- Research article
- Open access
- Published: 03 March 2016

Relationships between adverse childhood experiences and adult mental well-being: results from an English national household survey
- Karen Hughes 1 ,
- Helen Lowey 2 ,
- Zara Quigg 1 &
- Mark A. Bellis 3 , 4
BMC Public Health volume 16 , Article number: 222 ( 2016 ) Cite this article
42k Accesses
125 Citations
34 Altmetric
Metrics details
Individuals’ childhood experiences can strongly influence their future health and well-being. Adverse childhood experiences (ACEs) such as abuse and dysfunctional home environments show strong cumulative relationships with physical and mental illness yet less is known about their effects on mental well-being in the general population.
A nationally representative household survey of English adults ( n = 3,885) measuring current mental well-being (Short Edinburgh-Warwick Mental Well-being Scale SWEMWBS) and life satisfaction and retrospective exposure to nine ACEs.
Almost half of participants (46.4 %) had suffered at least one ACE and 8.3 % had suffered four or more. Adjusted odds ratios (AORs) for low life satisfaction and low mental well-being increased with the number of ACEs. AORs for low ratings of all individual SWEMWBS components also increased with ACE count, particularly never or rarely feeling close to others. Of individual ACEs, growing up in a household affected by mental illness and suffering sexual abuse had the most relationships with markers of mental well-being.
Conclusions
Childhood adversity has a strong cumulative relationship with adult mental well-being. Comprehensive mental health strategies should incorporate interventions to prevent ACEs and moderate their impacts from the very earliest stages of life.
Peer Review reports
Individuals’ childhood experiences are of paramount importance in determining their future outcomes. Research exposing the harmful effects that childhood adversity has on adult physical and mental health has advanced significantly over the past few decades. For instance, the Adverse Childhood Experiences (ACE) framework has provided a mechanism for retrospectively measuring childhood adversities and identifying their impact on health in later life [ 1 ]. ACEs include child maltreatment (e.g. physical, sexual and verbal abuse) and broader experiences of household dysfunction, such as witnessing violence in the home, parental separation and growing up in a household affected by substance misuse, mental illness or criminal behaviour. Studies show a dose-responsive relationship between ACEs and poor outcomes, with the more ACEs a person suffers the greater their risks of developing health harming behaviours (e.g. substance misuse, risky sexual behaviour), suffering poor adult health (e.g. obesity, cancer, heart disease) and ultimately premature mortality [ 1 – 6 ].
Much research on the long-term impacts of ACEs has focused on their relationships with mental illness. Thus, studies have found increasing numbers of ACEs to be associated with increasing risks of conditions including depression, anxiety, panic reactions, hallucinations, psychosis and suicide attempt, along with overall psychopathology, psychotropic medication use and treatment for mental disorders [ 2 , 3 , 7 – 11 ]. However the literature on the impact of ACEs on broader measures of mental health and well-being is less extensive. While definitions vary [ 12 ], mental well-being is widely recognised as being more than just the absence of mental illness; incorporating aspects of mental functioning, feelings and behaviours and having been simply described as feeling good and functioning well [ 13 ]. Positive mental well-being has been associated with better physical and mental health and with reduced mortality in both healthy and ill populations [ 14 , 15 ]. Correspondingly, the promotion of mental well-being has become a public and mental health priority both globally and in countries such as the UK [ 16 , 17 ].
Understanding how different factors impede mental well-being in adults is imperative to investing effectively and efficiently in its promotion. With little longitudinal data available, considerable focus has been placed on the associations between current conditions (e.g. social relationships, residential deprivation, physical exercise, health status) and mental well-being rather than longer-term drivers. However, a US study using the ACE framework found a cumulative relationship between childhood adversity and markers of mental well-being in the general population, including mentally healthy days and life satisfaction [ 18 ]. In England, we conducted a pilot ACE study in a local administrative area which found increased odds of low life satisfaction and low mental well-being in adults with increased ACEs [ 19 ]. Following this pilot, we undertook a national ACE study of adults across England that included validated measurements of mental well-being and life satisfaction. Here we explore relationships between levels of exposure to adversity during childhood and current mental well-being in adults. Finally, we discuss the convergence between the roots of poor physical health and poor mental well-being in early years and consequently, how poor mental well-being in one generation may adversely impact well-being in the next.
A target sample size of 4,000 adult residents of England was established based on the prevalence of ACEs identified in the pilot study [ 19 ]. Study inclusion criteria were: aged 18–69 years; resident in a selected LSOA; and cognitively able to participate in a face-to-face interview. Households were selected through random probability sampling stratified by English region ( n = 10, with inner and outer London treated as two regions) and then by small area deprivation using lower super output areas (LSOAs; geographic areas with a population mean of 1,500) [ 20 ]. Within each region, LSOAs were categorised into deciles of deprivation based on their ranking in the 2010 Index of Multiple Deprivation (IMD; a composite measure including 38 indicators relating to economic, social and housing issues) [ 21 ]. Two LSOAs were then randomly selected from each decile in each region and for each LSOA between 40 and 120 addresses were randomly selected for inclusion from the Postcode Address File ® . Sample sizes in each region were proportionate to their population to provide a sample representative of the English population, with a total of 16,000 households initially sampled to account for ineligibility, non-response and non-compliance.
Sampled households were sent a letter prior to researchers visiting providing information on the study and the opportunity to opt out; 771 (4.8 %) households opted out at this stage. Operating under the direction of the research team, a professional survey company visited households on differing days/times (seven days a week, 9:30 am to 8.30 pm) between April and July 2013. The protocol employed by the survey company was to remove households after four attempted visits with no contact. Where contact was made and more than one household member met the inclusion criteria, the eligible resident with the next birthday was selected for interview. Interviewers explained the purpose of the study, outlined its voluntary and anonymous nature and provided a second opportunity for individuals to opt out, with informed consent obtained verbally at the point of interview. Household visits ceased once the target sample size was achieved. Thus, 9,852 of the sampled households were visited of which 7,773 resulted in contact with a resident. Of these households, 2,719 (35.0 %) opted out, 1,044 (13.4 %) were ineligible and 4,010 completed a study questionnaire. Compliance was 59.6 % across eligible occupied households visited and 53.5 % when including those opting out at the letter stage.
The study used an established questionnaire covering demographics, lifestyle behaviours, health status, mental well-being, life satisfaction and exposure to ACEs before the age of 18 [ 19 ]. Participants were able to complete the questionnaire through a face-to-face interview using a hand held computer (with sensitive questions self-completed; n = 3,852), or to self-complete using paper questionnaires ( n = 158). Mental well-being was measured using the Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS) [ 22 ], which asks individuals how often over the past two weeks they have been: feeling optimistic about the future; feeling useful; feeling relaxed; dealing with problems well; thinking clearly; feeling close to other people; able to make up their own mind about things . Responses are scored from 1 (none of the time) to 5 (all of the time) and an overall mental well-being score is calculated, ranging from 7 (lowest possible mental well-being) to 35 (highest possible mental well-being). Life satisfaction was measured on a scale of 1–10 using the standard question: All things considered how satisfied are you with your life, with 1 being not at all satisfied and 10 very satisfied [ 23 ]. ACEs were measured using the Centers for Disease Control and Prevention short ACE tool [ 24 ] which comprises eleven questions covering nine ACE types: physical abuse; verbal abuse; sexual abuse (three questions); parental separation; exposure to domestic violence; and growing up in a household with mental illness, alcohol abuse, drug abuse or incarceration (for further information see [ 4 ]). Ethnicity was recorded using standard UK Census categories [ 25 ] and categorised as White, Asian and Other due to small numbers within individual ethnic groups. Respondents were allocated an IMD 2010 quintile of deprivation based on their LSOA of residence. Ethical approval for the study was obtained from Liverpool John Moores University’s Research Ethics Committee and the study adhered to the Declaration of Helsinki.
Analyses were undertaken using SPSS v20. Only individuals with complete data relating to all ACEs, age, sex, ethnicity, and IMD quintile were included in the analysis, resulting in a final sample size of 3,885. Bivariate analyses used chi-squared with backwards conditional logistic regression used to examine independent relationships between ACEs and adult mental well-being and life satisfaction. Consistent with other work including previous ACE studies [ 1 – 3 ] and the World Mental Health Surveys [ 26 – 28 ], the number of ACEs participants reported exposure to was summed into an ACE count (range 0 to 9) and here categorised into four groups for analysis: 0 ACEs ( n = 2,072), 1 ACE ( n = 879), 2–3 ACEs ( n = 594) and 4 + ACEs ( n = 322). We also explored relationships between outcome variables and individual ACEs, with analysis focusing on those with highly significant relationships. The seven individual components of SWEMWBS were each dichotomised to indicate poor ratings (never or rarely in the last two weeks). Overall SWEMWBS scores and life satisfaction (LS) ratings were dichotomised to indicate low scores as >1 standard deviation (SD) below the mean (SWEMWBS, mean 27.5, SD 4.4, low <23; LS, mean 7.7, SD 1.7, low <6).
The demographic breakdown of the sample is shown in Table 1 . Compared with the English population the sample overrepresented females (55.0 % v 50.3 % in England) and individuals aged 60–69 years (20.7 % v 16.1 %) and underrepresented those aged 18–29 (21.0 % v 24.2 %). There were no differences by deprivation quintile or ethnicity. Just under half of participants reported having suffered at least one ACE (46.4 %) with 15.4 % reporting 2–3 ACEs and 8.3 % 4+ ACEs. The proportion of participants with low measures (never or rarely in the last two weeks) for the individual components of SWEMWBS ranged from 2.5 % (able to make up own mind) to 14.5 % (feeling relaxed). Thirteen percent were categorised as having low SWEMWBS scores (<23) and 11.6 % as having low life satisfaction (score <6; Table 1 ).
Low SWEMWBS scores and LS were both associated with age, being most prevalent in the 50–59 year age group (Table 1 ). Significant relationships with age were also seen for all individual SWEMWBS components except feeling useful and dealing with problems. There were no relationships between gender and LS or overall SWEMWBS score, although among the individual SWEMWBS components more females had low scores for feeling relaxed and more males for feeling close to others. There were no significant relationships between ethnicity and either low SWEMWBS score or low LS. However both outcomes increased with deprivation, as did low levels of all individual SWEMWBS components except feeling relaxed.
There were strong associations between ACE count and all markers of low mental well-being. Thus the prevalence of low SWEMWBS score tripled from 9.5 % in those with 0 ACEs to 30.7 % in those with 4+ ACEs, while the prevalence of low LS more than tripled from 7.9 to 26.6 % respectively. These significant relationships remained after controlling for confounders in logistic regression analysis with adjusted odds ratios (AORs) for low SWEMWBS score and low LS increasing with ACE count and reaching 3.9 for both outcomes in those with 4+ ACEs (compared with 0 ACEs; Table 2 ). Importantly, while associations between both outcomes and age also remained in LR, running separate models for each age group showed the relationships between high ACE count and low mental well-being to be consistent across age groups. Thus, compared with individuals with no ACEs, AORs for low SWEBWBS scores in those with 4+ ACEs ranged from 3.08 in both 18–29 year olds (95 % CIs, 1.56–6.07) and 30–39 year olds (95 % CIs 1.66–5.72) to 5.34 (95 % CIs 2.10–13.57) in 60–69 year olds (all p < 0.001) and for low LS from 2.54 (95 % CIs 1.09–5.90, p = 0.030) in 18–29 year olds to 11.20 (95 % CIs 4.43–28.29, p < 0.001) in 60–69 year olds.
Figure 1 presents AORs for low scores for each component of SWEMWBS by increasing ACE count (all ages). All relationships were significant and cumulative with AORs for those with 4+ ACEs (compared with 0 ACEs) ranging from 2.23 (95 % CIs 1.22–4.10) for never or rarely being able to make up one’s own mind to 4.09 (2.70–6.20) for never or rarely feeling close to others.
Relationship between adverse childhood experience count and components of poor adult mental well-being (adjusted odds ratios and 95 % confidence intervals). Variables represent the individual component questions in the SWEMWBS scale. Adjusted odds ratios were calculated using logistic regression analysis. Additional independent variables included in the logistic regression were age, gender, deprivation and ethnicity. All relationships are significant with poor mental well-being components positively related to increasing ACE count ( p < 0.001, except ‘ability to make up own mind where p < 0.05). Ref = reference category
Table 3 shows the relationships between measures of mental well-being and the nine individual ACEs examined. Physical, sexual and emotional abuse, witnessing domestic violence, and living in a household affected by mental illness or drug abuse were significantly associated with low levels of all mental well-being measures and household alcohol misuse and incarceration with low levels of all except the ability to make one’s own mind up about things. However parental separation or divorce was only associated with two of the seven SWEMWBS components (feeling useful, feeling relaxed) and an overall low SWEMWBS score. For each marker of mental well-being, a logistic regression model was run that included individual ACE types significantly related to the marker (in bivariate analysis, see Table 3 ) and demographic variables. Here, household mental illness was found to have independent relationships with the most mental well-being marker, being associated with all except the SWEMWBS component of feeling relaxed (Table 4 ). Childhood sexual abuse was associated with all except the SWEMWBS components of feeling useful and feeling close to others. Emotional and physical abuse each had independent relationships with five of the nine measures and household alcohol problems with four. Feeling close to others (the SWEMWBS component with the strongest relationship with ACE count; Fig. 1 ), was independently associated with household mental illness, emotional abuse and physical abuse.
Promoting mental well-being has become a major public health priority as recognition of the links between well-being and broader health and social outcomes has grown. This has contributed to the emergence of broader policy approaches to mental health, both globally and nationally, that incorporate population-level prevention and promotion activity alongside traditional therapeutic responses to mental illness [ 16 , 17 ]. In England, motivation for increased investment in mental well-being promotion has centred around the notion that interventions to improve mental well-being at a population level could produce greater benefits than those to prevent mental illness in at-risk populations [ 29 , 30 ]. However, the evidence base on which such approaches are based is being questioned as broader measurements and studies of mental well-being emerge [ 12 ]. Thus, existing studies have largely associated mental well-being in adults with factors linked to their current circumstances, such as employment, residential deprivation, social participation, physical exercise, relationship satisfaction and health status [ 31 ]. Correspondingly, interventions have often focused on promoting individual behavioural change through, for example, increasing social connectedness and physical activity [ 32 , 33 ]. A life course perspective that incorporates the longer-term impact of childhood adversity has largely been absent from discussions on mental well-being.
Using a randomly selected national household sample of English adults, our study found a strong cumulative relationship between childhood adversities and two widely used measures of mental well-being. The more ACEs participants reported having suffered during their childhood the more likely they were to report low SWEMWBS scores and low life satisfaction (Table 1 ). These relationships remained after controlling for demographics, with odds of poor outcomes for both measures being elevated in those with even a single ACE and almost four times higher in those with four or more ACEs (compared with those with no ACEs; Table 2 ). We also found ACE count to be independently related to each of the seven individual components of SWEMWBS; individuals with higher ACE counts were more likely to report never or rarely (in the last two weeks) feeling optimistic, useful, relaxed or close to others, dealing with problems well, thinking clearly and being able to make up one’s own mind (Fig. 1 ).
A variety of mechanisms link ACEs to poor adult mental well-being. Critically, maltreatment and other stressors in childhood can affect brain development and have harmful, lasting effects on emotional functioning [ 2 , 34 ]. Children who are maltreated can develop attachment difficulties, including poor emotional regulation, lack of trust and fear of getting close to other people. They can also form negative self-images, lack self-worth and suffer feelings of incompetence, all of which can be retained into adulthood [ 2 , 34 , 35 ]. The relationships between ACEs and factors including poor educational attainment and the development of health-damaging behaviours mean that individuals who suffer ACEs can also face a range of risk factors for poor mental well-being in adulthood, such as poor health, low employment and social deprivation [ 2 , 4 , 36 ]. These effects can contribute to cycles of adversity and poor mental well-being whereby individuals that grew up in adverse conditions are less able to provide optimum childhood environments for their own offspring [ 37 ]. Here, and consistent with previous work [ 38 ], the SWEMWBS component with the strongest relationship with ACE count was never or rarely feeling close to others. Children whose parents show poor relationships with them are at greater risks of ACEs [ 39 ], thus individuals who cannot feel close to others as a result of their own ACE history may subsequently be more likely to expose their own children to ACEs. These relationships may also have implications for the implementation and effectiveness of interventions to improve mental well-being through social connectedness.
While analysis based on ACE count highlights the cumulative impact of childhood adversity on mental well-being, it is also useful to explore which ACEs may have particular effects. All ACE types showed significant bivariate relationships with low SWEMWEBS scores, and all except parental separation/divorce with low life satisfaction and most individual SWEMWBS components. In multivariate analyses, however, the ACEs with the most independent relationships with markers of low mental well-being were growing up in a household with someone affected by mental illness and suffering childhood sexual abuse.
The links between growing up in a household affected by mental illness in childhood and low mental well-being in adulthood may in part reflect genetic risk factors that make the offspring of individuals with mental disorders susceptible to poor mental health themselves [ 40 ]; although genetic explanations for the transmission of mental disorders are disputed [ 41 ]. Thus, parental mental illness can have broader impacts on children’s social and emotional development when parenting practices are affected by factors such as low emotional warmth, reduced responsiveness, impaired attention and unpredictable behavioural patterns [ 42 ]. An extensive body of research provides evidence that exposure to childhood adversity such as parental stress, disrupted care patterns and abuse increases risks of mental illness [ 43 ], while studies are increasingly identifying how exposure to such adversity can trigger epigenetic modifications to gene expressions, altering brain structure, stress reactivity and consequently vulnerability to both mental and physical ill health [ 44 ]. Childhood sexual abuse can have particularly damaging effects on individuals’ emotional development, having been linked to feelings of shame and self-blame, powerlessness, inappropriate sexual beliefs and difficulties forming and maintaining intimate relationships [ 45 , 46 ]. Correspondingly research has identified strong relationships between childhood sexual abuse and adult mental illness [ 11 ]. For example, in England sexual abuse in childhood has been attributed to 11 % of all common mental disorders, along with 7 % of alcohol dependence disorders, 10 % of drug dependence disorders, 15 % of eating disorders and 17 % of post-traumatic stress disorders [ 47 ].
The WHO Mental Health Action Plan 2013–2020 incorporates the promotion of mental well-being as part of its overarching goal: highlighting the need for a life course approach that intervenes early to prevent mental health difficulties; recognising the importance of reducing violence; and emphasising the importance of services being responsive to the needs of survivors of violence [ 17 ]. Interventions that seek to reduce ACEs, develop parenting skills and promote resilience in children should thus be considered essential elements in comprehensive mental health strategies. Starting at the very earliest stages of life, these can include measures to train midwives, health visitors and other early years professionals to enquire about parental mental well-being and identify and treat post-natal depression and other mental health concerns [ 48 ]. The ante- and post-natal periods also offer the opportunity to identify and address a broader range of ACEs including parental substance use and domestic violence as well as to increase parenting skills and knowledge. Effective interventions include home visiting and parenting programmes that promote parent-child bonding and develop parenting skills, along with social and emotional development programmes that strengthen life skills and thus resilience in children [ 49 , 50 ]. Measures should also be taken to ensure service providers across a broad range of disciplines are cognisant of the lasting damage that ACEs place on mental well-being and wider health and social outcomes, and are trained to recognise and respond appropriately to clients with adverse backgrounds [ 51 ]. In particular, professionals in mental health services should be trained to routinely enquire about childhood experiences during client assessments. Studies suggest such enquiry is often lacking, with mental health treatment typically based on a medical model that focuses on biological factors and ignores the profound influence of socio-environmental experiences on brain development and functioning [ 52 , 53 ].
While the ACE methodology has been widely employed [ 54 ] it remains vulnerable to issues associated with any cross-sectional and retrospective survey with, for example, results relying on accurate recall and willingness to report ACEs. While adults with low mental well-being may have more negative perceptions of their childhoods, studies suggest false-positive reports of ACEs are rare [ 55 ]. Measures of current mental well-being and life satisfaction were also self-reported and therefore vulnerable to subjectivity, while the exclusion of individuals cognitively unable to participate in a face-to-face survey may have created bias in our sample. The dichotomisation of well-being scales may also have resulted in loss of information, although we used a consistent method to identify low mental well-being of greater than one SD from the sample mean. We used a recognised tool to measure nine important ACEs yet other common adversities such as neglect, bullying and parental death were not recorded. We explored the independent associations between outcome variables and both ACE counts and individual ACEs. However, we had insufficient sample size to look at how interactions between the individual ACE types, different combinations of ACEs and demographics may have resulted in different relationships with mental wellbeing. Such limitations aside our analyses did include multiple statistical analyses potentially increasing risks of type I errors. Consequently, while we have presented all figures for transparency, discussion has focused on highly significant results [ 56 ]. Finally, our study did not measure resilience resources [ 57 ], and developing understanding of factors that promote resiliency in those affected by ACEs would be an important future research priority.
While the high prevalence of mental disorders in the most vulnerable children (e.g. those in child protection systems) and the continued risks of mental illness in adults who suffered ACEs are widely recognised, data linking childhood adversity to the development and persistence of low mental well-being in the broader population is scarce. Our study suggests that almost half of the general English population have experienced at least one ACE and over one in twelve have suffered four or more ACEs. Such childhood adversity places individuals at significantly increased risk of low mental well-being and may have implications for the implementation and success of interventions that seek to promote mental well-being in the general population. The strong links between ACEs and adult mental well-being emphasise the need for a life course approach to mental health with the drivers of poor mental and physical health outcomes rooted together in childhood issues. Many of the ACEs that impact on children’s long term health and well-being are linked to familial behaviours and mental health (e.g. mental illness, substance abuse, violent and aggressive behaviour) suggesting that the mental health impacts of ACEs are what pushes much of their cyclical nature. A life course approach suggests that preventing ACEs would contribute to better physical and mental health from childhood through to old age and thus improve mental well-being in future generations.
Availability of data and materials
Data sets and other materials used in this article can be accessed by request to Professor Karen Hughes.
Abbreviations
adverse childhood experience
adjusted odds ratio
confidence interval
Index of Multiple Deprivation
life satisfaction
lower super output area
Short Warwick and Edinburgh Mental Well-being Scale
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58.
Article CAS PubMed Google Scholar
Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256:174–86.
Article PubMed PubMed Central Google Scholar
Bellis MA, Hughes K, Leckenby N, Jones L, Baban A, Kachaeva M, et al. Adverse childhood experiences and associations with health-harming behaviours in young adults: surveys in eight eastern European countries. Bull World Health Organ. 2014;92:641–55.
Bellis MA, Hughes K, Leckenby N, Perkins C, Lowey H. National household survey of adverse childhood experiences and their relationship with resilience to health-harming behaviors in England. BMC Med. 2014;12:72.
Bellis MA, Hughes K, Leckenby N, Hardcastle KA, Perkins C, Lowey H. Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: a national survey. J Public Health (Oxf). 2014;37:445–54.
Article Google Scholar
Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, Giles WH. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37:389–96.
Article PubMed Google Scholar
Anda RF, Brown DW, Felitti VJ, Bremner JD, Dube SR, Giles WH. Adverse childhood experiences and prescribed psychotropic medications in adults. Am J Prev Med. 2007;32:389–94.
Clark C, Caldwell T, Power C, Stansfeld SA. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Ann Epidemiol. 2010;20:385–94.
Koskenvuo K, Koskenvuo M. Childhood adversities predict strongly the use of psychotropic drugs in adulthood: a population-based cohort study of 24 284 Finns. J Epidemiol Community Health. 2015;69:354–60.
Pirkola S, Isometsä E, Aro H, Kestilä L, Hämäläinen J, Veijola J, et al. Childhood adversities as risk factors for adult mental disorders: Results from the health 2000 study. Soc Psychiatry Psychiatri Epidemiol. 2005;40:769–77.
Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–71.
Davies SC, Mehta N, Murphy O, Lillford-Wildman C. Annual report of the Chief Medical Officer 2013, Public mental health priorities: investing in the evidence. London: Department of Health; 2014.
Google Scholar
Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43:207–22.
Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70:741–56.
Diener E, Chan MY. Happy people live longer: subjective wellbeing contributes to health and longevity. Appl Psychol: Health and Well-Being. 2010;3:1–43.
Department of Health. Closing the gap: priorities for essential change in mental health. London: Department of Health; 2014.
World Health Organization. Mental health action plan 2013–2020. Geneva: World Health Organization; 2013.
Nurius PS, Logan-Greene P, Green S. Adverse Childhood Experiences (ACE) within a social disadvantage framework: distinguishing unique, cumulative, and moderated contributions to adult mental health. J Prev Interv Community. 2012;40:278–90.
Bellis MA, Lowey H, Leckenby N, Hughes K, Harrison D. Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. J Public Health (Oxf). 2013;36:81–91.
Bates A. Methodology used for producing ONS’s small area population estimates. Popul Trends. 2006;12:30–6.
Department for Communities and Local Government. English indices of deprivation. 2010. London: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010 . Accessed 18 Aug 2015.
Stewart-Brown S, Tennant A, Tennant R, Platt S, Parkinson J, Weich S. Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): a Rasch analysis using data from the Scottish Health Education Population Survey. Health Qual Life Outcomes. 2009;7:15.
Waldron S. Measuring subjective wellbeing in the UK. Newport: Office for National Statistics; 2010.
Bynum L, Griffin T, Ridings DL, Wynkoop KS, Anda RF, Edwards VJ, et al. Adverse childhood experiences reported by adults --- five states, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:1609–13.
Office for National Statistics. Population estimates by ethnic group 2002–2009. http://www.ons.gov.uk/ons/rel/peeg/population-estimates-by-ethnic-group--experimental-/current-estimates/population-density--change-and-concentration-in-great-britain.pdf . Accessed 18 Aug 2015.
Scott KM, Von Korff M, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, et al. The association of childhood adversities and early onset mental disorders with adult onset chronic physical conditions. Arch Gen Psychiatry. 2011;68:838–44.
Bruffaerts R, Demyttenaere K, Borges G, Haro JM, Chiu WT, Hwang I, et al. Childhood adversities as risk factors for onset and persistence of suicidal behavior. Br J Psychiatry. 2010;197:20–7.
Kessler RC, McLaughln KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010;197:378–85.
Foresight Mental Capital and Wellbeing Project. Mental capital and wellbeing: making the most of ourselves in the 21st century. London: The Government Office for Science; 2008.
Huppert FA. A new approach to reducing disorder and improving well-being. Psychol Sci. 2009;4:108–11.
Chanfreau J, Lloyd C, Byron C, Roberts C, Craig R, De Feo D, McManus S. Predicting wellbeing. London: NatCen Social Research; 2013.
Aked J, Marks N, Cordon C, Thompson S. Five ways to wellbeing: the evidence. London: New Economics Foundation; 2008.
Aked J, Thompson S. Five ways to wellbeing: new applications, new ways of thinking. London: New Economics Foundations and NHS Confederation; 2011.
Danese A, McEwen BS. Adverse childhood experiences, allostatis, allostatic load, and age-related disease. Physiol Behav. 2012;106:29–39.
Riggs SA. Childhood emotional abuse and the attachment system across the life cycle: what theory and research tell us. J Aggress Maltreat Trauma. 2010;19:5–51.
Currie J, Widom CS. Long-term consequences of child abuse and neglect on adult economic well-being. Child Maltreat. 2010;15:111–20.
Read J, Bentall RP. Childhood experiences and mental health: theoretical, clinical and primary prevention implications. Br J Psychiatry. 2012;200:89–91.
Bellis MA, Hughes K, Jones A, Perkins C, McHale P. Childhood happiness and violence: a retrospective study of their impacts on adult well-being. BMJ Open. 2013;3:e003427.
Stith SM, Liu T, Davies LC, Boykin EL, Alder MC, Harris JM, et al. Risk factors in child maltreatment: a meta-analytical review of the literature. Aggress Violent Behav. 2009;14:13–29.
Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–9.
Article PubMed Central Google Scholar
Joseph J. Why the emporer (still) has no genes. In: Read J, Dillon J, editors. Models of madness: psychological, social and biological approaches to psychosis. Hove: Routledge; 2013.
Manning C, Gregoire A. Effect of parental mental illness on children. Psychiatry. 2008;8:7–9.
Read J, Fosse R, Moskowitz A, Perry B. The traumagenic neurodevelopmental model of psychosis revisited. Neuropsychiatry. 2014;4:65–79.
Vaiserman AM. Epigenetic programming by early-life stress: evidence from human populations. Dev Dyn. 2015;244:254–65.
Finkelhor D, Browne A. The traumatic impact of child sexual abuse: a conceptualization. Am J Orthopsych. 1985;4:530–41.
Lalor K, McElvaney R. Child sexual abuse, links to later sexual exploitation/high-risk sexual behavior, and prevention/treatment programs. Trauma Violence Abuse. 2010;11:159–77.
Jonas S, Bebbington P, McManus S, Meltzer H, Jenkins R, Kuipers E, et al. Sexual abuse and psychiatric disorder in England: results from the 2007 Adult Psychiatric Morbidity Survey. Psychol Med. 2011;41:709–19.
Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al. Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial. Health Technol Assess. 2009;13:30.
Sethi D, Bellis MA, Hughes K, Gilbert R, Mitis F, Galea G. European report on preventing child maltreatment. Copenhagen: World Health Organization Regional Office for Europe; 2013.
World Health Organization. Violence prevention: the evidence. Geneva: World Health Organization; 2010.
Kagi R, Regala D. Translating the Adverse Childhood Experiences (ACE) study into public policy: progress and possibility in Washington State. J Prev Interv Community. 2012;40:271–7.
Hepworth I, McGowan L. Do mental health professionals enquire about childhood sexual abuse during routine mental health assessment in acute mental health settings? A substantive literature review. J Psychiatr Ment Health Nurs. 2013;20:473–83.
Read J, Bentall RP, Fosse R. Time to abandon the bio-bio-bio model of psychosis: exploring the epigenetic and psychological mechanisms by which adverse life events lead to psychotic symptoms. Epidemiol Psichiatr Soc. 2009;18:299–310.
PubMed Google Scholar
Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. Am J Prev Med. 2010;39:93–8.
Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45:260–73.
Perneger TV. What’s wrong with Bonferroni adjustments. BMJ. 1998;316:1236–8.
Article CAS PubMed PubMed Central Google Scholar
Logan-Greene P, Green S, Nurius PS, Longhi D. Distinct contributions of adverse childhood experiences and resilience resources: a cohort analysis of adult physical and mental health. Soc Work Health Care. 2014;53:776–97.
Download references
Acknowledgments
We thank Nicola Leckenby for coordinating the study and preparing data for analysis, and Katie Hardcastle and Olivia Sharples for supporting study implementation. We are grateful to all the surveyors for their time and commitment to the project and to all the individuals who participated in the study.
Author information
Authors and affiliations.
Centre for Public health, Liverpool John Moores University, 15-21 Webster Street, Liverpool, L3 2ET, UK
Karen Hughes & Zara Quigg
Blackburn with Darwen Borough Council, Public Health Department, 10 Duke Street, Blackburn, BB2 1DH, UK
Helen Lowey
Bangor University, Normal Site, Bangor, LL57 2PZ, UK
Mark A. Bellis
Director of Policy, Research and International Development, Public Health Wales, Hadyn Ellis Building, Maindy Road, Cardiff, CF24 4HQ, UK
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Karen Hughes .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
KH supported study development and implementation, analysed the data and wrote the manuscript. HL supported study development and contributed to data analysis and manuscript writing. ZQ edited the manuscript. MAB designed the study, supported data analysis and contributed to manuscript writing. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Hughes, K., Lowey, H., Quigg, Z. et al. Relationships between adverse childhood experiences and adult mental well-being: results from an English national household survey. BMC Public Health 16 , 222 (2016). https://doi.org/10.1186/s12889-016-2906-3
Download citation
Received : 21 August 2015
Accepted : 22 February 2016
Published : 03 March 2016
DOI : https://doi.org/10.1186/s12889-016-2906-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adverse childhood experiences
- Child maltreatment
- Mental well-being
- Life satisfaction
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Q Improvement Lab
Essays, Learning and Insights
Q Community site
Print-friendly version
- Facebook Facebook
- LinkedIn Twitter
- Project two
Mental health and persistent pain: an introduction
Why this topic and why it is important for all those working across mental and physical health
- by Libby Keck
In September 2018, the Q Lab and Mind embarked on a year-long collaboration to understand how care can be designed to best meet the needs of people living with both mental health problems and persistent back and neck pain.
The Q Lab focuses on specific health and care challenges and brings together organisations and individuals, to pool what is known and uncover new insights and ideas.
For some, mental health and persistent back and neck pain may sound like a niche topic. In reality, the numbers of people impacted by mental health problems and persistent back and neck pain in the UK are significant, and they are the two most common reasons for people to be on long-term sick leave or unable to work. A lot of attention has been given to these as individual needs, but more needs to be done to bring them together.

