Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Topic collections
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 13, Issue 2
- Qualitative Research Methods in Mental Health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Sarah Peters
- Correspondence to : Dr Sarah Peters, School of Psychological Sciences, The University of Manchester, Coupland Building 1, Oxford Road M13 9PL, UK; sarah.peters{at}manchester.ac.uk
As the evidence base for the study of mental health problems develops, there is a need for increasingly rigorous and systematic research methodologies. Complex questions require complex methodological approaches. Recognising this, the MRC guidelines for developing and testing complex interventions place qualitative methods as integral to each stage of intervention development and implementation. However, mental health research has lagged behind many other healthcare specialities in using qualitative methods within its evidence base. Rigour in qualitative research raises many similar issues to quantitative research and also some additional challenges. This article examines the role of qualitative methods within mental heath research, describes key methodological and analytical approaches and offers guidance on how to differentiate between poor and good quality qualitative research.
https://doi.org/10.1136/ebmh.13.2.35
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
The trajectory of qualitative methods in mental health research
Qualitative methodologies have a clear home within the study of mental health research. Early and, arguably, seminal work into the study of mental illnesses and their management was based on detailed observation, moving towards theory using inductive reasoning. Case studies have been long established in psychiatry to present detailed analysis of unusual cases or novel treatments. Participant observation was the principle method used in Goffman's seminal study of psychiatric patients in asylums that informed his ideas about the institutionalising and medicalising of mental illness by medical practice. 1 However, the 20th century saw the ‘behaviourist revolution’, a movement where quantification and experimentation dominated. Researchers sought to identify cause and effects, and reasoning became more deductive – seeking to use data to confirm theory. The study of health and illness was determined by contemporary thinking about disease, taking a biomedical stance. Psychologists and clinical health researchers exploited natural science methodologies, attempting to measure phenomenon in their smallest entities and do so as objectively as possible. This reductionist and positivist philosophy shaped advances in research methods and meant that qualitative exploration failed to develop as a credible scientific approach. Indeed, ‘objectivity’ and the ‘discovery of truth’ have become synonymous with ‘scientific enquiry’ and qualitative methods are easily dismissed as ‘anecdotal’. The underlying epistemology of this approach chimes well with medical practice for which training is predominately in laboratory and basic sciences (such as physics and chemistry) within which the discourse of natural laws dominate. To this end, research in psychiatry still remains overwhelmingly quantitative. 2
Underlying all research paradigms are assumptions. However, most traditional researchers remain unaware of these until they start to use alternative paradigms. Key assumptions of quantitative research are that facts exist that can be quantified and measured and that these should be examined, as far as possible, objectively, partialling out or controlling for the context within which they exist. There are research questions within mental health where this approach can hold: where phenomenon of interest can be reliably and meaningfully quantified and measured, it is feasible to use data to test predictions and examine change. However, for many questions these assumptions prove unsatisfying. It is often not possible or desirable to try and create laboratory conditions for the research; indeed it would be ecologically invalid to do so. For example, to understand the experience of an individual who has been newly diagnosed with schizophrenia, it is clearly important to consider the context within which they live, their family, social grouping and media messages they are exposed to. Table 1 depicts the key differences between the two methodological approaches and core underlying assumptions for each.
- View inline
Comparison of underlying assumptions of quantitative and qualitative research approaches
It should be cautioned that it is easy to fall into the trap of categorising studies as either quantitative or qualitative. The two traditions are often positioned within the literature as opposing and in conflict. This division is unhelpful and likely to impede methodological advancement. Though, undeniably, there are differences in the two approaches to research, there are also many exceptions that expose this dichotomy to be simplistic: some qualitative studies seek to test a priori hypotheses, and some quantitative studies are atheoretical and exploratory. 3 Hence it is more useful to consider research methodologies as lying along a spectrum and that researchers should be familiar with the full range of methodologies, so that a method is chosen according to the research question rather than the researcher's ability.
Rationale for qualitative methods in current mental health research
There are a number of scientific, practical and ethical reasons why mental health is an area that can particularly benefit from qualitative enquiry. Mental health research is complex. Health problems are multifactorial in their aetiology and the consequences they have on the individual, families and societies. Management can involve self-help, pharmacological, educative, social and psychotherapeutic approaches. Services involved are often multidisciplinary and require liaison between a number of individuals including professionals, service-users and relatives. Many problems are exacerbated by poor treatment compliance and lack of access to, or engagement with, appropriate services. 4
Engagement with mental health research can also be challenging. Topics may be highly sensitive or private. Individuals may have impaired capacity or be at high risk. During the research process there may be revelations of suicidal ideation or criminal activity. Hence mental health research can raise additional ethical issues. In other cases scepticism of services makes for reluctant research participants. However, if we accept the case that meaningful research can be based in subjective enquiry then qualitative methods provide a way of giving voice to participants. Qualitative methods offer an effective way of involving service-users in developing interventions for mental health problems 5 ensuring that the questions asked are meaningful to individuals. This may be particularly beneficial if participants are stakeholders, for example potential users of a new service.
Qualitative methods are valuable for individuals who have limited literacy skills who struggle with pencil and paper measures. For example qualitative research has proved fruitful in understanding children's concepts of mental illness and associated services. 6
How qualitative enquiry is used within mental health research
There are a range of types of research question where qualitative methods prove useful – from the development and testing of theory, to the piloting and establishing efficacy of treatment approaches, to understanding issues around translation and implementation into routine practice. Each is discussed in turn.
Development and testing of theory
Qualitative methods are important in exploratory work and in generating understanding of a phenomenon, stimulating new ideas or building new theory. For example, stigma is a concept that is recognised as a barrier to accessing services and also an added burden to mental health. A focus-group study sought to understand the meaning of stigma from the perspectives of individuals with schizophrenia, their relatives and health professionals. 7 From this they developed a four-dimensional theory which has subsequently informed interventions to reduce stigma and discrimination that target not only engagement with psychiatric services but also interactions with the public and work. 7
Development of tools and measures
Qualitative methods access personal accounts, capturing how individuals talk about a lived experience. This can be invaluable for designing new research tools. For example, Mavaddat and colleagues used focus groups with 56 patients with severe or common mental health problems to explore their experiences of primary care management. 8 Nine focus groups were conducted and analysis identified key themes. From these, items were generated to form a Patient Experience Questionnaire, of which the psychometric properties were subsequently examined quantitatively in a larger sample. Not only can dimensions be identified, the rich qualitative data provide terminology that is meaningful to service users that can then be incorporated into question items.
Development and testing of interventions
As we have seen, qualitative methods can inform the development of new interventions. The gold-standard methodology for investigating treatment effectiveness is the randomised controlled trial (RCT), with the principle output being an effect size or demonstration that the primary outcome was significantly improved for participants in the intervention arm compared with those in the control/comparison arm. Nevertheless, what will be familiar for researchers and clinicians involved in trials is that immense research and clinical learning arises from these substantial, often lengthy and expensive research endeavours. Qualitative methods provide a means to empirically capture these lessons, whether they are about recruitment, therapy training/supervision, treatment delivery or content. These data are essential to improve the feasibility and acceptability of further trials and developing the intervention. Conducting qualitative work prior to embarking on an RCT can inform the design, delivery and recruitment, as well as engage relevant stakeholders early in the process; all of these can prevent costly errors. Qualitative research can also be used during a trial to identify reasons for poor recruitment: in one RCT, implementing findings from this type of investigation led to an increased randomisation rate from 40% to 70%. 9
Nesting qualitative research within a trial can be viewed as taking out an insurance policy as data are generated which can later help explain negative or surprising findings. A recent trial of reattribution training for GPs to manage medically unexplained symptoms demonstrated substantial improvements in GP consultation behaviour. 10 However, effects on clinical outcomes were counterintuitive. A series of nested qualitative studies helped shed light as to why this was the case: patients' illness models were complex, and they resisted engaging with GPs (who they perceived as having more simplistic and dualistic understanding) because they were anxious it would lead to non-identification or misdiagnosis of any potential future disease 11 , an issue that can be addressed in future interventions. Even if the insights are unsurprising to those involved in the research, the data collected have been generated systematically and can be subjected to peer review and disseminated. For this reason, there is an increasing expectation from funding bodies that qualitative methodologies are integral to psychosocial intervention research.
Translation and implementation into clinical practice
Trials provide limited information about how treatments can be implemented into clinical practice or applied to another context. Psychological interventions are more effective when delivered within trial settings by experts involved in their development than when they are delivered within clinical settings. 12 Qualitative methods can help us understand how to implement research findings into routine practice. 13
Understanding what stakeholders value about a service and what barriers exist to its uptake is another evidence base to inform clinicians' practice. Relapse prevention is an effective psychoeducation approach that helps individuals with bipolar disorder extend time to relapse. Qualitative methodologies identified which aspects of the intervention service-users and care-coordinators value, and hence, are likely to utilise in routine care. 14 The intervention facilitated better understanding of bipolar disorder (by both parties), demonstrating, in turn, a rationale for medication. Patients discovered new, empowering and less socially isolated ways of managing their symptoms, which had important impacts on interactions with healthcare staff and family members. Furthermore, care-coordinators' reported how they used elements of the intervention when working with clients with other diagnoses. The research also provided insights as to where difficulties may occur when implementing a particular intervention into routine care. For example, for care-coordinators this proved a novel way of working with clients that was more emotionally demanding, thus highlighting the need for supervision and managerial support. 14
Beginners guide to qualitative approaches: one size doesn't fit all
Just as there is a range of quantitative research designs and statistical analyses to choose from, so there are many types of qualitative methods. Choosing a method can be daunting to an inexperienced or beginner-level qualitative researcher, for it requires engaging with new terms and ways of thinking about knowledge. The following summary sets out analytic and data-generation approaches that are used commonly in mental health research. It is not intended to be comprehensive and is provided only as a point of access/familiarisation to researchers less familiar with the literature.
Data generation
Qualitative data are generated in several ways. Most commonly, researchers seek a sample and conduct a series of individual in-depth interviews, seeking participants' views on topics of interest. Typically these last upwards of 45 min and are organised on the basis of a schedule of topics identified from the literature or pilot work. This does not act as a questionnaire, however; rather, it acts as a flexible framework for exploring areas of interest. The researcher combines open questions to elicit free responses, with focused questions for probing and prompting participants to provide effective responses. Usually interviews are audio-recorded and transcribed verbatim for subsequent analysis.
As interviews are held in privately, and on one-to-one basis, they provide scope to develop a trusting relationship so that participants are comfortable disclosing socially undesirable views. For example, in a study of practice nurses views of chronic fatigue syndrome, some nurses described patients as lazy or illegitimate – a view that challenges the stereotype of a nursing professional as a sympathetic and caring person. 15 This gives important information about the education and supervision required to enable or train general nurses to ensure that they are capable of delivering psychological interventions for these types of problems.
Alternatively, groups of participants are brought together for a focus group, which usually lasts for 2 hours. Although it is tempting to consider focus groups as an efficient way of acquiring data from several participants simultaneously, there are disadvantages. They are difficult to organise for geographically dispersed or busy participants, and there are compromises to confidentiality, particularly within ‘captive’ populations (eg, within an organisation individuals may be unwilling to criticise). Group dynamics must be considered; the presence of a dominant or self-professed expert can inhibit the group and, therefore, prevent useful data generation. When the subject mater is sensitive, individuals may be unwilling to discuss experiences in a group, although it often promotes a shared experience that can be empowering. Most of these problems are avoided by careful planning of the group composition and ensuring the group is conducted by a highly skilled facilitator. Lester and colleagues 16 used focus-group sessions with patients and health professionals to understand the experience of dealing with serious mental illness. Though initially participants were observed via focus-group sessions that used patient-only and health professional only groups, subsequently on combined focus groups were used that contained both patients and health professionals. 16 The primary advantage of focus groups is that they enable generation of data about how individuals discuss and interact about a phenomenon; thus, a well-conducted focus group can be an extremely rich source of data.
A different type of data are naturally occurring dialogue and behaviours. These may be recorded through observation and detailed field notes (see ethnography in Table 2 ) or analysed from audio/ video-recordings. Other data sources include texts, for example, diaries, clinical notes, Internet blogs and so on. Qualitative data can even be generated through postal surveys. We thematically analysed responses to an open-ended question set within a survey about medical educators' views of behavioural and social sciences (BSS). 17 From this, key barriers to integrating BSS within medical training were identified, which included an entrenched biomedical mindset. The themes were analysed in relation to existing literature and revealed that despite radical changes in medical training, the power of the hidden curriculum persists. 17
Key features of a range of analytical approaches used within mental health research
Analysing qualitative data
Researchers bring a wide range of analytical approaches to the data. A comprehensive and detailed discussion of the philosophy underlying different methods is beyond the scope of this paper; however, a summary of the key analytical approaches used in mental health research are provided in Table 2 . An illustrative example is provided for each approach to offer some insight into the commonalities and differences between methodologies. The procedure for analysis for all methods involves successive stages of data familiarisation/immersion, followed by seeking and reviewing patterns within the data, which may then be defined and categorized as specific themes. Researchers move back and forth between data generation and analysis, confirming or disconfirming emerging ideas. The relationship of the analysis to theory-testing or theory-building depends on the methodology used.
Some approaches are more common in healthcare than others. Interpretative phenomenological (lPA) analysis and thematic analysis have proved particularly popular. In contrast, ethnographic research requires a high level of researcher investment and reflexivity and can prove challenging for NHS ethic committees. Consequently, it remains under used in healthcare research.
Recruitment and sampling
Quantitative research is interested in identifying the typical, or average. By contrast, qualitative research aims to discover and examine the breadth of views held within a community. This includes extreme or deviant views and views that are absent. Consequently, qualitative researchers do not necessarily (though in some circumstances they may) seek to identify a representative sample. Instead, the aim may be to sample across the range of views. Hence, qualitative research can comment on what views exist and what this means, but it is not possible to infer the proportions of people from the wider population that hold a particular view.
However, sampling for a qualitative study is not any less systematic or considered. In a quantitative study one would take a statistical approach to sampling, for example, selecting a random sample or recruiting consecutive referrals, or every 10th out-patient attendee. Qualitative studies, instead, often elect to use theoretical means to identify a sample. This is often purposive; that is, the researcher uses theoretical principles to choose the attributes of included participants. Healey and colleagues conducted a study to understand the reasons for individuals with bipolar disorder misusing substances. 18 They sought to include participants who were current users of each substance group, and the recruitment strategy evolved to actively target specific cases.
Qualitative studies typically use far smaller samples than quantitative studies. The number varies depending on the richness of the data yielded and the type of analytic approach that can range from a single case to more than 100 participants. As with all research, it is unethical to recruit more participants than needed to address the question at hand; a qualitative sample should be sufficient for thematic saturation to be achieved from the data.
Ensuring that findings are valid and generalisable
A common question from individuals new to qualitative research is how can findings from a study of few participants be generalised to the wider population? In some circumstances, findings from an individual study (quantitative or qualitative) may have limited generalisability; therefore, more studies may need to be conducted, in order to build local knowledge that can then be tested or explored across similar groups. 4 However, all qualitative studies should create new insights that have theoretical or clinical relevance which enables the study to extend understanding beyond the individual participants and to the wider population. In some cases, this can lead to generation of new theory (see grounded theory in Table 2 ).
Reliability and validity are two important ways of ascertaining rigor in quantitative research. Qualitative research seeks to understand individual construction and, by definition, is subjective. It is unlikely, therefore, that a study could ever be repeated with exactly the same circumstances. Instead, qualitative research is concerned with the question of whether the findings are trustworthy; that is, if the same circumstances were to prevail, would the same conclusions would be drawn?
There are a number of ways to maximise trustworthiness. One is triangulation, of which there are three subtypes. Data triangulation involves using data from several sources (eg, interviews, documentation, observation). A research team may include members from different backgrounds (eg, psychology, psychiatry, sociology), enabling a range of perspectives to be used within the discussion and interpretation of the data. This is termed researcher triangulation . The final subtype, theoretical triangulation, requires using more than one theory to examine the research question. Another technique to establish the trustworthiness of the findings is to use respondent validation. Here, the final or interim analysis is presented to members of the population of interest to ascertain whether interpretations made are valid.
An important aspect of all qualitative studies is researcher reflexivity. Here researchers consider their role and how their experience and knowledge might influence the generation, analysis and interpretation of the data. As with all well-conducted research, a clear record of progress should be kept – to enable scrutiny of recruitment, data generation and development of analysis. However, transparency is particularly important in qualitative research as the concepts and views evolve and are refined during the process.
Judging quality in qualitative research
Within all fields of research there are better and worse ways of conducting a study, and range of quality in mental health qualitative research is variable. Many of the principles for judging quality in qualitative research are the same for judging quality in any other type of research. However, several guidelines have been developed to help readers, reviewers and editors who lack methodological expertise to feel more confident in appraising qualitative studies. Guidelines are a prerequisite for the relatively recent advance of methodologies for systematic reviewing of qualitative literature (see meta-synthesis in Table 2 ). Box 1 provides some key questions that should be considered while studying a qualitative report.
Box 1 Guidelines for authors and reviewers of qualitative research (adapted from Malterud 35 )
▶ Is the research question relevant and clearly stated?
Reflexivity
▶ Are the researcher's motives and background presented?
Method, sampling and data collection
▶ Is a qualitative method appropriate and justified?
▶ Is the sampling strategy clearly described and justified?
▶ Is the method for data generation fully described
▶ Are the characteristics of the sample sufficiently described?
Theoretical framework
▶ Was a theoretical framework used and stated?
▶ Are the principles and procedures for data organisation and analysis described and justified?
▶ Are strategies used to test the trustworthiness of the findings?
▶ Are the findings relevant to the aim of the study?
▶ Are data (e.g. quotes) used to support and enrich the findings?
▶ Are the conclusions directly linked to the study? Are you convinced?
▶ Do the findings have clinical or theoretical value?
▶ Are findings compared to appropriate theoretical and empirical literature?
▶ Are questions about the internal and external validity and reflexivity discussed?
▶ Are shortcomings of the design, and the implications these have on findings, examined?
▶ Are clinical/theoretical implications of the findings made?
Presentation
▶ Is the report understandable and clearly contextualised?
▶ Is it possible to distinguish between the voices of informants and researchers?
▶ Are sources from the field used and appropriately referenced?
Conclusions and future directions
Qualitative research has enormous potential within the field of mental health research, yet researchers are only beginning to exploit the range of methods they use at each stage of enquiry. Strengths of qualitative research primarily lie in developing theory and increasing understanding about effective implementation of treatments and how best to support clinicians and service users in managing mental health problems. An important development in the field is how to integrate methodological approaches to address questions. This raises a number of challenges, such as how to integrate textual and numerical data and how to reconcile different epistemologies. A distinction can be made between mixed- method design (eg, quantitative and qualitative data are gathered and findings combined within a single or series of studies) and mixed- model study, a pragmatist approach, whereby aspects of qualitative and quantitative research are combined at different stages during a research process. 19 Qualitative research is still often viewed as only a support function or as secondary to quantitative research; however, this situation is likely to evolve as more researchers gain a broader skill set.
Though it is undeniable that there has been a marked increase in the volume and quality of qualitative research published within the past two decades, mental health research has been surprisingly slow to develop, compared to other disciplines e.g. general practice and nursing, with relatively fewer qualitative research findings reaching mainstream psychiatric journals. 2 This does not appear to reflect overall editorial policy; however, it may be partly due to the lack of confidence on the part of editors and reviewers while identifying rigorous qualitative research data for further publication. 20 However, the skilled researcher should no longer find him or herself forced into a position of defending a single-methodology camp (quantitative vs qualitative), but should be equipped with the necessary methodological and analytical skills to study and interpret data and to appraise and interpret others' findings from a full range of methodological techniques.
- Crawford MJ ,
- Cordingley L
- Dowrick C ,
- Edwards S ,
- ↵ MRC Developing and Evaluating Complex Interventions 2008
- Nelson ML ,
- Quintana SM
- Schulze B ,
- Angermeyer MC
- Mavaddat N ,
- Lester HE ,
- Donovan J ,
- Morriss R ,
- Barkham M ,
- Stiles WB ,
- Connell J ,
- Chew-Graham C ,
- England E ,
- Kinderman P ,
- Tashakkoria A ,
- Ritchie J ,
- Ssebunnya J ,
- Chilvers R ,
- Glasman D ,
- Finlay WM ,
- Strauss A ,
- Hodges BD ,
- Dobransky K
- Dixon-Woods M ,
- Fitzpatrick R ,
- Espíndola CR ,
Read the full text or download the PDF:
Qualitative Research in Mental Health and Mental Illness
Cite this chapter.

- Rebecca Gewurtz Ph.D. O.T. Reg. (Ont.) 6 ,
- Sandra Moll Ph.D. O.T. Reg. (Ont.) 6 ,
- Jennifer M. Poole M.S.W., Ph.D. 7 &
- Karen Rebeiro Gruhl Ph.D., M.Sc. O.T. OT. Reg. (Ont) 8
Part of the book series: Handbooks in Health, Work, and Disability ((SHHDW,volume 4))
4491 Accesses
5 Citations
In this chapter we present an overview of qualitative research in the mental health field. We provide an historical account of the vital role that qualitative methods have played in the development of theoretical and practice approaches of psychiatry, and their current use in contemporary mental health practice. We consider how different approaches to qualitative research are used to advance knowledge and understanding of mental health, mental illness, and related services and systems, as well as the contributions of qualitative research to the mental health field. We then provide a synthesis of evidence derived from qualitative research within the mental health sector, spanning four key areas: (1) recovery, (2) stigma, (3) employment, and (4) housing. We conclude this chapter with a review of the ongoing challenges facing qualitative researchers in this area.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
By Mad we are referring to a term now used by many individuals to self-identify their experiences with diagnosis, treatment and mental health services. As outlined in the new Canadian Mad Studies reader, Mad Matters (LeFrancois et al. 2013 ), Mad may refer to a movement, an identity, a stance, an act of resistance, a theoretical approach and a burgeoning field of study. There are many ways to take up a Mad analysis, and they may be informed by multiple ideas from Anti-oppressive social work practice (AOP), Intersectionality, Queer Studies, and the Social model of disability for instance.
Abberley, P. (2004). A critique of professional support and intervention. In J. Swain, S. French, C. Barnes, & C. Thomas (Eds.), Disabling barriers - - Enabling environments (2nd ed., pp. 239–244). London: Sage.
Google Scholar
Abbey, S. E., De Luca, E., Mauthner, O. E., McKeever, P., Shildrick, M., Poole, J. M., et al. (2011). Qualitative interviews vs standardized self-report questionnaires in assessing quality of life in heart transplant recipients. The Journal of Heart and Lung Transplantation, 30 (8), 963–966.
PubMed Google Scholar
Alverson, M., Becker, D., & Drake, R. (1995). An ethnographic study of coping strategies used by people with severe mental illness participating in supported employment. Psychosocial Rehabilitation Journal, 18 (4), 115–128.
Article Google Scholar
Auerbach, E. S., & Richardson, P. (2005). The long-term work experiences of persons with severe and persistent mental illness. Psychiatric Rehabilitation Journal, 28 , 267. doi: 10.2975/28.2005.267.273 .
Article PubMed Google Scholar
Baarnhielm, S., & Ekblad, S. (2002). Qualitative research, culture and ethics: A case discussion. Transcultural Psychiatry, 39 (4), 469–483.
Baines, D. (Ed.). (2007). Doing anti-oppressive practice: Building transformative, politicized social work . Halifax, NS: Fernwood.
Bassett, H., Lampe, J., & Lloyd, C. (1999). Parenting: Experiences and feelings of parents with a mental illness. Journal of Mental Health, 8 , 597. doi: 10.1080/09638239917067 .
Beresford, P., & Wallcraft, J. (1997). Psychiatric system survivors and emancipatory research: Issues, overlaps and differences. In C. Barnes & G. Mercer (Eds.), Doing disability research (pp. 66–87). Leeds: Disability Press.
Bertilsson, M., Petersson, E.-L., Ostlund, G., Waern, M., & Hensing, G. (2013). Capacity to work while depressed and anxious – A phenomenological study. Disability and Rehabilitation, 35 , 1705. doi: 10.3109/09638288.2012.751135 .
Blumer, H. (1986). Symbolic interactionism: Perspective and method . Berkeley, CA: University of California Press.
Borg, M., & Davidson, L. (2008). The nature of recovery as lived in everyday experience. Journal of Mental Health, 17 , 129. doi: 10.1080/09638230701498382 .
Bourdieu, P. (1990). In other words: Essays towards a reflexive sociology . Stanford, CA: Stanford University Press.
Bracken, P., Thomas, P., Timimi, S., Asen, E., Behr, G., Beuster, C., et al. (2012). Psychiatry beyond the current paradigm. The British Journal of Psychiatry, 201 , 430. doi: 10.1192/bjp.bp.112.109447 .
Campbell, M., & Gregor, F. (2008). Mapping social relations: A primer in doing institutional ethnography . Toronto, ON: University of Toronto Press.
Chamberlin, J. (1990). The ex-patients’ movement: Where we’ve been and where we’re going. Journal of Mind and Behaviour, 11 (3), 323–336.
Chamberlin, J. (2005). User/consumer involvement in mental health service delivery. Epidemiologia e Psichiatria Sociale, 14 (1), 10–14.
Charmaz, K. (2006). Constructing grounded theory: A practical guide through qualitative analysis . Thousand Oaks, CA: Sage Publications Ltd.
Cheek, J. (2011). The politics and practices of funding qualitative inquiry: Messages about messages about messages.... In N.K. Denzin & Y.S. Lincoln (Eds.), THe SAGE handbook of qualitative research (4th ed., pp. 251–268). Thousand Oaks, CA: SAGE publications, Inc.
Church, K. (1995). Forbidden narratives: Critical autobiography as social science . Amsterdam: International Publishers Distributors. Reprinted by Routledge, London.
Church, K. (1997). Because of where we’ve been: The business behind the business of psychiatric survivor economic development . Toronto, ON: Ontario Council of Alternative Businesses.
Church, K., & Reville, D. (2001). “First we take Manhattan”: Evaluation report on a community connections grant OCAB Regional Council Development . Toronto, ON: Ontario Council of Alternative Businesses.
Cohen, O. (2005). How do we recover? An analysis of psychiatric survivor oral histories. Journal of Humanistic Psychology, 45 (3), 333–354.
Costa, L., Voronka, J., Landry, D., Reid, J., McFarlane, B., Reville, D., et al. (2012). Recovering our stories: A small act of resistance. Studies in Social Justice, 6 (1), 85–101.
Crawford, M. J., Ghosh, P., & Keen, R. (2003). Use of qualitative research methods in general medicine and psychiatry: Publication trends in medical journals 1990–2000. International Journal of Social Psychiatry, 49 , 308. doi: 10.1177/0020764003494007 .
Cunningham, K., Wolbert, R., & Brockmeier, M. B. (2000). Moving beyond the illness: Factors contributing to gaining and maintaining employment. American Journal of Community Psychology, 28 , 481. doi: 10.1023/A:1005136531079 .
Dalgin, R. S., & Gilbride, D. (2003). Perspectives of people with psychiatric disabilities on employment disclosure. Psychiatric Rehabilitation Journal, 26 (3), 306–310.
Davidson, L., Ridgway, P., Kidd, S., Topor, A., & Borg, M. (2008). Using qualitative research to inform mental health policy. Canadian Journal of Psychiatry, 53 (3), 137–144.
Davidson, L., & Strauss, J. (1992). Sense of self in recovery from severe mental illness. British Journal of Medical Psychology, 65 (2), 131–145.
De Haene, L., Grietens, H., & Verschueren, K. (2010). Holding harm: Narrative methods in mental health research on refugee trauma. Qualitative Health Research, 20 , 1664. doi: 10.1177/1049732310376521 .
Deegan, P. E. (1988). Recovery: The lived experience of rehabilitation. Psychosocial Rehabilitation Journal, 11 (4), 11–19.
Deegan, P. E. (2005). The importance of personal medicine: A qualitative study of resilience in people with psychiatric disabilities. Scandinavian Journal Public Health Supplement, 66 , 29. doi: 10.1080/14034950510033345 .
Deegan, P. E. (2007). The lived experience of using psychiatric medicine in the recovery process and a shared decision making program to support it. Psychiatric Rehabilitation Journal, 31 (1), 62–69.
Devlin, R., & Pothier, D. (2006). Introduction: Toward a critical theory of dis-citizenship. In D. Pothier & R. Devlin (Eds.), Dis-ability. Critical disability theory: Essays in philosophy, politics, policy and law (1st ed., pp. 1–22). Vancouver, BC: UBC Press.
Dougherty, S., Campana, K., Kontos, R., Flores, M., Lockhart, R., & Shaw, D. (1996). Supported education: A qualitative study of the student experience. Psychiatric Rehabilitation Journal, 19 (3), 59–70.
Fabris, E. (2011). Tranquil prisons: Chemical incarceration under community treatment orders . Toronto, ON: University of Toronto Press.
Forrester-Jones, R., & Barnes, A. (2008). On being a girlfriend not a patient: The quest for an acceptable identity amongst people diagnosed with a severe mental illness. Journal of Mental Health, 17 , 153. doi: 10.1080/09638230701498341 .
Fossey, E. M., & Harvey, C. A. (2010). Finding and sustaining employment: A qualitative meta-synthesis of mental health consumer views. Canadian Journal of Occupational Therapy, 77 , 303. doi:10.2182/cjot.2010.77.5.6.
Foster-Fishman, P., & Nowell, B. (2005). Using methods that matter: The impact of reflection, dialogue and voice. American Journal of Community Psychology, 36 , 275. doi: 10.1007/s10464-005-8626-y .
Foucault, M. (1980). Power/Knowledge- selected interviews and other writings 1972-1977 . New York: Pantheon Books.
Frances, A. (2013). Saving normal . New York: Harper Collins.
Gardner, P. J., & Poole, J. M. (2009). One story at a time narrative therapy, older adults, and addictions. Journal of Applied Gerontology, 28 (5), 600–620.
Georgaca, E. (2013). Discourse analytic research on mental distress: A critical overview. Journal of Mental Health, 23 , 55. doi: 10.3109/09638237.2012.734648 .
Gewurtz, R. E., Cott, C., Rush, B., & Kirsh, B. (2012). The shift to rapid job placement for people living with mental illness: An analysis of consequences. Psychiatric Rehabilitation Journal, 35 , 428. doi: 10.1037/h0094575 .
Gewurtz, R., Kirsh, B., Jacobson, N., & Rappolt, S. (2006). The influence of mental illnesses on work potential and career development. Canadian Journal of Community Mental Health, 25 (2), 207–220.
Giddens, A. (1984). The constitution of society: Outline of the theory of structuration . Berkeley, CA: University of California Press.
Goering, P., Boydell, K. M., & Pignatiello, A. (2008). The relevance of qualitative research for clinical programs in psychiatry. Canadian Journal of Psychiatry, 53 (3), 145–151.
Goffman, E. (1961). Asylums: Essays on the social situation of mental patients and other inmates . New York: Doubleday.
Goffman, E. (1963). Stigma: Notes on the management of spoiled identity . Englewood Cliffs, NJ: Prentice-Hall.
Gold, E. (2007). From narrative wreckage to islands of clarity: Stories of recovery from psychosis. Canadian Family Physician, 53 (8), 1271–1275.
PubMed PubMed Central Google Scholar
Gould, A., DeSouza, S., & Rebeiro Gruhl, K. (2005). And then I lost that life: A shared narrative of young men with schizophrenia. British Journal of Occupational Therapy, 68 (10), 467–473.
Hall, J. M. (2011). Narrative methods in a study of trauma recovery. Qualitative Health Research, 21 , 3. doi: 10.1177/1049732310377181 .
Haw, K., & Hadfield, M. (2011). Video in social science research: Function and forms . New York: Routledge.
Henry, A., & Lucca, A. (2004). Facilitators and barriers to employment: The perspectives of people with psychiatric disabilities and employment service providers. Work, 22 (3), 169–182.
Holmes, D., Murray, S., Perron, A., & Rail, G. (2006). Deconstructing the evidence-based discourse in health sciences: Truth, power and fascism. International Journal of Evidence Based Healthcare, 4 , 180. doi: 10.1111/j.1479-6988.2006.00041.x .
Honey, A. (2004). Benefits and drawbacks of employment: Perspectives of people with mental illness. Qualitative Health Research, 14 , 381. doi: 10.1177/1049732303261867 .
Israel, B. A., Eng, E., Schulz, A. J., & Parker, E. A. (Eds.). (2005). Methods in community-based participatory research for health . San Francisco: Jossey-Bass.
Jacobson, N. (2001). Experiencing recovery: A dimensional analysis of recovery narratives. Psychiatric Rehabilitation Journal, 24 (3), 248–256.
Jacobson, N., Farah, D., & The Toronto and Cultural Diversity Community of Practice. (2010). Recovery through the lens of cultural diversity . Toronto, ON: The Wellesley Institute, Community Resources Connections of Toronto and the Centre for Addiction and Mental Health.
Johnson, M. (1998). Being mentally ill: A phenomenological inquiry. Archives of Psychiatric Nursing, 12 (4), 195–201.
Joseph, S., Beer, C., Forman, A., Pikersgill, M., Swift, J., Taylor, J., et al. (2009). Qualitative research into mental health: Reflections on epistemology. Mental Health Review Journal, 14 (1), 36–42.
Karnieli-Miller, O., Perlick, D. A., Nelson, A., Mattias, K., Corrigan, P., & Roe, D. (2013). Family members’ of persons living with a serious mental illness: Experiences and efforts to cope with stigma. Journal of Mental Health, 22 , 254. doi: 10.3109/09638237.2013.779368 .
Kartalova-O’Doherty, Y., Stevenson, C., & Higgins, A. (2012). Reconnecting with life: A grounded theory study of mental health recovery in Ireland. Journal of Mental Health, 21 , 135. doi: 10.3109/09638237.2011.621467 .
Kennedy-Jones, M., Cooper, J., & Fossey, E. (2005). Developing a worker role: Stories of four people with mental illness. Australian Occupational Therapy Journal, 52 , 116. doi: 10.1111/j.1440-1630.2005.00475.x .
Killeen, M. B., & O’Day, B. L. (2004). Challenging expectations: How individuals with psychiatric disabilities find and keep work. Psychiatric Rehabilitation Journal, 28 , 157. doi: 10.2975/28.2004.157.163 .
Kirsh, B. (1996). Influences on the process of work integration: The consumer perspective. Canadian Journal of Community Mental Health, 15 (1), 21–31.
Kirsh, B. (2000). Work, workers, and workplaces: A qualitative analysis of narratives of mental health consumers. Journal of Rehabilitation, 66 (4), 24–30.
Kirsh, B., Gewurtz, R., & Bakewell, R. A. (2011). Critical characteristics of supported housing: Resident and service provider perspectives. Canadian Journal of Community Mental Health, 30 (1), 15–30.
Kirsh, B., Krupa, T., Cockburn, L., & Gewurtz, R. (2010). A Canadian model of work integration for persons with mental illnesses. Disability and Rehabilitation, 32 , 1833. doi: 10.3109/09638281003734391 .
Knight, M., Wykes, T., & Hayward, P. (2003). ‘People don’t understand’: An investigation of stigma in schizophrenia using Interpretative Phenomenological Analysis (IPA). Journal of Mental Health, 12 , 209. doi: 10.1080/0963823031000118203 .
Krupa, T. (2004). Employment, recovery and schizophrenia: Integrating health and disorder at work. Psychiatric Rehabilitation Journal, 28 , 8. doi: 10.2975/28.2004.8.1 .
Krupa, T. (2008). Muriel Driver Memorial Lecture 2008: Part of the solution…or part of the problem? Addressing the stigma of mental illness in our midst. Canadian Journal of Occupational Therapy, 75 (4), 198–205.
Krupa, T., Kirsh, B., Cockburn, L., & Gewurtz, R. (2009). Understanding the stigma of mental illness in employment. Work, 33 , 413. doi: 10.3233/WOR-2009-0890 .
Krupa, T., Kirsh, B., Gewurtz, R., & Cockburn, L. (2005). Improving the employment prospects of people with serious mental illness: Five challenges for a national mental health strategy. Canadian Public Policy, 31 (s1), 59–64.
Lane, A. M. (2011). Placement of older adults from hospital mental health units into nursing homes: Exploration of the process, system issues and implications. Journal of Gerontological Nursing, 37 , 49. doi: 10.3928/00989134-20100730-07 .
Lather, P. (2004). Scientific research in education: A critical perspective. British Educational Research Journal, 30 (6), 759–772.
LeFrancois, B., Menzies, R., & Reaume, G. (Eds.). (2013). Mad matters: A critical reader in Canadian Mad Studies . Toronto, ON: Canadian Scholars Press.
Link, B. G., & Phelan, J. C. (2001). Conceptualizing stigma. Annual Review of Sociology, 27 , 363. doi: 10.1146/annurev.soc.27.1.363 .
Lord, J., Schnarr, A., & Hutchison, P. (1987). The voice of the people: Qualitative research and the needs of consumers. Canadian Journal of Community Mental Health, 6 (2), 25–36.
Lurie, S., Kirsh, B., & Hodge, S. (2007). Can ACT lead to more work? The Ontario experience. Canadian Journal of Community Mental Health, 26 (1), 161–171.
Mancini, M. (2007). A qualitative analysis of turning points in the recovery process. American Journal of Psychiatric Rehabilitation, 10 (3), 223–244.
Mental health recovery study working group. (2009). Mental health ‘recovery’: Users and refusers . Toronto, ON: The Wellesley Institute.
Michalak, E., Livingston, J., Hole, R., Suto, M., Hale, S., & Haddock, C. (2011). ‘It’s something that I manage but it is not who I am’: Reflections on internalized stigma in individuals with bipolar disorder. Chronic Illness, 7 , 209. doi: 10.1177/1742395310395959 .
Moll, S. (2012). Navigating political minefields: Partnerships in organizational case study research. Work: A Journal of Prevention, Treatment and Rehabilitation, 43 , 5. doi: 10.3233/WOR-2012-1442 .
Moll, S., Dick, R., Sherman, D., & Dahan, R. (2006). Photovoice: Transforming marginalized communities through photography. Presentation at the Making Gains in Mental Health and Addictions Conference. Toronto, ON, Canada.
Moll, S., Eakin, J. M., Franche, R. L., & Strike, C. (2013). When health care workers experience mental ill health: Institutional practices of silence. Qualitative Health Research, 23 , 167. doi: 10.1177/1049732312466296 .
Moran, G. S., Russinova, Z., Gidugu, V., Yim, J., & Sprague, C. (2012). Benefits and mechanisms of recovery among peer providers with psychiatric illnesses. Qualitative Health Research, 22 , 304. doi: 10.1177/1049732311420578 .
Morrow, M. (2013). Recovery: Progressive paradigm or neoliberal smokescreen? In B. LeFrancois, R. Menzies, & G. Reaume (Eds.), Mad matters: A critical reader in Canadian Mad Studies (pp. 323–333). Toronto, ON: Canadian Scholars’ Press.
Morse, J. M. (2009). Mixing qualitative methods. Qualitative Health Research, 19 , 1523. doi: 10.1177/1049732309349360 .
Morse, J.M. (2003). The adjudication of qualitative proposals. Qualitative Health Research, 13 (6), 739–742.
Moss, P. A., Phillips, D. C., Erickson, F. D., Floden, R. E., Lather, P. A., & Schneider, B. L. (2009). Learning from our differences: A dialogue across perspectives on quality in education research. Educational Research, 38 (7), 501–507.
Nelson, G., Clarke, J., Febbraro, A., & Hatzipantelis, M. (2005). A narrative approach to the evaluation of supportive housing: Stories of homeless people who have experienced serious mental illness. Psychiatric Rehabilitation Journal, 29 (2), 98–104.
Noordik, E., Nieuwenhuijsen, K., Varekamp, I., van der Klink, J. J., & van Dijk, F. J. (2011). Exploring the return-to-work process for workers partially returned to work and partially on long-term sick leave due to common mental disorders: A qualitative study. Disability and Rehabilitation, 33 (17-18), 1625–1635.
Ochocka, J., Nelson, G., & Janzen, R. (2005). Moving forward: Negotiating self and external circumstances in recovery. Psychiatric Rehabilitation Journal, 28 (4), 315–322.
Oliver, M. (2006). Social policy and disability: Some theoretical issues. In L. Barton (Ed.), Overcoming disabling barriers: 18 years of disability and society (pp. 7–20). Oxford: Routledge.
Pease, B. (2002). Rethinking empowerment: A postmodern reappraisal for emancipatory practice. British Journal of Social Work, 32 (2), 135–147.
