- Open access
- Published: 27 October 2021

A narrative review on the validity of electronic health record-based research in epidemiology
- Milena A. Gianfrancesco 1 &
- Neal D. Goldstein ORCID: orcid.org/0000-0002-9597-5251 2
BMC Medical Research Methodology volume 21 , Article number: 234 ( 2021 ) Cite this article
11k Accesses
47 Citations
5 Altmetric
Metrics details
Electronic health records (EHRs) are widely used in epidemiological research, but the validity of the results is dependent upon the assumptions made about the healthcare system, the patient, and the provider. In this review, we identify four overarching challenges in using EHR-based data for epidemiological analysis, with a particular emphasis on threats to validity. These challenges include representativeness of the EHR to a target population, the availability and interpretability of clinical and non-clinical data, and missing data at both the variable and observation levels. Each challenge reveals layers of assumptions that the epidemiologist is required to make, from the point of patient entry into the healthcare system, to the provider documenting the results of the clinical exam and follow-up of the patient longitudinally; all with the potential to bias the results of analysis of these data. Understanding the extent of as well as remediating potential biases requires a variety of methodological approaches, from traditional sensitivity analyses and validation studies, to newer techniques such as natural language processing. Beyond methods to address these challenges, it will remain crucial for epidemiologists to engage with clinicians and informaticians at their institutions to ensure data quality and accessibility by forming multidisciplinary teams around specific research projects.
Peer Review reports
The proliferation of electronic health records (EHRs) spurred on by federal government incentives over the past few decades has resulted in greater than an 80% adoption-rate at hospitals [ 1 ] and close to 90% in office-based practices [ 2 ] in the United States. A natural consequence of the availability of electronic health data is the conduct of research with these data, both observational and experimental [ 3 ], due to lower overhead costs and lower burden of study recruitment [ 4 ]. Indeed, a search on PubMed for publications indexed by the MeSH term “electronic health records” reveals an exponential growth in biomedical literature, especially over the last 10 years with an excess of 50,000 publications.
An emerging literature is beginning to recognize the many challenges that still lay ahead in using EHR data for epidemiological investigations. Researchers in Europe identified 13 potential sources of “bias” (bias was defined as a contamination of the data) in EHR-based data covering almost every aspect of care delivery, from selective entrance into the healthcare system, to variation in care and documentation practices, to identification and extraction of the right data for analysis [ 5 ]. Many of the identified contaminants are directly relevant to traditional epidemiological threats to validity [ 4 ]. Data quality has consistently been invoked as a central challenge in EHRs. From a qualitative perspective, healthcare workers have described challenges in the healthcare environment (e.g., heavy workload), imperfect clinical documentation practices, and concerns over data extraction and reporting tools, all of which would impact the quality of data in the EHR [ 6 ]. From a quantitative perspective, researchers have noted limited sensitivity of diagnostic codes in the EHR when relying on discrete codings, noting that upon a manual chart review free text fields often capture the missed information, motivating such techniques as natural language processing (NLP) [ 7 ]. A systematic review of EHR-based studies also identified data quality as an overarching barrier to the use of EHRs in managing the health of the community, i.e. “population health” [ 8 ]. Encouragingly this same review also identified more facilitators than barriers to the use of EHRs in public health, suggesting that opportunities outweigh the challenges. Shortreed et al. further explored these opportunities discussing how EHRs can enhance pragmatic trials, bring additional sophistication to observational studies, aid in predictive modeling, and be linked together to create more comprehensive views of patients’ health [ 9 ]. Yet, as Shortreed and others have noted, significant challenges still remain.
It is our intention with this narrative review to discuss some of these challenges in further detail. In particular, we focus on specific epidemiological threats to validity -- internal and external -- and how EHR-based epidemiological research in particular can exacerbate some of these threats. We note that while there is some overlap in the challenges we discuss with traditional paper-based medical record research that has occurred for decades, the scale and scope of an EHR-based study is often well beyond what was traditionally possible in the manual chart review era and our applied examples attempt to reflect this. We also describe existing and emerging approaches for remediating these potential biases as they arise. A summary of these challenges may be found in Table 1 . Our review is grounded in the healthcare system in the United States, although we expect many of the issues we describe to be applicable regardless of locale; where necessary, we have flagged our comments as specific to the U.S.
Challenge #1: Representativeness
The selection process for how patients are captured in the EHR is complex and a function of geographic, social, demographic, and economic determinants [ 10 ]. This can be termed the catchment of the EHR. For a patient record to appear in the EHR the patient must have been registered in the system, typically to capture their demographic and billing information, and upon a clinical visit, their health details. While this process is not new to clinical epidemiology, what tends to separate EHR-based records from traditional paper-based records is the scale and scope of the data. Patient data may be available for longer periods of time longitudinally, as well as have data corresponding to interactions with multiple, potentially disparate, healthcare systems [ 11 ]. Given the consolidation of healthcare [ 12 ] and aggregated views of multiple EHRs through health information networks or exchanges [ 11 ] the ability to have a complete view of the patients’ total health is increasing. Importantly, the epidemiologist must ascertain whether the population captured within the EHR or EHR-derived data is representative of the population targeted for inference. This is particularly true under the paradigm of population health and inferring the health status of a community from EHR-based records [ 13 ]. For example, a study of Clostridium difficile infection at an urban safety net hospital in Philadelphia, Pennsylvania demonstrated notable differences in risk factors in the hospital’s EHR compared to national surveillance data, suggesting how catchment can influence epidemiologic measures [ 14 ]. Even health-related data captured through health information exchanges may be incomplete [ 15 ].
Several hypothetical study settings can further help the epidemiologist appreciate the relationship between representativeness and validity in EHR research. In the first hypothetical, an EHR-based study is conducted from a single-location federally qualified health center, and in the second hypothetical, an EHR-based study is conducted from a large academic health system. Suppose both studies occur in the same geographic area. It is reasonable to believe the patient populations captured in both EHRs will be quite different and the catchment process could lead to divergent estimates of disease or risk factor prevalence. The large academic health system may be less likely to capture primary care visits, as specialty care may drive the preponderance of patient encounters. However, this is not a bias per se : if the target of inference from these two hypothetical EHR-based studies is the local community, then selection bias becomes a distinct possibility. The epidemiologist must also consider the potential for generalizability and transportability -- two facets of external validity that respectively relate to the extrapolation of study findings to the source population or a different population altogether -- if there are unmeasured effect modifiers, treatment interference, or compound treatments in the community targeted for inference [ 16 ].
There are several approaches for ascertaining representativeness of EHR-based data. Comparing the EHR-derived sample to Census estimates of demography is straightforward but has several important limitations. First, as previously described, the catchment process may be driven by discordant geographical areas, especially for specialty care settings. Second and third, the EHR may have limited or inaccurate information on socioeconomic status, race, and ethnicity that one may wish to compare [ 17 , 18 ], and conversely the Census has limited estimates of health, chiefly disability, fertility, and insurance and payments [ 19 ]. If selection bias is suspected as a result of missing visits in a longitudinal study [ 20 ] or the catchment process in a cross-sectional study [ 21 ], using inverse probability weighting may remediate its influence. Comparing the weighted estimates to the original, non-weighted estimates provides insight into differences in the study participants. In the population health paradigm whereby the EHR is used as a surveillance tool to identify community health disparities [ 13 ], one also needs to be concerned about representativeness. There are emerging approaches for producing such small area community estimates from large observational datasets [ 22 , 23 ]. Conceivably, these approaches may also be useful for identifying issues of representativeness, for example by comparing stratified estimates across sociodemographic or other factors that may relate to catchment. Approaches for issues concerning representativeness specifically as it applies to external validity may be found in these references [ 24 , 25 ].
Challenge #2: Data availability and interpretation
Sub-challenge #2.1: billing versus clinical versus epidemiological needs.
There is an inherent tension in the use of EHR-based data for research purposes: the EHR was never originally designed for research. In the U.S., the Health Information Technology for Economic and Clinical Health Act, which promoted EHRs as a platform for comparative effectiveness research, was an attempt to address this deficiency [ 26 ]. A brief history of the evolution of the modern EHR reveals a technology that was optimized for capturing health details relevant for billing, scheduling, and clinical record keeping [ 27 ]. As such, the availability of data for fundamental markers of upstream health that are important for identifying inequities, such as socioeconomic status, race, ethnicity, and other social determinants of health (SDOH), may be insufficiently captured in the EHR [ 17 , 18 ]. Similarly, behavioral risk factors, such as being a sexual minority person, have historically been insufficiently recorded as discrete variables. It is only recently that such data are beginning to be captured in the EHR [ 28 , 29 ], or techniques such as NLP have made it possible to extract these details when stored in free text notes (described further in “ Unstructured data: clinical notes and reports ” section).
As an example, assessing clinical morbidities in the EHR may be done on the basis of extracting appropriate International Classification of Diseases (ICD) codes, used for billing and reimbursement in the U.S. These codes are known to have low sensitivity despite high specificity for accurate diagnostic status [ 30 , 31 ]. Expressed as predictive values, which depend upon prevalence, presence of a diagnostic code is a likely indicator of a disease state, whereas absence of a diagnostic code is a less reliable indicator of the absence of that morbidity. There may further be variation by clinical domain in that ICD codes may exist but not be used in some specialties [ 32 ], variation by coding vocabulary such as the use of SNOMED for clinical documentation versus ICD for billing necessitating an ontology mapper [ 33 ], and variation by the use of “rule-out” diagnostic codes resulting in false-positive diagnoses [ 34 , 35 , 36 ]. Relatedly is the notion of upcoding, or the billing of tests, procedures, or diagnoses to receive inflated reimbursement, which, although posited to be problematic in EHRs [ 37 ] in at least one study, has not been shown to have occurred [ 38 ]. In the U.S., the billing and reimbursement model, such as fee-for-service versus managed care, may result in varying diagnostic code sensitivities and specificities, especially if upcoding is occurring [ 39 ]. In short, there is potential for misclassification of key health data in the EHR.
Misclassification can potentially be addressed through a validation study (resources permitting) or application of quantitative bias analysis, and there is a rich literature regarding the treatment of misclassified data in statistics and epidemiology. Readers are referred to these texts as a starting point [ 40 , 41 ]. Duda et al. and Shepherd et al. have described an innovative data audit approach applicable to secondary analysis of observational data, such as EHR-derived data, that incorporates the audit error rate directly in the regression analysis to reduce information bias [ 42 , 43 ]. Outside of methodological tricks in the face of imperfect data, researchers must proactively engage with clinical and informatics colleagues to ensure that the right data for the research interests are available and accessible.
Sub-challenge #2.2: Consistency in data and interpretation
For the epidemiologist, abstracting data from the EHR into a research-ready analytic dataset presents a host of complications surrounding data availability, consistency and interpretation. It is easy to conflate the total volume of data in the EHR with data that are usable for research, however expectations should be tempered. Weiskopf et al. have noted such challenges for the researcher: in their study, less than 50% of patient records had “complete” data for research purposes per their four definitions of completeness [ 44 ]. Decisions made about the treatment of incomplete data can induce selection bias or impact precision of estimates (see Challenges #1 , #3 , and #4 ). The COVID-19 pandemic has further demonstrated the challenge of obtaining research data from EHRs across multiple health systems [ 45 ]. On the other hand, EHRs have a key advantage of providing near real-time data as opposed to many epidemiological studies that have a specific endpoint or are retrospective in nature. Such real-time data availability was leveraged during COVID-19 to help healthcare systems manage their pandemic response [ 46 , 47 ]. Logistical and technical issues aside, healthcare and documentation practices are nuanced to their local environments. In fact, researchers have demonstrated how the same research question analyzed in distinct clinical databases can yield different results [ 48 ].
Once the data are obtained, choices regarding operationalization of variables have the potential to induce information bias. Several hypothetical examples can help demonstrate this point. As a first example, differences in laboratory reporting may result in measurement error or misclassification. While the order for a particular laboratory assay is likely consistent within the healthcare system, patients frequently have a choice where to have that order fulfilled. Given the breadth of assays and reporting differences that may differ lab to lab [ 49 ], it is possible that the researcher working with the raw data may not consider all possible permutations. In other words, there may be lack of consistency in the reporting of the assay results. As a second example, raw clinical data requires interpretation to become actionable. A researcher interested in capturing a patient’s Charlson comorbidity index, which is based on 16 potential diagnoses plus the patient’s age [ 50 ], may never find such a variable in the EHR. Rather, this would require operationalization based on the raw data, each of which may be misclassified. Use of such composite measures introduces the notion of “differential item functioning”, whereby a summary indicator of a complexly measured health phenomenon may differ from group to group [ 51 ]. In this case, as opposed to a measurement error bias, this is one of residual confounding in that a key (unmeasured) variable is driving the differences. Remediation of these threats to validity may involve validation studies to determine the accuracy of a particular classifier, sensitivity analysis employing alternative interpretations when the raw data are available, and omitting or imputing biased or latent variables [ 40 , 41 , 52 ]. Importantly, in all cases, the epidemiologists should work with the various health care providers and personnel who have measured and recorded the data present in the EHR, as they likely understand it best.
Furthermore and related to “Billing versus Clinical versus Epidemiological Needs” section, the healthcare system in the U.S. is fragmented with multiple payers, both public and private, potentially exacerbating the data quality issues we describe, especially when linking data across healthcare systems. Single payer systems have enabled large and near-complete population-based studies due to data availability and consistency [ 53 , 54 , 55 ]. Data may also be inconsistent for retrospective longitudinal studies spanning many years if there have been changes to coding standards or practices over time, for example due to the transition from ICD-9 to ICD-10 largely occurring in the mid 2010s or the adoption of the Patient Protection and Affordable Care Act in the U.S. in 2010 with its accompanying changes in billing. Exploratory data analysis may reveal unexpected differences in key variables, by place or time, and recoding, when possible, can enforce consistency.
Sub-challenge #2.3: Unstructured data: clinical notes and reports
There may also be scenarios where structured data fields, while available, are not traditionally or consistently used within a given medical center or by a given provider. For example, reporting of adverse events of medications, disease symptoms, and vaccinations or hospitalizations occurring at different facility/health networks may not always be entered by providers in structured EHR fields. Instead, these types of patient experiences may be more likely to be documented in an unstructured clinical note, report (e.g. pathology or radiology report), or scanned document. Therefore, reliance on structured data to identify and study such issues may result in underestimation and potentially biased results.
Advances in NLP currently allow for information to be extracted from unstructured clinical notes and text fields in a reliable and accurate manner using computational methods. NLP utilizes a range of different statistical, machine learning, and linguistic techniques, and when applied to EHR data, has the potential to facilitate more accurate detection of events not traditionally located or consistently used in structured fields. Various NLP methods can be implemented in medical text analysis, ranging from simplistic and fast term recognition systems to more advanced, commercial NLP systems [ 56 ]. Several studies have successfully utilized text mining to extract information on a variety of health-related issues within clinical notes, such as opioid use [ 57 ], adverse events [ 58 , 59 ], symptoms (e.g., shortness of breath, depression, pain) [ 60 ], and disease phenotype information documented in pathology or radiology reports, including cancer stage, histology, and tumor grade [ 61 ], and lupus nephritis [ 32 ]. It is worth noting that scanned documents involve an additional layer of computation, relying on techniques such as optical character recognition, before NLP can be applied.
Hybrid approaches that combine both narrative and structured data, such as ICD codes, to improve accuracy of detecting phenotypes have also demonstrated high performance. Banerji et al. found that using ICD-9 codes to identify allergic drug reactions in the EHR had a positive predictive value of 46%, while an NLP algorithm in conjunction with ICD-9 codes resulted in a positive predictive value of 86%; negative predictive value also increased in the combined algorithm (76%) compared to ICD-9 codes alone (39%) [ 62 ]. In another example, researchers found that the combination of unstructured clinical notes with structured data for prediction tasks involving in-hospital mortality and 30-day hospital readmission outperformed models using either clinical notes or structured data alone [ 63 ]. As we move forward in analyzing EHR data, it will be important to take advantage of the wealth of information buried in unstructured data to assist in phenotyping patient characteristics and outcomes, capture missing confounders used in multivariate analyses, and develop prediction models.
Challenge #3: Missing measurements
While clinical notes may be useful to recover incomplete information from structured data fields, it may be the case that certain variables are not collected within the EHR at all. As mentioned above, it is important to remember that EHRs were not developed as a research tool (see “ Billing versus clinical versus epidemiological needs ” section), and important variables often used in epidemiologic research may not be typically included in EHRs including socioeconomic status (education, income, occupation) and SDOH [ 17 , 18 ]. Depending upon the interest of the provider or clinical importance placed upon a given variable, this information may be included in clinical notes. While NLP could be used to capture these variables, because they may not be consistently captured, there may be bias in identifying those with a positive mention as a positive case and those with no mention as a negative case. For example, if a given provider inquires about homelessness of a patient based on knowledge of the patient’s situation or other external factors and documents this in the clinical note, we have greater assurance that this is a true positive case. However, lack of mention of homelessness in a clinical note should not be assumed as a true negative case for several reasons: not all providers may feel comfortable asking about and/or documenting homelessness, they may not deem this variable worth noting, or implicit bias among clinicians may affect what is captured. As a result, such cases (i.e. no mention of homelessness) may be incorrectly identified as “not homeless,” leading to selection bias should a researcher form a cohort exclusively of patients who are identified as homeless in the EHR.
Not adjusting for certain measurements missing from EHR data can also lead to biased results if the measurement is an important confounder. Consider the example of distinguishing between prevalent and incident cases of disease when examining associations between disease treatments and patient outcomes [ 64 ]. The first date of an ICD code entered for a given patient may not necessarily be the true date of diagnosis, but rather documentation of an existing diagnosis. This limits the ability to adjust for disease duration, which may be an important confounder in studies comparing various treatments with patient outcomes over time, and may also lead to reverse causality if disease sequalae are assumed to be risk factors.
Methods to supplement EHR data with external data have been used to capture missing information. These methods may include imputation if information (e.g. race, lab values) is collected on a subset of patients within the EHR. It is important to examine whether missingness occurs completely at random or at random (“ignorable”), or not at random (“non-ignorable”), using the data available to determine factors associated with missingness, which will also inform the best imputation strategy to pursue, if any [ 65 , 66 ]. As an example, suppose we are interested in ascertaining a patient's BMI from the EHR. If men were less likely to have BMI measured than women, the probability of missing data (BMI) depends on the observed data (gender) and may therefore be predictable and imputable. On the other hand, suppose underweight individuals were less likely to have BMI measured; the probability of missing data depends on its own value, and as such is non-predictable and may require a validation study to confirm. Alternatively to imputing missing data, surrogate measures may be used, such as inferring area-based SES indicators, including median household income, percent poverty, or area deprivation index, by zip code [ 67 , 68 ]. Lastly, validation studies utilizing external datasets may prove helpful, such as supplementing EHR data with claims data that may be available for a subset of patients (see Challenge #4 ).
As EHRs are increasingly being used for research, there are active pushes to include more structured data fields that are important to population health research, such as SDOH [ 69 ]. Inclusion of such factors are likely to result in improved patient care and outcomes, through increased precision in disease diagnosis, more effective shared decision making, identification of risk factors, and tailoring services to a given population’s needs [ 70 ]. In fact, a recent review found that when individual level SDOH were included in predictive modeling, they overwhelmingly improved performance in medication adherence, risk of hospitalization, 30-day rehospitalizations, suicide attempts, and other healthcare services [ 71 ]. Whether or not these fields will be utilized after their inclusion in the EHR may ultimately depend upon federal and state incentives, as well as support from local stakeholders, and this does not address historic, retrospective analyses of these data.
Challenge #4: Missing visits
Beyond missing variable data that may not be captured during a clinical encounter, either through structured data or clinical notes, there also may be missing information for a patient as a whole. This can occur in a variety of ways; for example, a patient may have one or two documented visits in the EHR and then is never seen again (i.e. right censoring due to lost to follow-up), or a patient is referred from elsewhere to seek specialty care, with no information captured regarding other external issues (i.e. left censoring). This may be especially common in circumstances where a given EHR is more likely to capture specialty clinics versus primary care (see Challenge #1 ). A third scenario may include patients who appear, then are not observed for a long period of time, and then reappear: this case is particularly problematic as it may appear the patient was never lost to follow up but simply had fewer visits. In any of these scenarios, a researcher will lack a holistic view of the patient’s experiences, diagnoses, results, and more. As discussed above, assuming absence of a diagnostic code as absence of disease may lead to information and/or selection bias. Further, it has been demonstrated that one key source of bias in EHRs is “informed presence” bias, where those with more medical encounters are more likely to be diagnosed with various conditions (similar to Berkson’s bias) [ 72 ].
Several solutions to these issues have been proposed. For example, it is common for EHR studies to condition on observation time (i.e. ≥n visits required to be eligible into cohort); however, this may exclude a substantial amount of patients with certain characteristics, incurring a selection bias or limiting the generalizability of study findings (see Challenge #1 ). Other strategies attempt to account for missing visit biases through longitudinal imputation approaches; for example, if a patient missed a visit, a disease activity score can be imputed for that point in time, given other data points [ 73 , 74 ]. Surrogate measures may also be used to infer patient outcomes, such as controlling for “informative” missingness as an indicator variable or using actual number of missed visits that were scheduled as a proxy for external circumstances influencing care [ 20 ]. To address “informed presence” bias described above, conditioning on the number of health-care encounters may be appropriate [ 72 ]. Understanding the reason for the missing visit may help identify the best course of action and before imputing, one should be able to identify the type of missingness, whether “informative” or not [ 65 , 66 ]. For example, if distance to a healthcare location is related to appointment attendance, being able to account for this in analysis would be important: researchers have shown how the catchment of a healthcare facility can induce selection bias [ 21 ]. Relatedly, as telehealth becomes more common fueled by the COVID-19 pandemic [ 75 , 76 ], virtual visits may generate missingness of data recorded in the presence of a provider (e.g., blood pressure if the patient does not have access to a sphygmomanometer; see Challenge #3 ), or necessitate a stratified analysis by visit type to assess for effect modification.
Another common approach is to supplement EHR information with external data sources, such as insurance claims data, when available. Unlike a given EHR, claims data are able to capture a patient’s interaction with the health care system across organizations, and additionally includes pharmacy data such as if a prescription was filled or refilled. Often researchers examine a subset of patients eligible for Medicaid/Medicare and compare what is documented in claims with information available in the EHR [ 77 ]. That is, are there additional medications, diagnoses, hospitalizations found in the claims dataset that were not present in the EHR. In a study by Franklin et al., researchers utilized a linked database of Medicare Advantage claims and comprehensive EHR data from a multi-specialty outpatient practice to determine which dataset would be more accurate in predicting medication adherence [ 77 ]. They found that both datasets were comparable in identifying those with poor adherence, though each dataset incorporated different variables.
While validation studies such as those using claims data allow researchers to gain an understanding as to how accurate and complete a given EHR is, this may only be limited to the specific subpopulation examined (i.e. those eligible for Medicaid, or those over 65 years for Medicare). One study examined congruence between EHR of a community health center and Medicaid claims with respect to diabetes [ 78 ]. They found that patients who were older, male, Spanish-speaking, above the federal poverty level, or who had discontinuous insurance were more likely to have services documented in the EHR as compared to Medicaid claims data. Therefore, while claims data may help supplement and validate information in the EHR, on their own they may underestimate care in certain populations.
Research utilizing EHR data has undoubtedly positively impacted the field of public health through its ability to provide large-scale, longitudinal data on a diverse set of patients, and will continue to do so in the future as more epidemiologists take advantage of this data source. EHR data’s ability to capture individuals that traditionally aren’t included in clinical trials, cohort studies, and even claims datasets allows researchers to measure longitudinal outcomes in patients and perhaps change the understanding of potential risk factors.
However, as outlined in this review, there are important caveats to EHR analysis that need to be taken into account; failure to do so may threaten study validity. The representativeness of EHR data depends on the catchment area of the center and corresponding target population. Tools are available to evaluate and remedy these issues, which are critical to study validity as well as extrapolation of study findings. Data availability and interpretation, missing measurements, and missing visits are also key challenges, as EHRs were not specifically developed for research purposes, despite their common use for such. Taking advantage of all available EHR data, whether it be structured or unstructured fields through NLP, will be important in understanding the patient experience and identifying key phenotypes. Beyond methods to address these concerns, it will remain crucial for epidemiologists and data analysts to engage with clinicians and informaticians at their institutions to ensure data quality and accessibility by forming multidisciplinary teams around specific research projects. Lastly, integration across multiple EHRs, or datasets that encompass multi-institutional EHR records, add an additional layer of data quality and validity issues, with the potential to exacerbate the above-stated challenges found within a single EHR. At minimum, such studies should account for correlated errors [ 79 , 80 ], and investigate whether modularization, or submechanisms that determine whether data are observed or missing in each EHR, exist [ 65 ].
The identified challenges may also apply to secondary analysis of other large healthcare databases, such as claims data, although it is important not to conflate the two types of data. EHR data are driven by clinical care and claims data are driven by the reimbursement process where there is a financial incentive to capture diagnoses, procedures, and medications [ 48 ]. The source of data likely influences the availability, accuracy, and completeness of data. The fundamental representation of data may also differ as a record in a claims database corresponds to a “claim” as opposed to an “encounter” in the EHR. As such, the representativeness of the database populations, the sensitivity and specificity of variables, as well as the mechanisms of missingness in claims data may differ from EHR data. One study that evaluated pediatric quality care measures, such as BMI, noted inferior sensitivity based on claims data alone [ 81 ]. Linking claims data to EHR data has been proposed to enhance study validity, but many of the caveats raised in herein still apply [ 82 ].
Although we focused on epidemiological challenges related to study validity, there are other important considerations for researchers working with EHR data. Privacy and security of data as well as institutional review board (IRB) or ethics board oversight of EHR-based studies should not be taken for granted. For researchers in the U.S., Goldstein and Sarwate described Health Insurance Portability and Accountability Act (HIPAA)-compliant approaches to ensure the privacy and security of EHR data used in epidemiological research, and presented emerging approaches to analyses that separate the data from analysis [ 83 ]. The IRB oversees the data collection process for EHR-based research and through the HIPAA Privacy Rule these data typically do not require informed consent provided they are retrospective and reside at the EHR’s institution [ 84 ]. Such research will also likely receive an exempt IRB review provided subjects are non-identifiable.
Conclusions
As EHRs are increasingly being used for research, epidemiologists can take advantage of the many tools and methods that already exist and apply them to the key challenges described above. By being aware of the limitations that the data present and proactively addressing them, EHR studies will be more robust, informative, and important to the understanding of health and disease in the population.
Availability of data and materials
All data and materials used in this review are described herein.
Abbreviations
Body Mass Index
Electronic Health Record
International Classification of Diseases
Institutional review board/ethics board
Health Insurance Portability and Accountability Act
Natural Language Processing
Social Determinants of Health
Socioeconomic Status
Adler-Milstein J, Holmgren AJ, Kralovec P, et al. Electronic health record adoption in US hospitals: the emergence of a digital “advanced use” divide. J Am Med Inform Assoc. 2017;24(6):1142–8.
Article PubMed PubMed Central Google Scholar
Office of the National Coordinator for Health Information Technology. ‘Office-based physician electronic health record adoption’, Health IT quick-stat #50. dashboard.healthit.gov/quickstats/pages/physician-ehr-adoption-trends.php . Accessed 15 Jan 2019.
Cowie MR, Blomster JI, Curtis LH, et al. Electronic health records to facilitate clinical research. Clin Res Cardiol. 2017;106(1):1–9.
Article PubMed Google Scholar
Casey JA, Schwartz BS, Stewart WF, et al. Using electronic health records for population health research: a review of methods and applications. Annu Rev Public Health. 2016;37:61–81.
Verheij RA, Curcin V, Delaney BC, et al. Possible sources of bias in primary care electronic health record data use and reuse. J Med Internet Res. 2018;20(5):e185.
Ni K, Chu H, Zeng L, et al. Barriers and facilitators to data quality of electronic health records used for clinical research in China: a qualitative study. BMJ Open. 2019;9(7):e029314.
Coleman N, Halas G, Peeler W, et al. From patient care to research: a validation study examining the factors contributing to data quality in a primary care electronic medical record database. BMC Fam Pract. 2015;16:11.
Kruse CS, Stein A, Thomas H, et al. The use of electronic health records to support population health: a systematic review of the literature. J Med Syst. 2018;42(11):214.
Shortreed SM, Cook AJ, Coley RY, et al. Challenges and opportunities for using big health care data to advance medical science and public health. Am J Epidemiol. 2019;188(5):851–61.
In: Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: confronting racial and ethnic disparities in health care. Washington (DC) 2003.
Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–52.
Cutler DM, Scott Morton F. Hospitals, market share, and consolidation. JAMA. 2013;310(18):1964–70.
Article CAS PubMed Google Scholar
Cocoros NM, Kirby C, Zambarano B, et al. RiskScape: a data visualization and aggregation platform for public health surveillance using routine electronic health record data. Am J Public Health. 2021;111(2):269–76.
Vader DT, Weldie C, Welles SL, et al. Hospital-acquired Clostridioides difficile infection among patients at an urban safety-net hospital in Philadelphia: demographics, neighborhood deprivation, and the transferability of national statistics. Infect Control Hosp Epidemiol. 2020;42:1–7.
Google Scholar
Dixon BE, Gibson PJ, Frederickson Comer K, et al. Measuring population health using electronic health records: exploring biases and representativeness in a community health information exchange. Stud Health Technol Inform. 2015;216:1009.
PubMed Google Scholar
Hernán MA, VanderWeele TJ. Compound treatments and transportability of causal inference. Epidemiology. 2011;22(3):368–77.
Casey JA, Pollak J, Glymour MM, et al. Measures of SES for electronic health record-based research. Am J Prev Med. 2018;54(3):430–9.
Polubriaginof FCG, Ryan P, Salmasian H, et al. Challenges with quality of race and ethnicity data in observational databases. J Am Med Inform Assoc. 2019;26(8-9):730–6.
U.S. Census Bureau. Health. Available at: https://www.census.gov/topics/health.html . Accessed 19 Jan 2021.
Gianfrancesco MA, McCulloch CE, Trupin L, et al. Reweighting to address nonparticipation and missing data bias in a longitudinal electronic health record study. Ann Epidemiol. 2020;50:48–51 e2.
Goldstein ND, Kahal D, Testa K, Burstyn I. Inverse probability weighting for selection bias in a Delaware community health center electronic medical record study of community deprivation and hepatitis C prevalence. Ann Epidemiol. 2021;60:1–7.
Gelman A, Lax J, Phillips J, et al. Using multilevel regression and poststratification to estimate dynamic public opinion. Unpublished manuscript, Columbia University. 2016 Sep 11. Available at: http://www.stat.columbia.edu/~gelman/research/unpublished/MRT(1).pdf . Accessed 22 Jan 2021.
Quick H, Terloyeva D, Wu Y, et al. Trends in tract-level prevalence of obesity in philadelphia by race-ethnicity, space, and time. Epidemiology. 2020;31(1):15–21.
Lesko CR, Buchanan AL, Westreich D, Edwards JK, Hudgens MG, Cole SR. Generalizing study results: a potential outcomes perspective. Epidemiology. 2017;28(4):553–61.
Westreich D, Edwards JK, Lesko CR, Stuart E, Cole SR. Transportability of trial results using inverse odds of sampling weights. Am J Epidemiol. 2017;186(8):1010–4.
Congressional Research Services (CRS). The Health Information Technology for Economic and Clinical Health (HITECH) Act. 2009. Available at: https://crsreports.congress.gov/product/pdf/R/R40161/9 . Accessed Jan 22 2021.
Hersh WR. The electronic medical record: Promises and problems. Journal of the American Society for Information Science. 1995;46(10):772–6.
Article Google Scholar
Collecting sexual orientation and gender identity data in electronic health records: workshop summary. Washington (DC) 2013.
Committee on the Recommended Social and Behavioral Domains and Measures for Electronic Health Records; Board on Population Health and Public Health Practice; Institute of Medicine. Capturing social and behavioral domains and measures in electronic health records: phase 2. Washington (DC): National Academies Press (US); 2015.
Goff SL, Pekow PS, Markenson G, et al. Validity of using ICD-9-CM codes to identify selected categories of obstetric complications, procedures and co-morbidities. Paediatr Perinat Epidemiol. 2012;26(5):421–9.
Schneeweiss S, Avorn J. A review of uses of health care utilization databases for epidemiologic research on therapeutics. J Clin Epidemiol. 2005;58(4):323–37.
Gianfrancesco MA. Application of text mining methods to identify lupus nephritis from electronic health records. Lupus Science & Medicine. 2019;6:A142.
National Library of Medicine. SNOMED CT to ICD-10-CM Map. Available at: https://www.nlm.nih.gov/research/umls/mapping_projects/snomedct_to_icd10cm.html . Accessed 2 Jul 2021.
Klabunde CN, Harlan LC, Warren JL. Data sources for measuring comorbidity: a comparison of hospital records and medicare claims for cancer patients. Med Care. 2006;44(10):921–8.
Burles K, Innes G, Senior K, Lang E, McRae A. Limitations of pulmonary embolism ICD-10 codes in emergency department administrative data: let the buyer beware. BMC Med Res Methodol. 2017;17(1):89.
Asgari MM, Wu JJ, Gelfand JM, Salman C, Curtis JR, Harrold LR, et al. Validity of diagnostic codes and prevalence of psoriasis and psoriatic arthritis in a managed care population, 1996-2009. Pharmacoepidemiol Drug Saf. 2013;22(8):842–9.
Hoffman S, Podgurski A. Big bad data: law, public health, and biomedical databases. J Law Med Ethics. 2013;41(Suppl 1):56–60.
Adler-Milstein J, Jha AK. Electronic health records: the authors reply. Health Aff. 2014;33(10):1877.
Geruso M, Layton T. Upcoding: evidence from medicare on squishy risk adjustment. J Polit Econ. 2020;12(3):984–1026.
Lash TL, Fox MP, Fink AK. Applying quantitative bias analysis to epidemiologic data. New York: Springer-Verlag New York; 2009.
Book Google Scholar
Gustafson P. Measurement error and misclassification in statistics and epidemiology: impacts and Bayesian adjustments. Boca Raton: Chapman and Hall/CRC; 2004.
Duda SN, Shepherd BE, Gadd CS, et al. Measuring the quality of observational study data in an international HIV research network. PLoS One. 2012;7(4):e33908.
Article CAS PubMed PubMed Central Google Scholar
Shepherd BE, Yu C. Accounting for data errors discovered from an audit in multiple linear regression. Biometrics. 2011;67(3):1083–91.
Weiskopf NG, Hripcsak G, Swaminathan S, et al. Defining and measuring completeness of electronic health records for secondary use. J Biomed Inform. 2013;46(5):830–6.
Kaiser Health News. As coronavirus strikes, crucial data in electronic health records hard to harvest. Available at: https://khn.org/news/as-coronavirus-strikes-crucial-data-in-electronic-health-records-hard-to-harvest/ . Accessed 15 Jan 2021.
Reeves JJ, Hollandsworth HM, Torriani FJ, Taplitz R, Abeles S, Tai-Seale M, et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. 2020;27(6):853–9.
Grange ES, Neil EJ, Stoffel M, Singh AP, Tseng E, Resco-Summers K, et al. Responding to COVID-19: The UW medicine information technology services experience. Appl Clin Inform. 2020;11(2):265–75.
Madigan D, Ryan PB, Schuemie M, et al. Evaluating the impact of database heterogeneity on observational study results. Am J Epidemiol. 2013;178(4):645–51.
Lippi G, Mattiuzzi C. Critical laboratory values communication: summary recommendations from available guidelines. Ann Transl Med. 2016;4(20):400.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Jones RN. Differential item functioning and its relevance to epidemiology. Curr Epidemiol Rep. 2019;6:174–83.
Edwards JK, Cole SR, Troester MA, Richardson DB. Accounting for misclassified outcomes in binary regression models using multiple imputation with internal validation data. Am J Epidemiol. 2013;177(9):904–12.
Satkunasivam R, Klaassen Z, Ravi B, Fok KH, Menser T, Kash B, et al. Relation between surgeon age and postoperative outcomes: a population-based cohort study. CMAJ. 2020;192(15):E385–92.
Melamed N, Asztalos E, Murphy K, Zaltz A, Redelmeier D, Shah BR, et al. Neurodevelopmental disorders among term infants exposed to antenatal corticosteroids during pregnancy: a population-based study. BMJ Open. 2019;9(9):e031197.
Kao LT, Lee HC, Lin HC, Tsai MC, Chung SD. Healthcare service utilization by patients with obstructive sleep apnea: a population-based study. PLoS One. 2015;10(9):e0137459.
Article PubMed PubMed Central CAS Google Scholar
Jung K, LePendu P, Iyer S, Bauer-Mehren A, Percha B, Shah NH. Functional evaluation of out-of-the-box text-mining tools for data-mining tasks. J Am Med Inform Assoc. 2015;22(1):121–31.
Canan C, Polinski JM, Alexander GC, et al. Automatable algorithms to identify nonmedical opioid use using electronic data: a systematic review. J Am Med Inform Assoc. 2017;24(6):1204–10.
Iqbal E, Mallah R, Jackson RG, et al. Identification of adverse drug events from free text electronic patient records and information in a large mental health case register. PLoS One. 2015;10(8):e0134208.
Rochefort CM, Verma AD, Eguale T, et al. A novel method of adverse event detection can accurately identify venous thromboembolisms (VTEs) from narrative electronic health record data. J Am Med Inform Assoc. 2015;22(1):155–65.
Koleck TA, Dreisbach C, Bourne PE, et al. Natural language processing of symptoms documented in free-text narratives of electronic health records: a systematic review. J Am Med Inform Assoc. 2019;26(4):364–79.
Wang L, Luo L, Wang Y, et al. Natural language processing for populating lung cancer clinical research data. BMC Med Inform Decis Mak. 2019;19(Suppl 5):239.
Banerji A, Lai KH, Li Y, et al. Natural language processing combined with ICD-9-CM codes as a novel method to study the epidemiology of allergic drug reactions. J Allergy Clin Immunol Pract. 2020;8(3):1032–1038.e1.
Zhang D, Yin C, Zeng J, et al. Combining structured and unstructured data for predictive models: a deep learning approach. BMC Med Inform Decis Mak. 2020;20(1):280.
Farmer R, Mathur R, Bhaskaran K, Eastwood SV, Chaturvedi N, Smeeth L. Promises and pitfalls of electronic health record analysis. Diabetologia. 2018;61:1241–8.
Haneuse S, Arterburn D, Daniels MJ. Assessing missing data assumptions in EHR-based studies: a complex and underappreciated task. JAMA Netw Open. 2021;4(2):e210184.
Groenwold RHH. Informative missingness in electronic health record systems: the curse of knowing. Diagn Progn Res. 2020;4:8.
Berkowitz SA, Traore CY, Singer DE, et al. Evaluating area-based socioeconomic status indicators for monitoring disparities within health care systems: results from a primary care network. Health Serv Res. 2015;50(2):398–417.
Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N Engl J Med. 2018;378(26):2456–8.
Cantor MN, Thorpe L. Integrating data on social determinants of health into electronic health records. Health Aff. 2018;37(4):585–90.
Adler NE, Stead WW. Patients in context--EHR capture of social and behavioral determinants of health. N Engl J Med. 2015;372(8):698–701.
Chen M, Tan X, Padman R. Social determinants of health in electronic health records and their impact on analysis and risk prediction: a systematic review. J Am Med Inform Assoc. 2020;27(11):1764–73.
Goldstein BA, Bhavsar NA, Phelan M, et al. Controlling for informed presence bias due to the number of health encounters in an electronic health record. Am J Epidemiol. 2016;184(11):847–55.
Petersen I, Welch CA, Nazareth I, et al. Health indicator recording in UK primary care electronic health records: key implications for handling missing data. Clin Epidemiol. 2019;11:157–67.
Li R, Chen Y, Moore JH. Integration of genetic and clinical information to improve imputation of data missing from electronic health records. J Am Med Inform Assoc. 2019;26(10):1056–63.
Koonin LM, Hoots B, Tsang CA, Leroy Z, Farris K, Jolly T, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic - United States, January-March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1595–9.
Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320(20):2147–9.
Franklin JM, Gopalakrishnan C, Krumme AA, et al. The relative benefits of claims and electronic health record data for predicting medication adherence trajectory. Am Heart J. 2018;197:153–62.
Devoe JE, Gold R, McIntire P, et al. Electronic health records vs Medicaid claims: completeness of diabetes preventive care data in community health centers. Ann Fam Med. 2011;9(4):351–8.
Schmajuk G, Li J, Evans M, Anastasiou C, Izadi Z, Kay JL, et al. RISE registry reveals potential gaps in medication safety for new users of biologics and targeted synthetic DMARDs. Semin Arthritis Rheum. 2020 Dec;50(6):1542–8.
Izadi Z, Schmajuk G, Gianfrancesco M, Subash M, Evans M, Trupin L, et al. Rheumatology Informatics System for Effectiveness (RISE) practices see significant gains in rheumatoid arthritis quality measures. Arthritis Care Res. 2020. https://doi.org/10.1002/acr.24444 .
Angier H, Gold R, Gallia C, Casciato A, Tillotson CJ, Marino M, et al. Variation in outcomes of quality measurement by data source. Pediatrics. 2014;133(6):e1676–82.
Lin KJ, Schneeweiss S. Considerations for the analysis of longitudinal electronic health records linked to claims data to study the effectiveness and safety of drugs. Clin Pharmacol Ther. 2016;100(2):147–59.
Goldstein ND, Sarwate AD. Privacy, security, and the public health researcher in the era of electronic health record research. Online J Public Health Inform. 2016;8(3):e207.
U.S. Department of Health and Human Services (HHS). 45 CFR 46. http://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html .
Download references
Acknowledgements
The authors thank Dr. Annemarie Hirsch, Department of Population Health Sciences, Geisinger, for assistance in conceptualizing an earlier version of this work.
Research reported in this publication was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number K01AR075085 (to MAG) and the National Institute Of Allergy And Infectious Diseases of the National Institutes of Health under Award Number K01AI143356 (to NDG). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and affiliations.
Division of Rheumatology, University of California School of Medicine, San Francisco, CA, USA
Milena A. Gianfrancesco
Department of Epidemiology and Biostatistics, Drexel University Dornsife School of Public Health, 3215 Market St., Philadelphia, PA, 19104, USA
Neal D. Goldstein
You can also search for this author in PubMed Google Scholar
Contributions
Both authors conceptualized, wrote, and approved the final submitted version.
Corresponding author
Correspondence to Neal D. Goldstein .
Ethics declarations
Ethics approval and consent to participate.
Not applicable
Consent for publication
Competing interests.
The authors have no competing interests to declare
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gianfrancesco, M.A., Goldstein, N.D. A narrative review on the validity of electronic health record-based research in epidemiology. BMC Med Res Methodol 21 , 234 (2021). https://doi.org/10.1186/s12874-021-01416-5
Download citation
Received : 02 July 2021
Accepted : 28 September 2021
Published : 27 October 2021
DOI : https://doi.org/10.1186/s12874-021-01416-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Electronic health records
- Data quality
- Secondary analysis
BMC Medical Research Methodology
ISSN: 1471-2288
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- TECHNOLOGY FEATURE
- 03 May 2022
Unlocking the potential of health data to help research and treatments
- Jyoti Madhusoodanan 0
Jyoti Madhusoodanan is a science writer in Portland, Oregon.
You can also search for this author in PubMed Google Scholar
Health-care workers check a patient’s electronic health records on a COVID-19 ward in Cremona, Italy. Credit: Marco Mantovani/Getty
For the gastrointestinal condition known as ulcerative colitis, some physicians recommend using a particular drug twice a day, others, three times. But which protocol is the best way to help people with the condition to avoid surgery? Instead of launching a clinical trial, Peter Higgins, a gastroenterologist at the University of Michigan at Ann Arbor, examined the data.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 605 , 182-183 (2022)
doi: https://doi.org/10.1038/d41586-022-01205-0
Related Articles

