Change Password
Your password must have 8 characters or more and contain 3 of the following:.
- a lower case character,
- an upper case character,
- a special character

Password Changed Successfully
Your password has been changed
- Sign in / Register
Request Username
Can't sign in? Forgot your username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
An Exploratory Study of Students with Depression in Undergraduate Research Experiences
- Katelyn M. Cooper
- Logan E. Gin
- M. Elizabeth Barnes
- Sara E. Brownell
*Address correspondence to: Katelyn M. Cooper ( E-mail Address: [email protected] ).
Department of Biology, University of Central Florida, Orlando, FL, 32816
Search for more papers by this author
Biology Education Research Lab, Research for Inclusive STEM Education Center, School of Life Sciences, Arizona State University, Tempe, AZ 85281
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect graduate student depression, we know of no studies that have explored the relationship between depression and undergraduate research. In this study, we sought to understand how undergraduates’ symptoms of depression affect their research experiences and how research affects undergraduates’ feelings of depression. We interviewed 35 undergraduate researchers majoring in the life sciences from 12 research-intensive public universities across the United States who identify with having depression. Using inductive and deductive coding, we identified that students’ depression affected their motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing in undergraduate research experiences. We found that students’ social connections, experiencing failure in research, getting help, receiving feedback, and the demands of research affected students’ depression. Based on this work, we articulate an initial set of evidence-based recommendations for research mentors to consider in promoting an inclusive research experience for students with depression.
INTRODUCTION
Depression is described as a common and serious mood disorder that results in persistent feelings of sadness and hopelessness, as well as a loss of interest in activities that one once enjoyed ( American Psychiatric Association [APA], 2013 ). Additional symptoms of depression include weight changes, difficulty sleeping, loss of energy, difficulty thinking or concentrating, feelings of worthlessness or excessive guilt, and suicidality ( APA, 2013 ). While depression results from a complex interaction of psychological, social, and biological factors ( World Health Organization, 2018 ), studies have shown that increased stress caused by college can be a significant contributor to student depression ( Dyson and Renk, 2006 ).
Depression is one of the top undergraduate mental health concerns, and the rate of depression among undergraduates continues to rise ( Center for Collegiate Mental Health, 2017 ). While we cannot discern whether these increasing rates of depression are due to increased awareness or increased incidence, it is clear that is a serious problem on college campuses. The percent of U.S. college students who self-reported a diagnosis with depression was recently estimated to be about 25% ( American College Health Association, 2019 ). However, higher rates have been reported, with one study estimating that up to 84% of undergraduates experience some level of depression ( Garlow et al. , 2008 ). Depression rates are typically higher among university students compared with the general population, despite being a more socially privileged group ( Ibrahim et al. , 2013 ). Prior studies have found that depression is negatively correlated with overall undergraduate academic performance ( Hysenbegasi et al. , 2005 ; Deroma et al. , 2009 ; American College Health Association, 2019 ). Specifically, diagnosed depression is associated with half a letter grade decrease in students’ grade point average ( Hysenbegasi et al. , 2005 ), and 21.6% of undergraduates reported that depression negatively affected their academic performance within the last year ( American College Health Association, 2019 ). Provided with a list of academic factors that may be affected by depression, students reported that depression contributed to lower exam grades, lower course grades, and not completing or dropping a course.
Students in the natural sciences may be particularly at risk for depression, given that such majors are noted to be particularly stressful due to their competitive nature and course work that is often perceived to “weed students out”( Everson et al. , 1993 ; Strenta et al. , 1994 ; American College Health Association, 2019 ; Seymour and Hunter, 2019 ). Science course instruction has also been described to be boring, repetitive, difficult, and math-intensive; these factors can create an environment that can trigger depression ( Seymour and Hewitt, 1997 ; Osborne and Collins, 2001 ; Armbruster et al ., 2009 ; Ceci and Williams, 2010 ). What also distinguishes science degree programs from other degree programs is that, increasingly, undergraduate research experiences are being proposed as an essential element of a science degree ( American Association for the Advancement of Science, 2011 ; President’s Council of Advisors on Science and Technology, 2012 ; National Academies of Sciences, Engineering, and Medicine [NASEM], 2017 ). However, there is some evidence that undergraduate research experiences can add to the stress of college for some students ( Cooper et al. , 2019c ). Students can garner multiple benefits from undergraduate research, including enhanced abilities to think critically ( Ishiyama, 2002 ; Bauer and Bennett, 2003 ; Brownell et al. , 2015 ), improved student learning ( Rauckhorst et al. , 2001 ; Brownell et al. , 2015 ), and increased student persistence in undergraduate science degree programs ( Jones et al. , 2010 ; Hernandez et al. , 2018 ). Notably, undergraduate research experiences are increasingly becoming a prerequisite for entry into medical and graduate programs in science, particularly elite programs ( Cooper et al. , 2019d ). Although some research experiences are embedded into formal lab courses as course-based undergraduate research experiences (CUREs; Auchincloss et al. , 2014 ; Brownell and Kloser, 2015 ), the majority likely entail working with faculty in their research labs. These undergraduate research experiences in faculty labs are often added on top of a student’s normal course work, so they essentially become an extracurricular activity that they have to juggle with course work, working, and/or personal obligations ( Cooper et al. , 2019c ). While the majority of the literature surrounding undergraduate research highlights undergraduate research as a positive experience ( NASEM, 2017 ), studies have demonstrated that undergraduate research experiences can be academically and emotionally challenging for students ( Mabrouk and Peters, 2000 ; Seymour et al. , 2004 ; Cooper et al. , 2019c ; Limeri et al. , 2019 ). In fact, 50% of students sampled nationally from public R1 institutions consider leaving their undergraduate research experience prematurely, and about half of those students, or 25% of all students, ultimately leave their undergraduate research experience ( Cooper et al. , 2019c ). Notably, 33.8% of these individuals cited a negative lab environment and 33.3% cited negative relationships with their mentors as factors that influenced their decision about whether to leave ( Cooper et al. , 2019c ). Therefore, students’ depression may be exacerbated in challenging undergraduate research experiences, because studies have shown that depression is positively correlated with student stress ( Hish et al. , 2019 ).
While depression has not been explored in the context of undergraduate research experiences, depression has become a prominent concern surrounding graduate students conducting scientific research. A recent study that examined the “graduate student mental health crisis” ( Flaherty, 2018 ) found that work–life balance and graduate students’ relationships with their research advisors may be contributing to their depression ( Evans et al. , 2018 ). Specifically, this survey of 2279 PhD and master’s students from diverse fields of study, including the biological/physical sciences, showed that 39% of graduate students have experienced moderate to severe depression. Fifty-five percent of the graduate students with depression who were surveyed disagreed with the statement “I have good work life balance,” compared to only 21% of students with depression who agreed. Additionally, the study highlighted that more students with depression disagreed than agreed with the following statements: their advisors provided “real” mentorship, their advisors provided ample support, their advisors positively impacted their emotional or mental well-being, their advisors were assets to their careers, and they felt valued by their mentors. Another recent study identified that depression severity in biomedical doctoral students was significantly associated with graduate program climate, a perceived lack of employment opportunities, and the quality of students’ research training environment ( Nagy et al. , 2019 ). Environmental stress, academic stress, and family and monetary stress have also been shown to be predictive of depression severity in biomedical doctoral students ( Hish et al. , 2019 ). Further, one study found that self-esteem is negatively correlated and stress is positively correlated with graduate student depression; presumably research environments that challenge students’ self-esteem and induce stress are likely contributing to depressive symptoms among graduate students ( Kreger, 1995 ). While these studies have focused on graduate students, and there are certainly notable distinctions between graduate and undergraduate research, the research-related factors that affect graduate student depression, including work–life balance, relationships with mentors, research environment, stress, and self-esteem, may also be relevant to depression among undergraduates conducting research. Importantly, undergraduates in the United States have reported identical levels of depression as graduate students but are often less likely to seek mental health care services ( Wyatt and Oswalt, 2013 ), which is concerning if undergraduate research experiences exacerbate depression.
Based on the literature on the stressors of undergraduate research experiences and the literature identifying some potential causes of graduate student depression, we identified three aspects of undergraduate research that may exacerbate undergraduates’ depression. Mentoring: Mentors can be an integral part of a students’ research experience, bolstering their connections with others in the science community, scholarly productivity, and science identity, as well as providing many other benefits ( Thiry and Laursen, 2011 ; Prunuske et al. , 2013 ; Byars-Winston et al. , 2015 ; Aikens et al. , 2016 , 2017 ; Thompson et al. , 2016 ; Estrada et al. , 2018 ). However, recent literature has highlighted that poor mentoring can negatively affect undergraduate researchers ( Cooper et al. , 2019c ; Limeri et al. , 2019 ). Specifically, one study of 33 undergraduate researchers who had conducted research at 10 institutions identified seven major ways that they experienced negative mentoring, which included absenteeism, abuse of power, interpersonal mismatch, lack of career support, lack of psychosocial support, misaligned expectations, and unequal treatment ( Limeri et al. , 2019 ). We hypothesize negative mentoring experiences may be particularly harmful for students with depression, because support, particularly social support, has been shown to be important for helping individuals with depression cope with difficult circumstances ( Aneshensel and Stone, 1982 ; Grav et al. , 2012 ). Failure: Experiencing failure has been hypothesized to be an important aspect of undergraduate research experiences that may help students develop some the most distinguishing abilities of outstanding scientists, such as coping with failure, navigating challenges, and persevering ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, experiencing failure and the stress and fatigue that often accompany it may be particularly tough for students with depression ( Aldwin and Greenberger, 1987 ; Mongrain and Blackburn, 2005 ). Lab environment: Fairness, inclusion/exclusion, and social support within one’s organizational environment have been shown to be key factors that cause people to either want to remain in the work place and be productive or to want to leave ( Barak et al. , 2006 ; Cooper et al. , 2019c ). We hypothesize that dealing with exclusion or a lack of social support may exacerbate depression for some students; patients with clinical depression react to social exclusion with more pronounced negative emotions than do individuals without clinical depression ( Jobst et al. , 2015 ). While there are likely other aspects of undergraduate research that affect student depression, we hypothesize that these factors have the potential to exacerbate negative research experiences for students with depression.
Depression has been shown to disproportionately affect many populations that are underrepresented or underserved within the scientific community, including females ( American College Health Association, 2018 ; Evans et al. , 2018 ), first-generation college students ( Jenkins et al. , 2013 ), individuals from low socioeconomic backgrounds ( Eisenberg et al. , 2007 ), members of the LGBTQ+ community ( Eisenberg et al. , 2007 ; Evans et al. , 2018 ), and people with disabilities ( Turner and Noh, 1988 ). Therefore, as the science community strives to be more diverse and inclusive ( Intemann, 2009 ), it is important that we understand more about the relationship between depression and scientific research, because negative experiences with depression in scientific research may be contributing to the underrepresentation of these groups. Specifically, more information is needed about how the research process and environment of research experiences may affect depression.
Given the high rate of depression among undergraduates, the links between depression and graduate research, the potentially challenging environment of undergraduate research, and how depression could disproportionately impact students from underserved communities, it is imperative to begin to explore the relationship between scientific research and depression among undergraduates to create research experiences that could maximize student success. In this exploratory interview study, we aimed to 1) describe how undergraduates’ symptoms of depression affect their research experiences, 2) understand how undergraduate research affects students’ feelings of depression, and 3) identify recommendations based on the literature and undergraduates’ reported experiences to promote a positive research experience for students with depression.
This study was done with an approved Arizona State University Institutional Review Board protocol #7247.
In Fall 2018, we surveyed undergraduate researchers majoring in the life sciences across 25 research-intensive (R1) public institutions across the United States (specific details about the recruitment of the students who completed the survey can be found in Cooper et al. (2019c) ). The survey asked students for their opinions about their undergraduate research experiences and their demographic information and whether they would be interested in participating in a follow-up interview related to their research experiences. For the purpose of this study, we exclusively interviewed students about their undergraduate research experiences in faculty member labs; we did not consider students’ experiences in CUREs. Of the 768 undergraduate researchers who completed the survey, 65% ( n = 496) indicated that they would be interested in participating in a follow-up interview. In Spring 2019, we emailed the 496 students, explaining that we were interested in interviewing students with depression about their experiences in undergraduate research. Our specific prompt was: “If you identify as having depression, we would be interested in hearing about your experience in undergraduate research in a 30–60 minute online interview.” We did not define depression in our email recruitment because we conducted think-aloud interviews with four undergraduates who all correctly interpreted what we meant by depression ( APA, 2013 ). We had 35 students agree to participate in the interview study. The interview participants represented 12 of the 25 R1 public institutions that were represented in the initial survey.
Student Interviews
We developed an interview script to explore our research questions. Specifically, we were interested in how students’ symptoms of depression affect their research experiences, how undergraduate research negatively affects student depression, and how undergraduate research positively affects student depression.
We recognized that mental health, and specifically depression, can be a sensitive topic to discuss with undergraduates, and therefore we tried to minimize any discomfort that the interviewees might experience during the interview. Specifically, we conducted think-aloud interviews with three graduate students who self-identified with having depression at the time of the interview. We asked them to note whether any interview questions made them uncomfortable. We also sought their feedback on questions given their experiences as persons with depression who had once engaged in undergraduate research. We revised the interview protocol after each think-aloud interview. Next, we conducted four additional think-aloud interviews with undergraduates conducting basic science or biology education research who identified with having depression to establish cognitive validity of the questions and to elicit additional feedback about any questions that might make someone uncomfortable. The questions were revised after each think-aloud interview until no question was unclear or misinterpreted by the students and we were confident that the questions minimized students’ potential discomfort ( Trenor et al. , 2011 ). A copy of the final interview script can be found in the Supplemental Material.
All interviews were individually conducted by one of two researchers (K.M.C. and L.E.G.) who conducted the think-aloud interviews together to ensure that their interviewing practices were as similar as possible. The interviews were approximately an hour long, and students received a $15 gift card for their participation.
Personal, Research, and Depression Demographics
All student demographics and information about students’ research experiences were collected using the survey distributed to students in Fall 2018. We collected personal demographics, including the participants’ gender, race/ethnicity, college generation status, transfer status, financial stability, year in college, major, and age. We also collected information about the students’ research experiences, including the length of their first research experiences, the average number of hours they spend in research per week, how they were compensated for research, who their primary mentors were, and the focus areas of their research.
In the United States, mental healthcare is disproportionately unavailable to Black and Latinx individuals, as well as those who come from low socioeconomic backgrounds ( Kataoka et al. , 2002 ; Howell and McFeeters, 2008 ; Santiago et al. , 2013 ). Therefore, to minimize a biased sample, we invited anyone who identified with having depression to participate in our study; we did not require students to be diagnosed with depression or to be treated for depression in order to participate. However, we did collect information about whether students had been formally diagnosed with depression and whether they had been treated for depression. After the interview, all participants were sent a link to a short survey that asked them if they had ever been diagnosed with depression and how, if at all, they had ever been treated for depression. A copy of these survey questions can be found in the Supplemental Material. The combined demographic information of the participants is in Table 1 . The demographics for each individual student can be found in the Supplemental Material.
a Students reported the time they had spent in research 6 months before being interviewed and only reported on the length of time of their first research experiences.
b Students were invited to report multiple ways in which they were treated for their depression; other treatments included lifestyle changes and meditation.
c Students were invited to report multiple means of compensation for their research if they had been compensated for their time in different ways.
d Students were asked whether they felt financially stable, particularly during the undergraduate research experience.
e Students reported who they work/worked with most closely during their research experiences.
f Staff members included lab coordinators or lab managers.
g Other focus areas of research included sociology, linguistics, psychology, and public health.
Interview Analysis
The initial interview analysis aimed to explore each idea that a participant expressed ( Charmaz, 2006 ) and to identify reoccurring ideas throughout the interviews. First, three authors (K.M.C., L.E.G., and S.E.B.) individually reviewed a different set of 10 interviews and took detailed analytic notes ( Birks and Mills, 2015 ). Afterward, the authors compared their notes and identified reoccurring themes throughout the interviews using open coding methods ( Saldaña, 2015 ).
Once an initial set of themes was established, two researchers (K.M.C. and L.E.G.) individually reviewed the same set of 15 randomly selected interviews to validate the themes identified in the initial analysis and to screen for any additional themes that the initial analysis may have missed. Each researcher took detailed analytic notes throughout the review of an interview, which they discussed after reviewing each interview. The researchers compared what quotes from each interview they categorized into each theme. Using constant comparison methods, they assigned quotes to each theme and constantly compared the quotes to ensure that each quote fit within the description of the theme ( Glesne and Peshkin, 1992 ). In cases in which quotes were too different from other quotes, a new theme was created. This approach allowed for multiple revisions of the themes and allowed the authors to define a final set of codes; the researchers created a final codebook with refined definitions of emergent themes (the final coding rubric can be found in the Supplemental Material). Once the final codebook was established, the researchers (K.M.C. and L.E.G.) individually coded seven additional interviews (20% of all interviews) using the coding rubric. The researchers compared their codes, and their Cohen’s κ interrater score for these seven interviews was at an acceptable level (κ = 0.88; Landis and Koch, 1977 ). One researcher (L.E.G.) coded the remaining 28 out of 35 interviews. The researchers determined that data saturation had been reached with the current sample and no further recruitment was needed ( Guest et al. , 2006 ). We report on themes that were mentioned by at least 20% of students in the interview study. In the Supplemental Material, we provide the final coding rubric with the number of participants whose interview reflected each theme ( Hannah and Lautsch, 2011 ). Reporting the number of individuals who reported themes within qualitative data can lead to inaccurate conclusions about the generalizability of the results to a broader population. These qualitative data are meant to characterize a landscape of experiences that students with depression have in undergraduate research rather than to make claims about the prevalence of these experiences ( Glesne and Peshkin, 1992 ). Because inferences about the importance of these themes cannot be drawn from these counts, they are not included in the results of the paper ( Maxwell, 2010 ). Further, the limited number of interviewees made it not possible to examine whether there were trends based on students’ demographics or characteristics of their research experiences (e.g., their specific area of study). Quotes were lightly edited for clarity by inserting clarification brackets and using ellipses to indicate excluded text. Pseudonyms were given to all students to protect their privacy.
The Effect of Depressive Symptoms on Undergraduate Research
We asked students to describe the symptoms associated with their depression. Students described experiencing anxiety that is associated with their depression; this could be anxiety that precedes their depression or anxiety that results from a depressive episode or a period of time when an individual has depression symptoms. Further, students described difficulty getting out of bed or leaving the house, feeling tired, a lack of motivation, being overly self-critical, feeling apathetic, and having difficulty concentrating. We were particularly interested in how students’ symptoms of depression affected their experiences in undergraduate research. During the think-aloud interviews that were conducted before the interview study, graduate and undergraduate students consistently described that their depression affected their motivation in research, their creativity in research, and their productivity in research. Therefore, we explicitly asked undergraduate researchers how, if at all, their depression affected these three factors. We also asked students to describe any additional ways in which their depression affected their research experiences. Undergraduate researchers commonly described five additional ways in which their depression affected their research; for a detailed description of each way students’ research was affected and for example quotes, see Table 2 . Students described that their depression negatively affected their productivity in the lab. Commonly, students described that their productivity was directly affected by a lack of motivation or because they felt less creative, which hindered the research process. Additionally, students highlighted that they were sometimes less productive because their depression sometimes caused them to struggle to engage intellectually with their research or caused them to have difficulty remembering or concentrating; students described that they could do mundane or routine tasks when they felt depressed, but that they had difficulty with more complex and intellectually demanding tasks. However, students sometimes described that even mundane tasks could be difficult when they were required to remember specific steps; for example, some students struggled recalling a protocol from memory when their depression was particularly severe. Additionally, students noted that their depression made them more self-conscious, which sometimes held them back from sharing research ideas with their mentors or from taking risks such as applying to competitive programs. In addition to being self-conscious, students highlighted that their depression caused them to be overly self-critical, and some described experiencing imposter phenomenon ( Clance and Imes, 1978 ) or feeling like they were not talented enough to be in research and were accepted into a lab by a fluke or through luck. Finally, students described that depression often made them feel less social, and they struggled to socially engage with other members of the lab when they were feeling down.
The Effect of Undergraduate Research Experiences on Student Depression
We also wanted to explore how research impacted students’ feelings of depression. Undergraduates described how research both positively and negatively affected their depression. In the following sections, we present aspects of undergraduate research and examine how each positively and/or negatively affected students’ depression using embedded student quotes to highlight the relationships between related ideas.
Lab Environment: Relationships with Others in the Lab.
Some aspects of the lab environment, which we define as students’ physical, social, or psychological research space, could be particularly beneficial for students with depression.
Specifically, undergraduate researchers perceived that comfortable and positive social interactions with others in the lab helped their depression. Students acknowledged how beneficial their relationships with graduate students and postdocs could be.
Marta: “I think always checking in on undergrads is important. It’s really easy [for us] to go a whole day without talking to anybody in the lab. But our grad students are like ‘Hey, what’s up? How’s school? What’s going on?’ (…) What helps me the most is having that strong support system. Sometimes just talking makes you feel better, but also having people that believe in you can really help you get out of that negative spiral. I think that can really help with depression.”
Kelley: “I know that anytime I need to talk to [my postdoc mentors] about something they’re always there for me. Over time we’ve developed a relationship where I know that outside of work and outside of the lab if I did want to talk to them about something I could talk to them. Even just talking to someone about hobbies and having that relationship alone is really helpful [for depression].”
In addition to highlighting the importance of developing relationships with graduate students or postdocs in the lab, students described that forming relationships with other undergraduates in the lab also helped their depression. Particularly, students described that other undergraduate researchers often validated their feelings about research, which in turn helped them realize that what they are thinking or feeling is normal, which tended to alleviate their negative thoughts. Interestingly, other undergraduates experiencing the same issues could sometimes help buffer them from perceiving that a mentor did not like them or that they were uniquely bad at research. In this article, we use the term “mentor” to refer to anyone who students referred to in the interviews as being their mentors or managing their research experiences; this includes graduate students, postdoctoral scholars, lab managers, and primary investigators (PIs).
Abby: “One of my best friends is in the lab with me. A lot of that friendship just comes from complaining about our stress with the lab and our annoyance with people in the lab. Like when we both agree like, ‘Yeah, the grad students were really off today, it wasn’t us,’ that helps. ‘It wasn’t me, it wasn’t my fault that we were having a rough day in lab; it was the grad students.’ Just being able to realize, ‘Hey, this isn’t all caused by us,’ you know? (…) We understand the stresses in the lab. We understand the details of what each other are doing in the lab, so when something doesn’t work out, we understand that it took them like eight hours to do that and it didn’t work. We provide empathy on a different level.”
Meleana: “It’s great to have solidarity in being confused about something, and it’s just that is a form of validation for me too. When we leave a lab meeting and I look at [another undergrad] I’m like, ‘Did you understand anything that they were just saying?’ And they’re like, ‘Oh, no.’ (…) It’s just really validating to hear from the other undergrads that we all seem to be struggling with the same things.”
Developing positive relationships with faculty mentors or PIs also helped alleviate some students’ depressive feelings, particularly when PIs shared their own struggles with students. This also seemed to normalize students’ concerns about their own experiences.
Alexandra: “[Talking with my PI] is helpful because he would talk about his struggles, and what he faced. A lot of it was very similar to my struggles. For example, he would say, ‘Oh, yeah, I failed this exam that I studied so hard for. I failed the GRE and I paid so much money to prepare for it.’ It just makes [my depression] better, like okay, this is normal for students to go through this. It’s not an out of this world thing where if you fail, you’re a failure and you can’t move on from it.”
Students’ relationships with others in the lab did not always positively impact their depression. Students described instances when the negative moods of the graduate students and PIs would often set the tone of the lab, which in turn worsened the mood of the undergraduate researchers.
Abby: “Sometimes [the grad students] are not in a good mood. The entire vibe of the lab is just off, and if you make a joke and it hits somebody wrong, they get all mad. It really depends on the grad students and the leadership and the mood that they’re in.”
Interviewer: “How does it affect your depression when the grad students are in a bad mood?”
Abby: “It definitely makes me feel worse. It feels like, again, that I really shouldn’t go ask them for help because they’re just not in the mood to help out. It makes me have more pressure on myself, and I have deadlines I need to meet, but I have a question for them, but they’re in a bad mood so I can’t ask. That’s another day wasted for me and it just puts more stress, which just adds to the depression.”
Additionally, some students described even more concerning behavior from research mentors, which negatively affected their depression.
Julie: “I had a primary investigator who is notorious in the department for screaming at people, being emotionally abusive, unreasonable, et cetera. (…) [He was] kind of harassing people, demeaning them, lying to them, et cetera, et cetera. (…) Being yelled at and constantly demeaned and harassed at all hours of the day and night, that was probably pretty bad for me.”
While the relationships between undergraduates and graduate, postdoc, and faculty mentors seemed to either alleviate or worsen students’ depressive symptoms, depending on the quality of the relationship, students in this study exclusively described their relationships with other undergraduates as positive for their depression. However, students did note that undergraduate research puts some of the best and brightest undergraduates in the same environment, which can result in students comparing themselves with their peers. Students described that this comparison would often lead them to feel badly about themselves, even though they would describe their personal relationship with a person to be good.
Meleana: “In just the research field in general, just feeling like I don’t really measure up to the people around me [can affect my depression]. A lot of the times it’s the beginning of a little spiral, mental spiral. There are some past undergrads that are talked about as they’re on this pedestal of being the ideal undergrads and that they were just so smart and contributed so much to the lab. I can never stop myself from wondering like, ‘Oh, I wonder if I’m having a contribution to the lab that’s similar or if I’m just another one of the undergrads that does the bare minimum and passes through and is just there.’”
Natasha: “But, on the other hand, [having another undergrad in the lab] also reminded me constantly that some people are invested in this and meant to do this and it’s not me. And that some people know a lot more than I do and will go further in this than I will.”
While students primarily expressed that their relationships with others in the lab affected their depression, some students explained that they struggled most with depression when the lab was empty; they described that they did not like being alone in the lab, because a lack of stimulation allowed their minds to be filled with negative thoughts.
Mia: “Those late nights definitely didn’t help [my depression]. I am alone, in the entire building. I’m left alone to think about my thoughts more, so not distracted by talking to people or interacting with people. I think more about how I’m feeling and the lack of progress I’m making, and the hopelessness I’m feeling. That kind of dragged things on, and I guess deepened my depression.”
Freddy: “Often times when I go to my office in the evening, that is when I would [ sic ] be prone to be more depressed. It’s being alone. I think about myself or mistakes or trying to correct mistakes or whatever’s going on in my life at the time. I become very introspective. I think I’m way too self-evaluating, way too self-deprecating and it’s when I’m alone when those things are really, really triggered. When I’m talking with somebody else, I forget about those things.”
In sum, students with depression highlighted that a lab environment full of positive and encouraging individuals was helpful for their depression, whereas isolating or competitive environments and negative interactions with others often resulted in more depressive feelings.
Doing Science: Experiencing Failure in Research, Getting Help, Receiving Feedback, Time Demands, and Important Contributions.
In addition to the lab environment, students also described that the process of doing science could affect their depression. Specifically, students explained that a large contributor to their depression was experiencing failure in research.
Interviewer: “Considering your experience in undergraduate research, what tends to trigger your feelings of depression?”
Heather: “Probably just not getting things right. Having to do an experiment over and over again. You don’t get the results you want. (…) The work is pretty meticulous and it’s frustrating when I do all this work, I do a whole experiment, and then I don’t get any results that I can use. That can be really frustrating. It adds to the stress. (…) It’s hard because you did all this other stuff before so you can plan for the research, and then something happens and all the stuff you did was worthless basically.”
Julie: “I felt very negatively about myself [when a project failed] and pretty panicked whenever something didn’t work because I felt like it was a direct reflection on my effort and/or intelligence, and then it was a big glaring personal failure.”
Students explained that their depression related to failing in research was exacerbated if they felt as though they could not seek help from their research mentors. Perceived insufficient mentor guidance has been shown to be a factor influencing student intention to leave undergraduate research ( Cooper et al. , 2019c ). Sometimes students talked about their research mentors being unavailable or unapproachable.
Michelle: “It just feels like [the graduate students] are not approachable. I feel like I can’t approach them to ask for their understanding in a certain situation. It makes [my depression] worse because I feel like I’m stuck, and that I’m being limited, and like there’s nothing I can do. So then I kind of feel like it’s my fault that I can’t do anything.”
Other times, students described that they did not seek help in fear that they would be negatively evaluated in research, which is a fear of being judged by others ( Watson and Friend, 1969 ; Weeks et al. , 2005 ; Cooper et al. , 2018 ). That is, students fear that their mentor would think negatively about them or judge them if they were to ask questions that their mentor thought they should know the answer to.