This topic – and what we’re learning as a result – is connected to the wider challenge of integrating care to meet people’s mental and physical health needs. The learning from the Q Lab and Mind’s work will provide useful insights for people interested in mental health problems and persistent back and neck pain, as well as individuals and organisations supporting people with combined physical and mental health needs and multiple long-term health conditions.
Over the coming months we will be sharing findings and resources. This essay offers a reminder of what the Q Lab is, the background and context for our work with Mind on this topic, and a flavour of what is to come.
What is the Q Improvement Lab?
The Q Lab – part of the Q initiative – provides an opportunity for individuals and organisations to collaborate and make progress on complex challenges that are affecting health and care in the UK.
The Q Lab works on a single challenge for 12 months – and in that time, convenes a group of people with experience and expertise in the topic (Lab participants). Together, we do research and sense-making, combining the best information and evidence about – and people’s experiences of – the challenge, and use this insight to support teams to develop and test ideas that have the potential to improve care. The Q Lab takes a developmental approach and aims to learn by doing, helping to build the skills and capabilities that are needed to deliver collaborative change.
The project on mental health and persistent pain is the Q Lab’s second project. The first project focussed on scaling patient-to-patient peer support and the learning and insights from this work are shared on this website. For more information on the Q Lab, take a look at What is the Q Improvement Lab? and Impact that counts essays.
Meeting the needs of people living with long-term physical and mental health problems
The Q Lab and Mind’s work aims to respond to the challenges of better meeting the needs of people living with long-term mental and physical health conditions.
Across the UK, long-term conditions are increasingly common. More than 15 million people (30% of the UK population) live with one or more long-term conditions (a condition for which there is no known cure, such as diabetes or arthritis). This will increase by another 3 million people by 2025. 1 Every week, 1 in 6 adults experiences a common mental health problem such as anxiety or depression. 2

Having either a physical or a mental health problem also makes you more likely to develop both – and this interrelationship goes both ways, with the conditions likely to interact and affect people in different ways.
Despite the interconnection of our mental and physical health (or more simply our minds and bodies), not enough people are receiving care that acknowledges and takes account of these needs at the same time.
This has a negative impact on individuals in lots of ways:
- Quality of life is worse for people with long-term conditions who also experience mental health problems. For example, people with long-term physical conditions are more likely to have lower wellbeing scores than those without. 3
- Health outcomes are also affected. Evidence shows that health screening is worse for people with mental health problems – which means fewer people benefit from interventions to improve their physical health, such as weight management, diet, nutrition and exercise advice. 4 There are also physical side effects of living with multiple conditions. For example, people with mental health problems regularly report that the physical side effects of their mental health medication have not been fully explained to them. 5
- The impact of both conditions can affect many areas of someone’s life – their sense of identity, emotional wellbeing, ability to perform and thrive at work – which can also affect relationships with families, friends and carers.
- Research tells us that despite this, people are not receiving joined-up care . For example, only 1 in 5 people with arthritis reports being asked about emotional or social issues by a rheumatology professional, even though almost half would like the opportunity. 6 The Mind Big Mental Health Survey 2017 found that less than half of the 8000+ respondents felt able to discuss a physical health issue at the same time as discussing their mental health, when attending primary care. 7
These issues impact the health and care system – increasing costs and pressures within services. It is estimated that the effect of poor mental health on people living with long-term physical conditions costs the NHS at least £8 billion a year. 8
Supporting and improving quality of life for people with mental and physical health needs is not just a priority for the NHS – it is also a public health issue. Increasingly people are living longer – but are doing so with greater health needs. In England, the economic and social burden from people living with disabilities is more significant than the impact of people dying young. 9 Increased disability drives demand for statutory services and reduces productivity and employment. It is the product of, and reinforced by, health inequalities.
Shifting the status quo
There is no easy fix for systematically supporting people’s mental and physical health needs. Whole-system change will involve adapting the way services are commissioned, designed and delivered, as well as how health care professionals are trained and supported to work together across professional and/or organisational boundaries. Despite these challenges, there is growing recognition of the need to change the status quo.

Increasingly, services are moving towards delivering care using the ‘Biopsychosocial Model’ – a model that acknowledges and recognises the combined biological, psychological and social factors that determine our health and wellbeing.
There is also a drive to increase provision of mental health services, and to support the delivery of better integrated services – through new models of care, strategic transformation partnerships, and the recent commitment in the NHS Long Term Plan that every area will be served by an integrated care system by 2021. Charity and campaigning organisations are collaborating to promote the importance of mental and physical health, for example the Equally Well UK initiative, and many organisations are developing and delivering holistic models of care, that meet people’s physical and mental health needs.
The Health Foundation, who deliver the Q Lab, have funded a wide portfolio of improvement projects that aim to provide more holistic and joined-up care for people living with long-term physical and mental health conditions, including the recent successful programme 3 Dimensions for Long-term Conditions . This programme has integrated mental, physical and social care support in long-term conditions across community and secondary services in London. Find out more at: www.health.org.uk/improvement-projects/integrating-mental-physical-and-social-care-in-long-term-conditions
From mental and physical health to persistent back and neck pain
When Mind and the Q Lab agreed to collaborate, we knew that improving care for people with mental and physical health was the right area to focus our work. It is an important topic that’s ripe for improvement.
It also allows us to build on the great work that’s happening already. For example, we drew on Mind’s work on reducing stigma for people with mental health through Time to Change (which works to end mental health discrimination by changing the way we all think and act about mental health problems) as well as their successful programme Building Health Futures that explored ways to improve the wellbeing, resilience and confidence of people with heart disease, diabetes and arthritis who may be at risk of developing mental health problems. 10
In order to undertake rapid research and develop and test ideas and solutions in practice in just 12 months, a more defined scope was needed. Through reviewing the evidence and speaking to a range of people in this field, a more focussed topic – improving care for people living with both mental health problems and persistent back and neck pain – was identified.
As you’ll go on to read in the next essay Challenges and opportunities to improve , many of the challenges and solutions we identify are either connected, or directly speak to, the challenges of bringing together physical and mental health care provision.
What we aim to achieve
The Q Lab and Mind have worked with others to understand the problem deeply, from a range of perspectives, drawing on data, evidence and experience. Our learning is shared in this essay collection to increase people’s awareness and understanding of the topic, and importantly to increase momentum for change – by highlighting opportunities and practical insights that are useful for people working in and with health and care.
The outputs take into account the evaluation of the Q Lab – conducted by the Innovation Unit – which has provided insights on the types of resources that are most useful for people working to improve health and care, in order to act on the findings.
(If you’d like to find out more about the impact we aim to achieve, take a look at the Impact that counts essay from our first project.)
What to expect from this essay collection
This essay collection presents the findings from the Q Lab and Mind, and the organisations and individuals who have worked with us on this challenge. The learning is shared as openly as possible, as we collectively seek to identify challenges and opportunities that have potential for use in services and organisations across the health and care system.
The next Lab essay in this collection – Challenges and opportunities to improve – brings together the outputs from surveys, workshops and interviews involving over 150 people. If you have lived or professional experience in mental health and persistent back and neck pain, the insights in this essay may be familiar to you and we hope it is a useful tool for you to share and build support for your work. If you are new to the topic – and want to understand more – this essay will provide an overview of the known problems and potential solutions and practical ideas that have worked elsewhere, that may be relevant for you to consider locally.

At the time of writing this essay, we have just started to work with four organisations – Health Innovation Network , Robert Jones and Agnes Hunt Orthopaedic Hospital , Powys Teaching Health Board and Keele University with Midlands Partnership NHS Foundation Trust – to build on our initial sense-making of the topic and translate that into practical actions to improve care.
Over the next six months you can also expect to see from us:
- Practical ideas and solutions to address this topic that have been shown to work elsewhere, with advice about how this could be translated to different contexts.
- Information on using design approaches to develop and test ideas in practice , curating learning from supporting four organisations to test ideas with the potential to improve care for people living with mental health problems and persistent pain.
- Ideas on developing skills for collaborative improvement – including a framework for the skills and attitudes for collaborative and creative problem solving (co-produced with Nesta ).
- Learning from delivering the Q Lab – with stories of how the Lab approach and ethos is helping to deliver impact to health and care in the UK – and what this means for others seeking to deliver change at scale, and for the evolution of the Lab in the coming year.
- Discover what the Q Lab and Mind have learned about mental health and persistent pain in Challenges and opportunities to improve
- Know someone who might be interested in this essay? Share it!
- To connect with people interested in transforming care for people with mental health and persistent back and neck pain, join the Q Lab online group .
- If you have ideas about what you’d like us to produce in the future, get in touch at [email protected]
Challenges and opportunities to improve
People's History of the NHS
- People's Encyclopaedia
- Virtual NHS Museum
- Encyclopaedia
Mental Health
A significant interest in something called mental health, not just mental illness, can be dated back in Britain to the interwar years. In other words, it was not a product of the new National Health Service. Indeed, hope that the new service might provide the opportunity for a vigorous state programme directed at mental health met disappointment. Recognition of the importance of mental health had been reinforced by lessons about military and civilian health in the Second World War, but the new NHS provided little in the way of new initiative. It certainly didn’t put mental health on the same footing as physical health. What’s more, the mentally ill continued to be housed in the same largely isolated, Victorian institutions that had been built up and down Britain over the past century: out of sight, out of mind.
As well as questioning the idea of 1948 as a turning point when it comes to mental health, we should also appreciate that a wholly negative account of the pre-NHS system of care needs some modification. In terms of public effort and investment, the building of this vast system of public institutions now seems impressive. In a sense this was a ‘National Asylum System’, well before the state accepted responsibility to provide free hospital care for the physically ill under the NHS. The problem was that so little could be done to cure those who ended up needing care in such places. Faced by a growing population of seemingly incurable patients, pessimism became pervasive. It was exacerbated as broader eugenic fears led to a parallel system of institutional care for people with mental disabilities – the ‘mentally defective’ as the new legislation of 1913 described them in a language that reflects the harsh attitudes of the time and the stigma that resulted from this. However, it was partly because these institutions seemed to have failed as sites of cure that an interest in the treatment of milder and early stages of mental illness advanced away from the site of asylum in the interwar years. This was often supported by charities. But in addition, local authorities began providing supervision in the community – community care in embryo. General hospitals began to offer outpatient care. Progressive general practitioners increasingly recognised that a large part of the physical illnesses they encountered had a psychological component. And child guidance and psychological clinics sprung up across the country. What’s more, with a boom in self-help literature, the public began to appreciate that mental health was a concern for the whole population. In other words, many of the pieces were in place for something far more ambitious in relation to mental health than was delivered in 1948.
Instead, 1948 saw more of the same. The old Victorian lunacy legislation remained largely in place. It had been modified in 1930 to allow some voluntary treatment in what were now to be termed mental hospitals rather than asylums. But this still left the mentally ill as a class apart, and this is how they were handled in the establishment of the new National Health Service. So, rather than a reversal, the decade after 1948 saw continued growth in the numbers ending up in these institutions to reach a peak of over 150,000 by the mid 1950s (40% of all beds in the NHS).
Reform of the legislation around mental illness had to wait until the Mental Health Act of 1959. The title of this piece of legislation symbolised the aspiration for integration into the NHS. At its heart was the decision to make entry to mental hospital an issue of medical rather than legal judgement. However, this was never going to be enough on its own to remove the stigma that surrounded these ageing institutions. The Act also signalled the intention of a move towards community care. This was given further momentum by a speech from Minister of Health Enoch Powell in 1961, which talked of getting rid of the Victorian asylums ‘brooded over by the gigantic water-tower and chimney combined, rising unmistakable and daunting out of the countryside’. The solution was to be twofold: on the one hand, moving the treatment of mental illness to the wards and wings of general hospitals; on the other, developing new services in the community supported by an expanding social work profession. This fundamental transformation was made much more feasible because of a new generation of drugs. However, in terms of bringing mental health care into the NHS, there was arguably a tension in this vision: at last there was a more hopeful medicine for mental illness; yet the vague talk of community care in fact signalled a future in which responsibility for the care of the mentally ill might largely lie elsewhere, in the field of social care.
In the long term, the vision of transformation was to be realised. Indeed, there has been perhaps no more fundamental shift in the whole history of NHS care than this move from hospital to community care for the mentally ill. In that sense, it provides a significant case study for those who have looked for a similar shift away from the centrality of the hospital in relation to physical health. But change was initially slow, and throughout the period there have been serious misgivings about the quality of the service that has resulted. In the late 1960s and early 1970s, the lack of dignity afforded to patients in some of the remaining large and overcrowded mental hospitals was publicised in several scathing public reports. Fashionable anti-psychiatric writing emerging out of the counter-culture added to the sense of unease. More significant still was the emerging service-user movement, which for the first time brought the experiences of those who suffered through the inadequacies of mental health care in the NHS to the fore.
Powell had talked of getting rid of the Victorian institutions, but although the bed numbers began to decline few hospitals were closed until the 1970s. From the 1980s the pace of change accelerated, with a dramatic 60% fall in mental hospital beds from 1987 to 2010. The challenge was ensuring that something more effective and humane was introduced in place of the asylum. However, there was a strong feeling from many at the time that such community care often proved hugely disappointing and an excuse for cuts in expenditure. From 1997, under New Labour, there was a significant increase in expenditure on mental health care, though this reflected a more general increase of expenditure on the NHS and in fact still fell behind the overall trend. One result of the closure of mental hospitals was a growing anxiety, sparked by a small number of well-publicised cases, about the danger of releasing seriously mentally ill patients into the community. In such a context, the residential settings that remained became targeted increasingly on patients deemed to be a ‘risk’ to the broader community. It also became clear that many such individuals were ending up in the country’s expanding prison system. What remained of the mental hospital system now offered no real solution to the demand for ‘asylum’ for those not deemed a danger, nor for the mounting problem of dementia which fell instead into the hands of families and an ailing system of social care.
The considerable challenges of the shift from hospital towards community care meant that it was the issue of mental illness rather than mental health that had remained central as a concern of policy through most of this period. However, it is tempting to argue that the 21st century is seeing something a new kind of transformation. Since the turn of the century, the issue of mental health finally began to come to the fore in debate about the future direction of the NHS. Influential research began to claim that there was a strong economic case for improving mental health, with problems of mental health a major cause of expenditure for the welfare state and of lost productivity. Politicians began to talk about improving happiness and about the neglect of mental health care within the NHS. And the Health and Social Care Act of 2012 made it a requirement for the NHS to place mental health on a par with physical health. A policy of IAPT – improving access to psychological therapy – provided the hope of a new kind of therapeutic armoury for the NHS which could be rolled out far beyond the population that had been the focus of psychiatric care for most of the period since 1948. Often deploying the tools of self-help, assisted by the revolution in communication brought about by the internet and by a greater openness in talking about mental health, the new approach was attractive as a way to overcome the dual problem that had always held back an expansion of mental health services: the inadequacy of both funding and expertise. However, these limitations continued to be exposed in the struggle to access professional services. At a time that the NHS was under so much pressure, putting mental health genuinely on a par with physical health was going to be a huge challenge.
Despite all its ongoing problems and limitations, it is tempting to conclude that the area of mental health care has nevertheless been one of the areas of most major transformation in the history of the NHS. This case rests firstly on the dramatic move from hospital to community care, and secondly on a belated but growing effort to address the mental health of the population as a whole. In 1948 the NHS was really a national physical health (and to a larger extent illness) service. It did inherit a national mental illness service (that huge population in the mental hospitals), but this was not well integrated and was largely hidden away from view. In subsequent efforts at integration, policy makers came to regard this decaying institutional system as having no place in a modern health service. Thereafter barriers were to some extent broken down, although the move from hospital to community care also saw responsibility to some extent passed on to the family, the social services, even eventually the penal system. More recently, there have been signs that the NHS is coming to see tackling mental health as just as much part of its responsibility as its longer term focus on physical health. Whether this is truly to be the case, and whether the developments in the relationship of the NHS towards mental illness and mental health are truly compatible, remains to be seen.
Read other posts:
6 thoughts on “ mental health ”.
‘Influential research began to claim that there was a strong economic case for improving mental health, with problems of mental health a major cause of expenditure for the welfare state and of lost productivity.’
This quotation really interested me because it links our understanding of mental health care to productivity. How far is our system of mental health care reproducing the precarious and tired “good neoliberal subject”?
Employers and Universities tell us to go and seek counselling, or to see the doctor, so we can improve ourselves – usually in our free time – and get back to producing as soon as possible. Therefore, how does this culture reinforce societal structures which exacerbate poor health and reproduce the good, productive, neoliberal citizen?
Yours, A good neoliberal subject
I am very interested in the idea that, as you put it above, ‘a wholly negative account of the pre-NHS system of care needs some modification’. Can we talk about the 1913 Mental Deficiency Act and the people who supported it as other than eugenic sympathisers whose main purpose was to segregate people with mental disabilities? Because of improvements in our current understanding of mental health we now seem to consider those who got involved in the past (including Ida Darwin) as doing more harm than good. Yet their work underpins the support that the NHS provides today.
So much was wrong about the system in the first half of the 20th century, that it may seem odd to talk about ‘positives’, but in the context of the time there was some progress. Areas included:
– Protection for the ‘mentally defective’ (ie care as well as control)
– Early treatment for the mentally ill on a voluntary and temporary basis to avoid the stigma of certification (Mental Treatment Act, 1930)
– The increasing influence of a range of talking therapies provided in clinics or in outpatient sections of hospitals, and reaching out also to children (child guidance clinics)
– Early forms of ‘community care’ via supervision but also licensing out of patients to half-way houses, guardianship schemes, and holiday homes (all particularly prevalent under the Mental Deficiency legislation
– New forms of physical therapy in the mental hospitals
– Efforts to educate the public and change attitudes
I have had a head enj and it’s can not be repair and in my childhood I spent more time in hospitals and I was taken tablets when l came to aduIt age I took myself of the tables because I had an illness EPL sorry I can’t spell the word and the people to whom adopted me could not understand my illness so I was beating but Iam very grateful for the help with the N H S with kind regards Derek Taylor
Hi, I thought you might be interested in this film about Fairfield Psychiatric Hospital in the 1980’s and my creative writing classes there.
https://www.youtube.com/watch?v=s13ARcXya7U&index=27&list=UUmSMyxoSbzMeR1leR8bC7-w
Please use and share as you wish.
David R Morgan
What is Normal ? What is Acceptable ? Behavoir or attitude . It’s ok to be different ? It’s not ok to appear the same but act upon others with harmful scheme or critism Consultation ,diagnosis ,therapy and treatment must be variable ,not the need to treat every patient to behave the same . Good vs evil drivers must be consulted in assessment of Behavoir. Not just Appearance and related fixed assumptions . Never judge a book by its cover. I to this day have no idea why i was detained under mental health act three to.es and heavily medicated ,without being a risk to myself or the general public. I now further my studies in psychology to psychiatry and mental health .With fascination !!!!
Should you wish to remove a comment you have made, please contact us
Twitter Feed

