We use some essential cookies to make this website work. We’d like to set some additional cookies to understand how you use the website and to improve it. We also use cookies set by other sites to help us deliver content from their services. You can read more about our cookies before you choose.
- Accept additional cookies
- Reject additional cookies
This is a new website – your feedback will help us to improve it.

Making the case
Making the case for evidence-based patient information: the importance of evidence to support shared decision-making and how NHS libraries can play a key role
On behalf of Health Education England and as part of a Senior Leadership Programme, a group of health library and knowledge specialists across England worked together on a shared project exploring how evidence is used in the creation and review of information for patients.
The project titled, ‘Making the case: evidence-based patient information’ explores the real need for patients and the public to have access to high quality, reliable health information.
As individuals are being encouraged to self-manage and be partners in their care they need access to a range of resources tailored to their literacy level.
The aims of the project were:
- influence and advocate the importance of evidence for health information for patients, carers and the public in healthcare settings
- identify key learning to support others in influencing the evidence base of patient leaflets in their local NHS settings.
As health librarians, we play a key role in providing evidence for patient care as part of our service to healthcare staff.
We have skills in finding the evidence, appraising it and making it readily available in formats needed by our healthcare colleagues.
The need for patient information to be evidence based is driven by a number of strategic priorities including:
- patient experience
- self-management
- shared decision-making
- health system sustainability
The project focused on the production of patient leaflets within NHS Trusts. These are usually written by local clinical staff for specific conditions or procedures.
We were looking at the current level of involvement by NHS KLS in the production and review of leaflets and the key stakeholders who play a role in this process.
Information was gathered from case studies of three NHS Trusts, through telephone interviews with NHS librarians delivering and supporting the production of patient information and a literature search on good quality patient information.
The findings of the work are outlined in the report, along with other useful resources highlighting:
- importance of KLS role in supporting evidence-based information
- key policy drivers
- influencing key stakeholders
- challenges of clinical language.
The report makes a number of recommendations including making patient information a part of our ‘offer’ as a service forming part of KLS existing role as champions of evidence-based practice within their organisations.
Key themes from the case studies and learning from networks were the significance of influencing skills and the importance of demonstrating the impact of this work and sharing best practice.
- Making the case; evidence-based patient information.’ A report of the findings
- Learning log
- Stakeholder map
Contact the Knowledge for Healthcare team on [email protected] for any of the resources in an accessible format.
There are other examples of best practice, highlighted to demonstrate the positive impact NHS libraries have experienced. It is another aspect of the work many NHS libraries are already engaged in as part of patient care.
If you have any queries about the project please contact a member of the project team:
Emily Hopkins, Health Education England Deena Maggs, The King’s Fund Victoria Treadway, NHS RightCare Vicki Veness, Royal Surrey County Hospital NHS Foundation Trust Jacqui Watkeys, Walsall Healthcare NHS Trust Suzanne Wilson, Northumberland, Tyne and Wear NHS Foundation Trust
Page last reviewed: 15 June 2021
Quality outcomes in NHS library and knowledge services
Performance Measurement and Metrics
ISSN : 1467-8047
Article publication date: 15 January 2021
Issue publication date: 16 August 2021
This paper aims to demonstrate the approach taken in delivering the quality and impact elements of Knowledge for Healthcare, the strategic development framework for National Health Service (NHS) library and knowledge services in England. It examines the work undertaken to enhance quality and demonstrate the value and impact of health library and knowledge services. It describes the interventions developed and implemented over a five-year period 2015–2020 and the move towards an outcome rather than process approach to impact and quality.
Design/methodology/approach
The case study illustrates a range of interventions that have been developed, including the outcomes of implementation to date. The methodology behind each intervention is informed by the evidence base and includes professional engagement.
The outcomes approach to the development and implementation of quality and impact interventions and assets provides evidence to demonstrate the value of library and knowledge staff to the NHS in England to both high-level decision-makers and service users.
Originality/value
The interventions are original concepts developed within the NHS to demonstrate system-wide impacts and change. The Evaluation Framework has been developed based on the impact planning and assessment (IPA) methodology. The interventions can be applied to other healthcare systems, and the generic learning is transferable to other library and knowledge sectors, such as higher education.
- Service improvement
Edwards, C. and Gilroy, D. (2021), "Quality outcomes in NHS library and knowledge services", Performance Measurement and Metrics , Vol. 22 No. 2, pp. 106-116. https://doi.org/10.1108/PMM-07-2020-0040
Emerald Publishing Limited
Copyright © 2020, Clare Edwards and Dominic Gilroy
Published by Emerald Publishing Limited. This article is published under the Creative Commons Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and non-commercial purposes), subject to full attribution to the original publication and authors. The full terms of this licence may be seen at http://creativecommons.org/licences/by/4.0/legalcode
Introduction
Health Education England (HEE) is the steward of development and investment in library and knowledge services on behalf of the National Health Service (NHS). HEE's Knowledge for Healthcare ( HEE, 2014 ) is the strategic development framework for NHS-funded library and knowledge services in England, which has set out an ambitious vision to ensure the use of the right knowledge and evidence at the right time. It calls for service transformation, redesign and collaboration ( Lacey Bryant et al. , 2018 ). One of the strategic work streams underpinning Knowledge for Healthcare is quality and impact.
Value and Impact Toolkit
Metrics for Success
Evaluation Framework
Quality Assurance Framework
Grieves and Pritchard (2018) note the importance of an outcomes and impact-centred model in developing an agile evidence base. This enables the library and knowledge staff to demonstrate to stakeholders that they “fully understand the value our customers place upon services, the contribution we make to strategic objectives, our value for money and the longer-term impact”. An outcomes focus has been adopted in the implementation of these interventions.
Methodology
The HEE Library and Knowledge Services team uses driver diagrams as a strategic planning tool. A driver diagram ( Figure 1 ) informed the development of interventions to be implemented by quality and impact group (QIG) to achieve the vision of Knowledge for Healthcare. In most instances, each intervention resulted in a project to oversee the development and implementation of a tool to improve service quality and demonstrate value and impact. In some instances, such as with the research and innovation aim, the intervention consisted of a range of projects and initiatives. Intervention and project were overseen by task and finish groups which included representatives from HEE, NHS-employed library and knowledge staff, higher education healthcare librarians and subject matter experts. An evidence-based approach was followed, including a literature review, piloting and evaluation processes.
Our next steps are to refresh the “impact” tool, promote widespread adoption and publish case studies in order to attract more decision makers to make the best use of the service ( HEE, 2014 ).
An initial intervention was to enhance the existing NHS library and knowledge services impact toolkit. This toolkit was based on sound evidence ( Weightman et al. , 2009 ); however, it was acute hospital focussed, and the evidence showed that many library and knowledge staff were not routinely measuring the impacts made by their service. Library and knowledge staff also often confused impact and user feedback ( Ayre et al. , 2018 ). A refresh of the original tool was required, grounded in current evidence of the type of positive impacts being demonstrated by health librarians ( Brettle et al. , 2016 ) and applicable to all healthcare settings.
A Value and Impact task and finish group was set up to review and update the Impact toolkit. The methodology used included a literature search, a baseline survey on the use of the existing toolkit and development and piloting of a questionnaire ( Ayre et al. , 2018 ).
The task and finish group used the standard methods and procedures for assessing the impact of libraries BS IS0 16439:2014 to define impact for NHS libraries as a difference or change in an individual or group resulting from the contact with library services. The group adopted Saracevic and Kantor’s (1997) definition of value as the perceived value approach which relies on an individual's own perception of the value of an impact.
The refreshed Impact Toolkit ( HEE, 2016b ) includes a generic questionnaire, an impact case study template and a resource that brings together a range of material useful in measuring value and impact. The main change to the questionnaire is the recommendation that impact is gathered in relation to one specific incident (or use) rather than overall use of the library ( Ayre et al. , 2018 ). The questionnaire focusses on impact as both immediate and probable future outcomes. Knock et al. (2017) provided an overview of the collaborative approach used in the development of the toolkit, its contents and intention to collate the outcomes of both the questionnaire and case studies nationally to provide a clear picture of the impact of health libraries in the NHS in England.
Since the launch of the toolkit, in 2016, there has been a considerable increase in the generation and sharing of impact evidence across England to demonstrate the value of the library and knowledge services to the NHS. Examples of this include Warrington and Halton Teaching Hospitals, where an impact mural was added in a prominent location within the teaching space, and University Hospitals Coventry and Warwickshire's Clinical Evidence-Based Information Service (CEBIS) which regularly use social media to tweet about their impact work.
A survey was carried out in spring 2019 to determine how many services had implemented the Impact toolkit. With a response rate of 100%, this survey showed that 75% of library and knowledge services were using the toolkit and of these, 80% were using the generic questionnaire, demonstrating progress towards the initial target in Knowledge for Healthcare of 95% of services using the toolkit.
The development of impact case studies has become the most powerful means of demonstrating the impact and value of services across England. Library and knowledge staff are encouraged to submit case studies to a national repository managed by the HEE team, with over 350 accepted to date. Many of these narratives have been developed into impact vignettes ( Plate 1 ).
Impact data only deliver their full potential value where they are used to evidence the critical functions that library and knowledge staff fulfil in the NHS and healthcare environment. Gilroy and Turner (2018) demonstrated how library and knowledge staff were championing their organisational impact at the local level, using impact evidence in a variety of ways including in annual reports and promotional materials to highlight their value to stakeholders.
The use of quotes from individual stakeholders and opinion leaders who have benefited from the use of services is an important part of the case study development. This recommendation is used in promotional material at the national and local level, ensuring the role of health library and knowledge services is visible to high-level decision-makers influencing thinking and policy.
Quality and Improvement Outcomes Framework (Outcomes Framework)
We will refresh the Library Quality Assurance Framework to ensure it continues to drive service improvement and is aligned with wider education and service monitoring (Knowledge for Healthcare, 2014).
An initial objective was to refresh the existing Library Quality Assurance Framework (LQAF), first introduced in 2010 ( De la Mano and Harrison, 2012 ). However, to align with the needs of Knowledge for Healthcare, it was decided to completely review the existing quality process. Many of the reasons for review were the same as those highlighted by Reid (2019) ; standards of service delivery had improved ( Lacey Bryant et al. , 2018 ); context had changed and the perception that it was becoming “too easy” to attain the highest ranking of excellence.
A key emphasis of the review was the focus on outcomes rather than process. Grey et al. (2012) highlighted that any future strategic development of health library services should promote the importance of quality improvement outcomes (rather than processes) as the key to improving services.
The development has been grounded in an evidence-based approach using the quality improvement methodology of plan, do, study, act (PDSA). The piloting stage and use of a range of methods, both evaluative and knowledge gathering, have been important to ensure the development of a robust framework for implementation ( Edwards and Gilroy, 2019 ).
All NHS organisations enable their workforce to freely access proactive library and knowledge services that meet organisational priorities within the framework of Knowledge for Healthcare.
All NHS decision-making is underpinned by high-quality evidence and knowledge mobilised by skilled library and knowledge specialists.
Library and knowledge specialists identify the knowledge and evidence needs of the workforce in order to deliver effective and proactive services.
All NHS organisations receive library and knowledge services provided by teams with the right skill mix to deliver on organisational and Knowledge for Healthcare priorities.
Library and knowledge specialists improve the quality of library and knowledge services using evidence from research, innovation and good practice.
Library and knowledge specialist demonstrate that their services make a positive impact on healthcare.
The maturity model has five levels from 0, which represents no development against the outcome, through to 4, a service that is highly developed and continually improving against the outcome.
Defining quality is difficult as there are multiple definitions which capture its myriad elements. Booth's (2003) analogy encourages consideration of as many different aspects, perspectives and types of evidence as possible to provide a realistic overview of quality. The evaluation of library and knowledge services against the levels for each of the outcomes therefore relies on a range of evidence to demonstrate progress. Based on the structure of the Public Library Improvement Model for Scotland ( 2017 ), the Outcomes Framework provides the scope, NHS strategic context, key questions to consider and examples of outcome-focussed evidence.
HEE's policy on NHS library and knowledge services in England ( HEE, 2016a ) emphasises the need for all NHS staff to be able to freely access library and knowledge services in order to use the right evidence and knowledge to deliver excellent healthcare and health improvement. To ensure that the NHS is engaged and delivering on this policy, the Outcomes Framework has taken an organisational approach. Outcomes 1 to 3 are focussed on the organisation to ensure that library and knowledge services are embedded and seen as business critical ( Lacey Bryant et al. , 2018 ). This ensures integration of the Outcomes Framework with the HEE Quality Framework ( HEE, 2019b ) covering the wider education and learning environment.
A baseline self-evaluation of the framework is being planned for submission by all NHS trusts across England in 2021. This differs from the LQAF for which only 70% of services carried out the initial baseline ( De la Mano and Harrison, 2012 ). To ensure consistency, a single national process is being established to validate the self-evaluation submissions. The result of this will be the first truly national and comparable review of quality within NHS-funded library and knowledge services in England.
The Outcomes Framework provides a structure to ensure services evolve to meet the changing needs of organisations and individuals. The framework should lead to increasing satisfaction and improved outcomes for users of the services. Grey et al. (2012) noted that quality improvement systems produce valuable outcomes including a positive impact on strategic planning, promotion, new and improved services and staff development.
Metrics and the impact evaluation framework
Metrics will be reviewed, and additional meaningful measures introduced, as part of action planning to implement the strategic framework (Knowledge for Healthcare, 2014).
A task and finish group carried out an extensive review of what makes a good metric and how these have been applied to library and knowledge services in the NHS. The methodology included a survey with library and knowledge staff about current approaches; a review of the history of metrics in NHS-funded libraries and a scoping literature search.
The resulting Principles for Metrics Report and Recommendations ( HEE, 2016c ) identifies a set of principles for good metrics for health library and knowledge services, as meaningful, actionable, reproducible and comparable. It defines metrics as “criteria against which something is measured” ( Showers, 2015 ). It also provides a template [1] to support the development and sharing of metrics that are adaptable across all service situations.
Fricker (EAHIL, 2017) emphasised how good metrics contribute to better engagement and understanding with stakeholders and highlighted the principles which will equip librarians to develop meaningful metrics in support of their service development and improvement.
This work has improved our understanding of metrics and has provided a major learning point since the production of Knowledge for Healthcare in 2014. This learning is now being used at the national level to inform the refresh of the strategy.
Working with Sharon Markless [2] , an impact Evaluation Framework ( HEE, 2017 ) was created to measure the progress and impact of delivery of the Knowledge for Healthcare vision. This used the impact planning and assessment (IPA) methodology and defined impact as “any effect of the service [or of an event or initiative] on an individual or group” ( Streatfield and Markless, 2009 ). This aligns well with the definition in the Value and Impact Toolkit.
The Evaluation Framework is based on the premise that it is very difficult to provide clear evidence of impact in complex systems such as healthcare. Therefore, the approach taken is to identify a series of indicators which, when taken together, suggest that progress is being made ( Streatfield and Markless, 2009 ). The overall emphasis in any evaluation framework is on achieving outcomes which show “changes in behaviour, relationships, activities or actions of people, groups and organisations with whom a programme works directly” ( Earl et al. , 2001 ).
Organisations are more effective in mobilising evidence and internally generated knowledge.
Patients, carers and the public are empowered to use information to make health and well-being choices.
Improved consistency and increased productivity and efficiency of healthcare library and knowledge services.
Enhanced quality of healthcare library and knowledge services.
Partnership working is the norm in delivering knowledge to healthcare.
Increased capability, confidence and capacity of library and knowledge services workforce.
It was important to ensure that appropriate evidence and data were available to demonstrate progress against the objectives. Most of the data and evidence required are generated by the activity carried out by the library and knowledge services delivering to the NHS at the local level, with additional evidence from national activity. A review resulted in the revision of existing NHS library service data sets and the development of some new processes.
A learning point has been to consider what data and evidence should be collected routinely compared to ad hoc requests for specific evidence requirements. A monitoring dashboard is being developed for review and reporting of the data sets against agreed metrics and to demonstrate trends and differences made against each of the objectives. The further goal is to have the significant longitudinal data and evidence to truly tell the story of the impact of the library and knowledge services in the NHS.
Overview of building the evidence base
As part of our commitment to quality, knowledge teams will continue to undertake and publish research in the field, thereby building the evidence base for service improvement and sharing best practice (Knowledge for Healthcare, 2014).
A range of initiatives have been taken forward by QIG towards achieving this aim with an emphasis on encouraging library and knowledge services to share good practice and innovation.
An important step had already been taken in promoting service improvement by recognising and rewarding innovation through the Sally Hernando Awards for Innovation [3] ( De la Mano and Harrison, 2012 ). These awards have been refined with more focus on the evaluation and impact of service innovation.
A key aim of Knowledge for Healthcare is to increase the numbers of clinical librarians within the NHS. Brettle et al. (2016) urged future researchers to build a significant and comprehensive international evidence base about the effectiveness and impact of clinical librarian services. QIG supported a national project to contribute to this evidence base. A task and finish group continued this research, demonstrating the impact of clinical librarians in assisting in decision-making surrounding patient safety, quality of care and efficiency ( Divall and James, 2019 ).
The Outcomes Framework also encourages library and knowledge staff to ensure developments are evidence based and to develop a research culture within the library service. This aligns to the work presented by Thorpe and Howlett (2019) on the development of an Australian maturity model for evidence-based practice.
The work of the QIG has produced a range of streamlined interventions that are applied and implemented nationally in a single consistent way. This approach to development and implementation is enabling the creation of an outcomes-focussed national evidence base to demonstrate the value and impact of library and knowledge services across the NHS system. Aligned to this is the use of the evidence and the interventions to support service improvement.
The impact vignettes have been used successfully with stakeholders to raise the profile of library and knowledge staff, a primary example being the A Million Decisions campaign [4] , delivered in partnership with the Chartered Institute of Library and Information Professionals (CILIP). Local services are using this effectively for both advocacy and promotion.
As Gann and Pratt (2013) conclude, there is a need for library and knowledge staff to identify ways to evaluate themselves and ensure current measures have meaning for those outside the library world and in the context of organisations' mission and objectives. Quality and impact tools facilitate this at a system level and allow for the development of policy. For example, the implementation of a library and knowledge staff ratio policy ( HEE, 2020 ) has been underpinned by the evidence from the use of the impact tools and collection of metrics and impact. In 2014, an unrealistic target was set of an increase in clinical librarians, from 58 to 80%, at this time, we have only reached 63%. However, the library and knowledge workforce metrics, impact on clinical librarians’ research and the impact vignettes have formed the evidence, that speaks clearly to stakeholders and employers, to enable a recommendation on an improved staffing ratio to increase the number of embedded librarians and knowledge specialist. The policy states that organisations should “strive to achieve a ratio of at least 1 qualified librarian or knowledge specialist per 1,250 WTE NHS staff”.
Although the different interventions can be used separately, the collective outputs provide a powerful narrative of the value of library and knowledge staff to the NHS from an impact and patient outcomes perspective.
The QIG driver diagram illustrates the primary aim of enhancing the quality and demonstrating the value of healthcare library and knowledge staff. The interventions described in this paper are enabling this change and have been used to demonstrate the system-wide value and impact of library and knowledge staff to the NHS in England.
In 2020, Knowledge for Healthcare will be reviewed and refreshed. Originally drafted to cover a 15-year time span and published as a five-year strategy, this is a useful juncture to take stock. The next steps for QIG will be for further evaluation of all the interventions. Effective knowledge services are business critical for the NHS. It follows that there are two crucial next steps: embedding the use of these evidence-based interventions in a consistent way in local NHS-funded library and knowledge services; generating the evidence base that allows NHS executives, clinicians and managers, as well as librarians and knowledge specialists, to tell the impact story to a range of different audiences and for different purposes, be that advocacy, promotion or sharing good practice and innovation.
Driver diagram
Examples of impact case study vignettes
https://kfh.libraryservices.nhs.uk/value-and-impact-toolkit/tools/metrics/
Sharon Markless, https://kclpure.kcl.ac.uk/portal/sharon.markless.html
The Sally Hernando Awards are for innovation in NHS library services are named in memory of Sally Hernando (1957–2010), formerly head of knowledge management and e-learning at NHS south-west. Sally led on many innovative national developments and was a great supporter of developing library services to their fullest potential.
A Million Decisions is a joint campaign led by HEE's Library and Knowledge Services team and the CILIP Health Libraries Group and with CILIP https://www.cilip.org.uk/general/custom.asp?page=AMillionDecisions
Ayre , S. , Brettle , A. , Gilroy , D. , Knock , D. , Mitchelmore , R. , Pattison , S. , Smith , S. and Turner , J. ( 2018 ), “ Developing a generic tool to routinely measure the impact of health libraries ”, Health Information and Libraries Journal , Vol. 35 No. 3 , pp. 227 - 245 , doi: 10.1111/hir.12223 .
Booth , A. ( 2003 ), “ What is quality and how can we measure it? ”, Scottish Health Information Network, SHINE , Vol. 43 , pp. 2 - 6 , available at: https://www.academia.edu/2723791/What_is_quality_and_how_can_we_measure_it .
Brettle , A. , Maden , M. and Payne , C. ( 2016 ), “ The impact of clinical librarian services on patients and health care organisations ”, Health Information and Libraries Journal , Vol. 33 No. 2 , pp. 100 - 120 , available at: https://onlinelibrary.wiley.com/doi/full/10.1111/hir.12136 .
De la Mano , M. and Harrison , J. ( 2012 ), “ Quality evaluation of health libraries in England: a new framework ”, Performance Measurement and Metrics , Vol. 13 No. 3 , pp. 139 - 153 .
Divall , P. and James , C. ( 2019 ), “ The impact of the clinical librarians in the NHS: findings of a national study ”, paper presented at 10th International Evidence Based Library and Information Practice (EBLIP 10) Conference , Glasgow, Scotland , 17-19 June , abstract available at: https://eblip10.org/Home/tabid/7677/Default.aspx .
Earl , S. , Carden , F. and Smutylo , T. ( 2001 ), “ Outcome mapping: building learning and reflection into development programs ”, International Development Research Centre , available at: https://www.idrc.ca/sites/default/files/openebooks/959-3/index.html .
Edwards , C. and Ferguson , L. ( 2015 ), “ Knowledge for healthcare – quality and impact ”, CILIP Update , Vol. 2015 November , pp. 35 - 37 .
Edwards , C. and Gilroy , D. ( 2019 ), “ The development and implementation of quality improvement standards for NHS library and knowledge services ”, Paper Presented at 10th International Evidence Based Library and Information Practice (EBLIP 10) Conference , Glasgow, Scotland , 17-19 June , abstract available at: https://eblip10.org/Home/tabid/7677/Default.aspx .
Fricker , A. ( 2017 ), “ Building better metrics – drive better conversations ”, Paper Presented at International Congress of Medical Librarianship (ICML) and European Association for Health Information and Libraries (EAHIL) Conference , Dublin, Ireland , 12-16 June , abstract available at: https://eahil2017.net/wp-content/uploads/2017/06/Abstracts-ICML-EAHIL-2017.pdf .
Gann , L.B. and Pratt , G.F. ( 2013 ), “ Using library search service metrics to demonstrate library value and manage workload ”, Journal of the Medical Library Association , Vol. 101 No. 3 , pp. 227 - 229 .
Gilroy , D. and Turner , J. ( 2018 ), “ Showcasing the impact of health libraries in England ”, Paper Presented at European Association for Health Information and Libraries (EAHIL) Conference , Cardiff, Wales , 9 - 13 July , abstract available at: https://eahilcardiff2018.wordpress.com/programme-2/ .
Grey , H. , Sutton , G. and Treadway , V. ( 2012 ), “ Do quality improvement systems improve health library services? A systematic review ”, Health Information and Libraries Journal , Vol. 29 No. 3 , pp. 180 - 196 , doi: 10.1111/j.1471-1842.2012.00996.x .
Grieves , K. and Pritchard , O. ( 2018 ), “ Articulating value and impact through outcome-centered service delivery: the student and learning support experience at the University of Sunderland ”, Performance Measurement and Metrics , Vol. 19 No. 1 , pp. 2 - 11 .
Health Education England ( 2014 ), “ Knowledge for healthcare: a development framework ”, available at: https://www.hee.nhs.uk/sites/default/files/documents/Knowledge_for_healthcare_a_development_framework_2014.pdf .
Health Education England ( 2016a ), “ NHS library and knowledge services in England policy ”, available at: https://www.hee.nhs.uk/sites/default/files/documents/NHS%20Library%20and%20Knowledge%20Services%20in%20England%20Policy.pdf .
Health Education England ( 2016b ), “ Value and impact toolkit ”, available at: https://kfh.libraryservices.nhs.uk/value-and-impact-toolkit/ .
Health Education England ( 2016c ), “ Principles for metrics report and recommendations ”, available at: http://kfh.libraryservices.nhs.uk/wp-content/uploads/2016/04/Metrics-Principles-Report-Final-2016.pdf .
Health Education England ( 2017 ), “ The evaluation framework ”, available at: https://kfh.libraryservices.nhs.uk/ef-intro/ef-view/ .
Health Education England ( 2019a ), “ Quality and improvement outcomes framework for NHS funded library and knowledge services in England ”, available at: https://www.hee.nhs.uk/sites/default/files/documents/HEE%20Quality%20and%20Improvement%20Outcomes%20Framework.pdf .
Health Education England , ( 2019b ), “ Quality framework ”, available at: https://healtheducationengland.sharepoint.com/Comms/Digital/Shared%20Documents/Forms/AllItems.aspx?id=%2FComms%2FDigital%2FShared%20Documents%2Fhee%2Enhs%2Euk%20documents%2FWebsite%20files%2FQuality%2FHEE%20Quality%20Framework%2Epdf&parent=%2FComms%2FDigital%2FShared%20Documents%2Fhee%2Enhs%2Euk%20documents%2FWebsite%20files%2FQuality&p=true&originalPath=aHR0cHM6Ly9oZWFsdGhlZHVjYXRpb25lbmd sYW5kLnNoYXJlcG9pbnQuY29tLzpiOi9nL0NvbW1zL0RpZ2l0YWwvRVhtRW85eU1fdUpOc lY0NzE1c3VqS3dCelRVbV9OM1hvWnZ0SE15a19yTnBEZz9ydGltZT0wM2tadUJXdTEwZw .
Health Education England ( 2020 ), “ HEE LKS staff ratio policy ”, available at: https://www.hee.nhs.uk/sites/default/files/documents/HEE%20LKS%20Staff%20Ratio%20Policy%20January%202020.pdf .
Knock , D. , Smith , S. , Gilroy , D. , Turner , J. , Ayre , S. and Brettle , A. ( 2017 ), “ Health Education Englands' library and knowledge services value and impact toolkit: a collaborative approach to demonstrating the impact of libraries within Europe's largest health provider ”, Paper Presented at International Congress of Medical Librarianship (ICML) and European Association for Health Information and Libraries (EAHIL) Conference , Dublin, Ireland , 12-16 June , abstract available at: https://eahil2017.net/wp-content/uploads/2017/06/Abstracts-ICML-EAHIL-2017.pdf .
Lacey Bryant , S. , Bingham , H. , Carlyle , R. , Day , A. , Ferguson , L. and Stewart , D. ( 2018 ), “ International perspectives and initiatives ”, Health Information and Libraries Journal , Vol. 35 No. 1 , pp. 70 - 77 , available at: https://search.proquest.com/docview/2007356955?accountid=26452 .
Reid , P.H. ( 2019 ), “ How good is our public library service? The evolution of a new quality standards framework for Scottish public libraries 2012-2017 ”, Journal of Librarianship and Information Science , (online) 3rd July , doi: 10.1177/0961000619855430 .
Saracevic , T. and Kantor , P.B. ( 1997 ), “ Studying the value of library and information services. Part I. establishing a theoretical framework ”, Journal of the American Society for Information Science , Vol. 48 No. 6 , pp. 527 - 542 , doi: 10.1002/(ISSN)1097-4571 .
Scottish Library and Information Council ( 2017 ), “ How good is our public library? A public library improvement model for Scotland ”, available at: https://scottishlibraries.org/advice-guidance/frameworks/how-good-is-our-public-library-service/ .
Showers , B. ( 2015 ), “ Metrics: counting what really matters ”, CILIP Update , February , pp. 42 - 44 .
Streatfield , D. and Markless , S. ( 2009 ), “ What is impact assessment and why is it important? ”, Performance Measurement and Metrics , Vol. 10 No. 2 , pp. 134 - 141 , doi: 10.1108/14678040911005473 .
Thorpe , C. and Howlett , A. ( 2019 ), “ Developing certainty via a maturity model for evidence-based library and information practice in university libraries ”, 10th International Evidence Based Library and Information Practice (EBLIP 10) Conference , Glasgow, Scotland , 17-19 June , abstract available at: https://eblip10.org/Home/tabid/7677/Default.aspx .
Weightman , A. , Urquhart , C. , Spink , S. and Thomas , R. ( 2009 ), “ The value and impact of information provided through library services for patient care: developing guidance for best practice ”, Health Information and Library Journal , Vol. 26 No. 1 , pp. 63 - 71 , available at: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1471-1842.2008.00782.x .
Further reading
Brettle , A. and Maden , M. ( 2016 ), What Evidence is There to Support the Employment of Professionally Trained Library, Information and Knowledge Workers? A Systematic Scoping Review of the Evidence , London , CILIP , (online) available at: https://www.researchgate.net/publication/301626933_What_evidence_is_there_to_support_the_employment_of_trained_and_professionally_registered_library_information_and_knowledge_workers_A_systematic_scoping_review_of_the_evidence .
Acknowledgements
Members of QIG: Linda Ferguson, Alan Fricker, Jenny Turner, Mic Heaton, Prof Alison Brettle and all those who contributed to the QIG task and finish groups. Sharon Markless, for facilitating the development of the Evaluation Framework, https://kclpure.kcl.ac.uk/portal/sharon.markless.html , HEE colleagues that have supported the QIG developments: Dr Ruth Carlyle, Sue Robertson, Holly Case-Wyatt.
Corresponding author
Related articles, we’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here

