- Quick Links
- Make An Appointment
- Our Services
- Price Estimate
- Price Transparency
- Pay Your Bill
- Patient Experience
- Careers at UH

Schedule an appointment today

Vaginoplasty: Male to Female (MTF) Genital Reconstructive Surgery
What is vaginoplasty.
Vaginoplasty is a surgical procedure during which surgeons remove the penis and testicles and create a functional vagina. This achieves resolution of gender dysphoria and allows for sexual activity with compatible genitalia. The highly sensitive skin and tissues from the penis are preserved and used to construct the vaginal lining and build a clitoris, resulting in genitals with appropriate sensations. Scrotal skin is used to increase the depth of the vaginal canal. Penile, scrotal and groin skin are refashioned to make the labia majora and minora, and the urethral opening is relocated to an appropriate female position. The final result is an anatomically congruent, aesthetically appealing, and functionally intact vagina. Unless there is a medical reason to do so, the prostate gland is not removed.
University Hospitals has the only reconstructive urology program in the region offering MTF vaginoplasty and other genital gender affirmation surgical procedures. Call 216-844-3009 to schedule a consultation.
Penile Inversion Technique for Vaginoplasty
Penile inversion is the most common type of vaginoplasty and is considered the gold standard for male to female genital reconstruction. This type of gender affirmation surgery can last from two to five hours and is performed with the patient under general anesthesia.
The skin is removed from the penis and inverted to form a pouch which is then inserted into the vaginal cavity created between the urethra and rectum. The urethra is partially removed, shortened and repositioned. Labia majora and labia minora (outer and inner lips), and a clitoris are created. After everything has been sutured in place, a catheter is inserted into the urethra and the area is bandaged. The bandages and catheter will typically remain in place for four to five days. For some patients, a shallow depth vaginoplasty is recommended. This allows for a functional vagina but removes the need for vaginal dilation and douching.
Outcomes after vaginoplasty are excellent, and patients can expect to have aesthetic outcomes and sexual functionality similar to that for cis-women (people that were assigned female sex characteristics at birth and identify as female).
Complications after vaginoplasty are rare, but patients are advised to talk to their doctor about postsurgical risks and how to best manage them.
Things to Consider Before Having a Penile Inversion Vaginoplasty
- Given that the skin used to construct the new vaginal lining may have abundant hair follicles, patients are recommended to undergo hair removal (either electrolysis or laser hair removal) prior to the vaginoplasty procedure to eliminate the potential for vaginal hair growth. A full course of hair removal can take several months.
- Patients with fertility concerns should talk to their doctor about ways to save and preserve their sperm before having a vaginoplasty.
- It is always recommended that patients talk with a therapist in the months leading up to surgery to ensure they are mentally prepared for the transition.
- In accordance with the World Professional Association of Transgender Health (WPATH) standards of care, patients are required be on appropriate cross-gender hormone therapy for a year, live in the gender-congruent role for a year, and have 2 mental health letters endorsing their suitability for surgery.
Postoperative Care of Your New Vagina
To ensure that your newly constructed vagina maintains the desired depth and width, your UH surgeon will give you a vaginal dilator to begin using as soon as the bandages are removed. Use the dilator regularly according to your surgeon’s recommendations. This will usually involve inserting the device for ten minutes several times per day for the first three months. After that, once per day for three months followed by two to three times a week until a full year has passed.
Furthermore, regular douching and cleaning of the vagina is recommended. Your surgeon will give you general guidelines for this as well. Approximately 1 out of 10 people who have a vaginoplasty end up requiring a second, minor surgery to correct some of the scarring from the first surgery and improve the function and cosmetic appearance.
Most genital gender affirmation surgeries are covered by insurance. In cases where they are not, your surgeon’s office will guide you through the self-pay options.
- Healthcare Services
- Find a Doctor
- Patient Portal
- Research and Education

Your recent searches
- Find a Location
- Nursing Careers
- Physical Therapy Careers
- Medical Education
- Research & Innovation
- Pay My Bill
- Billing & Insurance Questions
- For Healthcare Professionals
- News & Publications
- Classes & Events
- Philanthropy
Gender Affirmation Surgery
Browse this page

If you’re transgender, you may pursue hormone therapy or gender reassignment surgery to help align your body with your gender identity. Some transgender individuals also choose to pursue surgery to help reduce or enhance secondary sexual characteristics. For transgender men, this may include surgery to reduce breast size or remove the ovaries. Transgender women may elect for breast augmentation or facial feminization surgery to meet their needs. At MedStar Health, we offer the following procedures to help you be comfortable in your own skin. Types of gender reassignment surgery:
Feminizing vaginoplasty : Reconstructive surgery procedure that alters the structure of the genitals to create a vagina using penile or colon tissue. Dr. Del Corral uses a one-stage procedure, revisions can be necessary to enhance the final surgical result
Revision vaginoplasty (after loss of depth) : A secondary procedure allowing for revisions to the urethra, neovaginal canal, labia minora, and majora addressing asymmetries within the vagina, and scar revisions to help functionality. MedStar Center for Gender Affirmation specializes in revisional procedures after complications from primary vaginoplasty
Colon vaginoplasty : A different approach to an original vaginoplasty. The colon or small bowel can be used to line the vaginal wall to create depth, dilation, and providing a natural source of lubrication. At the MedStar Center for Gender Affirmation, we use a robotic-assisted approach to minimize incisions in the abdomen, and faster recovery while providing better access for the revision
Masculinizing phalloplasty/scrotoplasty : Reconstructive surgery that creates a penis using a free flap or pedicled flap of skin. These sections of the skin can be taken from the arm (radial forearm free-flap, RFF) or thigh (anterior lateral thigh pedicled flap phalloplasty, ALT). These procedures are performed in a combined team that include a reconstructive urologist and plastic surgeons
Metoidioplasty : The use of local tissue to create an enlargement to the penile area (clitoral release/enlargement, may include urethral lengthening)
Masculinizing chest surgery (“top” surgery) : Breast tissue is removed and the nipples and areolae are altered to help masculinize the chest
Facial feminization : Reconstructive surgery procedures that alters the shape and size of facial features to make them closer to typical female facial features — this may include a brow lift, forehead re-contouring, hairline correction, and rhinoplasty (nose reshaping)
Facial masculinization : Reconstructive surgery that alters the shape and size of facial features to make them more masculine — this may include forehead lengthening and augmentation, cheek augmentation, chin re-contouring, jaw contouring, thyroid cartilage enhancement (Adam’s apple surgery), and rhinoplasty (nose reshaping)
Reduction thyrochondroplasty (thyroid cartilage shave) : Reconstructive surgery that reduces the size of the thyroid cartilage, also known as the “Adam’s apple.” It is shaved down to create a more feminine appearance
Breast augmentation mammoplasty : Surgery to reshape, enlarge, and modify the breasts and achieve a more desired shape and look to the chest
Hysterectomy with bilateral salpingo-oophorectomy : Surgical removal of the uterus, cervix, ovaries, fallopian tubes, and surrounding structures
Orchiectomy : Reconstructive surgery to remove the testicles
Vaginectomy : Reconstructive surgery to remove all parts of the vagina
Gender surgery planning and recovery
What to expect.
You may need to meet a few requirements before qualifying for certain gender affirming procedure(s) at MedStar Health. The exact requirements will depend on your insurance coverage and may include one or more letters of referral from qualified mental health professionals, well-documented gender dysphoria, and/or one year of continuous hormone therapy. Procedures that are considered strictly cosmetic by your insurance plan will have fewer requirements.
After properly qualifying for surgery, you’ll meet with one of our surgeons. They will examine you and ask questions to determine if you physically qualify for surgery. If you qualify, you’ll discuss any risks and potential complications and walk through the steps involved. You’ll be given specific instructions to follow prior to your surgery.
On the day of surgery, your surgeon may use a variety of leading-edge techniques to achieve the best results, such as minimally invasive surgery to significantly reduce scarring.
Recovery from surgery
It’s important to follow your surgeon’s instructions for proper care of your body after surgery. You may have specific directions about taking medications and how to clean and care for the surgical site. Healing may take several weeks as swelling decreases.
Why choose us?
MedStar Health is the largest health care system in Maryland and the Washington, D.C., region. When you choose us for care, you’ll have access to our network of 10 hospitals and a team of more than 3,000 physicians and specialists.
If you choose MedStar Health for a breast augmentation or reduction procedure, you’ll be choosing to work with a nationally recognized leader in breast surgeries. Our breast surgeons have years of experience working exclusively in breast procedures and have developed their own techniques to help patients recover faster and have better results.
Our providers
Location: Change location Enter your location
Gabriel Alfonso Del Corral, MD
Microvascular Plastic Surgery, Gender Surgery, Reconstructive Plastic Surgery & Plastic Surgery
Laura Kate Tom, MD
Microvascular Plastic Surgery, Breast Surgery & Plastic Surgery
Our locations
Distance from Change location Enter your location
MedStar Health: Plastic Surgery at MedStar Washington Hospital Center
106 Irving St. NW POB North Ste. 3400 Washington, D.C., 20010
MedStar Franklin Square Medical Center
9000 Franklin Square Dr. Baltimore, MD 21237
Frequently asked questions
Do I need a referral?
If you’re exploring options for insurance coverage, you may need to request a referral from your primary care doctor, depending on your health insurance plan. Check with your carrier to see if medical coverage is an option for you and, if so, whether a referral is required.
How should I prepare?
Before surgery, you may be asked to get blood tests and take or adjust medications — this may include temporarily stopping hormone therapy. If you smoke, quitting will help you heal faster and avoid possible complications. You’ll also need to arrange for transportation to and from the hospital and for someone to stay with you the night after the surgery.
For more information visit Patient Resources or Preparing for Surgery
Dr. Gabriel Del Corral's Philosophy of Care

MedStar Center for Gender Affirmation: Vaginoplasty

Related services
Gender Health Services
We provide affirming, inclusive healthcare for adult transgender patients. Your goals and needs take center stage.
To help make your healthcare experience as positive as possible, we commit to:
- Listen first
- Remove barriers to your care
- Treat you with dignity and respect
- Make your well-being our top priority
UVA providers follow the clinical practice guidelines from the Endocrine Society . We've earned recognition from the Human Rights Campaign Foundation for our support of LGBTQ patients .
Gender Health Services at UVA
At UVA, we strive to offer the full spectrum of healthcare for our transgender patients. From primary care to gender-confirming surgery, from voice therapy to mental health services, we’re here to remove barriers from your care. View gender services transcript.
Gender Health & Transgender Health at UVA
We have skill and experience caring for patients who are transgender, nonbinary, intersex, genderfluid, and asexual. Gender-inclusive services include:
- Primary care
- Hormone therapy
- Mental health
- Voice therapy
- Gender-confirmation surgery
Surgical options include facial plastic surgery, procedures for trans men , and procedures for trans women .

Transgender Health Clinic
Find trans-friendly doctors providing hormone therapy, urological care, primary healthcare. Legal and wellness support also offered.
Transgender Support: Navigating the Experience
UVA Health strongly supports the LGBTQ community. We provide gender-affirming care, services, and support for patients going through gender transition. UVA Health doesn't discriminate, exclude, or treat differently patients or visitors based on their race, age, color, national origin, religion, disability, sexual orientation, gender, gender identity, or gender expression.
UVA Health is a community of healing, compassion, inclusion, and respect for all. Discrimination and prejudice have no place here. See our non-discrimination policy .
Find Local Transgender Support
From our family medicine and mental health providers, you can access:
- Family education and support
- Guidance on name and gender-marker changes on legal documents
- Financial advice about uncovered medical treatment
- A list of therapists who can write letters recommending hormone therapy
- Information about using and obtaining prosthetics, binders, other elements of gender expression
- A review of possible medical and surgical treatments and surgical referrals
Community Resources & Transgender Support
Find LGBTQ-friendly support:
- Transgender Health Alliance of Central Virginia
- UVA LGBTQ Center
- Transgender Health Services at the Virginia Department of Health

Support for Youth & Young Adults
Along with basic primary care, we provide therapy, family education, puberty blockers, more.
Make an Appointment

Unsurpassed Expertise, Quality, & Care

University of Virginia Plastic Surgery 1300 Jefferson Park Avenue 4th Floor Charlottesville, VA 22908 Phone: (434) 924-1234 Location Hours: Monday–Friday | 8 a.m.–5 p.m.
- Transgender Surgery
Individuals from Richmond and Roanoke, Virginia, and surrounding areas considering transgender surgery procedures, including female-to-male and male-to-female top and bottom surgery, choose UVA Plastic Surgery in Charlottesville, one of the leading providers of gender-confirming procedures in the region. Dr. John Stranix is a trusted plastic surgeon who combines exceptional surgical talent with an inclusive and compassionate demeanor to make your transition go as smoothly as possible.
Dr. Stranix is carrying on the legacy of the late Dr. Milton Edgerton, who established UVA Plastic Surgery and was one of a handful of pioneers in the field of transgender surgery.
How Is Gender Confirmation Surgery Performed?
Transgender surgical procedures include top surgery, bottom surgery, and facial plastic surgery. Each procedure involves specific techniques designed to help patients feel more comfortable physically by creating results that more closely resemble their identified gender.
What Is Top Surgery?
Top surgery directly addresses the chest’s appearance. Dr. Stranix customizes these surgical procedures based on the patient’s goals.
Male to Female (MTF)
MTF procedures use implants to create larger, more feminine breasts. In some cases, fat grafting can also help enhance the look and feel of the results or may be used as the primary method of augmentation alone. As with all breast augmentation procedures, the MTF top surgery can be customized based on the patient’s preferences. Many patients choose implants filled with silicone gel because they look and feel more like natural breasts than saline implants. Saline implants are also more prone to visible rippling. Dr. Stranix also offers autologous breast reconstruction for gender confirmation using tissue from the patient’s lower abdomen in a procedure referred to as a DIEP free flap. It is a technique often used for breast reconstruction .
During your initial consultation, Dr. Stranix discusses the details of each procedure, including the surgical technique, your breast implant options, and what to expect during the recovery.
Chest Feminization Before & After Photos
This feature contains nudity. Please click OK to confirm you are at least 18 years of age and are not offended by such material.
Chest Feminization Before & After Photos

Breast Augmentation with Fat Grafting
View Case Details
View All Cases
Keep in mind that each patient is unique and your results may vary.
Female to Male (FTM)
Creating a flatter chest involves removing breast tissue and, in many cases, reducing the size of the areolas and changing their position so they appear more masculine. The size of the patient’s breasts and the amount of skin, along with the size and position of the areolas, influence the specific surgical technique used during FTM top surgery.
A less invasive periareolar approach may be appropriate for patients with smaller breasts. This technique uses liposuction to remove breast tissue from behind the nipple and is often combined with an incision around the areola to reduce the areolar size.
For most patients with moderate to large breast volumes, Dr. Stranix utilizes the “double incision” technique. This method involves incisions above and below the areola along the inferior (lower) pole of the breast. This is designed so that the final incision follows the inferior border of the pectoralis major muscle—the most defining characteristic of a male chest. The nipple/areola are removed and then replaced in the appropriate position and size as free grafts after removal of all glandular breast tissue and excess chest skin. Liposuction may also be used as an adjunct in some cases as needed to optimize the result.
In both MTF and FTM top procedures, as with breast augmentation and breast reduction surgeries, Dr. Stranix tailors the surgical approach to provide the desired results while minimizing the appearance of scars. He provides detailed post-operative instructions for both MTF and FTM top procedures.
Chest Masculinization Before & After Photos
Chest masculinization before & after photos.

Chest Masculinization, Grade III Ptosis: Double incision with free nipple grafting

CHEST MASCULINIZATION: Double incision with free nipple grafting
Chest masculinization: circumareolar approach, chest masculinization: double incision without nipple reconstruction, chest masculinization, grade i ptosis: double incision with free nipple grafting, chest masculinization: double incision with free nipple grafting, what is bottom surgery.
Male-to-female and female-to-male sex reassignment surgeries use specific techniques to reconstruct patients’ genitalia to match that of their gender identity.
MTF Bottom Surgery
The goal of MTF bottom surgery is to create the most aesthetically appealing and functional vagina possible. Multiple procedures may be needed to reach these goals, including surgery designed to provide vaginal and clitoral sensation. These operations require the expertise of a multidisciplinary team that includes plastic surgery, urology, and sometimes colorectal surgery. Surgical procedures that may be involved in MTF bottom surgery include:
- Penile skin inversion vaginoplasty with or without scrotal skin grafting
- Revision vaginoplasty using small bowel or the rectosigmoid colon
- Secondary genital reconstruction
During a one-on-one consultation, Dr. Stranix explains these procedures in detail and the benefits they offer.
FTM Bottom Surgery
Surgery to create male genitalia can be performed using different techniques and may or may not be combined with a hysterectomy. One technique, called phalloplasty, uses tissue from either the forearm or the thigh to create a phallus and a urethra for standing urination. These procedures are usually performed in 2 stages. Dr. Stranix also performs metoidioplasty, which elongates the existing genital tissue to create a more defined phallus in a single stage.
The details of the procedure, the course of recovery, the expected outcomes, and the possible complications are covered in detail during your surgical consultation.
Facial Plastic Surgery
Your face can quickly communicate your gender identity to others. Dr. Black performs aesthetic procedures to make facial features appear either more feminine or more masculine. Because no single feature makes a face appear feminine or masculine, a range of surgical and nonsurgical approaches can be used to achieve these goals.
Facial Feminization
A feminine face is typically softer and more rounded than a masculine face. Lower face and neck lifts can help create this appearance by repositioning tissue and muscle using incisions made where they will be almost imperceptible. These techniques can produce a thinner, more feminine jawline and an overall heart-shaped facial structure.
Other procedures used for facial feminization include:
- Hairline/scalp modification
- Face lifting
- Facial volume enhancement using fat grafting or filler
- Brow reshaping including frontal bone contouring and frontal sinus setback
- Rhinoplasty
- Upper/lower eyelid surgery (blepharoplasty)
- Laser skin resurfacing
- Lip enhancement
- Laser hair removal
- Mandibular (lower jaw) angle contouring
- Chin setback (genioplasty) and narrowing
Facial Masculinization
A well-defined chin, chiseled jawline, and angular features define the masculine face. Dr. Black tailors his surgical plans based on the needs of each patient, but they usually involve a combination of procedures focused on sculpting the chin, jaw, and cheeks to appear more masculine.
Transgender Surgery FAQ
Is gender reassignment surgery safe.
While there are risks associated with all types of surgery, for optimal safety it’s important to choose a surgeon who specializes in gender confirmation surgery and has performed many of these procedures for a variety of patient needs. Dr. Stranix and his team perform a thorough evaluation to ensure each patient is a good candidate for surgery and minimize risks.
How common is gender reassignment surgery?
Gender reassignment (confirmation) surgery is more common in transgender men (42 to 54%) than transgender women (28%). Top (chest gender confirmation) surgery is performed approximately twice as often as bottom (genital) surgery. In studies that assessed transgender men and women as an aggregate, top surgery accounts for 8 to 25% and bottom surgery at 4 to 13%. Review study details .
How long does it take to transition to another gender?
Gender transitioning is a very personal and variable process that can take many months to many years, depending on the specific steps the individual chooses to take. The process can involve psychological assessment, hormone therapy, and gender reassignment surgery. For patients that decide to have surgery, some have only one surgery and others have a combination.
Can breasts grow back after top surgery?
Breast tissue does not grow back after it is removed. Dr. Stranix leaves some fat behind to create natural-looking chest contours. While this fat can enlarge like fat anywhere on the body, it likely will not take on a feminine appearance.
Are you ready to find out more?
Dr. Stranix, Dr. Black and Samantha Mason, PA-C, see transgender plastic surgery patients from throughout Virginia and as far as Tennessee, West Virginia, and North Carolina who travel to UVA Plastic Surgery for its track record of exceptional results. The experience is a deeply personal one, and our practice is thrilled to expand our services to provide even more opportunities for empowerment through plastic surgery.
To meet with Dr. Stranix or Dr. Black to discuss your options for transgender surgery in Charlottesville, request a consultation using the online form or call (434) 924-1234 to schedule an appointment.
Transgender Surgery Related Blog Posts
Top surgery recovery timeline: a guide for all transitions.
Recovering after top surgery is often an exciting, emotional journey. Whether you are embarking on an MTF or FTM transition (or seeking a nonbinary-affirming procedure), understanding what to expect during each stage of recovery can… Continue Reading
How Does Bottom Surgery Work (FTM): Consultation to Recovery
Embarking on the journey of FTM bottom surgery is more than a physical transformation; it's a deeply personal and profound step toward aligning your body with your true self. How does bottom surgery work for… Continue Reading
What Are Your Options for Male to Female (MTF) and Female to Male (FTM) Top Surgery? INFOGRAPHIC
You and your surgeon have many decisions to make when planning your gender-affirming top surgery One of these is the type of incision that will create the best and safest results from your surgery. Dr.… Continue Reading
- Fellowship-Trained Plastic Surgeon, Brittany J. Behar, MD
- Board-Certified Plastic Surgeon, Jonathan S. Black, MD, FACS
- Board-Certified Plastic Surgeon, Christopher A. Campbell, MD, FACS
- Plastic Surgeon, Brent R. DeGeorge Jr., MD, PhD
- Board-Certified Plastic Surgeon, Thomas J. Gampper, MD, FACS
- Board-Certified Oral Surgeon, Martin A. Hoard, DDS, MD, FACS
- Board-Certified Plastic Surgeon, Scott T. Hollenbeck, MD, FACS
- Plastic & Reconstructive Surgeon, John T. Stranix, MD
- Samantha Mason, PA-C
- Nichole Brooks, PA-C
- Ryan Evans, AGACNP-BC
- Marcelle Zimcosky-Murray, AGACNP-BC
- Breast Augmentation
- Breast Lift
- Breast Reduction
- Fat Grafting
- Male Breast Reduction
- Mommy Makeover
- Liposuction
- Facelift & Neck Lift
- Eyelid Surgery
- Request A Consultation
- Nonsurgical
- BOTOX® Cosmetic
- CoolSculpting®
- Dermal Fillers
- Peels & Facials
- Reconstructive & Clinical
- Breast Reconstruction Center
- Virginia Hand Center
- DeCamp Burn & Wound Healing Center
- Pediatric Plastic Surgery Center
- Migraine Surgery
- Skin Cancer Reconstruction
- Photo Gallery
- UVA Location
- University of Virginia Plastic Surgery, Augusta
- Patient Resources
- Blepharoplasty
- Breast Implants
- Breast Reconstruction
- CoolSculpting
- Mini Tummy Tuck
- Plastic Surgery
- February 2024
- January 2024
- December 2023
- September 2023
- August 2023
- January 2023
- December 2022
- November 2022
- September 2022
- August 2022
- February 2022
- January 2022
- August 2021
- December 2020
- November 2020
- September 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- February 2019
- January 2019
- December 2018
- November 2018
- September 2018
- August 2018
- February 2018
- (434) 924-1234
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Gender Affirmation Surgeries
Featured Expert:

Fan Liang, M.D.
Surgeries are not required for gender affirmation, but many patients choose to undergo one or more surgical procedures. Talk with your doctor to discuss what surgical options may be right for you. The following is an overview of gender affirmation surgeries.
- Penile construction (phalloplasty/metoidioplasty) : This surgical procedure can include removal of the vagina (vaginectomy), reconstruction of the urethra and penile reconstruction. Surgeons may use either vaginal tissue or tissue from another part of the body to construct the penis.
- Vaginal construction (vaginoplasty) : This surgical procedure is a multistage process during which surgeons may remove the penis (penectomy) and the testes (orchiectomy), if still present, and use tissues from the penis to construct the vagina, the clitoris (clitoroplasty) and the labia (labiaplasty).
- Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people.
- Facial gender surgery can include a variety of procedures to create more feminine features , like reshaping the nose; brow lift (or forehead lift); chin, cheek and jaw reshaping; Adam’s apple reduction; lip augmentation; hairline restoration; and earlobe reduction.
- Facial gender surgery can also include a series of procedures to create more masculine features , such as forehead lengthening and augmentation; cheek augmentation; reshaping the nose and chin; jaw augmentation ; and thyroid cartilage enhancement to construct an Adam’s apple.
- Hysterectomy : This surgical procedure includes the removal of the uterus and ovaries (oophorectomy). There are options for oocyte storage and fertility preservation that you may want to discuss with your doctor.
- Some people may combine this procedure with a scrotectomy , which is surgery to remove all or part of the scrotum. For others, the skin of the scrotum can be used in vulvoplasty or vaginoplasty ― the surgical construction of a vulva or vagina.
- The procedure reduces testosterone production and may eliminate the need for continuing therapy with estrogen and androgen-suppressing medications. Your health care practitioner will discuss options such as sperm freezing before orchiectomy that can preserve your ability to become a biological parent.
Recovery After Gender Affirmation Surgeries
Recovery time from a gender affirmation surgery or procedure varies, depending on the procedure. Talk to your doctor about what you can expect.
Treatment Caring for Transgender Patients
Fearing discrimination and hostility, transgender people are often reluctant to seek care. Discover how Paula Neira, Program Director of LGBTQ+ Equity and Education, Johns Hopkins Medicine Office of Diversity, Inclusion and Health Equity, is working to ensure that all patients — regardless of gender identity — are treated with dignity and respect.
Find a Doctor
Specializing In:
- Transgender Health
- Gender Affirmation Surgery
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
Find Additional Treatment Centers at:

Request an Appointment

Gender Affirmation: Do I Need Surgery?

Gender Affirmation Nonsurgical Services

Facial Masculinization Surgery
Related Topics
Do I need a referral to see a specialist? Learn more here . Explore the Department Directory Learn more about Telehealth Appointments Protect Yourself from West Nile Virus
How to schedule your APPOINTMENT at Denver Health: CURRENT PATIENTS: Login to MyChart to schedule appointments or call 303-436-4949 . NEW PATIENTS: Schedule an appointment online or call 303-436-4949 . NEED CARE? Schedule a Virtual Urgent Care appointment or click here to find an Urgent Care clinic .
MyChart Login
Login to MyChart
MyChart for Mobile
Download the MyChart mobile app for access to your healthcare information. Managing your healthcare has never been more simple. Download for iPhone and Android .
MyChart Sign Up
Learn about MyChart features , and sign up for an account .
Virtual Urgent Care Now Available for Denver Health MyChart Users
Denver Health MyChart users can now have a virtual urgent care visit with one of our expert providers. It’s easy and convenient to get the urgent care you need from the comfort of your home, using your smartphone, tablet or computer.
Click here for more details

- Departments & Services
- Conditions & Treatments
- Our Locations
- Find a Provider
- Pharmacy / Prescriptions
- Pay my bill
- Main Campus (303) 436-6000
- Appointments (303) 436-4949
- Lean Academy 855-888-5326
- Nurseline (303) 739-1211
- Pharmacy (303) 389-1390
- Telehealth (303) 436-4949
Contact LGBTQ Patient Navigator
Hours of operation, vaginoplasty.
Learn more about gender affirmation surgery:
Interested in this surgery?
Please complete the following surgical interest form and submit it to our LGBTQ+ Services team.
Surgical Interest Form
Overview of Vaginoplasty
Vaginoplasty is a gender-affirming, feminizing, lower surgery to create a vagina* and vulva (including mons, labia, clitoris, and urethral opening) and remove the penis, scrotal sac and testes.
What is the procedure for vaginoplasty?
- The scrotum and testes are removed.
- The glans is made into a clitoris.
- Space for the vagina is dissected between the bladder and the rectum.
- Skin from the shaft of the penis* is inverted to create the inner walls of your vagina.
- Extra skin may be taken from the scrotum* to line your vagina. The hair roots on the skin graft will be cauterized.
- The urethra is shortened.
- Vulva are created using scrotal and urethral tissue.
- A temporary urinary catheter is inserted into the bladder.
- A temporary prosthesis/stent is inserted in the vagina.
Do I need to have hair removal before vaginoplasty ?
Hair removal is highly encouraged and recommended prior to penile inversion vaginoplasty (full depth vaginoplasty). The scrotal skin will be used to make the neo vagina. If you do not do hair removal, there will be hair inside the vagina. This can make post operative care more difficult and place you at increased risk for post op infection. The surgeon will not do any hair removal during the surgical procedure. Ask an LGBTQ+ Patient Advocate about resources for hair removal.
** Hair removal is not required for minimal depth vaginoplasty.
Do I need to stop taking hormones before vaginoplasty?
Your surgeon will discuss this with you at your pre-visit.
How long will my hospital stay be?
You will be admitted to the hospital for 3 days following your surgery.
What medications will I be prescribed after surgery?
You will likely receive painkillers and antibiotics to prevent infection. Your surgeon will provide you with a list of medications to avoid for the first month. Do not resume taking hormones until your surgeon has advised you to do so.
What should I expect during the healing process?
- Bleeding during the first 48 hours following surgery
- Itchiness and small shooting electrical sensations as nerve endings heal
- Bruising can spread from your belly to your thighs and takes 3-4 weeks to settle down
- A bit of spraying when you urinate which usually improves over time
- Swelling of your labia which can take up to 6 weeks to resolve
- Brown/yellow vaginal discharge for the first 6-8 weeks
- Your vulva will approach its final appearance at 4 months
- Numbness that will improve over the first few months, and can take up to 18 months to resolve
- Red, dark pink or purple scars that take up to one year to fade
What will my post-operative routine look like?
A urinary catheter will be in place for the first five days after surgery to allow you to pass urine while your urethra heals. Sometimes people still aren’t able to urinate when the catheter comes out, due to swelling around the urethra. This situation can easily be resolved with a second catheter that will remain in place for a week and be removed by your physician when you go home. You’ll be encouraged to drink lots of fluids to prevent urinary tract infections.
A prosthesis/stent will be placed in your vagina during surgery and will remain there for 5 days to make sure the skin grafts stay in place. When it’s removed, you will begin dilating and douching. A vaginal douche is a process of rinsing the vagina by forcing water or another solution into the vagina to flush away vaginal discharge or other contents. You will be given a set of vaginal dilators of different sizes. You’ll use them to maintain vaginal depth and width and promote healing.
Initially, you’ll dilate several times a day and over the first year the amount of time spent dilating will be gradually reduced. After you have completely healed, you will only need to dilate about once a week. The frequency depends on how much penetrative sex you have. For the first two months after surgery, you will take sitz baths. A sitz bath is a way to soak your surgical site to keep it clean. You’ll want to wear thin maxi pads for about one month to manage post-operative bleeding and discharge.
What check-ups will be needed after my hospital stay?
The number of check-ups needed varies from person to person. If possible, see your primary care provider about a week after and then every 2-4 weeks for the first few months. When you visit your surgeon or primary care provider, they should check your surgical sites to make sure there are no infections or wound healing problems. They will ask questions about dilating, bleeding, vaginal discharge, fever, pain and how you are feeling emotionally and physically.
How long will it take for me to get back to my usual activities?
Recovery time varies from person to person, so always follow the advice of your surgeon. Many people begin to feel more comfortable during the second week after their surgery. You’ll need plenty of rest in the first two weeks. It’s common to be back to your usual activities, including work, in six to eight weeks. Some activities, such as driving, heavy lifting, exercise, sex and soaking in hot tubs, may be restricted in the post-operative period. Your surgeon will give you advice about when it is okay to resume these activities. Complete recovery can take up to one year.
What complications are associated with vaginoplasty?
All surgical procedures involve some risks, including negative reactions to anesthesia, blood loss, blood clots and infection. These complications can, in extreme cases, result in death. It’s important to discuss these risks in detail with your surgeon. Your surgical care team will take a wide variety of steps to prevent these problems, detect them if they arise and respond to them appropriately.
They will also inform you about what you can do to minimize your risks. The list below includes some of the complications associated with vaginoplasty in particular. It does not replace a thorough consultation with your surgeon.
This is when blood collects in the surgical site, causing pain, swelling and redness. Smaller hematomas can be drained, but larger ones require removal through surgery.
Abscess Formation
An abscess is a collection of pus. It’s caused by a bacterial infection. It can be treated with antibiotics or drained by the surgeon.
This is when clear fluid accumulates in the surgical site. Small seromas may need to be aspirated, or sucked out, once or more by the surgeon.
Loss of Sensation
You may have small areas of numbness. Your ability to achieve orgasm could decrease. Loss of clitoris is a remote possibility.
Rectovaginal fistula
This is when an abnormal path between the rectum and vagina is created. Surgery would be needed to correct this.
May be correctable with various treatments, including additional surgery.
Injury to the Nerves or Muscles in the Legs
Can lead to numbness or a change of sensation in the skin of the legs. In very rare cases, it can lead to difficulty moving the leg which needs correction through surgery.
Unsatisfactory Size or Shape of the Vagina, Clitoris or Labia
Outcomes that are quite different from what was expected may require surgical revision.
Urological Complications
Examples include:
- fistulas (flow of urine to areas other than urethra opening)
- stenosis (narrowing of the urethra, causing difficulties urinating)
- strictures (blockage of the urethra, causing difficulty urinating).
It is common to have spraying or dribbling when urinating until your swelling settles down. If these problems don’t resolve on their own, they may require additional surgery.
- 0 && newsLoaded" class="" data-id="{044698B9-FA04-4636-994D-47662155601F}" ref="news"> News
- 0 && blogLoaded" class="" data-id="{9AB9C6CB-06BD-4D71-867F-FAB69D88F93C}" ref="blog"> Blog Articles
- 0 && storiesLoaded" class="" data-id="{71E64EA2-1956-4F7C-A67D-579E0BB54378}" ref="stories"> Patient Stories
- May 29 Labor and Delivery Tour for Expectant Families
- Jun 5 Labor and Delivery Tour for Expectant Families
- Jun 8 Boot Camp for New Dads ®
- Jun 11 CPR Class for Mom and Partner (expectant parents only)

- Health Care Home
- Transgender Health Program
- Gender Affirmation Surgery
Vaginoplasty / Vulvoplasty
Wpath standards of care.
- Breast Augmentation
- Facial Feminization Surgery
- Orchiectomy
- Vaginoplasty / Vulvuplasty
Gender affirmation surgery for a transfeminine person is sometimes called bottom surgery. These are three surgeries that can help a patient feel more aligned with their gender identity. They are:
- vaginoplasty,
- vulvoplasty, and
- orchiectomy .
Criteria for Vaginoplasty Vulvoplasty in Transfeminine Patients
- Persistent, well documented gender dysphoria;
- Capacity to make a fully informed decision and to consent for treatment;
- be the age of majority in a given country;
- If significant medical or mental health concerns are present, they must be well controlled;
- 12 continuous months of hormone therapy as appropriate to the patient’s gender goals (unless the patient has a medical contraindication or is otherwise unable or unwilling to take hormones);
- 12 continuous months of living in a gender role that is congruent with their gender identity.
Vaginoplasty
During a vaginoplasty surgery, a surgeon creates both an outer and inner vagina by using skin and tissue from a penis.
- Your surgeon will use skin from the penis and scrotum to build the inner and outer labia of the vagina
- Your surgeon will create a new opening for the urethra (so you can urinate)
- Your surgeon will use tissue from your foreskin to build the new opening of the vagina (also called the introitus).
Vaginoplasty Procedure
During most vaginoplasties, your surgeon will use a skin graft to create a new vaginal canal (the inside wall of the vagina). To do this, your surgeon will take skin from your scrotum and thin it so it works well as a skin graft.
If there’s not enough skin from your scrotum to make your new vagina, then your surgeon can take extra skin from the sides of your abdomen where there won’t be a very noticeable scar.
To make your new vaginal canal, your surgeon will create a space between your rectum and bladder. Once your skin graft is inserted, your surgeon will place gauze or spongy material inside the new vaginal canal for 5 days. The gauze puts pressure on the skin graft so it grows like it should into the surrounding vaginal tissue.
Vaginoplasty & Orgasms
Many transfeminine people wonder if they’ll still be able to have orgasms after having a vaginoplasty.
Your surgeon will use skin from your penis to create a clitoris. This clitoris still has feeling, and most transgender women can have orgasm through clitoral stimulation.
How Long Will I Be in the Hospital After Vaginoplasty?
Patients are in the hospital for 5 days and mostly rest in bed. Resting will help your skin graft grow into the surrounding tissue in your vaginal canal.
Your surgeon will also place a compressive bandage on the outside of your vagina. After the outer and inner bandages are removed, most patients feel fine and can leave the hospital.
When Should I Start to Dilate my Vagina After Vaginoplasty?
Each patient’s situation is different, but we recommend waiting two weeks after your surgery before you start dilating your vagina. Waiting two weeks will let your vagina heal.
Your surgeon will give you vaginal dilators to use at home. You should dilate your vagina two to three times each day for the first six months after your surgery.
Read this instruction sheet on how to dilate your vagina after having a vaginoplasty .
Preparing for Vaginoplasty Surgery
There are several things that patients need to do before having a vaginoplasty.
Pursue hair reduction: The first thing you’ll need to do is have hair removal on your scrotum and lower penile skin. Your vaginoplasty surgeon will use this skin to create your new vaginal canal. If hair were to grow inside your new vagina, it would create hygiene problems.
Quit smoking: If you’re a smoker, it’s very important for you to quit. Smoking, vaping, or using any nicotine products decreases blood flow to the area around your genitals and will make it harder for you to heal after your surgery.
If you’re a recent smoker, we will give you a nicotine urine test to make sure you’ve been able to quit completely. Nicotine takes about a month to wash out of your system before the test results will be negative.
Weight considerations : Keep in mind that patients with a body mass index ( BMI *) greater than 35 are at a higher risk for wound healing problems and complications after surgery. However, we understand that BMI is not a perfect measure of your overall health. We will discuss how your weight may affect you and the potential benefits of losing weight before surgery. If our team decides that weight loss is the best pre-surgical option for you, we will refer you to our weight management program .
For some people, vaginoplasty or vulvoplasty may not be possible because of their body shape and weight.
Physical Therapy for Vaginoplasty
Both before and after having a vaginoplasty, your surgeon will recommend that you start seeing a physical therapist. Physical therapy can help you prepare for this surgery.
Vulvoplasty
The vulva is the outside part of the vagina. A vulvoplasty is a type of surgery that uses skin and tissue from a penis to create all of the outside parts of a vagina (except for the vaginal canal).
The steps of a vulvoplasty are the same as a vaginoplasty. During a vulvoplasty, your surgeon will:
- create a clitoris out of the glans (or head) of the penis,
- create an inner and outer labia from skin on the penis and scrotum,
- create the opening of the urethra so you can urinate, and
- create the introitus (opening of the vagina).
The only thing that’s different between a full vaginoplasty and a vulvoplasty is the internal part of the vaginal canal.
- Vaginoplasty creates a vaginal canal.
- Vulvoplasty creates all the parts of a vagina except for the vaginal canal.
After vulvoplasty, this means you won’t be able to have intercourse or insert a penis into your vagina.
How Do I Choose Between a Vulvoplasty vs. Vaginoplasty?
A vulvoplasty has a much easier recovery. For example, you won’t need to dilate (or stretch) your vagina.
Another reason to consider vulvoplasty instead of vaginoplasty is because of medical problems or complications. One serious complication after vaginoplasty is called rectal injury. In some cases, a rectal injury can create a hole between your rectum and vagina.
But your chances of developing a rectal injury are much lower if you have a vulvoplasty instead of a vaginoplasty.
Sex & Vaginal Intercourse
Some patients know that they’re not interested in having vaginal intercourse. For these patients, a vulvoplasty may be a better choice.
After a vulvoplasty, you can still have orgasms through clitoral stimulation, just like with vaginoplasty. During a vulvoplasty, your surgeon will create a clitoris from the glans or head of the penis.
How Long Will I Be in the Hospital After Vulvoplasty?
Patients usually are in the hospital for 3 days after having a vulvoplasty. Your surgical team will give you a compressive dressing that reduces inflammation (swelling) after your surgery.
Most patients rest in bed while they’re healing since the dressing is uncomfortable to walk with.
After your dressing is removed, you can leave the hospital, usually right at about 3 days.
Find a Surgeon
Post-surgery instructions, vaginal dilation instructions, hear from our patient.
"I definitely feel complete. I feel whole. But that doesn’t describe it… that doesn’t even begin to describe it,” beams Josie Jesse as she sits, finally comfortable, in her new body that reflects who she has always been.
Read Josie Jesse's Story

- Reference Manager
- Simple TEXT file
People also looked at
Original research article, male-to-female gender-affirming surgery: 20-year review of technique and surgical results.

