An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Integr Care
- v.18(3); Jul-Sep 2018


The Core Dimensions of Integrated Care: A Literature Review to Support the Development of a Comprehensive Framework for Implementing Integrated Care
Laura g. gonzález-ortiz.
1 Università della Svizzera Italiana, IdEP Institute, CH
Stefano Calciolari
Nick goodwin.
2 International Foundation for Integrated Care, UK
Viktoria Stein
As part of the EU-funded Project INTEGRATE, the research sought to develop an evidence-based understanding of the key dimensions and items of integrated care associated with successful implementation across varying country contexts and relevant to different chronic and/or long-term conditions. This paper identifies the core dimensions of integrated care based on a review of previous literature on the topic.
Methodology:
The research reviewed literature evidence from the peer-reviewed and grey literature. It focused on reviewing research articles that had specifically developed frameworks on integrated care and/or set out key elements for successful implementation. The search initially focused on three main scientific journals and was limited to the period from 2006 to 2016. Then, the research snowballed the references from the selected published studies and engaged leading experts in the field to supplement the identification of relevant literature. Two investigators independently reviewed the selected articles using a standard data collection tool to gather the key elements analyzed in each article.
A total of 710 articles were screened by title and abstract. Finally, 18 scientific contributions were selected, including studies from grey literature and experts’ suggestions. The analysis identified 175 items grouped in 12 categories.
Conclusions:
Most of the key factors reported in the literature derive from studies that developed their frameworks in specific contexts and/or for specific types of conditions. The identification and classification of the elements from this literature review provide a basis to develop a comprehensive framework enabling standardized descriptions and benchmarking of integrated care initiatives carried out in different contexts.
Introduction
This paper presents findings from the “International Check” work package of Project INTEGRATE that was funded within the EU 7 th Framework Program (EU Grant Agreement 305821; see http://projectintegrate.eu.com ). The overall purpose of the work package was to develop an evidence-based framework on the key dimensions and items of integrated care associated with successful implementation. Moreover, the purpose of such a framework was designed to support decision-makers in the effective design and implementation of integrated care programs[ 1 ].
Several studies have contributed to the development of theoretical frameworks for integrated care implementation (e.g. [ 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 ]). The articles and technical reports published on the topic identify factors or structures of elements fostering care integration, most often for people suffering from chronic and/or long-term conditions. In addition, most of these studies focus on a specific context of implementation (e.g. in coordinating services around people with a chronic illness) and so do not appreciate the influential role that contextual factors in care integration can play in determining outcomes (e.g. of finances, cultures, organizational forms etc.) [ 11 ]. In the former case, the resulting framework or list of key factors is likely to be tailored for the selected setting. In the latter case, it is hard to disentangle the context dependence of the analytical proposal.
Context is very important in evaluating the implementation of complex service innovations like integrated care and so any framework must be robust enough to understand the intricate interplay between multi-component interventions across contexts and settings [ 11 , 12 , 13 ]. The COMIC Model for the comprehensive evaluation of integrated care interventions [ 11 ], for example, has illustrated how the use or realistic synthesis to study the interplay between contexts, mechanisms and outcomes can bring insights into understanding how and why integrated care interventions succeed or fail.
Hence, to understand the complex and dynamic issues at play in the implementation of integrated care a more comprehensive framework is necessary that helps to benchmark initiatives across different contexts and condition-specific population groups. The task is a challenging one and cannot disregard the accumulated knowledge in the field. Therefore, as a first step in this direction, it is paramount to analyze and summarize the findings from previous studies in this respect. This can provide the basis for a more comprehensive approach to understanding how integrated care may be implemented by building on the evidence available in the extant literature of integrated care.
This paper presents a comprehensive, non-systematic, review of the extant literature on care integration design and implementation. Coherently with the objectives of Project INTEGRATE, this study purposefully focuses on initiatives targeting patients affected by chronic diseases (COPD and diabetes) and people living with geriatric and/or mental health conditions. The purpose of this paper, therefore, has been to build a more comprehensive understanding of the factors and elements associated with successful integrated care implementation as a precursor to the development of a new conceptual framework. The objectives of this paper are: (1) to identify the most important factors influencing the success of an initiative of care integration across different contexts; and (2) to classify and summarize the identified evidence according to the extant literature in the field.