The information is provided by us and while we endeavour to keep the information up to date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability or availability with respect to the website or the information, products, services, or related graphics contained on the website for any purpose. We only capture and store personal information with the prior consent of users. Any personal information collected as part of the user registration process or the submission of material (including, but not limited to, name, address, e-mail address) will be stored securely, and accessible only to members of the Cultural History of the NHS project team. We will not sell, license or trade your personal information to others. We do not provide your personal information to direct marketing companies or other such organizations. These opinions do not necessarily represent those of Warwick University or the Wellcome Trust.
This site would like to use cookies to track your usage of the site
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 5, Issue 6
- What is mental health? Evidence towards a new definition from a mixed methods multidisciplinary international survey
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Laurie A Manwell 1 , 2 ,
- Skye P Barbic 1 , 3 ,
- Karen Roberts 1 ,
- Zachary Durisko 1 ,
- Cheolsoon Lee 1 , 4 ,
- Emma Ware 1 ,
- Kwame McKenzie 1
- 1 Social Aetiology of Mental Illness Training Program , Centre for Addiction and Mental Health, University of Toronto , Toronto, Ontario , Canada
- 2 Department of Anatomy and Cell Biology , Schulich School of Medicine & Dentistry, University of Western , London, Ontario , Canada
- 3 Department of Psychiatry , University of British Columbia , Vancouver, British Columbia , Canada
- 4 Department of Psychiatry , Gyeongsang National University Hospital, School of Medicine, Gyeongsang National University , Jinju , Republic of Korea
- Correspondence to Dr Laurie A Manwell; lauriemanwell{at}gmail.com
Objective Lack of consensus on the definition of mental health has implications for research, policy and practice. This study aims to start an international, interdisciplinary and inclusive dialogue to answer the question: What are the core concepts of mental health?
Design and participants 50 people with expertise in the field of mental health from 8 countries completed an online survey. They identified the extent to which 4 current definitions were adequate and what the core concepts of mental health were. A qualitative thematic analysis was conducted of their responses. The results were validated at a consensus meeting of 58 clinicians, researchers and people with lived experience.
Results 46% of respondents rated the Public Health Agency of Canada (PHAC, 2006) definition as the most preferred, 30% stated that none of the 4 definitions were satisfactory and only 20% said the WHO (2001) definition was their preferred choice. The least preferred definition of mental health was the general definition of health adapted from Huber et al (2011). The core concepts of mental health were highly varied and reflected different processes people used to answer the question. These processes included the overarching perspective or point of reference of respondents (positionality), the frameworks used to describe the core concepts (paradigms, theories and models), and the way social and environmental factors were considered to act . The core concepts of mental health identified were mainly individual and functional, in that they related to the ability or capacity of a person to effectively deal with or change his/her environment. A preliminary model for the processes used to conceptualise mental health is presented.
Conclusions Answers to the question, ‘ What are the core concepts of mental health ?’ are highly dependent on the empirical frame used. Understanding these empirical frames is key to developing a useful consensus definition for diverse populations.
- MENTAL HEALTH
- mental illness
- social determinants of health
- human rights
- primary health care
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
https://doi.org/10.1136/bmjopen-2014-007079
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
Our study identifies a major obstacle for integrating mental health initiatives into global health programmes and health service delivery, which is a lack of consensus on a definition, and initiates a global, interdisciplinary and inclusive dialogue towards a consensus definition of mental health .
Despite the limitations of a small sample size and response saturation, our sample of global experts was able to demonstrate dissatisfaction with current definitions of mental health and significant agreement among subcomponents, specifically factors beyond the ‘ability to adapt and self-manage’, such as ‘diversity and community identity’ and creating distinct definitions, ‘one for individual and a parallel for community and society’.
This research demonstrates how experts in the field of mental health determine the core concepts of mental health, presenting a model of how empirical discourses shape definitions of mental health.
We propose a transdomain model of health to inform the development of a comprehensive definition capturing all of the subcomponents of health: physical, mental and social health.
Our study discusses the implications of the findings for research, policy and practice in meeting the needs of diverse populations.
Introduction
A major obstacle for integrating mental health initiatives into global health programmes and primary healthcare services is lack of consensus on a definition of mental health. 1–3 There is little agreement on a general definition of ‘mental health’ 4 and currently there is widespread use of the term ‘mental health’ as a euphemism for ‘mental illness’. 5 Mental health can be defined as the absence of mental disease or it can be defined as a state of being that also includes the biological, psychological or social factors which contribute to an individual’s mental state and ability to function within the environment. 4 , 6–11 For example, the WHO 12 includes realising one's potential, the ability to cope with normal life stresses and community contributions as core components of mental health. Other definitions extend beyond this to also include intellectual, emotional and spiritual development, 13 positive self-perception, feelings of self-worth and physical health, 11 , 14 and intrapersonal harmony. 8 Prevention strategies may aim to decrease the rates of mental illness but promotion strategies aim at improving mental health. The possible scope of promotion initiatives depends on the definition of mental health.
The purpose of this paper is to begin a global, interdisciplinary, interactive and inclusive series of dialogues leading to a consensus definition of mental health. It has been stimulated and informed by a recent debate about the need to redefine the term health . Huber et al 15 emphasised that health should encompass an individual's “ability to adapt and to self-manage” in response to challenges, rather than achieving “a state of complete wellbeing” as stated in current WHO 6 , 12 definitions. They also argued that a new definition must consider the demographics of stakeholders involved and future advances in science. 15 Responses to the article suggested the process of reconceptualising health be extended “beyond the esoteric world of academia and the pragmatic world of policy” 16 to include a “much wider lens to the aetiology of health” 17 along with patients and lay members of the public. Huber et al's 15 definition of health could include mental health but it is not clear that this would be satisfactory to patients, practitioners or researchers. We aimed to compare the satisfaction of mental health specialists, patients and the public with Huber et al ’s definition and other currently used definitions of mental health. We also asked them what they considered to be the core components of mental health.
Participants and procedures
A pool of 25 researchers in mental health was identified through literature/internet searches to capture expertise in (1) ‘community mental health’ and ‘public mental health’, (2) ‘human rights’ and ‘global mental health’, (3) ‘positive mental health’ and ‘resilience’, (4) ‘recovery’ and ‘mental health’, and (5) ‘natural selection’ and ‘evolutionary origins’ of ‘mental health’. Each of these five areas was assigned to an author with expertise in that area who then conducted a series of literature/internet searches using the key terms listed above. Proposed participants were identified based on their expert contributions, such as published papers, presentations, community outreach, and other evidence of work in their field that had implications for mental health. Each author presented their list to the research team which then narrowed the number to 5 per category for a total of 25 initial participants. An additional 31 individuals were added, which included people with lived experience of mental illness as well as the mentors of the Social Aetiology of Mental Illness (SAMI) Training Programme (funded by the Canadian Institutes of Health Research and includes a multidisciplinary group of experts with diverse interests, including biological, social and psychological sciences); all of these participants were identified through the SAMI/Centre for Addiction and Mental Health network. Fifty-six participants were sent the survey in the first round. Two subsequent rounds were completed using a snowballing technique: each person in round 1 was asked to indicate up to three other people they thought should receive the survey, which was then distributed to those identified individuals. This was repeated in round 2.
The ‘What is Mental Health?’ survey was created and distributed electronically using the SurveyMonkey platform. Respondents were asked to describe their areas of expertise, and list or describe the core concepts of mental health. Respondents ranked four definitions (without citations) of mental health 12 , 15 , 18 (McKenzie K. Community definition of Mental Health. What Is Mental Health Survey. Centre for Addiction and Mental Health, personal communication, 15 January 2014) and a fifth choice of ‘None of the existing definitions are satisfactory’ in order of preference (1=most preferred, 5=least preferred), and could rate multiple definitions as most and/or least preferred (see table 1 ). Respondents were asked to state, ‘What was missing and why?’ from these definitions.
- View inline
Current definitions of mental health and participant rank ordering from most to least preferred
Data analysis
Thematic analysis 19 was used to evaluate the core concepts of mental health, followed by triangulation (ie, multiple methods, analysts or theory/perspectives) to verify and validate the qualitative data analysis. 20
First, multiple analysts with knowledge from different disciplines reviewed the data. 20 Our collective areas of expertise encompass the following: animal models of human behaviour; arts; clinical, cognitive, political and social psychology; ecology; education; epidemiology; evolutionary theory; humanities; knowledge translation; measurement; molecular biology; neuroscience; occupational therapy; psychiatry; qualitative and quantitative research; social aetiology of mental illness; toxicology and transcultural health. All transcripts were reviewed by each coder first independently, then collectively, to become familiar with the data and create a mutually agreed on code book using NVivo 10. Codes were organised into themes, and compared and contrasted manually and through NVivo10 coding queries within each major theme and across response items. Initial models derived from the data were created and validated by the multidisciplinary research team.
Second, method triangulation was used to assess the consistency of our findings. 20 Preliminary results from the survey were presented and discussed at the 4th Annual Social Aetiology of Mental Illness Conference (20 May 2014) at the Centre for Addiction and Mental Health, University of Toronto (Toronto, Ontario, Canada). Attendees were divided into five focus groups of 10–12 people facilitated by a project leader and 2 trained note takers. The two consecutive 1 h focused discussions used the ORID method (Objective, Reflective, Interpretive and Decisional) 21 in order to elicit feedback on the methods and results of the survey. All responses from each of the five groups were transcribed by two recorders and disseminated to the research team for individual and collaborative review.
A second round of data analysis was conducted to validate the results according to key areas of interest and critique reported by the conference participants.
Survey respondents
Fifty-six surveys were distributed in the first round, 28 in the second and 38 in the third. Fifty people completed the survey (rounds 1, 2 and 3 had 32, 12 and 6 respondents, respectively) with a total response rate of 41%. Two-thirds of respondents (66%) were male and one-third were female (34%). Respondents’ current country of residence/employment included Canada (52%), UK (20%), USA (14%), Australia (6%), New Zealand (2%), Brazil (2%), South Africa (2%) and Togo (2%). The majority of respondents (72%) held academic positions at postsecondary institutions and were conducting research in the broad field of mental health. Sixty per cent were also involved in giving advice to mental health services or managing them. Thirty-four per cent of respondents were clinicians.
Survey items
Respondents had diverse expertise (see table 2 ). Forty-six per cent of respondents rated the Public Health Agency of Canada (PHAC) 18 definition as their most preferred. However, 30% stated that none were satisfactory. The WHO definition 12 was preferred by 20%. The least preferred definition of mental health was the general definition of health adapted from Huber et al 15 (see table 1 ).
Self-reported areas of expertise
Analysis of the three open-ended items established four major themes— Positionality, Social/Environmental Factors, Paradigms/Theories/Models and the Core Concepts of Mental Health —and five-directional relationships between them ( figure 1 ). Positionality represented the overarching perspective or point-of-reference from which the Core Concepts were derived; whereas Paradigms/Theories/Models represented the theoretical framework within which the Core Concepts were described. Core Concepts represented factors related to the individual; these were distinguishable from the Social/Environmental Factors related to society. Five significant relationships between these themes were established ( figure 1 ). First, respondents’ theoretical framework (Direction A) influenced the overarching point-of-reference they used to describe the core concepts and vice versa (Direction B). Positionality and Paradigms/Theories/Models significantly influenced the core concepts respondents provided and the corresponding descriptions (Direction C). Respondents described how social and environmental factors impacted the core concepts (Direction D) and reciprocally, how the core concepts could influence society (Direction E) ( tables 3 and 4 ). Feedback from the conference focus groups showed support for these five-directional relationships but questioned whether there was evidence for other direct relationships, specifically the impact of Social/Environmental Factors on both Paradigms/Theories/Models and Positionality . A second round of data analysis confirmed these relationships were not explicitly reported by respondents in the survey. Respondents did not discuss how social factors (ie, education or employment) would impact the adoption of a particular paradigm, theory or model (ie, quality of life, evolutionary theory or biomedical model).
Theme—Positionality
Theme—Core Concepts
- Download figure
- Open in new tab
- Download powerpoint
Themes of Positionality, Core Concepts, Social/Environmental Factors, and Paradigms/Theories/Models. *Indicates answers specifically from the third open-ended question asking respondents to state “what is missing” from the definitions provided for ranking.
The theme of Positionality demonstrated how respondents positioned their conceptualisations of mental health within an explicit or implicit framework of understanding ( table 3 , figures 2 and 3 ). Several respondents described the core concepts in terms of binary or conflicting dynamics or as categorical or continuous . Some respondents pointed to the mutual exclusivity of ‘mental health’ and ‘mental illness’ while others described these concepts as distinct points separated on a continuum or as overlapping. Respondents specified the complexity of mental health, for example, positioning mental health explicitly outside of, and specifically in between, the individual and society. Several respondents framed the core concepts of mental health as descriptive versus prescriptive , arguing that these must be empirically determined and defined (ie, describing what is ) rather than prescribed according to values and morals (ie, describing what should be ). In accordance with Hume's Law (ie, an ‘ought’ cannot be derived from an ‘is’), 22 several respondents cautioned that problems of living, such as ‘poverty, vices, social injustices and stupidity’, should not be defined ‘as medical problems’. Many respondents described mental health in relation to hierarchical levels , and/or temporal trajectories , and/or context ( table 3 , figure 3 ). Respondents articulated the multiple levels at which mental health can be understood (ie, from the basic unit of the gene, through the individual and up to the globe) and how meaning changes across time (ie, mental health described as functioning in line with our evolutionary ancestors, to current developmental mechanisms and including expectations of a peaceful death and spiritual existence) and across context (ie, from region, to race, to culture, to epistemology). In the second round of data analysis, we searched for bias in participants’ reporting of evidence-based models and bias against other sources of information; there was support for objective and subjective sources in conceptualising mental health.
Positionality. The overarching perspective or point-of-reference used to describe the constructs of mental health and illness.
Complexity. Descriptions of mental health in relation to hierarchical levels, and/or spatial directions, and/or temporal trajectories.
A second theme of Paradigms/Theories/Models developed as respondents discussed the need to perceive health through various frameworks (eg, recovery, resilience, human flourishing, quality of life, developmental and evolutionary theories, cultural psychiatry and ecology). Some respondents noted that current definitions of mental health treat problems of living as medical problems, rather than adaptive responses to the conditions that people experience, and that alternative explanations should be considered: “An evolutionary approach to these conditions suggests that anxiety and depression (as responses to social stressors) evolved to help the individual take corrective action that could ameliorate the negative effects of these stressors”. Some respondents emphasised that ‘low’ mental health did not equate to mental illness, but rather a state of hopelessness and lack of personal autonomy, whereas ‘high’ mental health was demonstrated by ‘meaningful participation, community citizenship, and life satisfaction’. Others referenced Westerhof and Keyes's 23 two-continuum model describing mental illness and mental health as related by two distinct dimensions.
The Core Concepts of mental health ( figure 1 , table 4 ) largely described factors relating to the individual—as opposed to society—that are observed in correlation with mental health and which are necessary, to some degree or another, but not normally sufficient on their own to achieve mental health. Concepts related to agency, autonomy and control appeared frequently in relation to an individual's ability or capacity to effectively deal with and/or create change in his or her environment (Directions D–E). Agency/autonomy/control reappeared as an essential component of other core concepts: agency may be required in order to engage in meaningful participation (eg, ‘sense of being part of a vibrant society, with agency to make change for you and others, and supportive relationships and governance’) and in dignity (eg, ‘a state of mind that allows one to lead one's life knowing that one’s dignity and integrity as a human being is respected by others’). A cluster of concepts describing the self signified (1) the subjective experience of the individual as fundamental to well-being and (2) the importance of one's ability, confidence and desire to live in accordance with one's own values and beliefs in moving towards the fulfilment of one's goals and ambitions ( figure 1 ).
Social and Environmental Factors reflected the societal factors external to the individual that affect mental health. Although many respondents listed the basic necessities for general health/mental health (eg, housing, food security, access to health services, equitable access to public resources, childcare, education, transportation, support for families, respect for diversity, opportunities for building resilience, self-esteem, personal and social efficacy, growth, meaning and purpose, and sense of safety and belonging, and employment), some also recommended approaches to achieving social equity (eg, “mental health needs to be protected by applying antiracism, antioppression, antidiscrimination lens to prevention and treatment”) ( figure 1 , Direction D). A distinct category of human rights developed from responses to the third open-ended question (eg, “What is missing?”) ( figure 1 ). Several respondents suggested that a basic standard, analogous to a legal definition, is required ( table 3 ) and/or that “a human rights, political, economic and ecosystem perspective” should be included.
The international exploratory ‘What is Mental Health?’ survey sought the opinions of individuals, across multiple modes of inquiry, on what they perceived to be the core concepts of mental health. The survey found dissatisfaction with current definitions of mental health. There was no consensus among this group on a common definition. However, there was significant agreement among subcomponents of the definitions, specifically factors beyond the ‘ability to adapt and self-manage’, such as ‘diversity and community identity’ and creating distinct definitions, “one for individual and a parallel for community and society.” The Core Concepts of mental health that participants identified were predominantly centred on factors relating to the individual, and one's capacity and ability for choice in interacting with society. The concepts of agency, autonomy and control were commonly mentioned throughout the responses, specifically in regard to the individual's ability or capacity to effectively deal with and/or create change in his or her environment. Similarly, respondents pointed to the self as an essential component of mental health, signifying the subjective experience of the individual as fundamental to well-being, particularly in relationship to achieving one's valued goals. Respondents suggested that mentally healthy individuals are socially connected through meaningful participation in valued roles (ie, in family, work, worship, etc), but that mental health may involve being able to disconnect by choice, as opposed to being excluded (eg, having the capacity and ability to reject social, legal and theological practices). In contrast, Social and Environmental Factors reflected respondents’ emphasis on factors that are external to the individual and which can influence the core concepts of mental health. Many respondents reiterated the basic necessities for general health/mental health, similar to the foundations of Maslow's hierarchy of needs, 24 and their recommendations for achieving social equity.
Descriptions of the core concepts of mental health were highly influenced by respondents’ Positionality and Paradigms/Theories/Models of reference, which often propelled the discourse of “What is mental health?” in opposing directions. The debate as to whether mental health and illness are distinct constructs, or points of reference on a continuum of being, was a common theme. Respondents were either, adamant in asserting the distinction between the descriptive or prescriptive nature of the core concepts, or, ardent in integrating them, producing ideas such as describing mental health as a life free of poverty, discrimination, oppression, human rights violations and war. Respondents’ made repeated references to human rights, suggesting that a basic standard, analogous to a legal definition, is required, and that ‘a human rights, political, economic and ecosystem perspective’ should be included. Again, in the tradition of Hume's ‘ought–is’ distinction, several respondents cautioned that problems of living, such as ‘poverty, vices and social injustices…’ should not be defined ‘as medical problems’. The significance of this issue cannot be understated: while we asked respondents what the core concepts of mental health are , overwhelmingly they answered in terms of what they should be. This finding is similar to other issues in public health policy that address instances of ‘conflating scientific evidence with moral argument’. 15 , 22 Indeed, a primary criticism of the WHO definition of health is that its declaration of “complete physical, mental, and social wellbeing” 6 is prescriptive rather than descriptive. 15 Such a definition “contributes to the medicalization of society” and excludes most people, most of the time, and has little practical value “because ‘complete’ is neither operational nor measurable.” 15
Accordingly, we propose a transdomain model of health ( figure 4 ) to inform the development of a comprehensive definition for all aspects of health. This model builds on the three domains of health as described by WHO 6 , 12 and Huber et al, 15 and expands these definitions to include four specific overlapping areas and the empirical, moral and legal considerations discussed in the current study. First, all three domains of health should have a basic legal standard of functioning and adaptation. Our findings suggest that for physical health, a standard level of biological functioning and adaptation would include allostasis (ie, homeostatic maintenance in response to stress), whereas for mental health, a standard level of cognitive–emotional functioning and adaptation would include sense of coherence (ie, subjective experience of understanding and managing stressors), similar to Huber et al 's 15 proposal. However, for social health, a standard level of interpersonal functioning and adaptation would include interdependence (ie, mutual reliance on, and responsibility to, others within society), rather than Huber et al 's 15 focus on social participation (ie, balancing social and environmental challenges). Our results provide further insight into how these domains interact to affect overall quality of life. Integration of mental and physical health can be defined by level of autonomy (ie, the capacity for control over one's self), whereas integration of mental and social health can be defined by a sense of ‘us’ (ie, capacity for relating to others); the integration of mental and physical health can be defined by control (ie, capacity for navigating social spaces). The highest degree of integration would be defined by agency , the ability to choose one's level of social participation (eg, to accept, reject or change social, legal or theological practices). Such a transdomain model of health could be useful in developing cross-cultural definitions of physical, social and mental health that are both inclusive and empirically valid. For example, Valliant's 25 seven models for conceptualizing mental health across cultures are all represented, to varying degrees, within the proposed transdomain model of health . The basic standard of functioning across domains which is proposed here is congruent with Valliant's 25 criteria for mental health to be ‘conceptualised as above normal’ and defined in terms of ‘multiple human strengths rather than the absence of weaknesses’, including maturity, resilience, positive emotionality and subjective well-being. In addition, Valliant's 25 conceptualisation of mental health as ‘high socio-emotional intelligence’ is also represented in the transdomain model's highest level of integration of the three areas for full individual autonomy. Finally, Valliant's 25 cautions for defining positive mental health—being culturally sensitive, recognising that population averages do not equate to individual normalcy and that state and trait functioning may overlap, and contextualising mental health in terms of overall health—are all addressed within the transdomain model .
Transdomain Model of Health. This model builds on the three domains of health as described by WHO 6 , 12 and Huber et al 15 and expands these definitions to include four specific overlapping areas and the empirical, moral, and legal considerations discussed in the current study. There are three domains of health (ie, physical, mental, and social), each of which would be defined in terms of a basic (human rights) standard of functioning and adaptation . There are four dynamic areas of integration or synergy between domains and examples of how the core concepts of mental health could be used to define them.
Strengths and limitations of the current study
We are unaware of any study to date that has asked this research question to a group of international experts in the broad field of mental health. Although our survey sample was small (N=50), it was diverse with regard to place of origin and expertise; it was also further validated by participants (N=58) at a day-long conference on mental health through discussion, debate and written responses. The current study included global experts who dedicate their research and professional lives to advancing the standards of mental health. Of particular note was that little to no consensus among the selected group of experts on any particular definition was found. In fact, this was simultaneously a limitation and strength of the study: the small sample size limited the scope of the core concepts of mental health, but indicated that it was sufficient to demonstrate that there are highly divergent definitions that are largely dependent on the respondents’ frame of reference. It is possible that saturation was not achieved in regards to the diversity of responses. Further, more than half of the survey respondents were from Canada, which may have influenced the preference towards the PHAC definition of mental health. Although there were advantages to using a snowball sampling method, another type of sampling method (eg, cluster sampling, stratified sampling) may have resulted in more varied responses to the survey items. The next logical step would be to survey experts in countries currently not represented and then ultimately survey members of the general public with regard to their conceptual and pragmatic understanding of mental health. One of the a priori objectives for the survey was to eventually create a consensus definition of mental health that could be used in public policy; this objective was not communicated in the survey, nor did we actually ask this question. Our results indicate that finding consensus on a definition of mental health will require much more convergence in the frame of reference and common language describing components of mental health. Even we, as authors, have been challenged by consensus. For example, some of us wish to emphasise that future work should focus on developing an operational definition that can be applied across disciplines and cultures. Others among us suggest further exploring what purpose a definition of mental health would or should serve, and why. In contrast, others among us wish to emphasise the process of conceptualising mental health versus the outcome or application of such a definition. What we hoped would be a straightforward, simple question, designed to create consensus for a definition of mental health, ultimately demonstrated the nuanced but crucial epistemological and empirical influences on the understanding of mental health. Based on the results of the survey and conference, we present a preliminary model for conceptualising mental health. Our study provides evidence that if we are to try to come to a common consensus on a definition of mental health, we will need to understand the frame of reference of those involved and try to parse out the paradigms, positionality and the social/environmental factors that are offered from the core concepts we make seek to describe. Future work may also need to distinguish between the scientific evidence of mental health and the arguments for mental health . Similar debates in bioethics 22 , 26–28 demonstrate the theoretical and practical limitations of science for proscribing human behaviour, especially with regard to individual freedom and social justice.
Conclusions
Our results suggest that any practical use of a definition of health will depend on the epistemological and moral framework through which it was developed, and that the mental and social domains may be differentially influenced than the physical domain. A definition of health, grounded solely in biology, may be more applicable across diverse populations. A definition of health encompassing the mental and social domains may vary more in application, particularly across systems, cultures or clinical practices that differ in values (eg, spiritual, religious) and ways of understanding and being (eg, epistemology). A universal (global) definition based on the physical domain could be parsed out separately from several unique (local) definitions based on the mental and social domains. Understanding the history and evolution of the concept of mental health is essential to understanding the problems it was intended to solve, and what it may be used for in the future.
Acknowledgments
The authors wish to extend their gratitude to their colleagues for their generous feedback, constructive critiques and recommendations for the project, and to the many volunteers who organised the conference. Special thanks to Nina Flora, Helen Thang, Andrew Tuck, Athena Madan, David Wiljer, Alex Jadad, Sean Kidd, Andrea Cortinois, Heather Bullock, Mehek Chaudhry and Anika Maraj.
- Whiteford HA ,
- Degenhardt L ,
- Rehn J , et al
- Belkin GS ,
- Chockalingham A , et al
- ↵ WHO . 2008 Policies and practices for mental health in Europe—meeting the challenges. http://www.euro.who.int/__data/assets/pdf_file/0006/96450/E91732.pdf .
- Carter JW ,
- Hidreth HM ,
- Knutson AL , et al
- ↵ WHO . 1948 Constitution of the World Health Organization , 2006 http://www.who.int/governance/eb/who_constitution_en.pdf
- ↵ WHO . Prevention of mental disorders . Geneva : 2004 . http://www.who.int/mental_health/evidence/en/prevention_of_mental_disorders_sr.pdf
- Sartorius N
- ↵ WHO . Mental health: strengthening mental health promotion, 2001 ; Fact Sheet No. 220 Geneva, Switzerland , 2001 . Updated August 2014: http://www.who.int/mediacentre/factsheets/fs220/en/
- ↵ Health Education Authority (HEA) . Mental health promotion: a quality framework. London : HEA , 1997 .
- ↵ Mental Health Foundation (MHF) . What works for you? London : MHF, 2008 .
- Knottnerus JA ,
- Green L , et al
- Macaulay AC
- ↵ Public Health Agency of Canada (PHAC) . The human face of mental health and mental illness in Canada 2006 . Ottawa, ON : Minister of Public Works and Government Services Canada , 2006 .
- Stanfield RB
- Westerhof GJ ,
- Valliant GE
Contributors All the authors contributed to the conceptualisation of the project. LAM wrote the manuscript. SB, KR, ZD, CL and KM contributed to the content and editing of the manuscript. LAM, SB, KR, ZD, CL and EW created the survey and conducted data analyses. SB, KR and LAM presented findings at the conference. LAM, SB, KR, ZD and EW led the focused discussion groups. KM supervised the project. LM is the guarantor.
Funding This work was performed with grants from the Canadian Institutes of Health Research (CIHR) for the Social Aetiology of Mental Illness Training Program at the Centre for Addiction and Mental Health.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement No additional are data available.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychol
Mental Health and Well-Being of University Students: A Bibliometric Mapping of the Literature
Daniel hernández-torrano.
1 Graduate School of Education, Nazarbayev University, Nur-Sultan, Kazakhstan
Laura Ibrayeva
Jason sparks, natalya lim.
2 Nazarbayev University School of Medicine, Nur-Sultan, Kazakhstan
Alessandra Clementi
Ainur almukhambetova, yerden nurtayev.
3 Psychological Counseling Center, Nazarbayev University, Nur-Sultan, Kazakhstan
Ainur Muratkyzy
Associated data.
The datasets generated for this study are available on request to the corresponding author.
The purpose of this study is to map the literature on mental health and well-being of university students using metadata extracted from 5,561 journal articles indexed in the Web of Science database for the period 1975–2020. More specifically, this study uses bibliometric procedures to describe and visually represent the available literature on mental health and well-being in university students in terms of the growth trajectory, productivity, social structure, intellectual structure, and conceptual structure of the field over 45 years. Key findings of the study are that research on mental health and well-being in university students: (a) has experienced a steady growth over the last decades, especially since 2010; (b) is disseminated in a wide range of journals, mainly in the fields of psychology, psychiatry, and education research; (c) is published by scholars with diverse geographical background, although more than half of the publications are produced in the United States; (d) lies on a fragmented research community composed by multiple research groups with little interactions between them; (e) is relatively interdisciplinary and emerges from the convergence of research conducted in the behavioral and biomedical sciences; (f) tends to emphasize pathogenic approaches to mental health (i.e., mental illness); and (g) has mainly addressed seven research topics over the last 45 years: positive mental health, mental disorders, substance abuse, counseling, stigma, stress, and mental health measurement. The findings are discussed, and the implications for the future development of the field are highlighted.
Introduction
The entrance to the university marks a period of transition for young people. Through this transition, students face new challenges, such as making independent decisions about their lives and studies, adjusting to the academic demands of an ill-structured learning environment, and interacting with a diverse range of new people. In addition, many students must, often for the first time, leave their homes and distance themselves from their support networks ( Cleary et al., 2011 ). These challenges can affect the mental health and well-being of higher education students. Indeed, there is evidence that a strain on mental health is placed on students once they start at the university, and although it decreases throughout their studies ( Macaskill, 2013 ; Mey and Yin, 2015 ), it does not return to pre-university levels ( Cooke et al., 2006 ; Bewick et al., 2010 ). Also, the probabilities of experiencing common psychological problems, such as depression, anxiety, and stress, increase throughout adolescence and reach a peak in early adulthood around age 25 ( Kessler et al., 2007 ) which makes university students a particularly vulnerable population.
The interest in mental health and well-being in university students has grown exponentially in the last decades. This is likely due to three interrelated challenges. First, although university students report levels of mental health similar to their non-university counterparts ( Blanco et al., 2008 ), recent studies suggest an increase and severity of mental problems and help-seeking behaviors in university students around the world in the last decade ( Wong et al., 2006 ; Hunt and Eisenberg, 2010 ; Verger et al., 2010 ; Auerbach et al., 2018 ; Lipson et al., 2019 ). Some researchers refer to these trends as an emerging “mental health crisis” in higher education ( Kadison and DiGeronimo, 2004 ; Evans et al., 2018 ). Second, psychological distress in early adulthood is associated with adverse short-term outcomes, such as poor college attendance, performance, engagement, and completion (e.g., King et al., 2006 ; Antaramian, 2015 ), and others in the long term, such as dysfunctional relationship ( Kerr and Capaldi, 2011 ), recurrent mental health problems, university dropout, lower rates of employment, and reduced personal income ( Fergusson et al., 2007 ). Third, there is a widespread agreement that higher education institutions offer unique opportunities to promote the mental health and well-being of young adults as they provide a single integrated setting that encompasses academic, professional, and social activities, along with health services and other support services ( Eisenberg et al., 2009 ; Hunt and Eisenberg, 2010 ). However, the majority of university students experiencing mental health problems and low levels of well-being are not receiving treatment ( Blanco et al., 2008 ; Eisenberg et al., 2011 ; Lipson et al., 2019 ) and, while universities continue to expand, there is a growing concern that the services available to provide support to students are not developing at an equivalent rate ( Davy et al., 2012 ).
In response to the increasing volume of research on the mental health and well-being of university students, there have been several attempts to synthesize the accumulating knowledge in the field and to provide an illustration of the theoretical core and structure of the field using traditional content analysis of the literature (e.g., Kessler et al., 2007 ; Gulliver et al., 2010 ; Hunt and Eisenberg, 2010 ; Sharp and Theiler, 2018 ). This study aims to extend the understanding of mental health in university students by providing a bird’s eye view of the research conducted in this field in recent decades using a bibliometric approach. Bibliometric overviews provide an objective and systematic approach to discover knowledge flows and patterns in the structure of a field ( Van Raan, 2014 ) reveal its scientific roots, identify emerging thematic areas and gaps in the literature ( Skute et al., 2019 ) and, ultimately, contribute to moving the field forward. Accordingly, this study employs several bibliometric indicators to explore the evolution of the field based on publication and citation trends, key actors and venues contributing to the advancement of research on mental health and well-being of university students, and the structure of the field in terms of patterns of scientific collaborations, disciplines underlying the foundations of the field, and recurrent research themes explored in the literature. This is important because, despite significant advances in the field, research on mental health and well-being remains a diverse and fragmented body of knowledge ( Pellmar and Eisenberg, 2000 ; Bailey, 2012 ; Wittchen et al., 2014a ). Indeed, mental health and well-being are nebulous concepts and their history and development are quite intricate, with a multitude of perspectives and contributions emerging from various disciplines and contexts (see section “Conceptualization of Mental Health, Mental Illness, and Well-Being: An Overview”). Therefore, mapping research on mental health and well-being in university students is essential to identify contributions and challenges to the development of the field, to help guide policy, research, and practice toward areas, domains, populations, and contexts that should be further explored, and to provide better care of students at higher education institutions ( Naveed et al., 2017 ).
Conceptualization of Mental Health, Mental Illness, and Well-Being: An Overview
This section provides an overview of the different perspectives adopted in the literature to conceptualize mental health, well-being, and other relevant constructs in order to identify the glossary of key terms that will be used in the search strategy to create a comprehensive corpus of documents on mental health and well-being in university students for this bibliometric review.
Perspectives on Mental Health and Mental Illness
There is no general agreement on the definition of mental health. For a long time, the term mental health has been used as a euphemism for mental illness ( Manwell et al., 2015 ). However, mental health and mental illness are regarded as distinct constructs nowadays and two main perspectives differentiating between mental health and illness are available in the literature. The continuum approach considers that mental health and mental illness are the two opposite poles of a continuum. Thus, there are various degrees of health and illness between these poles, with most of us falling somewhere in between. The categorical approach, on the other hand, represents mental health and illness as a dichotomy. People who manifest mental illness symptoms would belong to that category and labeled correspondingly, while those absent of these symptoms can be considered as mentally healthy ( Scheid and Brown, 2010 ).
Disciplinary Approaches to the Conceptualization of Mental Health/Illness
Conceptualizations of mental health/illness are largely dependent on the theoretical and paradigmatic foundations of the disciplines from which they emerge. In this context, the field has progressively evolved through the accumulation of knowledge generated in a diverse range of disciplines in the biomedical, behavioral, and social sciences. Biomedical disciplines are grounded in the medical paradigm focused on disease and (ab)normality and often emphasize dichotomous conceptions of mental health/illness ( Scheid and Brown, 2010 ). Research on mental health and well-being in this domain has been traditionally conducted from a psychiatric perspective, which aims to understand the dysfunctionality in the brain that leads to psychiatric symptoms and to also offer a pharmacological treatment to correct neuronal dysfunctions. Consequently, psychiatrists have historically considered mental health as a disease of the brain (e.g., depression), similar to any other physical disease, caused by genetic, biological, or neurological factors ( Schwartz and Corcoran, 2010 ). While the prevalence of psychiatric approaches to mental health is currently incontestable, the development of other biomedical disciplines has tremendously contributed to the progression of the field in recent decades. For example, Insel and Wang (2010) argue that insights gained from genetics and neuroscience contribute to the reconceptualization of “the disorders of the mind as disorders of the brain and thereby transform the practice of psychiatry.” (1979). In addition to that, other disciplines such as behavioral medicine have made important contributions to the field, although it has recently argued that mental health and behavioral medicine should be as two separate fields ( Dekker et al., 2017 ).
Within the behavioral sciences, the study of mental health focuses on the distinct psychological processes and mechanisms that prompt thoughts, feelings, and behaviors ( Peterson, 2010 ). Clinical psychology has the longest tradition in the psychological study of mental health and tends to focus on the assessment and treatment of mental illness and disorders that can alleviate psychological distress or promote positive states of being ( Haslam and Lusher, 2011 ). However, significant contributions to the field have also emerged from other branches of psychology less focused on psychopathology, including personality and social psychology, psychoanalysis, humanistic psychology, and cognitive psychology ( Peterson, 2010 ). Despite the diversity of theories, principles, and methodological approaches to understanding mental health within the behavioral sciences, these disciplines acknowledge that mental health have a biological basis and reside in the social context, and tend to prioritize continuum approaches to mental health ( Scheid and Brown, 2010 ).
Perspectives from the social sciences complement the biomedical and behavioral approaches by considering the influence of social and cultural environments in mental health/illness ( Horwitz, 2010 ). For example, sociologists are interested in how social circumstances (e.g., level of support available) affect levels of mental health/illness and how social structures shape the understanding and response to mental health issues [see Compton and Shim (2015) for an overview of the social determinants of mental health]. Similarly, medical anthropologists attend to the mental health beliefs and practices that form the cultural repertory within and across populations ( Foster, 1975 ). Beyond sociology and anthropology, social researchers in the fields of business and economics, family and ethnic studies, and educational research have also played a key role in advancing research on mental health in different directions.
The Importance of the Context in Mental Health
Certainly, most notions of mental health/illness in the literature derive from prevailing psychiatric and psychological traditions developed in Western countries ( Gopalkrishnan, 2018 ). However, cultural values and traditions do shape how mental health and mental illness are conceptualized across contexts ( Vaillant, 2012 ). In this regard, Eshun and Gurung (2009) pointed out that “culture influences how individuals manifest symptoms, communicate their symptoms, cope with psychological challenges, and their willingness to seek treatment.” (4). Fernando (2019) argued that issues related to the ‘mind’ developed and are often interpreted very differently in non-Western and Low- and Middle-Income Countries (LMICs). For example, cultures explain the manifestation of certain feelings and behaviors based on a range of motives including biological, psychological, social, religious, spiritual, supernatural, and cosmic. Failure to acknowledge alternative non-Western approaches to mental health and mental illness has resulted in imbalances of knowledge exchange and the permeation of dominating Western narratives into LMICs (i.e., so-called medical imperialism) ( Timimi, 2010 ; Summerfield, 2013 ). To address this issue, scholars have advocated for a greater willingness to embrace pluralism in the conceptualization of mental health and illness, which might help people to engage with particular forms of support that they deem to be appropriate for them, and to explore how knowledge and practices developed in LMICs can benefit those living in higher-income countries (i.e., knowledge “counterflow”) (see White et al., 2014 ).
Prioritizing Positive Mental Health: The Science of Well-Being
Despite the diversity of disciplinary and contextual approaches to mental health, current definitions of mental health have two things in common. First, mental health is considered from a biopsychosocial point of view that incorporates biological, psychological, and social factors. Second, mental health implies something beyond the absence of mental illness (e.g., Bhugra et al., 2013 ; Galderisi et al., 2015 ). An example is the definition by the World Health Organization which refers to mental health as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community” ( World Health Organization, 2004 ). This definition contributed to substantial progress in research and practice in the field as it expanded the notion of mental health beyond the absence of mental illness and integrated the presence of positive features ( Galderisi et al., 2015 ).
Research on positive mental health is relatively new but has grown rapidly in the last decades fueled by advocates of positive medicine and psychology, who have argued for a change of paradigm from medical and psychopathological-oriented models of mental health that focus on disorders and illness toward more strength-based approaches, which pay more attention to what is right about people and positive attributes and assets ( Kobau et al., 2011 ). In this regard, the term mental well-being has been progressively incorporated into the study of mental health to account for the positive aspects of mental health beyond the absence of negative factors. While there is not a universally accepted definition of well-being, two perspectives have dominated the discourses on well-being in the literature: subjective well-being (SBW) and psychological well-being (PWB). SWB is based on hedonic perspectives of pleasure and represents “people’s beliefs and feelings that they are living a desirable and rewarding life” ( Diener, 2012 ). SBW is strongly linked with the idea of happiness and is typically understood as the personal experience of high levels of positive affect, low levels of negative affect, and high satisfaction with one’s life ( Deci and Ryan, 2008 ). PWB is grounded in Aristotelian ideas about eudaimonia, i.e., self-realization, with the ultimate aim in life being to strive to realize one’s true potential ( Ryff and Singer, 2008 ). PWB has been broadly defined as a state of positive psychological functioning and encompasses six dimensions: purpose in life (i.e., the extent to which respondents felt their lives had meaning, purpose, and direction); autonomy (i.e., whether they viewed themselves as living in accord with their own convictions); personal growth (i.e., the extent to which they were making use of their personal talents and potential); environmental mastery (i.e., how well they were managing their life situations); positive relationships (i.e., the depth of connection they had in ties with significant others); and self-acceptance (i.e., the knowledge and acceptance they had of themselves, including awareness of personal limitations) ( Ryff, 1989 ).
Integrating Mental Health, Mental Illness, and Well-Being
The contribution of positive mental health frameworks to the advancement of the field has been undeniable. However, definitions that overemphasize positive emotions and productive functioning as key indicators of mental health have been recently challenged because of the potential they have to discriminate against individuals and groups that, for example, might not be able to work productively or function within the environment because of individual physical characteristics or contextual constraints ( Galderisi et al., 2015 ). To address these issues, Keyes has successfully integrated the notions of mental illness, mental health, well-being, and other related terms in the literature into a conceptual framework that allows for a more comprehensive understanding of mental health ( Keyes, 2005 , 2007 ; Keyes and Michalec, 2010 ). The model argues that neither pathogenic approaches focusing on the negative (e.g., mental illness) nor salutogenic approaches focusing on the positive (e.g., well-being) can alone accurately describe the mental health of a person ( Keyes and Michalec, 2010 ). Instead, the model proposes that mental illness and well-being represent two correlated but differentiated latent continua in defining mental health. More specifically, mental illness and well-being lie on two separate spectra, the first going from absent to present mental illness and the second running from low to high well-being ( Slade, 2010 ). The absence of mental illness, therefore, does not necessarily imply high levels of well-being. Correspondingly, low levels of well-being do not always indicate the presence of mental illness. Further, in this model, mental health is defined as not only the absence of mental illness, not the mere presence of high well-being. Complete mental health (i.e., flourishing) is a result of experiencing low mental illness and high levels of well-being. Incomplete mental health (i.e., languishing), on the other hand, refers to the absence of mental illness symptoms and low reported levels of well-being. Two other conditions are possible within this framework. Incomplete mental illness (i.e., struggling) refers to high levels of well-being accompanied by high mental illness symptoms. Lastly, complete mental illness (i.e., floundering) accounts for low levels of well-being and high mental illness symptoms ( Keyes and Lopez, 2002 ).
The Present Study
In light of the complexity of the constructs of mental health and well-being and the multiple theoretical, disciplinary, and contextual approaches to their conceptualization, this study seeks to map out the terrain of international research and scholarship on mental health and university students for the period 1975–2020. More specifically, this study aims to provide new insights into the development and current state of mental health research in university students by mapping and visually representing the literature on mental health and well-being of university students over the last 45 years in terms of the growth trajectory, productivity, and social, intellectual, and conceptual structure of the field. First, the study describes the development of research mental health and well-being in university students examining the trends in publication and citation data between 1975 and 2020 (i.e., growth trajectory). Second, the study identifies the core journals and the research areas contributing most to the development of the field, as well as the key authors and countries leading the generation and dissemination of research on mental health and well-being in university populations (i.e., productivity). Third, the study outlines the networks of scientific collaboration between authors, and countries (i.e., social structure). Fourth, the scientific disciplines underlying the intellectual foundations of research on mental health and well-being in university settings (i.e., intellectual structure) are uncovered. Fifth, the study elucidates the topical foci (i.e., conceptual structure) of the research on the mental health and well-being of university students over the last 45 years.
Materials and Methods
A bibliometric approach was used in this study to map the literature on mental health and well-being in university students over the last 45 years using metadata extracted from four indexes of the Web of Science (WoS): The Science Citation Index-Expanded (SCI-Expanded); the Social Sciences Citation Index (SSCI); the Arts & Humanities Citation Index (A&HCI); and the Emerging Sources Citation Index (ESCI). Several reasons justified the selection of the WoS database in this study. First, the WoS remains as the standard and most widely used for bibliometric analysis ( Meho and Yang, 2007 ). Second, the WoS is a multidisciplinary database and includes publications on mental health and well-being emerging from distinctive research areas and disciplines published in more than 20,000 journals ( McVeigh, 2009 ). Using specialized databases such as PubMed would introduce biases into the search strategy favoring biomedical research disciplines. Still, it is important to note that interdisciplinary databases such as WoS and Scopus discriminate against publications in the Social Sciences and Humanities and publications in languages other than the English language ( Mongeon and Paul-Hus, 2016 ), so the picture provided by WoS is still imperfect. Third, while other databases might provide wider coverage, WoS includes publication and citation information from 1900. For example, Scopus has complete citation information only from 1996 ( Li et al., 2010 ). Moreover, Google Scholar provides results of inconsistent accuracy in terms of citations, and citation analyses in PubMed are not available ( Falagas et al., 2008 ). Fourth, WoS has demonstrated better accuracy in its journal classification system compared to Scopus database ( Wang and Waltman, 2016 ).
The methodological approach used in this study is presented in Figure 1 and further elaborated in the following paragraphs.

