

Menstrual blood: no longer just a waste product
By Dr. Sara Naseri, Dr. Ryan Brewster and Professor Paul D. Blumenthal
For decades, glycated hemoglobin A1c (HbA1c) has been the diagnostic and prognostic standard for primary management of diabetes mellitus (DM). 1 It serves as an index of long-term glycemic control and a predictive indicator of preventable micro- and macrovascular complications, making routine monitoring an essential clinical practice. 2,3 To ensure timely therapeutic adjustments, guidelines advise biannual to quarterly HbA1c assessments, depending on the severity of the disease. Unfortunately, adherence to testing recommendations has been shown to be suboptimal. 4 Furthermore, the reasons for poor compliance are thought to be multifactorial, including logistical challenges and needle anxiety. Compared to men, women may face greater barriers to effective diabetes management, given known sex-based differences in cardiovascular risk factors, medication compliance, and access to treatment. 5
But what if there were another way to assess Hemoglobin A1C or for that matter, many other health markers that people, and particularly women, may benefit from knowing on a regular basis? One answer may lie in thinking about menstrual blood not just as a waste product, but rather as a clinical tool and a window into a variety of health or disease states. Indeed, menstrual blood is a complex fluid comprising whole blood, vaginal secretions, and cells of the uterine and cervical lining. To date, little is known about its characteristics at a molecular level. However, some recent analyses have revealed a profile similar to systemic blood, along with the presence of clinically-relevant indicators of uterine abnormalities. 6 A recent pilot study, for example, demonstrated high agreement between menstrual and systemic blood for common biomarkers. 7 HbA1c, among seven other biomarkers, was found to significantly correlate between the two sources. These results suggested that menstrual blood may be a safe, non-invasive, and cost-effective option for diagnostics, screening, and monitoring in women. Other preliminary work indicates that menstrual blood could also be leveraged in screening for HPV and other cancer biomarkers. 8
To assess this relationship more definitively, we performed a prospective, observational study to characterize the association between HbA1c levels measured in menstrual and systemic blood among diabetic and healthy women of reproductive age who regularly menstruate. The results of this project are now published in the BMJ-SRH. 9 One of the innovations applied here was the use of the the Q-Pad TM (Qurasense, Palo Alto USA), a modified menstrual pad containing a paper-based, dried blood spot (DBS) strip. The public might be most familiar with dried blood spots because they are commonly found at crime scenes and are often used to extract DNA and possibly lead to the identity of a perpetrator. DBS technology has been widely used for inherited metabolic disease screening in newborns and, more recently, in the measurement of numerous blood-based biomarkers, including HbA1c. 10-12 Importantly, the Q-Pad enables convenient (and non-messy!), acquisition and stabilization of menstrual blood specimens, which can then be sent to a lab for subsequent analysis.
In this project, 172 volunteers provided both menstrual blood and systemic blood specimens for analysis. And what did we find? Mean HbA1c levels were 6.53% for menstrual blood and 6.50% for systemic blood (Supplemental Table 2). There were no statistically significant differences in mean HbA1c between blood sources among the overall cohort (p=0.471) or among diabetic patients (p=0.272). When examining the data specifically among the diabetic women mean HbA1c levels in menstrual and systemic blood were not significantly different for patients with either type 1 (p=0.561) or type 2 (p=0.356) diabetes. In fact there was a “straight-line” relationship between Menstrual blood HbA1c and systemic blood HbA1c, meaning that in this study, the menstrual blood was really a window into the woman’s health!
Recent advances in self-care and point-of-care (POC) technologies highlight the advantages of more timely and convenient approaches to this kind of preventive screening 13 . This is particularly important for women, for whom the opportunity costs inherent in family and child-care responsibilities can make scheduling clinical appointments logistically challenging or inconvenient. It is also important to recognize novel uses of menstrual blood in the context of well-described gender disparities in diabetes management and outcomes 5 . Previous research indicates that women with diabetes experience disproportionately higher rates of cardiovascular complications and have poorer adherence to treatment regimens. 14-18 Based on our results, menstrual blood-based HbA1c monitoring could carry economic, clinical, and practical value analogous to POC testing.
Importantly, we found that the Q-Pad performed well with respect to sample acquisition, efficiency and processing. The DBS strip embedded in the Q-Pad was reliable for these purposes. With further validation, the Q-Pad has potential utility to facilitate further investigations and downstream clinical applications involving menstrual blood.
Of course, there are limitations to the present study. Menstrual and systemic blood specimens were subject to differential storage and transport conditions. An unbroken cold chain was maintained for serum samples, while the Q-Pad were left at ambient temperatures until processing. Further studies we will determine the possible effect of sample stability. Another limitation was that participants’ demographic information regarding race or ethnicity was not collected, which have shown to be important factors in HbA1c variability. 19 That said, there is little reason to suspect that menstrual or serum specimens themselves would behave differently by race or ethnicity.
In summary, leveraging the novel Q-Pad for self-collection, we found a high degree of concordance between HbA1c levels in menstrual blood and systemic blood in healthy and diabetic women of reproductive age. Future research is needed to establish menstrual blood-specific reference ranges for HbA1C and other biomarkers and more comprehensively assess both the user experience and the cost-effectiveness associated with Q-Pad usage. However, menstrual blood-based testing could become a safe, non-invasive, and potentially cost-effective alternative to conventional serum -based approaches to improve primary diabetes screening and management in women. More broadly, our findings open the possibility of transforming the significance of menstrual blood from a reproductive waste product to a valuable clinical tool with the potential to address sex-specific differences in healthcare access and outcomes and reduce menstrual stigma globally.
References:
- American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes—2018 . Diabetes Care 41 , S55–S64 (2018).
- Eberly, L. E., Cohen, J. D., Prineas, R., Yang, L., & Intervention Trial Research group. Impact of incident diabetes and incident nonfatal cardiovascular disease on 18-year mortality: the multiple risk factor intervention trial experience. Diabetes Care 26 , 848–854 (2003).
- Stamler, J., Vaccaro, O., Neaton, J. D. & Wentworth, D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care 16, 434–444 (1993).
- Lian, J. & Liang, Y. Diabetes management in the real world and the impact of adherence to guideline recommendations. Curr Med Res Opin 30, 2233–2240 (2014).
- The Lancet Diabetes & Endocrinology. Sex disparities in diabetes: bridging the gap. The Lancet Diabetes & Endocrinology 5, 839 (2017).
- Yang, H., Zhou, B., Prinz, M. & Siegel, D. Proteomic Analysis of Menstrual Blood. Molecular & Cellular Proteomics 11, 1024–1035 (2012).
- S, N., K, L. & Pd, B. Comparative Assessment of Serum versus Menstrual Blood for Diagnostic Purposes: A Pilot Study. Journal of Clinical and Laboratory Medicine 4, (2019).
- Wong, S. C. C. et al. Human Papillomavirus DNA Detection in Menstrual Blood from Patients with Cervical Intraepithelial Neoplasia and Condyloma Acuminatum. J. Clin. Microbiol. 48, 709–713 (2010).
- Naseri S, Brewster RCL, Blumenthal PD. Novel use of menstrual blood for monitoring glycaemic control in patients with diabetes: a proof-of-concept study. BMJ Sex Reprod Health. 2021 Nov 10:bmjsrh-2021-201211. doi: 10.1136/bmjsrh-2021-201211. Epub ahead of print. PMID: 34759003.
- Bhatti, P. et al. Blood spots as an alternative to whole blood collection and the effect of a small monetary incentive to increase participation in genetic association studies. BMC Medical Research Methodology 9, (2009).
- Mei, J. V., Alexander, J. R., Adam, B. W. & Hannon, W. H. Use of Filter Paper for the Collection and Analysis of Human Whole Blood Specimens. The Journal of Nutrition 131 , 1631S-1636S (2001).
- Parker, S. P. & Cubitt, W. D. The use of the dried blood spot sample in epidemiological studies. Journal of Clinical Pathology 52, 633–639 (1999).
- Schnell, O., Crocker, J. B. & Weng, J. Impact of HbA1c Testing at Point of Care on Diabetes Management. Journal of Diabetes Science and Technology 11, 611–617 (2017).
- Rust, G. et al. Point of care testing to improve glycemic control. International Journal of Health Care Quality Assurance 21, 325–335 (2008).
- Petersen, J. R. et al. Effect of Point-of-Care on Maintenance of Glycemic Control as Measured by A1C. Diabetes Care 30, 713–715 (2007).
- Raum, E. et al. Medication non-adherence and poor glycaemic control in patients with type 2 diabetes mellitus. Diabetes Research and Clinical Practice 97 , 377–384 (2012).
- Al-Salameh, A., Chanson, P., Bucher, S., Ringa, V. & Becquemont, L. Cardiovascular Disease in Type 2 Diabetes: A Review of Sex-Related Differences in Predisposition and Prevention. Mayo Clinic Proceedings 94 , 287–308 (2019).
- Siddiqui, M., Khan, M. & Carline, T. Gender Differences in Living with Diabetes Mellitus. Mater Sociomed 25 , 140 (2013).
- Herman, W. H. et al. Differences in A1C by Race and Ethnicity Among Patients With Impaired Glucose Tolerance in the Diabetes Prevention Program. Diabetes Care 30 , 2453–2457 (2007).
Read more: Novel use of menstrual blood for monitoring glycaemic control in patients with diabetes: a proof-of-concept study
Sara Naseri , MD is a native of Denmark and a graduate of Aarhus University. Her primary focus is on Women’s health and she is the founder of Qvin, a women’s health company focused on non-invasive health monitoring using menstrual blood.
Comment and Opinion | Open Debate
The views and opinions expressed on this site are solely those of the original authors. They do not necessarily represent the views of BMJ and should not be used to replace medical advice. Please see our full website terms and conditions .
All BMJ blog posts are posted under a CC-BY-NC licence
BMJ Journals
- Open access
- Published: 07 March 2022
Safety and efficacy study of allogeneic human menstrual blood stromal cells secretome to treat severe COVID-19 patients: clinical trial phase I & II
- Mina Fathi-Kazerooni 1 na1 ,
- Samrand Fattah-Ghazi 2 na1 ,
- Maryam Darzi 1 ,
- Jalil Makarem 2 ,
- Reza Nasiri 3 ,
- Faeze Salahshour 4 , 5 ,
- Seyed Ali Dehghan-Manshadi 6 &
- Somaieh Kazemnejad 1
Stem Cell Research & Therapy volume 13 , Article number: 96 ( 2022 ) Cite this article
3330 Accesses
24 Citations
10 Altmetric
Metrics details
Cell-free Mesenchymal stromal cells (MSCs) have been considered due to their capacity to modulate the immune system and suppress cytokine storms caused by SARS-CoV-2. This prospective randomized double-blind placebo-controlled clinical trial aimed to assess the safety and efficacy of secretome derived from allogeneic menstrual blood stromal cells (MenSCs) as a treatment in patients with severe COVID-19 .
Patients with severe COVID-19 were randomized (1:1) to either MenSC-derived secretome treatment or the control group. Subjects received five intravenous infusions of 5 mL secretome or the same volume of placebo for five days and were monitored for safety and efficacy for 28 days after treatment. Adverse events, laboratory parameters, duration of hospitalization, clinical symptom improvement, dynamic of O 2 saturation, lymphocyte number, and serial chest imaging were analyzed.
All safety endpoints were observed without adverse events after 72 h of secretome injection. Within 28 days after enrollment, 7 patients (50%) were intubated in the treated group versus 12 patients (80%) in the control group. Overall, 64% of patients had improved oxygen levels within 5 days of starting treatment ( P < 0.0001) and there was a survival rate of 57% in the treatment group compared to 28% in the control group was ( P < 0.0001). Laboratory values revealed that significant acute phase reactants declined, with mean C-reactive protein, ferritin, and D-dimer reduction of 77% ( P < 0.001), 43% ( P < 0.001), and 42% ( P < 0.05), respectively. Significant improvement in lymphopenia was associated with an increase in mean CD4 + and CD8 + lymphocyte counts of 20% ( P = 0.06) and 15% ( P < 0.05), respectively. Following treatment, percentage of pulmonary involvement showed a significant improvement in the secretome group ( P < 0.0001). This improvement differed significantly between survivors and those who were dying ( P < 0.005).
Conclusions
For the first time, this study demonstrated that in hospitalized patients with severe COVID-19, therapy with MenSCs-derived secretome leads to reversal of hypoxia, immune reconstitution, and downregulation of cytokine storm, with no adverse effects attributable to the treatment. Given these outcomes, it may be possible to use this type of treatment for serious inflammatory lung disease with a mechanism similar to COVID-19 in the future. However, it is necessary to evaluate the safety and efficacy of MenSCs-derived secretome therapy in clinical trials on a larger population of patients.
Trial registration : ClinicalTrials.gov Identifier: NCT05019287. Registered 24AGUEST 2021, retrospectively registered, https://clinicaltrials.gov/ct2/show/record/NCT05019287 . IRCT, IRCT20180619040147N6. Registered 04/01/2021.
Introduction
In late 2019, a new viral illness caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) began in China and quickly became a global pandemic [ 1 ]. To date, efforts have been made to treat acute respiratory distress syndrome (ARDS) caused by Coronavirus disease 2019 (COVID-19) with non-invasive supplemental O 2 and delay the intubation as long as possible. Several studies have demonstrated that in this group of patients, early therapeutic intervention may reduce the risk of developing the disease into hypoxia, which requires intubation and mechanical ventilation and is associated with a mortality rate of approximately 67–94% [ 2 , 3 , 4 ]. Available evidence suggests that uncontrolled excessive production of soluble inflammatory markers induces a “cytokine storm” playing a key role in the development of COVID-19ARDS [ 5 ]. In both types of classic ARDS and COVID-19ARDS, there are noticeable levels of pro-inflammatory biomarkers, increased capillary endothelial permeability, and a rise in inflammatory cells counts in the vascular and alveolar compartments [ 6 ]. Nevertheless, there are significant differences in the type of enhanced markers, so that less expression of IFNs and increased thrombotic mediators occurred in COVID-19 ARDS compared to classical ARDS [ 6 , 7 ]. High levels of pro-inflammatory cytokines such as interleukin (IL)-1β, IL-2, IL-6, IL-7, IL-8, IL-17, and tumor necrosis factor-α (TNF-α) have been reported in the serum of patients with severe COVID-19, which is associated with mortality risk [ 8 ]. Many scientists and researchers are now attempting to identify the most effective drug or combination against the disease in the context of randomized clinical trials. At present, several agents such as antivirals (including remdesivir), hydroxychloroquine, monoclonal antibodies, antisense RNA, corticosteroids, anticoagulants, and convalescent plasma are being assessed [ 9 , 10 ]; however, the efficacy of some of them, such as chloroquine or its hydroxyl analogue in treating this disease, is debatable in various studies [ 11 ]. In addition to these drug therapies, the use of MSC treatment because of its properties as adjunctive therapy has been considered by researchers in preclinical studies of lung diseases [ 12 , 13 ]. In several animal models of ARDS, demonstrated that paracrine release of different soluble products by MSC could induce anti-inflammatory, immunomodulatory, and anti-apoptotic effects, improve epithelial and endothelial cell recovery, enhance microbial and alveolar fluid clearance, and prevent tissue fibrosis thus resulting in improved lung and distal organ function and survival [ 14 , 15 , 16 , 17 ]. Furthermore, this type of cell therapy has been safe and effective in early-stage clinical trials. Despite limitations such as small sample sizes, heterogeneity of source, dose, route, and frequency of MSC administration, these clinical studies showed that MSC administration was safe and well tolerated and, in most cases, resulted in an improved hemodynamic and respiratory state associated with a reduction in pulmonary and systemic inflammatory biomarkers [ 18 , 19 , 20 , 21 , 22 ]. On the other hand, derivatives of these cells, including cell secretome with unique properties, have been evaluated in some studies [ 23 , 24 , 25 ]. The secretome of MSC is a complex mixture of soluble protein products consisting of growth factors, cytokines, microvesicles, and exosomes [ 26 ]. Trophic factors in the MSC secretome include tumor growth factor (TGF)-β, hepatocyte growth factor (HGF), vascular endothelial growth factor (VEGF), leukemia inhibitory factor (LIF), epidermal growth factor (EGF), nerve growth factor (NGF), Prostaglandin (PG) E2, interleukin-1 receptor antagonist (IL-1Ra), Metalloproteinase-processed-C motif chemokine ligand2 (mpCCL2), and brain-derived neurotrophic factor (BDNF) [ 27 , 28 , 29 ]. Because the soluble factors secreted by the MSCs appear to repair tissue damage, reduce inflammation, and increase tissue repair capacity, the current vision using cell-free strategies such as that proposed by the MSC secretome offers key benefits on cell transplantation [ 11 ]. The major advantage of using cell-free strategies is due to the ability of these products to exert similar effects of those from parental cells without a potential risk of immunogenicity (graft versus host disease [GvHD], for instance). Another important advantage of cell-free strategies is that the cells may form clusters and lead to thromboembolic events, which are especially important in dealing with people with severe COVID-19. Other benefits of using MSC-based cell-free derivatives include no worries about cell survival after transplantation, lower levels of cell surface protein expression, less immunity, and no need for large numbers of cells for injection (1 × 10 6 cells/kg/dose) and ultimately easier, more convenient and more cost-effective mass production with the possibility of monitoring the safety, effectiveness and dosage of the final product like conventional drugs [ 30 ]. Several preclinical studies have shown that MSC-secreted extracellular vesicles (EVs) function similarly or even more effectively than mesenchymal stem cells themselves in controlling of lung injury caused by inflammation [ 31 , 32 ]. These EVs are about 30–170 nM in size that express CD81, CD63, and tumor susceptibility gene (TSG) 101 [ 33 , 34 ].
Based on current knowledge about the therapeutic properties of MSC derivatives on inflammatory lung disease, an increasing number of experimental studies have examined the effectiveness of MSC-based cell-free products in COVID-19 patients in order to find an effective treatment to control severe inflammation in patients [ 35 ]. According to the data, we hypothesized MSC-derived secretome can be a new next-generation, multitarget biological agent that could be the key to cytokine storm regulation and the reversal of host antiviral defenses associated with COVID-19.
Among the different types of MSCs, menstrual blood-derived stromal cells (MenSCs) have been considered in numerous pre-clinical and clinical studies including treatment of pulmonary diseases in recent decades because of their unique characteristics, such as high proliferation rate, low immunogenicity, and non-invasive periodical collection [ 36 , 37 , 38 , 39 ]. Earlier studies conducted on the secretome content of MenSCs by this group within parallel with other groups demonstrated that these cells secrete plenty of bioactive molecules, especially anti-inflammatory interleukins and cytokines, growth factors and EVs [ 39 , 40 ] which proposes the potential effect of MenSCs derived secretome in treatment of various diseases and disorders including inflammatory and pulmonary diseases [ 41 ]. Therefore, this study focused on the compatibility of these cells in the treatment of COVID-19 patients. MenSC-derived secretion was tested for sterility and prepared in facilities that comply with current Good Manufacturing Practices (cGMP) and then was administered to 14 patients with severe Covid-19 pneumonia. After injecting five doses of MenSC-derived secretion intravenously, the safety of this type of treatment in patients was assessed by evaluating perfusion reactions and any side effects. The efficacy of secretome injection was also evaluated by assessment of overall condition, as demonstrated by blood oxygen saturation and oxygen requirements, degree of inflammation, and immunocompetence, indicated by levels of C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, ferritin, and cell counts of the cluster of differentiation (CD)4 + and CD8 + T lymphocytes.
Materials and methods
Trial design.
The patients were enrolled in Phase I and II randomized controlled clinical trial for evaluation of the safety and efficacy of infusions of secretome derived from the MenSCs. All patients with severe pneumonia due to COVID-19 were admitted to the intensive care unit (ICU) at the Imam Khomeini Hospital Complex from April 17 to June 7, 2021.
Written informed consent was obtained following the initial consultation with the patient. All the procedures in this clinical trial study were conducted according to Good Clinical Practice (GCP) or GMP guidelines approved by the Biomedical Research Ethics Committee of Academic Center for Education, Culture, and Research (ACECR) (Code:IR.ACECR.REC.1399.005). The study was registered at the Iranian Registry of Clinical Trials (IRCT20180619040147N6) and the cell manufacturing was performed by Zayabiotech Company (Tehran, Iran) in GMP cleanroom authorized by Iran food and drug administration authorities.
Participants
Subjects diagnosed with COVID-19 ARDS were eligible for inclusion if they met the eligibility criteria. The inclusion criteria were age 25–75 years, positive result on SARS-CoV-2 polymerase chain reaction (PCR), RR > 30 times/min, resting oxygen saturation of 90% or less, arterial partial pressure of oxygen/oxygen concentration ≤ 300 mmHg, and pulmonary infiltration greater than 50% in 24–48 h. Exclusion criteria were pregnancy or breastfeeding, history of drug reactions, pneumonia caused by bacteria, Mycoplasma, Chlamydia, Legionella, fungi or other viruses, airway obstruction due to lung cancer or unknown factors, Carcinoid syndrome, long-term use of immunosuppressive drugs, hemodialysis or peritoneal dialysis, creatinine clearance < 15 mL/min, moderate to severe liver disease (Child–Pugh score > 12), deep vein thrombosis (DVT) or pulmonary embolism over the past 3 years, being under high-frequency oscillatory ventilation support (ECMO),and patients with HIV, hepatitis B virus, or hepatitis C virus infections. All patients were already initiated on remdesivir, corticosteroid, and anticoagulants.
Randomization
A total of 36 patients were considered for eligibility; 30 patients who met the acceptance criteria were randomized 1:1 to receive either MenSCs-secretome ( n = 15) or the control (injectable normal saline) ( n = 15) (Fig. 1 ).In this study, a simple computer-assisted randomization method was used, in which a computer-generated list of numbers from 1 to 30 was prepared. Depending on the time of hospitalization, one of these numbers has been allocated to the patient, and based on the created list; patients were assigned to the treatment and control groups.
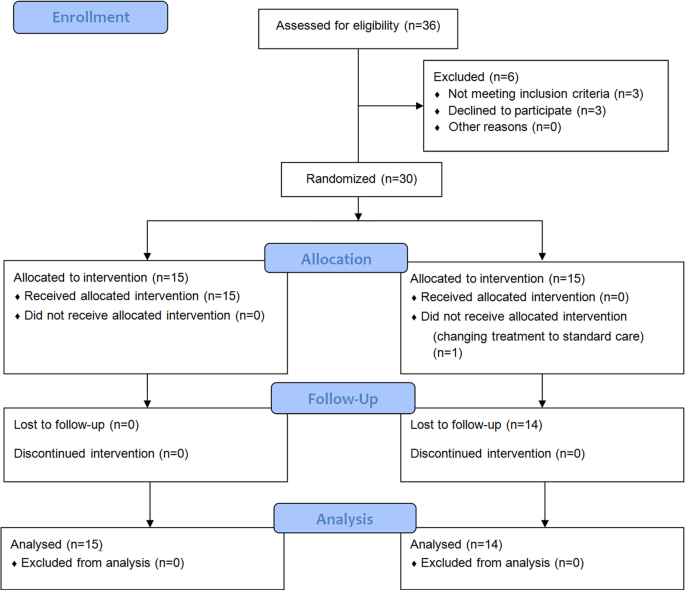
Flow diagram showing enrollment, allocation, follow up and analysis of patients
The study was double-blinded: the patients and the data analysts were blinded to group assignment.
MenSC-derived secretome investigational product
MenSCs were manufactured as previously described [ 37 ]. MenSCs were culture-expanded from a previously established and characterized master cell bank (MCB) derived from the menstrual blood collected from at least 5 healthy women [ 37 ]. The quality of the MenSCs stored in the bank was tested according to the applicable U.S. Food and Drug Administration (FDA) regulations for fungal and bacterial contamination using sterility by direct inoculation, mycoplasma assay by both culture and PCR (complaint with USP chapter 〈63〉 Mycoplasma Tests), endotoxin test (according to USP chapter 〈85〉 Bacterial Endotoxins Test), karyotyping with routine G-banded chromosomes analysis, and immunophenotyping assessment through expression analysis of CD73, CD44, CD90, and CD45.
In preparation for infusion, frozen MenSCs were quickly thawed and cultured up to 70% confluence in Dulbecco's Modified Eagle Medium/Nutrient Mixture F-12 (DMEM-F12) containing platelet lysate (PL). The medium was discarded and, following three washes with phosphate-buffered saline (PBS), the cells were incubated with red phenol-free DMEM-F12 at 5% CO 2 at 37 °C for 48 to 72 h. After that, the supernatant was aspirated, pooled, and sterile filtered through a 0.2-μm syringe filter (Membrane Solutions) and centrifuged at 2000 rpm for 5 min at RT. Finally, the supernatant was aspirated (soluble fraction) and packed in 5 mL microtubes.
Interventions
Subjects in the MenSC-derived secretome treatment group ( n = 14) received five intravenous infusions of 5 mL of MenSCs-derived secretome diluted in 100 mL of normal saline for 5 consecutive days for 60 min. The control group received five infusions of 100 mL of normal saline for 5 consecutive days. The best standard of care was provided in both groups, consistent with current institutional COVID-19 guidelines.
Assessments
Before starting the first infusion, the basic parameters including the following experiments were measured: CBC, PT/INR, LFT, ESR, CRP, ferritin, D-dimer, T lymphocyte panel, chest Computed tomography (CT)-scan, and ECG. During the injections and 1 h later, vital signs were recorded under the ICU standard protocol. Laboratory collection and clinical assessment were performed before each infusion and repeated daily up to 28 days following treatment or until the last day of hospitalization. The primary endpoint of the trial was safety: adverse events within six hours; cardiac arrest or death within 24 h of every infusion. Secondary endpoints included patient survival at 28 days after initial infusion and time to recovery.
Peripheral blood CD4 and CD8 markers were tested using flow cytometry procedure. Briefly, 100 µL of whole blood was poured into three separate test tubes, each containing 10 µL of Anti-Hu CD4 PE (Exbio, Czech Republic), CD8 FITC (Exbio, Czech Republic), and Anti-Hu antibodies. CD45 PerCP (Cytognos, Spain) was mixed well and incubated at room temperature for 30 min. The red blood cells were lysed using RBC lysis buffer solution (APRAD, Iran) for 5 min at 300 g. The supernatant was then discarded, and the cells were suspended with 0.3–0.5 mL PBS. The samples were immediately read using flow cytometry (SysmexPartec Pas III, Germany).
For evaluation of pulmonary involvement, chest CT scan images were obtained at the time of admission and discharge, lying on the back and fully inspired without contrast. Chest CT scan findings were recorded according to the Fleischner Society glossary and published literature on viral pneumonia [ 42 ]. Chest CT scan features included (a) predominant pattern: ground-glass opacification/opacity (GGO), consolidation, or mixed; (b) dominant distribution pattern: peripheral (peripheral one-third of the lung)/pleural based, peripheral/pleural sparing, axial (medial two-thirds of the lung), or diffuse; (c) the number of involved lobes; (d) other morphologies: crazy paving, reverse halo sign, intralesional traction bronchiectasis, parenchymal band, and Mesh-like opacity; and (e) additional findings: underlying pulmonary diseases such as bronchiectasis, emphysema, interstitial lung disease, cardiomegaly, pleural effusion (unilateral or bilateral), subsegmental atelectasis, mediastinal or hilar lymphadenopathy, pericardial effusion, and pleural thickening.
Statistical analysis
The study population consisted of all patients who had received all their treatment doses and whose clinical information was available for at least 10 days after starting treatment. The frequency tables were used to describe the individual data. Before and after treatment datasets were evaluated in each group using a paired t test analysis in GraphPad PRISM 6.0. Analysis of one variable at several intervals was performed by repeated-measures ANOVA test. Comparison between control and intervention groups was performed using an unpaired t test. The Kaplan-Meyer curve was used for survival analysis.
Baseline patient characteristics
Table 1 summarizes basic demographic and clinical characteristics for patients. 9 men and 6 women in the intervention group and 10 men and 5 women in the control group were enrolled in the study. One patient in the intervention group discontinued the study after receiving a dose of the secretome. In the intervention group, type 2 diabetic patients comprised 21.5% of the population whereas hypertension comprised 28.5%. In contrast, in the control group, 26.6% of patients had diabetes type 2 and 33.3% of patients had hypertension.
No allergic reactions to the injection or side effects were observed within the first five days of the treatment. Furthermore, no adverse effects attributed to the effects of secretome infusion were reported during the 28-day follow-up of patients. Side effects over the 28-day follow-up period include aggravating hypoxic respiratory failure requiring intubation ( n = 7), pulmonary embolism ( n = 3), myocardial infarction ( n = 1), sepsis ( n = 1), and death ( n = 6) that all these deaths occurred in intubated patients. After assessing the cause of death and the time interval of deaths from the time of injection, all events were logically related to the progression of COVID-19 disease and were not directly related to this type of treatment.
General clinical implications
The survival rate in this study was 57% in the intervention group and 20% in the control group, which differed significantly ( P < 0.001) as shown in the Kaplan Meyer diagram (Fig. 2 ). In total, all non-intubated patients, who constituted 50% of the patients, all improved (7/14) and were discharged from the hospital after an average of 12.3 ± 3.68 days after the first dose infusion. In total, 50% of patients with higher disease severity or underlying diseases, especially diabetes type 2, needed intubation and mechanical ventilation, one of whom was extubated and released and six died. By comparison, in the control group, out of 15 patients, only 3 patients recovered and were discharged from the hospital after a mean of 17.0 ± 4.35 days after the start of the intervention.
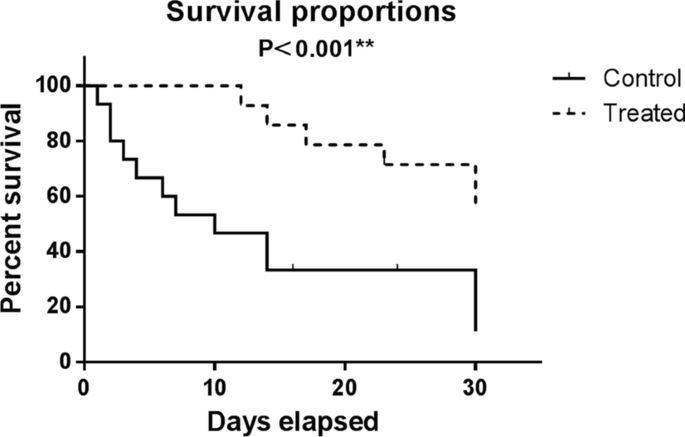
Kaplan–Meier survival curves for overall survival in control and treated groups which showed that the difference in survival rate between these two groups was statistically significant ( P < 0.001)
Oxygenation
Oxygenation was assessed by calculating the percentage of SpO 2 at room temperature, and then with oxygen support as well as tracking the oxygen demand first, on the days of the infusion and 28 days after the infusion of the first dose. Overall, 64% of patients had improved oxygen levels within 5 days of starting treatment. The average increase in the percentage of oxygenation from the beginning to the 14th day after the start of treatment or the last day of hospitalization was 21.3% ( P < 0.0001).
Laboratory data
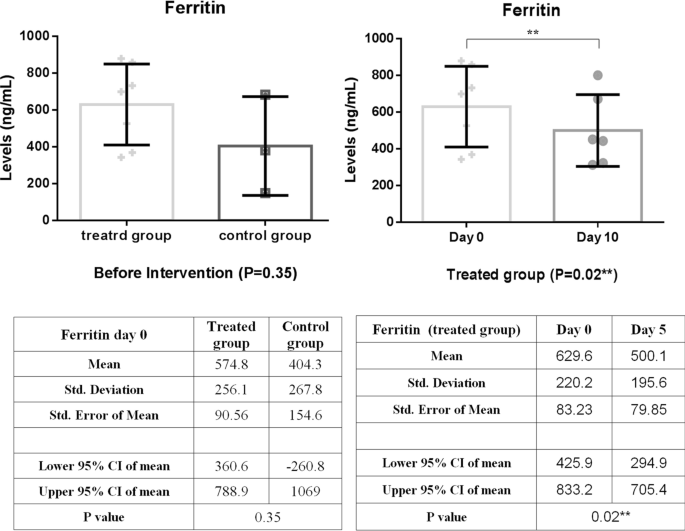
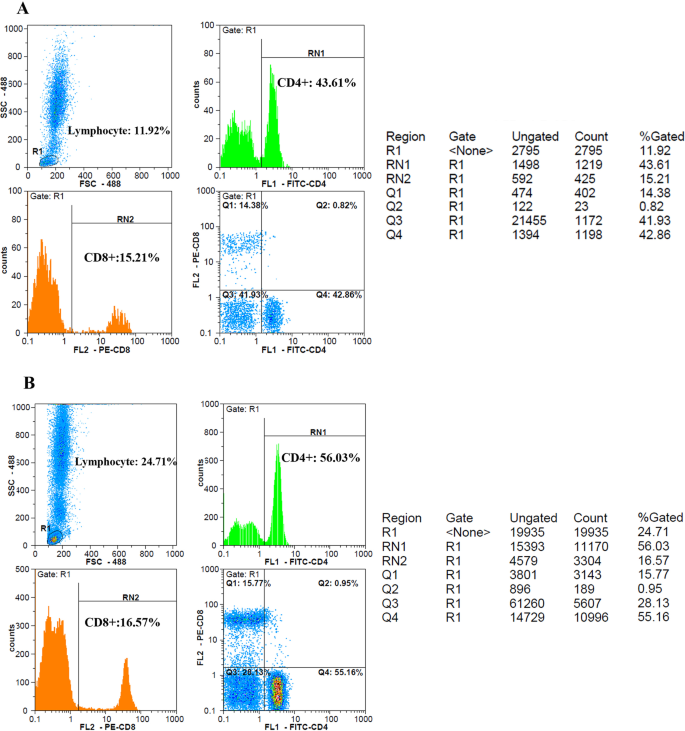
In comparison, between intervention and control groups, there was a significant reduction in CRP levels over the first five days of treatment, as shown in Fig. 3 ( P = 0.03). In addition, the CRP level of the intervention group decreased significantly ( P = 0.01) during the follow-up period with small fluctuations (Fig. 3 ). As shown in Fig. 4 , LDH concentration decreased more slowly than those of CRP in the treated group; as a result, a statistically significant decrease in LDH level was observed 10 days post-treatment ( P < 0.001). A similar reduction in D. Dimer level was observed in the intervention group within 5 days of treatment (Fig. 5 ). The decrease in serum ferritin concentration was the lowest among the serum markers in the treated group; a notable decrease in ferritin concentration occurred after 10 days, as shown in Fig. 6 ( P = 0.02). There was an increase in the number of lymphocytes including subsets staining positive for CD4 + and CD8 + on flow cytometry compared to baseline values with 10 days post secretome treatment, which is a statistically significant increase in the number of CD8 + lymphocytes ( P = 0.03, Fig. 7 ).
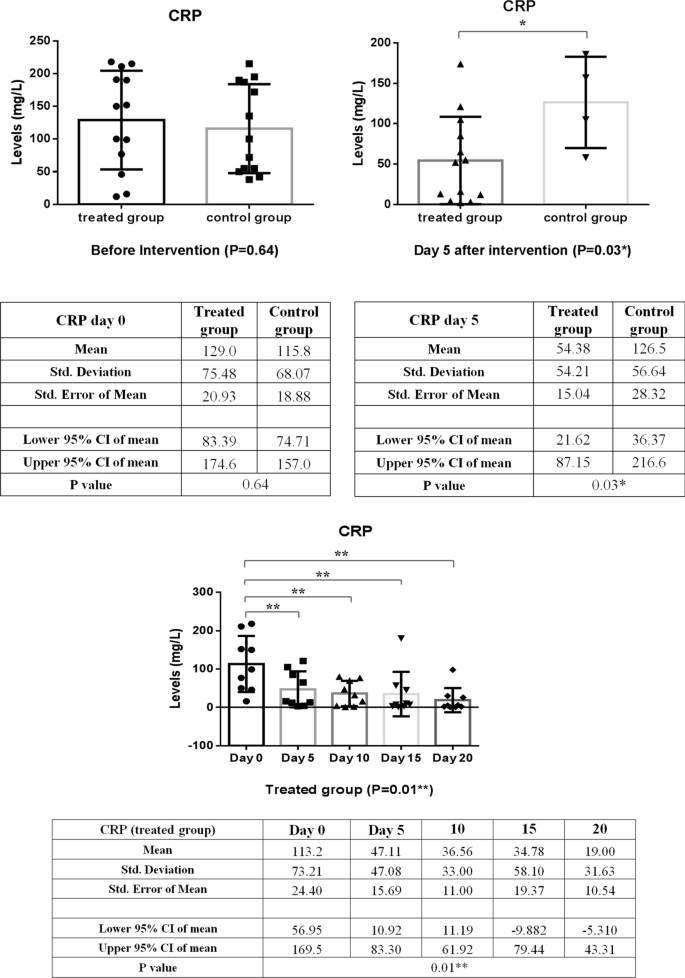
Change in acute phase reactant (CRP) levels before and after of secretome administration. Mean reduction of CRP in treated group was 77% ( P < 0.001)
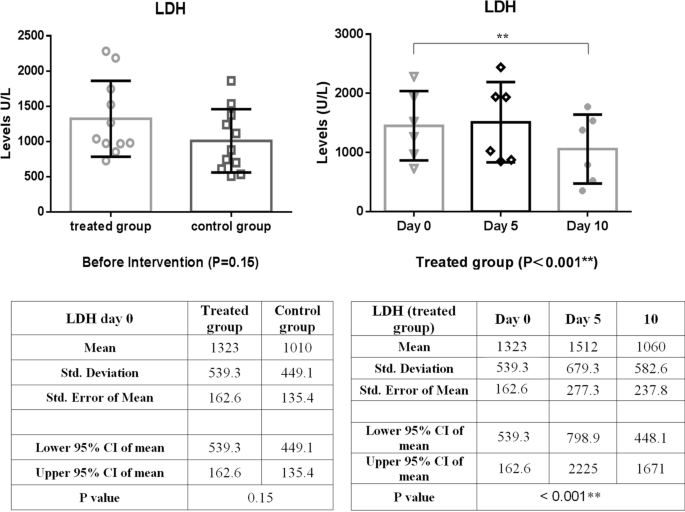
Decreasing trend of LDH level in the treated group within 10 days of starting treatment. A significant decrease in LDH levels was observed 10 days post-treatment ( P < 0.001)
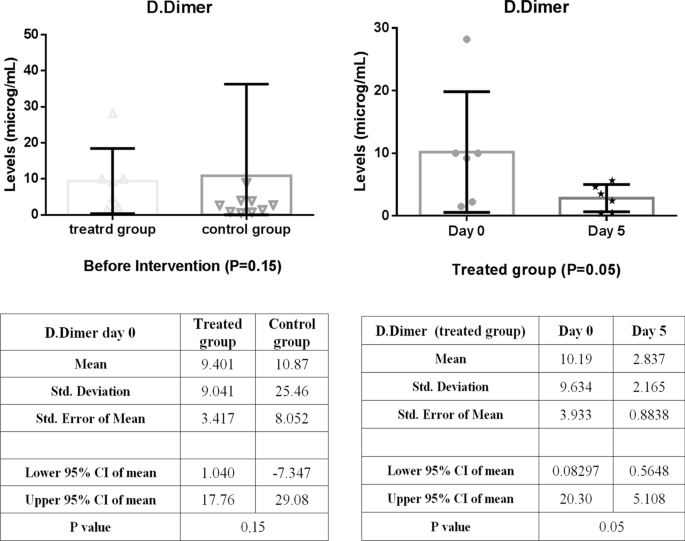
Decreasing trend of D.Dimer level in the treated group within 5 days of starting treatment. Mean reduction of D-dimer in treated group was 42% ( P < 0.05)
Decreased trend of ferritin level in the treated group within 5 days of starting treatment. Mean reduction of ferritin in treated group was 43% ( P < 0.001)
Flow cytometry gating strategy for CD4 + and CD8 + cells. Lymphocytes were first identified by R1 gate in forward scatter (FSC) and side scatter (SSC) graph. CD4 + and CD8 + T cells were then measured by means of anti CD4 and anti CD8 antibodies, labeled by FITC and PE respectively; as illustrated in the histogram graphs separately. A and B represent the changes in CD4 + and CD8 + lymphocyte counts between 5 and 10 days after secretome administration in a 35-year-old male patient, respectively
At the time of recruitment, a total of 28 CT scans [14 for the treated group and 14 for the control group] were performed. The most common finding was GGOs, appearing in 85.8% of the treated group and 66.7% of the control group ( P = 0.55), followed by consolidation in 2 patients (25.7%) in the first group and 1 patient (34.6%) in the second group ( P = 0.33). The dominant diffuse distribution was noted in 85.8% of patients of the treated group and 83.3% of patients of the control group ( P = 0.89). The crazy paving sign was observed in 78.6% of patients of the intervention group and 86.7% of patients of the control group ( P = 0.56). Parenchymal bands (57.1% vs. 40.0%, P = 0.36), bronchiectasis (12.3% vs. 20.0%, P = 0.74), subsegmental atelectasis (28.6% vs. 46.6%, P = 0.51), target sign (14.3 vs. 33.3, P = 0.23), and air bronchogram (14.3% vs. 40.0%, P = 0.12) were reported in treated and control group, respectively. Other findings include mosaic pattern, pulmonary emphysema, centrilobular nodules, bronchogenic carcinoma, peribronchial thickening, interlobular septal thickening, cavity, mediastinal lymphadenopathy, halo sign, alveolar collapse, pulmonary embolism, and infarction were seen neither in the treated nor in the control group.
At the outset of the study, there was no significant difference in the percentage of pulmonary involvement between the intervention and control groups (72.6 ± 11.3 vs. 66.8 ± 9.9, P = 0.33). However, following treatment, this rate showed a significant improvement in the MenSCs-derived secretome group (72.6 ± 11.3 vs. 28.7 ± 6.9, P < 0.0001) (Fig. 8 ). This improvement varied considerably between survivors and those dying (28.7 ± 6.9 vs. 46.7 ± 11.7, P = 0.002) (Fig. 9 ). Chest CT images of the two COVID-19 patients are demonstrated in Fig. 8 .
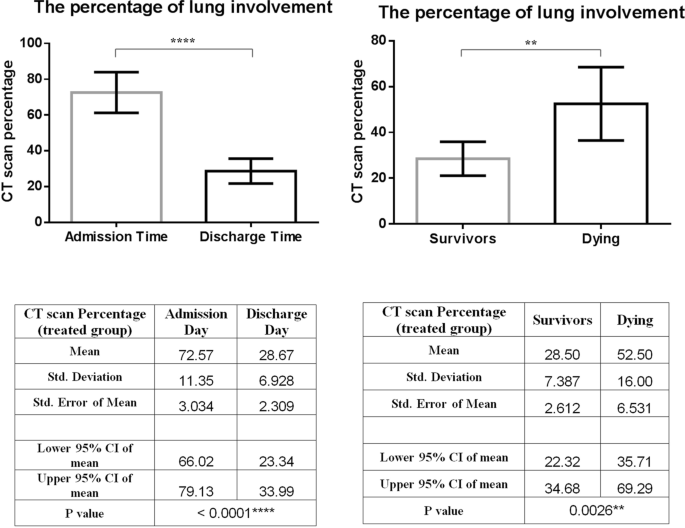
Change in the CT scan percentage of lung involvement before and after of secretome administration. This treatment significantly improved the lung involvement of patients when they were discharged from hospital. Furthermore, this effect was completely different in both groups of surviving and dying patients
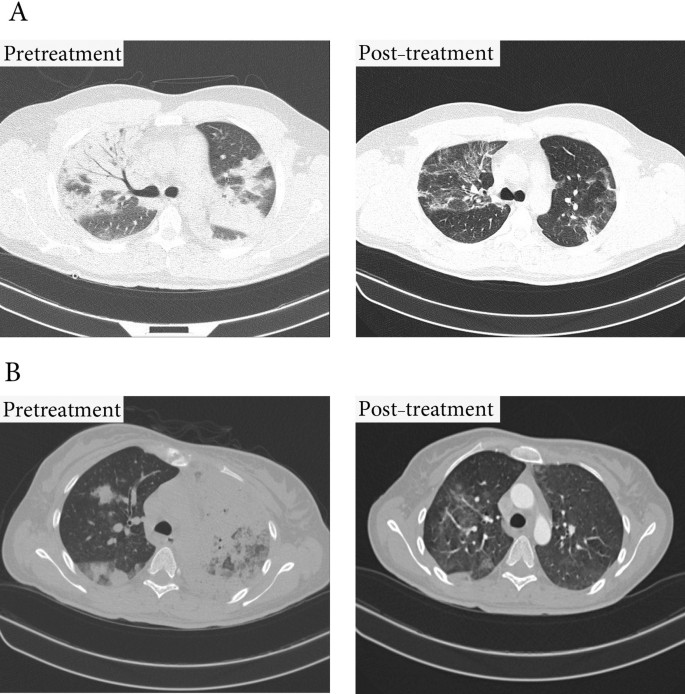
Lung CT scan. A Significant improvement in lung lesions within 10 days of starting treatment in a 37-year-old male patient B Significant improvement in lung lesions within 5 days of starting treatment in a 45-year-old female patient
The results of this prospective, double-blind clinical trial in patients with severe COVID-19 have demonstrated that the secretome of menstrual blood stromal cells can be safely administered by intravenous injection. In none of the patients, the injection of this cell-free product resulted in infusion reactions. We received no reports of immediate (< 6 h), intermediate (< 24 h), or delayed (< 72 h) adverse reactions. A review of adverse events after this period revealed that there was no association between the occurrence of these accidents and the therapeutic intervention of this product.
Reports of ICU mortality due to COVID-19 around the world showed that more than 70% of the patients with criteria of severe pneumonia will be intubated and need mechanical ventilation support [ 43 , 44 ], which will be associated with 50–97% mortality [ 1 ]. On the other hand, the risk of mortality in patients requiring noninvasive oxygen support is estimated as high as 60–79% [ 3 , 45 ]. Based on this data, along with the condition of our patients, we expected that most patients would require intubation within 24 to 48 h if treatment was not initiated. But evidence has shown that with the onset of treatment, only half of the 14 patients reached this stage. It can therefore be concluded that the use of the secretome can play a preventative role in the progression of the disease toward the need for invasive oxygen support and mechanical ventilation, although further studies at subsequent stages of this randomized controlled trial are necessary to prove efficacy. A total of 57% of treated patients (8/14) recovered, suggesting a profound reversal of disease progression and indicating the optimal time for administration of the MenSCs secretome is the early phase of the cytokines storm. Overall, treatment with this cell-free product has been linked to a significant 29% improvement in patient oxygenation ( P < 0.0001) and demonstrated a reduced need for oxygen support within 48–72 h of commencing treatment.
It should be noted that even in patients who eventually died in this study, several clinical parameters, including oxygenation and inflammatory markers, showed the optimal initial response to the injection, indicating the greatest reduction in the severity of inflammation following the third injection. This may suggest that booster doses may be necessary for these patients to achieve the desired anti-inflammatory response. Perhaps the short half-life of the secretome components [ 30 ] and the over-activity of the inflammatory system in these critically ill patients may be a justification for the need to infuse higher doses of this drug. However, in preclinical studies of exosome-based therapies, Evidence has been obtained of the alignment of the effect of circulating proteases on the inactivation of exosomal products at intervals from the time of injection [ 46 ].
In this study, changes such as a significant increase in the number of CD4 + and CD8 + T cells were observed, which led to a decrease in lymphopenia in patients, as well as a significant reduction in all acute inflammatory factors of serum and optimal improvement of pulmonary inflammation in patients. Infiltration of radiological images showed that, as expected, modulation of the hyperactive immune system is the most important mechanism of action of this cell-free treatment.
Exact mechanisms underlying efficiency of MenSCs derived secretome are not clear. However, it could be attributed to anti-inflammatory, anti-apoptotic and anti-fibrotic effects of the cytokines, interleukins, growth factors and EVs in the administrated secretome. In our study, to determine the underlying mechanisms of the proliferation of natural killer cells (NK) as a result of co-culture with MenSCs, relative concentrations of 41 different growth factors, their receptors, and binding proteins in the MenSCs secretome were tested using membrane-based antibody array. We have demonstrated that MenSCs secrete a large quantity of growth factors including EGF, fibroblast growth factor (FGF), platelet-derived growth factor (PDGF), TGF-β, VEGF, HGF, insulin-like growth factor (IGF)-1, and angiopoietin-1, which are essential components for immunoregulation and tissue repair by MenSCs [ 47 ]. Also, in an unpublished study conducted by this team, a comparison between the secretome content of MenSCs and BMSCs by Western blotting showed that MenSCs produced comparable amounts of HGF, VEGF, Stromal cell-derived factor (SDF)-1, Hypoxia-inducible factor (HIF)-1α, IL-1β, Angiopoietin (ANG)-1, and ANG-2 compared to the BMSCs. In this way, significantly higher levels of VEGF and HIF-1α and lower levels of IL-1β were found in the MenSCs secretome. Moreover, the MenSCs derived secretome contains lots of small EVs consisting of regulatory proteins, RNAs, and DNAs, lipids, and signaling peptides promoting regenerative repair of different tissues in various diseases including inflammatory diseases [ 48 ]. The secretome of endometrial-derived mesenchymal stromal cells contains about 900 proteins which 617 proteins are involved in activating various complement components, regulation of adaptive and innate immune reactions, antigen presentation, negative control of apoptosis, and different signaling pathway [ 49 ]. It consists certain functional immunomodulatory proteins such as colony-stimulating factor-1, PYCARD (PYD and CARD domain), and endoplasmic reticulum aminopeptidase 1 (ERAP1) that modulate immune reactions in interferon (IFN)-γ primed MenSC-derived small EVs [ 45 ]. Based on the studies, following the MenSCs license with pro-inflammatory cytokines such as IFN-γ modulations, the cargo of EV proteins was changed and the antigens processing and the presenting proteins and miRNA were increased. High levels of ICAM-1, angiogenin, angiopoetin-2, osteoprotegerin, and IL-8 have also been found in the EVs of MenSCs.
In a recent study, safety and efficacy of administration of exosomes from allogeneic BMSCs (ExoFloTM) in a small and non-randomized cohort study of patients with severe COVID-19 have been examined. This MSC-based cell free product demonstrated a good safety profile with no adverse events and was able to restore oxygenation, downregulate cytokine storm, and improve the biomarkers associated with inflammation [ 50 ]. We have shown that BMSCs and MenSCs secretome contained comparable amounts of growth factors and soluble growth factor receptors except for β-Nerve Growth Factor (NGF), VEGF-A, Insulin-like growth factor binding proteins (IGFBP)-1, IGFBP-2, IGFBP-3, and IGFBP-4 [ 46 ]. Due to some common secretory factors, close response of these two stem cells type (BMSCs and MenSCs) in therapeutic strategies is expected, while some differences observed in improvement levels of patients could be rationalized by the discrepancy in levels of mentioned growth factors in the secretome of these stem cell sources. Nevertheless, differences in age and condition of stem cells donors, dose and protocol of secretome preparation and administration procedure and route should not be ignored.
This is the first known clinical study to date using MenSCs-derived secretome as treatment of patients with severe COVID-19 pneumonia. Despite the significant advantages of stem cell secretome derivatives compared to stem cell, including greater ease of production and storage, and longer shelf life of the product, the lack of regulatory requirements related to manufacturing and quality control, along with the lack of familiarity of many physicians with this type of products has caused, despite having many capabilities to use them in many limited cases.
This study showed that the injection of MenSCs secretome was safe and well-tolerated by severely ill patients. Evaluation of the effectiveness of this treatment depicted that injecting five consecutive doses of MenSCs secretome, improved hypoxia, and pulmonary involvement, restored immune system function, and controlled cytokine storm in critically ill patients and hospitalized in the ICU. Given the mechanism of action of this type of treatment, MSC-derived secretome would be a feasible therapeutic strategy for the inflammatory state; however, it would be better if therapy was performed before this phase in order to prevent or alleviate multiorgan failure. Finally, we hope that the results of this study provide a new perspective on the use of menstrual blood stromal cell secretions in the treatment of many inflammatory processes such as ARDS, chronic obstructive pulmonary disease, sepsis, autoimmune diseases, and cancer [ 51 , 52 , 53 , 54 , 55 , 56 ]. Further clinical trials are necessary to examine safety and efficacy.
Availability of data and materials
All of the data generated and analyzed during this study are included in our manuscript.
Abbreviations
Mesenchymal stromal cells
Menstrual blood Stromal Cells
Severe acute respiratory syndrome coronavirus 2
Acute respiratory distress syndrome
Interleukin
Tumor necrosis factor-α
Tumor growth factor
Hepatocyte growth factor
Vascular endothelial growth factor
Leukemia inhibitory factor
Epidermal growth factor
Nerve growth factor
Prostaglandin
Interleukin-1 receptor antagonist
Metalloproteinase-Processed-C motif chemokine ligand2
Brain-derived neurotrophic factor
Graft versus host disease
Extracellular vesicle
Bone marrow
Fibroblast growth factor
Platelet-derived growth factor
Stromal cell-derived factor
Hypoxia-inducible factor
Angiopoietin
Endoplasmic reticulum aminopeptidase
Intercellular adhesion molecule
Natural killer
Insulin-like growth factor binding proteins
Current good manufacturing practices
C-reactive protein
Lactate dehydrogenase
Cluster of differentiation
Intensive care unit
Good clinical practice
Master cell bank
Food and drug administration
Polymerase chain reaction
Deep vein thrombosis
Dulbecco's modified eagle medium/nutrient mixture F-12
Platelet lysate
Phosphate-buffered saline
Complete blood count
Prothrombin time and international normalized ratio
Liver function tests
Erythrocyte sedimentation rate
Computed tomography
Ground-glass opacification/opacity
Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A novel coronavirus emerging in China—key questions for impact assessment. N Engl J Med. 2020;382(8):692–4.
Article CAS PubMed Google Scholar
Sun X, Wang T, Cai D, Hu Z, Liao H, Zhi L, et al. Cytokine storm intervention in the early stages of COVID-19 pneumonia. Cytokine Growth Factor Rev. 2020;53:38–42.
Article CAS PubMed PubMed Central Google Scholar
Yang X, Yu Y, Xu J, Shu H, Liu H, Wu Y, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–9.
Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The cytokine storm in COVID-19: an overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor Rev. 2020;53:25–32.
Matthay MA, Leligdowicz A, Liu KD. Biological mechanisms of COVID-19 acute respiratory distress syndrome. American Thoracic Society; 2020.
Lopes-Pacheco M, Silva PL, Cruz FF, Battaglini D, Robba C, Pelosi P, et al. Pathogenesis of multiple organ injury in COVID-19 and potential therapeutic strategies. Front Physiol. 2021;12:29.
Article Google Scholar
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506.
Article CAS Google Scholar
Gavriatopoulou M, Ntanasis-Stathopoulos I, Korompoki E, Fotiou D, Migkou M, Tzanninis I-G, et al. Emerging treatment strategies for COVID-19 infection. Clin Exp Med. 2020;21:167–79.
Article PubMed PubMed Central Google Scholar
Majumder J, Minko T. Recent developments on therapeutic and diagnostic approaches for COVID-19. AAPS J. 2021;23(1):1–22.
Das S, Ramachandran AK, Birangal SR, Akbar S, Ahmed B, Joseph A. The controversial therapeutic journey of chloroquine and hydroxychloroquine in the battle against SARS-CoV-2: a comprehensive review. Med Drug Discov. 2021;10:100085.
Mao YX, Xu JF, Seeley EJ, Tang XD, Xu LL, Zhu YG, et al. Adipose tissue-derived mesenchymal stem cells attenuate pulmonary infection caused by Pseudomonas aeruginosa via inhibiting overproduction of prostaglandin E2. Stem cells. 2015;33(7):2331–42.
Min F, Gao F, Li Q, Liu Z. Therapeutic effect of human umbilical cord mesenchymal stem cells modified by angiotensin-converting enzyme 2 gene on bleomycin-induced lung fibrosis injury. Mol Med Rep. 2015;11(4):2387–96.
Li H, Shen S, Fu H, Wang Z, Li X, Sui X, et al. Immunomodulatory functions of mesenchymal stem cells in tissue engineering. Stem Cells Int 2019; 2019.
Kavianpour M, Saleh M, Verdi J. The role of mesenchymal stromal cells in immune modulation of COVID-19: focus on cytokine storm. Stem Cell Res Ther. 2020;11(1):1–19.
Horie S, Gonzalez HE, Laffey JG, Masterson CH. Cell therapy in acute respiratory distress syndrome. J Thorac Dis. 2018;10(9):5607.
Lopes-Pacheco M, Robba C, Rocco PRM, Pelosi P. Current understanding of the therapeutic benefits of mesenchymal stem cells in acute respiratory distress syndrome. Cell Biol Toxicol. 2020;36(1):83–102.
Article PubMed Google Scholar
Zheng G, Huang L, Tong H, Shu Q, Hu Y, Ge M, et al. Treatment of acute respiratory distress syndrome with allogeneic adipose-derived mesenchymal stem cells: a randomized, placebo-controlled pilot study. Respir Res. 2014;15(1):1–10.
Wilson JG, Liu KD, Zhuo H, Caballero L, McMillan M, Fang X, et al. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet Respir Med. 2015;3(1):24–32.
Matthay MA, Calfee CS, Zhuo H, Thompson BT, Wilson JG, Levitt JE, et al. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial. Lancet Respir Med. 2019;7(2):154–62.
Simonson OE, Mougiakakos D, Heldring N, Bassi G, Johansson HJ, Dalén M, et al. In vivo effects of mesenchymal stromal cells in two patients with severe acute respiratory distress syndrome. Stem Cells Transl Med. 2015;4(10):1199–213.
Khoury M, Cuenca J, Cruz FF, Figueroa FE, Rocco PR, Weiss DJ. Current status of cell-based therapies for respiratory virus infections: applicability to COVID-19. Eur Respir J. 2020;55(6):2000858.
Eleuteri S, Fierabracci A. Insights into the secretome of mesenchymal stem cells and its potential applications. Int J Mol Sci. 2019;20(18):4597.
Article CAS PubMed Central Google Scholar
Ferreira JR, Teixeira GQ, Santos SG, Barbosa MA, Almeida-Porada G, Gonçalves RM. Mesenchymal stromal cell secretome: influencing therapeutic potential by cellular pre-conditioning. Front Immunol. 2018;9:2837.
Teixeira FG, Salgado AJ. Mesenchymal stem cells secretome: current trends and future challenges. Neural Regen Res. 2020;15(1):75.
Wangler S, Kamali A, Wapp C, Wuertz-Kozak K, Häckel S, Fortes C, et al. Uncovering the secretome of mesenchymal stromal cells exposed to healthy, traumatic, and degenerative intervertebral discs: a proteomic analysis. Stem Cell Res Ther. 2021;12(1):1–17.
Markov A, Thangavelu L, Aravindhan S, Zekiy AO, Jarahian M, Chartrand MS, et al. Mesenchymal stem/stromal cells as a valuable source for the treatment of immune-mediated disorders. Stem Cell Res Ther. 2021;12(1):1–30.
Rafei M, Campeau PM, Aguilar-Mahecha A, Buchanan M, Williams P, Birman E, et al. Mesenchymal stromal cells ameliorate experimental autoimmune encephalomyelitis by inhibiting CD4 Th17 T cells in a CC chemokine ligand 2-dependent manner. J Immunol. 2009;182(10):5994–6002.
Kim HS, Shin TH, Lee BC, Yu KR, Seo Y, Lee S, et al. Human umbilical cord blood mesenchymal stem cells reduce colitis in mice by activating NOD2 signaling to COX2. Gastroenterology. 2013;145(6):1392-403.e8.
Vizoso FJ, Eiro N, Cid S, Schneider J, Perez-Fernandez R. Mesenchymal stem cell secretome: toward cell-free therapeutic strategies in regenerative medicine. Int J Mol Sci. 2017;18(9):1852.
Article PubMed Central Google Scholar
Abreu SC, Weiss DJ, Rocco PR. Extracellular vesicles derived from mesenchymal stromal cells: a therapeutic option in respiratory diseases? Stem Cell Res Ther. 2016;7(1):1–10.
Phelps J, Sanati-Nezhad A, Ungrin M, Duncan NA, Sen A. Bioprocessing of mesenchymal stem cells and their derivatives: toward cell-free therapeutics. Stem Cells Int. 2018;2018:1–23.
Sanchez-Mata A, Gonzalez-Muñoz E. Understanding menstrual blood-derived stromal/stem cells: definition and properties: Are we rushing into their therapeutic applications? iScience. 2021;24:103501.
Doyle LM, Wang MZ. Overview of extracellular vesicles, their origin, composition, purpose, and methods for exosome isolation and analysis. Cells. 2019;8(7):727.
Abreu SC, Lopes-Pacheco M, Weiss DJ, Rocco PR. Mesenchymal stromal cell-derived extracellular vesicles in lung diseases: current status and perspectives. Front Cell Dev Biol. 2021;9:97.
Fathi-Kazerooni M, Tavoosidana G, Taghizadeh-Jahed M, Khanjani S, Golshahi H, Gargett CE, et al. Comparative restoration of acute liver failure by menstrual blood stem cells compared with bone marrow stem cells in mice model. Cytotherapy. 2017;19(12):1474–90.
Zafardoust S, Kazemnejad S, Darzi M, Fathi-Kazerooni M, Rastegari H, Mohammadzadeh A. Improvement of pregnancy rate and live birth rate in poor ovarian responders by Intraovarian Administration of autologous menstrual blood derived-Mesenchymal Stromal Cells: Phase I/II Clinical Trial. Stem Cell Rev Rep. 2020;16:755–63.
Chen L, Qu J, Xiang C. The multi-functional roles of menstrual blood-derived stem cells in regenerative medicine. Stem Cell Res Ther. 2019;10(1):1–10.
Bozorgmehr M, Gurung S, Darzi S, Nikoo S, Kazemnejad S, Zarnani A-H, et al. Endometrial and menstrual blood mesenchymal stem/stromal cells: biological properties and clinical application. Front Cell Dev Biol. 2020;8:497.
Murray LM, Krasnodembskaya AD. Concise review: intercellular communication via organelle transfer in the biology and therapeutic applications of stem cells. Stem Cells. 2019;37(1):14–25.
Chen X, Wu Y, Wang Y, Chen L, Zheng W, Zhou S, et al. Human menstrual blood-derived stem cells mitigate bleomycin-induced pulmonary fibrosis through anti-apoptosis and anti-inflammatory effects. Stem Cell Res Ther. 2020;11(1):1–19.
Hansell DM, Bankier AA, MacMahon H, McLoud TC, Muller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246(3):697–722.
Myers LC, Parodi SM, Escobar GJ, Liu VX. Characteristics of hospitalized adults with COVID-19 in an integrated health care system in California. JAMA. 2020;323(21):2195–8.
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region. Italy Jama. 2020;323(16):1574–81.
Peng F, Tu L, Yang Y, Hu P, Wang R, Hu Q, et al. Management and treatment of COVID-19: the Chinese experience. Can J Cardiol. 2020;36(6):915–30.
Hessvik NP, Llorente A. Current knowledge on exosome biogenesis and release. Cell Mol Life Sci. 2018;75(2):193–208.
Shokri M-R, Bozorgmehr M, Ghanavatinejad A, Falak R, Aleahmad M, Kazemnejad S, et al. Human menstrual blood-derived stromal/stem cells modulate functional features of natural killer cells. Sci Rep. 2019;9(1):1–13.
Chen L, Qu J, Mei Q, Chen X, Fang Y, Chen L, et al. Small extracellular vesicles from menstrual blood-derived mesenchymal stem cells (MenSCs) as a novel therapeutic impetus in regenerative medicine. Stem Cell Res Ther. 2021;12(1):1–15.
Marinaro F, Gómez-Serrano M, Jorge I, Silla-Castro JC, Vázquez J, Sánchez-Margallo FM, et al. Unraveling the molecular signature of extracellular vesicles from endometrial-derived mesenchymal stem cells: potential modulatory effects and therapeutic applications. Front Bioeng Biotechnol. 2019;7:431.
Sengupta V, Sengupta S, Lazo A, Woods P, Nolan A, Bremer N. Exosomes derived from bone marrow mesenchymal stem cells as treatment for severe COVID-19. Stem Cells Dev. 2020;29(12):747–54.
Harrell CR, Jovicic BP, Djonov V, Volarevic V. Therapeutic potential of mesenchymal stem cells and their secretome in the treatment of SARS-CoV-2-induced acute respiratory distress syndrome. Anal Cell Pathol. 2020;2020:1–11.
Bari E, Ferrarotti I, Torre ML, Corsico AG, Perteghella S. Mesenchymal stem/stromal cell secretome for lung regeneration: the long way through “pharmaceuticalization” for the best formulation. J Control Release. 2019;309:11–24.
Horak J, Nalos L, Martinkova V, Tegl V, Vistejnova L, Kuncova J, et al. Evaluation of mesenchymal stem cell therapy for sepsis: a randomized controlled porcine study. Front Immunol. 2020;11:126.
Rad F, Ghorbani M, Roushandeh AM, Roudkenar MH. Mesenchymal stem cell-based therapy for autoimmune diseases: emerging roles of extracellular vesicles. Mol Biol Rep. 2019;46(1):1533–49.
Wang J-H, Liu X-L, Sun J-M, Yang J-H, Xu D-H, Yan S-S. Role of mesenchymal stem cell derived extracellular vesicles in autoimmunity: a systematic review. World J Stem Cells. 2020;12(8):879.
Zimmerlin L, Park TS, Zambidis ET, Donnenberg VS, Donnenberg AD. Mesenchymal stem cell secretome and regenerative therapy after cancer. Biochimie. 2013;95(12):2235–45.
Download references
Acknowledgements
The authors would like to thank Dr. Hojjat Zeraati, Ph.D. for assistance with statistical analysis, Mrs. Mahin Rezapour, and Sedigheh Sharifinasab for their assistance with sample acquisition.
The Avicenna Research Institute (99/3436) and Zayabiotech Company supported this work.
Author information
Mina Fathi-Kazerooni and Samrand Fattah Ghazi equal first author
Authors and Affiliations
Nanobiotechnology Research Center, Avicenna Research Institute, ACECR, Tehran, Iran
Mina Fathi-Kazerooni, Maryam Darzi & Somaieh Kazemnejad
Department of Anesthesiology and Intensive Care, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
Samrand Fattah-Ghazi & Jalil Makarem
Avicenna Fertility Clinic, Avicenna Research Institute, ACECR, Tehran, Iran
Reza Nasiri
Department of Radiology, Advanced Diagnostic and Interventional Radiology Research Center (ADIR), Tehran University of Medical Sciences, Tehran, Iran
Faeze Salahshour
Liver Transplantation Research Center, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
Department of Infectious Diseases and Tropical Medicine, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
Seyed Ali Dehghan-Manshadi
You can also search for this author in PubMed Google Scholar
Contributions
MFK had collaboration in collecting data, and manuscript writing. SFG was responsible for conducting, taking care of the patients, and performing the follow-up checks. MD was responsible for production management. JM was responsible for monitoring the progress of the study and the follow-up of the patients. RN set up and performed molecular experiments. FS was responsible for CT scan imaging analyzing. SADM was responsible for supervising the clinical part of the study. SK proposed and designed the study, and edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Seyed Ali Dehghan-Manshadi or Somaieh Kazemnejad .
Ethics declarations
Ethics approval and consent to participate.
All the procedures in this clinical trial study were conducted according to Good Clinical Practice (GCP) or GMP guidelines approved by the Biomedical Research Ethics Committee of Academic Center for Education, Culture, and Research (Code:IR.ACECR.REC.1399.005). Written informed consent was obtained from each patient or the patient’s legally authorized surrogate before the conduct of study-specific procedures.
Consent for publication
Not relevant.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fathi-Kazerooni, M., Fattah-Ghazi, S., Darzi, M. et al. Safety and efficacy study of allogeneic human menstrual blood stromal cells secretome to treat severe COVID-19 patients: clinical trial phase I & II. Stem Cell Res Ther 13 , 96 (2022). https://doi.org/10.1186/s13287-022-02771-w
Download citation
Received : 26 October 2021
Accepted : 17 February 2022
Published : 07 March 2022
DOI : https://doi.org/10.1186/s13287-022-02771-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Menstrual blood stromal cells
- New treatment
Stem Cell Research & Therapy
ISSN: 1757-6512
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Menstrual blood banking