Meleana: “I would say [my depression] tends to come out more in being more reserved in asking questions because I think that comes more like a fear-based thing where I’m like, ‘Oh, I don’t feel like I’m good enough and so I don’t want to ask these questions because then my mentors will, I don’t know, think that I’m dumb or something.’”
Conversely, students described that mentors who were willing to help them alleviated their depressive feelings.
Crystal: “Yeah [my grad student] is always like, ‘Hey, I can check in on things in the lab because you’re allowed to ask me for that, you’re not totally alone in this,’ because he knows that I tend to take on all this responsibility and I don’t always know how to ask for help. He’s like, ‘You know, this is my lab too and I am here to help you as well,’ and just reminds me that I’m not shouldering this burden by myself.”
Ashlyn: “The graduate student who I work with is very kind and has a lot of patience and he really understands a lot of things and provides simple explanations. He does remind me about things and he will keep on me about certain tasks that I need to do in an understanding way, and it’s just because he’s patient and he listens.”
In addition to experiencing failure in science, students described that making mistakes when doing science also negatively affected their depression.
Abby: “I guess not making mistakes on experiments [is important in avoiding my depression]. Not necessarily that your experiment didn’t turn out to produce the data that you wanted, but just adding the wrong enzyme or messing something up like that. It’s like, ‘Oh, man,’ you know? You can get really down on yourself about that because it can be embarrassing.”
Commonly, students described that the potential for making mistakes increased their stress and anxiety regarding research; however, they explained that how other people responded to a potential mistake was what ultimately affected their depression.
Briana: “Sometimes if I made a mistake in correctly identifying an eye color [of a fly], [my PI] would just ridicule me in front of the other students. He corrected me but his method of correcting was very discouraging because it was a ridicule. It made the others laugh and I didn’t like that.”
Julie: “[My PI] explicitly [asked] if I had the dedication for science. A lot of times he said I had terrible judgment. A lot of times he said I couldn’t be trusted. Once I went to a conference with him, and, unfortunately, in front of another professor, he called me a klutz several times and there was another comment about how I never learn from my mistakes.”
When students did do things correctly, they described how important it could be for them to receive praise from their mentors. They explained that hearing praise and validation can be particularly helpful for students with depression, because their thoughts are often very negative and/or because they have low self-esteem.
Crystal: “[Something that helps my depression is] I have text messages from [my graduate student mentor] thanking me [and another undergraduate researcher] for all of the work that we’ve put in, that he would not be able to be as on track to finish as he is if he didn’t have our help.”
Interviewer: “Why is hearing praise from your mentor helpful?”
Crystal: “Because a lot of my depression focuses on everybody secretly hates you, nobody likes you, you’re going to die alone. So having that validation [from my graduate mentor] is important, because it flies in the face of what my depression tells me.”
Brian: “It reminds you that you exist outside of this negative world that you’ve created for yourself, and people don’t see you how you see yourself sometimes.”
Students also highlighted how research could be overwhelming, which negatively affected their depression. Particularly, students described that research demanded a lot of their time and that their mentors did not always seem to be aware that they were juggling school and other commitments in addition to their research. This stress exacerbated their depression.
Rose: “I feel like sometimes [my grad mentors] are not very understanding because grad students don’t take as many classes as [undergrads] do. I think sometimes they don’t understand when I say I can’t come in at all this week because I have finals and they’re like, ‘Why though?’”
Abby: “I just think being more understanding of student life would be great. We have classes as well as the lab, and classes are the priority. They forget what it’s like to be a student. You feel like they don’t understand and they could never understand when you say like, ‘I have three exams this week,’ and they’re like, ‘I don’t care. You need to finish this.’”
Conversely, some students reported that their research labs were very understanding of students’ schedules. Interestingly, these students talked most about how helpful it was to be able to take a mental health day and not do research on days when they felt down or depressed.
Marta: “My lab tech is very open, so she’ll tell us, ‘I can’t come in today. I have to take a mental health day.’ So she’s a really big advocate for that. And I think I won’t personally tell her that I’m taking a mental health day, but I’ll say, ‘I can’t come in today, but I’ll come in Friday and do those extra hours.’ And she’s like, ‘OK great, I’ll see you then.’ And it makes me feel good, because it helps me take care of myself first and then I can take care of everything else I need to do, which is amazing.”
Meleana: “Knowing that [my mentors] would be flexible if I told them that I’m crazy busy and can’t come into work nearly as much this week [helps my depression]. There is flexibility in allowing me to then care for myself.”
Interviewer: “Why is the flexibility helpful given the depression?”
Meleana: “Because sometimes for me things just take a little bit longer when I’m feeling down. I’m just less efficient to be honest, and so it’s helpful if I feel like I can only go into work for 10 hours in a week. It declutters my brain a little bit to not have to worry about all the things I have to do in work in addition the things that I need to do for school or clubs, or family or whatever.”
Despite the demanding nature of research, a subset of students highlighted that their research and research lab provided a sense of stability or familiarity that distracted them from their depression.
Freddy: “I’ll [do research] to run away from those [depressive] feelings or whatever. (…) I find sadly, I hate to admit it, but I do kind of run to [my lab]. I throw myself into work to distract myself from the feelings of depression and sadness.”
Rose: “When you’re sad or when you’re stressed you want to go to things you’re familiar with. So because lab has always been in my life, it’s this thing where it’s going to be there for me I guess. It’s like a good book that you always go back to and it’s familiar and it makes you feel good. So that’s how lab is. It’s not like the greatest thing in the world but it’s something that I’m used to, which is what I feel like a lot of people need when they’re sad and life is not going well.”
Many students also explained that research positively affects their depression because they perceive their research contribution to be important.
Ashlyn: “I feel like I’m dedicating myself to something that’s worthy and something that I believe in. It’s really important because it contextualizes those times when I am feeling depressed. It’s like, no, I do have these better things that I’m working on. Even when I don’t like myself and I don’t like who I am, which is again, depression brain, I can at least say, ‘Well, I have all these other people relying on me in research and in this area and that’s super important.’”
Jessica: “I mean, it just felt like the work that I was doing had meaning and when I feel like what I’m doing is actually going to contribute to the world, that usually really helps with [depression] because it’s like not every day you can feel like you’re doing something impactful.”
In sum, students highlighted that experiencing failure in research and making mistakes negatively contributed to depression, especially when help was unavailable or research mentors had a negative reaction. Additionally, students acknowledged that the research could be time-consuming, but that research mentors who were flexible helped assuage depressive feelings that were associated with feeling overwhelmed. Finally, research helped some students’ depression, because it felt familiar, provided a distraction from depression, and reminded students that they were contributing to a greater cause.
We believe that creating more inclusive research environments for students with depression is an important step toward broadening participation in science, not only to ensure that we are not discouraging students with depression from persisting in science, but also because depression has been shown to disproportionately affect underserved and underrepresented groups in science ( Turner and Noh, 1988 ; Eisenberg et al. , 2007 ; Jenkins et al. , 2013 ; American College Health Association, 2018 ). We initially hypothesized that three features of undergraduate research—research mentors, the lab environment, and failure—may have the potential to exacerbate student depression. We found this to be true; students highlighted that their relationships with their mentors as well as the overall lab environment could negatively affect their depression, but could also positively affect their research experiences. Students also noted that they struggled with failure, which is likely true of most students, but is known to be particularly difficult for students with depression ( Elliott et al. , 1997 ). We expand upon our findings by integrating literature on depression with the information that students provided in the interviews about how research mentors can best support students. We provide a set of evidence-based recommendations focused on mentoring, the lab environment, and failure for research mentors wanting to create more inclusive research environments for students with depression. Notably, only the first recommendation is specific to students with depression; the others reflect recommendations that have previously been described as “best practices” for research mentors ( NASEM, 2017 , 2019 ; Sorkness et al. , 2017 ) and likely would benefit most students. However, we examine how these recommendations may be particularly important for students with depression. As we hypothesized, these recommendations directly address three aspects of research: mentors, lab environment, and failure. A caveat of these recommendations is that more research needs to be done to explore the experiences of students with depression and how these practices actually impact students with depression, but our national sample of undergraduate researchers with depression can provide an initial starting point for a discussion about how to improve research experiences for these students.
Recommendations to Make Undergraduate Research Experiences More Inclusive for Students with Depression
Recognize student depression as a valid illness..
Allow students with depression to take time off of research by simply saying that they are sick and provide appropriate time for students to recover from depressive episodes. Also, make an effort to destigmatize mental health issues.
Undergraduate researchers described both psychological and physical symptoms that manifested as a result of their depression and highlighted how such symptoms prevented them from performing to their full potential in undergraduate research. For example, students described how their depression would cause them to feel unmotivated, which would often negatively affect their research productivity. In cases in which students were motivated enough to come in and do their research, they described having difficulty concentrating or engaging in the work. Further, when doing research, students felt less creative and less willing to take risks, which may alter the quality of their work. Students also sometimes struggled to socialize in the lab. They described feeling less social and feeling overly self-critical. In sum, students described that, when they experienced a depressive episode, they were not able to perform to the best of their ability, and it sometimes took a toll on them to try to act like nothing was wrong, when they were internally struggling with depression. We recommend that research mentors treat depression like any other physical illness; allowing students the chance to recover when they are experiencing a depressive episode can be extremely important to students and can allow them to maximize their productivity upon returning to research ( Judd et al. , 2000 ). Students explained that if they are not able to take the time to focus on recovering during a depressive episode, then they typically continue to struggle with depression, which negatively affects their research. This sentiment is echoed by researchers in psychiatry who have found that patients who do not fully recover from a depressive episode are more likely to relapse and to experience chronic depression ( Judd et al. , 2000 ). Students described not doing tasks or not showing up to research because of their depression but struggling with how to share that information with their research mentors. Often, students would not say anything, which caused them anxiety because they were worried about what others in the lab would say to them when they returned. Admittedly, many students understood why this behavior would cause their research mentors to be angry or frustrated, but they weighed the consequences of their research mentors’ displeasure against the consequences of revealing their depression and decided it was not worth admitting to being depressed. This aligns with literature that suggests that when individuals have concealable stigmatized identities, or identities that can be hidden and that carry negative stereotypes, such as depression, they will often keep them concealed to avoid negative judgment or criticism ( Link and Phelan, 2001 ; Quinn and Earnshaw, 2011 ; Jones and King, 2014 ; Cooper and Brownell, 2016 ; Cooper et al. , 2019b ; Cooper et al ., unpublished data ). Therefore, it is important for research mentors to be explicit with students that 1) they recognize mental illness as a valid sickness and 2) that students with mental illness can simply explain that they are sick if they need to take time off. This may be useful to overtly state on a research website or in a research syllabus, contract, or agreement if mentors use such documents when mentoring undergraduates in their lab. Further, research mentors can purposefully work to destigmatize mental health issues by explicitly stating that struggling with mental health issues, such as depression and anxiety, is common. While we do not recommend that mentors ask students directly about depression, because this can force students to share when they are not comfortable sharing, we do recommend providing opportunities for students to reveal their depression ( Chaudoir and Fisher, 2010 ). Mentors can regularly check in with students about how they’re doing, and talk openly about the importance of mental health, which may increase the chance that students may feel comfortable revealing their depression ( Chaudoir and Quinn, 2010 ; Cooper et al ., unpublished data ).
Foster a Positive Lab Environment.
Encourage positivity in the research lab, promote working in shared spaces to enhance social support among lab members, and alleviate competition among undergraduates.
Students in this study highlighted that the “leadership” of the lab, meaning graduate students, postdocs, lab managers, and PIs, were often responsible for establishing the tone of the lab; that is, if they were in a bad mood it would trickle down and negatively affect the moods of the undergraduates. Explicitly reminding lab leadership that their moods can both positively and negatively affect undergraduates may be important in establishing a positive lab environment. Further, students highlighted how they were most likely to experience negative thoughts when they were alone in the lab. Therefore, it may be helpful to encourage all lab members to work in a shared space to enhance social interactions among students and to maximize the likelihood that undergraduates have access to help when needed. A review of 51 studies in psychiatry supported our undergraduate researchers’ perceptions that social relationships positively impacted their depression; the study found that perceived emotional support (e.g., someone available to listen or give advice), perceived instrumental support (e.g., someone available to help with tasks), and large diverse social networks (e.g., being socially connected to a large number of people) were significantly protective against depression ( Santini et al. , 2015 ). Additionally, despite forming positive relationships with other undergraduates in the lab, many undergraduate researchers admitted to constantly comparing themselves with other undergraduates, which led them to feel inferior, negatively affecting their depression. Some students talked about mentors favoring current undergraduates or talking positively about past undergraduates, which further exacerbated their feelings of inferiority. A recent study of students in undergraduate research experiences highlighted that inequitable distribution of praise to undergraduates can create negative perceptions of lab environments for students (Cooper et al. , 2019). Further, the psychology literature has demonstrated that when people feel insecure in their social environments, it can cause them to focus on a hierarchical view of themselves and others, which can foster feelings of inferiority and increase their vulnerability to depression ( Gilbert et al. , 2009 ). Thus, we recommend that mentors be conscious of their behaviors so that they do not unintentionally promote competition among undergraduates or express favoritism toward current or past undergraduates. Praise is likely best used without comparison with others and not done in a public way, although more research on the impact of praise on undergraduate researchers needs to be done. While significant research has been done on mentoring and mentoring relationships in the context of undergraduate research ( Byars-Winston et al. , 2015 ; Aikens et al. , 2017 ; Estrada et al. , 2018 ; Limeri et al. , 2019 ; NASEM, 2019 ), much less has been done on the influence of the lab environment broadly and how people in nonmentoring roles can influence one another. Yet, this study indicates the potential influence of many different members of the lab, not only their mentors, on students with depression.
Develop More Personal Relationships with Undergraduate Researchers and Provide Sufficient Guidance.
Make an effort to establish more personal relationships with undergraduates and ensure that they perceive that they have access to sufficient help and guidance with regard to their research.
When we asked students explicitly how research mentors could help create more inclusive environments for undergraduate researchers with depression, students overwhelmingly said that building mentor–student relationships would be extremely helpful. Students suggested that mentors could get to know students on a more personal level by asking about their career interests or interests outside of academia. Students also remarked that establishing a more personal relationship could help build the trust needed in order for undergraduates to confide in their research mentors about their depression, which they perceived would strengthen their relationships further because they could be honest about when they were not feeling well or their mentors might even “check in” with them in times where they were acting differently than normal. This aligns with studies showing that undergraduates are most likely to reveal a stigmatized identity, such as depression, when they form a close relationship with someone ( Chaudoir and Quinn, 2010 ). Many were intimidated to ask for research-related help from their mentors and expressed that they wished they had established a better relationship so that they would feel more comfortable. Therefore, we recommend that research mentors try to establish relationships with their undergraduates and explicitly invite them to ask questions or seek help when needed. These recommendations are supported by national recommendations for mentoring ( NASEM, 2019 ) and by literature that demonstrates that both social support (listening and talking with students) and instrumental support (providing students with help) have been shown to be protective against depression ( Santini et al. , 2015 ).
Treat Undergraduates with Respect and Remember to Praise Them.
Avoid providing harsh criticism and remember to praise undergraduates. Students with depression often have low self-esteem and are especially self-critical. Therefore, praise can help calibrate their overly negative self-perceptions.
Students in this study described that receiving criticism from others, especially harsh criticism, was particularly difficult for them given their depression. Multiple studies have demonstrated that people with depression can have an abnormal or maladaptive response to negative feedback; scientists hypothesize that perceived failure on a particular task can trigger failure-related thoughts that interfere with subsequent performance ( Eshel and Roiser, 2010 ). Thus, it is important for research mentors to remember to make sure to avoid unnecessarily harsh criticisms that make students feel like they have failed (more about failure is described in the next recommendation). Further, students with depression often have low self-esteem or low “personal judgment of the worthiness that is expressed in the attitudes the individual holds towards oneself” ( Heatherton et al. , 2003 , p. 220; Sowislo and Orth, 2013 ). Specifically, a meta-analysis of longitudinal studies found that low self-esteem is predictive of depression ( Sowislo and Orth, 2013 ), and depression has also been shown to be highly related to self-criticism ( Luyten et al. , 2007 ). Indeed, nearly all of the students in our study described thinking that they are “not good enough,” “worthless,” or “inadequate,” which is consistent with literature showing that people with depression are self-critical ( Blatt et al. , 1982 ; Gilbert et al. , 2006 ) and can be less optimistic of their performance on future tasks and rate their overall performance on tasks less favorably than their peers without depression ( Cane and Gotlib, 1985 ). When we asked students what aspects of undergraduate research helped their depression, students described that praise from their mentors was especially impactful, because they thought so poorly of themselves and they needed to hear something positive from someone else in order to believe it could be true. Praise has been highlighted as an important aspect of mentoring in research for many years ( Ashford, 1996 ; Gelso and Lent, 2000 ; Brown et al. , 2009 ) and may be particularly important for students with depression. In fact, praise has been shown to enhance individuals’ motivation and subsequent productivity ( Hancock, 2002 ; Henderlong and Lepper, 2002 ), factors highlighted by students as negatively affecting their depression. However, something to keep in mind is that a student with depression and a student without depression may process praise differently. For a student with depression, a small comment that praises the student’s work may not be sufficient for the student to process that comment as praise. People with depression are hyposensitive to reward or have reward-processing deficits ( Eshel and Roiser, 2010 ); therefore, praise may affect students without depression more positively than it would affect students with depression. Research mentors should be mindful that students with depression often have a negative view of themselves, and while students report that praise is extremely important, they may have trouble processing such positive feedback.
Normalize Failure and Be Explicit about the Importance of Research Contributions.
Explicitly remind students that experiencing failure is expected in research. Also explain to students how their individual work relates to the overall project so that they can understand how their contributions are important. It can also be helpful to explain to students why the research project as a whole is important in the context of the greater scientific community.
Experiencing failure has been thought to be a potentially important aspect of undergraduate research, because it may provide students with the potential to develop integral scientific skills such as the ability to navigate challenges and persevere ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, in the interviews, students described that when their science experiments failed, it was particularly tough for their depression. Students’ negative reaction to experiencing failure in research is unsurprising, given recent literature that has predicted that students may be inadequately prepared to approach failure in science ( Henry et al. , 2019 ). However, the literature suggests that students with depression may find experiencing failure in research to be especially difficult ( Elliott et al. , 1997 ; Mongrain and Blackburn, 2005 ; Jones et al. , 2009 ). One potential hypothesis is that students with depression may be more likely to have fixed mindsets or more likely to believe that their intelligence and capacity for specific abilities are unchangeable traits ( Schleider and Weisz, 2018 ); students with a fixed mindset have been hypothesized to have particularly negative responses to experiencing failure in research, because they are prone to quitting easily in the face of challenges and becoming defensive when criticized ( Forsythe and Johnson, 2017 ; Dweck, 2008 ). A study of life sciences undergraduates enrolled in CUREs identified three strategies of students who adopted adaptive coping mechanisms, or mechanisms that help an individual maintain well-being and/or move beyond the stressor when faced with failure in undergraduate research: 1) problem solving or engaging in strategic planning and decision making, 2) support seeking or finding comfort and help with research, and 3) cognitive restructuring or reframing a problem from negative to positive and engaging in self encouragement ( Gin et al. , 2018 ). We recommend that, when undergraduates experience failure in science, their mentors be proactive in helping them problem solve, providing help and support, and encouraging them. Students also explained that mentors sharing their own struggles as undergraduate and graduate students was helpful, because it normalized failure. Sharing personal failures in research has been recommended as an important way to provide students with psychosocial support during research ( NASEM, 2019 ). We also suggest that research mentors take time to explain to students why their tasks in the lab, no matter how small, contribute to the greater research project ( Cooper et al. , 2019a ). Additionally, it is important to make sure that students can explain how the research project as a whole is contributing to the scientific community ( Gin et al. , 2018 ). Students highlighted that contributing to something important was really helpful for their depression, which is unsurprising, given that studies have shown that meaning in life or people’s comprehension of their life experiences along with a sense of overarching purpose one is working toward has been shown to be inversely related to depression ( Steger, 2013 ).
Limitations and Future Directions
This work was a qualitative interview study intended to document a previously unstudied phenomenon: depression in the context of undergraduate research experiences. We chose to conduct semistructured interviews rather than a survey because of the need for initial exploration of this area, given the paucity of prior research. A strength of this study is the sampling approach. We recruited a national sample of 35 undergraduates engaged in undergraduate research at 12 different public R1 institutions. Despite our representative sample from R1 institutions, these findings may not be generalizable to students at other types of institutions; lab environments, mentoring structures, and interactions between faculty and undergraduate researchers may be different at other institution types (e.g., private R1 institutions, R2 institutions, master’s-granting institutions, primarily undergraduate institutions, and community colleges), so we caution against making generalizations about this work to all undergraduate research experiences. Future work could assess whether students with depression at other types of institutions have similar experiences to students at research-intensive institutions. Additionally, we intentionally did not explore the experiences of students with specific identities owing to our sample size and the small number of students in any particular group (e.g., students of a particular race, students with a graduate mentor as the primary mentor). We intend to conduct future quantitative studies to further explore how students’ identities and aspects of their research affect their experiences with depression in undergraduate research.
The students who participated in the study volunteered to be interviewed about their depression; therefore, it is possible that depression is a more salient part of these students’ identities and/or that they are more comfortable talking about their depression than the average population of students with depression. It is also important to acknowledge the personal nature of the topic and that some students may not have fully shared their experiences ( Krumpal, 2013 ), particularly those experiences that may be emotional or traumatizing ( Kahn and Garrison, 2009 ). Additionally, our sample was skewed toward females (77%). While females do make up approximately 60% of students in biology programs on average ( Eddy et al. , 2014 ), they are also more likely to report experiencing depression ( American College Health Association, 2018 ; Evans et al. , 2018 ). However, this could be because women have higher rates of depression or because males are less likely to report having depression; clinical bias, or practitioners’ subconscious tendencies to overlook male distress, may underestimate depression rates in men ( Smith et al. , 2018 ). Further, females are also more likely to volunteer to participate in studies ( Porter and Whitcomb, 2005 ); therefore, many interview studies have disproportionately more females in the data set (e.g., Cooper et al. , 2017 ). If we had been able to interview more male students, we might have identified different findings. Additionally, we limited our sample to life sciences students engaged in undergraduate research at public R1 institutions. It is possible that students in other majors may have different challenges and opportunities for students with depression, as well as different disciplinary stigmas associated with mental health.
In this exploratory interview study, we identified a variety of ways in which depression in undergraduates negatively affected their undergraduate research experiences. Specifically, we found that depression interfered with students’ motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing. We also identified that research can negatively affect depression in undergraduates. Experiencing failure in research can exacerbate student depression, especially when students do not have access to adequate guidance. Additionally, being alone or having negative interactions with others in the lab worsened students’ depression. However, we also found that undergraduate research can positively affect students’ depression. Research can provide a familiar space where students can feel as though they are contributing to something meaningful. Additionally, students reported that having access to adequate guidance and a social support network within the research lab also positively affected their depression. We hope that this work can spark conversations about how to make undergraduate research experiences more inclusive of students with depression and that it can stimulate additional research that more broadly explores the experiences of undergraduate researchers with depression.
Important note
If you or a student experience symptoms of depression and want help, there are resources available to you. Many campuses provide counseling centers equipped to provide students, staff, and faculty with treatment for depression, as well as university-dedicated crisis hotlines. Additionally, there are free 24/7 services such as Crisis Text Line, which allows you to text a trained live crisis counselor (Text “CONNECT” to 741741; Text Depression Hotline , 2019 ), and phone hotlines such as the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK). You can also learn more about depression and where to find help near you through the Anxiety and Depression Association of American website: https://adaa.org ( Anxiety and Depression Association of America, 2019 ) and the Depression and Biopolar Support Alliance: http://dbsalliance.org ( Depression and Biopolar Support Alliance, 2019 ).
ACKNOWLEDGMENTS
We are extremely grateful to the undergraduate researchers who shared their thoughts and experiences about depression with us. We acknowledge the ASU LEAP Scholars for helping us create the original survey and Rachel Scott for her helpful feedback on earlier drafts of this article. L.E.G. was supported by a National Science Foundation (NSF) Graduate Fellowship (DGE-1311230) and K.M.C. was partially supported by a Howard Hughes Medical Institute (HHMI) Inclusive Excellence grant (no. 11046) and an NSF grant (no. 1644236). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF or HHMI.
