
Depression Detectives
A blog for the radical citizen science project Depression Detectives

Top 10 research questions

Our Depression Detectives have come up with 59 possible research questions and voted on their top ten. We are now discussing, narrowing and finetuning them, and finding ways how they could be researched. Every day, we are looking at one of the top ten questions. Then we will then have another vote to decide on the final favourite question, which will be the basis of our study.
THE TOP TEN
- Do people with depression feel that they predominantly receive help to treat their “symptoms“ vs “origins”? How could this be changed?
- What is the effectiveness of treatments on offer from GPs on the NHS (mainly anti-depressants and short-term counselling) and what proportion of patients recover with just this, what proportion go on to have a major crisis which enables them to access more in-depth treatment, and what proportion end up self-funding something which actually works in the long-term?
- How do people who say that they have recovered from depression describe their recovery: Do they think they are “cured” or just “coping better”, “able to spot triggers better”, etc.?
- How does chronic depression/dysphoria differ from, say a single episode, or discrete episodes of reactive depression? Are there markers (biological, psychological, behavioural, and current or in a person’s history e.g. trauma) that distinguish them?
- What would need to happen to make a wider range of support available, including more time-intensive interventions? How could access to psychological therapies be improved?
- What is the link between autism and depression? Misdiagnosis – are ‘symptoms’ of depression are actually ’traits’ of autism (being quiet, withdrawn and needing to shut yourself away from the stimulus of people and the outside world) which would explain why trying to get someone out and mixing with people as a way out of depression would not work and in fact make things 100x worse?
- How can others best support family members or friends with depression? What do people with depression find most helpful?
- What are the specific problems that emerge from having a parent with depression, and what can be done to help counter these effects?
- Can parents learn and teach healthy emotional behaviours and positive strategies (e.g. through therapy), even if they can’t always do them themselves?
- Can we ask GPs what training they received in mental health, whether they think it was adequate to prepare them for GP consultations, what more they would like to learn and what services do they wish they could refer patients to? Doing 6 months in inpatient psychiatry as an optional part of a rotation doesn’t really prepare you for dealing with the majority of mental health issues in the community.

One thought on “Top 10 research questions”
- Pingback: Working together to improve depression research – UKRI
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

HTML Text Top 10 research questions / Depression Detectives by blogadmin is licensed under a Creative Commons Attribution CC BY 3.0
Plain text Top 10 research questions by blogadmin @ is licensed under a Creative Commons Attribution CC BY 3.0
Report this page
To report inappropriate content on this page, please use the form below. Upon receiving your report, we will be in touch as per the Take Down Policy of the service.
Please note that personal data collected through this form is used and stored for the purposes of processing this report and communication with you.
If you are unable to report a concern about content via this form please contact the Service Owner .
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
7 Depression Research Paper Topic Ideas
Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
In psychology classes, it's common for students to write a depression research paper. Researching depression may be beneficial if you have a personal interest in this topic and want to learn more, or if you're simply passionate about this mental health issue. However, since depression is a very complex subject, it offers many possible topics to focus on, which may leave you wondering where to begin.
If this is how you feel, here are a few research titles about depression to help inspire your topic choice. You can use these suggestions as actual research titles about depression, or you can use them to lead you to other more in-depth topics that you can look into further for your depression research paper.
What Is Depression?
Everyone experiences times when they feel a little bit blue or sad. This is a normal part of being human. Depression, however, is a medical condition that is quite different from everyday moodiness.
Your depression research paper may explore the basics, or it might delve deeper into the definition of clinical depression or the difference between clinical depression and sadness .
What Research Says About the Psychology of Depression
Studies suggest that there are biological, psychological, and social aspects to depression, giving you many different areas to consider for your research title about depression.
Types of Depression
There are several different types of depression that are dependent on how an individual's depression symptoms manifest themselves. Depression symptoms may vary in severity or in what is causing them. For instance, major depressive disorder (MDD) may have no identifiable cause, while postpartum depression is typically linked to pregnancy and childbirth.
Depressive symptoms may also be part of an illness called bipolar disorder. This includes fluctuations between depressive episodes and a state of extreme elation called mania. Bipolar disorder is a topic that offers many research opportunities, from its definition and its causes to associated risks, symptoms, and treatment.
Causes of Depression
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic.
For instance, how does an imbalance in brain chemistry or poor nutrition relate to depression? Is there a relationship between the stressful, busier lives of today's society and the rise of depression? How can grief or a major medical condition lead to overwhelming sadness and depression?
Who Is at Risk for Depression?
This is a good research question about depression as certain risk factors may make a person more prone to developing this mental health condition, such as a family history of depression, adverse childhood experiences, stress , illness, and gender . This is not a complete list of all risk factors, however, it's a good place to start.
The growing rate of depression in children, teenagers, and young adults is an interesting subtopic you can focus on as well. Whether you dive into the reasons behind the increase in rates of depression or discuss the treatment options that are safe for young people, there is a lot of research available in this area and many unanswered questions to consider.
Depression Signs and Symptoms
The signs of depression are those outward manifestations of the illness that a doctor can observe when they examine a patient. For example, a lack of emotional responsiveness is a visible sign. On the other hand, symptoms are subjective things about the illness that only the patient can observe, such as feelings of guilt or sadness.
An illness such as depression is often invisible to the outside observer. That is why it is very important for patients to make an accurate accounting of all of their symptoms so their doctor can diagnose them properly. In your depression research paper, you may explore these "invisible" symptoms of depression in adults or explore how depression symptoms can be different in children .
How Is Depression Diagnosed?
This is another good depression research topic because, in some ways, the diagnosis of depression is more of an art than a science. Doctors must generally rely upon the patient's set of symptoms and what they can observe about them during their examination to make a diagnosis.
While there are certain laboratory tests that can be performed to rule out other medical illnesses as a cause of depression, there is not yet a definitive test for depression itself.
If you'd like to pursue this topic, you may want to start with the Diagnostic and Statistical Manual of Mental Disorders (DSM). The fifth edition, known as DSM-5, offers a very detailed explanation that guides doctors to a diagnosis. You can also compare the current model of diagnosing depression to historical methods of diagnosis—how have these updates improved the way depression is treated?
Treatment Options for Depression
The first choice for depression treatment is generally an antidepressant medication. Selective serotonin reuptake inhibitors (SSRIs) are the most popular choice because they can be quite effective and tend to have fewer side effects than other types of antidepressants.
Psychotherapy, or talk therapy, is another effective and common choice. It is especially efficacious when combined with antidepressant therapy. Certain other treatments, such as electroconvulsive therapy (ECT) or vagus nerve stimulation (VNS), are most commonly used for patients who do not respond to more common forms of treatment.
Focusing on one of these treatments is an option for your depression research paper. Comparing and contrasting several different types of treatment can also make a good research title about depression.
A Word From Verywell
The topic of depression really can take you down many different roads. When making your final decision on which to pursue in your depression research paper, it's often helpful to start by listing a few areas that pique your interest.
From there, consider doing a little preliminary research. You may come across something that grabs your attention like a new study, a controversial topic you didn't know about, or something that hits a personal note. This will help you narrow your focus, giving you your final research title about depression.
Remes O, Mendes JF, Templeton P. Biological, psychological, and social determinants of depression: A review of recent literature . Brain Sci . 2021;11(12):1633. doi:10.3390/brainsci11121633
National Institute of Mental Health. Depression .
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition . American Psychiatric Association.
National Institute of Mental Health. Mental health medications .
Ferri, F. F. (2019). Ferri's Clinical Advisor 2020 E-Book: 5 Books in 1 . Netherlands: Elsevier Health Sciences.
By Nancy Schimelpfening Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
- Media Center
- Events & Webinars
- Healthy Minds TV
- Email Signup
- Get Involved
- Anxiety Disorders
- Attention-Deficit Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder (ASD)
- Bipolar Disorder
- Borderline Personality Disorder (BPD)
- Eating Disorders
- Mental Illness (General)
- Inaccessible
- Obsessive-Compulsive Disorder (OCD)
- Post-Traumatic Stress Disorder (PTSD)
- Schizophrenia
- Suicide Prevention
- Other Brain-Related Illnesses
- Basic Research
- New Technologies
- Early Intervention/ Diagnostic Tools
- Next Generation Therapies
- Donate Today
- Make a Memorial/Tribute Gift
- Create an Event/Memorial Page
- Find an Event/Memorial Page
- Make a Stock/Securities Gift/IRA Charitable Rollover Gift
- Donate Cryptocurrency
- Other Giving Opportunities
- Monthly Giving
- Planned Giving
- Research Partners
- Donor Advised Funds
- Workplace Giving
- Team Up for Research!
- Sponsorship Opportunities
Frequently Asked Questions about Depression
Depression (major depressive disorder or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how you feel, think, and handle daily activities, such as sleeping, eating, or working. To be diagnosed with depression, the symptoms must be present for at least two weeks.
Impactful Depression Research Discoveries by Foundation Grantees:
- Rapid-Acting Antidepressant Heralded as Biggest Breakthrough in Depression Research in 50 years
- Development of TMS for Treatment-Resistant Depression
- Interactive Parent-Child Therapy Reduced Depression Symptoms in Very Young Children
- Foundation Grantee Shows Treating Inflammation May Improve Resistant Depression
Recent Depression Research Discoveries by Foundation Grantees:
- Impact of Mother’s Depressive Symptoms Just Before and After Childbirth Upon Child’s Brain Development
- Study Links Brain Connectivity Patterns with Response to Specific Antidepressant and Placebo
- Over Two Decades, 90 BBRF Grants Helped Build a Scientific Foundation for the First Rapid-Acting Antidepressants
- After 60 Years, Study Finds Children of Mothers with Bacterial Infections During Pregnancy Have Elevated Psychosis Risk
For more lay-friendly, summarized Depression Research Discoveries, click here .
Clinical depression is a serious condition that negatively affects how a person thinks, feels, and behaves. In contrast to normal sadness, clinical depression is persistent, often interferes with a person’s ability to experience or anticipate pleasure, and significantly interferes with functioning in daily life. Untreated, symptoms can last for weeks, months, or years; and if inadequately treated, depression can lead to significant impairment, other health-related issues, and in rare cases, suicide.
A person is diagnosed with a major depression when he or she experiences at least five of the symptoms listed below for two consecutive weeks. At least one of the five symptoms must be either (1) depressed mood or (2) loss of interest or pleasure. Symptoms include:
- Depressed mood most of the day, nearly every day
- Markedly diminished interest or pleasure in activities most of the day, nearly every day
- Changes in appetite that result in weight losses or gains unrelated to dieting
- Changes in sleeping patterns
- Loss of energy or increased fatigue
- Restlessness or irritability
- Feelings of anxiety
- Feelings of worthlessness, helplessness, or hopelessness
- Inappropriate guilt
- Difficulty thinking, concentrating, or making decisions
- Thoughts of death or attempts at suicide
The first step to being diagnosed is to visit a doctor for a medical evaluation. Certain medications, and some medical conditions such as thyroid disorder, can cause similar symptoms as depression. A doctor can rule out these possibilities by conducting a physical examination, interview and lab tests. If the doctor eliminates a medical condition as a cause, he or she can implement treatment or refer the patient to a mental health professional. Once diagnosed, a person with depression can be treated by various methods. The mainstays of treatment for depression are any of a number of antidepressant medications and psychotherapy, which can also be used in combination.
For severe, treatment-resistant depression, studies have been done showing Deep Brain Stimulation may be an option. Learn more in this webinar featuring Dr. Helen Mayberg :
Depression is twice as common among women as among men. About 20 percent of women will experience at least one episode of depression across their lifetime. Scientists are examining many potential causes for and contributing factors to women’s increased risk for depression. Biological, life cycle, hormonal and psychosocial factors unique to women may be linked to women’s higher depression rates. Researchers have shown, for example, that hormones affect brain chemistry, impacting emotions and mood. Before adolescence, girls and boys experience depression at about the same frequency. By adolescence, however, girls become more likely to experience depression than boys. Research points to several possible reasons for this imbalance. The biological and hormonal changes that occur during puberty likely contribute to the sharp increase in rates of depression among adolescent girls. In addition, research has suggested that girls are more likely than boys to continue feeling bad after experiencing difficult situations or events, suggesting they are more prone to depression.
Women are particularly vulnerable to depression after giving birth, when hormonal and physical changes and the new responsibility of caring for a newborn can be overwhelming. Many new mothers experience a brief episode of mild mood changes known as the “baby blues.” These symptoms usually dissipate by the 10th day. PPD lasts much longer than 10 days, and can go on for months following child birth. Acute PPD is a much more serious condition that requires active treatment and emotional support for the new mother. Some studies suggest that women who experience PPD often have had prior depressive episodes.
Menopause is defined as the state of an absence of menstrual periods for 12 months. Menopause is the point at which estrogen and progesterone production decreases permanently to very low levels. The ovaries stop producing eggs and a woman is no longer able to get pregnant naturally. During the transition into menopause, some women experience an increased risk for depression. Scientists are exploring how the cyclical rise and fall of estrogen and other hormones may affect the brain chemistry that is associated with depressive illness.
For older adults who experience depression for the first time later in life, other factors, such as changes in the brain or body, may be at play. For example, older adults may suffer from restricted blood flow, a condition called ischemia. Over time, blood vessels become less flexible. They may harden and prevent blood from flowing normally to the body’s organs, including the brain. If this occurs, an older adult with no family or personal history of depression may develop what some doctors call “vascular depression.” Those with vascular depression also may be at risk for a coexisting cardiovascular illness, such as heart disease or a stroke.
Researchers are looking for ways to better understand, diagnose and treat depression among all groups of people. Studying strategies to personalize care for depression, such as identifying characteristics of the person that predict which treatments are more likely to work, is an important goal.
The ability of ketamine to produce a rapid and efficacious antidepressant response by a completely novel mechanism is considered by many experts the most important finding in the depression field in 50 years. Originally developed as an anesthetic, ketamine is an antagonist of the NMDA receptor on a subset of brain cells. It often produces rapid (within hours) antidepressant actions in patients who have failed to respond to conventional antidepressants (i.e., are considered treatment-resistant). Ketamine is psychoactive and has potentially dangerous side effects; it has a past history of being abused as a street drug. Studies aimed at characterizing the mechanisms by which ketamine works rapidly and effectively in severely depressed individuals is likely to lead to novel targets and agents that are safer and more long-lasting, and could revolutionize the treatment of depression. Numerous BBRF Grants support this work , including a number that are attempting to develop ketamine analogs – compounds that act like ketamine but lack its side-effects.
Treatment-resistant depression (TRD) is a term used in clinical psychiatry to describe cases of major depressive disorder that do not respond to standard treatments (at least two courses of antidepressant treatments). For many people, antidepressant treatment and/or ‘talk’ therapy (such as Cognitive Behavioral Therapy) ease symptoms of depression, but with treatment-resistant depression, little to no relief is realized. Treatment-resistant depression symptoms can range from mild to severe and may require trying a number of approaches to identify what helps. (Source: Biological Psychiatry)
Treatment of resistant depression has most commonly been treated with electroconvulsive therapy (ECT). ECT has been modified to avoid the pain previously associated with it and is the most effective and quick-acting treatment for resistant depression. The downside is that it works by inducing brain seizures and can impair memory. Its therapeutic benefits can also fade over time. New methods of brain stimulation also offer the possibility of relief. These technologies exploit the fact that the brain is an electrical organ: it responds to electrical and magnetic stimulation to modulate brain circuits and change brain activity. Repetitive transcranial magnetic stimulation (rTMS), pioneered by Dr. Mark George with the support of NARSAD grants, was approved by the FDA in 2008 as a treatment for some otherwise untreatable depressions. rTMS is a noninvasive method that works through a coil held over the target area of the brain. A magnetic field passes through the skull to activate the appropriate brain circuit and no seizures are induced. Deep brain stimulation (DBS), a technique adapted for treating depression by Dr. Helen Mayberg with the support of NARSAD grants, works through electrodes planted deep in the brain. Another method, vagus nerve stimulation (VNS), stimulates the vagus nerve in the neck to therapeutically activate brain function. Magnetic seizure therapy (MST) combines rTMS and ECT to achieve a safer form of seizure therapy. MST has been supported through NARSAD Grants to Dr. Sarah Lisanby. Recently, Foundation grantees at the University of Pittsburgh have successfully experimented on a small number of patients with treatment-resistant depression, discovering underlying metabolic deficiencies and successfully treating these. In one subset of patients, a deficiency in cerebral folate was addressed by administering folinic acid. Patients’ depression symptoms declined significantly when these metabolic problems were treated. For some individuals, depression reached remission.
Learn more about TMS for depression in this webinar featuring Dr. Sarah Lisanby :
The first attempts at defining depression as a biologically-based illness hinged on a theory of a ‘chemical imbalance’ in the brain. It was thought that too much or too little of essential signal-transmitting chemicals—neurotransmitters—were present in the brain. This idea has been useful—that the brain is a kind of chemical soup in which there may be too much dopamine or too little serotonin, but it is now begin replaced by much more sophisticated knowledge about how the brain works, made possible by basic research. All the current antidepressants were developed during the period when the chemical-soup theory was in vogue. But now, many researchers are looking to understand in greater detail the brain biology that underlies depression’s symptoms so that novel therapies can be found.
Throughout this website you will find ideas for new depression treatments in greater detail. Efforts to create new classes of antidepressants, based on novel targets have borne fruit. A docking port on brain cells called the mu opioid receptor is the focus of one such effort. Other efforts focus not on the serotonin pathway, as do current “SSRI” drugs such as Prozac, but another pathway, that of another key neurotransmitter, called glutamate. A previously obscure brain area called the lateral habenula may be involved in depression pathology in some instances, due to glutamate hyperactivity. A drug able to specifically lower the activity in that region is a plausible drug discovery objective. Other researchers have been working on the idea that drugs that can mimic the biochemical and biological factors rendering certain people resilient to factors such as severe or chronic stress may have a future in depression treatment. A drug is now being tested that in preliminary trials has helped to reduce postpartum depression. Other researchers have been studying the ability to help women resist depression in the perinatal period through hormone treatments, or, in other work, via treatments that target the maternal immune system, which may be implicated in a subset of postpartum depression. Research has begun to see if administering certain strains of bacteria in depressed individuals might give a boost to their immune system and help reduce depression symptoms. Trying to alleviate depression via changes in diet – e.g., a Mediterranean diet, in one recent study – or omega-3 (“fish oil”) supplements is the subject of other Foundation-supported research. Yet another path that may lead to better outcomes in the future is bright-light therapy, which was first used to help people with seasonal affective disorder. It may have wider applications. It is also important to note research by grantees that has suggested the ability of even a short course of talk therapy to help alleviate depression in mothers with major depression, while at the same time helping their children. Such therapy worked best when it focused on the mother’s relationship with her child, the research revealed.
Dr. J. John Mann presented a webinar titled: Brain Plasticity: The Effects of Antidepressants on Major Depression in which he discusses why we need to better understand how antidepressants including SSRIs, lithium, and ketamine exert their therapeutic effects, so we can find newer more effective and rapidly acting treatments for depression:
Brain imaging has confirmed the biological nature of many psychiatric illnesses over the past twenty years. Yvette Sheline, M.D., in the mid-1990s, used functional magnetic resonance imaging (fMRI) to identify structural brain changes in depressed patients and established depression as a brain disease.
Using positron emission tomography (PET) scan images, Dr. Helen Mayberg of the Icahn School of Medicine at Mount Sinai, identified, in 2013, specific brain activity that can potentially predict whether people with major depressive disorder will best respond to an antidepressant medication or psychotherapy. This important new work offers a first potential imaging biomarker for treatment selection. A team of researchers including NARSAD Grantee Stefan G. Hoffman, Ph.D., of Boston University and Frida E. Polli, Ph.D., of Massachusetts Institute of Technology have used brain imaging to predict the success of cognitive behavioral therapy, a specific type of talk therapy often used to help treat a wide range of mental illnesses including anxiety disorders, depression, and schizophrenia. Research by Dr. Conor Liston of Weill Cornell Medical School, and colleagues, has used brain scans to identify four distinct “biotypes” of depression. Strikingly, patients in one of these four categories were about three times more likely to respond to a noninvasive treatment known as transcranial magnetic stimulation (TMS) than patients in two of the other categories. This is a good example of the power that biomarkers can have in the years just ahead to help direct people with depression to treatments most likely to help them.
Variations in genes – different kinds of DNA mutations, both common and rare – have been solidly linked to a number of serious psychiatric disorders including schizophrenia, bipolar disorder and autism. It is reasonable to wonder why similar progress has not been made yet in the study of the genetic factors contributing to depression. Researchers have made many attempts to search for such factors, but have not come up with results that statisticians consider “statistically meaningful.” One way of explaining the issue in studying depression concerns that very large number of people whom it affects. The power of massive genomic studies of patients (who are compared with unaffected individuals) evaporates if the people being compared have similar illnesses that have very different underlying genetic profiles. People with major depression might be grouped according to sex; whether or not they have recurrent depression; age at onset; symptom patterns; whether or not they were abused or under chronic stress early in life, for example. There is very good reason for progress on the genetic front, however. Foundation grantee Patrick Sullivan, M.D. and others have had success in finding the first reliable signals of commonly seen genetic variations in people with schizophrenia. To do so, they need to assemble a patient sample, across continents, numbering in the tens of thousands. They founded the Psychiatric Genomic Consortium to accomplish this. PGC scientists estimate that the inflection point in depression studies may be 75,000 to 100,000 study participants, a goal the PGC is working toward. It’s not that there is no genetic signal in depression, in other words. It’s a question of assembling a well-documented sample of patients of sufficient size to “tease out” the embedded genetic “signals,” which will point toward risk genes for the illness.
News and Events

Developing Biological Markers to Improve Clinical Care in Autism

ADVICE ON MENTAL HEALTH: Warning Signs & What to Look For: Anxiety and Depression in Childhood

‘Brains Within Brains’: Organoid Experiments Show How Pathologies Emerge in the Developing Brain

A RESEARCHER’S PERSPECTIVE: What Can We Do When Medicine is Not Enough in the Treatment of Schizophrenia?

2022 International Mental Health Research Symposium
OCD: Using Genome Data to Predict Risk, Symptoms and Treatment Response

Developing New Treatments for Mania Using Brain-Based Risk Markers

Self-Control Gone Awry: The Cognitive Neuroscience Behind Bulimia Nervosa
Cognitive Impairment in Psychosis: What it is and How it's Treated

Advice on Diagnosing and Treating Bipolar Disorder

2020 International Mental Health Research Symposium Presentations

Using Rapid-Acting Brain Stimulation for Treatment-Resistant Depression
Donations are welcome
100% of every dollar donated for research is invested in our research grants. Our operating expenses are covered by separate foundation grants.
The Brain & Behavior Research Foundation is a 501(c)(3) nonprofit organization, our Tax ID # is 31-1020010.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
April 23, 2024
Research in Context: Treating depression
Finding better approaches.
While effective treatments for major depression are available, there is still room for improvement. This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs.

Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness, anxiety, hopelessness, frustration, or guilt. You may not enjoy the activities you usually do. These feelings tend to be only temporary. Once circumstances change, and the source of stress goes away, your mood usually improves. But sometimes, these feelings don’t go away. When these feelings stick around for at least two weeks and interfere with your daily activities, it’s called major depression, or clinical depression.
In 2021, 8.3% of U.S. adults experienced major depression. That’s about 21 million people. Among adolescents, the prevalence was much greater—more than 20%. Major depression can bring decreased energy, difficulty thinking straight, sleep problems, loss of appetite, and even physical pain. People with major depression may become unable to meet their responsibilities at work or home. Depression can also lead people to use alcohol or drugs or engage in high-risk activities. In the most extreme cases, depression can drive people to self-harm or even suicide.
The good news is that effective treatments are available. But current treatments have limitations. That’s why NIH-funded researchers have been working to develop more effective ways to treat depression. These include finding ways to predict whether certain treatments will help a given patient. They're also trying to develop more effective drugs or, in some cases, find new uses for existing drugs.
Finding the right treatments
The most common treatments for depression include psychotherapy, medications, or a combination. Mild depression may be treated with psychotherapy. Moderate to severe depression often requires the addition of medication.
Several types of psychotherapy have been shown to help relieve depression symptoms. For example, cognitive behavioral therapy helps people to recognize harmful ways of thinking and teaches them how to change these. Some researchers are working to develop new therapies to enhance people’s positive emotions. But good psychotherapy can be hard to access due to the cost, scheduling difficulties, or lack of available providers. The recent growth of telehealth services for mental health has improved access in some cases.
There are many antidepressant drugs on the market. Different drugs will work best on different patients. But it can be challenging to predict which drugs will work for a given patient. And it can take anywhere from 6 to 12 weeks to know whether a drug is working. Finding an effective drug can involve a long period of trial and error, with no guarantee of results.
If depression doesn’t improve with psychotherapy or medications, brain stimulation therapies could be used. Electroconvulsive therapy, or ECT, uses electrodes to send electric current into the brain. A newer technique, transcranial magnetic stimulation (TMS), stimulates the brain using magnetic fields. These treatments must be administered by specially trained health professionals.
“A lot of patients, they kind of muddle along, treatment after treatment, with little idea whether something’s going to work,” says psychiatric researcher Dr. Amit Etkin.
One reason it’s difficult to know which antidepressant medications will work is that there are likely different biological mechanisms that can cause depression. Two people with similar symptoms may both be diagnosed with depression, but the causes of their symptoms could be different. As NIH depression researcher Dr. Carlos Zarate explains, “we believe that there’s not one depression, but hundreds of depressions.”
Depression may be due to many factors. Genetics can put certain people at risk for depression. Stressful situations, physical health conditions, and medications may contribute. And depression can also be part of a more complicated mental disorder, such as bipolar disorder. All of these can affect which treatment would be best to use.
Etkin has been developing methods to distinguish patients with different types of depression based on measurable biological features, or biomarkers. The idea is that different types of patients would respond differently to various treatments. Etkin calls this approach “precision psychiatry.”
One such type of biomarker is electrical activity in the brain. A technique called electroencephalography, or EEG, measures electrical activity using electrodes placed on the scalp. When Etkin was at Stanford University, he led a research team that developed a machine-learning algorithm to predict treatment response based on EEG signals. The team applied the algorithm to data from a clinical trial of the antidepressant sertraline (Zoloft) involving more than 300 people.

EEG data for the participants were collected at the outset. Participants were then randomly assigned to take either sertraline or an inactive placebo for eight weeks. The team found a specific set of signals that predicted the participants’ responses to sertraline. The same neural “signature” also predicted which patients with depression responded to medication in a separate group.
Etkin’s team also examined this neural signature in a set of patients who were treated with TMS and psychotherapy. People who were predicted to respond less to sertraline had a greater response to the TMS/psychotherapy combination.
Etkin continues to develop methods for personalized depression treatment through his company, Alto Neuroscience. He notes that EEG has the advantage of being low-cost and accessible; data can even be collected in a patient’s home. That’s important for being able to get personalized treatments to the large number of people they could help. He’s also working on developing antidepressant drugs targeted to specific EEG profiles. Candidate drugs are in clinical trials now.
“It’s not like a pie-in-the-sky future thing, 20–30 years from now,” Etkin explains. “This is something that could be in people’s hands within the next five years.”
New tricks for old drugs
While some researchers focus on matching patients with their optimal treatments, others aim to find treatments that can work for many different patients. It turns out that some drugs we’ve known about for decades might be very effective antidepressants, but we didn’t recognize their antidepressant properties until recently.
One such drug is ketamine. Ketamine has been used as an anesthetic for more than 50 years. Around the turn of this century, researchers started to discover its potential as an antidepressant. Zarate and others have found that, unlike traditional antidepressants that can take weeks to take effect, ketamine can improve depression in as little as one day. And a single dose can have an effect for a week or more. In 2019, the FDA approved a form of ketamine for treating depression that is resistant to other treatments.
But ketamine has drawbacks of its own. It’s a dissociative drug, meaning that it can make people feel disconnected from their body and environment. It also has the potential for addiction and misuse. For these reasons, it’s a controlled substance and can only be administered in a doctor’s office or clinic.
Another class of drugs being studied as possible antidepressants are psychedelics. These include lysergic acid diethylamide (LSD) and psilocybin, the active ingredient in magic mushrooms. These drugs can temporarily alter a person’s mood, thoughts, and perceptions of reality. Some have historically been used for religious rituals, but they are also used recreationally.
In clinical studies, psychedelics are typically administered in combination with psychotherapy. This includes several preparatory sessions with a therapist in the weeks before getting the drug, and several sessions in the weeks following to help people process their experiences. The drugs are administered in a controlled setting.
Dr. Stephen Ross, co-director of the New York University Langone Health Center for Psychedelic Medicine, describes a typical session: “It takes place in a living room-like setting. The person is prepared, and they state their intention. They take the drug, they lie supine, they put on eye shades and preselected music, and two therapists monitor them.” Sessions last for as long as the acute effects of the drug last, which is typically several hours. This is a healthcare-intensive intervention given the time and personnel needed.
In 2016, Ross led a clinical trial examining whether psilocybin-assisted therapy could reduce depression and anxiety in people with cancer. According to Ross, as many as 40% of people with cancer have clinically significant anxiety and depression. The study showed that a single psilocybin session led to substantial reductions in anxiety and depression compared with a placebo. These reductions were evident as soon as one day after psilocybin administration. Six months later, 60-80% of participants still had reduced depression and anxiety.
Psychedelic drugs frequently trigger mystical experiences in the people who take them. “People can feel a sense…that their consciousness is part of a greater consciousness or that all energy is one,” Ross explains. “People can have an experience that for them feels more ‘real’ than regular reality. They can feel transported to a different dimension of reality.”
About three out of four participants in Ross’s study said it was among the most meaningful experiences of their lives. And the degree of mystical experience correlated with the drug’s therapeutic effect. A long-term follow-up study found that the effects of the treatment continued more than four years later.
If these results seem too good to be true, Ross is quick to point out that it was a small study, with only 29 participants, although similar studies from other groups have yielded similar results. Psychedelics haven’t yet been shown to be effective in a large, controlled clinical trial. Ross is now conducting a trial with 200 people to see if the results of his earlier study pan out in this larger group. For now, though, psychedelics remain experimental drugs—approved for testing, but not for routine medical use.
Unlike ketamine, psychedelics aren’t considered addictive. But they, too, carry risks, which certain conditions may increase. Psychedelics can cause cardiovascular complications. They can cause psychosis in people who are predisposed to it. In uncontrolled settings, they have the risk of causing anxiety, confusion, and paranoia—a so-called “bad trip”—that can lead the person taking the drug to harm themself or others. This is why psychedelic-assisted therapy takes place in such tightly controlled settings. That increases the cost and complexity of the therapy, which may prevent many people from having access to it.
Better, safer drugs
Despite the promise of ketamine or psychedelics, their drawbacks have led some researchers to look for drugs that work like them but with fewer side effects.
Depression is thought to be caused by the loss of connections between nerve cells, or neurons, in certain regions of the brain. Ketamine and psychedelics both promote the brain’s ability to repair these connections, a quality called plasticity. If we could understand how these drugs encourage plasticity, we might be able to design drugs that can do so without the side effects.