To ensure a common understanding of the concept, Project INTEGRATE utilised Kodner and Spreeuwenberg’s definition of integrated care as: ‘a coherent set of methods and models on the funding, administrative, organisational, service delivery and clinical levels designed to create connectivity, alignment and collaboration within and between the cure and care sectors’ [ 14 ]. Hence, the main purpose of integrated care interventions consists of reducing fragmentations in service delivery and to foster both comprehensiveness of care and better care co-ordination around people’s needs. Many frameworks have been developed over time to understand the key elements, or building blocks, of integrated care [ 15 ].
One of the most well-known is the Chronic Care Model (CCM) that was developed from a Cochrane systematic review [ 10 ]. This work developed a comprehensive framework for the organization of healthcare to improve outcomes for people with chronic conditions. It identified six interrelated domains that should be considered to facilitate high-quality chronic disease care, thus improving health outcomes [ 3 ]. The CCM identifies the main areas of intervention to accomplish such a goal and enhance the health outcomes for specific target patients. In particular, its approach focuses on fostering an effective use of community resources; enabling patient self-management, nurturing evidence-based care and patient preferences, and leveraging on the use of supportive information technology [ 4 ].
Since the CCM focuses on the delivery of clinically oriented systems to patient it did not include many key aspects of care integration – for example, regarding health promotion and prevention, or indeed of rehabilitation and re-ablement. In this respect, Barr and colleagues proposed an evolution of the model, called the Expanded Chronic Model (ECCM) [ 2 ]. The ECCM includes elements specifically aimed to promote population health and encourage prevention by involving the community. Another variation is the Innovative Care for Chronic Conditions model (ICCC) [ 16 ]. Developed by the WHO as part of a ‘road map’ for health systems to deal with the rising burden of chronic illness, the ICCC placed a specific premium on prevention through ‘productive partnerships’ between patients and families, community partners and health care teams to create informed, prepared and motivated communities. In this respect, recent developments of integrated care initiatives, such as the patient-centred medical home (PCMH), have stressed the importance of delivering continuous, comprehensive and coordinated care in the context of people’s family and community [ 17 ].
The frameworks described above have primarily evolved from the USA and been confined in their thinking to within health systems. They have also not sought to identify key actions that decision-makers would need to implement integrated care effectively, such as governance and accountability, financing and incentives, or issues related to culture and values. However, other work has sought to address this. For example, a knowledge synthesis from Canada developed an influential paper entitled ‘ten principles of successful integrated systems’ [ 18 ].
More recently, Minkman et al. [ 7 ] carried out a study, based on a Delphi method, to identify and validate analytical key factors of care integration. The authors started by identifying elements from the literature. Then, they conducted a three-round Delphi study among a group of thirty-one experts, who provided comments to rank 175 elements in priority order. Then, the expert panel clustered the elements and discussed their content following a concept mapping procedure. Finally, the authors identified 89 relevant elements grouped into nine clusters. The results aim to develop a comprehensive quality management model for integrated care.
In another recent paper, Valentijn et al. [ 9 ] proposed a taxonomy to facilitate the description and comparison of different integrated care interventions. The taxonomy consists of 59 key elements resulting from a two-round Delphi study. This contribution is the development of a companion paper [ 8 ] in which the authors proposed a general model, known as the Rainbow Model of Integrated Care. Such model proposes six dimensions (in which the aforementioned 59 elements are grouped) and has a primary care perspective.
Compared to the CCM and the ECCM, the last two models are much more analytical in terms of the wider range of factors necessary to support the effective development of integrated care systems. Despite the differences they currently compete to propose an evidence-based perspective on the topic. Each has been developed for a different purpose and each varies in scope, for example, from the process of coordinating services around people with chronic conditions to enabling health and social care systems to operate more cohesively. For professionals and decision-makers tasked with designing and implementing integrated care for different client groups in a range of contexts and settings this potentially provides for confusion on the most appropriate frameworks and models they might use. This indicates that a more comprehensive framework – one that leverages the strengths of previously published studies but which enables an understanding of the core dimensions of integrated care across contexts and settings – is necessary to support decision-makers in the design and implementation of their integrated care programs across settings and differing client groups.
Methodology
The authors searched for scientific studies published in peer-reviewed journals and the most important contributions in the grey literature (research reports and conference presentations). The adopted search strategy aimed to be efficient and flexible enough to include also important seminal contributions on the topic. Therefore, the authors agreed on starting with three specialized journals where peer-reviewed articles presenting frameworks of integrated care would most likely be cited, namely: the International Journal of Integrated Care (IJIC), the Journal of Integrated Care (JIC), and the International Journal of Coordinated Care 1 (IJCC). The initial search was limited to the period 2006–2015.
