An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection


The coronavirus ( COVID ‐19) pandemic's impact on mental health
Bilal javed.
1 Faculty of Sciences, PMAS Arid Agriculture University, Rawalpindi Pakistan
2 Roy & Diana Vagelos Laboratories, Department of Chemistry, University of Pennsylvania, Philadelphia Pennsylvania, USA
Abdullah Sarwer
3 Nawaz Sharif Medical College, University of Gujrat, Gujrat Pakistan
4 Department of General Medicine, Allama Iqbal Memorial Teaching Hospital, Sialkot Pakistan
Erik B. Soto
5 Graduate School of Public Health, University of Pittsburgh, Pittsburgh Pennsylvania, USA
Zia‐ur‐Rehman Mashwani
Throughout the world, the public is being informed about the physical effects of SARS‐CoV‐2 infection and steps to take to prevent exposure to the coronavirus and manage symptoms of COVID‐19 if they appear. However, the effects of this pandemic on one's mental health have not been studied at length and are still not known. As all efforts are focused on understanding the epidemiology, clinical features, transmission patterns, and management of the COVID‐19 outbreak, there has been very little concern expressed over the effects on one's mental health and on strategies to prevent stigmatization. People's behavior may greatly affect the pandemic's dynamic by altering the severity, transmission, disease flow, and repercussions. The present situation requires raising awareness in public, which can be helpful to deal with this calamity. This perspective article provides a detailed overview of the effects of the COVID‐19 outbreak on the mental health of people.
1. INTRODUCTION
A pandemic is not just a medical phenomenon; it affects individuals and society and causes disruption, anxiety, stress, stigma, and xenophobia. The behavior of an individual as a unit of society or a community has marked effects on the dynamics of a pandemic that involves the level of severity, degree of flow, and aftereffects. 1 Rapid human‐to‐human transmission of the SARS‐CoV‐2 resulted in the enforcement of regional lockdowns to stem the further spread of the disease. Isolation, social distancing, and closure of educational institutes, workplaces, and entertainment venues consigned people to stay in their homes to help break the chain of transmission. 2 However, the restrictive measures undoubtedly have affected the social and mental health of individuals from across the board. 3
As more and more people are forced to stay at home in self‐isolation to prevent the further flow of the pathogen at the societal level, governments must take the necessary measures to provide mental health support as prescribed by the experts. Professor Tiago Correia highlighted in his editorial as the health systems worldwide are assembling exclusively to fight the COVID‐19 outbreak, which can drastically affect the management of other diseases including mental health, which usually exacerbates during the pandemic. 4 The psychological state of an individual that contributes toward the community health varies from person‐to‐person and depends on his background and professional and social standings. 5
Quarantine and self‐isolation can most likely cause a negative impact on one's mental health. A review published in The Lancet said that the separation from loved ones, loss of freedom, boredom, and uncertainty can cause a deterioration in an individual's mental health status. 6 To overcome this, measures at the individual and societal levels are required. Under the current global situation, both children and adults are experiencing a mix of emotions. They can be placed in a situation or an environment that may be new and can be potentially damaging to their health. 7
2. CHILDREN AND TEENS AT RISK
Children, away from their school, friends, and colleagues, staying at home can have many questions about the outbreak and they look toward their parents or caregivers to get the answer. Not all children and parents respond to stress in the same way. Kids can experience anxiety, distress, social isolation, and an abusive environment that can have short‐ or long‐term effects on their mental health. Some common changes in children's behavior can be 8 :
- Excessive crying and annoying behavior
- Increased sadness, depression, or worry
- Difficulties with concentration and attention
- Changes in, or avoiding, activities that they enjoyed in the past
- Unexpected headaches and pain throughout their bodies
- Changes in eating habits
To help offset negative behaviors, requires parents to remain calm, deal with the situation wisely, and answer all of the child's questions to the best of their abilities. Parents can take some time to talk to their children about the COVID‐19 outbreak and share some positive facts, figures, and information. Parents can help to reassure them that they are safe at home and encourage them to engage in some healthy activities including indoor sports and some physical and mental exercises. Parents can also develop a home schedule that can help their children to keep up with their studies. Parents should show less stress or anxiety at their home as children perceive and feel negative energy from their parents. The involvement of parents in healthy activities with their children can help to reduce stress and anxiety and bring relief to the overall situation. 9
3. ELDERS AND PEOPLE WITH DISABILITIES AT RISK
Elderly people are more prone to the COVID‐19 outbreak due to both clinical and social reasons such as having a weaker immune system or other underlying health conditions and distancing from their families and friends due to their busy schedules. According to medical experts, people aged 60 or above are more likely to get the SARS‐CoV‐2 and can develop a serious and life‐threatening condition even if they are in good health. 10
Physical distancing due to the COVID‐19 outbreak can have drastic negative effects on the mental health of the elderly and disabled individuals. Physical isolation at home among family members can put the elderly and disabled person at serious mental health risk. It can cause anxiety, distress, and induce a traumatic situation for them. Elderly people depend on young ones for their daily needs, and self‐isolation can critically damage a family system. The elderly and disabled people living in nursing homes can face extreme mental health issues. However, something as simple as a phone call during the pandemic outbreak can help to console elderly people. COVID‐19 can also result in increased stress, anxiety, and depression among elderly people already dealing with mental health issues.
Family members may witness any of the following changes to the behavior of older relatives 11 ;
- Irritating and shouting behavior
- Change in their sleeping and eating habits
- Emotional outbursts
The World Health Organization suggests that family members should regularly check on older people living within their homes and at nursing facilities. Younger family members should take some time to talk to older members of the family and become involved in some of their daily routines if possible. 12
4. HEALTH WORKERS AT RISK
Doctors, nurses, and paramedics working as a front‐line force to fight the COVID‐19 outbreak may be more susceptible to develop mental health symptoms. Fear of catching a disease, long working hours, unavailability of protective gear and supplies, patient load, unavailability of effective COVID‐19 medication, death of their colleagues after exposure to COVID‐19, social distancing and isolation from their family and friends, and the dire situation of their patients may take a negative toll of the mental health of health workers. The working efficiency of health professionals may decrease gradually as the pandemic prevails. Health workers should take short breaks between their working hours and deal with the situation calmly and in a relaxed manner. 5
5. STIGMATIZATION
Generally, people recently released from quarantine can experience stigmatization and develop a mix of emotions. Everyone may feel differently and have a different welcome by society when they come out of quarantine. People who recently recovered may have to exercise social distancing from their family members, friends, and relatives to ensure their family's safety because of unprecedented viral nature. Different age groups respond to this social behavior differently, which can have both short‐ and long‐term effects. 1
Health workers trying to save lives and protect society may also experience social distancing, changes in the behavior of family members, and stigmatization for being suspected of carrying COVID‐19. 6 Previously infected individuals and health professionals (dealing pandemic) may develop sadness, anger, or frustration because friends or loved ones may have unfounded fears of contracting the disease from contact with them, even though they have been determined not to be contagious. 5
However, the current situation requires a clear understanding of the effects of the recent outbreak on the mental health of people of different age groups to prevent and avoid the COVID‐19 pandemic.
6. TAKE HOME MESSAGE
- Understanding the effects of the COVID‐19 outbreak on the mental health of various populations are as important as understanding its clinical features, transmission patterns, and management.
- Spending time with family members including children and elderly people, involvement in different healthy exercises and sports activities, following a schedule/routine, and taking a break from traditional and social media can all help to overcome mental health issues.
- Public awareness campaigns focusing on the maintenance of mental health in the prevailing situation are urgently needed.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
AUTHOR CONTRIBUTIONS
B.J. and A.S. devised the study. B.J. collected and analyzed the data and wrote the first draft. E.B.S. edited and revised the manuscript. A.S. and Z.M. provided useful information. All the authors contributed to the subsequent drafts. The authors reviewed and endorsed the final submission.
Javed B, Sarwer A, Soto EB, Mashwani Z‐R. The coronavirus (COVID‐19) pandemic's impact on mental health . Int J Health Plann Mgmt . 2020; 35 :993–996. 10.1002/hpm.3008 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Open access
- Published: 11 April 2023
Effects of the COVID-19 pandemic on mental health, anxiety, and depression
- Ida Kupcova 1 ,
- Lubos Danisovic 1 ,
- Martin Klein 2 &
- Stefan Harsanyi 1
BMC Psychology volume 11 , Article number: 108 ( 2023 ) Cite this article
9084 Accesses
12 Citations
38 Altmetric
Metrics details
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact. According to the World Health Organization (WHO), anxiety and depression prevalence increased by 25% globally. In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population.
A cross-sectional study using an anonymous online-based 45-question online survey was conducted at Comenius University in Bratislava. The questionnaire comprised five general questions and two assessment tools the Zung Self-Rating Anxiety Scale (SAS) and the Zung Self-Rating Depression Scale (SDS). The results of the Self-Rating Scales were statistically examined in association with sex, age, and level of education.
A total of 205 anonymous subjects participated in this study, and no responses were excluded. In the study group, 78 (38.05%) participants were male, and 127 (61.69%) were female. A higher tendency to anxiety was exhibited by female participants (p = 0.012) and the age group under 30 years of age (p = 0.042). The level of education has been identified as a significant factor for changes in mental state, as participants with higher levels of education tended to be in a worse mental state (p = 0.006).
Conclusions
Summarizing two years of the COVID-19 pandemic, the mental state of people with higher levels of education tended to feel worse, while females and younger adults felt more anxiety.
Peer Review reports
Introduction
The first mention of the novel coronavirus came in 2019, when this variant was discovered in the city of Wuhan, China, and became the first ever documented coronavirus pandemic [ 1 , 2 , 3 ]. At this time there was only a sliver of fear rising all over the globe. However, in March 2020, after the declaration of a global pandemic by the World Health Organization (WHO), the situation changed dramatically [ 4 ]. Answering this, yet an unknown threat thrust many countries into a psycho-socio-economic whirlwind [ 5 , 6 ]. Various measures taken by governments to control the spread of the virus presented the worldwide population with a series of new challenges to which it had to adjust [ 7 , 8 ]. Lockdowns, closed schools, losing employment or businesses, and rising deaths not only in nursing homes came to be a new reality [ 9 , 10 , 11 ]. Lack of scientific information on the novel coronavirus and its effects on the human body, its fast spread, the absence of effective causal treatment, and the restrictions which harmed people´s social life, financial situation and other areas of everyday life lead to long-term living conditions with increased stress levels and low predictability over which people had little control [ 12 ].
Risks of changes in the mental state of the population came mainly from external risk factors, including prolonged lockdowns, social isolation, inadequate or misinterpreted information, loss of income, and acute relationship with the rising death toll. According to the World Health Organization (WHO), since the outbreak of the COVID-19 pandemic, anxiety and depression prevalence increased by 25% globally [ 13 ]. Unemployment specifically has been proven to be also a predictor of suicidal behavior [ 14 , 15 , 16 , 17 , 18 ]. These risk factors then interact with individual psychological factors leading to psychopathologies such as threat appraisal, attentional bias to threat stimuli over neutral stimuli, avoidance, fear learning, impaired safety learning, impaired fear extinction due to habituation, intolerance of uncertainty, and psychological inflexibility. The threat responses are mediated by the limbic system and insula and mitigated by the pre-frontal cortex, which has also been reported in neuroimaging studies, with reduced insula thickness corresponding to more severe anxiety and amygdala volume correlated to anhedonia as a symptom of depression [ 19 , 20 , 21 , 22 , 23 ]. Speaking in psychological terms, the pandemic disturbed our core belief, that we are safe in our communities, cities, countries, or even the world. The lost sense of agency and confidence regarding our future diminished the sense of worth, identity, and meaningfulness of our lives and eroded security-enhancing relationships [ 24 ].
Slovakia introduced harsh public health measures in the first wave of the pandemic, but relaxed these measures during the summer, accompanied by a failure to develop effective find, test, trace, isolate and support systems. Due to this, the country experienced a steep growth in new COVID-19 cases in September 2020, which lead to the erosion of public´s trust in the government´s management of the situation [ 25 ]. As a means to control the second wave of the pandemic, the Slovak government decided to perform nationwide antigen testing over two weekends in November 2020, which was internationally perceived as a very controversial step, moreover, it failed to prevent further lockdowns [ 26 ]. In addition, there was a sharp rise in the unemployment rate since 2020, which continued until July 2020, when it gradually eased [ 27 ]. Pre-pandemic, every 9th citizen of Slovakia suffered from a mental health disorder, according to National Statistics Office in 2017, the majority being affective and anxiety disorders. A group of authors created a web questionnaire aimed at psychiatrists, psychologists, and their patients after the first wave of the COVID-19 pandemic in Slovakia. The results showed that 86.6% of respondents perceived the pathological effect of the pandemic on their mental status, 54.1% of whom were already treated for affective or anxiety disorders [ 28 ].
In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population. This study aimed to assess the symptoms of anxiety and depression in the general public of Slovakia. After the end of epidemiologic restrictive measures (from March to May 2022), we introduced an anonymous online questionnaire using adapted versions of Zung Self-Rating Anxiety Scale (SAS) and Zung Self-Rating Depression Scale (SDS) [ 29 , 30 ]. We focused on the general public because only a portion of people who experience psychological distress seek professional help. We sought to establish, whether during the pandemic the population showed a tendency to adapt to the situation or whether the anxiety and depression symptoms tended to be present even after months of better epidemiologic situation, vaccine availability, and studies putting its effects under review [ 31 , 32 , 33 , 34 ].
Materials and Methods
This study utilized a voluntary and anonymous online self-administered questionnaire, where the collected data cannot be linked to a specific respondent. This study did not process any personal data. The questionnaire consisted of 45 questions. The first three were open-ended questions about participants’ sex, age (date of birth was not recorded), and education. Followed by 2 questions aimed at mental health and changes in the will to live. Further 20 and 20 questions consisted of the Zung SAS and Zung SDS, respectively. Every question in SAS and SDS is scored from 1 to 4 points on a Likert-style scale. The scoring system is introduced in Fig. 1 . Questions were presented in the Slovak language, with emphasis on maintaining test integrity, so, if possible, literal translations were made from English to Slovak. The questionnaire was created and designed in Google Forms®. Data collection was carried out from March 2022 to May 2022. The study was aimed at the general population of Slovakia in times of difficult epidemiologic and social situations due to the high prevalence and incidence of COVID-19 cases during lockdowns and social distancing measures. Because of the character of this web-based study, the optimal distribution of respondents could not be achieved.
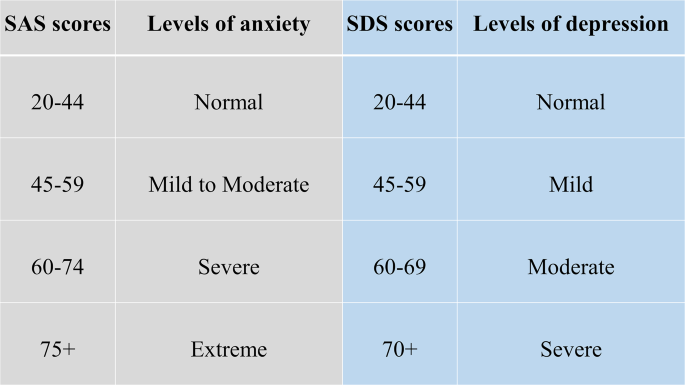
Categories of Zung SAS and SDS scores with clinical interpretation
During the course of this study, 205 respondents answered the anonymous questionnaire in full and were included in the study. All respondents were over 18 years of age. The data was later exported from Google Forms® as an Excel spreadsheet. Coding and analysis were carried out using IBM SPSS Statistics version 26 (IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY, USA). Subject groups were created based on sex, age, and education level. First, sex due to differences in emotional expression. Second, age was a risk factor due to perceived stress and fear of the disease. Last, education due to different approaches to information. In these groups four factors were studied: (1) changes in mental state; (2) affected will to live, or frequent thoughts about death; (3) result of SAS; (4) result of SDS. For SAS, no subject in the study group scored anxiety levels of “severe” or “extreme”. Similarly for SDS, no subject depression levels reached “moderate” or “severe”. Pearson’s chi-squared test(χ2) was used to analyze the association between the subject groups and studied factors. The results were considered significant if the p-value was less than 0.05.
Ethical permission was obtained from the local ethics committee (Reference number: ULBGaKG-02/2022). This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines. Due to the anonymous design of the study and by the institutional requirements, written informed consent for participation was not required for this study.
In the study, out of 205 subjects in the study group, 127 (62%) were female and 78 (38%) were male. The average age in the study group was 35.78 years of age (range 19–71 years), with a median of 34 years. In the age group under 30 years of age were 34 (16.6%) subjects, while 162 (79%) were in the range from 31 to 49 and 9 (0.4%) were over 50 years old. 48 (23.4%) participants achieved an education level of lower or higher secondary and 157 (76.6%) finished university or higher. All answers of study participants were included in the study, nothing was excluded.
In Tables 1 and 2 , we can see the distribution of changes in mental state and will to live as stated in the questionnaire. In Table 1 we can see a disproportion in education level and mental state, where participants with higher education tended to feel worse much more than those with lower levels of education. Changes based on sex and age did not show any statistically significant results.
In Table 2 . we can see, that decreased will to live and frequent thoughts about death were only marginally present in the study group, which suggests that coping mechanisms play a huge role in adaptation to such events (e.g. the global pandemic). There is also a possibility that living in times of better epidemiologic situations makes people more likely to forget about the bad past.
Anxiety and depression levels as seen in Tables 3 and 4 were different, where female participants and the age group under 30 years of age tended to feel more anxiety than other groups. No significant changes in depression levels based on sex, age, and education were found.
Compared to the estimated global prevalence of depression in 2017 (3.44%), in 2021 it was approximately 7 times higher (25%) [ 14 ]. Our study did not prove an increase in depression, while anxiety levels and changes in the mental state did prove elevated. No significant changes in depression levels go in hand with the unaffected will to live and infrequent thoughts about death, which were important findings, that did not supplement our primary hypothesis that the fear of death caused by COVID-19 or accompanying infections would enhance personal distress and depression, leading to decreases in studied factors. These results are drawn from our limited sample size and uneven demographic distribution. Suicide ideations rose from 5% pre-pandemic to 10.81% during the pandemic [ 35 ]. In our study, 9.3% of participants experienced thoughts about death and since we did not specifically ask if they thought about suicide, our results only partially correlate with suicidal ideations. However, as these subjects exhibited only moderate levels of anxiety and mild levels of depression, the rise of suicide ideations seems unlikely. The rise in suicidal ideations seemed to be especially true for the general population with no pre-existing psychiatric conditions in the first months of the pandemic [ 36 ]. The policies implemented by countries to contain the pandemic also took a toll on the population´s mental health, as it was reported, that more stringent policies, mainly the social distancing and perceived government´s handling of the pandemic, were related to worse psychological outcomes [ 37 ]. The effects of lockdowns are far-fetched and the increases in mental health challenges, well-being, and quality of life will require a long time to be understood, as Onyeaka et al. conclude [ 10 ]. These effects are not unforeseen, as the global population suffered from life-altering changes in the structure and accessibility of education or healthcare, fluctuations in prices and food insecurity, as well as the inevitable depression of the global economy [ 38 ].
The loneliness associated with enforced social distancing leads to an increase in depression, anxiety, and posttraumatic stress in children in adolescents, with possible long-term sequelae [ 39 ]. The increase in adolescent self-injury was 27.6% during the pandemic [ 40 ]. Similar findings were described in the middle-aged and elderly population, in which both depression and anxiety prevalence rose at the beginning of the pandemic, during the pandemic, with depression persisting later in the pandemic, while the anxiety-related disorders tended to subside [ 41 ]. Medical professionals represented another specific at-risk group, with reported anxiety and depression rates of 24.94% and 24.83% respectively [ 42 ]. The dynamic of psychopathology related to the COVID-19 pandemic is not clear, with studies reporting a return to normal later in 2020, while others describe increased distress later in the pandemic [ 20 , 43 ].
Concerning the general population, authors from Spain reported that lockdowns and COVID-19 were associated with depression and anxiety [ 44 ]. In January 2022 Zhao et al., reported an elevation in hoarding behavior due to fear of COVID-19, while this process was moderated by education and income levels, however, less in the general population if compared to students [ 45 ]. Higher education levels and better access to information could improve persons’ fear of the unknown, however, this fact was not consistent with our expectations in this study, as participants with university education tended to feel worse than participants with lower education. A study on adolescents and their perceived stress in the Czech Republic concluded that girls are more affected by lockdowns. The strongest predictor was loneliness, while having someone to talk to, scored the lowest [ 46 ]. Garbóczy et al. reported elevated perceived stress levels and health anxiety in 1289 Hungarian and international students, also affected by disengagement from home and inadequate coping strategies [ 47 ]. Wathelet et al. conducted a study on French University students confined during the pandemic with alarming results of a high prevalence of mental health issues in the study group [ 48 ]. Our study indicated similar results, as participants in the age group under 30 years of age tended to feel more anxious than others.
In conclusion, we can say that this pandemic changed the lives of many. Many of us, our family members, friends, and colleagues, experienced life-altering events and complicated situations unseen for decades. Our decisions and actions fueled the progress in medicine, while they also continue to impact society on all levels. The long-term effects on adolescents are yet to be seen, while effects of pain, fear, and isolation on the general population are already presenting themselves.
The limitations of this study were numerous and as this was a web-based study, the optimal distribution of respondents could not be achieved, due to the snowball sampling strategy. The main limitation was the small sample size and uneven demographic distribution of respondents, which could impact the representativeness of the studied population and increase the margin of error. Similarly, the limited number of older participants could significantly impact the reported results, as age was an important risk factor and thus an important stressor. The questionnaire omitted the presence of COVID-19-unrelated life-changing events or stressors, and also did not account for any preexisting condition or risk factor that may have affected the outcome of the used assessment scales.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to compliance with institutional guidelines but they are available from the corresponding author (SH) on a reasonable request.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Article PubMed PubMed Central Google Scholar
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Liu Y-C, Kuo R-L, Shih S-R. COVID-19: the first documented coronavirus pandemic in history. Biomed J. 2020;43:328–33.
Advice for the public on COVID-19 – World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public . Accessed 13 Nov 2022.
Osterrieder A, Cuman G, Pan-Ngum W, Cheah PK, Cheah P-K, Peerawaranun P, et al. Economic and social impacts of COVID-19 and public health measures: results from an anonymous online survey in Thailand, Malaysia, the UK, Italy and Slovenia. BMJ Open. 2021;11:e046863.
Article PubMed Google Scholar
Mofijur M, Fattah IMR, Alam MA, Islam ABMS, Ong HC, Rahman SMA, et al. Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustainable Prod Consum. 2021;26:343–59.
Article Google Scholar
Vlachos J, Hertegård E, Svaleryd B. The effects of school closures on SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci U S A. 2021;118:e2020834118.
Ludvigsson JF, Engerström L, Nordenhäll C, Larsson E, Open Schools. Covid-19, and child and teacher morbidity in Sweden. N Engl J Med. 2021;384:669–71.
Miralles O, Sanchez-Rodriguez D, Marco E, Annweiler C, Baztan A, Betancor É, et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: a report from six european countries. Eur Geriatr Med. 2021;12:193–204.
Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: a review of the global lockdown and its far-reaching effects. Sci Prog. 2021;104:368504211019854.
The Lancet null. India under COVID-19 lockdown. Lancet. 2020;395:1315.
Lo Coco G, Gentile A, Bosnar K, Milovanović I, Bianco A, Drid P, et al. A cross-country examination on the fear of COVID-19 and the sense of loneliness during the First Wave of COVID-19 outbreak. Int J Environ Res Public Health. 2021;18:2586.
COVID-19 pandemic. triggers 25% increase in prevalence of anxiety and depression worldwide. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide . Accessed 14 Nov 2022.
Bueno-Notivol J, Gracia-García P, Olaya B, Lasheras I, López-Antón R, Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int J Clin Health Psychol. 2021;21:100196.
Hajek A, Sabat I, Neumann-Böhme S, Schreyögg J, Barros PP, Stargardt T, et al. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: longitudinal evidence from the european COvid Survey (ECOS). J Affect Disord. 2022;299:517–24.
Piumatti G, Levati S, Amati R, Crivelli L, Albanese E. Trajectories of depression, anxiety and stress among adults during the COVID-19 pandemic in Southern Switzerland: the Corona Immunitas Ticino cohort study. Public Health. 2022;206:63–9.
Korkmaz H, Güloğlu B. The role of uncertainty tolerance and meaning in life on depression and anxiety throughout Covid-19 pandemic. Pers Indiv Differ. 2021;179:110952.
McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290:113104.
Funkhouser CJ, Klemballa DM, Shankman SA. Using what we know about threat reactivity models to understand mental health during the COVID-19 pandemic. Behav Res Ther. 2022;153:104082.
Landi G, Pakenham KI, Crocetti E, Tossani E, Grandi S. The trajectories of anxiety and depression during the COVID-19 pandemic and the protective role of psychological flexibility: a four-wave longitudinal study. J Affect Disord. 2022;307:69–78.
Holt-Gosselin B, Tozzi L, Ramirez CA, Gotlib IH, Williams LM. Coping strategies, neural structure, and depression and anxiety during the COVID-19 pandemic: a longitudinal study in a naturalistic sample spanning clinical diagnoses and subclinical symptoms. Biol Psychiatry Global Open Sci. 2021;1:261–71.
McCracken LM, Badinlou F, Buhrman M, Brocki KC. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. J Context Behav Sci. 2021;19:28–35.
Talkovsky AM, Norton PJ. Negative affect and intolerance of uncertainty as potential mediators of change in comorbid depression in transdiagnostic CBT for anxiety. J Affect Disord. 2018;236:259–65.
Milman E, Lee SA, Neimeyer RA, Mathis AA, Jobe MC. Modeling pandemic depression and anxiety: the mediational role of core beliefs and meaning making. J Affect Disorders Rep. 2020;2:100023.
Sagan A, Bryndova L, Kowalska-Bobko I, Smatana M, Spranger A, Szerencses V, et al. A reversal of fortune: comparison of health system responses to COVID-19 in the Visegrad group during the early phases of the pandemic. Health Policy. 2022;126:446–55.
Holt E. COVID-19 testing in Slovakia. Lancet Infect Dis. 2021;21:32.
Stalmachova K, Strenitzerova M. Impact of the COVID-19 pandemic on employment in transport and telecommunications sectors. Transp Res Procedia. 2021;55:87–94.
Izakova L, Breznoscakova D, Jandova K, Valkucakova V, Bezakova G, Suvada J. What mental health experts in Slovakia are learning from COVID-19 pandemic? Indian J Psychiatry. 2020;62(Suppl 3):459–66.
Rabinčák M, Tkáčová Ľ, VYUŽÍVANIE PSYCHOMETRICKÝCH KONŠTRUKTOV PRE, HODNOTENIE PORÚCH NÁLADY V OŠETROVATEĽSKEJ PRAXI. Zdravotnícke Listy. 2019;7:7.
Google Scholar
Sekot M, Gürlich R, Maruna P, Páv M, Uhlíková P. Hodnocení úzkosti a deprese u pacientů se zhoubnými nádory trávicího traktu. Čes a slov Psychiat. 2005;101:252–7.
Lipsitch M, Krammer F, Regev-Yochay G, Lustig Y, Balicer RD. SARS-CoV-2 breakthrough infections in vaccinated individuals: measurement, causes and impact. Nat Rev Immunol. 2022;22:57–65.
Accorsi EK, Britton A, Fleming-Dutra KE, Smith ZR, Shang N, Derado G, et al. Association between 3 doses of mRNA COVID-19 vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and Delta Variants. JAMA. 2022;327:639–51.