Dr. David Olson at the University of California, Davis studies how psychedelics work at the cellular and molecular levels. The drugs appear to promote plasticity by binding to a receptor in cells called the 5-hydroxytryptamine 2A receptor (5-HT2AR). But many other compounds also bind 5-HT2AR without promoting plasticity. In a recent NIH-funded study, Olson showed that 5-HT2AR can be found both inside and on the surface of the cell. Only compounds that bound to the receptor inside the cells promoted plasticity. This suggests that a drug has to be able to get into the cell to promote plasticity.
Moreover, not all drugs that bind 5-HT2AR have psychedelic effects. Olson’s team has developed a molecular sensor, called psychLight, that can identify which compounds that bind 5-HT2AR have psychedelic effects. Using psychLight, they identified compounds that are not psychedelic but still have rapid and long-lasting antidepressant effects in animal models. He’s founded a company, Delix Therapeutics, to further develop drugs that promote plasticity.
Meanwhile, Zarate and his colleagues have been investigating a compound related to ketamine called hydroxynorketamine (HNK). Ketamine is converted to HNK in the body, and this process appears to be required for ketamine’s antidepressant effects. Administering HNK directly produced antidepressant-like effects in mice. At the same time, it did not cause the dissociative side effects and addiction caused by ketamine. Zarate’s team has already completed phase I trials of HNK in people showing that it’s safe. Phase II trials to find out whether it’s effective are scheduled to begin soon.
“What [ketamine and psychedelics] are doing for the field is they’re helping us realize that it is possible to move toward a repair model versus a symptom mitigation model,” Olson says. Unlike existing antidepressants, which just relieve the symptoms of depression, these drugs appear to fix the underlying causes. That’s likely why they work faster and produce longer-lasting effects. This research is bringing us closer to having safer antidepressants that only need to be taken once in a while, instead of every day.
—by Brian Doctrow, Ph.D.
Related Links
- How Psychedelic Drugs May Help with Depression
- Biosensor Advances Drug Discovery
- Neural Signature Predicts Antidepressant Response
- How Ketamine Relieves Symptoms of Depression
- Protein Structure Reveals How LSD Affects the Brain
- Predicting The Usefulness of Antidepressants
- Depression Screening and Treatment in Adults
- Serotonin Transporter Structure Revealed
- Placebo Effect in Depression Treatment
- When Sadness Lingers: Understanding and Treating Depression
- Psychedelic and Dissociative Drugs
References: An electroencephalographic signature predicts antidepressant response in major depression. Wu W, Zhang Y, Jiang J, Lucas MV, Fonzo GA, Rolle CE, Cooper C, Chin-Fatt C, Krepel N, Cornelssen CA, Wright R, Toll RT, Trivedi HM, Monuszko K, Caudle TL, Sarhadi K, Jha MK, Trombello JM, Deckersbach T, Adams P, McGrath PJ, Weissman MM, Fava M, Pizzagalli DA, Arns M, Trivedi MH, Etkin A. Nat Biotechnol. 2020 Feb 10. doi: 10.1038/s41587-019-0397-3. Epub 2020 Feb 10. PMID: 32042166. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. J Psychopharmacol . 2016 Dec;30(12):1165-1180. doi: 10.1177/0269881116675512. PMID: 27909164. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. Agin-Liebes GI, Malone T, Yalch MM, Mennenga SE, Ponté KL, Guss J, Bossis AP, Grigsby J, Fischer S, Ross S. J Psychopharmacol . 2020 Feb;34(2):155-166. doi: 10.1177/0269881119897615. Epub 2020 Jan 9. PMID: 31916890. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Vargas MV, Dunlap LE, Dong C, Carter SJ, Tombari RJ, Jami SA, Cameron LP, Patel SD, Hennessey JJ, Saeger HN, McCorvy JD, Gray JA, Tian L, Olson DE. Science . 2023 Feb 17;379(6633):700-706. doi: 10.1126/science.adf0435. Epub 2023 Feb 16. PMID: 36795823. Psychedelic-inspired drug discovery using an engineered biosensor. Dong C, Ly C, Dunlap LE, Vargas MV, Sun J, Hwang IW, Azinfar A, Oh WC, Wetsel WC, Olson DE, Tian L. Cell . 2021 Apr 8: S0092-8674(21)00374-3. doi: 10.1016/j.cell.2021.03.043. Epub 2021 Apr 28. PMID: 33915107. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. Nature . 2016 May 26;533(7604):481-6. doi: 10.1038/nature17998. Epub 2016 May 4. PMID: 27144355.
Connect with Us
- More Social Media from NIH

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
- Download PDF
- Order a free hardcopy
What is depression?
Everyone feels sad or low sometimes, but these feelings usually pass. Depression (also called major depression, major depressive disorder, or clinical depression) is different. It can cause severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working.
Depression can affect anyone regardless of age, gender, race or ethnicity, income, culture, or education. Research suggests that genetic, biological, environmental, and psychological factors play a role in the disorder.
Women are diagnosed with depression more often than men, but men can also be depressed. Because men may be less likely to recognize, talk about, and seek help for their negative feelings, they are at greater risk of their depression symptoms being undiagnosed and undertreated. Studies also show higher rates of depression and an increased risk for the disorder among members of the LGBTQI+ community.
In addition, depression can co-occur with other mental disorders or chronic illnesses, such as diabetes, cancer, heart disease, and chronic pain. Depression can make these conditions worse and vice versa. Sometimes, medications taken for an illness cause side effects that contribute to depression symptoms as well.
What are the different types of depression?
There are two common types of depression.
- Major depression includes symptoms of depressed mood or loss of interest, most of the time for at least 2 weeks, that interfere with daily activities.
- Persistent depressive disorder (also called dysthymia or dysthymic disorder) consists of less severe depression symptoms that last much longer, usually for at least 2 years.
Other types of depression include the following.
- Seasonal affective disorder comes and goes with the seasons, with symptoms typically starting in the late fall and early winter and going away during the spring and summer.
- Depression with symptoms of psychosis is a severe form of depression in which a person experiences psychosis symptoms, such as delusions or hallucinations.
- Bipolar disorder involves depressive episodes, as well as manic episodes (or less severe hypomanic episodes) with unusually elevated mood, greater irritability, or increased activity level.
Additional types of depression can occur at specific points in a woman’s life. Pregnancy, the postpartum period, the menstrual cycle, and menopause are associated with physical and hormonal changes that can bring on a depressive episode in some people.
- Premenstrual dysphoric disorder is a more severe form of premenstrual syndrome, or PMS, that occurs in the weeks before menstruation.
- Perinatal depression occurs during pregnancy or after childbirth. It is more than the “baby blues” many new moms experience after giving birth.
- Perimenopausal depression affects some women during the transition to menopause. Women may experience feelings of intense irritability, anxiety, sadness, or loss of enjoyment.
What are the signs and symptoms of depression?
Common signs and symptoms of depression include:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness or pessimism
- Feelings of irritability, frustration‚ or restlessness
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Fatigue, lack of energy, or feeling slowed down
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, waking too early in the morning, or oversleeping
- Changes in appetite or unplanned weight changes
- Physical aches or pains, headaches, cramps, or digestive problems without a clear physical cause that do not go away with treatment
- Thoughts of death or suicide or suicide attempts
Depression can also involve other changes in mood or behavior that include:
- Increased anger or irritability
- Feeling restless or on edge
- Becoming withdrawn, negative, or detached
- Increased engagement in high-risk activities
- Greater impulsivity
- Increased use of alcohol or drugs
- Isolating from family and friends
- Inability to meet responsibilities or ignoring other important roles
- Problems with sexual desire and performance
Not everyone who is depressed shows all these symptoms. Some people experience only a few symptoms, while others experience many. Depression symptoms interfere with day-to-day functioning and cause significant distress for the person experiencing them.
If you show signs or symptoms of depression and they persist or do not go away, talk to a health care provider. If you see signs of depression in someone you know, encourage them to seek help from a mental health professional.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911 .
How is depression diagnosed?
To be diagnosed with depression, a person must have symptoms most of the day, nearly every day, for at least 2 weeks. One of the symptoms must be a depressed mood or a loss of interest or pleasure in most activities. Children and adolescents may be irritable rather than sad.
Although several persistent symptoms, in addition to low mood, are required for a depression diagnosis, people with only a few symptoms may benefit from treatment. The severity and frequency of symptoms and how long they last vary depending on the person.
If you think you may have depression, talk to a health care provider, such as a primary care doctor, psychologist, or psychiatrist. During the visit, the provider may ask when your symptoms began, how long they have lasted, how often they occur, and if they keep you from going out or doing your usual activities. It may help to take some notes about your symptoms before the visit.
Certain medications and medical conditions, such as viruses or thyroid disorders, can cause the same symptoms as depression. A provider can rule out these possibilities by doing a physical exam, interview, and lab tests.
Does depression look the same in everyone?
Depression can affect people differently depending on their age.
- Children may be anxious or cranky, pretend to be sick, refuse to go to school, cling to a parent, or worry that a parent may die.
- Older children and teens may get into trouble at school, sulk, be easily frustrated‚ feel restless, or have low self-esteem. They may have other disorders, such as anxiety, an eating disorder, attention-deficit/hyperactivity disorder, or substance use disorder. Older children and teens are also more likely to experience excessive sleepiness (called hypersomnia) and increased appetite (called hyperphagia).
- Young adults are more likely to be irritable, complain of weight gain and hypersomnia, and have a negative view of life and the future. They often have other disorders, such as generalized anxiety disorder, social phobia, panic disorder, or substance use disorder.
- Middle-aged adults may have more depressive episodes, decreased libido, middle-of-the-night insomnia, or early morning waking. They often report stomach problems, such as diarrhea or constipation.
- Older adults often feel sadness, grief, or other less obvious symptoms. They may report a lack of emotions rather than a depressed mood. Older adults are also more likely to have other medical conditions or pain that can cause or contribute to depression. Memory and thinking problems (called pseudodementia) may be prominent in severe cases.
Depression can also look different in men versus women, such as the symptoms they show and the behaviors they use to cope with them. For instance, men (as well as women) may show symptoms other than sadness, instead seeming angry or irritable.
For some people, symptoms manifest as physical problems (for example, a racing heart, tightened chest, chronic headaches, or digestive issues). Many men are more likely to see a health care provider about these physical symptoms than their emotional ones. While increased use of alcohol or drugs can be a sign of depression in any person, men are also more likely to use these substances as a coping strategy.
How is depression treated?
Depression treatment typically involves psychotherapy (in person or virtual), medication, or both. If these treatments do not reduce symptoms sufficiently, brain stimulation therapy may be another option.
Choosing the right treatment plan is based on a person’s needs, preferences, and medical situation and in consultation with a mental health professional or a health care provider. Finding the best treatment may take trial and error.
For milder forms of depression, psychotherapy is often tried first, with medication added later if the therapy alone does not produce a good response. People with moderate or severe depression usually are prescribed medication as part of the initial treatment plan.
Psychotherapy
Psychotherapy (also called talk therapy or counseling) can help people with depression by teaching them new ways of thinking and behaving and helping them change habits that contribute to depression. Psychotherapy occurs under the care of a licensed, trained mental health professional in one-on-one sessions or with others in a group setting.
Psychotherapy can be effective when delivered in person or virtually via telehealth. A provider may support or supplement therapy using digital or mobile technology, like apps or other tools.
Evidence-based therapies to treat depression include cognitive behavioral therapy and interpersonal therapy. Using other forms of psychotherapy, such as psychodynamic therapy, for a limited time also may help some people with depression.
- Cognitive behavioral therapy (CBT) : With CBT, people learn to challenge and change unhelpful thoughts and behaviors to improve their depressive and anxious feelings. Recent advances in CBT include adding mindfulness principles and specializing the therapy to target specific symptoms like insomnia.
- Interpersonal therapy (IPT) : IPT focuses on interpersonal and life events that impact mood and vice versa. IPT aims to help people improve their communication skills within relationships, form social support networks, and develop realistic expectations to better deal with crises or other issues that may be contributing to or worsening their depression.
Learn more about psychotherapy .
Antidepressants are medications commonly used to treat depression. They work by changing how the brain produces or uses certain chemicals involved in mood or stress.
Antidepressants take time—usually 4−8 weeks—to work, and problems with sleep, appetite, and concentration often improve before mood lifts. Giving a medication a chance to work is important before deciding whether it is right for you.
Treatment-resistant depression occurs when a person doesn’t get better after trying at least two antidepressants. Esketamine is a medication approved by the U.S. Food and Drug Administration (FDA) for treatment-resistant depression. Delivered as a nasal spray in a doctor’s office, clinic, or hospital, the medication acts rapidly, typically within a couple of hours, to relieve depression symptoms. People will usually continue to take an antidepressant pill to maintain the improvement in their symptoms.
Another option for treatment-resistant depression is to combine an antidepressant with a different type of medication that may make it more effective, such as an antipsychotic or anticonvulsant medication.
All medications can have side effects. Talk to a health care provider before starting or stopping any medication. Learn more about antidepressants .
Note : In some cases, children, teenagers, and young adults under 25 years may experience an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. The FDA advises that patients of all ages taking antidepressants be watched closely, especially during the first few weeks of treatment.
Information about medication changes frequently. Learn more about specific medications like esketamine, including the latest approvals, side effects, warnings, and patient information, on the FDA website .
Brain stimulation therapy
Brain stimulation therapy is an option when other depression treatments have not worked. The therapy involves activating or inhibiting the brain with electricity or magnetic waves.
Although brain stimulation therapy is less frequently used than psychotherapy and medication, it can play an important role in treating depression in people who have not responded to other treatments. The therapy generally is used only after a person has tried psychotherapy and medication, and those treatments usually continue. Brain stimulation therapy is sometimes used as an earlier treatment option when severe depression has become life-threatening, such as when a person has stopped eating or drinking or is at a high risk of suicide.
The FDA has approved several types of brain stimulation therapy. The most used are electroconvulsive therapy (ECT) and repetitive transcranial magnetic stimulation (rTMS). Other brain stimulation therapies are newer and, in some cases, still considered experimental. Learn more about brain stimulation therapies .
Natural products
The FDA has not approved any natural products for treating depression. Although research is ongoing and findings are inconsistent, some people report that natural products, including vitamin D and the herbal dietary supplement St. John’s wort, helped their depression symptoms. However, these products can come with risks, including, in some cases, interactions with prescription medications.
Do not use vitamin D, St. John’s wort, or other dietary supplements or natural products without first talking to a health care provider. Rigorous studies must test whether these and other natural products are safe and effective.
How can I take care of myself?
Most people with depression benefit from mental health treatment. Once you begin treatment, you should gradually start to feel better. Go easy on yourself during this time. Try to do things you used to enjoy. Even if you don’t feel like doing them, they can improve your mood.
Other things that may help:
- Try to get physical activity. Just 30 minutes a day of walking can boost your mood.
- Try to maintain a regular bedtime and wake-up time.
- Eat regular, healthy meals.
- Do what you can as you can. Decide what must get done and what can wait.
- Connect with people. Talk to people you trust about how you are feeling.
- Delay making important life decisions until you feel better. Discuss decisions with people who know you well.
- Avoid using alcohol, nicotine, or drugs, including medications not prescribed for you.
How can I find help for depression?
You can learn about ways to get help and find tips for talking with a health care provider on the NIMH website.
The Substance Abuse and Mental Health Services Administration (SAMHSA) also has an online tool to help you find mental health services in your area.
How can I help a loved one who is depressed?
If someone you know is depressed, help them see a health care provider or mental health professional. You also can:
- Offer support, understanding, patience, and encouragement.
- Invite them out for walks, outings, and other activities.
- Help them stick to their treatment plan, such as setting reminders to take prescribed medications.
- Make sure they have transportation or access to therapy appointments.
- Remind them that, with time and treatment, their depression can lift.
What are clinical trials and why are they important?
Clinical trials are research studies that look at ways to prevent, detect, or treat diseases and conditions. These studies help show whether a treatment is safe and effective in people. Some people join clinical trials to help doctors and researchers learn more about a disease and improve health care. Other people, such as those with health conditions, join to try treatments that aren’t widely available.
NIMH supports clinical trials across the United States. Talk to a health care provider about clinical trials and whether one is right for you. Learn more about participating in clinical trials .
For more information
Learn more about mental health disorders and topics . For information about various health topics, visit the National Library of Medicine’s MedlinePlus .
The information in this publication is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health NIH Publication No. 24-MH-8079 Revised 2024

