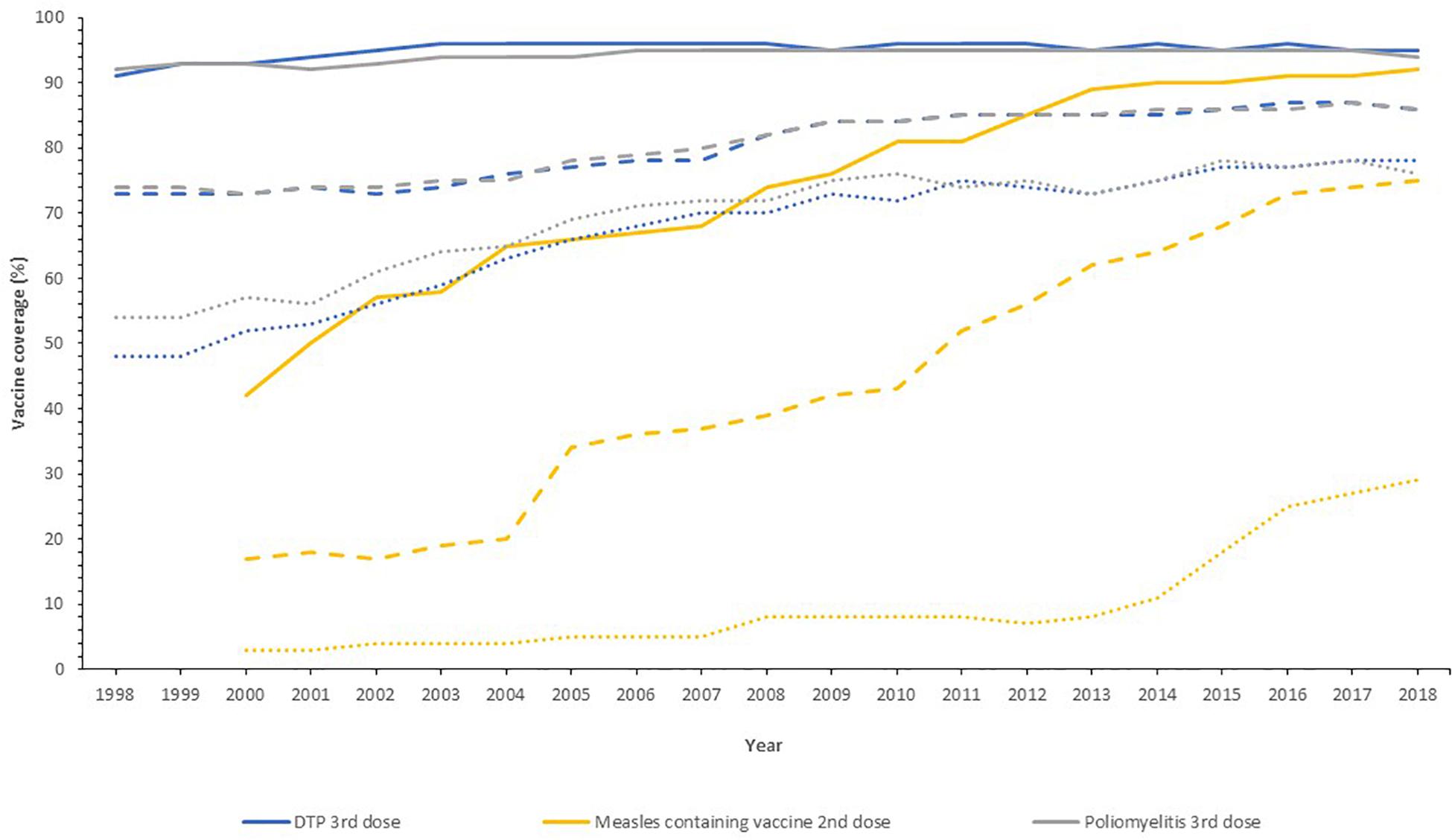
Figure 2. Vaccine uptake across different regions defined by economic status by the World Bank into high- (solid line), middle- (dashed line), and low-income countries (dotted line) for the past 20 years. Data from the World Health Organization and UNICEF dataset “Coverage Estimates Series” ( World Health Organization [WHO] and United Nations Children’s Fund [UNICEF], 2019 ).
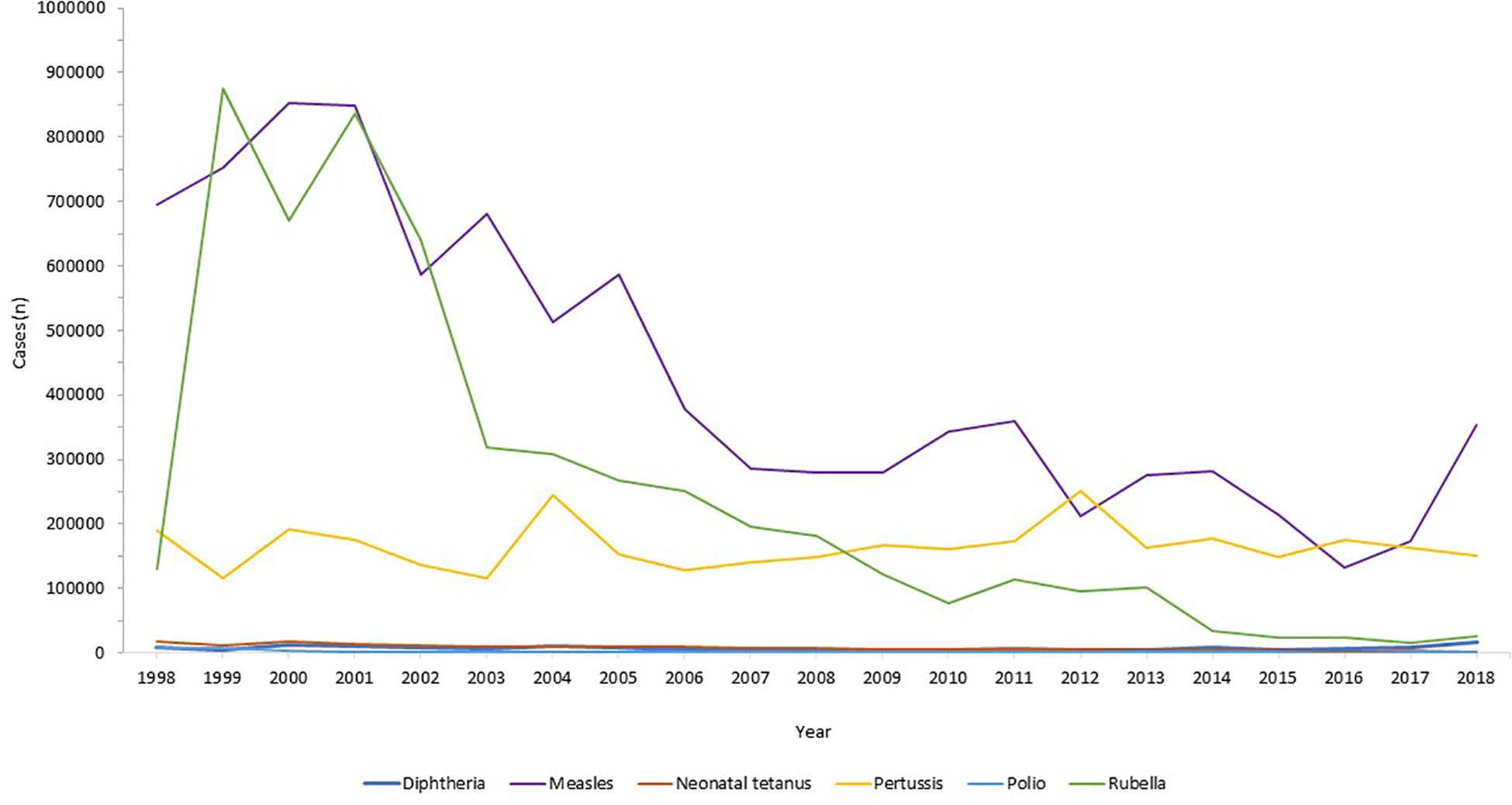
Figure 3. Reduction in infectious diseases globally. Across all world regions, data from the WHO, for the last 20 years showing the control of diphtheria and tetanus and the decline in rubella and congenital rubella syndrome (data not shown). Data from the World Health Organization dataset “Reported cases of vaccine-preventable diseases” ( World Health Organisation, 2019c ).
Eradication of Infectious Diseases
Global disease eradication can be achieved for pathogens that are restricted to human reservoirs. For eradication of infectious diseases, high levels of population immunity are required globally, to ensure no ongoing transmission in our well-connected world ( Andre et al., 2008 ). Furthermore, surveillance systems must be in place to monitor the decline in disease, with accurate and reliable diagnostic testing to monitor ongoing cases. At the time of writing, the only infectious disease that has been eradicated in humans by vaccination is smallpox. This disease had afflicted humans for millenia, with the earliest evidence found in Egyptian mummies from 1000 BC ( Geddes, 2006 ). Jenner’s successful development of the smallpox vaccine using vaccinia virus ( Jenner, 1798 ) led to the ultimate eradication of the disease through ring vaccination as announced by the World Health Assembly in 1980 ( Strassburg, 1982 ), which was an historic public health achievement. The second example of eradication was of the rinderpest virus in livestock, an infection that indirectly led to human loss of life through loss of agriculture leading to humanitarian crises through famine and poverty. Rinderpest virus infects cattle, buffalo and numerous other domestic species, with widespread disease affecting large parts of Africa and Europe in the 19th century ( Roeder et al., 2013 ). The Plowright tissue culture rinderpest vaccine, developed during the 1950s, was used for mass vaccination campaigns, alongside other public health measures, leading to eradication in 2011 ( Morens et al., 2011 ).
The next infection targeted for eradication is wild polio virus. This devastating paralytic disease routinely afflicted children and adults in both industrialized and developing settings, prior to the development of vaccines. Two polio vaccines, the inactivated polio vaccine (IPV) and the live-attenuated oral polio vaccine (OPV) became available in 1955 and 1963, respectively ( Plotkin, 2014 ), both able to protect against all three wild types of polio virus. Both vaccines have been used globally, with live-attenuated OPV much cheaper and easier to administer but carrying the risk of causing circulating vaccine-derived poliovirus (cVDPV) owing to back-mutation and re-acquisition of neurovirulence. Hence, due to its safety IPV was preferred in industrialized regions and those where the polio incidence was low. In 1998, the Global Polio Eradication Initiative, the largest public-private partnership led by national governments in partnership with the WHO, Rotary International, United States Centers for Disease Control and Prevention (CDC), and UNICEF was launched with the aim of global polio eradication by 2000. Although this target was not met due to lack of funding, political will, and competing health initiatives, there was a 99% reduction in polio incidence by 2000 ( Lien and Heymann, 2013 ). By 2003, there were only six endemic countries with new cases: Egypt, Niger, India, Nigeria, Afghanistan, and Pakistan, of which only the latter four had new cases by 2005. Eradication in India was problematic due to the high birth rates and poor sanitation amongst densely populated regions with marginalized communities and high population mobility ( Thacker et al., 2016 ). India was declared polio free in 2014. Wild polio virus type 2 was eradicated in 2015, the last case of wild type 3 was in 2012 and eradication announced in 2019, with wild type 1 virus remaining in two countries, Pakistan and Afghanistan ( World Health Organisation, 2019b ). In 2019, Nigeria was declared 3 years free of wild polio, the last country in Africa to declare any cases. In the first 6 months of 2020, there were 51 and 17 cases of wild type 1 polio reported in Pakistan and Afghanistan respectively ( Global Polio Eradication Initiative, 2019 ). Ongoing programs to roll out universal vaccination in both countries remain hindered by armed conflict, political instability, remote communities and underdeveloped infrastructure. The risk of the OPV recipients developing cVDPV disease, with transmission through the faeco-oral route to cause outbreaks of vaccine-derived paralytic poliomyelitis remains a concerning obstacle in the eradication process, requiring intensive surveillance.
Herd Immunity
The overriding health benefit perceived by most vaccine recipients is their personal, direct, protection. The added value of vaccination, on a population level, is the potential to generate herd immunity. Where a sufficiently high proportion of the population are vaccinated, transmission of the infecting agent is halted thereby protecting the unvaccinated, who may be those too young, too vulnerable, or too immunosuppressed to receive vaccines. Highly successful vaccination programs have been in place as part of the routine EPI, against encapsulated bacteria that are carried asymptomatically in the oropharynx but that can invade and cause septicemia and meningitis in all age groups. Vaccines against Neisseria meningitidis ( Gold and Artenstein, 1971 ), Streptococcus pneumoniae ( Austrian, 1989 ), and Hib ( Anderson et al., 1972 ) were developed in the 1960s, 1970s, and 1980s, respectively, using their polysaccharide capsules as vaccine antigens, which successfully induced protective immunity (direct protection). Conjugation of these polysaccharides to carrier proteins in the 1990s improved their efficacy by not only ensuring a T cell response and immune memory, but by reducing acquisition of pharyngeal carriage of these organisms, thus providing indirect protection and thereby preventing ongoing transmission ( Pollard et al., 2009 ). This was first observed in national carriage studies in the United Kingdom in 1999–2001 during a mass vaccination campaign against serogroup C N. meningitidis ( Maiden et al., 2008 ) and was a major contributing factor to the declining disease thereafter.
Herd (population) immunity requires high levels of vaccine uptake, to limit the number of unvaccinated people and the opportunity for pathogen transmission between them. The proportion of a given population required to induce herd immunity through vaccination is lower for the bacterial infections and conjugate polysaccharide vaccines, as their basic reproductive number (R 0 ) is lower than viral infections like measles, varicella or polio ( Table 2 ). Measles virus can cause devastating disease ranging from acute presentations with pneumonia or encephalitis, to immune amnesia and long-term complications such as subacute sclerosing panencephalitis ( Mina et al., 2015 , 2019 ; Moss, 2017 ; Petrova et al., 2019 ). The live-attenuated measles vaccine is highly efficacious and the first dose is recommended at 9–12 months of age. To protect those who cannot receive live vaccines (younger infants, pregnant women, the immunosuppressed) from acquiring measles in the community, at least 93–95% of the population is required to be vaccinated with two doses in order to interrupt measles virus transmission. In many countries in Europe and in the United States, this level of vaccination uptake is falling ( Wise, 2018 ), due to a combination of reduced accessibility to health services and vaccine misinformation. As a result, some countries, including the United Kingdom and United States, where elimination of measles had been declared have had a resurgence of disease ( Wise, 2019 ). For high-risk individuals who are unable to be vaccinated, herd immunity represents a life-saving protection strategy against many infections. An alternative strategy, cocooning, has been employed with limited success for pertussis and influenza ( Grizas et al., 2012 ), where their close/household contacts are vaccinated to prevent transmission.
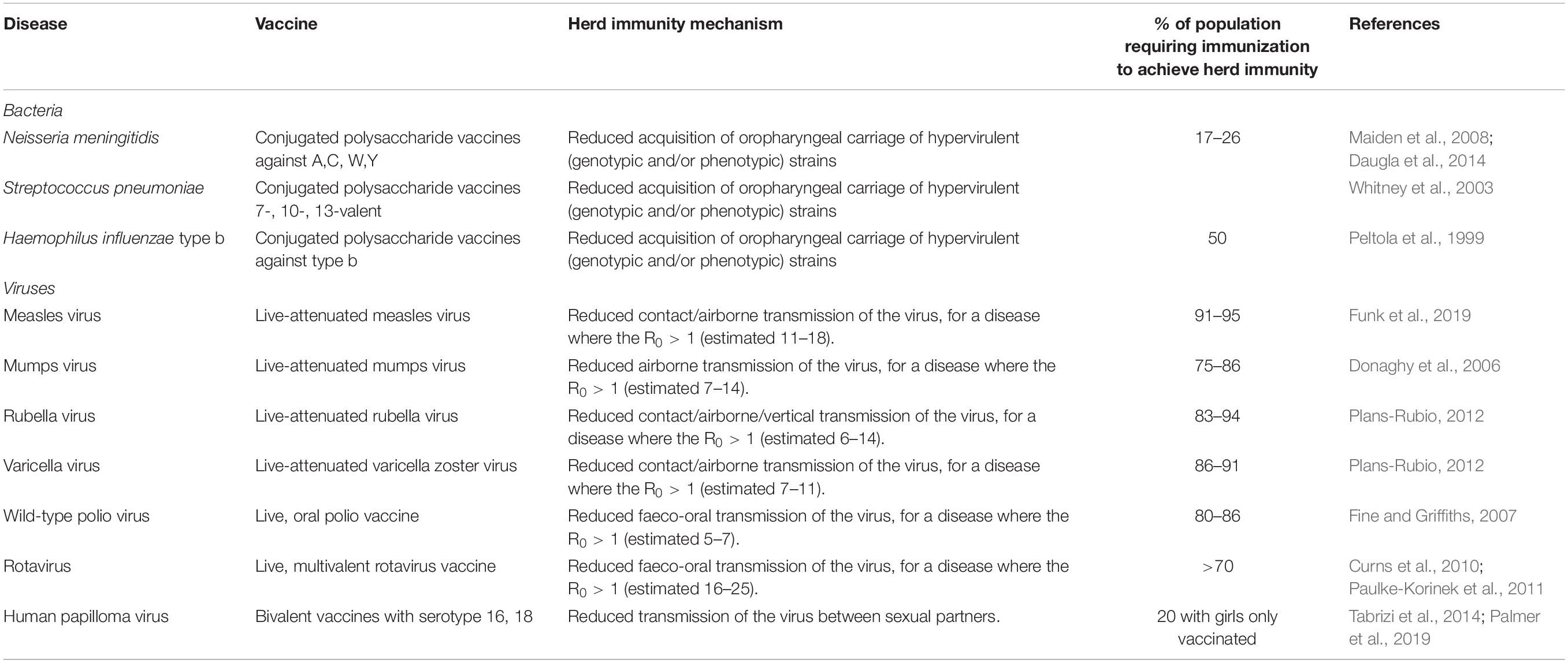
Table 2. Vaccines with the potential to induce herd immunity, with the infectious agent, vaccine type, and thresholds of population vaccination needed for herd immunity ( Peltola et al., 1999 ; Whitney et al., 2003 ; Donaghy et al., 2006 ; Fine and Griffiths, 2007 ; Maiden et al., 2008 ; Curns et al., 2010 ; Paulke-Korinek et al., 2011 ; Plans-Rubio, 2012 ; Daugla et al., 2014 ; Tabrizi et al., 2014 ; Funk et al., 2019 ; Palmer et al., 2019 ).
Herd immunity has been observed for gastrointestinal infections with vaccines against cholera (oral cholera vaccine) and rotavirus (oral rotavirus vaccines). Early adopters of rotavirus vaccines included the United States (2006) and Austria (2007) where there were dramatic reductions in disease observed in the vaccinated infant cohort, and also in the older age groups of children and adults ( Curns et al., 2010 ; Paulke-Korinek et al., 2011 ), suggesting that the reduction in disease and shedding of virus in the stool stopped transmission to healthy household contacts. For the OPV, herd protection may also be induced through vaccine virus shedding and spread to unvaccinated people ( Fine and Griffiths, 2007 ).
Reduction in Secondary Infections That Complicate Vaccine-Preventable Diseases
Vaccines can prevent diseases beyond the specific infection they are designed to target. Infections with pathogens, in particular viruses, can predispose to the acquisition of other bacterial infections. For example, influenza virus infection, both seasonal and pandemic, is frequently complicated by bacterial pneumonia and acute otitis media (OM), and infrequently Aspergillus pneumonia/pneumonitis. During the influenza pandemic of 1918–19, secondary bacterial bronchopneumonia with S. pneumoniae, Streptococcus pyogenes , H. influenzae , and Staphylococcus aureus identified at autopsy, likely contributed to the excess mortality observed amongst healthy children and adults ( Morens and Fauci, 2007 ). Influenza vaccinations can be beneficial in preventing these complications and also morbidity including acute OM in children; a systematic review demonstrated influenza vaccine efficacy against OM of 51% (21–70%) ( Manzoli et al., 2007 ). Further, there is evidence that inactivated influenza vaccines administered to pregnant women can reduce the hospital admission with acute respiratory illnesses in their infants up to 6 months of age ( Regan et al., 2016 ). Amongst pregnant, HIV-negative women in South Africa, infants (<3 months) were protected against hospitalization with all-cause lower respiratory tract infections with a vaccine efficacy of 43% ( p = 0.05), including primary viral and secondary bacterial causes ( Nunes et al., 2017 ). Additionally, in children pneumococcal conjugate vaccines were observed to reduce the incidence of influenza-associated hospital admissions in United States ( Simonsen et al., 2011 ), Spain ( Dominguez et al., 2013 ), and South Africa ( Madhi et al., 2004 ; Abadom et al., 2016 ), through the prevention of secondary bacterial infections following primary influenza infection.
The introduction of the live-attenuated measles vaccine in the 1970s was observed to reduce both measles and non-measles mortality in children ( Aaby et al., 2003 ). Measles causes severe pneumonia, encephalitis, and the long-term sequel of subacute sclerosing panencephalitis ( Moss, 2017 ), but the decline in mortality was not limited to preventing these alone ( Aaby et al., 2003 ). Mathematical modeling of vaccination and immunological research demonstrated that measles causes an immunological amnesia, eliminating B cell populations and thus immune memory, leaving measles survivors susceptible to all the infective agents they had previously developed immunity against; it is estimated to take 3 years for immune recovery to occur ( Mina et al., 2015 ).
Prevention of Cancer
Historically, vaccines were developed against very severe infections with major morbidity and mortality from acute disease. As non-communicable diseases, including cancer, become the most frequent causes of death in industrialized countries and some developing countries, vaccines are being used to prevent these too, when the infectious agents are involved in carcinogenesis. Hepatitis B prevalence is high in regions of East Asia, sub-Saharan Africa, and the Pacific Islands. Chronic hepatitis B infection can lead to liver cirrhosis and hepatocellular carcinoma ( Bogler et al., 2018 ). Vertical transmission of hepatitis B is problematic as 70–90% of babies born to HbsAg and HbeAg positive mothers will become infected without prophylaxis administered to babies; with ∼90% of infants developing chronic hepatitis ( Borgia et al., 2012 ; Gentile and Borgia, 2014 ). The chronic hepatitis B carriage status of mothers is routinely checked at the start of pregnancy, in order to assess the need to vaccinate the infant after birth. The use of both hepatitis B vaccine, containing hepatitis B surface antigen, and immunoglobulin containing hepatitis B antibody can be used to minimize vertical transmission, with evidence from a 20-year-long study in Thailand demonstrating 100% prevention of transmission ( Poovorawan et al., 2011 ).
The sexually transmitted HPV is responsible for genital tract and oropharyngeal infections as a precursor to causing oncological disease affecting the cervix, vagina, vulva, penis, anal tract, and pharynx in both men and women. Cervical cancer is the fourth most common cancer globally, with 528,000 new cases annually and peak incidence in young women aged 25–34 years ( Ferlay et al., 2012 ). The HPV serotypes 16 and 18 carry a high-risk for cervical cancer ( Wang et al., 2018 ) and vaccination against these specific serotypes has been available since 2006 through bivalent (16 and 18), quadrivalent (6, 11, 16, and 18), and nonavalent (6, 11, 16, 18, 31, 33, 45, 52, 58) vaccines, which are now available to individuals from the age of 9 years ( Gupta et al., 2017 ). A vaccination program started in the United Kingdom in 2008, and at the time of writing over 10.5 million doses had been given to girls ( Public Health England, 2018 ), with the aim of preventing primary infection with HPV. The vaccine coverage was 83.8% for 13–14 year old girls in England in 2017/18 ( Public Health England, 2019 ). In July 2018, the vaccine was approved for use in boys ( Public Health England, 2019 ). After a decade of use, there has been an observed decline in the genital infections caused by serotypes 16 and 18 ( Public Health England, 2018 ), with further time needed to observe the fall in cervical cancer incidence. However, the incidence of pre-invasive cervical diseases has been reduced by 79–89% in Scottish women over 20 who were vaccinated with bivalent HPV vaccine when aged 12–13 years, with evidence of herd protection ( Palmer et al., 2019 ), offering a promising outlook for the reduction of cervical cancer in the future. An additional benefit of HPV vaccines, is their impact on neonatal morbidity and mortality, through the reduction in surgical treatment of cervical neoplasias, and the related preterm births and complications ( Soergel et al., 2012 ).
Preventing Antibiotic Resistance
The rise in antimicrobial resistance (AMR) is a universal threat. The use of antibiotics in humans, exposes the bacteria that reside in our microbiota to selection pressures resulting in the development of AMR. As the bacteria constituting the host microbiota are frequently responsible for invasive diseases such as: meningitis, pneumonia, urinary tract, or abdominal infections, the risk of developing infections that are difficult or eventually impossible to treat is fast becoming a reality ( Brinkac et al., 2017 ). In regions where resistant pathogens are circulating at high frequency, such as India or regions of Europe ( Logan and Weinstein, 2017 ), patients will be faced with choosing between having elective surgical procedures or chemotherapy for malignancy, and the risk of acquiring potentially untreatable, multi-drug resistant bacterial infections ( Liu et al., 2016 ). Vaccination is crucial in mitigating this risk, by preventing people from developing viral and bacterial infections in the first instance, and therefore reducing the antibiotic burden to which their microbiota are exposed. The development of AMR in bacteria is a cumulative process with frequent, repeated exposure to broad spectrum antibiotics as a major driver. Children and the elderly who are at particular risk of infection can benefit from vaccines against common primary and secondary infections such as: pneumonia (prevented by PCV, PPSV, influenza, and measles vaccines), OM (PCV, Hib, and measles vaccines), cellulitis secondary to VZV (VZV vaccine), and typhoid fever (typhoid vaccine) which alleviates the need for antibiotics being prescribed or bought ( Kyaw et al., 2006 ; Palmu et al., 2014 ). The extent to which vaccination contributes to antimicrobial stewardship was highlighted by its inclusion in vaccine cost-effectiveness analyses as part of national United Kingdom policy ( Bonanni et al., 2015 ).
Economic Benefits
Cost savings.
Vaccines are highly beneficial on a population level and also cost-effective ( Shearley, 1999 ) in comparison to other public health interventions ( Bloom et al., 2005 ). Government departments are required to perform systematic economic analyses of vaccines and vaccine programs to justify their purchase in view of pressure on public and private finances globally, this was exacerbated by the 2008 financial crash. A vaccination program has clear direct costs including: vaccine purchase, infrastructure to run the program and maintain the cold chain, and healthcare/administration personnel. Governments, sometimes supported by charities and non-governmental organizations, invest in these with the intention of improving health. The reduction in morbidity and mortality associated with successful vaccine programs, through a combination of direct and indirect protection, has led to reduced incidence of diseases and their associated treatments and healthcare costs ( Deogaonkar et al., 2012 ). This potentially leads to economic growth, with less money spent owing to the costs averted through fewer medical tests, procedures, treatments and less time off work by patients/parents. Additionally, the use of combination vaccines e.g., DTaP/IPV/Hib/HepB provides protection against an increased number of diseases, with no additional infrastructure costs i.e. the same number of injections per child within existing immunization programs.
The cost-effectiveness analyses of vaccination programs demonstrate that they are overwhelmingly worth the investment, with most programs costing less than $50 per life gained, orders of magnitude less than prevention of diseases like hypertension ( Ehreth, 2003 ; Bloom et al., 2005 ). The returns on investment in vaccines, given their increasing provision through Gavi, have been estimated at 12–18% ( Bloom et al., 2005 ), but this is likely an underestimate. The monetary advantages of vaccination programs are important both to industrialized nations, such as the United States which obtains a net economic benefit of $69 billion, but also in 94 LMIC where investment of $34 billion, resulted in savings of $586 billion from the direct illness costs ( Ozawa et al., 2016 ; Orenstein and Ahmed, 2017 ). The net economic impact of eradication of disease has been estimated for both smallpox and polio. For smallpox, the eradication costs were over 100 million USD, but there are cost savings of 1.35 billion USD annually, with elimination of polio estimated to save 1.5 billion USD annually ( Barrett, 2004 ; Bloom et al., 2005 ). A less well-considered economic saving, not captured in cost-effectiveness or cost-benefit analyses, is from the prevention of long-term morbidity following acute infections ( Bloom et al., 2005 ), for example hearing impairment following pneumococcal meningitis or limb amputation following meningococcal disease, along with broader productivity gains ( Deogaonkar et al., 2012 ), which could have a major impact on LMIC adoption of vaccine programs.
Productivity Gains
The relationship between health and the economy is bidirectional, whereby economic growth enables funding in investments that improve health; and a healthy population contributes to and enhances an economy. These benefits of vaccinations and other public health interventions including sanitation, clean water, and antibiotics, are important for social as well as economic reasons. It has been suggested that the economic impact of vaccines should be considered more broadly than just the averted healthcare costs from prevented illness episodes and associated carer costs ( Deogaonkar et al., 2012 ; Barnighausen et al., 2014 ; Bonanni et al., 2015 ; Gessner et al., 2017 ; Wilder-Smith et al., 2017 ). Bärnighausen et al. (2011) , set out a framework to consider productivity gains measured by: outcome and behavior; community health and economic externalities; risk reduction; and health gains. Healthy children demonstrate improved educational attainment at school through better attendance and better cognitive performance ( Barham and Calimeria, 2008 ; Bloom et al., 2011 ; Deogaonkar et al., 2012 ). The impact of hearing loss from mumps, rubella or pneumococcal infections, or visual impairment from measles may require specific educational support, whereas the cognitive deficits from those childhood infections may require substantial remedial input. As more children survive to adulthood, a larger adult workforce is available, who when healthy can work for longer and more productively both physically and mentally ( Bloom and Canning, 2000 ; Bloom et al., 2005 ); though to date this has been observed largely following other health improvements, not vaccination specifically ( Jit et al., 2015 ). As a result of vaccination healthy and economically successful populations have lower fertility rates and smaller families ( Sah, 1991 ; Andre et al., 2008 ). With improved health and therefore life expectancy, there is a wider effect on families who may choose to invest more money in their future, for example to enhance their education or through savings ( Jit et al., 2015 ). Overall, vaccine programs should be viewed as an investment in human capital, providing enduring impact on economies worldwide.
Minimizing the Impact on Family
The economic impact of adult illness is evident from loss of productivity and pay for the duration of the illness and recovery period. The impact of childhood illness falls primarily on their adult carers, generally parents. In most industrialized regions, two-parent families are reliant on both parents undertaking at least part-time or full-time work. Therefore, when a child is unwell with childhood illnesses, which may or may not necessitate admission to hospital, the parent will invariably have to forego their paid employment to care for the child. In seven European countries one parent or carer required time off work in 39–91% of rotavirus gastroenteritis cases ( Van der Wielen et al., 2010 ). This loss of productivity in the parental workforce tends to disproportionately affect women, but loss of either parental attendance at work reduces overall employer productivity and in the short-term is rarely replaced. This argument was made for the impact of chicken pox on children, whereby the exclusion from school mandates parental caring at home for a period until the lesions are crusted over. VZV vaccines are estimated to have had a similar impact as rotavirus vaccine in United States studies ( Lieu et al., 1994 ). In many regions, mothers are still the primary carers, spending their days at home caring for children and maintaining the household; in these settings, the impact on this unpaid work is harder to determine.
It is of paramount importance to quantify and include productivity gains and the wider effects in analyses of impact for vaccines with only moderate efficacy, as calculated using traditional metrics. Vaccines such as the RTS,S/AS01 malaria vaccine, CYD-TDV dengue vaccine and rotavirus vaccine used in LMIC all have limited ability to broadly protect populations over a long duration but the public health benefits were important in vaccine implementation decisions in those countries ( Wilder-Smith et al., 2017 ). This suggests a paradigm for alternative regulatory requirements with a focus on public health outcomes ( Gessner et al., 2017 ).
Cost-Effective Preparedness for Outbreaks
As human populations grow and their use of the finite land resources increases, we are in increasingly close association with other living creatures, voluntarily or involuntarily. This interaction with natural reservoirs of potential infectious diseases increases the risk of zoonotic transmission of new infectious pathogens e.g., SARS, MERS-CoV, or known infectious pathogens with increased virulence e.g., influenza. Emerging infectious diseases disproportionately affect developing regions, where health infrastructure and surveillance are likely to be less well-established and robust. There were 1,307 epidemics of infectious diseases between 2011 and 2017, which cumulatively cost $60 billion annually to manage ( GHRF Commission, 2016 ). The unpredictability of outbreaks was highlighted by the Ebola epidemic in Western African countries of Liberia, Sierra Leone, and Guinea in 2014, which occurred in a period when public health was supposedly at its most advanced in recent history. However, a catalog of areas including: outbreak planning infrastructure; disease surveillance; local health services; escalation to international agencies were found to be lacking ( GHRF Commission, 2016 ). Although the WHO received criticism for its lack of escalation, in reality the global and interconnected infrastructure to prevent such epidemics taking lives and devastating societies is insufficient at the present time. The Zika virus epidemic in Latin America in 2015, first observed through an unexpectedly high incidence of microcephaly amongst newborns in Brazil’s northern regions ( Heukelbach et al., 2016 ), provide another example of how epidemics can have lasting impact, with the virus causing significant neurological damage to surviving infants ( Russo et al., 2017 ). The SARS-CoV-2 pandemic which began in 2019, was, at the time of writing, the largest infectious disease pandemic since the influenza pandemic of 1918/9. This global public health crisis highlighted stark societal inequalities persistent in many high-, middle- and low-income countries with direct and indirect impact on health outcomes from this infection. The cost-effectiveness of a vaccine in this setting was unquestionable, with economies and societies shut down for months in early 2020 and likely again in future. As it is not feasible or practical to be able to predict the location or nature of the next emerging threat, investment of an estimated $4.5 billion/year in healthcare systems could help speed up responses to infectious epidemics by prompt identification of the agent and effective control measures to limit the spread and consequences of disease ( GHRF Commission, 2016 ). The importance of this planning within the political landscape and the ongoing threat that infectious disease pose, may be appreciated more widely after 2020.
Establishing Programs for Vaccine Development
One effective infection control method is the use of vaccines in the course of an epidemic to halt transmission and to induce immunity to those as yet unaffected. The cost of vaccine development is a major challenge as there is little incentive for industry to invest in the design, testing and manufacture of vaccines that may never be needed, have a limited market, and, as previously eluded to, may be required in LMIC which cannot afford the upfront costs as an epidemic unfolds. The estimated costs for funding the development of infectious diseases vaccines for epidemics through phase 2a clinical trials are a minimum of $2.8-3.7 billion ( Gouglas et al., 2018 ). The CEPI alliance was established at the Davos World Economic Forum in 2017 as a global partnership between public, private and philanthropic organizations. In response to the conclusion that “a coordinated, international, and intergovernmental plan was needed to develop and deploy new vaccines to prevent future epidemics,” CEPI have identified the most important known global infectious threats and invested in the development of vaccines, stockpiling, and policies to allow equitable access to these ( Plotkin, 2017 ). Further, the establishment of research and development infrastructure pipelines will allow production of suitable vaccine candidates within 16 weeks of identification of a new pathogen antigen. The broader aims including: improving global epidemic responses; capacity building; and global regulation of outbreak management strategies are also within the remit of CEPI’s work. It is these types of preparedness plans that assisted vaccine development and global health collaborations to address the COVID-19 pandemic, though many regions of high-, middle-, and low-income countries alike were slow or resistant to pre-empt and prepare for this type of infectious disease threat.
Social Benefits
Equity of healthcare.
As a result of the combined effects of poverty, malnutrition, poor hygiene and sanitation, overcrowding, discrimination and poorer access to health-care, the underprivileged in society are disproportionately afflicted by infectious diseases. Over the 20th century, it has become a moral standpoint and a human right for every individual to be provided with access to safe vaccines. The provision of vaccination as part of the EPI on a national and international scale ( World Health Assembly, 1974 ) acted as a great leveler to start reducing the impact of infectious diseases to all, regardless of other disadvantages. Over the 15 years of the EPI, the vaccine coverage in developing countries increased from 5% to ∼80% ( Levine and Robins-Browne, 2009 ). The EPI was revolutionary for its time, an ambitious public health program that aimed to improve children’s life chances despite the country and situation in which they were born. The administration of vaccines by UNICEF was deemed so important that there have been at least seven ceasefires in civil conflicts to allow this to happen ( Hotez, 2001 ).
The impact of vaccines on the inequity of those living in poverty is marked. A study of over 16,000 children during the phased introduction of the measles vaccine in Bangladesh in 1982, demonstrated improved health outcome equity when measured by under-5 mortality ( Bishai et al., 2003 ). Further, modeling of the impact of the rotavirus vaccine in India across social strata, which are closely aligned to wealth, suggested that the vaccine program would provide the poor with both health and financial benefits ( Verguet et al., 2013 ). Including such equity impact in the health economic modeling of vaccines would allow policy decisions to be targeted to the most vulnerable in society ( Riumallo-Herl et al., 2018 ). Additional cost-effective benefits observed after the implementation of combined public health initiatives ( Deogaonkar et al., 2012 ; Gessner et al., 2017 ) include provision of vaccines, facilitation of healthcare, reduction of indoor air pollution and improvement of nutrition to prevent childhood pneumonia ( Niessen et al., 2009 ).
Strengthening Health and Social Care Infrastructure
To provide the EPI universally to infants and children, a significant degree of healthcare infrastructure is required ranging from primary care to public health. An example of the multiple facets of a successful vaccine program were outlined in the Mission Indradhanush in India, which planned to make life-saving vaccines available to all children and pregnant women by 2020 through programs with (i) national, (ii) state, (iii) district, and (iv) block/urban level input ( Hinman and McKinlay, 2015 ). National programs require governments to provide financial resources and set out policy for implementation. States needed to obtain the vaccines and to store them appropriately whilst eligible children were identified through public health messaging and outreach. Districts and urban areas recruited staff trained in vaccine delivery and communication to administer vaccines and to provide the aftercare where required. Establishing this degree of nationwide infrastructure to reach those in urban and rural areas, provides the basis for the provision of other health and social care services for all members of the community, in particular improving maternal and infant mortality in developing regions and in the elderly in industrialized regions ( Shearley, 1999 ). Public health infrastructure and personnel could be used to promote other important messages and health education ( Shearley, 1999 ), relating to malnutrition, hygiene and sanitation and preventable diseases such as malaria and HIV infection. Global drivers are also key, as demonstrated by the establishment of the EPI in 1974, when all countries were directed to provide these vaccines, thereby developing their primary- and public health-care infrastructure, with benefit beyond the vaccine program. Vaccination contributes to the UN Millennium Development Goals and later Sustainable Development Goals for achievement by 2030. Gavi, the Vaccine Alliance, has been an important provider of funds, vaccines and support for countries whose gross national income per capita was <£1000/year ( Hinman and McKinlay, 2015 ). The partnerships forged through the development of vaccine programs in LMIC, can be long-lasting and beneficial through other health and social care endeavors ( Shearley, 1999 ).
Impact of Life Expectancy and Opportunity
Vaccination programs provide a degree of social mobility, as poverty and the associated ill-health and mortality from infectious diseases are no longer the determinants of one’s life chances. Vaccine recipients have the potential for improved life-expectancy largely demonstrated by, but not confined to, infants and children ( Andre et al., 2008 ). It has become increasingly recognized that an aging population goes through the process of immunosenescence ( Fulop et al., 2017 ), and increased incidence and severity of infectious diseases. In many countries, therefore, older people are offered vaccines to prevent infections with high mortality and morbidity, including the influenza, pneumococcal, herpes zoster, and pertussis vaccines ( Bonanni et al., 2015 ). These prevent the development of pneumonia, admission to hospital and the subsequent associated risks of death from cardiac failure, as observed in Sweden ( Christenson et al., 2004 ).
The global and interconnected world of the 21st century provides opportunity to discover new cultures, new environments and their resident microbes. The safety of global travel has been greatly enhanced by the availability of vaccines that provide protection against organisms that are different to those in a person’s home setting. Movement of people may be through necessity when fleeing war and conflict, in the search of better life opportunities, or for leisure purposes. For mass movements of refugees vaccines are crucial to the aid and relief efforts to support these individuals ( Hermans et al., 2017 ), as measles and cholera can be highly problematic in refugee camps. Global mass cultural or religious gatherings, such as the Hajj pilgrimage ( Yezli et al., 2018 ) or the Chinese New Year ( Chen et al., 2018 ) have been implicated in the spread of meningococcal disease outbreaks. Pre-travel vaccines offer the optimal level of protection for those with scheduled travel plans and include protection against: yellow fever, hepatitis A and B, rabies, Japanese encephalitis, tick-borne encephalitis, typhoid, and cholera.
Empowerment of Women
The empowerment of women is both a driver and effect of vaccination programs. The degree of education, literacy and independence of girls and women varies considerably across the world and within countries. Where women have the information and autonomy to make health-related decision for their children, childhood immunization rates improve. In a study in Bihar State in rural India involving an empowerment program, where participating women were educated about health and hygiene, there was a higher rate of DTP, measles and BCG vaccination in their children compared to the non-participants in the villages running the program ( Janssens, 2011 ). Further, this information and autonomy served to improve the rates of vaccination in children of non-participants in the villages running the program compared to control villages not running the education program, through social or formal ongoing dialogue within the village community. A separate public health initiative in Haryana, India conducted between 2005 and 2012 to reduce maternal and child health inequalities, involved improving access and provision of health resources to rural areas, the poor in society, women and children. One significant outcome of this initiative was the equitable provision of immunizations to girls and boys, despite the male-favored disparity prior to starting the public health initiative ( Gupta et al., 2016 ).
By improving infant and childhood mortality from infection, more children will survive to adulthood with the potential to have productive and healthy lives. This has led to healthy and economically secure women having fewer children and less peripartum morbidity and mortality ( Sah, 1991 ; Shearley, 1999 ). Thus, women are able to spend more time with their children and on their development ( Shearley, 1999 ) as well as their own education and contribution to the workforce. The strategy of maternal vaccination has demonstrated great success at preventing diseases that afflict infants too young to be vaccinated against pertussis, influenza and tetanus ( Marchant et al., 2017 ). Factors influencing the uptake of maternal vaccination include women’s previous experiences with healthcare and vaccines, so it is crucial to provide the access and support required to enable them to make informed choices during their pregnancy ( Wilson et al., 2019 ).
The impact of vaccines is broad and far-reaching, though not consistently quantifiable, analyzed or communicated. Traditionally, the perceived benefits of vaccination were to reduce morbidity and mortality from infections, and those remain the drivers for the innovation of new vaccines, in particular in preparation for outbreaks or against infections that afflict the most disadvantaged in society. However, an increasing appreciation for the economic and social effects of vaccines is being included in the development and assessment of vaccine programs, potentially realizing a greater benefit to society and resulting in wider implementation. There remain challenges to delivering vaccines to all children and vulnerable people worldwide, in particular those in communities that are difficult to reach geographically, politically and culturally and these challenges can only be overcome with the continued commitment and dedication to this endeavor on an international, national and individual scale.
Author Contributions
SP conceptualized and designed the study. CR prepared the manuscript and figures. CR and SP contributed to literature search and revision and review of the final manuscript. Both authors contributed to the article and approved the submitted version.
Conflict of Interest
SP consults for many major vaccine manufacturers and biotechnology companies but this article was unfunded.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Aaby, P., Bhuiya, A., Nahar, L., Knudsen, K., de Francisco, A., and Strong, M. (2003). The survival benefit of measles immunization may not be explained entirely by the prevention of measles disease: a community study from rural Bangladesh. Intern. J. Epidemiol. 32, 106–116.
Google Scholar
Abadom, T. R., Smith, A. D., Tempia, S., Madhi, S. A., Cohen, C., and Cohen, A. L. (2016). Risk factors associated with hospitalisation for influenza-associated severe acute respiratory illness in South Africa: a case-population study. Vaccine 34, 5649–5655.
Anderson, P., Peter, G., Johnston, R. B. Jr., Wetterlow, L. H., and Smith, D. H. (1972). Immunization of humans with polyribophosphate, the capsular antigen of Hemophilus influenzae , type b. J. Clin. Invest. 51, 39–44.
Andre, F. E., Booy, R., Bock, H. L., Clemens, J., Datta, S. K., John, T. J., et al. (2008). Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull. World Health Organ. 86, 140–146.
Artenstein, M. S. (1975). Control of meningococcal meningitis with meningococcal vaccines. Yale J. Biol. Med. 48, 197–200.
Austrian, R. (1989). Pneumococcal polysaccharide vaccines. Rev. Infect. Dis. 11, (Suppl. 3), S598–S602.
Barham, T., and Calimeria, L. (2008). Long-term Effects of Family Planning and Child Health Interventions on Adolescent Cognition: Evidence from Matlab in Bangladesh. Boulder, CO: Univeristy of Colorado.
Barnighausen, T., Bloom, D. E., Cafiero-Fonseca, E. T., and O’Brien, J. C. (2014). Valuing vaccination. Proc. Nat. Acad. Sci. U.S.A. 111, 12313–12319.
Bärnighausen, T., Bloom, D. E., Canning, D., Friedman, A., Levine, O. S., O’Brien, J., et al. (2011). Rethinking the benefits and costs of childhood vaccination: the example of the Haemophilus influenzae type b vaccine. Vaccine 29, 2371–2380.
Barrett, S. (2004). Eradication versus control: the economics of global infectious disease policies. Bull. World Health Organ. 82, 683–688.
Bishai, D., Koenig, M., and Ali Khan, M. (2003). Measles vaccination improves the equity of health outcomes: evidence from Bangladesh. Health Econ. 12, 415–419.
Bloom, D. E., and Canning, D. (2000). Policy forum: public health. The health and wealth of nations. Science 287:1207.
Bloom, D. E., Canning, D., and Seiguer, E. (2011). The Effect of Vaccination on Children’s Physical and Cognitive Development in the Philippines. Boston, MA: Harvard School of Public Health.
Bloom, D. E., Canning, D., and Weston, M. (2005). The value of vaccination. World Econ. 6, 15–16.
Bogler, Y., Wong, R. J., and Gish, R. G. (2018). “Epidemiology and natural history of chronic hepatitis B virus infection,” in Hepatitis B Virus and Liver Disease , eds J.-H. Kao and D.-S. Chen (Berlin: Springer), 63–89.
Bonanni, P., Picazo, J. J., and Remy, V. (2015). The intangible benefits of vaccination - what is the true economic value of vaccination? J. Mark. Access Health Policy 3:10.3402/jmahv3.26964.
Borgia, G., Carleo, M. A., Gaeta, G. B., and Gentile, I. (2012). Hepatitis B in pregnancy. World J. Gastroenterol. 18, 4677–4683.
Brinkac, L., Voorhies, A., Gomez, A., and Nelson, K. E. (2017). The threat of antimicrobial resistance on the human microbiome. Microb. Ecol. 74, 1001–1008.
Calmette, A. (1927). La Vaccination Preìventive Contre La Tuberculose par le “BCG,”. Paris: Masson.
Centers for Disease Control and Prevention (2017). Reported Cases Of Notifiable Diseases And Rates Per 100,000, Excluding U.S. Territories, United States, 2017. Atlanta: Centers for Disease Control and Prevention.
Chan, J. F., Yuan, S., Kok, K. H., To, K. K., Chu, H., Yang, J., et al. (2020). A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395, 514–523.
Chen, M., Rodrigues, C. M. C., Harrison, O. B., Zhang, C., Tan, T., Chen, J., et al. (2018). Invasive meningococcal disease in Shanghai, China from 1950 to 2016: implications for serogroup B vaccine implementation. Sci. Rep. 8:12334.
Christenson, B., Hedlund, J., Lundbergh, P., and Ortqvist, A. (2004). Additive preventive effect of influenza and pneumococcal vaccines in elderly persons. Eur. Resp. J. 23, 363–368.
Clark, H. F., Offit, P. A., Plotkin, S. A., and Heaton, P. M. (2006). The new pentavalent rotavirus vaccine composed of bovine (strain WC3) -human rotavirus reassortants. Pediatr. Infect. Dis. J. 25, 577–583.
Curns, A. T., Steiner, C. A., Barrett, M., Hunter, K., Wilson, E., and Parashar, U. D. (2010). Reduction in acute gastroenteritis hospitalizations among US children after introduction of rotavirus vaccine: analysis of hospital discharge data from 18 US states. J. Infect. Dis. 201, 1617–1624.
Daugla, D. M., Gami, J. P., Gamougam, K., Naibei, N., Mbainadji, L., Narbe, M., et al. (2014). Effect of a serogroup A meningococcal conjugate vaccine (PsA-TT) on serogroup A meningococcal meningitis and carriage in Chad: a community study [corrected]. Lancet 383, 40–47.
Deogaonkar, R., Hutubessy, R., van der Putten, I., Evers, S., and Jit, M. (2012). Systematic review of studies evaluating the broader economic impact of vaccination in low and middle income countries. BMC Public Health 12:878. doi: 10.1186/s12916-017-0911-878
CrossRef Full Text | Google Scholar
Dominguez, A., Castilla, J., Godoy, P., Delgado-Rodriguez, M., Saez, M., Soldevila, N., et al. (2013). Benefit of conjugate pneumococcal vaccination in preventing influenza hospitalization in children: a case-control study. Pediatr. Infect. Dis. J. 32, 330–334.