Barda N, Dagan N, Cohen C, Hernán MA, Lipsitch M, Kohane IS, et al. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. 2021;398:2093–100.
Magen O, Waxman JG, Makov-Assif M, Vered R, Dicker D, Hernán MA, et al. Fourth dose of BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2022;386:1603–14.
Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021;301:113998.
Kok AAL, Pan K-Y, Rius-Ottenheim N, Jörg F, Eikelenboom M, Horsfall M, et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in dutch case-control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J Affect Disord. 2022;305:85–93.
Aknin LB, Andretti B, Goldszmidt R, Helliwell JF, Petherick A, De Neve J-E, et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. The Lancet Public Health. 2022;7:e417–26.
Prochazka J, Scheel T, Pirozek P, Kratochvil T, Civilotti C, Bollo M, et al. Data on work-related consequences of COVID-19 pandemic for employees across Europe. Data Brief. 2020;32:106174.
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239e3.
Zetterqvist M, Jonsson LS, Landberg Ã, Svedin CG. A potential increase in adolescent nonsuicidal self-injury during covid-19: a comparison of data from three different time points during 2011–2021. Psychiatry Res. 2021;305:114208.
Mooldijk SS, Dommershuijsen LJ, de Feijter M, Luik AI. Trajectories of depression and anxiety during the COVID-19 pandemic in a population-based sample of middle-aged and older adults. J Psychiatr Res. 2022;149:274–80.
Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110247.
Stephenson E, O’Neill B, Kalia S, Ji C, Crampton N, Butt DA, et al. Effects of COVID-19 pandemic on anxiety and depression in primary care: a retrospective cohort study. J Affect Disord. 2022;303:216–22.
Goldberg X, Castaño-Vinyals G, Espinosa A, Carreras A, Liutsko L, Sicuri E et al. Mental health and COVID-19 in a general population cohort in Spain (COVICAT study).Soc Psychiatry Psychiatr Epidemiol. 2022;:1–12.
Zhao Y, Yu Y, Zhao R, Cai Y, Gao S, Liu Y, et al. Association between fear of COVID-19 and hoarding behavior during the outbreak of the COVID-19 pandemic: the mediating role of mental health status. Front Psychol. 2022;13:996486.
Furstova J, Kascakova N, Sigmundova D, Zidkova R, Tavel P, Badura P. Perceived stress of adolescents during the COVID-19 lockdown: bayesian multilevel modeling of the Czech HBSC lockdown survey. Front Psychol. 2022;13:964313.
Garbóczy S, Szemán-Nagy A, Ahmad MS, Harsányi S, Ocsenás D, Rekenyi V, et al. Health anxiety, perceived stress, and coping styles in the shadow of the COVID-19. BMC Psychol. 2021;9:53.
Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors Associated with Mental Health Disorders among University students in France Confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2025591.
Download references
Acknowledgements
We would like to provide our appreciation and thanks to all the respondents in this study.
This research project received no external funding.
Author information
Authors and affiliations.
Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Ida Kupcova, Lubos Danisovic & Stefan Harsanyi
Institute of Histology and Embryology, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Martin Klein
You can also search for this author in PubMed Google Scholar
Contributions
IK and SH have produced the study design. All authors contributed to the manuscript writing, revising, and editing. LD and MK have done data management and extraction, SH did the data analysis. Drafting and interpretation of the manuscript were made by all authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Stefan Harsanyi .
Ethics declarations
Ethics approval and consent to participate.
Ethical permission was obtained from the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava (Reference number: ULBGaKG-02/2022). The need for informed consent was waived by the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava due to the anonymous design of the study. This study did not process any personal data and the dataset does not contain any direct or indirect identifiers of participants. This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kupcova, I., Danisovic, L., Klein, M. et al. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol 11 , 108 (2023). https://doi.org/10.1186/s40359-023-01130-5
Download citation
Received : 14 November 2022
Accepted : 20 March 2023
Published : 11 April 2023
DOI : https://doi.org/10.1186/s40359-023-01130-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Mental Health and COVID-19
- Mental Health Diversity, Equity, and Inclusion
- Origins of Mental Health
- Job Openings
- Faculty Profiles
- PET Alumni Profiles - Postdocs
- PET Alumni Profiles - Predocs
- Trainee Profiles
- NIMH T32 Mental Health Services and Systems Training Grant
- Funded Training Program in Data Integration for Causal Inference in Behavioral Health
- Aging and Dementia Funded Training Program
- COVID-19 and Mental Health Research
- Mental Health Resources During COVID-19
- News and Media
- Social Determinants of Mental and Behavioral Health
Our Work in Action
- Global Mental Health
- Related Faculty
- Courses of Interest
- Training and Funding Opportunities
- Mental Health in the Workplace: A Public Health Summit
- Autism and Developmental Disabilities
- Alumni Newsletters
- Alumni Updates
- Postdoctoral Fellows
- Doctor of Philosophy (PhD) Students in Mental Health
- Master of Health Science (MHS) Students in Mental Health
- In the News
- Past Seminars 2020-21 AY: Wednesday Seminar Series
- Make a Gift
- Available Datasets
The COVID-19 pandemic has had a huge impact on public health around the globe in terms of both physical and mental health, and the mental health implications of the pandemic may continue long after the physical health consequences have resolved. This research area aims to contribute to our understanding of the COVID-19 pandemics implications for mental health, building on a robust literature on how environmental crises, such as SARS or natural disasters, can lead to mental health challenges, including loneliness, acute stress, anxiety, and depression. The social distancing aspects of the COVID-19 pandemic may have particularly significant effects on mental health. Understanding how mental health evolves as a result of this serious global pandemic will inform prevention and treatment strategies moving forward, including allocation of resources to those most in need. Critically, these data can also serve as evidence-based information for public health organizations and the public as a whole.
Understanding the Mental Health Implications of a Pandemic

Introduction
The world is entering into a new phase with COVID-19 spreading rapidly. People will be studying various consequences of the COVID-19 pandemic and mental and behavioral health should be a core part of that effort. There is a robust literature on how environmental crises, such as SARS or natural disasters, can lead to mental health challenges, including loneliness, acute stress, anxiety, and depression. The social distancing aspects of the current pandemic may have particularly significant effects on mental health. Understanding how mental health evolves as a result of this serious global outbreak will inform prevention and treatment strategies moving forward, including allocation of resources to those most in need. Critically, these data can also serve as evidence-based information for public health organizations and the public as a whole.
The data will be leveraged to address many questions, such as:
- Which individuals are at greatest risk for high levels of mental health distress during a pandemic?
- As individuals spend more time inside and isolated, how does their mental health distress evolve?
- How do different behaviors (such as media consumption) relate to mental health?
Read more about how our experts are measuring mental distress amid a pandemic.
We have been working to ensure that measurement of mental health measures is a key part of large-scale national and international data collections relative to COVID-19.
Read more about conducting research studies on mental health during the pandemic.
Mental Health Resources
See our resources guide here.
Members of the COVID-19 Mental Health Measurement Working Group
- M. Daniele Fallin, JHSPH
- Calliope Holingue, Kennedy Krieger Institute, JHSPH
- Renee M. Johnson, JHSPH
- Luke Kalb, Kennedy Krieger Institute, JHSPH
- Frauke Kreuter, University of Maryland, University of Mannheim
- Courtney Nordeck, JHSPH
- Kira Riehm, JHSPH
- Emily J. Smail, JHSPH
- Elizabeth Stuart, JHSPH
- Johannes Thrul, JHSPH
- Cindy Veldhuis, Columbia University School of Nursing
The Johns Hopkins COVID-19 Mental Health Measurement Working Group developed key questions to add to existing large domestic and international surveys to measure the mental health impact of the pandemic.

ORIGINAL RESEARCH article
The effect of covid-19 on mental health and wellbeing in a representative sample of australian adults.
A correction has been applied to this article in:
Corrigendum: The Effect of COVID-19 on Mental Health and Wellbeing in a Representative Sample of Australian Adults
- Read correction

- 1 Research School of Psychology, The Australian National University, Canberra, ACT, Australia
- 2 Centre for Research on Ageing, Health and Wellbeing, Research School of Population Health, The Australian National University, Canberra, ACT, Australia
- 3 Centre for Mental Health Research, Research School of Population Health, The Australian National University, Canberra, ACT, Australia
- 4 Department of Global Health, Research School of Population Health, The Australian National University, Canberra, ACT, Australia
- 5 National Centre for Epidemiology and Population Health, Research School of Population Health, The Australian National University, Canberra, ACT, Australia
There is minimal knowledge about the impact of large-scale epidemics on community mental health, particularly during the acute phase. This gap in knowledge means we are critically ill-equipped to support communities as they face the unprecedented COVID-19 pandemic. This study aimed to provide data urgently needed to inform government policy and resource allocation now and in other future crises. The study was the first to survey a representative sample from the Australian population at the early acute phase of the COVID-19 pandemic. Depression, anxiety, and psychological wellbeing were measured with well-validated scales (PHQ-9, GAD-7, WHO-5). Using linear regression, we tested for associations between mental health and exposure to COVID-19, impacts of COVID-19 on work and social functioning, and socio-demographic factors. Depression and anxiety symptoms were substantively elevated relative to usual population data, including for individuals with no existing mental health diagnosis. Exposure to COVID-19 had minimal association with mental health outcomes. Recent exposure to the Australian bushfires was also unrelated to depression and anxiety, although bushfire smoke exposure correlated with reduced psychological wellbeing. In contrast, pandemic-induced impairments in work and social functioning were strongly associated with elevated depression and anxiety symptoms, as well as decreased psychological wellbeing. Financial distress due to the pandemic, rather than job loss per se , was also a key correlate of poorer mental health. These findings suggest that minimizing disruption to work and social functioning, and increasing access to mental health services in the community, are important policy goals to minimize pandemic-related impacts on mental health and wellbeing. Innovative and creative strategies are needed to meet these community needs while continuing to enact vital public health strategies to control the spread of COVID-19.
Introduction
The new coronavirus SARS-CoV-2 (COVID-19) pandemic is unprecedented in recent history, with global impacts including high rates of mortality and morbidity, and loss of income and sustained social isolation for billions of people. The effect this crisis will have on population mental health, both in the short- and long-term, is unknown. There is minimal evidence about the acute phase mental health impacts of large-scale epidemics across communities. Existing work has focused on those individuals most directly affected by disease (e.g., infected individuals and their families, healthcare workers ( 1 – 5 ) and examined mental health impacts across broader communities only after the acute phase has passed ( 1 ). In the acute phase however, fear about potential exposure to infection, loss of employment, and financial strain are also likely to increase psychological distress in the broader population ( 1 – 4 ). This distress may be further exacerbated in individuals who have experienced prior traumatic events ( 2 ). In the longer term, grief and trauma are likely to emerge ( 3 ) and, as financial and social impacts become entrenched, risk of depression and suicidality may increase ( 2 , 6 – 8 ).
Reports of the mental health impacts of previous severe health epidemics have focused primarily on disease survivors [e.g., of Ebola virus disease ( 2 ) and SARS ( 1 )]. Almost invariably, these studies show survivors experience greater psychological distress post-epidemic than others from affected communities ( 1 , 3 ). Risk for psychological distress may also be greater for people employed in occupations that potentially expose them to infection ( 4 , 5 ), and in those who have friends or family members who have been infected ( 3 ). However, in the acute phase of COVID-19, there are clear reasons to also expect that Government policies and physical distancing measures aimed at limiting disease spread will impact mental health in the broader community. For instance, loss of employment ( 6 ), financial strain ( 9 ), and social isolation ( 8 , 10 ) are all well-documented correlates of mental health problems. In many countries, physical distancing measures have already resulted in an enormous increase in unemployment ( 11 ), likely causing significant financial strain for many.
Gathering early evidence of the impacts of COVID-19 is vital for informing mental health service delivery as the pandemic and its extended effects continue. The present study surveyed a representative sample of Australians from 28 to 31 March 2020, during the acute phase of the pandemic in Australia. Figure 1 shows the number of confirmed cases in Australia had just started to escalate at this time, relative to global cases. A total of 19 deaths had been reported in Australia by the survey close, relative to over 36,500 across the globe. In the fortnight leading up to the survey, the Australian government had closed restaurants, bars, and churches, severely restricted the size of public and private gatherings, banned foreign nationals from entering Australia, and was enforcing strict quarantine measures for Australians returning from overseas.
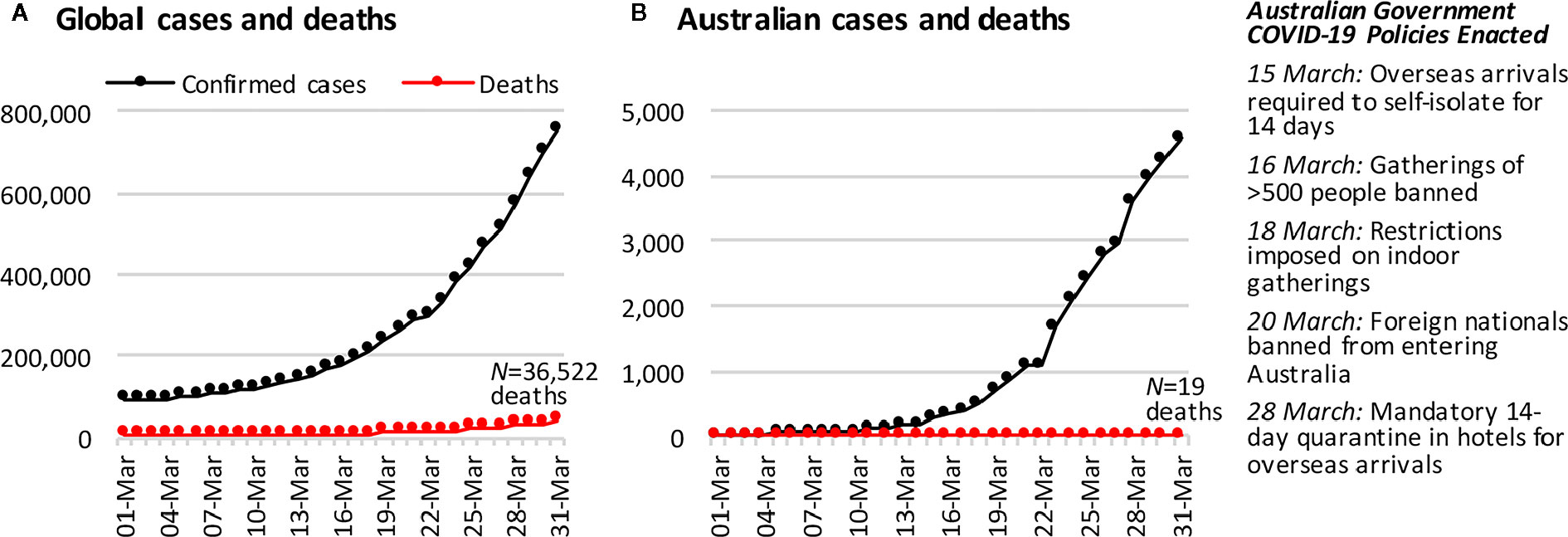
Figure 1 The cumulative number of COVID-19 confirmed cases and deaths (A) across the globe and (B) in Australia, in the month leading up to the first survey wave of this study. Case and death data are from https://covid19.who.int/ .
The present study aimed to document the initial mental health scenario across the Australian community and examine its association with exposure to the broad COVID-19 environment at this critical acute phase by: (1) measuring the current prevalence of clinically significant symptoms of generalized anxiety and depression, including associations with other recent adversities; and (2) investigating the degree to which symptom severity is associated with exposure to COVID-19, and pandemic-related impacts on employment, finances, and social functioning. We also accounted for exposure to the catastrophic bushfires that occurred across Australia in November 2019–January 2020. We hypothesized that greater exposure to COVID-19, and impairment in employment, finances, and social functioning, would be associated with higher psychological distress and decreased psychological wellbeing
Study Design and Sample
We established a new longitudinal study—The Australian National COVID-19 Mental Health, Behavior and Risk Communication (COVID-MHBRC) Survey—to investigate the impact of the COVID-19 pandemic on a representative sample of the Australian adult population (≥18 years). Participants were required to be able to respond to an online English language survey. The study comprises seven survey waves initiated online fortnightly, via Qualtrics Research Services. Recruitment was conducted using quota sampling to obtain a representative sample on the basis of age group, gender, and geographical location (State/Territory). Participants gave written informed consent after receiving a complete description of the study. The study was approved by The Australian National University Human Research Ethics Committee (number 2020/152). The full study protocol is available here: https://psychology.anu.edu.au/files/COVID_MHBRCS_protocol.pdf .
We report data (N = 1,296) from the first assessment (Wave 1, 28–31 March 2020). The sample size requirement estimate was based on planned power analyses for finding an effect of f 2 = 0.1 in linear and logistic regression models, setting 1 - β = .95 and α = .05, and taking into account variations in the prevalence of binary outcomes and attrition over the stages of the longitudinal survey, and an allowance for 10% unusable data. Our sample of N = 1,296 was only 2% less than our target sample of N = 1,320 (see Supplement S1 for additional details). Only 2–3% of the data were unusable for the present analyses.
Table 1 reports Wave 1 sample distributions by gender, age, and location. These distributions aligned well with population data from the Australian Bureau of Statistics ( 12 ), demonstrating that a representative sample of the Australian community was achieved.
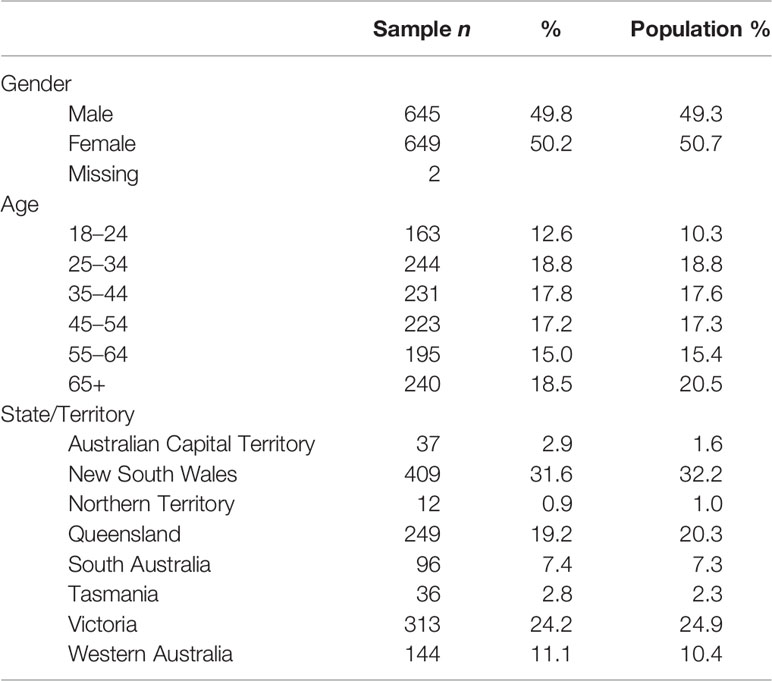
Table 1 Sample demographics and comparison with population data from the 2016 Australian Census ( 12 ).
Survey Measures
Symptoms of depression and anxiety over the last 2 weeks were assessed by the Patient Health Questionnaire-9 (PHQ-9) ( 13 ) and Generalized Anxiety Disorder-7 (GAD-7) ( 13 ) respectively. These measures align closely with diagnostic criteria for major depressive disorder and generalized anxiety disorder respectively ( 14 ). General psychological wellbeing over the last 2 weeks was measured using the World Health Organization Wellbeing Index (WHO-5) ( 15 ).
COVID-19 exposure was computed as the sum of self-reports of possible or actual exposures to the virus, of the related population health response, or of close social impact including: having been diagnosed with the virus, awaiting results from a test, having tested negative to the test, being in direct contact with a carrier of the virus, having had to isolate in the past, having chosen to isolate in the past, being currently forced to isolate, currently choosing to isolate, having a family member diagnosed with the virus, having a family member in isolation, knowing someone who was diagnosed, knowing someone in isolation, or being asked to work from home because of the virus.
Our measures of the work and social impacts of COVID-19 were whether someone had lost their job due to COVID-19 (yes/no); was working from home due to COVID-19 (yes/no); was experiencing financial distress due to COVID-19 (six-point Likert-type rating, from Not at all to Extremely); and the overall extent to which their work and social activities were impaired by COVID-19, measured using the Work and Social Adjustment Scale (WSAS) ( 16 ). For the WSAS, participants rated the level of impairment COVID-19 had caused (eight-point Likert-type rating, from Not at all impaired to Very severely impaired) for five work and social domains (ability to work, home management, social leisure activities, private leisure activities, and ability to form and maintain close relationships).
We also measured other background factors that could be associated with mental health: age (in years); gender (male/female/other); years of education; partner status (yes/no); living alone (yes/no); living with dependent children (yes/no); existing health, neurological, or psychological conditions, diagnosed by an appropriate clinician (yes/no); recent exposure to bushfire smoke (yes/no) or fire (yes/no); and impact of other recent adverse life events (five-point Likert-type rating, from Not at all to Extremely). Regarding the bushfire exposure variables, our reason for separating out smoke from fire is that many Australians who were exposed to smoke lived far away from the actual fires and their home/region was never under direct threat. The major impact for smoke-but-not-fire affected individuals was poor air quality, which prohibited people from spending time outside for several weeks over the Summer.
Statistical Analysis
Statistical analyses were conducted in R version 3.6.3 under RStudio version 1.1.456 ( 17 ). Multiple linear regression was the primary technique employed to assess correlates of poor mental health. Models were checked and showed an absence of multicollinearity, outliers, and non-normality in the residuals. However, as is typical in non-clinical samples, the PHQ-9 and GAD-7 variables had high frequencies at their lowest possible values, resulting in incorrigible skew. Therefore, compound Poisson-gamma (Tweedie distribution) generalized linear models ( 18 ) were estimated as a check on the linear models ( Supplement S2 ). Their results were consistent with the linear models. Likewise, the models included categorical predictors with small subsample sizes, so cross-validation was conducted to ensure that the models were stable ( Supplement S3 ). Overall, <1% of data were missing. Models reported in the main text dealt with these cases using listwise deletion. We also multiply imputed the missing values and reran the models, which produced the same pattern of findings ( Supplement S5 ).
Table 2 presents our sample characteristics. Overall, 20.3 and 16.4 of our sample scored above the clinical cut-offs on our depression (PHQ-9) and anxiety (GAD-7) measures respectively. Table 3 shows these rates are notably elevated compared to other community-based samples. Even among individuals without a current diagnosis, the rates remained elevated well above levels seen in other representative community-based samples.
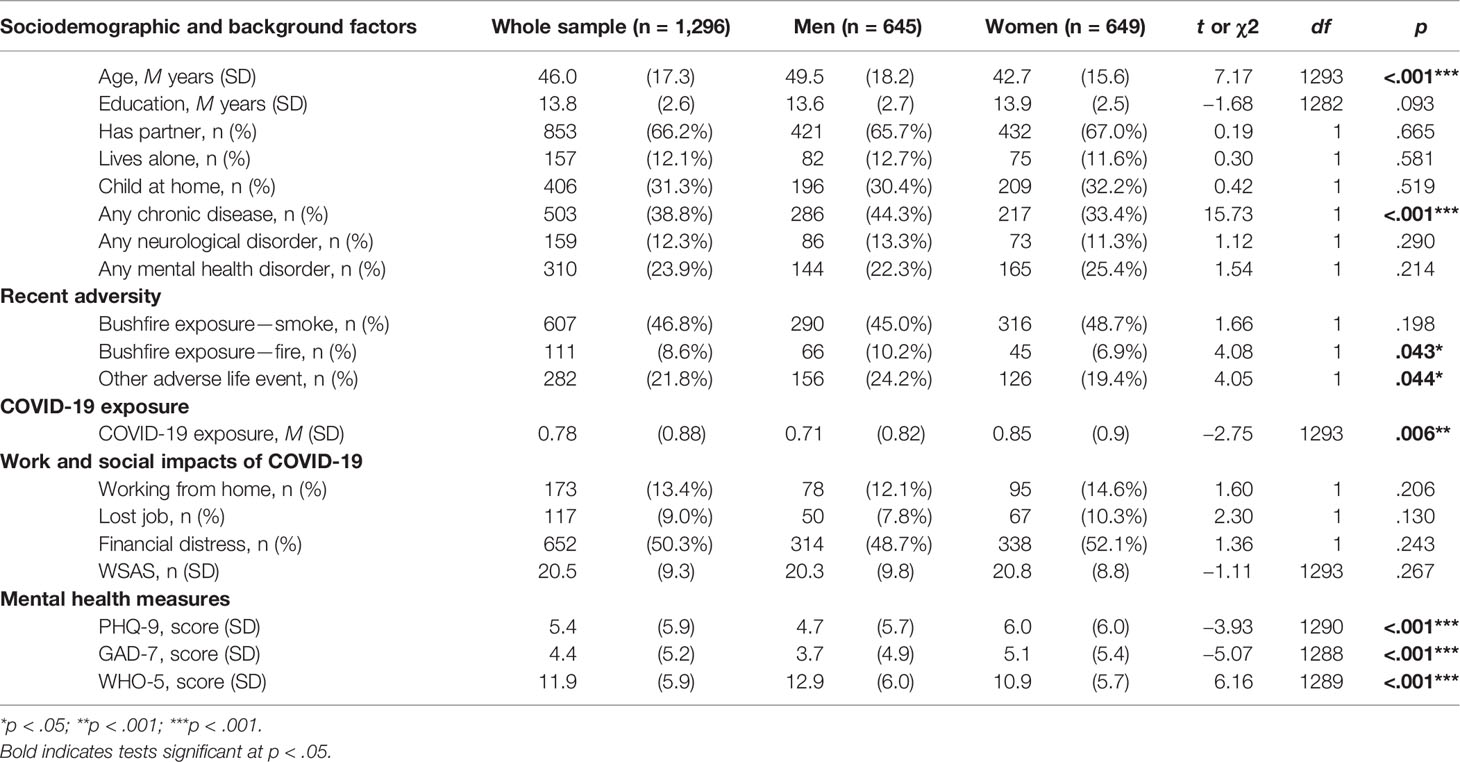
Table 2 Description of sample characteristics, including comparison of men and women.
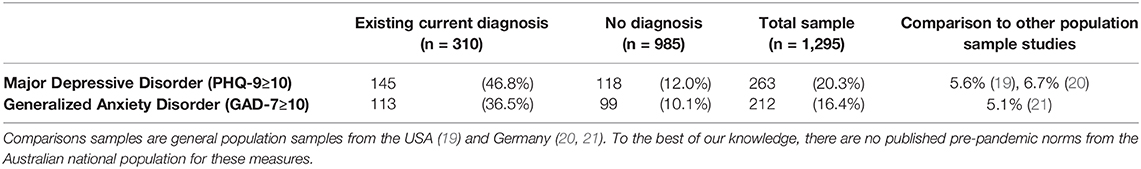
Table 3 Prevalence of depression and generalized anxiety based on self-reported current mental health diagnosis.
Investigation of the relationships between our predictor measures and three mental health outcome measures used a Bonferroni adjusted significance threshold of 0.17 to control for the three sets of comparisons, i.e., α = .05/3 = .017. Note, all three measures showed good reliability (see Supplement S6 ).
Our initial univariate tests revealed that higher levels of depression and anxiety symptoms, and lower psychological wellbeing (WHO-5), were all associated with job loss and financial distress, and overall work and social impairment due to COVID-19, as measured by the WSAS. Being required to work from home was not associated with any mental health effects at this acute stage of the pandemic, all ps > 0.27 (see Supplement S6 for all univariate results).
