This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search

Search menu
Critical thinking: what it is and why it counts. 2020. https://tinyurl.com/ybz73bnx (accessed 27 April 2021)
Faculty of Intensive Care Medicine. Curriculum for training for advanced critical care practitioners: syllabus (part III). version 1.1. 2018. https://www.ficm.ac.uk/accps/curriculum (accessed 27 April 2021)
Guerrero AP. Mechanistic case diagramming: a tool for problem-based learning. Acad Med.. 2001; 76:(4)385-9 https://doi.org/10.1097/00001888-200104000-00020
Harasym PH, Tsai TC, Hemmati P. Current trends in developing medical students' critical thinking abilities. Kaohsiung J Med Sci.. 2008; 24:(7)341-55 https://doi.org/10.1016/S1607-551X(08)70131-1
Hayes MM, Chatterjee S, Schwartzstein RM. Critical thinking in critical care: five strategies to improve teaching and learning in the intensive care unit. Ann Am Thorac Soc.. 2017; 14:(4)569-575 https://doi.org/10.1513/AnnalsATS.201612-1009AS
Health Education England. Multi-professional framework for advanced clinical practice in England. 2017. https://www.hee.nhs.uk/sites/default/files/documents/multi-professionalframeworkforadvancedclinicalpracticeinengland.pdf (accessed 27 April 2021)
Health Education England, NHS England/NHS Improvement, Skills for Health. Core capabilities framework for advanced clinical practice (nurses) working in general practice/primary care in England. 2020. https://www.skillsforhealth.org.uk/images/services/cstf/ACP%20Primary%20Care%20Nurse%20Fwk%202020.pdf (accessed 27 April 2021)
Health Education England. Advanced practice mental health curriculum and capabilities framework. 2020. https://www.hee.nhs.uk/sites/default/files/documents/AP-MH%20Curriculum%20and%20Capabilities%20Framework%201.2.pdf (accessed 27 April 2021)
Jacob E, Duffield C, Jacob D. A protocol for the development of a critical thinking assessment tool for nurses using a Delphi technique. J Adv Nurs.. 2017; 73:(8)1982-1988 https://doi.org/10.1111/jan.13306
Kohn MA. Understanding evidence-based diagnosis. Diagnosis (Berl).. 2014; 1:(1)39-42 https://doi.org/10.1515/dx-2013-0003
Clinical reasoning—a guide to improving teaching and practice. 2012. https://www.racgp.org.au/afp/201201/45593
McGee S. Evidence-based physical diagnosis, 4th edn. Philadelphia PA: Elsevier; 2018
Norman GR, Monteiro SD, Sherbino J, Ilgen JS, Schmidt HG, Mamede S. The causes of errors in clinical reasoning: cognitive biases, knowledge deficits, and dual process thinking. Acad Med.. 2017; 92:(1)23-30 https://doi.org/10.1097/ACM.0000000000001421
Papp KK, Huang GC, Lauzon Clabo LM Milestones of critical thinking: a developmental model for medicine and nursing. Acad Med.. 2014; 89:(5)715-20 https://doi.org/10.1097/acm.0000000000000220
Rencic J, Lambert WT, Schuwirth L., Durning SJ. Clinical reasoning performance assessment: using situated cognition theory as a conceptual framework. Diagnosis.. 2020; 7:(3)177-179 https://doi.org/10.1515/dx-2019-0051
Examining critical thinking skills in family medicine residents. 2016. https://www.stfm.org/FamilyMedicine/Vol48Issue2/Ross121
Royal College of Emergency Medicine. Emergency care advanced clinical practitioner—curriculum and assessment, adult and paediatric. version 2.0. 2019. https://tinyurl.com/eps3p37r (accessed 27 April 2021)
Young ME, Thomas A, Lubarsky S. Mapping clinical reasoning literature across the health professions: a scoping review. BMC Med Educ.. 2020; 20 https://doi.org/10.1186/s12909-020-02012-9
Advanced practice: critical thinking and clinical reasoning
Sadie Diamond-Fox
Senior Lecturer in Advanced Critical Care Practice, Northumbria University, Advanced Critical Care Practitioner, Newcastle upon Tyne Hospitals NHS Foundation Trust, and Co-Lead, Advanced Critical/Clinical Care Practitioners Academic Network (ACCPAN)
View articles
Advanced Critical Care Practitioner, South Tees Hospitals NHS Foundation Trust

Clinical reasoning is a multi-faceted and complex construct, the understanding of which has emerged from multiple fields outside of healthcare literature, primarily the psychological and behavioural sciences. The application of clinical reasoning is central to the advanced non-medical practitioner (ANMP) role, as complex patient caseloads with undifferentiated and undiagnosed diseases are now a regular feature in healthcare practice. This article explores some of the key concepts and terminology that have evolved over the last four decades and have led to our modern day understanding of this topic. It also considers how clinical reasoning is vital for improving evidence-based diagnosis and subsequent effective care planning. A comprehensive guide to applying diagnostic reasoning on a body systems basis will be explored later in this series.
The Multi-professional Framework for Advanced Clinical Practice highlights clinical reasoning as one of the core clinical capabilities for advanced clinical practice in England ( Health Education England (HEE), 2017 ). This is also identified in other specialist core capability frameworks and training syllabuses for advanced clinical practitioner (ACP) roles ( Faculty of Intensive Care Medicine, 2018 ; Royal College of Emergency Medicine, 2019 ; HEE, 2020 ; HEE et al, 2020 ).
Rencic et al (2020) defined clinical reasoning as ‘a complex ability, requiring both declarative and procedural knowledge, such as physical examination and communication skills’. A plethora of literature exists surrounding this topic, with a recent systematic review identifying 625 papers, spanning 47 years, across the health professions ( Young et al, 2020 ). A diverse range of terms are used to refer to clinical reasoning within the healthcare literature ( Table 1 ), which can make defining their influence on their use within the clinical practice and educational arenas somewhat challenging.
The concept of clinical reasoning has changed dramatically over the past four decades. What was once thought to be a process-dependent task is now considered to present a more dynamic state of practice, which is affected by ‘complex, non-linear interactions between the clinician, patient, and the environment’ ( Rencic et al, 2020 ).
Cognitive and meta-cognitive processes
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting. Facione (2020) described critical thinking as ‘purposeful reflective judgement’ that consists of six discrete cognitive skills: analysis, inference, interpretation, explanation, synthesis and self–regulation. Ross et al (2016) identified that critical thinking positively correlates with academic success, professionalism, clinical decision-making, wider reasoning and problem-solving capabilities. Jacob et al (2017) also identified that patient outcomes and safety are directly linked to critical thinking skills.
Harasym et al (2008) listed nine discrete cognitive steps that may be applied to the process of critical thinking, which integrates both cognitive and meta-cognitive processes:
- Gather relevant information
- Formulate clearly defined questions and problems
- Evaluate relevant information
- Utilise and interpret abstract ideas effectively
- Infer well-reasoned conclusions and solutions
- Pilot outcomes against relevant criteria and standards
- Use alternative thought processes if needed
- Consider all assumptions, implications, and practical consequences
- Communicate effectively with others to solve complex problems.
There are a number of widely used strategies to develop critical thinking and evidence-based diagnosis. These include simulated problem-based learning platforms, high-fidelity simulation scenarios, case-based discussion forums, reflective journals as part of continuing professional development (CPD) portfolios and journal clubs.
Dual process theory and cognitive bias in diagnostic reasoning
A lack of understanding of the interrelationship between critical thinking and clinical reasoning can result in cognitive bias, which can in turn lead to diagnostic errors ( Hayes et al, 2017 ). Embedded within our understanding of how diagnostic errors occur is dual process theory—system 1 and system 2 thinking. The characteristics of these are described in Table 2 . Although much of the literature in this area regards dual process theory as a valid representation of clinical reasoning, the exact causes of diagnostic errors remain unclear and require further research ( Norman et al, 2017 ). The most effective way in which to teach critical thinking skills in healthcare education also remains unclear; however, Hayes et al (2017) proposed five strategies, based on well-known educational theory and principles, that they have found to be effective for teaching and learning critical thinking within the ‘high-octane’ and ‘high-stakes’ environment of the intensive care unit ( Table 3 ). This is arguably a setting that does not always present an ideal environment for learning given its fast pace and constant sensory stimulation. However, it may be argued that if a model has proven to be effective in this setting, it could be extrapolated to other busy clinical environments and may even provide a useful aide memoire for self-assessment and reflective practices.
Integrating the clinical reasoning process into the clinical consultation
Linn et al (2012) described the clinical consultation as ‘the practical embodiment of the clinical reasoning process by which data are gathered, considered, challenged and integrated to form a diagnosis that can lead to appropriate management’. The application of the previously mentioned psychological and behavioural science theories is intertwined throughout the clinical consultation via the following discrete processes:
- The clinical history generates an initial hypothesis regarding diagnosis, and said hypothesis is then tested through skilled and specific questioning
- The clinician formulates a primary diagnosis and differential diagnoses in order of likelihood
- Physical examination is carried out, aimed at gathering further data necessary to confirm or refute the hypotheses
- A selection of appropriate investigations, using an evidence-based approach, may be ordered to gather additional data
- The clinician (in partnership with the patient) then implements a targeted and rationalised management plan, based on best-available clinical evidence.
Linn et al (2012) also provided a very useful framework of how the above methods can be applied when teaching consultation with a focus on clinical reasoning (see Table 4 ). This framework may also prove useful to those new to the process of undertaking the clinical consultation process.
Evidence-based diagnosis and diagnostic accuracy
The principles of clinical reasoning are embedded within the practices of formulating an evidence-based diagnosis (EBD). According to Kohn (2014) EBD quantifies the probability of the presence of a disease through the use of diagnostic tests. He described three pertinent questions to consider in this respect:
- ‘How likely is the patient to have a particular disease?’
- ‘How good is this test for the disease in question?’
- ‘Is the test worth performing to guide treatment?’
EBD gives a statistical discriminatory weighting to update the probability of a disease to either support or refute the working and differential diagnoses, which can then determine the appropriate course of further diagnostic testing and treatments.
Diagnostic accuracy refers to how positive or negative findings change the probability of the presence of disease. In order to understand diagnostic accuracy, we must begin to understand the underlying principles and related statistical calculations concerning sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios.