- Aikens, M. L., Robertson, M. M., Sadselia, S., Watkins, K., Evans, M., Runyon, C. R. , … & Dolan, E. L. ( 2017 ). Race and gender differences in undergraduate research mentoring structures and research outcomes . CBE—Life Sciences Education , 16 (2), ar34. Link , Google Scholar
- Aikens, M. L., Sadselia, S., Watkins, K., Evans, M., Eby, L. T., & Dolan, E. L. ( 2016 ). A social capital perspective on the mentoring of undergraduate life science researchers: An empirical study of undergraduate–postgraduate–faculty triads . CBE—Life Sciences Education , 15 (2), ar16. Link , Google Scholar
- Aldwin, C., & Greenberger, E. ( 1987 ). Cultural differences in the predictors of depression . American Journal of Community Psychology , 15 (6), 789–813. Medline , Google Scholar
- American Association for the Advancement of Science . ( 2011 ). Vision and change in undergraduate biology education: A call to action . Retrieved November 29, 2019, from http://visionandchange.org/files/2013/11/aaas-VISchange-web1113.pdf Google Scholar
- American College Health Association . ( 2018 ). Undergraduate reference group executive summary, Fall 2018 . Retrieved November 29, 2019, from www.acha.org/documents/ncha/NCHA-II_Fall_2018_Reference_Group_Executive_Summary.pdf Google Scholar
- American College Health Association . ( 2019 ). Retrieved November 29, 2019, from NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf www.acha.org/documents/ncha/NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf Google Scholar
- American Psychiatric Association . ( 2013 ). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. Google Scholar
- Aneshensel, C. S., & Stone, J. D. ( 1982 ). Stress and depression: A test of the buffering model of social support . Archives of General Psychiatry , 39 (12), 1392–1396. Medline , Google Scholar
- Anxiety and Depression Association of America . ( 2019 ). Home page . Retrieved November 29, 2019, from https://adaa.org Google Scholar
- Armbruster, P., Patel, M., Johnson, E., & Weiss, M. ( 2009 ). Active learning and student-centered pedagogy improve student attitudes and performance in introductory biology . CBE—Life Sciences Education , 8 (3), 203–213. Link , Google Scholar
- Ashford, S. J. ( 1996 ). Working with doctoral students: Rhythms of Academic Life: Personal Accounts of Careers in Academia . In Front, P. J.Taylor, M. S. (Eds.), Rhythms of Academic Life: Personal Accounts of Careers in Academia (pp. 153–158). Thousand Oaks, CA: Sage. Google Scholar
- Auchincloss, L. C., Laursen, S. L., Branchaw, J. L., Eagan, K., Graham, M., Hanauer, D. I. , … & Rowland, S. ( 2014 ). Assessment of course-based undergraduate research experiences: A meeting report . CBE—Life Sciences Education , 13 (1), 29–40. Link , Google Scholar
- Barak, M. E. M., Levin, A., Nissly, J. A., & Lane, C. J. ( 2006 ). Why do they leave? Modeling child welfare workers’ turnover intentions . Children and Youth Services Review , 28 (5), 548–577. Google Scholar
- Bauer, K. W., & Bennett, J. S. ( 2003 ). Alumni perceptions used to assess undergraduate research experience . Journal of Higher Education , 74 (2), 210–230. Google Scholar
- Birks, M., & Mills, J. ( 2015 ). Grounded theory: A practical guide . Thousand Oaks, CA: Sage. Google Scholar
- Blatt, S. J., Quinlan, D. M., Chevron, E. S., McDonald, C., & Zuroff, D. ( 1982 ). Dependency and self-criticism: Psychological dimensions of depression . Journal of Consulting and Clinical Psychology , 50 (1), 113. Medline , Google Scholar
- Brown, R. T., Daly, B. P., & Leong, F. T. ( 2009 ). Mentoring in research: A developmental approach . Professional Psychology: Research and Practice , 40 (3), 306. Google Scholar
- Brownell, S. E., Hekmat-Scafe, D. S., Singla, V., Seawell, P. C., Imam, J. F. C., Eddy, S. L. , … & Cyert, M. S. ( 2015 ). A high-enrollment course-based undergraduate research experience improves student conceptions of scientific thinking and ability to interpret data . CBE—Life Sciences Education , 14 (2), ar21. Link , Google Scholar
- Brownell, S. E., & Kloser, M. J. ( 2015 ). Toward a conceptual framework for measuring the effectiveness of course-based undergraduate research experiences in undergraduate biology . Studies in Higher Education , 40 (3), 525–544. Google Scholar
- Byars-Winston, A. M., Branchaw, J., Pfund, C., Leverett, P., & Newton, J. ( 2015 ). Culturally diverse undergraduate researchers’ academic outcomes and perceptions of their research mentoring relationships . International Journal of Science Education , 37 (15), 2533–2554. Medline , Google Scholar
- Cane, D. B., & Gotlib, I. H. ( 1985 ). Depression and the effects of positive and negative feedback on expectations, evaluations, and performance . Cognitive Therapy and Research , 9 (2), 145–160. Google Scholar
- Ceci, S. J., & Williams, W. M. ( 2010 ). Sex differences in math-intensive fields . Current Directions in Psychological Science , 19 (5), 275–279. Medline , Google Scholar
- Center for Collegiate Mental Health . ( 2017 ). Center for Collegiate Mental Health 2017 Annual Report . State College, PA: Penn State Universit. Google Scholar
- Charmaz, K. ( 2006 ). Constructing grounded theory: A practical guide through qualitative research . Thousand Oaks, CA: Sage. Google Scholar
- Chaudoir, S. R., & Fisher, J. D. ( 2010 ). The disclosure processes model: Understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity . Psychological Bulletin , 136 (2), 236. Medline , Google Scholar
- Chaudoir, S. R., & Quinn, D. M. ( 2010 ). Revealing concealable stigmatized identities: The impact of disclosure motivations and positive first-disclosure experiences on fear of disclosure and well-being . Journal of Social Issues , 66 (3), 570–584. Medline , Google Scholar
- Clance, P. R., & Imes, S. A. ( 1978 ). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention . Psychotherapy: Theory, Research & Practice , 15 (3), 241. Google Scholar
- Cooper, K. M., Ashley, M., & Brownell, S. E. ( 2017 ). A bridge to active learning: A summer bridge program helps students maximize their active-learning experiences and the active-learning experiences of others . CBE—Life Sciences Education , 16 (1), ar17. Link , Google Scholar
- Cooper, K. M., Blattman, J. N., Hendrix, T., & Brownell, S. E. ( 2019a ). The impact of broadly relevant novel discoveries on student project ownership in a traditional lab course turned CURE . CBE—Life Sciences Education , 18 (4), ar57. Link , Google Scholar
- Cooper, K. M., & Brownell, S. E. ( 2016 ). Coming out in class: Challenges and benefits of active learning in a biology classroom for LGBTQIA students . CBE—Life Sciences Education , 15 (3), ar37. https://doi.org/10.1187/cbe.16-01-0074 Link , Google Scholar
- Cooper, K. M., Brownell, S. E., & Gormally, C. C. ( 2019b ). Coming out to the class: Identifying factors that influence college biology instructor decisions about whether to reveal their LGBQ identity in class . Journal of Women and Minorities in Science and Engineering , 25 (3). Google Scholar
- Cooper, K. M., Downing, V. R., & Brownell, S. E. ( 2018 ). The influence of active learning practices on student anxiety in large-enrollment college science classrooms . International Journal of STEM Education , 5 (1), 23. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., Akeeh, B., Clark, C. E., Hunter, J. S., Roderick, T. B. , … & Brownell, S. E. ( 2019c ). Factors that predict life sciences student persistence in undergraduate research experiences . PLoS ONE , 14 (8). https://doi.org/10.1371/journal.pone.0220186 Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( 2019d ). Diagnosing differences in what introductory biology students in a fully online and an in-person biology degree program know and do regarding medical school admission . Advances in Physiology Education , 43 (2), 221–232. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( In press ). Depression as a concealable stigmatized identity: What influences whether students conceal or reveal their depression in undergraduate research experiences? International Journal of STEM Education , ( in press ). Google Scholar
- Depression and Biopolar Support Alliance . ( 2019 ). Home page . Retrieved November 28, 2019, from www.dbsalliance.org Google Scholar
- Deroma, V. M., Leach, J. B., & Leverett, J. P. ( 2009 ). The relationship between depression and college academic performance . College Student Journal , 43 (2), 325–335. Google Scholar
- Dweck, C. S. ( 2008 ). Mindset: The new psychology of success . New York, NY: Random House Digital. Google Scholar
- Dyson, R., & Renk, K. ( 2006 ). Freshmen adaptation to university life: Depressive symptoms, stress, and coping . Journal of Clinical Psychology , 62 (10), 1231–1244. Medline , Google Scholar
- Eddy, S. L., Brownell, S. E., & Wenderoth, M. P. ( 2014 ). Gender gaps in achievement and participation in multiple introductory biology classrooms . CBE—Life Sciences Education , 13 (3), 478–492. https://doi.org/10.1187/cbe.13-10-0204 Link , Google Scholar
- Eisenberg, D., Gollust, S. E., Golberstein, E., & Hefner, J. L. ( 2007 ). Prevalence and correlates of depression, anxiety, and suicidality among university students . American Journal of Orthopsychiatry , 77 (4), 534–542. Medline , Google Scholar
- Elliott, R., Sahakian, B. J., Herrod, J. J., Robbins, T. W., & Paykel, E. S. ( 1997 ). Abnormal response to negative feedback in unipolar depression: Evidence for a diagnosis specific impairment . Journal of Neurology, Neurosurgery & Psychiatry , 63 (1), 74–82. Medline , Google Scholar
- Eshel, N., & Roiser, J. P. ( 2010 ). Reward and punishment processing in depression . Biological Psychiatry , 68 (2), 118–124. Medline , Google Scholar
- Estrada, M., Hernandez, P. R., & Schultz, P. W. ( 2018 ). A longitudinal study of how quality mentorship and research experience integrate underrepresented minorities into STEM careers . CBE—Life Sciences Education , 17 (1), ar9. Link , Google Scholar
- Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., & Vanderford, N. L. ( 2018 ). Evidence for a mental health crisis in graduate education . Nature Biotechnology , 36 (3), 282. Medline , Google Scholar
- Everson, H. T., Tobias, S., Hartman, H., & Gourgey, A. ( 1993 ). Test anxiety and the curriculum: The subject matters . Anxiety, Stress, and Coping , 6 (1), 1–8. Google Scholar
- Flaherty, C. ( 2018 ). New study says graduate students’ mental health is a “crisis.” Retrieved November 29, 2019, from www.insidehighered.com/news/2018/03/06/new-study-says-graduate-students-mental-health-crisis Google Scholar
- Forsythe, A., & Johnson, S. ( 2017 ). Thanks, but no-thanks for the feedback . Assessment & Evaluation in Higher Education , 42 (6), 850–859. Google Scholar
- Garlow, S. J., Rosenberg, J., Moore, J. D., Haas, A. P., Koestner, B., Hendin, H., & Nemeroff, C. B. ( 2008 ). Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University . Depression and Anxiety , 25 (6), 482–488. Medline , Google Scholar
- Gelso, C. J., & Lent, R. W. ( 2000 ). Scientific training and scholarly productivity: The person, the training environment, and their interaction . In Brown, S. D.Lent, R. W. (Eds.), Handbook of counseling psychology (pp. 109–139). Hoboken, NJ: John Wiley & Sons Inc. Google Scholar
- Gilbert, P., Baldwin, M. W., Irons, C., Baccus, J. R., & Palmer, M. ( 2006 ). Self-criticism and self-warmth: An imagery study exploring their relation to depression . Journal of Cognitive Psychotherapy , 20 (2), 183. Google Scholar
- Gilbert, P., McEwan, K., Bellew, R., Mills, A., & Gale, C. ( 2009 ). The dark side of competition: How competitive behaviour and striving to avoid inferiority are linked to depression, anxiety, stress and self-harm . Psychology and Psychotherapy: Theory, Research and Practice , 82 (2), 123–136. Medline , Google Scholar
- Gin, L. E., Rowland, A. A., Steinwand, B., Bruno, J., & Corwin, L. A. ( 2018 ). Students who fail to achieve predefined research goals may still experience many positive outcomes as a result of CURE participation . CBE—Life Sciences Education , 17 (4), ar57. Link , Google Scholar
- Glesne, C., & Peshkin, A. ( 1992 ). Becoming qualitative researchers: An introduction . London, England, UK: Longman. Google Scholar
- Grav, S., Hellzèn, O., Romild, U., & Stordal, E. ( 2012 ). Association between social support and depression in the general population: The HUNT study, a cross-sectional survey . Journal of Clinical Nursing , 21 (1–2), 111–120. Medline , Google Scholar
- Guest, G., Bunce, A., & Johnson, L. ( 2006 ). How many interviews are enough? An experiment with data saturation and variability . Field Methods , 18 (1), 59–82. Google Scholar
- Hancock, D. R. ( 2002 ). Influencing graduate students’ classroom achievement, homework habits and motivation to learn with verbal praise . Educational Research , 44 (1), 83–95. Google Scholar
- Hannah, D. R., & Lautsch, B. A. ( 2011 ). Counting in qualitative research: Why to conduct it, when to avoid it, and when to closet it . Journal of Management Inquiry , 20 (1), 14–22. Google Scholar
- Heatherton, T. F., & Wyland, C. L. ( 2003 ). Assessing self-esteem . In Lopez, S. J.Snyder, C. R. (Eds.), Positive psychological assessment: A handbook of models and measures (pp. 219–233). Washington, DC: American Psychological Association. https://doi.org/10.1037/10612-014 . Google Scholar
- Henderlong, J., & Lepper, M. R. ( 2002 ). The effects of praise on children’s intrinsic motivation: A review and synthesis . Psychological Bulletin , 128 (5), 774. Medline , Google Scholar
- Henry, M. A., Shorter, S., Charkoudian, L., Heemstra, J. M., & Corwin, L. A. ( 2019 ). FAIL is not a four-letter word: A theoretical framework for exploring undergraduate students’ approaches to academic challenge and responses to failure in STEM learning environments . CBE—Life Sciences Education , 18 (1), ar11. Link , Google Scholar
- Hernandez, P. R., Woodcock, A., Estrada, M., & Schultz, P. W. ( 2018 ). Undergraduate research experiences broaden diversity in the scientific workforce . BioScience , 68 (3), 204–211. Google Scholar
- Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Applying the stress process model to stress–burnout and stress–depression relationships in biomedical doctoral students: A cross-sectional pilot study . CBE—Life Sciences Education , 18 (4), ar51. Link , Google Scholar
- Howell, E., & McFeeters, J. ( 2008 ). Children’s mental health care: Differences by race/ethnicity in urban/rural areas . Journal of Health Care for the Poor and Underserved , 19 (1), 237–247. Medline , Google Scholar
- Hysenbegasi, A., Hass, S. L., & Rowland, C. R. ( 2005 ). The impact of depression on the academic productivity of university students . Journal of Mental Health Policy and Economics , 8 (3), 145. Medline , Google Scholar
- Ibrahim, A. K., Kelly, S. J., Adams, C. E., & Glazebrook, C. ( 2013 ). A systematic review of studies of depression prevalence in university students . Journal of Psychiatric Research , 47 (3), 391–400. Medline , Google Scholar
- Intemann, K. ( 2009 ). Why diversity matters: Understanding and applying the diversity component of the National Science Foundation’s broader impacts criterion . Social Epistemology , 23 (3–4), 249–266. Google Scholar
- Ishiyama, J. ( 2002 ). Does early participation in undergraduate research benefit social science and humanities students? College Student Journal , 36 (3), 381–387. Google Scholar
- Jenkins, S. R., Belanger, A., Connally, M. L., Boals, A., & Durón, K. M. ( 2013 ). First-generation undergraduate students’ social support, depression, and life satisfaction . Journal of College Counseling , 16 (2), 129–142. Google Scholar
- Jobst, A., Sabass, L., Palagyi, A., Bauriedl-Schmidt, C., Mauer, M. C., Sarubin, N. , … & Zill, P. ( 2015 ). Effects of social exclusion on emotions and oxytocin and cortisol levels in patients with chronic depression . Journal of Psychiatric Research , 60 , 170–177. Medline , Google Scholar
- Jones, K. P., & King, E. B. ( 2014 ). Managing concealable stigmas at work: A review and multilevel model . Journal of Management , 40 (5), 1466–1494. Google Scholar
- Jones, M. T., Barlow, A. E., & Villarejo, M. ( 2010 ). Importance of undergraduate research for minority persistence and achievement in biology . Journal of Higher Education , 81 (1), 82–115. Google Scholar
- Jones, N. P., Papadakis, A. A., Hogan, C. M., & Strauman, T. J. ( 2009 ). Over and over again: Rumination, reflection, and promotion goal failure and their interactive effects on depressive symptoms . Behaviour Research and Therapy , 47 (3), 254–259. Medline , Google Scholar
- Judd, L. L., Paulus, M. J., Schettler, P. J., Akiskal, H. S., Endicott, J., Leon, A. C. , … & Keller, M. B. ( 2000 ). Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? American Journal of Psychiatry , 157 (9), 1501–1504. Medline , Google Scholar
- Kahn, J. H., & Garrison, A. M. ( 2009 ). Emotional self-disclosure and emotional avoidance: Relations with symptoms of depression and anxiety . Journal of Counseling Psychology , 56 (4), 573. Google Scholar
- Kataoka, S. H., Zhang, L., & Wells, K. B. ( 2002 ). Unmet need for mental health care among US children: Variation by ethnicity and insurance status . American Journal of Psychiatry , 159 (9), 1548–1555. Medline , Google Scholar
- Kreger, D. W. ( 1995 ). Self-esteem, stress, and depression among graduate students . Psychological Reports , 76 (1), 345–346. Medline , Google Scholar
- Krumpal, I. ( 2013 ). Determinants of social desirability bias in sensitive surveys: A literature review . Quality & Quantity , 47 (4), 2025–2047. Google Scholar
- Landis, J. R., & Koch, G. G. ( 1977 ). An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers . Biometrics , 33 (2), 363–374. Medline , Google Scholar
- Laursen, S., Hunter, A.-B., Seymour, E., Thiry, H., & Melton, G. ( 2010 ). Undergraduate research in the sciences: Engaging students in real science . Hoboken, NJ: Wiley. Google Scholar
- Limeri, L. B., Asif, M. Z., Bridges, B. H., Esparza, D., Tuma, T. T., Sanders, D. , … & Maltese, A. V. ( 2019 ). “Where’s my mentor?” Characterizing negative mentoring experiences in undergraduate life science research . CBE—Life Sciences Education , 18 (4), ar61. Link , Google Scholar
- Link, B. G., & Phelan, J. C. ( 2001 ). Conceptualizing stigma . Annual Review of Sociology , 27 (1), 363–385. Google Scholar
- Luyten, P., Sabbe, B., Blatt, S. J., Meganck, S., Jansen, B., De Grave, C. , … & Corveleyn, J. ( 2007 ). Dependency and self-criticism: Relationship with major depressive disorder, severity of depression, and clinical presentation . Depression and Anxiety , 24 (8), 586–596. Medline , Google Scholar
- Mabrouk, P. A., & Peters, K. ( 2000 ). Student perspectives on undergraduate research (UR) experiences in chemistry and biology . CUR Quarterly , 21 (1), 25–33. Google Scholar
- Maxwell, J. A. ( 2010 ). Using numbers in qualitative research . Qualitative Inquiry , 16 (6), 475–482. Google Scholar
- Mongrain, M., & Blackburn, S. ( 2005 ). Cognitive vulnerability, lifetime risk, and the recurrence of major depression in graduate students . Cognitive Therapy and Research , 29 (6), 747–768. Google Scholar
- Nagy, G. A., Fang, C. M., Hish, A. J., Kelly, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Burnout and mental health problems in biomedical doctoral students . CBE—Life Sciences Education , 18 (2), ar27. Link , Google Scholar
- National Academies of Sciences, Engineering, and Medicine (NASEM) . ( 2017 ). Undergraduate research experiences for STEM students: Successes, challenges, and opportunities . Washington, DC: National Academies Press. https://doi.org/10.17226/24622 Google Scholar
- NASEM . ( 2019 ). The science of effective mentorship in STEMM . Washington, DC: National Academies Press. Retrieved November 29, 2019, from www.nap.edu/download/25568 Google Scholar
- Osborne, J., & Collins, S. ( 2001 ). Pupils’ views of the role and value of the science curriculum: A focus-group study . International Journal of Science Education , 23 (5), 441–467. https://doi.org/10.1080/09500690010006518 Google Scholar
- Porter, S. R., & Whitcomb, M. E. ( 2005 ). Non-response in student surveys: The role of demographics, engagement and personality . Research in Higher Education , 46 (2), 127–152. Google Scholar
- President’s Council of Advisors on Science and Technology . ( 2012 ). Engage to excel: Producing one million additional college graduates with degrees in science, Technology, Engineering, and mathematics . Washington, DC: U.S. Government Office of Science and Technology. Google Scholar
- Prunuske, A. J., Wilson, J., Walls, M., & Clarke, B. ( 2013 ). Experiences of mentors training underrepresented undergraduates in the research laboratory . CBE—Life Sciences Education , 12 (3), 403–409. Link , Google Scholar
- Quinn, D. M., & Earnshaw, V. A. ( 2011 ). Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes . Social Issues and Policy Review , 5 (1), 160–190. Google Scholar
- Rauckhorst, W. H., Czaja, J. A., & Baxter Magolda, M. ( 2001 ). Measuring the impact of the undergraduate research experience on student intellectual development . Snowbird, UT: Project Kaleidoscope Summer Institute. Google Scholar
- Saldaña, J. ( 2015 ). The coding manual for qualitative researchers . Thousand Oaks, CA: Sage. Google Scholar
- Santiago, C. D., Kaltman, S., & Miranda, J. ( 2013 ). Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of Clinical Psychology , 69 (2), 115–126. Medline , Google Scholar
- Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., & Haro, J. M. ( 2015 ). The association between social relationships and depression: A systematic review . Journal of Affective Disorders , 175 , 53–65. Medline , Google Scholar
- Schleider, J., & Weisz, J. ( 2018 ). A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial . Journal of Child Psychology and Psychiatry , 59 (2), 160–170. Medline , Google Scholar
- Seymour, E., & Hewitt, N. M. ( 1997 ). Talking about leaving: Why undergraduates leave the sciences . Westview Press. Google Scholar
- Seymour, E., & Hunter, A.-B. ( 2019 ). Talking about leaving revisited . New York, NY: Springer. Google Scholar
- Seymour, E., Hunter, A.-B., Laursen, S. L., & DeAntoni, T. ( 2004 ). Establishing the benefits of research experiences for undergraduates in the sciences: First findings from a three-year study . Science Education , 88 (4), 493–534. Google Scholar
- Smith, D. T., Mouzon, D. M., & Elliott, M. ( 2018 ). Reviewing the assumptions about men’s mental health: An exploration of the gender binary . American Journal of Men’s Health , 12 (1), 78–89. Medline , Google Scholar
- Sorkness, C. A., Pfund, C., Ofili, E. O., Okuyemi, K. S., Vishwanatha, J. K., Zavala, M. E. , … & Deveci, A. ( 2017 ). A new approach to mentoring for research careers: The National Research Mentoring Network . BMC Proceedings , 11 , 22. Medline , Google Scholar
- Sowislo, J. F., & Orth, U. ( 2013 ). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies . Psychological Bulletin , 139 (1), 213. Medline , Google Scholar
- Steger, M. F. ( 2013 ). Experiencing meaning in life: Optimal functioning at the nexus of well-being, psychopathology, and spirituality . In Wong, P. T. P. (Ed.), The human quest for meaning (pp. 211–230). England, UK: Routledge. Google Scholar
- Strenta, A. C., Elliott, R., Adair, R., Matier, M., & Scott, J. ( 1994 ). Choosing and leaving science in highly selective institutions . Research in Higher Education , 35 (5), 513–547. Google Scholar
- Text Depression Hotline . ( 2019 ). Crisis text line . Retrieved November 29, 2019, from www.crisistextline.org/depression Google Scholar
- Thiry, H., & Laursen, S. L. ( 2011 ). The role of student–advisor interactions in apprenticing undergraduate researchers into a scientific community of practice . Journal of Science Education and Technology , 20 (6), 771–784. Google Scholar
- Thompson, J. J., Conaway, E., & Dolan, E. L. ( 2016 ). Undergraduate students’ development of social, cultural, and human capital in a networked research experience . Cultural Studies of Science Education , 11 (4), 959–990. Google Scholar
- Trenor, J. M., Miller, M. K., & Gipson, K. G. ( 2011 ). Utilization of a think-aloud protocol to cognitively validate a survey instrument identifying social capital resources of engineering undergraduates . 118th American Society for Engineering Education Annual Conference and Exposition, Vancouver, BC, Canada . Google Scholar
- Turner, R. J., & Noh, S. ( 1988 ). Physical disability and depression: A longitudinal analysis . Journal of Health and Social Behavior , 29 (1), 23–37. Medline , Google Scholar
- Watson, D., & Friend, R. ( 1969 ). Measurement of social-evaluative anxiety . Journal of Consulting and Clinical Psychology , 33 (4), 448. Medline , Google Scholar
- Weeks, J. W., Heimberg, R. G., Fresco, D. M., Hart, T. A., Turk, C. L., Schneier, F. R., & Liebowitz, M. R. ( 2005 ). Empirical validation and psychometric evaluation of the Brief Fear of Negative Evaluation Scale in patients with social anxiety disorder . Psychological Assessment , 17 (2), 179. Medline , Google Scholar
- World Health Organization . ( 2018 ). Depression . Retrieved November 29, 2019, from www.who.int/news-room/fact-sheets/detail/depression Google Scholar
- Wyatt, T., & Oswalt, S. B. ( 2013 ). Comparing mental health issues among undergraduate and graduate students . American Journal of Health Education , 44 (2), 96–107. Google Scholar
- Carly A. Busch ,
- Tala Araghi ,
- Jingyi He ,
- Katelyn M. Cooper , and
- Colin Harrison, Monitoring Editor
- Emma C. Goodwin ,
- Danielle Pais ,
- Logan E. Gin , and
- Derek Braun, Monitoring Editor
- Logan E. Gin ,
- Allyson Aeschliman ,
- Adwoa Kumi Afoakwa ,
- Bryttani A. Allred ,
- Sarah T. Avalle ,
- Amanda Bell ,
- Jessica Berkheimer ,
- Hannah Brzezinski ,
- Rachel Campos ,
- Hozhoo Emerson ,
- Savage Cree Hess ,
- Arron M. Montelongo ,
- Nereus Noshirwani ,
- W. Levi Shelton ,
- Emma M. Valdez ,
- Jennifer White ,
- Quinn White ,
- Ehren Wittekind ,
- Sheela Vemu, Monitoring Editor
- Baylee A. Edwards ,
- Chloe Bowen ,
- M. Elizabeth Barnes , and
- Tati Russo-Tait, Monitoring Editor
- Sara E. Grineski ,
- Danielle X. Morales , and
- Timothy W. Collins
- Carly A. Busch , and
- Tasneem F. Mohammed ,
- Erika M. Nadile ,
- Madison L. Witt ,
- Cindy Vargas ,
- Missy Tran ,
- Joseph Gazing Wolf ,
- Danielle Brister , and
- Sehoya Cotner, Monitoring Editor
- Katelyn M. Cooper ,
- Sarah L. Eddy , and
- Coping behavior versus coping style: characterizing a measure of coping in undergraduate STEM contexts 14 February 2022 | International Journal of STEM Education, Vol. 9, No. 1
- Lisa A. Corwin ,
- Michael E. Ramsey ,
- Eric A. Vance ,
- Elizabeth Woolner ,
- Stevie Maiden ,
- Nina Gustafson and
- Joseph A. Harsh
- Erin Shortlidge, Monitoring Editor
- K. Supriya ,
- Brian Sato, Monitoring Editor
- Clark Coffman, Monitoring Editor
- Nicholas J. Wiesenthal , and
- Maryrose Weatherton and
- Elisabeth E. Schussler
- Erika Offerdahl, Monitoring Editor
- Eight Recommendations to Promote Effective Study Habits for Biology Students Enrolled in Online Courses 29 Apr 2022 | Journal of Microbiology & Biology Education, Vol. 23, No. 1
- Fostering professional development through undergraduate research: supporting faculty mentors and student researchers 30 March 2022 | Mentoring & Tutoring: Partnership in Learning, Vol. 30, No. 2
- Jeffrey Maloy ,
- Monika B. Kwapisz , and
- Bryce E. Hughes
- Terrell Morton, Monitoring Editor
- Anxiety and depression among US college students engaging in undergraduate research during the COVID-19 pandemic 14 December 2021 | Journal of American College Health, Vol. 9
- Danielle Brister ,
- Sara E. Brownell ,
- Chade T. Claiborne ,
- Curtis Lunt ,
- Kobe M. Walker ,
- Tamiru D. Warkina ,
- Yi Zheng , and
- Rebecca Price, Monitoring Editor
- Dominant Learning Styles of Interior Design Students in Generation Z 26 July 2021 | Journal of Interior Design, Vol. 46, No. 4
- Linking Emotional Intelligence, Physical Activity and Aggression among Undergraduates 26 November 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 23
- Advancing undergraduate synthetic biology education: insights from a Canadian iGEM student perspective 1 Oct 2021 | Canadian Journal of Microbiology, Vol. 67, No. 10
- Frank A. Guerrero ,
- Sara E. Brownell , and
- Jennifer Momsen, Monitoring Editor
- Nicholas J. Wiesenthal ,
- Isabella Ferreira , and
- Grant Ean Gardner, Monitoring Editor
- Carolyn E. Clark ,
- Deanna B. Elliott ,
- Travis B. Roderick ,
- Rachel A. Scott ,
- Denisse Arellano ,
- Diana Ramirez ,
- Kimberly Velarde ,
- Michael Gerbasi ,
- Sophia Hughes ,
- Julie A. Roberts ,
- Quinn M. White ,
- Rachelle Spell, Monitoring Editor
- Christine Pfund ,
- Janet L. Branchaw ,
- Melissa McDaniels ,
- Angela Byars-Winston ,
- Steven P. Lee ,, and
- Bruce Birren
- Vladimir Anokhin ,
- MacKenzie J. Gray ,
- Daniel E. Zajic ,
- Jason E. Podrabsky , and
- Erin E. Shortlidge
- Depression as a concealable stigmatized identity: what influences whether students conceal or reveal their depression in undergraduate research experiences? 4 June 2020 | International Journal of STEM Education, Vol. 7, No. 1
Submitted: 4 November 2019 Revised: 24 February 2020 Accepted: 6 March 2020
© 2020 K. M. Cooper, L. E. Gin, et al. CBE—Life Sciences Education © 2020 The American Society for Cell Biology. This article is distributed by The American Society for Cell Biology under license from the author(s). It is available to the public under an Attribution–Noncommercial–Share Alike 3.0 Unported Creative Commons License (http://creativecommons.org/licenses/by-nc-sa/3.0).
Assessing the role of depression-related stigma in depression care in Malawi
Add to collection, downloadable content.
- Affiliation: Gillings School of Global Public Health, Department of Epidemiology
- Globally, depression is prevalent and burdensome. People with depression that hold stigmatizing beliefs related to their condition are at higher risk of never seeking treatment and/or falling out of treatment after initial engagement, posing significant risks to depression recovery. Research in the U.S. found a reduction in stigma after patients engaged in supportive counseling compared to other treatment methods for depression. There has not been much research on mental health stigma in Malawi. Therefore, using data from the Sub-Saharan Africa Regional Partnership (SHARP) for Mental Health Capacity Building scale-up trial, this dissertation expands upon ongoing depression-related implementation science research efforts in the region by exploring the role of stigma during depression care. Patients in the cohort (N=743) were largely treatment-naïve and had depressive symptoms indicated by the Patient Health Questionnaire-9. This dissertation aimed to 1) estimate the effect of baseline anticipated treatment-related stigma on the 3-month probability of depression remission and 2) estimate the association between referral to clinically appropriate problem-solving based therapy and internalized depression stigma three months later. We found that the probability of achieving depression remission at the 3-month interview among participants with high anticipated treatment-related stigma (0.31; 95% Confidence Interval [CI]: 0.23, 0.39)) was 10 percentage points lower than among patients who had low or neutral levels of anticipated treatment-related stigma (risk: 0.41; 95% CI: 0.36, 0.45; RD: -0.10; 95% CI: -0.19, -0.003). In our analysis of the effect of counseling referral on 3-month probability of having high internalized depression stigma, we found that the probability of high internalized stigma was 33 percentage points greater (95% Confidence Interval [CI]: 0.16, 0.50) among patients who were referred to counseling (0.43; 95% CI: 0.32, 0.55) compared to those who were not referred to counseling (0.10; 95% CI: -0.10, 0.30). Taken together, the results from this dissertation highlight 1) the critical role that treatment-related stigma plays in the path to depression recovery, 2) the lack of adequate solutions currently being implemented to address internalized stigma during depression treatment, and 3) the potential impact of an intervention targeting depression-related stigma among patients receiving depression care in Malawi.