- Medical research
- Research data

Innovative cancer therapies offer new hope
Outlook 29 MAY 24

Advances in highly targeted radiation treatment for cancer have ignited interest in a once obscure field

Randomized trials of cancer drugs are for yesterday
Trials that infected people with common colds can inform today’s COVID-19 challenge trials
Correspondence 21 MAY 24

A global pandemic treaty is in sight: don’t scupper it
Editorial 21 MAY 24

US halts funding to controversial virus-hunting group: what researchers think
News 16 MAY 24

The AI revolution is coming to robots: how will it change them?
News Feature 28 MAY 24
Standardized metadata for biological samples could unlock the potential of collections
Correspondence 14 MAY 24

A guide to the Nature Index
Nature Index 13 MAR 24
Postdoctoral and Visiting Scholar positions in Immunology, Stem Cells, and Cancer
Postdoctoral Research Fellow and Visiting Scholar positions in immunology, stem cells and cancer are immediately available at UConn in USA
Storrs Mansfield, Connecticut
University of Connecticut-Lai's Lab
Zhejiang Provincial Hospital of Chinese Medicine on Open Recruitment of Medical Talents and Postdocs
Director of Clinical Department, Professor, Researcher, Post-doctor
Hangzhou, Zhejiang, China
The First Affiliated Hospital of Zhejiang Chinese Medical University
Postdoc in Biomechanical Engineering (m/f/d)
The Muskuloskelettales Universitätszentrum München (MUM) on the Campus Großhadern invites applications for the department Orthopädie
Munich (Stadt), Bayern (DE)
PWG-LMU Klinikum
Assistant, Associate or Full Professor
The McLaughlin Research Institute and Touro University – Montana campus invite applications for open rank faculty positions.
McLaughlin Research Institute
Postdoctoral Associate- Neuroscience
Houston, Texas (US)
Baylor College of Medicine (BCM)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Focus Issue Archive
- Open Access Articles
- JAMIA Journal Club
- Author Guidelines
- Submission Site
- Open Access
- Call for Papers
- About Journal of the American Medical Informatics Association
- About the American Medical Informatics Association
- Journals Career Network
- Editorial Board
- Advertising and Corporate Services
- Self-Archiving Policy
- Dispatch Dates
- For Reviewers
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Materials and methods, acknowledgements, contributions, competing interests, provenance and peer review.
- < Previous
Patient access to medical records and healthcare outcomes: a systematic review
- Article contents
- Figures & tables
- Supplementary Data
Traber Davis Giardina, Shailaja Menon, Danielle E Parrish, Dean F Sittig, Hardeep Singh, Patient access to medical records and healthcare outcomes: a systematic review, Journal of the American Medical Informatics Association , Volume 21, Issue 4, July 2014, Pages 737–741, https://doi.org/10.1136/amiajnl-2013-002239
- Permissions Icon Permissions
Objectives We conducted a systematic review to determine the effect of providing patients access to their medical records (electronic or paper-based) on healthcare quality, as defined by measures of safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity.
Methods Articles indexed in PubMed from January 1970 to January 2012 were reviewed. Twenty-seven English-language controlled studies were included. Outcomes were categorized as measures of effectiveness (n=19), patient-centeredness (n=16), and efficiency (n=2); no study addressed safety, timeliness, or equity.
Results Outcomes were equivocal with respect to several aspects of effectiveness and patient-centeredness. Efficiency outcomes in terms of frequency of in-person and telephone encounters were mixed. Access to health records appeared to enhance patients' perceptions of control and reduced or had no effect on patient anxiety.
Conclusion Although few positive findings generally favored patient access, the literature is unclear on whether providing patients access to their medical records improves quality.
Engaging patients as partners in their own care has garnered growing interest as a method for improving the quality of healthcare delivery. 1–7 It is now widely acknowledged that a more patient-centered, collaborative approach is needed to foster patient engagement. 8 To date, research has shown a trend towards improved patient satisfaction, health behaviors, and health status in response to patient-centered practices. 9 , 10 One such practice is increasing patients' access to timely and accurate information. The Institute of Medicine (IOM) 11 advocates for unrestricted patient access to medical records. Furthermore, patients have a legal right to access their medical records, 12 and multiple studies have documented their general interest in doing so. 13–19
Providing patients access to their medical records may facilitate a more collaborative relationship between provider and patient. 20 Existing literature suggests that patient-accessible records can improve patient–provider communication, 21–25 self-management, 24 , 26 and patient satisfaction. 20 , 27 , 28 A 2003 narrative review on the effects of patient access to medical records found that access improves communication between provider and patient, patient adherence, patients' knowledge about their own health, and is unlikely to cause patient harm. 21 Despite these reassuring data, many providers are still wary of patient access to their records, fearing it may cause patient anxiety or increase provider workload. 14 , 21 , 29–31
The IOM has recommended six major aims for improving the quality of healthcare delivery: safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity. 11 Using the six IOM aims as a framework for assessing potential benefits and patient outcomes, we conducted a systematic review to determine the effects of interventions that provide patients access to their medical records. Our overall aim was to provide a timely synthesis of the growing body of literature on patient access to medical records in order to inform future policies and practices in this area.
Data sources and searches
English-language articles indexed in PubMed with publication dates between January 1970 and January 2013 were included. Potentially relevant studies were identified using a combination of medical subject headings and free text phrases (see figure 1 ). Furthermore, we reviewed the bibliographies of each article to identify additional potentially relevant articles.

Study search terms.
Study selection
Two investigators divided the task of screening the titles and abstracts of all articles retrieved through the medical subject headings and key phrase search. We included quantitative studies that assessed the effect of patient-accessible records (electronic or paper-based) on quality-related outcomes in adult populations. We defined medical records as any patient-specific information held by the physician and/or healthcare system (see figure 2 ). After the initial screening process, each investigator randomly selected and reviewed 10% of the other's articles in order to ensure consistency in the selection process. All discrepancies were resolved through consensus.

Study eligibility.
Data extraction and quality rating
One investigator extracted data from each article meeting the screening criteria and a second investigator extracted data for 10% of the articles in order to ensure reliability. Both reviewers scored each randomized controlled trial (RCT) using the quality of study rating form (QSRF). 32 , 33 The reviewer κ for the QSRF was 0.534 (95% CI 0.411 to 0.674). In the case of disagreement, the reviewers analyzed the paper together to reach consensus.
The PubMed search resulted in 1247 citations, and the bibliography review yielded 18 additional articles. The majority of citations were excluded based on abstract and title review ( figure 3 ). Twenty studies were RCT and seven were uncontrolled observational studies (see supplementary appendix tables 1 and 2 for study details, available online only). Almost half of the studies focused on patient populations with chronic diseases including diabetes, cancer, heart failure, and hypertension.