A new research has found that menstrual blood is a rich source of stem cells that have the ability to multiply and differentiate into any kind of cells. Stem cells in menstrual blood have similar regenerative capabilities as the stem cell in umbilical cord blood and bone marrow.
Related Papers
Regenerative Medicine
Nurjannah Achmad
The open stem cell journal
Natalie Yefimenko
We are in the beginning of the era of regenerative medicine and many researchers are testing adult stem cells to be used for tissue repair and regeneration in the human body. Many adult stem cells have been discovered since the late 1990's with more recently a novel adult stem cell described in menstrual blood. The menstrual blood is derived from shedding of the endometrial lining, specifically the functionalis layer, which contains highly proliferative cells used to prepare the female body for implementation of a fertilized egg. Cell characterization experiments of stromal stem cells discovered in menstrual blood have demonstrated cells to be multipotent which can successfully differentiate in vitro into cell lineages derived from the mesoderm and the ectoderm.When menstrual blood cells were seeded in culture the average number of adherent cells was 8.50 % with a range of 0.48% to 47.76%. Demonstrating longevity one cell line allowed to grow was subcultured 47 times before comp...
Peertechz Journals
Stem cells isolated from menstrual fluid have mesenchymal stem cell like properties and have multi lineage differentiation capacity. Menstrual fluid has ease of access in collection and repeated sampling is possible in a noninvasive manner. Also, rapid culture of these is possible in numbers that are sufficient for therapeutic use. They are, hence, looked upon as a novel innovation and are finding a place in the current medicine practice
Journal of Medical – Clinical Research & Reviews
Vincent Gallicchio
Journal of Zhejiang University SCIENCE B
julie allickson
Biology Open
Recently, menstrual blood-derived endometrial stem cells (MenSCs) have become attractive for stem cell based therapy due to their abundance, easy and non-invasive extraction and isolation process, high proliferative capacity and multi-lineage differentiation potential. MenSC-based therapies for various diseases are being extensively researched. However, the high death rate and poor engraftment in sites of damaged tissues reduce the therapeutic value of these stem cells for transplantation. In theory, periodic stem cell transplantation is an alternative strategy to overcome the challenge of the loss of beneficial stem cell-derived effects due to the rapid disappearance of the stem cells in vivo. However, periodic stem cell transplantation requires sufficient amounts of the desired stem cells with a low number of subculture passages. Our previous results have demonstrated that primary MenSCs mainly reside in the deciduous endometrium, and considerable amounts of deciduous endometrium ...
Cell Transplantation
The stromal stem cell fraction of many tissues and organs has demonstrated to exhibit stem cell properties such as the capability of self-renewal and multipotency, allowing for multilineage differentiation. In this study, we characterize a population of stromal stem cells derived from menstrual blood (MenSCs). We demonstrate that MenSCs are easily expandable to clinical relevance and express multipotent markers such as Oct-4, SSEA-4, and c-kit at the molecular and cellular level. Moreover, we demonstrate the multipotency of MenSCs by directionally differentiating MenSCs into chondrogenic, adipogenic, osteogenic, neurogenic, and cardiogenic cell lineages. These studies demonstrate the plasticity of MenSCs for potential research in regenerative medicine.
International Journal of Molecular Sciences
Raminta Baušytė
When looking for the causes and treatments of infertility, much attention is paid to one of the reproductive tissues—the endometrium. Therefore, endometrial stem cells are an attractive target for infertility studies in women of unexplained origin. Menstrual blood stem cells (MenSCs) are morphologically and functionally similar to cells derived directly from the endometrium; with dual expression of mesenchymal and embryonic cell markers, they proliferate and regenerate better than bone marrow mesenchymal stem cells. In addition, menstrual blood stem cells are extracted in a non-invasive and painless manner. In our study, we analyzed the characteristics and the potential for decidualization of menstrual blood stem cells isolated from healthy volunteers and women diagnosed with infertility. We demonstrated that MenSCs express CD44, CD166, CD16, CD15, BMSC, CD56, CD13 and HLA-ABC surface markers, have proliferative properties, and after induction of menstrual stem cell differentiation ...
Frontiers in Cell and Developmental Biology
Caroline Gargett
Frontiers in Genetics
Daniela Manica
RELATED PAPERS
Rafael flores garcia
Ulysses Fernandes
Kant's Lectures on Metaphysics: A Critical Guide
serena di nepi , manuele gianfrancesco
Monica Ceci , Riccardo Santangeli Valenzani
Murat Çekilmez
Las reliquias de Martioda
Gorka López de Munain
Jose Parsons
Gustavo Eugenio Elizondo Alanís
Dr. Irfan Ahmed
Analecta Cracoviensia
Paweł Ulman
The books' journal, τεύχ. 129, σελ. 58-59
DIMITRIOS KARABEROPOULOS
Statistika: Statistics and Economy Journal
Angela Digrandi
Revista Brasileira de Recursos Hídricos
Adilson Pinheiro
serdar budak
Frontiers in Psychology
Markus Pawelzik
IFIP Advances in Information and Communication Technology
Rodrigo Carlo Toloi
International Journal of Chemical Studies
Jadav Sarma
Word & World
Karl Jacobson
Aquatic Sciences
Verbum Vitae
ACM SIGMETRICS Performance Evaluation Review
Virgilio Almeida
Journal of Clinical Neuroscience
Marcus Stoodley
Seminar Nasional Aplikasi Teknologi Informasi
achmad ridok
Mansholt seminar on Consumer perspectives and globalising food provision, University of Wageningen, June 9, 2005
Natalia Yakovleva
Acta Oto-Laryngologica
Luiz Lavinsky
Critical Reviews in Biotechnology
Xunli Zhang
Chemistry & Biodiversity
Ana Sevcenco
REVISTA FOCO
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
ORIGINAL RESEARCH article
Knowledge, attitude, and practice of menstrual blood-derived mesenchymal stem cells among female healthcare workers in india.