elearning for healthcare
About the antimicrobial resistance and infections programme, amr toolkit, case studies, uti learning resources, further materials, further information, health education england project team, elearning team, antimicrobial stewardship for community pharmacy staff project team, antibiotic review kit – (ark), antimicrobial prescribing for common infections elearning session, how to access.

The Antimicrobial Resistance (AMR) and Infections programme has been designed to support health and care staff – both clinical and non-clinical – in a variety of settings to understand the threats posed by antimicrobial resistance, and the ways they can help to tackle this major health issue. This programme has been developed by Health Education England (HEE) in collaboration with Public Health England (PHE), NHS England and NHS Improvement, Care Quality Commission and National Institute for Health and Care Excellence.
Antibiotic (antimicrobial) resistance poses a major threat to everyday life and modern day medicine where lives could be lost as a result of antibiotics not working as they should. All health and care staff, as well as the public, have a very important role in preserving the power of antibiotics and in controlling and preventing the spread of infections. Amongst the approaches to reduce this threat includes adequate infection prevention and control practices, good antimicrobial stewardship and the use of diagnostics.
Visit HEE website for more information on our AMR work .
HEE has produced an AMR toolkit , making available credible and helpful resources relating to antimicrobial resistance, as well as learning about the management of infective states, infection prevention and control and antimicrobial stewardship.
Antimicrobial Prescribing for Urinary Tract Infections (UTIs)
The Antimicrobial Prescribing for Urinary Tract Infections (UTIs) elearning provides a quick overview on the key points to consider when prescribing antibiotics for UTIs, as outlined in the NICE guidance on managing common infections.
The session covers why the management of UTIs matter, what you need to know as a clinician, what you can do in your clinical practice and where can you find more information.
This bite-sized session is accompanied by an assessment and learners have the flexibility of assessing their knowledge before and/or after engaging with the session.
The AMR toolkit can support you in addressing any further learning needs you identify through completing this elearning.
Introduction to Antimicrobial Resistance
The Introduction to Antimicrobial Resistance session supports health and care staff, including non-clinical staff working for independent contractors within the NHS, as well as volunteers across health and care settings and service provision:
- discuss why there is such a concern about misuse of antibiotics and antimicrobial resistance.
- list the key risks for development of antimicrobial resistance.
- identify their role in tackling antimicrobial resistance.
It provides an overview for clinical and non-clinical staff. It will also be of benefit to all health and care staff, including those non-clinical staff working for independent contractors within the NHS, as well as volunteers across health and care settings and service provision.
ARK is an antimicrobial stewardship initiative that aims to safely reduce antibiotic use in hospitals by helping staff stop unnecessary antibiotic treatments. This protects patients from drug side-effects like Clostridium difficile and antibiotic resistant infections.
This elearning was developed in partnership with British Society of Antimicrobial Chemotherapy (BSAC) and covers the rationale for the Antibiotic Review Kit, presents the ARK Decision Aid and also includes some brief scenarios, with reflection questions to consolidate learning.
Antimicrobial Stewardship for Community Pharmacy staff
How Community Pharmacies Can Keep Antibiotics Working
This free elearning session addresses the impact of antimicrobial resistance and the hugely important role community pharmacy staff can play in it.
This elearning will help community pharmacy staff:
- understand the connection between antibiotic use and antibiotic resistance
- identify their role in optimising antibiotic use in the general population who visit their pharmacy
- use the Antibiotic Checklist to personalise patient advice when dispensing antibiotics
- improve their self-care/safety-netting advice using the Treat Antibiotics Responsibly, Guidance, Education, Tools (TARGET) Treating Your Infection leaflets
- be aware of the global impact of antibiotic resistance
This has been developed by Public Health England in partnership with British Society of Antimicrobial Chemotherapy (BSAC), Royal Pharmaceutical Society, University of Leeds, University of Nottingham. Graphic design provided by The Letter G.
Antimicrobial Stewardship for Pharmacy Staff – c ase study
The Royal Pharmaceutical Society supported key pharmacists within NHS Trusts and Sustainability and Transformation Partnerships (STPs) to develop the skills and behaviours to become effective antimicrobial clinicians, leaders and mentors via a pilot training programme in London and the south east of England.
You can view the individual case studies from the training here .
Action on AMR – case study
Action on AMR focussed on equipping teams with QI skills to deliver their improvement work and share successful initiatives, rather than demonstrating a significant reduction in Gram-negative bloodstream infections (GNBSI) rates in the region. It is hoped that infection rates will be reduced in future as the teams progress their improvement work using the skills and knowledge gained.
Antimicrobial Stewardship (AMS) change – case study
The University of Manchester – AMS change project developed a cohort of “AMS CHANGErs”: experts in behaviour change related to AMS, with the capability, opportunity and motivation to drive change in health professional practices related to AMS.
The following report – AMS Change: Practical training to apply behavioural science to antimicrobial stewardship , outlines the development and training that has been created. It can support the development of AMS Change projects in local areas.
AMR Public Awareness
This short animation is aimed at the public and has been produced in partnership with PHE, intended to be used by health and social care staff in a variety of settings with the aim of helping prescribers respond appropriately to patients requesting antibiotics without medical need. The creation of the animation was influenced by the work of the Wellcome Trust in understanding how the public responds to information about antimicrobial resistance.
AMR GP and Primary Care Awareness
Also developed is an introductory film entitled a guide for GPs on antimicrobial resistance aimed at GPs and primary care staff to provide an introduction into the risks associated with the over-use of antibiotics, and to encourage appropriate dispersion of the animation above. It supports a range of educational materials for GPs and other primary care prescribers called the TARGET toolkit .
Urinary Tract Infection Management in the Elderly
Surveillance shows that previous urinary tract (bladder) infections, urinary catheterisation, hospitalisation, being prescribed antibiotics in the previous month and old age are key risk factors for these infections in the out of hospital setting. This short film aims to support health and care workers looking after older adults with suspected urinary tract infections (UTIs) and introduces resources that can be used to diagnose, manage and prevent UTIs in the out of hospital setting. In particular Public Health England’s (PHE) diagnostic flowchart and a patient leaflet to facilitate the management of suspected UTIs in the older frail population. ‘To Dip Or Not To Dip’ has a network of health and social care professionals who are improving the management of UTI in older people in care settings throughout the UK. To join this community email [email protected]
Blood Culture Pathway Awareness
We collaborated with NHS England and NHS Improvement to produce 2 animated videos to improve antimicrobial stewardship by raising awareness and promoting an optimal blood culture pathway as set out by Public Health England.
The first animation is a general overview , designed to raise awareness of the issues and will explain the background of AMR, the importance of an optimal blood culture pathway in AMS, and some of the factors to consider in the pre-analytical, analytical and post-analytical phases.
The second animation is a step-by-step guide of good practice in taking a blood culture sample in the pre-analytical phase.
Improving the blood culture pathway
Blood culture pathway: Taking a blood culture
Primary Care Antibiotic Prescribing
This film is aimed at health and care staff who recommend, prescribe, dispense and supply antibiotics in primary care. It highlights processes, considerations and actions that should occur to support safe and effective antibiotic prescribing and signposts to further available resources. The film is based on the TARGET Toolkit and NICE Guidance on ‘Managing common infections and antimicrobial stewardship’.
This will help health and care staff to:
- understand the connection between antibiotic use and antibiotic resistance.
- identify their role in optimising antibiotic use and stewardship.
- ensure compliance with national guidance when recommending, prescribing, dispensing and administering antibiotics.
- improve their self-care/safety-netting advice to patients on the appropriate use of antibiotics.
Secondary Care Antibiotic Prescribing
This film is aimed at health and care staff who recommend, prescribe, dispense and supply antibiotics in secondary care. It highlights processes, considerations and actions that should occur to support safe and effective antibiotic prescribing and signposts to further available resources. The film is based on Public Health England’s ‘ Start Smart – Then Focus: Antimicrobial Stewardship Toolkit ’ and NICE Guidance on antimicrobial stewardship.
Educational resources for health and care workers
For care workers
- Urinary tract infections (UTIs)’ A leaflet for older adults and carers [ Word ; PDF and User Guide ] and leaflet for those under 65 years ‘Treating your infection – URINARY TRACT INFECTION’ [ Word ; PDF and Fully Referenced ].
- To Dip or Not to Dip? Training handbook ; elearning ; animation ; poster and leaflet .
- Oxford AHSN: Good hydration and urine infections (Part 1 , 2 , 3 , 4 , 5 & 6 ).
- Infection Control In Care Homes films.
- eLearning for Healthcare (elfh) Continence and Catheter Care ; Promoting Best Practice in Catheter Care and Management of Incontinence and Urinary Catheters .
For health workers
- Managing UTI eModule explains the importance and appropriateness of diagnostics and offers advice on how to assess and treat patients with a range of urinary symptoms.
- Webinar on UTIs highlights simple key actions to help improve your antibiotic prescribing while improving the patient experience and their self-care, therefore freeing up your time.
- Antibiotic presentation core slides lasts 60 minutes and includes a clinical scenario on UTIs, slide notes and references.
- PHE quick reference tools for diagnosis of UTIs including knowing when to use the microbiology laboratory and how to understand results.
- To Dip or Not to Dip? Presentation for GPs.
- NHSI Preventing Healthcare Associated Gram-Negative Bacterial Bloodstream Infections toolkit
- NICE: Urinary tract infection products
- HEE: Antimicrobial resistance – A training resources guide
Practical resources for health and care workers to share with patients and carers
- ‘Urinary tract infections (UTIs)’ A leaflet for older adults and carers [ Word ; PDF and User Guide ]
- Preventing Urinary Tract Infections Poster
- To Dip or Not to Dip? Leaflet [1] https://www.gov.uk/government/publications/government-response-the-review-on-antimicrobial-resistance [2] http://www.pulsetoday.co.uk/clinical/clinical-specialties/infectious-diseases/what-the-new-uti-guidance-means-for-gps/20036770.article
- TARGET leaflet ‘Treating your infection – URINARY TRACT INFECTION’ for those under 65 years [ Word ; PDF and Fully Referenced ].
TARGET (Treat Antibiotics Responsibly, Guidance, Education, Tools) helps influence prescribers’ and patients’ personal attitudes, social norms and perceived barriers to optimal antibiotic prescribing. It includes a range of resources that can each be used to support prescribers’ and patients’ responsible antibiotic use, helping to fulfil CPD and revalidation requirements. Free resources include:
- leaflets to share with patients (translated into more than 20 languages)
- resources for clinical and waiting areas
- audit toolkits, self-assessment and action planning
- training resources
Keep Antibiotics Working
Public Health England (PHE) first launched ‘ Keep Antibiotics Working ‘ national campaign in October 2017 across England. This was to support the government’s efforts to reduce inappropriate prescriptions for antibiotics by raising awareness of the issue of antimicrobial resistance and reducing demand from the public. The campaign’s key aims are:
- alert and inform the public to the issue of antimicrobial resistance (AMR) in a way that they understand, in a manner which they understand, and increase recognition of personal risk of inappropriate usage
- reduce public expectation for antibiotics by increasing understanding amongst patients about why they might not be given antibiotics, so reducing demand
- support healthcare professional (HCP) change by boosting support for alternatives to prescription
The messaging for the national campaign aims to move patients to a better understanding that taking antibiotics when you don’t need them means they are less likely to work for you in the future and to trust their doctors’ advice regarding the best appropriate treatment for them.
A free health education resource, e-Bug , is also available for health and care staff to reduce antibiotic resistance by helping children and young people understand infections and antibiotic use. It is a valuable resource, not only because it is free to access, but it’s also available in 27 languages, being used in 221 countries worldwide.
Antibiotic Guardian
Antibiotic Guardian , a campaign led by PHE, urges members of the public and healthcare professionals to take action in helping to slow antibiotic resistance and ensure our antibiotics work now and in the future. To become an Antibiotic Guardian, people choose 1 pledge about how they can personally prevent infections and make better use of antibiotics and help protect these vital medicines.
FutureLearn
Clinical staff who have an active interest and prior experience in the prevention, diagnosis and management of infectious disease should consider accessing the free, interactive 6 week online course on Antimicrobial Stewardship by the British Society for Antimicrobial Chemotherapy, University of Dundee and FutureLearn. For more information, please visit FutureLearn .
For more information on HEE’s work on antimicrobial resistance, please visit our website .

Antonio De Gregorio

Mohamed Sadak

Janet Flint

Dr Sanjiv Ahluwalia

Vanessa Petroni-Caesar

Diane Ashiru Oredope

Jon Collins

Tracy Watkins

Rashmi Chavda

Alex Drinkall

Louise Garrahan

Cliodna McNulty

Rosie Allison
Diane ashiru-oredope.

Philip Howard

Tracey Thornley

Sara Chapman

Dr Martin Llewelyn

Annie Joseph

Professor Jo Hart

Dr Lucie Byrne-Davis

Dr Tessa Lewis

Dr Donna Lecky
Available to all.
The Antimicrobial Resistance and Infections programme is freely available to access here . Please note your progress and completion of sessions will not be recorded and you will not be able to generate a record of completion. If you require evidence of learning, please register and then log in to access this programme on the elfh Hub.
If you already have an account with elfh, then you can enrol on to the Antimicrobial Resistance and Infections programme by logging in to the elfh Hub, selecting My Account > Enrolment and selecting the programme. You can then access the programme immediately in the My elearning section.
In order to access the Antimicrobial Resistance and Infections programme, you will need an elfh account. If you do not have one, then you can register by selecting the Register button below.
Register >
To view the Antimicrobial Resistance and Infections programme, select the View button below. If you already have an account with elfh, you will also be able to login and enrol on the programme from the View button.
NHS healthcare staff in England
The Antimicrobial Resistance and Infections programme is also available to NHS healthcare staff via the Electronic Staff Record (ESR). Accessing this elearning via ESR means that your completions will transfer with you throughout your NHS career.
Further details are available here .
Not an NHS organisation?
If you are not an NHS health or care organisation and therefore do not qualify for free access elfh Hub, you may be able to access the service by creating an OpenAthens account.
To check whether or not you qualify for free access via OpenAthens, you can view the eligibility criteria and register on the ‘ OpenAthens ’ portal.
Registering large numbers of users
If you are a HR, IT or Practice Manager and would like to register and enrol large numbers of staff within your organisation for access onto the Antimicrobial Resistance and Infections programme, please contact elfh directly.
Organisations wishing to use their own LMS
For HR departments wanting to know more about gaining access to courses using an existing Learning Management System please contact elfh directly to express interest.
Access for care home or hospice staff
To register for the Antimicrobial Resistance and Infections programme, select the ‘Register’ button above. Select the option ‘I am a care home or hospice worker’ then enter your care home / hospice name or postcode and select it from the options available in the drop down list. Finally enter your care home / hospice registration code and select ‘Register’. You may need to see your employer to get this code.
If your employer does not have a code, then they need to contact the elfh Support Team . The Support Team can either give the employer the Registration Code or arrange a bulk upload of all staff.
Access for social care professionals
Access to elfh content is available to all social care professionals in England whose employers are registered with the Skills for Care National Minimum Data Set for Social Care (NMDS-SC). Every employer providing NMDS-SC workforce information to Skills for Care has been given a user registration code for their staff. This code enables you to self-register for access to the Antimicrobial Resistance and Infections programme. Please contact your employer for more details about the registration code. For information about registering your organisation with the NMDS-SC your employer should access www.nmds-sc-online.org.uk or contact the Skills for Care Support Service on 0845 8730129. If you have a registration code select the ‘register’ button above.
More information
Please select the following link for more information on how to use the elfh Hub .
Advertisement

- Facebook Messenger
- Our Services
- Case Studies
- Get in Touch
User research about national library services for Health Education England
- User research
We were asked by Health Education England (HEE) to conduct a programme of research with users of NHS library and knowledge services.
Health Education England were considering options to provide new national services to support or replace the multitude of local tools, platforms and methods used by NHS staff to find and use evidence and information.
HEE had already led work to develop some ideas about possible improvements to national library services. But they had done this work from the perspective of NHS librarians, so they rightly wanted to better understand user behaviours and needs before proceeding.
We ran a programme of user research to understand how NHS staff access and use information, and to identify needs for a prospective national information service.
We conducted 26 one-to-one interviews with NHS staff from a diverse set of roles, ran a workshop with 5 end user role representatives to generate proto-personas and user journey scenarios, analysed 454 responses to our user needs survey, and conducted 2 field visits to observe users in their own context.
A particular challenge during this research was the breadth of end user roles amongst the 1.3 million NHS workforce. To address this, we worked with the HEE team to prioritise key user roles and to ensure that each role was represented in our research. These user roles included tutors, preceptors and mentors, practicing clinicians, staff in training, non-clinical staff and clinical researchers.
We presented our work (which included 38 validated and prioritised user needs) to Health Education England stakeholders, and our findings were used to inform their case to invest in national library and knowledge platforms.
Related Case Studies
Gathering evidence to inform wellcome connecting science's training programme strategy.
Wellcome Connecting Science (WCS) funds, develops anddelivers courses, conferences and other events across theworld. By engaging with WCS learning…
A critique of the leaver survey approach for HIT Training
HIT Training Ltd (HIT) is the leading specialist training and apprenticeship provider for the UK’s hospitality, catering and retail…
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Case studies: Perinatal Pelvic Health Services
Annex 1: Collected Case Studies from Early Implementer and Fast Follower Systems
The following case studies support the Implementation guidance: Perinatal Pelvic Health Services .

