Hospital Medicine Virtual Journal Club

Predictors of COVID-19 severity: A literature review
Link to article at PubMed
Rev Med Virol. 2020 Jul 30:e2146. doi: 10.1002/rmv.2146. Online ahead of print.
The coronavirus disease 2019 (COVID-19) pandemic is a rapidly evolving global emergency that continues to strain healthcare systems. Emerging research describes a plethora of patient factors-including demographic, clinical, immunologic, hematological, biochemical, and radiographic findings-that may be of utility to clinicians to predict COVID-19 severity and mortality. We present a synthesis of the current literature pertaining to factors predictive of COVID-19 clinical course and outcomes. Findings associated with increased disease severity and/or mortality include age > 55 years, multiple pre-existing comorbidities, hypoxia, specific computed tomography findings indicative of extensive lung involvement, diverse laboratory test abnormalities, and biomarkers of end-organ dysfunction. Hypothesis-driven research is critical to identify the key evidence-based prognostic factors that will inform the design of intervention studies to improve the outcomes of patients with COVID-19 and to appropriately allocate scarce resources.
PMID: 32845042 | DOI: 10.1002/rmv.2146
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Mastodon (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)
Leave a Reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Notify me of new posts by email.
- Open supplemental data
- Reference Manager
- Simple TEXT file
People also looked at
Systematic review article, chronic diseases as a predictor for severity and mortality of covid-19: a systematic review with cumulative meta-analysis.