- 1 Serviço de Urologia, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 2 Serviço de Psiquiatria, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 3 Serviço de Psiquiatria, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current study, a retrospective cohort, we report the 20-years outcomes of the gender-affirming surgery performed at a single Brazilian university center, examining demographic data, intra and postoperative complications. During this period, 214 patients underwent penile inversion vaginoplasty.
Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18–61 years); the average of operative time was 3.3 h (range 2–5 h); the average duration of hormone therapy before surgery was 12 years (range 1–39). The most commons minor postoperative complications were granulation tissue (20.5 percent) and introital stricture of the neovagina (15.4 percent) and the major complications included urethral meatus stenosis (20.5 percent) and hematoma/excessive bleeding (8.9 percent). A total of 36 patients (16.8 percent) underwent some form of reoperation. One hundred eighty-one (85 percent) patients in our series were able to have regular sexual intercourse, and no individual regretted having undergone GAS.
Conclusions: Findings confirm that it is a safety procedure, with a low incidence of serious complications. Otherwise, in our series, there were a high level of functionality of the neovagina, as well as subjective personal satisfaction.
Introduction
Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ( 1 ). The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ( 1 ). Gender identity-affirming care, for those who desire, can include hormone therapy and affirming surgeries, as well as other procedures such as hair removal or speech therapy ( 1 ).
Since 1998, the Gender Identity Program (PROTIG) of the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul, Brazil has provided public assistance to transsexual people, is the first one in Brazil and one of the pioneers in South America. Our program offers psychosocial support, health care, and guidance to families, and refers individuals for gender-affirming surgery (GAS) when indicated. To be eligible for this surgery, transsexual individuals must have been adherent to multidisciplinary follow-up for at least 2 years, have a minimum age of 21 years (required for surgical procedures of this nature), have a positive psychiatric or psychological report, and have a diagnosis of GD.
Gender-affirming surgery (GAS) is increasingly recognized as a therapeutic intervention and a medical necessity, with growing societal acceptance ( 2 ). At our institution, we perform the classic penile inversion vaginoplasty (PIV), with an inverted penis skin flap used as the lining for the neovagina. Studies have demonstrated that GAS for the management of GD can promote improvements in mental health and social relationships for these patients ( 2 – 5 ). It is therefore imperative to understand and establish best practice techniques for this patient population ( 2 ). Although there are several studies reporting the safety and efficacy of gender-affirming surgery by penile inversion vaginoplasty, we present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
Patients and Methods
Subjects and study setup.
This is a retrospective cohort study of Brazilian transgender women who underwent penile inversion vaginoplasty between January of 2000 and March of 2020 at the Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil. The study was approved by our institutional medical and research ethics committee.
At our institution, gender-affirming surgery is indicated for transgender women who are under assistance by our program for transsexual individuals. All transsexual women included in this study had at least 2 years of experience as a woman and met WPATH standards for GAS ( 1 ). Patients were submitted to biweekly group meetings and monthly individual therapy.
Between January of 2000 and March of 2020, a total of 214 patients underwent penile inversion vaginoplasty. The surgical procedures were performed by two separate staff members, mostly assisted by residents. A retrospective chart review was conducted recording patient demographics, intraoperative and postoperative complications, reoperations, and secondary surgical procedures. Informed consent was obtained from all individual participants included in the study.
Hormonal Therapy
The goal of feminizing hormone therapy is the development of female secondary sex characteristics, and suppression/minimization of male secondary sex characteristics.
Our general therapy approach is to combine an estrogen with an androgen blocker. The usual estrogen is the oral preparation of estradiol (17-beta estradiol), starting at a dose of 2 mg/day until the maximum dosage of 8 mg/day. The preferred androgen blocker is spironolactone at a dose of 200 mg twice a day.
Operative Technique
At our institution, we perform the classic penile inversion vaginoplasty, with an inverted penis skin flap used as the lining for the neovagina. For more details, we have previously published our technique with a step-by-step procedure video ( 6 ). All individuals underwent intestinal cleansing the evening before the surgery. A first-generation cephalosporin was used as preoperative prophylaxis. The procedure was performed with the patient in a dorsal lithotomy position. A Foley catheter was placed for bladder catheterization. A inverted-V incision was made 4 cm above the anus and a flap was created. A neovaginal cavity was created between the prostate and the rectum with blunt dissection, in the Denonvilliers space, until the peritoneal fold, usually measuring 12 cm in extension and 6 cm in width. The incision was then extended vertically to expose the testicles and the spermatic cords, which were removed at the level of the external inguinal rings. A circumferential subcoronal incision was made ( Figure 1 ), the penis was de-gloved and a skin flap was created, with the de-gloved penis being passed through the scrotal opening ( Figure 2 ). The dorsal part of the glans and its neurovascular bundle were bluntly dissected away from the penile shaft ( Figure 3 ) as well as the urethra, which included a portion of the bulbospongious muscle ( Figure 4 ). The corpora cavernosa was excised up to their attachments at the symphysis pubis and ligated. The neoclitoris was shaped and positioned in the midline at the level of the symphysis pubis and sutured using interrupted 5-0 absorbable suture. The corpus spongiosum was reduced and the urethra was shortened, spatulated, and placed 1 cm below the neoclitoris in the midline and sutured using interrupted 4-0 absorbable suture. The penile skin flap was inverted and pulled into the neovaginal cavity to become its walls ( Figure 5 ). The excess of skin was then removed, and the subcutaneous tissue and the skin were closed using continuous 3-0 non-absorbable suture ( Figure 6 ). A neo mons pubis was created using a 0 absorbable suture between the skin and the pubic bone. The skin flap was fixed to the pubic bone using a 0 absorbable suture. A gauze impregnated with Vaseline and antibiotic ointment was left inside the neovagina, and a customized compressive bandage was applied ( Figure 7 —shows the final appearance after the completion of the procedures).

Figure 1 . The initial circumferential subcoronal incision.

Figure 2 . The de-gloved penis being passed through the scrotal opening.

Figure 3 . The dorsal part of the glans and its neurovascular bundle dissected away from the penile shaft.
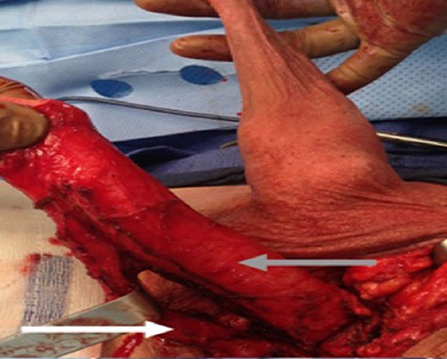
Figure 4 . The urethra dissected including a portion of the bulbospongious muscle. The grey arrow shows the penile shaft and the white arrow shows the dissected urethra.

Figure 5 . The inverted penile skin flap.
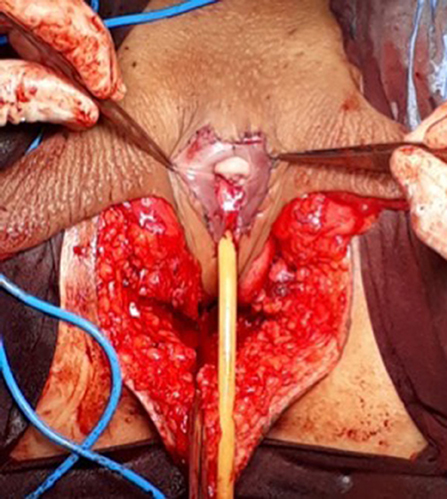
Figure 6 . The neoclitoris and the urethra sutured in the midline and the neovaginal cavity.
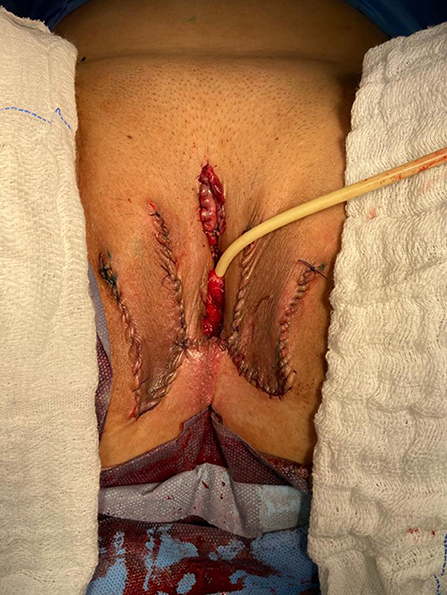
Figure 7 . The final appearance after the completion of the procedures.
Postoperative Care and Follow-Up
The patients were usually discharged within 2 days after surgery with the Foley catheter and vaginal gauze packing in place, which were removed after 7 days in an ambulatorial attendance.
Our vaginal dilation protocol starts seven days after surgery: a kit of 6 silicone dilators with progressive diameter (1.1–4 cm) and length (6.5–14.5 cm) is used; dilation is done progressively from the smallest dilator; each size should be kept in place for 5 min until the largest possible size, which is kept for 3 h during the day and during the night (sleep), if possible. The process is performed daily for the first 3 months and continued until the patient has regular sexual intercourse.
The follow-up visits were performed 7 days, 1, 2, 3, 6, and 12 months after surgery ( Figure 8 ), and included physical examination and a quality-of-life questionnaire.

Figure 8 . Appearance after 1 month of the procedure.
Statistical Analysis
The statistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Outcome measures were intra-operative and postoperative complications, re-operations. Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented as continuous variables. Frequencies and percentages are reported for dichotomous and ordinal variables.
Patient Demographics
During the period of the study, 214 patients underwent penile inversion vaginoplasty, performed by two staff surgeons, mostly assisted by residents ( Table 1 ). The average age at the time of surgery was 32.2 years (range 18–61 years). There was no significant increase or decrease in the ages of patients who underwent SRS over the study period (Fisher's exact test: P = 0.065; chi-square test: X 2 = 5.15; GL = 6; P = 0.525). The average of operative time was 3.3 h (range 2–5 h). The average duration of hormone therapy before surgery was 12 years (range 1–39). The majority of patients were white (88.3 percent). The most prevalent patient comorbidities were history of tobacco use (15 percent), human immunodeficiency virus infection (13 percent) and hypertension (10.7 percent). Other comorbidities are listed in Table 1 .
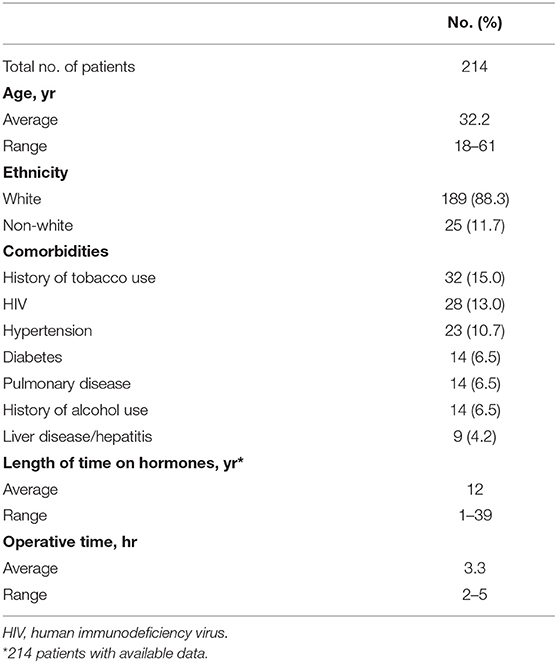
Table 1 . Patient demographics.
Multidisciplinary follow-up was comprised of 93.45% of patients following up with a urologist and 59.06% of patients continuing psychiatric follow-up, median follow-up time of 16 and 9.3 months after surgery, respectively.
Postoperative Results
The complications were classified according to the Clavien-Dindo score ( Table 2 ). The most common minor postoperative complications (Grade I) were granulation tissue (20.5 percent), introital stricture of the neovagina (15.4 percent) and wound dehiscence (12.6 percent). The major complications (Grade III-IV) included urethral stenosis (20.5 percent), urethral fistula (1.9 percent), intraoperative rectal injury (1.9 percent), necrosis (primarily along the wound edges) (1.4 percent), and rectovaginal fistula (0.9 percent). A total of 17 patients required blood transfusion (7.9 percent).
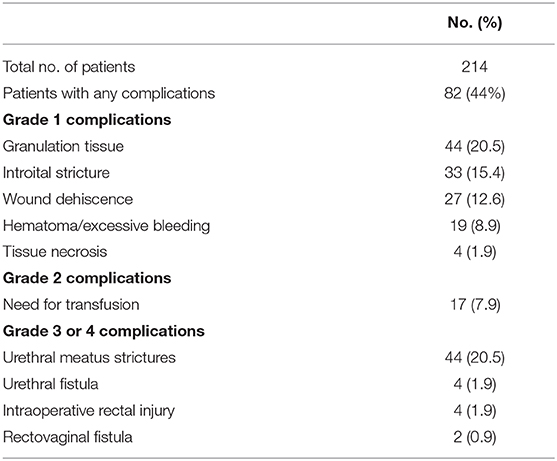
Table 2 . Complications after penile inversion vaginoplasty.
A total of 36 patients (16.8 percent) underwent some form of reoperation.
One hundred eighty-one (85 percent) patients in our series were able to have regular sexual vaginal intercourse, and no individual regretted having undergone GAS.
Penile inversion vaginoplasty is the gold-standard in gender-affirming surgery. It has good functional outcomes, and studies have demonstrated adequate vaginal depths ( 3 ). It is recognized not only as a cosmetic procedure, but as a therapeutic intervention and a medical necessity ( 2 ). We present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
The mean age of transsexual women who underwent GAS in our study was 32.2 years (range 18–61 years), which is lower than the mean age of patients in studies found in the literature. Two studies indicated that the mean ages of patients at time of GAS were 36.7 years and 41 years, respectively ( 4 , 5 ). Another study reported a mean age at time of GAS of 36 years and found there was a significant decrease in age at the time of GAS from 41 years in 1994 to 35 years in 2015 ( 7 ). According to the authors, this decrease in age is associated with greater tolerance and societal approval regarding individuals with GD ( 7 ).
There was no grade IV or grade V complications. Excessive bleeding noticed postoperatively occurred in 19 patients (8.9 percent) and blood transfusion was required in 17 cases (7.9 percent); all patients who required blood transfusions were operated until July 2011, and the reason for this rate of blood transfusion was not identified.
The most common intraoperative complication was rectal injury, occurring in 4 patients (1.9 percent); in all patients the lesion was promptly identified and corrected in 2 layers absorbable sutures. In 2 of these patients, a rectovaginal fistula became evident, requiring fistulectomy and colonic transit deviation. This is consistent with current literature, in which rectal injury is reported in 0.4–4.5 percent of patients ( 4 , 5 , 8 – 13 ). Goddard et al. suggested carefully checking for enterotomy after prostate and bladder mobilization by digital rectal examination ( 4 ). Gaither et al. ( 14 ) commented that careful dissection that closely follows the urethra along its track from the central tendon of the perineum up through the lower pole of the prostate is critical and only blunt dissection is encouraged after Denonvilliers' fascia is reached. Alternatively, a robotic-assisted approach to penile inversion vaginoplasty may aid in minimizing these complications. The proposed advantages of a robotic-assisted vaginoplasty include safer dissection to minimize the risk of rectal injury and better proximal vaginal fixation. Dy et al. ( 15 ) has had no rectal injuries or fistulae to date in his series of 15 patients, with a mean follow-up of 12 months.
In our series, we observed 44 cases (20.5 percent) of urethral meatus strictures. We credit this complication to the technique used in the initial 5 years of our experience, in which the urethra was shortened and sutured in a circular fashion without spatulation. All cases were treated with meatal dilatation and 11 patients required surgical correction, being performed a Y-V plastic reconstruction of the urethral meatus. In the literature, meatal strictures are relatively rare in male-to-female (MtF) GAS due to the spatulation of the urethra and a simple anastomosis to the external genitalia. Recent systematic reviews show an incidence of five percent in this complication ( 16 , 17 ). Other studies report a wide incidence of meatal stenosis ranging from 1.1 to 39.8 percent ( 4 , 8 , 11 ).
Neovagina introital stricture was observed in 33 patients (15.4 percent) in our study and impedes the possibility of neovaginal penetration and/or adversely affects sexual life quality. In the literature, the reported incidence of introital stenosis range from 6.7 to 14.5 percent ( 4 , 5 , 8 , 9 , 11 – 13 ). According to Hadj-Moussa et al. ( 18 ) a regimen of postoperative prophylactic dilation is crucial to minimize the development of this outcome. At our institution, our protocol for vaginal dilation started seven days after surgery and was performed three to four times a day during the first 3 months and was continued until the individual had regular sexual intercourse. We treated stenosis initially with dilation. In case of no response, we propose a surgical revision with diamond-shaped introitoplasty with relaxing incisions. In recalcitrant cases, we proposed to the patient a secondary vaginoplasty using a full-thickness skin graft of the lower abdomen.
One hundred eighty-one (85 percent) patients were classified as having a “functional vagina,” characterized as the capacity to maintain satisfactory sexual vaginal intercourse, since the mean neovaginal depth was not measured. In a review article, the mean neovaginal depth ranged from 10 to 13.5 cm, with the shallowest neovagina depth at 2.5 cm and the deepest at 18 cm ( 17 ). According to Salim et al. ( 19 ), in terms of postoperative functional outcomes after penile inversion vaginoplasty, a mean percentage of 75 percent (range from 33 to 87 percent) patients were having vaginal intercourse. Hess et al. found that 91.4% of patients who responded to a questionnaire were very satisfied (34.4%), satisfied (37.6%), or mostly satisfied (19.4%) with their sexual function after penile inversion vaginoplasty ( 20 ).
Poor cosmetic appearance of the vulva is common. Amend et al. reported that the most common reason for reoperation was cosmetic correction in the form of mons pubis and mucosa reduction in 50% of patients ( 16 ). We had no patient regrets about performing GAS, although 36 patients (16.8 percent) were reoperated due to cosmetic issues. Gaither et al. propose in order to minimize scarring to use a one-stage surgical approach and the lateralization of surgical scars to the groin ( 14 ). Frequently, cosmetic issues outcomes are often patient driven and preoperative patient education is necessary ( 14 ).
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) ( 21 ). The authors found that GAS promotes the improvement of psychological aspects and social relations. However, even 1 year after GAS, MtF persons continue to report problems in physical and difficulty in recovering their independence. In a systematic review and meta-analysis of QOL and psychosocial outcomes in transsexual people, researchers verified that sex reassignment with hormonal interventions more likely corrects gender dysphoria, psychological functioning and comorbidities, sexual function, and overall QOL compared with sex reassignment without hormonal interventions, although there is a low level of evidence for this ( 22 ). Recently, Castellano et al. assessed QOL in 60 Italian transsexuals (46 transwomen and 14 transmen) at least 2 years after SRS using the WHOQOL-100 (general QOL score and quality of sexual life and quality of body image scores) to focus on the effects of hormonal therapy. Overall satisfaction improved after SRS, and QOL was similar to the controls ( 23 ). Bartolucci et al. evaluated the perception of quality of sexual life using four questions evaluating the sexual facet in individuals with gender dysphoria before SRS and the possible factors associated with this perception. The study showed that approximately half the subjects with gender dysphoria perceived their sexual life as “poor/dissatisfied” or “very poor/very dissatisfied” before SRS ( 24 ).
Our study has some limitations. The total number of operated patients is restricted within the long follow-up period. This is due to a limitation in our health system, which allows only 1 sexual reassignment surgery to be performed per month at our institution. Neovagin depth measurement was not performed routinely in the follow-up of operated patients.
Conclusions
The definitive treatment for patients with gender dysphoria is gender-affirming surgery. Our series demonstrates that GAS is a feasible surgery with low rates of serious complications. We emphasize the high level of functionality of the vagina after the procedure, as well as subjective personal satisfaction. Complications, especially minor ones, are probably underestimated due to the nature of the study, and since this is a surgical population, the results may not be generalizable for all transgender MTF individuals.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Hospital de Clínicas de Porto Alegre. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM: conception and design, data acquisition, data analysis, interpretation, drafting the manuscript, review of the literature, critical revision of the manuscript and factual content, and statistical analysis. ML and TR: conception and design, data interpretation, drafting the manuscript, critical revision of the manuscript and factual content, and statistical analysis. DS, KS, AF, AC, PT, AG, and RC: conception and design, data acquisition and data analysis, interpretation, drafting the manuscript, and review of the literature. All authors contributed to the article and approved the submitted version.
This study was supported by the Fundo de Incentivo à Pesquisa e Eventos (FIPE - Fundo de Incentivo à Pesquisa e Eventos) of Hospital de Clínicas de Porto Alegre.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-non-conforming people, version 7. Int J Transgend. (2012) 13:165–232. doi: 10.1080/15532739.2011.700873
CrossRef Full Text | Google Scholar
2. Massie JP, Morrison SD, Maasdam JV, Satterwhite T. Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plast Reconstruct Surg. (2018) 141:911–921. doi: 10.1097/PRS.0000000000004427
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Pan S, Honig SC. Gender-affirming surgery: current concepts. Curr Urol Rep . (2018) 19:62. doi: 10.1007/s11934-018-0809-9
4. Goddard JC, Vickery RM, Qureshi A, Summerton DJ, Khoosal D, Terry TR. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int . (2007) 100:607–13. doi: 10.1111/j.1464-410X.2007.07017.x
5. Rossi NR, Hintz F, Krege S, Rübben H, Vom DF, Hess J. Gender reassignment surgery – a 13 year review of surgical outcomes. Eur Urol Suppl . (2013) 12:e559. doi: 10.1016/S1569-9056(13)61042-8
6. Silva RUM, Abreu FJS, Silva GMV, Santos JVQV, Batezini NSS, Silva Neto B, et al. Step by step male to female transsexual surgery. Int Braz J Urol. (2018) 44:407–8. doi: 10.1590/s1677-5538.ibju.2017.0044
7. Aydin D, Buk LJ, Partoft S, Bonde C, Thomsen MV, Tos T. Transgender surgery in Denmark from 1994 to 2015: 20-year follow-up study. J Sex Med. (2016) 13:720–5. doi: 10.1016/j.jsxm.2016.01.012
8. Perovic SV, Stanojevic DS, Djordjevic MLJ. Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. (2001) 86:843–50. doi: 10.1046/j.1464-410x.2000.00934.x
9. Krege S, Bex A, Lümmen G, Rübben H. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. (2001) 88:396–402. doi: 10.1046/j.1464-410X.2001.02323.x
10. Wagner S, Greco F, Hoda MR, Inferrera A, Lupo A, Hamza A, et al. Male-to-female transsexualism: technique, results and 3-year follow-up in 50 patients. Urol International. (2010) 84:330–3. doi: 10.1159/000288238
11. Reed H. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin PlasticSurg. (2011) 25:163–74. doi: 10.1055/s-0031-1281486
12. Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. (2015) 12:1837–45. doi: 10.1111/jsm.12936
13. Sigurjonsson H, Rinder J, Möllermark C, Farnebo F, Lundgren TK. Male to female gender reassignment surgery: surgical outcomes of consecutive patients during 14 years. JPRAS Open. (2015) 6:69–73. doi: 10.1016/j.jpra.2015.09.003
14. Gaither TW, Awad MA, Osterberg EC, Murphy GP, Romero A, Bowers ML, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. (2018) 199:760–5. doi: 10.1016/j.juro.2017.10.013
15. Dy GW, Sun J, Granieri MA, Zhao LC. Reconstructive management pearls for the transgender patient. Curr. Urol. Rep. (2018) 19:36. doi: 10.1007/s11934-018-0795-y
16. Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. (2013) 64:141–9. doi: 10.1016/j.eururo.2012.12.030
17. Horbach SER, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med . (2015) 12:1499–512. doi: 10.1111/jsm.12868
18. Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. (2018) 6:457–68.e2. doi: 10.1016/j.sxmr.2017.11.005
19. Salim A, Poh M. Gender-affirming penile inversion vaginoplasty. Clin Plast Surg. (2018) 45:343–50. doi: 10.1016/j.cps.2018.04.001
20. Hess J, Rossi NR, Panic L, Rubben H, Senf W. Satisfaction with male-to-female gender reassignment surgery. DtschArztebl Int. (2014) 111:795–801. doi: 10.3238/arztebl.2014.0795
21. Silva DC, Schwarz K, Fontanari AMV, Costa AB, Massuda R, Henriques AA, et al. WHOQOL-100 before and after sex reassignment surgery in brazilian male-to-female transsexual individuals. J Sex Med. (2016) 13:988–93. doi: 10.1016/j.jsxm.2016.03.370
22. Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol . (2010) 72:214–31. doi: 10.1111/j.1365-2265.2009.03625.x
23. Castellano E, Crespi C, Dell'Aquila C, Rosato R, Catalano C, Mineccia V, et al. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest . (2015) 38:1373–81. doi: 10.1007/s40618-015-0398-0
24. Bartolucci C, Gómez-Gil E, Salamero M, Esteva I, Guillamón A, Zubiaurre L, et al. Sexual quality of life in gender-dysphoric adults before genital sex reassignment surgery. J Sex Med . (2015) 12:180–8. doi: 10.1111/jsm.12758
Keywords: transsexualism, gender dysphoria, gender-affirming genital surgery, penile inversion vaginoplasty, surgical outcome
Citation: Moisés da Silva GV, Lobato MIR, Silva DC, Schwarz K, Fontanari AMV, Costa AB, Tavares PM, Gorgen ARH, Cabral RD and Rosito TE (2021) Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Front. Surg. 8:639430. doi: 10.3389/fsurg.2021.639430
Received: 17 December 2020; Accepted: 22 March 2021; Published: 05 May 2021.
Reviewed by:
Copyright © 2021 Moisés da Silva, Lobato, Silva, Schwarz, Fontanari, Costa, Tavares, Gorgen, Cabral and Rosito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriel Veber Moisés da Silva, veber.gabriel@gmail.com
This article is part of the Research Topic
Gender Dysphoria: Diagnostic Issues, Clinical Aspects and Health Promotion
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Semin Plast Surg
- v.25(3); 2011 Aug