Yearly paid plans are up to 65% off for the spring sale. Limited time only! 🌸
- Form Builder
- Survey Maker
- AI Form Generator
- AI Survey Tool
- AI Quiz Maker
- Store Builder
- WordPress Plugin
HubSpot CRM
Google Sheets
Google Analytics
Microsoft Excel
- Popular Forms
- Job Application Form Template
- Rental Application Form Template
- Hotel Accommodation Form Template
- Online Registration Form Template
- Employment Application Form Template
- Application Forms
- Booking Forms
- Consent Forms
- Contact Forms
- Donation Forms
- Customer Satisfaction Surveys
- Employee Satisfaction Surveys
- Evaluation Surveys
- Feedback Surveys
- Market Research Surveys
- Personality Quiz Template
- Geography Quiz Template
- Math Quiz Template
- Science Quiz Template
- Vocabulary Quiz Template
Try without registration Quick Start
Read engaging stories, how-to guides, learn about forms.app features.
Inspirational ready-to-use templates for getting started fast and powerful.
Spot-on guides on how to use forms.app and make the most out of it.
See the technical measures we take and learn how we keep your data safe and secure.
- Integrations
- Help Center
- Sign In Sign Up Free
- 45 Survey questions for a depression questionnaire (+templates)
.jpg)
Eren Eltemur
Maintaining mental health is important, and depression is a big problem in the modern world. With the highly developed technological world, humankind keeps getting lonelier day by day. For this reason, diagnosing depression has become important, and a depression questionnaire can help professionals as a powerful tool. It makes it easier to gather data from patients using depression survey questions.
Since it is so important to gather data from clients with depression test questions, in this article, we cover what a depression questionnaire is , how to create an online depression questionnaire , and 45 great survey questions examples to use in your depression questionnaire. So if you are a mental health professional or want to create a questionnaire about depression, you can use this article as a go-to guide.
- What is a depression questionnaire?
A depression questionary is a way of assessing the severity of depressive symptoms associated with depression . Even though it can help professionals, individuals also self-measure their depression with surveys. Although it cannot give definite answers to measuring depression , it can be a helpful tool.
It can consist of a series of questions related to their feelings, appetite, sleep patterns , and other topics, such as their interest in activities . The quality of life is improved by having good mental health and well-being. For this reason, readers should take a step and take action to measure their depression with these helpful questions.
The definition of depression questionnaire
- 45 survey question examples to use in your depression questionnaire
Since we are well aware of the necessity of adequate questions as forms.app, we gathered 45 great questions for the survey questionnaire about depression. You can use these questions in your depression research questionnaire to create well-developed and professional surveys. Since there are different types of depression questionnaire examples, these questions are separated into groups with their intended use. Including these questions will give you information about your potential clients and see:
- if they are having trouble staying asleep or sleeping too much
- if they are feeling down, depressed, or hopeless all the time
- if they had a diagnosis of depression or received treatments for depression earlier
- If they read too much newspaper or watch television
- if they lost their interest and pleasure in life
- or in extreme cases, if they are having trouble moving or speaking so slowly.
Self-report questionnaires
This type is specifically focused on individual experience. Individuals can measure themselves with questions related to their feelings, symptoms, sadness, loss of interest , and suicidal thoughts.
SELF-CARE/MOBILITY
1 - Have you experienced physical symptoms such as aches and pains, digestive issues, or changes in appetite?
2 - Have you noticed any changes in your sleep patterns, such as waking up too early or feeling unrested after a full night's sleep?
3 - Do you feel self-conscious or embarrassed about your movement or speech patterns?
4 - Do you feel like your movements or speech are slower than usual or that you have trouble getting your words out?
5 - How frequently did you feel drained of energy over the last two weeks?
USUAL ACTIVITIES
6 - How frequently did you struggle to fall asleep, stay asleep, or oversleep over the previous two weeks?
7 - Have you been crying more or more easily than usual?
8 - How frequently did you find it difficult to focus over the past two weeks on activities like reading the news or watching TV?
9 - Do you have difficulty falling asleep or staying asleep most nights?
10 - Are there any changes in your sexual desire compared to usual?
ANXIETY/ DEPRESSION
11 - How many times in the last two weeks have you felt dejected, miserable, or hopeless?
12 - How many times in the last two weeks have you felt little interest in or enjoyment from accomplishing things?
13 - How frequently have you felt inferior to yourself, like a failure, or like you have let yourself or your family down over the last two weeks?
14 - Do you consider yourself more impatient than usual?
15 - Have you been feeling self-conscious, like a failure, or having disappointed yourself or your family?
16 - Do you feel guilty about something you have done?
17 - Do you have any recent trust issues in your relationships?
18 - Have you been feeling bad or sad most days, or have you lost interest in activities that you once enjoyed?
19 - Have you had thoughts of self-harm or suicide?
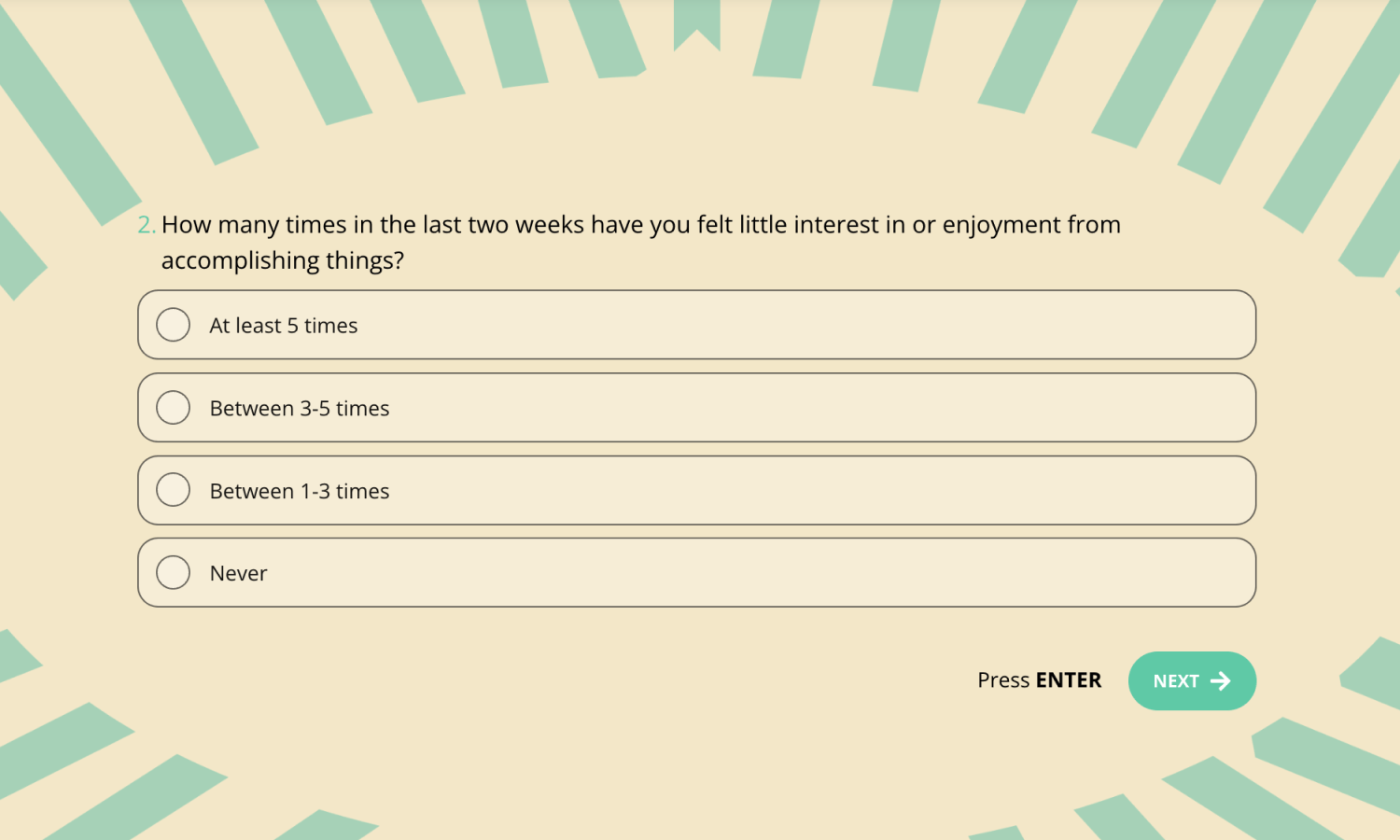
Self-report depression question example
Observer-Rated Questionnaires
20 - This type of questionnaire can be used by professionals or anyone other than the patient. Typically, they evaluate a variety of symptoms, such as alterations in mood, behavior, and physical health .
21 - Have you felt like your mental health issues are negatively affecting your ability to function at work, school, or in your personal life?
22 - Have you discussed your sleep problems with your primary care physician or another healthcare provider?
23 - Have you received any mental health care in the past year, such as counseling or medication management?
24 - Have you observed any changes in the individual's social functioning or engagement with others over the past week?
25 - Have you observed any changes in the individual's movement or speech patterns, such as slowing down or appearing agitated?
26 - How frequently has the individual reported feeling fatigued or lacking in energy over the past week?
27 - Over the past week, how frequently has the individual exhibited symptoms of sadness, hopelessness, or low mood?
28 - Over the past week, how frequently has the individual exhibited symptoms of irritability or restlessness?
29 - Have you observed any changes in the individual's ability to engage in social or recreational activities over the past week?
30 - Have you observed any changes in the individual's communication patterns or ability to express themselves effectively over the past week?
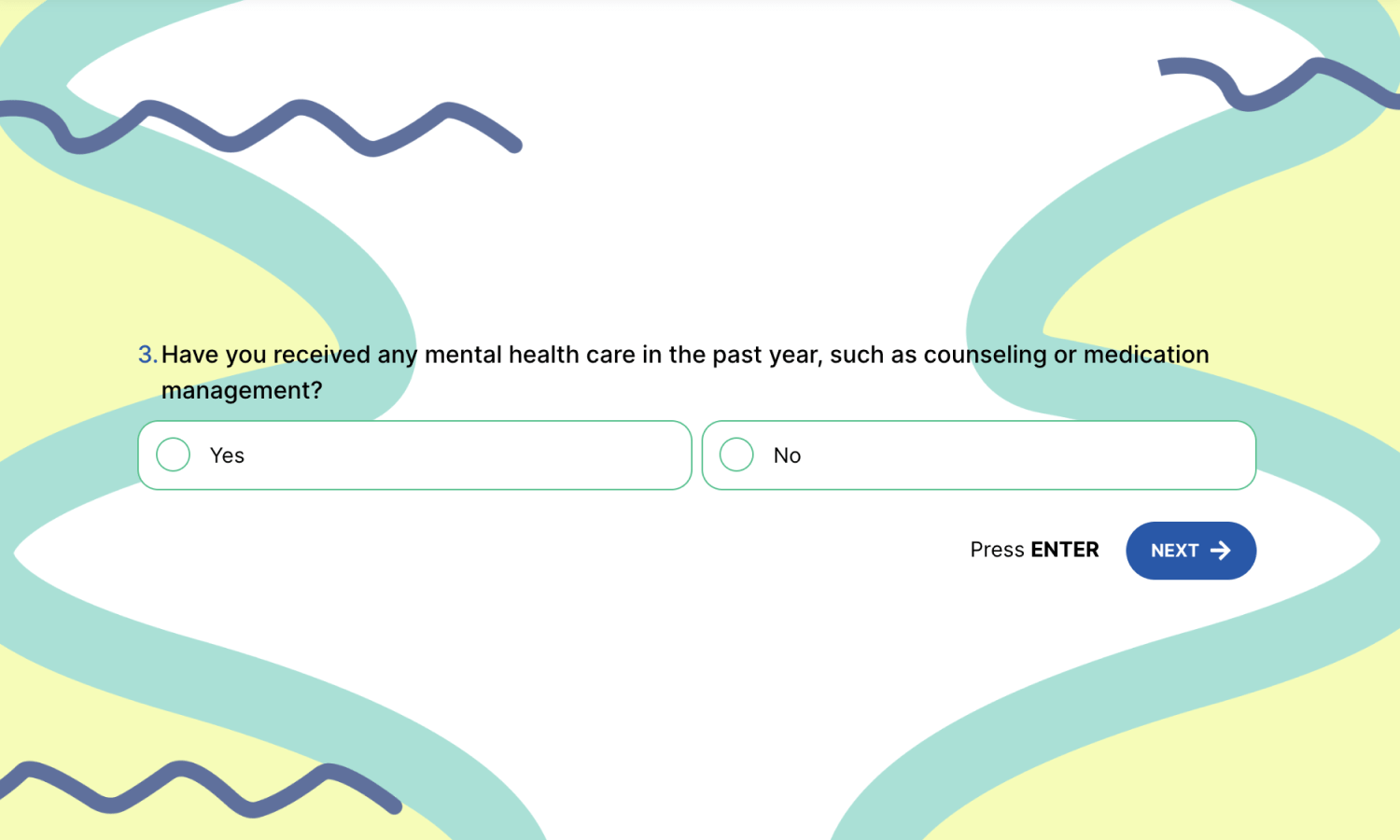
Observer-rated depression question example
Suicide risk questionnaires
This type of questionnaire focuses on suicidal intentions or attempts . It should be considered that these questions must be used by professionals but can also help to create awareness. It should be noted that patients may not be aware of their suicidal behavior. For this reason, creating awareness can help to save a life.
31 - Have you ever considered harming yourself or taking your own life?
32 - Have you thought about dying or getting killed?
33 - Have you ever considered suicide or attempted it before?
34 - Have you cut yourself or burned yourself? Or have you engaged in other self-harming behaviors?
35 - Have you been feeling more agitated, irritable, or anxious lately? Does this make you think about committing suicide?
36 - Have you had a substantial behavioral shift that would point to a possible suicide attempt, such as giving away possessions or saying goodbye to loved ones?
37 - Have your concentration or focus decreased as a result of having suicidal thoughts?
38 - Have you recently gone through a big loss or trauma that could have triggered feelings of hopelessness or thoughts of suicide?
39 - Have you ever felt guilty or unworthy, which could be motivating your suicidal thoughts?
40 - Have you experienced an increase in your use of drugs or alcohol as a way of coping with your depression symptoms?
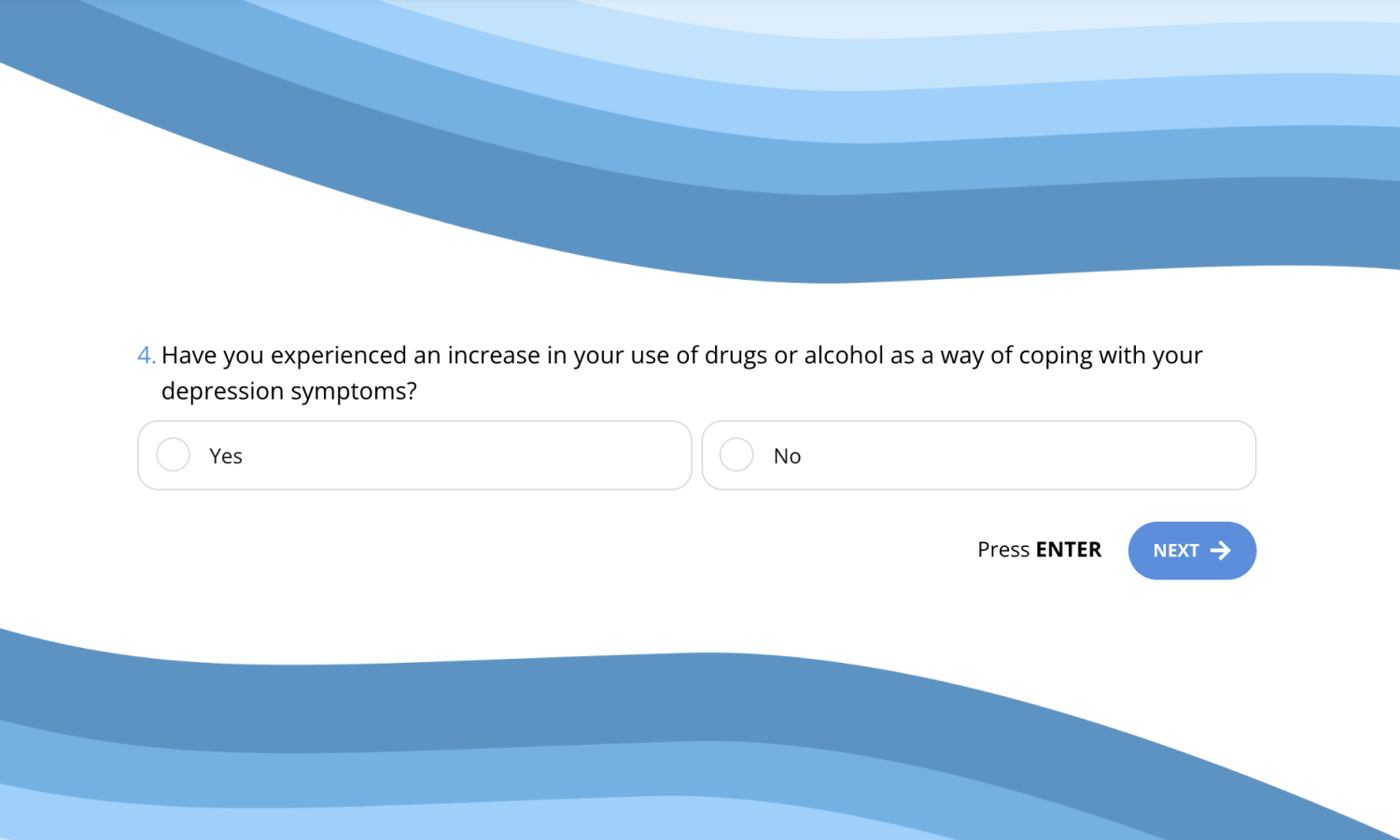
Suicide risk depression question example
- How to create an online depression questionnaire
Creating a depression questionnaire is an easy task with forms.app. You can customize pre-made depression questionnaires or create yours from scratch . You can create well-developed questionnaires using features like conditional logic and a calculator, and in addition to these, you can add multiple layers to your survey with different form fields. Here are some form fields you can use in your questionnaire to enrich your question variety:
- Single selection: Allows responders to pick up just one option.
- Multiple selections: Allow responders to select from a variety of alternatives.
- Picture selections: Enables responders with visual options to choose from.
- Selection matrix: Offers a graphic alternative for multiple or single choices.
- Short text: Short answer field for manual typing.
- Long text: Long answer field for manual typing.
- Yes/No: With only to possible outcomes, you can get conclusive responses.
How to automatically show results on your depression test
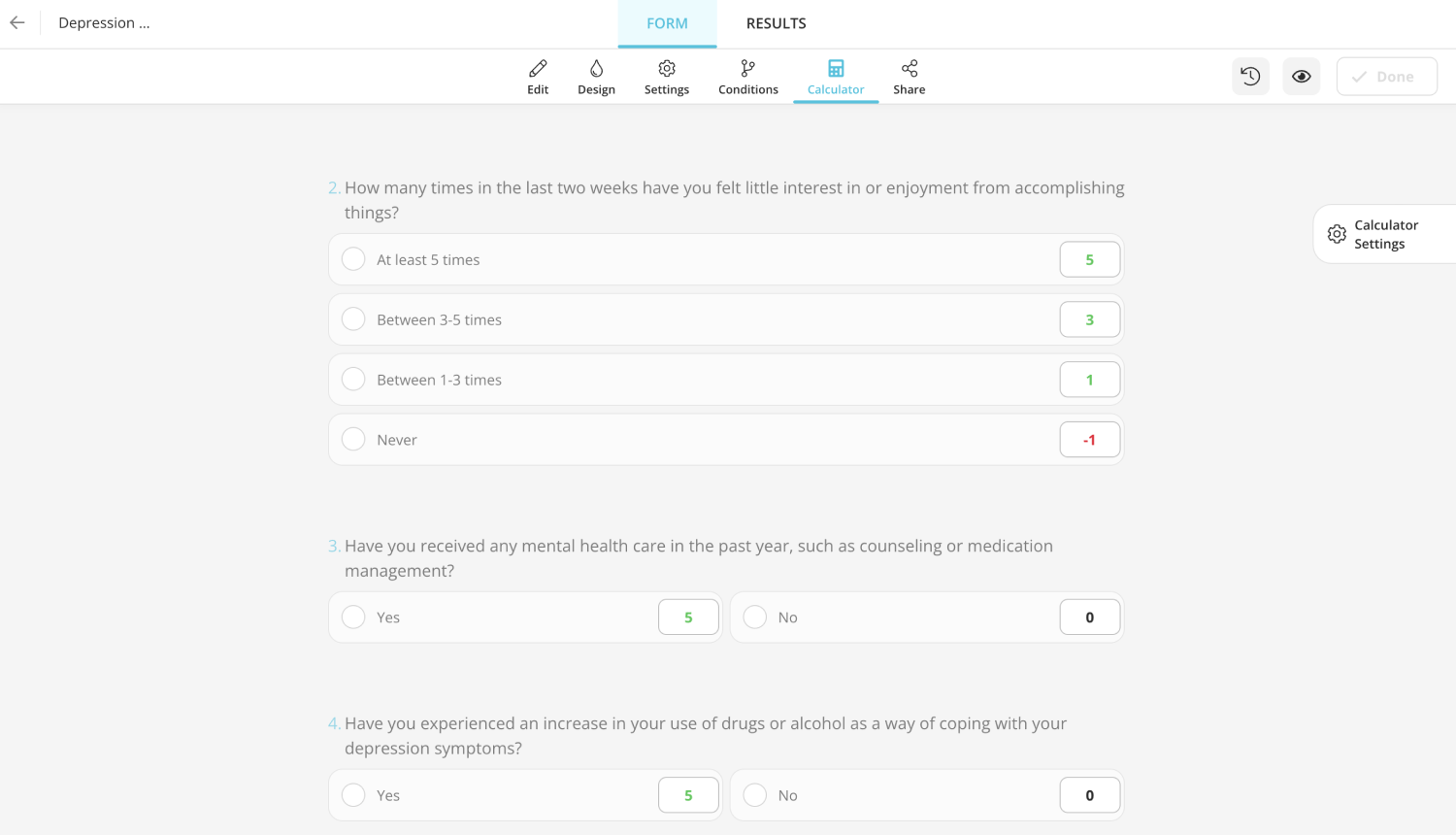
forms.app offers a calculator feature that can be used for measurement and showing results. You can give scores to each answer by setting up calculations. By assigning scores to necessary fields, you can get automated results for your depression surveys. Follow these 5 easy steps to use the calculator feature actively:
1 - Switch to the “Calculator” tab.
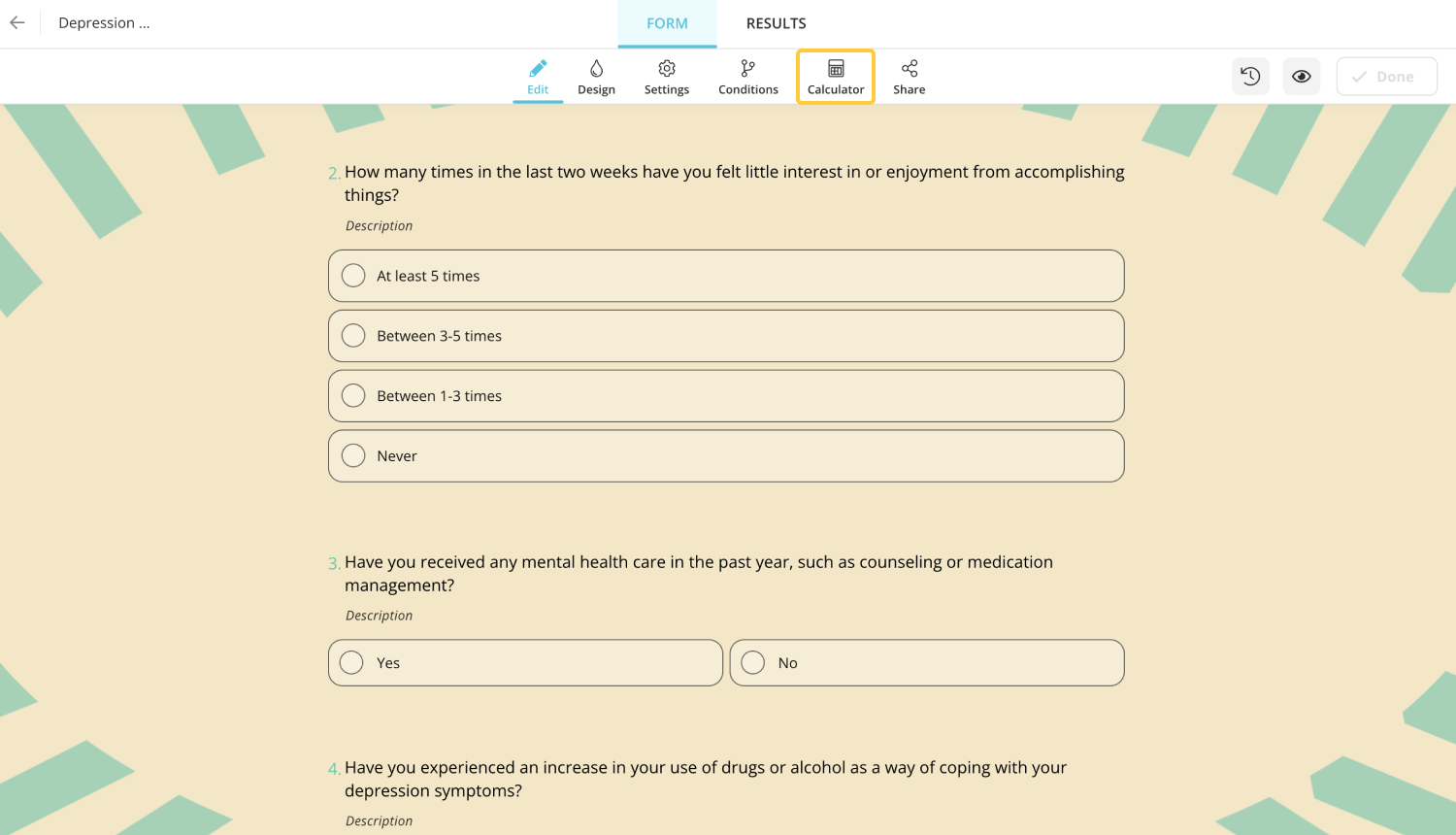
2 - Click on a score field of an option on the right side of each option.
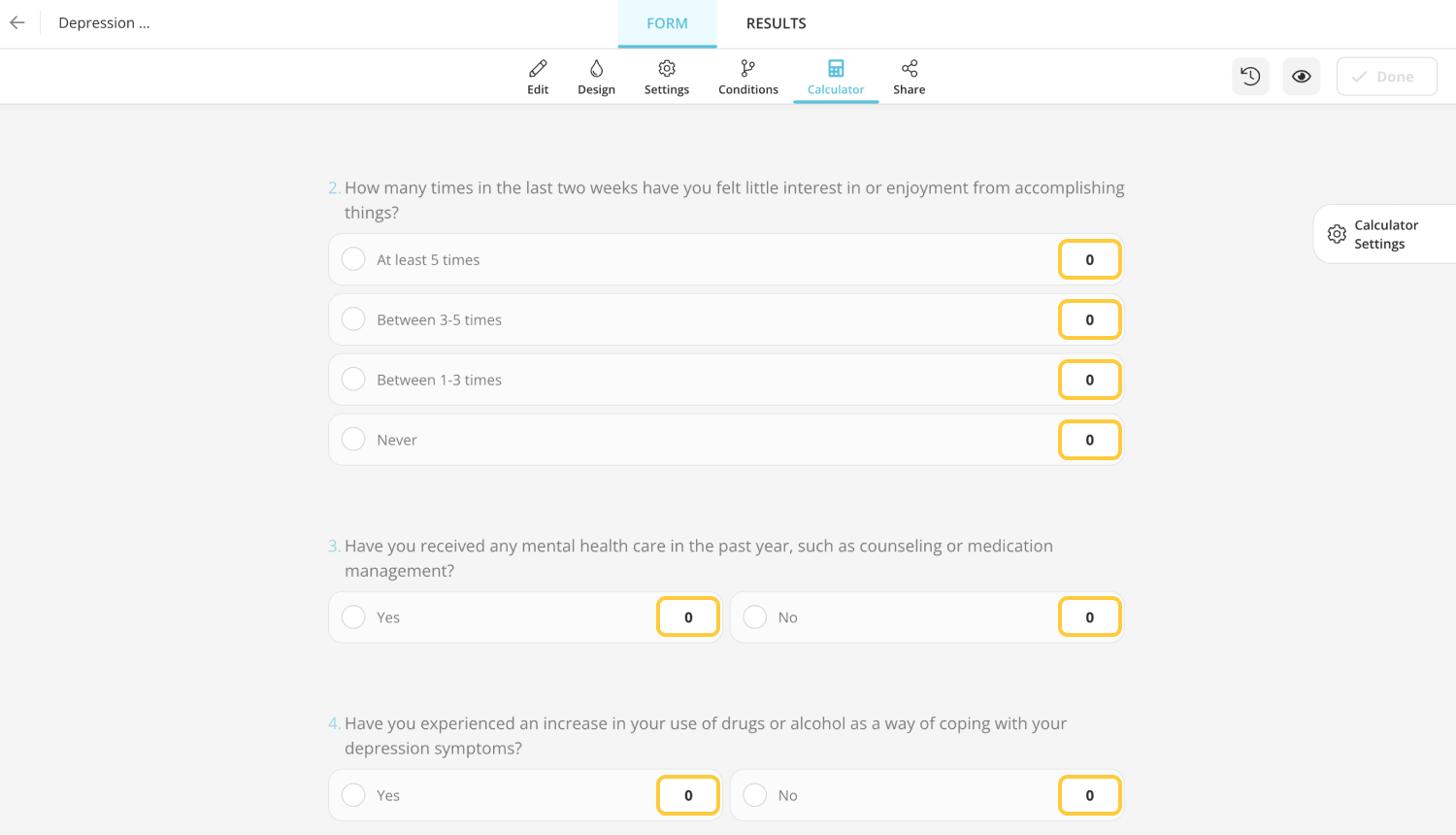
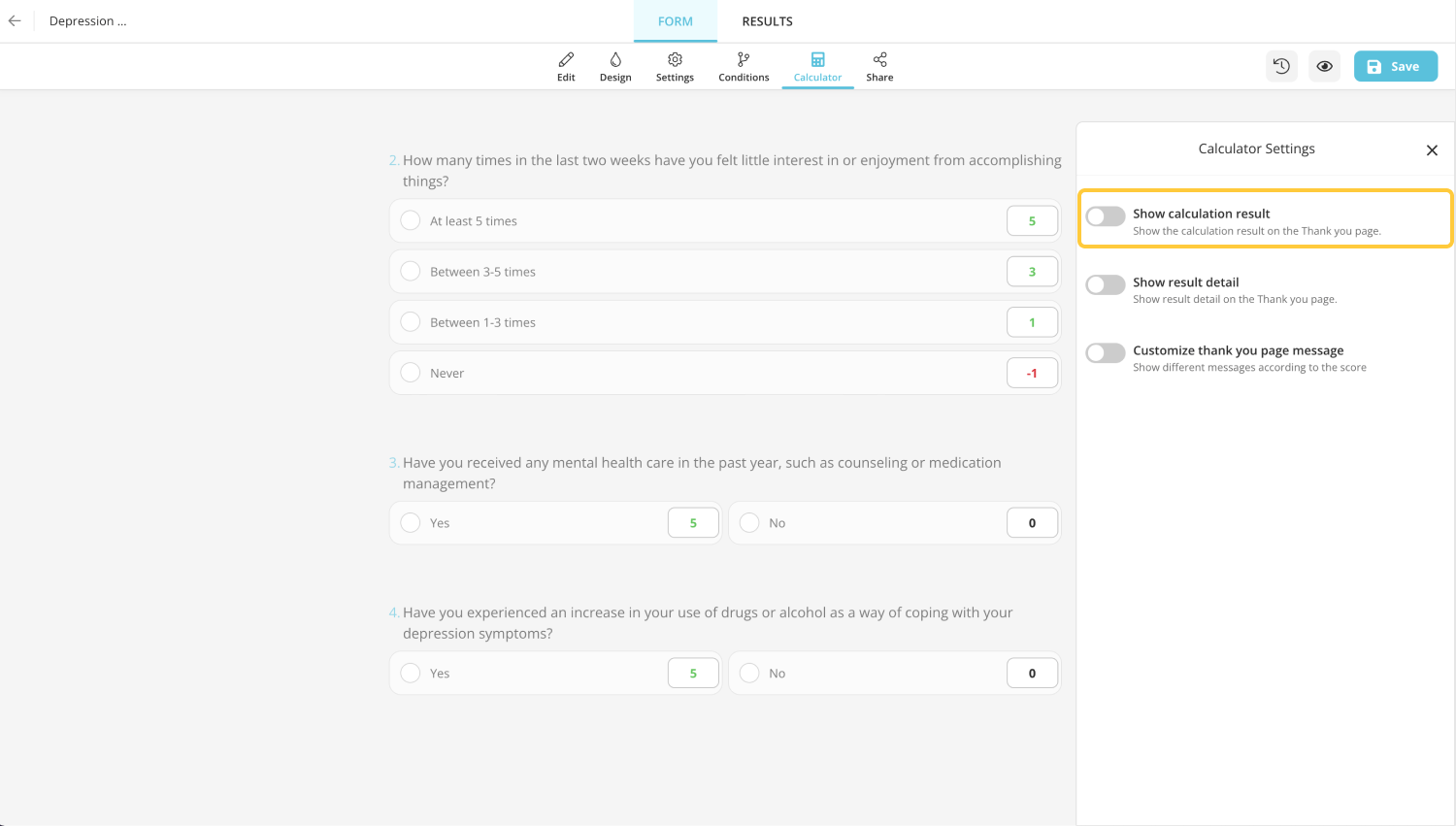
3 - Enter a positive value directly or a negative value
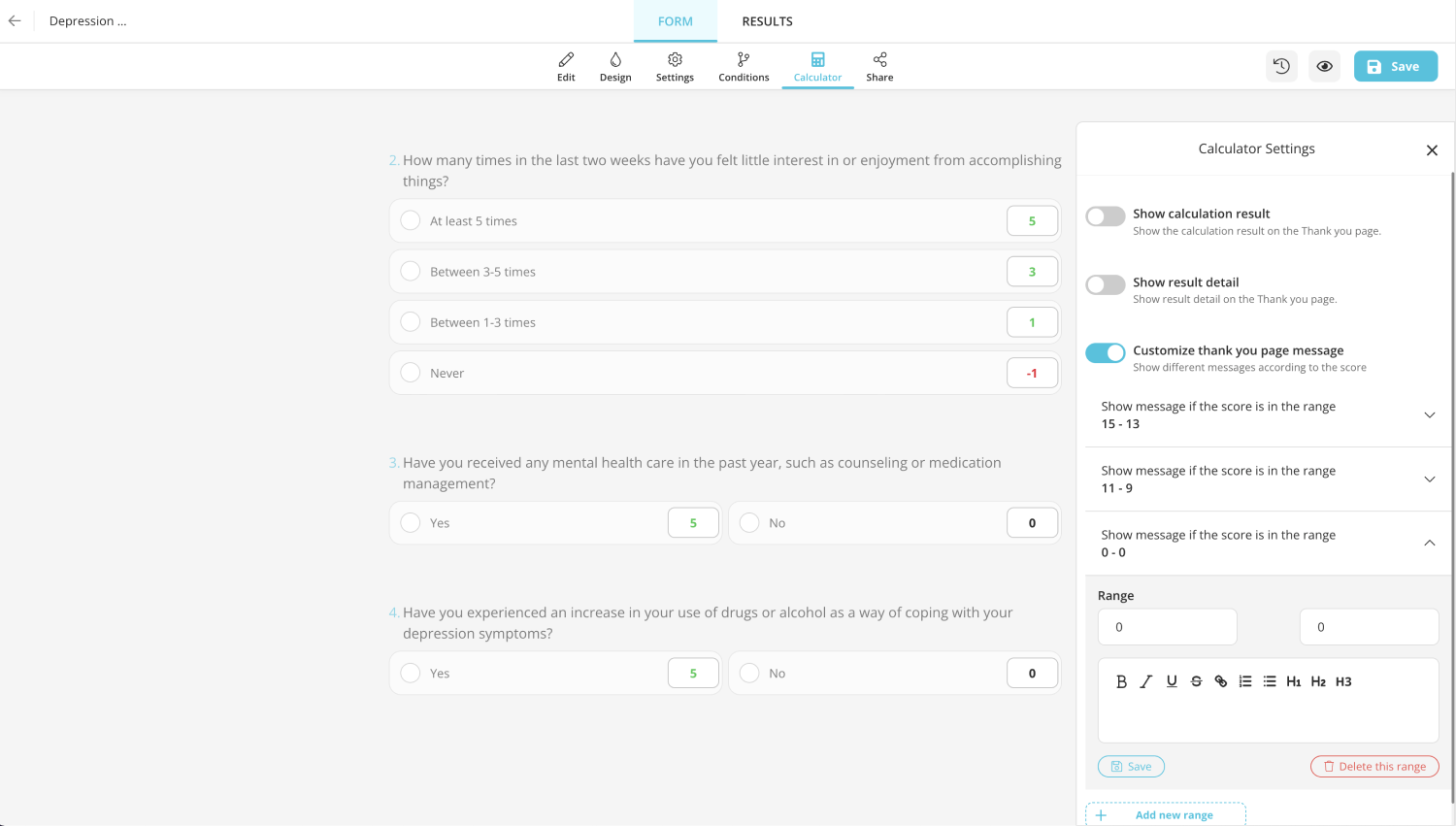
4 - On the calculation settings, click on “show calculation result” to show people their score
5 - Lastly, enable “Customize thank you page message” to add ranges and custom messages for people in a certain score range.
In conclusion, it is a fact that professionals must use these types of questions. But creating awareness and creating a short and easy way as the first step before professional support can also be helpful. forms.app offers a fast and easy way to create and customize depression questionnaires that focus on different aspects and topics.
- Form Features
- Data Collection
Table of Contents
Related posts.
Web surveys: Definition, types, examples & tips ( +free templates)
Işılay Kırbaş
Volunteer recruitment: A complete guide
Sevgi Soylu