- Public health
- Mental health
- https://doi.org/10.17615/0gj3-ya05
- Dissertation
- In Copyright - Educational Use Permitted
- Pence, Brian W
- Gaynes, Bradley N
- Hill, Sherika
- Aiello, Allison E
- Keil, Alexander
- Doctor of Philosophy
- University of North Carolina at Chapel Hill Graduate School
This work has no parents.
Select type of work
Master's papers.
Deposit your masters paper, project or other capstone work. Theses will be sent to the CDR automatically via ProQuest and do not need to be deposited.
Scholarly Articles and Book Chapters
Deposit a peer-reviewed article or book chapter. If you would like to deposit a poster, presentation, conference paper or white paper, use the “Scholarly Works” deposit form.
Undergraduate Honors Theses
Deposit your senior honors thesis.
Scholarly Journal, Newsletter or Book
Deposit a complete issue of a scholarly journal, newsletter or book. If you would like to deposit an article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
Deposit your dataset. Datasets may be associated with an article or deposited separately.
Deposit your 3D objects, audio, images or video.
Poster, Presentation, Protocol or Paper
Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 July 2021
Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students
- Emily N. Satinsky 1 ,
- Tomoki Kimura 2 ,
- Mathew V. Kiang 3 , 4 ,
- Rediet Abebe 5 , 6 ,
- Scott Cunningham 7 ,
- Hedwig Lee 8 ,
- Xiaofei Lin 9 ,
- Cindy H. Liu 10 , 11 ,
- Igor Rudan 12 ,
- Srijan Sen 13 ,
- Mark Tomlinson 14 , 15 ,
- Miranda Yaver 16 &
- Alexander C. Tsai 1 , 11 , 17
Scientific Reports volume 11 , Article number: 14370 ( 2021 ) Cite this article
88k Accesses
74 Citations
821 Altmetric
Metrics details
- Epidemiology
- Health policy
- Quality of life
University administrators and mental health clinicians have raised concerns about depression and anxiety among Ph.D. students, yet no study has systematically synthesized the available evidence in this area. After searching the literature for studies reporting on depression, anxiety, and/or suicidal ideation among Ph.D. students, we included 32 articles. Among 16 studies reporting the prevalence of clinically significant symptoms of depression across 23,469 Ph.D. students, the pooled estimate of the proportion of students with depression was 0.24 (95% confidence interval [CI], 0.18–0.31; I 2 = 98.75%). In a meta-analysis of the nine studies reporting the prevalence of clinically significant symptoms of anxiety across 15,626 students, the estimated proportion of students with anxiety was 0.17 (95% CI, 0.12–0.23; I 2 = 98.05%). We conclude that depression and anxiety are highly prevalent among Ph.D. students. Data limitations precluded our ability to obtain a pooled estimate of suicidal ideation prevalence. Programs that systematically monitor and promote the mental health of Ph.D. students are urgently needed.
Similar content being viewed by others
Prevalence of depression among Chinese university students: a systematic review and meta-analysis
A repeated cross-sectional analysis assessing mental health conditions of adults as per student status during key periods of the COVID-19 epidemic in France
Relationship between depression and quality of life among students: a systematic review and meta-analysis
Introduction.
Mental health problems among graduate students in doctoral degree programs have received increasing attention 1 , 2 , 3 , 4 . Ph.D. students (and students completing equivalent degrees, such as the Sc.D.) face training periods of unpredictable duration, financial insecurity and food insecurity, competitive markets for tenure-track positions, and unsparing publishing and funding models 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 —all of which may have greater adverse impacts on students from marginalized and underrepresented populations 13 , 14 , 15 . Ph.D. students’ mental health problems may negatively affect their physical health 16 , interpersonal relationships 17 , academic output, and work performance 18 , 19 , and may also contribute to program attrition 20 , 21 , 22 . As many as 30 to 50% of Ph.D. students drop out of their programs, depending on the country and discipline 23 , 24 , 25 , 26 , 27 . Further, while mental health problems among Ph.D. students raise concerns for the wellbeing of the individuals themselves and their personal networks, they also have broader repercussions for their institutions and academia as a whole 22 .
Despite the potential public health significance of this problem, most evidence syntheses on student mental health have focused on undergraduate students 28 , 29 or graduate students in professional degree programs (e.g., medical students) 30 . In non-systematic summaries, estimates of the prevalence of clinically significant depressive symptoms among Ph.D. students vary considerably 31 , 32 , 33 . Reliable estimates of depression and other mental health problems among Ph.D. students are needed to inform preventive, screening, or treatment efforts. To address this gap in the literature, we conducted a systematic review and meta-analysis to explore patterns of depression, anxiety, and suicidal ideation among Ph.D. students.
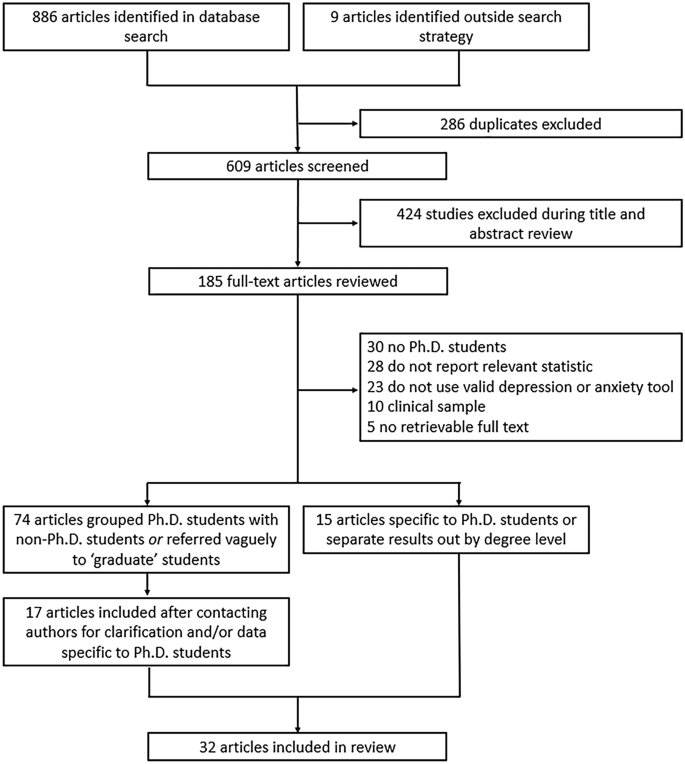
Flowchart of included articles.
The evidence search yielded 886 articles, of which 286 were excluded as duplicates (Fig. 1 ). An additional nine articles were identified through reference lists or grey literature reports published on university websites. Following a title/abstract review and subsequent full-text review, 520 additional articles were excluded.
Of the 89 remaining articles, 74 were unclear about their definition of graduate students or grouped Ph.D. and non-Ph.D. students without disaggregating the estimates by degree level. We obtained contact information for the authors of most of these articles (69 [93%]), requesting additional data. Three authors clarified that their study samples only included Ph.D. students 34 , 35 , 36 . Fourteen authors confirmed that their study samples included both Ph.D. and non-Ph.D. students but provided us with data on the subsample of Ph.D. students 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 . Where authors clarified that the sample was limited to graduate students in non-doctoral degree programs, did not provide additional data on the subsample of Ph.D. students, or did not reply to our information requests, we excluded the studies due to insufficient information (Supplementary Table S1 ).
Ultimately, 32 articles describing the findings of 29 unique studies were identified and included in the review 16 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 (Table 1 ). Overall, 26 studies measured depression, 19 studies measured anxiety, and six studies measured suicidal ideation. Three pairs of articles reported data on the same sample of Ph.D. students 33 , 38 , 45 , 51 , 53 , 56 and were therefore grouped in Table 1 and reported as three studies. Publication dates ranged from 1979 to 2019, but most articles (22/32 [69%]) were published after 2015. Most studies were conducted in the United States (20/29 [69%]), with additional studies conducted in Australia, Belgium, China, Iran, Mexico, and South Korea. Two studies were conducted in cross-national settings representing 48 additional countries. None were conducted in sub-Saharan Africa or South America. Most studies included students completing their degrees in a mix of disciplines (17/29 [59%]), while 12 studies were limited to students in a specific field (e.g., biomedicine, education). The median sample size was 172 students (interquartile range [IQR], 68–654; range, 6–6405). Seven studies focused on mental health outcomes in demographic subgroups, including ethnic or racialized minority students 37 , 41 , 43 , international students 47 , 50 , and sexual and gender minority students 42 , 54 .
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2 ; range, 10–47%). Of these, the most widely used depression scales were the PHQ-9 (9 studies) and variants of the Center for Epidemiologic Studies-Depression scale (CES-D, 4 studies) 63 , and all studies assessed clinically significant symptoms of depression over the past one to two weeks. Three of these studies reported findings based on data from different survey years of the same parent study (the Healthy Minds Study) 40 , 42 , 43 , but due to overlap in the survey years reported across articles, these data were pooled. Most of these studies were based on data collected through online surveys (13/16 [81%]). Ten studies (63%) used random or systematic sampling, four studies (25%) used convenience sampling, and two studies (13%) used multiple sampling techniques.
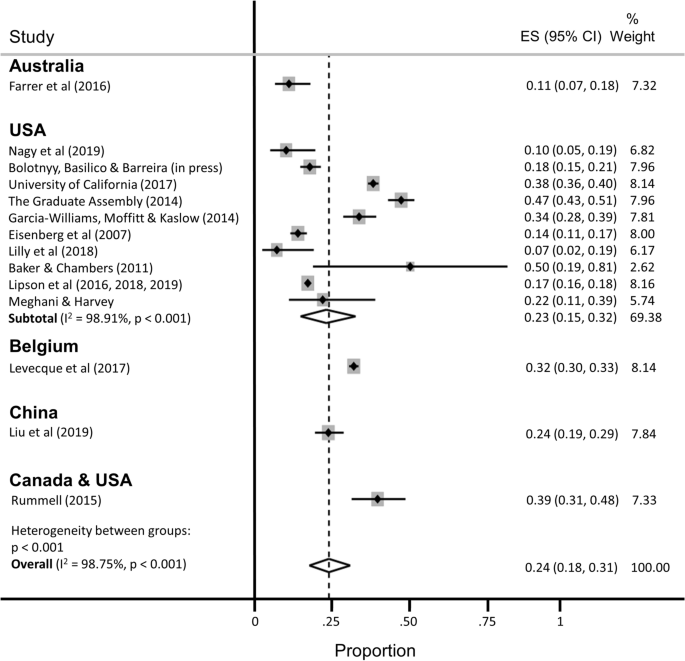
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of depression.
The estimated proportion of Ph.D. students assessed as having clinically significant symptoms of depression was 0.24 (95% confidence interval [CI], 0.18–0.31; 95% predictive interval [PI], 0.04–0.54), with significant evidence of between-study heterogeneity (I 2 = 98.75%). A subgroup analysis restricted to the twelve studies conducted in the United States yielded similar findings (pooled estimate [ES] = 0.23; 95% CI, 0.15–0.32; 95% PI, 0.01–0.60), with no appreciable difference in heterogeneity (I 2 = 98.91%). A subgroup analysis restricted to the studies that used the PHQ-9 to assess depression yielded a slightly lower prevalence estimate and a slight reduction in heterogeneity (ES = 0.18; 95% CI, 0.14–0.22; 95% PI, 0.07–0.34; I 2 = 90.59%).
Nine studies reported the prevalence of clinically significant symptoms of anxiety among a total of 15,626 Ph.D. students (Fig. 3 ; range 4–49%). Of these, the most widely used anxiety scale was the 7-item Generalized Anxiety Disorder scale (GAD-7, 5 studies) 64 . Data from three of the Healthy Minds Study articles were pooled into two estimates, because the scale used to measure anxiety changed midway through the parent study (i.e., the Patient Health Questionnaire-Generalized Anxiety Disorder [PHQ-GAD] scale was used from 2007 to 2012 and then switched to the GAD-7 in 2013 40 ). Most studies (8/9 [89%]) assessed clinically significant symptoms of anxiety over the past two to four weeks, with the one remaining study measuring anxiety over the past year. Again, most of these studies were based on data collected through online surveys (7/9 [78%]). Five studies (56%) used random or systematic sampling, two studies (22%) used convenience sampling, and two studies (22%) used multiple sampling techniques.
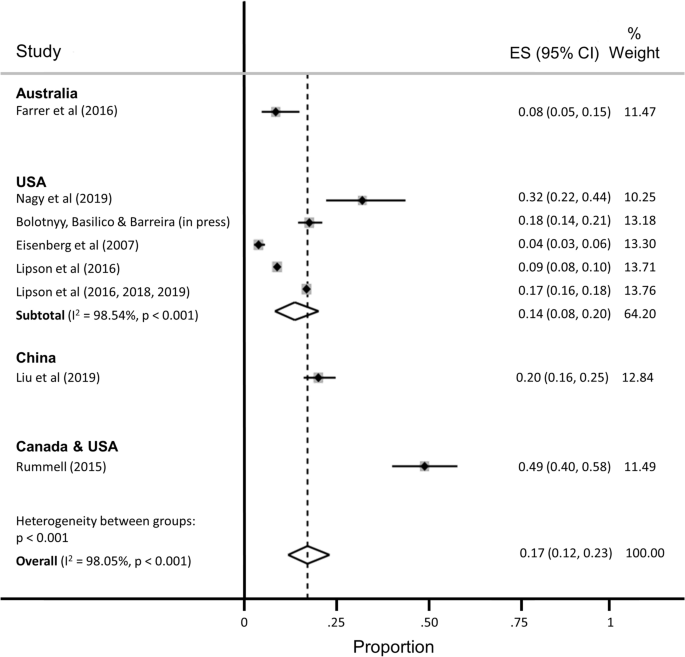
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of anxiety.
The estimated proportion of Ph.D. students assessed as having anxiety was 0.17 (95% CI, 0.12–0.23; 95% PI, 0.02–0.41), with significant evidence of between-study heterogeneity (I 2 = 98.05%). The subgroup analysis restricted to the five studies conducted in the United States yielded a slightly lower proportion of students assessed as having anxiety (ES = 0.14; 95% CI, 0.08–0.20; 95% PI, 0.00–0.43), with no appreciable difference in heterogeneity (I 2 = 98.54%).
Six studies reported the prevalence of suicidal ideation (range, 2–12%), but the recall windows varied greatly (e.g., ideation within the past 2 weeks vs. past year), precluding pooled estimation.
Additional stratified pooled estimates could not be obtained. One study of Ph.D. students across 54 countries found that phase of study was a significant moderator of mental health, with students in the comprehensive examination and dissertation phases more likely to experience distress compared with students primarily engaged in coursework 59 . Other studies identified a higher prevalence of mental ill-health among women 54 ; lesbian, gay, bisexual, transgender, and queer (LGBTQ) students 42 , 54 , 60 ; and students with multiple intersecting identities 54 .
Several studies identified correlates of mental health problems including: project- and supervisor-related issues, stress about productivity, and self-doubt 53 , 62 ; uncertain career prospects, poor living conditions, financial stressors, lack of sleep, feeling devalued, social isolation, and advisor relationships 61 ; financial challenges 38 ; difficulties with work-life balance 58 ; and feelings of isolation and loneliness 52 . Despite these challenges, help-seeking appeared to be limited, with only about one-quarter of Ph.D. students reporting mental health problems also reporting that they were receiving treatment 40 , 52 .
Risk of bias
Twenty-one of 32 articles were assessed as having low risk of bias (Supplementary Table S2 ). Five articles received one point for all five categories on the risk of bias assessment (lowest risk of bias), and one article received no points (highest risk). The mean risk of bias score was 3.22 (standard deviation, 1.34; median, 4; IQR, 2–4). Restricting the estimation sample to 12 studies assessed as having low risk of bias, the estimated proportion of Ph.D. students with depression was 0.25 (95% CI, 0.18–0.33; 95% PI, 0.04–0.57; I 2 = 99.11%), nearly identical to the primary estimate, with no reduction in heterogeneity. The estimated proportion of Ph.D. students with anxiety, among the 7 studies assessed as having low risk of bias, was 0.12 (95% CI, 0.07–0.17; 95% PI, 0.01–0.34; I 2 = 98.17%), again with no appreciable reduction in heterogeneity.
In our meta-analysis of 16 studies representing 23,469 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of depression was 24%. This estimate is consistent with estimated prevalence rates in other high-stress biomedical trainee populations, including medical students (27%) 30 , resident physicians (29%) 65 , and postdoctoral research fellows (29%) 66 . In the sample of nine studies representing 15,626 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of anxiety was 17%. While validated screening instruments tend to over-identify cases of depression (relative to structured clinical interviews) by approximately a factor of two 67 , 68 , our findings nonetheless point to a major public health problem among Ph.D. students. Available data suggest that the prevalence of depressive and anxiety disorders in the general population ranges from 5 to 7% worldwide 69 , 70 . In contrast, prevalence estimates of major depressive disorder among young adults have ranged from 13% (for young adults between the ages of 18 and 29 years in the 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions III 71 ) to 15% (for young adults between the ages of 18 and 25 in the 2019 U.S. National Survey on Drug Use and Health 72 ). Likewise, the prevalence of generalized anxiety disorder was estimated at 4% among young adults between the ages of 18 and 29 in the 2001–03 U.S. National Comorbidity Survey Replication 73 . Thus, even accounting for potential upward bias inherent in these studies’ use of screening instruments, our estimates suggest that the rates of recent clinically significant symptoms of depression and anxiety are greater among Ph.D. students compared with young adults in the general population.
Further underscoring the importance of this public health issue, Ph.D. students face unique stressors and uncertainties that may put them at increased risk for mental health and substance use problems. Students grapple with competing responsibilities, including coursework, teaching, and research, while also managing interpersonal relationships, social isolation, caregiving, and financial insecurity 3 , 10 . Increasing enrollment in doctoral degree programs has not been matched with a commensurate increase in tenure-track academic job opportunities, intensifying competition and pressure to find employment post-graduation 5 . Advisor-student power relations rarely offer options for recourse if and when such relationships become strained, particularly in the setting of sexual harassment, unwanted sexual attention, sexual coercion, and rape 74 , 75 , 76 , 77 , 78 . All of these stressors may be magnified—and compounded by stressors unrelated to graduate school—for subgroups of students who are underrepresented in doctoral degree programs and among whom mental health problems are either more prevalent and/or undertreated compared with the general population, including Black, indigenous, and other people of color 13 , 79 , 80 ; women 81 , 82 ; first-generation students 14 , 15 ; people who identify as LGBTQ 83 , 84 , 85 ; people with disabilities; and people with multiple intersecting identities.
Structural- and individual-level interventions will be needed to reduce the burden of mental ill-health among Ph.D. students worldwide 31 , 86 . Despite the high prevalence of mental health and substance use problems 87 , Ph.D. students demonstrate low rates of help-seeking 40 , 52 , 88 . Common barriers to help-seeking include fears of harming one’s academic career, financial insecurity, lack of time, and lack of awareness 89 , 90 , 91 , as well as health care systems-related barriers, including insufficient numbers of culturally competent counseling staff, limited access to psychological services beyond time-limited psychotherapies, and lack of programs that address the specific needs either of Ph.D. students in general 92 or of Ph.D. students belonging to marginalized groups 93 , 94 . Structural interventions focused solely on enhancing student resilience might include programs aimed at reducing stigma, fostering social cohesion, and reducing social isolation, while changing norms around help-seeking behavior 95 , 96 . However, structural interventions focused on changing stressogenic aspects of the graduate student environment itself are also needed 97 , beyond any enhancements to Ph.D. student resilience, including: undercutting power differentials between graduate students and individual faculty advisors, e.g., by diffusing power among multiple faculty advisors; eliminating racist, sexist, and other discriminatory behaviors by faculty advisors 74 , 75 , 98 ; valuing mentorship and other aspects of “invisible work” that are often disproportionately borne by women faculty and faculty of color 99 , 100 ; and training faculty members to emphasize the dignity of, and adequately prepare Ph.D. students for, non-academic careers 101 , 102 .
Our findings should be interpreted with several limitations in mind. First, the pooled estimates are characterized by a high degree of heterogeneity, similar to meta-analyses of depression prevalence in other populations 30 , 65 , 103 , 104 , 105 . Second, we were only able to aggregate depression prevalence across 16 studies and anxiety prevalence across nine studies (the majority of which were conducted in the U.S.) – far fewer than the 183 studies included in a meta-analysis of depression prevalence among medical students 30 and the 54 studies included in a meta-analysis of resident physicians 65 . These differences underscore the need for more rigorous study in this critical area. Many articles were either excluded from the review or from the meta-analyses for not meeting inclusion criteria or not reporting relevant statistics. Future research in this area should ensure the systematic collection of high-quality, clinically relevant data from a comprehensive set of institutions, across disciplines and countries, and disaggregated by graduate student type. As part of conducting research and addressing student mental health and wellbeing, university deans, provosts, and chancellors should partner with national survey and program institutions (e.g., Graduate Student Experience in the Research University [gradSERU] 106 , the American College Health Association National College Health Assessment [ACHA-NCHA], and HealthyMinds). Furthermore, federal agencies that oversee health and higher education should provide resources for these efforts, and accreditation agencies should require monitoring of mental health and programmatic responses to stressors among Ph.D. students.
Third, heterogeneity in reporting precluded a meta-analysis of the suicidality outcomes among the few studies that reported such data. While reducing the burden of mental health problems among graduate students is an important public health aim in itself, more research into understanding non-suicidal self-injurious behavior, suicide attempts, and completed suicide among Ph.D. students is warranted. Fourth, it is possible that the grey literature reports included in our meta-analysis are more likely to be undertaken at research-intensive institutions 52 , 60 , 61 . However, the direction of bias is unpredictable: mental health problems among Ph.D. students in research-intensive environments may be more prevalent due to detection bias, but such institutions may also have more resources devoted to preventive, screening, or treatment efforts 92 . Fifth, inclusion in this meta-analysis and systematic review was limited to those based on community samples. Inclusion of clinic-based samples, or of studies conducted before or after specific milestones (e.g., the qualifying examination or dissertation prospectus defense), likely would have yielded even higher pooled prevalence estimates of mental health problems. And finally, few studies provided disaggregated data according to sociodemographic factors, stage of training (e.g., first year, pre-prospectus defense, all-but-dissertation), or discipline of study. These factors might be investigated further for differences in mental health outcomes.
Clinically significant symptoms of depression and anxiety are pervasive among graduate students in doctoral degree programs, but these are understudied relative to other trainee populations. Structural and clinical interventions to systematically monitor and promote the mental health and wellbeing of Ph.D. students are urgently needed.
This systematic review and meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach (Supplementary Table S3 ) 107 . This study was based on data collected from publicly available bibliometric databases and did not require ethical approval from our institutional review boards.
Eligibility criteria
Studies were included if they provided data on either: (a) the number or proportion of Ph.D. students with clinically significant symptoms of depression or anxiety, ascertained using a validated scale; or (b) the mean depression or anxiety symptom severity score and its standard deviation among Ph.D. students. Suicidal ideation was examined as a secondary outcome.
We excluded studies that focused on graduate students in non-doctoral degree programs (e.g., Master of Public Health) or professional degree programs (e.g., Doctor of Medicine, Juris Doctor) because more is known about mental health problems in these populations 30 , 108 , 109 , 110 and because Ph.D. students face unique uncertainties. To minimize the potential for upward bias in our pooled prevalence estimates, we excluded studies that recruited students from campus counseling centers or other clinic-based settings. Studies that measured affective states, or state anxiety, before or after specific events (e.g., terrorist attacks, qualifying examinations) were also excluded.
If articles described the study sample in general terms (i.e., without clarifying the degree level of the participants), we contacted the authors by email for clarification. Similarly, if articles pooled results across graduate students in doctoral and non-doctoral degree programs (e.g., reporting a single estimate for a mixed sample of graduate students), we contacted the authors by email to request disaggregated data on the subsample of Ph.D. students. If authors did not reply after two contact attempts spaced over 2 months, or were unable to provide these data, we excluded these studies from further consideration.
Search strategy and data extraction
PubMed, Embase, PsycINFO, ERIC, and Business Source Complete were searched from inception of each database to November 5, 2019. The search strategy included terms related to mental health symptoms (e.g., depression, anxiety, suicide), the study population (e.g., graduate, doctoral), and measurement category (e.g., depression, Columbia-Suicide Severity Rating Scale) (Supplementary Table S4 ). In addition, we searched the reference lists and the grey literature.
After duplicates were removed, we screened the remaining titles and abstracts, followed by a full-text review. We excluded articles following the eligibility criteria listed above (i.e., those that were not focused on Ph.D. students; those that did not assess depression and/or anxiety using a validated screening tool; those that did not report relevant statistics of depression and/or anxiety; and those that recruited students from clinic-based settings). Reasons for exclusion were tracked at each stage. Following selection of included articles, two members of the research team extracted data and conducted risk of bias assessments. Discrepancies were discussed with a third member of the research team. Key extraction variables included: study design, geographic region, sample size, response rate, demographic characteristics of the sample, screening instrument(s) used for assessment, mean depression or anxiety symptom severity score (and its standard deviation), and the number (or proportion) of students experiencing clinically significant symptoms of depression or anxiety.
Risk of bias assessment
Following prior work 30 , 65 , the Newcastle–Ottawa Scale 111 was adapted and used to assess risk of bias in the included studies. Each study was assessed across 5 categories: sample representativeness, sample size, non-respondents, ascertainment of outcomes, and quality of descriptive statistics reporting (Supplementary Information S5 ). Studies were judged as having either low risk of bias (≥ 3 points) or high risk of bias (< 3 points).
Analysis and synthesis
Before pooling the estimated prevalence rates across studies, we first transformed the proportions using a variance-stabilizing double arcsine transformation 112 . We then computed pooled estimates of prevalence using a random effects model 113 . Study specific confidence intervals were estimated using the score method 114 , 115 . We estimated between-study heterogeneity using the I 2 statistic 116 . In an attempt to reduce the extent of heterogeneity, we re-estimated pooled prevalence restricting the analysis to studies conducted in the United States and to studies in which depression assessment was based on the 9-item Patient Health Questionnaire (PHQ-9) 117 . All analyses were conducted using Stata (version 16; StataCorp LP, College Station, Tex.). Where heterogeneity limited our ability to summarize the findings using meta-analysis, we synthesized the data using narrative review.
Woolston, C. Why mental health matters. Nature 557 , 129–131 (2018).
Article ADS CAS Google Scholar
Woolston, C. A love-hurt relationship. Nature 550 , 549–552 (2017).
Article Google Scholar
Woolston, C. PhD poll reveals fear and joy, contentment and anguish. Nature 575 , 403–406 (2019).
Article ADS CAS PubMed Google Scholar
Byrom, N. COVID-19 and the research community: The challenges of lockdown for early-career researchers. Elife 9 , e59634 (2020).
Article PubMed PubMed Central Google Scholar
Alberts, B., Kirschner, M. W., Tilghman, S. & Varmus, H. Rescuing US biomedical research from its systemic flaws. Proc. Natl. Acad. Sci. USA 111 , 5773–5777 (2014).
Article ADS CAS PubMed PubMed Central Google Scholar
McDowell, G. S. et al. Shaping the future of research: A perspective from junior scientists. F1000Res 3 , 291 (2014).
Article PubMed Google Scholar
Petersen, A. M., Riccaboni, M., Stanley, H. E. & Pammoli, F. Persistence and uncertainty in the academic career. Proc. Natl. Acad. Sci. USA 109 , 5213–5218 (2012).
Leshner, A. I. Rethinking graduate education. Science 349 , 349 (2015).
National Academies of Sciences Engineering and Medicine. Graduate STEM Education for the 21st Century (National Academies Press, 2018).
Google Scholar
Charles, S. T., Karnaze, M. M. & Leslie, F. M. Positive factors related to graduate student mental health. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1841207 (2021).
Riddle, E. S., Niles, M. T. & Nickerson, A. Prevalence and factors associated with food insecurity across an entire campus population. PLoS ONE 15 , e0237637 (2020).
Article CAS PubMed PubMed Central Google Scholar
Soldavini, J., Berner, M. & Da Silva, J. Rates of and characteristics associated with food insecurity differ among undergraduate and graduate students at a large public university in the Southeast United States. Prev. Med. Rep. 14 , 100836 (2019).
Clark, U. S. & Hurd, Y. L. Addressing racism and disparities in the biomedical sciences. Nat. Hum. Behav. 4 , 774–777 (2020).
Gardner, S. K. The challenges of first-generation doctoral students. New Dir. High. Educ. 2013 , 43–54 (2013).
Seay, S. E., Lifton, D. E., Wuensch, K. L., Bradshaw, L. K. & McDowelle, J. O. First-generation graduate students and attrition risks. J. Contin. High. Educ. 56 , 11–25 (2008).
Rummell, C. M. An exploratory study of psychology graduate student workload, health, and program satisfaction. Prof. Psychol. Res. Pract. 46 , 391–399 (2015).