Donaghy, M., Cameron, J. C., and Friederichs, V. (2006). Increasing incidence of mumps in Scotland: options for reducing transmission. J. Clin. Virol. 35, 121–129.
Ehreth, J. (2003). The global value of vaccination. Vaccine 21, 596–600.
Ferlay, J., Soerjomataram, I., Dikshit, R., Eser, S., Mathers, C., Rebelo, M., et al. (2012). Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN. Int. J. Cancer 136, E359–E386.
Fine, P. E., and Griffiths, U. K. (2007). Global poliomyelitis eradication: status and implications. Lancet 369, 1321–1322.
Fulop, T., Larbi, A., Dupuis, G., Le Page, A., Frost, E. H., Cohen, A. A., et al. (2017). Immunosenescence and inflamm-aging as two sides of the same coin: friends or foes? Front. Immunol. 8:1960. doi: 10.3389/fmicb.2018.01960
PubMed Abstract | CrossRef Full Text | Google Scholar
Funk, S., Knapp, J. K., Lebo, E., Reef, S. E., Dabbagh, A. J., Kretsinger, K., et al. (2019). Combining serological and contact data to derive target immunity levels for achieving and maintaining measles elimination. BMC Med. 17:180. doi: 10.1186/s12889-019-6655-180
Geddes, A. M. (2006). The history of smallpox. Clin. Dermatol. 24, 152–157.
Gentile, I., and Borgia, G. (2014). Vertical transmission of hepatitis B virus: challenges and solutions. Intern. J. Women Health 6, 605–611.
Gessner, B. D., Kaslow, D., Louis, J., Neuzil, K., O’Brien, K. L., Picot, V., et al. (2017). Estimating the full public health value of vaccination. Vaccine 35, 6255–6263.
GHRF Commission (2016). Commission on a Global Health Risk Framework for the Future). The Neglected Dimension of Global Security A Framework to Counter Infectious Disease Crises. Commission on Global Health Risk Framework for the Future. Available online at: https://nam.edu/wp-content/uploads/2016/01/Neglected-Dimension-of-Global-Security.pdf (September 24, 2019).
Glenny, A. T., and Hopkins, B. E. (1923). Diphtheria toxoid as an immunising agent. Br. J. Exp. Pathol. 4, 283–288.
Global Polio Eradication Initiative (2019). Polio this Week, Wild Poliovirus Type 1 And Circulating Vaccine-Derived Poliovirus Cases. Available online at: http://polioeradication.org/polio-today/polio-now/this-week/ (accessed June 25, 2020).
Gold, R., and Artenstein, M. S. (1971). Meningococcal infections. 2. Field trial of group C meningococcal polysaccharide vaccine in 1969-70. Bull. World Health Organ. 45, 279–282.
Gouglas, D., Thanh, Le, T., Henderson, K., Kaloudis, A., Danielsen, T., et al. (2018). Estimating the cost of vaccine development against epidemic infectious diseases: a cost minimisation study. Lancet Glob. Health 6:e001386-96.
Grizas, A. P., Camenga, D., and Vazquez, M. (2012). Cocooning: a concept to protect young children from infectious diseases. Curr. Opin. Pediatr. 24, 92–97.
Gupta, G., Glueck, R., and Patel, P. R. (2017). HPV vaccines: global perspectives. Hum. Vacc. Immunotherap. 13, 1–4.
Gupta, M., Angeli, F., Bosma, H., Rana, M., Prinja, S., Kumar, R., et al. (2016). Effectiveness of multiple-strategy community intervention in reducing geographical, socioeconomic and gender based inequalities in maternal and child health outcomes in Haryana, India. PLoS One 11:e0150537. doi: 10.1371/journal.pone.0150537
Hajjeh, R. (2011). Accelerating introduction of new vaccines: barriers to introduction and lessons learned from the recent Haemophilus influenzae type B vaccine experience. Philos. Trans. R. Soc. B. 366, 2827–2832.
Hermans, M. P. J., Kooistra, J., Cannegieter, S. C., Rosendaal, F. R., Mook-Kanamori, D. O., and Nemeth, B. (2017). Healthcare and disease burden among refugees in long-stay refugee camps at Lesbos. Greece. Eur. J. Epidemiol. 32, 851–854.
Heukelbach, J., Alencar, C. H., Kelvin, A. A., de Oliveira, W. K., and Pamplona de Goes, C. L. (2016). Zika virus outbreak in Brazil. J. Infect. Dev. Countr. 10, 116–120.
Hill, H. A., Elam-Evans, L. D., Yankey, D., Singleton, J. A., and Kang, Y. (2017). Vaccination coverage among children aged 19-35 Months - United States, 2016. MMWR Morb. Mort. Wkly Rep. 66, 1171–1177.
Hinman, A. R., and McKinlay, M. A. (2015). Immunization equity. Vaccine 33, (Suppl. 4), D72–D77.
Hotez, P. J. (2001). Vaccines as instruments of foreign policy. The new vaccines for tropical infectious diseases may have unanticipated uses beyond fighting diseases. EMBO Rep. 2, 862–868.
Janssens, W. (2011). Externalities in program evaluation: the impact of a Women’s empowerment program on immunization. J. Eur. Econ. Assoc. 9, 1082–1113.
Jenner, E. (1798). An Inquiry Into The Causes And Effects Of The Variolæ Vaccinæ, A Disease Discovered In Some Of The Western Counties Of England, Particularly Gloucestershire, And Known By The Name Of The Cow Pox. London: Sampson Low.
Jit, M., Hutubessy, R., Png, M. E., Sundaram, N., Audimulam, J., Salim, S., et al. (2015). The broader economic impact of vaccination: reviewing and appraising the strength of evidence. BMC Med. 13:209. doi: 10.1186/s12916-017-0911-209
Keja, K., Chan, C., Hayden, G., and Henderson, R. H. (1988). Expanded programme on immunization. World Health Stat. Q. 41, 59–63.
Kirnbauer, R., Booy, F., Cheng, N., Lowy, D. R., and Schiller, J. T. (1992). Papillomavirus L1 major capsid protein self-assembles into virus-like particles that are highly immunogenic. Proc. Nat. Acad. Sci. U.S.A. 89, 12180–12184.
Kyaw, M. H., Lynfield, R., Schaffner, W., Craig, A. S., Hadler, J., Reingold, A., et al. (2006). Effect of introduction of the pneumococcal conjugate vaccine on drug-resistant Streptococcus pneumoniae . New Engl. J. Med. 354, 1455–1463.
Levine, M. M., and Robins-Browne, R. (2009). Vaccines, global health and social equity. Immunol. Cell Biol. 87, 274–278.
Lien, G., and Heymann, D. L. (2013). The problems with polio: toward eradication. Infect. Dis. Ther. 2, 167–174.
Lieu, T. A., Cochi, S. L., Black, S. B., Halloran, M. E., Shinefield, H. R., Holmes, S. J., et al. (1994). Cost-effectiveness of a routine varicella vaccination program for US children. JAMA 271, 375–381.
Liu, Y. Y., Wang, Y., Walsh, T. R., Yi, L. X., Zhang, R., Spencer, J., et al. (2016). Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect. Dis. 16, 161–168.
Logan, L. K., and Weinstein, R. A. (2017). The epidemiology of carbapenem-resistant Enterobacteriaceae : the impact and evolution of a global menace. J. Infect. Dis. 215(Suppl._1), S28–S36.
Maassab, H. F., and DeBorde, D. C. (1985). Development and characterization of cold-adapted viruses for use as live virus vaccines. Vaccine 3, 355–369.
Madhi, S. A., Klugman, K. P., and Vaccine Trialist, G. (2004). A role for Streptococcus pneumoniae in virus-associated pneumonia. Nat. Med. 10, 811–813.
Maiden, M. C., Ibarz-Pavon, A. B., Urwin, R., Gray, S. J., Andrews, N. J., Clarke, S. C., et al. (2008). Impact of meningococcal serogroup C conjugate vaccines on carriage and herd immunity. J. Infect. Dis. 197, 737–743.
Manzoli, L., Schioppa, F., Boccia, A., and Villari, P. (2007). The efficacy of influenza vaccine for healthy children: a meta-analysis evaluating potential sources of variation in efficacy estimates including study quality. Pediatr. Infect. Dis. J. 26, 97–106.
Marchant, A., Sadarangani, M., Garand, M., Dauby, N., Verhasselt, V., Pereira, L., et al. (2017). Maternal immunisation: collaborating with mother nature. Lancet. Infect. Dis. 17, e197–e208. doi: 10.1016/S1473-3099(17)30229-3
Mina, M. J., Kula, T., Leng, Y., Li, M., de Vries, R. D., Knip, M., et al. (2019). Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Science 366, 599–606.
Mina, M. J., Metcalf, C. J., de Swart, R. L., Osterhaus, A. D., and Grenfell, B. T. (2015). Long-term measles-induced immunomodulation increases overall childhood infectious disease mortality. Science 348, 694–699.
Morens, D. M., and Fauci, A. S. (2007). The 1918 influenza pandemic: insights for the 21st century. J. Infect. Dis. 195, 1018–1028.
Morens, D. M., Holmes, E. C., Davis, A. S., and Taubenberger, J. K. (2011). Global rinderpest eradication: lessons learned and why humans should celebrate too. J. Infect. Dis. 204, 502–505.
Moss, W. J. (2017). Measles. Lancet 390, 2490–2502.
Munira, S. L., and Fritzen, S. A. (2007). What influences government adoption of vaccines in developing countries? A policy process analysis. Soc. Sci. Med. 65, 1751–1764.
Needham, J. (2000). Science and Civilisation in China: Volume 6, Biology and Biological Technology. Cambridge: Cambridge University Press.
Niessen, L. W., ten Hove, A., Hilderink, H., Weber, M., Mulholland, K., and Ezzati, M. (2009). Comparative impact assessment of child pneumonia interventions. Bull. World Health Organ. 87, 472–480.
Nunes, M. C., Cutland, C. L., Jones, S., Downs, S., Weinberg, A., Ortiz, J. R., et al. (2017). Efficacy of maternal influenza vaccination against all-cause lower respiratory tract infection hospitalizations in young infants: results from a randomized controlled trial. Clin. Infect. Dis. 65, 1066–1071.
Orenstein, W. A., and Ahmed, R. (2017). Simply put: vaccination saves lives. Proc. Nat. Acad. Sci. U.S.A. 114, 4031–4033.
Ozawa, S., Clark, S., Portnoy, A., Grewal, S., Brenzel, L., and Walker, D. G. (2016). Return On investment from childhood immunization in low- and middle-income countries, 2011-20. Health Aff. 35, 199–207.
Palmer, T., Wallace, L., Pollock, K. G., Cuschieri, K., Robertson, C., Kavanagh, K., et al. (2019). Prevalence of cervical disease at age 20 after immunisation with bivalent HPV vaccine at age 12-13 in Scotland: retrospective population study. BMJ 365:l1161.
Palmu, A. A., Jokinen, J., Nieminen, H., Rinta-Kokko, H., Ruokokoski, E., Puumalainen, T., et al. (2014). Effect of pneumococcal Haemophilus influenzae protein D conjugate vaccine (PHiD-CV10) on outpatient antimicrobial purchases: a double-blind, cluster randomised phase 3-4 trial. Lancet Infect. Dis. 14, 205–212.
Pasteur, L. (1880). De l’attenuation du virus du choléra des poules. Comptes Rendus De l’Acad. Sci. 91, 673–680.
Pasteur, L. (1881). Sur la vaccination charbonneuse. Comptes Rendus De l’Acad. Sci. 92, 1378–1383.
Pasteur, L. (1885). Mèthode pour prévenir la rage apres morsure. Comptes Rendus De l’Acad. Sci. 101, 765–772.
Paulke-Korinek, M., Kundi, M., Rendi-Wagner, P., de Martin, A., Eder, G., Schmidle-Loss, B., et al. (2011). Herd immunity after two years of the universal mass vaccination program against rotavirus gastroenteritis in Austria. Vaccine 29, 2791–2796.
Peltola, H., Aavitsland, P., Hansen, K. G., Jonsdottir, K. E., Nokleby, H., and Romanus, V. (1999). Perspective: a five-country analysis of the impact of four different Haemophilus influenzae type b conjugates and vaccination strategies in Scandinavia. J. Infect. Dis. 179, 223–229.
Petrova, V. N., Sawatsky, B., Han, A. X., Laksono, B. M., Walz, L., Parker, E., et al. (2019). Incomplete genetic reconstitution of B cell pools contributes to prolonged immunosuppression after measles. Sci. Immunol. 4:eaay6125.
Plans-Rubio, P. (2012). Evaluation of the establishment of herd immunity in the population by means of serological surveys and vaccination coverage. Hum. Vacc. Immunotherap. 8, 184–188.
Plotkin, S. (2014). History of vaccination. Proc. Natl. Acad. Sci. U.S.A. 111, 12283–12287.
Plotkin, S. A. (2017). Vaccines for epidemic infections and the role of CEPI. Hum. Vacc. Immunotherap. 13, 2755–2762.
Plotkin, S. A., and Mortimer, E. A. (1988). Vaccines. Philadelphia, PA: Saunders.
Pollard, A. J., Perrett, K. P., and Beverley, P. C. (2009). Maintaining protection against invasive bacteria with protein-polysaccharide conjugate vaccines. Nat. Rev. Immunol. 9, 213–220.
Poovorawan, Y., Chongsrisawat, V., Theamboonlers, A., Leroux-Roels, G., Kuriyakose, S., Leyssen, M., et al. (2011). Evidence of protection against clinical and chronic hepatitis B infection 20 years after infant vaccination in a high endemicity region. J. Viral Hepat. 18, 369–375.
Public Health England (2018). Public Health Matters Ten Years On Since The Start Of The HPV Vaccine Programme – What Impact Is It Having? London: Public Health England.
Public Health England (2019). Human Papillomavirus (HPV) Vaccination Coverage In Adolescent Females In England: 2017/18. London: Public Health England.
Regan, A. K., de Klerk, N., Moore, H. C., Omer, S. B., Shellam, G., and Effler, P. V. (2016). Effect of maternal influenza vaccination on hospitalization for respiratory infections in newborns: a retrospective cohort study. Pediatr. Infect. Dis. J. 35, 1097–1103.
Riumallo-Herl, C., Chang, A. Y., Clark, S., Constenla, D., Clark, A., Brenzel, L., et al. (2018). Poverty reduction and equity benefits of introducing or scaling up measles, rotavirus and pneumococcal vaccines in low-income and middle-income countries: a modelling study. BMJ Glob. Health 3:e000613.
Roeder, P., Mariner, J., and Kock, R. (2013). Rinderpest: the veterinary perspective on eradication. Philos. Trans. R. Soc. B 368:20120139.
Roush, S. W., and Murphy, T. V. (2007). Vaccine-preventable disease table working G. historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA 298, 2155–2163.
Russo, F. B., Jungmann, P., and Beltrao-Braga, P. C. B. (2017). Zika infection and the development of neurological defects. Cell. Microbiol. 19: 12744.
Sah, R. K. (1991). The effects of child-mortality changes on fertility choice and parental welfare. J. Polit. Econ. 99, 582–606.
Sato, Y., and Sato, H. (1999). Development of acellular pertussis vaccines. Biologicals 27, 61–69.
Schneerson, R., Barrera, O., Sutton, A., and Robbins, J. B. (1980). Preparation, characterization, and immunogenicity of Haemophilus influenzae type b polysaccharide-protein conjugates. J. Exp. Med. 152, 361–376.
Serruto, D., Bottomley, M. J., Ram, S., Giuliani, M. M., and Rappuoli, R. (2012). The new multicomponent vaccine against meningococcal serogroup B, 4CMenB: immunological, functional and structural characterization of the antigens. Vaccine 30, (Suppl. 2), B87–B97.
Shearley, A. E. (1999). The societal value of vaccination in developing countries. Vaccine 17, (Suppl. 3), S109–S112.
Simonsen, L., Taylor, R. J., Young-Xu, Y., Haber, M., May, L., and Klugman, K. P. (2011). Impact of pneumococcal conjugate vaccination of infants on pneumonia and influenza hospitalization and mortality in all age groups in the United States. mBio 2:e00309-10.
Soergel, P., Makowski, L., Schippert, C., Staboulidou, I., Hille, U., and Hillemanns, P. (2012). The cost efficiency of HPV vaccines is significantly underestimated due to omission of conisation-associated prematurity with neonatal mortality and morbidity. Hum. Vacc. Immunother. 8, 243–251.
Strassburg, M. A. (1982). The global eradication of smallpox. Am. J. Infect. Control 10, 53–59.
Tabrizi, S. N., Brotherton, J. M., Kaldor, J. M., Skinner, S. R., Liu, B., Bateson, D., et al. (2014). Assessment of herd immunity and cross-protection after a human papillomavirus vaccination programme in Australia: a repeat cross-sectional study. Lancet Infect.ous Dis. 14, 958–966.
Thacker, N., Vashishtha, V. M., and Thacker, D. (2016). Polio eradication in India: the lessons learned. Pediatrics 138:e20160461.
Thanh Le, T., Andreadakis, Z., Kumar, A., Gomez Roman, R., Tollefsen, S., Saville, M., et al. (2020). The COVID-19 vaccine development landscape. Nat. Rev. Drug Discov. 19, 305–306.
Theiler, M., and Smith, H. H. (1937a). The effect of prolonged cultivation in vitro upon the pathogenicity of yellow fever virus. J. Exp. Med. 65, 767–786.
Theiler, M., and Smith, H. H. (1937b). The use of yellow fever virus modified by in vitro cultivation for human immunization. J. Exp. Med. 65, 787–800.
Turner, H. C., Thwaites, G. E., and Clapham, H. E. (2018). Vaccine-preventable diseases in lower-middle-income countries. Lancet Infect. Dis. 18, 937–939.
United Nations Department of Economic and Social Affairs (2019). Population Division. World Population Prospects 2019. New York, NY: United Nations Department of Economic and Social Affairs.
Van der Wielen, M., Giaquinto, C., Gothefors, L., Huelsse, C., Huet, F., Littmann, M., et al. (2010). Impact of community-acquired paediatric rotavirus gastroenteritis on family life: data from the REVEAL study. BMC Fam. Pract. 11:22. doi: 10.1186/s12916-017-0911-22
Verguet, S., Murphy, S., Anderson, B., Johansson, K. A., Glass, R., and Rheingans, R. (2013). Public finance of rotavirus vaccination in India and Ethiopia: an extended cost-effectiveness analysis. Vaccine 31, 4902–4910.
Wang, X., Huang, X., and Zhang, Y. (2018). Involvement of human papillomaviruses in cervical cancer. Front. Microbiol. 9:2896. doi: 10.3389/fmicb.2018.02896
Whitney, C. G., Farley, M. M., Hadler, J., Harrison, L. H., Bennett, N. M., Lynfield, R., et al. (2003). Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. New Engl. J. Med. 348, 1737–1746.
Wilder-Smith, A., Longini, I., Zuber, P. L., Barnighausen, T., Edmunds, W. J., Dean, N., et al. (2017). The public health value of vaccines beyond efficacy: methods, measures and outcomes. BMC Med. 15:138. doi: 10.1186/s12916-017-0911-8
Wilson, R., Paterson, P., and Larson, H. J. (2019). Strategies to improve maternal vaccination acceptance. BMC Public Health 19:342. doi: 10.1186/s12889-019-6655-y
Wise, J. (2018). Child vaccination rates drop in England as MMR uptake falls for fourth year. BMJ 362:k3967.
Wise, J. (2019). MMR vaccine: johnson urges new impetus to increase uptake as UK loses measles-free status. BMJ 366:l5219.
World Bank (2019). Immunization, DPT (% of Children Ages 12-23 Months). Washington, DC: World Bank.
World Health Assembly (1974). The expanded programme on immunization: the 1974 resolution by the world health assembly. Assign. Child. 1985, 87–88.
World Health Organisation (2019a). Immunization Coverage. Geneva: World Health Organisation.
World Health Organisation (2019b). Polio Eradication. Geneva: World Health Organisation.
World Health Organisation (2019c). Reported Cases of Selected Vaccine Preventable Diseases (VPDs). Geneva: World Health Organisation.
World Health Organization [WHO], United Nations Children’s Fund [UNICEF] (2019). WHO/UNICEF Estimates of National Immunization Coverage (WUENIC) 1980-2018. Geneva: WHO.
Yezli, S., Gautret, P., Assiri, A. M., Gessner, B. D., and Alotaibi, B. (2018). Prevention of meningococcal disease at mass gatherings: lessons from the Hajj and Umrah. Vaccine 36, 4603–4609.
Zhou, F., Shefer, A., Wenger, J., Messonnier, M., Wang, L. Y., Lopez, A., et al. (2009). Economic evaluation of the routine childhood immunization program in the United States. Pediatrics 133, 577–585.
Zhu, N., Zhang, D., Wang, W., Li, X., Yang, B., Song, J., et al. (2020). A novel coronavirus from patients with pneumonia in China, 2019. New Engl. J. Med. 382, 727–733.
Keywords : immunization, vaccines, infectious diseases, infection, children, health economics
Citation: Rodrigues CMC and Plotkin SA (2020) Impact of Vaccines; Health, Economic and Social Perspectives. Front. Microbiol. 11:1526. doi: 10.3389/fmicb.2020.01526
Received: 09 April 2020; Accepted: 12 June 2020; Published: 14 July 2020.
Reviewed by:
Copyright © 2020 Rodrigues and Plotkin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stanley A. Plotkin, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
COVID-19 and vaccine hesitancy: A longitudinal study
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Rady School of Management, University of California San Diego, La Jolla, California, United States of America
Roles Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing
- Ariel Fridman,
- Rachel Gershon,
- Ayelet Gneezy

- Published: April 16, 2021
- https://doi.org/10.1371/journal.pone.0250123
- Peer Review
- Reader Comments
How do attitudes toward vaccination change over the course of a public health crisis? We report results from a longitudinal survey of United States residents during six months (March 16 –August 16, 2020) of the COVID-19 pandemic. Contrary to past research suggesting that the increased salience of a disease threat should improve attitudes toward vaccines, we observed a decrease in intentions of getting a COVID-19 vaccine when one becomes available. We further found a decline in general vaccine attitudes and intentions of getting the influenza vaccine. Analyses of heterogeneity indicated that this decline is driven by participants who identify as Republicans, who showed a negative trend in vaccine attitudes and intentions, whereas Democrats remained largely stable. Consistent with research on risk perception and behavior, those with less favorable attitudes toward a COVID-19 vaccination also perceived the virus to be less threatening. We provide suggestive evidence that differential exposure to media channels and social networks could explain the observed asymmetric polarization between self-identified Democrats and Republicans.
Citation: Fridman A, Gershon R, Gneezy A (2021) COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE 16(4): e0250123. https://doi.org/10.1371/journal.pone.0250123
Editor: Valerio Capraro, Middlesex University, UNITED KINGDOM
Received: November 12, 2020; Accepted: February 14, 2021; Published: April 16, 2021
Copyright: © 2021 Fridman et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All data and code are publicly available on the Open Science Framework at https://osf.io/kgvdy/ .
Funding: UC San Diego Global Health Initiative (GHI): awarded to all authors; Project number: 1001288. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. https://medschool.ucsd.edu/som/medicine/divisions/idgph/research/Global-Health/grant-recipients/2019-2020/Pages/Faculty-Postdoc-Travel-and-Research.aspx .
Competing interests: The authors have declared that no competing interests exist.
Introduction
Vaccinations are among the most important public health tools for reducing the spread and harm caused by dangerous diseases [ 1 ]. The World Health Organization estimates that vaccines prevented at least 10 million deaths between 2010–2015 worldwide [ 2 ]. Despite considerable evidence showing vaccines are safe [ 3 , 4 ], there is increasing skepticism toward vaccination [ 5 , 6 ]. Vaccine hesitancy has led to a decline in vaccine uptake and to an increase in the prevalence of vaccine-preventable diseases (VPDs) [ 7 , 8 ]. Ironically, the objection to vaccines is commonly a consequence of their effectiveness—because individuals have lower exposure to VPDs, they are less concerned about contracting them [ 9 ], which consequently leads to greater vaccine hesitancy [ 10 ]. The COVID-19 pandemic has created a new reality where individuals are faced with a previously unknown disease and its effects, providing a unique opportunity to investigate vaccine attitudes during a period of heightened disease salience. The present research reports findings from a longitudinal study conducted during the COVID-19 health crisis, in which we measured changes in attitudes toward a prospective vaccine, as well as shifts in vaccine attitudes in general.
Factors influencing vaccine attitudes and behaviors
Past research has identified a variety of situational and individual-level factors that influence vaccine attitudes and behavior, the most prominent of which are risk perceptions and demographic characteristics.
Assessments of risk are influenced by both cognitive evaluations (i.e., objective features of the situation such as probabilities of outcomes) and affective reactions [ 11 ], as well as by contextual factors (e.g., the information that is most available or salient at the time [ 12 ]). For example, research shows that media coverage plays a significant role in determining the extent to which we take threats seriously [ 13 ]. When individuals perceive heightened risk of a threat, they become more favorable toward interventions that mitigate that threat, including vaccination (for a meta-analysis on the effect of perceived risk on intentions and behaviors, see [ 14 ]). In the case of COVID-19, this would suggest more positive attitudes toward a vaccine and greater likelihood to get vaccinated. Indeed, research suggests that individuals should exhibit a greater interest in vaccinations during a pandemic because disease threat is more salient [ 15 ].
Past efforts to improve vaccine attitudes have had limited success or even backfired; for example, messages refuting claims about the link between vaccines and autism, as well as messages featuring images of children who were sick with VPDs, had negative effects on vaccine attitudes among those who were already hesitant to vaccinate [ 16 ]. In contrast, messaging that increases disease threat salience has shown promise in reducing vaccine hesitancy [ 5 ], and there is evidence suggesting that increased threat salience for a particular disease may also increase intentions to vaccinate for other diseases [ 17 ]. Building on these findings, we expected to find an increase in pro-vaccine attitudes and in individuals’ interest in a COVID-19 vaccine when the perceived threat of the COVID-19 virus increased.
Vaccine attitudes are also influenced by a variety of demographic and ideological factors (for a review, see [ 18 ]). For example, perceptions of vaccine risk differ among individuals of different ethnic backgrounds [ 19 ], and there is extant work demonstrating a positive correlation between socioeconomic status (SES) and vaccine hesitancy [ 20 , 21 ]. Socio-demographic factors are also linked to vaccine-related behaviors: among college students, those whose parents have attained a higher level of education are more likely to get immunized [ 22 ], and researchers have identified age as a predictor for receiving the influenza vaccine [ 23 ].
Political ideology is another well-documented determinant of vaccine-related attitudes and behaviors. Despite a common belief that liberals tend toward anti-vaccination attitudes in the United States, there is strong evidence that this trend is more present among conservatives [ 24 , 25 ]. According to a recent Gallup Poll, Republicans are twice as likely to believe the widely debunked myth that vaccines cause autism [ 26 ]. Recent work has shown that exposure to anti-vaccination tweets by President Trump—the first known U.S. president to publicly express anti-vaccination attitudes—has led to increased concern about vaccines among his supporters [ 27 ]. Based on these findings, and in conjunction with the sentiments expressed by the White House that diminished the significance of the pandemic [ 28 ], we expected to find diverging trends between Democrats and Republicans.
The current research
We collected vaccine-related attitudes of individuals living in the U.S. over a six-month period. Beginning in March 2020, we elicited attitudes from a cohort of the same individuals every month. We began data collection before any COVID-19 lockdown measures were in place (i.e., prior to the nation’s first shelter-in-place order [ 29 ]). Hence, our data spans the early phase of the pandemic, when there were fewer than 2,000 total confirmed cases in the U.S., through the following six months, at which point cumulative cases reached over 5.3 million [ 30 ].
Despite our prediction—that a public health crisis would increase disease threat, consequently increasing pro-vaccine attitudes and interest in vaccination—our data show an overall decrease in favorable attitudes toward vaccines. A closer look at the data revealed that political orientation explains more variance than any other socio-demographic variable. Specifically, participants who identify as Republican showed a decrease in their intention to get the COVID-19 vaccine and the influenza vaccine as well as a general decrease in pro-vaccine attitudes, whereas Democrats’ responses to these measures did not show a significant change during this period.
Our work is the first, to our knowledge, to longitudinally measure individuals’ attitudes toward vaccines. In doing so, our findings advance the understanding of how vaccine attitudes might change during an unprecedented public health crisis, revealing a strong association between political party affiliation and vaccine attitudes.
Participants
We recruited a panel of U.S. residents on Amazon’s Mechanical Turk platform to respond to multiple survey waves. To incentivize completion of all waves, we informed participants their payment would increase for subsequent surveys. Participants were paid 30 cents for wave 1, 40 cents for wave 2, and 60 cents for waves 3 and 4, $1.00 for wave 5, and $1.20 for wave 6. In addition, participants were informed that those who completed the first three waves would enter a $100 raffle. The median survey completion time was 5.5 minutes. The sample size for the first wave was 1,018, and the number of participants ranged from 608–762 on subsequent waves (see S1 Table for attrition details). This project was certified as exempt from IRB review by the University of California, San Diego Human Research Protections Program (Project #191273XX).
Our panel represents the broad and diverse population of the United States. The first wave sample included participants from all 50 states (except Wyoming) and Washington D.C., with an age range of 18 to 82 years old (mean = 38.48, median = 35). Approximately half (53%) identified as male, 46% as female, and.6% as other. The racial makeup in our sample was: 80% White, 9% Asian, 6% Black or African American, 4% multiple racial or ethnic identities, and 1% other. Relative to the U.S. Census (2019) [ 31 ] estimates, our sample over-represents White and Asian individuals, and under-represents Black or African American individuals and other racial groups.
We elicited political affiliation using a 6-point Likert scale, ranging from Strongly Republican to Strongly Democratic. In wave 1, 62% identified as Democrats and 38% identified as Republican, which is consistent with results from the most recent General Social Survey (GSS) [ 32 ]. There was no significant change in mean political identity from wave 1 to waves 2–6 (see S2 Table ). We classified participants as Democrats or Republicans using wave 1 political party affiliation. See S2 Appendix for additional details about the correlation of political party affiliation with age, gender, and SES.
Questions and measures
Our primary measure of interest was participants’ stated intention to get the COVID-19 vaccine when it becomes available. We were also interested in their perceptions of COVID-19 threat, general vaccination attitudes, and intention to get the flu shot. For all measures, except flu shot intentions, we combined multiple items to create a composite measure (see S2 Table for specific questions and construct compositions). Questions designed to measure general vaccination attitudes were adapted from prior work [ 33 ].
Additional measures of interest were participants’ trust in broad institutions (media, local government, and federal government). These trust measures followed different trends from each other, and therefore were not combined. At the end of the survey, participants responded to demographic questions. We retained all questions used in wave 1 throughout all six waves (our survey included additional items not reported in this paper; see S2 and S3 Tables for a complete list of measured items).
Data and analysis plan
Only participants with non-missing and non-duplicated responses were included in the analyses (see S1 Appendix for additional details). For all outcomes of interest, we tested for linear trends over time using a fixed effects regression specification [ 34 ]. All regression results include individual-level fixed effects, and standard errors are clustered at the individual level, to adjust for within-person correlation. We used this approach to control for the impact of omitted or unobserved time-invariant variables. P-values are not adjusted for multiple testing (see [ 35 ]). All analyses were conducted using R (version 4.0.2), and regressions were run using the package “fixest” (version 0.6.0). All materials, data, and additional analyses including robustness checks can be found here: https://osf.io/kgvdy/ .
We report results for three different vaccination-related measures: attitudes toward a COVID-19 vaccine, general vaccination attitudes, and flu shot intentions. All measures showed a decreasing trend (Ps < .001, except flu shot intentions where p = .05) for the 6-month duration of the study, indicating a reduction in pro-vaccination attitudes and intention to get vaccinated (COVID-19 and influenza vaccines). See S4 Table for full results of all regressions.
Heterogeneity in trend by political party
To better understand whether the decline in vaccine attitudes over time was driven by a particular factor, we used a data-driven approach, regressing all demographic characteristics on vaccine attitudes, in separate regressions. These demographics included education, income, SES, race, gender, an item measuring whether participants considered themselves to be a minority, whether the participant has children, and political party. Education, income, and SES were median split; race and gender were dummy coded; and political party affiliation was dichotomized into Democrat or Republican. Among all demographic characteristics, separating time trends by political affiliation (by adding an interaction term) attained the greatest adjusted within-R 2 in explaining vaccination attitude measures. In other words, political party affiliation explains the greatest within-individual variation in vaccine attitudes over time.
An analysis of responses by political affiliation revealed that the observed decreasing trend in all three vaccine measures was mostly driven by participants who identified as Republican (all Ps < .05), whereas Democrats’ responses showed either no significant trend (for COVID-19 vaccination and flu shot intentions: Ps >.67) or a significantly less negative time trend (general vaccination: p < .001). For these regressions, and moving forward, all results included interactions between wave and political party as well as interactions for wave and age, and wave and SES, to control for potentially different time trends associated with these variables. In each regression we also tested whether the strength of political affiliation moderates the observed results, and we reported the result when it did. We also conducted ANOVAs to compare mean responses for the outcomes of interest between Democrats and Republicans, separately for each wave (see S5 Table ).
COVID-19 vaccination attitudes ( Fig 1 , Panel A).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Points represent means, and error bars represent 95% confidence intervals. All scale responses range from 1 to 7.
https://doi.org/10.1371/journal.pone.0250123.g001
A two-item construct ( r = .78) was created, with greater values corresponding to more favorable responses.
In wave 1, Democrats ( M = 5.39, SD = 1.55) had more favorable attitudes toward a COVID-19 vaccine than Republicans ( M = 4.57, SD = 1.76; t = -7.38, p < .001, d = -.48, 95% CI = [-.61, -.35]). Among Democrats, there was no significant time trend ( β = .02, SE = .04, p >.67) whereas Republicans’ responses followed a decreasing time trend ( β = -.09, SE = .05, p = .046). These trends were significantly different from each other ( β = -.11, SE = .02, p < .001).
General vaccination attitudes ( Fig 1 , Panel B).
A ten-item construct ( α = .95) was created, with greater values corresponding to a more positive attitude toward vaccination in general.
In wave 1, Democrats ( M = 5.83, SD = 1.15) expressed more favorable general vaccination attitudes than Republicans ( M = 5.17, SD = 1.31; t = -7.91, p < .001, d = -.52, 95% CI = [-.66, -.39]). Although both Democrats and Republicans had a decreasing time trend (Democrats: β = -.04, SE = .02, p = .029; Republicans: β = -.09, SE = .02, p < .001), the trend for Republicans was significantly more negative ( β = -.04, SE = .01, p < .001).
Flu shot intentions ( Fig 1 , Panel C).
We asked participants whether they plan to get the flu shot next year, with greater values indicating greater intentions.
In wave 1, Democrats ( M = 4.84, SD = 2.34) indicated greater intentions to vaccinate against the flu than Republicans ( M = 4.35, SD = 2.39; t = -3.15, p = .002, d = -.21, 95% CI = [-.34, -.08]). Among Democrats, there was no significant time trend ( β = .01, SE = .04, p = .86), suggesting their vaccination intentions remained largely stable. Republicans’ responses, however, revealed a decreasing time trend ( β = -.12, SE = .04, p = .005), and the two trends were significantly different from each other ( β = -.12, SE = .02, p < .001).
Our analyses revealed an interaction with political affiliation strength among Republicans, whereby participants who identified as more strongly Republican had a more negative time trend ( β = -.05, SE = .02, p = .027). This interaction was not significant for Democrats ( β = -.02, SE = .01, p = .19).
Perceived threat of COVID-19 ( Fig 2 ).
https://doi.org/10.1371/journal.pone.0250123.g002
A three-item construct ( α = .82) was created, with greater perceived threat about COVID-19.
In wave 1, Democrats ( M = 4.26, SD = 1.25) expressed greater perceived threat of COVID-19 than Republicans ( M = 3.90, SD = 1.39; t = -4.14, p < .001, d = -.40, 95% CI = [-.27, -.14]). Democrats’ responses showed an increasing time trend ( β = .08, SE = .04, p = .033), indicating they became increasingly concerned about the threat posed by the virus over time. Among Republicans, there was no significant time trend ( β = -.01, SE = .04, p = .83). These trends were significantly different from each other ( β = -.09, SE = .02, p < .001). While our data does not render causal claims, it is possible that the divergence in COVID-19 threat perceptions over time among Republicans and Democrats contributes to the divergence in vaccine attitudes between these groups over time. We revisit this proposition in the General Discussion.
Our analyses revealed an interaction with political affiliation strength among Democrats—participants who identified as more strongly Democrat had a more positive time trend ( β = .03, SE = .01, p = .019), suggesting an increasing threat perception over time. This interaction was not significant for Republicans ( β = .01, SE = .02, p = .61).
Trust in broad institutions.
The measures of trust in media, local government, and federal government were not highly correlated ( α = .66), and were therefore analyzed separately.
Trust in media ( Fig 3 , Panel A) . In wave 1, Democrats ( M = 3.61, SD = 1.66) reported greater trust in the media than Republicans ( M = 2.73, SD = 1.65; t = -8.12, p < .001, d = -.53, 95% CI = [-.66, -.39]). There was no significant time trend for either Democrats ( β = .02, SE = .04, p = .57) or Republicans ( β = -.05, SE = .04, p = .20). However, the trend for Republicans was significantly more negative ( β = -.07, SE = .02, p < .001). The different trends we observe for Democrats and Republicans with respect to trust in the media may explain the divergence in perceived threat and vaccine attitudes between these groups over time (see General discussion ).
https://doi.org/10.1371/journal.pone.0250123.g003
Trust in local government ( Fig 3 , Panel B) . In wave 1, Democrats ( M = 4.07, SD = 1.60) indicated lower trust in local government than Republicans ( M = 4.28, SD = 1.60; t = 2.01, p = .045, d = .13, 95% CI = [.003,.26]). Among Democrats, there was no significant time trend ( β = -.06, SE = .04, p = .18), though among Republicans, there was a decreasing time trend ( β = -.11, SE = .05, p = .015). These trends were significantly different from each other ( β = -.06, SE = .02, p = .004).
Trust in federal government ( Fig 3 , Panel C) . In wave 1, Democrats ( M = 2.96, SD = 1.67) expressed lower trust in the federal government than Republicans ( M = 4.08, SD = 1.60; t = 10.52, p < .001, d = .68, 95% CI = [.55,.82]). Both Democrats and Republicans had decreasing time trends (Democrats: β = -.08, SE = .04, p = .036; Republicans: β = -.10, SE = .04, p = .025). These trends were not significantly different from each other ( β = -.02, SE = .02, p = .37).
To rule out differential attrition, we tested whether the composition of our sample (i.e., age, gender, and political party) changed over time (see S1 Table ). Specifically, we tested whether participants who responded to waves 2–6 were significantly different at baseline (wave 1) from the full sample at baseline. The only significant change detected (Ps < .05) was with respect to participants’ age, though the differences were small—the average age was 38.5 at baseline, and remained between 39.9 and 40.8 at baseline among participants who responded to subsequent waves. We found no other systematic pattern of attrition among our participants.
General discussion
Over the course of six months of the COVID-19 pandemic, beginning with a relatively early phase prior to any U.S. directives to stay home (March 2020) and continuing through a cumulation of over 5 million cases (August 2020), we found a decrease in pro-vaccine attitudes and COVID-19 vaccination intentions, as well as reduced intentions to get the influenza vaccine. These findings are contrary to our prediction that increased salience of COVID-19 would improve attitudes toward vaccines.
Our analyses identify political ideology as the best predictor of the decreasing time trend across our three vaccine-related attitudes and intentions measures. In particular, we found that while Democrats’ responses remained fairly stable over time, Republicans shifted away from their lower initial responses and from Democrats’ responses, leading to increased polarization throughout the six-month period.
Contrary to the polarization observed in our data, social and behavioral scientists have long argued that groups facing threats often come together, demonstrating stronger social cohesion [ 36 ], and more cooperative behaviors [ 37 , 38 ]. Researchers have also found that individuals’ sense of shared identity plays a role in promoting cooperative behavior in response to threat [ 39 – 41 ]. Considering our results in the context of these findings might suggest that our respondents’ sense of shared identity was dominated by their political ideology, as opposed to a broader (e.g. American) identity.
What might be going on?
Although the nature of our data does not render causal claims, it highlights potential explanations. First, we note that participants’ ratings of perceived COVID-19 threat followed a similar diverging pattern by party affiliation to our three vaccine-related measures during the study period. Democrats perceived COVID-19 threat to be greater at the start of the study than Republicans did, and this gap widened significantly as the study progressed. This trend is consistent with previous research showing that vaccine hesitancy is related to perceived risk of a threat; when a VPD threat level is low, individuals are less motivated to take preventative action (i.e., immunize; for a review, see [ 42 ]).
Our data offers one potential explanation for the polarization of threat perception: Republican and Democratic participants in our study reported consuming different sources of information. The most commonly checked news source for Republicans was Fox News (Republicans: 50%, Democrats: 8%; χ 2 = 164.55, p < .001) and for Democrats was CNN (Democrats: 47%, Republicans: 23%, χ 2 = 43.08, p < .001, see S6 Table ). Corroborating this proposition, a Pew Research Center poll conducted in March 2020 found that 56% of respondents whose main news source is Fox News believed that “the news media have greatly exaggerated the risks about the Coronavirus outbreak,” whereas this was only true for 25% of those whose main news source is CNN [ 43 ]. Of note, Facebook and Instagram, were also in the top four most consumed news sources for participants affiliated with either party. Extant work describes these platforms as echo chambers [ 44 , 45 ], which may exacerbate partisan exposure to news and information.
Another trend highlighted by our data shows that similar to vaccine attitudes, Republicans’ trust in the media decreased significantly more during our study than Democrats’, suggesting these patterns might be related. According to Dr. Heidi Larson, an expert on vaccine hesitancy and founder of the Vaccine Confidence Project, misinformation regarding vaccinations is more likely to take root when individuals do not trust the information source [ 46 ]. Future research might further examine the role of trust in the media on vaccine attitudes.
While trust in media or media exposure may be driving COVID-19 threat perceptions and vaccine attitudes, there are many other possible explanatory factors that are not captured by our data or analyses. For example, it is possible that threat perceptions were influenced by how a respondents’ county or state was affected by COVID-19; up until June 2020, COVID-19 cases were more common in Democrat-leaning states [ 47 ], which might have amplified its salience early on and influenced attitudes and behavior. Further, although we included individual-level fixed-effects which control for all time invariant participant characteristics, and controlled for different trends by age and SES, we cannot rule out the possibility that other factors (e.g., educational attainment or population density) may have influenced the observed trends. Finally, as our data collection began after the onset of COVID-19, it is possible that the trend we observe for Republicans represents a return to a pre-pandemic baseline of vaccine-related attitudes.
Contributions
This work advances our understanding of how health-related attitudes evolve over time. Our focus on vaccine-related attitudes and intentions is important because experts agree that having enough people vaccinate against COVID-19 is key to stemming the pandemic [ 48 ]. More broadly, negative attitudes toward vaccination in general, and reduced vaccine uptake, is increasingly a public health concern [ 49 ]. This research provides insight into the trends of such vaccine hesitancy, underlining the importance of risk salience and its roots in ideology and media exposure.
This work also contributes to our understanding of political parties and polarization. Numerous anecdotes and reports have demonstrated a partisan divide in Americans’ response to the COVID-19 pandemic. For example, research found greater negative affective responses to wearing a face covering among politically right (vs. left) leaning individuals [ 50 ]. Here, we show that although these observations are valid, the reality is more nuanced. For example, our analyses reveal that polarization on vaccine measures—both attitudes and intentions—is driven primarily by self-identified Republicans’ gradual movement away from their initial responses whereas Democrats’ responses remained largely stable. This insight has important practical implications: It informs us about the dynamics of individuals’ attitudes, bringing us closer to understanding the underlying factors that influence attitudes and behaviors. Equipped with this knowledge, one could design more effective communications and interventions.
Note on methodology and data availability
The present study contributes to a small but growing literature in the social sciences using longitudinal data [ 51 ]. Using a longitudinal methodology allowed us to track individual-level changes over time. Merely observing a single point in time would allow us to observe across-group differences, but would lack the bigger picture of how polarization between these groups evolved. Another key advantage of panel data is that it allows us to include individual-level fixed effects, which control for the impact of omitted or unobserved time-invariant variables. Finally, panel data allows for more accurate inference of model parameters [ 52 ].
While the focus of this paper is vaccine attitudes, our broad dataset offers a unique opportunity to understand attitudes and behavior over time. Due to the richness of our data, its unique nature, and its timeliness, we believe it is important to make it available to other researchers interested in exploring it and publishing additional findings. The complete dataset is available at https://osf.io/kgvdy/ (see S2 and S3 Tables for all items collected).
Supporting information
S1 appendix. additional information about sample exclusions..
https://doi.org/10.1371/journal.pone.0250123.s001
S2 Appendix. Additional information about political party affiliation.
https://doi.org/10.1371/journal.pone.0250123.s002
S1 Table. Attrition table.
https://doi.org/10.1371/journal.pone.0250123.s003
S2 Table. Summary table of measures and constructs included in the text.
https://doi.org/10.1371/journal.pone.0250123.s004
S3 Table. Summary table of measures excluded from the text.
https://doi.org/10.1371/journal.pone.0250123.s005
S4 Table. Regression results.
https://doi.org/10.1371/journal.pone.0250123.s006
S5 Table. Outcome measures by political party affiliation.
https://doi.org/10.1371/journal.pone.0250123.s007
S6 Table. Summary of news sources.
https://doi.org/10.1371/journal.pone.0250123.s008
- View Article
- Google Scholar
- 2. World Health Organization. The Power of Vaccines: Still not fully utilized. WHO; 2020. https://www.who.int/publications/10-year-review/vaccines/en/ .
- 4. Immunization Safety Review Committee. Immunization safety review: vaccines and autism. National Academies Press; 2004 Sep 30.
- PubMed/NCBI
- 25. Luton R, Hare C. Conservatives are more likely to believe that vaccines cause autism. The Washington Post. 2015 March 1. https://www.washingtonpost.com/news/monkey-cage/wp/2015/03/01/conservatives-are-more-likely-to-believe-that-vaccines-cause-autism/ .
- 26. Reinhart R. Fewer in US continue to see vaccines as important. 2020 Jan 24. https://news.gallup.com/poll/276929/fewer-continue-vaccines-important.aspx .
- 28. Summers, Juana Timeline: How Trump Has Downplayed The Coronavirus Pandemic. NPR. 2020 October 2, 2020. https://www.npr.org/sections/latest-updates-trump-covid-19-results/2020/10/02/919432383/how-trump-has-downplayed-the-coronavirus-pandemic
- 29. Ortiz J, Hauck G. Coronavirus in the US. USA Today. 2020 March 30, 2020. https://www.usatoday.com/story/news/nation/2020/03/30/coronavirus-stay-home-shelter-in-place-orders-by-state/5092413002/ .
- 30. Elflein J. State of Health. World Health Organization. 2020 October 5. https://www.statista.com/statistics/1103185/cumulative-coronavirus-covid19-cases-number-us-by-day/ .
- 31. United States Census Bureau. Quick Facts. 2019. https://www.census.gov/quickfacts/fact/table/US/PST045219 .
- 32. Smith TW, Davern M, Freese J, Morgan S. General Social Surveys, National Science Foundation. 2020. gssdataexplorer.norc.org
- 34. Wooldridge JM. Econometric analysis of cross section and panel data. MIT press; 2010 Oct 1.
- 46. Anderson J. She Hunts Viral Rumors about Real Viruses. The New York Times. 2020 October 13. https://www.nytimes.com/2020/10/13/health/coronavirus-vaccine-hesitancy-larson.html .
- 47. Bump P. Coronavirus has come to Trump country. The Washington Post. 2020 June 17. https://www.washingtonpost.com/politics/2020/06/17/coronavirus-has-come-trump-country/ .
- 48. Quinn M. Fauci warns U.S. "unlikely" to reach Herd Immunity if too Many Refuse Vaccine. CBS News. 2020 June 29. https://www.cbsnews.com/news/fauci-herd-immunity-coronavirus-vaccine/ .
- 49. World Health Organization. Improving vaccination demand and addressing hesitancy. WHO; 2019. [cited 2020 November 3]. https://www.who.int/immunization/programmes_systems/vaccine_hesitancy/en/ .
Effectiveness and Safety of COVID-19 Vaccinations: An Umbrella Meta-Analysis
Affiliations.
- 1 Evidence-Based Medicine Center, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Linhai, Zhejiang, China.
- 2 Institute for Hospital Management, Tsinghua University, Shenzhen, China.
- 3 Department of Health Policy Management, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States.
- 4 Shanghai Bluecross Medical Science Institute, Shanghai, China.
- 5 Department of Hematology, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Linhai, Zhejiang, China.