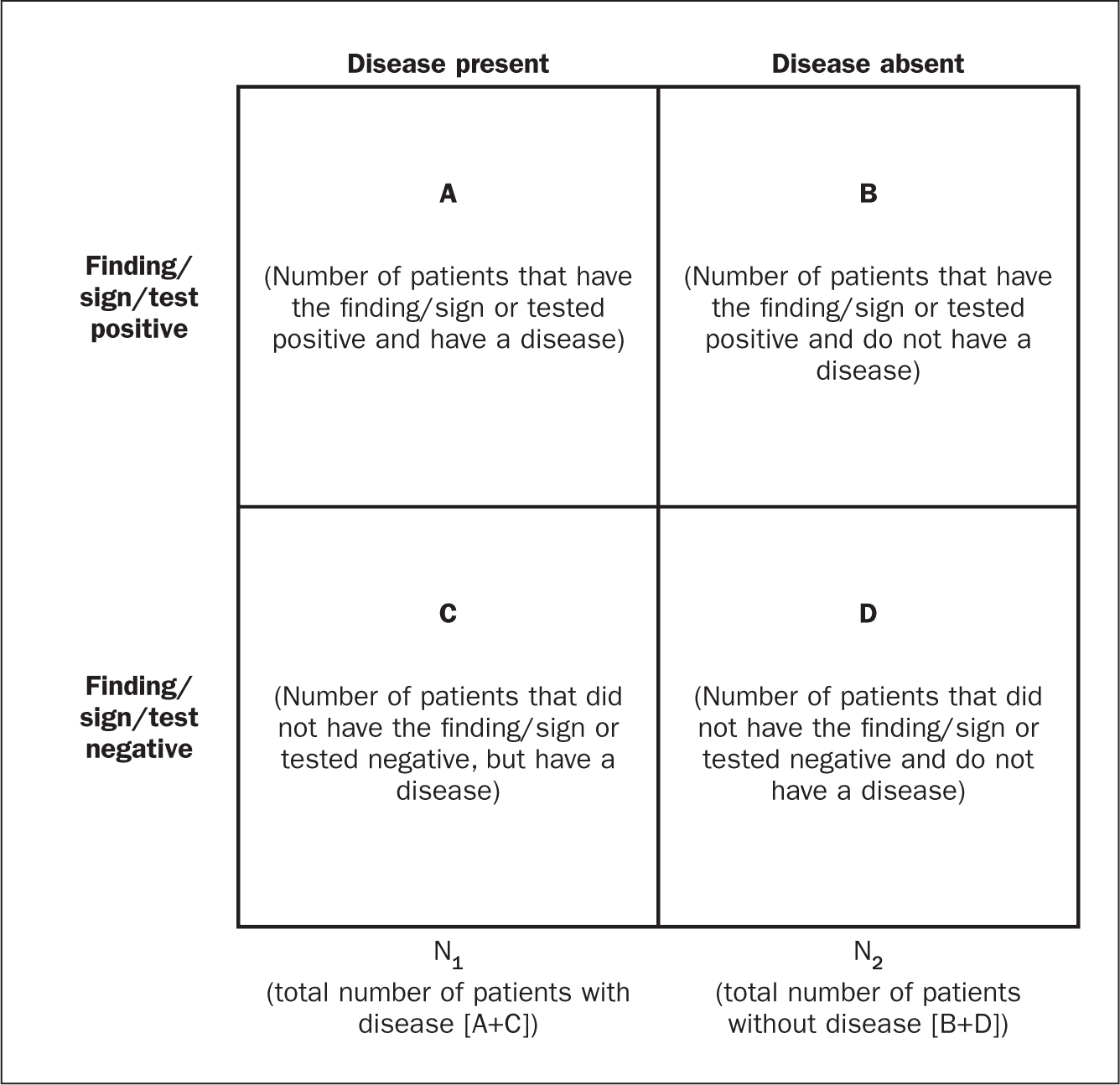
The construction of a two-by-two square (2 x 2) table ( Figure 1 ) allows the calculation of several statistical weightings for pertinent points of the history-taking exercise, a finding/sign on physical examination, or a test result. From this construct we can then determine the aforementioned statistical calculations as follows ( McGee, 2018 ):
- Sensitivity , the proportion of patients with the diagnosis who have the physical sign or a positive test result = A ÷ (A + C)
- Specificity , the proportion of patients without the diagnosis who lack the physical sign or have a negative test result = D ÷ (B + D)
- Positive predictive value , the proportion of patients with disease who have a physical sign divided by the proportion of patients without disease who also have the same sign = A ÷ (A + B)
- Negative predictive value , proportion of patients with disease lacking a physical sign divided by the proportion of patients without disease also lacking the sign = D ÷ (C + D)
- Likelihood ratio , a finding/sign/test results sensitivity divided by the false-positive rate. A test of no value has an LR of 1. Therefore the test would have no impact upon the patient's odds of disease
- Positive likelihood ratio = proportion of patients with disease who have a positive finding/sign/test, divided by proportion of patients without disease who have a positive finding/sign/test OR (A ÷ N1) ÷ (B÷ N2), or sensitivity ÷ (1 – specificity) The more positive an LR (the further above 1), the more the finding/sign/test result raises a patient's probability of disease. Thresholds of ≥ 4 are often considered to be significant when focusing a clinician's interest on the most pertinent positive findings, clinical signs or tests
- Negative likelihood ratio = proportion of patients with disease who have a negative finding/sign/test result, divided by the proportion of patients without disease who have a positive finding/sign/test OR (C ÷ N1) ÷ (D÷N1) or (1 – sensitivity) ÷ specificity The more negative an LR (the closer to 0), the more the finding/sign/test result lowers a patient's probability of disease. Thresholds <0.4 are often considered to be significant when focusing clinician's interest on the most pertinent negative findings, clinical signs or tests.
There are various online statistical calculators that can aid in the above calculations, such as the BMJ Best Practice statistical calculators, which may used as a guide (https://bestpractice.bmj.com/info/toolkit/ebm-toolbox/statistics-calculators/).
Clinical scoring systems
Evidence-based literature supports the practice of determining clinical pretest probability of certain diseases prior to proceeding with a diagnostic test. There are numerous validated pretest clinical scoring systems and clinical prediction tools that can be used in this context and accessed via various online platforms such as MDCalc (https://www.mdcalc.com/#all). Such clinical prediction tools include:
- 4Ts score for heparin-induced thrombocytopenia
- ABCD² score for transient ischaemic attack (TIA)
- CHADS₂ score for atrial fibrillation stroke risk
- Aortic Dissection Detection Risk Score (ADD-RS).
Conclusions
Critical thinking and clinical reasoning are fundamental skills of the advanced non-medical practitioner (ANMP) role. They are complex processes and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories. There are multiple constructs to guide these processes, not all of which will be suitable for the vast array of specialist areas in which ANMPs practice. There are multiple opportunities throughout the clinical consultation process in which ANMPs can employ the principles of critical thinking and clinical reasoning in order to improve patient outcomes. There are also multiple online toolkits that may be used to guide the ANMP in this complex process.
- Much like consultation and clinical assessment, the process of the application of clinical reasoning was once seen as solely the duty of a doctor, however the advanced non-medical practitioner (ANMP) role crosses those traditional boundaries
- Critical thinking and clinical reasoning are fundamental skills of the ANMP role
- The processes underlying clinical reasoning are complex and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories
- Through the use of the principles underlying critical thinking and clinical reasoning, there is potential to make a significant contribution to diagnostic accuracy, treatment options and overall patient outcomes
CPD reflective questions
- What assessment instruments exist for the measurement of cognitive bias?
- Think of an example of when cognitive bias may have impacted on your own clinical reasoning and decision making
- What resources exist to aid you in developing into the ‘advanced critical thinker’?
- What resources exist to aid you in understanding the statistical terminology surrounding evidence-based diagnosis?

Clinical Nurse Educators' LibGuide
- Keeping up to date This link opens in a new window
- Recent articles from the Journal of Nursing Education and Practice
- Critical thinking and clinical reasoning
- LibGuides Homepage This link opens in a new window
Library support
Library staff can assist you with:
- Literature searching
- Research skills training and support
- EndNote training
- Advice regarding getting published
- Document delivery to obtain full text of journal articles
- And more... see the Library website
Contact or visit your local CLIN Library to find out more about our full range of services and for assistance with your research project.
Some articles on critical thinking in nursing practice
- Fero, L. J., et al. (2009). "Critical thinking ability of new graduate and experienced nurses." Journal of Advanced Nursing 65(1): 139-148. This paper is a report of a study to identify critical thinking learning needs of new and experienced nurses. Concern for patient safety has grown worldwide as high rates of error and injury continue to be reported. In order to improve patient safety, nurses must be able to recognize changes in patient condition, perform independent nursing interventions, anticipate orders and prioritize. Conclusion. Patient safety may be compromised if a nurse cannot provide clinically competent care. Assessments such as the Performance Based Development System can provide information about learning needs and facilitate individualized orientation targeted to increase performance level. © 2008 Blackwell Publishing Ltd.
- Jacob, E., et al. (2018). "Development of an Australian nursing critical thinking tool using a Delphi process." Journal of Advanced Nursing. AIM To develop a critical thinking assessment tool for Australian undergraduate nurses. BACKGROUND Critical thinking is an important skill but difficult to assess in nursing practice. There are often many responses a nurse can make to a clinical problem or situation. Some responses are more correct than others and these decisions have an impact on a patient's care and safety. Differences in a response can relate to the depth of knowledge, experience and critical thinking ability of the individual nurse. DESIGN This study used a Delphi process to develop five clinical case studies together with the most appropriate clinical responses to 25 clinical questions. RESULTS Four rounds of Delphi questions were required to reach consensus on the correct wording and answers for the scenarios. Five case studies have been developed with nursing responses to patient management in rank order from most correct to least correct. CONCLUSION Use of the tool should provide confidence that a nurse has met a certain level of critical thinking ability.
- Ludin, S. M. (2017). "Does good critical thinking equal effective decision-making among critical care nurses? A cross-sectional survey."Intensive and Critical Care Nursing. v. 44 https://doi.org/10.1016/j.iccn.2017.06.002 Background: A critical thinker may not necessarily be a good decision-maker, but critical care nurses are expected to utilise outstanding critical thinking skills in making complex clinical judgements. Studies have shown that critical care nurses' decisions focus mainly on doing rather than reflecting. To date, the link between critical care nurses' critical thinking and decision-making has not been examined closely in Malaysia.
- Simpson, E. and M. Courtney (2002). "Critical thinking in nursing education: literature review." International journal of nursing practice 8(2): 89-98. The need for critical thinking in nursing has been accentuated in response to the rapidly changing health-care environment. Nurses must think critically to provide effective care while coping with the expansion in role associated with the complexities of current health-care systems. This literature review will present a history of inquiry into critical thinking and research to support the conclusion that critical thinking is necessary not only in the clinical practice setting, but also as an integral component of nursing-education programmes to promote the development of nurses' critical-thinking abilities. The aims of this paper are to: (i) review the literature on critical thinking; (ii) examine the dimensions of critical thinking; (iii) investigate the various critical thinking strategies for their appropriateness to enhance critical thinking in nurses; and (iv) examine issues relating to the evaluation of critical-thinking skills in nursing.
- Turner, P. (2005) "Critical thinking in nursing education and practice as defined in the literature". Nursing Education Perspectives 26(5): 272-277. Critical thinking is frequently discussed in nursing education and nursing practice literature. This article presents an analysis of the concept of critical thinking as it applies to nursing, differentiating its use in education and practice literature. Three computerized databases (CINAHL, MEDLINE, and EBSCO) were searched for the years 1981 to 2002, using the keywords critical thinking. References were stratified into two 11-year periods (1981-1991, 1992-2002) to identify changes in the concept over time and integration of the concept differentially into nursing education and nursing practice. A random sample of literature from each stratum was coded for definitions, attributes, surrogate terms, referents, antecedents, and consequences of critical thinking. Critical thinking as a nursing concept has matured since its first appearance in the literature. It is well defined and has clear characteristics. However, antecedents and consequences are not well defined, and many consequences are identical to attributes and surrogate terms. Additional work is needed to clarify the boundaries of the concept of critical thinking in nursing.
Books on critical thinking and clinical reasoning
- << Previous: Recent articles from the Journal of Nursing Education and Practice
- Next: LibGuides Homepage >>
- Last Updated: May 1, 2024 11:54 AM
- URL: https://swslhd.libguides.com/CNE
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Perspect Med Educ
- v.11(2); 2022 Mar

Advancing the assessment of clinical reasoning across the health professions: Definitional and methodologic recommendations
David gordon.
1 Division of Emergency Medicine, Duke University, Durham, NC USA
Joseph J. Rencic
2 Department of Medicine, Boston University School of Medicine, Boston, MA USA
Valerie J. Lang
3 Division of Hospital Medicine, University of Rochester School of Medicine and Dentistry, Rochester, NY USA
Aliki Thomas
4 School of Physical and Occupational Therapy, Institute of Health Sciences Education, McGill University, Montreal, QC Canada
Meredith Young
5 Department of Medicine and Institute of Health Sciences Education, McGill University, Montreal, QC Canada
Steven J. Durning
6 Department of Medicine, Uniformed Services University of the Health Sciences, Bethesda, MD USA
The importance of clinical reasoning in patient care is well-recognized across all health professions. Validity evidence supporting high quality clinical reasoning assessment is essential to ensure health professional schools are graduating learners competent in this domain. However, through the course of a large scoping review, we encountered inconsistent terminology for clinical reasoning and inconsistent reporting of methodology, reflecting a somewhat fractured body of literature on clinical reasoning assessment. These inconsistencies impeded our ability to synthesize across studies and appropriately compare assessment tools. More specifically, we encountered: 1) a wide array of clinical reasoning-like terms that were rarely defined or informed by a conceptual framework, 2) limited details of assessment methodology, and 3) inconsistent reporting of the steps taken to establish validity evidence for clinical reasoning assessments. Consolidating our experience in conducting this review, we provide recommendations on key definitional and methodologic elements to better support the development, description, study, and reporting of clinical reasoning assessments.
Clinical reasoning broadly entails the cognitive processes that enable clinicians to observe, collect, and analyze information, resulting in decisions and actions that seek to improve patients’ well-being while considering their specific circumstances and preferences [ 1 , 2 ]. Clinical reasoning is a multidimensional construct that is inherently complex [ 2 ], comprised of different components (e.g., data gathering, problem representation) [ 3 ], and undergirded by varied theoretical frameworks and epistemologies [ 1 ]. More recently, the conceptualization of diagnosis as a team-based activity has emerged, emphasizing clinical reasoning as a collaborative effort between health care professionals, patients, and families [ 4 , 5 ].