The linear regression models, presented in Table 4 , established that the effects of financial distress and overall work and social impairment were independent, and not better accounted for by demographic or other background factors. Job loss however did not have a significant independent association with mental health after accounting for financial distress and other covariates, all ps > 0.25.
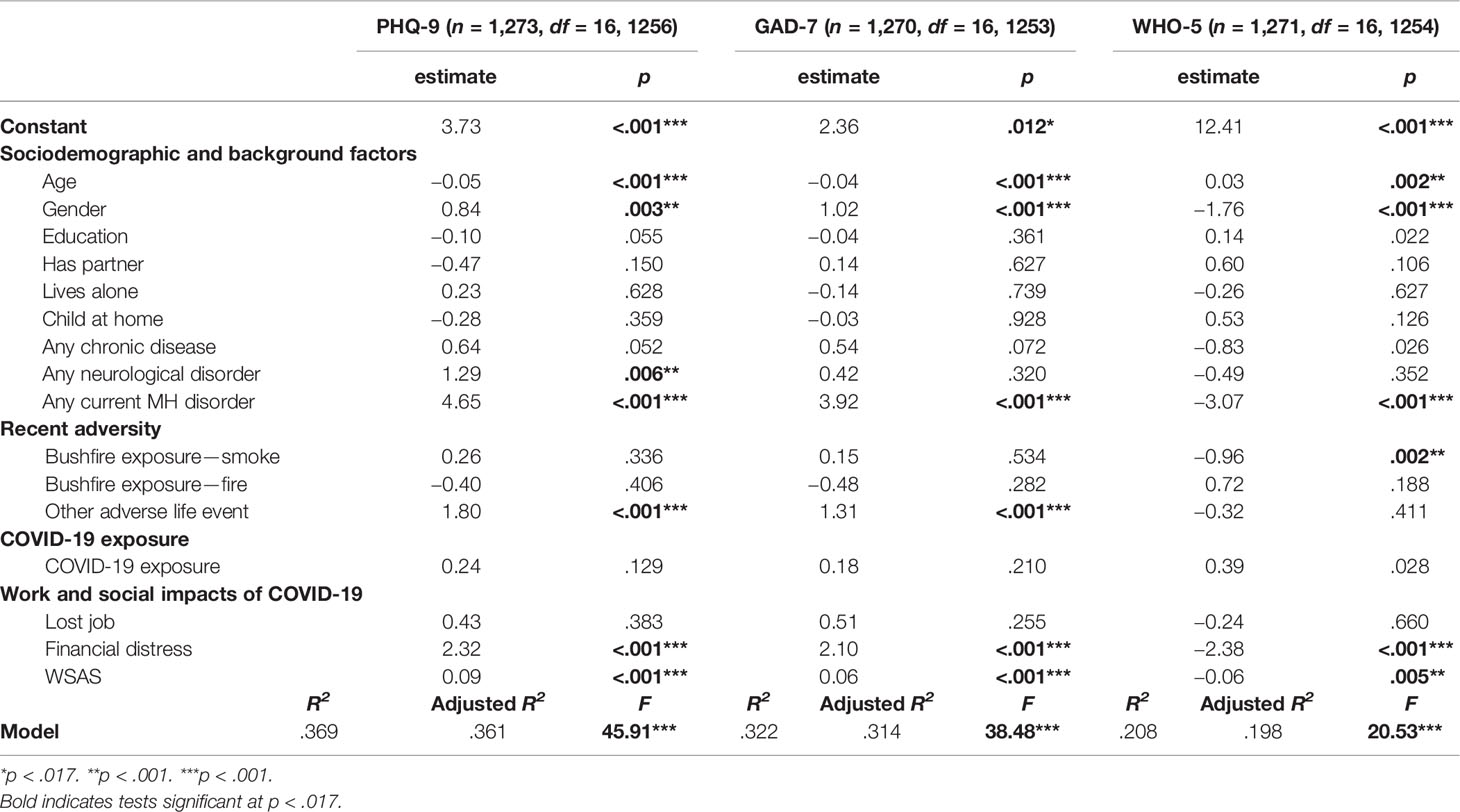
Table 4 Linear regression models for each mental health outcome.
In contrast, the regression analyses found no significant unique association between exposure to COVID-19 and depression or anxiety symptoms, or wellbeing.
Depression and anxiety symptoms were also elevated in people who had experienced other recent adversities, although this did not include direct exposure to the recent catastrophic Australian bushfires. Exposure to bushfire smoke was however associated with decreased wellbeing.
Finally, within these regression models, we also found that younger age, identifying as female, and having at least one current mental health disorder were each independently associated with higher levels of depression and anxiety, and decreased wellbeing.
We found the social, work, and financial disruptions induced by the acute phase of the COVID-19 pandemic were associated with considerable impairments in community mental health in Australian adults. In contrast, exposure to COVID-19 was not found to predict mental health in this cohort. A key strength of this study was the testing of a representative community sample early in the pandemic, providing rapid evidence of population mental health status. The results highlight that epidemics may cause serious problems for community mental health in the acute phase of disease.
Indeed, our results suggest that, at a population level, changes to social and work functioning due to COVID-19 were more strongly associated with decrements in mental health than amount of disease contact. This finding is consistent with a recent UK-based finding that their citizens were more concerned about how societal changes will impact their psychological and financial wellbeing, than becoming unwell with the virus ( 7 ). This finding is also consistent with emergent work indicating that loneliness is playing a central role in the observed mental health impacts of the COVID-19 pandemic ( 22 – 24 ). Altogether then, it is evident that the necessary public health arrangements surrounding the pandemic are having serious implications for community mental health, via their disruption to social and work functioning.
However, this does not mean the mental health costs of pandemic-related social changes will inevitably be greater than those caused by exposure to disease. In Australia, mortality rates were very low at the time of this study, and the health system had capacity to meet demand. The relatively low case rates were also reflected in our sample; although the majority of the sample had some exposure, such as needing to self-isolate, only 36 participants reported direct exposure to the virus (self or close contact diagnosed). The short-term mental health impacts of disease contact may be considerably greater in communities that have high mortality rates, and health systems over-burdened by disease. In the longer-term, disease contact may also lead to elevated levels of trauma and grief for affected individuals ( 3 ).
The elevated levels of psychological distress observed in this study indicate mental health services are likely to experience increased demand during pandemics. Following recommended physical distancing guidelines, these will need to be delivered flexibly, leveraging resources for telehealth and internet-based Cognitive Behavior Therapy (CBT) programs, which have been shown to be effective in preventing and treating common mental disorders ( 7 , 25 , 26 ). There may also be an increased role for community cohesion strategies ( 27 ) and peer support ( 28 ), for instance, drawing on the experience and knowledge of people already living with mental health issues to support those experiencing these issues for the first time.
The findings also provide clear evidence that minimizing social and financial disruption during the COVID-19 pandemic should be a central goal of public health policy. A key challenge is how to best achieve this goal without compromising public safety by, for instance, relaxing physical distancing restrictions too early. Our results suggest policy approaches that target financial support to those experiencing financial strain may be useful, rather than on the basis of lost employment alone. We also found that well-established risk factors for poorer mental health—younger age, identifying as female, and having a pre-existing mental health condition—continue to be associated with increased risk within the pandemic context. Governments should consider additional measures to monitor and support these at-risk groups. Psychosocial interventions to support multiple aspects of wellbeing, including minimizing financial debt, may have positive impacts on depression and anxiety in the community ( 29 ). Clinicians should also remain vigilant for potential added social and financial impacts that existing clients in primary care and psychological settings may be experiencing.
A possible limitation of the present study is the use of self-report scales that may not characterize mental health status with the accuracy of structured clinical interviews, although both the PHQ-9 and GAD-7 have previously demonstrated strong alignment with clinical diagnosis in population samples ( 14 ), and the WHO-5 is also well-validated ( 15 ). Another potential issue is the influence of selection bias on the prevalence of mental health problems seen in this sample, however, the likelihood of this is low. We were careful to ensure the recruitment advertisement did not mention the topic or nature of our survey (e.g., no mention of mental health or COVID-19 at all), and the service we used also recruits participants for non-psychological research (i.e., market research panel). Most importantly, we did obtain a sample that was representative of the Australian population by age, gender, and location. It is however important to note that online survey methods may bias samples towards people who have good internet literacy and access ( 30 ). This type of bias may have a disproportionate impact on subsections of the population, such as older adults.
Finally, this initial report of our work is cross-sectional. The observed associations may not reflect causal effects, and the nature of any causal relationships may be more complicated than our interpretation suggests (e.g., possible bi-directional effects between psychological distress and social/occupational functioning). We intend to balance the necessity of providing our first wave findings in a timely fashion, to rapidly inform ongoing global responses to the pandemic, by reporting longitudinal outcomes as they become available in the coming months. Examination of population subgroups within our sample may also be possible in longitudinal analyses, although additional targeted studies may be required to provide greater insight into how specific vulnerable groups are affected. These findings should also be considered in combination with other studies that survey the mental health impacts of COVID-19 in communities that have adopted different approaches to managing the pandemic and/or have differing social structures (e.g., low GDP) to Australia.
In conclusion, the current study provides a snapshot of the acute phase impact of COVID-19 on the mental health of the Australian adult community. The findings are concerning, suggesting markedly elevated rates of depression and anxiety, even among individuals with no current diagnosis. This worsening of mental health may also have been exacerbated by the recent severe bushfire season Australians had experienced in the months leading up to the pandemic, although bushfire exposure was controlled for in our analyses. Overall, the findings suggest that interventions to counteract the social, financial and role disruptions induced by COVID-19, particularly among people with existing health conditions, are likely to have the greatest impact on community mental health and wellbeing.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Australian National University Human Research Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors contributed to the design and conceptualization of the study, which was coordinated by AD. AD, PJB, and LMF contributed to the literature review. AD, PJB, YS, MS, and NC contributed to the data analyses and formulation of the manuscript, with input from all other authors. AD, PJB, NC, and MS drafted the manuscript and all authors critically revised the manuscript. All authors contributed to the article and approved the submitted version.
This study was funded by the ANU College of Health and Medicine, ANU Research School of Psychology, and ANU Research School of Population Health. PJB is supported by National Health and Medical Research Council (NHMRC) Fellowship 1158707. ALC is supported by NHMRC Fellowships 1122544 and 1173146. LMF is supported by Australian Research Council Discovery Early Career Researcher Award (ARC DECRA) DE190101382. YS is supported by ARC DECRA DE180100015. AG and ARM are supported by funding provided by the ACT Health Directorate for ACACIA: The ACT Consumer and Carer Mental Health Research Unit.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Patrice Ford for assistance with preparing this manuscript and Georgia Baines for media monitoring.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.579985/full#supplementary-material
1. Gardner PJ, Moallef P. Psychological impact on SARS survivors: Critical review of the English language literature. Can Psychology/Psychologie Can (2015) 56:123–35. doi: 10.1037/a0037973
CrossRef Full Text | Google Scholar
2. James PB, Wardle J, Steel A, Adams J. Post-Ebola psychosocial experiences and coping mechanisms among Ebola survivors: a systematic review. Trop Med Int Health (2019) 24:671–91. doi: 10.1111/tmi.13226
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Van Bortel T, Basnayake A, Wurie F, Jambai M, Koroma AS, Muana AT, et al. Psychosocial effects of an Ebola outbreak at individual, community and international levels. Bull World Health Organ (2016) 94:210–4. doi: 10.2471/BLT.15.158543
4. Ricci-Cabello I, Meneses-Echavez JF, Serrano-Ripoll MJ, Fraile-Navarro D, Fiol de Roque MA, Moreno GP, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review. medRxiv (2020). doi: 10.1101/2020.04.02.20048892
5. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The Psychological Impact of the SARS Epidemic on Hospital Employees in China: Exposure, Risk Perception, and Altruistic Acceptance of Risk. Can J Psychiatry (2009) 54:302–31. doi: 10.1177/070674370905400504
6. Kim TJ, von dem Knesebeck O. Perceived job insecurity, unemployment and depressive symptoms: a systematic review and meta-analysis of prospective observational studies. Int Arch Occup Environ Health (2016) 89:561–73. doi: 10.1007/s00420-015-1107-1
7. Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
8. Ma J, Batterham PJ, Calear AL, Han J. A systematic review of the predictions of the Interpersonal-Psychological Theory of Suicidal Behavior. Clin Psychol Rev (2016) 46:34–45. doi: 10.1016/j.cpr.2016.04.008
9. Fitch C, Hamilton S, Bassett P, Davey R. The relationship between personal debt and mental health: a systematic review. Ment Health Rev J (2011) 16:153–66. doi: 10.1108/13619321111202313
10. Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health (2017) 152:157–71. doi: 10.1016/j.puhe.2017.07.035
11. U.N. News. COVID-19: impact could cause equivalent of 195 million job losses, says ILO chief . U.N. News (2020). Available at: https://news.un.org/en/story/2020/04/1061322 .
Google Scholar
12. Australian Bureau of Statistics, 2016 Census QuickStats. Australian Bureau of Statistics (2016). Available at: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/036
13. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
14. Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry (2010) 32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006
15. Topp CW, Ostergaard SD, Sondergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom (2015) 84:167–76. doi: 10.1159/000376585
16. Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale:a simple measure of impairment in functioning. Br J Psychiatry (2002) 180:461–4. doi: 10.1192/bjp.180.5.461
17. R.C. Team. R: A language and environment for statistical computing . Vienna, Austria: R Foundation for Statistical Computing: Vienna, Austria (2013).
18. Smithson M, Shou Y. Generalized linear models for bounded and limited quantitative variables . Belmont, CA: SAGE Publications (2019).
19. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Internal Med (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
20. Kocalevent RD, Hinz A, Brahler E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry (2013) 35:551–5. doi: 10.1016/j.genhosppsych.2013.04.006
21. Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
22. González-Sanguino C, Ausín B, ÁngelCastellanos M, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun (2020) 87:172–6. doi: 10.1016/j.bbi.2020.05.040
23. Li LZ, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res (2020) 291:113267. doi: 10.1016/j.psychres.2020.113267
24. Palgi Y, Shrira A, Ring L, Bodner E, Avidor S, Bergman Y, et al. The loneliness pandemic: Loneliness and other concomitants of depression, T anxiety and their comorbidity during the COVID-19 outbreak. J Affect Disord (2020) 275:109–11. doi: 10.1016/j.jad.2020.06.036
25. Batterham PJ, Mackinnon AJ, Christensen H. The panic disorder screener (PADIS): Development of an accurate and brief population screening tool. Psychiatry Res (2015) 228:72–6. doi: 10.1016/j.psychres.2015.04.016
26. Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med (2007) 37:319–28. doi: 10.1017/S0033291706008944
27. Townshend I, Awosoga O, Kulig J, Fan H. Social cohesion and resilience across communities that have experienced a disaster. Natural Hazards (2014) 76:913–38. doi: 10.1007/s11069-014-1526-4
28. Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health (2011) 20:392–411. doi: 10.3109/09638237.2011.583947
29. Jenkins R, Bhugra D, Bebbington P, Brugha T, Farrell M, Coid J, et al. Debt, income and mental disorder in the general population. Psychol Med (2008) 38:1485–93. doi: 10.1017/S0033291707002516
30. Lourenco SF, Tasimi A. No participant left behind: Conducting science during COVID-19. Trends Cogn Sci (2020) 24:583–4. doi: 10.1016/j.tics.2020.05.003
Keywords: coronavirus, COVID-19, bushfire, mental health, anxiety, depression, financial strain
Citation: Dawel A, Shou Y, Smithson M, Cherbuin N, Banfield M, Calear AL, Farrer LM, Gray D, Gulliver A, Housen T, McCallum SM, Morse AR, Murray K, Newman E, Rodney Harris RM and Batterham PJ (2020) The Effect of COVID-19 on Mental Health and Wellbeing in a Representative Sample of Australian Adults. Front. Psychiatry 11:579985. doi: 10.3389/fpsyt.2020.579985
Received: 03 July 2020; Accepted: 07 September 2020; Published: 06 October 2020.
Reviewed by:
Copyright © 2020 Dawel, Shou, Smithson, Cherbuin, Banfield, Calear, Farrer, Gray, Gulliver, Housen, McCallum, Morse, Murray, Newman, Rodney Harris and Batterham. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amy Dawel, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Stress, anxiety, depression and sleep disturbance among healthcare professional during the COVID-19 pandemic: An umbrella review of 72 meta-analyses
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Fatima College of Health Sciences, Al Ain, United Arab Emirates
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing
Affiliation Faculty of Pharmacy, Department of Clinical Pharmacy and Therapeutics, Applied Science Private University, Amman, Jorden
Affiliation Institute of Nursing and Health Research School of Health Sciences, Ulster University, Belfast, United Kingdom
Affiliation University of Texas MD Anderson Cancer Center, Houston, Texas, United States of America
* E-mail: [email protected]
Affiliations Midwifery and Health Faculty of Health and Life Sciences, Mental Health Nursing Department of Nursing, Northumbria University, Newcastle-Upon-Tyne, United Kingdom, Adjunct Professor Western Sydney University, Parramatta, NSW, Australia
- Mohammed Al Maqbali,
- Ahmad Alsayed,
- Ciara Hughes,
- Eileen Hacker,
- Geoffrey L. Dickens

- Published: May 9, 2024
- https://doi.org/10.1371/journal.pone.0302597
- Peer Review
- Reader Comments
The outbreak of SARS-CoV-2, which causes COVID-19, has significantly impacted the psychological and physical health of a wide range of individuals, including healthcare professionals (HCPs). This umbrella review aims provide a quantitative summary of meta-analyses that have investigated the prevalence of stress, anxiety, depression, and sleep disturbance among HCPs during the COVID-19 pandemic. An umbrella review of systematic reviews and meta-analyses reviews was conducted. The search was performed using the EMBASE, PubMed, CINAHL, MEDLINE, PsycINFO, and Google Scholar databases from 01 st January 2020 to 15 th January 2024. A random-effects model was then used to estimate prevalence with a 95% confidence interval. Subgroup analysis and sensitivity analyses were then conducted to explore the heterogeneity of the sample. Seventy-two meta-analyses involved 2,308 primary studies were included after a full-text review. The umbrella review revealed that the pooled prevalence of stress, anxiety, depression, and sleep disturbance among HCPs during the COVID-19 pandemic was 37% (95% CI 32.87–41.22), 31.8% (95% CI 29.2–34.61) 29.4% (95% CI 27.13–31.84) 36.9% (95% CI 33.78–40.05) respectively. In subgroup analyses the prevalence of anxiety and depression was higher among nurses than among physicians. Evidence from this umbrella review suggested that a significant proportion of HCPs experienced stress, anxiety, depression, and sleep disturbance during the COVID-19 pandemic. This information will support authorities when implementing specific interventions that address mental health problems among HCPs during future pandemics or any other health crises. Such interventions may include the provision of mental health support services, such as counseling and peer support programs, as well as the implementation of organizational strategies to reduce workplace stressors.
Citation: Al Maqbali M, Alsayed A, Hughes C, Hacker E, Dickens GL (2024) Stress, anxiety, depression and sleep disturbance among healthcare professional during the COVID-19 pandemic: An umbrella review of 72 meta-analyses. PLoS ONE 19(5): e0302597. https://doi.org/10.1371/journal.pone.0302597
Editor: Fadwa Alhalaiqa, Qatar University College of Nursing, QATAR
Received: January 21, 2024; Accepted: April 8, 2024; Published: May 9, 2024
Copyright: © 2024 Al Maqbali et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All data are in the paper and/or supporting information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
1. Introduction
In December 2019, the coronavirus disease 2019 (COVID-19) pandemic emerged in Wuhan, China. The disease quickly spread worldwide, and the WHO declared a global health emergency in March 2020 [ 1 ]. Due to the COVID-19 pandemic, many countries implemented various measures to prevent the spread of the disease. These included implementing a partial or complete lockdown and social distancing strategies of varying intensity. The measures taken by these countries also affected the livelihood of individuals, an occurrence which might directly or indirectly also increase psychological morbidities. Undoubtedly, pandemics have a long history of impacting physical and mental health for different population groups, and HCPs are typically the most affected group in terms of bearing the burden of these illnesses [ 2 ]. In addition, several researchers have shown that work-related psychological disorders, including stress, anxiety, depression, and burnout, had already negatively affected the healthcare system before the COVID-19 pandemic, leading to low-quality care and high malpractice litigation [ 3 – 5 ].
As a result of the pandemic, HCPs experienced various changes in their personal and professional lives. For some, these included being given more responsibility, having to re-learn how to effectively control the infection, and dealing with the emotional impact of caring for infected and dying COVID-19 patients [ 6 ]. The alteration in their work environment, as well as the likelihood that they might acquire the infection themselves, can also affect their personal mental health. It is almost inevitable that the experiences of HCPs went through during the pandemic put them at heightened risk of stress, anxiety, depression, and sleep disturbance [ 7 , 8 ]. It is important to understand the effects of the pandemic on the mental health and well-being of HCPs in order to help plan strategies to prevent these individuals from experiencing detrimental effects, and to ensure that they can continue to deliver healthcare services.
During previous viral outbreaks including the Severe Acute Respiratory Syndrome (SARS) and the Middle East Respiratory Syndrome (MERS) epidemics, HCPs were placed under extraordinary amounts of pressure [ 9 , 10 ]. Indeed, evidence suggested that HCPs suffered from high levels of stress, anxiety, depression and sleep disturbance during these outbreaks [ 11 , 12 ]. A high prevalence of mental health problems can adversely impact the quality of life of HCPs, increase disability, turnover, absenteeism, and errors, and can deleteriously affect patient outcomes which may lead to low patient satisfaction [ 13 ]. Further, it might increase suicidal ideation or self-harming among HCPs [ 14 ].
In the present review, four phenomena were addressed. Sleep disturbance refers to a range of sleep-related problems, including disruptions in the body’s natural sleep-wake cycle, insufficient or poor-quality sleep, and sleep disorders [ 15 ]. The anxiety symptoms were defined as a state of excessive fear that translates to behavioural disturbances [ 16 ]. Major depressive disorder is a set of symptoms that includes depressed mood, loss of pleasure or interest, fatigue, changes in sleep and activity levels, and other symptoms, with a minimum duration of two weeks and at least five or more symptoms present according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [ 16 ]. Cohen et al., [ 17 ] define stress as “the degree to which individuals appraise situations in their lives as stressful”. In this umbrella review, stress, anxiety, depression, and sleep disturbance symptoms were defined based on the validated scales/questionnaires that assess each phenomenon in the original studies.
Several primary studies and, subsequently, systematic reviews and meta-analyses have been carried out to identify the prevalence of mental health problems among HCPs during the COVID-19 pandemic. Additionally, three umbrella reviews of meta-analyses [ 18 – 20 ] have been published previously, but the number of meta-analyses included in both cases did not exceed twenty. Since their publication, further meta-analyses have estimated the prevalence of stress, anxiety, depression, and sleep disturbance during the COVID-19 pandemic. The advantages of umbrella reviews include their ability to provide a comprehensive analysis of the literature, in this case about the prevalence of various mental disorders in HCPs during the COVID-19 pandemic. In addition, the results can then be used to make policy-level decisions to improve the quality of clinical care in terms of making clinical risk predictions and can inform future research priorities. Therefore, the aim of this umbrella review is to quantify meta-analytic findings aimed at estimating the prevalence symptoms of stress, anxiety, depression, and sleep disturbance among HCPs during the COVID-19 pandemic.
The umbrella review and meta-analysis were carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [ 21 ]. The review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) database and can be accessed online (CRD42022364721).
2.1 Search strategy
A systematic search was conducted to identify relevant meta-analyses in various electronic databases published between 1 st January 2020 and 15 th January 2024. The databases searched were PubMed, CINAHL, MEDLINE, EMBASE, PsycINFO, and Google Scholar. The search terms strategy used Medical Subject Headings (MeSH) and free text words with Boolean operators and truncations (AND/OR/NOT). The key search terms included (MH "Coronavirus Infections+") OR "COVID-19” OR "COVID” OR "coronavir* OR "Coronavirus" OR "SARS-COV2" AND "Health care provider" OR "health care professional" OR "healthcare provider*" OR (MH "Nurses+") OR (MH "Medical Staff") OR (MH "Physician") OR (MH "Medical Doctor") OR (MH "Staff Nurses") OR "nursing staff" OR "health personnel or health professional or nurse" OR "health personnel or health professional or nurse" AND "Stress" OR "post-traumatic stress disorder" OR "panic disorder" OR "obsessive compulsive disorder OR "anxi*" OR (MH "Anxiety Disorders+") OR (MH "Anxiety+") OR (MH "Depression+") OR "depress*" OR (MH "Affective Symptoms+") OR (MH "Affective Disorders+") OR (MH "Bipolar Disorder+") OR "affective" OR "mood" OR "mental" OR (MH "Mental Disorders+") OR (MH "Mental OR "psycho*" OR (MH "Insomnia+") OR (MH "Circadian Rhythm+") OR (MH "Sleep Disorders+") OR (MH "Insomnia+") OR (MH "Sleep+") AND "Systematic Review" OR "Meta-Analysis" OR "Meta-Analytic". Additionally, the reference lists were searched to find any other studies.
2.2 Study selection
Two reviewers (A.M.; A.A.) independently extracted the data from the search, scrutinizing all titles and abstracts for eligibility against the inclusion and exclusion criteria. A third reviewer (G.D.) was available to resolve any disagreements through discussion. Systematic reviews incorporating meta-analyses were included according to the following criteria. The studies: (1) examined the prevalence of stress or anxiety or depression or sleep disturbance symptoms; (2) presented results for HCPs as a group or separately (e.g., nurses or physicians only); further, studies involving non-HCPs must have presented results for HCPs separately and not pooled with non-HCPs.; (3) were conducted during the COVID-19 pandemic; (4) were published in English; (5) involved a systematic review with meta-analysis. Studies were excluded if (1) these consisted of a systematic review without meta-analysis; (2) consisted of a literature review or a narrative review (3) the participants were general population or non-HCPs.
2.3 Quality assessment
The methodological quality assessment of each meta-analysis was blindly rated by two reviewers using the Assessment of Multiple Systematic Reviews (AMSTAR-2) tool [ 22 ]. This scale consists of 16 items that evaluate the risk of bias of a systematic review. Items 1, 3, 5, 6, 10, 13, 14, and 16 are evaluated with either a "Yes" or "No" response. Items 2, 4, 7, 8, and 9 are evaluated with "Yes," "Partial Yes," or "No" responses. Items 11, 12, and 15 are evaluated with "Yes," "No," or "No meta-analysis conducted" responses. The overall rating can be rated as "High," "Moderate," "Low," or "Critically low."
2.4 Credibility of evidence
The credibility of the evidence of each association provided was evaluated by the Fusar-Poli and Radua [ 23 ] classification criteria. The level of evidence as convincing (class I) when specific criteria were met, including more than 1000 cases, p<10 −6 , I 2 higher than 50%, 95% prediction intervals excluding the null, no small-study effects, and no publication bias. If the number of cases exceeded 1000, p<10 −6 , the largest study showed a statistically significant effect, but not all class I criteria were satisfied; the evidence level was considered highly suggestive (class II). When there were over 1000 cases, p<10 −3 , but no other class I or II criteria were met, the evidence level was termed suggestive (class III). If no class I-III criteria were met, the evidence level was classified as weak (class IV). The fourth level, termed weak evidence (class IV), included associations with a p ≤0.05, but these associations did not meet the criteria for class I, class II, or class III. The fifth level, denoted as non-significant (NS), comprised associations with a p˃0.05.