The two authors from USI retrieved all the abstracts published in the selected period. Then, each one read half of the abstracts of all the articles to decide which contributions should be further analyzed. At this stage, the preliminary inclusion criteria consisted of two simple questions: (a) Does the contribution propose or analyze any framework aimed to explain the success or describe the implementation of integrated care initiatives? (b) Does the article propose or analyze any important aspect/s explaining the success of integrated care initiatives?
Each of the two researchers crosschecked the list of abstracts selected by her/his colleague until they reached an agreement. Afterwards, the two researchers read separately the full text of the selected articles to confirm their inclusion. They looked for contributions defining and operationalizing relevant elements of care integration or discussing the relationships between elements of care integration (inclusion criteria). They also applied the following exclusion criteria: (1) Limited to motivating the importance and goals of integrated care; (2) Limited to describing care integration properties and/or principles; (3) Limited to problems/gaps pf a specific case or national context; (4) Limited to a specific means/technology of integration (e.g. integrated care pathways); (5) Not normative (hard to use for assessing an initiative); (6) Limited to assessment of results of integrated care (not elements/strategies of care integration); (7) Review not based on a specific framework; (8) Not focused on chronic diseases or long-term conditions; (9) Non enough details (to allow for operationalization); (10) Based on another framework/model (and with no significant additional contribution); (11) Too much focused on a specific target population (e.g., elderly, minors, diabetic patients). Then, the two researchers compared the results of their selective analysis and found agreement when it was necessary to reconcile differences.
After this step, the two researchers analyzed the references of the included contributions looking for further relevant articles (snowballing). This approach was designed to identify previously published frameworks (including in the grey literature). The complete list of the identified contributions was sent to the other two authors from IFIC, who confirmed each item and suggested relevant contributions not included. All the researchers agreed on the new list. Then they performed hand searches looking for further articles/documents in selected databases (ScienceDirect, PubMed, and Medline) and collected suggestions from experts in the field. This range of experts included those within the research consortium plus the 13 members of the Advisory Board of Project INTEGRATE comprising leading academics, policy-makers, professional and commissioners across health, social care and public health disciplines (see: www.projectintegrate.eu.com/integrated-care-purpose ).
Once all the authors agreed on the final list (with the earlies selected article published in 2002), the two researchers from USI carefully analyzed each selected contribution to identify the elements of the proposed framework or relevant aspects reported as factors fostering care integration. In some cases, the framework and/or the elements were quite evident, since they were listed or presented in a schematic way. For instance, Lyngsø et al. [ 6 ] categorized and listed the key elements in a table. In other contributions, the elements had to be meticulously identified into the text and extracted by the researchers. In such cases, both researchers independently identified and coded the elements from each selected document. Then, they cross-checked the results and found agreement on eventual differences.
The identified elements (hereafter referred as “items”) were gathered in a comprehensive list. Each item was written down textually to avoid misunderstandings in the next phase (validation). Supported by existing dimensions of the CCM, we drafted a table and placed each identified item into a corresponding category. Each item was associated with a consecutive number and the article/document where it was identified. Elements not fitting in any of the CCM dimensions were listed at the bottom of the table to be afterwards grouped into additional categories proposed by the researchers. It is important to mention that, in this study, we went for inclusiveness. Therefore, items quite similar but with non-identical wording were reported as a different item.
The database search, spanning over a decade in the publication history of the three selected journals, retrieved 710 peer-reviewed articles. The majority of these studies were subsequently excluded (679 articles) based on their title or abstract, because they did not meet the inclusion criteria. Therefore, we focused on the remaining 31 articles eligible for inclusion. After full text reading, based on the aforementioned exclusion criteria, 14 studies remained.
We found articles written by the same author(s) and discussing elements to foster integrated care already proposed in preceding companion(s) paper(s). In this case, we included only the most recent article, which generally confirms or further develops ideas/notions proposed in the previous one/s. We did not include any study from the references search (snowballing), because none of the identified articles did actually meet the predefined eligibility criteria.