The health professions encompass a broad array of practices which share a common commitment to the study, diagnosis, treatment, and prevention of human illness and injury [ 6 ]. In fulfilling this purpose, the health professions have recognized the centrality of clinical reasoning and its assessment, as represented in multiple competency-based educational frameworks [ 7 – 10 ]. From the patient safety perspective, faulty reasoning has been identified as a major cause of diagnostic error [ 11 ], and thus strategies to improve clinical reasoning education and assessment and reduce clinical reasoning errors have been highlighted as an important area for health professions education (HPE) and research [ 12 , 13 ].
To understand how clinical reasoning is assessed across the health professions, our group of clinical educators and researchers undertook a scoping review of the HPE literature [ 14 ], which in turn led to additional work on how clinical reasoning is variably defined and conceptualized [ 15 , 16 ]. In the process of synthesizing the vast body of literature across multiple health professions we encountered multiple challenges which prompted us to reflect on our experience and identify opportunities for better definitional and methodologic clarity in clinical reasoning assessment research and reporting. Clinical reasoning is a topic that often feels familiar (or even obvious) as it permeates health professions education, however, as we observed, this sense of familiarity may be masking important differences in how it is understood, operationalized, and assessed.
The overarching aim of this eye opener is to share the challenges we had in synthesizing a large, and somewhat fractured, body of literature on a multidimensional construct and then propose recommendations to better support the development, description, study, and reporting of assessments. The recommendations that we include in this eye-opener are generated based on our collective experience but draw from and align with sound research and assessment practices in terms of the importance of conceptual frameworks [ 1 , 17 – 19 ], detailed assessment methodology [ 20 , 21 ], and sources of validity evidence [ 22 – 24 ] in modern educational assessments. While our experiences were deeply embedded in the clinical reasoning context, we believe that similar complexities are likely encountered when synthesizing other multidimensional constructs in health professions education, and as such, our recommendations may be of value in other literature spaces.
Following a description of the challenges we experienced synthesizing literature in clinical reasoning assessments, we present resultant experienced-based and best-practices-linked recommendations. Through this synthesis, we seek to bring new perspective and collective insight into the current state and future direction of clinical reasoning assessment by first illustrating the need for greater clarity in the HPE literature followed by proposing a roadmap for how this can be achieved.
Observations from a scoping review of clinical reasoning assessment
Our author team conducted a large scoping review on clinical reasoning assessment. A scoping review is a methodology well suited to mapping literature that may be evolving, disperse, or contain a variety of different conceptualizations [ 25 – 27 ]. We used a mapping approach for our synthesis given the diversity of clinical reasoning assessment approaches—from knowledge-based exams to workplace-based assessments. While we expected the literature on clinical reasoning assessment to be varied, we found its synthesis particularly challenging because: 1) clinical reasoning is a multidimensional construct with varied conceptualizations and definitions, 2) method sections often lacked adequate detail, and 3) there was a paucity of validity evidence supporting a particular clinical reasoning assessment approach.
Several observations regarding the conceptualization of clinical reasoning have emerged [ 14 ]. The presence of multiple conceptualizations can result in different boundaries as to what is considered clinical reasoning, different terms being used that refer to the broad construct of clinical reasoning, and the same term being used with different intended interpretations. First, different understandings of what “counts” as relevant to clinical reasoning exist, which can result in different definitions, and influences what might be a relevant target for assessment [ 15 ]. For example, conceptualizations that focus on the cognitive processes within individuals can lead to one definition with one set of targets for assessment, while those that emphasize the interplay between provider, patient, and environment can result in another definition and create a different set of targets. Second, numerous terms have emerged in the literature that relate to clinical reasoning. One study identified 110 different terms used in reference to the construct of clinical reasoning [ 16 ]. Some of these terms, such as “clinical skills” and “competence,” are very broad and, without an accompanying clear definition, require inferences on the part of a reader to determine the intended assessment focus. More specifically, these broad terms make it challenging to determine how clinical reasoning has been operationalized into a target for assessment, or whether an ability traditionally regarded as a different domain—like procedural or communication skills [ 7 , 8 , 15 ]—is the focus of the assessment. Lastly, the same term can take on different meanings. For instance, in the field of surgery, “judgment” has been used to represent “respect for tissue” and assessed by measuring the amount of force applied [ 28 ]. In other medical fields, judgment has been used to represent sound problem solving and decision making within a given clinical context [ 29 ]. In further contrast, in the field of nursing, the emphasis has been placed on judgment as the outcome of a reasoning process [ 10 ]. Therefore, the same term has been used to refer to a specific subskill, a transferable set of approaches, and an outcome of the reasoning process. This multiplicity of meanings across contexts, especially when not accompanied by an explicit definition, makes the mechanisms of synthesis challenging, and more importantly relies heavily on a reader being aware of, and responding to, different contextually-bound uses of the same term.
Our scoping review also provided insight into the methodological and reporting rigor in literature describing clinical reasoning assessments. One key means of documenting the potential value of an assessment tool is attending to, collecting, and reporting on validity evidence. Despite its importance, few papers in our review used any explicit validity framework or provided validity evidence to support the use of their assessment. The infrequency of validity evidence included in an assessment paper in the HPE literature is not unique to clinical reasoning. Others have reported similar findings of limited validity evidence in technology-enhanced simulation-based assessments—primarily focused on procedural skills but also used to evaluate communication and teamwork skills [ 30 ]—and in professionalism assessments [ 31 ].
Many key concepts in HPE are complex and often multidimensional. Clinical reasoning is not unique in its complexity but provided us with some deeply grounded experience in synthesizing the literature on an important but often inconsistently operationalized focus of assessment in HPE. Considering our experience, we would like to suggest a series of experience-based and best-practices-linked recommendations focused on the use of more explicit terminology, incorporation of theoretical framework(s), increased methodologic detail, and the provision of validity evidence. We believe that these recommendations developed in the context of clinical reasoning assessment may provide helpful guidance for others who study, teach, or assess other broad concepts (e.g., professionalism, expertise) in HPE.
Recommendations
Define the construct of interest.
Clearly defining a construct is essential to assessment development and validation [ 20 , 23 ]. When considering a broad concept like clinical reasoning, it is important that authors provide an explicit definition of clinical reasoning (or synonym) or a clear description of the target construct used in their assessment. This recommendation does not imply that there is one universally “correct” definition of clinical reasoning [ 32 , 33 ], but rather it emphasizes the importance of providing a clear description of the specific construct of interest. This clear description will promote appropriate understanding, defensible application, and meaningful integration of the assessment method.
In developing a construct of clinical reasoning for assessment, an important consideration to specify is whether clinical reasoning is being assessed as an outcome, process, or combination thereof [ 15 ]. This clarification of clinical reasoning as an outcome, process, or both leads to the use of different forms of assessment. For example, an assessment concerned with diagnostic accuracy may treat clinical reasoning as an outcome (i.e., a defined output) while another assessment concerned with data gathering may emphasize clinical reasoning as a process (i.e., a sequence of steps). How well the assessment distinguishes between process and outcome, and how that relates to the construct definition, will have important implications in understanding the strengths and limitations of a given assessment approach.
If an assessment is a process-oriented assessment (i.e., focused on clinical reasoning as a process rather than an outcome), authors should clearly define the clinical reasoning subprocesses of interest [ 3 , 14 ]. Some assessments focus on information gathering and differential diagnosis (e.g., OSCEs); other methods are geared towards the assessment of problem representation (e.g., concept maps) [ 14 ]. Specifying the clinical reasoning subprocesses or components targeted by a given assessment approach will make it clear if, how, and in which manner the assessment method is capturing clinical reasoning performance.
Clinical reasoning has been studied using a variety of lenses, and several theories have been mobilized to better understand this complex construct. Given that clinical reasoning can be considered a process or outcome, a deeply cognitive or collaborative activity, we recommend that authors describe the theoretical framework(s) that shape how they understand the construct of clinical reasoning, and the perspectives that ground the assessment and study design [ 34 ]. Multiple theoretical frameworks exist that highlight the multiple understandings of clinical reasoning, and different frameworks provide different rationales for selecting certain assessment approaches over others [ 19 ]. For example, use of dual-process theory as a conceptual framework may lead researchers to discriminate between and assess both unconscious/automated cognitive processes and conscious/analytical processes [ 35 ]. Alternatively, relying on situated cognition theories may lead to emphasizing a contextual dimension to clinical reasoning—as a process that emerges from interactions between physician factors, patient factors, and practice environment factors [ 36 ]. If these two different theoretical stances are carried forward to assessment design, one could imagine a situated cognition researcher focusing an assessment approach on how the diagnostic accuracy of a learner is affected by an angry patient, whereas a researcher using dual process theory might focus on the cognitive processes a learner uses to navigate diagnostic ambiguity. Explicitly stating the theoretical framework and definition of clinical reasoning in an article allows the reader to understand the rationale for the assessment methodology and discussion of the results.
Describe the assessment tool
In addition to an explicit definition or articulated construct, a clearly described assessment development and validation approach is critical to understanding the nature, purpose, quality, and potential utility of the assessment. Clinical reasoning assessments can vary by their setting (classroom versus clinical), type of encounter (simulated versus workplace), clinical reasoning component of interest, and a variety of other factors [ 14 , 37 , 38 ]. Additional important components of an assessment include the instruments used to collect examinee responses (i.e., assessment format), the method used to score those responses, the intended use of the scores generated by the assessment, and, when applicable, the background or training of the raters who conduct the scoring.
In conducting our review on assessments of clinical reasoning, our research group focused on data reported about an assessment that included: the stimulus format (i.e., what necessitated a response), response format (i.e., how a learner could respond to the assessment), and scoring activity (i.e., how a learner response was transformed into an assessment score). We found these elements helpful in structuring our analysis of existing literature [ 14 ] and suggest reporting these characteristics would increase clarity for the development and description of new research on clinical reasoning assessment.
Stimulus format describes the way in which an examinee is presented with a clinical scenario [ 21 ]. Examples include a real patient, standardized patient, computer-based virtual patient, or a written clinical vignette. Providing detail on how these stimuli are chosen or constructed, their level of complexity, and their degree of intended ambiguity or uncertainty will help promote understanding of the development, scope, and application of the assessment and contribute to building a validity argument in support of score interpretation [ 38 ].
An examinee’s choices or series of actions in response to the stimulus format need to be recorded, and this component is captured in response format [ 21 ]. Responses can be selected in which an examinee chooses from a list of provided answers or constructed in which an examinee responds verbally or in writing to open prompts [ 21 ]. Furthermore, constructed responses can exist in different formats such as essays, diagrams, and post-encounter documentation. We recommend authors describe how response instruments were either created or selected to meet the goals of the assessment and—particularly if novel—whether they were piloted to see if examinees understood the question, response options, and mechanics of the collection instrument.
Scoring activity is the process by which examinee’s responses are converted into a performance result. It can be quantitative or qualitative. It refers to both “answer key” generation and application, and in certain assessment approaches includes rater training. Scoring activities can occur pre-, intra-, and/or post-assessment and should be explicitly described. Answer key generation typically occurs pre-assessment, when a group develops a clinical question or scenario and determines the “correct” response. Information on how consensus was achieved for the answer key (if relevant) should be provided.
Intra-assessment scoring occurs primarily during direct observation. Authors should provide the details about the tool with accompanying rationale for why a particular scoring approach is used (e.g., checklist vs global; complete/incomplete vs. Likert-scale). Intra-assessment scoring activity is challenging because of the multi-tasking required of the assessor. Thus, authors should provide details about rater qualifications, experience, training, and inter- or intra-rater reliability. Information should also be provided about the time needed to complete the assessment activity.
Post-assessment scoring can involve grading selected or constructed responses. Depending on the format, it may be automated or by hand. Like intra-assessment scoring, providing background information on the scorers and/or technology and time needed to complete the activity will allow for determinations about the feasibility of an assessment method.
In summary, to better support transparent reporting, we suggest papers describing assessments of clinical reasoning include a clear definition of the construct of interest, describe the theoretical framework underpinning the assessment, and describe the stimulus format, response format, and scoring activity.