Salzer, M. S. A comparative study of campus experiences of college students with mental illnesses versus a general college sample. J. Am. Coll. Health 60 , 1–7 (2012).
Hysenbegasi, A., Hass, S. & Rowland, C. The impact of depression on the academic productivity of university students. J. Ment. Health Policy Econ. 8 , 145–151 (2005).
PubMed Google Scholar
Harvey, S. et al. Depression and work performance: An ecological study using web-based screening. Occup. Med. (Lond.) 61 , 209–211 (2011).
Article CAS Google Scholar
Eisenberg, D., Golberstein, E. & Hunt, J. B. Mental health and academic success in college. BE J. Econ. Anal. Policy 9 , 40 (2009).
Lovitts, B. E. Who is responsible for graduate student attrition--the individual or the institution? Toward an explanation of the high and persistent rate of attrition. In: Annual Meeting of the American Education Research Association (New York, 1996). Available at: https://eric.ed.gov/?id=ED399878.
Gardner, S. K. Student and faculty attributions of attrition in high and low-completing doctoral programs in the United States. High. Educ. 58 , 97–112 (2009).
Lovitts, B. E. Leaving the Ivory Tower: The Causes and Consequences of Departure from Doctoral Study (Rowman & Littlefield Publishers, 2001).
Rigler Jr, K. L., Bowlin, L. K., Sweat, K., Watts, S. & Throne, R. Agency, socialization, and support: a critical review of doctoral student attrition. In: Proceedings of the Third International Conference on Doctoral Education: Organizational Leadership and Impact , University of Central Florida, Orlando, (2017).
Golde, C. M. The role of the department and discipline in doctoral student attrition: Lessons from four departments. J. High. Educ. 76 , 669–700 (2005).
Council of Graduate Schools. PhD Completion and Attrition: Analysis of Baseline Program Data from the PhD Completion Project (Council of Graduate Schools, 2008).
National Research Council. A Data-Based Assessment of Research-Doctorate Programs in the United States (The National Academies Press, 2011).
Akhtar, P. et al. Prevalence of depression among university students in low and middle income countries (LMICs): A systematic review and meta-analysis. J. Affect. Disord. 274 , 911–919 (2020).
Mortier, P. et al. The prevalence of suicidal thoughts and behaviours among college students: A meta-analysis. Psychol. Med. 48 , 554–565 (2018).
Article CAS PubMed Google Scholar
Rotenstein, L. S. et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: A systematic review and meta-analysis. JAMA 316 , 2214–2236 (2016).
Tsai, J. W. & Muindi, F. Towards sustaining a culture of mental health and wellness for trainees in the biosciences. Nat. Biotechnol. 34 , 353–355 (2016).
Levecque, K., Anseel, F., De Beuckelaer, A., Van der Heyden, J. & Gisle, L. Work organization and mental health problems in PhD students. Res. Policy 46 , 868–879 (2017).
Nagy, G. A. et al. Burnout and mental health problems in biomedical doctoral students. CBE Life Sci. Educ. 18 , 1–14 (2019).
Garcia-Williams, A., Moffitt, L. & Kaslow, N. J. Mental health and suicidal behavior among graduate students. Acad. Psychiatry 28 , 554–560 (2014).
Sheldon, K. M. Emotionality differences between artists and scientists. J. Res. Pers. 28 , 481–491 (1994).
Lightstone, S. N., Swencionis, C. & Cohen, H. W. The effect of bioterrorism messages on anxiety levels. Int. Q. Community Health Educ. 24 , 111–122 (2006).
Clark, C. R., Mercer, S. H., Zeigler-Hill, V. & Dufrene, B. A. Barriers to the success of ethnic minority students in school psychology graduate programs. School Psych. Rev. 41 , 176–192 (2012).
Eisenberg, D., Gollust, S. E., Golberstein, E. & Hefner, J. L. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am. J. Orthopsychiatry 77 , 534–542 (2007).
Farrer, L. M., Gulliver, A., Bennett, K., Fassnacht, D. B. & Griffiths, K. M. Demographic and psychosocial predictors of major depression and generalised anxiety disorder in Australian university students. BMC Psychiatry 16 , 241 (2016).
Lipson, S. K., Zhou, S., Wagner, B. III., Beck, K. & Eisenberg, D. Major differences: Variations in undergraduate and graduate student mental health and treatment utilization across academic disciplines. J. Coll. Stud. Psychother. 30 , 23–41 (2016).
Lilly, F. R. W. et al. The influence of racial microaggressions and social rank on risk for depression among minority graduate and professional students. Coll. Stud. J. 52 , 86–104 (2018).
Lipson, S. K., Raifman, J., Abelson, S. & Reisner, S. L. Gender minority mental health in the U.S.: Results of a national survey on college campuses. Am. J. Prev. Med. 57 , 293–301 (2019).
Lipson, S. K., Kern, A., Eisenberg, D. & Breland-Noble, A. M. Mental health disparities among college students of color. J. Adolesc. Health 63 , 348–356 (2018).
Baker, A. J. L. & Chambers, J. Adult recall of childhood exposure to parental conflict: Unpacking the black box of parental alienation. J. Divorce Remarriage 52 , 55–76 (2011).
Golberstein, E., Eisenberg, D. & Gollust, S. E. Perceived stigma and mental health care seeking. Psychiatr. Serv. 59 , 392–399 (2008).
Hindman, R. K., Glass, C. R., Arnkoff, D. B. & Maron, D. D. A comparison of formal and informal mindfulness programs for stress reduction in university students. Mindfulness 6 , 873–884 (2015).
Hirai, R., Frazier, P. & Syed, M. Psychological and sociocultural adjustment of first-year international students: Trajectories and predictors. J. Couns. Psychol. 62 , 438–452 (2015).
Lee, J. S. & Jeong, B. Having mentors and campus social networks moderates the impact of worries and video gaming on depressive symptoms: A moderated mediation analysis. BMC Public Health 14 , 1–12 (2014).
Corral-Frias, N. S., Velardez Soto, S. N., Frias-Armenta, M., Corona-Espinosa, A. & Watson, D. Concurrent validity and reliability of two short forms of the mood and anxiety symptom questionnaire in a student sample from Northwest Mexico. J. Psychopathol. Behav. Assess. 41 , 304–316 (2019).
Meghani, D. T. & Harvey, E. A. Asian Indian international students’ trajectories of depression, acculturation, and enculturation. Asian Am. J. Psychol. 7 , 1–14 (2016).
Barry, K. M., Woods, M., Martin, A., Stirling, C. & Warnecke, E. A randomized controlled trial of the effects of mindfulness practice on doctoral candidate psychological status. J. Am. Coll. Health 67 , 299–307 (2019).
Bolotnyy, V., Basilico, M. & Barreira, P. Graduate student mental health: lessons from American economics departments. J. Econ. Lit. (in press).
Barry, K. M., Woods, M., Warnecke, E., Stirling, C. & Martin, A. Psychological health of doctoral candidates, study-related challenges and perceived performance. High. Educ. Res. Dev. 37 , 468–483 (2018).
Boyle, K. M. & McKinzie, A. E. The prevalence and psychological cost of interpersonal violence in graduate and law school. J. Interpers. Violence 36 , 6319-6350 (2021).
Heinrich, D. L. The causal influence of anxiety on academic achievement for students of differing intellectual ability. Appl. Psychol. Meas. 3 , 351–359 (1979).
Hish, A. J. et al. Applying the stress process model to stress-burnout and stress-depression relationships in biomedical doctoral students: A cross-sectional pilot study. CBE Life Sci. Educ. 18 , 1–11 (2019).
Jamshidi, F. et al. A cross-sectional study of psychiatric disorders in medical sciences students. Mater. Sociomed. 29 , 188–191 (2017).
Liu, C. et al. Prevalence and associated factors of depression and anxiety among doctoral students: The mediating effect of mentoring relationships on the association between research self-efficacy and depression/anxiety. Psychol. Res. Behav. Manag. 12 , 195–208 (2019).
Sverdlik, A. & Hall, N. C. Not just a phase: Exploring the role of program stage on well-being and motivation in doctoral students. J. Adult Contin. Educ. 26 , 1–28 (2019).
University of California Office of the President. The University of California Graduate student Well-Being Survey Report (University of California, 2017).
The Graduate Assembly. Graduate Student Happiness & Well-Being Report (University of California at Berkeley, 2014).
Richardson, C. M., Trusty, W. T. & George, K. A. Trainee wellness: Self-critical perfectionism, self-compassion, depression, and burnout among doctoral trainees in psychology. Couns. Psychol. Q. 33 , 187-198 (2020).
Radloff, L. S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1 , 385–401 (1977).
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Lowe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 166 , 1092–1097 (2006).
Mata, D. A. et al. Prevalence of depression and depressive symptoms among residents physicians: A systematic review and meta-analysis. JAMA 314 , 2373–2383 (2015).
Gloria, C. T. & Steinhardt, M. A. Flourishing, languishing, and depressed postdoctoral fellows: Differences in stress, anxiety, and depressive symptoms. J. Postdoct. Aff. 3 , 1–9 (2013).
Levis, B. et al. Patient Health Questionnaire-9 scores do not accurately estimate depression prevalence: Individual participant data meta-analysis. J. Clin. Epidemiol. 122 , 115-128.e111 (2020).
Tsai, A. C. Reliability and validity of depression assessment among persons with HIV in sub-Saharan Africa: Systematic review and meta-analysis. J. Acquir. Immune Defic. Syndr. 66 , 503–511 (2014).
Baxter, A. J., Scott, K. M., Vos, T. & Whiteford, H. A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 43 , 897–910 (2013).
Ferrari, A. et al. Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychol. Med. 43 , 471–481 (2013).
Hasin, D. S. et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry 75 , 336–346 (2018).
US Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2020).
Kessler, R. C. et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62 , 593–602 (2005).
Working Group report to the Advisory Committee to the NIH Director. Changing the Culture to End Sexual Harassment (U. S. National Institutes of Health, 2019).
National Academies of Sciences Engineering and Medicine. Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine (The National Academies Press, 2018).
Wadman, M. A hidden history. Science 360 , 480–485 (2018).
Hockfield, S., Magley, V. & Yoshino, K. Report of the External Review Committee to Review Sexual Harassment at Harvard University (External Review Committee to Review Sexual Harassment at Harvard University, 2021).
Bartlett, T. & Gluckman, N. She left Harvard. He got to stay. Chronicle High. Educ. 64 , A14 (2021). Available at: https://www.chronicle.com/article/she-left-harvard-he-got-to-stay/.
Tseng, M. et al. Strategies and support for Black, Indigenous, and people of colour in ecology and evolutionary biology. Nat. Ecol. Evol. 4 , 1288–1290 (2020).
Williams, D. R. et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch. Gen. Psychiatry 64 , 305–315 (2007).
Wu, A. H. Gender bias in rumors among professionals: An identity-based interpretation. Rev. Econ. Stat. 102 , 867–880 (2020).
Kessler, R. C. Epidemiology of women and depression. J. Affect. Disord. 74 , 5–13 (2003).
Mattheis, A., Cruz-Ramirez De Arellano, D. & Yoder, J. B. A model of queer STEM identity in the workplace. J. Homosex 67 , 1839–1863 (2020).
Semlyen, J., King, M., Varney, J. & Hagger-Johnson, G. Sexual orientation and symptoms of common mental disorder or low wellbeing: Combined meta-analysis of 12 UK population health surveys. BMC Psychiatry 16 , 1–19 (2016).
Lark, J. S. & Croteau, J. M. Lesbian, gay, and bisexual doctoral students’ mentoring relationships with faculty in counseling psychology: A qualitative study. Couns. Psychol. 26 , 754–776 (1998).
Jaremka, L. M. et al. Common academic experiences no one talks about: Repeated rejection, imposter syndrome, and burnout. Perspect Psychol Sci 15 , 519–543 (2020).
Allen, H. K. et al. Substance use and mental health problems among graduate students: Individual and program-level correlates. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1725020 (2020).
Turner, A. & Berry, T. Counseling center contributions to student retention and graduation: A longitudinal assessment. J. Coll. Stud. Dev. 41 , 627–636 (2000).
Dyrbye, L. N., Thomas, M. R. & Shanafelt, T. D. Medical student distress: Causes, consequences, and proposed solutions. Mayo Clin. Proc. 80 , 1613–1622 (2005).
Tija, J., Givens, J. L. & Shea, J. A. Factors associated with undertreatment of medical student depression. J. Am. Coll. Health 53 , 219–224 (2005).
Dearing, R., Maddux, J. & Tangney, J. Predictors of psychological help seeking in clinical and counseling psychology graduate students. Prof. Psychol. Res. Pract. 36 , 323–329 (2005).
Langin, K. Amid concerns about grad student mental health, one university takes a novel approach. Science https://doi.org/10.1126/science.caredit.aay7113 (2019).
Guillory, D. Combating anti-blackness in the AI community. arXiv , arXiv:2006.16879 (2020).
Galán, C. A. et al. A call to action for an antiracist clinical science. J. Clin. Child Adolesc. Psychol 50 , 12-57 (2021).
Wyman, P. A. et al. Effect of the Wingman-Connect upstream suicide prevention program for air force personnel in training: A cluster randomized clinical trial. JAMA Netw Open 3 , e2022532 (2020).
Knox, K. L. et al. The US Air Force Suicide Prevention Program: Implications for public health policy. Am. J. Public Health 100 , 2457–2463 (2010).
Inclusive Climate Subcommittee of the Government Department Climate Change Committee. Government Department Climate Change: Final Report and Recommendations (Government Department, Harvard University, 2019).
Inclusive Climate Subcommittee of the Government Department Climate Change Committee. Government Department Climate Survey Report (Government Department, Harvard University, 2019).
Magoqwana, B., Maqabuka, Q. & Tshoaedi, M. “Forced to care” at the neoliberal university: Invisible labour as academic labour performed by Black women academics in the South African university. S. Afr. Rev. Sociol. 50 , 6–21 (2019).
Jones, H. A., Perrin, P. B., Heller, M. B., Hailu, S. & Barnett, C. Black psychology graduate students’ lives matter: Using informal mentoring to create an inclusive climate amidst national race-related events. Prof. Psychol. Res. Pract. 49 , 75–82 (2018).
Mathur, A., Meyers, F. J., Chalkley, R., O’Brien, T. C. & Fuhrmann, C. N. Transforming training to reflect the workforce. Sci. Transl. Med. 7 , 285 (2015).
Scharff, V. Advice: Prepare your Ph.D.s for diverse career paths. Chronicle High. Educ. 65 , 30 (2018).
Beattie, T. S., Smilenova, B., Krishnaratne, S. & Mazzuca, A. Mental health problems among female sex workers in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 17 , e1003297 (2020).
Ismail, Z. et al. Prevalence of depression in patients with mild cognitive impairment: A systematic review and meta-analysis. JAMA Psychiatry 74 , 58–67 (2017).
Lim, G. Y. et al. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 8 , 1–10 (2018).
Article ADS Google Scholar
Jones-White, D. R., Soria, K. M., Tower, E. K. B. & Horner, O. G. Factors associated with anxiety and depression among U.S. doctoral students: Evidence from the gradSERU survey. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1865975 (2021).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 151 , 264–269 (2009).
Helmers, K. F., Danoff, D., Steinert, Y., Leyton, M. & Young, S. N. Stress and depressed mood in medical students, law students, and graduate students at McGill University. Acad. Med. 72 , 708–714 (1997).
Rabkow, N. et al. Facing the truth: A report on the mental health situation of German law students. Int. J. Law Psychiatry 71 , 101599 (2020).
Bergin, A. & Pakenham, K. Law student stress: Relationships between academic demands, social isolation, career pressure, study/life imbalance and adjustment outcomes in law students. Psychiatr. Psychol. Law 22 , 388–406 (2015).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25 , 603–605 (2010).
Freeman, M. F. & Tukey, J. W. Transformations related to the angular and the square root. Ann. Math. Stat. 21 , 607–611 (1950).
Article MathSciNet MATH Google Scholar
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 7 , 177–188 (1986).
Wilson, E. B. Probable inference, the law of succession, and statistical inference. J. Am. Stat. Assoc. 22 , 209–212 (1927).
Newcombe, R. G. Two-sided confidence intervals for the single proportion: Comparison of seven methods. Stat. Med. 17 , 857–872 (1998).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21 , 1539–1558 (2002).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 16 , 606–613 (2001).
Download references
Acknowledgements
We thank the following investigators for generously sharing their time and/or data: Gordon J. G. Asmundson, Ph.D., Amy J. L. Baker, Ph.D., Hillel W. Cohen, Dr.P.H., Alcir L. Dafre, Ph.D., Deborah Danoff, M.D., Daniel Eisenberg, Ph.D., Lou Farrer, Ph.D., Christy B. Fraenza, Ph.D., Patricia A. Frazier, Ph.D., Nadia Corral-Frías, Ph.D., Hanga Galfalvy, Ph.D., Edward E. Goldenberg, Ph.D., Robert K. Hindman, Ph.D., Jürgen Hoyer, Ph.D., Ayako Isato, Ph.D., Azharul Islam, Ph.D., Shanna E. Smith Jaggars, Ph.D., Bumseok Jeong, M.D., Ph.D., Ju R. Joeng, Nadine J. Kaslow, Ph.D., Rukhsana Kausar, Ph.D., Flavius R. W. Lilly, Ph.D., Sarah K. Lipson, Ph.D., Frances Meeten, D.Phil., D.Clin.Psy., Dhara T. Meghani, Ph.D., Sterett H. Mercer, Ph.D., Masaki Mori, Ph.D., Arif Musa, M.D., Shizar Nahidi, M.D., Ph.D., Arthur M. Nezu, Ph.D., D.H.L., Angelo Picardi, M.D., Nicole E. Rossi, Ph.D., Denise M. Saint Arnault, Ph.D., Sagar Sharma, Ph.D., Bryony Sheaves, D.Clin.Psy., Kennon M. Sheldon, Ph.D., Daniel Shepherd, Ph.D., Keisuke Takano, Ph.D., Sara Tement, Ph.D., Sherri Turner, Ph.D., Shawn O. Utsey, Ph.D., Ron Valle, Ph.D., Caleb Wang, B.S., Pengju Wang, Katsuyuki Yamasaki, Ph.D.
A.C.T. acknowledges funding from the Sullivan Family Foundation. This paper does not reflect an official statement or opinion from the County of San Mateo.
Author information
Authors and affiliations.
Center for Global Health, Massachusetts General Hospital, Boston, MA, USA
Emily N. Satinsky & Alexander C. Tsai
San Mateo County Behavioral Health and Recovery Services, San Mateo, CA, USA
Tomoki Kimura
Department of Epidemiology and Population Health, Stanford University, Palo Alto, CA, USA
Mathew V. Kiang
Center for Population Health Sciences, Stanford University School of Medicine, Palo Alto, CA, USA
Harvard Society of Fellows, Harvard University, Cambridge, MA, USA
Rediet Abebe
Department of Electrical Engineering and Computer Science, University of California Berkeley, Berkeley, CA, USA
Department of Economics, Hankamer School of Business, Baylor University, Waco, TX, USA
Scott Cunningham
Department of Sociology, Washington University in St. Louis, St. Louis, MO, USA
Department of Microbiology, Immunology, and Molecular Genetics, Institute for Quantitative and Computational Biosciences, University of California Los Angeles, Los Angeles, CA, USA
Xiaofei Lin
Departments of Newborn Medicine and Psychiatry, Brigham and Women’s Hospital, Boston, MA, USA
Cindy H. Liu
Harvard Medical School, Boston, MA, USA
Cindy H. Liu & Alexander C. Tsai
Centre for Global Health, Edinburgh Medical School, Usher Institute, University of Edinburgh, Edinburgh, Scotland, UK
Department of Psychiatry, University of Michigan, Ann Arbor, MI, USA
Department of Global Health, Institute for Life Course Health Research, Stellenbosch University, Cape Town, South Africa
Mark Tomlinson
School of Nursing and Midwifery, Queens University, Belfast, UK
Fielding School of Public Health, Los Angeles Area Health Services Research Training Program, University of California Los Angeles, Los Angeles, CA, USA
Miranda Yaver
Mongan Institute, Massachusetts General Hospital, Boston, MA, USA
Alexander C. Tsai
You can also search for this author in PubMed Google Scholar
Contributions
A.C.T. conceptualized the study and provided supervision. T.K. conducted the search. E.N.S. contacted authors for additional information not reported in published articles. E.N.S. and T.K. extracted data and performed the quality assessment appraisal. E.N.S. and A.C.T. conducted the statistical analysis and drafted the manuscript. T.K., M.V.K., R.A., S.C., H.L., X.L., C.H.L., I.R., S.S., M.T. and M.Y. contributed to the interpretation of the results. All authors provided critical feedback on drafts and approved the final manuscript.
Corresponding authors
Correspondence to Emily N. Satinsky or Alexander C. Tsai .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Satinsky, E.N., Kimura, T., Kiang, M.V. et al. Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students. Sci Rep 11 , 14370 (2021). https://doi.org/10.1038/s41598-021-93687-7
Download citation
Received : 31 March 2021
Accepted : 24 June 2021
Published : 13 July 2021
DOI : https://doi.org/10.1038/s41598-021-93687-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
How to improve academic well-being: an analysis of the leveraging factors based on the italian case.
- Alice Tontodimamma
- Emiliano del Gobbo
- Antonio Aquino
Quality & Quantity (2024)
Suicidal affective risk among female college students: the impact of life satisfaction
- Dawei Huang
- Xianbin Wang
Current Psychology (2024)
A single-center assessment of mental health and well-being in a biomedical sciences graduate program
- Sarah K. Jachim
- Bradley S. Bowles
- Autumn J. Schulze
Nature Biotechnology (2023)
Mental Health Problems Among Graduate Students in Turkey: a Cross-Sectional Study
- Cafer Kılıç
- Faika Şanal Karahan
International Journal for the Advancement of Counselling (2023)
A study in University of Ruhuna for investigating prevalence, risk factors and remedies for psychiatric illnesses among students
- Patikiri Arachchige Don Shehan Nilm Wijesekara
Scientific Reports (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
7 Depression Research Paper Topic Ideas
Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
In psychology classes, it's common for students to write a depression research paper. Researching depression may be beneficial if you have a personal interest in this topic and want to learn more, or if you're simply passionate about this mental health issue. However, since depression is a very complex subject, it offers many possible topics to focus on, which may leave you wondering where to begin.
If this is how you feel, here are a few research titles about depression to help inspire your topic choice. You can use these suggestions as actual research titles about depression, or you can use them to lead you to other more in-depth topics that you can look into further for your depression research paper.
What Is Depression?
Everyone experiences times when they feel a little bit blue or sad. This is a normal part of being human. Depression, however, is a medical condition that is quite different from everyday moodiness.
Your depression research paper may explore the basics, or it might delve deeper into the definition of clinical depression or the difference between clinical depression and sadness .
What Research Says About the Psychology of Depression
Studies suggest that there are biological, psychological, and social aspects to depression, giving you many different areas to consider for your research title about depression.
Types of Depression
There are several different types of depression that are dependent on how an individual's depression symptoms manifest themselves. Depression symptoms may vary in severity or in what is causing them. For instance, major depressive disorder (MDD) may have no identifiable cause, while postpartum depression is typically linked to pregnancy and childbirth.
Depressive symptoms may also be part of an illness called bipolar disorder. This includes fluctuations between depressive episodes and a state of extreme elation called mania. Bipolar disorder is a topic that offers many research opportunities, from its definition and its causes to associated risks, symptoms, and treatment.
Causes of Depression
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic.
For instance, how does an imbalance in brain chemistry or poor nutrition relate to depression? Is there a relationship between the stressful, busier lives of today's society and the rise of depression? How can grief or a major medical condition lead to overwhelming sadness and depression?
Who Is at Risk for Depression?
This is a good research question about depression as certain risk factors may make a person more prone to developing this mental health condition, such as a family history of depression, adverse childhood experiences, stress , illness, and gender . This is not a complete list of all risk factors, however, it's a good place to start.
The growing rate of depression in children, teenagers, and young adults is an interesting subtopic you can focus on as well. Whether you dive into the reasons behind the increase in rates of depression or discuss the treatment options that are safe for young people, there is a lot of research available in this area and many unanswered questions to consider.
Depression Signs and Symptoms
The signs of depression are those outward manifestations of the illness that a doctor can observe when they examine a patient. For example, a lack of emotional responsiveness is a visible sign. On the other hand, symptoms are subjective things about the illness that only the patient can observe, such as feelings of guilt or sadness.
An illness such as depression is often invisible to the outside observer. That is why it is very important for patients to make an accurate accounting of all of their symptoms so their doctor can diagnose them properly. In your depression research paper, you may explore these "invisible" symptoms of depression in adults or explore how depression symptoms can be different in children .
How Is Depression Diagnosed?
This is another good depression research topic because, in some ways, the diagnosis of depression is more of an art than a science. Doctors must generally rely upon the patient's set of symptoms and what they can observe about them during their examination to make a diagnosis.
While there are certain laboratory tests that can be performed to rule out other medical illnesses as a cause of depression, there is not yet a definitive test for depression itself.
If you'd like to pursue this topic, you may want to start with the Diagnostic and Statistical Manual of Mental Disorders (DSM). The fifth edition, known as DSM-5, offers a very detailed explanation that guides doctors to a diagnosis. You can also compare the current model of diagnosing depression to historical methods of diagnosis—how have these updates improved the way depression is treated?
Treatment Options for Depression
The first choice for depression treatment is generally an antidepressant medication. Selective serotonin reuptake inhibitors (SSRIs) are the most popular choice because they can be quite effective and tend to have fewer side effects than other types of antidepressants.
Psychotherapy, or talk therapy, is another effective and common choice. It is especially efficacious when combined with antidepressant therapy. Certain other treatments, such as electroconvulsive therapy (ECT) or vagus nerve stimulation (VNS), are most commonly used for patients who do not respond to more common forms of treatment.
Focusing on one of these treatments is an option for your depression research paper. Comparing and contrasting several different types of treatment can also make a good research title about depression.
A Word From Verywell
The topic of depression really can take you down many different roads. When making your final decision on which to pursue in your depression research paper, it's often helpful to start by listing a few areas that pique your interest.
From there, consider doing a little preliminary research. You may come across something that grabs your attention like a new study, a controversial topic you didn't know about, or something that hits a personal note. This will help you narrow your focus, giving you your final research title about depression.
Remes O, Mendes JF, Templeton P. Biological, psychological, and social determinants of depression: A review of recent literature . Brain Sci . 2021;11(12):1633. doi:10.3390/brainsci11121633
National Institute of Mental Health. Depression .
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition . American Psychiatric Association.
National Institute of Mental Health. Mental health medications .
Ferri, F. F. (2019). Ferri's Clinical Advisor 2020 E-Book: 5 Books in 1 . Netherlands: Elsevier Health Sciences.
By Nancy Schimelpfening Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
10 New Thesis Statement about Depression & Anxiety | How to Write One?
Did you know according to the National Institute of Mental Health; it is estimated that approximately 8.4% of adults are patients of major depression in the US? Well, depression is a common illness globally that affects a lot of people. Yet, the reasons for this psychological sickness vary from person to person and numerous studies are being conducted to discover more about depression.
Therefore, college and university students are currently assigned to write research papers, dissertations, essays, and a thesis about depression. However, writing essays on such topics aims to increase the awareness of physical and mental well-being among youth and help them find solutions.
However, a lot of students find it pretty challenging to write a thesis statement about depression and seek someone to write my essay . No worries! In this article, you will learn about what is a good thesis statement about mental health and some effective methods and approaches to write a killer headline and compose an astonishing essay about depression.
5 Thesis Statement About Depression:
- “The complexity of depression, which includes biological, psychological, and environmental components, emphasizes the need for individualized treatment plans that consider each person’s particular requirements.”
- “Depression in the workplace not only affects an individual’s productivity but also carries economic implications, emphasizing the importance of fostering a mental health-friendly work environment.”
- “Alternative, holistic approaches to mental health care have the potential to be more successful as the link between creative expressions, such as art therapy, and depression management becomes more commonly recognized.”
- “It is critical to enhance geriatric mental health treatment and reduce the stigma associated with mental illness in older people since depression in senior populations is typically underdiagnosed and mistreated.”
- “The link between early childhood adversity and the risk of developing depression later in life accentuates the importance of early intervention and support systems for children exposed to adverse experiences.”
5 Thesis Statements about Anxiety & Depression :
- “Depression and anxiety Co-occurring disorders are a major concern in mental health, necessitating integrated treatment options that meet the unique challenges that co-occurring diseases provide.”
- “The utilization of technology-driven therapies, such as smartphone apps and telehealth services, is a realistic approach of addressing persons suffering from anxiety and depression, while also increasing access to mental health care.”