- 1 Department of Medical Informatics, Medical School of Nantong University, Nantong, China
- 2 Department of Emergency Medicine, Affiliated Hospital of Nantong University, Nantong, China
- 3 Library and Reference Department, Zhejiang University School of Medicine First Affiliated Hospital, Hangzhou, China
- 4 Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston, MA, United States
Introduction: Given the ongoing coronavirus disease 2019 (COVID-19) pandemic and the consequent global healthcare crisis, there is an urgent need to better understand risk factors for symptom deterioration and mortality among patients with COVID-19. This systematic review aimed to meet the need by determining the predictive value of chronic diseases for COVID-19 severity and mortality.
Methods: We searched PubMed, Embase, Web of Science, and Cumulative Index to Nursing and Allied Health Complete to identify studies published between December 1, 2019, and December 31, 2020. Two hundred and seventeen observational studies from 26 countries involving 624,986 patients were included. We assessed the risk of bias of the included studies and performed a cumulative meta-analysis.
Results: We found that among COVID-19 patients, hypertension was a very common condition and was associated with higher severity, intensive care unit (ICU) admission, acute respiratory distress syndrome, and mortality. Chronic obstructive pulmonary disease was the strongest predictor for COVID-19 severity, admission to ICU, and mortality, while asthma was associated with a reduced risk of COVID-19 mortality. Patients with obesity were at a higher risk of experiencing severe symptoms of COVID-19 rather than mortality. Patients with cerebrovascular disease, chronic liver disease, chronic renal disease, or cancer were more likely to become severe COVID-19 cases and had a greater probability of mortality.
Conclusions: COVID-19 patients with chronic diseases were more likely to experience severe symptoms and ICU admission and faced a higher risk of mortality. Aggressive strategies to combat the COVID-19 pandemic should target patients with chronic diseases as a priority.
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The COVID-19 outbreak was declared as a public health emergency of international concern by the World Health Organization (WHO) on January 30, 2020 ( 1 ). Since then, the disease has been spreading quickly around the world, reaching 9.296 million cases and 479,133 deaths as of June 25, 2020 ( 2 ). The ongoing COVID-19 pandemic has led to a rapidly growing demand for healthcare facilities and healthcare workers, leaving healthcare systems in many countries overstretched and unable to perform effectively ( 3 ).
The COVID-19 symptoms range from very mild to severe problems. While it was reported that the majority of COVID-19 cases were mild and required limited treatment ( 4 ), those patients with severe COVID-19 might need hospitalization or intensive care and have worse outcomes, such as death. Identifying risk factors for serious cases and mortality can be helpful in guiding public health interventions for protecting the most vulnerable groups of the population from COVID-19. For example, the risk factor information can be used to design risk stratification tools and clinical pathways, thus establishing more effective early intervention strategies and resource allocation policies.
COVID-19 is a serious global health threat, with more than 99% of confirmed cases currently coming from countries outside China. However, the vast majority of the published review articles relied almost exclusively on the studies conducted in China ( 5 – 11 ). In fact, several published reviews included data from only few countries outside China ( 12 – 14 ). Consequently, the limited information prevented decision-makers and patients from better recognizing the global evidence about risk factors for adverse COVID-19 outcomes. In addition, there is a serious concern about the validity and generalizability of the evidence on risk factors in COVID-19 patients generated by the published review articles, which failed to address the clinical heterogeneity of patients with COVID-19 among the observational studies. For instance, a meta-analysis ( 11 ) combined data from intensive care unit (ICU) admission and mortality into a single effect measure to find risk factors for progression of COVID-19, while another meta-analysis ( 8 ) pooled data from patients with severe COVID-19 symptoms and those who were admitted to the ICU into one group. Further systematic reviews are needed to address this issue of patient heterogeneity to improve the validity and generalizability of the evidence.
This paper aimed to fill the gap by conducting a systematic review with meta-analysis to determine the predictive value of chronic diseases for the severity and mortality of COVID-19. Our analysis examined global evidence to generate systematic and robust findings. To our knowledge, this study represented the most comprehensive meta-analysis of COVID-19 severity, mortality, ICU admission, and acute respiratory distress syndrome (ARDS). Furthermore, it was the first study to determine the associations between several chronic conditions, including obesity, asthma, and hyperlipidemia, with clinical outcomes of COVID-19 patients. We also included only studies from the peer-reviewed journals to ensure the validity of conclusions, while some meta-analyses used manuscripts in preprint servers to increase the sample size ( 9 , 15 – 17 ).
Methods for this systematic review were developed according to the recommendations from the MOOSE statement ( 18 ) and PRISMA statement ( 19 ) for reporting of systematic review and meta-analysis.
Criteria for Considering Studies for This Review
Observational studies that focused on adult patients (aged over 16 years) with COVID-19 and investigated the association between chronic diseases and severity, ICU admission, mortality, and ARDS of COVID-19 were included.
The following types of studies were excluded: (1) studies that only included infants, children, and pregnant women; (2) studies that only included decedents (only death patients were enrolled in each group); (3) studies that did not classify patients into different groups by severity, type of hospital wards (i.e., general wards, ICU), mortality, or ARDS; (4) studies that did not have enough statistical information to be extracted from each group of patients; (5) duplicated publication of the same research results, i.e., data from the same hospitals within the same period; and (6) descriptive reviews, systematic review, meta-analysis, opinion, editorial, comments, and conference abstracts without full article publication.
Study Outcomes
The primary outcome measure was the association between chronic diseases and the severity of COVID-19 patients. Secondary outcomes included the association between chronic diseases and mortality, ICU admission, and ARDS of COVID-19 hospitalized patients. The chronic diseases in our review were hypertension, diabetes, pulmonary disease [chronic obstructive pulmonary disease (COPD), asthma, and unspecified type], cardiovascular disease (coronary heart disease, heart failure, and unspecified type), cerebrovascular disease, hyperlipidemia, obesity, chronic liver disease, chronic renal disease, cerebrovascular disease, and cancer. The association between Charlson comorbidity index and the clinical outcomes of COVID-19 patients was also analyzed.
Search Strategy
Studies were identified by searching PubMed, Embase, Science Citation Index Expanded (Web of Science), and Cumulative Index to Nursing and Allied Health (CINAHL) Complete. Our search strategy is listed in Appendix 1 in Supplementary Material. References from the retrieved papers were also searched. Studies published between December 1, 2019, and December 31, 2020 were included.
Study Selection and Data Extraction
In accordance with the defined inclusion criteria, two reviewers independently read the title and abstract of each study retrieved by the search. The reviewers excluded studies that did not meet the inclusion criteria. After screening the title and abstract of each study, the full texts of eligible citations were then assessed by the two reviewers independently.
A third reviewer was consulted when the two reviewers could not agree on selecting a study. The reviewers developed a data extraction form and used it to extract data to reflect the characteristics of each included study. If the data from the same hospitals in the same period were published several times, only the paper with the largest sample size was included.
The included studies varied in their classification of disease severity, ranging from mild, moderate, severe, to critical severe. We categorized mild and moderate cases into the non-severe group and severe and critical severe cases into the severe group. We considered the following cases as the ICU groups—ICU admission and requiring invasive mechanical ventilation, and critical cases of illness that were admitted to the ICU.
Risk of Bias Assessment
We used the tools developed by the Joanna Briggs Institute (JBI) ( 20 – 23 ) to assess the risk of bias of the included studies. The JBI critical appraisal tools for cohort studies, case series, case–control studies, and cross-sectional studies included 11, 10, 10, and 8 items, respectively. The appraisal tools addressed the internal validity and risk of bias of the study design, particularly confounding, selection, and information bias, in addition to the importance of clear reporting.
Statistical Analysis
We conducted a meta-analysis when data from more than one study could be combined. We calculated pooled estimates of odds ratio (OR) and 95% confidence interval (CI) by the generic inverse variance method using STATA 14.2 (STATA Corporation, College Station, TX, USA). We tested the heterogeneity of effective measures using the I 2 statistic. We defined I 2 values greater than 50% as considerable or substantial heterogeneity ( 24 ). For data with substantial heterogeneity, a random-effects model using the method developed by DerSimonian and Laird ( 25 ) was specified to address heterogeneity among the studies. For data with unsubstantial heterogeneity, a fixed-effects model with the inverse variance method was used to synthesize the data.
For the most prevalent chronic diseases including hypertension, diabetes, COPD, coronary heart disease, cerebrovascular disease, and cancer, we conducted the cumulative meta-analysis according to the season of admission of the patients and the increasing sample size of the included studies within each season. A cumulative meta-analysis is helpful to assess the dynamics of how the summary results change with a newly added study ( 26 ). R 4.0.3 (The R Foundation for Statistical Computing, Vienna, Austria) was used to conduct a cumulative meta-analysis.
Literature Search and Study Selection
Two hundred and seventeen observational studies ( 27 – 243 ) with 624,986 patients met the inclusion criteria in our systematic review. A PRISMA flowchart summarized our search results and study selection procedure ( Figure 1 ).
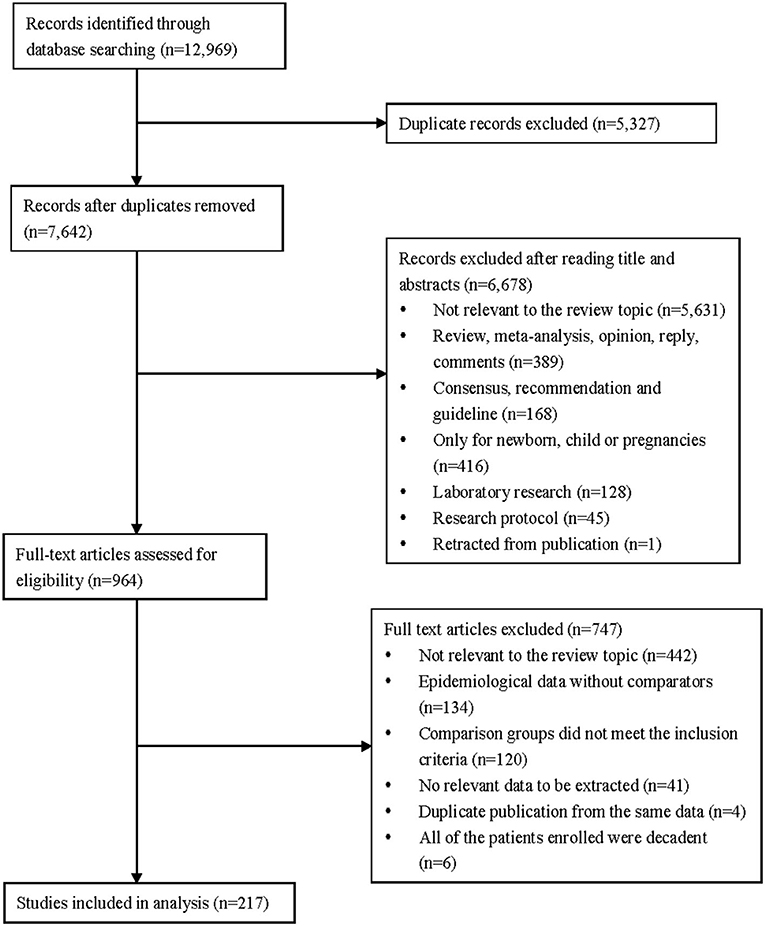
Figure 1 . Flow diagram of the study selection for inclusion in the systematic review.
Characteristics and Quality of the Included Studies
Table 1 presents the characteristics of the 217 included studies. The studies were carried out in 26 countries, 83 (38.25%) of them were performed in multicenters, 123 (56.68%) were case series, and 82 (37.79%) were cohort studies. The date of admission of the patients was from December 11, 2019, to August 1, 2020. Most of the outcome variables were about mortality (48.39%) and severity (34.10%). Details of the characteristics are shown in Appendix 2 in Supplementary Material.
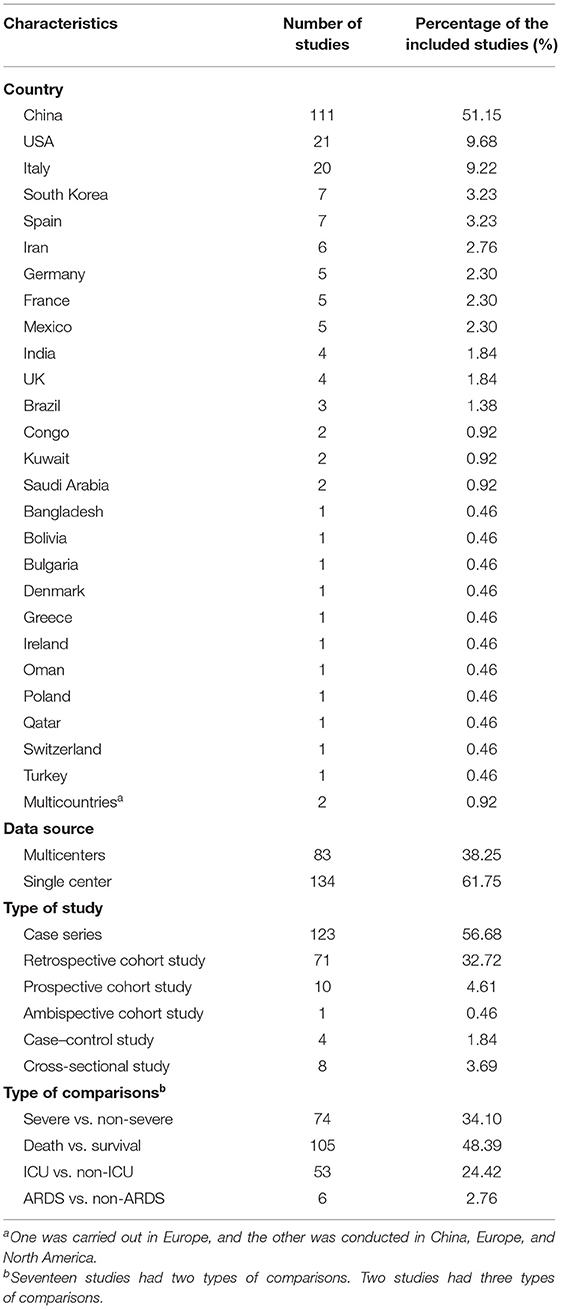
Table 1 . Characteristics of the included studies.
The quality assessment score for the case series ranged from 6 to 10 (9.13 ± 0.84) with 102 of them (82.93%) having a score higher than 8 (10 indicates the best quality). Among the case series, 48 studies (39.02%) did not indicate a consecutive inclusion of patients, and 45 studies (36.59%) did not have a complete inclusion of patients.
The score of cohort studies ranged from 6 to 11 (10.04 ± 0.92) with 62 cohort studies (75.61%) having a score more than 9 (11 indicates the best quality). Length of follow-up was not mentioned in 34 cohort studies, and the reasons for losses to follow-up were not described in 6 studies. In addition, we were not sure whether patients across different centers had similar characteristics in relation to exposure (27 studies). Appendix 3 in Supplementary Material presents details of the risk of bias assessment.
Association Between Chronic Diseases and Severity of COVID-19
We identified 74 studies of COVID-19 severity, involving a total of 32,213 patients and 8,433 cases of severe COVID-19. Among these studies, 65 of them were performed in China, 3 in the USA, and 1 in Bulgaria, Congo, Kuwait, Saudi Arabia, South Korea, and Spain, respectively.
As shown in Table 2 , the prevalence of patients with any type of chronic disease in the group of severe COVID-19 was substantially higher than that of the non-severe group (60.71 vs. 31.81%; OR 3.70, 95% CI 2.98–4.61). Hypertension (OR 3.05, 95% 2.60–3.59), diabetes (OR 2.55, 95% CI 2.14–3.03), COPD (OR 3.91, 95% CI 3.05–5.02), asthma (OR 1.93, 95% CI 1.53–2.42), unspecified type of pulmonary disease (OR 2.48, 95% CI 2.03–3.03), coronary heart disease (OR 2.04, 95% CI 1.72–2.42), unspecified type of cardiovascular disease (OR 3.01, 95% CI 2.64–3.43), cerebrovascular disease (OR 2.32, 95% CI 1.83–2.94), obesity (OR 2.63, 95% CI 1.70–4.07), chronic liver disease (OR 1.96, 95% CI 1.64–2.35), chronic renal disease (OR 2.09, 95% 1.52–2.87), and cancer (OR 2.33, 95% 1.90–2.87) were all associated with significantly higher risk of severity among COVID-19 patients. There were only two types of the study chronic diseases (i.e., heart failure and hyperlipidemia) that were not significantly associated with the severity of COVID-19 ( P > 0.05). However, the prevalence of heart failure or hyperlipidemia was only reported in three studies.
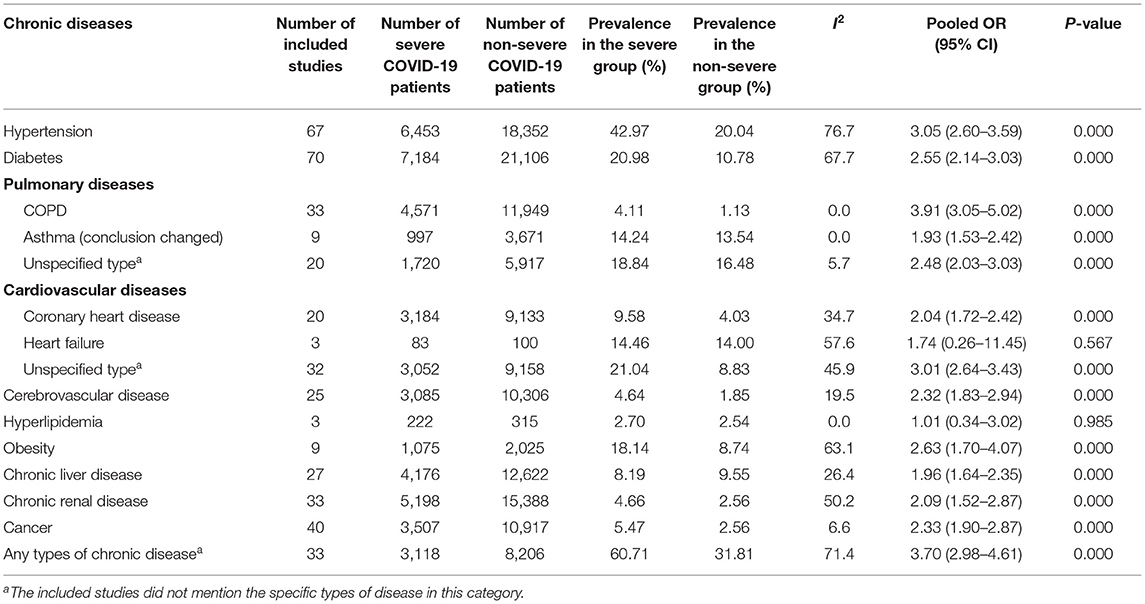
Table 2 . Associations between chronic diseases and severity of COVID-19.
Appendix 4 in Supplementary Material presents the forest plots of cumulative meta-analysis for major types of chronic diseases. Subsequent studies increased the precision of the point estimate, and no change occurred in the direction of the effect size.
Association Between Chronic Diseases and Mortality of COVID-19
We found that 105 studies with a total of 350,522 patients and 68,157 deaths presented data on mortality. Among the studies, 40 of them were carried out in China, 12 in Italy, 11 in the USA, 6 in Iran, 6 in Spain, 4 in India, 4 in the UK, 3 in Brazil, 3 in South Korea, 2 in France, 2 in Mexico, and 1 in Bangladesh, Bolivia, Congo, German, Greece, Ireland, Kuwait, Saudi Arabia, Switzerland, and Turkey, respectively. We also found two studies that were conducted in multicountries.
As shown in Table 3 , 36.49% of patients who died had at least one type of chronic disease. Hyperlipidemia (52.80%) was the most common chronic condition among patients who died, followed by hypertension (37.53%) and unspecified type of cardiovascular disease (28.56%). Hypertension (OR 2.31, 95% CI 2.04–2.61), diabetes (OR 1.99, 95% CI 1.82–2.18), COPD (OR 2.95, 95% CI 2.48–3.50), unspecified type of pulmonary disease (OR 2.05, 95% CI 1.83–2.31), coronary heart disease (OR 2.46, 95% CI 2.14–2.82), heart failure (OR 2.74, 95% CI 2.21–3.40), unspecified type of cardiovascular disease (OR 2.59, 95% CI 2.24–3.00), cerebrovascular disease (OR 2.46, 95% CI 2.08–2.91), hyperlipidemia (OR 1.72, 95% CI 1.07–2.77), chronic liver disease (OR 1.52, 95% CI 1.30–1.77), chronic renal disease (OR 2.85, 95% CI 2.44–3.33), and cancer (OR 2.11, 95% CI 1.85–2.42) were associated with a higher risk of mortality.
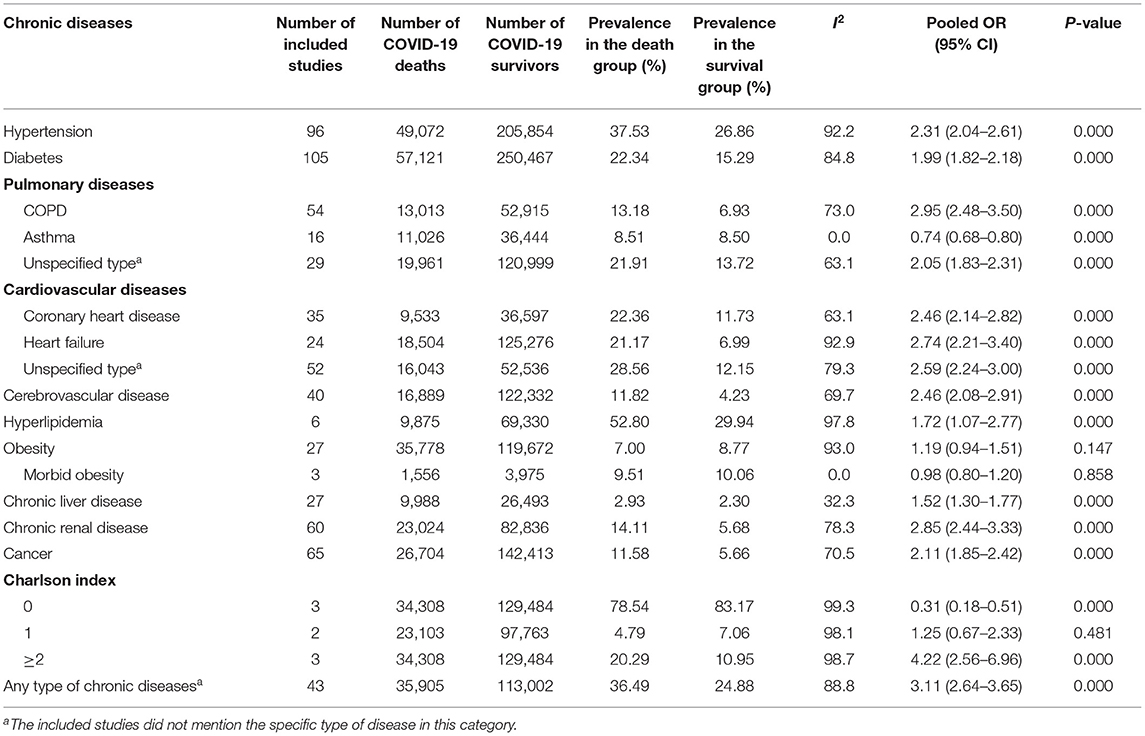
Table 3 . Associations between chronic diseases and mortality of COVID-19.
We found no significant correlation between obesity (OR 1.19, 95% CI 0.94–1.51) and death. We also did the subgroup analysis for morbid obesity (BMI ≥ 40 kg/m 2 ), and the results were not statistically significant (OR 0.98, 95% CI 0.80–1.20). Our meta-analysis showed that asthma was associated with a reduced risk of mortality (OR 0.74, 95% CI 0.68–0.80). The Charlson index score equals to 0 seemed to be a protective factor for mortality (OR 0.31, 95% CI 0.18–0.51), while a score ≥2 might be consistent with the higher likelihood of death (OR 4.22, 95% CI 2.56–6.96).
The cumulative meta-analysis showed that the sample size increased; the CI for hypertension, diabetes, COPD, coronary heart disease, and cancer became increasingly narrower; and statistical significance was more common ( Appendix 4 in Supplementary Material). However, the subgroup of cerebrovascular disease with the admission date of patients in summer was not significant ( P > 0.05), probably due to only two studies were included.
Association Between Chronic Diseases and ICU Admission of COVID-19
Fifty-three studies involving a total of 260,465 patients and 12,233 cases of ICU admission were included. Of these studies, 14 were conducted in China; 9 in the USA; 6 in Italy; 4 in South Korea; 3 in France, Germany, and Mexico, respectively; 2 in Kuwait; and 1 in Denmark, India, Iran, Oman, Poland, Qatar, Saudi Arabia, Spain, and Turkey, respectively.
We found that 73.62% of the ICU patients had at least one type of chronic disease, which was significantly higher than that in the non-ICU group (OR 2.82, 95% CI 2.23–3.56) ( Table 4 ). Hypertension (OR 2.24, 95% CI 1.90–2.63), diabetes (OR 2.50, 95% CI 2.18–2.87), COPD (OR 2.76, 95% CI 1.99–3.82), unspecified type of pulmonary disease (OR 1.40, 95% CI 1.26–1.56), coronary heart disease (OR 2.16, 95% CI 1.56–2.99), heart failure (OR 1.80, 95% CI 1.44–2.55), unspecified type of cardiovascular disease (OR 2.38, 95% CI 1.92–2.96), hyperlipidemia (OR 1.53, 95% CI 1.22–1.93), obesity (OR 1.86, 95% CI 1.49–2.31), chronic renal disease (OR 2.25, 95% CI 1.73–2.94), and cancer (OR 1.57, 95% CI 1.39–1.77) were significant predictive factors for admission to ICU. On the other hand, asthma and chronic liver disease were not significantly associated with ICU admission ( P > 0.05). The association between cerebrovascular disease and ICU admission was not very obvious ( P = 0.048).
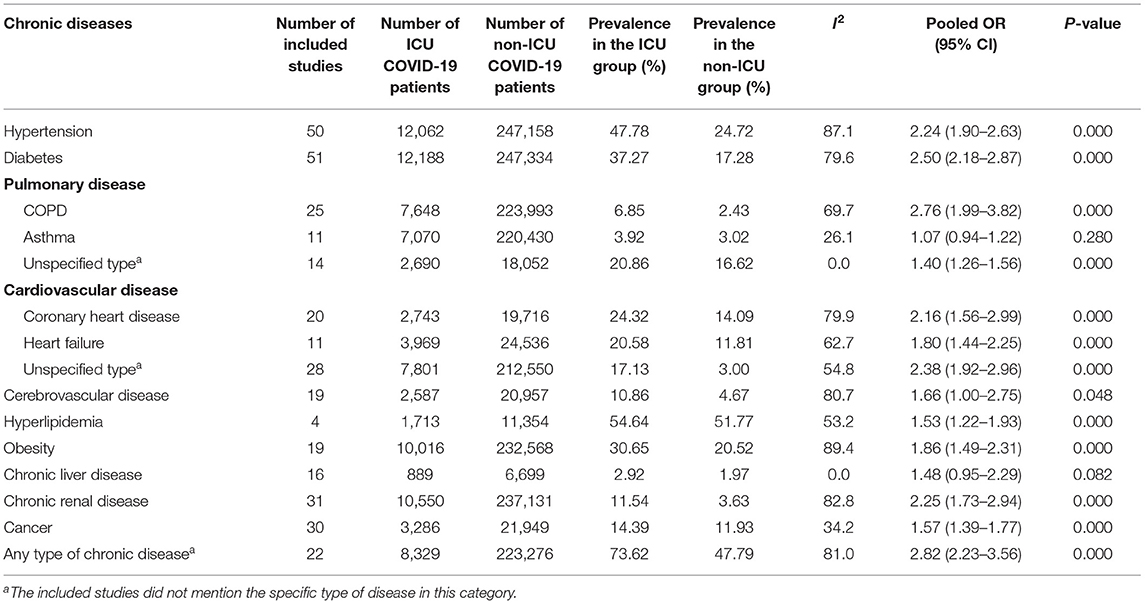
Table 4 . Associations between chronic diseases and ICU admission of COVID-19.
The cumulative meta-analysis showed that the statistical significance of hypertension, diabetes, COPD, coronary heart disease, and cancer had the tendency of becoming evident with increasing sample size ( Appendix 4 in Supplementary Material).
Association Between Chronic Diseases and ARDS of COVID-19
Six studies involving a total of 2,128 patients and 635 cases of ARDS admission were included. Two of them were conducted in China, two in Italy, and 1 in Germany and the USA, respectively.
We found a significant association between hypertension (OR 2.17, 95% CI 1.78–2.66), diabetes (OR 2.32, 95% CI 1.70–3.17), coronary heart disease (OR 1.96, 95% CI 1.32–2.92), unspecified type of cardiovascular disease (OR 2.35, 95% CI 1.24–4.47), obesity (OR 2.25, 95% CI 1.18–4.28), chronic renal disease (OR 1.63, 95% CI 1.14–2.33), and occurrence of ARDS ( Table 5 ). COPD, heart failure, and cerebrovascular disease were not significantly correlated with the risk of ARDS ( P > 0.05).
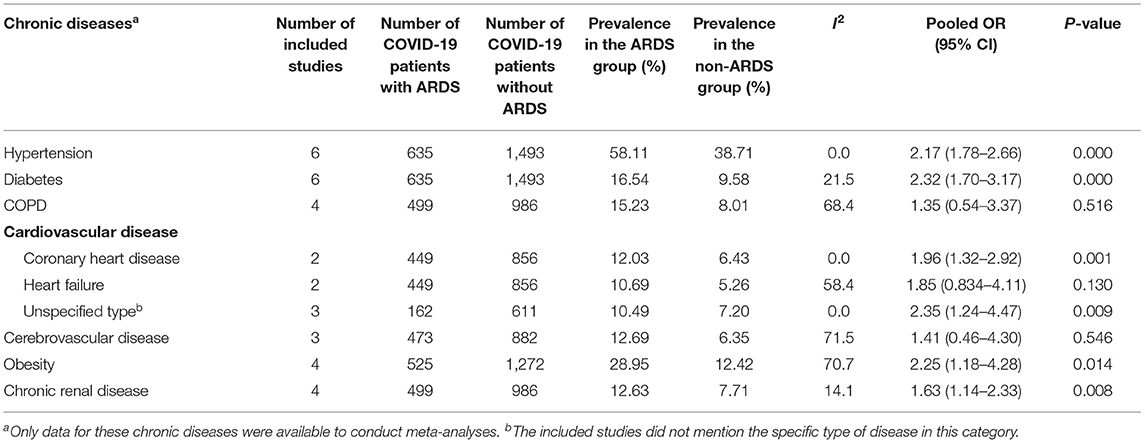
Table 5 . Associations between chronic diseases and ARDS of COVID-19.
Given the ongoing COVID-19 pandemic and the consequent global healthcare crisis, there is an urgent need to better understand risk factors for symptom deterioration and identify the vulnerable populations at higher risk for COVID-19 mortality. Our meta-analysis aimed to meet the need by examining global evidence, including 217 studies from 26 countries with 624,986 COVID-19 patients. Compared with a prior meta-analysis that showed that among COVID-19 patients, 20.3% required ICU admission and 32.8% had ARDS ( 244 ), our analysis provided further data on the association between chronic diseases and the different clinical prognoses of COVID-19 patients. According to our findings, COVID-19 patients with chronic diseases were more likely to have severe symptoms, ICU admissions, and an increased risk of mortality.
On the contrary, a meta-analysis found that pre-existing chronic conditions were not correlated with COVID-19 mortality (OR 2.09, 95% CI 0.26 to 16.67) ( 12 ). However, the conclusion of that meta-analysis was not reliable due to the fact that it only included three studies with a small sample size (453). In comparison, our meta-analysis had a much large sample size and identified the significant associations between a variety of chronic conditions and COVID-19 mortality, such as hypertension, diabetes, COPD, unspecified type of pulmonary disease, coronary heart disease, heart failure, unspecified type of cardiovascular disease, cerebrovascular disease, hyperlipidemia, chronic liver disease, chronic renal disease, and cancer.
We found that among COVID-19 patients, hypertension was a common comorbidity and was associated with COVID-19 severity, ICU admission, ARDS, and mortality. We found that COPD was the strongest predictive comorbidity for COVID-19 severity, ICU admission, and mortality, a finding that is consistent with prior research results, confirming that COPD patients are particularly vulnerable for very severe or critical COVID-19 cases ( 6 ).
Whereas, the published COVID-19 systematic reviews used the term “cardiovascular disease” generally ( 11 , 13 , 245 ), merely merged different types of cardiovascular diseases into a single measure, or only used the data from “unspecified type of cardiovascular diseases” as the outcome ( 6 , 11 , 13 ), we categorized cardiovascular diseases into three groups—coronary heart disease, heart failure, and unspecified type of cardiovascular diseases—to provide specific evidence for decision-makers. We found that coronary heart disease was a potential risk factor for the severity, ICU admission, mortality, and ARDS of COVID-19, while heart failure could increase the probability of ICU admission and mortality.
According to our results, cerebrovascular disease was an important comorbidity for COVID-19 mortality. We also identified cerebrovascular disease as a risk factor for severity of COVID-19 patients, which was consistent with other meta-analyses ( 14 , 245 ). However, we found that there was a weak association between cerebrovascular disease and the risk of ICU admission, a finding that was different from a meta-analysis showing that cardio-cerebrovascular diseases were about 3-fold higher in ICU patients than in their non-ICU counterparts ( 17 ). However, only six studies were included in that meta-analysis, and its method was problematic as it calculated relative risk despite the fact that it included retrospective studies. Furthermore, cardiovascular disease and cerebrovascular disease were combined into a single outcome measure in the previous meta-analysis.
Asthma is a chronic disease of the air passages of the lungs which inflames and narrows them. Both its prevalence and mortality increased in recent decades, accounting for 272.68 million cases (3.57%) and 0.49 million deaths (0.006%) in the year 2017 ( 246 ). A multicenter retrospective study in 10 US hospitals found that asthma did not lead to an increased risk of hospitalization (RR 0.96, 95% CI 0.77–1.19) for COVID-19 patients after adjusting for age, sex, gender, and comorbidities ( 247 ). However, we found that asthma was associated with the severity of COVID-19 but tended to become a protective factor to reduce mortality risk. On the other hand, a published meta-analysis demonstrated that asthma patients were not predisposed to severe COVID-19 infections ( 248 ). It should be noted that the meta-analysis searched for articles published from January 1, 2020, to August 28, 2020, which was even shorter than our study, and only five studies were included in that meta-analysis.
The prevalence of obesity in many countries has been increasing rapidly in recent decades. We found that obese patients were at a higher risk of developing severe COVID-19 symptoms. However, the association between obesity (BMI ≥ 28 or 30 kg/m 2 ) and mortality was not statistically significant. We did not find a significant relationship between morbid obesity (BMI ≥ 40 kg/m 2 ) and mortality.
Hyperlipidemia involves an imbalance of cholesterol levels, including low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C) in the blood. It has become common in many countries ( 249 ), especially in the USA where low HDL-C among adults aged 20 and over was 17.2% ( 250 ) and roughly 53% of adults had elevated LDL-C levels ( 251 ). Our results showed that hyperlipidemia was associated with increased ICU admission and mortality of COVID-19 patients.
A meta-analysis revealed an insignificant correlation between the increased risk of severe COVID-19 and liver disease, cancer, or renal disease ( 245 ). The insignificant results were probably due to the small number of studies included in the analysis—only five studies were included and all of them were from China. In contrast, our large sample size from multiple countries enabled us to find that those COVID-19 patients with chronic liver disease, cancer, or chronic renal disease were more likely to become severe cases and had a higher risk of mortality.
Our results emphasize the need for enhanced vigilance, priority for detection and testing, and aggressive COVID-19 therapy for patients with chronic diseases. Given our findings that COVID-19 patients with various chronic diseases were more likely to experience severe symptoms and ICU admissions and faced a higher risk of mortality, policymakers across different countries need to target patients with chronic diseases as a priority of their strategies to combat the COVID-19 pandemic. In particular, measures should be taken to protect the vulnerable groups with specific types of chronic disease, such as hypertension, diabetes, cardiovascular disease, and hyperlipidemia, each of which has a high prevalence in the general population.
For some of the less common chronic conditions, a targeted and intensive health protection strategy is also warranted. For example, although COPD is a less common condition among the general population, our analysis indicated that it is strongly associated with COVID-19 severity, ICU admission, and mortality. We also found that cerebrovascular disease, a less common condition that is the leading cause of serious long-term disability, was a significant comorbidity predicting mortality in COVID-19 patients. Thus, patients with COPD and/or cerebrovascular diseases should receive special attention from both policymakers and healthcare professionals.
Finally, our analysis suggested that more adequately powered studies should be conducted to investigate how the severity and mortality of COVID-19 are associated with morbid obesity and hyperlipidemia, and a composite measure of comorbidity such as the Charlson comorbidity index must be utilized. The risk factors for ARDS in patients with severe COVID-19 are also worthy of further analysis in the future.
The results of our systematic review should be interpreted in the context of its limitations. First, we did not include studies that only analyzed children, pregnancies, and healthcare professionals in order to ensure the homogeneity and representativeness of the general population. The existing systematic reviews found that children seemed to have a milder disease course and better prognosis than adults ( 252 ) and that vertical transmission of COVID-19 from pregnancies to newborns could not be ruled out ( 253 ). Second, there was a limited sample size on risk factors for ARDS, and future observational studies are still needed on this topic. Third, the predictive value of concurrent multiple chronic diseases for the prognosis of COVID-19 patients remains unclear. Fourth, we were unable to conduct subgroup analysis according to community dwellings and institutionalized individuals due to a lack of data from the included studies. The association between chronic diseases and severity of COVID-19 should be further analyzed in community care and institutional care, respectively. Finally, further observational studies and meta-analyses are still needed to explore the impacts of chronic diseases on the severity and mortality in later waves of the COVID-19 pandemic.
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material , further inquiries can be directed to the corresponding author.
Author Contributions
HY and JG designed the protocol. JG, XC, and CL performed the literature search and screening. XYu, HB, ZF, JZ, and XC extracted the data and did the quality assessment. JG and YC checked the data. XYuan took part in the interpretation of the data. JG and HY contributed to the meta-analysis and interpretation of the results and drafted the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by National Natural Science Foundation of China (Grant No. 71603138), Jiangsu Overseas Visiting Scholar Program for University Prominent Young & Middle-aged Teachers and Presidents, and Primary Healthcare Research Project in Nantong (Grant No. 2020JCC003). The funders had no role in the design, literature search, data extraction, statistical analysis, data interpretation, or writing of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
At the time of drafting the manuscript, JG was a fellow at the Fellowship in Health Policy and Insurance Research, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Healthcare Institute. We sincerely acknowledge the comments and suggestions from the reviewers.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.588013/full#supplementary-material
1. World Health Organization. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV) . (2020). Available online at: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (accessed June 2, 2020).
Google Scholar
2. World Health Organization. Coronavirus disease (COVID-19) Situation Report-157 . (2020). Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200625-covid-19-sitrep-157.pdf?sfvrsn=423f4a82_2 (accessed June 2, 2020).
3. Stevens MP, Doll M, Pryor R, Godbout E, Cooper K, Bearman G. Impact of COVID-19 on traditional healthcare-associated infection prevention efforts. Infect Control Hosp Epidemiol. (2020) 41:946–7. doi: 10.1017/ice.2020.141
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the chinese center for disease control and prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
5. Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emergency Med. (2020) 8:e35. doi: 10.22037/aaem.v8i1.600
6. Jain V, Yuan JM. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int J Public Health. (2020) 65:533–46. doi: 10.1007/s00038-020-01390-7
7. Li X, Guan B, Su T, Liu W, Chen M, Bin Waleed K, et al. Impact of cardiovascular disease and cardiac injury on in-hospital mortality in patients with COVID-19: a systematic review and meta-analysis. Heart. (2020) 106:1142–7. doi: 10.1136/heartjnl-2020-317062
8. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. (2020) 94:91–5. doi: 10.1016/j.ijid.2020.03.017
9. Zhang J, Wu J, Sun X, Xue H, Shao J, Cai W, et al. Association of hypertension with the severity and fatality of SARS-CoV-2 infection: a meta-analysis. Epidemiol Infect. (2020) 148:e106. doi: 10.1017/s095026882000117x
10. Zhao Q, Meng M, Kumar R, Wu Y, Huang J, Lian N, et al. The impact of COPD and smoking history on the severity of COVID-19: a systemic review and meta-analysis. J Med Virol. (2020) 92:1915–21. doi: 10.1002/jmv.25889
11. Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. (2020) 81:e16–25. doi: 10.1016/j.jinf.2020.04.021
12. Liu H, Chen S, Liu M, Nie H, Lu H. Comorbid chronic diseases are strongly correlated with disease severity among COVID-19 patients: a systematic review and meta-analysis. Aging Dis. (2020) 11:668–78. doi: 10.14336/ad.2020.0502
13. Parohan M, Yaghoubi S, Seraji A, Javanbakht MH, Sarraf P, Djalali M. Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Aging Male. (2020) 23:1416–24. doi: 10.1080/13685538.2020.1774748
14. Tian W, Jiang W, Yao J, Nicholson CJ, Li RH, Sigurslid HH, et al. Predictors of mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. J Med Virol. (2020) 92:1875–83. doi: 10.1002/jmv.26050
15. Pranata R, Lim MA, Huang I, Raharjo SB, Lukito AA. Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: a systematic review, meta-analysis and meta-regression. J Renin Angiotensin Aldosterone Syst. (2020) 21:1470320320926899. doi: 10.1177/1470320320926899
16. Zhu J, Ji P, Pang J, Zhong Z, Li H, He C, et al. Clinical characteristics of 3062 COVID-19 patients: a meta-analysis. J Med Virol. (2020) 92:1902–14. doi: 10.1002/jmv.25884
17. Jiang SW, Gao H, Wu L, Wang GW, Cen FL, Li JX, et al. [Clinical feature changes of a COVID-19 patient from mild to critical condition and cardiopulmonary pathological results]. Zhonghua Xin Xue Guan Bing Za Zhi. (2020) 48:580–6. doi: 10.3760/cma.j.cn112148-20200304-00155
18. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
19. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
20. The Joanna Briggs Institute. Critical Appraisal Tools for Use in JBI Systematic Reviews: Checklist for Cohort Studies . (2020). Available online at: http://joannabriggs.org/research/critical-appraisal-tools.html (accessed June 16, 2021).
21. The Joanna Briggs Institute. Critical Appraisal Tools for Use in JBI Systematic Reviews: Checklist for Case Series . (2020). Available online at: http://joannabriggs.org/research/critical-appraisal-tools.html . (accessed June 16, 2021).
22. The Joanna Briggs Institute. Critical Appraisal Tools for Use in JBI Systematic Reviews: Checklist for Case-Control Studies . (2020). Available online at: http://joannabriggs.org/research/critical-appraisal-tools.html . (accessed June 16, 2021).
23. The Joanna Briggs Institute. Critical Appraisal Tools for Use in JBI Systematic Reviews: Checklist for Analytical Cross Sectional Studies . (2020). Available online at: http://joannabriggs.org/research/critical-appraisal-tools.html . (accessed June 16, 2021).
24. Higgins J, Wells G. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Collaboration . (2019). Available online at: https://training.cochrane.org/handbook/current . (accessed June 16, 2020).
PubMed Abstract | Google Scholar
25. DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
26. Feng H, Zhao Y, Jing T, Ma J, Zhao Y, Zhang J, et al. Traditional and cumulative meta-analysis: Chemoradiotherapy followed by surgery versus surgery alone for resectable esophageal carcinoma. Mol Clin Oncol. (2018) 8:342–51. doi: 10.3892/mco.2017.1534
27. Abohamr SI, Abazid RM, Aldossari MA, Amer HA, Badhawi OS, Aljunaidi OM, et al. Clinical characteristics and in-hospital mortality of COVID-19 adult patients in Saudi Arabia. Saudi Med J. (2020) 41:1217–26. doi: 10.15537/smj.2020.11.25495
28. Aggarwal S, Garcia-Telles N, Aggarwal G, Lavie C, Lippi G, Henry BM. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): early report from the United States. Diagnosis. (2020) 7:91–6. doi: 10.1515/dx-2020-0046
29. Ali S, H DA, Arash M, Alireza A, Mehdi K, Saman H, et al. Novel coronavirus disease 2019: predicting prognosis by using a computed tomography severity score and clinicolaboratory data. Polish Arch Intern Med. (2020) 130:629–34. doi: 10.20452/pamw.15422
30. Allameh SF, Nemati S, Ghalehtaki R, Mohammadnejad E, Aghili SM, Khajavirad N, et al. Clinical characteristics and outcomes of 905 COVID-19 patients admitted to imam khomeini hospital complex in the capital city of Tehran, Iran. Arch Iran Med. (2020) 23:766–75. doi: 10.34172/aim.2020.102
31. Alqahtani AM, AlMalki ZS, Alalweet RM, Almazrou SH, Alanazi AS, Alanazi MA, et al. Assessing the severity of illness in patients with coronavirus disease in Saudi Arabia: a retrospective descriptive cross-sectional study. Front Public Health. (2020) 8:593256. doi: 10.3389/fpubh.2020.593256
32. Al-Sabah S, Al-Haddad M, Al-Youha S, Jamal M, Almazeedi S. COVID-19: impact of obesity and diabetes on disease severity. Clin Obes. (2020) 10:e12414. doi: 10.1111/cob.12414
33. Alshukry A, Ali H, Ali Y, Al-Taweel T, Abu-Farha M, AbuBaker J, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) patients in Kuwait. PLoS ONE. (2020) 15:e0242768. doi: 10.1371/journal.pone.0242768
34. Argenziano MG, Bruce SL, Slater CL, Tiao JR, Baldwin MR, Barr RG, et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. (2020) 369:m1996. doi: 10.1136/bmj.m1996
35. Attaway AA, Zein J, Hatipoglu US. SARS-CoV-2 infection in the COPD population is associated with increased healthcare utilization: an analysis of Cleveland clinic's COVID-19 registry. EClinicalMedicine. (2020) 26:100515. doi: 10.1016/j.eclinm.2020.100515
36. Bahl A, Van Baalen MN, Ortiz L, Chen NW, Todd C, Milad M, et al. Early predictors of in-hospital mortality in patients with COVID-19 in a large American cohort. Intern. Emergency Med. (2020) 15:1485–99. doi: 10.1007/s11739-020-02509-7
37. Bartoletti M, Giannella M, Scudeller L, Tedeschi S, Rinaldi M, Bussini L, et al. Development and validation of a prediction model for severe respiratory failure in hospitalized patients with SARS-CoV-2 infection: a multicentre cohort study (PREDI-CO study). Clin Microbiol Infect. (2020) 26:1545–53. doi: 10.1016/j.cmi.2020.08.003
38. Bellan M, Patti G, Hayden E, Azzolina D, Pirisi M, Acquaviva A, et al. Fatality rate and predictors of mortality in an Italian cohort of hospitalized COVID-19 patients. Sci Rep. (2020) 10:20731. doi: 10.1038/s41598-020-77698-4
39. Bepouka BI, Mandina M, Makulo JR, Longokolo M, Odio O, Mayasi N, et al. Predictors of mortality in COVID-19 patients at Kinshasa University Hospital, Democratic Republic of the Congo, from March to June 2020. Pan Afr Med J. (2020) 37:105. doi: 10.11604/pamj.2020.37.105.25279
40. Berenguer J, Ryan P, Rodríguez-Baño J, Jarrín I, Carratalà J, Pachón J, et al. Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain. Clin Microbiol Infect. (2020) 26:1525–36. doi: 10.1016/j.cmi.2020.07.024
41. Bhargava A, Fukushima EA, Levine M, Zhao W, Tanveer F, Szpunar SM, et al. Predictors for severe COVID-19 infection. Clin Infect Dis. (2020) 71:1962–8. doi: 10.1093/cid/ciaa674
42. Boari GEM, Chiarini G, Bonetti S, Malerba P, Bianco G, Faustini C, et al. Prognostic factors and predictors of outcome in patients with COVID-19 and related pneumonia: a retrospective cohort study. Biosci Rep. (2020) 40:BSR20203455. doi: 10.1042/bsr20203455
43. Borobia AM, Carcas AJ, Arnalich F, Álvarez-Sala R, Monserrat-Villatoro J, Quintana M, et al. A cohort of patients with COVID-19 in a major teaching hospital in Europe. J Clin Med. (2020) 9:1733. doi: 10.3390/jcm9061733
44. Brill SE, Jarvis HC, Ozcan E, Burns TLP, Warraich RA, Amani LJ, et al. COVID-19: a retrospective cohort study with focus on the over-80s and hospital-onset disease. BMC Med. (2020) 18:194. doi: 10.1186/s12916-020-01665-z
45. Buckner FS, McCulloch DJ, Atluri V, Blain M, McGuffin SA, Nalla AK, et al. Clinical features and outcomes of 105 hospitalized patients with COVID-19 in Seattle, Washington. Clin Infect Dis. (2020) 71:2167–73. doi: 10.1093/cid/ciaa632
46. Cai Q, Huang D, Ou P, Yu H, Zhu Z, Xia Z, et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. (2020) 75:1742–52. doi: 10.1111/all.14309
47. Caliskan T, Saylan B. Smoking and comorbidities are associated with COVID-19 severity and mortality in 565 patients treated in Turkey: a retrospective observational study. Rev Assoc Med Bras. (2020) 66:1679–84. doi: 10.1590/1806-9282.66.12.1679
48. Cao J, Tu WJ, Cheng W, Yu L, Liu YK, Hu X, et al. Clinical features and short-term outcomes of 102 patients with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. (2020) 71:748–55. doi: 10.1093/cid/ciaa243
49. Cao Y, Han X, Gu J, Li Y, Liu J, Alwalid O, et al. Prognostic value of baseline clinical and HRCT findings in 101 patients with severe COVID-19 in Wuhan, China. Sci Rep. (2020) 10:17543. doi: 10.1038/s41598-020-74497-9
50. Carrillo-Vega MF, Salinas-Escudero G, García-Peña C, Gutiérrez-Robledo LM, Parra-Rodríguez L. Early estimation of the risk factors for hospitalization and mortality by COVID-19 in Mexico. PLoS ONE. (2020) 15:e0238905. doi: 10.1371/journal.pone.0238905
51. Cattelan AM, Di Meco E, Trevenzoli M, Frater A, Ferrari A, Villano M, et al. Clinical characteristics and laboratory biomarkers changes in COVID-19 patients requiring or not intensive or sub-intensive care: a comparative study. BMC Infect Dis. (2020) 20:934. doi: 10.1186/s12879-020-05647-7
52. Cen Y, Chen X, Shen Y, Zhang XH, Lei Y, Xu C, et al. Risk factors for disease progression in patients with mild to moderate coronavirus disease 2019-a multi-centre observational study. Clin Microbiol Infect. (2020) 26:1242–7. doi: 10.1016/j.cmi.2020.05.041
53. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. (2020) 130:2620–9. doi: 10.1172/jci137244
54. Chen Q, Zheng Z, Zhang C, Zhang X, Wu H, Wang J, et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Taizhou, Zhejiang, China. Infection. (2020) 48:543–51. doi: 10.1007/s15010-020-01432-5
55. Chen R, Liang W, Jiang M, Guan W, Zhan C, Wang T, et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. (2020) 158:97–105. doi: 10.1016/j.chest.2020.04.010
56. Chen T, Dai Z, Mo P, Li X, Ma Z, Song S, et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: a single-centered, retrospective study. J Gerontol A Biol Sci Med Sci. (2020) 75:1788–95. doi: 10.1093/gerona/glaa089
57. Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. (2020) 368:m1091. doi: 10.1136/bmj.m1091
58. Chinnadurai R, Ogedengbe O, Agarwal P, Money-Coomes S, Abdurrahman AZ, Mohammed S, et al. Older age and frailty are the chief predictors of mortality in COVID-19 patients admitted to an acute medical unit in a secondary care setting- a cohort study. BMC Geriatr. (2020) 20:409. doi: 10.1186/s12877-020-01803-5
59. Ciceri F, Castagna A, Rovere-Querini P, De Cobelli F, Ruggeri A, Galli L, et al. Early predictors of clinical outcomes of COVID-19 outbreak in Milan, Italy. Clin Immunol. (2020) 217:108509. doi: 10.1016/j.clim.2020.108509
60. Cocconcelli E, Biondini D, Giraudo C, Lococo S, Bernardinello N, Fichera G, et al. Clinical features and chest imaging as predictors of intensity of care in patients with COVID-19. J Clin Med. (2020) 9:2990. doi: 10.3390/jcm9092990
61. Colombi D, Bodini FC, Petrini M, Maffi G, Morelli N, Milanese G, et al. Well-aerated lung on admitting chest CT to predict adverse outcome in COVID-19 pneumonia. Radiology. (2020) 296:E86–96. doi: 10.1148/radiol.2020201433
62. Cortés-Tellés A, López-Romero S, Mancilla-Ceballos R, Ortíz-Farías DL, Núñez-Caamal N, Figueroa-Hurtado E. Risk factors for mortality in hospitalized patients with COVID-19: an overview in a mexican population. Tubercul Respir Dis. (2020) 83(Suppl. 1):S46–54. doi: 10.4046/trd.2020.0095
63. Covino M, De Matteis G, Santoro M, Sabia L, Simeoni B, Candelli M, et al. Clinical characteristics and prognostic factors in COVID-19 patients aged ≥80 years. Geriatr Gerontol Int. (2020) 20:704–8. doi: 10.1111/ggi.13960
64. de Andrade CLT, Pereira CCA, Martins M, Lima SML, Portela MC. COVID-19 hospitalizations in Brazil's Unified Health System (SUS). PLoS ONE. (2020) 15:e0243126. doi: 10.1371/journal.pone.0243126