Collect validity evidence
Validity refers to the evidence provided to support the interpretation of the assessment results and the decisions that follow [ 23 ]. Evidence of validity is essential to ensure the defensible use of assessment scores and is an important component of assessment literature [ 39 ]. A common misassumption that we encountered in our scoping review was that validity is a dichotomous feature (i.e., that an assessment is either valid or not valid). This notion of validity as a characteristic of a test has been reported elsewhere and is not limited to the clinical reasoning assessment literature [ 40 ]. In more current conceptualizations of validity, an assessment may have varying strengths of evidence in an argument supporting the use of its scores to make specific inferences about specific populations. In other words, evidence of validity does not “travel” with an assessment tool and should be collected each time an assessment is used in a different context or population and for each different score use (i.e., formative feedback vs. summative decisions). For example, validity evidence collected for an examination to determine whether medical students demonstrate a minimum level of competence in their clinical reasoning to pass the pediatrics clerkship would not be sufficient to justify using the examination to determine whether pediatric residents should be licensed to practice independently. In summary, validity evidence must be collected for a clinical reasoning assessment supporting the intended score use and the decisions that result.
We recommend that authors use an explicit validity framework to collect and report the validity evidence. There are multiple approaches, but in HPE, two major validity frameworks are frequently used: Messick’s unified framework of construct validity [ 41 ] and Kane’s validity argument framework [ 42 ]. Messick’s framework, as modified by Downing [ 23 ], identifies five categories of evidence to support score interpretation and use. These categories (adapted in the Standards for educational and psychological testing [ 39 ]) are: content (e.g., blueprinting an examination or ensuring workplace assessments are performed aligned with the definition of clinical reasoning adopted), response process (e.g., ensuring those being assessed and those assessing understand the assessment as intended), internal structure (e.g., analysis of difficulty and discrimination of items/cases and how that aligns with the definition of clinical reasoning adopted), relationship to other variables (e.g., relationship with another assessment that assesses a similar or different aspect of clinical reasoning), and consequences (e.g., whether decisions made based on results of the assessment are justified for the individual and the institution). Notably, reliability is included as one piece of evidence supporting validity (part of internal structure), rather than treated as a separate construct from validity. In summary, Messick’s approach focuses on the types of evidence that help us determine whether a decision based on assessment data is sound, or, in other words, whether a score interpretation (e.g., pass/fail) is defensible.
As described by Schuwirth and van der Vleuten, Kane’s framework involves organizing categories of evidence into a logical argument to justify that the units of assessment can be translated into an inference about the population being assessed [ 24 ]. The four links in the logic chain are scoring (translation of an observation into a score), generalization (using a score to reflect performance in a particular setting), extrapolation (using the score to reflect performance in the real-world setting), and implications (using the score to make a decision about the learner). Through this lens, sequential inferences are made about the learner’s clinical reasoning. For example, a workplace-based assessment may begin with a chart-stimulated recall [ 43 ] of a resident’s clinical reasoning about a case (a supervisor translates that observation into a score), followed by generalization of that score to make an inference about the resident’s clinical reasoning performance in the outpatient clinic within their patient population, followed by extrapolation to their clinical reasoning ability for outpatients in general, and ending in a decision to allow the resident to make clinical decisions without supervision.
Our recommendations and resources for developing, describing, and documenting an assessment of clinical reasoning are summarized in Tab. 1 . Where Messick’s approach focuses on types of evidence, Kane focuses on the types of inference that are made moving from an assessment to judgment such as “competent.” Thus, these two frameworks are complementary and have been combined in order to think comprehensively about the validity of assessment score interpretation [ 44 ].
Summary of recommendations for developing and detailing an assessment of clinical reasoning
We hope these recommendations can assist investigators in their conception and execution of new studies on the assessment of clinical reasoning. Similarly, these recommendations can guide educators in analyzing the quality of existing studies in order to decide whether to incorporate an assessment approach into their own educational program. Towards this end, these recommendations offer a structured approach to question the utility of an assessment paper based on whether a clear definition of clinical reasoning has been provided in order to evaluate if the study is generalizable to one’s context, a theory was utilized to shed insight into the perspectives and assumptions behind the study, sufficient methodological detail is available for the assessment to be reproduced accurately and reliably, and the validity evidence provides adequate justification for pass/fail or promotion decisions.
Potential future implications of our reflections and proposed recommendations include the creation of formal guidelines to be used in reporting of studies on the assessment of clinical reasoning, similar to PRISMA guidelines for systematic reviews and metanalysis [ 48 ]. Our recommendations require further review and discussion by experts in clinical reasoning and assessment research as well as additional empirical examination, but we hope this manuscript can serve as an important conversation starter for developing formal guidelines. As the volume of articles on clinical reasoning assessment continues to rapidly expand [ 16 ], we worry that the literature will become even more fragmented, further impeding the ability to synthesize, reproduce, and generalize research in this critical domain. An increasingly fragmented literature may limit our ability to effectively share innovative approaches to assessment, and limit constructive engagement with how to best assess, or how to best combine multiple assessments, to effectively capture clinical reasoning performance.
The future of clinical reasoning
As health care delivery continues to evolve, so likely will the dimensions of clinical reasoning. The emergence of health systems science as a third pillar in medical education will place increased emphasis on systems thinking and caring for both populations and individuals [ 49 ]. With the growth of electronic health records and big data, computational thinking and data literacy can be expected to be of increased importance in clinical decision making [ 50 ]. Telehealth has provided a new environment in which clinical reasoning can be situated [ 51 ]. These expanded possibilities of what clinical reasoning entails and the contexts in which it can occur will require ongoing discussion on how different conceptualizations of clinical reasoning can be captured and assessed. This evolution of clinical reasoning further stresses the importance for definitional and methodologic clarity in future studies on clinical reasoning assessment to facilitate synthesis across research and promote cohesion in the HPE literature.
To better support researchers, educators, and assessors, we suggest a variety of means to increase the quality of reporting on assessments of clinical reasoning. Including an explicit definition, a description of the theoretical frameworks being applied, and organizing validity evidence within a recognized framework will better support communication about assessments of clinical reasoning and hopefully support more consistent implementation and use of novel approaches to assessment. Our recommendations represent the application of several general principles of educational assessments to the design, documentation, and reporting of clinical reasoning assessments. They can easily be applied to other domains of study in HPE, particularly those involving constructs that are broad in their scope, open to different interpretations, and comprised of multiple components.
Acknowledgements
The authors would like to thank all members of the research team for their expertise and contributions to this project.
M. Young received support from the Fonds de Recherche du Quebec—Sante as a Chercheur Boursier Junior 1.
Conflict of interest
D. Gordon, J.J. Rencic, V.J. Lang, A. Thomas, M. Young and S.J. Durning declare that they have no competing interests. The views expressed herein are those of the authors and not necessarily those of the U.S. Department of Defense or other U.S. federal agencies.
Critical Thinking and Clinical Reasoning in Undergraduate Medical Course: A Mixed-Methods Study in a Medical College in Kolkata, West Bengal, India
Affiliations.
- 1 School of Higher Education & Research, Datta Meghe Institute of Higher Education & Research, Sawangi (Meghe), Maharashtra, 442107, India.
- 2 Community Medicine, College of Medicine and Sagore Dutta Hospital, Kolkata, West Bengal, 700058, India.
- 3 Community Medicine, Jawaharlal Nehru Medical College, Sawangi (Meghe), Maharashtra, 442107, India.
- PMID: 38779311
- PMCID: PMC11109580
- DOI: 10.12688/f1000research.146009.1
Critical thinking is considered as the essential set of skills for medical practice, particularly during emergencies. However, there is lack of conceptual clarity around it and it was not explicitly included in the undergraduate medical curriculum in India. The present study has been planned to assess the critical thinking disposition and clinical reasoning skills among medical undergraduate students in a medical college in West Bengal, India. The perceived definition and attributes of critical thinking in medical education will be explored and the contexts where application of critical thinking skills may be crucial for medical practice will be identified. The content validity index, test-retest agreement; internal consistency and construct validity of the Critical Thinking Disposition Assessment Questionnaire (CTDAQ) will be assessed through step-by-step procedure. CTDAQ and the case-based objective-type questions for the clinical reasoning skills will be applied to around 200 medical undergraduate students. Their perception and experience on critical thinking in medical education will be assessed with structured open-ended questions. In-depth interviews with medical teachers of the second and third phases of undergraduate medical curriculum will be conducted to assess their perception and experiences on critical thinking. The quantitative analysis will be conducted with MS excel and R software using the relevant packages. The qualitative data will be transcribed and translated in English, close to the participants' verbatim. The thematic analysis will be conducted with inductive coding and memoing. The study will be conducted maintaining ethical standards for epidemiological studies. The present study, one of the first a few studies in India, will help to meet the conceptual gap in understanding the attributes of critical thinking, its association with clinical reasoning and the contexts of preferred application in medical practice.
Keywords: Clinical reasoning; Critical thinking; Education; Medical; Medical Students; Undergraduate.
Copyright: © 2024 Mukhopadhyay DK and Choudhari SG.
- Clinical Competence
- Clinical Reasoning*
- Education, Medical, Undergraduate* / methods
- Students, Medical*
- Surveys and Questionnaires
Grants and funding
- Open access
- Published: 24 May 2024
Integration of case-based learning and three-dimensional printing for tetralogy of fallot instruction in clinical medical undergraduates: a randomized controlled trial
- Jian Zhao 1 na1 ,
- Xin Gong 1 na1 ,
- Jian Ding 1 ,
- Kepin Xiong 2 ,
- Kangle Zhuang 3 ,
- Rui Huang 1 ,
- Shu Li 4 &
- Huachun Miao 1
BMC Medical Education volume 24 , Article number: 571 ( 2024 ) Cite this article
164 Accesses
Metrics details
Case-based learning (CBL) methods have gained prominence in medical education, proving especially effective for preclinical training in undergraduate medical education. Tetralogy of Fallot (TOF) is a congenital heart disease characterized by four malformations, presenting a challenge in medical education due to the complexity of its anatomical pathology. Three-dimensional printing (3DP), generating physical replicas from data, offers a valuable tool for illustrating intricate anatomical structures and spatial relationships in the classroom. This study explores the integration of 3DP with CBL teaching for clinical medical undergraduates.
Sixty senior clinical medical undergraduates were randomly assigned to the CBL group and the CBL-3DP group. Computed tomography imaging data from a typical TOF case were exported, processed, and utilized to create four TOF models with a color 3D printer. The CBL group employed CBL teaching methods, while the CBL-3DP group combined CBL with 3D-printed models. Post-class exams and questionnaires assessed the teaching effectiveness of both groups.
The CBL-3DP group exhibited improved performance in post-class examinations, particularly in pathological anatomy and TOF imaging data analysis ( P < 0.05). Questionnaire responses from the CBL-3DP group indicated enhanced satisfaction with teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities ( P < 0.05). These findings underscore the potential of 3D printed models to augment the effectiveness of CBL, aiding students in mastering instructional content and bolstering their interest and self-confidence in learning.
The fusion of CBL with 3D printing models is feasible and effective in TOF instruction to clinical medical undergraduates, and worthy of popularization and application in medical education, especially for courses involving intricate anatomical components.
Peer Review reports
Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart disease(CHD) [ 1 ]. Characterized by four structural anomalies: ventricular septal defect (VSD), pulmonary stenosis (PS), right ventricular hypertrophy (RVH), and overriding aorta (OA), TOF is a focal point and challenge in medical education. Understanding anatomical spatial structures is pivotal for learning and mastering TOF [ 2 ]. Given the constraints of course duration, medical school educators aim to provide students with a comprehensive and intuitive understanding of the disease within a limited timeframe [ 3 ].
The case-based learning (CBL) teaching model incorporates a case-based instructional approach that emphasizes typical clinical cases as a guide in student-centered and teacher-facilitated group discussions [ 4 ]. The CBL instructional methods have garnered widespread attention in medical education as they are particularly appropriate for preclinical training in undergraduate medical education [ 5 , 6 ]. The collection of case data, including medical records and examination results, is essential for case construction [ 7 ]. The anatomical and hemodynamic consequences of TOF can be determined using ultrasonography, computed tomography (CT), and magnetic resonance imaging techniques. However, understanding the anatomical structures from imaging data is a slow and challenging psychological reconstruction process for undergraduate medical students [ 8 ]. Three-dimensional (3D) visualization is valuable for depicting anatomical structures [ 9 ]. 3D printing (3DP), which creates physical replicas based on data, facilitates the demonstration of complex anatomical structures and spatial relationships in the classroom [ 10 ].
