
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.
Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Zink is a board-certified emergency medicine physician with expertise in the wilderness and global medicine.
Breech Position: What It Means if Your Baby Is Breech
Medical review policy, latest update:.
Medically reviewed for accuracy.
What does it mean if a baby is breech?
What are the different types of breech positions, what causes a baby to be breech, recommended reading, how can you tell if your baby is in a breech position, what does it mean to turn a breech baby, how can you turn a breech baby, how does labor usually start with a breech baby.
If your cervix dilates too slowly, if your baby doesn’t move down the birth canal steadily or if other problems arise, you’ll likely have a C-section. Talk your options over with your practitioner now to be prepared. Remember that though you may feel disappointed things didn’t turn out exactly as you envisioned, these feelings will melt away once your bundle of joy safely enters the world.
Updates history
Jump to your week of pregnancy, trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
- Breech presentation occurs in three to four per cent of term deliveries and is more common in nulliparous women.
- External cephalic version (ECV) from 37 weeks has been shown to decrease the incidence of breech presentation at term and the subsequent elective caesarean section (ELCS) rate.
- Vaginal breech birth increases the risk of low Apgar scores and more serious short-term complications, but evidence has not shown an increase in long-term morbidity.
- Emergency caesarean section (EMCS) is needed in approximately 40 per cent of women planning a vaginal breech birth.
- 0.5/1000 with ELCS for breech >39 weeks gestation
- 2.0/1000 planned vaginal breech birth >39/40
- 1.0/1000 with planned cephalic birth.
- A reduction in planned vaginal breech birth followed publication of the Term Breech Trial (TBT) in 2001.
- Acquisition of skills necessary to manage breech presentation (for example, ECV) is important to optimise outcomes.
Clinical suspicion of breech presentation
- Abdominal palpation: if the presenting part is irregular and not ballotable or if the fetal head is ballotable at the fundus
- Pelvic examination: head not felt in the pelvis
- Cord prolapse
- Very thick meconium after rupture of membranes
- Fetal heart heard higher in the abdomen
In cases of extended breech, the breech may not be ballotable and the fetal heart may be heard in the same location as expected for a cephalic presentation.
If breech presentation is suspected, an ultrasound examination will confirm diagnosis.
Cord prolapse is an obstetric emergency. Urgent delivery is indicated after confirming gestation and fetal viability.
Diagnosis: preterm ≤36+6 weeks
- Breech presentation is a normal finding in preterm pregnancy.
- If diagnosed at the 35-36 week antenatal visit, refer the woman for ultrasound scan to enable assessment prior to ECV.
- Mode of birth in a breech preterm delivery depends on the clinical circumstances.
Diagnosis: ≥37+0 weeks
- determine type of breech presentation
- determine extension/flexion of fetal head
- locate position of placenta and exclude placenta praevia
- exclude fetal congenital abnormality
- calculate amniotic fluid index
- estimate fetal weight.
Practice points
- Offer ECV if there are no contraindications.
- If ECV is declined or unsuccessful, provide counselling on risks and benefits of a planned vaginal birth versus an ELCS.
- Inform the woman that there are fewer maternal complications with a successful vaginal birth, however the risk to the woman increases significantly if there is a need for an EMCS.
- Inform the woman that caesarean section increases the risk of complication in future pregnancies, including the risk of a repeat caesarean section and the risk of invasive placentation.
- If the woman chooses an ELCS, document consent and organise booking for 39 weeks gestation.
Information and decision making
Women with a breech presentation should have the opportunity to make informed decisions about their care and treatment, in partnership with the clinicians providing care.
Planning for birth requires careful assessment for risk of poor outcomes relating to planned vaginal breech birth. If any risk factors are identified, inform the woman that an ELCS is recommended due to increased perinatal risk.
Good communication between clinicians and women is essential. Treatment, care and information provided should:
- take into account women's individual needs and preferences
- be supported by evidence-based, written information tailored to the needs of the individual woman
- be culturally appropriate
- be accessible to women, their partners, support people and families
- take into account any specific needs, such as physical or cognitive disabilities or limitations to their ability to understand spoken or written English.
Documentation
The following should be documented in the woman's hospital medical record and (where applicable) in her hand-held medical record:
- discussion of risks and benefits of vaginal breech birth and ELCS
- discussion of the woman's questions about planned vaginal breech birth and ELCS
- discussion of ECV, if applicable
- consultation, referral and escalation
External cephalic version (ECV)
- ECV can be offered from 37 weeks gestation
- The woman must provide written consent prior to the procedure
- The success rate of ECV is 40-60 per cent
- Approximately one in 200 ECV attempts will lead to EMCS
- ECV should only be performed by a suitably trained, experienced clinician
- continuous electronic fetal monitoring (EFM)
- capability to perform an EMCS.
Contraindications
Table 1. Contraindications to ECV
Precautions
- Hypertension
- Oligohydramnios
- Nuchal cord
Escalate care to a consultant obstetrician if considering ECV in these circumstances.
- Perform a CTG prior to the procedure - continue until RANZCOG criteria for a normal antenatal CTG are met.
- 250 microg s/c, 30 minutes prior to the procedure.
- Administer Anti-D immunoglobulin if the woman is rhesus negative.
- Do not make more than four attempts at ECV, for a suggested maximum time of ten minutes in total.
- Undertake CTG monitoring post-procedure until RANZCOG criteria for a normal antenatal CTG are met.
Emergency management
Urgent delivery is indicated in the event of the following complications:
- abnormal CTG
- vaginal bleeding
- unexplained pain.
Initiate emergency response as per local guidelines.
Alternatives to ECV
There is a lack of evidence to support the use of moxibustion, acupuncture or postural techniques to achieve a vertex presentation after 35 weeks gestation.
Criteria for a planned vaginal breech birth
- Documented evidence of counselling regarding mode of birth
- Documentation of informed consent, including written consent from the woman
- Estimated fetal weight of 2500-4000g
- Flexed fetal head
- Emergency theatre facilities available on site
- Availability of suitably skilled healthcare professional
- Frank or complete breech presentation
- No previous caesarean section.
- Cord presentation
- Fetal growth restriction or macrosomia
- Any presentation other than a frank or complete breech
- Extension of the fetal head
- Fetal anomaly incompatible with vaginal delivery
- Clinically inadequate maternal pelvis
- Previous caesarean section
- Inability of the service to provide experienced personnel.
If an ELCS is booked
- Confirm presentation by ultrasound scan when a woman presents for ELCS.
- If fetal presentation is cephalic on admission for ELCS, plan ongoing management with the woman.
Intrapartum management
Fetal monitoring.
- Advise the woman that continuous EFM may lead to improved neonatal outcomes.
- Where continuous EFM is declined, perform intermittent EFM or intermittent auscultation, with conversion to EFM if an abnormality is detected.
- A fetal scalp electrode can be applied to the breech.
Position of the woman
- The optimal maternal position for birth is upright.
- Lithotomy may be appropriate, depending on the accoucheur's training and experience.
Pain relief
- Epidural analgesia may increase the risk of intervention with a vaginal breech birth.
- Epidural analgesia may impact on the woman's ability to push spontaneously in the second stage of labour.
Induction of labour (IOL)
See the IOL eHandbook page for more detail.
- IOL may be offered if clinical circumstances are favourable and the woman wishes to have a vaginal birth.
- Augmentation (in the absence of an epidural) should be avoided as adequate progress in the absence of augmentation may be the best indicator of feto-pelvic proportions.
The capacity to offer IOL will depend on clinician experience and availability and service capability.
First stage
- Manage with the same principles as a cephalic presentation.
- Labour should be expected to progress as for a cephalic presentation.
- If progress in the first stage is slow, consider a caesarean section.
- If an epidural is in situ and contractions are less than 4:10, consult with a senior obstetrician.
- Avoid routine amniotomy to avoid the risk of cord prolapse or cord compression.
Second stage
- Allow passive descent of the breech to the perineum prior to active pushing.