- “The examination of the gut-brain connection and its potential role in anxiety and depression showcases a burgeoning area of research that could lead to novel treatments emphasizing nutrition and gut health.”
- “Adolescents who experience both anxiety and depression face a serious issue that calls for comprehensive school-based mental health programs and preventative measures to promote young people’s mental health.”
- “Exploring the impact of sociocultural factors and the role of community support systems in the experience of anxiety and depression provides insights into the development of culturally sensitive mental health interventions.”

GET ACADEMIC WRITING HELP
Your assignment won’t be delivered on time: you’ll get it beforehand. Review your work immediately and ask for free revisions right away. Get extensive help in:

Follow 7 Proven Methods to Compose Thesis Statement about Depression
A thesis is the overview of the concepts and ideas that you will write in your research paper or in the essay. Yet, a thesis statement about anxiety focuses more on the stress and depression topics for the paper you’re working on, which can be written by following the tips given below.
Nonetheless, you can compose an outline by covering the points mentioned below:
1. Pick a good study topic and perform a basic reading. Look for some intriguing statistics and try to come up with creative ways to approach your subject. Examine a few articles for deficiencies in understanding.
2. Make a list of your references and jot down when you come across a noteworthy quotation. You can cite them in your paper as references. Organize all of the information you’ve acquired in one location.
3. In one phrase, state the purpose of your essay. Consider what you want to happen when other people read your article.
4. Examine your notes and construct a list of all the key things you wish to emphasize. Make use of brainstorming strategies and jot down any ideas that come to mind.
5. Review and revise the arguments and write a thesis statement for a research paper or essay about depression.
6. Organize your essay by organizing the list of points. Arrange the points in a logical sequence. Analyze all elements to ensure that they are all relevant to your goal.
7. Reread all of your statements and arrange your outline in a standard manner, such as a bulleted list.

Final Words
So, what is an ideal way to write a thesis statement about depression for your research paper or essay? We hope you have a thorough idea of the essay you’re writing before picking a thesis statement about mental well-being. That will assist you in developing the greatest thesis for our essay.
But don’t get too worked up over your thesis statement for a research paper on mental disorders. Our professional subject experts have produced a list of thesis statements about mental health and depression themes for research paper writing, so you’ve got your job cut out for you. For your essay assignments or assignments, we will also offer appropriate thesis statements.
If you’re still confused about which statement to use, contact us right away. We have a staff of highly qualified and seasoned writers who can assist you with your essay or research work and guarantee that you receive the highest possible score.
Related Posts

Can You Go to Jail for Plagiarism?
- July 17, 2023
ChatGPT Writer Extension: Boosting Your Writing Efficiency
- June 23, 2023

ChatGPT Plagiarism Detection: Ensuring Originality in AI-Generated Content
- May 29, 2023
Home — Essay Samples — Nursing & Health — Psychiatry & Mental Health — Depression
Essays About Depression
Depression essay topic examples.
Explore topics like the impact of stigma on depression, compare it across age groups or in literature and media, describe the emotional journey of depression, discuss how education can help, and share personal stories related to it. These essay ideas offer a broad perspective on depression, making it easier to understand and engage with this important subject.
Argumentative Essays
Argumentative essays require you to analyze and present arguments related to depression. Here are some topic examples:
- 1. Argue whether mental health stigma contributes to the prevalence of depression in society.
- 2. Analyze the effectiveness of different treatment approaches for depression, such as therapy versus medication.
Example Introduction Paragraph for an Argumentative Essay: Depression is a pervasive mental health issue that affects millions of individuals worldwide. This essay delves into the complex relationship between mental health stigma and the prevalence of depression in society, examining the barriers to seeking help and the consequences of this stigma.
Example Conclusion Paragraph for an Argumentative Essay: In conclusion, the analysis of mental health stigma's impact on depression underscores the urgent need to challenge and dismantle the stereotypes surrounding mental health. As we reflect on the far-reaching consequences of stigma, we are called to create a society that fosters empathy, understanding, and open dialogue about mental health.
Compare and Contrast Essays
Compare and contrast essays enable you to examine similarities and differences within the context of depression. Consider these topics:
- 1. Compare and contrast the symptoms and risk factors of depression in adolescents and adults.
- 2. Analyze the similarities and differences between the portrayal of depression in literature and its depiction in modern media.
Example Introduction Paragraph for a Compare and Contrast Essay: Depression manifests differently in various age groups and mediums of expression. This essay embarks on a journey to compare and contrast the symptoms and risk factors of depression in adolescents and adults, shedding light on the unique challenges faced by each demographic.
Example Conclusion Paragraph for a Compare and Contrast Essay: In conclusion, the comparison and contrast of depression in adolescents and adults highlight the importance of tailored interventions and support systems. As we contemplate the distinct challenges faced by these age groups, we are reminded of the need for age-appropriate mental health resources and strategies.
Descriptive Essays
Descriptive essays allow you to vividly depict aspects of depression, whether it's the experience of the individual or the societal impact. Here are some topic ideas:
- 1. Describe the emotional rollercoaster of living with depression, highlighting the highs and lows of the experience.
- 2. Paint a detailed portrait of the consequences of untreated depression on an individual's personal and professional life.
Example Introduction Paragraph for a Descriptive Essay: Depression is a complex emotional journey that defies easy characterization. This essay embarks on a descriptive exploration of the emotional rollercoaster that individuals with depression experience, delving into the profound impact it has on their daily lives.
Example Conclusion Paragraph for a Descriptive Essay: In conclusion, the descriptive portrayal of the emotional rollercoaster of depression underscores the need for empathy and support for those grappling with this condition. Through this exploration, we are reminded of the resilience of the human spirit and the importance of compassionate understanding.
Persuasive Essays
Persuasive essays involve arguing a point of view related to depression. Consider these persuasive topics:
- 1. Persuade your readers that incorporating mental health education into the school curriculum can reduce the prevalence of depression among students.
- 2. Argue for or against the idea that employers should prioritize the mental well-being of their employees to combat workplace depression.
Example Introduction Paragraph for a Persuasive Essay: The prevalence of depression underscores the urgent need for proactive measures to address mental health. This persuasive essay asserts that integrating mental health education into the school curriculum can significantly reduce the prevalence of depression among students, offering them the tools to navigate emotional challenges.
Example Conclusion Paragraph for a Persuasive Essay: In conclusion, the persuasive argument for mental health education in schools highlights the potential for early intervention and prevention. As we consider the well-being of future generations, we are called to prioritize mental health education as an essential component of a holistic education system.
Narrative Essays
Narrative essays offer you the opportunity to tell a story or share personal experiences related to depression. Explore these narrative essay topics:
- 1. Narrate a personal experience of overcoming depression or supporting a loved one through their journey.
- 2. Imagine yourself in a fictional scenario where you advocate for mental health awareness and destigmatization on a global scale.
Example Introduction Paragraph for a Narrative Essay: Personal experiences with depression can be transformative and enlightening. This narrative essay delves into a personal journey of overcoming depression, highlighting the challenges faced, the support received, and the lessons learned along the way.
Example Conclusion Paragraph for a Narrative Essay: In conclusion, the narrative of my personal journey through depression reminds us of the resilience of the human spirit and the power of compassion and understanding. As we reflect on our own experiences, we are encouraged to share our stories and contribute to the ongoing conversation about mental health.
Holden Caulfield Symptoms
Depression is depression an actual illness, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Ileana Chivescu Case Study
The epidemic of depression among students and teenagers, the effects of depression in your body and its treatment, the issue of depression and its reality nowadays, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Overview of Biological Predispositions and Risk Factors Associated with Depression
How to overcome depression and anxiety, depression: definition, risks, symptoms and treatment, the best way to help someone who is depressed, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
The Issue of Depression: Mental Battle
What is a depression, living in depression: a firsthand account, teen depression - symptoms and causes, adolescent depression and its contribution to teenage suicides, the issue of depression and its affect in an emerging adulthood, depression: definition and ways of resolving caused problems, depression in teenagers: causes and ways to overcome, depression and its main causes, genetic disorder report: clinical depression, the way teachers can help their students to overcome anxiety and depression, depression and its effects of mind and body, the effectiveness of cognitive behavioural therapy (cbt) for treating individuals with depression and anxiety, how to overcome teenage depression, depression as the reason of serious health problems and suicide, a depressing world with different obstacles, the link between self-esteem and adolescent depression, darwinian psychology and depression: the gender differential hypothesis, prevention of depression, anxiety and burnout in resident doctors – a systematic review, dysregulated processing of negative and positive responses in depression.
Depression, known as major depressive disorder or clinical depression, is a psychological condition characterized by enduring feelings of sadness and a significant loss of interest in activities. It is a mood disorder that affects a person's emotional state, thoughts, behaviors, and overall well-being.
Its origin can be traced back to ancient civilizations, where melancholia was described as a state of sadness and melancholy. In the 19th century, depression began to be studied more systematically, and terms such as "melancholic depression" and "nervous breakdown" emerged. The understanding and classification of depression have evolved over time. In the early 20th century, Sigmund Freud and other psychoanalysts explored the role of unconscious conflicts in the development of depression. In the mid-20th century, the Diagnostic and Statistical Manual of Mental Disorders (DSM) was established, providing a standardized criteria for diagnosing depressive disorders.
Biological Factors: Genetic predisposition plays a role in depression, as individuals with a family history of the disorder are at a higher risk. Psychological Factors: These may include a history of trauma or abuse, low self-esteem, pessimistic thinking patterns, and a tendency to ruminate on negative thoughts. Environmental Factors: Adverse life events, such as the loss of a loved one, financial difficulties, relationship problems, or chronic stress, can increase the risk of depression. Additionally, living in a socioeconomically disadvantaged area or lacking access to social support can be contributing factors. Health-related Factors: Chronic illnesses, such as cardiovascular disease, diabetes, and chronic pain, are associated with a higher risk of depression. Substance abuse and certain medications can also increase vulnerability to depression. Developmental Factors: Certain life stages, including adolescence and the postpartum period, bring about unique challenges and changes that can contribute to the development of depression.
Depression is characterized by a range of symptoms that affect an individual's emotional, cognitive, and physical well-being. These characteristics can vary in intensity and duration but generally include persistent feelings of sadness, hopelessness, and a loss of interest or pleasure in activities once enjoyed. One prominent characteristic of depression is a noticeable change in mood, which can manifest as a constant feeling of sadness or emptiness. Individuals may also experience a significant decrease or increase in appetite, leading to weight loss or gain. Sleep disturbances, such as insomnia or excessive sleepiness, are common as well. Depression can impact cognitive functioning, causing difficulties in concentration, decision-making, and memory recall. Negative thoughts, self-criticism, and feelings of guilt or worthlessness are also common cognitive symptoms. Furthermore, physical symptoms may arise, including fatigue, low energy levels, and a general lack of motivation. Physical aches and pains, without an apparent medical cause, may also be present.
The treatment of depression typically involves a comprehensive approach that addresses both the physical and psychological aspects of the condition. It is important to note that the most effective treatment may vary for each individual, and a personalized approach is often necessary. One common form of treatment is psychotherapy, which involves talking to a mental health professional to explore and address the underlying causes and triggers of depression. Cognitive-behavioral therapy (CBT) is a widely used approach that helps individuals identify and change negative thought patterns and behaviors associated with depression. In some cases, medication may be prescribed to help manage depressive symptoms. Antidepressant medications work by balancing neurotransmitters in the brain that are associated with mood regulation. It is crucial to work closely with a healthcare provider to find the right medication and dosage that suits an individual's needs. Additionally, lifestyle changes can play a significant role in managing depression. Regular exercise, a balanced diet, sufficient sleep, and stress reduction techniques can all contribute to improving mood and overall well-being. In severe cases of depression, when other treatments have not been effective, electroconvulsive therapy (ECT) may be considered. ECT involves administering controlled electric currents to the brain to induce a brief seizure, which can have a positive impact on depressive symptoms.
1. According to the World Health Organization (WHO), over 264 million people worldwide suffer from depression, making it one of the leading causes of disability globally. 2. Depression can affect people of all ages, including children and adolescents. In fact, the prevalence of depression in young people is increasing, with an estimated 3.3 million adolescents in the United States experiencing at least one major depressive episode in a year. 3. Research has shown that there is a strong link between depression and other physical health conditions. People with depression are more likely to experience chronic pain, cardiovascular diseases, and autoimmune disorders, among other medical conditions.
The topic of depression holds immense significance and should be explored through essays due to its widespread impact on individuals and society as a whole. Understanding and raising awareness about depression is crucial for several reasons. Firstly, depression affects a significant portion of the global population, making it a pressing public health issue. Exploring its causes, symptoms, and treatment options can contribute to better mental health outcomes and improved quality of life for individuals affected by this condition. Additionally, writing an essay about depression can help combat the stigma surrounding mental health. By promoting open discussions and providing accurate information, essays can challenge misconceptions and foster empathy and support for those experiencing depression. Furthermore, studying depression allows for a deeper examination of its complex nature, including its psychological, biological, and sociocultural factors. Lastly, essays on depression can highlight the importance of early detection and intervention, promoting timely help-seeking behaviors and reducing the burden of the condition on individuals and healthcare systems. By shedding light on this critical topic, essays have the potential to educate, inspire action, and contribute to the overall well-being of individuals and society.
1. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. 2. World Health Organization. (2017). Depression and other common mental disorders: Global health estimates. World Health Organization. 3. Kessler, R. C., Bromet, E. J., & Quinlan, J. (2013). The burden of mental disorders: Global perspectives from the WHO World Mental Health Surveys. Cambridge University Press. 4. Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression. Guilford Press. 5. Nierenberg, A. A., & DeCecco, L. M. (2001). Definitions and diagnosis of depression. The Journal of Clinical Psychiatry, 62(Suppl 22), 5-9. 6. Greenberg, P. E., Fournier, A. A., Sisitsky, T., Pike, C. T., & Kessler, R. C. (2015). The economic burden of adults with major depressive disorder in the United States (2005 and 2010). Journal of Clinical Psychiatry, 76(2), 155-162. 7. Cuijpers, P., Berking, M., Andersson, G., Quigley, L., Kleiboer, A., & Dobson, K. S. (2013). A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian Journal of Psychiatry, 58(7), 376-385. 8. Hirschfeld, R. M. A. (2014). The comorbidity of major depression and anxiety disorders: Recognition and management in primary care. Primary Care Companion for CNS Disorders, 16(2), PCC.13r01611. 9. Rush, A. J., Trivedi, M. H., Wisniewski, S. R., Nierenberg, A. A., Stewart, J. W., Warden, D., ... & Fava, M. (2006). Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. American Journal of Psychiatry, 163(11), 1905-1917. 10. Kendler, K. S., Kessler, R. C., Walters, E. E., MacLean, C., Neale, M. C., Heath, A. C., & Eaves, L. J. (1995). Stressful life events, genetic liability, and onset of an episode of major depression in women. American Journal of Psychiatry, 152(6), 833-842.
Relevant topics
- Mental Health
- Eating Disorders
- Drug Addiction
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Write my thesis
- Thesis writers
- Buy thesis papers
- Bachelor thesis
- Master's thesis
- Thesis editing services
- Thesis proofreading services
- Buy a thesis online
- Write my dissertation
- Dissertation proposal help
- Pay for dissertation
- Custom dissertation
- Dissertation help online
- Buy dissertation online
- Cheap dissertation
- Dissertation editing services
- Write my research paper
- Buy research paper online
- Pay for research paper
- Research paper help
- Order research paper
- Custom research paper
- Cheap research paper
- Research papers for sale
- Thesis subjects
- How It Works
What Is a Good Thesis Statement About Depression?

Do you need to compose an informative or an argumentative essay on depression? One of the vital parts of your paper is a thesis statement on depression. Note there are various types of thesis statements, and what you use depends on the type of essay you are writing. A thesis summarizes the concept that you write on your research paper or the bottom line that you will write in your essay. It should elaborate more on the depression topics for the research paper you are working on. But at times, you might have a hard time writing your thesis statement.
Good Thesis Statement about Teenage Depression
Bipolar disorder thesis statements about depression, interesting thesis statements about depression, interesting thesis statement about diagnosis and treatment of depression, thesis statement about stress and depression, free thesis statements about depression and anxiety, get help with your depression research paper.
Here is a list of thesis statements to have an easier time writing your essay. They cover different topics, making it easy to select what excites you. Here we go!
Are you writing about teenagers and how they are always overthinking about their future, and they end up getting depressed? You need to write a good thesis statement for a depression research paper. That will help your depression argumentative essay stand out. Here are some thesis statement for depression to check out.
- There is a link between depression and alcohol among teenagers and the various ways to control it.
- Teenagers dealing with mood disorders eat and sleep more than usual, getting less interested in regular activities.
- Mediation is an effective way to reach out to adolescents that show heightened symptoms of depression.
- Self-blaming attributions are social cognitive mechanisms among adolescents.
- Peer victimization causes high-stress levels among adolescents and has negative psychological consequences.
Choosing a good depression thesis statement on bipolar disorder can be hectic. Research on bipolar will require a good thesis statement for mental health. Choose a thesis statement about mental health awareness here.
- People with Bipolar depression have more difficulties getting quality sleep.
- Bipolar disorder influences every aspect of a person’s life and changes their quality of life.
- Bipolar disorder causes depressive moods or lows of mental disorder.
- Bipolar is a severe mental issue that can negatively impact your moods, self-esteem, and behavior.
- Psychological evaluations play a significant role in diagnosing bipolar disorder.
When writing your essay, ensure that the thesis statement for mental health is fascinating. You will impress your professors if you get the right depression research paper outline as your thesis statement. Here is a depression thesis statement you can use.
- The effects of human psychology are viewed in the form of depression.
- Clinical psychology can help to bring outpatients who have depression.
- Treating long-term depression in bipolar patients is possible.
- Bipolar patients are drained to the roots of depression.
- Well-established rehabilitation centers can help bring drug addicts from depression.
Are you thinking of writing a thesis on depression and how to treat it? If so, you need to have an excellent thesis statement about mental health that will impress your professor. Read this list to find a thesis you need for your research paper.
- There are different ways to diagnose and treat depression from its early stage.
- People who show signs of depression from an early stage and seek treatment are likely to recover instead of those who do not show early signs.
- After you receive treatment for depression, putting the right measure in place is one of the best and effective ways to ensure that you do not get it again for the second time.
- Anxiety can interfere with daily living, and it can get anyone from children to adults.
- Besides medication, you need a lifestyle change and acceptance to treat depression.
Is your research about stress and how it can impact mental health? Getting a thesis statement for depression research paper that impresses your examiners can be challenging. Choose a thesis statement for your mental illness research paper below.
- Although it is normal for various situations to cause stress, having constant stress can have detrimental effects.
- To survive the modern industrial society, you need to have stress management strategies.
- The challenges of understanding and adapting to the changing environment can lead to stress.
- Lack of proper stress management will lead to inefficiency in everything people do.
- Stress does not come unless there are underlying stressors in your life.
Our team of writers is well-conversant about a free thesis statement about anxiety you can use. The best anxiety thesis statement will help you get the best grades. Here is a list of statements that stands out:
- Many factors can lead to early anxiety, but the leading cause of anxiety in adolescents is directly linked to families.
- Anxiety is a severe mental disorder that can occur without any apparent triggers.
- Long-term depression and anxiety can impact your mental health, but you can recover if you seek treatment.
- Depression and anxiety are not interlinked, and it is essential to learn how to differentiate them on practical grounds.
- Society has a role to play in helping people come out of depression and anxiety.
How do you write a research paper about depression and how it affects mental health? Before choosing a thesis statement on mental health, have a clear understanding of the essay that you are writing. That will help you get the best thesis to make our essay stand out.
But don’t keep stressing out about your thesis statement for mental illness research paper. We have your work cut out because our skilled writers have compiled a list of thesis statements about mental health and depression topics for research paper writing. We will also suggest correct thesis statements for your essay homework or assignment.
If you are still unsure of the statement to use, get in touch with us today. We have a team of skilled and experienced writers that can help you with your essay or research project and ensure that you get the best grades.
Leave a Reply Cancel reply
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Curr Neuropharmacol
- v.13(4); 2015 Jul
The Effects of Psychological Stress on Depression
Longfei yang.
a Jilin Provincial Key Laboratory on Molecular and Chemical Genetic;
Yinghao Zhao
b Department of Thoracic Surgery, Second Hospital of Jilin University, Changchun 130024, China
Xingyi Zhang
Major depressive disorder is a serious mental disorder that profoundly affects an individual's quality of life. Although the aetiologies underlying this disorder remain unclear, an increasing attention has been focused on the influence imposed by psychological stress over depression. Despite limited animal models of psychological stress, significant progress has been made as to be explicated in this review to elucidate the physiopathology underlying depression and to treat depressive symptoms. Therefore, we will review classical models along with new methods that will enrich our knowledge of this disorder.
INTRODUCTION
As the commonest cause of disability affecting nearly 16% of the global population [ 1 ], major depressive disorder (MDD) attracts increasing attention while the underlying mechanism of this disorder is largely uncharacterized. In accordance with published reports from the World Health Organizaton (WHO), MDD is projected to be a major reason for disability in the world by 2030 [ 2 ]. In the United States, about 10% of the whole population (that is 14 million people) at any time is inflicted with depression [ 1 ].
The cardinal symptoms of MDD include depressed mood (reduced motivation or hopelessness), anhedonia (diminished ability to experience pleasurable activity such as food, sex and social interactions), anergia, irritability, difficulty in concentrating, disrupted sleep, appetite and cognition and tendency to suicide [ 3 ]. Depression is not only highly comorbid with anxiety disorders [ 4 ], but is also closely associated with dementia [ 5 ], type 2 diabetes, coronary artery disease [ 6 ], Parkinson’s disease, epilepsy, pain, cancers [ 7 ], aging [ 8 ], osteoporosis [ 9 ] and irritable bowel syndrome [ 10 ]. Unfortunately, the chronic and debilitating nature of depression makes the prognosis of many chronic diseases complicated and aggravates the situation of disease and disability in the world [ 11 ].
Although much attention has been focused on this multifactorial and heterogeneous disorder, the aetiologies of depression remain hitherto poorly understood. While risk loci for many other common diseases have been identified by genetic analysis, the true “depression genes” which are responsible for the onset and the cure of depression and could be manipulated to produce models of depression in rodents, have not been identified [ 11 , 12 ]. Even so, genetic factors (about 40% [ 11 ]), together with external environmental factors (stressful events in particular such as losing jobs and beloved ones), are considered to be involved in the onset of depression [ 11 , 13 ]. The environmental risk factors associated with depression include endocrine abnormalities (hyper- or hypo-thyroidism), cancers (for example, pancreatic adenocarcinoma and breast cancers), adverse effects of drugs (such as recombinant interferons [ 14 ] and isotretinion [ 11 ]), and stressful events [ 11 ] and other factors will be detailed further in this review.
Stressful life events could induce a series of psychological and physiological changes including activation of hypothalamic-pituitary-adrenal (HPA) axis and sympathetic nervous system [ 15 ], which could be referred to as psychological stress responses. Here, recent approaches and effects dedicated to uncovering the interconnections between psychological stress and depression will be briefly reviewed.
PSYCHOLOGICAL STRESS
Psychological stress has been increasingly featured in scientific works as well as in popular media such as internet, newspapers and TV due to terrorism, war [ 16 ], divorce and unemployment [ 17 ]. Psychological stress which is an adaptation to the fight-or-flight response during evolution, can induce a constellation of physiological responses (including nervous, endocrine and immune systems) which otherwise could be harmful under some conditions [ 17 ]. Among those responses, hyperactivity of HPA axis is one of the commonest neurobiological changes in depressive patients (dysfunction of HPA axis is manifested in about 70% patients of depression [ 18 ]) as is revealed by researches over the last 40 years [ 19 ].
According to the duration of stress, psychological stresses may be divided into two classes: acute psychological stress (surgical operation and examination, for example) and chronic psychological stress (such as anxiety about children, financial problems and periodic headaches) which could be subdivided into disconnected and persistent psychological stress [ 20 ].
Animal models are useful tools for investigating the neurobiology of psychological stress as well as mental diseases such as depression and anxiety [ 21 ]. Several animal models of psychological stress are listed in Table 1 1 .
Animal models and involved factors discussed in brief.
Abbreviation in the table: ΔFosB, a highly stable isoform of FosB which is a component of transcription factor-activator protein-1 (AP-1); BDNF, brain-derived neurotrophic factor; CRF, corticotrophin releasing factor; HPA, hypothalamic-pituitary-adrenal; IL-1β, interleukin-1β; IL-6, interleukin-6; LHb, lateral hebenula; mPFC, medial prefrontal cortex; PFC, prefrontal cortex; SNS, sympathetic nervous system; TNF-α, tumor necrosis factor-α; VTA, ventral tegmental area.
In response to psychological stress, impulses stemming from the higher cortical areas of the brain are transmitted to the hypothalamus through the limbic system [ 29 ]. Neurotransmitters such as serotonin, norepinephrine (NE), and acetylcholine are released, and certain cells of paraventricular nucleus (PVN) at the hypothalamus are activated to synthesize and secrete corticotrophin releasing factor (CRF) [ 3 , 12 , 29 ]. Subsequently, CRF enters the hypothalamic portal venous system and stimulates the corticotrophs located at the anterior pituitary gland to synthesize proopiomelanocortin (POMC) [ 19 , 29 ]. Just as proinsulin cleaves to produce insulin and C-peptide, the polyprotein POMC subsequently splits to produce adrenocorticotropic hormone (ACTH) and alpha melanocyte-stimulating hormone (α-MSH) [ 29 ]. CRF from parvocellular neurons also stimulates the release of arginine vasopressin (AVP) from PVN which together with CRF synergistically stimulates the release of ACTH [ 3 , 30 ]. ACTH stimulates the zone fasciculate and reticularis of the adrenal cortex to produce and release glucocorticoids (GCs, cortisol and corticosterone in human and rodent, respectively) [ 19 , 29 , 30 ], which together with catecholamine released by sympathetic nervous system (SNS) are the main stress hormones [ 20c , 29 ]. GCs exert their effects on the multiple aspects of the brain function, such as survival of neurons, neurogenesis, hippocampal size and emotional events, and the peripheral functions including metabolism and immunity [ 3 , 19 ]. By binding to glucocorticoid receptors (GRs) in the hypothalamus, the pituitary and the medial prefrontal cortex (mPFC), which will result in a decrease in CRF secretion and subsequent reduced release of ACTH from the pituitary, these GCs inhibit activity of HPA axis through negative feedback mechanism to sustain homeostasis [ 3 , 13b , 19 , 20b , 21a , 31 ].
BRAIN REGIONS INVOLVED IN DEPRESSION
Signals from environmental stressors such as danger to life, social stressors and responses to injuries in the body are firstly transduced by sensory nervous systems, and then the sequent information is processed by so-called emotional circuits in the brain [ 16 ]. Although so far we have no clear understanding of the neural loops underlying the pathology of depression, the diverse symptoms of depression imply that many brain regions could be involved in the affection disorders [ 12 ]. Human brain imaging researches have demonstrated alterations of hemorheology and related parameters in brain regions such as amygdala, thalamus, striatum, hippocampus, prefrontal and cingulate cortex and so on, and many abnormities in those regions have been evidenced by studies on brains of depressive patients on autopsy [ 12 ].
The most frequently reported findings obtained by brain-imaging technology are diminished grey-matter volumes and reduced glial densities of hippocampus and prefrontal cortex (PFC) in depressive patients [ 11 ], while it is still inconclusive whether these alterations in hippocampus and PFC represent a precipitating factor or are just a result of major depression [ 32 ].
Prefrontal Cortex
Reduced neuronal activity of medial PFC (mPFC) is found in social defeat-induced depression mice models despite its unclear pro-depressant mechanism [ 21b ]. Degeneration of astrocytes in the PFC of rat induced depressive symptoms [ 33 ] and glial loss in PFC could effectively generate behaviors similar to depression [ 34 ]. The activity of ERK1/2 MAPK pathway as well as levels of mRNA expression and protein of ERK1/2 significantly declined in the PFC of depressant people who committed suicide [ 35 ]. The antidepressant action of ATP was evidenced to be modulated by P2X2 receptors in PFC [ 36 ].
Recent studies showed that transcription factor ΔFosB in mPFC, the prelimbic area in particular, regulates the vulnerability to stressful events and its overexpression exerts an enhancing effect on vulnerability to stress, in part via suppressing activity of cholecystokinin (CCK)-Breceptor [ 21b ]. Blocking CCKB receptor in mice generates a pliable phenotype while the ligand CCK administered into mPFC in mice produces depressive symptoms similar to those induced by social defeat stress [ 21b ].
These results suggest that CCKB and ΔFosB may be novel potent targets for preventing and/or curing depression [ 21b ]. However, optogenetic stimulation of mPFC projections to basolateral amygdala or nucleus accumbens (NAc) after CCK infusion in mPFC can block the anxiogenic effect of CCK but no other antidepressant-like effect was observed in social defeat stress models [ 21b ], which indicates that more detailed underpinnings of those effects need to be mapped out.