65. de Souza CD, de Arruda Magalhães AJ, Lima AJ, Nunes DN, de Fátima Machado Soares É, de Castro Silva L, et al. Clinical manifestations and factors associated with mortality from COVID-19 in older adults: retrospective population-based study with 9807 older Brazilian COVID-19 patients. Geriatr Gerontol Int. (2020) 20:1177–81. doi: 10.1111/ggi.14061
66. Deng M, Qi Y, Deng L, Wang H, Xu Y, Li Z, et al. Obesity as a potential predictor of disease severity in young COVID-19 patients: a retrospective study. Obesity. (2020) 28:1815–25. doi: 10.1002/oby.22943
67. Deng Y, Liu W, Liu K, Fang YY, Shang J, Zhou L, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: a retrospective study. Chin Med J. (2020) 133:1261–7. doi: 10.1097/cm9.0000000000000824
68. Di Castelnuovo A, Bonaccio M, Costanzo S, Gialluisi A, Antinori A, Berselli N, et al. Common cardiovascular risk factors and in-hospital mortality in 3,894 patients with COVID-19: survival analysis and machine learning-based findings from the multicentre Italian CORIST Study. Nutr Metab Cardiovasc Dis. (2020) 30:1899–913. doi: 10.1016/j.numecd.2020.07.031
69. Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. (2020) 369:m1985. doi: 10.1136/bmj.m1985
70. Dreher M, Kersten A, Bickenbach J, Balfanz P, Hartmann B, Cornelissen C, et al. The characteristics of 50 hospitalized COVID-19 patients with and without ARDS. Deutsch Arzteblatt Int. (2020) 117:271–8. doi: 10.3238/arztebl.2020.0271
71. Du H, Pan X, Liu N, Chen J, Chen X, Werring DJ, et al. The effect of vascular risk factor burden on the severity of COVID-19 illness, a retrospective cohort study. Respir Res. (2020) 21:241. doi: 10.1186/s12931-020-01510-0
72. Du RH, Liang LR, Yang CQ, Wang W, Cao TZ, Li M, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARSCoV- 2: a prospective cohort study. Eur Respir J. (2020) 55:2000524. doi: 10.1183/13993003.00524-2020
73. Du RH, Liu LM, Yin W, Wang W, Guan LL, Yuan ML, et al. Hospitalization and critical care of 109 decedents with COVID-19 Pneumonia in Wuhan, China. Ann Am Thorac Soc. (2020) 17:839–46. doi: 10.1513/AnnalsATS.202003-225OC
74. Duan J, Wang X, Chi J, Chen H, Bai L, Hu Q, et al. Correlation between the variables collected at admission and progression to severe cases during hospitalization among patients with COVID-19 in Chongqing. J Med Virol. (2020) 92:2616–22. doi: 10.1002/jmv.26082
75. Ebinger JE, Achamallah N, Ji H, Claggett BL, Sun N, Botting P, et al. Pre-existing traits associated with Covid-19 illness severity. PLoS ONE. (2020) 15:e0236240. doi: 10.1371/journal.pone.0236240
76. Efrén M, Xóchitl T, Miguel H, Mónica R, Oliver M. Male gender and kidney illness are associated with an increased risk of severe laboratory-confirmed coronavirus disease. BMC Infect Dis. (2020) 20:674. doi: 10.1186/s12879-020-05408-6
77. Eliana F, Paolo GR, Stefania SA, Gianluca T, Gisella P, Olivia L, et al. Survival of hospitalized COVID-19 patients in Northern Italy: a population-based cohort study by the ITA-COVID-19 network. Clin Epidemiol. (2020) 12:1337–46. doi: 10.2147/CLEP.S271763
78. El-Solh AA, Lawson Y, Carter M, El-Solh DA, Mergenhagen KA. Comparison of in-hospital mortality risk prediction models from COVID-19. PLoS ONE. (2020) 15:e0244629. doi: 10.1371/journal.pone.0244629
79. Escalera-Antezana JP, Lizon-Ferrufino NF, Maldonado-Alanoca A, Alarcon-De-la-Vega G, Alvarado-Arnez LE, Balderrama-Saavedra MA, et al. Risk factors for mortality in patients with Coronavirus Disease 2019 (COVID-19) in Bolivia: an analysis of the first 107 confirmed cases. Le Infezioni Med. (2020) 28:238–42.
80. Feng Y, Ling Y, Bai T, Xie Y, Huang J, Li J, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med. (2020) 201:1380–8. doi: 10.1164/rccm.202002-0445OC
81. Ferguson J, Rosser JI, Quintero O, Scott J, Subramanian A, Gumma M, et al. Characteristics and outcomes of coronavirus disease patients under nonsurge conditions, Northern California, USA, March-April 2020. Emerg Infect Dis. (2020) 26:1679–85. doi: 10.3201/eid2608.201776
82. Fumagalli C, Rozzini R, Vannini M, Coccia F, Cesaroni G, Mazzeo F, et al. Clinical risk score to predict in-hospital mortality in COVID-19 patients: a retrospective cohort study. BMJ Open. (2020) 10:e040729. doi: 10.1136/bmjopen-2020-040729
83. Gao C, Cai Y, Zhang K, Zhou L, Zhang Y, Zhang X, et al. Association of hypertension and antihypertensive treatment with COVID-19 mortality: a retrospective observational study. Eur Heart J. (2020) 41:2058–66. doi: 10.1093/eurheartj/ehaa433
84. Gao J, Huang X, Gu H, Lou L, Xu Z. Predictive criteria of severe cases in COVID-19 patients of early stage: a retrospective observational study. J Clin Lab Anal. (2020) 34:e23562. doi: 10.1002/jcla.23562
85. Genet B, Vidal JS, Cohen A, Boully C, Beunardeau M, Marine Harlé L, et al. COVID-19 in-hospital mortality and use of renin-angiotensin system blockers in geriatrics patients. J Am Med Direct Assoc. (2020) 21:1539–45. doi: 10.1016/j.jamda.2020.09.004
86. Giacomelli A, Ridolfo AL, Milazzo L, Oreni L, Bernacchia D, Siano M, et al. 30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: a prospective cohort study. Pharmacol Res. (2020) 158:104931. doi: 10.1016/j.phrs.2020.104931
87. Goodall JW, Reed TAN, Ardissino M, Bassett P, Whittington AM, Cohen DL, et al. Risk factors for severe disease in patients admitted with COVID-19 to a hospital in London, England: a retrospective cohort study. Epidemiol Infect. (2020) 148:e251. doi: 10.1017/s0950268820002472
88. Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. (2020) 180:1345–55. doi: 10.1001/jamainternmed.2020.3539
89. Gu T, Chu Q, Yu Z, Fa B, Li A, Xu L, et al. History of coronary heart disease increased the mortality rate of patients with COVID-19: a nested case-control study. BMJ Open. (2020) 10:e038976. doi: 10.1136/bmjopen-2020-038976
90. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. NEngl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
91. Gupta N, Ish P, Kumar R, Dev N, Yadav SR, Malhotra N, et al. Evaluation of the clinical profile, laboratory parameters and outcome of two hundred COVID-19 patients from a tertiary centre in India. Monaldi Arch Chest Dis. (2020) 90:675–82. doi: 10.4081/monaldi.2020.1507
92. Gupta S, Hayek SS, Wang W, Chan L, Mathews KS, Melamed ML, et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. (2020) 180:1436–47. doi: 10.1001/jamainternmed.2020.3596
93. Hajifathalian K, Sharaiha RZ, Kumar S, Krisko T, Skaf D, Ang B, et al. Development and external validation of a prediction risk model for short-term mortality among hospitalized U.S. COVID-19 patients: a proposal for the COVID-AID risk tool. PLoS ONE. (2020) 15:e0239536. doi: 10.1371/journal.pone.0239536
94. Harrison SL, Fazio-Eynullayeva E, Lane DA, Underhill P, Lip GYH. Comorbidities associated with mortality in 31,461 adults with COVID-19 in the United States: a federated electronic medical record analysis. PLoS Med. (2020) 17:e1003321. doi: 10.1371/journal.pmed.1003321
95. He F, Ding XF, Cao M, Gong HY, Fu XZ, Luo J, et al. Comparative analysis of 95 patients with different severity in the early outbreak of COVID-19 in Wuhan, China. Can J Infect Dis Med Microbiol. (2020) 2020:4783062. doi: 10.1155/2020/4783062
96. He F, Luo Q, Lei M, Fan L, Shao X, Huang G, et al. Risk factors for severe cases of COVID-19: a retrospective cohort study. Aging. (2020) 12:15730–40. doi: 10.18632/aging.103803
97. He XW, Lai JS, Cheng J, Wang MW, Liu YJ, Xiao ZC, et al. Impact of complicated myocardial injury on the clinical outcome of severe or critically ill COVID-19 patients. Zhonghua Xin Xue Guan Bing Za Zhi. (2020) 48:456–60. doi: 10.3760/cma.j.cn112148-20200228-00137
98. Hernández-Galdamez DR, González-Block M, Romo-Dueñas DK, Lima-Morales R, Hernández-Vicente IA, Lumbreras-Guzmán M, et al. Increased risk of hospitalization and death in patients with COVID-19 and pre-existing noncommunicable diseases and modifiable risk factors in Mexico. Arch Med Res. (2020) 51:683–9. doi: 10.1016/j.arcmed.2020.07.003
99. Hong KS, Lee KH, Chung JH, Shin KC, Choi EY, Jin HJ, et al. Clinical features and outcomes of 98 patients hospitalized with SARS-CoV-2 infection in Daegu, South Korea: a brief descriptive study. Yonsei Med J. (2020) 61:431–7. doi: 10.3349/ymj.2020.61.5.431
100. Hou H, Zhang B, Huang H, Luo Y, Wu S, Tang G, et al. Using IL-2R/lymphocytes for predicting the clinical progression of patients with COVID-19. Clin Exp Immunol. (2020) 201:76–84. doi: 10.1111/cei.13450
101. Hu L, Chen S, Fu Y, Gao Z, Long H, Ren HW, et al. Risk factors associated with clinical outcomes in 323 coronavirus disease 2019 (COVID-19) hospitalized patients in Wuhan, China. Clin Infect Dis. (2020) 71:2089–98. doi: 10.1093/cid/ciaa539
102. Hu X, Hu C, Yang Y, Chen J, Zhong P, Wen Y, et al. Clinical characteristics and risk factors for severity of COVID-19 outside Wuhan: a double-center retrospective cohort study of 213 cases in Hunan, China. Ther Adv Respir Dis. (2020) 14:1753466620963035. doi: 10.1177/1753466620963035
103. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/s0140-6736(20)30183-5
104. Huang J, Cheng A, Kumar R, Fang Y, Chen G, Zhu Y, et al. Hypoalbuminemia predicts the outcome of COVID-19 independent of age and co-morbidity. J Med Virol. (2020) 92:2152–8. doi: 10.1002/jmv.26003
105. Huang Q, Deng X, Li Y, Sun X, Chen Q, Xie M, et al. Clinical characteristics and drug therapies in patients with the common-type coronavirus disease 2019 in Hunan, China. Int J Clin Pharm. (2020) 42:837–45. doi: 10.1007/s11096-020-01031-2
106. Huang R, Zhu L, Xue L, Liu L, Yan X, Wang J, et al. Clinical findings of patients with coronavirus disease 2019 in Jiangsu province, China: a retrospective, multi-center study. PLoS Negl Trop Dis. (2020) 14:e0008280. doi: 10.1371/journal.pntd.0008280
107. Huh K, Lee R, Ji W, Kang M, Hwang IC, Lee DH, et al. Impact of obesity, fasting plasma glucose level, blood pressure, and renal function on the severity of COVID-19: a matter of sexual dimorphism? Diabetes Res Clin Pract. (2020) 170:108515. doi: 10.1016/j.diabres.2020.108515
108. Hwang J, Ryu HS, Kim HA, Hyun M, Lee JY, Yi HA. Prognostic factors of COVID-19 infection in elderly patients: a multicenter study. J Clin Med. (2020) 9:3932. doi: 10.3390/jcm9123932
109. Hwang JM, Kim JH, Park JS, Chang MC, Park D. Neurological diseases as mortality predictive factors for patients with COVID-19: a retrospective cohort study. Neurol Sci. (2020) 41:2317–24. doi: 10.1007/s10072-020-04541-z
110. Iaccarino G, Grassi G, Borghi C, Ferri C, Salvetti M, Volpe M. Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian society of hypertension. Hypertension. (2020) 76:366–72. doi: 10.1161/hypertensionaha.120.15324
111. Ioannou GN, Locke E, Green P, Berry K, O'Hare AM, Shah JA, et al. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US veterans with SARS-CoV-2 infection. JAMA Netw Open. (2020) 3:e2022310. doi: 10.1001/jamanetworkopen.2020.22310
112. Islam MZ, Riaz BK, Islam A, Khanam F, Akhter J, Choudhury R, et al. Risk factors associated with morbidity and mortality outcomes of COVID-19 patients on the 28th day of the disease course: a retrospective cohort study in Bangladesh. Epidemiol Infect. (2020) 148:e263. doi: 10.1017/s0950268820002630
113. Israelsen SB, Kristiansen KT, Hindsberger B, Ulrik CS, Andersen O, Jensen M, et al. Characteristics of patients with COVID-19 pneumonia at Hvidovre Hospital, March-April 2020. Danish Med J. (2020) 67:A05200313.
114. Jiang Y, Abudurexiti S, An MM, Cao D, Wei J, Gong P. Risk factors associated with 28-day all-cause mortality in older severe COVID-19 patients in Wuhan, China: a retrospective observational study. Sci Rep. (2020) 10:22369. doi: 10.1038/s41598-020-79508-3
115. Jiménez E, Fontán-Vela M, Valencia J, Fernandez-Jimenez I, Álvaro-Alonso EA, Izquierdo-García E, et al. Characteristics, complications and outcomes among 1549 patients hospitalised with COVID-19 in a secondary hospital in Madrid, Spain: a retrospective case series study. BMJ Open. (2020) 10:e042398. doi: 10.1136/bmjopen-2020-042398
116. Jourdes A, Lafaurie M, Martin-Blondel G, Delobel P, Faruch M, Charpentier S, et al. Clinical characteristics and outcome of hospitalized patients with SARS-CoV-2 infection at Toulouse University hospital (France). Results from the Covid-clinic-Toul cohort. La Revue Med Interne. (2020) 41:732–40. doi: 10.1016/j.revmed.2020.08.006
117. Kalligeros M, Shehadeh F, Mylona EK, Benitez G, Beckwith CG, Chan PA, et al. Association of obesity with disease severity among patients with coronavirus disease 2019. Obesity. (2020) 28:1200–4. doi: 10.1002/oby.22859
118. Karagiannidis C, Mostert C, Hentschker C, Voshaar T, Malzahn J, Schillinger G, et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. (2020) 8:853–62. doi: 10.1016/s2213-2600(20)30316-7
119. Kayina CA, Haritha D, Soni L, Behera S, Nair PR, Gouri M, et al. Epidemiological & clinical characteristics & early outcome of COVID-19 patients in a tertiary care teaching hospital in India: a preliminary analysis. Indian J Med Res. (2020) 152:100–4. doi: 10.4103/ijmr.IJMR_2890_20
120. Khamis F, Al-Zakwani I, Al Naamani H, Al Lawati S, Pandak N, Omar MB, et al. Clinical characteristics and outcomes of the first 63 adult patients hospitalized with COVID-19: an experience from Oman. J Infect Public Health. (2020) 13:906–13. doi: 10.1016/j.jiph.2020.06.002
121. Kim SR, Nam SH, Kim YR. Risk factors on the progression to clinical outcomes of COVID-19 patients in South Korea: using national data. Int J Environ Res Public Health. (2020) 17:8847. doi: 10.3390/ijerph17238847
122. Klang E, Kassim G, Soffer S, Freeman R, Levin MA, Reich DL. Severe obesity as an independent risk factor for COVID-19 mortality in hospitalized patients younger than 50. Obesity. (2020) 28:1595–9. doi: 10.1002/oby.22913
123. Kokoszka-Bargieł I, Cyprys P, Rutkowska K, Madowicz J, Knapik P. Intensive care unit admissions during the first 3 months of the COVID-19 pandemic in Poland: a single-center, cross-sectional study. Med Sci Monit. (2020) 26:e926974. doi: 10.12659/msm.926974
124. Kunal S, Sharma SM, Sharma SK, Gautam D, Bhatia H, Mahla H, et al. Cardiovascular complications and its impact on outcomes in COVID-19. Indian Heart J. (2020) 72:593–8. doi: 10.1016/j.ihj.2020.10.005
125. Labenz C, Kremer WM, Schattenberg JM, Wörns MA, Toenges G, Weinmann A, et al. Clinical Frailty Scale for risk stratification in patients with SARS-CoV-2 infection. J Invest Med. (2020) 68:1199–202. doi: 10.1136/jim-2020-001410
126. Lagi F, Piccica M, Graziani L, Vellere I, Botta A, Tilli M, et al. Early experience of an infectious and tropical diseases unit during the coronavirus disease (COVID-19) pandemic, Florence, Italy, February to March 2020. Euro Surveill. (2020) 25:2000556. doi: 10.2807/1560-7917.es.2020.25.17.2000556
127. Lee JY, Kim HA, Huh K, Hyun M, Rhee JY, Jang S, et al. Risk factors for mortality and respiratory support in elderly patients hospitalized with COVID-19 in Korea. J Korean Med Sci. (2020) 35:e223. doi: 10.3346/jkms.2020.35.e223
128. Lei F, Liu YM, Zhou F, Qin JJ, Zhang P, Zhu L, et al. Longitudinal association between markers of liver injury and mortality in COVID-19 in China. Hepatology. (2020) 72:389–98. doi: 10.1002/hep.31301
129. Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. (2020) 21:100331. doi: 10.1016/j.eclinm.2020.100331
130. Li G, Liu Y, Jing X, Wang Y, Miao M, Tao L, et al. Mortality risk of COVID-19 in elderly males with comorbidities: a multi-country study. Aging. (2020) 13:27–60. doi: 10.18632/aging.202456
131. Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. (2020) 55:327–31. doi: 10.1097/rli.0000000000000672
132. Li T, Lu L, Zhang W, Tao Y, Wang L, Bao J, et al. Clinical characteristics of 312 hospitalized older patients with COVID-19 in Wuhan, China. Arch Gerontol Geriatr. (2020) 91:104185. doi: 10.1016/j.archger.2020.104185
133. Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. (2020) 146:110–8. doi: 10.1016/j.jaci.2020.04.006
134. Li Y, Liu T, Tse G, Wu M, Jiang J, Liu M, et al. Electrocardiograhic characteristics in patients with coronavirus infection: a single-center observational study. Ann Noninvasive Electrocardiol. (2020) 25:e12805. doi: 10.1111/anec.12805
135. Li YK, Peng S, Li LQ, Wang Q, Ping W, Zhang N, et al. Clinical and transmission characteristics of Covid-19 - a retrospective study of 25 cases from a single thoracic surgery department. Curr Med Sci. (2020) 40:295–300. doi: 10.1007/s11596-020-2176-2
136. Liang W, Liang H, Ou L, Chen B, Chen A, Li C, et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med. (2020) 180:1081–9. doi: 10.1001/jamainternmed.2020.2033
137. Liao Y, Feng Y, Wang B, Wang H, Huang J, Wu Y, et al. Clinical characteristics and prognostic factors of COVID-19 patients progression to severe: a retrospective, observational study. Aging. (2020) 12:18853–65. doi: 10.18632/aging.103931
138. Liu D, Cui P, Zeng S, Wang S, Feng X, Xu S, et al. Risk factors for developing into critical COVID-19 patients in Wuhan, China: a multicenter, retrospective, cohort study. EClinicalMedicine. (2020) 25:100471. doi: 10.1016/j.eclinm.2020.100471
139. Liu D, Wang Y, Wang J, Liu J, Yue Y, Liu W, et al. Characteristics and outcomes of a sample of patients with COVID-19 identified through social media in Wuhan, China: observational study. J Med Internet Res. (2020) 22:e20108. doi: 10.2196/20108
140. Liu F, Zhang Q, Huang C, Shi C, Wang L, Shi N, et al. CT quantification of pneumonia lesions in early days predicts progression to severe illness in a cohort of COVID-19 patients. Theranostics. (2020) 10:5613–22. doi: 10.7150/thno.45985
141. Liu J, Li S, Liu J, Liang B, Wang X, Wang H, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine. (2020) 55:102763. doi: 10.1016/j.ebiom.2020.102763
142. Liu M, Han S, Liao Q, Chang L, Tan Y, Jia P, et al. Outcomes and prognostic factors in 70 non-survivors and 595 survivors with COVID-19 in Wuhan, China. Transbound Emerg Dis. (2020). doi: 10.1111/tbed.13969
143. Liu S, Luo H, Wang Y, Cuevas LE, Wang D, Ju S, et al. Clinical characteristics and risk factors of patients with severe COVID-19 in Jiangsu province, China: a retrospective multicentre cohort study. BMC Infect Dis. (2020) 20:584. doi: 10.1186/s12879-020-05314-x
144. Liu SP, Zhang Q, Wang W, Zhang M, Liu C, Xiao X, et al. Hyperglycemia is a strong predictor of poor prognosis in COVID-19. Diabetes Res Clin Pract. (2020) 167:108338. doi: 10.1016/j.diabres.2020.108338
145. Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thrombosis Res. (2020) 191:9–14. doi: 10.1016/j.thromres.2020.04.024
146. Lu Y, Sun K, Guo S, Wang J, Li A, Rong X, et al. Early warning indicators of severe COVID-19: a single-center study of cases from Shanghai, China. Front Med. (2020) 7:432. doi: 10.3389/fmed.2020.00432
147. Luo X, Zhou W, Yan X, Guo T, Wang B, Xia H, et al. Prognostic value of C-reactive protein in patients with coronavirus 2019. Clin Infect Dis. (2020) 71:2174–9. doi: 10.1093/cid/ciaa641
148. Zamanian M, Foroozanfar Z, Izadi Z, Jafari S, Derakhshankhah H, Salimi M. Association of underlying diseases and clinical characteristics with mortality in patients with 2019 novel coronavirus in Iran. Arch Clin Infect Dis. (2020) 15:1–9. doi: 10.5812/archcid.104621
149. Ma X, Li A, Jiao M, Shi Q, An X, Feng Y, et al. Characteristic of 523 COVID-19 in Henan Province and a death prediction model. Front Public Health. (2020) 8:475. doi: 10.3389/fpubh.2020.00475
150. Macedo MCF, Pinheiro IM, Carvalho CJL, Fraga H, Araujo IPC, Montes SS, et al. Correlation between hospitalized patients' demographics, symptoms, comorbidities, and COVID-19 pandemic in Bahia, Brazil. PLoS ONE. (2020) 15:e0243966. doi: 10.1371/journal.pone.0243966
151. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. (2020) 77:683–90. doi: 10.1001/jamaneurol.2020.1127
152. Mendes A, Serratrice C, Herrmann FR, Genton L, Périvier S, Scheffler M, et al. Predictors of in-hospital mortality in older patients with COVID-19: the COVIDAge study. J Am Med Direct Assoc. (2020) 21:1546–54. doi: 10.1016/j.jamda.2020.09.014
153. Monteiro AC, Suri R, Emeruwa IO, Stretch RJ, Cortes-Lopez RY, Sherman A, et al. Obesity and smoking as risk factors for invasive mechanical ventilation in COVID-19: a retrospective, observational cohort study. PLoS ONE. (2020) 15:e0238552. doi: 10.1371/journal.pone.0238552
154. Nachega JB, Ishoso DK, Otokoye JO, Hermans MP, Machekano RN, Sam-Agudu NA, et al. Clinical characteristics and outcomes of patients hospitalized for COVID-19 in Africa: early insights from the democratic republic of the Congo. Am J Trop Med Hyg. (2020) 103:2419–28. doi: 10.4269/ajtmh.20-1240
155. Nikpouraghdam M, Jalali Farahani A, Alishiri G, Heydari S, Ebrahimnia M, Samadinia H, et al. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: a single center study. J Clin Virol. (2020) 127:104378. doi: 10.1016/j.jcv.2020.104378
156. Okoh AK, Sossou C, Dangayach NS, Meledathu S, Phillips O, Raczek C, et al. Coronavirus disease 19 in minority populations of Newark, New Jersey. Int J Equity Health. (2020) 19:93. doi: 10.1186/s12939-020-01208-1
157. Omrani AS, Almaslamani MA, Daghfal J, Alattar RA, Elgara M, Shaar SH, et al. The first consecutive 5000 patients with Coronavirus Disease 2019 from Qatar; a nation-wide cohort study. BMC Infect Dis. (2020) 20:777. doi: 10.1186/s12879-020-05511-8
158. Ortiz-Brizuela E, Villanueva-Reza M, González-Lara MF, Tamez-Torres KM, Román-Montes CM, Díaz-Mejía BA, et al. Clinical and epidemiological characteristics of patients diagnosed with COVID-19 in a tertiary care center in Mexico city: a prospective cohort study. Rev Invest Clin. (2020) 72:252–8. doi: 10.24875/ric.20000334
159. Pan F, Yang L, Li Y, Liang B, Li L, Ye T, et al. Factors associated with death outcome in patients with severe coronavirus disease-19 (COVID-19): a case-control study. Int J Med Sci. (2020) 17:1281–92. doi: 10.7150/ijms.46614
160. Peng XP, Hua TR, Song L, Yue ZZ, Bin F, Ming WX, et al. Risk factors for adverse clinical outcomes with COVID-19 in China: a multicenter, retrospective, observational study. Theranostics. (2020) 10:6372–83. doi: 10.7150/thno.46833
161. Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. (2020) 369:m1966. doi: 10.1136/bmj.m1966
162. Polverino F, Stern DA, Ruocco G, Balestro E, Bassetti M, Candelli M, et al. Comorbidities, cardiovascular therapies, and COVID-19 mortality: a nationwide, Italian Observational Study (ItaliCO). Front Cardiovasc Med. (2020) 7:585866. doi: 10.3389/fcvm.2020.585866
163. Popov GT, Baymakova M, Vaseva V, Kundurzhiev T, Mutafchiyski V. Clinical characteristics of hospitalized patients with COVID-19 in Sofia, Bulgaria. Vector Borne Zoonot Dis. (2020) 20:910–5. doi: 10.1089/vbz.2020.2679
164. Rastad H, Karim H, Ejtahed HS, Tajbakhsh R, Noorisepehr M, Babaei M, et al. Risk and predictors of in-hospital mortality from COVID-19 in patients with diabetes and cardiovascular disease. Diabetol Metab Syndr. (2020) 12:57. doi: 10.1186/s13098-020-00565-9
165. Rath D, Petersen-Uribe Á, Avdiu A, Witzel K, Jaeger P, Zdanyte M, et al. Impaired cardiac function is associated with mortality in patients with acute COVID-19 infection. Clin Res Cardiol. (2020) 109:1491–9. doi: 10.1007/s00392-020-01683-0
166. Ren H, Yang Y, Wang F, Yan Y, Shi X, Dong K, et al. Association of the insulin resistance marker TyG index with the severity and mortality of COVID-19. Cardiovasc Diabetol. (2020) 19:58. doi: 10.1186/s12933-020-01035-2
167. Renieris G, Katrini K, Damoulari C, Akinosoglou K, Psarrakis C, Kyriakopoulou M, et al. Serum hydrogen sulfide and outcome association in pneumonia by the SARS-CoV-2 coronavirus. Shock. (2020) 54:633–7. doi: 10.1097/shk.0000000000001562
168. Rivera-Izquierdo M, Del Carmen Valero-Ubierna M, JL Rd, Fernández-García M, Martínez-Diz S, Tahery-Mahmoud A, et al. Sociodemographic, clinical and laboratory factors on admission associated with COVID-19 mortality in hospitalized patients: a retrospective observational study. PLoS ONE. (2020) 15:e0235107. doi: 10.1371/journal.pone.0235107
169. Rodilla E, Saura A, Jiménez I, Mendizábal A, Pineda-Cantero A, Lorenzo-Hernández E, et al. Association of hypertension with all-cause mortality among hospitalized patients with COVID-19. J Clin Med. (2020) 9:3136. doi: 10.3390/jcm9103136
170. Rokni M, Ahmadikia K, Asghari S, Mashaei S, Hassanali F. Comparison of clinical, para-clinical and laboratory findings in survived and deceased patients with COVID-19: diagnostic role of inflammatory indications in determining the severity of illness. BMC Infect Dis. (2020) 20:869. doi: 10.1186/s12879-020-05540-3
171. Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E, Sánchez-Larsen Á, Layos-Romero A, García-García J, et al. Neurologic manifestations in hospitalized patients with COVID-19: The ALBACOVID registry. Neurology. (2020) 95:e1060–70. doi: 10.1212/wnl.0000000000009937
172. Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Netw Open. (2020) 3:e2029058. doi: 10.1001/jamanetworkopen.2020.29058
173. Russo V, Di Maio M, Attena E, Silverio A, Scudiero F, Celentani D, et al. Clinical impact of pre-admission antithrombotic therapy in hospitalized patients with COVID-19: a multicenter observational study. Pharmacol Res. (2020) 159:104965. doi: 10.1016/j.phrs.2020.104965
174. Lapthorne S, Faller E, Barry R, O'sullivan M, Finnegan P, Everard C, et al. Clinical characteristics and factors associated with severity in patients admitted with SARS-CoV-2 infection. Irish Med J. (2020) 113:1–11.
175. Saleh A, Matsumori A, Abdelrazek S, Eltaweel S, Salous A, Neumann FJ, et al. Myocardial involvement in coronavirus disease 19. Herz. (2020) 45:719–25. doi: 10.1007/s00059-020-05001-2
176. Salvatore P, Andrea D, Elia V, Devis B, Massimo M, G GC, et al. Abnormal liver function tests predict transfer to intensive care unit and death in COVID-19. Liver Int. (2020) 40:2394–406. doi: 10.1111/liv.14565
177. Sanchez-Pina JM, Rodríguez Rodriguez M, Castro Quismondo N, Gil Manso R, Colmenares R, Gil Alos D, et al. Clinical course and risk factors for mortality from COVID-19 in patients with haematological malignancies. Eur J Haematol. (2020) 105:597–607. doi: 10.1111/ejh.13493
178. Shah C, Grando DJ, Rainess RA, Ayad L, Gobran E, Benson P, et al. Factors associated with increased mortality in hospitalized COVID-19 patients. Ann Med Surg. (2020) 60:308–13. doi: 10.1016/j.amsu.2020.10.071
179. Shang W, Dong J, Ren Y, Tian M, Li W, Hu J, et al. The value of clinical parameters in predicting the severity of COVID-19. J Med Virol. (2020) 92:2188–92. doi: 10.1002/jmv.26031
180. Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. (2020) 28:1195–9. doi: 10.1002/oby.22831
181. Smadja DM, Guerin CL, Chocron R, Yatim N, Boussier J, Gendron N, et al. Angiopoietin-2 as a marker of endothelial activation is a good predictor factor for intensive care unit admission of COVID-19 patients. Angiogenesis. (2020) 23:611–20. doi: 10.1007/s10456-020-09730-0
182. Smith AA, Fridling J, Ibrahim D, Porter PS Jr. Identifying patients at greatest risk of mortality due to COVID-19: a new england perspective. Western J Emergency Med. (2020) 21:785–9. doi: 10.5811/westjem.2020.6.47957
183. Sun L, Shen L, Fan J, Gu F, Hu M, An Y, et al. Clinical features of patients with coronavirus disease 2019 from a designated hospital in Beijing, China. J Med Virol. (2020) 92:2055–66. doi: 10.1002/jmv.25966
184. Tambe MP, Parande MA, Tapare VS, Borle PS, Lakde RN, Shelke SC. An epidemiological study of laboratory confirmed COVID-19 cases admitted in a tertiary care hospital of Pune, Maharashtra. Indian J Public Health. (2020) 64(Suppl.):S183–7. doi: 10.4103/ijph.IJPH_522_20
185. Trecarichi EM, Mazzitelli M, Serapide F, Pelle MC, Tassone B, Arrighi E, et al. Clinical characteristics and predictors of mortality associated with COVID-19 in elderly patients from a long-term care facility. Sci Rep. (2020) 10:20834. doi: 10.1038/s41598-020-77641-7
186. Vrillon A, Hourregue C, Azuar J, Grosset L, Boutelier A, Tan S, et al. COVID-19 in older adults: a series of 76 patients aged 85 years and older with COVID-19. J Am Geriatr Soc. (2020) 68:2735–43. doi: 10.1111/jgs.16894
187. Wan S, Xiang Y, Fang W, Zheng Y, Li B, Hu Y, et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. (2020) 92:797–806. doi: 10.1002/jmv.25783
188. Wang A, Gao G, Wang S, Chen M, Qian F, Tang W, et al. Clinical characteristics and risk factors of acute respiratory distress syndrome (ARDS) in COVID-19 patients in Beijing, China: a retrospective study. Med Sci Monit. (2020) 26:e925974. doi: 10.12659/msm.925974
189. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. doi: 10.1001/jama.2020.1585
190. Wang D, Yin Y, Hu C, Liu X, Zhang X, Zhou S, et al. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan, China. Crit Care. (2020) 24:188. doi: 10.1186/s13054-020-02895-6
191. Wang F, Yang Y, Dong K, Yan Y, Zhang S, Ren H, et al. Clinical characteristics of 28 patients with diabetes and COVID-19 in Wuhan, China. Endocr Pract. (2020) 26:668–74. doi: 10.4158/ep-2020-0108
192. Wang J, Guo S, Zhang Y, Gao K, Zuo J, Tan N, et al. Clinical features and risk factors for severe inpatients with COVID-19: a retrospective study in China. PLoS ONE. (2020) 15:e0244125. doi: 10.1371/journal.pone.0244125
193. Wang L, He W, Yu X, Hu D, Bao M, Liu H, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. (2020) 80:639–45. doi: 10.1016/j.jinf.2020.03.019
194. Wang Q, Zhao H, Liu LG, Wang YB, Zhang T, Li MH, et al. Pattern of liver injury in adult patients with COVID-19: a retrospective analysis of 105 patients. Milit Med Res. (2020) 7:28. doi: 10.1186/s40779-020-00256-6
195. Wang Y, Lu X, Li Y, Chen H, Chen T, Su N, et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. (2020) 201:1430–4. doi: 10.1164/rccm.202003-0736LE
196. Wei X, Su J, Yang K, Wei J, Wan H, Cao X, et al. Elevations of serum cancer biomarkers correlate with severity of COVID-19. J Med Virol. (2020) 92:2036–41. doi: 10.1002/jmv.25957
197. Wei Y, Zeng W, Huang X, Li J, Qiu X, Li H, et al. Clinical characteristics of 276 hospitalized patients with coronavirus disease 2019 in Zengdu District, Hubei Province: a single-center descriptive study. BMC Infect Dis. (2020) 20:549. doi: 10.1186/s12879-020-05252-8
198. Wendel Garcia PD, Fumeaux T, Guerci P, Heuberger DM, Montomoli J, Roche-Campo F, et al. Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: initial report of the international RISC-19-ICU prospective observational cohort. EClinicalMedicine. (2020) 25:100449. doi: 10.1016/j.eclinm.2020.100449
199. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. (2020) 180:934–43. doi: 10.1001/jamainternmed.2020.0994
200. Wu J, Li W, Shi X, Chen Z, Jiang B, Liu J, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Intern Med. (2020) 288:128–38. doi: 10.1111/joim.13063
201. Xia X, Wen M, Zhan S, He J, Chen W. An increased neutrophil/lymphocyte ratio is an early warning signal of severe COVID-19. Nan Fang Yi Ke Da Xue Xue Bao. (2020) 40:333–6. doi: 10.12122/j.issn.1673-4254.2020.03.06
202. Xiao LS, Zhang WF, Gong MC, Zhang YP, Chen LY, Zhu HB, et al. Development and validation of the HNC-LL score for predicting the severity of coronavirus disease 2019. EBioMedicine. (2020) 57:102880. doi: 10.1016/j.ebiom.2020.102880
203. Xie H, Zhao J, Lian N, Lin S, Xie Q, Zhuo H. Clinical characteristics of non-ICU hospitalized patients with coronavirus disease 2019 and liver injury: a retrospective study. Liver Int. (2020) 40:1321–6. doi: 10.1111/liv.14449
204. Xie J, Wu W, Li S, Hu Y, Hu M, Li J, et al. Clinical characteristics and outcomes of critically ill patients with novel coronavirus infectious disease (COVID-19) in China: a retrospective multicenter study. Intensive Care Med. (2020) 46:1863–72. doi: 10.1007/s00134-020-06211-2
205. Xie Y, You Q, Wu C, Cao S, Qu G, Yan X, et al. Impact of cardiovascular disease on clinical characteristics and outcomes of coronavirus disease 2019 (COVID-19). Circ J. (2020) 84:1277–83. doi: 10.1253/circj.CJ-20-0348
206. Xiong S, Lin L, Feng L, Jinhu S, Lei H, Huijian L, et al. Clinical characteristics of 116 hospitalized patients with COVID-19 in Wuhan, China: a single-centered, retrospective, observational study. BMC Infect Dis. (2020) 20:787. doi: 10.1186/s12879-020-05452-2
207. Xu J, Yang X, Yang L, Zou X, Wang Y, Wu Y, et al. Clinical course and predictors of 60-day mortality in 239 critically ill patients with COVID-19: a multicenter retrospective study from Wuhan, China. Crit Care. (2020) 24:394. doi: 10.1186/s13054-020-03098-9
208. Yan X, Han X, Peng D, Fan Y, Fang Z, Long D, et al. Clinical characteristics and prognosis of 218 patients with COVID-19: a retrospective study based on clinical classification. Front Med. (2020) 7:485. doi: 10.3389/fmed.2020.00485
209. Yan Y, Yang Y, Wang F, Ren H, Zhang S, Shi X, et al. Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res Care. (2020) 8:e001343. doi: 10.1136/bmjdrc-2020-001343
210. Yang Q, Xie L, Zhang W, Zhao L, Wu H, Jiang J, et al. Analysis of the clinical characteristics, drug treatments and prognoses of 136 patients with coronavirus disease 2019. J Clin Pharm Ther. (2020) 45:609–16. doi: 10.1111/jcpt.13170
211. Yang Q, Zhou Y, Wang X, Gao S, Xiao Y, Zhang W, et al. Effect of hypertension on outcomes of adult inpatients with COVID-19 in Wuhan, China: a propensity score-matching analysis. Respir Res. (2020) 21:172. doi: 10.1186/s12931-020-01435-8
212. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. (2020) 8:475–81. doi: 10.1016/s2213-2600(20)30079-5
213. Yao Q, Wang P, Wang X, Qie G, Meng M, Tong X, et al. A retrospective study of risk factors for severe acute respiratory syndrome coronavirus 2 infections in hospitalized adult patients. Pol Arch Intern Med. (2020) 130:390–9. doi: 10.20452/pamw.15312
PubMed Abstract | CrossRef Full Text
214. Ye C, Zhang S, Zhang X, Cai H, Gu J, Lian J, et al. Impact of comorbidities on patients with COVID-19: a large retrospective study in Zhejiang, China. J Med Virol. (2020) 92:2821–9. doi: 10.1002/jmv.26183
215. Yi P, Yang X, Ding C, Chen Y, Xu K, Ni Q, et al. Risk factors and clinical features of deterioration in COVID-19 patients in Zhejiang, China: a single-centre, retrospective study. BMC Infect Dis. (2020) 20:943. doi: 10.1186/s12879-020-05682-4
216. Yu C, Lei Q, Li W, Wang X, Liu W, Fan X, et al. Clinical characteristics, associated factors, and predicting COVID-19 mortality risk: a retrospective study in Wuhan, China. Am J Prev Med. (2020) 59:168–75. doi: 10.1016/j.amepre.2020.05.002
217. Yuan M, Yin W, Tao Z, Tan W, Hu Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS ONE. (2020) 15:e0230548. doi: 10.1371/journal.pone.0230548
218. Yun K, Lee JS, Kim EY, Chandra H, Oh BL, Oh J. Severe COVID-19 illness: risk factors and its burden on critical care resources. Front Med. (2020) 7:583060. doi: 10.3389/fmed.2020.583060
219. Zeng JH, Wu WB, Qu JX, Wang Y, Dong CF, Luo YF, et al. Cardiac manifestations of COVID-19 in Shenzhen, China. Infection. (2020) 48:861–70. doi: 10.1007/s15010-020-01473-w
220. Zhang G, Zhang J, Wang B, Zhu X, Wang Q, Qiu S. Analysis of clinical characteristics and laboratory findings of 95 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a retrospective analysis. Respir Res. (2020) 21:74. doi: 10.1186/s12931-020-01338-8
221. Zhang J, Wang X, Jia X, Li J, Hu K, Chen G, et al. Risk factors for disease severity, unimprovement, and mortality in COVID-19 patients in Wuhan, China. Clin Microbiol Infect. (2020) 26:767–72. doi: 10.1016/j.cmi.2020.04.012
222. Zhang J, Yu M, Tong S, Liu LY, Tang LV. Predictive factors for disease progression in hospitalized patients with coronavirus disease 2019 in Wuhan, China. J Clin Virol. (2020) 127:104392. doi: 10.1016/j.jcv.2020.104392
223. Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. (2020) 75:1730–41. doi: 10.1111/all.14238
224. Zhang N, Xu X, Zhou LY, Chen G, Li Y, Yin H, et al. Clinical characteristics and chest CT imaging features of critically ill COVID-19 patients. Eur Radiol. (2020) 30:6151–60. doi: 10.1007/s00330-020-06955-x
225. Zhang R, Ouyang H, Fu L, Wang S, Han J, Huang K, et al. CT features of SARS-CoV-2 pneumonia according to clinical presentation: a retrospective analysis of 120 consecutive patients from Wuhan city. Eur Radiol. (2020) 30:4417–26. doi: 10.1007/s00330-020-06854-1
226. Zhang S, Liu L, Yang B, Li R, Luo J, Huang J, et al. Clinical characteristics of 134 convalescent patients with COVID-19 in Guizhou, China. Respir Res. (2020) 21:314. doi: 10.1186/s12931-020-01580-0
227. Zhang SX, Li J, Zhou P, Na JR, Liu BF, Zheng XW, et al. The analysis of clinical characteristics of 34 novel coronavirus pneumonia cases in Ningxia Hui autonomous region. Zhonghua Jie He He Hu Xi Za Zhi. (2020) 43:431–6. doi: 10.3760/cma.j.cn112147-20200219-00121
228. Zhang SY, Lian JS, Hu JH, Zhang XL, Lu YF, Cai H, et al. Clinical characteristics of different subtypes and risk factors for the severity of illness in patients with COVID-19 in Zhejiang, China. Infect Dis Poverty. (2020) 9:85. doi: 10.1186/s40249-020-00710-6
229. Zhang Y, Cui Y, Shen M, Zhang J, Liu B, Dai M, et al. Association of diabetes mellitus with disease severity and prognosis in COVID-19: a retrospective cohort study. Diabetes Res Clin Pract. (2020) 165:108227. doi: 10.1016/j.diabres.2020.108227
230. Zhang YT, Deng AP, Hu T, Chen XG, Zhuang YL, Tan XH, et al. [Clinical outcomes of COVID-19 cases and influencing factors in Guangdong province]. Zhonghua liu xing bing xue za zhi. (2020) 41:1999–2004. doi: 10.3760/cma.j.cn112338-20200318-00378
231. Zhao S, Lin Y, Zhou C, Wang L, Chen X, Clifford SP, et al. Short-term outcomes of patients with COVID-19 undergoing invasive mechanical ventilation: a retrospective observational study from Wuhan, China. Front Med. (2020) 7:571542. doi: 10.3389/fmed.2020.571542
232. Zhao X, Wang K, Zuo P, Liu Y, Zhang M, Xie S, et al. Early decrease in blood platelet count is associated with poor prognosis in COVID-19 patients-indications for predictive, preventive, and personalized medical approach. Epma J. (2020) 11:1–7. doi: 10.1007/s13167-020-00208-z
233. Zhao XY, Xu XX, Yin HS, Hu QM, Xiong T, Tang YY, et al. Clinical characteristics of patients with 2019 coronavirus disease in a non-Wuhan area of Hubei Province, China: a retrospective study. BMC Infect Dis. (2020) 20:311. doi: 10.1186/s12879-020-05010-w
234. Zhao Y, Nie HX, Hu K, Wu XJ, Zhang YT, Wang MM, et al. Abnormal immunity of non-survivors with COVID-19: predictors for mortality. Infect Dis Poverty. (2020) 9:108. doi: 10.1186/s40249-020-00723-1
235. Zheng F, Tang W, Li H, Huang YX, Xie YL, Zhou ZG. Clinical characteristics of 161 cases of corona virus disease 2019 (COVID-19) in Changsha. Eur Rev Med Pharmacol Sci. (2020) 24:3404–10. doi: 10.26355/eurrev_202003_20711
236. Zheng Y, Xiong C, Liu Y, Qian X, Tang Y, Liu L, et al. Epidemiological and clinical characteristics analysis of COVID-19 in the surrounding areas of Wuhan, Hubei Province in 2020. Pharmacol Res. (2020) 157:104821. doi: 10.1016/j.phrs.2020.104821
237. Zheng Y, Xu H, Yang M, Zeng Y, Chen H, Liu R, et al. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID-19 in Chengdu. J Clin Virol. (2020) 127:104366. doi: 10.1016/j.jcv.2020.104366
238. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/s0140-6736(20)30566-3
239. Zhou W, Ye S, Wang W, Li S, Hu Q. Clinical features of COVID-19 patients with diabetes and secondary hyperglycemia. J Diabetes Res. (2020) 2020:3918723. doi: 10.1155/2020/3918723
240. Zhou Y, He Y, Yang H, Yu H, Wang T, Chen Z, et al. Development and validation a nomogram for predicting the risk of severe COVID-19: a multi-center study in Sichuan, China. PLoS ONE. (2020) 15:e0233328. doi: 10.1371/journal.pone.0233328
241. Zhu Z, Cai T, Fan L, Lou K, Hua X, Huang Z, et al. Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019. Int J Infect Dis. (2020) 95:332–9. doi: 10.1016/j.ijid.2020.04.041
242. Zou L, Dai L, Zhang Y, Fu W, Gao Y, Zhang Z, et al. Clinical characteristics and risk factors for disease severity and death in patients with coronavirus disease 2019 in Wuhan, China. Front Med. (2020) 7:532. doi: 10.3389/fmed.2020.00532
243. Zou X, Li S, Fang M, Hu M, Bian Y, Ling J, et al. Acute physiology and chronic health evaluation II score as a predictor of hospital mortality in patients of coronavirus disease 2019. Crit Care Med. (2020) 48:e657–65. doi: 10.1097/ccm.0000000000004411
244. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. (2020) 34:101623. doi: 10.1016/j.tmaid.2020.101623
245. Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging. (2020) 12:6049–57. doi: 10.18632/aging.103000
246. Mattiuzzi C, Lippi G. Worldwide asthma epidemiology: insights from the Global Health Data Exchange database. Int Forum Allergy Rhinol. (2020) 10:75–80. doi: 10.1002/alr.22464
247. Chhiba KD, Patel GB, Vu THT, Chen MM, Guo A, Kudlaty E, et al. Prevalence and characterization of asthma in hospitalized and nonhospitalized patients with COVID-19. J Allergy Clin Immunol. (2020) 146:307–14.e4. doi: 10.1016/j.jaci.2020.06.010
248. Wu T, Yu P, Li Y, Wang J, Li Z, Qiu J, et al. Asthma does not influence the severity of COVID-19: a meta-analysis. J Asthma. (2021) 1–7. doi: 10.1080/02770903.2021.1917603
249. Huang Y, Gao L, Xie X, Tan SC. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control. Popul Health Metr. (2014) 12:28. doi: 10.1186/s12963-014-0028-7
250. Carroll MD, Fryar CD. Total and high-density lipoprotein cholesterol in adults: United States, 2015–2018. NCHS Data Brief, no 363. Hyattsville, MD: National Center for Health Statistics (2020). Available online at: https://www.cdc.gov/nchs/data/databriefs/db363-h.pdf
251. Tóth PP, Potter D, Ming EE. Prevalence of lipid abnormalities in the United States: the National Health and Nutrition Examination Survey 2003-2006. J Clin Lipidol. (2012) 6:325–30. doi: 10.1016/j.jacl.2012.05.002
252. Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. (2020) 109:1088–95. doi: 10.1111/apa.15270
253. Zaigham M, Andersson O. Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstetr Gynecol Scand. (2020) 99:823–9. doi: 10.1111/aogs.13867
Keywords: chronic diseases, COVID-19, systematic review, cumulative meta-analysis, severity, mortality
Citation: Geng J, Yu X, Bao H, Feng Z, Yuan X, Zhang J, Chen X, Chen Y, Li C and Yu H (2021) Chronic Diseases as a Predictor for Severity and Mortality of COVID-19: A Systematic Review With Cumulative Meta-Analysis. Front. Med. 8:588013. doi: 10.3389/fmed.2021.588013
Received: 28 July 2020; Accepted: 05 August 2021; Published: 01 September 2021.
Reviewed by:
Copyright © 2021 Geng, Yu, Bao, Feng, Yuan, Zhang, Chen, Chen, Li and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: JinSong Geng, gjs@ntu.edu.cn
This article is part of the Research Topic
Infectious Disease Surveillance: Applying Cooperative Research to Recent Outbreaks including COVID-19
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (43,954,836 articles, preprints and more)
- Free full text
- Citations & impact
- Similar Articles
Predictors of COVID-19 severity: a systematic review and meta-analysis.
Author information, affiliations.
- Mudatsir M 1
- Fajar JK 1, 5
- Harapan H 1
- Wulandari L 2
- Soegiarto G 3
- Ilmawan M 4
- Purnamasari Y 4
- Suhendra S 4
- Alluza HHD 4
- Rosida NA 4
- Mayasari M 4
- Mustofa M 4
- Prastiwi F 4
- Nugroho RA 4
- Jayanto GD 5
ORCIDs linked to this article
- Purnamasari Y | 0000-0001-5830-3571
- Setianingsih YA | 0000-0001-6186-7976
- Mahdi BA | 0000-0001-6634-6088
- Nugroho RA | 0000-0001-6888-1850
- Dhama K | 0000-0001-7469-4752
F1000research , 09 Sep 2020 , 9: 1107 https://doi.org/10.12688/f1000research.26186.2 PMID: 33163160 PMCID: PMC7607482
Abstract
Free full text .