2.5 Data analyses
There are two methods exist for deriving effect size estimates from existing meta-analyses. The first approach involves conducting a meta-analysis on the effect size estimates taken from individual studies included in multiple prior meta-analyses [ 24 ]. However, this method demands significant time and resources. Furthermore, it contradicts the primary purpose of an umbrella review because it requires return to the original studies.
The second approach employs a statistical technique to efficiently summarize data from previous meta-analyses without the need to go back to the individual studies. This method relies solely on the summary effect sizes and their associated variances provided in the original meta-analyses [ 25 ]. It calculates an overall effect size for the combined meta-analyses by computing a weighted average of the summary effect sizes, with the weights determined by the inverse of the variances [ 26 ]. This approach is similar to the methods used in meta-analyses of primary studies. Although the second approach (combining summary effect sizes) may not achieve the same level of precision as the first method (combining all individual studies), empirical tests have confirmed its ability to generate a statistically valid estimate for the overall effect size [ 27 , 28 ]. In this umbrella review, we employed the second approach, which entailed the utilization of aggregate data derived from the meta-analyses.
The analyses were conducted using R software, version 4.3.1 (R Foundation for Statistical Computing), with packages used ‘meta’ [ 29 ], ‘metafore’ [ 30 ] and ‘metaumbrella’[ 31 ]. Pooled estimates prevalence with 95% Confidence Intervals (CIs) was conducted using random effect models, and the results were reported on a forest plot. In addition, the I-squared (I 2 ) test was used to assess the statistical heterogeneity of the included meta-analyses. A value of I 2 < 25% was considered low, 25–50% moderate, and ˃ 50% high [ 32 ]. Subgroup analyses were performed when there were at least four meta-analyses per subgroup.
Publication bias was assessed using Egger’s test with a p < 0.10 indicates a statistically significant small-study effect [ 33 ]. Statistical significance was set at p<0.05. If publication bias was identified, trim and fill methods were used to adjust the publication bias [ 34 ]. A sensitivity analysis was conducted in which individual meta-analyses were systematically removed one at a time to assess how they affected the overall combined prevalence of the remaining meta-analyses [ 35 ], with the aim of clarifying the stability and reliability of the finding [ 36 ].
A total of 1,987 papers were identified through the database search. Out of these, 1,843 were excluded at the abstract and title screening stage for the following reasons: 786 were duplicates, 443 did not include a meta-analysis, 392 lacked information about prevalence, 139 lacked information about HCP status, and 83 were not conducted during the period of the COVID-19 pandemic. A further 72 papers were excluded during the full text review process. As a result, 72 meta-analyses were eligible for umbrella review ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0302597.g001
3.1 General characteristics of the studies included
The included 72 meta-analyses [ 37 – 108 ]. Fifty-four of the meta-analyses dealt with HCPs in general, whereas two meta-analyses reported the situation only with regard to physicians or nurses [ 44 , 59 ], three meta-analyses dealt with nurses [ 49 , 79 , 91 ], and one dealt with physicians [ 88 ], while 17 meta-analyses included a mixed population (General and HCPs),(Only data specifically related to healthcare professionals were included in the umbrella review analysis). The most commonly used statistical software was STATA (n = 32), R (n = 17) and comprehensive meta-analysis (n = 11). Twenty-four meta-analyses used the Newcastle–Ottawa scale to assess the quality of the studies. Forty-six meta-analyses included mixed studies from different countries, twenty-five meta-analyses were conducted in specifical geographical areas: 10 for China, five for India, four for Asia two for Bangladesh and Ethiopia and one for each of the following: Egypt, South Asia, and Vietnam. The detailed characteristics of the studies including meta-analyses are shown in Table 1 .
https://doi.org/10.1371/journal.pone.0302597.t001
3.2 Quality appraisal
Each meta-analysis was assessed using the AMSTAR-2 tool. Twenty- nine meta-analyses were classified as moderate quality and thirty-seven as low quality. Only six meta-analyses were classified as critically low quality [ 37 , 44 , 45 , 76 , 97 , 101 ].
3.3 Prevalence of stress
Stress was reported in 42 meta-analyses among HCPs. The estimation of prevalence for stress varied between 11% [ 72 ] and 66.6% [ 58 ] ( Fig 2 : Forest Plots). The pooled prevalence of stress from was 37% (292,245/854,852 participants, 95% CI 32.87–41.22) with 95% PI: 14.86–66.3. There was significant heterogeneity between meta-analyses when it came to estimating the prevalence of stress ( p < 0.0001, I 2 = 99.9%). In the subgroup analysis, the prevalence of anxiety among nurses was determined to be 42.6% (n = 5; 95% CI = 30.49–55.27, I 2 = 99%), as shown in Fig 3 : Forest Plots. However, the analysis for physicians was not conducted due to an insufficient number of available meta-analyses. In sensitivity analysis, none of the meta-analyses resulted in changes to the pooled prevalence estimates greater than a 2%. The prevalence rate estimates for stress were considered to be suggestive evidence (class III) (Seen Table 2 ).
https://doi.org/10.1371/journal.pone.0302597.g002
https://doi.org/10.1371/journal.pone.0302597.g003
https://doi.org/10.1371/journal.pone.0302597.t002
3.4 Prevalence of anxiety
Fifty-five meta-analyses estimated the prevalence of anxiety among HCPs, and ranged from 11.4% [ 40 ] to 71.9% [ 58 ]. The pooled prevalence of anxiety was 31.8% (734,036/2,310,774 participants, 95% CI 29.2–34.61) with 95% PI: 15.24–54.83 ( Fig 4 : Forest Plots) among all HCPs and there was considerable heterogeneity ( p < 0.0001, I 2 = 99.9%). In the subgroup analyses, in terms of professional status, the pooled prevalence of anxiety was 31.6% (n = 12; 95% CI = 28.33–35.14, I 2 = 99%) and 26.3% (n = 9; 95% CI = 22.89–30.10, I 2 = 99%) for nurses, and physicians respectively (Figs 5 and 6 : Forest Plots). A sensitivity analysis, specifically a leave-one-out analysis, revealed that none of the meta-analyses had an impact on the global prevalence estimate of anxiety symptoms greater than 1%. Suggestive evidence (class III) was found for the estimated prevalence of anxiety in the case of HCPs, nurses and physicians.
https://doi.org/10.1371/journal.pone.0302597.g004
https://doi.org/10.1371/journal.pone.0302597.g005
https://doi.org/10.1371/journal.pone.0302597.g006
3.5 Prevalence of depression
A total of 54 meta-analyses examined the prevalence of depression among HCPs during the COVID-19 pandemic and results ranged from 14% [ 52 ] to 65.6% [ 58 ]. The pooled prevalence was 29.4% (698,808/2,349,613 participants, 95% CI 27.13–31.84) with 95% PI: 15.01–49.62 ( Fig 7 : Forest Plots) and there was a significant result in terms of the study heterogeneity ( p < 0.0001, I 2 = 99.9%). In subgroups analyses, the prevalence of depression was higher among nurses 32% (n = 11; 95% CI = 28–36.35, I 2 = 99%) compared with physicians 28.4% (n = 8; 95% CI = 24.32–32.78, I 2 = 99%) (Figs 8 and 9 : Forest Plots). In the sensitivity analysis, the pooled prevalence remained stable when one meta-analysis was excluded at a time, with variations of less than 1%. Class III evidence revealed suggestive findings regarding the estimated prevalence of depression among HCPs, nurses, and physicians.
https://doi.org/10.1371/journal.pone.0302597.g007
https://doi.org/10.1371/journal.pone.0302597.g008
https://doi.org/10.1371/journal.pone.0302597.g009
3.6 Prevalence of sleep disturbance
Sleep disturbance was assessed in 36 meta-analyses, with a calculated pooled prevalence of 36.9% (191,673/502,780 participants, 95% CI 33.78–40.05) with 95% PI: 19.99–57.70 ( Fig 10 : Forest Plots) with significant differences in terms of the meta-analyses heterogeneity presented (p< 0.0001, I 2 = 99.7%). The prevalence of sleep disturbance ranged from 15.01% [ 93 ] to 47.3% [ 95 ]. In subgroup analyses, the prevalence of sleep disturbance was found to be higher among nurses at 37.1% (n = 5; 95% CI = 30.71–44.1, I 2 = 99%) compared to physicians, where it was 30.6% (n = 4; 95% CI = 20.04–43.77, I 2 = 99%) (Figs 11 and 12 : Forest Plots). The estimated prevalence rate of sleep disturbance was deemed to be suggestive evidence (Class III). The pooled prevalence did not change in sensitivity analysis by excluding one meta-analyses each time by less than 3%.
https://doi.org/10.1371/journal.pone.0302597.g010
https://doi.org/10.1371/journal.pone.0302597.g011
https://doi.org/10.1371/journal.pone.0302597.g012
3.7 Publication bias
The result of Egger’s regression test for all pooled prevalence indicates that publication bias was insignificant, showing no evidence of publication bias Table 2 .
4. Discussion
To the best of our knowledge, this is the first umbrella review to provide a comprehensive synthesis of the estimate of the aggregate data prevalence symptoms of stress, anxiety, depression, and sleep disturbance among HCPs, physicians, and nurses during the entire COVID-19 pandemic.
In the present umbrella review, which utilizes aggregate data from 71 meta-analyses, the most prevalent problems among healthcare professionals (HCPs) were found to be stress (37%), followed by sleep disturbance (36.9%), anxiety (31.8%), and depression (29.4%). The findings among HCPs are slightly higher than the prevalence estimates from the general population (prevalence estimates of 27% for sleep disturbance; 36% for stress; 26% for anxiety and 28% for depression) during the COVID-19 pandemic [ 109 ]. In addition, a report by the World Health Organization prior to the COVID-19 pandemic estimated that the global prevalence of anxiety and depression was 4.4% and 3.6% respectively [ 110 ]. While some of this disparity may result from different methodological approaches used, the prevalence of depression and anxiety during the COVID-19 pandemic appears to have been higher than before the outbreak. The rise in mental health problems among HCPs may have been triggered by the uncertainty surrounding the pandemic, increased workload, and the fear of family transmission, any, or all of which may also contribute to the higher prevalence of these conditions.
The results of this umbrella review revealed higher prevalence rates compared with two previous reviews of meta-analyses [ 18 , 20 ]. These include 10 meta-analyses which reported prevalence rates during COVID-19 among HCPs: 25% for anxiety and 24% for depression [ 18 ]. Another umbrella review involving 18 meta-analyses found stress in 36% of the sample, depression in 26%, anxiety in 27% and sleep disturbance in 32% among HCPs during the COVID-19 pandemic [ 20 ]. It is important to highlight that the previous reviews included meta-analyses published before March 2021, while this current review included studies published until January 2024. As a result, the current umbrella review includes more meta-analyses compared to the two previous umbrella reviews [ 18 , 20 ]. This umbrella review therefore extends the scientific knowledge of the impact of COVID on mental health of HCPs.
The results of our study suggest that the psychological trauma experienced by HCPs during the SARS and MERS epidemics was lower than that experienced during the COVID-19 pandemic [ 111 – 114 ]. However, the difference between COVID-19 and previous pandemics could be explained by the high mortality rate and infectious potential of the COVID-19 pandemic. The results of this study suggest that the COVID-19 pandemic has had a significant negative effect on the psychological health of HCPs. One important lesson that should be learned is that early detection and treatment are carried out to prevent these types of psychological issues developing into more complex ones.
The result of this analysis demonstrates a higher level of anxiety, depression and sleep disturbance among nurses compared to physicians. One explanation for this may be that nurses are involved in more prolonged and closer contact to COVID-19 patients than physicians [ 115 – 117 ]. Another possible reason might be due to the higher number of nurses included in original studies.
The current review found that the overall pooled prevalence varied between the meta-analyses, for example ranging between 1% [ 72 ] and 66.6% [ 58 ] for stress, 11.% [ 40 ] and 71.9% [ 58 ] for anxiety, 14% [ 52 ] and 65.6% [ 58 ] for depression, and 15% [ 93 ] and 47.3% [ 95 ] for sleep disturbance. This could be linked to the varying COVID-19 infection and mortality rates in the countries in which the studies were conducted. Other possible reasons might relate to the healthcare system, cultural norms of HCPs, and their perceptions of stress, anxiety, depression, and sleep disturbance which in turn might be influenced by their working conditions, exposure to pandemics, intensity of lockdown and social distancing strategies, and perceived support. For instance, the result of the meta-analysis by El-Qushayri [ 58 ] showed the highest prevalent rate in terms of stress, anxiety and depression. This may be because this meta-analysis included only HCPs from Egypt, which in turn might indicate that the Egyptian healthcare system was severely affected by COVID-19 compared to other countries [ 118 ].
The finding of this umbrella review highlights significant negative effect that the COVID-19 pandemic has had on the psychological health of HCPs, further emphasizing the need for regular mental health assessment and management in this population. Due to the increasing number of complex traumas that HCPs are experiencing, special attention should be paid to the development of positive traumatic growth. The higher prevalence of stress, anxiety, depression, and sleep disturbance among HCPs have important implications for both the policies and practices of the healthcare system under consideration. It is important to identify effective interventions for HCPs such as the behavioural and educational interventions that have been suggested, including the development of a sense of coherence, positive thinking, and social support [ 119 – 121 ]. Currently there is a lack of evidence about the effectiveness of some psychological interventions that were adapted for use during COVID-19 pandemic specifically for healthcare workers [ 122 , 123 ].
Heterogeneity was significant in the majority of the analyses; several reasons can be attributed to this prominence. Firstly, the individual studies within each meta-analysis might differ substantially in terms of their design, sample sizes, interventions or exposures, and outcome measures. These variations can lead to differing effect sizes or conclusions, making the integration of results into a cohesive summary more complex. Furthermore, heterogeneity can arise from variations in the quality of these studies. While some research might have been meticulously conducted with strict inclusion criteria and rigorous methodologies, other studies on healthcare workers may have inherent biases or confounding factors due to the rapidly changing nature of the pandemic, the pressures of lockdowns, and their effects.
The unique characteristics and experiences of healthcare workers during the COVID-19 crisis, compounded by the challenges of lockdown measures, have the potential to further amplify this variability. Factors such as age, gender, ethnicity, and underlying health conditions, when combined with the stress, increased workload, and challenges of the pandemic and lockdown situations, can significantly influence study outcomes. Additionally, methodological differences in individual studies, like the use of a wide variety of questionnaires to measure symptoms, varied cut-off points, and severity thresholds, as well as the absence of a consistent ’gold standard’ for diagnostic interviews, can contribute to increased heterogeneity. In the context of the umbrella review, synthesizing findings from such a diverse collection of meta-analyses, particularly those focused on healthcare workers during this unparalleled period marked by fluctuating lockdown measures, poses a formidable challenge. Such complexity may constrain the robustness and precision of the conclusions drawn.
One of the most critical factors that policymakers need to consider when it comes to implementing effective interventions is the availability of organizational support. This can be done through various work-based interventions such as implementing shorter working hours and having buddy systems [ 124 ]. In addition, other measures such as providing mental health consultants and tele counselling can also help reduce the impact of the outbreak of disease on the well-being of staff members [ 125 , 126 ].
4.1 Limitations
Several limitations must be taken into consideration when interpreting the results of this umbrella review even though one strength of this methodology is that it provides comprehensive evidence regarding the mental health problems that were faced by HCPs during the COVID-19 pandemic, First, there is a possibility of selection bias. For example, non-English language meta-analyses were not included in this umbrella review, and this may introduce a selection bias. Second, it may be the case that some meta-analyses may have included the same primary studies and that there is consequently a significant study overlap between the meta-analyses included in this review. However, since the results of the studies were then combined with other studies, and a new result was presented, these were regarded as being new studies [ 25 ]. Further, several researchers address overlapping by removing some of the reviews with higher rates of overlapping [ 26 , 127 ]. Although removing the overlapping meta-analyses solves the problem of dependent effects, it might introduce a bias of its own. Excluding one of two overlapping meta-analyses from an umbrella review will bias the overall estimate [ 128 , 129 ]. In addition, Hennessy and Johnson [ 127 ] clearly mention that the overlap of primary studies included in a meta-review is not necessarily a bias but often can be a benefit.
Third, the various methodologies of the primary studies that were included in the meta-analyses, in terms of sampling methods, assessment tools, operational definitions of the symptoms and study length, might have affected the sensitivity and specificity with regard to detecting the prevalence estimations of stress, anxiety, depression, and sleep disturbance [ 130 ]. Finally, it should be noted that stress, anxiety, depression, and sleep disturbance varied between the HCPs studied. Therefore, future research should focus on the difference contexts of estimation prevalence between HCPs and should report the prevalence in each group.
5. Conclusion
In summary, this umbrella review systematically analyses the currently available evidence on the prevalence of stress, anxiety, depression, and sleep disturbance among HCPs in relation to COVID-19. It revealed that the incidence of these symptoms is high in the HCP population. However, there is wide variation in the degree of these conditions among this HCP population. This may be due to the varying experiences of COVID-19 and the cultural differences in the countries where the studies have been carried out. It is clear from the current evidence that strategies involving multi-level interventions are required to develop effective interventions that can help improve the mental health and well-being of HCPs and foster post-traumatic growth. Further research needs to address the limitations of the existing literature, in order to enable the authorities, providers, and patients to improve the quality of mental health on the part of HCPs.
Supporting information
S1 checklist. prisma 2020 checklist..
https://doi.org/10.1371/journal.pone.0302597.s001
S1 Table. Quality assessment result of meta analysis using the AMSTAR-2 (N = 72).
https://doi.org/10.1371/journal.pone.0302597.s002
- View Article
- Google Scholar
- PubMed/NCBI
- 15. National Institutes of Health. National institutes of health sleep disorders research plan. Maryland, USA: National Institutes of Health; 2011 pp. 1–34. Available: https://www.nhlbi.nih.gov/files/docs/ncsdr/201101011NationalSleepDisordersResearchPlanDHHSPublication11-7820.pdf .
- 16. Association American Psychiatric. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. 5th edition. Washington, D.C: American Psychiatric Publishing; 2013.
- 25. Pollock M, Fernandes RM, Becker LA, Pieper D, Butler LD. Chapter V: Overviews of Reviews. 2nd ed. In: Higgins JP, Thomas J, Chandel J, Cumpston M, Li T, Page M, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions 63. 2nd ed. Chichester (UK): John Wiley & Sons; 2022. Available: www.training.cochrane.org/handbook .
- 29. Schwarzer G, Carpenter JR, Rücker G. Meta-Analysis with R. Cham: Springer International Publishing; 2015. https://doi.org/10.1007/978-3-319-21416-0
- 110. WHO. World Health Organization: Depression and Other Common Global Health Estimates. Geneva.Swizerland: World Health Organization; 2017 pp. 1–24. Available: https://scholar.google.com/scholar_lookup?title=Depression%20and%20Other%20Common%20Mental%20Disorders%3A%20Global%20Health%20Estimates&publication_year=2017 .
- Open access
- Published: 15 June 2022
COVID-19 and mental health in Australia – a scoping review
- Yixuan Zhao 1 ,
- Liana S. Leach 1 ,
- Erin Walsh 1 ,
- Philip J. Batterham 1 ,
- Alison L. Calear 1 ,
- Christine Phillips 2 ,
- Anna Olsen 2 ,
- Tinh Doan 1 ,
- Christine LaBond 1 &
- Cathy Banwell 1
BMC Public Health volume 22 , Article number: 1200 ( 2022 ) Cite this article
8348 Accesses
11 Citations
58 Altmetric
Metrics details
The COVID-19 outbreak has spread to almost every country around the world and caused more than 3 million deaths. The pandemic has triggered enormous disruption in people’s daily lives with profound impacts globally. This has also been the case in Australia, despite the country’s comparative low mortality and physical morbidity due to the virus. This scoping review aims to provide a broad summary of the research activity focused on mental health during the first 10 months of the pandemic in Australia.
A search of the Australian literature was conducted between August-November 2020 to capture published scientific papers, online reports and pre-prints, as well as gaps in research activities. The search identified 228 unique records in total. Twelve general population and 30 subpopulation group studies were included in the review.
Conclusions
Few studies were able to confidently report changes in mental health driven by the COVID-19 context (at the population or sub-group level) due to a lack of pre-COVID comparative data and non-representative sampling. Never-the-less, in aggregate, the findings show an increase in poor mental health over the early period of 2020. Results suggest that young people, those with pre-existing mental health conditions, and the financially disadvantaged, experienced greater declines in mental health. The need for rapid research appears to have left some groups under-researched (e.g. Culturally and Linguistically Diverse populations and Indigenous peoples were not studied), and some research methods under-employed (e.g. there was a lack of qualitative and mixed-methods studies). There is a need for further reviews as the follow-up results of longitudinal studies emerge and understandings of the impact of the pandemic are refined.
Peer Review reports
The outbreak of COVID-19, an infectious disease causing severe acute respiratory syndrome, led the Director-General of the World Health Organisation (WHO) to declare a public health emergency of international concern on the 30 th January 2020 [ 72 ]. By April 2021, the disease had spread to almost every country around the world, and caused more than 3 million deaths [ 74 ]. The pandemic has triggered enormous disruption in people’s daily lives and has undoubtedly had a widespread and profound global impact.
Australia has managed to date to achieve low total numbers of local infection, partly because of its geographic isolation (i.e. all borders are surrounded by sea) and also because of early interventions to contain the virus. Following the first confirmed case on the 25 th January 2020 [ 34 ], the Federal Government quickly introduced border controls, quarantine measures and urged the public to take precautions in response to the virus. By March 2020, a series of stringent containment measures were put in place by the state and territory governments to stop the spread of the virus and protect people’s lives. These included requirements to stay at home (except for specific reasons), business closures, restrictions on social gatherings and interstate travel, as well as a ban on all international travel. Residents in the state of Victoria experienced particularly stringent restrictions (e.g. a nightly curfew, a 5 km-limit for all activities, and mandatory mask-wearing [ 6 ]) during a second wave of COVID from June-October, 2020. To date, these restrictions have proven to be successful at reducing the transmission of the virus in Australia [ 16 , 13 ]. However, they have come at a considerable economic and health cost to individuals, businesses, communities and the nation. Government data shows that during June-July, 2020, the Australian Gross Domestic Product fell by a record 7% and the unemployment rate hit 7.5%—the highest it had been in over 20 years. Reassuringly, after July, the Australian economy started to improve in all states except Victoria [ 3 ].
Despite the successful management of the pandemic to date and the ongoing economic recovery, there are indications that Australians’ mental health declined in the early months of the pandemic and that this reduction has been somewhat sustained. Data from the Australian Bureau of Statistics (ABS) shows that in January 2021 22% of Australians reported that their mental health was ‘worse’ or ‘much worse’ than in March 2020; comparatively only 0.1% of people in Australia have been infected with COVID-19. Similarly, 21% reported that their mental health was ‘fair’ or ‘poor’ in January 2021—higher than the 14.4% who reported this in July 2020 [ 2 , 4 ]. Although this self-report data is not based on validated mental health measures, it demonstrates the importance of investigating the widespread and potentially enduring impact of the pandemic on mental health in Australia. Mental health experts have stated that increases in mental health problems are likely due to risk factors attributable to the virus itself (e.g. fear of contracting the virus, concerns about the lack of treatment options and/or being in a high-risk group for mortality, and uncertainty about when the virus will be controlled) as well as risk factors attributable to the lockdowns aimed at combating the virus (e.g. interrupted daily routines, unemployment and underemployment, loss of income, reduced social support, financial distress, and loneliness) [ 38 ]. The latter are well-established risk factors for poor mental health generally, let alone within the complex context of a global pandemic [ 50 , 32 ].
The Australian context is unusual in terms of the focus on individuals’ and communities’ mental health in 2020. In part, because the prevalence of COVID-19 has been relatively low in Australia compared to other countries, discussion regarding the more distal mental health impacts of COVID has been prominent alongside concerns about the proximal physical impacts. Justifiably, the research community (and the media) in Australia has paid tremendous attention to the potential mental health impacts of the outbreak. An influx of studies have been conducted in the past year (mainly from March to September 2020) to understand people’s experiences and gauge any increase in mental health problems during the pandemic. While many of these studies are still ongoing, numerous results have been published reporting on the prevalence and severity of mental health problems during this time (mostly common experiences such as psychological distress, depression and anxiety), and the vulnerability of different groups. For context, it is also important to note that the COVID pandemic closely followed the Black Summer bushfires. From September 2019 to February 2020, large swathes of Australia were burnt, accompanied by destruction of life, property, the natural environment and wildlife [ 11 ] (although most COVID-focused studies have not considered the population’s possible lingering emotional responses to the bushfires).
Despite the influx of research activity in Australia investigating mental health during 2020, comprehensive summaries of what has been done and what has been found are scarce (for an international review and meta-analyses see Prati & Mancini [ 56 ]). Given it has been over a year since the outbreak began, the current scoping review provides a timely summary of the Australian research conducted in 2020 during the early phase of the COVID-19 outbreak. The review also aimed to identify gaps in research activities, knowledge and understanding of how the pandemic is affecting Australian’s mental health.
Study design
In this review, the use of the term ‘mental health’ goes beyond the presence/absence of diagnosed mental illness and instead focuses on the most common psychological symptoms experienced in the community, such as distress, anxiety, and depression. Because this review aimed to be inclusive, and also considering much research regarding the pandemic is ongoing (with some research reports and online pre-prints not yet available in peer-reviewed scientific journals), we deemed a descriptive broader scoping review more appropriate than a traditional systematic review [ 44 , 64 ]. This review follows the PRISMA-ScR checklist, an extension of the PRISMA statement for conducting scoping reviews [ 66 , 51 ].

Eligibility criteria
While this scoping review was necessarily broad, clear well-defined eligibility criteria and research questions were still required. Following the JBI recommendations [ 51 ] we define our population as Australians, our context as Australia during the first 10 months of the COVID-19 pandemic, and our concept as mental health prevalence (or outcomes) and risk factors during this window of time.
Publications (reports, non-reviewed pre-prints of papers and peer-reviewed articles) were eligible to be included if they were focused on mental health during the COVID-19 pandemic, reported original research findings/results (i.e. media releases, editorials, opinion pieces, commentaries, protocol papers or general text summaries within reports (with no detailed findings) were excluded), were conducted within the Australian population, and were written in English.
Literature search and data extraction
Searches of the literature were conducted between August-November 2020 to capture research with a focus on COVID-19 and mental health in Australia. The search included three elements:
Four databases (PsycINFO, PubMed, Scopus and Web of Science) were searched using key words to capture published peer-reviewed articles focused on COVID-19 and mental health in Australia. These keywords were COVID AND ("mental health" OR "psychological dis*" OR "mental dis*" OR depress* OR anxiety OR wellbeing OR well-being OR "well being" OR worr* OR fear OR lonel* OR "alcohol use" OR "substance use” OR stress OR confus* OR anger OR optimism OR pessimism OR "mental ill*" OR mood OR panic) AND Australia *. The search was generally within the title and abstract field (in some databases, keywords and author information were also included). The document type was limited to “article” where possible so that other types of publications such as reviews, study protocols, editorials, commentaries, viewpoints, letters to editors, and dissertations, were excluded.
The online search engine Google was searched using the phrase “COVID mental health research survey Australia” to capture research findings not yet published in scientific journals. The results were limited to records within one year, verbatim, and pages published in or originating from Australia. Reports, online papers and pre-prints that included mental health/wellbeing measures or interview questions (and sufficient information about study methods) were identified and recorded. In addition, we checked the reference lists of identified publications and reached out to our existing research networks to identify relevant pre-prints or recently accepted publications.