Top 100 prize ideas for your online giveaways & contests
Şeyma Beyazçiçek
227 Depression Research Topics & Essay Titles + Examples
If you’re looking for a good depression research title, you’re at the right place! StudyCorgi has prepared a list of titles for depression essays and research questions that you can use for your presentation, persuasive paper, and other writing assignments. Read on to find your perfect research title about depression!
🙁 TOP 7 Depression Title Ideas
🏆 best research topics on depression, ❓ depression research questions, 👍 depression research topics & essay examples, 📝 argumentative essay topics about depression, 🌶️ hot depression titles for a paper, 🔎 creative research topics about depression, 🎓 most interesting depression essay topics, 💡 good titles for depression essays.
- Teenage Depression: Causes and Symptoms
- Depression: Case Conceptualization and Treatment Planning
- Depression and Solutions in Psychiatry
- The Concept of Postpartum Depression
- Depression in the Contemporary Society
- Depression: Psychoeducational Intervention
- Theories in Depression Treatment
- Depression as It Relates to Obesity This paper will argue that there is a positive correlation between depression and obesity. The paper will make use of authoritative sources to reinforce this assertion.
- Depression Among Rich People Analysis Among the myriad differences between rich and poor people is the manner in which they are influenced by and respond to depression.
- Impact of Depression on a Family The article makes a very powerful argument about the effects of depression on the relatives of the patient by identifying the major factors that put the family into a challenging position.
- Action Research in Treating Depression With Physical Exercise Depression is one of the most common mental health disorders in the United States. The latest statistics showed that depression does not discriminate against age.
- Depression and Depressive Disorders Depression is one of the leading causes of disability in the world. Symptoms are feelings of sadness and guilt, changes in sleeping patterns changes in appetite, and other.
- Social Media as a Cause of Anxiety and Depression Anxiety and depression are considerable problems for world society. Numerous studies have linked high social media use with high levels of anxiety and depression.
- Evidence-Based Pharmacology: Major Depression In this paper, a certain attention to different treatment approaches that can be offered to patients with depression will be paid, including the evaluation of age implications.
- Major Types of Depression This paper will review and analyze two scholarly articles concerning depression, its sings in male and female patients, and its connection and similarity to other disorders.
- Transition Phase of Depression and Its’ Challenges Providing psychoeducation to people with mild to moderate depression, strategies for recognizing and addressing conflict and reluctance are discussed in this paper
- Depression Treatment and Management Treatment could be started only after patient is checked whether he has an allergy to the prescribed pills or not. If he is not allergic, he should also maintain clinical tests for depression.
- Post-Stroke Anxiety and Depression The purpose of the given study is to ascertain how cognitive behavior therapy affects individuals with post-stroke ischemia in terms of depression reduction.
- Literature Evaluation on the Depression Illness The evaluation considers the articles that study such medical illness as depression from different planes of its perception.
- Application of Analysis of Variance in the Analysis of HIV/AIDS-Related Depression Cases Analysis of variance (ANOVA) is a commonly used approach in the testing of the equality of various means using variance.
- Does Social Media Use Contribute to Depression? Social media is a relatively new concept in a modern world. It combines technology and social tendencies to enhance interaction through Internet-based gadgets and applications.
- Depression and Other Antecedents of Obesity Defeating the inertia about taking up a regular programme of sports and exercise can be a challenging goal. Hence, more advocacy campaigns focus on doing something about obesity with a more prudent diet.
- Adolescent Mental Health: Depression This paper includes depression background discussion, including its signs, prevalence, diagnosis, and treatment, and a plan of treatment with three interventions to address this chronic health disease.
- Impact of COVID-19 on Depression and Suicide Rates among Adolescents and Young People The purpose of this paper is to explore the influence of coronavirus on these tragic numbers.
- Depression in Older Adults Depression is one of the most common mental illnesses in the world. Evidence-based holistic intervention would provide more effective treatment for elderly patients with depression.
- Smoking Cessation and Depression It was estimated that nicotine affects the human’s reward system. As a result, smoking cessation might lead to depression and other mental disorder.
- The Causes of Depression and How to Overcome It In this self-reflection essay, the author describes the causes of his depression and the steps he is taking to overcome it.
- Depression: Symptoms, Causes and Treatment Depression interferes with daily routine, wasting valuable time and lowering production. Persistent downs or blues, sadness, and anger may be signs of depression.
- Geriatric Depression Scale, Clock Drawing Test and Mini-Mental Status Examination Depression is a common condition among geriatric patients. Around 5 million older adults in the US experience significant morbidity from depression.
- Postpartum Depression: Evidence-Based Practice Postpartum or postnatal depression refers to a mood disorder that can manifest in a large variety of symptoms and can range from one person to another.
- Baby Blues: What We Know About Postpartum Depression The term Postpartum Depression describes a wide variety of physical and emotional adjustments experienced by a significant number of new mothers.
- Anxiety, Depression, and Post-Traumatic Stress Disorder Currently, many people experience anxiety, depression, and post-traumatic stress disorder that affect their general health.
- Depression and Anxiety in Mental Health Nurses Depression and anxiety are the most common mental diseases in humans. Nurses who work in mental health are at significant risk of getting psychiatric illnesses.
- “Yoga for Depression” Article by The Minded Institute One can say that depression is both the biological and mental Black Death of modern humanity in terms of prevalence and negative impact on global health.
- What Are the Characteristics and Causes of Depression?
- Why Are Athletes Vulnerable to Depression?
- Why and How Adolescents Are Affected by Generalized Anxiety Disorder and Clinical Depression?
- Does Depression Assist Eating Disorders?
- What Should You Know About Depression?
- How Can Mother Nature Lower Depression and Anxiety?
- How Can Video Games Relieve Stress and Reduce Depression?
- When Does Teacher Support Reduce Depression in Students?
- Why Are Teenagers Affected by Depression?
- How Teens and Depression Today?
- Are Mental Health Issues Like Depression Related to Race?
- What Does Depression Mean?
- How Did the Depression Affect France?
- How Does Depression Stop?
- When Postpartum Depression Leads to Psychosis?
- How Do Medication and Therapy Combat Depression?
- What Are the Leading Causes of Depression?
- What About Drugs for Anxiety and Depression?
- What’s the Big Deal About Anxiety and Depression in Students?
- How Should Childhood Depression and Anxiety Be?
- How Do Gender Stereotypes Warp Our View of Depression?
- What Are the Signs of Teenage Depression?
- Are Testosterone Levels and Depression Risk Linked Based on Partnering and Parenting?
- How Psychology Helps People With Depression?
- How Should Childhood Depression and Anxiety Be Treated or Dealt With?
- Relation Between the COVID-19 Pandemic and Depression The paper is to share an insight into the detrimental effects of the COVID-19 pandemic on the mental health of thousands of people and provide advice on how to reduce its impact.
- How Covid-19 Isolation Contributed to Depression and Adolescent Suicide The pandemic affected adolescents because of stringent isolation measures, which resulted in mental challenges such as depression and anxiety, hence suicidal thoughts.
- The Rise of Depression in the Era of the Internet Understanding how the Internet affects human lives is essential in ascertaining the reasons for the growing loneliness in the intrinsically connected world.
- Mitigating Postnatal Depression in New Mothers: A Recreational Program Plan Post-natal depression is a popular form of depression in women. This paper presents an activity plan for the use of leisure as a therapeutic response to post-natal depression.
- History and Treatment of Depression Depression is currently one of the most common medical conditions among the adult population in the US. The paper aims to investigate the history and treatment of depression.
- Effects of Music Therapy on Depressed Elderly People Music therapy has been shown to have positive effects among people, and thus the aim was to assess the validity of such claims using elderly people.
- Components of the Treatment of Depression The most effective ways of treating people with depression include pharmacotherapy, psychotherapy or a combination of both.
- Adult Depression Treatment in the United States This study characterizes the treatment of adult depression in the US. It is prompted by the findings of earlier studies, which discover the lack of efficient depression care.
- Homelessness and Depression Among Illiterate People There are various myths people have about homelessness and depression. For example, many people believe that only illiterate people can be homeless.
- Depression and Workplace Violence The purpose of this paper is to provide an in-depth analysis how can workplace violence and verbal aggression be reduced or dealt with by employees.
- Treating Mild Depression: Psychotherapy and Pharmacotherapy The project intends to investigate the comparative effectiveness of the treatments that are currently used for mild depression.
- Patients with Depression’ Care: Betty Case Betty, a 45 years old woman, is referred to a local clinic because of feeling depressed. She has a history of three divorces and thinks that she is tired of living the old way.
- Major Depression’ Symptoms and Treatment – Psychology A continuous sense of tiredness, unhappiness, and hopelessness are key signs of clinical or major depression. Such mood changes alter the daily life programs of an individual for sometimes.
- Women’s Mental Health Disorder: Major Depression The mental health disorder paper aims to explore major depression, its symptoms, assessment, and intervention strategies appropriate for women.
- Depression in Young Adults: Annotated Bibliography The purpose of this study was to discover sociodemographic and health traits related to depression sufferers’ usage of various mental health services.
- Depression in Middle-Aged African Women The research study investigates depression in middle-aged African women because the mental health of the population is a serious concern of the modern healthcare sector.
- Detecting Depression in Young Adults: Literature Review The paper shows a need for early identification of depression symptoms in primary care practice. PHQ-2 and PHQ-9 are useful tools for portraying symptoms.
- Predicting Barriers to Treatment for Depression Mental health issues such as depression and drug abuse are the most frequent among teenagers and young adults. In this age range, both disorders tend to co-occur.
- Early Diagnosis of Depression: Public Health Depression in young adults has become a significant health problem across the US. It causes persistent feelings of loss of interest in activities and sadness.
- Depression and Social Media in Scientific vs. Popular Articles The damage can come in the form of misinformation, which can result in an unjustified and unnecessary self-restriction of social media.
- Depression in Adolescence: Causes and Treatment Depression amongst young adults at the puberty stage comes in hand with several causes that one cannot imagine, and depression happens or is triggered by various reasons.
- Addressing Depression Among Native Youths The current paper aims to utilize a Medicine Wheel model and a social work paradigm to manage depression among Native American Indian youths.
- Psychological Assessments and Intervention Strategies for Depression The article presents two case studies highlighting the importance of psychological assessments and intervention strategies for individuals experiencing depression.
- The Impact of Postpartum Maternal Depression on Postnatal Attachment This paper examines the influence of postpartum maternal depression on postnatal infant attachment, discusses the adverse effects of depression on attachment.
- Marijuana Effects on Risk of Anxiety and Depression The current paper aims to find out whether medical cannabis can positively affect anxiety and depression and the process of their treatment.
- Cognitive Behavioral Therapy for Anxiety and Depression Cognitive behavioral therapy analyzes the unconscious processes influencing the normal functioning of the human body, causing different pathologies.
- Hypnotherapy as an Effective Method for Treating Depression This paper explores the use of hypnotherapy as a treatment for depression and highlights the advantages of hypnosis in addressing depressive symptoms.
- Depression and Anxiety: Mary’s Case Mary’s husband’s death precipitated her depression and anxiety diagnosis. She feels lonely and miserable as she struggles with her daily endeavors with limited emotional support.
- Postpartum Depression in Women and Men The focus of the paper is health problems that affect women after giving birth to a child, such as depression. The author proposes that men also experience postpartum depression.
- Repression and Depression in “The Yellow Wallpaper” by Charlotte Perkins Gilman In “The Yellow Wallpaper” by Charlotte Perkins Gilman, the author highlighted the connection between repression and depression.
- Men and Depression: Signs, Symptoms, Causes, and Treatment Depression in men and women has several incompatibilities as males suffer from health problems more often than women as they rarely express their emotions.
- Promotion of Change Regarding Adolescent Depression In the essay, the author describes the methods to evaluate the symptoms of a patient who has been referred for counseling with depression.
- Interventions to Cope With Depression Depression is characterized by sadness, anxiety, feelings of worthlessness, and helplessness. These feelings do not necessarily relate to life events.
- Bipolar Depression and Bipolar Mania Although all bipolar disorders are characterized by periods of extreme mood, the main difference between them is the severity of the condition itself.
- Is depression a biological condition or a result of unrealistic expectations?
- Should employers be legally required to provide support to workers with depression?
- Do the media portrayals of depression accurately reflect people’s experiences?
- Social media contributes to depression rates by eliciting the feeling of loneliness.
- Should mental health screening be mandatory in schools?
- Should depression be reclassified as a neurological disorder?
- Antidepressants are an overused quick-fix solution to depression.
- Should non-pharmacological treatments for depression be prioritized?
- Should depression be considered a disability?
- The use of electroconvulsive therapy for depression should be banned.
- Depression and Anxiety Management The medical staff will investigate the treatment modalities currently being utilized for the large population of patients experiencing symptoms of anxiety and depression.
- Depression in Hispanic Culture There are different ways in which culture or ethnicity can impact the treatment of the development of mental health disorders.
- Impacts of Stress of Low Income on the Risk of Depression in Children Socioeconomic hardships lead to a decline in the quality of parenting and the development of psychological and behavioral problems in children.
- African American Children Suffering From Anxiety and Depression Depression and anxiety are common among African American children and adolescents, and they face significant barriers to receiving care and treatment.
- Depression: Diagnostics and Treatment Depression, when it remains unchecked, can cause detrimental effects to individuals, such as suicide, which will eventually equate to mental disorders.
- Psychedelics in Depression and Anxiety Treatment Mental illnesses have become an essential part of health in the last few decades, with sufficient attention being devoted to interventions that resolve them.
- Depression and Anxiety Among African-American Children Depression and anxiety are common among African-American children and adolescents, but they face significant barriers to receiving care and treatment due to their age and race.
- Why Are Physical Activities Treatments for Depression? In this paper, the connection between physical activities and depression will be analyzed, and the common counterargument will be discussed.
- Depression in the Older Population The paper discusses depression is an actual clinical disorder for older people with specific reasons related to their age.
- Nutrition and Depression: A Psychological Perspective When discussing nutrition in toddlers and certain behavioral patterns, one of the first standpoints to pay attention to is the humanistic perspective.
- Social Media and Depression in Adolescents: The Causative Link This paper explores how social media causes depression in adolescents during the social-emotional stage of life.
- Physical Activities as Treatment for Depression This paper will discuss what factors are improved via physical exercise and how they help with treating depression.
- Therapeutic Interventions for the Older Adult With Depression and Dementia The paper researches the therapeutic interventions which relevant for the older people with depression and dementia nowadays.
- Depression Among Patients With Psoriasis Considering psoriasis as the cause of the development of depressive disorders, many researchers assign a decisive role to the severe skin itching that accompanies psoriasis.
- Qi Gong Practices’ Effects on Depression Qi Gong is a set of physical and spiritual practices aimed at the balance of mind, body, and soul and the article demonstrates whether it is good or not at treating depression.
- The Effects of Forgiveness Therapy on Depression for Women The study analyzes the impact of forgiveness therapy on the emotional state of women who have experienced emotional abuse.
- Post-operative Breast Cancer Patients With Depression: Annotated Bibliography This paper is an annotated bibliography about risk reduction strategies at the point of care: Post-operative breast cancer patients who are experiencing depression.
- Depression and Anxiety in Older Generation Depression and anxiety represent severe mental disorders that require immediate and prolonged treatment for patients of different ages.
- Coping with Depression After Loss of Loved Ones This case is about a 60-year-old man of African American origin. He suffered from depression after his wife’s death, which made him feel lonely and isolated.
- Postpartum Depression Screening Program Evaluation In order to manage the depression of mothers who have just delivered, it is important to introduce a routine postpartum depression-screening program in all public hospitals.
- Is Creativity A Modern Panacea From Boredom and Depression? Communication, daily life, and working patterns become nothing but fixed mechanisms that are deprived of any additional thoughts and perspectives.
- Adolescent Males With Depression: Poly-Substance Abuse Depression is the most crucial aspect that makes young males indulge in poly-substance abuse. There are various ways in which male adolescents express their depression.
- The Health of the Elderly: Depression and Severe Emotional Disturbance This study is intended for males and females over the age of 50 years who are likely to suffer from depression and severe emotional disturbance.
- Suicidal Ideation & Depression in Elderly Living in Nursing Home vs. With Family This paper attempts to compare the incidence of suicidal ideation and depression among elderly individuals living in nursing homes and those living with family in the community.
- Major Depression: Symptoms and Treatment Major depression is known as clinical depression, which is characterized by several symptoms. There are biological, psychological, social, and evolutionary causes of depression.
- Health Disparity Advocacy: Clinical Depression in the U.S. Recent statistics show that approximately more than 10 million people suffer from severe depression each year in the U.S..
- Serum Neurotrophic Factors in Adolescent Depression by Pallavi et al. The research hypothesis of the article is to compare the serum concentration of neurotrophic factors in depression patients and healthy control.
- The Treatment of Anxiety and Depression The meta-analysis provides ample evidence, which indicates that CES is not only effective but also safe in the treatment of anxiety and depression.
- Depression Intervention Among Diabetes Patients The research examines the communication patterns used by depression care specialist nurses when communicating with patients suffering from diabetes.
- Postnatal Depression in New Mothers and Its Prevention Leisure activities keep new mothers suffering from postnatal depression busy and enable them to interact with other members of the society.
- Treatment of Major Depression The purpose of the paper is to identify the etiology and the treatment of major depression from a psychoanalytic and cognitive perspective.
- Edinburgh Depression Screen for Treating Depression Edinburgh Depression screen is also known as Edinburgh Postnatal Depression Scale which is used to screen pregnant and postnatal women for emotional distress.
- Depression Treatment Variants in the US There is a debate regarding the best formula for depression treatment whereby some argue for using drugs, whereas others are advocating for therapy.
- Depression in the Elderly: Treatment Options Professionals may recommend various treatment options, including the use of antidepressants, psychotherapy such as cognitive-behavioral therapy.
- Can physical exercise alone effectively treat depression?
- Art therapy as a complementary treatment for depression.
- Is there a link between perfectionism and depression?
- The influence of sleep patterns on depression treatment outcomes.
- Can exposure to nature and green spaces decrease depression rates in cities?
- The relationship between diet and depression symptoms.
- The potential benefits of psychedelic-assisted therapy in treating depression.
- The role of outdoor experiences in alleviating depression symptoms.
- The relationship between depression and physical health in older adults.
- The role of workplace culture in preventing employee depression.
- Depression Treatments and Therapeutic Strategies This article examines the effectiveness of different depression treatments and reviews the therapeutic strategies, which can be helpful if the initial treatment fails.
- Depression and the Nervous System Depression is a broad condition that is associated with failures in many parts of the nervous system. It can be both the cause and the effect of this imbalance.
- Depression: Types, Symptoms, Etiology & Management Depression differs from other disorders, connected with mood swings, and it may present a serious threat to the individual’s health condition.
- The Effect of Music Therapy on Depression One major finding of study is that music therapy alleviates depression among the elderly. Music therapy could alleviate depression.
- Post-Natal Depression as an Affective Disorder Postpartum or post-natal depression (PPD) is a serious issue that can potentially be destructive to both infant and mother.
- “Neighborhood Racial Discrimination and the Development of Major Depression” by Russell The study investigates how neighborhood racial discrimination influences this severe mental disorder among African American Women.
- Adolescent Depression and Physical Health Depression in adolescents and young people under 24 is a factor that affects their physical health negatively and requires intervention from various stakeholders.
- Family Support to a Veteran With Depression Even the strongest soldiers become vulnerable to multiple health risks and behavioral changes, and depression is one of the problems military families face.
- Alcohol and Depression Article by Churchill and Farrell The selected article for this discussion is “Alcohol and Depression: Evidence From the 2014 Health Survey for England” by Sefa Awaworyi Churchill and Lisa Farrell.
- Negative Effects of Depression in Adolescents on Their Physical Health Mental disorders affect sleep patterns, physical activity, digestive and cardiac system. The purpose of the paper to provide information about adverse impacts of depression on health.
- Elderly Depression: Symptoms, Consequences, Behavior, and Therapy The paper aims to identify symptoms, behavioral inclinations of older adults, consequences of depression, and treatment ways.
- Depression in Feminist Literature of the 1890s The aim of the work is to analyze the cause of female sickness, which is their inability to express themselves and the pitiful place of a female in the society of that time.
- Major Depression Disorder: Causes and Treatment Loss in weight and appetite are some of the symptoms that a patient diagnosed with Major Depression Disorder could manifest.
- Mood Disorders: Depression Concepts Description The essay describes the nature of depression, its causes, characteristics, consequences, and possible ways of treatment.
- Geriatric Depression Diagnostics Study Protocol The research question is: how does the implementation of the National Institute for Health and Care Excellence guidelines affect the accuracy of diagnosing of depression?
- Mental Health Association of Depression and Alzheimer’s in the Elderly Depression can be a part of Alzheimer’s disease. Elderly people may have episodes of depression, but these episodes cannot be always linked to Alzheimer’s disease.
- Protective Factors Against Youthful Depression Several iterations of multiple correlation, step-wise and hierarchical regression yielded inconclusive results about the antecedents of youthful depression.
- Depression and Related Psychological Issues Depression as any mental disorder can be ascribed, regarding the use of psychoanalysis, to a person`s inability to control his destructive or sexual instincts or impulses.
- Television Habituation and Adolescent Depression The paper investigates the theory that there is a link between heavy TV viewing and adolescent depression and assess the strength of association.
- Physiological Psychology. Postpartum Depression Depression is a focal public health question. In the childbearing period, it is commoner in females than in males with a 2:1 ratio.
- Adolescent Depression: Modern Issues and Resources Teenagers encounter many challenging health-related issues; mental health conditions are one of them. This paper presents the aspects of depression in adolescents.
- Occupational Psychology: Depression Counselling The case involves a 28-year-old employee at Data Analytics Ltd. A traumatic event affected his mental health, causing depression and reduced performance.
- Psychotherapeutic Group: Treatment of Mild-To-Moderate Depression The aim of this manual is to provide direction and employ high-quality sources dedicated to mild-to-moderate depression and group therapy to justify the choices made for the group.
- “Depression and Ways of Coping With Stress” by Orzechowska et al. The study “Depression and Ways of Coping With Stress” by Orzechowska et al. aimed the solve an issue pertinent to nursing since depression can influence any patient.
- Effectiveness of Telenursing in Reducing Readmission, Depression, and Anxiety The project is dedicated to testing the effectiveness of telenursing in reducing readmission, depression, and anxiety, as well as improving general health outcomes.
- Nurses’ Interventions in Postnatal Depression Treatment This investigation evaluates the effect of nurses’ interventions on the level of women’s postnatal depression and their emotional state.
- Postpartum Depression: Evidence-Based Care Outcomes In this evidence-based study, the instances of potassium depression should be viewed as the key dependent variable that will have to be monitored in the course of the analysis.
- Postpartum Depression: Diagnosis and Treatment This paper aims to discuss the peculiarities of five one-hour classes on depression awareness, to implement this intervention among first-year mothers, and to evaluate its worth during the first year after giving birth.
- Postpartum Depression In First-time Mothers The most common mental health problem associated with childbirth remains postpartum depression, which can affect both sexes, and negatively influences the newborn child.
- The Diagnosis and Treatment of Postpartum Depression Postpartum depression has many explanations, but the usual way of referring to this disease is linked to psychological problems.
- What Is Postpartum Depression? Causes, Symptoms, and Treatment The prevalence of postpartum depression is quite high as one in seven new American mothers develops this health issue.
- Depression in Adolescence as a Contemporary Issue Depression in adolescents is not medically different from adult depression but is caused by developmental and social challenges young people encounter.
- Predictors of Postpartum Depression The phenomenon of postpartum depression affects the quality of women’s lives, as well as their self-esteem and relationships with their child.
- Depression and Self-Esteem: Research Problem Apart from descriptively studying the relationship between depression and self-esteem, a more practical approach can be used to check how interventions for enhancing self-esteem might affect depression.
- The Relationship Between Depression and Self-Esteem The topic which is proposed to be studied is the relationship between depression and self-esteem. Self-esteem can be defined as individual’s subjective evaluation of his or her worth.
- The Impact of Depression on Motherhood This work studies the impact of depression screening on prenatal and posts natal motherhood and effects on early interventions using a literature review.
- Self-Esteem and Depression in Quantitative Research The topic that has been proposed for quantitative research pertains to the problem of the relationship between self-esteem and depression.
- Depression in Female Cancer Patients and Survivors Depression is often associated with fatigue and sleep disturbances that prevent females from thinking positively and focusing on the treatment and its outcomes.
- Depression in Cardiac or Diabetic Patients The paper develops a framework through which risk factors associated with the development of MDD among adult patients with heart disease or diabetes can be easily identified.
- The Geriatric Population’s Depression This paper discusses how does the implementation of National Institute for Health and Care guidelines affect the accuracy of diagnosing of depression in the geriatric population.
- Problem of Depression: Recognition and Management Depression is a major health concern, which is relatively prevalent in the modern world. Indeed, in the US, 6.7 % of adults experienced an episode of the Major Depressive Disorder in 2015.
- Health and Care Excellence in Depression Management The introduction of the National Institute for Health and Care Excellence guidelines can affect the accuracy of diagnosing and quality of managing depression.
- Mild Depression: Psychotherapy or Pharmacotherapy The research question in this paper is: in psychiatric patients with mild depression, what is the effect of psychotherapy on health compared with pharmacotherapy?
- Postpartum Bipolar Disorder and Depression The results of the Mood Disorder Questionnaire screening of a postpartum patient suggest a bipolar disorder caused by hormonal issues and a major depressive episode.
- Bipolar Disorder or Manic Depression Bipolar disorder is a mental illness characterized by unusual mood changes that shift from manic to depressive extremes. In the medical field, it`s called manic depression.
- The Improvement of Depression Management The present paper summarizes the context analysis that was prepared for a change project aimed at the improvement of depression management.
- Depression Management in US National Guidelines The project offers the VEGA medical center to implement the guidelines for depression management developed by the National Institute for Health and Care Excellence.
- Women’s Health and Major Depression Symptoms The client’s complaints refer to sleep problems, frequent mood swings (she gets sad a lot), and the desire to stay away from social interactions.
- Predictors of Postpartum Depression: Who Is at Risk? The article “Predictors of Postpartum Depression” by Katon, Russo, and Gavin focuses on the identification of risk factors related to postnatal depression.
- Depression and Its Treatment: Racial and Ethnic Disparities The racial and ethnic disparities in depression treatment can be used for the development of quality improvement initiatives aimed at the advancement of patient outcomes.
- Lamotrigine for Bipolar Depression Management Lamotrigine sold as Lamictal is considered an effective medication helping to reduce some symptoms that significantly affect epileptic and bipolar patients’ quality of life.
- Citalopram, Methylphenidate in Geriatric Depression Citalopram typically ranges among 10-20 antidepressants for its cost-effectiveness and positive effect on patients being even more effective than reboxetine and paroxetine.
- Depression and Self-Esteem Relationship Self-esteem can be defined as an “individual’s subjective evaluation of his or her worth as a person”; it does not necessarily describe one’s real talents.
- Postpartum Depression: Methods for the Prevention Postpartum depression is a pressing clinical problem that affects new mothers, infants, and other family members. The prevalence of postpartum depression ranges between 13 and 19 percent.
- Anxiety and Depression Among Females with Cancer The study investigated the prevalence of and the potential factors of risk for anxiety and/or depression among females with early breast cancer during the first 5 years.
- Post-Partum Depression and Perinatal Dyadic Psychotherapy Post-partum depression affects more than ten percent of young mothers, and a method Perinatal Dyadic Psychotherapy is widely used to reduce anxiety.
- VEGA Medical Center: Detection of Depression Practice guidelines for the psychiatric evaluation of adults, and they can be employed to solve the meso-level problem of the VEGA medical center and its nurses.
- The Postnatal (Postpartum) Depression’ Concept Postnatal or postpartum depression (PPD) is a subtype of depression which is experienced by women within the first half a year after giving birth.
- Depression in Obstetrics and Gynecology: Research This essay analyzes a clinical research article “Improving care for depression in obstetrics and gynecology: A randomized controlled trial” by Melville et al.
- Postpartum Depression, Prevention and Treatment Postpartum depression is a common psychiatric condition in women of the childbearing age. They are most likely to develop the disease within a year after childbirth.
- Smoking Cessation and Depression Problem The aim of the study is to scrutinize the issues inherent in the process of smoking cessation and align them with the occurrence of depression in an extensive sample of individuals.
- The Efficacy of Medication in Depression’ Treatment This paper attempts to provide a substantial material for the participation in an argument concerning the clinical effectiveness of antidepressant medications.
- Depression and Cognitive Psychotherapy Approaches Cognitive psychotherapy offers various techniques to cope with emotional problems. This paper discusses the most effective cognitive approaches.
- Treatment of Depression in Lesbians The aim of this paper is to review a case study of 45 years old lesbian woman who seeks treatment for depression and to discuss the biophysical, psychological, sociocultural, health system.
- Women’s Health: Predictors of Postpartum Depression The article written by Katon, Russo, and Gavin is focused on women’s health. It discusses predictors of postpartum depression (PPD), including sociodemographic and clinic risk factors.
- Depression and Thyroid Issues in Young Woman Young people are busy at studies or at work and do not pay much attention to primary symptoms unless they influence the quality of life.
- Counseling Depression: Ethical Aspects This paper explores the ethical aspects required to work with a widower who diminished passion for food, secluding himself in the house, portraying signs of depression.
- Postpartum Depression as Serious Mental Health Problem The research study aimed to evaluate the effectiveness of a two-step behavioral and educational intervention on the symptoms of postpartum depression in young mothers.
- European Alliances, Wars, Dictatorships and Depression The decades leading to World War I had unusual alignments. The European nations were still scrambling for Asia, Africa and parts of undeveloped Europe.
- Women’s Health: Depression as a Psychological Factor Women who identify themselves as lesbian are likely to experience depression. Biophysical, psychological, sociocultural, behavioral, and health system factors should be taken into consideration.
- Childhood Obesity and Depression Intervention The main intervention to combat depressive moods in adolescents should be linked to improving the psychological health of young people in cooperation with schools.
- Postnatal Depression Prevalence and Effects The paper analyzes the prevalence and risk factors of Postnatal (Postpartum) Depression as well as investigates the effect on the newborns whose mothers suffer from this condition.
- Placebo and Treatments for Depression Natural alternative treatments for depression actually work better than the biochemical alternatives like antidepressants.
- Care for Depression in Obstetrics and Gynecology This work analyzes the article developed by Melville et al. in which discusses the theme of depression in obstetrics and gynecology and improving care for it.
- Depression Screening in Primary Care Screening for depression in patients suffering from long term conditions (LTCs) or persistent health problems of the body, could largely be erroneous.
- Clinical Depression Treatment: Issues and Solvings The paper describes and justifies the design selected for research on depression treatment. It also identifies ethical issues and proposes ways of addressing them.
- Depression in Older Persons – Psychology This article presents the research findings of a study conducted in Iran to assess how effective integrative and instrumental therapies are in the management of depression in older persons.
- Depression in the Elderly – Psychology This paper discusses how a person would know whether a relative had clinical depression or was sad due to specific changes or losses in life.
- Depression in the Elderly Depression can be defined as a state of anxiety, sadness, hopelessness, and worthlessness. It can affect people across all ages, who present with diverse signs and symptoms
- Postnatal Depression: Prevalence of Postnatal Depression in Bahrain The study was aimed at estimating the prevalence of postnatal depression among 237 Bahraini women who attended checkups in 20 clinical centres over a period of 2 months.
Cite this post
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2021, September 9). 227 Depression Research Topics & Essay Titles + Examples. https://studycorgi.com/ideas/depression-essay-topics/
"227 Depression Research Topics & Essay Titles + Examples." StudyCorgi , 9 Sept. 2021, studycorgi.com/ideas/depression-essay-topics/.
StudyCorgi . (2021) '227 Depression Research Topics & Essay Titles + Examples'. 9 September.
1. StudyCorgi . "227 Depression Research Topics & Essay Titles + Examples." September 9, 2021. https://studycorgi.com/ideas/depression-essay-topics/.
Bibliography
StudyCorgi . "227 Depression Research Topics & Essay Titles + Examples." September 9, 2021. https://studycorgi.com/ideas/depression-essay-topics/.
StudyCorgi . 2021. "227 Depression Research Topics & Essay Titles + Examples." September 9, 2021. https://studycorgi.com/ideas/depression-essay-topics/.
These essay examples and topics on Depression were carefully selected by the StudyCorgi editorial team. They meet our highest standards in terms of grammar, punctuation, style, and fact accuracy. Please ensure you properly reference the materials if you’re using them to write your assignment.
This essay topic collection was updated on January 22, 2024 .

Frequently Asked Questions
What is Depression?
Major Depression, also known as clinical or unipolar depression, is one of the most common mental illnesses. Over 9 million American adults suffer from clinical depression each year. This estimate is likely to be higher since depression commonly remains undiagnosed and untreated in a large percentage of the U.S. population. Major Depression is more than a temporary state of feeling sad; rather, it is a persistent state that can significantly impair an individual's thoughts, behavior, daily activities, and physical health.
Major Depressive Disorder impacts all racial, ethnic, and socioeconomic groups and can occur at any age. The average lifetime prevalence of depression is 17%: 26% for women and 12% for men. The mean age for a first episode is in the thirties. Demographic differences show that rates are higher in urban rather than in rural areas. No racial significance has been noted. Along gender lines, women suffer from depression at twice the rate of men. Statistics have shown that one out of every seven women will experience at least one depressive episode in their lifetime. This gender difference is best explained by looking at the interplay between biological, genetic, psychological, social, and environmental factors.
Classified as mood disorders, major depression, along with other depressive disorders such as dysthymia (a chronic less severe form of depression), and bipolar disorder (manic depression) fall along a spectrum. On one end of the spectrum is unipolar or major depression and on the opposite is bipolar disorder or manic depression, both with varying degrees of severity and duration. Along this spectrum, there are several categories of mood disorders, such as postpartum depression, seasonal affective disorder (SAD) and psychotic depression, as well as variants of bipolar disorder. Bipolar disorder is characterized by severe and disabling cycles of depression and mania.
Mood disorders are highly treatable conditions, with each type requiring different treatment approaches and modalities. Antidepressant medications and psychotherapies offer useful treatment approaches and are commonly employed in treating the debilitating effects of depression. However, if mood disorders are left untreated for long periods of time, the debilitating effects of depression can lead to suicide.
SYMPTOMS OF MAJOR DEPRESSIVE DISORDER
Symptoms of Major Depression represent a significant change from the individual's normal level of functioning. Together the symptoms cause significant distress or impairment in the individual's life and his/her ability to function. Depression symptoms can occur with either a sudden onset or in a more gradual fashion, with the severity of symptoms ranging from mild to severe.
A Major Depressive Episode is defined as having five or more of the following symptoms present for the same two-week period, and represents a change from the individual's normal level of functioning when well. At least one of the five required symptoms must be (1) depressed mood or (2) loss of interest.
1. depressed mood experienced most of the day, nearly every day;
2. diminished interest or pleasure in all or almost all activities most of the day, nearly every day;
3. significant change in appetite (increase or decrease) or weight (loss or gain);
4. insomnia or hypersomnia nearly every day;
5. observable psychomotor agitation (feeling restless or fidgety) or retardation (feeling slowed down) nearly every day;
6. loss of energy or fatigue nearly every day;
7. feelings of worthlessness, or excessive or inappropriate guilt, nearly every day (not merely self reproach about being sick);
8. diminished ability to think or concentrate, or indecisiveness, nearly every day (either subjective account or observed by others);
9. recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
What are the Symptoms of Major Depression with Psychotic Features (PMD)?
Symptoms of major depression with psychotic features include all of the symptoms of major depressive disorder listed above. In addition, patients experience delusions and/or hallucinations. Examples of these latter symptoms include feelings as though other people are out to harm them, feeling as though one has special powers to do things that other people cannot do, feeling overwhelmed with guilt, or hearing voices that put one down.
In psychotic major depression, the delusions and/or hallucinations only occur when the person is also experiencing significant depression. These symptoms do not occur when the person is no longer depressed. If one experiences these psychotic symptoms when they are not depressed, there are other diagnoses that would need to be considered.
What are the Symptoms of Dysthymic Disorder?
The differentiation of dysthymic disorder from major depressive disorder can be difficult. Key features of dysthymia are a mild to moderate depressed mood that has a chronic course (greater than 2 years). Dysthymia is characterized by the following:
1. Depressed mood for most of the day, for more days than not, for at least two years.
2. While depressed, there must be present 2 or more of the following: poor appetite or over-eating, insomnia or hypersomnia, low energy/fatigue,
low self-esteem, poor concentration or difficulty making decisions, feelings of hopelessness.
3. During the two-year period, the patient has never been without the symptoms in number 1 or 2 for more than 2 months at a time.
4. No history of a major depressive episode, manic episode, mixed episode, hypomanic episode or cyclothymic disorder.
5. The symptoms cause significant impairment or distress.
What are the Symptoms of Bipolar Disorder?
SYMPTOMS OF BIPOLAR DISORDER
Bipolar Disorder is a spectrum of disorders that are distinguished from Major Depressive Disorder by the presence of manic or hypomanic episodes. During the depressed periods, patients experience symptoms of major depression (see above). Contrasted by the manic periods where patients experience mania episodes. A manic episode is characterized as follows:
Manic Episode
1. Distinct period of abnormally and persistently elevated, expansive or irritable mood, lasting for at least one week (or any duration if hospitalization is
necessary).
2. During the period of mood disturbance, three (or more) of the following symptoms (four if the mood is only irritable) have been present to a significant
degree:
a. inflated self-esteem or grandiosity
b. decreased need for sleep
c. more talkative than usual or pressure to keep talking
d. disconnected or racing thoughts
e. distractibility
f. increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation
g. excessive involvement in inappropriate social behavior
3. The mood symptoms cause significant impairment or distress, or severity of illness requires hospitalization to prevent harm to self or others,
or there are psychotic features.
For more information on Bipolar Disorder: http://www.ndmda.org/
What are Causes of Depression?
The exact etiology of depression is yet to be determined; however, multiple factors, including biological, psychological, and environmental factors are involved in the presentation of depression. For example, an individual who has a first-degree relative with depression has a four times higher risk of developing depression than the general population. Twin studies have shown that an individual with a monozygotic twin with depression has as high as a fifty percent chance of developing the disorder.
Major depression is caused by imbalance of certain neurotransmitters (chemical messengers) in the brain, such as serotonin, norepinephrine, and dopamine. Antidepressants work either by changing the sensitivity of the receptors or by increasing the availability of neurotransmitters in the brain.
In addition to genetic components, there are many psychosocial factors that contribute to the development of mood disorders. For example, an individual with little or no social support will have fewer resources to handle stress and thereby will be at a greater risk of developing a mood disorder.
What are Treatments for Depression?
Major depression is a highly treatable illness. Between 80 to 90% of individuals who suffer from severe depression are effectively treated and return to a normal level of functioning. Treatment of depression depends on the individual as well as the severity and duration of the illness. Basic types of treatment for depression include antidepressant medications, psychotherapy, or electroconvulsive therapy (ECT). Often these basic treatment approaches are used in combination. Antidepressants are one of the largest groups of pharmaceuticals produced in the world and the second largest produced in the United States. Currently, over two-dozen antidepressants are on the market.
Antidepressants are successful in 60-80% of patients. No single antidepressant drug has been shown to be more effective than another. Antidepressants work by correcting imbalances in neurotransmitters. Generally, antidepressants take several weeks and up to months to show efficacy and each has their own side effect profile.
Additionally, several methods of short-term, goal-oriented psychotherapy have proven successful in the treatment of depression, such as cognitive behavioral therapy (CBT) and interpersonal therapy. Cognitive behavioral therapy addresses the negative thinking and behavioral patterns associated with depression, and teaches the individual to recognize and target the self-defeating behavioral patterns that contribute to their depression. In contrast, interpersonal therapy has a focus on improving disturbed or unhealthy personal relationships, which may be contributing to the individual's depression.
The final treatment approach, electroconvulsive therapy (ECT), is employed in cases of severe treatment-resistant depression. An electric current is passed through the brain to produce a seizure, thereby affecting chemical activity in all regions of the brain. It is believed that, with repeated treatments, chemical changes build upon one another to help restore the normal chemical balance in the brain and help to alleviate symptoms of depression.
For more information about ECT and other treatment approaches: http://www.mayoclinic.com/health/electroconvulsive-therapy/MY00129
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts
- PMC10723193

Revisiting the theoretical and methodological foundations of depression measurement
Eiko i. fried.
1 Department of Clinical Psychology, Leiden University, Leiden, The Netherlands
Jessica K. Flake
2 Department of Psychology, McGill University, Montreal, Quebec, Canada
Donald J. Robinaugh
3 Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts, US
4 Department of Applied Psychology, Northeastern University, Boston, Massachusetts, US
Author contributions
Associated Data
Depressive disorders are among the leading causes of global disease burden, but there has been limited progress in understanding the causes and treatments for these disorders. In this Perspective, we suggest that such progress crucially depends on our ability to measure depression. We review the many problems with depression measurement, including limited evidence of validity and reliability. These issues raise grave concerns about common uses of depression measures, such as diagnosis or tracking treatment progress. We argue that shortcomings arise because depression measurement rests on shaky methodological and theoretical foundations. Moving forward, we need to break with the field’s tradition that has, for decades, divorced theories about depression from how we measure it. Instead, we suggest that epistemic iteration, an iterative exchange between theory and measurement, provides a crucial avenue for depression measurement to progress.
Introduction
Major Depressive Disorder (MDD)—a prevalent, debilitating, and often recurrent mental disorder of episodic nature—is one of the most frequently measured constructs in the scientific literature. More than 280 measures of this mental health condition have appeared in the literature in the past century. 1 These include three scales which are among the 100 most cited papers across all fields of science: 2 the Hamilton Rating Scale for Depression (HRSD) 3 , the Beck Depression Inventory (BDI) 4 , and the Centre for Epidemiological Studies Depression Scale (CES-D). 5 These papers have a combined 81,000 citations since 1960 (see Supplementary Figure 1 and Supplementary Note 1 ); according to Web of Science, each has been cited in more than 140 distinct disciplines. Papers introducing abbreviated, translated, and adapted versions of these scales contribute thousands more citations.
With so much empirical research on depression, one would expect there to have been considerable advances in understanding depression and the ability to treat it. Unfortunately, progress has been limited. The prevalence rate and global disease burden of MDD have not decreased over the past 3 decades. 6 Despite sizeable efforts, researchers have been unable to identify actionable biomarkers for MDD that explain sufficient variance in diagnosis to be useful in clinical settings. 7 , 8 Further, efficacies of both psychological and pharmacological treatments remain limited. 9 , 10
In this Perspective, we take the position that progress in understanding, predicting, and treating depression crucially depends on the ability to measure it. We first provide a brief history of depression measurement. Next, we describe the many problems with depression measurement, including limited evidence of validity and reliability. We argue that these problems arise because the measurement of depression rests on shaky methodological and theoretical foundations. We conclude by offering ideas for moving methodological and theoretical aspects of depression measurement into the 21 st century.
A brief history
In the middle of the 20 th century, psychoanalytic theory and practice dominated psychiatry. 11 , 12 Diagnoses were defined by narrative descriptions and assessed by unstructured interviews, leaving considerable room for subjectivity. 13 Perhaps not surprisingly, the agreement of two psychiatrists on whether a patient had a given mental disorder was barely above chance. 14 , 15
During the 1960s and 1970s, there was a concerted effort to increase diagnostic reliability by developing diagnostic criteria sets: lists of readily observable or reportable experiences with explicit algorithms for determining the presence or absence of a disorder based on these signs and symptoms. 16 This effort culminated in 1980 with the third edition of the Diagnostic and Statistical Manual (DSM-III), American psychiatry’s authoritative publication on the diagnosis of mental disorders. 17 DSM-III leaned heavily on recently developed criteria sets and aimed to be theoretically agnostic, focusing on symptoms rather than etiology or underlying mechanisms.
In this context, the most commonly used depression scales such as HRSD, BDI and CES-D were developed and began to take hold in the field. Diagnostic interviews (for example, based on DSM criteria) aim to determine the presence or absence of MDD. By contrast, scales such as HRSD, BDI and CES-D were developed to assess the severity of current depressive symptoms, with scores above a certain threshold indicating potential MDD. The various depression scales that arose during this era differ in several ways, including the number and nature of assessed symptoms and mode of assessment; for example, BDI and CES-D are self-rated, whereas HRSD is observer-rated. However, they share a common approach: measuring depression severity by adding together the symptoms of depression, such as depressed mood, sleep problems, and suicidal ideation. This approach based on symptoms and sum-scores is identical in virtually all of the depression instruments that have appeared in the literature, including self-report and observer-rated scales as well as clinician-rated diagnostic criteria. 1 , 18
In the decades since this shift toward diagnostic criteria and standardized scales, depression research has thrived, but the measurement of depression has remained strikingly unchanged. Since the HRSD was published over half a century ago, scientists put a man on the Moon, invented the internet, and created powerful computers small enough to fit in people’s pockets. Yet, the HRSD remains the gold-standard scale for depression, used in over 90% of antidepressant trials. 19 Given the enormous amount of depression research and the substantial gains made in psychological measurement practices in the last few decades, it is worth taking stock of depression measurement. We focus our investigation on the most important aspects of validity and reliability. These and other key terms are defined in Box 1 .
Key terms and definitions.
Alpha (coefficient alpha, cronbach’s alpha):.
Internal consistency is often summarized with coefficient alpha. Alpha ranges from 0–1, with higher numbers indicating more consistency. Alpha does not provide information about scale validity, and is often not appropriate for depression instruments due to strict assumptions that are rarely met. 147
Depression instrument:
A depression instrument is a measure of depression. Common instruments include self-rated and observer-rated scales typically used to assess depression severity, and structured or semi-structured clinical interviews typically used to assess the presence of Major Depressive Disorder.
Depression scale:
A depression scale is a particular type of instrument to measure depression severity. Depression scales can be self-rated or observer-rated. These scales typically include a list of depression symptoms rated on a brief ordinal scale indicating frequency (how common is a symptom), intensity (how severe is a symptom), relativity (compared to usual, how is the symptom expression), or a mix of the above.
Diagnostic interview:
A diagnostic interview is a particular type of instrument to measure the presence of Major Depressive Disorder. Diagnostic interviews are usually structured or semi-structured. They typically include a list of depression symptoms coded as present or absent, and a question about impairment of functioning. A specific algorithm determines presence of the disorder.