Perlin, M. L. (1992). On sanism. SMULaw Review, 46 , 373.
Perry, B., Taylor, D., & Shaw, S. (2007). “You’ve got to have a positive state of mind”: An interpretative phenomenological analysis of hope and first episode psychosis. Journal of Mental Health, 16 , 781. doi: 10.1080/09638230701496360 .
Pescosolido, B. A., Martin, J. K., Lang, A., & Olafsdottir, S. (2008). Rethinking theoretical approaches to stigma: A Framework Integrating Normative Influences on Stigma (FINIS). Social Science and Medicine, 67 , 431. doi: 10.1016/j.socscimed.2008.03.018 .
Peters, S. (2010). Qualitative research methods in mental health. Evidence Based Mental Health, 13 , 35. doi: 10.1136/ebmh.13.2.35 .
Phillips, N., & Hardy, C. (2002). Discourse analysis . Thousand Oaks, CA: Sage Publications.
Piat, M., & Lal, S. (2012). Service providers’ experiences and perspectives on recovery-oriented mental health system reform. Psychiatric Rehabilitation Journal, 35 (4), 289–296.
Pickens, J. (1999). Living with serious mental illness: The desire for normalcy. Nursing Science Quarterly, 12 (3), 233–239.
Pink, S. (2006). Doing visual ethnography . London: Sage Press.
Polvere, L., Macnaughton, E., & Piat, M. (2013). Participant perspectives on housing first and recovery: Early findings from the at home/chez soi project. Psychiatric Rehabilitation Journal, 36 , 110. doi: 10.1037/h0094979 .
Poole, J. (2011). Behind the rhetoric: Mental health recovery in Ontario . Halifax, NS: Fernwood.
Poole, J. M., Jivraj, T., Arslanian, A., Bellows, K., Chiasson, S., Hakimy, H., et al. (2012). Sanism, ‘mental health’, and social work/education: A review and call to action. Intersectionalities: A Global Journal of Social Work Analysis, Research, Polity, and Practice, 1 (1), 20–36.
Poole, J. M., Shildrick, M., De Luca, E., Abbey, S. E., Mauthner, O. E., McKeever, P. D., et al. (2011). The obligation to say ‘Thank You’: Heart transplant recipients’ experience of writing to the donor family. American Journal of Transplantation, 11 (3), 619–622.
Poole, J., & Ward, J. (2013). ‘Breaking open the bone’: Storying, sanism and mad grief. In B. LeFrancois, R. Menzies, & G. Reaume (Eds.), Mad matters: A critical reader in Canadian Mad Studies (pp. 94–104). Toronto, ON: Canadian Scholars’ Press.
Rebeiro, K. (1999). The labyrinth of community mental health: In search of meaningful occupation. Psychiatric Rehabilitation Journal, 23 (2), 143–152.
Rebeiro Gruhl, K. L. (2011). An exploratory study of the influence of place on access to employment for persons with serious mental illness residing in northeastern Ontario . (Unpublished doctoral dissertation). School of Rural and Northern Health, Laurentian University, Sudbury, ON.
Rebeiro Gruhl, K. L., Kauppi, C., Montgomery, P., & James, S. (2012a). “Stuck in the mud”: Limited employment success of persons with serious mental illness in northeastern Ontario. Canadian Journal of Community Mental Health, 31 (2), 67–81.
Rebeiro Gruhl, K. L., Kauppi, C., Montgomery, P., & James, S. (2012b). Consideration of the influence of place on access to employment for persons with serious mental illness in northeastern Ontario. Rural and Remote Health, Spring/Summer, 36 (1), 11–17.
Rebeiro, K. L., Day, D. G., Semeniuk, B., O’Brien, M. C., & Wilson, B. (2001). NISA: An occupation-based, mental health program. American Journal of Occupational Therapy, 55 (5), 493–500.
Ridgway, P. (2001). ReStorying psychiatric disability: Learning from first person recovery narratives. Psychiatric Rehabilitation Journal, 24 (4), 335–343.
Rioux, M., & Valentine, F. (2006). Does theory matter? Exploring the nexus between disability, human rights and public policy. In D. Pothier & R. Devlin (Eds.), Dis ability. Critical disability theory: Essays in philosophy, politics, policy and law (1st ed., pp. 47–69). Vancouver, BC: UBC Press.
Rose, L. (1998). Gaining control: Family members relate to persons with severe mental illness. Research in Nursing & Health, 21 (4), 363–373.
Ross, H., Abbey, S., De Luca, E., Mauthner, O., McKeever, P., Shildrick, M., et al. (2010). What they say versus what we see: “Hidden” distress and impaired quality of life in heart transplant recipients. The Journal of Heart and Lung Transplantation, 29 (10), 1142–1149.
Rothgeb, C. L. (1971). Abstracts of the standard edition of the complete psychological works of Sigmund Freud . Bethesda, MD: National Institute of Mental Health.
Book Google Scholar
Sandelowski, M. (2000). Focus on research methods: Combining qualitative and quantitative sampling, data collection, and data analysis techniques in mixed-method studies. Research in Nursing & Health, 23 (3), 246–255.
Schulze, B. (2008). Qualitative research methods in psychiatric science. European Psychiatry, 23 , S48. doi: 10.1016/j.eurpsy.2008.01.174 .
Schulze, B., & Angermeyer, M. (2003). Subjective experiences of stigma. A focus group study of schizophrenic patients, their relatives and mental health professionals. Social Science & Medicine, 56 (2), 299–312.
Secker, J., Armstrong, C., & Hill, M. (1999). Young people’s understanding of mental illness. Health Education Research, 14 , 729–739. doi: 10.1093/her/14.6.729 .
Shankar, J. (2005). Improving job tenure for people with psychiatric disabilities through ongoing employment. Australian e-Journal for the Advancement of Mental Health, 4 (1), 1–11. Retrieved from www.ausienet.com/journal/vol4iss1/shankar.pdf
Smith, D. (2006). Institutional ethnography: A sociology for the people . Oxford: AltaMira.
Stapleton, J. (2010). “Zero Dollar Linda”: A mediation on Malcolm Gladwell’s “Million D ollar Murray,” the Linda Chamberlain Rule, and the Auditor General of Ontario. The Metcalf Foundation. Available at http://www.openpolicyontario.com/ZeroDollarLindaf.pdf
Strauss, J. S. (1989). Subjective experiences of schizophrenia: Towards a new dynamic psychiatry – II. Schizophrenia Bulletin, 15 (2), 179–187.
Streiner, D. L. (2008). Qualitative research in psychiatry. Canadian Journal of Psychiatry, 53 (3), 135–136.
Sutton, D. J., Hocking, C. S., & Smythe, L. A. (2012). A phenomenological study of occupational engagement in recovery from mental illness. Canadian Journal of Occupational Therapy, 79 , 142. doi: 10.2182/cjot.2012.79.3.3 .
Sveinbjarnardottir, E., & de Casterle, B. (1997). Mental illness in the family: An emotional experience. Issues in Mental Health Nursing, 18 (1), 45–56.
Tashakkori, A., & Teddlie, C. (Eds.). (2003). Handbook of mixed methods in social and behavioral research . Thousand Oaks, CA: Sage Publications Inc.
The Standing Senate Committee on Social Affairs, Science and Technology. (2006). Out of the shadows at last: Transforming mental health, mental illness and addiction services in Canada . Available at http://www.parl.gc.ca/Content/SEN/Committee/391/soci/rep/rep02may06-e.htm
Townsend, E. (1998). Good intentions over-ruled: A critique of empowerment in the routine organization of mental health services . Toronto, ON: University of Toronto Press.
Twohig, P. L. (2007). Written on the landscape: Health and region in Canada. Journal of Canadian Studies, 41 (3), 5–17.
Wang, C., & Burris, M. A. (1997). Photovoice: Concept, methodology, and use for participatory needs assessment. Health Education & Behavior, 24 , 369. doi: 10.1177/109019819702400 .
Wang, C., Cash, J. L., & Powers, L. S. (2000). Who knows the streets as well as the homeless? Promoting personal and community action through photovoice. Health Promotion Practice, 1 , 81. doi: 10.1177/152483990000100113 .
Weiner, E. (1999). The meaning of education for university students with a psychiatric disability: A grounded theory analysis. Psychiatric Rehabilitation Journal, 22 (4), 403–409.
Whitley, R., Harris, M., & Drake, R. (2008). Safety and security in small-scale recovery housing for people with severe mental illness: An inner-city case study. Psychiatric Services, 59 (2), 165–169.
Wiersma, E. C. (2011). Using Photovoice with people with early-stage Alzheimer’s disease: A discussion of methodology. Dementia, 10 , 203. doi: 10.1177/1471301211398990 .
Young, S., & Ensing, D. (1999). Exploring recovery from the perspective of people with psychiatric disabilities. Psychiatric Rehabilitation Journal, 22 (3), 219–231.
Young, N. L., Wabano, M. J., Burke, T. A., Ritchie, S. D., Mishibinijima, D., & Corbiere, R. G. (2013). A process for creating the Aboriginal Children’s Health and Well-being Measure (ACHWM). Canadian Journal of Public Health, 104 (2), 136–141.
Zolnierek, C. D. (2011). Exploring lived experiences of persons with severe mental illness: A review of the literature. Issues in Mental Health Nursing, 32 , 46. doi:10.3109/01612840.2010.522755.
Download references
Author information
Authors and affiliations.
School of Rehabilitation Science, McMaster University, IAHS Bldg, 4th Floor, 1400 Main St. W., Hamilton, ON, Canada, L8S 1C7
Rebecca Gewurtz Ph.D. O.T. Reg. (Ont.) & Sandra Moll Ph.D. O.T. Reg. (Ont.)
School of Social Work, Faculty of Community Services, Ryerson University, 350 Victoria Street, Toronto, ON, Canada, M5B 2K3
Jennifer M. Poole M.S.W., Ph.D.
Community Mental Health and Addictions Program, Health Sciences North, 127 Cedar Street, Sudbury, ON, Canada, P3E 1B1
Karen Rebeiro Gruhl Ph.D., M.Sc. O.T. OT. Reg. (Ont)
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Rebecca Gewurtz Ph.D. O.T. Reg. (Ont.) .
Editor information
Editors and affiliations.
Faculty of Nursing, University of Alberta, Edmonton, Alberta, Canada
Karin Olson
Department of Educational and Counseling Psychology, and Special Education, University of British Columbia, Vancouver, British Columbia, Canada
Richard A. Young
Izabela Z. Schultz
Rights and permissions
Reprints and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Gewurtz, R., Moll, S., Poole, J.M., Gruhl, K.R. (2016). Qualitative Research in Mental Health and Mental Illness. In: Olson, K., Young, R., Schultz, I. (eds) Handbook of Qualitative Health Research for Evidence-Based Practice. Handbooks in Health, Work, and Disability, vol 4. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2920-7_13
Download citation
DOI : https://doi.org/10.1007/978-1-4939-2920-7_13
Publisher Name : Springer, New York, NY
Print ISBN : 978-1-4939-2919-1
Online ISBN : 978-1-4939-2920-7
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Open access
- Published: 13 October 2023
A qualitative exploration of young people’s mental health needs in rural and regional Australia: engagement, empowerment and integration
- Christiane Klinner ORCID: orcid.org/0000-0001-9313-6799 1 ,
- Nick Glozier 1 , 2 ,
- Margaret Yeung 1 ,
- Katrina Conn ORCID: orcid.org/0000-0002-0476-9146 1 , 3 &
- Alyssa Milton ORCID: orcid.org/0000-0002-4326-0123 1 , 2
BMC Psychiatry volume 23 , Article number: 745 ( 2023 ) Cite this article
2967 Accesses
1 Citations
Metrics details
Australian rural and regional communities are marked by geographic isolation and increasingly frequent and severe natural disasters such as drought, bushfires and floods. These circumstances strain the mental health of their inhabitants and jeopardise the healthy mental and emotional development of their adolescent populations. Professional mental health care in these communities is often inconsistent and un-coordinated. While substantial research has examined the barriers of young people’s mental health and help-seeking behaviours in these communities, there is a lack of research exploring what adolescents in rural and regional areas view as facilitators to their mental health and to seeking help when it is needed. This study aims to establish an in-depth understanding of those young people’s experiences and needs regarding mental health, what facilitates their help-seeking, and what kind of mental health education and support they want and find useful.
We conducted a qualitative study in 11 drought-affected rural and regional communities of New South Wales, Australia. Seventeen semi-structured (14 group; 3 individual) interviews were held with 42 year 9 and 10 high school students, 14 high school staff, and 2 parents, exploring participants’ experiences of how geographical isolation and natural disasters impacted their mental health. We further examined participants’ understandings and needs regarding locally available mental health support resources and their views and experiences regarding mental illness, stigma and help-seeking.
Thematic analysis highlighted that, through the lens of participants, young people’s mental health and help-seeking needs would best be enabled by a well-coordinated multi-pronged community approach consisting of mental health education and support services that are locally available, free of charge, engaging, and empowering. Participants also highlighted the need to integrate young people’s existing mental health supporters such as teachers, parents and school counselling services into such a community approach, recognising their strengths, limitations and own education and support needs.
Conclusions
We propose a three-dimensional Engagement, Empowerment, Integration model to strengthen young people’s mental health development which comprises: 1) maximising young people’s emotional investment (engagement); 2) developing young people’s mental health self-management skills (empowerment); and, 3) integrating mental health education and support programs into existing community and school structures and resources (integration).
Peer Review reports
Mental health service use is considerably lower in rural and regional communities than in urban areas in both Australia [ 1 , 2 ] and internationally [ 3 , 4 , 5 ]. Young people (YP) in particular have been reluctant to seek formal mental health support, which has been attributed to stigma and negative beliefs towards mental health services and professionals [ 6 , 7 ]. Such reluctance is particularly pronounced in rural and regional communities where mental health stigma rapidly spreads through social networks and “sticks” to the individual [ 3 ]. This phenomenon has been associated with higher levels of socio-economic disadvantage [ 8 ], social conservatism [ 9 ] and social visibility in these communities resulting in reduced privacy [ 10 , 11 ], with lack of confidentiality cited as a major concern of YP when considering accessing mental health services [ 8 ]. Professional mental health care in rural and regional areas is often inconsistent and un-coordinated [ 3 , 12 ], with help-seekers being required to travel large distances [ 13 ] and experiencing lengthy service waitlist [ 14 ]. The wellbeing of these communities is also more affected by increasingly severe and prevalent natural disasters. Prolonged drought, for example, coupled with feelings of isolation has been shown to impact YP’s mental health, making them feel overwhelmed and worry about their families, friends, money and their futures [ 15 , 16 ].
While there is substantial research examining the barriers of YP’s mental health help-seeking behaviour in drought-affected rural and regional areas, less is known about what types of supports, programs and education facilitates their help-seeking [ 17 ]. In a recent systematic review on the barriers, facilitators and interventions for mental health help-seeking behaviours in adolescents, only 19 of 56 studies identified help-seeking facilitators [ 6 ]. These included previous positive experience with health services and higher levels of mental health literacy. Most research examining enablers of YP’s help-seeking is from the perspective of adults, parents and teachers (e.g., [ 14 , 18 , 19 , 20 , 21 , 22 ]). There is a lack of research examining what YP in rural and regional areas view as facilitators to seeking help when it is needed. The few studies that have examined help-seeking facilitators report that confidentiality and accessibility of mental health services [ 23 ], for the availability of more school counselling services [ 24 ], and YP desire to develop mental health self-management skills [ 15 ] to support the mental health help-seeking process.
This research program had 2 overarching aims. The first aim, which is reported in this article, was to establish a more in-depth understanding of YP’s experiences and needs regarding their mental health help-seeking, and explore mental health education, support and programs in rural and regional communities, complemented by the views of their teachers and parents. The second aim, which is reported elsewhere [ 25 ], was to evaluate the batyr@school program which was to be delivered at the participating schools within the year. The schools were selected to participate in the program by the New South Wales Department of Education as they were identified as communities which had, at the time of establishing the research, been experiencing severe drought — a recurring natural event in Australia that has been linked to adverse mental health outcomes in the affected communities [ 26 , 27 ]. The primary research question for the research reported in this article was: What are the attitudes and needs of young people, their teachers and parents regarding mental health and help-seeking in drought affected r ural and regional areas of Australia?
Study design
This study used qualitative pre- and post-intervention data from an evaluation of the batyr@school intervention [ 28 ] delivered to YP, teachers and parents in drought affected communities in Australia [ 25 ]. Semi-structured interviews (group and individual) were conducted to enable an in-depth exploration of participants’ views, experiences and needs about this sensitive topic [ 29 , 30 ]. While acknowledging its limitations [ 31 ], we used the COnsolidated criteria for REporting Qualitative research checklist (COREQ checklist [ 32 ], See Supplementary File ).
Ethical approval for this study was provided by the University of Sydney Human Research Ethics Committee (Protocol number 2020/607). Subsequent approval was provided via the NSW State Education Research Applications Process (SERAP Number 2020373).
Setting, participants and recruitment
The participants comprised three stakeholder groups: high school students aged 14–15 years (grade 9 and 10 in Australia; n = 42; 24 females, 18 males), high school staff (primarily teachers but also administrators and Wellbeing Officers) ( n = 14; 10 females, 4 males) and two parents of high school students ( n = 2; females). Detailed participant demographics and inclusion criteria are available as a Supplementary File . Participants were recruited through 11 participating high schools who were willing to take part in the qualitative research component of the wider batyr@school evaluation. In total, 26 rural and regional school communities from drought-affected areas of New South Wales were invited to participate in focus groups or individual interviews. Focus groups were selected as the main form of data collection as this reduced the administrative burden on schools in supporting the research. Individual interviews were also offered depending on the needs of the participant (eg. time constraints, unable to attend a focus group, personal preference, accessibility issues). Of these schools, 20 participated in the mixed methods evaluation, and 11 consented to conducting the qualitative research component. Of the six schools that did not participate, 5 cited that they were under too much administrative burden to take part, and one school had experienced a recent mental health trauma so felt the timing was not appropriate.
Participants for the focus groups and interviews were recruited through a combination of passive recruitment (via distribution of info sheets through the participating schools’ communication channels to staff, parents and students) [ 33 ] and snowball sampling [ 34 ]. The intention was to minimise perceived pressure to participate whilst utilising the schools’ social networks [ 35 ]. Written informed consent was obtained from all participants.
Data collection
From June 2021 to June 2022, the chief investigator (a qualitative researcher and psychologist), supported by a postgraduate student, conducted 14 group and three individual interviews with a total of 57 participants. The group interview size ranged from 2 to 5 participants. Of the 11 student interviews, three included the active participation of a teacher. Some schools considered the presence of a teacher necessary because the student interviews were conducted during school hours. Sixteen interviews were held via Zoom, and one parent interview via telephone. The sessions lasted between 20 and 115 min (mean duration 50 min). All interviews were audio-recorded, transcribed verbatim, de-identified and checked for accuracy. One teacher who was unable to participate in an interview provided a one-page written feedback on the interview questions, which was included in the data set.
Two of the research team members, both with extensive experience in qualitative research, reviewed the transcripts alongside data gathering and adapted the interview guide for further interviews as initial themes evolved and the need for more data in particular topic areas emerged [ 36 ]. This reflexive iteration between data gathering and analysis also served to refine focus and understanding of the data, and to determine when theme saturation was achieved [ 37 ]. The interviews explored 4 questions: 1) participants’ views on how drought impacted their local community from a mental health perspective, 2) participants’ understanding of locally available mental health support resources, 3) YP’s help-seeking experiences including what participants would do if a(nother) YP reached out to them for mental health support, and 4) participants’ views on their communities’ attitudes and beliefs about mental ill health, stigma and help-seeking. Participants were also asked for improvement suggestions in all 4 focus areas. The final interview guide is available as a Supplementary File .
In the process of reviewing the interview transcripts and listening to the audio files, one qualitative researcher developed an extensive analytical memo. This memo initially contained rich descriptions of preliminary themes identified inductively as important relative to the research question, interspersed reflexive comments on their potential meaning and relationships to each other [ 38 ]. This expansive phase of memo-writing followed a process of structuring and abstraction of the data in which themes and sub-themes were consolidated in team discussions, using a critical realist approach [ 39 ]. As a result of this process, the analytic memo had transformed into a framework that was used to report the results. The authors (who had a diverse mix of backgrounds including: qualitative researchers, mental health professionals, a teacher, a university student and an expert by experience; two of the research team were young people themselves (i.e. aged under 25 years [ 40 ]) and one was residing in a regional community) collaboratively refined the written results in several rounds of discussion and editing. The findings were also triangulated with the initial qualitative findings of an internal batyr @school baseline evaluation report [ 25 ], which had previously been analysed, interpreted and iteratively refined by the same team excluding one qualitative researcher who led this study’s analysis. This collaborative approach to analysis encourages high levels of reflexivity based on comparisons between the multiple personal and professional perspectives of all involved.
Terminology
This study was set in a high school environment. Therefore, the term ‘student’ is used when referring to the YP who participated in this study and the term ‘young person/people (YP)’ in reference to adolescents generally. The term ‘participants’ is used when referring to all three study participant groups. Otherwise, the participant group is specified; for example, ‘Students said…’.
In the following results section YP’s perspectives, experiences and needs regarding mental health help-seeking, stigma, and education and support services in drought-affected rural and regional communities are described. This is complemented by the views of their teachers and parents. The participants’ descriptions of the barriers to each of these above areas relating to their community, family, school, peers and individuals are provided. Importantly, these barriers are followed by their suggested solutions and facilitators to help-seeking and support. The most salient participant quotes are included in the text and ancillary quotes illustrating the findings further are presented in a Supplementary File .
Barriers to mental wellbeing and coping mechanisms
Community level.
Students vividly described their communities’ existential stressors caused by drought and other recurring natural events such as floods, bushfires and mice plagues, all straining the community’s mental wellbeing (See Supplementary File , Quote 1). In some communities these stressors coincided with high levels of social disadvantage, substance abuse and domestic violence (Quote 2). Participants described how these existential and economic stressors affected YPs’ mental health (Quote 3). Long distances to the nearest healthcare services (GPs, specialists, hospitals), long wait times to obtain an appointment and a lack of local youth mental health services made it difficult for YP and their families to access professional help when they needed it (Quote 4a-4b). Both students and teachers summarised the, at times, complete absence of accessible mental health services and contrasted them to those perceived to be available in urban areas (Quote 5 and below):
In [capital city], there was a lot of resources; and when I come here, there's nothing […] There's a whole lot of issues with suicide and attempted suicide. I think there's a headspace, but I don't know where that is. I think it might be in [nearest city, two hours’ drive away]. Which is nowhere near here. We're in the middle of nowhere. It seems to me like there's a really high, a lot higher incidence of sexual assault and suicidal ideation here. I mean, it's really hard to compare these two populations, but it does seem that way to me. And there's no services. [Teacher_B4]
Mental health services that were provided as one-off visits to rural and regional schools were seen as lacking coordination and continuity, impacting their effectiveness (Quote 6). Students also emphasised the absence of suitable places outside of home and school where they could socialise and informally support each other’s mental health. Community events that provided social opportunities were limited, and youth and community centres were perceived as lacking essential infrastructure and personnel (Quote 7–8), and were not viewed as desirable for 14–15-year-olds to attend – being more suited to pre-adolescent children (Quotes 7–8).
Family level
With limited access to professional mental health and youth support services in the community, good relationships with parents were pivotal to students’ mental wellbeing (Quote 9). Some students valued talking with their parents about mental health, and felt understood and supported when a parent with lived experience of mental ill health shared their experience with them (Quote 10). However, participants described parents, especially fathers, often as time-poor, absent from home, and/or struggling with their own mental health in the face of the rural challenges (Quotes 11–13). Students (and one parent) highlighted that as parents were often lacking mental health literacy and skills, they tended to ignore or dismiss their children’s mental health concerns (Quote 14–16). This lack of knowledge was attributed to stigma, open conversations about mental health being a relatively new phenomenon, fear of appearing weak, stress, or hoping the issue would just go away (Quote 14–16). Students also reported how, at times, mental health issues entrusted to their parents leaked into the community (Quote 17). Others described how parents acted out their mental health struggles via physical aggression, which was viewed as role-modelling unhelpful behaviours to their children:
S1: I've seen parents who have engaged in their children's, like, dramas […] And it's so hard, because a lot of the behavioural issues do come from parents. Like, it often stems from like your roots […] S2: And how their parents deal with their own issues, there’s like, a lot of physical fighting in our community too. I definitely notice. [Female Student_B1]
Some students described situations where they or their friends had felt invalidated by their parents (or carers) when trying to share. YP withdrew from sharing their mental health issues with their parents due to negative experiences with it. This also put up a barrier for some students to access online mental health support in case it was witnessed by their parents (Quotes 18–19). Other YP described that this feeling of reluctance, combined with a lack of local mental health services, made it difficult for YP to seek non-local professional help as they relied on parental support to physically get to an appointment (Quotes 20–22). One teacher also described some parents’ lack of cooperation regarding their adolescent children’s mental health treatment in situations when it was initiated by the school (Quote 23).
School level
Students reported strongly valuing the educational mental health programs that had been provided at school by visiting services (e.g., batyr@school [an interactive mental health program for high school students in years 9 to 12 delivered by facilitators and young people with lived experience of mental ill health that aims to reduce stigma, and educate and empower students to reach out for help when needed ( www.batyr.com.au )]; Tomorrow Man, Tomorrow Woman [a mental health program for year 10 high school students that aims to cultivate awareness among emerging young women and men of the pressures that come from gender stereotypes. The program aims to grow emotional literacy and develops skills around cultivating mental wellbeing for themselves and others ( https://leonsec.vic.edu.au/tomorrow-man-tomorrow-woman/ )]; Elephant Ed [a sex education workshops for year 5 to year 12 students ( www.elephanted.com.au )]), but considered this to be a drop in the ocean. Participants felt that a whole-of-community approach was needed, which extended to including educating parents and other adults in the community (Quote 35 and 35a). Some students had not experienced any school-based mental health programs (noting a batyr@school program was scheduled for delivery at their school over the following months as it was part of the research evaluation).
The majority of schools had local school counselling services which provided what was described by students and school staff as essential and sought-after mental health support for students. School counselling, however, was extremely under resourced and not meeting demand — as it was commonly only available one day per week, was often booked out for weeks in advance, and follow up appointments were difficult to obtain (Quote 36 and below):
We've actually got massive waiting lists at the moment for students to see people with mental health training, counsellors, we've got, we've got an undersupply. We've got a school psychologist who's got waiting lists, we got a school counsellor who's got waiting lists and we've got a student support officer who's got a waiting list. [Teacher_F6]
A teacher described how their school self-funded a psychologist whose work had markedly improved the mental wellbeing of students over years (Quote 37). As part of this, parents were included in the counselling services to YP and given support how to parent YP with mental health issues which was also viewed as effective approach (Quote 37). Other teachers commented on their school counsellors’ limits and, at times, inadequate qualifications (Quote 38–39). A minority of students were unaware that their school provided a counselling service (“ Do we even have a school counsellor?” [Male Student_F3]); some students were reluctant to visit their school counsellor out of fear of being singled out by the school community (Quote 40).
Both students and teachers described teachers as essential for YPs’ mental wellbeing. Students trusted their teachers and relied on their ability to help. Teachers were highly committed, and often proud, to provide mental health support to their students (Quotes 42–44). Teachers —particularly those with student wellbeing support briefs in their roles like Physical Education teachers, Wellbeing Officers, Year Advisors and Principals — provided mental health counselling to students when school counselling services were unavailable or when approached by students, both formally and informally (Quotes 45–46). They also provided emergency mental health services for students to support and bridge gaps in the chain of professional and home care (Quotes 47–48), and they supported and educated parents (Quotes 49–50). At the same time, teachers expressed feeling overwhelmed by the extent to which a growing number of students needed acute mental health support. They described this as navigating on the edge between feeling obliged, and wanting, to provide mental health support on one hand and being at their limits on the other. These limits, as reported by teachers, included feeling overstretched and often unable to balance the time to fit mental health education and support in with their multiple teaching responsibilities (Quotes 51–53 and below):
[Teachers] have got so much on their plate with what they've got to do in learning outcomes and all that sort of stuff. They don't really have time to think about these things [referring to students’ mental health] as well. [Teacher_F11]
Teachers also emphasised that they sometimes felt ill-equipped regarding their mental health knowledge and skills to help students with complex mental health needs (Quotes 55 and below):
I feel on edge when I try to give the kids advice because I'm not trained in that, like I know myself, I've raised three kids, you know. I've done heaps in my life experience. But at the end of the day, I'm not a counsellor, I'm not a psychologist […] and yet we’re expected to be. [Teacher_B5]
Teachers felt uncertain where to draw the line between YPs’ privacy versus their caring responsibility as teachers (Quote 56); and also reported that, despite their best intentions, their own patience and empathy was challenged in regard to students with behavioural disorders:
We’ll have empathy for kids that have got really obvious issues, but then there's the other sort of kids that’ll be in your class, that exhibit disruptive sort of behaviour, and there might be some sort of issue behind that. And people are much less understanding of that, I mean, I find myself I’m much less understanding of that sort of behaviour than I was previously. [Teacher_B4]
Peer friendship and mutual support were of utmost importance to students (Quote 67). One student, for example, enthusiastically spoke of the mental health benefits of having initiated a boys social media chat group for the purpose of mutual support (Quote 68). Concurrently, students were acutely aware of their limitations regarding supporting each other’s mental health. They felt weighted down by the responsibility that came with giving, offering, or even just intending to support their friends, and were extremely keen to learn how to help each other more effectively (Quotes 69–71). A parent described YP’s attempts to help each other as “ the blind leading the blind ” (Quote 72).
Individual level
Participants reported above-mentioned existential stressors on the community, stretched and insufficiently equipped parents and teachers, a collective silencing (i.e., not talking about) of mental health issues, and a lack of local mental health support weighed on YP at an individual level. This culminated in students knowing when ‘something’ was wrong with their mental health, but often did not know how to describe let alone deal with ‘it’ effectively (Quotes 58–59). Participants described a variety of unhelpful mental health coping mechanisms that they had used themselves or observed in peers. These included: accepting mental health issues as normal (Quote below) and suppressing negative feelings (Quote 60).
Our feelings are so normalized that it's OK to be sad a lot of the time. It's OK to be angry all the time, which you don't want to be angry and sad all the time. That's not, it's OK to be sad and angry sometimes, but we don't want to do it all the time. And I think that's another issue. We don't register that something is wrong, you know […] it kind of doesn't process that it's not that's not how it has to be, like you can get help. But I don't think we realize that we need it. [Female Student_B1]
When the weight of bottling up mental health issues became overwhelming, some YP relieved their mental stress in maladaptive ways, making their social surroundings obscurely yet acutely aware that they were not coping. Such ‘concealed cries for help’ ranged from attention seeking behaviour (Quote 61), physical aggression against teachers (Quote 62), towards each other (Quote 63), and towards themselves in form of self-harm and suicide, with self-harm incidents at times being shared with peers on social media. The latter was described by students and teachers as concealed cries for attention and/or support:
Suicidal self-harm, which self-harm just seems to periodically go with depression and anxiety, now, that's just how this coping strategy that young people have developed like they don't know what else to do that puts them in this next level. [Teacher_F8]
YPs’ maladaptive stress relief behaviours further increased the mental stress load on other YP and their social circles. Examples given by participants were students’ and teachers’ anxiety coming to school out of fear of being the target of physical aggression (Quote 64), and getting distressed by seeing peers’ self-harm stories on social media (Quote 65). Posted self-harm stories were also perceived as problematic by some participating YP as they thought to be normalising self-harm as a legitimate means of mental stress relief:
The whole idea of social media has become kind of destroyed by that image that like to have depression, you've got to be self-harming. [Female Student_B1]
However, participants also reported YPs’ constructive attempts of dealing with mental distress where parental and professional support were lacking, or unwanted out of concern of being dismissed or singled out. These attempts centred around YP helping (and seeking help from) each other as described in section ‘ Peer level ’. Several students knew of the availability of online mental health resources from school advertisements (Quote 41). The uptake of these online mental health services, however, was mixed. Some students valued the anonymity that online help offered; others hesitated to use it because of “ the security risk associated with putting stuff out on the internet” [MS_B3], or because they preferred talking face-to-face with someone (MS_B3). Others hadn’t considered accessing online help at all for themselves (M + FS_F12).
Impact of COVID-19 compared to other stressors and major events
While the data gathering for this study was conducted during the height of the COVID pandemic (June 2021 to June 2022), and the impact of the pandemic was touched on in the occasional interview/focus group (mostly prompted by the interviewer), we found that the pandemic did not significantly impact, exacerbate, or otherwise change the nature of young people’s mental health needs. Geographic remoteness, long-term drought, and other natural disasters such as floods and bush fires were together much deeper and complex existential stressors on rural and regional YP and their mental health than the comparatively shorter restrictions to urban areas that came with COVID-19. Social distancing and lockdown restrictions for example were viewed as a non-issue in communities without COVID cases. Moreover, remoteness, social distance and isolation were well-known factors that all participants reported to navigate long before the pandemic started, with its restrictions not incurring a substantial difference to day-to-day life.
Mental health stigma
In all interviews, participants described the presence of stigma in the community limiting addressing mental health issues and accessing appropriate support, including in the school playground and at home. Mental health self-stigma was characterised by (a fear of) being seen as weird or weak – the latter more so among boys and men; being ashamed to be different; and being (scared of getting) judged negatively (Quotes 24–28). Students and teachers reported how fear-based negative connotations around mental ill health prevented YP and their families from talking about their feelings and seeking mental health support, especially in smaller communities where everyone knew each other (Quotes 29–32 and below):
They don’t feel comfortable but yeah, or they think oh, that's a shame. I'm not going to be going to ask for help, like, people might tease me. [Female Student_B1]
Students described how a lack of mental health awareness in the community perpetuated the mental health stigma (Quote 33), and noted that being educated about “awkward” themes made it easier for them to talk about them (Quote 34).
Mental health solutions
Multi-pronged approach to mental health education.
All participant groups emphasised the need to take a multi-pronged approach to mental health education and support, with programs and services not only for YP, but also for parents and teachers and the community as a whole (Quote 73-74a), to tackle the communal mental health stigma and enable managing mental health issues without shame (Quote 75). Students in particular stressed the importance of educating parents and teachers (Quote 76). They wanted their parents to gain more mental health awareness, know how to identify mental ill health, act appropriately when their adolescent child displayed signs of mental ill health, know where to get help and how to keep mental health issues confidential (Quotes 77–80). Indeed, students yearned for their parents’ mental health understanding and appropriate behaviour (Quote 81). It was rare for students to report that their parents already had “ a really good idea of what to do ” (FS_F5). Educating parents was also a high priority for teacher and parent participants (Quotes 82–83). All participant groups also stressed the need to upskill teachers on how to identify and support YP with mental health issues (Quotes 84–86). Several teachers wanted mental health education to be part of the core teacher training (Quote 87).
Local, face-to-face, free of charge mental health services
Participants wanted mental health services to be offered locally, that is, in their community, to overcome the access barrier and to get personal face-to-face support. They wanted mental health services to be offered free of charge, especially during times of financial hardship caused by recurring natural events (Quotes 88–93). Some participants also emphasised a need to review how school counselling services operate including how well their training addressed the needs of school communities (Quotes 94–95). One teacher considered mental health education as the foundation for other learning to happen and suggested implementing it into the school curriculum (Quote 96).
Relatable, engaging, and inspiring mental health programs
Relatability was the desired mental health intervention characteristic that participants referred to most often and most passionately. Specifically, students wanted mental health programs to be tailored to their local circumstances, with demonstrations of empathy and understanding for them (Quote 97). More importantly, participants found programs extremely relatable and effective when they portrayed the perspective of YP with lived mental ill health experience, as in the batyr @school program (Quotes 98–99 and below).
I think it was really good that [Y9 students] heard […] the story of that young girl […] she wasn't going anywhere. She had no money. She was homeless, living in a car […]. But the kids, really, they were captivated by her. I remember looking around when she was speaking and they were just staring at her, like, in awe, yeah. And a lot of kids, when they had to write a message about the program, wrote about her on their piece of paper. [Teacher_F10]
Students contrasted this with mental health programs that only consisted of standard lecture format presentations, rated these as “ disengaging ” (Quote 100–101). Students also opened up when mental health programs included interactive elements such as group discussions and physical activity games. They found these highly engaging as they could contribute their opinions and experiences, release stress while physically engaging in fun activities, and maintain focus (Quotes 102–104). Group discussions were most accepted when the groups were small and homogenous regarding YPs’ age, gender and mental health needs (Quotes 105–108).
Empowering YP
Students highly valued peer friendships, if not depending on them in the face of the rural and regional challenges. They often preferred providing mental health support to each other over approaching their parents or teachers or accessing professional mental health support (Quotes 109–110), especially mental health services with whom they had no pre-existing relationship (see next section). Obtaining practical strategies how to help each other and increasing their confidence in talking about mental health were therefore top priorities for students, rarely addressed by the existing mental health support options available to them (Quotes 111–113). Some of the more outspoken students, and students with a lived experience of mental ill health, also valued opportunities where they could act as mental health ambassadors to give their peers “ that little push to come out ” (MS_B3), pass on their experiences and inspire other YP (Quotes 114–115).
Confidentiality and trust
Confidentiality around using mental health support was extremely important to students. Many of them were deeply afraid of being identified as in need of mental health support (due to the stigma identified above); they were only prepared to open up if they felt it was absolutely safe to do so and they could trust their helper (Quotes 116–117). Trust, confidentiality and safety for them developed with knowing the helper, preferably in person, being able to relate to them, and having a positive personal relationship with them. For the students who participated in our study, these criteria tended to be met mostly by peers and teachers, less so by parents and school counselling services, and least by health professionals and online helplines not previously known to students. Face-to-face contact, relatability, engagement and empowerment of YP all contributed to enhancing YP’s trust, as detailed in the earlier parts of this section.
Early and ongoing preventative mental health education
All participant groups emphasised that mental health education for YP should start early and be taught throughout all high school years, with some participants wanting mental health education to start in primary school (Quotes 118–122). Similar to the mental health education goals for parents and teachers (see section Multi-pronged approach above), participants suggested that mental health programs for YP should raise mental health awareness, teach how to recognise mental ill health, develop mental health self-help strategies, and address and break through stigma and stereotypes that were detrimental to YP’s mental health (Quotes 123–127).
This was the first known Australian qualitative study to explore the barriers, needs and solutions of 14 to 15 year-old YP in drought-affected rural and regional communities regarding MH education, help-seeking and support, specifically focussing on how to facilitate help-seeking. The key findings through the lens of YP, their teachers and parents were that help-seeking would best be enabled by a multi-pronged community approach to mental health education and support. More specifically, they wanted such mental health education and support to be locally available to all community members, free of charge, relatable, engaging, and empowering. Participants felt the need for mental health education to take a preventative approach, emphasise the development of mental health self-management skills, start in early school years, and be offered throughout all high school years to both YP and parents. For teachers in rural and regional areas, facilitating help-seeking for YP with mental health problems led to a tension between being students’ trusted, first point of call for mental health support on one hand and feeling overwhelmed and under-skilled regarding providing this support on the other. Following, a three-dimensional approach to improving the MH situation for YP in rural and regional communities in Australia by facilitating Engagement, Empowerment and Integration is discussed in context with existing literature (See Supplementary File : Principles and Facilitators).
Emotional engagement is crucial in the effectiveness of mental health programs, as for example shown by the literature on contact-based interventions [ 41 , 42 ]. Our study adds to this literature by demonstrating how relatability facilitates emotional engagement and, at least temporarily, this can break through stigma in rural and regional communities and improve YPs’ mental health help-seeking behaviour. Hearing the lived experience mental health stories of other YP, a contact-based intervention and core component of the batyr @school program [ 28 ], was by YP, their teachers and parents perceived as particularly relatable, engaging and meaningful. Our findings demonstrate how the perceived relatability of this intervention emotionally opened up YP towards sharing their own mental health stories. Given the high acceptance of this type of interventions from this sample, more research needs be conducted into how lived experience storytelling can be harnessed as a tool to make mental health programs relatable, and thus maximise YPs engagement and help-seeking behaviour. Further research into this area could be a valuable contribution to the currently inconclusive literature in the field of contact-based interventions [ 43 ].
An important variable in the relatability of lived experience storytelling and, more broadly, a mental health education intervention as a whole, is the delivery mode. While in this study, participants preferred face-to-face over online delivery, citing trust, confidentiality and interactivity as limiting factors of online programs, systematic review evidence suggests that online interventions can provide similarly effective anti-stigma results as face-to-face sessions [ 44 ]. More studies are needed to consolidate these findings. In any case, digital delivery has a potential to add extra scaffolding to face-to-face, providing further information and support to those who want it or don’t have access to face-to-face programs, for example, due to their geographical remoteness.