- 1 Amity Institute of Public Health, Amity University, Noida, India
- 2 SRM Medical College Hospital and Research Centre, SRM University, Kattankulathur, India
- 3 Apollo Hospital, Chennai, India
Introduction: Mesenchymal stem cells (MSCs) are pluripotent progenitor cells that can be differentiated into a variety of specialized cell types. Menstrual blood, such as umbilical cord blood and bone marrow stem cells, is a rich source of MSCs with proliferative properties. This research was conducted to understand the knowledge, attitude, and practice of menstrual blood donation regarding menstrual blood-derived mesenchymal stem cells (MenSCs) among female healthcare workers in India.
Methodology: A cross-sectional online and offline survey was conducted at the national level between 20 November 2021 and 10 March 2022. A self-constructed semi-structured questionnaire was distributed through Google Forms on various social media platforms. The questionnaire was self-administered, and data were collected using the purposive sampling technique.
Results: A total of 499 respondents completed the questionnaire. Nearly 49% of the respondents had adequate knowledge, 54% showed a positive attitude, and 45% reported adequate practices regarding menstrual blood donation and the usage of related products. The educational background, occupational status, and monthly income of the participants were found to be significantly associated with their attitude toward MenSCs.
Conclusion: There is a need to promote interactive sessions on MenSCs among healthcare professionals in order to bridge the gap between general populations and the healthcare setting. Enhancing knowledge and awareness regarding the potential benefits of MenSCs would help in dissipating the age-old myths associated with menstruation and will benefit society as a whole.
Introduction
Mesenchymal stem cells (MSCs) are pluripotent progenitor cells capable of differentiating into a variety of specialized cell types such as osteoblasts, chondrocytes, and adipocytes ( 1 , 2 ). MSCs can be extracted from a range of adult tissues including, but not limited to, the bone marrow, peripheral blood, adipose tissue, umbilical cord, placenta, and menstrual blood ( 3–5 ). Over the last 12 years, MSCs have gained attention from researchers worldwide owing to their high proliferative rate, low immunogenicity, non-invasive collection techniques, high abundance, unlimited availability, and fewer ethical issues ( 6 , 7 ). MSCs are a novel and easily accessible therapeutic tool for regenerative medicine and tissue engineering. The use of MSCs for the treatment of different ailments is progressing at a rapid pace, and their potential applications are expanding.
Menstrual blood is an expandable source of such stem cells with a high proliferative capacity and restorative properties compared to umbilical cord blood and bone marrow stem cells. Researchers have successfully retrieved stem cells from menstrual blood, and this makes the concept of stem cell preservation viable for all women, even those who never give birth ( 8 ).
The identification of stem cells in the menstrual blood will give women a new perspective on menstruation, which has been stigmatized in low-and middle-income countries (LMICs) such as India ( 9–11 ). This type of novel revelation can be a boon for the Indian scenario, where approximately 355 million menstruating girls and women reside. Unfortunately, the issue of menstruation has been a taboo for centuries in India, with menstruating women deemed filthy and forced to live under harsh limitations, prohibited from social and religious gatherings, temples, and shrines ( 9 ).
Therefore, it is imperative to raise awareness and knowledge among women from all strata regarding menstrual blood-derived mesenchymal stem cells (MenSCs). Although menstrual blood is a cost-effective, convenient, and easily accessible source of stem cells, minimal research has been conducted to assess the knowledge gap as well as the perception of women toward MenSCs. This becomes particularly important among healthcare workers as they are the link connecting healthcare centers and community resources. Hence, this research was conducted to understand the knowledge, attitude, and practice of donating menstrual blood among female healthcare workers in India.
Methodology
Participants and recruitment.
A cross-sectional online and offline survey was conducted at the national level between 20 November 2021 and 10 March 2022. The purposeful sampling technique was used for data collection. The questionnaire was distributed through Google Forms and physical copies to a total of 550 participants for filling the questionnaire after reading a descriptive introduction on the topic. The link to the Google Forms was shared on various social media platforms. Women above the age of 18 years who were in the healthcare profession being a student or a worker were included. Healthcare workers who had menopause and who identified themselves as males were excluded from the study. No incentive was provided for questionnaire completion. This research was approved by the SRM Medical and Research Ethics Clearance Subcommittee. After taking informed consent, women aged 18 years and above were recruited from various colleges and healthcare setups to complete the questionnaire.
A self-constructed semi-structured questionnaire was made based on an extensive review of relevant literature ( 12 , 13 ). A pilot study was conducted among 15 participants, who volunteered and gave informed consent after going through the study objectives, to gain inputs from the participants to improve the clarity and ensure the validity of the questionnaire. However, the participants enrolled in the pilot study were not part of the survey, and their responses were not incorporated in the results of this manuscript. The questionnaire was further validated by a gynecologist and then used in the survey. The questionnaire covered questions related to socio-demographic characteristics and the assessment of knowledge, attitude, and practice regarding MenSCs. The survey was anonymous, and ethical clearance was obtained from the institutional ethical clearance committee. This questionnaire was copyrighted by the authors with the diary number 32063/2021-CO/L.
Data analysis
Data were entered in an Excel sheet, and statistical analysis was performed using SPSS software version 25. Descriptive statistics, such as frequency, were used to present the socio-demographic characteristics of the respondents and various factors included in the assessment of knowledge, attitude, and practice regarding MenSCs. Pearson’s chi-square test was performed to find the significant associations between socio-demographic characteristics and the factors included in this study.
Out of 550 participants, a total of 499 participants completed the questionnaire. In total, 67% of the participants were from 18 to 24 years ( Table 1 ). Out of the 499 female participants, 78% of the respondents were either pursuing or had completed their bachelor’s degree; 63% of the respondents were from the medical or allied health sciences department, while 37% had a paramedical background. The majority of the respondents were students (57.5%), and 35% had private-sector jobs. A total of 53% of the respondents earned 10 to 29,000 rupees per month, whereas only 16% earned 50,000–1,00,000 rupees per month. The proportion of unmarried respondents in our study was 76%, and only 22% were reported to be married. In total, 69% of the participants were practicing Hinduism, and a majority of the respondents were from the southern region of India (52.1%), followed by northern India (39.2%).
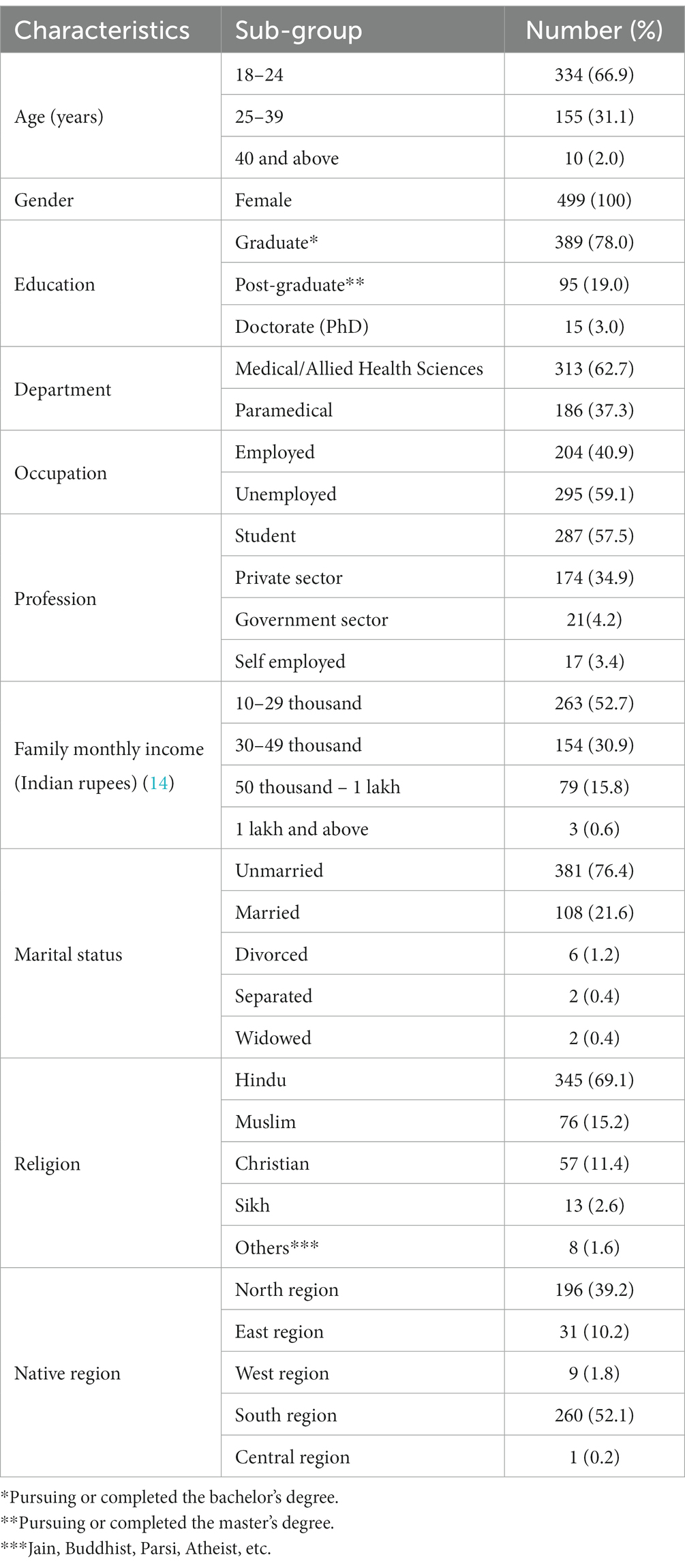
Table 1 . Socio-demographic characteristics of the respondents ( n = 499).
A total of 49% of the respondents in our study had adequate knowledge regarding MenSCs ( Figure 1 ). However, 53% of the respondents were unaware that menstrual blood can be donated ( Table 2 ). Educational courses were the predominant source of obtaining knowledge related to MenSCs (50.6%). Only 31% of the respondents were familiar with the notion that MenSCs can be utilized for various therapeutic purposes. Similarly, 43% of the respondents were unaware of the novel regenerative properties of the MenSCs, and 24% were unaware of mesenchymal stem cell banking in India. In addition, 83% of the respondents showed an interest toward enhancing their knowledge with respect to MenSCs.
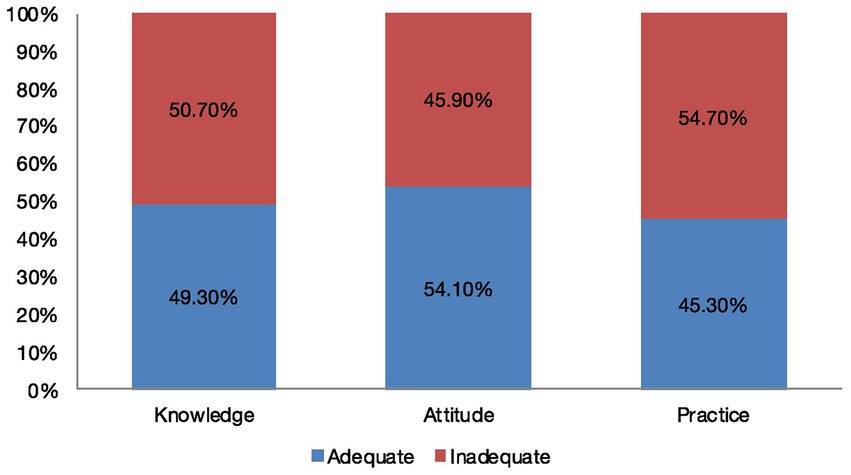
Figure 1 . Knowledge, attitude, and practice level among respondents regarding menstrual blood-derived stem cells. This figure depicts the level of knowledge, attitude, and practice among 499 respondents toward MenSCs. In total, 49% of the respondents had an adequate knowledge level, 54% showed a positive attitude, and 45% reported adequate practices regarding menstrual blood donation and the usage of related products.
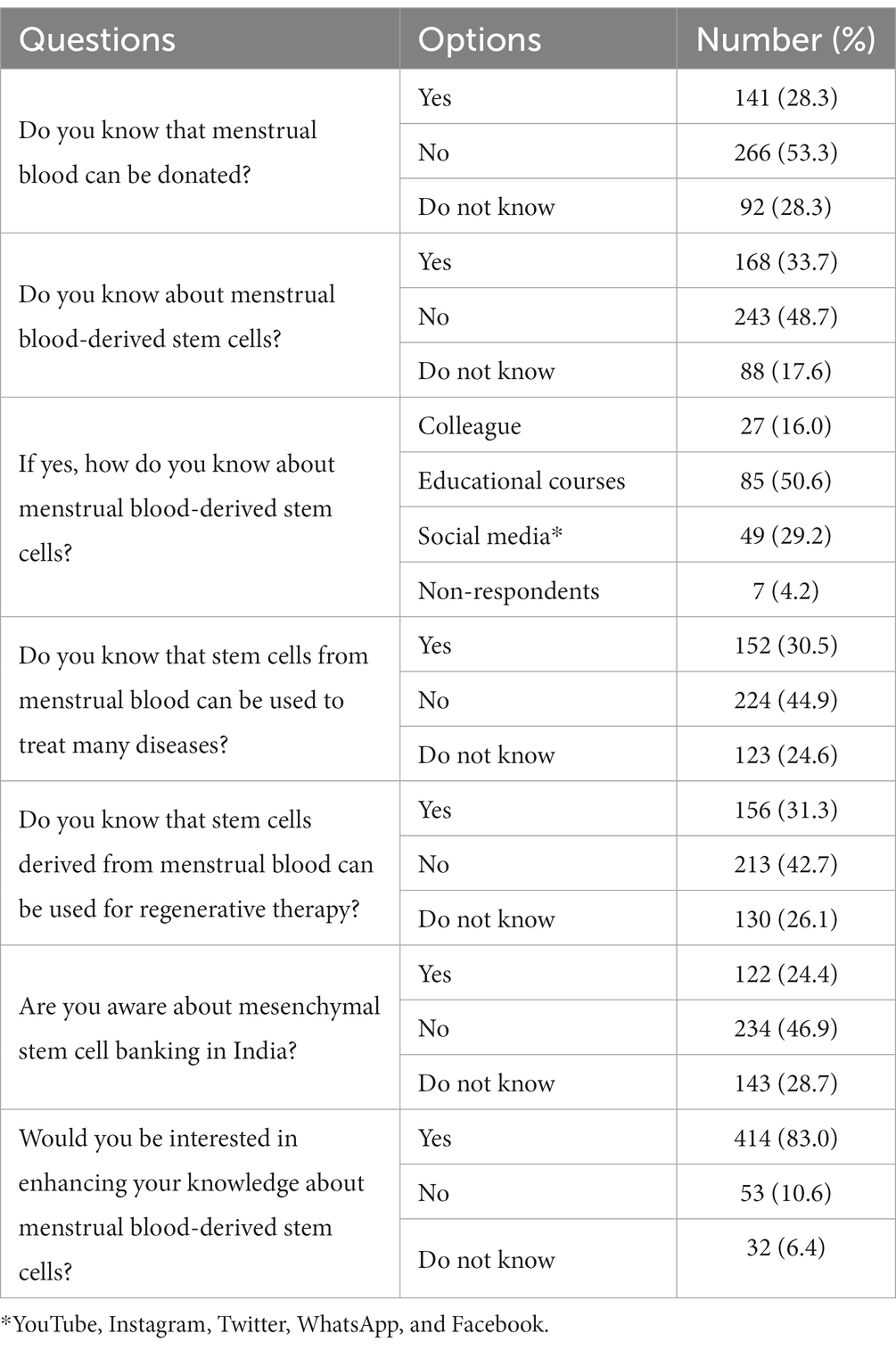
Table 2 . Knowledge of the respondents regarding menstrual blood-derived stem cells.
In total, 54% of the respondents in our study were reported to have a positive attitude toward menstrual blood donation and the utilization of MenSCs for therapeutic purposes ( Figure 1 ). Impressively, 65% of the respondents agreed that menstrual blood donation can be a boon to society, 73% supported the fact that menstrual blood for MSC collection should be promoted, and 82% felt that government should take proactive actions toward increasing MenSCs awareness ( Table 3 ). Being healthcare professionals, 82% of the respondents thought that competency in knowledge regarding stem cells is very crucial, 34% of the respondents favored that MenSCs can be beneficial for the treatment of heart-related disorders, and 47% believed that MenSCs could be a potential therapeutic tool for ovarian-related diseases ( Table 3 ).
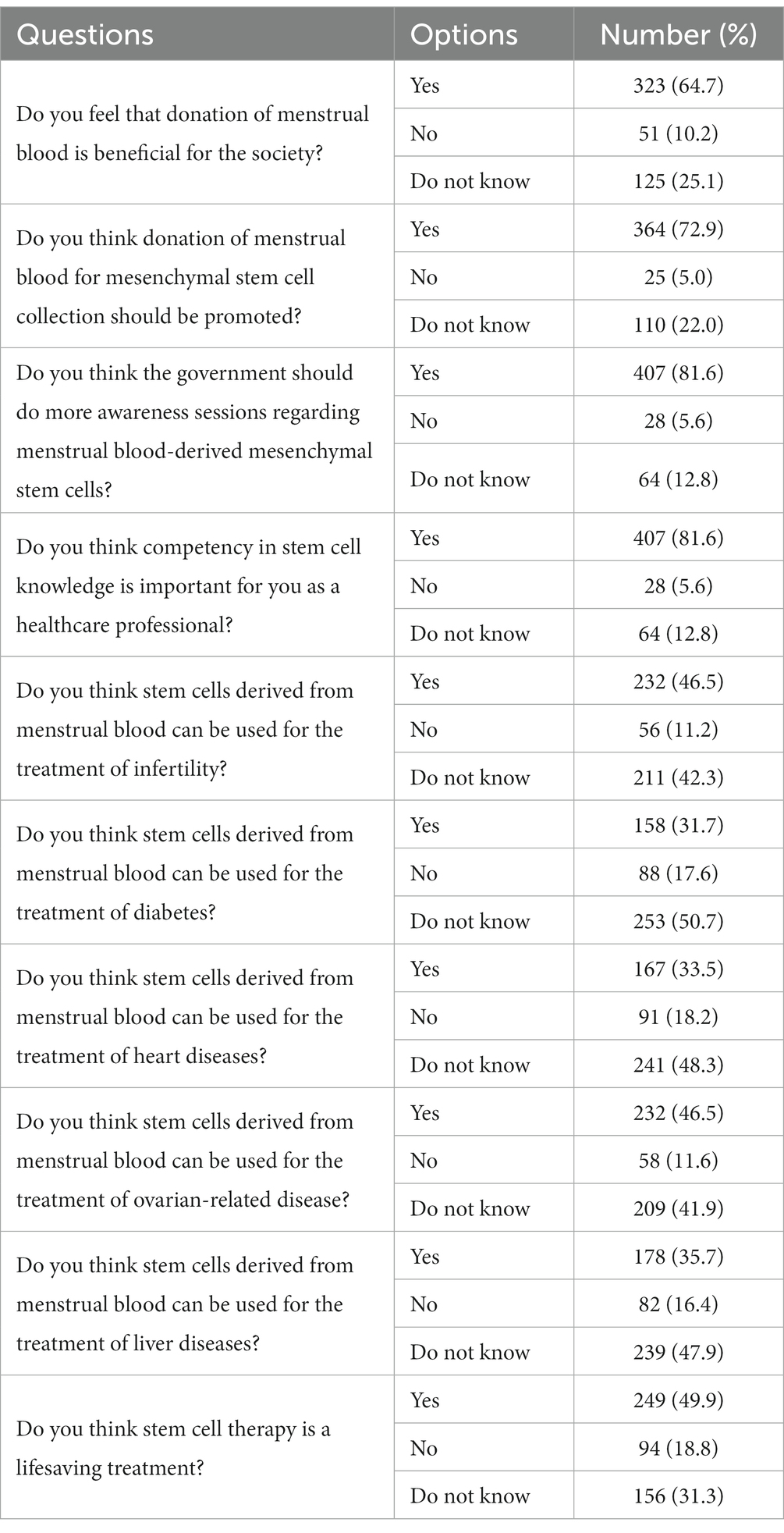
Table 3 . The attitude of the respondents regarding menstrual blood-derived stem cells.
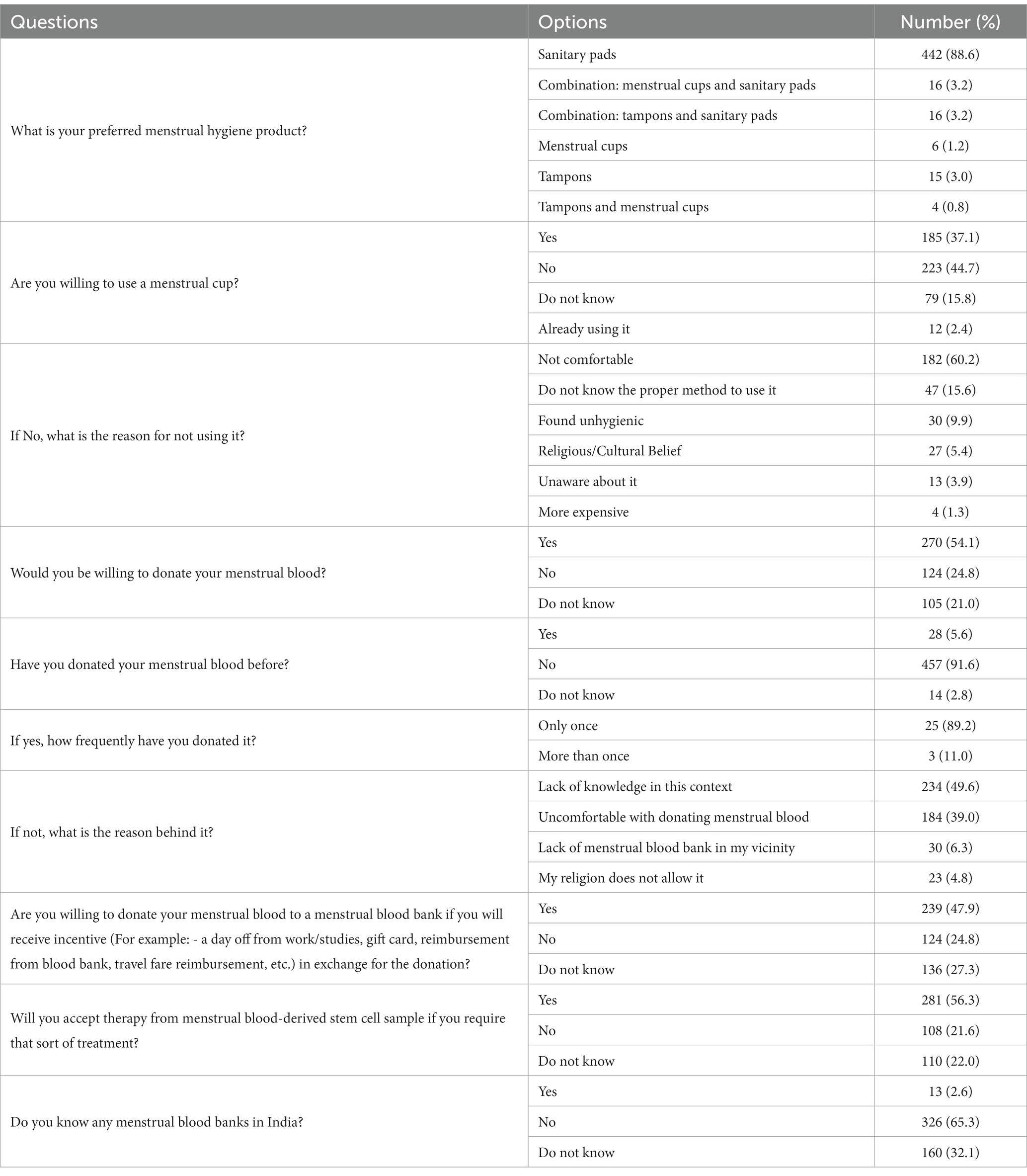
Table 4 . Practices of the respondents regarding menstrual blood-derived stem cells.
In our study, adequate practices toward menstrual blood donation and the usage of related products were reported by 45% of the respondents ( Figure 1 ). For 89% of the respondents, sanitary pads were the most preferred menstrual hygiene product. A total of 45% of the respondents showed unwillingness toward using menstrual cups and 60% of the respondents expressed discomfort while wearing was the primary factor for not using menstrual cups followed by a lack of knowledge regarding their proper usage (15.6%). Although 54% of the respondents showed willingness toward menstrual blood donation, the majority had not donated menstrual blood before (91.6%). Willingness toward donating menstrual blood to a menstrual blood bank was reported by 48% of the respondents provided they received incentives in the form of gift cards, reimbursements from the blood bank, and work/studies day off. Although 56% of the respondents showed acceptance toward therapy from MenSCs, only 3% of respondents had knowledge regarding menstrual blood banks in India.
Upon bivariate analysis ( Table 5 ), the educational qualification of the respondents was found to be significantly associated ( p , 0.002) with the respondent’s perceived attitude toward MenSCs. Respondents from the department of the medical or paramedical were found to have a significant impact ( p , 0.033) on their knowledge about MenSCs. The occupational status of the respondents ( p < 0.001) along with their profession ( p < 0.001) and monthly earnings ( p , 0.042) was also found to be significantly associated with the respondent’s attitude toward menstrual blood donation and utilization of MenSCs for therapeutic purposes.
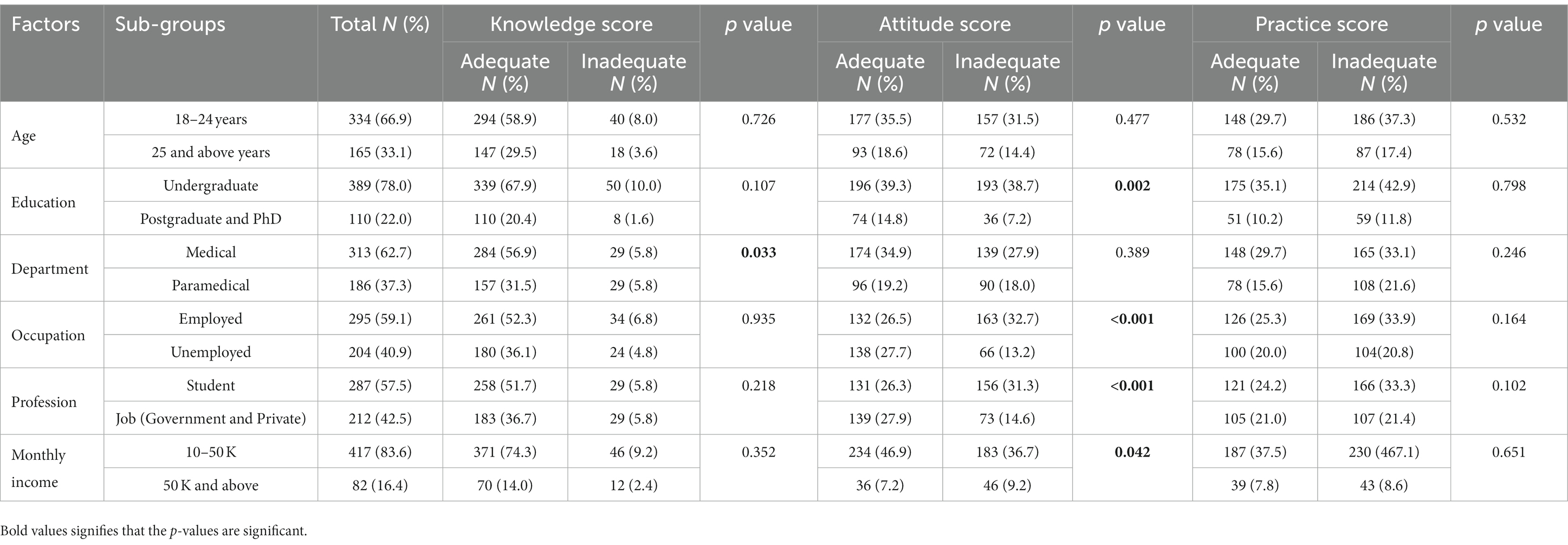
Table 5 . Factors associated with knowledge, attitude, and practice level of the respondents.
MenSCs are pluripotent cells with the potential to replicate every 24–36 h. It is crucial to note that MenSCs exhibit characteristics associated with embryonic stem cells, giving them the apparent ability to differentiate into a variety of healthy cell types. These cells have unique characteristics that can be used as a novel therapeutic modality for the treatment of various diseases in the future including rare diseases such as amyotrophic lateral sclerosis and Alzheimer’s disease (AD) ( 15 , 16 ). Hence, the purpose of this study was to assess the level of knowledge, perceived attitude, and practice of Indian healthcare professionals regarding MenSCs. To the best of our knowledge, this is the first research study in India to evaluate the awareness level and perspective of MenSCs among female healthcare professionals and to highlight the existing gaps. According to the current study conducted among Indian female healthcare workers, 49% of the respondents had knowledge regarding MenSCs. A similar study conducted among staff nurses in Tamil Nadu reported that 30% of the respondents had moderate knowledge regarding MenSCs ( 17 ), whereas a study conducted among nursing students in Government Nursing College, Jodhpur, reported a higher level of knowledge (64%) ( 18 ). A possible explanation for the variations in the level of knowledge could be the difference in the geographic region, varied sample sizes, and socio-demographic characteristics. In our study, 24% of the female healthcare workers were aware of menstrual blood banking in India. A similar study conducted among female healthcare professionals at Manipal University, Karnataka, reported that 13% of the respondents were aware of menstrual blood banks ( 19 ). On the other hand, a study conducted in Amritsar assessed both pre-test and post-test knowledge to determine the effectiveness of a teaching program among nursing students regarding menstrual blood banking and reported that during the pre-test, 93% of the respondents had just an average knowledge of menstrual blood banking, while post-test 89% had a good knowledge ( 20 ).
In total, 54% of the respondents in our study were reported to perceive a positive attitude toward the utilization of MenSCs, 65% of the respondents supported menstrual blood donation and considered it to be beneficial for society, and 73% felt it should be encouraged. Furthermore, 50% of the respondents believed that the therapeutic properties of stem cells can become a life-saving treatment modality. These findings are supported by a cross-sectional study performed in Kelantan, Malaysia, among nurses with midwifery and neonatology expertise in a tertiary teaching hospital. They found that 87% of the respondents had moderate knowledge regarding the utilization of stem cells in medicinal therapy, while 61% of the nurses reported a positive attitude toward the therapeutic potential of stem cells in medicine ( 21 ). Even though a majority of the respondents in our study were receptive toward enhancing their knowledge regarding MenSCs, some of the respondents (5.0%) were not in favor of promoting menstrual blood donation. This attitude could be due to age-old religious beliefs, socio-cultural myths, and misconceptions associated with menstrual blood that are deeply rooted in India ( 22 ).
Though the proportion of willingness regarding menstrual blood donation was found to be 54% in our study, the majority of the respondents had not donated menstrual blood before (91.6%). The major reason behind this was the lack of knowledge in the concerned field as stated by 47%. Thus, it is essential to implement multiple strategies to enhance knowledge among women regarding the donation of menstrual blood for MSCs in the form of awareness sessions, health camps, as well as interactive classes. This will not only result in a larger participation in menstrual blood donation but will also support the development of MSC therapy. This conclusion is supported by the fact that the predominant number of respondents in our study was positive toward the acceptance of therapies from MenSCs (56.3%). Similarly, a study conducted in the United Kingdom among women from local universities also showed that the majority of the women (91%) had a positive response toward acceptance of therapy derived from menstrual blood ( 12 ). The designated department of the respondents in our study (medical or paramedical) was found to have a significant association ( p = 0.033) with knowledge regarding MenSCs. Other socio-demographic factors, such as level of education ( p = 0.002), occupation ( p < 0.001), and profession ( p < 0.001), as well as monthly income ( p = 0.042) of the respondents, were significantly associated with the attitude perceived toward MenSCs. Thus, we conclude that the occupational environment where the participants are working or studying should also be sensitized with the beneficial aspects of menstrual blood and the advantages of using its related products. This can be a potential strategy to address the misconceptions related to menstruation in the Indian scenario thereby limiting the stigma associated with it.
As the most preferred menstrual hygiene product was sanitary pads, which was reported by 89% of the respondents, 45% of the respondents showed unwillingness toward the usage of menstrual cups. Their predominant reason was discomfort, as reported by 60% of the respondents. However, because a significant proportion of female healthcare workers were willing toward menstrual blood donation, they should be encouraged and educated regarding the application and the superadded benefits of a menstrual cup. A preliminary study reported that women who were learning the menstrual cup application for the first time showed better experience outcomes with guidance and positive support ( 23 ). Therefore, providing a menstrual cup with assistance during the initial use might result in a more favorable first-hand experience for Indian women who have never used a menstrual cup before and may increase their likelihood of using the product on a regular basis. MenSC donation should be promoted as it can benefit society as a whole as well as make individual women feel positive toward this normal physiological process.
Limitations
This study was conducted specifically among female healthcare professionals, which are limiting factors. Focusing on one particular profession or community will not be enough to determine the gravity of the scenario. Another limitation of this study was the social desirability bias that can be introduced due to the self-constructed nature of the questionnaire. To avoid such a bias, validated subscales should be developed to assess the knowledge, attitude, and practice of the general populace regarding important public health issues prevalent in the LMICs such as menstrual hygiene and sanitation. Furthermore, due to the cross-sectional design, this study cannot provide the longitudinal impact on the attitude and practice affecting the knowledge of the participants regarding MenSCs as it lacks follow-up surveys. Therefore, more extensive studies should be conducted at all socio-demographic levels covering all genders from all economical strata, which will depict the actual picture regarding the awareness and the perceived attitude toward menstrual blood donation and MenSCs.
This study highlights that there is only limited knowledge regarding MenSCs among women healthcare workers with a lack of adequate practice for the same. In order to encourage women to menstrual blood donation, healthcare workers must know how to foster a good attitude toward menstruation both among themselves and within the community. As a future practice, the key focus will be to instigate female healthcare workers with adequate knowledge and awareness about MenSCs because they are the key representatives in promoting new life-saving modalities and treatments in the community. The responses of the female healthcare workers in our study toward MenSCs should be taken as a positive factor to initiate further studies that are required in the general population to assess and improve the knowledge and attitude toward MenSCs. This will eventually encourage researchers to work on MSCs, their storage, and therapeutic use. The enhancement of knowledge and awareness regarding the potential benefits of MenSCs would not only help in dissipating the age-old myths associated with menstruation but will also benefit society as a whole.
Implications
The results of this study showed that there is a need to create awareness regarding MenSCs therapy because a majority of the women showed willingness toward menstrual blood donation. The healthcare personnel should be equipped in conducting various health education programs and camps at the community level for reinforcement of knowledge, positive attitude, and positive practice associated with menstruation and its related products.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by SRM Medical and Research Ethics Clearance Subcommittee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
KK: conceptualization. DN: data analysis. LM: draft writing. SS: data collection. MS: visualization. ST: validation. RJ: supervisor. KR: writing, reviewing and editing. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Andrzejewska, A, Lukomska, B, and Janowski, M. Concise review: mesenchymal stem cells: from roots to boost. Stem Cells . (2019) 37:855–64. doi: 10.1002/stem.3016
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Uccelli, A, Moretta, L, and Pistoia, V. Mesenchymal stem cells in health and disease. Nat Rev Immunol . (2008) 8:726–36. doi: 10.1038/nri2395
CrossRef Full Text | Google Scholar
3. Allickson, JG. Recent studies assessing the proliferative capability of a novel adult stem cell identified in menstrual blood. Open Stem Cell J . (2011) 3:4–10. doi: 10.2174/1876893801103010004
4. Lee, OK, Kuo, TK, Chen, WM, Lee, KD, Hsieh, SL, and Chen, TH. Isolation of multipotent mesenchymal stem cells from umbilical cord blood. Blood . (2004) 103:1669–75. doi: 10.1182/blood-2003-05-1670
5. Zuk, PA, Zhu, M, Ashjian, P, de Ugarte, DA, Huang, JI, Mizuno, H, et al. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell . (2002) 13:4279–95. doi: 10.1091/mbc.e02-02-0105
6. Liu, Y, Niu, R, Yang, F, Yan, Y, Liang, S, Sun, Y, et al. Biological characteristics of human menstrual blood-derived endometrial stem cells. J Cell Mol Med . (2017) 22:1627–39. doi: 10.1111/jcmm.13437
7. Du, X, Yuan, Q, Qu, Y, Zhou, Y, and Bei, J. Endometrial mesenchymal stem cells isolated from menstrual blood by adherence. Stem Cells Int . (2016) 2016:1–8. doi: 10.1155/2016/3573846
8. Podder, L. Assessment of knowledge regarding menstrual blood stem cell bank ing among nursing students. Nurs J India . (2019) 13:243–7. doi: 10.48029/nji.2019.cx601
9. Menstrual Health in India. Country Landscape Analysis. (2023). Available at: https://menstrualhygieneday.org/wp-content/uploads/2016/04/FSG-Menstrual-Health-Landscape_India.pdf . (Accessed January 30, 2023)
Google Scholar
10. Jui-Che, T, Ting-Yun, L, and Yi-Ting, L. Women’s cognition and attitude with eco-friendly menstrual products by consumer lifestyle. Int J Environ Res Public Health . (2021) 18:5534. doi: 10.3390/ijerph18115534
11. Kuhlmann, A, Kaysha, H, and Lewis, WL. Menstrual hygiene management in resource-poor countries. Obstet Gynecol Surv . (2017) 72:356–76. doi: 10.1097/ogx.0000000000000443
12. Manley, H, Sprinks, J, and Breedon, P. Menstrual blood-derived mesenchymal stem cells: women’s attitudes, willingness, and barriers to donation of menstrual blood. J Women’s Health . (2019) 28:1688–97. doi: 10.1089/jwh.2019.7745
13. Ngente, ER, Chaudhari, V, Fodekar, N, Gathe, P, Ghume, S, Jambhulkar, S, et al. Protocol on effect of planned teaching on knowledge regarding menstrual blood banking among nursing students. J Pharm Res Int . (2021) 33:220–4. doi: 10.9734/jpri/2021/v33i58A34109
14. Role and Pay. WageIndicator Foundation. (2023). Available at: https://paycheck.in/career-tips/role-income/india-community-health-workers . (Accessed January 30, 2023)
15. Allickson, JG. Recent studies assessing the proliferative capability of a novel adult stem cell identified in menstrual blood. Open Stem Cell J . (2011) 3:4–10. doi: 10.2174/1876893801103010004
16. Rosy, MM. Menstrual blood banking-a review. Int J Nurs Educ Res . (2017) 5:213. doi: 10.5958/2454-2660.2017.00046.1
17. Sasikala, P. Descriptive study to assess the knowledge on menstrual stem cell among staff nurses. Int J Appl Res . (2021) 7:8–10.
18. Dhaka, G. A descriptive study to assess the knowledge regarding menstrual blood banking among nursing students at Jodhpur. EPRA Int J Res Dev . (2021) 6:328–32. doi: 10.36713/epra8574
19. Jomon, CU, Barboza, L, and Sara, GL. Knowledge and attitude regarding menstrual blood banking. Indian J Public Health Res Dev . (2019) 10:68. doi: 10.5958/0976-5506.2019.00262.6
20. Hans, N, and Kaur, S. Effectiveness of structured teaching programme on knowledge regarding menstrual blood stem cells banking among nursing students. Int J Reprod Contracept Obstet Gynecol . (2016) 5:3137–40. doi: 10.18203/2320-1770.ijrcog20163001
21. Leng, LJ, Keng, SL, WanAhmad, WAN, and Cheng, TS. Association between nurses’ knowledge and attitudes toward stem cell application in medicine. Malays J Nurs . (2016) 7:3–9.
22. Anand, T, and Garg, S. Menstruation related myths in India: strategies for combating it. J Fam Med Primary Care . (2015) 4:184–6. doi: 10.4103/2249-4863.154627
23. Manley, HL. The potential for menstrually-derived stem cell banking in the UK. J Undergrad Res NTU . (2018) 1:1–18.
Keywords: public health, women health, stem cell, health care profession, mesenchymal stem cells, India
Citation: Kaur KN, Nandi D, Ramachandran K, Mohanan L, Subhashini S, Segan M, Tripathy S and Janardhanan R (2023) Knowledge, attitude, and practice of menstrual blood-derived mesenchymal stem cells among female healthcare workers in India. Front. Public Health 11:1102016. doi: 10.3389/fpubh.2023.1102016
Received: 18 November 2022; Accepted: 04 April 2023; Published: 04 May 2023.
Reviewed by:
Copyright © 2023 Kaur, Nandi, Ramachandran, Mohanan, Subhashini, Segan, Tripathy and Janardhanan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rajiv Janardhanan, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
The Real Reason Studying Menstrual Blood Is So Important
Long overlooked, menstrual stem cells could have important medical applications, including diagnosing endometriosis.