Methodological framework.
Search Strategy
To create a comprehensive corpus of documents on the mental health and well-being of university students, three parallel searches were performed, which accounted for the multiple approaches and perspectives that have been used in the field, as identified in the Section “Conceptualization of Mental Health, Mental Illness, and Well-Being: An Overview.” All the searches were conducted in the last week of January 2020. The first search aimed at capturing research on mental health broadly and included one single keyword in the topic field: [“mental health”]. The second search was implemented to capture research focusing on pathogenic approaches to mental health. Key terms used in the literature to refer to the negative side of mental health, as well as the most frequent mental health problems experienced by university students, were introduced in this search in the title field: [“mental illness,” “mental disorder ∗ ,” “mental distress,” “psychological distress,” “psychopathology,” “depression,” “anxiety,” “stress,” “suicide,” “eating disorder ∗ ,” “substance use”]. In the third search, keywords reflecting salutogenic approaches to mental health were input. These included terms related to mental health from a positive mental health perspective (i.e., well-being). These key terms were added in the title field and included the following: [“well-being,” “wellbeing,” “wellness,” “life satisfaction,” “happiness,” “positive affect,” “purpose in life,” “personal growth,” “self-determination”].
To retrieve research relevant only to higher education students, another set of keywords was imputed in all three searches in the title field. These included: [“university,” “college,” “higher education,” “tertiary education,” “post-secondary education,” “postsecondary education,” “undergrad ∗ student,” “grad ∗ student,” “master’s student,” “doctoral student,” “Ph.D. student”]. The Boolean operator OR was used between keywords in all the three searches to secure a higher number of relevant hits. Also, asterisks were used as wildcards to account for multiple variations in several keywords (e.g., disorder and disorder-s). All searches were limited to journal articles published between 1975 and 2020 (both inclusive). No restrictions on language were implemented in the search.
The search strategy retrieved a total of 6,356 hits ( n search 1 = 2782; n search 2 = 2814, n search 3 = 760). After the removal of duplicates, 5,561 research articles were finally selected and retained for the study. For each of the documents obtained in the search, the authors extracted metadata about the title of the paper, the year of publication, the journal, the number of citations, and the authors’ name, organization, and country. Also, the title, the abstract, the author’s keywords, and cited references were retrieved.
Data Analysis Procedures
The corpus of the literature was then analyzed using descriptive and bibliometric approaches to provide an overall picture of the evolution and current state of the research on mental health and wellbeing in university settings. Frequency counts of the number of publications and citations per year were obtained to describe the growth trajectory of research on the mental health and well-being of university students. Rank ordered tables were produced to describe the productivity of the field in terms of core journals and research areas, as well as leading scholars and countries contributing to the development of the field.
Bibliometric analyses in VOSViewer software were implemented to examine and visually represent the social, intellectual, and conceptual structure of the field. VOSViewer is a freely available computer software for viewing and constructing bibliometric maps 1 . In VOSViewer, the units of analysis are journals, publications, citations, authors, or countries, depending on the focus of the analysis. The units of analysis are represented in the maps as circular nodes. The size of the node accounts for volume (e.g., number of publications in the dataset by an author) and the position represents the similarity with other nodes in the map. Closer nodes are more alike than nodes far apart from each other. The lines connecting nodes represent the relationship between nodes and their thickness indicates the strength of that relationship. Finally, the color of the node denotes the cluster to which each node has been allocated. Nodes are clustered together based on relatedness ( Van Eck et al., 2010 ). The software uses a distance-based approach to constructing the bibliometric maps in three steps ( Van Eck and Waltman, 2014 ). In the first step, the software normalizes the differences between nodes. In the second step, the software builds a two-dimensional map where the distance between the nodes reflects the similarity between these nodes. In the third step, VOSViewer groups closely related nodes into clusters ( Van Eck and Waltman, 2014 ).
A series of co-authorship analyses were performed to examine the social structure of research on mental health and well-being in university students. In these analyses, the units of analysis were authors and countries/territories. Each node in the map represents an author or a country/territory and the lines connecting them reflect the relationship between nodes. Clusters represent networks of scientific collaboration, which might be interpreted as groups of authors or countries frequently publishing together (e.g., research groups in the case of authors).
Co-citation analysis of journals was implemented to explore the intellectual structure of the field. Here, the units of analysis were journals in the dataset and the map reflects co-citation relationships between journals. Two journals are co-cited if there is a third journal citing these two. The more times a pair of journals are cited by other journals, the stronger their co-citation relationship will be. Frequently co-cited journals are assumed to share theoretical and semantical grounds. Therefore, in our study, clusters of frequently co-cited journals can be interpreted as disciplines underlying the foundations of research on mental health and well-being in university students.
Finally, a co-occurrence analysis of keywords was used to uncover the conceptual structure of the field. The units of analysis, in this case, were the authors’ keywords. The more often two keywords appear in the same record, the stronger their co-occurrence relationship. Clusters of co-occurring keywords represent in this study the topical foci (i.e., knowledge base) that have been addressed in the literature in mental health and well-being in university students in the last 45 years.
Findings and Discussion
Growth trajectory: evolution of publications and citations in the field.
The developmental patterns of a particular field can be well demonstrated by trends in publications and citations. The 5,561 publications in the dataset have been cited 87,096 times, with an average of 15.6 citations per item. Figure 2 shows the growth trajectory of publication data of research on mental health and well-being in university students from 1975 to January 2020. Overall, the trends demonstrate a gradual increase in the scholarly interest in the mental health of university students over the last 45 years that can be organized in three stages: an emergence stage, in which publications rose slowly (1975–2000); a fermentation stage, with a notable increase in publications in the field (2000–2010); and a take-off stage, during which the number of records published per year in the field has almost risen 10 times (2010–2020). The steady increase of publications in the last 15 years coincides with the first calls for attention on the increase and severity of mental problems and help-seeking behaviors of college students ( Kadison and DiGeronimo, 2004 ; Evans et al., 2018 ), potentially indicating a growing interest in exploring the epidemiology of mental disorders and the role of universities in promoting the mental health and well-being of students. A similar pattern has also been observed in a recent bibliometric study examining global research on mental health both in absolute terms and as a proportion of all papers published in medicine and across disciplines, which certainly reflects an increase in the general interest in the field ( Larivière et al., 2013 ).