Case study 1: South East London – Engagement with diverse groups
South East London PPHS engaged with diverse groups in the local community to increase awareness of pelvic health conditions and offer women knowledge, skills and confidence to manage their pelvic health in the perinatal period.
Joint Strategic Needs Assessments (JSNAs) were reviewed for each borough in the LMNS to identify the make-up of the overall population and the female population by ethnicity and languages spoken. 22 key local groups were identified.
The Lead Pelvic Health Physio and Project Manager ran virtual coffee mornings via Zoom. Open questions were used to understand the groups’ experiences of pelvic floor care. Women that attended were also taught how and when to refer, and how to self-manage their condition. Sessions with the local Latin-American community were run in Spanish and information leaflets were also shared in Spanish. Findings from these outreach sessions included:
- Some women did not know there were services that offer help
- Some women thought it was normal to be incontinent after childbirth or were embarrassed about their symptoms.
- Many of the women did not know the differences between the roles of healthcare professionals in the UK for example, Midwives versus Health Visitors
- Women did not know that pelvic health physiotherapists can provide care and treatment for pelvic floor issues.
- Women also expressed a desire to have more sessions to discuss other health care topics and like the idea of having consultations in their own communities.
From these community outreach sessions, the team found that building networks in local communities takes time and healthcare professionals need to be prepared to travel to places where communities meet. Collaborating with other groups, even if not within the same geographical footprint, can be useful. It also helps to have health professionals from the same background as the community running the session and, if not, the use of interpreters is vital.
Case study 3: Norfolk and Waveney – Antenatal and postnatal information
Norfolk and Waveney identified inconsistencies in the antenatal and postnatal information provided to women across their three Trusts. The PPHS now ensures that all women using maternity services are signposted to standardised information.
An initial scoping meeting and service user survey was carried out with the local MNVP to guide content. Service users asked for video content and interactive online sessions, as well as a mobile app. Feedback also indicated that patient choice was important, as well as separating antenatal and postnatal information so that women can easily access suitable information at different time points.
A website was developed for pelvic health education and information , as well as the single point of access. The webpages include videos, resources, functionality to book onto monthly pelvic health webinars, and advice on how to self-refer to pelvic health physiotherapy.
A suite of communications resources were also developed, including: postcards signposting how to book appointments; paper leaflets containing pelvic health information; posters and banners for spaces pregnant women visit, such as continuity of carer hubs; and social media templates. Clinical stakeholder meetings and service user focus groups were held prior to launch to gather feedback on the materials.
A free mobile application is also offered to all pregnant women following the dating scan to support them with pelvic floor exercises. The clinical team run antenatal and postnatal pelvic health sessions to help women adhere to pelvic floor exercises, as well as to provide general pelvic health advice. These sessions are held at various community locations including continuity of carer hubs, libraries, and family hubs.
Case study 4: Herefordshire and Worcestershire – Public health campaign
Herefordshire and Worcestershire co-produced a public health campaign and online platform to raise awareness of pelvic floor dysfunction and provide information on how to do pelvic floor exercises.
The campaign was co-produced with the MNVP and focus groups were held to understand what content needed to be included. A website ( www.squeezelifthold.co.uk ) was developed, which includes information on the pelvic floor, a workout programme, and a monthly blog. Content is added regularly to ensure that it is up to date with evidence-based information. It also includes a tool to translate the content into different languages. Newsletters, social media, and paid advertising have been successfully used to increase traffic to the website.
Case study 5: Norfolk and Waveney – Self-assessment facilitating self-referral
Perinatal pelvic health self-referral varied across the Norfolk and Waveney LMNS, with only one of the three providers offering self-referral prior to the PPHS.
To plan for the implementation of self-referral and a single point of access across the System, meetings were held with the MNVP, clinical stakeholders, allied health professionals, contracts and commissioning, and the local Just One Norfolk platform led by Children and Young people services.
The LMNS procured the ePAQ-Pelvic Floor Patient Reported Outcome Measure. Women are invited to complete the self-assessment questionnaire antenatally following the dating scan and again four to six months after giving birth. Women receive instant access to their own pelvic floor questionnaire report, and the results are also stored in their maternity records and postnatally on acute Trust health records, and copied to the GP if problems are identified. The results are triaged by a pelvic health physiotherapist who then places women on the following pathways:
- No concerns: Signpost to self-management information on the website and invite to monthly advice sessions
- Mild symptoms: One-to-one advice session with a therapy assistant practitioner and guided use of a mobile application
- Symptoms of pelvic floor dysfunction: Referral to a specialist physiotherapist or, where required, consultant care.
An LMNS-wide standard operating pathway for ePAQ-Pelvic Floor was put in place and is regularly reviewed and updated. ePAQ-Pelvic Floor is also being written into Trust Guidelines (e.g. for bladder care). Clinical review meetings of ePAQ-pelvic floor are held regularly at each Trust.
Since implementing ePAQ, Norfolk and Waveney are seeing an improved rate of identification of sensitive issues such as anal incontinence and referrals are being made earlier in pregnancy, which is enabling more time to treat antenatally. Physiotherapists are asked to complete an evaluation to identify whether referrals via the triage system are appropriate, and so far none have been inappropriate.
Case study 6: South East London – PFE education classes
Standardised face-to-face and virtual antenatal pelvic floor education classes have been implemented across South East London, to offer women support to build the knowledge, skills, and confidence required to manage their own pelvic health in the perinatal period.
An online survey was conducted to understand what content would be useful to service users, and morning coffee sessions were held with community groups. Before launch, maternity staff were invited to attend a drop-in session and information about the classes and other interventions are also shared with midwives on their mandatory pelvic health training.
Women with risk factors for pelvic floor dysfunction (in line with NICE clinical guidelines) are advised to attend the classes and women who do not have symptoms are welcome to attend if they would like to. GPs and Health Visitors are also aware of this service and can advise patients to attend.
The classes last one and a half hours and are delivered online by a pelvic health midwife and/or pelvic health physiotherapist. A minimum of 12 classes a month are available, with one class a week per maternity provider. Some classes are held in the evening. Women book onto classes online and those who attend are sent post-class resources, including links to pelvic health videos and an evaluation survey.
Posters for the classes are available on information boards across providers and there are virtual links to the posters on local perinatal apps. Classes are further publicised via social media and relevant local organisations. Evaluation results have been positive overall, with 85.7% of attendees feeling confident about their knowledge of pelvic floor symptoms and how to find advice and support in their maternity unit and 100% feeling confident on what to do to prevent pelvic floor issues. Further, 89% of participants felt more confident about how to do PFE and 96.4 % reporting that the class has motivated them to practice PFE regularly during pregnancy.
Case study 7: Frimley – Risk assessment tool
Prior to the development of a PPHS in Frimley, few women were referred to pelvic health physiotherapy services perinatally. The PPHS therefore wanted to improve identification of both those with symptoms, but also those that are at risk of developing issues.
The team therefore created a pelvic floor risk assessment tool that enables the pathway to be individualised according to a woman’s risk. The tool also helps to prompt discussion, sharing of information and signposting for all women.
The tool was developed based on a review of evidence for pregnancy and birth related risk factors for pelvic floor dysfunction. Items for inclusion in the tool were discussed and agreed with the steering group, community matrons and midwifery team leads, with sign off via local governance groups.
The tool was initially trialled with one midwifery team and then implementation was phased across providers, with support provided by PPHS leads, including training sessions, resources, and guidance.
The tool is conducted at booking and at 10 days postnatally. A short version is also completed at 28 weeks if a woman begins to experience symptoms. Results are recorded in the new maternity electronic patient record and women receive support accordingly:
- Low risk of pelvic floor dysfunction: directed to resources on the pelvic health website.
- Medium/high risk of pelvic floor dysfunction: offered a group pelvic health workshop led by a Pelvic Health Physiotherapy Associate Practitioner (band 4). Virtual workshops are offered for those who cannot attend in person. Women who do not speak English have the option to view a recording with a family member or to attend an online meeting with a translation function, with advice to direct questions to their midwife at their next appointment where a translator is present.
- Symptoms of pelvic floor dysfunction: one-to-one physiotherapy according to the agreed pathway.
As the assessment takes place at booking, and some women will subsequently experience a miscarriage, a ‘non-pregnancy’ virtual pelvic floor class is also offered for women who have had a miscarriage. Use of the tool has raised awareness of pelvic health among midwives and encouraged better collaboration between physiotherapy and maternity departments. Referral numbers to pelvic health physiotherapy services for pelvic floor dysfunction antenatally and within a year of birth have increased significantly since its introduction.
Case study 8: Birmingham and Solihull – Implementation of the OASI Care Bundle
Birmingham and Solihull have two maternity providers, but the OASI Care Bundle had only been implemented in one prior to the PPHS. To ensure equity across the System footprint, the PPHS worked with the other maternity provider to implement the Care Bundle.
Initially, staff were surveyed on their knowledge and understanding of perineal protection techniques. The perineal specialist midwife also had conversations with staff on perineal protection, which helped them understand staff views and enthusiasm for perineal protection.
The following activities were carried out to support implementation of the OASI Care Bundle:
- An interactive e-learning package on ‘Perineal Protection and Repair’ was created, with videos demonstrating perineal repair and protection techniques.
- Perineal protection displays were put up on the labour ward.
- Electronic notes were updated to include OASI Care Bundle documentation, including an antenatal discussions leaflet.
- OASI Care Bundle education was incorporated into community midwifery pelvic health training sessions.
- The PPHS perineal specialist midwife spent a day on the labour ward each week for staff to drop-in and practice techniques or discuss perineal protection.
- A ‘Spotlight on’ video training series was developed, with each video providing information on a different aspect of perineal protection.
- Facebook posts with information and evidence for perineal protection techniques are regularly shared.
Since implementation of the OASI Care bundle there has been an increase in the use of warm compress in vaginal births from 9% to 50%.
Case study 9: Lancashire and South Cumbria – Implementation of the OASI Care Bundle
Lancashire and South Cumbria wanted to ensure the OASI Care Bundle was implemented across the System to reduce the risk of third- and fourth-degree tears and improve outcomes for pelvic health.
Implementation teams were formed and collaboration was established with the maternity education team. The education team also worked closely with university training providers to support student midwives with OASI training. Throughout implementation, focus groups were held with local MNVPs about plans and the resources.
All relevant staff were emailed the OASI care bundle manual and there was an OASI Care Bundle ‘learning bus’ to raise awareness pre-launch. Throughout the launch month regular ‘on-the-job’ training sessions were held and OASI badges were given to staff after they had attended training to increase visibility. A train the trainer model was applied, so initially all band 7 midwife coordinators and consultant/mid-grade doctors were trained. In response to feedback that some staff, particularly those working in the community, lacked confidence performing episiotomy and suturing, a multi-disciplinary ‘OASI Care bundle and suturing workshop’ was also developed. The workshops were successful and have therefore been opened to all midwifery staff. A refresher training package facilitated by the maternity education team has been built into maternity mandatory training days and at each departmental induction.
Case study 10: South East London – Education and training for health care professionals
South East London PPHS undertook a gap analysis across all providers in the LMNS to assess what education was currently available for health professionals on pelvic health care. The analysis found wide variation in the type of training available, the frequency and regularity of training opportunities, who attended and whether training was mandatory. It was subsequently agreed across all providers that a standard package of mandatory Pelvic Health Training needed to be developed for the whole LMNS.
An Education and Learning programme was developed by the PPHS delivery group, which included an obstetrician, urogynaecologist, MNVP chairs, pelvic health physiotherapist, consultant midwife, project manager, and a consultant nurse in urogynaecology.
The group oversaw the development of a mandatory training session for maternity staff and a separate session for Doctors, GPs and Health Visitors. The sessions include the key themes identified from a service user survey, as well as information from services users with lived experience. The content of the training session was peer reviewed by a psychologist who is leading the local Maternal Mental Health Service pilot to ensure that emotional and psychological elements are included.
Mandatory training has now been rolled out across all three maternity providers. The objectives of this mandatory training are for staff to:
- Understand the anatomy and function of the pelvic floor musculature,
- Identify pelvic floor dysfunction and know when to refer to the PPHS,
- Understand the NICE recommendations for the prevention and management of pelvic floor problems,
- Understand the impact of pelvic floor dysfunction in women,
- Teach a basic pelvic floor exercise programme, and
- Provide pelvic health care.
The sessions are 45 minutes to an hour and delivered by a Pelvic Health Midwife or Pelvic Health Physiotherapist twice a month at each of the providers. Where possible, the training is multi-professional. Ad-hoc sessions with Obstetrics and Gynaecology trainees and maternity support workers are also delivered, with a recommendation for them to also complete the pelvic health e-learning module developed by Health Education England (HEE) . GP sessions have been organised via GP training Hubs and Health Visitor sessions have been organised with specialist Health Visitor practice educators across all boroughs. These sessions are delivered by the PPHS project manager and the pelvic health physiotherapy lead.
Case study 11: Frimley – Pelvic health champions
Frimley LMNS implemented a new initiative to identify perinatal patients with pelvic floor dysfunction within the wider community workforce. They provided education awareness sessions for GP’s, Midwives, Mental Health Teams and Health Visitors to increase pelvic health education within the area and awareness of how the PPHS was changing access to perinatal physiotherapy care.
Engagement with GPs was focused on sharing the care pathway and referral system for perinatal mothers to ensure they are referred into the service. Mental Health teams and Health Visitors were offered training on pelvic floor dysfunction, including on identification of symptoms and how to access and refer to the PPHS.
The development of Pelvic Health Champions, who are specifically trained to use the local risk assessment tool and support women with perinatal pelvic floor problems, began within community midwifery teams. This joint working between physiotherapists and midwives in practice has strengthened interprofessional relationships. A pilot team started the initiative which enabled learning on how the process could be successfully embedded across more teams. The service has observed an increase in appropriate perinatal referrals, but not in the significant numbers they were expecting. Empowering other staff to support women has improved awareness of how to access care within a changing system.
Case study 12: Birmingham and Solihull – Staff training
Birmingham and Solihull identified that workforce training in prevention, early recognition and treatment for pelvic health was needed for all health care providers who have contact with women during the perinatal period to ‘Make Every Contact Count’.
A workforce survey was carried out which established several key themes, including that there are a variety of barriers to delivering pelvic health information, which include: time restraints, lack of confidence in the subject, lack of awareness of treatment options, and having other priorities. Many professionals surveyed also did not feel confident in optimising bowel health or best bladder care during labour, birth, and the immediate postnatal period.
It was agreed that the aims of the training should be:
- Prevention, early recognition, and treatment of pelvic health dysfunction in the perinatal period.
- To elicit knowledge about PPHS, new pathways, what resources are available currently and what is being developed.
- Engagement, input, and feedback on the development of the PPHS.
The clinical project team created a multi-disciplinary training package open to all healthcare professionals in contact with women in the perinatal period. It is a two-hour in person or online training which includes practical elements and group discussion and is led by a pelvic health physiotherapist and a specialist perineal trauma midwife. The training is provided in a variety of locations across the System and evaluations are collected to facilitate ongoing improvement.
The training covers: early recognition, prevention, and treatment of pelvic floor dysfunction; PFE; perineal protection and the OASI Care Bundle; the PPHS pathway; and key resources and how to access them. An e-learning on suturing has also been developed by a specialist perineal protection midwife. [Continues on next page]
As part of the training strategy, the PPHS also run a session for undergraduate physiotherapy students at a local university, which they are expanding to medics and nurses, master’s students, and other local universities. The training has been well received and supported, with 100% of attendees reporting that they are somewhat or extremely confident discussing how to do PFE with women; 95% are confident discussing perineal protection methods; and 95% are confident in directing women to resources.
Case study 13: Bristol, North Somerset and South Gloucestershire – Midwifery training
Bristol, North Somerset and South Gloucestershire wanted to ensure pelvic health was embedded into routine midwifery care to help break cultural stigmas and beliefs, with a focus on empowerment and prevention of pelvic floor dysfunction, as well as good physiotherapy care. The PPHS project is led clinically by physiotherapists but with a midwifery project manager. It was recognised that many midwives’ knowledge of pelvic health was low, and this needed to be addressed.
The PPHS carried out midwifery and service user surveys and focus groups to understand:
- What pelvic health knowledge and support service users wanted and in what format and who they wanted it from; and
- What knowledge midwives didn’t have and what their training needs were.
Findings from the surveys were used to develop midwifery training and resources. It was agreed that it was important to enable and empower midwives to have regular pelvic health discussions with service users and to have the knowledge to give correct first line advice, while not overburdening them.
The midwifery outreach and training programme involves:
- Face-to-face physiotherapy-led midwifery training is provided at both providers. This is a mandatory, bi-annual 30-minute session.
- Midwives were involved in the development of local screening tools. Midwives complete screening with all service users at booking and at 28 weeks in pregnancy.
- Local maternity antenatal care guidelines have been updated to include PPHS screening and discussion.
- Relevant pelvic health requirements have been integrated into the maternity electronic patient record.
- Sessions have been held with community midwives to update, involve, and inform them of PPHS project developments.
- Physiotherapy drop-in sessions on postnatal wards are helping to create multidisciplinary working across midwifery and physiotherapy departments.
Case study 14: North West London – Fully integrated multidisciplinary clinic
Hillingdon Hospital is one of four Trusts that are part of North West London PPHS. One of the elements of the PPHS has been the development of a ‘one-stop’ appointment for mothers with obstetric anal sphincter injuries (OASI).
It was identified that asymptomatic women who had sustained an OASI were not being referred for physiotherapy and therefore not taught PFE. Those with symptoms were referred to the physiotherapy team, however some of the physiotherapists were not fully competent assessing women anorectally and therefore were not assessing the sphincter during appointments.
Hillingdon have therefore set up a weekly interprofessional perinatal outpatient clinic run by a collaborative team made up of a Pelvic Health Physiotherapist and specialist midwife, who are supported by a consultant and registrar. When attending their postnatal consultant appointment, women can jointly see a physiotherapist and consultant on the same day, with a midwife also present to address any other concerns (e.g. lactation or wound care advice).
Collaboration between the specialists within the clinic ensures their knowledge and skills are shared inter-professionally, aligning their skills to the needs of the patient. They provide perinatal assessment and treatments within the clinic tailored to the patient’s needs. As an example, assessments such as detailed pelvic floor muscle assessment is taught to doctors and midwives via the physiotherapist, while the midwife and doctors train the physiotherapist in catheterisation and wound care. This learning environment creates a trusting, open atmosphere for the professionals to manage the most complex cases of wound care and pelvic floor dysfunction following birth.
“our PPHS has provided a really safe space to do follow-up for wounds and develop extended scope specialist skills in a safe, collaborative environment”
As all members are aware of each other’s skills, women in the area are now receiving more timely access to urgent postnatal care by experts.
Evaluations indicate that the service provides patient and staff satisfaction, and the staff feel they can provide the care needed to women in the local area. The team also regularly meet to discuss what went well and not so well and to continuously improve the service.
“This clinic now has become so much more…right there in one appointment we are able to offer a holistic approach to a woman’s body, mental health support, and support her journey through motherhood”
Case study 15: Frimley – Single point of access
Frimley has one acute Trust, with two sites providing maternity care and 9,000 births a year. Prior to the PPHS they had a very low number of referrals to pelvic health physiotherapy services for pelvic floor dysfunction in antenatal or postnatal period.
To improve the consistency of service provision and ensure compliance with NICE guidance, a new pathway was created for referral to the PPHS. Alongside this, a new telephone triage service for antenatal and postnatal women was launched and included referral to PPHS.
Engagement activities were carried out, including a staff focus group, service user focus group and a survey. These activities revealed variation in where GPs referred women with pelvic floor dysfunction following birth.
The aims, criteria, and pathways were designed with input from Gynaecology, Urogynaecology, PPHS physiotherapy leads and then approved via local clinical governance. This process initiated wider discussions regarding the adult female incontinence pathway.