- PMC7607482.1 ; 2020 Sep 9
- ➤ PMC7607482.2; 2021 Jan 6
Predictors of COVID-19 severity: a systematic review and meta-analysis
Mudatsir mudatsir.
1 Department of Microbiology, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Aceh, 23111, Indonesia
Jonny Karunia Fajar
2 Brawijaya Internal Medicine Research Center, Department of Internal Medicine, Faculty of Medicine, Universitas Brawijaya, Malang, East Java, 65145, Indonesia
Laksmi Wulandari
3 Department of Pulmonology and Respiratory Medicine, Faculty of Medicine, Universitas Airlangga, Surabaya, East Java, 60286, Indonesia
Gatot Soegiarto
4 Department of Internal Medicine, Faculty of Medicine, Universitas Airlangga, Surabaya, Easy Java, 60286, Indonesia
Muhammad Ilmawan
5 Faculty of Medicine, Universitas Brawijaya, Malang, East Java, 65145, Indonesia
Yeni Purnamasari
Bagus aulia mahdi, galih dwi jayanto, suhendra suhendra, yennie ayu setianingsih.
6 Department of Urology, Faculty of Medicine, Universitas Airlangga, Surabaya, East Java, 60285, Indonesia
Romi Hamdani
7 Department of Orthopedic Surgery, Faculty of Medicine, Universitas Brawijaya, Malang, East Java, 65145, Indonesia
Daniel Alexander Suseno
8 Department of Obstetry and Gynecology, Faculty of Medicine, Universitas Brawijaya, Malang, East Java, 65145, Indonesia
Kartika Agustina
9 Department of Neurology, Faculty of Medicine, Universitas Brawijaya, Malang, East Java, 65145, Indonesia
Hamdan Yuwafi Naim
10 Department of Urology, Faculty of Medicine, Universitas Brawijaya, Malang, East Java, 65145, Indonesia
Muchamad Muchlas
11 Faculty of Animal Science, Universitas Brawijaya, Malang, East Java, 65145, Indonesia
Hamid Hunaif Dhofi Alluza
Nikma alfi rosida, mayasari mayasari, mustofa mustofa, adam hartono.
12 Faculty of Medicine, Universitas Negeri Sebelas Maret, Surakarta, Surakarta, 57126, Indonesia
Richi Aditya
Firman prastiwi, fransiskus xaverius meku, monika sitio, abdullah azmy, anita surya santoso.
13 Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Brawijaya, Malang, East Java, 65145, Indonesia
Radhitio Adi Nugroho
Camoya gersom, ali a. rabaan.
14 Molecular Diagnostic Laboratory, Johns Hopkins Aramco Healthcare, Dhahran, Dhahran, 31311, Saudi Arabia
Sri Masyeni
15 Department of Internal Medicine, Faculty of Medicine and Health Science, Universitas Warmadewa, Denpasar, Bali, 80235, Indonesia
Firzan Nainu
16 Faculty of Pharmacy, Hasanuddin University, Makassar, Makassar, 90245, Indonesia
Abram L. Wagner
17 Department of Epidemiology, University of Michigan, Ann Arbor, MI, 48109, USA
Kuldeep Dhama
18 Division of Pathology, Indian Veterinary Research Institute, Izatnagar, Uttar Pradesh, 243 122, India
Harapan Harapan
19 Medical Research Unit, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Aceh, 23111, Indonesia
Associated Data
Underlying data.
All data underlying the results are available as part of the article and no additional source data are required.
Reporting guidelines
Figshare: PRISMA checklist for ‘Predictors of COVID-19 severity: a systematic review and meta-analysis’, https://doi.org/10.6084/m9.figshare.12813683.v1 94
Data are available under the terms of the Creative Commons Attribution 4.0 International license (CC-BY 4.0).
Version Changes
Revised. amendments from version 1.
In the revised version of our current article, we provided the revision of method, the limitation, and the clinical implication of our study.
Peer Review Summary
Background : The unpredictability of the progression of coronavirus disease 2019 (COVID-19) may be attributed to the low precision of the tools used to predict the prognosis of this disease.
Objective : To identify the predictors associated with poor clinical outcomes in patients with COVID-19.
Methods : Relevant articles from PubMed, Embase, Cochrane, and Web of Science were searched as of April 5, 2020. The quality of the included papers was appraised using the Newcastle-Ottawa scale (NOS). Data of interest were collected and evaluated for their compatibility for the meta-analysis. Cumulative calculations to determine the correlation and effect estimates were performed using the Z test.
Results : In total, 19 papers recording 1,934 mild and 1,644 severe cases of COVID-19 were included. Based on the initial evaluation, 62 potential risk factors were identified for the meta-analysis. Several comorbidities, including chronic respiratory disease, cardiovascular disease, diabetes mellitus, and hypertension were observed more frequent among patients with severe COVID-19 than with the mild ones. Compared to the mild form, severe COVID-19 was associated with symptoms such as dyspnea, anorexia, fatigue, increased respiratory rate, and high systolic blood pressure. Lower levels of lymphocytes and hemoglobin; elevated levels of leukocytes, aspartate aminotransferase, alanine aminotransferase, blood creatinine, blood urea nitrogen, high-sensitivity troponin, creatine kinase, high-sensitivity C-reactive protein, interleukin 6, D-dimer, ferritin, lactate dehydrogenase, and procalcitonin; and a high erythrocyte sedimentation rate were also associated with severe COVID-19.
Conclusion : More than 30 risk factors are associated with a higher risk of severe COVID-19. These may serve as useful baseline parameters in the development of prediction tools for COVID-19 prognosis.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a global crisis across health, economic, and educational dimensions 1 , 2 . The disease has spread rapidly, can cause severe illness, and is characterized by a high mortality rate in certain groups. Mortality is particularly high in the absence of proven effective standard management measures 3 . One of the problems with the management of this disease is the absence of standardized methods for diagnosis and the inability to estimate prognosis based on clinical features. Certain reports have shown that poor prognostic prediction has correlated with high mortality among patients with COVID-19 4 , 5 . Among patients with similar clinical characteristics and with similar treatment regiments, there may be a diversity in clinical outcomes 6 . Therefore, the development and use of an accurate predictor for COVID-19 prognosis will be beneficial for the clinical management of patients with COVID-19, and will help reduce the mortality rate. Successful implementation of such a prediction mechanism could have a large public health impact. Better understanding of clinical progression could also improve public health messaging, particularly as many individuals may consider COVID-19 to not be severe.
Prognostic tools for the prediction of COVID-19 severity in patients have been in development since January 2020. At least nine studies proposed the use of prognostic tools for the prediction of COVID-19 severity 7 – 15 . However, a recent systematic review and critical appraisal study evaluated the accuracy of these tools using prediction model risk of bias assessment tool (PROBAST) and reported a high risk of bias 16 . The establishment of a prediction model for the estimation of disease prognosis may help health workers segregate patients according to prediction status. However, the high risk of bias in these prediction tools might lead to inaccurate prediction of COVID-19 severity. A comprehensive study of the identification of risk factors that might play a significant role in determining the severity of patients with COVID-19 is necessary. We performed a systematic review and meta-analysis to assess the risk factors associated with poor clinical outcomes among patients with COVID-19. To the best of our knowledge, this is the first meta-analysis to assess the comprehensive risk factors that might affect the severity of COVID-19 in patients. The results of our study might serve as preliminary data for the compilation or improvement of the scoring system in the prediction of COVID-19 severity.
Study design
We performed a systematic review and meta-analysis to evaluate potential risk factors that might influence the severity of COVID-19. These risk factors include comorbidities, clinical manifestations, and laboratory findings. Accordingly, we searched the relevant studies from major scientific websites and databases to collect the data of interest, and determined the association and effect estimates by calculating the combined odds ratio (OR) and 95% confidence intervals (95% CI). The protocols for the systematic review and meta-analysis were similar to those used in previous studies 17 – 23 , as well as to those recommended by Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 24 .
Eligibility criteria
Studies were included in this review if they met the following inclusion criteria: (1) assessed the clinical manifestations and laboratory findings of patients with mild to severe COVID-19; (2) provided adequate data for the calculation of OR and 95% CI (event per sample size or mean ± SD in both case and control groups), (3) written inEnglish. Review articles, articles with non-standard data presentation, and duplicate publications were excluded.
Search strategy and data extraction
Major scientific databases (PubMed, Embase, Cochrane, and Web of Science) were searched for articles as of April 5, 2020. Moreover, we also searched in google scholar for the additional database. A comprehensive initial search was performed to identify the potential predictors, and a final search was performed to identify the relevant papers that could be included in the meta-analysis. We used the keywords adapted from medical subject headings: ["COVID-19" or "Coronavirus disease-19" or "SARS-CoV-2"] and ["mild" or "severe" or "prognosis" or "clinical outcome"] and ["clinical manifestation" or "morbidity" or "laboratory findings"]. Only studies written in English were included. If a duplicate publication was found, the article with the larger sample size was included. We also searched for relevant studies from the reference lists in the articles. During data extraction, the following information of interest was extracted: (1) first author name; (2) publication year; (3) country of origin, (4) sample size of mild and severe cases, (5) clinical manifestations, (6) morbidities, and (7) laboratory findings. Data extraction was performed by two independent investigators (JKF and MI) using a pilot form. If the disagreement was found, we performed a discussion to resolve the disagreement.
Assessment of the methodological quality
Before inclusion in the meta-analysis, the methodological quality of the articles was assessed using the New Castle-Ottawa scale (NOS). NOS scores range from 0 to 9 and consider three items: selection of patients (4 points), comparability of the groups (2 points), and ascertainment of exposure (3 points). Each study was interpreted to be of low quality (for scores ≤ 4), moderate quality (for scores between 5–6), or high quality (for scores ≥ 7) 25 . Articles with moderate to high quality were included in the analysis. The study assessment was conducted by two independent investigators (MI and YP) using a pilot form. The discrepancies between the findings of the two investigators were solved by consulting with another investigator (JKF).
Study measures
The outcome measure of the study was the severity of COVID-19 (mild vs . severe). The risk factors or predictors included three major groups: comorbidities, clinical manifestations, and laboratory parameters. Comorbid factors such as chronic kidney disease, chronic liver disease, chronic respiratory disease, cerebrovascular accident, cardiovascular disease, diabetes mellitus, hypertension, and malignancy were compatible with the analysis. For clinical manifestations, fever, cough, dry cough, expectoration, sore throat, dyspnea, diarrhea, myalgia, nasal congestion, anorexia, abdominal pain, fatigue, dizziness, headache, fever, heart rate, respiratory rate, systolic blood pressure, and diastolic blood pressure were included in this study. Among laboratory characteristics, the presence of leukocytosis, leukocytopenia, anemia, lymphocytopenia; the levels or the counts of white blood cell (WBC), hemoglobin, neutrophil, lymphocyte, monocyte, platelet, activated partial thromboplastin time (aPTT), partial thromboplastin time (PTT), aspartate aminotransferase (AST), alanine aminotransferase (ALT), total bilirubin, albumin, serum creatinine, blood urea nitrogen (BUN), high-sensitivity (Hs)-troponin I, creatine kinase, high-sensitivity C-reactive protein (Hs-CRP), C-reactive protein (CRP) >8 mg/L, interleukin 6 (IL-6), glucose, D-dimer, serum ferritin, sodium, potassium, lactate dehydrogenase, and procalcitonin, CD4 and CD8; erythrocyte sedimentation rate (ESR); elevated IL-16; and elevated ESR were all included.
Statistical analysis
The significant risk factors that might govern the severity of COVID-19 were determined by the calculation of a pooled OR and 95% CI. The significance of the pooled ORs was determined using the Z test (p<0.05 was considered statistically significant). Prior to identification of the significant risk factors, data were evaluated for heterogeneity and potential publication bias. The heterogeneity among included studies was evaluated using the Q test. If heterogeneity existed (p<0.10), a random effect model was adopted; if not, a fixed effect model was adopted. Egger’s test and a funnel plot were used to assess the reporting or publication bias (p<0.05 was considered statistically significant). Furthermore, we performed a moderator analysis to identify the independent predictors of poor clinical outcomes among patients with COVID-19. The data were analyzed using Review Manager version 5.3 (Revman Cochrane, London, UK). To prevent analytical errors, statistical analysis was performed by two authors (JKF and MI). The cumulative calculation was presented in a forest plot.
Eligible studies
Our searches yielded 6,209 potentially relevant studies, of which 6,170 studies were excluded after assessment of the titles and abstracts. Subsequently, further review of the complete texts was performed for 39 potential studies. In the full text review, we excluded 20 studies because they were reviews articles (n = 9), inadequacy of data for the calculation of OR and 95% CI (n = 7), and poor quality (n = 4). Eventually, 19 papers were included in our meta-analysis 26 – 42 The paper selection process adopted in our study is summarized in Figure 1 , and the characteristics of studies included in our analysis are outlined in Table 1 .