- If breech is not visible within one hour of passive descent, a caesarean section is normally recommended.
- Active second stage should be ½ hour for a multigravida and one hour for a primipara.
- All midwives and obstetricians should be familiar with the techniques and manoeuvres required to assist a vaginal breech birth.
- Ensure a consultant obstetrician is present for birth.
- Ensure a senior paediatric clinician is present for birth.
VIDEO: Maternity Training International - Vaginal Breech Birth
- Encouragement of maternal pushing (if at all) should not begin until the presenting part is visible.
- A hands-off approach is recommended.
- Significant cord compression is common once buttocks have passed the perineum.
- Timely intervention is recommended if there is slow progress once the umbilicus has delivered.
- Allow spontaneous birth of the trunk and limbs by maternal effort as breech extraction can cause extension of the arms and head.
- Grasp the fetus around the bony pelvic girdle, not soft tissue, to avoid trauma.
- Assist birth if there is a delay of more than five minutes from delivery of the buttocks to the head, or of more than three minutes from the umbilicus to the head.
- Signs that delivery should be expedited also include lack of tone or colour or sign of poor fetal condition.
- Ensure fetal back remains in the anterior position.
- Routine episiotomy not recommended.
- Lovset's manoeuvre for extended arms.
- Reverse Lovset's manoeuvre may be used to reduce nuchal arms.
- Supra-pubic pressure may aide flexion of the fetal head.
- Maricueau-Smellie-Veit manoeuvre or forceps may be used to deliver the after coming head.
Undiagnosed breech in labour
- This occurs in approximately 25 per cent of breech presentations.
- Management depends on the stage of labour when presenting.
- Assessment is required around increased complications, informed consent and suitability of skilled expertise.
- Do not routinely offer caesarean section to women in active second stage.
- If there is no senior obstetrician skilled in breech delivery, an EMCS is the preferred option.
- If time permits, a detailed ultrasound scan to estimate position of fetal neck and legs and estimated fetal weight should be made and the woman counselled.
Entrapment of the fetal head
This is an extreme emergency
This complication is often due to poor selection for vaginal breech birth.
- A vaginal examination (VE) should be performed to ensure that the cervix is fully dilated.
- If a lip of cervix is still evident try to push the cervix over the fetal head.
- If the fetal head has entered the pelvis, perform the Mauriceau-Smellie-Veit manoeuvre combined with suprapubic pressure from a second attendant in a direction that maintains flexion and descent of the fetal head.
- Rotate fetal body to a lateral position and apply suprapubic pressure to flex the fetal head; if unsuccessful consider alternative manoeuvres.
- Reassess cervical dilatation; if not fully dilated consider Duhrssen incision at 2, 10 and 6 o'clock.
- A caesarean section may be performed if the baby is still alive.
Neonatal management
- Paediatric review.
- Routine observations as per your local guidelines, recorded on a track and trigger chart.
- Observe for signs of jaundice.
- Observe for signs of tissue or nerve damage.
- Hip ultrasound scan to be performed at 6-12 weeks post birth to monitor for developmental dysplasia of the hip (DDH). See Neonatal eHandbook - Developmental dysplasia of the hip .
More information
Audit and performance improvement.
All maternity services should have processes in place for:
- auditing clinical practice and outcomes
- providing feedback to clinicians on audit results
- addressing risks, if identified
- implementing change, if indicated.
Potential auditable standards are:
- number of women with a breech presentation offered ECV
- success rate of ECV
- ECV complications
- rate of planned vaginal breech birth
- breech birth outcomes for vaginal and caesarean birth.
For more information or assistance with auditing, please contact us via [email protected]
- Bue and Lauszus 2016, Moxibustion did not have an effect in a randomised clinical trial for version of breech position. Danish Medical Journal 63(2), A599
- Coulon et.al. 2014, Version of breech fetuses by moxibustion with acupuncture. Obstetrics and Gynecology 124(1), 32-39. DOI: 10.1097/AOG.0000000000000303
- Coyle ME, Smith CA, Peat B 2012, Cephalic version by moxibustion for breech presentation. Cochrane Database of Systematic Reviews 2012, Issue 5. Art. No.: CD003928. DOI: 10.1002/14651858.CD003928.pub3
- Evans J 2012, Essentially MIDIRS Understanding Physiological Breech Birth Volume 3. Number 2. February 2012
- Hoffmann J, Thomassen K, Stumpp P, Grothoff M, Engel C, Kahn T, et al. 2016, New MRI Criteria for Successful Vaginal Breech Delivery in Primiparae. PLoS ONE 11(8): e0161028. doi:10.1371/journal.pone.0161028
- Hofmeyr GJ, Kulier R 2012, Cephalic version by postural management for breech presentation. Cochrane Database of Systematic Reviews 2012, Issue 10. Art. No.: CD000051. DOI: 10.1002/14651858.CD000051.pub2
- New South Wales Department of Health 2013, Maternity: Management of Breech Presentation HNELHD CG 13_01, NSW Government; 2013
- Royal College of Obstetricians and Gynaecologists 2017, External Cephalic Version and Reducing the Incidence of Term Breech Presentation. Green-top Guideline No. 20a . London: RCOG; 2017
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) 2016, Management of breech presentation at term , July 2016 C-Obs-11:
- The Royal Women's Hospital 2015, Management of Breech - Clinical Guideline
- Women's and Newborn Health Service, King Edward Memorial Hospital 2015, Complications of Pregnancy Breech Presentation
Abbreviations
Get in touch, version history.
First published: November 2018 Due for review: November 2021
Uncontrolled when downloaded
Related links.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
- Management of breech presentation
Evidence review M
NICE Guideline, No. 201
National Guideline Alliance (UK) .
- Copyright and Permissions
Review question
What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy?
Introduction
Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman’s and the baby’s health. The aim of this review is to determine the most effective way of managing a breech presentation in late pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics of this review.
Summary of the protocol (PICO table).
For further details see the review protocol in appendix A .
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014 . Methods specific to this review question are described in the review protocol in appendix A .
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Clinical evidence
Included studies.
Thirty-six randomised controlled trials (RCTs) were identified for this review.
The included studies are summarised in Table 2 .
Three studies reported on external cephalic version (ECV) versus no intervention ( Dafallah 2004 , Hofmeyr 1983 , Rita 2011 ). One study reported on a 4-arm trial comparing acupuncture, sweeping of fetal membranes, acupuncture plus sweeping, and no intervention ( Andersen 2013 ). Two studies reported on postural management versus no intervention ( Chenia 1987 , Smith 1999 ).
Seven studies reported on ECV plus anaesthesia ( Chalifoux 2017 , Dugoff 1999 , Khaw 2015 , Mancuso 2000 , Schorr 1997 , Sullivan 2009 , Weiniger 2010 ). Of these studies, 1 study compared ECV plus anaesthesia to ECV plus other dosages of the same anaesthetic ( Chalifoux 2017 ); 4 studies compared ECV plus anaesthesia to ECV only ( Dugoff 1999 , Mancuso 2000 , Schorr 1997 , Weiniger 2010 ); and 2 studies compared ECV plus anaesthesia to ECV plus a different anaesthetic ( Khaw 2015 , Sullivan 2009 ).
Ten studies reported ECV plus a β2 receptor agonist ( Brocks 1984 , Fernandez 1997 , Hindawi 2005 , Impey 2005 , Mahomed 1991 , Marquette 1996 , Nor Azlin 2005 , Robertson 1987 , Van Dorsten 1981 , Vani 2009 ). Of these studies, 5 studies compared ECV plus a β2 receptor agonist to ECV plus placebo ( Fernandez 1997 , Impey 2005 , Marquette 1996 , Nor Azlin 2005 , Vani 2009 ); 1 study compared ECV plus a β2 receptor agonist to ECV alone ( Robertson 1987 ); and 4 studies compared ECV plus a β2 receptor agonist to no intervention ( Brocks 1984 , Hindawi 2005 , Mahomed 1991 , Van Dorsten 1981 ).