Another variable relating to emotional engagement in this sample of YP was the depth of insight mental health program facilitators had of the local communities they worked with. This included insight into the specific economic and environmental challenges rural and regional communities faced and how these challenges impacted their members. YP for example connected better with counsellors who “ understood drought ” [ 15 ] or who had experienced bushfires. Following this rationale, it seems advantageous to deliver locally tailored mental health education and support by professionals who are familiar with the culture and needs of individual communities [ 10 , 24 ]. Further research into the importance of this aspect is indicated.
Empowerment
While emotionally engaging YP is important, it is not enough. Corroborating with existing literature, the present study found that YP wanted to feel a sense of empowerment and active participation in the process of learning about and managing their mental health, and seeking help [ 10 , 45 , 46 ]. This sample of YP asked to be equipped with more confidence and skills around talking about and managing their mental health. They described wanting to feel a sense of choice and self-determination. Further, a desire for empowerment was raised by YP alongside their preference for informal, especially peer-based mental health support, which is also a common theme in the literature [ 11 , 45 , 47 , 48 ] as is the finding that such informal sources are notoriously under-resourced and under-qualified (e.g., [ 11 ]). Further investigation into whether (and how) YPs’ desire for self-determination and peer-based mental health support can be harnessed is warranted. For example, in the context of developing mental health youth ambassadors — as done in the Student Chapter of the batyr @school program [ 28 ] and the Canadian Stop Now and Plan (SNAP®) Boys (e.g., [ 49 ]). This could be especially useful in rural and regional communities where professional mental health services are scarce and YP rely on strong peer friendships. With appropriate professional guidance, there is potential for YP to grow into role models for ‘good’ mental health management, building from the bottom up a positive mental health culture in their social networks including on social media to reshape current, often maladaptive, mental ill health models and discourses [ 50 , 51 ]. YP’s desire for more educated parents also speaks to a bottom-up empowerment approach to tackling mental health issues in rural and regional communities where parents are often found to feel helpless when it comes to understanding and supporting their children’s mental health [ 14 , 19 , 20 ]. Clearly, empowerment is unlikely to result from one-off interventions. It rather needs a systematic, well-coordinated and integrated mental health approach as outlined following.
Integration
In line with existing literature, our findings highlight the need for a multi-dimensional integration and coordination approach to the provision of mental health education and support in rural and regional communities. An integrated approach requires first and foremost better coordination between school- and non-school-based mental health services so that YP are offered seamless and ongoing mental health education and support solutions rather than uncoordinated or one-off piecemeal [ 3 , 12 ]. The current findings also show that embedding mental health education in school curricula earlier, more prominently and consistently throughout schooling years was requested by participants as a way to equip YP with mental health knowledge and management skills before mental health issues arise. While this may not be unique to rural and regional areas, it could be an important avenue to tackling mental health stigma and increasing help-seeking when needed, particularly because these communities can be underpinned by social conservatism and lack anonymity [ 9 , 10 , 11 ].
Intensifying school-based mental health education and support, however, has its own issues. Teachers, including welfare officers, have been shown to increasingly navigate at the edge of their time availability and mental health competence, calling for training and resources on how to identify and provide early mental health support for students [ 18 , 21 , 52 , 53 , 54 ]. Recent nation-wide surveys of teachers and the public have shown a link between teachers’ mental health care role and burnout: as teachers assume an increasingly influential role in developing YPs’ social and emotional development, with the public relying on them to do so [ 55 ], teacher burnout and exodus of the profession is rising [ 56 ]. Furthermore, school counselling services cannot completely meet the burgeoning demands for students’ mental health support in rural and regional Australia. Frequently covering multiple rural and regional communities, school counselling services often operate on a one-day-per week basis, are booked out well in advance and, regularly stretched for time, experience concerning levels of burnout [ 57 , 58 ]. We recommend more research be done on the role that external/visiting mental health programs can play in rural and regional areas and thus build on selective studies that have shown that such programs can relieve school staff and emotionally engage YP in unique and novel ways that cannot easily be replicated by schools who are bound to rather uniform structures, curricula and lesson formats [ 25 ]. There might also be a place for the integration of social workers into a multi-pronged mental health approach with the aim to strengthen social connections and support between YP and their families, schools and communities [ 59 , 60 ].
Whichever integration model is chosen, attention must be given to the careful coordination of school-based with community-based and visiting services to ensure smooth transitions, consistency and continuation of mental health education and support for YP throughout their formative high school years and beyond [ 17 ]. Co-design, also known as participatory design, with key stakeholders including YP, teachers, parents and mental health organisations, could be an important way of ensuring mental health education and support programs meet the needs and wants of (school) communities and the YP they are targeting. Participatory design places stakeholders at the centre of the design process and is part of a paradigm shift towards collaborative bottom-up engagement whereby stakeholders jointly explore and create solutions to program design and service delivery [ 61 ]. Recommendations for best practice in clinical mental health service design already emphasise the need to involve YP in the planning, implementation and evaluation of services [ 62 ] and this must be extended to community-based interventions [ 63 , 64 , 65 ].
Strengths and limitations
A key strength of this study was the recruitment of a large sample of YP from a diverse range of rural and regional areas of Australia. Their perspectives were complemented and triangulated with those of rural and regional teachers and two parents. However, due to the conservative recruitment methods we used, our sample was likely biased towards participants with a certain familiarity with, and confidence in talking about, mental health issues. Other limitations of this study relating to the participants include the presence of a teacher in 4 out of 7 student interviews, possibly inducing some students to say different things to what they would have shared had they been interviewed without the presence of their teacher. Further to this, three adult participants were interviewed individually, as they needed to be conducted at a time that was convenient to them in order to participate. It is acknowledged that these interviews may glean more information and depth, compared to the focus groups. Further, although we followed processes to establish theme saturation [ 37 ], it is acknowledged that only two parents participated, and their views were not drastically distinct to other participating adults. Given the constraints of the evaluation, a greater focus on student recruitment was prioritised, however more diverse set of parent voices could have consolidated our finding on parental support of YP in drought affected rural and regional Australia.
The design of the evaluation research was such that some of the focus groups were conducted prior to the implementation of the batyr @school program to address the first research aim (i.e. to understand experiences and needs regarding mental health help-seeking, and explore mental health education, support and programs in rural and regional communities) and some were conducted after the batyr @school program was implemented as part of the program evaluation’s second aim. As both sets of focus groups were used in data analysis, results are interpreted through a lens of school-based mental health programs. This is important as although eco-systemic enablers to help-seeking (such as service provision models, family environment, community attitudes) are addressed in the findings and elsewhere in research focusing on rural and regional areas (e.g., [ 14 , 18 , 19 , 20 , 21 , 22 ]), the solutions presented in this discussion centre around what schools and the schooling systems can do in practice to enable better mental health education, programs and support. Further to this, topic guide development was influenced by the evaluation questions, not necessarily the literature concerning young people's help-seeking or general mental health and help-seeking when impacted by drought.
Another limitation is that for the focus groups that were conducted after batyr @school program implementation, the voices of students who had not attended the batyr @school program, and YP outside of the school system were lacking. There is evidence that such unheard voices form a significant portion of YP who need but don’t reach out for mental health support [ 47 , 66 , 67 ]. There is a need for further research into understanding how to engage and support these “silent” adolescent populations to best identify how to facilitate and support help-seeking. Further to this, future studies should consider investigating the needs of young people outside the 14–15 year age range, and seek to compare perspectives based on different demographics including young people who identify with minority groups such as young people with an Aboriginal and Torres Strait Islander background, LGBTQIA + young people, and young people who have a non-English speaking background, particularly those who have arrived as refugees.
Our study highlights important facilitators of mental health education and support for YP in drought-affected rural and regional areas of Australia. These include a multi-pronged, preventative, local community approach with an emphasis on early and ongoing development of YP’s self-management skills. We propose a three-dimensional Engagement, Empowerment, Integration approach which comprises: 1) maximising YP’s emotional engagement; 2) empowering YP to manage their mental health through developing practical coping skills; and, 3) integrating MH education and support programs into existing community and school structures and resources. Integration needs to be well coordinated in respect to time, place and capacity-related factors. Particular regard should be given to the important support roles teachers, school counselling services, social workers and parents can and already do play in the social and emotional development of YP.
Terms and abbreviations used
YP: Young person or young people. This term is used interchangeably with ‘adolescents’ and refers in this study to 14–15 year-old students who are enrolled in the high school years 9 and 10. The cited literature (Background and Discussion sections) refers to adolescents using a variety of age groups, ranging from age 10 to 19 years (reference [ 6 ]), to 14–18 years (reference [ 7 ]) and 12–18 years (reference [ 8 ]).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Handley TE, Kay-Lambkin FJ, Inder KJ, Lewin TJ, Attia JR, Fuller J, et al. Self-reported contacts for mental health problems by rural residents: predicted service needs, facilitators and barriers. BMC Psychiatry. 2014;14(1):249.
PubMed PubMed Central Google Scholar
Bowman S, McKinstry C, McGorry P. Youth mental ill health and secondary school completion in Australia: time to act. Early Interv Psychiatry. 2017;11(4):277–89.
PubMed Google Scholar
Gamm L, Stone S, Pittman S. Mental health and mental disorders—a rural challenge: a literature review. Rural Healthy People. 2010;2(1):97–114.
Google Scholar
Morales DA, Barksdale CL, Beckel-Mitchener AC. A call to action to address rural mental health disparities. J Clin Transl Sci. 2020;4(5):463–7.
Anderson JK, Howarth E, Vainre M, Jones P, Humphrey A. A scoping literature review of service-level barriers for access and engagement with mental health services for children and young people. Child Youth Serv Rev. 2017;77:164–76.
Aguirre Velasco A, Cruz ISS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? a systematic review. BMC Psychiatry. 2020;20(1):293.
Hudson J, Ingram V. Stigma-reduction & help-seeking in Australian classrooms. Sydney: Macquarie University, Centre for Emotional Health; 2017.
Quine S, Bernard D, Booth M, Kang M, Usherwood T, Alperstein G, et al. Health and access issues among Australian adolescents: a rural-urban comparison. Rural Remote Health. 2003;3(4):1–11.
Vanderbeck RM, Dunkley CM. Young people’s narratives of rural-urban difference. Child Geogr. 2003;1(2):241–59.
Waid C, Steven S, Sinclair L, Priest L, Petrie S, Carson DB, Peter, P. Report: Interventions for Rural and Remote Youth Mental Health. Carlton University; 2019. p. 1–9. https://doi.org/10.22215/sdhlab/2019.4 .
Francis K, Boyd C, Aisbett D, Newnham K, Newnham K. Rural adolescents’ attitudes to seeking help for mental health problems. Youth Stud Aust. 2006;25(4):42–9.
Salinas-Perez JA, Gutierrez-Colosia MR, Furst MA, Suontausta P, Bertrand J, Almeda N, et al. Patterns of mental health care in remote areas: Kimberley (Australia), Nunavik (Canada), and Lapland (Finland): Modèles de soins de santé mentale dans les régions éloignées: Kimberley (Australie), Nunavik (Canada) et Laponie (Finlande). Can J Psychiatr. 2020;65(10):721–30.
Aisbett D, Boyd CP, Francis KJ, Newnham K. Understanding barriers to mental health service utilization for adolescents in rural Australia. Rural Remote Health. 2007;7(1):1–10.
Salamone-Violi GM, Chur-Hansen A, Winefield HR. In this day and age why is it still so hard to find the right type of help? Carers’ perspectives regarding child and adolescent mental health services: a qualitative study. Adv Ment Health. 2017;15(1):58–70.
Carnie TL, Berry HL, Blinkhorn SA, Hart CR. In their own words: young people’s mental health in drought-affected rural and remote NSW. Aust J Rural Health. 2011;19(5):244–8.
Dean JG, Stain HJ. Mental health impact for adolescents living with prolonged droughtajr_1107 32.. 37. Aust J Rural Health. 2010;18:32–7.
Perkins A, Clarke J, Smith A, Oberklaid F, Darling S. Barriers and enablers faced by regional and rural schools in supporting student mental health: a mixed-methods systematic review. Aust J Rural Health. 2021;29(6):835–49.
Graham A, Phelps R, Maddison C, Fitzgerald R. Supporting children’s mental health in schools: teacher views. Teach Teach. 2011;17(4):479–96.
Boydell KM, Pong R, Volpe T, Tilleczek K, Wilson E, Lemieux S. Family perspectives on pathways to mental health care for children and youth in rural communities. J Rural Health. 2006;22(2):182–8.
Reardon T, Harvey K, Baranowska M, O’Brien D, Smith L, Creswell C. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? a systematic review of qualitative and quantitative studies. Eur Child Adolesc Psychiatr. 2017;26(6):623–47.
Trudgen M, Lawn S. What is the threshold of teachers’ recognition and report of concerns about anxiety and depression in students? an exploratory study with teachers of adolescents in regional Australia. J Psychol Couns Sch. 2011;21(2):126–41.
Jorm AF, Kitchener BA, Sawyer MG, Scales H, Cvetkovski S. Mental health first aid training for high school teachers: a cluster randomized trial. BMC Psychiatry. 2010;10(1):51.
Ivancic L, Cairns K, Shuttleworth L, Welland L, Fildes J, Nicholas M. Lifting the weight: Understanding young people’s mental health and service needs in regional and remote Australia. 2018.
Boyd CP, Hayes L, Nurse S, Aisbett D, Francis K, Newnham K, et al. Preferences and intention of rural adolescents toward seeking help for mental health problems. Rural Remote Health. 2011;11(1):122–34.
Milton A, Yeung M, Conn K, Glozier N. batyr@school in Drought Affected Regional School Communities. Sydney: University of Sydney; 2021.
Vins H, Bell J, Saha S, Hess JJ. The mental health outcomes of drought: a systematic review and causal process diagram. Int J Environ Res Public Health. 2015;12(10):13251–75.
Edwards B, Gray M, Hunter B. The impact of drought on mental health in rural and regional Australia. Soc Indic Res. 2015;121(1):177–94.
batyr. batyr@school info pack. online at https://www.batyr.com.au/batyr-school/ : batyr; 2019.
Fielding N. Qualitative interviewing. In: Gilbert. N, editor. Researching social life (2nd edition). London: Sage; 2001. p. 123–44.
Brinkmann S. Qualitative interviewing: Oxford university press; 2013.
Buus N, Perron A. The quality of quality criteria: Replicating the development of the Consolidated Criteria for Reporting Qualitative Research (COREQ). Int J Nurs Stud. 2020;102: 103452.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Khatamian FP. Challenges of recruitment and retention of university students as research participants: lessons learned from a pilot study. J Aust Libr Inf Assoc. 2018;67(3):278–92.
Biernacki P, Waldorf D. Snowball sampling: problems and techniques of chain referral sampling. Sociol Methods Res. 1981;10(2):141–63.
Miller WE, Kreiner DS. Student perception of coercion to participate in psychological research. N Am J Psychol. 2008;10(1).
Srivastava P, Hopwood N. A practical iterative framework for qualitative data analysis. Int J Qual Methods. 2009;8(1):76–84.
Francis JJ, Johnston M, Robertson C, Glidewell L, Entwistle V, Eccles MP, et al. What is an adequate sample size? operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25(10):1229–45.
Birks M, Chapman Y, Francis K. Memoing in qualitative research: probing data and processes. J Res Nurs. 2008;13(1):68–75.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Gao CX, Filia KM, Bedi G, Menssink JM, Brown E, Rickwood DJ, et al. Understanding the complexity, patterns, and correlates of alcohol and other substance use among young people seeking help for mental ill-health. Soc Psychiatry Psychiatr Epidemiol. 2023:1–11.
Cooper J, Hunter C, Owen-Smith A, Gunnell D, Donovan J, Hawton K, et al. “Well it’s like someone at the other end cares about you.” a qualitative study exploring the views of users and providers of care of contact-based interventions following self-harm. Gen Hosp Psychiatry. 2011;33(2):166–76.
Chen S-P, Sargent E, Stuart H. Effectiveness of school-based interventions on mental health stigmatization. Handbook of school-based mental health promotion: Springer; 2018. p. 201–12.
Jorm AF. Effect of contact-based interventions on stigma and discrimination: a critical examination of the evidence. Psychiatr Serv. 2020;71(7):735–7.
Janoušková M, Tušková E, Weissová A, Trančík P, Pasz J, Evans-Lacko S, et al. Can video interventions be used to effectively destigmatize mental illness among young people? a systematic review. Eur Psychiatry 2017;41(1):1–9.
Martínez-Hernáez A, DiGiacomo SM, Carceller-Maicas N, Correa-Urquiza M, Martorell-Poveda MA. Non-professional-help-seeking among young people with depression: a qualitative study. BMC Psychiatr. 2014;14(1):124.
Orlowski S, Lawn S, Antezana G, Venning A, Winsall M, Bidargaddi N, et al. A rural youth consumer perspective of technology to enhance face-to-face mental health services. J Child Fam Stud. 2016;25(10):3066–75.
Rothì DM, Leavey G. Mental health help-seeking and young people: a review. Pastor Care Educ. 2006;24(3):4–13.
Rickwood D, Deane FP, Wilson CJ, Ciarrochi J. Young people’s help-seeking for mental health problems. Aust E-J Adv Mental Health. 2005;4(3):218–51.
Sewell KM, Fredericks K, Mohamud A, Kallis J, Augimeri LK. Youth experiences in evaluating the Canadian SNAP® Boys youth leadership program. Child Adolesc Soc Work J. 2020;37(3):301–14.
Jadayel R, Medlej K, Jadayel JJ. Mental disorders: a glamorous attraction on social media. J Teach Educ. 2017;7(1):465–76.
O’Reilly M, Dogra N, Whiteman N, Hughes J, Eruyar S, Reilly P. Is social media bad for mental health and wellbeing? exploring the perspectives of adolescents. Clin Child Psychol Psychiatry. 2018;23(4):601–13.
Rothì DM, Leavey G, Best R. On the front-line: Teachers as active observers of pupils’ mental health. Teach Teach Educ. 2008;24(5):1217–31.
Shelemy L, Harvey K, Waite P. Supporting students’ mental health in schools: what do teachers want and need? Emot Behav Diffic. 2019;24(1):100–16.
Loades ME, Mastroyannopoulou K. Teachers’ recognition of children’s mental health problems. Child Adolesc Mental Health. 2010;15(3):150–6.
Heffernan A, Bright D, Longmuir F, Magyar B. Perceptions of Australian schooling: What matters in 2021. Monash University; 2021.
Longmuir F, Gallo Cordoba B, Phillips M, Allen KA, Moharami M. Australian Teachers’ Perceptions of their Work in 2022. Monash University, https://bridges.monash.edu/articles/report/Australian_Teachers_Perceptions_of_their_Work_in_2022/21212891 ; 2022.
Earle K-M. Burnout in NSW school counsellors: relationships between mindfulness, career-sustaining practices and work setting. J Stud Engagem Educ Matters. 2017;7(1):71–96.
King C, Subotic-Kerry M, O’Dea B. An exploration of the factors associated with burnout among NSW secondary school counsellors. J Psychol Couns Sch. 2018;28(2):131–42.
Maple M, Pearce T, Gartshore S, MacFarlane F, Wayland S. Social work in rural New South Wales school settings: addressing inequalities beyond the school gate. Aust Soc Work. 2019;72(2):219–32.
Smith J. Locational disadvantage and the role of school counsellors and social workers: “Doing whatever it takes” to support children, families and communities. Commun Child Fam Aus. 2018;12(1):43–63.
Milton AC, Stewart E, Ospina-Pinillos L, Davenport T, Hickie IB. Participatory design of an activities-based collective mentoring program in after-school care settings: connect, promote, and protect program. JMIR Pediatr Parent. 2021;4(2):e22822.
Early Psychosis Guidelines Working Group. Australian clinical guidelines for early psychosis. Melbourne, Australia: Orygen The National Centre of Excellence in Youth Mental Health; 2016.
Corrigan P. Effect of contact-based interventions on stigma and discrimination. Psychiatr Serv. 2020;71(12):1324–5.
Freebairn L, Occhipinti J-A, Song YJC, Skinner A, Lawson K, Lee GY, et al. Participatory methods for systems modeling of youth mental health: implementation protocol. JMIR Res Protoc. 2022;11(2):e32988.
Milton A, Zelalem M, Ballesteros K, McClean T, Hartog S, Bray-Rudkin L, et al. Supporting children’s social connection and well-being in school-age care: mixed methods evaluation of the connect, promote, and protect program. JMIR Pediatr Parent. 2023;6:e44928.
O’Connor PJ, Martin B, Weeks CS, Ong L. Factors that influence young people’s mental health help-seeking behaviour: a study based on the health belief model. J Adv Nurs. 2014;70(11):2577–87.
Rickwood DJ, Deane FP, Wilson CJ. When and how do young people seek professional help for mental health problems? Med J Aust. 2007;187(S7):S35–9.
Download references
Acknowledgements
We thank the students, staff and families from the participating NSW public schools. We also thank batyr and their enthusiastic team who have helped on this project including.
Amy Brown, India Smith, Zoe Dunnill, Sarah Morris and Tom Riley. We would also like to extend our thanks the Department of Education team for their ongoing support of this research.
This study was funded by a grant from the Australian Department of Education and batyr, and was partially supported by the Australian Government through the Australian Research Council's Centre of Excellence for Children and Families over the Life Course (Project ID CE200100025).
Author information
Authors and affiliations.
Central Clinical School, Faculty of Medicine and Health, The University of Sydney, Sydney, Australia
Christiane Klinner, Nick Glozier, Margaret Yeung, Katrina Conn & Alyssa Milton
Australian Research Council (ARC), Centre of Excellence for Children and Families over the Life Course, Sydney, Australia
Nick Glozier & Alyssa Milton
NSW Department of Education, NSW, Australia
Katrina Conn
You can also search for this author in PubMed Google Scholar
Contributions
AM conceived this study. AM and NG designed this study. AM conducted the interviews oversaw the interpretation of the data at all stages. MY supported the interviews and conducted a preliminary analysis of data with AM, KC and NG. CK analysed the data and drafted the manuscript. CK and AM refined and revised the manuscript with the help of NG, MY and KC.
Corresponding author
Correspondence to Alyssa Milton .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this study was provided by the University of Sydney Human Research Ethics Committee (Protocol number 2020/607). Subsequent approval was provided via the NSW State Education Research Applications Process (SERAP Number 2020373). All participants provided written informed consent. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., additional file 3., additional file 4., additional file 5., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Klinner, C., Glozier, N., Yeung, M. et al. A qualitative exploration of young people’s mental health needs in rural and regional Australia: engagement, empowerment and integration. BMC Psychiatry 23 , 745 (2023). https://doi.org/10.1186/s12888-023-05209-6
Download citation
Received : 12 April 2023
Accepted : 21 September 2023
Published : 13 October 2023
DOI : https://doi.org/10.1186/s12888-023-05209-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Youth mental health
- High school students
- Help-seeking
- Mental health education and support
- Rural and regional Australia
- Qualitative research
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 01 July 2020
Lived experiences: a focus group pilot study within the MentALLY project of mental healthcare among European users
- Malin Axelsson ORCID: orcid.org/0000-0001-5493-8334 1 ,
- Viktor Schønning 2 , 3 ,
- Claudi Bockting 4 ,
- Ann Buysse 5 ,
- Mattias Desmet 6 ,
- Alexis Dewaele 5 ,
- Theodoros Giovazolias 7 ,
- Dewi Hannon 5 ,
- Konstantinos Kafetsios 8 ,
- Reitske Meganck 6 ,
- Spyridoula Ntani 7 ,
- Kris Rutten 9 ,
- Sofia Triliva 7 ,
- Laura Van Beveren 9 ,
- Joke Vandamme 5 ,
- Simon Øverland 3 , 10 &
- Gunnel Hensing 2
BMC Health Services Research volume 20 , Article number: 605 ( 2020 ) Cite this article
7612 Accesses
5 Citations
1 Altmetric
Metrics details
Mental healthcare is an important component in societies’ response to mental health problems. Although the World Health Organization highlights availability, accessibility, acceptability and quality of healthcare as important cornerstones, many Europeans lack access to mental healthcare of high quality. Qualitative studies exploring mental healthcare from the perspective of people with lived experiences would add to previous research and knowledge by enabling in-depth understanding of mental healthcare users, which may be of significance for the development of mental healthcare. Therefore, the aim of the current study was to describe experiences of mental healthcare among adult Europeans with mental health problems.
In total, 50 participants with experiences of various mental health problems were recruited for separate focus group interviews in each country. They had experiences from both the private and public sectors, and with in- and outpatient mental healthcare. The focus group interviews ( N = 7) were audio recorded, transcribed verbatim and analysed through thematic analysis. The analysis yielded five themes and 13 subthemes.
The theme Seeking and trying to find help contained three subthemes describing personal thresholds for seeking professional help, not knowing where to get help, and the importance of receiving help promptly. The theme Awaiting assessment and treatment contained two subthemes including feelings of being prioritized or not and feelings of being abandoned during the often-lengthy referral process. The theme Treatment: a plan with individual parts contained three subthemes consisting of demands for tailored treatment plans in combination with medications and human resources and agreement on treatment. The theme Continuous and respectful care relationship contained two subthemes describing the importance of continuous care relationships characterised by empathy and respect. The theme Suggestions for improvements contained three subthemes highlighting an urge to facilitate care contacts and to increase awareness of mental health problems and a wish to be seen as an individual with potential.
Facilitating contacts with mental healthcare, a steady contact during the referral process, tailored treatment and empathy and respect are important aspects in efforts to improve mental healthcare. Recommendations included development of collaborative practices between stakeholders in order to increase general societal awareness of mental health problems.
Peer Review reports
Mental health problems are among the dominant causes of non-fatal health loss in Europe [ 1 ] affecting 17.3% ( n = 84 million) of the European population [ 2 ]. The high prevalence of mental health problems and associated needs for mental healthcare pose a significant challenge for politicians and healthcare providers all over Europe [ 2 , 3 ]. Still, a large proportion of Europeans lack access to high quality mental healthcare. Delayed or ineffective treatment of mental health problems has negative consequences for the individual but also for society, as it affects work participation and contributes to increased sickness absence [ 3 ].
The World Health Organization (WHO) has developed a framework, Availability, Accessibility, Acceptability and Quality of healthcare (AAAQ), as an analytic tool to clarify how the right to health [ 4 ], as stated in the United Nations (UN) declaration of universal human rights §25 [ 5 ], can be understood in terms of provision of healthcare (Table 1 ). The possibility to provide healthcare of high AAAQ standards is related to the overall healthcare system in each country, which in turn depends both on the economic situation and on political decisions [ 4 ]. The individual’s right to mental healthcare is in any case indisputable and ratified by the UN, the WHO and the European Union (EU) levels [ 4 ]. However, according to a report from the Organisation for Economic Co-operation and Development (OECD) many individuals with mental health problems do not receive necessary treatment, indicating an international treatment gap of approximately 50% depending on the type of mental health problem [ 2 ]. In a cross-sectional study conducted in six European countries aimed at estimating the unmet need for mental healthcare at population level, 3.1% of the adult general population reported an unmet need for mental healthcare and 6.5% of those having mental problems were defined as being in need of mental healthcare [ 6 ]. Europeans with mental health problems who have received treatment regarded the effectiveness of mental healthcare as low [ 7 ]. Concerns regarding the quality of mental healthcare provided in primary care have also been raised by patients who experienced that they were stuck with ineffective medication treatments instead of being provided psychosocial care [ 8 ]. This coincides with Barbato and colleagues [ 9 ] who state that Europeans seeking help for their mental health problems are often prescribed ineffective treatments. Importantly, if patients experience the mental health treatment as ineffective they are more likely to discontinue their treatment [ 10 ], which in turn could jeopardize their recuperation.
There are different factors leading to delay in mental healthcare seeking, such as, structural barriers in terms of availability of mental healthcare [ 10 , 11 ], economic barriers [ 10 , 12 ], and transportation [ 12 ]. Attitudes in terms of a wish to deal with the problem yourself [ 10 ] and self-stigma constitute other barriers in seeking professional help for mental problems [ 10 , 12 , 13 , 14 , 15 ]. Rüsch et al. [ 16 ] made a distinction between social stigma and the self-stigma that can occur because of the negative attitudes held by other people. Self-stigma has been associated with both less openness to and less perceived value of professional treatment for mental problems [ 17 ]. Another phenomenon that has been forwarded as relevant to help-seeking behaviour is mental health literacy [ 18 ]. Indeed, Xu and colleagues [ 19 ] reviewed the effectiveness of interventions aimed at promoting help-seeking for mental health problems and found that increasing mental health literacy had a positive effect on professional help-seeking.
Important perspectives have emerged from previous qualitative studies. Newman et al. [ 11 ] as well as Gilburt et al. [ 20 ] have highlighted that the relationship between service users and professionals within mental healthcare is important as it form a basis for interaction and support, which is important to combat mental health problems. A qualitative study on mental health services provided to immigrants in 16 European countries [ 21 ] found consistent challenges to ensure optimal treatment for this marginalized group. The authors further suggest that recommendation for best practice may be appropriate at a European level. The majority of previous qualitative studies in this field capturing experiences from people with lived experiences have emerged from single countries, such as the United Kingdom and Ireland. Qualitative studies add to the research field but few studies take a cross-country perspective.
In summary, the burden of mental health problems in Europe challenges healthcare to offer high-standard mental healthcare corresponding to the AAAQ framework but quality improvement should be a continuous effort [ 4 ]. So far, most studies and reports of mental healthcare provision in Europe are based on quantitative data. The European Mental Health Action Plan 2013–2020 [ 3 ] stipulates that research in mental health assessing needs is to be supported and proposes that persons with mental health problems and their families are involved in quality control. Therefore, conducting qualitative studies that elicit an in-depth exploration of the perspectives of people with lived experiences of mental health problems and the use of mental health services would add to previous research and knowledge by increasing awareness and utilizing the expertise of this group. This can contribute to an in-depth understanding that can inspire and form the basis for quality improvement and development of mental healthcare in Europe.
The aim of this study was to describe experiences of mental healthcare among adult Europeans with mental health problems.
The current study is part of MentALLY - Together for better mental healthcare - a European collaborative effort between Belgium, Cyprus, Greece, the Netherlands, Norway and Sweden. MentALLY is a pilot project that has received funding from the European Parliament and the intention of the project is to gather qualitative data to improve European mental healthcare ( http://mentally-project.eu ). The current study is based on qualitative focus group interviews.
Participants
The total number of participants ( N = 50) were adults recruited for separate focus group interviews in the six countries. All participants had personal experiences of mental health problems and treatment from the mental healthcare services in their countries. The participants’ experiences were varied in type, length and time of contacts with the health care. Table 2 summarizes the recruitment procedures in each country and presents the study population. In all countries, the recruitment was done in several different ways to reach persons that might be interested in sharing their experiences. In all countries the initial contact was followed by written information about the MentALLY project after which the persons made their decision to participate.
Data collection
Data were collected through focus group interviews between April and November 2018. In total seven focus groups lasting between 73 and 141 min were conducted, each consisting of 4–14 participants (Table 2 ). MentALLY is a pilot project including six countries to test whether the study design and methods were useful in a cross-country approach. We therefore choose to limit the data collection to one focus group per country with one exception in Cyprus where two focus groups were conducted. The focus groups were facilitated by a social psychologist and a clinical psychologist in Greece, by a social psychologist in Cyprus, by a psychologist in Belgium, by registered nurses in Sweden, by a clinical psychologist, a psychology student and a physiotherapist in Norway and in the Netherlands by a communication scientist supervised by a clinical psychologist. Number of facilitators in each focus groups are accounted for in the Table 2 . All focus groups were held in the native language of each country.
A special effort was made to create a pleasant and hospitable atmosphere. Each focus group discussion began by providing information about the MentALLY pilot project and the interview procedures. Permission to audio record the interview was provided by the participants. They also provided written informed consent and demographic information including their age, sex, mental health problems and type of mental healthcare they had experienced. Registration of diagnoses or treatment site was not included in the ethics approval application in Norway, and this information was therefore not gathered at individual level.
The focus group interviews followed an interview guide that was developed in English by the MentALLY teams in collaboration. Thereafter the interview guide was translated into the different native languages using back-translation techniques [ 22 ]. The interview guide is presented in Table 3 . The interviews started with opening questions regarding positive and negative experiences with mental healthcare to inspire the participants to start talking and thinking about their experiences of mental healthcare. Gradually the questions became more focused relating to the organization of mental healthcare, changes needed to reach the goal of optimal mental healthcare and questions relating to the participants’ experiences of access to mental healthcare, issues related to diagnosis and referral, as well as treatment and collaboration. The interviews ended with questions about uncovered topics and the most important aspects of mental healthcare were discussed [ 23 ]. The audiotaped interview material was transcribed verbatim and translated into English in each country. Each participant was given a code to preserve confidentiality.
The initial analysis of the transcripts in the native language was conducted by the MentALLY teams in each country separately, except for the data from Cyprus and the Netherlands that were analysed by the Greek and Belgian teams, respectively. The transcripts and the analysis from each country were then translated into English to enable the creation of a common result covering all countries. The analyses followed the thematic analysis as described by Braun and Clark [ 24 ]. Adhering to a common analysis template in all MentALLY teams, the analysis was driven by an analytic interest to acquire a more detailed understanding [ 24 ] of experiences of access, diagnosis and referral, treatment and collaboration regarding mental healthcare.
Ethical considerations
Ethical approvals were granted from the Review Boards at Ghent University in Belgium, the University of Crete in Greece (Επι.Δ.Ε. i.e. Ethical Committee, 6/2018/16-05-2018) and the Regional Ethical Review board in Gothenburg in Sweden (474–18). In Cyprus, the Mental Health Services of the Ministry of Health gave permission to conduct the study (4.2.09.37/7). In the Netherlands, an application was sent to the Medical Ethical Committee of Academic Medical Hospital of the University of Amsterdam and an exemption was given as all subjects were healthy and non-invasive procedures were used (no number was given due to the exemption). The Regional Committees for Medical and Health Research Ethics in Norway deemed the project outside the realm of medical ethics assessment. Therefore, an assessment and approval from data protection officer at the Norwegian Institute of Public Health was collected. Following written and verbal information about the study, all participants signed an informed consent before the focus group interviews started.
The results are based on the thematic analyses of focus group interviews where a total of 50 participants with lived experiences of mental health problems and of receiving mental healthcare participated. As a group, the focus group participants had experiences from mental healthcare in both private and public sectors, and from in- and outpatient mental healthcare for various mental health problems. The participants had experiences of a wide range of mental healthcare treatment offers. Figure 1 depicts the experiences across five themes and 13 subthemes.
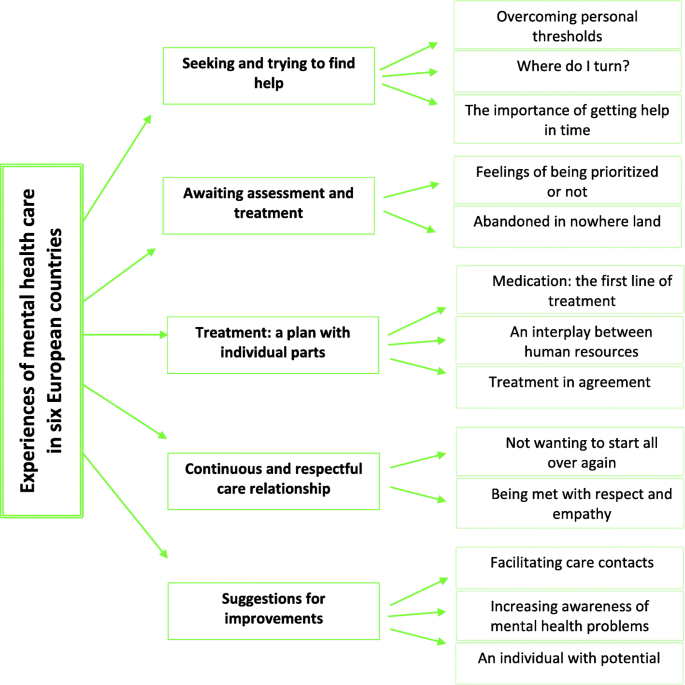
Illustration of themes and subthemes describing experiences of mental healthcare in six European countries
Seeking and trying to find help
The participants shared their experiences of what hindered or helped them in seeking and trying to find help for their mental health problems. Some of these experiences were related to accessibility to mental healthcare.
Overcoming personal thresholds
To seek help for mental health problems was described as a process in which the participants had to overcome different personal thresholds. According to some of the participants, one of the first thresholds to overcome was to accept and acknowledge that they were facing mental health problems that required professional care. Furthermore, they needed to be courageous enough to make a decision to contact a healthcare provider, which for some was an easier threshold to overcome than for others.
“You admit to yourself that something is wrong, and you go to a psychiatrist – the way you go to a GP or any other doctor. Why not? If you have a problem, you need to do that in order to get well”. (3 Cyprus).
“There is a threshold for having the courage to contact the care system to begin with.” (4 Sweden)
“The first time I came with a very deep depression, it was difficult to seek help, it was shameful.” (4 Norway).
This process and its thresholds consisted of both internal and external aspects, which could delay or even prevent the participants from seeking mental healthcare. Some were experienced in a context of negative attitudes, stereotypes and other aspects of public stigma surrounding mental health problems.
“In Cyprus, people with mental health issues are stigmatized” … // … “This is a big problem in Cyprus. Someone may suffer from a mild depression and leave it without treatment because of what society is going to think”. (1 Cyprus).
“...// … break through certain taboos, because I believe it is the biggest problem in Belgium. To break through the taboo of psychic health.” (1 Belgium).
Besides a process of acceptance and courage lived in a context of public stigma, there were other personal thresholds for seeking mental healthcare. For some of the participants these thresholds were related to previous negative experiences with the use of mental healthcare, while others had problems affording the care they needed and consequently were prevented from accessing necessary mental healthcare.
“ … // … this is a very important thing, that you...that there are far too many people who are terrified to have anything to do with mental healthcare, because...and then they have been there, and they know what they are talking about.” (1 Sweden).
“Ah yes just financial accessibility for everyone he, because that is the first block for many people because we may have now...// … many people may be lucky enough to have an insurance or I don’t know, but there are also people who have no insurance and mutuality that is refunded … // … ”(2 Belgium).
“I couldn’t get an appointment in the public sector. I went to the private sector. … // … There are people that haven’t got the financial resources to get help (in the private sector)”. (4 Greece)
“ … // … you don’t have the money to go to a clinic. So what can you do? Where can you go?” (6 Cyprus).
Where do I turn?
Related to the above described difficulties uncertainties about where to turn to seek care and treatment i.e. access to mental healthcare were brought up in the focus group discussions. Experiences of not finding the way through “the wilderness” of healthcare offers was mentioned and, as was to not know at all where to turn to receive help. Some found information by chance or by persons in their network. A common experience in the studied countries was the lack of easy found information about how to access mental healthcare.
“ I found it by myself. Circumstances helped me, a higher power if you want. I went to an event, found a pamphlet and I started going there. ” (1 Greece).
“A friend told me about it – I had no idea such a facility existed. ” (2 Cyprus).
“Well, I am thinking about when you don’t know exactly where to turn to. Where do I go, what should I do, who should I talk to? It does seem pretty unclear. Where do I begin, where do I call?” (2 Sweden).
“I think it is a... a wilderness, that you don’t know where to go.” (3 Belgium).
“And plenty exist, but we need to find what is what and what exists,” (1 Norway).
“Sometimes unfortunately you get tips that have worked for other, but did not help me. But I do notice that, I have been helped a lot by these tips by others.” (1 Netherlands).
The importance of getting help in time
To get help just in time was brought up as an important aspect of access to mental healthcare. Quite some time could pass before contact with a healthcare provider was made. Reasons were associated with the thresholds of acceptance, courage and public stigma that had to be overcome before help was sought, and in addition was the time it took to figure out where to find help. There were also acute situations when urgent contact with mental healthcare was made. Nonetheless, immediate access to mental healthcare was always regarded as crucial. When they contacted a healthcare provider the situation was described as acute or highly open in the sense that the need for help and the wish to get help was combined. This was described as important to combat the mental health problems with support of professionals. However, there were disagreements regarding waiting times as the participants had different experiences of waiting times when contacting mental healthcare. Some had very good experiences of getting help in time and had not been confronted with waiting times.
“...I haven’t been confronted with waiting times.” (5 Belgium).
“I called in the morning, made an appointment and came here (mental healthcare) on the same day. It was all very easy ”. (3 Cyprus).