Note: ICU, intensive care unit; CT, computed tomography; NOS, Newcastle Ottawa Scale.
Risk factors of severe COVID-19
We found that eight comorbidities, 19 clinical manifestations, and 35 laboratory parameters were available for the meta-analysis ( Table 2 and Table 3 ). Among the comorbid factors, chronic respiratory disease (OR: 2.48; 95% CI: 1.44, 4.27), cardiovascular disease (OR: 1.70; 95% CI: 1.05, 2.78), diabetes mellitus (OR: 2.10; 95% CI: 1.33, 3.34), and hypertension (OR: 2.33; 95% CI: 1.42, 3.81) were associated with a greater risk of severe COVID-19 ( Figure 2A–D ).
Note, Value, data were presented in number [%] or mean ± SD; NS, number of studies; pE, p Egger; pHet, p heterogeneity; OR, odd ratio; CI, confidence interval; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Note: Value, data were presented in number [%] or mean ± SD; NS, number of studies; pE, p Egger; pHet, p heterogeneity; OR, odd ratio; CI, confidence interval; CBC, complete blood count; WBC, white blood cells; AST, aspartate transaminase; ALT, alanine transaminase; aPTT, activated partial thromboplastin time; PTT, partial thromboplastin time; BUN, blood urea nitrogen; Hs-CRP, high sensitivity C reactive protein; ESR, erythrocyte sedimentation rate; IL, interleukin.