- PMID: 37485047
- PMCID: PMC10361396
- DOI: 10.3389/ijph.2023.1605526
Objectives: This umbrella meta-analysis aims to provide comprehensive and synthesized evidence regarding the effectiveness and safety of COVID-19 vaccinations based on current studies. Methods: Studies from the Cochrane Library, PubMed, and EMBASE, published before 10 December 2021, were included in the analysis. The pooled results of effectiveness and safety were estimated and shown in forest plots. Results: We included nineteen studies (fifteen studies regarding safety and nine regarding effectiveness) in the analysis. The mRNA vaccines, adenovirus vector vaccines, subunit vaccines, and inactivated vaccines were found to be effective; however, mRNA vaccines, adenovirus vector vaccines and subunit vaccines were associated with local adverse events and systemic events when compared with inactivated vaccines. Conclusion: Our study suggested that till date, COVID-19 vaccination is still a preferred pharmaceutical way to control the widespread pandemic. However, all reported adverse events should be revisited to provide further evidence for mass vaccinations.
Keywords: COVID-19; effectiveness; safety; umbrella meta-analysis; vaccination.
Copyright © 2023 Jiesisibieke, Liu, Yang, Chien and Tung.
Publication types
- Meta-Analysis
- Adenovirus Vaccines*
- COVID-19 Vaccines / adverse effects
- COVID-19* / prevention & control
- RNA, Messenger
- Vaccination / adverse effects
- COVID-19 Vaccines
- Adenovirus Vaccines
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- JME Commentaries
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 47, Issue 2
- Good reasons to vaccinate: mandatory or payment for risk?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1691-6403 Julian Savulescu 1 , 2 , 3
- 1 Faculty of Philosophy , University of Oxford , Oxford , UK
- 2 Murdoch Childrens Research Institute , Parkville , Victoria , Australia
- 3 Melbourne Law School , University of Melbourne , Melbourne , Victoria , Australia
- Correspondence to Professor Julian Savulescu, Faculty of Philosophy, University of Oxford, Oxford, UK; julian.savulescu{at}philosophy.ox.ac.uk
Mandatory vaccination, including for COVID-19, can be ethically justified if the threat to public health is grave, the confidence in safety and effectiveness is high, the expected utility of mandatory vaccination is greater than the alternatives, and the penalties or costs for non-compliance are proportionate. I describe an algorithm for justified mandatory vaccination. Penalties or costs could include withholding of benefits, imposition of fines, provision of community service or loss of freedoms. I argue that under conditions of risk or perceived risk of a novel vaccination, a system of payment for risk in vaccination may be superior. I defend a payment model against various objections, including that it constitutes coercion and undermines solidarity. I argue that payment can be in cash or in kind, and opportunity for altruistic vaccinations can be preserved by offering people who have been vaccinated the opportunity to donate any cash payment back to the health service.
- behaviour modification
- technology/risk assessment
- philosophical ethics
- public health ethics
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/medethics-2020-106821
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
We are in the midst of a global pandemic with COVID-19 and there is a race to develop a vaccine. At the time of writing, there are 53 vaccines in clinical trials on humans (plus five that have bypassed the full trial process) and at least 92 preclinical vaccines under active investigation in animals. There are a number of different approaches: (1) genetic—using mRNA to cause the body to produce viral proteins; (2) viral vector—using genetically modified viruses such as adenovirus to carry sections of coronavirus genetic material; (3) protein—delivering viral proteins (but not genetic material) to provoke an immune response; (4) inactivated or attenuated coronavirus; (5) repurposing existing vaccines, eg, BCG (bacillus Calmette–Guérin). 1
Given the mounting number of deaths globally, and the apparent failure of many countries to contain the pandemic without severely damaging or problematic lockdowns and other measures, there have been calls to make a vaccine, if it were approved, mandatory. 2 Mandatory vaccination has not been ruled out within the UK. 3
The first part of this article asks when, if ever, a vaccine should be mandatory. I will create a set of criteria and a decision algorithm for mandatory vaccination. I will argue that in the case of COVID-19, some of these criteria may not be satisfied. The second part of the article argues that in the case of COVID-19, it may be ethically preferable to incentivise vaccine uptake. I will justify incentivisation and discuss different kinds of incentives.
Ethics of mandatory COVID-19 vaccination
There is a large body of literature on the justification for the use of coercion in public health and infectious disease in particular. Mandatory vaccination is typically justified on Millian grounds: harm to others. According to John Stuart Mill, the sole ground for the use of state coercion (and restriction of liberty) is when one individual risks harming others. 4 The most prominent arguments from bioethicists appeal to preventing harm to others. 5–7 In the case of children, significant risk of harm to the child is also a ground for state protection. Bambery et al 8 give the example of a child taking a box of toxic bleach to school, potentially harming himself and other children. Teachers are entitled to restrain the child and remove the poison both because of risk to the child and to other children. 8 Flanigan uses a similar example of a person shooting a gun into a crowd. 5
The Nuffield Council of Bioethics produced an influential report on public health which considers when coercion and mandatory vaccination might be justified:
When assessing whether more directive policies are acceptable, the following factors should be taken into account: the risks associated with the vaccination and with the disease itself, and the seriousness of the threat of the disease to the population. In the case of incentivised policies, the size of the incentive involved should be appropriate so that it would not unduly compromise the voluntariness of consent. We identified two circumstances in which quasi-mandatory vaccination measures are more likely to be justified. First, for highly contagious and serious diseases, for example with characteristics similar to smallpox. Second, for disease eradication if the disease is serious and if eradication is within reach. 9
I will elaborate on these brief suggestions and provide a novel structured algorithm for when vaccination should be mandatory.
COVID-19 is almost unique because of the gravity of the problem at the global level: not only is there cost in terms of lives from COVID-19, there is also the extraordinary economic, health and well-being consequences of various virus-control measures, including lockdown, which will extend into the future. Probably never before has a vaccine been developed so rapidly and the pressure to use it so great, at least at the global level.
There is a strong case for making any vaccination mandatory (or compulsory) if four conditions are met:
There is a grave threat to public health
The vaccine is safe and effective
Mandatory vaccination has a superior cost/benefit profile compared with other alternatives
The level of coercion is proportionate.
Each of these conditions involves value judgements.
Grave threat to public health
So far, there have been over 1 million deaths attributed to COVID-19 globally (as of 30 September 2020). 10 In the UK alone, it was predicted in influential early modelling that 500 000 would have died if nothing was done to prevent its spread. Even with the subsequent introduction of a range of highly restrictive lockdown measures (measures which could themselves come at a cost of 200 000 non-COVID-19 lives according to a recent UK government report), 11 more than 42 000 (as of 30 September 2020) 12 have died in the UK within 28 days of a positive test.
The case fatality rate was originally estimated to be as high as 11%, but (as is typical with new diseases) this was quickly scaled down to 1.5% or even lower. 13 The infection fatality rate (IFR, which accounts for asymptomatic and undiagnosed cases) is lower still as it has become clear that there are a large number of asymptomatic and mild cases. For example, the Centre for Evidence Based Medicine reports that “In Iceland, where the most testing per capita has occurred, the IFR lies somewhere between 0.03% and 0.28%”. 14
Of course, how you define “grave” is a value judgement. One of the worst-affected countries in the world in terms of COVID-19-attributed deaths per million is Belgium. The mortality is (at the time of writing) around 877 per million population, which is still under 0.1%, and the average age of death is 80. Of course, Belgium and most other countries have taken strict measures to control the virus and so we are not seeing the greatest possible impact the virus could have. Yet others such as Brazil and Sweden have intervened to a much lesser degree, yet (currently) have rates of 687 and 578 deaths per million respectively. Sweden’s April all-cause deaths and death rate at the peak of its pandemic so far, while extremely high, were surpassed by months in 1993 and 2000. 15
The data are complex and difficult to compare with different testing rates, and ways of assigning deaths and collecting data differing from country to country. For example, Belgium counts deaths in care homes where there is a suspicion that COVID-19 was the cause (without the need for a positive test) and, until recently, the UK counted a death which followed any time from a COVID-19 positive test as a COVID-19 death. Moreover, there have been huge behavioural changes even in countries without legally enforced lockdowns. Furthermore, the IFR varies wildly by age-group and other factors. Even among survivors, there is emerging evidence that there may be long-term consequences for those who have been infected but survived. Long COVID-19 health implications may present a grave future public health problem. Nevertheless, some might still argue that this disease has not entered the “grave” range that would warrant mandatory vaccination. The Spanish influenza killed many more (50–100 million), 16 and it afflicted younger rather than older people, meaning even more “life years” were lost. It is not difficult to imagine a Superflu, or bioengineered bug, which killed 10% across all ages. This would certainly be a grave public health emergency where it is likely mandatory vaccination would be employed.
Deciding whether COVID-19 is sufficiently grave requires both more data than we have and also a value judgement over the gravity that would warrant this kind of intervention. But let us grant for the sake of argument that COVID-19 is a grave public health emergency.
Vaccine is safe and effective
There are concerns that testing has been rushed and the vaccine may not be safe or effective. 17
First, although the technology being used in many of these vaccine candidates has been successfully used in other vaccines, no country has ever produced a safe and effective vaccine against a coronavirus. So in one way, we are all in uncharted waters.
Second, any vaccine development will be accelerated in the context of a grave public health emergency.The inherent probabilistic nature of the development of any biologic means that no vaccine could be said to be 100% safe. There will be risks and those risks are likely to be greater than with well-established vaccines.
Thirdly, some side effects may take time to manifest.
This is not to support the anti-vaccination movement. Vaccines are one of the greatest medical accomplishments and a cornerstone of public health. There are robust testing procedures in place in most jurisdictions to ensure that licensed COVID-19 vaccines are both effective and safe. It is only to acknowledge that everything, including vaccination, has risks. Perhaps the biggest challenge in the development of a vaccine for COVID-19 will be to be honest about the extent of those risks and convey the limitations of confidence in safety and efficacy relative to the evidence accrued.
There is an ethical balance to be struck: introducing a vaccine early and saving more lives from COVID-19, but risking side effects or ineffectiveness versus engaging in longer and more rigorous testing, and having more confidence in safety and efficacy, but more people dying of COVID-19 while such testing occurs. There is no magic answer and, given the economic, social and health catastrophe of various anti-COVID-19 measures such as lockdown, there will be considerable pressure to introduce a vaccine earlier.
To be maximally effective, particularly in protecting the most vulnerable in the population, vaccination would need to achieve herd immunity (the exact percentage of the population that would need to be immune for herd immunity to be reached depends on various factors, but current estimates range up to 82% of the population). 18
There are huge logistical issues around finding a vaccine, proving it to be safe, and then producing and administering it to the world’s population. Even if those issues are resolved, the pandemic has come at a time where there is another growing problem in public health: vaccine hesitancy.
US polls “suggest only 3 in 4 people would get vaccinated if a COVID-19 vaccine were available, and only 30% would want to receive the vaccine soon after it becomes available.” 18
Indeed, vaccine refusal appears to be going up. A recent Pew survey suggested 49% of adults in the USA would refuse a COVID-19 vaccine in September 2020. 19
If these results prove accurate then even if a safe and effective vaccine is produced, at best, herd immunity will be significantly delayed by vaccine hesitancy at a cost both to lives and to the resumption of normal life, and at worst, it may never be achieved.
There remain some community concerns about the safety of all pre-existing vaccines, including many that have been rigorously tested and employed for years.
In the case of COVID-19, the hesitancy may be exacerbated by the accelerated testing and approval process which applies not only to Sputnik V (the controversial “Russian vaccine”). Speaking about America’s vaccine programme, Warp Speed, Donald Trump applauded its unprecedented pace:
…my administration cut through every piece of red tape to achieve the fastest-ever, by far, launch of a vaccine trial for this new virus, this very vicious virus. And I want to thank all of the doctors and scientists and researchers involved because they’ve never moved like this, or never even close. 20
The large impact on society means the vaccine will be put to market much more quickly than usual, perhaps employing challenge studies or other innovative designs, or by condensing or running certain non-safety critical parts of the process in parallel (for example, creating candidate vaccines before its approval).
While the speed is welcomed by politicians and some members of the public, the pressure to produce a candidate vaccine, and the speed at which it has been done, may be also perceived (perhaps unfairly) to increase the likelihood of the kind of concerns that lead to vaccine hesitancy: concerns over side-effects that are unexpected or rare, or that take longer to appear than the testing process allows for, or that for another reason may be missed in the testing process.
The job to be done will not only be to prove scientifically that the vaccine is safe and effective, but also to inform and reassure the public, especially the group who are willing to take the vaccine in theory—but only after others have tried it out first.
The question remains of how safe is safe enough to warrant mandatory vaccination. It is vanishingly unlikely that there will be absolutely no risk of harm from any biomedical intervention, and the disease itself has dramatically different risk profiles in different groups of the population. In an ideal world, the vaccine would be proven to be 100% safe. But there will likely be some risk remaining. Any mandatory vaccination programme would therefore need to make a value judgement about what level of safety and what level of certainty are safe and certain enough. Of course, it would need to be very high, but a 0% risk option is very unlikely.
A COVID-19 vaccine may be effective in reducing community spread and/or preventing disease in individuals. Mandatory vaccination is most justifiable when there are benefits to both the individual and in terms of preventing transmission. If the benefits are only to individual adults, it is more difficult to support mandatory vaccination. One justification would be to prevent exhaustion of healthcare services in an emergency (eg, running out of ventilators), which has been used a basis of restriction of liberty (it was the main justification for lockdown). It could also be justified in the case of protection of children and others who cannot decide for themselves, and of other adults who either cannot be vaccinated for medical reasons.
Better than the alternatives
It is a standard principle of decision theory that the expected utility of a proposed option must be compared with the expected utility of relevant alternatives. There are many alternatives to mandatory vaccination. See figure 1 for a summary of the range of strategies for preventing infectious disease.
- Download figure
- Open in new tab
- Download powerpoint
Strategies for prevention of infectious disease.
A popular position, especially among medical professionals, 7 is that we don’t need mandatory vaccination because people are self-interested or altruistic enough to come forward for vaccination. We can reach herd immunity without mandatory vaccination.
If this were true, all well and good, but the surveys mentioned above cast doubt on this claim with regard to the future COVID-19 vaccine. Moreover, reaching herd immunity is not good enough.
First, how fast we reach herd immunity is also important. In a pandemic, time is lives. If it takes a year to reach herd immunity, that could be thousands or tens of thousands of lives in one country.
Second, herd immunity is necessary because some people cannot be vaccinated for medical reasons: they have allergies, immune problems, or other illnesses. The elderly often don’t mount a strong immune response (that is why it is better to vaccinate children for influenza because they are the biggest spreaders of that disease 7 —although COVID-19 appears to be different on the current evidence). And immunity wanes over time—so even people previously vaccinated may become vulnerable.
Even when national herd immunity is achieved, local areas can fall below that level over time, causing outbreaks, as happened with measles recently. This is especially likely to happen where people opposed to vaccines tend to cluster toghether—for example, in the case of certain religious communities. So ideally we need better than herd immunity to ensure that people are protected both over time and in every place.
These are thus reasons to doubt whether a policy of voluntary vaccination will be good enough, though it remains to be seen.
There are other policies that might obviate the need for mandatory vaccination. South Korea has kept deaths down to about 300 (at the time of writing) with a population of 60 000 000 with a vigorous track and trace programme (although it was criticised for exposing extra-marital affairs and other stigmatised behaviours). 21 Other countries have enforced quarantine with tracking devices. There could be selective lockdown of certain groups, 22 or for intermittent periods of time.
The long-term costs and benefits of such policies would have to be evaluated. That is, we should calculate the expected utility of mandatory vaccination (in combination with other policies) and compare it to alternative strategies (or some other combination of these). How utility should be evaluated is an ethical question. Should we count deaths averted (no matter how old), life years lost or lost well-being (perhaps measured by quality adjusted life years)? 23 Should we count loss of liberty or privacy into the other side the equation?
It may be that a one-off mandatory vaccination is a significantly smaller loss of well-being or liberty than these other complex resource intensive strategies.
So we cannot say whether a mandatory policy of COVID-19 vaccination is ethically justified until we can assess the nature of the vaccine, the gravity of the problem and the likely costs/benefit of alternatives. But it is certainly feasible that it could be justified.
It is important to recognise that coercive vaccination can be justified. This is easy to see by comparing it to other coercive interventions in the public interest.
Conscription in war
In the gravest emergencies, where the existence and freedom of the whole population is at stake, people are conscripted to serve their country, often with high risk of death or permanent injury. We often analogise the pandemic to a war: we are fighting the virus. If people can be sent to war against their will, in certain circumstances some levels of coercion are justified in the war on the virus. Notably, in conditions of extreme emergency in past wars (graver than currently exist for COVID-19), imprisonment or compulsion have even been employed. 24
A more mundane example is the payment of taxes. Taxes benefit individuals because tax revenue allows the preservation of public goods. But if sufficient numbers of others are paying their taxes, it is in a person’s self-interest to free ride and avoid taxes. Indeed, paying taxes may result in harm in some circumstances. 24 In the USA, where there is a large private healthcare sector, paying your taxes may mean you cannot pay for lifesaving medical care that you would otherwise have been able to afford. Still, taxes are mandatory based on considerations of fairness and utility.
Seat belts are mandatory in the UK and many other countries, whereas they were previously voluntary. Interestingly, 50% or so of Americans initially opposed making seat belts mandatory, but now 70% believe mandatory laws are justified. 25
Seat belts reduce the chance of death if you are involved in a car accident by 50%. They are very safe and effective. Notably, they do cause injuries (seat belt syndrome) and even, very occasionally, death. But the chances of being benefitted by wearing them vastly outweigh these risks, so they are mandatory, with enforcement through fines . I have previously likened vaccination to wearing a seat belt. 25
Pre-existing mandatory vaccination
Mandatory vaccination policies are already in place in different parts of the world. Mandatory vaccination policies are those that include a non-voluntary element to vaccine consent and impose a penalty or cost for unjustified refusal (justified refusal includes those who have a contraindicating medical condition, or those who already have natural immunity). There are a range of possible penalties or costs which can coerce people. Australia has the “No Jab, No Pay” scheme which withholds child benefits if the child is not vaccinated, and a “No Jab, No Play” scheme which withholds kindergarten childcare benefits. Italy introduced fines for unvaccinated children who attend school. In the USA, state regulations mandate that children cannot attend school if they are not vaccinated, and healthcare workers are required to vaccinate. Some US states (eg, Michigan) make exemptions difficult to obtain by requiring parents to attend immunisation education courses 26 (see also 27 28 ).
Figure 2 summarises the range of coercive policies that can constitute mandatory vaccination.
Cost of mandatory/coercive vaccination.
Coercion is proportionate
In public health ethics, there is a familiar concept of the “least restrictive alternative”. 28 The least restrictive alternative is the option which achieves a given outcome with the least coercion (and least restriction of liberty).
This is a very weak principle: it uses liberty as tie breaker between options with the same expected utility. More commonly, however, we need to weigh utility against liberty. That is, a more restrictive policy will achieve more expected utility—but is it justified?
According to a principle of proportionality, the additional coercion or infringement in liberty is justified if it is proportionate to the gain in expected utility of the more coercive intervention compared with next best option. That is, additional coercion is justified when the restriction of liberty is both minimised and proportionate to the expected advantages offered by the more coercive policy.
As we can see from the previous section and figure 2, there are a variety of coercive measures. (The Nuffield Council has created a related “Intervention Ladder”, 29 though this includes education and incentives, as well as coercive measures.) Penalties can be high. In war, those who conscientiously objected to fighting went to jail or were forced to perform community service (or participate in medical research). In France, parents were given a suspended prison sentence for refusing to vaccinate their child. 30
While there are legitimate concerns that the effectiveness of these policies in different contexts has been inadequately investigated, a number of these policies have been shown to increase vaccination rates. 31
Notably, the fine or punishment for avoiding taxes varies according to the gravity of the offence. The fine for not wearing a seat belt is typically small. A modest penalty for not being vaccinated in a grave public health emergency could be justifiable. For example, a fine or restriction of movement might be justified.
Figure 3 combines these four factors into an algorithm for justified mandatory vaccination.
Algorithm for mandatory vaccination.
These four factors can be justified in several ways. They represent a distillation and development of existing principles in public health ethics, for example, the least restrictive alternative. They can also be justified by the four principles of biomedical ethics.
For example, justice is about the distribution of benefits and burdens across a population in a fair manner. Justice and beneficence, in the context of vaccination policies, both require that the problem addressed is significant and vaccination is an effective means of addressing it. Non-maleficence requires that the risk imposed on individuals be small. Respect for autonomy and justice both require that coercion be applied only if necessary and that it be proportionate to additional utility of mandatory vaccination (and that such coercion be minimised, which is a feature of proportionality).
It is important to recognise that vaccines may have benefits both to the individual and to others (the community). If the vaccine has an overall net expected utility for the individual, beneficence supports its administration.
How great a sacrifice (loss of liberty or risk) can be justified? The most plausible account is provided by a duty of easy rescue: when the cost to an individual is small of some act, but the benefit or harm to another is large, then there is a moral obligation to perform that act. I have elsewhere argued for a collective duty of easy rescue: where the cost of some act to an individual is small, and the benefit of everyone doing that act to the collective is large, there is a collective duty of easy rescue. 32 Such a principle appropriately balances respect for autonomy with justice.
Whether mandatory vaccination for any disease can be justified will depend on precise facts around the magnitude of the problem, the nature of the disease and vaccination, the availability and effectiveness of alternative strategies and the level of coercion. Elsewhere I compare mandatory vaccination for influenza and COVID-19 in more detail. 27
Better than coercion? Payment for risk
Given the risks, or perceived risks, of a novel COVID-19 vaccine, it would be practically and perhaps ethically problematic to introduce a mandatory policy, at least initially (when uncertainty around safety will be greater). Is there a more attractive alternative?
The arguments in favour of vaccination, particularly for those at lower risk (children, young people and those previously infected) can be based on a principle of solidarity. After all, “We are in this together” has been a recurrent slogan supporting pandemic measures in different countries. Those at low risk are asked to do their duty to their fellow citizens, which is a kind of community service. Yet they have little to personally gain from vaccination. The risk/benefit profile looms large for those at lowest risk.
However, another way of looking at this is that those at low risk are being asked to do a job which entails some risk., so they should be paid for the risk they are taking for the sake of providing a public good. And although it may be unlikely to influence so-called 'anti-vaxxers', it may influence a good portion of the 60% of American adults who responded in a March 2020 poll that they would either delay vaccination or didn’t know about vaccination. 33
I have previously argued that we should reconceive live organ donation and participation in risky research, including challenge studies, 34 as jobs where risk should be remunerated, much like we pay construction workers and other dangerous professions both for the job and for the risk involved. 35 36 While the risk profile for approved vaccinations means that it differs from these examples, it could be compared to a job such as social work as a further argument in favour of payment. People may legitimately be incentivised to take on risks, as the Nuffield Council recognises in its Intervention Ladder. 29
The advantage of payment for risk is that people are choosing voluntarily to take it on. As long as we are accurate in conveying the limitations in our confidence about the risks and benefits of a vaccine, then it is up to individuals to judge whether they are worth payment.
Of course, that is a big ask. It would require government to be transparent, explicit and comprehensive in disclosure of data, what should be inferred and the limitations on the data and confidence. This has often not been the case—one only has to remember the denial of the risks of bovine spongiform encephalopathy (BSE) at the height of the crisis by the British government, when in 1990 the Minister for Agriculture, Fisheries and Food, John Gummer proudly fed his 4-year-old daughter, Cordelia, a hamburger in front of the world’s media, declaring British beef safe. (Gummer was awarded a peerage in 2010 and is now Lord Deben.) 37
There is also a danger that payment might signal lack of confidence in safety. That is a real risk and one that I will address in the “payment in kind” section below.
But the basic ethical point (public acceptability aside) is that, if a vaccine is judged to be safe enough to be used without payment, then it is safe enough to be used with payment. 36 Payment itself does not make a vaccine riskier. If a vaccine is considered too risky to be administered to the population, then it should not be administered, no matter whether coercively, through incentives, or through some other policy.
A standard objection to payment for risk (whether it is risky research or live organ donation) is that it is coercive: it forces people to take risks against their better judgement. In Macklin’s words:
The reason for holding that it is ethically inappropriate to pay patients to be research subjects is that it is likely to be coercive, violating the ethical requirement that participation in research should be fully voluntary. 38
As I have previously argued, 39 this demonstrates deep conceptual confusion. Coercion exists when an option which is either desired or good is removed or made very unappealing. The standard example is a robber who demands “Your money or your life”. This removes the most desired and best option: your money and your life. The Australian “No Jab, No Pay”scheme arguably does constitute coercion as it removes an option that one is entitled to, that is, non-vaccination with the “Pay”. So too is the Italian scheme of fines coercive.
However, paying people is not coercive. Adding an option, like payment, without affecting the status quo is not coercive. If a person chooses that option, it is because they believe that overall their life will go better with it, in this case, with the vaccination and the payment. The gamble may not pay off: some risk might eventuate and then it wasn’t worth it. But that is life—and probability.
It is true that the value of the option might exercise force over our rational capacities, but that is no different from offering a lot of money to attract a favoured job applicant.
What can be problematic about offers is exploitation. Exploitation exists where one offers less than a fair deal and a person only accepts it because of vulnerability from background injustice.
There are two ways to prevent exploitation. First, we can correct any background injustice that might cause it. In this case, the person would have little reason to accept the offer. Second, we can pay a fair minimum price for risk, as when we pay construction workers danger money. Paradoxically, this requires paying more, rather than less. 40
But there is an important additional feature of vaccination. If a vaccine were deemed to be safe enough to offer on a voluntary basis without payment, it must be safe enough to incentivise with payment because the risks are reasonable. It may be that those who are poorer may be more inclined to take the money and the risk, but this applies to all risky or unpleasant jobs in a market economy. It is not necessarily exploitation if there are protections in place such as a minimum wage or a fair price is paid to take on risk.
So payment for vaccination which passes independent safety standards (and could reasonably be offered without payment) is not exploitation, if the payment is adequate.
Undue influence?
A related concern is undue influence. Undue influence means that because of the attractiveness of the offer, I can’t autonomously and rationally weigh up the risks and benefits. It is sometimes understood as “were it not for the money, he would not do it”.
But that formulation is too broad—were it not for the money, many people would not go to work. Rather what the concept of ‘undue influence’ intends to capture is that the offer, usually money, bedazzles a person so that he or she makes a mistake in weighing up the risks and benefits. Someone offers Jones a million dollars to take on a risk of 99.99% of dying in a dangerous experiment. He just focuses on the money and takes a deal which is unfair and unreasonable. However, taking such an offer might be rational. If Jones’ daughter is about to die without a million dollars and he values her life more than his own, it might be both autonomous and rational to take the deal.
Because we cannot get into people’s minds, it is difficult in practice to unravel whether undue influence is occurring—how can you differentiate it from a rational decision? In practice, if it would be acceptable to be vaccinated for nothing, it is acceptable to do it for money. Concerns about undue influence are best met by implementing procedures to minimise bias and irrational decision making, such as cooling off periods, information reframing, and so on.
There remains a lurking concern that a decision where payment is involved may not be fully autonomous or authentic. For example, racial and ethnic minorities are among the groups most gravely affected by COVID-19, but given concerns about systemic racism in research and medicine, these communities may have good reason to distrust the medical machine. Is it acceptable to use payment to get over those concerns?
All we can do practically to address concerns about autonomy and authenticity is to redouble efforts: to ensure we do know the risks and they are reasonable (and that the underpinning research is not itself subject to concerns about systemic racism), and try to foster trust with such public education campaigns. This can work alongside a payment scheme. People still need to understand what the facts are. They still need to make as autonomous and authentic a decision as possible.
Practical advantages
A payment model could also be superior to a mandatory model from a practical point of view. There may be considerable resistance to a mandatory model which may make it difficult, expensive and time-consuming to implement, with considerable invasion of liberty. In a payment model, people are doing what they want to do.
A payment model could also be very cheap, compared with the alternatives. The cost of the UK’s furlough scheme is estimated to reach £60 billion by its planned end in October, 41 and the economic shut down is likely to cost many billions more, as well as the estimated 200 000 lives expected to be lost as a result. 11 It would make economic sense to pay people quite a lot to incentivise them to vaccinate sooner rather than later—which, for example, would speed up their full return to work.
It may be that payment is only required to incentivise certain groups. For example, it may be that young people require incentivising because they are at lower risk from the disease itself. On the other hand, justice might require payment for all taking the risk. Although the elderly and those at higher risk have more to gain personally, they are also providing a service by being vaccinated and not using limited health resources. (There is an enormous backlog of patients in the NHS—another grave threat to public health.)
One particularly difficult case is paying parents to vaccinate their children. It is one thing to pay people to take on risk for themselves; it is quite another to pay them to enable their children to take on risks, particularly when the children have little to gain as they are at lowest risk. In part, the answer to this issue is determined by how safe the vaccine is and how confident we can be in that assessment. If it were safe, to a level that even a mandatory programme would be justified, it may be appropriate to instead incentivise parents to volunteer their children for vaccination. If safety is less certain, payment for risk in this group is the most problematic.
It is true that some mandatory vaccination programmes already fine parents for failure to vaccinate their children. However, in those cases vaccination is clearly in the child’s best interest, as the child receives the benefit of immunity to diseases such as measles, that pose a greater risk to that child than we currently believe COVID-19 does. Moreover, they are for vaccines that have been in place for many years and have a well-established safety profile.
A standard objection to paying people to do their duty, particularly civic duty, is that it undermines solidarity, trust, reciprocity and other community values. This is the argument given by Richard Titmuss for a voluntary blood donation scheme. 42
The UK does not pay donors for blood or blood products, but does purchase blood products from other countries, including Austria where donors are paid a “travel allowance” for plasma donation. In Australia, which runs a donor system, more than 50% of the plasma comes from paid donors in the USA. 43 Altruism is insufficient. Germany recently moved to paying for plasma donors. It does not appear to have undermined German society.
In the end, the policy we should adopt towards COVID-19 vaccination will depend on the precise risks and benefits of the vaccine (and our confidence in them), the state of the pandemic, the nature of the alternatives, and particularly the public appetite for a vaccine.
In the right circumstances, mandatory vaccination could be ethically justified, if the penalty is suitably proportionate.
Payment for vaccination, perhaps, has even more to be said for it.
For those attached to the gift of altruism, the vaccinated could be offered the opportunity to donate their fee back to the NHS (or similar health service provider). This combined “payment-donation” model would be a happy marriage of ethics and economics. It would give altruists a double chance to be altruistic: first by vaccinating and second by donating the fee. It would also couple self-interest with morality for free-riders (as they would have greater self-interest to do what is moral), and it would give those who face obstacles to vaccination an additional reason to overcome these.
Payment in kind
Of course, benefits can come in cash or kind. An alternative “payment” model is to pay those who vaccinate in kind. This could take the form of greater freedom to travel, opportunity to work or socialise. With some colleagues, I have given similar arguments in favour of immunity passports. 44
One attractive benefit would be the freedom to not wear a mask in public places if you carried a vaccination certificate, and not to socially distance. Currently, everyone has to wear a mask and practise social distancing. Relaxing this requirement for those who have been vaccinated (or otherwise have immunity) would be an attractive benefit. Moreover, it would help ameliorate the risks the unvaccinated would pose to others.
Payment in kind has one advantage over cash in that it might not send the signal that vaccination is perceived to be unsafe. A cash payment may paradoxically undermine vaccination uptake by introducing unwarranted suspicion (though this is an intuition that may need to be tested). Benefits in kind are less susceptible to this concern because they are directly linked to the benefit provided by the vaccine itself: the vaccinated person is no longer a threat to others.
Some might object that this represents a form of shaming the non-vaccinators (some of whom might be excluded from vaccination for health reasons), just as presenting those who evaded conscription with a white feather was a method of shaming perceived free-riders. But this could be managed through an education campaign about the justification for face covering requirements. There is a good reason to require the non-vaccinated to continue to wear masks and practice social distancing, regardless of whether their refusal is justified—they do represent a greater direct threat to others.
It is quite possible that some mixture of altruism, financial and non-financial benefits will obviate the need to introduce mandatory vaccination. It is better that people voluntarily choose on the basis of reasons to act well, rather than being forced to do so. Structuring the rewards and punishments in a just and fair way is one way of giving people reasons for action.
Mandatory vaccination can be ethically justified (see figure 3), but when risks are more uncertain, payment for vaccination (whether in cash or kind) may be an ethically superior option.
Acknowledgments
This piece builds on a previous piece I published on the JME blog, Good Reasons to Vaccinate: COVID19 Vaccine, Mandatory or Payment Model? [ https://blogs.bmj.com/medical-ethics/2020/07/29/good-reasons-to-vaccinate-covid19-vaccine-mandatory-or-payment-model/ ]. I would like to thank an anonymous reviewer for very many helpful and constructive comments. I would also like to thank Alberto Giubilini for his help.
- Zimmer C , et al
- Bambery B ,
- Douglas T ,
- Selgelid MJ , et al
- Selgelid M ,
- Maslen H , et al
- Nuffield Council on Bioethics
- Worldometer
- ↵ Gov.uk. coronavirus (COVID-19) in the UK . Available: https://coronavirus.data.gov.uk/ [Accessed 30 Sep 2020 ].
- Rajgor DD ,
- Archuleta S , et al
- Johnson S ,
- Greenberger M
- Schaffer DeRoo S ,
- Pudalov NJ ,
- Johnson C ,
- Whitehouse.gov
- Savulescu J ,
- Persson I ,
- Wilkinson D
- Giubilini A
- Giubilini A ,
- Savulescu J
- Sabin Vaccine Institute
- MacDonald NE ,
- Dube E , et al
- LX Morning Consult
- Weijer C , et al
- Anomaly J ,
- Grimwade O ,
- Giubilini A , et al
- Brown RCH ,
- Williams B , et al
Supplementary materials
- Press release
Contributors Sole authorship.
Funding JS is supported by the Uehiro Foundation on Ethics and Education. He received funding from the Wellcome Trust WT104848 and WT203132. Through his involvement with the Murdoch Children’s Research Institute, he has received funding through from the Victorian State Government through the Operational Infrastructure Support (OIS) Program.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement No data are available.
Linked Articles
- Response Persuasion, not coercion or incentivisation, is the best means of promoting COVID-19 vaccination Susan Pennings Xavier Symons Journal of Medical Ethics 2021; 47 709-711 Published Online First: 27 Jan 2021. doi: 10.1136/medethics-2020-107076
Read the full text or download the PDF:
Other content recommended for you.
- Spoonful of honey or a gallon of vinegar? A conditional COVID-19 vaccination policy for front-line healthcare workers Owen M Bradfield et al., Journal of Medical Ethics, 2021
- The unintended consequences of COVID-19 vaccine policy: why mandates, passports and restrictions may cause more harm than good Kevin Bardosh et al., BMJ Global Health, 2022
- Exploring vaccine hesitancy in care home employees in North West England: a qualitative study Amelia Dennis et al., BMJ Open, 2022
- Persuasion, not coercion or incentivisation, is the best means of promoting COVID-19 vaccination Susan Pennings et al., Journal of Medical Ethics, 2021
- COVID-19 vaccine boosters for young adults: a risk benefit assessment and ethical analysis of mandate policies at universities Kevin Bardosh et al., Journal of Medical Ethics, 2022
- Vaccine mandates for healthcare workers beyond COVID-19 Alberto Giubilini et al., Journal of Medical Ethics, 2022
- No Jab, No Job? Ethical Issues in Mandatory COVID-19 Vaccination of Healthcare Personnel Rachel Gur-Arie et al., BMJ Global Health, 2021
- Evaluating potential unintended consequences of COVID-19 vaccine mandates and passports Maxwell J Smith, BMJ Global Health, 2022
- Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review Mei Li et al., Postgraduate Medical Journal, 2021
- Covid-19: Is the UK heading towards mandatory vaccination of healthcare workers? Jacqui Wise, BMJ, 2021
- Research article
- Open access
- Published: 17 August 2020
A systematic review of studies that measure parental vaccine attitudes and beliefs in childhood vaccination
- Amalie Dyda ORCID: orcid.org/0000-0003-2806-4834 1 , 2 ,
- Catherine King 3 , 4 ,
- Aditi Dey 3 , 5 ,
- Julie Leask 6 , 3 &
- Adam G. Dunn 7 , 1
BMC Public Health volume 20 , Article number: 1253 ( 2020 ) Cite this article
17k Accesses
50 Citations
12 Altmetric
Metrics details
Acceptance of vaccines is an important predictor of vaccine uptake. This has public health implications as those who are not vaccinated are at a higher risk of infection from vaccine preventable diseases. We aimed to examine how parental attitudes and beliefs towards childhood vaccination were measured in questionnaires through a systematic review of the literature .
We systematically reviewed the literature to identify primary research studies using tools to measure vaccine attitudes and beliefs, published between January 2012 and May 2018. Studies were included if they involved a quantitative survey of the attitudes and beliefs of parents about vaccinations recommended for children. We undertook a synthesis of the results with a focus on evaluating the tools used to measure hesitancy.
A total of 116 studies met the inclusion criteria, 99 used a cross sectional study design, 5 used a case control study design, 4 used a pre-post study design and 8 used mixed methods study designs. Sample sizes of included studies ranged from 49 to 12,259. The most commonly used tool was the Parent Attitudes about Childhood Vaccines (PACV) Survey ( n = 7). The most common theoretical framework used was the Health Belief Model ( n = 25). Questions eliciting vaccination attitudes and beliefs varied widely.
Conclusions
There was heterogeneity in the types of questionnaires used in studies investigating attitudes and beliefs about vaccination in parents. Methods to measure parental attitudes and beliefs about vaccination could be improved with validated and standardised yet flexible instruments. The use of a standard set of questions should be encouraged in this area of study.
Peer Review reports
Childhood vaccination rates vary widely by country and region, and the reasons for these variations are likely to be context-specific [ 1 , 2 , 3 ]. While access to vaccination is a perennial challenge, acceptance also remains an issue of importance to uptake which is affected by an individual’s feelings, attitudes and beliefs about vaccination [ 4 ]. There is a spectrum of attitudes towards vaccination, including those who are pro-vaccination and accept all vaccines, those who have many concerns but may fully or partially vaccinate, and those who refuse all vaccines [ 5 ]. Those who have questions and concerns have been shown to have lower levels of vaccination uptake [ 6 ] which may have a substantial impact on vaccination coverage and increases the risk of outbreaks [ 7 ]. Not only are unvaccinated individuals at higher risk of infection and adverse health outcomes, but under-vaccinated populations are at higher risk of more severe outbreaks [ 8 , 9 , 10 ].
A range of questionnaires have been developed and tested for measuring vaccination attitudes and beliefs [ 11 ]. The largest recent questionnaires in the area include The Vaccine Confidence Project [ 12 ] which collected 65,819 responses across 67 countries [ 13 ], and the Wellcome Global Monitor 2018 [ 14 ], which collected more than 140,000 responses from 140 countries. Both were based on the same set of questions, which included items about vaccine importance, effectiveness, safety, and religious compatibility.
Studies using questionnaires to understand vaccine attitudes and beliefs often modify existing items to incorporate the local context of a specific country or region. There is high variability with respect to use of behavioural theories to inform constructs and items and the comprehensiveness of validation, such as whether the items predict vaccination uptake. Moreover, high variability in how constructs such as vaccine confidence are measured between different questionnaires makes it difficult to assess how attitudes and beliefs vary globally.
Our aim was to examine how parental attitudes and beliefs towards childhood vaccination were measured in questionnaires through a systematic review of the literature.
Inclusion criteria
Studies were included if they were quantitative primary studies investigating parental vaccine attitudes and/or beliefs, regardless of whether they considered one or a combination of vaccines or vaccine-preventable diseases. For the purpose of this review studies on vaccine hesitancy were included, with vaccine hesitancy defined as “a motivational state of being conflicted about, or opposed to, getting vaccinated” [ 15 ]. Vaccine hesitancy can result in “a delay in acceptance or refusal of vaccines despite availability of vaccination services” [ 16 ]. Studies published after January 2012 were included. Studies were excluded if they investigated vaccination barriers not associated with attitudes or beliefs (e.g. measuring access other than as a factor affecting convenience), adult and adolescent vaccination, or if they were not reported in English. We applied no geographical constraints.
Search strategy
This review was developed in line with the PRISMA guidelines [ 17 ]. Key bibliographic databases were searched to identify relevant articles. The 19 databases searched included: OVID Medline, PsycINFO and Database of Systematic Reviews (see Additional File 1 for the full list of databases searched) Search terms included thesaurus terms (where available) such as ‘Immunization’, ‘Immunization programs’, ‘Vaccines’, ‘Decision Making’, ‘Decision Theory’, ‘Attitude to Health’, ‘Health Behavior’, ‘Risk Assessment’, ‘Trust’, ‘Uncertainty’, ‘Vaccination Refusal’, ‘Anti-Vaccination movement’, ‘Child, Preschool’ and ‘Infant’ These were used with relevant associated text terms. Truncation was utilised to ensure all variant spelling endings of text words were retrieved. The searches were limited to items published from 2012 and ‘Humans’. (see Additional File 1 for the full search strategy). The last search was conducted on 19 May 2018. Articles reviewed for inclusion were limited from January 2012 to May 2018 to avoid duplicating the findings of a 2014 systematic review that reviewed the global literature on vaccine hesitancy [ 5 ].
All titles and abstracts or executive summaries found through the search strategy were screened independently by two authors (Adam Dunn and Amalie Dyda) to determine if they were relevant to the review. The full text of those articles that appeared to meet the inclusion criteria were retrieved and reviewed for relevance independently by the same two authors. The reference lists of all included items were searched to identify any additional items for inclusion.
Data extraction and synthesis
Data were extracted by one author (Amalie Dyda) and confirmed by a second author (Adam Dunn). A standard data extraction form developed by the authors was used. For each study, study design information extracted from the articles included the method of recruitment and the location and type of participants, the number of participants recruited (and completing the study, where appropriate), the vaccine or set of vaccines of relevance to the study, and details of the questions used to measure attitudes and belief about vaccination including any description of behavioural theories used to inform the questionnaire design, and whether the questions were taken directly or adapted from existing instruments. We defined validated questionnaires as those that followed “the process of establishing that a survey item or measure serves the intended purpose. This process can include establishing whether it measures the intended construct using qualitative means (advice from experts, cognitive testing with lay people) and quantitative means (convergent, discriminant, predictive validity)” [ 18 ]. Data extracted from each study were tabulated and grouped by study type and study characteristics including sample size, recruitment method, and location.
The initial search strategy returned 41,570 titles and abstracts, of which 23,201 were removed as duplicates. Title and abstract screening identified 673 full text items for review. Of these, 116 met the inclusion criteria (Fig. 1 ). A review of the reference lists of included articles did not identify any additional items for inclusion.
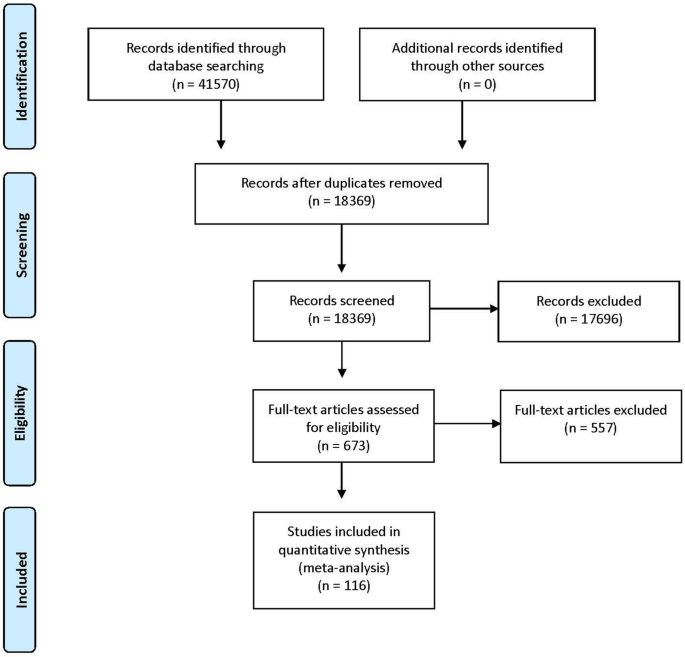
Summary of the search strategy results and set of included studies
Summary of included studies
Of the included studies, 99 (85.3%) used a cross sectional study design (Additional File 2 ). Sample sizes across all 116 included studies ranged from 49 to 12,259 participants, with a median of 455 participants. Parental attitudes and beliefs about childhood vaccines in general were studied in 57 (49.1%) studies, and attitudes and beliefs about influenza vaccination (including pandemic H1N1 influenza) in 35 (30.2%). The other 24 (20.7%) studies asked participants about attitudes and beliefs for other specific vaccines, such as polio and rotavirus vaccines.
Thirty-four countries were represented in the included studies (Fig. 2 ). The most common country in which studies were conducted was the United States ( n = 36), followed by Canada ( n = 9) and the United Kingdom ( n = 8). When aggregated by the number of participants, the United States included the largest number (40,155 participants), followed by Canada (7200 participants), and the United Kingdom (3273 participants).
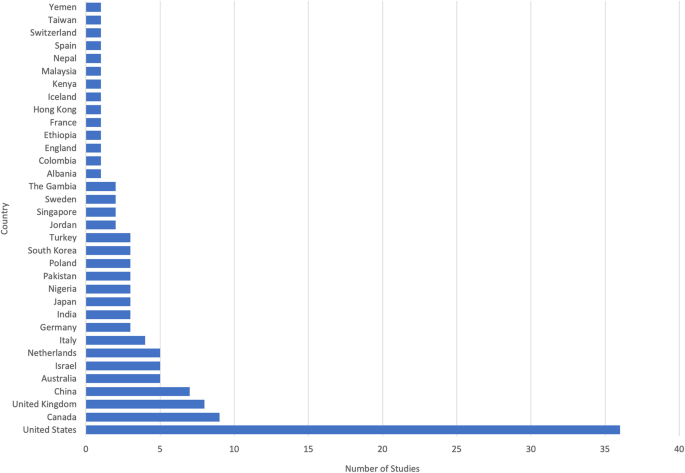
Among the set of 116 included studies, 34 countries were represented
Questionnaires and survey instruments
One hundred and fourteen studies used a survey design, with the two remaining studies using interviews. The questions asked of participants varied substantially across the set of included studies. There was heterogeneity both in terms of the specific questions asked of participants as well as the provenance of those questions in theory or from standardised questionnaire sets. Sixty three studies reported at least one aspect of validation.
The most commonly used standard questionnaire was the Parent Attitudes about Childhood Vaccines (PACV) Survey Tool ( n = 7), used in 4 studies with its full format with 15 questions [ 19 , 20 , 21 , 22 ]. In some studies, the PACV questions were adapted to match the local context or study population, such as in Malaysia [ 21 ] and for expectant parents in the United States [ 19 ]. In 3 studies, a subset of the PACV questions were used [ 23 , 24 , 25 ]. Other questionnaires used included 6 studies based on national immunisation surveys or health department questionnaires [ 26 , 27 , 28 , 29 , 30 , 31 ], 1 study based on the Parental Attitudes toward MMR Vaccine and Trust in Medical Authority questionnaire [ 32 ], and 1 that used the Vaccine Safety, Attitudes, Training and Communication measures [ 33 ].
A total of 62 (53.4%) included studies developed questionnaires using previous literature or previously developed questionnaires, 7 developed questionnaires with experts in the field, 1 used a self-developed scale, and 6 conducted a qualitative data to elicit appropriate questions. The remaining 40 studies did not report having used previous examples as the basis for the designs of their questionnaires.
A variety of theoretical frameworks were used to inform the design of the questionnaires used in the studies. The most common was the Health Belief Model (HBM), which was explicitly stated as having been used to inform the questions in 25 (19.0%) studies [ 30 , 32 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 ], followed by the Theory of Planned Behaviour, which was used in 5 (4.3%) studies [ 58 , 59 , 60 , 61 , 62 , 63 ]. Other studies that were adapted from existing questionnaires may have implicitly been based on these or other theoretical frameworks as a consequence of having adapted from other questionnaires but did not explicitly claim the theoretical framework as a basis for their questions.
Questions about intention to vaccinate
Of the 116 included studies, 38 (32.8%) included questions in which parents were directly asked about their vaccination intentions for one or more antigens. The specific questions that were asked varied across the set of studies. Examples included, “If you had another infant today, would you want him or her to get all the recommended shots?, “I would get a flu vaccine for my child under 5, every year, if it was free?”, and “If your child were offered it at some point in the future, would you vaccinate them against swine flu?”. This variation precluded a synthesis of the results, and the proportion of participants responding in the affirmative varied substantially across the set of studies.
Of the 38 studies which asked about vaccination intentions for one or more antigens, 16 (13.8%) of these specifically asked about whether they would have children vaccinated for all childhood vaccines. The percentages in these studies ranged from 75% in a study involving 200 parents in the United States [ 64 ] to 98% in a study involving 54 parents in Canada [ 35 ]. For the 9 (7.8%) studies that asked about intentions in relation to influenza vaccination, the percentages ranged from 29% in a study involving 236 parents in Canada [ 65 ] to 92% in a before and after study at a clinic involving 5284 and 5755 different groups of parents in rural Kenya [ 66 ].