“I didn’t have the same experience. My psychiatrist immediately helped me.” (3 Netherlands).
For others it was more difficult to access mental healthcare due to long waiting times, which appeared to be very common. They described the waiting as being in a desperate situation characterised as a matter of survival or death. Additionally, the long waiting times for treatment resulted in strenuous and unbearable situations for their relatives.
“Yes, I had to wait several times for a long time. But at the same time, 3 weeks are hellish as well. When you are suicidal for 3 weeks, it becomes too much.” (1 Netherlands).
“ There are people who have died waiting to be put on the waiting list (to enter a rehabilitation program for their addiction). There are mothers who are really begging out there (in the rehabilitation centre) elderly people praying and crying. ” (3 Greece).
Even as a patient within the psychiatric care system, it was not easy to access the care they needed to deal with their mental health problems. During the experienced long waiting times feelings of resignation emerged. The open window of a need and wish for help seemed to be time dependent.
“You cannot find the doctors and the professionals when you need them. They are not there when you need them. You need them and you feel they have abandoned you.” (2 Greece).
“ … and when I looked for care through the care system, I didn’t even get an appointment with a psychologist before I gave up and began to self-medicate instead, sort of thing. It is these waiting times that I would emphasize have really been a major obstacle for me.” (3 Sweden)
Awaiting assessment and treatment
Other experiences of the mental healthcare in the focus groups performed in six different European countries were related to how the mental healthcare functioned. When the participants eventually got in contact with healthcare and asked for help to fight their mental health problems, some of them experienced that their health problems were not prioritized and not always carefully assessed while others had experiences of being prioritized and properly cared for. When being referred to another level of care, feelings of being abandoned arose for some participants during the waiting time, because they experienced that no one cared for them. According to these participants, there seemed to be a lack of support in between the appointments and different levels of care. On the contrary, other participants described a smoother referral process to the level of care they deemed correct.
Feelings of being prioritized or not
Some participants expressed that healthcare professionals did not take mental health problems as seriously as somatic conditions. That experience led in turn to the feeling that healthcare providers did not prioritize mental health problems. In contrast, other participants shared experiences of being prioritized and thus being more or less immediately assessed and referred to correct level of care. Thus, the feelings of being or not being prioritized in care were individual experiences but also understood as structural differences. Some participants felt that they had to exaggerate their problems, and especially the risk of committing suicide, to receive help when being in need. In opposition, other participants shared their positive experiences of how well they had been cared for.
“I am aware that it isn’t something that is seen with the eye, but still if others can see it, a caregiver should as well. I find that so hard to understand. When it comes to physical problems, they do not just send someone home, they do not say yes, it’s cancer, just rest up a bit and perhaps the tumour goes away.” (1 Netherlands).
“I would want it to be easier to get help. Because I have said so many times that I want help, but then I do not get it. And they say to the patients: “have you tried taking your own life”, and “no, then you do not get to be admitted”. But you need to be admitted before you get so sick, in order to avoid getting sick.” (1 Norway).
“I think that I have received a lot of good help, actually. I have been treated in the mental health system for many, many, many years, in periods … // … I am still in contact with a psychiatrist for medication and stuff, and I think that I have received a lot of help and support … //...well, mainly through the open mental health system .” (6 Sweden)
“I have a few positive stories. For me, I was always referred to a good institute or caregiver. Well not always, but most of the time. And when I was sent to the wrong place, they would send me through to the correct place quite quickly. It never ended up being terrible. Sometimes you hear those stories of how it turns out bad. But it went well, even with files. The referrals in general were good.” (1 Netherlands).
“I’ve also been admitted to the psychiatric ward of the general hospital. That was very nice. Everything was ready and waiting for you.” (4 Cyprus).
Experiences that nurtured the perception of not being a priority were related also to the quality of mental healthcare, and related negative experiences. It was discussed that a careful anamnesis was required to diagnose mental health problems accurately and that preferably a psychiatrist should be involved from the beginning of the diagnostic process. However, the experience of the diagnostic procedure did not always correspond to these requirements. It was argued that time limitations and associated deficiencies in diagnostics and referrals from general practitioners were a major problem, and better support for general practitioners was mentioned as important.
“When the doctor saw me, he said “you have schizophrenia”. He just looked at me! He did not examine me for more than one minute and he diagnosed me with schizophrenia.” (1 Greece).
“ … // … that the patient is heard, and seen and gets good help on time, and gets good referrals. The primary doctors need to be strengthened so the patient gets the correct help in the specialist healthcare service that is very, very important.” (2 Norway).
Abandoned in nowhere land
The referral process was experienced as long and tiresome with long gaps between inpatient and outpatient care by some of the participants. Without a functional care chain, some experiences concerned feelings of being trapped and abandoned in nowhere land struggling with the mental health problems without support from any healthcare professionals.
“That it is very difficult, that you must just keep on nagging and fighting, to fight a lot and you don’t have the strength to do that. I find that it is a huge problem, when you are waiting, because you are in the care queue and waiting for a referral, and waiting for something to happen with the referral, and then you just have to keep at them, you have to call, you have to nag, and you don’t have the strength, so you just wait, quiet and being nice. So not much happens. That’s my experience.” (2 Sweden).
“It can take a long time before the assessment happens, and in the meantime the patient sits around and is not getting the help he should have.” (6 Norway).
“I had experienced it as different islands at the same time. No contact between general practitioner and therapist … // … There was no contact in general between anyone. They all just did their thing, and without me having any say.” (6 Netherlands).
Treatment: a plan with different parts
The participants shared their experiences of what aspects in the treatment for their mental health problems that had helped and hindered their recuperation. As previously mentioned, there were thresholds to overcome aggravated by public stigma. Once overcome the time was described as crucial since care was often sought late and when symptoms were severe, and in some cases even life threatening. But also in less severe situations the window between need and motivation to seek help could be closed due to experiences of unfair treatment or feelings of being abandoned. However, the participants also experienced it as a long process to recuperate from the mental health problems. During the discussions in all focus groups, the participants highlighted that it required a combination of different kinds of help and treatment to get better. Depending on individual needs, it seemed important that the treatment was individually planned and that a combination of treatments was the most effective.
Medication: the first line of treatment
Although the participants argued that an individualized treatment entailing different parts was needed to recuperate, some of them seemed to experience that medication was usually the first line of treatment prescribed. However, there was a variation of experiences regarding the medication treatment. On one hand, some of the participants recognized the importance of medication because either it had improved their condition or because it helped them to avoid negative outcomes i.e. relapses. On the other hand, some of them argued that there was an over-prescription of medication – sometimes against their will.
“I would be unable to function right now without the medication. I’d be much worse if I didn’t take it. Much worse. The medication I’m taking helps me a lot. If it weren’t for it, I’d take drugs, or start drinking. Taking it is in my best interest – not the doctor’s or the pharmacist’s.” (4 Cyprus).
“ … // … they press in more and more medicines, and if you try to say, wait a bit, I want some form of therapy or tool so that I can get somewhere with my problem, well then they just prescribe more medication that they don’t follow up and it just gets worse and they don’t check up, sort of thing, whether those medicines work together.” (2 Sweden).
An interplay between human resources
In all focus groups, the participants emphasized that medication regimens were not the only solution and therefore they discussed the elements in mental healthcare that they regarded as necessary for them to get better besides medications. Naturally, there was a variation of what elements that was considered as beneficial to get better from the mental health problems. They discussed that different resources were needed to meet their treatment needs and an interplay between resources was seen as treating the patient as a whole person. Among the resources mentioned to be involved in the treatment was healthcare professionals with experiences and competencies from different specializations. Additionally, patients themselves should also play an active part and participate in the treatment planning.
“In principle, we cannot treat someone with medications without psychological support. I think that everyone must do their part. That is, a person arrives at the doctor, that is, the psychiatrist, he will do his own work, and there must be a psychologist. What does this person have behind him? He has family, children, and legal issues? There should be a social worker who has a different role from the psychologist. It is a different job. … // … There should be different specialties.” (3 Greece).
“I think there is much in being able to take part in your own treatment, that you are a part of planning the treatment, and actually writing your own treatment together with your therapist, what sort of treatment you want, what is written in the journal, to be a part of planning the treatment course. However, it will probably be like that now in the set clinical pathways, that you are able to take part in your own treatment.” (3 Norway).
The continued discussion focused on the benefits and challenges with involvement of significant others in the treatment. Some participants considered significant others as an essential resource. Without them they risked fighting the mental health problems on their own. They argued that their next of kin should be invited to be involved so they could have a better understanding of the situation but also so they could provide the necessary support. In contrast, the involvement of significant others was also experienced as challenging as they could contribute to further distress by being unsupportive. Another challenge, highlighted by some of participants, was to be open about mental health problems and talk with their significant others about their problems.
“Perhaps professionals could require you bring someone with you during the visit. Things such as a visit from the GP. You first visit a specialist and you forget half of it so that they ask you to make a checklist. Because you are in such a bad place. I have had that problem for my whole life, making a list but never finishing it. Take your mother with you, is how I would describe it. That should become a standard. It is a smart thing to do.” (5 Netherlands)
“And it’s also a little hard to hear people tell you that it’s nothing and you’ll get over it. Personally, I had to face that too. My environment didn’t realize I was going through something serious … // … I had to fight on my own in order to make it”. (3 Cyprus).
“ … // … the word taboo, as long as we don’t break through it and don’t dare to talk with our children and our relatives” (1 Belgium).
Another element in the treatment that was regarded as essential and helpful to get better was inclusion of people who were experts by experience.
“Actually the best therapists are those who have experienced it themselves … and sometimes I wonder that is a kind of … if my psychiatrist is sitting in front of me, that is book knowledge … that person can never know what a depression is, that person can never know what an eating disorder is, he knows it but just due to experience, but that person cannot … at first-hand experience it. And the biggest help I got was actually from people with the same problems.” (1 Belgium).
An important part in the treatment, which facilitated for them to get better was the encouragement of social health i.e., contacts with their social context and labour market. When struggling with mental health problems, it was sometimes difficult to maintain one’s social health. Getting help to maintain or re-establish contacts with the labour market and social networks was considered essential.
“But it is important to address all problems the person is presenting. It is not certain that the psychiatry or the substance abuse is the worst. It could be economy, it could be living conditions, there are many other things that play a role, it is not only psychiatry”. (1 Norway)
“...// … even if the Social Insurance Agency is outside the care system it is an extremely important part of care, because it is the whole reason that you have security in being able to pay your bills and stuff.” (1 Sweden).
Treatment in agreement
The importance of consent in different stages of the therapeutic process was discussed during the focus groups. The option to interrupt the therapy and voice concerns towards their care provider was emphasized. Moreover, experiences of involuntary hospitalization and treatment had left some of the participants traumatized and very critical about the practices and the legislation that support these types of interventions. Negative experiences were also related to the reluctance to seek care discussed above.
“I think that is also still a big problem that a lot of people don’t dare to take a step themselves to … to stop with that... and say, ‘he isn’t doing anything for me, I have to go to somebody else.” (7 Belgium).
“This distressed me too much because they took me with handcuffs; they took me in a patrol car as if I was some criminal … // … I have yet to recover from that hospitalization. I have completely compromised; I have fully complied with what the doctor said I did what she told me but deep inside me I am not well to be honest. I’m not well. And this hospitalization was a horrible experience for me. And I have not been able to overcome it and I will never overcome it. They brought me in with handcuffs as though I was a criminal. There should be a court hearing when there is an involuntary hospitalization. No one has called me to defend myself in any court or trial. These things happen only in Greece. This only happens in Greece”. (1 Greece).
Continuous and respectful care relationship
When combatting the mental health problems, the participants described that they were in an extremely vulnerable situation. They had overcome the first reluctance to admit their problem and recognized a need to get help as soon as possible. For some of the participants, earlier negative experiences had to be set aside. During this period participants experienced that they were quite dependent on the relationship with the healthcare professionals, who represented the possibility to get better. Thus the characteristics of the care relationship was important to help them recuperate from the mental health problems.
Not wanting to start all over again
The importance of continuity in care relationships was underlined because that was regarded as helpful in contrast to having to explain everything all over again when meeting new healthcare professionals. Continuity was described as having a steady care contact with one or a few healthcare professionals who were very involved in their care process and who oversaw the whole process and took the necessary steps in the direction of recuperation. The process of needing to start all over again, every time a new treatment started or when having to meet new healthcare professionals, was experienced as exhausting and a hinder to get better.
“Then just to have a person...yes, partly to one who is...sort of like a coach for that person, a little like a mentor or coach, and that it is one person, so that they are not replaced all the time so you get new people, even if you do not have this first input, it is also important that you have regular staff, ...// … ” (1 Sweden).
“With my second depression, after my first child, my counsellor, took the initiative, as she saw it was going, left, to come together with me and my general practitioner and my social worker. This instead of having me tell my story over and over again.” (3 Netherlands).
Being met with respect and empathy
The situation of being vulnerable was a highlighted experience related to the fact that it was very difficult to stand up for yourself while struggling with mental health problems. However, being met as unique human beings in a respectful manner by healthcare professionals eased the situation. In contrast, stigmatizing attitudes and the often-oppressive way mental health professionals imposed a therapy or a course of intervention was experienced as the opposite: unhelpful and did not promote the collaboration.
“Everyone should be treated as a person, as a distinct individual as all of us are” (3 Greece).
“ I wrote a list before I came here and at the top of the list is respect for the individual and ...yes, I totally agree. I experience strongly that you...just like that you didn’t have a voice any longer, I am used to be listened to and taken seriously. Suddenly, I just felt that, aha, here comes a new mental case.” (1 Sweden).
“I wish for better attitudes among healthcare professionals, especially when it comes to the most serious diagnoses. There is a lot of prejudice and stigma, and you often get treated as a diagnosis, and I think that is condemnable.” (6 Norway).
“They (the psychiatrists) continue to oppress me. They would tell me you will take it (the medication) or you will go in, or I‘ll go back into the psychiatric hospital” (1 Greece).
The healthcare professionals’ empathic ability was emphasized as a necessary ingredient in the care relationship. The participants reasoned that empathy made the healthcare professionals able to put themselves in the position of their patients and understand them better, which in turn influenced the quality of care. They wanted to feel a willingness on behalf of the healthcare professionals to help them to get better. A feeling that they were authentically cared for instead of feeling as if they just were a number on a list for the healthcare professional.
“It means empathy; being able to understand the problem so you can help. It means therapists themselves should be able to feel what each one of us is going through. Because if you don’t, you can’t help”. (5 Cyprus).
“After a while I got the feeling I was number five of the day. They would have gaps in knowledge about me and then I would be like ‘Yes, but last time we agreed on this and this.’ I call it empathic ability. They lacked that.” (7 Netherlands).
“It is like a conveyor belt, you feel like that when you walk in, so I almost never go to the doctor. But when I go, I have gathered some things and when I get to point three, he does not have more time, and then we have to take it next time, and then it is two months to the next time, if it is not urgent. They have too many patients on their lists.” (1 Norway).
Suggestions for improvements
During the discussions of experiences of mental healthcare, the participants came up with different suggestions, which they thought would contribute to quality improvement of mental healthcare and to increase awareness of mental health problems in society.
Facilitating care contacts
Based on the challenges of getting in contact with the mental healthcare system, the participants discussed several creative suggestions, which were seen as important future possibilities to improve availability and accessibility. One suggestion was an emergency reception like the immediate help available for somatic health problems. This help should be adjusted to the kind of mental health problems the patients are struggling with and be based on a correct diagnosis. Besides an emergency reception, the participants also suggested care contact in the form of a knowledgeable contact point that could navigate the care seeker to the correct mental healthcare. Additionally, the availability of an informative website for finding help was regarded as good practice.
“It would like to have a kind of basic post for mental healthcare. Kind of like an EHBO (First aid), where you could go for help. It would help lots of people. There would be a faster process, instead of the long waiting lists. It would cost the taxpayer less as well.” (1 Netherlands).
“I was thinking that if there was...well, you have Contact Point in mental health, if that could have a double function so that you call there, explain that you are feeling ill with this and that, but I don’t know where to turn. If they had the knowledge to then direct you onwards, like railway points in some way. Not just that you can book appointments there, but also that you call there and sort of...I don’t know, where do I go now, and they can help you and direct you onwards, that could be a good thing to have, if you could just talk on the phone.” (2 Sweden).
Another suggestion was that healthcare professionals should send patients in the right direction by explaining different types of available treatments for their specific problems and the purpose of these treatments. It could be described as an expectation that professionals work not only for their own type of treatment but is aware of and have knowledge in other type of treatments and willing to refer patients further.
“There are infinite psychologists but if you are no psychologist you don’t know... // … cognitive behaviour therapy what does that include, you have a psychologist that works in a certain manner...but we are not aware of it and I believe that they should explain to us everything that exists”. (5 Belgium).
“ … // … I also think about this thing about...there has been a lot of focus on CBT, cognitive behavioural therapy, now, and it...I have received another type of therapy, and also have had CBT, and I feel it like this, that CBT is not always suitable, just that, it is very narrowly focused. A lot of people need a completely different type of therapy, but it is just that everybody needs to fit in the same folder today. And I don’t think that it is good. It must be changed.” (6 Sweden).
Other resources that would presumably improve accessibility to mental healthcare are having a better geographical spread of mental healthcare services or an expansion of mobile teams providing home consultations on demand.
“I think that, instead of having a bigger building, the facility should spread to other cities … // … We need to have such facilities close to us. It’s not enough for me to come here and see a doctor for 10 or 30 minutes. Or to have to wait for 3 months, for 2 months at least or for 1 month until the date of my appointment comes ”. (2 Cyprus).
“And then there are these mobile teams, … //... if you have established a contact they can come on home visits, and that is...// … and that is exactly a step that I think would help very many people,” (4 Sweden).
Increasing awareness of mental health problems
The participants discussed their wishes for more proactive efforts in society aimed at reducing stigma and increasing knowledge about mental health. Suitable arenas for such initiatives were for example schools and workplaces. It was suggested that mental health promotion should start already in primary schools as a way of increasing awareness and understanding about mental health problems.
“So, I think there should be an education campaign. … // … we need to get to young people in schools. So that young people know what can happen to anyone. Because what’s happening to me may happen tomorrow to my neighbour. They should know how to handle it, know how to deal with it. Now there are drugs, treatments, and institutions. There are many good and remarkable doctors. So, I think people need to be informed”. (3 Greece).
“One thing is that, I think that we touched on it earlier, but that you could also work quite a lot proactively on public health and have more healthy living thoughts that have more focus on the mental health parts, too, that you can hear about it in school at an early age, and I think that it would be an incredibly important tool for public health. As we said earlier, building up this knowledge, too, that you can sort of...I don’t want to say normalise, because I think that would give a negative connotation, but in some way still normalise mental illness.” (3 Sweden)
Some participants described the usefulness of experts with experience being involved in team meetings, in meetings with politicians, in education for healthcare professionals. They described that involving former patients might broaden up new perspectives above and beyond theoretical knowledge. By being involved in these things, they wanted care providers and policy makers to understand what mental health problems are really like.
“I think that it’s very important that there is uhm good education but there is still a big difference between book knowledge and experience knowledge and if both sectors would cooperate I think that...//... that there would be more understanding, much more indeed... as (name participant) said about changing that mentality or saying ‘politics’ or so, that doesn’t go … doesn’t go so easily but we, from our difficult things we can convert it in that positive one and work with that, witness, to inform people correctly.” (9 Belgium).
An individual with potential
The focus group discussions had a clear message that it was important to be treated as individuals with potential, with strengths in addition to vulnerabilities and with ability to strengthen their health. This was something that the participants meant could improve treatment for mental health problems. Some participants also suggested that alternative treatment options which they meant could facilitate for them to recuperate from the mental health problems were included in the treatment. Importantly, the treatment should not focus solely on the mental health problems but also on the healthy parts that could be strengthened.
“It is important that the care providers look at what our talents are, our powerful points and not just at what is going wrong.” (8 Belgium).
“ … // … to treat an illness is also to...you need to sort of treat the people who are ill … // … strengthening the healthy, because focusing too much on the illness makes you more ill, and then it is easy to be, sort of...it goes in a ring, a downward spiral. And exactly that somewhere in care...exactly that thing about the individual, empowered, not just focusing on the illness but also ensuring that you do things that strengthen and retain function. I think, that is how it works in the somatic world, strengthening and retaining, and that should also exist in mental healthcare, I think. And that should be of political interest, too.” (4 Sweden).
The aim of this study was to describe experiences of mental healthcare among adult Europeans with mental health problems. Focus groups were chosen as a suitable form of data collection allowing the participants to share and discuss their experiences of mental healthcare. Experiences of seeking and trying to find help were related to overcoming personal threshold of accepting the problems and need for care, not knowing where to turn and to get help in time. Awaiting assessment and treatment included feelings of being prioritized or not and feelings of being abandoned. Experiences of treatment disclosed a need for more tailored treatment plans including more pieces than medication treatment. Continuity in mental healthcare and being met with respect and empathy were raised as crucial in care relationships. Possibilities for future improvements were put forward entailing suggestions to increase the societal awareness of mental health problems.
The AAAQ framework refers to availability, accessibility, acceptability and quality in healthcare [ 4 ]. Interestingly, all aspects of this framework came up in different ways in the focus group interviews. This was of particular interest since the study was not designed with AAAQ in mind, it did not guide the focus group interviews and it was not used as an analytical tool during the analysis of the interviews. However, the AAAQ were used as a tool to discuss the findings and mirror the users’ experiences in a framework based in rights and expert opinions. Availability was the least discussed aspect, but several suggestions of mental healthcare facilities that were non-existing were mentioned such as a special first aid emergency unit for persons with common mental health problems, since fast and good quality support was seen as helpful in general. It was considered a way to secure the emotional ground and as a help to get well. Mental health first aid programmes introduced by Kitchner and Jorm [ 25 ] have been evaluated as effective for provision of first aid support for individuals developing mental health problems [ 26 ]. This started as an effort to educate lay persons to recognize and provide a first support for someone with mental health problems prior to a professional care contact being established [ 25 ]. Mental health first aid can be a form of available help for individuals developing mental health problems, but it needs to be aligned with available professional mental healthcare that is easily accessible.
Experiences of accessing mental healthcare were clearly addressed during the focus group interviews. Accessibility refers mainly to the idea that healthcare should be easy to access, affordable and geographically close [ 4 ]. The current results showed that some participants experienced structural barriers in terms of difficulties in accessing mental healthcare but also barriers related to personal economic conditions, which is in accordance with previous research highlighting insufficient accessibility [ 11 ] as obstructing mental healthcare seeking. Geographical closeness of mental healthcare facilities was seen as important by the participants and they gave creative suggestions to improve access. One suggestion was mobile teams that could do home visits on demand. Mobile mental health units have been proven successful in remote areas in Greece by reducing hospitalizations. These units also seem to encourage patients with psychosis to receive treatment thanks to accessibility and non-restrictive care [ 27 ]. A similar French initiative in terms of a mobile mental intensive care unit has been evaluated as functional for individuals with their first episode of psychosis and those being at risk of mental health problems [ 28 ]. Another suggestion was to build smaller units throughout a region instead of large hospitals in urban areas. Thus, moving mental healthcare closer to those in need instead of centralizing might be one option to increase both availability and accessibility.
Accessibility also stipulates that information about healthcare should be provided in an understandable way [ 4 ] but importantly, the participants displayed a need for information about mental healthcare. An interesting angle to this was brought up by the focus groups participants who wanted a broader information on accessible treatment methods. They had experienced that professionals often were devoted to a specific type of care (cognitive behaviour therapy or medication to mention two) while participants wanted a broader palette to choose from. This is particularly interesting in the ongoing development of evidence based healthcare; certain types of treatments receive less attention or are more difficult to investigate which give them a disadvantage on the healthcare market, be it private or public.
Furthermore, the experiences regarding accessibility also contained expressions of uncertainty about where to turn when having overcome the threshold to actually seek mental healthcare. This expressed need for information about how to access mental healthcare and different treatment methods could be understood as a need for better mental health literacy. Mental health literacy has been described as relevant for seeking mental healthcare [ 18 ] and interventions aimed at increasing mental health literacy have shown a favourable effect on seeking mental healthcare [ 19 ]. A suggestion from the focus group participants was that web-based tools could be used to improve access information. Web-based interventions targeting mental health literacy have been proven effective if they contain a structured program, are directed towards a specific population, provide evidence-based content in a pedagogical manner and are interactive [ 29 ].
The current results also demonstrated a wish for more proactive efforts in society aimed at reducing stigma and increasing general awareness of mental health problems in society, which could be interpreted as a plea for better general mental health literacy. Information campaigns in schools were suggested, which is in line with previous research showing that efforts to improve mental health literacy in schools are effective among adolescents. Campaigns both in the community and in schools can improve mental health literacy in general leading to improved readiness to act on mental health problems [ 30 , 31 ]. It could be argued that the current results point towards a clear harmony between experiential knowledge from the perspective of people with lived experiences and scientific evidence, but there is a gap without a firm bridge connecting these knowledge practices. One scope of the European mental health action plan is to establish accessible care that meets peoples’ needs [ 4 ]. Hence, initiatives focusing on improving mental health literacy may be one notion for policymakers to consider. This corresponds to both patients’ experiences and scientific evidence as well as the AAAQ framework which emphasizes the importance of evidence-based knowledge regarding treatment, and service as a quality criterion [ 4 ]. In fact, it can be hypothesized that an improved population mental health literacy in the population will reduce stigma and improve individual mental health literacy. Policymakers, mental healthcare and healthcare professionals are obviously important drivers in such a process.
It was obvious that there were thresholds to overcome before seeking mental healthcare. The first was to acknowledge that one had mental health problems and then to ignore stigmatizing attitudes. These experiences are in accordance with the results in a review by Newman et al. [ 11 ] showing that seeking mental healthcare is a complex effort involving aspects such as overcoming stigma but also prolonged suffering among individuals who did not admit that they needed help. Regarding stigma, reviews show that stigma is associated with mental healthcare seeking [ 13 , 14 , 15 ]. It was evident that stigma prevailed in all countries included in the present study both as social- and self-stigma and perhaps of outmost importance stigmatizing attitudes from healthcare professionals. Because stigma appears to influence mental healthcare seeking [ 12 , 13 , 14 ] and as a result most likely delay initiation of treatment or perhaps even worsen the mental health condition, actions are urgent. Unmet needs for mental healthcare can lead to secondary negative consequences such as reduced capacity to work and sickness absence. Essentially, our study also showed that third parties i.e. next of kin are affected by worries, responsibilities and reduced quality of life. Before Europe can move towards a better mental healthcare, stigmatizing attitudes need to be combatted on all levels in society.
From the experiences shared in the focus groups, it was clear that individualized care was requested containing different parts tailored to each patient’s problems and needs. Being treated as a routine patient was not supportive in the process of combatting the mental health problems according to the participants in the current study. In fact, person-centred care with healthcare professionals working in teams involving patients and their families has been put forward as a future direction of mental healthcare [ 32 ], which is also in line with acceptability in the AAAQ framework underlining placing the patient/person in the centre [ 4 ]. Among the needs that focus group participants mentioned were social treatment including support to become knowledgeable of how society works and being prepared to make contacts with authorities. Participants mentioned the vulnerable situation a person with mental health problems encounters and that this vulnerability can be a major barrier. Mental health problems impact on ability to participate in the labour market [ 2 ] and may even postpone return to work [ 33 ]. It is therefore of vital importance to remember social health when planning treatment for persons with mental health problems. An enhanced collaboration between mental healthcare, social authorities and policymakers is most likely an urgent matter to develop strategies aimed at supporting individuals with mental health problems to improve their social health and to act on exclusion from the labour market and society in general. In this respect, empowerment could play an important role as previous research has demonstrated associations between empowerment and occupational engagement among persons with mental health problems [ 34 ]. It was brought up during the focus group discussions that is was important to be seen as an individual with potential, which can be interpreted as a wish to be empowered. The WHO action plan [ 3 ] has also emphasized that empowerment is one important value to defend among persons with mental health problems. It has also been argued by McAllistar and colleagues [ 35 ] that empowerment serves as an essential outcome measure for patients with long-term health conditions. Because empowerment is associated with both well-being and rehabilitation among persons with mental health problems [ 36 , 37 ] efforts to enhance empowerment is suggested as one crucial part of mental health treatment.
Another aspect of acceptability is the provision of a respectful encounter [ 4 ] which may be related to the results illustrating the importance of continuity and a desire to be met in a respectful empathic way by the healthcare professionals. Continuity has been discussed in many healthcare contexts and both patients and healthcare professionals ask for better continuity [ 38 ]. Again, patients with mental health problems might be more vulnerable to a lack of continuity since trust, confidence and treatment alliances between the healthcare professional and the patient are fundamental ingredients in mental healthcare. Continuity in mental healthcare is a prerequisite in order to build care relationships [ 11 ] and having a trusting care relationship with one or a few healthcare professionals has been considered as good continuity because it means personal stories do not have to be recounted every time [ 39 ]. This is in line with the current results showing that the participants asked for better continuity because they did not want to start all over again when contacting mental healthcare. Moreover, being met in an empathic respectful way was also essential because struggling with mental health problems was experienced as being in a very vulnerable situation, often without the resources to make one’s voice heard. Moreover, negative experiences from former care contacts seemed to nurture a negative expectation spiral leading to delays in taking new contacts when their mental health worsened. This delay may lead to impaired prognosis and poorer opportunity to recuperate and in turn to potential higher costs for society in terms of sick leave and healthcare. Thus, a respectful and empathic encounter was called for which has also been found in previous research with persons who have experienced mental health problems [ 40 ]. It seems important to develop competence in healthcare professionals to manage their own negative attitudes to mental illness and promote supportive behaviour. Therefore, the current study strongly suggests that syllabuses in educations leading to professions within healthcare and social services contain learning activities focusing on patient/person centred care and empathic and respectful communication and encounters.
Quality in healthcare, which refers to evidence or knowledge-based treatment and services [ 4 ], was not explicitly framed in the experiences in the current study, but aspects of quality were embedded in the discussions, for instance in relation to the treatment. In accordance with previous research [ 8 ], the participants raised concerns regarding treatment. They experienced that medication was the first line of treatment prescribed and that over-prescriptions occurred. Although they acknowledged the value of medications, they asked for a treatment entailing different parts and not medication alone. Cuijpers et al. [ 41 ], showed that combining pharmacotherapy with psychotherapy in adults with common mental health problems appears to be more effective than pharmacotherapy alone. Another suggested part of the treatment that could be related to quality was to involve significant others in terms of persons with experiences of mental health problems and next of kin. Persons with their own experiences, so called peers, were regarded as trustworthy because they shared similar experiences as the participants. In fact, peers can help to combat stigma and being part of a peer support network can offer space to focus on other aspects than mental illness [ 42 ]. Concerning involvement of next of kin, it has been suggested that families are invited to be involved in the treatment [ 43 ]. Family involvement has for instance resulted in reduced relapses and hospitalizations for individuals with schizophrenia [ 44 ]. Cohen et al. [ 45 ] found that many individuals with mental health problems wanted their families to be involved but that it could interfere with privacy and integrity and therefore needed to be individually negotiated. The participants in the current study displayed an openness to involve next of kin because thanks to their support they avoided fighting the mental health problems on their own. Furthermore, involving next of kin when receiving information from healthcare professionals was regarded as a quality check because the information was sometimes difficult to remember and understand. In light of the fact that approximately 84 million Europeans have mental health problems [ 2 ], even more are affected as next of kin, which may point towards a shift from patient/person centred to family focused mental healthcare comprising treatment with different parts individually determined. Thoughts about a more multifaceted treatment, which was raised in the focus group discussions, can of course be seen in relation to available resources in the society and within mental healthcare. However, a treatment that does not lead to improved mental health is not profitable neither from an individual perspective nor from a societal perspective. Based on the current study, there is a need for more flexible and individualized treatment for persons with mental health problems. Of course, this must be seen in relation to realistic resources but also in relation to costs of treatment failure. As a suggestion, more intervention studies are needed to evaluate the effect of more flexible or person-centred mental health treatments with individual recuperation and cost effectiveness as outcome measures.
Methodological considerations
A strength of the current study is that the participants represent several European countries and that there is a variation in age, mental health problems and experiences from different forms of mental healthcare. Another strength is that different ways of recruiting were used to ensure a good spread in patient experiences. For example, if participants had only been recruited from psychiatric specialist clinics the experiences would probably have been less varied. Another aspect regarding the recruitment is that all focus group interviews were conducted in urban areas which may indicate that most experiences are related to mental healthcare in larger cities. However, no information about geographical location of the received mental healthcare was collected, which could be regarded as a short-coming and interfere with the applicability of the results. Nevertheless, future studies should preferably address experiences of mental healthcare outside larger cities. As previously described, MentALLY is a pilot project including six countries to test whether the study design and methods were useful in a cross-country approach, which is to be considered as a strength. But a limitation is that only one focus group was performed in each country, except from in Cyprus where two were conducted. As in all qualitative research it is important that the results are not interpreted as possible to generalize in a similar sense as for quantitative studies. The transferability of the findings would have been strengthened with more focus groups in each country not related to mere numbers but rather to a broader patterns of experiences represented in the groups. Comparisons between countries have been avoided.
Moreover, because the participants were recruited through a self-selection process, the findings might not reflect the broader population of people with lived experiences of mental healthcare. To ensure trustworthiness of the results, the analysis was first conducted in each country in the native languages in order to reduce the risk of misinterpretations. The analysis was also supported with verbatim quotations, which could be considered as a strength. As the focus group interviews were held in the native languages, nuances might have been lost in the translation process, an inherent challenge in studies relying on different languages. Regarding trustworthiness, during the analysis, preliminary findings have been presented and discussed with stakeholders from non-governmental network organizations connected to the MentALLY pilot project. Another potential limitation may be that the Dutch data were analysed by the MentALLY team in Belgium but the team in the Netherlands scrutinized the content of the results. It is to be noted that all teams have read the results and contributed with intellectual and critical input. The focus group interviews were conducted adhering to a strict study protocol including an interview guide for conformity between the six MentALLY teams. The interview guide was not pilot tested, which could be regarded as a shortcoming. This and the fact that the analysis followed an analysis template and was driven by what Braun and Clark [ 24 ] refer to as an analytic interest to acquire a more detailed analysis of preconceived aspects could have resulted in aspects of experiences of mental healthcare not being covered in this study. Still, the intention with qualitative research is to gain an in-depth understanding of a phenomenon in this case mental healthcare with focus on access, diagnosis and referral, treatment and collaboration in six European countries from a patient perspective and this intention is regarded as reached.
The present study is limited as it involved a small sample of people with lived experiences from each of the involved countries. However, qualitative studies as the present are not designed for wide generalizability, but to gain a rich and deeper understanding of variations of human experiences [ 46 ], and our results should be appraised accordingly. As this study is a pilot project to explore experiences of mental healthcare across countries and potentially learn from these, detailed analyses linking their experiences to the specific healthcare infrastructures in each country were beyond the scope of the current study. However, based on the current study, we suggest at least three methodological adjustments would be beneficial: First, we would suggest a mixed method approach comparing experiences from patients to a detailed overview of the treatment modalities and capacity in mental health care. Second, we would recommend an immersed qualitative study to explore questions and findings related to stigma further. This includes stigma from health care personnel, which the participants reported across all focus groups. Third, we would aim to also include survey data to approach a wider sense of generalizations and comparisons of key findings between countries. The findings from the current pilot project has been important to illustrate that a cross-country comparison study with a qualitative approach is feasible. The results indicate that there are similar and cross-cutting experiences and questions in mental health care that should be addressed for several European countries.
The following suggestions emerged: Mental healthcare can become more accessible through mobile teams and e-health, a steady contact can facilitate the process of diagnosis and referral, mental health treatment needs to be tailored for each individual containing more parts than medication but with the addition of an empathic respectful encounter. Increased collaboration between stakeholders to act on stigma and improvement of mental health literacy is warranted.
Availability of data and materials
The data collected and analysed during the current study are not publicly available due to research ethical reasons.
Abbreviations
Availability, accessibility, acceptability and quality of healthcare
European union
Organisation for economic co-operation and development
United Nations
World health organization
Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. GBD 2017 DALYs and HALE collaborators. Lancet. 2018. https://doi.org/10.1016/S0140-6736(18)32335-3 .
OECD/EU (2018 Health at a glance: Europe 2018: state of health in the EU cycle, OECD publishing, Paris 2018. https://doi.org/ https://doi.org/10.1787/health_glance_eur-2018-en . Accessed 27 June 2019.
WHO 2015. The European Mental Health Action Plan 2013-2020. 2015; http://www.euro.who.int/en/publications/abstracts/european-mental-health-action-plan-20132020-the . Accessed 27 June 2019.
WHO. Gender, equity and human rights. Availability, accessibility, acceptability, quality. 2016; https://www.who.int/gender-equity-rights/knowledge/aaaq-infographic/en/ . Accessed 27 June 2019.
United Nations. Universal Declaration of Human Rights. https://www.un.org/en/universal-declaration-human-rights/ . [].
Alonso, et al. Population level of unmet need for mental healthcare in Europe. Br J Psychiatry. 2007;190:299–306.
Article Google Scholar
Ten haven M, et al. Are attitudes towards mental health help-seeking associated with service use? results from the european study of epidemiology of mental disorders. Soc Psychiat Epidemiol. 2010. https://doi.org/10.1007/s00127-009-0050-4 .
Cerimele JM, Fortneya JC, Pyne JM, Curran GM. Bipolar disorder in primary care: a qualitative study of clinician and patient experiences with diagnosis and treatment. Fam Pract. 2018. https://doi.org/10.1093/fampra/cmy019 .
Barbato A, Vallarino M, Rapisarda F, Lora A, and Caldas de Almeida JM. Access to mental health care in Europe 2014. https://ec.europa.eu/health/sites/health/files/mental_health/docs/ev_20161006_co02_en.pdf . Accessed 27 June 2019.
Andrade LH, Alonso J, Mneimneh Z, Wells JE, Al-Hamzawi A, Borges G, Bromet E, Bruffaerts R, de Girolamo G, de Graaf R, Florescu S, Gureje O, Hinkov HR, Hu C, Huang Y, Hwang I, Jin R, Karam EG, Kovess-Masfety V, Levinson D, Matschinger H, O'Neill S, Posada-Villa J, Sagar R, Sampson NA, Sasu C, Stein DJ, Takeshima T, Viana MC, Xavier M, Kessler RC. Barriers to mental health treatment: results from the WHO world mental health surveys. Psychol Med. 2014;44:1303–17.
Article CAS Google Scholar
Newman D. O’Reilly, lee S H, Kennedy C. mental health service users’ experiences of mental healthcare: an integrative literature review. J Psychiatr Ment Health Nurs. 2015;22:171–82.
Packness A, Halling A, Simonsen E, Waldorff FB, Hastrup LH. Are perceived barriers to accessing mental healthcare associated with socioeconomic position among individuals with symptoms of depression? Questionnaire-results from the Lolland-Falster health study, a rural Danish population study. BMJ Open. 2019. https://doi.org/10.1136/bmjopen-2018-023844 .
Clement S, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015. https://doi.org/10.1017/S0033291714000129 .
Schnyder N, Panczak R, Groth N, Schultze-Lutter F. Association between mental health-related stigma and active help-seeking: systematic review and meta-analysis. Br J Psychiatry. 2017. https://doi.org/10.1192/bjp.bp.116.189464 .
Ali K, Farrer L, Fassnacht DB, Gulliver A, Bauer S, Griffiths KM. Perceived barriers and facilitators towards help-seeking for eating disorders: a systematic review. Int J Eat Disord. 2017;50(1):9–21. https://doi.org/10.1002/eat.22598 Epub 2016 Aug 16.
Article PubMed Google Scholar
Rüsch N, Angermeyer MC, Corrigan PW. Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. Eur Psychiatry. 2005;20(8):529–39.
Coppens E, et al. Public attitudes toward depression and help-seeking in four European countries baseline survey prior to the OSPI-Europe intervention. J Affect Disord. 2013;150:320–9.
Schomerus G, Angermeyer MC. Stigma and its impact on help-seeking for mental disorders: what do we know? Epidemiol Psichiatr Soc. 2008;17:31–7.
Xu Z, Huang F, Kösters M, Staiger T, Becker T, Thornicroft G, Rüsch N. Effectiveness of interventions to promote help-seeking for mental health problems: systematic review and metaanalysis. Psychol Med 2018. https://doi.org/ https://doi.org/10.1017/S0033291718001265 . Accessed 27 June 2019.