A ) Chronic respiratory disease; B ) Cardiovascular diease; C ) Diabetes mellitus; D ) Hypertension.
Among the clinical manifestations, dyspnea (OR: 3.28; 95% CI: 2.09, 5.15), anorexia (OR: 1.83; 95% CI: 1.00, 3.34), fatigue (OR: 2.00; 95% CI: 1.25, 3.20), and dizziness (OR: 2.67; 95% CI: 1.18, 6.01) were associated with severe COVID-19 ( Figure 3A–D ). In addition, increased respiratory rate (OR: 2.85; 95% CI: 1.28, 6.33) and increased systolic blood pressure (OR: 1.84; 95% CI: 1.31, 2.60) were also associated with severe COVID-19 ( Figure 4A and B ). Compared to productive cough, dry cough was associated with a lower risk of severe COVID-19 (OR: 0.66; 95% CI: 0.44, 0.97).

A ) Dyspnea; B ) Anorexia; C ) Fatique; D ) Dizziness.

A ) Respiratory rate; B ) Systolic blood pressure.
Among laboratory characteristics, severe COVID-19 was associated with elevated WBC count (OR: 4.92; 95% CI: 2.12, 11.31), increased neutrophil count (OR: 5.45; 95% CI: 2.04, 14.54), lymphocytopenia (OR: 3.19; 95% CI: 1.14, 7.07), and decreased hemoglobin levels (OR: 0.76; 95%CI: 0.58, 1.00) ( Figure 5A–D ). Elevated levels of AST, ALT, and serum creatinine increased the risk for severe manifestations of COVID-19 (ORs 4.91, 3.23, and 2.14, respectively; Figure 6A–C ). Elevated levels of BUN (OR: 6.15; 95% CI: 3.05, 12.37), Hs-troponin I (OR: 9.25; 95% CI: 3.51, 24.37), creatine kinase (OR: 2.44; 95% CI: 1.65, 3.62), Hs-CRP (OR: 14.27; 95% CI: 5.13, 39.71), IL-6 (OR: 6.68; 95% CI: 3.20, 13.94), D-dimer (OR: 6.19; 95% CI: 4.22, 9.08), ferritin (OR: 1.96; 95% CI: 1.06, 3.62), lactate dehydrogenase (OR: 8.28; 95% CI: 4.75, 14.46), procalcitonin (OR: 6.62; 95% CI: 3.32, 13.21), ESR (OR: 4.45; 95% CI: 2.56, 7.76), and CRP >8 (OR: 8.34; 95% CI: 1.85, 37.62) were also associated with severe COVID-19 ( Figure 7 – Figure 9 ). A low risk of severe COVID-19 was associated with low leukocyte levels (OR: 0.59; 95% CI: 0.41, 0.87) and elevated lymphocyte levels (OR: 0.34; 95% CI: 0.23, 0.50).

A ) White blood cells; B ) Neutrophil count; C ) Lymphocytopenia; D ) Hemoglobin.

A forest plot of the association between the risk of severe COVID-19 and the levels of AST ( A ), ALT ( B ), and serum creatinine ( C ).

A forest plot of the association between the risk of severe COVID-19 and the levels of BUN ( A ), Hs-troponin ( B ), and creatine kinase ( C ).

A forest plot of the association between the risk of severe COVID-19 and the levels of CRP ( A ), Hs-CRP ( B ), ESR ( C ), and IL-6 ( D ).

A forest plot of the association between the risk of severe COVID-19 and the levels of D-dimer ( A ), serum ferritin ( B ), lactate dehydrogenase ( C ), and procalcitonin ( D ).
Source of heterogeneity
Heterogeneity was detected in the data of chronic kidney disease, cerebrovascular disease, cardiovascular disease, diabetes mellitus, hypertension, and malignancy among the comorbid factors analyzed. Therefore, we used the random effect model to analyze the data. The fixed effect model was used to analyze the data on chronic liver disease and chronic respiratory disease, as there was no evidence of heterogeneity. For clinical manifestations, the data on fever, cough, sore throat, dyspnea, diarrhea, anorexia, fatigue, temperature >38°C, respiratory rate, and diastolic blood pressure were analyzed using the random effect model while the rest of clinical manifestation data were analyzed using the fixed effect model.
Among laboratory parameters, evidence of heterogeneity was found in count of WBC, neutrophil, monocyte, lymphocyte, platelet, CD4, and CD8; the presence of lymphocytopenia and anemia; the levels of AST, ALT, total bilirubin, albumin, aPTT, PTT, serum creatinine, BUN, Hs-Troponin I, creatine kinase, IL-6, Hs-CRP, glucose, D-dimer, sodium, potassium, lactate dehydrogenase, and procalcitonin; elevated CRP; and ESR. Accordingly, the data were analyzed using the random effect model. The data for the remaining parameters were analyzed using the fixed effect model.
Potential publication bias
We used Egger's test to assess the potential publication bias. Our cumulative calculation revealed that reporting or publication bias (p<0.05) existed with respect to chronic liver disease, expectoration, myalgia, abdominal pain, heart rate, leukocytosis, elevated ESR, and elevated IL-6 levels.
Our data suggest that comorbidities, such as chronic respiratory disease, cardiovascular disease, diabetes, and hypertension, were associated with a higher risk of severe COVID-19, among which, hypertension was the strongest risk factor. These results are consistent with those of previous meta-analyses 43 , 44 that indicated that chronic respiratory disease, cardiovascular disease, diabetes, and hypertension are significantly associated with higher COVID-19 mortality. Hypertension and diabetes are also associated with higher mortality among patients with dengue fever, West Nile virus infection, Zika virus infection, and yellow fever 45 . To date, no study has reported details of the primary mechanism underlying the association between severe COVID-19 and comorbid factors. However, immune responses might be the most crucial factor underlying this association. Patients with comorbidities such as cardiovascular disease, chronic respiratory disease, hypertension, and diabetes were observed to have a lower immunity status than healthy individuals 46 – 48 . Since COVID-19 primarily affects the respiratory tract 49 , patients with chronic respiratory diseases might be at a higher risk of contracting severe COVID-19. In addition, endothelial dysfunction might also play a pivotal role 50 .
COVID-19 is a novel disease, and the immune response of this disease is not completely understood. Our data suggest that elevated leukocyte and neutrophil levels and reduced lymphocyte levels are associated with severe COVID-19. In other viral infections, such as influenza, elevated leukocyte and neutrophil levels serve as important predictors of disease severity 51 . The role of leukocytes in the pathogenesis of COVID-19 is conflicting. In most cases, viral infections have been observed to cause leukopenia 52 . Furthermore, a study also reported that leukopenia was observed at a significantly higher frequency among COVID-19 patients than among non-COVID-19 patients 53 . However, in our present study, we did not compare COVID-19 and non-COVID-19 patients. The major factor that seemed to affect our findings was the occurrence of cytokine storm in patients. In COVID-19, there is an immune system overreaction, which results in a cytokine storm. In this condition, leukocytes might be over-activated, which might lead to the release of high levels of cytokines 54 . Consistent with our data, a study has confirmed that cytokine storm is significantly associated with severe COVID-19 55 . The theory underlying the role of neutrophils in COVID-19, as reported in our study, remains unclear. The speculations might be attributed to the involvement of neutrophil extracellular traps (NETs). While no study has assessed the precise role of NETs in COVID-19 pathogenesis, certain researchers speculate that SARS-CoV-2 might stimulate neutrophils to produce NETs, similar to several other viral pathogens 56 . Furthermore, this might lead to neutrophil infiltration in pulmonary capillaries, organ damage, and the development of acute respiratory distress syndrome 57 .
Low lymphocyte levels were observed in patients with severe COVID-19 compared with those with mild COVID-19. In the context of the immunological mechanism, our results might be contradictory. Lymphocyte subsets are known to play an important role in the action against bacterial, viral, fungal, and parasitic infections 58 ; therefore, the levels of circulating lymphocytes should increase. The immunological response in COVID-19 is unique and remains unclear. However, certain propositions might help describe our findings. First, coronaviruses infect human cells through ACE2 receptors 59 . Since ACE2 receptors are also expressed by lymphocytes 60 , the coronaviruses may enter lymphocytes and induce apoptosis. Second, the feedback mechanism between pro-inflammatory cytokines (such as IL-6) and lymphocytes might also explain our results. A study revealed that elevation in the levels of pro-inflammatory cytokines correlated with reduction in the levels of lymphocytes 61 . Moreover, our findings also confirmed the significant elevation in the levels of IL-6. Third, ACE2 receptors are expressed by cells from various organs, including the thymus and spleen 62 . As coronaviruses infect human cells through the ACE2 receptors, the spleen and thymus might also be damaged in patients with COVID-19, which would lead to lower levels of lymphocyte production. Fourth, lymphocyte proliferation requires a balanced metabolism, and metabolic disorders such as hyperlactic acidemia have been reported to disturb lymphocyte proliferation 63 . Hyperlactic acidemia has been observed in patients with severe COVID-19 64 .
The studies included in this systematic review also suggest that the levels of D-dimer were significantly higher in patients with severe COVID-19. Coagulation in patients with COVID-19 has been a major concern, and the lack of reliable data and meta-analyses prevents a holistic comparison. Certain infectious diseases that cause abnormal coagulation have been associated with poor clinical outcomes 65 . The theory behind this mechanism is not understood clearly. It is widely known that ACE2 receptors are important for the infection of host cells by SARS-CoV-2, and ACE2 receptors are expressed in various cells in the human body, including endothelial cells 66 . Consequently, a massive inflammatory reaction may occur in endothelial cells owing to SARS-CoV-2 infection 67 , which may lead to increased coagulation, disseminated intravascular coagulation 68 , and increased fibrin degradation 69 . High fibrin degradation leads to elevated levels of fibrinogen and D-dimer 70 , which might also explain the occurrence of venous thromboembolism in critical patients of COVID-19 71 . In addition, a study with a short follow-up period also reported the existence of a dynamic correlation between the D-dimer levels and the severity of COVID-19 72 . Furthermore, pulmonary embolism and deep vein thrombosis were also observed in patients with severe COVID-19 73 , 74 , which suggests that D-dimer might play a prominent role in governing the severity of COVID-19 patients.
We also observed that inflammatory markers, including elevated levels of CRP, ESR, and IL-6, were found both in patients with severe and mild COVID-19, with a significant increase detected in patients with severe COVID-19. Other variables associated with adverse outcomes, such as ferritin, lactate dehydrogenase, and procalcitonin levels, were found to be elevated predominantly in patients with severe COVID-19. Our findings were consistent with those of a previous meta-analysis 75 , and indicated that high levels of CRP, lactate dehydrogenase, and ESR were associated with adverse outcomes in COVID-19. Another meta-analysis had also confirmed that elevated levels of IL-6 were observed in patients with COVID-19 who exhibited poor clinical outcomes 76 . Therefore, the levels of CRP, ESR, IL-6, ferritin, procalcitonin, and lactate dehydrogenase can serve as potential markers for the evaluation of COVID-19 prognosis.
The high mortality rate and treatment failure in patients with COVID-19 can be attributed to the fact that COVID-19 affects multiple organs, including the lung, heart, kidney, and liver 77 . Our data suggest that elevated levels of urea and creatinine, and not chronic kidney disease, were associated with severe COVID-19, which indicates that acute inflammation might be caused by SARS-CoV-2 infection. Previous meta-analyses have also reported findings consistent with our results 78 , 79 . Moreover, anatomical studies have reported significant renal inflammation in patients with severe COVID-19 75 , 80 , 81 . There might be two mechanisms by which SARS-CoV-2 induces renal inflammation. First, SARS-CoV-2 might directly infect renal tubular epithelial cells and podocytes through ACE2 receptors, which facilitates the targeted infection of certain cells by the virus. Consequently, acute tubular necrosis, podocytopathy, microangiopathy, and collapsing glomerulopathy might occur owing to the massive inflammation in renal tubular epithelial cells and podocytes 82 , 83 . Second, the binding between SARS-CoV-2 and ACE2 receptors might activate angiotensin II and induce cytokine production, which may lead to hypercoagulopathy and microangiopathy, and eventually cause renal hypoxia 84 , 85 .
Conversely, with respect to liver function, we observed that the levels of liver enzymes were higher in patients with severe COVID-19. Previous studies in this context have elucidated that ACE2 receptors are highly expressed in bile duct cells; therefore, infection of these cells by coronaviruses might lead to abnormalities in the levels of liver enzymes 86 . However, a recent anatomical study on liver biopsy specimens from patients with severe COVID-19 revealed that moderate microvascular steatosis and mild lobular and portal activities were observed 87 . These data suggest that it cannot be determined clearly whether the elevated levels of liver enzymes in patients with severe COVID-19 are caused by direct infection or by drug-induced liver injury. Therefore, further studies are required to elucidate the precise mechanism underlying the elevation of liver enzymes levels in patients with severe COVID-19.
Meta-analyses on this topic have been performed previously 43 , 44 , 75 , 76 , 88 – 91 . However, compared to previous studies, our study has the following strengths. The previous studies only reported limited factors, such as clinical manifestations 43 , 88 , 90 , 91 , laboratory findings 76 , 89 , or a combination of only clinical manifestations and laboratory findings 75 . In our study, we included all comorbidities, clinical manifestations, and laboratory characteristics. Additionally, compared to previous studies, this study has a larger sample size; the data on 1,934 patients with mild and 1,644 patients with severe COVID-19 treated across 19 hospitals were retrieved. However, this study also has certain limitations. Certain crucial factors that might play an important role in the pathogenesis of COVID-19, including secondary infection, treatment, and immunological status were not controlled for. Our current findings should be interpreted with caution because the majority of studies included were cross-sectional, and the samples corresponding to the data analyzed originated only in China. Moreover, in our study, we did not perform the sub-group analysis according to the transmission area. As already reported, the transmission of COVID-19 in China was also affected by the transmission area 92 . Therefore, this limitation might also affect the final findings of our study. Longitudinal studies may reveal more long-term impacts of SARS-CoV-2 infection 93 .
COVID-19 is an emergent infectious disease, and the major problem associated with it is the unknown pattern of disease development. We identified 34 factors that are associated with severe COVID-19. This might improve our understanding of COVID-19 progression and provide baseline data to compile or improve the prediction models for the estimation of COVID-19 prognosis. Moreover, our current findings may also contribute to guide the prioritization of high-risk target populations for vaccination.
Data availability
[version 2; peer review: 2 approved]
Funding Statement
We thank to Lembaga Pengelola Dana Pendidikan (LPDP) Republik Indonesia for supporting this project.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Morteza Arab-Zozani
1 Social Determinants of Health Research Center, Birjand University of Medical Sciences, Birjand, Iran
The authors responded to my comments clearly and the manuscript is accepted for publication in your journal.
Are the rationale for, and objectives of, the Systematic Review clearly stated?
Is the statistical analysis and its interpretation appropriate?
Are sufficient details of the methods and analysis provided to allow replication by others?
Are the conclusions drawn adequately supported by the results presented in the review?
Reviewer Expertise:
I confirm that I have read this submission and believe that I have an appropriate level of expertise to confirm that it is of an acceptable scientific standard.
Annelies Wilder-Smith
1 Heidelberg Institute of Global Health, University of Heidelberg, Heidelberg, Germany
The strength of this paper is the meta-analysis in terms of effect estimates. The weakness is the focus of data from China, while we should learn more from global data including the comparison between HIC and LMIC.
In China, severity was also found to correlate with the force of infection, eg those in high transmission areas had more severe disease outcomes than those from lower transmission areas in China, see: Exposure to SARS-CoV-2 in a high transmission setting increases the risk of severe COVID -19 compared with exposure to a low transmission setting?
Chen D, Hu C, Su F, Song Q, Wang Z. J Travel Med . 2020 Aug 20;27(5):taaa094. 10.1093/jtm/taaa094. 1
The authors highlight the need for a scoring system for the prediction of severity. There is another reason why it is important to identify risk factors for severe disease: to guide prioritization of high risk target populations for vaccination
COVID-19, Zika and dengue
In this meta-analysis, you investigated the predictors of COVID-19 severity through the literature. You considered a topic of interest and provided a well-written manuscript. However, there are some things that will improve your reporting.
Abstract, method section, please insert detail about critical/quality appraisal of the included studies.
Abstract, method section, line 1, please remove " and extracted" from the text. It maybe causes a misunderstanding between this step and the data extraction step.
Method section, please remove line five. "the protocols for the ...". Mentioning the PRISMA is enough.
Method section, eligibility criteria, (2) please mention the type of data for adequate data. what is adequate data?
Method section, search strategy, why is Scopus not searched? You may have missed some articles that are only indexed in Scopus.
Method section, search strategy, this sentence not related to this section. If you limit the search to EN publication then you need to change the verb. If not this sentence related to inclusion criteria.
Method section, search strategy, based on PRISMA, add at least one search strategy for one database as a supplement.
Method section, data extraction, please added the country of origin for each study. The predictors may be different from one setting to another setting.
Method section, data extraction, please add details about how resolved disagreement between reviewers.
Method section, how did you handle the publication bias?
Result section, there is some problem in figure 1. Please fill it considering other related studies. The number for "record screened" is incorrect.
Result section, table 1, all studies are from China. If all studies are from China it is better to change the title. these are a predictor of severity in China. In my opinion, this is a limitation of your study.
Systematic review and meta-analysis in health and medical intervention
Full text links
Read article at publisher's site: https://doi.org/10.12688/f1000research.26186.2
Citations & impact
Impact metrics, citations of article over time, alternative metrics.

Smart citations by scite.ai Smart citations by scite.ai include citation statements extracted from the full text of the citing article. The number of the statements may be higher than the number of citations provided by EuropePMC if one paper cites another multiple times or lower if scite has not yet processed some of the citing articles. Explore citation contexts and check if this article has been supported or disputed. https://scite.ai/reports/10.12688/f1000research.26186.2
Article citations, risk factors associated with severe covid-19 outcomes in jamaica: a cross-sectional study of national surveillance data..
Webster-Kerr K , Grant A , Harris A , Thorpe R , Rowe D , Henningham D , Mullings T , Wellington I , Wiggan J , Gordon-Johnson KA , Lord C , Dawkins-Beharie T , Azille-Lewis J , Duncan J
Rev Panam Salud Publica , 48:e36, 04 Apr 2024
Cited by: 0 articles | PMID: 38576843 | PMCID: PMC10993815

Comparison of ELISA with automated ECLIA for IL-6 determination in COVID-19 patients: An Italian real-life experience.
Romano F , Lanzilao L , Russo E , Infantino M , Nencini F , Cappelli G , Dugheri S , Manfredi M , Fanelli A , Amedei A , Mucci N
Pract Lab Med , 39:e00392, 01 Mar 2024
Cited by: 0 articles | PMID: 38617587 | PMCID: PMC11015480
Quantification of hs-Troponin Levels and Global Longitudinal Strain among Critical COVID-19 Patients with Myocardial Involvement.
Alsagaff MY , Wardhani LFK , Nugraha RA , Putra TS , Khrisna BPD , Al-Farabi MJ , Gunadi RI , Azmi Y , Budianto CP , Fagi RA , Luthfah N , Subagjo A , Oktaviono YH , Lefi A , Dharmadjati BB , Alkaff FF , Pikir BS
J Clin Med , 13(2):352, 08 Jan 2024
Cited by: 0 articles | PMID: 38256486 | PMCID: PMC10816186
Correlation between interleukin-6 expression in post-mortem core liver biopsy and degree of liver injury in patients with fatal COVID-19.
Maimunah U , Maharani AR , Soegiarto G , Rahniayu A , Gunawan VA , Wiratama PA , Djuanda SN , Supriadi S , Marhana IA , Semedi BP , Lefi A , Kusumastuti EH , Suyanto E , Lilihata JG , Anggoro A , Rinjani LG , Rosyid AN , Wahyu D , Fauziah D , [...] Nugraha RA
Narra J , 3(3):e463, 06 Dec 2023
Cited by: 0 articles | PMID: 38455630 | PMCID: PMC10919438
Exploring the relationship between SARS-CoV-2 variants, illness severity at presentation, in-hospital mortality and COVID-19 vaccination in a low middle-income country: A retrospective cross-sectional study.
Mushtaq MZ , Nasir N , Mahmood SF , Khan S , Kanji A , Nasir A , Syed MA , Aamir UB , Hasan Z
Health Sci Rep , 6(12):e1703, 01 Dec 2023
Cited by: 2 articles | PMID: 38045627 | PMCID: PMC10690835
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Prognostic factors for severity and mortality in patients infected with COVID-19: A systematic review.
Izcovich A , Ragusa MA , Tortosa F , Lavena Marzio MA , Agnoletti C , Bengolea A , Ceirano A , Espinosa F , Saavedra E , Sanguine V , Tassara A , Cid C , Catalano HN , Agarwal A , Foroutan F , Rada G
PLoS One , 15(11):e0241955, 17 Nov 2020
Cited by: 337 articles | PMID: 33201896 | PMCID: PMC7671522
Meta-analysis investigating the relationship between clinical features, outcomes, and severity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia.
Li J , He X , Yuan Yuan , Zhang W , Li X , Zhang Y , Li S , Guan C , Gao Z , Dong G
Am J Infect Control , 49(1):82-89, 12 Jun 2020
Cited by: 79 articles | PMID: 32540370 | PMCID: PMC7292004
Laboratory features of severe vs. non-severe COVID-19 patients in Asian populations: a systematic review and meta-analysis.
Ghahramani S , Tabrizi R , Lankarani KB , Kashani SMA , Rezaei S , Zeidi N , Akbari M , Heydari ST , Heydari ST , Akbari H , Nowrouzi-Sohrabi P , Ahmadizar F
Eur J Med Res , 25(1):30, 03 Aug 2020
Cited by: 149 articles | PMID: 32746929 | PMCID: PMC7396942
Biomarkers of cytokine storm as red flags for severe and fatal COVID-19 cases: A living systematic review and meta-analysis.
Melo AKG , Milby KM , Caparroz ALMA , Pinto ACPN , Santos RRP , Rocha AP , Ferreira GA , Souza VA , Valadares LDA , Vieira RMRA , Pileggi GS , Trevisani VFM
PLoS One , 16(6):e0253894, 29 Jun 2021
Cited by: 75 articles | PMID: 34185801 | PMCID: PMC8241122
Risk factors and predictors associated with the severity of COVID-19 in China: a systematic review, meta-analysis, and meta-regression.
Zhang T , Huang WS , Guan W , Hong Z , Gao J , Gao G , Wu G , Qin YY
J Thorac Dis , 12(12):7429-7441, 01 Dec 2020
Cited by: 27 articles | PMID: 33447431 | PMCID: PMC7797827
Funding
Funders who supported this work.
Lembaga Pengelola Dana Pendidikan
Europe PMC is part of the ELIXIR infrastructure
Exploring Micronutrient Dynamics in COVID-19 Severity and Mortality: Unraveling the Roles of Vitamin D, Calcium, Phosphorus, Magnesium and ALP
- ORIGINAL RESEARCH ARTICLE
- Published: 21 April 2024
Cite this article