Dimensionality:
A unidimensional instrument is one that can aptly describe or summarize the relations among items of a construct with only one score (that is, one dimension, factor, or component). It is defensible to add up all items to one total score, which reflects the single dimension, in such scales. Depression instruments are often multidimensional, meaning that more than one score is required to describe the relations among items adequately.
Inter-rater reliability:
In the context of depression measurement, inter-rater reliability is the degree to which independent observers (usually two) agree on whether a person should receive a diagnosis of Major Depressive Disorder or not.
Internal consistency:
Internal consistency quantifies how consistent responses to items on a scale are. A scale is internally consistent if all its items produce similar scores.
Measurement invariance:
If an instrument measures the same construct in the same way across populations or time, it has the psychometric property of measurement invariance. This property is necessary to compare scores across populations or time.
Kappa coefficient:
Inter-rater reliability is commonly assessed using the kappa coefficient, which ranges from 0–1. Higher numbers indicate more agreement.
Reliability:
Reliability or precision denotes the consistency of scores across instances of the testing procedure, such as raters, time, items, and context. Reliability is necessary but not sufficient for validity.
Response process:
The response process denotes the cognitive processes engaged in by people using an instrument. In depression research, these people can be the participants filling out self-rated instruments or being interviewed; observers scoring observer-rated scales; or clinicians administering an interview.
Test score:
The test score is the resulting score from depression instruments, usually a continuous sum-score indicating depression severity, or a categorical score with two groups, healthy versus depressed.
As defined by the Standards of Educational and Psychological Testing, 25 validity “…refers to the degree to which evidence and theory support the interpretations of test scores for proposed uses of tests […]. The process of validation involves accumulating relevant evidence to provide a sound scientific basis for the proposed score interpretations.”
Validity and reliability
The most fundamental question for any measure concerns its validity: does it measure what it purports to measure? 20 This question turns out to be difficult to answer, and there are many theoretical and methodological frameworks for evaluating validity. 16 , 21 – 24 Here, we adopt the perspective taken by the Standards for Educational and Psychological Testing and consider validity to be the degree to which the evidence supports the interpretation and use of a test score for a specific purpose. 25 Examples of such purposes include using DSM-5 criteria to diagnose a person with an episode of MDD or using the BDI to track treatment progress over time. Validation entails accumulating evidence to form a sound scientific basis for using instruments for these purposes.
We will consider three sources of evidence for validity—content, internal structure, and response processes—and will evaluate whether the evidence supports common uses of depression instruments. These three sources do not represent distinct types of validity; instead, they together support the intended interpretation of scores for a given use. 25 We also discuss reliability—the consistency of instruments across raters, contexts, and time. Reliability does not provide evidence of validity, given that a score can be consistent but not hold the intended interpretation. Reliability is therefore necessary, but not sufficient, for validity.
One source of evidence for the valid use of depression instruments is its content. A valid score must reflect all of the content needed to describe a construct, avoiding construct under-representation (omitting important content) and construct contamination (including construct-irrelevant content). 26 Evidence of adequate content is critical for many uses of depression instruments, such as communication: If a diagnosed patient is referred from one therapist to another, the diagnosis is only useful to the new therapist if the instrument used for diagnosis actually captures content relevant to depression. Appropriate content coverage is also required for many other purposes, such as accurately determining whether treatment is needed or progressing well.
The development of diagnostic criteria sets and scales in the middle of the 20 th century provided significant clarity about the content being assessed relative to earlier unstructured interviews. Accordingly, these instruments supported clearer communication and provided standard criteria for determining the need for treatment. However, there is a surprising level of disagreement about the content depression measures ought to assess. A review of seven commonly used scales for depression, 18 , 27 including CES-D, BDI, and HRSD, found that they contain 52 disparate symptoms, 40% of which appear in only one of the scales. The CES-D—the most used depression scale in history (see Supplementary Figure 1 )—has the lowest mean overlap with other scales (Jaccard similarity index of 31%), with half of all CES-D items not appearing in any of the six other scales. Content overlap between common scales and DSM-5 criteria for MDD is only moderate ( Figure 1 ).

Colored circles for a symptom indicate that a scale directly assesses that symptom, whereas empty circles indicate that a scale indirectly measures a symptom. For instance, IDS assesses item 4 ‘hypersomnia’ directly; BDI measures ‘hypersomnia’ indirectly via a general question on sleep problems; and SDS does not capture ‘hypersomnia’ at all. Note that the 9 QIDS items analyzed correspond to the DSM-5 criterion symptoms for MDD. IDS: Inventory of Depressive Symptoms 80 ; BDI-II: Beck Depression Inventory 119 ; SDS: Zung Self-Rating Depression Scale 145 ; HRSD: Hamilton Rating Scale for Depression 3 ; CES-D: Center of Epidemiological Studies Depression Scale 5 ; QIDS: Quick Inventory of Depressive Symptoms 81 ; MADRS: Montgomery-Åsberg Depression Rating Scale 35 . Figure reprinted with permission from Fried et al. 2017 18
If the 52 distinct symptoms are considered to reflect the full breadth of the depression construct for diagnosing, monitoring, and studying depression, no one scale can be said to have adequate content converage. 25 And the seven scales mentioned above are just a small minority: Over 280 instruments have been developed to assess depression, 1 and a recent review of 30 clinical trials in adolescents found 19 different primary outcome measures for depression. 28 Additionally, there is evidence that none of these scales assess important features of depression. In a recent study of over 3,000 patients, informal caregivers, and healthcare professionals from 52 countries, mental pain was commonly mentioned as an important feature of depression; 29 but common depression scales do not include this experience. 18
Scales therefore seem to measure different ‘depressions’. This conclusion is supported by different content and the fact that correlations among scales are often only around 0.5 (and regularly much lower). 30 – 33 Small to moderate correlations are not surprising, as depression instruments were constructed absent a unifying theory and by scholars working in distinct settings and towards distinct goals. The HRSD was developed for severely depressed inpatients who were already diagnosed and relies heavily on clinical, observable signs such as weight loss and slowing of speech rather than self-reported symptoms. The BDI focuses on cognitive and affective symptoms, such as worthlessness and pessimism, central to Beck’s theory of depression. 34 The CES-D was developed for depression screening in general population settings and captures problems such as feeling bothered or lonely that are more common in non-clinical settings than BDI or HRSD symptoms. Items on the Montgomery-Åsberg Depression Rating Scale (MADRS) 35 were selected because they were found to change during treatment, providing a scale sensitive to change. 35
Despite these key differences in content, scales such as BDI, HRSD, and MADRS are used interchangeably to, for example, track treatment progress in clinical trials. Clinical trials usually report how many patients respond to and remit during treatment. However, there are systematic differences in the measurement of pharmacological interventions (mostly observer-rated; HRSD and MADRS most common) versus behavioral interventions (mostly self-rated; Patient Health Questionnaire (PHQ-9) most common). 36 Comparing treatments based on different measures is problematic due to content differences and because observer-rated scales result in larger pre-post treatment effect sizes than self-report scales. 36 Different treatments are thus confounded with different types of measurement, biasing their comparison.
Another problem of interchangeable use is when scales are used to diagnose participants. The PHQ-9 developers, for instance, encourage doing so, 37 despite evidence that scales like the PHQ-9 produce substantially higher rates of MDD diagnosis compared to clinical interviews. 36 , 38 Important decisions about whether people are diagnosed with MDD, enrolled into a clinical trial, or considered remitted after treatment depend to a considerable degree on the instruments used by researchers and clinicians. This state of affairs leaves much to be desired.
Response processes
A second important source of validity evidence is the response processes when people complete a measure. A score is valid when people respond to an instrument in a way that corresponds to the construct being assessed. 39 For example, when developing a test of mathematical reasoning, questions should not be so rote as to render the test a measure of one’s memory for facts, or so verbose as to render the test a measure of reading comprehension.
There is very little research on the processes engaged when people score self-rated or observer-rated depression instruments, but there is reason to think they influence depression measurement. Generally, scores on self-reported depression scales tend to differ from those on observer-rated instruments: studies based on observer ratings find greater efficacy of depression treatments than studies relying on self-report 31 , 36 , and self-reported symptoms tend to be more severe than observer ratings. 38 , 40 These differences may be due to different response processes. Clinicians may not score some symptoms endorsed in self-report scales if these symptoms can be attributed to external causes. For example, a single parent getting little sleep due to a newborn may endorse sleep problems in a self-report scale, but a clinician may not score that as a depression symptom in a diagnostic interview, leading to differences in scores. Alternatively, it might be that participants report more honestly in self-rated instruments and are less candid in clinical interviews. 41 , 42 Or differences might arise because observers are vulnerable to certain kinds of cognitive biases, including overconfidence bias (overestimating one’s knowledge and therefore acting without sufficient information), confirmation bias (selectively engaging with confirming rather than refuting evidence), attribution error (when a serious medical condition is misdiagnosed as psychiatric diagnosis), or diagnosis momentum (even if a diagnosis is erroneously attached to a patient, it tends to stick). 43
Although the DSM-5 is explicitly atheoretical, clinical judgements are made within the context of implicit and explicit conceptual frameworks, which influence response and measurement processes. 44 A 2007 survey showed that clinicians are acutely aware that these frameworks contribute to clinical decision-making: 86% of participating clinicians stated that psychiatric diagnoses are unreliable. When asked about the reasons for this lack of reliability, clinician-related factors such as differences in training, biases, and interview style were the most common explanations for discrepancies between raters (63.5%), rather than patient characteristics (21.6%) or nosological issues (14.9%). 45
Overall, we know very little about how participants or observers interpret items or select responses on depression instruments. Differences in response processes could explain consistent differences between scale types (such as self-report versus observer-report), but this is an area that urgently needs more research.
Internal structure
The third source of validity evidence comes from an instrument’s internal structure: the extent to which the relationships among test items are consistent with one’s theory about the construct being assessed. 39 Unfortunately, efforts to evaluate whether the relationships among depression symptoms are consistent with theoretical expectations face an immediate challenge: such expectations are often unclear. The measurement of depression has developed largely independently from theories. The DSM, which is explicitly atheoretical, is one of many examples.
However, many tacit theoretical assumptions about the nature of depression are evident in clinical and research practices. Accordingly, whether an instrument’s internal structure conforms to expectations can be evaluated based on assumptions that underlie how this instrument is used. We discuss assumptions of taxonicity, dimensionality, measurement invariance, and inter-rater reliability.
Researchers and clinicians use instruments to separate people with MDD from people without MDD, implying a belief that depression is taxonic (that is, categorical) in nature. In the DSM-5, MDD is diagnosed if participants meet 5 of 9 symptom criteria, for two weeks, along with significant impairment of functioning. 46 Similarly, on the HRSD, BDI, and CES-D, researchers commonly sum all items and use thresholds to determine the presence of MDD. 36 However, there is considerable evidence that depression is not categorical, but rather exists on a continuum from healthy to severely depressed. 47 – 50 If MDD were categorical, one would expect an area of the distribution of depression severity with relatively few individuals—a zone of rarity—that divides those with and without depression ( Figure 2a ). However, this is not present in observed data ( Figure 2b and and2c 2c ).

a) Expected distributions if a disorder is categorical, featuring a ‘zone of rarity’ between cases and controls. Such distributions are not observed in depression data. b) Empirical distribution of depressive symptoms in an online sample, n=12613, based on the 14-item depression subscale of the Depression Anxiety Stress Scale (DASS-42); 146 due to the nature of an online convenience dataset, depression scores are considerably higher than those in representative samples. c) Empirical distribution of depressive symptoms from an individual participant data meta-analysis consisting of 54 data sets with n=12613, based on the 9-item Patient Health Questionnaire (PHQ-9). 37 See Supplementary Note 2 for further details, and data and code for reproducing this figure.
The data shown in Figure 2 explains why many different MDD thresholds exist for each of the most commonly used scales. It is much more difficult to clearly demarcate healthy from sick in the real data presented in Figures 2b and and2c, 2c , compared to the common conceptualization of depression as a taxon in Figure 2a (that is not supported by evidence). An analysis of 350 clinical trials for depression using the MADRS identified that 28 different thresholds were used to determine whether patients have MDD and should therefore be included in a given trial; thresholds ranged from total scores of 5 to 34 points. 36 Similarly, a review of 29 trials for adolescent MDD identified 47 unique definitions of remission, with only a minority of trials providing a rationale for their cutoffs. 51 Overall, this illustrates that the internal structure of the most commonly used depression instruments does not support the use of cutoffs to identify the presence versus absence of MDD.
Dimensionality
Another common use for depression scales is adding up equally weighted symptoms to derive a single score representing depression severity. This practice is valid if all items measure one construct (rather than three or five), and if items are interchangeable, that is, if they contribute roughly equally to depression severity. 52 , 53 If these assumptions are met, data from depression instruments will be best described by a unidimensional factor model in which item loadings are roughly equal. However, statistical analyses often do not produce this result. Many depression scales are multidimensional, measuring more than one construct. In fact, 1 to 7 factors have been extracted for BDI, HRSD, and CES-D. 33 , 54 , 55 Notably, replication of factor structures is poor across instruments 56 ; poor within instruments across samples; 33 , 54 – 61 and poor even within the same instrument in different subsets of the same sample. 62 Thus, depression sum scores not only often fail to measure a single construct, but the number and nature of those constructs shift across context, time, and people. The assumption that items are interchangeable is similarly untenable given a broad set of empirical studies showing that individual symptoms differ in their relations to risk factors, 63 , 64 impact on functioning, 65 – 67 and biological markers, 68 – 74 and are differentially predicted by life events. 75 – 79 Together, this severely limits the use of sum scores to denote one underlying construct. 52
Further evidence against the validity of sum-scores comes from the internal consistency of depression instruments: the extent to which people respond similarly across all instrument items. For depression scales, there is a wide range of internal consistency estimates, with reported alpha coefficients as low as 0.4 to as high as 0.9. 31 , 33 , 80 , 81 . Acceptable internal consistency (alpha > 0.7) is usually observed in general population samples, whereas alpha is often substantially lower in clinical populations. 31 , 33 , 80 , 81 This phenomenon is particularly visible in clinical trials for depression where, using the same scale in the same sample, alpha often increases considerably within a few weeks as the sample gets healthier (for the HRSD, often from 0.4 to 0.8). 80 , 81
Issues of multidimensionality and inadequate internal consistency might be related to the heterogeneity of the MDD phenotype. An analysis of depression symptoms of 3,703 MDD patients identified over 1,000 unique empirical symptom profiles; around half of these profiles were endorsed by only a single individual 82 (see ref 83 for similar findings). There have been attempts to tackle the massive heterogeneity of MDD by proposing more homogeneous depression subtypes or specifiers, such as melancholic or atypical depression that come with specific symptoms. 84 – 86 However, subtyping efforts have largely failed to result in categories that support clear demarcation of patients, higher treatment specificity, or higher temporal stability. 84 – 96 Seasonal Affective Disorder is a possible exception. 97 – 99
Some of the limits of total scores were understood a long time ago. Hamilton referred to the sum of symptoms assessed by the HRSD as ‘total crude score’ and focused his analysis on four subscales assessing narrower phenotypes, such as ‘anxiety’ and ‘agitated depression.’ 3 Yet today, the total crude score is used in nearly all studies that utilize the HRSD. As reviewed here, the six decades since Hamilton developed his scale have provided ample psychometric evidence regarding dimensionality and internal consistency of depression instruments, raising questions about the common use of adding depression symptoms to a single score.
Measurement invariance
Researchers use depression scales to compare scores for different groups of people, implying a belief that depression is invariant across contexts. Accordingly, the measurement of depression should be similarly invariant. Measurement invariance is necessary for common research questions, such as whether depression rates are similar in women and men. If an instrument does not measure the same construct in two groups, it cannot be used to compare groups regarding this construct. Measurement invariance across groups has several levels, including invariance at the structural level (the same number of factors can be extracted in different groups) and invariance of factor loadings (factor loadings of items in one group are similar to those in another group). The more the psychometric properties of an instrument (such as factor loadings) remain consistent across groups, the more the instrument can be said to exhibit measurement invariance, 100 that is, to measure the same construct across groups.
Some level of measurement invariance has been established for certain depression instruments across certain groups; for example, the nine DSM-IV depression symptoms exhibit measurement invariance in women assessed across samples collected in the US, Europe, and China, 101 as do PHQ-9 scores across women and men in a community sample in Hong Kong. 102 However, in other situations and data, depression instruments do not meet the level of measurement invariance required to compare groups on depression scores. Significant differences in the psychometric properties of depression instruments have been observed across groups defined by socioeconomic status 103 , ethnicity, 104 sex, 105 and age, 106 among others. Thus, common uses of depression instruments, such as comparing depression scores across groups, might not be valid, depending on the instrument and situation.
The same issue applies to measurement invariance across time: Some studies found that so-called temporal measurement invariance of depression scales held, which means that a score in a sample at time 1 holds the same meaning as a score in the same sample at time 2 because it measures the same construct. 107 But many other studies have demonstrated a lack of temporal invariance. 33 , 58 , 108 This raises serious concerns about using depression scales to track treatment progress. If temporal measurement invariance is violated, a BDI score of 20 points for a sample at treatment entry, and 10 points for the same sample 8 weeks later, do not measure the same construct, limiting the ability to assess treatment efficacy. 33
Inter-rater reliability
Finally, diagnoses in clinical or research settings are usually given by one rater, implying a belief that diagnoses are sufficiently reliable that multiple assessors are unnecessary. Indeed, much of the motivation to move toward diagnostic criteria and standardized scales was to enhance reliability: the consistency of scores obtained in depression instruments across raters, contexts, and time. 25 Here, we focus on inter-rater reliability (the extent to which independent raters produce similar scores), which is required to support the common clinical and research practice of using one rater to assign a depression diagnosis. Inter-rater reliability is important because prevalence rates derived from diagnoses inform mental health policy, and because both over-diagnosis and under-diagnosis of MDD can have dramatic consequences for a person’s life. There are three broad sets of findings related to inter-rater reliability.
Some studies for DSM diagnoses and observer-rated scales have noted very high agreement among raters, at times exceeding 0.90. 109 , 110 However, such high agreement is usually obtained when interviews are not conducted independently (for example, both raters watch the same interview tape), which inflates agreement among raters. To properly assess inter-rater reliability, different clinicians must conduct their interviews separately.
Studies using separate, structured clinical interviews show moderate agreement between raters. For example, a study in which different clinicians conducted structured interviews reported a kappa coefficient of 0.62. 111 Although MDD had the lowest inter-rater reliability of the 20 assessed diagnoses, the result suggests that such interviews can produce substantial agreement. Unfortunately, only an estimated 15% of clinical psychologists and psychiatrists make use of structured interviews. 112
Finally, studies examining how diagnostic criteria perform in routine clinical practice are troubling; the DSM-5 field trials are a prominent example. Such field trials are conducted when new versions of official psychiatric nosologies such as International Classification of Diseases (ICD) or DSM are released, with the goal to assess the reliability of psychiatric diagnoses in clinical practice. In the DSM-5 field trials, interviewers had a minimum of 2 years of psychiatric post-graduate training, and for each participant, independent psychiatric assessments were conducted by two interviewers within 4 to 48 hours of each other; interviews relied on usual clinical interview procedures to “mirror the circumstances in which most diagnosing takes place.” 113 Strikingly, despite using criteria designed explicitly to promote reliability, 114 inter-rater reliability for a diagnosis of MDD was just 0.28, placing it among the least reliable diagnoses in the DSM. We illustrate the severe impact of this level of inter-rater reliability on diagnostic outcomes (both false positives and false negatives) in Figure 3 . For comparison, kappa values (see Box 1 ) for bipolar disorder and post-traumatic stress disorder were 0.56 and 0.67, respectively. 111 Reliability for MDD is even lower (kappa = 0.16) when interviews are carried out by general practitioners 115 who are responsible for a substantial proportion of MDD diagnoses worldwide. 116