A substantial number of studies quantitatively examine the childhood vaccination attitudes and beliefs of parents across a broad range of countries. A large number of studies did not report using a validated questionnaire. The countries in which the highest number of studies were conducted were the United States, Canada and the United Kingdom, with most other countries having either none or only a small number of studies. There were significant differences in the way in which questionnaires were developed and the questions asked in each of the studies, making synthesis or comparison of findings a challenge. The use of standardised questionnaires globally would allow findings across countries to be compared and help track longitudinal trends.
The geographical distribution of primary studies included in the review was generally consistent with a previous review on attitudes and beliefs regarding vaccination [ 5 ], in which most included studies were conducted in North America and Europe. Among the subset of studies that used standardised questionnaires, there was no clear difference in rates of vaccine hesitancy between countries, nor any clear pattern in the attitudes and beliefs that exhibited the strongest associations with intention. Given that only a relatively small subset used standardised questionnaires, this result is a reflection of the small number of studies rather than evidence of consistency in what matters most to parents exhibiting vaccine hesitancy.
There was little consistency in the provenance of the questions used to measure attitudes and beliefs across studies. A number of studies did not report how the questionnaire or survey instrument was developed, making comparison of these studies difficult. The majority of studies reported construct and item development methods such as basing the questionnaire on previous literature, expert opinion or the use of previously developed surveys.
The use of qualitative evidence is best practice for forming constructs [ 67 ] and the use of a previously validated questionnaire is the most appropriate methodology as this ensures that items have content, construct and predictive validity. Previously developed questionnaires which are not validated may not accurately capture information, which is then repeated if these questionnaires are reused [ 18 ]. However, as there is no agreed upon gold standard survey instrument, a wide range of sources were used for development, resulting in heterogeneity of questionnaires. The most commonly used standard questionnaire was the PACV Survey Tool, which has been validated in two different settings and been shown to identify vaccine hesitant parents. The questionnaire focuses on the domains of ‘Safety and efficacy’, ‘General attitudes’ and ‘Behaviour’ [ 68 , 69 ]. The use of this questionnaire for studies investigating vaccine hesitancy should be encouraged to better allow for comparison across studies.
For theoretical frameworks, we found that the HBM was most commonly used to support the development of questionnaires, which was consistent with previous reviews [ 5 ]. The HBM posits that perceptions of susceptibility, severity, benefit and barriers, cues to action and self-efficacy predict behaviour. This and other models place emphasis on risk appraisals as important predictors of vaccination. Use of the HBM is complicated by the fact that all related perceptions could apply to vaccination uptake as much as disease outcomes. Since these models look at individual psychological factors by design, they are weaker at measuring other factors like false contraindications, social influence, or access to services or vaccines, which are more likely to be effective in increasing uptake, if they are addressed [ 15 ]. Further, many models fail to measure trust, yet trust in vaccination arises as a relevant phenomenon in both qualitative accounts of under-vaccination and the influence of vaccine safety scares [ 15 ]. Trust is often “ill-defined and a loosely measured concept” [ 70 ]. Recent work on the moral foundations of behaviour suggests that measuring constructs such as contamination and liberty are also relevant [ 71 , 72 ]. Further work is needed to incorporate moral foundations, other feelings and attitudes and beliefs and trust into a single model of vaccination behaviour and test its robustness.
Future studies in this area may benefit from considering standardised questions on vaccine attitudes and beliefs and other barriers or facilitators [ 11 ]. Large international surveys based on a standardised set of questions may be useful for providing international comparisons with context-specific additional questions. To consider the local context, qualitative investigations could supplement the broad based quantitative knowledge from surveys. Both forms of data collection are useful but are also resource intensive and relatively slow to report.
Current outbreaks of measles in the US highlight the importance of monitoring and measuring attitudes and beliefs about vaccinations. From 1st January to 18th July 2019 there were a total of 1148 cases of measles identified in the US which is the largest number of infections reported since 1992. Outbreaks are occurring across a number of states, with an outbreak in Rockland County, reporting the majority (78.4%) of cases have not been vaccinated [ 73 ].
The development of the internet has increased the speed with which information and misinformation can spread in the community. This may outpace our ability to measure and report on attitudes and beliefs using current survey methods which are time and resource intensive. Due to the time lag involved, using these methods may limit the ability to support the rapid design of evidence-informed and localised interventions for debunking or mitigating the impact of misinformation.
There were several limitations to the review approach and conduct. The first limitation was that the geographical distribution of the studies included in the review may be biased by the exclusion of studies not written in English. In addition, parental beliefs and attitudes towards influenza vaccination often differ from routine childhood vaccinations [ 74 ]. This childhood vaccine was included as some countries recommend annual influenza vaccination, but this is unlikely to affect the findings regarding tools used to monitor attitudes and beliefs about vaccination.
Despite the number of studies investigating parental attitudes and beliefs about childhood vaccination which were conducted in at least 36 countries, there was heterogeneity in survey designs. Methods to measure parental attitudes and beliefs about vaccination could be improved with validated and standardised yet flexible instruments, supplemented with qualitative investigations. The use of a standard set of validated questions should be encouraged in this area of study to identify, track, and monitor longitudinal trends using quality data.
Availability of data and materials
Not applicable.
Abbreviations
Health belief model
Parent attitudes about childhood vaccines
Hill HA, Elam-Evans LD, Yankey D, Singleton JA, Kang Y. Vaccination coverage among children aged 19-35 months - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(40):1123–8.
Article PubMed PubMed Central Google Scholar
International Institute for Population Sciences (IIPS) and ICF. National family health survey (nfhs-4), 2015–16: India. Mumbai: IIPS; 2017.
Google Scholar
National Centre for Immunisation Research and Surveillance. Coverage data and reports 2019 [Available from: http://www.ncirs.org.au/health-professionals/coverage-data-and-reports .
Larson HJ. The biggest pandemic risk? Viral misinformation. Nature. 2018;562:309.
Article CAS PubMed Google Scholar
Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32(19):2150–9.
Article PubMed Google Scholar
Damnjanović K, Graeber J, Ilić S, Lam WY, Lep Ž, Morales S, et al. Parental decision-making on childhood vaccination. Front Psychol. 2018;9:735.
Smith LE, Amlot R, Weinman J, Yiend J, Rubin GJ. A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017;35(45):6059–69.
Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association between vaccine refusal and vaccine-preventable diseases in the United States: a review of measles and pertussis. JAMA. 2016;315(11):1149–58.
Article CAS PubMed PubMed Central Google Scholar
Omer SB, Enger KS, Moulton LH, Halsey NA, Stokley S, Salmon DA. Geographic clustering of nonmedical exemptions to school immunization requirements and associations with geographic clustering of pertussis. Am J Epidemiol. 2008;168(12):1389–96.
Salathe M, Bonhoeffer S. The effect of opinion clustering on disease outbreaks. J R Soc Interface. 2008;5(29):1505–8.
Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R. Beyond confidence: Development of a measure assessing the 5c psychological antecedents of vaccination. Plos One. 2018;13(12):e0208601-e.
Larson HJ. The state of vaccine confidence. Lancet. 2018;392(10161):2244–6.
Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, et al. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301.
Gallup (2019) wellcome global monitor– first wave findings. 2019.
Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18(3):149–207.
World Health Organization. Report of the SAGE working group on vaccine hesitancy. Geneva: World Health Organization; 2014.
Prisma- preferred reporting items for systematic reviews and meta-analyses 2013 [Available from: http://www.prisma-statement.org/ .
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. 2018;6:149.
Cunningham RM, Minard CG, Guffey D, Swaim LS, Opel DJ, Boom JA. Prevalence of vaccine hesitancy among expectant mothers in Houston, Texas. Acad Pediatr. 2018;18(2):154–60.
Henrikson NB, Anderson ML, Opel DJ, Dunn J, Marcuse EK, Grossman DC. Longitudinal trends in vaccine hesitancy in a cohort of mothers surveyed in washington state, 2013–2015. Public Health Rep. 2017;132(4):451–4 Available from: http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/885/CN-01400885/frame.html .
Mohd Azizi FS, Kew Y, Moy FM. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35(22):2955–61.
Orr C, Beck AF. Measuring vaccine hesitancy in a minority community. Clin Pediatr. 2017;56(8):784–8.
Article Google Scholar
Oladejo O, Allen K, Amin A, Frew PM, Bednarczyk RA, Omer SB. Comparative analysis of the parent attitudes about childhood vaccines (pacv) short scale and the five categories of vaccine acceptance identified by gust et al. Vaccine. 2016;34(41):4964–8.
Schoeppe J, Cheadle A, Melton M, Faubion T, Miller C, Matthys J, et al. The immunity community: a community engagement strategy for reducing vaccine hesitancy. Health Promot Pract. 2017;18(5):654–61.
Cataldi JR, Dempsey AF, O'Leary ST. Measles, the media, and mmr: impact of the 2014-15 measles outbreak. Vaccine. 2016;34(50):6375–80.
LaVail KH, Kennedy AM. The role of attitudes about vaccine safety, efficacy, and value in explaining parents' reported vaccination behavior. Health Educ Behav. 2013;40(5):544–51.
Luthy KE, Beckstrand RL, Meyers CJH. Common perceptions of parents requesting personal exemption from vaccination. J Sch Nurs. 2013;29(2):95–103.
Schönberger K, Ludwig MS, Wildner M, Kalies H. Timely mmr vaccination in infancy: influence of attitudes and medical advice on the willingness to vaccinate. Klin Padiatr. 2012;224(7):437–42.
Shrestha S, Shrestha M, Wagle RR, Bhandari G. Predictors of incompletion of immunization among children residing in the slums of Kathmandu valley, Nepal: a case-control study. BMC Public Health. 2016;16:970.
Smith PJ, Marcuse EK, Seward JF, Zhao Z, Orenstein WA. Children and adolescents unvaccinated against measles: geographic clustering, parents' beliefs, and missed opportunities. Public Health Rep. 2015;130(5):485–504.
Walsh S, Thomas DR, Mason BW, Evans MR. The impact of the media on the decision of parents in south wales to accept measles-mumps-rubella (mmr) immunization. Epidemiol Infect. 2015;143(3):550–60.
Leonard W. Parental Confidence in U.S. Government and Medical Authorities, Measles (Rubeloa) Knowledge, and MMR Vaccine Compliance (2015). Walden Dissertations and Doctoral Studies; 1718.
Umeh GC, Nomhwange TI, Shamang AF, Zakari F, Musa AI, Dogo PM, et al. Attitude and subjective wellbeing of non-compliant mothers to childhood oral polio vaccine supplemental immunization in northern Nigeria. BMC Public Health. 2018;18(1):231.
Armitage ET, Camara J, Bah S, Forster AS, Clarke E, Kampmann B, et al. Acceptability of intranasal live attenuated influenza vaccine; influenza knowledge and vaccine intent in the Gambia. Vaccine. 2018;36(13):1772–80.
Atkinson KM, Ducharme R, Westeinde J, Wilson SE, Deeks SL, Pascali D, et al. Vaccination attitudes and mobile readiness: a survey of expectant and new mothers. Hum Vaccin Immunotherapeutics. 2015;11(4):1039–45.
Ben Natan M, Kabha S, Yehia M, Hamza O. Factors that influence israeli muslim Arab parents' intention to vaccinate their children against influenza. J Pediatr Nurs-Nurs Care Children Fam. 2016;31(3):293–8.
Chen CH, Chiu PJ, Chih YC, Yeh GL. Determinants of influenza vaccination among young taiwanese children. Vaccine. 2015;33(16):1993–8.
Cheung S, Wang HL, Mascola L, El Amin AN, Pannaraj PS. Parental perceptions and predictors of consent for school-located influenza vaccination in urban elementary school children in the United States. Influenza Other Respir Viruses. 2015;9(5):255–62.
Chun Chau JP, Lo SHS, Chow Choi K, Kin Chau MH, Tong DWK, Kwong T, et al. Factors determining the uptake of influenza vaccination among children with chronic conditions. Pediatr Infect Dis J. 2017;36(7):e197-e202.
He L, Liao QY, Huang YQ, Feng S, Zhuang XM. Parents' perception and their decision on their children's vaccination against seasonal influenza in Guangzhou. Chin Med J. 2015;128(3):327–41.
Hwang JH, Lim CH, Kim DH, Eun BW, Jo DS, Song YH, et al. A survey of parental perception and pattern of action in response to influenza-like illness in their children: including healthcare use and vaccination in Korea. J Korean Med Sci. 2017;32(2):204–11.
Janks M, Cooke S, Odedra A, Kang H, Bellman M, Jordan RE. Factors affecting acceptance and intention to receive pandemic influenza a h1n1 vaccine among primary school children: A cross-sectional study in Birmingham, UK. Influenza Res Treat. 2012;2012:182565.
Kempe A, Daley MF, Pyrzanowski J, Vogt TM, Campagna EJ, Dickinson LM, et al. School-located influenza vaccination with third-party billing: what do parents think? Acad Pediatr. 2014;14(3):241–8.
Lau JT, Mo PK, Cai YS, Tsui HY, Choi KC. Coverage and parental perceptions of influenza vaccination among parents of children aged 6 to 23 months in hong kong. BMC Public Health. 2013;13:1026.
Malosh R, Ohmit SE, Petrie JG, Thompson MG, Aiello AE, Monto AS. Factors associated with influenza vaccine receipt in community dwelling adults and their children. Vaccine. 2014;32(16):1841–7.
Mergler MJ, Omer SB, Pan WKY, Navar-Boggan AM, Orenstein W, Marcuse EK, et al. Association of vaccine-related attitudes and beliefs between parents and health care providers. Vaccine. 2013;31(41):4591–5.
Morin A, Lemaître T, Farrands A, Carrier N, Gagneur A. Maternal knowledge, attitudes and beliefs regarding gastroenteritis and rotavirus vaccine before implementing vaccination program: which key messages in light of a new immunization program? Vaccine. 2012;30(41):5921–7.
O'Leary ST, Barnard J, Lockhart S, Kolasa M, Shmueli D, Dickinson LM, et al. Urban and rural differences in parental attitudes about influenza vaccination and vaccine delivery models. J Rural Health. 2015;31(4):421–30.
Paek HJ, Shin KA, Park K. Determinants of caregivers' vaccination intention with respect to child age group: A cross-sectional survey in south korea. BMJ Open. 2015;5:e008342.
Saitoh A, Sato I, Shinozaki T, Kamiya H, Nagata S. Improved parental attitudes and beliefs through stepwise perinatal vaccination education. Hum Vaccin Immunother. 2017;13(11):2639–45.
Tsuchiya Y, Shida N, Machida K. Flu vaccination acceptance among children and awareness of mothers in japan. In: Spier R, editor. 7th Vaccine & ISV Annual Global Congress, vol. 8: Procedia in Vaccinology. 2014. p. 12–7.
Wagner AL, Boulton ML, Sun X, Mukherjee B, Huang Z, Harmsen IA, et al. Perceptions of measles, pneumonia, and meningitis vaccines among caregivers in shanghai, China, and the health belief model: a cross-sectional study. BMC Pediatr. 2017;17.
Wu CST, Kwong EWY, Wong HT, Lo SH, Wong ASW. Beliefs and knowledge about vaccination against ah1n1pdm09 infection and uptake factors among chinese parents. Int J Environ Res Public Health. 2014;11(2):1989–2002.
Tsuchiya Y, Shida N, Izumi S, Ogasawara M, Kakinuma W, Tsujiuchi T, et al. Factors associated with mothers not vaccinating their children against mumps in Japan. Public Health. 2016;137:95–105.
Schollin Ask L, Hjern A, Lindstrand A, Olen O, Sjögren E, Blennow M, et al. Receiving early information and trusting swedish child health Centre nurses increased parents’ willingness to vaccinate against rotavirus infections. Acta Paediatr. 2017;106(8):1309–16.
Scheuerman O, Zilber E, Davidovits M, Chodick G, Levy I. Nephrologists need to play a key role in improving annual influenza vaccination rates in children with kidney disease. Acta Paediatr. 2017;106(5):812–8.
Peleg N, Zevit N, Shamir R, Chodick G, Levy I. Seasonal influenza vaccination rates and reasons for non-vaccination in children with gastrointestinal disorders. Vaccine. 2015;33(1):182–6.
Dubé E, Bettinger JA, Halperin B, Bradet R, Lavoie F, Sauvageau C, et al. Determinants of parents' decision to vaccinate their children against rotavirus: results of a longitudinal study. Health Educ Res. 2012;27(6):1069–80.
Dube E, Gagnon D, Ouakki M, Bettinger JA, Witteman HO, MacDonald S, et al. Measuring vaccine acceptance among Canadian parents: a survey of the Canadian immunization research network. Vaccine. 2018;36(4):545–52.
Fadel CW, Colson ER, Corwin MJ, Rybin D, Heeren TC, Wang CL, et al. Maternal attitudes and other factors associated with infant vaccination status in the united states, 2011–2014. J Pediatr. 2017;185:136.
Harmsen IA, Lambooij MS, Ruiter RAC, Mollema L, Veldwijk J, van Weert Y, et al. Psychosocial determinants of parents' intention to vaccinate their newborn child against hepatitis b. Vaccine. 2012;30(32):4771–7.
MacDougall DM, Halperin BA, Langley JM, MacKinnon-Cameron D, Li L, Halperin SA, et al. Knowledge, attitudes, beliefs, and behaviors of parents and healthcare providers before and after implementation of a universal rotavirus vaccination program. Vaccine. 2016;34(5):687–95.
Thorpe EL, Zimmerman RK, Steinhart JD, Lewis KN, Michaels MG. Homeschooling parents' practices and beliefs about childhood immunizations. Vaccine. 2012;30(6):1149–53.
Weiner JL, Fisher AM, Nowak GJ, Basket MM, Gellin BG. Childhood immunizations first-time expectant mothers' knowledge, beliefs, intentions, and behaviors. Vaccine. 2015;33:D92–D8.
Dubé E, Gagnon D, Huot C, Paré R, Jacques S, Kossowski A, et al. Influenza immunization of chronically ill children in pediatric tertiary care hospitals. Hum Vaccin Immunotherapeutics. 2014;10(10):2935–41.
Oria PA, Arunga G, Lebo E, Wong JM, Emukule G, Muthoka P, et al. Assessing parents' knowledge and attitudes towards seasonal influenza vaccination of children before and after a seasonal influenza vaccination effectiveness study in low-income urban and rural Kenya, 2010-2011. BMC Public Health. 2013;13.
Opel DJ, Mangione-Smith R, Taylor JA, Korfiatis C, Wiese C, Catz S, et al. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum Vaccin. 2011;7(4):419–25.
Opel DJ, Taylor JA, Mangione-Smith R, Solomon C, Zhao C, Catz S, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29(38):6598–605.
Abd Halim H, Abdul-Razak S, Md Yasin M, Isa MR. Validation study of the parent attitudes about childhood vaccines (PACV) questionnaire: the Malay version. Hum Vaccin Immunother. 2020;16(5):1040–9.
Larson HJ, Clarke RM, Jarrett C, Eckersberger E, Levine Z, Schulz WS, et al. Measuring trust in vaccination: a systematic review. Hum Vaccin Immunotherapeutics. 2018;14(7):1599–609.
Amin AB, Bednarczyk RA, Ray CE, Melchiori KJ, Graham J, Huntsinger JR, et al. Association of moral values with vaccine hesitancy. Nat Hum Behav. 2017;1(12):873–80.
Luz PM, Brown HE, Struchiner CJ. Disgust as an emotional driver of vaccine attitudes and uptake? A mediation analysis. Epidemiol Infect. 2019;147:e182-e.
Centers for Disease Control and Prevention. Measles cases and outbreaks. 2019.
C.S. Mott Children’s Hospital. Inferiority complex? Parents rate flu lower than other vaccines. Mott Poll Rep. 2016;26(1).
Download references
Acknowledgements
This project was funded by the Australian National Health and Medical Research Council (NHMRC) Project Grant APP1128968. The funding body played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and affiliations.
Centre for Health Informatics, Australian Institute of Health Innovation, Macquarie University, Sydney, NSW, Australia
Amalie Dyda & Adam G. Dunn
Department of Health Systems and Populations, Faculty of Medicine, Health and Human Sciences, Macquarie University, Sydney, NSW, Australia
Amalie Dyda
National Centre for Immunisation Research & Surveillance, Sydney, NSW, Australia
Catherine King, Aditi Dey & Julie Leask
The University of Sydney, Children’s Hospital at Westmead Clinical School, Faculty of Medicine and Health, Sydney, NSW, Australia
Catherine King
The University of Sydney, School of Medicine, Faculty of Medicine and Health, Sydney, NSW, Australia
The University of Sydney, Susan Wakil School of Nursing and Midwifery, Sydney, NSW, Australia
Julie Leask
The University of Sydney, Discipline of Biomedical Informatics and Digital Health, School of Medical Sciences, Faculty of Medicine and Health, Sydney, NSW, Australia
Adam G. Dunn
You can also search for this author in PubMed Google Scholar

Contributions
A.Dyda led the design and coordination of the review. CK designed and conducted the literature searches and was a contributor in writing the manuscript. A. Dey assisted in the design of the review and provided critical intellectual content throughout. JL was a major contributor to the design of the review and provided critical intellectual content throughout. A. Dunn was also was a major contributor to the design of the review, and assisted with removing duplicates and screening of titles, abstracts and full review of papers for inclusion. All authors contributed to the revision of the manuscript and provided intellectual content. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Amalie Dyda .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Search strategy. Detailed description of search strategy used for review.
Additional file 2: Table 1.
Summary of included studies. Summary table of each included study with details about study characteristics.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dyda, A., King, C., Dey, A. et al. A systematic review of studies that measure parental vaccine attitudes and beliefs in childhood vaccination. BMC Public Health 20 , 1253 (2020). https://doi.org/10.1186/s12889-020-09327-8
Download citation
Received : 16 June 2020
Accepted : 02 August 2020
Published : 17 August 2020
DOI : https://doi.org/10.1186/s12889-020-09327-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Immunization/immunisation
- Vaccination
- Vaccines, questionnaire
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
MANDATORY VACCINATION: WHY WE STILL GOT TO GET FOLKS TO TAKE THEIR SHOTS
Ben Balding
Class of 2006
April 27, 2006
This paper is submitted in satisfaction of the Food and Drug Law course paper and the Harvard Law School 3L Written Work Requirement
Vaccination is widely considered one of the greatest medical achievements of modern civilization. Childhood diseases that were commonplace less than a generation ago are now increasingly rare because of vaccines. In order to be effective at eliminating communicable diseases, vaccines must be administered to sufficient levels of persons in the community. Because of this, public health officials have mandated vaccination for certain diseases as a condition to school attendance. The overwhelming effectiveness of vaccination programs may lead individuals to ignore the benefits of vaccination and focus more on the risk of side effects. Moreover, some have criticized the coercive nature of these programs. These objections may lead to an unacceptably high number of exemptions, which can compromise vaccination programs and leave the population susceptible to outbreaks.
This paper explores vaccination programs with an eye toward greater public safety without ignoring the reality of a small but committed group of vaccine critics. The paper begins with a discussion of the historical development of mandatory vaccination policies and the issues posed by exemptions. It then addresses some of these issues in the context of vaccine safety. It also seeks solution by framing the discussion in economic terms. It concludes by recommending stricter enforcement of mandatory requirements for most vaccines and greater dissemination of information on the continued importance of vaccination.
TABLE OF CONTENTS
Introduction.
Vaccination is widely considered one of the greatest medical achievements of modern civilization. Childhood diseases that were commonplace less than a generation ago are now increasingly rare because of vaccines. The smallpox vaccine has eradicated a disease that was responsible for centuries of outbreaks and had a 30% fatality rate. [1] Physical handicaps resulting from polio can still be observed on some of those who were children before Jonas Salk developed a vaccine in 1955. Formerly common childhood diseases are now rarely observed. Even ear infections may soon be prevented by vaccination. [2] The widespread success of vaccinations has led one medical report to comment that “[n]ext to clean water, no single intervention has had so profound an effect on reducing mortality from childhood diseases as has the widespread introduction of vaccines.” [3]
The story of modern vaccination begins with Edward Jenner’s development of the vaccine for smallpox, one of the most feared diseases in recent history. At first, vaccination was optional and not everyone chose to vaccinate. [4] In time, states would allow municipalities to mandate vaccination in time of outbreak in order to protect the public from epidemics. [5] A further step was taken when states imposed smallpox vaccination as a prerequisite for attending public schools. [6] These requirements were amended in time as new vaccines were developed. [7] At some point actual outbreaks and epidemics ceased to be the trigger for mandatory vaccination, and prevention became the overriding justification. [8] Most states today require vaccination for a multitude of childhood diseases, including measles, diphtheria, pertussis, polio, and now even chickenpox. [9]
Because of the success and the mandatory nature of vaccination, most people would probably not consider vaccination an optional method of medical treatment. For most parents, the “decision” to vaccinate is equivalent to the “decision” to feed one’s child. [10] Typically, a doctor informs parents of the school vaccination schedule and the parents consent to having their child vaccinated. Since the vaccination schedule usually corresponds to the scheduled doctor visits for infants, full compliance with mandatory vaccination schedules is typically not a problem and can usually be substantially accomplished by age two. [11]
For some parents, however, vaccination is no routine matter. [12] From the time of Jenner’s smallpox vaccine, vaccination has had its critics. [13] In the two centuries since that time, many different types of objections have been raised. Some have questioned the scientific qualifications of mass immunization. [14] Others have focused on the personal liberty interests at stake and have objected to the paternalistic nature of government imposition of what is viewed as a personal medical choice. [15] Still others have opposed vaccination for personal or religious reasons. [16]
Today, some parents raise similar objections. The idea that a potentially harmful substance is being placed directly into the bloodstream raises a red flag for some. Additionally, the decline of many diseases for which vaccination is still mandated may make some parents skeptical of the continued wisdom of subjecting a child to a vaccine, even if the vaccine is considered extremely safe. This skepticism grows when some point to the correlation between vaccinations and conditions such as SIDS and autism. Whether or not such a correlation is scientifically significant, many parents simply wonder if it is wise to vaccinate against a disease unlikely to afflict their child if any chance exists that the vaccine will cause autism, SIDS, or any other side effect. [17]
Since the efficacy of a particular vaccine corresponds directly with the percentage of a given population that has been vaccinated, proponents of mandatory vaccination have sought to convince those with reservations about vaccines that vaccination is the right choice. The Center for Disease Control has attempted to allay possible reservations parents may have with vaccinations by rebutting some of the commonly held fears about vaccines. [18] The CDC has pointed out, for example, that most adverse effects from vaccines are “minor and temporary, such as a sore arm or mild fever.” [19] Because vaccination often involves the introduction of a harmful live (although seriously weakened) organism into the patient, vaccination can never be 100% safe. Serious side effects usually occur only between one per thousands to one per millions of doses, while some serious reactions and death occur so rarely that accurate risk assessment is difficult. [20] The CDC has also responded to many of the other concerns raised about the need for vaccination, and the FDA continually works to ensure vaccine safety and efficacy, but many still harbor reservations toward vaccination.
This paper will endeavor to discuss some of the most common objections to vaccination programs in general while trying to shed light on the veracity and tenability of these objections. Part I will discuss the nature of mandatory vaccination programs in this country; both scientific and historical issues will play a key part in this discussion. Part II will describe the role of the FDA and other governmental bodies in the overall vaccination picture. Part III will attempt to utilize multiple analytical tools in search of possible solutions to the dangers posed by those who may attempt to opt out of vaccination programs. It will first examine vaccination through the lens of an old television show episode. It will then adopt an economic analytical framework to discuss the balance between individual and general welfare in the context of vaccination. Part IV will conclude with some observations on how the goal of greater public health might be achieved without completely neglecting the concerns of many in the community regarding the prudence of using a medical technique that by definition relies on a degree of coercion.
I. MANDATORY VACCINATION
Historical background.
Jenner’s smallpox vaccine led to the research and development of vaccines for other widespread and epidemic diseases. The twentieth century saw the development of vaccines for such diseases as polio, diphtheria, tetanus, pertussis, measles, and others. [21] As with the smallpox vaccine, many of these vaccines soon found their way into vaccination programs mandated by the government, albeit through a somewhat different pathway.
Mandatory smallpox vaccination programs typically arose through state police power legislation authorizing municipalities to deal with outbreaks. [22] Typically, when a local municipality decided that the threat of outbreak was sufficient to exercise this authority it would require vaccination of everyone in the community (with a possible exception for individuals who could demonstrate uncommonly high health risks from receiving the vaccine, although this exception sometimes applied only to children) and fine and/or quarantine those who refused to be vaccinated. [23] When other diseases became preventable by vaccination, outbreak ceased to be the trigger for mandatory vaccination. Rather, because of their cost-efficiency and their ability to reduce and ultimately eliminate disease, vaccination programs became an important part of general public health policy. [24]
Most of the time, vaccination programs are accomplished through the dual efforts of national entities (which tend to develop and recommend vaccines) and state legislatures and local boards of health (which usually implement these recommended vaccines through vaccination programs). [25] It is not entirely accurate to refer to this as “mandatory vaccination,” as typically individual states will not criminally punish parents for not vaccinating their children or forcefully subject individuals to vaccination. [26] Instead, states typically condition school enrollment on proof of vaccination. [27] Though it may be a high price to pay, home schooling is usually an available means parents have if they wish to bypass these vaccination requirements. Moreover, most states grant exemptions to vaccination requirements for religious reasons and some even grant exemptions for philosophical reasons (in addition, every state exempts from school vaccination requirements individuals who cannot be vaccinated for medical reasons). [28]
The connection between school enrollment and vaccination programs may now seem obvious. Public health officials, faced with a means of protecting the general population from the harmful disease smallpox, realized that mass vaccination could lead to a sufficient level of immunity to eliminate the risk of outbreak, even for those in the community unable to vaccinate (because of medical reasons, for instance). [29] Because of the concept of herd immunity, public health officials considering the proper utilization of vaccines were dealing with a medical procedure quite out of the ordinary. Since vaccination itself does not typically provide 100% immunity to a disease, vaccinated individuals can still contract the disease. [30] Yet because of herd immunity, if a sufficient level of vaccination within a population is attained, the entire population will no longer be susceptible to the disease. In this way, vaccination came to be viewed not only as a personal medical choice but also as a step taken to improve the overall health of the population.
With the rise of public schooling in the mid- to late-nineteenth century, cities decided to condition public school attendance on smallpox vaccination. [31] By the latter part of the century, many states had adopted this practice. [32] Such a policy makes sense when one considers the increased risk of infectious disease in public areas like cities in general and schools in particular. By mandating vaccination for school attendance, of course, the state would eventually have ensured the vaccination of the entire population by the time the initially vaccinated generation became the oldest living one.
These vaccination schemes have faced challenges, both legal and social, throughout their existence. [33] The reasons for such challenges have ranged from personal liberty interests to doubts about the efficacy of vaccines. [34] State courts in the nineteenth century typically upheld both the enactment of mandatory vaccination programs and the delegation of power to local authorities. [35] More importantly for the future of mandatory vaccination policy, two important Supreme Court decisions in the early part of the twentieth century affirmed the power of state governments both to mandate vaccination and to delegate a broad degree of authority to local municipalities and health boards to carry out particular vaccination programs.
Judicial Approval
In 1905 the Court held in Jacobson v. Massachusetts [36] that the general police power of states is broad enough to overcome a Due Process claim brought by an individual who claimed his personal liberty interests were unconstitutionally invaded by the mandatory smallpox vaccination program in question. [37] In an opinion by Justice Harlan, the Court ruled that the constitutional guarantee of liberty “does not import an absolute right in each person, to be, at all times and in all circumstances wholly free from restraint.” [38]
This case still represents the initial constitutional basis of most mandatory vaccination legislation. Many states still provide for the governor or a public health official to mandate vaccination for all in the event of an outbreak. [39] Individuals who cannot vaccinate for health reasons or who refuse to vaccinate may be quarantined in order to protect the population in some states. [40] These laws gained greater relevance following the terrorist attacks of 9/11 and the increased public concerns regarding bioterrorism. For the most part, however, mandatory vaccination laws in the name of outbreak control have given way to vaccination requirements as a prerequisite for school attendance.
The issue of school vaccination came before the Court nearly two decades after Jacobson . In Zucht v. King [41] , the plaintiff challenged a general grant of authority from Texas to local boards of health to condition school entry on proof of vaccination. [42] To differentiate the case from Jacobson , the plaintiff noted that the San Antonio ordinances mandated vaccination even in the absence of evidence of outbreak. [43] The Court, speaking this time through Justice Brandeis, upheld the validity of the ordinances as well as the broad grant of authority to local health boards. [44] On the issue of the state’s power to mandate vaccination, he merely cited Jacobson : “[l]ong before this suit was instituted, Jacobson v. Massachusetts...had settled that it is within the police power of a state to provide for compulsory vaccination.” [45] As for entrusting a broad degree of authority on local health officials, he noted that Jacobson and other cases had affirmed that a state may “delegate to a municipality authority to determine under what conditions health regulations shall become operative.” [46] This delegation includes the permission to vest municipal officials with “broad discretion in matters affecting the application and enforcement of a health law.” [47] In summary, the Court found that these ordinances were valid assignments of “that broad discretion required for the protection of the public health.” [48] The language of the opinion emphasizes the importance of the public health as the key justification for mandatory vaccination.
Zucht , along with Jacobson , thus became the legal foundation for the mandatory vaccination laws of the twentieth century. Modern school vaccination laws and policies have grown from early mandatory smallpox vaccination laws:
The early successes of school vaccination laws against most political, legal, and social challenges helped lay the foundation for modern immunization statutes. Since the introduction of smallpox vaccination policies in the mid-to-late 1800s, states have amended them to include additional diseases as new vaccines become available. [49]
Though various amendments and additions have been made to mandatory vaccination laws throughout their history, the past half century has experienced the true culmination of mandatory vaccination policy. Public health officials have been able to institute a scheme for near-universal vaccination:
Many existing school vaccination laws were enacted in response to the transmission of measles in schools in the 1960s and 1970s. State legislatures at that time were influenced by the significantly lower incidence rates of measles among school children in states that strictly enforced vaccination requirements and school exclusions in outbreak situations without significant community opposition. Rather than having health departments require immunization in emergency conditions, legislatures acted to prevent disease by mandatory immunization as a condition of enrollment or attendance in schools or licensed day care facilities. [50]
Moreover, states have not been completely left to implement the recommended immunization schedule. [51] Though school requirements are still a state matter, national public health officials are typically able to enact their recommendations through federally funded immunization plans. [52] These plans require states to implement and enforce federally recommended immunization requirements before the states can receive federal funds. [53] The current recommended vaccination schedule appears below.
Recommended Childhood and Adolescent Immunization Schedule [54]
Challenges and concessions.
While school vaccination requirements have been credited with bringing about the control and elimination of many devastating childhood diseases, critics have continued to voice concerns and raise legal and political challenges to the entire process of mandatory vaccination.
Personal Liberty Concerns
One key argument against mandatory school vaccination has always focused on government intrusion into what is considered a personal medical choice. [55] Just as the government cannot force a person to have surgery to repair a torn ligament, for example, the government should not be able to force parents to vaccinate their children if the parents believe that vaccination is not the best medical decision. One prominent critic of mandatory vaccination has stated her organization’s goal as simply providing parents with choices: “[w]e believe that health care consumers should have the right to choose the type of preventive health care that they want to use – including choosing whether to use one, ten, or no vaccines.” [56] Other objections along similar bases argue that mandatory vaccination violates the medical ethic of informed consent or even that school district control over mandatory vaccination policies amounts to the unlawful practice of medicine without a license. [57]
The typical counterargument given by the public health officials is to point out that one’s decision to vaccinate, unlike one’s decision whether to undergo surgery, affects the health of others in the community. [58] To allow parents the right to choose not to vaccinate is to infringe on the ability of other parents to raise their children in a society free of certain deadly diseases. From a legal standpoint, Jacobson still seems to have settled the issue that at least under some circumstances, the government may force an individual to receive a vaccination.
Although public health officials have the legal authority to mandate vaccination for the public health under Jacobson, they should be very mindful of the personal liberty concerns just stated. Those with such views often cling to them vigorously. [59] As certain vaccine-preventable diseases decline, such concerns become even stronger. For this reason, it is important for public health officials to support their mandatory vaccination programs with justifiable arguments rather than simply citing legal precedent or historical tradition in support of their exercise of power. Fortunately for public health officials, the benefits provided by vaccination programs can be utilized to justify the existence of such programs.
Safety Accountability Concerns
A variation on the consumer choice challenge to mandatory school vaccination requirements tends to accuse the public health community of conspiring with or at least willfully acquiescing to powerful vaccine manufacturers at the expense of citizens. [60] Mandatory programs, the argument goes, eliminate any accountability from vaccine manufacturers that the free market might otherwise provide. [61] Both the safety and efficacy of vaccines fail to improve because manufacturers do not have to respond to consumer concerns. [62] Mandatory programs thus prevent better vaccines. A prominent critic of these programs has stated that if mandatory vaccination programs are ended, “we will have the ability to put economic pressure on the drug companies and on the health agencies to do a better job with vaccine safety and efficacy.” [63]
The strength of this argument lies in its apparent lack of hostility toward vaccines per se. Given the historical success of vaccination in eradicating smallpox and in reducing or eliminating the risk of other childhood diseases, any critique of mandatory vaccination programs that focuses on the use of vaccines generally is likely to be dismissed by those in the field of public health. By focusing on the economic drawbacks inherent in a mandatory vaccination program and how those drawbacks can negatively affect the quality of vaccines, this argument may gain more traction. Indeed, all sides of this debate claim to desire both safer and more effective vaccines.
The response to this argument, I would imagine, would be to emphasize the drawbacks of opening up the “market” in this case. Because vaccination programs depend on a sufficient percentage of the community being vaccinated, complete consumer choice carries with it problems that might be absent in a standard market. As for vaccine quality, FDA regulation is in place to ensure a sufficient level of safety and efficacy to accomplish the goals of vaccination. [64] The pressure faced by vaccine manufacturers to obtain and maintain FDA approval should provide a check sufficient to guarantee proper vaccine quality. If not, the answer should be to raise FDA standards, rather than to jettison the entire mandatory vaccination process and with it the likelihood of maintaining a sufficient level of immunity among the population.
This response might be unacceptable to those concerned. If the connection between public health officials entrusted with implementing the mandatory vaccination schedule and FDA regulators entrusted with ensuring the safety and efficacy of vaccines is seen as too close, proposing higher FDA standards as a solution may not allay concerns. The independence and integrity of FDA is therefore critical in this arena, just as it is in other areas of public health.
Concern of Unknown Risks
In what may be a combination of the two challenges previously discussed, many individuals challenge vaccine programs because of a lack of information about vaccines. [65] Many people, for example, legitimately question the wisdom of forced vaccination before long-term effects of a vaccine are studied. One website that purports “to provide a wide range of news and views on vaccination and vaccination policy” has summarized this challenge to vaccines simply as opposing the idea of “a parent, any parent, being forced to do something that has even a remote chance of harming their child.” [66] Since long-term (ten or more years down the road) and low-risk (on the order of one-per-million or less, for example) side effects may truly be unknown, this concern does present a challenge for public health officials. [67]
Unfortunately, even the best studies are unable to fully determine all long-term consequences of vaccination. In addition, “[t]here is no such thing as a ‘perfect’ vaccine which protects everyone who receives it AND is entirely safe for everyone.” [68] Therefore, it is true that mandatory vaccination probably forces some parents to inject their children with a substance that will cause some unknown harm.
As with the other objections to mandatory vaccination, however, this objection suffers from a critical flaw. Mandatory school vaccination requirements are not justified solely on the benefit they provide to the recipient. Instead, it is the benefit they provide to the community as a whole by ensuring a sufficient level of vaccination to prevent outbreak that justifies their intrusive nature on individual medical decision-making. [69] For this reason, if public health officials did not enact the mandatory vaccination program, they would be forcing on parents a system that had at least a “remote chance of harming their child.” [70] Because the decision to enact a community-wide vaccination program must be made at the general level if it is to be made at all, and because some children will undoubtedly suffer some health consequences regardless of which policy is chosen, individuals will always be able to raise this argument against mandatory vaccination programs.
A better critique of these programs would focus on whether mandatory vaccination causes more overall harm than a voluntary system; that is, is it better when viewed at the general, rather than the individual, level? Ironically, the very success of vaccination programs in reducing the incidence of once-prominent diseases has led some to ignore the overall and continuing benefit of community vaccination (herd immunity). [71] But for parents to decry the “remote chance” of harm from vaccination while ignoring the very real chance of outbreak in an under-vaccinated population is to reframe the issue entirely.
Other Concerns
Other challenges to vaccination laws have cited strongly held religious or philosophical positions against vaccination in general. Such challenges require a different type of response from public health officials; often the options are limited to overriding such objections and excluding children of parents adhering to such positions from public schools (which is constitutionally permissible under Jacobson and its progeny) or creating exemptions to vaccination requirements (which is detrimental to the overall goals of mandatory vaccination if a sufficient number of exemptors exist). Reactions to such religious and philosophical concerns vary from state to state, with a general trend toward greater accommodation of objectors.
In response to these and other challenges to mandatory vaccination laws, states have enacted various exemptions to vaccination requirements for school entry. Actual enforcement varies by state.
All states provide exemptions for those with medical risks associated with vaccines. [72] If certain contraindications indicate a likelihood of harm from a particular vaccine, the exemption will be allowed. [73] Because such cases are rare and exemptions relatively easy to enforce, there usually is very little risk of compromising the efficacy of the overall vaccination program by granting these exemptions. [74] The ability to grant medical exemptions while still maintaining sufficient levels of vaccination to provide community-wide immunity is one of the great accomplishments of the vaccination system. [75]
In addition to medical exemptions, almost every state grants religious exemptions for those with sincere religious beliefs opposing vaccination. [76] Individual states tend to vary with regard to the level of religious conviction necessary to obtain a religious exemption. Such exemptions reflect the sometimes uneasy balance between mandatory vaccination programs and First Amendment Free Exercise rights, even though the Supreme Court has validated the right of states to mandate vaccination without providing for such exemptions. [77] West Virginia, for example, does not provide religious exemptions. [78]
Some religious exemption statutes have spurred challenges on Establishment Clause grounds by those who claim they favor organized or recognized religions over the sincerely held religious views of others. [79] These challenges, if successful, would lead to the invalidation of many religious exemption statutes. Rather than decrease the number of religious exemptors, however, this may actually lead to more religious exemptors. The political climate of our day, along with the experience of a few states already (such as Arkansas), suggests that legislatures may respond to invalidation of religious exemption statutes that require adherence to an organized religion by drafting more general and expansive religious exemption statutes. [80] By subjugating religion to compulsory vaccination, courts may actually be helping to bring about a system with even more religious exemptors, thereby harming the very vaccination programs to which religious objections had been subordinated. [81]
Philosophical
The possibility that some parents who strongly oppose vaccination for other than religious reasons has led to other means of exempting from mandatory vaccination programs. In some states, people may avoid vaccination requirements by way of philosophical exemptions. [82] In California, for example, a parent need only “submit a letter or affidavit stating that the immunization is contrary to his or her beliefs” to exempt their child from vaccination requirements. [83] “Where available, parents are taking advantage of such exemptions with growing regularity; and in states offering both exemptions, the number of philosophical exemptions far exceeds the number of religious and medical exemptions.” [84]
States without philosophical exemptions, moreover, are often lax with their enforcement of religious exemptions. [85] Because of this, parents in these states can usually submit insincere affidavits purporting to object to vaccination for religious reasons and local health officials, unconcerned with delving into the sincerity of such affidavits, will widely grant exemptions. [86] In most states, therefore, persistent parents can usually find some way to exempt their children from vaccination requirements. If all else fails and vaccination is still regarded as unacceptable to the parent, the option of home schooling may provide a final avenue of evading these school vaccination requirements.
Dangers of Widespread Exemptions
The ease with which non-medical exemptions can typically be obtained has raised concerns among many that the benefits of widespread immunization are being compromised. [87] Because of the nature of medical exemptions, unvaccinated persons in a community with only medical exemptions would be expected to be few and dispersed. Herd immunity can be attained, and protection is ensured for both the vaccinated majority and the unvaccinated few. [88] Broadly granted philosophical and religious exemptions make herd immunity more difficult to attain and increase the risk to the community. This risk is exacerbated by the fact that many of those who apply for such exemptions “will cluster together in one geographic area.” [89] This cluster effect tends to increase the likelihood of serious outbreaks:
Recent studies have shown that clusters of exemptors, who are significantly more susceptible to contracting vaccine preventable illnesses, pose an increased risk of spread of diseases not only to their unimmunized peers, but also to the surrounding, largely vaccinated population. [90]
Given that many childhood diseases seem to be in decline, exemptors may fail to realize the continued value of vaccination. As the mumps outbreak in Iowa makes clear, however, vaccination programs take time and are at risk if vaccination rates fall. Other diseases are still prevalent in other parts of the world, and outbreaks can still occur in this country due to the prevalence of international travel. Ever though measles is rarely observed in the US, for example, the World Health Organization has reported that nearly 900,000 measles-related deaths occurred in developing countries in 1999. [91] Until diseases are eradicated globally, it may be necessary to continue vaccination.
Because many of the aforementioned risks are frequently underappreciated by those who seek exemptions, some have suggested a combination of stricter enforcement of exemption requirements and increased public knowledge of the reasons underlying childhood vaccination requirements. [92] Knowledge is indeed essential to the resolution of this problem. The easier it is to obtain an exemption, the less likely individuals are to understand and appreciate the importance of widespread participation to the success of a vaccination program. Greater public appreciation of the need for such participation (even for diseases that seem to be in retreat), along with greater information on the safety of vaccines can go a long way toward increasing public health in this area. [93]
Partial Exemptors – A Modern Phenomenon
The availability of exemptions has led to other interesting developments in the vaccination debate. Recently, for example, challenges have been raised against the need for mandatory chickenpox and hepatitis B vaccines. Diseases such as these, which are either not greatly feared (chickenpox) or transmitted primarily through voluntary rather than involuntary contact (hepatitis B), do not fit neatly into the typical justification for mandatory vaccination. [94] Nevertheless, public health officials have decided that recently-developed vaccines for these diseases should be placed on the recommended schedule. This has given rise to a significant number of partial exemptors – those who are not opposed to vaccination requirements per se, but who oppose particular vaccines on the schedule. Such a position may not have been comprehended by those who drafted the religious and philosophical exemptions, which seem to assume that a parent’s opposition is to vaccination generally, rather than to a specific vaccine. [95]
Because the religious exemption is usually constructed to apply to those who oppose vaccination generally because of sincere religious beliefs, would-be partial exemptors have difficulty fulfilling their optimal desires. In states without a philosophical objection, parents must choose either to accept the entirety of the recommended schedule of vaccines or to obtain a religious exemption for all vaccinations. [96] Parents who live in states with a philosophical exemption are much more able to tailor their objection to those vaccines with which they disagree. [97]
From the standpoint of a public health official, this presents two possible worlds. In the world with traditional religious exemptors but no philosophical exemptors, overall percentages of vaccinations would be relatively equal from vaccine to vaccine, and higher vaccination rates would be obtained for diseases associated with more objectionable vaccines at the expense of lower vaccination rates for diseases associated with less objectionable vaccines. [98] By contrast, in the world with philosophical exemptors, the public health official would observe higher vaccination rates for the less objectionable vaccines and lower vaccination rates for the more objectionable vaccines. [99]
The difference between these two worlds can have far-reaching implications. If parents are forced to make the all-or-nothing choice, a significant enough number could choose to forego vaccines (including some which they would otherwise accept) that herd immunity is lost, even for less objectionable vaccinations. On the other hand, a significant enough number could accept the more objectionable vaccinations to bring about herd immunity for those diseases. Though the public health official might prefer a world in which neither religious nor philosophical exemptions exist, such a world may not be possible. Therefore, the official should determine which of the two possible worlds provides a greater overall level of safety for the society. In addition, potential public reaction to a vaccine should cause the public health official to consider the ramifications the addition of a vaccine to the schedule will have on those vaccines already on the schedule.
Because partial exemptors have the potential to sway the balance between herd immunity and vulnerability, public health officials must take account of their concerns. Unlike in years past, today the development of a new vaccine presents public health officials with a choice that can affect other vaccines on the recommended schedule. Though the possibility for a chickenpox- and Hepatitis-B-free nation may seem tempting, officials should now consider the possible consequences of mandating such “borderline” vaccines. Parents who might otherwise vaccinate according to the old schedule might have second thoughts about the new vaccines on the schedule and seek means of avoiding the new requirements. If no means exist for avoiding the new vaccines other than complete exemption on religious grounds, parents who would subsequently pursue such exemptions would bring about a lower level of immunization for older diseases.
Studies may be necessary in the above situation to determine whether herd immunity status could be in jeopardy for those diseases for which vaccines are already on the schedule. While one solution might be to provide parents with greater ability to tailor their individual vaccination desires, such a solution would undermine the efficacy of newly scheduled vaccines. In addition, greater levels of flexibility in vaccination choice would undermine public understanding of the community-based nature of vaccination. I think it might be worth sacrificing the efficacy of the newer vaccines in order to maintain that of the more established ones. The public might be willing to suffer the possibility of chickenpox outbreaks, for example, in order to prevent an even minor epidemic of diphtheria or the measles.