Flow diagrams of study report selection.
Twenty RCT were evaluated using the QSRF tool. The average score was 71 points (range 67–86).
Studies of effectiveness
Physical health outcomes.
Seven studies included variables measuring biological outcomes such as laboratory values, body mass index, and blood pressure. Of these, four studies included diabetes-specific quality measures. 34–37 Although glycated hemoglobin A 1C improved overall in three RCT, the difference between the intervention and control groups was significant only in one trial. 34–36 An observational study suggested an association between personal health record (PHR) use and improved laboratory values (glycated hemoglobin A 1C and low-density lipoprotein cholesterol), blood pressure, and health maintenance screening in patients with diabetes; 37 however, blood pressure and low-density lipoprotein cholesterol were not significantly different between intervention and control conditions in one of the aforementioned RCT. 34 Two additional prospective studies examined the effect of PHR access on blood pressure control in patients with chronic disease and found no impact. 38 , 39
Psychosocial health outcomes
Five studies addressed psychosocial variables including depression, anxiety, contentment, and quality of life. All five studies included an anxiety variable. 40–44 Three studies found no significant differences in anxiety between groups, 40 , 41 , 43 while two studies found that anxiety decreased with access to medical information. 42 , 44 Two studies evaluated self-reported depression and contentment in patients and found no significant differences between the intervention and control groups. 40 , 43 Only one study measured quality of life and found that providing a paper copy of the medical record resulted in no significant improvement. 41
Health behaviors and adherence outcomes
Four studies included measures of patient health behaviors, and outcomes were mixed. 38 , 45–47 Two studies found no significant impact on adherence. 45 , 47 A third study found that patients who received only a computer-generated health summary were more likely to attend their next routine appointment than those in the other groups receiving only a written PHR with health promotion advice, both the computer-generated health summary and the written PHR, or neither. 38 That study also measured other health behavior; recipients of the written PHR were significantly more likely to report drinking less alcohol, whereas those who received only the summary were significantly more likely to say that they did not feel the need to change their alcohol use. In a follow-up RCT, the use of medications, tobacco, and alcohol, and awareness of health maintenance did not appear to be influenced by access to a computer-generated health summary. 46
Recall of medical information
Two studies addressed patient recall of medical information as an outcome of patient access to medical records, and the results were mixed. 43 , 48
Usage of PHR
Three RCT compared usage of informational resources when given computer access to either personalized medical information or general health information, and found that access to personalized information increased the likelihood of usage. 49–51
Accuracy of the medical record
One uncontrolled observational study evaluated the influence of a secure web-based patient portal on the accuracy of medication lists in the electronic health record, and found no significant differences. 52
Perceived usefulness of access to medical records
One trial randomly assigned pregnant patients to use an internet-based pregnancy resource either with or without additional access to personal antenatal health records. 51 Although both groups found the information easy to access and useful, there was no significant difference in perceived usefulness.
Studies of patient-centeredness
Patient satisfaction.
Eleven studies included primary outcomes related to satisfaction with various aspects of the patient experience, including care provided, 36 , 40 , 42 , 47 , 53 , 54 provider–patient communication, 18 information provided, 49 , 51 consultation, 55 and perceived quality of care. 39 In eight studies, no significant differences were found when patients were given access to their medical information via the internet, on a USB stick, or in paper form as compared to no access or access to general information only. 18 , 39–42 , 51 , 53 , 54 Only three found a moderate improvement in patient satisfaction when given access to physician notes, 47 , 55 a copy of the letter sent from their specialist to their general practitioner, or a computerized medical record summary. 49
‘Informed’ patient
Three studies measured pregnant women's perceptions of being informed when provided with access to their medical records, 40 , 54 , 56 of which two found a significant effect. 54 , 56
Patient involvement in care
Seven studies measured various aspects of patients' involvement in their care. In two, there was no significant difference in self-efficacy between the intervention and control groups 18 , 44 whereas in a third study, patients with type 1 diabetes reported greater diabetes-related self-efficacy when provided access to the entire health record compared to a web-based diabetes case management program only. 35 Studies of pregnant women found that patients who carried their full antenatal records endorsed greater perceptions of control of their pregnancies 40 , 56 and greater ease in talking to doctors and midwives than control group participants. 40 An RCT to study the effect of PHR access on patients undergoing in-vitro fertilization found no effect on measures of patient empowerment. 57 Another RCT evaluating the effect of PHR access found a statistically significant, although clinically negligible, difference in empowerment scores among patients with hypertension in the intervention group. 39
Studies of efficiency
Two observational studies included measures of efficiency, telephone and office visit rates, among PHR users and non-users. One measured the frequency of primary care office visits and documented telephone contacts after PHR adoption. 58 While both groups experienced a decrease in annual primary care office visit rates, the effect was significantly greater in the PHR user group. Telephone call rates significantly increased in both groups, but more so among non-users. The second study found that PHR users increased office visits and telephone contacts in the year following activation compared to the year before activation, while non-users showed decreased office and telephone encounters during a similar 2-year period. 59 PHR users as a group had significantly more after-hours clinic visits, emergency department visits, and hospital visits.
Our systematic review found that studies of interventions that provided patients access to their medical records have addressed three of six IOM quality domains: effectiveness, patient-centeredness, and efficiency. The effects of patients' access to medical records on measures of safety, timeliness, and equity remain understudied.
Despite concerns that might have been raised about patient access to medical records such as the potential for patient anxiety and confusion, our review found no current evidence to substantiate any negative patient outcomes resulting from access to health information. Notably, access to medical information did not increase patient anxiety, 42 , 44 a common fear endorsed by physicians. 44 , 60 , 61 Conversely, the effects of PHR access on workload and system efficiency merit further evaluation. For instance, a better understanding of how PHR and related technologies increase or decrease system burden can help with resource allocation decisions related to managing patients who use these tools.
Future research in this area should focus on interventions that target and measure actual health record usage and engagement in care. For example, some of the studies measured outcomes among patients who were already PHR users, primarily white, and with higher incomes and private insurance compared to PHR non-users. 37 PHR use may thus be a marker for characteristics related to better health outcomes, and providing access alone is unlikely to be sufficient to improve outcomes for all types of patients. For PHRs to be widely used for routine patient communication, or as ‘backup systems' to mitigate care delays, 62 issues of equity in PHR adoption and use need to be addressed. 63 Conversely, certain design features of the PHR may be able to influence patient engagement. For instance, we found that patients given access to personalized information accessed electronic resources more frequently than those given only general educational information. 49–51 Whether carefully targeted PHR design can enhance equity and engagement among groups at higher risk of negative health outcomes remains to be seen.
Our review covered a relatively small group of studies in an emerging area of enquiry, and as such we erred in the direction of including smaller and less methodologically rigorous studies. The heterogeneity of study populations, intervention content, and measurement strategies varied, making it difficult to synthesize the evidence. The possibility of selective reporting and publication bias cannot be excluded. Fairly restrictive search criteria were used to address primary study aims, and thus we may have excluded papers not classified under our search terms. We attempted to minimize this problem by reviewing bibliographies to locate additional articles not identified through database search.
In conclusion, our systematic review examined the effects of patients' medical record access and revealed few overarching trends. There was minimal evidence of psychological harm to patients. Limited evidence suggests that patients with access to medical records have improved levels of satisfaction, but evidence was less clear for other aspects of quality, and was absent for effects on patient safety, timeliness, and equity. Although few positive findings generally favored patient access, in light of mounting pressures to make medical records transparent to patients, 64 more rigorous research is needed to evaluate this practice.
The authors would like to thank Annie Bradford, PhD for assistance with medical editing.
TDG contributed to the conception and design of the project, acquisition of data, and the analysis and interpretation of the data. She drafted the article, worked with the team on revisions, and gave final approval of the version to be published. SM contributed to the acquisition of data, analysis and interpretation of the data, provided critical revisions, and gave final approval of the version to be published. DP contributed to the conception and design of the project and the analysis and interpretation of the data. She provided critical revisions and gave final approval of the version to be published. DFS contributed to the conception and design of the project, provided critical revisions, and gave final approval of the version to be published. HS contributed to the conception and design of the project and the analysis and interpretation of the data. He provided critical revisions, and gave final approval of the version to be published.
This work was supported by the VA National Center of Patient Safety and in part by the Houston VA Center for Innovations in Quality, Effectiveness and Safety (CIN 13-413). These sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Not commissioned; externally peer reviewed.
Schwappach DL . Review: engaging patients as vigilant partners in safety: a systematic review . Med Care Res Rev 2010 ; 67 : 119 – 48 .
Google Scholar
Peat M Entwistle V Hall J et al. .; PIPS Group . Scoping review and approach to appraisal of interventions intended to involve patients in patient safety . J Health Serv Res Policy 2010 ; 15 ( Suppl. 1 ): 17 – 25 .
Koutantji M Davis R Vincent C et al. . The patient's role in patient safety: engaging patients, their representatives, and health professionals . Clin Risk 2005 ; 11 : 99 – 104 .
Hall J Peat M Birks Y et al. . Effectiveness of interventions designed to promote patient involvement to enhance safety: a systematic review . Qual Saf Health Care 2010 ; 19 : e10 .
Davis RE Jacklin R Sevdalis N et al. . Patient involvement in patient safety: what factors influence patient participation and engagement? Health Expect 2007 ; 10 : 259 – 67 .
Davis RE Koutantji M Vincent CA . How willing are patients to question healthcare staff on issues related to the quality and safety of their healthcare? An exploratory study . Qual Saf Health Care 2008 ; 17 : 90 – 6 .
Davis RE Sevdalis N Vincent CA . Patient involvement in patient safety: how willing are patients to participate? Qual Saf Health Care 2011 ; 20 : 108 – 14 .
Epstein RM Fiscella K Lesser CS et al. . Why the nation needs a policy push on patient-centered health care . Health Aff (Millwood) 2010 ; 29 : 1489 – 95 .
Lewin SA Skea ZC Entwistle V et al. . Interventions for providers to promote a patient-centred approach in clinical consultations . Cochrane Database Syst Rev 2001 ;( 4 ): CD003267 .
Dwamena F Holmes-Rovner M Gaulden CM et al. . Interventions for providers to promote a patient-centred approach in clinical consultations . Cochrane Database Syst Rev 2012 ;( 12 ): CD003267 .
Institute of Medicine . Crossing the quality chasm: a new health system for the 21st century . Washington, DC : National Academies Press , 2001 .
Google Preview
CFR Parts 160 and 164 Standards for Privacy of Individually Identifiable Health Information; Final Rule . Fed Regist 2000 ; 65 : 82462 – 829 .
Cho AH Arar NH Edelman DE et al. . Do diabetic veterans use the Internet? Self-reported usage, skills, and interest in using My HealtheVet Web portal . Telemed J E Health 2010 ; 16 : 595 – 602 .
Delbanco T Walker J Bell SK et al. . Inviting patients to read their doctors' notes: a quasi-experimental study and a look ahead . Ann Intern Med 2012 ; 157 : 461 – 70 .
Fowles JB Kind AC Craft C et al. . Patients' interest in reading their medical record: relation with clinical and sociodemographic characteristics and patients' approach to health care . Arch Intern Med 2004 ; 164 : 793 – 800 .
Hassol A Walker JM Kidder D et al. . Patient experiences and attitudes about access to a patient electronic health care record and linked web messaging . J Am Med Inform Assoc 2004 ; 11 : 505 – 13 .
Pyper C Amery J Watson M et al. . Access to electronic health records in primary care-a survey of patients' views . Med Sci Monit 2004 ; 10 : SR17 – 22 .
Ross SE Moore LA Earnest MA et al. . Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial . J Med Internet Res 2004 ; 6 : e12 .
Tang PC Newcomb C . Informing patients: a guide for providing patient health information . J Am Med Inform Assoc 1998 ; 5 : 563 – 70 .
Tang PC Ash JS Bates DW et al. . Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption . J Am Med Inform Assoc 2006 ; 13 : 121 – 6 .
Ross SE Lin CT . The effects of promoting patient access to medical records: a review . J Am Med Inform Assoc 2003 ; 10 : 129 – 38 .
Baldry M Cheal C Fisher B et al. . Giving patients their own records in general practice: experience of patients and staff . BMJ (Clin Res Ed) 1986 ; 292 : 596 – 8 .
Cimino JJ Patel VL Kushniruk AW . The patient clinical information system (PatCIS): technical solutions for and experience with giving patients access to their electronic medical records . Int J Med Inform 2002 ; 68 : 113 – 27 .
Honeyman A Cox B Fisher B . Potential impacts of patient access to their electronic care records . Inform Prim Care 2005 ; 13 : 55 – 60 .
Cimino JJ Patel VL Kushniruk AW . What do patients do with access to their medical records? Stud Health Technol Inform 2001 ; 84 : 1440 – 4 .
Fisher B Bhavnani V Winfield M . How patients use access to their full health records: a qualitative study of patients in general practice . J R Soc Med 2009 ; 102 : 539 – 44 .
Matheny ME Gandhi TK Orav EJ et al. . Impact of an automated test results management system on patients' satisfaction about test result communication . Arch Intern Med 2007 ; 167 : 2233 – 9 .
Tang PC Lansky D . The missing link: bridging the patient-provider health information gap . Health Aff (Millwood) 2005 ; 24 : 1290 – 5 .
Johnson AJ Frankel RM Williams LS et al. . Patient access to radiology reports: what do physicians think? J Am Coll Radiol 2010 ; 7 : 281 – 9 .
Ross AP . The case against showing patients their records . BMJ (Clin Res Ed) 1986 ; 292 : 578 .
Siteman E Businger A Gandhi T et al. . Clinicians recognize value of patient review of their electronic health record data . AMIA Annu Symp Proc 2006 ; 1101 .
Gibbs L . Evidence-based practice for the helping professions: a practical guide with the integrated multimedia . Pacific Grove, CA : Brooks/Cole–Thomson Learning , 2003 .
Gibbs LE . Quality of study rating form: an instrument for synthesizing evaluation studies . J Soc Work Educ 1989 ; 25 : 55 – 67 .
Grant RW Wald JS Schnipper JL et al. . Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial . Arch Intern Med 2008 ; 168 : 1776 – 82 .
McCarrier KP Ralston JD Hirsch IB et al. . Web-based collaborative care for type 1 diabetes: a pilot randomized trial . Diabetes Technol Ther 2009 ; 11 : 211 – 17 .
Ralston JD Hirsch IB Hoath J et al. . Web-based collaborative care for type 2 diabetes: a pilot randomized trial . Diabetes Care 2009 ; 32 : 234 – 9 .
Tenforde M Nowacki A Jain A et al. . The association between personal health record use and diabetes quality measures . J Gen Intern Med 2012 ; 27 : 420 – 4 .
Liaw T Lawrence M Rendell J . The effect of a computer-generated patient-held medical record summary and/or a written personal health record on patients' attitudes, knowledge and behaviour concerning health promotion . Fam Pract 1996 ; 13 : 289 – 93 .
Wagner PJ Dias J Howard S et al. . Personal health records and hypertension control: a randomized trial . J Am Med Inform Assoc 2012 ; 19 : 626 – 34 .
Elbourne D Richardson M Chalmers I et al. . The Newbury Maternity Care Study: a randomized controlled trial to assess a policy of women holding their own obstetric records . Br J Obstet Gynaecol 1987 ; 94 : 612 – 19 .
Gravis G Protiere C Eisinger F et al. . Full access to medical records does not modify anxiety in cancer patients: results of a Randomized Study . Cancer 2011 ; 117 : 4796 – 804 .
Spodik M Goldman J Merli K et al. . Providing an endoscopy report to patients after a procedure: a low-cost intervention with high returns . Gastrointest Endosc 2008 ; 67 : 103 – 11 .
Stevens DP Stagg R Mackay IR . What happens when hospitalized patients see their own records . Ann Intern Med 1977 ; 86 : 474 – 7 .
Wiljer D Leonard KJ Urowitz S et al. . The anxious wait: assessing the impact of patient accessible EHRs for breast cancer patients . BMC Med Inform Decis Mak 2010 ; 10 : 46 .
Banet GA Felchlia MA . The potential utility of a shared medical record in a “first-time” stroke population . J Vasc Nurs 1997 ; 15 : 29 – 33 .
Liaw ST Radford AJ Maddocks I . The impact of a computer generated patient held health record . Aust Fam Physician 1998 ; 27 ( Suppl. 1 ): S39 – 43 .
Maly RC Bourque LB Engelhardt RF . A randomized controlled trial of facilitating information giving to patients with chronic medical conditions: effects on outcomes of care . J Fam Pract 1999 ; 48 : 356 – 63 .
Rubin DT Ulitsky A Poston J et al. . What is the most effective way to communicate results after endoscopy? Gastrointest Endosc 2007 ; 66 : 108 – 12 .
Jones R Pearson J McGregor S et al. . Randomised trial of personalised computer based information for cancer patients . BMJ 1999 ; 319 : 1241 – 7 .
Ross SE Haverhals LM Main DS et al. . Adoption and use of an online patient portal for diabetes (Diabetes-STAR) . AMIA Annu Symp Proc 2006 ; 1080 .
Shaw E Howard M Chan D et al. . Access to web-based personalized antenatal health records for pregnant women: a randomized controlled trial . J Obstet Gynaecol Can 2008 ; 30 : 38 – 43 .
Staroselsky M Volk LA Tsurikova R et al. . An effort to improve electronic health record medication list accuracy between visits: patients' and physicians' response . Int J Med Inform 2008 ; 77 : 153 – 60 .
Wackerle A Blochlinger-Wegmann B Burkhardt T et al. . Notes on a stick: use and acceptability of woman-held maternity notes . Eur J Obstet Gynecol Reprod Biol 2010 ; 152 : 156 – 9 .
Lovell A Zander LI James CE et al. . The St. Thomas's Hospital maternity case notes study: a randomised controlled trial to assess the effects of giving expectant mothers their own maternity case notes . Paediatr Perinat Epidemiol 1987 ; 1 : 57 – 66 .
Saunders NC Georgalas C Blaney SP et al. . Does receiving a copy of correspondence improve patients' satisfaction with their out-patient consultation? J Laryngol Otol 2003 ; 117 : 126 – 9 .
Homer CS Davis GK Everitt LS . The introduction of a woman-held record into a hospital antenatal clinic: the bring your own records study . Aust N Z J Obstet Gynaecol 1999 ; 39 : 54 – 7 .
Tuil WS Verhaak CM Braat DD et al. . Empowering patients undergoing in vitro fertilization by providing Internet access to medical data . Fertil Steril 2007 ; 88 : 361 – 8 .
Zhou YY Garrido T Chin HL et al. . Patient access to an electronic health record with secure messaging: impact on primary care utilization . Am J Manag Care 2007 ; 13 : 418 – 24 .
Palen TE Ross C Powers JD et al. . Association of online patient access to clinicians and medical records with use of clinical services . JAMA 2012 ; 308 : 2012 – 19 .
Moyer CA Stern DT Dobias KS et al. . Bridging the electronic divide: patient and provider perspectives on e-mail communication in primary care . Am J Manag Care 2002 ; 8 : 427 – 33 .
Sung S Forman-Hoffman V Wilson MC et al. . Direct reporting of laboratory test results to patients by mail to enhance patient safety . J Gen Intern Med 2006 ; 21 : 1075 – 8 .
Giardina TD King BJ Ignaczak A et al. . Root cause analysis reports help identify common factors in delayed diagnosis and treatment of outpatients . Health Aff 2013 ; 32 .
Yamin CK Emani S Williams DH et al. . The digital divide in adoption and use of a personal health record . Arch Intern Med 2011 ; 171 : 568 – 74 .
Giardina TD, Singh H. Should patients get direct access to their laboratory test results? An answer with many questions. JAMA 2011;306:2502–3.
Supplementary data
Email alerts, companion article.
- Networking the country to promote health and scientific discovery
Citing articles via
- Recommend to your Library
Affiliations
- Online ISSN 1527-974X
- Copyright © 2024 American Medical Informatics Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Research article
- Open access
- Published: 02 March 2020
A systematic review of patient access to medical records in the acute setting: practicalities, perspectives and ethical consequences
- Stephanie N. D’Costa 1 ,
- Isla L. Kuhn 2 &
- Zoë Fritz ORCID: orcid.org/0000-0001-9403-409X 2
BMC Medical Ethics volume 21 , Article number: 18 ( 2020 ) Cite this article
12k Accesses
21 Citations
11 Altmetric
Metrics details
Internationally, patient access to notes is increasing. This has been driven by respect for patient autonomy, often recognised as a primary tenet of medical ethics: patients should be able to access their records to be fully engaged with their care. While research has been conducted on the impact of patient access to outpatient and primary care records and to patient portals, there is no such review looking at access to hospital medical records in real time, nor an ethical analysis of the issues involved in such a change in process.
This study employed a systematic review framework in two stems, to integrate literature identified from two searches: Medline, CINAHL and Scopus databases were conducted, (for (1) hospitalised patients, patient access to records and its effects on communication and trust within the doctor-patient relationship; and (2) patient access to medical records and the ethical implications identified). The qualitative and quantitative results of both searches were integrated and critically analysed.
3954 empirical and 4929 ethical studies were identified; 18 papers representing 16 studies were identified for review (12 empirical and 6 ethical). The review reveals a consensus that our current approach to giving information to patients – almost exclusively verbally – is insufficient; that patient access to notes is a welcome next step for patient-centred care, but that simply allowing full access, without explanation or summary, is also insufficient. Several ethical implications need to be considered: increased information could improve patient trust and knowledge but might transfer an (unwelcome) sense of responsibility to patients; doctors and patients have conflicting views on how much information should be shared and when; sharing written information might increase the already significant disparity in access to health care, and have unforeseen opportunity costs. The impact on medical practice of sharing notes in real time will also need to be evaluated.
Conclusions
The review presents encouraging data to support patient access to medical notes. However, sharing information is a critical part of clinical practice; changing how it is done could have significant empirical and ethical impacts; any changes should be carefully evaluated.
Peer Review reports
It is unusual for patients to request access to their medical hospital records, despite their legal right to do so [ 1 ]. The U.K. government mandated that patients should be able to readily access their electronic medical record by 2018, a promise which has not been fulfilled, mostly due to logistical difficulties [ 2 ]. This mandate was built on respect for patient autonomy as a primary tenet of medical ethics: patients should be able to access their records to be fully engaged with their care. Access to records allows patients to be more informed which may increase opportunities for them to question their care plans and request second opinions.
Internationally, patients are more readily able to access their notes, and there has been evidence of positive outcomes in maternity records [ 3 ]; in primary care [ 4 , 5 ]; for specific diseases, [ 6 , 7 ] and for specific interventions [ 8 , 9 ]. A 2003 (Ross and Lin) [ 10 ] and 2007 (Ferreira et al) [ 11 ] review of the literature in these fields found that patient access was unlikely to cause harm and can improve doctor-patient communication and relations; the latter review also identified the potential for patients to spot and correct mistakes in their records.
More recently, the use of patient ‘portals’ – an electronic route to targeted parts of the medical record – has become more common. Several systematic reviews on the design, use and impact of such portals have been conducted [ 12 , 13 , 14 ]. Patients are generally enthusiastic about the possibility of accessibility, and positive or neutral health outcomes were observed. However, it was noted that clinician contact for portal users increased, and, perhaps related to this, disparity of uptake among different ethnic and socioeconomic groups was noted.
While these reviews demonstrate significant bodies of research on the impact of patient access to outpatient and primary care records and to patient portals (see Table 1 for a summary table of the systematic reviews in these domains), there is no such review looking at access to hospital medical records in real time, nor an ethical analysis of the issues involved in such a change in process.
Real-time access to medical records (particularly as they are currently written) may have unintended consequences on patient care both directly and indirectly – for example, by altering how things are recorded in the notes.
In this paper, we focus on adult access to notes in the medical acute care setting. We define this as the environment which comprises an adult medical patient’s presentation to hospital and their initial (up to 5 days) in-patient stay. This is a busy environment in which a sick patient generally only receives verbal communication, and in which decisions need to be made quickly, often by or with clinicians unfamiliar to the patient. In this context, access to notes may serve a different purpose than in the chronic disease or outpatient setting. Our aim was to review empirical papers relating to patient access and contribution to medical records, and consider the ethical issues raised by this proposed change in practice to fully appreciate the consequences of access to notes in real time.
Our review therefore set out to answer two questions:
1) What studies have there been of sharing records with medical patients in the in-patient setting, and in particular on the impact on trust and communication between patients and doctors?
2) What are the ethical issues associated with sharing records with medical patients?
This study employed a systematic review framework in two stems, to integrate literature identified from two searches surrounding our research questions. This ensured a robust, replicable searching strategy from which we could extract data clearly defined by inclusion and exclusion criteria (an initial attempt to search ethical issues relating to sharing medical records in acute care yielded no relevant results). We conducted critical interpretive synthesis [ 16 ] to the data extracted, an application of qualitative enquiry that allowed us to critically analyse and integrate both the qualitative and quantitative results of both searches into main themes.
The review was registered on the PROSPERO database (registration ID CRD42018114125). PRISMA guidelines have been used to inform the methodology and write up.
Identification of studies
A replicable search strategy was developed to answer our two research questions, using two literature searches, on the Medline via OVID, CINAHL via Ebsco and Scopus databases (See Appendix 1 for the full search strategies for both searches). Searches were run on the 23rd February 2018. Reference lists of included studies were reviewed for additional papers. A complete record of all identified articles was kept on a managed reference database.
Literature search of the empirical data
Search words, phrases and subject headings (including MeSH) were used to search for literature surrounding the topics of (1) hospitalised patients, (2) patient access to records and (3) its effects on communication and trust within the doctor-patient relationship.
The inclusion criteria limited the literature to studies about adult, hospitalised patients in the acute setting. Limits were applied for English language papers published since 1997 were included. Exclusion criteria consisted of paediatric, disease-specific studies and those focussed on confidentiality and data sharing. Studies relating to the design of a system allowing patient access to records were also excluded.
Literature search of the ethical issues
The second search consisted of a range of terms for (1) patient access to records and (2) ethical implications. This search therefore did not specify hospitalised patients or the effect access to notes has on communication and trust and was run from inception to the search date. The exclusion criteria remained the same.
Study selection
For each search, the titles and abstracts of references were screened by one reviewer (either SD or ZF) who selected those appropriate for full text analysis. 100 references in every 1000 were independently screened by both reviewers to assess for concordance and prevent drift, refining the inclusion criteria if needed. Any references where there was ambiguity were discussed by both authors and a decision made. Reference lists of included studies were screened by both authors. The results of the study selection are shown in Fig. 1 .
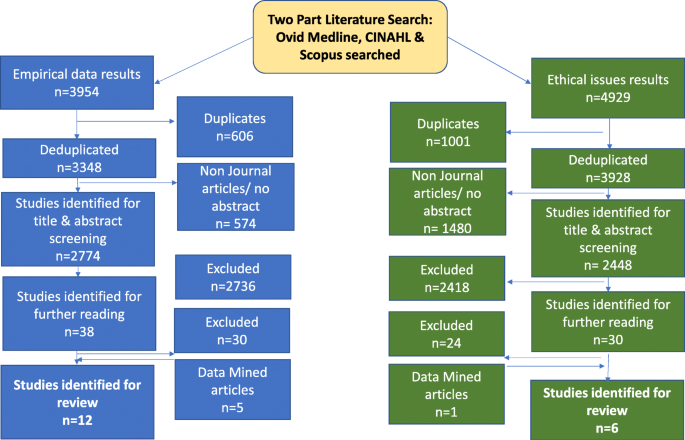
PRISMA Article Selection Flow chart
Data extraction and risk of bias
SD extracted the following data from the included studies: setting, nature of study, sample size, nature and contribution of participants, nature of analysis and summary of results, shown in Table 1 . Both researchers conducted thematic analysis on the papers, identifying four major themes.
Planned methods of analysis
Meta-analysis was inappropriate for the heterogenous nature of the search results and therefore a critical interpretive synthesis [ 16 ] was undertaken to discover emerging themes from the literature. Analysis of the papers was followed by extraction of data and discussion between the two authors, to consider the themes underlying these results. The ethics literature, which encompassed a wider range of settings than the empirical literature, was examined for themes which would be applicable across health care settings. An iterative process was utilised, examining and grouping them into overarching themes that both organised and illustrated the findings of the review.
Of the 3954 empirical and 4929 ethical studies identified through the two searches, 18 papers representing 16 studies were identified for review (12 empirical and 6 ethical) see Fig. 1 .
Two studies used questionnaires [ 17 , 18 ]; four used interviews or focus groups [ 19 , 20 , 21 , 22 , 23 , 24 ]; two used mixed methods [ 25 , 26 ]. One note analysis, [ 27 ] one portal analysis [ 28 ] and one clinical trial [ 29 , 30 ] was conducted, and six analysis articles were identified [ 31 , 32 , 33 , 34 , 35 , 36 ]. One empirical study came from each of Israel [ 19 ], Norway [ 20 , 21 ] and Canada [ 18 ]; the rest originated from the USA. No papers looked at perspectives of the multidisciplinary team. The data extraction is summarised in Table 2 .
Four main themes emerged on analysis: Impact on patient care; Conflicts between patient and physician perspective; divergent views on doctor and patient roles; cultural differences and societal risks.
Impact on patient care
Sharing notes was seen to empower patients by improving trust and knowledge [ 30 ], facilitating patients to work with doctors [ 28 ]. Communication of written information was considered superior to verbal explanations; one patient was reported as saying “Yeah, they come and update me but..I mean I can’t keep track of it all. That’s why I like this.” [ 24 ] No studies revealed objective changes in care such as reduced length of stay. Access to their own notes might enable patients to correct inaccuracies, [ 21 , 36 ] although this raised the possibility of patients feeling responsible if something was missed: [ 20 , 32 ]
“patients could end up feeling they are to blame for their own poor outcomes.” [ 32 ]
Some participants thought written information might ‘facilitate verbal communication’. [ 26 ] Others were concerned that a written note might supplant face-to-face interaction [ 22 ]; this did not manifest in the only study to trial giving patients a written daily summary [ 17 ].
Conflict between doctor and patient perspectives
Patients and doctors had discordant perceptions of how accessing the medical record might affect care: whilst doctors were concerned access to notes will overwhelm or unnecessarily worry patients, [ 17 , 24 ] patients were reassured by the shared information [ 37 ]. Grossman et al suggested that ‘it may be prudent to omit or explain potentially alarming information that carries a low degree of certainty such as a cancer on a differential diagnosis list” [ 28 ] .
A reoccurring conflict was the release of lab (and other) results in real time – patients strongly supported this whereas doctors preferred a delay, [ 24 , 29 , 31 ] in part so they could interpret them appropriately, offer support and create a future healthcare plan. Without this, some participants theorised that results could be prone to misinterpretation and unnecessary anxiety could be provoked [ 32 ]. As a physician participant said: “one of the primary duties of a physician is not only to alert the patient to abnormal results but also to educate them on their condition and appraise them of the follow up that will be needed” [ 32 ] . If delayed release did exist, however, there was a question about who would take responsibility for this [ 31 ].. Interestingly, this was not mentioned in the papers reporting direct experience.
There was also debate about whether patients should be co-creators of notes: Doctors, again hypothesising, were concerned that patients editing their own record might make them less reliable [ 34 , 35 ].
Divergent views on doctor and patient roles
A range of alternative approaches have been developed to share non-verbal information, and they reveal a variety of implicit perspectives about the role of the patient and the doctor. Tools designed to ensure patient choice and satisfaction are for those who perceive the patient as client ; one participant was quoted as saying: “I would like to be able to see background information [ about my doctor] like where they went to school” [ 25 ]. Providing information in the hope that patients will become more actively involved in their care see the patient as collaborator [ 22 , 29 ]. The different perspectives influence the purpose (and extent) of information sharing.
Cultural difference and societal risks
Different healthcare systems worldwide vary in their approach and concerns regarding access to notes – one study set in Israel found that the doctors more willing to share notes with patients originated from English-speaking countries, suggesting a cultural influence towards this [ 19 ]. In some countries such as the USA and Norway, liability seems to be more of a concern for the doctors and more of a motive for patients to access notes [ 21 , 24 ].
Across geographical boundaries, however, there was a recognition that there would be variation in patients’ willingness and ability to access notes, and that this might lead to disparity in health care, [ 22 , 35 ] with those from lower socioeconomic groups less likely to engage despite an often greater need; ‘{to] what extent should less engaged individuals be punished for their ‘ignorance’ [ 35 ] . As Lyles et al stated : “there is an ethical imperative to work to reduce the potential for the emergence or amplification of health disparities with respect to portal use’ [ 33 ] . Large screens, simple formats and buttons will help accessibility for some [ 26 , 38 ]; empirical research assessing the impact on access to health care or impact on different socioeconomic groups was not identified.
Finally, the questions of privacy and security of patient notes were raised, although papers focussing solely on this issue were excluded from the study. Some patients were concerned about the security of having information on their own devices, [ 26 ] while others did not voice privacy concerns [ 25 ]. Patients need to be able to trust their details are stored and shared securely, so they can contribute to them in a transparent manner [ 35 ].
The review reveals a consensus that our current approach to giving information to patients – almost exclusively verbally – is insufficient; that patient access to notes is a welcome next step for patient-centred care, but that simply allowing full access, without explanation or summary, is also insufficient. Several ethical implications need to be considered: increased information could improve patient trust and knowledge but might transfer an (unwelcome) sense of responsibility to patients; doctors and patients have conflicting views on how much information should be shared and when; sharing written information might increase the already significant disparity in access to health care, and have unforeseen opportunity costs.
It is also clear that we need to consider the impact that sharing notes in real time will have on medical practice.
Trust and the medical record
Although trust, both in doctors individually and generally, is often measured, it is rarely sufficiently specified in the medical literature. Trust is necessary when there is a degree of uncertainty and vulnerability (Becker 1996), both of which are present in the patient-doctor relationship; uncertainty about diagnosis and treatment, vulnerability not only because the patient is physically unwell, but because of the anxiety which often accompanies illness, and which can affect judgment. Trust is often described as a ‘three place relation’: ‘A’ trusts ‘B’ with ‘C’ [ 39 ].
In healthcare, the factors which can determine trust can relate to the patient (‘A’) and the doctor (‘B’), as well as what is entrusted (‘C’), namely the patient’s care [ 40 ]. Since the degree of care required is related to the severity and circumstances of the illness, these are also factors which can affect the patient’s vulnerability and need to trust. While trust is necessary for a functioning patient-doctor relationship, too much trust could be detrimental [ 41 ]. It may lead to reduced patient involvement in decision-making, or fewer questions being asked, leading to the possibility of sub-standard patient care.
What we want to achieve is well-placed patient trust, a concept O’Neil refers to as trust of the trustworthy, [ 42 ] where a patient can be confident that their trust in their clinician is justified and thus can reasonably entrust decisions and actions about their care to him or her. This places an obligation on clinicians to be trustworthy, but it also requires patients to be able to ask questions to satisfy themselves that their trust is well-placed. Providing access to medical records enables patients to determine what they are entrusting (more about what is wrong with them, and more about what treatments and investigations are planned) and enables them to place their trust well (or withhold it). Patients reading their own records might in turn alter physicians’ behaviours to be more trustworthy: they may, as they have done with clinic letters, modulate their language and ensure better verbal communication to avoid misconstruction of what is written.
Increased knowledge, increased responsibility?
While trust is important, the relationship between trust and autonomy has been well explored [ 43 ]. In medical ethics analysis of the last 40 years, autonomy has been given primacy [ 44 , 45 ]; part of respecting patient autonomy is ensuring that they have sufficient information to participate in shared decision-making [ 46 ]. There appears to be a recognition that the current approach – of only relaying verbal information to patients until their discharge – is inadequate. Patients forget, [ 47 ] relatives are concerned, questions are not asked [ 48 ].
It is thus unsurprising that imparting more (or more accessible) information to patients was welcomed by both patients and doctors. However, concerns were expressed that giving more information to patients also transferred responsibility to them: responsibility to check for errors; to deal with uncertainty; to worry about results. This responsibility may not always be desired by the patient. As Alfred Taubert says: “In the so-called co-operative mode, guidance dominates to the point where most patients, realistically and appropriately, want the doctor to take responsibility for their health.” By giving patients increased information, we may be removing their choice to defer responsibility – and associated ‘emotional work’ [ 49 ] or worry - to their physician.
Too much information, too soon?
A specific example of emotional work or worry related to receiving test results in real time: whilst patients expressed a strong desire for this, doctors’ concerns are two-fold. Firstly, they were concerned that patients lack the medical expertise to gauge the clinical importance of results. Secondly, they were worried that they (the doctor) would not be present to offer support and interpretation if the patient receives distressing news. Receiving emotional support from their doctor was a primary reason found for why patients audio-record consultations [ 50 ]; getting results without the doctor present would deprive them of that immediate support. Outside the acute setting, Milliat-Guittard showed that 21% of breast cancer patients did not want to hold records; they did not want to come across a comment that they were not expecting. Instead, they wished to come to terms with the disease in their own way [ 51 ].
Unintended worsening of inequality
Some interventions unintentionally increase inequalities by disproportionately benefiting less disadvantaged groups [ 52 ]. Giving patients access to records might be one such intervention: clinical teams acknowledged that they were working in a stretched system - an intervention which could divert resources to those who could read and understand their medical notes (or who had the confidence to ask questions) might lead to disparities. Awareness of this, and establishing and testing ways to mitigate this risk would be an important element to consider when introducing shared medical records.
Impact on medical practice
Medical records are not only a patient narrative – of their presentation, their investigations and their progress - but a working medical document which reflects dynamic thinking, [ 53 ] consultations, and acts as a tool for handover and for training [ 54 ]. If doctors do not reflect concerns clearly in the notes for fear of worrying the patient, handover could be compromised, impacting negatively on the patient’s care and training of future doctors.
Strengths and limitations
This review synthesised a wide range of papers from medical, nursing and ethical literatures, and was rigorously conducted. However, it identified only papers written in western cultures, and in English, and the conclusions made here should not be extrapolated to other environments. In addition, 7/10 of the studies were carried out in the USA, where the patient doctor relationship also includes a transactional component – doctors need to ensure that patients know what they are paying for. In other health systems represented in these studies (Canada, Norway, Israel) this is not the case, and so the motivations and repercussions of information sharing may be different.
Conclusions and future directions