Aesthetic and Functional Genital and Perineal Surgery: Male
Sex reassignment surgery in the female-to-male transsexual, stan j. monstrey.
1 Department of Plastic Surgery, Ghent University Hospital, Gent, Belgium

Peter Ceulemans
Piet hoebeke.
2 Department of Urology, Ghent University Hospital, Gent, Belgium
In female-to-male transsexuals, the operative procedures are usually performed in different stages: first the subcutaneous mastectomy which is often combined with a hysterectomy-ovarectomy (endoscopically assisted). The next operative procedure consists of the genital transformation and includes a vaginectomy, a reconstruction of the horizontal part of the urethra, a scrotoplasty and a penile reconstruction usually with a radial forearm flap (or an alternative). After about one year, penile (erection) prosthesis and testicular prostheses can be implanted when sensation has returned to the tip of the penis. The authors provide a state-of-the-art overview of the different gender reassignment surgery procedures that can be performed in a female-to-male transsexual.
Transsexual patients have the absolute conviction of being born in the wrong body and this severe identity problem results in a lot of suffering from early childhood on. Although the exact etiology of transsexualism is still not fully understood, it is most probably a result of a combination of various biological and psychological factors. As to the treatment, it is universally agreed that the only real therapeutic option consists of “adjusting the body to the mind” (or gender reassignment) because trying to “adjust the mind to the body” with psychotherapy has been shown to alleviate the severe suffering of these patients. Gender reassignment usually consists of a diagnostic phase (mostly supported by a mental health professional), followed by hormonal therapy (through an endocrinologist), a real-life experience, and at the end the gender reassignment surgery itself.
As to the criteria of readiness and eligibility for these surgical interventions, it is universally recommended to adhere to the Standards of Care (SOC) of the WPATH (World Professional association of Transgender Health) 1 . It is usually advised to stop all hormonal therapy 2 to 3 weeks preoperatively.
The two major sex reassignment surgery (SRS) interventions in the female-to-male transsexual patients that will be addressed here are (1) the subcutaneous mastectomy (SCM), often combined with a hysterectomy/ ovariectomy; and (2) the actual genital transformation consisting of vaginectomy, reconstruction of the fixed part of the urethra (if isolated, metoidioplasty), scrotoplasty and phalloplasty. At a later stage, a testicular prostheses and/or erection prosthesis can be inserted.
SUBCUTANEOUS MASTECTOMY
General principles.
Because hormonal treatment has little influence on breast size, the first (and, arguably, most important) surgery performed in the female-to-male (FTM) transsexual is the creation of a male chest by means of a SCM. This procedure allows the patient to live more easily in the male role 2 , 3 , 4 , 5 and thereby facilitates the “real-life experience,” a prerequisite for genital surgery.
The goal of the SCM in a FTM transsexual patient is to create an aesthetically pleasing male chest, which includes removal of breast tissue and excess skin, reduction and proper positioning of the nipple and areola, obliteration of the inframammary fold, and minimization of chest-wall scars. 4 , 5 Many different techniques have been described to achieve these goals and most authors agree that skin excess , not breast volume, is the factor that should determine the appropriate SCM technique. 2 , 3 , 4 , 5 Recently, the importance of the skin elasticity has also been demonstrated and it is important to realize that in this patient population, poor skin quality can be exacerbated when the patient has engaged in years of “breast binding” (Fig. 1 ). 6

(A,B) Result of long-term “breast binding.”
In the largest series to date, Monstrey et al 6 described an algorithm of five different techniques to perform an aesthetically satisfactory SCM (Fig. 2 ). Preoperative parameters to be evaluated include breast volume, degree of excess skin, nipple-areola complex (NAC) size and position, and skin elasticity.

Algorithm for choosing appropriate subcutaneous mastectomy technique.
Regardless of the technique, it is extremely important to preserve all subcutaneous fat when dissecting the glandular tissue from the flaps. This ensures thick flaps that produce a pleasing contour. Liposuction is only occasionally indicated laterally, or to attain complete symmetry at the end of the procedure. Postoperatively, a circumferential elastic bandage is placed around the chest wall and maintained for a total of 4 to 6 weeks.
The semicircular technique (Fig. 3 ) is essentially the same procedure as that described by Webster in 1946 7 for gynecomastia. It is useful for individuals with smaller breasts and elastic skin. A sufficient amount of glandular tissue should be left in situ beneath the NAC to avoid a depression. The particular advantage of this technique is the small and well-concealed scar which is confined to (the lower half of) the nipple-areola complex. The major drawback is the small window through which to work, making excision of breast tissue and hemostasis more challenging.

Semicircular technique. (A) Incisions and scar; (B) preoperative; (C) postoperative.
In cases of smaller breasts with large prominent nipples, the transareolar technique (Fig. 4 ) is used. This is similar to the procedure described by Pitanguy in 1966 8 and allows for subtotal resection and immediate reduction of the nipple. The resulting scar traverses the areola horizontally and passes around the upper aspect of the nipple.

Transareolar technique. (A,B) Incisions and scar; (C) preoperative; (D) postoperative.
The concentric circular technique (Fig. 5 ) is similar to that described by Davidson in 1979. 9 It is used for breasts with a medium-sized skin envelope (B cup), or in the case of smaller breasts with poor skin elasticity. The resulting scar will be confined to the circumference of the areola. The concentric incision can be drawn as a circle or ellipse, enabling deepithelialization of a calculated amount of skin in the vertical or horizontal direction. 4 , 5 Access is gained via an incision in the inferior aspect of the outer circle leaving a wide pedicle for the NAC. A purse-string suture is placed and set to the desired areolar diameter (usually 25–30 mm). The advantage of this technique is that it allows for reduction and/or repositioning of the areola, where required, and for the removal of excess skin.

Concentric circular technique. (A) incisions; (B) preoperative; (C) postoperative.
The extended concentric circular technique (Fig. 6 ) is similar to the concentric circular technique, but includes one or two additional triangular excisions of skin and subcutaneous tissue lateral and/ or medial. This technique is useful for correcting skin excess and wrinkling produced by large differences between the inner and outer circles. The resulting scars will be around the areola, with horizontal extensions onto the breast skin, depending on the degree of excess skin.

Extended concentric circular technique. (A) Incisions and scar; (B) preoperative preoperative; (C) postoperative.
The free nipple graft technique (Fig. 7 ) has been proposed by several authors for patients with large and ptotic breasts. 2 , 3 , 10 , 11 , 12 It consists of harvesting the NAC as a full-thickness skin graft; amputating the breast; and grafting the NAC onto its new location on the chest wall. Our preference is to place the incision horizontally 1 to 2 cm above the inframammary fold, and then to move upwards laterally below the lateral border of the pectoralis major muscle. The placement of the NAC usually corresponds to the 4th or 5th intercostal space. Clinical judgment is most important, however, and we always sit the patient up intraoperatively to check final nipple position. The advantages of the free nipple graft technique are easy chest contouring, excellent exposure and more rapid resection of tissue, as well as nipple reduction, areola resizing, and repositioning. The disadvantages are the long residual scars, NAC pigmentary and sensory changes, and the possibility of incomplete graft take.

Free nipple graft technique. (A) Incisions and scar; (B) preoperative; (C) postoperative.
Complications
Postoperative complications include hematoma (most frequent, despite drains and compression bandages), (partial) nipple necrosis, and abscess formation. This underscores the importance of achieving good hemostasis intraoperatively. Smaller hematomas and seromas can be evacuated through puncture, but for larger collections surgical evacuation is required.
Another not infrequent complication consists of skin slough of the NAC, which can be left to heal by conservative means. The exceptional cases of partial or total nipple necrosis may require a secondary nipple reconstruction. Even in the patients without complications, ~25% required an additional procedure to improve the aesthetic results. The likelihood of an additional aesthetic correction should be discussed with the patient in advance. 13 Tattoo of the areola may be performed for depigmentation.
The recommendations of the authors are summarized in their algorithm (Fig. 2 ), which clearly demonstrates that a larger skin envelope and a less elastic skin will require progressively a longer-incision technique. The FTM transsexual patients are rightfully becoming a patient population that is better informed and more demanding as to the aesthetic outcomes.
Finally, it is important to note that there have been reports of breast cancer after bilateral SCM in this population 14 , 15 , 16 because in most patients the preserved NAC and the always incomplete glandular resection leave behind tissue at risk of malignant transformation.
PHALLOPLASTY
In performing a phalloplasty for a FTM transsexual, the surgeon should reconstruct an aesthetically appealing neophallus, with erogenous and tactile sensation, which enables the patient to void while standing and have sexual intercourse like a natural male, in a one-stage procedure. 17 , 18 The reconstructive procedure should also provide a normal scrotum, be predictably reproducible without functional loss in the donor area, and leave the patient with minimal scarring or disfigurement.
Despite the multitude of flaps that have been employed and described (often as Case Reports), the radial forearm is universally considered the gold standard in penile reconstruction. 17 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28
In the largest series to date (almost 300 patients), Monstrey et al 29 recently described the technical aspects of radial forearm phalloplasty and the extent to which this technique, in their hands approximates the criteria for ideal penile reconstruction.
For the genitoperineal transformation (vaginectomy, urethral reconstruction, scrotoplasty, phalloplasty), two surgical teams operate at the same time with the patient first placed in a gynecological (lithotomy) position. In the perineal area, a urologist may perform a vaginectomy, and lengthen the urethra with mucosa between the minor labiae. The vaginectomy is a mucosal colpectomy in which the mucosal lining of the vaginal cavity is removed. After excision, a pelvic floor reconstruction is always performed to prevent possible diseases such as cystocele and rectocele. This reconstruction of the fixed part of the urethra is combined with a scrotal reconstruction by means of two transposition flaps of the greater labia resulting in a very natural looking bifid scrotum.
Simultaneously, the plastic surgeon dissects the free vascularized flap of the forearm. The creation of a phallus with a tube-in-a-tube technique is performed with the flap still attached to the forearm by its vascular pedicle (Fig. 8A ). This is commonly performed on the ulnar aspect of the skin island. A small skin flap and a skin graft are used to create a corona and simulate the glans of the penis (Fig. 8B ).

(A–D) Phallic reconstruction with the radial forearm flap: creation of a tube (urethra) within a tube (penis).
Once the urethra is lengthened and the acceptor (recipient) vessels are dissected in the groin area, the patient is put into a supine position. The free flap can be transferred to the pubic area after the urethral anastomosis: the radial artery is microsurgically connected to the common femoral artery in an end-to-side fashion and the venous anastomosis is performed between the cephalic vein and the greater saphenous vein (Fig. 8C ). One forearm nerve is connected to the ilioinguinal nerve for protective sensation and the other nerve of the arm is anastomosed to one of the dorsal clitoral nerves for erogenous sensation. The clitoris is usually denuded and buried underneath the penis, thus keeping the possibility to be stimulated during sexual intercourse with the neophallus.
In the first 50 patients of this series, the defect on the forearm was covered with full-thickness skin grafts taken from the groin area. In subsequent patients, the defect was covered with split-thickness skin grafts harvested from the medial and anterior thigh (Fig. 8D ).
All patients received a suprapubic urinary diversion postoperatively.
The patients remain in bed during a one-week postoperative period, after which the transurethral catheter is removed. At that time, the suprapubic catheter was clamped, and voiding was begun. Effective voiding might not be observed for several days. Before removal of the suprapubic catheter, a cystography with voiding urethrography was performed.
The average hospital stay for the phalloplasty procedure was 2½ weeks.
Tattooing of the glans should be performed after a 2- to 3-month period, before sensation returns to the penis.
Implantation of the testicular prostheses should be performed after 6 months, but it is typically done in combination with the implantation of a penile erection prosthesis. Before these procedures are undertaken, sensation must be returned to the tip of the penis. This usually does not occur for at least a year.
The Ideal Goals of Penile Reconstruction in FTM Surgery
What can be achieved with this radial forearm flap technique as to the ideal requisites for penile reconstruction?
A ONE-STAGE PROCEDURE
In 1993, Hage 20 stated that a complete penile reconstruction with erection prosthesis never can be performed in one single operation. Monstrey et al, 29 early in their series and to reduce the number of surgeries, performed a (sort of) all-in-one procedure that included a SCM and a complete genitoperineal transformation. However, later in their series they performed the SCM first most often in combination with a total hysterectomy and ovariectomy.
The reason for this change in protocol was that lengthy operations (>8 hours) resulted in considerable blood loss and increased operative risk. 30 Moreover, an aesthetic SCM is not to be considered as an easy operation and should not be performed “quickly” before the major phalloplasty operation.
AN AESTHETIC PHALLUS
Phallic construction has become predictable enough to refine its aesthetic goals, which includes the use of a technique that can be replicated with minimal complications. In this respect, the radial forearm flap has several advantages: the flap is thin and pliable allowing the construction of a normal sized, tube-within-a-tube penis; the flap is easy to dissect and is predictably well vascularized making it safe to perform an (aesthetic) glansplasty at the distal end of the flap. The final cosmetic outcome of a radial forearm phalloplasty is a subjective determination, but the ability of most patients to shower with other men or to go to the sauna is the usual cosmetic barometer (Fig. 9A-C ).

(A–C) Late postoperative results of radial forearm phalloplasties.
The potential aesthetic drawbacks of the radial forearm flap are the need for a rigidity prosthesis and possibly some volume loss over time.
TACTILE AND EROGENOUS SENSATION
Of the various flaps used for penile reconstruction, the radial forearm flap has the greatest sensitivity. 1 Selvaggi and Monstrey et al. always connect one antebrachial nerve to the ilioinguinal nerve for protective sensation and the other forearm nerve with one dorsal clitoral nerve. The denuded clitoris was always placed directly below the phallic shaft. Later manipulation of the neophallus allows for stimulation of the still-innervated clitoris. After one year, all patients had regained tactile sensitivity in their penis, which is an absolute requirement for safe insertion of an erection prosthesis. 31
In a long-term follow-up study on postoperative sexual and physical health, more than 80% of the patients reported improvement in sexual satisfaction and greater ease in reaching orgasm (100% in practicing postoperative FTM transsexuals). 32
VOIDING WHILE STANDING
For biological males as well as for FTM transsexuals undergoing a phalloplasty, the ability to void while standing is a high priority. 33 Unfortunately, the reported incidences of urological complications, such as urethrocutaneous fistulas, stenoses, strictures, and hairy urethras are extremely high in all series of phalloplasties, as high as 80%. 34 For this reason, certain (well-intentioned) surgeons have even stopped reconstructing a complete neo-urethra. 35 , 36
In their series of radial forearm phalloplasties, Hoebeke and Monstrey still reported a urological complication rate of 41% (119/287), but the majority of these early fistulas closed spontaneously and ultimately all patients were able to void through the newly reconstructed penis. 37 Because it is unknown how the new urethra—a 16-cm skin tube—will affect bladder function in the long term, lifelong urologic follow-up was strongly recommended for all these patients.
MINIMAL MORBIDITY
Complications following phalloplasty include the general complications attendant to any surgical intervention such as minor wound healing problems in the groin area or a few patients with a (minor) pulmonary embolism despite adequate prevention (interrupting hormonal therapy, fractioned heparin subcutaneously, elastic stockings). A vaginectomy is usually considered a particularly difficult operation with a high risk of postoperative bleeding, but in their series no major bleedings were seen. 30 Two early patients displayed symptoms of nerve compression in the lower leg, but after reducing the length of the gynecological positioning to under 2 hours, this complication never occurred again. Apart from the urinary fistulas and/or stenoses, most complications of the radial forearm phalloplasty are related to the free tissue transfer. The total flap failure in their series was very low (<1%, 2/287) despite a somewhat higher anastomotic revision rate (12% or 34/287). About 7 (3%) of the patients demonstrated some degree of skin slough or partial flap necrosis. This was more often the case in smokers, in those who insisted on a large-sized penis requiring a larger flap, and also in patients having undergone anastomotic revision.
With smoking being a significant risk factor, under our current policy, we no longer operate on patients who fail to quit smoking one year prior to their surgery.
NO FUNCTIONAL LOSS AND MINIMAL SCARRING IN THE DONOR AREA
The major drawback of the radial forearm flap has always been the unattractive donor site scar on the forearm (Fig. 10 ). Selvaggi et al conducted a long-term follow-up study 38 of 125 radial forearm phalloplasties to assess the degree of functional loss and aesthetic impairment after harvesting such a large forearm flap. An increased donor site morbidity was expected, but the early and late complications did not differ from the rates reported in the literature for the smaller flaps as used in head and neck reconstruction. 38 No major or long-term problems (such as functional limitation, nerve injury, chronic pain/edema, or cold intolerance) were identified. Finally, with regard to the aesthetic outcome of the donor site, they found that the patients were very accepting of the donor site scar, viewing it as a worthwhile trade-off for the creation of a phallus (Fig. 10 ). 38 Suprafascial flap dissection, full thickness skin grafts, and the use of dermal substitutes may contribute to a better forearm scar.