All the records in the databases for the Research Tracker and Facilitator for Assessment of COVID-19 Experiences and Mental Health project [ 14 ] were checked for any additional studies not already identified. This project aims to track research being undertaken on COVID-19 and mental health by Australian researchers.
General description of studies included
The search and selection process is outlined in Fig. 1 . As the manual search of reference lists did not yield any more records beyond the records identified through other search methods, this was not specified in Fig. 1 . The records identified through the database searches were reviewed by two researchers (YZ and LL) independently. Any disagreements regarding the eligibility of articles were resolved via broader discussion with the project team. Overall, 42 articles were identified as eligible for inclusion in the scoping review. Two reviewers (YZ and EW) independently assessed the full-texts of the 42 articles and extracted and recorded relevant data (including sample characteristics, whether the study included pre-COVID comparisons, mental health outcomes and measures, study key findings, and any main risk or protective factors identified). All discrepancies regarding data extraction were resolved through discussion.
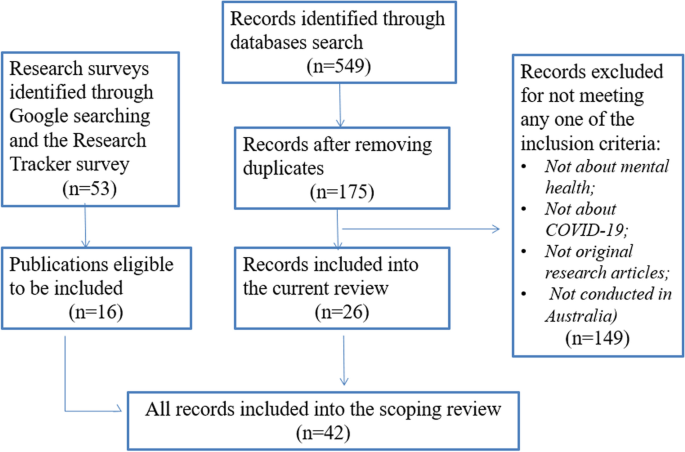
Search and selection process for the review
The characteristics of the 42 included studies are outlined in Tables 1 and 2 (see Additional file 1 ).
Study time-frame and geographical coverage
The majority of the eligible studies were conducted between the end of March and early June 2020, covering the time period when the whole country was under stringent stay-at-home measures, with strict restrictions placed on social gatherings. Seven studies included data collected after this period, when the restrictions were beginning to relax across Australia (except for Victoria) [ 9 , 10 , 30 , 36 , 39 , 40 , 57 ]. All but one [ 39 ] of these seven studies included data from every state including Victoria after the second wave’s containment measures. However, Griffiths et al. [ 30 ] was the only study that made direct comparisons between Victoria and the rest of Australia.
Study populations
Out of the 42 research studies, 12 were conducted among the general Australian adult population, while the remaining 30 focused on a specific group within the population (e.g. parents of young children, health workers, people with an existing health or mental health condition, or young people). The characteristics and key findings for the general population studies are summarized in Table 1 and for specific group studies in Table 2 . Three studies [ 10 , 52 , 68 ] drew a subsample of data from surveys conducted among the general population. However, because the aims and findings of these studies focused on specific subpopulation groups, they were included as research conducted among specific groups.
Pre-COVID comparisons
Of the total 42 studies, nine studies were longitudinal or repeated cross-sectional and had data collection points covering the time period before and during the COVID-19 outbreak (with comparative data collection methods and mental health measures employed) [ 7 , 8 , 15 , 22 , 39 , 43 , 63 , 65 , 67 ]. These studies were more robustly able to compare participants’ mental health during the COVID-19 pandemic to a pre-COVD level. In other words, the evidence provided in these studies was higher quality than other studies with no baseline pre-COVID comparison. Ten further studies compared the results of their studies to norms or results of similar studies conducted before the pandemic. Four studies asked the participants to self-report on whether, and to what extent, their mental health had changed since the onset of the pandemic (these studies are susceptible to recall misjudgements). Several studies used more than one mental health measure and the pre-COVID comparison for each measure sometimes varied. Twenty studies did not report any pre-COVID comparison data, making it difficult to draw confident conclusions about changes in mental health due to COVID.
Research on the general population in Australia
Study sampling and data sources.
In the 12 general population studies (Table 1 ), the participants were usually required to be aged over 18 and currently living in Australia. Four of the 12 studies were based on representative samples of Australian population – 1 & 2. ANUpoll study (Life in Australia™) Footnote 1 [ 7 , 8 ]; 3. Taking the Pulse of the Nation Survey Footnote 2 [ 9 ]; 4. The Australian National COVID-19 Mental Health, Behaviour and Risk Communication (COVID-MHBRC) Survey [ 18 ]. Six studies recruited participants online via social media (e.g. through Facebook advertisements) – 1 & 2. Fisher et al. [ 27 ] and Owen et al. [ 48 ] drew data from the Living with COVID-19 restrictions in Australia survey Footnote 3 ; 3. Rossell et al. [ 58 ] used data from the COVID-19 and you: Mental health in Australia now survey (COLLATE) Footnote 4 ; 4. Gurvich et al. [ 31 ] used data drawn from the COVID-19 and Mental Health Survey Footnote 5 ; 5. Newby et al. [ 45 ] used data from the Mental Health and Coronavirus Study conducted by UNSW and the Black Dog Institute (approval number 3330); 6. Survey data used by Stanton, To & Khalesi et al. [ 62 ] (approval number 22332). The sample representativeness when recruiting participants via online platforms varies greatly in published research [ 53 ]. It is generally accepted that studies based on random and/or representative samples are higher quality with more generalisable findings. However, online methodologies are considered feasible and efficient for broadly summarising population experiences and for correlational research, as they provide timely access to a significant number of individuals [ 40 ]. The two remaining studies in Table 1 [ 21 , 25 ] were based on analyses of online content. Given the ubiquity of internet use, analysing online content offers researchers an avenue to understand public sentiments and opinions [ 21 , 25 ].
During-COVID/Pre-COVID study comparisons
Most of the surveys investigating the COVID-19 outbreak and mental health have collected, or intend to collect, follow-up data to understand changes in the public’s experiences and mental health symptomology as the pandemic evolves, but currently available publications mostly report baseline data. In other words, the majority of studies are cross-sectional and the longitudinal results are not yet available. Out of the 12 studies included in Table 1 , four report changes in participants’ mental health over time during the pandemic. These studies correlate changes in mental health symptomology with varying case rates of COVID-19, as well as changes in social and economic policies and other life circumstances in the first few months of the pandemic [ 7 , 9 , 21 , 25 ].
In terms of pre-COVID comparisons, we identified no studies tracking mental health from pre-COVID and into the COVID period using the same sample/cohort over time. However, six of the 12 studies made comparisons between current COVID results and results from a pre-COVID sample in Australia. Biddle et al. [ 7 ] and [ 8 ] compared their current results with previous waves of the same survey, although the same cohort of respondents was not tracked individually. Four studies compared their results with findings from various representative studies conducted prior to COVID [ 9 , 18 , 27 , 58 ]. These comparisons provided some information about whether, and how, people’s mental health changed during COVID, but the comparisons are less rigorous than if pre-COVID data were available from longitudinal cohort studies tracking temporal changes in individuals.
Mental health outcome measures
Studies generally focused on psychological distress, depression and anxiety. These mental health problems were primarily examined using validated psychometric scales – demonstrating good quality, robust measurement. The most common measures included the Kessler 6 (K6) scale (used by Biddle et al., [ 7 , 8 ] as an indicator for general psychological distress; Patient Health Questionnaire-9 (PHQ-9) (used by Dawel et al. [ 18 ]; Fisher et al. [ 27 ]; Owen et al. [ 48 ]) to assess depression symptoms, suicidality and eating patterns; Generalized Anxiety Disorder-7 (GAD-7) (used by Dawel et al. [ 18 ]; Fisher et al. [ 27 ] to measure anxiety and irritability; and the 21-item Depression Anxiety Stress Scales (DASS-21) (used by Gurvich et al. [ 31 ]; Newby et al. [ 45 ]; Rossell et al. [ 58 ]; Stanton et al. 62 ]) to measure dimensions of depression and anxiety symptoms. Gurvich et al. [ 31 ] also reported on suicidal thoughts using the relevant items in Beck Depression Inventory (BDI). Among the two studies analysing online content, Du et al. [ 21 ] selected the terms “fear”, “panic”, “worry” to represent fear-related emotions as they showed high consistency with each other, while Ewing & Vu [ 25 ] harvested public sentiments through researchers’ interpretations of the tweet data from Twitter.
Overall study findings
The results of the four nationally representative studies (Biddle, et al. [ 7 , 8 ], Botha et al. [ 9 ], Dawel et al. [ 18 ] all showed an increase in mental health problems compared to pre-pandemic published statistics. Three of the remaining general population studies also found an elevation in mental health problems when comparing their results with pre-pandemic norms [ 27 , 45 , 58 ]. Du et al. [ 21 ] tracked the internet searches for fear-related emotions, protective behaviours, health-related knowledge, and panic buying by Australian throughout March, and Ewing &Vu [ 25 ] analysed 3-weeks of tweets by Australian in April. They both found a decline in positive emotions, which matched the deterioration of the COVID-19 situation over time. The three studies by Gurvich et al. [ 31 ], Owen et al. [ 48 ] and Stanton et al. [ 62 ] had no pre-COVID comparisons, and provided no evidence about whether mental health deteriorated during the pandemic. Instead, these studies identified a series of risk and protective factors for mental health during COVID-19. Despite the reports of pessimism in the population, some optimistic feelings were also identified – Biddle et al. [ 8 ] found a significant increase in social cohesion and trust to fellow Australians in the population and Fisher et al. [ 27 ] found that on average Australians were optimistic about the future.
Several studies identified demographic and socio-economic characteristics associated with mental health during COVID-19. For example, Newby et al. [ 45 ], Biddle et al. [ 7 ] and Dawel et al. [ 18 ] all found that younger people reported poorer mental health during the pandemic relative to older groups. Those who experienced job loss, reductions in work hours, and financial hardship during COVID were also more likely to record mental health problems (e.g. [ 7 , 9 ]). Another important factor was pre-existing mental health conditions. Participants with a prior mental health diagnosis were more likely to report worse mental health during COVID-19 [ 18 , 45 , 58 , 62 ].
Studies also showed that people who were worried about contracting COVID-19 were more likely to report poorer mental health [ 27 , 45 , 48 ]. Surprisingly, Dawel et al. [ 18 ] found that direct COVID-19 exposure was not associated with mental health problems. Instead, impairments in work and social functioning and financial distress due to COVID-19 were more strongly associated with poorer mental health. Dawel et al.’s study [ 18 ] also considered the experience of bushfire exposure during the 2019–2020 fires. The results showed that exposure to the fire was not associated with mental health symptomology, but exposure to the bushfire smoke was associated with decreased wellbeing.
Research on specific subpopulation groups
The 30 studies with a focus on specific subpopulations included 25 quantitative studies (with the majority based on survey data and five based on administrative data), four qualitative studies and one mix-method study. Two of the four qualitative studies (Digby et al., 2021; [ 19 , 24 ]) reported the qualitative findings of mixed-methods research, with the quantitative findings reported elsewhere.
Study samples and populations of interest
Of these 30 studies, 20 studies collected data from participants across the nation (although one comprised largely of people living in Victoria (88.2%)) [ 57 ]. Only Sollis et al. [ 61 ] and Broadway et al. [ 10 ] were based on survey data analysed from nationally representative samples, and Johnston et al. [ 36 ] pre-stratified their data/sample to approximate a nationally representative sample. The remaining ten studies focused on specific states or cities. One focused on South Australian [ 67 ]; one on Queensland [ 39 ]; two studies were conducted in Western Australia [ 22 , 41 ]; and two studies in Sydney or New South Wales [ 43 , 60 ]. Four studies were conducted in Melbourne or Victoria [ 15 ]; Digby et al. 2020; [ 20 , 33 ].
People with a particular vulnerability were a major focus of these studies. They included patients presenting to and/or staying in hospital due to poor health or mental health in the study period [ 15 , 22 , 60 ]; people with a pre-existing physical or mental health disorder [ 52 , 68 ]; and people accessing mental health services [ 63 , 65 , 67 ]. Leske et al. [ 39 ] studied suicide rates and motives during the pandemic. Hospital staff, whose physical and mental health may have been more vulnerable during the pandemic, were the population of interest in three studies (Digby et al., 2021, [ 19 , 20 , 33 ]. Other potential participant vulnerabilities included being an adolescent or young adult [ 40 , 41 , 43 ], in self-isolation/quarantine [ 35 ], living alone [ 46 ] and having higher dysmorphic concern [ 55 ].
Families with young children were considered vulnerable and therefore a population of interest in nine studies. Six studies drew data from the COVID-19 Pandemic Adjustment Survey which was conducted among parents of children under the age of 18 (see Table 2 ). Two studies drew data from other nationwide surveys [ 36 , 10 ]. Additionally, Chivers et al. [ 17 ] conducted a qualitative research on new and expecting parents.
Pre-COVID/ during-COVID study comparisons
As indicated in Table 2 , 15 of the 30 studies reported on changes in mental health and other wellbeing indicators before and during the COVID-19 outbreak. Most studies investigating specific populations were cross-sectional and compared current results with the results or statistics from pre-COVID studies that used similar samples (or comparable admissions/administrative data). Other studies asked participants to self-report on the differences in their mental health before and during the pandemic. Four studies reporting administrative data from health services [ 15 , 22 , 63 , 65 ] selected data collected during the corresponding period of 2019 as their pre-COVID comparisons (to avoid the period immediately before the pandemic when Australia experienced the severe bushfire crisis). One longitudinal study tracking the same cohort of participants [ 43 ] adopted a cut-off date to compare mental health before and after the implementation of the COVID-19 restrictions. Separate from the pre-COVID comparisons, four studies [ 15 , 22 , 30 , 63 ] compared mental health across multiple time points during the pandemic, linking changes in participants’ mental health to changes in case rates for COVID-19 in Australia.
Mental health measures
Similar to studies focused on the whole general population, most of the subpopulation studies measured participants’ mental health and wellbeing using validated scales such as the K6, K10, PHQ-9, GAD-7 and the DASS-21. A series of other mental health measures were also adopted (see Table 2 ). Apart from the validated mental health measures, behaviours related to mental health, including eating and exercise behaviours [ 52 ], and appearance-focused behaviours [ 55 ], were also adopted as mental health indicators. Several studies examined public or administrative records, including emergency department presentations [ 15 , 22 ], suicide registers [ 39 ] and website visits and call centre traffic for mental health services [ 65 , 63 ]. A small number of studies did not use validated measures and instead asked participants to self-report on their mental health, lowering the quality of mental health measurement in these studies (e.g. [ 10 , 35 , 36 , 41 , 43 ]). None of the sub-group studies assessed the widespread and likely traumatic impact of the 2019–20 bushfires (a significant individual and community-level pre-pandemic vulnerability).
Five studies qualitatively assessed participants’ descriptions of their experiences and feelings during the COVID-19 pandemic [ 17 ], Digby et al., 2021; [ 19 , 24 , 46 , 60 ] to gain a deeper understanding into participants’ psychological wellbeing in relation to their specific contexts. Of the five studies, Chivers et al. [ 17 ] analysed posts related to COVID-19 in an online parenting forum to understand perinatal distress. Shaban et al. [ 60 ] conducted bedside interviews of COVID-19 patients to explore their lived experiences and perceptions. The other three studies added open-ended questions asking about participants’ concerns related to COVID-19 in their surveys.
In general, the studies investigating specific subpopulation groups showed similar patterns to the findings of the studies on the general population – mental health and wellbeing deteriorated with the emergence of the COVID-19 pandemic and associated restrictions. This trend is consistent across the different populations of interest. However, it is also apparent that important population groups, such as Indigenous and CALD (Culturally and Linguistically Diverse) groups were not researched, limiting our knowledge for these groups. Psychological distress was reported widely among hospital staff in the two studies that measured hospital workers’ mental health [ 20 , 33 ]. Three studies focusing on adolescents and university students consistently showed higher psychological distress and lower subjective wellbeing since the COVID-19 outbreak [ 40 , 41 , 43 ]. Studies focusing on parents with young children identified a range of mental health challenges and risks during the COVID-19 period, and the three studies that included a pre-COVID comparison indicated that psychological distress increased [ 10 , 70 , 71 ]. The themes identified from the qualitative studies differed as they were specific to the experiences of each subpopulation group. However, participants in these studies acknowledged the impact and the challenges brought by the COVID-19 pandemic and expressed worry and concerns (refer to Table 2 for details).
The two studies [ 30 , 63 ] reporting on participants’ mental health several times across the pandemic showed similar results to Biddle et al.’s [ 7 ] study of the general population. Griffiths et al. [ 30 ] focused on working adults and Staples et al. [ 63 ] focused on consecutive users of digital mental health services during the pandemic. Corresponding with Biddle et al. [ 7 ], both studies found that declines in mental health appeared to be more significant during March to April, and then improved in later months (returning normal levels) (except for the Victorian participants in Griffiths et al. [ 30 ]).
In contrast to the consistent findings from survey data showing increases in common mental health problems (i.e. psychological distress, depression and anxiety), two studies analysed data on emergency department (ED) presentations during the pandemic and showed varying results. Cheek et al. [ 15 ] found that mental health presentations potentially increased,while Dragovic et al. [ 22 ] found that the total number of mental health presentations decreased and that the trend varied depending on the reasons for the presentation. A decrease in ED presentations is not surprising given that face-to-face access to many health services declined during the pandemic (as people restricted their mobility) [ 5 ] – and thus, actual service use during this time does not likely reflect the need for services in the community. Importantly, according to data from AIHW [ 5 ], mental health related services, particularly services delivered online or via phone showed heightened service usage since the restrictions were introduced. The contrast between the two studies is likely because they were based on data from two different states with different COVID-19 responses, and Cheek et al. [ 15 ] only included paediatric patients.
In terms of suicidal intention, plans or behaviours, data from Queensland showed no change in suspected suicides [ 39 ] and in Western Australia, the presentations to emergency departments due to suicide or self-harm decreased significantly during this period [ 22 ]. On a national level, those who accessed digital mental health services during the pandemic also showed no changes regarding suicidal thoughts or plans [ 63 ].
Several potentially positive experiences related to the COVID-19 situation were identified from existing studies. Many individuals and families practicing isolation/social distancing reported some “silver linings”, such as strengthening relationships with their families, enjoying spending time at home, and developing new hobbies [ 24 , 35 ]. Patients with COVID-19 who were in isolation also reported some positive factors [ 60 ]. For example, although patients reported that they were disconnected from the outside world, lost track of time, and had limited mobility, some saw this as a reflection of the professionalism and quality of care provided. This enhanced their confidence and helped to ameliorate their initial concerns about being infected. Positive experiences were also identified as potential indicators of resilience and helped to mitigate the negative effect of the pandemic and restrictions on mental health [ 20 , 35 , 42 , 24 ]. For example, Oliva & Johnston’s study [ 24 ], showed the mental health benefits of having a dog during the lockdown, likely because it encouraged exercise and provided an opportunity to socialize with other people.
Several studies made comparisons between specific population groups and the general population, or other population groups. These studies provide insights into which population groups might be at greater risk of experiencing mental health problems, and what factors were protective during the pandemic. Specifically, Broadway et al. [ 10 ] showed the protective effect of having two earners in the family in times of uncertainty. Phillipou et al. [ 52 ] found that individuals previously diagnosed with eating disorders experienced more mental health problems compared to the general population while people with high and low dysmorphic concern displayed different psychological and behaviour responses to the shutdown of the beauty industry in the COVID-19 lockdown [ 55 ].
In summary, we found that Australians in general experienced poorer mental health during the early stages of the pandemic in 2020 compared to pre-COVID. However, the absence of robust longitudinal cohort studies with pre-pandemic baseline data with makes this difficult to conclude definitively. Despite variation in the prevalence of and responses to COVID in individual countries, internationally research similarly indicates there has been a consistent deterioration in mental health and wellbeing levels around the world (see Findlay et al. [ 26 ] (Canada), Fitzpatrick et al. [ 28 ] (US), Pierce, Hope & Ford et al. [ 54 ] (UK). For example, the results of a meta-analysis [ 56 ] of longitudinal studies and natural experiments regarding the psychological impact of COVID-19 pandemic lockdowns internationally, aligns with our findings, showing an increase in psychological symptoms such as depression and anxiety, but no changes in suicidal risk. However, it is worth mentioning that all studies above were conducted in relatively high-income countries. Low-to-middle income countries have experienced even greater impacts during the pandemic, because of their inadequate and underprepared health systems and the uncertainty of their economies. Therefore the mental health impacts of COVID-19 are possibly more serious in the low-to-middle income countries and worthy of specific attention [ 1 , 12 ].
Apart from this general trend, some other key issues regarding the impact of the COVID-19 pandemic on mental health were also evident from the research findings. First, a series of demographic and socio-economic characteristics were identified as risk factors for adverse mental health outcomes. Most clearly, mental health and wellbeing levels seemed to deteriorate in younger age groups – while adolescents and young adults are at greater risk of poor mental health at any time (i.e. outside of pandemic conditions) the deterioration in their mental health during COVID appeared greater than for older age groups [ 7 ]. One explanation is that age is associated with other mental health risk factors that were heightened during the pandemic – such as employment and financial status. In April 2020, the underemployment rate in Australia was 13.8% while the youth underemployment rate hit 23.6% [ 3 ]. Along with employment and financial insecurity, young people are also more likely to have precarious housing and be more reliant on social and peer support which diminished during the pandemic [ 69 ]. As a consequence, it appears there has been a disproportional impact on younger adult’s mental health, despite their relative physical robustness [ 73 ]. Another important risk factor identified was pre-existing mental health problems. Earlier in 2020, Galletly [ 29 ] stated that the pandemic would be a difficult time for people with chronic mental illness. This is echoed by research showing that participants with a prior mental health diagnosis had poorer mental health during the pandemic – however the lack of studies reporting pre-COVID comparative data makes it difficult to determine the extent to which mental health decline for this group comparative to those with no pre-existing mental health problems.
The current review found that people reported some positive mental health and wellbeing experiences that emerged during the early stages of the pandemic. Potentially positive experiences reported by the participants in the reviewed studies included strengthening relationship with family and increased confidence in healthcare system [ 24 , 60 ]. Identifying the positive aspects of peoples’ experience during this challenging time is as important as identifying risk factors in terms of grasping a holistic understanding of what approaches and strategies are most useful to mitigate the negative impact of the pandemic on mental health.
Shortcomings in the research response
The current scoping review demonstrates that many Australian mental health researchers, like researchers internationally, responded rapidly to the pandemic. While this swift response captures a highly valuable snapshot of the impacts of this worldwide disaster, there are shortcomings in terms of design and the reliability and validity of findings. One key gap highlighted in this review is the lack of longitudinal studies with comparative pre-COVID data from the same cohort. Consequently, conclusions about how mental health changed over the course of the pandemic (from pre-pandemic levels), how people adapted during COVID, and whether trajectories varied for different groups are currently limited. A number of important national Australian studies (longitudinal and repeated cross-sectional) are yet to release data collected towards the end of 2020 (e.g. the Longitudinal Study of Australian Children wave 9C1; the ABS Intergenerational Health and Mental Health Study) – we expect these and other studies still to be published will go some way to addressing this knowledge gap. A further shortcoming is that the impact of the 2019–2020 Australian bushfires has rarely been considered.
The small number of qualitative and mixed method studies indicates another gap in the available research. There is value in adding qualitative research components to the mix that can elucidate contextual factors and lived experience particularly for specific and vulnerable groups which may assist in better provision of services to them. As COVID-19 is a novel virus leading to unprecedented challenges and experiences, qualitative research may contribute to a deeper understanding of the complexities (and emerging issues) of mental health and wellbeing pathways during the pandemic, and its potentially lasting impact on mental health once the pandemic has subsided.
These possibilities suggest that we need to fund good quality longitudinal research, as well as turn to rigorous and multi-faceted research. There is a need to gather baseline and follow-up data (including the use of administrative data, longitudinal, mixed-methods studies, and in-depth qualitative research). On a practical note, while the practicalities and mechanics of research are not the focus of the current review, it is important to note that the pandemic has revealed some of the barriers to conducting high quality mental health research that is responsive and has longevity. The time sensitivity of the pandemic, and its rapidly evolving nature highlighted delays related to need to for prompt ethics clearances across multiple institutions in Australia (under-resourced ethics committees were inundated with requests that needed to be expedited). The formal requirements of funding bodies are not well suited to rapidly evolving pandemics either, with funding for COVID-19 mental health research announced in November 2020 after the most restrictive lockdowns had ended. While Australia is a success story compared to similar wealthy western nations, the mental health impacts of COVID-19 (and the current gaps in this body of research) suggests that efforts to address current research practices and resource constraints may improve the country’s responsiveness to comprehensively study future challenges.
Research still to come….
The studies included in this review were conducted generally between April–May 2020. However, the COVID experience in Australia and worldwide is rapidly evolving: it has been contained in some Australian locations while additional outbreaks have occurred elsewhere. It is anticipated that Australian research results from studies conducted in the second half of 2020 and early 2021 will be different from those reported in the current review as efforts to contain the virus have been also evolving across the states and territories. The vaccine program rollout, currently being implemented, may have a significant impact. Research on the long-term mental health effects of disasters suggest that people’s responses evolve considerably [ 59 ]. However, the health nature of this pandemic may differentiate it from natural disasters, and comparative literature is not currently available.
While most existing studies show that COVID-19 containment measures have impacted negatively on the mental health of the general population and on specific vulnerable groups, it is anticipated that the population’s mental health outlook will improve as the vaccination program takes hold and lockdown measures are no longer needed [ 30 ]. However, the discontinuation of the national Job-keeper program (a federally funded program paid to businesses to keep their employees) and the Coronavirus Supplement payment for Job-seekers (an unemployment payment) [ 23 ] by end of March 2021 may trigger job and income losses, leading to declines in mental health for some. Financial insecurity is an important risk factor for poorer mental health—the Taking the Pulse of the Nation survey showed mental distress (depression or anxiety) was closely aligned with financial stress throughout 2021 [ 10 ]. Concerns remain for those with pre-existing mental health conditions, for those who may experience financial hardship over a long period, and for those who experience future lockdowns. For example, it appears that the mental health of residents in Victoria varied from the rest of Australia [ 30 ] as they were subjected to a second lengthy and severe lockdown period when the virus re-emerged that delayed re-entry to employment, schooling and services.
The COVID-19 pandemic may have a delayed impact on mental health in subpopulation groups in myriad interactive and cumulative ways. One example is the mental health of those who were pregnant during the early phases of the pandemic, who in 2021 will have infants and be in the postnatal phase and may have added vulnerability to postnatal depression and anxiety. In addition, as we note above, some vulnerable population groups are under-represented in the existing studies with implications for the management of the pandemic. For example, media reports at the time suggested that some CALD and socially and economically disadvantaged groups may have had different COVID-19 experiences and may have missed out on mainstream messaging; consequently, there may be discrimination that impacts the mental health for different ethnic groups for some time to come. The mental health status of healthcare workers, who have been on the frontline of this crisis, also requires further attention from the research community. The existing studies on the mental health of healthcare workers identified in this review were only conducted among hospital staff in several health services in Melbourne – not nearly enough to cover the experience of this population group in Australia. Fear of transmitting the virus to family, community perception of frontline workers as potential disease carriers, extreme workloads, limited availability of protective equipment and moral dilemmas have all added extra burdens to the mental health of the healthcare workers (Digby et al., 2021) [ 19 ]. A systematic review and meta-analysis of studies conducted in other countries has found high prevalence of mood and sleep disturbances among this specific group [ 49 ]. These future possibilities and identified research gaps demonstrate the need for ongoing research to better understand what happened to mental health both during the pandemic phase and in the aftermath.