Growth of research on mental health and well-being of university students.
Productivity I: Core Journals and Research Areas
In total, 1,560 journals published the 5,561 records included in the dataset. Table 1 presents the ten core journals in the field. The Journal of American College stands out as the main publication venue in the field, accumulating around 5% of the publications in the dataset ( n = 270). Psychological Reports and Journal of College Student Development also stand out, publishing 119 and 102 studies, respectively. The Journal of Counseling Psychology ranks fourth in the list with 83 records. Despite being an interdisciplinary and relatively young journal, Plos One appears in the top five journal publishing research on mental health and well-being in university students.
Core journals ranked by number of records.
The top research areas contributing to the publication of research on the mental health and well-being of university students are presented in Table 2 . Nearly half of the records in the dataset are published in psychology journals. Another influential research area in the field is psychiatry , which captures almost 20% of the publications. Journals on education and educational research also accumulate a considerable number of publications in the field (15%). Other relevant research areas in the field are connected with health and medicine, including public environmental occupational health , substance abuse , general internal medicine , neurosciences neurology , health care sciences services , and nursing . Finally, the field is also grounded, although to a lower extent, in the publications emerging from journals in the social sciences , family studies , and social work research.
Top research areas ranked by number of records.
All in all, the productivity analysis for journals and research areas showed that most research on mental health and well-being in university students is disseminated in journals in the “psy disciplines”’ (i.e., psychology and psychiatry) ( McAvoy, 2014 ), which is consistent with previous research on mental health in general populations (e.g., Haslam and Lusher, 2011 ). However, our findings demonstrated that the volume of research in psychology doubles that of research emerging from psychiatric journals. This contrasts with the findings by Haslam and Lusher (2011) , who demonstrated that psychiatry journals had a greater influence on mental health research compared to clinical psychology journals and that psychiatry journals accumulate a higher volume of research and citations on mental health research. This is probably because our study includes publications emerging from all branches of psychology, unlike the study by Haslam and Lusher, which included only journals in the field of clinical psychology. Additionally, mental health services in higher education are typically provided by counseling centers led and staffed by non-medical professionals (e.g., psychologists, social workers, counselors, and family therapists) who tend to adopt developmental models of practice grounded in the behavioral sciences and focused on adjustment issues, vocational training, employment, and other personal needs rather than diagnosis and symptom reduction, more common in the biomedical sciences (i.e., psychiatry) ( LeViness et al., 2018 ; Mitchell et al., 2019 ).
Productivity II: Leading Authors and Countries/Territories
The 5,561 publications in the dataset were published by a total of 16,161 authors from 119 countries worldwide. Table 3 shows the researchers with the highest number of publications in the field. D. Eisenberg appears as the most productive researcher, followed by K. Peltzer and S. Pengpid. Authors on the list come from diverse geographical backgrounds. Five of the authors work at three different American universities (University of Michigan, Harvard Medical School, and Boston University), two researchers work at KU Leuven University (Belgium), and two other authors are affiliated to the same two universities in Thailand and South Africa. Other prolific researchers are affiliated with higher education institutions in the Netherlands, Egypt, and Germany.
Leading authors ranked by number of records.
Countries and territories leading research on mental health and well-being of university students are presented in Table 4 . The United States is the indisputable leader in this field, publishing more than half of the records in the dataset. This is nearly 10 times the number of publications produced in China, which occupies the second position in the ranking and accounts for nearly 6% of the volume of research in the dataset. Three predominantly English speaking countries/territories complete the top five of the ranking: Canada (265 records), Australia (254), and England (243). The rest of the countries in the list are situated in Europe (Spain, Germany, Turkey), Western Asia (Iran), Africa (South Africa), and East Asia (Japan), which demonstrates that research on college students’ mental health and well-being is a matter of concern in different regions of the world, at least to some extent.
Leading countries/territories ranked by number of records.
Overall, the productivity analysis for authors and countries indicated that the research of mental health and well-being of university students occurs in a variety of locations around the world, especially in developed countries, and in a very prominent way, in the United States. This is not surprising since it is in those countries where better infrastructures and more abundant resources for research are available ( Wong et al., 2006 ), and a more lasting tradition in the study of mental health, in general, exists ( Gopalkrishnan, 2018 ). However, Larivière et al. (2013) found that the productivity of the United States on mental health research has dropped significantly and remained stable in other two English speaking countries (the United Kingdom and Canada) since 1980. On the contrary, the number of publications from European countries and the five major emerging national economies (Brazil, Russia, India, China, and South Africa), has experienced remarkable growth, and collectively account nearly for half of the publications in the field. Still, the predominance of knowledge generated in the developed world today, which tends to be grounded on psychiatric and psychological perspectives, might be eclipsing non-traditional views on mental health and well-being that are popular in other regions of the world and, therefore, limiting the development of effective initiatives that align better with local norms, values, and needs in LMICs ( Timimi, 2010 ; Summerfield, 2013 ).

Social Structure: Networks of Scientific Collaboration
Research collaboration is regarded as an indicator of quality research and a means to improve research productivity and academic impact (i.e., citations) ( Kim, 2006 ; Abramo et al., 2009 ). In particular, international research collaboration is considered a key contributor to the social construction of science and the evolution of scientific disciplines ( Coccia and Wang, 2016 ). There is recent evidence that national and international research collaborations have been accelerating in recent years ( Gazni et al., 2012 ; Wagner et al., 2015 ), especially in applied fields such as medical and psychological disciplines ( Coccia and Bozeman, 2016 ). In this study, co-authorship analyses were performed to find out patterns in the scientific collaboration between researchers and countries/territories on the mental health and well-being of university students.
Figure 3 demonstrates collaborative ties among authors who published at least 5 articles in the dataset ( n = 179). The map shows the existence of multiple productive collaborative networks of five or more researchers contributing to the development of the field. The largest collaboration network (red cluster) represents an international research group composed of 15 scholars affiliated to universities in the United States, Belgium, and Netherlands. This cluster groups some of the leading scholars in the field, including R. P. Auerbach, R. Brauffaerts, R. C. Kressler, and P. Cuijpers. Moreover, researchers in this cluster lead The WHO World Mental Health International College Student (WMH-ICS) Initiative, a large scale international project aimed at promoting the mental health and well-being of college students around the world through generating epidemiological data of mental health issues in university students worldwide, designing web-based interventions for the prevention and promotion of mental health, and disseminating evidence-based interventions ( Cuijpers et al., 2019 ). The second biggest cluster (green) represents an intra-national research network that includes 10 researchers from eight different higher education institutions in the United States. The dark blue cluster represents an institutional collaborative network, including nine researchers from the School of Public Health, Puerto Rico. Other prominent clusters in the map represent collaborative research networks between eight (olive color) and seven researchers (turquoise, violet, orange, and mellow mauve). This contrasts, however, with the limited collaboration that exists between clusters. Only four of the clusters on the map demonstrate some kind of scientific collaboration in the field (light blue, pink, brown, and yellow).

Collaborative research networks between researchers. Only researchers with five or more publications were considered in the analysis ( n = 179).
Cross-country collaboration networks in mental health and well-being of university students study are presented in Figure 4 . Research collaborations between countries with 20 or more publications were considered in this analysis ( n = 45). The United States occupies the central position of the map and shares collaborative ties with all other countries/territories, forming a cluster together with China, South Korea, and Taiwan. Overall, the results suggest that international collaborations in the field are framed to a large extent by cultural, linguistic, and geographical proximity. For instance, the largest cluster (red) is formed by two European countries (Spain and Portugal) and other South American countries with whom they share historical and cultural backgrounds. Other European countries form the purple cluster. Similarly, the blue cluster clearly brings together predominantly English-speaking countries and territories, while the green cluster agglomerates a range of Asian countries.

Collaborative research networks between countries and territories. Only countries with 20 or more publications were considered in the analysis ( n = 45).
Collectively, the results of our study suggest that research collaboration in the field of mental health and well-being in university students remains relatively scarce and localized to date. The social structure of the field at the author level could be described as an archipelago formed by a large number of islands (research groups) of different composition and size but with few bridges connecting them, which suggests a relatively fragmented research community. Moreover, while the existence of international collaborative networks was evident in the analysis, they seem to be formed within national borders, between researchers in neighboring countries/territories, or between countries that share cultural, linguistic, and historical heritages. This may be due to the important role that cultural and traditional values play in the conceptualization of mental health and well-being across contexts ( Eshun and Gurung, 2009 ; Vaillant, 2012 ; Fernando, 2019 ). Also, language differences, divergent cross-national institutional and organizational traditions, and increased costs of extramural collaboration, have been found to complicate the formation and continuity of research partnerships in health research ( Hooper et al., 2005 ; Freshwater et al., 2006 ). Nevertheless, limited within- and between-country research collaboration arguably poses challenges to the development of a field in terms of lost opportunities to challenge assumptions taken for granted and move toward fresh perspectives, push boundaries in methods and techniques, meet diverse groups of people from differing cultures and get immersed in those cultures, share information, resources, and skills, and address common mental health problems through the pooling of resources ( Rolfe et al., 2004 ; Freshwater et al., 2006 ).
Intellectual Structure: Disciplines Underlying the Foundations of the Field
Interdisciplinarity is considered as a valuable approach to address the complex and multidimensional nature of health and well-being ( Mabry et al., 2008 ). Buckton (2015) argues that the integration of medical, psychological, and social sciences have contributed to generate “new insights into theory, practice, and research in mental health and development.” (3). To examine the disciplines underlying research on the mental health and well-being of university students, a journal co-citation analysis was performed. In this analysis, only journals with at least 50 citations were considered ( n = 593). The nodes on the map represent journals and their size reflects the number of co-citation relationships with other journals. Colors account for journal clusters, which agglutinate journals with higher co-citation relationships and stronger semantic connectedness. Clusters were interpreted and labeled accounting for the WoS categorization of the journals with the highest co-citation links within each cluster. For example, if the Journal of Personality and Social Psychology , the Journal of Counseling Psychology , and Personality and Individual Differences clustered together, this group was interpreted as the personality, social, and counseling psychology cluster.
In general, the findings of this study suggest that research on mental health and well-being in university students is interdisciplinary, to a certain extent, and mainly emerges from the convergence of research conducted in the behavioral and biomedical sciences, as it has been suggested elsewhere ( Schumann et al., 2014 ; Wittchen et al., 2014b ). More specifically, the map shows that the research in the mental health and well-being of university students is constructed through the integration of knowledge generated in five interconnected disciplines (see Figure 5 ). To the left of the map, the red cluster integrates journals on personal, social, and counseling psychology . To the right, the blue cluster represents the contribution of psychiatric journals to research to the formation and development of the field. At the top, the yellow cluster groups journals on substance abuse and issues related to alcohol consumption, addiction, and interpersonal violence. At the bottom of the map, journals covering topics on eating behaviors, sleep, and other issues related to physical health converge on the green cluster. At the center of the map is the purple cluster, which includes journals in the area of clinical psychology and behavioral therapy .

Map of clustered network journals based on co-citation data. Only publications with 50 or more citations were considered in the analysis ( n = 593).
More broadly, the findings suggest that biomedical sciences contribute to a large extent to the composition of the field. Psychiatric research emerged in our study as an obvious building block in the study of university students’ mental health and well-being, which is not surprising considering the historical contributions of biomedical disciplines to mental health research ( Schwartz and Corcoran, 2010 ). Within the behavioral sciences, personality and social psychology, which explores processes and mechanisms through which social phenomena influence mental health and well-being ( Sánchez Moreno and Barrón López de Roda, 2003 ), appears as a key discipline underlying the foundations of the field. Surprisingly, clinical psychology journals occupy a central position in the map and demonstrate co-citation relationships with journals from all other clusters but make up the most dispersed network and account for a considerably lower volume of co-citation relationships in the field. This suggests that clinical psychology journals are more subordinate to journals in other disciplines in terms of citations flows, and ultimately, play a less unique role in research on the mental health and well-being of university students, as suggested by Haslam and Lusher (2011) . Interestingly, research arising from the social sciences (e.g., sociology and anthropology) does not seem to make a distinctive contribution to the intellectual structure of the field, which suggests that the influence of social contexts and cultures on university students’ mental health and well-being (e.g., inequality, social norms, public policies, cultural beliefs, and values) is an underexplored research area. Still, the density of co-citation network relationships within and between clusters is particularly noteworthy, considering the lack of common language between disciplines, the absence of a shared philosophy of practice on mental health, and the tensions between medical, psychological, and social explanations of mental distress ( Bailey, 2012 ).
Conceptual Structure: Topical Foci Addressed in the Literature Over the Last 45 Years
The topical foci of research on the mental health and well-being of university students during the 1975–January 2020 period are presented in Figure 6 . The map offers a visual representation of the co-occurrence analysis of author keywords of all the publications included in the dataset. Only the most frequently occurring keywords (25+ occurrences) were considered in the analysis ( n = 84). Items that were not related to others and do not belong to the existing clusters were excluded. The size of the nodes indicates the occurrence of author keywords in the dataset and the thickness of edges represents the co-occurrence strength between pairs of keywords.