One study reported on ECV plus Ca 2+ channel blocker versus ECV plus placebo ( Kok 2008 ). Two studies reported on ECV plus β2 receptor agonist versus ECV plus Ca 2+ channel blocker ( Collaris 2009 , Mohamed Ismail 2008 ). Four studies reported on ECV plus a µ-receptor agonist ( Burgos 2016 , Liu 2016 , Munoz 2014 , Wang 2017 ), of which 3 compared against ECV plus placebo ( Liu 2016 , Munoz 2014 , Wang 2017 ) and 1 compared to ECV plus nitrous oxide ( Burgos 2016 ).
Four studies reported on ECV plus nitroglycerin ( Bujold 2003a , Bujold 2003b , El-Sayed 2004 , Hilton 2009 ), of which 2 compared it to ECV plus β2 receptor agonist ( Bujold 2003b , El-Sayed 2004 ) and compared it to ECV plus placebo ( Bujold 2003a , Hilton 2009 ). One study compared ECV plus amnioinfusion versus ECV alone ( Diguisto 2018 ) and 1 study compared ECV plus talcum powder to ECV plus gel ( Vallikkannu 2014 ).
One study was conducted in Australia ( Smith 1999 ); 4 studies in Canada ( Bujold 2003a , Bujold 2003b , Hilton 2009 , Marquette 1996 ); 2 studies in China ( Liu 2016 , Wang 2017 ); 2 studies in Denmark ( Andersen 2013 , Brocks 1984 ); 1 study in France ( Diguisto 2018 ); 1 study in Hong Kong ( Khaw 2015 ); 1 study in India ( Rita 2011 ); 1 study in Israel ( Weiniger 2010 ); 1 study in Jordan ( Hindawi 2005 ); 5 studies in Malaysia ( Collaris 2009 , Mohamed Ismail 2008 , Nor Azlin 2005 , Vallikkannu 2014 , Vani 2009 ); 1 study in South Africa ( Hofmeyr 1983 ); 2 studies in Spain ( Burgos 2016 , Munoz 2014 ); 1 study in Sudan ( Dafallah 2004 ); 1 study in The Netherlands ( Kok 2008 ); 2 studies in the UK ( Impey 2005 , Chenia 1987 ); 9 studies in US ( Chalifoux 2017 , Dugoff 1999 , El-Sayed 2004 , Fernandez 1997 , Mancuso 2000 , Robertson 1987 , Schorr 1997 , Sullivan 2009 , Van Dorsten 1981 ); and 1 study in Zimbabwe ( Mahomed 1991 ).
The majority of studies were 2-arm trials, but there was one 3-arm trial ( Khaw 2015 ) and two 4-arm trials ( Andersen 2013 , Chalifoux 2017 ). All studies were conducted in a hospital or an outpatient ward connected to a hospital.
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K .
Summary of clinical studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 2 .
Summary of included studies.
See the full evidence tables in appendix D and the forest plots in appendix E .
Quality assessment of clinical outcomes included in the evidence review
See the evidence profiles in appendix F .
Economic evidence
A systematic review of the economic literature was conducted but no economic studies were identified which were applicable to this review question.
A single economic search was undertaken for all topics included in the scope of this guideline. See supplementary material 2 for details.
Economic studies not included in this review are listed, and reasons for their exclusion are provided in appendix K .
Summary of studies included in the economic evidence review
No economic studies were identified which were applicable to this review question.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Evidence statements
Clinical evidence statements, comparison 1. complementary therapy versus control (no intervention), critical outcomes, cephalic presentation in labour.
No evidence was identified to inform this outcome.

Method of birth
Caesarean section.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.74 (95% CI 0.38 to 1.43).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 1.29 (95% CI 0.73 to 2.29).
Admission to SCBU/NICU
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.19 (95% CI 0.02 to 1.62).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.40 (0.08 to 2.01).
Fetal death after 36 +0 weeks gestation
Infant death up to 4 weeks chronological age, important outcomes, apgar score <7 at 5 minutes.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.32 (95% CI 0.01 to 7.78).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.33 (0.01 to 8.09).
Birth before 39 +0 weeks of gestation
Comparison 2. complementary therapy versus other treatment.
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.64 (95% CI 0.34 to 1.22).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.57 (95% CI 0.30 to 1.07).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 1.13 (95% CI 0.66 to 1.94).
- Very low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.33 (95% CI 0.03 to 3.12).
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.48 (95% CI 0.04 to 5.22).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.69 (95% CI 0.12 to 4.02).
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 3. ECV versus no ECV
- Moderate quality evidence from 2 RCTs (N=680) showed that there is clinically important difference favouring ECV over no ECV on cephalic presentation in labour in pregnant women with breech presentation: RR 1.83 (95% CI 1.53 to 2.18).
Cephalic vaginal birth
- Very low quality evidence from 3 RCTs (N=740) showed that there is a clinically important difference favouring ECV over no ECV on cephalic vaginal birth in pregnant women with breech presentation: RR 1.67 (95% CI 1.20 to 2.31).
Breech vaginal birth
- Very low quality evidence from 2 RCTs (N=680) showed that there is no clinically important difference between ECV and no ECV on breech vaginal birth in pregnant women with breech presentation: RR 0.29 (95% CI 0.03 to 2.84).
- Very low quality evidence from 3 RCTs (N=740) showed that there is no clinically important difference between ECV and no ECV on the number of caesarean sections in pregnant women with breech presentation: RR 0.52 (95% CI 0.23 to 1.20).
- Very low quality evidence from 1 RCT (N=60) showed that there is no clinically important difference between ECV and no ECV on admission to SCBU//NICU in pregnant women with breech presentation: RR 0.50 (95% CI 0.14 to 1.82).
- Very low evidence from 3 RCTs (N=740) showed that there is no statistically significant difference between ECV and no ECV on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: Peto OR 0.29 (95% CI 0.05 to 1.73) p=0.18.
- Very low quality evidence from 2 RCTs (N=120) showed that there is no clinically important difference between ECV and no ECV on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.28 (95% CI 0.04 to 1.70).
Comparison 4. ECV + Amnioinfusion versus ECV only
- Very low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.74 (95% CI 0.74 to 4.12).
- Low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.95 (95% CI 0.75 to 1.19).
Comparison 5. ECV + Anaesthesia versus ECV only
- Very low quality evidence from 2 RCTs (N=210) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.16 (95% CI 0.56 to 2.41).
- Very low quality evidence from 5 RCTs (N=435) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.16 (95% CI 0.77 to 1.74).
- Very low quality evidence from 1 RCT (N=108) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on breech vaginal birth in pregnant women with breech presentation: RR 0.33 (95% CI 0.04 to 3.10).
- Very low quality evidence from 3 RCTs (N=263) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.76 (95% CI 0.42 to 1.38).
- Moderate quality evidence from 1 RCT (N=69) showed that there is a clinically important difference favouring ECV plus anaesthesia over ECV alone on admission to SCBU/NICU in pregnant women with breech presentation: MD −1.80 (95% CI −2.53 to −1.07).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 6. ECV + Anaesthesia versus ECV + Anaesthesia
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.13 (95% CI 0.73 to 1.74).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 0.05mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.69 (95% CI 0.37 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.19 (95% CI 0.79 to 1.79).
- Low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.92 (95% CI 0.68 to 1.24).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.08 (95% CI 0.78 to 1.50).
- Very low evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.70 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.17 (95% CI 0.86 to 1.61).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.03 (95% CI 0.77 to 1.37).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.88 (95% CI 0.64 to 1.20).
Comparison 7. ECV + β2 agonist versus Control (no intervention)
- Moderate quality evidence from 2 RCTs (N=256) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on cephalic presentation in labour in pregnant women with breech presentation: RR 4.83 (95% CI 3.27 to 7.11).