With regard to the grey literature and expert suggestions, we selected four studies. This resulted in 18 studies ultimately included in our review [ 4 , 5 , 6 , 8 , 11 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 ]. From each of the selected contributions, we identified and extracted items considered influential for care integration. We obtained a comprehensive list consisting of 175 items categorized in 12 domains. The first six domains are those proposed by the CCM: health care system, community resources and policies, self-management support, delivery system design, decision support, and clinical information system. In addition, we defined six further categories (leadership, governance, performance monitoring, organizational culture, contextual factors, and social capital) to group those elements that did not fit with any of the CCM domains. Figure Figure1 1 summarizes the selection process followed in the search and Table Table1 1 the results of the search across the 12 domains.

Flowchart of the literature selection process.
Results of the search across the identified 12 conceptual domains.
| Domain | No. | Element/item | Reference |
|---|---|---|---|
| 1 | Universal coverage or enrolled population with care free at point of use | [ , ] | |
| 2 | Emphasis on chronic and long-term care | [ , ] | |
| 3 | Emphasis on population health management | [ , , ] | |
| 4 | Alignment of regulatory frameworks with goals of integrated care | [ , , ] | |
| 5 | Data on chronic illnesses (eg. registries) | [ ] | |
| 6 | Understand needs and priorities of local populations | [ , , , ] | |
| 7 | Mobilize and coordinate resources | [ , ] | |
| 8 | Adequate financing system linked with quality improvement | [ , , ] | |
| 9 | Funding payment flexibilities to promote integrated care | [ ] | |
| 10 | Allocating financial budgets for the implementation and maintenance of integrated care | [ , ] | |
| 11 | Funding of a program or service | [ ] | |
| 12 | Changes to funding arrangements | [ ] | |
| 13 | Finances for implementation and maintenance | [ ] | |
| 14 | Reaching agreements on the financial budget for integrated care | [ ] | |
| 15 | Prepaid capitation at various levels | [ ] | |
| 16 | Financing mechanism allowing for pooling of funds across services | [ , , ] | |
| 17 | Creating financial and regulatory incentives that encourage cooperation among health care providers | [ ] | |
| 18 | Integrate policies: collaboration/coordination across health-related policy fields (eg. environment, education, transportation, housing) | [ , , ] | |
| 19 | Location policy | [ ] | |
| 20 | Inter-organisational strategy | [ , , ] | |
| 21 | Creating interdependence between organisations | [ , ] | |
| 22 | Reaching agreements on introducing and integrating new partners in the care chain | [ ] | |
| 23 | Formal connections between organisations: varying from linkage with community to merging of organisations | [ , , , , , ] | |
| 24 | Achieving adjustments among care partners | [ ] | |
| 25 | Reaching agreements about letting go care partner domains | [ ] | |
| 26 | Reaching agreements among care partners on the consultation of experts and professionals | [ ] | |
| 27 | Reaching agreements among care partners on managing client preferences | [ ] | |
| 28 | Reaching agreements among care partners on scheduling client examinations and treatment | [ ] | |
| 29 | Reaching agreements among care partners on discharge planning | [ ] | |
| 30 | Making transparent the effects of the collaboration on the production of the care partners | [ ] | |
| 31 | Structural meetings with external parties such as insurers, local governments and inspectorates | [ ] | |
| 32 | Structural meetings of leaders of care-chain organizations | [ , ] | |
| 33 | Role of volunteers and third sector to support needs of patients and carers | [ , ] | |
| 34 | Building systems of care at the neighborhood level | [ , ] | |
| 35 | Building community awareness and trust with services (gives legitimacy to new approaches to care, and increase likelihood of appropriate, and earlier, referrals) | [ ] | |
| 36 | Family caregivers (involvement and support) | [ , , , , ] | |
| 37 | Coordinated home and community health | [ , ] | |
| 38 | Build resilience among carers to promote home-based care | [ , ] | |
| 39 | Raise awareness and reduce stigma | [ ] | |
| 40 | Social value creation | [ ] | |
| 41 | Provide complementary services | [ ] | |
| 42 | Patient education | [ , ] | |
| 43 | Patient empowerment | [ ] | |
| 44 | Using self-management support methods as a part of integrated care | [ , , , ] | |
| 45 | Patient engagement and participation, i.e. patients provide input on various levels | [ , , , ] | |
| 46 | Electronic tools for patients to be engaged and active in self-management | [ , ] | |