During the classroom session, 3D-printed models offer a convenient means for hands-on demonstration and communication, similar to facing a patient, enhancing the efficiency and specificity of intra-team communication and discussion [ 11 ]. In this study, we printed TOF models based on case imaging data, integrated them into CBL teaching, and assessed the effectiveness of classroom instruction.
Research participants
The study employed a prospective, randomized controlled design which received approval from the institutional ethics committee. Senior undergraduate students majoring in clinical medicine at Wannan Medical College were recruited for participation based on predefined inclusion criteria. The researchers implemented recruitment according to the recruitment criteria by contacting the class leaders of the target classes they had previously taught. Notably, these students were in their third year of medical education, with anticipation of progressing to clinical courses in the fourth year, encompassing Internal Medicine, Surgery, Obstetrics, Gynecology, and Pediatrics. Inclusion criteria for participants encompassed the following: (1) proficient communication and comprehension abilities, (2) consistent attendance without absenteeism or truancy, (3) absence of failing grades in prior examinations, and (4) capability to conscientiously fulfill assigned learning tasks. Exclusion criteria were (1) absence from lectures, (2) failure to complete pre-and post-tests, and (3) inadequate completion of questionnaires. For their participation in the study, Students were provided access to the e-book “Localized Anatomy,” authored by the investigators, as an incentive for their participation. Voluntary and anonymous participation was emphasized, with participants retaining the right to withdraw from the study at any time without providing a reason.
The study was conducted between May 1st, 2023, and June 30, 2023, from recruitment to completion of data collection. Drawing upon insights gained from a previous analogous investigation which yielded an effect size of 0.95 [ 10 ]. Sample size was computed, guided by a statistical consultant, with the aim of 0.85 power value, predicated on an effect size of 0.8 and a margin of error set at 0.05. A minimum of 30 participants per group was calculated using G*Power software (latest ver. 3.1.9.7; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany), resulting in the recruitment of a total of 60 undergraduate students. Each participant was assigned an identification number, with codes placed in boxes. Codes drawn from the boxes determined allocation to either the CBL group or the CBL-3DP group. Subsequently, participants were randomly assigned to either the CBL group, receiving instruction utilizing the CBL methodology, or the CBL-3DP group, which received instruction integrating both CBL and 3D Printed models.
Printing of TOF models
Figure 1 A shows the printing flowchart of the TOF models. A typical TOF case was collected from the Yijishan Hospital of Wannan Medical College. The CT angiography imaging data of the case was exported. Mimics Research 20.0 software (Mimics Innovation Suite version 20, Materialize, Belgium) was used for data processing. The cardiovascular module of the CT-Heart tool was employed to adjust the threshold range, independently obtain the cardiac chambers and vessels, post-process the chambers and vessels to generate a hollow blood pool, and merge it with the myocardial volume to construct a complete heart model. The file was imported into Magics 24.0 software (version 24.0; Materialize, Belgium) for correction using the Shell tool page. After repairs, the model entered the smoothing page, where tools such as triangular surface simplification, local smoothing, refinement and smoothing, subdivision of components, and mesh painting were utilized to achieve varying degrees of smoothness. Finally, optimized data were obtained and exported as stereolithography (STL) files. An experienced cardiothoracic surgeon validated the anatomical accuracy of the digital model.
The STL files were imported into a 3D printer (J401Pro; Sailner 3D Technology, China) for model printing. This printer can produce full-color medical models using different materials. The models were fabricated using two distinct materials: rigid and flexible. Both materials are suitable for the observational discussion of the teaching objectives outlined in our study. From the perspective of observing pathological changes in the TOF, there is no significant difference between the two materials.
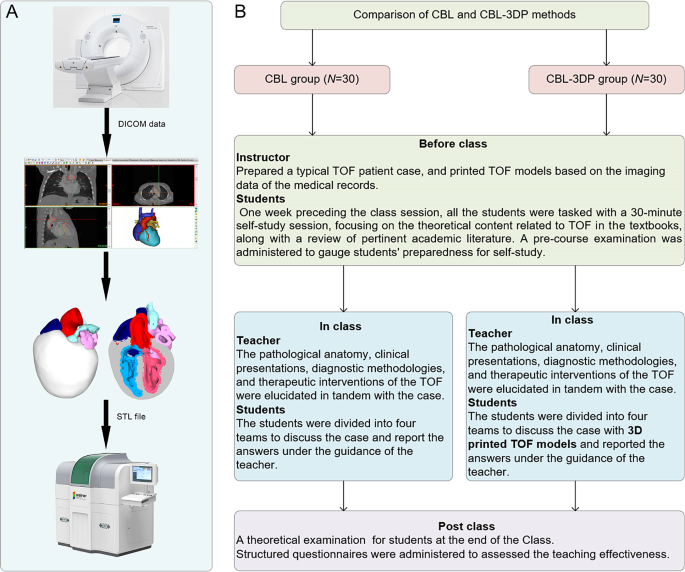
Experimental flow chart of this study. A TOF model printing flow chart. B The instructional framework
Teaching implementation
Figure 1 B illustrates the instructional framework employed in this study. One week preceding the class session, all the students were tasked with a 30-minute self-study session, focusing on the theoretical content related to TOF as outlined in the Pediatrics and Surgery textbooks, along with a review of pertinent academic literature. Both groups received co-supervision from two basic medicine lecturers boasting over a decade of teaching experience, alongside a senior cardiothoracic surgeon. Teaching conditions remained consistent across groups, encompassing uniform assessment criteria and adherence to predefined teaching time frames, all conducted in a Project-Based Learning (PBL) classroom at Wannan Medical College. Additionally, a pre-course examination was administered to gauge students’ preparedness for self-study.
In adherence to the curriculum guidelines, the teaching objectives aimed to empower students to master TOF’s clinical manifestations, diagnostic modalities, and differential diagnoses, while acquainting them with treatment principles and surgical methodologies. Additionally, the objectives sought to cultivate students’ clinical reasoning abilities and problem-solving skills. the duration of instruction for the TOF theory session was standardized to 25 min. The didactic content was integrated with the TOF case study to construct a coherent pedagogical structure.
During the instructional session, both groups underwent teaching utilizing the CBL methodology. Clinical manifestations and case details of TOF cases were presented to stimulate students’ interest and curiosity. Subsequently, the theory of TOF, including its etiology, pathogenesis, pathologic anatomy, clinical manifestations, diagnostic methods, and therapeutic interventions, was briefly elucidated. Emphasis was then placed on the case, wherein selected typical TOF cases were explained, guiding students in analysis and discussion. Students were organized into four teams under the instructors’ supervision, fostering cooperative learning and communication, thereby deepening their understanding of the disease through continuous inquiry and exploration (Fig. 2 L). In the routinely equipped PBL classroom with standard heart models (Fig. 2 J, K), all students had prior exposure to human anatomy and were familiar with these models. Both groups were provided with four standard heart models for reference, while the CBL-3DP group received additional four 3D-printed models depicting TOF anomalies, enriching their learning experience (Fig. 2 D, G). After the lesson, summarization, and feedback sessions were conducted to consolidate group discussions’ outcomes, evaluate teaching effectiveness, and assess learning outcomes.
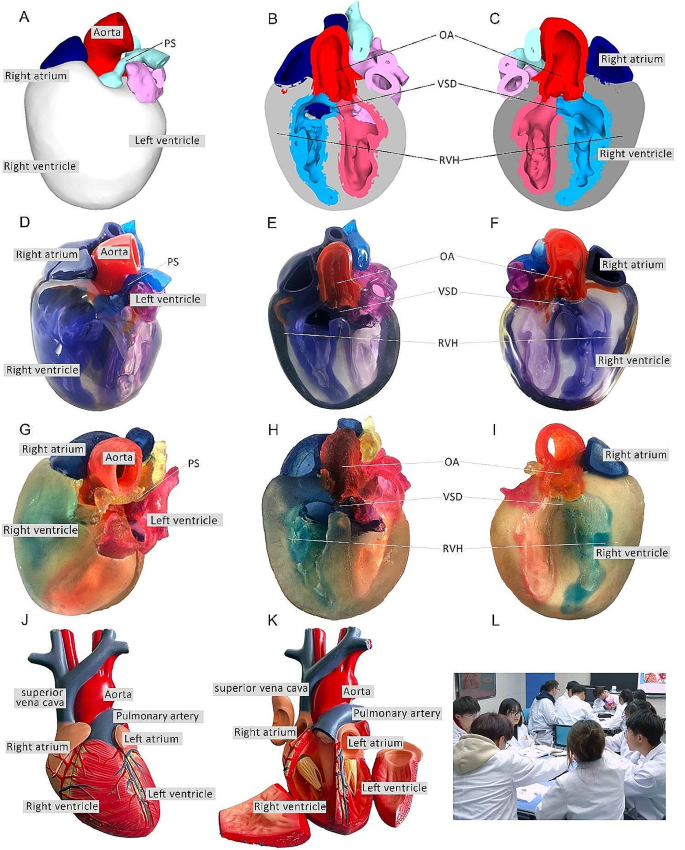
Heart models utilized in instructional sessions. A External perspective of 3D digital models. B, C Cross-sectional views following trans-septal sagittal dissection of the 3D digital model (PS: Pulmonary Stenosis; OA: Overriding Aorta; VSD: Ventricular Septal Defect; RVH: Right Ventricular Hypertrophy). D External depiction of rigid 3D printed model. E, F Sagittal sections of the rigid 3D printed model. G External portrayal of flexible 3D printed model. H, I Sagittal sections of the flexible 3D printed model. J, K The normal heart model employed in the instruction of the CBL group. L Ongoing classroom session
Teaching effectiveness assessment
Following the instructional session, participants from the two groups underwent a theoretical examination to assess their comprehension of the taught material. This assessment covered domains such as pathological anatomy, clinical manifestations, imaging data interpretation, diagnosis, and treatment relevant to TOF. Additionally, structured questionnaires were administered to evaluate the efficacy of the pedagogical approach employed. The questionnaire consisted of six questions designed to gauge participants’ understanding of the teaching content, enhancement of diagnostic skills, cultivation of critical thinking and clinical reasoning abilities, bolstering of confidence in managing TOF cases, satisfaction with the teaching mode, and satisfaction with the CBL methodology.
The questionnaire employed a 5-point Likert scale to gauge responses, with 5 indicating “strongly satisfied/agree,” 4 for “satisfied/agree,” 3 denoting “neutral,” 2 reflecting “dissatisfied/disagree,” and 1 indicating “strongly dissatisfied/disagree.” It comprised six questions, with the initial two probing participants’ knowledge acquisition, questions 3 and 4 exploring satisfaction regarding enhanced competence, and the final two assessing satisfaction with teaching methods and modes. Additionally, participants were encouraged to provide suggestions at the end of the questionnaire. To ensure the questionnaire’s validity, five esteemed lecturers in basic medical sciences with more than 10 years of experience verified its content and assessed its Content Validity Ratio and Content Validity Index to ensure alignment with the study’s objectives.
Statistical analysis
Statistical analyses were conducted utilizing GraphPad Prism 9.0 software. Aggregate score data for both groups were presented as mean ± standard deviation (x ± s). The gender comparisons were analyzed with the chi-square (χ2) test, while the other variables were compared using the Mann-Whitney U test. The threshold for determining statistical significance was set at P < 0.05.

Three-dimensional printing models
After configuring the structural colors of each component (Fig. 2 A, B, C), we printed four color TOF models using both rigid and flexible materials, resulting in four life-sized TOF models. Two color TOF models were created using rigid materials (Fig. 2 D, E, F). These models, exhibiting resistance to deformation, and with a firm texture, smooth and glossy surface, and good transparency, allowing visibility of the internal structures, were deemed conducive to teaching and observation. We also fabricated two color TOF models using flexible materials (Fig. 2 G, H, I), characterized by soft texture, opacity, and deformability, allowing for easy manipulation and cutting. It has potential utility beyond observational purposes. It can serve as a valuable tool for simulating surgical interventions and may be employed to create tomographic anatomical specimens. In this study, both material models were suitable for observation in the classroom. The participants were able to discern the four pathological changes characteristic of TOF from surface examination or cross-sectional analysis.
Baseline characteristics of the students
In total, 60 students were included in this study. The CBL group comprised 30 students (14 males and 16 females), with an average age of (21.20 ± 0.76) years. The CBL-3DP group consisted of 30 students (17 males and 13 females) with an average age of 20.96 years. All the students completed the study procedures. There were no significant differences in age, sex ratio, or pre-class exam scores between the two groups ( P > 0.05), indicating that the baseline scores between the two groups were comparable (Table 1 ).