- Very low quality evidence from 3 RCTs (N=265) showed that there no clinically important difference between ECV plus β2 agonist and control (no intervention) on cephalic vaginal birth in pregnant women with breech presentation: RR 2.03 (95% CI 0.22 to 19.01).
- Very low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on breech vaginal birth in pregnant women with breech presentation: RR 0.38 (95% CI 0.20 to 0.69).
- Low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.53 (95% CI 0.41 to 0.67).
- Very low quality evidence from 1 RCT (N=48) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RD 0.00 (95% CI −0.08 to 0.08).
- Very low quality evidence from 3 RCTs (N=208) showed that there is no statistically significant difference between ECV plus β2 agonist and control (no intervention) on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD −0.01 (95% CI −0.03 to 0.01) p=0.66.
- Very low quality evidence from 2 RCTs (N=208) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.80 (95% CI 0.31 to 2.10).
Comparison 8. ECV + β2 agonist versus ECV only
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on cephalic vaginal birth in pregnant women with breech presentation: RR 1.32 (95% CI 0.67 to 2.62).
- Very low quality evidence from 1 RCT (N=58) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on breech vaginal birth in pregnant women with breech presentation: RR 0.75 (95% CI 0.22 to 2.50).
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 0.79 (95% CI 0.27 to 2.28).
- Very low quality evidence from 1 RCT (N=114) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.00 (95% CI 0.21 to 4.75).
Comparison 9. ECV + β2 agonist versus ECV + Placebo
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.54 (95% CI 0.24 to 9.76).
- Very low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 1.27 (95% CI 0.41 to 3.89).
- Very low quality evidence from 2 RCTs (N=227) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on breech vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.33 to 2.97).
- Low quality evidence from 4 RCTs (N=532) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.81 (95% CI 0.72 to 0.92)
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.78 (95% CI 0.17 to 3.63).
- Very low quality evidence from 1 RCT (N=124) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 10. ECV + Ca 2+ channel blocker versus ECV + Placebo
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.87 to 1.48).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.90 (95% CI 0.73 to 1.12).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 1.11 (95% CI 0.88 to 1.40).
- High quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: MD −0.20 (95% CI −0.70 to 0.30).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no statistically significant difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.01 to 0.01) p=1.00.
- Low quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.52 (95% 0.05 to 5.02).
Comparison 11. ECV + Ca2+ channel blocker versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=90) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on cephalic presentation in labour in pregnant women with breech presentation: RR 0.62 (95% CI 0.39 to 0.98).
- Very low quality evidence from 2 RCTs (N=126) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 1.26 (95% CI 0.55 to 2.89).
- Very low quality evidence from 2 RCTs (N=132) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on the number of caesarean sections in pregnant women with breech presentation: RR 1.42 (95% CI 1.06 to 1.91).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on admission to SCBU/NICU in pregnant women with breech presentation: Peto OR 0.53 (95% CI 0.05 to 5.22).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 12. ECV + µ-receptor agonist versus ECV only
- High quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.80 to 1.24).
- Low quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 1.00 (95% CI 0.42 to 2.40).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 13. ECV + µ-receptor agonist versus ECV + Placebo
Cephalic vaginal birth after successful ecv.
- High quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on cephalic vaginal birth after successful ECV in pregnant women with breech presentation: RR 1.00 (95% CI 0.86 to 1.17).
Caesarean section after successful ECV
- Low quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after successful ECV in pregnant women with breech presentation: RR 0.97 (95% CI 0.33 to 2.84).
Breech vaginal birth after unsuccessful ECV
- High quality evidence from 3 RCTs (N=186) showed that there is a clinically important difference favouring ECV plus µ-receptor agonist over ECV plus placebo on breech vaginal birth after unsuccessful ECV in pregnant women with breech presentation: RR 0.10 (95% CI 0.02 to 0.53).
Caesarean section after unsuccessful ECV
- Moderate quality evidence from 3 RCTs (N=186) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after unsuccessful ECV in pregnant women with breech presentation: RR 1.19 (95% CI 1.09 to 1.31).
- Low quality evidence from 1 RCT (N=137) showed that there is no statistically significant difference between ECV plus µ-receptor agonist and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03) p=1.00.
Comparison 14. ECV + µ-receptor agonist versus ECV + Anaesthesia
- Moderate quality evidence from 1 RCT (N=92) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on cephalic vaginal birth in pregnant women with breech presentation: RR 1.04 (95% CI 0.84 to 1.29).
- Very low quality evidence from 2 RCTs (N=212) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on the number of caesarean sections in pregnant women with breech presentation: RR 0.90 (95% CI 0.61 to 1.34).
- Very low quality evidence from 1 RCT (N=129) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on admission to SCBU/NICU in pregnant women with breech presentation: RR 2.30 (95% CI 0.21 to 24.74).
- Low quality evidence from 2 RCTs (N=255) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 15. ECV + Nitric oxide donor versus ECV + Placebo
- Very low quality evidence from 3 RCTs (N=224) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.59 to 2.16).
- Low quality evidence from 1 RCT (N=99) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.78 (95% CI 0.49 to 1.22).
- Low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.83 (95% CI 0.68 to 1.01).
Comparison 16. ECV + Nitric oxide donor versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=74) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus nitric oxide donor on cephalic presentation in labour in pregnant women with breech presentation: RR 0.56 (95% CI 0.29 to 1.09).
- Very low quality evidence from 2 RCTs (N=97) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 0.98 (95% CI 0.47 to 2.05).
- Very low quality evidence from 1 RCT (N=59) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on the number of caesarean sections in pregnant women with breech presentation: RR 1.07 (95% CI 0.73 to 1.57).
Comparison 17. ECV + Talcum powder versus ECV + Gel
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic presentation in labour in pregnant women with breech presentation: RR 1.02 (95% CI 0.68 to 1.53).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic vaginal birth in pregnant women with breech presentation: RR 1.08 (95% CI 0.67 to 1.74).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.67 to 1.33).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.96 (95% CI 0.38 to 10.19).
Comparison 18. Postural management versus No postural management
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic presentation in labour in pregnant women with breech presentation: RR 1.26 (95% CI 0.70 to 2.30).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic vaginal birth in pregnant women with breech presentation: RR 1.11 (95% CI 0.59 to 2.07).
Breech vaginal delivery
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on breech vaginal delivery in pregnant women with breech presentation: RR 1.15 (95% CI 0.67 to 1.99).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on the number of caesarean sections in pregnant women with breech presentation: RR 0.69 (95% CI 0.31 to 1.52).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.24 (95% CI 0.03 to 2.03).
Comparison 19. Postural management + ECV versus ECV only
- Moderate quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 1.05 (95% CI 0.80 to 1.38).
- Low quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.13 (95% CI 0.00 to 6.55).
Economic evidence statements
No economic evidence was identified which was applicable to this review question.
The committee’s discussion of the evidence
Interpreting the evidence, the outcomes that matter most.
Provision of antenatal care is important for the health and wellbeing of both mother and baby with the aim of avoiding adverse pregnancy outcomes and enhancing maternal satisfaction and wellbeing. Breech presentation in labour may be associated with adverse outcomes for the fetus, which has contributed to an increased likelihood of caesarean birth. The committee therefore agreed that cephalic presentation in labour and method of birth were critical outcomes for the woman, and admission to SCBU/NICU, fetal death after 36 +0 weeks gestation, and infant death up to 4 weeks chronological age were critical outcomes for the baby. Apgar score <7 at 5 minutes and birth before 39 +0 weeks of gestation were important outcomes for the baby.
The quality of the evidence
The quality of the evidence for interventions for managing a longitudinal lie fetal malpresentation (that is breech presentation) in late pregnancy ranged from very low to high, with most of the evidence being of a very low or low quality.
This was predominately due to serious overall risk of bias in some outcomes; imprecision around the effect estimate in some outcomes; indirect population in some outcomes; and the presence of serious heterogeneity in some outcomes, which was unresolved by subgroup analysis. The majority of included studies had a small sample size, which contributed to imprecision around the effect estimate.