Gilburt H, Rose D, Slade M. The importance of relationships in mental health care: a qualitative study of service users' experiences of psychiatric hospital admission in the UK. BMC Health Serv Res. 2008;8:92. https://doi.org/10.1186/1472-6963-8-92 .
Article PubMed PubMed Central Google Scholar
Sandhu S, Bjerre NV, Dauvrin M, Dias S, Gaddini A, Greacen T, Ioannidis E, Kluge U, Jensen NK, Lamkaddem M, Puigpinós i Riera R, Kósa Z, Wihlman U, Stankunas M, Straßmayr C, Wahlbeck K, Welbel M, Priebe S. Experiences with treating immigrants: a qualitative study in mental health services across 16 European countries. Soc Psychiatry Psychiatr Epidemiol. 2013;48(1):105–16. https://doi.org/10.1007/s00127-012-0528-3 Epub 2012 Jun 20.
Brislin RW. Back-translation for cross-cultural research. J Cross-Cult Psychol. 1970;1:185–216.
Krueger R, Casey A-M, Focus groups. A practical guide for applied research. Thousand Oaks: SAGE Publications Inc.; 2009.
Google Scholar
Braun V, Clark V. Using thematic analysis in psychology. Qual Res Psychol. 2008;3(2):77–101.
Kitchener BA, Jorm AF. Mental health first aid: an international programme for early intervention. Early Interv Psychiatry. 2008;2:55–61.
Morgan AJ, Ross A, Reavley NJ. Systematic review and meta-analysis of mental health first aid training: effects on knowledge, stigma, and helping behaviour. PLoS One. 2018. https://doi.org/10.1371/journal.pone.0197102 .
Peritogiannis V, Manthopoulou T, Gogou A, Mavreas V. Mental healthcare delivery in rural Greece: a 10-year account of a Mobile mental health unit. J Neurosci Rural Pract. 2017. https://doi.org/10.4103/jnrp.jnrp_142_17 .
Lecardeur L, Meunier-Cussac S, Dollfus S. Mobile intensive care unit: a case management team dedicated to early psychosis in France. Early Interv Psychiatry. 2018. https://doi.org/10.1111/eip.12674 .
Brijnath B, Protheroe J, Mahtani KR, Antoniades J. Do web-based mental health literacy interventions improve the mental health literacy of adult consumers? results from a systematic review. J Med Internet Res. 2016. https://doi.org/10.2196/jmir.5463 .
Skre I, Friborg O, Breivik C, Johnsen LI, Arnesen Y, Wang CE. A school intervention for mental health literacy in adolescents: effects of a non-randomized cluster controlled trial. BMC Public Health. 2013. https://doi.org/10.1186/1471-2458-13-873 .
Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. 2012. https://doi.org/10.1037/a0025957 .
Gask L, Coventry P. Person-centred mental health care: the challenge of implementation. Epidemiol Psychiatr Sci. 2012. https://doi.org/10.1017/S2045796012000078 .
Hensing G, Bertilsson M, Ahlborg G Jr, Waern M, Vaez M. Self-assessed mental health problems and work capacity as determinants of return to work: a prospective general population-based study of individuals with all-cause sickness absence. BMC Psychiatry. 2013. https://doi.org/10.1186/1471-244X-13-259 .
Hultqvist J, Eklund M, Leufstadius C. Empowerment and occupational engagement among people with psychiatric disabilities. Scand J Occup Ther. 2015;22(1):54–61. https://doi.org/10.3109/11038128.2014.934916 .
McAllister M, Dunn G, Payne K, Davies L, Todd C. Patient empowerment: the need to consider it as a measurable patient-reported outcome for chronic conditions. BMC Health Serv Res. 2012;12:157 http://www.biomedcentral.com/1472-6963/12/157 .
Johanson S, Bejerholm U. The role of empowerment and quality of life in depression severity among unemployed people with affective disorders receiving mental healthcare. Disabil Rehabil. 2017;39(18):1807–13. https://doi.org/10.1080/09638288.2016.1211758 .
Grealish A, Tai S, Hunter A, Emsley R, Murrells T, Morrison AP. Does empowerment mediate the effects of psychological factors on mental health, well-being, and recovery in young people? Psychol Psychother. 2017;90(3):314–35. https://doi.org/10.1111/papt.12111 .
Parker G, Corden A, Heaton J. Experiences of and influences on continuity of care for service users and carers: synthesis of evidence from a research programme. Health Soc Care Community. 2011. https://doi.org/10.1111/j.1365-2524.2011.01001.x .
Biringer E, Hartveit M, Sundfør B, Ruud T, Borg M. Continuity of care as experienced by mental health service users - a qualitative study. BMC Health Serv Res. 2017. https://doi.org/10.1186/s12913-017-2719-9 .
Porter S, Lexén A, Johanson S, Bejerholm U. Critical factors for the return-to-work process among people with affective disorders: voices from two vocational approaches. Work. 2018;60:221–34. https://doi.org/10.3233/WOR-182737 .
Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF 3rd. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry. 2013. https://doi.org/10.1002/wps.20038 .
Huggett C, Birtel MD, Awenat YF, Fleming P, Wilkes S, Williams S, Haddock G. A qualitative study: experiences of stigma by people with mental health problems. Psychol Psychother. 2018. https://doi.org/10.1111/papt.12167 .
Doody O, Butler MP, Lyons R, Newman D. Families' experiences of involvement in care planning in mental health services: an integrative literature review. J Psychiatr Ment Health Nurs. 2017. https://doi.org/10.1111/jpm.12369 .
Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database Syst Rev. 2010. https://doi.org/10.1002/14651858.CD000088.pub2 .
Cohen AN, Drapalski AL, Glynn SM, Medoff D, Fang LJ, Dixon LB. Preferences for family involvement in care among consumers with serious mental illness. Psychiatr Serv. 2013. https://doi.org/10.1176/appi.ps.201200176 .
Polit DF, Beck CT. Generalization in quantitative and qualitative research: myths and strategies. Int J Nurs Stud. 2010;47(11):1451–8. https://doi.org/10.1016/j.ijnurstu.2010.06.004 Epub 2010 Jul.
Download references
Acknowledgements
All participants are acknowledged for contributing with their time and lived experiences to enable the study.
The study was funded by the European Parliament (Pilot Project Grant PP-2-2016, Topic: PP-2-2-2016). The funding body had no role in or influence over the study design, the execution of the study, the data analysis or the writing of the study. Open access funding provided by Malmö University.
Author information
Authors and affiliations.
Department of Care Science, Faculty of Health and Society, Malmö University, Jan Waldenströms gata 25 – F416, SE-205 06, Malmö, Sweden
Malin Axelsson
Department of Public Health and Community Medicine, Institute of Medicine, The Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden
Viktor Schønning & Gunnel Hensing
Department of Health Promotion, Division of Mental and Physical Health, Norwegian Institute of Public Health, Bergen, Norway
Viktor Schønning & Simon Øverland
Amsterdam UMC, Department of Psychiatry (AMC) and Institute for Advanced Studies, University of Amsterdam, Amsterdam, the Netherlands
Claudi Bockting
Department of Experimental Clinical and Health Psychology, Faculty of Psychology and Educational Sciences, Ghent University, Ghent, Belgium
Ann Buysse, Alexis Dewaele, Dewi Hannon & Joke Vandamme
Department of Psychoanalysis and Clinical Consulting, Faculty of Psychology and Educational Sciences, Ghent University, Ghent, Belgium
Mattias Desmet & Reitske Meganck
Department of Psychology, University of Crete, Rethymno, Crete, Greece
Theodoros Giovazolias, Spyridoula Ntani & Sofia Triliva
Aristotle University of Thessaloniki, Thessaloniki, Greece
Konstantinos Kafetsios
Department of Educational Studies, Faculty of Psychology and Educational Sciences, Ghent University, Ghent, Belgium
Kris Rutten & Laura Van Beveren
Division of Mental and Physical Health, Norwegian Institute of Public Health & Department of Psychosocial Science, University of Bergen, Bergen, Norway
Simon Øverland
You can also search for this author in PubMed Google Scholar
Contributions
The MentALLY teams in each country (Belgium: AB, MD, AD, DH, RM, KR, LVB, JV; Greece: TG, KK, SN, ST; Netherlands: CB; Norway: VS, SØ; Sweden: MA, GH) applied for ethical approvals, invited participants, organized the focus group interviews and collected the data. Initial analyses of the transcripts in the native languages were conducted by the MentALLY teams in each country separately (Belgium: AB, MD, AD, DH, RM, KR, LVB, JV; Greece: TG, KK, SN, ST; Netherlands: CB; Norway: VS, SØ; Sweden: MA, GH), except for the data from the Netherlands and Cyprus that were analysed by the team in Belgium (AB, MD, AD, DH, RM, KR, LVB, JV) and Greece (TG, KK, SN, ST) respectively. The MentALLY themes in Norway and Sweden (VS, SØ, MA, GH,) then created a common result covering all countries and drafted the manuscript. All MentALLY teams have contributed by critically revising the manuscript for important intellectual content (MA, VS, CB, AB, MD, AD, TG, DH, KK, RM, SN, KR, ST, LVB, JV, SØ, GH). All authors (MA, VS, CB, AB, MD, AD, TG, DH, KK, RM, SN, KR, ST, LVB, JV, SØ, GH) have read and approved the final manuscript.
Corresponding author
Correspondence to Malin Axelsson .
Ethics declarations
Ethics approval and consent to participate.
Ethical approvals were granted from the Review Boards at Ghent University in Belgium, the University of Crete in Greece (Επι.Δ.Ε. i.e. Ethical Committee, 6/2018/16-05-2018) and the Regional Ethical Review board in Gothenburg in Sweden (474–18). In Cyprus, the Mental Health Services of the Ministry of Health gave permission to conduct the study (4.2.09.37/7). In the Netherlands, an application was sent to the Medical Ethical Committee of Academic Medical Hospital of the University of Amsterdam and an exemption was given as all subjects were healthy and non-invasive procedures were used (no number was given due to the exemption). The Regional Committees for Medical and Health Research Ethics in Norway found the project outside the realm of medical ethics assessment. Therefore, an assessment and approval from a data protection officer at the Norwegian Institute of Public Health was collected. Following written and verbal information about the study, all participants signed an informed consent before the focus group interviews started.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Axelsson, M., Schønning, V., Bockting, C. et al. Lived experiences: a focus group pilot study within the MentALLY project of mental healthcare among European users. BMC Health Serv Res 20 , 605 (2020). https://doi.org/10.1186/s12913-020-05454-5
Download citation
Received : 18 September 2019
Accepted : 22 June 2020
Published : 01 July 2020
DOI : https://doi.org/10.1186/s12913-020-05454-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Collaboration
- Lived experiences
- Mental health literacy
- Service-users
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

A Qualitative Study Exploring Access to Mental Health and Substance Use Support among Individuals Experiencing Homelessness during COVID-19
Emma a. adams.
1 Population Health Sciences Institute, Newcastle University, Newcastle upon Tyne NE3 4ES, UK; [email protected] (C.S.); [email protected] (C.M.); [email protected] (A.O.); [email protected] (E.K.); [email protected] (S.E.R.)
Jeff Parker
2 HeathNow, Crisis, City House 1 City Road, Newcastle upon Tyne NE1 2AF, UK
3 Pathway, 4th Floor East, 250 Euston Road, London NW1 2PG, UK
4 Crisis Pie Team, 66 Commercial Street, London E1 6LT, UK
Tony Jablonski
Joanne kennedy.
5 Expert by Experience Network, Fulfilling Lives Newcastle Gateshead, Gateshead NE8 4DY, UK
Fiona Tasker
Desmond hunter, katy denham.
6 Newcastle University Medical School, Newcastle University, Newcastle upon Tyne NE2 4HH, UK; [email protected]
Claire Smiles
Cassey muir, amy o’donnell, emily widnall.
7 Population Health Sciences, Bristol Medical School, University of Bristol, Bristol BS8 2PS, UK; [email protected]
Kate Dotsikas
8 Division of Psychiatry, UCL, London W1T 7BN, UK; [email protected]
Eileen Kaner
Sheena e. ramsay, associated data.
Summaries of the data presented in the study are available on request from the corresponding author. The data are not publicly available due to containing potentially identifiable information about participants.
People experiencing homelessness have higher rates of mental ill-health and substance use and lower access to health services compared to the general population. The COVID-19 pandemic led to changes in service delivery across health and social care services, with many adopting virtual or telephone support for service users. This paper explores the experiences of access to community-based mental health and substance use support for people experiencing homelessness during the COVID-19 pandemic. Qualitative telephone interviews were conducted with 10 women and 16 men (ages 25 to 71) who self-identified as experiencing homelessness in North East England between February and May 2021. With five individuals with lived experience, results were analysed using inductive reflexive thematic analysis. Reactive changes to support provision often led to inadvertent exclusion. Barriers to access included: physical locations, repetition of recovery stories, individual readiness, and limited availability. Participants suggested creating services reflective of need and opportunities for choice and empowerment. Community mental health and substance use support for people experiencing homelessness should ensure the support is personalised, responsive to need, inclusive, and trauma-informed. The findings of this research have important implications for mental health and substance use policy and practice for individuals who experience homelessness during a public health crisis.
1. Introduction
The COVID-19 pandemic has amplified health inequalities and adversity among people who were already facing social and material disadvantage [ 1 , 2 , 3 ]. Indeed, historical evidence indicates that some groups are more susceptible to harm than others during pandemics and comparable crises [ 3 , 4 , 5 ], for example, individuals experiencing homelessness. However, fear of negative impacts from COVID-19 extend beyond having the infection to impacts on mental health (such as anxiety, isolation, and becoming mentally unwell, access to support) [ 6 ]. Early longitudinal evidence suggests that in the general population the prevalence of anxiety, depression, and other psychological impacts remained relatively unchanged [ 7 , 8 ]. For people experiencing homelessness, there is the potential that lockdowns and social distancing measures could negatively impact their mental health due to existing fears around forced incarceration and hospitalization [ 9 ]. The longer-term impacts to mental health from COVID-19 for this population remain unknown [ 10 ]. This is a particular concern since homelessness often co-exists with mental ill-health, substance use, and offending [ 11 ]. This co-occurrence of vulnerabilities is broadly defined as multiple complex needs, multiple exclusion homelessness, and severe and multiple disadvantage [ 12 , 13 , 14 ]. This co-occurrence and their interactions create a mutually reinforcing cycle, leading to further marginalisation and making it harder to access support [ 11 , 15 , 16 , 17 , 18 ].
People experiencing homelessness face disproportionately high rates of substance use and mental ill-health compared to the general population [ 11 , 19 , 20 ], yet have some of the lowest rates of engagement when it comes to accessing support [ 21 , 22 , 23 ]. Although provision is not always integrated, support for mental health and substance use crosses statutory health, social care, and voluntary sectors [ 24 ]. Examples of support may include, but is not limited to: specialist mental health services, assertive outreach, peer support, housing first, street support, assessment, trauma-informed care, psychologically informed environments, psychotherapy, street, support, and detox services [ 24 , 25 , 26 , 27 ]. Despite the variety of services, a survey found that essential mental health and addictions services are often unavailable in most areas and access is becoming increasingly difficult [ 25 ]. Epidemiological data has shown that people with co-occurring mental health and substance use (dual diagnosis) are less likely to access and use treatment [ 28 , 29 , 30 ]. It is likely that these rates would be even lower for homeless people, whose lack of a stable or permanent address can be a barrier to appointment-based care, where letters are sent to addresses or service provision is based on geographical regions [ 31 ].
Evidence demonstrating the disproportionate health and social care need and barriers to access people experiencing homelessness face is abundant [ 11 , 32 , 33 , 34 , 35 ]. An integrative literature review including qualitative and quantitative studies exploring access to treatment among individuals with dual diagnosis found two categories of barriers: personal characteristics and structural factors [ 36 ]. Personal characteristics barriers encompassed personal vulnerabilities (such as diagnosis-related symptoms associated with co-occurring substance use and mental ill health) and personal beliefs (such as lack of institutional trust, cultural beliefs, stigma) [ 37 , 38 , 39 , 40 ]. Whereas structural factors focus on availability, lack of appropriate diagnosis, and structural barriers to service provision (such as long waiting lists and gender-specific treatment options) [ 32 , 36 , 41 , 42 ]. Prior negative care experiences and lack of knowledge about the benefits of accessing health and social care support were continued barriers even after receiving housing accommodation [ 32 ]. However, most studies around barriers to accessing support for mental health and substance use by people experiencing homelessness have been quantitative. There remains a need for qualitative studies to better understand the experiences of homeless people on accessing support for mental ill-health and substance use.
Measures introduced to limit the spread of COVID-19 from March 2020 onwards led to substantial changes to daily life in the UK and elsewhere. Measures included social distancing, mandating people to ‘stay home’, and the closure of non-essential businesses and many face-to-face services. This meant many health and social care providers who traditionally offered support in-person transitioned to reduced capacity [ 43 ], socially distanced and remote support (such as telephone, Zoom, Skype, or Microsoft Teams) [ 43 , 44 , 45 , 46 ], and in some cases stopping services for periods of time [ 46 ]. The creative responses to offer support remotely demonstrated the ability of organisations to recover and adapt to the dynamic situation; effective adaption is essential for resilience with mental health and substance use services [ 47 ]. In cases where service provision was stopped, the organisation lacked resiliency and was ill-prepared/equipped for the changing circumstances.
For individuals experiencing homelessness, the initiatives introduced during COVID-19 focused on preventing disease transmission and providing temporary accommodation to house individuals sleeping rough [ 48 ]. Low substance use treatment rates coupled with high drug related deaths during COVID-19 suggests initiatives did not address the substance use needs of people experiencing homelessness [ 49 ]. This suggests that the health system was likely ill-prepared/equipped to meet these needs of people experiencing homelessness during the pandemic. Recent COVID-19 studies have highlighted a gap in understanding the depth of experiences for those who were dealing with mental health and substance use and particularly among people experiencing homelessness [ 45 , 46 , 49 , 50 ].
To better understand access to community-based mental health and substance use services, we conducted a qualitative study with people who experienced homelessness in North East England. We explored their experiences during the COVID-19 pandemic with accessing support, perceptions of barriers to access, and on what they might change to make support more accessible. Findings from this study will provide valuable information for building a more resilient healthcare system, which are better able to respond to current and future crises [ 47 ].

2. Materials and Methods
This qualitative study was informed by participatory action research approaches to ensure the study, findings, and recommendations were grounded in the experiences of those who are directly affected by the topic of the research [ 51 , 52 , 53 , 54 ]. Eligibility criteria were lived experience of homelessness, substance use, and/or mental ill-health. Initial interest was by male Experts by Experience, so the lead researcher made a specific request for females. After individuals expressed interest, E.A.A met with each person individually to clarify any concerns, explain expectations, and confirm participation. Experts by Experience then became part of the core project team and assisted in the design of the study, understanding of interviews, and sharing of findings. Approaches were based on best practices for community-based research with vulnerable populations [ 54 ]. To build rapport and reduce power imbalances between the lead researcher (E.A.A) and the Experts by Experience, Experts by Experience suggested the days and location (either Zoom or in-person) for meetings, refreshments (e.g., tea/coffee, cookies, and health snacks) were offered at all in-person meetings, and feedback was encouraged and listened to [ 55 ]. Using a cross-sectional design, semi-structured interviews were conducted over the phone between February and May 2021 during the COVID-19 pandemic.
2.1. Recruitment, Procedures, and Data Collection
Recruitment used purposive sampling through gatekeepers in housing and charity sectors alongside ‘Experts by Experience’ networks, followed by snowballing among participants. Individuals self-identified as experiencing homelessness during the COVID-19 pandemic, over 18 years of age, and wanting to access community mental health and addiction support within the region. Individuals did not need to have engaged with the support over the last year but did need to express an interest in seeking help. A broad definition of homelessness was used, including different types of homelessness, (e.g., rough sleeping, those in temporary accommodations such as hostels, those staying with friends or sofa surfing, and those who approach the local authority for housing) [ 56 ]. Given the frequently changing contexts and complex health and social care needs experienced by individuals within this population, efforts were made to accommodate re-scheduling interviews, calling different telephone numbers, and providing individuals with multiple opportunities to participate if they were initially unresponsive [ 57 ]. Thirty-one individuals expressed interest and a total of 26 participated; 2 could not be reached following multiple attempts to contact via hostels or referrer; 1 passed away before participating; 1 withdrew prior to data collection, and 1 moved on from their current hostel and did not have follow-up contact details. Participant recruitment continued until data sufficiency had been reached, no new themes, and anyone who had expressed interest previously was given an opportunity to participate.
Prior to participating, individuals were given an information sheet, assured anonymity and confidentiality, the option to withdraw at any time, an opportunity to ask any questions, and provided verbal or written consent. E.A.A conducted individual, telephone semi-structured interviews using a topic guide that covered the following areas: types of community-based mental health and addiction and interest in accessing them; experiences of access during the pandemic; and suggestions for improvement. The topic guide was developed with input from Experts by Experience and those who support people experiencing homelessness. Interviews ranged from 20 min in length to 80 min depending on what an individual was willing to share or their personal experiences. Individuals received a £30 voucher for a grocery store as a thank you for participating.
Ethics approval was granted by the Faculty of Medical Sciences Research Ethics Committee, part of Newcastle University’s Research Ethics Committee (ref: 2034/6698/2020.)
2.2. Analysis
Interviews were digitally recorded, transcribed, anonymised, and checked for accuracy. Analysis was informed by Braun and Clarke’s inductive reflexive thematic analysis [ 58 ]. The recursive process and nonlinear stages enabled shared meaning in the data focused on a central concept to be conceptualised as themes early in the analysis [ 59 ]. Led by the lead researcher (E.A.A), the analysis applied participatory approaches to work with five ‘Experts by Experience’ (J.P., T.J., J.K., F.T., D.H.) through a series of 10 Zoom and in-person workshops. We began by reading, listening, and re-reading transcripts followed by initial coding development for each transcript (all were done by E.A.A, and a portion were done by the five ‘Experts by Experience’). Preliminary themes were developed collectively based on initial coding and reviewed to determine patterns of shared meaning across transcripts. Naming and defining of themes and subthemes were refined with ‘Experts by Experience’ and discussed with all co-authors. The participatory approaches enhanced the quality of the research, as the ongoing reflective engagement led to richer and more nuanced understanding of the data and construction of themes [ 60 ]. All participants were given pseudonyms to maintain anonymity.
Sixteen men and 10 women participated in the study, with ages ranging from 25 to 71 years (mean 40.7, standard deviation 11.4). All individuals self-identified as White British. No further demographic information was collected. Individuals reported a combination of mental health challenges (anxiety, depression, and other diagnosed conditions) and alcohol and drug use (cocaine, heroin, synthetic cannabinoids (spice), and marijuana) and diverse and multiple experiences of homelessness (ranging from sleeping on streets (rough sleeping) and staying with friends (couch surfing) to hostels and supported accommodation) during the COVID-19 pandemic. Table 1 presents an overview of the three main themes developed.
Themes and subthemes related to access to community mental health and substance use support for people experiencing homelessness during the COVID-19 pandemic.
3.1. Inadvertent Exclusion
Participants reported that service provision had drastically changed over the course of the COVID-19 pandemic. Changes that were often made reactively to create support, led to inherent forms of exclusion.
3.1.1. Mental Health Is Not 9-to-5
One of the most evident ways people felt overlooked was the fact that many providers only offered support between normal business hours; yet, people frequently felt that late at night was when they most needed support as ‘no one is awake’ and that was often when they hit ‘rock bottom’. Although this was not necessarily unique to COVID-19, individuals explained they wanted to be able to access some type of support during non-business hours; suggesting either a telephone line or texting service to ensure ‘somebody is there’ so you were never alone.
“Aye, it should be open when you are feeling the worst. Sometimes when you are feeling your worst it is very late. Ya know, it’s dark, and it’s that’s when you feel your most loneliness. Like after 10 o’clock at night ya know, when there is no one around. People are in bed”. — Keith, 45
“I want support 24/7”. — Lily, 33
Individuals reflected on a reduction in services during the pandemic and discussed how support they could normally access out-of-hours had been cut.
“There’s an organisation [name removed] who I’ve sought help from in the past, but at this moment in time, they’re only open Monday to Friday, 10:00 a.m. to 4:00 p.m. If you’re having any episodes or if you need support outside of those hours, you can’t turn to them, where you used to be able to. They used to be open all sorts of hours and they even offered an emergency line for the weekends, but that’s all cut off now”. — Mike, 33
3.1.2. Digital Exclusion
When speaking about experiences accessing services, individuals reflected on the pre-pandemic in-person support with general positivity although recognising it was not without its faults. Barriers included balancing the costs of travelling to appointments with having a meal or not feeling confident enough to meet people face-to-face. With social distancing restrictions coming into effect across England in response to COVID-19, there was a rapid transition to remote care provision to prevent services from closing their doors. Although this approach to care suited some people, others expressed frustration around feeling excluded. Exclusion took multiple forms including lack of device access and lack of digital literacy. Individuals expressed frustration around unspoken expectations that were required to access support.
“He rang and went, “Right, if you join this Zoom link.” Obviously, I’m sat there as if to say, “Well what am I supposed to do? I haven’t got credit, I can’t ring up to say I can’t join the Zoom link.” Obviously, after I’d missed the Zoom link meeting, he rang me on the phone and went, “Why haven’t you joined?” I went, “Because I don’t have internet, I don’t have a laptop, I don’t have credit on my phone to get internet to do it.” He went, “Oh right, well we’ll do it over the phone now then.” It’s like, “Well why didn’t you ask about it?””. — Danny, 29
“They expect you all to have these phones that do everything and we haven’t”. — Sam, 37
Across the interviews, conversations around not having access to Wi-Fi, laptops, or smart phones were plentiful. Where organisations provided devices for people experiencing homelessness, they spoke about issues of theft and the need for training to address gaps in digital literacy.
“I dread to think how many phones I’ve had and they’ve been stolen or whatever. You couldn’t leave your phone lying anywhere. Everything goes. If you had a spit, it would be gone before it hit the floor”. — Hannah, 43
“Computer illiterate. I’ve been on courses and that for it, but I get no further forward two weeks later from the first minute. I can’t log any technology in my head”. — Alan, 54
3.1.3. Awareness of What Support Is out There
Knowledge of available care and support and who provides it was one of the most powerful barriers or facilitators to accessing support. Moreover, public spaces like libraries and coffee shops are typical locations to access information, however, COVID-19 lockdown restrictions had presented new barriers to accessing information from these locations. Participants suggested that information about support needed to be shared widely and not solely online, something that was heavily relied on during COVID-19.
“Once you’re in that vicious circle, it can be very hard to access anything, you don’t know who to go to or who to speak to or who to contact, it’s just extremely difficult to know what to do”. — Ian, 53
“Well, I think somebody coming out and actually talking to the girls, somebody being informed that there are services out there. The key is getting out into the hostels and knocking on the doors and saying, “This is what we’re offering, and would you like to be involved in it?” You’re not aware". — Hannah, 43
For those who accessed support, experiences depicted the variety of ways they found out about support (e.g., online, football match adverts, hostel workers, friends, bulletin boards, providers) and the fact that sometimes they were not looking for support when they found information about available support.
“I just googled. Yeah it was um, I was googling how to kill myself and it came up with that. And I ended up using it. I’ve been using it for months”. — Andrea, 25
3.2. Barriers to Recovery
People shared negative experiences and barriers accessing support before and during COVID-19. These experiences shaped their attitudes towards accessing future support.
3.2.1. Lack of Space for Recovery
With a push to house everyone sleeping rough during the pandemic, individuals reflected on their experiences of being provided with accommodation. Group accommodation was often provided to both current and ex-substance users. This group offering was often a negative experience and sometimes resulted in past users being targeted by drug dealers and facing behaviours they had moved on from. Participants also expressed frustration around experiencing this when accessing support in person.
“They knew there was Spice use in this hostel. They shouldn’t have put me there. I was clean for seven months”. — Sam, 37
“[treatment location] It’s not a nice place to go to when you’re trying to recover from drugs. They’re trying to sell you things outside, and inside the building to be honest. There’s always somebody trying to push something onto you. When you’re trying to recover yourself, it’s hard when people are putting things in your face”. — Hannah, 43
“I don’t like going, but you got-you have to. Because, I’ve got away from it all, and yet you’re walking in and seeing people who are still using and they try and get you to buy some and things like that. [contrast to pandemic] While the pandemic is on, it’s all been changed to differently. You can’t go, they keep away and people get in touch with you over the phone. That would make it alright if it was always like that. That way you don’t have to bump into them”. — Alan, 54
These negative environments created further social isolation as individuals would try to isolate themselves from others to maintain their sobriety.
“When I got put into shared accommodation it was quite hard because every one of the neighbours was on hard drugs like heroin and crack and stuff like that. Obviously, I’m no longer using. It’s like they try to pull you in, so I had to pretty much isolate myself when I was in there”. — Danny, 29
During COVID-19, support offered remotely often took place while individuals were in their shared accommodation. Individuals highlighted the importance of space and place during recovery and shared that their ideal location would be reflective of their current recovery stage, have ample space, and be supportive and welcoming.
3.2.2. Disjointed Care and Repetition of Recovery Stories
Many people shared disconnected care experiences and discontinuity of care due to staff turnover, perhaps exacerbated by COVID-19 constraints. The constant need to repeat their stories caused many people to relive experiences.
“I know. I am sick of getting new workers and having to explain again. Explaining me story to workers. You should get one worker. I’m sick. … I have done this for 17 years and I can’t do it anymore. I can’t”. — Clare, 32
You know you get tired of times of saying—you just want to live a normal life again, you know. You explain your situation to one person, then you’ve, I’ve got to do it over and over and over again. It just seems like it’s never ending". — Keith, 45
One of the perceived solutions was creating an integrated system with increased collaboration and co-working across organisations. A few people shared experiences of how the pandemic led to providers working collaboratively to make sure people did not slip through the cracks.
“Before lockdown, it was a bit of a jigsaw puzzle, everything was here, there and everywhere. Nobody was really communicating well enough together. But since lockdown, people have really honed in on their skills and they’ve had to learn to cope with different ways of doing things. I’ve got literally an appointment almost every day now, and I’ve got such a good routine going on, it’s amazing". — Emily, 39
3.2.3. Not Ready for Recovery
Feeling ready to access support was perceived as extremely personal. Many people explained they were not ready to get help for their substance use or mental health as they had other priorities during COVID-19, including getting housed, a job, or their children back if they had been taken into state care. Individuals could not always articulate what could help them become ‘ready’.
“I don’t know if the support is there but I’m not ready to ask for help”. — Clare, 32
“When you’re feeling down like that and you’re wanting to go with stuff…”. — Danny, 29
Many felt they should be given adequate space and time and not be pressured into seeking help as it may lead to disengagement.
3.2.4. Prioritization When Resources Are Scarce
A common thread across interviews was that people often met ‘brick walls’ when trying to access support. This felt even harder during the pandemic where services appeared fewer and farther between. Examples included waiting lists, requirements around referral pathways, not meeting eligibility criteria around ‘being sick enough,’ or being passed around between services.
“I rung the Crisis team a lot. I was on the phone to them nine times in one night before they actually came out. […later explains] the Crisis team is pretty much the wrong name for them I would say”. — Mike, 33
A shared experience across interviews was the fact that accessing support was often challenging.
“If you’re determined to climb to the top of that mountain, you’re going to get there. But it’s really, really difficult. So, you just have to shout and scream and try as hard as you can”. — Emily, 39
Experiences of being ignored or frequently passed from one place to another led to people feeling reluctant to access support.
“They say “ah we can do this, we can do that” but it never seems to come off, or the supports not really that good or it’s bad for you, it’s not good for you. Most of them just leave you to do what you are doing. … Promises, false promises and it doesn’t happen”. — Tommy, 38
3.3. Building a System Responsive to Needs
Across the interviews, participants highlighted that before and during COVID-19, support was frequently offered using a structured approach that was disempowering for people experiencing homelessness.
3.3.1. Disconnect between Service Provision and Needs
Amplified by frustration around the lack of support during COVID-19, people often felt services did not understand their needs. This meant not recognising or understanding the complex interaction of mental health and substance use. One suggestion was to include peer-led or peer supported approaches within services. This was a perceived opportunity to leverage lived experience knowledge to design services to reflect the complex needs faced by people experiencing homelessness.
“Because they say, “Oh, you have to reduce your drinking,” but I can’t. I’ve got deep psychological issues, I can’t- So, I need the therapy in line with the reduction of alcohol. I need them in conjunction, that’s my biggest hurdle at the minute. It’s a vicious cycle, isn’t it?”. — Emily, 39
“…it would have helped because we’d all be in the same boat anyway, so we could help each other with our own experiences. [later goes on to say] Yes, it would be somebody on your own level that has actually been through alcoholism or drug use”. — Glen, 62
Individuals reflected on how the complexity of co-occurring mental health and substance use meant there was uncertainty over when they would need help with mental health or substance use. This was a particular concern during COVID-19 where lives felt dominated by uncertainty around when things would return to ‘normal’. The best experiences of access were when individuals felt that providers recognised this uncertainty and supported individuals with constant reviews and check-ins.
“Just because I’m feeling good this month, it doesn’t mean that in a month or two’s time, I am still feeling great. There are constant reviews and chats and contacts and stuff, which is great”. — Liam, 26
3.3.2. Choice and an Active Voice
During COVID-19 people felt they lost control of their circumstances and were frustrated with being offered limited and no flexibility in options. One of the easiest ways to create a more positive experience of access was through giving individuals choice in their care. In the context of COVID-19, choice was offered by providing support through a variety of mediums; for example, face-to-face, online, in groups, or one-to-one.
“Everyone’s different. So, a lot of people loved the Zoom, a lot of people like going to different meetings, a lot of people need a lot more support than other people. So, it’s about tailoring it or catering for the individual isn’t it, I suppose”. — Andy, 46
One of the key messages shared during interviews was that individuals need to be asked what they want, to be involved in decision making, and to feel empowered to be active participants in their care.
“Like when people are saying, like they don’t want to be here, or anything in the mental health bag—don’t just hoy a prescription in their face. Like sit down with them and look at what they need". — Carlie, 25
“Ask the person, ask the individual how they want to be helped, that’s the way forward for them, what help do they need”. — Darren, 36
4. Discussion
The urgent response to the global COVID-19 pandemic has led to new ways of working, which presented an opportunity to change how mental health and substance use support is provided. This study explored the experiences of access to community-based mental health and substance use support in people experiencing homelessness during the pandemic. The experiences of access shared took place while there were constraints to the mental health and substance use system (such as reduced service provision and staffing) brought about by the pandemic and pre-existing austerity. Although many experiences of access were negative, individuals did share some positive experiences or suggestions for service improvement.
Although this study focused on experiences during the pandemic, our findings illustrated some known barriers to accessing mental health and substance use support that existed prior to the pandemic and align with pre-pandemic research findings. These included services being restricted to business hours, repeating recovery stories, and limited support [ 61 , 62 , 63 , 64 , 65 ], suggesting an opportunity to improve service provision irrespective of times of austerity and crisis. Negative experiences and barriers to access highlight the need for a resilient mental health and substance use system that is responsive to the needs and circumstances of vulnerable groups such as people experiencing homelessness.
Experiences of exclusion took many forms across interviews. Many people felt they could not access mental health support when they needed it most (e.g., in the evening) or in the most suitable form for their needs or abilities. This echoes research prior to COVID-19 [ 61 , 62 ]. During conversations about remote out-of-hours support many discussed access issues surrounding not having smartphones, internet, or feeling uncomfortable accessing support online or transitioning to online support. Remote solutions therefore need to consider these barriers to ensure appropriate and inclusive access [ 46 ], but this also suggests that more creative out-of-hours provision solutions are needed.
Our findings emphasise that when additional needs (such as past negative experiences, dual diagnosis, material disadvantage) are not recognised, people experiencing homelessness are often unable to appropriately access support. Prior research has extensively explored the complex structural and individual circumstances surrounding people experiencing homelessness [ 33 , 34 , 61 , 66 ]. Our findings suggest that the instability around circumstances and needs requires recognition from service providers during times of heightened adversity. Participants’ suggestions of hiring and training people with lived experience could be one way to better target provision; existing evidence demonstrates improved treatment outcomes in mental health and substance use support when lived experience is integrated within care provision [ 27 , 67 , 68 ].
One of the most crucial messages within interviews was the need to have a choice in one’s care, particularly during the pandemic where people felt their loss of autonomy and control had worsened. The notion of rebuilding control has previously been highlighted within trauma-informed care approaches for homelessness [ 69 ]. In line with autonomy and control, our findings highlighted that not everyone is ready to access support but that continuing to increase awareness and knowledge of current support would equip individuals with the necessary information to access support at the right time for them. This knowledge is essential considering knowing where to go to access support is a central issue for people experiencing homelessness [ 70 , 71 ].
Negative environments for accessing support (such as high presence of drugs, lack of safety) were a source of frustration and led to subsequent care avoidance; a consequence seen in other studies [ 23 , 72 ]. Telephone support to accommodate COVID-19 restrictions meant some people finally felt comfortable accessing support as the environment changed. Like existing mental health and homeless literature [ 63 , 64 , 65 ], participants shared frustration around repeating their stories; likely a consequence of a siloed system of care/support. In a few cases, individuals shared how the pandemic was the first time they found services working collaboratively to support them—echoing other emerging evidence [ 66 ]. Lessons from providers on mechanisms for coordination across the system during COVID-19, could allow future approaches to be more bespoke and coordinated to ensure that the specific needs of people experiencing homelessness are addressed [ 73 ]. Finally, our findings highlight that many struggled to access support, particularly with the reduced service provision and increased waiting lists during COVID-19. Recognising that reduced service provision was perhaps unavoidable given the context, it is important to consider the impact these negative experiences have on future access and experiences.
4.1. Strengths and Limitations
A key strength to this study is its application of participatory approaches, which meaningfully brings the voice of people with lived experience to the study design, methodology and interpretation of findings. Involving individuals with lived experience throughout each phase of the data analysis meant that some of the initial codes were created based on their suggestions and theme refinement was influenced by their rich insights. Lived experience involvement also led to an action-oriented interpretation with a desire to improve future experiences of access, provision, and policy around community mental health and substance use support.
The study is limited by its localised recruitment in Newcastle and Gateshead; however, preliminary conversations with providers in other regions suggest the findings echo their experiences. Despite active recruitment effort, we were unable to recruit anyone who did not self-identify as White British, however, the proportion of individuals in North East England who do not identify as White British is less than 8% in the general population [ 74 ]. Discussions with local providers emphasised that contrary to other regions in England, most individuals who experience homelessness in North East England self-identify as White British. The study employed solely remote approaches to data collection due to the COVID-19 restrictions. Although research has shown the acceptability of remote data collection [ 75 ], the potential of sampling bias remains due to not reaching out to those without telephone or internet access or potentially those sleeping rough [ 76 ]. We attempted to mitigate this bias through working closely with hostels to ensure individuals had access to communal phones.
4.2. Implications for Practice and Research
Our findings suggest several actionable solutions for policymakers and providers in health, social care, and housing that are transferable outside the context of pandemics and times of crisis. These include providing choice (e.g., offer someone a choice between service provision online or in-person or offering choices for the time of day for provision), lived experience representation within support, making information about services accessible (e.g., communicating using simple and clear language [ 23 ]), ensuring appropriate and inclusive digital solutions (e.g., working with individuals with lived experience to co-create solutions or providing smartphones with internet access [ 46 ]), creating a safe space for accessing support (e.g., a service that feels safe, private, and is not overly crowded [ 23 ]), and creating bespoke and integrated care pathways. Research is needed to investigate the difference and factors associated with digital confidence and literacy among people experiencing homelessness. In all cases, solutions should be designed, implemented, and delivered with individuals with lived experience to ensure it is acceptable and appropriate for this population. Ensuring that provision is responsive and appropriate to those most in need is vital for integrated care systems across England.
Through working with individuals with lived experience, we were able to better understand the experiences of participants while being open to seeing solutions to challenges. Further research should look to understand the perspectives of those providing support and co-developing solutions that are equally acceptable to providers and those who experience homelessness.
5. Conclusions
COVID-19 presented an opportunity to learn from changes in service provision and has drawn attention to the need for more accessible and bespoke support for people experiencing homelessness. This study provided rich accounts on the (in)accessibility of mental health and substance use support, which have implications for developing future policy and practice responses. These implications are potentially beneficial for post-pandemic efforts to improve access to and increase the resilience of mental health and substance use support for people experiencing homelessness.
Acknowledgments
We would like to thank participants and the community organisations who supported recruitment efforts.