| 47 | Patient navigation/clinical pathways | [ ] | |
| 48 | Reminders for patients | [ , ] | |
| 49 | Paradigm shift from acute to chronic care and from reactive to proactive care delivery | [ , ] | |
| 50 | Population-based needs assessment: focus on defined population | [ , , , ] | |
| 51 | Defining the targeted client group | [ , ] | |
| 52 | Developing care programmes for relevant client subgroups | [ ] | |
| 53 | Designing care for clients with multi- or co-morbidities | [ ] | |
| 54 | Understand best ways to organize and implement care | [ ] | |
| 55 | Collaborative involvement in planning, policy development and patient care delivery | [ ] | |
| 56 | Service characteristics | [ ] | |
| 57 | Co-location of services | [ , , , , ] | |
| 58 | Specialized clinic or centres | [ ] | |
| 59 | Patient-centered philosophy (focus on patients’ need) | [ , , ] | |
| 60 | Promotion of functional independence and wellbeing, not just the management or treatment of medical symptoms (holistic focus) | [ , , ] | |
| 61 | Commitment to the view that the patient is the customer | [ ] | |
| 62 | Interaction between professional and client | [ ] | |
| 63 | Care plans including collaborative goal setting between patients and clinicians | [ , , ] | |
| 64 | Centralized information, referral and intake | [ , ] | |
| 65 | Single point of entry and a single point of contact for patients and carers | [ , , ] | |
| 66 | Case management (relational continuity with a named coordinator) | [ , , , , , , , , ] | |
| 67 | Case management | [ ] | |
| 68 | Arrangements for priority access to another service | [ ] | |
| 69 | Disease management | [ ] | |
| 70 | Professional attitude and fulfilment of work as drivers of integration | [ ] | |
| 71 | Multidisciplinary teamwork | [ , , , , , , , ] | |
| 72 | Developing a multi-disciplinary care pathway | [ , , ] | |
| 73 | Creating interdependence between professionals (inter-professional networks) | [ , , , , ] | |
| 74 | Teamwork (joint working) and care coordination | [ ] | |
| 75 | Arrangements for facilitating communication | [ , ] | |
| 76 | Information sharing, planned/organised meetings | [ ] | |
| 77 | Using a uniform language in the care chain | [ ] | |
| 78 | Using uniform client-identification numbers within the care chain | [ ] | |
| 79 | Shared assessment | [ , ] | |
| 80 | Coordinated or joint consultations | [ ] | |
| 81 | Using feedback and reminders by professionals for improving care | [ , , ] | |
| 82 | Agreements on referrals, discharge and transfer of clients through the care chain | [ , , , ] | |
| 83 | Clinical follow-up | [ ] | |
| 84 | Continuity of care | [ , , , ] | |
| 85 | Assisted living/care support at home | [ , ] | |
| 86 | Service management (e.g., collective telephone numbers, counter assistance and 24-hour access) | [ , , ] | |
| 87 | Medication management | [ ] | |
| 88 | Essential and new pharmaceuticals and medical devices | [ ] | |
| 89 | Collaboratively assessing bottlenecks and gaps in care | [ ] | |
| 90 | An adequate workforce (in terms of number, competencies and distribution) | [ , , , ] | |
| 91 | Workforce educated and skilled in chronic care (graduate) | [ , , , ] | |
| 92 | Cross-training of staff (to ensure staff culture, attitudes, skills are complementary) | [ , , , , , ] | |
| 93 | Reaching agreements among care partners on tasks, responsibilities and authorizations | [ , ] | |
| 94 | Establishing the roles and tasks of multidisciplinary team members | [ , , ] | |
| 95 | Professionals in the care chain are informed/aware of each other’s expertise and tasks | [ , , , ] | |
| 96 | Education for professionals (continuous education) | [ , , , , ] | |
| 97 | Training (joint or relating to collaboration) | [ , , ] | |
| 98 | Inter-professional education | [ , , , , ] | |
| 99 | Stimulating a learning culture and continuous improvement in the care chain | [ ] | |
| 100 | Share registries and/or methods to track care/health | [ , , , ] | |
| 101 | Implementing care process-supporting clinical information systems | [ , ] | |
| 102 | Shared decision support | [ ] | |
| 103 | Support/supervision for clinicians | [ ] | |
| 104 | Clear communication strategies and protocols | [ ] | |
| 105 | Standardised diagnostic and eligibility criteria | [ , , ] | |
| 106 | Multidisciplinary and comprehensive assessment | [ , ] | |
| 107 | Developing criteria for assessing client’s urgency | [ ] | |
| 108 | Case finding and use of risk stratification | [ ] | |
| 109 | Common decision-support tools (practice guidelines, protocols) | [ , , , ] | |
| 110 | Multidisciplinary guidelines and protocols | [ , , ] | |
| 111 | Existence of evidence-based clinical practice guidelines with automated tools to enforce their use | [ , , , ] | |