Again, information should play a key role in the resolution of this issue. Many of the websites urging parents to carefully consider the vaccination decision do not inform parents that their decision to vaccinate may affect the overall health of the community. [100] The CDC, for its part, does urge parents to take note of this concern. [101] The very persons who most need to know of this concern (those seeking exemptions), however, are often those most likely to distrust CDC publications. For supposed citizen-oriented websites to urge individuals to make vaccination choices without considering how such decisions affect the community is irresponsible, especially given the scientific stability of the concept of herd immunity.
II. THE ROLE OF THE FEDERAL GOVERNMENT
Some of the problems posed to vaccination programs by exemptors and others could be partially solved through greater public awareness of the stringent safety and efficacy testing done on vaccines before they may enter the market. This section summarizes the role of FDA in the context of vaccination programs. In addition, this section will discuss other ways in which the federal government gets involved in the vaccination issue, concluding with a brief synopsis of the no-fault compensation scheme enacted pursuant to the National Childhood Vaccine Injury Act of 1986. [102]
FDA Regulation
Though state governments determine which vaccinations are mandatory for school attendance, the federal government plays a key role in vaccination. Perhaps most importantly, the federal government regulates the safety and effectiveness of all vaccines. The FDA’s Center for Biologics Evaluation and Research (CBER) is charged with this critical task. [103] The role of CBER ranges from pre-approval testing of potential vaccines to facility inspection to continued oversight and sampling after approval. [104] Regulation of vaccines can be more stringent than for other biologics or drugs. [105] Even after a vaccine is licensed, for example, FDA oversight is prevalent. [106] Since vaccines are derived from living organisms and are particularly susceptible to contamination and other environmental factors, manufacturers usually must submit samples of each vaccine lot for testing before release. [107]
Before a vaccine can even be licensed for distribution and use, it must go through an extensive testing process relatively similar to that of drugs and other biologics. [108] First, a new vaccine must be tested for safety on animals. [109] The vaccine manufacturer next must file an Investigational New Drug application (IND) with the FDA. [110] Studies are then undertaken to ensure safety before any human testing takes place. [111] In addition, the IND must describe the studies intended for humans. [112]
Once these initial steps are completed, proposed vaccines must undergo three phases of clinical trials, in which the vaccine is tested on humans. [113] Phase 1 testing looks only for very serious or very common problems. [114] A small number of subjects (usually less than 100) are closely monitored, usually for only a few months. [115] Testing expands in Phase 2 to begin evaluating efficacy, as well as to further test safety. [116] Phase 2 trials can last up to two years and typically include hundreds of subjects. [117] The final stage of testing, Phase 3, further studies safety and effectiveness. [118] Thousands of people may be involved in this stage of testing, and if successful it can lead to application for FDA licensing. [119]
Once the clinical trials are completed, the FDA can examine the results of the tests to determine whether the vaccine is safe and effective enough to be placed on the market. [120] At any point in the process, the FDA may halt ongoing studies if safety concerns require such action. [121] The FDA also reviews the data from the studies and inspects the manufacturing facility. [122] At this point the vaccine may be licensed.
As stated above, the FDA’s role in protecting the safety and effectiveness of vaccines does not end at the licensing stage. [123] Before any vaccines from a particular lot can be released, the manufacturer must typically submit samples for potency, safety, and purity testing. [124] Periodic facility inspections also continue for the duration of the license. [125] Furthermore, formal post-market studies may be conducted in order to identify problems that would not show up in pre-market clinical testing. [126] These tests are referred to as Phase 4 tests and are not mandatory, but can help identify problems that may only occur very infrequently. [127] Post-marketing surveillance programs are important because manufacturers are “never going to be able to do studies big enough to detect risks that might happen at a level of one in 100,000 or one in 1 million.” [128]
The Vaccine Adverse Event Reporting System (VAERS) is another valuable tool in identifying problems with a vaccine once it has been approved for the market. [129] VAERS was developed following Congress’s enactment of the National Childhood Vaccine Injury Act of 1986 and has become a very useful tool for identifying possible adverse effects that would otherwise escape detection. [130] VAERS allows anyone to report a problem that may be associated with any vaccine. [131]
It is important to keep in mind that VAERS is simply a reporting system. Experts and others use the data in VAERS to attempt to determine whether a vaccine actually causes a particular adverse effect, but the events that VAERS documents are not all caused by vaccines. It is therefore easy to understand why VAERS encourages doctors and others to report any adverse event that may be related to a vaccine. “VAERS is designed to detect signals or warnings that there might be a problem rather than to answer questions about what caused the adverse event.” [132] It is important to keep these facts in mind when looking at VAERS data, as many of the adverse effects may be completely unrelated to the vaccine in question. Often the effects are correlated with, but unrelated to, vaccination simply because many of the problems reported are those usually associated with events happening during the vaccination period (the first few years of life). [133]
Used correctly, VAERS can lead to useful studies and the discovery of potentially rare adverse effects. [134] VAERS can also be used to monitor individual lots of a vaccine. [135] Unfortunately, by encouraging individuals to report any adverse effect that may possibly have been caused by a vaccine, VAERS can provide ammunition for those claiming a definite link between a vaccine and a particular adverse effect, even if the data is silent on whether such a link exists. [136] While VAERS is in place to help identify actual risks associated with vaccines, these risks cannot be accurately assessed solely on the basis of reported incidents of adverse effects. [137]
The real value of VAERS lies in the testing and hypotheses that are developed in response to the data that has been reported. Because of the serious adverse effects already occurring during the typical vaccination period, it will often be easy and convenient to point to the correlation between vaccines and reported adverse events. Lost in the picture is the foundational proposition that VAERS is, at its core, a data collection system. To forego scientific inquiry and point instead to simple correlation may be convenient, but it is unwise. [138]
The recent public discussion surrounding the use of thimerosal as a preservative in vaccines helps to illustrate the importance of the FDA and other factors in furthering the goals of vaccine safety and public confidence in the entire safety regulatory process. Thimerosal is a mercury-containing organic compound that for many years has been used as a preservative in vaccines to help prevent contamination with microbes that could potentially be fatal. [139] Recently, fears that mercury at very low levels may be toxic to the brain have raised concern among many in the public about allowing the use of thimerosal in vaccines. [140] Many began to fear a connection between thimerosal and autism. [141] Standard FDA testing of lots, as well as studies measuring the amount of mercury contained in the standard immunization schedule versus accepted safe amounts, did not lead to safety concerns sufficient to pull thimerosal from the market. [142] Though one committee (the Immunization Safety Review Committee, commissioned by the Institute of Medicine) concluded that a theoretical link between thimerosal and autism was biologically plausible, most health experts continue to assert that there simply is no scientific evidence of a link between the two. [143]
During this time period FDA performed additional tests to verify or refute the supposed link between thimerosal and autism. [144] In 1999, FDA performed a comprehensive study and review of thimerosal use in vaccines for children. This review revealed no risk from thimerosal use, other than “local hypersensitivity reactions.” [145] Indeed, none of the standard safety protocols in place suggested or required that FDA pull thimerosal from the market. This is not to say, however, that no risk existed. As is clear from the foregoing summary of FDA vaccine approval, not all adverse effects will be known from clinical trials. [146] It may take years or longer to assess some of the risks of vaccines, including the risk of thimerosal as a preservative. [147]
Continued public concern over the safety of thimerosal caused FDA to begin to work with vaccine manufacturers in order to reduce or eliminate thimerosal from vaccines as a precautionary measure. [148] About this time, the American Academy of Pediatrics and the Public Health Service urged the removal of thimerosal from vaccines. [149] Today, with the exception of the inactivated influenza vaccine, all recommended childhood vaccines are either thimerosal free or contain only trace amounts of the compound. [150] Even though the risk may not have been as great as feared by the public or even existent at all, if the new vaccines are equally effective, the elimination of thimerosal from vaccines can probably be seen as a safety improvement, albeit at the expense of the added research and development needed to create the new thimerosal-free vaccines.
Rather than quell the existing safety concerns, this action led many of those who had decried the use of thimerosal to accuse FDA of participating in a cover-up to protect vaccine manufacturers. [151] Government agencies, for their part, continue to claim that vaccines with thimerosal are as safe as thimerosal-free vaccines, suggesting that the added development may have been superfluous. [152] While this may be so, the availability and now prevalence of thimerosal-free vaccines does provide the scientific and medical community with a new means of assessing the possible autism-causing effects of thimerosal. Namely, since thimerosal is suspected to cause autism within the first few years of life (the routine vaccination calendar), those who were vaccinated in the years since thimerosal-free vaccines have comprised the overwhelming majority of vaccines (that is, those born after 2001) would be expected to experience lower incidences of autism than the groups vaccinated with thimerosal-containing vaccines. [153]
In spite of the potentially costly decision to encourage the development of thimerosal-free vaccines when there is no sufficient safety concern to pull thimerosal from the market, FDA and other government officials have had little success in assuaging the fears and concerns of thimerosal critics. [154] Scientific arguments often fail to persuade, either because they are inconclusive or because of a perceived bias favoring vaccine manufacturers. [155] To back up their own arguments, thimerosal critics rarely point to scientific studies. [156] Instead, their reasoning seems to stem more from anecdotal evidence and comparison of thimerosal (which contains ethyl-mercury) to methyl-mercury-containing fish. [157] Representative Dan Burton (R-Indiana), a key supporter of the fight against thimerosal, explained that his belief in the toxicity of thimerosal stemmed from a personal episode: “[m]y grandson received nine shots in one day, seven of which contained thimerosal, which is 50 percent mercury as you know, and he became autistic a short time later.” [158] Others point to the rise in autism rates in the past twenty years and put the onus on the medical community to prove that this rise is not due to thimerosal. [159]
The response of health officials has been to ask why the burden should be placed on them to disprove a link between thimerosal and autism; cell phones, ultrasound, or diet soda could just as easily be the culprit. [160] Indeed, the typical response to those charging vaccination with causing many of the adverse effects occurring in life’s first few years is to point out that usually such accusations are based on nothing more than the temporal proximity of the vaccine and the illness. Some have suggested that the rates of autism may be on the rise not because of thimerosal, but because of generally more accurate diagnosis of the affliction. [161] In the past, an autistic child may have been wrongfully diagnosed with other mental disorders. [162] Figures showing a correlation between the rise in autism and the drop in other diagnosed mental disorders bolster such assertions, and suggest that vaccination may simply be a convenient scapegoat. [163]
As the thimerosal issue makes clear, vaccines often provoke strong feelings amongst various segments of the population. [164] Proper consideration of public reaction to its actions is a delicate aspect of FDA regulation of vaccine safety. To complicate matters further, one can easily imagine an equally vehement response and similar claims of conspiracy had the FDA not worked to reduce thimerosal from vaccines as a precautionary measure. Indeed, public confidence in the safety of vaccines is often influenced by factors outside the typical FDA calculus. Though FDA must act in the interests of the general safety regardless of public opinion, it may sometimes be necessary for FDA to consider public opinion, at least when exercising discretionary oversight. After all, the entire VAERS system is to a large extent dependant on public cooperation. Nevertheless, when the choice is between FDA popularity and doing what is right for the safety of Americans, the FDA should not allow itself to be swayed by a misinformed public.
Vaccine Injury Compensation Program
Congressional reaction to safety concerns goes beyond the adverse reporting system VAERS. The National Childhood Vaccine Injury Act of 1986, which created VAERS, also created a no-fault compensation scheme for people injured or killed by vaccines as an alternative to the traditional tort system. [165] This system was intended to efficiently and rapidly compensate those who are actually injured by vaccines while maintaining an environment in which further vaccine research and safety improvement could exist. The situation giving rise to this compensation program sounds remarkably similar to the more recent concerns surrounding thimerosal:
In the early 1980's, reports of harmful side effects following the DTP (diphtheria, tetanus, pertussis) vaccine posed major liability concerns for vaccine companies and health care providers, and caused many to question the safety of the DTP vaccine. Parents began filing many more lawsuits against vaccine companies and health care providers. Vaccination rates among children began to fall and many companies that develop and produce vaccines decided to leave the marketplace, creating significant vaccine shortages and a real threat to the Nation’s health. [166]
Funding for the no-fault compensation scheme initially came from Congressional grants of federal tax dollars totaling $110 million per year. [167] Since October 1, 1988, funding has proceeded from the Vaccine Injury Compensation Trust Fund, which is funded by a $0.75 excise tax on all doses of vaccines covered under the program. [168]
One may wonder what makes vaccines worthy of an alternative dispute resolution system. Perhaps it is the result of the power of the vaccine manufacturing lobby or simply an attempt by Congress to pass some legislation in the face of strong public sentiment. Although these reasons may appear plausible, it seems more likely to me that the Act created this no-fault compensation scheme because of the mandatory nature of vaccination. For those injured by other medical devices or drugs, the traditional tort system or medical insurance seem the proper means of addressing the issue. When people are told to undertake a medical procedure they may not agree with because it helps further a public goal, however, it may make sense to have a system in place whereby they can obtain relief quickly if harmed by the procedure. Moreover, because certain vaccines may be closely associated with particular adverse effects, the efficiency of a no-fault scheme may trump the standard fact-finding processes of the legal system. The government has chosen to enact such a no-fault scheme, and err on the side of compensation.
III. ANALYTICAL MEANS OF ADDRESSING THE ISSUE
The concerns and problems raised in the context of mandatory vaccination programs do not readily suggest a simple answer. In examining the issue, I came across two particularly useful tools for analyzing the problem. The first comes from an old episode of The Andy Griffith Show in which a local farmer refused to accept a vaccination from the local nurse. In addition to providing substantial entertainment to the viewer, the characters can be viewed metaphorically to represent the various parties in the mandatory vaccination debate. The episode’s solution, in turn, sheds some light on the current debate.
This section will also utilize the analytical framework of economic analysis. Though not as enjoyable a topic as The Andy Griffith Show, economic theory helps to reshape the vaccination discussion and greatly facilitates the process of assessing the various positions.
“We got to get folks to take their shots” – Sheriff Andy Taylor [169]
The Andy Griffith Show addressed the concept of popular resistance to universal vaccination over forty years ago. In “The County Nurse,” Sheriff Andy Taylor confronted a local nurse who was trying to bring everyone up to date on their tetanus shots. Not surprisingly, at least to Andy, many of the mountain farmers had not been inoculated. The naïve nurse would soon discover the reason for the low vaccination rate.
Rafe Hollister, one of the leading farmers in Mayberry, had little use for modern medicine or doctors in general. “We don’t need any nurse, nobody gets sick up here.” [170] Thermometers? “I know when I got a fever, I’m hot.” [171] Stethoscopes? “I know my heart’s beating, I’m alive ain’t I?” [172] But his strongest objection was saved for vaccinations: “I ain’t never been jabbed and I ain’t fixin’ to be.” [173] Such were the views that the nurse was up against in her attempt to achieve 100% vaccination rates.
Rafe Hollister
Rafe Hollister’s reasons for opposing vaccination went beyond his desire to avoid getting “jabbed.” He was a farmer who lived off the land, and when he got sick he let his body fight the sickness naturally. His daddy had lived to the age of hundred and he aimed to do the same. [174] The concept of a vaccination was certainly something foreign to him, as was the idea that a health official could force him to do anything. Even in the wake of the nurse’s impassioned plea to accept a shot that could someday save his life, he retorted simply, “I done alright before you come around and I’m doing alright now.” [175]
Although the county nurse was not acting pursuant to a mandatory vaccination program, under the circumstances her attempts to get Rafe inoculated were pretty forceful. The nurse was accompanied by the local sheriff to Rafe’s farm to try to convince him to take the shot, and when he refused, the sheriff and nurse continued to attempt to make him acquiesce. When Deputy Barney Fife heard of Rafe’s stubbornness, he insisted the nurse return to Rafe’s farm with him to force Rafe to take the shot. After all, boasted the deputy, “Rafe Hollister’s like a child and he’s gotta be treated like one...I’ll make him take his shot.” [176] When the deputy arrived at Rafe’s farm yelling that he was forcing Rafe to accept the vaccination, Rafe decided to fight the mandatory vaccination by drawing his rifle and forcing the deputy to leave the farm.
In a classic manifestation of the early spirit of the television series, Sheriff Andy Taylor finally convinced Rafe to take the shot through a little reverse psychology. Andy began by facetiously praising Rafe’s refusal to take the shot as stemming from Rafe’s desire for immortality. Namely, by refusing to take the shot, Rafe was sure to become the impetus for all the other townspeople not to neglect to take their shots. Unfortunately for Rafe, this heroic stature would only be achieved posthumously, as he will have succumbed to a violent and painful death from tetanus. As Andy explained to Rafe, someday, after getting cut by a rusty saw or bitten by an animal, without the shot he’ll “be a cinch to go.” [177] Eschewing the chance to be a dead hero, Rafe finally took the shot.
Sheriff Andy Taylor
Vaccination has changed the modern world. Indeed, it has led to the elimination or significant decline of many diseases that once posed significant and potentially deadly health risks. Public health officials in the United States have managed to institute a program that, though subject to variations on a state by state basis, essentially mandates certain vaccinations as a requirement for school attendance. While these vaccination programs are touted by most public health officials, a significant number of people oppose mandatory vaccination. The County Nurse episode helps illuminate the perspectives of the various sides of the issue, as well as one possible solution.
The nurse herself represents the public health officials. Though she is not implementing a mandatory vaccination program, her stated goal is to inoculate 100% of the population. [178] As mentioned above, she has the assistance of local law enforcement and she is quite persistent. Rafe Hollister, the stubborn farmer, represents those within the community who oppose or resist mandatory vaccination programs. His reasons initially rest on a general reluctance to stray from natural medicine. In this way he represents the contingent of society that scientists and medical researchers will always find difficult to convince of any developments in the medical field. In many ways, he is comparable to the plaintiff in Jacobson . Andy and Barney can be seen as the arms of the state that are entrusted with carrying out the general vaccination plan. Their varying styles can be seen as varying state requirements and enforcement options for vaccination.
Though these comparisons may seem elementary and of little value, the character development that the characters undertake during the episode greatly increases the episode’s usefulness as a surrogate for real world concerns and issues. Rafe resists the shot initially not only because he distrusts medicine in general, but also because he resents the idea that a county nurse can make him do anything. Many who resist mandatory vaccination schemes do so because of personal liberty concerns; they do not want the government to tell them what to do, especially in the context of personal medical decisions. Just as Rafe’s stance becomes more vehement the harder the nurse attempts to convince him, many who oppose mandatory vaccination see the persistence of the medical community as evidence of blind adherence to a potentially dangerous system, or worse yet as an active promotion of the special interests of the vaccine manufacturers. [179] The episode does not paint the nurse in this way at all, however. Rather, after seeing how strongly Rafe opposes vaccination, the nurse passionately pleads with him to reconsider. Her stance truly seems to stem from a genuine concern that he not suffer the potentially terrible effects of the disease. [180] As before, he refuses; this seems to illustrate that the stance of some may be so strong that they will never accept vaccination on the basis of arguments advanced by government officials.
Barney Fife’s insistence that Rafe accept the shot demonstrates the lack of understanding among many in the government and in the general population as to the vehemence with which those opposing mandatory vaccination hold to their views. His paternalistic stand only serves to exacerbate the situation with Rafe. Indeed, Barney Fife helps to illustrate that there cannot be a one-way solution to the issue of mandatory vaccination.
Andy Taylor’s method of convincing, which eventually carried the day, may not be very conducive to real-world implementation. After all, it is unrealistic to think that reverse psychology will convince those currently opposed to vaccination programs to change their minds. What I think is important to notice, however, is the role information can play in this issue. Andy finally convinces Rafe Hollister to take his shot after describing the horrible effects of the disease and how likely Rafe is to contract it. Similarly, any solution to the issue of mandatory vaccination holdouts must rely on increased information dissemination. That the information in the episode came from a trustworthy source may also have been crucial, which seems to imply that public health officials may need to work more closely with local personnel in order to obtain higher vaccination rates.
Because this episode deals with the vaccine for tetanus, a non-communicable disease, the usual community-based arguments in favor of vaccination do not enter the equation. Extra-personal consequences of Rafe’s decision to vaccinate do exist, however. Most importantly, as the unofficial leader of the farming community, his decision will be followed by the other farmers. This is shown both in Andy’s assurances to the nurse that Rafe is the most important of the farmers to convince on the issue and later, after Rafe has decided to get the shot, in his promise to the nurse that all she has to do is come with him and he’ll get all the farmers to take their shots. Perhaps those parents who support vaccination can help bring about higher vaccination rates by being more vocal and persistent with their neighbors who oppose vaccination programs.
Economic Analysis
Economic analysis [181] provides a useful theoretical basis for evaluating the competing sides of the vaccination debate. Arguments regarding the wisdom of the current vaccination policy can often be recast as economic questions involving a cost-benefit analysis.
When an epidemic breaks out, for example, the benefits of vaccination (protection from the disease both for the individual and for society through herd immunity) seem more clearly to outweigh the costs (potential side effects of the vaccine, decreased ability of the immune system to defend the body from variant strands of the disease, or personal or religious objection). Vaccination rates would, therefore, be expected to be highest during such epidemics. Consequently, those few who continue to oppose vaccination during such epidemics would be expected to do so for only the strongest reasons. This is due to the fact that in economic terms, the opponent of vaccination would have to believe that the benefits of vaccination still do not outweigh the costs, even during an epidemic. This might stem from a relative undervaluation of the benefits of vaccination (perhaps due to a belief that contracting the disease would not be so bad) or a relative overvaluation of the costs of vaccination (possibly due to the greater cost to the conscience of the personal or religious opponent of vaccination) or some combination of both. Medical exemptions directly illustrate this cost-benefit analysis: for a person likely to suffer serious side effects from a vaccine, the cost of vaccination is much greater than the cost to the average individual. Even in a time of epidemic, therefore, vaccination might not be rational for such an individual.
This economic analysis of vaccination is well illustrated by the facts of Jacobson v. Massachusetts [182] , the first Supreme Court case addressing the constitutionality of mandatory vaccination legislation. The case involved a Massachusetts statute allowing local authorities to mandate vaccination for smallpox if necessary for the public health and safety. [183] Subsequently, and upon a determination that smallpox was “prevalent to some extent” and “continues to increase,” the city of Cambridge passed a mandatory vaccination ordinance. [184] This ordinance represented the economic determination that the benefit of mandatory vaccination outweighed the cost of supplying vaccines, finding and prosecuting holdouts (such as Jacobson), and the decreased liberty of individuals to be permitted to decide whether to vaccinate.
Jacobson subsequently challenged his prosecution under the ordinance by claiming it to be an unconstitutional denial of his liberty under the 14th Amendment (as well as in violation of the Preamble and the “spirit” of the Constitution, arguments that were summarily dismissed). [185] In economic terms, this may simply indicate that he viewed the cost of accepting a forced vaccination (perhaps of any kind, in any circumstance) as greater than any possible benefit. A closer look at his arguments, however, suggests that he may have performed a more detailed cost-benefit analysis. One can easily convert the various arguments he attempted to advance into economic costs. Among these arguments were the likelihood of vaccination to bring about “serious and permanent injury” and occasional death, the inability of an individual to assess the risk of vaccination in a particular case, and the potential impurity of vaccines and inability to test such impurity, among others. [186] At the very least, it would appear that Jacobson attributed a greater than average cost to vaccination.
The statute also provided that ordinances mandating vaccination provide an exception for “children who present a certificate, signed by a registered physician, that they are unfit subjects for vaccination.” [187] This reflects the state’s determination that the cost of forcing vaccination upon those more likely to suffer adverse side effects outweighed the benefit of completely universal vaccination. Given the determination that near-universal vaccination was required to provide the desired benefit, one would expect that the state expected to grant relatively few medical exemptions (or at least few enough not to seriously compromise the goal of providing protection against smallpox through vaccination).
In rejecting Jacobson’s liberty challenge to the ordinance, the Court endorsed the concept that the State’s cost-benefit analysis can supersede that of the individual, at least in the area of public health. The Court’s decision, in fact, makes irrelevant any individual cost-benefit analysis in the face of a comprehensive mandatory vaccination program.
Various vaccination-related developments in the century since Jacobson can also be cast in an economic analytical framework. Certainly the benefit from vaccination disappears when a disease has been eradicated, which explains why the smallpox vaccine is no longer mandated. Any cost greater than zero (the likely benefit of smallpox vaccination at this point, barring of course a reintroduction of the disease using laboratory samples) will suffice to outweigh this benefit. [188] The success of vaccination policies, however, may lead to an undervaluation of the benefit of continuing to vaccinate due to the lack of visible instances of the disease. [189] This problem may be compounded when vaccines are mandated for diseases which are not associated with high mortality rates, such as chickenpox. A further complication to the cost-benefit analysis arises when assessing vaccination policy for diseases such as Hepatitis B, which is spread typically through voluntary contact. In such a case, an individual who feels highly unlikely to engage in the behavior giving rise to the risk of the disease might rationally see very minimal benefit from vaccination, while the state may view widespread vaccination as the most cost-effective method of dealing with the disease. [190]
Altruism and Free Riding
Given the continuing policy of vaccinating for diseases that have become relatively rare in recent decades, one might expect individual cost-benefit analyses to increasingly come into conflict with the societal policy. Several factors, however, serve to counteract this possibility. Perhaps most significantly, it is likely that many parents defer on the question of vaccination and accept the cost-benefit analysis of the state (communicated to the individual through the vaccination schedule and through doctor’s recommendations) as their own. Along the same lines, many individuals might not strongly consider the pros and cons involved in vaccinating; if the possibility exists for contracting a disease, and a vaccination is available, the decision may already be made. [191] A third possibility implicates a factor that I have not yet mentioned in relation to the individual cost-benefit analysis: altruism.
Some have proposed that altruism may bridge the gap between incompatible cost-benefit analyses of states and individuals. [192] Whereas typical medical decisions affect only the patient making the decision, it is pointed out, medical decisions regarding vaccine-preventable diseases usually implicate outside interests. [193] A patient thinking only of his own interests may forego vaccination if he feels the risk from vaccination outweighs the personal benefit. Altruism, it is argued, may present a separate benefit for such an individual. [194] Though the individual may not consider the risk of contracting the disease high enough by itself to justify vaccination, he may still vaccinate in order to help accomplish the public goal of eliminating the threat of an epidemic. Public health officials hope that comprehensive vaccination will produce herd immunity. [195] Thus the individual who may otherwise forego vaccination might undertake it in order to “do his part” for the community at large. Individuals who cannot vaccinate are particularly dependent on this sort of altruistic behavior, as they often have no other protection from the disease. [196]
Working against this altruistic behavior is the temptation of individuals to enjoy the benefit conferred on them by herd immunity without undertaking the cost of being vaccinated personally. [197] This is widely referred to as “free riding,” and greatly undermines the goal of comprehensive vaccination. Since herd immunity is supposed to create a level of protection sufficient for even those few who are not vaccinated, a small number of free riders might not pose a significant problem. As described earlier in this paper, comprehensive vaccination programs are designed to work even though some members of society cannot be vaccinated. [198] The problem arises when the number of free riders becomes sufficiently high to compromise the ability of the society to achieve herd immunity. Since the average citizen (one with no greater reason to avoid vaccination than any other member of society) could always choose to free ride if immunization were voluntary, herd immunity might never be achieved. This is one of the key arguments advanced in support of government mandated vaccinations. [199]
Ex Ante Versus Ex Post
The concepts of altruism and especially free riding emphasize the importance of ex ante (before the fact) versus ex post (after the fact) decision making in the context of vaccination. One of the main benefits of economic analysis is that it requires decisions to be justified ex ante. Public health officials, for example, are faced with the decision of whether to mandate vaccination for a particular disease at a time when all adverse effects cannot be known. They must weigh the possible consequences of allowing a disease to continue against the possible known and unknown adverse effects of a vaccine that may have just entered the market. When this decision is made properly, the benefit of the vaccination program will have outweighed the cost. The benefit is manifested in lower or no occurrences of the disease, while the cost is seen most directly in those children who have actually experienced adverse effects as a result of the vaccine. If the benefit is greater than the cost from an ex ante perspective, to the economist there should be no second-guessing of the vaccination program. [200]
The economist, of course, is not the parent. Parents who decry mandatory vaccination as the cause of their child’s adverse reaction are typically viewing the situation ex post. That the program has been implemented assumes that the sum of these adverse reactions was an acceptable alternative to non-implementation, and should therefore not be allowed to undermine public confidence in the program. When one surveys the landscape of the vaccination issue, however, objections are usually of the ex post variety. Since it is harder to appreciate the absence of an epidemic than the presence of a child suffering a vaccine-related injury, it is easy to look at the issue solely ex post. In the interests of public safety, such reasoning should be avoided.
This is not to imply that all critics of mandatory vaccination are on unsound theoretical footing. In fact, those whose objections are marked by a distrust of the government authorities in charge of implementing vaccination programs can be seen as questioning only the ex ante judgment of the officials. If this is so, they are actually on firmer ground than those who object to the programs because they feel their child was harmed by the vaccine. Ex ante critiques are valuable because they can bring about change in the system at a time when it can still prove useful.
The National Vaccine Injury Compensation Program represents a theoretically sound program under these criteria. Economically, it represents the idea that some of the costs of mandatory vaccination programs known only ex post will be compensated by all those who share the benefits ex ante. The excise tax, paid ex ante by all who receive the vaccine, is used to compensate anyone who experiences certain adverse effects ex post. This is simply an example of the government distributing the costs of the vaccination program across the spectrum of those who receive the benefit, rather than an ex post complaint by those on whom the costs have fallen.
Other Issues
The modern trend toward more widely-granted exemptions represents government acquiescence toward a certain degree of free riding. Should such exemptions proliferate too widely, herd immunity may indeed be lost and a recalculation of the cost-benefit analysis of individuals will be necessary. In the face of a greater potential to contract disease, the benefit of vaccination grows significantly, while the cost of accepting the vaccine remains the same. Likewise, from the standpoint of the government, the cost of allowing widespread exemptions will eventually overtake the benefit of permitting such exemptions if that cost suddenly includes serious risk of epidemic.
The risks associated with non-vaccination can be illustrated through a rather simplified mathematical example. [201] Suppose a school with 1,000 students is exposed to a measles outbreak. 990 of the students have received all of their measles shots, and so are fully immunized. Suppose further that the measles vaccine is 99% effective; that is, it produces complete immunity in 99% of patients. [202] Therefore, 10 out of the 990 who have been fully immunized will be susceptible to the disease. In addition, all 10 of the 1,000 students who had not been fully immunized will be susceptible to measles. Therefore, 20 out of 1,000 students will get the disease. Although the number of infected students who were vaccinated is equal to the number who were not, this example demonstrates that vaccination can be very effective even if it sometimes does not produce immunity in an individual. If no one had been vaccinated, 980 more students would probably have caught the measles. It is also important to note that this example assumes an epidemic; in reality, herd immunity would probably be attained at this level of inoculation and none of the 1,000 students would have caught the disease.
IV. CONCLUSION
Vaccines have immeasurably improved our quality of life. They have led to the eradication of deadly diseases like smallpox and the near elimination of diseases such as diphtheria, polio, and measles. Outbreaks of vaccine-preventable diseases, such as mumps, are infrequent and are also quite newsworthy on the rare occasion that they do occur. And people like Rafe Hollister can survive a run-in with a rusty saw or an animal bite.
The life-saving benefits of vaccination often overshadow the vast economic and personal benefits it has helped provide. Jonas Salk’s cure for polio has spared generations from a life hindered by the devastating physical handicaps of that terrible affliction. Children no longer must miss vast stretches of school to overcome a debilitating battle with pertussis (although there is no doubt that some children lament this decline in excused absences from school). Parents no longer have to spend restless hours worrying as their children suffer the body’s natural response to disease. In economic terms, this translates directly into fewer missed hours of work and less administrative difficulty, leading to a generally more productive society.
For all the benefits of vaccines, of course, it is important not to ignore the costs. The National Vaccine Injury Compensation Program is one way of dealing with the economic costs of vaccination, but this may provide little solace to the parent of a child who has been injured by a vaccine for a disease that is seemingly in decline. Side effects with very low probability will sometimes occur; though from a community-wide view this possibility is acceptable, for the individual who experiences the adverse effect the vaccination may not have been the best medical decision. Many who view natural immunity as a rite of passage for children might not desire a means of bypassing the disease entirely.
Some may accuse public health officials of dreaming for an unreachable day when all diseases are controlled by vaccination. Zeal on the part of public health officials, however, should not overshadow the actual benefits of vaccination generally. Soon may come the day when diphtheria, like smallpox, will be eradicated globally. At that point, it can be removed from the vaccination schedule and future generations will reap the benefits of vaccination while undertaking none of the costs.
This prospect, I think, sheds light on the ultimate solution to vaccination issues that have been discussed in this paper. Highly communicable and especially terrible diseases should continue on the vaccination schedule until they are virtually eliminated. The eventual elimination of these scourges will someday make vaccination unnecessary, and the costs of vaccination will drop to zero. Until that time, officials should seek stricter enforcement of the mandatory vaccination laws and should tighten down on non-medical exemptions. At the same time, information campaigns should be considered in the interest of reminding the public of the continued importance and relevance of vaccine programs. Though risks are unavoidable when dealing with vaccines, parents should constantly be reminded that immunity depends on a high level of cooperation. This will hopefully keep immunization rates high, at least for the most harmful diseases.
Meanwhile, public health officials may be wise to consider an alternate stance toward somewhat less-important vaccines such as Hepatitis B and varicella (chickenpox). [203] With such diseases it may be worthwhile to wait longer before placing the vaccines on the recommended schedule. This will undoubtedly make herd immunity more difficult if not impossible to attain, while simultaneously announcing to parents that undertaking the vaccine in question is a personal medical decision. Most of those who choose to vaccinate (and accept the risk of adverse effects from these newer vaccines) will still acquire immunity. Without a mandatory program in place, however, one would still expect to see regular occurrences of the disease. Given the relatively high likelihood of outbreak under these circumstances, a percentage of those who vaccinate will probably get the disease. They will likely turn to those who did not vaccinate at all and see them as the cause of the outbreak. In time, social pressures may lead to greater vaccination rates, and the time may be ripe for greater acceptance of mandatory vaccination for the disease.
One significant benefit to this approach lies in its natural tendency to point out to parents the importance of receiving the more important vaccines. When some vaccines are mandatory and others are not, the distinction between the two types of vaccines is impossible to neglect. It would hopefully make parents think more carefully before attempting to gain an insincere exemption. This approach would fail to satisfy those who want parents to have the option to choose “one, ten, or no vaccines,” [204] but it would at least allow an element of choice for some vaccines while hopefully maintaining a sufficient level of immunization for the more important vaccines. It is also important to remember that parents with serious reservations about any vaccines will usually have the option of home schooling. Overall, this approach might have the advantage of winning over those who only partially object to the vaccination schedule, thus helping bring about a greater chance of herd immunity for diseases associated with less objectionable vaccines.
Vaccination certainly is unique among medical treatments, both for its incredible potential and its coercive nature. It is unfortunate that questionable evidence has led many concerned parents to question the wisdom of vaccination programs that still serve important goals. Given the importance of public support for the achievement of these goals, however, public health officials must account for sometimes questionable concerns in determining vaccination policy. Greater information dissemination, combined with more sharply drawn (and potentially vaccine-specific) guidelines, can hopefully further the important goals of vaccination policy.
[1] Center for Disease Control, “Smallpox Disease Overview,” at http://www.bt.cdc.gov/agent/smallpox/overview/disease-facts.asp (last visited April 27, 2006).
[2] GlaxoSmithKline is currently developing an ear infection vaccine and plans to seek regulatory approval shortly. Jessica Said, “Vaccine Could End Children’s Ear Infections,” CNN online article, March 3, 2006 (on file with author).
[3] Institute of Medicine. CP Howson, et al. eds. Adverse Effects of Pertussis and Rubella Vaccines. Washington, DC: National Academy Press; 1991, at 1.
[4] James G. Hodge, Jr. and Lawrence O. Gostin, School Vaccination Requirements: Historical, Social, and Legal Perspectives , 90 Ky. L. J. 831, 867 (2001).
[5] See, e.g., Jacobson v. Massachusetts , 197 U.S. 11 (1905).
[6] Hodge and Gostin, supra note 4, at 867.
[7] Id. at 868.
[8] “Rather than having health departments require immunization in emergency conditions, legislatures acted to prevent disease by mandatory immunization as a condition of enrollment or attendance in schools or licensed day care facilities.” Id.
[9] See id. ; see also infra Part I (chart describing the current recommended vaccination schedule).
[10] The Center for Disease Control has gone so far as to suggest that “to have a medical intervention as effective as vaccination in preventing disease not use it would be unconscionable.” Center for Disease Control, National Immunization Program publication, “Six Common Misconceptions About Vaccination and How to Respond to Them,” at http://www.cdc.gov/nip/publications/6mishome.htm (last visited April 27, 2006) (hereinafter “Six Common Misconceptions”).
[11] Center for Disease Control, National Immunization Program publication, “Ten Things You Need to Know about Immunizations,” at http://www.cdc.gov/nip/publications/fs/gen/shouldknow.htm (last visited April 27, 2006).
[12] This is not to imply that parents who vaccinate without carefully considering the pros and cons of vaccination are in the wrong. The health and safety of a child is of paramount importance to most parents, and every parent must make decisions that affect the welfare of the child. Most parents approach such decisions with a sincere desire to promote the child’s best interests, and this desire is no different in the context of vaccination.
[13] “Despite its utility, vaccination has provoked popular resistance from the beginning.” Hodge and Gostin, supra note 4, at 834.
[14] “Some opponents express valid scientific objections about effectiveness or need for mass vaccinations; some fear harmful effects arising from the introduction of foreign particles into the human body; and others worry that vaccination actually transmits, rather than prevents, disease, or weakens the immune system.” Id.
[15] See, e.g. , Jacobson v. Massachusetts , 197 U.S. 11 (1905) (constitutional challenge to government mandated smallpox vaccination); “Six Common Misconceptions,” supra note 10 (“[s]ome see mandatory vaccination as interference by the government into what they believe should be a personal choice”).
[16] “Six Common Misconceptions,” supra note 10.
[17] A more detailed explanation of this subject appears in Part I of this paper.
[21] See, e.g. , “Ten Things You Need to Know about Immunizations,” supra note 11.
[22] Angie A. Welborn, “Mandatory Vaccinations: Precedent and Current Laws,” CRS Report for Congress, at http://www.fas.org/sgp/crs/RS21414.pdf (last updated Jan. 18, 2005).
[23] For a typical scenario of public health response to outbreak, see the facts of Jacobson v. Massachusetts , 197 U.S. 11 (1905).
[24] Hodge and Gostin, supra note 4, at 833-34.
[25] Id. at 867-68.
[26] Id. at 833.
[29] This level of immunity is often referred to as “herd immunity,” the concept that not everyone in a population must be vaccinated in order for the entire population to be protected. Abi Berger, “How Does Herd Immunity Work?” 319 BMJ 1466 (1999). “As long as a sufficient number of children are immunised against each disease for which there is a vaccine, protection against that disease will be conferred on everybody.” Id. Also, the level of vaccination necessary to attain herd immunity increases as the infectivity of the disease increases. Id. Highly infectious diseases, therefore, require higher levels of immunity for herd immunity to occur. Id. The concept of herd immunity will arise throughout this paper, with particular emphasis in Part III.
[30] This is evidenced by the fact that in time of outbreak, the vaccinated population can still be susceptible to the disease, although usually the vaccinated population is far less susceptible to the disease than the unvaccinated population. Vaccines typically produce the desired antibody in an individual around 90% of the time, with actual percentages varying from vaccine to vaccine. Some vaccines, moreover, lose their efficacy and require boosters. These concepts will be further developed throughout this paper.
[31] Hodge and Gostin, supra note 4, at 850-51.
[32] Id. at 851.
[33] Id. at 834.
[34] Id. at 834-35.
[35] See, e.g. , Duffield v. Sch. Dist. , 29 A. 742 (Penn. 1894).
[36] 197 U.S. 11 (1905).
[38] Id. at 26.
[39] Welborn, supra note 22.
[41] 260 U.S. 174 (1922).
[42] Id. at 175.
[43] Id. (“[t]he bill charges that there was then no occasion for requiring vaccination” and that the ordinances “in effect, mak[e] vaccination compulsory”).
[45] Id. at 176.
[48] Id. at 177.
[49] Hodge and Gostin, supra note 4, at 867-68.
[50] Id. at 868.
[51] The schedule of immunizations is published by the Center for Disease Control, and follows the recommendations of the Advisory Committee on Immunizations Practices, the American Academy of Pediatrics’ Committee on Infectious Diseases, and the American Academy of Family Physicians. Id.
[52] Id. at 869.
[54] Based on chart publicized by Center for Disease Control, approved by Advisory Committee on Immunization Practices, American Academy of Pediatrics, American Academy of Family Physicians, available at http://www.cispimmunize.org/IZSchedule_2006.pdf (last visited April 27, 2006).
[55] Indeed, the law in Jacobson was challenged for this reason.
[56] Statement of Barbara Fisher, founder of National Vaccine Information Center, quoted in Neenyah Ostrom, “First Do No Harm,” at http://www.chronicillnet.org/online/Fisher.html (last visited April 27, 2006).
[57] K.N.O.W. Vaccines, Vaccine Awareness of Florida fact sheet, at http://www.know-vaccines.org/vaccine_fact.html (last visited April 27, 2006).
[58] The most direct way in which this occurs surrounds the concept of herd immunity, as discussed elsewhere throughout this paper. If a sufficient number of persons in the community does not vaccinate, herd immunity may be unattainable and others may be put at risk.
[59] See, e.g. , the discussion in Part III involving The Andy Griffith Show.
[60] See Statement of Barbara Fisher, quoted in Ostrom, supra note 56. See also “Autism and Vaccines: Activists Wage a Nasty Campaign to Silence Scientists,” Wall Street Journal, February 16, 2004, at http://www.opinionjournal.com/forms/printThis.html?id=110004700 (last visited April 27, 2006) (citing vaccination critics who had accused the vaccination-defending writers of “having an ‘industry profit promoting agenda’”).
[61] See Statement of Barbara Fisher, quoted in Ostrom, supra note 56.
[64] See the discussion in Part II regarding vaccine safety.
[65] See, e.g. , “Six Common Misconceptions,” supra note 10.
[66] Mission Statement of Vaccination News website, at http://www.vaccinationnews.com (last visited April 27, 2006).
[67] As the discussion in Part II on vaccine safety demonstrates, pre-licensing testing for very rare adverse effects cannot take place if vaccines are ever to reach the market. Phase 4 post-licensing testing does exist, but may take years to discover extremely rare adverse effects.
[68] World Health Organization Immunization Safety page, “Adverse Events Following Immunization,” at http://www.who.int/immunization_safety/aefi/en/ (last visited April 27, 2006).
[69] As the recent mumps outbreak in Iowa demonstrates, not everyone who receives a vaccine develops immunity to the disease. For this reason, the success of vaccination depends on a sufficient level of vaccination in the community. When a significant percentage of the population has not received the vaccine, an outbreak can occur and even threaten some of those who have been vaccinated. See David Pitt, “Iowa Mumps Epidemic Continues to Broaden,” Associated Press, April 13, 2006, at http://www.breitbart.com/news/2006/04/13/D8GVGL600.html (last visited April 27, 2006). See also the above discussion of the history of vaccination.
[70] Mission Statement of Vaccination News website, supra note 66.
[71] See, e.g. , Ross D. Silverman, “No More Kidding Around: Restructuring Non-Medical Childhood Immunization Exemptions to Ensure Public Health Protection,” 12 Annals Health L. 277, 278-79 (2003).
[A]s risks of contracting many deadly and crippling diseases continue to decline to near negligible levels, and rates of childhood immunization continue to reach record levels, the public today places greater attention on the relative weaknesses and dangers of immunizations, and the systems through which they are administered.
[72] Hodge and Gostin, supra note 4, at 874.
[73] Usually this requires physician certification. Id.
[74] Indeed, the CDC itself presupposes the existence of medical exemptors in any broad mandatory vaccination program. See “Six Common Misconceptions,” supra note 10 (noting that the mandatory vaccination program can work to protect even those few who cannot vaccinate because of the possibility of adverse medical reactions).
[76] Hodge and Gostin, supra note 4, at 874.
[77] Jacobson v. Massachusetts , 197 U.S. 11 (1905). See also Employment Division v. Smith , 494 U.S. 872 (1990) (permitting neutral laws of general applicability that incidentally affect religion); Boone v. Boozman , 217 F.Supp.2d 938 (E.D. Ark. 2002) (“constitutionally-protected free exercise of religion does not excuse an individual from compulsory immunization...the right to free exercise of religion and parental rights are subordinated to society’s interest in protecting against the spread of disease”).
[78] W. Va. Code Sec. 16-3-4 (2004).
[79] See, e.g. , Boone v. Boozman , 217 F.Supp.2d 938 (E.D. Ark. 2002). The challenged Arkansas immunization statute exempted “individuals for whom ‘immunization conflicts with the religious tenets and practices of a recognized church or religious denomination of which [they are] an adherent or member.’” The statute was struck down under the Establishment Clause using the test laid out in Lemon v. Kurtzman , 403 U.S. 602 (1971). 217 F.Supp.2d at 950. The Arkansas legislature subsequently amended the exemption generally to allow for religious or philosophical objections without regard to recognized churches. Ark. Code Sec. 6-18-702(d).
[80] See Silverman, supra note 71, at 290-93.
[81] See id.
[82] Hodge and Gostin, supra note 4, at 874.
[83] Cal. Health and Safety Code Sec. 120365 (2003).
[84] Silverman, supra note 71, at 284.
[85] Id. at 285.
[87] See id.
[88] Recall that for those unable to vaccinate for medical reasons, herd immunity provides the only protection from the disease. See “Six Common Misconceptions,” supra note 10.
[89] Silverman, supra note 71, at 285.
[90] Id. The recent mumps outbreak may directly demonstrate this. Officials have pointed out that vaccination only confers immunity on 95% of patients, and of those affected in the recent outbreak, 25% have been vaccinated. See Pitt, supra note 69. The strong implication is that the 75% of those inflicted who were not vaccinated have put the entire community at risk.
[91] Center for Disease Control, National Immunization Program publication, “What Would Happen If We Stopped Vaccinations?” at http://www.cdc.gov/nip/publications/fs/gen/WhatIfStop.htm (last visited April 27, 2006).
[92] Silverman, supra note 71, at 293.
[93] Silverman suggests that eliminating philosophical and religious exemptions would do more harm than good. This approach, he believes, “would exacerbate feelings of animosity and skepticism toward vaccination and the public health system in general.” Id. at 293. On this score he is probably correct, and I agree that wider knowledge, at the very least, is a better initial response to this problem.
[94] Incidentally, it is worth mentioning that of the more longstanding vaccines, the tetanus vaccine stands out as unique. Tetanus is a very harmful disease with about a 20% fatality rate. “What Would Happen If We Stopped Vaccinations?” supra note 91. What makes it unique in the vaccine schedule is that tetanus is not contagious. That is, herd immunity is not attainable and cannot be used to justify mandatory tetanus vaccination. The reason for the general acceptance of the tetanus vaccine seems to stem both from the high risk of the disease and the fact that tetanus can only be prevented by immunization. In addition, the tetanus vaccine for infants has been combined with the vaccines for diphtheria and pertussis. On strictly public health grounds, however, the status of the tetanus shot on the compulsory vaccination schedule comes closest to government fiat of individual health decisions.
[95] Because medical risks may vary from vaccine to vaccine, and thus the justification for such exemptions remains even if the risk is to some but not all vaccines, medical exemptions are somewhat outside the scope of this discussion.
[96] Sean Coletti, Taking Account of Partial Exemptors in Vaccination Law, Policy, and Practice , 36 Conn. L. Rev. 1341, 1344 (2004).
[98] This follows directly from the all-or-nothing nature of the vaccination decision in this world.
[99] Again, this follows directly from the nature of the decision.
[100] See, e.g. , National Vaccine Information Center, at http://www.nvic.org (last visited April 27, 2006) (urging parents to consider eight questions before vaccinating, none of which inform parents of the effect their decision may have on others).
[101] See “Six Common Misconceptions,” supra note 10.
[102] 42 U.S.C. §§ 300aa-1 to 300aa-34.
[103] U.S. Food and Drug Administration, Center for Biologics Evaluation and Research, “Vaccine Product Approval Process,” updated July 27, 2002, at http://www.fda.gov/cber/vaccine/vacappr.htm (last visited April 27, 2006) (hereinafter “Vaccine Product Approval Process”).
[104] See id.
[105] See, e.g. , Isadora Stehlin, “How FDA Works to Ensure Vaccine Safety,” FDA Consumer magazine (December 1995), at http://www.fda.gov/fdac/features/095_vacc.html (last visited April 27, 2006).
[106] “Licensing of a vaccine is only the beginning of FDA’s oversight.” Id.