Author Contributions
Conceptualisation, E.A.A., C.S., C.M., A.O., E.W., K.D. (Kate Dotsikas), E.K. and S.E.R.; data collection, E.A.A.; analysis led by E.A.A. with support from J.P., T.J., F.T., J.K. and D.H.; validation of analysis, all co-authors; literature review, E.A.A. and K.D. (Katy Denham); writing—original draft preparation, E.A.A.; writing, reviewing, and editing, all co-authors. All authors have read and agreed to the published version of the manuscript.
This research was funded by the National Institute for Health Research (NIHR) School for Public Health Research (SPHR) development fund for early career researchers (ECRs). E.A.A and Kate D. are supported by the NIHR SPHR Pre-doctoral Fellowship Funding Scheme, Grant Reference Number PD-SPH-2015 and C.M. is being supported by the NIHR SPHR PhD studentship (SPHR-PHD-FUS-002). A.O. is an NIHR Advanced Fellow. E.K. is supported by an NIHR Senior Investigator award and is Director of the NIHR Applied Research Collaboration North East and North Cumbria. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Institutional Review Board Statement
Ethics approval was granted by the Faculty of Medical Sciences Research Ethics Committee, part of Newcastle University’s Research Ethics Committee (ref: 2034/6698/2020 including amendment 2034_1.)
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study, including consent to publish.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Open access
- Published: 03 June 2024
The use of evidence to guide decision-making during the COVID-19 pandemic: divergent perspectives from a qualitative case study in British Columbia, Canada
- Laura Jane Brubacher ORCID: orcid.org/0000-0003-2806-9539 1 , 2 ,
- Chris Y. Lovato 1 ,
- Veena Sriram 1 , 3 ,
- Michael Cheng 1 &
- Peter Berman 1
Health Research Policy and Systems volume 22 , Article number: 66 ( 2024 ) Cite this article
Metrics details
The challenges of evidence-informed decision-making in a public health emergency have never been so notable as during the COVID-19 pandemic. Questions about the decision-making process, including what forms of evidence were used, and how evidence informed—or did not inform—policy have been debated.
We examined decision-makers' observations on evidence-use in early COVID-19 policy-making in British Columbia (BC), Canada through a qualitative case study. From July 2021- January 2022, we conducted 18 semi-structured key informant interviews with BC elected officials, provincial and regional-level health officials, and civil society actors involved in the public health response. The questions focused on: (1) the use of evidence in policy-making; (2) the interface between researchers and policy-makers; and (3) key challenges perceived by respondents as barriers to applying evidence to COVID-19 policy decisions. Data were analyzed thematically, using a constant comparative method. Framework analysis was also employed to generate analytic insights across stakeholder perspectives.
Overall, while many actors’ impressions were that BC's early COVID-19 policy response was evidence-informed, an overarching theme was a lack of clarity and uncertainty as to what evidence was used and how it flowed into decision-making processes. Perspectives diverged on the relationship between 'government' and public health expertise, and whether or not public health actors had an independent voice in articulating evidence to inform pandemic governance. Respondents perceived a lack of coordination and continuity across data sources, and a lack of explicit guidelines on evidence-use in the decision-making process, which resulted in a sense of fragmentation. The tension between the processes involved in research and the need for rapid decision-making was perceived as a barrier to using evidence to inform policy.
Conclusions
Areas to be considered in planning for future emergencies include: information flow between policy-makers and researchers, coordination of data collection and use, and transparency as to how decisions are made—all of which reflect a need to improve communication. Based on our findings, clear mechanisms and processes for channeling varied forms of evidence into decision-making need to be identified, and doing so will strengthen preparedness for future public health crises.
Peer Review reports
The challenges of evidence-informed decision-making Footnote 1 in a public health emergency have never been so salient as during the COVID-19 pandemic, given its unprecedented scale, rapidly evolving virology, and multitude of global information systems to gather, synthesize, and disseminate evidence on the SARS-CoV-2 virus and associated public health and social measures [ 1 , 2 , 3 ]. Early in the COVID-19 pandemic, rapid decision-making became central for governments globally as they grappled with crucial decisions for which there was limited evidence. Critical questions exist, in looking retrospectively at these decision-making processes and with an eye to strengthening future preparedness: Were decisions informed by 'evidence'? What forms of evidence were used, and how, by decision-makers? [ 4 , 5 , 6 ].
Scientific evidence, including primary research, epidemiologic research, and knowledge synthesis, is one among multiple competing influences that inform decision-making processes in an outbreak such as COVID-19 [ 7 ]. Indeed, the use of multiple forms of evidence has been particularly notable as it applies to COVID-19 policy-making. Emerging research has also documented the important influence of ‘non-scientific’ evidence such as specialized expertise and experience, contextual information, and level of available resources [ 8 , 9 , 10 ]. The COVID-19 pandemic has underscored the politics of evidence-use in policy-making [ 11 ]; what evidence is used and how can be unclear, and shaped by political bias [ 4 , 5 ]. Moreover, while many governments have established scientific advisory boards, the perspectives of these advisors were reportedly largely absent from COVID-19 policy processes [ 6 ]. How evidence and public health policy interface—and intersect—is a complex question, particularly in the dynamic context of a public health emergency.
Within Canada, a hallmark of the public health system and endorsed by government is evidence-informed decision-making [ 12 ]. In British Columbia (BC), Canada, during the early phases of COVID-19 (March—June 2020), provincial public health communication focused primarily on voluntary compliance with recommended public health and social measures, and on supporting those most affected by the pandemic. Later, the response shifted from voluntary compliance to mandatory enforceable government orders [ 13 ]. Like many other jurisdictions, the government’s public messaging in BC asserted that the province took an approach to managing the COVID-19 pandemic and developing related policy that was based on scientific evidence, specifically. For example, in March 2021, in announcing changes to vaccination plans, Dr. Bonnie Henry, the Provincial Health Officer, stated, " This is science in action " [ 14 ]. As a public health expert with scientific voice, the Provincial Health Officer has been empowered to speak on behalf of the BC government across the COVID-19 pandemic progression. While this suggests BC is a jurisdiction which has institutionalized scientifically-informed decision-making as a core tenet of effective public health crisis response, it remains unclear as to whether BC’s COVID-19 response could, in fact, be considered evidence-informed—particularly from the perspectives of those involved in pandemic decision-making and action. Moreover, if evidence-informed, what types of evidence were utilized and through what mechanisms, how did this evidence shape decision-making, and what challenges existed in moving evidence to policy and praxis in BC’s COVID-19 response?
The objectives of this study were: (1) to explore and characterize the perspectives of BC actors involved in the COVID-19 response with respect to evidence-use in COVID-19 decision-making; and (2) to identify opportunities for and barriers to evidence-informed decision-making in BC’s COVID-19 response, and more broadly. This inquiry may contribute to identifying opportunities for further strengthening the synthesis and application of evidence (considered broadly) to public health policy and decision-making, particularly in the context of future public health emergencies, both in British Columbia and other jurisdictions.
Study context
This qualitative study was conducted in the province of British Columbia (BC), Canada, a jurisdiction with a population of approximately five million people [ 15 ]. Within BC’s health sector, key actors involved in the policy response to COVID-19 included: elected officials, the BC Government’s Ministry of Health (MOH), the Provincial Health Services Authority (PHSA), Footnote 2 the Office of the Provincial Health Officer (PHO), Footnote 3 the BC Centre for Disease Control (BCCDC), Footnote 4 and Medical Health Officers (MHOs) and Chief MHOs at regional and local levels.
Health research infrastructure within the province includes Michael Smith Health Research BC [ 16 ] and multiple post-secondary research and education institutions (e.g., The University of British Columbia). Unlike other provincial (e.g., Ontario) and international (e.g., UK) jurisdictions, BC did not establish an independent, formal scientific advisory panel or separate organizational structure for public health intelligence in COVID-19. That said, a Strategic Research Advisory Council was established, reporting to the MOH and PHO, to identify COVID-19 research gaps and commission needed research for use within the COVID-19 response [ 17 ].
This research was part of a multidisciplinary UBC case study investigating the upstream determinants of the COVID-19 response in British Columbia, particularly related to institutions, politics, and organizations and how these interfaced with, and affected, pandemic governance [ 18 ]. Ethics approval for this study was provided by the University of British Columbia (UBC)’s Institutional Research Ethics Board (Certificate #: H20-02136).
Data collection
From July 2021 to January 2022, 18 semi-structured key informant interviews were conducted with BC elected officials, provincial and regional-level health officials, and civil society actors (e.g., within non-profit research organizations, unions) (Table 1 ). Initially, respondents were purposively sampled, based on their involvement in the COVID-19 response and their positioning within the health system organizational structure. Snowball sampling was used to identify additional respondents, with the intent of representing a range of organizational roles and actor perspectives. Participants were recruited via email invitation and provided written informed consent to participate.
Interviews were conducted virtually using Zoom® videoconferencing, with the exception of one hybrid in-person/Zoom® interview. Each interview was approximately one hour in duration. One to two research team members led each interview. The full interview protocol focused on actors’ descriptions of decision-making processes across the COVID-19 pandemic progression, from January 2020 to the date of the interviews, and they were asked to identify key decision points (e.g., emergency declaration, business closures) [see Additional File 1 for the full semi-structured interview guide]. For this study, we used a subset of interview questions focused on evidence-use in the decision-making process, and the organizational structures or actors involved, in BC's early COVID-19 pandemic response (March–August 2020). Questions were adapted to be relevant to a respondent’s expertise and particular involvement in the response. ‘Evidence’ was left undefined and considered broadly by the research team (i.e., both ‘scientific’/research-based and ‘non-scientific’ inputs) within interview questions, and therefore at the discretion of the participant as to what inputs they perceived and described as ‘evidence’ that informed or did not inform pandemic decision-making. Interviews were audio-recorded over Zoom® with permission and transcribed using NVivo Release 1.5© software. Each transcript was then manually verified for accuracy by 1–2 members of the research team.
Data analysis
An inductive thematic analysis was conducted, using a constant comparative method, to explore points of divergence and convergence across interviews and stakeholder perspectives [ 19 ]. Transcripts were inductively coded in NVivo Release 1.5© software, which was used to further organize and consolidate codes, generate a parsimonious codebook to fit the data, and retrieve interview excerpts [ 20 ]. Framework analysis was also employed as an additional method for generating analytic insights across stakeholder perspectives and contributed to refining the overall coding [ 21 ]. Triangulation across respondents and analytic methods, as well as team collaboration in reviewing and refining the codebook, contributed to validity of the analysis [ 22 ].
How did evidence inform early COVID-19 policy-making in BC?
Decision-makers described their perceptions on the use of evidence in policy-making; the interface between researchers and policy-makers; and specific barriers to evidence-use in policy-making within BC’s COVID-19 response. In discussing the use of evidence, respondents focused on ‘scientific’ evidence; however, they noted a lack of clarity as to how and what evidence flowed into decision-making. They also acknowledged that ‘scientific’ evidence was one of multiple factors influencing decisions. The themes described below reflect the narrative underlying their perspectives.
Perceptions of evidence-use
Multiple provincial actors generally expressed confidence or had an overall impression that decisions were evidence-based (IDI5,9), stating definitively that, "I don’t think there was a decision we made that wasn’t evidence-informed" (IDI9) and that "the science became a driver of decisions that were made" (IDI5). However, at the regional health authority level, one actor voiced skepticism that policy decisions were consistently informed by scientific evidence specifically, stating, "a lot of decisions [the PHO] made were in contrast to science and then shifted to be by the science" ( IDI6). The evolving nature of the available evidence and scientific understanding of the virus throughout the pandemic was acknowledged. For instance, one actor stated that, "I’ll say the response has been driven by the science; the science has been changing…from what I’ve seen, [it] has been a very science-based response" (IDI3).
Some actors narrowed in on certain policy decisions they believed were or were not evidence-informed. Policy decisions in 2020 that actors believed were directly informed by scientific data included the early decision to restrict informal, household gatherings; to keep schools open for in-person learning; to implement a business safety plan requirement across the province; and to delay the second vaccine dose for maximum efficacy. One provincial public health actor noted that an early 2020 decision made, within local jurisdictions, to close playgrounds was not based on scientific evidence. Further, the decision prompted public health decision-makers to centralize some decision-making to the provincial level, to address decisions being made 'on the ground' that were not based on scientific evidence (IDI16). Similarly, they added that the policy decision to require masking in schools was not based on scientific evidence; rather, "it's policy informed by the noise of your community." As parents and other groups within the community pushed for masking, this was "a policy decision to help schools stay open."
Early in the pandemic response, case data in local jurisdictions were reportedly used for monitoring and planning. These "numerator data" (IDI1), for instance case or hospitalization counts, were identified as being the primary mode of evidence used to inform decisions related to the implementation or easing of public health and social measures. The ability to generate epidemiological count data early in the pandemic due to efficient scaling up of PCR testing for COVID-19 was noted as a key advantage (IDI16). As the pandemic evolved in 2020, however, perspectives diverged in relation to the type of data that decision-makers relied on. For example, it was noted that BCCDC administered an online, voluntary survey to monitor unintended consequences of public health and social measures and inform targeted interventions. Opinions varied on whether this evidence was successfully applied in decision-making. One respondent emphasized this lack of application of evidence and perceived that public health orders were not informed by the level and type of evidence available, beyond case counts: "[In] a communicable disease crisis like a pandemic, the collateral impact slash damage is important and if you're going to be a public health institute, you actually have to bring those to the front, not just count cases" (IDI1).
There also existed some uncertainty and a perceived lack of transparency or clarity as to how or whether data analytic ‘entities’, such as BCCDC or research institutions, fed directly into decision-making. As a research actor shared, "I’m not sure that I know quite what all those channels really look like…I’m sure that there’s a lot of improvement that could be driven in terms of how we bring strong evidence to actual policy and practice" (IDI14). Another actor explicitly named the way information flowed into decision-making in the province as "organic" (IDI7). They also noted the lack of a formal, independent science advisory panel for BC’s COVID-19 response, which existed in other provincial and international jurisdictions. Relatedly, one regional health authority actor perceived that the committee that was convened to advise the province on research, and established for the purpose of applying research to the COVID-19 response, "should have focused more on knowledge translation, but too much time was spent commissioning research and asking what kinds of questions we needed to ask rather than looking at what was happening in other jurisdictions" (IDI6). Overall, multiple actors noted a lack of clarity around application of evidence and who is responsible for ensuring evidence is applied. As a BCCDC actor expressed, in relation to how to prevent transmission of COVID-19:
We probably knew most of the things that we needed to know about May of last year [2020]. So, to me, it’s not even what evidence you need to know about, but who’s responsible for making sure that you actually apply the evidence to the intervention? Because so many of our interventions have been driven by peer pressure and public expectation rather than what we know to be the case [scientifically] (IDI1).
Some described the significance of predictive disease modelling to understand the COVID-19 trajectory and inform decisions, as well as to demonstrate to the public the effectiveness of particular measures, which "help[ed] sustain our response" (IDI2). Others, however, perceived that "mathematical models were vastly overused [and] overvalued in decision-making around this pandemic" (IDI1) and that modellers stepped outside their realm of expertise in providing models and policy recommendations through the public media.
Overall, while many actors’ impressions were that the response was evidence-informed, an overarching theme was a lack of clarity and uncertainty with respect to how evidence actually flowed into decision-making processes, as well as what specific evidence was used and how. Participants noted various mechanisms created or already in place prior to COVID-19 that fed data into, and facilitated, decision-making. There was an acknowledgement that multiple forms of evidence—including scientific data, data on public perceptions, as well as public pressure—appeared to have influenced decision-making.
Interface between researchers and policy-makers
There was a general sense that the Ministry supported the use of scientific and research-based evidence specifically. Some actors identified particular Ministry personnel as being especially amenable to research and focused on data to inform decisions and implementation. More broadly, the government-research interface was characterized by one actor as an amicable one, a "research-friendly government", and that the Ministry of Health (MOH), specifically, has a research strategy whereby, "it’s literally within their bureaucracy to become a more evidence-informed organization" (IDI11). The MOH was noted to have funded a research network intended to channel evidence into health policy and practice, and which reported to the research side of the MOH.
Other actors perceived relatively limited engagement with the broader scientific community. Some perceived an overreliance on 'in-house expertise' or a "we can do that [ourselves] mentality" within government that precluded academic researchers’ involvement, as well as a sense of "not really always wanting to engage with academics to answer policy questions because they don’t necessarily see the value that comes" (IDI14). With respect to the role of research, an actor stated:
There needs to be a provincial dialogue around what evidence is and how it gets situated, because there’s been some tension around evidence being produced and not used or at least not used in the way that researchers think that it should be (IDI11).
Those involved in data analytics within the MOH acknowledged a challenge in making epidemiological data available to academic researchers, because "at the time, you’re just trying to get decisions made" (IDI7). Relatedly, a research actor described the rapid instigation of COVID-19 research and pivoting of academic research programs to respond to the pandemic, but perceived a slow uptake of these research efforts from the MOH and PHSA for decision-making and action. Nevertheless, they too acknowledged the challenge of using research evidence, specifically, in an evolving and dynamic pandemic:
I think we’ve got to be realistic about what research in a pandemic situation can realistically contribute within very short timelines. I mean, some of these decisions have to be made very quickly...they were intuitive decisions, I think some of them, rather than necessarily evidence-based decisions (IDI14).
Relatedly, perspectives diverged on the relationship between 'government' and public health expertise, and whether or not public health actors had an independent voice in articulating evidence to inform governance during the pandemic. Largely from Ministry stakeholders, and those within the PHSA, the impressions were that Ministry actors were relying on public health advice and scientific expertise. As one actor articulated, "[the] government actually respected and acknowledged and supported public health expertise" (IDI9). Others emphasized a "trust of the people who understood the problem" (IDI3)—namely, those within public health—and perceived that public health experts were enabled "to take a lead role in the health system, over politics" (IDI12). This perspective was not as widely held by those in the public health sector, as one public health actor expressed, "politicians and bureaucrats waded into public health practice in a way that I don't think was appropriate" and that, "in the context of a pandemic, it’s actually relatively challenging to bring true expert advice because there’s too many right now. Suddenly, everybody’s a public health expert, but especially bureaucrats and politicians." They went on to share that the independence of public health to speak and act—and for politicians to accept independent public health advice—needs to be protected and institutionalized as "core to good governance" (IDI1). Relatedly, an elected official linked this to the absence of a formal, independent science table to advise government and stated that, "I think we should have one established permanently. I think we need to recognize that politicians aren't always the best at discerning scientific evidence and how that should play into decision-making" (IDI15).
These results highlight the divergent perspectives participants had as to the interface between research and policy-making and a lack of understanding regarding process and roles.
Challenges in applying evidence to policy decisions
Perspectives converged with respect to the existence of numerous challenges with and barriers to applying evidence to health policy and decision-making. These related to the quality and breadth of available data, both in terms of absence and abundance. For instance, as one public health actor noted in relation to health policy-making, "you never have enough information. You always have an information shortage, so you're trying to make the best decisions you can in the absence of usually really clear information" (IDI8). On the other hand, as evidence emerged en masse across jurisdictions in the pandemic, there were challenges with synthesizing evidence in a timely fashion for 'real-time' decision-making. A regional health authority actor highlighted this challenge early in the COVID-19 pandemic and perceived that there was not a provincial group bringing new synthesized information to decision-makers on a daily basis (IDI6). Other challenges related to the complexity of the political-public health interface with respect to data and scientific expertise, which "gets debated and needs to be digested by the political process. And then decisions are made" (IDI5). This actor further expressed that debate among experts needs to be balanced with efficient crisis response, that one has to "cut the debate short. For the sake of expediency, you need to react."
It was observed that, in BC’s COVID-19 response, data was gathered from multiple sources with differing data collection procedures, and sometimes with conflicting results—for instance, 'health system data' analyzed by the PHSA and 'public health data' analyzed by the BCCDC. This was observed to present challenges from a political perspective in discerning "who’s actually getting the 'right' answers" (IDI7). An added layer of complexity was reportedly rooted in how to communicate such evidence to the public and "public trust in the numbers" (IDI7), particularly as public understanding of what evidence is, how it is developed, and why it changes, can influence public perceptions of governance.
Finally, as one actor from within the research sector noted, organizationally and governance-wise, the system was "not very well set up to actually use research evidence…if we need to do better at using evidence in practice, we need to fix some of those things. And we actually know what a lot of those things are." For example , "there’s no science framework for how organizations work within that" and " governments shy away from setting science policy " (IDI11). This challenge was framed as having a macro-level dimension, as higher-level leadership structures were observed to not incentivize the development and effective use of research among constituent organizations, and also micro-level implications. From their perspective, researchers will struggle without such policy frameworks to obtain necessary data-sharing agreements with health authorities, nor will they be able to successfully navigate other barriers to conducting action-oriented research that informs policy and practice.
Similarly, a research actor perceived that the COVID-19 pandemic highlighted pre-existing fragmentation, "a pretty disjointed sort of enterprise" in how research is organized in the province:
I think pandemics need strong leadership and I think pandemic research response needed probably stronger leadership than it had. And I think that’s to do with [how] no one really knew who was in charge because no one really was given the role of being truly in charge of the research response (IDI14).
This individual underscored that, at the time of the interview, there were nearly 600 separate research projects being conducted in BC that focused on COVID-19. From their perspective, this reflected the need for more centralized direction to provide leadership, coordinate research efforts, and catalyze collaborations.
Overall, respondents perceived a lack of coordination and continuity across data sources, and a lack of explicit guidelines on evidence-use in the decision-making process, which resulted in a sense of fragmentation. The tension between the processes involved in research and the need for rapid decision-making was perceived as a barrier to using evidence to inform policy.
This study explored the use of evidence to inform early COVID-19 decision-making within British Columbia, Canada, from the perspectives of decision-makers themselves. Findings underscore the complexity of synthesizing and applying evidence (i.e., ‘scientific’ or research-based evidence most commonly discussed) to support public health policy in 'real-time', particularly in the context of public health crisis response. Despite a substantial and long-established literature on evidence-based clinical decision-making [ 23 , 24 ], understanding is more limited as to how public health crisis decision-making can be evidence-informed or evidence-based. By contributing to a growing global scholarship of retrospective examinations of COVID-19 decision-making processes [ 25 , 26 , 27 , 28 ], our study aimed to broaden this understanding and, thus, support the strengthening of public health emergency preparedness in Canada, and globally.
Specifically, based on our findings on evidence-based public health practice, we found that decision-makers clearly emphasized ‘evidence-based’ or ‘evidence-informed’ as meaning ‘scientific’ evidence. They acknowledged other forms of evidence such as professional expertise and contextual information as influencing factors. We identified four key points related to the process of evidence-use in BC's COVID-19 decision-making, with broader implications as well:
Role Differences: The tensions we observed primarily related to a lack of clarity among the various agencies involved as to their respective roles and responsibilities in a public health emergency, a finding that aligns with research on evidence-use in prior pandemics in Canada [ 29 ]. Relatedly, scientists and policy-makers experienced challenges with communication and information-flow between one another and the public, which may reflect their different values and standards, framing of issues and goals, and language [ 30 ].
Barriers to Evidence-Use: Coordination and consistency in how data are collected across jurisdictions reportedly impeded efficiency and timeliness of decision-making. Lancaster and Rhodes (2020) suggest that evidence itself should be treated as a process, rather than a commodity, in evidence-based practice [ 31 ]. Thus, shifting the dialogue from 'barriers to evidence use' to an approach that fosters dialogue across different forms of evidence and different actors in the process may be beneficial.
Use of Evidence in Public Health versus Medicine: Evidence-based public health can be conflated with the concept of evidence-based medicine, though these are distinct in the type of information that needs to be considered. While ‘research evidence’ was the primary type of evidence used, other important types of evidence informed policy decisions in the COVID-19 public health emergency—for example, previous experience, public values, and preferences. This concurs with Brownson’s (2009) framework of factors driving decision-making in evidence-based public health [ 32 ]. Namely, that a balance between multiple factors, situated in particular environmental and organizational context, shapes decision-making: 1) best available research evidence; 2) clients'/population characteristics, state, needs, values, and preferences; and 3) resources, including a practitioner’s expertise. Thus, any evaluation of evidence-use in public health policy must take into consideration this multiplicity of factors at play, and draw on frameworks specific to public health [ 33 ]. Moreover, public health decision-making requires much more attention to behavioural factors and non-clinical impacts, which is distinct from the largely biology-focused lens of evidence-based medicine.
Transparency: Many participants emphasized a lack of explanation about why certain decisions were made and a lack of understanding about who was involved in decisions and how those decisions were made. This point was confirmed by a recent report on lessons learned in BC during the COVID-19 pandemic in which the authors describe " the desire to know more about the reasons why decisions were taken " as a " recurring theme " (13:66). These findings point to a need for clear and transparent mechanisms for channeling evidence, irrespective of the form used, into public health crisis decision-making.
Our findings also pointed to challenges associated with the infrastructure for utilizing research evidence in BC policy-making, specifically a need for more centralized authority on the research side of the public health emergency response to avoid duplication of efforts and more effectively synthesize findings for efficient use. Yet, as a participant questioned, what is the realistic role of research in a public health crisis response? Generally, most evidence used to inform crisis response measures is local epidemiological data or modelling data [ 7 ]. As corroborated by our findings, challenges exist in coordinating data collection and synthesis of these local data across jurisdictions to inform 'real-time' decision-making, let alone to feed into primary research studies [ 34 ].
On the other hand, as was the case in the COVID-19 pandemic, a 'high noise' research environment soon became another challenge as data became available to researchers. Various mechanisms have been established to try and address these challenges amid the COVID-19 pandemic, both to synthesize scientific evidence globally and to create channels for research evidence to support timely decision-making. For instance: 1) research networks and collaborations are working to coordinate research efforts (e.g., COVID-END network [ 35 ]); 2) independent research panels or committees within jurisdictions provide scientific advice to inform decision-making; and 3) research foundations, funding agencies, and platforms for knowledge mobilization (e.g., academic journals) continue to streamline funding through targeted calls for COVID-19 research grant proposals, or for publication of COVID-19 research articles. While our findings describe the varied forms of evidence used in COVID-19 policy-making—beyond scientific evidence—they also point to the opportunity for further investments in infrastructure that coordinates, streamlines, and strengthens collaborations between health researchers and decision-makers that results in timely uptake of results into policy decisions.
Finally, in considering these findings, it is important to note the study's scope and limitations: We focused on evidence use in a single public health emergency, in a single province. Future research could expand this inquiry to a multi-site analysis of evidence-use in pandemic policy-making, with an eye to synthesizing lessons learned and best practices. Additionally, our sample of participants included only one elected official, so perspectives were limited from this type of role. The majority of participants were health officials who primarily referred to and discussed evidence as ‘scientific’ or research-based evidence. Further work could explore the facilitators and barriers to evidence-use from the perspectives of elected officials and Ministry personnel, particularly with respect to the forms of evidence—considered broadly—and other varied inputs, that shape decision-making in the public sphere. This could include a more in-depth examination of policy implementation and how the potential societal consequences of implementation factor into public health decision-making.
We found that the policy decisions made during the initial stages of the COVID-19 pandemic were perceived by actors in BC's response as informed by—not always based on—scientific evidence, specifically; however, decision-makers also considered other contextual factors and drew on prior pandemic-related experience to inform decision-making, as is common in evidence-based public health practice [ 32 ]. The respondents' experiences point to specific areas that need to be considered in planning for future public health emergencies, including information flow between policy-makers and researchers, coordination in how data are collected, and transparency in how decisions are made—all of which reflect a need to improve communication. Furthermore, shifting the discourse from evidence as a commodity to evidence-use as a process will be helpful in addressing barriers to evidence-use, as well as increasing understanding about the public health decision-making process as distinct from clinical medicine. Finally, there is a critical need for clear mechanisms that channel evidence (whether ‘scientific’, research-based, or otherwise) into health crisis decision-making, including identifying and communicating the decision-making process to those producing and synthesizing evidence. The COVID-19 pandemic experience is an opportunity to reflect on what needs to be done to guild our public health systems for the future [ 36 , 37 ]. Understanding and responding to the complexities of decision-making as we move forward, particularly with respect to the synthesis and use of evidence, can contribute to strengthening preparedness for future public health emergencies.
Availability of data and materials
The data that support the findings of this study are not publicly available to maintain the confidentiality of research participants.
The terms 'evidence-informed' and 'evidence-based' decision-making are used throughout this paper, though are distinct. The term 'evidence-informed' suggests that evidence is used and considered, though not necessarily solely determinative in decision-making [ 38 ].
The Provincial Health Services Authority (PHSA) works with the Ministry of Health (MOH) and regional health authorities to oversee the coordination and delivery of programs.
The Office of the Provincial Health Officer (PHO) has binding legal authority in the case of an emergency, and responsibility to monitor the health of BC’s population and provide independent advice to Ministers and public offices on public health issues.
The British Columbia Centre for Disease Control (BCCDC) is a program of the PHSA and provides provincial and national disease surveillance, detection, treatment, prevention, and consultation.
Abbreviations
British Columbia
British Columbia Centre for Disease Control
Coronavirus Disease 2019
Medical Health Officer
Ministry of Health
Provincial Health Officer
Provincial Health Services Authority
Severe Acute Respiratory Syndrome Coronavirus—2
University of British Columbia
Rubin O, Errett NA, Upshur R, Baekkeskov E. The challenges facing evidence-based decision making in the initial response to COVID-19. Scand J Public Health. 2021;49(7):790–6.
Article PubMed Google Scholar
Williams GA, Ulla Díez SM, Figueras J, Lessof S, Ulla SM. Translating evidence into policy during the COVID-19 pandemic: bridging science and policy (and politics). Eurohealth (Lond). 2020;26(2):29–48.
Google Scholar
Vickery J, Atkinson P, Lin L, Rubin O, Upshur R, Yeoh EK, et al. Challenges to evidence-informed decision-making in the context of pandemics: qualitative study of COVID-19 policy advisor perspectives. BMJ Glob Heal. 2022;7(4):1–10.
Piper J, Gomis B, Lee K. “Guided by science and evidence”? The politics of border management in Canada’s response to the COVID-19 pandemic. Front Polit Sci. 2022;4
Cairney P. The UK government’s COVID-19 policy: what does “Guided by the science” mean in practice? Front Polit Sci. 2021;3(March):1–14.
Colman E, Wanat M, Goossens H, Tonkin-Crine S, Anthierens S. Following the science? Views from scientists on government advisory boards during the COVID-19 pandemic: a qualitative interview study in five European countries. BMJ Glob Heal. 2021;6(9):1–11.
Salajan A, Tsolova S, Ciotti M, Suk JE. To what extent does evidence support decision making during infectious disease outbreaks? A scoping literature review. Evid Policy. 2020;16(3):453–75.
Article Google Scholar
Cairney P. The UK government’s COVID-19 policy: assessing evidence-informed policy analysis in real time. Br Polit. 2021;16(1):90–116.
Lancaster K, Rhodes T, Rosengarten M. Making evidence and policy in public health emergencies: lessons from COVID-19 for adaptive evidence-making and intervention. Evid Policy. 2020;16(3):477–90.
Yang K. What can COVID-19 tell us about evidence-based management? Am Rev Public Adm. 2020;50(6–7):706–12.
Parkhurst J. The politics of evidence: from evidence-based policy to the good governance of evidence. Abingdon: Routledge; 2017.
Office of the Prime Minister. Minister of Health Mandate Letter [Internet]. 2021. https://pm.gc.ca/en/mandate-letters/2021/12/16/minister-health-mandate-letter
de Faye B, Perrin D, Trumpy C. COVID-19 lessons learned review: Final report. Victoria, BC; 2022.
First Nations Health Authority. Evolving vaccination plans is science in action: Dr. Bonnie Henry. First Nations Health Authority. 2021.
BC Stats. 2021 Sub-provincial population estimates highlights. Vol. 2021. Victoria, BC; 2022.
Michael Smith Health Research BC [Internet]. 2023. healthresearchbc.ca. Accessed 25 Jan 2023.
Michael Smith Health Research BC. SRAC [Internet]. 2023. https://healthresearchbc.ca/strategic-provincial-advisory-committee-srac/ . Accessed 25 Jan 2023.
Brubacher LJ, Hasan MZ, Sriram V, Keidar S, Wu A, Cheng M, et al. Investigating the influence of institutions, politics, organizations, and governance on the COVID-19 response in British Columbia, Canada: a jurisdictional case study protocol. Heal Res Policy Syst. 2022;20(1):1–10.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
DeCuir-Gunby JT, Marshall PL, McCulloch AW. Developing and using a codebook for the analysis of interview data: an example from a professional development research project. Field Methods. 2011;23(2):136–55.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(117):1–8.
Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory Pract. 2000;39(3):124–30.
Sackett D. How to read clinical journals: I. Why to read them and how to start reading them critically. Can Med Assoc J. 1981;1245:555–8.
Evidence Based Medicine Working Group. Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA Netw. 1992;268(17):2420–5.
Allin S, Fitzpatrick T, Marchildon GP, Quesnel-Vallée A. The federal government and Canada’s COVID-19 responses: from “we’re ready, we’re prepared” to “fires are burning.” Heal Econ Policy Law. 2022;17(1):76–94.
Bollyky TJ, Hulland EN, Barber RM, Collins JK, Kiernan S, Moses M, et al. Pandemic preparedness and COVID-19: an exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, from Jan 1, 2020, to Sept 30, 2021. Lancet. 2022;6736(22):1–24.
Kuhlmann S, Hellström M, Ramberg U, Reiter R. Tracing divergence in crisis governance: responses to the COVID-19 pandemic in France, Germany and Sweden compared. Int Rev Adm Sci. 2021;87(3):556–75.
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–80.
Article CAS PubMed Google Scholar
Rosella LC, Wilson K, Crowcroft NS, Chu A, Upshur R, Willison D, et al. Pandemic H1N1 in Canada and the use of evidence in developing public health policies—a policy analysis. Soc Sci Med. 2013;83:1–9.
Article PubMed PubMed Central Google Scholar
Saner M. A map of the interface between science & policy. Ottawa, Ontario; 2007. Report No.: January 1.
Lancaster K, Rhodes T. What prevents health policy being “evidence-based”? New ways to think about evidence, policy and interventions in health. Br Med Bull. 2020;135(1):38–49.
Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health. 2009;30:175–201.
Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health. 2002;56:119–27.
Article CAS PubMed PubMed Central Google Scholar
Khan Y, Brown A, Shannon T, Gibson J, Généreux M, Henry B, et al. Public health emergency preparedness: a framework to promote resilience. BMC Public Health. 2018;18(1):1–16.
COVID-19 Evidence Network to Support Decision-Making. COVID-END [Internet]. 2023. https://www.mcmasterforum.org/networks/covid-end . Accessed 25 Jan 2023.
Canadian Institutes of Health Research. Moving forward from the COVID-19 pandemic: 10 opportunities for strengthening Canada’s public health systems. 2022.
Di Ruggiero E, Bhatia D, Umar I, Arpin E, Champagne C, Clavier C, et al. Governing for the public’s health: Governance options for a strengthened and renewed public health system in Canada. 2022.
Adjoa Kumah E, McSherry R, Bettany-Saltikov J, Hamilton S, Hogg J, Whittaker V, et al. Evidence-informed practice versus evidence-based practice educational interventions for improving knowledge, attitudes, understanding, and behavior toward the application of evidence into practice: a comprehensive systematic review of undergraduate studen. Campbell Syst Rev. 2019;15(e1015):1–19.
Download references
Acknowledgements
We would like to extend our gratitude to current and former members of the University of British Columbia Working Group on Health Systems Response to COVID-19 who contributed to various aspects of this study, including Shelly Keidar, Kristina Jenei, Sydney Whiteford, Dr. Md Zabir Hasan, Dr. David M. Patrick, Dr. Maxwell Cameron, Mahrukh Zahid, Dr. Yoel Kornreich, Dr. Tammi Whelan, Austin Wu, Shivangi Khanna, and Candice Ruck.
Financial support for this work was generously provided by the University of British Columbia's Faculty of Medicine (Grant No. GR004683) and Peter Wall Institute for Advanced Studies (Grant No. GR016648), as well as a Canadian Institutes of Health Research Operating Grant (Grant No. GR019157). These funding bodies were not involved in the design of the study, the collection, analysis or interpretation of data, or in the writing of this manuscript.
Author information
Authors and affiliations.
School of Population and Public Health, University of British Columbia, Vancouver, Canada
Laura Jane Brubacher, Chris Y. Lovato, Veena Sriram, Michael Cheng & Peter Berman
School of Public Health Sciences, University of Waterloo, Waterloo, Canada
Laura Jane Brubacher
School of Public Policy and Global Affairs, University of British Columbia, Vancouver, Canada
Veena Sriram
You can also search for this author in PubMed Google Scholar
Contributions
CYL, PB, and VS obtained funding for and designed the study. LJB, MC, and PB conducted data collection. LJB and VS analyzed the qualitative data. CYL and LJB collaboratively wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Laura Jane Brubacher .
Ethics declarations
Ethics approval and consent to participate.
This case study received the approval of the UBC Behavioural Research Ethics Board (Certificate # H20-02136). Participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Semi-structured interview guide [* = questions used for this specific study]
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Brubacher, L.J., Lovato, C.Y., Sriram, V. et al. The use of evidence to guide decision-making during the COVID-19 pandemic: divergent perspectives from a qualitative case study in British Columbia, Canada. Health Res Policy Sys 22 , 66 (2024). https://doi.org/10.1186/s12961-024-01146-2
Download citation
Received : 08 February 2023
Accepted : 29 April 2024
Published : 03 June 2024
DOI : https://doi.org/10.1186/s12961-024-01146-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decision-making
- Public health
- Policy-making
- Qualitative
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Case Study Research Method in Psychology
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews).
The case study research method originated in clinical medicine (the case history, i.e., the patient’s personal history). In psychology, case studies are often confined to the study of a particular individual.
The information is mainly biographical and relates to events in the individual’s past (i.e., retrospective), as well as to significant events that are currently occurring in his or her everyday life.
The case study is not a research method, but researchers select methods of data collection and analysis that will generate material suitable for case studies.
Freud (1909a, 1909b) conducted very detailed investigations into the private lives of his patients in an attempt to both understand and help them overcome their illnesses.
This makes it clear that the case study is a method that should only be used by a psychologist, therapist, or psychiatrist, i.e., someone with a professional qualification.
There is an ethical issue of competence. Only someone qualified to diagnose and treat a person can conduct a formal case study relating to atypical (i.e., abnormal) behavior or atypical development.
Famous Case Studies
- Anna O – One of the most famous case studies, documenting psychoanalyst Josef Breuer’s treatment of “Anna O” (real name Bertha Pappenheim) for hysteria in the late 1800s using early psychoanalytic theory.
- Little Hans – A child psychoanalysis case study published by Sigmund Freud in 1909 analyzing his five-year-old patient Herbert Graf’s house phobia as related to the Oedipus complex.
- Bruce/Brenda – Gender identity case of the boy (Bruce) whose botched circumcision led psychologist John Money to advise gender reassignment and raise him as a girl (Brenda) in the 1960s.
- Genie Wiley – Linguistics/psychological development case of the victim of extreme isolation abuse who was studied in 1970s California for effects of early language deprivation on acquiring speech later in life.
- Phineas Gage – One of the most famous neuropsychology case studies analyzes personality changes in railroad worker Phineas Gage after an 1848 brain injury involving a tamping iron piercing his skull.
Clinical Case Studies
- Studying the effectiveness of psychotherapy approaches with an individual patient
- Assessing and treating mental illnesses like depression, anxiety disorders, PTSD
- Neuropsychological cases investigating brain injuries or disorders
Child Psychology Case Studies
- Studying psychological development from birth through adolescence
- Cases of learning disabilities, autism spectrum disorders, ADHD
- Effects of trauma, abuse, deprivation on development
Types of Case Studies
- Explanatory case studies : Used to explore causation in order to find underlying principles. Helpful for doing qualitative analysis to explain presumed causal links.
- Exploratory case studies : Used to explore situations where an intervention being evaluated has no clear set of outcomes. It helps define questions and hypotheses for future research.
- Descriptive case studies : Describe an intervention or phenomenon and the real-life context in which it occurred. It is helpful for illustrating certain topics within an evaluation.
- Multiple-case studies : Used to explore differences between cases and replicate findings across cases. Helpful for comparing and contrasting specific cases.
- Intrinsic : Used to gain a better understanding of a particular case. Helpful for capturing the complexity of a single case.
- Collective : Used to explore a general phenomenon using multiple case studies. Helpful for jointly studying a group of cases in order to inquire into the phenomenon.
Where Do You Find Data for a Case Study?
There are several places to find data for a case study. The key is to gather data from multiple sources to get a complete picture of the case and corroborate facts or findings through triangulation of evidence. Most of this information is likely qualitative (i.e., verbal description rather than measurement), but the psychologist might also collect numerical data.