A landing page, pathway and referral form for the PPHS was developed, with relevant referrals seen by physiotherapists and referred on to Urogynaecology Nurse Specialists or Consultants if required. The launch of this pathway was communicated by the GP communications team and a webinar event was held.
Case study 16: Dorset – Self-referral
Dorset has three Trusts, two maternity units and 7,500 births per year. One site has provided self-referral to antenatal and postnatal women since 2013 and has confidence in this process. The ambition of the PPHS is to move self-referral to a digital format and expand it to women at all three Trusts to:
- Ensure equity across the PPHS footprint;
- Facilitate timely referral;
- Improve the accuracy of triage through improved referral information;
- Offer service users a choice of location to receive physiotherapy treatment;
- Reduce the workload of Midwives and GPs; and
- Reduce urgent phone calls to physiotherapy.
The existing referral form has had nine years of use and staff using it felt confident in the uptake, demand, and opportunities to triage from the data received. Prior to roll-out to the other areas, the screening questions were reviewed by local pelvic health physiotherapists, midwives and the local MNVP.
Pathways were developed for urgent and routine cases, with possible appointments either as one-to-one or group sessions and either virtual or face-to-face. Physiotherapists also reviewed the format of the received self-referral to ensure it facilitates triage appropriately and enables a ‘RAG’ rating for urgency.
The self-referral form was made available on an LMNS webpage. As this took some time, in the interim digital midwife leads constructed a bespoke form on the maternity electronic patient record for urgent cases. Referrals arrive at an email inbox where an administrator logs them into a department and episode. Triage is always undertaken by a specialist pelvic health physiotherapist. The administrator then assigns them to an appointment or group depending on the outcome of the triage and sends an appointment letter. The administrator also answers phone calls relating to questions or changes to appointments.
Case study 17: South East London – Collaboration with the MMHS
South East London is ethnically and socially diverse with areas with high levels of deprivation. The LMNS was an Early Implementer PPHS and a Fast Follower Maternal Mental Health Service and the leads for these services identified several common themes between their services, including: the need to understand the local population and gaps in care, coproduction and reducing health inequalities, trauma in the context of maternity, and a focus on prevention as well as access to treatment.
Given these connections, the leads agreed that it would be useful to work together and have been doing so in the following ways:
- Participating in each other’s steering groups and working parties.
- Swapping notes regarding local data (e.g. on physical health, mental health, ethnicity, deprivation, risk factors).
- Sharing resources and relationships (e.g. with psychosexual services).
- Assisting each other with recruitment of staff, which has enabled the recruitment of staff that can treat women holistically, integrating both pelvic health and mental health.
- Facilitating joint awareness events for stakeholders, including an event on holistic wellbeing which was attended equally by healthcare professionals and service users.
- Engaging and educating healthcare professionals and service users, particularly in relation to seldom heard from communities.
- Upskilling both the PPHS and MMHS workforce and increasing training for the wider maternity workforce.
- Developing a clear referral pathway between the services.
- Evaluating women’s experiences of referral pathways.
- Improving data quality together.
Case study 18: Lancashire and South Cumbria – Collaboration with the MMHS
Lancashire and South Cumbria identified early in the PPHS project the opportunity to connect with the local MMHS. Data gathered from the MMHS was used to develop plans for the PPHS, which ensured there was shared learning between the two projects from the offset. The services have also collaborated in the following ways:
- The leads for each service attend each other’s steering groups which facilitates good communication and opportunities to share lessons learnt and avoid duplication.
- There are regular catch-ups between MMHS and PPHS teams, as well as other organisations such as psychosexual services, health visitors, and the charity sector.
- A joint staff training programme has been put in place.
- The Local Maternity Hub (hosted by the local LMNS) provides a space for MMHS and PPHS to collaborate.
- The local electronic maternity system enables both PPHS and MMHS staff to add notes to a single patient record.
- An informal referral pathway between the services has been put in place to ensure that referral between the two services is as seamless as possible for women.
Case Study 19: North West London – Internal training and development of pelvic health physiotherapists
Imperial College Hospital within North West London has developed an internal training programme for their pelvic health team that facilitates sustainability and succession planning. This development programme helps bring new staff into the service, offers a collaborative approach to shared learning, and enables advanced practice development within perinatal services.
Rotational perinatal posts within pelvic health are provided in both inpatient and outpatient services. A range of rotational roles have been established, including a band 5 rotation, a band 6 pelvic health rotation or a split musculoskeletal/pelvic health rotation. These offer an introduction to perinatal services, an opportunity for training, and allow rehabilitative care to be provided along the whole perinatal patient pathway. Those training within these roles typically apply for permanent roles in pelvic health.
“We’ve got one rotational band 5. This rotational post is the reason why we’re constantly able to recruit into band 6 pelvic health roles. We have a lot of band 5s who come, enjoy pelvic health and want to progress further, when the opportunities arise, they apply for band 6 roles.”
Band 5 and 6 physiotherapists are supported to learn enhanced clinical practice within pelvic health. There is an in-service training that the team complete together to discuss complex patients and learn new practical skills, in addition to the completion of competencies that standardise the quality of care and service provided.
“If rotational staff want to do pelvic floor, we’re really supportive and we’ll get them trained up as soon as they start with us. We complete in-house competencies, which provides standardisation across our team and allows the band 7’s to teach others their skills”.
For the more advanced staff within the service, physiotherapists are supported to complete master’s modules and develop advanced practice skills. The team have several trainee prescribers and physiotherapists within point of care ultrasound, in addition to those with additional pelvic health skills such as utilisation of vaginal pessaries, rectal irrigation and biofeedback. The service has also utilised the NHS advanced practice apprenticeship to support the development of the staff. The service provides an internal, supportive training environment for entry level physiotherapists and supports the development of advanced practice to enable physiotherapists to provide high quality care to patients, as well as to share their knowledge to train and develop the team.
Case study 20: Frimley – Physiotherapy assistant practitioner hybrid role
To improve consistency in service provision and ensure compliance with NICE guidance at Frimley, a new pathway was created for referral to the PPHS. Alongside this pathway, a telephone triage service for antenatal and postnatal women was launched that enables referral into the PPHS.
Frimley created two Band 4 Physiotherapy Assistant Practitioner hybrid roles with maternity, which are both community and ward based. The Band 4’s work on the postnatal ward and offer initial advice to inpatients after OASI, rectus abdominis diastasis, over distension injury, Pelvic Girdle Pain, as well as advice to women with risk factors for developing pelvic floor dysfunction such as forceps birth, shoulder dystocia, baby over 4kg, twins, and maternal age of over 35 at first birth. The ward staff have found it beneficial to have a consistent ‘specialist’ team member present.
They additionally run perinatal workshops virtually and in-person on pelvic health and anatomy, and prevention and treatment strategies. They have attended a course in perinatal Pilates and now see any one-to-one patient referred by a pelvic health team member. The Physiotherapy Assistant Practitioners also assist with administrative responsibilities such as data collection, booking patients, documentation, and technical support. This has alleviated pressure on other staff members.
Case study 21: Norfolk and Waveney – Band 4 therapy assistant practitioners
Perinatal pelvic health care provision varied across the three trusts in Norfolk and Waveney, so one of the aims of the PPHS was to provide greater consistency of care to service users across the LMNS. To help build capacity across the footprint, a new band 4 Therapy Assistant Practitioner (TAP) role was created.
TAPs go through extensive training before being signed off to work within the service. Their responsibilities in the PPHS include:
- Assisting with the screening questionnaire, including triaging referrals and bookings,
- Running pelvic health advice sessions
- Providing one-to-one support sessions for those with mild symptoms or those who are at risk of problems,
- Monitoring use of the mobile application that which is provided to every pregnant woman,
- Handing out surveys, and
- Collating data, including service user feedback.
Norfolk and Waveney have found that TAPs have fitted into the service well. Trusts with Continuity of Carer in place have had a better uptake of care and this is thought to be due to TAPs being present in maternity hubs.
Case study 22: Dorset – Physiotherapy leadership
Dorset has recruited a band 8a pelvic health clinical lead who has supported the development of the PPHS but also manages the overarching pelvic health physiotherapy team. This has worked well in this rural area, because it has helped ensure the sustainability of the service by facilitating the development a larger workforce and appropriate training for all within perinatal and pelvic health services.
“We have a workforce of lots of part-time staff, and I know how important it is that in the end all staff can do almost everything in pelvic health, so we have resilience when somebody is off sick, and knowledge across the team”.
In a rural area that has smaller numbers of perinatal patients that are widely spread out, this model is beneficial, as it has enabled the smaller allocation of funding for perinatal care to be embedded within the larger pelvic health service by spreading the education and patient allocation amongst all staff. The pelvic health lead prioritised and provided training within the wider perinatal service in addition to the pelvic health service.
At an 8a staffing level, the leader can escalate the appropriate learning needs for their team, rather than their specialist needs sitting under a musculoskeletal physiotherapy service, where the allocation of training is unsuitable for the pelvic health service.
A flexible recruitment strategy implemented by the pelvic health lead ensured that support and training to enter the pelvic health workforce was provided. This was done by highlighting experience as desirable rather than necessary within pelvic health. This is different from other areas that would always ensure that high amounts of experience are necessary to apply for a band 6 and 7 role. The experienced pelvic health leader is aware of the service’s needs as well as the training needs of the team, so that they are able to make strategic decisions that support the management of services in addition to the recruitment and sustainability of the workforce.
- Open access
- Published: 15 May 2024
Learning together for better health using an evidence-based Learning Health System framework: a case study in stroke
- Helena Teede 1 , 2 na1 ,
- Dominique A. Cadilhac 3 , 4 na1 ,
- Tara Purvis 3 ,
- Monique F. Kilkenny 3 , 4 ,
- Bruce C.V. Campbell 4 , 5 , 6 ,
- Coralie English 7 ,
- Alison Johnson 2 ,
- Emily Callander 1 ,
- Rohan S. Grimley 8 , 9 ,
- Christopher Levi 10 ,
- Sandy Middleton 11 , 12 ,
- Kelvin Hill 13 &
- Joanne Enticott ORCID: orcid.org/0000-0002-4480-5690 1
BMC Medicine volume 22 , Article number: 198 ( 2024 ) Cite this article
228 Accesses
1 Altmetric
Metrics details
In the context of expanding digital health tools, the health system is ready for Learning Health System (LHS) models. These models, with proper governance and stakeholder engagement, enable the integration of digital infrastructure to provide feedback to all relevant parties including clinicians and consumers on performance against best practice standards, as well as fostering innovation and aligning healthcare with patient needs. The LHS literature primarily includes opinion or consensus-based frameworks and lacks validation or evidence of benefit. Our aim was to outline a rigorously codesigned, evidence-based LHS framework and present a national case study of an LHS-aligned national stroke program that has delivered clinical benefit.
Current core components of a LHS involve capturing evidence from communities and stakeholders (quadrant 1), integrating evidence from research findings (quadrant 2), leveraging evidence from data and practice (quadrant 3), and generating evidence from implementation (quadrant 4) for iterative system-level improvement. The Australian Stroke program was selected as the case study as it provides an exemplar of how an iterative LHS works in practice at a national level encompassing and integrating evidence from all four LHS quadrants. Using this case study, we demonstrate how to apply evidence-based processes to healthcare improvement and embed real-world research for optimising healthcare improvement. We emphasize the transition from research as an endpoint, to research as an enabler and a solution for impact in healthcare improvement.
Conclusions
The Australian Stroke program has nationally improved stroke care since 2007, showcasing the value of integrated LHS-aligned approaches for tangible impact on outcomes. This LHS case study is a practical example for other health conditions and settings to follow suit.
Peer Review reports
Internationally, health systems are facing a crisis, driven by an ageing population, increasing complexity, multi-morbidity, rapidly advancing health technology and rising costs that threaten sustainability and mandate transformation and improvement [ 1 , 2 ]. Although research has generated solutions to healthcare challenges, and the advent of big data and digital health holds great promise, entrenched siloes and poor integration of knowledge generation, knowledge implementation and healthcare delivery between stakeholders, curtails momentum towards, and consistent attainment of, evidence-and value-based care [ 3 ]. This is compounded by the short supply of research and innovation leadership within the healthcare sector, and poorly integrated and often inaccessible health data systems, which have crippled the potential to deliver on digital-driven innovation [ 4 ]. Current approaches to healthcare improvement are also often isolated with limited sustainability, scale-up and impact [ 5 ].
Evidence suggests that integration and partnership across academic and healthcare delivery stakeholders are key to progress, including those with lived experience and their families (referred to here as consumers and community), diverse disciplines (both research and clinical), policy makers and funders. Utilization of evidence from research and evidence from practice including data from routine care, supported by implementation research, are key to sustainably embedding improvement and optimising health care and outcomes. A strategy to achieve this integration is through the Learning Health System (LHS) (Fig. 1 ) [ 2 , 6 , 7 , 8 ]. Although there are numerous publications on LHS approaches [ 9 , 10 , 11 , 12 ], many focus on research perspectives and data, most do not demonstrate tangible healthcare improvement or better health outcomes. [ 6 ]
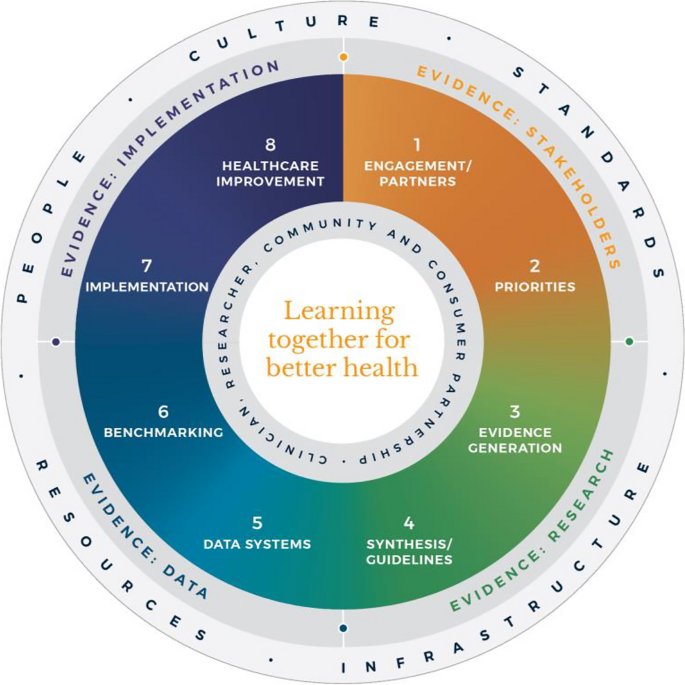
Monash Learning Health System: The Learn Together for Better Health Framework developed by Monash Partners and Monash University (from Enticott et al. 2021 [ 7 ]). Four evidence quadrants: Q1 (orange) is evidence from stakeholders; Q2 (green) is evidence from research; Q3 (light blue) is evidence from data; and, Q4 (dark blue) is evidence from implementation and healthcare improvement
In developed nations, it has been estimated that 60% of care provided aligns with the evidence base, 30% is low value and 10% is potentially harmful [ 13 ]. In some areas, clinical advances have been rapid and research and evidence have paved the way for dramatic improvement in outcomes, mandating rapid implementation of evidence into healthcare (e.g. polio and COVID-19 vaccines). However, healthcare improvement is challenging and slow [ 5 ]. Health systems are highly complex in their design, networks and interacting components, and change is difficult to enact, sustain and scale up. [ 3 ] New effective strategies are needed to meet community needs and deliver evidence-based and value-based care, which reorients care from serving the provider, services and system, towards serving community needs, based on evidence and quality. It goes beyond cost to encompass patient and provider experience, quality care and outcomes, efficiency and sustainability [ 2 , 6 ].
The costs of stroke care are expected to rise rapidly in the next decades, unless improvements in stroke care to reduce the disabling effects of strokes can be successfully developed and implemented [ 14 ]. Here, we briefly describe the Monash LHS framework (Fig. 1 ) [ 2 , 6 , 7 ] and outline an exemplar case in order to demonstrate how to apply evidence-based processes to healthcare improvement and embed real-world research for optimising healthcare. The Australian LHS exemplar in stroke care has driven nationwide improvement in stroke care since 2007.
An evidence-based Learning Health System framework
In Australia, members of this author group (HT, AJ, JE) have rigorously co-developed an evidence-based LHS framework, known simply as the Monash LHS [ 7 ]. The Monash LHS was designed to support sustainable, iterative and continuous robust benefit of improved clinical outcomes. It was created with national engagement in order to be applicable to Australian settings. Through this rigorous approach, core LHS principles and components have been established (Fig. 1 ). Evidence shows that people/workforce, culture, standards, governance and resources were all key to an effective LHS [ 2 , 6 ]. Culture is vital including trust, transparency, partnership and co-design. Key processes include legally compliant data sharing, linkage and governance, resources, and infrastructure [ 4 ]. The Monash LHS integrates disparate and often siloed stakeholders, infrastructure and expertise to ‘Learn Together for Better Health’ [ 7 ] (Fig. 1 ). This integrates (i) evidence from community and stakeholders including priority areas and outcomes; (ii) evidence from research and guidelines; (iii) evidence from practice (from data) with advanced analytics and benchmarking; and (iv) evidence from implementation science and health economics. Importantly, it starts with the problem and priorities of key stakeholders including the community, health professionals and services and creates an iterative learning system to address these. The following case study was chosen as it is an exemplar of how a Monash LHS-aligned national stroke program has delivered clinical benefit.
Australian Stroke Learning Health System
Internationally, the application of LHS approaches in stroke has resulted in improved stroke care and outcomes [ 12 ]. For example, in Canada a sustained decrease in 30-day in-hospital mortality has been found commensurate with an increase in resources to establish the multifactorial stroke system intervention for stroke treatment and prevention [ 15 ]. Arguably, with rapid advances in evidence and in the context of an ageing population with high cost and care burden and substantive impacts on quality of life, stroke is an area with a need for rapid research translation into evidence-based and value-based healthcare improvement. However, a recent systematic review found that the existing literature had few comprehensive examples of LHS adoption [ 12 ]. Although healthcare improvement systems and approaches were described, less is known about patient-clinician and stakeholder engagement, governance and culture, or embedding of data informatics into everyday practice to inform and drive improvement [ 12 ]. For example, in a recent review of quality improvement collaborations, it was found that although clinical processes in stroke care are improved, their short-term nature means there is uncertainty about sustainability and impacts on patient outcomes [ 16 ]. Table 1 provides the main features of the Australian Stroke LHS based on the four core domains and eight elements of the Learning Together for Better Health Framework described in Fig. 1 . The features are further expanded on in the following sections.
Evidence from stakeholders (LHS quadrant 1, Fig. 1 )
Engagement, partners and priorities.
Within the stroke field, there have been various support mechanisms to facilitate an LHS approach including partnership and broad stakeholder engagement that includes clinical networks and policy makers from different jurisdictions. Since 2008, the Australian Stroke Coalition has been co-led by the Stroke Foundation, a charitable consumer advocacy organisation, and Stroke Society of Australasia a professional society with membership covering academics and multidisciplinary clinician networks, that are collectively working to improve stroke care ( https://australianstrokecoalition.org.au/ ). Surveys, focus groups and workshops have been used for identifying priorities from stakeholders. Recent agreed priorities have been to improve stroke care and strengthen the voice for stroke care at a national ( https://strokefoundation.org.au/ ) and international level ( https://www.world-stroke.org/news-and-blog/news/world-stroke-organization-tackle-gaps-in-access-to-quality-stroke-care ), as well as reduce duplication amongst stakeholders. This activity is built on a foundation and culture of research and innovation embedded within the stroke ‘community of practice’. Consumers, as people with lived experience of stroke are important members of the Australian Stroke Coalition, as well as representatives from different clinical colleges. Consumers also provide critical input to a range of LHS activities via the Stroke Foundation Consumer Council, Stroke Living Guidelines committees, and the Australian Stroke Clinical Registry (AuSCR) Steering Committee (described below).
Evidence from research (LHS quadrant 2, Fig. 1 )
Advancement of the evidence for stroke interventions and synthesis into clinical guidelines.
To implement best practice, it is crucial to distil the large volume of scientific and trial literature into actionable recommendations for clinicians to use in practice [ 24 ]. The first Australian clinical guidelines for acute stroke were produced in 2003 following the increasing evidence emerging for prevention interventions (e.g. carotid endarterectomy, blood pressure lowering), acute medical treatments (intravenous thrombolysis, aspirin within 48 h of ischemic stroke), and optimised hospital management (care in dedicated stroke units by a specialised and coordinated multidisciplinary team) [ 25 ]. Importantly, a number of the innovations were developed, researched and proven effective by key opinion leaders embedded in the Australian stroke care community. In 2005, the clinical guidelines for Stroke Rehabilitation and Recovery [ 26 ] were produced, with subsequent merged guidelines periodically updated. However, the traditional process of periodic guideline updates is challenging for end users when new research can render recommendations redundant and this lack of currency erodes stakeholder trust [ 27 ]. In response to this challenge the Stroke Foundation and Cochrane Australia entered a pioneering project to produce the first electronic ‘living’ guidelines globally [ 20 ]. Major shifts in the evidence for reperfusion therapies (e.g. extended time-window intravenous thrombolysis and endovascular clot retrieval), among other advances, were able to be converted into new recommendations, approved by the Australian National Health and Medical Research Council within a few months of publication. Feedback on this process confirmed the increased use and trust in the guidelines by clinicians. The process informed other living guidelines programs, including the successful COVID-19 clinical guidelines [ 28 ].
However, best practice clinical guideline recommendations are necessary but insufficient for healthcare improvement and nesting these within an LHS with stakeholder partnership, enables implementation via a range of proven methods, including audit and feedback strategies [ 29 ].
Evidence from data and practice (LHS quadrant 3, Fig. 1 )