These studies - and the timing of their publication - reveal that there is significant growth in the approach of sharing more medical information with patients, and significant variation in the type and quantity of information which is being shared. Empirical work with integrated ethical analysis is needed examining the impact of sharing medical records on patient-doctor and multi-disciplinary team communication, on patient trust, on physician training and on resources. The overarching question is what changes will occur to the role of doctor and patient as a result of routinely sharing more information, and, normatively, if there is a “right” amount of information to share with patients in the hospital setting.
Sharing information is a critical part of clinical practice; changing how it is done could have significant empirical and ethical impacts. This review has highlighted what those potential impacts might be. We recommend that careful evaluation of what is recorded and what care is given – both at individual and societal levels – need to be conducted when changes are made to how information is shared.
Availability of data and materials
There are no further data to present other than that which is presented here.
Abbreviations
Cumulative index of nursing and allied health literature
Elton B Stephens Company (A database search database)
Medical subject headings
United Kingdom
United States of America
Access to Health Records Act 1990, available at https://www.legislation.gov.uk/ukpga/1990/23/contents . Accessed 22 Feb 2020.
House of Commons Library. Legislation and guidance relating to medical records explained by House of Commons Library. NHS Confederation 2015, available at https://www.nhsconfed.org/resources/2015/10/legislation-and-guidance-relating-to-medical-records-explained-by-house-of-commonslibrary%20 . Accessed 22 Feb 2020.
Elbourne D, Richardson M, Chalmers I, Waterhouse I, Holt E. The Newbury maternity care study: a randomized controlled trial to assess a policy of women holding their own obstetric records. Br J Obstet Gynaecol. 1987;94(7):612–9.
Article Google Scholar
Liaw T, Lawrence M, Rendell J. The effect of a computer-generated patient-held medical record summary and/or a written personal health record on patients’ attitudes, knowledge and behaviour concerning health promotion. Fam Pract. 1996;13(3):289–93.
Walker J, Leveille SG, Ngo L, Vodicka E, Darer JD, Dhanireddy S, et al. Inviting patients to read their doctors’ notes: patients and doctors look ahead: patient and physician surveys. Ann Intern Med. 2011;155(12):811–9.
Dijkstra RF, Braspenning JC, Huijsmans Z, Akkermans RP, van Ballegooie E, ten Have P, et al. Introduction of diabetes passports involving both patients and professionals to improve hospital outpatient diabetes care. Diabetes Res Clin Pract. 2005;68(2):126–34.
Ayana M, Pound P, Lampe F, Ebrahim S. Improving stroke patients’ care: a patient held record is not enough. BMC Health Serv Res. 2001;1:1.
Volk RJ, Cass AR, Spann SJ. A randomized controlled trial of shared decision making for prostate cancer screening. Arch Fam Med. 1999;8(4):333–40.
Katz SJ, Lantz PM, Janz NK, Fagerlin A, Schwartz K, Liu L, et al. Patient involvement in surgery treatment decisions for breast cancer. J Clin Oncol. 2005;23(24):5526–33.
Ross SE, Lin CT. The effects of promoting patient access to medical records: a review. J Am Med Inform Assoc. 2003;10(2):129–38.
Ferreira A, Correia A, Silva A, Corte A, Pinto A, Saavedra A, et al. Why facilitate patient access to medical records. Stud Health Technol Inform. 2007;127:77–90.
Google Scholar
Goldzweig CL, Orshansky G, Paige NM, Towfigh AA, Haggstrom DA, Miake-Lye I, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013;159(10):677–87.
Kelly MM, Coller RJ, Hoonakker PL. Inpatient portals for hospitalized patients and caregivers: a systematic review. J Hosp Med. 2017;20:20.
Prey JE, Woollen J, Wilcox L, Sackeim AD, Hripcsak G, Bakken S, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Inform Assoc. 2014;21(4):742–50.
Vermeir P, Degroote S, Vandijck D, Van Tiggelen H, Peleman R, Verhaeghe R, et al. The patient perspective on the effects of medical record accessibility: a systematic review. Acta Clin Belg. 2017;72(3):186–94.
Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35.
Weinert C. Giving Doctors’ daily Progress notes to hospitalized patients and families to improve patient experience. Am J Med Qual. 2017;32(1):58–65.
Urowitz S, Wiljer D, Apatu E, Eysenbach G, Delenardo C, Harth T, et al. Is Canada ready for patient accessible electronic health records? A national scan. BMC Medical Informatics & Decision Making. 2008;8:33.
Weiss M. For doctors’ eyes only: medical records in two Israeli hospitals. Culture Med Psychiat. 1997;21(3):283–302.
Wibe T, Ekstedt M, Helleso R, Slaughter L. Why do people want a paper copy of their electronic patient record? Stud Health Technol Inform. 2010;160(Pt 1):676–80.
Wibe T, Helleso R, Slaughter L, Ekstedt M. Lay people's experiences with reading their medical record. Soc Sci Med. 2011;72(9):1570–3.
Dykes PC, Carroll DL, Hurley AC, Benoit A, Chang F, Pozzar R, et al. Building and testing a patient-centric electronic bedside communication center. J Gerontol Nurs. 2013;39(1):15–9.
Wilcox LG, Gatewood J, Morris D, Tan DS, Feiner S, Horvitz E. Physician attitudes about patient-facing information displays at an urban emergency department. AMIA Annu Symp Proc. 2010;2010:887–91.
Wilcox L, Morris D, Tan D, Gatewood J. Designing patient-centric information displays for hospitals. Proc SIGCHI Conf Hum Factor Comput Syst. 2010;2010:2123–32.
Vawdrey DK, Wilcox LG, Collins SA, Bakken S, Feiner S, Boyer A, et al. A tablet computer application for patients to participate in their hospital care. AMIA Annu Symp Proc. 2011;2011:1428–35.
Collins SA, Rozenblum R, Leung WY, Morrison CR, Stade DL, McNally K, et al. Acute care patient portals: a qualitative study of stakeholder perspectives on current practices. J Am Med Inform Assoc. 2017;24(e1):e9–e17.
Lee EH, Patel JP, Fortin AHV. Patient-centric medical notes: identifying areas for improvement in the age of open medical records. Patient Educ Couns. 2017;100(8):1608–11.
Grossman LV, Choi SW, Collins S, Dykes PC, O'Leary KJ, Rizer M, et al. Implementation of acute care patient portals: recommendations on utility and use from six early adopters. J Am Med Inform Assoc. 2017;04:04.
O'Leary KJ, Lohman ME, Culver E, Killarney A, Randy Smith G Jr, Liebovitz DM. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. J Am Med Inform Assoc. 2016;23(1):159–65.
O'Leary KJ, Sharma RK, Killarney A, O'Hara LS, Lohman ME, Culver E, et al. Patients’ and healthcare providers’ perceptions of a mobile portal application for hospitalized patients. BMC Med Inform Decis Mak. 2016;16(1):123.
Beard L, Schein R, Morra D, Wilson K, Keelan J. The challenges in making electronic health records accessible to patients. J Am Med Inform Assoc. 2012;19(1):116–20.
Davis KA, Smith LB. Ethical considerations about EHR-mediated results disclosure and pathology information presented via patient portals. AMA J Ethics. 2016;18(8):826–32.
Lyles CR, Fruchterman J, Youdelman M, Schillinger D. Legal, practical, and ethical considerations for making online patient portals accessible for all. Am J Public Health. 2017;107(10):1608–11.
Gu Y, Orr M, Warren J, Humphrey G, Day K, Tibby S, et al. Why a shared care record is an official medical record. N Z Med J. 2013;126(1384):109–17.
Spriggs M, Arnold MV, Pearce CM, Fry C. Ethical questions must be considered for electronic health records. J Med Ethics. 2012;38(9):535–9.
Gilhooly ML, McGhee SM. Medical records: practicalities and principles of patient possession. J Med Ethics. 1991;17(3):138–43.
Wibe T, Slaughter L. Patients reading their health records - what emotional factors are involved? Studies in Health Technol Inform. 2009;146:174–8.
Dykes PC, Stade D, Chang F, Dalal A, Getty G, Kandala R, et al. Participatory design and development of a patient-centered toolkit to engage hospitalized patients and care partners in their plan of care. AMIA Annu Symp Proc. 2014;2014:486–95.
Baier A. Trust and Antitrust Ethics. 1986;96:231–60.
Zaner RM. The phenomenon of trust in the patient-physician relationship. In: Pellegrino V, editor. Ethics, trust and the professionals: philosophical and cultural Apects. Langan: Georgetown University Press; 1991.
Lee YY, Lin JL. Trust but verify: the interactive effects of trust and autonomy preferences on health outcomes. Health Care Anal. 2009;17(3):244–60.
O'Neill O. Trust with accountability? J Health Serv Res Policy. 2003;8(1):3–4.
O’Neill O. Autonomy and Trust in Bioethics. Cambridge: Cambridge University Press; 2002.
Book Google Scholar
Entwistle VA, Carter SM, Cribb A, McCaffery K. Supporting patient autonomy: the importance of clinician-patient relationships. J Gen Intern Med. 2010;25(7):741–5.
Childress JF. The place of autonomy in bioethics. Hast Cent Rep. 1990;20(1):12–7.
Sandman L, Munthe C. Shared decision-making and patient autonomy. Theor Med Bioeth. 2009;30(4):289–310.
McGuire LC. Remembering what the doctor said: organization and adults’ memory for medical information. Exp Aging Res. 1996;22(4):403–28.
Judson TJ, Detsky AS, Press MJ. Encouraging patients to ask questions: how to overcome “white-coat silence”. JAMA. 2013;309(22):2325–6.
Watt L. “Her life rests on your shoulders”: doing worry as emotion work in the care of children with diabetes. Glob Qual Nurs Res. 2017;4:2333393617743638.
Elwyn G, Barr PJ, Grande SW. Patients recording clinical encounters: a path to empowerment? Assessment by mixed methods. BMJ Open. 2015;5(8):e008566.
Milliat-Guittard L, Charlois AL, Letrilliart L, Favrel V, Galand-Desme S, Schott AM, et al. Shared medical information: expectations of breast cancer patients. Gynecol Oncol. 2007;107(3):474–81.
Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health. 2013;67(2):190–3.
Mamykina L, Vawdrey DK, Stetson PD, Zheng K, Hripcsak G. Clinical documentation: composition or synthesis? J Am Med Inform Assoc. 2012;19(6):1025–31.
Rowlands S, Coverdale S, Callen J. Documentation of clinical care in hospital patients’ medical records: a qualitative study of medical students’ perspectives on clinical documentation education. Health Inf Manag. 2016;45(3):99–106.
Download references
Acknowledgments
We would like to thank Anne-Marie Slowther for helpful conversations which guided us during this research.
Zoe Fritz is funded by the Wellcome trust Grant reference numbers: 208213/Z/17/Z, and WT100577MA. The funding body had no role in the design of the study, collection, analysis, interpretation of data, or of the writing the manuscript.
Author information
Authors and affiliations.
Gonville and Caius College, Cambridge University, Trinity Street, Cambridge, CB2 1TA, UK
Stephanie N. D’Costa
THIS Institute (The Healthcare Improvement Studies Institute), Cambridge University, Clifford Allbutt Building, Cambridge, CB2 0AH, UK
Isla L. Kuhn & Zoë Fritz
You can also search for this author in PubMed Google Scholar
Contributions
The Authors have contributed in the following way: ZF conceived of the study, and designed the research questions. SND and IK constructed the literature search; IK refined it and preformed deduplications. SND and ZF screened all papers and identified those for inclusion. ZF and SND drafted different parts of the manuscript. All three authors reviewed, edited and approved the final manuscript.
Corresponding author
Correspondence to Zoë Fritz .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Full search strategies for both literature searches.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
D’Costa, S.N., Kuhn, I.L. & Fritz, Z. A systematic review of patient access to medical records in the acute setting: practicalities, perspectives and ethical consequences. BMC Med Ethics 21 , 18 (2020). https://doi.org/10.1186/s12910-020-0459-6
Download citation
Received : 28 March 2019
Accepted : 17 February 2020
Published : 02 March 2020
DOI : https://doi.org/10.1186/s12910-020-0459-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]
- Research article
- Open access
- Published: 06 January 2021
Electronic medical record implementation in tertiary care: factors influencing adoption of an electronic medical record in a cancer centre
- Anna Janssen ORCID: orcid.org/0000-0001-6611-9651 1 , 2 ,
- Candice Donnelly 1 , 2 ,
- Elisabeth Elder 3 ,
- Nirmala Pathmanathan 3 &
- Tim Shaw 1 , 2
BMC Health Services Research volume 21 , Article number: 23 ( 2021 ) Cite this article
10k Accesses
14 Citations
1 Altmetric
Metrics details
Electronic Medical Records (EMRs) are one of a range of digital health solutions that are key enablers of the data revolution transforming the health sector. They offer a wide range of benefits to health professionals, patients, researchers and other key stakeholders. However, effective implementation has proved challenging.
A qualitative methodology was used in the study. Interviews were conducted with 12 clinical and administrative staff of a cancer centre at one-month pre-launch and eight clinical and administrative staff at 12-months post-launch of an EMR. Data from the interviews was collected via audio recording. Audio recordings were transcribed, de-identified and analysed to identify staff experiences with the EMR.
Data from the pre-implementation interviews were grouped into four categories: 1) Awareness and understanding of EMR; 2) Engagement in launch process; 3) Standardisation and completeness of data; 4) Effect on workload. Data from the post-launch interviews were grouped into six categories: 1) Standardisation and completeness of data; 2) Effect on workload; 3) Feature completeness and functionality; 4) Interaction with technical support; 5) Learning curve; 6) Buy-in from staff. Two categories: Standardisation and completeness of data and effect on workload were common across pre and post-implementation interviews.
Findings from this study contribute new knowledge on barriers and enablers to the implementation of EMRs in complex clinical settings. Barriers to successful implementation include lack of technical support once the EMR has launched, health professional perception the EMR increases workload, and the learning curve for staff adequately familiarize themselves with using the EMR.
Peer Review reports
Digital technologies are being widely adopted in the healthcare, leading to a widespread transformation of the sector. This transformation has included an increase in the personalisation of health care [ 1 , 2 ] and potential for new approaches to facilitate research quality improvement initiatives and patient driven care [ 3 ]. Lately, digital technologies have been adopted by health sectors often for its better functioning and Electronic Medical Records (EMRs). EMRs are computerized information systems which collect, store and display patients’ information and typically replace paper-based medical records [ 4 ].
EMRs are key enablers of the data revolution transforming the health sector [ 5 ]. They incorporate a wide range of functionalities but can be broadly described as systems for presenting health, clinical or medical records in a digitised format [ 6 ]. The literature has acknowledged a number of benefits of using EMRs for healthcare professionals, patients, organisations and other stakeholders. Benefits include improving the quality of care for patients [ 6 ], improving timely access to data, and to potentially facilitate knowledge exchange for collaboration in multidisciplinary teams (MDTs) [ 7 ].
In spite of the wide range of potential benefits, physicians and other healthcare staffs can harness these supports only if EMRs are implemented [ 4 ]. However, it has been noted in the literature that there is a notable gap in understanding about the best ways to implement digital health [ 8 , 9 ]. The implementation of EMRs is particularly complex and requires a range of technical, human and organisational factors to be considered [ 7 ]. A comprehensive review of the literature identified eight categories of barriers to EMR adoption: Financial, Technical, Time, Psychological, Social, Legal, Organizational and Change process [ 4 ]. Financial, time/workload and technical barriers are the most frequently cited challenges in the literature [ 7 ].
Although the literature has identified some of the barriers and enablers to implementing EMRs in healthcare, much of this research has focused on primary care [ 10 ]. There is currently a dearth of literature on the implementation of EMRs in cancer care, which is a unique setting for implementing technology. The gold standard for the delivery of cancer care is the use of MDTs. MDTs describe a group of health professionals from a range of specialties who work together on a regular basis to deliver evidence-based care to patients [ 11 ]. Successful implementation of EMRs in a multidisciplinary setting requires consideration of the unique challenges to implementing EMRs for health professionals across a range of specialties, and for administrative staff.
This study described in this manuscript aimed to explore the barriers and enablers to implementing an EMR in a metropolitan tertiary cancer service.
Study design
A qualitative methodology was used to collect data on the experiences of clinical and administrative staff at pre- and post- launch of a new EMR.
Participants and study setting
The EMR was implemented in November 2017 in a breast cancer service within Western Sydney Local Health District. The cancer service is located across three hospitals within Western Sydney Local Health District (LHD). The main centre is co-located with a screening clinic and registers approximately 500 new breast cancer patients per year. Staff at the cancer centre had used another EMR platform for 10 years prior to the launch of the new EMR investigated in this study. The existing platform was a bespoke SQL database that no longer met the needs of the service. This EMR was predominantly used by administrative staff who entered data from paper records completed by clinical staff as well as clinicians doing follow-up with patients, had restricted interoperability with the main hospital EMR (Cerner) and was not used widely across the various disciplines within the service. The new EMR was developed in a Cerner Millennium platform with bespoke built multidisciplinary breast cancer fields for data entry at point-of-care. The development was a collaboration between key clinical representatives of the breast cancer centre and the LHD Information Communication and Technology service over a period of several years.
All clinical and administrative staff within the service were eligible to participate in the study, but due to the size of the center not all staff opted to participate. A purposeful sample were recruited to participate in 30–60 min phone interviews about their experiences with the EMR. A total of 12 participants consented to participate in the pre-launch interviews, three in administrative or research roles and nine in clinical roles. A total of eight participants consented to participate in the post-launch interviews, two in administrative or research roles and six in clinical roles. Participants were from a range of disciplines including medical oncology, radiation oncology, surgery, pathology, nursing and clinical administration.
Potential participants were recruited via email to participate in the study. Consent was provided either through return of a signed consent form, or via confirmation in the email response. At the start of each interviewee consent to participate in the interview and consent to record the interview was once again confirmed.
Interviews were conducted with staff within the cancer centre one-month pre-launch and twelve months post-launch of the EMR. Potential participants for the pre-implementation interviews were identified by members of the Advisory Committee that oversee the development of data improvement projects within the organisation. A member of the research team contacted all eligible participants via email and scheduled a pre-launch interview. All participants who completed a pre-launch interview were invited to participate in an interview post-launch.
Both pre and post launch interviews were conducted face to face or via phone at a time convenient to the participant. Interviews took between 30 and 60 min and were conducted by a researcher experienced in qualitative methods. Interviews were audio recorded. Audio recordings were transcribed by a commercial transcription service, prior to de-identification by one member of the research team.
Refer to Additional file 1 to see the interview guide.
Analysis was conducted to identify key themes and subthemes. These themes were then refined to reduce redundancy and emphasise prominent groupings. During analysis, illustrative quotes were identified and grouped them by themes and sub-themes.
The study was granted ethical approval by the Western Sydney Local Health District Human Research Ethics Committee’s Executive Committee (protocol/approval number:4678). All participants provided written consent to participate in the study by return of an email, verbal consent was confirmed at the start of each interview.
Pre-implementation interview findings
Pre-implementation interview findings were grouped into 4 categories, awareness and understanding of electronic medical record, engagement in launch process, effect on workload, standardisation and completeness of data.
Refer to Table 1 for exemplar quotes related to these themes.
All participants were aware of the upcoming EMR launch within the service. The majority of participants were enthusiastic about the potential of the EMR, but many acknowledged uncertainty in what the additional capabilities and functionalities of the new EMR would be.
The participants who held the greatest knowledge of the functionality of the new EMR had been involved in the design and implementation of the EMR. Outside of this group, almost all participants indicated a basic understanding that the EMR would replace the current process of using paper records at point of care with digitised data entry into the EMR. It was also widely understood that the new EMR would change the data entry process to be completed by clinical staff rather than administrative staff. Some participants also indicated that the new EMR would replace the existing database used to store clinical notes, anticipating that this would be useful for research and quality improvement activities.
Finally, a number of participants discussed the use of the new EMR in MDT meetings instead of the existing process where administrative staff manually extract and collate relevant patient information for discussion. Most of the participants who understood this application of the EMR were clinical staff. Most participants thought the use of the EMR in MDT meetings would be beneficial, particularly for early career clinicians who would be able to learn from the process of using the record in meetings.
All participants indicated that they had been engaged on some level during the implementation process for the new EMR. Most participants had been involved in training sessions in the weeks prior to the EMR launch, or had been provided an opportunity to participate even if they hadn’t attended. A minority of participants indicated they had an active role in the design of the new EMR in the 18-month development period.
Although participants were happy with the level of engagement they had with the development and implementation of the EMR, the majority weren’t sure whether their needs had been captured in the final EMR design. A minority of participants indicated that features they had requested were not being made available in the initial launch of the EMR, but anticipated the inclusion of those features in the future. Other participants felt their requests for particular EMR features had been included, but were not sure how what they had requested would function once the EMR was made available to them. This was because request for features were often made prior to using the EMR or when there had only been limited use of the EMR. It was anticipated that there would be a need to refine the design once the EMR had launched in order to align it with the needs of the service.
Participants perceived the EMR to be beneficial for improving the quality of clinical data collected within their centre in the future. This was one of the most consistently stated benefits of implementing a new EMR. The anticipated benefits of the improved data collection and quality varied across participants, but included a reduction in incomplete data entry for patient records due to mandatory fields, a more holistic view of the patient record and opportunities to access data for research purposes.
A minority of participants raised concerns about the EMR’s effect on standardisation and data completeness. Some participants raised concerns that the EMR was not integrated with other clinical data repositories within the local health district (outside of the NSW Health EMR) and that interoperability would continue to be an issue. Another participant raised concern about the limitations of the EMR to capture data that was appropriate for their discipline specialty.
The majority of participants discussed the perceived effect of the EMR on their workload. Generally, participants were concerned that the EMR may negatively impact workload, particularly for clinical staff who would be required to complete data entry tasks. Although workload concerns were raised frequently, multiple participants also acknowledged that this issue was likely to resolve after launch when both clinical and administrative staff became more familiar with the technology and integrated it into their routine.
Although most participants felt the EMR would increase workload, a minority of participants felt that the EMR implementation could decrease their workload. Currently, a number of participants described having to manage and search through a large number of paper files to access information. Participants anticipated that being able to access information digitally would be more efficient. Other participants felt it would be beneficial to be able to access data in the EMR remotely allowing more flexibility over where work was undertaken.
Post-launch interview findings
Post-implementation interview findings were grouped into 5 categories, feature completeness and functionality, learning curve, buy-in from staff.
Refer to Table 2 for exemplar quotes related to these themes.
A total of eight interviews were conducted with staff within the cancer center. Of these interviews, three were undertaken with administrative staff and five were undertaken with clinical staff. Clinical staff represented a range of specialties including radiation oncology, surgery and pathology.
Data analysed from the interviews was classified into six categories: 1) Standardisation of documentation and completeness of data; 2) Effect on workload; 3) Feature completeness and functionality; 4) Interaction with technical support; 5) Learning curve; 6) Buy-in from staff.
Both administrative and clinical staff indicated benefits of interoperability with the main hospital EMR and centre-wide access to the same information in the EMR. This was valuable when patients had been transferred to the centre from other hospital departments as patient information was easily accessible, enabling more efficient internal transfer for patients. It was also noted as a useful reference for finding initial consult information for returning patients that the clinical staff had not seen for a long time.
The EMR was noted as valuable for improving completeness of data on MDT recommendations. The new process of live data entry during MDT meetings allows all members to ensure the accuracy of the data in real-time, thus reducing recall bias that may have occurred when data was entered from notes after the MDT meeting. The centre had also installed three large LCD screens in the MDT meeting room to easily visualise patient information from multiple systems at the same time as viewing the EMR. One participant noted that data entry during the MDT meeting led to increased recording of longer-term recommendations for patients.
The EMR was perceived to have both positive and negative impacts on workload. A participant reported that the EMR increased efficiency by making information more accessible. Once familiar with the platform, it was described as relatively easy to navigate the EMR and input patient data. With regards to follow-up patients, data entry was noted as particularly efficient, only taking a few minutes, though it was more time consuming for new patients. Other benefits included decreased time in finding and reviewing information prior to a patient consultation, when compared with the previous process of manually searching through paper records.
Participants noted increased efficiency and reduced risk of errors in the new process of clinical staff entering data directly into the EMR rather than the previous process of administrative staff transcribing paper records. One participant noted the increased accountability for clinical staff to input data into the EMR. However, concerns were raised that some senior clinicians had experienced an increased workload as they complete EMR data entry themselves, due to uncertainty regarding whether early career doctors were inputting data consistently.
Although some participants felt the EMR was more efficient, others felt it increased workload. Concern was also raised about the unexpected issues when the new EMR did not allow staff to complete simple tasks that were previously automated, including the inability to bulk-print letters. The EMR was described as having increased workload for administrative staff due to increased time spent on auditing and completing the letters automatically generated from the EMR, following-up clinical staff for completion of data needed to generate the letters and repetitively scanning documents in to the EMR.
A number of participants raised concerns about issues with features, or functionality of features in the EMR, and ranged in degree of severity, from usability to issues effecting data quality and workload. Some of these issues included not having drop down menus to select a doctor or provider name in the EMR or generating letters from the incorrect clinical encounter. Letter generation was a largely cited concern. Participants noted that the process of letter generation was cumbersome and often the letter contained the incorrect content. Furthermore, the letter layout was described as unprofessional by some interviewees as the template put constraints on the content and structure on the letter, preventing clinicians to generate their patient letters in a preferred style.
A significant concern, was the lack of the patient summary page which provided a single-page overview of the patients treatment and other clinical interactions in the EMR. The inclusion of a patient summary view was an important feature of the new EMRs design, and its sub-optimal implementation was a perceived barrier to use of the new EMR. This feature was intended for quick and easy access to pertinent patient information in one instance. The patient summary was also intended to be used for MDT meetings. Participants noted that due to a lack of the ‘patient summary’ page, the required navigation across tabs to retrieve all the information needed was time consuming.
Another major functionality issue was lack of auto completion of fields in the EMR. Concerns were raised about GP information not auto-populating as it did in the previous system. As this functionality was also not successfully executed, an unexpected technical issue that occurred was that patient information did not transfer across clinical encounters. There were some issues that occurred in the first 3 months of implementation when forms were not auto-populating and there was a loss of data. Finally, some participants noted that not all forms suited the type of appointment e.g. second appointment for surgical decision, making it difficult to know where the data should be entered appropriately. Another highlighted issue was the lack of flexibility in the EMR drop-down menus or pre-set tick box options. One clinical staff member noted this was particularly concerning as these options should incorporate emerging evidence, such as new drugs.
There were some concerns about the difficulty in remembering how to enter data into the new EMR fields, particularly for staff that didn’t interact with it regularly. The platform was different to that found in other clinical settings which also meant new staff had a learning curve to familiarise themselves with how to use the system. However, it was noted that it had typically taken one to 2 weeks to overcome the learning curve. After this time, the EMR usability was reported positively. One participant noted that the EMR may be challenging to learn to use for relief staff who may only use it for one or 2 weeks.
Some participants raised concerns about lack of buy-in to the EMR across clinical disciplines that work within and in collaboration within the centre, which led to gaps in available information. There were also concerns that some people had ceased using the EMR because of issues with the data fields. These issues included drop down menus in the EMR not including treatment options the clinicians wanted to use, and other issues relating to navigating the EMR.
This study presents findings describing the implementation of EMR in a cancer care centre. The findings are broadly aligned with the literature on barriers to implementation of EMRs, particularly in regard to the central role of Information Technology (IT) support during the post-implementation period [ 2 , 7 ]. However, findings from this study suggested that staff were prepared to overlook challenges in functionality or technical support due to a perception the system would become beneficial over time as system errors would be addressed.
Findings from this study showed that prior to launch, study participants were generally enthusiastic about the EMR and optimistic it would improve processes. A core component of this enthusiasm was the perceived engagement during the pre-implementation process. A number of participants were provided an opportunity to be involved in the design of the EMR, and all participants noted they had an opportunity to participate in EMR training sessions. Whilst research has showed the value of involving health professionals in EMR to improve uptake [ 12 ], there is little research describing the important role of delivering flexible training to staff on the use of the new system in the lead up to implementation. The value of using education and training as a tool in successful implementation has been acknowledged in the literature [ 12 ], with findings from this study showing it is as important when implementing digital technologies as in other areas.
The literature has shown that clinician resistance is a major barrier to EMR implementation as they are the largest user group of EMR systems [ 4 ]. However, findings from this study identified some perceived benefits that have not previously been recognized in the literature. The EMR was particularly well received by early career doctors who had found it easier for documentation, time saving, effective for improving record completeness and beneficial for guiding clinical consultations in highlighting what should be recorded. Clinical staff also felt the EMR enabled senior specialists to act in a more traditional consultant role, with early career doctors completing data entry. By incorporating the EMR into MDT meetings there was a perceived benefit to early career doctors as they had an opportunity to engage more actively with patient records and ask questions about treatment decisions. The central role of informal education opportunities in the training and mentorship of early career doctors has been acknowledged in the literature [ 13 , 14 ]. Furthermore, there literature on health professions education has acknowledged the untapped potential of EMR data and other clinical data sets for supporting high-quality learning environments [ 15 ]. Findings from this study suggest placing an emphasis on these benefits when implementing digital technologies to enhance EMR uptake.
Although findings from this study identified benefits of the EMR, there were also a number of challenges identified which acted as barriers to engagement with the new system. These challenges included feature completeness and reliability, as well as poor communication from IT regarding feasibility of achieving required program features and in addressing EMR issues once implemented. Interestingly, the major challenges implementing the EMR were external to the control of the clinical team implementing the system. The literature has noted that lack of infrastructure and technical supports is a major barrier preventing the harnessing of EMR data by the staff [ 16 ], and for making health data actionable more broadly [ 15 ]. Findings from this study emphasise the enormity of overcoming resourcing and infrastructure challenges if digital technologies are to be effectively implemented and sustained in the health sector. Finally, the challenges faced when successfully implementing an EMR in this study highlight the need for technical and clinical experts to collaborate closely from the outset when developing digital technologies for healthcare, in order for those technologies to capture the complexity of clinical care.
A limitation of this study is that, although all staff at the study site were invited to participate, not all chose to. As a result the perspectives of these staff members might not have been captured in this study. Further, not all participants who participated in pre-implementation interviews chose to participate in post-implementation interviews. As such some of the perspectives of interviewees pre-implementation are not captured in the post-implementation findings.
Digital technologies such as EMRs have great potential to improve the quality, equity and cost of healthcare. However, the health sector is still struggling to implement these technologies in a way that leads to sustained use. Barriers to successful implementation of EMRs include lack of technical support, perceived increase in workload and a learning curve to adequately familiarise with the feature set of the EMR. Enablers of successful implementation include clinician engagement in the design and roll-out of the EMR, and training and upskilling of all end-users of the EMR. Although there may be challenges in the usability of EMRs right after its implementation, staff will be encouraged to use it if they perceive improved features of EMR are imminent and has potential benefit to patient care and workflow. However, it is important that continuous supports are provided to ensure buy-in from health professional is not lost.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Electronic Medical Record/s
Clauser SB, Wagner EH, Bowles EJA, Tuzzio L, Greene SM. Improving modern cancer care through information technology. Am J Prev Med. 2011;40(5):S198–207.
Article Google Scholar
Miller RH, Sim I. Physicians’ use of electronic medical records: barriers and solutions. Health Aff. 2004;23(2):116–26.
Baldwin JL, Singh H, Sittig DF, Giardina TD. Patient portals and health apps: Pitfalls, promises, and what one might learn from the other. Healthcare. 2017: Elsevier;2017:81–5.
Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res. 2010;10(1):231.
Kayyali B, Knott D, Van Kuiken S. The big-data revolution in US health care: accelerating value and innovation. Mc Kinsey Co. 2013;2(8):1–13.
Google Scholar
Nguyen L, Bellucci E, Nguyen LT. Electronic health records implementation: an evaluation of information system impact and contingency factors. Int J Med Inform. 2014;83(11):779–96.
McGinn CA, Grenier S, Duplantie J, Shaw N, Sicotte C, Mathieu L, Leduc Y, Légaré F, Gagnon M-P. Comparison of user groups' perspectives of barriers and facilitators to implementing electronic health records: a systematic review. BMC Med. 2011;9(1):46.
Devlin AM, McGee-Lennon M, O’Donnell CA, Bouamrane M-M, Agbakoba R, O’Connor S, Grieve E, Finch T, Wyke S, Watson N. Delivering digital health and well-being at scale: lessons learned during the implementation of the Dallas program in the United Kingdom. J Am Med Inform Assoc. 2016;23(1):48–59.
Murray E, Burns J, May C, Finch T, O'Donnell C, Wallace P, Mair F. Why is it difficult to implement e-health initiatives? A qualitative study. Implement Sci. 2011;6(1):6.
Fleming NS, Culler SD, McCorkle R, Becker ER, Ballard DJ. The financial and nonfinancial costs of implementing electronic health records in primary care practices. Health Aff. 2011;30(3):481–9.
Janssen A, Brunner M, Keep M, Hines M, Nagarajan SV, Kielly-Carroll C, Dennis S, McKeough Z, Shaw T. Interdisciplinary eHealth practice in cancer care: a review of the literature. Int J Environ Res Public Health. 2017;14(11):1289.
Bain E, Bubner T, Ashwood P, Van Ryswyk E, Simmonds L, Reid S, Middleton P, Crowther CA. Barriers and enablers to implementing antenatal magnesium sulphate for fetal neuroprotection guidelines: a study using the theoretical domains framework. BMC Pregnancy Childbirth. 2015;15(1):176.
Cowan F, Flint S. The importance of mentoring for junior doctors. BMJ. 2012;345:e7813.
Fournier M, Tourian L. “A peer mentoring initiative across medical residency programs”. Mental Health and Social Inclusion. 2019;24(1):33–40. https://doi.org/10.1108/MHSI-09-2019-0027 .
Wang YC, DeSalvo K. Timely, granular, and actionable: informatics in the public health 3.0 era. Am J Public Health. 2018;108(7):930–4.
Tolar M, Balka E. Beyond individual patient care: enhanced use of EMR data in a primary care setting. ITCH. 2011;2011:143–7.
Janssen A, Donnelly C, Elder E, Pathmanathan N, Shaw T. Factors Influencing Implementation of an Electronic Medical Record in a Tertiary Cancer Centre. Stud Health Technol Inform. 2019;266:95–100. https://doi.org/10.3233/SHTI190779 .
Download references
Acknowledgements
The authors wish to thank the cancer MDT leaders and members for volunteering their time to participate in the study.
Preliminary results of this study where presented at the Health Informatics Conference 2019 [ 17 ].
All authors listed in this publication conducted the research as part of the salaried position supported by their hiring organisation. No additional funding was provided for this research study.
Author information
Authors and affiliations.
Faculty of Medicine and Health, Charles Perkins Centre, The University of Sydney, Level 2, Charles Perkins Centre D17, Sydney, NSW, Australia
Anna Janssen, Candice Donnelly & Tim Shaw
Sydney West Translational Cancer Research Centre, Westmead Hospital, Sydney, NSW, Australia
Westmead Breast Cancer Institute, Western Sydney Local Health District, Sydney, NSW, Australia
Elisabeth Elder & Nirmala Pathmanathan
You can also search for this author in PubMed Google Scholar
Contributions
Authors AJ and CD wrote where involved in study design, data collection and coordination of manuscript drafting. Authors TS, EE and NP where involved in study design and manuscript drafting. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Anna Janssen .
Ethics declarations
Ethics approval and consent to participate.
Permission to conduct this study was granted by human research ethics committees of the University of Sydney, the Western Sydney Local Health District, and the Nepean Blue Mountains Local Health District. Participants were consented to participate, as per the requirements of the ethics approval. Potential participants were recruited via email to participate in the study. Consent was provided either through return of a signed consent form, or via confirmation in the email response. At the start of each interviewee consent to participate in the interview and consent to record the inter-view was once again confirmed. All authors have read and approved the manuscript.
Consent for publication
Consent for publication is not necessary for this publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Janssen, A., Donnelly, C., Elder, E. et al. Electronic medical record implementation in tertiary care: factors influencing adoption of an electronic medical record in a cancer centre. BMC Health Serv Res 21 , 23 (2021). https://doi.org/10.1186/s12913-020-06015-6
Download citation
Received : 04 June 2020
Accepted : 13 December 2020
Published : 06 January 2021
DOI : https://doi.org/10.1186/s12913-020-06015-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Multidisciplinary care
- Clinical informatics
- Electronic medical records
- Implementation
- Digital health
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Electronic Medical Records implementation in hospital: An empirical investigation of individual and organizational determinants
Contributed equally to this work with: Anna De Benedictis, Emanuele Lettieri
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Current address: Department of Healthcare Professions, University Hospital Campus Bio-Medico, Rome, Italy
Affiliations Department of Healthcare Professions, University Hospital Campus Bio-Medico, Rome, Italy, Faculty of Medicine & Surgery, University Campus Bio-Medico, Rome, Italy
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
Current address: Department of Economics, Management and Industrial Engineering, Politecnico of Milan, Milan, Italy
Affiliation Department of Economics, Management and Industrial Engineering, Politecnico of Milan, Milan, Italy
Roles Conceptualization, Data curation, Methodology, Writing – review & editing
Roles Conceptualization, Methodology, Writing – review & editing
Roles Formal analysis, Investigation, Project administration
Affiliation Department of Healthcare Professions, University Hospital Campus Bio-Medico, Rome, Italy
Roles Conceptualization, Writing – review & editing
- Anna De Benedictis,
- Emanuele Lettieri,
- Luca Gastaldi,
- Cristina Masella,
- Alessia Urgu,
- Daniela Tartaglini