1. Primary sources
- Interviews – Interviewing key people related to the case to get their perspectives and insights. The interview is an extremely effective procedure for obtaining information about an individual, and it may be used to collect comments from the person’s friends, parents, employer, workmates, and others who have a good knowledge of the person, as well as to obtain facts from the person him or herself.
- Observations – Observing behaviors, interactions, processes, etc., related to the case as they unfold in real-time.
- Documents & Records – Reviewing private documents, diaries, public records, correspondence, meeting minutes, etc., relevant to the case.
2. Secondary sources
- News/Media – News coverage of events related to the case study.
- Academic articles – Journal articles, dissertations etc. that discuss the case.
- Government reports – Official data and records related to the case context.
- Books/films – Books, documentaries or films discussing the case.
3. Archival records
Searching historical archives, museum collections and databases to find relevant documents, visual/audio records related to the case history and context.
Public archives like newspapers, organizational records, photographic collections could all include potentially relevant pieces of information to shed light on attitudes, cultural perspectives, common practices and historical contexts related to psychology.
4. Organizational records
Organizational records offer the advantage of often having large datasets collected over time that can reveal or confirm psychological insights.
Of course, privacy and ethical concerns regarding confidential data must be navigated carefully.
However, with proper protocols, organizational records can provide invaluable context and empirical depth to qualitative case studies exploring the intersection of psychology and organizations.
- Organizational/industrial psychology research : Organizational records like employee surveys, turnover/retention data, policies, incident reports etc. may provide insight into topics like job satisfaction, workplace culture and dynamics, leadership issues, employee behaviors etc.
- Clinical psychology : Therapists/hospitals may grant access to anonymized medical records to study aspects like assessments, diagnoses, treatment plans etc. This could shed light on clinical practices.
- School psychology : Studies could utilize anonymized student records like test scores, grades, disciplinary issues, and counseling referrals to study child development, learning barriers, effectiveness of support programs, and more.
How do I Write a Case Study in Psychology?
Follow specified case study guidelines provided by a journal or your psychology tutor. General components of clinical case studies include: background, symptoms, assessments, diagnosis, treatment, and outcomes. Interpreting the information means the researcher decides what to include or leave out. A good case study should always clarify which information is the factual description and which is an inference or the researcher’s opinion.
1. Introduction
- Provide background on the case context and why it is of interest, presenting background information like demographics, relevant history, and presenting problem.
- Compare briefly to similar published cases if applicable. Clearly state the focus/importance of the case.
2. Case Presentation
- Describe the presenting problem in detail, including symptoms, duration,and impact on daily life.
- Include client demographics like age and gender, information about social relationships, and mental health history.
- Describe all physical, emotional, and/or sensory symptoms reported by the client.
- Use patient quotes to describe the initial complaint verbatim. Follow with full-sentence summaries of relevant history details gathered, including key components that led to a working diagnosis.
- Summarize clinical exam results, namely orthopedic/neurological tests, imaging, lab tests, etc. Note actual results rather than subjective conclusions. Provide images if clearly reproducible/anonymized.
- Clearly state the working diagnosis or clinical impression before transitioning to management.
3. Management and Outcome
- Indicate the total duration of care and number of treatments given over what timeframe. Use specific names/descriptions for any therapies/interventions applied.
- Present the results of the intervention,including any quantitative or qualitative data collected.
- For outcomes, utilize visual analog scales for pain, medication usage logs, etc., if possible. Include patient self-reports of improvement/worsening of symptoms. Note the reason for discharge/end of care.
4. Discussion
- Analyze the case, exploring contributing factors, limitations of the study, and connections to existing research.
- Analyze the effectiveness of the intervention,considering factors like participant adherence, limitations of the study, and potential alternative explanations for the results.
- Identify any questions raised in the case analysis and relate insights to established theories and current research if applicable. Avoid definitive claims about physiological explanations.
- Offer clinical implications, and suggest future research directions.
5. Additional Items
- Thank specific assistants for writing support only. No patient acknowledgments.
- References should directly support any key claims or quotes included.
- Use tables/figures/images only if substantially informative. Include permissions and legends/explanatory notes.
- Provides detailed (rich qualitative) information.
- Provides insight for further research.
- Permitting investigation of otherwise impractical (or unethical) situations.
Case studies allow a researcher to investigate a topic in far more detail than might be possible if they were trying to deal with a large number of research participants (nomothetic approach) with the aim of ‘averaging’.
Because of their in-depth, multi-sided approach, case studies often shed light on aspects of human thinking and behavior that would be unethical or impractical to study in other ways.
Research that only looks into the measurable aspects of human behavior is not likely to give us insights into the subjective dimension of experience, which is important to psychoanalytic and humanistic psychologists.
Case studies are often used in exploratory research. They can help us generate new ideas (that might be tested by other methods). They are an important way of illustrating theories and can help show how different aspects of a person’s life are related to each other.
The method is, therefore, important for psychologists who adopt a holistic point of view (i.e., humanistic psychologists ).
Limitations
- Lacking scientific rigor and providing little basis for generalization of results to the wider population.
- Researchers’ own subjective feelings may influence the case study (researcher bias).
- Difficult to replicate.
- Time-consuming and expensive.
- The volume of data, together with the time restrictions in place, impacted the depth of analysis that was possible within the available resources.
Because a case study deals with only one person/event/group, we can never be sure if the case study investigated is representative of the wider body of “similar” instances. This means the conclusions drawn from a particular case may not be transferable to other settings.
Because case studies are based on the analysis of qualitative (i.e., descriptive) data , a lot depends on the psychologist’s interpretation of the information she has acquired.
This means that there is a lot of scope for Anna O , and it could be that the subjective opinions of the psychologist intrude in the assessment of what the data means.
For example, Freud has been criticized for producing case studies in which the information was sometimes distorted to fit particular behavioral theories (e.g., Little Hans ).
This is also true of Money’s interpretation of the Bruce/Brenda case study (Diamond, 1997) when he ignored evidence that went against his theory.
Breuer, J., & Freud, S. (1895). Studies on hysteria . Standard Edition 2: London.
Curtiss, S. (1981). Genie: The case of a modern wild child .
Diamond, M., & Sigmundson, K. (1997). Sex Reassignment at Birth: Long-term Review and Clinical Implications. Archives of Pediatrics & Adolescent Medicine , 151(3), 298-304
Freud, S. (1909a). Analysis of a phobia of a five year old boy. In The Pelican Freud Library (1977), Vol 8, Case Histories 1, pages 169-306
Freud, S. (1909b). Bemerkungen über einen Fall von Zwangsneurose (Der “Rattenmann”). Jb. psychoanal. psychopathol. Forsch ., I, p. 357-421; GW, VII, p. 379-463; Notes upon a case of obsessional neurosis, SE , 10: 151-318.
Harlow J. M. (1848). Passage of an iron rod through the head. Boston Medical and Surgical Journal, 39 , 389–393.
Harlow, J. M. (1868). Recovery from the Passage of an Iron Bar through the Head . Publications of the Massachusetts Medical Society. 2 (3), 327-347.
Money, J., & Ehrhardt, A. A. (1972). Man & Woman, Boy & Girl : The Differentiation and Dimorphism of Gender Identity from Conception to Maturity. Baltimore, Maryland: Johns Hopkins University Press.
Money, J., & Tucker, P. (1975). Sexual signatures: On being a man or a woman.
Further Information
- Case Study Approach
- Case Study Method
- Enhancing the Quality of Case Studies in Health Services Research
- “We do things together” A case study of “couplehood” in dementia
- Using mixed methods for evaluating an integrative approach to cancer care: a case study
Related Articles
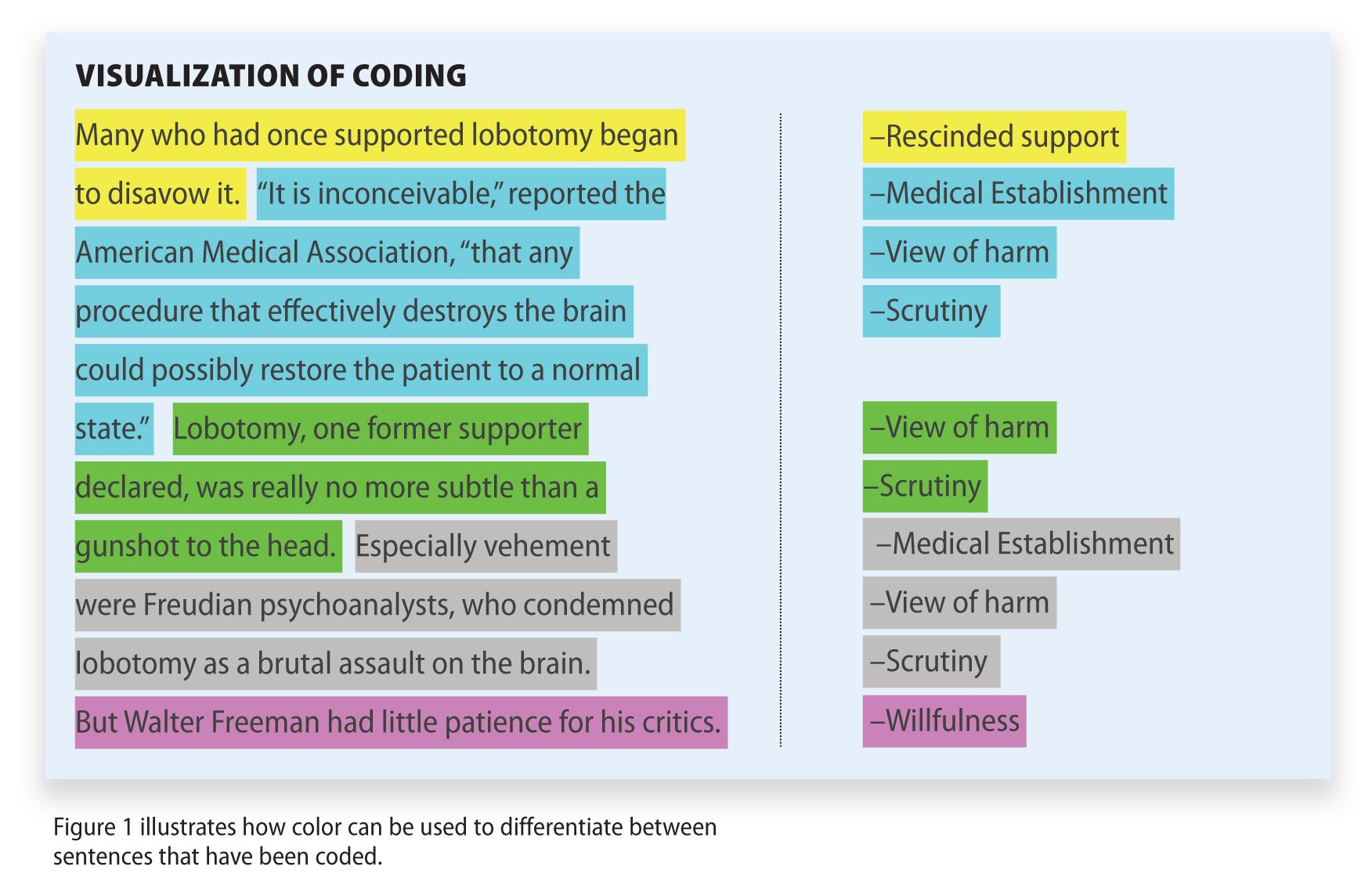
Research Methodology
Qualitative Data Coding

What Is a Focus Group?
Cross-Cultural Research Methodology In Psychology

What Is Internal Validity In Research?

Research Methodology , Statistics
What Is Face Validity In Research? Importance & How To Measure

Criterion Validity: Definition & Examples
Loading metrics
Open Access
Peer-reviewed
Research Article
Process evaluation of the HIV+D intervention for integrating the management of depression in routine HIV care in Uganda
Roles Conceptualization, Formal analysis, Methodology, Writing – original draft
* E-mail: [email protected]
Affiliation Medical Research Council/Uganda Virus Research Institute & London School of Hygiene and Tropical Medicine Uganda Research Unit, Mental Health Research Unit, Entebbe, Uganda
Roles Validation, Writing – review & editing
Roles Methodology, Project administration
Roles Methodology, Supervision, Writing – review & editing
Affiliations Medical Research Council/Uganda Virus Research Institute & London School of Hygiene and Tropical Medicine Uganda Research Unit, Mental Health Research Unit, Entebbe, Uganda, Butabika National Referral Mental Hospital, Kampala, Uganda
Roles Investigation, Supervision, Writing – review & editing
Roles Conceptualization, Supervision
Affiliation Mental Health Division, Ministry of Health, Kampala, Uganda
Roles Conceptualization, Funding acquisition, Resources
Roles Conceptualization, Resources, Supervision
Affiliation Department of Global Health and Social Medicine, Harvard Medical School, Boston, Massachusetts, United States of America
Roles Conceptualization, Funding acquisition, Project administration, Supervision, Validation
- Joshua Ssebunnya,
- Rutakumwa Rwamahe,
- Richard Mpango,
- Leticia Kyohangirwe,
- Christine Tusiime,
- Hafsa Sentongo,
- Pontiano Kaleebu,
- Vikram Patel,
- Eugene Kinyanda

- Published: June 4, 2024
- https://doi.org/10.1371/journal.pmen.0000009
- Peer Review
- Reader Comments
HIV/AIDS continues to be one of the leading global health challenges, having claimed over 40 million lives so far. People infected with HIV are more likely to develop depression, leading to several negative behavioural and clinical outcomes. Studies have reported exceptionally high prevalence of depressive symptoms among people living with HIV/AIDS (PLWHA), making a case for integrating mental healthcare in routine HIV care. The HIV+D program was implemented in Uganda as an intervention model for integrating the management of depression in HIV care. Process evaluation was carried out to understand the contextual factors and explain the outcomes of the intervention. This was a qualitative study, conducted in 28 out of the 40 public health facilities in 3 districts, where the intervention was undertaken. A total of 82 participants, including the implementers and beneficiaries of the intervention were purposively selected for key informant interviews and focus group discussions. Conventional content analysis was done focusing on 6 aspects including reach, effectiveness, acceptability, implementation fidelity, maintenance (sustainability) and contextual factors that affected the intervention. The intervention was well received and believed to address a real need of the intended beneficiaries; many of whom described it as a program for helping the depressed PLWHA to deal with their depression. The implementers were said to have adhered to the intervention protocol, without major program adaptations, suggesting strong implementation fidelity. The respondents cited several positive health outcomes that resulted from the intervention, for both the beneficiaries and the implementers. Several contextual factors affected the implementation. Although it met the beneficiaries’ approval, and was considered relevant and acceptable, they expressed uncertainty over sustainability of the intervention in a health system characterized by understaffing, resource constraints and several other challenges. The intervention was generally implemented as intended, resulting in several positive health outcomes.
Citation: Ssebunnya J, Rwamahe R, Mpango R, Kyohangirwe L, Tusiime C, Sentongo H, et al. (2024) Process evaluation of the HIV+D intervention for integrating the management of depression in routine HIV care in Uganda. PLOS Ment Health 1(1): e0000009. https://doi.org/10.1371/journal.pmen.0000009
Editor: Justus Uchenna Onu, Nnamdi Azikiwe University, NIGERIA
Received: December 11, 2023; Accepted: March 17, 2024; Published: June 4, 2024
Copyright: © 2024 Ssebunnya et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: De-identified data from which this manuscript has been produced will be made available upon request, but the full data set may not be shared due to the qualitative and potentially identifiable nature of the raw data (eg, transcripts). Request for data access should be made to the UVRI – REC Chairperson: Mr. Tom Lutalo, [email protected] and committee member, Mr. Wilber Ssembajjwe, [email protected] .
Funding: The study was supported by an unrestricted grant from the Wellcome Trust through a Senior Research Fellowship in Public Health and Tropical Medicine to EK, reference number 205069/Z/16/Z. The funders had no influence on the design or conduct of the study and were not involved in data collection or analysis, in the writing of the manuscript, or in the decision to submit it for publication.
Competing interests: The authors have declared that no competing interests exist.
Introduction
HIV/AIDS is one of the most devastating illnesses that humans have ever suffered. It remains a major public health issue impacting communities all over the world, having claimed over 40 million lives so far, and with an estimated 39 million people living with HIV globally, as at the end of 2022 [ 1 ]. Eastern and Southern Africa, an under-resourced region with significant health system constraints [ 2 ], remains the region most heavily affected, with an estimated 20.6 million people living with HIV [ 1 , 3 ]. Several studies have shown that depression is one of the most common comorbid conditions in people infected with HIV, with approximately 8–50% of persons living with HIV reported to have suffered from depressive disorders [ 4 – 8 ]. In Uganda, a recent meta-analysis found a pooled depression prevalence of 28.2% among people living with HIV/AIDS (PLWHA), nearly ten times higher than the prevalence estimates in the general population [ 9 ].
Depression in PLWHA worsens the existing disease states, as it not only affects the quality of life [ 10 ], but has been associated with poorer health outcomes such as hastening the progression to AIDS [ 11 – 13 ], poor adherence to HIV treatment, risky sexual behaviour and increased utilization of health facilities [ 14 – 16 ] and elevated risk of mortality [ 5 , 17 ]. Although an estimated 76% of the PLWHA globally are on antiretroviral (ARV) treatment, the majority of HIV care providers in sub-Saharan Africa do not routinely provide mental health services to address the problem of depression [ 3 ]. However, there is growing evidence of specific treatments for depression among PLWHA, associated with anti-retroviral therapy (ART) adherence and reduced HIV disease progression [ 18 – 20 ]. This makes a case for integrating such treatments in routine HIV care [ 21 – 23 ].
With an estimated 1.4 million people living with HIV/AIDS in Uganda, studies have reported exceptionally high prevalence of depressive symptoms among PLWHA, posing a major challenge in HIV care, despite the success in the scale up of anti-retroviral therapy. This consequently increases mortality [ 14 , 24 ]. To address the absence of mental health care in HIV programs, the Uganda National HIV and AIDS Strategic Plan (2020/21–2024/25) called for the integration of mental health and other chronic conditions in HIV care so as to further improve the quality of care and treatment. In a similar vein, the 2016 Ministry of Health policy initiative and guidelines called for the assessment and management of depression in PLWHA [ 25 ].
In response to the above calls, the Mental Health Section of the Medical Research Council (MRC)/Uganda Virus Research Institute (UVRI) & London School of Hygiene and Tropical Medicine (LSHTM) Uganda Research Unit, in partnership with the STD/AIDS Control Program of the Ministry of Health, Uganda Implemented the HIV+D intervention model. This was a 5 year project implemented in 3 districts within Uganda. The intervention model consisted of psychoeducation, Behavioural Activation, antidepressant medication and referral to mental health workers; delivered in a stepped care fashion. The therapies have previously been shown to be effective against depression in primary care settings including in HIV care [ 26 – 29 ].
Process evaluation, which is carried out during or after the intervention to evaluate and explain the outcomes has become a dominant part of clinical trials [ 30 ]. It focuses on how and why the intervention works or does not work in the context of the trial [ 31 , 32 ]. Process evaluation is critical for interpreting the outcomes of trials of complex interventions and aids in the understanding of contextual factors associated with intervention and implementation effectiveness; which can influence potential replication in different settings as well as scale up [ 33 , 34 ].
It is on this basis that we set out to conduct a process evaluation for the HIV+D intervention.
The aim of the study therefore was to assess and report results of the process evaluation of the HIV+D intervention. This was deemed necessary so as to understand whether the intervention was implemented as intended and received similarly across all sites; and to understand the variation in outcomes, breadth and depth in effectiveness; thereby differentiating intervention failure from implementation failure. The process evaluation would justify any variability in the intervention outcomes and inform strategies to integrate the management of depression in HIV care.
Overview of the intervention
The HIV + D intervention model was based on therapies that have been shown to be effective against depressive disorder in primary care settings including in HIV care, namely: psychoeducation, behavioural activation-the Healthy Activity Program (HAP) [ 29 ] and antidepressant medications [ 27 ]. These were delivered in a stepped care format and overseen by an HIV counsellor (Lay Health Worker). Recruitment of participants in the study started on Monday 3rd May 2021 and ended on Friday 31st December 2021.
Recruitment would start with a health talk about depression, given by a trained Lay Health Worker (LHW) to PLWHs sitting in the triage area of the participating Public Health Care Facilities. Thereafter, consecutive attenders would be approached and requested to be screened for the study. The screening would be done by the trained LHW using the PHQ-2 (a two-item questionnaire that assess for ‘depressed mood’ and ‘loss of interest in typically pleasurable activities’). Those screening positive (PHQ-2 score ≥ 3) would be invited for further evaluation by the trained LHW for trial eligibility and consent. The eligibility assessment would include confirmation of depressive symptoms using the PHQ-9 tool [ 35 ]. The eligible respondents would be recruited into the intervention. Those with suicidal ideation (endorsing item 9 on the PHQ-9) would immediately be referred to the supervisor for further assessment and then referral to a mental health specialist (Psychiatric Clinical Officer) for further management.
The intervention was delivered in 4 steps. Step 1: (initiation of treatment), patients with PHQ-9 scores of 10–19 would be told of their scores and offered psychoeducation by a LHW. Step 2: (management of moderate to severe cases), patients who remained symptomatic at follow up (PHQ-9 score ≥ 5 after 4 weeks) would be offered Behavioural Activation (BA); 4–10 bi-weekly sessions) by a LHW. Step 3: (monitoring outcomes), if after 6 sessions of BA, one still scored 10 and above on PHQ-9, they would continue BA sessions to completion and add antidepressant medication (Fluoxetine 20 mg/day for 6 months), initiated by the HIV clinician. Step 4: (referral to mental health worker), if there was no improvement (PHQ-9 ≥ 5) after step 3 or at eligibility assessment PHQ-9 ≥ 20, or if someone had a moderate to high suicide risk (based on suicide risk assessment by the supervisor), they would continue all existing treatment and be referred to a mental health worker. This is summarized in the appended CONSORT flow diagram ( S1 Fig ) and CONSORT checklist ( S1 Checklist ).
The interventions were delivered to the recruited PLWHA in the intervention sites, while those in the control sites received enhanced usual care following mental health Gap Action Plan (mhGAP) treatment guidelines. Full details of the intervention are described elsewhere in the HIV+D protocol paper, appended as supporting information ( S1 Text ) [ 36 ].
Conceptual framework for implementation outcomes
The process evaluation was designed in line with the MRC guidelines for process evaluations [ 30 ]; specifically using the RE-AIM framework [ 37 ]. This is a framework that guides planning and evaluation of programs, focusing on 5 key dimensions: (i) reach (the extent to which the intervention was received by the targeted group), (ii) efficacy/effectiveness (effects of the intervention on health outcomes), (iii) acceptability (extent to which participants found the intervention relevant, acceptable and satisfactory), (iv) implementation fidelity (extent to which the intervention was delivered as planned), (v) maintenance (extent to which the intervention can be integrated within the existing structure and sustained over time). Thus, in this paper, we report on the above 5 implementation outcomes, which formed the basis of our process evaluation. Although not part of the framework, we also report on context (environmental aspects of the intervention setting) as an additional dimension that has been acknowledged as a key dimension [ 32 ].
The specific objectives of the study were thus:
- To assess and determine the extent to which the intervention reached the target group.
- To document the effects of the intervention on the health outcomes in the target population.
- To determine the extent to which the participants found the intervention relevant and satisfactory.
- To determine the extent to which the intervention was implemented as intended across the different intervention sites.
- To explore the perceived sustainability and integration of the intervention within the existing HIV care system
- To describe the contexts in which the intervention was delivered and explore contextual factors that have influenced the delivery and outcomes of the intervention.
The HIV+D program was implemented in 40 public health facilities, which were randomly selected across the 3 study districts of Wakiso and Masaka (semi-urban and rural), and Kalungu (predominantly rural). These are all in central Uganda. All the facilities were running active HIV/AIDS clinics. This process evaluation was a qualitative study, conducted in 28 of the 40 public health facilities (14 intervention sites and 14 control sites) between June 2021 and April 2022.
Study participants and sampling
We set out to conduct the process evaluation in all the 40 health facilities and involve purposively selected participants who could provide in-depth and detailed information on the topic under investigation. These included the health workers who delivered the intervention, the study data collectors, lay health workers, persons living with HIV/AIDS and carers (treatment supporters). However, the data collection went on until we reached saturation and further data collection was deemed redundant; after covering 28 health facilities, with a total of 82 participants.
Data collection
Data was collected through key informant interviews (KIIs) and focus group discussions (FGDs) to understand the context and process, characteristics of the intervention, effectiveness, facilitating factors and challenges from the perspective of different stakeholders. An interview guide with items covering these aspects was developed for this purpose. A total of 58 KIIs and 6 FGDs were conducted with the different stakeholders, as summarized in Table 1 below. All interviews and FGDs were audio-recorded. The interviews with health workers and data collectors were conducted in English, while those with the LHWs, PLWHA and carers were conducted in Luganda (the local language) and translated during the transcription. The transcription and translation were done by the first author and one of the research assistants, both being very conversant with the 2 languages, and having strong experience in qualitative data collection methods.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmen.0000009.t001
Data analysis
After the transcription, conventional content analysis was done by the 2 researchers who have expertise in qualitative research and data analysis, to ensure rigour. They subjectively interpreted the content of the transcripts through coding and identifying themes [ 38 , 39 ]. The initial coding of the transcripts was undertaken by the first author, guided by predefined themes and sub-themes derived from the study objectives. These were amended along the way based on the transcription data. The coded transcripts were shared with the first co-author for common interpretation, improvement and consensus. A data analysis matrix sheet was then used to generate a concise summary of the key results.
Ethical considerations
Ethical approval was obtained from the UVRI Research and Ethics Committee (07 th April, 2020), the LSHTM Ethics Committee (17 th September, 2020) and the Uganda National Council for Science and Technology (ethical clearance number: HS645ES) (07 th July, 2020). All study participants gave written informed consent to participate in the study.
The results are presented below, under 5 themes: effectiveness, acceptability, implementation fidelity, maintenance (sustainability) and contextual factors that affected the intervention. Given the study design, it was not possible to meaningfully assess “reach”.
Acceptability
The key implementers for the program at the primary health care facilities included health workers (clinical staff), lay health workers (members of the Village Health Teams), data collectors. Some of the respondents could not give a very precise description of the program, but indicated that it was a program for treating depressed PLWHA. The non-health care professionals (LHWs and data collectors) termed it as “a program for helping PLWHA who were depressed to deal with their depression, as part of their HIV treatment program, so as to live positively.”
It emerged that the counselling provided in the routine HIV clinics mostly focused on the importance of adherence to treatment (taking ARVs), rarely addressing the clients’ psychosocial concerns and depressive feelings. However, the PLWHA reiterated that under the HIV+D intervention, they received a kind of counselling they had never received before, which helped them dealing with their psychosocial problems; although many did not know that depression is an illness; and its term in the local language was not familiar to them.
Aspects of acceptability included the respondents’ level of interest in the HIV+D program and perceptions about its relevance and usefulness as well as the level of satisfaction. The intervention and its content met the respondents’ approval, and was generally considered relevant and acceptable. The participating health workers and supervisors commented on the appropriateness of the intervention, affirming that the program addressed a real need of the target population and was much needed, given the agony, health and socio-economic challenges associated with being HIV positive. They further reported having a sense of contentment that the intervention provided for helping the depressed PLWHA more meaningfully. On the other hand, some of the PLWHA admitted that at the time of this intervention, they were still struggling to come to terms with their HIV status; and the program had greatly helped them in this aspect. There were reports of increased awareness and recognition of depression as a common health problem among PLWHA, for which they ought to seek help. One PLWHA stated:
“… Before , it was like I was in my own world , because of my HIV status . I had nothing to do to earn some money . It also seems there was another disease , inside me and I had so many thoughts … so many questions … || … I was taking the medicine (ARVs) but it wasn’t working for me … and that was mentioned by the health workers , that if you have so many thoughts , the medicine you’re taking will not work for you . Personally , I was depressed and doing badly ” (KII 40, PLWHA, Busawamanze HC III).
A health worker affirmed:
“… at first they did not even know that depression is an illness , some would tell us : ‘Nurse I did not know that to feel like this , it’s an illness . Someone can have problems , move with them every day but does not know that it is an illness’ . So patients got to know that there is a solution to those problems and one does not have to be depressed .” (FGD 06, health workers, Busawamanze HCIII).
The respondents across the different health facilities gave reports indicating high levels of patient satisfaction with the service. For example, one supervisor said:
“… Someone comes and say “nurse you have helped me a lot . Those things sessions that been through have helped me understand myself , I feel better . It means that the patient is appreciative and feels helped , I am satisfied and feel it ” (Respondent 1, FGD 02, Supervisors).
Patient satisfaction was further confirmed by the fact that some of the PLWHA and carers identified and referred fellow PLWHA in their communities, whom they believed to be depressed, for recruitment into the program. Similarly, the health workers at the facilities offering the intervention reported an increase in the number of clients seeking treatment at these facilities, attracted by the program.
Implementation fidelity
According to the protocol, the implementation would start with a health talk on depression, delivered by a lay health worker, followed by screening for depressive symptoms. The screen positive would be further subjected to an eligibility assessment to confirm the depressive symptoms before consenting for enrollment. In their accounts, most respondents affirmed that screening for depressive symptoms would be done using the PHQ-9, followed by testing for eligibility before recruitment into the program. The screen positives would initially receive psychoeducation and those whose symptoms persisted be recruited to receive Behavioural Activation therapy, which was the main intervention for the program. These would attend bi-weekly BA sessions until full remission of the symptoms. At the control sites, they would assess for depression and any other physical condition such as high blood pressure and then give medication accordingly; though not giving the clients much time, as was the case at intervention sites. However, there were some variations and confusion in some of the respondents’ description of the intervention design and components, as they seemed to confuse the procedure and order of the steps and to confuse the initial health talk that would be given, with psychoeducation which was offered as part of the therapy.
It was noted that at all health facilities, the implementers duly adhered to the intervention protocol, conducting the activities according to the plan, without major program adaptations or alterations of any critical components relating to the content, activities or delivery of the program. The process evaluation thus revealed strong implementation fidelity.
Effect of the intervention on health outcomes of the target population
The intervention was said to have been delivered with excellent facilitation skills, enthusiasm and positive attitude across the implementation sites, which resulted in positive outcomes. It was noted that the intervention resulted in increased awareness and recognition of depression as a health problem, awakening the health workers’ awareness to focus beyond presenting complaints and symptoms while handling patients.
Apparently many of the PLWHA with depressive symptoms did not know that they were having a health problem that warranted clinical intervention. The health workers on the other hand confessed that they were previously not offering adequate help because they were less confident in assessing for depression, and did not give it consideration, as reflected in the quote below:
“… we the health workers did not know these symptoms . We were not assessing the clients for depression because we did not have that knowledge … and we did not know it was important anyway ” (KII 46, Health facility manager/supervisor)
The intervention was reported to have resulted in increased competence and confidence to detect and treat depression associated with HIV or any other causes. Similarly, the health workers appreciated the importance of giving the patients more time and conducting a detailed assessment to inquire about patients’ psychosocial problems.
“… What I observed in this study if you have not talked to the person you cannot know what they are going through but when you talk with them at length , you discover that people have problems . You watch the person coming in to the clinical room as usual things seem normal but if you start a conversation with that person and give him/her time , you find that they are depressed ” (Respondent 2, FGD 01, study supervisors).
Another health worker echoed:
“… even us health workers in ART clinic , we were not emphasizing depression treatment so much . We would only ask them about how many tablets the patient is left with . And if one is not the taking medicine , we only asked “why” , but we could not go deep to find out whether the client is depressed or not ” (KII 44, Health worker)
It was reported that by design, the intervention strengthened the bond between the health workers and PLWHA, resulting in improved Patient-Health worker relationship, empathy and compassion. The improved relationship was said to have contributed to increased disclosure by the PLWHA to the health workers as well as the family members, for those who were living in denial or struggling to keep their HIV status a secret, resulting in increased adherence to treatment. This is reflected in the voices below:
“… Before [the intervention] , we would come to the facility but never got a chance to sit with a health worker to talk like we are doing now . O . k the nurse would ask whether you have anything bothering you , whether you are taking the medicine …. but doing so in a rush . You could see that she is after clearing the long queue . So , it would be hard to disclose important information ” (KII 054, PLWHA, Mpugwe HCIII).
One health worker also affirmed:
“… So , because of the good relationship we have now , they don’t miss on their appointments . And sometimes a client comes just to greet you . But before [the intervention] , that could not happen for a patient to come and say “nurse I have this problem” the moment you give them medicine , they would just walk away . Sometimes this patient may be going through hardships and you the health worker can never know about it unless the patient discloses ” (Respondent 01, FGD 06, PHC workers)
The PLWHA anticipated that the improved relationship they developed with the health workers in the course of the program would be an opportunity to leverage on and serve as a potential buffer against likely psychosocial problems long after the project.
The health workers at various health facilities reported an increase in prescription and consumption of the anti-depressant medication, which would previously expire at some of the facilities. Consequently, there was a reduction in the depressive symptoms among the beneficiaries. This was further exemplified by the significant drop in the clients’ PHQ-9 scores on the subsequent visits.
One of the remarkable outcomes reported was the improvement in adherence to treatment and positive living. Some of the PLWHA confessed that they previously deliberately defaulted on treatment and could not see the point in continuing with medication that would not lead to absolute healing. However, they had resumed taking their ARVs following the intervention.
“… before this program , I would come pick the medicine , but I was not taking it … would just keep it home waiting for death …. || … when I came and had a health talk with the health worker , I went home picked the tins of medicine and brought them back to the health facility . I confessed that I was not taking the medicine . Actually some tins had expired , so they were thrown away . But now , am taking the medicine and have not skipped even a day ” (KII 054, PLWHA, Mpugwe HCIII).
It emerged that for some PLWHA, defaulting on taking their ARV medication was driven by their suicidal ideation, wishing they could die in the process. Indeed, some of them shared testimonies indicating how they had contemplated suicide at some point, because of their HIV status and how they had deliberately defaulted on ARV medication, hoping it would be an easy gateway to death without having to use the more obvious means of committing suicide. There were reports of several PLWHA who were previously very depressed and contemplating suicide, but had improved tremendously following the intervention.
Another key outcome proving the efficacy of the intervention relates to the reported noticeable increase in viral load suppression among PLWHA at several health facilities. The health workers reported on several cases of PLWHA who had failed to suppress the viral load despite taking their ARVs for some time, but were able to achieve the suppression in the course of this intervention.
The respondents also cited some noteworthy unintended effects of the intervention. One such effect was the gain in terms of capacity building for the lay health workers who were trained in delivering BA intervention. They affirmed that delivering the intervention was in some way a learning experience for them as well, having acquired more knowledge and skills in counselling in the process, which could potentially enable sustainability of the intervention.
One such effect was the reported improvement in the welfare of some PLWHA, attributable to the small financial support they received as transport refund whenever they attended therapy sessions. One respondent revealed:
“… There are some two women in their 50s who said they had given up on life . One of them said ‘this money they give us , now I was able to buy a hoe or shoes . Because previously , I was walking bare-footed . I was even able to buy cups and plates for the home . Previously , one would have to take tea and wash the cup so that another one can also take . We did not have enough cups and plates . We would get maize from the garden , cook it and put on banana leaves and take water as soup . But you have helped us a lot . Now everyone has a plate and a cup’ . So , you realize that the program has helped this person financially ”. (KII 028, Expert Client, Kyanamukaaka HCIV).
Sustainability
The health workers were optimistic that the intervention could be adopted and incorporated into the existing HIV/AIDS care system. However, they expressed uncertainty over continuity of the intervention and sustainability of the gains, due to challenges such as understaffing and resource constraints. The PLWHA and carers too were skeptical that the quality of service would remain the same under the mainstream health care system, given the resource requirements. They thus maintained that adoption of such an intervention would necessitate scaling up of the staffing in light of the fact that the intervention entails health workers giving patients adequate time. The health workers further expressed willingness to continue delivering the intervention even after the end of the trial.
Contextual factors
The context and mode of operation at all the health facilities was generally the same, save for some difference in the staffing levels. However, several contextual factors relating to health worker’s attitude and skills, resources, organizational norms etc affected the implementation and the outcomes.
The respondents affirmed that the intervention addressed an actual need and was long overdue. The PLWHA and carers specifically commented on the humility, compassion and the positive attitude of the health workers who delivered the intervention as key facilitating factors that enabled smooth running of the intervention. The warm patient-health worker relationship has been key in fostering adherence and recovery. This was further backed by teamwork and a good working relationship that the implementers exhibited.
According to the health workers, the training they received to deliver the intervention was thorough, backed by close supervision by other project staff, which enabled them to appreciate the intervention well. In addition, they showed commitment towards the work, and were motivated by the incentive; thereby giving the program adequate time.
The transport refund given to the PLWHA recruited into therapy was also cited as a major motivating factor for patients’ attendance. Apparently, many of them previously did not show interest to turn up for the counseling sessions in the routine HIV care. Relatedly, it was reported that the beneficiaries of the intervention (PLWHA) had high expectations, in terms of material support at the time of recruitment. This was believed to have influenced their compliance and consistence in attending the therapy sessions.
There were also a few contextual factors that negatively affected implementation. Most notable of these was the nearly 2 years of Covid-19 lockdown characterized by high levels of anxiety, restriction of movement and disruption of work and people’s lives. Implementation was mostly around that timing, and necessitated conducting some of the therapy sessions on phone.
Like in any study setting, there was a limit on the number of clients to recruit at the health facilities, to a maximum of 30 PLWHA. According to some of the respondents, the limit meant leaving out some other potentially depressed clients who would actually have benefited from the service.
One major challenge in the implementation of the intervention was to do with the screening and testing clients for eligibility. It emerged that by design, the program involved too much paperwork right from assessment of individuals for eligibility, recruitment into therapy and other processes. This was considered to be practically cumbersome if the intervention is to be replicated or rolled out under normal circumstances (outside a research study context).
“… we talked about the long questionnaires … time . Some of the patients would get impatient . And our patients would always want their visits to coincide with the day for picking their drugs . Time was a major concern ” (FGD 02, Health workers, Bukakata HC III)
Related to the above, there was a possible risk of some of the PLWHA answering questions just for the sake, when already tired of the so many questions, thereby giving wrong information. Furthermore, some of the lay health workers and expert clients thought the idea of using screening tools in recruiting clients into therapy was superficial, arguing that all PLWHA have psychosocial problems and ideally should benefit from the service.
The HIV+D process evaluation findings indicated that the intervention reached the target population and was generally implemented and received as intended. Most stakeholders described the intervention as “a program for helping PLWHA who were depressed to deal with their depression”; an indicator that they were clear about the goal of the intervention and the target population. Importantly, the PLWHA acknowledged the fact that they received a form of counselling quite different from the usual HIV counselling delivered in the HIV clinics. The fact that most of them initially did not consider depression to be an illness is of particular concern, as it has implications on the likelihood of seeking help.
The intervention received approval from the implementers (health workers) as well as the recipients (PLWHA and carers); who considered it to be acceptable and very necessary. Importantly, several respondents, including health workers believed that all PLWHA would ideally benefit from the intervention in light of the fact that acquiring HIV can be a serious psychological trauma, predisposing one to psychological distress and different mental disorders [ 40 , 41 ]. This was further confirmed by health workers who cited several examples of PLWHA who earlier on seemed to be doing well, but turned out to be harboring serious distressing problems which were unearthed during the therapy sessions, much to the surprise of the health workers. This could be one reason why at the time of this evaluation, most respondents wished for continuity of the program and expressed disappointment to learn of its impending closure.
Fidelity was a function of the implementers and encompassed both the quality and quantity of delivery [ 42 ]. As earlier noted, not all respondents could accurately describe the intervention and give a perfect narration of how it was implemented from the onset. However, their summative description indicated that the health workers endeavoured to comply with the procedure and activities as set out in the intervention protocol, with no significant adaptations.
It is worth noting that both the implementers and recipients of the intervention expressed concern over the much paperwork involved, especially in the screening and recruitment process. While this was a procedural requirement as per the design of the intervention, and also important for scientific rigor (for the research aspect), it may be rather cumbersome and not practically viable in the normal clinical setting. Indeed, this emerged as one of the challenges encountered during the implementation, and would need to be considered critically while making arrangements for scaling up the intervention.