Based on the inter-rater reliability (kappa coefficient) of 0.28 for Major Depressive Disorder reported in the DSM-5 field trials, we simulated data for two clinicians and 100 people, 30 of whom have depression. The left column shows accurate agreement between clinicians in 71% of the 70 non-depressed cases (green), 26% disagreement (blue), and 3% inaccurate agreement (purple). For the 30 depressed participants (right column), diagnostic performance was particularly poor, with only 43% accurate agreement (green), 40% disagreement (blue), and 17% inaccurate agreement (purple). See Supplementary Note 3 for a complete description of the simulation underlying this figure.
In summary, the historical shift of DSM-III towards more objective criteria improved reliability, especially when structured interviews are used to assess signs and symptoms. However, the results from studies attempting to approximate measurement of MDD typical in clinical contexts are discouraging, to the degree that the head of the DSM-5 task force had to concede that the “relatively low reliability of major depressive disorder […] is a concern for clinical decision-making.” 113
Shaky Foundations
By the standards commonly applied in psychological research, the evidence does not support many of the common uses of depression instruments. Next, we discuss two potential explanations of these shortcomings rooted in the foundations of depression measurement.
Methodological Foundations
One explanation for the validity and reliability problems of common depression instruments is that they were not developed following modern best practices. Today, the development and validation of psychometric instruments is a thorough process that occurs in three phases. 117 In phase 1, the substance of the construct is explored (for example, clarifying its nature, breadth, and depth). In phase 2, the structure of the instrument is investigated (for example, using item analyses and factor analysis). Finally, in phase 3, the relation between the instrument and external constructs is researched (for example, by testing its ability to discriminate between groups known to be distinct). Critically, each phase includes iterative revisions until the instrument meets desired criteria. 118 These practices were not widely established when common depression instruments were developed. Although much individual validation research has been published, for example regarding the factor structure of depression instruments, 33 , 54 , 55 , 107 , it remains a cause for concern that the majority of studies focused on phases 2 and 3 rather than the foundational phase 1, and that findings have not led to substantial iterative development of depression measurement (the BDI is one of few scales that has been updated over the years 119 ).
Rather than a rigorous exploration of the construct to be measured via item development, expert reviews, or focus groups, scale developers often developed depression instruments based on their clinical experiences and personal views. For example, Hamilton developed the HRSD based on his experiences and knowledge working with inpatients, not from an explicated theory that defined depression. 3 Other scale developers sidestepped theoretical considerations altogether, often via statistical procedures. For example, to obtain an “empirically founded scale” 35 the MADRS items were chosen by dropping items from a prior scale on which 64 patients did not improve significantly after receiving antidepressant drugs. This procedure raises questions about what the scale measures. As a recent historical analysis notes, the MADRS is really a measure of emotions that change over a few weeks in drug trials, rather than a measure of depression. 120
Further, the content of depression instruments was often shaped not by theory or to support valid scores, but by what Lilienfeld called “centrifugal antiscientific forces”, 121 including practical constraints such as ease of clinical use as well as continuity (for example with previous DSM editions). The former emphasizes brief instruments and thereby presents a considerable obstacle toward adequate content representation, while the latter severely constrains opportunities for iterative development.
Overall, given these various shortcomings and constraints, it should not be surprising that validity evidence does not support many of the common uses of depression measurement.
Theoretical Foundations
A second, related explanation for validity and reliability problems of common depression instruments is that most depression instruments were developed without clear and explicit theories about the nature of depression. Without a clear theory of depression, it is unclear what researchers aim to measure, and how we can evaluate whether they have succeeded. 122 – 124 However, the absence of explicit theories does not mean depression measurement is atheoretical: Many implicit beliefs about depression such as taxonicity are embedded in measures. Unfortunately, these latent theories 125 do not align well with decades of empirical research, and one of the most fundamental latent theories is the notion that depression symptoms arise from a common cause.
Mental health research leans heavily on medicine and psychology in its approach to measurement. Medicine has symptom checklists indicating diseases, and psychologists measure constructs such as mathematical ability or personality via tests and questionnaires. Critically, using items to indicate underlying diseases or constructs only works under the assumption that constructs cause item responses. Medical symptoms can indicate an underlying disorder because symptoms are caused by the disorder (for example, measles causes Koplik’s spots). Similarly, tests for mathematical ability use items like ‘17×39’ because an individual’s performance on this item is thought to be caused by their mathematical ability.
The common cause theory—all symptoms have a shared origin—implicitly underlies the scoring and use of nearly all psychiatric assessments, including depression instruments, and justifies practices such as summing items. 126 , 127 The field uses the term ‘symptom’ to refer to items of depression instruments, implying (by definition of the word symptom) an independent disease entity that gives rise to the symptoms. 128 The common cause theory presupposes a homogeneous, categorical, unitary construct with interchangeable symptoms. The common cause theory also explains common statistical practices in psychiatric research, including the notion that ‘good’ scales should be unidimensional (they measure one construct) and have high internal consistency (items measure the same construct).
In contrast to the common cause framework, there is increasingly widespread recognition that depression is a highly heterogeneous, multifactorial, and complex phenotype. 129 , 130 Depression has fuzzy boundaries, and features both multifinality (the same constellation of variables can lead to different outcomes) and equifinality (different constellations can lead to the same outcome). 131 Depression also shows pronounced inter-individual differences, such that two people diagnosed with MDD may not share a single symptom, 82 , 83 and the disorder may be categorical for some but continuous for others. 132 Indeed, the lack of validity evidence for commonly used instruments for measuring depression can be interpreted as evidence that there is a mismatch between the nature of depression and the common cause theory implicit in these instruments. Importantly, if the common cause theory had been explicit when these instruments were developed, the failure to observe evidence for validity would have immediately signaled that something was wrong, either with the instrument or with the theory of depression. However, because theories about depression have largely remained latent and are only implied through research and clinical practices, these discrepancies were less salient, and opportunities to improve depression instruments were missed.
The state of depression measurement today resembles that of thermometry in the 17 th century. Although objective measures of temperature are now taken for granted, just a few centuries ago there were many different thermometers developed by many different scientists, all claiming to measure temperature, with “standards kept by each workman, without any agreement or reference to one another” (Halley, 1693, referenced in 133 ). Everyone could agree that these thermometers were assessing something, but the precise nature of the thing was unclear.
Progress in thermometry was made possible by epistemic iteration, a series of successive approximations in which advances in thermometry afforded advances in understanding temperature that, in turn, allowed for further improvement in thermometry. 133 Central to this framework is the notion that fallible measures, despite their imperfections, can provide enough advance in knowledge that there is an opportunity for further advances in measurement.
Despite the obvious differences between depression and temperature, the idea of an ongoing exchange between advances in knowledge and improvements in measurement provides a crucial framework for considering how the measurement of depression can move forward. We provide a list of concrete suggestions for improving depression measurement ( Box 2 ), based on two fundamental principles.
Towards better depression measurement
We suggest several steps for iterative improvement of depression measurement.
Development and iteration
1. develop explicit theories of depression..
Without a clear theory, it is unclear what we ought to measure, and how to evaluate whether we have succeeded in doing so. Explicit theories spell out core beliefs or assumptions about the nature of depression in detail and, in the best case, do so in formalized ways. 123 , 125 , 148
2. Epistemic iteration.
Progress in depression measurement comes from successive approximations in which each stage moves us closer to our epistemic goals. 133 Fallible depression instruments, such as HRSD or BDI, can provide advances in knowledge which, in turn, enable advances in measurement. This iterative exchange between theory and measurement provides an avenue for science to progress, but critically relies on having explicated theories in the first place.
3. Experience experts and cross-cultural aspects.
Common depression instruments were predominantly designed by WEIRD (Western, educated, industrialized, rich and democratic) clinicians, and validated in WEIRD samples. It is crucial to involve people with lived experiences and their caregivers, and people from non-WEIRD cultures and countries, in this process. 29
4. Response processes.
There is a lack of research on how self-rated and observer-rated scales are scored. Response processes should be investigated when developing new (or improving existing) instruments via tools such as the Response Process Evaluation method (a type of cognitive interview which elucidates how participants interpret items and select responses). 149 – 153
5. Use scales for appropriate purposes.
Not all instruments are appropriate for all purposes. 154 Hamilton wrote in 1960 that his scale ought to be used only in already diagnosed patients as a measure of severity, 3 but HRSD is commonly used today to distinguish depressed from healthy participants. Researchers and clinicians should use instruments for the purposes for which they were developed and validated, and justify their choice of depression instrument. In the immediate future, this might mean developing and using different instruments for different uses, for example, one for determining whether treatment is warranted and another for tracking progress. We note that this suggestion is opposed to recent initiatives by NIH and Wellcome Trust to mandate the PHQ-9 as a universal depression measure for all contexts and uses. 154
6. Robustness.
Especially for data-driven research, researchers should consider utilizing multiple depression instruments and investigating whether they lead to robust results, or whether results depend on the use of one particular instrument. 52 , 154
7. Symptomics.
Depression severity and MDD are highly heterogeneous phenotypes, such that it can be unclear what scores on these phenotypes represent. Investigating individual symptoms of depression scales, such as insomnia or suicidal ideation, might represent more valid and reliable phenotypes than symptom sum-scores or categorical diagnoses. 52 , 127 , 129
8. Continuous analyses.
Consistent with psychometric evidence that depression data is best described as continuous ( Figure 2 ), 47 – 50 researchers should avoid arbitrary cutoffs whenever not strictly necessary, and conceptualize and analyze depression as a continuum rather than a taxon.
9. Increase transparency of measure use.
The 12 versions of the HRSD differ in the number of items (6 to 36), 155 , 156 and some have dozens of translations. Although these versions differ in crucial aspects such as content and psychometric properties, approximately half of the studies using HRSD provide no information about the version used. 155 In intervention trials published in clinical psychology journals, only 1 in 7 studies pre-register their measures, 157 leaving these studies vulnerable to selecting which measures to report post-hoc, a practice especially prevalent in studies with industry funding. 158 Similarly, only 18 of 32 reviewed randomized controlled trials of adolescent depression featured an identifiable, single, primary outcome. 159 This lack of transparency when administering instruments creates fertile ground for questionable measurement practices, and muddies the inferences that can be drawn. We recommend answering the six questions to promote transparent reporting of measurement listed in ref. 122
First, we cannot divorce our measures of depression from our theories about what depression is. In contrast to current practices, where measures are often expressly atheoretical but infused with implicit theories (such as that MDD is categorical), it will be essential to ground measurement in strong theories that explicate core assumptions about the nature of depression. Grounding measurement in clearly explicated theory will enable researchers to identify the limits of existing measures and take steps to improve them. 123 Developing such theories will be challenging given the complex, dynamic, and heterogeneous nature of MDD. But, doing so is crucial due to the central role of theory development in advancing scientific knowledge. To this end, clinical sciences can draw on tools and frameworks from fields with rigorous approaches to modeling processes of interest. 123 , 125 , 134
Second, improving depression measurement requires iterative development. Despite evidence of the shortcomings of common instruments that have been in use for many decades, there has been minimal effort to move beyond these measures. Evidence of shortcomings is not a criticism of original scale developers; we doubt that Hamilton would have wanted his scale used uncritically and without any revisions for over 60 years. Moreover, reluctance to move beyond these measures is not unfounded. There is clear value in having consistency of measurement across time and contexts for an applied field like psychiatry. Nonetheless, whatever advantages there are to be gained by adherence to precedent, they are outweighed by the gains to be made by genuine progress in our ability to measure and therefore understand, diagnose, prevent, and treat depression. Given the shortcomings reviewed here, we should develop better depression measures, but these must be rooted in what we have learned from existing instruments. 133
To illustrate these core principles, consider the theory that depression syndrome emerges from a complex system of causal interactions among the physiological, cognitive, emotional, and behavioral experiences we commonly refer to as symptoms. 135 – 138 This theory emerged because data gathered from existing measures were inconsistent with the common cause theory on which they are implicitly based. Now, to measure depression as a complex system we need new measures, which will require at least two innovations.
First, each component in the system must be measured rigorously, which is not the case in current depression measures that typically only provide very rough assessments of individual elements. 52 Common depression symptoms like guilt, suicidal ideation and sleep problems are themselves complex phenotypes, but are usually assessed only with a single item each. In addition, measures could encompass a broader set of elements than symptoms alone, including variables conceptualized as risk factors, maintenance factors, and outcomes, such as stress or adversity, and impairment and quality of life. 139 – 142 It will be critical to engage scientific and experiential experts in characterizing the system of elements that drive depression. 29 , 143
Second, according to this systems theory, symptoms (such as sad mood) do not merely indicate depression; they are active causal agents that influence other symptoms (such as sleep, concentration, or suicidal ideation). Thus, individual system elements and their relationships must be measured, necessitating a move away from static, retrospective assessments and toward instruments that can assess the dynamic unfolding of depression within individuals over time. For example, smartphone apps and other digital tools that utilize ecological momentary assessment to query people multiple times per day regarding their thoughts, feelings, behaviors, and experiences 144 have the potential to reveal dynamic information about depression, including the development of individual system elements and relationships among them.
Importantly, establishing the components of a system and their relations can promote new insights into depression. From a systems perspective, someone is at risk for depression if the system, once sufficiently perturbed, is likely to fall into a self-sustaining depressed state. The key to this determination is in the system’s attractor states. An attractor state can be thought of as a valley in a landscape, with a ball representing the system’s current state resting on the surface. If an individual is healthy, the landscape is flat and only has a single valley, which is their healthy attractor state where elements of depression are absent. Perturbations (such as life stress) may push the ball up the slope of this valley, but it will always return to this healthy attractor state. By contrast, if an individual is at risk for depression, the landscape features a second valley where many elements of depression are active. In this landscape, a perturbation can push the ball up the slope, out of the healthy valley and into the depressed one. Critically, system elements and their causal relationships determine the shape of a person’s stability landscape (and, thus, the presence of attractor states). Accordingly, accurately measuring elements and relationships can identify the presence of a harmful attractor, providing a novel measure of depression. From this perspective, depression is determined by the presence of a harmful attractor state, as well as the shape of the stability landscape (for example, how steep the valleys are), rather than just the number of symptoms. This shift has substantial implications for how we think about measuring depression risk, depression severity, and depression recovery. Identifying people vulnerable for depression means measuring the system thoroughly to determine if a depressed attractor is present before the person ever falls into it; measuring depression severity means to assess the shape of the stability landscape in detail; and assessing treatment efficacy might involve measuring the flattening or elimination of the harmful attractor, changing the stability landscape into one that has a single healthy valley. Working from a theory that clearly specifies the nature of the phenomenon we are assessing affords clear new paths for how to measure it.
Our example is not meant to show that the systems approach is the one right theoretical path forward, but rather that grounding measurement in theories can provide insight into how to advance depression measurement. Measuring depression from a systems perspective would initially exhibit substantial shortcomings, but advances in the theory would enable improvements in measurement, which, in turn, may equip us to interrogate further and advance the theory. Through this iterative exchange we can improve the measurement of depression 133 , and in doing so, improve our ability to study, diagnose, treat, and prevent it.
Supplementary Material
Supplementary materials, acknowledgements.
The authors thank Dr Melissa Gordon Wolf, Dr Nancy Butcher, and Dr Zachary Cohen for comments on earlier versions of this manuscript.
Competing interests
The authors declare no competing interests.
Supplementary information
Supplementary information for this paper is available at https://osf.io/7dp5s/
What Is Depression? Symptoms, Causes, Diagnosis, Treatment, and Prevention
While everyone has experienced sadness, not everyone has experienced depression. In fact, if you’ve never been depressed, chances are that you don’t have a real grasp on what living with this complex mental illness is like.
Depression is insidious. It affects not only your mood, but also your ability to feel, think, and function. It blunts sensations of pleasure, closes off connectedness, stifles creativity, and, at its worst, shuts down hope. It also often causes deep emotional pain not only to the person experiencing it, but to that person’s close family and friends.
Common Questions & Answers
Signs and symptoms of depression.
If sadness alone isn’t a good gauge of depression, what is? According to the American Psychiatric Association’s (APA) current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) , which is the diagnostic guide used by most mental health professionals, if you’ve experienced at least five of the following symptoms most of the day, nearly every day, for at least two weeks, you may be diagnosed with major depressive disorder (MDD) , also known as clinical depression.
- Tearfulness, emptiness, or worthlessness
- Little interest or pleasure in your work, hobbies, friends, family, and other things you once enjoyed
- Dramatic changes up or down in your appetite or your weight not related to dieting
- Feelings of listlessness or fatigue for no obvious reason
- Trouble concentrating or making decisions
- Anxious restlessness that manifests in ways like pacing or wringing your hands — or the opposite, moving or speaking more slowly than usual
- Insomnia or sleeping too much
- Recurrent thoughts of suicide or death
Causes and Risk Factors of Depression
No one knows for sure why some people become depressed and others do not. Depression can occur spontaneously, without any obvious cause. And it’s well documented that once you’ve had one depressive episode, your risk of having another later in life increases.
Psychiatrists today generally look at depression in “bio-psycho-social” terms, meaning that they see it as a complex disorder most likely triggered by overlapping biological, psychological, and social (also referred to as environmental) factors, according to a study published in August 2019 in Psychiatric Times .
Among the potential contributors to depression are:
- Genetics Many studies suggest that depression can spring from a genetic predisposition, including one international study involving more than 807,000 people, published in the February 2019 issue of the journal Nature Neuroscience , that linked 269 genes to depression. Genes alone are not believed to write your destiny, however. Scientists think that while some genes may increase risk, other factors are needed to trigger symptoms.
- Neurotransmitters The long-held idea that depression is caused by low levels of certain neurotransmitters (chemical messengers that communicate between neurons) has been debunked, according to a systematic review published in July 2022 in Molecular Psychiatry . But, it’s clear that neurotransmitters play a role, at least for some people. Experts’ current belief is that the relationship between depression and neurotransmitters is complex and may be related to nerve cell connections, nerve cell growth, or the functioning of nerve circuits, Harvard Medical School states.
- Inflammation Multiple studies indicate that disease-related or stress-related inflammation may create chemical changes in the brain that can trigger or worsen depression in certain people and influence how a person responds to drug therapy, according to a study published May 2018 in Psychiatric Times .
- Hardship There’s growing evidence, according to the World Health Organization , that psychological and social factors like a history of abuse, poor health and nutrition, unemployment, social isolation or loneliness, low socioeconomic status, or stressful life events (divorce or money worries, for example) can play a decisive role in the onset of depression. For example, adults with MDD have double the rate of childhood trauma compared with people without MDD, a study published May 3, 2016, in the journal Translational Psychiatry showed.
- Traumatic Brain Injury (TBI) Another all-too-common cause of depression is TBI. In 2019, more than 223,000 people were hospitalized for TBIs (aka concussions ) following a bump or blow to the head from things like falls, assaults, car accidents, and workplace and sports-related injuries, according to the Centers for Disease Control and Prevention . And more than half of those patients will meet the criteria for major depression three months after their injury, suggests a study published November 30, 2017, in the journal Brain Injury .
How Is Depression Diagnosed?
To be diagnosed with MDD, one of your symptoms must be a persistent low mood or a loss of interest or pleasure, the DSM-5 states. Your symptoms must also not be due to substance abuse or a medical condition, such as thyroid problems , a brain tumor , or a nutritional deficiency.
Of course, it’s normal to have any or all of these symptoms temporarily (for hours or even days) from time to time. The difference with depression is that the symptoms persist and make it difficult to function normally.
If you suspect you may be depressed, the best first step is to reach out to your primary care doctor, a psychiatrist , or a psychotherapist. Also, know that depression screenings may now be a part of routine checkups. As of June 2023, the U.S. Preventive Services Task Force (USPSTF) recommends that primary care providers screen all adults for depression, including pregnant and postpartum people and older adults.
If you’re reluctant to consult a professional, type “depression” or “clinical depression” into Google on your cellphone or computer and you’ll find links to a clinically validated depression test known as the PHQ-9 patient health questionnaire . Although designed to be administered by a healthcare professional, this test is short and straightforward. Take it and you can immediately see if your score indicates you may have depression.
Important: If you suspect you have depression, or if you’re feeling troubled by your symptoms, have suicidal thoughts, just need to talk, want some advice, or need a referral for treatment, call the Suicide and Crisis Lifeline (formerly known as the National Suicide Prevention Lifeline) at the three-digit code 988 , or the National Substance Abuse and Mental Health Services Administration Helpline at 1-800-662-HELP (4357). Both are free and available 24/7, 365 days a year.
Learn More About Depression Symptoms
What Are the Different Types of Depression?
In addition to MDD, there are several other kinds of depression, including:
- Persistent depressive disorder (PDD), previously known as dysthymia, is diagnosed in people who have at least two of the symptoms of major depression for at least two years at a time, according to Cleveland Clinic . It’s possible to fluctuate between severe and less-severe symptoms, and to have both PDD and MDD at the same time, a condition called double depression. People with PDD are often perceived as cranky, sullen, changeable, or pessimistic rather than being recognized as having a treatable disorder.
- Bipolar disorder, formerly called manic depressive disease, is characterized by moods that cycle between extreme highs (mania) and lows (depression), often with periods of normal mood in between, according to the American Psychiatric Association . Bipolar disorder affects 2.8 percent of U.S. adults, according to the National Institute of Mental Health .
- Seasonal affective disorder (SAD) is depression that occurs at the same time each year, usually beginning in fall and persisting through winter, according to Mayo Clinic . SAD is associated with changes in sunlight, and is often accompanied by increased sleep, weight gain, and cravings for foods high in carbohydrates.
- Premenstrual dysphoric disorder (PMDD) is a more serious form of premenstrual syndrome (PMS). PMDD usually develops a week or two before a woman’s period and passes two or three days after menstruation starts, according to the Office of Women’s Health .
- Postpartum (or perinatal) depression (PPD) is diagnosed in mothers who experience symptoms of major depression shortly after giving birth (or during pregnancy), the American College of Obstetricians and Gynecologists states. PPD is usually related to a combination of factors, including sharp changes in hormone levels following childbirth. Feelings of intense sadness, anxiety, or exhaustion are much stronger, and last longer, than the “baby blues” — the relatively mild symptoms of depression and anxiety that many new mothers experience in the first few days after childbirth.
Learn More About Perinatal Depression
Learn More About SAD
Learn More About Bipolar Disorder
Learn More About Postpartum Depression
Depression: Recognizing Unusual Symptoms
One reason depression can be hard to identify is that its signs can vary widely from person to person and sometimes be masked by atypical symptoms. For example, some people who are depressed may show it by acting disgruntled, resentful, or irritable. In fact, aggression — including outright acts of violence — can be indicative of “hidden” depression, according to a report published in February 2017 in Psychiatric Times . Depression masquerading as anger may seem surprising at first, but not when you consider that several underlying factors, including alcohol or substance abuse and childhood trauma, have been linked to both.
Similarly, although it’s not clear why, a person who experiences anxiety is at high risk for developing depression, and vice versa. The National Alliance on Mental Illness reports that as many as 60 percent of people with anxiety will also have symptoms of depression; the same goes for people with depression having symptoms of anxiety . Experts say there is often a genetic predisposition for these co-occurring disorders, according to Hartgrove Behavioral Health System .
Depression may also manifest psychosomatically, meaning that instead of presenting first and foremost as a mood disorder, the dominant symptom may be things like vague aches, dizziness , headaches, digestive problems , or back pain , according to a review published in the Journal of Clinical Psychiatry . Complicating matters is that it’s often hard to know whether depression is causing the physical symptoms, or if the physical symptoms are causing depression.
Duration of Depression
How long depression lasts varies from person to person, but according to the DSM-5 , a depressive episode lasts at least two weeks.
Untreated depressive episodes appear to last 6 to 12 months, according to StatPearls . Depression also tends to be chronic, with episodes happening again in about half of people who’ve experienced one depressive episode, 70 percent of people who’ve had two episodes, and 90 percent of people who’ve had three episodes. But some people never experience another episode after the first one.
How Do I Know if My Antidepressants Are Working?
Next up video playing in 10 seconds
Treatment and medication options for depression.
If you suspect that depression is interfering with your life, talking about what you’re experiencing and discussing treatment options with a medical professional is essential. As actress Taraji P. Henson, who describes her depression as “suffocating” darkness, recently explained in an interview with Self , “When you’re quiet, things aren’t fixed. It gets worse.”
The good news is that there’s abundant evidence that people with depression who seek treatment will find significant relief from talk therapy (psychotherapy), medication, lifestyle changes, or a combination of all efforts, according to the Anxiety and Depression Association of America .
Read our reviews and expert recommendations for the best online therapy , including programs like Betterhelp, Talkspace, and Brightside.
Which Types of Talk Therapy Work Best for Depression?
The Society of Clinical Psychology rates several types of psychotherapy as highly effective treatments for depression :
- Behavioral Activation Therapy The aim of this type of therapy is to reverse the downward spiral of depression by encouraging you to seek out experiences and activities that give you joy.
- Cognitive Behavioral Therapy (CBT) CBT focuses on changing specific negative thought patterns so that you are able to better respond to challenging and stressful situations.
- Interpersonal Therapy This very structured, time-limited form of therapy focuses on identifying and improving problematic personal relationships and circumstances directly related to your current depressive mood.
- Problem-Solving Therapy This therapy is a form of CBT that teaches take-charge skills that help you solve real-life problems and stressors , big and small, that contribute to depression.
- Self-Management or Self-Control Therapy This type of behavioral therapy trains you to lessen your negative reactions to events and reduce your self-punishing behaviors and thoughts.
What Are the Different Antidepressants and How Do They Work?
The most commonly prescribed antidepressants cause changes in brain chemistry that affect how neurons communicate. Exactly how this improves mood remains somewhat of a mystery, but the fact that they do often work is well-established. If you’re thinking about trying antidepressants, talk to your doctor about whether these treatments could be right for you.
- SSRIs (Selective Serotonin Reuptake Inhibitors) This category of drug includes fluoxetine (Prozac) , citalopram (Celexa) , and sertraline (Zoloft) and targets serotonin , a neurotransmitter that helps control mood, appetite, and sleep.
- SNRIs (Serotonin and Norepinephrine Reuptake Inhibitors) SNRIs include drugs like duloxetine (Cymbalta) , desvenlafaxine (Pristiq) , and venlafaxine (Effexor XR) , which block the reabsorption of both serotonin and another neurotransmitter, norepinephrine .
- NDRIs (Norepinephrine-Dopamine Reuptake Inhibitors) This class of medications includes bupropion .
- TCAs (Tricyclic Antidepressants) TCAs include such drugs as imipramine (Tofranil) and nortriptyline (Pamelor) . These drugs were among the earliest antidepressants to come on the market. These days, doctors generally only turn to them when treatment with SSRIs , SNRIs, and NDRIs has failed.
- MAOIs (Monoamine Oxidase Inhibitors) MAOIs, including phenelzine (Nardil) and isocarboxazid (Marplan) , were the first antidepressants developed. They’re rarely used today, in part because people who take them require careful monitoring to prevent negative interactions with certain foods and other medications.
All antidepressants can have side effects, but some may be more problematic than others. You may need to try several different medications, or a combination, guided by your doctor, before you find what works best for you.
In addition, it may take some patience before you see results. The full benefits of the drugs may not be realized until you’ve taken them for as long as three months, according to the the STAR*D trial , the largest, longest study on antidepressant treatment, which ended in 2006.
Sometimes, other medications may be added to your regimen, depending on the form of depression, severity of your symptoms, and your response to other therapies. These might include a mood stabilizer, such as lithium (sold under several brand names) or valproic acid (Depakene, Depakote) . If symptoms of psychosis (having delusions or seeing or hearing voices that are not real, for example) are present, a doctor may prescribe an antipsychotic medication, such as haloperidol (Haldol) , risperidone (Risperdal) , ziprasidone (Geodon) , aripiprazole (Abilify) , and olanzapine (Zyprexa) .
Some experts believe that using an antipsychotic in combination with an antidepressant may be more effective for depressive disorders than antidepressants alone, according to a review published in Shanghai Archives of Psychiatry .
Learn More About Depression Treatment
Lifestyle Changes for Depression
Lifestyle changes, such as making art, journaling, exercising more, and practicing yoga or mindfulness, can also alleviate depression and the stress that can heighten it. Alternative treatments like massage, acupuncture , and light therapy may also help.
Diet changes, too, can uplift your mood by reducing inflammation and helping to ensure your brain gets the nutrients it needs to function at its best.
One small randomized controlled study, published October 9, 2019, in the journal PLoS One , found that self-reported symptoms of depression dropped significantly in just three weeks in young adults who changed from a highly processed, high-carbohydrate diet to a Mediterranean diet focused on vegetables, whole grains, lean proteins, unsweetened dairy, nuts and seeds, olive oil, and the spices turmeric and cinnamon. In contrast, the depression scores didn’t budge in a control group of people who didn’t change their diet.
Should You Worry About Antidepressant Withdrawal?
No, but it’s easy to see why some people might think so, because of a medical condition called antidepressant discontinuation syndrome (ADS), which can occur if you abruptly stop taking medication rather than tapering off as is generally advised. ADS is marked by a wide range of responses, including but not limited to flu-like symptoms, insomnia, worsening mood, and stomach distress, according to a report published March 11, 2019, in Psychiatric Times .
Current estimates are that up to 40 percent of patients who’ve taken an antidepressant for at least a month will experience ADS symptoms if they abruptly stop their medication instead of lowering their dose gradually, according to a study published December 2018 in The American Journal of Psychiatry . (Conversely, more than 60 percent of patients who stop taking an SSRI will have no significant symptoms.) Tapering under the care of a doctor can prevent ADS by allowing the brain to adjust to changes in neurotransmitter levels.
More to the point, while you should slowly stop your antidepressant with the help of your doctor, antidepressants do not cause dependence and withdrawal like other substances. Unlike substances that are known to cause addiction, such as alcohol, opioids , and barbiturates , people don't crave antidepressants. You don’t get “high” from them, and they aren’t intentionally or compulsively overused. Serious reactions like the seizures and agitation that can follow sudden withdrawal from addictive substances are “unheard of when these antidepressants are tapered gradually,” note the authors of the Psychiatric Times report.
What Is Treatment Resistant Depression and Is There Any Help for It?
If you’ve tried at least two different antidepressants and your depression hasn’t improved, you may be diagnosed with treatment-resistant depression (TRD) . TRD is a serious condition that has been highly associated with suicidal ideation and suicide attempts. Thirty percent of people with TRD attempt suicide in their lifetime, more than double the rate of their treatment-responsive peers, according to a review published in April 2018 in the Journal of Affective Disorders . It is not, however, a hopeless condition. A number of alternative treatment approaches are available, including:
- Esketamine A nasal spray marketed under the name Spravato, esketamine won FDA approval on March 5, 2019, as a new treatment for TRD. It is derived from ketamine , a veterinary anesthetic best known as the street drug “Special K.” Because of safety concerns, Spravato must be administered in a medical office and should be taken along with an oral antidepressant.
- Electroconvulsive Therapy (ECT) ECT is the modern-day version of electroshock therapy. It involves a brief electrical stimulation of the brain while the patient is under anesthesia. According to the APA , ECT rapidly provides substantial improvement in approximately 80 percent of patients with severe, uncomplicated major depression. Like any medical procedure, ECT is associated with side effects — most commonly, issues with memory. In most cases, this is short-term; however, some people can experience permanent gaps in memory, per the APA. Nevertheless, current ECT has far fewer side effects than electroshock therapy of the past.
- Transcranial Magnetic Stimulation (TMS) TMS uses rapidly alternating magnetic fields to change activity in specific areas of the brain. Although researchers don’t fully understand how exactly TMS affects the brain, it appears to influence how the brain is operating and, in turn, improve mood and decrease depressive symptoms, according to Mayo Clinic .
- Vagus Nerve Stimulation This therapy involves implanting a tiny device in the chest that provides regular mild electrical pulses to the longest of the nerves that arise from the brain. A study published on August 21, 2018, in the Journal of Clinical Psychiatry involving nearly 600 patients with TRD found that vagus nerve stimulation significantly improved quality of life for many patients.
- Psychedelic Drugs While not yet FDA approved, microdosing with psychedelic drugs to produce a more positive mood in people with chronic depression is the focus of a flurry of research worldwide, including at the Johns Hopkins Center for Psychedelic and Consciousness Research. The possibilities appear vast and promising. For example, one of the latest Johns Hopkins studies, published March 1, 2019, in The American Journal of Drug and Alcohol Abuse , found that a synthetic form of a psychedelic derived from the venom of certain toads provided fast-acting relief from depression and anxiety. However, according to a July 2022 position statement from the APA , there’s not enough evidence yet to endorse the use of psychedelics for the treatment of any mental health condition except during approved investigational studies, and more research is needed in this field.
Prevention of Depression
If you’re wondering how to prevent depression, unfortunately there’s no surefire way. But according to Mayo Clinic, these steps could help:
- If you suspect you have depression, get professional help early on to keep it from getting worse.
- Lean on your family or friends for support.
- Consider long-term treatment to prevent your depressive symptoms from coming back even after you feel better.
Try your best to curb stress in your life.
Complications of Depression
Depression can worsen and take a significant toll on your mental and physical health if it’s not properly treated, according to Mayo Clinic . Potential complications of depression include:
- Misuse of alcohol or drugs
- Anxiety disorders
- Social isolation
- Family or relationship difficulties
- Work or school issues
- Excess weight, which can lead to diabetes or heart disease
- Self-harm or suicide
- Early death from other medical conditions
Research and Statistics: How Many People Have Depression?
Unfortunately, there are plenty of people who know exactly what it means to be depressed. In 2020, an estimated 21 million, or 8.4 percent, of adults in the United States had at least one major depressive episode in the past year, according to the National Institute of Mental Health , making it one of the most common mental illnesses in the United States.
What’s more, a recent report from Mental Health America, a nonprofit founded in 1909, offers startling statistics pertaining to one of depression's most disturbing symptoms: thoughts of suicide.
According to its 2023 State of Mental Health in America report , suicidal ideation among adults has reached 4.84 percent (more than 12.1 million people).
There is a bright side. Although there is no one-size-fits-all cure for depression, there are many effective treatment options, one of which is bound to help you heal if you’re struggling with the illness. This cannot be emphasized enough, given that roughly two-thirds of people living with depression do not receive the care they need, according to a report published online February 22, 2019, in the journal Neuropsychiatric Disease and Treatment .
Depression and Gender: Is It Different in Men and Women?
When it comes to depression, there is a distinct gender gap. Depression is nearly twice as common in women as in men, according to data from the National Center for Health Statistics . Hormonal and other biological factors play a role in this disparity. After all, only cisgender women and people with a uterus can have premenstrual or postpartum depression. The same is true of antepartum (or perinatal) depression — depression during pregnancy — which the American College of Obstetricians and Gynecologists estimates affects 1 in 10 pregnant women.
Have You Ever Experienced Antidepressant Withdrawal?
How are people of color affected by depression.
Research on depression within communities of color has revealed a number of differences in the symptoms, diagnosis, and treatment between people of color and white communities.
The symptoms of depression may appear differently among people of color compared with white people, according to the study from February 2019 in Neuropsychiatric Disease and Treatment . For instance, while white people are more likely to have acute depressive episodes, African American people are more likely to experience depression that’s more chronic, prolonged, and debilitating.
In another study, published in December 2022 in Nursing Research , which was focused primarily on Black and African American mothers, participants were more likely to report self-blame, irritability, difficulty sleeping, and an inability to experience pleasure than some of the hallmark symptoms of depression, such as feelings of hopelessness or sadness.
Importantly, the authors of the study noted, traditional depression screening tools may not capture these symptoms, meaning depression may go undetected in some Black and African American women.
Among Black and Hispanic people, major depression goes undiagnosed and is undertreated at a much greater rate than among white people, according to a report published in May 2022 by Blue Cross Blue Shield . When these communities do receive treatment, prescription medication and counseling are utilized less often than in white communities, the report noted.
When it comes to treatment, Asian American and Pacific Islander (AAPI) communities are the least likely racial group to seek professional mental health services, according to Mental Health America . That’s often due to factors like a lack of accessible resources, language barriers, and cultural stigmas surrounding mental health issues.
Learn More About Suicide Risk and Prevention
Related Conditions
When your provider evaluates you for depression, it’s important that they rule out any other potential conditions that could be causing your symptoms. Conditions that may overlap with MDD, according to StatPearls, include:
- Bipolar disorder
- Eating disorders
- Grief or bereavement
- Schizoaffective disorder
- Schizophrenia
- Substance- or medication-induced depressive disorder
Importantly, some people may have at least one of the above conditions in addition to depression, according to research published in February 2015 in the Journal of Medical Internet Research . Having multiple mental health conditions at the same time is what’s known as psychiatric comorbidity.
Suicide Discussion

Resources We Trust
- Mayo Clinic: Depression (Major Depressive Disorder)
- Cleveland Clinic: Depression
- Families for Depression Awareness: Help Prevent Suicides
- Depression and Bipolar Support Alliance: Depression
- Anxiety & Depression Association of America: What Is Depression?
Editorial Sources and Fact-Checking
Everyday Health follows strict sourcing guidelines to ensure the accuracy of its content, outlined in our editorial policy . We use only trustworthy sources, including peer-reviewed studies, board-certified medical experts, patients with lived experience, and information from top institutions.
- Major Depression. National Institute of Mental Health . January 2022.
- The State of Mental Health in America 2023. Mental Health America . 2023.
- Bailey RK, Mokonogho, J, Kumar A. Racial and Ethnic Differences in Depression: Current Perspectives. Neuropsychiatric Disease and Treatment . February 22, 2019.
- What Is Depression? American Psychiatric Association . October 2020.
- Persistent Depressive Disorder (PDD). Cleveland Clinic . March 8, 2021.
- What Are Bipolar Disorders? American Psychiatric Association . January 2021.
- Bipolar Disorder. National Institute of Mental Health .
- Seasonal Affective Disorder (SAD). Mayo Clinic . December 14, 2021.
- Premenstrual Dysphoric Disorder (PMDD). Office on Women's Health . February 22, 2021.
- Postpartum Depression. American College of Obstetricians and Gynecologists . December 2021.
- Krakowski M, Nolan K. Depressive Symptoms Associated With Aggression. Psychiatric Times . February 27, 2017.
- Salcedo B. The Comorbidity of Anxiety and Depression. National Alliance on Mental Illness . January 19, 2018.
- Tjornehoj T. The Relationship Between Anxiety and Depression. Hartgrove Behavioral Health System .
- Trivedi MH. The Link Between Depression and Physical Symptoms. Primary Care Companion to the Journal of Clinical Psychiatry . February 2004.
- Pies RW. Debunking the Two Chemical Imbalance Myths, Again. Psychiatric Times . August 2, 2019.
- Howard DM, Adams MJ, McIntosh AM, et al. Genome-Wide Meta-Analysis of Depression Identifies 102 Independent Variants and Highlights the Importance of the Prefrontal Brain Regions. Nature Neuroscience . February 4, 2019.
- Moncrieff J, Cooper RE, Stockmann T, et al. The Serotonin Theory of Depression: A Systematic Umbrella Review of the Evidence. Molecular Psychiatry . July 20, 2022.
- What Causes Depression? Harvard Medical School . January 10, 2022.
- Pariante CM. Why Are Depressed Patients Inflamed? A New Path to Personalized Treatment in Psychiatry. Psychiatric Times. May 31, 2018.
- Social Determinants of Mental Health. World Health Organization . 2014.
- Williams LM, Debattista C, Duchemin A-M, et al. Childhood Trauma Predicts Antidepressant Response in Adults With Major Depression: Data From the Randomized International Study to Predict Pptimized Treatment for Depression. Translational Psychiatry . May 3, 2016.
- TBI Data. Centers for Disease Control and Prevention . April 24, 2023.
- Singh R, Mason S, Lecky F, Dawson J. Prevalence of Depression After TBI in a Prospective Cohort: The SHEFBIT Study. Brain Injury . November 30, 2017.
- Brody DJ, Pratt LA, Hughes JP. Prevalence of Depression Among Adults Aged 20 and Over: United States, 2013–2016. Centers for Disease Control and Prevention . February 2018.
- Depression During Pregnancy. American College of Obstetricians and Gynecologists . May 2023.
- Kennedy Bailey R, Mokonogho J, Kumar A. Racial and Ethnic Differences in Depression: Current Perspectives. Neuropsychiatric Disease and Treatment . February 22, 2019.
- Perez NB, D’Eramo Melkus G, Wright F, et al. Latent Class Analysis of Depressive Symptom Phenotypes Among Black/African American Mothers. Nursing Research . March/April 2023.
- Racial Disparities in Diagnosis and Treatment of Major Depression. Blue Cross Blue Shield . May 31, 2022.
- Asian American / Pacific Islander Communities and Mental Health. Mental Health America .
- Taraji P. Henson on Living With Depression and Anxiety. Self . December 3, 2019.
- Salcedo B. Depression Treatment — It Works. Anxiety and Depression Association of America . May 29, 2018.
- Francis HM, Stevenson RJ, Chambers JR, et al. A Brief Diet Intervention Can Reduce Symptoms of Depression in Young Adults – A Randomized Controlled Trial. PLoS One . October 9, 2019.
- Treatment Target: Depression. Society of Clinical Psychology .
- Questions and Answers about the NIMH Sequenced Treatment Alternatives to Relieve Depression (STAR*D) Study — All Medication Levels. National Institute of Mental Health . November 2006.
- Wang P, Si T. Use of Antipsychotics in the Treatment of Depressive Disorders. Shanghai Archives of Psychiatry . June 25, 2013.
- Pies RW, Osser DN. Sorting Out the Antidepressant “Withdrawal” Controversy. Psychiatric Times . March 11, 2019.
- Jha MK, Rush AJ, Trivedi MH. When Discontinuing SSRI Antidepressants Is a Challenge: Management Tips. American Journal of Psychiatry . December 1, 2018.
- Bergfeld IO, Mantione M, Figee M, et al. Treatment-Resistant Depression and Suicidality. Journal of Affective Disorders . August 1, 2018.
- FDA Approves New Nasal Spray Medication for Treatment-Resistant Depression; Available Only at a Certified Doctor’s Office or Clinic. U.S. Food and Drug Administration . March 5, 2019.
- What Is Electroconvulsive Therapy (ECT)? American Psychiatric Association . January 2023.
- Transcranial Magnetic Stimulation. Mayo Clinic . April 7, 2023.
- Conway CR, Kumar A, Xiong W, et al. Chronic Vagus Nerve Stimulation Significantly Improves Quality of Life in Treatment-Resistant Major Depression. The Journal of Clinical Psychiatry . 2018.
- Davis AK, So S, Lancelotta R, et al. 5-Methoxy-N,N-Dimethyltryptamine (5-MeO-DMT) Used in a Naturalistic Group Setting Is Associated With Unintended Improvements in Depression and Anxiety. The American Journal of Drug and Alcohol Abuse . March 1, 2019.
- Position Statement on the Use of Psychedelic and Empathogenic Agents for Mental Health Conditions. American Psychiatric Association . July 2022.
- Kavan MG, Barone EJ. Grief and Major Depression — Controversy Over Changes in DSM-5 Diagnostic Criteria. American Family Physician . November 15, 2014.
- Depression (Major Depressive Disorder): Symptoms & Causes. Mayo Clinic . October 14, 2022.
- Major Depressive Disorder. StatPearls . April 10, 2023.
- AL-Asadi AM, Klein B, Meyer D, et al. Multiple Comorbidities of 21 Psychological Disorders and Relationships With Psychosocial Variables: A Study of the Online Assessment and Diagnostic System Within a Web-Based Population. Journal of Medical Internet Research . February 26, 2015.