- Published: June 4, 2020
- https://doi.org/10.1371/journal.pone.0234108
- Reader Comments
The implementation of hospital-wide Electronic Medical Records (EMRs) is still an unsolved quest for many hospital managers. EMRs have long been considered a key factor for improving healthcare quality and safety, reducing adverse events for patients, decreasing costs, optimizing processes, improving clinical research and obtaining best clinical performances. However, hospitals continue to experience resistance from professionals to accepting EMRs. This study combines institutional and individual factors to explain which determinants can trigger or inhibit the EMRs implementation in hospitals, and which variables managers can exploit to guide professionals’ behaviours. Data have been collected through a survey administered to physicians and nurses in an Italian University Hospital in Rome. A total of 114 high-quality responses had been received. Results show that both, physicians and nurses, expect many benefits from the use of EMRs. In particular, it is believed that the EMRs will have a positive impact on quality, efficiency and effectiveness of care; handover communication between healthcare workers; teaching, tutoring and research activities; greater control of your own business. Moreover, data show an interplay between individual and institutional determinants: normative factors directly affect perceived usefulness (C = 0.30 **), perceived ease of use (C = 0.26 **) and intention to use EMRs (C = 0.33 **), regulative factors affect the intention to use EMRs (C = -0.21 **), and perceived usefulness directly affect the intention to use EMRs (C = 0.33 **). The analysis carried out shows that the key determinants of the intention to use EMRs are the normative ones (peer influence) and the individual ones (perceived usefulness), and that perceived usefulness works also as a mediator between normative factors and intention to use EMRs. Therefore, Management can leverage on power users to motivate, generate and manage change.
Citation: De Benedictis A, Lettieri E, Gastaldi L, Masella C, Urgu A, Tartaglini D (2020) Electronic Medical Records implementation in hospital: An empirical investigation of individual and organizational determinants. PLoS ONE 15(6): e0234108. https://doi.org/10.1371/journal.pone.0234108
Editor: Stefano Triberti, University of Milan, ITALY
Received: September 16, 2019; Accepted: May 19, 2020; Published: June 4, 2020
Copyright: © 2020 De Benedictis et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Healthcare is the most complex and fast-moving industry that exists. New digital technologies are constantly being developed, all with the potential to support the clinical practice by bringing many advantages into the healthcare sector [ 1 ]. Nevertheless, the healthcare industry has lagged behind other sectors in the adoption of Information Technology (IT) in the workplace [ 2 ]. Electronic Medical Records (EMRs) have long been considered a key factor for improving healthcare quality and safety, reducing adverse events for patients, decreasing costs, optimizing processes, improving clinical research and obtaining best clinical performance [e.g., 3 – 5 ]. However, the pace of adoption of EMRs–as other digital technologies–in healthcare continues to lag [ 2 , 6 ], and hospitals continue to experience resistance from professionals to accepting digital technology [ 7 ]. Though many research and development programs exist and venture capital investment has been growing, successful IT projects in healthcare continue to be rare, and a plan to accelerate innovation is needed beginning with a diagnosis of the problem [ 2 ]. Some studies analyzed both individual and organizational factors that affect the acceptance and implementation of technology [ 8 ], but they have generated mixed results [ 9 ]. Indeed, mechanisms that drive the adoption and implementation of IT in hospitals remain unclear. Organizational studies conceive organizations as strongly institutionalized settings in which individual behaviours are influenced by regulations, social norms and cultural systems [ 10 , 11 ]. In contrast, Information Science has mostly adopted user acceptance models, which emphasise individuals’ rational and volitional assessment of the costs and benefits they would attain from the new digital technology [ 11 ].
Hospitals are highly institutionalized and regulated contexts, in terms of regulatory oversight and professional roles, and are operationally and technically complex [ 12 ]. Physicians and nurses have a high level of professionalism and they often affiliate within their specialities via professional training and participation in speciality-focused organizations [ 13 ]. Successful adoption or perceived usefulness of EMRs by others within their specialities may influence hospital professionals’ decisions, particularly if they are uncertain about individual benefits. Nevertheless, the majority of academic research in IT adoption in healthcare focused on the individual level [ 14 ]. The most widely used model to explore issues related to the acceptance of technology is the Technology Acceptance Model (TAM) [ 15 ], which identifies two main antecedents the perceived usefulness and the perceived ease of use of technology. The TAM has been validated in multiple settings [e.g. 16 – 18 ]. In its basic framework, the end user’s attitudes and perceptions regarding the use of new technology determine the user’s behavioural intention to use it. Institutional theory, instead, is based on the assumption that individual behaviours are modelled by regulations, social norms and meaning systems and that institutions embodied in routines rely on automatic cognition and uncritical processing of existing schemata and privilege consistency with stereotypes and speed over accuracy [ 19 ]. Thus, in this theory, normative and cultural conditions are co-determinants of the adoption of new technologies [ 20 ]. The use of institutional theory in Information Science is rare compared to other fields such as organization science [ 21 ]. However, several studies have used an institutional approach for exploring the adoption of technology considering institutional forces as crucial to shaping organizational actions and the opinions of the decision-makers [ 22 , 23 , 24 ].
Both institutional theory and user acceptance models have independently tried to incorporate elements of the other theory to enrich their explanatory power [ 2 ]. User acceptance models have incorporated the direct effects of social influences and organizational conditions on individuals’ behavioural intention [ 25 , 26 ], and institutional studies have demonstrated that even when professionals are subject to institutional influences, their self-determination plays an important role even in highly-institutionalized and regulated settings such as hospitals [ 27 ]. Previous studies about technology acceptance and adoption compared individual and social levels including environmental factors [ 22 , 28 – 30 ], typically based on the diffusion of innovation theory (DOI) [ 31 ] or the TOE (technology, organization, and environment) framework [ 32 ]. Moreover, only a few studies have tested both explanations (institutional and individual) in an integrative framework [ 23 ] to explain the behaviour of organizations.
The main purpose of this study was to explore which are the main determinants of hospital professionals’ intention to use EMRs through a novel theoretical model that combines organizational theories and technology acceptance models. By combining these theories, this study investigated the interplay between organizational and individual factors, thus offering novel insights on the determinants of hospital professionals’ acceptance of digital technology by showing how and to what extent the interplay between individual and organizational determinants might trigger or inhibit the acceptance of digital technology. This study focused on perceived usefulness and perceived ease of use as explanatory factors at the individual level, and on inter-hospital normative and regulative forces as explanatory factors at the organizational level. Intention to use has been preferred to repetitive use as the dependent variable. This choice is because of the still relatively low adoption rate of EMRs in many Countries such as Italy, where this study is located. In the specific case of Italy, a recent report issued by the Politecnico di Milano within the research activities of the Permanent Observatory of Digital Transformation in Health Care [ 33 ] pointed out that only 53% of Italian hospitals have in place an EMRs for therapy management, only 30% of Italian hospitals have in place an EMRs that collects vital parameters and informed consensus, and only 19% of Italian hospitals have in place an EMRs that supports clinical decision-making. In this view, a large number of Italian hospitals–as well as hospitals from other Countries who are still lagging in the adoption of EMRs–is expected to commit in the next years to adopt EMRs and the understanding of which individual or organizational factors might shape hospital professionals’ intention to use EMRs might contribute to the successful adoption and implementation of such and other digital technologies. In this view, the results of this study might be valuable for hospital managers and professionals of different countries who are going to invest in the digital transformation of their hospitals.