Theoretical examination results
All students completed the research procedures as planned. The post-class theoretical examination encompassed assessment of pathological anatomy, clinical presentations, imaging data interpretation, diagnosis, and treatment pertinent to TOF. Notably, no statistically significant disparities were observed in the scores on clinical manifestations, diagnosis and treatment components between the cohorts, as delineated in Table 2 . Conversely, discernible distinctions were evident whereby the CBL-3DP group outperformed the CBL group notably in pathological anatomy, imaging data interpretation, and overall aggregate scores ( P < 0.05).
Results of the questionnaires
All the 60 participants submitted the questionnaire. Comparing the CBL and CBL-3DP groups, the scores from the CBL-3DP group showed significant improvements in many areas. This included satisfaction with the teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities (Fig. 3 B, C, D, E). All of which improved significantly ( P < 0.05 for the first aspects and P < 0.01 for the rest). However, the two groups were not comparable ( P > 0.05) in terms of understanding of the teaching content and Satisfaction with the CBL methodology (Fig. 3 A, F).
Upon completion of the questionnaires, participants were invited to proffer recommendations. Notably, in the CBL group, seven students expressed challenges in comprehending TOF and indicated a need for additional time for consolidation to enhance understanding. Conversely, within the CBL-3DP group, twelve students advocated for the augmentation of model repertoire and the expansion of disease-related data collection to bolster pedagogical efficacy across other didactic domains.
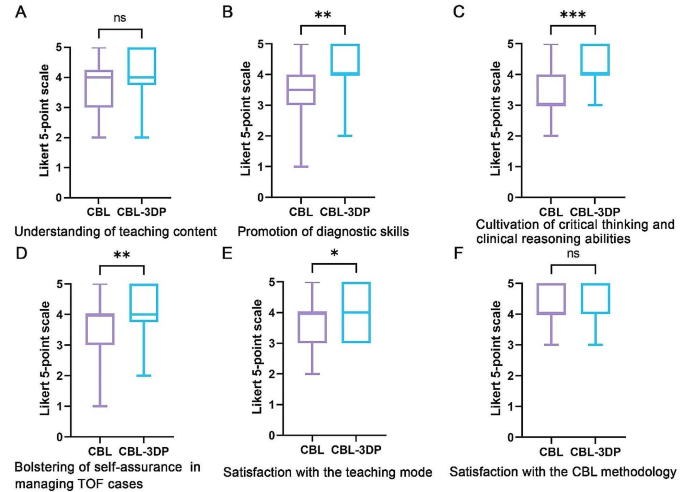
Five-point Likert scores of students’ attitudes in CBL ( n = 30) and CBL-3DP ( n = 30) groups. A Understanding of teaching content. B Promotion of diagnostic skills. C Cultivation of critical thinking and clinical reasoning abilities. D Bolstering of self-assurance in managing TOF cases. E Satisfaction with the teaching mode. F Satisfaction with the CBL methodology. ns No significant difference, * p < 0.05, ** p < 0.01, *** p < 0.001
TOF presents a significant challenge in clinical practice, necessitating a comprehensive understanding for effective diagnosis and treatment [ 12 ]. Traditional teaching methods in medical schools have relied on conventional resources such as textbooks, 2D illustrations, cadaver dissections, and radiographic materials to impart knowledge about complex conditions like TOF [ 13 ]. However, the limitations of these methods in fully engaging students and bridging the gap between theoretical knowledge and practical application have prompted a need for innovative instructional approaches.
CBL has emerged as a valuable tool in medical education, offering students opportunities to engage with authentic clinical cases through group discussions and inquiry-based learning [ 14 ]. By actively involving students in problem-solving and decision-making processes, CBL facilitates the application of theoretical knowledge to real-world scenarios, thus better-preparing students for future clinical practice [ 15 ]. Our investigation revealed that both groups of students exhibited comparable levels of satisfaction with the CBL methodology, devoid of discernible disparities.
CHD presents a formidable challenge due to the intricate nature of anatomical anomalies, the diverse spectrum of conditions, and individual variations [ 16 ]. Utilizing 3D-printed physical models, derived from patient imaging data, can significantly enhance comprehension of complex anatomical structures [ 17 ]. These models have proven invaluable in guiding surgical planning, providing training for junior or inexperienced pediatric residents, and educating healthcare professionals and parents of patients [ 18 ]. Studies indicate that as much as 50% of pediatric surgical decisions can be influenced by the insights gained from 3D printed models [ 19 ]. By providing tangible, anatomically accurate models, 3D printing offers a unique opportunity for people to visualize complex structures and enhance their understanding of anatomical intricacies. Our study utilized full-color, to-scale 3D printed models to illustrate the structural abnormalities associated with TOF, thereby enriching classroom sessions and facilitating a deeper comprehension of the condition.
Comparative analysis between the CBL-3DP group and the CBL group revealed significant improvements in post-test performance, particularly in pathological anatomy and imaging data interpretation. Additionally, questionnaire responses indicated higher levels of satisfaction and confidence among students in the CBL-3DP group, highlighting the positive impact of incorporating 3D printed models into the learning environment, improving the effectiveness of CBL classroom instruction. Despite the merits, our study has limitations. Primarily, participants were exclusively drawn from the same grade level within a single college, possibly engendering bias owing to shared learning backgrounds. Future research could further strengthen these findings by expanding the sample size and including long-term follow-up to assess the retention of knowledge and skills. Additionally, the influence of the 3D models depicting a normal heart on the learning process and its potential to introduce bias into the results warrants consideration, highlighting a need for scrutiny in subsequent studies.
As medical science continues to advance, the need for effective teaching methods becomes increasingly paramount. Our study underscores the potential of combining active learning approaches like CBL with innovative technologies such as 3D printing to enhance teaching effectiveness, improve knowledge acquisition, and foster students’ confidence and enthusiasm in pursuing clinical careers. Moving forward, further research and integration of such methodologies are essential for meeting the evolving demands of medical education, especially in areas involving complex anatomical understanding.
Conclusions
Integrating 3D-printed models with the CBL method is feasible and effective in TOF instruction. The demonstrated success of this method warrants broad implementation in medical education, particularly for complex anatomical topics.
Data availability
All data supporting the conclusions of this research are available upon reasonable request from the corresponding author.
Apitz C, Webb GD, Redington AN. Tetralogy of Fallot. Lancet. 2009;374:1462–71.
Article Google Scholar
Ghosh RM, Jolley MA, Mascio CE, Chen JM, Fuller S, Rome JJ, et al. Clinical 3D modeling to guide pediatric cardiothoracic surgery and intervention using 3D printed anatomic models, computer aided design and virtual reality. 3D Print Med. 2022;8:11.
Chakrabarti R, Wardle K, Wright T, Bennie T, Gishen F. Approaching an undergraduate medical curriculum map: challenges and expectations. BMC Med Educ. 2021;21:341.
Donkin R, Yule H, Fyfe T. Online case-based learning in medical education: a scoping review. BMC Med Educ. 2023;23:564.
Novack JP. Designing cases for case-based immunology teaching in large medical school classes. Front Immunol. 2020;11:995.
Chen HC, Van Den Broek WES, Ten Cate O. The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90:431–6.
Wang M, Sun Z, Jia M, Wang Y, Wang H, Zhu X, et al. Intelligent virtual case learning system based on real medical records and natural language processing. BMC Med Inf Decis Mak. 2022;22:60.
Yoo S-J, Thabit O, Kim EK, Ide H, Yim D, Dragulescu A, et al. 3D printing in medicine of congenital heart diseases. 3D Print Med. 2015;2:3.
Yammine K, Violato C. A meta-analysis of the educational effectiveness of three-dimensional visualization technologies in teaching anatomy. Anat Sci Educ. 2015;8:525–38.
Miao H, Ding J, Gong X, Zhao J, Li H, Xiong K, et al. Application of 3D-printed pulmonary segment specimens in experimental teaching of sectional anatomy. BMC Surg. 2023;23:109.
Sun Z, Wong YH, Yeong CH. Patient-specific 3D-printed low-cost models in medical education and clinical practice. Micromachines (Basel). 2023;14:464.
Downing TE, Kim YY. Tetralogy of Fallot: general principles of management. Cardiol Clin. 2015;33:531–41. vii–viii.
Jia X, Zeng W, Zhang Q. Combined administration of problem- and lecture-based learning teaching models in medical education in China: a meta-analysis of randomized controlled trials. Med (Baltim). 2018;97:e11366.
McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3:JMECD.S20377.
Zeng N, Lu H, Li S, Yang Q, Liu F, Pan H, et al. Application of the combination of CBL teaching method and SEGUE framework to improve the doctor-patient communication skills of resident physicians in otolaryngology department. Bmc Med Educ. 2024;24:201.
Sun Z. Patient-specific 3D-printed models in pediatric congenital heart disease. Children. 2023;10:319.
Meyer-Szary J, Luis MS, Mikulski S, Patel A, Schulz F, Tretiakow D, et al. The role of 3D printing in planning complex medical procedures and training of medical professionals—cross-sectional multispecialty review. IJERPH. 2022;19:3331.
Sun Z, Wee C. 3D printed models in cardiovascular disease: an exciting future to deliver personalized medicine. Micromachines-basel. 2022;13:1575.
Valverde I, Gomez-Ciriza G, Hussain T, Suarez-Mejias C, Velasco-Forte MN, Byrne N, et al. Three-dimensional printed models for surgical planning of complex congenital heart defects: an international multicentre study. Eur J Cardio-thorac. 2017;52:1139–48.
Download references
Acknowledgements
We extend our sincere appreciation to the instructors and students whose invaluable participated in this study.
This paper received support from the Education Department of Anhui Province, China (Grant Numbers 2022jyxm1693, 2022jyxm1694, 2022xskc103, 2018jyxm1280).
Author information
Jian Zhao and Xin Gong are joint first authors.
Authors and Affiliations
Department of Human Anatomy, Wannan Medical College, No.22 West Wenchang Road, Wuhu, 241002, China
Jian Zhao, Xin Gong, Jian Ding, Rui Huang & Huachun Miao
Department of Cardio-Thoracic Surgery, Yijishan Hospital of Wannan Medical College, Wuhu, China
Kepin Xiong
Zhuhai Sailner 3D Technology Co., Ltd., Zhuhai, China
Kangle Zhuang
School of Basic Medical Sciences, Wannan Medical College, Wuhu, China
You can also search for this author in PubMed Google Scholar
Contributions
Jian Zhao and Huachun Miao designed the research. Jian Zhao, Xin Gong, Jian Ding, Kepin Xiong designed the tests and questionnaires. Kangle Zhuang processed the imaging data and printed the models. Xing Gong and Kepin Xiong implemented the teaching. Jian Zhao and Rui Huang collected the data and performed the statistical analysis. Jian Zhao and Huachun Miao prepared the manuscript. Shu Li and Huachun Miao revised the manuscript. Shu Li provided the Funding acquisition. All authors reviewed and approved the final manuscript.
Corresponding authors
Correspondence to Shu Li or Huachun Miao .
Ethics declarations
Ethics approval and consent to participate.
This investigation received ethical approval from the Ethical Committee of School of Basic Medical Sciences, Wannan Medical College (ECBMSWMC2022-1-12). All methodologies adhered strictly to established protocols and guidelines. Written informed consent was obtained from the study participants to take part in the study.
Consent for publication
Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhao, J., Gong, X., Ding, J. et al. Integration of case-based learning and three-dimensional printing for tetralogy of fallot instruction in clinical medical undergraduates: a randomized controlled trial. BMC Med Educ 24 , 571 (2024). https://doi.org/10.1186/s12909-024-05583-z
Download citation
Received : 03 March 2024
Accepted : 21 May 2024
Published : 24 May 2024
DOI : https://doi.org/10.1186/s12909-024-05583-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Case-based learning
- 3D printing
- Tetralogy of fallot
- Medical undergraduates
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Critical Thinking
Ai generator.