[109] “Vaccine Product Approval Process,” supra note 103.
[112] Stehlin, supra note 105.
[115] Id. ; “Vaccine Product Approval Process,” supra note 103.
[116] Stehlin, supra note 105.
[118] “Vaccine Product Approval Process,” supra note 103.
[121] Id. ; Stehlin, supra note 105.
[123] Indeed, the National Immunization Program has confidently pointed to the FDA’s role in continued oversight of vaccines:
FDA would recall a lot of vaccine at the first sign of problems. There is no benefit to either the FDA or the manufacturer in allowing unsafe vaccine to remain on the market. The American public would not tolerate vaccines if they did not have to conform to the most rigorous safety standards. The mere fact that a vaccine lot [is] still in distribution says that the FDA considers it safe.
“Six Common Misconceptions,” supra note 10.
[124] “Vaccine Product Approval Process,” supra note 103.
[127] Stehlin, supra note 105.
[128] So states Susan Ellenberg, Ph.D., director of CBER’s division of biostatistics and epidemiology. Id.
[129] “Vaccine Product Approval Process,” supra note 103.
[130] Stehlin, supra note 105.
[136] See, e.g. , “Six Common Misconceptions,” supra note 10 (“[o]nly some of the reported health conditions are side effects related to vaccines. A certain number of VAERS reports of serious illnesses or death do occur by chance alone among persons who have been recently vaccinated”).
[137] “VAERS reports have many limitations since they often lack important information, such as laboratory results, used to establish a true association with the vaccine.” Id.
[138] “In summary, scientists are not able to identify a problem...based on VAERS reports alone without scientific analysis of other factors and data.” Id.
[139] U.S. Food and Drug Administration, Center for Biologics Evaluation and Research, “Thimerosal in Vaccines,” at http://www.fda.gov/Cber/vaccine/thimerosal.htm (last updated Sept. 6, 2005).
[141] See, e.g. , Gardiner Harris and Anahad O’Connor, “On Autism’s Cause, It’s Parents vs. Research,” New York Times, June 25, 2005, at http://www.nytimes.com/2005/06/25/science/25autism.html (last visited April 27, 2006) (reporting the ongoing tension between parents of autistic children and the medical community over the use of thimerosal in vaccines).
[142] See, e.g. , Center for Disease Control, National Immunization Program publication, “Mercury and Vaccines (Thimerosal),” at http://www.cdc.gov/nip/vacsafe/concerns/thimerosal/default.htm (last visited April 27, 2006) (studies have failed to find any association between exposure to thimerosal in vaccines and autism); “On Autism’s Cause, It’s Parents vs. Research,” supra (noting that the amount of ethyl mercury in each childhood vaccine was once about the same as the amount of methyl mercury, a more toxic compound, found in an average tuna sandwich).
[143] “Thimerosal in Vaccines,” supra note 139.
[146] Stehlin, supra note 105.
[149] “On Autism’s Cause, It’s Parents vs. Research,” supra note 141.
[150] “Thimerosal in Vaccines,” supra note 139; see also “On Autism’s Cause, It’s Parents vs. Research,” supra note 141 (“[b]y 2001, no vaccine routinely administered to children in the United States had more than half a microgram of mercury – about what is found in an infant’s daily supply of breast milk”).
[151] “Autism and Vaccines: Activists Wage a Nasty Campaign to Silence Scientists,” Wall Street Journal editorial, February 16, 2004, at http://www.opinionjournal.com/forms/printThis.html?id=110004700 (last visited April 27, 2006).
[152] “On Autism’s Cause, It’s Parents vs. Research,” supra note 141.
[153] Indeed, one recent study has suggested that neurological disorders have decreased with the removal of thimerosal from most vaccines. See David A. Geier and Mark R. Geier, “Early Downward Trends in Neurodevelopmental Disorders Following Removal of Thimerosal-Containing Vaccines,” 11 J. Am. Physicians and Surgeons 8 (2006). This study should be taken with a grain of salt, however, as the Geiers are widely known thimerosal critics. Years before this study, Dr. Mark Geier called thimerosal use in vaccines the world’s “greatest catastrophe that’s ever happened, regardless of cause.” “On Autism’s Cause, It’s Parents vs. Research,” supra note 141. A witness in many vaccine cases, a judge once ruled that he was “a professional witness in areas for which he has no training, expertise and experience.” Id. Scientists have criticized his prior studies and even called his methods “voodoo science.” Id.
[155] See id.
[156] See “The Politics of Autism: Lawsuits and Emotion vs. Science and Childhood Vaccines,” Wall Street Journal editorial, Dec. 29, 2003, at http://www.opinionjournal.com/forms/printThis.html?id=110004487 (last visited April 27, 2006) (characterizing the position of thimerosal critics as “scientifically untenable”).
[157] See generally “On Autism’s Cause, It’s Parents vs. Research,” supra note 141.
[161] “The Politics of Autism,” supra note 156.
[162] Id. ; “Study: Autism Rise from Labeling, Not Epidemic,” April 3, 2006, at http://www.cnn.com/2006/EDUCATION/04/03/health.autism.reut/index.html (last visited April 27, 2006) (noting rise in diagnosed cases of autism since 1994 is correlated with fall in diagnosed cases of mental retardation and learning disabilities).
[163] The Politics of Autism,” supra note 156.
[164] See, e.g. , “Six Common Misconceptions,” supra note 10 (noting that many anti-vaccine publications claim vaccines are unsafe on the basis of sheer numbers of reports to VAERS without noting that many of them may not represent actual vaccine side-effects).
[165] National Vaccine Information Center, “The Vaccine Injury Compensation Program,” at http://www.909shot.com/Issues/Comp_Summary.htm (last visited April 27, 2006).
[166] Center for Disease Control, National Vaccine Program Office, Vaccine Fact Sheets, “National Vaccine Injury Compensation Program,” at http://www.hhs.gov/nvpo/factsheets/fs_tableIV_doc1.htm (last visited April 27, 2006).
[167] See National Vaccine Injury Compensation Program, at http://www.hrsa.gov/vaccinecompensation/ (last visited April 27, 2006).
[169] The Andy Griffith Show: The County Nurse (CBS television broadcast, March 19, 1962).
[177] Id. That is, there will be a high probability of death.
[179] See the discussion above in Part I of this paper.
[180] For example, she begs Rafe to consider his family and what his decision could mean to them. She literally appears to be on the verge of tears as he refuses.
[181] In utilizing the theoretical framework of economic analysis, it is useful to keep in mind a few foundational concepts. First, a policy or program (in this case mandatory vaccination) is desirable if the overall benefit to society as a whole outweighs the cost of the program, where benefits and costs include both monetary and non-monetary factors. Second, individuals making rational choices regarding vaccination will vaccinate when the benefits of vaccination outweigh the risks or costs of non-vaccination to the individual. This decision-making process can be skewed by externalities, such as an unforeseeable decrease in the effectiveness of a vaccine due to a reduction in vaccination by others unknown to the individual at the time of the decision.
[182] 197 U.S. 11 (1905).
[183] Id. at 12.
[185] Id. at 13, 22.
[186] Id. at 36.
[187] Id. at 12.
[188] As the CDC itself explains, “[e]ven one serious adverse effect in a million doses of vaccine cannot be justified if there is no benefit from the vaccination.” “Six Common Misconceptions,” supra note 10.
[189] In Japan in the 1970s, for instance, pertussis vaccination coverage fell from 80% to 20%, leading to an outbreak in 1979 resulting in 13,000 cases and 41 deaths. “What Would Happen If We Stopped Vaccinations?” supra note 91.
[190] Judge Richard Posner has suggested that this difference between sexually transmitted diseases and air- and water-borne diseases may imply a lesser imperative to eliminate sexually transmitted diseases:
[T]he externality created by sexually transmitted diseases is smaller than in the case of other contagious diseases. Sexually transmitted disease is spread primarily by voluntary contact, implying (to the economist) that a person is compensated...for assuming the risk of contracting the disease. Hence the number of cases of sexually transmitted diseases may be closer to the optimum than in the usual air-borne or water-borne or insect-borne epidemics.
Posner, Economic Analysis of Law 162. (6th Ed. 2003).
[191] Additionally, if vaccination rates are high, these individuals may assume that those in society who have already made the choice to vaccinate have performed a similar cost-benefit analysis. These individuals choose to vaccinate based simply on vaccination rates in the community. See John C. Hershey et al., The Roles of Altruism, Free Riding, and Bandwagoning in Vaccination Decisions , 59 Organizational Behavior and Human Processes 177, 178 (1994).
[192] See, e.g. , id. (behavioral survey studying various factors individuals use to make vaccination decisions).
[194] See id. at 178 (“[i]f a patient believes vaccination is in his own best interests, then he has two reasons to vaccinate. One is selfish, in that he will improve his own well being. The other is altruistic, in that he can improve the health prospects of those around him who might otherwise become infected if he is not vaccinated himself”).
[195] The concept of herd immunity is discussed in Part I. Note that “[i]n economic terms, herd immunity is a positive externality of vaccination. Altruistic individuals who recognize and value this externality may undergo vaccination partly to help others in addition to themselves.” Id. See also Berger, supra note 29 (“‘[h]erd immunity’...is the concept that not everybody in a population has to be immunised to protect everyone in that population. As long as a sufficient number of children are immunised against each disease for which there is a vaccine, protection against that disease will be conferred on everybody”).
[196] The CDC has pointed to this as one of the two most important reasons to vaccinate:
There is a small number of people who cannot be vaccinated (because of severe allergies to vaccine components, for example), and a small percentage of people don’t respond to vaccines. These people are susceptible to disease, and their only hope of protection is that people around them are immune and cannot pass disease along to them. A successful vaccination program, like a successful society, depends on the cooperation of every individual to ensure the good of all.
[197] In economic terms, “[w]idening vaccine use decreases each individual’s benefit from being vaccinated, but leaves unchanged each individual’s risk from the vaccination itself.” Hershey, supra note 191, at 178.
[198] “Six Common Misconceptions, supra note 10.
[199] Hershey, supra note 191, at 178.
[200] Suppose, for sake of example, that a vaccination program, if implemented, would save ten lives out of a thousand that would otherwise have perished without the program. Unfortunately, the vaccine will randomly cause death to five persons out of a thousand. From an ex ante perspective, the vaccination program should be implemented as it will save five lives overall. Concerns or complaints from those five persons who die (or their estates) represent ex post objections, and, though unfortunate, should not affect evaluations of the soundness of the program.
[201] This mathematical explanation is a slight variation of that found at CDC, “Six Common Misconceptions,” supra note __.
[202] Note that no vaccine is 100% effective, and vaccination efficacy rates for most childhood vaccinations range from 85 to 95%. Id. As stated in an earlier section, herd immunity is relied upon to protect those who do not develop full immunity from the vaccine.
[203] Given that these particular vaccines are already on the schedule, I think it would be unwise to remove them now. My analysis applies to comparable vaccines that may arise in the future – vaccines for those communicable diseases that do not pose relatively significant health risks. The definition of such diseases, of course, would be a matter of debate. Vaccines for noncommunicable diseases like ear infections would also fall within this rubric.
[204] Statement of Barbara Fisher, quoted in Ostrom, supra note 56.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 23 March 2021
Vaccination strategies against COVID-19 and the diffusion of anti-vaccination views
- Rafael Prieto Curiel ORCID: orcid.org/0000-0002-0738-2633 1 &
- Humberto González Ramírez ORCID: orcid.org/0000-0002-3988-534X 2
Scientific Reports volume 11 , Article number: 6626 ( 2021 ) Cite this article
24k Accesses
65 Citations
66 Altmetric
Metrics details
- Applied mathematics
- Risk factors
Misinformation is usually adjusted to fit distinct narratives and propagates rapidly through social networks. False beliefs, once adopted, are rarely corrected. Amidst the COVID-19 crisis, pandemic-deniers and people who oppose wearing face masks or quarantine have already been a substantial aspect of the development of the pandemic. With the vaccine for COVID-19, different anti-vaccine narratives are being created and are probably being adopted by large population groups with critical consequences. Assuming full adherence to vaccine administration, we use a diffusion model to analyse epidemic spreading and the impact of different vaccination strategies, measured with the average years of life lost, in three network topologies (a proximity, a scale-free and a small-world network). Then, using a similar diffusion model, we consider the spread of anti-vaccine views in the network, which are adopted based on a persuasiveness parameter of anti-vaccine views. Results show that even if anti-vaccine narratives have a small persuasiveness, a large part of the population will be rapidly exposed to them. Assuming that all individuals are equally likely to adopt anti-vaccine views after being exposed, more central nodes in the network, which are more exposed to these views, are more likely to adopt them. Comparing years of life lost, anti-vaccine views could have a significant cost not only on those who share them, since the core social benefits of a limited vaccination strategy (reduction of susceptible hosts, network disruptions and slowing the spread of the disease) are substantially shortened.
Similar content being viewed by others
Evolution of resistance to COVID-19 vaccination with dynamic social distancing
COVID-19 vaccination strategies depend on the underlying network of social interactions

Modelling the effects of social distancing, antiviral therapy, and booster shots on mitigating Omicron spread
Introduction.
Major disruptions have been suffered at all social levels due to the COVID-19 pandemic. With over 10,000 daily confirmed casualties directly related to the virus during December 2020, and an increase of deaths related to other illnesses due to weakened healthcare systems 1 , it will be among one of the leading causes of death of 2020 and it will have long-lasting economic and social consequences. Surveys conducted in heavily affected cities suggest that a small part of the population has acquired COVID-19 antibodies 2 , implying that we are far from reaching herd immunity through natural infection 3 . Furthermore, considering a conservative infection fatality ratio and an optimistic herd immunity threshold, several thousand casualties would still be suffered 3 . With many vaccines already approved, the biggest and most ambitious vaccination campaign in history has already begun.
The production and mass distribution of a COVID-19 vaccine will still be a major challenge. For example, Robert Redfield, the Director of the US Centers for Disease Control and Prevention (CDC), mentioned on a US Senate hearing (September 16th, 2020) that he expects that with the availability of the vaccine the US public will return to their “regular life” around the third quarter 2021 4 . In most parts of the world, mass immunisation will not happen any time soon, and therefore, a targeted vaccination will be a key element to optimise the limited number of vaccines and to mitigate the impacts of the pandemic. Under this scenario, unvaccinated individuals will still benefit from the immunity of those vaccinated, since the reduction of susceptible hosts limits the spread of the disease 5 . Considering the global demand for the vaccine, distinct vaccination strategies, prioritising population groups with higher exposure to the virus or higher risk of severe disease or death, will be a key policy, particularly during the early stages of the vaccine distribution.
Beyond the limitations related to the logistics of the vaccine, opposition to vaccination will become central to any strategy for coping with the pandemic. Already for COVID-19, the use of a non-invasive item such as the mask has been highly polarising and rejected by some groups, and protests and demonstrations around the world against the responses to the pandemic are frequent. Anti-lockdown protesters and conspiracy theorists have already demonstrated against the possibility of a mandatory vaccine, as is the case with pandemic sceptics and so-called “anti-vaxxers” in London 6 , whilst some conspiracy theorists burned 5G towers in the United Kingdom 7 . A survey conducted in 27 countries indicates that 1 in 4 people would not get a COVID-19 vaccine due to concerns about side effects and doubts about its effectiveness 8 , and another survey suggests that around half of the population would rather let others receive the vaccine first 9 , which could indicate both fears and solidarity with others. Also, some people fear more a mandatory vaccine for COVID-19 than the virus itself 10 . Vaccine opposition views have already reduced vaccination coverage in some places, causing the re-emergence of previously controlled diseases 11 , as happened for measles in 2019 12 . Anti-vaccination views offer a wide range of narratives, such as safety concerns, conspiracy theories and the use of alternative medicine, and it has been predicted that these views could dominate in a decade 13 . Different narratives about the virus itself 14 and against the vaccine would friction vaccination strategies, which could greatly influence their coverage and the time needed to eliminate transmission 15 .
Either because of logistic restrictions or because people refuse to be vaccinated, strategies in which some people—perhaps a small percentage—are immunised, need to be considered in order to reduce the impacts of the pandemic. Here, we consider a network-based population model and five vaccination strategies varying the proportion of the population that has received the vaccine. A modified version of the SIR model, SVIR (due to the existence of the Vaccine) is used to detect the long-term behaviour of a pandemic, where the efficiency of each vaccination strategy is measured using the years of life lost and the time to eliminate transmission. Simulating the evolution of the pandemic under different network topologies allows us to compare vaccination strategies and detect successful immunisation strategies. Using a similar technique, we consider the dispersion of anti-vaccination views on a network, which pass through individuals with a certain level of persuasiveness . Assuming that all individuals are equally likely to adopt anti-vaccination views after being exposed to them, we demonstrate that individuals who are central in the network are much more likely to adopt these views. Considering that individuals who share anti-vaccination views will refuse a vaccine, we quantify the burden that anti-vaccination narratives have on optimal vaccination strategies.
Modelling vaccination and anti-vaccination views on a network
Dealing with non-universal vaccination.
Vaccinations changed our health and quality of life dramatically. Yearly cases of measles, mumps, or smallpox decreased by more than 98% since introducing a vaccine 5 . Formerly fearsome diseases are now rare in many parts of the world thanks to vaccination programs 11 . Yet, due to a limited number of vaccines, their cost, views against vaccines and many more reasons, including the fact that with more vaccines, the spreading of a virus slows down, which in turn, tends to discourage more people from participating in the vaccination campaign 16 , universal vaccination is almost impossible. Thus, understanding the impact of limited vaccination is critical, as it plays a relevant role during the COVID-19 pandemic.
Vaccination strategies have two core objectives: lower and delay the peak size (“flattening the curve”) and reduce the final infected population to limit morbidity 17 . There are, however, many challenges for designing a vaccination strategy. Deaths can be prevented by first targeting highly vulnerable populations 3 (such as elderly people, with severe morbidity, or vulnerable communities, including prison and homeless populations 18 ). Yet, targeting vulnerable populations might not reduce the viral circulation and might not reduce the final infected population, particularly if the targeted population has limited social contacts. Another strategy is to target highly exposed people, such as health-care workers or with frequent social contacts, as it could slow down the overall exposure to the virus. Other strategies, for instance, targeting young people (as more years of life are saved with each vaccine) or random individuals (as means of some distributive fairness) could also be proposed for a variety of reasons. Thus, the relevance of being able to compare the expected outcomes of different vaccination strategies.
Modelling immunisation in a population
One of the first mathematical models in epidemiology was concerned with immunisation. In 1760, Daniel Bernoulli predicted the impact of immunisation with cowpox upon the expectation of life of the immunised population 19 . Since then, many models of immunisation have been constructed. Remarkably, the Susceptible, Infected and Recovered (SIR) compartments model proposed in 1927 by William Ogilvy Kermack and Anderson Gray McKendrick 20 has been extended for the application of a vaccine (SVIR) 17 , 21 , 22 , 23 , 24 .
Nearly 100 years ago, the lack of computational power meant that dealing with a high number of variables was nearly impossible and obtaining numerical results was very costly and so compartmental models in epidemiology were translated, under many assumptions, into differential equations. Algebraic solutions were more accessible than numerical results and gave rudimentary insights into the general behaviour of the dynamics of the disease 25 . For instance, this basic model can provide us with a rough idea of the number of individuals that would need to be infected to achieve herd immunity 18 . In the case of a vaccine, it was showed that uniform vaccination is always less effective than targeted vaccinations, and the optimal strategy involves vaccinating specific individuals first 26 .
Many of the implications of the SIR and the SVIR models rely on simplifying assumptions, such as an homogeneous population mixing and uniform recovery rate. In recent years, thanks to the gain of computational power and the development of specific tools and frameworks, some of these assumptions have been relaxed, particularly assuming an homogeneous population with homogeneous contacts. The use of networks in epidemiology is a powerful tool to relax both as tagged nodes allow considering disease dynamics for heterogeneous population groups 27 , and different distribution of the edges allows considering distinct types of contacts. For example, in the case of a sexually transmitted infection, the sexual partnership network is a natural framework for modelling the disease 28 . The contact network among people is frequently modelled as a strongly connected small-world-like graph 29 , 30 , meaning that the path in the network needed to connect any two nodes is rather small, or with many short-cut connections 31 , with a well-defined scale for the degree distribution of the number of contacts of each node 32 . The network structure has a major impact on the spread of infectious diseases and therefore, on successful vaccination strategies 5 , 28 , 33 , 34 . The basis of the disease models on a network is a compartments model (as with the SIR and SVIR model), but minor changes on the network’s connectivity might alter results significantly. Furthermore, the network structure appropriate for a given setting not only depends on the structure of the contacts of the population (which likely changes over time) but on the infection itself 28 .
Designing successful immunisation strategies need to consider the inhomogeneous connectivity properties of the network 35 . An infected person, even with a reduced number of contacts, can pass the virus between separate clusters, particularly if any of such contacts is a short-cut connection in the network 32 . On a small-world network, all individuals, even if they have a small number of contacts, are within a few infections to be infected themselves. On a different network structure, some nodes (often called “hubs”) have many more connections than others, and the network as a whole has a power-law degree distribution, as in the case of the network of sexual contacts, which exhibits scale-free features 35 , referred to as a scale-free network 36 . On a scale-free network, uniform vaccination is always less effective than targeted vaccination 28 . Scale-free networks are resilient to a few disconnections but are strongly affected by selective node damage. If a few of the most connected nodes are removed, the infection suffers a substantial reduction in its ability to propagate 35 . Control programs should be targeted towards the highly connected nodes, and such programs will be much more effective than those that target nodes at random 37 .
These strategies, however, assume that all individuals would accept the vaccine if offered. A targeted vaccination towards the most connected nodes will be highly ineffective if, for any reason, some of the central nodes refuse a vaccine. The impact of those who reject a treatment has been analysed among distinct demographic groups 15 , showing that non-adherence to a treatment, such as a vaccine, can greatly influence the needed coverage to eliminate transmission. In the case of network structures, the impact of non-adherence has not been explored, and it is likely to play a significant role during the COVID-19 vaccination program.
Opinion dynamics and anti-vaccination views
An idea or an opinion, such as views in favour or against a vaccine, is transmitted—frequently as an intentional act—from one person to another 38 . Through distinct types of interactions, people want to persuade others to adopt an opinion 39 . The views of others might have an impact on individual beliefs 40 who update their own opinion. Different ways to model, not only different perceptions or ideas but to also the updating process of those ideas—obtained through interactions with others or with some externalities—aim at capturing why opposing views (which could be the acceptance of a vaccine), can emerge and co-exist in a society, even if all individuals try to reach a consensus.
Opinion dynamics has been modelled through a variety of angles and techniques, for instance, kinetic models of opinion formation 41 , mean-field analysis, which usually leads to a system of differential equations 42 , agent-based models and even epidemiological models 38 . Frequently, two opposing opinions are assigned to the extremes of an interval, say, \([-1,1]\) , individual opinions are modelled as a number s in that interval, according to the position with respect to the two opinions, and through interactions, individuals have some compromise (opinions get closer) and other elements, such as memory loss 43 , the presence of leaders 42 , the ability to convince others with a different opinion 44 , varying levels of assertiveness 45 , the fact that more extreme opinions are more difficult to change 46 . Also, confrontation with distinct views and opinions does not happen at random. Either because of the dynamic process through which opinions are updated 44 , or because of preferential interactions, people tend to be surrounded by others with similar views 45 .
As in the diffusion of a virus, different network structures are a natural framework to analyse opinion dynamics. Ideas and opinions tend to propagate on a network between adjacent nodes 47 . For instance, opinion leaders, who have a greater impact, can be the hubs of the social (scale-free) network 42 , whereas the distribution of online contents can pass through highly connected nodes on a (small-world) network 48 . The results observed of complex opinion dynamics are that a population might have relevant levels of polarisation or fragmentation 49 , people tend to have more interactions with others with similar views, so they are more frequently exposed to the information that aligns to their values (confirmation bias) 48 . Users tend to aggregate in communities of interest, which causes reinforcement and fosters confirmation bias, segregation, and polarisation and leads to the proliferation of biased narratives fomented by unsubstantiated rumours, mistrust, and paranoia 48 . Existent communities adopt new narratives and work as echo chambers, limiting the information their members receive to what they agree with and discarding contradicting points of view, thus reinforcing their beliefs. Moreover, repeated exposition to similar content increases the chances of believing it, even when its plausibility is low 50 . For example, it was detected that political ideology predicts perceptions of COVID-19 threat 51 .
Massive misinformation is becoming one of the main threats to our society 12 , 48 and they have rapidly become central in terms of COVID-19 52 . Already for COVID-19, most of the misinformation detected involves reconfigurations, where existing (often true) facts are twisted or adjusted to fit different narratives 53 . With a vaccine for COVID-19, opposing views towards immunisation will become the crucial element, especially if the propagation of the virus itself and if vaccination strategies are, in any way, entangled within the network of individuals who refuse it.
Anti-vaccination views
Opposition to vaccination is as old as vaccines themselves. The reasons behind anti-vaccine views are diverse, including religious 54 and political beliefs 55 , as well as concerns about their safety and effectiveness, that are often based on misinformation. Perhaps, the most cited case in the last decades is the theory that falsely links autism in children with the MMR vaccine, a theory that has been debunked by several studies 56 , but that is still used as an argument against vaccination by some groups. The origin and motivation behind fake narratives are often unclear, but they usually create a certain panic in the readers and encourage action, such as sharing the “news” with family and friends 57 . Perceived altruism and solidarity with others is one of the main reasons people share unverified and often fake content 52 , 58 . Vaccine safety concerns receive more public attention than vaccination effectiveness 11 . People share false claims about COVID-19 and its vaccine since it is often difficult to detect whether some content is accurate 59 .
According to a 2018 study in 140 countries 60 , 79% of the global population perceive vaccines as safe, and 84% as effective. However, these percentages vary greatly from region to region, representing less than two-thirds of the population in some areas, especially Europe. And, in the case of a COVID-19 vaccine, a study published in August 2020 in 27 countries found that nearly one in four adults would not get a vaccine for COVID-19 8 and in some countries, more than half of the population would not get it, including Poland and France. The main reasons cited for not taking the vaccine were adverse secondary effects and doubts about its effectiveness. Misinformation, amplified by social networks, have eroded the public confidence on vaccination, causing an increase in the number of outbreaks of diseases that were already controlled, as happened for measles in 2019 13 .
Currently, there are still some critical questions concerning the COVID-19 vaccines. Still, we do not know whether the immunisation of a vaccine would wane over time and so how long the acquired immunity would last 18 . Even with a vaccine, if reinfection could occur, persistent herd immunity may never be attained, which then could lead to cyclic outbreaks and cyclic vaccination 18 , 61 . Finally, we do not know if a sufficiently large population would reject the vaccine delaying even more the process of obtaining herd immunity.
A population of N individuals is constructed with two attributes: current age (or simply age) and age at death (or simply death). Both age and death are sampled from a scaled Beta distribution: \(100Beta(\alpha _a, \beta _a)\) with \(\alpha _a =2\) and \(\beta _a= 3\) for age, and \(100Beta(\alpha _d, \beta _d)\) with \(\alpha _d =5\) and \(\beta _d= 2\) for age at the moment of death 62 . Individuals with death smaller than age are resampled, resulting in a simulated population with a median age of nearly 35 years and a median age at the moment of death of 75 years (close to the median age and expected life in Mexico City).
Three network topologies are considered, where the nodes represent the individuals and the edges their contacts, either concerning their vaccine views or their physical contacts, so they might pass the virus between them. Firstly, a proximity network, where nodes are located randomly on a square and pairs at a distance smaller than a certain threshold d are connected. The proximity network tends to have a large network diameter since nodes only contact others located nearby. Secondly, a small-world network with a rewiring probability r . The small-world network has shortcuts between the nodes, meaning that the network diameter is much smaller than the proximity network. Thirdly, a scale-free network with power p . The scale-free network has “hubs”, meaning some nodes with a much larger number of adjacent neighbours. The three networks have the same average node degree so that between different topologies, only the structure of the network is altered. Although very young or elderly people tend to have fewer contacts, we construct age and network independently, for simplicity.
An SVIR model is constructed in the network as follows. Firstly, some randomly-selected nodes are infected, and the rest of the nodes are susceptible. After the initial infection process, a percentage \(\nu\) of the individuals are vaccinated, called the vaccination rate . If the individual is susceptible, she or he gains permanent immunity and is no longer capable of passing the virus, but if the person was already infected, the vaccine does nothing (a scenario which could happen for individuals who are asymptomatic and receive a vaccine). Each time step, which could be considered a day, susceptible individuals in contact with an infected person are also infected, with probability \(\pi\) . When a node is infected, it is moved to the recovered state after \(\tau\) steps, counting from the moment of infection. A recovered node no longer passes the virus to others. The process stops when the population has no infected nodes, and that time is noted as T , i.e., T is the duration of the epidemic. See the Appendix for more details on the parameters of the model.
After infection, some of the individuals who “recover” might not survive. It has been noted that, in the case of COVID-19, lethality increases with age. For simplicity, we consider a linear impact of age, so that a person with age y years does not survive with a probability of \(\phi y\) , for some \(\phi >0\) . The average number of years of life lost due to the pandemic, denoted by D , is computed as the sum of the number of years that people who passed away lost (that is, their death minus their current age), divided by the population size N .
Vaccination strategies
Five vaccination strategies, based on targeting people by their age or their position on the contact network, are considered. For the proportion \(\nu\) of individuals receiving the vaccine:
Degree —target the top \(\nu\) nodes with a higher degree. More connected nodes receive the vaccine first.
Centrality —vaccinate the top \(\nu\) nodes with the highest node betweenness.
Peripheral —apply the vaccine to nodes with the lowest node betweenness.
Age —vaccinate the top \(\nu\) nodes with highest age (elderly population) first.
Random —select a portion \(\nu\) of the individuals at random.
The first three strategies (Degree, Centrality and Peripheral) are based on network attributes, meaning that nodes are sorted depending on their degree or the node betweenness and the top \(\nu\) nodes are vaccinated. The Age strategy is based on node attributes (their age), and the last strategy (Random) uses no information about the nodes.
Even though the vaccination strategies (in the case of the COVID-19) differ by country, they are mainly based on prioritising vulnerable groups, defined as those with significantly higher risk of severe disease or death, and those with high risk of contracting and transmitting the virus. The first group comprises elderly and adults with comorbidities; the second, health and education workers, as well as low-income persons living in dense urban neighbourhoods for which social distancing is difficult 63 , 64 . Three of the strategies that we test try to emulate the above vaccination guidelines. We identify the Age strategy (elderly first), with the group of higher risk of severe disease, and the Degree and Centrality strategies (prioritising people with many contacts or high betweenness centrality) with the group of population with a high risk of infection and transmission. It is worth mentioning that, in practice, individuals with a high degree can be identified by their activity (those with many contacts) but identifying those with high betweenness centrality is more complicated. For example, we could think of a university professor, who is in contact with several groups of students, or, at a larger scale, of individuals who make inter-city commute trips, thus acting as the bridge between different subnetworks. Finally, we define the Random and Peripheral strategies for comparison reasons since they are unlikely to be put into practice.
Comparing vaccination strategies
We consider two distinct metrics for comparing vaccination strategies. Firstly, from the population of N individuals from which a small group is initially infected, vaccines are applied according to some strategy, and the SVIR dynamic is simulated until no individuals are infected. From the recovered individuals, the casualties are simulated and the average number of years of life lost D is computed as the sum of the difference between death and age from individuals who passed away, divided by the population size N . Although it is possible to simply count the number of casualties, measuring instead the average years of life lost distinguishes between the death of an elderly person, with a reduced number of years to live and the death of a young person. A second metric to understand the impact of distinct vaccination strategies is the time needed for the dynamic to stop, T , i.e., the time after the population has no infected nodes. Both D and T are computed for a vaccination strategy and for a certain vaccination rate \(\nu\) , so that \(D_{Age}(\nu )\) and \(T_{Age}(\nu )\) are reported for the Age strategy with a vaccination rate of \(\nu\) , and likewise for other strategies.
For a given network and a fixed vaccination rate and a (non-random) strategy, results might vary for two reasons. Firstly, because the initial infected population is sampled from the population. Secondly, because of the transmission of the virus itself: susceptible individuals who are adjacent to an infected node are infected with a probability \(\pi\) on each time step, and so the progression of the virus might change between different realisations, even with the same initial conditions. For this reason, we simulate each vaccination strategy 500 times for different vaccination rates \(\nu\) and report the intervals which contain \(D_{S}(\nu )\) and \(T_{S}(\nu )\) for the different strategies S .
Here, we consider a perfect vaccine that grants permanent immunity, although, in reality, the level of antibodies of an immune person may drop below a critical threshold (waning immunity), which could take individuals back into being susceptible 19 , 23 .
Diffusion of anti-vaccine views
The diffusion process of anti-vaccine views plays a relevant role in the vaccination process and therefore, in the evolution and the burden of the pandemic. The social network is a crucial part of the diffusion process, as anti-vaccine views are spread through contacts, convincing other individuals of their views of the vaccine.
We construct a diffusion process on a network, similar to the SIR model, but for the adoption of an idea 38 as follows. Initially, all individuals are susceptible to anti-vaccine views, and some randomly selected individuals have already these views. Although some individuals could be considered more susceptible (for instance, those who engage more with social media 52 ), we assume that all individuals are equally susceptible. At each time step, individuals with anti-vaccine views share them with all their contacts. Individuals exposed for the first time to anti-vaccine views make a permanent decision based on the persuasiveness \(\theta\) of the ideas, where \(\theta \in [0,1]\) are the chances that an anti-vaccine view persuades the exposed individual. A small value of \(\theta\) means that most individuals are not convinced by anti-vaccine views and the opposite for a high value of \(\theta\) . Since we assume that the decisions of people are permanent, then on the first step, only the neighbours of those who initially share anti-vaccine views are exposed to them, then, at each time step, only the neighbours of individuals who were convinced on the previous step are exposed for the first time to anti-vaccine views and make a decision. On the second step, only the neighbours of individuals who were convinced on the previous step are then exposed to anti-vaccine views, and so on. Each time step, only the neighbours of individuals who were convinced on the previous step are exposed for the first time to anti-vaccine views and make a permanent decision. The dynamic stops when no new individuals are convinced of anti-vaccine views.
At the final stage of this dynamic, some individuals have anti-vaccine views, some have been exposed to anti-vaccine views but do not support them, and some individuals (potentially a large group or none, depending on the persuasiveness of \(\theta\) ) were never exposed to anti-vaccine views. We assume that only individuals who share anti-vaccine views reject a vaccine, and the rest, whether they were exposed or not to the views, will accept to be immunised if a vaccine is offered. A similar SIR model for the COVID-19 social media infodemic was constructed, although not based on a network, but based on the spreading parameters 65 .
Considering a scale-free network with \(N = 5000\) individuals and 250 infected individuals at time \(t = 0\) , targeted vaccinations yield drastically distinct results than a random vaccination strategy (Fig. 1 ). Applying the vaccine to central nodes not only protects them from receiving the virus, but also slows down its diffusion process, allowing nearby infected nodes to recover and stop passing the infection to others (as it has beenobserved previously 35 , 37 ). The final size of the recovered population varies considerably. For example, considering a random vaccination strategy with a proportion of immunised people of \(\nu = 20\%\) , a large part of the population would be infected at a point. With targeted vaccinations, the size of the infected population drops drastically, and therefore most of the individuals remain susceptible, even with the same (small) vaccination rate \(\nu = 20\%\) .
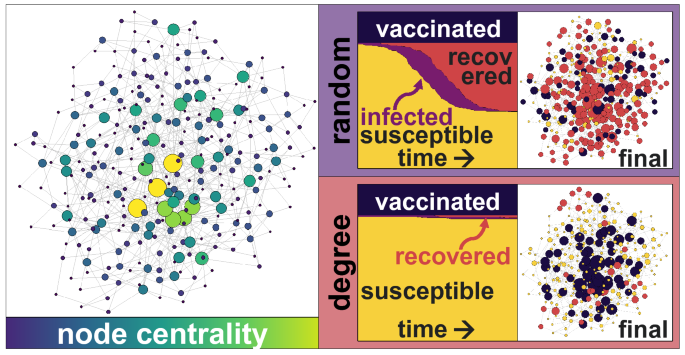
Schematic representation of a scale-free network with power \(p=1\) (left) with larger and brighter nodes displaying their node betweenness. The evolution of the SVIR model for the Random and Degree vaccination strategies (centre), with the same vaccination rate \(\nu = 20\%\) , shows that the majority of the population will remain susceptible under the targeted Degree vaccination strategy, but that a large part of the population will be infected and recovered under the Random strategy. The final state of the nodes (right) shows that many nodes are recovered (red) with a Random strategy, but most remain susceptible (yellow) with a Degree strategy.
Without a vaccine, the simulations show that the population expects to suffer up to 4.7 years of life lost due to the pandemic. With a universal vaccine, the loss is negligible. Yet, a Random vaccination strategy with rate \(\nu = 60\%\) has the same impact, in terms of life saved, than a Degree or Centrality strategy with \(\nu = 30\%\) . In a population in which some individuals are much more connected than others (a scale-free network), or one in which individuals are just a few nodes away from each other (a small-world network), targeting nodes with a high number of neighbours (Degree strategy) or nodes with a high betweenness (Centrality strategy) yields similar results in terms of the years of life saved (Fig. 2 top panel). On a proximity network, which has no nodes with a high number of neighbours or shortcuts, the life lost due to the pandemic is smaller as the virus propagates slower and among fewer nodes, nonetheless, a Degree strategy still reduces the burden of the pandemic, particularly if the vaccination rate is small (Fig. 2 ).
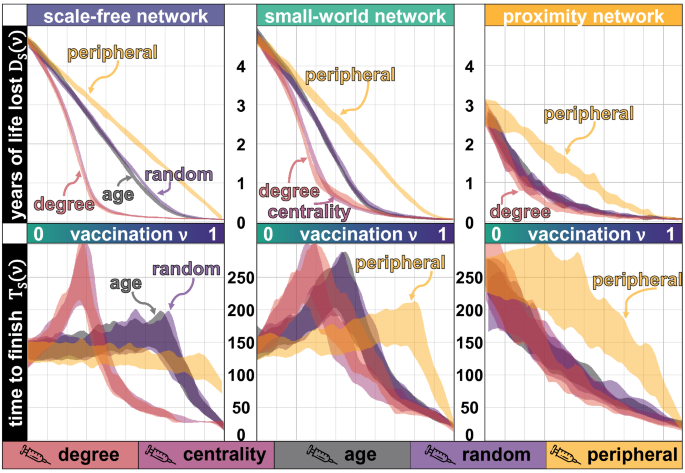
Years of life lost \(D_{S}(\nu )\) (vertical axis) for different vaccination rates \(\nu\) (in the top panel), and the corresponding time \(T_{S}(\nu )\) (vertical axis) with the same vaccination rate (in the bottom panel). Three network topologies are tested, a scale-free network in the left (with power \(p=1\) ), a small-world network in the middle (where the rewiring probability is \(r=0.1\) ) and a proximity network in the right, all networks with an average node degree of 6. Each strategy is simulated 500 times with \(N = 5000\) individuals, with a probability of infecting neighbouring nodes at each step of \(\pi =0.05\) and with a varying vaccination rate \(\nu\) . The lethality of the virus increases with \(\phi = 0.05\) , meaning that a person with y years does not survive after being infected with a probability of 0.05 y .
Surprisingly, targeting the most vulnerable population (in our model, elderly population, who are more likely to pass away after the infection) does not give better results in terms of the years of life lost than a random strategy, as it does not slow down the diffusion process of the virus as much as the Degree of the Centrality strategy. The Peripheral strategy gives the worst results in terms of the years of life saved, as it targets the nodes less capable of slowing down the virus’s diffusion or decreasing the number of deaths. The Age strategy does perform better than the Random strategy in terms of the number of casualties, but not in terms of the years of life lost. Measuring only casualties does not give sufficient information, and the demographics (age) of the population who passed away should be taken into account. The Age strategy targets individuals who are more likely to pass away, but it does not save much more years of life than the Random strategy, as it prevents casualties from people with a shorter remaining life expectancy, provided that the potential correlations between age and centrality are ignored. However, elderly people tend to have fewer contacts 3 , so targeting them with a low vaccination rate could imply some peripheral vaccination as well.
Vaccination, particularly with a low rate \(\nu\) , slows down the virus’s evolution, and thus it also slows down the time for the process to finish (Fig. 2 , bottom panel). Without vaccination, it takes around 130 steps for the virus to spread across the population and for them to recover. Applying a vaccine to the most connected or the most central nodes (Degree and Central strategy) prevents the virus from spreading to many nodes, however, it still moves through the network between less central nodes, taking up to twice as many steps for the pandemic to end, compared to the case with no vaccine. The Age and the Random strategy also friction the evolution of the virus and, therefore, it also takes longer for the pandemic to end. With Degree, Centrality, Age and even the Random strategy, applying the vaccine to only some individuals (more than half of the individuals in some cases) delays the end of the pandemic. Only if a very large part of the population gets vaccinated, the pandemic finishes faster than without any vaccine.
The Peripheral strategy on a scale-free network accelerates the end of the pandemic (with all vaccination rates), since it immunises individuals who would be infected last, as opposed to the case of a small-world network. On a small-world network, less connected nodes still pass the virus to their neighbours. Therefore, low vaccination rates delay the epidemic process, increasing the duration of the pandemic \(T_{S}(\nu )\) .
Notice that although the SVIR model is a dynamic process, it is based on a static network of individuals, meaning that no new connections are formed. However, if the vaccine process takes longer, it is likely that new contacts (more edges) are added to the network, with its possible implications in terms of the years of life lost \(D_{S}(\nu )\) and the time \(T_{S}(\nu )\) .
The topology of the network
The topology of the social network plays a relevant role in detecting the optimal vaccination strategy and its impacts on saving lives and speeding the pandemic process. Targeting the most central or the most connected nodes on a scale-free network rapidly decreases the years of life lost for some vaccination rates, but it is slightly less effective on a small-world network and has a limited impact on a proximity network, compared to other strategies.
Qualitatively speaking, except for the Peripheral vaccination strategy, a small-world and a scale-free network show similar results. Targeting the vaccine to the most central or the most connected nodes reduces the casualties, although, for low vaccination rates, it increases the time for the pandemic to end. Targeting the most vulnerable individuals (even assuming that they are as central or connected as other individuals, which might not be true) has an impact as reduced as the Random vaccination strategy and, for low vaccination rates, both will increase the time \(T_{S}(\nu )\) . When central nodes are removed through vaccination, fewer individuals will be infected, but the virus takes longer to propagate, so the time \(T_{S}(\nu )\) nearly doubles as compared to the scenario with no vaccination.
A strategy targeting the younger nodes could also be designed, but due to their small lethality, that strategy saves fewer years of life and prevents fewer casualties than any other strategy. The time \(T_{S}(\nu )\) of such strategy follows the same patterns than the Age and the Random strategies since none of those strategies uses the network properties.
Anti-vaccine views
Anti-vaccine views strongly depend on the persuasiveness \(\theta\) . For small values of \(\theta\) , the idea dies fast, and only a few individuals ever share those views (Fig. 3 ). As with an infection, most of the individuals remain “susceptible”. For medium values of \(\theta\) , many individuals will have heard of anti-vaccination views, although many of them will not be convinced by them. Only with high values of \(\theta\) , anti-vaccination views percolate the network. The final size of the anti-vaccination community depends, in a non-linear way, on the persuasiveness \(\theta\) and the network’s topology.
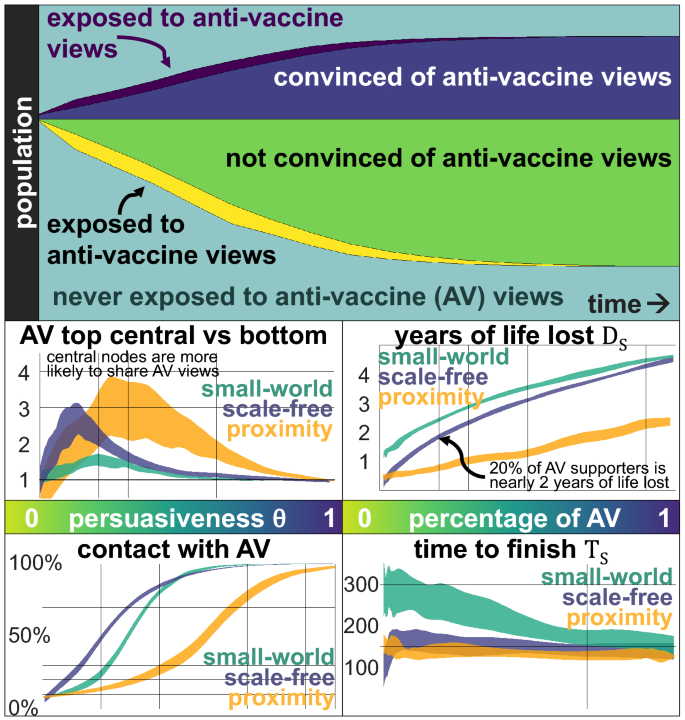
Anti-vaccine views are shared on a network of \(N=5000\) individuals, where some randomly-selected nodes initially share the views. The top panel shows the evolution of those who are exposed for the first time to anti-vaccine views (dark purple) and are convinced by them (dark blue), those who are exposed for the first time (yellow) but do not adopt them (green) and individuals who never have contact with them (light blue). The odds of a person sharing anti-vaccine views, comparing the top 10% most central nodes against the bottom 10% (central left panel) shows that for extreme values of \(\theta\) , centrality does not have an impact (since all individuals share similar views), but for values in between, the most central nodes are two or more times more likely to share anti-vaccination views since they are more likely to be exposed. Since individuals are equally likely to adopt the views after their first exposure, more central individuals are more likely to adopt them. The impact is more pronounced on a proximity network (yellow) even when the network does not have nodes with a high degree, and a scale-free network (blue) than on a small-world network (green). By the end of the diffusion process of the anti-vaccination views (bottom left panel), even with a small persuasiveness \(\theta\) , most individuals will have contact with those views. On a scale-free network, with persuasiveness of \(\theta = 0.3\) , around 70% of the population has contact with the views (even if most of them reject them and do not pass them onwards). The impact of the size of the anti-vaccine community (AV) is relevant in terms of the years of life lost \(D_{S}(\nu )\) (central right) and has some impact in terms of the time to finish \(T_{S}(\nu )\) , considering a vaccination rate of 30%. Assuming a Degree vaccination strategy, we see that if 20% of the people support anti-vaccination views, nearly two years of life are lost (so that \(D_{S}(0.3) \approx 2\) years). However, with a vaccination rate of 0.3 and the Degree vaccination strategy, only 0.3 years of life are lost.
More central nodes are more exposed to anti-vaccination views than peripheral nodes (Fig. 3 ). In turn, assuming that nodes are equally likely to adopt anti-vaccination views the first time they are exposed to them, more central nodes are also more likely to share anti-vaccination opinions. The top 10% most central nodes are between two and three times more likely to share anti-vaccination views than the 10% least central nodes for a small persuasiveness \(\theta\) .
For small values of persuasiveness \(\theta\) , most individuals have contact with the anti-vaccination views, even if they reject them and do not pass them onwards (bottom left panel of Fig. 3 ). This can be particularly challenging, as anti-vaccine views have many narratives, including different conspiracy theories, safety concerns, the use of alternative medicine or medical risks such as autism 66 . Each narrative might follow similar dynamics, reaching most individuals but convincing only some, triggering collective narratives and creating echo chambers which reinforce themselves. Thus, the diffusion of distinct anti-vaccination narratives could also be conceived as many realisations of the same dynamic, each for separate views that convince different susceptible individuals.
The final size of the anti-vaccine community is directly related to the persuasiveness parameter \(\theta\) , and the number of steps needed for the dynamic to stop is surprisingly short. With a small persuasiveness \(\theta\) , the idea dies fast; with a large \(\theta\) , the idea percolates in just a few steps. Only with intermediate values of \(\theta\) , there is some delay, but it is still a fast process (around 10% of the steps needed for the virus dynamics). A virus might propagate fast, but fake news and misinformation propagate many times more quickly.
Finally, assuming that the network in which opinions are shared is the same in which the virus propagates, the anti-vaccination views’ impact is highly relevant and interferes with vaccination strategies. Considering a vaccination rate of 30% and a Degree vaccination strategy, 0.3 years of life are lost on a scale-free network and little more than a year on a small-world network, but that could increase to nearly two years if only 20% of the population shares anti-vaccination views (Fig. 3 , right panels). More central individuals are the key aspect of optimal vaccination strategies, as they slow down the diffusion process of the virus, but their centrality also places them as nodes more likely to share anti-vaccination views, thus, having a substantial cost on the vaccination strategy. A larger anti-vaccination community reduces the time to finish \(T_S\) as the virus propagates faster, except for a small range on a scale-free network only.