(A,B) Aspect of the donor site after a phalloplasty with a radial forearm flap.
NORMAL SCROTUM
For the FTM patient, the goal of creating natural-appearing genitals also applies to the scrotum. As the labia majora are the embryological counterpart of the scrotum, many previous scrotoplasty techniques left the hair-bearing labia majora in situ, with midline closure and prosthetic implant filling, or brought the scrotum in front of the legs using a V-Y plasty. These techniques were aesthetically unappealing and reminiscent of the female genitalia. Selvaggi in 2009 reported on a novel scrotoplasty technique, which combines a V-Y plasty with a 90-degree turning of the labial flaps resulting in an anterior transposition of labial skin (Fig. 11 ). The excellent aesthetic outcome of this male-looking (anteriorly located) scrotum, the functional advantage of fewer urological complications and the easier implantation of testicular prostheses make this the technique of choice. 39

Reconstruction of a lateral looking scrotum with two transposition flaps: (A) before and (B) after implantation of testicular prostheses.
SEXUAL INTERCOURSE
In a radial forearm phalloplasty, the insertion of erection prosthesis is required to engage in sexual intercourse. In the past, attempts have been made to use bone or cartilage, but no good long-term results are described. The rigid and semirigid prostheses seem to have a high perforation rate and therefore were never used in our patients. Hoebeke, in the largest series to date on erection prostheses after penile reconstruction, only used the hydraulic systems available for impotent men. A recent long-term follow-up study showed an explantation rate of 44% in 130 patients, mainly due to malpositioning, technical failure, or infection. Still, more than 80% of the patients were able to have normal sexual intercourse with penetration. 37 In another study, it was demonstrated that patients with an erection prosthesis were more able to attain their sexual expectations than those without prosthesis (Fig. 12 ). 32

(A,B) Phalloplasty after implantation of an erection prosthesis.
A major concern regarding erectile prostheses is long-term follow-up. These devices were developed for impotent (older) men who have a shorter life expectancy and who are sexually less active than the mostly younger FTM patients.
Alternative Phalloplasty Techniques
Metaidoioplasty.
A metoidioplasty uses the (hypertrophied) clitoris to reconstruct the microphallus in a way comparable to the correction of chordee and lengthening of a urethra in cases of severe hypospadias. Eichner 40 prefers to call this intervention “the clitoris penoid.” In metoidioplasty, the clitoral hood is lifted and the suspensory ligament of the clitoris is detached from the pubic bone, allowing the clitoris to extend out further. An embryonic urethral plate is divided from the underside of the clitoris to permit outward extension and a visible erection. Then the urethra is advanced to the tip of the new penis. The technique is very similar to the reconstruction of the horizontal part of the urethra in a normal phalloplasty procedure. During the same procedure, a scrotal reconstruction, with a transposition flap of the labia majora (as previously described) is performed combined with a vaginectomy.
FTM patients interested in this procedure should be informed preoperatively that voiding while standing cannot be guaranteed, and that sexual intercourse will not be possible (Fig. 13 ).

Results of a metoidioplasty procedure.
The major advantage of metoidioplasty is the complete lack of scarring outside the genital area. Another advantage is that its cost is substantially lower than that of phalloplasty. Complications of this procedure also include urethral obstruction and/or urethral fistula.
It is always possible to perform a regular phalloplasty (e.g., with a radial forearm flap) at a later stage, and with substantially less risk of complications and operation time.
FIBULA FLAP
There have been several reports on penile reconstruction with the fibular flap based on the peroneal artery and the peroneal vein. 27 , 41 , 42 It consists of a piece of fibula that is vascularized by its periosteal blood supply and connected through perforating (septal) vessels to an overlying skin island at the lateral site of the lower leg. The advantage of the fibular flap is that it makes sexual intercourse possible without a penile prosthesis. The disadvantages are a pointed deformity to the distal part of the penis when the extra skin can glide around the end of fibular bone, and that a permanently erected phallus is impractical.
Many authors seem to agree that the fibular osteocutaneous flap is an optimal solution for penile reconstruction in a natal male. 42
NEW SURGICAL DEVELOPMENTS: THE PERFORATOR FLAPS
Perforator flaps are considered the ultimate form of tissue transfer. Donor site morbidity is reduced to an absolute minimum, and the usually large vascular pedicles provide an additional range of motion or an easier vascular anastomosis. At present, the most promising perforator flap for penile reconstruction is the anterolateral thigh (ALT) flap. This flap is a skin flap based on a perforator from the descending branch of the lateral circumflex femoral artery, which is a branch from the femoral artery. It can be used both as a free flap 43 and as a pedicled flap 44 then avoiding the problems related to microsurgical free flap transfer. The problem related to this flap is the (usually) thick layer of subcutaneous fat making it difficult to reconstruct the urethra as a vascularized tube within a tube. This flap might be more indicated for phallic reconstruction in the so-called boys without a penis, like in cases of vesical exstrophy (Fig. 14 ). However, in the future, this flap may become an interesting alternative to the radial forearm flap, particularly as a pedicled flap. If a solution could be found for a well-vascularized urethra, use of the ALT flap could be an attractive alternative to the radial forearm phalloplasty. The donor site is less conspicuous, and secondary corrections at that site are easier to make. Other perforator flaps include the thoracodorsal perforator artery flap (TAP) and the deep inferior epigastric perforator artery flap (DIEP). The latter might be an especially good solution for FTM patients who have been pregnant in the past. Using the perforator flap as a pedicled flap can be very attractive, both financially and technically.

Penile reconstruction with a pedicled anterolateral thigh flap. (A) Preoperative and (B) postoperative results.
The Importance of a Multidisciplinary Approach
Gender reassignment, particularly reassignment surgery, requires close cooperation between the different surgical specialties. In phalloplasty, the collaboration between the plastic surgeon, the urologist, and the gynecologist is essential. 45 The actual penile reconstruction is typically performed by the plastic and reconstructive surgeon, and the contribution of the gynecologist, who performs a hysterectomy and a BSO (preferably through a minimal endoscopic access in combination with SCM), should not be underestimated.
However, in the long term, the urologist's role may be the most important for patients who have undergone penile reconstruction, especially because the complication rate is rather high, particularly with regard to the number of urinary fistulas and urinary stenoses. The urologist also reconstructs the fixed part of the urethra. He or she is likely the best choice for implantation and follow-up of the penile and/or testicular prostheses. They must also address later sequelae, including stone formation. Moreover, the surgical complexity of adding an elongated conduit (skin-tube urethra) to a biological female bladder, and the long-term effects of evacuating urine through this skin tube, demand lifelong urological follow-up.
Therefore, professionals who unite to create a gender reassignment program should be aware of the necessity of a strong alliance between the plastic surgeon, the urologist, mental health professional and the gynecologist. In turn, the surgeons must commit to the extended care of this unique population, which, by definition, will protract well into the future.
- Meyer W J, III, Bockting W O, Cohen-Kettenis P, et al. The Standards of Care for Gender Identity Disorders, 6th Version. J Psychol Human Sex. 2002; 13 :1–30. [ Google Scholar ]
- Lindsay W RN. Creation of a male chest in female transsexuals. Ann Plast Surg. 1979; 3 (1):39–46. [ PubMed ] [ Google Scholar ]
- Eicher W. Transsexualismus. Vol. 1992. Stuttgart: Fisher Verlag; pp. 120–123. [ Google Scholar ]
- Hage J J, Bloem J J. Chest wall contouring for female-to-male transsexuals: Amsterdam experience. Ann Plast Surg. 1995; 34 (1):59–66. [ PubMed ] [ Google Scholar ]
- Hage J J, Kesteren P J van. Chest-wall contouring in female-to-male transsexuals: basic considerations and review of the literature. Plast Reconstr Surg. 1995; 96 (2):386–391. [ PubMed ] [ Google Scholar ]
- Monstrey S, Selvaggi G, Ceulemans P, et al. Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast Reconstr Surg. 2008; 121 (3):849–859. [ PubMed ] [ Google Scholar ]
- Webster J P. Mastectomy for gynecomastia through a semicircular intra-areolar incision. Ann Surg. 1946; 124 :557–575. [ PubMed ] [ Google Scholar ]
- Pitanguy I. Transareolar incision for gynecomastia. Plast Reconstr Surg. 1966; 38 (5):414–419. [ PubMed ] [ Google Scholar ]
- Davidson B A. Concentric circle operation for massive gynecomastia to excise the redundant skin. Plast Reconstr Surg. 1979; 63 (3):350–354. [ PubMed ] [ Google Scholar ]
- Kluzák R. Sex conversion operation in female transsexualism. Acta Chir Plast. 1968; 10 (3):188–198. [ PubMed ] [ Google Scholar ]
- Hoopes J E. Surgical construction of the male external genitalia. Clin Plast Surg. 1974; 1 (2):325–334. [ PubMed ] [ Google Scholar ]
- Kenney J G, Edgerton M T. Reduction mammoplasty in gender dysphoria. Abstract presented at the 11th Symposium of the Harry Benjamin International Gender Dysphoria Association; septerber20–23, 1989; Cleveland, Ohio.
- Beer G M, Budi S, Seifert B, Morgenthaler W, Infanger M, Meyer V E. Configuration and localization of the nipple-areola complex in men. Plast Reconstr Surg. 2001; 108 (7):1947–1952. discussion 1953. [ PubMed ] [ Google Scholar ]
- Symmers W S. Carcinoma of breast in trans-sexual individuals after surgical and hormonal interference with the primary and secondary sex characteristics. BMJ. 1968; 2 (5597):83–85. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Secreto G, Toniolo P, Berrino F, et al. Increased androgenic activity and breast cancer risk in premenopausal women. Cancer Res. 1984; 44 (12 Pt 1):5902–5905. [ PubMed ] [ Google Scholar ]
- Burcombe R J, Makris A, Pittam M, Finer N. Breast cancer after bilateral subcutaneous mastectomy in a female-to-male trans-sexual. Breast. 2003; 12 (4):290–293. [ PubMed ] [ Google Scholar ]
- Gilbert D A, Horton C E, Terzis J K, Devine C J, Jr, Winslow B H, Devine P C. New concepts in phallic reconstruction. Ann Plast Surg. 1987; 18 (2):128–136. [ PubMed ] [ Google Scholar ]
- Hage J J, Bouman F G, de Graaf F H, Bloem J J. Construction of the neophallus in female-to-lake transsexuals: the Amsterdam experience. J Urol. 1993; 6 :1463–1468. [ PubMed ] [ Google Scholar ]
- Chang T S, Hwang W Y. Forearm flap in one-stage reconstruction of the penis. Plast Reconstr Surg. 1984; 74 (2):251–258. [ PubMed ] [ Google Scholar ]
- Hage J J, De Graaf F H. Addressing the ideal requirements by free flap phalloplasty: some reflections on refinements of technique. Microsurgery. 1993; 14 (9):592–598. [ PubMed ] [ Google Scholar ]
- Fang R H, Kao Y S, Ma S, Lin J T. Phalloplasty in female-to-male transsexuals using free radial osteocutaneous flap: a series of 22 cases. Br J Plast Surg. 1999; 52 (3):217–222. [ PubMed ] [ Google Scholar ]
- Biemer E. Penile construction by the radial arm flap. Clin Plast Surg. 1988; 15 (3):425–430. [ PubMed ] [ Google Scholar ]
- Koshima I, Tai T, Yamasaki M. One-stage reconstruction of the penis using an innervated radial forearm osteocutaneous flap. J Reconstr Microsurg. 1986; 3 (1):19–26. [ PubMed ] [ Google Scholar ]
- Meyer R, Daverio P J. One-stage phalloplasty without sensory deprivation in female transsexuals. World J Urol. 1987; 5 :9–13. [ Google Scholar ]
- Upton J, Mutimer K L, Loughlin K, Ritchie J. Penile reconstruction using the lateral arm flap. J R Coll Surg Edinb. 1987; 32 (2):97–101. [ PubMed ] [ Google Scholar ]
- Harashina T, Inoue T, Tanaka I, Imai K, Hatoko M. Reconstruction of penis with free deltoid flap. Br J Plast Surg. 1990; 43 (2):217–222. [ PubMed ] [ Google Scholar ]
- Sadove R C, Sengezer M, McRoberts J W, Wells M D. One-stage total penile reconstruction with a free sensate osteocutaneous fibula flap. Plast Reconstr Surg. 1993; 92 (7):1314–1323. discussion 1324–1325. [ PubMed ] [ Google Scholar ]
- Santanelli F, Scuderi N. Neophalloplasty in female-to-male transsexuals with the island tensor fasciae latae flap. Plast Reconstr Surg. 2000; 105 (6):1990–1996. [ PubMed ] [ Google Scholar ]
- Monstrey S, Hoebeke P, Selvaggi G, et al. Penile reconstruction: is the radial forearm flap really the standard technique? Plast Reconstr Surg. 2009; 124 (2):510–518. [ PubMed ] [ Google Scholar ]
- Weyers S, Selvaggi G, Monstrey S, et al. Two-stage versus one-stage sex reassignment surgery in female-to-male transsexual individuals. Gynecol Surg. 2006; 3 :190–194. [ Google Scholar ]
- Selvaggi G, Monstrey S, Ceulemans P, T'Sjoen G, De Cuypere G, Hoebeke P. Genital sensitivity after sex reassignment surgery in transsexual patients. Ann Plast Surg. 2007; 58 (4):427–433. [ PubMed ] [ Google Scholar ]
- De Cuypere G, T'Sjoen G, Beerten R, et al. Sexual and physical health after sex reassignment surgery. Arch Sex Behav. 2005; 34 (6):679–690. [ PubMed ] [ Google Scholar ]
- Hage J J, Bout C A, Bloem J J, Megens J A. Phalloplasty in female-to-male transsexuals: what do our patients ask for? Ann Plast Surg. 1993; 30 (4):323–326. [ PubMed ] [ Google Scholar ]
- Vriens J P, Acosta R, Soutar D S, Webster M H. Recovery of sensation in the radial forearm free flap in oral reconstruction. Plast Reconstr Surg. 1996; 98 (4):649–656. [ PubMed ] [ Google Scholar ]
- Felici N, Felici A. A new phalloplasty technique: the free anterolateral thigh flap phalloplasty. J Plast Reconstr Aesthet Surg. 2006; 59 (2):153–157. [ PubMed ] [ Google Scholar ]
- Matti B A, Matthews R N, Davies D M. Phalloplasty using the free radial forearm flap. Br J Plast Surg. 1988; 41 (2):160–164. [ PubMed ] [ Google Scholar ]
- Hoebeke P, Selvaggi G, Ceulemans P, et al. Impact of sex reassignment surgery on lower urinary tract function. Eur Urol. 2005; 47 (3):398–402. [ PubMed ] [ Google Scholar ]
- Selvaggi G, Monstrey S, Hoebeke P, et al. Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast Reconstr Surg. 2006; 118 (5):1171–1177. [ PubMed ] [ Google Scholar ]
- Hoebeke P, de Cuypere G, Ceulemans P, Monstrey S. Obtaining rigidity in total phalloplasty: experience with 35 patients. J Urol. 2003; 169 (1):221–223. [ PubMed ] [ Google Scholar ]
- Eicher W. Surgical Treatment of Female-to-Male Transsexuals. In: Echer W, editor. Plastic Surgery in the Sexually Handicapped. Vol. 1989. Berlin: Springer; pp. 106–112. [ Google Scholar ]
- Hage J J, Winters H A, Lieshout J Van. Fibula free flap phalloplasty: modifications and recommendations. Microsurgery. 1996; 17 (7):358–365. [ PubMed ] [ Google Scholar ]
- Sengezer M, Oztürk S, Deveci M, Odabaşi Z. Long-term follow-up of total penile reconstruction with sensate osteocutaneous free fibula flap in 18 biological male patients. Plast Reconstr Surg. 2004; 114 (2):439–450. discussion 451–452. [ PubMed ] [ Google Scholar ]
- Felici N. Phalloplasty with Free Anterolateral Thigh Flap. Paper presented the XIX Biennial Symposium of the Harry Benjamin International Gender Dysphoria Association (HBIGDA); April 6–9, 2005; Bologna, Italy.
- Ceulemans P. The Pedicled Anterolateral Thigh Flap (ALT) Perforator Flap: A New Technique for Phallic Reconstruction. Paper presented at the XIV Biennial Symposium of the Harry Benjamin International Gender Dysphoria Association (HBIGDA); April 6–9, 2005; Bologna, Italy.
- Monstrey S, Hoebeke P, Dhont M, et al. Surgical therapy in transsexual patients: a multi-disciplinary approach. Acta Chir Belg. 2001; 101 (5):200–209. [ PubMed ] [ Google Scholar ]
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
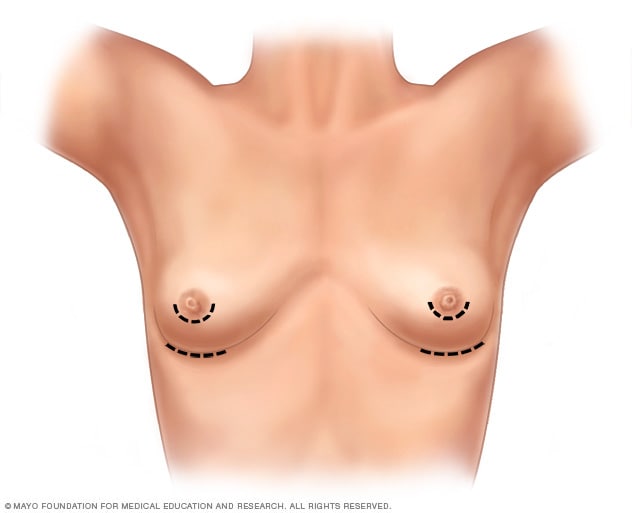
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
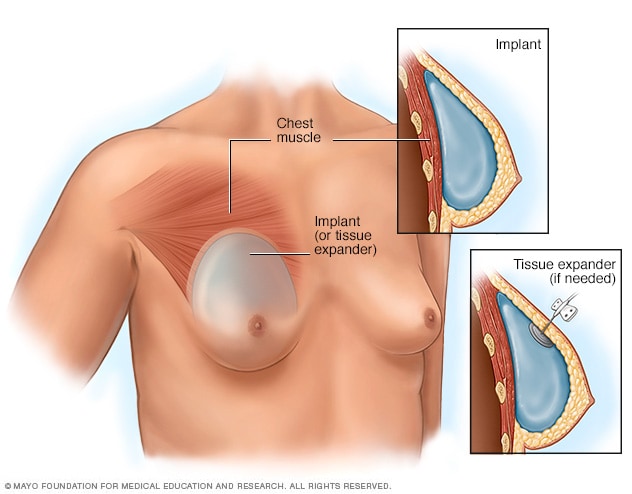
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
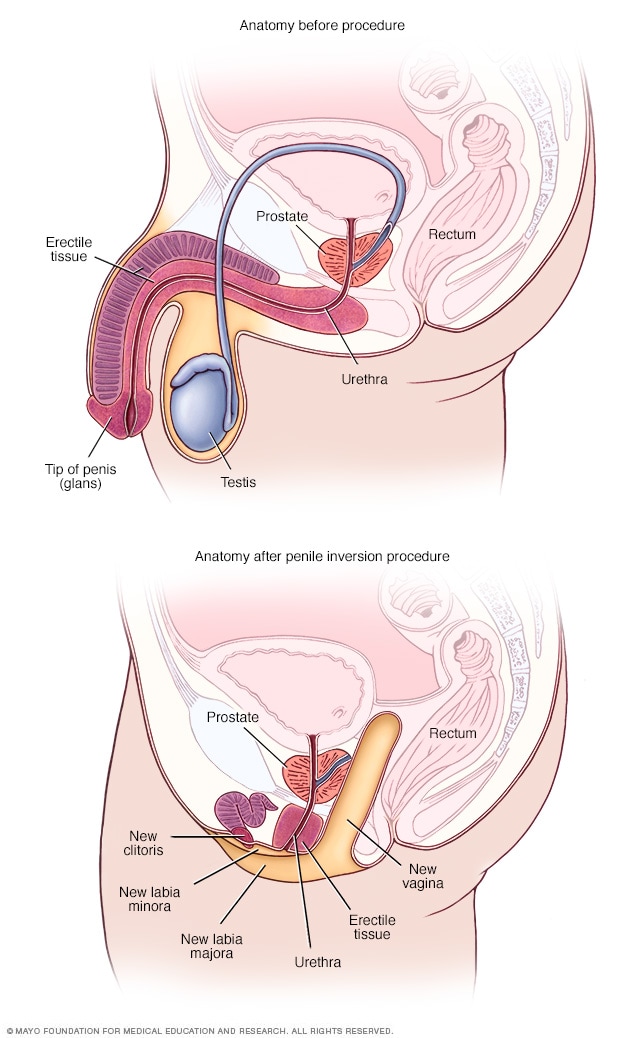
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
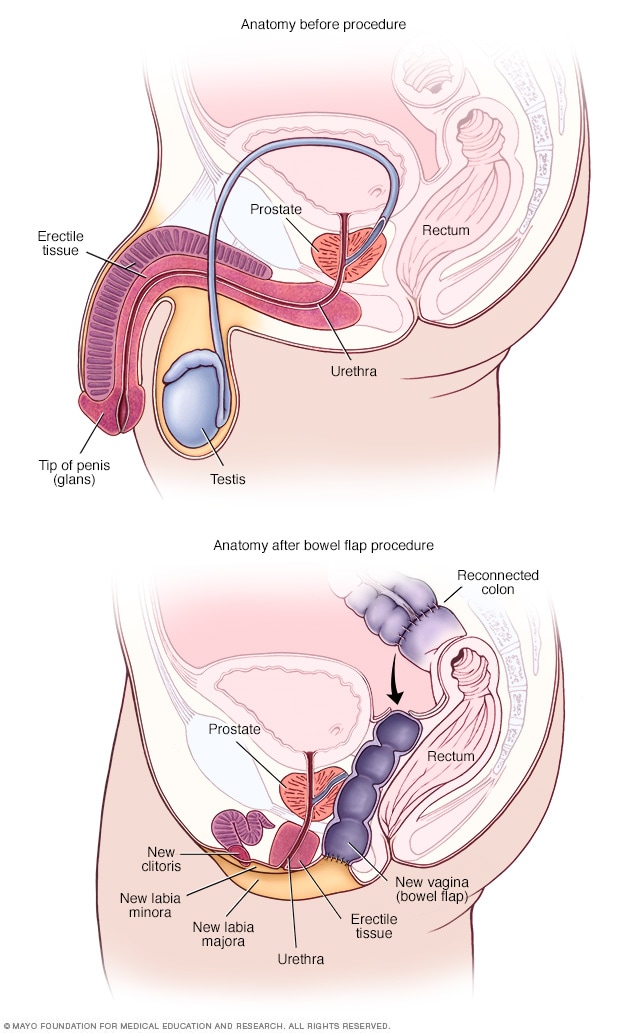
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
The Christian Post
To enjoy our website, you'll need to enable JavaScript in your web browser. Please click here to learn how.
You are using an outdated browser. Please upgrade your browser to improve your experience.
Recommended