| 112 | Join planning | [ , , , , , , ] | |
| 113 | Using a single client-monitoring record accessible for all care partners | [ ] | |
| 114 | Using a protocol for the systematic follow-up of clients | [ ] | |
| 115 | Information sharing, planned/organised meetings | [ ] | |
| 116 | Shared decision-making and problem solving | [ ] | |
| 117 | Shared-care protocols and evidence based practice guidelines | [ , , , , , , , ] | |
| 118 | Shared clinical records | [ , , ] | |
| 119 | Integrated clinical pathways | [ ] | |
| 120 | Decision aids to patients | [ ] | |
| 121 | Providing understandable and client-centered information | [ ] | |
| 122 | Assistance in accessing primary health care | [ ] | |
| 123 | Intelligence systems for data collection | [ , , , ] | |
| 124 | Centralised system-wide computerised patient record system (data accessibility from anywhere in the system) | [ , , ] | |
| 125 | Integrated electronic health records | [ , , , , , , , , ] | |
| 126 | Electronic registry for planning care and risk-stratifying patients | [ ] | |
| 127 | Technologies that support continuous and remote patient monitoring | [ , , ] | |
| 128 | Reminders to clinicians and patients (e.g., medication management) | [ , ] | |
| 129 | Local leadership and long-term commitments | [ , , , ] | |
| 130 | Leaders with a clear vision on integrated care | [ ] | |
| 131 | Distributed leadership | [ , , , , ] | |
| 132 | Managerial leadership | [ , , , , ] | |
| 133 | Visionary leadership | [ ] | |
| 134 | Clinical leadership | [ , , ] | |
| 135 | Organisational leadership for providing optimal chronic care | [ ] | |
| 136 | Conflict management | [ ] | |
| 137 | Reputation | [ ] | |
| 138 | Good governance | [ , , , ] | |
| 139 | Inter-organisational governance | [ ] | |
| 140 | Inter-professional governance | [ ] | |
| 141 | Action oriented to understand and support more effective ways for improving quality and enabling change | [ , , , , ] | |
| 142 | Collaborative learning in the care chain in order to innovate integrated care | [ ] | |
| 143 | Involving leaders in improvement efforts in the care chain | [ ] | |
| 144 | Involving client representatives by monitoring the performance of the care chain | [ ] | |
| 145 | Using a systematic procedure for the evaluation of agreements, approaches and results | [ , , , , , ] | |
| 146 | Reaching agreements about the uniform use of performance indicators in the chain care | [ ] | |
| 147 | Establishing quality targets for the performance of care partners | [ ] | |
| 148 | Establishing quality targets for the performance of the whole care chain | [ ] | |
| 149 | Installing improvement teams at care-chain level | [ ] | |
| 150 | Evaluate outcomes | [ ] | |
| 151 | Client satisfaction | [ , , ] | |
| 152 | Performance management (common outcomes evaluation, performance indicator) | [ , , , , , , ] | |
| 153 | Monitoring successes and results during the development of the integrated care chain | [ , ] | |
| 154 | Regular feedback of performance indicators | [ ] | |
| 155 | Shared accountability/risk and responsibility for care | [ , ] | |
| 156 | Integrating incentives for rewarding the achievement of quality targets | [ , , , , ] | |
| 157 | Gathering financial performance data for the care chain | [ ] | |
| 158 | Gathering data on client logistics (e.g. volumes, waiting periods and throughput times) in the care chain | [ , ] | |
| 159 | Monitoring and analysing mistakes/near-mistakes in the care chain | [ ] | |
| 160 | Monitoring whether the care delivered corresponds with evidence-based guidelines | [ ] | |
| 161 | Shared vision and values for the purpose of integrated care | [ , , , , , ] | |
| 162 | An integration culture institutionalised through policies and procedures | [ , , , , , ] | |
| 163 | Organisational culture for providing optimal chronic care | [ , ] | |
| 164 | Striving towards an open culture for discussing possible improvements for care partners | [ ] | |
| 165 | Linking cultures | [ ] | |
| 166 | Population features (e.g., demographic composition) | [ , ] | |
| 167 | Advocacy | [ ] | |
| 168 | Rurality of the area | [ ] | |
| 169 | Environmental climate | [ ] | |
| 170 | Environmental awareness | [ ] | |
| 171 | Labour market | [ , ] | |
| 172 | Quality features of the informal collaboration | [ ] | |
| 173 | Trust (on colleagues, caregivers and organisations) | [ , , , ] | |
| 174 | Reputation | [ ] | |
| 175 | Interpersonal characteristics | [ ] | |
From a quantitative point of view, about one third of the items (58) are supported by at least three contributions. Considering that some items are quite similar in the list, this is a conservative measure of the level of overlapping of the research findings and it can be interpreted as a degree of convergence on some important factors.