No evidence was identified to inform the outcomes of infant death up to 4 weeks chronological age and birth before 39 +0 weeks of gestation.
There was no publication bias identified in the evidence. However, the committee noted the influence pharmacological developers may have in these trials as funders, and took this into account in their decision making.
Benefits and harms
The committee discussed that in the case of breech presentation, a discussion with the woman about the different options and their potential benefits, harms and implications is needed to ensure an informed decision. The committee discussed that some women may prefer a breech vaginal birth or choose an elective caesarean birth, and that her preferences should be supported, in line with shared decision making.
The committee discussed that external cephalic version is standard practice for managing breech presentation in uncomplicated singleton pregnancies at or after 36+0 weeks. The committee discussed that there could be variation in the success rates of ECV based on the experience of the healthcare professional providing the ECV. There was some evidence supporting the use of ECV for managing a breech presentation in late pregnancy. The evidence showed ECV had a clinically important benefit in terms of cephalic presentations in labour and cephalic vaginal deliveries, when compared to no intervention. The committee noted that the evidence suggested that ECV was not harmful to the baby, although the effect estimate was imprecise relating to the relative rarity of the fetal death as an outcome.
Cephalic (head-down) vaginal birth is preferred by many women and the evidence suggests that external cephalic version is an effective way to achieve this. The evidence suggested ECV increased the chance for a cephalic vaginal birth and the committee agreed that it was important to explain this to the woman during her consultation.
The committee discussed the optimum timing for ECV. Timing of ECV must take into account the likelihood of the baby turning naturally before a woman commences labour and the possibility of the baby turning back to a breech presentation after ECV if it is done too early. The committee noted that in their experience, current practice was to perform ECV at 37 gestational weeks. The majority of the evidence demonstrating a benefit of ECV in this review involved ECV performed around 37 gestational weeks, although the review did not look for studies directly comparing different timings of ECV and their relative success rates.
The evidence in this review excluded women with previous complicated pregnancies, such as those with previous caesarean section or uterine surgery. The committee discussed that a previous caesarean section indicates a complicated pregnancy and that this population of women are not the focus of this guideline, which concentrates on women with uncomplicated pregnancies.
The committee’s recommendations align with other NICE guidance and cross references to the NICE guideline on caesarean birth and the section on breech presenting in labour in the NICE guideline on intrapartum care for women with existing medical conditions or obstetric complications and their babies were made.
ECV combined with pharmacological agents
There were some small studies comparing a variety of pharmacological agents (including β2 agonists, Ca 2+ channel blockers, µ-receptor agonists and nitric oxide donors) given alongside ECV. Overall the evidence typically showed no clinically important benefit of adding any pharmacological agent to ECV except in comparisons with a control arm with no ECV where it was not possible to isolate the effect of the ECV versus the pharmacological agent. The evidence tended toward benefit most for β2 agonists and µ-receptor agonists however there was no consistent or high quality evidence of benefit even for these agents. The committee agreed that although these pharmacological agents are used in practice, there was insufficient evidence to make a recommendation supporting or refuting their use or on which pharmacological agent should be used.
The committee discussed that the evidence suggesting µ-receptor agonist, remifentanil, had a clinically important benefit in terms reducing breech vaginal births after unsuccessful ECV was biologically implausible. The committee noted that this pharmacological agent has strong sedative effects, depending on the dosage, and therefore studies comparing it to a placebo had possible design flaws as it would be obvious to all parties whether placebo or active drug had been received. The committee discussed that the risks associated with using remifentanil such as respiratory depression, likely outweigh any potential added benefit it may have on managing breech presentation.
There was some evidence comparing different anaesthetics together with ECV. Although there was little consistent evidence of benefit overall, one small study of low quality showed a combination of 2% lidocaine and epinephrine via epidural catheter (anaesthesia) with ECV showed a clinically important benefit in terms of cephalic presentations in labour and the method of birth. The committee discussed the evidence and agreed the use of anaesthesia via epidural catheter during ECV was uncommon practice in the UK and could be expensive, overall they agreed the strength of the evidence available was insufficient to support a change in practice.
Postural management
There was limited evidence on postural management as an intervention for managing breech presentation in late pregnancy, which showed no difference in effectiveness. Postural management was defined as ‘knee-chest position for 15 minutes, 3 times a day’. The committee agreed that in their experience women valued trying interventions at home first which might make postural management an attractive option for some women, however, there was no evidence that postural management was beneficial. The committee also noted that in their experience postural management can cause notable discomfort so it is not an intervention without disadvantages.
Cost effectiveness and resource use
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question.
The committee’s recommendations to offer external cephalic version reinforces current practice. The committee noted that, compared to no intervention, external cephalic version results in clinically important benefits and that there would also be overall downstream cost savings from lower adverse events. It was therefore the committee’s view that offering external cephalic version is cost effective and would not entail any resource impact.
Andersen 2013
Brocks 1984
Bujold 2003
Burgos 2016
Chalifoux 2017
Chenia 1987
Collaris 2009
Dafallah 2004
Diguisto 2018
Dugoff 1999
El-Sayed 2004
Fernandez 1997
Hindawi 2005
Hilton 2009
Hofmeyr 1983
Mahomed 1991
Mancuso 2000
Marquette 1996
Mohamed Ismail 2008
NorAzlin 2005
Robertson 1987
Schorr 1997
Sullivan 2009
VanDorsten 1981
Vallikkannu 2014
Weiniger 2010
Appendix A. Review protocols
Review protocol for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 260K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 281K)
Appendix C. Clinical evidence study selection
Clinical study selection for: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 113K)
Appendix D. Clinical evidence tables
Clinical evidence tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.2M)
Appendix E. Forest plots
Forest plots for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 678K)
Appendix F. GRADE tables
GRADE tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.0M)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix h. economic evidence tables, economic evidence tables for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix i. economic evidence profiles, economic evidence profiles for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix j. economic analysis, economic evidence analysis for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No economic analysis was conducted for this review question.
Appendix K. Excluded studies
Excluded clinical and economic studies for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, clinical studies, table 24 excluded studies.
View in own window
Economic studies
No economic evidence was identified for this review.
Appendix L. Research recommendations
Research recommendations for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No research recommendations were made for this review question.
Evidence reviews underpinning recommendation 1.2.38
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page National Guideline Alliance (UK). Management of breech presentation: Antenatal care: Evidence review M. London: National Institute for Health and Care Excellence (NICE); 2021 Aug. (NICE Guideline, No. 201.)
- PDF version of this title (2.2M)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 201: Antenatal care
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Health economics (PDF)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Identification of breech presentation: Antenatal care: Evidence review L [ 2021] Review Identification of breech presentation: Antenatal care: Evidence review L National Guideline Alliance (UK). 2021 Aug
- Vaginal delivery of breech presentation. [J Obstet Gynaecol Can. 2009] Vaginal delivery of breech presentation. Kotaska A, Menticoglou S, Gagnon R, MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Jun; 31(6):557-566.
- Review Cephalic version by moxibustion for breech presentation. [Cochrane Database Syst Rev. 2005] Review Cephalic version by moxibustion for breech presentation. Coyle ME, Smith CA, Peat B. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD003928. Epub 2005 Apr 18.
- [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. [Gynecol Obstet Fertil Senol. 2...] [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. Riethmuller D, Ramanah R, Mottet N. Gynecol Obstet Fertil Senol. 2018 Dec; 46(12):937-947. Epub 2018 Oct 28.
- Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. [J Obstet Gynaecol Br Emp. 1961] Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. BAINBRIDGE MN, NIXON WC, SMYTH CN. J Obstet Gynaecol Br Emp. 1961 Oct; 68:748-54.
Recent Activity
- Management of breech presentation Management of breech presentation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
What to know if your baby is breech
Find out what breech position means, how to turn a breech baby, and what having a breech baby means for your labor and delivery.