Ventral Tegmental Area
Dopamine neurons in ventral tegmental area (VTA) determine vulnerability versus resilience to social defeat stress, while vulnerable phenotype will manifest depressive behaviors [ 23a ]. Induction of phasic rather than tonic firing by optogenetic methods in VTA dopamine neurons (projecting to NAc rather than to mPFC) of mice which experienced a social defeat stress beneath the threshold, caused a rapid vulnerable phenotype evidenced by increased social avoidance and reduced sucrose preference [ 24 ]. Optogenetic induction of VTA phasic firing also transformed resilient mice that underwent repeated social defeat stress previously into a vulnerable phenotype. Optogenetic suppression of the VTA-NAc dopamine projections generated resilience while suppression of VTA-mPFC dopamine projection induced vulnerability [ 24 ]. These projection-specific and fire-pattern-specific findings improve our understanding regarding roles of VTA dopamine neurons in susceptibility to stress and in pathology of depression [ 24 ].
Hippocampus
Structural and neurochemical changes of the hippocampus such as hippocampal neurons atrophy [ 37 ] and decreased ERK1/2 MAP kinase activity (detected in the post-mortem hippocampus of depressed persons [ 35 ]) are among the characteristics of major depression. Chronic stress exposure induces reduced hippocampal volume and diminished expression of neurotrophic factors and inhibits neurogenesis occurring in dentate gyrus in the adult brain [ 38 ]. Those alterations could be reversed by antidepressants [ 38c ]. In psychological stress induced rat model of depression, levels of total zinc and mRNA expression of zinc transporting-associated proteins decreased in the hippocampus, while zinc functioned as cofactor for enzymes which are critical for biochemical processes especially in the brain [ 39 ]. Supplements with zinc or treatment with antidepressants could reverse the changes that are mentioned above [ 39 ]. Both drugs (such as resveratrol) and antidepressants (fluoxetine for example) could enhance the levels of BDNF mRNA and protein in the hippocampus and the mPFC [ 21a ]. The ATP abundance in interstitial fluid derived from the hippocampus and PFC of the mice vulnerable to chronic social defeat stress was lower than that from the resilient mice [ 36 ]. The phospholipidomic profile (such as catalase, superoxide dismutase (SOD) and glutathione reductase) in the hippocampus was changed in mice exposed to chronic unpredictable stress [ 28a ]. Micro-RNAs in the hippocampus such as miR-16 and miR-598-5p could be targeted to generate antidepressant behavior effects [ 40 ]. All those studies corroborate that the hippocampus may play diverse roles in the psychopathology of depression and much more details need to be further explored.
ENDOCRINE SYSTEM AND DEPRESSION
Glucocorticoids.
Upon activation of HPA axis by the psychological stress, more GCs are released into the blood. Elevated concentrations of cortisol in the blood, saliva and urine, as well as bigger size and increased activity of adrenal gland, are found in a large part of depressive patients [ 41 ]. Hypercortisolemia can cause excitotoxicity to pyramidal neurons in the hippocampus and can lead to spine loss and atrophy of dendrites, as well as inhibition of neurogenesis in the dentate gyrus of the hippocampus [ 12 ]. Redundant GCs may also reduce the volume of hippocampus [ 42 ] thus affecting the function of brain areas related to emotion and reward circuitry. Many of these alterations could be rescued by antidepressant drugs [ 12 ]. Under normal conditions, GCs contribute to the termination of the stressful reaction via complicated feedback loops which involve the participation of hippocampus and paraventricular nucleus [ 12 , 19 ]. However, the dysregulation of GC-mediated feedback loops, such as decreased function of glucocorticoid receptor (GR) in HPA axis, peripheral blood mononuclear cells (PBMC) and skin cells, was identified in depressive patients by a series of studies [ 19 , 26a ].
The abnormalities in GR may explain the hyperactivity of HPA axis in depression, and antagonists of GR (such as mifepristone) and GC synthesis inhibitors (for example, metyrapone) exhibit some therapeutic efficacy on depressive symptoms [ 43 ]. However, different effects of GCs and GR on depressive symptoms remain to be further explored.
Corticotrophin Releasing Factor
Evidence for the important role played by CRF in depression increased over the past decade. Acting as a neurotransmitter in the central nucleus of amygdala and bed nucleus of stria terminalis, concentrations of CRF in those areas, as well as the number of CRF-secreting neurons in the hypothalamus and locus coeruleus, were found elevated in patients with depression [ 12 , 31 , 44 ]. CRF overexpression in transgenic mice induced depressive behaviors and histonic signatures such as hypercortisolemia, anorexia, weight loss and decreased libido, which could also be achieved by infusion of CRF into CNS [ 31 ].
CRF exerts its physiological function by binding to its G-protein coupled receptors, CRF 1 and CRF 2 , to activate the downstream cAMP signaling [ 31 , 45 ]. CRF 1 receptors are highly expressed in the pituitary and the limbic areas where they modulate the activity of HPA axis [ 46 ]. Selective deletion of CRF 1 receptors in limbic areas leads to antidepressant-like behaviors in mice subjected to stress while antagonists of CRF 1 receptors could attenuate a series of depressive behaviors generated by withdrawal of drugs of abuse, but inconsistent results still exist [ 12 , 31 ]. A major frustration about developing antagonists of CRF 1 receptors as antidepressants is the pharmacokinetic issue as well as hepatotoxicity [ 12 ]. The major function of CRF 2 receptors might be keeping the HPA axis response, rather than activating the HPA axis when exposed to stress, by functioning as auto-receptors on some neurons in paraventricular nucleus (PVN) [ 47 ]. Genetic deletion of CRF 2 receptors induces anxiety-like symptoms in mice and antagonists exhibit anxiolytic effects, and some antagonists even exhibit antidepressant effects in chronic mild stress model [ 12 ]. With less side effects compared to antagonists of CRF 1 receptors, exploring antagonistsof CRF 2 receptors is of great interest to treat depression even though there are much more efforts to be made [ 12 , 31 , 47 ]. For more detailed knowledge about CRF, please see Reference 31.
Vasopressin
Synthesized in and secreted from paraventricular and supraoptic hypothalamic nuclei, this neuropeptide along with CRF stimulates the release of ACTH from corticotropes located at anterior pituitaryand thus tunes the activity of the HPA axis when exposed to stress [ 12 , 13b ]. After binding to vasopressin V1a and V1b receptors which are also GPCRs [ 48 ], the activated complex exerts its influence throughout the limbic brain system, especially in the amygdala and bed nucleus of the stria terminalis [ 12 ]. The physiological effects of vasopressin include regulating water balance, blood pressure stress and anxiety among others [ 48 , 49 ]. Vasopressin exerts driving influence on HPA axis related to chronic psychological stress by interacting with its V1b receptors which are widely distributed in the limbic brain regions [ 48 , 50 ]. Concentrations of vasopressin were elevated in depressive patients which might conduce to the hyperactivity of the HPA axis in those patients, while SSRI drugs treatment reverses this kind of alterations [ 48 , 51 ]. The quantities of V1b receptor-expressing neurons in depressive patients are larger than those of the healthy ones [ 48 ]. Antagonists of vasopressin V1b receptors of non-peptide property exhibit antidepressant action while conflicting results about the antidepressant effects of genetic deletion of V1b receptor gene in mice have been found [ 48 , 52 ]. These confusing results need more detailed explanation by more well-designed experiments.
As a major excitatory neurotransmitter in the central nervous system, glutamate functions by binding metabotropic glutamate receptors (mGluR) and ionotropic glutamate receptors (iGluR) localized on both neurons and non-neuronal cells to produce rapid synapses-crossing transmission [ 53 ]. The levels of glutamate (or glutamine) in patients with depression were found elevated in the brain, cerebrospinal fluid and plasma [ 33 , 54 ]. Exposure to stress leads to the release of glutamate from presynaptic neurons, which subsequently binds to iGluRs (such as N-methyl-D-aspartate (NMDA) receptors, kainite receptors and α-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid (AMPA) receptors on the postsynaptic neurons), as well as mGluRs located on both presynaptic and postsynaptic cells, and activates the downstream signaling pathways [ 54 , 55 ].
NMDA Receptors
Two NR1 subunits, combined with either two NR2 subunits (the NR2 subunits could be subdivided into NR2A to NR2D subunits) or two NR3 subunits (NR3A to NR3B, less common), form the tetrameric NMDA receptors [ 54 , 56 ]. They play important roles in learning and cognition and are closely associated with depression [ 57 ] while NMDA receptor antagonists are attractive drug candidates for refractory depression therapy [ 58 ].
Despite the fact that supportive results from clinical trials for the use of NMDA receptor antagonists remain weak, the diminished function of the receptors still shows antidepressant-like activity in the animal models [ 12 ]. The low status of NMDA receptor function could also prevent the morphological changes in hippocampal neurons induced by psychological stress and NMDA receptors expression could also be repressed by the marketed antidepressants [ 12 ]. By inhibiting glutamate activity, antagonists of NMDA receptors such as ketamine exhibited rapid antidepressant properties in both animal models and depressive patients [ 59 ]. However, ketamine could risk a series of side effects which set a limit to its use [ 33 ]. But another non-competitive and low-affinity antagonist of NMDA receptor, memantine, failed to produce rapid antidepressant-like responses until a high dose [ 54 ], which imply the complicated mechanism underlying the pathology of depression. Genetic deletion of NMDA receptor ε4 subunit (GluRε4, also named as NR2D) could generate antidepressant-like effects in mice [ 60 ]. The specific antagonists of NMDA receptors containing NR2B subunits may present good candidates considering that the NR2B subunits are mainly localized in the depression-associated brain regions such as the hippocampus [ 54 ] but there are also results showing that NR2B and NR2A levels are reduced in the PFC of depressive patients [ 56 ], which is confusing. However, the identified X-ray crystal structure of NMDA will shed more light on the depression treatments based on NMDA receptors [ 61 ].
AMPA Receptors
After binding with glutamate, the activated APMA receptors elevate the expression of BDNF in the hippocampus leading to fast neurogenesis and sprouting of hippocampal neurons [ 12 ]. Positive allosteric modulators (such as piracetam, aniracetam and cyclothiazide [ 54 ]) exhibit antidepressant profiles alike to tricyclic drugs and SSRIs in several animal paradigms without fast desensitization of AMPA receptors which are often observed with full agonists [ 54 ]. In forced swim and tail suspension paradigms of mice, inhibitors of AMPA receptors may suppress the antidepressant-like behaviors induced by ICV administration of lithium, which could also elevate the protein level of glutamate receptor 1 (GluR1) and GluR2 in the mice hippocampus [ 62 ]. There is also an evidence proving that antidepressant drugs may be attributed to the biological effects of AMPA receptors [ 12 ].
Metabotropic Glutamate Receptors
Adverse effects of NMDA receptor antagonists resulting from direct suppression of glutamatergic function turned our focus to metabotropic glutamate receptors (mGluR, (class C G-protein-coupled receptors (GPCR)) [ 33 ]. Highly expressed in the hippocampus, cortex, striatum, caudate nucleus and NAc, mGluR5 are mainly localized on postsynaptic membrane [ 33 ] and drugs targeted at this receptor to cure depression, anxiety and fragile X syndrome are experiencing clinical trials [ 53b ]. Antagonists of group II metabotropic glutamate (mGlu2/3) receptor exhibit acute and sustained antidepressant-like actions in tail suspension and novelty-suppressed feeding paradigms [ 63 ]. Antidepressant effects in behavior could also be induced by mGluR5 antagonists such as MTEP [ 33 ]. The structure of mGluR5 transmembrane domain helps greatly in understanding the pathologies of neuropsychiatric disorders [ 53b ].
Gamma-aminobutyric Acid (GABA)
It is postulated that the imbalance between glutamate and GABA with glutamatergic hyperactivity is involved in the neurobiology of major depression disorder [ 33 ]. GABA is the major inhibitory transmitter in the central nervous system and some brain regions (such as PFC, hippocampus, NAc, amygdala, VTA and hypothalamus) closely related to depression have GABAergic neuronal projections [ 12 ]. Therefore, there is a hypothesis that the activation of the GABA receptors may produce antidepressant effects [ 33 ]. The α2/α3 GABA A receptor modulators are supposed to probably serve as novel antidepressant candidates [ 64 ]. However, GABA receptor antagonist bicuculline can reverse the depression-like behaviors generated by ICV administered neuronostatin [ 65 ]. The resolved three-dimensional structure of GABA A receptor will further explore our understanding of depression and the design of potential drugs [ 66 ].
Serotonin and its receptors are among the major targets for depression therapeutic drugs such as tricyclics, selective serotonin re-uptake inhibitors (SSRIs) and serotonin and noradrenaline re-uptake inhibitors (SNRIs) [ 12 ]. Serotonin from the dorsal raphe (DR) located in the periaqueductal grey area and other raphe nucleus innervates many brain areas involved in depression such as the amygdala, the NAc and the PFC [ 67 ]. Elevated levels of serotonin contribute to the antidepressant effect [ 68 ]. By binding to serotonin receptors, serotonin activates a series of signaling pathways including cAMP-PKA-CREB pathway to generate antidepressant effects [ 55 ]. The X-ray structure of 5-HT 3 receptor in complex with stabilizing nanobodies [ 69 ] may help us understand the antidepressant effects of drugs at the molecular level and reasonably design drugs targeted at this receptors with less side effects.
These structures of transmitters receptors involved in the pathology of depression will help us to study the antidepressant molecular mechanism and to design more rational chemical drugs with specific target sites.
Brain-derived Neurotrophic Factor
Neurotrophic factors play important roles in the regulation of neurogenesis, synaptic and structural plasticity, which are involved in the pathology of depression [ 37 , 70 ].
Stressful exposure could induce reduced hippocampal neurogenesis and lower expression of brain-derived neuro-trophic factor (BDNF) in limbic structures [ 70 ] and declined BDNF concentration in serum, the source of which is still disputed [ 11 ]. Neurotrophic factors such as BDNF (one member of nerve growth factor (NGF) family) play central roles in the survival, function and neuronal plasticity of the brain of adults as well as in the development of nervous system [ 55 ]. The binding of BDNF with its receptor tropomyosin-related kinase B (TrkB, a membrane-spanning protein with tyrosine kinase site at the cytoplasmic side) activates a series of downstream signaling pathways including phosphatidyl inositol-3 kinase (PI3K)-Akt (protein kinase B or serine threonine kinase) pathway, Ras-mitogen activated protein kinase (MAPK) pathway and phospholipase Cγ (PLCγ)-Ca 2+ pathway (which splits afterwards into 1,4,5-triphosphate inositol (IP3)-Ca 2+ -Ca 2+ /calmoludin-dependent protein kinase (CAMK) signaling and diacylglycerol (DAG)-PKC signaling) [ 55 ]. The NMDA receptor antagonist 7-chlorokynurenic acid could generate fast antidepressant effects such as elevated sucrose preference via alterations in expressions of microRNA that are involved in TrkB-ERK/Akt signaling in a chronic mild stress model of mice [ 40 ]. The activation of these pathways convergently promotes the survival, growth, synaptic plasticity and/or differentiation [ 55 ].
Consistent with the decreased BDNF in the hippocampus and prefrontal cortex (PFC) caused by stress, protein levels of the PI3K-Akt and Ras-MAPK signaling pathways decline, and this effect could be reversed by antidepressant treatments [ 71 ]. Meanwhile, the rapid antidepressant action of NMDA receptor antagonist 7-chlorokynurenic acid could be blocked by the MAPK/Akt inhibitors in the animal models [ 40 ]. Antidepressant drug ketamine (another NMDA receptor antagonist) could increase the level of BDNF, and BDNF conditional deletion in mice could block the antidepressant action of ketamine [ 72 ]. The fact that BDNF could effectively generate antidepressant-like behaviors in the animal paradigms of depression and antidepressant effects of drugs could be blocked by genetic deletion of BDNF [ 37 ] leads to the thought that BDNF and downstream elements of BDNF signaling may render some therapeutic targets different from those targeted by monoamine re-uptake inhibitors.
However, the fact that genetic deletion of BDNF in rodent models is insufficient to cause depressive symptoms [ 55 ], suggests that BDNF is not the main cause for depression or maybe there is an alternative unknown factor leading to depression in parallel with BDNF and probably components downstream of BDNF are better targets [ 55 ].
Although blockade of IP3 receptors in PFC of stressed mice could improve the cognitive function involved in depression [ 73 ], the pervasive expression of such signaling pathways hinders the research and application of potential drugs (for example, activation of MAP kinase in cingular cortex and paraventricular hypothalamus generated different effects [ 74 ]), which is probably the leading cause of few literatures about depression and the aforementioned signaling pathways downstream of BDNF.
Glial Cell-derived Neurotrophic Factor
Exposure to chronic stress reduced the mRNA transcription and protein synthesis of glial cell-derived neurotrophic factor (GDNF) in NAc in stress-susceptible BALB/c (BALB) mice strain but increased those in stress-resilient C57BL/6 (B6) mice [ 75 ], but sequences of the GDNF promoters between the two strains showed no differences [ 13a , 76 ]. This led to the finding that chronic ultra-mild stress (CUMS) enhances DNA methylation at the CpG site 2 and the binding level of methyl-CpG binding protein 2 (MeCP2) to the CpG2 site 2 [ 13a ]. The complex together with histone deacetylase2 (HDAC2) represses acetylation of Histone 3 (H3) and subsequently inhibits the GDNF transcription and finally results in depression-vulnerable phenotype in BALB mice [ 13a ]. While in B6 mice subjected to CUMS, although enhanced methylation and binding status of MeCP2 were also detected in NAc, the levels of GDNF expression and H3 acetylation were higher [ 13a ]. These demonstrated that MeCP2-cyclic AMP response element binding protein (CREB) complex binds to methylated site on GNDF promoters in resilient B6 mice [ 13a ].
These results suggest that different epigenetic signatures may affect the adaptive ability to stress [ 13a , 76 ]. It is interesting that in depressive patients, GDNF levels in serum are lower [ 77 ] while elevated GDNF levels are reported in drug-resistant depressive patients after electroconvulsive therapy [ 78 ]. This may be of prognostic importance to individuals from families historically involved in depression.
IMMUNE SYSTEM IN DEPRESSION
Increasing studies suggest that psychological stress has an important effect on the immune system [ 17 , 79 ], while researches showing that components of immune system such as interleukin-1β (IL-1β), IL-6, soluble IL-2 receptors and tumor necrosis factor-alpha (TNF-α) were elevated in depressive patients [ 80 ] indicate that the immune system is closely associated with depression. Peripheral inducers of immune cytokines may generate symptoms of depression [ 81 ] and in the brain, these inducers may decrease monoamine levels [ 82 ] that most current antidepressants aim to increase.
As an important regulator of brain-body interaction, immune mediators such as cytokines affect diverse central nervous system (CNS) functions involved in depression such as cognition, sleep and reward [ 83 ].
Expressed in the hypothalamus (mainly), hippocampus, cerebral cortex and thalamus, IL-1β (derived from microglia, astrocytes and neurons [ 84 ]) functions through interaction with its receptor, IL-1R1, which is expressed in several areas of the brain with more prominent expression in the hippocampus [ 85 ]. The binding of IL-1β to IL-1R1 activates a triad of signaling pathways including nuclear factor (NF)-κB, MAPK and JNK to function as host defenders [ 84 ]. Exposure to psychological stress will increase IL-1β in the hypothalamus and hippocampus while the administration of IL-1β will induce effects similar to stress response including activation of HPA axis, suppression of hippocampal long-term potentiation and down-regulated expression of BDNF [ 86 ]. Blockade of IL-1β signaling by administration of IL-1β receptors antagonists reversed stress-like symptoms induced by IL-1β at both cellular and behavioral levels [ 86 ]. IL-1β can also regulate the expression of the serotonin transporter gene [ 87 ], which is involved in the treatment of depression. This implicates the potential of IL-1β antagonists as a new candidate for depression therapy.
Although IL-1β plays a necessary and sufficient role in the cytostatic effect of stress on hippocampal progenitor cells, IL-6 may also conduce to the inhibition of proliferation [ 86 ]. This may be consistent with the hypothesis that hippocampal neurogenesis is necessary for the treatment of depression [ 38a ]. Furthermore, mice with IL-6 gene deleted manifested resistance to the development of depressive symptoms induced by stress [ 88 ], which could be adopted as a tool to study the mechanism underlying the pathology of depression and to screen potential antidepressant drugs.
TNF-α could activate HPA axis [ 89 ] and directly activate indoleamine-2,3-dioxygenase, which is expressed in macrophages and dendritic cells in the brain and could through kynurenine pathway catabolize tryptophan which is the substrate for serotonin synthesis [ 90 ]. Succeeding studies identified that via p38 MAPK signaling, TNF-α, as well as IL-1β, promotes the serotonin uptake in mice midbrain and striatal synaptosomes by activating serotonin transporters [ 68 ]. This kind of serotonin-decreasing effect of TNF-α may suggests that blocking the TNF-α signaling may contribute to ameliorate the depressive symptoms, which have the same target as the selective serotonin reuptake inhibitors (SSRIs): to inhibit the re-uptake of serotonin [ 68 ]. Studies showing that genetic deletion of either TNF-α receptor 1 (TNFR1) or TNFR2 generates a series of antidepressant-like behaviors in several animal models [ 91 ] while administration of TNF-α induced depression-like behaviors which could be prevented by antidepressant drug such as fluoxetine [ 89 ] corroborate the thought above.
The existence of those cytokines in both central nervous system and peripheral organs may explain, at least partly, the concomitance of mental and somatic symptoms in depressive patients [ 3 , 12 ]. Future researches about relationship between depression and cytokines may focus on the largely undiscovered neural circuits underlying the somatic and behavioral effects and the more detailed interaction among cells in brain.
NEW APPROACHES
Voltage-sensitive dyes (VSD) can be incorporated into cytoplasmic membranes and thus reflect the alteration of membrane potential [ 92 ]. With the help of suitable VSD, macroscopes and high-frequency cameras connected to computers, VSD imaging (VSDI) provides a quantitative method to quickly analyze neuronal activity involved in psychiatric diseases such as depression and anxiety at millisecond level, with a micrometer-level spatial resolution and a range spanning whole brain network [ 92 , 93 ]. This method is useful for investigating the dynamics of neuronal networks, especially in the animal models of stress [ 93b ]. However, this technology could only investigate the exposed areas which do not include deep brain regions. Other methods such as two-photon microendoscopy, will make up for that limitation [ 92 ].
3D anatomical and phenotypical maps are important for us to understand the relationships between structures and functions at cellular, circuit and organic levels [ 94 ]. Clearing tissues are the basis for the imaging of the whole body or whole organ, which is required for the identification and analysis of neuronal circuits in the brain [ 94 , 95 ]. Using passive clarity technique (PACT) followed by perfusion associated agent release in situ (PARS) method, optical access into intact tissues could be easily obtained, so the target tissues labeled with fluorescent probes could be readily detected in the premise of preserving tissue morphology [ 94 ]. With cellular and subcellular resolution, this kind of improved CLARITY technology, could make the study of intercellular spatial relationship and neuronal connectivity in the brain much easier, and thus improve the animal models of depression [ 94 , 96 ]. The CUBIC (clear, unobstructedbrain imaging cocktails and computational analysis) method could also be used to generate whole-brain image with single-cell resolution quickly, and in combination with other protocols, this method could also be utilized to visualizes and quantify the neuronal activities induced by ambient stimulation [ 95 ]. Those whole-body clearing technologies will provide insights into the neuronal circuits underlying the pathophysiology of depression.
As an outstanding example for the combination of genetics and optical methods, optical stimulation plus genetic engineering (optogenetics) could rapidly and precisely control specific function (gain or loss) of precisely defined biological processes in living tissues, especially in the central nervous system [ 97 ]. This kind of effect is based on light-activated ion channels and pumps (mainly channelrhodopsin 2, ChR2) which could be expressed in neurons and used to manipulate the firing rate and duration of neurons [ 24 , 98 ]. Using this technology, stimulation imposed upon cells can be manipulated at the speed of millisecond scale with precision of cell type level (such as stimulating or suppressing dopamine neurons in VTA projecting to NAc [ 97 ]). The well-designed manipulations could be made upon specific neural circuits in awake and freely moving animals and present us precise results with good repeatability, compared to other approaches in neuroscience such as lesions and pharmacological interventions [ 97 , 99 ]. Moreover, optogenetics could be used for behavioral controlling for a long period, which is important for identifying new neural loops involved in chronic stress [ 99 ]. Although optogenetic manipulations have been performed on the ex vivo retina (one kind of living human neural tissue), the major influence of this technology on human health comes from using it as a tool to gain insights into complex tissue function in diseases such as depression and Parkinson`s disease [ 97 ].
Magnetite nanoparticles could be used to generate heat under an alternating magnetic field, and heat could induce expression of some genes. When the heat-induced genes and magnetic nanoparticles are introduced into tumor xenografts, the expression of these genes could be controlled in a temporally and spatially selective manner, by altering the magnetic field [ 100 ]. The remote control of gene expression without lesions is very useful in animal models, especially models of mental diseases such as depression. With the improvement of this method, more insights into genes in neuronal circuits underlying the pathophysiology of depression will be obtained, although there is still much to do to achieve this purpose.
Although more and more focus has been laid on the brain research, especially the “ BRAIN Project ” launched by the national institutes of health (NIH) which will invest more money and energy into this area, our understanding about how the brain deals with the external information and how mental diseases especially depression and schizophrenia occur, remains to be further explored. However, the VSDI, optogenetic, CLARITY, PACT-PARS and CUBIC technologies will shed more light on our researches on the pathology of depression, or even more diseases such as cancer.
ACKNOWLEDGEMENTS
This work was supported by the Natural Science Foundation of China (31171123; 31300850; 81328011; 31471120); Jilin Provincial Department of Human Resources and Social Security Project ([2012]39); Jilin Science and Technology Agency funding (20110726).
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
What is depression?
Depression (also known as major depression, major depressive disorder, or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working.
To be diagnosed with depression, the symptoms must be present for at least 2 weeks.
There are different types of depression, some of which develop due to specific circumstances.
- Major depression includes symptoms of depressed mood or loss of interest, most of the time for at least 2 weeks, that interfere with daily activities.
- Persistent depressive disorder (also called dysthymia or dysthymic disorder) consists of less severe symptoms of depression that last much longer, usually for at least 2 years.
- Perinatal depression is depression that occurs during pregnancy or after childbirth. Depression that begins during pregnancy is prenatal depression, and depression that begins after the baby is born is postpartum depression.
- Seasonal affective disorder is depression that comes and goes with the seasons, with symptoms typically starting in the late fall or early winter and going away during the spring and summer.
- Depression with symptoms of psychosis is a severe form of depression in which a person experiences psychosis symptoms, such as delusions (disturbing, false fixed beliefs) or hallucinations (hearing or seeing things others do not hear or see).
People with bipolar disorder (formerly called manic depression or manic-depressive illness) also experience depressive episodes, during which they feel sad, indifferent, or hopeless, combined with a very low activity level. But a person with bipolar disorder also experiences manic (or less severe hypomanic) episodes, or unusually elevated moods, in which they might feel very happy, irritable, or “up,” with a marked increase in activity level.
Other depressive disorders found in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5-TR) include disruptive mood dysregulation disorder (diagnosed in children and adolescents) and premenstrual dysphoric disorder (that affects women around the time of their period).
Who gets depression?
Depression can affect people of all ages, races, ethnicities, and genders.
Women are diagnosed with depression more often than men, but men can also be depressed. Because men may be less likely to recognize, talk about, and seek help for their feelings or emotional problems, they are at greater risk of their depression symptoms being undiagnosed or undertreated.
Studies also show higher rates of depression and an increased risk for the disorder among members of the LGBTQI+ community.
What are the signs and symptoms of depression?
If you have been experiencing some of the following signs and symptoms, most of the day, nearly every day, for at least 2 weeks, you may have depression:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness or pessimism
- Feelings of irritability, frustration, or restlessness
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Fatigue, lack of energy, or feeling slowed down
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, waking too early in the morning, or oversleeping
- Changes in appetite or unplanned weight changes
- Physical aches or pains, headaches, cramps, or digestive problems without a clear physical cause that do not go away with treatment
- Thoughts of death or suicide or suicide attempts
Not everyone who is depressed experiences all these symptoms. Some people experience only a few symptoms, while others experience many. Symptoms associated with depression interfere with day-to-day functioning and cause significant distress for the person experiencing them.