Roughly 20 years ago, a biologist named Caroline Gargett went in search of some remarkable cells in tissue that had been removed during hysterectomy surgeries. The cells come from the endometrium, which lines the inside of the uterus. When Gargett cultured the cells in a petri dish, they looked like round clumps surrounded by a clear, pink medium. But examining them with a microscope, she saw what she was looking for — two kinds of cells, one flat and roundish, the other elongated and tapered, with whisker-like protrusions.
Gargett strongly suspected that the cells were adult stem cells — rare, self-renewing cells, some of which can give rise to many different types of tissues. She and other researchers had long hypothesized that the endometrium contained stem cells, given its remarkable capacity to regrow itself each month. The tissue, which provides a site for an embryo to implant during pregnancy and is shed during menstruation, undergoes roughly 400 rounds of shedding and regrowth before a woman reaches menopause. But although scientists had isolated adult stem cells from many other regenerating tissues — including bone marrow, the heart, and muscle — “no one had identified adult stem cells in the endometrium,” Gargett says.
Such cells are highly valued for their potential to repair damaged tissue and treat diseases such as cancer and heart failure. But they exist in low numbers throughout the body and can be tricky to obtain, requiring surgical biopsy or extracting bone marrow with a needle. The prospect of a previously untapped source of adult stem cells was thrilling on its own, says Gargett. And it also raised the exciting possibility of a new approach to long-neglected women’s health conditions such as endometriosis.
Before she could claim that the cells were truly stem cells, Gargett and her team at Monash University in Australia had to put them through a series of rigorous tests. First, they measured the cells’ ability to proliferate and self-renew and found that some of them could divide into about 100 cells within a week. They also showed that the cells could indeed differentiate into endometrial tissue and identified certain telltale proteins that are present in other types of stem cells.
Gargett , who is now also with Australia’s Hudson Institute of Medical Research, and her colleagues went on to characterize several types of self-renewing cells in the endometrium . But only the whiskered cells, called endometrial stromal mesenchymal stem cells , were truly “multipotent,” with the ability to be coaxed into becoming fat cells, bone cells, or even the smooth muscle cells found in organs such as the heart.
Around the same time, two independent research teams made another surprising discovery: Some endometrial stromal mesenchymal stem cells could be found in menstrual blood . Gargett was surprised that the body would so readily shed its precious stem cells. Since they are so important for the survival and function of organs, she didn’t think the body would “waste” them by shedding them. But she immediately recognized the finding’s significance: Rather than relying on an invasive surgical biopsy to obtain the elusive stem cells she’d identified in the endometrium, she could collect them via menstrual cup.
More detailed studies of the endometrium have since helped to explain how a subset of these precious endometrial stem cells — dubbed menstrual stem cells — end up in menstrual blood. The endometrium has a deeper basal layer that remains intact and an upper functional layer that sloughs off during menstruation. During a single menstrual cycle, the endometrium thickens as it prepares to nourish a fertilized egg, then shrinks as the upper layer sloughs away.
Gargett’s team has shown that these special stem cells are present in both the lower and upper layers of the endometrium. The cells are typically wrapped around blood vessels in a crescent shape, where they are thought to help stimulate vessel formation and play a vital role in repairing and regenerating the upper layer of tissue that gets shed each month during menstruation. This layer is crucial to pregnancy, providing support and nourishment for a developing embryo. The layer and the endometrial stem cells that produce its growth also appear to play an important role in infertility: An embryo can’t implant if the layer doesn’t thicken enough.
Endometrial stem cells have also been linked to endometriosis , a painful condition that affects roughly 190 million women and girls worldwide. Although much about the condition isn’t fully understood, researchers hypothesize that one contributor is the backflow of menstrual blood into a woman’s fallopian tubes, the ducts that carry the egg from the ovaries into the uterus. This backward flow takes the blood into the pelvic cavity, a funnel-shaped space between the bones of the pelvis. Endometrial stem cells that get deposited in these areas may cause endometrial-like tissue to grow outside of the uterus, leading to lesions that can cause excruciating pain, scarring, and, in many cases, infertility.
Researchers are still developing a reliable, noninvasive test to diagnose endometriosis, and patients wait an average of nearly seven years before receiving a diagnosis. However, studies have shown that stem cells collected from the menstrual blood of women with endometriosis have different shapes and patterns of gene expression than cells from healthy women. Several labs are working on ways to use these differences in menstrual stem cells to identify women at higher risk of the condition, which could lead to faster diagnosis and treatment. Menstrual stem cells may also have therapeutic applications. Some researchers working on mice, for example, have found that injecting menstrual stem cells into the rodents’ blood can repair the damaged endometrium and improve fertility.
Other research in lab animals suggests that menstrual stem cells could have therapeutic potential beyond gynecological diseases. In a couple of studies, for example, injecting menstrual stem cells into diabetic mice stimulated the regeneration of insulin-producing cells and improved blood sugar levels . In another, treating injuries with stem cells or their secretions helped heal wounds in mice .
A handful of small but promising clinical trials have found that menstrual stem cells can be transplanted into humans without adverse side effects. Gargett’s team is also attempting to develop human therapies. She and her colleagues are using endometrial stem cells — those taken directly from endometrial tissue rather than menstrual blood — to engineer a mesh to treat pelvic organ prolapse, a common, painful condition in which the bladder, rectum, or uterus slips into the vagina due to weak or injured muscles.
The condition is often caused by childbirth. Existing treatments use synthetic meshes to reinforce and support weak pelvic tissues. However, adverse immune reactions to these materials have led these meshes to be withdrawn from the market. Gargett’s research — so far conducted only in animal models — suggests that using a patient’s own endometrial stem cells to coat biodegradable meshes could yield better results .
Despite the relative convenience of collecting adult multipotent stem cells from menstrual blood, research exploring and utilizing the stem cells’ power — and their potential role in disease — still represents a tiny fraction of stem cell research, says Daniela Tonelli Manica , an anthropologist at Brazil’s State University of Campinas. As of 2020, she found, menstrual stem cell research accounted for only 0.25 percent of all mesenchymal cell research, while bone marrow stem cells represented 47.7 percent.
Manica attributes the slow adoption of menstrual stem cells in part to misogynistic ideas that uteruses are outside the norm and to reactions of disgust. “There’s certainly something of an ‘ick factor’ associated with menstrual blood,” agrees Victoria Male , a reproductive immunologist at Imperial College London who coauthored an article about uterine immune cells in the 2023 Annual Review of Immunology .
Cultural taboos surrounding menstruation — and a general lack of investment in women’s health research — can make it difficult to get funding, says Gargett. Immunologist Male has faced similar challenges — it was easier to obtain funding when she used to study immune cells in liver transplantation than it is now that she works on immune cells in the uterus, she says.
“If we want more research on menstrual fluid, we need more funding,” says Male, noting that the logistics of collecting menstrual fluid over multiple days can be expensive. For that to happen, “we have to tackle sex and gender bias in research funding.” Through more equitable investments, she and others hope, menstruation will be recognized as an exciting new frontier in regenerative medicine — not just a monthly inconvenience.
This article originally appeared in Knowable Magazine , an independent journalistic endeavor from Annual Reviews. Sign up for the newsletter .
- Research article
- Open access
- Published: 22 August 2018
A systematic review of methods to measure menstrual blood loss
- Julia L. Magnay 1 ,
- Shaughn O’Brien 1 , 2 ,
- Christoph Gerlinger 3 , 4 &
- Christian Seitz ORCID: orcid.org/0000-0003-2315-9148 3
BMC Women's Health volume 18 , Article number: 142 ( 2018 ) Cite this article
23k Accesses
54 Citations
13 Altmetric
Metrics details
Since the publication over 50 years ago of the alkaline hematin method for quantifying menstrual blood loss (MBL) many new approaches have been developed to assess MBL. The aim of this systematic review is to determine for methods of measuring MBL: ability to distinguish between normal and heavy menstrual bleeding (HMB); practicalities and limitations in the research setting; and suitability for diagnosing HMB in routine clinical practice.
Embase®™, MEDLINE®, and ClinicalTrials.gov were screened for studies on the development/validation of MBL assessment methods in women with self-perceived HMB, actual HMB or uterine fibroids, or patients undergoing treatment for HMB. Studies using simulated menstrual fluid and those that included women with normal MBL as controls were also eligible for inclusion. Extracted data included study population, results of validation, and advantages/disadvantages of the technique.
Seventy-one studies fulfilled the inclusion criteria. The sensitivity and/or specificity of diagnosing HMB were calculated in 16 studies of methods involving self-perception of MBL (11 pictorial), and in one analysis of the menstrual-fluid-loss (MFL) method; in 13 of these studies the comparator was the gold standard alkaline hematin technique. Sensitivity and specificity values by method were, respectively: MFL model, 89, 98%; pictorial blood loss assessment chart (PBAC), 58–99%, 7.5–89%; menstrual pictogram, 82–96%, 88–94%; models/questionnaires, 59–87%, 62–86%, and complaint of HMB, 74, 74%. The power of methods to identify HMB was also assessed using other analyses such as comparison of average measurements: statistical significance was reported for the PBAC, MFL, subjective complaint, and six questionnaires. In addition, PBAC scores, menstrual pictogram volumes, MFL, pad/tampon count, iron loss, and output from three questionnaires correlated significantly with values from a reference method in at least one study. In general, pictorial methods have been more comprehensively validated than questionnaires and models.
Conclusions
Every method to assess MBL has limitations. Pictorial methods strike a good balance between ease of use and validated accuracy of MBL determination, and could complement assessment of HMB using quality of life (QoL) in the clinical and research setting.
Trial registration
PRISMA registration number: CRD42016032956 .
Peer Review reports
Heavy menstrual bleeding (HMB; menorrhagia) is defined by the National Institute for Health and Care Excellence (NICE) in the United Kingdom as excessive menstrual blood loss (MBL) that interferes with a woman’s physical, emotional, social, and material quality of life (QoL). Up to 50% of women of reproductive age (18–54 years) can experience HMB [ 1 , 2 ], which may cause anemia [ 3 ], lead to limitations in social, physical, and leisure activities [ 1 , 4 ], and be associated with increased healthcare resource use and costs [ 5 ].
In clinical practice, the impact of HMB on a woman’s QoL is currently used to guide treatment [ 1 ]. However, it is acknowledged that self-perception of MBL can be inaccurate [ 6 ], and this may result in surgical intervention in women who are distressed by menses that are actually defined as low volume. General health questionnaires have been found to be inappropriate for use in women with HMB [ 7 ], and there is an absence of recommendations for HMB-specific QoL tools [ 1 , 8 , 9 ]. Thus, a method is needed to complement QoL assessments of HMB. Evaluation of MBL informs patient choice by providing context and clarity; for example, the finding of MBL within the normal range may reassure a woman with perceived HMB to the extent that she chooses not to seek further treatment [ 10 , 11 , 12 , 13 ]. Also, determination of MBL can be important when establishing the etiology of cases of anemia, and changes in MBL are often used to evaluate treatment efficacy in clinical trials.
The alkaline hematin technique, which involves chemically measuring the blood content of used sanitary products, is considered the “gold standard” for MBL determination and has traditionally been used to diagnose HMB as a loss of more than 80 mL of blood per cycle [ 14 , 15 ]. However, as a result of its practical limitations, its use is mainly confined to the research setting. Consequently, many new approaches to measuring MBL have been developed since publication of the alkaline hematin method more than 50 years ago [ 16 , 17 , 18 ]. During this time, sanitary wear has evolved from cotton-based sanitary products to superabsorbent-polymer-containing (SAP-c) ultraslim towels containing granules that can absorb many times their own weight in fluid [ 19 ] hence there is a requirement to validate any method for measuring MBL with the same types/brands of sanitary product that the method is intended to be used with. A summary of the validity and merits of existing measurement techniques, including details of the specific products for which they are validated, would be of great benefit to healthcare providers, clinical scientists, and policy makers. To this end, we performed a systematic review with the specific aims of determining: (1) the degree to which methods for measuring MBL are validated to distinguish between normal bleeding and HMB, (2) the practicalities and limitations of each method in the research setting, and (3) whether any of the methods could be used in routine clinical practice to diagnose HMB.
The systematic review protocol was registered at PROSPERO ( https://www.crd.york.ac.uk/PROSPERO ) in March, 2016, with the registration number CRD42016032956 . Embase®™ and MEDLINE® were searched using Ovid® on 2 March, 2016, and again on 2 November, 2016. The search for articles concerned with validation/development of methods for assessing MBL was based on strategies used to develop the NICE HMB guidelines [ 1 ]. Further terms were added to broaden the range of techniques for assessing MBL among retrieved articles. The search terms can be found in Additional file 1 . A search was also performed in ClinicalTrials.gov for relevant ongoing and recently completed clinical trials that investigated methods to measure MBL. The search terms are shown in Additional file 2 . Following removal of duplicates, retrieved articles were manually screened based on title then abstract.
Articles were selected for inclusion in the study if the main focus was the development or validation of a measure for assessing MBL in women with self-perceived HMB, actual HMB (MBL > 80 mL per cycle), or uterine fibroids, or in women undergoing treatment for HMB. Validation/development studies that used simulated menstrual fluid and those that included women with normal MBL as controls were also eligible for inclusion. Studies investigating only health-related QoL measures or questionnaires were not specifically sought in the original searches to maintain the focus of the review, but were considered for inclusion during screening. To ensure the capture of methods for which published validation data may not yet be available, we included articles that presented novel or modified methods even if validation was not the main focus. To guarantee that original validation studies were included there were no date limits. Similarly, because some early validation studies had only a few participants, no limitations to population size were applied.
Exclusion criteria were studies that only considered an application rather than the development or validation of a technique, those with non-English abstracts, or articles on irrelevant outcome measures or of an inappropriate publication type; for example, preclinical studies and letters. For each included study, the following data were extracted and independently checked: full reference, study type, setting, population, measurement technique, type of validation, statistical output, advantages/disadvantages of the technique (including sensitivity/specificity scores for measuring MBL, discriminatory power for assessing normal versus high MBL, and additional advantages/disadvantages), and any information on the risk of bias. Inter-cycle and internal consistency were also assessed.
On 2 November, 2016, 1438 records were retrieved from Embase®™ and MEDLINE®, including key predefined references [ 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ]. Of these articles, 70 fulfilled the inclusion criteria (Fig. 1 ; Additional file 3 ) [ 6 , 8 , 10 , 11 , 14 , 19 , 20 , 21 , 22 , 23 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 ]. Up to 25 January, 2017, 123 relevant entries were retrieved from ClinicalTrials.gov . One trial, NCT01643304, fulfilled the inclusion criteria [ 85 ].
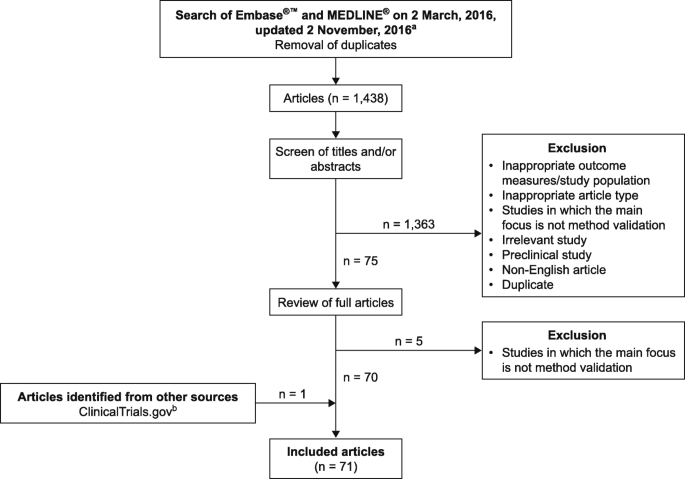
Systematic search and selection process. a See Additional file 1 for search terms. b See Additional file 2 for search terms
Among these studies, population sizes ranged from 2 [ 14 ] to 4506 [ 80 ]. The risk of bias was rarely formally acknowledged in the included studies, which were also subject to different types of bias. Inter-cycle consistency was assessed in six studies [ 11 , 14 , 25 , 42 , 44 , 86 ], with variable results (Additional file 4 ). Internal consistency, measured using a variety of methods, was generally good in the 18 studies in which it was considered (Additional file 4 ). The sensitivity and specificity of diagnosing HMB, or a specified change in MBL, were calculated in 16 studies of tools involving self-perception of MBL (11 pictorial), and in one analysis of the menstrual fluid loss (MFL) method (Table 1 ). In studies reporting both sensitivity and specificity, the Youden’s statistic, a measure of test performance with an optimal score of 1.0, ranged from 0.33 [ 20 ] to 0.88 [ 26 ].
As many women now prefer to use ultraslim towels with enhanced absorbency properties [ 19 ], the most relevant methods for measuring MBL in current clinical use and research are those validated for SAP-c products. The validity of measuring MBL with selected SAP-c products was investigated for the alkaline hematin technique, weight assessment of MFL, the pictorial blood loss assessment chart (PBAC), and the menstrual pictogram [ 19 , 27 , 33 , 38 , 39 ].
Alkaline hematin method
The original alkaline hematin method was developed for cotton-based sanitary products. It was concurrently validated in one study, showing good agreement with an iron isotope activity method in three phases of one woman’s menstrual cycle (Additional files 3 and 5 ) [ 14 ]. Modified versions of the alkaline hematin method were concurrently validated in two studies. In the first study, mean MBL measured with an automated alkaline hematin method in an Indian population was similar to that determined using a precursor alkaline hematin method in a US population [ 36 , 40 , 41 ]. With the advent of SAP-c sanitary products, the method was revalidated by comparing a semi-automated version for use with a selected brand of SAP-c towels to a manual reference method ( r 2 = 0.991; P < .0001, n = 63) (Additional files 3 and 4 ) [ 39 ]. The power to discriminate between normal bleeding and HMB was assessed for four methods and found to be reasonable, but statistical significance was not given (Additional file 6 ) [ 10 , 35 , 41 , 42 ].
The efficiency of blood extraction from sanitary products using the alkaline hematin method was investigated in 10 studies (Additional file 4 ) [ 10 , 14 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. In the original alkaline hematin method, blood recovery was 96.3% after a 20-h incubation [ 14 ]. With modifications to improve speed and usability, efficiencies of recovering various volumes of blood from a selection of sanitary products ranged from 74.8% [ 42 ] to 107% [ 41 ]. Adaptation of the method for a selected brand of SAP-c towels resulted in recovery of at least 90% (≥85% with automation) of simulated menstrual fluid volumes [ 38 , 39 ].
Menstrual fluid loss, pad counts, and duration of period
Fluid weight (MFL) has been investigated as a simple alternative to the assessment of MBL by the alkaline hematin method [ 44 ]. The measure can be expressed gravimetrically (g) or converted directly to volume (mL), based on the assumption that the specific gravity of menstrual fluid equals one [ 28 , 44 ]. The relationship between MBL and MFL was considered in four studies, three of which used the alkaline hematin method as the comparator [ 27 , 44 , 48 ]. In all four studies, including one that validated MFL measurements with a selected brand of SAP-c towels [ 46 ], there was a correlation between MFL and either MBL or change in MBL ( r = 0.88–0.97; P = .001–.0001; Additional file 5 ) [ 27 , 44 , 46 , 48 ]. In a fifth study, MBL estimated from MFL correlated, but was not interchangeable, with MBL measured by the alkaline hematin method ( r = 0.73; P < .00001; Additional file 5 ) [ 84 ].
In the study by Fraser and colleagues, the sensitivity and specificity of diagnosing HMB with a regression model to estimate MBL from MFL were 89 and 98%, respectively. It was also shown that the blood content in MFL was similar in women with moderately heavy (60–100 mL) and excessive (> 100 mL) MBL (48 and 50%, respectively) [ 44 ]. In a later study using SAP-c towels, establishment of a normal range for MFL was prohibited because of overlap of MFL between women with normal and those with excessive MBL, and blood fraction was found to increase progressively with MFL volume [ 27 ].
The association of MBL with duration of menstruation was investigated in four studies (Additional files 5 and 6 ). There was a modest correlation in a study of 207 women complaining of HMB ( r = 0.35, P < .01) [ 82 ], whereas no relationship was observed in the other three studies, which included women with a range of MBL volumes [ 11 , 27 , 43 ]. In a study of women with self-perceived HMB, period duration was not significantly different for the lightest versus the heaviest periods [ 6 ]. Information on the length of periods was requested in some questionnaires [ 62 , 66 ], and this parameter forms part of both the PBAC and menstrual pictogram methods of assessing MBL [ 23 , 32 ].
The association of MBL with counts of sanitary items was considered in eight studies. Higham and Shaw and Warner et al. found that MBL was associated with the total number of pads and tampons used ( r = 0.61 and 0.30; P < .005 and P < .001, respectively) [ 68 , 82 ]. Chimbira et al. found that the median MBL was greater in women using 10 or fewer pads per period than in those using 31–40 pads, but there was a wide scatter of MBL in each group [ 34 ]. Five studies found no significant or overall correlation between pad/tampon count and MBL (Additional file 5 : Table S5) [ 6 , 27 , 32 , 42 , 82 ]. A question about the number of pads used by women was included in seven questionnaires [ 61 , 62 , 65 , 68 , 71 , 74 , 83 ]; information about the frequency of changing pads was requested in three questionnaires [ 28 , 63 , 79 ].
Measurement of iron/labelled red blood cells
The discriminatory power of three methods to measure iron/labelled blood in pads [ 31 ], from menstrual products [ 43 ], or in the whole body [ 29 ] was assessed: all of the techniques were able to discriminate between normal and high MBL, or between non-anemic and anemic women, but statistical significance was not reported (Additional file 6 ). In a fourth study, the amount of iron lost in pads strongly correlated with MFL [ 47 ] (Additional file 5 ).
Pictorial methods
The validation of pictorial methods was the focus of 19 articles (Additional file 3 ). These studies evaluated either the PBAC, which uses a scoring system that is proportional but not equivalent to MBL, or the menstrual pictogram, which measures MBL in milliliters and is directly comparable to the alkaline hematin method.
Pictorial blood loss assessment chart (PBAC)
Fourteen of the included articles reported on the PBAC/modified PBAC (Additional file 3 ). In one study, the PBAC was validated for a selected brand of SAP-c products [ 33 ]. Sensitivity and specificity of the PBAC were determined in seven studies (Table 1 ). In six studies these related to diagnosis of a measured MBL > 80 mL [ 20 , 22 , 23 , 25 , 30 , 33 ], and in one study they related to diagnosis of self-perceived HMB [ 54 ]. For the diagnosis of MBL > 80 mL, sensitivity was 58–99% and specificity was 7.5–89%. For the diagnosis of self-perceived HMB, sensitivity was 78.5% and specificity was 75.8%. Specificity and sensitivity data generated with a single PBAC cut-off of 100 were presented in three studies [ 22 , 23 , 30 ]. Sensitivity and specificity data derived from a PBAC cut-off of 50 were provided in one study [ 20 ]. In three studies, data using multiple cut-off values, including those > 100, were reported [ 25 , 33 , 54 ].
The discriminatory power of PBAC was assessed in nine studies (Additional file 6 ). Statistically significant results were reported for the difference in PBAC scores between patients in heavy, normal, and light bleeding categories [ 54 , 56 ], those with and without menstrual disorder [ 52 ], individuals before and after treatment [ 81 ], and treated patients and active controls [ 48 ]. The association of PBAC with MBL (or change in MBL) was assessed in five studies. The range in correlation coefficients across four studies was 0.4659–0.847 (Additional file 5 ). The generalizability of the PBAC beyond the United Kingdom population of adult women in which it was originally validated was considered in seven studies (Additional file 4 ). The method was used successfully in populations of adolescents [ 56 , 76 ], users and non-users of oral contraceptives [ 55 ], and Iranian and Turkish women [ 51 , 52 , 81 ]. However, the PBAC may overestimate MBL in the general community [ 53 ]. Inter-cycle consistency was assessed with PBAC in two studies and found to be high [ 25 , 54 ].
- Menstrual pictogram
The menstrual pictogram/modified menstrual pictogram were the focus of five included articles (Additional file 3 ). The sensitivity and specificity of the menstrual pictogram were determined in one investigation for a specified decrease in MBL, and in three studies in terms of diagnosing MBL > 80 mL. In one study in which the menstrual pictogram was evaluated as part of the Symptometrics device, the reference method was the paper menstrual pictogram (Table 1 ) [ 26 , 27 , 32 , 59 ]. Across these four studies, the sensitivity was 82–96% and the specificity was 88–94%. A menstrual pictogram specifically designed for use with a particular brand of SAP-c towels (Fig. 2 ) was endorsed in one of these studies [ 27 ]. The predictive power of the menstrual pictogram at diagnosing HMB was presented in one report (positive, 91%; negative, 83%) [ 26 ].
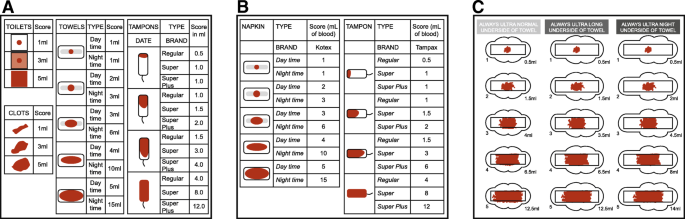
a Representation of the original menstrual pictogram. Reprinted from Fertility and Sterility , 76, Wyatt KM et al., Determination of total menstrual blood loss, pp125–31, Copyright 2001, with permission from Elsevier [ 32 ]. b A modified version of the menstrual pictogram. Larsen L et al., Reproductive Sciences , 20 (6), pp680–7, Copyright © 2013, Reprinted by permission of SAGE publications [ 26 ]. c The menstrual pictogram validated for use with towels containing superabsorbent polymers. Reprinted from Fertility and Sterility , 101, Magnay, JL et al., Validation of a new menstrual pictogram (superabsorbent polymer-c version) for use with ultraslim towels that contain superabsorbent polymers, pp515–21, Copyright 2014, with permission from Elsevier [ 27 ]
Menstrual pictogram/modified menstrual pictogram values correlated highly with MFL assessed by the weight method, and with MBL or change in MBL from baseline assessed by the alkaline hematin method (Additional file 5 ). The original menstrual pictogram (Fig. 2 ) was validated in the United Kingdom in untreated women with self-perceived, normal, or heavy MBL [ 32 ]. External validation of a modified version of the tool (Fig. 2 ) was performed in North American women treated for HMB associated with leiomyomata [ 26 ] (Additional file 4 ).
Self-perception
The specificity and sensitivity of self-perception methods were investigated in six studies, including some questionnaires (Table 1 ). Complaint of HMB was able to diagnose an MBL > 80 mL with both a specificity and a sensitivity of 74% and a positive predictive value of 56% [ 25 ]. A model including diary entries of both self-perceived bleeding intensity and clinical parameters diagnosed MBL > 80 mL with a sensitivity and specificity of 87 and 70% respectively [ 84 ]. A questionnaire including a Record and a Recall method for estimating MBL, both of which had a subjective element, resulted in sensitivities of 66 and 59%, respectively. Recall method and Record method tertiles had significantly different mean MFL values [ 62 ]. With the Menorrhagia Impact Questionnaire (MIQ), the specificity and sensitivity of changes in MIQ items corresponding to either a meaningful change in perceived MBL [ 69 ] or an optimal reduction in MBL measured by the alkaline hematin method [ 4 ] were 63–82%. In a study of the Menstrual Evaluation Questionnaire, which includes questions on the self-perceived heaviness of periods, the sensitivity and specificity of diagnosing MBL > 80 mL were 60 and 86% respectively, and women who rated their periods as “very heavy” had a significantly higher mean MBL than the remainder of the women [ 68 ].
There was low-to-moderate correlation of 36-Item Short Form Survey (SF-36) score, log discharge rate, ferritin score or PBAC score with scores from four questionnaires: the Menstrual Bleeding Questionnaire [MBQ], the Mansfield–Voda–Jorgensen menstrual bleeding scale, an MBL questionnaire, and a QoL questionnaire (Additional file 5 ) [ 8 , 28 , 73 , 83 ]. All four surveys, as well as the Health Utilities Index questionnaire [ 75 ], were able to discriminate between women with and without HMB, with statistical significance attained for the MBQ, the QoL questionnaire, and the Health Utilities Index (Additional file 6 ). The Portuguese SF-36 did not correlate with PBAC scores [ 70 ].
A questionnaire was used in 1547 women to self-grade MBL heaviness and assess the effects of self-perceived HMB on daily life and the Swedish SF-36 [ 85 ]. The daily lives of women with self-perceived HMB were affected much more than those of women with normal MBL (Additional file 6 ). Women with self-perceived HMB also had significantly worse health-related QoL in all domains of the Swedish SF-36 compared with women with normal menstrual bleeding.
The percentage of women with self-perceived HMB and a measured MBL of 80 mL or more was assessed in nine studies and found to range from 26 to 76% [ 6 , 11 , 27 , 30 , 32 , 34 , 35 , 68 , 82 ] (Additional file 6 ). For three methods involving self-perception of MBL, positive establishment of face and content validity was reported (Additional file 3 ) [ 57 , 71 , 78 ].
Additional advantages and disadvantages
The additional advantages and disadvantages of methods for measuring MBL are summarized in Table 2 . A more detailed overview is provided in Additional file 3 .
We present the results of a systematic review of the development and validation of methods for measuring MBL. We summarize the data available and list other key advantages and disadvantages of the various procedures.
The alkaline hematin method has been well validated in terms of the efficiency of blood recovery from sanitary items, including towels that contain superabsorbent polymers as the absorptive agent. It is widely recognized as the most objective technique with which to measure MBL, and can be required by regulatory bodies to assess the efficacy of new treatments for HMB. However, to be suitable for the clinical setting, a test must be quick, easy to conduct, and accepted by patients. In this respect, the alkaline hematin method is less appropriate for use in the general population than the PBAC, menstrual pictogram, or a questionnaire, especially the electronic versions. Despite extensive development to make it more practical and widely applicable, the original inherent disadvantages of the method remain; namely, the need to collect, store and then send all used sanitary items to a laboratory for analysis. In addition, the method is limited to documentation of MBL collected on sanitary items. To overcome this drawback it would be necessary to either carefully capture all extraneous blood loss or use a simultaneous diary to take extraneous blood loss into account. Nonetheless, the alkaline hematin method is widely recognized to be the “gold standard” in terms of accuracy. Ideally, all methods to measure MBL would be validated against alkaline hematin. However, this can be challenging in practice, in part due to the abovementioned disadvantages of the alkaline hematin technique.
Correlations were observed between MFL and MBL, and it is argued that MFL matters more to women concerned with flooding than MBL [ 48 ]. However, MBL estimated using MFL is not interchangeable with MBL measured using the alkaline hematin method [ 84 ]. Furthermore, variation in the proportion of the non-blood fraction, particularly at extremes of menstrual loss, limits the validity of using MFL to diagnose HMB [ 27 , 87 , 88 ]. Therefore, we do not consider MFL to be a reliable validator of MBL. The MFL method also requires women to store and submit carefully all used products for analysis, which may not be acceptable or feasible, resulting in reduced compliance. In principle, the use of menstrual cups to collect large volumes of MFL is simple. In reality, many women report that spillage and leakage is common and the technique has thus proved unsuitable for measuring MBL.
The hypothesis that menstrual duration alone can be used to predict HMB is not supported by current evidence. It is also not possible to accurately correlate MBL with the number of feminine items used during a menstrual period, and extreme examples have been cited of women with HMB using far fewer towels than those with light menstrual flow [ 6 , 27 , 82 ]. In addition to the brand and absorbency of the product, many variables affect the frequency with which items are changed, including rate and composition of menstrual flow, individual anatomy, ambient humidity, physical activity, posture, and personal fastidiousness in changing sanitary garments. Some patient-reported outcome instruments have attempted to incorporate product absorbencies, albeit that towel absorbency ratings are arbitrary and unregulated [ 28 , 62 , 71 , 83 ]. However, the degree of saturation and/or brands of products are not always taken into account [ 28 , 71 , 83 ].
In general, the discriminatory power and sensitivity/specificity scores are reasonably high for the PBAC/modified PBAC, but because some low scores have been recorded the robustness of this test has been queried [ 20 , 25 , 30 , 89 ]. The PBAC is not as accurate as the alkaline hematin method for determination of HMB, but it is nevertheless superior to using clinical history or a simple bleeding diary. Moreover, it has been validated for use with selected SAP-c products, does not require laboratory facilities, and has undergone much external validation. The menstrual pictogram has consistently high (> 80%) sensitivity and specificity in diagnosing HMB, including when validated with a SAP-c product. Furthermore, it correlates well with the alkaline hematin method [ 26 , 27 , 32 , 59 ], although only five menstrual pictogram validation studies were retrieved. In contrast to the PBAC, the original menstrual pictogram includes a greater range of icons and differentiates between absorbency ratings of sanitary items [ 32 ].
Self-assessment of MBL yields a number of false negatives and positives when compared with more objective measurements. The concept that some women have a distorted perception of their MBL is corroborated by data from a 16-study meta-analysis [ 90 ]. Among measures of MBL involving self-perception, a mixed linear model based on a menstrual diary and laboratory parameters had the highest sensitivity score (87%), but to date the model has only been tested in a single trial in women with HMB.
Various articles on questionnaires were reviewed. All the questionnaires contained items related to self-perception of MBL or its impact on QoL. Concurrent validation was performed in fewer than half of the questionnaires included, with mixed results [ 8 , 28 , 62 , 69 , 70 , 72 , 73 , 75 , 76 , 85 , 86 ], but three questionnaires showed promise in terms of ability to discriminate between heavy and normal MBL [ 8 , 73 , 75 ].
Importantly, of all the methods reviewed, only the alkaline hematin method, the PBAC, and the menstrual pictogram are validated for measuring MBL with selected SAP-c products [ 19 , 27 , 33 , 38 , 39 ]. In addition to the statistical analyses described above, treatment-induced changes in MBL that were also detected by a reference technique were reported for four methods: the menstrual pictogram, PBAC, MFL, and MIQ [ 26 , 48 , 54 , 69 , 72 , 81 ] (Table 1 ; Additional files 5 and 6 ).
MBL is only one aspect of the menstrual experience. Pain, pattern, and predictability of timing can all influence a woman’s perception of her period. QoL is recognized to be an important clinical indicator of the effects of menstruation on women [ 17 , 85 , 91 ]. However, QoL is influenced by many factors other than HMB, such as undernourishment and depression [ 70 ]. Given that treatment of HMB may incur significant psychological, physical, and financial costs [ 28 ], and – as discussed above – validated, quick, economical, and easy methods for assessing MBL are available, future evaluation of a clinical technique that combines a pictorial method validated for modern sanitary products with a daily (preferably electronic) menstrual diary of specific health-related QoL items would be beneficial.
A limitation of this review is that comprehensive comparisons of the different techniques were limited because of the heterogeneity of validation methods and result formats. The definition of HMB was not the same for all methods and there was a lack of consistency in the comparator employed (Table 1 and Additional file 5 ). With the PBAC, different cut-off values were used to diagnose HMB. Often the PBAC or menstrual pictogram was not used or evaluated in the way in which it was originally validated [ 50 , 51 , 52 , 54 ], and none of the amendments has been recertified by the alkaline hematin assay. The risk of bias was seldom formally acknowledged in the articles reviewed, and different types of study were subject to different types of bias. Blinding of investigators/gynecologists to participant data was acknowledged in all studies in which investigator–participant agreement was assessed (Additional file 4 ) [ 19 , 23 , 25 , 27 , 39 , 48 , 59 ].
Our searches identified articles that were excluded because they primarily described the application of an existing method for measuring MBL rather than any form of method validation [ 92 , 93 , 94 , 95 , 96 , 97 ]. A recent systematic review analyzing the frequency of use of MBL measurement tools in randomized controlled trials found that PBAC score was the most commonly used primary outcome [ 16 ]. The menstrual pictogram did not feature, perhaps because it has been used less frequently than the PBAC, but in our systematic review four non-validation studies were identified in which the menstrual pictogram assessed MBL [ 92 , 93 , 95 , 97 ]. As a result of the search terms used in our review there may have been incomplete retrieval of reports relating to questionnaires and QoL studies [ 7 , 98 , 99 , 100 , 101 , 102 , 103 ]. It would be well beyond the scope of this review to expand the existing search strategy to identify all questionnaires relating to MBL. However, it should be considered for a follow-up analysis because there is a need to standardize the validation of questionnaires and QoL tools for measuring MBL [ 9 , 104 ].
Despite these limitations, we hope that by summarizing all of the available data on the different methods together this review will inform researchers evaluating new techniques of the standard types of validation required. This in turn should help policy makers conduct a robust appraisal of available methods for measuring MBL.
Every available method to assess MBL has limitations. Pictorial methods strike a good balance between ease of use and validated accuracy of MBL determination; of these methods, the menstrual pictogram has several advantages, not least that it considers different absorbency levels of sanitary items and has an output of MBL volume in milliliters. Currently, clinicians usually base their diagnosis of HMB on a patient’s reported QoL. However, there are drawbacks, particularly in research trials, to relying entirely on health-related QoL devices, which are essentially subjective measures of HMB. A compromise would be to consider MBL alongside QoL when deciding how to diagnose HMB and assess effectiveness of treatments.
Abbreviations
- Heavy menstrual bleeding
- Menstrual blood loss
Menstrual bleeding questionnaire
Menstrual fluid loss
Menorrhagia impact questionnaire
National Institute for Health and Care Excellence
Pictorial blood loss assessment chart; superabsorbent-polymer-containing
Quality of life
36-item short form survey, SF-36
National Evidence Based Clinical Guidelines. Heavy menstrual bleeding. https://www.nice.org.uk/guidance/cg44?unlid=84830935220164267953 . Accessed 16 Nov 2016.
Shapley M, Jordan K, Croft PR. An epidemiological survey of symptoms of menstrual loss in the community. Br J Gen Pract. 2004;54:359–63.
PubMed PubMed Central Google Scholar
Peuranpaa P, Heliovaara-Peippo S, Fraser I, Paavonen J, Hurskainen R. Effects of anemia and iron deficiency on quality of life in women with heavy menstrual bleeding. Acta Obstet Gynecol Scand. 2014;93:654–60.
Article PubMed CAS Google Scholar
Lukes AS, Baker J, Eder S, Adomako TL. Daily menstrual blood loss and quality of life in women with heavy menstrual bleeding. Women’s Health (Lond). 2012;8:503–11.
Copher R, Le Nestour E, Law A, Pocoski J, Zampaglione E. Retrospective analysis of variation in heavy menstrual bleeding treatments by age and underlying cause. Curr Med Res Opin. 2013;29:127–39.
Fraser IS, McCarron G, Markham R. A preliminary study of factors influencing perception of menstrual blood loss volume. Am J Obstet Gynecol. 1984;149:788–93.
Jenkinson C, Peto V, Coulter A. Making sense of ambiguity: evaluation in internal reliability and face validity of the SF 36 questionnaire in women presenting with menorrhagia. Qual Health Care. 1996;5:9–12.
Article PubMed PubMed Central CAS Google Scholar
Matteson KA, Scott DM, Raker CA, Clark MA. The menstrual bleeding questionnaire: development and validation of a comprehensive patient-reported outcome instrument for heavy menstrual bleeding. Br J Obstet Gynaecol. 2015;122:681–9.
Article CAS Google Scholar
Clark TJ, Khan KS, Foon R, Pattison H, Bryan S, Gupta JK. Quality of life instruments in studies of menorrhagia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2002;104:96–104.
Article PubMed Google Scholar
Gannon MJ, Day P, Hammadieh N, Johnson N. A new method for measuring menstrual blood loss and its use in screening women before endometrial ablation. Br J Obstet Gynaecol. 1996;103:1029–33.
Haynes PJ, Hodgson H, Anderson AB, Turnbull AC. Measurement of menstrual blood loss in patients complaining of menorrhagia. Br J Obstet Gynaecol. 1977;84:763–8.
Higham J, Reid P. A preliminary investigation of what happens to women complaining of menorrhagia but whose complaint is not substantiated. J Psychosom Obstet Gynaecol. 1995;16:211–4.
Rees MC. Role of menstrual blood loss measurements in management of complaints of excessive menstrual bleeding. Br J Obstet Gynaecol. 1991;98:327–8.
Hallberg L, Nilsson L. Determination of menstrual blood loss. Scand J Clin Lab Invest. 1964;16:244–8.
Hallberg L, Hogdahl AM, Nilsson L, Rybo G. Menstrual blood loss - a population study. Variation at different ages and attempts to define normality. Acta Obstet Gynecol Scand. 1966;45:320–51.
Herman MC, Penninx J, Geomini PM, Mol BW, Bongers MY. Choice of primary outcomes evaluating treatment for heavy menstrual bleeding. Br J Obstet Gynaecol. 2016;123:1593–8.
Quinn SD, Higham J. Outcome measures for heavy menstrual bleeding. BMC Women’s Health. 2016;12:21–6.
Warrilow G, Kirkham C, Ismail K, Wyatt K, Dimmock P, O'Brien S. Quantification of menstrual blood loss. Obstet Gynecol. 2004;6:88–92.
Magnay JL, Nevatte TM, Seitz C, O'Brien S. A new menstrual pictogram for use with feminine products that contain superabsorbent polymers. Fertil Steril. 2013;100:1715–21. e1–4
Barr F, Brabin L, Agbaje O. A pictorial chart for managing common menstrual disorders in Nigerian adolescents. Int J Gynecol Obstet. 1999;66:51–3.
Cheyne GA, Shepherd MM. Comparison of chemical and atomic absorption methods for estimating menstrual blood loss. J Med Lab Technol. 1970;27:350–4.
PubMed CAS Google Scholar
Deeny M, Davis JA. Assessment of menstrual blood loss in women referred for endometrial ablation. Eur J Obstet Gynecol Reprod Biol. 1994;57:179–80.
Higham JM, O'Brien PMS, Shaw RW. Assessment of menstrual blood loss using a pictorial chart. Br J Obstet Gynaecol. 1990;97:734–9.
Holt JM, Mayet FG, Warner GT, Callender ST. Measurement of blood loss by means of a whole-body counter. Br Med J. 1967;4:86–8.
Janssen CAH, Scholten PC, Heintz APM. A simple visual assessment technique to discriminate between menorrhagia and normal menstrual blood loss. Obstet Gynecol. 1995;85:977–82.
Larsen L, Coyne K, Chwalisz K. Validation of the menstrual pictogram in women with leiomyomata associated with heavy menstrual bleeding. Reprod Sci. 2013;20:680–7.
Magnay JL, Nevatte TM, O'Brien S, Gerlinger C, Seitz C. Validation of a new menstrual pictogram (superabsorbent polymer-c version) for use with ultraslim towels that contain superabsorbent polymers. Fertil Steril. 2014;101:515–22. e5
Mansfield PK, Voda A, Allison G. Validating a pencil-and-paper measure of perimenopausal menstrual blood loss. Women’s Health Issues. 2004;14:242–7.
Price DC, Forsyth EM, Cohn SH, Cronkite EP. The study of menstrual and other blood loss, and consequent iron deficiency, by Fe 59 whole-body counting. Can Med Assoc J. 1964;90:51–4.
PubMed PubMed Central CAS Google Scholar
Reid PC, Coker A, Coltart R. Assessment of menstrual blood loss using a pictorial chart: a validation study. Br J Obstet Gynaecol. 2000;107:320–2.
Tauxe WN. Quantitation of menstrual blood loss: a radioactive method utilizing a counting dome. J Nucl Med. 1962;3:282–7.
Wyatt KM, Dimmock PW, Walker TJ, O'Brien PMS. Determination of total menstrual blood loss. Fertil Steril. 2001;76:125–31.
Zakherah MS, Sayed GH, El-Nashar SA, Shaaban MM. Pictorial blood loss assessment chart in the evaluation of heavy menstrual bleeding: diagnostic accuracy compared to alkaline hematin. Gynecol Obstet Investig. 2011;71:281–4.
Article Google Scholar
Chimbira TH, Anderson ABM, Turnbull AC. Relation between measured menstrual blood loss and patient's subjective assessment of loss, duration of bleeding, number of sanitary towels used, uterine weight and endometrial surface area. Br J Obstet Gynaecol. 1980;87:603–9.
van Eijkeren MA, Scholten PC, Christiaens GC, Alsbach GP, Haspels AA. The alkaline hematin method for measuring menstrual blood loss - a modification and its clinical use in menorrhagia. Eur J Obstet Gynecol Reprod Biol. 1986;22:345–51.
Desai H, Raghavan KS, Mapa MK, Gupta AN. Quantitative estimation of menstrual blood loss. Ind J Med Res. 1982;75:827–30.
CAS Google Scholar
Hurskainen R, Teperi J, Turpeinen U, Grenman S, Kivela A, Kujansuu E, et al. Combined laboratory and diary method for objective assessment of menstrual blood loss. Acta Obstet Gynecol Scand. 1998;77:201–4.
Magnay JL, Nevatte TM, Dhingra V, O'Brien S. Menstrual blood loss measurement: validation of the alkaline hematin technique for feminine hygiene products containing superabsorbent polymers. Fertil Steril. 2010;94:2742–6.
Magnay JL, Schonicke G, Nevatte TM, O'Brien S, Junge W. Validation of a rapid alkaline hematin technique to measure menstrual blood loss on feminine towels containing superabsorbent polymers. Fertil Steril. 2011;96:394–8.
Newton J, Barnard G, Collins W. A rapid method for measuring menstrual blood loss using automatic extraction. Contraception. 1977;16:269–82.
Shaw ST Jr, Aaronson DE, Moyer DL. Quantitation of menstrual blood loss - further evaluation of the alkaline hematin method. Contraception. 1972;5:497–513.
Vasilenko P, Kraicer PF, Kaplan R, deMasi A, Freed N. A new and simple method of measuring menstrual blood loss. J Reprod Med Obstet Gynecol. 1988;33:293–7.
Baldwin RM, Whalley PJ, Pritchard JA. Measurements of menstrual blood loss. Am J Obstet Gynecol. 1961;81:739–42.
Fraser IS, Warner P, Marantos PA. Estimating menstrual blood loss in women with normal and excessive menstrual fluid volume. Obstet Gynecol. 2001;98:806–14.
Gleeson N, Devitt M, Buggy F, Bonnar J. Menstrual blood loss measurement with Gynaeseal. Aus New Zeal J Obstet Gynaecol. 1993;33:79–80.
Gudmundsdottir BR, Hjaltalin EF, Bragadottir G, Hauksson A, Geirsson RT, Onundarson PT. Quantification of menstrual flow by weighing protective pads in women with normal, decreased or increased menstruation. Acta Obstet Gynecol Scand. 2009;88:275–9.
Napolitano M, Dolce A, Celenza G, Grandone E, Perilli MG, Siragusa S, et al. Iron-dependent erythropoiesis in women with excessive menstrual blood losses and women with normal menses. Ann Hematol. 2014;93:557–63.
Reid PC, Virtanen-Kari S. Randomised comparative trial of the levonorgestrel intrauterine system and mefenamic acid for the treatment of idiopathic menorrhagia: a multiple analysis using total menstrual fluid loss, menstrual blood loss and pictorial blood loss assessment charts. Br J Obstet Gynaecol. 2005;112:1121–5.
Stewart K, Greer R, Powell M. Women's experience of using the Mooncup. J Obstet Gynaecol. 2010;30:285–7.
Barrington JW, Bowen-Simpkins P. The levonorgestrel intrauterine system in the management of menorrhagia. Br J Obstet Gynaecol. 1997;104:614–6.
Biri A, Bozkurt N, Korucuoglu U, Yilmaz E, Tiras B, Guner H. Use of pictorial chart for managing menorrhagia among Turkish women. J Turk Ger Gynecol Assoc. 2007;9:35–7.
Google Scholar
Nahidi F, Bagheri L, Jannesari S, Majd HA. Relationship between delivery type and menstrual disorders: a case-control study. J Res Health Sci. 2011;11:83–90.
PubMed Google Scholar
Shapley M, Redman CWE. Assessment of menstrual blood loss using a pictorial chart and endometrial sampling within the community. J Obstet Gynaecol. 1995;15:123–4.
Hald K, Lieng M. Assessment of periodic blood loss: interindividual and intraindividual variations of pictorial blood loss assessment chart registrations. J Min Invas Gynecol. 2014;21:662–8.
MacEachern K, Kaur H, Toukh M, Mumal I, Hamilton A, Scovil S, et al. Comprehensive evaluation of hemostasis in normal women: impact on the diagnosis of mild bleeding disorders. Clin Appl Thromb Hemost. 2015;21:72–81.
Sanchez J, Andrabi S, Bercaw JL, Dietrich JE. Quantifying the PBAC in a pediatric and adolescent gynecology population. Pediatr Hematol Oncol. 2012;29:479–84.
Shaw RW, Brickley MR, Evans L, Edwards MJ. Perceptions of women on the impact of menorrhagia on their health using multi-attribute utility assessment. Br J Obstet Gynaecol. 1998;105:1155–9.
Sowter M, Bidgood K, Richardson J. A comparative randomised trial of the effect of preoperative endometrial inhibition on the long-term outcome of transcervical endometrial resection. Gynaecol Endosc. 1997;6:33–7.
Wyatt KM, Dimmock PW, Hayes-Gill B, Crowe J, O'Brien PMS. Menstrual symptometrics: a simple computer-aided method to quantify menstrual cycle disorders. Fertil Steril. 2002;78:96–101.
Côté I, Jacobs P, Cumming D. Work loss associated with increased menstrual loss in the United States. Obstet Gynecol. 2002;100:683–7.
Harlow B, Missmer S, Cramer D, Barbieri R. Does tubal sterilization influence the subsequent risk of menorrhagia or dysmenorrhea? Fertil Steril. 2002;77:754–60.
Heath ALM, Skeaff CM, Gibson RS. Validation of a questionnaire method for estimating extent of menstrual blood loss in young adult women. J Trace Elem Med Biol. 1999;12:231–5.
Hodgson DA, Feldberg IB, Sharp N, Cronin N, Evans M, Hirschowitz L. Microwave endometrial ablation: development, clinical trials and outcomes at three years. Br J Obstet Gynaecol. 1999;106:684–94.
Johannes CB, Crawford SL, Woods J, Goldstein RB, Tran D, Mehrotra S, et al. An electronic menstrual cycle calendar: comparison of data quality with a paper version. Menopause. 2000;7:200–8.
Lee LK, Chen PCY, Lee KK, Kaur J. Menstruation among adolescent girls in Malaysia: a cross-sectional school survey. Singap Med J. 2006;47:869–74.
Santer M, Warner P, Wyke S. A Scottish postal survey suggested that the prevailing clinical preoccupation with heavy periods does not reflect the epidemiology of reported symptoms and problems. J Clin Epidemiol. 2005;58:1206–10.
Shapley M, Jordan K, Croft PR. Increased vaginal bleeding: the reasons women give for consulting primary care. J Obstet Gynaecol. 2003;23:48–50.
Warner PE, Critchley HOD, Lumsden MA, Campbell-Brown M, Douglas A, Murray GD. Menorrhagia I: measured blood loss, clinical features, and outcome in women with heavy periods - a survey with follow-up data. Am J Obstet Gynecol. 2004;190:1216–23.
Bushnell DM, Martin ML, Moore KA, Richter HE, Rubin A, Patrick DL. Menorrhagia impact questionnaire: assessing the influence of heavy menstrual bleeding on quality of life. Curr Med Res Opin. 2010;26:2745–55.
de Souza SS, Camargos AF, Ferreira MC, de Assis Nunes Pereira F, de Rezende CP, Araujo CA, et al. Hemoglobin levels predict quality of life in women with heavy menstrual bleeding. Arch Gynecol Obstet. 2010;281:895–900.
Deal LS, Williams VS, Fehnel SE. Development of an electronic daily uterine fibroid symptom diary. Patient. 2011;4:31–44.
Lukes AS, Muse K, Richter HE, Moore KA, Patrick DL. Estimating a meaningful reduction in menstrual blood loss for women with heavy menstrual bleeding. Curr Med Res Opin. 2010;26:2673–8.
Pawar A, Krishnan R, Davis K, Bosma K, Kulkarni R. Perceptions about quality of life in a school-based population of adolescents with menorrhagia: implications for adolescents with bleeding disorders. Haemophilia. 2008;14:579–83.
Pisoni CN, Cuadrado MJ, Khamashta MA, Hunt BJ. Treatment of menorrhagia associated with oral anticoagulation: efficacy and safety of the levonorgestrel releasing intrauterine device (Mirena coil). Lupus. 2006;15:877–80.
Rae C, Furlong W, Horsman J, Pullenayegum E, Demers C, St-Louis J, et al. Bleeding disorders, menorrhagia and iron deficiency: impacts on health-related quality of life. Haemophilia. 2013;19:385–91.
Revel-Vilk S, Paltiel O, Lipschuetz M, Ilan U, Hyam E, Shai E, et al. Underdiagnosed menorrhagia in adolescents is associated with underdiagnosed anemia. J Pediatr. 2012;160:468–72.
Sambrook AM, Elders A, Cooper KG. Microwave endometrial ablation versus thermal balloon endometrial ablation (MEATBall): 5-year follow up of a randomised controlled trial. Br J Obstet Gynaecol. 2014;121:747–53.
Santer M, Wyke S, Warner P. What aspects of periods are most bothersome for women reporting heavy menstrual bleeding? Community survey and qualitative study. BMC Women’s Health. 2007;7:8.
Bruinvels G, Burden R, Brown N, Richards T, Pedlar C. The prevalence and impact of heavy menstrual bleeding (menorrhagia) in elite and non-elite athletes. PLoS One. 2016;11:e0149881.
Fraser IS, Mansour D, Breymann C, Hoffman C, Mezzacasa A, Petraglia F. Prevalence of heavy menstrual bleeding and experiences of affected women in a European patient survey. Int J Gynaecol Obstet. 2015;128:196–200.
Goshtasebi A, Mazari Z, Behboudi Gandevani S, Naseri M. Anti-hemorrhagic activity of Punica granatum L. flower (Persian Golnar) against heavy menstrual bleeding of endometrial origin: a double-blind, randomized controlled trial. Med J Islam Repub Iran. 2015;29:199.
Higham JM, Shaw RW. Clinical associations with objective menstrual blood volume. Eur J Obstet Gynecol Reprod Biol. 1999;82:73–6.
Toxqui L, Perez-Granados AM, Blanco-Rojo R, Wright I, Vaquero MP. A simple and feasible questionnaire to estimate menstrual blood loss: relationship with hematological and gynecological parameters in young women. BMC Women’s Health. 2014;14:71.
Schumacher U, Schumacher J, Mellinger U, Gerlinger C, Wienke A, Endrikat J. Estimation of menstrual blood loss volume based on menstrual diary and laboratory data. BMC Women’s Health. 2012;12:24.
Karlsson TS, Marions LB, Edlund MG. Heavy menstrual bleeding significantly affects quality of life. Acta Obstet Gynecol Scand. 2014;93:52–7.
Warner PE, Critchley HO, Lumsden MA, Campbell-Brown M, Douglas A, Murray GD. Menorrhagia II: is the 80-mL blood loss criterion useful in management of complaint of menorrhagia? Am J Obstet Gynecol. 2004;190:1224–9.
Fraser IS, McCarron G, Markham R, Resta T. Blood and total fluid content of menstrual discharge. Obstet Gynecol. 1985;65:194–8.
Reid PC. Assessment of menorrhagia by total menstrual fluid loss. J Obstet Gynaecol. 2006;26:438–41.
El-Nashar SA. Pictorial blood loss assessment chart for quantification of menstrual blood loss: a systematic review. Gynecol Surg. 2015;12:157–63.
Bowering J, Sanchez AM. A conspectus of research on iron requirements of man. J Nutr. 1976;106:985–1074.
Hasson KA. From bodies to lives, complainers to consumers: measuring menstrual excess. Soc Sci Med. 2012;75:1729–36.
Brolmann H, Bongers M, Garza-Leal JG, Gupta J, Veersema S, Quartero R, et al. The FAST-EU trial: 12-month clinical outcomes of women after intrauterine sonography-guided transcervical radiofrequency ablation of uterine fibroids. Gynecol Surg. 2016;13:27–35.
Dasharathy SS, Mumford SL, Pollack AZ, Perkins NJ, Mattison DR, Wactawski-Wende J, et al. Menstrual bleeding patterns among regularly menstruating women. Am J Epidemiol. 2012;175:536–45.
Article PubMed PubMed Central Google Scholar
Donnez J, Tatarchuk TF, Bouchard P, Puscasiu L, Zakharenko NF, Ivanova T, et al. Ulipristal acetate versus placebo for fibroid treatment before surgery. N Engl J Med. 2012;366:409–20.
Fathima A, Sultana A. Clinical efficacy of a Unani formulation 'Safoof Habis' in menorrhagia: a randomized controlled trial. Eur J Integr Med. 2012;4:e315–22.
Fraser IS, Critchley HO, Broder M, Munro MG. The FIGO recommendations on terminologies and definitions for normal and abnormal uterine bleeding. Semin Reprod Med. 2011;29:383–90.
Mirabi P, Dolatian M, Mojab F, Namdari M. Effects of valerian on bleeding and systemic manifestations of menstruation. J Med Plants. 2012;11:155–63.
Pattison H, Daniels JP, Kai J, Gupta JK. The measurement properties of the menorrhagia multi-attribute quality-of-life scale: a psychometric analysis. Br J Obestet Gynaecol. 2011;118:1528–31.
Ruta DA, Garratt AM, Chadha YC, Flett GM, Hall MH, Russell IT. Assessment of patients with menorrhagia: how valid is a structured clinical history as a measure of health status? Qual Life Res. 1995;4:33–40.
Moos RH. The development of a menstrual distress questionnaire. Psychosom Med. 1968;30:853–67.
Habiba M, Julian S, Taub N, Clark M, Rashid A, Baker R, et al. Limited role of multi-attribute utility scale and SF-36 in predicting management outcome of heavy menstrual bleeding. Eur J Obstet Gynecol Reprod Biol. 2010;148:81–5.
Lamping DL, Rowe P, Clarke A, Black N, Lessof L. Development and validation of the menorrhagia outcomes questionnaire. Br J Obstet Gynaecol. 1998;105:766–79.
Harding G, Coyne KS, Thompson CL, Spies JB. The responsiveness of the uterine fibroid symptom and health-related quality of life questionnaire (UFS-QOL). Health Qual Life Outcomes. 2008;6:99.
Matteson KA, Boardman LA, Munro MG, Clark MA. Abnormal uterine bleeding: a review of patient-based outcome measures. Fertil Steril. 2009;92:205–16.
Download references
Acknowledgements
The authors thank Dr. Lucy Bomphrey of Oxford PharmaGenesis for data extraction and writing support.
This review was funded by Bayer AG, Berlin, Germany. Data extraction, medical writing and editorial support were provided by Oxford PharmaGenesis, funded by Bayer AG, Berlin, Germany. Bayer AG did not contribute to the design of this review, the collection, analysis and interpretation of the data, or writing of the manuscript beyond providing financial support.
Availability of data and materials
Datasets analyzed during the current study are presented in the main paper or as additional supporting files. A completed PRISMA checklist for the manuscript is provided as Additional file 7 . Please note that the page numbers herein refer to the original submission file and not the final print version.
Author information
Authors and affiliations.
Institute for Science and Technology in Medicine, Guy Hilton Research Centre, Hartshill, Stoke-on-Trent, UK
Julia L. Magnay & Shaughn O’Brien
Department of Obstetrics & Gynaecology, Keele University School of Medicine, Stoke-on-Trent, UK
Shaughn O’Brien
Bayer AG, 13342, Berlin, Germany
Christoph Gerlinger & Christian Seitz
Gynecology, Obstetrics and Reproductive Medicine, University of Saarland Medical School, Homburg/Saar, Germany
Christoph Gerlinger
You can also search for this author in PubMed Google Scholar
Contributions
JLM, SO’B, CG and CS contributed substantially to the conception and design of the review, and to the analysis and interpretation of the data. All the authors reviewed the article critically for important intellectual content and approved the final version for publication.
Corresponding author
Correspondence to Christian Seitz .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
J.L.M. has received payment for consulting and medical writing services from Bayer AG for this and other work. S.O’B. has received a grant to his institution from Bayer AG for Menstrual Pictogram Research and from Advantage West Midlands for Symptometrics, a company involved in the development of an electronic version of premenstrual syndrome charts, pain charts and an alternative menstrual pictogram. He has received payment from Asarina Pharma for consultancy work and to act as Chief Investigator for an RCT on Premenstrual Syndrome, and from Bayer for consulting services and expert testimony for the licensing of and lectures on OC Yaz. He has also been an unpaid Chairman for the International Society for Premenstrual Disorders (ISPMD) and received payment for intellectual property issues unrelated to the work in this manuscript. C.G. and C.S. are employees of Bayer AG, Berlin, Germany. C.S. holds stock in Bayer AG.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
Table S1. Full electronic search strategy of Embase®™ and Medline. (PDF 44 kb)
Additional file 2:
Table S2. Advanced search of the ClinicalTrials.gov website. (PDF 32 kb)
Additional file 3:
Table S3. Overview of types of validation performed, practicalities, and limitations of methods. (PDF 232 kb)
Additional file 4:
Table S4. Further validation of methods. (PDF 171 kb)
Additional file 5:
Table S5. Correlations of methods with established standards. (PDF 168 kb)
Additional file 6:
Table S6. Assessment of discriminatory power of methods for assessing MBL. (PDF 148 kb)
Additional file 7:
Completed PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) checklist. (PDF 133 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Magnay, J.L., O’Brien, S., Gerlinger, C. et al. A systematic review of methods to measure menstrual blood loss. BMC Women's Health 18 , 142 (2018). https://doi.org/10.1186/s12905-018-0627-8
Download citation
Received : 05 December 2017
Accepted : 27 July 2018
Published : 22 August 2018
DOI : https://doi.org/10.1186/s12905-018-0627-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Alkaline hematin
- Alkaline haematin
- Menorrhagia
- Pictorial blood loss assessment chart
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Help & FAQ