Data systems and benchmarking : revealing the disparities in care between health services. A national system for standardized stroke data collection was established as the National Stroke Audit program in 2007 by the Stroke Foundation [ 30 ] following various state-level programs (e.g. New South Wales Audit) [ 31 ] to identify evidence-practice gaps and prioritise improvement efforts to increase access to stroke units and other acute treatments [ 32 ]. The Audit program alternates each year between acute (commencing in 2007) and rehabilitation in-patient services (commencing in 2008). The Audit program provides a ‘deep dive’ on the majority of recommendations in the clinical guidelines whereby participating hospitals provide audits of up to 40 consecutive patient medical records and respond to a survey about organizational resources to manage stroke. In 2009, the AuSCR was established to provide information on patients managed in acute hospitals based on a small subset of quality processes of care linked to benchmarked reports of performance (Fig. 2 ) [ 33 ]. In this way, the continuous collection of high-priority processes of stroke care could be regularly collected and reviewed to guide improvement to care [ 34 ]. Plus clinical quality registry programs within Australia have shown a meaningful return on investment attributed to enhanced survival, improvements in quality of life and avoided costs of treatment or hospital stay [ 35 ].
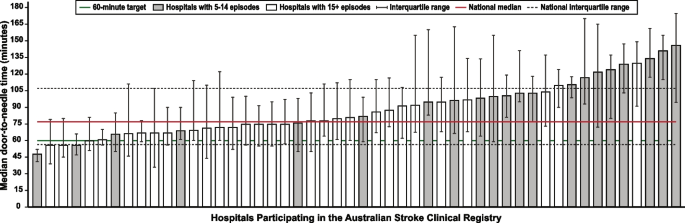
Example performance report from the Australian Stroke Clinical Registry: average door-to-needle time in providing intravenous thrombolysis by different hospitals in 2021 [ 36 ]. Each bar in the figure represents a single hospital
The Australian Stroke Coalition endorsed the creation of an integrated technological solution for collecting data through a single portal for multiple programs in 2013. In 2015, the Stroke Foundation, AuSCR consortium, and other relevant groups cooperated to design an integrated data management platform (the Australian Stroke Data Tool) to reduce duplication of effort for hospital staff in the collection of overlapping variables in the same patients [ 19 ]. Importantly, a national data dictionary then provided the common data definitions to facilitate standardized data capture. Another important feature of AuSCR is the collection of patient-reported outcome surveys between 90 and 180 days after stroke, and annual linkage with national death records to ascertain survival status [ 33 ]. To support a LHS approach, hospitals that participate in AuSCR have access to a range of real-time performance reports. In efforts to minimize the burden of data collection in the AuSCR, interoperability approaches to import data directly from hospital or state-level managed stroke databases have been established (Fig. 3 ); however, the application has been variable and 41% of hospitals still manually enter all their data.
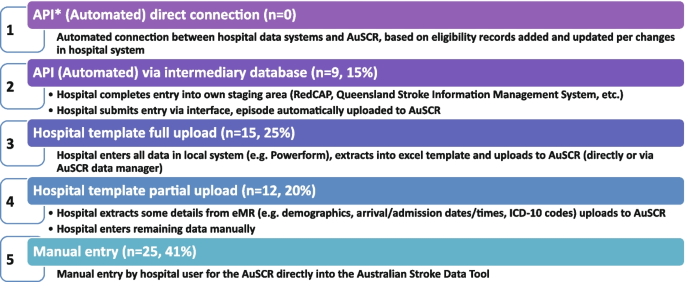
Current status of automated data importing solutions in the Australian Stroke Clinical Registry, 2022, with ‘ n ’ representing the number of hospitals. AuSCR, Australian Stroke Clinical Registry; AuSDaT, Australian Stroke Data Tool; API, Application Programming Interface; ICD, International Classification of Diseases; RedCAP, Research Electronic Data Capture; eMR, electronic medical records
For acute stroke care, the Australian Commission on Quality and Safety in Health Care facilitated the co-design (clinicians, academics, consumers) and publication of the national Acute Stroke Clinical Care Standard in 2015 [ 17 ], and subsequent review [ 18 ]. The indicator set for the Acute Stroke Standard then informed the expansion of the minimum dataset for AuSCR so that hospitals could routinely track their performance. The national Audit program enabled hospitals not involved in the AuSCR to assess their performance every two years against the Acute Stroke Standard. Complementing these efforts, the Stroke Foundation, working with the sector, developed the Acute and Rehabilitation Stroke Services Frameworks to outline the principles, essential elements, models of care and staffing recommendations for stroke services ( https://informme.org.au/guidelines/national-stroke-services-frameworks ). The Frameworks are intended to guide where stroke services should be developed, and monitor their uptake with the organizational survey component of the Audit program.
Evidence from implementation and healthcare improvement (LHS quadrant 4, Fig. 1 )
Research to better utilize and augment data from registries through linkage [ 37 , 38 , 39 , 40 ] and to ensure presentation of hospital or service level data are understood by clinicians has ensured advancement in the field for the Australian Stroke LHS [ 41 ]. Importantly, greater insights into whole patient journeys, before and after a stroke, can now enable exploration of value-based care. The LHS and stroke data platform have enabled focused and time-limited projects to create a better understanding of the quality of care in acute or rehabilitation settings [ 22 , 42 , 43 ]. Within stroke, all the elements of an LHS culminate into the ready availability of benchmarked performance data and support for implementation of strategies to address gaps in care.
Implementation research to grow the evidence base for effective improvement interventions has also been a key pillar in the Australian context. These include multi-component implementation interventions to achieve behaviour change for particular aspects of stroke care, [ 22 , 23 , 44 , 45 ] and real-world approaches to augmenting access to hyperacute interventions in stroke through the use of technology and telehealth [ 46 , 47 , 48 , 49 ]. The evidence from these studies feeds into the living guidelines program and the data collection systems, such as the Audit program or AuSCR, which are then amended to ensure data aligns to recommended care. For example, the use of ‘hyperacute aspirin within the first 48 h of ischemic stroke’ was modified to be ‘hyperacute antiplatelet…’ to incorporate new evidence that other medications or combinations are appropriate to use. Additionally, new datasets have been developed to align with evidence such as the Fever, Sugar, and Swallow variables [ 42 ]. Evidence on improvements in access to best practice care from the acute Audit program [ 50 ] and AuSCR is emerging [ 36 ]. For example, between 2007 and 2017, the odds of receiving intravenous thrombolysis after ischemic stroke increased by 16% 9OR 1.06 95% CI 1.13–1.18) and being managed in a stroke unit by 18% (OR 1.18 95% CI 1.17–1.20). Over this period, the median length of hospital stay for all patients decreased from 6.3 days in 2007 to 5.0 days in 2017 [ 51 ]. When considering the number of additional patients who would receive treatment in 2017 in comparison to 2007 it was estimated that without this additional treatment, over 17,000 healthy years of life would be lost in 2017 (17,786 disability-adjusted life years) [ 51 ]. There is evidence on the cost-effectiveness of different system-focussed strategies to augment treatment access for acute ischemic stroke (e.g. Victorian Stroke Telemedicine program [ 52 ] and Melbourne Mobile Stroke Unit ambulance [ 53 ]). Reciprocally, evidence from the national Rehabilitation Audit, where the LHS approach has been less complete or embedded, has shown fewer areas of healthcare improvement over time [ 51 , 54 ].
Within the field of stroke in Australia, there is indirect evidence that the collective efforts that align to establishing the components of a LHS have had an impact. Overall, the age-standardised rate of stroke events has reduced by 27% between 2001 and 2020, from 169 to 124 events per 100,000 population. Substantial declines in mortality rates have been reported since 1980. Commensurate with national clinical guidelines being updated in 2007 and the first National Stroke Audit being undertaken in 2007, the mortality rates for men (37.4 deaths per 100,000) and women (36.1 deaths per 100,0000 has declined to 23.8 and 23.9 per 100,000, respectively in 2021 [ 55 ].
Underpinning the LHS with the integration of the four quadrants of evidence from stakeholders, research and guidelines, practice and implementation, and core LHS principles have been addressed. Leadership and governance have been important, and programs have been established to augment workforce training and capacity building in best practice professional development. Medical practitioners are able to undertake courses and mentoring through the Australasian Stroke Academy ( http://www.strokeacademy.com.au/ ) while nurses (and other health professionals) can access teaching modules in stroke care from the Acute Stroke Nurses Education Network ( https://asnen.org/ ). The Association of Neurovascular Clinicians offers distance-accessible education and certification to develop stroke expertise for interdisciplinary professionals, including advanced stroke co-ordinator certification ( www.anvc.org ). Consumer initiative interventions are also used in the design of the AuSCR Public Summary Annual reports (available at https://auscr.com.au/about/annual-reports/ ) and consumer-related resources related to the Living Guidelines ( https://enableme.org.au/resources ).
The important success factors and lessons from stroke as a national exemplar LHS in Australia include leadership, culture, workforce and resources integrated with (1) established and broad partnerships across the academic-clinical sector divide and stakeholder engagement; (2) the living guidelines program; (3) national data infrastructure, including a national data dictionary that provides the common data framework to support standardized data capture; (4) various implementation strategies including benchmarking and feedback as well as engagement strategies targeting different levels of the health system; and (5) implementation and improvement research to advance stroke systems of care and reduce unwarranted variation in practice (Fig. 1 ). Priority opportunities now include the advancement of interoperability with electronic medical records as an area all clinical quality registry’s programs needs to be addressed, as well as providing more dynamic and interactive data dashboards tailored to the need of clinicians and health service executives.
There is a clear mandate to optimise healthcare improvement with big data offering major opportunities for change. However, we have lacked the approaches to capture evidence from the community and stakeholders, to integrate evidence from research, to capture and leverage data or evidence from practice and to generate and build on evidence from implementation using iterative system-level improvement. The LHS provides this opportunity and is shown to deliver impact. Here, we have outlined the process applied to generate an evidence-based LHS and provide a leading exemplar in stroke care. This highlights the value of moving from single-focus isolated approaches/initiatives to healthcare improvement and the benefit of integration to deliver demonstrable outcomes for our funders and key stakeholders — our community. This work provides insight into strategies that can both apply evidence-based processes to healthcare improvement as well as implementing evidence-based practices into care, moving beyond research as an endpoint, to research as an enabler, underpinning delivery of better healthcare.
Availability of data and materials
Not applicable
Abbreviations
Australian Stroke Clinical Registry
Confidence interval
- Learning Health System
World Health Organization. Delivering quality health services . OECD Publishing; 2018.
Enticott J, Braaf S, Johnson A, Jones A, Teede HJ. Leaders’ perspectives on learning health systems: A qualitative study. BMC Health Serv Res. 2020;20:1087.
Article PubMed PubMed Central Google Scholar
Melder A, Robinson T, McLoughlin I, Iedema R, Teede H. An overview of healthcare improvement: Unpacking the complexity for clinicians and managers in a learning health system. Intern Med J. 2020;50:1174–84.
Article PubMed Google Scholar
Alberto IRI, Alberto NRI, Ghosh AK, Jain B, Jayakumar S, Martinez-Martin N, et al. The impact of commercial health datasets on medical research and health-care algorithms. Lancet Digit Health. 2023;5:e288–94.
Article CAS PubMed PubMed Central Google Scholar
Dixon-Woods M. How to improve healthcare improvement—an essay by Mary Dixon-Woods. BMJ. 2019;367: l5514.
Enticott J, Johnson A, Teede H. Learning health systems using data to drive healthcare improvement and impact: A systematic review. BMC Health Serv Res. 2021;21:200.
Enticott JC, Melder A, Johnson A, Jones A, Shaw T, Keech W, et al. A learning health system framework to operationalize health data to improve quality care: An Australian perspective. Front Med (Lausanne). 2021;8:730021.
Dammery G, Ellis LA, Churruca K, Mahadeva J, Lopez F, Carrigan A, et al. The journey to a learning health system in primary care: A qualitative case study utilising an embedded research approach. BMC Prim Care. 2023;24:22.
Foley T, Horwitz L, Zahran R. The learning healthcare project: Realising the potential of learning health systems. 2021. Available from https://learninghealthcareproject.org/wp-content/uploads/2021/05/LHS2021report.pdf . Accessed Jan 2024.
Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Washington: The National Academies Press; 2013.
Google Scholar
Zurynski Y, Smith CL, Vedovi A, Ellis LA, Knaggs G, Meulenbroeks I, et al. Mapping the learning health system: A scoping review of current evidence - a white paper. 2020:63
Cadilhac DA, Bravata DM, Bettger J, Mikulik R, Norrving B, Uvere E, et al. Stroke learning health systems: A topical narrative review with case examples. Stroke. 2023;54:1148–59.
Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: The 60–30-10 challenge. BMC Med. 2020;18:1–8.
Article Google Scholar
King D, Wittenberg R, Patel A, Quayyum Z, Berdunov V, Knapp M. The future incidence, prevalence and costs of stroke in the UK. Age Ageing. 2020;49:277–82.
Ganesh A, Lindsay P, Fang J, Kapral MK, Cote R, Joiner I, et al. Integrated systems of stroke care and reduction in 30-day mortality: A retrospective analysis. Neurology. 2016;86:898–904.
Lowther HJ, Harrison J, Hill JE, Gaskins NJ, Lazo KC, Clegg AJ, et al. The effectiveness of quality improvement collaboratives in improving stroke care and the facilitators and barriers to their implementation: A systematic review. Implement Sci. 2021;16:16.
Australian Commission on Safety and Quality in Health Care. Acute stroke clinical care standard. 2015. Available from https://www.safetyandquality.gov.au/our-work/clinical-care-standards/acute-stroke-clinical-care-standard . Accessed Jan 2024.
Australian Commission on Safety and Quality in Health Care. Acute stroke clinical care standard. Sydney: ACSQHC; 2019. Available from https://www.safetyandquality.gov.au/publications-and-resources/resource-library/acute-stroke-clinical-care-standard-evidence-sources . Accessed Jan 2024.
Ryan O, Ghuliani J, Grabsch B, Hill K, G CC, Breen S, et al. Development, implementation, and evaluation of the Australian Stroke Data Tool (AuSDaT): Comprehensive data capturing for multiple uses. Health Inf Manag. 2022:18333583221117184.
English C, Bayley M, Hill K, Langhorne P, Molag M, Ranta A, et al. Bringing stroke clinical guidelines to life. Int J Stroke. 2019;14:337–9.
English C, Hill K, Cadilhac DA, Hackett ML, Lannin NA, Middleton S, et al. Living clinical guidelines for stroke: Updates, challenges and opportunities. Med J Aust. 2022;216:510–4.
Cadilhac DA, Grimley R, Kilkenny MF, Andrew NE, Lannin NA, Hill K, et al. Multicenter, prospective, controlled, before-and-after, quality improvement study (Stroke123) of acute stroke care. Stroke. 2019;50:1525–30.
Cadilhac DA, Marion V, Andrew NE, Breen SJ, Grabsch B, Purvis T, et al. A stepped-wedge cluster-randomized trial to improve adherence to evidence-based practices for acute stroke management. Jt Comm J Qual Patient Saf. 2022.
Elliott J, Lawrence R, Minx JC, Oladapo OT, Ravaud P, Jeppesen BT, et al. Decision makers need constantly updated evidence synthesis. Nature. 2021;600:383–5.
Article CAS PubMed Google Scholar
National Stroke Foundation. National guidelines for acute stroke management. Melbourne: National Stroke Foundation; 2003.
National Stroke Foundation. Clinical guidelines for stroke rehabilitation and recovery. Melbourne: National Stroke Foundation; 2005.
Phan TG, Thrift A, Cadilhac D, Srikanth V. A plea for the use of systematic review methodology when writing guidelines and timely publication of guidelines. Intern Med J . 2012;42:1369–1371; author reply 1371–1362
Tendal B, Vogel JP, McDonald S, Norris S, Cumpston M, White H, et al. Weekly updates of national living evidence-based guidelines: Methods for the Australian living guidelines for care of people with COVID-19. J Clin Epidemiol. 2021;131:11–21.
Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7:50.
Harris D, Cadilhac D, Hankey GJ, Hillier S, Kilkenny M, Lalor E. National stroke audit: The Australian experience. Clin Audit. 2010;2:25–31.
Cadilhac DA, Purvis T, Kilkenny MF, Longworth M, Mohr K, Pollack M, et al. Evaluation of rural stroke services: Does implementation of coordinators and pathways improve care in rural hospitals? Stroke. 2013;44:2848–53.
Cadilhac DA, Moss KM, Price CJ, Lannin NA, Lim JY, Anderson CS. Pathways to enhancing the quality of stroke care through national data monitoring systems for hospitals. Med J Aust. 2013;199:650–1.
Cadilhac DA, Lannin NA, Anderson CS, Levi CR, Faux S, Price C, et al. Protocol and pilot data for establishing the Australian Stroke Clinical Registry. Int J Stroke. 2010;5:217–26.
Ivers N, Jamtvedt G, Flottorp S, Young J, Odgaard-Jensen J, French S, et al. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev . 2012
Australian Commission on Safety and Quality in Health Care. Economic evaluation of clinical quality registries. Final report. . 2016:79
Cadilhac DA, Dalli LL, Morrison J, Lester M, Paice K, Moss K, et al. The Australian Stroke Clinical Registry annual report 2021. Melbourne; 2022. Available from https://auscr.com.au/about/annual-reports/ . Accessed 6 May 2024.
Kilkenny MF, Kim J, Andrew NE, Sundararajan V, Thrift AG, Katzenellenbogen JM, et al. Maximising data value and avoiding data waste: A validation study in stroke research. Med J Aust. 2019;210:27–31.
Eliakundu AL, Smith K, Kilkenny MF, Kim J, Bagot KL, Andrew E, et al. Linking data from the Australian Stroke Clinical Registry with ambulance and emergency administrative data in Victoria. Inquiry. 2022;59:469580221102200.
PubMed Google Scholar
Andrew NE, Kim J, Cadilhac DA, Sundararajan V, Thrift AG, Churilov L, et al. Protocol for evaluation of enhanced models of primary care in the management of stroke and other chronic disease (PRECISE): A data linkage healthcare evaluation study. Int J Popul Data Sci. 2019;4:1097.
CAS PubMed PubMed Central Google Scholar
Mosalski S, Shiner CT, Lannin NA, Cadilhac DA, Faux SG, Kim J, et al. Increased relative functional gain and improved stroke outcomes: A linked registry study of the impact of rehabilitation. J Stroke Cerebrovasc Dis. 2021;30: 106015.
Ryan OF, Hancock SL, Marion V, Kelly P, Kilkenny MF, Clissold B, et al. Feedback of aggregate patient-reported outcomes (PROs) data to clinicians and hospital end users: Findings from an Australian codesign workshop process. BMJ Open. 2022;12:e055999.
Grimley RS, Rosbergen IC, Gustafsson L, Horton E, Green T, Cadigan G, et al. Dose and setting of rehabilitation received after stroke in Queensland, Australia: A prospective cohort study. Clin Rehabil. 2020;34:812–23.
Purvis T, Middleton S, Craig LE, Kilkenny MF, Dale S, Hill K, et al. Inclusion of a care bundle for fever, hyperglycaemia and swallow management in a national audit for acute stroke: Evidence of upscale and spread. Implement Sci. 2019;14:87.
Middleton S, McElduff P, Ward J, Grimshaw JM, Dale S, D’Este C, et al. Implementation of evidence-based treatment protocols to manage fever, hyperglycaemia, and swallowing dysfunction in acute stroke (QASC): A cluster randomised controlled trial. Lancet. 2011;378:1699–706.
Middleton S, Dale S, Cheung NW, Cadilhac DA, Grimshaw JM, Levi C, et al. Nurse-initiated acute stroke care in emergency departments. Stroke. 2019:STROKEAHA118020701.
Hood RJ, Maltby S, Keynes A, Kluge MG, Nalivaiko E, Ryan A, et al. Development and pilot implementation of TACTICS VR: A virtual reality-based stroke management workflow training application and training framework. Front Neurol. 2021;12:665808.
Bladin CF, Kim J, Bagot KL, Vu M, Moloczij N, Denisenko S, et al. Improving acute stroke care in regional hospitals: Clinical evaluation of the Victorian Stroke Telemedicine program. Med J Aust. 2020;212:371–7.
Bladin CF, Bagot KL, Vu M, Kim J, Bernard S, Smith K, et al. Real-world, feasibility study to investigate the use of a multidisciplinary app (Pulsara) to improve prehospital communication and timelines for acute stroke/STEMI care. BMJ Open. 2022;12:e052332.
Zhao H, Coote S, Easton D, Langenberg F, Stephenson M, Smith K, et al. Melbourne mobile stroke unit and reperfusion therapy: Greater clinical impact of thrombectomy than thrombolysis. Stroke. 2020;51:922–30.
Purvis T, Cadilhac DA, Hill K, Reyneke M, Olaiya MT, Dalli LL, et al. Twenty years of monitoring acute stroke care in Australia from the national stroke audit program (1999–2019): Achievements and areas of future focus. J Health Serv Res Policy. 2023.
Cadilhac DA, Purvis T, Reyneke M, Dalli LL, Kim J, Kilkenny MF. Evaluation of the national stroke audit program: 20-year report. Melbourne; 2019.
Kim J, Tan E, Gao L, Moodie M, Dewey HM, Bagot KL, et al. Cost-effectiveness of the Victorian Stroke Telemedicine program. Aust Health Rev. 2022;46:294–301.
Kim J, Easton D, Zhao H, Coote S, Sookram G, Smith K, et al. Economic evaluation of the Melbourne mobile stroke unit. Int J Stroke. 2021;16:466–75.
Stroke Foundation. National stroke audit – rehabilitation services report 2020. Melbourne; 2020.
Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. 2023. Webpage https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts/contents/about (accessed Jan 2024).
Download references
Acknowledgements
The following authors hold National Health and Medical Research Council Research Fellowships: HT (#2009326), DAC (#1154273), SM (#1196352), MFK Future Leader Research Fellowship (National Heart Foundation #105737). The Funders of this work did not have any direct role in the design of the study, its execution, analyses, interpretation of the data, or decision to submit results for publication.
Author information
Helena Teede and Dominique A. Cadilhac contributed equally.
Authors and Affiliations
Monash Centre for Health Research and Implementation, 43-51 Kanooka Grove, Clayton, VIC, Australia
Helena Teede, Emily Callander & Joanne Enticott
Monash Partners Academic Health Science Centre, 43-51 Kanooka Grove, Clayton, VIC, Australia
Helena Teede & Alison Johnson
Stroke and Ageing Research, Department of Medicine, School of Clinical Sciences at Monash Health, Monash University, Level 2 Monash University Research, Victorian Heart Hospital, 631 Blackburn Rd, Clayton, VIC, Australia
Dominique A. Cadilhac, Tara Purvis & Monique F. Kilkenny
Stroke Theme, The Florey Institute of Neuroscience and Mental Health, University of Melbourne, Heidelberg, VIC, Australia
Dominique A. Cadilhac, Monique F. Kilkenny & Bruce C.V. Campbell
Department of Neurology, Melbourne Brain Centre, Royal Melbourne Hospital, Parkville, VIC, Australia
Bruce C.V. Campbell
Department of Medicine, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia
School of Health Sciences, Heart and Stroke Program, University of Newcastle, Hunter Medical Research Institute, University Drive, Callaghan, NSW, Australia
Coralie English
School of Medicine and Dentistry, Griffith University, Birtinya, QLD, Australia
Rohan S. Grimley
Clinical Excellence Division, Queensland Health, Brisbane, Australia
John Hunter Hospital, Hunter New England Local Health District and University of Newcastle, Sydney, NSW, Australia
Christopher Levi
School of Nursing, Midwifery and Paramedicine, Australian Catholic University, Sydney, NSW, Australia
Sandy Middleton
Nursing Research Institute, St Vincent’s Health Network Sydney and and Australian Catholic University, Sydney, NSW, Australia
Stroke Foundation, Level 7, 461 Bourke St, Melbourne, VIC, Australia
Kelvin Hill
You can also search for this author in PubMed Google Scholar
Contributions
HT: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. DAC: conception, design and initial draft, provided essential literature and case study examples, approved the submitted version. TP: revised the manuscript critically for important intellectual content, approved the submitted version. MFK: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. BC: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. CE: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. AJ: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. EC: revised the manuscript critically for important intellectual content, approved the submitted version. RSG: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. CL: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. SM: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. KH: revised the manuscript critically for important intellectual content, provided essential literature and case study examples, approved the submitted version. JE: conception, design and initial draft, developed the theoretical formalism for learning health system framework, approved the submitted version. All authors read and approved the final manuscript.
Authors’ Twitter handles
@HelenaTeede
@DominiqueCad
@Coralie_English
@EmilyCallander
@EnticottJo
Corresponding authors
Correspondence to Helena Teede or Dominique A. Cadilhac .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Teede, H., Cadilhac, D.A., Purvis, T. et al. Learning together for better health using an evidence-based Learning Health System framework: a case study in stroke. BMC Med 22 , 198 (2024). https://doi.org/10.1186/s12916-024-03416-w
Download citation
Received : 23 July 2023
Accepted : 30 April 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12916-024-03416-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Evidence-based medicine
- Person-centred care
- Models of care
- Healthcare improvement
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Blog The Education Hub
https://educationhub.blog.gov.uk/2024/05/13/before-and-after-school-childcare-what-is-wraparound-childcare/
Wraparound childcare: Everything you need to know about before and after school childcare