Adults who undergo trans surgeries at 12 times higher risk of attempting suicide: report

Sadie Robertson Huff on overcoming her exposure to porn: ‘Freedom on the other side’

Travis Kelce defends Harrison Butker amid backlash: 'I cherish him'

Louisiana House passes bill to punish abusers for poisoning women with abortion drugs

National Park Service changes course, will allow Knights of Columbus Memorial Day mass

The Christian’s duty in a revolutionary age (part 2)

Ask Chuck: Struggling to pay for senior care

Rebuilding a safe, pro-learning culture at an inner-city school

Is the Electoral College 'un-American?'

Why Piers Morgan doesn't need 'Catholic guilt'

Trans-identifying adults who underwent body-mutilating surgeries as part of an effort to look like the opposite sex had an elevated suicide attempt risk, according to a recent study.
The study , titled “Risk of Suicide and Self-Harm Following Gender-Affirmation Surgery,” was published in April in the medical science journal Cureus. Researchers conducted the study by assessing over 90 million adults aged 18 to 60.
According to the study, individuals who underwent “gender-affirming surgery” had a 12-fold higher suicide attempt risk than those who did not. The researchers found that 3.5% of people who had an elective trans surgery were treated for attempting suicide. As the study reported, 0.3% of patients who did not undergo a surgical procedure did not attempt suicide.

Get Our Latest News for FREE
One critic of the study, trans-identified journalist Erin Reed, published an analysis on his Substack page, Erin in The Morning, refuting its findings. The analysis claims that the authors' methodology raises questions about the study's accuracy.
Reed questioned the study’s results, taking issue with the research because, he claimed, it compared people who had trans surgeries to non-trans-identifying individuals to determine if said surgeries increased the risk of suicide.
“To accurately assess whether transgender surgeries increase suicide risk, the correct control group would be transgender people who did not have surgery or, even more accurately, those who were denied surgery,” Reed wrote. “It would be like judging the effectiveness of a new teaching method by comparing college students using the new method to those who never went to college, rather than to college students using the old method.”
Dietrich Jehle, one of the study’s authors, said in a statement to The Christian Post that they “looked at associations with outcomes rather than causation in a large propensity matched retrospective study.” Jehle serves as professor and chair of the Sealy Department of Emergency Medicine at the University of Texas Medical Branch in Galveston, Texas.
“We did not look at the effect of surgery — just the outcomes of the population that had gender affirmation surgery,” Jehle told CP, adding that trans-identifying individuals typically have higher rates of depression.
“[I should emphasize] that we did not use individuals that wanted gender affirmation surgery and were not granted the surgery as a control as patients are required to undergo at least two psychiatric evaluations in order to qualify for surgery (i.e., patients who qualify for surgery are at lower suicide risk than the group who wants surgery but does not qualify regardless of whether the group that qualifies undergoes surgery),” Jehle added.
According to the researcher, the “key point” of the study is that individuals who have undergone a trans surgery “need comprehensive psychiatric care in the years following the surgery.”
“Our conclusion might be better worded: Patients who undergo gender-affirming surgery are associated with significantly elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support,” Jehle said.
He further told CP that researchers used "Z87.890" for the study, which is a code used in medical records to indicate whether someone has a history of undergoing trans procedures.
Regarding the methodology, the study consisted of four separate cohorts. The first Cohort, A, consisted of 1,501 adults aged 18 to 60, who underwent a trans surgery and later sought emergency care for suicidal ideation. Cohort B was intended to serve as the study’s control group, and it consisted of adults aged 18 to 60 who had gone to an emergency room for mental health concerns but had no history of having undergone a sex-change operation.
Another group, Cohort C, served as the study’s second control group, and it consisted of adults aged 18 to 60, who went to the ER and had tubal litigation (surgery performed on women to prevent pregnancy) or a vasectomy but they did not undergo “gender-affirmation surgery.”
“A secondary analysis involving a control group with pharyngitis, referred to as cohort D, was conducted to validate the results from cohort C,” the study stated.
The study concluded, “Gender-affirming surgery is significantly associated with elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support.”
Brandon Showalter, a social commentator for The Christian Post, who has done extensive research on the topic of gender dysphoria and so-called gender-affirming surgeries, noted that there can be a variety of factors that cause a person to feel compelled to end his or her life.
"While I'm not surprised to see these higher numbers in this latest research, the prevailing challenge for critics of these procedures is to make visible the harms of this experimental medicalization and irreversible surgeries, which are numerous aside from any consideration about how those medical practices might contribute to suicide," Showalter stated.
Discussions about the effectiveness of so-called “gender-affirming care” and the potentially negative impact on an individual’s mental health are ongoing.
In October 2019, a study published in the American Journal of Psychiatry initially highlighted the mental health benefits associated with “gender-affirming” surgeries. Researchers analyzed the records of 9.7 million Swedes in the national population registry. Between 2005 and 2015, 1018 of the 2,679 individuals diagnosed with "gender incongruence" underwent surgery to remove their genitals or permanently alter their bodies.
The study authors highlighted a supposed 8% decrease in mood and anxiety disorders for postoperative patients each year after the surgery. The authors later posted a correction after several media outlets reported on the finding, stating their data “demonstrated no advantage of surgery in relation to subsequent mood or anxiety disorder-related health care visits or prescriptions or hospitalizations following suicide attempts.”
A separate extensive long-term study conducted in Sweden by scholars at the Karolinska Institute and Gothenburg University concluded that "after sex reassignment, [trans-identified individuals] have considerably higher risks for mortality, suicidal behavior, and psychiatric morbidity than the general population."
The study analyzed 324 individuals (191 male-to-female, 133 female-to-male) for over 30 years after a sex-change surgery from a period of 1973 to 2003.
Samantha Kamman is a reporter for The Christian Post. She can be reached at: [email protected] . Follow her on Twitter: @Samantha_Kamman
Was this article helpful?
Help keep The Christian Post free for everyone.
By making a recurring donation or a one-time donation of any amount, you're helping to keep CP's articles free and accessible for everyone.
We’re sorry to hear that.
Hope you’ll give us another try and check out some other articles. Return to homepage.
Psychiatry journal issues major correction to study on trans surgeries effect on mental health
44% of trans-identified individuals report ‘serious psychological distress,' one-third experienced homelessness, aclu sues ohio over law banning sex-change surgeries for minors, men in women's sports, appeals court says wva, nc can’t bar medicaid coverage for elective trans surgeries, most popular.

'Blasphemous': 4 reactions to UN, US honoring fallen Iranian president

After setting record for baptisms in California, pastor wants to baptize America, then the world

Pastor Matthew Queen charged with obstructing DOJ, FBI investigation of SBC

Bishop Robert Barron clarifies Catholic teaching amid 'kerfuffle' over papal interview

Millions see duet performance of 'Goodness of God' on 'American Idol' finale
More articles.

Nikki Haley says she is voting for Trump: 'Biden has been a catastrophe'

Ted Cruz torches Biden judicial nominee for recommending male rapist in women's prison
Group of brands.
Breaking News
RELIST WATCH
Restrictions on gender-affirming medical care – and assault weapons.

The Relist Watch column examines cert petitions that the Supreme Court has “relisted” for its upcoming conference. A short explanation of relists is available here .
After going two conferences without any new relists, the Supreme Court ended the relist drought this week with a vengeance. We have 12 new relists, several of which are potential blockbusters if the court grants review.
Gender-affirming care
Three of the cases involve constitutional challenges brought against state prohibitions on providing gender-affirming care to minors: United States v. Skrmetti , L. W. v. Skrmetti , and Jane Doe 1 v. Kentucky ex rel. Cameron . Last year, Tennessee and Kentucky were among a group of more than 20 states that enacted laws that prohibit giving transgender youths under the age of 18 medical treatment to align their appearance with their gender identity.
Tennessee’s law forbids medical treatments that are intended to allow a minor “to identify with, or live as, a purported identity inconsistent with the minor’s sex” or to treat “purported discomfort or distress from a discordance between the minor’s sex and asserted identity.” Kentucky’s law prohibits medical treatments “for the purpose of attempting to alter the appearance of, or to validate a minor’s perception of, [a] minor’s sex.” Both provisions outlaw a range of treatments, including gender-reassignment surgery. But the challenges before the court specifically concern two nonsurgical treatments: the administration of puberty blockers to stop physical changes brought on by puberty; and hormone therapy, which seeks to produce physiological changes to conform physical appearance with gender identity.
Transgender youths and their parents in both states quickly brought constitutional challenges in federal court, seeking to enjoin the laws before they went into effect. The challengers first argue that the restrictions discriminate on the basis of sex and therefore violate the 14th Amendment’s equal protection clause. They contend that the laws allow the use of puberty blockers and hormone therapy to conform a minor’s appearance to their birth sex, while barring transgender minors from using the same treatments. Second, the challengers argue that the prohibitions violate the 14th Amendment’s due process clause by infringing upon parents’ rights to make medical decisions for their children. The Biden administration intervened on the challengers’ side in the Tennessee case.
Federal district courts in both states granted the challengers’ requests to block the laws from going into effect. Kentucky and Tennessee then asked the U.S. Court of Appeals for the 6th Circuit to lift those orders while they appealed. The court of appeals refused, instead expediting argument. By a split vote, the 6th Circuit then reversed the lower courts’ rulings , concluding that the states were likely to win their appeals. The court thus allowed the laws go into effect.
The Biden administration, together with the Tennessee and Kentucky families, seek reversal of the 6th Circuit’s ruling. All three challengers maintain that the laws violate the equal protection clause, arguing that under Bostock v. Clayton County (in which the Supreme Court held that firing transgender employees on the basis of their gender identity violates federal employment discrimination laws) drawing distinctions on the basis of gender identity constitute prohibited action on the basis of sex. The private challengers also argue that the laws violate the due process clause because the Supreme Court has repeatedly struck down state restrictions on parents’ ability to raise their children as they see fit.
Just last month, the Supreme Court granted Idaho’s request for a partial stay of a lower-court injunction, thus permitting the state’s ban on gender-affirming care to go into effect until the court rules on any cert petition – although the injunction still remained in force as to the plaintiffs in that case, thus permitting the plaintiffs there to receive treatment.
There are some differences in the case – in the Idaho case, the district court’s decision to grant relief beyond the plaintiffs – a so-called “universal injunction” – was more prominent. But the grant of a stay suggests that a majority of the court believes the issue is certworthy and that the state is likely to succeed. A grant in this case would make next term very interesting indeed.
Assault weapons
In early 2023, Illinois adopted the Protect Illinois Communities Act, which prohibits the possession of assault weapons and high-capacity magazines. The state law’s definition of “assault weapon” essentially followed the federal-law definition. The act prohibits possession of certain semiautomatic pistols and rifles. A semiautomatic rifle falls under the law’s proscriptions if it has a detachable magazine and one or more of the following features: a pistol grip or thumbhole stock; any feature capable of functioning as a protruding grip for the non-trigger hand; a folding, telescoping, thumbhole, or detachable stock or a stock that otherwise enhances the concealability of the weapon; a flash suppressor; a grenade launcher; or a barrel shroud. The definition also includes a semiautomatic rifle with a fixed magazine capacity of more than 10 rounds (except those that accept only .22 caliber rimfire ammunition). Finally, there is a lengthy list of particular models that fall within the scope of the statute, notably all “AK” weapons (modeled after the Russian AK-47) and all “AR” weapons (those modeled after the AR-15). People who owned such weapons before the effective date of the law are permitted to retain them, subject to some geographic restrictions on use; otherwise, possession is a crime. Several Illinois municipalities adopted similar legislation.
Gun owners, dealers, and interest groups brought a number of lawsuits arguing that the law violated their rights under the Second Amendment to keep and bear arms and sought to block the state from enforcing the law. Roughly speaking, plaintiffs in northern Illinois, which is more urban, lost; plaintiffs in southern Illinois, which is more rural, were successful, and a judge there held that the statute was unconstitutional in all its applications and barred the state from enforcing it.
In a consolidated appeal, a divided panel of the U.S. Court of Appeals for the 7th Circuit affirmed the denial of relief for the northern cases and reversed the grant of relief for the southern ones. The panel said that, “[u]sing the tools of history and tradition to which the Supreme Court directed us in [ District of Columbia v. ] Heller and [ New York State Rifle & Pistol Ass’n v. ] Bruen ,” which instructed courts to look for analogous laws in history when considering the constitutionality of restrictions on the personal right to bear arms, “the state and the affected subdivisions have a strong likelihood of success in the pending litigation.” The 7th Circuit reasoned that “these assault weapons and high-capacity magazines are much more like machineguns and military-grade weaponry” that are not protected by the Second Amendment “than they are like the many different types of firearms that are used for individual self-defense,” and thus they can be regulated or banned.
Six petitions have been filed seeking review of that determination: Harrel v. Raoul , Herrera v. Raoul , Barnett v. Raoul , National Association for Gun Rights v. City of Naperville, Illinois , Langley v. Kelly , and Gun Owners of America, Inc. v. Raoul . Given the ubiquity of AR- and AK-type firearms, this case will likely be a blockbuster if granted.
Environmental law
The Clean Water Act of 1972 regulates the discharge of pollutants into regulated waters. The city and county of San Francisco received a permit from the EPA under the law’s National Pollutant Discharge Elimination System that allowed San Francisco to discharge from its wastewater treatment facility into the Pacific Ocean. San Francisco challenged the terms of its permit, arguing that the permit contained terms so vague that it failed to tell the city how much it needed to limit or treat its discharges to comply with the act, while simultaneously exposing it to liability for violating the permit provisions. After exhausting administrative remedies, San Francisco petitioned the U.S. Court of Appeals for the 9th Circuit for review.
A divided panel of the 9th Circuit denied San Francisco’s petition , concluding that the provisions are not unduly vague and are “consistent with the CWA and its implementing regulations.” In dissent, Judge Daniel Collins concluded that those provisions were “inconsistent with the text of the CWA.” He argued that the permit violated the CWA by making the permittee responsible for maintaining water quality standards without specifying what limitations on discharges would satisfy its responsibility.
San Francisco now seeks review , arguing that the 9th Circuit’s decision conflicts with decisions of the U.S. Court of Appeals for the 2nd Circuit and the Supreme Court itself. The government denies that there’s any such split.
Yes, that Michael Avenatti
Michael Avenatti enjoyed his 15 minutes of fame representing porn star Stormy Daniels in her suit against then-President Donald Trump. Afterwards, while representing youth basketball coach Gary Franklin in sponsorship negotiations with sports clothing company Nike, Avenatti threatened to disclose certain documents (that his client had not authorized him to disclose) unless Nike paid him and a colleague more than $10 million to do an “internal investigation” into sports corruption. Based on the conduct, Avenatti was convicted in federal court of extortion and fraud for depriving his client of his “honest services,” prohibited by 18 U.S.C. § 1346. The U.S. Court of Appeals for the 2nd Circuit affirmed his conviction.
In his petition in Avenatti v. United States , Avenatti raises two claims . First, he argues that 18 U.S.C. § 1346 is void “both on its face and” as applied to him because, as Justice Neil Gorsuch said in his concurring opinion in last year’s Percoco v. United States , “[t]o this day, no one knows what ‘honest-services fraud’ encompasses.” Avenatti claims that he did not defraud his client – he “at worst … abus[ed] his fiduciary duty as Franklin’s attorney by leveraging Franklin’s claims to pursue compensation for himself.” Second, he argues that most courts besides the 2nd Circuit have held that civil litigation conduct — and in particular, an attorney’s settlement demand — cannot support federal criminal extortion liability. Avenetti argues that under the 2nd Circuit’s rule, what would normally be handled by bar discipline is converted into a 20-year felony. The government responds that Avenatti raised neither claim before the court of appeals and that they are therefore procedurally defaulted; and even if they weren’t, those claims are meritless.
The Surpeme Court has long been skeptical of the honest-services fraud statute and the risks of overcriminalizing sharp business dealings, so one or more of the justices is surely taking a close look at this case.
Last up is a capital case, Medrano v. Texas . Rodolfo Medrano was a member of a south Texas gang charged with capital murder for the shooting deaths of six rival gang members during a robbery. When Medrano was arrested, he invoked his Miranda rights and told police he wanted to speak to an attorney. Police then spoke to Medrano’s wife and told her (falsely) that he was not believed to be involved and would be released if he spoke to police. She persuaded Medrano to talk, and he confessed to providing the guns. Medrano protested that he only provided guns for a robbery and was not present and did not expect the shootings to occur, but the jury found him criminally responsible. That testimony was then introduced against him at trial, and he was convicted of murder and sentenced to death. His conviction and sentence were affirmed on appeal, and his first petition for state post-conviction relief was denied.
Medrano then filed a second petition for state post-conviction relief, alleging that his Miranda rights were violated because police responded to his invocation of his right to silence by persuading his wife to talk to him. He also argued that expert testimony introduced against him violated his due process rights. The Texas Court of Criminal Appeals concluded that Medrano’s application failed to satisfy a state rule of criminal procedure governing successive petitions, and therefore dismissed his application as an “abuse of the writ” of habeas corpus.
In his petition , Medrano renews his argument that law enforcement officers violated his Miranda rights by using his wife to circumvent his invocation of his right to silence. He also argues that the rule invoked by the Texas Court of Criminal Appeals was not actually an “adequate and independent state ground” precluding review of his petition on the merits. He explains that the rule itself permitted a subsequent petition if the defendant could make a showing that but for a violation of the Constitution, no rational juror could have found him guilty. That condition is satisfied here, Medrano says, because the principal evidence introduced against him was the confession he says was improperly procured. In a supplemental brief , Medrano says that his second question is related to an issue the court will be considering next term in Glossip v. Oklahoma , so at minimum, the court should hold his petition for resolution of that case.
We’ll know more soon. Until next time!
New Relists
L.W. v. Skrmetti , 23-466 Issues : (1) Whether Tennessee’s Senate Bill 1 , which categorically bans gender-affirming healthcare for transgender adolescents, triggers heightened scrutiny and likely violates the 14th Amendment’s equal protection clause; and (2) whether Senate Bill 1 likely violates the fundamental right of parents to make decisions concerning the medical care of their children guaranteed by the 14th Amendment’s due process clause. (rescheduled before the Mar. 15, Mar. 22, Mar. 28, Apr. 12, Apr. 19, Apr. 26 and May 9 conferences; relisted after the May 16 conference)
United States v. Skrmetti , 23-477 Issue : Whether Tennessee Senate Bill 1 , which prohibits all medical treatments intended to allow “a minor to identify with, or live as, a purported identity inconsistent with the minor’s sex” or to treat “purported discomfort or distress from a discordance between the minor’s sex and asserted identity,” violates the equal protection clause of the 14th Amendment. (rescheduled before the Mar. 15, Mar. 22, Mar. 28, Apr. 12, Apr. 19, Apr. 26 and May 9 conferences; relisted after the May 16 conference)
Jane Doe 1 v. Kentucky ex rel. Coleman, Attorney General , 23-492 Issues : (1) Whether, under the 14th Amendment’s due process clause, Kentucky Revised Statutes Section 311.372(2) , which bans medical treatments “for the purpose of attempting to alter the appearance of, or to validate a minor’s perception of, the minor’s sex, if that appearance or perception is inconsistent with the minor’s sex,” should be subjected to heightened scrutiny because it burdens parents’ right to direct the medical treatment of their children; (2) whether, under the 14th Amendment’s equal protection clause, § 311.372(2) should be subjected to heightened scrutiny because it classifies on the basis of sex and transgender status; and (3) whether petitioners are likely to show that § 311.372(2) does not satisfy heightened scrutiny. (rescheduled before the Mar. 15, Mar. 22, Mar. 28, Apr. 12, Apr. 19, Apr. 26 and May 9 conferences; relisted after the May 16 conference)
City and County of San Francisco v. Environmental Protection Agency , 23-753 Issue : Whether the Clean Water Act allows the Environmental Protection Agency (or an authorized state) to impose generic prohibitions in National Pollutant Discharge Elimination System permits that subject permit-holders to enforcement for violating water quality standards without identifying specific limits to which their discharges must conform. (relisted after the May 16 conference)
Harrel v. Raoul , 23-877 Issues : (1) Whether the Constitution allows the government to prohibit law-abiding, responsible citizens from protecting themselves, their families, and their homes with semiautomatic firearms that are in common use for lawful purposes; (2) whether the Constitution allows the government to prohibit law-abiding, responsible citizens from protecting themselves, their families, and their homes with ammunition magazines that are in common use for lawful purposes; and (3) whether enforcement of Illinois’s semiautomatic firearm and ammunition magazine bans should be enjoined. (relisted after the May 16 conference)
Herrera v. Raoul , 23-878 Issues : (1) Whether semiautomatic rifles and standard handgun and rifle magazines do not count as “Arms” within the ordinary meaning of the Second Amendment’s plain text; and (2) whether there is a broad historical tradition of states banning protected arms and standard magazines from law-abiding citizens’ homes. (relisted after the May 16 conference)
Barnett v. Raoul , 23-879 Issue : Whether Illinois’ sweeping ban on common and long-lawful arms violates the Second Amendment. (relisted after the May 16 conference)
National Association for Gun Rights v. City of Naperville, Illinois , 23-880 Issues : (1) Whether the state of Illinois’ ban of certain handguns is constitutional in light of the holding in District of Columbia v. Heller that handgun bans are categorically unconstitutional; (2) whether the “in common use” test announced in Heller is hopelessly circular and therefore unworkable; and (3) whether the government can ban the sale, purchase, and possession of certain semi-automatic firearms and firearm magazines that are possessed by millions of law-abiding Americans for lawful purposes when there is no analogous Founding-era regulation. (relisted after the May 16 conference)
Langley v. Kelly , 23-944 Issues : (1) Whether the state of Illinois’ absolute ban of certain commonly owned semi-automatic handguns is constitutional in light of the holding in District of Columbia v. Heller that handgun bans are categorially unconstitutional; (2) whether the state of Illinois’ absolute ban of all commonly owned semi-automatic handgun magazines over 15 rounds is constitutional in light of the holding in Heller that handgun bans are categorially unconstitutional; and (3) whether the government can ban the sale, purchase, possession, and carriage of certain commonly owned semi-automatic rifles, pistols, shotguns, and standard-capacity firearm magazines, tens of millions of which are possessed by law-abiding Americans for lawful purposes, when there is no analogous historical ban as required by Heller and New York State Rifle & Pistol Ass’n, Inc. v. Bruen . (relisted after the May 16 conference)
Gun Owners of America, Inc. v. Raoul , 23-1010 Issue : Whether Illinois’ categorical ban on millions of the most commonly owned firearms and ammunition magazines in the nation, including the AR-15 rifle, violates the Second Amendment. (relisted after the May 16 conference)
Medrano v. Texas , 23-5597 Issues : (1) Whether under all the circumstances, including an officer’s knowing and deliberate deployment of Petitioner’s wife to elicit statements from Petitioner while he was in custody, the falsity of the information the officer gave her to convey to the petitioner, the strength of the incentive he proffered to induce the Petitioner to speak, and the fact that similar tactics were deliberately employed to obtain confessions Petitioner’s codefendants, introduction of the resulting statement Petitioner’s Fifth and Fourteenth Amendment rights under Miranda v. Arizona, 384 U.S. 436 (1966); (2) Whether the Texas Court of Criminal Appeals’ determination that the Petitioner’s subsequent petition failed to satisfy the requirements of Article 11.071, § 5(a)(2) was an adequate and independent state ground precluding merits review of his claim where that provision authorizes a subsequent petition when “by a preponderance of the evidence, but for a violation of the United States Constitution no rational juror could have found the applicant guilty beyond a reasonable doubt” and the confession whose constitutionality Petitioner is challenging was the only significant evidence linking him to the capital murder with which he was charged. (relisted after the May 16 conference)
Avenatti v. United States , 23-6753 Issues : (1) whether 18 U.S.C. § 1346, making it a crime to engage in “honest services fraud,” is void for vagueness; (2); whether civil litigation conduct – in particular, an attorney’s settlement demand – can support federal criminal extortion liability. (relisted after the May 16 conference)
Returning Relists
Hamm v. Smith , 23-167 Issues : (1) Whether Hall v. Florida and Moore v. Texas mandate that courts deem the standard of “significantly subaverage intellectual functioning” for determining intellectual disability in Atkins v. Virginia satisfied when an offender’s lowest IQ score, decreased by one standard error of measurement, is 70 or below; and (2) whether the court should overrule Hall and Moore , or at least clarify that they permit courts to consider multiple IQ scores and the probability that an offender’s IQ does not fall at the bottom of the lowest IQ score’s error range. (relisted after the Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22, Mar. 28, Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Cunningham v. Florida , 23-5171 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Nov. 17, Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Guzman v. Florida , 23-5173 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Crane v. Florida , 23-5455 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Arellano-Ramirez v. Florida , 23-5567 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Jackson v. Florida , 23-5570 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Sposato v. Florida , 23-5575 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Morton v. Florida , 23-5579 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Aiken v. Florida , 23-5794 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (rescheduled before the Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Enrriquez v. Florida , 23-5965 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (rescheduled before the Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Bartee v. Florida , 23-6143 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Manning v. Florida , 23-6049 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (rescheduled before the Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Tillman v. Florida , 23-6304 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (relisted after the Apr. 19, Apr. 26, May 9 and May 16 conferences)
Sanon v. Florida , 23-6289 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (relisted after the Apr. 19, Apr. 26, May 9 and May 16 conferences)
Posted in Featured , Cases in the Pipeline
Cases: United States v. Skrmetti , Avenatti v. United States , Jane Doe 1 v. Kentucky ex rel. Coleman, Attorney General , City and County of San Francisco v. Environmental Protection Agency , Harrel v. Raoul , Herrera v. Raoul , Barnett v. Raoul , National Association for Gun Rights v. City of Naperville, Illinois , Langley v. Kelly , Hamm v. Smith , Gun Owners of America, Inc. v. Raoul , L. W. v. Skrmetti , Medrano v. Texas
Recommended Citation: John Elwood, Restrictions on gender-affirming medical care – and assault weapons , SCOTUSblog (May. 24, 2024, 10:49 AM), https://www.scotusblog.com/2024/05/restrictions-on-gender-affirming-medical-care-and-assault-weapons/
Privacy Overview