What does it mean when a baby is breech?
Signs of a breech baby, why are some babies breech, how to turn a breech baby: is it possible, will i need a c-section if my baby is breech, how to turn a breech baby naturally.
Breech is a term used to describe your baby's position in the womb. Breech position means your baby is bottom-down instead of head-down.
Babies are often active in early pregnancy, moving into different positions. But by around 8 months, there's not much room in the uterus. Most babies maximize their cramped quarters by settling in head down, in what's known as a cephalic or vertex presentation. But if you have a breech baby, it means they're poised to come out buttocks and/or feet first. At 28 weeks or less, about a quarter of babies are breech, and at 32 weeks, 7 percent are breech. By the end of pregnancy, only 3 to 4 percent of babies are in breech position. At term, a baby in breech position is unlikely to turn on their own.
There are several types of breech presentations:
- Frank breech (bottom first with feet up near the head)
- Complete breech (bottom first with legs crossed)
- Incomplete or footling breech (one or both feet are poised to come out first)
(In rare cases, a baby will be sideways in the uterus with their shoulder, back, or arm presenting first – this is called a transverse lie.)
See what these breech presentations look like .
If your baby is in breech position, you may feel them kicking in your lower belly. Or you may feel pressure under your ribcage, from their head.
By the beginning of your third trimester , your practitioner may be able to tell what position your baby is in by feeling your abdomen and locating the baby's head, back, and bottom.
If your baby's position isn't clear during an abdominal exam at 36 weeks, your caregiver may do an internal exam to try to feel what part of the baby is in your pelvis. In some cases, they may use ultrasound to confirm the baby's position.
We don't usually know why some babies are breech – in most cases it seems to be chance. While sometimes a baby with certain birth defects may not turn to a head-down position, most babies in breech position are perfectly fine. Here are some things that might increase the risk of a breech presentation:
- You're carrying multiples
- You've been pregnant before
- You've had a breech presentation before
- There's too much amniotic fluid or not enough amniotic fluid
- You have placenta previa (the placenta is covering all of part of the opening of the uterus)
- Your baby is preterm
- Your uterus is shaped abnormally or has growths, such as fibroids
- The umbilical cord is short
- You were a breech delivery, or your sibling or parent was a breech delivery
- Advanced maternal age (especially age 45 and older)
- Your baby is a low weight at delivery
- You're having a girl
There is a procedure for turning a breech baby. It's called an external cephalic version (ECV). An ob/gyn turns your baby by applying pressure to your abdomen and manually manipulating the baby into a head-down position. Some women find it very uncomfortable or even painful.
An EVC has about a 58 percent success rate, and it's more likely to work if this isn't your first baby. It's not for everyone – you can't have the procedure if you're carrying multiples or if you have too little amniotic fluid or placental abruption , for example. Your provider also won't attempt to turn your breech baby if your baby has any health problems.
The procedure is done after 36 weeks and in the hospital, where your baby can be monitored and where you'll be near a delivery room should any complications arise.
It depends, and it's something you'll want to talk with your caregiver about ahead of time. Discuss your preferences, the advantages and risks of each option ( vaginal and cesarean delivery of a breech presentation), and their experience. The biggest risk of a breech delivery is when the body delivers but the head stays entrapped within the cervix.
In the United States, most breech babies are delivered via cesarean. You may wind up having a vaginal breech delivery if your labor is so rapid that you arrive at the hospital just about to deliver. Another scenario is if you have a twin pregnancy where the first baby is in the head-first position and the second baby is not. A baby who delivers head-first will make room for the breech baby.
However, the vast majority of babies who remain breech arrive by c-section. If a c-section is planned, it will usually be scheduled at 39 weeks. To make sure your baby hasn't changed position in the meantime, you'll have an ultrasound at the hospital to confirm their position just before the surgery.
If you go into labor or your water will break s before your planned c-section, be sure to call your provider right away and head for the hospital.
In rare circumstances, if you're at low risk of complications and your caregiver is experienced delivering breech babies vaginally, you may choose to have what is called a "trial of vaginal birth." This means that you can attempt to deliver vaginally but should be prepared to have a cesarean delivery if labor isn't progressing well. You and your baby will be closely monitored during labor.
In addition to ECV, there are some alternative, natural ways to try to turn your baby. There's no proof that any of them work – or that all of them are safe. Consult your practitioner before trying them.
There's no conclusive proof that the mother's position has any effect on the baby's position, but the idea is to employ gravity to help your baby somersault into a head-down position. A few tips:
- Get into one of the following positions twice a day, starting at around 32 weeks.
- Be sure to do these moves on an empty stomach, lest your lunch comes back up.
- Make sure there's someone around to help you get up if you start feeling lightheaded.
- If you find these positions uncomfortable, stop doing them.
Position 1: Lie flat on your back and raise your pelvis so that it's 9 to 12 inches off the floor. Support your hips with a pillow and stay in this position for five to 15 minutes. Position 2: Kneel down, with your forearms on the floor in front of you, so that your bottom sticks up in the air. Stay in this position for five to 15 minutes. Sleeping position
Many women wonder if there are sleeping positions to turn a breech baby. But the positions you use to try to coax your baby head down for a short time shouldn't be used while you're sleeping. (It's not safe to sleep flat on your back in late pregnancy, for example, because the weight of your baby may compress the blood vessels that provide oxygen and nutrients to them.)
The best position for sleeping during pregnancy is on your side. Placing a pillow between your legs in this position may help open your pelvis, giving your baby room to move more easily. Support your back with plenty of pillows, too. Again, there's no proof that this works, but since it's the best sleeping position for you and your baby, you may as well give it a try.
Moxibustion
This ancient Chinese technique burns herbs to stimulate key acupressure points. To help turn a breech baby, an acupuncturist or other practitioner burns mugwort near the acupressure point of your pinky toes. According to Chinese medicine, this should stimulate your baby's activity enough that they may change position on their own. Some studies show that moxibustion in combination with acupuncture and/or positioning methods may be of some benefit. Others show moxibustion to provide no help in coaxing a baby into cephalic position. If you've discussed it with your caregiver and want to give it a try, contact your state acupuncture or Chinese medicine association and ask for the names of licensed practitioners.
One small study found that women who are regularly hypnotized into a state of deep relaxation at 37 to 40 weeks are more likely to have their baby turn than other women. If you're willing to try this technique, look for a licensed hypnotherapist with experience working with pregnant women.
Chiropractic care
There's a technique – called The Webster Breech Technique – that aims to reduce stress on the pelvis by relaxing the uterus and surrounding ligaments. The idea is that a breech baby can turn more naturally in a relaxed uterus, but research is limited as to the risks and benefits of this technique. If you're interested, talk with your provider about working with a chiropractor who's experienced with the technique.
This is a safe – and again, unproven – method based on the fact that your baby can hear sounds outside the womb. Simply play music close to the lower part of your abdomen (some women use headphones) to encourage your baby to move in the direction of the sound.
Learn more:
- C-section recovery
- Third trimester pregnancy guide and checklist
- Hospital bag checklist
Was this article helpful?
Breech, posterior, transverse lie: What position is my baby in?