We’re supporting working families through the UK government’s biggest ever investment in childcare, to make it more affordable, available and flexible.
As part of this announcement, we’re expanding wraparound care for primary school children across England by increasing the number of places available, to support working families.
But what exactly is wraparound childcare? We explain everything you need to know, from what it is to how you can access it.
What is wraparound childcare?
Wraparound childcare is before and after school care for primary school aged children in England during term time, such as and regular afterschool provision that runs until 6pm or later.
The childcare should be available every school day outside of regular school hours and is aimed at helping parents access more childcare and work the hours they want to.
This is different from out-of-school activities, or school clubs, which are less frequent and can be a one-off activity.
Around 60 percent of primary schools across England offer wraparound childcare, both before and after school.
Private, voluntary, and independent providers, including childminders and early years settings, are also able to offer wraparound childcare. Often, it’s run on a school site or another setting in the local area.
How do I find wraparound childcare near me?
Parents looking for childcare options for their primary school child should speak to their child’s school or the Family Information Service run by their local authority to find out what wraparound childcare is currently available in the area.
From September 2024, parents can expect to see an increase in the number of wraparound childcare places available across the country.
We expect all parents who need it to have access to wraparound childcare, either from their school or from another provider in their local area, by September 2026.
We encourage parents to talk to their child’s school or the Family Information Service in their local authority about their need for wraparound childcare, even if it’s not currently available.
Who will be eligible for wraparound childcare?
Our ambition is that all parents in England with primary school aged children will be able to access wraparound care in their local area by September 2026.
How much will it cost and is financial support available ?
Providers will set their own fees for wraparound places, so prices will vary.
Parents will pay their wraparound childcare provider directly for their child’s place.
Parents eligible for Tax-Free Childcare or Universal Credit Childcare will be able to use the support to help pay for wraparound care.
Tax-Free Childcare could save eligible parents up to £2,000 per year for children aged up to 11, or £4,000 per year for children aged up to 17 with disabilities.
Universal Credit Childcare could save eligible parents up to 85% of their childcare costs for children aged up to 16.
To check if you are eligible for Tax-Free Childcare or Universal Credit Childcare, visit the Childcare Choices website.
What if wraparound childcare is not available in my area ?
If you live in England you can request that your child’s school consider setting up wraparound childcare for your child if they don’t already provide it.
You should write to your child’s school by letter or e-mail and include when you most need wraparound childcare, detailing the days and times you need it. The school will get back to you with a decision within a school-term.
How are we supporting local authorities to deliver the wraparound childcare expansion?
To make more available wraparound care possible, local authorities will receive a share of £289 million to help map out and accommodate the needs of parents in their area.
They will also be able to use the funds to test different ways to increase their wraparound options, including working with local private providers or partnering with schools.
We’re also giving local authorities a share of a further £100 million to ensure childcare settings in the area – including both early years and wraparound settings – have enough physical space to roll out the programme from next year.
What else are we doing to improve access to childcare for under 5s for working parents ?
We’re doubling the amount we are investing in childcare over the next few years from around £4 billion to around £8 billion each year.
As part of this investment, by September 2025, working parents will be able to claim 30 hours childcare a week, over 38 weeks of the year, all the way through from nine months up to their child starting school.
Nurseries are also set to receive a £204 million cash boost which they can use to ease cost pressures such as staffing costs, training and bills.
You can read more about how we’re investing in childcare in England on the Education Hub .
You may also be interested in:
- Thousands of parents of two-year-olds benefit from 15 hours free childcare - here's how
- Free childcare: How we are tackling the cost of childcare
- How to apply for 30 hours free childcare and find out if you’re eligible
Tags: After school childcare , Before school childcare , Breakfast Clubs , Childcare , What is wraparound care , What is wraparound childcare , Wraparound care , wraparound childcare
Sharing and comments
Share this page, related content and links, about the education hub.
The Education Hub is a site for parents, pupils, education professionals and the media that captures all you need to know about the education system. You’ll find accessible, straightforward information on popular topics, Q&As, interviews, case studies, and more.
Please note that for media enquiries, journalists should call our central Newsdesk on 020 7783 8300. This media-only line operates from Monday to Friday, 8am to 7pm. Outside of these hours the number will divert to the duty media officer.
Members of the public should call our general enquiries line on 0370 000 2288.
Sign up and manage updates
Follow us on social media, search by date, comments and moderation policy.
- Share on twitter
- Share on facebook
Education research funding shortfall exposed by learned societies
Royal society and british academy back increase in education research spending after study reveals funding gap compared to health.
- Share on linkedin
- Share on mail