Knowledge and attitude regarding menstrual blood banking
- Department of Fundamentals of Nursing, Manipal College of Nursing, Manipal
- Manipal College of Nursing, Manipal
Research output : Contribution to journal › Article › peer-review
Introduction or Background: The menstrual blood is being discharged by the female every month considering it is useless. But researchers found out that it contains plenty of self-renewing stem cells. Stem cells are master cells that have the capability of turning into any sort of cell in the body. They are very proliferative and have the unique capacity to form into different sorts of healthy cells such as cells of blood, heart, bones, skin, muscles, and brain cells. Objective of this study is to assess the knowledge and attitude of female health care professionals regarding menstrual blood banking. Method and Material: The study was carried out in various departments of Manipal University, Manipal. Descriptive survey design was used. Using purposive sampling method 220 female health care professionals were selected for the study. Structured knowledge questionnaire and attitude scale was used for data collection. Descriptive statistics was used for analysis. Findings: The study identified that 75 (34.1%) had poor, 116 (52.7%) had average and 29(13.2%) had good knowledge regarding menstrual blood banking among female health care professionals. The attitude of female health care professionals shows that 76 (34.5%) has favorable, and 144 (65.5%) has unfavorable attitude towards menstrual blood banking. Conclusions: The study results shows that the majority of the subjects had unfavorable attitude. Hence incidental teaching was given to improve their knowledge and change their attitude and making known about the facts to the public remains challenging but the present research should show its possibility and gain its momentum.
All Science Journal Classification (ASJC) codes
- Public Health, Environmental and Occupational Health
This output contributes to the following UN Sustainable Development Goals (SDGs)
Access to Document
- 10.5958/0976-5506.2019.00262.6
Other files and links
- Link to publication in Scopus
- Link to the citations in Scopus
Fingerprint
- blood INIS 100%
- attitudes INIS 100%
- Health Care Personnel Nursing and Health Professions 100%
- Dihydrotachysterol Pharmacology, Toxicology and Pharmaceutical Science 100%
- females INIS 71%
- stem cells INIS 28%
- Sampling Nursing and Health Professions 25%
- Attitude Scale Nursing and Health Professions 25%
T1 - Knowledge and attitude regarding menstrual blood banking
AU - Jomon, C. U.
AU - Barboza, Laveena Anitha
AU - George, Linu Sara
N1 - Publisher Copyright: © 2019, Indian Journal of Public Health Research and Development. All rights reserved.
PY - 2019/2
Y1 - 2019/2
N2 - Introduction or Background: The menstrual blood is being discharged by the female every month considering it is useless. But researchers found out that it contains plenty of self-renewing stem cells. Stem cells are master cells that have the capability of turning into any sort of cell in the body. They are very proliferative and have the unique capacity to form into different sorts of healthy cells such as cells of blood, heart, bones, skin, muscles, and brain cells. Objective of this study is to assess the knowledge and attitude of female health care professionals regarding menstrual blood banking. Method and Material: The study was carried out in various departments of Manipal University, Manipal. Descriptive survey design was used. Using purposive sampling method 220 female health care professionals were selected for the study. Structured knowledge questionnaire and attitude scale was used for data collection. Descriptive statistics was used for analysis. Findings: The study identified that 75 (34.1%) had poor, 116 (52.7%) had average and 29(13.2%) had good knowledge regarding menstrual blood banking among female health care professionals. The attitude of female health care professionals shows that 76 (34.5%) has favorable, and 144 (65.5%) has unfavorable attitude towards menstrual blood banking. Conclusions: The study results shows that the majority of the subjects had unfavorable attitude. Hence incidental teaching was given to improve their knowledge and change their attitude and making known about the facts to the public remains challenging but the present research should show its possibility and gain its momentum.
AB - Introduction or Background: The menstrual blood is being discharged by the female every month considering it is useless. But researchers found out that it contains plenty of self-renewing stem cells. Stem cells are master cells that have the capability of turning into any sort of cell in the body. They are very proliferative and have the unique capacity to form into different sorts of healthy cells such as cells of blood, heart, bones, skin, muscles, and brain cells. Objective of this study is to assess the knowledge and attitude of female health care professionals regarding menstrual blood banking. Method and Material: The study was carried out in various departments of Manipal University, Manipal. Descriptive survey design was used. Using purposive sampling method 220 female health care professionals were selected for the study. Structured knowledge questionnaire and attitude scale was used for data collection. Descriptive statistics was used for analysis. Findings: The study identified that 75 (34.1%) had poor, 116 (52.7%) had average and 29(13.2%) had good knowledge regarding menstrual blood banking among female health care professionals. The attitude of female health care professionals shows that 76 (34.5%) has favorable, and 144 (65.5%) has unfavorable attitude towards menstrual blood banking. Conclusions: The study results shows that the majority of the subjects had unfavorable attitude. Hence incidental teaching was given to improve their knowledge and change their attitude and making known about the facts to the public remains challenging but the present research should show its possibility and gain its momentum.
UR - http://www.scopus.com/inward/record.url?scp=85064178825&partnerID=8YFLogxK
UR - http://www.scopus.com/inward/citedby.url?scp=85064178825&partnerID=8YFLogxK
U2 - 10.5958/0976-5506.2019.00262.6
DO - 10.5958/0976-5506.2019.00262.6
M3 - Article
AN - SCOPUS:85064178825
SN - 0976-0245
JO - Indian Journal of Public Health Research and Development
JF - Indian Journal of Public Health Research and Development
[email protected]
- li:not(.tcb-excluded-from-group-item)"> Home
- li:not(.tcb-excluded-from-group-item)"> Journals list
- li:not(.tcb-excluded-from-group-item)"> Latest Publications
- For Authors
- For Reviewer
- manuscript-guidelines
- Open-Access
- Peer Review Policy
- Publication and Ethics
- Special issues
- li:not(.tcb-excluded-from-group-item)"> Contact
- li.menu-item.menu-item-4"> Login
- li.menu-item.menu-item-7"> Logout
Effectiveness of Structured Teaching Programme on Knowledge and Attitude Regarding Menstrual Blood Banking and Its Usage Among Nursing Staff
Aswathy ga, r. rajesh, and kavitha. p, journal menu, this is a popup.
Contact Us Name * First Last * Last Email * Subject * Message * If you are human, leave this field blank. Submit
Introduction: Menstruation is the monthly expulsion of the uterine endometrial lining when ovulation does not result in fertilisation. Recently, menstrual blood has garnered attention as a valuable source due to the presence of versatile stem cells, making it a prospective resource for future applications. This study seeks to examine the understanding and perspectives of staff nurses concerning menstrual blood banking. Aim: To evaluate the understanding and perspective concerning menstrual blood banking among staff nurses in designated hospitals in Kolar. Materials and Methods : A preliminary study was conducted on 60 nursing staff members at R. Jalappa Hospital and Research Centre in Kolar. Non-probability convenience sampling was employed to select participants, with data collection taking place from March 17th to July 16th, 2023, utilising structured knowledge questionnaires and attitude scales. The data were analysed using both descriptive and inferential statistical methods. Result: The study findings indicate that a majority (78.03%) of the staff nurses possessed moderate knowledge concerning menstrual blood banking. Additionally, the research demonstrated a notable correlation between the level of knowledge and various socio-demographic variables. Moreover, the respondents exhibited a favourable attitude towards menstrual blood banking, with most expressing positivity. Furthermore, a significant relationship was observed between knowledge and attitude towards menstrual blood banking. Conclusion: It can be emphasised that nursing staffs possess a moderate level of knowledge concerning menstrual blood banking and exhibit a favourable attitude towards it. Moreover, there exists a correlation between the knowledge and attitude towards menstrual blood banking .
Keywords: Attitude, knowledge, menstrual blood banking, menstruation, fertilisation
- Neelam Hans, et al. Effectiveness of structured teaching programme on knowledge regarding menstrual blood stem cells banking among nursing students. Int. J Reprod. Contracept. Obstet. Gynecol. 2016 Sept; 5(9): 3137–3140.
- Verma N. Menstrual blood banking: Scope and future. PM Health in Focus; 2012.
- Manley H, Sprinks J, Breedon P. Menstrual blood-derived mesenchymal stem cells: Women’s attitudes, willingness, and barriers to donation of menstrual blood. J Womens Health (Larchmt). 2019 Dec; 28(12): 1688–1697p. DOI: 10.1089/jwh.2019.7745.
- com. (2024). Banking menstrual stem cells. (monograph online). [Online] Available from: http://www.cryo-cell.com/menstrual/stem-cells .
- Francis F, Joel S E, Mathew A. Menstrual blood banking: A concept ‘best out of waste’ in the area of stem cell research. Journal of Medical Biomedical and Applied Sciences. 2016; 3(1): 48. [Online] Available at: www.jmbm.in.
- Hida N, Nishiyama N, Miyoshi S, Kira S, Segawa K, Uyama T, et al. Novel cardiac precursor-like cells from human menstrual blood-derived mesenchymal cells. Stem Cells. 2008; 26(7): 1695–1704.
- Sethia PP. Development and commercialization of menstrual blood stem cells banking. Chennai: Case Western Reserve University; 2011.
- Hans N, Kaur S. Effectiveness of structured teaching programme on knowledge regarding menstrual blood stem cells banking among nursing students. Int. J Rerod. Contracept Obstet Gynecol. 2016 Sept; 5(9): 3137–3140.
- Keng SI, Ahmad WANW, Cheng TS, Leng LJ. Association between nurses’ knowledge and attitudes toward stem cell application in medicine. The Malaysian Journal of Nursing. 2016; 7(3): 3–9.
- Mohammed HS, Sayed HA EL. Knowledge and attitude of maternity nurses regarding cord blood collection and stem cells: An education and practice. Journal of Nursing Education and Practice. 2015; 5(4): 58–69. [Online] Available at: www.sciedu.ca/jnep.
- Azzazy HM, Mohamed HF. Effect of educational intervention on knowledge and attitude of nursing students regarding stem cells therapy. IOSR Journal of Nursing and Health Science. 2016; 5(2): 75–80p. [Online] Available at: www.iosrjournals.org.
- Allickson JG, Sanchez A, Yefimenko N, Borlongan CV, Sanberg PR. Recent studies assessing the proliferative capability of a novel adult stem cell identified in menstrual blood. Open Stem Cell J. 2011; 3(2011): 4–10p. DOI: 10.2174/1876893801103010004.
- Rosy MM. Menstrual blood banking: A review. Int. J Nurs. Educ. Res. 2017; 5(2): 213–217. DOI: 10.5958/2454-2660.2017.00046.1
- Sasikala P. Descriptive study to assess the knowledge on menstrual stem cell among staff nurses. Int. J Appl. Res. 2021; 7: 8–10.
- Dhaka G. A descriptive study to assess the knowledge regarding menstrual blood banking among nursing students at Jodhpur. EPRA Int. J Res Dev. 2021; 6: 328–32. DOI: 10.36713/epra8574.
- Jomon CU, Barboza L, Sara GL. Knowledge and attitude regarding menstrual blood banking. Indian J Public Health Res Dev. 2019; 10: 68. doi: 10.5958/0976-5506.2019.00262.6
- Hans N, Kaur S. Effectiveness of structured teaching programme on knowledge regarding menstrual blood stem cells banking among nursing students. Int J Reprod Contracept Obstet Gynecol. 2016; 5(9): 3137–41p. doi: 10.18203/2320-1770.ijrcog20163001.
- Leng LJ, Keng SL, WanAhmad WAN, Cheng TS. Association between nurses’ knowledge and attitudes toward stem cell application in medicine. Malays J Nurs. 2016; 7(3): 3–9.
- Anand T, Garg S. Menstruation related myths in India: strategies for combating it. J Fam. Med Primary Care. 2015; 4(2): 184–186p. DOI: 10.4103/2249-4863.154627.
- Manley HL. The potential for menstrually-derived stem cell banking in the UK. J Undergrad Res NTU. 2018; 1(1): 1–18.
Log into Your Account
I HAVE FORGOTTEN MY PASSWORD
Password Reset
Please enter your email address. You will receive a link to create a new password via email
Back to login
The instructions to reset your password are sent to the email address you provided. If you did not receive the email, please check your spam folder as well
You are already logged in
Create a new account.
Already have an account? Login
August 22, 2023
No One Studied Menstrual Product Absorbency Realistically until Now
A new study reveals the absorbency of pads, tampons and other menstrual products is significantly different than labels suggest
By Joanna Thompson