Some of the health workers cited some examples of PLWHA who disclosed during the therapy sessions that they had earlier contemplated suicide because of their HIV status, but had not responded affirmatively to the suicide item during the assessment. Several earlier studies have asserted that suicidal behaviours are much more pronounced in PLWHA [ 43 – 46 ], citing the relationship between HIV-related stigma, depression and suicidal ideation among PLWHA [ 47 ]. This therefore speaks to the likely concealment of the suicidal ideation during the screening and the need for thorough assessment so as to respond and intervene appropriately. One of the striking findings was the revelation by some of the PLWHA, that they deliberately defaulted on their ARV medication, with the ulterior motive of dying in the process. Several studies have found PLWHA to have a higher likelihood of suicidal ideation due to a significant burden of disease they have to contend; often mediated by several psychosocial variables such as high perceived stigma, low self-esteem, social support and resilience [ 48 – 50 ].
The findings further alluded to effectiveness of the intervention. According to the respondents, the intervention resulted in several positive treatment outcomes (both direct and indirect), demonstrating the importance of giving PLWHA in therapy adequate time to assess their psychosocial wellbeing and understand their plight. The intervention was thus considered a success despite being implemented during the difficult times of Covid-19 lockdown, associated with numerous challenges causing distress to communities. The observed efficacy is in support of other earlier studies that have reported on the effectiveness of Behaviour Activation therapy in treating depression, even though little is known about its working mechanisms [ 51 , 52 ]. The beneficiaries appreciated the intervention, as it apparently gave them something beyond what they ordinarily received under the usual HIV care system; illustrating the effectiveness of psychological treatments for depression.
Several contextual factors were reported to have affected the implementation of the intervention. It should be noted that both the implementers (health workers) and the beneficiaries (PLWHA and their carers) overemphasized the facilitation in terms of transport refund as having been key to their participation and consistence. Given the high poverty levels, some would even endure walking the long distances, so as to save the money and support their financial needs.
This seems to suggest that many of them were mostly driven by some extrinsic motivation, instead of their underlying condition; implying that their attendance and consistence would probably have been difficult if there was not such facilitation, as a motivating factor. This casts doubt on the sustainability of the intervention at health facility level under the current health system, characterized by inadequate staffing and resource constraints. Nevertheless, the health system ought to devise strategies for scaling up or integrating the intervention in the mainstream HIV care in light of its potential positive effects.
In light of the above findings, we reasonably conclude that the intervention was generally implemented as planned, and considered acceptable and satisfactory by the implementers and beneficiaries. All respondents concurred with the fact that the intervention was beneficial and feasible; calling for its integration into the mainstream HIV/AIDS care system.
Lessons learnt and recommendations
Some of the lessons learnt in the course of the implementation, which could potentially inform the scale up of the intervention include:
- The importance of a warm patient-health worker relationship and its potential impact on treatment outcomes.
- The importance of supervising the implementers very closely when rolling out such an intervention
- The role played by stigma and discrimination in non-adherence to treatment and loss to follow up among PLWHA.
- Poverty is a strong mediating factor leading to depression among the PLWHA.
In light of the above, we make the following recommendations:
- The need to prioritize training of all health workers involved in HIV care in mental healthcare, to be able to assess for, detect and manage the less obvious psychosocial problems and their manifestation among PLWHA.
- While there were reports of stigma and discrimination against the PLWHA, the participants’ revelations apparently pointed towards more of self-perceived (internalizing stigma). Interventions for PLWHA should therefore not overlook this problem.
- The need for special consideration of the PLWHA who are socio-economically disadvantaged, prioritizing them in economic support programs such as the Social Assistance Grants for Empowerment (SAGE) program.
Limitations of the study
The intervention had to go on during the COVID-19 pandemic. The lock-down that ensued and the associated restrictions certainly reduced activity and participation rates; implying that the overall impact of the intervention could have been more significant had it not been the disruptions by the COVID-19 pandemic. However, the process evaluation did not assess for the effect of the pandemic on the programme.
One other limitation of the study is the fact that we relied on qualitative measurements, collecting data from a relatively small sample of individuals, which may affect the generalization of the findings. Furthermore, we did not do any quantitative assessment of the intervention outputs; making it hard to assess and demonstrate rigour.
Supporting information
S1 checklist. spirit checklist (consort checklist)..
Standards of how the HIV+D trial was designed, analyzed and interpreted.
https://doi.org/10.1371/journal.pmen.0000009.s001
S1 Fig. HIV+D Consort flow diagram.
Visual representation of the steps involved (progress and phases) for the HIV+D trial.
https://doi.org/10.1371/journal.pmen.0000009.s002
S1 Text. HIV+D protocol paper.
Article about the HIV+D study, highlighting the rationale and objectives of the study, methodology, data management and analysis.
https://doi.org/10.1371/journal.pmen.0000009.s003
- 1. UNAIDS. IN DANGER: UNAIDS Global AIDS Update 2022 [Internet]. Geneva: Joint United Nations Programme on HIV/AIDS; 2022 July 27 [cited 2023 July 16]. 376p. Report. https://www.unaids.org/sites/default/files/media_asset/2022-global-aids-update_en.pdf .
- View Article
- PubMed/NCBI
- Google Scholar
- 24. Uganda AIDS Commission [Internet]. Kampala: Uganda AIDS Commission; 2022. Facts on HIV and AIDS in Uganda, 2022 [cited 2023 October 11]. https://uac.go.ug/media/attachments/2023/01/12/hiv-aids-factsheet-2022.pdf .
- 25. Uganda AIDS Commission [Internet]. Kampala: Uganda AIDS Commission; 2015. The Uganda National HIV and AIDS Strategic Plan 2015/2016–2019/2020 [cited 2023 June 19]. http://library.health.go.ug/publications/service-delivery-diseases-control-prevention-communicable-diseases/hivaids/national-h-1 .
Barriers to Accessing Mental Health Care Under the Mental Health Services Act: A Qualitative Case Study in Orange County, California
Affiliations.
- 1 College of Social Work, University of Utah, Salt Lake City, UT, USA. [email protected].
- 2 Herbert Wertheim School of Public Health and Human Longevity Sciences, University of California San Diego, La Jolla, CA, USA.
- PMID: 36121527
- DOI: 10.1007/s10597-022-01016-7
Despite progress made under California's Mental Health Services Act, limited access to care for cultural and linguistic minority groups remains a serious issue in community mental health. In this qualitative study we report findings from a large-scale community-level assessment that explored barriers to accessing care from the perspectives of multiple stakeholders including county advisors, advocates, community members, and consumers representing a range of cultural and linguistic communities in Orange County, California. We conducted 14 focus groups with N = 112 participants. Qualitative analysis revealed that system fragmentation, limited availability of linguistically appropriate care, and stigma continue to undermine access to mental health care. Peer health navigation and culturally responsive peer support are potential ways to promote service engagement with persons from cultural and linguistic minority groups that encounter barriers when accessing mental health services.
Keywords: Access to mental health services; Community mental health; Cultural and linguistic diversity; Mental health equity; Qualitative.
© 2022. The Author(s), under exclusive licence to Springer Science+Business Media, LLC, part of Springer Nature.
- Focus Groups
- Health Services Accessibility
- Mental Health Services*
- Mental Health*
- Qualitative Research
Grants and funding
- Orange County Department of Mental Health/Orange County Department of Mental Health
- Open access
- Published: 29 May 2024
The Retrospective Stressor Analysis (RSA): a novel qualitative tool for identifying causes of burnout and mitigation strategies during residency
- Kristin L. Chrouser 1 ,
- Laura Zebib 1 ,
- Blake F. Webb 2 ,
- Tandi Bagian 2 &
- Timothy Arnold 3 , 4
BMC Medical Education volume 24 , Article number: 591 ( 2024 ) Cite this article
128 Accesses
3 Altmetric
Metrics details
Resident physicians are at an increased risk of burnout due to their high-pressure work environments and busy schedules which can lead to poor mental health outcomes and decreased performance quality. Given variability among training programs and institutions across the United States, stressors likely differ, and interventions must be tailored to the local context, but few tools exist to assist in this process.
A tool commonly used in adverse event analysis was adapted into a “retrospective stressor analysis” (RSA) for burnout prevention. The RSA was tested in a group of chief residents studying quality improvement and patient safety in veteran’s hospitals across the United States. The RSA prompted them to identify stressors experienced during their residencies across four domains (clinical practice, career development, personal life, and personal health), perceived causes of the stressors, and potential mitigation strategies.
Fifty-eight chief residents completed the RSA. Within the clinical domain, they describe the stress of striving for efficiency and clinical skills acquisition, all while struggling to provide quality care in high pressure environments. In the career domain, identifying mentors and opportunities for research engagement was stressful. Within their personal lives, a lack of time-constrained their ability to maintain hobbies, relationships, and attend meaningful social events while also reducing their engagement in healthy behaviors such as exercise, optimal nutrition, and attending medical appointments. Within each of these domains, they identified and described stress mitigation strategies at the individual, departmental, and national levels.
The RSA is a novel tool that can identify national trends in burnout drivers while simultaneously providing tailored prevention strategies for residents and their training sites.
Peer Review reports
Resident physicians are vital to the US healthcare system, but burnout rates among residents range from 17–94%, with variation by specialty and program [ 1 , 2 ]. Burnout is characterized by emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment.[ 3 ] External factors like demanding work environments, high patient care standards, long hours, poor work-life balance, lack of mental health support, and mistreatment in the workplace, combined with internal factors such as perfectionist personality, neuroticism, and previous mental health diagnosis, heighten the risk of burnout [ 1 , 4 , 5 , 6 ].
Burnout can be detrimental to resident physicians’ personal and professional well-being, leading to decreased job satisfaction, increasing attrition, depression, substance use, and suicide [ 7 , 8 , 9 ]. Burnout can also have clinical implications, negatively affecting patient access and quality of care. Burned-out physicians are more likely to make medical errors, exhibit increased implicit and explicit biases, and become less productive [ 9 , 10 , 11 , 12 ]. Meta-analyses find that burnout among healthcare providers is associated with reduced patient satisfaction, quality indicators, and perceived patient safety [ 13 , 14 ]. Thus, patient safety, quality of care, and physician wellbeing are inextricably linked. Consequently, the Accreditation Council for Graduate Medical Education (ACGME) has enhanced requirements for residency program accreditation, emphasizing monitoring and maintaining well-being during residency training [ 15 ].
A recent review of interventions to reduce resident burnout notes the current literature is of marginal quality and results are inconclusive [ 16 ]. While self-care initiatives have been shown to alleviate burnout in some small samples, such interventions emphasize modification of internal factors. This shifts the responsibility onto residents and does not address the systemic and environmental factors that promote burnout. Studies suggest that interventions addressing external factors such as work-hour limitations, structured mentorship programs, and access to mental health programs are associated with decreased burnout among residents [ 16 , 17 , 18 , 19 ]. Bakker’s Job Demands-Job Resources Conceptual Model illustrates that burnout is a consequence of chronic work-related stress, when job demands exceed job resources and individuals can no longer cope [ 20 ]. Therefore, effective burnout prevention requires reduction of job demands and/or augmentation of job resources, and should address both internal and external risk factors unique to each specialty and residency program.
Given the ACGME’s interest in burnout prevention, many residency programs use standardized surveys to monitor resident burnout rates. Tailored information can be gleaned from measures such as the Mini ReZ, which assesses the impact of several common residency stressors (e.g., electronic health record, interruptions, sleep impairment) [ 21 , 22 ]. However, causes of burnout will likely change rapidly over time as institutions adopt new technologies, face novel challenges (like COVID-19), or respond to regulatory changes.[ 23 ] For example, the advent of the electronic health record (EHR) rapidly changed documentation processes and created new stressors that increased physician burnout [ 24 ]. In the context of a constantly changing environment, surveys that identify sources of burnout based on the existing literature may fail to promptly capture ever-shifting stressors. Surveys are confined to capturing trends in explicitly asked topics. This limits our ability to capture emerging or unknown stressors. Furthermore, there is a paucity of data on residents’ perceptions of the causes of burnout. Therefore, we need tools that can elucidate burnout drivers and potential prevention strategies in rapidly changing environments from the perspective of impacted individuals. This will aid resource allocation for high-yield improvements.
The adaptation of an adverse event analysis tool can leverage methods that are already familiar to residents in order to generate an understanding of burnout drivers and potential interventions. With growing evidence of the negative impact of burnout on providers, trainees, and patient care, institutions need innovative tools to monitor for new causes of burnout in changing environments. This will allow them to rapidly shift burnout prevention strategies when appropriate. This study aims to 1) characterize recent residency graduates’ perceptions of the drivers of burnout, 2) identify potential interventions for mitigating resident burnout, and 3) assess the utility of the RSA (retrospective stressor analysis) as a novel tool to identify a wider breadth of sources of resident burnout than found in the current literature as well as generate practical strategies to mitigate these causes.
Root-cause analysis (RCA) is a methodology to identify underlying causes of an adverse event and has been used in healthcare to characterize and help prevent future adverse outcomes [ 25 ]. Residents are typically familiar with RCA methodology, including the “five whys” and fishbone diagrams from their patient safety and quality improvement training. The final deliverable of an RCA is a list of “action items” to address or eliminate these underlying causes and prevent similar future problems. Similar to an RCA, this Retrospective Stressor Analysis (RSA) was designed to identify potential underlying causes of stressors and list possible corrective actions/prevention strategies (see Appendix A). The RSA has dual utility to 1) be used by institutions to explore resident perceptions of causes as a cohort and implement resident-derived interventions and 2) be used by residents as an opportunity for self-reflection on their own individual perceived burnout causes and identify actions they can personally take to mitigate burnout and improve resilience.
In March 2022, 87 VA Chief Residents in Quality Improvement and Patient Safety (CRQS) across 67 Veterans Affairs Healthcare Centers were given a homework assignment on Building Resilience/Preventing Burnout. Participants were instructed to recall stressors experienced during their residencies across four domains (clinical practice, career development, personal life, and personal health) that they felt increased their risk of burnout. Then they listed perceived causes of these stressors and potential prevention and mitigation strategies. After aggregating the deidentified data, we coded stressors and mitigation strategies and identified themes within each of the four domains (clinical practice, career development, personal life, and personal health). Evaluating each entry’s content and context, one author (KC) developed codes using thematic analysis. After compiling the initial codebook, a second coder (TA) coded 20% of the entries in each domain. Co-analysis agreement was > 80%, and disagreements were resolved by discussion. Given the large dataset, codes for stressors were then ranked by frequency within each domain and the top 15 illustrated as word clouds. Conceptual themes were identified within each domain.
Preventive strategies for each domain were compiled and categorized by intervention level (personal, departmental, national) and themes were identified. Participants received a deidentified compilation of prevention strategies as a resource to share with their medical education community. The University of Michigan Institutional Review Board reviewed this study and determined it to be exempt and waived ethical approval and consent to participate. The data are available from the corresponding author, Dr. Kristin Chrouser, upon request.
In 2022, 58 chief residents (67%) completed the RSA assignment. All responses were deidentified, so demographic information is not available. Participants identified 1020 stressors (306 clinical, 262 career, 247 personal life, and 205 personal health) and 569 mitigation strategies (165 clinical, 136 career, 133 personal life, and 135 personal health). Qualitative analysis of stressors and mitigation strategies revealed several themes within the four domains.
Themes from clinical practice domain stressors
Participants describe the stresses related to their clinical work (Fig. 1 ), such as high patient volume, patient acuity, challenging patient interactions, poor outcomes, and systems issues, including EHR frustrations, documentation hassles, administrative burden, and lack of backup. They highlighted challenges regarding the management of clinical work, such as striving for efficiency, admitting a lack of knowledge/experience, and asking for help. They were stressed by their adjustments to gaining seniority over the course of training related to role transition, acquiring leadership and teaching skills, and delegation challenges. They describe challenges related to their role as learners, such as time to study, gaining clinical knowledge, and learning procedures. They also describe their emotional experience/response to the stresses of their clinical role, including experiencing imposter syndrome, worry, the weight of responsibilities, emotion management, coping with mistakes, and facing inadequacies.
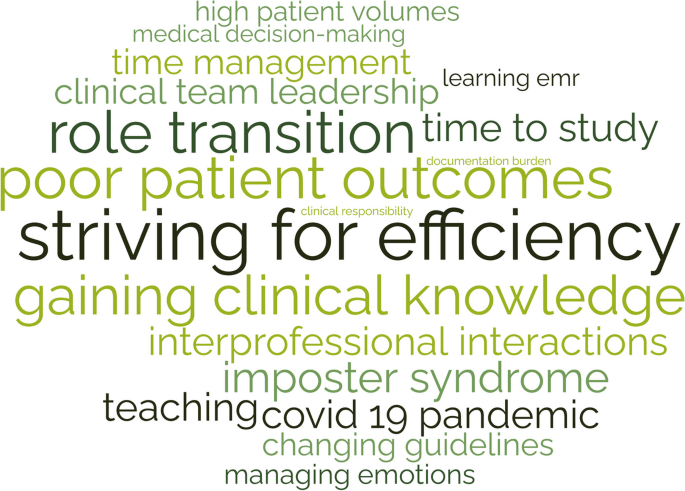
Clinical Practice Domain: Stressors that increased burnout risk*
*Size of word correlates with frequency of theme
Themes from the career development domain stressors
Participants describe various aspects of career development they considered stressful—such as research, publishing, presentations, teaching, committees, and professional relationships (Fig. 2 ). Many find career planning and career choices difficult, including fellowship decisions. They also recognize challenges in finding and becoming good mentors. Balancing academic and personal priorities and time management were common struggles. They also describe the additional stress of learning to cope with bias, competitiveness, failure, burnout, and performance anxiety.

Career Domain: Stressors that increased burnout risk*
Themes from the personal life domain stressors
Participants describe challenges in maintaining their personal lives as residents (Fig. 3 ). Lack of time is a common complaint, leading to difficulty separating work and home lives while describing concerns with a lack of opportunity to unwind from the stressors of residency. This includes inadequate time to invest in social life and maintain relationships with family and friends, eventually leading to erosion of social support. Social isolation was exacerbated by geographic separation from family support, moving to a new city, and COVID-19 restrictions.

Personal Life Domain: Stressors that increased burnout risk*
Many felt that long work hours led to difficulty coping with home stressors such as caregiving for children, family, and pets. Schedule inflexibility during residency led to missing important social events and being unavailable to manage family emergencies. They also recognized the difficulty of home maintenance, finances, and chores due to a lack of time. Residents described their emotional experience/response to these stresses in their personal lives as leading to guilt and feeling overwhelmed.
Themes from the personal health domain stressors
Participants described various challenges in maintaining their personal health as residents (Fig. 4 ). They described that a lack of time led to an inability to maintain healthy habits such as exercise, nutritious meals, proper hydration, and adequate sleep. Accessing physical and mental healthcare for themselves was difficult due to their schedules and social pressure to prioritize work over healthcare needs. Similarly, due to the demands and expectations of residency, many found it difficult to take a day off when ill.

Personal Health Domain: Stressors that increased burnout risk*
The struggle to cope and manage stress was a common complaint. Many participants noted this was exacerbated by the physical and mental stress of pregnancy and parenthood. They also described various emotional experiences related to their health: fear of COVID-19, feeling out of control, anxiety, and guilt for taking a sick day.
Mitigation strategies at the personal level
Table 1 outlines potential interventions to reduce burnout at various levels. For mitigation strategies on a personal level, many emphasized the importance of maintaining productivity through intentional organization within all domains. For example, within the clinical and career domains, their self-identified need for ongoing clinical learning could be achieved through setting clear goals and creating consistent study schedules, and within the personal domain, by scheduling designated time for relaxation, vacation, hobbies, and quality time with family. Interestingly, this also included creating time to prioritize one’s own health and attend medical appointments. Residents stressed the importance of determining clear personal goals, priorities, and setting expectations both at work and with family members. Many described the need to outsource home tasks, including house cleaning, grocery shopping, and childcare. Also, they described behaviors to automate healthy choices such as meal prepping, not purchasing unhealthy snacks, tracking water intake, and organizing resident meals with healthy options to maintain personal wellness.
Many residents commented on the importance of creating a team-like atmosphere in the work environment, including learning what tasks to delegate and consistently coordinating debrief sessions after adverse patient outcomes. They also discussed the importance of leveraging specific relationships, such as nursing staff, specialists, hospital resources, and asking for help from senior residents or faculty. Many advised the importance of adapting one’s mindset, such as adopting a reflective mindfulness practice, being vulnerable with peers and mentors, and reframing success and failure. A common theme was the importance of peer-to-peer relationships in discussing potential hurdles such as imposter syndrome and creating a culture where open discussion was encouraged.
Mitigation strategies at the departmental level
At the departmental level, participants emphasized the importance of mentorship and coaching. While some encouraged the importance of individually reaching out to potential mentors early and the utility of building peer relationships, others described the role institutions can play in creating mentorship programming. They desired mentors who would discuss imposter syndrome and failure and guide mentees through career and personal decisions. Many felt a need for significant shifts in culture to encourage open communication, sharing failures, and enhancing feedback mechanisms.
Some advised significant changes to patient care responsibilities, such as reduced work hours, capping the number of patients, and reduced note writing. Others described a need for greater standardization of clinical expectations such as templates for best practices, patient handoffs, consults, checklists, and “guides” for workflows in different clinic settings. Many described the need for augmenting the curriculum to include robust mechanisms for research support and increased training during orientation on communication skills, efficiency in the workplace, teaching, navigating difficult cases, managing imposter syndrome, and coping with failure.
Mitigation strategies at the national level
The most cited mitigation strategy across all domains was reducing resident duty hours. While many emphasized the role of institutions in complying with duty hour restrictions, further adjustments to duty hours require top-down implementation by the ACGME. Residents stated that there was a need for greater flexibility to utilize wellness days or sick leave. Given the stressors associated with family planning, many felt the ACGME and/or institutions should provide information and resources for cryopreservation, parental leave, and lactation. Lastly, increasing resident income was suggested as an effective strategy to alleviate resident budgetary stressors, accurately reflect work hours, and compensate some for the added stress of challenging work schedules such as jeopardy call schedules and night-float.
Burnout’s impact on physician well-being and quality of care is well established, and current rates are concerning [ 1 , 5 ]. Therefore, we need tools for ongoing assessment of the underlying causes of resident burnout and identification of potential interventions within local work environments. In this study, we describe the successful use of a novel tool, the retrospective stressor analysis (RSA), informed by the familiar RCA process, to characterize residents’ perceptions of burnout causes and potential mitigation strategies. To our knowledge, the field currently lacks alternatives to survey-based tools that will identify new sources of burnout and provide individuals and institutions with intervention strategies.
Participants in our study highlight how lack of time impacts their well-being in all four domains. This is not surprising as previous studies have shown a significant difference in the burnout rates of residents based on adherence to work-hour restrictions [ 26 ]. Similar to our findings, Mian et al., identified several common stressors among trainees that lead to burnout, such as overwork/sleep deprivation, emotional drain of caring for sick patients, lack of time for personal life outside training, and residency coinciding with major life events such as parenthood [ 27 ]. Related, Linzer et al. found burnout correlated with work-related conditions such as value alignment, teamwork, work control, and time pressures [ 22 ]. The RSA identified similar themes among participants. In addition, the RSA also provided greater context across the four domains to elucidate previously unacknowledged sources of stress, such as career decision-making, acquisition of leadership roles, and coping with adverse patient outcomes. To our knowledge, these have not been previously identified as potential sources of burnout within the resident population. Moreover, participants provided highly specific stressors, such as “variability in clinical preferences among attendings”, and potential mitigation strategies that program directors might find useful when restructuring expectations or generating standardized workflows.
While the RSA may be a novel resource for understanding burnout, there were some challenges with using it in practice. Despite clear instructions to list multiple causes, some participants did not identify more than one potential cause of their stressors, even though this is a common step used in root cause analysis. Failure to identify a variety of causes can reduce the diversity of proposed interventions. Despite this potential limitation, our cohort of residents still generated a large range of interventions for burnout prevention and mitigation. However, if RSA is used in smaller resident samples in the future without encouraging participants to provide a range of causes, this might generate a reduced range of interventions, thus limiting impact. The “personal life” domain was listed prior to “personal health,” so often participants included many factors in the personal life domain that would have been more appropriate under personal health, which made analysis of frequency by domain more challenging.
Moreover, proposed preventive strategies overwhelmingly focused on personal actions, although some participants suggested departmental/institutional/national policy reforms. The Institute for Healthcare Improvement’s Action Hierarchy Tool is used to assist RCA teams in identifying interventions with the strongest effect for sustained and successful system improvement [ 28 ]. Stronger actions are those that do not rely on human memory, such as architectural changes, forced functioning, removing unnecessary steps, and tangible involvement of leadership; while weaker actions, such as trainings and new procedures, rely on humans to remember to perform an action. Many of the recommended interventions identified using the RSA would be classified as weaker actions, as they rely on residents to remember and make time to perform specific tasks such as exercise, mindfulness, studying, and delegating in the clinical space. Future iterations of the tool should encourage the development of stronger intervention actions.
Although these challenges with RSA had minimal effect on data and analysis, our group refined the RSA tool for future data collection. Refinements included adjusting domain order to reduce categorization errors, adding reminders of QI tools useful in collecting a broader range of potential causes (5 whys, fishbone diagram), and providing examples of systemic preventive strategies (e.g., programs, policies). The revised RSA is available in Appendix B. Although our sample size was more than adequate to reach saturation for a qualitative study, the RSA’s usability, generalizability, and utility of our findings may vary among residents. The Chief Residents in Quality Improvement and Patient Safety were already familiar with RCA tools and methods, but this might not be the case for all residents, and future iterations may be informed by piloting the tool in varied resident populations. Participants also provided this data via a homework assignment, and even though they were assured their responses were confidential, fear of being identified by course directors may have influenced their responses. Demographics of participants were not collected, precluding any analysis based on specialty or gender. This is a limitation as burnout causes and mitigation recommendations might differ based on demographic categories.
The RSA provided findings consistent with factors known to contribute to burnout in the literature while generating a broader range of stressors than previously reported. RSA utilization can allow residency programs to identify emerging burnout drivers as medicine changes rapidly and provides a wealth of intervention ideas appropriate to the local context. Engaging residents in developing implementation strategies can serve the dual purpose of reinforcing skills applicable to adverse event analysis techniques and helping prevent resident burnout. Qualitative data assessment from the RSA could also be used by national associations to identify novel stressors and then generate new quantitative survey questions more appropriate for measurement within a larger population.
We adapted a familiar patient safety tool, root cause analysis (RCA), to create the retrospective stressor analysis (RSA) for burnout prevention. This novel tool allowed recent residency graduates to identify stressors they believe increased their risk of burnout and generate practical preventive strategies at personal, institutional, and national levels. Common themes highlighted the difficulty of inflexible schedules and lack of time invested in protective factors such as social support, mentorship, and healthy habits. The RSA is a novel tool that can identify national trends in the drivers of burnout while providing tailored prevention strategies for individuals, training sites, and the ACGME to consider for future implementation.
Disclaimers
The opinions expressed in this presentation are the authors’ own and do not necessarily reflect the view of the Department of Veterans Affairs or the United States government.
Availability of data and materials
The data are available from the corresponding author, Dr. Kristin Chrouser, upon request.
Abbreviations
Retrospective Stressor Analysis
American Council for Graduate Medical Education
Kratzke IM, Woods LC, Adapa K, et al. The Sociotechnical Factors Associated With Burnout in Residents in Surgical Specialties: A Qualitative Systematic Review. J Surg Educ. 2022May 1;79(3):614–23.
Article Google Scholar
Rodrigues H, Cobucci R, Oliveira A, et al. Burnout syndrome among medical residents: A systematic review and meta-analysis. PLoS One. 2018;13(11):e0206840.
Nene Y, Tadi P. Resident Burnout. StatPearls Publishing. 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553176/ . Cited 2023 Feb 24.
Zhou AY, Panagioti M, Esmail A, et al. Factors associated with burnout and stress in trainee physicians: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(8):e2013761.
Ferguson C, Low G, Shiau G. Resident physician burnout: insights from a Canadian multispecialty survey. Postgrad Med J. 2020Jun 1;96(1136):331–8.
McManus I, Keeling A, Paice E. Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: A twelve year longitudinal study of UK medical graduates. BMC Med. 2004Dec;2(1):29.
Chaukos D, Chad-Friedman E, Mehta DH, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41(2):189–94.
van der Heijden F, Dillingh G, Bakker A, et al. Suicidal thoughts among medical residents with burnout. Arch Suicide Res. 2008;12(4):344–6.
West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018Jun;283(6):516–29.
Dewa CS, Loong D, Bonato S, Trojanowski L, et al. The relationship between resident burnout and safety-related and acceptability-related quality of healthcare: a systematic literature review. BMC Med Educ. 2017Nov 9;17(1):195.
Scheepers RA, Boerebach BCM, Arah OA, et al. A systematic review of the impact of physicians’ occupational well-being on the quality of patient care. Int J Behav Med. 2015;22(6):683–98.
Dyrbye L, Herrin J, West CP, Wittlin NM, et al. Association of racial bias with burnout among resident physicians. JAMA Netw Open. 2019J 3;2(7):e197457.
Salyers MP, Bonfils KA, Luther L, et al. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis. J Gen Intern Med. 2017Apr 1;32(4):475–82.
Tawfik DS, Scheid A, Profit J, Shanafelt T, et al. Evidence relating health care provider burnout and quality of care. Ann Intern Med. 2019;171(8):555–67.
American Medical Association. ACGME seeks to transform residency to foster wellness. 2015. Available from: https://www.ama-assn.org/medical-residents/medical-resident-wellness/acgme-seeks-transform-residency-foster-wellness . Cited 2023 Feb 24.
Busireddy KR, Miller JA, Ellison K, et al. Efficacy of Interventions to Reduce Resident Physician Burnout: A Systematic Review. J Grad Med Educ. 2017Jun 1;9(3):294–301.
Mullins CH, Gleason F, Wood T, et al. Do internal or external characteristics more reliably predict burnout in resident physicians: a multi-institutional study. J Surg Educ. 2020;77(6):e86-93.
Leung VWY, Konci X, Meterissian S. Is there a role for formal mentorship programs in reducing burnout in surgical residency?: a literature review. Available from: https://www.ijsed.com/article/25104.pdf . Cited 2023 Feb 25.
Clough BA, March S, Chan RJ, et al. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev. 2017Jul 17;6(1):144.
Bakker AB, Demerouti E. The job demands-resources model: state of the art. J Manag Psychol. 2007;22(3):309–28.
Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory: Third edition. In: Zalaquett CP, editor. Evaluating stress: A book of resources. Lanham, MD, US: Scarecrow Education, xvii; 1997. p. 191–218. Available from: https://psycnet.apa.org/fulltext/1997-09146-011.pdf .
Linzer M, Shah P, Nankivil N, et al. The Mini Z Resident (Mini ReZ): Psychometric Assessment of a Brief Burnout Reduction Measure. J Gen Intern Med. 2023Feb;38(2):545–8.
Cravero AL, Kim NJ, Feld LD, et al. Impact of exposure to patients with COVID-19 on residents and fellows: an international survey of 1420 trainees. Postgrad Med J. 2021;97(1153):706–15.
Yan Q, Jiang Z, Harbin Z, et al. Exploring the relationship between electronic health records and provider burnout: A systematic review. J Am Med Inform Assoc. 2021Apr 23;28(5):1009–21.
Williams PM. Techniques for root cause analysis. Proc. 2001;14(2):154–7.
Google Scholar
Marchalik D, Brems J, Rodriguez A, et al. The Impact of Institutional Factors on Physician Burnout: A National Study of Urology Trainees. Urology. 2019Sep;1(131):27–35.
Mian A, Dahye K, Duane C, et al. Medical student and resident burnout: a review of causes, effects, and prevention. J Fam Med Dis Prev. 2018;31:4.
RCA2: Improving root cause analyses and actions to prevent harm. National Patient Safety Foundation. Available from: https://www.ashp.org/-/media/assets/policy-guidelines/docs/endorsed-documents/endorsed-documents-improving-root-cause-analyses-actions-prevent-harm.ashx . Cited 2023 Jun 19.
Download references
Acknowledgements
Maria Lennox, MS assisted with collating the raw data.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Urology, University of Michigan, Ann Arbor, MI, USA
Kristin L. Chrouser & Laura Zebib
VHA National Center for Patient Safety, Ann Arbor, MI, USA
Blake F. Webb & Tandi Bagian
Human Factors Engineering Division, Clinical Informatics and Data Management, Office of Health Informatics, Veterans Health Administration, Washington, DC, USA
Timothy Arnold
College of Pharmacy, University of Michigan, Ann Arbor, MI, USA
You can also search for this author in PubMed Google Scholar
Contributions
KC, TB, and TA conceptualized, developed, and designed the research study and tools. KC, TA, LZ, and BW analyzed and organized data. KC and LZ wrote the first draft. All authors edited manuscript drafts, read, and approved the final manuscript.
Corresponding author
Correspondence to Kristin L. Chrouser .
Ethics declarations
Ethical approval and consent to participate.
The University of Michigan Institutional Review Board reviewed this study and determined it to be exempt from ethical approval and consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chrouser, K.L., Zebib, L., Webb, B.F. et al. The Retrospective Stressor Analysis (RSA): a novel qualitative tool for identifying causes of burnout and mitigation strategies during residency. BMC Med Educ 24 , 591 (2024). https://doi.org/10.1186/s12909-024-05571-3
Download citation
Received : 09 February 2024
Accepted : 17 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1186/s12909-024-05571-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality improvement
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
This qualitative study explores the lived experience of mental distress within college. student identity. The purposes of this study is to: (1) address a gap in extant literature on mental. health as an aspect of college identity from students' own voice, (2) add to literature that.
As the evidence base for the study of mental health problems develops, there is a need for increasingly rigorous and systematic research methodologies. Complex questions require complex methodological approaches. Recognising this, the MRC guidelines for developing and testing complex interventions place qualitative methods as integral to each stage of intervention development and ...
Research indicates that mental health services delivered via telehealth are as effective as in-person services for a range of mental health ... lessons learned from four case studies. ... Parker J, et al. Remote care for mental health: qualitative study with service users, carers and staff during the COVID-19 pandemic. BMJ Open 2021; 11 ...
Qualitative case studies, interviews, and observational studies form the foundation of many theoretical and practice approaches in mental health and psychiatry. For example, Freud's approach to psychoanalysis was grounded in qualitative case studies with his patients (Rothgeb 1971 ; Streiner 2008 ).
Qualitative mental health services research are often iterative in nature in which there is a constant back and forth between data ... Norman I, Redfern S, Jones R. Exposing the key functions of a complex intervention for share care in mental health: Case study of a process evaluation. BMC Health Services Research. 2008; 8:274. doi: 10. ...
This chapter builds on the systematic review of qualitative research into the meaning of quality of life for people with mental health problems reported in Chapter 5 . The review identified six major themes: well-being and ill-being; control, autonomy and choice; self-perception; belonging; activity; and hope and hopelessness. One limitation of the review was that available studies focused on ...
1. Introduction. Discourse and policies around COVID-19 disproportionately focus on the adverse effects of the public health crisis on adults. Research shows that depression, anxiety, and post-traumatic stress are the most common psychological reactions to the pandemic in adults []; however, the impact of COVID-19 on young people is not fully understood.
The topic of stigma was examined using two focus groups of thirteen people with experience of mental health problems and stigma. Results: Two main themes and five subthemes were identified. Participants believed that (1) the 'hierarchy of labels' has a profound cyclical impact on several levels of society: people who experience mental health ...
This qualitative research was employed in this study to gather an in-depth understanding of the impact faced by the family members when providing care for relatives with mental illness. It will also provide a touch of emotion concerning the research environment, and in addition it could demonstrate a more holistic approach of the phenomena ...
This also put up a barrier for some students to access online mental health support in case it was witnessed by their parents (Quotes 18-19). ... Carers' perspectives regarding child and adolescent mental health services: a qualitative study. Adv Ment Health. 2017;15(1):58-70. Google Scholar
A case study is one of the most commonly used methodologies of social research. This article attempts to look into the various dimensions of a case study research strategy, the different epistemological strands which determine the particular case study type and approach adopted in the field, discusses the factors which can enhance the effectiveness of a case study research, and the debate ...
Mental healthcare is an important component in societies' response to mental health problems. Although the World Health Organization highlights availability, accessibility, acceptability and quality of healthcare as important cornerstones, many Europeans lack access to mental healthcare of high quality. Qualitative studies exploring mental healthcare from the perspective of people with lived ...
Here we present results from an interview study with semi-structured questions. In qualitative content analysis, the researchers strive to make the participants' voices heard . The rationale behind adopting a qualitative study design is to capture variations in experiences within a population, in this case, adolescents with ADHD.
Methods: A qualitative, case study in a large, urban healthcare organization was conducted in order to explore the perceptions and experiences of employees across the organization. In-depth interviews were conducted with eight healthcare workers who had experienced mental health issues at work as well as eight workplace stakeholders who ...
Mental health nursing is acknowledged internationally as being a demanding profession; however, little is known about the range of experience and complexity of workplace challenges or their impacts on mental health nurses (MHN). This qualitative descriptive study aimed to examine and describe the range of challenging workplace situations ...
An instrumental case-study approach was used to gather information (Creswell, 2013; Stake, 2005; Yazan, 2015; Yin, 2014) in an attempt to shed light on the issue of mental health in teacher preparation and how student teachers live with a mental health condition. This type of study was supported in the literature to
Study design: The study employed a qualitative, comparative case study design. We developed a framework, based on existing evidence and the experiential insight of the team, which conceptualised the challenges and facilitators of introducing peer worker roles into mental health services.
The web of silence: A qualitative case study of early intervention and support for healthcare workers with mental ill-health February 2014 BMC Public Health 14(1):138
Given the prevalence of children's mental health disorders, teachers' roles have expanded to include identifying students with mental health needs and delivering mental health interventions. ... Teachers' perspectives on educator mental health competencies: A qualitative case study. American Journal of Qualitative Research, 2(1), 22-40 ...
2. Materials and Methods. This qualitative study was informed by participatory action research approaches to ensure the study, findings, and recommendations were grounded in the experiences of those who are directly affected by the topic of the research [51,52,53,54].Eligibility criteria were lived experience of homelessness, substance use, and/or mental ill-health.
a study that reviewed mental-health services in Australia, Ireland, and the UK, it was reported that access to mental-health services was the poorest for children and youth (McGorry, Bates, & Birchwood, 2013). As was indicated in the results of these studies, there is a global need to identify and support students with mental-health disorders.
Whether this is also the case in other areas of the country and across other youth mental health services warrants further investigation. The findings from this qualitative study are summarized in Table 1 and have been grouped into concordant and discordant themes for contrast and comparison. It is noteworthy that both clinicians and clients ...
Study context. This qualitative study was conducted in the province of British Columbia (BC), Canada, a jurisdiction with a population of approximately five million people [].Within BC's health sector, key actors involved in the policy response to COVID-19 included: elected officials, the BC Government's Ministry of Health (MOH), the Provincial Health Services Authority (PHSA), Footnote 2 ...
Qualitative Health Research (QHR) is a peer-reviewed monthly journal that provides an international, interdisciplinary forum to enhance health care and further the development and understanding of qualitative research in health-care settings.QHR is an invaluable resource for researchers and academics, administrators and others in the health and social service professions, and graduates who ...
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews). The case study research method originated in clinical medicine (the case history, i.e., the patient's personal history). In psychology, case studies are ...
Given the large mental health treatment gap in low- and middle-income countries (LMICs), particularly in post-conflict settings like Sierra Leone, and the limited healthcare infrastructure, understanding the wider benefits of evidence-based mental health interventions within households is critical. This study explored potential mental health spillover effects - the phenomenon of beneficial ...
This was a qualitative study, conducted in 28 out of the 40 public health facilities in 3 districts, where the intervention was undertaken. ... PLOS Mental Health is an inclusive journal addressing challenges and gaps in the field of mental health research, ... Grant A, Bugge C, Wells M. Designing process evaluations using case study to explore ...
Despite progress made under California's Mental Health Services Act, limited access to care for cultural and linguistic minority groups remains a serious issue in community mental health. ... Barriers to Accessing Mental Health Care Under the Mental Health Services Act: A Qualitative Case Study in Orange County, California Community Ment Health ...
Resident physicians are at an increased risk of burnout due to their high-pressure work environments and busy schedules which can lead to poor mental health outcomes and decreased performance quality. Given variability among training programs and institutions across the United States, stressors likely differ, and interventions must be tailored to the local context, but few tools exist to ...
Background: Anxiety problems are common in children, yet few affected children access evidence-based treatment. Digitally augmented psychological therapies bring potential to increase availability of effective help for children with mental health problems. This study aimed to establish whether therapist-supported, digitally augmented, parent-led cognitive behavioural therapy (CBT) could ...