Education research in UK universities requires a “significant uplift” as it is significantly lagging behind other sectors, a joint report by the British Academy and Royal Society has recommended.
While health research accounts for 1.7 per cent of all spending on public health in Britain, education research represents only 0.05 per cent of funds invested in education, explains the study published on 21 May.
Put differently, that means just £1 in every £2,000 spent on education goes on research, whereas the equivalent sum for £2,000 of health spending is £34.
Overall, universities receive about £55 million annually via the Research Excellence Framework to undertake education research, which, according to the report, was described by a sub-panel for REF 2021 as “a very small amount in the context of annual public spending on education”.
Education research received about £22.7 million in charity and industry donations in 2021-22, the paper adds, comparing this sum with the £1.4 billion received by health research from these sectors in the same year.
“The comparison made to health here is not to suggest that educational research spending should match that in the health sector in absolute terms, nor that one is necessarily more important than the other,” says the report, titled ‘ Investing in a 21st century educational research system ’
“But there is an argument that, as a vital public service, investment in education research should be in line with health research as a proportion of overall health spending,” it continues.
The policy briefing – the culmination of longstanding collaboration between the British Academy and the Royal Society – recommends that “government should increase funding for educational research, bringing it into line with other important public service research funding”.
It also calls on research funders to include more long-term research funding opportunities and support for underrepresented and emerging research themes to provide deeper insight into important questions and into the effectiveness of policy changes.
Noting a lack of longitudinal research, the report observes that two thirds of grants awarded by research councils between 2010 and 2020 were for less than three years.
Ulrike Tillmann, chair of the Royal Society’s education committee, said that “if the UK is to become a science superpower, we need to understand better the long-term effects of education”.
“We can no longer rely solely on short-term evaluation and learning gains – we need forward-thinking research that looks at the enduring impact of education on an individual’s lifelong growth to build a healthier education system that benefits us all,” he added.
Register to continue
Why register?
- Registration is free and only takes a moment
- Once registered, you can read 3 articles a month
- Sign up for our newsletter
Or subscribe for unlimited access to:
- Unlimited access to news, views, insights & reviews
- Digital editions
- Digital access to THE’s university and college rankings analysis
Already registered or a current subscriber? Login
Related articles