Topical foci in mental health and well-being of university students research. Only keywords with 25 or more occurrences were considered in the analysis ( n = 84).
The most frequent keywords in the dataset, excluding students’ descriptors (e.g., college students and university students), refer to common mental health challenges experienced by university students such as depression ( n = 612), anxiety ( n = 353), and stress ( n = 341). Salutogenic-related keywords such as well-being and life satisfaction occurred less often ( n = 138, n = 113, respectively), suggesting that pathogenic approaches to the exploration of mental health issues in higher education are more widespread. More broadly, seven general themes seem to summarize the topical foci of interest in the field of mental health and well-being of university students over the last 45 years. First, there has been a general interest in positive mental health , as denoted by frequently co-occurring key terms such as well-being, self-esteem, life satisfaction, social support, emotional intelligence, and happiness (red cluster). Second, mental disorders stand as another theme widely addressed in the literature, with a special emphasis on depression, anxiety, and to a lesser extent, suicide and suicidal ideation (green cluster). A third topical area in this field has been substance abuse , most predominantly alcohol consumption (blue cluster). The fourth theme reflects college counseling for mental health , including interventions and protective factors such as mindfulness, stress management, spirituality, and help-seeking (yellow cluster). Other topics reflected in the map are mental illness stigma (purple), stress (e.g., psychological distress and coping) (light blue), and mental health measurement (orange).
This study provides a comprehensive overview of the research on university students’ mental health and well-being in the last 45 years using bibliometric indicators. In general, the results reveal interesting trends in the evolution of the field over the last four decades and promising scientific patterns toward a better understanding of the mental health and well-being of university students internationally. First, the interest in the mental health and well-being of university students has grown in the last decades and in a very significant way during the last 10 years, indicating that this area has not still reached its maturity period and will continue developing in the future. Second, research in the field is relatively interdisciplinary and emerges from the convergence of research conducted in several disciplines within the behavioral and biomedical sciences. Third, research in this field is produced by a community of productive researchers coming from several regions around the world, most notably in the United States, which secures a generation of scholars that will continue shaping the field in the years to come. Fourth, over the last 45 years, researchers have been able to address a multitude of research topics in the field, including positive mental health, mental disorders, substance abuse, counseling, stigma, stress, and mental health measurement.
However, this study also identified some issues that could be hindering the development of the study of the mental health and well-being of university students. For example, the research available overrepresents theoretical and disciplinary approaches from the developed world. Additional studies on the field from developing economies and LMICs are needed to provide a more comprehensive picture and ensure a fair representation of the multiple perspectives available in the field. Such studies would inform administrators and practitioners on how to broaden and enrich available programs and initiatives to promote mental health and well-being in higher education contexts in order to offer alternative forms of support that university students find appropriate for their social and cultural values. Moreover, the research community contributing to the development of the field is relatively fragmented. There are multiple research groups but little research collaborations between them and, at the international level, these connections tend to be limited by geographic, cultural, and language proximity. In this context, more actions like the WMH-ICS Initiative could provide a partial solution to this problem by strengthening national and international research partnerships and facilitating knowledge exchange across regions. Also, special issues in the core journals in the field inviting cross-cultural studies on the topic could contribute to promoting research collaboration across regions and research in less represented countries. The field would also benefit from a greater volume of research from the social sciences and humanities exploring the influence of social, cultural, economic, and educational factors on the conceptualization, manifestation, and experience of mental health and well-being. Moreover, more studies emerging from disciplines such as sociology, anthropology, business, and education, would likely increase the permeability of positive mental health concepts into the field and contribute to the promotion of salutogenic approaches to the study of mental health and well-being of university students.
This study has several limitations. First, publications were retrieved only from the WoS database, which limits the generalizability of the findings. Second, WoS provides stronger coverage of Life Sciences, Biomedical Sciences, and Engineering, and includes a disproportionate number of publications in the English language ( Mongeon and Paul-Hus, 2016 ). This could partially explain the low number of publications emerging from the Social Sciences, the Arts, and the Humanities, and research conducted in non-English speaking countries in the present study. Third, only journal articles were retrieved for analysis, excluding other relevant publications in the field such as reviews, book chapters, and conference proceedings. Future studies could replicate the findings of this study using alternative databases (e.g., Scopus and PubMed) or a combination of them, as well as different filters in the search strategy, to provide an alternative coverage of research conducted in the field. Nevertheless, we believe that the bibliometric approach used in this study offers novel insights about the development and current status of the field and some of the challenges that undermine its progression.
Data Availability Statement
Author contributions.
DH-T and LI contributed to conception and design of the study, organized the database, and performed the statistical analysis. DH-T, LI, and JS wrote the first draft of the manuscript. NL, AC, AA, YN, and AM wrote the sections of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. This research was funded by the Nazarbayev University Faculty-Development Competitive Research Grants Program (Reference Number 240919FD3902).
1 www.vosviewer.com
- Abramo G., D’Angelo C. A., Di Costa F. (2009). Research collaboration and productivity: Is there correlation? High. Educ. 57 155–171. 10.1007/s10734-008-9139-z [ CrossRef ] [ Google Scholar ]
- Antaramian S. (2015). Assessing psychological symptoms and well-being: application of a dual-factor mental health model to understand college student performance. J. Psychoeduc. Assess. 33 419–429. 10.1177/0734282914557727 [ CrossRef ] [ Google Scholar ]
- Auerbach R. P., Mortier P., Bruffaerts R., Alonso J., Benjet C., Cuijpers P., et al. (2018). WHO world mental health surveys international college student project: prevalence and distribution of mental disorders. J. Abnorm. Psychol. 127 623–638. 10.1037/abn0000362 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bailey D. (2012). Interdisciplinary Working in Mental Health. Basingstoke: Palgrave Macmillan. [ Google Scholar ]
- Bewick B. M., Koutsopoulou G., Miles J., Slaa E., Barkham M. (2010). Changes in undergraduate students’ psychological wellbeing as they progress through university. Stud. High. Educ. 35 633–645. 10.1080/03075070903216643 [ CrossRef ] [ Google Scholar ]
- Bhugra D., Till A., Sartorius N. (2013). What is mental health? Int. J. Soc. Psychiatr. 59 3–4. 10.1177/0020764012463315 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blanco C., Okuda M., Wright C., Hasin D. S., Grant B. F., Liu S. M., et al. (2008). Mental health of college students and their non-college-attending peers: results from the national epidemiologic study on alcohol and related conditions. Arch. Gen. Psychiatry 65 1429–1437. 10.1001/archpsyc.65.12.1429 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buckton A. (2015). Conversations between anthropology and psychiatry: drawing out the best from interdisciplinarity in global mental health. Australas. Psychiatry 23 3–5. 10.1177/1039856215608291 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cleary M., Walter G., Jackson D. (2011). Not always smooth sailing: mental health issues associated with the transition from high school to college. Issues Ment. Health Nurs. 32 250–254. 10.3109/01612840.2010.548906 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coccia M., Bozeman B. (2016). Allometric models to measure and analyze the evolution of international research collaboration. Scientometrics 108 1065–1084. 10.1007/s11192-016-2027-x [ CrossRef ] [ Google Scholar ]
- Coccia M., Wang L. (2016). Evolution and convergence of the patterns of international scientific collaboration. Proc. Natl. Acad. Sci. U.S.A. 113 2057–2061. 10.1073/pnas.1510820113 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Compton M. T., Shim R. S. (2015). The social determinants of mental health. Focus 13 419–425. 10.1176/appi.focus.20150017 [ CrossRef ] [ Google Scholar ]
- Cooke R., Bewick B. M., Barkham M., Bradley M., Audin K. (2006). Measuring, monitoring and managing the psychological well-being of first year university students. Br. J. Guid. Couns. 34 505–517. 10.1080/03069880600942624 [ CrossRef ] [ Google Scholar ]
- Cuijpers P., Auerbach R. P., Benjet C., Bruffaerts R., Ebert D., Karyotaki E., et al. (2019). The world health organization world mental health international college student initiative: an overview. Int. J. Methods Psychiatr. Res. 28 : e1762 . 10.1002/mpr.1761 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davy C., Dobson A., Lawrence-Wood E., Lorimer M., Moores K., Lawrence A., et al. (2012). The Middle East Area of Operations (MEAO) Health Study: Prospective Study Report. Adelaide: University of Adelaide. [ Google Scholar ]
- Deci E. L., Ryan R. M. (2008). Self-determination theory: a macrotheory of human motivation, development, and health. Can. Psychol. 49 182–185. 10.1037/a0012801 [ CrossRef ] [ Google Scholar ]
- Dekker J., Stauder A., Penedo F. J. (2017). Proposal for an update of the definition and scope of behavioral medicine. Int. J. Behav. Med. 24 1–4. 10.1007/s12529-016-9610-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Diener E. (2012). New findings and future directions for subjective well-being research. Am. Psychol. 67 590–597. 10.1037/a0029541 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eisenberg D., Downs M. F., Golberstein E., Zivin K. (2009). Stigma and help seeking for mental health among college students. Med. Care Res. Rev. 66 522–541. 10.1177/1077558709335173 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eisenberg D., Hunt J., Speer N., Zivin K. (2011). Mental health service utilization among college students in the United States. J. Nerv. Ment. Dis. 199 301–308. 10.1097/NMD.0b013e3182175123 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eshun S., Gurung A. R. (2009). “ Introduction to culture and psychopathology ,” in Culture and Mental Health: Sociocultural Influences, Theory, and Practice , eds Eshun S., Gurung R. A. R. (Hoboken, NJ: Wiley and Sons; ), 3–18. [ Google Scholar ]
- Evans T. M., Bira L., Gastelum J. B., Weiss L. T., Vanderford N. L. (2018). Evidence for a mental health crisis in graduate education. Nat. Biotechnol. 36 282–284. 10.1038/nbt.4089 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Falagas M. E., Pitsouni E. I., Malietzis G. A., Pappas G. (2008). Comparison of PubMed, Scopus, web of science, and Google scholar: strengths and weaknesses. FASEB J. 22 338–342. 10.1096/fj.07-9492LSF [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fergusson D. M., Boden J. M., Horwood L. J. (2007). Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. Br. J. Psychiatry 191 335–342. 10.1192/bjp.bp.107.036079 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fernando S. (2019). Developing mental health services in the global south. Int. J. Ment. Health 48 338–345. 10.1080/00207411.2019.1706237 [ CrossRef ] [ Google Scholar ]
- Foster G. M. (1975). Medical anthropology: some contrasts with medical sociology. Soc. Sci. Med. 9 427–432. 10.1016/0037-7856(75)90070-0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Freshwater D., Sherwood G., Drury V. (2006). International research collaboration: issues, benefits and challenges of the global network. J. Res. Nurs. 11 295–303. 10.1177/1744987106066304 [ CrossRef ] [ Google Scholar ]
- Galderisi S., Heinz A., Kastrup M., Beezhold J., Sartorius N. (2015). Toward a new definition of mental health. World Psychiatry 14 231–233. 10.1002/wps.20231 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gazni A., Sugimoto C. R., Didegah F. (2012). Mapping world scientific collaboration: authors, institutions, and countries. J. Am. Soc. Inf. Sci. Technol. 63 323–335. 10.1002/asi.21688 [ CrossRef ] [ Google Scholar ]
- Gopalkrishnan N. (2018). Cultural diversity and mental health: considerations for policy and practice. Front. Public Health 6 : 179 . 10.3389/fpubh.2018.00179 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gulliver A., Griffiths K. M., Christensen H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry 10 : 113 . 10.1186/1471-244X-10-113 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haslam N., Lusher D. (2011). The structure of mental health research: networks of influence among psychiatry and clinical psychology journals. Psychol. Med. 41 2661–2668. 10.1017/S0033291711000821 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hooper T. I., Smith T. C., Gray G. C., Al Qahtani M. S., Memish Z. A., Barrett D. H., et al. (2005). Saudi Arabia–United States collaboration in health research: a formula for success. Am. J. Infect. Control 33 192–196. 10.1016/j.ajic.2005.01.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Horwitz A. V. (2010). “ An overview of sociological perspectives on the definitions, causes, and responses to mental health and illness ,” in A Handbook for the Study of Mental Health: Social Contexts, Theories and Systems , eds Scheid T. L., Brown T. N. (Cambridge: Cambridge University Press; ), 6–19. 10.1017/9781316471289.004 [ CrossRef ] [ Google Scholar ]
- Hunt J., Eisenberg D. (2010). Mental health problems and help-seeking behaviors among college students. J. Adolesc. Health 46 3–10. 10.1016/j.jadohealth.2009.08.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Insel T. R., Wang P. S. (2010). Rethinking mental illness. JAMA 303 1970–1971. [ PubMed ] [ Google Scholar ]
- Kadison R., DiGeronimo T. F. (2004). College of the Overwhelmed: The Campus Mental Health Crisis and What to do About It. San-Francisco, CA: Jossey-Bass. [ Google Scholar ]
- Kerr D. C., Capaldi D. M. (2011). Young men’s intimate partner violence and relationship functioning: long-term outcomes associated with suicide attempt and aggression in adolescence. Psychol. Med. 41 759–769. 10.1017/S0033291710001182 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kessler R. C., Amminger G. P., Aguilar-Gaxiola S., Alonso J., Lee S., Ustun T. B. (2007). Age of onset of mental disorders: a review of recent literature. Curr. Opin. Psychiatr. 20 359–364. 10.1097/YCO.0b013e32816ebc8c [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Keyes C. L. (2005). Mental illness and/or mental health? Investigating axioms of the complete state model of health. J. Consult. Clin. Psychol. 73 539–548. 10.1037/0022-006X.73.3.539 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Keyes C. L. (2007). Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am. Psychol. 62 95–108. 10.1037/0003-066X.62.2.95 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Keyes C. L., Lopez S. J. (2002). “ Toward a science of mental health ,” in Handbook of Positive Psychology , eds Synder C. R., Lopez S. J. (Oxford: Oxford University Press; ), 45–62. [ Google Scholar ]
- Keyes C. L. M., Michalec B. (2010). “ Viewing mental health from the complete state paradigm ,” in A Handbook for the Study of Mental Health: Social Contexts, Theories and Systems , eds Scheid T. L., Brown T. N. (Cambridge: Cambridge University Press; ), 125–134. 10.1017/cbo9780511984945.010 [ CrossRef ] [ Google Scholar ]
- Kim K. W. (2006). Measuring international research collaboration of peripheral countries: taking the context into consideration. Scientometrics 66 231–240. 10.1007/s11192-006-0017-0 [ CrossRef ] [ Google Scholar ]
- King K. M., Meehan B. T., Trim R. S., Chassin L. (2006). Marker or mediator? The effects of adolescent substance use on young adult educational attainment. Addiction 101 1730–1740. 10.1111/j.1360-0443.2006.01507.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kobau R., Seligman M. E., Peterson C., Diener E., Zack M. M., Chapman D., et al. (2011). Mental health promotion in public health: perspectives and strategies from positive psychology. Am. J. Public Health 101 e1–e9. 10.2105/AJPH.2010.300083 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Larivière V., Diepeveen S., Chonaill S. N., Macaluso B., Pollitt A., Grant J. (2013). International comparative performance of mental health research, 1980–2011. Eur. Neuropsychopharm. 23 1340–1347. 10.1016/j.euroneuro.2013.01.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- LeViness P., Bershad C., Gorman K., Braun L., Murray T. (2018). The Association for University and College Counseling Center Directors Annual Survey. Available online at: https://www.aucccd.org/assets/documents/Survey/2018%20AUCCCD%20Survey-Public-June%2012-FINAL.pdf (accessed February 24, 2020). [ Google Scholar ]
- Li J., Burnham J. F., Lemley T., Britton R. M. (2010). Citation analysis: comparison of Web of Science, Scopus, SciFinder, and Google Scholar. J. Electron. Resour. Med. Lib. 7 196–217. 10.1080/15424065.2010.505518 [ CrossRef ] [ Google Scholar ]
- Lipson S. K., Lattie E. G., Eisenberg D. (2019). Increased rates of mental health service utilization by US college students: 10-year population-level trends (2007–2017). Psychiatr. Serv. 70 60–63. 10.1176/appi.ps.201800332 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mabry P. L., Olster D. H., Morgan G. D., Abrams D. B. (2008). Interdisciplinarity and systems science to improve population health: a view from the NIH Office of Behavioral and Social Sciences Research. Am. J. Prev. Med. 35 S211–S224. 10.1016/j.amepre.2008.05.018 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Macaskill A. (2013). The mental health of university students in the United Kingdom. Br. J. Guid. Couns. 41 426–441. 10.1080/03069885.2012.743110 [ CrossRef ] [ Google Scholar ]
- Manwell L. A., Barbic S. P., Roberts K., Durisko Z., Lee C., Ware E., et al. (2015). What is mental health? Evidence towards a new definition from a mixed methods multidisciplinary international survey. BMJ Open 5 1–11. 10.1136/bmjopen-2014-007079 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McAvoy J. (2014). “ Psy disciplines ,” in Encyclopedia of Critical Psychology , ed. Teo T. (New York, NY: Springer; ), 1527–1529. 10.1007/978-1-4614-5583-7_611 [ CrossRef ] [ Google Scholar ]
- McVeigh M. (2009). “ Citation indexes and the Web of Science ,” in Encyclopedia of Library and Information Sciences , 3rd Edn, eds Bates M. J., Maack M. N. (Cambridge: Chandos Publishing; ), 1027–1037. 10.1081/e-elis3-120044569 [ CrossRef ] [ Google Scholar ]
- Meho L. I., Yang K. (2007). Impact of data sources on citation counts and rankings of LIS faculty: web of science versus Scopus and Google scholar. J. Am. Soc. Inf. Sci. Technol. 58 2105–2125. 10.1002/asi.20677 [ CrossRef ] [ Google Scholar ]
- Mey S. C., Yin C. J. (2015). Mental health and wellbeing of the undergraduate students in a research university: a Malaysian experience. Soc. Indic. Res. 122 539–551. 10.1007/s11205-014-0704-9 [ CrossRef ] [ Google Scholar ]
- Mitchell S. L., Oakley D. R., Dunkle J. H. (2019). White paper: a multidimensional understanding of effective university and college counseling center organizational structures. J. Coll. Stud. Psychother. 33 89–106. 10.1080/87568225.2019.1578941 [ CrossRef ] [ Google Scholar ]
- Mongeon P., Paul-Hus A. (2016). The journal coverage of Web of Science and Scopus: a comparative analysis. Scientometrics 106 213–228. 10.1007/s11192-015-1765-5 [ CrossRef ] [ Google Scholar ]
- Naveed S., Waqas A., Majeed S., Zeshan M., Jahan N., Sheikh M. H. (2017). Child psychiatry: a scientometric analysis 1980-2016. F1000Res . 6 : 1293 . 10.12688/f1000research.12069.1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pellmar T. C., Eisenberg L. (2000). Bridging Disciplines in the Brain, Behavioral, and Clinical Sciences. Washington, DC: IOM. [ PubMed ] [ Google Scholar ]
- Peterson P. (2010). “ Psychological approaches to mental illness ,” in A Handbook for the Study of Mental Health: Social Contexts, Theories and Systems , eds Scheid T. L., Brown T. N. (Cambridge: Cambridge University Press; ), 106–124. [ Google Scholar ]
- Rolfe M. K., Bryar R. M., Hjelm K., Apelquist J., Fletcher M., Anderson B. L. (2004). International collaborations to address common problems in healthcare: processes practicalities and power. Int. Nurs. Rev. 51 140–148. 10.1111/j.1466-7657.2004.00237.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ryff C. D. (1989). Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Pers. Soc. Psychol. 57 1069–1081. 10.1037/0022-3514.57.6.1069 [ CrossRef ] [ Google Scholar ]
- Ryff C. D., Singer B. H. (2008). Know thyself and become what you are: a eudaimonic approach to psychological well-being. J. Happiness Stud. 9 13–39. 10.1007/s10902-006-9019-0 [ CrossRef ] [ Google Scholar ]
- Sánchez Moreno E., Barrón López de Roda A. (2003). Social psychology of mental health: the social structure and personality perspective. Span. J. Psychol. 6 3–11. 10.1017/s1138741600005163 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Scheid T. L., Brown T. N. (2010). A Handbook for the Study of Mental Health: Social Contexts, Theories and Systems. Cambridge: Cambridge University Press. [ Google Scholar ]
- Schumann G., Binder E., Holte A., de Kloet E. R., Odegaard K. J., Robbins T. W., et al. (2014). Stratified medicine for mental disorders. Eur. Neuropsychopharm. 24 5–50. 10.1016/j.euroneuro.2013.09.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwartz S., Corcoran C. (2010). “ Biological theories of psychiatric disorders: a sociological approach ,” in A Handbook for the Study of Mental Health: Social Contexts, Theories and Systems , eds Scheid T. L., Brown T. N. (Cambridge: Cambridge University Press; ), 64–88. 10.1017/cbo9780511984945.007 [ CrossRef ] [ Google Scholar ]
- Sharp J., Theiler S. (2018). A review of psychological distress among university students: pervasiveness, implications and potential points of intervention. Int. J. Adv. Couns. 40 193–212. 10.1007/s10447-018-9321-7 [ CrossRef ] [ Google Scholar ]
- Skute I., Zalewska-Kurek K., Hatak I., de Weerd-Nederhof P. (2019). Mapping the field: a bibliometric analysis of the literature on university-industry collaborations. J. Technol. Transfer 44 916–947. 10.1007/s10961-017-9637-1 [ CrossRef ] [ Google Scholar ]
- Slade M. (2010). Mental illness and well-being: the central importance of positive psychology and recovery approaches. BMC Health Serv. Res. 10 : 26 . 10.1186/1472-6963-10-26 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Summerfield D. (2013). Global mental health is an oxymoron and medical imperialism. Br. Med. J. 346 : f3509 . 10.1136/bmj.f3509 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Timimi S. (2010). The McDonaldization of childhood: children’s mental health in neo-liberal market cultures. Transcult. Psychiatry 47 686–706. 10.1177/1363461510381158 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vaillant G. E. (2012). Positive mental health: Is there a cross-cultural definition? World Psychiatry 11 93–99. 10.1016/j.wpsyc.2012.05.006 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van Eck N. J., Waltman L. (2014). “ Visualizing bibliometric networks ,” in Measuring Scholarly Impact: Methods and Practice , eds Ding Y., Rousseau R., Wolfram D. (Cham: Springer; ), 285–320. 10.1007/978-3-319-10377-8_13 [ CrossRef ] [ Google Scholar ]
- Van Eck N. J., Waltman L., Noyons E. C. M., Buter R. K. (2010). Automatic term identification for bibliometric mapping. Scientometrics 82 581–596. 10.1007/s11192-010-0173-0 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van Raan A. F. (2014). “ Advances in bibliometric analysis: research performance assessment and science mapping ,” in Bibliometrics: Use and Abuse in the Review of Research Performance , Vol. 3 eds Blockmans W., Engwall L., Weaire D. (London: Portland Press Ltd; ), 17–28. [ Google Scholar ]
- Verger P., Guagliardo V., Gilbert F., Rouillon F., Kovess-Masfety V. (2010). Psychiatric disorders in students in six French universities: 12-month prevalence, comorbidity, impairment and help-seeking. Soc. Psychiatry Psychiatr. Epidemiol. 45 189–199. 10.1007/s00127-009-0055-z [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wagner C. S., Park H. W., Leydesdorff L. (2015). The continuing growth of global cooperation networks in research: a conundrum for national governments. PLoS One 10 : e0131816 . 10.1371/journal.pone.0131816 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang Q., Waltman L. (2016). Large-scale analysis of the accuracy of the journal classification systems of Web of Science and Scopus. J. Informetr. 10 347–364. 10.1016/j.joi.2016.02.003 [ CrossRef ] [ Google Scholar ]
- White R., Jain S., Giurgi-Oncu C. (2014). Counterflows for mental well-being: what high-income countries can learn from low and middle-income countries. Int. Rev. Psychiatr. 26 602–606. 10.3109/09540261.2014.939578 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wittchen H. U., Knappe S., Andersson G., Araya R., Banos Rivera R. M., Barkham M., et al. (2014a). The need for a behavioural science focus in research on mental health and mental disorders. Int. J. Methods Psychiatr. Res. 23 28–40. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wittchen H. U., Knappe S., Schumann G. (2014b). The psychological perspective on mental health and mental disorder research: introduction to the ROAMER work package 5 consensus document. Int. J. Methods Psychiatr. Res. 23 15–27. 10.1002/mpr.1408 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wong J. G., Cheung E. P., Chan K. K., Ma K. K., Wa Tang S. (2006). Web-based survey of depression, anxiety and stress in first-year tertiary education students in Hong Kong. Aust. N. Z. J. Psychiatry 40 777–782. 10.1080/j.1440-1614.2006.01883.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization (2004). Promoting Mental Health: Concepts, Emerging Evidence, Practice (Summary Report). Geneva: World Health Organization. [ Google Scholar ]
- Our Process

Mental Health Essay Topics with Outline & Examples
Published by Ellie Cross at April 5th, 2022 , Revised On January 3, 2024
Mental health studies are a discipline that looks into various mental illnesses to see how they affect people, their causes, and what we can do about them. On the other hand, selecting the right topic for an argumentative essay is crucial to addressing a specific mental health issue. In other words, mental health essay topics have equal importance as the idea of mental health itself.
Students who have a real passion for any particular area of mental health should spend considerable time searching and finding the right topic for their essays.
This article presents many good mental health essay topics for your argumentative essay that you can use right away. These unique ideas will make it easier for students to address unique mental health issues through their arguments.
Mental Health Essay Topics to Write About
Everyone is affected by a mental illness at some stage in their lives. So how do you explain what other people in the world are going through without feeling their pain, emotions and anxiety? The success of your argumentative essay largely depends on the quality and uniqueness of the topic. Here are some exciting and intriguing mental health essay topics you can consider:
- The relationship between obesity and mental health
- The relationship between teenagers and self-harm
- How does a returning soldier deal with his mental health problems?
- The causes of post-traumatic stress disorder in soldiers and its treatment
- What does anorexia nervosa mean?
- It is recognising and addressing indicators of a loved one’s mental health.
- What do you think about people who have “dark” thoughts?
- What does ADHD mean, and what factors may play a role in its development?
- An analysis of gender with most of the mental health problems
- The possible treatment options for obsessive-compulsive disorder
- The most common mental disorders in geriatric people
- The treatments that are used most frequently in depressed patients
- Identifying the main influences on brain screening
- The impact of depression on overall mental wellbeing
- Differences between anxiety disorders and key protective factors for mental health
- Do video games have an impact on a person’s mental health?
- How does music affect mental health?
- How do graphic images affect mental health?
- The effects of obsessive-compulsive disorder on human activity
- How to identify mental illness
- What makes you feel anxious?
- How can stress cause depression?
- What are anxieties, and why do people fear everyday objects?
- Examine the mental health of Holocaust survivors.
- Postpartum depression is a real problem.
- What are the benefits of a cognitive health crisis?
- How does poverty affect mental health?
- The importance of improving psychological and emotional health
- Common mental health problems of women and men
- What role do school programs play in addressing mental health?
Grave Mental Health Essay Topics
You may also write about some more serious mental health topics. However, acing a mental health essay on a grave mental health issue will require you to relate your content to people’s real-life experiences and start accumulating arguments to support your claims. Here are some interesting but super specific mental health essay topics.
- Identify and discuss the role of physiotherapy in maintaining mental health.
- Sigmund Freud’s contributions to mental health
- What role does parenting stress play in depression?
- The influence of nightmares on depression
- The contribution of insomnia to depression
- Is it possible to keep the brain healthy to protect its health?
- Is it possible to forget painful memories?
- What educational credentials are required to practice psychiatry?
- What role do horror films play in anxiety?
- Why do people watch scary films?
- Discuss the relationship between mental health and therapy
- What measures are taken to treat mental health problems in the UK?
- Why are so many artists mentally ill?
- Do you think that living in the limelight causes mental illness?
- Discuss COVID-19 and mental health.
- How can you tell if someone is suffering from anxiety?
- An unintended consequence of online learning
- The impact of divorce on children’s mental health
- Why dropping out can harm a student’s mental health
- There is a link between physical violence and mental illness. Discuss
Has a difficult essay got you down? No problem!
With EssaysUK you get:
- Expert UK Writers
- Plagiarism-free Content
- Timely Delivery
- Thorough Research
- Rigorous Quality Control

Topics on Mental Illness Argumentative Essay
- Writing about a mental illness in your essay will require you to have an in-depth understanding of the illness you will investigate. If you pursue one of those in-depth mental health topics, you can surely impress your professor. TV shows that can benefit people with mental illnesses
- In the LGBTQ community, mental illness is common.
- Why are the people of the black community facing more mental illness?
- How can child abuse lead to mental illness?
- How is substance abuse related to mental illness?
- What are coping mechanisms most prevalent in mental illness?
- What is the impact of trauma on mental health?
- School-based programs to support students with mental health problems will be considered.
- What is the most common mental illness faced by raped victims? Discuss each of them.
- How lack of confidence can affect mental health
- Discuss the most recent developments in the field of clinical depression
- Anxiety caused by sexual assault in the metaverse
- How does anxiety affect the ability to cope with your daily life activities?
- Does women’s mental health matter in the nation?
- What are the most common mental illnesses faced by children?
- How can mental health be promoted at colleges and universities?
- How did music come to be associated with mental health?
- Mental health and its connection with peer groups
- How images of homeless people can affect a person’s mental health
- How can people on low incomes receive mental health care?
- The value of forgiveness for mental health
- Name and explain why one of the countries in the world has the highest rate of mental illness.
- The role of society in mental health problems
- Can a change of environment improve mental wellbeing?
- How can love help people who have a mental illness, and how can it not?
Good Essay Topics on Mental Health
- The role of extremists in the deterioration of mental health care in their holy places
- What happens when parents ignore their children, and how does it affect their mental health?
- The difference between religious counselling and professional counselling
- What does it mean to be anti-social, and how can you change or support someone who is?
- Recognise and explain the role of chronic stress and anxiety disorders in long-term loneliness. Discuss the impact of remote working on mental health and how to manage it.
- Talk about ways to deal with unhappy feelings to avoid slipping into chronic mental health problems.
- How can you tell if a person’s mental health is okay?
- How can you empower a handicapped person to pursue their goals without becoming depressed because of physical limitations?
- How can the general public best respond to someone suffering from a mental illness?
Cause-Effect Essay Topics on Mental Health
- What role does physical health play in maintaining mental health?
- The effects of post-traumatic stress disorder are severe. Explain why?
- Does emotional stress affect the immune system?
- How can break-ups help or hurt your mental health?
- How does early retirement affect or worsen mental health?
- What can a child do if they are diagnosed with schizophrenia, and how can they be helped?
- What are some of the potentially harmful behaviours that can exacerbate mental illness?
Argumentative Essay Topics on Mental Health
- People who are mentally ill are not religious. Argue on this perception
- Religion has both negative and positive influences on an individual’s mental health
- Anxiety is influenced by discrimination
- Depression can also be caused by self-awareness
- There are five reasons why mental illness is so prevalent
- Depression is a common problem among young people and is never taken seriously
- Suicide is a result of ignoring mental illness at its early stages. Argue
So now, when you have an opportunity to dazzle your teachers by working on these unique mental health essay topics, you must also know about the basic structure of a mental health essay. We have created a brief outline for you guys to understand the structure before delving into the topics.
Outline of the Essay
It would be best to write down what you want to cover in your essay after conducting your research on a topic. Do not forget to find and review different academic sources when writing a mental health essay.
Mental Health Essay Introduction
Your essay must have a hook that attracts the reader. Next, you need to establish a thesis statement to show you understand the significance of the topic you are exploring. You can also use your introduction to tell a story or share an experience.
Use proverbs, statistics, or anything that you feel is relevant to your topic in an introduction. Before concluding your introduction, give background information about your essay so that the reader knows what it is about.
The body is divided into paragraphs that support your thesis with evidence and arguments. In general, the body should consist of five paragraphs . However, each sentence must contain a topic sentence linked to independent thought on the topic of mental health. You can also write each sentence with a definite purpose, convincing arguments, supporting details, and examples.
The conclusion sums up the content that you have presented in your essay. You can include a statement of your thesis at the end of your conclusion, and you can even ask a rhetorical question about the future of mental health. However, it would help if you did not make any new arguments in conclusion.
Important Tips when Writing Mental Health Essay
- Present sufficient knowledge of the actual topic
- Know the difference between mental health/illness and emotions
- A generalisation of the term “Mentally Ill” should be avoided
- Use neutral terms, be precise in your arguments/claims
- Emphasis on the treatment and positive vibes through your content
- Get professional assistance if you struggle with your medical or nursing essay.
Frequently Asked Questions
How to write an excellent essay on mental health.
To write an excellent essay on mental health, research the topic thoroughly, provide personal insights, use a clear structure, support your arguments with evidence, and offer practical solutions. Prioritize empathy and awareness throughout.
You May Also Like
‘Commemorate’ comes from Latin commemorat, which means ‘to remember collectively.’ A commemorative speech, therefore, is a kind of spoken discourse where the speaker is trying to do one or all the following
Qualitative research involves describing or explaining an event or a phenomenon without heavily relying on statistical or mathematical practices.
Looking for some unique and workable argumentative essay topics? Need to select a topic for your argumentative essay but unsure where to begin?
Ready to Place an Order?
USEFUL LINKS
LEARNING RESOURCES
COMPANY DETAILS