Korolkoff/Getty Images
Most convenience stores or pharmacies have an aisle dedicated to “feminine hygiene” filled with shelves of various menstrual products such as tampons, pads, cups and discs. On the side of each package, you’ll find a small “absorbency” label proclaiming how much liquid blood the product is designed to hold.
But that number can be misleading, according to a recent paper published on August 7 in BMJ Sexual & Reproductive Health . A team of researchers at Oregon Health & Science University found that many menstrual products had a much lower or higher liquid capacity than advertised when real blood was used instead of a saline solution—a mixture of water, salt and bicarbonate that is more commonly employed in the product development process. This is the first known study to test the absorbency of period products with blood, the researchers say. The results suggest that doctors may be underdiagnosing heavy menstrual bleeding, which can be a sign of certain medical conditions.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Study co-author Bethany Samuelson Bannow, a clinician and an assistant professor of hematology, started to investigate menstrual product capacity after she noticed an increase in the number of her patients who opted for reusable menstrual discs and cups—insertable products shaped like shallow bowls and narrower cups, respectively, that rest below the cervix and collect blood—in place of disposable pads and tampons. These patients switched partly to reduce waste, but Samuelson Bannow suspects they also did so to better deal with heavy menstrual flow. “We realized that there wasn’t really a metric for diagnosing heavy menstrual bleeding in folks who use those products,” she says.
Estimates of the capacities of many products were based on decades-old tampon research. In the 1980s, a tampon task force was convened to help develop safer menstrual products after a particular brand of tampons was found to slightly increase the risk of toxic shock syndrome, a serious medical condition that occurs when certain strains of bacteria from outside the circulatory system enter the bloodstream and release toxins that can cause severe organ damage or death. This research set the standard for modern tampon absorbency. Additionally, many of those initial studies used a saline solution rather than menstrual blood. Saline solutions are still predominantly employed to test menstrual products today.
Blood and saline solution have very different viscosities, meaning they are absorbed at different rates. “The saying ‘blood is thicker than water’ is technically true,” Samuelson Bannow says. “We really felt that [the absorbency metric] needed to be updated.”
Saline solution is a homogenous mixture that is only slightly more viscous than distilled water. Blood, however, is not homogenous. It is full of cells and platelets, as well as proteins and other molecules that move around and vary in concentration depending on a myriad of factors, such as how hydrated a person is. Menstrual blood is even more variable than circulating blood because it also contains vaginal secretions and tissue that has been shed from the uterine wall. Its viscosity can change from person to person and even hour to hour.
These characteristics make it hard for manufacturers to accurately approximate the amount of blood a given period product will absorb based on tests that primarily use saline. In the new study, Samuelson Bannow and her team tested 21 different menstrual products, including discs, tampons, pads, period underwear and cups. They found that menstrual underwear products were the least absorbent ones on the market, soaking up one to three milliliters of blood, depending on size. “Light” pads were slightly more absorbent, maintaining 3 to 4 ml. Tampons held between 20 and 34 ml, depending on the brand and flow rating, and “heavy” pads, which advertised 10- to 20-ml capacity, could hold up to 52 ml. Menstrual discs held the most blood—61ml on average—with one brand holding up to 80 ml.
The results startled researchers. Doctors typically diagnose heavy bleeding based on either a visual chart—called the pictorial blood loss assessment chart (PBAC)—or the frequency with which an individual needs to change their period product. Using two or more tampons that absorb 20 ml of blood within a two-hour time frame is considered a heavy flow. But a heavy bleeding metric based on menstrual discs—which can hold about four times as much as a tampon and are used by many people with intense periods—hasn’t been established.
This could mean “we’re probably missing a lot of heavy menstrual bleeding,” Samuelson Bannow says. It’s important to catch this type of excessive bleeding, she adds, because this can be a sign of more serious conditions, including bleeding disorders, certain types of cancer and fibroids—smooth muscle tumors in the lining of the uterus. It can also lead to anemia, which manifests as extreme fatigue. Heavy bleeding during menstruation is also “really a mental health and quality of life issue,” says Candace Tingen, a researcher at the Gynecologic Health and Disease Branch at the National Institute of Child Health and Development, who was not involved in the study.
So why don’t period product manufacturers test absorbency with blood for better accuracy?
Blood is a precious commodity. Approximately five million people in the U.S. need a blood transfusion every year, according to the National Institutes of Health . Even though about 6.8 million individuals donate blood annually, not all of those donations are compatible with the blood types of those who need them, and donations have a short shelf life (six weeks for red blood cells and five days for platelets). Frequent blood shortages in hospitals make it difficult to justify using donations for anything other than transfusions. The fluid is also considered a potential biohazard. Researchers who handle blood in the lab must undergo training and take special precautions to work with it safely. In contrast, “you don’t have to have any special training to work with saline,” Tingen says. Additionally, blood—and artificial blood—is expensive. A 10-ml vial of research-quality human blood costs around $100. Meanwhile 200 ml of high-quality synthetic blood—a lab-made mixture of amino acids and hemoglobin—can run upward of $150 . In contrast, labs can buy a full liter of saline solution for $45.
These barriers don’t mean that period product companies shouldn’t update their standards, however—or that doctors shouldn’t update their charts for diagnosing heavy bleeding. “I think these results are very good justification for revisiting the PBAC and making it more applicable,” Tingen says. “The science isn’t settled.”
Tingen and Samuelson Bannow say these types of studies can help break down the stigma around menstruation. Discussing menstrual health can lead to better care, the development of better products and improved gender equity in health care, Samuelson Bannow says. “The main thing is just to get people talking about their periods,” she adds.
- Open access
- Published: 07 May 2024
Effects of improved amino acid balance diet on lysine mammary utilization, whole body protein turnover and muscle protein breakdown on lactating sows
- Sai Zhang 1 , 2 ,
- Juan C. Marini 3 ,
- Vengai Mavangira 4 ,
- Andrew Claude 4 ,
- Julie Moore 1 ,
- Mahmoud A. Mohammad 3 &
- Nathalie L. Trottier 1 , 5
Journal of Animal Science and Biotechnology volume 15 , Article number: 65 ( 2024 ) Cite this article
256 Accesses
Metrics details
The study objective was to test the hypothesis that low crude protein (CP) diet with crystalline amino acids (CAA) supplementation improves Lys utilization efficiency for milk production and reduces protein turnover and muscle protein breakdown. Eighteen lactating multiparous Yorkshire sows were allotted to 1 of 2 isocaloric diets (10.80 MJ/kg net energy): control (CON; 19.24% CP) and reduced CP with “optimal” AA profile (OPT; 14.00% CP). Sow body weight and backfat were recorded on d 1 and 21 of lactation and piglets were weighed on d 1, 14, 18, and 21 of lactation. Between d 14 and 18, a subset of 9 sows (CON = 4, OPT = 5) was infused with a mixed solution of 3-[methyl- 2 H 3 ]histidine (bolus injection) and [ 13 C]bicarbonate (priming dose) first, then a constant 2-h [ 13 C]bicarbonate infusion followed by a 6-h primed constant [1- 13 C]lysine infusion. Serial blood and milk sampling were performed to determine plasma and milk Lys enrichment, Lys oxidation rate, whole body protein turnover, and muscle protein breakdown.
Over the 21-d lactation period, compared to CON, sows fed OPT had greater litter growth rate ( P < 0.05). Compared to CON, sows fed OPT had greater efficiency of Lys ( P < 0.05), Lys mammary flux ( P < 0.01) and whole-body protein turnover efficiency ( P < 0.05). Compared to CON, sows fed OPT tended to have lower whole body protein breakdown rate ( P = 0.069). Muscle protein breakdown rate did not differ between OPT and CON ( P = 0.197).
Feeding an improved AA balance diet increased efficiency of Lys and reduced whole-body protein turnover and protein breakdown. These results imply that the lower maternal N retention observed in lactating sows fed improved AA balance diets in previous studies may be a result of greater partitioning of AA towards milk rather than greater body protein breakdown.
The increasing availability of crystalline amino acid (CAA) at competitive costs relative to protein ingredients allows for reduction of excessive dietary nitrogen (N) and improving AA balance [ 1 ]. Several studies have shown that improving dietary AA balance in lactating sows leads to greater milk casein yield [ 2 , 3 ] and utilization efficiency of N and essential amino acid (EAA) [ 4 , 5 ] while dramatically mitigating N losses and ammonia emissions to the environment [ 2 ]. Lysine efficiency values previously reported [ 4 , 5 , 6 ] were estimated based on lean mass change during lactation. This approach yielded similar efficiency estimates for Val based on isotopic method [ 7 ]. Lysine utilization efficiency values in lactation using an isotopic approach have not been reported.
The increased apparent AA efficiency may be at the expense of sow body weight (BW) loss and reduced maternal N retention whereby partitioning of dietary AA and energy towards the mammary glands appears to be favoured [ 3 , 5 , 8 ]. Preserving maternal N pool during the lactation period is important since maternal body protein and lipid loss can affect subsequent production performance. Loss in performances may include delayed estrus [ 9 ], reduction of piglet birth weight and litter uniformity [ 10 , 11 ], and prolonged interval from weaning to successful pregnancy [ 12 ], thus compromising the overall life span production efficiency. It is unknown whether the reduced maternal N retention previously reported [ 3 , 5 ] in sows fed an improved AA balance diet was a result of greater maternal body protein breakdown. In addition, whole body and muscle protein breakdown rates in lactating sows are unknown and such values are critical to assess at a mechanistic level the impact of improved dietary AA balance on body protein dynamic. Isotope technique allows for better mechanistic understanding of protein dynamics, including protein turnover rate, AA flux and muscle protein breakdown in humans [ 13 ] and animals [ 14 ].
We hypothesized that low CP diet with improved AA balance would increase milk yield through improving efficiency of Lys for milk and increasing maternal body and muscle protein breakdown. The objectives were to (1) measure whole body protein dynamics and (2) estimate Lys utilization efficiency for milk synthesis.
Materials and methods
Dietary treatments.
The NRC model [ 6 ] was used to estimate requirements for AA, net energy (NE), calcium (Ca) and phosphorus (P). The requirements were predicted based on the following parameters: sow BW of 210 kg after parturition, parity number of 2 and above, average daily intake of 6 kg/d, litter size of 10, piglet average daily gain (ADG) of 280 g/d over a 21-d lactation period, and an ambient temperature of 20 °C. The model predicted a minimum sow BW loss of 7.5 kg and the protein to lipid ratio in the model was adjusted to the minimum allowable value of near zero. The model predicted SID Lys requirement of 0.90% and NE requirement of 2,580 kcal/kg.
A control diet (CON) was formulated using corn and soybean meal as the only sources of Lys to meet the SID Lys requirement (0.90%) and consequently contained 19.24% CP and a SID Val concentration 0.77% which was near the NRC (2012) requirement of 0.79%. All other EAA SID contents were in excess relative to NRC (2012). The SID AA values of feed ingredients were referred to NRC (2012). A second diet was formulated to improve AA balance [ 5 ], and referred to as optimal diet (OPT) throughout the manuscript. Fermentable fiber was high in CON due to high content of soybean meal with 24.88% fermentable fiber [ 6 ]. Thus, the same fiber source (soy hulls) was supplemented in OPT, and levels of fermentable fiber were consistent between CON and OPT. Ingredients and calculated nutrient composition of CON and OPT diets are presented in Table 1 . Analyzed total (hydrolysate) and free AA concentrations are presented in Table 2 , in order to verify the precision of diet formulation. The analyzed N concentration corresponded to a CP% of 18.44 compared to a calculated value of 19.24% CP. Therefore, the analyzed CP concentration value is used in the heading for the remainder of tables.
Animals and feeding
The study was conducted at the Michigan State University Swine Teaching and Research Center. A total of 18 purebred multiparous (parity 2+) Yorkshire sows were moved to conventional farrowing crates between d 105 and 107 of gestation, grouped by parity, and randomly assigned to 1 of 2 dietary treatments within parity groups (CON, n = 9; OPT, n = 9). The study was conducted over 3 blocks of time, with 6, 6, and 5 sows in each block, respectively. One sow in CON from block 3 was removed due to poor feed intake that was deemed unrelated to the dietary treatments. Sows were adapted to the experimental diets (2.2 kg/d) 4 to 6 d before the expected farrowing date. Following farrowing, sows feed allowance progressively increased from 1.88 kg/d on d 1 to 7.44 kg/d at d 21, according to the NRC model [ 6 ], with a targeted ADFI of 6.0 kg/d over the 21-d lactation period. Feed was provided daily in 3 equal meals (0700, 1300, and 1900) with feed intake and refusal recorded daily before the morning meal. On infusion days (between d 14 and 18), the 0700 and 1300 meals were divided into 6 aliquots fed every 2 h from 0700 to 1700. Water was freely accessible to sows and piglets. Litters were aimed to be standardized to 11 piglets within the first 24 h after farrowing with the objective of weaning 10 piglets per sow. Injection of iron and surgical castration of male were conducted on d 1 and 7, respectively, according to the institutional research farm protocol. No creep feed was supplied to the piglets. Body weight and backfat thickness [ 5 ] of sows were recorded on d 1 and 21, and litter weights were recorded on d 1, 14, 18 and 21. Milk yield was estimated for peak lactation (between d 14 and 18) [ 5 ]. Prediction equation for milk yield during peak lactation is as follows [ 15 ]: \(\mathrm{Daily}\;\mathrm{milk}\;\mathrm{yield}\;(\text{g}/\text{d})=\mathrm{littersize}\times(582+1.168\times\text{ADG}+0.00425\times\text{ADG}^2)\)
Bilateral ear vein catheterization
A subset of 10 sows (5 sows per treatment) was used for the catheterization and infusion protocol. An ear vein catheter was placed in each ear, with one ear serving as the infusion line and the other as the sampling line. For the length of the catheterization procedure, piglets were removed and transferred to an empty adjacent stall with a heat lamp. The sows were restrained with a rope snare and remained in their farrowing stall where sedation was induced. For sedation, Telazol was reconstituted with 2.5 mL of 100 mg/mL ketamine and 2.5 mL of 100 mg/mL xylazine to a volume of 5 mL. This sedative mixture was administered i.m. in the brachiocephalicus muscle approximately 6 cm caudal to the ear, at a dosage of 0.1 mL/4.537 kg body weight. Sows were carefully assisted to facilitate laying in ventral recumbence. Sedation lasted for 45 to 60 min. The depth of anesthesia was monitored by the degree of muscle relaxation and respiration rate (i.e., 10 to 25 breaths/min).
The entire dorsal surface of both ears was prepared for aseptic placement of the ear vein catheters. The skin was scrubbed gently with 10% betadine solution followed with 70% isopropyl alcohol. The hair covering the skin area caudal to the ear and dorsal to the neck was clipped using a professional clipper to ensure a good adhesion of veterinary adhesive tape to the skin (described below).
A pre-cut 61-cm, round tip, medical grade microbore intravascular tubing (1.65 mm o.d., 1.02 mm i.d.) with hydromer coating (Access Technology Corp., Skokie, IL, USA) was prefilled at the time of catheterization with heparinized saline (30 IU/mL) before insertion. A hand tourniquet was applied at the base of the ear to distend the medial and lateral branches of the auricular vein. Either vein was used for catheterization. A short-term stylet catheter (14G, 5.08 cm, Safety IV catheter; B. Braun Melsungen AG, Germany) was inserted into the vein with the needle bevel facing up. Upon appearance of blood, the vein was gently occluded, and the needle rotated 180° to angle the bevel facing down. While holding the needle in place, the stylet catheter was gently pushed into the vein through the needle. Once the stylet was in place, the needle was removed, and the intravascular tubing was inserted through the stylet and pushed for approximately 30 cm caudally to reach the external jugular vein, and the catheter verified for patency at this point. Small sections of tape (5.1 cm wide, ZONAS® porous tape, Johnson & Johnson Consumer Companies, Inc., Skillman, NJ, USA) were affixed to the remaining section of intravascular tubing and sutured to the skin to secure the tubing in place. The stylet catheter was also sutured (Monocryl, CP-1, 36 mm, 1/2c; Ethicon Inc., USA) to the skin at the point of entry. Gauze was placed over each sutured sites and held in position by wrapping the ear with elastic adhesive tape. A connector was used to join the intravascular tubing to a long tubing extension (approximately 120 cm). A blunt-end needle adapter with an adaptor injection cap and a male luer lock was placed onto the distal end of the tubing extension. The same vein catheterization procedure was done on the other ear. A final layer of elastic adhesive tape (7.5 cm wide, 3M veterinary adhesive tape) was used to wrap each ear into a gently folded cone shape and to affix extension tubing directly onto the clipped skin surface. The extension tubing ran from the ears to the dorsal region of the neck, caudally to the ears and cranial to the shoulders and the free end (approximately 100 cm) rolled up and placed in a handmade denim protective pouch mounted on 4.0-cm thick foam material. The pouch was kept in place by gluing the foam directly onto the skin with Livestock ID Tag Cement (W.J. Ruscoe Company, Akron, OH, USA). Catheters were verified for patency once more and the lines were filled with sterile saline, coiled, and placed in the pouch until used for infusion and blood sampling. The entire procedure was done following sterile techniques and lasted 45 to 90 min per sow. As soon as sows were able to stand, 15-cm wide elastic bandage (Novation ® , Hartmann USA, Inc., Rock Hill, SC, USA) was wrapped over the pouch and around the neck and thorax in at least 3 layers in the shape of a life vest (crisscross) to protect the pouch. Thereafter, the catheters were verified for patency and flushed with sterilized heparinized saline (30 IU/mL) twice per day.
Catheters were removed after all infusions and blood sampling were completed (blood sampling lasted for 3 d for 3MH; Fig. 1 ). The elastic bandaging was removed, and the elastic adhesive tape was carefully pulled to expose the sutures. The sutures were cut with small surgical scissors, the catheters were gently pulled out of the ear veins, and pressure was applied over the insertion sites to accelerate coagulation. The remaining adhesive tape was then carefully removed, and the pouch was freed from the foam which remained on the sow. Rectal temperature was recorded from the day of catheterization and for 3 d following removal of catheters.
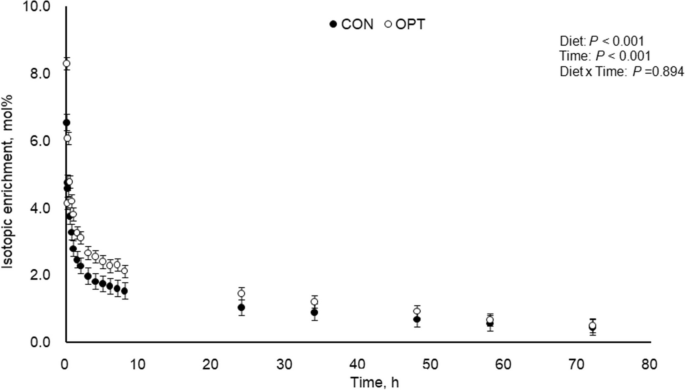
Plasma isotopic enrichment of 3-[methyl- 2 H 3 ]histidine following 3-[methyl- 2 H 3 ]histidine bolus infusion during peak lactation (between d 14 and 18) for sows fed control (CON; 18.4% CP; n = 4) and optimal (OPT; 14.0% CP; n = 4) diets. Plasma isotopic enrichment of 3-[methyl- 2 H 3 ]histidine differed between diets ( P < 0.001) and time points ( P < 0.001), with no interaction between diet and time ( P = 0.894). Standard error of the mean (SEM) = 0.214
Preparation of isotope solutions
Tracers were weighed, dissolved in saline and the solution sterilized by filtration through Millipore Steriflip filters (0.22 μm). For each sow, the following stock solutions were prepared: 3-[methyl- 2 H 3 ]histidine (183 μmol in 20 mL saline for bolus injection), [ 13 C]bicarbonate (368 μmol in 20 mL saline for prime and 736 μmol in 30 mL saline for 2-h infusion), and [1- 13 C]lysine (1.28 mmol in 30 mL saline for prime and 9.00 mmol in 60 mL saline for 6-h infusion). The bolus dose of 3-[methyl- 2 H 3 ]histidine (3MH) was calculated based on 20% pool size of 3MH in sows [ 16 , 17 ]. The infusion rate of [1- 13 C]lysine was calculated based on average flux of lysine (25 mmol/h) in lactating sows [ 7 ] with the aim of 2% enrichment. The priming dose of [1- 13 C]lysine was aiming for 1.5 mmol (1 h of infusion), and 1.28 mmol was the actual amount according to weight balance.
The solution of [ 13 C]bicarbonate was freshly prepared to minimize loss of 13 CO 2 . Specifically, [ 13 C]bicarbonate was weighed and dissolved in 20-mL 3-[methyl- 2 H 3 ]histidine solution in the morning of infusion day (Fig. 2 ). The 3-[methyl- 2 H 3 ]histidine (3MH) was used to estimate muscle protein breakdown, and the [ 13 C]bicarbonate was used to prime the CO 2 pool to accelerate the estimation of lysine oxidation rate. The primed-constant infusion of [1- 13 C]lysine was used to estimate lysine utilization by the mammary gland and the lysine flux in the whole body.
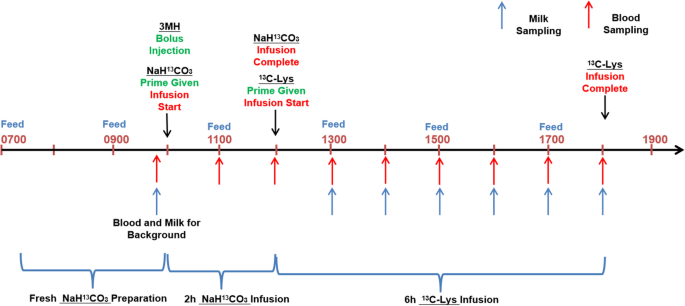
Timeline of isotope infusion and sampling (infusion day was within d 18–21)
Infusion protocol
The timeline for infusion is presented in Fig. 2 . Actual infusion day varied between d 14 and 18 due to real time patency of catheter. For lysine balance (Table 3 ) and body protein kinetics (Table 6 ), the actual infusion days were 17.0 ± 1.0 for CON and 17.0 ± 1.4 for OPT. For 3MH kinetics, the actual infusion days were 17.3 ± 1.0 for CON and 16.8 ± 1.5 for OPT. Pumps (Genie Touch TM , Kent Scientific Corp, Torrington, CT, USA) and syringes were placed on a large and stable plastic board laid above the farrowing stall. Following the priming dose, the infusion line was immediately attached to the syringe mounted to the pump to begin the constant infusion. The sampling line was coiled and stored in the pouch until used for blood sampling.
The mixed 20 mL saline solution containing 3-[methyl- 2 H 3 ]histidine (183 μmol) and [ 13 C]bicarbonate (368 μmol) was given through the infusion line as a bolus injection. The [ 13 C]bicarbonate in this infusate was used as a priming dose. After bolus injection, a constant 2-h infusion of [ 13 C]bicarbonate (368 μmol/h) began. The 2-h [ 13 C]bicarbonate infusion was followed by a 6-h primed constant [1- 13 C]lysine infusion (1.50 mmol/h) (Fig. 2 ).
Blood sampling
The timeline for blood sampling is presented in Fig. 2 . For analysis of plasma 3-[methyl- 2 H 3 ]histidine concentrations and estimation of muscle protein breakdown rate, blood samples were collected through the sampling line at 0 (immediately after termination of the bolus infusion), 5, 10, 15, 30 and 45 min and 1, 2, 3, 4, 5, 6, 7, 8, 24, 34, 48, 58 and 72 h post bolus infusion. Blood samples (0.5 mL) were transferred into 500-μL BD microtainer tubes (K 2 EDTA) and centrifuged (1,500 × g at 4 °C for 5 min). The plasma was extracted and stored in 1.5-mL microcentrifuge tubes at −20 °C until analysis.
For analysis of plasma [1- 13 C]lysine concentrations and estimation of whole-body Lys flux, blood samples (0.5 mL) were collected prior to infusion for background enrichment and at 1, 2, 3, 4, 5 and 6 h from the start of [1- 13 C]lysine infusion (Fig. 2 ).
For analysis of blood CO 2 concentrations, blood samples (2 mL) were collected prior to [ 13 C]bicarbonate-prime infusion for background, and at 1, 2, 3, 4, 5, 6, 7 and 8 h following the prime infusion. Blood samples were injected into evacuated vacutainer tubes (Becton Dickinson, Plymouth, UK) previously prepared with 2 mL of phosphoric acid, immediately mixed, and cooled to room temperature. The CO 2 was then transferred from evacuated vacutainers to Exetainer tubes (Labco Breath Tube, UK) by using pure nitrogen gas as medium until analysis.
Milk sampling protocol
The timeline for milk sampling is presented in Fig. 2 . Milk samples were taken between d 14 and 18 during the infusion protocol. Milk was sampled before infusion for background enrichment, and at 1, 2, 3, 4, 5 and 6 h of primed constant infusion of Lys.
For each milk sampling period, piglets were separated from the sows for 1 h in an empty adjacent farrowing crate with no access to water, and sows were administered 1 mL of oxytocin (20 IU/mL oxytocin, sodium chloride 0.9% w/v, and chlorobutanol 0.5% w/v, VetTek, Blue Springs, MO, USA) through the sampling catheter immediately after blood sampling. The catheter was rinsed with 2 mL of saline solution to ensure oxytocin reached the blood circulation. A total of 30-mL milk was manually collected across all glands and stored in 2 separate 15-mL tubes (polypropylene centrifuge tubes with screw cap, Denville Scientific, Swedesboro, NJ, USA). Piglets were immediately returned to sows to complete nursing and empty the mammary glands. Piglets were removed after nursing and kept separate from the sow until the next milk sampling time, 1 h later.
Isotope analysis
Plasma and milk [1- 13 C]lysine and 3-[methyl- 2 H 3 ]histidine (after acid hydrolysis) were determined as their dansyl derivatives by HESI LC-MS as previously described [ 18 ]. The following m/z transitions were monitored: 613→379 and 614→380 for [1- 13 C]lysine and 403→124 and 406→127 for 3-[methyl- 2 H 3 ]histidine. Determination of blood 13 CO 2 enrichment was performed by IRMS (Delta+XL IRMS coupled with GasBench-II peripheral device, Thermo-Quest Finnigan, Bremen, Germany) as previously described [ 19 ].
Nutrient analysis
Feed samples were analyzed for gross energy (GE) by bomb calorimetry (Parr Instrument Inc., Moline, IL, USA). Dry matter and N in feed samples were analyzed as previously described [ 5 ]. Dietary AA analysis [AOAC Official Method 982.30 E (a,b,c), 45.3.05, 2006] was performed by the Agricultural Experiment Station Chemical Laboratories (University of Missouri-Columbia, Columbia, MO, USA) as outlined in previous reports [ 5 ].
Calculations
The following assumptions were made during calculation:
Priming dose of isotope was assumed to mix with pool instantly.
The appearance of unlabeled bicarbonate was constant during the time of primed-constant infusion of bicarbonate (2 h) and that of [1- 13 C]lysine (6 h).
[1- 13 C]lysine cannot be synthesized once 1-carbon was lost to CO 2 , thus rate of lysine decarboxylation represented rate of lysine breakdown.
Kinetics of plasma lysine was an indicator of kinetics of whole body protein.
The indicator AA (lysine) was assumed to be oxidised for maintenance or incorporated into milk protein without other metabolic pathway.
Lysine oxidation
The enrichment of CO 2 during the period of primed-constant infusion of [ 13 C]bicarbonate was calculated as follows (Eq. 1 ):
Where “infusion \({\text{rate}}_{\text{H}{}^{13}\text{CO}_3^-}\) ” represents the infusion rate (368 μmol/h) of [ 13 C]bicarbonate, and “ \(\text{Ra}_{\text{HCO}_{3}^-}\) ” represents the rate of appearance of unlabeled bicarbonate (baseline) in the body.
The enrichment of CO 2 during the period of primed-constant infusion of [1- 13 C]lysine was calculated as follows (Eq. 2 ):
Where “ \({\text{Ra}}_{\text{H}{}^{13}\text{CO}_3^-}\) ” represents the rate of appearance of labeled bicarbonate from [1- 13 C]lysine oxidation, and “ \(\text{Ra}_{\text{HCO}_{3}^-}\) ” represents the rate of appearance of unlabeled bicarbonate (baseline) in the body as in Eq. 1 .
The enrichment of lysine during the period of primed-constant infusion of [1- 13 C]lysine was calculated as follows (Eq. 3 ):
Where Ra Lys represents the rate of appearance of unlabeled lysine in the body.
Lysine oxidation was estimated as follows (Eq. 4 ):
Whole body protein breakdown and synthesis
Whole body protein breakdown (PB) and synthesis (PS) were mirrored by Lys dynamics (Table 3 and Fig. 3 ).
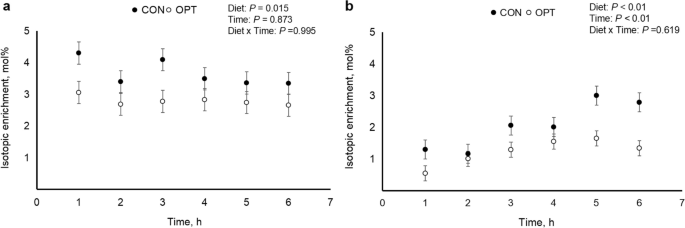
Isotopic enrichment of [1- 13 C]lysine in plasma (panel a ) and milk (panel b ) over 6 h during peak lactation (d 14 to 18) for sows fed control (CON; 18.4% CP; n = 3) and optimal (OPT; 14.0% CP; n = 5) diets
The PB and PS were calculated as follows (Eqs. 5 and 6 ):
Where 146.19 g/mol is the molar weight of isotopic Lys, 6.74% is the average weight percentage of Lys in the sow’s body protein [ 6 ].
The average milk protein concentration of 5.16% was used [ 6 ]. Milk yield was estimated according to Theil et al. [ 15 ].
Muscle protein breakdown
Data was expressed as tracer to tracee ratio (TTR). Multiexponential models were fitted to the data (Eq. 10 and Fig. 1 ). Residual inspection and pseudo-R 2 were used to determine the most parsimonious model that best fitted the data from each individual sow. Area under the curve (AUC; TTR•h) was calculated using the parameters from the multiexponential equation (Eq. 11 and Table 4 ) and 3MH rate of appearance (Ra; μmol/kg/h) was calculated by dividing the dose administered (μmol/kg) by AUC (Eq. 12 and Table 4 ). Half-life (h) was determined using the rate constant corresponding to the tail of the curve (Eq. 13 , Table 4 , and Fig. 1 ).
Muscle protein breakdown rate (%/d) was calculated as follows (Eq. 14 ):
Where total protein bound 3MH pool = muscle protein mass (g) × 3.8742 μmol 3MH/g protein and muscle protein mass = 8.21% × sow BW (kg) [ 20 ].
Muscle protein breakdown (g/d), was calculated as follows (Eq. 15 ):
Efficiency of lysine for lactation
Lysine utilization efficiency for lactation was calculated as follows (Eq. 16 ):
Statistical analysis
Data were confirmed for homogeneity of residual variance and normality of residuals by Mixed Procedures and Univariate Procedures of SAS 9.4 (SAS Inst. Inc., Cary, NC, USA) before ANOVA analysis (Mixed model procedures).
For the lysine balance and protein kinetic estimation, two sows from CON were removed from the data set. In one case, both ear vein catheters lost patency at the time of infusion, and in the other case, one of the 2 ear vein catheters lost patency. The latter sow, however, was used for the estimation of muscle protein breakdown, which only required one catheter. Therefore, the number of sows for the lysine balance data and protein kinetic estimation were 5 and 3 for OPT and CON, respectively.
For the analysis of lysine enrichment in plasma and milk, the following model was used:
The Enrichment of lysine depended on the fixed effects of diet ( OPT vs. CON ) , and sampling hour, with hour included as repeated measurement. The random effects included block and individual sow . The interactive effect of diet × hour was also included .
For the analysis of lysine balance, body protein breakdown and synthesis, and muscle protein breakdown rate, identified as “Response”, the following model was used:
The Response depended on the fixed effects of diet ( OPT vs. CON ) . The random effects included block and individual sow .
Differences between treatments were declared at P < 0.05 and tendencies at P ≤ 0.1.
Lactation performance
Lactation performance during the 21-d period and milk yield and nutrient concentrations between d 14 and 18 are presented in Table 5 . Sow initial BW and ADFI did not differ between OPT and CON diets. Litter growth rate of sows fed OPT diet was greater than those fed CON diet ( P < 0.05).
Lysine balance and efficiency of utilization
Lysine balance values are presented in Table 3 . The SID Lys intake, Lys oxidation, flux and Lys associated with protein synthesis did not differ between OPT and CON diets (Table 3 ). Compared to sows fed CON, those fed OPT had greater efficiency of Lys (0.62 vs. 0.50; P < 0.05) and tended to have a lower ( P = 0.069) released Lys associated with protein breakdown.
Whole body protein synthesis, whole body protein breakdown and fractional muscle protein breakdown
Whole body protein breakdown rate and synthesis rate tended to be lower ( P = 0.069 and P = 0.109, respectively) and protein turnover efficiency (synthesis: breakdown) tended to be greater ( P = 0.060) in sows fed OPT compared to those fed CON (Table 6 ). Whole body protein net synthesis (i.e., whole body protein synthesis − whole body protein breakdown) did not differ between OPT and CON diets.
For estimation of muscle protein breakdown rate, an additional sow in OPT treatment lost patency of both catheters, therefore the number of sows was 4 in each of the treatment. A 3-exponential model best fitted the 3MH decaying curve (Fig. 1 ) and pseudo- R 2 were > 0.995. Muscle protein breakdown rate and fractional muscle protein breakdown rate (%) did not differ ( P = 0.197) between sows fed OPT and CON diets (4.84% and 5.59%, respectively) (Table 6 ).
Enrichment of lysine
Lysine enrichment in plasma (panel a) and milk (panel b) is presented in Fig. 3 . The lysine enrichment in plasma did not differ between diets and time. Lysine enrichment in milk was lower ( P < 0.01) in sows fed OPT compared to sows fed CON diets and differed over time ( P < 0.01). There was no interaction between diets and time.
fDynamics of 3-[methyl- 2 H 3 ]histidine
Plasma isotopic enrichment of 3-MH following 3-MH bolus infusion is presented in Fig. 1 , and relevant dynamic parameters are presented in Table 4 . Plasma isotopic enrichment of 3-MH of sows fed CON was lower ( P < 0.001) than that for OPT diet. Time effects of 3-MH were significant ( P < 0.001) in both treatments of CON and OPT, and no interaction effect between diet and time ( P = 0.894) was detected.
Previous studies showed that lactating sows fed low CP diets with CAA supplementation had greater milk casein yield [ 2 , 3 ], and utilization efficiency of N and EAA [ 4 , 5 ]. The improvement of milk yield however was at the expense of sow BW and maternal N retention [ 3 , 5 ]. Zhang et al. [ 8 ] suggested that feeding diets with improved AA balance triggered nutrient repartitioning to milk at the expense of maternal adipose tissue rather than protein tissue. Maternal body fat loss affects subsequent reproductive performance and compromises the overall production efficiency during the sow’s life span [ 21 ]. Therefore, commercial implementation of diets with aggressing reduction in CP with CAA supplementation to achieve improved AA balance will not only depend on their impact on lactation performance and production efficiency but also on ensuring that long-term maternal body protein and lipid reserves are not compromised.
The mechanisms behind the reduced maternal N retention in sows fed improved AA balance diets reported in earlier studies [ 4 , 5 ] are unclear. Reduced maternal body protein synthesis, greater body protein breakdown, or a combination of thereof can dictate maternal N balance during lactation. In this study however, BW and backfat change during lactation did not differ between OPT and CON sows. Of note, sows fed OPT had no change in BW with a small loss in backfat while sows fed CON gained 5.5 kg with no change in backfat. Body protein kinetics in this study (Table 6 ) dictated that whole body protein net synthesis (whole body protein synthesis − whole body protein breakdown) of sows fed CON and OPT were close (1,041.72 vs. 1,022.90 g/d), but note that whole body protein net synthesis of lactating sows included milk protein yield and maternal protein deposition. Milk protein yield was greater in OPT than CON as mirrored by litter growth rate (Table 5 ). Consequently, maternal protein deposition was greater in CON than OPT which aligns with the observation that body weight increased in sows fed CON while there was no change of body weight in sows fed OPT (Table 5 ). In addition, increased milk production in sows fed OPT suggest that OPT diet led sows to partition more dietary nutrient towards milk than maternal reserves, in other words, sows fed OPT were more motivated to produce milk even at the expense of maternal deposition.
This study used Lys as representative AA of body protein to analyze whole body protein turnover. In essence, Lys flux in the blood was contributed by dietary Lys intake and Lys released by body protein breakdown, and free Lys in the blood could be directed to either Lys oxidation or Lys incorporation into body protein (Fig. 4 ). Thus, body protein breakdown and synthesis could be estimated by measuring Lys flux in blood and Lys oxidation. The carbon dioxide released by Lys oxidation remains in the blood bicarbonate pool and mixed with carbon dioxide from other substrate oxidation (Fig. 5 ). By priming the bicarbonate pool, the baseline production rate of carbon dioxide can be estimated based on bicarbonate enrichment and constant infusion rate of labeled bicarbonate during prime-constant infusion of bicarbonate (Eq. 1 ). The release of labeled carbon dioxide due to labeled Lys oxidation was proportional to the baseline production rate of carbon dioxide according to enrichment of bicarbonate during prime-constant infusion of Lys (Eqs. 2 and 3 ).
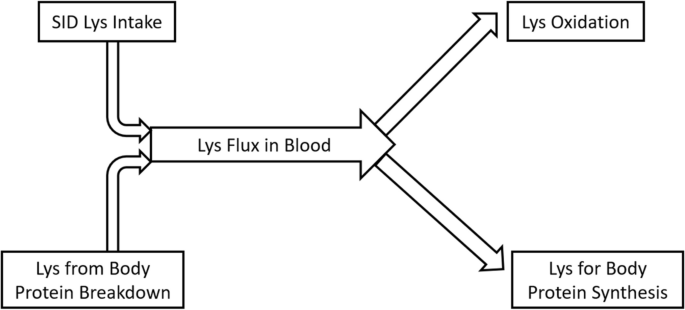
Diagram of lysine balance in lactating sows at fed state
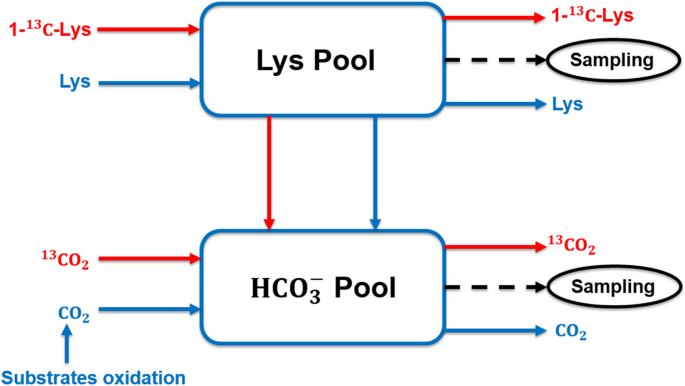
Representation of a two-pool model to estimate lysine oxidation
Milk protein synthesis represents the difference between whole body protein synthesis and breakdown, assuming that maternal protein retention is close to zero, since maternal tissue mobilization is majorly comprised of body fat rather than body protein [ 5 , 8 ]. According to this assumption, milk protein output rate measured by isotopic technique (Eq. 8 ) was 1,023 to 1,042 g/d, which aligns well with a previous study where 957 g/d milk protein synthesis was reported using a N balance approach [ 5 ]. When compared to traditional method where milk protein synthesis is the product of milk yield and milk protein concentration (645 to 675 g/d; Eq. 9 ), the isotopic-predicted milk protein synthesis (1,023 to 1,042 g/d) appears overestimated. Guan et al. [ 7 ] reported milk protein synthesis of 575 g/d as the net balance between sow whole mammary protein synthesis (975 g/d) and breakdown rate (400 g/d), corroborating the values reported here (645–675 g/d) using the traditional method. Nitrogen balance techniques tend to overestimate actual nitrogen retention [ 22 , 23 ], as observed herein with the isotope technique (Eq. 8 ). Note that the estimated muscle protein breakdown rate according to 3MH method in this study was 960 to 1,261 g/d (Eq. 15 ), which was greater than the protein breakdown rate (650 to 1,051 g/d; Eq. 8 ) based on the Lys flux. On the other hand, milk protein synthesis rate per metabolic BW (BW 0.75 ) were 10.25 and 9.85 g/d/kg 0.75 for OPT and CON, respectively in this study, supporting a previously reported value of 11.57 g/d/kg 0.75 (using Val as representative AA) [ 24 ]. Thus, overestimation of milk protein synthesis (Eq. 8 ) was majorly attributed to an underestimation of protein breakdown rather than overestimation of protein synthesis. The underestimation of body protein breakdown according to Lys flux (Eq. 5 ) may be partially due to the tendency to overestimate feed intake [ 23 ], although feed waste was minimized in this study. Nevertheless, it is also important to note that estimated muscle protein breakdown (15.4 to 17.8 μmol/kg/d; Eq. 15 ; Table 6 ) and fractional breakdown (4.84–5.59%/d; Eq. 14 ; Table 6 ) in this study was greater than those reported for lactating gilt (3.4%/d, 12.0 μmol/kg/d) using the same 3MH method [ 17 ]. It is speculated that the multiparous lactating sow may mobilize body protein more readily compared to the lactating gilt.
In this study, milk protein yield of lactating sows fed OPT diet did not differ from those fed control diet neither when an isotopic method nor the traditional method were used. Although there was no difference between whole body protein synthesis and breakdown, the absolute values of protein synthesis and breakdown were both lower in sows fed OPT diet compared to CON diet, suggesting less whole-body protein turnover in sows fed the OPT diet. In support of this view, previous studies also showed a decreased protein breakdown rate reflected by lower urea nitrogen output when sows were fed reduced protein diets [ 3 , 5 ]. The biological process of protein turnover is energetically costly [ 1 , 25 ]. Zhang et al. [ 5 ] reported feeding sows with an improved AA balance diet was associated with higher energy efficiency, lending support to the current observation.
The Lys efficiency for sows fed different levels of dietary protein based on the NRC [ 6 ] approach was previously determined [ 4 , 5 ], with greater efficiency values (0.68 and 0.66, respectively) found during peak lactation (d 14–18) in sows fed low CP diets balanced with CAA. Herein, greater Lys utilization efficiency values, determined using a different approach, were also found in sows fed OPT (0.62) compared to CON (0.50). The estimation of Lys utilization efficiency was based on Lys balance parameters, i.e., Lys flux in blood, SID Lys intake and Lys oxidation (Fig. 4 ), and the assumption that net protein synthesis (protein synthesis − protein breakdown) represents milk protein synthesis, with negligible maternal body retention. The true Lys utilization efficiency is the ratio between “Lys in milk” and “Lys for milk”, thus Lys utilized for maintenance should be excluded in the denominator [ 6 ] as follows:
In this study, the whole-body Lys flux was corrected by excluding Lys oxidation (Eq. 16 ), which corresponds to the Lys requirement for maintenance. Guan et al. [ 7 ] reported that Lys flux partitioned to the mammary glands as percentage of whole-body Lys flux was 56% in sows fed a conventional diet, which is comparable to the Lys efficiency values of 50% to 62% observed in this study.
Feeding lactation sows with an improved AA balance diet did not affect milk protein yield and reduced whole-body protein turnover. The reduced whole-body protein turnover resulted from a decrease in both whole-body protein synthesis and breakdown rate, with a tendency for greater protein synthesis to protein breakdown ratio (2.65 vs. 2.02).
Efficiency of Lys was also greater during peak lactation, together suggesting higher efficiency of energy use. These results imply that the lower maternal N retention observed in lactating sows fed improved AA balance diets in previous studies may be a result of greater partitioning of AA towards milk rather than greater body protein breakdown.
Availability of data and materials
All data generated or analyzed during this study are available from the corresponding author on request.
Abbreviations
Average daily gain
Area under the curve
Body weight
Crystalline amino acid
Crude protein
Essential amino acid
Standard error of the mean
Standardized ileal digestibility
3-[methyl- 2 H 3 ]histidine
Zhang S, Trottier NL. Dietary protein reduction improves the energetic and amino acid efficiency in lactating sows. Anim Prod Sci. 2019;59:1980–90.
Article CAS Google Scholar
Chamberlin DP. Impacts of reducing dietary crude protein with crystalline amino acid supplementation on lactating sow performance, nitrogen utilization and heat production. East Lansing: MS Thesis, Michigan State University; 2017.
Google Scholar
Huber L, de Lange CFM, Krogh U, Chamberlin D, Trottier NL. Impact of feeding reduced crude protein diets to lactating sows on nitrogen utilization. J Anim Sci. 2015;93:5254–64.
Article CAS PubMed Google Scholar
Huber L, de Lange CFM, Ernst CW, Krogh U, Trottier NL. Impact of improving dietary amino acid balance for lactating sows on efficiency of dietary amino acid utilization and transcript abundance of genes encoding lysine transporters in mammary tissue. J Anim Sci. 2016;94:4654–65.
Zhang S, Qiao M, Trottier NL. Feeding a reduced protein diet with a near ideal amino acid profile improves amino acid efficiency and nitrogen utilization for milk production in sows. J Anim Sci. 2019;97:3882–97.
Article PubMed PubMed Central Google Scholar
NRC. Nutrient requirements of swine. 11th ed. Washington, DC: National Academy Press; 2012.
Guan X, Bequette BJ, Calder G, Ku PK, Ames KN, Trottier NL. Amino acid availability affects amino acid flux and protein metabolism in the porcine mammary gland. J Nutr. 2002;132:1224–34.
Zhang S, Johnson JS, Qiao M, Trottier NL. Reduced protein diet with near ideal amino acid profile improves energy efficiency and mitigate heat production associated with lactation in sows. J Anim Sci Biotechno. 2020;11:4.
Article Google Scholar
Quesnel H. Nutritional and lactational effects on follicular development in the pig. In: Rodriguez Martinez H, Vallet JL, Ziecik AJ, editors. Control of pig reproduction VIII. Nottingham: Notthingham University Press; 2009. p. 121–34.
Wientjes JGM, Soede NM, van den Brand H, Kemp B. Nutritionally induced relationships between insulin levels during the weaning-to-ovulation interval and reproductive characteristics in multiparous sows: I. Luteinizing hormone, follicle development, oestrus and ovulation. Reprod Domest Anim. 2012;47:53–61.
Wientjes JGM, Soede NM, van den Brand H, Kemp B. Nutritionally induced relationships between insulin levels during the weaning-to-ovulation interval and reproductive characteristics in multiparous sows: II. Luteal development, progesterone and conceptus development and uniformity. Reprod Domest Anim. 2012;47:62–8.
Wientjes JGM, Soede NM, Knol EF, van den Brand H, Kemp B. Piglet birth weight and litter uniformity: effects of weaning-to-pregnancy interval and body condition changes in sows of different parities and crossbred lines. J Anim Sci. 2013;91(5):2099–107.
Kim IY, Schutzler S, Schrader A, Spencer H, Kortebein P, Deutz NEP, et al. Quantity of dietary protein intake, but not pattern of intake, affects net protein balance primarily through differences in protein synthesis in older adults. Am J Physiol-Endoc M. 2015;308(1):E21.
CAS Google Scholar
Claydon AJ, Thom MD, Hurst JL, Beynon RJ. Protein turnover: measurement of proteome dynamics by whole animal metabolic labelling with stable isotope labelled amino acids. Proteomics. 2012;12(8):1194–206.
Theil PK, Nielsen TT, Kristensen NB, Labouriau R, Danielsen V, Lauridsen C, et al. Estimation of milk production in lactating sows by determination of deuterated water turnover in three piglets per litter. Acta Agric Scand. 2002;52:221–32.
Rathmacher JA, Link GA, Nissen SL. Measuring of 3-methylhistidine production in lambs by using compartmental-kinetic analysis. Br J Nutr. 1993;69:1.
Trottier NL. Protein metabolism in the lactating sow. Urbana-Champaign: PhD Dissertation, University of Illinois; 1995.
Marini JC. Quantitative analysis of 15 N-labeled positional isomers of glutamine and citrulline via electrospray ionization tandem mass spectrometry of their dansyl derivatives. Rapid Commun Mass Spectrom. 2011;25(9):1291–6.
Verbruggen S, Sy J, Gordon WE, Hsu J, Wu M, Chacko S, et al. Ontogeny of methionine utilization and splanchnic uptake in critically ill children. Am J Physiol Endocrinol Metab. 2009;297(5):E1046–55.
Article CAS PubMed PubMed Central Google Scholar
Rathmacher JA, Nissen SL, Paxton RE, Anderson DB. Estimation of 3-methylhistidine production in pigs by compartmental analysis. J Anim Sci. 1996;74(1):46–56.
De Rensis F, Gherpelli M, Superchi P, Kirkwood RN. Relationships between backfat depth and plasma leptin during lactation and sow reproductive performance after weaning. Anim Reprod Sci. 2005;90(1–2):95–100.
Article PubMed Google Scholar
Kopple JD. Uses and limitations of the balance technique. JPEN J Parenter Enteral Nutr. 1987;11(5 Suppl):79S–85S.
CAS PubMed Google Scholar
Spanghero M, Kowalski ZM. Updating analysis of nitrogen balance experiments in dairy cows. J Dairy Sci. 2021;104(7):7725–37.
Hanigan MD, France J, Mabjeesh SJ, McNabb WC, Bequette BJ. High rates of mammary tissue protein turnover in lactating goats are energetically costly. J Nutr. 2009;139(6):1118–27.
Wolfe RR. Radioactive and stable isotope tracers in biomedicine: principles and practice of kinetic analysis. Somerset, NJ: John Wiley & Sons Inc; 1992.
Download references
This work was financially supported by funds from the USDA-NIFA (award number 2014-67015-21832).
Author information
Authors and affiliations.
Department of Animal Science, Michigan State University, East Lansing, 48824, USA
Sai Zhang, Julie Moore & Nathalie L. Trottier
State Key Laboratory of Swine and Poultry Breeding Industry, Key Laboratory of Animal Nutrition and Feed Science in South China, Ministry of Agriculture and Rural Affairs, Guangdong Provincial Key Laboratory of Animal Breeding and Nutrition, Institute of Animal Science, Guangdong Academy of Agricultural Sciences, Guangzhou, 510640, PR China
USDA/ARS Children’s Nutrition Research Center and Pediatric Critical Care Medicine, Department of Pediatrics, Baylor College of Medicine, Houston, TX, 77030, USA
Juan C. Marini & Mahmoud A. Mohammad
Department of Large Animal Clinical Sciences, Michigan State University, East Lansing, MI, 48824, USA
Vengai Mavangira & Andrew Claude
Present address: Department of Animal Science, Cornell University, Frank Morrison Hall, 507 Tower Road, Ithaca, NY, 14853-4801, USA
Nathalie L. Trottier
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, NLT and SZ; Methodology, NLT, SZ, JCM, VM, AC, JM, and MAM; Formal analysis, SZ and JCM; Writing, SZ and NLT; Supervision, NLT; Funding acquisition, NLT.
Corresponding author
Correspondence to Nathalie L. Trottier .
Ethics declarations
Ethics approval and consent to participate.
All procedures were approved by the Michigan State University Institutional Animal Care and Use Committee (AUF # 05/16-091-00) and followed the American Association for Laboratory Animal Science guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhang, S., Marini, J.C., Mavangira, V. et al. Effects of improved amino acid balance diet on lysine mammary utilization, whole body protein turnover and muscle protein breakdown on lactating sows. J Animal Sci Biotechnol 15 , 65 (2024). https://doi.org/10.1186/s40104-024-01020-9
Download citation
Received : 07 December 2023
Accepted : 05 March 2024
Published : 07 May 2024
DOI : https://doi.org/10.1186/s40104-024-01020-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lactating sows
- Protein breakdown
- Protein turnover
- Reduced protein diet
Journal of Animal Science and Biotechnology
ISSN: 2049-1891
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Womens Health