Education research should be central to the academy. Why isn’t it?
Our report suggests the discipline is struggling in the UK amid low funding and methodological clashes, say four academics

Black academics ‘give up’ on UKRI research funding
Number of black principal investigators applying to UK research councils halves year-on-year

China research at ‘crisis point’, Australian scholars warn
No projects are funded because nobody has the expertise to appraise them, letter claims

Charity’s ‘alarm’ over heart disease research funding shortfall
British Heart Foundation says cardiovascular disease research faces shortfall of more than £250 million to 2035

Mixed reaction to Australian research and development review
We should improve the system while we’re examining it, critics argue
Featured jobs
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Adverse Childhood Experiences
- Risk and Protective Factors
- Program: Essentials for Childhood: Preventing Adverse Childhood Experiences through Data to Action
- Adverse childhood experiences can have long-term impacts on health, opportunity and well-being.
- Adverse childhood experiences are common and some groups experience them more than others.

What are adverse childhood experiences?
Adverse childhood experiences, or ACEs, are potentially traumatic events that occur in childhood (0-17 years). Examples include: 1
- Experiencing violence, abuse, or neglect.
- Witnessing violence in the home or community.
- Having a family member attempt or die by suicide.
Also included are aspects of the child’s environment that can undermine their sense of safety, stability, and bonding. Examples can include growing up in a household with: 1
- Substance use problems.
- Mental health problems.
- Instability due to parental separation.
- Instability due to household members being in jail or prison.
The examples above are not a complete list of adverse experiences. Many other traumatic experiences could impact health and well-being. This can include not having enough food to eat, experiencing homelessness or unstable housing, or experiencing discrimination. 2 3 4 5 6
Quick facts and stats
ACEs are common. About 64% of adults in the United States reported they had experienced at least one type of ACE before age 18. Nearly one in six (17.3%) adults reported they had experienced four or more types of ACEs. 7
Preventing ACEs could potentially reduce many health conditions. Estimates show up to 1.9 million heart disease cases and 21 million depression cases potentially could have been avoided by preventing ACEs. 1
Some people are at greater risk of experiencing one or more ACEs than others. While all children are at risk of ACEs, numerous studies show inequities in such experiences. These inequalities are linked to the historical, social, and economic environments in which some families live. 5 6 ACEs were highest among females, non-Hispanic American Indian or Alaska Native adults, and adults who are unemployed or unable to work. 7
ACEs are costly. ACEs-related health consequences cost an estimated economic burden of $748 billion annually in Bermuda, Canada, and the United States. 8
ACEs can have lasting effects on health and well-being in childhood and life opportunities well into adulthood. 9 Life opportunities include things like education and job potential. These experiences can increase the risks of injury, sexually transmitted infections, and involvement in sex trafficking. They can also increase risks for maternal and child health problems including teen pregnancy, pregnancy complications, and fetal death. Also included are a range of chronic diseases and leading causes of death, such as cancer, diabetes, heart disease, and suicide. 1 10 11 12 13 14 15 16 17
ACEs and associated social determinants of health, such as living in under-resourced or racially segregated neighborhoods, can cause toxic stress. Toxic stress, or extended or prolonged stress, from ACEs can negatively affect children’s brain development, immune systems, and stress-response systems. These changes can affect children’s attention, decision-making, and learning. 18
Children growing up with toxic stress may have difficulty forming healthy and stable relationships. They may also have unstable work histories as adults and struggle with finances, jobs, and depression throughout life. 18 These effects can also be passed on to their own children. 19 20 21 Some children may face further exposure to toxic stress from historical and ongoing traumas. These historical and ongoing traumas refer to experiences of racial discrimination or the impacts of poverty resulting from limited educational and economic opportunities. 1 6
Adverse childhood experiences can be prevented. Certain factors may increase or decrease the risk of experiencing adverse childhood experiences.
Preventing adverse childhood experiences requires understanding and addressing the factors that put people at risk for or protect them from violence.
Creating safe, stable, nurturing relationships and environments for all children can prevent ACEs and help all children reach their full potential. We all have a role to play.
- Merrick MT, Ford DC, Ports KA, et al. Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. MMWR Morb Mortal Wkly Rep 2019;68:999-1005. DOI: http://dx.doi.org/10.15585/mmwr.mm6844e1 .
- Cain KS, Meyer SC, Cummer E, Patel KK, Casacchia NJ, Montez K, Palakshappa D, Brown CL. Association of Food Insecurity with Mental Health Outcomes in Parents and Children. Science Direct. 2022; 22:7; 1105-1114. DOI: https://doi.org/10.1016/j.acap.2022.04.010 .
- Smith-Grant J, Kilmer G, Brener N, Robin L, Underwood M. Risk Behaviors and Experiences Among Youth Experiencing Homelessness—Youth Risk Behavior Survey, 23 U.S. States and 11 Local School Districts. Journal of Community Health. 2022; 47: 324-333.
- Experiencing discrimination: Early Childhood Adversity, Toxic Stress, and the Impacts of Racism on the Foundations of Health | Annual Review of Public Health ( annualreviews.org).
- Sedlak A, Mettenburg J, Basena M, et al. Fourth national incidence study of child abuse and neglect (NIS-4): Report to Congress. Executive Summary. Washington, DC: U.S. Department of Health an Human Services, Administration for Children and Families.; 2010.
- Font S, Maguire-Jack K. Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse Negl. 2016;51:390-399.
- Swedo EA, Aslam MV, Dahlberg LL, et al. Prevalence of Adverse Childhood Experiences Among U.S. Adults — Behavioral Risk Factor Surveillance System, 2011–2020. MMWR Morb Mortal Wkly Rep 2023;72:707–715. DOI: http://dx.doi.org/10.15585/mmwr.mm7226a2 .
- Bellis, MA, et al. Life Course Health Consequences and Associated Annual Costs of Adverse Childhood Experiences Across Europe and North America: A Systematic Review and Meta-Analysis. Lancet Public Health 2019.
- Adverse Childhood Experiences During the COVID-19 Pandemic and Associations with Poor Mental Health and Suicidal Behaviors Among High School Students — Adolescent Behaviors and Experiences Survey, United States, January–June 2021 | MMWR
- Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics. 2004 Feb;113(2):320-7.
- Miller ES, Fleming O, Ekpe EE, Grobman WA, Heard-Garris N. Association Between Adverse Childhood Experiences and Adverse Pregnancy Outcomes. Obstetrics & Gynecology . 2021;138(5):770-776. https://doi.org/10.1097/AOG.0000000000004570 .
- Sulaiman S, Premji SS, Tavangar F, et al. Total Adverse Childhood Experiences and Preterm Birth: A Systematic Review. Matern Child Health J . 2021;25(10):1581-1594. https://doi.org/10.1007/s10995-021-03176-6 .
- Ciciolla L, Shreffler KM, Tiemeyer S. Maternal Childhood Adversity as a Risk for Perinatal Complications and NICU Hospitalization. Journal of Pediatric Psychology . 2021;46(7):801-813. https://doi.org/10.1093/jpepsy/jsab027 .
- Mersky JP, Lee CP. Adverse childhood experiences and poor birth outcomes in a diverse, low-income sample. BMC pregnancy and childbirth. 2019;19(1). https://doi.org/10.1186/s12884-019-2560-8.
- Reid JA, Baglivio MT, Piquero AR, Greenwald MA, Epps N. No youth left behind to human trafficking: Exploring profiles of risk. American journal of orthopsychiatry. 2019;89(6):704.
- Diamond-Welch B, Kosloski AE. Adverse childhood experiences and propensity to participate in the commercialized sex market. Child Abuse & Neglect. 2020 Jun 1;104:104468.
- Shonkoff, J. P., Garner, A. S., Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. https://doi.org/10.1542/peds.2011-2663
- Narayan AJ, Kalstabakken AW, Labella MH, Nerenberg LS, Monn AR, Masten AS. Intergenerational continuity of adverse childhood experiences in homeless families: unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsych. 2017;87(1):3. https://doi.org/10.1037/ort0000133.
- Schofield TJ, Donnellan MB, Merrick MT, Ports KA, Klevens J, Leeb R. Intergenerational continuity in adverse childhood experiences and rural community environments. Am J Public Health. 2018;108(9):1148-1152. https://doi.org/10.2105/AJPH.2018.304598.
- Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta-analysis. J Adolesc Health. 2013;53(4 Suppl):S32-38. https://doi.org/10.1016/j.jadohealth.2013.05.004 .
Adverse Childhood Experiences (ACEs)
ACEs can have a tremendous impact on lifelong health and opportunity. CDC works to understand ACEs and prevent them.

IMAGES
VIDEO
COMMENTS
A series of case studies can be found in the Related documents section below. Further case studies will be published in due course. To help ensure health and care services are built around the needs of people in their own communities, the NHS Five Year Forward View asked local providers, commissioners and other partners in the health and care ...
Case studies deemed to meet the 4th and 5th criteria may be escalated to NHSE library leads for awareness with impact vignettes created for use. Go to the review team quality checklist. Contact the Knowledge for Healthcare team on [email protected] for the quality checklist in an accessible format.
Health Education England NHS England Health literacy toolkit Case studies Prepared by Health Education England, NHS England, Public Health England, and the Community Health and Learning Foundation . Health literacy toolkit: case studies *Names and identifying details have been changed to protect individuals' identity 2
Submit an impact case study. Frequently asked questions. Impact case studies help share best practice and learnings from across the NHS. Health librarians and knowledge specialists, working closely with staff and organisations within the NHS and wider health sector, bring tangible benefits, including: savings in time. costs.
The Children & Young People's Health Partnership: Full LHS . 7 . The Secure Anonymised Information Linkage (SAIL) Databank: Data . 8 . Informatics Consult: Data . 9 . Towards a national learning health system for asthma in Scotland: Data . 10 . Reducing the health burden of diabetes with artificial intelligence-powered clinical decision tools ...
The project fulfils the ethos of the Health Education Mandate (2015/16), Health Education North West Strategic Plan (2015/16), Francis Report (2013), Keogh Review (2013), Willis Report (2012), Berwick Report (2013), Cavendish Review (2013) and NHS 5 Year Plan. These reports all highlight the need to develop a workforce fit for
Over 350 case studies have been collected by Health Education England's National Knowledge and Library Service team. These provide an important addition to the evidence base around the impact of knowledge and library specialists. Many of these case studies detail the impacts of specific instances of evidence search provision (Citation 8). As ...
Children's education, health, and welfare are at the heart of coherent policies and ... This case study is confined to the country of England, the largest of the four countries in the United Kingdom. ... International Case Studies of Innovative Early Childhood Systems: England . Part 1 Introduction . 1. e. Finland Australia.
On behalf of Health Education England and as part of a Senior Leadership Programme, a group of health library and knowledge specialists across England worked together on a shared project exploring how evidence is used in the creation and review of information for patients. The project titled, 'Making the case: evidence-based patient ...
Case Study | Healthcare Health Education England Technology Enhanced Learning (HEE TEL) provides over 500 elearning programmes to the healthcare workforce in England with its elearning for healthcare (elfh) offering. Insight mapped HEE TEL's processes and created detailed job role personas for hosting its elearning infrastructure, designing
The development of impact case studies has become the most powerful means of demonstrating the impact and value of services across England. Library and knowledge staff are encouraged to submit case studies to a national repository managed by the HEE team, with over 350 accepted to date. ... Health Education England, (2019b), ...
Case studies Antimicrobial Stewardship for Pharmacy Staff - case study. The Royal Pharmaceutical Society supported key pharmacists within NHS Trusts and Sustainability and Transformation Partnerships (STPs) to develop the skills and behaviours to become effective antimicrobial clinicians, leaders and mentors via a pilot training programme in London and the south east of England.
Health Education England Share. X Linkedin Email Facebook Facebook Messenger ... Case Studies Team About Company Details ...
Case Studies. User research about expert NHS searchers for Health Education England. User research; We were asked by Health Education England (HEE) to conduct some research on the user needs of highly skilled information searchers, or expert searchers, in the NHS.
We were asked by Health Education England (HEE) to conduct a programme of research with users of NHS library and knowledge services. Health Education England were considering options to provide new national services to support or replace the multitude of local tools, platforms and methods used by NHS staff to find and use evidence and information.
The following case studies support the Implementation guidance: Perinatal Pelvic Health Services.. Case study 1: South East London - Engagement with diverse groups. South East London PPHS engaged with diverse groups in the local community to increase awareness of pelvic health conditions and offer women knowledge, skills and confidence to manage their pelvic health in the perinatal period.
Background In the context of expanding digital health tools, the health system is ready for Learning Health System (LHS) models. These models, with proper governance and stakeholder engagement, enable the integration of digital infrastructure to provide feedback to all relevant parties including clinicians and consumers on performance against best practice standards, as well as fostering ...
mediaofficer, 16 May 2024 - Relationships and Sex Education. Relationships, Sex and Heath Education (RSHE) is a subject taught at both primary and secondary school. In 2020, Relationships and Sex Education was made compulsory for all secondary school pupils in England, and Health Education compulsory for all pupils in state-funded schools.
The Education Hub is a site for parents, pupils, education professionals and the media that captures all you need to know about the education system. ... You can read more about how we're investing in childcare in England on the Education Hub. ... straightforward information on popular topics, Q&As, interviews, case studies, and more. Please ...
Overall, universities receive about £55 million annually via the Research Excellence Framework to undertake education research, which, according to the report, was described by a sub-panel for REF 2021 as "a very small amount in the context of annual public spending on education". Education research received about £22.7 million in charity ...
Educating health care providers and changing treatment practices. To prevent antibiotic-resistance gonorrhea, health care providers should update their treatment practices to be consistent with CDC's current STI Treatment Guidelines, 2021).Previous evaluations show that health care providers are aware of when CDC publishes new STD treatment guidelines and update their practices as needed. 3 4 ...
Health Education England Graduate and Student Placement Scheme: Case studies from current graduates and placement students 6 Joe Lemmens HR and OD Placement Student Started at HEE in September 2020 A little bit about me and my university studies… Hi there! My name is Joe and I am from Liverpool. I have completed two years at
Quick facts and stats. ACEs are common. About 64% of adults in the United States reported they had experienced at least one type of ACE before age 18. Nearly one in six (17.3%) adults reported they had experienced four or more types of ACEs. Preventing ACEs could potentially reduce many health conditions.