10 Good Questions About Depression And Their Answers
D epression is a disorder of mood, so what does it feel like to live with depression? The answers to these 10 questions about depression and their answers will provide you with a better understanding of the condition.
1. What is depression?
Depression is a mood disorder that affects one's ability to feel pleasure and derive satisfaction from life. It's a serious illness that affects millions of people, yet it remains misunderstood by many in the general population. This can lead to negative stereotypes and stigma surrounding those who suffer from depression, which can make it even more difficult for them to get help.
It is not caused by feelings of sadness or grief at a specific point in time, but rather a pervasive sense of hopelessness and despair that lingers over time. It can be sparked by an event or series of events, such as the death of a loved one or divorce. But while these events may trigger depressive symptoms, they are usually not the root cause themselves. Instead, they are often just triggers for an underlying condition that has been building up over time.
2. What is a common misconception about depression?
One of the most common misconceptions about depression is that it’s a sign of weakness. People who are depressed often feel like they need to hide their feelings, even from their friends and family. The stigma surrounding mental illness has led to negative stereotypes, which makes it even more difficult for people to discuss their struggles openly.
Depression isn’t something you can just snap out of. Because it’s a serious medical condition, people who experience clinical depression need professional treatment from trained mental health professionals in order to get better. If you have symptoms of depression, never try to treat yourself without first consulting with your doctor or therapist. Untreated depression can lead to serious consequences such as substance abuse and suicide attempts or completions.
3. What are some of the symptoms of depression?
Depressed people may feel sad, anxious, empty, hopeless, worried, helpless or worthless. Depression can interfere with normal daily activities and cause problems in relationships and at work.
If you have symptoms of depression, talk to your doctor about treatment options. Treatment for depression includes antidepressant medications and psychotherapy (talk therapy). Your doctor may recommend that you try several different medications to find the right one for you.
Antidepressants are not addictive and are not the same as street drugs like cocaine or heroin. They don't make you high or groggy and they typically don't cause withdrawal symptoms when you stop taking them. Most antidepressants take three to five weeks before they start working.
4. How is depression different from grief, sadness, or disappointment?
When you're grieving, you're processing the loss of something or someone important to you, which can be similar to depression but is temporary and has an end-point. Sadness is a normal reaction to a situation that's upsetting, but it doesn't last long. It's a feeling that comes and goes quickly as part of the process of moving on.
Disappointment happens when things don't go your way, like missing out on something or failing to achieve something. Depression can be caused by many different things: genetic factors, childhood trauma, an illness like cancer or heart disease, stress at work or home and the list goes on!
5. How can I help someone who is depressed?
First, tell them that you're there for them and that you care about them. They may feel like they have no one else in their life who cares about them, so hearing that someone does can really help.
Second, don't be afraid to ask questions—you might not know what's going on in your head, but asking questions will show that you're interested and trying to understand. You can also let them know if they start talking about something that makes you uncomfortable or that you don't want to talk about (like suicide), so they know they can trust you with those kinds of things without fear of judgment or shame.
Thirdly, be patient! It might take some time for them to open up about what's going on with them emotionally—you'll have better results if you just listen when they do start talking. Don't push too hard or pressure them into sharing more than they're comfortable sharing (or even at all).
6. Why does it seem like some people get depressed more often than others?
A person's risk of depression is heavily influenced by their genes, but it's also affected by environmental factors.
Genes have a very strong influence on whether or not you get depressed, but environmental factors are also important.
If you've ever wondered why some people seem to suffer from more depression than others, it could all be down to their genes. In fact, scientists have found that depression is strongly influenced by genetics — a person's genetic makeup can play an important role in whether or not they develop the condition. However, it's important to remember that there are many other factors involved as well.
There are two main types of genes associated with depression: those that code for neurotransmitters and those that code for something called cytokines. Neurotransmitters are chemicals produced by nerve cells (neurons) that allow them to communicate with one another; cytokines are proteins released by immune cells that help them signal infection or injury within the body.
Neurotransmitter genes may predispose people towards depression because they make it difficult for certain neurotransmitters (such as serotonin) to function properly in the brain.
7. Can anyone get depressed? If so, who?
Anyone at any age — women, men, teens, and children — can get depression. But it's more likely to happen as you get older.
Women are twice as likely to develop depression as men are. Women are also more likely than men to have repeated episodes of depression over time or get depressed again after they've gone through treatment.
Most people with depression will experience only one episode in their lifetime, but some people may have more than one episode over their lifetime.
Depression is more common among young people ages 15-24 than any other age group; however, it can occur at any age.
8. How long does it take for someone to get better after they're diagnosed with depression?
The answer to this question depends on the severity of the depression and how long it has been present. Depression can come on suddenly and be severe, or it can develop gradually over time. The more severe or chronic your depression is, the longer it will take to recover.
If your depression is mild or moderate in nature, you may begin to feel better within a few weeks or months. If your depression is more severe or chronic, it might take longer for your symptoms to subside. In some cases, people with severe depression may require treatment for many years before they feel back to normal.
In addition to the length of time it takes for someone to recover from depression, there's also a wide range of individual responses to treatment. Some people respond very quickly while others may need additional treatment after initial responses wear off over time.
9. What causes depression? Is there a cure for it? Are there other treatments besides medication?
There are many different causes for depression, including genetics, the environment, personality traits, and life experiences. Sometimes it can be caused by a medical condition like hypothyroidism or an underactive pituitary gland.
One of the most common treatments for depression is medication. Although there are many different medications to treat depression, they all work in different ways and have varying side effects. For example, some medications affect serotonin levels in the brain while others affect norepinephrine levels in the brain; some medications have side effects like weight gain while others have side effects like drowsiness and dry mouth; some medications are used only if other treatments haven't been effective in treating your symptoms.
There are also non-medical treatments for depression like therapy (talk therapy) or supportive counseling (listening). These therapies help you learn how to deal with stressors in your life so they don't cause you more distress than necessary which can lead to more depressive episodes down the road.
10. What should I do if I think someone I know is depressed or suicidal?
If you think someone you know is depressed or suicidal, the first thing to do is talk to them. It's important to let them know that you're concerned about them and that you want to help. If they don't open up to you, try again later.
If they are open to your questions, you can ask if they're thinking about hurting themselves. If so, suggest getting professional help immediately. You can offer to go with them or help make an appointment for them at a local clinic or hospital.
However, if they're not thinking about suicide but are still struggling with depression, encourage them to get professional help as well. Depression can be treated with therapy or medication, and it's important for people who suffer from depression to get treatment so that they can feel better and get back on track with their lives.
If you are experiencing the symptoms described in this article, please take the time to talk to a trained medical professional. You don't have to go through this alone.
For more helpful and informative insights.
The post 10 Good Questions About Depression And Their Answers appeared first on Things That Make People Go Aww .

124 Great Depression Topics to Write about & Examples
Welcome to our list of the Great Depression topics! Here, you will find writing ideas about the causes and effects of the Great Depression. You can also pick plenty of related issues to debate.
🔝 Top 10 Great Depression Topics to Write About
🏆 best great depression topic ideas & essay examples, 💡 good great depression essay topics, ⭐ interesting topics to write about great depression, ❓ great depression essay questions, 🔎 great depression research topics.
- The Stock Market Crash of 1929
- What Triggered the Great Depression?
- Lessons Learned from the Great Depression
- The Dust Bowl Disaster and Its Role in the Depression
- How Banks Caused the Collapse of the Economy
- Government’s Response to the Great Depression
- The Great Depression and International Relations
- Unemployment and Poverty During the Depression
- Hardship and Resilience in Literature of the Great Depression
- The Impact of the Great Depression on Population Movements
- Cause and Effects of The Great Depression The economic devastation of the 1920s led to the Great Depression and brought a tragedy for the whole society. Crash of stock market The crash of the stock market in 1929 ushered in the Great […]
- The History of Great Depression The Great Depression was the most severe recession of the past centuries. It affected the whole world and lasted for approximately 12 years.
- The Impact of the Great Depression on Canada Some of the measures that Bennett put in place included camps to support the old and sick as well as the distribution of aid to the unemployed and disadvantaged in the country.
- The Reality of the Great Depression in Steinbeck’s “The Grapes of Wrath” The journey of the Joad family and other significant characters in the story who played the roles in building the whole context take the path of meeting miserable economic situations.
- The Great Depression in Canada Before the onset of the Great Depression from the years 1919-1929, Canada had the fastest growing economy amongst the developing nations and the only blip to this record was the slight recession they suffered during […]
- John Steinbeck’s “The Grapes of Wrath” and the Great Depression The Grapes of Wrath begins by describing an occurrence of soil erosion in Dust Bowl Oklahoma that led to the destruction of crops, a decline in farming and farm produce and the migration of farmers […]
- How the Great Depression Changed Americans During the depression, the population experienced intense pain and extensive misery and the event has been blamed for leading to calamities such as World War II and the rising to power of Adolf Hitler.
- How New Deal Represented Minorities and Ended the Great Depression The Civilian Conservation Corps and the Works Progress Administration were some of the many programs representing minorities in the New Deal.
- Public Enemies During the Great Depression In the 1930’s most people in America were feeling the impact of the Great Depression due to the crashed economy. During the great depression, most people were facing the challenges of starving and losing their […]
- Great Depression: Annotated Bibliography This is a secondary source, written in 2020, and its main idea is that shocks of uncertainty had the main effect on the changes during the Great Depression, which contributed to the fall in production.
- President Hoover’s Role During the Great Depression Although a significant percentage of the causative constituents emanated from the previous government’s economic strategies, President Hoover elevated the conditional outlier.
- Impact of the Great Depression and the New Deal on Minorities However, despite the intention to promote democracy and equality in the United States, the impact of the Great Depression was devastating, and the New Deal did not solve most problems among minorities.
- Social Work During the Great Depression and COVID-19 Pandemic Social workers during the COVID-19 pandemic were faced with a series of novice challenges similar to their counterparts in the Great Depression.
- The Great Depression: Prerequisites, Essence, and Consequences As a result of the crisis and the rise of protectionism, according to the League of Nations, world trade fell threefold from 1929 to 1933.
- The Concepts of Freedom and the Great Depression Furthermore, blacks were elected to construct the constitution, and black delegates fought for the rights of freedpeople and all Americans. African-Americans gained the freedom to vote, work, and be elected to government offices during Black […]
- Economic History of the US: The Great Depression The government’s immediate and unprecedented action brought the state out of the crisis and preserved the system of capitalism. In order to restore the security of Americans in the new deal, Congress and the President […]
- The Contribution of Former U.S. Presidents in Overcoming the Great Depression The Great Depression presents an event in which the U.S.developed progressive leadership policies to improve living standards. Modern politics in the U.S.has caused social divisions similar to the period of Unravelling.
- Great Depression and Cold War: Making of Modern America This paper will explore the causes of the Great Depression, the measures implemented within the New Deal, Cold War tensions, and the changes to the American society by the civil rights movement.
- American History: Great Depression and Other Issues One of the causes of the Great Depression was the international economic woes of the United States of America. One of the actions taken by the Hoover administration to combat the depression was urging the […]
- The Great Depression, Volatility and Employee Morale A?” The purpose of the present investigation study is to understand the morale of employees in corporate America on how it affects the way the economy functions in the United States.
- Stories From the Great Depression: President Roosevelt At the same time, the era of the Great Depression was the time when many Americans resorted to their wit and creativity.
- Gender, Family, and Unemployment in Ontario’s Great Depression The introduction and all the background that Campbell gives are firmly in line with the goals of this course. The first part of the study is the business and the economic history.
- How Did the Great Depression Affect Americans? The Great Depression can be fairly supposed to have been the harshest time in the history of the United States after The Civil War.
- The Causes of the Great Depression: Black Tuesday and Panic Historians relate the end of the great depression to the start of the second-word war. The government then came up with packages that sought to lessen the effects of the depression.
- The Actions of the Roosevelt on Great Depression S president and his efforts to save the country from the effects of the great depression were futile. The deal consisted of recovery programs which were targeted to be initiated into the economy in the […]
- The Great Depression of 1929 This was the program that opened the eyes of the people to the fact that the depression era did not affect just the low bracket of society and that if they were to overcome it, […]
- The Great Depression in the United States’ History This great depression was considered as the major reason of the war and in the initial stages the world was ignorant about the disasters of the war.
- The Great Depression Period Analysis The main causes for the Great Depression were a combination of unequally distributed wealth, the stock market crash, and eventually the bank failures.
- Great Depression and the American People’s Relationship With Their Government In this essay, I will try to trace the effects of the depression not just on the people who lived it but also among the present Americans.
- America in 1920s: Great Depression Regarding the issue of credit exploration in the 1920s, and the contribution of the credit’s expansion into the process of onset of the Great Depression, it is necessary to refer to the facts from American […]
- History of the Great Depression and the New Deal According to the prominent American economist John Keyne, the main cause of the Great Depression was the shortage of money supply, which was dependant on the gold reserve, in the meantime, the industry output significantly […]
- Great Depression of Canada and Conscription During World War I in Canada Due to the depression in the United States, the people across the border were not able to buy the wheat produced and cultivated in Canada and as a result, the exports declined.
- The Great Depression in Steinbeck’s “The Grapes of Wrath” The family adjusted to the codes of conduct in the camp, and Tom even managed to find a job picking fruits at a local farm.
- The Great Depression: Time of Crisis in America This was a time of immeasurable economic instability, and as many of us have read, the depression started with the atrocious crash of the stock market in 1929.
- Presidential Policy During the Great Depression During the early part of the Great Depression, the economy had ground to a halt as a result of the stock market crashing and the unemployment rates skyrocketed as businesses shut down.
- Great Depression in “A Worn Path” by Eudora Welty The first few paragraphs of the story are dedicated specifically to painting the image of the old Afro-American woman in the mind of the reader by providing details on her appearance, closing, her manners of […]
- Great Depression in the United States The Great Depression of the 1930’s is the most significant economic crises in the history of the modern world and the United States, in particular.
- American Great Depression and New Deal Reforms What is definitely certain is that many factors like the shifting of the economy, unstable credit and financial system, poor government decisions, and the fact that the international economy was still recovering from ruinous effects […]
- Great Depression’ History: Causes and Regulations The Great Depression that happened in the 1930s was the gravest and prolonged economic downturn in the history of the developed Western world.
- Child Labor, Great Depression and World War II in Photographs The impression is of isolation and yearning for daylight, freedom, and a childhood foregone, in the midst of a machine-dominated world.
- The Great Depression in the US and Its Causes It was believed at the time that even if a person failed to pay back their loan, the seizure of assets to cover the cost of the loan in the form of stocks would have […]
- Women’s Rights in the Great Depression Period The pursuit of the workplace equality and the protection of women from unfair treatment by the employers were quite unsuccessful and slow due to the major division in the opinions.
- Great Depression – American History However, though the thicket of sarcasm and irony, one can see despair and disbelief in the power of art, as well as the doubt if art can actually be produced under the name of Hollywood: […]
- The Great Depression and the New Deal Phenomenon With time, due to the highly unequal distribution of income, as well as to the depression in farming regions, the buying capacity of Americans decreased significantly; this led to the inability to purchase the goods […]
- Gardens Role in Great Depression Although the main causes of the great depression are still vague and contentious to date, the overall outcome was unexpected and resulted in the universal loss of trust in the economic future.
- The Great Depression in Amercia Form the war in Japan to the Vietnamese war, and many other political modifications, these changes destined to cross over into the 1970s and 1980s.
- Roosevelt’s Plan to End the Great Depression When he assumed the presidency in 1932, Franklin acknowledged the challenges of the nation, and also the way to get them out of the great depression.
- Lessons From the Great Depression and Postwar Global Economy: A Critical Analysis The economic slump that hit industrialized economies of the world, starting in the U.S.and later spreading to Europe, began in earnest in 1929 and lasted until about 1941, making it the longest and most ruthless […]
- Franklin D. Roosevelt’s Plans to End the Great Depression in His Presidency President Franklin Roosevelt rose to power at the time when the U.S.was facing hardships in the economy with the great depression badly affecting the economic activities of the country.
- Franklin Delano Roosevelt’s Plans to Combat the Great Depression He came to power in 1933 when the United States was in the middle of the Great Depression, and left in 1945 when the world, including the USA, was grappling with the effects of the […]
- US’s Economic Recovery in the Aftermath of the Great Depression The efforts to US’s economic recovery in the aftermath of the Great Depression of the 1930s sparked a series of economic programs under an umbrella name, the ‘New Deal.’ The mission of the ‘New Deal’ […]
- Causes of Great Depression: Canada Great Depression Causes of great depression The fundamental causes of great depression in Canada were the decline in the spending. Crash in the stock market in the United State and Canada contributed to the great depression.
- Is the U.S. Headed Towards the Second Great Depression? This is one of the indicators economists observe to foresee the possibility of the economy diving in to a recession, or is already on the way to recession.
- Repercussion of Great Depression The US mortgage crisis that was the genesis of the financial crisis is blamed on the laxity of law enforcers or failure of the laws that have governed the financial market in the US.
- Why the Great Depression Occurred – a Public Budgeting Stand Point As observed by Romer, “the great depression took place in the late 1920s to the late 1930s and was the longest and most severe depression ever experienced in the industrialized Western world”.
- The Great Depression: A Diary The book covers very little on the normal lifestyle of the people in Youngstown before the crisis; all that it documents are the hardships that describe Ohio as a hopeless place to live.
- The Great Depression’ Influence on the World His book looks at the factors that have caused and prolonged the issues that have deprived many people of jobs and ability to come out of the atrocious conditions.
- In the Eye of the Great Depression It led to the formation of groupings in society due to their similarities in their plight to restore dignity and compassion to their lives.
- Causes of the Great Depression This was due to a prediction of the end of rise in the stock market thus; there was a nationwide stampede to unload the stocks.
- The Great Depression and the New Deal The Great Depression of 1929-40s refers to the collapse of the world economy. For instance, a democrat entitled as Glass believed in the dominance of the white, budget devoid of deficits, the statutory rights, as […]
- Monetary and Fiscal Policy during the Great Depression An expansionary monetary policy is any action by the Fed that results in an increase to the total output or aggregate demand in an economy.
- Economic Depression in USA The Depression of 1873-1879 This depression was as a result of the bankruptcy of the railroad investment firm of Jay Cooke and company and particularly the restrictive monetary policy of the federal government; this is […]
- The Actual Causes of the Great Depression In the period between the end of First World War and the onset of the great depression, United States enjoyed relatively stable economic conditions under the leadership of a string of republican presidents.
- Government Policy Interventions and the Great Depression Monetary policy is the process where the government intervenes by administering and controlling the amount of money in the economy using the Central Bank in many countries and the Federal Reserve in the United States.
- Problem of USA Exposed by the Great Depression The recession was triggered by various fiscal features such as the vast margin between the poor and the wealthy, government debts and surplus production of commodities only to mention a few.
- The Great Depression Effects on American Economy The main problem behind the stated Great Depression experienced in the United States in 1929 was the mismatch between the consuming capacity of the population of the United States and the production capacity of the […]
- Great Depression as a Worldwide Economic Decline Many people ceased to buy products leading to low production of the products. This led to lose of market for American industries and led to trade disagreements among nations.
- The Great Depression Crisis Other causes that led to a reduction in aggregate demand followed throughout the depression period and the effects were transmitted from the United States which was in essence the ‘epicenter’ of the depression to the […]
- The Great Depression in Latin America Leaders in Latin America acknowledged the need to change economic policies and promoted the discarding of the free-market model in favor of import substitution.
- The Causal-Effect Connection of the Great Depression According to majority of the authors and scholars, The Great Depression is the worst economic downturn in the history of the United States of America.
- The Three Main Causes of Great Depression This paper sheds light on the causes that led to the great depression in America According to Bordo and White, the great depression begun in 1929 and many people suffered because all the businesses had […]
- Did Bank Distress Stifle Innovation During the Great Depression?
- How Does “The Cinderella Man” Depict Life During the Great Depression?
- Could the FED Have Prevented the Great Depression?
- How Did the Great Depression Affect a Generation?
- Did American Welfare Capitalists Breach Their Implicit Contracts During the Great Depression?
- How Does the Great Depression Affect the World Economy?
- Could the Great Depression Be Describes a Time of Desperation?
- How Did the Great Depression Pave the Road for Hitler?
- Did France Cause the Great Depression?
- How Did Demographics Cause the Great Depression?
- Did Hayek and Robbins Deepen the Great Depression?
- How Did Black People Face the Great Depression Differently?
- Did International Economic Forces Cause the Great Depression?
- How Did Governments Deal With Problems Caused by the Great Depression?
- Did Korekiyo Takahashi Rescue Japan From the Great Depression?
- How Did Great Britain, France, and the United States Respond to the Great Depression?
- Did Monetary Forces Cause the Great Depression?
- How Did the Great Depression Completely Destroy America?
- Did Sunspot Forces Cause the Great Depression?
- How Did WWII End the Great Depression?
- Did Technology Shocks Drive the Great Depression?
- How Does the Current Global Economic Recession Compare to the Great Depression?
- Did the Canadian Government Do Enough During the Great Depression?
- How Franklin Delano Roosevelt Handled the Great Depression in the U.S.?
- Did the Commercial Paper Funding Facility Prevent a Great Depression Style Money Market Meltdown?
- How Great Was the Great Depression?
- Did the Great Depression Affect Educational Attainment in the US?
- How Has Homelessness Changed Since the Great Depression?
- Did the New Deal Prolong or Worsen the Great Depression?
- How Did Income Inequality Lead to the Great Depression?
- The Agricultural Crisis During the Great Depression
- Government Relief Programs of the Depression Era
- How the Great Depression Impacted Minority Communities
- The Political Consequences of the Stock Market Crash
- Hoover vs. Roosevelt’s Approaches to Economic Recovery
- The Psychological Effects of the Great Depression on People and Families
- The Role of Government in Economic Recovery during the Great Depression
- The Legacy of Labor Unions and Workers’ Rights of the Depression Era
- Gender Roles, Employment, and Social Changes During the Depression Era
- The Legacy of the Great Depression as Seen in the Modern Economic Policy
- Economic Topics
- Cold War Topics
- Private Equity Research Ideas
- Social Democracy Essay Titles
- International Politics Questions
- Macroeconomics Topics
- American Revolution Topics
- Franklin Roosevelt Questions
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 27). 124 Great Depression Topics to Write about & Examples. https://ivypanda.com/essays/topic/great-depression-essay-examples/
"124 Great Depression Topics to Write about & Examples." IvyPanda , 27 Feb. 2024, ivypanda.com/essays/topic/great-depression-essay-examples/.
IvyPanda . (2024) '124 Great Depression Topics to Write about & Examples'. 27 February.
IvyPanda . 2024. "124 Great Depression Topics to Write about & Examples." February 27, 2024. https://ivypanda.com/essays/topic/great-depression-essay-examples/.
1. IvyPanda . "124 Great Depression Topics to Write about & Examples." February 27, 2024. https://ivypanda.com/essays/topic/great-depression-essay-examples/.
Bibliography
IvyPanda . "124 Great Depression Topics to Write about & Examples." February 27, 2024. https://ivypanda.com/essays/topic/great-depression-essay-examples/.
- Warning Signs and Symptoms
- Mental Health Conditions
- Common with Mental Illness
- Mental Health By the Numbers
- Individuals with Mental Illness
- Family Members and Caregivers
- Kids, Teens and Young Adults
- Maternal & New Parent Mental Health
- Veterans & Active Duty
- Identity and Cultural Dimensions
- Frontline Professionals
- Mental Health Education
- Support Groups
- NAMI HelpLine
- Publications & Reports
- Podcasts and Webinars
- Video Resource Library
- Justice Library
- Find Your Local NAMI
- Find a NAMIWalks
- Attend the NAMI National Convention
- Fundraise Your Way
- Create a Memorial Fundraiser
- Pledge to Be StigmaFree
- Awareness Events
- Share Your Story
- Partner with Us
- Advocate for Change
- Policy Priorities
- NAMI Advocacy Actions
- Policy Platform
- Crisis Intervention
- State Fact Sheets
- Public Policy Reports
- About Mental Illness
Depressive disorder, frequently referred to simply as depression, is more than just feeling sad or going through a rough patch. It’s a serious mental health condition that requires understanding and medical care. Left untreated, depression can be devastating for those who have it and their families. Fortunately, with early detection, diagnosis and a treatment plan consisting of medication, psychotherapy and healthy lifestyle choices, many people can and do get better.
Some will only experience one depressive episode in a lifetime, but for most, depressive disorder recurs. Without treatment, episodes may last a few months to several years.
About 21 million U.S. adults— 8.4% of the population—had at least one major depressive episode in 2020. People of all ages and all racial, ethnic and socioeconomic backgrounds experience depression, but it does affect some groups more than others.
Personal Perspectives On Major Depressive Disorder
In this 2-part podcast series, NAMI Chief Medical Officer Dr. Ken Duckworth guides discussions on major depressive disorder that offer insights from individuals, family members and mental health professionals. Read the transcript . Note: Content includes discussions on topics such as suicide attempts and may be triggering.
Depression can present different symptoms, depending on the person. But for most people, depressive disorder changes how they function day-to-day, and typically for more than two weeks. Common symptoms include:
- Changes in sleep
- Changes in appetite
- Lack of concentration
- Loss of energy
- Lack of interest in activities
- Hopelessness or guilty thoughts
- Changes in movement (less activity or agitation)
- Physical aches and pains
- Suicidal thoughts
Depression does not have a single cause. It can be triggered by a life crisis, physical illness or something else—but it can also occur spontaneously. Scientists believe several factors can contribute to depression:
- Trauma . When people experience trauma at an early age, it can cause long-term changes in how their brains respond to fear and stress. These changes may lead to depression.
- Genetics . Mood disorders, such as depression, tend to run in families.
- Life circumstances . Marital status, relationship changes, financial standing and where a person lives influence whether a person develops depression.
- Brain changes . Imaging studies have shown that the frontal lobe of the brain becomes less active when a person is depressed. Depression is also associated with changes in how the pituitary gland and hypothalamus respond to hormone stimulation.
- Other medical conditions . People who have a history of sleep disturbances, medical illness, chronic pain, anxiety and attention-deficit hyperactivity disorder (ADHD) are more likely to develop depression. Some medical syndromes (like hypothyroidism) can mimic depressive disorder. Some medications can also cause symptoms of depression.
- Drug and alcohol misuse . Adults with a substance use disorder are at significantly higher risk for experiencing a major depressive episode. Co-occurring disorders require coordinated treatment for both conditions, as alcohol can worsen depressive symptoms.
To be diagnosed with depressive disorder, a person must have experienced a depressive episode lasting longer than two weeks. The symptoms of a depressive episode include:
- Loss of interest or loss of pleasure in all activities
- Change in appetite or weight
- Sleep disturbances
- Feeling agitated or feeling slowed down
- Feelings of low self-worth, guilt or shortcomings
- Difficulty concentrating or making decisions
- Suicidal thoughts or intentions
Although depressive disorder can be a devastating illness, it often responds to treatment. The key is to get a specific evaluation and treatment plan. Safety planning is important for individuals who have suicidal thoughts. After an assessment rules out medical and other possible causes, a patient-centered treatment plans can include any or a combination of the following:
- Psychotherapy including cognitive behavioral therapy, family-focused therapy and interpersonal therapy.
- Medications including antidepressants, mood stabilizers and antipsychotic medications.
- Exercise can help with prevention and mild-to-moderate symptoms.
- Brain stimulation therapies can be tried if psychotherapy and/or medication are not effective. These include electroconvulsive therapy (ECT) for depressive disorder with psychosis or repetitive transcranial magnetic stimulation (rTMS) for severe depression.
- Light therapy , which uses a light box to expose a person to full spectrum light in an effort to regulate the hormone melatonin.
- Alternative approaches including acupuncture, meditation, faith and nutrition can be part of a comprehensive treatment plan.
Reviewed August 2017
Many treatment options are available for depression, but how well treatment works depends on the type of depression and its severity. For most people, psychotherapy and medications give better results together than either alone, but this is something to review with your mental health care provider.
Psychotherapy
Psychotherapy (or talk therapy) has an excellent track record of helping people with depressive disorder. While some psychotherapies have been researched more than others, many types can be helpful and effective. A good relationship with a therapist can help improve outcomes.
Many clinicians are trained in more than one kind of psychotherapy, so ask your clinician what kind of psychotherapy they practice and how it can help you. A few examples include:
- Cognitive behavioral therapy (CBT) has a strong research base to show it helps with symptoms of depression. This therapy helps assess and change negative thinking patterns associated with depression. The goal of this structured therapy is to recognize negative thoughts and to teach coping strategies. CBT is often time-limited and may be limited to 8–16 sessions in some instances.
- Interpersonal therapy (IPT) focuses on improving problems in personal relationships and other changes in life that may be contributing to depressive disorder. Therapists teach individuals to evaluate their interactions and to improve how they relate to others. IPT is often time-limited like CBT.
- Psychodynamic therapy is a therapeutic approach rooted in recognizing and understanding negative patterns of behavior and feelings that are rooted in past experiences and working to resolve them. Looking at a person’s unconscious processes is another component of this psychotherapy. It can be done in short-term or longer-term modes.
Psychoeducation And Support Groups
Psychoeducation involves teaching individuals about their illness, how to treat it and how to recognize signs of relapse. Family psychoeducation is also helpful for family members who want to understand what their loved one is experiencing.
Support groups, meanwhile, provide participants an opportunity to share experiences and coping strategies. Support groups may be for the person with the mental health condition, for family/friends or a combination of both. Mental health professionals lead some support groups, but groups can also be peer-led.
Explore NAMI’s nationwide offerings of free educational programs and support groups that provide outstanding education, skills training and support.
Medications
For some people, antidepressant medications may help reduce or control symptoms. Antidepressants often take 2-4 weeks to begin having an effect and up to 12 weeks to reach full effect. Most people will have to try various doses or medications to find what works for them. Here are some antidepressants commonly used to treat depression:
Selective serotonin reuptake inhibitors (SSRIs) act on serotonin, a brain chemical. They are the most common medications prescribed for depression.
- Fluoxetine (Prozac)
- Sertraline (Zoloft)
- Paroxetine (Paxil)
- Citalopram (Celexa)
- Escitalopram (Lexapro)
Serotonin and norepinephrine reuptake inhibitors (SNRIs) are the second most common antidepressants. These medications increase serotonin and norepinephrine.
- Venlafaxine (Effexor)
- Desvenlafazine (Pristiq)
- Duloxetine (Cymbalta)
Norepinephrine-dopamine reuptake inhibitors (NDRIs) increase dopamine and norepinephrine. Bupropion (Wellbutrin) is a popular NDRI medication, which causes fewer (and different) side effects than other antidepressants. For some people, bupropion causes anxiety symptoms, but for others it is an effective treatment for anxiety.
Mirtazapine (Remeron) targets specific serotonin and norepinephrine receptors in the brain, thus indirectly increasing the activity of several brain circuits. Mirtazapine is used less often than newer antidepressants (SSRIs, SNRIs and bupropion) because it is associated with more weight gain, sedation and sleepiness. However, it appears to be less likely to result in insomnia, sexual side effects and nausea than the SSRIs and SNRIs.
- Bupropion (Wellbutrin)
- Mirtazapine (Remeron)
Second-generation antipsychotics (SGAs) , or “atypical antipsychotics,” treat schizophrenia, acute mania, bipolar disorder and bipolar mania and other mental illnesses. SGAs can be used for treatment-resistant depression.
- Aripiprazole (Abilify)
- Quetiapine (Seroquel)
Tricyclic antidepressants (TCAs) are older medications, seldom used today as initial treatment for depression. They work similarly to SNRIs but have more side effects. They are sometimes used when other antidepressants have not worked. TCAs may also ease chronic pain.
- Amitriptyline (Elavil)
- Desipramine (Norpramin)
- Doxepin (Sinequan)
- Imipramine (Tofranil)
- Nortriptyline (Pamelor, Avantyl)
- Protriptyline (Vivactil)
Monoamine oxidase inhibitors (MAOIs) are less used today because newer, more effective medications with fewer side effects have been found. These medications can never be used in combination with SSRIs. MAOIs can sometimes be effective for people who do not respond to other medications.
- Phenelzine (Nardil)
- Isocarboxazid (Marplan)
- Tranylcypromine Sulfate (Parnate)
- Selegiline patch (Emsam)
Brain Stimulation Therapies
For some, brain stimulation therapies may be effective, typically after other treatments have not been effective.
- Electroconvulsive Therapy (ECT) involves transmitting short electrical impulses into the brain. ECT does cause some side effects, including memory loss. Individuals should understand the risks and benefits of this intervention before beginning a treatment trial.
- Repetitive Transcranial Magnetic Stimulation (rTMS) is a relatively new type of brain stimulation that uses a magnet instead of an electrical current to activate the brain. It is not effective as a maintenance treatment.
- Vagus Nerve Stimulation (VNS) has a complex history. For a fuller understanding of this treatment, read the NIMH summary of this and other brain stimulation interventions.
Complementary And Alternative Medicine (CAM)
Relying solely on CAM methods is not enough to treat depression, but they may be useful when combined with psychotherapy and medication. Discuss your ideas of CAM interventions with your health care professional to be sure they will not cause side effects or adverse reactions.
The National Center for Complementary and Integrative Health reviews research on complementary treatments. You can search for each intervention on their website .
- Exercise. Studies show that aerobic exercise can help treat mild depression because it increases endorphins and stimulates norepinephrine, which can improve a person’s mood.
- Folate . Some studies have shown that when people with depression lack folate (also called folic acid or vitamin B9), they may not be receiving the full benefit from any antidepressants they may be taking. Studies suggest that in some situations taking L-methylfolate (an active form of folate) can be an additional treatment with other psychiatric medications.
- St John’s Wort. This supplement has similar chemical properties to some SSRIs. Risks of combining St John’s Wort with SSRIs and other medications are well-known and substantial.
Experimental Treatments
These following treatments are not FDA-approved but are being researched:
- Ketamine. Ketamine, which may offer a new model in treating depression, may have potentially quick and short-term impact on depression and suicidal thoughts. Ketamine is an anesthetic with a street value (special K) that has not been studied for long-term use. It can make psychosis worse and is not an ideal choice for people with substance use disorders.
- Deep Brain Stimulation . This treatment has been used to treat Parkinson’s disease. See the NIMH page on brain stimulation for more information .
- I Think I Might Be Gay
Coping with depression isn’t easy, but if you, a family member or a friend is struggling, there is help. NAMI is there to provide support and resources for you and your family.
Helping Yourself
Leading a balanced lifestyle can help you manage symptoms of depression. Here are some suggestions from people who have lived experience with depression:
Learn all you can . Learn about the many treatment options available. Connect with other people experiencing depression in support groups or meetings. Attend local conferences and conventions. Build a personal library of useful websites and helpful books.
Recognize early symptoms . Identify possible warning signs and triggers that may aggravate your depression symptoms. With this knowledge, you can recognize an emerging episode and get the help you need as soon as possible. Don’t be afraid to ask your friends and family for help—they can help you monitor your symptoms and behavior.
Partner with your health care providers . Give your health care provider all the information he or she needs to help you recover—including any reactions to medications, your symptoms or any triggers you notice. Develop trust and communicate openly.
Know what to do in a crisis . Be familiar with your community’s crisis hotline or emergency walk-in center. Know how to contact them and keep the information handy.
Find emotional support from others who experience depression . Share your story , thoughts, fears and questions with other people who have the same condition. Connect through online message boards or peer-education programs like NAMI Peer-to-Peer or support groups like NAMI Connection .
Avoid drugs and alcohol . These substances can disturb emotional balance and interact with medications. You may think using alcohol or drugs will help you feel better, but using them can hinder your recovery or make symptoms worse.
Get physically healthy . Eat well and exercise. To relieve stress, try activities like meditation, yoga or Tai Chi.
Helping A Family Member Or Friend
When someone you love and care about experiences the symptoms of mental illness, you face unique challenges yourself, including complex family dynamics, social isolation and often unpredictable behavior. Getting support for yourself is essential for you to be able to be helpful for the person you care about.
Learn more about your loved one’s condition . Learning about the condition your loved one experiences will help you better understand and support them. Read personal accounts of lived experience, full of tips and advice on the NAMI Blog :
- Depression is an Illness, Not a Weakness
- Living with Depression: How to Keep Working
Recognize early symptoms . Depression often has warning signs, such as a low mood, feeling fatigued or having trouble sleeping. Discuss your friend or family member’s past episodes with them to help them improve their ability to recognize the signs early.
Communicate . Speak honestly and kindly . Don’t scold or blame people with depression or urge them to “try harder” to “just be happy.” Instead, make specific offers of help and follow through with those offers. Tell the person you care about them. Ask them how they feel and truly listen.
React calmly and rationally . Even if your family member or friend is in a crisis, it’s important to remain calm. Listen to their concerns and make them feel understood—then take the next step toward getting help.
Find emotional support from others . Share your thoughts, fears and questions with other people who have loved ones with similar conditions. Connect with others through online message boards or NAMI peer-education programs .