The categories with the highest concentration of elements are the Delivery system design (51), Community resources & policies (24), Decision support (23), Performance & quality (20), Healthcare system (17). While Governance (3), Social capital (4) Organizational culture (5), Contextual factors (6), and Clinical information system (6) show the lowest concentration.
More specifically, the category with the largest number of items concerns features of the service delivery design. This suggests that processes, logistics, and human resources management (e.g., multidisciplinary teamwork, staffing of professionals, training) have been widely investigated and represent a cornerstone of care integration. In addition, 43% (or 22) of the items classified in Delivery system design are identified by at least three different contributions. This is the highest level of convergence after Leadership (44%) and Clinical information system (67%); however, each of these last two categories groups a much lower number of items. One might conclude that research has already reported convincing evidence on some important aspects that should guide the design of service delivery to integrate care.
Focusing more on the contents, on the one hand several items grouped in the Delivery system design indicate the importance of centering service delivery on the needs of the patients (e.g. #53, 59, 60–63, 66). On the other hand, several items emphasize the need for standardizing (or foster uniformity of) specific aspects/tools that are paramount to ensure care quality and coordination across organizational boundaries and settings (e.g., #64, 65, 68, 72, 75, 77, 78), together with multi-/inter-professional collaboration (e.g., #71, 73, 74, 76, 79, 80).
At the system level two relevant policy areas are clearly identified: funding/financing mechanisms and priority setting coherent with the needs of the population (e.g., chronic conditions, older people) and the pillars of integrated care (e.g., cooperation between providers, synergic mobilization of community resources). The items grouped in the Contextual factors category reinforce importance of fine tuning interacting policies (e.g. health, environment, labor) with the actual needs and conditions of the population (e.g., demographic composition, orographic configuration of locations).
The categories Decision support and Community resources & policies group items that seem to point at setting the best conditions – by introducing changes and specific tools – to foster collaboration between professionals and organizations involved in the care delivery and help such actors to focus on patients’ needs and priorities.
The category Performance & Quality includes items that, rather than proposing specific technical solutions, indicate the need for fostering shared accountability on the results of the “care chain”. The few cases where end-points are proposed, they range from patient experience (e.g., satisfaction) to outcomes. This aspect, reinforced by the categories directly focused on soft aspects (i.e., Organizational culture and Social capital), suggests the importance of developing shared values to foster care integration.
Conclusions
The literature evidence reviewed here has uncovered a range of elements and factors associated with successful care integration over the last decade. Moreover, the development of conceptual frameworks to understand and guide thinking on integrated care has grown and evolved over time.
However, the majority of contributions provide recommendations related to a smaller number of specific aspects that were found to be influential. Moreover, these were often derived in specific contexts/settings or with defined target patients, especially to those with chronic illnesses as opposed to those with comorbidities or wider health and social care needs. Few studies propose, and eventually validate, frameworks indicating key areas of intervention and/or analytical aspects to consider in order to foster care integration. They are mostly lists of key building blocks to integrated care, rather than frameworks supporting the process of implementation. In addition, the retrieved frameworks generally build on the findings of previous research, but each of them assumes either a diverse (though not necessarily alternative) perspective or different analytical degree. Interestingly, despite that our review focused on forms of integrated care addressing patients with chronic diseases and long-term conditions, we found that recent frameworks (more or less explicitly) assume a population health rather than a disease-based perspective. This dramatically increases the need for accurately defining client groups or populations, including people with non-medical conditions, profiling their needs and specificities, and manage the complexity resulting from this broad perspective.