+44 (0) 141 628 7445 +44 7388 619137 8am - 8pm Monday - Friday and 10am - 4pm Saturday and Sunday.
- How It Works
- Skip to content
- Skip to navigation
- News and stories
- News and views
- A mental health system in crisis v social causes of mental illness
A mental health system in crisis V social causes of mental illness
Until we address the issues under the surface, we will continue to see increased demand on overstretched public services.
Help us get the mental health conversation moving .
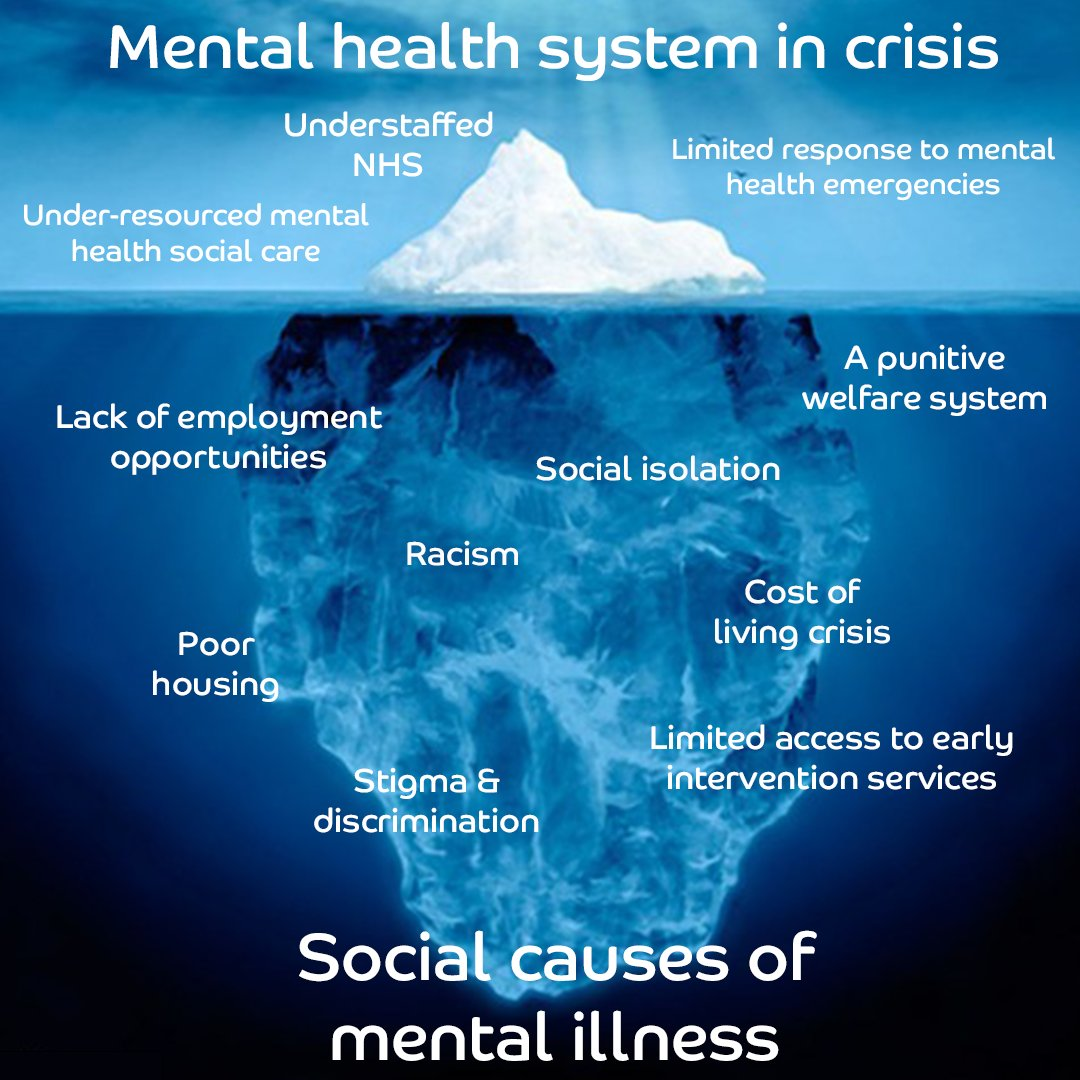
Advertisement
Analysis and Health
Could mental health conditions be 'transmitted' among teen classmates.
Having just one person in a school class with a mental health condition has been linked to a higher risk of such a diagnosis among their peers, but the potential reasons for this are hard to pin down
By Clare Wilson
22 May 2024

People with mental health conditions are often advised to talk things over with people they are close to
Maskot/Getty Images
If there is one thing most people know about teenagers and their mental health, it is that things are getting worse. Rates of several mental health conditions are on the rise in this group, especially in the US, but also in Australia, the UK and many other European countries.
While several possible causes have been debated, further evidence has emerged for an alarming possibility that has long been suspected, but has been hard…
Sign up to our weekly newsletter
Receive a weekly dose of discovery in your inbox! We'll also keep you up to date with New Scientist events and special offers.
To continue reading, subscribe today with our introductory offers
No commitment, cancel anytime*
Offer ends 2nd of July 2024.
*Cancel anytime within 14 days of payment to receive a refund on unserved issues.
Inclusive of applicable taxes (VAT)
Existing subscribers
More from New Scientist
Explore the latest news, articles and features
One-day mental health workshop improves teenagers' mood for six months
Uk schools are teaching teenagers about mental health in the wrong way.
Subscriber-only
Suppressing worrying thoughts may improve our mental health
Why being more open about mental health could be making us feel worse, popular articles.
Trending New Scientist articles
How to practice self-compassion and build a stable sense of confidence, according to experts
Being kinder to yourself pushes you to make positive changes

Feeling really, truly good about yourself may seem like a straightforward goal, but it's actually the result of developing both self-compassion and confidence.
Building the latter usually means improving your self-esteem—an internal judgment of your self-worth or 'an evaluation of worthiness,' says Kristin Neff, PhD, an associate professor of educational psychology at the University of Texas at Austin.
Perhaps the most talked-about method for pumping yourself up is to tip the needle in the direction you want, telling yourself to work harder, get stronger, and develop grit. But now, psych experts are poking holes in that theory, noting that while elevating your self-esteem can certainly be a pathway to more confidence, it has its pitfalls.
Self-esteem is tied to external validation, like compliments at work or likes on an IG post, so it’s fragile, says Christopher Germer, PhD, a lecturer in psychiatry at Harvard Medical School. When things don’t go right, comparison, feelings of isolation, and criticism creep in.
Say you’re falling behind on your marathon-training plan and angry with yourself about it. You might think, I’ll try harder because I feel inadequate. In the short term, that may work. But in the long run? Nope. When you get down on yourself, you wind up doubting yourself, which makes it harder to take risks, learn, and grow. You become afraid of failure, and you’re more likely to give up than to try again.
An alternate way to a more assertive you: self-compassion, which involves showing yourself kindness when you’re struggling, failing, or noticing something you don’t love about yourself. Self-compassion isn’t about measuring up to expectations; it’s a way of relating to yourself as a human. By caring and expressing concern for yourself during hard times, you’re able to persevere and create changes.
.css-1cugboc{margin:0rem;font-size:2.125rem;line-height:1.2;font-family:Domaine,Domaine-roboto,Domaine-local,Georgia,Times,Serif;color:#f7623b;font-weight:bold;}.css-1cugboc em,.css-1cugboc i{font-style:italic;font-family:inherit;}.css-1cugboc b,.css-1cugboc strong{font-family:inherit;font-weight:bold;} 'We tend to think of self-compassion as passive, even unproductive, but that could not be further from the truth'
Well, yeah, feels kind of obvious, right? Let’s go back to the training scenario to paint the picture a little more clearly: With self-compassion, you’ll think, I’m going to try because I care about myself and I don’t want to suffer . That kind of motivation 'leads to more self-confidence,' Neff says. When you can sit with your pain and think through what you might need to achieve your goal—like waking up earlier for runs or scheduling them on your phone calendar—instead of spiralling over all the ways you’re failing, you’ll overcome challenges, building confidence and belief in yourself as you go. It’s a subtle change in reaction, but it makes a huge difference. 'Self-compassion gives you a stable source of self-competence, as opposed to a "sugar high,"' Neff says.
We tend to think of self-compassion as passive, even unproductive ('If I’m easy on myself, I’ll become complacent'). But that could not be further from the truth. There are two sides to self-compassion, Neff says. The tender side embodies the idea that although you are innately flawed, you are still worthy. And the fierce side says if you truly care about yourself, you accept yourself but don’t accept all of your behaviours, especially harmful ones. 'Part of caring for yourself means taking active steps to change,' says Neff. That’s where the power of self-compassion comes in.
But none of this is easy. We tend to be waaay nicer to others than we are to ourselves—and we’re quick to judge our shortcomings and failures. The good news is this is a trainable skill. 'It’s a muscle you can build,' says Neff.
What is self-compassion?
'Self-compassion is to accept yourself and give [yourself] the same grace and understanding you would give others,' says Reena B. Patel, BCBA, a board-certified behavioural analyst and positive psychologist. This can be especially hard since we often set high goals, standards, and ideals for ourselves, but self-compassion is accepting the current situation and not beating yourself up when things go awry, she adds.
In other words, self-compassion is gently accepting when you make a mistake and giving yourself room to fail, says Diana Gasperoni, LCSW-R, a licensed clinical social worker and founder of New York-based BeWELL Psychotherapy. 'Self-compassion will allow us to pick ourselves up and try again,' she explains. 'It allows us to grow and flourish.'
Self-compassion exercises to try
These six methods create a deeper understanding of self-compassion and will help you feel your best today and for years to come. Motivation, a better mood, and, yep, alllll the feel-good feelings, right this way…
1. Ask yourself: What do I need?
This is the question that guides the whole self-compassion cultivation agenda, says Germer. Say you missed a deadline and are being hard on yourself about it. Instead of spiralling into negative self-talk, figure out what you need—a few more hours of childcare, writing daily to-do lists—to problem-solve. This inquiry (part of the fierce side of self-compassion) provides resources and tools for change, eventually generating self-confidence as you’re able to learn and grow.
2. Put a hand on your heart.
Touching your heart or your cheek 'is probably the most widely used, simple, and physiologically transformative experience toward self-compassion,' says Germer. (You’re likely already doing it—when you receive bad news, you may instinctively put your hand on your heart!) This self-touch lowers cortisol levels, according to research published in Comprehensive Psychoneuroendocrinology . Also, when you rub your chest, specifically, you may activate your vagus nerve, the main nerve of your parasympathetic (or 'rest and digest') system, Germer says.
3. Figure out when you just *don’t* have it in you.
Pinpoint times when you lack self-compassion, says Pooja Lakshmin, MD, author of Real Self-Care . Do you get in your head when you see an email from a certain coworker, or does negative self-talk bubble up every time you and your partner fight? Homing in on self-kindness in these moments can push you toward the type of change you’re looking for.
4. Reflect on how you speak to yourself.
Is the voice in your head positive or negative? 'Talking to ourselves in a positive way, especially when facing difficulties, is a great place to start with practicing self-compassion because you’re literally giving yourself grace and understanding when working through and accepting difficult situations,' says Patel.
When you make a mistake, shift your perspective, and reflect on what you can learn. 'It’s all about how you emotionally respond to yourself and how those responses affect your overall well-being and outlook on life.'
5. Acknowledge the small wins.
Set achievable goals and acknowledge the small wins, says Gasperoni. This can be as simple as setting a bedtime and sticking to it, or reading 10 pages of a book a day, she explains. Big changes often start with small steps, and this is also true for how we embody self-compassion and perceive and talk to ourselves, adds Patel.
6. Practice gratitude—for yourself.
If you’re disappointed in yourself, it can be hard to let go and move on. But instead of spiralling with negative self-talk, let yourself forgive and move on, says Patel. 'Be kind to yourself and practice self-love and gratitude ,' she explains. 'Expressing gratitude to yourself is being aware of the things that are affecting you and responding with appreciation.'
How to practice positive self-talk
The way you talk to yourself can fuel compassion, but acing positive self-talk is not simply telling yourself, 'Everything’s great!' Here's how to change your tune:
Notice the negativity
An easy way to cultivate a little TLC toward yourself is to practice a meditation tailored by Neff for this purpose: Focus on the mistakes or flaws that have been bothering you lately, then find where the emotions about them tend to end up in your body, like a tightness in your jaw or tension in your shoulders. Allow those feelings to sit in your body instead of resisting or rejecting them. This lets you get in touch with the suffering caused by your criticisms or the belief that you have to be perfect.
Make a wish
Germer favors the use of wishes over positive self-statements (like 'I’m getting stronger!'). Wishes, such as 'May I accept every part of me,' are like 'surrounding yourself with sacred company rather than the nasty chatter in our own minds,' he says. Plus, they encourage growth.
Replace the word should
Ever find yourself 'shoulding' all over yourself? ( Ugh, I should have done this earlier. ) It’s a common form of self-criticism, one that’s not exactly self-compassionate, says Dr. Lakshmin. Try subbing for your shoulds anything that fosters curiosity ( Could I have chosen to do X instead? Or: I wonder what held me back most this week? ). Curiosity is kinder and more productive than shoulding, she says.
How practicing self-esteem can boost your confidence
'Loving yourself is the first step in boosting your confidence,' says Patel. 'If you don't love yourself, feelings of insecurity and inadequacy will creep up and your self-confidence will lower,' she explains.
Additionally, practicing self-esteem can build up your sense of self-worth, says Gasperoni. Acknowledge your strengths, take pride in your accomplishments, and give yourself room to fail, she explains. 'Self-esteem is the cornerstone of confidence.'
More empowering relationship stories..
- 'I tried a "delusion week" to become the most confident version of myself'
- Dr. Tara advises how one divorcee can rediscover her sexual confidence after 20 years of marriage
- Do injectables really boost self confidence?
Relationships

What it means to be in a sexless relationship

18 signs you’re in an unhappy relationship

Honeymoon phase over? Don't fret—help is here

How to be more vulnerable in your relationship

Do you initiate sex differently from your partner?

Are your relationship expectations unrealistic?

66 signs of an abusive relationship

What is a polycule?

Here's how to set boundaries in your relationship

What to do if you're in a one-sided relationship

20 gaslighting examples and how to handle them
Blog Teaching
https://teaching.blog.gov.uk/2024/05/14/a-whole-school-approach-to-mental-health-and-wellbeing/
A whole school approach to mental health and wellbeing: Part 1
Jayne Kumi is the designated safeguarding lead and senior mental health lead at Woodmansterne School and Sixth Form, an all-through school in London. She reflects on her leadership role in the journey to implement a whole school approach to mental health and wellbeing .

Implementing a whole-school approach to mental health is a journey, rather than a task with an end point. At the beginning of the journey, I asked myself, ‘what is our vision for a whole-school approach - and how can I ensure that both senior and middle leaders buy into this vision?’
We began by setting up a trained mental health team to coordinate mental health and wellbeing activities across the school. In efforts to make mental health and wellbeing visible throughout the school, we posted images of the team in all classrooms and put a mental health display board in the foyer. Each member of the team also started wearing a specially designed T-shirt at key events with bold print on the front and back stating "Mental Health, Let's talk about it".
We operate an open-door policy for new ideas and suggestions which is essential to an effective whole-school approach that everybody feels ownership of. A recent suggestion was regarding a school therapy dog, and following consultation, we now have Pepper in school 2-3 days per week, providing a calm, stress release experience for children.

I completed a 12-week DfE funded senior mental health training with Place2Be which gave access to invaluable resources and a chat room for networking. There are a number of providers for the course, and I would recommend that settings seek to identify a course relevant to their needs using the Carnegie ‘select a course tool’.
Following the training, SLT undertook a mental health audit of our existing provision and the findings were presented to teaching and non-teaching staff. The audit helped identify our strengths and served as a foundation for confidence and growth and areas for development. As a result of the training, I am more confident and proactive in in my role. I have put in place a mental health framework which provides tiered and context-based guidance for school staff on how to be involved with mental health. The framework enables staff to understand their role in promoting mental health in everyday activities, identifying potential concerns, listening and referring on.
Supporting the wellbeing of staff through the work of our staff wellbeing committee is also key. We often remind staff of the importance of ‘putting your oxygen mask on first’, to ensure they are mentally well and able to support our children. This is true of our parents and carers also; hence we work hard to engage them with resources, workshops, fairs, and an open-door policy.
Our senior leadership team have achieved so much through our continuous efforts to involve the whole school, including staff, pupils, parents and carers in our approach. This is a continuous journey, and we remain open to learning and growing as we further develop our approach.
Matthew Bradley is the headteacher and mental health lead at Newton Farm Nursery, Infant and Junior school in London. He talks about how the senior leadership team worked together to review and develop their approach to supporting mental health and wellbeing throughout the school.

Mental health is an interesting and challenging problem for any school. It poses complex questions that we feel need to be managed by senior members of staff.
At our school, the deputy headteachers and I are senior mental health leads (SMHL). In order to better understand the issues, we undertook training through the DfE’s senior mental health lead training grant .
Following the training, we spent a day together, discussing what we had learned, and developing our strategic thinking to come up with a plan that would be understood, accepted and genuinely embedded across the school. To ensure whole school buy-in, SLT have championed efforts to promote mental health and wellbeing by promoting several core principles:
- Understanding that mental health and wellbeing are closely related and ensuring that we have early support in place to promote wellbeing.
- Making sure staff feel valued and are supported to have good mental wellbeing and that workload is manageable.
- Understanding that good mental health and wellbeing benefits everybody leading to better outcomes against our core goals such as improved attainment, attendance, and behaviour, as well as happier, more confident and resilient children and staff.
We reviewed all our mental health initiatives and increased their visibility. We made changes to common strategies:
- Staff surveys: We conduct weekly surveys which consist of one open-ended question, normally generated by staff. The results are shared in every SLT meeting. This keeps the issue of staff wellbeing “live” and changes can be implemented quickly, and transparently giving staff more agency over their wellbeing.
- Learning mentors: We reduced one to one mentoring sessions and implemented small group sessions so that we can offer support to more children. These groups, led by our SENCO and administered by teaching assistants, support children who are identified as having early signs of a wellbeing need.
- Pupil check ins: Each day the senior mental health leads pick a few children from our school register to have a brief wellbeing conversation with. Pupils are selected where there has been little prior interaction. This has resulted in us being able to identify a number of safeguarding concerns early.
The management changes we have introduced ensure that our whole school approach is understood and actively supported by staff. We maintain the profile of mental health by ensuring that some element of wellbeing is discussed in each of our weekly “All Hands” meetings. This means staff feel involved in the decision-making processes, and their concerns are understood. The investment of time and energy made by working together has resulted in a happier and more productive school - and a journey well worth engaging in for any SLT.
Fur ther reading:
- Schools and colleges can access a £1,200 Department for Education senior mental health lead training grant to help develop and implement a whole school or college approach to mental health and wellbeing.
- Access a new resource hub to help mental health leads embed a whole school or college approach to mental health & wellbeing.
- A new targeted mental wellbeing support toolkit is also available. This provides a practical guide and filterable tool to help schools and colleges review, refresh and develop effective targeted support for pupils and learners with social, emotional and mental health needs.
- Access a recently launched resources page for teachers, parents and carers to support pupils experiencing mental health & wellbeing difficulties to attend school or college.
Sharing and comments
Share this page, leave a comment.
Cancel reply
By submitting a comment you understand it may be published on this public website. Please read our privacy notice to see how the GOV.UK blogging platform handles your information.
Related content and links
About the teaching blog.
A Department for Education blog for teachers, by teachers.
Covering everything from reducing workload , to pupil premium , school leadership and pupil wellbeing .
Find out more about the blog and sign up to receive email updates when new posts are added.
- DfE on Twitter
- DfE on Facebook
- DfE on Instagram
- DfE on YouTube
- DfE on LinkedIn
Sign up and manage updates
Recent posts.
- A whole school approach to mental health and wellbeing: Part 2 17 May 2024
- A whole school approach to mental health and wellbeing: Part 1 14 May 2024
- Keeping pupils active to support their wellbeing 10 May 2024
- Breaking barriers: School’s drive to close the attainment gap using tutoring 8 May 2024
- Offering wraparound childcare at our schools 17 April 2024
Comments and moderation policy
- Find out more
- Members area
- Members registration
Medically Assisted Reproduction and Mental Health in Adolescence

Posted on 20 May 2024
DOI: 10.13056/acamh.27597
In this Papers Podcast, Maria Palma and Associate Professor Alice Goisis discuss their co-authored JCPP paper ‘Medically assisted reproduction and mental health in adolescence: evidence from the UK Millennium Cohort Study’ ( https://doi.org/10.1111/jcpp.13877 ).
There is an overview of the paper, methodology, key findings, and implications for practice.
Discussion points include:
- What the UK Millennium Cohort Study is.
- The differences in parental reports on adolescent mental health between MAR (medically assisted reproduction) adolescents and naturally conceived adolescents.
- The differences between adolescent self-reports and parental reports on adolescent mental health.
- The association between MAR conception and mental health outcomes in adolescents.
- Implications for clinical practice and researchers.
In this series, we speak to authors of papers published in one of ACAMH’s three journals. These are The Journal of Child Psychology and Psychiatry (JCPP) ; The Child and Adolescent Mental Health (CAMH) journal ; and JCPP Advances .
#ListenLearnLike
Subscribe to ACAMH mental health podcasts on your preferred streaming platform. Just search for ACAMH on; SoundCloud , Spotify , CastBox , Deezer , Google Podcasts, Podcastaddict, JioSaavn, Listen notes , Radio Public, and Radio.com (not available in the EU). Plus we are on Apple Podcasts visit the link or click on the icon, or scan the QR code.
Maria is a Research Fellow at the UCL Centre for Longitudinal Studies working on European Research Council Grant to study the effects of Medically Assisted Reproduction (MAR) on children and adults (MARTE). She investigates the long-term associations between MAR and health and educational outcomes using the Millennium Cohort Studies and Finnish register data.
Maria is also studying a PhD in Social Sciences in the same department. Her supervisors are John Jerrim and Lindsay Macmillan, and her PhD works aims to build a better understanding of impact that educational policies have had on educational inequalities and highlight the potential of administrative data to lead to better informed policy decisions.