In today’s dynamic and fast-paced world, critical thinking stands out as an essential competency, seamlessly bridging the gap between soft and hard skills . As we navigate complex challenges and make informed decisions, the ability to think critically enhances our overall skill set. Critical thinking stands at the core of effective decision-making and problem-solving in today’s complex world. It involves analyzing information, evaluating evidence, and considering multiple perspectives to make informed judgments. In a society flooded with information, the ability to think critically ensures that individuals can distinguish between credible sources and misinformation. It empowers people to approach challenges logically and creatively, fostering innovation and resilience. By honing critical thinking skills, individuals enhance their capacity to navigate personal and professional landscapes with clarity and confidence.
What is Critical Thinking?
Critical thinking is the process of actively and skillfully analyzing, evaluating, and synthesizing information gathered from various sources, including observations , experiences, and communication. It involves using logic and reasoning to identify connections, draw conclusions, and make informed decisions, while remaining open-minded and aware of potential biases.
Critical Thinking Examples
- Analyzing News Reports : Evaluating the credibility of sources, checking for biases, and verifying facts before accepting news stories as true.
- Problem-Solving in the Workplace : Identifying the root cause of a problem, considering multiple solutions, and weighing the pros and cons before deciding on the best course of action.
- Scientific Research : Formulating hypotheses, designing experiments to test them, analyzing data objectively, and drawing conclusions based on evidence.
- Budgeting : Assessing income and expenses, prioritizing spending, and making informed decisions to stay within budget while saving for future needs.
- Reading Literature : Interpreting themes, symbols, and character motivations in a novel or poem, and considering how they relate to broader societal issues.
- Debating : Constructing logical arguments, anticipating counterarguments, and using evidence to support one’s position while also listening to and understanding opposing views.
- Medical Diagnosis : Doctors evaluating symptoms, considering possible conditions, ordering tests, and interpreting results to make accurate diagnoses and treatment plans.
- Educational Assessment : Teachers designing fair and effective assessments that measure student understanding and skills, and using the results to improve teaching strategies.
- Ethical Decision-Making : Weighing the moral implications of actions, considering the impact on stakeholders, and making choices that align with ethical principles.
- Legal Analysis : Lawyers analyzing case law, statutes, and evidence to build strong legal arguments and anticipate the strategies of opposing counsel.
- Marketing Strategy : Analyzing market trends, customer needs, and competitor actions to develop effective marketing campaigns that resonate with target audiences.
- Programming : Writing efficient code by understanding the problem, breaking it into smaller parts, and testing and debugging to ensure it works correctly.
- Urban Planning : Evaluating the needs of a community, considering environmental impact, and planning sustainable and functional urban spaces.
- Historical Analysis : Examining historical events, considering the context, and understanding the causes and effects while avoiding presentism (judging the past by today’s standards).
- Personal Decision-Making : Weighing the benefits and drawbacks of significant life choices, such as career changes or moving to a new city, and making decisions based on careful consideration and long-term goals.
For Students
- Activity : Organize debates on current events or controversial topics.
- Example : Have students debate the pros and cons of renewable energy sources versus fossil fuels.
- Activity : Present students with complex problems to solve in groups.
- Example : Task students with designing a plan to reduce plastic waste in their school.
- Activity : Analyze case studies relevant to their subjects.
- Example : In a business class, analyze a company’s decision-making process during a crisis.
- Activity : Conduct Socratic seminars where students discuss philosophical or ethical questions.
- Example : Discuss the ethical implications of artificial intelligence in society.
- Activity : Facilitate brainstorming sessions to generate creative solutions to problems.
- Example : Brainstorm ideas for a community service project to help local residents.
- Activity : Assign research projects requiring critical analysis of sources.
- Example : Research the impact of social media on teenage mental health and present findings.
- Activity : Engage students in role-playing exercises to explore different perspectives.
- Example : Role-play a historical event, with each student taking on the role of a key figure.
- Activity : Use logic puzzles and games to develop reasoning skills.
- Example : Solve Sudoku puzzles or play strategy games like chess.
- Activity : Encourage students to write reflectively about their learning experiences.
- Example : Write an essay on how their views on a topic have changed after a class discussion.
- Activity : Analyze the techniques used in advertisements to influence consumers.
- Example : Evaluate an advertisement’s claims and discuss the strategies used to persuade the audience.
In the Workplace
- Problem Solving : Analyzing the root cause of a recurring issue in production and developing a sustainable solution.
- Decision Making : Evaluating the pros and cons of two potential suppliers based on cost, quality, and reliability.
- Strategic Planning : Assessing market trends to develop a new product line that meets future consumer demands.
- Conflict Resolution : Mediating a disagreement between team members by understanding both perspectives and finding common ground.
- Process Improvement : Reviewing workflow inefficiencies and implementing new procedures to increase productivity.
- Risk Management : Identifying potential risks in a project and devising strategies to mitigate them.
- Customer Service : Addressing a customer complaint by understanding the underlying issue and providing a satisfactory resolution.
- Innovation : Brainstorming and evaluating new ideas for improving a product or service.
- Performance Evaluation : Analyzing employee performance data to provide constructive feedback and development plans.
- Budgeting : Reviewing and adjusting the department budget to ensure financial efficiency without compromising quality.
In the Classroom
- Critical Reading : Analyzing a text to understand the author’s argument, purpose, and use of evidence.
- Scientific Inquiry : Designing and conducting experiments to test hypotheses and draw conclusions based on data.
- Mathematical Problem Solving : Applying logical reasoning to solve complex math problems and explaining the solution process.
- Historical Analysis : Evaluating historical events and their impact from multiple perspectives.
- Debate : Constructing and defending arguments on various topics using evidence and reasoning.
- Project-Based Learning : Developing a research project by identifying a problem, gathering information, and presenting findings.
- Creative Writing : Critiquing peers’ work to provide constructive feedback and suggestions for improvement.
- Ethical Dilemmas : Discussing moral questions and justifying decisions based on ethical principles.
- Literary Analysis : Interpreting themes, symbols, and character development in literature.
- Collaborative Learning : Working in groups to solve problems, share ideas, and reach consensus.
In Everyday Life
- Financial Planning : Creating a budget to manage expenses, savings, and investments.
- Nutrition and Health : Analyzing dietary choices to improve overall health and wellness.
- Time Management : Prioritizing tasks and activities to make efficient use of time.
- Consumer Decisions : Comparing product reviews and prices before making a purchase.
- Home Maintenance : Troubleshooting and fixing household issues, such as plumbing or electrical problems.
- Travel Planning : Researching destinations, comparing travel options, and creating itineraries.
- Parenting : Making informed decisions about children’s education, health, and activities.
- Conflict Resolution : Resolving disputes with family or friends by understanding different viewpoints and finding compromises.
- Personal Development : Setting and pursuing personal goals, such as learning a new skill or improving fitness.
- Community Involvement : Analyzing community issues and participating in local initiatives to address them.
In Healthcare
- Diagnosis : Interpreting patient symptoms and medical history to diagnose conditions accurately.
- Treatment Planning : Developing individualized treatment plans based on patient needs and evidence-based practices.
- Ethical Decision-Making : Addressing ethical dilemmas in patient care, such as end-of-life decisions.
- Patient Communication : Explaining complex medical information to patients and families clearly and compassionately.
- Interdisciplinary Collaboration : Working with other healthcare professionals to provide comprehensive care.
- Medical Research : Designing and conducting research studies to advance medical knowledge and treatments.
- Healthcare Policy Analysis : Evaluating healthcare policies and their impact on patient care and outcomes.
- Clinical Judgment : Assessing and prioritizing patient care needs in emergency situations.
- Quality Improvement : Implementing strategies to improve patient safety and care quality.
- Continuing Education : Staying updated on medical advancements and integrating new knowledge into practice.
In Business
- Market Analysis : Evaluating market trends and consumer behavior to make informed business decisions.
- Strategic Planning : Developing long-term goals and strategies to achieve business objectives.
- Financial Management : Analyzing financial statements to make sound investment and budgeting decisions.
- Risk Assessment : Identifying and mitigating potential business risks.
- Negotiation : Using persuasive arguments and data to negotiate contracts and deals.
- Product Development : Assessing customer needs and market gaps to create new products.
- Customer Feedback Analysis : Collecting and analyzing customer feedback to improve products and services.
- Supply Chain Management : Optimizing supply chain processes to reduce costs and increase efficiency.
- Leadership : Making decisions that motivate and guide employees toward achieving company goals.
- Corporate Social Responsibility : Evaluating the social and environmental impact of business practices and implementing sustainable strategies.
- Research Projects : Conducting independent research, analyzing data, and presenting findings.
- Critical Essays : Writing essays that critically analyze texts, arguments, and ideas.
- Group Projects : Collaborating with classmates to complete assignments and solve problems.
- Class Discussions : Participating in discussions by presenting well-reasoned arguments and listening to others.
- Case Studies : Analyzing real-world scenarios to understand complex issues and propose solutions.
- Exam Preparation : Developing study plans and strategies to prepare for exams effectively.
- Internships : Applying classroom knowledge to real-world situations during internships and reflecting on experiences.
- Time Management : Balancing academic, social, and personal responsibilities.
- Library Research : Using library resources to find credible sources for research papers.
- Extracurricular Activities : Engaging in activities that develop leadership, teamwork, and problem-solving skills.
Critical Thinking scenarios
Here are some critical thinking scenarios along with questions and answers to help you practice and enhance your critical thinking skills:
Scenario 1: Workplace Conflict
Scenario: You are a manager at a company. Two of your team members, John and Lisa, have been having frequent disagreements. These conflicts are starting to affect the team’s productivity and morale.
- What steps would you take to address the conflict between John and Lisa?
- How would you ensure that the resolution is fair and satisfactory for both parties?
- What strategies would you implement to prevent similar conflicts in the future?
- Schedule a private meeting with John and Lisa to discuss the issue.
- Listen to both sides without taking sides to understand the root cause of the conflict.
- Facilitate a mediation session where both parties can express their concerns and work towards a resolution.
- Agree on specific actions that both parties will take to avoid future conflicts.
- Ensure that both John and Lisa feel heard and respected during the mediation process.
- Identify common ground and mutual interests to build a foundation for resolution.
- Set clear expectations and follow-up actions for both parties.
- Monitor the situation and provide support to ensure the conflict does not resurface.
- Foster an open and inclusive team culture where concerns can be raised early.
- Provide regular team-building activities to strengthen relationships.
- Implement conflict resolution training for all team members.
- Establish clear communication channels and protocols for addressing grievances.
Scenario 2: Ethical Dilemma
Scenario: You are a journalist working on a high-profile story. You discover that one of your sources has provided you with information that could harm their reputation if published. However, this information is crucial to your story and serves the public interest.
- What factors would you consider before deciding whether to publish the information?
- How would you balance the public interest with the potential harm to your source?
- What steps would you take to verify the accuracy of the information before publication?
- The significance of the information to the public interest.
- The potential consequences for the source if the information is published.
- The ethical guidelines and professional standards of journalism.
- Any possible legal implications of publishing the information.
- Evaluate whether the public’s right to know outweighs the potential harm to the source.
- Consider anonymizing the source or redacting sensitive details to protect their identity.
- Seek advice from colleagues or an ethics committee to make an informed decision.
- Cross-check the information with other reliable sources.
- Review any documentation or evidence provided by the source.
- Conduct interviews with other individuals who can corroborate the information.
- Ensure that the information is presented in context to avoid misrepresentation.
Scenario 3: Environmental Impact
Scenario: Your company is planning to build a new factory in a rural area. This project promises economic growth and job creation but also raises concerns about environmental impact and the displacement of local wildlife.
- What are the potential environmental impacts of the new factory?
- How would you address the concerns of the local community and environmental groups?
- What measures would you implement to minimize the environmental impact of the factory?
- Air and water pollution from factory emissions and waste.
- Habitat destruction and displacement of local wildlife.
- Increased traffic and noise pollution in the area.
- Strain on local resources such as water and energy.
- Organize community meetings to discuss the project and listen to concerns.
- Collaborate with environmental groups to assess the impact and find solutions.
- Provide transparent information about the factory’s operations and mitigation plans.
- Offer compensation or relocation assistance to affected residents if necessary.
- Implement eco-friendly technologies and practices to reduce emissions and waste.
- Develop a comprehensive environmental management plan.
- Create buffer zones and wildlife corridors to protect local habitats.
- Invest in renewable energy sources to power the factory.
- Improved Problem Solving: Critical thinking helps in analyzing problems systematically and making better decisions.
- Enhanced Communication: It allows for clear expression and understanding of ideas.
- Better Decision Making: Critical thinking leads to more informed and logical choices.
- Adaptability: It enables individuals to adapt to new situations and challenges effectively.