- myWHRO Login
The Vatican says surrogacy and gender theory are 'grave threats' to human dignity

Updated April 8, 2024 at 5:55 PM ET
The Vatican has released a new document calling poverty, war and the plight of migrants "threats to human dignity." But it also calls abortion, surrogacy and gender theory "grave threats" facing humanity today.
The document, titled " Infinite Dignity " says that each person's dignity comes from the love of the creator "who has imprinted the indelible features of his image on every person." This language is familiar to Christians accustomed to hearing that humans are all made in God's image.
The document goes on to say that this dignity is inalienable, beyond any circumstance or situation the person might encounter. Simply put, because a person exists, a human has intrinsic dignity.
"Infinite Dignity" details a long list of what it calls grave threats to that dignity, some of which might be expected given other Catholic teachings. It talks about the drama of poverty and how the unequal distribution of wealth denies humans their God-given dignity. It also describes war, the abuse of migrants, sexual abuse, violence against women, the marginalizing of people with disabilities, assisted suicide and abortion all as affronts to human dignity.
But then the document turns to other issues that have become more highly politicized in recent years: surrogacy, gender theory, and what it calls "sex change."
The document's framework holds that if a person is made in God's image, gender theory and gender reassignment surgery call into question why God would create a person with the wrong gender.
It says that the understanding of humanity as divided into two sexes — male and female — is biblical and deeply meaningful, especially in terms of procreation. Gender theory argues that a person's gender can be different from the sex that person was assigned at birth.
"Infinite Dignity" says the concept of human dignity can be misused to justify what it calls an "arbitrary proliferation of new rights," describing those, rather, as "individual preference" or "desire." That language is very similar to how conservatives often talk about being transgender as a choice, which is something major medical and psychological groups dispute.
The document makes a clear distinction between the issue of sexual orientation (whether a person is gay, lesbian or bisexual) and the issue of gender identity (whether a person's sex assigned at birth matches what that person understands his or her gender to be).
The document will be seen by some more conservative Catholic as a win after years of feeling embattled during Pope Francis's leadership. Just last year, the Vatican said priests could baptize transgender Catholics and allowed for priests to bless people in same-sex relationships .
But many transgender Catholics and their families as well as more progressive Catholics are displeased with "Infinite Dignity."
Executive director of the LGBTQ Catholic group New Ways Ministry, Francis DeBernardo says of the document, "When it gets to the section on people who are transgender or non-binary, it doesn't apply the principles of human dignity to them."
New Ways Ministry's mission is, in part, to help pastors and religious teachers better understand gender identity and sexuality. It also fosters, "holiness and wholeness within the Catholic LGBTQ+ community."
DeBernardo argues "Infinite Dignity" does not live up to its own name. "In a sense, it's not infinite dignity," he says. "It's a very limited dignity that the church is offering."
He fears this document will be used to further persecute transgender people, and he thinks it will cause transgender Catholics and their families to leave the church.
DeBernardo also worries the sections on gender theory and what it calls "sex change" will eclipse what he describes as the very good parts of the document on war, poverty and migrants.
The group Catholics for Choice, is also disappointed and calls into question how the document was created. "Yet again," said the group's president Jamie Manson in a written statement, "a group of all-male, celibate clergymen are telling women and gender-expansive people that their lived experiences are not real or valid."
Catholics for Choice advocates within the church on a variety of issues regarding sexual and reproductive health, including abortion rights. The group holds – and argues that Catholic teaching supports – people's individual consciences should be their guide in such decisions.
"It is clear to me that the women and trans people who continue to identify as Catholic — despite documents like this completely disregarding our experiences — only do so because of a deep love for our faith and its traditions," continues Manson in her statement. "It is devastating that our leaders do not offer the same respect and love in return."
Copyright 2024 NPR. To see more, visit https://www.npr.org.

International Commentary

Lack of Jurisdiction and Biased Indictment: ICC’s Imaginary Case Against Israel
Education Commentary

The Most Important Trait for Yale’s Next President: Courage
Security News

Rand Paul: Fauci ‘Could Be Indicted’ for Deleting Records
Politics Commentary

Democrats, Not Republicans Are Capitol Hill’s True Extremists

Reason No. 3 the Left Wants Open Borders—Extortion for Amnesty: The BorderLine
Politics News

Border Bill Goes Down in Flames on Senate Floor
Security News

GOP Senators Label Border Bill an ‘Election Year Political Stunt’
Law News

Illegal Alien Convicted of Killing 2 Children Released Despite ICE Detainer
International News

These GOP Senators Rip ‘Neocon’ Foreign Policy on Both Sides
International News

China Launches ‘Punishment’ Drills Around Taiwan After President’s Inauguration
Health Care Commentary

In COVID-19 Oversight, House Republicans Deliver a Win for Accountability

Who Is Running Congress?
Politics News

Up to 2.7 Million Noncitizens Could Vote Illegally in November, Study Warns

‘PRIVILEGE’: What the White House Doesn’t Think You Should Know About Biden’s Order on Mobilizing Voters

EXCLUSIVE: HHS Chief Routinely Checked Progress of Biden Election-Meddling Directive, Records Show

‘A Travesty of Justice’: House Speaker Dissects the Left’s ‘Lawfare’ Campaign Against Trump
Politics Analysis

EXCLUSIVE: Ted Cruz Sets the Record Straight After SPLC Claims He Spread ‘Antisemitic Trope’
Society Analysis

EXCLUSIVE: Federal Farm Credit Agency Plows Ahead With DEI, ‘Queer’ Farming

EXCLUSIVE: DOJ’s Kristen Clarke Testified She Was Never Arrested. Court Records and Text Messages Indicate She Was.

EXCLUSIVE: She Survived a Death Camp. Facing Biden DOJ Charges, She Is Prepared to Die in Prison
Education News

Omar Shrugs Off Harassment of Jewish Student, Faults UCLA for Not Protecting Anti-Israel Protesters
Politics Analysis

69% of Elites Want to Restrict Voting to College Graduates Only
International Analysis

It’s ‘in Hamas’ Interest’ to Create ‘Situation of Misery and Starvation’ in Gaza, Columbia University Professor Says

Trump, Biden, and CNN: What to Know About the First Presidential Debate
International Analysis

How Taiwan’s New President May Change His Country’s Tense Relationship With China
Society Analysis
THE WPATH TAPES: Behind-Scenes Recordings Reveal What Top Gender Doctors Really Think About Sex-Change Procedures
Megan Brock / @MegEBrock / Kate Anderson / @kliseanderson / May 15, 2024
Recordings from meetings of the World Professional Association for Transgender Health reveal doctors pushing risky sex-change procedures for children, contradicting the organization's own guidelines. (Photo illustration: Anastassiya Bezhekeneva/Getty Images)

Get your FREE digital copy of The Heritage Foundation’s Founders’ Almanac.
The World Professional Association for Transgender Health , or WPATH, is the leading authority in the field of gender medicine. Its guidance is routinely used by top medical associations in the U.S. and abroad, while its standards of care inform insurance companies’ approach to coverage policies.
But behind closed doors, top WPATH doctors discussed, and at times seemed to challenge, the organization’s own published guidelines for sex-change procedures and acknowledged pushing experimental medical interventions that can have devastating and irreversible complications, according to exclusive footage obtained by the Daily Caller News Foundation.