Raspberry leaf tea is popular during pregnancy – but possible benefits aren't proven

Too much amniotic fluid (polyhydramnios)

C-section recovery: Timeline, aftercare tips, and expectations

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
ACOG. 2019. If your baby is breech. FAQ. The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/if-your-baby-is-breech Opens a new window [Accessed November 2021]
ACOG. 2018. Mode of term singleton breech delivery. Committee opinion number 745. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/mode-of-term-singleton-breech-delivery Opens a new window [Accessed November 2021]
Brici P et al. 2019. Turning foetal breech presentation at 32-35 weeks of gestational age by acupuncture and moxibustion. Evidence-based Complementary and Alternative Medicine https://www.hindawi.com/journals/ecam/2019/8950924/ Opens a new window [Accessed November 2021]
Ekeus C et al. 2019. Vaginal breech delivery at term and neonatal morbidity and mortality — a population-based cohort study in Sweden. Journal of Maternal Fetal Neonatal Medicine 32(2):265. https://pubmed.ncbi.nlm.nih.gov/28889774/ Opens a new window [Accessed November 2021]
Fruscalzo A et al 2014. New and old predictive factors for breech presentation: our experience in 14433 singleton pregnancies and a literature review. Journal of Maternal Fetal Neonatal Medicine 27(2): 167-72. https://pubmed.ncbi.nlm.nih.gov/23688372/ Opens a new window [Accessed November 2021]
Garcia MM et al. 2019 Effectiveness and safety of acupuncture and moxibustion in pregnant women with noncephalic presentation: An overview of systematic reviews. Evidence Based Complementary Alternative Medicine 7036914. https://pubmed.ncbi.nlm.nih.gov/31885661/ Opens a new window [Accessed November 2021]
Gray C. 2021. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed November 2021]
Meaghan M et al. 2021. External cephalic version. NCBI StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK482475/ Opens a new window [Accessed November 2021]
MedlinePlus. 2020. Breech - series - Types of breech presentation. https://medlineplus.gov/ency/presentations/100193_3.htm Opens a new window [Accessed November 2020]
Noli SA et al. 2019. Preterm birth, low gestational age, low birth weight, parity, and other determinants of breech presentation: Results from a large retrospective population-based study. Biomed Research International https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6766171/ Opens a new window [Accessed November 2021]
Pistolese RA. 2002. The Webster Technique: A chiropractic technique with obstetric implications. Journal of Manipulative and Physiological Therapeutics 25(6): E1-9. https://pubmed.ncbi.nlm.nih.gov/12183701/ Opens a new window [Accessed November 2021]

Where to go next

What happens if your baby is breech?
Babies often twist and turn during pregnancy, but most will have moved into the head-down (also known as head-first) position by the time labour begins. However, that does not always happen, and a baby may be:
- bottom first or feet first (breech position)
- lying sideways (transverse position)
Bottom first or feet first (breech baby)
If your baby is lying bottom or feet first, they are in the breech position. If they're still breech at around 36 weeks' gestation, the obstetrician and midwife will discuss your options for a safe delivery.
Turning a breech baby
If your baby is in a breech position at 36 weeks, you'll usually be offered an external cephalic version (ECV). This is when a healthcare professional, such as an obstetrician, tries to turn the baby into a head-down position by applying pressure on your abdomen. It's a safe procedure, although it can be a bit uncomfortable.
Giving birth to a breech baby
If an ECV does not work, you'll need to discuss your options for a vaginal birth or caesarean section with your midwife and obstetrician.
If you plan a caesarean and then go into labour before the operation, your obstetrician will assess whether it's safe to proceed with the caesarean delivery. If the baby is close to being born, it may be safer for you to have a vaginal breech birth.
The Royal College of Obstetricians and Gynaecologists (RCOG) website has more information on what to expect if your baby is still breech at the end of pregnancy .
The RCOG advises against a vaginal breech delivery if:
- your baby's feet are below its bottom – known as a "footling breech"
- your baby is larger or smaller than average – your healthcare team will discuss this with you
- your baby is in a certain position – for example, their neck is very tilted back, which can make delivery of the head more difficult
- you have a low-lying placenta (placenta praevia)
- you have pre-eclampsia
Lying sideways (transverse baby)
If your baby is lying sideways across the womb, they are in the transverse position. Although many babies lie sideways early on in pregnancy, most turn themselves into the head-down position by the final trimester.
Giving birth to a transverse baby
Depending on how many weeks pregnant you are when your baby is in a transverse position, you may be admitted to hospital. This is because of the very small risk of the umbilical cord coming out of your womb before your baby is born (cord prolapse). If this happens, it's a medical emergency and the baby must be delivered very quickly.
Sometimes, it's possible to manually turn the baby to a head-down position, and you may be offered this.
But, if your baby is still in the transverse position when you approach your due date or by the time labour begins, you'll most likely be advised to have a caesarean section.
Video: My baby is breech. What help will I get?
In this video, a midwife describes what a breech position is and what can be done if your baby is breech.
Page last reviewed: 1 November 2023 Next review due: 1 November 2026
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
For patients who present in labor with a breech fetus, cesarean birth is the preferred approach in many hospitals in the United States and elsewhere. Cesarean is performed for over 90 percent of breech presentations, and this rate has increased worldwide [ 1,2 ]. However, even in institutions with a policy of routine cesarean birth for breech presentation, vaginal breech births occur because of situations such as patient preference, precipitous birth, out-of-hospital birth, and lethal fetal anomaly or fetal death. Therefore, it is essential for clinicians to maintain familiarity with the techniques required to assist in a vaginal breech birth.
In addition, some clinicians and patients consider vaginal breech birth preferable to cesarean birth. Recent trends, particularly in central Europe, support vaginal breech birth [ 3-5 ]. In selected cases, as described below and depicted in the algorithm ( algorithm 1 ), it is associated with a low risk of complications. The American College of Obstetricians and Gynecologists has opined that "Planned vaginal delivery of a term singleton breech fetus may be reasonable under hospital-specific protocol guidelines for eligibility and labor management" [ 6 ].
This topic will focus on vaginal birth of breech singletons, with a brief discussion of breech delivery at cesarean. Choosing the best route of birth for the fetus in breech presentation and delivery of the breech first or second twin are reviewed separately.
● (See "Overview of breech presentation", section on 'Approach to management at or near term' .)

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Breech - series—Types of breech presentation
- Go to slide 1 out of 7
- Go to slide 2 out of 7
- Go to slide 3 out of 7
- Go to slide 4 out of 7
- Go to slide 5 out of 7
- Go to slide 6 out of 7
- Go to slide 7 out of 7
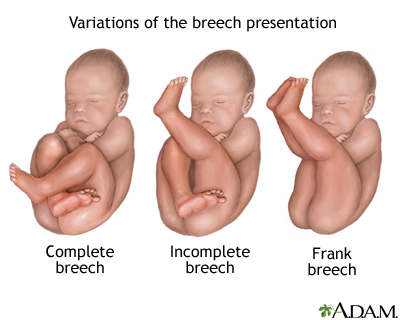
There are three types of breech presentation: complete, incomplete, and frank.
Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal.
Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Frank breech is when the baby's legs are folded flat up against his head and his bottom is closest to the birth canal.
There is also footling breech where one or both feet are presenting.
Review Date 11/21/2022
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems
- Patient Care & Health Information
- Diseases & Conditions
- Neuroblastoma
Adrenal glands
Located on top of each kidney, the adrenal glands make hormones that help regulate metabolism, the immune system, blood pressure and other important functions. Although small, these glands control much of what happens in the body.
Neuroblastoma is a cancer that develops from immature nerve cells found in several areas of the body.
Neuroblastoma most commonly arises in and around the adrenal glands, which have similar origins to nerve cells and sit atop the kidneys. However, neuroblastoma can also develop in other areas of the abdomen and in the chest, neck and near the spine, where groups of nerve cells exist.
Neuroblastoma most commonly affects children age 5 or younger, though it may rarely occur in older children.
Some forms of neuroblastoma go away on their own, while others may require multiple treatments. Your child's neuroblastoma treatment options will depend on several factors.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Signs and symptoms of neuroblastoma vary depending on what part of the body is affected.
Neuroblastoma in the abdomen — the most common form — may cause signs and symptoms such as:
- Abdominal pain
- A mass under the skin that isn't tender when touched
- Changes in bowel habits, such as diarrhea or constipation
Neuroblastoma in the chest may cause signs and symptoms such as:
- Changes to the eyes, including drooping eyelids and unequal pupil size
Other signs and symptoms that may indicate neuroblastoma include:
- Lumps of tissue under the skin
- Eyeballs that seem to protrude from the sockets (proptosis)
- Dark circles, similar to bruises, around the eyes
- Unexplained weight loss
When to see a doctor
Contact your child's doctor if your child has any signs or symptoms that worry you. Mention any changes in your child's behavior or habits.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get Mayo Clinic cancer expertise delivered to your inbox.