Limitations
As noted, there are a number of limitations to this scoping review that need to be briefly acknowledged. The first relates to the rapidly changing and emergence of new published results. This review only provides a snapshot of the research available during the period when the existing literature was searched and it is possible that some information published online has been missed. Further updated reviews need to be conducted to continue to synthesize research findings. Second, while the current review did not perform a quality rating of the studies included in the review, discussion of study quality is included throughout and Tables 1 and 2 list detailed information about the characteristics of each study—including document type, sample size and representativeness, as well as whether pre-COVID comparisons were made. This information provides a reference for making judgements about the strengths and weaknesses (quality) of each study. We do conclude that studies published in peer-reviewed journals, based on a nationally representative sample of Australian population, with a pre-COVID comparison sample from the Australian population are the highest quality. We also make the point that prospective longitudinal studies including baseline (pre-COVID) data from the same sample or cohort are the most robust, but are rare. Third, an analysis of publication bias was not undertaken given that the body of literature is still so new – an analysis of publication bias that extends to considering those vulnerable groups that may have been missed (or difficult to access during COVID-19) would be worthwhile once a more substantial body of literature exists.
The review does not provide detailed data on prevalence rates and statistical associations for each study as many of them did not provide this information. Therefore, we instead aimed to scope the breadth of research conducted and provide a narrative overview (in the text and the Tables) of the findings. Future reviews will provide a comparative summary of the prevalence rates and associations (such as meta-analyses), once this information is obtained. Although the range of differences between studies (e.g. measures used, timing of survey within 2020) that we have observed is likely to make it challenging to combine the data to obtain comparative estimates.
The current scoping review provides a detailed record of the studies published online and in the academic literature investigating mental health during the COVID-19 pandemic in Australia. Our findings suggest that despite the comparatively low prevalence of the disease in the population, mental health problems (i.e. psychological distress, anxiety, depression, poor wellbeing) increased during the early part of the COVID pandemic in 2020. This finding points to the need to focus on mental health problems once the physical health impacts are reduced in countries where the pandemic has been widespread. However, limitations associated with many of the studies in the review, preclude reaching a more definite finding. Young people, those with fewer socio-economic resources and those with pre-existing mental health conditions showed the strongest associations with poor mental health during this time. The review highlights the importance of considering particular vulnerable groups, including health and hospital workers, those in quarantine or isolation, adolescents, parents of children, and people with a pre-existing mental health condition or who were accessing services. Heightened impact on these vulnerable groups suggests that policy attention needs to be given to their economic and psycho-social health to reduce the pandemic’s potentially long-lasting regressive effect. There is a need for further reviews as the follow-up results of longitudinal studies emerge and estimates and understandings of the impact of the pandemic are refined. There is also an important opportunity to consider the limitations of the research available and identify what resources are needed to ensure future timely responses to major disruptions to our way of life to understand the mental health impacts.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
https://www.srcentre.com.au/services/life-in-australia-panel
https://melbourneinstitute.unimelb.edu.au/data/COVID-19-tracker
https://www.monash.edu/medicine/living-with-COVID-19-restrictions-survey
https://www.researchgate.net/project/COVID-19-and-you-mentaL-heaLth-in-AusTralia-now-survEy-COLLATE-project
https://www.maprc.org.au/COVID19-mental-health
Aborode AT, Hasan MM, Jain S, Okereke M, Adedeji OJ, Karra-Aly A, Fasawe AS. Impact of poor disease surveillance system on COVID-19 response in Africa: time to rethink and rebuilt. Clinical Epidemiology and Global Health. 2021;12:100841.
Article PubMed PubMed Central Google Scholar
ABS. Household Impacts of COVID-19 Survey, 6–10 July 2020 Household Impacts of COVID-19 Survey, 6–10 July 2020 | Australian Bureau of Statistics (abs.gov.au). 2020. Accessed 25 Apr 2021.
Google Scholar
ABS. One year of COVID-19: Aussie jobs, business and the economy. 2021. https://www.abs.gov.au/articles/one-year-covid-19-aussie-jobs-business-and-economy Accessed 25 Apr 2021.
ABS. Household Impacts of COVID-19 Survey, January 2021 Household Impacts of COVID-19 Survey, January 2021 | Australian Bureau of Statistics (abs.gov.au). 2021. Accessed 26 Apr 2021.
AIHW. How COVID-19 changed the way Australians used health services in 2019–20 [Media Release]. 2020. https://www.aihw.gov.au/news-media/media-releases/2020/december/how-covid-19-changed-the-way-australians-used-heal . Accessed 26 Apr 2020.
Andrews D. Premier’s statement on changes to Melbourne’s restrictions. Department of Health and Human Services Victoria. 2020. https://www.dhhs.vic.gov.au/updates/coronavirus-covid-19/premiers-statement-changes-melbournes-restrictions-2-august-2020 . Accessed 25Apr 2020.
Biddle N, Edwards B, Gray M, Sollis K. Mental health and relationships during the COVID-19 pandemic. ANU Centre for Social Research. 2020. https://csrm.cass.anu.edu.au/sites/default/files/docs/2020/7/Mental_health_and_relationships.pdf .
Biddle N, Edwards B, Gray M, Sollis K. Hardship, distress, and resilience: The initial impacts of COVID-19 in Australia. ANU Centre for Social Research. 2020. https://csrm.cass.anu.edu.au/sites/default/files/docs/2020/5/The_initial_impacts_of_COVID-19_in_Australia_2020_3.pdf
Botha F, Butterworth P, Wilkins R. Chapter 4: Heightened mental distress: Can addressing financial stress help? In Broadway B, Payne A, Salamanca N. (Eds), Coping with Covid-19: Rethinking Australia. Melbourne Institute: Applied Economic & Social Research, the University of Melbourne. 2020. https://melbourneinstitute.unimelb.edu.au/__data/assets/pdf_file/0004/3562906/Coping-with-COVID-19-Rethinking-Australia.pdf
Broadway B, Méndez S, Moschion J. Chapter 5: Help! High levels of parents' mental distress In Broadway B, Payne A, Salamanca N. (Eds), Coping with Covid-19: Rethinking Australia. Melbourne Institute: Applied Economic & Social Research, the University of Melbourne. 2020. https://melbourneinstitute.unimelb.edu.au/__data/assets/pdf_file/0004/3562906/Coping-with-COVID-19-Rethinking-Australia.pdf
Burgess T, Burgmann JR, Hall S, Holmes D, Turner E. Black Summer: Australian newspaper reporting on the nation’s worst bushfire season, Monash Climate Change Communication Research Hub, Monash University, Melbourne, 2020: 30. https://www.monash.edu/__data/assets/pdf_file/0009/2121111/Black-Summer-Australian-newspaper-reporting-of-the-nations-worst-bushfire-season.pdf
Castro-de-Araujo LFS, Machado DB. Impact of COVID-19 on mental health in a Low and Middle-Income Country. Cien Saude Colet. 2020;25:2457–60.
Article PubMed Google Scholar
Chang SL, Harding N, Zachreson C, Cliff OM, Prokopenko M. Modelling transmission and control of the COVID-19 pandemic in Australia. Nat Commun. 2020;11(1):1–13.
Article CAS Google Scholar
Chapman C, Sunderland M, Slade T, Batterham P, Ross K, Teesson M. Research Tracker and Facilitator for Assessment of COVID-19 Experiences and Mental Health. 2020. https://osf.io/6vtph/ Accessed 26 Apr 2020.
Cheek JA, Craig SS, West A, Lewena S, Hiscock H. Emergency department utilisation by vulnerable paediatric populations during the COVID-19 pandemic. Emerg Med Australas. 2020;32(5):870–1.
Chin KL, Ofori-Asenso R, Jordan KA, Jones D, Liew D. Early signs that COVID-19 is being contained in Australia. J Infect. 2020;81(2):318–56.
Article CAS PubMed PubMed Central Google Scholar
Chivers BR, Garad RM, Boyle JA, Skouteris H, Teede HJ, Harrison CL. Perinatal distress during COVID-19: thematic analysis of an online parenting forum. J Med Internet Res. 2020;22(9):e22002.
Dawel A, Shou Y, Smithson M, Cherbuin N, Banfield M, Calear AL, Farrer LM, Gray D, Gulliver A, Housen T, McCallum SM, Morse AR, Murray K, Newman E, Rodney Harris RM, Batterham PJ. The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Front Psych. 2020;11:1026.
Digby R, Winton-Brown T, Finlayson F, Dobson H, Bucknall T. Hospital staff well-being during the first wave of COVID-19: Staff perspectives. Int J Ment Health Nurs. 2021;30:440–50.
Dobson H, Malpas CB, Burrell AJ, Gurvich C, Chen L, Kulkarni J, Winton-Brown T. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas Psychiatry 2020. https://doi.org/10.1177/1039856220965045 .
Du H, Yang J, King RB, Yang L, Chi P. COVID-19 increases online searches for emotional and health-related terms. Appl Psychol Health Well Being. 2020;12(4):1039–53.
Dragovic M, Pascu V, Hall T, Ingram J, Waters F. Emergency department mental health presentations before and during the COVID-19 outbreak in Western Australia. Australas Psychiatry. 2020;28(6):627–31.
DSS. Government response to Coronavirus Government response to Coronavirus | Social Security Guide (dss.gov.au). 2021. Accessed 26 Apr 2021.
Evans S, Mikocka-Walus A, Klas A, Olive L, Sciberras E, Karantzas G, Westrupp EM. From ‘It has stopped our lives’ to ‘Spending more time together has strengthened bonds’: The varied experiences of Australian families during COVID-19. Front Psychol. 2020;11:2906.
Article Google Scholar
Ewing LA, Vu HQ. Navigating ‘home schooling’during COVID-19: Australian public response on Twitter. Media Int Aust. 2021;178(1):77–86.
Findlay LC, Arim R, Kohen D. Understanding the perceived mental health of Canadians during the COVID-19 pandemic. Health Rep. 2020;31(4):22–7.
PubMed Google Scholar
Fisher JR, Tran TD, Hammargerg K, Sastry J, Nguyen H, Rowe H, Popplestone S, Stocker R, Stubber C, Kirkman M. Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med J Aust. 2020;213(10):458–64.
Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychol Trauma Theory Res Pract Policy. 2020;12(S1):S17–21.
Galletly C. Psychiatry in the COVID-19 Era. Aust N Z J Psychiatry. 2020;54(5):447–8.
Griffiths D, Sheehan L, van Vreden C, Petrie D, Sim M, Collie A. The Community Lockdown in Victoria, Australia (July-October 2020): Implications For Health During The Second COVID-19 Wave. Insurance Work and Health Group, Faculty of Medicine Nursing and Health Sciences, Monash University (2020). https://bridges.monash.edu/articles/report/_/13289570
Gurvich C, Thomas N, Thomas EH, Hudaib AR, Sood L, Fabiatos K, Sutton K, Isaacs A, Arunogiri S, Sharp G, Kulkarni J. Coping styles and mental health in response to societal changes during the COVID-19 pandemic. Int J Soc Psychiatry. 2020;0020764020961790:1–10.
Henssler J, Stock F, van Bohemen J, Walter H, Heinz A, Brandt L. Mental health effects of infection containment strategies: quarantine and isolation—A systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2020;271:223–34.
Holton S, Wynter K, Trueman M, Bruce S, Sweeney S, Crowe S, Dabscheck A, Eleftheriou P, Booth S, Hitch D, Said CM, Haines KJ, Said CM. Psychological well-being of Australian hospital clinical staff during the COVID-19 pandemic. Aust Health Rev. 2020. https://doi.org/10.1071/AH20203 .
Hunt G. First confirmed case of novel coronavirus in Australia [Media release]. Department of Health. 2020. https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/first-confirmed-case-of-novel-coronavirus-in-australia . Accessed 25 Apr 2021
Ji J, Basanovic J, MacLeod C, Johnson P, David F. The Covid-19 Care Study: Initial survey report. 2020. https://www.thecarestudy.com/uploads/1/3/1/5/131561714/thecarestudy_initialsurveyreport_web.pdf .
Johnston RM, Mohammed A, Van Der Linden C. Evidence of exacerbated gender inequality in child care obligations in Canada and Australia during the COVID-19 pandemic. Politics Gend. 2020: 1–16.
Karantzas G, Chesterman S, Ferguson E, Knox L, Lawless N, Mullins E, Romano DA, Toumbourou JW, Stokes M A, Westrupp E. Parent’s Relationship Wellbeing and Lonelines during COVID-19: A Test of the Vulnerability-Stress and Stress-Buffering Hypotheses. PRE-PRINT. 2020.
Lakhan R, Agrawal A, Sharma M. Prevalence of depression, anxiety, and stress during COVID-19 pandemic. J Neurosci Rural Pract. 2020;11(4):519.
Leske S, Kõlves K, Crompton D, Arensman E, De Leo D. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry. 2020;8:58–63.
Li S, Beames J, Newby J, Maston K, Christensen H, Werner-Seidler A. The impact of COVID-19 on the lives and mental health of Australian adolescents. 2020. PRE-PRINT.
Lyons Z, Wilcox H, Leung L, Dearsley O. COVID-19 and the mental well-being of Australian medical students: impact, concerns and coping strategies used. Australas Psychiatry. 2020;8(6):649–52.
Mikocka-Walus A, Stokes MA, Evans S, Olive L, Westrupp E. Finding the power within: is resilience protective against symptoms of stress, anxiety, and depression in Australian parents during the COVID-19 pandemic? 2020. PRE-PRINT.
Munasinghe S, Sperandei S, Freebairn L, Conroy E, Jani H, Marjanovic S, Page A. The impact of physical distancing policies during the COVID-19 pandemic on health and well-being among Australian adolescents. J Adolesc Health. 2020;67(5):653–61.
Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):1–7.
Newby JM, O’Moore K, Tang S, Christensen H, Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS One. 2020;15(7):e0236562.
Oliva JL, Johnston KL. Puppy love in the time of Corona: dog ownership protects against loneliness for those living alone during the COVID-19 lockdown. 2020 Int J Soc Psychiatry: 1-11. https://doi.org/10.1177/0020764020944195
Olive L, Sciberras E, Berkowitz TS, Hoare E, Telford R, Mikocka-Walus A, Evans S, Hutchinson D, McGillivray JA, Teague SJ, Wood AG, Olsson C, Westrupp E. Child and parent physical activity, sleep and screen time during COVID-19 compared to pre-pandemic nationally representative data and associations with mental health. 2020. PRE-PRINT.
Owen AJ, Tran T, Hammarberg K, Kirkman M, Fisher JRW. Poor appetite and overeating reported by adults in Australia during the coronavirus-19 disease pandemic: a population-based study. Public Health Nutr. 2020;24(2):275–81.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–7.
Paul KI, Moser K. Unemployment impairs mental health: Meta-analyses. J Vocat Behav. 2009;74(3):264–82.
Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil, H. Chapter 11: Scoping Reviews (2020 version). In: Aromataris E, Munn Z (Editors). JBI Manual Evid Synth, 2020. Available from https://synthesismanual.jbi.global . https://doi.org/10.46658/JBIMES-20-12
Phillipou A, Meyer D, Neill E, Tan EJ, Toh WL, Van Rheenen TE, Rossell SL. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int J Eat Disord. 2020;53(7):1158–65.
Pierce M, McManus S, Jessop C, John A, Hotopf M, Ford T, Hatch S, Wessely S, Abel KM. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7(7):567–8.
Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, Kontopantelis E, Webb R, Wessely S, McManus S, Abel KM. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–92.
Pikoos TD, Buzwell S, Sharp G, Rossell SL. The COVID-19 pandemic: psychological and behavioral responses to the shutdown of the beauty industry. Int J Eat Disord. 2020;53:1993–2002.
Prati, G, Mancini A. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. 2021. PRE-PRINT.
Rahman MA, Hoque N, Alif SM, Salehin M, Islam SMS, Banik B, Sharif A, Nazim NB, Sultana F, Cross W. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Glob Health. 2020;16(1):1–15.
Rossell SL, Neill E, Phillipou A, Tan EJ, Toh WL, Van Rheenen TE, Meyer D. An overview of current mental health in the general population of Australia during the COVID-19 pandemic: results from the COLLATE project. Psychiatry Res. 2021;296:113660.
Article CAS PubMed Google Scholar
Royal Australian and New Zealand College of Psychiatrists (RANZCP). Addressing the mental health impacts of natural disasters and climate change-related weather events. Position Statement 35. 2020. https://www.ranzcp.org/news-policy/policy-and-advocacy/position-statements/addressing-mental-health-impacts-natural-disasters Accessed 26 Apr 2021
Shaban RZ, Nahidi S, Sotomayor-Castillo C, Li C, Gilroy N, O’Sullivan MV, Sorrel TC, White E, Hackett K, Bag S. SARS-CoV-2 infectinon and COVID-19: the lived experience and perceptions of patients in isolation and care in an Australian healthcare setting. Am J Infect Control. 2020;48(12):1445–50.
Sollis K, Biddle N, Edwards B, Herz D. Improved wellbeing or distress? Measuring the impacts of participation in a COVID-19 survey on participant wellbeing. ANU Centre for Social Research. 2020. https://csrm.cass.anu.edu.au/sites/default/files/docs/2020/6/Improved_wellbeing_or_distress_Measuring_the_impacts_of_participation_in_a_COVID-19_survey_Final.pdf
Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, Fenning AS, Vandelanotte C. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17(11):4065.
Article CAS PubMed Central Google Scholar
Staples L, Nielssen O, Kayrouz R, Cross S, Karin E, Ryan K, Dear B, Titov N. Rapid report 2: symptoms of anxiety and depression during the first 12 weeks of the Coronavirus (COVID-19) pandemic in Australia. Internet Interv. 2020;22:100351.
Sucharew H, Macaluso M. Progress notes: methods for research evidence synthesis: the scoping review approach. J Hosp Med. 2019;14(7):416–8.
Titov N, Staples L, Kayrouz R, Cross S, Karin E, Ryan K, Dear B, Nielssen O. Rapid report: Early demand, profiles and concerns of mental health users during the coronavirus (COVID-19) pandemic. Internet Interv. 2020;21:100327.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMAScR): checklist and explanation. Ann Intern Med. 2018;169:467–73. https://doi.org/10.7326/M18-0850 .
van Agteren J, Bartholomaeus J, Fassnacht DB, Iasiello M, Ali K, Lo L, Kyrios M. Using Internet-Based psychological measurement to capture the deteriorating community mental health profile during COVID-19: observational study. JMIR Mental Health. 2020;7(6):e20696.
Van Rheenen TE, Meyer D, Neill E, Phillipou A, Tan EJ, Toh WL, Rossell SL. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. J Affect Disord. 2020;275:69–77.
Article PubMed PubMed Central CAS Google Scholar
Verick S. Who is hit hardest during a financial crisis? The vulnerability of young men and women to unemployment in an economic downturn. 2009.IZA Discussion Paper No. 4359, Available at SSRN: https://ssrn.com/abstract=1455521 .
Westrupp E, Stokes MA, Fuller-Tyszkiewicz M, Berkowitz TS, Capic T, Khor S, et al. Subjective wellbeing in parents during the COVID-19 Pandemic in Australia. 2020. PRE-PRINT.
Westrupp E, Bennett C, Berkowitz TS, Youssef G, Toumbourou J, Tucker R., et al. Child, parent, and family mental health and functioning in Australia during COVID-19: comparison to pre-pandemic data. 2020. PRE-PRINT.
WHO. Timeline: WHO’s COVID-19 response. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline# ! Accessed 25 Apr 2021.
WHO. COVID-19: vulnerable and high risk groups. 2020. https://www.who.int/westernpacific/emergencies/covid-19/information/high-risk-groups Accessed 26 Apr 2021.
WHO. Coronavirus disease (COVID-19) pandemic. 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Accessed 25 Apr 2021.
Download references
Acknowledgements
Not applicable.
This scoping review was supported by funding from the Australian National Mental Health Commission. The findings and views reported are those of the authors and should not be attributed to the National Mental Health Commission.
Author information
Authors and affiliations.
The Research School of Population Health (RSPH), College of Health and Medicine, The Australian National University, Canberra, ACT, Australia
Yixuan Zhao, Liana S. Leach, Erin Walsh, Philip J. Batterham, Alison L. Calear, Tinh Doan, Christine LaBond & Cathy Banwell
The ANU Medical School, College of Health and Medicine, The Australian National University, Canberra, ACT, Australia
Christine Phillips & Anna Olsen
You can also search for this author in PubMed Google Scholar
Contributions
L.L., C.B., YZ., P.B., formulated the research approach. Y.Z., undertook the search, L.L., screened articles and P.B. and A.C., assessed quality. Y.Z. wrote the article with L.L. and C.B. All authors participated in critical revisions and approved the final draft.
Corresponding author
Correspondence to Yixuan Zhao .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Table 1 Research conducted among general Australian adult population [ 37 , 47 ]. Table 2 Research conducted among specific subgroups in the population.
Additional file 2.
PRISMA-ScR Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhao, Y., Leach, L.S., Walsh, E. et al. COVID-19 and mental health in Australia – a scoping review. BMC Public Health 22 , 1200 (2022). https://doi.org/10.1186/s12889-022-13527-9
Download citation
Received : 18 June 2021
Accepted : 29 April 2022
Published : 15 June 2022
DOI : https://doi.org/10.1186/s12889-022-13527-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Systematic review
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- For Patients
- For Providers
- Pregnancy Loss
- Pregnancy Complications
- Early Pregnancy Loss
- Estimated Placental Volume
- Behind Every
INFORMATION FOR
- Residents & Fellows
- Researchers
Polimanti Receives NIMH Grant To Study Internalizing Disorders, COVID-19
Renato Polimanti, PhD, assistant professor of psychiatry at Yale School of Medicine, has received a 3-year grant from the National Institute of Mental Health (NIMH) to evaluate the association of internalizing disorders with the risk, onset, and vulnerability of COVID-19.
The $3.69 million R01 grant aims to address urgent, time-sensitive mental health research questions related to COVID-19, according to the NIMH.
Many uncertainties about the COVID-19 pandemic remain although understanding of the virus has improved and effective vaccines have been developed, Polimanti said. There are also many consequences to be faced post-pandemic due to the pervasive impact of COVID-19 on individuals and society. Polimanti said the lack of reliable information to guide health care professionals and policymakers has been particularly difficult over the last two years.
“Mental health is surely one of the health domains that are being more strongly affected by COVID-19 outcomes. Isolation, psychological stress, and ‘free-time’ boredom induced by COVID-19 restrictions have been consistently associated with increased internalizing symptoms, including anxiety and depression. Additionally, traumatic experiences related to COVID-19 have been also linked to posttraumatic stress disorder. In a vicious circle, internalizing disorders have been associated with an increased risk of infection and COVID-19 severe symptoms, hospitalization, and mortality,” Polimanti explained.
Researchers plan to identify the latent factors linking the internalizing spectrum, such as anxiety, major depressive disorder, and post-traumatic stress disorder, and COVID-19 outcomes, including infection, hospitalization, and critical illness, and investigate the regulatory mechanisms. They will also test the interaction of the internalizing spectrum with blood-based transcriptomic and epigenomic changes associated with COVID-19 morbidity and psychological stress.
“Our findings will provide a multi-dimensional perspective on the processes underlying the associations between COVID-19 outcomes and internalizing disorders,” Polimanti said.
- Mental Health
Featured in this article
- Renato Polimanti, PhD, MSc Associate Professor of Psychiatry; Associate Professor on Term, Chronic Disease Epidemiology
- Understanding Infant and Caregiver…
Understanding Infant and Caregiver Mental Health: What is the Impact of the COVID-19 Pandemic and Systemic Racism?
Date posted:.
Mental Health Awareness Month offers an opportunity to reflect on the importance of our health and well-being—including for the littlest amongst us. The first five years of life are a critically important period of physical, social, cultural, and emotional development in the lives of children and their families that sets the foundation for young children’s future health, development, and well-being. Importantly, all events that occur in the child’s life at this early stage are likely to have a significant impact as they develop.
Over the last several decades, we have learned that social determinants of health—including where children and families live, work, and play—are crucial in understanding how contexts impact health, and in the case of incredibly young children, their development.
Additionally, the well-being of young children depends heavily on the mental and physical health of their parents and caregivers. Thus, it is crucial to prioritize the mental well-being of these adults and the environments in which children are nurtured to address the challenges impacting infants, toddlers and preschoolers.
Amid this landscape of supports and challenges for families with young children, the past 4 years have been particularly difficult for many families with the rise of the COVID-19 pandemic and simultaneous increasing national awareness and discussion of long-standing racial inequities. Racism is a known social determinant of health which affects the mental health and well-being of families, particularly pregnant and postpartum individuals and their children.
As we have continued to wrestle with the COVID-19 pandemic, there have been increased efforts to better understand the impacts of this global event with racialized components on communities that have historically lacked access, services, and care. Our team’s Prenatal to Preschool (P2P) study , described below, is one such example of a project that originated during the pandemic with the explicit goal to better understand how this global crisis differentially impacted the mental health of families in our Philadelphia community.
Prenatal to Preschool (P2P): How are we understanding the mental health of very young children and their families?
P2P evaluates the simultaneous effects of the pandemic, stressors, and multiple forms of racism on mothers and their developing children, providing important insight into risk and resilience factors in early development and the peripartum period.
In the context of a major U.S. city, Philadelphia, like many others, is marked by pronounced neighborhood disparities, such that our group found it imperative for public health and policy efforts to better understand how known inequities impact the mental well-being of the city's thousands of very young children and their families. We are doing this by examining cross-cultural differences and experiences faced by Black and non-Latinx White families.
Our team began talking to families participating in the study when they were pregnant at the very beginning of the pandemic when the world shut down in April 2020. Over the last four years, as our global and local experiences of the pandemic changed, caregivers have answered questions about their health and well-being, as well as that of their growing child’s, and their partners in child-rearing. Questions have covered topics including depression, anxiety, parenting stress, social supports, experiences of multiple forms of racism, their child’s development, and COVID-related worries.
Our initial findings underscore the importance of supporting families with very young children in a variety of ways and amongst unprecedented challenges.
We hope that this project will set the foundation for future work to continue fostering diversity and equity in research, along with promoting the well-being of children and families impacted by the pandemic.
As the P2P families continue to participate as their children turn four, we will be able to look at the past four years with an additional goal to create individualized, culturally informed preventative interventions for all families. We aim to ensure that the work we are doing joins the work of so many others in achieving mental health equity for all young children and their families in our region and across the nation.
Latest Blog Posts

Recognizing Cross-sector Collaborations That Can Improve Financial Wellness and Educational Opportunities in 200 Words
Education pays. That truth underlies the role education plays in addressing poverty, and is part of why education has been acknowledged as a …
Utilizing Behavioral Health Research to Inform Policy: A Conversation with Dr. Rhonda Boyd
As the youth behavioral health crisis has grown in the past several years, members of PolicyLab’s Behavioral Health portfolio have continued to think…

Syringe Services Programs Are Critical for Adolescents and Young Adults: Research and Clinical Perspectives
As physicians who take care of young people with substance use disorders, we recognize the significance of harm reduction approaches in helping…
Check out our new Publications View Publications
Adolescent Health & Well-Being
Behavioral health, population health sciences, health equity, family & community health.