Depression can also involve other changes in mood or behavior that include:
- Increased anger or irritability
- Feeling restless or on edge
- Becoming withdrawn, negative, or detached
- Increased engagement in high-risk activities
- Greater impulsivity
- Increased use of alcohol or drugs
- Isolating from family and friends
- Inability to meet the responsibilities of work and family or ignoring other important roles
- Problems with sexual desire and performance
Depression can look different in men and women. Although people of all genders can feel depressed, how they express those symptoms and the behaviors they use to cope with them may differ. For example, men (as well as women) may show symptoms other than sadness, instead seeming angry or irritable. And although increased use of alcohol or drugs can be a sign of depression in anyone, men are more likely to use these substances as a coping strategy.
In some cases, mental health symptoms appear as physical problems (for example, a racing heart, tightened chest, ongoing headaches, or digestive issues). Men are often more likely to see a health care provider about these physical symptoms than their emotional ones.
Because depression tends to make people think more negatively about themselves and the world, some people may also have thoughts of suicide or self-harm.
Several persistent symptoms, in addition to low mood, are required for a diagnosis of depression, but people with only a few symptoms may benefit from treatment. The severity and frequency of symptoms and how long they last will vary depending on the person, the illness, and the stage of the illness.
If you experience signs or symptoms of depression and they persist or do not go away, talk to a health care provider. If you see signs or symptoms of depression in someone you know, encourage them to seek help from a mental health professional.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911 .
What are the risk factors for depression?
Depression is one of the most common mental disorders in the United States . Research suggests that genetic, biological, environmental, and psychological factors play a role in depression.
Risk factors for depression can include:
- Personal or family history of depression
- Major negative life changes, trauma, or stress
Depression can happen at any age, but it often begins in adulthood. Depression is now recognized as occurring in children and adolescents, although children may express more irritability or anxiety than sadness. Many chronic mood and anxiety disorders in adults begin as high levels of anxiety in childhood.
Depression, especially in midlife or older age, can co-occur with other serious medical illnesses, such as diabetes, cancer, heart disease, chronic pain, and Parkinson’s disease. These conditions are often worse when depression is present, and research suggests that people with depression and other medical illnesses tend to have more severe symptoms of both illnesses. The Centers for Disease Control and Prevention (CDC) has also recognized that having certain mental disorders, including depression and schizophrenia, can make people more likely to get severely ill from COVID-19.
Sometimes a physical health problem, such as thyroid disease, or medications taken for an illness cause side effects that contribute to depression. A health care provider experienced in treating these complicated illnesses can help determine the best treatment strategy.
How is depression treated?
Depression, even the most severe cases, can be treated. The earlier treatment begins, the more effective it is. Depression is usually treated with psychotherapy , medication , or a combination of the two.
Some people experience treatment-resistant depression, which occurs when a person does not get better after trying at least two antidepressant medications. If treatments like psychotherapy and medication do not reduce depressive symptoms or the need for rapid relief from symptoms is urgent, brain stimulation therapy may be an option to explore.
Quick tip : No two people are affected the same way by depression, and there is no "one-size-fits-all" treatment. Finding the treatment that works best for you may take trial and error.
Psychotherapies
Several types of psychotherapy (also called talk therapy or counseling) can help people with depression by teaching them new ways of thinking and behaving and helping them change habits that contribute to depression. Evidence-based approaches to treating depression include cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT). Learn more about psychotherapy .
The growth of telehealth for mental health services , which offers an alternative to in-person therapy, has made it easier and more convenient for people to access care in some cases. For people who may have been hesitant to look for mental health care in the past, virtual mental health care might be an easier option.
Medications
Antidepressants are medications commonly used to treat depression. They work by changing how the brain produces or uses certain chemicals involved in mood or stress. You may need to try several different antidepressants before finding the one that improves your symptoms and has manageable side effects. A medication that has helped you or a close family member in the past will often be considered first.
Antidepressants take time—usually 4–8 weeks—to work, and problems with sleep, appetite, and concentration often improve before mood lifts. It is important to give a medication a chance to work before deciding whether it’s right for you. Learn more about mental health medications .
New medications, such as intranasal esketamine , can have rapidly acting antidepressant effects, especially for people with treatment-resistant depression. Esketamine is a medication approved by the U.S. Food and Drug Administration (FDA) for treatment-resistant depression. Delivered as a nasal spray in a doctor’s office, clinic, or hospital, it acts rapidly, typically within a couple of hours, to relieve depression symptoms. People who use esketamine will usually continue taking an oral antidepressant to maintain the improvement in their symptoms.
Another option for treatment-resistant depression is to take an antidepressant alongside a different type of medication that may make it more effective, such as an antipsychotic or anticonvulsant medication. Further research is needed to identify the role of these newer medications in routine practice.
If you begin taking an antidepressant, do not stop taking it without talking to a health care provider . Sometimes people taking antidepressants feel better and stop taking the medications on their own, and their depression symptoms return. When you and a health care provider have decided it is time to stop a medication, usually after a course of 9–12 months, the provider will help you slowly and safely decrease your dose. Abruptly stopping a medication can cause withdrawal symptoms.
Note : In some cases, children, teenagers, and young adults under 25 years may experience an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. The FDA advises that patients of all ages taking antidepressants be watched closely, especially during the first few weeks of treatment.
If you are considering taking an antidepressant and are pregnant, planning to become pregnant, or breastfeeding, talk to a health care provider about any health risks to you or your unborn or nursing child and how to weigh those risks against the benefits of available treatment options.
To find the latest information about antidepressants, talk to a health care provider and visit the FDA website .
Brain stimulation therapies
If psychotherapy and medication do not reduce symptoms of depression, brain stimulation therapy may be an option to explore. There are now several types of brain stimulation therapy, some of which have been authorized by the FDA to treat depression. Other brain stimulation therapies are experimental and still being investigated for mental disorders like depression.
Although brain stimulation therapies are less frequently used than psychotherapy and medication, they can play an important role in treating mental disorders in people who do not respond to other treatments. These therapies are used for most mental disorders only after psychotherapy and medication have been tried and usually continue to be used alongside these treatments.
Brain stimulation therapies act by activating or inhibiting the brain with electricity. The electricity is given directly through electrodes implanted in the brain or indirectly through electrodes placed on the scalp. The electricity can also be induced by applying magnetic fields to the head.
The brain stimulation therapies with the largest bodies of evidence include:
- Electroconvulsive therapy (ECT)
- Repetitive transcranial magnetic stimulation (rTMS)
- Vagus nerve stimulation (VNS)
- Magnetic seizure therapy (MST)
- Deep brain stimulation (DBS)
ECT and rTMS are the most widely used brain stimulation therapies, with ECT having the longest history of use. The other therapies are newer and, in some cases, still considered experimental. Other brain stimulation therapies may also hold promise for treating specific mental disorders.
ECT, rTMS, and VNS have authorization from the FDA to treat severe, treatment-resistant depression. They can be effective for people who have not been able to feel better with other treatments; people for whom medications cannot be used safely; and in severe cases where a rapid response is needed, such as when a person is catatonic, suicidal, or malnourished.
Additional types of brain stimulation therapy are being investigated for treating depression and other mental disorders. Talk to a health care provider and make sure you understand the potential benefits and risks before undergoing brain stimulation therapy. Learn more about these brain stimulation therapies .
Natural products
The FDA has not approved any natural products for treating depression. Although research is ongoing and findings are inconsistent, some people use natural products, including vitamin D and the herbal dietary supplement St. John’s wort, for depression. However, these products can come with risks. For instance, dietary supplements and natural products can limit the effectiveness of some medications or interact in dangerous or even life-threatening ways with them.
Do not use vitamin D, St. John’s wort, or other dietary supplements or natural products without talking to a health care provider. Rigorous studies must be conducted to test whether these and other natural products are safe and effective.
Daily morning light therapy is a common treatment choice for people with seasonal affective disorder (SAD). Light therapy devices are much brighter than ordinary indoor lighting and considered safe, except for people with certain eye diseases or taking medications that increase sensitivity to sunlight. As with all interventions for depression, evaluation, treatment, and follow-up by a health care provider are strongly recommended. Research into the potential role of light therapy in treating non-seasonal depression is ongoing.
How can I find help for depression?
A primary care provider is a good place to start if you’re looking for help. They can refer you to a qualified mental health professional, such as a psychologist, psychiatrist, or clinical social worker, who can help you figure out next steps. Find tips for talking with a health care provider about your mental health.
You can learn more about getting help on the NIMH website. You can also learn about finding support and locating mental health services in your area on the Substance Abuse and Mental Health Services Administration (SAMHSA) website.
Once you enter treatment, you should gradually start to feel better. Here are some other things you can do outside of treatment that may help you or a loved one feel better:
- Try to get physical activity. Just 30 minutes a day of walking can boost your mood.
- Try to maintain a regular bedtime and wake-up time.
- Eat regular, healthy meals.
- Break up large tasks into small ones; do what you can as you can. Decide what must get done and what can wait.
- Try to connect with people. Talk with people you trust about how you are feeling.
- Delay making important decisions, such as getting married or divorced, or changing jobs until you feel better. Discuss decisions with people who know you well.
- Avoid using alcohol, nicotine, or drugs, including medications not prescribed for you.
How can I find a clinical trial for depression?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions, including depression. The goal of a clinical trial is to determine if a new test or treatment works and is safe. Although people may benefit from being part of a clinical trial, they should know that the primary purpose is to gain new scientific knowledge so that others can be better helped in the future.
Researchers at NIMH and around the country conduct many studies with people with and without depression. We have new and better treatment options today because of what clinical trials have uncovered. Talk to a health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- Clinical Trials – Information for Participants : Information about clinical trials, why people might take part in a clinical trial, and what people might experience during a clinical trial
- Clinicaltrials.gov: Current Studies on Depression : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
- Join a Study: Depression—Adults : List of studies currently recruiting adults with depression being conducted on the NIH campus in Bethesda, MD
- Join a Study: Depression—Children : List of studies currently recruiting children with depression being conducted on the NIH campus in Bethesda, MD
- Join a Study: Perimenopause-Related Mood Disorders : List of studies on perimenopause-related mood disorders being conducted on the NIH campus in Bethesda, MD
- Join a Study: Postpartum Depression : List of studies on postpartum depression being conducted on the NIH campus in Bethesda, MD
Where can I learn more about depression?
Free brochures and shareable resources.
- Chronic Illness and Mental Health: Recognizing and Treating Depression : This fact sheet provides information about the link between depression and chronic disease. It describes what a chronic disease is, symptoms of depression, and treatment options, and presents resources to find help for yourself or someone else.
- Depression : This brochure provides information about depression, including different types of depression, signs and symptoms, how it is diagnosed, treatment options, and how to find help for yourself or a loved one.
- Depression in Women: 4 Things to Know : This fact sheet provides information about depression in women, including signs and symptoms, types of depression unique to women, and how to get help.
- Perinatal Depression : This brochure provides information about perinatal depression, including how it differs from “baby blues,” causes, signs and symptoms, treatment options, and how to find help for yourself or a loved one.
- Seasonal Affective Disorder : This fact sheet provides information about seasonal affective disorder, including signs and symptoms, how it is diagnosed, causes, and treatment options.
- Seasonal Affective Disorder (SAD): More Than the Winter Blues : This infographic provides information about how to recognize the symptoms of SAD and what to do to get help.
- Teen Depression: More Than Just Moodiness : This fact sheet is for teens and young adults and provides information about how to recognize the symptoms of depression and what to do to get help.
- Digital Shareables on Depression : These digital resources, including graphics and messages, can be used to spread the word about depression and help promote depression awareness and education in your community.
Federal resources
- Depression (MedlinePlus - also en español )
- Moms’ Mental Health Matters: Depression and Anxiety Around Pregnancy ( Eunice Kennedy Shriver National Institute of Child Health and Human Development)
Research and statistics
- Journal Articles : This webpage provides articles and abstracts on depression from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Major Depression : This webpage provides the statistics currently available on the prevalence and treatment of depression among people in the United States.
- Depression Mental Health Minute : Take a mental health minute to watch this video on depression.
- NIMH Experts Discuss the Menopause Transition and Depression : Learn about the signs and symptoms, treatments, and latest research on depression during menopause.
- NIMH Expert Discusses Seasonal Affective Disorder : Learn about the signs and symptoms, treatments, and latest research on seasonal affective disorder.
- Discover NIMH: Personalized and Targeted Brain Stimulation Therapies : Watch this video describing repetitive transcranial magnetic stimulation and electroconvulsive therapy for treatment-resistant depression. Brain stimulation therapies can be effective treatments for people with depression and other mental disorders. NIMH supports studies exploring how to make brain stimulation therapies more personalized while reducing side effects.
- Discover NIMH: Drug Discovery and Development : One of the most exciting breakthroughs from research funded by NIMH is the development of a fast-acting medication for treatment-resistant depression based on ketamine. This video shares the story of how ketamine infusions meaningfully changed the life of a participant in an NIMH clinical trial.
- Mental Health Matters Podcast: Depression: The Case for Ketamine : Dr. Carlos Zarate Jr. discusses esketamine—the medication he helped discover—for treatment-resistant depression. The podcast covers the history behind the development of esketamine, how it can help with depression, and what the future holds for this innovative line of clinical research.
Last Reviewed: March 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
The Impact of Social Media on Mental Health: Understanding Depression
This essay is about how social media can contribute to depression. It examines factors such as the culture of comparison, cyberbullying, and the impact on sleep and self-esteem. Social media often promotes idealized images that lead to unfavorable comparisons, causing feelings of inadequacy. Cyberbullying on these platforms can result in severe emotional distress. Additionally, social media can disrupt sleep patterns, a known risk factor for depression, and affect self-esteem and body image by setting unrealistic beauty standards. The essay suggests that mindful and moderated use of social media can help mitigate these negative effects.
How it works
The ubiquitous presence of social media in contemporary society has intricately woven itself into the fabric of everyday life, serving as a conduit for global connectivity and facilitating instantaneous communication and dissemination of information. Nonetheless, amidst its myriad benefits, mounting evidence suggests that the excessive consumption of social media may exacerbate mental health concerns, notably depression. Comprehending the mechanisms through which social media engenders depression entails a nuanced examination of several interconnected factors, including the culture of comparison, cyberbullying, and the ramifications on sleep patterns and self-esteem.
One of the foremost conduits through which social media precipitates depression is the pervasive culture of comparison it cultivates. Platforms such as Instagram, Facebook, and TikTok incentivize users to showcase the highlights of their lives, often presenting a curated facade of reality. Consequently, this engenders a distorted perception wherein others appear perpetually happier, more accomplished, and aesthetically superior. Prolonged exposure to these meticulously curated portrayals fosters a proclivity among individuals to unfavorably juxtapose their own lives, thereby instigating sentiments of inadequacy, diminished self-worth, and ultimately, depression. Empirical research indicates that individuals who frequently engage in social comparisons on social media platforms exhibit heightened susceptibility to depressive symptomatology.
Cyberbullying stands as another salient factor linking social media utilization to depression. Unlike conventional forms of bullying, cyberbullying transcends temporal and spatial barriers, manifesting as relentless dissemination of derogatory messages or imagery that can rapidly achieve wide circulation. Victims of cyberbullying often experience a profound sense of powerlessness and isolation, precipitating acute emotional anguish. The anonymity afforded by the digital realm emboldens individuals to engage in callous conduct that they might eschew in face-to-face interactions. Particularly among adolescents and young adults, who constitute among the most avid consumers of social media, cyberbullying poses deleterious repercussions on mental well-being, escalating the risk of depression and even suicidal ideation.
Moreover, the deleterious impact of social media on sleep patterns assumes a pivotal role in precipitating depression. A considerable cohort, notably adolescents, habitually devote extensive nocturnal hours to digital engagement, thereby impinging upon their sleep hygiene. The emission of blue light by screens disrupts the secretion of melatonin, a hormone pivotal in regulating circadian rhythms. Poor sleep quality and inadequate sleep duration are well-documented precursors to depression. Furthermore, the addictive allure of social media imparts formidable impediments to disengagement, precipitating chronic sleep deprivation and attendant mental health adversities.
Furthermore, social media exerts a pernicious influence on self-esteem and body image, thereby fostering a milieu conducive to depression. The proliferation of retouched and embellished imagery propounds unrealistic benchmarks of beauty and flawlessness. Particularly among young women, users contend with heightened pressure to conform to these idealized standards, thereby incurring dissatisfaction with body image and diminished self-regard. The incessant exposure to idealized portrayals engenders a warped conception of normalcy and attainability, exacerbating sentiments of inadequacy and fostering depressive symptomatology.
Social media’s role in fomenting depression is further compounded by the phenomenon colloquially termed “FOMO,” or fear of missing out. The incessant deluge of updates pertaining to peers’ engagements and experiences breeds a palpable anxiety and a pervasive sense of exclusion among those who perceive themselves as peripheral to the fray. This apprehension precipitates compulsive monitoring of social media platforms, thereby reinforcing feelings of isolation and despondency. The compulsive need for perpetual connectivity engenders a preclusion from authentic, real-world interactions, thereby further alienating individuals and precipitating deleterious effects on mental well-being.
Notwithstanding these perils, it behooves us to acknowledge that social media is not inherently deleterious. Indeed, it avails invaluable opportunities for social interconnectedness, communal support, and expressive freedom. However, judicious moderation and discerning engagement are imperative to ameliorating its adverse consequences. Encouraging individuals to cultivate intermittent reprieves from social media, partake in offline pursuits, and avail themselves of support networks can redound to a mitigation of depression risk. Parents and educators wield pivotal agency in cultivating healthy social media habits among youths, underscoring the primacy of genuine interpersonal connections and self-care.
In summation, whilst social media has revolutionized interpersonal dynamics and communication modalities, it concurrently engenders a panoply of challenges for mental well-being, particularly in the realm of depression. The culture of comparison, cyberbullying, disrupted sleep patterns, and impacts on self-esteem and body image coalesce as multifaceted factors that precipitate depressive symptomatology. By comprehensively delineating these mechanisms and advocating for judicious social media utilization, we can attenuate its deleterious repercussions and foster enhanced mental health outcomes for all stakeholders.
Cite this page
The Impact of Social Media on Mental Health: Understanding Depression. (2024, Jun 01). Retrieved from https://papersowl.com/examples/the-impact-of-social-media-on-mental-health-understanding-depression/
"The Impact of Social Media on Mental Health: Understanding Depression." PapersOwl.com , 1 Jun 2024, https://papersowl.com/examples/the-impact-of-social-media-on-mental-health-understanding-depression/
PapersOwl.com. (2024). The Impact of Social Media on Mental Health: Understanding Depression . [Online]. Available at: https://papersowl.com/examples/the-impact-of-social-media-on-mental-health-understanding-depression/ [Accessed: 4 Jun. 2024]
"The Impact of Social Media on Mental Health: Understanding Depression." PapersOwl.com, Jun 01, 2024. Accessed June 4, 2024. https://papersowl.com/examples/the-impact-of-social-media-on-mental-health-understanding-depression/
"The Impact of Social Media on Mental Health: Understanding Depression," PapersOwl.com , 01-Jun-2024. [Online]. Available: https://papersowl.com/examples/the-impact-of-social-media-on-mental-health-understanding-depression/. [Accessed: 4-Jun-2024]
PapersOwl.com. (2024). The Impact of Social Media on Mental Health: Understanding Depression . [Online]. Available at: https://papersowl.com/examples/the-impact-of-social-media-on-mental-health-understanding-depression/ [Accessed: 4-Jun-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers

OBSTETRICIAN-GYNECOLOGISTS’ KNOWLEDGE, PRACTICES, AND DECISION-MAKING REGARDING DEPRESSION DURING PERIMENOPAUSE
Depression in women is more common during perimenopause (the time period around and during menopause) than pre- and postmenopause. Obstetrician/gynecologists (ob-gyns) play a vital role in the detection and management of depression symptoms in women because for many women ob-gyns are the first and most frequent point of medical contact. As such, this study assessed ob-gyns' knowledge and practice patterns regarding depression in perimenopause as well as specific decision making biases and heuristics (decision making shortcuts) that may impact physicians’ screening and treatment practices. Fellows of the American College of Obstetricians and Gynecologists (ACOG) were selected randomly from a nationally representative sample from the ACOG database and completed an electronic or paper version of the survey. Higher quality education about depression, respondent sex, and personal experience with depression were associated with higher rates of screening for depression during perimenopause, but not greater diagnostic accuracy. Fewer than half of respondents were able to correctly diagnose vignettes depicting a major depressive episode with a somatic presentation, and their confidence ratings were not good indicators of the accuracy of their diagnoses. Findings suggest that respondents may engage in ambiguity avoidance and the availability heuristic when answering questions about depression during perimenopause.
Usage metrics

Navigation Menu
Search code, repositories, users, issues, pull requests..., provide feedback.
We read every piece of feedback, and take your input very seriously.
Saved searches
Use saved searches to filter your results more quickly.
To see all available qualifiers, see our documentation .
- Notifications You must be signed in to change notification settings
Thesis on Depression Analysis
emankhadim/bsc_thesis
Folders and files, repository files navigation.
Mental health problems are considered as serious health issues all over the world because these problems can lead to severe outcomes like suicide, violence, abuse or murder. Majority of people with mental health problems are either untreated or undiagnosed. People who end up having schizophrenia, depression, bipolar or OCD for more than a year might undergo mental disability (Government Digital Service (GDS), 2014). There is a need to identify such problems before it gets worse. Fortunately, social media is as a platform where people express their feelings and problems openly. Data science can extract and analyze these statements to perform verity of functions for people suffering from mental health problems. This dissertation contributes to the psychology field by providing a system which depicts the Twitter users who are potentially suffering/ suffered from depression, bipolar disorder and schizophrenia in US, UAE and Singapore. Different numbers of tweets are extracted from twitter using keywords and hashtags in these three countries. Snscraper was used to extract tweets from twitter. These tweets are then filtered out to people who convey signs of mental health problems only. Data is extracted from four timestamps within 2019-2022 to find the impact of Covid19 among twitter users. The dissertation includes all the methods, tools and techniques used in the project to achieve its aim and objectives
- Jupyter Notebook 100.0%

IMAGES
VIDEO
COMMENTS
INTRODUCTION. Depression is described as a common and serious mood disorder that results in persistent feelings of sadness and hopelessness, as well as a loss of interest in activities that one once enjoyed (American Psychiatric Association [APA], 2013).Additional symptoms of depression include weight changes, difficulty sleeping, loss of energy, difficulty thinking or concentrating, feelings ...
Abstract. The current paper critically evaluates Beck and Bredemeier's (2016) Unified Model of Depression (UMD) and explores some of the wider issues it raises about explanations of depression ...
Taken together, the results from this dissertation highlight 1) the critical role that treatment-related stigma plays in the path to depression recovery, 2) the lack of adequate solutions currently being implemented to address internalized stigma during depression treatment, and 3) the potential impact of an intervention targeting depression ...
Depression is a mental health condition in part characterized by sadness and changes in thinking. One ... Thesis of an undergraduate student, Alan Rheaume, who assisted with collecting and analyzing data for this study, and he is a second author on this manuscript. Dr. Louis Schmidt (McMaster University), who
As a result, individuals in modern societies continually store excess energy as their bodies prepare for a famine that never arrives. Deteriorating health of modern populations via the obesity epidemic ( Flegal et al., 2010) is a likely contributing factor to a rising prevalence of depression. Compared to normal-weight peers, obese individuals ...
Abstract. Major depression is a mood disorder characterized by a sense of inadequacy, despondency, decreased activity, pessimism, anhedonia and sadness where these symptoms severely disrupt and ...
thesis was thus to expand upon previous research and enhance the knowledge about social and gender differences in depression among young people in Sweden. Three different materials were used to capture a broad picture of the role of social position, gender and depression, in adolescence (13-17 year olds) and in young adulthood (18-32 year olds).
College students treated for depression have reported significantly more stress than students without a diagnosis (Aselton, 2012). Rates of suicide are also prevalent in this population, with studies indicating that 1 in 10 college students with depression have endorsed suicidal thoughts (Woodhead et al., 2020). Pedrelli et al. (2015)
In a recent study by Midgley and colleagues (2015), a British sample of 77 adolescents (11-17 years) who had been diagnosed with depression and were entering outpatient psychotherapy, were interviewed about the individual experience of depression as part of a large randomized controlled trial, the Improving Mood With Psychoanalytic and ...
In the second study of this thesis, we followed more than 1.5 million individuals from birth up until age 31. Of these, 338,251 (22.5%) experienced early-life infections, 67,630 (4.5%) received a diagnosis of depression, and 25,651 (1.7%) were diagnosed with or died by self-harm.
Introduction. Depression is the principal cause of illness and disability in the world. The World Health Organization (WHO) has been issuing warnings about this pathology for years, given that it affects over 300 million people all over the world and is characterized by a high risk of suicide (the second most common cause of death in those aged between 15 and 29) [World Health Organization ...
level of anxiety, depression, and stress and second one to measure Emotional stability using a self-reported scale. The collected data was analyzed using SPSS version 22 to find result for this thesis. The results of the study outlined that there is a negative but significant correlation among depression, anxiety, and stress with emotional ...
Depression, Anxiety, and Self-Concept (TITLE) BY . Emily Baker THESIS . SUBMIITED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF . Master of Arts in Clinical Psychology . IN THE GRADUATE SCHOOL, EASTERN ILLINOIS UNIVERSITY CHARLESTON, ILLINOIS . 2019 . YEAR . I HEREBY RECOMMEND THAT THIS THESIS BE ACCEPTED AS FULFILLING
INTRODUCTION. In 2018, researchers found that graduate students were more than six times as likely to report experiencing depression and anxiety compared with the general population and subsequently declared a "graduate student mental health crisis" (Evans et al., 2018; Flaherty, 2018).Calls to identify which factors exacerbate graduate student mental health problems followed ("The ...
Depression is a common and debilitating mental health condition whose underlying aetiology and pathophysiology is still relatively poorly understood. In this article, we first turn to the past and briefly review what neuroscientific investigations have taught us so far about depression. In doing so, we cover neurochemical, neuroendocrine ...
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2; range, 10-47%).Of these, the most widely used depression scales were the PHQ-9 (9 studies ...
Bisson, Katherine H., "The Effect of Anxiety and Depression on College Students' Academic Performance: Exploring Social Support as a Moderator" (2017). Digital Commons @ ACU, Electronic Theses and Dissertations. Paper 51. This Thesis is brought to you for free and open access by the Electronic Theses and Dissertations at Digital Commons @ ACU.
Treatment Options for Depression. The first choice for depression treatment is generally an antidepressant medication. Selective serotonin reuptake inhibitors (SSRIs) are the most popular choice because they can be quite effective and tend to have fewer side effects than other types of antidepressants.
5 Thesis Statements about Anxiety & Depression: "Depression and anxiety Co-occurring disorders are a major concern in mental health, necessitating integrated treatment options that meet the unique challenges that co-occurring diseases provide.". "The utilization of technology-driven therapies, such as smartphone apps and telehealth ...
Argumentative Essays. Argumentative essays require you to analyze and present arguments related to depression. Here are some topic examples: 1. Argue whether mental health stigma contributes to the prevalence of depression in society. 2. Analyze the effectiveness of different treatment approaches for depression, such as therapy versus medication.
Here is a depression thesis statement you can use. The effects of human psychology are viewed in the form of depression. Clinical psychology can help to bring outpatients who have depression. Treating long-term depression in bipolar patients is possible. Bipolar patients are drained to the roots of depression.
Abstract. Major depressive disorder is a serious mental disorder that profoundly affects an individual's quality of life. Although the aetiologies underlying this disorder remain unclear, an increasing attention has been focused on the influence imposed by psychological stress over depression. Despite limited animal models of psychological ...
Depression (also known as major depression, major depressive disorder, or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working. To be diagnosed with depression, the symptoms must be present for at least 2 ...
Thesis Statement Generator . Generate thesis statement for me . ... Social media's role in fomenting depression is further compounded by the phenomenon colloquially termed "FOMO," or fear of missing out. The incessant deluge of updates pertaining to peers' engagements and experiences breeds a palpable anxiety and a pervasive sense of ...
Higher quality education about depression, respondent sex, and personal experience with depression were associated with higher rates of screening for depression during perimenopause, but not greater diagnostic accuracy. Fewer than half of respondents were able to correctly diagnose vignettes depicting a major depressive episode with a somatic ...
Data science can extract and analyze these statements to perform verity of functions for people suffering from mental health problems. This dissertation contributes to the psychology field by providing a system which depicts the Twitter users who are potentially suffering/ suffered from depression, bipolar disorder and schizophrenia in US, UAE ...
Reports the retraction of "Predictors of depression among school adolescents in Northwest, Ethiopia, 2022: Institutional based cross-sectional" by Aklile Tsega Chekol, Mastewal Aschale Wale, Agmas Wassie Abate, Eyerusalem Abebe Beo, Eman Ali Said and Berhan Tsegaye Negash (BMC Psychiatry, 2023[Jun][14], Vol 23[1][429]). The Editors have retracted this article after concerns were raised.