- PVSN Kiran Kumar 1 ,
- Pradeep Japa 2 ,
- Sojit Tomo 2 ,
- Shrimanjunath Sankanagoudar 2 ,
- Purvi Purohit 2 ,
- Jayakaran Charan 3 ,
- Abhishek Purohit 4 ,
- Vijaya Lakshmi Nag 5 ,
- Pradeep Kumar Bhatia 6 ,
- Kuldeep Singh 7 ,
- Naveen Dutt 8 ,
- Mahendra Kumar Garg 9 ,
- Sanjeev Misra 10 ,
- Praveen Sharma 2 &
- Dharamveer Yadav ORCID: orcid.org/0000-0002-7109-8039 2
Explore all metrics
The COVID-19 pandemic has underscored the critical importance of understanding the intricate relationship between micronutrient levels and disease outcomes. This study explores the impact of Vitamin D, calcium, phosphorus, magnesium, and alkaline phosphatase (ALP) on COVID-19 severity and mortality. The study involves 200 participants (100 COVID-19 patients, 100 controls), we meticulously analyzed micronutrient dynamics. Calcium, phosphorus, magnesium and ALP was measured spectrophotometrically. Vitamin D was measured using Chemiluminescent method. The study reveals that diminished levels of calcium, phosphorus, magnesium, and with elevated ALP, are significantly associated with COVID-19 cases. Whereas the Vitamin D levels in severe group was increased when compared to mild cases but decreased than control group. Disease severity correlated with declining calcium (r = − 0.35, p < 0.01), phosphorus (r = − 0.26, p < 0.05), and magnesium (r = − 0.21, p < 0.05), and increased ALP (r = 0.42, p < 0.001). Post-discharge, calcium ( p < 0.05) and phosphorus ( p < 0.01) showed positive trends, while ALP ( p < 0.001) decreased. Notably, calcium (OR = 0.63, p < 0.05) and ALP (OR = 1.87, p < 0.001) emerged as significant predictors of disease severity. The findings not only illuminate potential therapeutic avenues but also emphasize the need to optimize nutrient levels, including magnesium, for COVID-19 prevention and management. Given the complexities of these relationships, further rigorous exploration, including well-designed trials and understanding underlying mechanisms, is imperative to unravel the dynamics of these nutrient interactions in the context of COVID-19.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Hiscott J, Alexandridi M, Muscolini M, Tassone E, Palermo E, Soultsioti M, et al. The global impact of the coronavirus pandemic. Cytokine Growth Factor Rev. 2020;53:1–9.
Article CAS PubMed PubMed Central Google Scholar
Brandily P, Brébion C, Briole S, Khoury L. A poorly understood disease? The impact of COVID-19 on the income gradient in mortality over the course of the pandemic. Eur Econ Rev. 2021;140:103923.
Article PubMed PubMed Central Google Scholar
Sundar R, Bhagavandas Rai A, Naveen Kumar J, Devang DD. The role of Vitamin D as an adjunct for bone regeneration: a systematic review of literature. Saudi Dent J. 2023;35:220–32.
Martiniakova M, Babikova M, Mondockova V, Blahova J, Kovacova V, Omelka R. The role of macronutrients, micronutrients and flavonoid polyphenols in the prevention and treatment of osteoporosis. Nutrients. 2022;14:523.
Orchard TS, Larson JC, Alghothani N, Bout-Tabaku S, Cauley JA, Chen Z, et al. Magnesium intake, bone mineral density, and fractures: results from the women’s health initiative observational study. Am J Clin Nutr. 2014;99:926–33.
Yang C, Ma X, Wu J, Han J, Zheng Z, Duan H, et al. Low serum calcium and phosphorus and their clinical performance in detecting COVID-19 patients. J Med Virol. 2021;93:1639–51.
Article CAS PubMed Google Scholar
Pvsn KK, Tomo S, Purohit P, Sankanagoudar S, Charan J, Purohit A, et al. Comparative analysis of serum zinc, copper and magnesium level and their relations in association with severity and mortality in SARS-CoV-2 patients. Biol Trace Elem Res. 2023;201:23–30.
Dharmalingam K, Birdi A, Tomo S, Sreenivasulu K, Charan J, Yadav D, et al. Trace elements as immunoregulators in SARS-CoV-2 and other viral infections. Indian J Clin Biochem. 2021;36:1–11.
Article Google Scholar
Yadav D, Pvsn KK, Tomo S, Sankanagoudar S, Charan J, Purohit A, et al. Association of iron-related biomarkers with severity and mortality in COVID-19 patients. J Trace Elem Med Biol. 2022;74:127075.
Yadav D, Birdi A, Tomo S, Charan J, Bhardwaj P, Sharma P. Association of vitamin D status with COVID-19 infection and mortality in the Asia Pacific region: a cross-sectional study. Indian J Clin Biochem. 2021;36:1–6.
Tomo S, Karli S, Dharmalingam K, Yadav D, Sharma P. The clinical laboratory: a key player in diagnosis and management of COVID-19. EJIFCC. 2020;31:326–46.
CAS PubMed PubMed Central Google Scholar
Clinical Spectrum [Internet]. COVID-19 Treatment guidelines. [cited 2024 Mar 30]. Available from: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/
Zayed NE, Abbas A, Lutfy SM. Criteria and potential predictors of severity in patients with COVID-19. Egypt J Bronchol. 2022;16:11.
Tomo S, Kumar KP, Roy D, Sankanagoudar S, Purohit P, Yadav D, et al. Complement activation and coagulopathy - an ominous duo in COVID19. Expert Rev Hematol. 2021;14:155–73.
Tomo S, Kiran Kumar P, Yadav D, Sankanagoudar S, Charan J, Purohit A, et al. Association of serum complement C3 levels with severity and mortality in COVID 19. Ind J Clin Biochem. 2023;38:447–56.
Article CAS Google Scholar
Dramé M, Cofais C, Hentzien M, Proye E, Coulibaly PS, Demoustier-Tampère D, et al. Relation between vitamin D and COVID-19 in aged people: a systematic review. Nutrients. 2021;13:1339.
Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12:988.
Ali N. Role of vitamin D in preventing of COVID-19 infection, progression and severity. J Infect Public Health. 2020;13:1373–80.
Ginde AA, Blatchford P, Breese K, Zarrabi L, Linnebur SA, Wallace JI, et al. High dose monthly vitamin D for prevention of acute respiratory infection in older long-term care residents: a randomized clinical trial. J Am Geriatr Soc. 2017;65:496–503.
Article PubMed Google Scholar
Shekhawat J, Gauba K, Gupta S, Purohit P, Mitra P, Garg M, et al. Interleukin-6 perpetrator of the COVID-19 cytokine storm. Indian J Clin Biochem. 2021;36:1–11.
Anghel L, Manole C, Nechita A, Tatu AL, Ștefănescu BI, Nechita L, et al. Calcium, phosphorus and magnesium abnormalities associated with COVID-19 infection, and beyond. Biomedicines. 2023;11:2362.
Povaliaeva A, Bogdanov V, Pigarova E, Dzeranova L, Katamadze N, Malysheva N, et al. Impaired vitamin D metabolism in hospitalized COVID-19 patients. Pharmaceuticals (Basel). 2022;15:906.
Abobaker A, Alzwi A. The effect of COVID-19 on parathyroid glands. J Infect Public Health. 2021;14:724–5.
di Filippo L, Frara S, Doga M, Giustina A. The osteo-metabolic phenotype of COVID-19: an update. Endocrine. 2022;78:247–54.
Kerschan-Schindl K, Dovjak P, Butylina M, Rainer A, Mayr B, Röggla V, et al. Moderate COVID-19 disease is associated with reduced Bone turnover. J Bone Miner Res. 2023;38:943–50.
Tang J. COVID-19 pandemic and osteoporosis in elderly patients. Aging Dis. 2022;13:960–9.
Kerner A, Avizohar O, Sella R, Bartha P, Zinder O, Markiewicz W, et al. Association between elevated liver enzymes and c-reactive protein. Arterioscler Thromb Vasc Biol. 2005;25:193–7.
Clark R, Waters B, Stanfill AG. Elevated liver function tests in COVID-19. Nurse Pract. 2021;46:21–6.
Vargas-Mendoza N, García-Machorro J, Angeles-Valencia M, Martínez-Archundia M, Madrigal-Santillán EO, Morales-González Á, et al. Liver disorders in COVID-19, nutritional approaches and the use of phytochemicals. World J Gastroenterol. 2021;27:5630–65.
Xu Y, Baylink DJ, Chen C-S, Reeves ME, Xiao J, Lacy C, et al. The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19. J Transl Med. 2020;18:322.
van Kempen TATG, Deixler E. SARS-CoV-2: influence of phosphate and magnesium, moderated by vitamin D, on energy (ATP) metabolism and on severity of COVID-19. Am J Physiol Endocrinol Metab. 2021;320:E2-6.
Bego T, Meseldžić N, Prnjavorac B, Prnjavorac L, Marjanović D, Azevedo R, et al. Association of trace element status in COVID-19 patients with disease severity. J Trace Elem Med Biol. 2022;74:127055.
Download references
This research has received support from an intramural project grant provided by the All India Institute of Medical Sciences Jodhpur.
Author information
Authors and affiliations.
Department of Biochemistry, Andhra Medical College, Visakhapatnam, India
PVSN Kiran Kumar
Department of Biochemistry, All India Institute of Medical Sciences, Basni, Jodhpur, Rajasthan, 342005, India
Pradeep Japa, Sojit Tomo, Shrimanjunath Sankanagoudar, Purvi Purohit, Praveen Sharma & Dharamveer Yadav
Department of Pharmacology, All India Institute of Medical Sciences, Jodhpur, India
Jayakaran Charan
Department of Pathology & Lab Medicine, All India Institute of Medical Sciences, Jodhpur, India
Abhishek Purohit
Department of Microbiology, All India Institute of Medical Sciences, Jodhpur, India
Vijaya Lakshmi Nag
Department of Anaesthesiology and Critical Care, All India Institute of Medical Sciences, Jodhpur, India
Pradeep Kumar Bhatia
Department of Paediatrics, All India Institute of Medical Sciences, Jodhpur, India
Kuldeep Singh
Department of Pulmonary Medicine, All India Institute of Medical Sciences, Jodhpur, India
Naveen Dutt
Department of General Medicine, All India Institute of Medical Sciences, Jodhpur, India
Mahendra Kumar Garg
Department of Surgical Oncology, All India Institute of Medical Sciences, Jodhpur, India
Sanjeev Misra
You can also search for this author in PubMed Google Scholar
Contributions
Material preparation, data collection, and analysis were expertly handled by PVSN KK, PJ, ST, DY, PP and SS. The initial draft of the manuscript was crafted by PVSN KK, DY, and PP, with insightful comments and revisions from all authors. The final manuscript was reviewed and approved by all contributors.
Corresponding author
Correspondence to Dharamveer Yadav .
Ethics declarations
Ethics approval.
This study was conducted in strict adherence to the principles outlined in the Declaration of Helsinki. Approval for the study was obtained from the institutional ethics committee.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 14 kb)
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Kumar, P.K., Japa, P., Tomo, S. et al. Exploring Micronutrient Dynamics in COVID-19 Severity and Mortality: Unraveling the Roles of Vitamin D, Calcium, Phosphorus, Magnesium and ALP. Ind J Clin Biochem (2024). https://doi.org/10.1007/s12291-024-01225-9
Download citation
Received : 12 January 2024
Accepted : 07 April 2024
Published : 21 April 2024
DOI : https://doi.org/10.1007/s12291-024-01225-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Phosphorous
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 18 April 2024
The predictive power of data: machine learning analysis for Covid-19 mortality based on personal, clinical, preclinical, and laboratory variables in a case–control study
- Maryam Seyedtabib ORCID: orcid.org/0000-0003-1599-9374 1 ,
- Roya Najafi-Vosough ORCID: orcid.org/0000-0003-2871-5748 2 &
- Naser Kamyari ORCID: orcid.org/0000-0001-6245-5447 3
BMC Infectious Diseases volume 24 , Article number: 411 ( 2024 ) Cite this article
137 Accesses
1 Altmetric
Metrics details
Background and purpose
The COVID-19 pandemic has presented unprecedented public health challenges worldwide. Understanding the factors contributing to COVID-19 mortality is critical for effective management and intervention strategies. This study aims to unlock the predictive power of data collected from personal, clinical, preclinical, and laboratory variables through machine learning (ML) analyses.
A retrospective study was conducted in 2022 in a large hospital in Abadan, Iran. Data were collected and categorized into demographic, clinical, comorbid, treatment, initial vital signs, symptoms, and laboratory test groups. The collected data were subjected to ML analysis to identify predictive factors associated with COVID-19 mortality. Five algorithms were used to analyze the data set and derive the latent predictive power of the variables by the shapely additive explanation values.
Results highlight key factors associated with COVID-19 mortality, including age, comorbidities (hypertension, diabetes), specific treatments (antibiotics, remdesivir, favipiravir, vitamin zinc), and clinical indicators (heart rate, respiratory rate, temperature). Notably, specific symptoms (productive cough, dyspnea, delirium) and laboratory values (D-dimer, ESR) also play a critical role in predicting outcomes. This study highlights the importance of feature selection and the impact of data quantity and quality on model performance.
This study highlights the potential of ML analysis to improve the accuracy of COVID-19 mortality prediction and emphasizes the need for a comprehensive approach that considers multiple feature categories. It highlights the critical role of data quality and quantity in improving model performance and contributes to our understanding of the multifaceted factors that influence COVID-19 outcomes.
Peer Review reports
Introduction
The World Health Organization (WHO) has declared COVID-19 a global pandemic in March 2020 [ 1 ]. The first cases of SARSCoV-2, a new severe acute respiratory syndrome coronavirus, were detected in Wuhan, China, and rapidly spread to become a global public health problem [ 2 ]. The clinical presentation and symptoms of COVID-19 may be similar to those of Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS), however the rate of spread is higher [ 3 ]. By December 31, 2022, the pandemic had caused more than 729 million cases and nearly 6.7 million deaths (0.92%) were confirmed in 219 countries worldwide [ 4 ]. For many countries, figuring out what measures to take to prevent death or serious illness is a major challenge. Due to the complexity of transmission and the lack of proven treatments, COVID-19 is a major challenge worldwide [ 5 , 6 ]. In middle- and low-income countries, the situation is even more catastrophic due to high illiteracy rates, a very poor health care system, and lack of intensive care units [ 5 ]. In addition, understanding the factors contributing to COVID-19 mortality is critical for effective management and intervention strategies [ 6 ].
Numerous studies have shown several factors associated with COVID-19 outcomes, including socioeconomic, environmental, individual demographic, and health factors [ 7 , 8 , 9 ]. Risk factors for COVID -19 mortality vary by study and population studied [ 10 ]. Age [ 11 , 12 ], comorbidities such as hypertension, cardiovascular disease, diabetes, and COPD [ 13 , 14 , 15 ], sex [ 13 ], race/ethnicity [ 11 ], dementia, and neurologic disease [ 16 , 17 ], are some of the factors associated with COVID-19 mortality. Laboratory factors such as elevated levels of inflammatory markers, lymphopenia, elevated creatinine levels, and ALT are also associated with COVID-19 mortality [ 5 , 18 ]. Understanding these multiple risk factors is critical to accurately diagnose and treat COVID-19 patients.
Accurate diagnosis and treatment of the disease requires a comprehensive assessment that considers a variety of factors. These factors include personal factors such as medical history, lifestyle, and genetics; clinical factors such as observations on physical examinations and physician reports; preclinical factors such as early detection through screening or surveillance; laboratory factors such as results of diagnostic tests and medical imaging; and patient-reported signs and symptoms. However, the variety of characteristics associated with COVID-19 makes it difficult for physicians to accurately classify COVID-19 patients during the pandemic.
In today's digital transformation era, machine learning plays a vital role in various industries, including healthcare, where substantial data is generated daily [ 19 , 20 , 21 ]. Numerous studies have explored machine learning (ML) and explainable artificial intelligence (AI) in predicting COVID-19 prognosis and diagnosis [ 22 , 23 , 24 , 25 ]. Chadaga et al. have developed decision support systems and triage prediction systems using clinical markers and biomarkers [ 22 , 23 ]. Similarly, Khanna et al. have developed a ML and explainable AI system for COVID-19 triage prediction [ 24 ]. Zoabi has also made contributions in this field, developing ML models that predict COVID-19 test results with high accuracy based on a small number of features such as gender, age, contact with an infected person and initial clinical symptoms [ 25 ]. These studies emphasize the potential of ML and explainable AI to improve COVID-19 prediction and diagnosis. Nonetheless, the efficacy of ML algorithms heavily relies on the quality and quantity of data utilized for training. Recent research has indicated that deep learning algorithms' performance can be significantly enhanced compared to traditional ML methods by increasing the volume of data used [ 26 ]. However, it is crucial to acknowledge that the impact of data volume on model performance can vary based on data characteristics and experimental setup, highlighting the need for careful consideration and analysis when selecting data for model training. While the studies emphasize the importance of features in training ML algorithms for COVID-19 prediction and diagnosis, additional research is required on methods to enhance the interpretability of features.
Therefore, the primary aim of this study is to identify the key factors associated with mortality in COVID -19 patients admitted to hospitals in Abadan, Iran. For this purpose, seven categories of factors were selected, including demographic, clinical and conditions, comorbidities, treatments, initial vital signs, symptoms, and laboratory tests, and machine learning algorithms were employed. The predictive power of the data was assessed using 139 predictor variables across seven feature sets. Our next goal is to improve the interpretability of the extracted important features. To achieve this goal, we will utilize the innovative SHAP analysis, which illustrates the impact of features through a diagram.
Materials and methods
Study population and data collection.
Using data from the COVID-19 hospital-based registry database, a retrospective study was conducted from April 2020 to December 2022 at Ayatollah Talleghani Hospital (a COVID‑19 referral center) in Abadan City, Iran.
A total of 14,938 patients were initially screened for eligibility for the study. Of these, 9509 patients were excluded because their transcriptase polymerase chain reaction (RT-PCR) test results were negative or unspecified. The exclusion of patients due to incomplete or missing data is a common issue in medical research, particularly in the use of electronic medical records (EMRs) [ 27 ]. In addition, 1623 patients were excluded because their medical records contained more than 70% incomplete or missing data. In addition, patients younger than 18 years were not included in the study. The criterion for excluding 1623 patients due to "70% incomplete or missing data" means that the medical records of these patients did not contain at least 30% of the data required for a meaningful analysis. This threshold was set to ensure that the dataset used for the study contained a sufficient amount of complete and reliable information to draw accurate conclusions. Incomplete or missing data in a medical record may relate to key variables such as patient demographics, symptoms, lab results, treatment information, outcomes, or other data points important to the research. Insufficient data can affect the validity and reliability of study results and lead to potential bias or inaccuracies in the findings. It is important to exclude such incomplete records to maintain the quality and integrity of the research findings and to ensure that the conclusions drawn are based on robust and reliable data. After these exclusions, 3806 patients remained. Of these patients, 474 died due to COVID -19, while the remaining 3332 patients recovered and were included in the control group. To obtain a balanced sample, the control group was selected with a propensity score matching (PSM). The PSM refers to a statistical technique used to create a balanced comparison group by matching individuals in the control group (in this case, the survived group) with individuals in the case group (in this case, the deceased group) based on their propensity scores. In this study, the propensity scores for each person represented the probability of death (coded as a binary outcome; survived = 0, deceased = 1) calculated from a set of covariates (demographic factors) using the matchit function from the MatchIt library. Two individuals, one from the deceased group and one from the survived group, are considered matched if the difference between their propensity scores is small. Non-matching participants are discarded. The matching aims to reduce bias by making the distribution of observed characteristics similar between groups, which ultimately improves the comparability of groups in observational studies [ 28 ]. In total, the study included 1063 COVID-19 patients who belonged to either the deceased group (case = 474) or the survived group (control = 589) (Fig. 1 ).
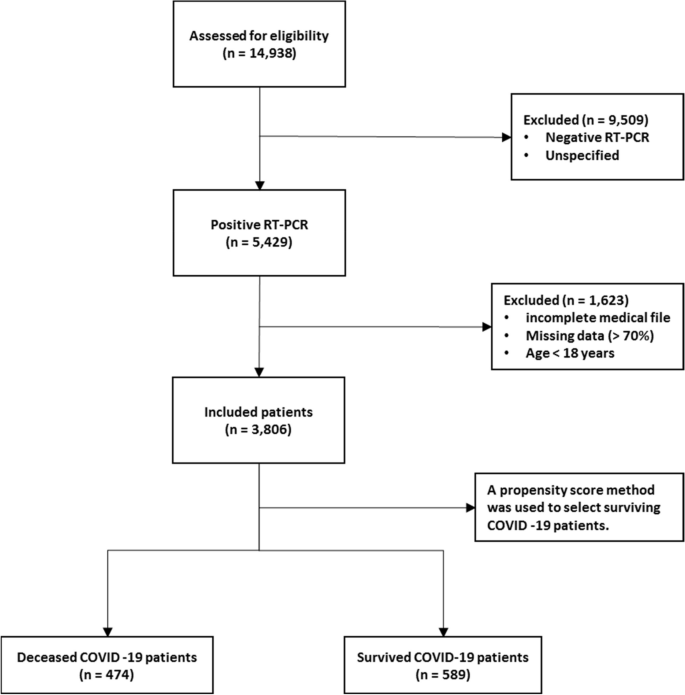
Flowchart describing the process of patient selection
In the COVID‑19 hospital‑based registry database, one hundred forty primary features in eight main classes including patient’s demographics (eight features), clinical and conditions features (16 features), comorbidities (18 features), treatment (17 features), initial vital sign (14 features), symptoms during hospitalization (31 features), laboratory results (35 features), and an output (0 for survived and 1 for deceased) was recorded for COVID-19 patients. The main features included in the hospital-based COVID-19 registry database are provided in Appendix Table 1 .
To ensure the accuracy of the recorded information, discharged patients or their relatives were called and asked to review some of the recorded information (demographic information, symptoms, and medical history). Clinical symptoms and vital signs were referenced to the first day of hospitalization (at admission). Laboratory test results were also referenced to the patient’s first blood sample at the time of hospitalization.
The study analyzed 140 variables in patients' records, normalizing continuous variables and creating a binary feature to categorize patients based on outcomes. To address the issue of an imbalanced dataset, the Synthetic Minority Over-sampling Technique (SMOTE) was utilized. Some classes were combined to simplify variables. For missing data, an imputation technique was applied, assuming a random distribution [ 29 ]. Little's MCAR test was performed with the naniar package to assess whether missing data in a dataset is missing completely at random (MCAR) [ 30 ]. The null hypothesis in this test is that the data are MCAR, and the test statistic is a chi-square value.
The Ethics Committee of Abadan University of Medical Science approved the research protocol (No. IR.ABADANUMS.REC.1401.095).
Predictor variables
All data were collected in eight categories, including demographic, clinical and conditions, comorbidities, treatment, initial vital signs, symptoms, and laboratory tests in medical records, for a total of 140 variables.
The "Demographics" category encompasses eight features, three of which are binary variables and five of which are categorical. The "Clinical Conditions" category includes 16 features, comprising one quantitative variable, 12 binary variables, and five categorical features. " Comorbidities ", " Treatment ", and " Symptoms " each have 18, 17, and 30 binary features, respectively. Also, there is one quantitative variable in symptoms category. The "Initial Vital Signs" category features 11 quantitative variables, two binary variables, and one categorical variable. Finally, the "Laboratory Tests" category comprises 35 features, with 33 being quantitative, one categorical, and one binary (Appendix Table 1 ).
Outcome variable
The primary outcome variable was mortality, with December 31, 2022, as the last date of follow‐up. The feature shows the class variable, which is binary. For any patient in the survivor group, the outcome is 0; otherwise, it is 1. In this study, 44.59% ( n = 474) of the samples were in the deceased group and were labeled 1.
Data balancing
In case–control studies, it is common to have unequal size groups since cases are typically fewer than controls [ 31 ]. However, in case–control studies with equal sizes, data balancing may not be necessary for ML algorithms [ 32 ]. When using ML algorithms, data balancing is generally important when there is an imbalance between classes, i.e., when one class has significantly fewer observations than the other [ 33 ]. In such cases, balancing can improve the performance of the algorithm by reducing the bias in favor of the majority class [ 34 ]. For case–control studies of the same size, the balance of the classes has already been reached and balancing may not be necessary. However, it is always recommended to evaluate the performance of the ML algorithm with the given data set to determine the need for data balancing. This is because unbalanced case–control ratios can cause inflated type I error rates and deflated type I error rates in balanced studies [ 35 ].
Feature selection
Feature selection is about selecting important variables from a large dataset to be used in a ML model to achieve better performance and efficiency. Another goal of feature selection is to reduce computational effort by eliminating irrelevant or redundant features [ 36 , 37 ]. Before generating predictions, it is important to perform feature selection to improve the accuracy of clinical decisions and reduce errors [ 37 ]. To identify the best predictors, researchers often compare the effectiveness of different feature selection methods. In this study, we used five common methods, including Decision Tree (DT), eXtreme Gradient Boosting (XGBoost), Support Vector Machine (SVM), Naïve Bayes (NB), and Random Forest (RF), to select relevant features for predicting mortality of COVID -19 patients. To avoid overfitting, we performed ten-fold cross-validation when training our dataset. This approach may help ensure that our model is optimized for accurate predictions of health status in COVID -19 patients.
Model development, evaluation, and clarity
In this study, the predictive models were developed with five ML algorithms, including DT, XGBoost, SVM, NB, and RF, using the R programming language (v4.3.1) and its packages [ 38 ]. We used cross-validation (CV) to tune the hyperparameters of our models based on the training subset of the dataset. For training and evaluating our ML models, we used a common technique called tenfold cross validation [ 39 ]. The primary training dataset was divided into ten folding, each containing 10% of the total data, using a technique called stratified random sampling. For each of the 30% of the data, a ML model was built and trained on the remaining 70% of the data. The performance of the model was then evaluated on the 30%-fold sample. This process was repeated 100 times with different training and test combinations, and the average performance was reported.
Performance measures include sensitivity (recall), specificity, accuracy, F1-score, and the area under the receiver operating characteristics curve (AUC ROC). Sensitivity is defined as TP / (TP + FN), whereas specificity is TN / (TN + FP). F1-score is defined as the harmonic mean of Precision and Recall with equal weight, where Precision equals TP + TN / total. Also, AUC refers to the area under the ROC curve. In the evaluation of ML techniques, values were classified as poor if below 50%, ok if between 50 and 80%, good if between 80 and 90%, and very good if greater than 90%. These criteria are commonly used in reporting model evaluations [ 40 , 41 ].
Finally, the shapely additive explanation (SHAP) method was used to provide clarity and understanding of the models. SHAP uses cooperative game theory to determine how each feature contributes to the prediction of ML models. This approach allows the computation of the contribution of each feature to model performance [ 42 , 43 ]. For this purpose, the package shapr was used, which includes a modified iteration of the kernel SHAP approach that takes into account the interdependence of the features when computing the Shapley values [ 44 ].
Patient characteristics
Table 1 shows the baseline characteristics of patients infected with COVID-19, including demographic data such as age and sex and other factors such as occupation, place of residence, marital status, education level, BMI, and season of admission. A total of 1063 adult patients (≥ 18 years) were enrolled in the study, of whom 589 (55.41%) survived and 474 (44.59%) died. Analysis showed that age was significantly different between the two groups, with a mean age of 54.70 ± 15.60 in the survivor group versus 65.53 ± 15.18 in the deceased group ( P < 0.001). There was also a significant association between age and survival, with a higher proportion of patients aged < 40 years in the survivor group (77.0%) than in the deceased group (23.0%) ( P < 0.001). No significant differences were found between the two groups in terms of sex, occupation, place of residence, marital status, and time of admission. However, there was a significant association between educational level and survival, with a lower proportion of patients with a college degree in the deceased group (37.2%) than in the survivor group (62.8%) ( P = 0.017). BMI also differed significantly between the two groups, with the proportion of patients with a BMI > 30 (kg/cm 2 ) being higher in the deceased group (56.5%) than in the survivor group (43.5%) ( P < 0.001).
Clinical and conditions
Important insights into the various clinical and condition characteristics associated with COVID-19 infection outcomes provides in Table 2 . The results show that patients who survived the infection had a significantly shorter hospitalization time (2.20 ± 1.63 days) compared to those who died (4.05 ± 3.10 days) ( P < 0.001). Patients who were admitted as elective cases had a higher survival rate (84.6%) compared to those who were admitted as urgent (61.3%) or emergency (47.4%) cases. There were no significant differences with regard to the number of infections or family infection history. However, patients who had a history of travel had a lower decease rate (40.1%).
A significantly higher proportion of deceased patients had cases requiring CPR (54.7% vs. 45.3%). Patients who had underlying medical conditions had a significantly lower survival rate (38.3%), with hyperlipidemia being the most prevalent condition (18.7%). Patients who had a history of alcohol consumption (12.5%), transplantation (30.0%), chemotropic (21.4%) or special drug use (0.0%), and immunosuppressive drug use (30.0%) also had a lower survival rate. Pregnant patients (44.4%) had similar survival outcomes compared to non-pregnant patients (55.6%). Patients who were recent or current smokers (36.4%) also had a significantly lower survival rate.
Comorbidities
Table 3 summarizes the comorbidity characteristics of COVID-19 infected patients. Out of 1063 patients, 54.84% had comorbidities. Chi-Square tests for individual comorbidities showed that most of them had a significant association with COVID-19 outcomes, with P -values less than 0.05. Among the various comorbidities, hypertension (HTN) and diabetes mellitus (DM) were the most prevalent, with 12% and 11.5% of patients having these conditions, respectively. The highest fatality rates were observed among patients with cardiovascular disease (95.5%), chronic kidney disease (62.5%), gastrointestinal (GI) (93.3%), and liver diseases (73.3%). Conversely, patients with neurology comorbidities had the lowest fatality rate (0%). These results highlight the significant role of comorbidities in COVID-19 outcomes and emphasize the need for special attention to be paid to patients with pre-existing health conditions.
The treatment characteristics of the COVID-19 patients and the resulting outcomes are shown in Table 4 . The table shows the frequency of patients who received different types of medications or therapies during their treatment. According to the results, the use of antibiotics (35.1%), remdesivir (29.6%), favipiravir (36.0%), and Vitamin zinc (33.5%) was significantly associated with a lower mortality rate ( P < 0.001), suggesting that these medications may have a positive impact on patient outcomes. On the other hand, the use of Heparin (66.1%), Insulin (82.6%), Antifungal (89.6%), ACE inhibitors (78.1%), and Angiotensin II Receptor Blockers (ARB) (83.8%) was significantly associated with increased mortality ( P < 0.001), suggesting that these medications may have a negative effect on the patient's outcome. Also, It seems that taking hydroxychloroquine (51.0%) is associated with a worse outcome at lower significance ( P = 0.022). The use of Atrovent, Corticosteroids and Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) did not show a significant association with survival or mortality rates. Similarly, the use of Intravenous Immunoglobulin (IVIg), Vitamin C, Vitamin D, and Diuretic did not show a significant association with the patient’s outcome.
Initial vital signs
Table 5 provides initial vital sign characteristics of COVID-19 patients, including heart rate, respiratory rate, temperature, blood pressure, oxygen therapy, and radiography test result. The findings shows that deceased patients had higher HR (83.03 bpm vs. 76.14 bpm, P < 0.001), lower RR (11.40 bpm vs. 16.25 bpm, P < 0.001), higher temperature (37.43 °C vs. 36.91 °C, P < 0.001), higher SBP (128.16 mmHg vs. 123.33 mmHg, P < 0.001), and higher O 2 requirements (invasive: 75.0% vs. 25.0%, P < 0.001) compared to the survived patients. Additionally, deceased patients had higher MAP (99.35 mmHg vs. 96.08 mmHg, P = 0.005), and lower SPO 2 percentage (81.29% vs. 91.95%, P < 0.001) compared to the survived patients. Furthermore, deceased patients had higher PEEP levels (5.83 cmH2O vs. 0.69 cmH2O, P < 0.001), higher FiO2 levels (51.43% vs. 8.97%, P < 0.001), and more frequent bilateral pneumonia (63.0% vs. 37.0%, P < 0.001) compared to the survived patients. There appears to be no relationship between diastolic blood pressure and treatment outcome (83.44 mmHg vs. 85.61 mmHg).
Table 6 provides information on the symptoms of patients infected with COVID-19 by survival outcome. The table also shows the frequency of symptoms among patients. The most common symptom reported by patients was fever, which occurred in 67.0% of surviving and deceased patients. Dyspnea and nonproductive cough were the second and third most common symptoms, reported by 40.4% and 29.3% of the total sample, respectively. Other common symptoms listed in the Table were malodor (28.7%), dyspepsia (28.4%), and myalgia (25.6%).
The P -values reported in the table show that some symptoms are significantly associated with death, including productive cough, dyspnea, sore throat, headache, delirium, olfactory symptoms, dyspepsia, nausea, vomiting, sepsis, respiratory failure, heart failure, MODS, coagulopathy, secondary infection, stroke, acidosis, and admission to the intensive care unit. Surviving and deceased patients also differed significantly in the average number of days spent in the ICU. There was no significant association between patient outcomes and symptoms such as nonproductive cough, chills, diarrhea, chest pain, and hyperglycemia.
Laboratory tests
Table 7 shows the laboratory values of COVID-19 patients with the average values of the different laboratory results. The results show that the deceased patients had significantly lower levels of red blood cells (3.78 × 106/µL vs. 5.01 × 106/µL), hemoglobin (11.22 g/dL vs. 14.10 g/dL), and hematocrit (34.10% vs. 42.46%), whereas basophils and white blood cells did not differ significantly between the two groups. The percentage of neutrophils (65.59% vs. 62.58%) and monocytes (4.34% vs. 3.93%) was significantly higher in deceased patients, while the percentage of lymphocytes and eosinophils did not differ significantly between the two groups. In addition, deceased patients had higher levels of certain biomarkers, including D-dimer (1.347 mgFEU/L vs. 0.155 mgFEU/L), lactate dehydrogenase (174.61 U/L vs. 128.48 U/L), aspartate aminotransferase (93.09 U/L vs. 39.63 U/L), alanine aminotransferase (74.48 U/L vs. 28.70 U/L), alkaline phosphatase (119.51 IU/L vs. 81.34 IU/L), creatine phosphokinase-MB (4.65 IU/L vs. 3.33 IU/L), and positive troponin I (56.5% vs. 43.5%). The proportion of patients with positive C-reactive protein was also higher in the deceased group.
Other laboratory values with statistically significant differences between the two groups ( P < 0.001) were INR, ESR, BUN, Cr, Na, K, P, PLT, TSH, T3, and T4. The surviving patients generally had lower values in these laboratory characteristics than the deceased patients.
Model performance and evaluation
Five ML algorithms, namely DT, XGBoost, SVM, NB, and RF, were used in this study to build mortality prediction models COVID -19. The models were based on the optimal feature set selected in a previous step and were trained on the same data set. The effectiveness of the models was evaluated by calculating sensitivity, specificity, accuracy, F1 score, and AUC metrics. Table 8 shows the results of this performance evaluation. The average values are expressed from the test set as the mean (standard deviation).
The results show that the performance of the models varies widely in the different feature categories. The Laboratory Tests category achieved the highest performance, with all models scoring 100% in all metrics. The Symptoms and initial Vital Signs categories also show high performance, with XGBoost achieving the highest accuracy of 98.03% and DT achieving the highest sensitivity of 92.79%.
The Clinical and Conditions category also showed high performance, with all models showing accuracy above 91%. XGBoost achieved the highest sensitivity and specificity of 92.74% and 92.96%, respectively. In contrast, the Demographics category showed the lowest performance, with all models achieving less than 66.5% accuracy.
In summary, the results suggest that certain feature categories may be more useful than others in predicting mortality from COVID-19 and that some ML models may perform better than others depending on the feature category used.
Feature importance
SHapley Additive exPlanations (SHAP) values indicate the importance or contribution of each feature in predicting model output. These values help to understand the influence and importance of each feature on the model's decision-making process.
In Fig. 2 , the mean absolute SHAP values are shown to depict global feature importance. Figure 2 shows the contribution of each feature within its respective group as calculated by the XGBoost prediction model using SHAP. According to the SHAP method, the features that had the greatest impact on predicting COVID-19 mortality were, in descending order: D-dimer, CPR, PEEP, underlying disease, ESR, antifungal treatment, PaO2, age, dyspnea, and nausea.
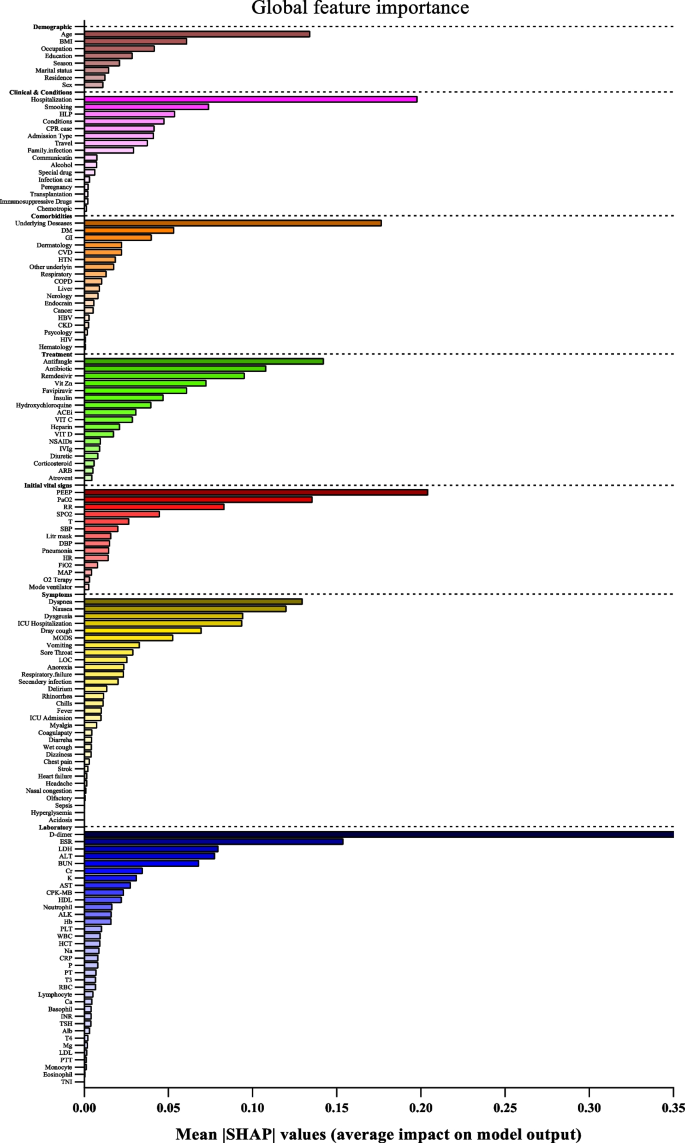
Feature importance based on SHAP-values. The mean absolute SHAP values are depicted, to illustrate global feature importance. The SHAP values change in the spectrum from dark (higher) to light (lower) color
On the other hand, Fig. 3 presents the local explanation summary that indicates the direction of the relationship between a variable and COVID-19 outcome. As shown in Fig. 3 (I to VII), older age and very low BMI were the two demographic factors with the greatest impact on model outcome, followed by clinical factors such as higher CPR, hospitalization, and hyperlipidemia. Higher mortality rates were associated with patients who smoked and had traveled in the past 14 days. Patients with underlying diseases, especially HTN, died more frequently. In contrast, the use of remdesivir, Vit Zn, and favipiravir is associated with lower mortality. Initial vital signs such as high PEEP, low PaO2 and RR had the greatest impact, as did symptoms such as dyspnea, MODS, sore throat and LOC. A higher risk of mortality is observed in patients with higher D-dimer levels and ESR as the most consequential laboratory tests, followed by K, AST and CPK-MB.
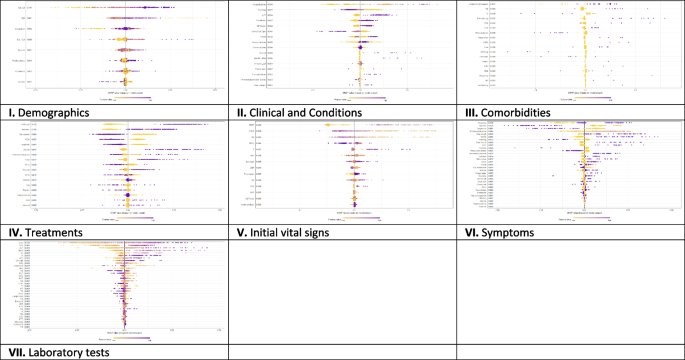
The SHAP-based feature importance of all categories (I to VII) for COVID‑19 mortality prediction, calculated with the XGBoost model. The local explanatory summary shows the direction of the relationship between a feature and patient outcome. Positive SHAP values indicate death, whereas negative SHAP values indicate survival. As the color scale shows, higher values are blue while lower values are orenge
Using the feature types listed in Appendix Table 1 , Fig. 4 shows that the performance of ML algorithms can be improved by increasing the number of features used in training, especially in distinguishing between symptoms, comorbidities, and treatments. In addition, the amount and quality of data used for training can significantly affect algorithm performance, with laboratory tests being more informative than initial vital signs. Regarding the influence of features, quantitative features tend to have a more positive effect on performance than qualitative features; clinical conditions tend to be more informative than demographic data. Thus, both the amount of data and the type of features used have a significant impact on the performance of ML algorithms.
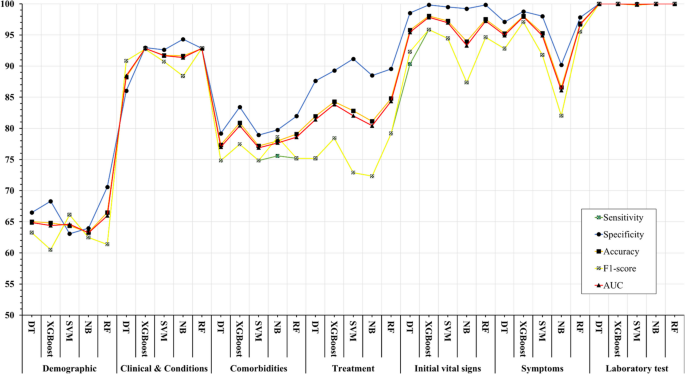
Association between feature sets and performance of machine learning algorithms in predicting COVID-19’s mortality
The COVID-19 pandemic has presented unprecedented public health challenges worldwide and requires a deep understanding of the factors contributing to COVID-19 mortality to enable effective management and intervention. This study used machine learning analysis to uncover the predictive power of an extensive dataset that includes wide range of personal, clinical, preclinical, and laboratory variables associated with COVID-19 mortality.
This study confirms previous research on COVID-19 outcomes that highlighted age as a significant predictor of mortality [ 45 , 46 , 47 ], along with comorbidities such as hypertension and diabetes [ 48 , 49 ]. Underlying conditions such as cardiovascular and renal disease also contribute to mortality risk [ 50 , 51 ].
Regarding treatment, antibiotics, remdesivir, favipiravir, and vitamin zinc are associated with lower mortality [ 52 , 53 ], whereas heparin, insulin, antifungals, ACE, and ARBs are associated with higher mortality [ 54 ]. This underscores the importance of drug choice in COVID -19 treatment.
Initial vital signs such as heart rate, respiratory rate, temperature, and oxygen therapy differ between surviving and deceased patients [ 55 ]. Deceased patients often have increased heart rate, lower respiratory rate, higher temperature, and increased oxygen requirements, which can serve as early indicators of disease severity.
Symptoms such as productive cough, dyspnea, and delirium are significantly associated with COVID-19 mortality, emphasizing the need for immediate monitoring and intervention [ 56 ]. Laboratory tests show altered hematologic and biochemical markers in deceased patients, underscoring the importance of routine laboratory monitoring in COVID-19 patients [ 57 , 58 ].
The ML algorithms were used in the study to predict mortality COVID-19 based on these multilayered variables. XGBoost and Random Forest performed better than other algorithms and had high recall, specificity, accuracy, F1 score, and AUC. This highlights the potential of ML, particularly the XGBoost algorithm, in improving prediction accuracy for COVID-19 mortality [ 59 ]. The study also highlighted the importance of drug choice in treatment and the potential of ML algorithms, particularly XGBoost, in improving prediction accuracy. However, the study's findings differ from those of Moulaei [ 60 ], Nopour [ 61 ], and Mehraeen [ 62 ] in terms of the best-performing ML algorithm and the most influential variables. While Moulaei [ 60 ] found that the random forest algorithm had the best performance, Nopour [ 61 ] and Ikemura [ 63 ] identified the artificial neural network and stacked ensemble models, respectively, as the most effective. Additionally, the most influential variables in predicting mortality varied across the studies, with Moulaei [ 60 ] highlighting dyspnea, ICU admission, and oxygen therapy, and Ikemura [ 63 ] identifying systolic and diastolic blood pressure, age, and other biomarkers. These differences may be attributed to variations in the datasets, feature selection, and model training.
However, it is important to note that the choice of algorithm should be tailored to the specific dataset and research question. In addition, the results suggest that a comprehensive approach that incorporates different feature categories may lead to more accurate prediction of COVID-19 mortality. In general, the results suggest that the performance of ML models is influenced by the number and type of features in each category. While some models consistently perform well across different categories (e.g., XGBoost), others perform better for specific types of features (e.g., SVM for Demographics).
Analysis of the importance of characteristics using SHAP values revealed critical factors affecting model results. D-dimer values, CPR, PEEP, underlying diseases, and ESR emerged as the most important features, highlighting the importance of these variables in predicting COVID-19 mortality. These results provide valuable insights into the underlying mechanisms and risk factors associated with severe COVID-19 outcomes.
The types of features used in ML models fall into two broad categories: quantitative (numerical) and qualitative (binary or categorical). The performance of ML methods can vary depending on the type of features used. Some algorithms work better with quantitative features, while others work better with qualitative features. For example, decision trees and random forests work well with both types of features [ 64 ], while neural networks often work better with quantitative features [ 65 , 66 ]. Accordingly, we consider these levels for the features under study to better assess the impact of the data.
The success of ML algorithms depends largely on the quality and quantity of the data on which they are trained [ 67 , 68 , 69 ]. Recent research, including the 2021 study by Sarker IH. [ 26 ], has shown that a larger amount of data can significantly improve the performance of deep learning algorithms compared to traditional machine learning techniques. However, it should be noted that the effect of data size on model performance depends on several factors, such as data characteristics and experimental design. This underscores the importance of carefully and judiciously selecting data for training.
Limitations
One of the limitations of this study is that it relies on data collected from a single hospital in Abadan, Iran. The data may not be representative of the diversity of COVID -19 cases in different regions, and there may be differences in data quality and completeness. In addition, retrospectively collected data may have biases and inaccuracies. Although the study included a substantial number of COVID -19 patients, the sample size may still limit the generalizability of the results, especially for less common subgroups or certain demographic characteristics.
Future works
Future studies could adopt a multi-center approach to improve the scope and depth of research on COVID-19 outcomes. This could include working with multiple hospitals in different regions of Iran to ensure a more diverse and representative sample. By conducting prospective studies, researchers can collect data in real time, which reduces the biases associated with retrospective data collection and increases the reliability of the results. Increasing sample size, conducting longitudinal studies to track patient progression, and implementing quality assurance measures are critical to improving generalizability, understanding long-term effects, and ensuring data accuracy in future research efforts. Collectively, these strategies aim to address the limitations of individual studies and make an important contribution to a more comprehensive understanding of COVID-19 outcomes in different populations and settings.
Conclusions
In summary, this study demonstrates the potential of ML algorithms in predicting COVID-19 mortality based on a comprehensive set of features. In addition, the interpretability of the models using SHAP-based feature importance, which revealed the variables strongly correlated with mortality. This study highlights the power of data-driven approaches in addressing critical public health challenges such as the COVID-19 pandemic. The results suggest that the performance of ML models is influenced by the number and type of features in each feature set. These findings may be a valuable resource for health professionals to identify high-risk patients COVID-19 and allocate resources effectively.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
World Health Organization
Middle east respiratory syndrome
Severe acute respiratory syndrome
Reverse transcription polymerase chain reaction
Propensity score matching
Synthetic minority over-sampling technique
Missing completely at random
Decision tree
EXtreme gradient boosting
Support vector machine
Naïve bayes
Random forest
Cross-validation
True positive
True negative
False positive
False negative
- Machine learning
Artificial Intelligence
Shapely additive explanation
Cardiopulmonary Resuscitation
Hypertension
Diabetes mellitus
Cardiovascular disease
Chronic Kidney disease
Chronic obstructive pulmonary disease
Human immunodeficiency virus
Hepatitis B virus
Such as influenza, pneumonia, asthma, bronchitis, and chronic obstructive airways disease
Gastrointestinal
Such as epilepsy, learning disabilities, neuromuscular disorders, autism, ADD, brain tumors, and cerebral palsy
Such as fatty liver disease and cirrhosis
Blood disease
Skin diseases
Mental disorders
Intravenous immunoglobulin
Non-steroidal anti-Inflammatory drugs
Angiotensin converting enzyme inhibitors
Angiotensin II receptor blockers
Beats per minute
Respiratory rate
Temperatures
Systolic blood pressure
Diastolic blood pressure
Mean arterial pressure
Oxygen saturation
Partial pressure of oxygen in the alveoli
Positive end-expiratory pressure
Fraction of inspired oxygen
Radiography (X-ray) test result
Smell disorders
Indigestion
Level of consciousness
Multiple organ dysfunction syndrome
Coughing up blood; Coagulopathy: bleeding disorder
High blood glucose
Intensive care unit
Red blood cell
White blood cell
Low-density lipoprotein
High-density lipoprotein
Prothrombin time
Partial thromboplastin time
International normalized ratio
Erythrocyte sedimentation rate
C-reactive-protein
Lactate dehydrogenase
Aspartate aminotransferase
Alanine aminotransferase
Alkaline phosphatase
Creatine phosphokinase-MB
Blood urea nitrogen
Thyroid stimulating hormone
Triiodothyronine
Coronavirus disease (COVID-19) pandemic. Available from: https://www.who.int/europe/emergencies/situations/covid-19 . [cited 2023 Sep 5].
Moolla I, Hiilamo H. Health system characteristics and COVID-19 performance in high-income countries. BMC Health Serv Res. 2023;23(1):1–14. https://doi.org/10.1186/s12913-023-09206-z . [cited 2023 Sep 5].
Article Google Scholar
Peeri NC, Shrestha N, Rahman MS, Zaki R, Tan Z, Bibi S, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020;49(3):717–26.
Article PubMed Google Scholar
WHO Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data. Available from: https://covid19.who.int/ . [cited 2023 Sep 5].
Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21(1):1–28. https://doi.org/10.1186/s12879-021-06536-3 . [cited 2023 Sep 5].
Article CAS Google Scholar
Wong ELY, Ho KF, Wong SYS, Cheung AWL, Yau PSY, Dong D, et al. Views on Workplace Policies and its Impact on Health-Related Quality of Life During Coronavirus Disease (COVID-19) Pandemic: Cross-Sectional Survey of Employees. Int J Heal Policy Manag. 2022;11(3):344–53. Available from: https://www.ijhpm.com/article_3879.html .
Google Scholar
Drefahl S, Wallace M, Mussino E, Aradhya S, Kolk M, Brandén M, et al. A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat Commun. 2020;11(1):5097.
Article CAS PubMed PubMed Central Google Scholar
Islam N, Khunti K, Dambha-Miller H, Kawachi I, Marmot M. COVID-19 mortality: a complex interplay of sex, gender and ethnicity. Eur J Public Health. 2020;30(5):847–8.
Sarmadi M, Marufi N, Moghaddam VK. Association of COVID-19 global distribution and environmental and demographic factors: An updated three-month study. Environ Res. 2020;188:109748.
Aghazadeh-Attari J, Mohebbi I, Mansorian B, Ahmadzadeh J, Mirza-Aghazadeh-Attari M, Mobaraki K, et al. Epidemiological factors and worldwide pattern of Middle East respiratory syndrome coronavirus from 2013 to 2016. Int J Gen Med. 2018;11:121–5.
Risk of COVID-19-Related Mortality. Available from: https://www.cdc.gov/coronavirus/2019-ncov/science/data-review/risk.html . [cited 2023 Aug 26].
Bhaskaran K, Bacon S, Evans SJW, Bates CJ, Rentsch CT, MacKenna B, et al. Factors associated with deaths due to COVID-19 versus other causes: population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Reg Heal. 2021;6:100-9.
Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21(1):855. https://doi.org/10.1186/s12879-021-06536-3 .
Talebi SS, Hosseinzadeh A, Zare F, Daliri S, JamaliAtergeleh H, Khosravi A, et al. Risk Factors Associated with Mortality in COVID-19 Patient’s: Survival Analysis. Iran J Public Health. 2022;51(3):652–8.
PubMed PubMed Central Google Scholar
Singh J, Alam A, Samal J, Maeurer M, Ehtesham NZ, Chakaya J, et al. Role of multiple factors likely contributing to severity-mortality of COVID-19. Infect Genet Evol J Mol Epidemiol Evol Genet Infect Dis. 2021;96:105101.
CAS Google Scholar
Bhaskaran K, Bacon S, Evans SJ, Bates CJ, Rentsch CT, MacKenna B, et al. Factors associated with deaths due to COVID-19 versus other causes: population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Reg Heal - Eur. 2021;6:100109. Available from: https://www.pmc/articles/PMC8106239/ . [cited 2023 Aug 26].
Ge E, Li Y, Wu S, Candido E, Wei X. Association of pre-existing comorbidities with mortality and disease severity among 167,500 individuals with COVID-19 in Canada: A population-based cohort study. PLoS One. 2021;16(10):e0258154. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0258154 . [cited 2023 Aug 26].
Tian S, Liu H, Liao M, Wu Y, Yang C, Cai Y, et al. Analysis of mortality in patients with COVID-19: clinical and laboratory parameters. Open Forum Infect Dis. 2020;7(5). Available from: https://dx.doi.org/10.1093/ofid/ofaa152 . [cited 2023 Aug 26].
Rashidi HH, Tran N, Albahra S, Dang LT. Machine learning in health care and laboratory medicine: General overview of supervised learning and Auto-ML. Int J Lab Hematol. 2021;43:15–22.
Najafi-Vosough R, Faradmal J, Hosseini SK, Moghimbeigi A, Mahjub H. Predicting hospital readmission in heart failure patients in Iran: a comparison of various machine learning methods. Healthc Inform Res. 2021;27(4):307–14.
Article PubMed PubMed Central Google Scholar
Alanazi A. Using machine learning for healthcare challenges and opportunities. Informatics Med Unlocked. 2022;100924:1–5.
Chadaga K, Prabhu S, Sampathila N, Chadaga R, Umakanth S, Bhat D, et al. Explainable artificial intelligence approaches for COVID-19 prognosis prediction using clinical markers. Sci Rep. 2024;14(1):1783.
Chadaga K, Prabhu S, Bhat V, Sampathila N, Umakanth S, Chadaga R, et al. An explainable multi-class decision support framework to predict COVID-19 prognosis utilizing biomarkers. Cogent Eng. 2023;10(2):2272361.
Khanna VV, Chadaga K, Sampathila N, Prabhu S, Chadaga R. A machine learning and explainable artificial intelligence triage-prediction system for COVID-19. Decis Anal J. 2023;100246:1–14.
Zoabi Y, Deri-Rozov S, Shomron N. Machine learning-based prediction of COVID-19 diagnosis based on symptoms. npj Digit Med. 2021;4(1):1–5.
IH Sarker 2021 Machine Learning: Algorithms, Real-World Applications and Research Directions SN Comput Sci. 2 3 160 Available from: https://doi.org/10.1007/s42979-021-00592-x .
Jones JA, Farnell B. Missing and Incomplete Data Reduces the Value of General Practice Electronic Medical Records as Data Sources in Research. Aust J Prim Health. 2007;13(1):74–80. Available from: https://www.publish.csiro.au/py/py07010 . [cited 2023 Dec 16].
Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res. 2011;46(3):399–424.
Torjusen H, Lieblein G, Næs T, Haugen M, Meltzer HM, Brantsæter AL. Food patterns and dietary quality associated with organic food consumption during pregnancy; Data from a large cohort of pregnant women in Norway. BMC Public Health. 2012;12(1):1–11.
Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83(404):1198–202.
Tenny S, Kerndt CC, Hoffman MR. Case Control Studies. Encycl Pharm Pract Clin Pharm Vol 1-3 [Internet]. 2023;1–3:V2-356-V2-366. [cited 2024 Apr 14] Available from: https://www.ncbi.nlm.nih.gov/books/NBK448143/ .
Stanfill B, Reehl S, Bramer L, Nakayasu ES, Rich SS, Metz TO, et al. Extending Classification Algorithms to Case-Control Studies. Biomed Eng Comput Biol. 2019;10:117959721985895. Available from: https://www.pmc/articles/PMC6630079/ .[cited 2023 Sep 3].
Mulugeta G, Zewotir T, Tegegne AS, Juhar LH, Muleta MB. Classification of imbalanced data using machine learning algorithms to predict the risk of renal graft failures in Ethiopia. BMC Med Inform Decis Mak. 2023;23(1):1–17. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-023-02185-5 . [cited 2023 Sep 3].
Sadeghi S, Khalili D, Ramezankhani A, Mansournia MA, Parsaeian M. Diabetes mellitus risk prediction in the presence of class imbalance using flexible machine learning methods. BMC Med Inform Decis Mak. 2022;22(1):36. https://doi.org/10.1186/s12911-022-01775-z .
Zhou W, Nielsen JB, Fritsche LG, Dey R, Gabrielsen ME, Wolford BN, et al. Efficiently controlling for case-control imbalance and sample relatedness in large-scale genetic association studies. Nat Genet. 2018;50(9):1335. Available from: https://www.pmc/articles/PMC6119127/ . [cited 2023 Sep 3].
Miao J, Niu L. A Survey on Feature Selection. Procedia Comput Sci. 2016;91(1):919–26.
Remeseiro B, Bolon-Canedo V. A review of feature selection methods in medical applications. Comput Biol Med. 2019;112:103375.
Article CAS PubMed Google Scholar
R Studio Team. A language and environment for statistical computing. R Found Stat Comput. 2021;1.
Training Sets, Test Sets, and 10-fold Cross-validation - KDnuggets. Available from: https://www.kdnuggets.com/2018/01/training-test-sets-cross-validation.html . [cited 2023 Sep 4].
Hossin M, Sulaiman MN. A review on evaluation metrics for data classification evaluations. Int J data Min Knowl Manag Process. 2015;5(2):1.
Seyedtabib M, Kamyari N. Predicting polypharmacy in half a million adults in the Iranian population: comparison of machine learning algorithms. BMC Med Inform Decis Mak. 2023;23(1):84. https://doi.org/10.1186/s12911-023-02177-5 .
Lundberg SM, Lee S-I. A unified approach to interpreting model predictions. Adv Neural Inf Process Syst. 2017;30:4765–74.
Greenwell B. Fastshap: Fast approximate shapley values. Man R Packag v0 05. 2020;9–12. https://www.CRANR-projectorg/package=fastshap . Last accessed.
Aas K, Jullum M, Løland A. Explaining individual predictions when features are dependent: More accurate approximations to Shapley values. Artif Intell. 2021;298:103502.
Mesas AE, Cavero-Redondo I, Álvarez-Bueno C, Sarriá Cabrera MA, de Maffei Andrade S, Sequí-Dominguez I, et al. Predictors of in-hospital COVID-19 mortality: A comprehensive systematic review and meta-analysis exploring differences by age, sex and health conditions. PLoS One. 2020;15(11):e0241742.
Yanez ND, Weiss NS, Romand J-A, Treggiari MM. COVID-19 mortality risk for older men and women. BMC Public Health. 2020;20(1):1–7.
Sasson I. Age and COVID-19 mortality. Demogr Res. 2021;44:379–96.
Huang I, Lim MA, Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia–a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr Clin Res Rev. 2020;14(4):395–403.
Albitar O, Ballouze R, Ooi JP, Ghadzi SMS. Risk factors for mortality among COVID-19 patients. Diabetes Res Clin Pract. 2020;166:108293.
Di Castelnuovo A, Bonaccio M, Costanzo S, Gialluisi A, Antinori A, Berselli N, et al. Common cardiovascular risk factors and in-hospital mortality in 3,894 patients with COVID-19: survival analysis and machine learning-based findings from the multicentre Italian CORIST Study. Nutr Metab Cardiovasc Dis. 2020;30(11):1899–913.
Ssentongo P, Ssentongo AE, Heilbrunn ES, Ba DM, Chinchilli VM. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PLoS ONE. 2020;15(8):e0238215.
Beran A, Mhanna M, Srour O, Ayesh H, Stewart JM, Hjouj M, et al. Clinical significance of micronutrient supplements in patients with coronavirus disease 2019: A comprehensive systematic review and meta-analysis. Clin Nutr ESPEN. 2022;48:167–77.
Perveen RA, Nasir M, Murshed M, Nazneen R, Ahmad SN. Remdesivir and favipiravir changes hepato-renal profile in COVID-19 patients: a cross sectional observation in Bangladesh. Int J Med Sci Clin Inven. 2021;8(1):5196–201.
El-Arif G, Khazaal S, Farhat A, Harb J, Annweiler C, Wu Y, et al. Angiotensin II Type I Receptor (AT1R): the gate towards COVID-19-associated diseases. Molecules. 2022;27(7):2048.
Ikram AS, Pillay S. Admission vital signs as predictors of COVID-19 mortality: a retrospective cross-sectional study. BMC Emerg Med. 2022;22(1):1–10.
Martí-Pastor A, Moreno-Perez O, Lobato-Martínez E, Valero-Sempere F, Amo-Lozano A, Martínez-García M-Á, et al. Association between Clinical Frailty Scale (CFS) and clinical presentation and outcomes in older inpatients with COVID-19. BMC Geriatr. 2023;23(1):1.
Lippi G, Plebani M. Laboratory abnormalities in patients with COVID-2019 infection. Clin Chem Lab Med. 2020;58(7):1131–4.
Naghashpour M, Ghiassian H, Mobarak S, Adelipour M, Piri M, Seyedtabib M, et al. Profiling serum levels of glutathione reductase and interleukin-10 in positive and negative-PCR COVID-19 outpatients: A comparative study from southwestern Iran. J Med Virol. 2022;94(4):1457–64.
Sharifi-Kia A, Nahvijou A, Sheikhtaheri A. Machine learning-based mortality prediction models for smoker COVID-19 patients. BMC Med Inform Decis Mak. 2023;23(1):1–15.
Moulaei K, Shanbehzadeh M, Mohammadi-Taghiabad Z, Kazemi-Arpanahi H. Comparing machine learning algorithms for predicting COVID-19 mortality. BMC Med Inform Decis Mak. 2022;22(1):2. https://doi.org/10.1186/s12911-021-01742-0 .
Nopour R, Erfannia L, Mehrabi N, Mashoufi M, Mahdavi A, Shanbehzadeh M. Comparison of Two Statistical Models for Predicting Mortality in COVID-19 Patients in Iran. Shiraz E-Medical J 2022 236 [Internet]. 2022;23(6):119172. [cited 2024 Apr 14] Available from: https://brieflands.com/articles/semj-119172 .
Mehraeen E, Karimi A, Barzegary A, Vahedi F, Afsahi AM, Dadras O, et al. Predictors of mortality in patients with COVID-19–a systematic review. Eur J Integr Med. 2020;40:101226.
Ikemura K, Bellin E, Yagi Y, Billett H, Saada M, Simone K, et al. Using Automated Machine Learning to Predict the Mortality of Patients With COVID-19: Prediction Model Development Study. J Med Internet Res [Internet]. 2021;23(2):e23458. Available from: https://www.jmir.org/2021/2/e23458 .
Breiman L. Random forests. Mach Learn. 2001;45:5–32.
Hinton G, Srivastava N, Swersky K. Neural networks for machine learning lecture 6a overview of mini-batch gradient descent. Cited on. 2012;14(8):2.
Zheng A, Casari A. Feature Engineering for Machine Learning: Principles and Techniques for Data Scientists. O’Reilly [Internet]. 2018;218. [cited 2024 Apr 14] Available from: https://www.amazon.com/Feature-Engineering-Machine-Learning-Principles/dp/1491953241 .
Adamson AS, Smith A. Machine Learning and Health Care Disparities in Dermatology. JAMA Dermatology. 2018;154(11):1247–8. Available from: https://jamanetwork.com/journals/jamadermatology/fullarticle/2688587 . [cited 2023 Sep 15].
Kavakiotis I, Tsave O, Salifoglou A, Maglaveras N, Vlahavas I, Chouvarda I. Machine Learning and Data Mining Methods in Diabetes Research. Comput Struct Biotechnol J. 2017;1(15):104–16.
Schmidt J, Marques MRG, Botti S, Marques MAL. Recent advances and applications of machine learning in solid-state materials science. Comput Mater. 2019;5(1):83. https://doi.org/10.1038/s41524-019-0221-0 .
Download references
Acknowledgements
We thank the Research Deputy of the Abadan University of Medical Sciences for financially supporting this project.
Summary points
∙ How can datasets improve mortality prediction using ML models for COVID-19 patients?
∙ In order, quantity and quality variables have more effect on the model performances.
∙ Intelligent techniques such as SHAP analysis can be used to improve the interpretability of features in ML algorithms.
∙ Well-structured data are critical to help health professionals identify at-risk patients and improve pandemic outcomes.
This research was supported by grant No. 1456 from the Abadan University of Medical Sciences. However, the funding source did not influence the study design, data collection, analysis and interpretation, report writing, or decision to publish the article.
Author information
Authors and affiliations.
Department of Biostatistics and Epidemiology, School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Maryam Seyedtabib
Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
Roya Najafi-Vosough
Department of Biostatistics and Epidemiology, School of Health, Abadan University of Medical Sciences, Abadan, Iran
Naser Kamyari
You can also search for this author in PubMed Google Scholar
Contributions
MS: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Data curation, Writing–original draft, writing—review & editing, Visualization, Project administration. RNV: Conceptualization, Data curation, Formal analysis, Investigation, Writing–original draft, writing—review & editing. NK: Conceptualization, Methodology, Software, Validation, Formal analysis, Investigation, Resources, Data curation, Writing–original draft, writing—review & editing, Visualization, Supervision.
Corresponding author
Correspondence to Naser Kamyari .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Research Ethics Committee (REC) of Abadan University of Medical Sciences under the ID number IR.ABADANUMS.REC.1401.095. Methods used complied with all relevant ethical guidelines and regulations. The Ethics Committee of Abadan University of Medical Sciences waived the requirement for written informed consent from study participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Seyedtabib, M., Najafi-Vosough, R. & Kamyari, N. The predictive power of data: machine learning analysis for Covid-19 mortality based on personal, clinical, preclinical, and laboratory variables in a case–control study. BMC Infect Dis 24 , 411 (2024). https://doi.org/10.1186/s12879-024-09298-w
Download citation
Received : 22 December 2023
Accepted : 05 April 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12879-024-09298-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Predictive model
- Coronavirus disease
- Data quality
- Performance
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]
A Review of Clinical and Laboratory Predictors of Severe COVID-19 Disease
Affiliations.
- 1 From the Department of Family Medicine, Fort Belvoir Community Hospital, Fort Belvoir, VA (All authors). [email protected].
- 2 From the Department of Family Medicine, Fort Belvoir Community Hospital, Fort Belvoir, VA (All authors).
- PMID: 33622836
- DOI: 10.3122/jabfm.2021.S1.200165
Introduction: In late December 2019, the coronavirus 2 (SARS-CoV-2) emerged in Wuhan, China. It quickly spread and emerged as a global pandemic with far-reaching impacts on society. As clinical research on this novel virus emerges, there is a limited amount of data that review clinical and laboratory predictors of severe disease. We present a case of a patient with severely elevated inflammatory markers who remained clinically stable during his hospital course.
Case discussion: A 53-year-old male presented to the emergency room with 11 days of persistent fevers and new-onset anterior chest tightness. He was admitted to the hospital due to a reported oxygen desaturation at home to 87% (taken by his spouse, a healthcare professional) and ambulatory oxygen desaturation down to 87%. He was noted to have severely elevated inflammatory markers, lymphopenia, and computed tomography pulmonary angiograph findings consistent with COVID-19. He remained on room air and clinically stable throughout his 3-day hospital course. While his C-reactive protein levels improved, his ferritin and erythrocyte sedimentation rate continued to elevate. He was discharged home and was symptom-free within 4 days of hospital discharge.
Discussion: COVID-19 has proven to be a viral disease with a high transmission rate, that has caused over 100,000 deaths in the United States, thus far. The decision to admit a patient must balance the risks of transmission with the benefit of being readily available to provide urgent supportive care should the patient develop complications. Thus, there is a significant benefit to being able to predict poor outcomes. We performed a targeted review of the literature, focusing on clinical and laboratory predictors of poor outcomes in COVID-19. Our case report and narrative review outline these findings within the context of our case.
Keywords: Blood Sedimentation; C-reactive protein; COVID-19; Communicable Diseases; Erythrocyte sedimentation rate; Ferritins; Fever; Lymphopenia; Pandemics.
© Copyright 2021 by the American Board of Family Medicine.
Publication types
- Case Reports
- COVID-19 / diagnosis*
- Diagnostic Tests, Routine
- Disease Progression
- Lung / diagnostic imaging
- Lung / pathology
- Middle Aged
- Severity of Illness Index
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Risk factors for Covid-19 severity and fatality: a structured literature review
Dominik wolff.
Peter L. Reichertz Institute for Medical Informatics of TU Braunschweig and Hannover Medical School, Hannover, Germany
Natalie Sandy Hickey
Michael marschollek, associated data.
All data used is publicly available either by PubMed or CORD-19.
The python code used for preprocessing and search in CORD-19 will be made available upon request.
Covid-19 is a global threat that pushes health care to its limits. Since there is neither a vaccine nor a drug for Covid-19, people with an increased risk for severe and fatal courses of disease particularly need protection. Furthermore, factors increasing these risks are of interest in the search of potential treatments. A systematic literature review on the risk factors of severe and fatal Covid-19 courses is presented.
The review is carried out on PubMed and a publicly available preprint dataset. For analysis, risk factors are categorized and information regarding the study such as study size and location are extracted. The results are compared to risk factors listed by four public authorities from different countries.
The 28 records included, eleven of which are preprints, indicate that conditions and comorbidities connected to a poor state of health such as high age, obesity, diabetes and hypertension are risk factors for severe and fatal disease courses. Furthermore, severe and fatal courses are associated with organ damages mainly affecting the heart, liver and kidneys. Coagulation dysfunctions could play a critical role in the organ damaging. Time to hospital admission, tuberculosis, inflammation disorders and coagulation dysfunctions are identified as risk factors found in the review but not mentioned by the public authorities.
Factors associated with increased risk of severe or fatal disease courses were identified, which include conditions connected with a poor state of health as well as organ damages and coagulation dysfunctions. The results may facilitate upcoming Covid-19 research.
Introduction
In the end of 2019, a novel respiratory disease, the coronavirus disease 2019 (Covid-19), occurred. The pathogen causing the disease was identified by next-generation sequencing as a novel coronavirus closely related to the SARS-coronavirus discovered in 2003 [ 1 ]. According to the WHO guidelines [ 2 ], this novel coronavirus was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). First cases of Covid-19 were reported from the Chinese city Wuhan located in the province Hubei in December 2019 [ 3 ]. The disease is spreading worldwide and was classified as a pandemic by the WHO in March 2020 [ 4 ]. The virus is transmissible from human to human [ 5 ] and the number of infected people increases at an exponential rate, exceeding 1 mio. cases on 02.04.2020 and 1.5 mio. cases in 184 countries only a week later [ 6 , 7 ]. At various disease hotspots such as New York, the health care system reaches its limits.
For diagnosis, the virus is mainly detected by real-time quantitative polymerase chain reaction (rt-PCR) in throat swabs [ 8 , 9 ]. Due to limited test capacities, which require a special equipped laboratory, patients showing symptoms are tested only. On the onset of Covid-19 typical symptoms are fever, cough, myalgia and fatigue, while headache, sputum production, hemoptysis and diarrhea are less common. In the course of disease a subset of patients show pneumonia with abnormal findings on chest CT [ 10 ]. Severe cases are transferred to an intensive care unit (ICU) and frequently require artificial ventilation. The disease’s case fatality rate is estimated between 3.4% and 11% [ 11 ]. Although, it depends to a large extent on the number of tests carried out as well as the quality and occupancy rate of local health care.
Until a vaccine is available, an increase in the number of infections must be expected and if not being controlled Covid-19 will exceed the limits of health care systems. Since some groups appear to be at higher risk of serious disease progression and increased mortality, they should be given special protection against an infection. This is particularly important in the context of the much-discussed relaxation of restrictions, such as the prohibition of contact. To identify these vulnerable groups, the risk factors for severe and fatal disease progression must be found. Additionally, the identification of risk factors can contribute to research into the pathophysiological processes of Covid-19 from which possible treatment strategies can be developed. However, information on this is scattered and based on rather small studies. For connecting these, this publication describes a structured literature review on the risk factors of Covid-19 for severe and fatal disease courses. Additionally, the review’s results are compared to the risk factors mentioned by four public authorities.
Publications of interest describe clinical studies on Covid-19 identifying factors for increased risks of severe or fatal disease courses. The review focusses on studies whose patients were diagnosed positive by rt-PCR. The diagnosis by rt-PCR shows a low false-positive rate, but is criticized for a quite high false-negative rate [ 12 , 13 ]. The inclusion of rt-PCR diagnoses only reduces the number of false diagnoses to a minimum. Since the disease is new and has only been present since December 2019, the search is carried out on PubMed as well as on the Covid-19 Open Research Dataset (CORD-19) [ 14 ] containing mostly yet unpublished publications, so called preprints.
To identify publications of interest, MESH Terms and synonyms for Covid-19 and risk factors are combined leading to the following search term:
- ("risk factor" OR "determinant" OR "disposition" OR "increased risk" OR "population at risk" OR "health risk behavior") AND ("covid-19" OR "sars-cov-2" OR "covid19" OR "2019-nCov" OR "severe acute respiratory syndrome coronavirus 2 " OR "covid 19").
- Furthermore, the search is limited to the English language. It was performed on PubMed on 25.03.2020 and was updated on 17.04.2020. Search results were documented as file export including search term and date.
The Covid-19 Open Research Dataset (CORD-19) was created by the Allen Institute for AI in partnership with the Chan Zuckerberg Initiative, Georgetown University’s Center for Security and Emerging Technology, Microsoft Research, and the National Library of Medicine-National Institutes of Health, in coordination with the White House Office of Science and Technology Policy. It is freely available and updated weekly. The data provided is intended to facilitate the application of natural language processing to generate new insights in support of the fight against Covid-19. The dataset contains more than 51,000 scholarly articles on SARS-CoV-2 and related coronaviruses such as SARS-CoV and the Middle East Respiratory Syndrome (MERS) Coronavirus including over 40,000 full texts [ 14 ]. Beside these documents, a file containing the publications’ metadata, is provided. It contains information such as title, DOI, PubMed ID and the abstract, but is not limited to these. In a first step the metadata is preprocessed and a keyword search is performed to identify publications of interest. Afterwards, the typical literature review procedure is carried out, including screening of title and abstract for eligibility and accessing the full texts.
For preprocessing of the data, a simple algorithmic pipeline was applied to the metadata file. First, information of interest (PubMed ID, title, abstract, availability of the full text) are extracted. In the next steps, all articles without a full text, with abstracts shorter than 20 words and with abstracts in a different language than English are excluded. Afterwards, the abstracts and keywords are transformed to lower case characters to perform an algorithmic keyword search analog to the above-mentioned search term. The search was performed on 25.03.2020 and updated on 21.04.2020.
Analytical methods
In a first step the identified publications’ titles and abstracts are screened for eligibility. For publications describing literature reviews or meta-studies, the references are checked for eligibility. Full texts of suitable publications are then analyzed regarding the inclusion criteria. Both steps were executed by multiple researchers.
The analysis centers on the identification of risk factors for severe and fatal disease progression. Risk factors found are categorized into lifestyle factors, demographic factors, pre-existing comorbidities, due to Covid-19 developed comorbidities, symptoms and clinical factors. Additionally, information on the studies are extracted including study size, location, duration, mono- or multicentricity and whether the data collected is available. For characterization of the articles, the publication status is recorded. To ensure the quality of preprints, the comprehensibility and correctness of the study design and statistical analysis is evaluated. In the event of uncertainty, the decision is to exclude the record. P-values smaller than 0.05 are regarded as significant.
In the search 213 papers were identified (67 PubMed, 131 CORD, 15 referenced literature). After the removal of duplicates 204 records were screened based on title and abstract. In this step, 125 records were excluded. The remaining records’ full texts were assessed and 51 records were excluded for not describing risk factors backed by a clinical study or not diagnosing patients by rt-PCR. Thus 28 records were included (see Fig. 1 ).