Social online training can help against loneliness and depression
M ental health problems, loneliness among young people, and polarization are rapidly increasing, especially after the COVID-19 pandemic. A new large-scale research study, the CovSocial project, led by Tania Singer from the Max Planck Society, is helping people to reconnect with themselves, others and society at large.
Recent findings reveal that a ten-week, partner-based mental online training program boosted resilience, empathy and compassion, and deepened social connections. At the same time, these short daily, app-based practices done with another person, so-called Dyads, decreased loneliness, depression, anxiety and a negative outlook in life. Researchers hope that this training can be scaled worldwide to overcome loneliness and social divisions.
The work is published in the Journal of Affective Disorders .
Singer, a psychologist, social neuroscientist and scientific head of the Max Planck Society's Social Neuroscience Lab in Berlin, Germany, has for many years been developing mental intervention programs based on partner-based daily exercises, known as "Contemplative Dyads" as they resemble a mindfulness meditation done together with a partner in your daily life.
Unlike solitary mindfulness-based meditation practices, Dyads involve structured interactions between pairs of individuals who are taking turn in exploring loudly specific questions while the other is empathically listening without judging and interrupting in any way. The basic Affect Dyad for example consists of two questions that are aiming at both exploring and cultivating a deeper understanding and acceptance of challenging emotions as well as building resilience through the cultivation of gratitude and care.
More tolerance and less prejudice
These daily Dyads are done over ten weeks as a social skill learning program and the practice is supported by teacher-led weekly coaching sessions to help deepen the daily practice. People are randomly paired every week with a new partner to help increase tolerance, help reduce prejudice, overcome boundaries, and foster a sense of common humanity. With roots in ancient meditation traditions and recent advancements in social neuroscience, dyadic practices have emerged as a powerful tool for cultivating social skills and promoting resilience in diverse populations.
Science is now revealing the benefits of such social practices. The CovSocial Project, a large-scale mental health study spearheaded by Singer at the Social Neuroscience Lab of the Max Planck Society and performed during the years of the COVID-19 pandemic, has revealed in its first phase--by tracking thousands of Berliners recruited from a random draw of the Berlin city register--that loneliness, stress, depression and anxiety increased, with each lockdown showing severe lockdown fatigue effects.
To reduce this suffering, the team therefore decided to offer a second-phase mental online training program to those still participating in the study. The team compared the efficiency of two 10-week online mental training programs: a classic mindfulness-based and a partner-based socio-emotional Dyad intervention program.
Daily contemplative exercises are effective
A growing body of research is now published, giving impressive evidence that these daily social contemplative exercises done with another person are indeed effective in supporting participants mental well-being and health by reducing depression, anxiety and emotion regulation difficulties while at the same time increasing social skills such as empathy, self and other-related compassion. These findings give hope that such social mental practices could help overcome social divides, reducing loneliness, and improving human-to-human social connection.
The recently published paper showed that the ten-week online Dyad program could indeed reduce depression, anxiety and emotion-regulation difficulties while at the same time improving resilience. Interestingly, participants also showed a significant reduction in their "negative interpretation bias"—the likelihood of interpreting other people or situations in a negative way—and this decrease in negativity could actually account for the observed mental health benefits.
This means that internalized knee-jerk anxieties about life or different groups or individuals can be tackled and a more positive worldview and outlook on life can be trained.
Singer comments on these findings, "While both interventions could decrease mental health problems, it was interesting to see that only in the dyadic social practices the reduction in negative interpretation bias was a strong candidate mechanism underlying the observed decrease in depression. We think that practicing daily gratitude during a Dyad with a partner may help boost this more positive outlook onto life and in turn strengthen one's resilience and mental health."
Increasing social connections
In another mental training study from the CovSocial project just published, first author Hannah Matthaeus and colleagues revealed that again only the socio-emotional Dyad practice program, but not the classic mindfulness practice program focusing on meditations done alone, could significantly reduce loneliness.
Singer concludes, "As in a previous large-scale mental training study, the ReSource project, we could confirm again that these daily relational practices are a powerful tool to increase social connections and facilitate people to share their difficulties and vulnerability.
"In the recent study, we could extend these previous findings in showing that even if practicing Dyads only online and only for ten weeks, we can find this deepening of social connections and even reduce loneliness. This offers real hope that recent alarming trends towards social isolation, loneliness and division can be reversed by scaling such interrelational mental training programs based on Dyads."
As the evidence for the effectiveness of this Dyad intervention builds, the study's authors hope that they can develop ways to scale it so that these Dyad training programs can be brought to society at large and especially to domains which suffer mostly under high burn-out rates and stress such as the health-care or educational systems. Their next programs, Edu:Social School and Health will focus on exactly this: testing the effects of such Dyad programs in the context of the classroom and hospitals in the hope to increase not only the resilience of teachers and health care providers but also boost classroom climate and team spirits and social cohesion.
Singer, the principal investigator of the CovSocial study, concludes, "At a time when policymakers are grappling with a rising tide of poor public mental health and increasing loneliness and social divisions, our study shows it is possible to bring communities back together and promote positive, healthy human interactions. This is what our societies need urgently. People are crying out for a sense of belonging, community, care, and true social connections.
"I hope we can take the lessons of this study and begin to scale and amplify such interrelation mental training programs to benefit society. This is why we started now a follow-up study, the Edu:Social project, to bring these practices into the fields of education and health care."
More information: Malvika Godara et al, Training-related improvements in mental well-being through reduction in negative interpretation bias: A randomized trial of online socio-emotional dyadic and mindfulness interventions, Journal of Affective Disorders (2024). DOI: 10.1016/j.jad.2024.03.037
Provided by Max Planck Society

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 06 May 2024
The mental health toll among healthcare workers during the COVID-19 Pandemic in Malawi
- Limbika Maliwichi 1 ,
- Fiskani Kondowe 1 ,
- Chilungamo Mmanga 2 ,
- Martina Mchenga 3 ,
- Jimmy Kainja 1 ,
- Simunye Nyamali 1 &
- Yamikani Ndasauka 1
Scientific Reports volume 14 , Article number: 10327 ( 2024 ) Cite this article
375 Accesses
4 Altmetric
Metrics details
- Health care
- Occupational health
- Public health
The COVID-19 pandemic has affected the mental health of healthcare workers worldwide, with frontline personnel experiencing heightened rates of depression, anxiety, and posttraumatic stress. This mixed-methods study aimed to assess the mental health toll of COVID-19 on healthcare workers in Malawi. A cross-sectional survey utilising the Generalized Anxiety Disorder (GAD-7), Patient Health Questionnaire (PHQ-9), and Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) was conducted among 109 frontline healthcare workers. Additionally, in-depth interviews were conducted with 16 healthcare workers to explore their experiences and challenges during the pandemic. The results indicated a high prevalence of COVID-19-related depression (31%; CI [23, 41]), anxiety (30%; CI [22, 40]), and PTSD (25%; CI [17, 34]) among participants. Regression analysis revealed significantly higher rates of depression, anxiety, and PTSD among healthcare workers in city referral hospitals compared to district hospitals. Qualitative findings highlighted the emotional distress, impact on work and personal life, and experiences of stigma and discrimination faced by healthcare workers. The stress process model provided a valuable framework for understanding the relationship among pandemic-related stressors, coping resources, and mental health outcomes. The findings underscore the urgent need for interventions and support systems to mitigate the mental health impact of COVID-19 on frontline healthcare workers in Malawi. Policymakers should prioritise the assessment and treatment of mental health problems among this critical workforce to maintain an effective pandemic response and build resilience for future crises.
Similar content being viewed by others

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

MDMA-assisted therapy for moderate to severe PTSD: a randomized, placebo-controlled phase 3 trial

MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study
Introduction.
This study aims to assess the mental health toll of COVID-19 on healthcare workers in Malawi. In March 2020, the World Health Organization (WHO) declared COVID-19 a global pandemic, given its rapid worldwide spread 1 . Malawi registered its first case of COVID-19 in March 2020. According to statistics from the World Health Organization 2 , Malawi has registered approximately 89,000 confirmed cases of COVID-19, resulting in 2,686 deaths. While these numbers are relatively low compared to many other countries, the pandemic nevertheless placed immense strain on Malawi's healthcare system, which was already struggling with limited resources and infrastructure before the crisis.
COVID-19 has affected mental health worldwide, with the general population and healthcare workers experiencing heightened rates of depression, anxiety and posttraumatic stress 3 , 4 . COVID-19-related mental health challenges in frontline health personnel could negatively impact healthcare provision, compounding the pandemic's strain on health systems. Pandemics can generate multifaceted stressors, including fear of infection, financial loss, work disruptions, and social isolation, which may adversely impact the population's mental health 3 .
One of the most striking findings across studies is the high prevalence of mental health problems among healthcare workers during the COVID-19 pandemic in LMICs. Systematic reviews and meta-analyses by Chen, et al. 5 and Luo, et al. 6 provide an overview of the magnitude of the issue, with pooled prevalence rates ranging from 31.6% to 43.6% for depression, 37.2% to 37.3% for anxiety, and 31.4% to 49.5% for post-traumatic stress disorder (PTSD) among healthcare workers in Africa and other LMICs. These rates are considerably higher than those reported in the general population, underscoring the disproportionate psychological burden experienced by frontline health personnel in resource-constrained settings.
Studies focused on specific countries within sub-Saharan Africa, such as Zimbabwe 7 , Malawi 8 , 9 , South Africa 10 , 11 , Nigeria 12 , 13 , and Uganda 14 , consistently report high levels of psychological distress, anxiety, depression, and PTSD among healthcare workers. For instance, Chingono, et al. 7 found that over 53% of healthcare workers in Zimbabwe experienced moderate to severe psychological distress. At the same time, Erinoso, et al. 12 reported high rates of anxiety (40%) and depression (40%) among frontline nurses in Nigeria. These findings are not limited to sub-Saharan Africa, as studies from other LMICs, such as Pakistan 15 and Nepal 16 , have yielded similar results. The pervasive nature of the mental health impact across different regions highlights the global scale of the problem and the need for urgent action to support healthcare workers in resource-constrained settings.
Further, the high prevalence of mental health problems among healthcare workers can be attributed to a complex interplay of occupational and personal stressors. Studies identify several key occupational stressors that contribute to psychological distress, including increased workload, lack of personal protective equipment (PPE), fear of infection, and exposure to patient suffering and death. Qualitative studies provide valuable insights into the emotional toll of these occupational stressors on frontline health personnel. For example, Dawood, Tomita and Ramlall 11 found that healthcare workers in South Africa's KwaZulu-Natal Province felt unheard and unsupported by their employers and the government, leading to feelings of burnout, anxiety, and depression. Similarly, Mahlangu, et al. 10 reported that healthcare workers in South Africa experienced memories of traumatic experiences, such as witnessing patient deaths and fearing for their safety. In Nigeria, Kwaghe, et al. 13 highlighted the role of stigma and lack of support from communities and employers in exacerbating the psychological impact of the pandemic on healthcare workers. Participants in this study reported experiencing fear, anxiety, and emotional distress due to the risk of infection, stigma, and inadequate support systems.
Personal stressors, such as concerns for the well-being of family members, have also emerged as significant contributors to mental health challenges among healthcare workers. Sia-Morenike, et al. 17 found that frontline health personnel in Sierra Leone experienced anxiety and fear not only for their health but also for the safety of their loved ones. The challenges of balancing professional duties with personal and family responsibilities have added to the psychological burden healthcare workers face during the pandemic. The interplay of occupational and personal stressors is further complicated by the resource constraints and systemic challenges faced by healthcare systems in sub-Saharan Africa and other LMICs. Lack of adequate resources, such as PPE, medical equipment, and trained personnel, has increased workload and heightened stress among frontline health workers 17 . Furthermore, pre-existing issues such as underfunded health systems, limited mental health infrastructure, and social stigma associated with seeking psychological support have exacerbated the mental health impact of the pandemic on healthcare workers in these regions.
In addition, findings from studies underscore the urgent need for targeted interventions and support systems to mitigate the mental health impact of the COVID-19 pandemic on healthcare workers in sub-Saharan Africa and other LMICs. Moitra, et al. 18 and Oyat, et al. 19 emphasise the importance of providing stress management training, peer support, and access to psychological services to support healthcare workers' mental health. Munyenyembe and Chen 9 and Oyat, et al. 19 provide valuable insights into the coping strategies used by healthcare workers, such as seeking social support, engaging in leisure activities, and relying on faith. However, these studies also highlight the barriers to coping, including lack of resources and stigma associated with seeking mental health support. These findings suggest that interventions should focus not only on enhancing individual coping capacities but also on addressing the structural and systemic factors that contribute to psychological distress.
The current study employed a mixed-methods approach integrating quantitative screening instruments with qualitative interviews to address these knowledge gaps. Combining these methodologies allowed for assessing depression, anxiety and PTSD prevalence while also capturing nuanced insights into healthcare workers' pandemic experiences. The qualitative component was critical for understanding how Malawian healthcare workers made sense of the unprecedented crisis and its mental health ramifications. In-depth interviews explored healthcare workers' responses and perspectives on mental health within their socio-cultural context. This qualitative lens complemented quantitative findings, enabling a more comprehensive, contextually-grounded analysis. The stress process model provides a valuable framework for examining how pandemic-related stressors may impact mental health 20 . This model posits that stressors arising from social circumstances can precipitate psychological distress, with coping resources potentially mitigating adverse effects. The model also recognises both the direct impacts of stressors and indirect effects via the erosion of coping mechanisms. COVID-19 represents an acute, society-wide stressor that has dramatically transformed healthcare workers' occupational and social realities. Findings can inform interventions to support this critical workforce and guide mental health responses to COVID-19 in similar contexts. More broadly, this study highlights the need to invest in mental health infrastructure and prioritise psychological support within the pandemic preparedness in LMICs.
Materials and methods
The stress process model.
There are several models that researchers may consider using in COVID-19 research to explore the interplay of stress, coping, and resilience in individuals and communities. Some of these models include the transactional model of stress and coping, which emphasises the dynamic relationship between individuals and their environment during the stress-coping process. The biopsychosocial model considers biological, psychological, and social factors influencing health and well-being. The social-ecological model examines how the environment multiple levels of their environment influence individuals. The resilience model emphasises individuals' capacity to adapt and bounce back from adversity. Each model offers unique insights and perspectives that can contribute to a comprehensive understanding of the psychological and social impacts of the pandemic.
This study utilises the stress process model because it offers a comprehensive framework for studying the interplay among stressors, coping mechanisms, and outcomes in COVID-19. The stress process model 20 provides a valuable framework for examining how exposure to pandemic-related stressors may impact mental health outcomes in healthcare workers. This model posits that stressors arise from individuals' social circumstances and roles. Prolonged or intense stressors can manifest mental health symptoms through processes like the erosion of positive coping resources. Researchers have applied this model to examine chronic stressors' impact on doctoral students' mental health outcomes 21 . The study revealed academic stressors to be the strongest predictors of burnout, while family and monetary stressors were most closely associated with depression. It also found that the relationship between stress and burnout was partially mediated by mastery and advisor support, whereas the relationship between stress and depression was partially mediated by mastery. Likewise, Gilster 22 used the stress process model to investigate the neighbourhood stress process, particularly exploring racial and ethnic variations in the associations between neighbourhood stressors, mastery, and depressive symptoms within a multi-ethnic sample population. The study found that mastery partially mediates the relationship between perceived and observed neighbourhood stressors and depressive symptoms but does not provide a buffering effect against neighbourhood stressors.
In this study, the COVID-19 pandemic represents an acute and enduring stressor event that has fundamentally altered the social circumstances and occupational roles of frontline healthcare workers in Malawi and other LMICs. Specific pandemic-related stressors include heightened risk of infection, resource shortages, heavy workloads, loss of patients, and moral distress. The stress process model would suggest that these stressors can directly impact healthcare workers' mental health. Guided by the stress process model, this study analyses the relationships between pandemic stressor exposure, availability of coping resources, and mental health to determine predictive pathways. The framework recognises the pandemic's role as a significant stressor while accounting for individual and systemic protective factors that may confer resilience despite circumstances.
Study design, setting and participants
This cross-sectional study was conducted from May to June 2021 and utilised a mixed methods approach by combining quantitative and qualitative methods. The study was conducted in 4 districts (Blantyre, Mangochi, Lilongwe and Karonga) from the four regions of Malawi. We selected these districts because two are cities with large central hospitals handling severe and most COVID-19 cases (Lilongwe and Blantyre), one is a Lake District (Mangochi), which may be affected by dropped levels of tourism due to COVID-19, and finally a boarder district (Karonga) which is a possible entry point for imported COVID-19 cases. For qualitative data, we targeted frontline health workers with first-hand knowledge of the COVID-19 situation in hospitals and supervisors/managers who are believed to have a better idea of the situation in the four hospitals. Key Informant Interviews (KIIs) were conducted with four chief nursing officers or matrons. 12 In-depth Interviews (IDIs) were conducted with frontline health workers, three from each of the four hospitals. The data collected provided in-depth information to address the study objectives. Those who participated in the qualitative interviews did not participate in the quantitative survey and were purposively selected from hospital health workers on the data collection days. The sample of n = 119 was estimated using the sample size calculation formula for an unknown total population 23 . We used probability proportional to size (PPS) so that each hospital contributes a proportional sample depending on the number of health workers. Convenience sampling was used to select the respondents. However, 109 frontline clinicians and nurses from the four hospitals were interviewed to assess the prevalence of depression, anxiety and PTSD, representing a 91.5% response rate.
Interview guides and interviewer-administered questionnaires were used to collect qualitative and quantitative data. With practical experience and expertise in the mental health field for content and construct validity, the research team developed and reviewed the interview guide, which explored the experiences of frontline health workers. This guide was administered in English and Chichewa, and the interviews were conducted by research supervisors who had experience conducting key informant interviews. To assess the mental health status of participants, the study utilised the Generalized Anxiety Disorder (GAD-7), Patient Health Questionnaire (PHQ-9) and the Primary Care Post Traumatic Symptom Disorder Screen for DSM-5 (PC-PTSD-5). The three questionnaires have been used in various populations as brief screening measures for depression and anxiety 24 , 25 . Additionally, the PHQ-9 has been used before in Malawi 26 . PHQ-9 has nine items which measure depressive symptoms in the past two weeks on a scale of 1–27. The GAD-7 measures anxiety symptoms in the past two weeks and has seven questions with options ranging from 0 (not at all) to 3 (nearly every day) with an overall scale of 0–21. The PC-PTSD-5 is a 5-item questionnaire that measures posttraumatic symptoms in the past month on a scale of 1–5. The higher the scores, the more severe the symptoms were on all three questionnaires.
Data analysis
Quantitative data were analysed using STATA version 14. Scores were calculated for depression, anxiety and PTSD. Depression was measured by PHQ-9 on a scale of 0–27 and was classified into the following five groups: minimal (1–4), mild (5–9), moderate (10–14), moderately severe (15–19), and severe (20–27). The GAD-7 anxiety questionnaire had an overall score range of 0–21, which was classified into the following four categories: no anxiety or minimal (< 5), mild anxiety (5–9), moderate anxiety (10–14), and severe anxiety (> 15). PTSD was measured using a PC-PTSD-5 questionnaire on a scale of 1–5, with a cut-off of 3 points, i.e. PTSD was reported as observed for scores > 2. Binary outcomes are reported as depressed (score < 5) or not depressed (score > = 5), anxious (score < 5) or not anxious (score > = 5), PTSD (score < 3) or no PTSD (score > = 3). We tested the differences in proportions within population characteristics and the outcomes of interest using the Mc-Nemas chi-square test for proportions. We used binary logistic regression to explore factors associated with the three binary outcomes. All tests were conducted at a 95% confidence level.
Qualitative data were analysed using thematic analysis from a constructivist perspective. The study utilised the six phases of thematic analysis. The first step was data familiarisation, which involved reading and re-reading all KIIs and IDIs transcripts. Secondly, we generated initial codes from the data set identifying essential features relevant to answering the research question. Thirdly, we collated initial codes to identify significant broader patterns of meaning (potential themes) and review the viability of each theme. Fourth, we examined the themes to check if they addressed the research question. Some themes were split, combined, or discarded. Fifth, we defined and named the themes and worked out the scope and focus of each theme. Finally, we drafted the paper using triangulated quantitative and qualitative data, paying attention to context and the existing literature. The draft manuscript was circulated to the team members for their final review before consolidating all the revisions and submitting the finalised paper.
Ethics approval and consent to participate
The study fully adhered to ethical standards expressed in the Declaration of Helsinki. Before the commencement of the study, relevant authorisation and approval were sought from the University of Malawi Research Ethics Committee (UNIMAREC) (No. P/03/21/53), Mangochi, Blantyre, Lilongwe and Karonga District Health Officers (DHOs) and hospital directors. Participants who were above eighteen years old and agreed to participate in the study provided written informed consent to participate.
Demographic characteristics
Table 1 shows the basic demographic details of the study participants.
According to Table 1 , most study participants were female, 57% (n = 62), while males comprised 42% (n = 46). The age range of participants was from 21 to 65 years old, with a mean age of 33 (SD = 7.9) years old, and the majority aged below 40 years old, 80% (n = 87). Almost half of the participants were from Blantyre, 46% (n = 50). Most respondents, 77% (n = 84), were from city referral hospitals of Blantyre and Lilongwe, while only 23% (n = 25) were from the district hospitals of Mangochi and Karonga).
Prevalence of COVID-19-related depression, anxiety and PTSD
Table 2 . shows the point prevalence of COVID-19-related depression segregated by demographic factors.
The results of this study (Table 2 ) indicated an overall high prevalence of COVID-19-related depression (31%; CI [23, 41]), anxiety (30%; CI [22, 40]) and PTSD (25%; CI [17, 34]) among health care workers. However, most respondents had mild depression (18.4%) or anxiety (20.2%), as highlighted in Fig. 1 .
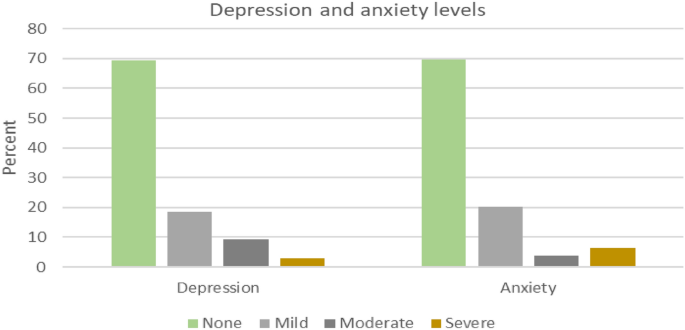
Levels of depression and anxiety for sampled health care workers.
A high proportion of depression was observed in Blantyre (n = 20, 40%) and among female health workers (n = 24, 39%). On the other hand, a high proportion of anxiety was observed in Lilongwe (n = 15, 44%) and among female health workers (n = 22, 35%). Furthermore, a high proportion of PTSD incidence was observed in Lilongwe (n = 12, 35%) and among female health workers (n = 18, 29%).
Despite the observed differences in depression, anxiety and PTSD prevalence for different variable groups, the regression results reveal that these differences are not statistically significant (Table 3 ).
The qualitative data analysis revealed three main themes that encapsulate the experiences and challenges faced by healthcare workers in Malawi during the COVID-19 pandemic: 1) Mental health symptoms and emotional distress, 2) Impact on work and personal life, and 3) Stigma and discrimination.
Mental health symptoms and emotional distress
The healthcare workers across the four districts reported experiencing a wide range of concerning mental health symptoms related to depression, anxiety, and posttraumatic stress disorder (PTSD). Regarding depressive symptoms, many workers described persistent sadness, hopelessness, loss of interest in everyday activities, fatigue, worthlessness or guilt, difficulty concentrating, and recurrent thoughts of death or suicide. The healthcare workers highlighted excessive worry, restlessness, difficulty relaxing, irritability, muscle tension, sleep disturbances, and panic attacks as some of the anxiety-related symptoms they had been experiencing. Additionally, the workers reported PTSD-associated symptoms, including unwanted distressing memories of treating COVID-19 patients and emotional and physical reactions when reminded of traumatic pandemic experiences. This avoidance of people or situations triggers recollections of trauma, hypervigilance, and exaggerated startle response. "Memories of the dead from Covid-19 haunted most of us. Most of the night, I failed to sleep. Some health workers reported the same to me. They would come for help, but I could only give them sleeping pills" (Matron, Karonga). "Sometimes, you just wish you could just shut down. Just forget everything. It was too much for us; too much sadness" (Matron, Lilongwe) .
According to the healthcare workers' accounts, these mental health symptoms had persisted for several months since the onset of the COVID-19 pandemic and significantly impacted their daily functioning and quality of life. Some workers reported being unable to get out of bed in the morning due to depression, while others described intense anxiety preventing them from being able to focus at work. The intrusive re-experiencing symptoms of PTSD were causing some workers substantial distress. Several workers tearfully recalled traumatic events such as holding the hands of dying COVID patients. These traumatic memories now haunted the healthcare workers, causing sleep disturbances and emotional anguish. In addition, traumatic experiences related to COVID-19 patient care also led to PTSD symptoms, such as intrusive memories and emotional numbing. A nurse in Lilongwe recounted, " I can still hear the sound of the ventilator alarms and see the faces of the patients who passed away. It is like a constant reminder of the tragedy we witnessed. "
In addition to the associated symptoms, healthcare workers also described profound emotional distress from their experiences of rapid patient deterioration and death in COVID-19 cases. As one clinician from Mangochi district poignantly recounted: "Most people say medical personnel are used to that, but with that disease, it is not easy to see people who were okay suddenly got the disease, it gets worse, and suddenly they die; it was too much to accept it." (Clinician, Mangochi). Further, anxiety symptoms were also prevalent, with healthcare workers mentioning excessive worry, restlessness, and sleep disturbances. A clinician in Karonga remarked, " I would lie awake at night, my mind racing with thoughts of all the patients I could not save and the constant fear of bringing the virus home to my family. "
These clinicians’ accounts provide insight into the trauma and moral injury inflicted on healthcare workers by the stark severity and frequent fatalities of COVID-19. It exemplifies the psychological impact of experiencing rapid patient declines and deaths first-hand, sometimes without adequate resources to prevent grievous outcomes. The sentiment expressed by this frontline worker in Mangochi district was similarly echoed by many others who struggled to come to terms with the sudden loss of life amongst their patients. One nurse from Karonga shared, " I felt so overwhelmed and helpless seeing patients deteriorate despite our best efforts. It was like a never-ending nightmare ." These experiences likely contributed to the substantial burden of depressive, anxiety, and PTSD symptoms endorsed by the healthcare workers amid Malawi's COVID-19 response.
Impact on work and personal life
Participants reported that frontline health workers were overwhelmed with work due to an increase in patient numbers and a reduction in the number of health workers. However, in Mangochi, respondents reported a general decrease in patient numbers, approximately from 60 patients per day to 30 per day; this did not translate to a lower workload since there was also a reduction in health workers for various reasons such as unexplained absenteeism, sickness and transfers. One nurse from Mangochi shared, " We were stretched thin, working endless hours with little rest. It was physically and emotionally draining." The same applied to Karonga, where healthcare workers were expected to work continuously for two weeks, followed by a week's holiday. This work overload may have contributed to "burnout", as reported by most participants. "The workload has increased, as you know. The pandemic, especially the second wave, hit us hard, so the workload just increased suddenly" (Nurse, Karonga).