A systematic review of methods to measure menstrual blood loss
Julia l. magnay.
1 Institute for Science and Technology in Medicine, Guy Hilton Research Centre, Hartshill, Stoke-on-Trent, UK
Shaughn O’Brien
2 Department of Obstetrics & Gynaecology, Keele University School of Medicine, Stoke-on-Trent, UK
Christoph Gerlinger
3 Bayer AG, 13342 Berlin, Germany
4 Gynecology, Obstetrics and Reproductive Medicine, University of Saarland Medical School, Homburg/Saar, Germany
Christian Seitz
Associated data.
Datasets analyzed during the current study are presented in the main paper or as additional supporting files. A completed PRISMA checklist for the manuscript is provided as Additional file 7 . Please note that the page numbers herein refer to the original submission file and not the final print version.
Since the publication over 50 years ago of the alkaline hematin method for quantifying menstrual blood loss (MBL) many new approaches have been developed to assess MBL. The aim of this systematic review is to determine for methods of measuring MBL: ability to distinguish between normal and heavy menstrual bleeding (HMB); practicalities and limitations in the research setting; and suitability for diagnosing HMB in routine clinical practice.
Embase®™, MEDLINE®, and ClinicalTrials.gov were screened for studies on the development/validation of MBL assessment methods in women with self-perceived HMB, actual HMB or uterine fibroids, or patients undergoing treatment for HMB. Studies using simulated menstrual fluid and those that included women with normal MBL as controls were also eligible for inclusion. Extracted data included study population, results of validation, and advantages/disadvantages of the technique.
Seventy-one studies fulfilled the inclusion criteria. The sensitivity and/or specificity of diagnosing HMB were calculated in 16 studies of methods involving self-perception of MBL (11 pictorial), and in one analysis of the menstrual-fluid-loss (MFL) method; in 13 of these studies the comparator was the gold standard alkaline hematin technique. Sensitivity and specificity values by method were, respectively: MFL model, 89, 98%; pictorial blood loss assessment chart (PBAC), 58–99%, 7.5–89%; menstrual pictogram, 82–96%, 88–94%; models/questionnaires, 59–87%, 62–86%, and complaint of HMB, 74, 74%. The power of methods to identify HMB was also assessed using other analyses such as comparison of average measurements: statistical significance was reported for the PBAC, MFL, subjective complaint, and six questionnaires. In addition, PBAC scores, menstrual pictogram volumes, MFL, pad/tampon count, iron loss, and output from three questionnaires correlated significantly with values from a reference method in at least one study. In general, pictorial methods have been more comprehensively validated than questionnaires and models.
Conclusions
Every method to assess MBL has limitations. Pictorial methods strike a good balance between ease of use and validated accuracy of MBL determination, and could complement assessment of HMB using quality of life (QoL) in the clinical and research setting.
Trial registration
PRISMA registration number: CRD42016032956 .
Electronic supplementary material
The online version of this article (10.1186/s12905-018-0627-8) contains supplementary material, which is available to authorized users.
Heavy menstrual bleeding (HMB; menorrhagia) is defined by the National Institute for Health and Care Excellence (NICE) in the United Kingdom as excessive menstrual blood loss (MBL) that interferes with a woman’s physical, emotional, social, and material quality of life (QoL). Up to 50% of women of reproductive age (18–54 years) can experience HMB [ 1 , 2 ], which may cause anemia [ 3 ], lead to limitations in social, physical, and leisure activities [ 1 , 4 ], and be associated with increased healthcare resource use and costs [ 5 ].
In clinical practice, the impact of HMB on a woman’s QoL is currently used to guide treatment [ 1 ]. However, it is acknowledged that self-perception of MBL can be inaccurate [ 6 ], and this may result in surgical intervention in women who are distressed by menses that are actually defined as low volume. General health questionnaires have been found to be inappropriate for use in women with HMB [ 7 ], and there is an absence of recommendations for HMB-specific QoL tools [ 1 , 8 , 9 ]. Thus, a method is needed to complement QoL assessments of HMB. Evaluation of MBL informs patient choice by providing context and clarity; for example, the finding of MBL within the normal range may reassure a woman with perceived HMB to the extent that she chooses not to seek further treatment [ 10 – 13 ]. Also, determination of MBL can be important when establishing the etiology of cases of anemia, and changes in MBL are often used to evaluate treatment efficacy in clinical trials.
The alkaline hematin technique, which involves chemically measuring the blood content of used sanitary products, is considered the “gold standard” for MBL determination and has traditionally been used to diagnose HMB as a loss of more than 80 mL of blood per cycle [ 14 , 15 ]. However, as a result of its practical limitations, its use is mainly confined to the research setting. Consequently, many new approaches to measuring MBL have been developed since publication of the alkaline hematin method more than 50 years ago [ 16 – 18 ]. During this time, sanitary wear has evolved from cotton-based sanitary products to superabsorbent-polymer-containing (SAP-c) ultraslim towels containing granules that can absorb many times their own weight in fluid [ 19 ] hence there is a requirement to validate any method for measuring MBL with the same types/brands of sanitary product that the method is intended to be used with. A summary of the validity and merits of existing measurement techniques, including details of the specific products for which they are validated, would be of great benefit to healthcare providers, clinical scientists, and policy makers. To this end, we performed a systematic review with the specific aims of determining: (1) the degree to which methods for measuring MBL are validated to distinguish between normal bleeding and HMB, (2) the practicalities and limitations of each method in the research setting, and (3) whether any of the methods could be used in routine clinical practice to diagnose HMB.
The systematic review protocol was registered at PROSPERO ( https://www.crd.york.ac.uk/PROSPERO ) in March, 2016, with the registration number CRD42016032956 . Embase®™ and MEDLINE® were searched using Ovid® on 2 March, 2016, and again on 2 November, 2016. The search for articles concerned with validation/development of methods for assessing MBL was based on strategies used to develop the NICE HMB guidelines [ 1 ]. Further terms were added to broaden the range of techniques for assessing MBL among retrieved articles. The search terms can be found in Additional file 1 . A search was also performed in ClinicalTrials.gov for relevant ongoing and recently completed clinical trials that investigated methods to measure MBL. The search terms are shown in Additional file 2 . Following removal of duplicates, retrieved articles were manually screened based on title then abstract.
Articles were selected for inclusion in the study if the main focus was the development or validation of a measure for assessing MBL in women with self-perceived HMB, actual HMB (MBL > 80 mL per cycle), or uterine fibroids, or in women undergoing treatment for HMB. Validation/development studies that used simulated menstrual fluid and those that included women with normal MBL as controls were also eligible for inclusion. Studies investigating only health-related QoL measures or questionnaires were not specifically sought in the original searches to maintain the focus of the review, but were considered for inclusion during screening. To ensure the capture of methods for which published validation data may not yet be available, we included articles that presented novel or modified methods even if validation was not the main focus. To guarantee that original validation studies were included there were no date limits. Similarly, because some early validation studies had only a few participants, no limitations to population size were applied.
Exclusion criteria were studies that only considered an application rather than the development or validation of a technique, those with non-English abstracts, or articles on irrelevant outcome measures or of an inappropriate publication type; for example, preclinical studies and letters. For each included study, the following data were extracted and independently checked: full reference, study type, setting, population, measurement technique, type of validation, statistical output, advantages/disadvantages of the technique (including sensitivity/specificity scores for measuring MBL, discriminatory power for assessing normal versus high MBL, and additional advantages/disadvantages), and any information on the risk of bias. Inter-cycle and internal consistency were also assessed.
On 2 November, 2016, 1438 records were retrieved from Embase®™ and MEDLINE®, including key predefined references [ 20 – 35 ]. Of these articles, 70 fulfilled the inclusion criteria (Fig. 1 ; Additional file 3 ) [ 6 , 8 , 10 , 11 , 14 , 19 – 23 , 25 – 84 ]. Up to 25 January, 2017, 123 relevant entries were retrieved from ClinicalTrials.gov . One trial, {"type":"clinical-trial","attrs":{"text":"NCT01643304","term_id":"NCT01643304"}} NCT01643304 , fulfilled the inclusion criteria [ 85 ].