- Informed Opinions: Critical thinkers can form well-grounded opinions and defend them logically.
What are the critical thinking skills?
- Analysis: Breaking down complex information into smaller parts to understand it better.
- Interpretation: Understanding and explaining the meaning of information or an event.
- Inference: Drawing logical conclusions from available information.
- Evaluation: Assessing the credibility and relevance of information and arguments.
- Explanation: Clearly and concisely articulating your reasoning and evidence.
- Self-Regulation: Reflecting on and adjusting one’s own thought processes and biases.
Concepts of critical thinking
- Clarity: Ensuring that the information and arguments are clear and understandable.
- Accuracy: Ensuring that information is true and free from errors.
- Precision: Providing enough detail to understand the specific context.
- Relevance: Ensuring that information and arguments are directly related to the issue at hand.
- Depth: Addressing the complexities and underlying factors of an issue.
- Breadth: Considering different perspectives and alternatives.
- Logic: Ensuring that the reasoning is coherent and follows a logical sequence.
- Fairness: Being open-minded and impartial in evaluating information and arguments.
- Identify the Problem or Question: Clearly define what you are trying to solve or understand.
- Gather Information: Collect relevant data, evidence, and viewpoints.
- Analyze the Information: Break down the information to understand the relationships and implications.
- Evaluate the Evidence: Assess the quality, credibility, and relevance of the evidence.
- Formulate Conclusions: Draw reasoned conclusions based on the analysis and evaluation.
- Communicate the Conclusion: Clearly express your findings and reasoning.
- Reflect and Reassess: Continuously reflect on the process and outcomes to improve your critical thinking skills.
Basics of critical thinking
- Open-Mindedness: Being willing to consider new ideas and perspectives.
- Curiosity: Having a strong desire to learn and understand.
- Skepticism: Questioning the validity of information and not taking things at face value.
- Objectivity: Striving to remain unbiased and impartial.
- Rationality: Basing decisions on logical reasoning rather than emotions.
- Socratic Questioning: Asking a series of probing questions to explore complex ideas and uncover underlying assumptions.
- Mind Mapping: Visually organizing information to see connections and relationships.
- Brainstorming: Generating a wide range of ideas and solutions without immediate judgment.
- Role Playing: Considering different perspectives by imagining oneself in another person’s position.
- SWOT Analysis: Evaluating the strengths, weaknesses, opportunities, and threats related to a particular situation or decision.
- Thought Experiments: Imagining hypothetical scenarios to explore potential outcomes and implications.
How to Practice and Use Critical Thinking
The critical thinking process incorporates various other logical soft skills that will help you analyze and interpret all the information to create an informed decision. These soft skills include observational skills, problem-solving, communication skills, and analytical thinking. If you sharpen all of these elements and characteristics you will inadvertently enhance your critical thinking.
Step 1: Practice One’s Observational and Perception Skills
We use our senses to perceive the world around us, whether it would be sight, smell, a, and sensations. One should practice utilizing these senses to create logical inferences and deductions that will help out brain unconsciously absorb and analyze these types of information. The more one practices their senses the better their thinking process will be.
Step 2: Enhance One’s Problem-Solving Skills
Logic and problem-solving allow the person to deduce and connect information that the environment or circumstance presents to the said person. You need to practice your problem-solving skills via puzzles, logical reasoning tests, and ethical dilemmas. Practicing one’s problem-solving skills will allow the person to efficiently establish cause-and-effect reasoning or properly create logical decisions.
Step 3: Prepare and Practice One’s Communication Skills
Communication is a pivotal skill we often use when interacting with other people. This type of skill includes body language , assertive communication , concise language, and other communication skills. In critical thinking, a person must be able to properly communicate their thoughts and thinking process to other people, which will create a collaborative environment. Other times, the perfect solution might not be present without the need for communication.
Step 4: Practice Analysis of the Situation
One’s analytical thinking skills allow the person to take note of various elements and characteristics of the situation and analyze these elements’ contribution to the current situation or circumstance. You need to practice your analytical thinking to properly process the current situation or circumstance you find yourself in.
Why Do Employers Value Critical Thinking Skills?
Employers value critical thinking skills because they enable employees to analyze situations, make informed decisions, and solve problems effectively. Critical thinkers can evaluate information from various sources, identify logical connections, and foresee potential consequences, which leads to better strategic planning and innovation. These skills also enhance communication and collaboration, as critical thinkers can present their ideas clearly and consider different perspectives. Ultimately, critical thinking contributes to improved productivity, adaptability, and competitiveness in the workplace.
What is critical thinking?
Critical thinking involves analyzing and evaluating information to make reasoned, logical decisions, and judgments. It emphasizes evidence-based reasoning and problem-solving.
Why is critical thinking important?
Critical thinking enhances decision-making, problem-solving, and the ability to analyze complex situations. It is crucial for personal and professional growth.
How can I improve my critical thinking skills?
Improve critical thinking by questioning assumptions, seeking diverse perspectives, practicing problem-solving, and engaging in reflective thinking regularly.
What are the key components of critical thinking?
Key components include analysis, evaluation, inference, explanation, and self-regulation. These skills help in understanding and assessing arguments and evidence.
How does critical thinking benefit students?
Students benefit from critical thinking by improving academic performance, enhancing research skills, and fostering independent thinking and creativity.
What role does critical thinking play in the workplace?
In the workplace, critical thinking aids in decision-making, innovation, conflict resolution, and improving productivity and efficiency.
Can critical thinking be taught?
Yes, critical thinking can be taught through targeted educational programs, exercises, and practice that focus on developing analytical and evaluative skills.
What is an example of critical thinking in everyday life?
An example is evaluating news sources for credibility before accepting information as true. This involves analyzing evidence and assessing biases.
How does critical thinking relate to problem-solving?
Critical thinking is integral to problem-solving as it involves analyzing the problem, evaluating options, and making reasoned decisions based on evidence.
What are common barriers to critical thinking?
Common barriers include cognitive biases, emotional influences, lack of relevant information, and social pressures. Overcoming these requires awareness and deliberate practice.
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting

IMAGES
VIDEO
COMMENTS
Improving clinical reasoning techniques is the right way to facilitate decision-making from prognostic, diagnostic, and therapeutic points of view. However, the process to do that is to fill knowledge gaps by studying and growing experience and knowing some cognitive aspects to raise the awareness of thinking mechanisms to avoid cognitive ...
Critical thinking underlies independent and interdependent decision making. Critical thinking includes questioning, analysis, synthesis, interpretation, inference, inductive and deductive reasoning, intuition, application, and creativity 8 (p. 9). Course work or ethical experiences should provide the graduate with the knowledge and skills to:
Clinical reasoning is a multi-faceted and complex construct, the understanding of which has emerged from multiple fields outside of healthcare literature, primarily the psychological and behavioural sciences. ... Advanced practice: critical thinking and clinical reasoning Br J Nurs. 2021 May 13;30(9):526-532. doi: 10.12968/bjon.2021.30.9.526 ...
During the search, the terms clinical reasoning, critical thinking, and clinical judgement were used interchangeably since clinical judgement is part of clinical reasoning and is defined by the decision to act. ... Still, it is necessary to add another teaching method to increase the efficacy of clinical simulations. Therefore, nursing schools ...
Clinical reasoning is a complex process in which one identifies and prioritizes pertinent clinical data to develop a hypothesis and a plan to confirm or refute that hypothesis. Clinical reasoning is related to and dependent on critical thinking skills, which are defined as one's capacity to engage in higher cognitive skills such as analysis ...
Critical thinking is a general reasoning process that informs a discipline and context-specific clinical reasoning process, and both are used in the complex process of clinical judgment (Bowles, 2000; Klenke-Borgmann et al., 2020; Victor-Chmil, 2013). For example, critical thinking informs our common day-to-day decision-making, such as ...
After completing this chapter, you should be able to: 1. Describe critical thinking (CT), clinical reasoning, and clinical judgment in your own words, based on the descriptions in this chapter. 2. Give at least three reasons why CT skills are essential for stu- dents and nurses. 3.
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting.
critical thinking, clinical reasoning, and clinical decision-making. In the purest form, health profession educators are referencing the cognitive abilities of a clinician to transfer thinking skills from an academic to a clinical setting. The problem with teaching clinical reasoning in health professions is that the ability to transfer knowledge and skill to patient care is often inefficient ...
Critical thinking skills are necessary to engage in effective patient care in the ICU, and clinicians and educators can help learners develop their reasoning skills by emphasizing the role of inductive reasoning in clinical practice, asking effective questions (using "how" and "why'), acknowledging the impact of cognitive biases in ...
In nursing, the concepts of critical thinking, clinical reasoning, and clinical judgment are typically interrelated sets of processes that are important for the nursing process (Victor-Chmil, Citation 2013). Young et al. (Citation 2020) conducted a qualitative analysis of the literature to identify terms describing clinical reasoning. They ...
Here are five ways to nurture your critical-thinking skills: Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice. That knowledge helps you make informed decisions in stressful moments. Practice reflection.
Teaching clinical reasoning is challenging, particularly in the time-pressured and complicated environment of the ICU. Clinical reasoning is a complex process in which one identifies and prioritizes pertinent clinical data to develop a hypothesis and a plan to confirm or refute that hypothesis. Clinical reasoning is related to and dependent on critical thinking skills, which are defined as one ...
This literature review will present a history of inquiry into critical thinking and research to support the conclusion that critical thinking is necessary not only in the clinical practice setting, but also as an integral component of nursing-education programmes to promote the development of nurses' critical-thinking abilities.
This review intends to reveal the current status of the instructional practices used to enhance Critical Thinking (CrT), Clinical Reasoning and Clinical Judgement (CJ) skills and dispositions in Health Sciences Higher Education programmes. After a three-step filtering process, 28 empirical studies on the effectiveness of the instructional ...
We examine the literature that questions the benefits of teaching clinical reasoning skills to increase diagnostic accuracy, and we identify methodological problems with those studies. ... Learners should be encouraged to understand the role of all these processes to mature and develop their critical thinking and clinical reasoning skills.
Abstract. Clinical reasoning is a complex cognitive process that is essential to evaluate and manage a patient's medical problem. The aim of this paper was to provide a critical review of the research literature on clinical reasoning theories and models. To conduct our study, we applied the process of conducting a literature review in four ...
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood ...
Clinical reasoning differs slightly from critical thinking. Clinical reasoning is the systematic process by which nurses collect and use clinical information to form nursing judgements (Liaw et al., 2018). Therefore, clinical reasoning is a prerequisite for developing critical thinking (Liaw et al., 2018).
Abstract. Physiotherapists require clinical reasoning and critical thinking skills in order to perform as effective, first-line practitioners. Concept maps were incorporated into an existing ...
In recent decades, approaches to critical thinking have generally taken a practical turn, pivoting away from more abstract accounts - such as emphasizing the logical relations that hold between statements (Ennis, 1964) - and moving toward an emphasis on belief and action.According to the definition that Robert Ennis (2018) has been advocating for the last few decades, critical thinking is ...
CBS is used to increase clinical judgment, critical thinking skills, and clinical reasoning in onsite and online educational settings. Learners assess the scenario and then using their own experiences, they then analyze the provided cues, implement prioritization, accurately find solutions, and take immediate action.
Define the construct of interest. Clearly defining a construct is essential to assessment development and validation [20, 23].When considering a broad concept like clinical reasoning, it is important that authors provide an explicit definition of clinical reasoning (or synonym) or a clear description of the target construct used in their assessment.
Clinical reasoning is a complex, evolving, non-linear, context-driven, and content-specific construct which arguably cannot be assessed at one point in time or with a single method. ... and increase in learners' agency. Repeated exposure and measurement are critical to develop a clinical reasoning assessment narrative, thus the assessment ...
The present study has been planned to assess the critical thinking disposition and clinical reasoning skills among medical undergraduate students in a medical college in West Bengal, India. The perceived definition and attributes of critical thinking in medical education will be explored and the contexts where application of critical thinking ...
Comparing the CBL and CBL-3DP groups, the scores from the CBL-3DP group showed significant improvements in many areas. This included satisfaction with the teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities (Fig. 3B, C, D
In today's dynamic and fast-paced world, critical thinking stands out as an essential competency, seamlessly bridging the gap between soft and hard skills.As we navigate complex challenges and make informed decisions, the ability to think critically enhances our overall skill set. Critical thinking stands at the core of effective decision-making and problem-solving in today's complex world.