Subscribe for free and receive an in-depth guide to coping with cancer, plus helpful information on how to get a second opinion. You can unsubscribe at any time. Click here for an email preview.
Error Select a topic
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Your in-depth coping with cancer guide will be in your inbox shortly. You will also receive emails from Mayo Clinic on the latest about cancer news, research, and care.
If you don’t receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
In general, cancer begins with a genetic mutation that allows normal, healthy cells to continue growing without responding to the signals to stop, which normal cells do. Cancer cells grow and multiply out of control. The accumulating abnormal cells form a mass (tumor).
Neuroblastoma begins in neuroblasts — immature nerve cells that a fetus makes as part of its development process.
As the fetus matures, neuroblasts eventually turn into nerve cells and fibers and the cells that make up the adrenal glands. Most neuroblasts mature by birth, though a small number of immature neuroblasts can be found in newborns. In most cases, these neuroblasts mature or disappear. Others, however, form a tumor — a neuroblastoma.
It isn't clear what causes the initial genetic mutation that leads to neuroblastoma.
Risk factors
Children with a family history of neuroblastoma may be more likely to develop the disease. Yet, familial neuroblastoma is thought to comprise a very small number of neuroblastoma cases. In most cases of neuroblastoma, a cause is never identified.
Complications
Complications of neuroblastoma may include:
- Spread of the cancer (metastasis). Neuroblastoma may spread (metastasize) to other parts of the body, such as the lymph nodes, bone marrow, liver, skin and bones.
- Spinal cord compression. Tumors may grow and press on the spinal cord, causing spinal cord compression. Spinal cord compression may cause pain and paralysis.
- Signs and symptoms caused by tumor secretions. Neuroblastoma cells may secrete certain chemicals that irritate other normal tissues, causing signs and symptoms called paraneoplastic syndromes. One paraneoplastic syndrome that occurs rarely in people with neuroblastoma causes rapid eye movements and difficulty with coordination. Another rare syndrome causes abdominal swelling and diarrhea.
Neuroblastoma care at Mayo Clinic
Living with neuroblastoma?
Connect with others like you for support and answers to your questions in the Blood Cancers & Disorders support group on Mayo Clinic Connect, a patient community.
Blood Cancers & Disorders Discussions

26 Replies Thu, May 16, 2024

380 Replies Wed, May 15, 2024

67 Replies Tue, May 14, 2024
- Shohet J, et al. Clinical presentation, diagnosis, and staging evaluation of neuroblastoma. https://www.uptodate.com/contents/search. Accessed Oct. 12, 2018.
- Shohet J, et al. Treatment and prognosis of neuroblastoma. https://www.uptodate.com/contents/search. Accessed Oct. 12, 2018.
- Hay WW, et al., eds. Neoplastic disease. In: Current Diagnosis & Treatment: Pediatrics. 24th ed. New York, N.Y.: McGraw-Hill Education; 2018. https://accessmedicine.mhmedical.com. Accessed Oct. 12, 2018.
- Neuroblastoma treatment (PDQ). National Cancer Institute. https://www.cancer.gov/types/neuroblastoma/patient/neuroblastoma-treatment-pdq. Accessed Oct. 12, 2018.
- National Library of Medicine. Neuroblastoma. Genetics Home Reference. https://ghr.nlm.nih.gov/condition/neuroblastoma. Accessed Oct. 12, 2018.
- Kliegman RM, et al. Neuroblastoma. In: Nelson Textbook of Pediatrics. 20th ed. Philadelphia, Pa.: Elsevier; 2016. https://www.clinicalkey.com. Accessed June 26, 2018.
- Niederhuber JE, et al., eds. Pediatric solid tumors. In: Abeloff's Clinical Oncology. 5th ed. Philadelphia, Pa.: Churchill Livingstone Elsevier; 2014. https://www.clinicalkey.com. Accessed June 26, 2018.
- Types of cancer treatment. National Cancer Institute. https://www.cancer.gov/about-cancer/treatment/types. Accessed Oct. 16, 2018.
Associated Procedures
- Bone marrow biopsy
- Bone marrow transplant
- Chemotherapy
- Radiation therapy
News from Mayo Clinic
- Mayo Clinic Q and A: Cancer of the nerve cells July 27, 2023, 03:20 p.m. CDT
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been ranked among the best Neurology & Neurosurgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

IMAGES
VIDEO
COMMENTS
Presentation refers to the part of the fetus's body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way. Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput ...
A fetus is typically breech at some point during pregnancy. But a breech position matters when you approach 36 weeks of pregnancy. Up until this point, fetuses often move into a head down position. Your provider will feel your belly during your appointments in the third trimester of pregnancy to check if the fetus is in a breech position.
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse. Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position. Abnormal fetal lie, presentation, or position may occur with. Fetopelvic disproportion (fetus too large for the pelvic inlet)
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
In the last weeks of pregnancy, a fetus usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation.A breech presentation occurs when the fetus's buttocks, feet, or both are in place to come out first during birth. This happens in 3-4% of full-term births.
However, not every fetus makes this turn to head south in the womb. About 3 to 4 percent of babies still hang out head-up by the time they're full-term. ... Very rarely, a problem with the baby's muscular or central nervous system can cause a breech presentation. Having an abnormally short umbilical cord may also limit your baby's ...
Breech presentation, which occurs in approximately 3 percent of fetuses at term, describes the fetus whose presenting part is the buttocks and/or feet. Although most breech fetuses have normal anatomy, this presentation is associated with an increased risk for congenital malformations and mild deformations, torticollis, and developmental ...
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered. ... the fetus's health will be monitored, and an ECV is often performed ...
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Up to 25% of all preterm deliveries are iatrogenic due to antenatal complications, such as pre-eclampsia, fetal growth restriction and antepartum haemorrhage. 57 For women requiring planned delivery for maternal and/or fetal compromise with a viable fetus in breech presentation, elective caesarean section is recommended. Evidence level 4
Breech and external cephalic version. Breech presentation is when the fetus is lying longitudinally and its buttocks, foot or feet are presenting instead of its head. Figure 1. Breech presentations. Breech presentation occurs in three to four per cent of term deliveries and is more common in nulliparous women.
Introduction. Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman's and the baby's health. The aim of this review is to determine the most ...
A breech presentation at delivery occurs when the fetus does not turn to a cephalic presentation. ... breech births in which the sacrum is the fetal denominator can be classified by the position of a fetus. Thus sacro-anterior, ...
How to turn a breech baby naturally. Get into one of the following positions twice a day, starting at around 32 weeks. Be sure to do these moves on an empty stomach, lest your lunch comes back up. Make sure there's someone around to help you get up if you start feeling lightheaded. If you find these positions uncomfortable, stop doing them.
Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of births at term.
Turning a breech baby. If your baby is in a breech position at 36 weeks, you'll usually be offered an external cephalic version (ECV). This is when a healthcare professional, such as an obstetrician, tries to turn the baby into a head-down position by applying pressure on your abdomen. It's a safe procedure, although it can be a bit uncomfortable.
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
INTRODUCTION. Vaginal breech birth is associated with increased neonatal morbidity and mortality compared with vaginal birth of a cephalic presentation. External cephalic version of a breech fetus is an effective approach to increasing the number of patients who present in labor with cephalic presentation and is the approach that we recommend.
Overview. There are three types of breech presentation: complete, incomplete, and frank. Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal. Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Neuroblastoma begins in neuroblasts — immature nerve cells that a fetus makes as part of its development process. As the fetus matures, neuroblasts eventually turn into nerve cells and fibers and the cells that make up the adrenal glands. Most neuroblasts mature by birth, though a small number of immature neuroblasts can be found in newborns.