Diffusion of anti-vaccination views and the virus on different networks
Opinions and anti-vaccine views are frequently shared on social media among distant individuals. Therefore, the network in which anti-vaccine views propagate does not match the network in which the virus infects more people, although there could be some interdependence. If a person rejects a vaccine, then the people with whom they have physical contact with are more likely to reject it as well, as they will probably be exposed to anti-vaccine views. Therefore, clusters of individuals will form who reject the vaccine and in which the virus spreads easily. To detect the impact of different network structures on the process of vaccination and the propagation of anti-vaccine views, first, we construct the opinion network according to some topology (proximity, small-world or scale-free). Then by dropping edges, rewiring them, or changing the topology completely, we construct the contact network in which the virus is passed.
Dropping some randomly selected edges from the opinion network to construct the contact network happens, for example, if two individuals are connected to each other through social media, but they do not have any physical contact and thus the edge between them should be dropped for the contagion process. Formally, the opinion network is constructed (as before, with some pre-determined topology and parameters) and then, each edge in the network is kept with a probability \(\rho\) in the contact network. With \(\rho = 1\) , the contact network remains the same as the opinion network, with a value of \(\rho = 0\) the contact network is empty, but with values of \(\rho \in (0,1)\) , the resulting contact network keeps some of the aspects of the opinion network, such as hubs, but with fewer edges. Results show that dropping random edges considerably decreases the speed at which the virus spreads in the network, thus reducing the final size of the recovered population and the life lost (Fig. 4 , top panel).
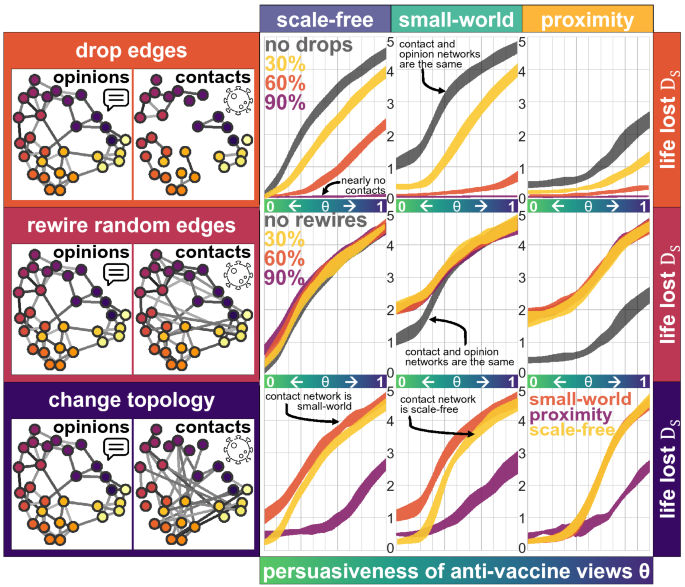
Anti-vaccine views are shared on a network of \(N=5000\) individuals on a scale-free network (left), a small-world network (middle) and a proximity network (right), where some randomly-selected nodes initially are exposed to the views and share them according to the persuasiveness \(\theta\) of the anti-vaccination views (horizontal axis). The contact network is constructed based on the opinion network by dropping edges (top panel), rewiring some edges (middle panel) or by changing the topology completely (bottom panel). The number of years of life lost at the end of the pandemic are measured, considering a vaccination rate of 30% and applying a Degree strategy, based on the degree of the contact network (vertical axis, \(D_{S}(0.3)\) ).
Rewiring some randomly-selected edges of the opinion network to construct the contact network maintains some structure from the opinion network, but creates shortcuts between nodes 29 , increasing the burden of the pandemic (Fig. 4 middle panel). This could happen if, for example, two individuals have some physical contact (on the elevator or at the market), so that the virus can pass between them, but they do not interact in terms of their opinions or views concerning the vaccine. Formally, the opinion network is constructed as before, with some pre-determined topology and parameters. Then, each edge in the graph is maintained with a probability \(\rho\) , and it is rewired in any of the two extremes with a probability \(1-\rho\) to a randomly selected node (ignoring loops and duplicated edges). For values of \(\rho = 1\) the contact network is identical to the opinion network, but with smaller values of \(\rho\) , the contact network exhibits some perturbations. Even for values of \(\rho \approx 0\) a node with a high degree is expected to keep a high degree after rewiring, meaning that part of the structure of the network is kept. Rewiring, even a small number of edges, creates contacts between nodes which are far away and increases the years of life lost. This is observed specially on the proximity network, in which clusters of anti-vaccine individuals get in touch with others who may not have exposure to such views, decreasing the collective benefit from the vaccination strategy. On a small-world network, only with a small persuasiveness \(\theta\) of anti-vaccine views, rewiring creates contacts between anti-vaccine clusters and nodes that were not exposed, so there is a high cost on rewiring.
Considering that the propagation of the virus and the anti-vaccine views on distinct networks is the case when, for example, most of the debate regarding views in favour or against a vaccine happens online and rarely in person. Results show that the proximity network reduces the years of life lost when anti-vaccine views have a high level of persuasiveness, but that with a small level of persuasiveness, the scale-free network reduces the life loss since even a low vaccination rate minimises the propagation of the virus drastically (Fig. 4 bottom panel). If anti-vaccine views are seductive and they tend to propagate through a highly-connected network with hubs and shortcuts (almost all social media platforms) most people will be exposed to such views. If, in addition, there is a limited number of vaccines, applying them to the most central nodes which are not against the vaccine, will reduce the total burden of the pandemic. Further, preventing shortcuts in the contact network (such as people travelling over long distances) and hubs (people with too many contacts) lowers the number of years of life lost and the number of casualties, even with a limited number of vaccines and seductive anti-vaccination views.
A vaccine for COVID-19 will not be a silver bullet to end the pandemic and mitigate its impact. Beyond the logistics related to producing and distributing billions of vaccines worldwide, most countries will face limited availability of the vaccine, especially at early stages. Still, outbreaks can be contained by a strategy of targeted vaccination combined with early detection 32 .
Our simulations cannot be used to estimate the years of life lost we would experience due to COVID-19 for different vaccination rates since that requires considering comorbidities, access to health services and many more factors. Still, with a simulated population and pandemic, we obtain a qualitative description of how the process might evolve, considering a limited vaccination and anti-vaccination views.
The main benefit of a person being vaccinated does not rest just on the immunity that they gain, but also on the fact that they stop spreading the virus to others. As such, targeting vaccination to more exposed people or with a high centrality on the network (such as a person who works at a shop, a barber or a taxi driver, as they have frequent contact with many different clusters of people) reduces the final size of the recovered population and the expected years of life lost as well.
Anti-vaccine views will be highly relevant
Anti-vaccine views and in general, fake news related to the virus are a second pandemic to defeat. Convincing individuals that a vaccine designed in a specific country (say the US or Russia, for instance) will feed conspiracy theories and other narratives, including its potential lack of testing and fast-track design. A vaccine for COVID-19 would raise many questions, and people often find miss-guiding, incomplete or entirely wrong answers to all of them on social media. Anti-vaccination narratives offer a wide range of attractive and seductive explanations which could pull undecided individuals, with genuine questions and concerns about the vaccine, into their anti-vaccination views.
Strictly enforced vaccination would blend perfectly with many of the conspiracy theories created around COVID-19 and would create massive chaos, considering the reactions against a non-invasive element, such as a face mask. If universal vaccination in a country is offered, still many individuals will likely opt to refuse it. In turn, the time needed to reach herd immunity might increase substantially.
Although pandemic-denying, opposing quarantines or face masks and anti-vaccine views are substantially different and are not necessarily shared by the same people, a pandemic-denier, for instance, will most likely oppose being vaccinated against COVID-19. A person with anti-vaccine views likely has as many contacts as she or he had before the pandemic and, without keeping some physical distance to others or adopting safety measures (such as a face mask), would still pass on the virus (to as many contacts) if they get infected.
One of the severe challenges with anti-vaccine views is that they might be shared by individuals with high centrality in the social network, as they are more exposed to them. Our results suggest that individuals with higher centrality are more likely to share anti-vaccination views, which is detrimental for the results of an optimal vaccination strategy. Central nodes play a highly relevant role in the diffusion of anti-vaccination views and the pandemic evolution.
Clear and concise evidence-based communication to the broad audience will be crucial to fighting against anti-vaccination views. Thus, it is worth considering an efficient communication campaign as having a similar impact as a vaccination strategy among the most central nodes. During the Ebola crisis, for example, religious leaders across faiths in Sierra Leone advocated for practices such as hand washing and safe burials and their engagement was considered a turning point in the epidemic response 67 . Social media celebrities, Instagram influencers or YouTube stars, could help promote evidence-based views about the vaccine but could also act as hubs of misinformation. An effective communication strategy, targeting central nodes with shreds of evidence about vaccines in general, and about COVID-19, could be viewed as an immunisation strategy against fake news which could percolate the network.
Data availability
Code for simulating the SVIR dynamics and the propagation of anti-vaccine views, using 68 , 69 , is available at https://github.com/rafaelprietocuriel/vaccination .
Roser, M., Ritchie, H., Ortiz-Ospina, E., & Hasell, J. Coronavirus pandemic (COVID-19). Our World in Data (2020). https://ourworldindata.org/coronavirus .
Byambasuren, O. et al. Estimating the seroprevalence of SARS-CoV-2 infections: Systematic review. medRxiv 20 , 20 (2020).
Google Scholar
Fontanet, A. & Cauchemez, S. COVID-19 herd immunity: Where are we?. Nat. Rev. Immunol. 20 , 1–2 (2020).
Article CAS Google Scholar
Lovelace, B. & Higgins-Dunn, N. CDC says U.S. should have enough coronavirus vaccine to return to ‘regular life’ by third quarter of 2021 (2020).
Ma, J., van den Driessche, P. & Willeboordse, F. H. The importance of contact network topology for the success of vaccination strategies. J. Theor. Biol. 325 , 12–21 (2013).
Article MathSciNet PubMed PubMed Central MATH Google Scholar
Gayle, D. & Blackall, M. Coronavirus sceptics, conspiracy theorists and anti-vaxxers protest in London (2020).
Ahmed, W., Vidal-Alaball, J., Downing, J. & Seguí, F. L. COVID-19 and the 5G conspiracy theory: Social network analysis of Twitter data. J. Med. Intern. Res. 22 (5), e19458 (2020).
Boyon, N. Three in four adults globally say they would get a vaccine for COVID-19 (2020).
Campos, R. Coronavirus en México [36 encuesta] (2020).
Martin, B. Texas anti-vaxxers fear mandatory COVID-19 vaccines more than the virus itself (2020).
Andre, F. E. et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull. World Health Organ. 86 , 140–146 (2008).
Article CAS PubMed Google Scholar
Larson, H. J. A lack of information can become misinformation (2020).
Johnson, N. F. et al. The online competition between pro-and anti-vaccination views. Nature 20 , 1–4 (2020).
CAS Google Scholar
Larson, H. J. Blocking information on COVID-19 can fuel the spread of misinformation. Nature 20 , 306–306 (2020).
Article ADS CAS Google Scholar
Hardwick, R. J. et al. Dynamics of individual adherence to mass drug administration in a conditional probability model. medRxiv 20 , 20 (2020).
Cai, C.-R., Zhi-Xi, W. & Guan, J.-Y. Effect of vaccination strategies on the dynamic behavior of epidemic spreading and vaccine coverage. Chaos Solitons Fractals 62 , 36–43 (2014).
Article ADS MathSciNet PubMed PubMed Central MATH Google Scholar
Feng, Z., Towers, S. & Yang, Y. Modeling the effects of vaccination and treatment on pandemic influenza. AAPS J. 13 (3), 427–437 (2011).
Article CAS PubMed PubMed Central Google Scholar
Randolph, H. E. & Barreiro, L. B. Herd immunity: Understanding COVID-19. Immunity 52 (5), 737–741 (2020).
Scherer, A. & McLean, A. Mathematical models of vaccination. Br. Med. Bull. 62 (1), 187–199 (2002).
Article PubMed Google Scholar
Husein, I. et al. Modelling infectious disease in dynamic networks considering vaccine. Syst. Rev. Pharmacy 11 , 2 (2020).
Liu, X., Takeuchi, Y. & Iwami, S. SVIR epidemic models with vaccination strategies. J. Theor. Biol. 253 (1), 1–11 (2008).
Article MathSciNet PubMed MATH Google Scholar
El Koufi, A., Adnani, J., Bennar, A. & Yousfi, N. Analysis of a stochastic SIR model with vaccination and nonlinear incidence rate. Int. J. Differ. Equ. 2019 , 20 (2019).
MathSciNet MATH Google Scholar
Ehrhardt, M., Gašper, J. & Kilianová, S. SIR-based mathematical modeling of infectious diseases with vaccination and waning immunity. J. Comput. Sci. 37 , 101027 (2019).
Article MathSciNet Google Scholar
Luong, T. H. Mathematical modeling of vaccinations: Modified SIR model, vaccination effects, and herd immunity. University Honors Theses. Paper 695 (2019).
Chauhan, S., Misra, O. P. & Dhar, J. Stability analysis of SIR model with vaccination. Am. J. Comput. Appl. Math. 4 (1), 17–23 (2014).
Anderson, R. M. & May, R. M. Infectious Diseases of Humans: Dynamics and Control (Oxford University Press, 1991).
Nasution, H., Jusuf, H., Ramadhani, E. & Husein, I. Model of spread of infectious diseases. Syst. Rev. Pharm. 11 , 2 (2020).
Lloyd, A. L. & Valeika, S. Network models in epidemiology: An overview. In Complex Population Dynamics: Nonlinear Modeling in Ecology, Epidemiology and Genetics 189–214 (World Scientific, 2007).
Chapter Google Scholar
Watts, D. J. & Strogatz, S. H. Collective dynamics of ‘small-world’ networks. Nature 393 (6684), 440–442 (1998).
Article ADS CAS PubMed MATH Google Scholar
Newman, M., Barabási, A.-L. & Watts, D. J. The Structure and Dynamics of Networks (Princeton University Press, 2006).
MATH Google Scholar
Mosbah, O., Zekri, N., Mokhtari, M. & Sahraoui, S. Dynamics of disease spread. effect of the characteristic times. arXiv:1906.11556 (arXiv preprint) (2019).
Eubank, S. et al. Modelling disease outbreaks in realistic urban social networks. Nature 429 (6988), 180–184 (2004).
Article ADS CAS PubMed Google Scholar
Hartvigsen, G., Dresch, J. M., Zielinski, A. L., Macula, A. J. & Leary, C. C. Network structure, and vaccination strategy and effort interact to affect the dynamics of influenza epidemics. J. Theor. Biol. 246 (2), 205–213 (2007).
Article MathSciNet CAS PubMed MATH Google Scholar
Zhao, Y. & Roberts, M. Simulating epidemics on networks. Res. Lett. Inform. Math. Sci 6 , 101–103 (2007).
Pastor-Satorras, R. & Vespignani, A. Immunization of complex networks. Phys. Rev. E 65 (3), 036104 (2002).
Barabási, A.-L. & Albert, R. Emergence of scaling in random networks. Science 286 (5439), 509–512 (1999).
Article ADS MathSciNet PubMed MATH Google Scholar
May, R. M. & Lloyd, A. L. Infection dynamics on scale-free networks. Phys. Rev. E 64 (6), 066112 (2001).
Bettencourt, L. M. A., Cintrón-Arias, A., Kaiser, D. I. & Castillo-Chávez, C. The power of a good idea: Quantitative modeling of the spread of ideas from epidemiological models. Phys. A 364 , 513–536 (2006).
Article Google Scholar
Curtis, J. P. & Smith, F. T. The dynamics of persuasion. Int. J. Math. Models Methods Appl. Sci. 2 (1), 115–122 (2008).
Latané, B. The psychology of social impact. Am. Psychol. 36 (4), 343 (1981).
Galam, S., Gefen, Y. & Shapir, Y. Sociophysics: A new approach of sociological collective behaviour. I. mean-behaviour description of a strike. J. Math. Sociol. 9 (1), 1–13 (1982).
Article MATH Google Scholar
Düring, B., Markowich, P., Pietschmann, J.-F. & Wolfram, M.-T. Boltzmann and Fokker–Planck equations modelling opinion formation in the presence of strong leaders. Proc. R. Soc. Lond. A Math. Phys. Eng. Sci. 465 (2112), 3687–3708 (2009).
ADS MathSciNet MATH Google Scholar
Prieto Curiel, R. & Bishop, S. R. Modelling the fear of crime. Proc. R. Soc. Lond. A Math. Phys. Eng. Sci. 473 , 2203 (2017).
Castellano, C., Fortunato, S. & Loreto, V. Statistical physics of social dynamics. Rev. Mod. Phys. 81 (2), 591 (2009).
Article ADS Google Scholar
Düring, B. & Wolfram, M.-T. Opinion dynamics: Inhomogeneous Boltzmann-type equations modelling opinion leadership and political segregation. Proc. R. Soc. Lond. A Math. Phys. Eng. Sci. 471 , 2182 (2015).
Toscani, G. Kinetic models of opinion formation. Commun. Math. Sci. 4 (3), 481–496 (2006).
Article MathSciNet MATH Google Scholar
Deffuant, G., Neau, D., Amblard, F. & Weisbuch, G. Mixing beliefs among interacting agents. Adv. Complex Syst. 3 (4), 87–98 (2000).
Del Vicario, M. et al. The spreading of misinformation online. Proc. Natl. Acad. Sci. 113 (3), 554–559 (2016).
Article ADS PubMed CAS PubMed Central Google Scholar
Hegselmann, R. & Krause, U. Opinion dynamics and bounded confidence models, analysis, and simulation. J. Artif. Soc. Soc. Simul. 5 , 3 (2002).
Pennycook, G., Cannon, T. D. & Rand, D. G. Prior exposure increases perceived accuracy of fake news (2018).
Calvillo, D. P., Ross, B. J., Garcia, R. J. B., Smelter, T. J. & Rutchick, A. M. Political ideology predicts perceptions of the threat of COVID-19 (and susceptibility to fake news about it). Soc. Psychol. Personal. Sci. 20 , 1948550620940539 (2020).
Apuke, O. D. & Omar, B. Fake news and COVID-19: Modelling the predictors of fake news sharing among social media users. Telemat. Inform. 20 , 101475 (2020).
Brennen, J. S., Simon, F., Howard, P. N. & Nielsen, R. K. Types, sources, and claims of COVID-19 misinformation. Reuters Inst. 7 , 3–1 (2020).
Stein-Zamir, C., Abramson, N., Shoob, H. & Zentner, G. An outbreak of measles in an ultra-orthodox Jewish community in Jerusalem, Israel, 2007—an in-depth report. Eurosurveillance 13 (8), 5–6 (2008).
Bernstein, J. The case against libertarian arguments for compulsory vaccination. J. Med. Ethics 43 (11), 792–796 (2017).
Plotkin, S., Gerber, J. S. & Offit, P. A. Vaccines and autism: A tale of shifting hypotheses. Clin. Infect. Dis. 48 (4), 456–461 (2009).
O’Connor, C. & Murphy, M. Going viral: Doctors must tackle fake news in the COVID-19 pandemic. BMJ 24 (369), m1587 (2020).
Orso, D., Federici, N., Copetti, R., Vetrugno, L. & Bove, T. Infodemic and the spread of fake news in the COVID-19-era. Eur. J. Emerg. Med. 20 , 20 (2020).
Pennycook, G., McPhetres, J., Zhang, Y., Lu, J. G. & Rand, D. G. Fighting COVID-19 misinformation on social media: Experimental evidence for a scalable accuracy-nudge intervention. Psychol. Sci. 31 (7), 770–780 (2020).
Gallup. How does the world feel about science and health? Wellcome Global Monitor 2018: How does the world feel about science and health? 1–132 (2019).
Kissler, S. M., Tedijanto, C., Goldstein, E., Grad, Y. H. & Lipsitch, M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 368 (6493), 860–868 (2020).
Silva, P. C. L. et al. COVID-ABS: An agent-based model of COVID-19 epidemic to simulate health and economic effects of social distancing interventions. Chaos Solitons Fractals 139 , 110088 (2020).
Article MathSciNet PubMed PubMed Central Google Scholar
Strategic Advisory Group of Experts on Immunization (SAGE). WHO SAGE roadmap for prioritizing uses of COVID-19 vaccines in the context of limited supply. Technical report, World Health Organization (2020).
European Centre for Disease Prevention and Control. Overview of COVID-19 vaccination strategies and vaccine deployment plans in the EU/EEA and the UK. Technical report, ECDC (2020).
Cinelli, M., Quattrociocchi, W., Galeazzi, A., Valensise, C. M., Brugnoli, E., Schmidt, A. L., Zola, P., Zollo, F., Scala, A. The COVID-19 social media infodemic. arXiv:2003.05004 (arXiv preprint) (2020).
Weatherspoon, D. Anti vaxxers: Understanding opposition to vaccines (2017).
Van Bavel, J. J. et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Human Behav. 20 , 1–12 (2020).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2020).
Csardi, G. & Nepusz, T. The igraph software package for complex network research. Int. J. Complex Syst. 20 , 1695 (2006).
Download references
Acknowledgements
This article was completed with support from the PEAK Urban programme, funded by UKRI’s Global Challenge Research Fund, Grant Ref: ES/P011055/1. We thank the reviewers for their suggestions and insights.
Author information
Authors and affiliations.
Centre for Advanced Spatial Analysis, University College London, Gower Street, London, WC1E 6BT, UK
Rafael Prieto Curiel
University Gustave Eiffel, LICIT, 69518, Lyon, France
Humberto González Ramírez
You can also search for this author in PubMed Google Scholar
Contributions
R.P.C. designed the study. H.G.R. analysed the results. Both authors wrote the manuscript.
Corresponding author
Correspondence to Rafael Prieto Curiel .
Ethics declarations
Competing interest.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Parameter calibration
The models presented here for the diffusion of a virus and the propagation of anti-vaccine views are based on simplifying a complex reality. The diffusion of the virus and the way it is shared among infected individuals who recover after some days and the gain in popularity of anti-vaccination views are both severe social issues for which no model will ever capture all aspects at an individual and a collective level. Social models are frequently incomplete and inaccurate, aiming to capture emergent behaviours at a collective level, often reducing most elements of the process to its minimal expression. Here, the propagation of anti-vaccine views, for instance, is modelled as some permanent individual decision shared on some network. The propagation model depends on some assumptions, such as the fact that all anti-vaccine narratives can be grouped and modelled within the same dynamics, the fact that individuals make a permanent choice to adopt or reject the views or the fact that opinions are shared on a network between adjacent nodes. The main parameters of the model were selected to mimic, to an extent, the COVID-19 pandemic, including the propagation of the virus and the anti-vaccine views related to it, expecting to obtain a general description of both issues, but not hoping to obtain trends or forecasts concerning the pandemic (Fig. 5 ).
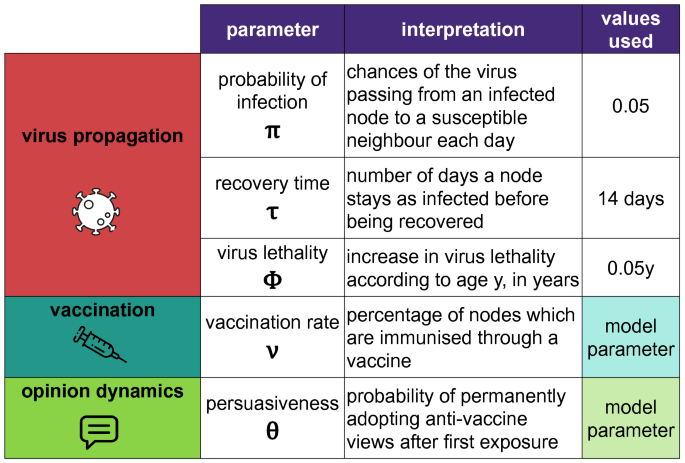
Main parameters used to model the propagation of some virus on a network, under some vaccination rate and strategy, where some individuals adopt anti-vaccination views. In terms of the virus, the three parameters are the probability of infection \(\pi\) , the recovery time \(\tau\) and the lethality \(\phi\) and are somehow related. The probability that a susceptible person is infected by an adjacent infected node is \(1 - (1-\pi )^\tau \approx 0.51\) (for the values of the parameters used) since they have interactions for a period of \(\tau\) days. The model parameters, which are used to detect the impact of anti-vaccine views and to measure the results of a vaccination strategy are the vaccination rate \(\nu\) and the persuasiveness of the views \(\theta\) , which are considered for all of its potential values in the [ \({0, 1}\) ] interval.
Other parameters, particularly concerning the three network topologies and the rewiring algorithm, were calibrated to keep the networks comparable in terms of their connectivity since a diffusion process would, in general, happen faster and have a larger recovered population on a network with higher connectivity. Thus, the topologies used help us test a network with a large diameter (the proximity network), the presence of shortcuts (the small-world network) and of hubs (the scale-free network) considering the case in which nodes have the same average number of neighbours.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Prieto Curiel, R., González Ramírez, H. Vaccination strategies against COVID-19 and the diffusion of anti-vaccination views. Sci Rep 11 , 6626 (2021). https://doi.org/10.1038/s41598-021-85555-1
Download citation
Received : 19 October 2020
Accepted : 02 March 2021
Published : 23 March 2021
DOI : https://doi.org/10.1038/s41598-021-85555-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Investigation of personal variables, technology usage, vaccine-related variables, social media-specific epistemological beliefs, media literacy, social impact strategies variables affecting vaccine hesitancy beliefs in the covid-19 pandemic.
- Hatice Yildiz Durak
- Zeynep Şimşir Gökalp
- Aykut Durak
Journal of Public Health (2024)
Deepfakes and scientific knowledge dissemination
- Christopher Doss
- Jared Mondschein
- Conrad Tucker
Scientific Reports (2023)
Can the Content of Social Networks Explain Epidemic Outbreaks?
- Alexandre Gori Maia
- Jose Daniel Morales Martinez
- Luiz Gustavo Sereno
Population Research and Policy Review (2023)
Risk assessment of COVID-19 epidemic resurgence in relation to SARS-CoV-2 variants and vaccination passes
- Tyll Krueger
- Krzysztof Gogolewski
- Ewa Szczurek
Communications Medicine (2022)
Modelling pandemic behaviour using an economic multiplayer game
- Simon T. van Baal
- Lukasz Walasek
- Jakob Hohwy
Scientific Reports (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: AI and Robotics newsletter — what matters in AI and robotics research, free to your inbox weekly.
- Share full article
Advertisement
Supported by
Guest Essay
Bird Flu Is Already Here. Just Look at the Millions Killed.

By Alex Tey
Ms. Tey is a freelance reporter studying journalism and the environment at New York University.
We don’t yet know if H5N1 bird flu will spill over from animals to infect a large number of humans. Based on the few cases of transmission so far, the World Health Organization has expressed concerns that infection in humans “can cause severe disease with a high mortality rate.”
But already it has wrought devastation upon so many lives. The deaths of millions of birds and mammals around the globe in the last few years directly and indirectly from this outbreak should be enough to spur urgent action to stop the spread of the virus, as well as remind us of the role humans play in the proliferation of infectious diseases.
It’s my belief that humans have an obligation to the nonhuman life we share this planet with to mitigate the harm we’ve enabled this virus to cause. Our unsustainable activities — factory farming, climate-warming emissions and habitat destruction, to name a few — have helped turn bird flu from a natural phenomenon into an anthropogenic disaster. But even if you don’t share that conviction, it is still in our best interest to keep this virus from spreading.
Disease has always been part of avian natural history. Wild birds are routinely exposed to mild viruses, but are seldom killed by them. Humans, however, have introduced factors that favor disease: A warming climate can weaken avian immune systems, and infections spread more easily when birds come into more frequent contact while sharing what little habitat remains.
And factory farming makes things even worse. When farm animals are kept in large numbers and close quarters in poultry and dairy farms, viruses can spread and mutate more easily. It’s a human-facilitated training ground for diseases. The progenitor of today’s H5N1 strain, for example, emerged in 1996 when a virus infecting farmed geese in Guangdong Province in southern China spilled back into wild populations.
Maintaining the health of their animal holdings and their businesses — not to mention the potential risk to farm workers and the ever-present threat of human spillover — requires farmers to act quickly. And when bird flu hits farms, often the only real way to contain it is the precautionary culling of entire flocks, which has resulted in tens of millions of dead hens since 2022. The United States Department of Agriculture recommends that farms use killing methods that avoid suffering. But as many as 66 million chickens and turkeys have been culled with a technique that animal welfare groups call unnecessarily cruel: ventilation shutdown, which kills over several hours through overheating.
Given the animal suffering at stake, minimizing interactions between wild and captive birds is all the more important in preventing the spread of bird flu in both populations. But it’s a daunting task for the agriculture industry, given how difficult it can be to isolate dense animal populations kept in close quarters. When biosecurity measures at farms fail — or aren’t even properly attempted — wild populations take an extremely hard hit.
Though wild bird deaths are harder to tally than poultry culls, the numbers that we do have are disturbing. The strain of bird flu coursing through North America ignited a season of plague for Atlantic seabirds when it first appeared in late 2021 at a Newfoundland farm. From April to September 2022, bird flu killed about 41,000 wild birds in Canada. At least 17 percent of northwestern Europe’s breeding population of Sandwich terns — over 20,000 birds — died. And from November 2022 to January 2023, the virus killed thousands of wild Ross’s and snow geese in North Dakota , Kansas , Indiana and California .
The overall death toll may lie in the millions , with millions more threatened by potential infection thanks to the long-range migrations of waterfowl.
Under normal circumstances, most bird populations can bounce back from die-offs. But climate-warming human activity could impair future recoveries in North America.
When bird flu caused “ unprecedented reproductive failure ” at a Newfoundland breeding colony of northern gannets in 2022, it was probably worsened by a marine heat wave that coincided with the outbreak. Heat stress weakens birds’ immune responses , and is likely to become more common as the planet warms. Warmer temperatures can also make recovery from H5N1 more difficult by deepening the effects of decreased food supplies, pollution and habitat loss.
None of this is encouraging for North American birds, which have already lost billions in the last half-century because of habitat loss and other forces. We contributed to the conditions that helped bird flu mutate into a highly pathogenic form. “Now it’s taken off, and it’s totally out of our control,” said Samantha Gibbs, the lead wildlife veterinarian at the U.S. Fish and Wildlife Service.
Worse may lie in store. If the virus spreads unencumbered, it could spell further disaster for species like the beloved Atlantic puffin or the regionally endangered roseate tern. Colony-nesting seabirds like these nest in close quarters and in high numbers, reducing predation but magnifying the effects of disease. Recent asymptomatic cases in Adélie penguins on the Antarctic Peninsula have spurred fears of outbreaks in tight-knit penguin colonies. The blurring of the lines between the wild and the domestic, as infections spill over and back again, also heightens the threats to livestock — and humans.
But to fret only about the prospect of human infection betrays an ecological narcissism. We must not ignore the nonhuman suffering for which, through factory farming, anthropogenic climate change and habitat destruction, we are responsible.
While you most likely need not worry about catching bird flu from meat, eggs or dairy, this is as good a time as any to cut down on products that contribute to climate change (like greenhouse gas-intensive beef) or perpetrate cruelty (like eggs from caged chickens). The same factory farms that cause excessive animal suffering can also function as a reservoir for disease.
An enduring commitment to nonhuman life on Earth would bring down the risk of zoonotic disease spreading to humans. But saving the planet for our own benefit is only by degrees less shortsighted than destroying it to our own detriment. As its most influential and destructive denizens, we owe a duty of care to all of nature — not just its human inhabitants.
Alex Tey is an editor at large of New York University’s student newspaper, Washington Square News.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Oxford University Press - PMC COVID-19 Collection

In Defense of Vaccine Mandates: An Argument from Consent Rights
Daniel a wilkenfeld.
Department of Acute and Tertiary Care, University of Pittsburgh School of Nursing, USA
Christa M Johnson
Department of Philosophy, University of Dayton, United States of America
This article will focus on the ethical issues of vaccine mandates and stake claim to the relatively extreme position that outright requirements for people to receive the vaccine are ethically correct at both the governmental and institutional levels. One novel strategy employed here will be to argue that deontological considerations pertaining to consent rights cut as much in favor of mandating vaccines as against them. The presumption seems to be that arguments from consent speak semi-definitively against forcing people to inject something into their bodies, and so any argument in favor of mandates must produce different and overriding logical and ethical considerations. Our central claim will be that the same logic that might seem to prohibit vaccine mandates as violations of consent actually supports such mandates when viewed from the perspective of the potential bystander who might otherwise be exposed to COVID-19.
Introduction
Recently, the question has arisen of the ethics of pressuring people into getting one of the COVID-19 vaccines. Debates exist along several crisscrossing axes, including:
- The acceptable form of any potential mandate: incentives vs. outright requirement.
- The acceptable locus of any potential mandate: governmental vs. institutional.
- Legal vs. ethical vs. policy considerations with respect to any potential mandate.
This article will focus on the ethical issues and stake claim to the relatively extreme position that outright requirements for people to receive the COVID-19 vaccine are ethically correct at both the governmental and institutional levels. By ‘outright requirement’, we do not mean to suggest that people will be forcibly vaccinated, but rather that some penalty will be assessed for most of those who choose to forgo a vaccine. One novel strategy employed here will be to argue that deontological considerations–and consent rights in particular—cut as much in favor of mandating vaccines as against them. To make allowances for a (narrow) realm of vaccine refusal, we do carve out an exception for those who are willing to take what we call Maximal Preventive Measures (MPMs): doing all of masking, social distancing and providing evidence of a negative test whenever they go into a public space; this carve-out would be sufficiently onerous for most people that it would act as another form of mandate, while allowing for certain legitimate exceptions. Note that our thesis is specifically applicable only to COVID-19 vaccines; we will however explore to what extent our argument might generalize to other vaccines. Even more precisely, our argument was originally formed in the context of variants of COVID-19 through delta. We comment below on how circumstances have changed with omicron (though not in a way that invalidates our argument), but of course given the likelihood that facts on the ground will continue to evolve, it is possible that some of our arguments might prove outdated. Even should that be the case, we maintain that the following ethical analysis of vaccine mandates in the era through delta (and to a lesser extent omicron) still has value in manifesting general argumentative positions that will likely apply to future variants or other viruses altogether.
We take it that one of the strongest arguments against requiring vaccines is that people generally have a right to refuse consent to any infringement on bodily integrity. We frequently hear vaccine opponents invoking the language of medical choice or informed consent. The presumption seems to be that arguments from consent speak semi-definitively against forcing people to inject something into their bodies, and so any argument in favor of mandates must produce different and overriding logical and ethical considerations.
Other defenses of vaccine mandates in the literature have generally taken this structure of rights vs. some other good. For example, they have focused on the unvaccinated’s contribution to a collective harm ( Brennan, 2018 ), the protection of the general public ( Flanigan, 2014 ; Savulescu, 2021 ), the protection of the otherwise unvaccinated ( Giubilini and Savulescu, 2019 ), herd immunity ( Giubilini, 2020 ) and considerations of fairness ( Giubilini, 2020 ). In most of these arguments, the general idea is that the considerations in favor of the mandate outweigh whatever claims or rights an unvaccinated person has to remain unvaccinated. The exception to this strategy is Brennan’s (2018) libertarian argument. Since the libertarian does not allow that considerations of the wellbeing of others can ever outweigh one’s right to liberty, a mandate will only be viable if the mandate falls outside the scope of one’s liberty rights. As such, Brennan argues that the unvaccinated contributes to a collective harm that the government is justified in preventing via vaccine mandate.
Our argument comes closest to Brennan’s in that we also do not focus on benefits of the vaccine mandate outweighing any harms or rights to the otherwise unvaccinated. Where it differs, however, is that our focus is not on a contribution to a collective harm that a government may protect against, but rather on a conflict of rights between the would-be unvaccinated and individuals with an interest in people with whom they interact being vaccinated. Indeed, our central claim is that this is a conflict of the very same right, i.e. one’s purported right to remain unvaccinated is undergirded by the same deontological logic of consent rights that we contend motivate the right of a potential bystander to not be unnecessarily exposed to COVID-19. As a catch-all term, we speak of a general right to engage in the world free of harms imposed on one’s body without consent; we mean by this construal to pick out whichever right or rights vaccine refusers and bystanders alike seek to invoke. The crux of the argument is that when one defends one’s right to remain unvaccinated, one inevitably also accepts infringement upon a bystander’s right to not be exposed to COVID-19 by the unvaccinated. What justifies a vaccine mandate, or so we will argue, is how this conflict of rights in kind gets settled.
We will be focusing our arguments exclusively on the justification of mandates for vaccines in Western cultures. We suspect that the strongest case against individual mandates can be made for a Western culture such as that of the USA, for two reasons. First, given their emphasis on individualism and individual rights, one would suspect a stronger cultural norm against essentially overriding individual decision making. Second—and we will return to this in the objections and replies—given the emphasis in at least the more liberal corners of Western culture on bodily integrity in support of reproductive rights, we might expect similar logic to speak in favor of preserving bodily integrity in the case of vaccine refusal.
We will also largely be omitting one standard argument in favor of vaccine mandates, as hinted to above. One might think that the sheer scope of the COVID-19 pandemic would justify overriding what would normally be ethical rights for the sake of avoiding catastrophe. While the scope of the pandemic will play a role in our argument, we do not intend to argue that otherwise unethical action is justified in this case on purely utilitarian (i.e. outcome-based) grounds. Rather, we argue that—properly thought of—mandating COVID-19 vaccines is not unethical in the first place. While others (especially Brennan, 2018 ) have argued that vaccine mandates do not violate general constraints against government restriction, we take our advance to be framing the defense of mandates in the very language of rights and consent most commonly used by their opponents.
For purposes of this paper, we begin with three assumptions. First, we assume the extreme safety and relative efficacy of the COVID vaccines. More specifically, we assume that there are very low odds of unforeseen serious side-effects ( Blumenthal et al. , 2021 , Klein et al. , 2021 ), that being vaccinated reduces one’s odds of acquiring COVID-19 ( Thompson et al. , 2021 ) and that being vaccinated greatly reduces the odds of transmitting COVID-19 to other people. This could be true because it reduces viral load ( Petter et al. , 2021 ; Vitiello et al. , 2021 ) or because it reduces the length of one’s contagion ( Thompson et al. , 2021 ), but if nothing else it follows as at least plausible from the fact that vaccinated individuals are less likely to be infected in the first place ( Centers for Disease Control and Prevention, 2021b ). Obviously many people who oppose vaccines on any level are likely to dispute this assumption, arguing either that vaccines are unsafe or that they are ineffective. However, the fact that people argue something does not in itself imply that it is a plausible position, and so—given the overwhelming empirical evidence—in this case it is reasonable to simply set aside for the purposes of ethical analysis claims that deny the vaccine’s (general) safety and effectiveness, so long as there is support for those who suffer side effects, as well as a very limited set of exceptions for those with legitimate medical reasons not to get the vaccine. That said, while the safety of the vaccines is unlikely to change, the soundness of the assumption that they reduce infection and transmission might wax and wane as new variants become dominant. For example, when this paper was drafted the dominant variant was delta (see citations above), but during revision the omicron strain became responsible for almost all infections in the USA ( Centers for Disease Control and Prevention, 2022 ). While the omicron variant exhibits significantly more vaccine escape than earlier variants ( Lyngse et al. , 2022 ), preliminary results indicate that vaccines are still somewhat effective at reducing infection and transmission ( Lyngse et al. , 2022 ) Perhaps by the time this paper is published or read the situation will have changed sufficiently that our underlying assumptions are no longer sound. If so, we present our arguments as pre-emptive considerations for how to treat vaccine mandates in the face of future variants or pandemics where these assumptions do apply.
Second, we assume that in the absence of a mandate there will be a large number of people who do not get the vaccine and that in the presence of a mandate this number will go down. The former claim is undeniably empirically accurate—there are as of this writing large swaths of the population who refuse to get the vaccine. The latter point is more speculative—it is possible that a mandate would somehow backfire and lead to fewer total vaccinations. However, evidence suggests that at least at the institutional level when mandates are enacted people become more likely to get the vaccine ( Greyson et al. , 2019 ; Gostin, 2021 ); so this seems like a reasonable assumption. (We do not however commit to how many more people would be likely to get it.) Finally, we assume that the vaccine is readily available—obviously it would be unjust to mandate someone get something that there is no way for them to get.
Note also that the exception for people taking MPMs discussed above (masking + distancing + testing whenever entering a shared public space) also entails that our discussion only applies to people who enter shared public spaces. If one really lives one’s entire life in a wholly insular fashion (as in a hermit in the woods), then one can trivially satisfy the mandate by doing nothing new (since one is not entering publicly shared spaces). In addition, there is likely a gray area where one has such minimal contact with outsiders—perhaps in a rural farming community—that taking MPMs is sufficiently doable that it represents a reasonable alternate path such that the vaccine is in some sense no longer ‘mandated’. Given how interconnected most people are (even those who spend most time in isolated locations generally have some need of interacting with the broader population) we thus focus our discussion on those who have some interest in regularly being in shared public spaces.
The structure of this paper is as follows. The next section provides the major arguments in the paper, showing how the very same deontological considerations that might speak against mandating vaccines in support of the consent rights of the recipient also speak in favor of mandating vaccines in support of the consent rights of those who might potentially be exposed. We will then discuss how to address these competing rights-claims and argue that the best resolution is to favor the rights of potential victims of COVID-19. In the following section, we will build on well-known analogies from clinical/medical/nursing ethics—this is intended merely to be illustrative. We then expand the argument from governmental mandates also to defend on similar grounds institutional mandates at effectively any sort of institution. We conclude with objections and replies.
Rights-Based Arguments for and against Mandates
Vaccines and individual rights.
When someone makes a decision not to get a COVID-19 vaccine, they are of course making a decision pertaining to their own healthcare. However, what is sometimes overlooked is that they are making a decision pertaining to others’ healthcare as well. Though there is no guarantee that anyone who is not vaccinated will be exposed to COVID-19 and will pass it on, not being vaccinated makes it more likely that they will do so (see above). In that way, they affect the rights of future people with whom they interact. By analogy, it is clearly wrong to put toxic chemicals in someone else’s water; we can then consider a person or company that allows potentially (but not certainly) dangerous chemicals into a local water supply. They might not know that they are putting anyone in danger and certainly would not be able to point to a specific individual who will be harmed. However, the potentially more diffuse nature of the wrong in not knowing whom will be hit seems on the surface almost exactly counterbalanced by the very real possibility that they will harm multiple people. In the same way, while we cannot point to a specific individual Y who will get COVID-19 as a result of person X’s decision not to get vaccinated, there are a whole host of individuals Y 1 – Y n who suddenly find themselves in unwanted harm’s way. It is also worth noting that some of the Y i s might not be able to get the vaccine themselves, either due to overriding medical reasons or the simple fact that (as of this writing) it is not yet approved for or available to all populations. In the case of pollutants, the right being violated is Y’s ability to live their life and assume a certain level of safety in their water supply, or more generally the right to engage in the world free of harms imposed on one’s body without consent.
What right then is being violated with respect to a person who is forced to get a vaccine? The clearest answer is the same as above, i.e. one’s right to engage in the world free of harms imposed on their bodies without their consent. This suggests we look at the literature on consent to ascertain whether their rights are more sacrosanct than the victims of any potential COVID-19 exposures. In the remainder of this section, we speak as if there is one particular person who will be exposed to COVID-19 as a result of an individual’s vaccine refusal—as pursuant to the previous paragraph, we take this to be morally similar to the more realistic scenario where there are multiple people with massively increased potential exposure.
Sources of Consent Rights
In this section, we will go over some common justifications for people’s right to refuse interventions on their bodies and argue that those same justifications provide at least some prima facie reason to think that they in most cases do not have a right to refrain from getting a COVID-19 vaccine. The key to this strategy is arguing not that there are conflicting kinds of rights, but rather that the very same kind of right that would justify vaccine refusal also justifies vaccine mandates.
For example, the right to refuse interventions is most frequently grounded in autonomy, which is literally the right to make laws for oneself. Spelling out precisely why this is the case is complicated by the fact that philosophers have no clear unified conception of autonomy ( Buss and Westlund, 2018 ). We do not need a full account of autonomy however to note that one necessary condition for autonomy is the liberty to decide for oneself how to live one’s life free of unnecessary externally imposed impediments. It is this liberty criterion that vaccine mandates are often thought to violate, but we will argue that the absence of mandates is responsible for violations of that same liberty criterion. For approximately as long as philosophers have discussed anything like autonomy or liberty there has been a general recognition that liberty rights can conflict in such a way as to make it impossible for everyone to have maximal liberty all of the time. Hobbes (2016 /1651, Chapter 13) famously observed that if everyone were free to do as they would, life for everyone would be ‘nasty, brutish, and short’, and even John Stuart Mill’s (2011 /1859) most famed statement of maximal individual freedoms in ‘On Liberty’ acknowledged that one’s liberty always needs be curtailed when its exercise would infringe upon the liberty of others. Yet—given our assumptions about the effectiveness of the vaccine and the need for common areas—this seems like a paradigmatic example of where one person’s liberty would limit another’s. My liberty to be able to engage in society without being ‘assaulted’ by a vaccine is no more obviously sacrosanct than your liberty to be able to engage in society without being ‘assaulted’ unnecessarily by deadly virus. I cannot govern myself as I will when I am willfully exposed to COVID-19.
Two notes are in order. First, some would argue that the battery of having a needle puncture your body violates one’s rights in a way that an increased risk of contracting COVID-19 does not (for one such argument, see Kowalik, 2021 ). For the most part we simply reject the reasonableness of this distinction on several grounds. First, on the actuality of the harm the needle causes vs. the mere possibility of contracting COVID-19, we note that the harm of the needle itself is quite minimal and that is the only harm 100% guaranteed. The reception of the vaccine itself is not a harm, unless there are adverse side effects, which are simply an added risk—not unlike the added risk of contracting COVID-19. Thus, if we step back and look at the overall expected utility of the actual needle jab and the possibility of adverse side effects of the vaccine with the overall expected utility of the increased risk of COVID-19 exposure, we contend that the latter is much worse. The risks of COVID-19 include unpleasant symptoms [ Ma et al. (2021) recently provided a headline-generating result that 40% of cases are asymptomatic, but that suggests that 60% might not be], ‘Long COVID’ ( Crook et al. , 2021 ), hospitalization ( Scobie et al. , 2021 , especially Figure 2) and death. The seeming similarity in kind and relative seriousness of potential harms from the virus as compared to the risks of the vaccine ( Blumenthal et al. , 2021 ; Klein et al. , 2021 ) + the actual harm of the jab make it seem like the rights violation are minimally of a piece (leading to our discussion in the next section of how they should be adjudicated). Second, focusing on the unwanted foreign agent itself, whether one receives an unwanted vaccine or an unwanted infection, the issue is that an unwanted foreign agent is entering one’s body without one’s consent–drawing a sharp distinction based on the foreign agent’s mode of entry would suggest that a vaccine mandate would be ethically worse than making the vaccine airborne and spreading it throughout the country. We suspect that most of those we have encountered who argue against mandates on the grounds that they do not consent to the intervention of a shot would be unlikely to accept the intervention being thrust on them via a different and more pervasive mechanism such as being omnipresent in the atmosphere. Finally, one might argue that there are different levels of consent violations–an unapproved cheek swab is an ethical problem, but clearly a smaller one than an unapproved surgery. Precisely what makes one violation worse than another is beyond the scope of this paper, but presumably one vector of evaluation is the expected harm done (as measured in the severity of possible outcomes multiplied by the likelihood of those outcomes obtaining). As just discussed, the calculus of expected harms speaks in favor of mandating a vaccine—the point here is that this same calculus might well also speak to the severity of a rights violation in exposing someone to that harm without consent relative to the consent violation of being mandated to get an unwanted vaccine.
Of course, one might argue that we are underestimating vaccine risks and overestimating how severe COVID-19 is to everyone. After all, there have been cases of reactions to COVID-19 vaccines (Centers for Disease Control and Prevention, 2021a) and there are populations for whom severe cases of COVID-19 are rare ( American Academy of Pediatrics, 2021 ). On the first issue, (of underestimating vaccine risks) we make three points. First, we began with the assumption that the vaccines are safe. To that end, it may be that certain vaccines, e.g. Johnson and Johnson or AstraZeneca, may not be ethically mandated due to their increased safety risks and lower efficacy ( Centers for Disease Control and Prevention, 2021c ). Second, we remind the reader that the mandate we propose does include MPMs as an alternative to receiving the vaccine. Those unwilling to receive the jab may choose N95 masking, distancing and testing as an alternate route to avoid violating the consent rights of bystanders. Third, we would agree that we can set aside the relatively rare instances of vaccine side effects, so long as there are accommodations for those who have side effects, as well as an exemption for legitimate medical reasons. The idea here is that when there are indeed side effects from the vaccine received due to a mandate, the ethical mandate will include provisions for compensation. On the latter issue of overestimating the severity of COVID-19, we again make three points. First, there are cases of severe COVID-19 across all age-groups, even if prevalence of cases is lower in certain age-groups ( American Academy of Pediatrics, 2021 ). Indeed, the prevalence of severe COVID-19 across groups is higher than the prevalence of severe reactions to COVID-19 vaccines (compare Centers for Disease Control and Prevention, 2021d to Delahoy et al ., 2021 for cases of adverse reactions to the vaccine to COVID-19 hospitalizations). Second, unless the unvaccinated can be sure only to interact with individuals from those groups who do not regularly suffer from severe COVID-19, it will not matter that some individuals fall into that camp. The unvaccinated will inevitably interact with those for whom severe COVID-19 has a higher prevalence. Finally, while it is possible to offer compensation and accommodation to those few who react poorly to the vaccine, a parallel proposal for those who ultimately suffer from severe COVID-19 is untenable. That is, it seems much more plausible to make whole those who have bad side effects from the vaccine mandate than to make whole those who suffer severe COVID-19 due to the lack of a vaccine mandate.