Systematic search and selection process. a See Additional file 1 for search terms. b See Additional file 2 for search terms
Among these studies, population sizes ranged from 2 [ 14 ] to 4506 [ 80 ]. The risk of bias was rarely formally acknowledged in the included studies, which were also subject to different types of bias. Inter-cycle consistency was assessed in six studies [ 11 , 14 , 25 , 42 , 44 , 86 ], with variable results (Additional file 4 ). Internal consistency, measured using a variety of methods, was generally good in the 18 studies in which it was considered (Additional file 4 ). The sensitivity and specificity of diagnosing HMB, or a specified change in MBL, were calculated in 16 studies of tools involving self-perception of MBL (11 pictorial), and in one analysis of the menstrual fluid loss (MFL) method (Table 1 ). In studies reporting both sensitivity and specificity, the Youden’s statistic, a measure of test performance with an optimal score of 1.0, ranged from 0.33 [ 20 ] to 0.88 [ 26 ].
Sensitivity and specificity of methods for measuring MBL
a N = study population size; n = number of cycles studied
AH alkaline hematin, MBL menstrual blood loss, MEQ Menstrual Evaluation Questionnaire, MFL menstrual fluid loss, MIQ Menorrhagia Impact Questionnaire, NR not reported, PBAC pictorial blood loss assessment chart, SAP superabsorbent polymer
As many women now prefer to use ultraslim towels with enhanced absorbency properties [ 19 ], the most relevant methods for measuring MBL in current clinical use and research are those validated for SAP-c products. The validity of measuring MBL with selected SAP-c products was investigated for the alkaline hematin technique, weight assessment of MFL, the pictorial blood loss assessment chart (PBAC), and the menstrual pictogram [ 19 , 27 , 33 , 38 , 39 ].
Alkaline hematin method
The original alkaline hematin method was developed for cotton-based sanitary products. It was concurrently validated in one study, showing good agreement with an iron isotope activity method in three phases of one woman’s menstrual cycle (Additional files 3 and 5 ) [ 14 ]. Modified versions of the alkaline hematin method were concurrently validated in two studies. In the first study, mean MBL measured with an automated alkaline hematin method in an Indian population was similar to that determined using a precursor alkaline hematin method in a US population [ 36 , 40 , 41 ]. With the advent of SAP-c sanitary products, the method was revalidated by comparing a semi-automated version for use with a selected brand of SAP-c towels to a manual reference method ( r 2 = 0.991; P < .0001, n = 63) (Additional files 3 and 4 ) [ 39 ]. The power to discriminate between normal bleeding and HMB was assessed for four methods and found to be reasonable, but statistical significance was not given (Additional file 6 ) [ 10 , 35 , 41 , 42 ].
The efficiency of blood extraction from sanitary products using the alkaline hematin method was investigated in 10 studies (Additional file 4 ) [ 10 , 14 , 35 – 42 ]. In the original alkaline hematin method, blood recovery was 96.3% after a 20-h incubation [ 14 ]. With modifications to improve speed and usability, efficiencies of recovering various volumes of blood from a selection of sanitary products ranged from 74.8% [ 42 ] to 107% [ 41 ]. Adaptation of the method for a selected brand of SAP-c towels resulted in recovery of at least 90% (≥85% with automation) of simulated menstrual fluid volumes [ 38 , 39 ].
Menstrual fluid loss, pad counts, and duration of period
Fluid weight (MFL) has been investigated as a simple alternative to the assessment of MBL by the alkaline hematin method [ 44 ]. The measure can be expressed gravimetrically (g) or converted directly to volume (mL), based on the assumption that the specific gravity of menstrual fluid equals one [ 28 , 44 ]. The relationship between MBL and MFL was considered in four studies, three of which used the alkaline hematin method as the comparator [ 27 , 44 , 48 ]. In all four studies, including one that validated MFL measurements with a selected brand of SAP-c towels [ 46 ], there was a correlation between MFL and either MBL or change in MBL ( r = 0.88–0.97; P = .001–.0001; Additional file 5 ) [ 27 , 44 , 46 , 48 ]. In a fifth study, MBL estimated from MFL correlated, but was not interchangeable, with MBL measured by the alkaline hematin method ( r = 0.73; P < .00001; Additional file 5 ) [ 84 ].
In the study by Fraser and colleagues, the sensitivity and specificity of diagnosing HMB with a regression model to estimate MBL from MFL were 89 and 98%, respectively. It was also shown that the blood content in MFL was similar in women with moderately heavy (60–100 mL) and excessive (> 100 mL) MBL (48 and 50%, respectively) [ 44 ]. In a later study using SAP-c towels, establishment of a normal range for MFL was prohibited because of overlap of MFL between women with normal and those with excessive MBL, and blood fraction was found to increase progressively with MFL volume [ 27 ].
The association of MBL with duration of menstruation was investigated in four studies (Additional files 5 and 6 ). There was a modest correlation in a study of 207 women complaining of HMB ( r = 0.35, P < .01) [ 82 ], whereas no relationship was observed in the other three studies, which included women with a range of MBL volumes [ 11 , 27 , 43 ]. In a study of women with self-perceived HMB, period duration was not significantly different for the lightest versus the heaviest periods [ 6 ]. Information on the length of periods was requested in some questionnaires [ 62 , 66 ], and this parameter forms part of both the PBAC and menstrual pictogram methods of assessing MBL [ 23 , 32 ].
The association of MBL with counts of sanitary items was considered in eight studies. Higham and Shaw and Warner et al. found that MBL was associated with the total number of pads and tampons used ( r = 0.61 and 0.30; P < .005 and P < .001, respectively) [ 68 , 82 ]. Chimbira et al. found that the median MBL was greater in women using 10 or fewer pads per period than in those using 31–40 pads, but there was a wide scatter of MBL in each group [ 34 ]. Five studies found no significant or overall correlation between pad/tampon count and MBL (Additional file 5 : Table S5) [ 6 , 27 , 32 , 42 , 82 ]. A question about the number of pads used by women was included in seven questionnaires [ 61 , 62 , 65 , 68 , 71 , 74 , 83 ]; information about the frequency of changing pads was requested in three questionnaires [ 28 , 63 , 79 ].
Measurement of iron/labelled red blood cells
The discriminatory power of three methods to measure iron/labelled blood in pads [ 31 ], from menstrual products [ 43 ], or in the whole body [ 29 ] was assessed: all of the techniques were able to discriminate between normal and high MBL, or between non-anemic and anemic women, but statistical significance was not reported (Additional file 6 ). In a fourth study, the amount of iron lost in pads strongly correlated with MFL [ 47 ] (Additional file 5 ).
Pictorial methods
The validation of pictorial methods was the focus of 19 articles (Additional file 3 ). These studies evaluated either the PBAC, which uses a scoring system that is proportional but not equivalent to MBL, or the menstrual pictogram, which measures MBL in milliliters and is directly comparable to the alkaline hematin method.
Pictorial blood loss assessment chart (PBAC)
Fourteen of the included articles reported on the PBAC/modified PBAC (Additional file 3 ). In one study, the PBAC was validated for a selected brand of SAP-c products [ 33 ]. Sensitivity and specificity of the PBAC were determined in seven studies (Table (Table1). 1 ). In six studies these related to diagnosis of a measured MBL > 80 mL [ 20 , 22 , 23 , 25 , 30 , 33 ], and in one study they related to diagnosis of self-perceived HMB [ 54 ]. For the diagnosis of MBL > 80 mL, sensitivity was 58–99% and specificity was 7.5–89%. For the diagnosis of self-perceived HMB, sensitivity was 78.5% and specificity was 75.8%. Specificity and sensitivity data generated with a single PBAC cut-off of 100 were presented in three studies [ 22 , 23 , 30 ]. Sensitivity and specificity data derived from a PBAC cut-off of 50 were provided in one study [ 20 ]. In three studies, data using multiple cut-off values, including those > 100, were reported [ 25 , 33 , 54 ].
The discriminatory power of PBAC was assessed in nine studies (Additional file 6 ). Statistically significant results were reported for the difference in PBAC scores between patients in heavy, normal, and light bleeding categories [ 54 , 56 ], those with and without menstrual disorder [ 52 ], individuals before and after treatment [ 81 ], and treated patients and active controls [ 48 ]. The association of PBAC with MBL (or change in MBL) was assessed in five studies. The range in correlation coefficients across four studies was 0.4659–0.847 (Additional file 5 ). The generalizability of the PBAC beyond the United Kingdom population of adult women in which it was originally validated was considered in seven studies (Additional file 4 ). The method was used successfully in populations of adolescents [ 56 , 76 ], users and non-users of oral contraceptives [ 55 ], and Iranian and Turkish women [ 51 , 52 , 81 ]. However, the PBAC may overestimate MBL in the general community [ 53 ]. Inter-cycle consistency was assessed with PBAC in two studies and found to be high [ 25 , 54 ].
Menstrual pictogram
The menstrual pictogram/modified menstrual pictogram were the focus of five included articles (Additional file 3 ). The sensitivity and specificity of the menstrual pictogram were determined in one investigation for a specified decrease in MBL, and in three studies in terms of diagnosing MBL > 80 mL. In one study in which the menstrual pictogram was evaluated as part of the Symptometrics device, the reference method was the paper menstrual pictogram (Table (Table1) 1 ) [ 26 , 27 , 32 , 59 ]. Across these four studies, the sensitivity was 82–96% and the specificity was 88–94%. A menstrual pictogram specifically designed for use with a particular brand of SAP-c towels (Fig. 2 ) was endorsed in one of these studies [ 27 ]. The predictive power of the menstrual pictogram at diagnosing HMB was presented in one report (positive, 91%; negative, 83%) [ 26 ].

a Representation of the original menstrual pictogram. Reprinted from Fertility and Sterility , 76, Wyatt KM et al., Determination of total menstrual blood loss, pp125–31, Copyright 2001, with permission from Elsevier [ 32 ]. b A modified version of the menstrual pictogram. Larsen L et al., Reproductive Sciences , 20 (6), pp680–7, Copyright © 2013, Reprinted by permission of SAGE publications [ 26 ]. c The menstrual pictogram validated for use with towels containing superabsorbent polymers. Reprinted from Fertility and Sterility , 101, Magnay, JL et al., Validation of a new menstrual pictogram (superabsorbent polymer-c version) for use with ultraslim towels that contain superabsorbent polymers, pp515–21, Copyright 2014, with permission from Elsevier [ 27 ]
Menstrual pictogram/modified menstrual pictogram values correlated highly with MFL assessed by the weight method, and with MBL or change in MBL from baseline assessed by the alkaline hematin method (Additional file 5 ). The original menstrual pictogram (Fig. (Fig.2) 2 ) was validated in the United Kingdom in untreated women with self-perceived, normal, or heavy MBL [ 32 ]. External validation of a modified version of the tool (Fig. (Fig.2) 2 ) was performed in North American women treated for HMB associated with leiomyomata [ 26 ] (Additional file 4 ).
Self-perception
The specificity and sensitivity of self-perception methods were investigated in six studies, including some questionnaires (Table (Table1). 1 ). Complaint of HMB was able to diagnose an MBL > 80 mL with both a specificity and a sensitivity of 74% and a positive predictive value of 56% [ 25 ]. A model including diary entries of both self-perceived bleeding intensity and clinical parameters diagnosed MBL > 80 mL with a sensitivity and specificity of 87 and 70% respectively [ 84 ]. A questionnaire including a Record and a Recall method for estimating MBL, both of which had a subjective element, resulted in sensitivities of 66 and 59%, respectively. Recall method and Record method tertiles had significantly different mean MFL values [ 62 ]. With the Menorrhagia Impact Questionnaire (MIQ), the specificity and sensitivity of changes in MIQ items corresponding to either a meaningful change in perceived MBL [ 69 ] or an optimal reduction in MBL measured by the alkaline hematin method [ 4 ] were 63–82%. In a study of the Menstrual Evaluation Questionnaire, which includes questions on the self-perceived heaviness of periods, the sensitivity and specificity of diagnosing MBL > 80 mL were 60 and 86% respectively, and women who rated their periods as “very heavy” had a significantly higher mean MBL than the remainder of the women [ 68 ].
There was low-to-moderate correlation of 36-Item Short Form Survey (SF-36) score, log discharge rate, ferritin score or PBAC score with scores from four questionnaires: the Menstrual Bleeding Questionnaire [MBQ], the Mansfield–Voda–Jorgensen menstrual bleeding scale, an MBL questionnaire, and a QoL questionnaire (Additional file 5 ) [ 8 , 28 , 73 , 83 ]. All four surveys, as well as the Health Utilities Index questionnaire [ 75 ], were able to discriminate between women with and without HMB, with statistical significance attained for the MBQ, the QoL questionnaire, and the Health Utilities Index (Additional file 6 ). The Portuguese SF-36 did not correlate with PBAC scores [ 70 ].
A questionnaire was used in 1547 women to self-grade MBL heaviness and assess the effects of self-perceived HMB on daily life and the Swedish SF-36 [ 85 ]. The daily lives of women with self-perceived HMB were affected much more than those of women with normal MBL (Additional file 6 ). Women with self-perceived HMB also had significantly worse health-related QoL in all domains of the Swedish SF-36 compared with women with normal menstrual bleeding.
The percentage of women with self-perceived HMB and a measured MBL of 80 mL or more was assessed in nine studies and found to range from 26 to 76% [ 6 , 11 , 27 , 30 , 32 , 34 , 35 , 68 , 82 ] (Additional file 6 ). For three methods involving self-perception of MBL, positive establishment of face and content validity was reported (Additional file 3 ) [ 57 , 71 , 78 ].
Additional advantages and disadvantages
The additional advantages and disadvantages of methods for measuring MBL are summarized in Table 2 . A more detailed overview is provided in Additional file 3 .
Additional advantages and disadvantages of methods to measure menstrual blood loss
MBL menstrual blood loss, MFL menstrual fluid loss, PBAC pictorial blood loss assessment chart, QoL quality of life, SAP-c superabsorbent polymer-containing
We present the results of a systematic review of the development and validation of methods for measuring MBL. We summarize the data available and list other key advantages and disadvantages of the various procedures.
The alkaline hematin method has been well validated in terms of the efficiency of blood recovery from sanitary items, including towels that contain superabsorbent polymers as the absorptive agent. It is widely recognized as the most objective technique with which to measure MBL, and can be required by regulatory bodies to assess the efficacy of new treatments for HMB. However, to be suitable for the clinical setting, a test must be quick, easy to conduct, and accepted by patients. In this respect, the alkaline hematin method is less appropriate for use in the general population than the PBAC, menstrual pictogram, or a questionnaire, especially the electronic versions. Despite extensive development to make it more practical and widely applicable, the original inherent disadvantages of the method remain; namely, the need to collect, store and then send all used sanitary items to a laboratory for analysis. In addition, the method is limited to documentation of MBL collected on sanitary items. To overcome this drawback it would be necessary to either carefully capture all extraneous blood loss or use a simultaneous diary to take extraneous blood loss into account. Nonetheless, the alkaline hematin method is widely recognized to be the “gold standard” in terms of accuracy. Ideally, all methods to measure MBL would be validated against alkaline hematin. However, this can be challenging in practice, in part due to the abovementioned disadvantages of the alkaline hematin technique.
Correlations were observed between MFL and MBL, and it is argued that MFL matters more to women concerned with flooding than MBL [ 48 ]. However, MBL estimated using MFL is not interchangeable with MBL measured using the alkaline hematin method [ 84 ]. Furthermore, variation in the proportion of the non-blood fraction, particularly at extremes of menstrual loss, limits the validity of using MFL to diagnose HMB [ 27 , 87 , 88 ]. Therefore, we do not consider MFL to be a reliable validator of MBL. The MFL method also requires women to store and submit carefully all used products for analysis, which may not be acceptable or feasible, resulting in reduced compliance. In principle, the use of menstrual cups to collect large volumes of MFL is simple. In reality, many women report that spillage and leakage is common and the technique has thus proved unsuitable for measuring MBL.
The hypothesis that menstrual duration alone can be used to predict HMB is not supported by current evidence. It is also not possible to accurately correlate MBL with the number of feminine items used during a menstrual period, and extreme examples have been cited of women with HMB using far fewer towels than those with light menstrual flow [ 6 , 27 , 82 ]. In addition to the brand and absorbency of the product, many variables affect the frequency with which items are changed, including rate and composition of menstrual flow, individual anatomy, ambient humidity, physical activity, posture, and personal fastidiousness in changing sanitary garments. Some patient-reported outcome instruments have attempted to incorporate product absorbencies, albeit that towel absorbency ratings are arbitrary and unregulated [ 28 , 62 , 71 , 83 ]. However, the degree of saturation and/or brands of products are not always taken into account [ 28 , 71 , 83 ].
In general, the discriminatory power and sensitivity/specificity scores are reasonably high for the PBAC/modified PBAC, but because some low scores have been recorded the robustness of this test has been queried [ 20 , 25 , 30 , 89 ]. The PBAC is not as accurate as the alkaline hematin method for determination of HMB, but it is nevertheless superior to using clinical history or a simple bleeding diary. Moreover, it has been validated for use with selected SAP-c products, does not require laboratory facilities, and has undergone much external validation. The menstrual pictogram has consistently high (> 80%) sensitivity and specificity in diagnosing HMB, including when validated with a SAP-c product. Furthermore, it correlates well with the alkaline hematin method [ 26 , 27 , 32 , 59 ], although only five menstrual pictogram validation studies were retrieved. In contrast to the PBAC, the original menstrual pictogram includes a greater range of icons and differentiates between absorbency ratings of sanitary items [ 32 ].
Self-assessment of MBL yields a number of false negatives and positives when compared with more objective measurements. The concept that some women have a distorted perception of their MBL is corroborated by data from a 16-study meta-analysis [ 90 ]. Among measures of MBL involving self-perception, a mixed linear model based on a menstrual diary and laboratory parameters had the highest sensitivity score (87%), but to date the model has only been tested in a single trial in women with HMB.
Various articles on questionnaires were reviewed. All the questionnaires contained items related to self-perception of MBL or its impact on QoL. Concurrent validation was performed in fewer than half of the questionnaires included, with mixed results [ 8 , 28 , 62 , 69 , 70 , 72 , 73 , 75 , 76 , 85 , 86 ], but three questionnaires showed promise in terms of ability to discriminate between heavy and normal MBL [ 8 , 73 , 75 ].
Importantly, of all the methods reviewed, only the alkaline hematin method, the PBAC, and the menstrual pictogram are validated for measuring MBL with selected SAP-c products [ 19 , 27 , 33 , 38 , 39 ]. In addition to the statistical analyses described above, treatment-induced changes in MBL that were also detected by a reference technique were reported for four methods: the menstrual pictogram, PBAC, MFL, and MIQ [ 26 , 48 , 54 , 69 , 72 , 81 ] (Table (Table1; 1 ; Additional files 5 and 6 ).
MBL is only one aspect of the menstrual experience. Pain, pattern, and predictability of timing can all influence a woman’s perception of her period. QoL is recognized to be an important clinical indicator of the effects of menstruation on women [ 17 , 85 , 91 ]. However, QoL is influenced by many factors other than HMB, such as undernourishment and depression [ 70 ]. Given that treatment of HMB may incur significant psychological, physical, and financial costs [ 28 ], and – as discussed above – validated, quick, economical, and easy methods for assessing MBL are available, future evaluation of a clinical technique that combines a pictorial method validated for modern sanitary products with a daily (preferably electronic) menstrual diary of specific health-related QoL items would be beneficial.
A limitation of this review is that comprehensive comparisons of the different techniques were limited because of the heterogeneity of validation methods and result formats. The definition of HMB was not the same for all methods and there was a lack of consistency in the comparator employed (Table (Table1 1 and Additional file 5 ). With the PBAC, different cut-off values were used to diagnose HMB. Often the PBAC or menstrual pictogram was not used or evaluated in the way in which it was originally validated [ 50 – 52 , 54 ], and none of the amendments has been recertified by the alkaline hematin assay. The risk of bias was seldom formally acknowledged in the articles reviewed, and different types of study were subject to different types of bias. Blinding of investigators/gynecologists to participant data was acknowledged in all studies in which investigator–participant agreement was assessed (Additional file 4 ) [ 19 , 23 , 25 , 27 , 39 , 48 , 59 ].
Our searches identified articles that were excluded because they primarily described the application of an existing method for measuring MBL rather than any form of method validation [ 92 – 97 ]. A recent systematic review analyzing the frequency of use of MBL measurement tools in randomized controlled trials found that PBAC score was the most commonly used primary outcome [ 16 ]. The menstrual pictogram did not feature, perhaps because it has been used less frequently than the PBAC, but in our systematic review four non-validation studies were identified in which the menstrual pictogram assessed MBL [ 92 , 93 , 95 , 97 ]. As a result of the search terms used in our review there may have been incomplete retrieval of reports relating to questionnaires and QoL studies [ 7 , 98 – 103 ]. It would be well beyond the scope of this review to expand the existing search strategy to identify all questionnaires relating to MBL. However, it should be considered for a follow-up analysis because there is a need to standardize the validation of questionnaires and QoL tools for measuring MBL [ 9 , 104 ].
Despite these limitations, we hope that by summarizing all of the available data on the different methods together this review will inform researchers evaluating new techniques of the standard types of validation required. This in turn should help policy makers conduct a robust appraisal of available methods for measuring MBL.
Every available method to assess MBL has limitations. Pictorial methods strike a good balance between ease of use and validated accuracy of MBL determination; of these methods, the menstrual pictogram has several advantages, not least that it considers different absorbency levels of sanitary items and has an output of MBL volume in milliliters. Currently, clinicians usually base their diagnosis of HMB on a patient’s reported QoL. However, there are drawbacks, particularly in research trials, to relying entirely on health-related QoL devices, which are essentially subjective measures of HMB. A compromise would be to consider MBL alongside QoL when deciding how to diagnose HMB and assess effectiveness of treatments.
Additional files
Table S1. Full electronic search strategy of Embase®™ and Medline. (PDF 44 kb)
Table S2. Advanced search of the ClinicalTrials.gov website. (PDF 32 kb)
Table S3. Overview of types of validation performed, practicalities, and limitations of methods. (PDF 232 kb)
Table S4. Further validation of methods. (PDF 171 kb)
Table S5. Correlations of methods with established standards. (PDF 168 kb)
Table S6. Assessment of discriminatory power of methods for assessing MBL. (PDF 148 kb)
Completed PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) checklist. (PDF 133 kb)
Acknowledgements
The authors thank Dr. Lucy Bomphrey of Oxford PharmaGenesis for data extraction and writing support.
This review was funded by Bayer AG, Berlin, Germany. Data extraction, medical writing and editorial support were provided by Oxford PharmaGenesis, funded by Bayer AG, Berlin, Germany. Bayer AG did not contribute to the design of this review, the collection, analysis and interpretation of the data, or writing of the manuscript beyond providing financial support.
Availability of data and materials
Abbreviations, authors’ contributions.
JLM, SO’B, CG and CS contributed substantially to the conception and design of the review, and to the analysis and interpretation of the data. All the authors reviewed the article critically for important intellectual content and approved the final version for publication.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Competing interests.
J.L.M. has received payment for consulting and medical writing services from Bayer AG for this and other work. S.O’B. has received a grant to his institution from Bayer AG for Menstrual Pictogram Research and from Advantage West Midlands for Symptometrics, a company involved in the development of an electronic version of premenstrual syndrome charts, pain charts and an alternative menstrual pictogram. He has received payment from Asarina Pharma for consultancy work and to act as Chief Investigator for an RCT on Premenstrual Syndrome, and from Bayer for consulting services and expert testimony for the licensing of and lectures on OC Yaz. He has also been an unpaid Chairman for the International Society for Premenstrual Disorders (ISPMD) and received payment for intellectual property issues unrelated to the work in this manuscript. C.G. and C.S. are employees of Bayer AG, Berlin, Germany. C.S. holds stock in Bayer AG.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Julia L. Magnay, Email: moc.sulp.noradla@yangamlj .
Shaughn O’Brien, Email: ku.shn.mnhu@neirb'o.nhguahs .
Christoph Gerlinger, Email: [email protected] .
Christian Seitz, Phone: +49 30 468 15539, Email: [email protected] .
- Medical Devices

Covaxin side-effects: Period-related abnormalities, musculoskeletal disorders reported among recipients
Meanwhile, a new study has found that covishield can cause another vaccine-induced immune thrombocytopenia and thrombosis (vitt)—a rare but fatal blood clotting disorder..

Covaxin side-effects: Days after panic over Covishield’s side-effects and AstraZeneca’s decision to withdraw the vaccine, a new study has highlighted the adverse effects reported among people who took Bharat Biotech’s Covaxin .
The observational study has found that nearly a third of the participants reported experiencing adverse events of special interest (AESI) following vaccination.

The study led by Sankha Shubhra Chakrabarti and his team at Banaras Hindu University was published in on SpringerLink, an integrated platform for journals and other materials published by Springer.

Finally our long term safety data of BBV152 vaccine is onlinehttps://t.co/7JtLXMl96o — Dr Sankha Shubhra Chakrabarti (@sankha_shubhra) May 14, 2024
According to the study, female adolescents and those with a history of allergy are at a higher risk of AESI after receiving Covaxin. It is noteworthy that a majority of the of the AESI persisted at the one-year follow-up, the researchers found.
What are the side-effect of Covaxin?
1024 people enrolled in the study. Out of which researchers managed to follow up with 635 adolescents and 291 adults over the course of one year. Among the reported adverse events, viral upper respiratory tract infections were prevalent among both adolescents and adults.
The study also found that new-onset skin and subcutaneous disorders, general disorders, and nervous system disorders were commonly observed AESIs were reported among adolscents. Similarly, among adults, general disorders, musculoskeletal disorders, and nervous system disorders were frequently found.
Shockingly, female participants of the study reported menstrual abnormalities. Some participants also eported ocular abnormalities and hypothyroidism were observed in a smaller percentage of participants. Moreover, serious AESIs such as stroke and Guillain-Barre Syndrome were identified in a fraction of the participants.
According to the researchers, adolescents, females, and those with a history of allergies or post-vaccination typhoid were at higher risk of experiencing AESIs. Additionally, people with comorbidities, were at increased risk of persistent AESIs. Among adults, those with co-morbidities such as hypertension were at more than two times higher risk of AESIs and persistent AESIs.
‘More surveillance required’
The researchers found that the patterns of adverse events developing after Covaxin differed from those reported with other COVID-19 vaccines, as well as between adolescents and adults.
The researchers emphasised on the need for extended surveillance of COVID-19 vaccinated individuals to understand the course and outcomes of late-onset adverse events.
“Relationship of AESIs with sex, co-morbidities, pre-vaccination COVID-19 and non-COVID illnesses should be explored in future studies,” the researchers noted.
Last week, AstraZeneca has initiated a global withdrawal of its COVID-19 vaccine. This came days after it was reported that the British pharmaceutical company admitted that the jab can cause rare side effects like Thrombotic Thrombocytopenic Syndrome (TTS).
Meanwhile, another study has found that AstraZeneca’s Covid-19 vaccine can increase the risk of vaccine-induced immune thrombocytopenia and thrombosis (VITT) — a rare but fatal blood clotting disorder. The new findings, published in the New England Journal of Medicine, also have important implications for improving vaccine safety.
Get live Share Market updates, Stock Market Quotes , and the latest India News and business news on Financial Express. Download the Financial Express App for the latest finance news.
- Stock Market Stats
Related News
Senior Citizen FDs are tailored for individuals above 60 years, offering higher interest rates and regular income. They are stable and predictable, making them ideal for risk-averse seniors. They also offer tax benefits and flexible payout options. To maximize returns, consider factors like interest rates, tenure, and diversification.
Photo Gallery
9 Scorching heatwaves: States issue guidelines advising people to stay indoors – PHOTOS
7 Kashmir: Freshly harvested strawberries! First fruit of the season is here – PHOTOS
9 Rs 50, Rs 200, Rs 500 and Rs 2000 notes images: Here are the new currency notes released by RBI
Latest News

Famine is an immediate risk in Gaza: UN aid chief

NTA successfully conducts day 2 of CUET UG – 2024 examination

IPL 2024 MI vs LSG Dream 11 Predictions: Match 67 preview, possible playing XI, head-to-head stats

Toshiba announces to cut 4,000 jobs amid intensified restructuring efforts

IPL 2024 Playoffs, Final Tickets: NPCI launches exclusive offer for RuPay cardholders – details here
Trending topics.
- Mutual Funds
- IPO’s Open and Upcoming 5
- Top Indices Performance
- Stock Analysis
- Financial Literacy
- Gold Rate Today
- NSE Top Gainers 1475
- NSE Top Losers 1050
- BSE Top Gainers 2289
- BSE Top Losers 1786
- NSE 52-Week High 106
- NSE 52-Week Low 12
- BSE 52-Week High 196
- BSE 52-Week Low 32
- NSE Price Shocker
- NSE Volume Shocker
- BSE Price Shocker
- BSE Volume Shocker
- NSE Sellers
- BSE Sellers
- Silver Rate Today
- Petrol Rate Today
- Diesel Rate Today

COMMENTS
On the other hand, a study conducted in Amritsar assessed both pre-test and post-test knowledge to determine the effectiveness of a teaching program among nursing students regarding menstrual blood banking and reported that during the pre-test, 93% of the respondents had just an average knowledge of menstrual blood banking, while post-test 89% ...
However, some recent analyses have revealed a profile similar to systemic blood, along with the presence of clinically-relevant indicators of uterine abnormalities. 6 A recent pilot study, for example, demonstrated high agreement between menstrual and systemic blood for common biomarkers. 7 HbA1c, among seven other biomarkers, was found to ...
MenSCs were culture-expanded from a previously established and characterized master cell bank (MCB) derived from the menstrual blood collected from at least 5 healthy women . The quality of the MenSCs stored in the bank was tested according to the applicable U.S. Food and Drug Administration (FDA) regulations for fungal and bacterial ...
Menstrual blood banking. A new research has found that menstrual blood is a rich source of stem cells that have the ability to multiply and differentiate into any kind of cells. Stem cells in menstrual blood have similar regenerative capabilities as the stem cell in umbilical cord blood and bone marrow. We are in the beginning of the era of ...
On the other hand, a study conducted in Amritsar assessed both pre-test and post-test knowledge to determine the effectiveness of a teaching program among nursing students regarding menstrual blood banking and reported that during the pre-test, 93% of the respondents had just an average knowledge of menstrual blood banking, while post-test 89% ...
Findings: The study identified that 75 (34.1%) had poor, 116 (52.7%) had average and 29 (13.2%) had good knowledge regarding menstrual blood banking among female health care professionals. The ...
This research was conducted to understand the knowledge, attitude, and practice of menstrual blood donation regarding menstrual blood-derived mesenchymal stem cells (MenSCs) among female ...
Plasticity of human menstrual blood stem cells derived from the endometrium. Menstrual blood-derived stem cells (MenSCs) provide an alternative source of adult stem cells for research and application in regenerative medicine and the multipotent properties and the plasticity and safety of the acquired cells have been demonstrated in many studies.
PHASES OF MENSTRUAL CYCLE: The day count for menstrual cycle begins on the first day of menstruation when blood starts to come out of the vagina. In this section, the length of menstrual cycle has been assumed to be 28 days (which is the average among women). The entire duration of a Menstrual cycle can be divided into four main phases:2.
As of 2020, she found, menstrual stem cell research accounted for only 0.25 percent of all mesenchymal cell research, while bone marrow stem cells represented 47.7 percent.
menstrual blood bank Eachlaboratory where it is processed, ... In the present study, analysis of data regarding menstrual blood stem cells banking among nursing students related to post-test knowledge revealed that majority (88.5%) of nursing students had good knowledge and only (11.5%)
1. Journal of Medical Biomedical and Applied Sciences, Jan (2016). Contents lists available at www .jmbm.in. JOURNAL OF MEDICAL BIOMEDICAL AND APPLIED SCIENCES. Menstrual Blood Banking: A concept ...
Background Since the publication over 50 years ago of the alkaline hematin method for quantifying menstrual blood loss (MBL) many new approaches have been developed to assess MBL. The aim of this systematic review is to determine for methods of measuring MBL: ability to distinguish between normal and heavy menstrual bleeding (HMB); practicalities and limitations in the research setting; and ...
Background of the study: Menstrual blood stem cell banking is a process of collection and storage of menstrual blood under required condition for the purpose of future therapeutic use. Aims and Objectives: To determine the effectiveness of structured teaching program on menstrual blood stem cells banking among
Findings: The study identified that 75 (34.1%) had poor, 116 (52.7%) had average and 29(13.2%) had good knowledge regarding menstrual blood banking among female health care professionals. The attitude of female health care professionals shows that 76 (34.5%) has favorable, and 144 (65.5%) has unfavorable attitude towards menstrual blood banking.
Result: The study findings indicate that a majority (78.03%) of the staff nurses possessed moderate knowledge concerning menstrual blood banking. Additionally, the research demonstrated a notable correlation between the level of knowledge and various socio-demographic variables. Moreover, the respondents exhibited a favourable attitude towards ...
Menstrual blood banking is a process for collection of menstrual blood by using tampon or a silicone cup and is inserted in the vagina on the day of heaviest flow. The cup needs to be placed inside the vagina for at least three hours so as to collect approximately 20 milliliters of blood.In this study, menstrual blood banking refers to ...
The menstrual blood was transferred by the study participants to a 50‐mL Falcon tube prefilled with 5 mL cell medium containing heparin, penicillin/streptomycin, gentamicin, and gluconazole as previously described. 19 Menstrual blood samples were kept refrigerated until processed and frozen down.
In the new study, Samuelson Bannow and her team tested 21 different menstrual products, including discs, tampons, pads, period underwear and cups. They found that menstrual underwear products were ...
Menstrual blood banking is a process of storing the menstrual blood of a woman to use the stem cells present in it in future. Stem cells which are present in menstrual blood are having multipotency.
Although menstrual blood banking is still new and lots of research is still going on menstrual blood, if its benefits are utilized, it can prove to be very beneficial for all women who want to give themselves the gift of good health[6]. It can be said that menstrual blood banking has a vast scope in future and is the next big thing in the ...
The study objective was to test the hypothesis that low crude protein (CP) diet with crystalline amino acids (CAA) supplementation improves Lys utilization efficiency for milk production and reduces protein turnover and muscle protein breakdown. Eighteen lactating multiparous Yorkshire sows were allotted to 1 of 2 isocaloric diets (10.80 MJ/kg net energy): control (CON; 19.24% CP) and reduced ...
In one study in which the menstrual pictogram was evaluated as part of the Symptometrics device, the reference method was the paper menstrual pictogram (Table (Table1) 1) [26, 27, 32, 59]. Across these four studies, the sensitivity was 82-96% and the specificity was 88-94%.
Meanwhile, a new study has found that Covishield can cause another vaccine-induced immune thrombocytopenia and thrombosis (VITT)—a rare but fatal blood clotting disorder.