Material and methods
Ethics statement.
The study has been approved by the Ethics Board of the University Hospital Campus Bio-Medico of Rome. (Approval number: 61/16 OSS ComEt CBM), and written consent has been obtained by professionals involved in the study.
Theoretical background
To evaluate the potential interplay between individual and institutional variables, a research framework has been created ( Fig 1 ). The framework integrates into a coherent view of two theories that belong to two different bodies of literature:
- The Technology Acceptance Model (TAM), from Information Science, that has been widely used in the last decades in healthcare to understand what leads professionals or patients to accept or reject Information Technology [ 15 ];
- The Institutional Theory, from Public Management, that has been largely adopted in the last decades to assess how institutional factors shape professionals’ behaviours [ 34 – 36 ].
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0234108.g001
Technology acceptance model.
Davis introduced the TAM in 1989 [ 15 ]. The main problem raised by the author was to understand what leads people to accept or reject Information Technology. In this regards, two main variables have been identified: the perceived usefulness and the ease of use. Perceived usefulness measures “the degree to which a person believes that using a particular system would enhance his or her job performance” [ 15 ], and therefore induces individuals to use technology as it allows to obtain better results. On the other hand, the ease of use measures “the degree to which a person believes that using a system would be free of effort” [ 15 ] and induces the potential users to use a certain technology since it requires low energy expenditure while it may bring advantages. The first one induces an individual to use technology as it allows to obtain better results in his work; the ease of use, on the other hand, stimulates potential users to use a certain technology since many advantages are supported with low energy expenditure.
Institutional theory.
The Institutional Theory refers to a line of organizational research that recognize the significant organizational effects that are associated with the increase of cultural and social forces. According to Scott [ 34 – 36 ], “Institutions are made up of cultural-cognitive, normative and regulative elements, which together with associated activities and resources offer stability and meaning to social life.” These three forces are present in totally developed institutional systems, with economists and political scientists emphasizing regulative, sociological and normative factors, and anthropologists and organizational theorists emphasizing cognitive-cultural factors. According to this perspective, individuals are embedded in institutional pillars that limit the scope of their rational assessment and direct the engagement of specific behaviours [ 34 – 36 ]. Scott [ 34 – 36 ] defines the three institutional pillars as follows:
- regulative pillars : which regard the existence of regulations, rules and processes whose breach is monitored and sanctioned;
- normative pillars : which introduce a social dimension of appropriate behaviours in the organization;
- cultural pillars : which emphasize the use of common schemas, frames, and other shared symbolic representations that create an attachment to the ‘appropriate’ behaviour.
Research framework
Consistently to our research questions, we combined the two theories described above to develop an original, comprehensive research framework where individual and institutional determinants have been interlinked to explore their potential interplay in explaining hospital professionals’ intention to use an EMR. Coherently to past researches about user acceptance of new technologies [ 36 , 37 ], we considered age and job seniority as key control variables. Additionally, to narrow the knowledge gap about how hospital professionals belonging to either different profession (e.g., physicians vs. nurses) or different speciality (e.g., cardiology vs. orthopaedics) might be interested to use an EMR, we included clinical speciality and profession as control variables. Fig 1 offers a synoptic view of our research framework, where the independent variable (i.e., the intention to use an EMR) is explained by individual factors from TAM (i.e., perceived usefulness and perceived ease of use) as well as by institutional factors from Institutional Theory (i.e., regulative factors that refer to the degree of adhesion to hospital managers’ goals, and normative factors that explain the peer influence among hospital colleagues. Control variables have been also displayed.
According to the research questions and the research framework, the following research hypotheses (H) were stated: H1: Individual factors (perceived usefulness, perceived ease of use) directly affect the intention to use EMRs; H2: Organizational factors (normative and regulative factors) directly affect individual factors and the intention to use EMRs; H3: Some control variables (age, seniority, clinical specialities and different professions) directly affect individual factors and the intention to use EMRs.
Setting and research methodology
Given the explorative nature of this study, a single case study research design has been adopted. The choice of a single case study offers the opportunity to eliminate potential confounding factors due to the heterogeneity–in terms of strategy, legacy, professionals’ behaviours and technology infrastructure–that different hospitals might show. We selected the Teaching Hospital Campus Bio-Medico (CBM) in Rome (Italy) as an adequate setting for investigating our research questions. This hospital is mid-size (around 300 beds), many-disciplines, teaching and private. Being a teaching hospital, there is more room for divergent goals between professionals and managers, thus creating the correct setting where to investigate the interplay between individual and organizational factors. Being many-discipline, there is room to study the potential conflict among professionals from different disciplines concerning the intention to use EMRs. Finally, being mid-size, CBM is a valid setting to observe the potential divergence between nurses and doctors in the intention to use EMRs. A quantitative study has been performed using a survey administered to hospital professionals (physicians and nurses). The questionnaire has been designed based on the scales identified in the literature and reviewed in detail by the authors. Moreover, a pilot test of the questionnaire has been carried out before the survey. The initial questionnaire comprised 20 items that were reviewed for face validity by a panel of four experts, consisting of one nurse and one physician—with more than 9 years of work experience -, and two engineers with expertise in Information Science. Panel members were asked to evaluate each statement for clarity, ease of use and appropriateness. Based on their comments and suggestions, five items were removed and changes were made in the wording of several items to increase clarity.
This 15-item questionnaire was tested for content validity by 10 experts not involved in the preceding phase to identify its ability to measure the determinants of the intention to use EMRs in hospitals and to identify, for each item, utility, consistency with the research objectives, easy of reply and other important aspects to take into account. Audio-recorded individual interviews using a semi-structured grid were carried out with 10 experts including two nurses, three head nurses, two managers and three physicians. The interviews lasted 60 minutes on average and were conducted in a designated room by three researchers: one acted as the interviewer, the other two helped with audio-recording and with filling out the grid for item evaluation. Based on the expert evaluation, three items were modified.
The questionnaire consists of two main sections: scales and constructs of the proposed model; control variables and characteristics of respondents. Eleven items evaluated individual variables, in particular, the scale for the measurement of perceived usefulness has been adapted from the studies of Venkatesh [ 38 , 39 ]. Organizational variables were explored through 4 items related to normative and regulative factors. The scale for the measurement of normative and regulative factors has been adapted from the study of Scott [ 20 ]. The survey items are available in Annex ( S1 Table ). Additional questions have been designed to gather demographic and sample information. All questionnaire items related to the constructs of the proposed model were explored using a 7 point Likert scale with 1 indicating “strongly disagree” and 7 “strongly agree”. The first re-call has been made one week after the expiration date for compilation. Three days after the first follow-up, the second recall has been sent. Finally, three days after, the third recall has been sent.
The statistical analysis was performed using the software Stata 14.1®. The internal consistency was evaluated through Cronbach’s Alpha coefficients, the path analysis was performed to test the proposed model considering a p-value of <0.05 as significant. The correlation between profession (doctors vs. nurses) and the answers provided for each item was analyzed through the Fisher’s test; a p-value of <0.05 was considered significant.
The study has been approved by the General Management and the Ethics Board of CBM. The link for the online questionnaire was sent by e-mail to 380 nurses and 250 physician representatives of different clinical areas. All questionnaires were filled out anonymously in a period between February and September 2018. The final sample included 114 hospital professionals (response rate 19%), composed by 78 (68%) nurses and 36 (32%) physicians. They were 84 (74%) females and 30 (36%) males, aged 37.4 years on average (range 23–66, SD 9.6), with a mean work experience of 13.24 (range 0.5–41, SD 8.73). The sample of respondents has been compared–in terms of age, gender and clinical experience–to the whole population of doctors and nurses enrolled at CBM confirming the absence of potential response biases related to the non-respondents.
Questionnaire’s internal consistency
The internal consistency of constructs was evaluated through Cronbach's Alpha coefficients, values greater than or equal to 0.7 were considered acceptable. (α ≥ 0.90 were considered excellent; 0.8 ≤ α < 0.9 good; 0.7 ≤ α < 0.8 acceptable; 0.6 ≤ α < 0.7 questionable; 0.5 ≤ α < 0.6 poor; α < 0.5 unacceptable) ( Table 1 ).
https://doi.org/10.1371/journal.pone.0234108.t001
Determinants of current behaviours
Data show that both physicians and nurses expect many benefits from the use of EMRs. In particular, they think EMRs will have a positive impact on relevant factors such as quality, efficiency and effectiveness of care; handover communication among healthcare workers; teaching, tutoring and research activities; greater control of their tasks. Data confirm that perceived usefulness (C = 0.33**) directly affects the intention to use EMRs. Concerning the organizational factors, data prove that there does exist an interplay between them and individual determinants. In fact, normative factors directly affect perceived usefulness (C = 0.30**), perceived ease of use (C = 0.26**) and intention to use EMRs (C = 0.33**). Regulative factors affect the intention to use EMRs, with a negative sign (C = -0.21**). Control variables (i.e., age, seniority, clinical area and profession) have no impact on other variables in our model. Fig 2 offers a graphical representation of our results.
https://doi.org/10.1371/journal.pone.0234108.g002
Moreover, the findings show a significant correlation between being a nurse or a physician and the perceived ease of use and intention to use EMRs. In particular, more nurse than physicians perceive EMRs as easy to use (p = 0.019 for the item “the EMR will be easy to use”) and state that they would like to use it (p = 0.01 for the item “if I had the opportunity I would use the EMR for most of my work’s processes”).
This study sought to better clarify the relationship between organizational and individual determinants of the intention to use EMRs in a hospital setting by nurses and physicians. Previous studies [ 40 – 46 ] have focused mainly on either the barriers or the facilitators that might impact on the implementation of EMRs, but, to the best of authors’ knowledge, it has never been deepened if and how organizational and individual factors do interact and affect jointly hospital professionals’ motivation to use EMRs. Findings confirmed the positive role played by the perceived usefulness as driving individual factor to the intention to use EMRs and shed light on the significant positive role played by the normative (peer influence) factors [ 2 ], both with direct and indirect effects. In this view, hospital managers can leverage on lead peer influence (i.e., innovation champions) to motivate, generate and manage change and generate a virtuous circle inside the hospital to motivate the use of EMRs. The EMRs implementation process should take into account that professionals need proper time to re-establish control over their tasks and processes. The introduction of EMRs in daily clinical practice changes the status quo and, if, on one hand, it allows many new opportunities, on the other hand, it involves changes that can have different effects on hospital professionals also based on their own characteristics, knowledge, skills and work type. In general, this is what happens in the case of effective implementation, while the consequences of poorly managed implementation can be very complex and involve a greater expenditure of time, energy and money to restart the processes at the previous speed and functionality. In this sense, to increase the motivation of users in all phases of the project represent an essential point for effective management of change. This study confirms the importance of involving front-line professionals, as soon as the hospital decides to start the implementation phase to increase their motivation to use EMRs. In fact, as a result of their involvement, professionals will better understand the rationale of this technological shift and their perception of usefulness will increase consequently. Moreover, it is important to consider that, as reported by Gastaldi et al. [ 2 ] in the absence of coercive mechanisms, institutional pressures toward EMR use are primarily normative and/or mimetic [ 2 ].
In the study, the construct “Regulative factor” has been derived from the Institutional theory and is aimed at exploring the pressure that a hospital professional might perceive from the goals set by hospital managers. This pressure is intended to be independent of the specific strategy/initiative and to be a general availability of a hospital professional to align his/her behaviour to the goals set by hospital managers. An example of a question is: “I very much agree with most of the objectives of the management”. The regulative factor should be analyzed together with the construct “Normative factor” that crystallizes the perceived pressure from peers. Hospitals are intended as professional bureaucracies where professionals feel more the pressures from peers rather than from apex managers. What is interesting is that the regulative factor affects negatively the intention to use, meaning that more the general agreement with managers’ goals less the intention to use an EMR. This finding might appear as counter-intuitive and contrary to what has been found in other studies [ 47 ]. This result cannot be explained by the potential misalignment between hospitals managers’ goals and those of physicians and nurses, being the former more focused on the efficiency and the latter on the effectiveness of care delivery. Managers at CBM have proved to be committed to the quality of care and not to efficiency strategies that might reduce the effectiveness of care. This context is quite typical in Italy, where the tensions between “medicine” and “management” are less evident than in other countries, such as in the US. We think that the negative impact of the regulative factors on the perception of usefulness is because hospital managers did not detail enough their goals about the digital transformation of care delivery, thus impacting negatively on hospital professionals’ perception about the usefulness of an EMR. Being these goals enough general–e.g., providing support to research activities and care delivery, promoting efficiency and process redesign–while the linkage between the regulative factors and the perception of usefulness failed to materialize, the linkage between the regulative factors and the intention to use EMRs became negative as hospital professionals lost the connection between EMR usage and managers’ goals. In this view, more contextualized goals about the usage of EMR are expected to positively affect the intention to use it among those professionals who are more willing to be adherent to managers’ goals. This finding should be tested and confirmed by further replication studies that might capture more in detail the relationships between regulative factors and either the perceived usefulness or the intention to use. For instance, it might be valuable to understand whether and how the co-development of hospitals goals between managers and professionals might impact these relationships as well as the specific content of hospital goals (financial vs. quality of care, operative vs. research).
This study offers original insights to further the ongoing debate about the digital transformation of hospitals, with a focus to EMRs. Our results show that there is an interplay between individual and organizational factors in shaping hospital professionals’ intention to use EMRs. The study showed that the main determinants of the intention to use EMRs are the normative ones (peer influence) and the individual ones (perceive usefulness).
From an academic viewpoint, the study offers an original perspective and a new theoretical framework, which combines organizational theories and technology acceptance models to explain hospital professionals’ acceptance of EMRs. In particular, the results confirm the importance of individual variables, not only as directly related to the acceptance of new technology, but also as important mediators between institutional variables and acceptance, thus highlight and confirming the importance of the connections between organizational studies and information science.
Despite the original contributions, this study suffers at least two limitations that should be addressed by future research. First, the research design is based on a single case study. Further research should consider a multi-centre design, thus allowing the generalization of our results. Moreover, a multi-centre study will allow exploring the role that hospital characteristics–in terms of strategy, legacy, etc.–might have on shaping both the organizational and individual factors investigated in this study. Second, this study investigated the intention to use EMRs as the dependent variable. Further research should consider hospitals where EMRs are already mature technologies, thus allowing the investigation of the actual use and which factors might facilitate/inhibit the translation of the intention to use into actual use.
Supporting information
S1 table. questionnaire..
https://doi.org/10.1371/journal.pone.0234108.s001
S2 Table. Perceived usefulness.
https://doi.org/10.1371/journal.pone.0234108.s002
S3 Table. Perceived ease of use.
https://doi.org/10.1371/journal.pone.0234108.s003
S4 Table. Intention to use.
https://doi.org/10.1371/journal.pone.0234108.s004
S5 Table. Normative factors (Peer influence).
https://doi.org/10.1371/journal.pone.0234108.s005
S6 Table. Regulative factors (Adhesion to the management objectives).
https://doi.org/10.1371/journal.pone.0234108.s006
Acknowledgments
We want to thank Dr Federica Segato for her valuable comments in all phases of this study.
- 1. Barlow J. Managing Innovation in Healthcare. World Scientific Publishing Europe. London; 2017.
- View Article
- PubMed/NCBI
- Google Scholar
- 10. Scott W.R., & Davis G. Organizations and organizing: rational, natural and open systems perspectives. New Jersey: Prentice Hall; 2008.
- 12. Scott W.R., Ruef P., Mendel P., Caronna C. Institutional change and healthcare organizations: from professional dominance to managed care. University of Chicago Press. Chicago; 2000.
- 19. Lawrence T.B., Suddaby R. and Leca B. Institutional Work: Actors and Agency in Institutional Studies of Organizations. Cambridge University Press, Cambridge, UK; 2009.
- 27. Leca, B., Battilana, J. and Boxenbaum, E. Agency and Institutions: A Review of Institutional Entrepreneurship, Working Paper 08–096, Harvard Business School; 2008.
- 31. Rogers E. Diffusion of Innovations. 4th ed., Free Press, New York; 1995.
- 32. Tornatzky L., Fleischer M. The Process of Technology Innovation, Lexington Books, Lexington, MA; 1990.
- 33. https://www.osservatori.net/it_it/pubblicazioni/rapporti/sanita-digitale-italia-stato-dell-arte-e-trend .
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
Toward a smarter electronic health record
Press contact :, media download.

*Terms of Use:
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."

Previous image Next image
Electronic health records have been widely adopted with the hope they would save time and improve the quality of patient care. But due to fragmented interfaces and tedious data entry procedures, physicians often spend more time navigating these systems than they do interacting with patients.
Researchers at MIT and the Beth Israel Deaconess Medical Center are combining machine learning and human-computer interaction to create a better electronic health record (EHR). They developed MedKnowts, a system that unifies the processes of looking up medical records and documenting patient information into a single, interactive interface.
Driven by artificial intelligence, this “smart” EHR automatically displays customized, patient-specific medical records when a clinician needs them. MedKnowts also provides autocomplete for clinical terms and auto-populates fields with patient information to help doctors work more efficiently.
“In the origins of EHRs, there was this tremendous enthusiasm that getting all this information organized would be helpful to be able to track billing records, report statistics to the government, and provide data for scientific research. But few stopped to ask the deep questions around whether they would be of use for the clinician. I think a lot of clinicians feel they have had this burden of EHRs put on them for the benefit of bureaucracies and scientists and accountants. We came into this project asking how EHRs might actually benefit clinicians,” says David Karger, professor of computer science in the Computer Science and Artificial Intelligence Laboratory (CSAIL) and senior author of the paper.
The research was co-authored by CSAIL graduate students Luke Murray, who is the lead author, Divya Gopinath, and Monica Agrawal. Other authors include Steven Horng, an emergency medicine attending physician and clinical lead for machine learning at the Center for Healthcare Delivery Science of Beth Israel Deaconess Medical Center, and David Sontag, associate professor of electrical engineering and computer science at MIT and a member of CSAIL and the Institute for Medical Engineering and Science, and a principal investigator at the Abdul Latif Jameel Clinic for Machine Learning in Health. It will be presented at the Association for Computing Machinery Symposium on User Interface Software and Technology next month.
A problem-oriented tool
To design an EHR that would benefit doctors, the researchers had to think like doctors.
They created a note-taking editor with a side panel that displays relevant information from the patient’s medical history. That historical information appears in the form of cards that are focused on particular problems or concepts.
For instance, if MedKnowts identifies the clinical term “diabetes” in the text as a clinician types, the system automatically displays a “diabetes card” containing medications, lab values, and snippets from past records that are relevant to diabetes treatment.
Most EHRs store historical information on separate pages and list medications or lab values alphabetically or chronologically, forcing the clinician to search through data to find the information they need, Murray says. MedKnowts only displays information relevant to the particular concept the clinician is writing about.
“This is a closer match to the way doctors think about information. A lot of times, doctors will do this subconsciously. They will look through a medications page and only focus on the medications that are relevant to the current conditions. We are helping to do that process automatically and hopefully move some things out of the doctor’s head so they have more time to think about the complex part, which is determining what is wrong with the patient and coming up with a treatment plan,” Murray says.
Pieces of interactive text called chips serve as links to related cards. As a physician types a note, the autocomplete system recognizes clinical terms, such as medications, lab values, or conditions, and transforms them into chips. Each chip is displayed as a word or phrase that has been highlighted in a certain color depending on its category (red for a medical condition, green for a medication, yellow for a procedure, etc.)
Through the use of autocomplete, structured data on the patient’s conditions, symptoms, and medication usage is collected with no additional effort from the physician.
Sontag says he hopes the advance will “change the paradigm of how to create large-scale health datasets for studying disease progression and assessing the real-world effectiveness of treatments.”
In practice
After a year-long iterative design process, the researchers tested MedKnowts by deploying the software in the emergency department at Beth Israel Deaconess Medical Center in Boston. They worked with an emergency physician and four hospital scribes who enter notes into the electronic health record.
Deploying the software in an emergency department, where doctors operate in a high-stress environment, involved a delicate balancing act, Agrawal says.
“One of the biggest challenges we faced was trying to get people to shift what they currently do. Doctors who have used the same system, and done the same dance of clicks so many times, form a sort of muscle memory. Whenever you are going to make a change, there is a question of is this worth it? And we definitely found that some features had greater usage than others,” she says.
The Covid-19 pandemic complicated the deployment, too. The researchers had been visiting the emergency department to get a sense of the workflow, but were forced to end those visits due to Covid-19 and were unable to be in the hospital while the system was being deployed.
Despite those initial challenges, MedKnowts became popular with the scribes over the course of the one-month deployment. They gave the system an average rating of 83.75 (out of 100) for usability.
Scribes found the autocomplete function especially useful for speeding up their work, according to survey results. Also, the color-coded chips helped them quickly scan notes for relevant information.
Those initial results are promising, but as the researchers consider the feedback and work on future iterations of MedKnowts, they plan to proceed with caution.
“What we are trying to do here is smooth the pathway for doctors and let them accelerate. There is some risk there. Part of the purpose of bureaucracy is to slow things down and make sure all the i’s are dotted and all the t’s are crossed. And if we have a computer dotting the i’s and crossing the t’s for doctors, that may actually be countering the goals of the bureaucracy, which is to force doctors to think twice before they make a decision. We have to be thinking about how to protect doctors and patients from the consequences of making the doctors more efficient,” Karger says.
A longer-term vision
The researchers plan to improve the machine learning algorithms that drive MedKnowts so the system can more effectively highlight parts of the medical record that are most relevant, Agrawal says.
They also want to consider the needs of different medical users. The researchers designed MedKnowts with an emergency department in mind — a setting where doctors are typically seeing patients for the first time. A primary care physician who knows their patients much better would likely have some different needs.
In the longer-term, the researchers envision creating an adaptive system that clinicians can contribute to. For example, perhaps a doctor realizes a certain cardiology term is missing from MedKnowts and adds that information to a card, which would update the system for all users.
The team is exploring commercialization as an avenue for further deployment.
“We want to build tools that let doctors create their own tools. We don’t expect doctors to learn to be programmers, but with the right support they might be able to radically customize whatever medical applications they are using to really suit their own needs and preferences,” Karger says.
This research was funded by the MIT Abdul Latif Jameel Clinic for Machine Learning in Health.
Share this news article on:
Related links.
- David Karger
- David Sontag
- Computer Science and Artificial Intelligence Laboratory
- Abdul Latif Jameel Clinic for Machine Learning in Health
- Institute for Medical Engineering and Science
- Department of Electrical Engineering and Computer Science
Related Topics
- Health care
- Artificial intelligence
- Electrical Engineering & Computer Science (eecs)
- Computer Science and Artificial Intelligence Laboratory (CSAIL)
- Institute for Medical Engineering and Science (IMES)
Related Articles
3 Questions: John Van Reenen on the impact of technology on health care workers
Algorithm reduces use of riskier antibiotics for UTIs

How well can computers connect symptoms to diseases?