As a second note on the liberty argument, Brennan (2018) has already argued that variants of Mill’s harm principle are sufficient to justify vaccine mandates. Our approach is subtly different in that Mill’s harm principle is characterized as a general limit on person X’s liberty whereas we are grounding our argument in the very same rights justifying vaccine refusal (e.g. liberty). This has an advantage that it defends against those who might think that unwanted medical interventions are a different kind of consent violation that cannot be overridden by Brennan’s ‘clean hands principle’—we argue that those the very same principles that support the vaccine refuser’s argument also undermine it. (Brennan’s approach has other advantages in engaging with specific libertarian concerns–as such we consider the two complementary rather than in competition.)
Similar strategies of looking at the question of rights from the potential of the prospective victim of COVID-19 exposure suffices to defray many other concerns with other intrusions on bodily integrity without consent. For example, some people ground the right to refuse intrusions in the fact that we own our own bodies (Eyal, 2012: 14). But just as my ownership right to a field gives me a claim against a neighbor whose conduct polluting risks dropping soot on my crops, so my ownership of my body gives me a claim against someone whose conduct risks dropping unnecessary SARS-CoV-2 droplets in my breathing area. Likewise, while your bodily integrity is undermined by receiving an unwanted shot, mine is undermined by receiving an unwanted COVID exposure.
One final worry worthy of special mention is that allowing the right to refuse bodily infringements is necessary to prevent abuse at the hands of authority figures ( Manson and O’Neill, 2007 ). In this case, one might worry that allowing the government the authority to mandate one shot will open the door for allowing future governments to mandate shots for more nefarious purposes. Another version of this concern might be a ‘slippery slope’ objection, which acknowledges that a vaccine mandate might be justified in this case but that allowing one would open the door to instances where such a mandate would be unjustified. However, the proper response to this is perhaps the standard one to most slippery slope arguments, which is that if the current action is justified but a future later one might not be then we need a mechanism in place that pulls the brakes right at the juncture between the justified and the unjustified. The way to prevent unjustified behavior is not to ban justified behavior, but rather to be vigilant regarding when one might cross the relevant boundary. This objection reasonably speaks against giving the government carte blanche authority to institute vaccine mandates but does not speak against allowing it to mandate this specific one. We would in effect require a new analysis to be done for each prospective vaccine. For example, current flu vaccines might not be amenable to mandates, as they violate the assumptions of strong effectiveness and high likelihood of spread and conceivably alter the calculation of expected harm that might be relevant for weighing consent violations against each other. As the effectiveness of flu vaccines increases and if the contagiousness and severity of flu infections increase the case will approach to COVID-19; our current situation provides a clear case against which other vaccine mandates could be compared—if the harms of the virus and safety/effectiveness of the vaccine are at least as great as they are for COVID-19, then a mandate is justified. Anything less must be evaluated on a case-by-case basis.
Competing Rights Claims
Suppose one accepts as above that there are competing rights claims—of the same kind—between potential unwilling vaccine recipients and potential unwilling victims of COVID-19 exposure. The next question is how we adjudicate between such conflicting rights claims. One move that would be reasonable here would be to reinvoke the societal costs of COVID-19 and argue the default should be the permissibility of a vaccine mandate unless there is a rights-based argument against having one. If the rights-based arguments all turn out to counterbalance, that would leave in place the default need to protect society of a rampaging pandemic. We think this would be a perfectly reasonable argument; however, as the ‘consequentialism vs. deontology’ argument (basically an argument between achieving positive outcomes at the cost of violating ethical ‘rules’) is well-trod ground, we table that line of reasoning in favor of arguing that a consideration of rights on their own terms favors vaccine mandates.
It is of course well beyond the scope of this paper to consider every way in which one might resolve conflicts among different people’s rights. We will thus argue from a framework inspired by Rawls’ landmark A Theory of Justice (1971/1999), widely considered to be the dominant work of political philosophy of the last century. We believe that the choice of this framework is not necessary for our ultimate conclusion and that virtually any system for trading off rights would get the same result—however, we obviously save proving this claim for future work. We will however entertain the possibility that this whole approach is wrong-headed and that a proper deontological (i.e. rule-based rather than outcome based) perspective demands that rights cannot really be weighed against each other or traded off in the first place.
Rawls’ central innovation is the ‘Veil of Ignorance’, wherein people in an ‘Original Position’ determine what is just by what one would agree to if one did not know exactly who one was. The basic idea is to imagine a group of people setting the rules for a new society, in particular the allocation of primary goods [including (at least in our version) such ‘goods’ as rights]. However, no one in that room has any idea who they are in the society; they do not know their race, gender, economic status, or any other identifying feature. Since they do not know who they are, anyone can be reasonably expected to represent all of humankind. Rawls, for his part, concludes that two principles of justice fall out of this setup. However, there is a wealth of literature debating whether Rawls is correct about what principles would fall out of the Original Position as well as how and to what those principles should apply, if correct. We do not wish to get bogged down in Rawlsian interpretation here. For our purposes, we instead turn to a Rawlsian lesson: the contractarian under-pinning of moral principles.
In envisioning the social contract, we need to discern what we would all agree to if we were fully rational and free of prejudice. This is what the Original Position and Veil of Ignorance are meant to establish. Though individual public health issues go beyond the scope of Rawls’s vision, we can use his thought experiment to develop one way of thinking through how a society ought to trade off rights when they conflict. We maintain that when setting up a society, if you do not know who you will be in that society, it is in your interest to protect those worst-off, in case you are one of those people. As such, when an issue arises in which not everyone’s rights can be met, one way of thinking through how to resolve the conflict of rights is to focus on protecting the rights of whoever would be worse off for the violation. Getting back to COVID-19 vaccine mandates, we contend that this reasoning speaks fairly clearly in favor of mandates. Given that we carve out exceptions for those with legitimate medical needs, the person who gets a vaccine they did not want is significantly better positioned than the person who gets COVID-19 exposure they did not want.
Given our use of Rawls’s setup, it is worth considering some of the push back it has received. First, some ( MacIntyre, 1981 ; Sandel, 1982 ) have argued that it is problematic to deny people in the original position all knowledge about their identity. How can I make a rational choice if I have no knowledge about my values or aims? If what is rational is whatever is in my best interest, I need to know what interests I have. Minimally, one should be offered their probability of belonging to a particular group that has particular interests. For example, if one knew that there was only a 1/7,000,000,000 chance of being a single person picked out for human sacrifice in a world where everyone else is obscenely rich, one might reasonably choose to take one’s chances. However, providing knowledge of probabilities would only make the case for mandating vaccines that much stronger, since one is much more likely to be harmed by exposure to COVID-19 from an unvaccinated individual than to receive any harm from the vaccine (see previous section). Others ( Harsanyi, 1975 ) have worried that even in the absence of probabilities Rawls (and in turn we) overestimates how risk averse people either are or should be. Psychologically speaking, perhaps people would be willing to risk a low well-being floor in the hopes of achieving a high well-being ceiling. This may be true, but notice that in this case, since one’s well-being floor and ceiling both go up if there are vaccine mandates (with suitable narrow medical exemptions), for each individual person in the population one’s odds of harm are greater if there is no mandate than if there is a mandate. Thus—whomever one thinks one might be—one is better off with the mandate. And the same math works for average utility. Given that the question of rights was a wash, this suggests that anyone in the Original Position should opt for a mandate.
One might at this point object that this entire section is based on a faulty assumption that rights claims can be traded off at all. One might think that certain rights are inviolate, even if respecting them involves a greater infringement on the rights of others ( Thomson, 1990 ; Kamm, 1996 ). There are countless cases used to show that one may not harm an individual to prevent harm to others. For instance, many argue that one may not push a hiker off a footbridge to stop an out-of-control trolley from killing five others ( Thomson, 1976 ). Likewise, it is argued that one may not kidnap an innocent person and harvest their organs to save the lives of five people in need of organ transplants ( Foot, 1967 ). To generalize the point, if there is an existing threat to some group of people, it is wrong to introduce a new threat to a third party to protect the group already under threat (or so the argument goes). In the case of COVID-19, one might argue that those who might get COVID-19 are already under threat and that the vaccine mandate introduces a new threat to the unvaccinated to protect the group already under threat. However, there is a clear disanalogy here insofar as the unvaccinated individuals are the threat. There is a morally important difference between putting an individual at risk when an out-of-control trolley will possibly cost lives and putting an individual at risk when that very individual will possibly cost lives.
There is another way to see the case, however. We have been arguing that there is a conflict of rights in the vaccine mandate case. Yet, the trolley and surgeon cases above are not necessarily conflicts of rights. These cases involve violating a right to save people, and few actually argue that individuals have a genuine right to be saved from harm. Many do argue, however, that one may not infringe a right to prevent others from having their rights violated ( Kamm, 1989 ; Heuer, 2011 ; Johnson, 2019 ). Indeed, one may not even do so when the same right is at issue. That is, I am not permitted to kill one even if it would stop five others from being killed. In the literature, this particular case has been dubbed the ‘paradox of deontology’. After all, it seems a bit odd that one would think killing is bad, yet not try to minimize them ( Nozick, 1974 ; Scheffler, 1988 ). However, deontologists (i.e. ethicists who focus on rules rather than outcomes) have argued at length, and in many ways, that we are not permitted to treat an individual as a mere means to an end. In these cases, violating that one right would be akin to using that individual as a mere means to the end of preventing other rights violations. Bringing this back to the vaccine mandate, it seems that we have a case of violating an individual’s liberty/consent rights (as characterized above) to prevent the violation of the liberty/consent rights of others, a clearly impermissible action according to these deontologists.
In response, again we can see a disanalogy. In ordinary cases discussed in the literature, there are a number of people whose rights will be violated, unless the rights of a neutral third party are violated. In the vaccine mandate case, however, the unvaccinated individual is not a neutral third party. Rather, the unvaccinated individual is the one who, if their rights are not violated, will violate the rights of the masses. To summarize, we have two parties at issue (the potential COVID-19 getter and the unvaccinated) and two possible situations (mandate or no mandate). Both parties have the potential to have their rights violated, depending on the situation. However, it is only the unvaccinated that would become a rights violator (in the no mandate situation). As such, this is not an ordinary conflict of rights. Rather, we have an innocent party at risk from a potential guilty party. And, although one might argue that seen this way, the mandate constitutes a sort of Pre-Crime preventative justice measure, a safe and effective vaccine can hardly be seen as a punishment, and prior to vaccination, we would argue that the unvaccinated is already violating the rights of potential COVID-19 getters. As such, it is not merely preventative. This marks a key area where our argument reaches farther than Brennan’s (2018) —since that piece was not addressed to deontologists, it (quite reasonably) does not consider the position of those who would take certain specific rights to be inviolable even to protect the rights of others. Our argument does so. (In a sense, our task has been made much easier by the sheer virulence of COVID-19 allowing us to assign individual culpability rather than rely upon concerns relating to collective action.)
There is another disanalogy worth mentioning before moving on. In the cases deontologists normally discuss, it is an ordinary bystander that we imagine either initiating the new threat or else violating the rights of the individual. Deontologists then argue that a bystander is not morally permitted to perform such acts to prevent harm or rights violations. However, in the vaccine mandate case, we do not have a mere bystander, we are considering government and institutional mandates. A bystander has no special obligation to the persons whom they would protect. Governments do have such special obligations, and some institutions might as well. So, not only do the stakes change insofar as the unvaccinated individual is the threat or potential rights violator, but the Government or institution who would infringe the rights of the unvaccinated via a mandate also have a special obligation to all parties involved to do what is necessary to protect them.
While one might seem to have a liberty/consent right not to be forced to get a vaccine, refraining from getting a vaccine makes one a perpetrator violating the liberty/consent rights of others. As such, it is legitimate for the government to prohibit one from doing so.
Analogies: Rights Violations and the Protection of Others
In this section, we point out that not only are there other circumstances (even in the medical domain) where we think that it is acceptable to infringe on what seem to be the rights of someone to protect the rights of others, but that (again) the same logic applies even more forcefully in the case of mandating COVID-19 vaccines. Some of the claims in this section will be controversial, so we note that our central argument in the previous section can (and should) be accepted independently of the analogies presented here. However, we believe the present analogies are still instructive regarding when it might be acceptable to infringe on what seem to be the rights of X for the sake of protecting the rights of Y.
To take perhaps the most obvious example, psychiatrists are required (legally and presumably also ethically) to break what is otherwise a strong right of confidentiality if not doing so would endanger the health and safety of a potential victim of violence ( Kahn, 2020 ). That case on the surface is fairly analogous to the present one, where mere potential harm to someone else suffices to override someone’s rights. Nor do we think the ethical calculus changes dramatically if—instead of threatening a specific individual—a psychiatric patient ‘just’ threatens to put potentially toxic chemicals into a shared water reserve—a diffuse risk of harm to a large number of anonymous people seems just as ethically relevant as a more specific risk of harm to a named individual.
However, one might believe that confidentiality rights are somehow more contingent or defeasible than consent rights, and so we turn to a second analogy perhaps more closely aligned with vaccine mandates. Parents generally have a right to decide for their children whether or not they will receive a medical intervention ( Wilkinson and Savulescu, 2018 ). However, the default view of ethicists in the relevant domains is that there are generally some (limited) circumstances where it is acceptable to override those rights for the sake of protecting someone else’s—in this case the child’s. For example, it is generally believed (e.g. Conti et al. , 2018 ) that it is acceptable to provide blood transfusions for the children of Jehovah’s Witnesses, even if the parents believe that doing so will cost the child their soul. If this position is correct (and we think that it is), then by itself it shows that we can override X’s rights for the sake of Y’s health. One might object that in this case the parental right is really just the child’s right by proxy, and hence, the cases are not relevantly analogous. However, there is still a conflict of autonomous individuals even in this case. While parents have default decisional authority on behalf of their children, the child still has a liberty interest of their own, which the parent is potentially violating by making a decision that has the potential to harm the child. (For more on the distinction between decisional authority and children’s liberty/autonomy, see Wilkenfeld and McCarthy, 2020 ). Seen as a potential conflict of liberty rights, we argue that a recent look at the best logic behind overriding parental rights also suggests overriding the apparent right to refuse a vaccine.
A recent article by Brummett (2021) makes the point that despite ethicists’ best efforts, it is not really plausible to ground the acceptability of overriding parental refusal in terms of neutral criteria like ‘minimizing harm’ ( Salter, 2012 ) or demanding internal consistency ( Bester, 2018 ). Brummett’s insight is that if one really took seriously the prospect that receiving a blood transfusion might cost a child their soul, then one could not reasonably maintain that doing so minimizes harm or in some way enforces consistency. Rather, we override the parent’s judgment not based on neutral procedural grounds, but based on our firm conviction that they believe a metaphysical claim that is simply false. If Brummett has correctly identified the justification for overriding parental rights, then it applies one thousand-fold to the question of vaccine mandates. The reason is that while we might believe that Jehovah’s Witnesses are wrong about blood transfusions costing children’s souls, it is hard to reasonably claim that we could possibly know it, and impossible to reasonably claim that we could ever prove it. However, per our assumptions, we do know that beliefs about the dangers of vaccines are simply incorrect and we have already proven it. Thus, if X’s endangering Y being based on a false belief is reason to override X’s rights, then the case is significantly stronger here than it is in the case of blood transfusions. Lest one worry that this logic could prove too much by allowing clinicians to paternalistically override patients’ wishes whenever those wishes are based on a provably false belief, note that when X’s decision only endangers himself there is no competing rights claim and the issue never arises in the first place.
Institutional Mandates
If the case has been successfully made that government vaccine mandates are ethically acceptable, then most of the logic applies doubly to institutional mandates, such as a university requiring vaccination as a condition of enrollment (subject to legitimate medical exemptions and corresponding precautions for those cases). The concern with government mandated vaccines is that they infringe on someone’s rights; however, if we are correct that doing so is part of the best system of overall rights protection then it is just as legitimate for institutions to respect potential victims’ rights in the same way.
In addition, there is the obvious point that groups of people are—with various exceptions—ethically free to associate as they see fit, and so they are likely entitled to demand people waive certain genuine rights as a condition of association. Presumably people have a right against being tackled by others, yet it is reasonable for professional sports associations such as the National Football League to demand that athletes waive that right to participate in on-field activities. It is their game, so they get to set the rules—if one does not want to waive that right, one always has the options not to play or to start one’s own group.
There are several lines of resistance one could put up to this argument. First, one might argue that some institutions (e.g. hospitals) have an ethical obligation to be open to the public, and so logic gleaned from a football organization does not apply. One might also point out that if every institution instituted a mandate then there would be nowhere else for people who did not want vaccines to go. However, in both cases the answer is the same—at the limit, the most restrictive institutional mandates can be is akin to government mandates, depriving individuals of a choice regardless of their own decisions to associate. If we have already established that government mandates are acceptable, at most these arguments show that there are no additional reasons in support of institutional mandates.
Another objection might be that similar logic to that used to defend institutional mandates above (i.e. freedom to associate) has historically been used for pernicious ends such as refusing minorities service (e.g. by refusing to make wedding cakes for gay marriages). For the most part, the ethics of allowing refusal of service based on minority status are complex and beyond the scope of this paper. However, there are two clear disanalogies between requiring that (for example) students receive vaccines and requiring that wedding cake customers be heterosexual. First, in the bakery case there would be a concern that if all bakeries had similar policies, then it would be impossible for gay couples to get wedding cakes at all. However, in this case, one can acquire the services simply by getting the vaccine, so there is no risk of being shut out simply in virtue of one’s identity. (We do assume that a gay person cannot just choose to be heterosexual, but even if they somehow could, it would be metaphysically impossible for this gay couple qua gay couple to somehow be heterosexual.) Second, we suspect (though will not here defend) that part of the issue with the bakery example is that refusing service on the grounds of sexual orientation is a capricious reason to do so—it seems exclusionary for no legitimate reason. Since there are clearly strong legitimate reasons that an institution would want its students/workers/customers/etc. to be vaccinated, there is no worry about capriciousness here.
Objections and Replies
Objection 1: If one can be required to waive bodily rights for the sake of another person, that will be used as a reason to limit abortion rights. That functions as a reductio against the original argument.
Reply 1: First, let us grant for the sake of argument that the fetus is a fully rights-bearing person. Note that if it is anything less than fully rights-bearing then there is no conflict of rights among equals, and the arguments above never get off the ground. But in any event the argument still does not go through, because the translation of our original premise that the vaccine is safe is simply false ( Kazemi et al. , 2017 ). Many pregnancies go relatively smoothly, but even then the woman is severely restricted for roughly nine months. And quite a lot of pregnancies do not go smoothly. Women can develop wrenching and dangerous nausea ( Bustos et al. , 2017 ), heart problems ( Iftikhar and Biswas, 2019 ), blood clots ( Devis and Knuttinen, 2017 ), etc. So there is simply no analogy between mandating a vaccine and mandating a continued pregnancy. One might get the result that if a fetus is fully rights-bearing and if a woman can do so without cost or danger and if no one else can do so then she might have some minimal obligation to aid the safe extraction of a post-viability fetus. But such a triply conditional conclusion does not seem like an obvious reductio. Arguably it is just a restatement of famed abortion rights philosopher Judith Jarvis Thomson’s (1976) concession that the right to an abortion is the right to end a pregnancy rather than a right to a dead baby. Note also that the limited conclusion might not allow for an enforcement mechanism as readily as would a vaccine mandate—knowing in the first place who is pregnant and what they are doing for their fetus would require a level of invasion of every woman’s privacy (even those not actually pregnant) that has no analogy in the case where everyone is required to get vaccinated (or show evidence of MPMs) to enter public spaces.
Objection 2: Institutional mandates risk unintended consequences. For example, if a hospital mandates that nurses get the vaccine, then nurses might quit and go work at a less well-regulated care facility where still more vulnerable people will be exposed to the virus.
Reply 2: We consider this a very real concern, though note that it has only limited application. While unvaccinated nurses congregating at less well-regulated nursing homes might be a risk, there is no reason to expect (for example) unvaccinated students would gather anywhere vulnerable and less well-regulated. This is also more of a policy question than an ethical one, where what really needs be resolved is not whether institutional mandates are ethical but rather how we can make sure that the absence of mandates are not disproportionately burdensome on particular populations. Interestingly this very objection strengthens the case for a government mandate, as one of the points of government action is to make sure that we avoid a race-to-the-bottom where some institutions see advantages in refusing to enact vaccine mandates.
Objection 3: We do (and presumably should?) let people take all sorts of actions that pose risks to others, such as driving. Similarly, we should let people walk around unvaccinated.
Reply 3: This objection is potentially more potent in the wake of omicron than it was upon drafting this paper. As mentioned at the start, vaccines are potentially less effective against the omicron variant than past variants. If the vaccine is not as effective, then one might to tempted to think that we might as well allow people to walk around unvaccinated at this stage in the pandemic. Unless we are endorsing a strict lockdown, people’s rights to not be assaulted by COVID-19 will be infringed, vaccine or not. To reiterate the objection, we allow people to take all sorts of actions that post risks to other, so why not the act of walking around unvaccinated? There are several disanalogies between cases like being allowed to drive and being allowed to refuse a vaccine. First, there are legitimate societal reasons for wanting people to be able to drive. Even if sometimes people drive for no discernible reason, it is still at least potentially in everyone’s interests for people to be able to drive generally. Returning to the Original Position, if no one were allowed to drive that would severely hamper one’s unknown self’s potential well-being in a way that being forced to receive a particular vaccine would not. Second, as Giubilini et al. (2021) argues, even in the case of driving, there is massive government regulation regarding how precisely it must be done. We cannot (and should not be able to) just drive as we see fit—if one wants to enter the sphere of drivers, there are certain rules. In fact, to even enter the sphere of drivers at all one needs to meet a certain government-imposed requirement (getting a license)—in the same way, to enter the sphere of societal interaction one might need to meet another condition. One might argue that one could simply refuse to drive, but the foregoing is still sufficient to address the issue that we simply allow people to risk the lives of others. We can also see from this example why general lockdowns are less ethically justifiable than vaccine mandates, even in the face of a more transmissible variant such as omicron. The vast majority of people would be significantly harmed by being barred from public spaces altogether, so it is unlikely people would choose such an option from our version of the original position. As with driving, allowing and regulating the valuable activity is significantly more justifiable than simply banning it outright.
Objection 4: One reviewer notes that we generally countenance communities running risks of spreading the common cold or the flu, so we have no principled reason to deny localities the right to run the risk of spreading COVID-19.
Reply 4: As noted above, there are several disanologies between COVID-19 and the flu (and a fortiori even more disanlogies with the common cold). The flu is not analogous to COVID-19 in terms of either virulence or severity, and the vaccines are not analogous in terms of effectiveness (even in the era of omicron). As such, the diseases/vaccines are different in kind and a reasonable individual within a community with high disease risk tolerance could more justly complain of their neighbors’ actions with regard to COVID-19 than the flu. We remain neutral on where the line is at which point an individual’s objectively defensible claim to a rights violation become decisive, but COVID-19 is clearly on one side of it. Note that this is particularly true where high risk tolerance of a particular disease is based on false empirical beliefs about its severity (e.g. that COVID-19 is no worse than the flu), as this undermines the validity of everyone’s consent to take the risk.
Objection 5: Once herd immunity nears or is reached, the risk of contracting COVID-19 in public spaces is reduced to the point that the conflict of rights ought to favor the unvaccinated, i.e. mandates are no longer permissible ( Giubilini, 2020 ; Williams, 2021 ).
Reply 5: This objection is interesting insofar as it may grant our argument up to a point. What our argument gets thus far is that when the risk of COVID-19 (or some other infectious disease) is sufficiently high, the consent rights of the bystander trump the consent rights of the would-be unvaccinated. One goal of vaccination is to achieve herd immunity, such that a disease is unable to find a host, and eventually the spread peters out. This is especially important in protecting those that cannot be vaccinated due to age or medical conditions. Our argument largely set herd immunity aside, insofar as we were not defending a mandate as a way to achieve herd immunity. Here, however, it is important to acknowledge that herd immunity is indeed a hopeful and likely result of a successful vaccine mandate. Yet, once herd immunity is reached, and the risk of COVID-19 exposure diminishes, it seems that the bystander’s right can no longer be said to trump the right of the would-be unvaccinated individual, such that the mandate is no longer ethical based on our argument.
A number of points are worth noting in response. First, as of this writing, herd immunity with respect to COVID-19 is far from becoming a reality. As new variants continue to emerge, the prospect of reaching herd immunity anytime soon continues to dwindle. As such, our argument stands strong for a COVID-19 vaccine mandate for the immediate and likely protracted future, even if not for all times. Second, removing a vaccine mandate once herd immunity has been reached invites new outbreaks and a general breakdown of the herd immunity. That is, it remains plausible that the risks of being unvaccinated, even once herd immunity is reached, continue to be high, insofar as herd immunity can easily be lost. We are seeing this occur presently with measles outbreaks and the prediction of many more to come in 2022 ( Center for Disease Control and Prevention, 2020 ; World Health Organization, 2021 ). Finally, if herd immunity is reached in such a way that a disease is eliminated entirely, with no clear risk of reemergence, then we concede our argument for a vaccine mandate has concluded—as we are making specific claims about the applied ethics of a particular policy in a particular context, the fact that it would no longer be applicable in a radically different context is no objection.
In summation, we think the case is extremely strong for requiring everyone who is able to receive a COVID-19 vaccine, ideally at the level of governmental mandate and also at the level of individual institutions. This case is strong even without looking at the utilitarian arguments that allowing the virus to spread and mutate can have catastrophic consequences, which arguments seem fairly impressive on their own. Rather, we argue that the same logic of a deontological right to consent or not to bodily infringements that speaks in favor of not requiring people to be injected with a vaccine also speaks in favor of not requiring people to be unnecessarily exposed to COVID-19, and so a full reckoning will involve a tradeoff of rights that will speak in favor of vaccine mandates.
Acknowledgments
We would like to thank Allison McCarthy for extensive comments and feedback and Dean Jacqueline Dunbar-Smith for the original impetus for this project.
This work was not supported by any particular funding mechanism.
Conflict of Interest
None declared.
Contributor Information
Daniel A Wilkenfeld, Department of Acute and Tertiary Care, University of Pittsburgh School of Nursing, USA.
Christa M Johnson, Department of Philosophy, University of Dayton, United States of America.
- American Academy of Pediatrics (2021). Children and Covid-19: State-Level Data Report , available from: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report [accessed 30 December 2021].
- Bester J. C. (2018). The Harm Principle Cannot Replace the Best Interest Standard: Problems with Using the Harm Principle for Medical Decision Making for Children . The American Journal of Bioethics , 18 , 9–19. [ PubMed ] [ Google Scholar ]
- Blumenthal K. G., Phadke N. A., Bates D. W. (2021). Safety Surveillance of COVID-19 mRNA Vaccines through the Vaccine Safety Datalink . JAMA , 326 , 1375. [ PubMed ] [ Google Scholar ]
- Brennan J. (2018). A Libertarian Case for Mandatory Vaccination . Journal of Medical Ethics , 44 , 37–43. [ PubMed ] [ Google Scholar ]
- Brummett A. L. (2021). Defending, Improving, Expanding, and Applying a Moral-Metaphysical Proceduralism for Secular Clinical Ethics . The American Journal of Bioethics , 21 , W6–W9. [ PubMed ] [ Google Scholar ]
- Buss, S., and Westlund, A. (2018). Personal Autonomy. In E. N. Zalta (ed.), Stanford Encyclopedia of Philosophy. Metaphysics Research Lab, Stanford University. https://plato.stanford.edu/archives/spr2018/entries/personal-autonomy/ [accessed 25 March 2022]. , [ Google Scholar ]
- Bustos M., Venkataramanan R., Caritis S. (2017). Nausea and Vomiting of Pregnancy—What’s New? Autonomic Neuroscience , 202 , 62–72. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention (2020). Measles (Rubeola) , available from: https://www.cdc.gov/measles/index.html [accessed 30 December 2021].
- Centers for Disease Control and Prevention (2021a). Selected Adverse Events Reported after COVID-19 Vaccination , available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/adverse-events.html [accessed 30 December 2021].
- Centers for Disease Control and Prevention (2021b). Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-Biontech COVID-19 Vaccine—United States, December 14–23, 2020 , available from: https://www.cdc.gov/mmwr/volumes/70/wr/mm7002e1.htm?s_cid=mm7002e1_w [accessed 30 December 2021].
- Centers for Disease Control and Prevention (2021c). CDC COVID-19 Study Shows MRNA Vaccines Reduce Risk of Infection by 91 Percent for Fully Vaccinated People , available from: https://www.cdc.gov/media/releases/2021/p0607-mrna-reduce-risks.html [accessed 30 December 2021].
- Centers for Disease Control and Prevention (2021d). Updates on Thrombosis with Thrombocytopenia Thrombocytopenia Syndrome (TTS) , available from: https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-12-16/02-COVID-See-508.pdf [accessed 30 December 2021].
- Centers for Disease Control and Prevention (2022). COVID Data Tracker Weekly Review, 25 February , available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html [accessed 1 March 2022].
- Conti A., Capasso E., Casella C., Fedeli P., Salzano F. A., Policino F., Terracciano L., Delbon P. (2018). Blood Transfusion in Children: The Refusal of Jehovah’s Witness Parents . Open Medicine , 13 , 101–104. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crook H., Raza S., Nowell J., Young M., Edison P. (2021). Long Covid—Mechanisms, Risk Factors, and Management . BMJ 374:n1648 http://dx.doi.org/10.1136/bmj.n1648 [ PubMed ] [ Google Scholar ]
- Delahoy M. J., , UjamaaD., , WhitakerM., , O'HalloranA., , AnglinO., , BurnsE., , CummingsC., , HolsteinR., , KambhampatiA. K., , MiluckyJ., , PatelK., , PhamH., , TaylorC. A., , ChaiS. J., , ReingoldA., , AldenN. B., , KawasakiB., , MeekJ., , Yousey-HindesK., , AndersonE. J., , OpenoK. P., , TenoK., , WeigelA., , KimS., , LeegwaterL., , ByeE., , Como-SabettiK., , RoppS., , RudinD., , MuseA., , SpinaN., , BennettN. M., , PophamK., , BillingL. M., , ShiltzE., , SuttonM., , ThomasA., , SchaffnerW., , TalbotH. K., , CrosslandM. T., , McCaffreyK., , HallA. J., , FryA. M., , McMorrowM., , ReedC., , GargS., and , Havers F. P. (2021). Hospitalizations Associated with COVID-19 AMONG Children and Adolescents- COVID-NET, 14 States, March 1, 2020-August 14, 2021 . MMWR. Morbidity and Mortality Weekly Report , 70 , 1255–1260. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Devis P., Knuttinen M. G. (2017). Deep Venous Thrombosis in Pregnancy: Incidence, Pathogenesis and Endovascular Management . Cardiovascular Diagnosis and Therapy , 7 (Suppl 3 ), S309. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Flanigan J. (2014). A Defense of Compulsory Vaccination . In HEC Forum , Vol. 26 . Springer, pp. 5–25. [ PubMed ] [ Google Scholar ]
- Foot P. (1967). The Problem of Abortion and the Doctrine of the Double Effect . Oxford Review , 5–15. [ Google Scholar ]
- Giubilini A. (2020). An Argument for Compulsory Vaccination: The Taxation Analogy . Journal of Applied Philosophy , 37 , 446–466. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Giubilini A., Minerva F., Schuklenk U., Savulescu J. (2021). The ‘Ethical’ COVID-19 Vaccine Is the One That Preserves Lives: Religious and Moral Beliefs on the COVID-19 Vaccine . Public Health Ethics , 14 , 242–255. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Giubilini A., Savulescu J. (2019). Vaccination, Risks, and Freedom: The Seat Belt Analogy . Public Health Ethics , 12 , 237–249. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gostin L. O. (2021). Vaccine Mandates Are Lawful, Effective and Based on Rock-Solid Science , Scientific American , available from: https://www.scientificamerican.com/article/vaccine-mandates-are-lawful-effective-and-based-on-rock-solid-science/ [accessed 13 September 2021].
- Greyson D., Vriesema-Magnuson C., Bettinger J. A. (2019). Impact of School Vaccination Mandates on Pediatric Vaccination Coverage: A Systematic Review . CMAJ Open , 7 , E524–E536. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harsanyi J. C. (1975). Can the Maximin Principle Serve as a Basis for Morality? A Critique of John Rawls’s Theory . American Political Science Review , 69 , 594–606. [ Google Scholar ]
- Heuer U. (2011) The Paradox of Deontology, Revisited. In Oxford Studies of Normative Ethics . New York: Oxford University Press. [ Google Scholar ]
- Hobbes T. (2016). Thomas Hobbes: Leviathan (Longman Library of Primary Sources in Philosophy) . New York: Routledge. [ Google Scholar ]
- Iftikhar S. F., Biswas M. Cardiac Disease In Pregnancy. In: StatPearls. StatPearls Publishing, Treasure Island (FL) PMID: 30725946. [ PubMed ]
- Johnson C. M. (2019). The Intrapersonal Paradox of Deontology . Journal of Moral Philosophy , 16 , 279–301. [ Google Scholar ]
- Kahn J. H. (2020). Confidentiality and Capacity . Emergency Medicine Clinics of North America , 38 , 283–296. [ PubMed ] [ Google Scholar ]
- Kamm F. M. (1989). Harming Some to save Others . Philosophical Studies , 57 , 227–260. [ Google Scholar ]
- Kamm F. M. (1996). Morality Mortality . New York: Oxford University Press. [ PubMed ] [ Google Scholar ]
- Kazemi F., Nahidi F., Kariman N. (2017). Disorders Affecting Quality of Life during Pregnancy: A Qualitative Study . Journal of Clinical and Diagnostic Research , 11 , QC06–QC10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Klein N. P., Lewis N., Goddard K., Fireman B., Zerbo O., Hanson K. E., Donahue J. G., Kharbanda E. O., Naleway A., Nelson J. C., Xu S., Yih W. K., Glanz J. M., Williams J. T. B., Hambidge S. J., Lewin B. J., Shimabukuro T. T., DeStefano F., Weintraub E. S. (2021). Surveillance for Adverse Events after COVID-19 mRNA Vaccination . JAMA , 326 , 1390. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kowalik M. (2022). Ethics of vaccine refusal. Journal of Medical Ethics , 48 , 240. https://doi.org/10.1136/medethics-2020-107026. [ PubMed ] [ Google Scholar ]
- Lyngse, F. P., Kirkeby, C. T., Denwood, M., Christiansen, L. E., Mølbak, K., Møller, C. H., Skov, R. L., Krause, T. G., Rasmussen, M., Sieber, R. N., Johannesen, T. B., Lillebaek, T., Fonager, J., Fomsgaard, A., Møller, F. T., Stegger, M., Overvad, M., Spiess, K., and Mortensen, L. H. (2022). Transmission of SARS-CoV-2 Omicron VOC subvariants BA.1 and BA.2: Evidence from Danish Households. MedRxiv , 2022.01.28.22270044. https://doi.org/10.1101/2022.01.28.22270044 [ Google Scholar ]
- Ma Q., Liu J., Liu Q., Kang L., Liu R., Jing W., Wu Y., Liu M. (2021). Global Percentage of Asymptomatic SARS-CoV-2 Infections among the Tested Population and Individuals with Confirmed COVID-19 Diagnosis: A Systematic Review and Meta-Analysis . JAMA Network Open , 4 , e2137257. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- MacIntyre A. (1981). After Virtue. Notre Dame: Notre Dame.
- Manson N. C., O’Neill O. (2007). Rethinking Informed Consent in Bioethics . New York: Cambridge University Press. [ Google Scholar ]
- Mill J. S. (2011). On Liberty. Project Guttenberg. https://www.gutenberg.org/files/34901/34901-h/34901-h.htm . [accessed 25 March 2022]. [ Google Scholar ]
- Nozick R. (1974). Anarchy, State, and Utopia . New York: Basic Books. [ Google Scholar ]
- Petter E., Mor, O., Zuckerman, N., Oz-Levi, D., Younger, A., Aran, D., and Erlich, Y. (2021). Initial Real World Evidence for Lower Viral Load of Individuals Who Have Been Vaccinated by BNT162b2 . medRxiv . [ Google Scholar ]
- Rawls J. (1999). A Theory of Justice: Revised Edition . New York: Harvard University Press. [ Google Scholar ]
- Salter E. K. (2012). Deciding for a Child: A Comprehensive Analysis of the Best Interest Standard . Theoretical Medicine and Bioethics , 33 , 179–198. [ PubMed ] [ Google Scholar ]
- Sandel M. (1982). Liberalism and the Limits of Justice . Cambridge: Cambridge University Press. [ Google Scholar ]
- Savulescu J. (2021). Good Reasons to Vaccinate: Mandatory or Payment for Risk? Journal of Medical Ethics , 47 , 78–85. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scheffler S. (1988). Agent-Centered Restrictions, Rationality, and the Virtues. In Scheffler S. (ed.) Consequentialism and Its Critics . New York: Oxford University Press, ; pp. 243–260. [ Google Scholar ]
- Scobie H. M., Johnson A. G., Suthar A. B., Severson R., Alden N. B., Balter S., Bertolino D., Blythe D., Brady S., Cadwell B., Cheng I., Davidson S., Delgadillo J., Devinney K., Duchin J., Duwell M., Fisher R., Fleischauer A., Grant A., Griffin J., Haddix M., Hand J., Hanson M., Hawkins E., Herlihy R. K., Hicks L., Holtzman C., Hoskins M., Hyun J., Kaur R., Kay M., Kidrowski H., Kim C., Komatsu K., Kugeler K., Lewis M., Lyons B. C., Lyons S., Lynfield R., McCaffrey K., McMullen C., Milroy L., Meyer S., Nolen L., Patel M. R., Pogosjans S., Reese H. E., Saupe A., Sell J., Sokol T., Sosin D., Stanislawski E., Stevens K., Vest H., White K., Wilson E., MacNeil A., Ritchey M. D., Silk B. J. (2021). Monitoring Incidence of COVID-19 Cases, Hospitalizations, and Deaths, by Vaccination Status—13 US Jurisdictions, April 4–July 17, 2021 . Morbidity and Mortality Weekly Report , 70 , 1284–1290. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thompson M. G., Burgess J. L., Naleway A. L., Tyner H. L., Yoon S. K., Meece J., Olsho L. E. W., Caban-Martinez A. J., Fowlkes A., Lutrick K., Kuntz J. L., Dunnigan K., Odean M. J., Hegmann K. T., Stefanski E., Edwards L. J., Schaefer-Solle N., Grant L., Ellingson K., Groom H. C., Zunie T., Thiese M. S., Ivacic L., Wesley M. G., Lamberte J. M., Sun X., Smith M. E., Phillips A. L., Groover K. D., Yoo Y. M., Gerald J., Brown R. T., Herring M. K., Joseph G., Beitel S., Morrill T. C., Mak J., Rivers P., Harris K. M., Hunt D. R., Arvay M. L., Kutty P., Fry A. M., Gaglani M. (2021). Interim Estimates of Vaccine Effectiveness of BNT162b2 and mRNA-1273 COVID-19 Vaccines in Preventing SARS-CoV-2 Infection among Health Care Personnel, First Responders, and Other Essential and Frontline Workers—Eight US Locations, December 2020–March . Morbidity and Mortality Weekly Report , 70 , 495–500. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thompson M. G., Burgess J. L., Naleway A., Tyner, H. L., Yoon, S. K., Meece, J., Olsho, L. E. W., Caban-Martinez, A. J., Fowlkes, A. L., Lutrick, K., Groom, H. C., Dunnigan, K., Odean, M. J., Hegmann, K. T., Stefanski, E., Edwards, L. J., Schaefer-Solle, N., Grant, L., Ellingson, K., Kuntz J. L., Zunie, T., Thiese, M. S., Ivacic, L., Wesley, M. G., Lamberte, J. M., Sun, X., Smith, M. E., Phillips, A. L., Groover, K. D., Yoo, Y. M., Gerald, J., Brown, R. T., Herring, M. K., Joseph, G., Beitel, S., Morrill, T. C., Mak, J., Rivers, P., Lynch, B., Zhou, Y., Zhang, J., Kelleher, A., Li, Y., Dickerson, M., Hanson, E., Guenther, K., Tong, S., Bateman, A., Reisdorf, E., Barnes, J., Azziz-Baumgartner, E., Hunt, D. R., Arvay, M. L., Kutty, P., Fry, A. M., and Gaglani, M. (2021). Prevention and Attenuation of COVID-19 by BNT162b2 and mRNA-1273 Vaccines . medRxiv . [ Google Scholar ]
- Thomson J. J. (1976). Killing, Letting Die, and the Trolley Problem . The Monist , 59 , 204–217. [ PubMed ] [ Google Scholar ]
- Thomson J. J. (1990). The Realm of Rights . Cambridge, MA: Harvard University Press. [ Google Scholar ]
- Vitiello A., Ferrara F., Troiano V., La Porta R. (2021). COVID-19 Vaccines and Decreased Transmission of SARS-CoV-2 . Inflammopharmacology , 29 , 1357–1354. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wilkenfeld D. A., McCarthy A. (2020). Ethical Concerns with Applied Behavior Analysis for Autism Spectrum Disorder . Kennedy Institute of Ethics Journal , 30 , 31–69. [ PubMed ] [ Google Scholar ]
- Wilkinson D., Savulescu J. (2018). Ethics, Conflict and Medical Treatment for Children: From Disagreement to Dissensus . Poland: Elsevier. [ PubMed ] [ Google Scholar ]
- Williams B. M. (2021). The Ethics of Selective Mandatory Vaccination for COVID-19 . Public Health Ethics . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- World Health Organization (2021). Global Progress against Measles Threatened Amidst COVID-19 Pandemic , available from: https://www.who.int/news/item/10-11-2021-global-progress-against-measles-threatened-amidst-covid-19-pandemic [accessed 30 December 2021].

IMAGES
VIDEO
COMMENTS
Thesis Summary . Vaccines are one of the world's most impactful medical therapies. They are cost-effective, successfully proven, and one of the quickest treatment options available today (Clark et al., 2016). They save millions of lives every year and have eliminated certain diseases on a
Two doses of the vaccine or placebo were given 21 days apart to the respective groups. 21 The mean age of the participants was 45.3 years, and the majority of participants were Caucasian (98.5%). 21 From 21 days after the first dose of the vaccine, efficacy against symptomatic COVID-19 illness was 91.6% ...
In less than a year, an array of vaccines was developed to bring an end to the SARS-CoV-2 pandemic. As impressive as the speed of development was the efficacy of vaccines such as Moderna and ...
The numbers of cases and deaths from coronavirus disease 2019 (COVID-19) are continuously increasing. Many people are concerned about the efficacy and safety of the COVID-19 vaccines. We performed a comprehensive analysis of the published trials of COVID-19 vaccines and the real-world data from the Vaccine Adverse Event Reporting System.
vaccination decisions, especially within the context of COVID-19 vaccines. Vaccination decision making has considered the known apprehensions that vaccination carries, but not as broadly as uncertainty around the virus and consequently the vaccine. This thesis aims to explore nurses' decision-making around COVID-19 vaccination, with
A vaccination program started in the United Kingdom in 2008, and at the time of writing over 10.5 million doses had been given to girls (Public Health England, 2018), with the aim of preventing primary infection with HPV. The vaccine coverage was 83.8% for 13-14 year old girls in England in 2017/18 (Public Health England, 2019).
Vaccination is a safe, simple, and effective way of protecting a person against COVID-19. By the end of August 2021, only 24.6% of the world population has received two doses of a COVID-19 vaccine. Since the emergence of COVID-19, several COVID-19 vaccines have been developed and approved for emergency use. Current vaccines have shown efficacy ...
Introduction. Vaccinations are among the most important public health tools for reducing the spread and harm caused by dangerous diseases [].The World Health Organization estimates that vaccines prevented at least 10 million deaths between 2010-2015 worldwide [].Despite considerable evidence showing vaccines are safe [3, 4], there is increasing skepticism toward vaccination [5, 6].
COVID-19 vaccines in the context of limited vaccine supply includes HW as a priority group for vaccination. This recommendation was further supported by the European Technical Advisory Group on immunizations in November 2020 (3). Evaluating the real-world COVID-19 vaccine performance is critical for understanding the risks and
vaccines at minimum age and with minimum intervals ensure rapid protectionwould against vaccine-preventable diseases. 5. Minimizing risk of COVID-19 transmission during routine and catch-up vaccination sessions Most people with COVID-19 develop mild or uncomplicated illness, and in some cases, infected ...
Objectives: This umbrella meta-analysis aims to provide comprehensive and synthesized evidence regarding the effectiveness and safety of COVID-19 vaccinations based on current studies.Methods: Studies from the Cochrane Library, PubMed, and EMBASE, published before 10 December 2021, were included in the analysis. The pooled results of effectiveness and safety were estimated and shown in forest ...
However, vaccination coverage remains a significant concern in many developing countries. While previous studies have linked community engagement to positive health outcomes, there is a gap in ...
Mandatory vaccination, including for COVID-19, can be ethically justified if the threat to public health is grave, the confidence in safety and effectiveness is high, the expected utility of mandatory vaccination is greater than the alternatives, and the penalties or costs for non-compliance are proportionate. I describe an algorithm for justified mandatory vaccination. Penalties or costs ...
DRAFT Prepared by the SAGE Working Group on COVID-19 Vaccines 22 December 2020 5 . even death. Several occupational risks for health workers emerged or were amplified by the COVID-
An additional aspect of vaccines many parents are troubled with is the increase in suggested vaccines for young children. "Today, the CDC recommends that children receive vaccines for 10 diseases — plus the flu vaccine — by age 6, which can mean up to 37 separate shots. That compares to five vaccines for the same age group in 1995 ...
Childhood vaccination rates vary widely by country and region, and the reasons for these variations are likely to be context-specific [1,2,3].While access to vaccination is a perennial challenge, acceptance also remains an issue of importance to uptake which is affected by an individual's feelings, attitudes and beliefs about vaccination []. ...
Vaccine hesitancy is a major threat to the success of COVID-19 vaccination programs. The present cross-sectional online survey of adult Poles (n = 1020) expressing a willingness to receive the COVID-19 vaccine was conducted between February and March 2021 and aimed to assess (i) the general trust in different types of vaccines, (ii) the level of acceptance of the COVID-19 vaccines already in ...
The 1800s. In 1872, despite enduring a stroke and the death of 2 of his daughters to typhoid, Louis Pasteur creates the first laboratory-produced vaccine: the vaccine for fowl cholera in chickens. In 1885, Louis Pasteur successfully prevents rabies through post-exposure vaccination. The treatment is controversial.
Vaccination is widely considered one of the greatest medical achievements of modern civilization. Childhood diseases that were commonplace less than a generation ago are now increasingly rare because of vaccines. In order to be effective at eliminating communicable diseases, vaccines must be administered to sufficient levels of persons in the community.
In a human challenge vaccine study, healthy volunteers are given an experimental vaccine, and then deliberately exposed to the organism causing the disease to see if the vaccine works. Some scientists believe that this approach could accelerate COVID-19 vaccine development, in part because it would require far fewer volunteers than a typical study.
A recent economic analysis of 10 vaccines for 94 low- and middle-income countries estimated that an investment of $34 billion for the immunization programs resulted in savings of $586 billion in reducing costs of illness and $1.53 trillion when broader economic benefits were included ( 5 ). The only human disease ever eradicated, smallpox, was ...
This paper introduces the different types of vaccines and the effects of vaccines in the body and provides an examination of a case study of the 2019 Pacific Northwest measles outbreak. The outbreak is modeled using a proposed modified SIR model and solved using the Fourth-Order Runge-Kutta method. The results suggest that around day 20, almost ...
Considering a vaccination rate of 30% and a Degree vaccination strategy, 0.3 years of life are lost on a scale-free network and little more than a year on a small-world network, but that could ...
Ms. Tey is a freelance reporter studying journalism and the environment at New York University. We don't yet know if H5N1 bird flu will spill over from animals to infect a large number of humans ...
Vaccine mandates risk treating individuals as a means to an end and risk running afoul of the second categorical imperative. Utilitarian advocates would argue for a vaccine mandate as it provides the greatest well-being for the most people possible. The utilitarian argument that vaccine mandates are doing the best for the most falls flat when ...
Investment thesis. Since the publication of my last article on January ... The main difference between these two vaccines is that Gardasil 9 protects against nine types of HPV (6, 11, 16, 18, 31 ...
Note that our thesis is specifically applicable only to COVID-19 vaccines; we will however explore to what extent our argument might generalize to other vaccines. Even more precisely, our argument was originally formed in the context of variants of COVID-19 through delta. ... Vaccine Mandates Are Lawful, Effective and Based on Rock-Solid ...