Overview of the publication selection process
Table Table1 1 shows a description of the studies found in the records included. From the 28 included records 17 are published and 11 are preprints. The studies described took place at the end of 2019 and in the first months of 2020. The last inclusion of a patient was on 05.04.2020 in [ 40 ]. Most studies found were conducted in China ( n = 24), while the remaining five studies were conducted in Italy, France and the USA (see Fig. 2 ). Eighteen studies were carried out at a single place, while twelve studies were multicentric, involving between 2 and 575 hospitals. The patient numbers of the individual studies range between 25 and 62,843, with small studies with up to 200 patients being the norm.
Overview of the records included

Number of studies found by location
Risk factors for severity
Risk factors for disease severity were identified in 20 records, which are described in Table Table2. 2 . Smoking [ 33 ], a higher body mass index (obesity) [ 40 ] and a longer waiting time to hospital admission [ 19 , 20 ] are lifestyle factors related to a higher risk for disease severity. The most frequently mentioned demographic factor increasing the risk for a severe course of disease is higher age [ 16 , 17 , 19 , 21 , 27 , 30 , 31 , 33 , 35 , 41 , 42 ], followed by male gender [ 19 , 21 , 25 ], post menopausality [ 25 ] and higher age in females [ 25 ]. Some publications specify the age for increased risk as > 64 [ 31 ] or > 65 [ 33 ] years. The most common pre-existing comorbidities are hypertension [ 16 , 19 , 27 , 35 , 40 , 42 ] and diabetes [ 16 , 28 , 33 , 35 , 40 , 42 ] with six records each, followed by cardiovascular disease with three records [ 16 , 19 , 35 ]. Occasionally, correlations of the severity and cerebrovascular disease [ 16 ], chronic obstructive pulmonary disease [ 35 ], chronic renal disease [ 35 ] or tuberculosis [ 36 ] were found. For eight comorbidities developed during the Covid-19 infection a significant impact on disease severity was found. These are organ failure [ 19 ], immunological dysfunction [ 19 ], acute liver injury [ 26 ], hypoproteinemia [ 26 ], Acute Respiratory Distress Syndrome (ARDS) [ 36 ], severe pneumonia [ 42 ], uncontrolled inflammation response [ 42 ] and hypercoagulable state [ 42 ]. With nine mentions, the most common abnormal clinical factor is decreased lymphocytes, followed by an increased d -dimer level (six records), increased leucocytes (four records), increased neutrophil count (four records), increased aspartate aminotransferase (AST) (four records), increased c-reactive protein (CRP) (four records), increased alanine aminotransferase (ALT) (three records) and low oxygen saturation (three records). Increased blood urea nitrogen (BUN), decreased thrombocytes, increased CT severity score and increased interleukin 6 (IL-6) level are each identified as risk factors for severity in two records. There are 23 other clinical features such as decreased blood sodium or decreased erythrocytes count each mentioned in one record only (see Table Table2). 2 ). In addition to the factors already mentioned, the symptoms fever (> 38.5 °C) [ 18 , 35 ] and dyspnea [ 18 , 35 ] are associated with severe disease progression.
Listing of the factors found that influence the severity of the disease
Risk factors of fatal disease courses
Thirteen records describe risk factors for fatal Covid-19 disease courses. They are listed in Table Table3. 3 . The most common identified risk factor is high age with eight denominations. The other demographic factor influencing Covid-19 mortality is male gender, which was found significant in three records. Furthermore, pre-existing comorbidities frequently show an influence in the publications included. Most common with three mentions each are hypertension, diabetes and coronary heart disease. Cardiovascular diseases are found significant in two records. Seven other pre-existing diseases were each significant in one record, including acute liver injury, kidney disease, chronic illnesses and cerebrovascular disease. For comorbidities developed during the infection, kidney injuries (four records), heart injuries (three records) and liver injuries (two records) are mentioned most often. Other developed complications are cardiac death, acute respiratory distress syndrome, hospital acquired infections, thrombocytopenia and hypoxemia. Only one record identified a symptom, dyspnea, as a risk factor. The most common clinical factors associated with mortality are increased creatinine (four records), increased c-reactive protein (CRP), increased procalcitonin (PCT), decreased lymphocytes and increased blood urea nitrogen (BUN) (three records each). Other clinical factors associated with fatal disease courses include increased neutrophils, increased leucocytes or increased d -dimer but are not limited to these. For the full list of clinical factors found in the records please refer to Table Table3 3 .
Listing of the factors found with an influence on fatal disease courses
Typically, a severe course of the disease occurs before the death of a Covid-19 patient. Of course, this is not true for all fatal courses, but it should be true for most of them and therefore be visible in the statistical significance. The risk factors for fatal courses should be approximately a subset of the factors for severe courses. Therefore, risk factors for fatal disease progression, which are not mentioned for severe disease progression, are of particular interest. For pre-existing comorbidities these are coronary heart disease, hypoproteinemia, cholestasis, acute liver injury and hypercholesterolemia, while hypoproteinemia and acute liver injury are also mentioned as developed comorbidities in severe courses. Developed comorbidities found with an influence on fatal courses but not on severe courses are heart damage, kidney damage, thrombocytopenia, hospital acquired infections, hypoxemia and cardiac death.
Disease specific laboratory values
Some laboratory values found are predictive for specific diseases. Most common are markers for liver, renal and heart function. Increased ALT, AST, lactic acid, procalcitonin, total, direct and indirect bilirubin as well as decreased albumin indicate liver injuries [ 43 ]. The same applies for increased blood urea nitrogen and creatinine as well as proteinuria and hematuria for renal injuries [ 44 ]. Heart specific markers found in the publications are increased creatine kinase, troponin C and myohemoglobin levels as well as a decreased platelet count [ 45 ]. It is also noticeable that an increased number of coagulation factors such as decreased platelets, increased d -dimer level and increased fibrinogen [ 46 ] as well as inflammatory parameters such as c-reactive protein [ 47 ] and increased leucocyte level are associated with severity and fatality.
This review shows a high exclusion rate (176/204), which is mainly caused by including studies identifying Covid-19 infections explicitly by rt-PCR only. However, a high significance of the results can be guaranteed, as other diseases, such as bacterial pneumonia, are clearly excluded by the rt-PCR identification. Identification by rt-PCR has also become the standard diagnostic procedure. Nevertheless, it must be assumed that a selection bias exists in the results obtained, since most studies do not provide a representative sample. Among other things, differences in the recruitment rate and different test procedures have an influence on this. Relying on rt-PCR based studies only enhances this effect. A portion of the included papers are preprints, which were not yet peer-reviewed. This allows early scientific results to be incorporated into the analysis performed in this record. Even though a quality review by the authors has been carried out, which includes the comprehensibility and correctness of the study design as well as the statistical analysis, the results of these preprinted studies should be used with caution in further decisions concerning Covid-19. The publication status of the preprints should be reviewed at a later date.
Most records included describe studies carried out in China. This is presumably since the disease first broke out in China and spread around the world only within the next weeks and months. Data from Chinese Covid-19 patients is available earlier and can therefore be analyzed and published earlier. When comparing the data on the level of the number of patients or facilities, a different picture arises. The majority of patients included in this review are from Italy (64,434), followed by China (7656), USA (4157) and France (1715). Therefore, statements for specific ethnicity cannot be made and the results should be generally interpreted. It should be noted that a doubling of patients between studies cannot be excluded. This is especially relevant for some of the Chinese publications, which show an overlapping of the author list and the recruitment time, potentially reducing the real number of patients. Based on the number of publications and the number of patients, it seems that Italy is trying to centralize research on Covid-19, while China tends to produce smaller individual studies. Both approaches have advantages and disadvantages. Individual studies can deliver results more quickly and be transferred to the community, while centralization allows linking the data so that statements of higher quality can be made. The rather small proportion of studies from the USA and Europe could be linked to the date the search was carried out and the course of the disease’s global spread. We expect to see more studies from these countries as well as other Asian countries in the future. Concerning the number of patients, publication [ 30 ] is particularly noteworthy as it summarizes all cases in Italy until the beginning of March. Unfortunately, the data of this study are not published as a complete data set. However, the publication rate of the collected data is quite high among the studies included as data of eight studies is publicly available or available upon request.
Since no special drug for treating Covid-19 exists, a longer waiting time to hospital admission is an eye-catching risk factor for severity. This indicates that the treatment of symptoms in an early disease stage can be effective and positively influence the disease’s course. Regarding other demographic and lifestyle factors found interdependencies are very likely. First, younger women will not be menopausal and therefore post menopausality is equivalent to higher age, which is the most named risk factor in this analysis. Second, with higher age comorbidities are getting more likely to be present while the immune systems is getting weaker [ 48 ]. This means higher age (approximately > 60 years) is very likely correlated with comorbidities such as hypertension, cardiovascular diseases and diabetes, which are the most common comorbidities in this review. Third, hypertension is a risk factor for cardiovascular diseases [ 49 ] and, since cardiovascular disease appear to be a risk factor for Covid-19, hypertension is a risk factor for Covid-19 as well. Although multivariate regression analyses are performed in 16 records, those dependencies could not be confirmed. More research and testing on interdependence of risk factors should to be carried out.
Typically, for a disease that primarily affects the lungs, it would be expected that lung-damaging behaviors, such as smoking, or pre-existing lung diseases increase the risk for severe courses. It is very striking that smoking shows a significant influence in only one publication as well as lung diseases not being commonly listed as risk factors for either severe or fatal disease progression. This may be related to the fact that the definition of a severe disease course is based on severe pneumonia and is therefore not listed. However, other pre-existing lung diseases such as chronic obstructive pulmonary disease (COPD) are only named in a few records. For nicotine on the other hand the ability to downregulate the ACE-2 level, which is a functional receptor for SARS-CoV-2 [ 1 ], was shown [ 50 ]. Furthermore, a mouse study [ 51 ] suggests that nicotine protects against acute inflammation in lung tissue by activating nicotinic acetylcholine receptors on immune cells which inhibits the release of pro-inflammatory cytokines. However, nicotine’s influence on the course of Covid-19 needs further research.
Regarding disease predictive clinical factors liver, renal and heart damage are most common, which are also present as comorbidities associated with increased risk. It can be assumed that Covid-19 damages these organs and pre-existing damages further promote the impact. Eleven records found coagulation factors positively associated with severity or fatality but only two ([ 23 ] and [ 42 ]) mention them directly in the publication. Therefore, the influence of coagulation disorders and their treatments on the course of the disease should be further examined. It is also possible that the above-mentioned organ damage is promoted or triggered by Covid-19 induced coagulation disorders. A newer pathological study with twelve deceased Covid-19 patients found high incidence of thromboembolic events suggesting an important role of Covid-19 - induced coagulopathy. Even more, 5 of the 12 patients showed high viral RNA titers in the liver, kidney, or heart [ 52 ]. In addition, laboratory values indicating heart, liver and renal damages are significant in the included records for fatal disease courses but not for severe ones. This suggests that organ damages, specifically heart, kidney and liver damages, are symptoms occurring in the late phase of Covid-19 infections.
For some risk factors found, it cannot be entirely excluded that they are manifestations of the disease itself and not real risk factors. This is especially the case for risk factors that are very close to the clinical picture of Covid-19, such as low oxygen saturation or ARDS. For cardinal symptoms of a severe disease, statistical significance is very likely to be found. Even if a significant influence on the severity of the disease has been found in several studies, it must be understood that causality does not necessarily follow from statistical significance.
Still, there are limitations to this review. Due to the exclusive focus on PCR diagnostics it is possible that some important factors are dismissed, which were found in studies relying on clinical diagnostics. However, the focus on PCR diagnosis increases the recall and hence the results’ expressiveness. Furthermore, records in which significant influencing factors for the severity or fatality are shown, but which are not called risk factors in the title or abstract, cannot be identified by the search strategy. An example of this is [ 53 ]. It must be assumed that other risk factors for serious and fatal injuries and publications on them exist which are not covered in this review. The studies found only took place in four countries meaning ethnic differences in the course of the disease cannot be considered. A certain bias can also arise from the timing of the search. The search was last updated on 21.04.2020, so that rather early publications are to be expected.
Comparison with official sites
Table Table4 4 shows the risk factors for severe disease courses form different public authorities. The Robert Koch Institute is Germany’s leading Public Health facility, whereas the Johns Hopkins University is one of the world’s leading facilities for Covid-19 updates. Furthermore, risk factors declared by the United States’ Centers for Disease Control and Prevention and the National Health Service of the United Kingdom are shown. The lists of the different institutions largely overlap. High age (from about 60 years), heart, renal, liver and respiratory diseases as well as diabetes and obesity are frequently mentioned factors. Other factors mentioned include immune compression, male sex, organ receptivity, pregnancy, smoking, secondary diseases, such as cancer or conditions affecting the brain or nerves, and African American ethnicity.
Overview of risk factors reported by leading institutions
On the most frequently mentioned points, the risk factors indicated by public authorities coincide with the results of the review. These are liver, heart, renal and respiratory diseases as well as diabetes, obesity, higher age, male gender, comorbidities and even conditions affecting brain and nerves. Risk factors mentioned by public authorities which were not present in this review include multimorbidity, immunosuppression, being an organ transplant recipient, asthma, living in a nursing home, African American ethnicity, blood or bone cancer as well as pregnancy. Even if these could not be confirmed by the review, most of them seem to be very reasonable. Conditions resulting in a diminished immune system such as cancer, immunosuppression or being an organ transplant recipient weaken the body's own immune response to SARS-CoV-2. Another factor is expected to be the prevalent viral pressure, which is high in places where many partly immune-deficient people share little space such as nursing homes. Although studies from the USA were included, no justification for African American ethnicity being a risk factor was found in this review.
This review identified some risk factors not mentioned by public authorities. Mostly these are waiting time to hospital admission, tuberculosis, inflammation disorders and coagulation factors. It is possible that for these factors, especially coagulation factors, not enough evidence is present yet to be support by public authorities.
Most of the 28 records included in this review describe studies conducted in China. However, regarding the number of patients Italy is outstanding. Conditions and comorbidities potentially connected to a poor state of health such as high age, obesity, diabetes and hypertension were identified as risk factors for severe and fatal disease courses. It was found that severe and even more fatal courses of disease are associated with organ damages mainly affecting the heart, the liver and the kidneys. Further, inflammation and coagulation dysfunctionality were identified as risk factors. For coagulation factors, laboratory values were significantly different in Covid-19 patients but were mostly not mentioned as risk factors in the records’ texts. A prospective study with 12 deceased Covid-19 patients supports this finding. Therefore, the influence of coagulation disorders developed during a SARS-CoV-2 infection should be further investigated.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by DW, SN and NSH. The first draft of the manuscript was written by DW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Open Access funding provided by Projekt DEAL. The authors declare that no funding was received for the review.
Data availability
Code availability, compliance with ethical standards.
The authors declare that there is no conflict of interest.

IMAGES
COMMENTS
Emerging research describes a plethora of patient factors-including demographic, clinical, immunologic, hematological, biochemical, and radiographic findings-that may be of utility to clinicians to predict COVID-19 severity and mortality. We present a synthesis of the current literature pertaining to factors predictive of COVID-19 clinical ...
The coronavirus disease 2019 (COVID-19) pandemic is a rapidly evolving global emergency that continues to strain healthcare systems. Emerging research describes a plethora of patient factors—including demographic, clinical, immunologic, hematological, biochemical, and radiographic findings—that may be of utility to clinicians to predict COVID-19 severity and mortality.
Predictors of COVID-19 severity: A literature review. July 2020; Reviews in Medical Virology; DOI:10.1002/rmv.2146. ... be particularly strong predictors for COVID-19 severity, even though.
A synthesis of the current literature pertaining to factors predictive of COVID‐19 clinical course and outcomes shows findings associated with increased disease severity and/or mortality include age, multiple pre‐existing comorbidities, hypoxia, specific computed tomography findings indicative of extensive lung involvement, diverse laboratory test abnormalities, and biomarkers of end ...
More than 30 risk factors are associated with a higher risk of severe COVID-19, and these may serve as useful baseline parameters in the development of prediction tools for CO VID-19 prognosis. Background: The unpredictability of the progression of coronavirus disease 2019 (COVID-19) may be attributed to the low precision of the tools used to predict the prognosis of this disease. Objective ...
Background: The unpredictability of the progression of coronavirus disease 2019 (COVID-19) may be attributed to the low precision of the tools used to predict the prognosis of this disease.Objective: To identify the predictors associated with poor clinical outcomes in patients with COVID-19.Methods: Relevant articles from PubMed, Embase, Cochrane, and Web of Science were searched as of April 5 ...
Predictors of COVID-19 severity: a systematic review and meta-analysis [version 2; peer review: 2 approved] Mudatsir Mudatsir, ... To identify the predictors associated with poor clinical outcomes in patients with COVID-19. Methods: Relevant articles from PubMed, Embase, Cochrane, and Web of Science were searched as of April 5, 2020. ...
The coronavirus disease 2019 (COVID-19) pandemic is a rapidly evolving global emergency that continues to strain healthcare systems. Emerging research describes a plethora of patient factors-including demographic, clinical, immunologic, hematological, biochemical, and radiographic findings-that may be of utility to clinicians to predict COVID ...
Common clinical symptoms of COVID-19 include fever, dry cough, and fatigue. Less common symptoms include headache, dizziness, abdominal pain, nausea, and vomiting.5Patients may present with anosmia (loss of smell), dysgeusia (distortion or loss of taste), nausea, and diarrhea a few days prior to the fever. Although fever is an impor- tant clue ...
The COVID-19 pandemic has caused huge socio-economic losses and continues to threat humans worldwide. With more than 4.5 million deaths and more than 221 million confirmed COVID-19 cases, the impact on physical, mental, social and economic resources is immeasurable. During any novel disease outbreak, one of the primary requirements for effective mitigation is the knowledge of clinical ...
Introduction: Given the ongoing coronavirus disease 2019 (COVID-19) pandemic and the consequent global healthcare crisis, there is an urgent need to better understand risk factors for symptom deterioration and mortality among patients with COVID-19. This systematic review aimed to meet the need by determining the predictive value of chronic diseases for COVID-19 severity and mortality.Methods ...
The coronavirus disease 2019 (COVID-19) pandemic is a rapidly evolving global emergency that continues to strain healthcare systems. Emerging research describes a plethora of patient factors—including demographic, clinical, immunologic, hematological, biochemical, and radiographic findings—that may be of utility to clinicians to predict COVID-19 severity and mortality.
Background: The unpredictability of the progression of coronavirus disease 2019 (COVID-19) may be attributed to the low precision of the tools used to predict the prognosis of this disease.Objective: To identify the predictors associated with poor clinical outcomes in patients with COVID-19.Methods: Relevant articles from PubMed, Embase, Cochrane, and Web of Science were searched as of April 5 ...
Risk Factors. SARS-CoV-2. The COVID-19 pandemic has caused huge socio-economic losses and continues to threat humans worldwide. With more than 4.5 million deaths and more than 221 million confirmed COVID-19 cases, the impact on physical, mental, social and economic resources is immeasurable. During any novel disease outbreak ….
The COVID-19 pandemic has underscored the critical importance of understanding the intricate relationship between micronutrient levels and disease outcomes. This study explores the impact of Vitamin D, calcium, phosphorus, magnesium, and alkaline phosphatase (ALP) on COVID-19 severity and mortality. The study involves 200 participants (100 COVID-19 patients, 100 controls), we meticulously ...
Abstract. Current evidence on COVID-19 prognostic models is inconsistent and clinical applicability remains controversial. We performed a systematic review to summarize and critically appraise the available studies that have developed, assessed and/or validated prognostic models of COVID-19 predicting health outcomes.
The COVID-19 pandemic has presented unprecedented public health challenges worldwide. Understanding the factors contributing to COVID-19 mortality is critical for effective management and intervention strategies. This study aims to unlock the predictive power of data collected from personal, clinical, preclinical, and laboratory variables through machine learning (ML) analyses.
Perceived severity and self-efficacy are very strong predictors of unusual purchase intention, suggesting that a major reason people made unusual purchases during the second wave of COVID-19 was to prepare themselves against the ill effects of the disease. ... Saparman M. S., & Rahim N. Z. A. (2021). Marketing strategy and implementation in the ...
COVID-19 has proven to be a viral disease with a high transmission rate, that has caused over 100,000 deaths in the United States, thus far. ... We performed a targeted review of the literature, focusing on clinical and laboratory predictors of poor outcomes in COVID-19. Our case report and narrative review outline these findings within the ...
However, information on this is scattered and based on rather small studies. For connecting these, this publication describes a structured literature review on the risk factors of Covid-19 for severe and fatal disease courses. Additionally, the review's results are compared to the risk factors mentioned by four public authorities.