Model improves prediction of mortality risk in ICU patients
Previous item Next item
More MIT News

New MIT-LUMA Lab created to address climate challenges in the Mediterranean region
Read full story →

MIT Press releases Direct to Open impact report

Modeling the threat of nuclear war
Modular, scalable hardware architecture for a quantum computer

Looking for a specific action in a video? This AI-based method can find it for you

Controlled diffusion model can change material properties in images
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
Electronic Medical Records Management and Administration: Current Trends, Issues, Solutions, and Future Directions
- Review Article
- Published: 20 April 2024
- Volume 5 , article number 460 , ( 2024 )
Cite this article

- Umar Abdulkadir ORCID: orcid.org/0000-0002-8118-0626 1 ,
- Victor Onomza Waziri 1 ,
- John Kolo Alhassan ORCID: orcid.org/0000-0002-9289-0404 2 &
- Idris Ismaila 1
65 Accesses
Explore all metrics
Electronic Medical Records (EMR) is often used to refer to as electronic personal health (EPH) records or electronic healthcare records (EHR). These are considered vivacious assets of health facilities and patients. The relevance of the EMRs has motivated diverse innovations in the collecting, organizing, managing and administering for purpose of treatment primarily and other reasons. There are various concerns raised about legitimate usages, reproducibility, accuracy, and privacy breaches of EMRs across majority of health and medical facilities globally. This phenomenon became popular due to its support of electronic devices, wireless links, transmission and storage of data in the cloud, and communication across a gateway (or central-point). Therefore, physicians and medical facilities were empowered to undertake virtual consultations to patients through telemedicine applications for the remote treatment and diagnosis. Internet of Things (IoT) systems, medical wearable objects, and sensors were the basic components that collect and transmit patient data on real-time basis to a base station or centralized servers managed by hospitals. However, there is the need to improve creation and adoption of EMRs not without understanding their roles and shortfalls as well possible means of improvement. Consequently, this study conducts a systematic literature review on electronic medical records management and administration under current trends, issues, solutions and future directions. To this end, eighty-one (81) peer-reviewed articles including conferences and journals papers were included in the final stage of the study after applying Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRIMA-P) methodology of records selection. The contributions of this study include: the recognition of the informed consent strategy as the best solution to illegitimate access to patient electronic records; the use of permissioned access strategies provided by blockchain technology as most recent attempt for privacy preservations; the use of lightweight cryptosystems with greater emphasis on Lattice systems; and the need to scale beyond theoretical frameworks to real-life implementations.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
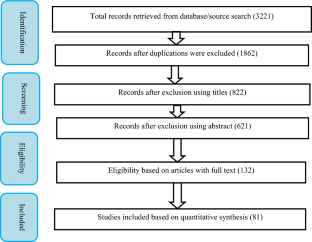
Similar content being viewed by others

Big data in healthcare: management, analysis and future prospects

Blockchain for healthcare data management: opportunities, challenges, and future recommendations
Cybersecurity, Data Privacy and Blockchain: A Review
Data availability.
Not applicable.
Code Availability
Abunadi I, Kumar RL. BSF-EHR: blockchain security framework for electronic health records of patients. Sensors. 2021;21(2865):1–10.
Google Scholar
Aghili SF, Mala H, Shojafar M, Peris-Lopez P. LACO: lightweight three-factor authentication, access control and ownership transfer scheme for e-health systems in IoT. Futur Gener Comput Syst. 2019;96:410–24. https://doi.org/10.1016/j.future.2019.02.020 .
Article Google Scholar
Alami J, Hammonds C, Hensien E, Khraibani J, Borowitz S, Hellems M, Riggs SL. Usability challenges with electronic health records (EHRs) during prerounding on pediatric inpatients. JAMIA Open. 2022;5(1):1–6.
Alamri M, Jhanjhi NZ, Humayun M. Blockchain for Internet of Things (IoT) research issues challenges & future directions: a review. Int J Comput Sci Newt Secur. 2019;19(5):244–58.
Albreiki H, Alqassem L, Salah K, Rehman MH, Svetinovic D. Decentralized Access control for IoT Data using blockchain and trusted oracles. IEEE Int Conf Ind Internet. 2019;2019:248–57. https://doi.org/10.1109/ICII.2019.00051 .
Al Mamun A, Azam S, Gritti C. Blockchain-based electronic health records management: a comprehensive review and future research direction. IEEE Access. 2022;10:5768–89.
Alfa AA, Alhassan JK, Olaniyi OM, Olalere M. Blockchain technology in IoT systems: current trends, methodology, problems, applications, and future directions. J Reliable Intell Environ. 2020. https://doi.org/10.1007/s40860-020-00116-z .
Alonso SG, Arambarri J, López-Coronado M, de la Torre-Díez I. Proposing new blockchain challenges in eHealth. J Med Syst. 2019;43(3):64. https://doi.org/10.1007/s10916-019-1195-7 .
Andola N, Prakash S, Venkatesan S, Verma S. SHEMB: a secure approach for healthcare management system using blockchain. In: 2019 IEEE conference on information and communication technology; 2019. p. 1–6. https://doi.org/10.1109/CICT48419.2019.9066237
Assenza, G, Fioravanti C, Guarino S, Petrassi V. New perspectives on wearable devices and electronic health record systems. In: 2020 IEEE international workshop on metrology for industry 4.0 and IoT; 2020. p. 740–5. https://doi.org/10.1109/MetroInd4.0IoT48571.2020.9138170 .
Azaria A, Ekblaw A, Vieira T, Lippman A. MedRec: using blockchain for medical data access and permission management. In: 2016 IEEE 2nd international conference on open and big data; 2016. p. 25–30. https://doi.org/10.1109/OBD.2016.11
Belfrage S, Helgesson G, Lynøe N. Trust and digital privacy in healthcare: a cross-sectional descriptive study of trust and attitudes towards uses of electronic health data among the general public in Sweden. BMC Med Ethics. 2022;23(19):1–8. https://doi.org/10.1186/s12910-022-00758-z .
Benil T, Jasper J. Cloud based security on outsourcing using blockchain in E-health systems. Comput Netw. 2020;178: 107344. https://doi.org/10.1016/j.comnet.2020.107344 .
Boumezbeur I, Zarour K. Privacy preservation and access control for sharing electronic health records using blockchain technology. Acta Inf Pragensia. 2022;11(1):105–22. https://doi.org/10.18267/j.aip.176 .
Brogan J, Baskaran I, Ramachandran N. Authenticating health activity data using distributed ledger technologies. Comput Struct Biotechnol J. 2018;16:257–66. https://doi.org/10.1016/j.csbj.2018.06.004 .
Charanya R, Saravanaguru RAK, Aramudhan M. Sefra: a secure framework to manage ehealth records using blockchain technology. Int J E-Health Med Commun. 2020;11(1):1–16. https://doi.org/10.4018/IJEHMC.2020010101 .
Chen HS, Jarrell JT, Carpenter KA, Cohen DS, Huang X. Blockchain in healthcare: a patient-centered model. Biomed J Sci Tech Res. 2019;20(3):15017–22. https://doi.org/10.26717/bjstr.2019.20.003448 .
Chukwu E, Garg L. A systematic review of blockchain in healthcare: frameworks, prototypes, and implementations. IEEE Access. 2020;8:21196–214. https://doi.org/10.1109/ACCESS.2020.2969881 .
Cichosz SL, Stausholm MN, Kronborg T, Vestergaard P, Hejlesen O. How to use blockchain for diabetes health care data and access management: an operational concept. J Diabetes Sci Technol. 2019;13(2):248–53. https://doi.org/10.1177/1932296818790281 .
Coppola L, Cianflone A, Grimaldi AM, Incoronato M, Bevilacqua P, Messina F, et al. Biobanking in health care: evolution and future directions. J Transl Med. 2019;17(1):1–18. https://doi.org/10.1186/s12967-019-1922-3 .
Cunningham J, Ainsworth J. Enabling patient control of personal electronic health records through distributed ledger technology. Stud Health Technol Inf. 2017;245:45–8. https://doi.org/10.3233/978-1-61499-830-3-45 .
Daraghmi E, Daraghmi YA, Yuan SM. MedChain: a design of blockchain-based system for medical records access and permissions management. IEEE Access. 2019;7:164595–613. https://doi.org/10.1109/ACCESS.2019.2952942 .
Ding S, Cao J, Li C, Fan K, Li H. A novel attribute-based access control scheme using blockchain for IoT. IEEE Access. 2019;7:38431–41. https://doi.org/10.1109/ACCESS.2019.2905846 .
Dubovitskaya A, Novotny P, Xu Z, Wang F. Applications of blockchain technology for data-sharing in oncology: results from a systematic literature review. Oncology. 2020;98(6):403–11. https://doi.org/10.1159/000504325 .
El Majdoubi D, El Bakkali H, Sadki S, Maqour Z, Leghmid A. The systematic literature review of privacy-preserving solutions in smart healthcare environment. Secur Commun Netw. 2022;2022:1–26.
El Sayed, A. I. Abdelaziz, M. Megahed, H. and M. Azeem HA. A new supervision strategy based on blockchain for electronic health records. In: 2020 12th international conference on electrical engineering (ICEENG); 2020. p. 151–6. https://doi.org/10.1109/ICEENG45378.2020.9171765 .
Faber B, Michelet GC, Weidmann N, Mukkamala RR, Vatrapu R. BPDIMS: a blockchain-based personal data and identity management system. In: Proceedings of the 52nd Hawaii International conference on system sciences; 2019. https://doi.org/10.24251/hicss.2019.821
Fatokun T, Nag A, Sharma S. Towards a blockchain assisted patient owned system for electronic health records. Electronics. 2021;10(580):1–14.
Fu J, Wang N, Cai Y. Privacy-preserving in healthcare blockchain systems based on lightweight message sharing. Sensors. 2020;20(7):1–16. https://doi.org/10.3390/s20071898 .
Ghazvini A, Shukur Z. Security challenges and success factors of electronic healthcare system. Procedia Technol. 2013;11:212–9. https://doi.org/10.1016/j.protcy.2013.12.183 .
Gong J, Zhao L. Blockchain application in healthcare service mode based on Health Data Bank. Front Eng Manag. 2020;7(4):605–14. https://doi.org/10.1007/s42524-020-0138-9 .
Article MathSciNet Google Scholar
Guan Z, Zhang Y, Wu L, Wu J, Li J, Ma Y, Hu J. APPA: an anonymous and privacy preserving data aggregation scheme for fog-enhanced IoT. J Netw Comput Appl. 2019;125:82–92. https://doi.org/10.1016/j.jnca.2018.09.019 .
Hang L, Choi E, Kim D. A Novel EMR Integrity management based on a medical blockchain platform in hospital. Electronics. 2019;8(467):1–27.
Hardin T, Kotz D. Blockchain in health data systems: a survey. In: 2019 6th international conference on internet of things: systems, management and security. IEEE; 2019. p. 490–7.
Hasselgren A, Kralevska K, Gligoroski D, Pedersen SA, Faxvaag A. Blockchain in healthcare and health sciences—a scoping review. Int J Med Inf. 2020;134: 104040. https://doi.org/10.1016/j.ijmedinf.2019.104040 .
Hoy MB. An introduction to the blockchain and its implications for libraries and medicine. Medical Ref Serv Quart. 2017. https://doi.org/10.1080/02763869.2017.1332261 .
Irving G, Holden J. How blockchain-timestamped protocols could improve the trustworthiness of medical science [version 3; referees: 3 approved]. F1000Research. 2017;5(1):1–7. https://doi.org/10.12688/f1000research.8114.1 .
Ismail L, Materwala H, Zeadally S. Lightweight blockchain for healthcare. IEEE Access. 2019;7:149935–51. https://doi.org/10.1109/ACCESS.2019.2947613 .
Jaiswal P, Agarwal S. Blockchain based safe electronic medical records. Int J Creat Res Thoughts. 2021;9(7):503–10.
Jayabalan M, Daniel TO. Access control and privilege management in electronic health record: a systematic literature review. J Med Syst. 2016;40(12):1–9. https://doi.org/10.1007/s10916-016-0589-z .
Jiang S, Wu H, Wang L. Patients-controlled secure and privacy-preserving EHRs sharing scheme based on consortium blockchain. In: 2019 IEEE global communications conference; 2019. p. 1–6. https://doi.org/10.1109/GLOBECOM38437.2019.9013220
Khatoon A. A blockchain-based smart contract system for healthcare management. Electronics. 2020;9(1):94. https://doi.org/10.3390/electronics9010094 .
Kim M, Yu S, Lee J, Park Y, Park Y. Design of secure protocol for cloud-assisted electronic health record system using blockchain. Sensors. 2020;20(10):1–21. https://doi.org/10.3390/s20102913 .
Kitchenham B, Brereton OP, Budgen D, Turner M, Bailey J, Linkman S. Systematic literature reviews in software engineering—a systematic literature review. Inform Softw Technol. 2009;51(1):7–15.
Koshechkin KA, Klimenko GS, Ryabkov IV, Kozhin PB. Scope for the application of blockchain in the public healthcare of scope for the application of blockchain in the public healthcare of the russian federation the russian federation. Procedia Comput Sci. 2018;126:1323–8. https://doi.org/10.1016/j.procs.2018.08.082 .
Li J, Dun W. Range query in blockchain-based data sharing model for electronic medical records. J Phys: Conf Ser. 2020;1634(1):1–8. https://doi.org/10.1088/1742-6596/1634/1/012035 .
Magyar G. Blockchain: Solving the privacy and research availability tradeoff for EHR data: a new disruptive technology in health data management. In: 2017 IEEE 30th Neumann Colloquium Budapes; 2017. p. 000135–000140. https://doi.org/10.1109/NC.2017.8263269 .
Margheri A, Masi M, Miladi A, Sassone V, Rosenzweig J. Decentralised provenance for healthcare data. Int J Med Inf. 2020;141: 104197. https://doi.org/10.1016/j.ijmedinf.2020.104197 .
Marques ICP, Ferreira JJM. Digital transformation in the area of health: systematic review of 45 years of evolution. Health Technol. 2020;10:575–86. https://doi.org/10.1007/s12553-019-00402-8 .
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Mohsin AH, Zaidan AA, Zaidan BB, Albahri OS, Albahri AS, Alsalem MA, Mohammed KI. Computer standards & interfaces blockchain authentication of network applications: taxonomy, classification, capabilities, open challenges, motivations, recommendations and future directions. Comput Standards Interfaces. 2019;64:41–60. https://doi.org/10.1016/j.csi.2018.12.002 .
Nagasubramanian G, Sakthivel RK, Patan R, Gandomi AH, Sankayya M, Balusamy B. Securing e-health records using keyless signature infrastructure blockchain technology in the cloud. Neural Comput App. 2020;32(3):639–47. https://doi.org/10.1007/s00521-018-3915-1 .
Nazir S, Khan S, Khan HU, Ali S, García-Magariño I, Atan RB, Nawaz M. A comprehensive analysis of healthcare big data management, analytics and scientific programming. IEEE Access. 2020;8:95714–33. https://doi.org/10.1109/ACCESS.2020.2995572 .
Nguyen DC, Pathirana PN, Ding M, Seneviratine A. Blockchain for secure EHRs sharing of mobile cloud based E-health systems. IEEE Access. 2019;7:66792–806. https://doi.org/10.1109/ACCESS.2019.2917555 .
Niu S, Chen L, Wang J, Yu F. Electronic health record sharing scheme with searchable attribute-based encryption on blockchain. IEEE Access. 2020;8:7195–204. https://doi.org/10.1109/ACCESS.2019.2959044 .
Noel R, Taramasco C, Marquez G. Standards, processes, and tools used to evaluate the quality of health information systems: systematic literature review. J Med Internet Res. 2022;24(3):1–11. https://doi.org/10.2196/26577 .
Nortey RN, Yue L, Agdedanu PR, Adjeisah M. Privacy module for distributed electronic health records(EHRs) using the blockchain. In: 2019 4th IEEE international conference on big data analytics; 2019. p. 369–74. https://doi.org/10.1109/ICBDA.2019.8713188
Pandey P, Litoriya R. Securing and authenticating healthcare records through blockchain technology. Cryptologia. 2020;44(4):341–56. https://doi.org/10.1080/01611194.2019.1706060 .
Premkamal PK, Pasupuleti SK, Alphonse PJ. A new verifiable outsourced ciphertext-policy attribute based encryption for big data privacy and access control in cloud. J Ambient Intell Humaniz Comput. 2019;10(7):2693–707. https://doi.org/10.1007/s12652-018-0967-0 .
Qin D, Ji P, Yang S, Berhane TM. An efficient data collection and load balance algorithm in wireless sensor networks. Wireless Netw. 2018;25(7):3703–14. https://doi.org/10.1007/s11276-017-1652-5 .
Quaini T, Roehrs A, da Costa CA, Righi RR. A Model for Blockchain-Based Distributed Electronic Health Records. IADIS Int J WWW/Internet. 2019;16(2):66–79.
Rajput AR, Li Q, Ahvanooey MT, Masood I. EACMS: emergency access control management system for personal health record based on blockchain. IEEE Access. 2019;7:84304–17. https://doi.org/10.1109/ACCESS.2019.2917976 .
Ramachandran S, Ramasamy A, Mukherjee S. Management of electronic health records. In: Proceedings of the international conference on smart electronics and communication. IEEEXplore; 2020. p. 341–346.
Riadi I, Ahmad T, Sarno R, Purwono P, Ma’arif A. Developing data integrity in an electronic health record system using blockchain and interplanetary file system (case study: COVID-19 data). Emerg Sci J. 2022;4:190–206.
Roehrs A, da Costa CA, da Rosa RR, da Silva VF, Goldim JR, Schmidt DC. Analyzing the performance of a blockchain-based personal health record implementation. J Biomed Inform. 2019;92:1–9. https://doi.org/10.1016/j.jbi.2019.103140 .
Roehrs A, Da Costa CA, Da Rosa RR, De Oliveira KSF. Personal health records: A systematic literature review. J Med Internet Res. 2017;19(1):1–22. https://doi.org/10.2196/jmir.5876 .
Shamshad S, Mahmood K, Kumari S, Chen CM. A secure blockchain-based e-health records storage and sharing scheme. J Inf Secur App. 2020;55: 102590. https://doi.org/10.1016/j.jisa.2020.102590 .
Shen B, Guo J, Yang Y. MedChain: efficient healthcare data sharing via blockchain. Appl Sci. 2019;9(6):1207.
Sun J, Ren L, Wang S, Yao X. A blockchain-based framework for electronic medical records sharing with fine-grained access control. PLoS ONE. 2020;15(10):1–23. https://doi.org/10.1371/journal.pone.0239946 .
Sun Y, Zhang R, Wang X, Gao K, Liu L. A decentralizing attribute-based signature for healthcare blockchain. In: 2018 27th international conference on computer communication and networks; 2018. pp. 1–9. https://doi.org/10.1109/ICCCN.2018.8487349
Tang F, Ma S, Xiang Y, Lin C. An efficient authentication scheme for blockchain-based electronic health records. IEEE Access. 2019;7:41678–89. https://doi.org/10.1109/ACCESS.2019.2904300 .
Tanwar S, Parekh K, Evans R. Blockchain-based electronic healthcare record system for healthcare 4.0 applications. J Inf Secur App. 2020;50:102407. https://doi.org/10.1016/j.jisa.2019.102407 .
Tith D, Lee J, Suzuki H, Wijesundara WMAB, Taira N, Obi T, Ohyama N. Patient consent management by a purpose-based consent model for electronic health record based on blockchain technology. Healthc Inf Res. 2020;26(4):265–73.
Tripathi G, Ahad MA, Paiva S. S2HS—a blockchain based approach for smart healthcare system. Healthcare. 2020;8(1): 100391. https://doi.org/10.1016/j.hjdsi.2019.100391 .
Uddin MA, Stranieri A, Gondal I, Balasubramanian V. Continuous patient monitoring with a patient centric agent: a block architecture. IEEE Access. 2018;6:32700–26. https://doi.org/10.1109/ACCESS.2018.2846779 .
Usman M, Qamar U. Secure electronic medical records storage and sharing using blockchain technology. Procedia Comput Sci. 2020;174:321–7. https://doi.org/10.1016/j.procs.2020.06.093 .
Verdonck M, Poels G. Architecture and value analysis of a blockchain-based electronic health record permission management system. In: 14th international workshop on value modelling and business ontologies; 2020. 2574:16–24.
Vora J, Nayyar A, Tanwar S, Tyagi S, Kumar, N., Obaidat, MS, Rodrigues, JJPC. BHEEM: a blockchain-based framework for securing electronic health records. In: 2018 IEEE Globecom Workshops. IEEE; 2018. p. 1–6.
Wang S, Wang J, Wang X, Qiu T, Yuan Y, Ouyang L, et al. Blockchain-powered parallel healthcare systems based on the ACP approach. IEEE Trans Comput Soc Syst. 2018. https://doi.org/10.1109/TCSS.2018.2865526 .
Wehbe Y, Zaabi MAl, Svetinovi D, Member S. Blockchain AI framework for healthcare records management : constrained goal model. In: 2018 26th telecommunications forum (TELFOR); 2018. p. 420–5.
Wu S, Du J. Electronic medical record security sharing model based on blockchain. ACM international conference proceeding series; 2019. p. 13–17. https://doi.org/10.1145/3309074.3309079
Yang G, Li C, Marstein KE. A blockchain-based architecture for securing electronic health record systems. Concurr Comput Pract Exp. 2021;33:1–10. https://doi.org/10.1002/cpe.5479 .
Yang J, Onik MH, Lee N, Ahmed M, Kim C. Proof-of-familiarity: a privacy-preserved blockchain scheme for collaborative medical decision-making. Appl Sci. 2019;9(1370):1–24. https://doi.org/10.3390/app9071370 .
Yang X, Li T, Pei X, Wen L, Wang C. Medical data sharing scheme based on attribute cryptosystem and blockchain technology. IEEE Access. 2020;8:45468–76. https://doi.org/10.1109/ACCESS.2020.2976894 .
Yim W, Wheeler AJ, Curtin C, Wagner TH. Secondary use of electronic medical records for clinical research: challenges and opportunities Secondary use of electronic medical records for clinical research: challenges and opportunities. Convergent Sci Phys Oncol. 2018;4:1–11. https://doi.org/10.1088/2057-1739/aaa905 .
Zhang A, Lin X. Towards secure and privacy-preserving data sharing in e-health systems via consortium blockchain. J Med Syst. 2018. https://doi.org/10.1007/s10916-018-0995-5 .
Zhao H, Zhang Y, Peng Y, Xu R. Lightweight backup and efficient recovery scheme for health blockchain keys. In: 2017 IEEE 13th international symposium on autonomous decentralized systems; 2017. p. 229–34. https://doi.org/10.1109/ISADS.2017.22
Zheng X, Mukkamala RR., Vatrapu R, Ordieres-Mere J. Blockchain-based Personal Health Data Sharing System Using Cloud Storage. In: 2018 IEEE 20th international conference on e-health networking, applications and services. IEEE; 2018. p. 1–6. https://doi.org/10.1109/HealthCom.2018.8531125
Zhou L, Wang L, Sun Y. MIStore: a blockchain-based medical insurance storage system. J Med Syst. 2018;42(8):1–7.
Zou R, Lv X, Zhao J. SPChain: blockchain-based medical data sharing and privacy-preserving eHealth system; 2020. arXiv preprint arXiv:2009.09957 .
Download references
Acknowledgements
We sincere acknowledge our reviewers for their candid and valuable contributions to the manuscript.
Author information
Authors and affiliations.
Department of Cyber Security Science, Federal University of Technology, Minna, Nigeria
Umar Abdulkadir, Victor Onomza Waziri & Idris Ismaila
Department of Computer Science, Federal University of Technology, Minna, Nigeria
John Kolo Alhassan
You can also search for this author in PubMed Google Scholar
Contributions
Corresponding author.
Correspondence to Umar Abdulkadir .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the topical collection “Security and Privacy 2020” guest edited by Pantelimon Stanica, Odelu Vanga and Sumit Kumar Debnath.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Abdulkadir, U., Waziri, V.O., Alhassan, J.K. et al. Electronic Medical Records Management and Administration: Current Trends, Issues, Solutions, and Future Directions. SN COMPUT. SCI. 5 , 460 (2024). https://doi.org/10.1007/s42979-024-02803-7
Download citation
Received : 28 September 2021
Accepted : 16 March 2024
Published : 20 April 2024
DOI : https://doi.org/10.1007/s42979-024-02803-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical records
- Access permission scheme
- Data administration
Advertisement
- Find a journal
- Publish with us
- Track your research
- All Publications
- Priorities Magazine Spring 2018
- The Next Plague and How Science Will Stop It
- Priorities Magazine Winter 2018
- Priorities Magazine Fall 2017
- Little Black Book of Junk Science
- Priorities Magazine Winter 2017
- Should You Worry About Artificial Flavors Or Colors?
- Should You Worry About Artificial Sweeteners?
- Summer Health and Safety Tips
- How Toxic Terrorists Scare You With Science Terms
- Adult Immunization: The Need for Enhanced Utilization
- Should You Worry About Salt?
- Priorities Magazine Spring 2016
- IARC Diesel Exhaust & Lung Cancer: An Analysis
- Teflon and Human Health: Do the Charges Stick?
- Helping Smokers Quit: The Science Behind Tobacco Harm Reduction
- Irradiated Foods
- Foods Are Not Cigarettes: Why Tobacco Lawsuits Are Not a Model for Obesity Lawsuits
- The Prevention and Treatment of Osteoporosis: A Review
- Are "Low Dose" Health Effects of Chemicals Real?
- The Effects of Nicotine on Human Health
- Traditional Holiday Dinner Replete with Natural Carcinogens - Even Organic Thanksgiving Dinners
- A Primer On Dental Care: Quality and Quackery
- Nuclear Energy and Health And the Benefits of Low-Dose Radiation Hormesis
- Priorities in Caring for Your Children: A Primer for Parents
- Endocrine Disrupters: A Scientific Perspective
- Good Stories, Bad Science: A Guide for Journalists to the Health Claims of "Consumer Activist" Groups
- A Comparison of the Health Effects of Alcohol Consumption and Tobacco Use in America
- Moderate Alcohol Consumption and Health
- Irradiated Foods Fifth Edition
- Media/Contact
- Write For Us
Thinking Out Loud: Electronic Health Records
Related articles.
Electronic Health Records (EHRs) were once hailed as the solution to streamlining healthcare processes, but their implementation has brought forth a host of challenges. From increased work burden and clinician burnout to facilitated medical errors, the journey of EHRs has been tumultuous. With billions invested and a staggering increase in adoption rates, we find ourselves retrofitting the system, but this isn't just about optimizing technology; it's about preserving the heart of healthcare.

“The implementation of EHR technology may be the root cause of some of these issues, [increased work burden, negative clinician emotions, burnout, and facilitated medical errors] beginning with developers designing a product based upon an organizational strategic vision, which routinely desires regulation compliance, billing productivity, and organizational growth.”
Now, after 15 years, $27 billion in “incentives,” and an 11-fold increase in electronic health record (EHR) implementations, we are left to fix “the plane as it continues to fly.” A new study looks at how one health system tried to optimize their EHR usability. In conjunction with the health systems IT group, a family medicine department created teams to look at daily workflow, including care coordination, communications, reception, medication, notes, nursing, order and referrals, and revenue. The study looks at what changes were made and how the metrics improved.
Those metrics tell the entire story. The included
“Monthly departmental measurements of productivity (number of departmental visits, charges, and payments).”
While the researchers' concerns do include increased work burden, which can be measured by productivity, none of these measures, all of which serve revenue, address burnout, negative clinical emotions or facilitated medical error. The problem with EHRs, primarily billing algorithms with a side effect of documentation, remains a feature, not a bug.
Changes included:
- 34% were accommodations – workflow adjustments made to human workflows for the EHR’s design
- 10% were creations – new workflows added by IT
- 43% were discovery – workflows already present but previously unknown to the department
- 11% were modifications – workflow adjustments made to the EHR for human needs
The workgroups made three times as many changes to how healthcare workers did their work to meet the needs of the EHR than to how the EHR worked to meet human needs. As the researcher conclude
“Sadly, the second largest proportion of optimizations (35%) were accommodations by the department adjusting workflow issues outside of the EHR. … Accepting the limitations within the EHR and working around them …”
As to the changes the EHR has made to human behavior,
“The IT-remedied interventions [Modifications] were surprisingly few in number …changes were predominately compiling department-specific order entry preference lists (i.e., medications … and orders) based on the most utilized departmental options … [ameliorating] the fundamental issue of clinicians having an overabundance of options, which resulted in orders being abandoned.”
It makes you wonder who the tool is.
The other significant change was in the discovery of workflow that was already present and previously unknown to the system users. The researchers described this as a “disconnect,” a “well-established problem” that continually occurs. The value of the EHR as a new tool comes from its full implementation. That this is a “well-established problem” speaks to the failure of the companies feeding from that $27 billion to provide a usable product.
But all is not lost; all three revenue-related outcomes, visits, charges, and payments ultimately increased. The fundamental role of the EHR, a documentation and billing system, remains undeterred.
I would like to mention my conflict of interest in these issues. I was part of the workgroups attempting to implement an EHR in my hospital. None of these user issues were unknown at the time, now well over a decade ago. It is dispiriting but unsurprising that they remain uncorrected. The headlong rush to AI is another chapter in this IT transformation of health care. Silicon Valley is known for “Move fast and break things,” that is what it has done to health care in implementing EHRs. It is what they are doing now as they rush AI into any number of interfaces between physicians, nurses, and patients. It is breaking the canaries in the healthcare mines, so burnout has increasingly become a concern for physicians and nurses. The IT companies that, in conjunction with the government, have imposed these ill-designed, poorly implemented systems upon us need to be held accountable. Unfortunately, like Boeing, they are too influential to fail.
Source: Optimization of Electronic Health Record Usability Through a Department-Led Quality Improvement Process Annals of Family Medicine DOI: 0.1370/afm.3073
View the discussion thread.