Alice Goisis is an Associate Professor in Demography and Research Director at the Centre for Longitudinal Studies located in the UCL Social Research Institute. Her research interests span a number of substantive areas in social demography and epidemiology. My research has examined the association between advanced maternal age and child well-being, with a particular focus on whether and how it varies across different groups of the population and time periods. Dr Goisis is currently the PI of an ERC Starting Grant investigating families the effects of Medically Assisted Reproduction on children, adults and families. More generally, I am interested in whether, and if so how, family processes are associated with children and adults’ well-being.
[00:00:01.339] Jo Carlowe: Hello. Welcome to the Papers Podcast series for the Association for Child and Adolescent Mental Health, or ACAMH for short. I’m Jo Carlowe , a Freelance Journalist with a specialism in psychology. In this series, we speak to authors of papers published in one of ACAMH’s three journals. These are the Journal of Child Psychology and Psychiatry, commonly known as JCPP, the Child & Adolescent Mental Health, known as CAMH, and JCPP Advances .
Today, I’m interviewing Maria Palma , Research Fellow at the Centre for Longitudinal Studies, Social Research Institute, University College London, and Alice Goisis , Associate Professor of Demography and Research Director at UCL’s Centre for Longitudinal Studies. Maria and Alice are co-authors of the paper, “Medically Assisted Reproduction and Mental Health in Adolescence: Evidence from the UK Millennium Cohort Study,” recently published in the JCPP.
This paper will be the focus of today’s podcast. If you’re a fan of our Papers Podcast series, please subscribe on your preferred streaming platform, let us know how we did, with a rating or review, and do share with friends and colleagues. Maria and Alice, thank you for joining me. Can you start with an introduction about who you are and what you do?
[00:01:18.490] Associate Professor Alice Goisis: Good morning. Thank you for having us. First of all, my name is Alice Goisis . I am a Family Demographer at the Centre for Longitudinal Studies at UCL. Over the past five years, I’ve been the PI of a project which aims to investigate different aspects of the life of families who are formed via medically assisted reproduction. For example, we have looked at the family’s mental health before, during and after the treatments, how it affects their relationships and whether the lives of children who are conceived through medically assisted reproduction are any different from those of the likes of children conceived naturally.
[00:01:54.700] Jo Carlowe: Brilliant, and Maria, could you introduce yourself too, please?
[00:01:58.090] Maria Palma: Of course. Hey, my name is Maria Palma . I’m a Research Fellow on our latest MARTE project and I am the Lead Author of the study and also a PhD student at the UCL Social Research Institute.
[00:02:09.300] Jo Carlowe: Great, thank you very much. So, today we are looking at your JCPP paper, “Medically Assisted Reproduction and Mental Health in Adolescence: Evidence from the UK Millennium Cohort Study.” Can you start with an overview of the paper? What did you look at and why?
[00:02:26.200] Maria Palma: The paper examines several mental health outcomes of adolescents conceived through medically assisted reproduction and whether they differ compared to those of adolescents who are conceived naturally. So, we are interested in MAR children, short for medically assisted reproduction children, because the number and proportion of children conceived via MAR has increased steadily over the last decades, and yet the evidence under mental health is inconclusive. So, we look at mental health outcomes reported by both the adolescents themselves and their parents to investigate if there are differences in the report.
[00:03:02.310] Jo Carlowe: Thank you. Can you tell us a little about the methodology used for this study?
[00:03:07.050] Maria Palma: Yes. The study uses data from the Millennium Cohort Study, a nationally representative longitudinal dataset that has followed around 18,000 babies born in the 2000s throughout their lives. This is important because it allows us to get informations on the children’s parents, such as education and other characteristics that might be relevant to explain differences in mental health by type of conception. And in our study, we focus on wave seven from MCS and altogether we follow almost 10,000 individuals up until they are aged 16/17.
We use linear and logistic estimations to investigate whether adolescents conceived through MAR are more or less likely than their naturally conceived peers to have mental health problems. So, to do so, we look at differences in different questionnaires, such as the SDQ, the Strengths and Difficulties Questionnaire, Kessler Psychological Distress Scale, and information that was self-reported by the adolescents on their antisocial behaviours, whether they have attempted suicide, have hurt themselves on purpose or have had substance abuse problems. So, we think that relying on several measures provide us with a comprehensive view on the cohort members’ levels of mental health and socioemotional wellbeing.
[00:04:29.060] Jo Carlowe: Thank you very much. What key findings from the paper would you like to highlight?
[00:04:32.880] Associate Professor Alice Goisis: We think that the main finding is that we find no differences by mode of conception in adolescents’ self-reported mental health. In other words, children who are conceived through medically assisted reproduction do not report to have more mental health problems than children who are conceived naturally. In contrast, when we look at the parents’ reports, we find small differences between adolescents conceived naturally and those conceived through medically assisted reproduction. In other words, based on the parental reports, parents of MAR adolescents report a slightly higher level of mental health problems than parents whose adolescents were conceived naturally.
[00:05:16.680] Jo Carlowe: What do you make of that discrepancy? So, what you’ve just highlighted is that based on parental reports, one might consider adolescents conceived through medically assisted reproduction to be at higher risk of suffering from mental health problems, but that was not supported by the adolescents’ own reports. How do you explain that? What do you – how do you interpret it?
[00:05:38.100] Associate Professor Alice Goisis: We think that this discrepancy might reflect differences in parental concerns, might reflect their underlying anxiety towards those children, since it was so difficult to conceive them and to have them, and possibly also, their relationship or closeness with their children. However, we think it’s important to highlight that the differences that we observe when looking at the parental reports are quite small and therefore, considering that the magnitude of the differences in the parental reports are small and we find no differences when we look at the cohort members’ reports, we interpret the findings as an indication of no meaningful, or clinically relevant, differences in MAR adolescents mental health outcomes compared to the mental health outcomes of adolescents conceived naturally.
[00:06:31.330] Jo Carlowe: What else in the paper would you like to highlight?
[00:06:35.000] Maria Palma: We think it’s relevant to highlight that before taking into consideration any of the parental characteristics that, for example, we know MAR children are – come from more advantaged families, we see that the unadjusted results show lack of differences in the association between MAR conception and the mental health outcomes for all of the outcomes. which means we observed no differences between children who were conceived via MAR or naturally. And then, when we adjusted for family sociodemographic characteristics, the results show MAR adolescents score slightly higher, but again, only when looking on three SCQ scales, which were reported by the parents, not by the adolescents themselves.
This suggests that the more selected and advantaged profiles of MAR families may protect against the risk of poor mental health outcomes. And the results did not change on adjustment for potential mediators, such as parental mental health, number of siblings in the household and parental household structure.
[00:07:29.099] Jo Carlowe: So, given your findings, what are the implications for clinical practice?
[00:07:32.230] Maria Palma: We urge that the finding of small long-term differences between MAR and naturally conceived adolescents should be part of the conversation between the Doctor and the couple when discussing the risks of fertility treatments. Also, they should be considered by Therapists when dealing with parents who conceived via this way and adolescent patients who were conceived via medical assisted reproduction. Still, the result suggest that the mode of conception is unlikely on average to play a major role in explaining mental health problems amongst adolescents.
[00:08:04.710] Jo Carlowe: Given that it’s not thought to play a major role, why does it still feel important then for Clinicians to ask?
[00:08:12.970] Maria Palma: We think it’s something that the Clinicians should have into consideration because – mostly because of the discrepancy in the report between parents and adolescents themselves. So, there could be that these parents have higher concerns, are more anxious and this could be affecting their relationships or their mental health, basically.
[00:08:31.150] Jo Carlowe: Right, thank you. Yeah, that’s very clear. What are the implications of your findings for Researchers?
[00:08:35.770] Associate Professor Alice Goisis: Previous studies looking at the mental health of children conceived by medically assisted reproduction have shown mixed results, with some studies finding an association and other studies finding a lack of an association. Based on our results, we hypothesised that this could be related to the fact that some of the previous studies have relied on the adolescent’s report and some of the previous studies have relied on the parental report. And so, the discrepancy in the responses between the adolescents’ reports and the parents’ reports suggest that future research should consider the views of different family members, but also that future research should evaluate a broad set of outcomes, if possible.
[00:09:13.860] Jo Carlowe: Maria and Alice, are you planning any follow-up research, or is there anything else in the pipeline for either of you that you would like to share with us?
[00:09:24.790] Associate Professor Alice Goisis: Another paper that we’re currently working on, which is aiming to shed light on why we observe that children who are conceived through medically assisted reproduction tend, on average, to come from highly advantaged families. So, the previous argument is that this might be related to differences in need for medically assisted reproductions. So, more advantaged women invest in their education and careers, postpone childbearing and therefore, are more likely to need medically assisted reproduction to conceive. But we challenged this assumption as there is evidence showing that less privileged women are less likely to access and undergo medically assisted reproduction, but actually, are not less likely to experience infertility.
Therefore, there could be barriers which prevent more disadvantaged women from accessing and succeeding in having a live birth via medically assisted reproduction. So, previous findings from our work support this hypothesis and this idea and show that amongst women who access and undergo medically assisted reproduction, the least advantaged, for example, women who have lower level of education, have a lower probability of having a live birth via medically assisted reproduction than women who are more advantaged. So, we argue that part of the social differences that we observe in medically assisted reproduction birth do not reflect, or are not fully explained by differences in needs between more and less advantaged women.
[00:10:44.350] Jo Carlowe: Sounds very interesting. What’s the timescale on the new study?
[00:10:48.110] Associate Professor Alice Goisis: Well, it’s difficult to tell. We are currently doing – we’re still in, sort of, analysis phase. So, we – and we are starting to write the paper, but we are hoping to submit it to a journal before the summer break and then the timeline is – that will be out of our hands after that, so – but several months.
[00:11:16.389] Jo Carlowe: Okay. Good luck with that.
[00:11:19.720] Associate Professor Alice Goisis: Thank you.
[00:11:22.570] Jo Carlowe: Finally, a question to both of you. What are your take-home messages for our listeners?
[00:11:29.720] Associate Professor Alice Goisis: Taken together, our research shows that most children who are conceived through medically assisted reproduction are healthy and develop normally. For outcomes such as education, we find that MAR conceived children have better outcomes than children who are conceived naturally, which is explained by the fact that MAR conceived children tend to grow up in socioeconomically advantaged families. And although the findings of this study looking at mental health could be a cause of concern, as highlighted before, the differences that we find are very small and this is reassuring evidence. At the same time, our research shows that the process of medically assisted reproduction can be highly stressful and can take a toll on women’s mental health, especially for those for whom the treatments are unsuccessful and do not result in a live birth.
[00:12:56.959] Jo Carlowe: Both of you, thank you ever so much. For more details on Maria Palma and Alice Goisis , please visit the ACAMH website, www.acamh.org and Twitter @acamh . ACAMH is spelled A-C-A-M-H, and don’t forget to follow us on your preferred streaming platform, let us know if you enjoyed the podcast, with a rating or review, and do share with friends and colleagues.
Your email address will not be published. Required fields are marked *
NEWS... BUT NOT AS YOU KNOW IT
Could ‘unhappiness leave’ make for a better work environment?

Share this with

Over the course of her career, Sonya Barlow constantly felt pressured to ‘show up’ – but in all the wrong ways.
Suffering from chronic migraines which would often flare up ‘significantly’ and impact her ability to work, Sonya also has attention deficit hyperactivity disorder (ADHD), which can disrupt sleep, mental health and emotional sensitivity, and these days is often supported through workplace adjustments.
However, she never felt confident calling in sick, even when she felt unwell, uncomfortable and generally unhappy at work.
‘As a woman of colour, I used to mask the pain and smile into work,’ Sonya, who is 31 and lives in London , tells Metro.co.uk.
Her colleagues often wouldn’t believe her if she reported feeling unwell, and her managers often made ‘snarky comments.’
‘I would come into work around 7.30am when my start time was 9am to avoid rush hour and leave around 4pm but the comments were often that I was doing a “half day” or “not taking it seriously”,’ she recalls.

‘I was also told, despite being sick, that I had to come in for an interview for a job at work because mine was under the possibility of redundancy.’
The only way that Sonya felt comfortable to take a day off – or even to be believed – was through a doctor’s note, which she found difficult to obtain but she ‘kept a log’ of her pain to make the process easier.
Subsequently, Sonya left the corporate space and started her own business, largely so that she could have freedom over her own calendar and take days off not just when she was feeling sick physically – but also when she was struggling with her mental health.
Now, as a boss with her own team, she actively encourages ‘duvet days’, particularly if they’re struggling with feelings of unhappiness.

She said: ‘From these experiences, I learnt what I didn’t want to become as a manager and also how important it was to create a relevant culture of trust, honesty and respect – because people will do their work and show up as their best selves, as long as you’re giving them the tools and resources to do so.’
Sonya’s approach to the world of work echoes a new policy coined by one regional Chinese supermarket chain, Pang Dong Lai. The company’s founder, Yu Donglai, has introduced a policy through which employees are entitled to 10 days of ‘unhappiness leave’ each year – for which they don’t need a doctor’s note.
‘I want every staff member to have freedom. Everyone has times when they’re not happy, so if you’re not happy, do not come to work,’ he told the South China Morning Post. ‘We want our employees to have a healthy and relaxed life so that the company will be too.’
Pang Dong Lai’s new policy has prompted discussions surrounding ‘unhappiness leave’ and overall workplace culture, which, in most circles, is generally moving towards an increased focus on employee wellbeing.
However, last month Rishi Sunak announced that he would be trialling a new policy that would see GPs stripped of their power to sign people off work in a wider stance against ‘sick note culture.’ This prompted outrage from the authors of workplace wellbeing initiatives, concerned workers and the disability community, with many arguing that Sunak’s plans were suggestive of anything but inclusivity.

But Sunak’s plans for the workforce aside, what benefits could ‘unhappiness leave’ have on employees and wider workplace culture? And how could they be enforced?
As Simon Miller, International Partnerships Director at Headspace points out, according to a survey by the company, 78% of UK employees have said that work stress has negatively impacted their physical health, while 76% reported that work stress has caused a personal relationship to end.
Elsewhere, 40% of employees disclosed that work stress has contributed to serious mental health challenges, such as substance use or suicidal ideation – highlighting the need for greater transparency around health and wellbeing, as potentially signified by ‘unhappiness leave’ policies.
‘By offering mental health or mental well-being days, we can help to reduce some of these alarming statistics, by creating a work culture in which employees feel like their mental health is valued and where they can openly seek support when it’s needed,’ Simon tells Metro.co.uk.
‘Setting time where employees can take time for themselves can help employees better understand how to set healthy boundaries for themselves. At Headspace we offer every other Friday as a MINDay, intended to create a four-day work week every other week to allow people to invest time in their own positive mental well-being – whatever form that might take,’ he adds.
What are the benefits of ‘unhappiness leave’?
So, what are the potential benefits of policies like ‘unhappiness leave’? And do these policies go far enough in furthering employee wellbeing?

‘”Unhappiness leave” policies are frequently introduced as a means for employers to prioritise the wellbeing and mental health of their workforce,’ Simon explains.
‘Some of the proven benefits of these initiatives include alleviating employee burnout, enhancing retention, improving productivity, and even combating the stigma surrounding mental health discussions in the workplace.’
And, as career coach and author Hannah Salton points out, these policies can improve relationships both in and outside the workplace.
‘The benefits of an ‘unhappiness leave’ policy could include feeling happier and more engaged at work and having better and more rewarding personal and professional relationships,’ Hannah adds.
Likewise, introducing such policies can highlight mental health struggles that, otherwise, might not have been addressed between an employer and an employee, as Naomi Humber, Head of Mental Wellbeing at Bupa UK , explains.
‘Introducing specialised work leave options could encourage staff to share mental health struggles with their line manager that may have otherwise been missed if they’d taken sick leave,’ Naomi highlights.
Are there any drawbacks to ‘unhappiness leave’?
However, as Hannah explains, there’s no ‘quick fix’ when it comes to employee wellbeing – change has to be meaningful, and suitable on an individual level.

‘Different things work for different people. Offering unhappiness days – if implemented correctly – could certainly help employees feel they are being looked after by their employer and improve overall workplace wellbeing.’
Though seemingly a productive move towards improving employee wellbeing, ‘unhappiness leave’ policies could see employees with mental health conditions downplaying their symptoms.
‘It’s important that those suffering from conditions such as anxiety and depression don’t feel pressure to minimise their conditions and just take unhappiness leave when more support is required,’ Hannah details.
How might employers roll out ‘unhappiness leave’?
‘It’s important for employers to take individual circumstances into account, and not take a one size fits all approach. It would need to be pre-agreed upon how much notice – if any – employees need to give to take unhappiness leave,’ Hannah advises.
‘It could also be helpful if other support is offered to employees feeling unhappy, to try and address the cause rather than the symptom. This could involve counselling, private health care, or vouchers to spend on wellbeing activities.’
And, when it comes to rolling out the policy, smaller companies might struggle.
‘Not all workplaces are the same – it may be more difficult for smaller companies to implement formal mental health policies for their staff if they don’t have their own HR function. It may be useful for businesses to look at what others are doing within their sector to help frame a policy,’ Naomi adds.
More from Metro

Run clubs have become our new nightclubs – here’s why
‘Formal unhappiness leave policies are best drawn up with an all-rounded approach. This means that it should be written down, and cover how staff will be supported if they experience poor mental health, with the stipulations of how many days’ leave they’re entitled to, each year, and how to request it. It may be useful to seek input from employees to ensure they’re fully engaged.’
Do you have a story to share?
Get in touch by emailing [email protected] .
MORE : This ‘tranquil’ UK city has been crowned the best for relaxing walks
MORE : I spoke to a free online therapist and came away feeling ripped off
MORE : School sent letter highlighting boy’s poor attendance despite knowing he was seriously ill
Sign up to our guide to what’s on in London, trusted reviews, brilliant offers and competitions. London’s best bits in your inbox
By ticking this box, you confirm you are over the age of 18*. Privacy Policy »

To the lady buying coffee, wearing a green leather jacket at South Ealing…
You were tall, dark and handsome and dressed smartly for work, with a…
Enter your birthday for your free daily horoscope sent straight to your inbox!
Get us in your feed
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Health and social care
- National Health Service
Mental Health Services Monthly Statistics, Performance May 2024
This publication provides the most timely statistics available relating to NHS funded secondary mental health, learning disabilities and autism services in England. This information will be of use to people needing access to information quickly for operational decision making and other purposes.
Is this page useful?
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. Please fill in this survey (opens in a new tab) .

IMAGES
VIDEO
COMMENTS
Mental health is a term that encompasses a range of experiences and situations. It can be an on going experience from mental wellbeing through to a severe and enduring mental illness affecting a person's overall emotional and psychological condition. Incidents in life such as bereavement, financial and personal happiness such as the way we ...
People who have good health can still have underlying emotional problems and mental problems. This can be caused by a physical imbalance in the brain, stress, family problems and stressful work/education can make it worse. These mental and physical feelings can cause the individual to become divided and live a separate life from others in society.
The nature of mental illness has been the subject of passionate discussion throughout history. In ancient Greece Plato, 1, 2 promoting a mentalist definition of mental illness, was the first to coin the term "mental health," which was conceived as reason aided by temper and ruling over passion. At around the same time, Hippocrates, 3 taking a more physicalist approach, defined different ...
Friday, 14 February 2014 Amy. Amy shares her experience of living with depression. Depression... it just eats you up from the inside out. It's like a monster inside your head that takes over. The worst thing is to know that my family and friends were doing all they could yet I still felt so lonely. Anything that was said to me, I managed to ...
'mental illness' or 'mental health issues' describe your experiences better, or are easier to explain to other people in your life. However you understand your own experiences, and whatever terms you prefer to use, we hope that you will find the information in these pages useful when considering different options for care and support.
Introduction. In developed countries such as the UK, most people diagnosed with mental illnesses receive their healthcare mainly via primary care (Cunningham, 2009; Care Quality Commission, 2015).In England, between 2013 and 2014, there were nearly 3 million adults on local general practice (GP) registers experiencing depression and approximately 500 000 were diagnosed with severe mental ...
Different perspectives on mental health and mental illness. There are various approaches to mental health and mental illness around the world. Most health professionals in the UK agree on a similar set of clinical diagnoses and treatments for mental health problems. We have chosen to reflect this approach in our information, as these are the terms and treatment models that you are most likely ...
Background Individuals' childhood experiences can strongly influence their future health and well-being. Adverse childhood experiences (ACEs) such as abuse and dysfunctional home environments show strong cumulative relationships with physical and mental illness yet less is known about their effects on mental well-being in the general population. Methods A nationally representative household ...
Mental health problems are common, with 1 in 6 adults reporting a common mental health disorder, such as anxiety, and there are close to 551,000 people in England with more severe mental illness ...
The Q Lab takes a developmental approach and aims to learn by doing, helping to build the skills and capabilities that are needed to deliver collaborative change. The project on mental health and persistent pain is the Q Lab's second project. The first project focussed on scaling patient-to-patient peer support and the learning and insights ...
Covid-19 understandi, 2020 ). A majority (86%) of the population in England and Wales identify. themselves as white and the remaining are Black, Asian and Minority. Ethnic (BAME) according to the ...
Search for more papers by this author. Darren Moore, Darren Moore. Graduate School of Education, University of Exeter, Exeter, UK. Search for more papers by this author. ... For example, a well-known UK mental health voluntary organisation refers to CYP's 'mental health and well-being' without details about their relationship (Young Minds ...
In 1948 the NHS was really a national physical health (and to a larger extent illness) service. It did inherit a national mental illness service (that huge population in the mental hospitals), but this was not well integrated and was largely hidden away from view. In subsequent efforts at integration, policy makers came to regard this decaying ...
Introduction. A major obstacle for integrating mental health initiatives into global health programmes and primary healthcare services is lack of consensus on a definition of mental health.1-3 There is little agreement on a general definition of 'mental health'4 and currently there is widespread use of the term 'mental health' as a euphemism for 'mental illness'.5 Mental health ...
Abstract. The purpose of this study is to map the literature on mental health and well-being of university students using metadata extracted from 5,561 journal articles indexed in the Web of Science database for the period 1975-2020. More specifically, this study uses bibliometric procedures to describe and visually represent the available ...
The success of your argumentative essay largely depends on the quality and uniqueness of the topic. Here are some exciting and intriguing mental health essay topics you can consider: The relationship between obesity and mental health. The relationship between teenagers and self-harm. How does a returning soldier deal with his mental health ...
The Mental Health Act is made up of different sections relating to treatment of mental patients against their will. The detention of such patients is also specified and the length of detention can range from 28 days (s.2) to six month (s.3) with the prospect of further renewals. We shall examine each section below.
National mental health charity: information, services & a strong voice for everyone affected by mental illness - challenging attitudes and changing lives. ... The first UK-wide mental health and money advice service dedicated to supporting people affected by mental health and money issues. Follow us: Modern Slavery Statement ...
It is an integral component of health and well-being that underpins our individual and collective abilities to make decisions, build relationships and shape the world we live in. Mental health is a basic human right. And it is crucial to personal, community and socio-economic development. Mental health is more than the absence of mental disorders.
The overall number of people reporting mental health problems has been going up in recent years. The amount of people with common mental health problems went up by 20% between 1993 to 2014, in both men and women . The percentage of people reporting severe mental health symptoms in any given week rose from 7% in 1993, to over 9% in 2014 .
Rates of several mental health conditions are on the rise in this group, especially in the US, but also in Australia, the UK and many other European countries.
Young people have been sharing their experiences of struggling with the pressures of finding housing, jobs and dealing with mental health. The latest data, external shows 28% of young adults aged ...
Reflective Essay on depression and mental illness. Depression is the commonest mental illness in the world yet only a few can tell you what exactly it is. Most people can well enough to recognise signs and symptoms of heart attack, diabetes, breast cancer and many more medical conditions. This statement is not only true for the general ...
Mental Health. How to practice self-compassion and build a stable sense of confidence, according to experts ... ©2024 Hearst UK is the trading name of the National Magazine Company Ltd, 30 Panton ...
Matthew Bradley is the headteacher and mental health lead at Newton Farm Nursery, Infant and Junior school in London. He talks about how the senior leadership team worked together to review and develop their approach to supporting mental health and wellbeing throughout the school. Mental health is an interesting and challenging problem for any ...
In this Papers Podcast, Maria Palma and Associate Professor Alice Goisis discuss their co-authored JCPP paper 'Medically assisted reproduction and mental health in adolescence: evidence from the UK Millennium Cohort Study'.
78% of UK employees have had work stress impact their physical health (Picture: Getty Images) ... 'By offering mental health or mental well-being days, we can help to reduce some of these ...
This publication provides the most timely statistics available relating to NHS funded secondary mental health, learning disabilities and autism services in England. This information will be of use ...
Mental illnesses linked to 'junk DNA' embedded with viruses inherited from our ancestors Mysterious genetic code now thought to trigger susceptibility to schizophrenia, bipolar disorder and ...