Know the warning signs of mental illness

Learn more about common mental health conditions
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264 , text “helpline” to 62640 , or chat online. In a crisis, call or text 988 (24/7).
- Student Program
- Sign Up for Free

How to Create a Survey
42 questions to ask in a depression survey
According to the Anxiety & Depression Association of America (ADAA) , 264 million people across the globe live with depression, yet many adults who experience this condition don’t receive treatment. Depression isn’t just a feeling of sadness, it’s a medical condition that can be treated successfully with interventions like psychotherapy, medication, and other modalities.
A depression screening survey is often the first step in identifying and assessing common symptoms of depression and determining the best treatment options. There are two main types of screening survey: self-rated and observer- or clinician-rated. These surveys can be used separately or in tandem.
In this article, we’ll explain what a depression survey is and how it’s used, share 42 depression survey question examples, and discuss how to use Jotform to create an online depression survey.
A brief overview of depression surveys and how clinicians use them
A depression survey is a self-administered or clinician-administered test that helps screen for depression symptoms. Depression survey questions gather information about a patient’s appetite, energy levels, sleep, mood, concentration, weight fluctuations, interest in daily activities, and other factors that contribute to overall mental health.
Clinicians use this screening method to help diagnose depression, understand its severity, and determine the type of depression a patient may have, but it does not, on its own, diagnose depression. Once a patient completes a depression survey, a healthcare provider will assess the responses and advise on next steps, including further evaluation or a possible treatment plan.
It’s important to keep in mind that while a self-rated test can help a person determine if they need to seek further guidance about their condition, the ratings from either a self-administered or a clinician- or observer-administered test on their own don’t constitute a clinical diagnosis made in consultation with a mental health professional.
42 depression survey question examples
A healthcare provider can ask a patient to answer depression survey questions, in which case they’re referred to as observer-rated or clinician-rated questions. An individual can administer a depression survey themselves; the questions in this type of survey are known as self-reported questions.
Initial observer- or clinician-rated depression survey questions
Healthcare providers often use the following two questions at the outset of an evaluation to determine whether to ask additional questions:
- During the past month, have you been bothered by feeling down, depressed, or hopeless?
- During the past month, have you been bothered by little interest or pleasure in doing things?
Follow-up observer-rated or clinician-rated depression survey questions
The following 16 assessments are based on the Hamilton Depression Rating Scale (HAM-D) ,available in the public domain. A healthcare professional should administer these questions. They’re related to the presence of symptoms, as well as their frequency or severity.
Depressed mood
(Gloomy attitude, pessimism about the future, feeling of sadness, tendency to weep)
1 = Sadness, etc.
2 = Occasional weeping
3 = Frequent weeping
4 = Extreme symptoms
Feelings of guilt
1 = Self-reproach, feels he/she has let people down
2 = Ideas of guilt
3 = Present illness is a punishment; delusions of guilt
4 = Hallucinations of guilt
1 = Feels life is not worth living
2 = Wishes he/she were dead
3 = Suicidal ideas or gestures
4 = Attempts at suicide
Insomnia — initial
(Difficulty in falling asleep)
1 = Occasional
2 = Frequent
Insomnia — middle (complaints of being restless and disturbed during the night; waking during the night)
Insomnia — delayed (waking in early hours of the morning and being unable to fall asleep again)
Work and interests
0 = No difficulty
1 = Feelings of incapacity, listlessness, indecision, and vacillation
2 = Loss of interest in hobbies, decreased social activities
3 = Productivity decreased
4 = Unable to work. Stopped working because of present illness only. (Absence from work after treatment or recovery may rate a lower score.)
Agitation (restlessness associated with anxiety)
Anxiety — psychic
1 = Tension and irritability
2 = Worrying about minor matters
3 = Apprehensive attitude
Anxiety — somatic (gastrointestinal issues, digestion problems, cardiovascular issues, palpitations, headaches, respiratory issues, genito-urinary problems, etc.)
2 = Moderate
4 = Incapacitating
Somatic symptoms — gastrointestinal (loss of appetite, heavy feeling in abdomen, constipation)
Somatic symptoms — general (heaviness in limbs, back, or head; diffuse backache; loss of energy and fatigability)
Genital symptoms (loss of libido, menstrual disturbances)
Hypochondriasis
0 = Not present
1 = Self-absorption (bodily)
2 = Preoccupation with health
3 = Querulous attitude
4 = Hypochondriacal delusions
Weight loss
0 = No weight loss
2 = Obvious or severe
Insight (Insight must be interpreted in terms of the patient’s understanding and background.)
0 = No loss
1 = Partial or doubtful loss
2 = Loss of insight
Self-reported depression survey questions
The following 10 questions are based on the Patient Health Questionnaire (PHQ-9) , which is available in the public domain. Individuals can administer it themselves, or healthcare professionals can use it.
In the past few weeks, how often have you experienced the following:
Little interest or pleasure in doing things
- Several days
- More than half of the days
- Nearly every day
Feeling down, depressed, or hopeless
Trouble falling or staying asleep or sleeping too much
Feeling tired or having little energy
Poor appetite or overeating
- More than half the days
Feeling bad about yourself or that you are a failure or have let yourself or your family down
Trouble concentrating on things, such as reading the newspaper or watching television
Moving or speaking so slowly that other people could have noticed
Thoughts that you would be better off dead or of hurting yourself
If you’ve had any days with the issues above, how difficult have these problems made it for you at work, home, school, or with other people?
- Not difficult at all
- Somewhat difficult
- Very difficult
- Extremely difficult
Additional self-administered depression survey questions
The following 14 questions come from the Beck Depression Inventory (BDI) which includes self-reported items in a multiple-choice format.
Please select the response that best describes how you’ve been feeling during the past two weeks:
- I don’t feel sad.
- I feel sad.
- I’m sad all the time and can’t snap out of it.
- I’m so sad and unhappy that I can’t stand it.
- I’m not particularly discouraged about the future.
- I feel discouraged about the future.
- I feel I have nothing to look forward to.
- I feel the future is hopeless and that things can’t improve.
Past failure
- I don’t feel like a failure.
- I feel I have failed more than the average person.
- As I look back on my life, all I can see is a lot of failures.
- I feel I’m a complete failure as a person.
Loss of pleasure
- I get as much satisfaction out of things as I used to.
- I don’t enjoy things the way I used to.
- I don’t get real satisfaction out of anything anymore.
- I’m dissatisfied or bored with everything.
- I don’t feel particularly guilty.
- I feel guilty a good part of the time.
- I feel quite guilty most of the time.
- I feel guilty all of the time.
Self-regard
- I don’t feel disappointed in myself.
- I’m disappointed in myself.
- I’m disgusted with myself.
- I hate myself.
Self-criticism
- I don’t feel I’m any worse than anybody else.
- I’m critical of myself for my weaknesses or mistakes.
- I blame myself all the time for my faults.
- I blame myself for everything bad that happens.
- I don’t cry any more than usual.
- I cry more now than I used to.
- I cry all the time now.
- I used to be able to cry, but now I can’t cry even though I want to.
Irritation level
- I’m no more irritated by things than I ever was.
- I’m slightly more irritated now than usual.
- I’m quite annoyed or irritated much of the time.
- I feel irritated all the time.
Interest in others
- I haven’t lost interest in other people.
- I’m less interested in other people than I used to be.
- I’ve lost most of my interest in other people.
- I’ve lost all of my interest in other people.
Decisiveness
- I make decisions about as well as I ever could.
- I put off making decisions more than I used to.
- I have greater difficulty with making decisions now than I used to.
- I can’t make decisions at all anymore.
- I don’t feel that I look any worse than I used to.
- I’m worried that I look old or unattractive.
- I feel there are permanent changes in my appearance that make me look unattractive.
- I believe that I look ugly.
- I can work about as well as before.
- It takes an extra effort to get started at doing something.
- I have to push myself very hard to do anything.
- I can’t do any work at all.
Health concerns
- I’m no more worried about my health than usual.
- I’m worried about physical problems like aches, pains, upset stomach, or constipation.
- I’m very worried about physical problems, and it’s hard to think of much else.
- I’m so worried about my physical problems that I can’t think of anything else.
Again, it’s important to remember that a depression rating on its own is not a formal diagnosis, but rather an indication that an individual may have some of the symptoms of depression. While a self-reported depression assessment can be useful for determining whether someone should seek professional help, only a qualified mental health practitioner can diagnose depression and other mental health conditions.
Tips for creating an online depression survey with Jotform
Creating an online depression survey is simple with Jotform. You can use this depression assessment template or this depression screening survey to screen patients online for depression. Jotform’s drag-and-drop functionality makes it easy to customize your survey to fit your needs. You can add different types of survey questions, set up conditional logic, and integrate your survey with over 100 apps, like Google Drive, Dropbox, or Airtable.
You can also create a form from scratch using different question types to collect the exact data you need. Jotform question types include open-ended , closed-ended , single-choice, multiple-choice , short text, long text, yes/no , ranking questions, demographic questions , and many more.
Filling out these surveys is also easy for patients, as they’re accessible on any device. You can easily track form submissions in Jotform Tables , which allows you to collect, organize, and manage data in an all-in-one workspace. Plus, you can share the submissions in one click for seamless collaboration or you can send them to a psychiatrist or clinician to sign off on via Jotform Approvals .
When you need to review and assess survey responses, you can use our free Form Calculation widget to measure numerical answers. Simply choose the fields you’d like to add, subtract, multiply, or divide, and the widget will automatically perform the calculation and display the result.
Photo by Timur Weber
Thank you for helping improve the Jotform Blog. 🎉

RECOMMENDED ARTICLES

14 best SurveyMonkey alternatives in 2024

How to add a signature in SurveyMonkey

How to make Google Forms anonymous

14 political survey questions to gauge public opinion

How to ask someone to take a survey via email

Basic product survey questions to ask customers

How to automate survey follow-up emails

16 best survey tools worth checking out

How to create an NPS® survey email that gets results

What are ambiguous survey questions, and how do you avoid asking them?

How to write a survey report

20 business survey questions to ask your customers

Survey data collection: 5 best practices

15 of the best Refiner.io alternatives in 2024

How to create a survey in Google Forms
6 best survey tools for research

What you need to know about SurveyMonkey pricing

How to improve survey accuracy

Top 20 team collaboration survey questions

How to embed a survey in a website

How many questions to include in an online survey

SurveyMonkey vs SurveySparrow

The 6 best customer satisfaction survey tools
8 of the best WordPress survey plug-ins

25 post-training survey questions to ask employees

4 survey design tips to get more accurate results

How to turn survey results into a great presentation

5 UX survey tools to help you create a winning user experience

Top survey questions to ask kids

10 of the best StrawPoll alternatives

80 survey question examples and when to use them

How to analyze survey data

Pre-sales surveys: How to focus on your best leads
How to create an employee pulse survey

How to close a survey on SurveyMonkey

30 insightful hotel survey questions

8 leading Survicate alternatives for customer feedback in 2024

20 psychology survey questions to ask your clients

How to add a popup survey on your website

How to write a survey reminder email

How to use a survey dashboard effectively

The 3 best Checkbox Survey alternatives

What is the smiley face rating scale?

One question at a time: The best strategy for a survey

20 essential human resources (HR) survey questions

Social media survey questions: Examples and best practices

5 types of questionnaires

4 types of survey questions to engage your audience

What is a survey?

Top podcast survey questions to ask guests and listeners

Best training survey questions to evaluate effectiveness

20 religion survey questions to ask your church community

Survey report examples with informative visuals

6 EmailMeForm alternatives to build powerful surveys in 2024

A Guide to Creating the Perfect Survey Form

Top 7 KwikSurveys alternatives in 2024

What is a good Net Promoter Score® (NPS®)?

Types of survey bias and ways to avoid them

5 tips for creating great qualitative surveys
How to send Mailchimp surveys easily

How to set up and send a Constant Contact survey

65+ e-commerce survey questions for valuable business insights
Announcing Jotform’s free Student Survey Program

Top diversity and inclusion questions to ask employees

Webinar: How to use surveys and email marketing to gain key insights

Exit survey questions to ask your former employees

Top 21 brand survey questions

How to send surveys: 7 survey distribution methods

How to create an anonymous survey for employees

How to write unbiased survey questions

9 examples of ranking survey questions

Survey vs questionnaire: Which one should you use for your next project?

How to write a research question

50 mental health survey questions to ask employees

11 top survey incentive ideas

How to write good survey questions

Top 3 Key Survey alternatives in 2024

What is a good survey response rate?

10 AidaForm alternatives that make data collection a breeze in 2024

How to create a survey in Microsoft Word

10 questions to ask in your membership survey

CRM survey benefits, best practices, and example questions

How to ask someone to fill out a survey

SurveyMonkey vs Alchemer (Formerly SurveyGizmo)

Offline surveys: How to collect data anywhere

Qualtrics vs SurveyMonkey: Which should you choose?

How to use open-ended survey questions

How to calculate the Net Promoter Score® (NPS®)

7 important user experience survey questions you should ask
How to embed a survey in an email

How to increase survey response rate

How to create a survey on Facebook
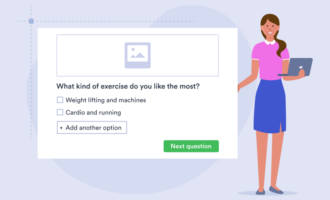
The 5 most powerful Bucket.io alternatives for 2024

12 employee-of-the-month survey questions you should ask

How to collect secure survey data

Top 6 QuestionPro alternatives in 2024

Ordinal Scale Questions: Definition and Examples

How to create an inviting welcome screen for online forms

Top 14 demographic survey questions to ask
Send Comment :
Why we don't exercise
We know that moving our bodies is good for us. So what keeps us from doing it?
For the better part of a year in 2017, I could barely will myself to leave my house. I was experiencing a prolonged depressive episode with daily, sometimes hourly, panic attacks, and I couldn't see the point in continuing on.
Many things helped me survive. Talking it through in therapy several times a week was like opening a pressure valve in my brain — it kept me functioning just enough to get by. Medication had mixed results — I felt less panicky, but also less joy, excitement, and other essential emotions. Crying to friends provided temporary catharsis. But it wasn't until I discovered Muay Thai, a form of kickboxing , that it felt as if day-to-day life might provide something other than hopelessness.
Every other form of healing I'd tried had focused my mind — its disordered thoughts and supposed chemical imbalances. What I hadn't tried was getting out of it altogether. When firm but well-meaning coaches yelled at me to fix my form, do five more pushups, and kick the bag until my shins were red and nearly bleeding, it jump-started my nervous system. It made me feel human again.
It's a trope to say you should not tell a depressed person to go outside, take a walk, or go for a run. Doing so would dismiss the severity and reality of their illness, like telling someone with a broken arm to go play catch. To some extent, this is true: It's probably not the best idea to tell someone struggling deeply with mental illness to simply suck it up and walk it off. But it's also true that when someone encouraged me to get out there and use my body, it was precisely what I needed at my lowest moment. I ended up at the gym only because my friends repeatedly encouraged me to come with them to a class until one day I finally did. It wasn't a cure-all, but it made me believe that a solution might exist.
Many of our collective crises — depression , anxiety , unhealthiness, and loneliness — are made worse by the same thing: our tendency toward a sedentary, shut-in lifestyle . We live in a society that makes it extremely difficult to find the time and space to be active. An abundance of research shows that exercise is good for depression , and yet most of the time when I hear people talk about the mental-health crisis — on TikTok, on X, and in real life — it is rarely mentioned. In my experience, it's much more common to hear people talk about finding the right diagnosis, the right medication, and the right kind of therapy than it is to see people encouraging their loved ones to get the heck outside.
Related stories
Many of us know exercise is good for us. All that's left is getting up off our asses.
The evidence is overwhelming that physical activity is good for both our bodies and our brains. A meta-review of studies that included 128,000 participants found that exercise of any kind significantly reduced symptoms of anxiety and depression . There are several theories as to why this is — exercise could increase the availability of neurotransmitters like dopamine in the brain, or it could help the brain form new neural pathways that are helpful to escaping cycles of depression. Either way, moving is good for our brains.
And the physical consequences of not moving enough are well-documented: heart disease, diabetes, high blood pressure, cancer, and a host of other maladies are linked to low physical activity. It is also bad for our mental health: A 2014 meta-analysis of more than 100,000 people found that increased sedentary time was positively correlated with rates of depression. A study from the beginning of COVID found that it was harder for people to stop being depressed if they spent too much time sitting.
Depression is a vicious cycle; it pits your brain against itself.
Despite the research, Americans have become less active over time. By one estimate, we're getting 27 fewer minutes of physical activity on average each day than we did 200 years ago. And for the past several decades, only about a quarter of American adults have met the recommended guidance of at least 20 minutes of exercise a day, according to the Centers for Disease Control and Prevention. One 2019 study found that we spent 82% of our time sedentary.
For kids, who need even more physical activity, the decline is stark. A 2022 Report Card on Physical Activity for Children and Youth gave the US a D- score, concluding that America, while never sufficiently supportive of physical activity, had become even worse at making the space and time for it. In 2007, an estimated 30% of adolescents completed the recommended 60 minutes of moderate-to-vigorous activity every day. By 2020 that number had fallen below 9%. Far fewer kids participate in team sports or walk or bike to school than did in the past, the report found. In Canada, as one study put it, pediatricians are so concerned about the decline in physical activity that they are encouraging parents to let kids engage in "thrilling and exciting forms of free play that involve uncertainty of outcome and a possibility of physical injury."
Instead of getting enough exercise, we're stuck lounging around on our phones. We've replaced real-world, bodily stimulation with mental stimulation from our screens. Meanwhile, our brains are rotting. In one study, nearly half of Americans ages 18 to 29 reported experiencing depression or anxiety in 2023. And over the past few decades, mental illness for teens and children has been on the rise.
Instead of looking at the situation and concluding that we all need to exercise more, some people are doing the opposite. Certain trends circulating social media emphasize not using your body: " hurkle-durkle ," aka "bed rotting," involves wrapping yourself in comfy clothes and bed linens and staying in bed way past the time you should be waking up. But while there is a time and place for doing nothing and relaxing, Americans aren't actually getting more rest. Much of the country is chronically underslept .
In this trend, I see the logic of depression — the sense that nothing can or will change so there's no point in trying. Much of America, it seems, has given up on trying to be active.
Over time, my year from hell faded from my mind. But eventually, my exercise routine went with it. I didn't need to work out to stay sane, I thought, and so I stopped committing to it. Then I moved away from the Muay Thai gym and completely fell out of the routine. After a few years, the depression caught up to me. It wasn't as catastrophic as before, more of a persistent ennui that was hard to shake. I tried to figure it out in therapy. I tried to intellectualize it. I tried to excuse it: There was no point in trying anything, life was just inherently bad, the political state of the world was scary, the outside world was too expensive. It wasn't working.
I've gotten to the point where exercise — being in my body, sweating — is more important to me than more mind-oriented forms of therapy.
Then one day, early in the pandemic when I was prone to languishing in my room for hours on end, a roommate suggested I come to the tennis court with them for an hour. I was immediately hooked. Playing tennis with friends several times a week wasn't just fun, and it didn't just help get me into shape — it became a main focal point of my life. It provided me with a new relationship to my body and mind. I'd forgotten that exercise, while not a cure for my mental illness, was a necessary precursor to my mental wellness. After years of intellectualizing my sadness and discomfort, I once again had something that got me into my body, got my endorphins going, and, most important, got me to stop thinking about anything other than where to place the ball on the other side of the court.
Depression is a vicious cycle; it pits your brain against itself. When I was at my worst, the usual advice of "don't tell a depressed person what to do" wasn't helpful to me because I needed someone to help me break that cycle by telling me to stop repeating the same patterns. What saved me was friends who helped me get out of the house, suggested I join the gym with them, or encouraged me to do anything to get me out of my head.
I still sometimes get depressed. I still struggle with mental health. But I now feel as if I have a reliable way to help myself out of it. I've gotten to the point where exercise — being in my body, sweating — is more important to me than more mind-oriented forms of therapy . It's not a magic cure, but I now see it as a fundamental baseline. If I'm not moving, nothing will help my sad state.
SSRI prescriptions continue to rise and more people are seeking therapy , but depression and anxiety rates remain sky-high. If you've tried nearly everything else, why not simply get moving?
P.E. Moskowitz runs Mental Hellth , a newsletter on psychology, psychiatry, and modern society. They are also the author of the forthcoming book Rabbit Hole, a combination of memoir and reportage about the role drugs play in our happiness.
About Discourse Stories
Through our Discourse journalism, Business Insider seeks to explore and illuminate the day’s most fascinating issues and ideas. Our writers provide thought-provoking perspectives, informed by analysis, reporting, and expertise. Read more Discourse stories here .

More from Health
Most popular
- Main content
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Psychedelic drug MDMA faces questions as FDA considers approval for PTSD
This photo provided by the Center for Psychedelic Therapy Research shows a Yehuda Lab MDMA-assisted therapy treatment room at the James J. Peters Department of Veterans Affairs Medical Center in the Bronx borough of New York. On Friday, May 31, 2024, the Food and Drug Administration posted its initial review of MDMA, the mind-altering club drug, as a treatment for PTSD. In their assessment, FDA scientists said that patients who received MDMA and talk therapy showed “rapid, clinically meaningful, durable improvements in their PTSD symptoms,.” But they also called the research “challenging to interpret,” and questioned how long the benefits might last. (OH Prema, Center for Psychedelic Therapy Research via AP)
- Copy Link copied
WASHINGTON (AP) — Federal health regulators are questioning the safety and evidence behind the first bid to use MDMA, the mind-altering club drug, as a treatment for PTSD, part of a decadeslong effort by advocates to move psychedelic drugs into the medical mainstream.
The Food and Drug Administration posted its initial review of the drug Friday, ahead of a meeting of outside advisers who could help decide whether MDMA — currently illegal under federal law — becomes the first drug of its kind to win U.S. approval as a medication.
In their assessment, FDA scientists said that patients who received MDMA and talk therapy showed “rapid, clinically meaningful, durable improvements in their PTSD symptoms.” But they also called the research “challenging to interpret,” and questioned how long the benefits might last.
They said it’s difficult to know how much of the improvement came from MDMA versus simply undergoing intensive therapy, and also raised several safety concerns, including MDMA’s heart risks and potential for abuse.
The outside experts will take a nonbinding vote on the drug’s overall benefits and risks during Tuesday’s meeting. The FDA will make the final decision, likely in August.
Antidepressants are now the only FDA-approved drugs for post-traumatic stress disorder, which is closely linked to depression, anxiety and suicidal thinking and is more prevalent among women and veterans.
If approved, MDMA would be reclassified as a prescription medicine and made available to specially certified doctors and therapists. Currently, the drug is in the same ultra-restrictive category as heroin and other substances the federal government deems prone to abuse and devoid of any medical use.
MDMA, also known as ecstasy or molly, is the first in a series of psychedelics that are expected to be reviewed by the FDA in coming years. It’s part of a resurgence of research into the potential of psychedelics for hard-to-treat conditions like depression , addiction and anxiety. MDMA’s main effect is triggering feelings of intimacy, connection and euphoria.
Companies are studying MDMA, psilocybin, LSD and other mind-expanding drugs for numerous mental health problems .
Until recently, psychedelic research was mainly funded by a handful of nonprofit advocacy groups, including Multidisciplinary Association for Psychedelic Studies, or MAPS. The company seeking approval for MDMA, Lykos Therapeutics, is essentially a corporate spinoff of MAPS, which conducted all the studies submitted for FDA review.
In two studies, patients received MDMA as part of an intensive, four-month course of talk therapy lasting more than a dozen sessions, only three of which involved taking the drug. The drug is thought to help patients come to terms with their trauma and let go of disturbing thoughts and memories.
The approach was studied in nearly 195 adults with moderate-to-severe PTSD who were randomly assigned to undergo the therapy with MDMA or with a dummy pill. Following treatment, patients who received MDMA had significantly lower PTSD scores and were more likely to be in remission.
But FDA reviewers noted that the vast majority of patients correctly guessed whether they had received MDMA or a dummy pill, making it “nearly impossible” to maintain the so-called “blinded” objectivity considered essential for high-quality drug research. The agency also questioned how long the drug’s benefits might last. The studies tracked some patients for up to two years, but reviewers noted that about a quarter of patients quickly dropped out of the follow-up study, limiting the usefulness of the results.
The most common side effects of MDMA included headache, nausea, muscle tightness and decreased appetite. More serious issues included heart palpitations and elevated blood pressure, which FDA reviewers said had the “potential to trigger” life-threatening heart problems.
They also raised concerns about the potential for patients to abuse MDMA, which functions similarly to amphetamines and other stimulants.
While MDMA would be a first-of-a-kind approval, U.S. doctors and the FDA itself have already laid some of the groundwork for working with drugs that can cause intense, psychological experiences.
Hundreds of clinics across the U.S. already offer ketamine — the powerful anesthetic sometimes used as a party drug — to treat a host of ailments, including depression, anxiety, chronic pain and PTSD. The FDA has only formally approved the drug for use during surgery, but its availability allows doctors to prescribe it “off-label” for various mental and physical ailments.
In 2019, the FDA approved Johnson & Johnson’s proprietary form of the drug, Spravato, a nasal spray that treats severe depression . Similar to ketamine, the drug is offered at doctor’s offices and clinics where patients usually spend several hours reclining in a chair.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.

IMAGES
VIDEO
COMMENTS
Top 10 research questions. Our Depression Detectives have come up with 59 possible research questions and voted on their top ten. We are now discussing, narrowing and finetuning them, and finding ways how they could be researched. Every day, we are looking at one of the top ten questions. Then we will then have another vote to decide on the ...
This is a good research question about depression as certain risk factors may make a person more prone to developing this mental health condition, ... This is another good depression research topic because, in some ways, the diagnosis of depression is more of an art than a science. Doctors must generally rely upon the patient's set of symptoms ...
Depression is a major public health issue in Canada. 1 About 8% of adults aged 25-64 years are projected to experience major depression at some time in their lives. 2 Depression is estimated to account for at least $32.3 billion of direct and indirect costs to this nation annually. 3 Continued investment in research that explores prevention and treatment is needed, 4, 5 in particular through ...
Frequently Asked Questions about Depression. Depression (major depressive disorder or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how you feel, think, and handle daily activities, such as sleeping, eating, or working. To be diagnosed with depression, the symptoms must be present for at least ...
n = 47 studies on heterogeneous research questions were included, ... = 12). A total of 38.3% of the studies were rated as "good", 55.3% as "fair" and 6.4% as "poor" in the quality assessment. 3.3. Overview of Studies on the Association between Anxiety/Depression as Independent Variables and QoL Outcomes ... Depression as ...
Depression is a prevalent psychiatric disorder that often leads to poor quality of life and impaired functioning. Treatment during the acute phase of a major depressive episode aims to help the patient reach a remission state and eventually return to their baseline level of functioning. Pharmacotherapy, especially selective serotonin reuptake ...
This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs. Choat / Adobe Stock. Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness ...
The research questions guided our analyses. In this sense, we were particularly looking for data where the YP spoke about their experience of depression, the impact that depression might have on their lives, and their journey into therapy—but we did not in any way pre-determine that themes might emerge in relation to these research questions.
Depression (also known as major depression, major depressive disorder, or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working. To be diagnosed with depression, the symptoms must be present for at least 2 ...
There are two common types of depression. Major depression includes symptoms of depressed mood or loss of interest, most of the time for at least 2 weeks, that interfere with daily activities.; Persistent depressive disorder (also called dysthymia or dysthymic disorder) consists of less severe depression symptoms that last much longer, usually for at least 2 years.
1. Is depression a mental illness? Yes, clinical depression is a serious, but treatable, mental illness. It is a medical condition, not a personal weakness. It is also very common. Major ...
45 survey question examples to use in your depression questionnaire. Since we are well aware of the necessity of adequate questions as forms.app, we gathered 45 great questions for the survey questionnaire about depression.You can use these questions in your depression research questionnaire to create well-developed and professional surveys.
Major Types of Depression. This paper will review and analyze two scholarly articles concerning depression, its sings in male and female patients, and its connection and similarity to other disorders. Depression in the Elderly. Depression can be defined as a state of anxiety, sadness, hopelessness, and worthlessness.
Depression Treatments for Adults. APA's Clinical Practice Guideline recommends seven psychotherapy interventions as well as a second-generation antidepressant (selective serotonin reuptake inhibitors — SSRIs — serotonin-norepinephrine reuptake inhibitors — SNRIs — or norepinephrine/dopamine reuptake inhibitors — NDRIs) for the ...
Treatment of depression depends on the individual as well as the severity and duration of the illness. Basic types of treatment for depression include antidepressant medications, psychotherapy, or electroconvulsive therapy (ECT). Often these basic treatment approaches are used in combination. Antidepressants are one of the largest groups of ...
The Geriatric Depression Scale (GDS) is specifically designed to screen and measure depression in older adults. It contains 30 forced-choice "yes" or "no" questions, a format that is helpful for individuals with cognitive dysfunction. Questions relate to how an individual has felt in a specified time frame.
1. How common is depression? About 4% of the population has what we call major depressive disorder, the most severe kind of depression, at any one time. Less severe depressions are probably more common. It is important to note that everyone gets a low mood at times, but most pull out of this within a couple of days. 2.
Researchers use depression scales to compare scores for different groups of people, implying a belief that depression is invariant across contexts. Accordingly, the measurement of depression should be similarly invariant. Measurement invariance is necessary for common research questions, such as whether depression rates are similar in women and ...
Depression is a serious medical illness. It's more than just a feeling of being sad or blue for a few days. If you are one of the more than 19 million teens and adults in the United States who have depression, the feelings do not go away. They persist and interfere with your everyday life. AHRQ has research, tools and resources on depression and how clinicians can help their patients with ...
Depression may also manifest psychosomatically, meaning that instead of presenting first and foremost as a mood disorder, the dominant symptom may be things like vague aches, dizziness, headaches ...
10 common questions about depression, answered. There are a lot of misconceptions surrounding depression. Freestyle Releasing. Depression is a common mood disorder that can make even daily ...
The first question asks for a ready-made solution, and is not focused or researchable. The second question is a clearer comparative question, but note that it may not be practically feasible. For a smaller research project or thesis, it could be narrowed down further to focus on the effectiveness of drunk driving laws in just one or two countries.
The answer to this question depends on the severity of the depression and how long it has been present. Depression can come on suddenly and be severe, or it can develop gradually over time.
Cause and Effects of The Great Depression. The economic devastation of the 1920s led to the Great Depression and brought a tragedy for the whole society. Crash of stock market The crash of the stock market in 1929 ushered in the Great […] The History of Great Depression. The Great Depression was the most severe recession of the past centuries.
Scientists believe several factors can contribute to depression: Trauma. When people experience trauma at an early age, it can cause long-term changes in how their brains respond to fear and stress. These changes may lead to depression. Genetics. Mood disorders, such as depression, tend to run in families. Life circumstances. Marital status ...
42 depression survey question examples. A healthcare provider can ask a patient to answer depression survey questions, in which case they're referred to as observer-rated or clinician-rated questions. An individual can administer a depression survey themselves; the questions in this type of survey are known as self-reported questions.
An abundance of research shows that exercise is good for depression, and yet most of the time when I hear people talk about the mental-health crisis — on TikTok, on X, and in real life — it is ...
WASHINGTON (AP) — Federal health regulators are questioning the safety and evidence behind the first bid to use MDMA, the mind-altering club drug, as a treatment for PTSD, part of a decadeslong effort by advocates to move psychedelic drugs into the medical mainstream.. The Food and Drug Administration posted its initial review of the drug Friday, ahead of a meeting of outside advisers who ...
Reports the retraction of "Predictors of depression among school adolescents in Northwest, Ethiopia, 2022: Institutional based cross-sectional" by Aklile Tsega Chekol, Mastewal Aschale Wale, Agmas Wassie Abate, Eyerusalem Abebe Beo, Eman Ali Said and Berhan Tsegaye Negash (BMC Psychiatry, 2023[Jun][14], Vol 23[1][429]). The Editors have retracted this article after concerns were raised.