By Chuck Dinerstein, MD, MBA
Director of Medicine
Dr. Charles Dinerstein, M.D., MBA, FACS is Director of Medicine at the American Council on Science and Health. He has over 25 years of experience as a vascular surgeon.
Latest from Chuck Dinerstein, MD, MBA :
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Mortality in Patients Hospitalized for COVID-19 vs Influenza in Fall-Winter 2023-2024
- 1 Clinical Epidemiology Center, VA St Louis Health Care System, St Louis, Missouri
In the first year of the COVID-19 pandemic, risk of death in people hospitalized for COVID-19 was substantially higher than in people hospitalized for seasonal influenza. 1 , 2 The risk of death due to COVID-19 has since declined. In fall-winter 2022-2023, people hospitalized for COVID-19 had a 60% higher risk of death compared with those hospitalized for seasonal influenza. 3 New variants of SARS-CoV-2 have continued to appear, including the emergence of JN.1, the predominant variant in the US since December 24, 2023. 4 This study evaluated the risk of death in a cohort of people hospitalized for COVID-19 or seasonal influenza in fall-winter 2023-2024.
Read More About
Xie Y , Choi T , Al-Aly Z. Mortality in Patients Hospitalized for COVID-19 vs Influenza in Fall-Winter 2023-2024. JAMA. Published online May 15, 2024. doi:10.1001/jama.2024.7395
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Frontiers in Cardiovascular Medicine
- Thrombosis and Haemostasis
- Research Topics
The Current Role of Inflammatory and Thrombotic Biomarkers in Myocardial Infarction
Total Downloads
Total Views and Downloads
About this Research Topic
Coronary artery disease (CAD) is the leading cause of death worldwide with acute myocardial infarction. (MI) representing the clinical condition associated with the greatest morbidity and mortality, up to 30% of in-hospital deaths. Prompt reperfusion with percutaneous coronary intervention (PCI), advances in acute cardiovascular care and more effective medical therapy have improved the prognosis of patients with MI in the last years. This increased survival revealed a previously unrecognized short- and long-term risk of recurrent cardiovascular events despite optimal medical therapy. Indeed, almost one-fifth of MI patients suffer from rehospitalization within 1 year, and 10% from recurrent MI. There is, therefore, a growing need for a more accurate risk stratification of MI patients to identify those at higher risk for adverse events and worse prognosis. Current guidelines of the American Heart Association and the European Society of Cardiology highlighted the lack of useful biomarkers to predict in-hospital complications and short/long term prognosis of patients with MI, recommending for this purpose only to measure troponin and brain natriuretic peptide (BNP) serum levels, with the latter associated with a low level of evidence. During the last decades, several studies, mostly conducted in the 90s before the routine use of dual antiplatelet therapy, described the pivotal and prognostic role of coronary thrombosis and hypercoagulable state in the pathophysiology of MI, correlating increased inflammatory and coagulation activity with recurrent event and poor outcome after MI. Despite many studies published, conclusive data on the real usefulness and additional value of biomarkers in the management of patients with MI are lacking. The aim of this article collection is to provide new evidence and summarize current evidence on the potential prognostic role of inflammatory and thrombotic biomarkers in patients with acute coronary syndrome.
Keywords : biomarkers, myocardial infarction, thrombosis, thrombotic biomarkers, coronary artery disease
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, submission deadlines, participating journals.
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Fam Physician
- v.61(10); 2015 Oct
Do electronic medical records improve quality of care?
Electronic medical records (EMRs) have had a positive effect on patient care and the work lives of family physicians.
Over the past few decades our medical knowledge has increased. More investigative and treatment options are available; as a result our patients are living longer and we are dealing with more chronic conditions. Family physicians cannot “know all things” nor can we be “all things to all patients.” To adequately address our patients’ complex needs, we need good sources of information and good relationships, including access to a multidisciplinary team of professionals and other specialists. We need tools that improve access to information and relationships. We have had to transform how we practise, and the EMR, with its associated information technology, has facilitated that transformation. It is no longer the early adopters or innovators who are using the EMR, as 75% of physicians responding to the 2014 National Physician Survey were using EMRs. 1 Of those, 65% indicated that patient care improved and less than 5% indicated a negative effect on the quality of care they provided. 1 However, there are still a few laggards who will argue against using EMRs. They will argue that there is no evidence EMRs have a positive effect on the health of their patients, or that implementing EMRs in their practices will reduce efficiency and negatively affect their patient flow.
Better informed
The EMR technology gives health care providers information in formats that were not possible with paper charts. Primary care providers can now view and print graphs of values such as weight, cholesterol levels, and blood pressure, tracking changes over time. The EMR improves attainment of chronic disease management, prevention, and screening targets, as shown in studies that demonstrated improved quality measures. 2 Electronic medical records can provide treatment goals or alerts to remind providers when certain prevention and screening maneuvers are due or out of date. The EMR also provides access to information and resources that point primary care providers toward the best approach to the various conditions they encounter in practice. With improved access to laboratory data there is a reduction in duplication and costs. 3 Disease outcomes can be improved, as shown by a randomized clinical trial of 21 practices that demonstrated a reduction in blood pressure in patients with hypertension who received screening for and advice on high-risk drinking, alcohol abuse, or alcohol dependence through an EMR intervention. 4 Numerous resources and tools, such as assessments for drug interactions, Framingham calculators, and body mass index calculators, can be accessed quickly to better inform clinicians and their patients. These benefits are not lost on patients, as patients’ perceptions of the quality of care that they receive have been positively associated with the use of EMRs. 5
The structured EMR data provide the potential to access point-of-care data that can be used to inform practice and conduct research. With meaningful use, including standard and consistent data entry in specific fields, the EMR data provide the physician with valuable practice-level information. This information can be used for practice-level interventions such as identifying patients who have not received bowel cancer screening or mammograms. The information provides feedback to the primary care providers about the quality of their care, such as screening rates and preventive target achievements. Point-of-care EMR data can be used to study issues in primary care, as demonstrated by the work of the Canadian Primary Care Sentinel Surveillance Network. Detailed analysis of EMR data on medications used in the primary care setting provides new information such as drug repurposing signals, as demonstrated in a recent study that identified a decrease in mortality in cancer patients treated with metformin. 6
Improved relationships
The EMR improves communication and relationships between family physicians and their multidisciplinary team members. 7 Chart summaries, medical notes, and consultation letter templates provide consultants and various team members with legible, structured information. The prescriptions are in a clear and structured format, which reduces medical errors in prescribing. 3 Electronic medical records facilitate requests and task assignment to various team members. Booking schedules are easily accessed by clinical staff, clinicians, and, in some cases, patients who might be able to book appointments remotely. Electronic medical records might also improve communication with patients through the use of patient portals and personal health records, which more effectively engage patients in managing their own care. 8
Beneficial effect on work flow
The effect of EMRs on the work lives of family physicians has been positive, as demonstrated by physicians’ largely favourable perceptions of EMRs. 1 , 9 Although the implementation of an EMR can lead to a subjective feeling of increased time requirements by family physicians, studies have found that implementation does not result in a significant decrease in patient access 3 or a loss of billings. 10 Canadian EMR research suffers from variation in vendors, study context, methods, and outcome measures. However, despite these deficiencies, studies are emerging that demonstrate numerous benefits of the EMR. 3 The EMR allows clinicians to see a larger number of patients through better access to comprehensive patient histories that include clinical data, which might help physicians spend less time searching for results and reports. 3 The perceived benefits include remote access to patient charts, improved laboratory result availability, medication error alerts, and reminders for preventive care.
We now have a critical mass of EMR users. 1 We are at a tipping point and the positive effect will escalate with increased knowledge of how to use EMR systems in a meaningful way to their full potential, as well as improved system interoperability, with seamless exchange of information from one system to another. 1
CLOSING ARGUMENTS — YES
Donna P. Manca md Mc l s c fcfp
- Electronic medical records improve quality of care, patient outcomes, and safety through improved management, reduction in medication errors, reduction in unnecessary investigations, and improved communication and interactions among primary care providers, patients, and other providers involved in care.
- Electronic medical records improve the work lives of family physicians despite some subjective concerns about implementation costs and time. Electronic medical records have been demonstrated to improve efficiencies in work flow through reducing the time required to pull charts, improving access to comprehensive patient data, helping to manage prescriptions, improving scheduling of patient appointments, and providing remote access to patients’ charts.
- Electronic medical records capture point-of-care data that inform and improve practice through quality improvement projects, practice-level interventions, and informative research.
Cet article se trouve aussi en français à la page 850 .
Competing interests
None declared
The parties in these debates refute each other’s arguments in rebuttals available at www.cfp.ca . Join the discussion by clicking on Rapid Responses at www.cfp.ca .
- Open access
- Published: 29 May 2024
Ethnic disparities in complete and partial molar pregnancy incidence: a retrospective analysis of arab and jewish women in single medical center
- Ala Aiob 1 , 2 ,
- Dina Gumin 1 ,
- Inna Zilberfarb 1 ,
- Karina Naskovica 1 ,
- Inshirah Sgayer 1 , 2 ,
- Susana Mustafa Mikhail 1 , 2 ,
- Avishalom Sharon 1 , 2 &
- Lior Lowenstein 1 , 2
BMC Public Health volume 24 , Article number: 1440 ( 2024 ) Cite this article
Metrics details
Molar pregnancies, encompassing complete and partial moles, represent a rare and enigmatic gestational disorder with potential ethnic variations in incidence. This study aimed to investigate relations of ethnicity with risks of complete and partial molar pregnancies within an Israeli population while accounting for age differences.
A retrospective study was conducted of data recorded during 2007–2021 in an academic medical center in Israel. The study population comprised 167 women diagnosed with complete or partial moles, for whom data were obtained through histological examination and P57 immunostaining. Maternal age and ethnicity were extracted from electronic medical records. Incidence rates were calculated per 10,000 live births, and a nested case-control study compared demographic characteristics and molar pregnancy incidences between Arab and Jewish women. Statistical analyses included age-adjusted comparisons, relative risk calculations and multivariate logistic regression.
The overall risk of molar pregnancy was 22 per 10,000 live births (95% confidence interval [CI] 18–25). Among Arab women, the overall risk was 21 (95% CI 17–25), and for PM and CM: 14 (95% CI 11–17) and 7 (95% CI 5–10), respectively. Among Jewish women, the overall risk was 23 (95% CI 18–29), and for PM and CM: 12 (95% CI 8–17) and 11 (95% CI 7–16), respectively. Among Arab women compared to Jewish women, the proportion of all the partial moles was higher: (65.3% vs. 51.6%, p = 0.05). The incidence of partial mole was higher among Arab than Jewish women, aged 35–39 years (26 vs. 8 per 10,000, p = 0.041), and did not differ in other age groups. After adjusting for age, the relative risk of partial moles was lower among Jews than Arabs (0.7, 95% CI 0.4-1.0, p = 0.053). For Arab compared to Jewish women, the mean age at molar pregnancies was younger: 31.0 vs. 35.1 years. However, other factors did not differ significantly between Arab and Jewish women with molar pregnancies. In multivariate analysis, Jewish ethnicity was significantly associated with a higher risk of complete molar pregnancies (OR = 2.19, 95% CI 1.09–4.41, p = 0.028).
This study highlights ethnic differences in molar pregnancy risk within the Israeli population. Jewish ethnicity was associated with a higher risk of complete molar pregnancies, while Arab women had a significantly higher risk of partial moles. These findings underscore the need to consider ethnicity when studying gestational disorders. Further research should seek to elucidate the underlying factors contributing to these differences.
Peer Review reports
Molar pregnancy is a rare and enigmatic gestational disorder that is classified into two distinct entities: complete mole (CM) and partial mole (PM). These classifications are rooted in differences in gross morphology, histopathology and genetic characteristics [ 1 , 2 , 3 ]. A CM arises from either monospermic or dispermic fertilization of an anuclear oocyte, and is characterized by the absence of fetal tissue and marked trophoblastic hyperplasia [ 3 , 4 ]. Conversely, a PM results from dispermous fertilization of a normal ovum; and manifests focal trophoblastic hyperplasia, villous swelling and the presence of identifiable fetal tissue [ 1 , 2 , 3 , 4 , 5 ]. Despite the intricate classifications and increasing awareness, the incidence of molar pregnancy demonstrates substantial geographic variation. This raises the potential of underlying factors such as genetics, nutrition, socioeconomic status and methodological discrepancies, as have been described in previous studies [ 6 , 7 , 8 ].
The role of race and ethnicity in molar pregnancy risk remains an area of limited understanding. While early investigations noted an increased prevalence among Asian women residing in Hawaii [ 10 ], other studies have yielded inconclusive results regarding ethnic associations [ 9 , 11 ]. Furthermore, data about black and Hispanic women are notably sparse [ 12 , 13 , 14 , 15 ]. Notably, many of the relevant studies were conducted before the availability of advanced diagnostic tools, such as flow cytometry and immunohistochemical staining for p57. These tools have revolutionized diagnosing CM and PM accurately, especially in instances of equivocal histological findings [ 16 , 17 , 18 ].
In light of the abovementioned complexities and gaps in knowledge, we embarked on a rigorous hospital-based retrospective study within the confines of an academic medical center in Israel. Our primary objective was to explore the potential relations of ethnicity with the risks of CM and PM pregnancies. Given the well-established association between maternal age and molar pregnancy risk [ 19 , 20 , 21 ], we meticulously conducted an age-adjusted analysis to mitigate the confounding effects of variations in the age distribution of pregnant women across ethnicity groups.
Before commencing this research, we received approval from the Institutional Review Board (Helsinki Committee) of Galilee Medical Center and the Israeli Ministry of Health (authorization number 0147-21-NHR in 01/02/2022).
The study population encompassed all the women diagnosed during 2007–2021 with CM or PM at the Obstetrics and Gynecologic Department of Galilee Medical Center, Israel, a regional medical center. In all instances of surgical uterine evacuation, whether due to spontaneous or induced abortion, the products of conception underwent histological examination. The diagnoses were established by pathologists at our institution based on histopathological features. P57 immunostaining was performed in all samples of hydatidiform mole (HM). We excluded from the analysis women who were of another ethnicity or who were referred to our center due to persistent elevation of human chorionic gonadotropin or for treating gestational trophoblastic neoplasia. Molar pregnancies that occurred in conjunction with twin pregnancies were also excluded. To calculate the incidence of molar pregnancy per live birth, we identified in our hospital obstetrical database all the singleton live births that occurred during 2007–2021. Maternal age and ethnicity data were extracted from electronic medical records, with ethnicity categories defined as Arab, Jewish and another.
The primary aim of this retrospective cohort study was to determine the incidence of molar pregnancies in our population, focusing on live births over a specified period. The data accessed from medical files, encompassing an examination of demographic characteristics, gravidity, parity, pathology reports, ultrasonographic reports, and laboratory data for all the women included. The incidence of hydatidiform moles was calculated per the total number of deliveries at our institution during the study period. Molar pregnancies identified within the specified timeframe were juxtaposed against the total number of live births recorded. This enabled calculating molar pregnancy incidence rates per a specific unit of the population (e.g., per 10,000 live births).
In a nested case-control study, our aim was to assess potential risk factors associated with molar pregnancies, and to compare between Arab and Jewish women. In particular, we compared between these groups, demographic characteristics, including age distribution (< 20 years, 20–24 years, 25–29 years, 30–34 years, 35–39 years, and 40 years and over), and incidences of CM and PM. Ethnicity-specific risk estimates of CM and PM per 10,000 live births were calculated, accompanied by corresponding 95% Poisson confidence intervals (CIs). This facilitated assessing both the incidence and risk factors associated with molar pregnancies within the study population.
Statistical analysis: Categorical data are summarized using frequencies and percentages, and continuous variables with normal distributions are presented as means ± standard deviations. We reported median values and ranges for variables not adhering to the standard distribution assumption. We employed the chi-square or Fisher’s exact test to compare categorical variables between groups when the expected frequency was less than 5. To compare continuous variables between groups, we used the independent t-test when the data displayed a normal distribution, as determined by a histogram of the variable’s distribution shape. A significance level of P < 0.05 was deemed statistically significant. Categorical and ordinal variables were compared using the χ2 test. Crude and age-adjusted relative risks (RR) for CM and PM were estimated using univariate and multivariate logistic regression, respectively. The age group was included as a covariate in the multivariate analysis. Women of unknown/other races were included in the models, but the results were not reported due to their limited numbers and heterogeneous nature. Odds ratios (ORs) were assumed to be a suitable approximation of relative risk for these uncommon outcomes. The referent group for all the calculations of RR was the group of Arab women, given its larger size. We conducted all the statistical analyses using SPSS Version 27.0 software.
We identified 167 women who were followed for a molar pregnancy during the study period. Of them, 101 had PM and 66 had CM; 101 were Arab women, 64 were Jewish, and two were of another ethnicity. During the study period, 78,665 singleton live births were recorded.
The risk of any molar pregnancy (CM and PM) for the entire population was 22 per 10,000 live births (95% confidence interval [CI] 18–25). The risk of a CM was 9 per 10,000 live births (95% CI 7–11); and for a PM, 13 per 10,000 live births (95% CI 11–16). Among Arab women, the risk of any molar pregnancy (CM or PM) was 21 per 10,000 live births (95% CI 17–25). The risks of PM and CM were 14 (95% CI 11–17) and 7 (95% CI 5–10), respectively, per 10,000 live births. Among Jewish women, the risk of any molar pregnancy was 23 per 10,000 live births (95% CI 18–29). The risks of PM and CM were 12 (95% CI 8–17) and 11 (95% CI 7–16), respectively, per 10,000 live births.
Tables 1 and 2 compare the incidences of CM and PM between Arab and Jewish women according to six age groups (< 20 years, 20–24 years, 25–29 years, 30–34 years, 35–39 years, and 40 years and over). The incidence of PM was significantly higher among Arab than Jewish women in the age group of 35–39 years (26 vs. 8 per 10,000, p = 0.041), while no differences were observed in other age groups. The incidence of CM was higher among Jewish than Arab women in the age group of 25–29 years, although this difference only reached marginal significance (10 vs. 4 per 10,000, p = 0.083, one-sided 0.054).
Crude and age-adjusted relative risks (RRs) for CM and PM (considering Arab women as the reference group) are presented in Table 3 . After adjustment for age, Jewish compared to Arab women were less likely to have a PM (RR 0.7, 95% CI 0.4-1.0, p = 0.053). Compared to Arab women, Jewish women did not have a significantly higher risk of a CM (RR 1.3, 95% CI 0.8–2.2, p = 0.275).
Table 4 presents the characteristics of Arab and Jewish women who had molar pregnancies (CM and PM). The mean age of the Arab women with molar pregnancies was younger than that of the Jewish women: (31.0 vs. 35.1 years, p < 0.001). Among the Arab women, 65.3% of the molar pregnancies were PM and 34.7% were CM. Among the Jewish women, 51.6% of the molar pregnancies were PM and 48.4% were CM.
The gestational age at presentation with molar pregnancies did not differ between the Arab and Jewish women (9.4 ± 2.1 vs. 10 ± 2.5 weeks, p = 0.146). Neither did the groups differ in BMI, smoking habits, gravity, parity, history of abortions, or history of molar pregnancies. Beta human chorionic gonadotropin levels were also similar at presentation.
In multivariate analysis, considering mole type as the dependent variable, and ethnicity and age as independent variables, ethnicity was significantly associated with the risk of a CM pregnancy. The risk of a CM was higher among Jewish than Arab women (OR = 2.19, 95% CI 1.09–4.41, p = 0.028).
In this retrospective single-center study, the overall risk of molar pregnancies was 22 per 10,000 live births, with a breakdown of 9 for CM and 13 for PM. We identified differences between Arab and Jewish women in incidences of molar pregnancies, according to the type of molar pregnancy and age groups. The mean age was younger for Arab than Jewish women (31 vs. 35 years).
The incidence of PM was higher among Arab than Jewish women, in the 35-39-year age group. The incidence of CM moles was higher among Jewish than Arab women, in the 25-29-year age group, but the statistical significance of this difference was only marginal. After adjusting for age, Arab women had a significantly higher risk of PM. In multivariable analysis, the risk of a CM was more than two times higher among Jews than Arabs.
The incidence of molar pregnancy has been shown to vary across studies, including some that reported rates similar to ours. For example, Melamed et al. reported an incidence rate of 24 per 10,000 live births for any molar pregnancy, and 13 and 11 per 10,000 live births for CM and PM, respectively [ 22 ]. Others reported higher [ 6 ] or lower rates; 14 and 12 moles per 10,000 live births were reported in the Netherlands and Sweden, respectively [ 7 , 23 ]. These variations might be due to differences in population demographics, study methodologies and diagnostic criteria.
Regarding the younger age of Arab compared to Jewish women with molar pregnancies, we suggest that this may be due to cultural and social differences, including marriages at an early age among Arabs. This contrasts with a U.S. study by Lurain et al. [25] that did not find significant differences in the age distribution of molar pregnancies between ethnic groups (Caucasian and African American). Taken together, the data suggest that the ethnic differences in age distribution observed in our study may be specific to the Arab and Jewish populations under investigation.
We report differences between Arabs and Jews in mole types. Arab women tended to have a higher proportion of PM (65.3%), while Jewish women tended to have a higher proportion of CM (51.6%). Though these differences were marginally significant, they could indicate a possible role of ethnic background in the type of molar pregnancy.
The known correlation between molar pregnancy and age led us to perform an age-adjusted analysis and to compare Arabs and Jews. We identified significant differences between Arabs and Jews in the incidences of molar pregnancies across age groups. Specifically, for the ages 35–39 years, the incidence of PM was higher among Arab women; while for ages 25–29 years, the incidence of CM was higher among Jewish women. In a crude analysis, Jewish women had a higher risk of CM than Arab women, but this difference did not persist after adjusting for age.However, after adjusting for age, Arab compared to Jewish women had a significantly higher risk of PM.
In a multivariate analysis that considered the mole type as the dependent variable, and ethnicity and age as independent variables, ethnicity was significantly associated with the risk of CM pregnancy. Jewish women had a higher risk of a CM than Arab women, OR = 2.19. These findings are consistent with studies that showed correlations between ethnicity and molar pregnancy incidence; Melamed et al. revealed ethnic disparities between women in the United States. Asian compared to white women exhibited a higher likelihood of developing CM but were less likely to develop PM. Blacks were less likely than whites to develop PM and marginally less likely to develop CM. Similarly, Hispanics were less likely than whites to develop both CM and PM [ 22 ].. However, other studies found no significant differences in the incidence of molar pregnancies between ethnic groups [ 14 , 15 ]. These discrepancies may be due to variations in population characteristics and geographic regions.
To our knowledge, this is the first report to describe the difference in molar pregnancy incidence between Arab and Jewish women. Notably, the vast majority of women in the area of our medical center give birth and are treated there. Additionally, these two ethnic groups, Arab and Jewish Israelis, live in a relatively small defined geographic area in northern Israel (The Galilee); this can neutralize the geographic bias. Moreover, in all instances of surgical uterine evacuation for termination of pregnancy in our department, the product of conception was sent for histological evaluation for HM. This increases the accuracy of the incidence, although the reported rate approximates HM incidence. Nonetheless, the ideal incidence of HM should be calculated as a percentage of pregnancies and not only live births.
Certain limitations of our study should be acknowledged; foremost is its retrospective design. The study’s sample size and potential biases should be considered when interpreting the results. The marginally significant findings should be interpreted cautiously and definitive conclusions cannot be reached due to the relatively small sample size. Additional multicenter studies with larger sample sizes are needed. Notably, as our medical center is a regional referral center, the patient population may not represent the entire patient population. This raises the possibility of referral bias.
Overall, our findings suggest a possible relation between ethnicity and the risk of molar pregnancies, particularly CM. Jewish women had a higher risk of a CM than Arab women. In parallel, Arab women had a higher risk of PM after age adjustment. However, it is important to note that while these findings are intriguing, further research with larger sample size is needed to explore the underlying factors that might contribute to these differences and to determine whether similar patterns exist in other populations.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- Complete mole
- Partial mole
Hydatidiform mole
Berkowitz RS, Goldstein DP. Molar Pregnancy N Engl J Med. 2009;360:1639–45.
Article CAS PubMed Google Scholar
Seckl MJ, Sebire NJ, Berkowitz RS. Gestational trophoblastic disease. Lancet. 2010;376:717–29.
Article PubMed Google Scholar
Lewis GH, DeScipio C, Murphy KM, Haley L, Beierl K, Mosier S, Tandy S, Cohen DS, Lytwyn A, Elit L, Vang R, Ronnett BM. Characterization of androgenetic/biparental mosaic/chimeric conceptions, including those with a molar component: morphology, p57 immnohistochemistry, molecular genotyping, and risk of persistent gestational trophoblastic disease. Int J Gynecol Pathol. 2013;32(2):199–214. https://doi.org/10.1097/PGP.0b013e3182630d8c . PMID: 23370656.
Buza N, Hui P. Genotyping diagnosis of gestational trophoblastic disease: frontiers in precision medicine. Mod Pathol. 2021;34(9):1658–1672. https://doi.org/10.1038/s41379-021-00831-9 . Epub 2021 Jun 4. PMID: 34088998.
Fisher RA, Maher GJ. Genetics of gestational trophoblastic disease. Best Pract Res Clin Obstet Gynaecol. 2021;74:29–41. https://doi.org/10.1016/j.bpobgyn.2021.01.004 . Epub 2021 Feb 2. PMID: 33685819.
Lurain JR, Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole, Am. J. Obstet. Gynecol. 203 (, Altieri S, Franceschi J, Ferlay J, Smith C. La Vecchia, Epidemiology and etiology of gestational trophoblastic diseases, Lancet Oncol. 4 (2003) 670–678.
Lurain JR. Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol. 2010;203(6):531–9. Epub 2010 Aug 21. PMID: 20728069.
Gockley AA, Joseph NT, Melamed A, Sun SY, Goodwin B, Bernstein M, Goldstein DP, Berkowitz RS, Horowitz NS. Effect of race/ethnicity on clinical presentation and risk of gestational trophoblastic neoplasia in patients with complete and partial molar pregnancy at a tertiary care referral center. Am J Obstet Gynecol. 2016;215(3):334e. 1-6. Epub 2016 Apr 26. PMID: 27130239.
Article Google Scholar
Matsuura J, Chin D, Jacobs PA, et al. Complete hydatidiform mole in Hawaii: an epidemiological study. Genet Epidemiol. 1984;1:271–84.
Atrash HK, Hogue CJ, Grimes DA. Epidemiology of hydatidiform mole during early gestation. Am J Obstet Gynecol. 1986;154:906–9.
Yen S, MacMahon B. Epidemiologic features of trophoblastic disease. Am J Obstet Gynecol. 1968;101:126–32.
Hayashi K, Bracken MB, Freeman DH Jr., Hellenbrand K. Hydatidiform mole in the United States (1970–1977): a statistical and theoretical analysis. Am J Epidemiol. 1982;115:67–77.
Smith HO, Hilgers RD, Bedrick EJ, Qualls CR, Wiggins CL, Rayburn WF, et al. Ethnic differences at risk for gestational trophoblastic disease in New Mexico: a 25-year population-based study. Am J Obstet Gynecol. 2003;188:357–66.
Drake RD, Rao GG, McIntire DD, Miller DS, Schorge JO. Gestational trophoblastic disease among hispanic women: a 21-year hospital-based study. Gynecol Oncol. 2006;103:81–6.
Lund H, Nielsen S, Grove A, Vyberg M, Sunde L. p57 in Hydatidiform moles: evaluation of antibodies and expression in various cell types. Appl Immunohistochem Mol Morphol. 2020;28(9):694–701. https://doi.org/10.1097/PAI.0000000000000807 . PMID: 31567274; PMCID: PMC7664962.
Castrillon DH, Sun D, Weremowicz S, Fisher RA, Crum CP, Genest DR. Discrimination of complete hydatidiform mole from its mimics by immunohistochemistry of the paternally imprinted gene product p57kip2, am. J Surg Pathol. 2001;25:1225–30.
Article CAS Google Scholar
Atabaki Pasdar F, Khooei A, Fazel A, Rastin M, Tabasi N, Peirouvi T, Mahmoudi M. DNA flow cytometric analysis in variable types of hydropic placentas. Iran J Reprod Med. 2015;13(5):269–74. PMID: 26221125; PMCID: PMC4515233.
PubMed PubMed Central Google Scholar
Savage PM, Sita-Lumsden A, Dickson S, Iyer R, Everard J, Coleman R, Fisher RA, et al. The relationship of maternal age to molar pregnancy incidence, risks for chemotherapy and subsequent pregnancy outcome. J Obstet Gynecol. 2013;33:406–11.
Parazzini F, La Vecchia C, Pampallona S. Parental age and risk of complete and partial hydatidiform mole. Br J Obstet Gynecol. 1986;93:582–5.
Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews MS. Births: Final data for 2013. National vital statistics reports; vol 64 no 1. Hyattsville, MD: National Center for Health Statistics, 2015 (Available on line at http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_01.pdf accessed on November 9, 2015).
Melamed A, Gockley AA, Joseph NT, Sun SY, Clapp MA, Goldstein DP, Berkowitz RS, Horowitz NS. Effect of race/ethnicity on risk of complete and partial molar pregnancy after adjustment for age. Gynecol Oncol. 2016;143(1):73–6. Epub 2016 Jul 30. PMID: 27486130.
Eysbouts YK, Bulten J, Ottevanger PB, et al. Trends in incidence for gestational trophoblastic disease over the last 20 years in a population-based study. Gynecol Oncol. 2016;140:70–5.
Salehi S, Eloranta S, Johansson AL, Bergstrom M, Lambe M. Reporting and incidence trends of hydatidiform mole in Sweden 1973–2004. Acta Oncol. 2011;50:367–72.
Download references
Acknowledgements
Not applicable.
No external funding sources were utilized in support of this research. The study was conducted independently, and there were no contributions from any funding body in the design, data collection, analysis, interpretation, or manuscript writing.
Author information
Authors and affiliations.
Department of Obstetrics and Gynecology, Galilee Medical Center, POB 21, 22100, Nahariya, Israel
Ala Aiob, Dina Gumin, Inna Zilberfarb, Karina Naskovica, Inshirah Sgayer, Susana Mustafa Mikhail, Avishalom Sharon & Lior Lowenstein
Department of Obstetrics and Gynecology, Azrieli Faculty of Medicine, Bar Ilan University, Safed, Israel
Ala Aiob, Inshirah Sgayer, Susana Mustafa Mikhail, Avishalom Sharon & Lior Lowenstein
You can also search for this author in PubMed Google Scholar
Contributions
AA: Planning, Protocol development, data management, data analysis, manuscript writing and editing. DG: Protocol development, collection and management. IZ: Protocol development, data collection and management. KN: data collection and management. IS: Protocol development, data collection and management. SMM: Protocol development, data management, data analysis. AS; Protocol development, data management, data analysis, manuscript revision. LL: Protocol development, data management, data analysis, manuscript revision. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Ala Aiob .
Ethics declarations
Ethics approval and consent to participate.
We confirm that all experimental protocols conducted in this study have received approval from the Institutional Review Board (Helsinki Committee) of Galilee Medical Center and the Israeli Ministry of Health. The approval is documented with the reference number 0147-21-NHR, issued on 01/02/2022.
We confirm that all methods in this study align with the ethical standards outlined in the Declaration of Helsinki and its subsequent amendments.
In accordance with the retrospective nature of this study, informed consent was deemed unnecessary. The research involves the analysis of existing data without direct interaction with participants, and all data used are anonymized to ensure confidentiality. The Institutional Review Board (Helsinki Committee) of Galilee Medical Center and the Israeli Ministry of Health reviewed and approved this approach, reference number 0147-21-NHR.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Aiob, A., Gumin, D., Zilberfarb, I. et al. Ethnic disparities in complete and partial molar pregnancy incidence: a retrospective analysis of arab and jewish women in single medical center. BMC Public Health 24 , 1440 (2024). https://doi.org/10.1186/s12889-024-18276-5
Download citation
Received : 09 January 2024
Accepted : 05 March 2024
Published : 29 May 2024
DOI : https://doi.org/10.1186/s12889-024-18276-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Molar pregnancy
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Open access
- Published: 24 May 2024
Sex differences in electrolyte abnormalities indicating refeeding syndrome risk among hospitalized adolescents and young adults with eating disorders
- Jason M. Nagata 1 na1 ,
- Anthony Nguyen 1 na1 ,
- Ruben Vargas 1 ,
- Amanda E. Downey 1 , 2 ,
- Anita V. Chaphekar 1 ,
- Kyle T. Ganson 3 ,
- Sara M. Buckelew 1 &
- Andrea K. Garber 1
Journal of Eating Disorders volume 12 , Article number: 67 ( 2024 ) Cite this article
126 Accesses
11 Altmetric
Metrics details
Refeeding syndrome is the gravest possible medical complication in malnourished patients undergoing refeeding in the hospital. We previously reported that males with malnutrition secondary to eating disorders required more calories and had longer hospital stays than females; however, sex differences in electrolyte abnormalities indicating refeeding syndrome risk remain unknown. The objective of this study was to assess differences in electrolyte abnormalities indicating refeeding syndrome risk among male and female adolescents and young adults with eating disorders hospitalized for medical instability.
We retrospectively reviewed the electronic medical records of 558 patients aged 9–25 years admitted to the University of California, San Francisco Eating Disorders Program for medical instability between May 2012 and August 2020. Serum was drawn per standard of care between 5 and 7 am each morning and electrolyte abnormalities indicating refeeding syndrome risk were defined as: hypophosphatemia (< 3.0 mg/dL), hypokalemia (< 3.5 mEq/L), and hypomagnesemia (< 1.8 mg/dL). Logistic regression was used to assess factors associated with electrolyte abnormalities indicating refeeding syndrome risk.
Participants included 86 (15.4%) males and 472 (84.6%) females, mean (SD) age 15.5 (2.8) years. Rates of refeeding hypophosphatemia (3.5%), hypokalemia (8.1%), and hypomagnesemia (11.6%) in males hospitalized with eating disorders were low, with no statistically significant differences from females. Older age was associated with higher odds of refeeding hypophosphatemia and hypomagnesemia. Lower percent median body mass index and greater weight suppression at admission were associated with higher odds of refeeding hypophosphatemia.
Conclusions
Rates of electrolyte abnormalities indicating refeeding syndrome risk were low in males hospitalized for eating disorders and rates did not significantly differ from females. Together with our finding that males have higher caloric requirements and longer hospital length of stay, the finding that electrolyte abnormalities indicating refeeding syndrome risk were not greater in males than females supports future research to evaluate the safety and efficacy of higher calorie and/or faster advancing refeeding protocols for males.
Plain English Summary
Refeeding syndrome may arise as a life-threatening consequence of rapid refeeding in the setting of malnutrition. Most of the current literature and subsequent treatment protocols for managing nutritional rehabilitation and the risk of refeeding syndrome are focused on female populations. We previously showed that, compared to females, adolescent males with eating disorders need larger caloric requirements to restore medical stability. Here, we studied refeeding electrolyte abnormalities and did not find differences in male and female risk of developing refeeding electrolyte abnormalities. Older age was associated with higher odds of developing low phosphorus and low magnesium. Greater degree of malnutrition and greater weight suppression at admission were associated with higher odds of developing low phosphorus. Further studies are warranted to examine higher calorie and/or faster advancing refeeding protocols in males to assess for safety regarding development of electrolyte abnormalities indicating refeeding syndrome risk.
Introduction
Males with eating disorders face under-recognition and undertreatment leading to medical complications, inpatient hospitalizations, and high mortality rates [ 1 – 5 ]. While a growing body of literature highlights the need for screening and treatment strategies among males with eating disorders, data are limited to inform sex-specific guidelines for healthcare providers [ 6 , 7 , 8 ]. While the impact of refeeding strategies in adolescents and young adults is an area of rigorous study, only one study to date examined sex differences in refeeding outcomes and lengths of stay [ 9 ].
During inpatient medical hospitalization, patients with malnutrition undergo refeeding treatment to restore medical stability [ 10 ]. We showed that this process requires more kilocalories (kcal) in males than females [ 9 , 11 ]. However, the potential benefits of higher calorie refeeding protocols must be weighed against the risk of developing the refeeding syndrome, defined as a reduction in phosphorous, potassium, and/or magnesium, and subsequent organ dysfunction during the acute renourishment process [ 10 , 12 , 13 ]. Life-threatening organ dysfunction from refeeding syndrome can include cardiac failure, respiratory insufficiency, rhabdomyolysis, hemolysis, and seizures. While hypophosphatemia is viewed as a hallmark electrolyte abnormality associated with the risk of developing refeeding syndrome, hypomagnesemia appears more frequently and hypokalemia can also occur [ 13 , 14 , 15 , 16 , 17 ]. In a randomized control trial comparing the safety and efficacy of refeeding protocols, hypomagnesemia was the most common electrolyte shift, occurring at four times the rate of hypophosphatemia among individuals with low-calorie refeeding diets [ 12 ]. The American Society for Parenteral and Enteral Nutrition (ASPEN) recently defined the refeeding syndrome by the relative decrease in serum phosphorus, magnesium, and/or potassium, stratified as mild (10% decrease), moderate (20-30% decrease), and severe (> 30% decrease) [ 14 ]. Lack of a universally accepted definition has hampered the comparison of refeeding syndrome risk across studies and refeeding protocols [ 12 , 15 ].
Prior research on refeeding syndrome has identified low weight as a predictor of refeeding syndrome in patients with anorexia nervosa (AN) [ 20 , 21 , 22 ]; however, these study populations were predominantly female samples and could not stratify by sex [ 20 , 21 , 22 ]. Studies of refeeding syndrome in males with eating disorders have been limited to small sample sizes and case studies [ 19 , 23 ]. Studies are needed to fill this gap in the literature and support the development of clinical practice guidance for males with eating disorders [ 24 ]. The objective of this study was to determine the prevalence of refeeding hypophosphatemia, hypokalemia, and hypomagnesemia among a sample of male adolescents and young adults hospitalized for eating disorders and to compare sex differences in electrolyte abnormalities indicating refeeding syndrome risk. In the current study, we focus on the electrolyte abnormalities indicating refeeding syndrome risk rather than direct measures of organ dysfunction.
Study population
We reviewed the electronic medical records (EMRs) of 601 adolescents and young adults admitted for medical instability to an inpatient eating disorder service located at a tertiary care hospital in Northern California between May 22, 2012, and August 31, 2020. Patients ranged from age 9 to 25 at time of admission. Each patient met criteria for inpatient hospitalization based on guidelines set by the Society for Adolescent Health and Medicine, including low median body mass index (BMI) ≤ 75% for age and sex, severe bradycardia (< 50 beats/minute daytime, or < 45 beats/minute at night), hypotension (< 90/45 mmHg), hypothermia (< 96 °F, < 35.6 °C), and/or orthostasis (sustained increase in heart rate > 30 beats per minute in adults aged > 19 years, > 40 beats per minute in adolescents aged < 19 years, or sustained decreased blood pressure > 20 mmHg or > 10 mmHg diastolic) [ 7 , 24 ]. Eating disorder diagnoses were made by a clinical psychologist or psychiatrist using DSM-5 criteria. Prior to May 2013, a subset of our population was diagnosed with eating disorders using DSM-IV criteria (8% of patients). These diagnoses were subsequently reclassified by the study team to an appropriate DSM-5 diagnosis upon review of clinical and psychological characteristics. All patients admitted to our medical stabilization unit meet medical admission criteria as per guidance from the Society of Adolescent Health and Medicine (e.g. vital sign instability or malnutrition criteria) [ 7 ]. Exclusion criteria included patients who did not meet DSM-5 diagnostic criteria for an eating disorder during their hospitalization ( n = 43). The final sample included 558 patients.
Sociodemographic data, anthropometric measurements, illness characteristics, and weight history were documented in the EMR for each participant during their hospitalization as part of standard clinical care. Serum was typically drawn in the morning between 5 and 7 am within 24 h of hospital admission and then daily, including phosphorus, potassium, and magnesium levels. Initial height and weight at admission were used to calculate BMI, kg/m 2 . Calculated BMI and median BMI for age and sex were used to calculate the patient’s percent of median BMI. Weight suppression was defined as the difference between the patient’s highest reported weight per chart review and their admission weight, divided by patient’s highest reported weight.
Nutritional rehabilitation protocol
The Eating Disorders Program at the University of California, San Francisco follows specific protocols regarding admission criteria, laboratory evaluation, caloric prescriptions and diet escalation, food macronutrient content, physical activity allowance, and discharge criteria, in line with clinical guidance from the Society for Adolescent Health and Medicine [ 7 ]. Most patients commenced at 2,000 kcal/day and advanced by 200 kcal each day; we previously reported that average (SD) starting diet prescription was 1985 (233) kcal [ 9 ]. Electrolytes were checked daily in the morning for a minimum of seven days to evaluate for risk of developing refeeding syndrome (unless the patient was discharged in under seven days) [ 12 ]. Refeeding hypophosphatemia, hypokalemia, or hypomagnesemia were defined as phosphorus (< 3 mg/dL), potassium (< 3.5 mEq/L), or magnesium (< 1.8 mg/dL); combined refeeding risk refers to the presence of any one of these abnormalities. Refeeding syndrome risk was indicated by the incidence of electrolyte abnormalities beginning on day 2 in the hospital, after one full day of refeeding in the hospital (i.e., low potassium, magnesium, or phosphorus present at admission prior to the onset of the refeeding protocol were not included towards the classification of electrolyte abnormalities indicating refeeding syndrome risk, but the patients were still included in the study to evaluate for subsequent laboratory abnormalities). All laboratory samples were collected using a standardized protocol and analyzed at a Clinical Laboratory Improvement Amendments (CLIA)-certified laboratory, following federal standards and regulations [ 12 ]. In order to minimize electrolyte abnormalities due to purging, several protocols and precautions are implemented for any patient with a history of purging, including a patient care attendant observing the patient during all meals/snacks and for a period following the completion of the meal/snack, taping/sealing sinks in the room, and limiting showers to early mornings before meals.
This retrospective chart review involving human participants was approved by the Institutional Review Board (IRB) of the University of California, San Francisco (20-30323). All study components are in accordance with the ethical standards set by the 1963 Helsinki Declaration, its later amendments, and the institutional and national research committee.
Statistical analysis
Statistical data analysis was conducted using Stata 15.1 (StataCorp LP, College Station, TX). Unadjusted sex differences in continuous variables (e.g., age, BMI) were compared using independent sample t-tests. Unadjusted sex differences in categorical variables (e.g., race/ethnicity, eating disorder diagnosis) were compared using Chi-squared or Fisher’s exact tests. We examined rates of electrolyte abnormalities indicating refeeding syndrome risk in the entire sample and in the subsample with anorexia nervosa, restricting subtype.
We first ran simple logistic regression models to determine unadjusted associations between independent variables (male sex, age, ethnicity, eating disorder diagnosis, duration of illness, percent median BMI, weight suppression at admission, prescribed kcal at admission, and prescribed kcal at discharge) with refeeding hypophosphatemia, hypokalemia, hypomagnesemia, or a combined electrolyte abnormality variable separately. Additional logistic regression models adjusted for percent median BMI, which is standardized across sex and age and previously shown to relate to the risk of developing refeeding syndrome, were conducted for each outcome, respectively.
Table 1 describes the demographic and clinical characteristics of 86 (15.4%) male and 472 (84.6%) female study participants, stratified by sex. Mean age was 15.5 years, 59.7% identified as non-Hispanic white, and 63.6% had anorexia nervosa. Mean (SD) percent median BMI was 87.5 (14.2). Admission serum phosphorus, potassium, and magnesium did not differ by sex. Incidence of electrolyte abnormalities indicating refeeding syndrome risk were 8.1% hypophosphatemia, 10.6% hypokalemia, and 19.2% hypomagnesemia, with a combined risk of 26.5%. Although rates of refeeding hypophosphatemia (M = 3.5%, F = 8.9%, p = 0.090), hypokalemia (M = 8.1%, F = 11.0%, p = 0.425), hypomagnesemia (M = 11.6%, F = 20.6%, p = 0.053), and combined risk (M = 19.8%, F = 27.8%, p = 0.123) were lower in males than in females, the differences were not statistically significant and the effect sizes for the differences were small. Findings in the subsample with anorexia nervosa, restricting subtype were similar (Appendix A).
Table 2 identifies the factors associated with refeeding hypophosphatemia, hypokalemia, hypomagnesemia, and combined risk in both unadjusted models and models adjusted for percent median BMI. There were no significant associations with male (compared to female) sex. In unadjusted logistic regression models, older age (OR 1.18, 95% CI 1.06–1.30, p = 0.001), greater weight suppression at admission (OR 1.04, 95% CI 1.01–1.07, p = 0.003), and percent median BMI (OR 0.96, 95% CI 0.94–0.99, p = 0.004) were associated with refeeding hypophosphatemia. In models adjusted for percent median BMI in the same model, older age (OR 1.15, 95% CI 1.03–1.27, p = 0.009) and greater weight suppression at admission (OR 1.04, 95% CI 1.00–1.07, p = 0.024) remained associated with higher odds of refeeding hypophosphatemia. Older age was associated with refeeding hypomagnesemia in both unadjusted models (OR 1.10, 95% CI 1.02–1.18, p = 0.012) and models adjusted for percent median BMI (OR 1.09, 95% CI 1.02–1.18, p = 0.018). Additionally, older age showed an association with combined refeeding syndrome risk in both unadjusted models (OR 1.09, 95% CI 1.02–1.16, p = 0.012) and models adjusted for percent median BMI (OR 1.08, 95% CI 1.01–1.16, p = 0.025). None of the investigated factors were found to be associated with refeeding hypokalemia.
In this study of 558 adolescents and young adults, we did not find significant sex differences in electrolyte abnormalities as indicators of risk for developing the refeeding syndrome. Overall, rates of refeeding hypophosphatemia (3.5%), hypokalemia (8.1%), and hypomagnesemia (11.6%) in males hospitalized with eating disorders were similar to patients undergoing higher calorie refeeding (starting 2000 kcal) in a clinical trial [ 12 ]. This was expected given that this study population received a very similar refeeding approach, starting at 2016 kcal in males and 1978 kcal in females and the same electrolyte monitoring and replacement protocol was used. Notably higher rates of electrolyte abnormalities in prior studies [ 25 ] were due to overestimation by counting patients who received prophylactic electrolyte supplementation or treatment of declining (but not low) serum levels as having had an electrolyte abnormality. Use of a standardized protocol to monitor and replace only serum levels below prespecified thresholds in the present study likely gives a more accurate representation of refeeding risk.
The incidence of electrolyte abnormalities indicative of refeeding syndrome risk is of particular interest in male patients as males have higher refeeding goal diets and longer hospital stays than females, and therefore may be at added risk of developing refeeding syndrome [ 9 ]. We did not find statistically significant differences in rates of electrolyte abnormalities indicative of refeeding syndrome. Although the rates of electrolyte abnormalities indicative of refeeding syndrome in males were qualitatively lower than in females, the effect sizes were small. A greater degree of malnutrition has traditionally been associated with higher refeeding risk based on historical studies in patients with AN [ 26 ]. Indeed, we did find that lower percent median BMI was associated with higher odds of refeeding hypophosphatemia. However, when controlling for presentation percent median BMI, we then showed that greater weight suppression was independently associated with higher odds of refeeding hypophosphatemia. These findings reinforce the importance of weight history in assessing risk and are consistent with prior studies in atypical AN showing that weight suppression predicts medical risk [ 27 , 28 ].
We showed that older age was associated with higher odds of refeeding hypophosphatemia and hypomagnesemia [ 29 ]. This may be explained by the longer duration of illness in older adolescents and young adults when compared to younger adolescents. A prior study in patients with AN and atypical AN demonstrated an association between longer duration of weight loss and lower serum phosphorus at presentation [ 27 ]. However, in a study of hypophosphatemia during the course of refeeding, Whitelaw et al. (2018) did not find associations with duration or recency of weight loss [ 27 ]. Thus, although it is plausible that total body mineral stores become increasingly depleted over longer illness duration, more studies are needed to determine whether this contributes to more frequent electrolyte abnormalities during renourishment. Perhaps the most important implication of this finding is that patients with delayed or missed diagnoses will be at higher risk due to longer duration of illness. This puts males at particular risk given studies showing inadequate assessment of eating disorders in male patients and delayed referrals to specialty care.
Although males and females were prescribed similar kcals on admission, males overall required higher daily caloric requirements by discharge (3777 kcals) compared to females (3005 kcals) to establish medical stability. We previously showed that this contributed to longer hospitalizations in males [ 9 , 30 ]. While this did not translate into greater electrolyte abnormalities indicating refeeding syndrome risk, extended duration of stays confers greater financial costs and increases the risk of hospital-acquired conditions for patients [ 31 ]. Thus, future research is needed to optimize refeeding outcomes in male patients, particularly among samples with greater sex parity to increase power for detecting potential sex differences. Although higher caloric refeeding strategies have been shown to restore medical stability and shorten hospital stay, these strategies were not sex-stratified [ 12 ]. Potential trials in adolescent and young adult males with eating disorders may include either a larger initial caloric diet or more aggressive caloric advances while monitoring electrolytes to optimize treatment protocols in malnutrition-associated medical instability.
Limitations and strengths
Limitations of this retrospective study include its observational nature which limits inferences of causality. With findings conducted at a single site from a tertiary care hospital in Northern California, generalizability may be limited to other populations given differences in regional sociodemographic factors and diets. As patients were aged 9 to 25 at time of admission, findings of this study may not be applicable to older adult populations. Patients who met DSM-IV criteria also met DSM-5 criteria but were diagnosed prior to the publication of DSM-5. To elucidate sex differences, we retained individuals originally diagnosed with DSM-IV criteria to maximize power, ensuring as large of a male sample size as possible. There are limitations to the use of BMI and percent median BMI as they cannot differentiate body composition (e.g., fat mass, lean mass), which may differ by sex among adolescents with eating disorders [ 32 ]. Despite these limitations, we report the percent median BMI in this study as the Society for Adolescent Health and Medicine recommends the use of percent median BMI to classify degree of malnutrition in patients with restrictive eating disorders [ 7 ].
Strengths of this study include a robust patient sample over the course of 8 years and a relatively high male clinical sample ( n = 86, 15%). This is the first study to our knowledge that evaluates the association of sex with refeeding hypophosphatemia, hypokalemia, or hypomagnesemia, and we adjusted regression analyses for percent median BMI. The lack of sex differences in both individual and compound variables of electrolyte abnormalities indicating refeeding syndrome risk show great promise towards tailoring current refeeding protocols towards more aggressive treatment and advancement of diets in adolescent male populations with eating disorders.
Males continue to be underrepresented in eating disorder research and often receive treatment based on data derived from predominantly female samples despite their higher caloric requirements and longer hospitalizations [33]. Higher initial caloric diets and rapid advancement of diet is associated with faster restoration of medical stability and shorter hospital stays, but such studies are not sex stratified [ 12 ]. Our findings that males and females with eating disorders do not have statistically significant electrolyte abnormalities indicating risk of refeeding syndrome suggests that higher or more aggressive refeeding protocols in male populations may be warranted, though future studies are needed.
Data availability
The data that support the findings of this study are available on request from the corresponding author, J.M.N. The data are not publicly available due to confidentiality restrictions (e.g., their containing information that could compromise the privacy of research participants).
Abbreviations
Clinical Laboratory Improvement Amendments
Electronic medical records
Body Mass Index
Murray SB, Nagata JM, Griffiths S, Calzo JP, Brown TA, Mitchison D, et al. The enigma of male eating disorders: a critical review and synthesis. Clin Psychol Rev. 2017;57:1–11.
Article PubMed Google Scholar
Nagata JM, Ganson KT, Murray SB. Eating disorders in adolescent boys and young men: an update. Curr Opin Pediatr. 2020;32:476–81.
Article PubMed PubMed Central Google Scholar
Forrest LN, Smith AR, Swanson SA. Characteristics of seeking treatment among U.S. adolescents with eating disorders. Int J Eat Disord. 2017;50:826–33.
Nagata JM, Ganson KT, Golden NH. Medical complications of eating disorders in boys and men. Eating disorders in boys and men. Cham: Springer Int Publishing; 2021.
Quadflieg N, Strobel C, Naab S, Voderholzer U, Fichter MM. Mortality in males treated for an eating disorder—A large prospective study. Int J Eat Disord. 2019;52:1365–9.
National Guideline Alliance (UK). Eating disorders: recognition and treatment. London: National Institute for Health and Care Excellence (NICE);2017. https://www.nice.org.uk/guidance/ng69/chapter/Recommendations-for-research . Accessed 1 Apr 2024.
Society for Adolescent Health and, Medicine, Golden NH, Katzman DK, Sawyer SM, Ornstein RM, Rome ES, et al. Position paper of the Society for Adolescent Health and Medicine: medical management of restrictive eating disorders in adolescents and young adults. J Adolesc Health. 2015;56:121–5.
Article Google Scholar
The American psychiatric association practice guideline for the treatment of patients with eating disorders. https://psychiatryonline.org/doi/epdf/10.1176/appi.books.9780890424865 . Accessed 1 Apr 2024.
Nagata JM, Bojorquez-Ramirez P, Nguyen A, Ganson KT, Machen VI, Cattle CJ, et al. Sex differences in Refeeding among hospitalized adolescents and young adults with eating disorders. Int J Eat Disord. 2022;55:247–53.
Strandjord SE, Sieke EH, Richmond M, Khadilkar A, Rome ES. Medical stabilization of adolescents with nutritional insufficiency: a clinical care path. Eat Weight Disord. 2016;21:403–10.
Whitelaw M, Nagata JM. Nutritional considerations for boys and men with eating disorders. Eating disorders in boys and men. Cham: Springer Int Publishing; 2021.
Google Scholar
Garber AK, Cheng J, Accurso EC, Adams SH, Buckelew SM, Kapphahn CJ et al. Short-term outcomes of the study of refeeding to optimize Inpatient gains for patients with Anorexia Nervosa. JAMA Pediatr. 2021;175.
Whitelaw M, Gilbertson H, Lam P-Y, Sawyer SM. Does aggressive refeeding in hospitalized adolescents with anorexia nervosa result in increased hypophosphatemia? J Adolesc Health. 2010;46:577–82.
da Silva JSV, Seres DS, Sabino K, Adams SC, Berdahl GJ, Citty SW, et al. ASPEN Consensus recommendations for Refeeding Syndrome. Nutr Clin Pract. 2020;35:178–95.
Friedli N, Odermatt J, Reber E, Schuetz P, Stanga Z. Refeeding syndrome: update and clinical advice for prevention, diagnosis and treatment. Curr Opin Gastroenterol. 2020;36:136–40.
Persaud-Sharma D, Saha S, Trippensee AW. In: StatPearls, editor. Refeeding syndrome. Treasure Island (FL): StatPearls Publishing; 2024.
Reber E, Friedli N, Vasiloglou MF, Schuetz P, Stanga Z. Management of Refeeding Syndrome in Medical inpatients. J Clin Med. 2019;8:2202.
Tresley J, Sheean PM. Refeeding syndrome: recognition is the key to Prevention and Management. J Am Diet Assoc. 2008;108:2105–8.
Funayama M, Koreki A, Mimura Y, Takata T, Ogino S, Kurose S, et al. Restrictive type and infectious complications might predict nadir hematological values among individuals with anorexia nervosa during the refeeding period: a retrospective study. J Eat Disorders. 2022;10:64.
Kells M, Gregas M, Wolfe BE, Garber AK, Kelly-Weeder S. Factors associated with refeeding hypophosphatemia in adolescents and young adults hospitalized with anorexia nervosa. Nutr Clin Pract. 2022;37:470–8.
Brown CA, Sabel AL, Gaudiani JL, Mehler PS. Predictors of hypophosphatemia during refeeding of patients with severe anorexia nervosa. Int J Eat Disord. 2015;48:898–904.
Sabel AL, Rosen E, Mehler PS. Severe anorexia nervosa in males: clinical presentations and Medical Treatment. Eat Disord. 2014;22:209–20.
Society for Adolescent Health and Medicine. Medical management of restrictive eating disorders in adolescents and young adults. J Adolesc Health. 2022;71:648–54.
O’Connor G, Nicholls D. Refeeding hypophosphatemia in adolescents with anorexia nervosa: a systematic review. Nutr Clin Pract. 2013;28:358–64.
Society for Adolescent Health and Medicine. Refeeding Hypophosphatemia in Hospitalized adolescents with Anorexia Nervosa. J Adolesc Health. 2022;71:517–20.
Garber AK, Cheng J, Accurso EC, Adams SH, Buckelew SM, Kapphahn CJ, et al. Weight loss and illness severity in adolescents with atypical Anorexia Nervosa. Pediatrics. 2019;144:e20192339.
Whitelaw M, Lee K, Gilbertson H, Sawyer S. Predictors of complications in Anorexia Nervosa and atypical Anorexia Nervosa: degree of underweight or extent and recency of weight loss? J Adolesc Health. 2018;63:717–23.
Raj KS, Keane-Miller C, Golden NH. Hypomagnesemia in adolescents with eating disorders hospitalized for medical instability. Nutr Clin Pract. 2012;27:689–94.
Nagata JM, Vargas R, Sanders AE, Stuart E, Downey AE, Chaphekar AV, et al. Clinical characteristics of hospitalized male adolescents and young adults with atypical anorexia nervosa. Int J Eat Disord. 2024;57:1008-19.
Tipton K, Leas BF, Mull NK, Siddique SM, Greysen SR, Lane-Fall MB, et al. Interventions to decrease hospital length of Stay. Agency for Healthcare Research and Quality (AHRQ); 2021.
Nagata JM, Golden NH, Peebles R, Long J, Murray SB, Leonard MB, et al. Assessment of sex differences in body composition among adolescents with anorexia nervosa. J Adolesc Health. 2017;60:455–9.
Medical Management of Restrictive Eating. Disorders in adolescents and young adults. J Adolesc Health. 2022;71:648–54.
Download references
Acknowledgements
We thank Paola Bojorquez-Ramirez for assistance with the UCSF Eating Disorder Database. We thank Anthony Kung and Zain Memon for editorial assistance.
J.M.N. was funded by the National Heart, Lung, and Blood Institute (K08HL159350) and the National Institute of Mental Health (R01MH135492). A.K.G was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD082166).
Author information
Jason M. Nagata, Anthony Nguyen contributed equally to this work.
Authors and Affiliations
Department of Pediatrics, University of California, San Francisco, 550 16th Street, 4th Floor, Box 0503, San Francisco, CA, 94143, USA
Jason M. Nagata, Anthony Nguyen, Ruben Vargas, Amanda E. Downey, Anita V. Chaphekar, Sara M. Buckelew & Andrea K. Garber
Department of Psychiatry and Behavioral Sciences, University of California, San Francisco, 550 16th Street, 4th Floor, Box 0503, San Francisco, CA, 94143, USA
Amanda E. Downey
Factor-Inwentash Faculty of Social Work, University of Toronto, 246 Bloor Street W, Toronto, ON, M5S 1V4, Canada
Kyle T. Ganson
You can also search for this author in PubMed Google Scholar
Contributions
J.N. conceptualized and designed the study, developed the methodology, conducted the analyses, drafted parts of the initial manuscript, and reviewed and revised the manuscript. A.N. contributed to the data extraction, conducted the literature review, drafted parts of the initial manuscript, and reviewed and revised the manuscript. R.V. performed the initial statistical analysis, and reviewed and revised the manuscript. A.C., A.D., K.G., and S.B. critically reviewed and revised the manuscript. A.G. helped conceptualize the study and reviewed and revised the manuscript.
Corresponding author
Correspondence to Jason M. Nagata .
Ethics declarations
Ethics approval and consent to participate.
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Review Board (IRB) of the University of California, San Francisco approved this study. This research study was conducted retrospectively from data obtained for clinical purposes. We consulted extensively with the IRB of the University of California, San Francisco who determined that our study did not need informed consent.
Consent for publication
Not Applicable.
Competing interest
The authors have no conflict to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nagata, J.M., Nguyen, A., Vargas, R. et al. Sex differences in electrolyte abnormalities indicating refeeding syndrome risk among hospitalized adolescents and young adults with eating disorders. J Eat Disord 12 , 67 (2024). https://doi.org/10.1186/s40337-024-01012-0
Download citation
Received : 21 November 2023
Accepted : 24 April 2024
Published : 24 May 2024
DOI : https://doi.org/10.1186/s40337-024-01012-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Refeeding syndrome
- Electrolytes
- Feeding and eating disorders
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Research article. First published online March 3, 2022. A Qualitative Analysis of the Impact of Electronic Health Records (EHR) on Healthcare Quality and Safety: Clinicians' Lived Experiences ... Schrijvers A, Boonstra A, Roes K. Medical specialists' perspectives on the influence of electronic medical record use on the quality of hospital ...
Overview of electronic health records. Broadly defined, EHRs represent longitudinal data (in electronic format) that are collected during routine delivery of health care [].EHRs generally contain demographic, vital statistics, administrative, claims (medical and pharmacy), clinical, and patient-centered (e.g., originating from health-related quality-of-life instruments, home-monitoring devices ...
A 2019 poll by the Henry J. Kaiser Family Foundation, a non-profit health-care advocacy organization in San Francisco, California, found that 45% of US citizens think that electronic health ...
Henry David Thoreau's prophetic statement in Walden (1854) - "Men have become the tools of their tools", has come to be completely realized in the 21 st century, specifically concerning human interface with information technology. The interaction of physicians with electronic medical records (EMR) is the most relevant example of how our inventions have enslaved us.
The proliferation of electronic health records (EHRs) spurred on by federal government incentives over the past few decades has resulted in greater than an 80% adoption-rate at hospitals [] and close to 90% in office-based practices [] in the United States.A natural consequence of the availability of electronic health data is the conduct of research with these data, both observational and ...
This review is an update of 2 previous literature analyses on the benefits and costs of electronic medical records (EMRs), based on articles from 1966 to January 2004 ... structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform. 2008 May; 77 (5):291-304. doi: 10.1016/j.ijmedinf ...
et. al., 2023, Gopal, et. al., 2019, Kumar, M., & Mos tafa, 2020). The purpose of this review is to provide a comprehensive overvi ew of the role of EHRs in modern healthcare and their. impact on ...
Some of the widely accepted benefits of implementation Electronic Health Record (EHR) systems into health organizations include secure clinical information, improved hospital administrative affairs, availability of e-prescription, and better management of patients and hospital staff . 1,2 Multi-aspects operations of the patient and extensive management of hospital staff make the prevalent ...
Only a few papers addressed the prerequisite for informed consent when electronic medical records are for clinical and research purposes [26], [27]. Analysis showed that 33% (n=8/24) of the papers screened and discussed the ethical principles of beneficence (Table 1). Similarly, the authors of 25% (n=6/24) of the article discussed non ...
Medical records can be tricky to access because of confidentiality and variability, but data-sharing efforts are helping to overcome these hurdles — without compromising patient privacy.
Results. On the basis of responses from 63.1% of hospitals surveyed, only 1.5% of U.S. hospitals have a comprehensive electronic-records system (i.e., present in all clinical units), and an ...
Abstract. Objectives We conducted a systematic review to determine the effect of providing patients access to their medical records (electronic or paper-based) on healthcare quality, as defined by measures of safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity.. Methods Articles indexed in PubMed from January 1970 to January 2012 were reviewed.
The budget of the National Institutes of Health, for example, was $20,298 million in 2001, having more than doubled from a budget of $9,218 million 10 years before. This growing body of research includes increased efforts to use stored medical records as a source of data for health services, epidemiologic, and clinical studies.
Background Internationally, patient access to notes is increasing. This has been driven by respect for patient autonomy, often recognised as a primary tenet of medical ethics: patients should be able to access their records to be fully engaged with their care. While research has been conducted on the impact of patient access to outpatient and primary care records and to patient portals, there ...
Background Electronic Medical Records (EMRs) are one of a range of digital health solutions that are key enablers of the data revolution transforming the health sector. They offer a wide range of benefits to health professionals, patients, researchers and other key stakeholders. However, effective implementation has proved challenging. Methods A qualitative methodology was used in the study ...
The implementation of hospital-wide Electronic Medical Records (EMRs) is still an unsolved quest for many hospital managers. EMRs have long been considered a key factor for improving healthcare quality and safety, reducing adverse events for patients, decreasing costs, optimizing processes, improving clinical research and obtaining best clinical performances. However, hospitals continue to ...
The misuse of medical records is not only revealed on paper-based medical records but also occurs in electronic medical record. According to the research from (Harande, 2018), the medical records ...
This research was funded by the MIT Abdul Latif Jameel Clinic for Machine Learning in Health. MedKnowts, a "smart" electronic health record system, can help doctors work more efficiently by presenting relevant information from a patient's medical history, autocompleting medical terms as a clinician types, and auto-populating repetitive ...
the first author were obtained. The types of specialties and types of research were analyzed. To understand the conditions for the use of medical records, the retrospective research using hospital's medical records were analyzed. Each article was read in entirety to realize the use and number of patients and the medical record items. Results: Among the 362 articles first-authored by TVGH ...
The budget of the National Institutes of Health, for example, was $20,298 million in 2001, 1 having more than doubled from a budget of $9,218 million 10 years before. 2 This growing body of research includes increased efforts to use stored medical records as a source of data for health services, epidemiologic, and clinical studies.
Electronic Medical Records (EMR) is often used to refer to as electronic personal health (EPH) records or electronic healthcare records (EHR). These are considered vivacious assets of health facilities and patients. The relevance of the EMRs has motivated diverse innovations in the collecting, organizing, managing and administering for purpose of treatment primarily and other reasons. There ...
But the price of that could be that we have to share more of our medical information. After all, researchers can't collect large amounts of data if people aren't willing to part with that data ...
Electronic Health Records (EHRs) were once hailed as the solution to streamlining healthcare processes, but their implementation has brought forth a host of challenges. From increased work burden and clinician burnout to facilitated medical errors, the journey of EHRs has been tumultuous. With billions invested and a staggering increase in adoption rates, we find ourselves retrofitting the ...
In the first year of the COVID-19 pandemic, risk of death in people hospitalized for COVID-19 was substantially higher than in people hospitalized for seasonal influenza. 1,2 The risk of death due to COVID-19 has since declined. In fall-winter 2022-2023, people hospitalized for COVID-19 had a 60% higher risk of death compared with those hospitalized for seasonal influenza. 3 New variants of ...
Coronary artery disease (CAD) is the leading cause of death worldwide with acute myocardial infarction.(MI) representing the clinical condition associated with the greatest morbidity and mortality, up to 30% of in-hospital deaths. Prompt reperfusion with percutaneous coronary intervention (PCI), advances in acute cardiovascular care and more effective medical therapy have improved the ...
Background: The coronavirus disease 2019 (COVID-19) pandemic has significantly impacted public health globally, with particular attention on the effects on children, adolescents, and young adults. This study aimed to investigate the potential relationship between COVID-19 and caries risk in this age group. Methods: A retrospective chart review was conducted on 120 patients between the ages of ...
Electronic medical records capture point-of-care data that inform and improve practice through quality improvement projects, practice-level interventions, and informative research. Footnotes Cet article se trouve aussi en français à la page 850 .
The research involves the analysis of existing data without direct interaction with participants, and all data used are anonymized to ensure confidentiality. The Institutional Review Board (Helsinki Committee) of Galilee Medical Center and the Israeli Ministry of Health reviewed and approved this approach, reference number 0147-21-NHR.
Suicides reached record levels in the United States in 2022, with nearly 49,500 suicide deaths. Since 2011, around 540,000 people in the U.S. have died by suicide. ... These investments into medical research have made the US the leader in medical innovation, measured either in terms of revenue or the number of new drugs and devices introduced ...
Background Refeeding syndrome is the gravest possible medical complication in malnourished patients undergoing refeeding in the hospital. We previously reported that males with malnutrition secondary to eating disorders required more calories and had longer hospital stays than females; however, sex differences in electrolyte abnormalities indicating refeeding syndrome risk remain unknown. The ...