Respondents also reported reduced face-to-face interaction with fellow workers, mainly due to new work protocols. COVID-19 measures, such as social distancing and the frequent use of Personal Protective Equipment (PPE, reduced their sense of connectedness. In addition, work output was negatively affected; participants attributed this to increased absenteeism, attrition and application of leave days, which was attributed to workers' fear of contracting COVID-19 at the workplace. Participants reported more panic and fear during the first wave than in the second since the healthcare workers might have developed strategies and coping mechanisms. "… so, there was less panic and fear in responding to the second wave because we had now learnt what we should do” (Matron, Lilongwe). Further, the fear of contracting the virus and infecting loved ones also took a toll on healthcare workers' family dynamics. " I had to isolate myself from my family for months, unable to hug my children or comfort them when they needed me the most. It was a painful sacrifice " (Clinician, Blantyre).
The COVID-19 pandemic also disrupted healthcare workers' family relationships and social connections in numerous ways. Many participants described the constant terror of spreading the virus to loved ones. This led some workers to agonise to isolate themselves entirely from family to avoid potential transmission. One matron from Lilongwe explained: " There was a time I thought I should send my wife and children home so that I should remain alone ." Sacrificing these crucial family bonds during an already stressful period exacted deep emotional pain, leaving workers feeling alone when support was most needed. Even for those who did not entirely self-isolate, the spectre of viral transmission strained family dynamics. Workers reported feeling unable to embrace loved ones, attend important events like weddings and funerals, or find comfort in casual physical affection. Families are vital for mental health; this constant stress and distance in relationships took a substantial psychological toll. Further, healthcare workers also expressed grief over the loss of colleagues and the impact on team morale. " Losing our coworkers to COVID-19 was devastating. It felt like a part of our family was gone, and the void they left behind was immense " (Nurse, Karonga).
Stigma and discrimination
Healthcare workers faced significant stigma and discrimination from their communities due to their occupation. Many reported instances of social isolation, harassment, and even violence. One nurse from Mangochi recounted, " People would yell at me on the street, calling me a virus carrier. They would cross the road to avoid passing by me as if I were a walking biohazard. " The stigma also extended to their living situations, with some healthcare workers being evicted from their homes by landlords who feared they would spread the virus. " I was kicked out of my rental apartment because the landlord found out I worked in a COVID-19 unit. I had nowhere to go and felt utterly betrayed " (Nurse, Lilongwe).
Participants described pervasive stigma from the community that damaged their social lives and sense of self. Many healthcare workers felt ostracised by the communities they sought to serve. Friends and neighbours avoided interacting with them in public due to transmission fears. This social stigma made healthcare workers increasingly isolated from previous social supports. For some healthcare workers, the stigma escalated to threats of physical violence. Multiple accounts emerged of community members throwing rocks at visiting health workers or barricading them from entering villages to administer vaccines. Workers feared that misinformation linking them to virus transmission had provoked this aggression. The social rejection, housing discrimination, and violence described by participants illustrate the heavy emotional toll of stigma during public health crises. Health workers felt hurt and afraid in the very communities they sacrificed to protect. This mistreatment exacerbated an already isolating and stressful pandemic working environment.
Many healthcare workers experienced self-stigma and were reluctant to seek mental health support despite the availability of some psychosocial support services. They feared further stigmatisation from colleagues who might perceive them as weak or incapable of handling their job responsibilities. A clinician in Blantyre admitted, " I was afraid to admit I needed mental health support. I did not want my colleagues to think I was weak or incapable of handling my job ." In addition to the fear of stigmatisation, many workers were unaware of the existence of in-house counselling or support services. Heavy workloads also left them little time to pursue such services, even when they knew their availability.
This study assessed the toll of COVID-19 on the mental health of frontline health workers and explored the experiences of these health workers in Malawi. The results showed relatively higher depressive, anxiety and PTSD symptoms due to COVID-19. This may be due to increased levels of work and fear for self and family. Whilst healthcare workers enjoyed a heroic reception in some parts of the world, they were discriminated against in Malawi. This added a toll on the mental health of healthcare workers.
On depression, a recent meta-analysis of a combined total of 33,062 participants showed a depression pooled prevalence rate of 22·8% 27 . Another review of 25 systematic reviews on primary studies with healthcare workers and other vulnerable groups showed that depression prevalence rates range from 20 to 51% 28 . This study found a depression prevalence rate of 31%. This higher rate may partly be explained by the unique challenges faced by the health workers in Malawi during the COVID-19 pandemic. One of the significant identified challenges highlighted in this study was the availability of limited resources in hospitals. These resources include Personal Protective Equipment (PPEs), syringes and blood bags that are crucial for healthcare workers' ability to effectively assist patients while preventing the transmission of diseases, including COVID-19. Inadequate human resources due to staff turnover and attrition leading to long working hours of the available health workers was another unique identified challenge.
Additionally, reduced face-to-face interaction with fellow workers, mainly due to new work protocols, decreased their sense of connectedness. Finally, stigmatisation and discrimination of health workers by the community resulted in reduced interaction between health workers and the community, thereby enhancing depressive symptoms. Likewise, stigmatising health workers experiencing mental health problems by their fellow health workers/colleagues may have negatively affected help-seeking behaviours, thereby worsening their condition 29 .
The high prevalence rate of COVID-19-related anxiety among health workers found in this study is slightly higher than the one reported in another recent study on nurses in Malawi, which found a prevalence rate of 25.5% on 26 nurses using the CAS 8 . However, the same study reported a slightly higher prevalence of COVID-19-related anxiety among hospital nurses (36.2%, n = 21). The slight differences may be attributed to differences in study design, anxiety measurement tools, cadre of health workers and time of data collection about COVID-19 waves. We collected our data in May 2021, four months after the pick of the second wave, when health workers were more confident in handling COVID-19 cases and were more aware of myths and misconceptions about the mode of COVID-19 transmission. These results contrast the low-pooled anxiety prevalence of 23·2% 5 , 30 .
Another review of 25 systematic reviews on primary studies with healthcare workers and other vulnerable groups showed that anxiety prevalence rates range from 12 to 45% 29 . The anxiety symptoms experienced by the healthcare workers in Malawi may be explained by their fear of contracting COVID-19 at the workplace. Likewise, the healthcare workers were also afraid of going home after work, fearing the possibility of transmitting the virus to their families. This explains the increased absenteeism, attrition and application of leave days. However, there was more panic and fear during the first wave compared to the second wave since the healthcare workers might have better understood the COVID-19 mode of transmission and prevention and developed better-coping mechanisms and strategies.
The PTSD prevalence rate of 24% found in this study is comparable to the results of other studies. A recent review of 25 systematic reviews on primary studies with healthcare workers and other vulnerable groups showed PTSD prevalence rates range from 19 to 51% 29 . The PTSD symptoms may be attributed to the health workers witnessing sudden deaths of COVID-19 patients. Even though the study did not find any case of healthcare workers with PTSD in Mangochi, there is evidence that some healthcare workers are experiencing PTSD symptoms, as reported by key informants.
Another significant finding of this study was that there are more healthcare workers with depression, anxiety and PTSD in city referral hospitals compared to district hospitals. These results may be attributed to several factors, including a higher workload for health workers due to increased COVID-19 patients in city referral hospitals than in district hospitals. As the most significant urban centres in the country, Blantyre and Lilongwe have higher population densities than rural districts. This demographic factor likely contributed to more COVID-19 cases in these cities, as crowded living conditions can facilitate the spread of the virus. Consequently, the referral hospitals in Blantyre and Lilongwe experienced a more significant influx of COVID-19 patients than district hospitals, placing a considerable burden on the healthcare workers in these facilities. These facilities also managed the most severe COVID-19 cases across Malawi. This concentration of critically ill patients likely exposed healthcare workers in these facilities to heightened levels of stress, trauma, and moral distress. Witnessing high rates of patient deterioration and death, coupled with the need to make difficult triage decisions amidst resource constraints, may have exacerbated the psychological toll on frontline staff in these urban referral hospitals. In contrast, some district hospitals, such as Mangochi, reported a significant decrease in patient numbers across all departments during the pandemic. This trend could be attributed to reduced health-seeking behaviour due to fear of contracting COVID-19 and the diversion of healthcare resources towards the pandemic response. While a decline in patient volume may have alleviated some workload pressures, it also raises concerns about potential unmet health needs and delayed care for non-COVID conditions in these rural districts.
Some of the identified challenges experienced by healthcare workers during the pandemic included limited resources such as PPEs, syringes and blood bags, inadequate human resources, long working hours, lack of awareness of available services such as counselling, staff turnover and attrition 31 . In addition, re-assigning most healthcare workers to work in COVID-19 centres created gaps in other departments that overwhelmed the remaining staff. Despite the several challenges faced due to the COVID-19 pandemic, respondents identified some opportunities that COVID-19 brought to mental health in Malawi. Firstly, more health workers were recruited in response to COVID-19. For example, a healthcare worker in Karonga reported receiving additional nurses during the first and second waves of the pandemic. Secondly, the government directed funds towards mental health and recruited more mental health workers, such as psychosocial counsellors. This is the first time in Malawi that the government has employed this particular cadre of health workers. Thirdly, public and private sectors offered several trainings to health workers, including those focusing on COVID-19 safety and management. Finally, both formal and informal psychosocial interventions were available. However, the utilisation of such interventions by health workers could have been more extensive. This was mainly attributed to fear of stigmatisation and lack of knowledge of such in-house services.
Even before the COVID-19 pandemic, healthcare workers in Malawi faced significant psychosocial challenges and resource constraints that likely heightened their vulnerability to the mental health consequences of the crisis. A 2018 study found that 62% of Malawian healthcare workers reported burnout, with emotional exhaustion being a shared experience 32 . Inadequate staffing, heavy workloads, lack of essential medical supplies, and low salaries contribute to healthcare worker burnout and job dissatisfaction 32 . These pre-existing issues, coupled with Malawi's critical shortage of healthcare personnel, created a context of chronic occupational stress and under-resourcing. The country has long struggled to train and retain an adequate health workforce, with a deficient number of physicians and nursing/midwifery personnel per 1,000 population 33 . This shortage has been compounded by the uneven distribution of health workers across urban and rural areas, high rates of attrition, and the burden of HIV/AIDS 34 . Consequently, when the COVID-19 pandemic struck, Malawian healthcare workers were already grappling with intense workloads, resource deficits, and psychosocial strain, potentially amplifying the mental health repercussions of pandemic-related stressors documented in this study.
The quantitative and qualitative results align closely with the stress process model's premise that exposure to stressors emerging from one's social circumstances can precipitate mental health symptoms without protective resources. The pandemic undoubtedly represented an abrupt stressor event that dramatically transformed participants' work environments and responsibilities. Quantitatively, high rates of depressive, anxiety and PTSD symptoms were documented. While not conclusively diagnostic, these screening results suggest a substantial burden of psychological distress consistent with other studies of frontline workers during COVID-19. Qualitative accounts provided vivid examples of pandemic-related stressors frequently cited in stress process model research as risk factors for poor mental health, including lack of personal protective equipment, heavy workloads, loss of co-workers and patients to illness, and the constant risk of infection. Witnessing the sheer human toll exacted by the virus profoundly impacted participants.
The stress process model recognises both the direct effects of stressors and indirect impacts via the erosion of positive coping resources. Participants described isolation and how fear of infecting loved ones kept them from family and social gatherings that previously provided support. The stigmatisation of healthcare workers also emerged as a prominent theme, aligning with literature on mental illness stigma as a barrier to help-seeking.
Study limitation
One of the main limitations of this study is the use of convenience sampling, which may limit the generalisability of the findings to the broader population of healthcare workers in Malawi. Convenience sampling relies on recruiting participants who are easily accessible and available. This non-probability sampling method can introduce bias, as the sample may not accurately reflect the characteristics and experiences of the entire healthcare workforce. Additionally, the study's cross-sectional design provides only a snapshot of the mental health status of healthcare workers at a single point in time. This approach does not allow for examining causal relationships or changes in mental health outcomes throughout the pandemic. Furthermore, the study relied on self-reported measures of mental health symptoms, which may be subject to social desirability bias or recall bias. Healthcare workers may have underreported their symptoms due to stigma or fear of professional consequences, or they may have had difficulty accurately recalling their experiences and emotions during the height of the pandemic. In addition, the study collected data from 109 out of 119 participants. This may affect the representativeness of the findings.
This mixed-methods study provides insights into the toll of the COVID-19 pandemic on mental health outcomes amongst frontline healthcare workers in Malawi. Utilising validated screening tools and in-depth interviews, the study revealed depression, anxiety, and posttraumatic stress disorder symptoms among clinicians and nurses across multiple districts. Qualitative findings contextualised these results, with participants recounting traumatic experiences of resource shortages, excessive workloads, stigmatisation and witnessing frequent patient deaths. These results align closely with the stress process model, emphasising the hazardous effects of acute stressor events and potential moderating resources. As Malawi continues battling COVID-19, implementing policies to support healthcare workers' mental health and capacity must be an urgent priority. Bolstering counselling services, reducing stigma, implementing self-care practices and peer support groups and allowing brief recuperative breaks could help strengthen coping. More broadly, this study exemplifies the pressing need for more investment in mental healthcare in Malawi and similar low-resource health systems. Protecting the mental well-being of healthcare workers through proactive interventions will be essential to maintaining an effective pandemic response and building resilience for future crises.
Based on the findings of this study, there are several recommendations that the researchers and governments of low-resource settings like Malawi can consider to better prepare for and mitigate the mental health toll on healthcare workers during public health crises like the COVID-19 pandemic:
Integrate mental health support into emergency response plans: Governments should proactively include mental health considerations and interventions as a core component of their emergency preparedness and response strategies. This includes allocating dedicated resources for mental health services, training healthcare workers in psychological first aid, and establishing clear protocols for accessing support.
Strengthen mental health infrastructure and workforce: Investing in developing mental health infrastructure and expanding the mental health workforce is crucial to ensure adequate capacity to meet the increased demand for services during crises. This may involve training more mental health professionals, integrating mental health into primary care, and leveraging digital platforms to improve access to care.
Governments should prioritise the well-being of frontline healthcare workers. They should recognise the unique challenges and stressors faced by healthcare workers during public health emergencies and prioritise their well-being. This includes ensuring adequate PPE provision, implementing reasonable work hours and rotations, and offering tailored mental health support services, such as counselling and peer support groups.
Address stigma and promote help-seeking behaviours: Governments should actively work to reduce mental health stigma and encourage healthcare workers to seek support when needed. This can be achieved through public awareness campaigns, education and training initiatives, and fostering a culture of openness and compassion within healthcare settings.
Conduct further research and monitoring: Governments should support ongoing research to better understand the mental health impacts of public health emergencies on healthcare workers and evaluate the effectiveness of interventions. Regular monitoring and assessment of mental health outcomes can inform policy decisions and guide the allocation of resources.
Data availability
Data for this report is only available upon request. To request the data, contact the corresponding author at [email protected].
Xu, B. & Kraemer, M. U. G. Open access epidemiological data from the COVID-19 outbreak. Lancet Infect. Dis. 20 (5), 534 (2020).
Article CAS PubMed PubMed Central Google Scholar
WHO, Novel coronavirus (2019-nCoV): Situation report-13 . 2023, World Health Organisation.
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 395 (10227), 912–920 (2020).
Nelson, B. W. et al. Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample. PLoS One 15 (11), e0241990 (2020).
Chen, J. et al. Mental health during the COVID-19 crisis in Africa: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 18 (20), 10604 (2021).
Luo, M. et al. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public-A systematic review and meta-analysis. Psychiatr. Res. 291 , 113190 (2020).
Article CAS Google Scholar
Chingono, R. M. S. et al. Psychological distress among healthcare workers accessing occupational health services during the COVID-19 pandemic in Zimbabwe. Compr. Psychiatr. 116 , 152321–152321 (2022).
Article Google Scholar
Chorwe-Sungani, G. Assessing COVID-19-related anxiety and functional impairment amongst nurses in Malawi. Afr. J. Prim. Health Care Fam. Med. 13 (1), e1–e6 (2021).
Article PubMed Google Scholar
Munyenyembe, B. & Chen, Y.-Y. COVID-19 anxiety-coping strategies of frontline health workers in a low-income country Malawi: A qualitative inquiry. J. Workplace Behav. Health 37 (1), 47–67 (2022).
Mahlangu, P. et al. “I Carry the Trauma and Can Vividly Remember”: Mental health impacts of the COVID-19 pandemic on frontline health care workers in South Africa. Int. J. Environ. Res. Public Health 20 (3), 2365 (2023).
Article PubMed PubMed Central Google Scholar
Dawood, B., Tomita, A. & Ramlall, S. ‘Unheard’, ‘uncared for’ and ‘unsupported’: The mental health impact of Covid-19 on healthcare workers in KwaZulu-Natal Province, South Africa. PloS One 17 (5), e0266008–e0266008 (2022).
Erinoso, O. et al. Effect of COVID-19 on mental health of frontline health workers in Nigeria: A preliminary cross-sectional study. J. Psychosom. Res. 139 , 110288–110288 (2020).
Kwaghe, A. V. et al. Stigmatization and psychological impact of COVID-19 pandemic on frontline healthcare Workers in Nigeria: A qualitative study. BMC Psychiatr. 21 (1), 1–518 (2021).
Muzyamba, C., Makova, O. & Mushibi, G. S. Exploring health workers’ experiences of mental health challenges during care of patients with COVID-19 in Uganda: A qualitative study. BMC Res. Notes 14 (1), 1–286 (2021).
Sandesh, R. et al. Impact of COVID-19 on the mental health of healthcare professionals in Pakistan. Cureus 12 (7), e8974 (2020).
PubMed PubMed Central Google Scholar
Gupta, A. K. et al. Prevalence of anxiety and depression among the healthcare workers in Nepal during the COVID-19 pandemic. Asian J. Psychiatr. 54 , 102260 (2020).
Sia Morenike, T. et al. Psychosocial impact of COVID-19 pandemic on front-line healthcare workers in Sierra Leone: An explorative qualitative study. BMJ Open 13 (8), e068551 (2023).
Moitra, M. et al. Mental health consequences for healthcare workers during the COVID-19 pandemic: A scoping review to draw lessons for LMICs. Front. Psychiatr. 12 , 602614–602614 (2021).
Oyat, F. W. D. et al. The psychological impact, risk factors and coping strategies to COVID-19 pandemic on healthcare workers in the sub-Saharan Africa: A narrative review of existing literature. BMC Psychol. 10 (1), 284–316 (2022).
Pearlin, L. I. et al. The stress process. J. Health Soc. Behav. 22 (4), 337–356 (1981).
Article CAS PubMed Google Scholar
Hish, A. J. et al. Applying the stress process model to stress-burnout and stress-depression relationships in biomedical doctoral students: A cross-sectional pilot study. CBE Life Sci. Educ. 18 (4), 51 (2019).
Gilster, M. E. Neighborhood stressors, mastery, and depressive symptoms: Racial and ethnic differences in an ecological model of the stress process in Chicago. J. Urban Health 91 (4), 690–706 (2014).
Cochran, W. G. Sampling techniques 3rd edn. (Wiley, 1977).
Google Scholar
Mmanga, C. et al. The world is coming to an end! COVID-19, depression, and anxiety among adolescents in Malawi. Front. Psychiatr. 13 , 1024793 (2022).
Khanal, P. et al. Mental health impacts among health workers during COVID-19 in a low resource setting: A cross-sectional survey from Nepal. Global Health 16 (1), 89 (2020).
Udedi, M. The prevalence of depression among patients and its detection by primary health care workers at Matawale Health Centre (Zomba). Malawi Med. J. 26 (2), 34–37 (2014).
Aymerich, C. et al. COVID-19 pandemic effects on health worker’s mental health: Systematic review and meta-analysis. Eur. Psychiatr. 65 (1), e10 (2022).
Iob, E., Steptoe, A. & Zaninotto, P. Mental health, financial, and social outcomes among older adults with probable COVID-19 infection: A longitudinal cohort study. Proc. Natl. Acad. Sci. U S A 119 (27), e2200816119 (2022).
Magner, C. et al. The psychological impact of COVID-19 on frontline healthcare workers “From Heartbreak to Hope”. J. Clin. Nurs. 30 (13–14), e53–e55 (2021).
Ghahramani, S. et al. Health care workers’ mental health in the face of COVID-19: A systematic review and meta-analysis. Int. J. Psychiatr. Clin. Pract. 27 (2), 208–217 (2023).
AlAteeq, D. A. et al. Mental health among healthcare providers during coronavirus disease (COVID-19) outbreak in Saudi Arabia. J. Infect. Public Health 13 (10), 1432–1437 (2020).
Kim, M. H. et al. Burnout and self-reported suboptimal patient care amongst health care workers providing HIV care in Malawi. PLoS One 13 (2), e0192983 (2018).
World Bank, Nurses and midwives (per 1,000 people) -Malawi . 2017.
Chimwaza, W. et al. What makes staff consider leaving the health service in Malawi?. Hum. Resour. Health 12 (1), 17 (2014).
Download references
This study was carried out under the Covid-19 Africa Rapid Grant Fund (Grant no. COV19200603527586), supported under the auspices of the Science Granting Councils Initiative in Sub-Saharan Africa (SGCI) and administered by South Africa's National Research Foundation (NRF) in collaboration with Canada's International Development Research Centre (IDRC), the Swedish International Development Cooperation Agency (SIDA), South Africa's Department of Science and Innovation (DSI), the Fonds de Recherche du Québec (FRQ), the United Kingdom's Department of International Development (DFID), United Kingdom Research and Innovation (UKRI) through the Newton Fund, and the SGCI participating councils across 15 countries in sub-Saharan Africa.
Author information
Authors and affiliations.
University of Malawi, Zomba, Malawi
Limbika Maliwichi, Fiskani Kondowe, Jimmy Kainja, Simunye Nyamali & Yamikani Ndasauka
Kamuzu University of Health Sciences, Lilongwe, Malawi
Chilungamo Mmanga
University of Cape Town, Cape Town, South Africa
Martina Mchenga
You can also search for this author in PubMed Google Scholar
Contributions
L.M., Y.N., J.K., S.N., F.K., M.M., and C.M. conceptualised the idea and reviewed the manuscript. L.M., M.M., J.K., C.M. and F.K. analysed the data. L.M., Y.N., and F.K. drafted the paper. All authors contributed to the article and approved the submitted version.
Corresponding author
Correspondence to Yamikani Ndasauka .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Maliwichi, L., Kondowe, F., Mmanga, C. et al. The mental health toll among healthcare workers during the COVID-19 Pandemic in Malawi. Sci Rep 14 , 10327 (2024). https://doi.org/10.1038/s41598-024-61216-x
Download citation
Received : 08 October 2023
Accepted : 02 May 2024
Published : 06 May 2024
DOI : https://doi.org/10.1038/s41598-024-61216-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Post-traumatic stress disorder
- Healthcare workers
- Mixed methods
- Stress process model
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
COMMENTS
COVID‐19 can also result in increased stress, anxiety, and depression among elderly people already dealing with mental health issues. Family members may witness any of the following changes to the behavior of older relatives 11 ; Irritating and shouting behavior. Change in their sleeping and eating habits.
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic ...
SUBMIT PAPER. Socius: Sociological Research for a Dynamic World ... although this study was focused primarily on internalized mental health, we acknowledge research by Rosenfield and ... van Wijngaarden-Cremers Patricia J. M. 2020. "Women's Mental Health in the Time of COVID-19 Pandemic." Frontiers in Global Women's Health 1:588372 ...
Mental health professionals can help craft messages to be delivered by trusted leaders. 4. The Covid-19 pandemic has alarming implications for individual and collective health and emotional and ...
The COVID-19 pandemic has had a severe impact on the mental health and wellbeing of people around the world while also raising concerns of increased suicidal behaviour. In addition access to mental health services has been severely impeded. However, no comprehensive summary of the current data on these impacts has until now been made widely ...
We collected data on 8 million calls from 19 countries, focusing on the COVID-19 crisis. Call volumes peaked six weeks after the initial outbreak, at 35% above pre-pandemic levels. The increase ...
This paper also relates to the broader research on the determinants of mental health (26 ... The consequences of COVID-19 for mental health have been dire, as highlighted in a May 2020 United Nations policy brief urging the international community to protect vulnerable populations . Among those identified as a specific population of concern ...
3. the risk of infection, severe illness and death from COVID-19 for people living with mental disorders 4. the impact of the COVID-19 pandemic on mental health services 5. the effectiveness of psychological interventions adapted to the COVID-19 pandemic to prevent or reduce mental health problems and/or maintain access to mental health services.
The good news is that by October, 2020, mental health was top of the charts in terms of published papers and preprints on the effects of COVID-19. The bad news is that the quantity of papers is not matched by quality. In March, 2020, Holmes and colleagues outlined the priorities for mental health research during the pandemic. How much have we ...
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint ...
Background The COVID-19 pandemic triggered vast governmental lockdowns. The impact of these lockdowns on mental health is inadequately understood. On the one hand such drastic changes in daily routines could be detrimental to mental health. On the other hand, it might not be experienced negatively, especially because the entire population was affected. Methods The aim of this study was to ...
In The Lancet Psychiatry, Matthias Pierce and colleagues 1,2 identify the importance of sampling in studying mental health effects of COVID-19. We found that a mental health survey 3 using a commercial panel (of approximately 20 000 people) overrepresented mentally unhealthy respondents by approximately 2·5 times. This overrepresentation ...
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact.
In this section. The COVID-19 pandemic has had a huge impact on public health around the globe in terms of both physical and mental health, and the mental health implications of the pandemic may continue long after the physical health consequences have resolved. This research area aims to contribute to our understanding of the COVID-19 ...
The present study aimed to document the initial mental health scenario across the Australian community and examine its association with exposure to the broad COVID-19 environment at this critical acute phase by: (1) measuring the current prevalence of clinically significant symptoms of generalized anxiety and depression, including associations with other recent adversities; and (2 ...
Health and social care workers (HSCWs) continue to play a vital role in our response to the COVID-19 pandemic. It is known that HSCWs exhibit high rates of pre-existing mental health (MH) disorders [1,2,3] which can negatively impact on the quality of patient care [].Studies from previous infectious outbreaks [5, 6] suggest that this group may be at risk of experiencing worsening MH during an ...
The outbreak of SARS-CoV-2, which causes COVID-19, has significantly impacted the psychological and physical health of a wide range of individuals, including healthcare professionals (HCPs). This umbrella review aims provide a quantitative summary of meta-analyses that have investigated the prevalence of stress, anxiety, depression, and sleep disturbance among HCPs during the COVID-19 pandemic.
Publications (reports, non-reviewed pre-prints of papers and peer-reviewed articles) were eligible to be included if they were focused on mental health during the COVID-19 pandemic, reported original research findings/results (i.e. media releases, editorials, opinion pieces, commentaries, protocol papers or general text summaries within reports ...
The $3.69 million R01 grant aims to address urgent, time-sensitive mental health research questions related to COVID-19, according to the NIMH. Many uncertainties about the COVID-19 pandemic remain although understanding of the virus has improved and effective vaccines have been developed, Polimanti said. There are also many consequences to be ...
Racism is a known social determinant of health which affects the mental health and well-being of families, particularly pregnant and postpartum individuals and their children.As we have continued to wrestle with the COVID-19 pandemic, there have been increased efforts to better understand the impacts of this global event with racialized ...
The present study aimed to understand the long-term cognitive, neurological, and psychiatric impact of COVID-19 and the brain alterations in long-term COVID patients two years after SARS-CoV-2 ...
Mental health problems, loneliness among young people, and polarization are rapidly increasing, especially after the COVID-19 pandemic. A new large-scale research study, the CovSocial project, led ...
The COVID-19 pandemic has affected the mental health of healthcare workers worldwide, with frontline personnel experiencing heightened rates of depression, anxiety, and posttraumatic stress. This ...