WPATH published highly influential clinical guidance called “Standards of Care for the Health of Transgender and Gender Diverse People, Version 8,” or SOC 8, which recommends the use of invasive medical interventions such as puberty blockers, cross-sex hormones and sex change surgeries, calling them “safe and effective.”
The Daily Caller News Foundation filed a series of public records requests to the World Professional Association for Transgender Health’s SOC 8 co-authors who are employed at taxpayer-funded institutions, making their emails subject to open records laws.
Buried in more than 100 pages of responsive records from the University of Nevada was a series of emails sent in 2022 among prominent WPATH members and leaders , including WPATH Global Education Institute Co-Chair Gail Knudson.
In one email, Knudson sent a colleague the link to a folder containing nearly 30 hours of recordings from WPATH’s Global Education Institute summit in September 2022 in Montreal, Canada, which included sessions on mental health, puberty blockers, cross-sex hormones, and sex-change surgery.
These sessions provided WPATH members with in-depth education on the clinical application of topics addressed in the SOC 8 treatment guidelines. However, the footage reveals WPATH-affiliated doctors advocating that children undergo risky sex-change procedures and even pushing for these treatments for patients struggling with severe mental health issues.
Several sessions were dedicated exclusively to treating children and included recommendations for minors to receive puberty blockers, cross-sex hormones, and surgeries.
For instance, WPATH guidance recommends addressing a patient’s mental health issues before giving him or her sex-change medical interventions. However, in one recorded session, a WPATH faculty member and gender doctor claimed that mental health issues don’t necessarily affect a patient’s ability to receive cross-sex hormones.
In another video, a doctor told attendees that children should be informed that cross-sex hormones will likely make them infertile. but admitted that he would prescribe them anyway if a child says he or she wants the treatment, regardless of future consequences.
A surgeon euphemistically referred to a phalloplasty procedure, a surgical series that includes obliterating the vaginal cavity and creating a fake penis with harvested tissue, as an “adventure” for young people. He did this despite later admitting that those same procedures “definitely” will have “complications,” such as permanent issues with bladder function and tissue death.
One physician called the entire field of cross-sex hormones “off-label,” referring to the concept of drugs being used for alternative purposes than what they were approved for. The doctor went on to say that female patients might actually appreciate drug side effects that cause them to lose hair, because they’d look “more like men.”
The U.S. Food and Drug Administration says that when it approves a drug, health care providers generally may prescribe that drug for an unapproved use, or off-label, when “they judge that it is medically appropriate for their patient.”
In several other videos, doctors argued in favor of transitioning patients who experience psychotic episodes. One admitted that some of his patients with schizophrenia have to be careful how much cross-sex hormones they take or they can’t “keep the voices down.”
The Daily Caller News Foundation consulted medical professionals from respected organizations, such as Do No Harm, who all argued that the comments from WPATH-affiliated doctors show that the transgender medical industry doesn’t have patients’ best interests at heart.
While the average person, nationally and internationally, likely never has heard of the World Professional Association for Transgender Health, the modern medical industry is deeply tied to the organization and relies on it to dictate the standards of care for transgender medicine.
WPATH’s guidelines are cited as criteria for obtaining insurance coverage by both private insurance companies and tax-funded insurance plans , positioning them as a lynchpin of the sex reassignment industry.
Additionally, WPATH’s guidelines help inform policy statements from major medical and professional organizations, such as the American Academy of Pediatrics , the American Psychological Association , and the Endocrine Society .
The American Academy of Pediatrics is being sued by Isabelle Ayala, a former patient who was medically transitioned as a child and claims she was rushed through sex-change medical procedures.
There’s been an explosion in the number of young people, including children, being put on hormones and puberty blockers and getting sex-change surgeries, according to a study published in August 2023 by the JAMA Network.
This surge has been fueled, in part, by groups such as Planned Parenthood, which distributes cross-sex hormones to patients as young as 16. Planned Parenthood saw a roughly 125% jump in the number of transgender services it provided between 2020 and 2022.
Twenty-three states, however, have enacted legislation preventing doctors from performing sex-change surgeries on minors amid backlash from concerned parents and doctors who don’t subscribe to the WPATH-endorsed “gender-affirming care” model. Gender-affirming care is another euphemism used by medical professionals to describe the idea that doctors should affirm a patient’s wish to live as the opposite biological sex through social transitioning, hormone therapy, and even surgery.
The SOC 8 was released just days ahead of the 2022 symposium and contained several significant changes to how doctors and medical institutions implemented transgender medical treatment. For instance, WPATH removed minimum age requirements that established when a child can or should receive transgender medical services such as puberty blockers, cross-sex hormones, and sex-reassignment surgeries.
The World Professional Association for Transgender Health’s previous guidelines recommended that hormone therapy be given once a patient was over the age of 16, but the updated version removed this barrier and suggests hormone therapy begin at the first signs of sexual maturity.
The videos obtained by the Daily Caller News Foundation give the first glimpse at how doctors and mental health professionals discussed implementing the new guidelines. To highlight the most significant portions of the content obtained in the records requests, the foundation has decided to publish a series of articles collectively called “The WPATH Tapes.”
Following this release, the Daily Caller News Foundation intends to publish all of the videos in their entirety to provide the public with necessary information about WPATH’s approach to medical care and shine a light on an influential organization that has largely remained anonymous until now.
“The WPATH Tapes” Table of Contents
- Video Shows Prominent Doctors Acknowledging, And Even Challenging, The Experimental Nature Of Sex Change Drugs
- Top Psychiatrist Argues Schizophrenic Patients Can Consent To Sex Change Surgeries
- ‘Keep The Voices Down’: In Unearthed Video, Doctors Discuss Putting Mentally Ill Patients, Including Kids, On Hormones
- Gender Doctor Calls Genital Surgery An ‘Adventure’ For Young People While Describing Grisly Complications
- ‘No Idea About Their Fertility’: Gender Doctors Shed Light On Grim Reality Facing Kids Considering Sex Changes
- Leader Of Gender Medicine Org Says Binary Sex ‘Doesn’t Really Hold True,’ Cheers On ‘Deconstructed’ Biology
- Private Footage Reveals Leading Medical Org’s Efforts To ‘Normalize’ Gender Ideology
Originally published by the Daily Caller News Foundation
Join the millions of people who benefit from The Daily Signal’s fair, accurate, trustworthy reporting with direct access to:
- Intelligence from inside Washington
- Deep policy understanding from over 100 experts
Don’t have time to read the Washington Post or New York Times? Then get The Morning Bell, an early morning edition of the day’s most important political news, conservative commentary and original reporting from a team committed to following the truth no matter where it leads.
Ever feel like the only difference between the New York Times and Washington Post is the name? We do. Try the Morning Bell and get the day’s most important news and commentary from a team committed to the truth in formats that respect your time…and your intelligence.
South Carolina Gov. McMaster signs bill outlawing transgender care for trans youth
South Carolina Gov. Henry McMaster signed a bill banning certain medical care for transgender youth on Tuesday.
House Bill 4624, called the “Help not Harm” bill by legislators, prohibits anyone under the age of 18 from receiving gender reassignment surgery or any form of puberty-blocking or hormone therapy. The bill became effective immediately.
The bill also makes it a felony to perform gender reassignment surgery on those under the age of 18.
McMaster said a ceremonial bill signing with legislators would take place in the Upstate next week.
Under the new bill, minors can still be prescribed puberty blockers or hormone therapy to treat certain conditions like precocious puberty or endometriosis.
The new law also bans the South Carolina Medicaid program from providing coverage for gender reassignment surgery or hormone therapy to adults and minors.
The bill passed on the last day of the legislative session after the House agreed to accept the Senate’s changes to the law. The Senate's major change was an amendment requiring public school principals and vice principals to report students to parents if their child informed officials that they were identifying as a different gender from their assigned sex or using different pronouns.
More: As SC legislature winds down, bill banning transgender youth medical care returns to House
Opponents of the amendment argued the measure would be a forced outing and worried it could put a child in an uncomfortable or potentially dangerous situation if their parent or guardian were not accepting. Supporters of the amendment said parents have a right to know if their children are identifying as transgender or requesting to change their pronouns.
Dr. Elizabeth Mack, president of the South Carolina chapter of the American Academy of Pediatrics testified against the bill during a Senate medical affairs subcommittee in February, noting there are “less than 2,000 trans kids in the state.”
Still, supporters of the bill pushed for it, saying its intention was to protect children, while others say it does the opposite.
“We stand in grief and solidarity with LGBTQ South Carolinians, who are increasingly under attack by our own government,” Executive Director of ACLU South Carolina Jace Woodrum said in a statement on X, formerly known as Twitter. “We can put to rest the notion that the government cares about limited government and personal freedom. With a stroke of a pen, he (McMaster) has chosen to insert the will of politicians into healthcare decisions, trample on the liberties of trans South Carolinians, and deny the rights of the parents of trans minors.”
South Carolina joins 25 states to outlaw transgender care for minors. It was also one of the only states that did not have a ban on transgender care in the South, with Virginia now being the lone Southern state with access.
Savannah Moss covers politics for the Greenville News. Reach her at [email protected] or follow her on X @Savmoss.
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My watchlist
- Stock market
- Biden economy
- Personal finance
- Stocks: most active
- Stocks: gainers
- Stocks: losers
- Trending tickers
- World indices
- US Treasury bonds
- Top mutual funds
- Highest open interest
- Highest implied volatility
- Currency converter
- Basic materials
- Communication services
- Consumer cyclical
- Consumer defensive
- Financial services
- Industrials
- Real estate
- Mutual funds
- Credit cards
- Balance transfer cards
- Cash back cards
- Rewards cards
- Travel cards
- Online checking
- High-yield savings
- Money market
- Home equity loan
- Personal loans
- Student loans
- Options pit
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
Bills limiting transgender rights, boosting parental rights head to NH governor’s desk
- Oops! Something went wrong. Please try again later. More content below
The Senate met May 16 for a whirlwind day of bills, taking up legislation relating to transgender rights, bail reform, cannabis, voter ID law, and more. (Ethan DeWitt / New Hampshire Bulletin)
As a transgender girl, Sarah Huckman’s experience joining girls’ sports in high school wasn’t automatic, her father Tom Huckman recalled. Because she had not undergone gender reassignment surgery, she needed to appeal to the New Hampshire Interscholastic Athletic Association for an exception, a process that involved writing letters with the help of GLBTQ Legal Advocates & Defenders.
But once Sarah started participating in cross-country running, Nordic skiing, and track, she was quickly accepted by her friends and peers, Tom Huckman, of Ossipee, said at a press conference earlier this week.
“She’s a very social, gregarious person, and sports was absolutely one of the best things for her for her mental well-being,” Huckman said.
On Thursday, the New Hampshire Senate passed a measure that would prohibit such participation and sent the legislation to Gov. Chris Sununu ’s desk.
The chamber voted to advance House Bill 1205 , a bill that would bar transgender girls in grades five through 12 from participating in girls’ sports in public school, in a party-line vote opposed by Democrats.
While Sununu has indicated he supports the bill’s intentions, it is not clear whether he will sign it. At a press conference Wednesday, Sununu declined to directly answer that question. But in other comments, he has made his position clear.
“I fundamentally don’t believe that biological boys should be competing in girls’ sports. I think it’s dangerous,” Sununu told WMUR in March. He declined to say then whether he would sign the bill.
On Wednesday, he said he would “potentially” sign a bill banning that participation but would need to review the final language.
“I think the voices around fairness and safety are being heard not just here in New Hampshire, but all across the country,” Sununu said. “And something that we’re going to take very seriously.”
The bill is one of several the Senate took up Thursday that would reduce the rights of transgender people in the state. The chamber also passed House Bill 619 , which would bar those under 18 from receiving gender reassignment surgeries, and House Bill 1312 , which would allow parents to opt their children out of any public school instruction in “sexual orientation, gender, gender identity, or gender expression.”
Republicans argued that barring transgender girls from girls’ sports teams would restore safety and fairness.
HB 1205 would require public schools to determine a student’s biological gender by requesting the student produce a birth certificate. If that were not available, it would require the student to “provide other evidence indicating the student’s sex at the time of birth.”
The bill would prevent athletic associations, such as the NHIAA, from entertaining complaints or investigating schools for enforcing gender separation on its sports teams.
And it would give any student who had suffered direct or indirect harm as a result of a school not enforcing the ban on transgender students the right to sue the school for injunctive relief or damages.
Supporters of the legislation have argued that transgender students born biologically male have physiologies that can favor them over cisgender students who were born biologically female.
“Rights should not be created for some at the expense of others,” said Senate President Jeb Bradley, a Wolfeboro Republican, speaking from the Senate floor. “And unfortunately, if we don’t pass this bill, we are allowing that to happen.”
Opponents have disputed that, noting that many transgender students have undergone hormone therapies that reduce or eliminate that advantage. And they’ve said the bill would discriminate against students who identify with or have transitioned to another gender and don’t feel comfortable playing on the teams associated with their biological sex at birth.
Sen. Cindy Rosenwald argued that high school sports teams were meant to be about more than winning and losing.
“Sports teaches you lessons that are about how to be part of a group,” she said. “And (they) also teach you how to lose gracefully.”
HB 1205 passed, 13-10. Because it was not amended by the Senate, it does not need to return to the House for another vote, and is now on its way through the enrollment process and on to Sununu’s desk.
Republicans said House Bill 1312 , which also passed on a 13-10 vote, would give parents more control over their child’s classroom. The bill expands on the existing state law allowing parents to opt out of sex education classes, as long as parents and the school district agree on alternative instruction arranged by the parents. HB 1312 would add instruction on gender, gender identity, and sexual orientation to that list and would require teachers to give two weeks’ written notice to parents before teaching anything that instructed in those topics.
“If schools are going to teach these sensitive subjects, parents ought to have the ability to review the material and make informed decisions about their child’s education,” said Sen. Tim Lang, a Sanbornton Republican.
Democrats countered that the bill was broad and vague, and argued it could require teachers to give notice that they were teaching the children’s book “Make Way for Ducklings” because it deals with gender.
“This bill is one of the reasons why nobody wants to go into teaching,” said Sen. Lou D’Allesandro, a Manchester Democrat and former teacher.
Lang has argued the opt-out would apply only to materials that are designed to instruct on gender and sexual orientation directly, not materials that happen to include it.
Because the Senate added no amendments, HB 1312 will also head directly to the governor’s desk.
In passing House Bill 619, Senate Republicans said they were attempting to block procedures that transgender teenagers might regret later in life. The bill would ban physicians from conducting metoidioplasties, phalloplasties, or vaginoplasties for people under 18, and would prevent doctors from making referrals to facilities out of state.
“HB 619 will protect New Hampshire children from making a permanent decision that they’re too young to make,” said Sen. Daryl Abbas, a Salem Republican. “And it’s a life-altering procedure that is irreversible.”
But Democrats countered that the law interfered with families’ ability to make personal decisions, and could stop children from making changes that could boost their well-being.
“ I’m not sure we should be legislating on this,” said Sen. David Watters, a Dover Democrat. “I think we should leave it to the medical profession, and parents, and minors to work through what seems appropriate in the light of medical information.”
Thursday’s string of votes were denounced by LGBTQ+ advocacy groups and civil rights organizations, including the American Civil Liberties Union of New Hampshire and 603 Equality.
“Today the Senate turned its back on New Hampshire values and sent an extremely harmful message to all New Hampshire youth,” said Chris Erchull, a staff attorney at GLBTQ Legal Advocates & Defenders. “…Transgender students need the opportunity to play sports for the same reason other kids do: to learn essential life skills as part of a team where they feel like they belong.”
Huckman said his daughter, who has since graduated, would have been “devastated” if she were barred from the girls’ teams in high school.
“It’s really the adults that have the problem, not the kids,” he said.
This story was first published in New Hampshire Bulletin, which is part of the nonprofit States Newsroom, a national network of news bureaus supported by grants and donors and includes Maine Morning Star.
SUPPORT NEWS YOU TRUST.
The post Bills limiting transgender rights, boosting parental rights head to NH governor’s desk appeared first on Maine Morning Star .
Recommended Stories
This week in bidenomics: 4 more years … of inflation.
Voters don't just blame Biden for current inflation. They think he'll cause future inflation, too.
2024 Indy 500: TV channels, streaming, starting grid, news, weather more
The "Greatest Spectacle in Racing" is scheduled to take place Sunday with the 108th running of the Indianapolis 500.
Junkyard Gem: 1989 Ford Ranger Just Do It Edition
A 1989 Ford Ranger pickup covered with handmade Nike "Just Do It" decoration, found in a North Carolina junkyard.
'The tummy control works': This flattering one-piece is just $25 right now
Strategically placed ruching means you get coverage where you need it.
Nintendo is finally opening a second US store
Nintendo is opening its second official US store in San Francisco next year. The original New York location opened all the way back in 2005.
Psst ... Amazon has a secret coupon page — save up to 50% on everything from air fryers to robot vacs
Score deep discounts on home goods, tech, clothing and more.
Evaluating 2024's one-and-dones, under-the-radar prospects and a way-too-early look at the 2025 Draft | On the Clock with Krysten Peek
Yahoo Sports NBA draft expert Krysten Peek is joined by Rob Cassidy, national basketball analyst at our sister site, Rivals, to evaluate some of the players who hope to make a name for themselves in the NBA in the years to come.
Amazon Memorial Day sale: The 40+ best deals on Apple, Sony, Le Creuset, Shark and more
Save up to 85% on everything from vacuums and tech finds to outdoor essentials for summer.
US pharma giant Cencora says Americans' health information stolen in data breach
U.S. pharmaceutical giant Cencora says it is notifying affected individuals that their personal and highly sensitive medical information was stolen during a cyberattack and data breach earlier this year. In letters to affected individuals sent out this week, Cencora said that the data from its systems includes patient names, their postal address and date of birth, as well as information about their health diagnosis and medications. The pharma giant said it had initially obtained patients' data through partnerships with the drug makers it works with "in connection with its patient support programs."
Monaco Grand Prix 2024: How to watch the next F1 race without cable
Everything you need to know about streaming the next Formula 1 Grand Prix.
Peyton Manning has 1 wish for drafted QBs: Break his rookie interception record
The Hall of Famer was joking. We think.
Daniel Jones 'wasn't fired up about' Giants’ attempts to draft his replacement
Jones heard the chatter about the Giants’ interest in other QBs, but the team passed on drafting one. That means Jones' job is safe. For now.
Groovy! Sarah Jessica Parker just made these iconic Dr. Scholl's sandals cool again
What's old is new: Follow in the stylish star's footsteps with a pair of versatile, supportive slides.
Ryan Garcia threatens to quit boxing, 'swallow all steroids' after B samples reportedly return 2 positives
Garcia's earlier samples also tested positive for the banned PED Ostarine.
These are the most comfortable walking sandals for women in 2024
Shoppers, editors and podiatrists agree that Birkenstock Arizonas are the comfiest sandals around.
West Ham's Lucas Paquetá charged by English FA for allegedly breaching betting rules
The charges are related to four matches over his first two seasons with the club.
'No more mis-steaks': This smart meat thermometer is down to its lowest price ever and makes a 'grill'-iant Father's Day gift
A gadget with 32,000+ fans that pairs with your phone for perfectly cooked food every time? That gets a 'Yes, chef!'
Scottie Scheffler incident: Louisville police release findings of investigation into police officer
Louisville police have disciplined the police officer whose body camera was not active during Scheffler's arrest.
'Built for the DIY enthusiast, priced for the hobbyist': Get this powerful Dewalt drill for over 40% off
Don't get screwed by an extortionate contractor — nail this deal down now and get fixin'!
The 1TB 14-inch MacBook Pro M3 is cheaper than ever right now
The 1TB 14-inch MacBook Pro M3 is cheaper than ever right now. It’s available on Amazon for $200 off.

IMAGES
VIDEO
COMMENTS
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Call or Visit the Clinic. Call 434.924.5078. Everyone wants to feel authentic and comfortable in their own skin. For some people, that means having the physical look and feel of their gender identity. Transgender surgery includes several types of gender-affirmation procedures that can help you feel at ease in your body.
Your surgeon will give you general guidelines for this as well. Approximately 1 out of 10 people who have a vaginoplasty end up requiring a second, minor surgery to correct some of the scarring from the first surgery and improve the function and cosmetic appearance. Most genital gender affirmation surgeries are covered by insurance.
Types of gender reassignment surgery: Feminizing vaginoplasty: Reconstructive surgery procedure that alters the structure of the genitals to create a vagina using penile or colon tissue. Dr. Del Corral uses a one-stage procedure, revisions can be necessary to enhance the final surgical result. Revision vaginoplasty (after loss of depth): A ...
Gender reassignment (confirmation) surgery is more common in transgender men (42 to 54%) than transgender women (28%). Top (chest gender confirmation) surgery is performed approximately twice as often as bottom (genital) surgery. In studies that assessed transgender men and women as an aggregate, top surgery accounts for 8 to 25% and bottom ...
Gender Health Services. We provide affirming, inclusive healthcare for adult transgender patients. Your goals and needs take center stage. To help make your healthcare experience as positive as possible, we commit to: Listen first. Remove barriers to your care. Treat you with dignity and respect. Make your well-being our top priority.
To meet with Dr. Stranix or Dr. Black to discuss your options for transgender surgery in Charlottesville, request a consultation using the online form or call (434) 924-1234 to schedule an appointment.
Great care is taken to limit the external scars from a vaginoplasty by locating the incisions appropriately and with meticulous closure. Typical depth is 15 cm (6 inches), with a range of 12-16cm (5-6.5 inches); in comparison, typical vaginal depth in non-transgender females is between 9-12cm (3.5 to 5 inches).
Gender affirmation surgery is paramount in the treatment of gender dysphoria for transgender individuals. For transgender women, vaginoplasty offers the opportunity for removal of masculine-appearing genitalia and replacement with a gender-congruent appearance. ... Krege S, et al. Gender reassignment surgery--a 13 year review of surgical ...
Featured Expert: Fan Liang, M.D. Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including: Creating the penis. Lengthening the urethra so you are able to stand to urinate. Creating the tip (glans) of the penis. Creating the scrotum.
Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people. Facial gender surgery: While hormone replacement therapy can help achieve gender affirming changes to the face, surgery may help. Facial gender surgery can include a variety ...
Please tell your medical provider the words you use to describe your body. Vaginoplasty is a gender-affirming, feminizing, lower surgery (transgender surgery; gender reassignemnt surgery; sex change surgery) to create a vagina and vulva (including mons, labia, clitoris, and urethral opening) and remove the penis, scrotal sac and testes.
A vulvoplasty is a type of surgery that uses skin and tissue from a penis to create all of the outside parts of a vagina (except for the vaginal canal). The steps of a vulvoplasty are the same as a vaginoplasty. During a vulvoplasty, your surgeon will: create the introitus (opening of the vagina).
Reconstructive surgery experts near you. If you have questions about gender-affirming surgery or other reconstructive surgery procedures, please call 206-223-6831. Virginia Mason Franciscan Health offers a full spectrum of gender-affirming surgery and high-quality, accessible care to trans and nonbinary patients.
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current ...
Gender affirmation surgery may help in those areas where your gender feels out of sync with your body. Surgery can enable you to become more satisfied with your: Appearance, including changes in the way your face, chest or genitals look. Gender expression, including how you look, sound and do routine things (like peeing standing up or sitting ...
The two major sex reassignment surgery (SRS) interventions in the female-to-male transsexual patients that will be addressed here are (1) the subcutaneous mastectomy (SCM), often combined with a hysterectomy/ ovariectomy; and (2) the actual genital transformation consisting of vaginectomy, reconstruction of the fixed part of the urethra (if ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Transgender rights in Iran are limited, with a narrow degree of official recognition of transgender identities by the government, but with trans individuals facing very high levels of discrimination, from the law, the state, and from the wider society. [citation needed]Before the Islamic Revolution in 1979, the issue of transgender identity in Iran had never been officially addressed by the ...
This includes a requirement to complete and submit the Gender Dysphoria Service Authorization Form (DMAS-P264) and all specified clinical documentation, and specify an F64 ICD-10 diagnosis code. Contact information for the DMAS Medical Support Unit is: Fax: 804-452-5450, Phone: 804-786-8056. Managed Care Organizations (MCOs) contracted with ...
A hand holds up a small transgender pride flag. The blue and pink stripes represent the colors for a boy and girl, while the white stripe represents self-declared gender identities, such as transitioning, intersex, neutral and undefined gender. | Getty Images Trans-identifying adults who underwent body-mutilating surgeries as part of an effort to look like the opposite sex had an elevated ...
People dressing and living differently from their sex assignment at birth and contributing to various aspects of British history and culture have been documented from the 14th century to the present day. In the 20th century, advances in medicine, social and biological sciences and transgender activism have influenced transgender life in the UK.
Both provisions outlaw a range of treatments, including gender-reassignment surgery. But the challenges before the court specifically concern two nonsurgical treatments: the administration of puberty blockers to stop physical changes brought on by puberty; and hormone therapy, which seeks to produce physiological changes to conform physical ...
Gender transition is the process of changing one's gender presentation or sex characteristics to accord with one's internal sense of gender identity - the idea of what it means to be a man or a woman, or to be non-binary, genderqueer, bigender, or pangender, or to be agender (genderless). For transgender and transsexual people, this process commonly involves reassignment therapy (which may ...
But then the document turns to other issues that have become more highly politicized in recent years: surrogacy, gender theory, and what it calls "sex change." The document's framework holds that if a person is made in God's image, gender theory and gender reassignment surgery call into question why God would create a person with the wrong gender.
Paying for private gender reassignment surgery. Of course, if you can afford the costs, private surgery is significantly quicker. The cost of a straightforward male to female surgery is approximately £20,000, a figure that includes aftercare. Female to male surgery is very expensive and can easily cost more than £60,000.
The World Professional Association for Transgender Health, or WPATH, is the leading authority in the field of gender medicine. Its guidance is routinely used by top medical associations in the U.S ...
The bill also makes it a felony to perform gender reassignment surgery on those under the age of 18. McMaster said a ceremonial bill signing with legislators would take place in the Upstate next week.
The chamber also passed House Bill 619, which would bar those under 18 from receiving gender reassignment surgeries, and House Bill 1312, which would allow parents to opt their children out of any ...