When streamlining all the aspects identified in the available relevant literature, on the one hand, it is striking the high number of factors deserving attention; however, on the other hand, there is a clear area of convergence identified by those factors mentioned in several contributions. The two findings can be considered, respectively, evidence of dynamism and indicator of the degree of maturity the research field.
Researchers seem to have concentrated their attention on the service delivery design of integrated care, with a recent shift toward the notion of person-centeredness as a way of shaping any aspect of processes and interaction with patients and their caregivers. Nevertheless, contextual aspects seem to rank more and more high in the priorities of experts in the field. Perhaps, this is the result of the aforementioned shift toward a population health perspective that tends to increase the interdependencies between the different components of a health (and social) care system. It may also be that many experts view care integration as primarily a systemic or organizational activity rather than an approach (as defined) that co-ordinates care with and around people’s needs at the clinical and service level.
A limitation of our contribution is that we searched studies that propose frameworks or key factors for integrated care starting from three selected journals specialized in the field. This could have limited our capacity to identify all available studies related to the objective of this article. However, we privileged the pertinence of the scientific source and tried to compensate the aforementioned bias by snowballing the references of the included contributions and by involving some external scholars/experts to fill eventual gaps based on their extensive knowledge.
Our selectivity allowed us to perform an exhaustive, careful review of all the included material. The extracted key elements offer a useful basis for describing and/or reflecting on integrated care initiatives for chronic illnesses and long-term conditions set in different contexts. Nevertheless, it may be difficult to obtain accurate information on all of the important aspects so far identified. Therefore, it would be useful to develop a comprehensive framework that could synthetically describe care integration initiatives implemented in different contexts and allow for efficient comparisons highlighting relevant variabilities and context-dependencies.
Acknowledgements
The study is part of Project INTEGRATE ( http://projectintegrate.eu.com ) that was funded within the EU 7 th Framework Program (EU Grant Agreement 305821).
Formerly, International Journal of Care Pathways.
Dr Teresa Burdett, Lecturer in Integrated Health Care, Professional Lead for Interprofessional Learning and Education, Unit Lead for Foundations of Integrated Care and Person Centred Services, Bournemouth University, UK.
One anonymous reviewer.
Competing Interests
The authors have no competing interests to declare.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals
You are here
- Volume 19, Issue 1
- Reviewing the literature
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Joanna Smith 1 ,
- Helen Noble 2
- 1 School of Healthcare, University of Leeds , Leeds , UK
- 2 School of Nursing and Midwifery, Queens's University Belfast , Belfast , UK
- Correspondence to Dr Joanna Smith , School of Healthcare, University of Leeds, Leeds LS2 9JT, UK; j.e.smith1{at}leeds.ac.uk
https://doi.org/10.1136/eb-2015-102252
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Implementing evidence into practice requires nurses to identify, critically appraise and synthesise research. This may require a comprehensive literature review: this article aims to outline the approaches and stages required and provides a working example of a published review.
Are there different approaches to undertaking a literature review?
What stages are required to undertake a literature review.
The rationale for the review should be established; consider why the review is important and relevant to patient care/safety or service delivery. For example, Noble et al 's 4 review sought to understand and make recommendations for practice and research in relation to dialysis refusal and withdrawal in patients with end-stage renal disease, an area of care previously poorly described. If appropriate, highlight relevant policies and theoretical perspectives that might guide the review. Once the key issues related to the topic, including the challenges encountered in clinical practice, have been identified formulate a clear question, and/or develop an aim and specific objectives. The type of review undertaken is influenced by the purpose of the review and resources available. However, the stages or methods used to undertake a review are similar across approaches and include:
Formulating clear inclusion and exclusion criteria, for example, patient groups, ages, conditions/treatments, sources of evidence/research designs;
Justifying data bases and years searched, and whether strategies including hand searching of journals, conference proceedings and research not indexed in data bases (grey literature) will be undertaken;
Developing search terms, the PICU (P: patient, problem or population; I: intervention; C: comparison; O: outcome) framework is a useful guide when developing search terms;
Developing search skills (eg, understanding Boolean Operators, in particular the use of AND/OR) and knowledge of how data bases index topics (eg, MeSH headings). Working with a librarian experienced in undertaking health searches is invaluable when developing a search.
Once studies are selected, the quality of the research/evidence requires evaluation. Using a quality appraisal tool, such as the Critical Appraisal Skills Programme (CASP) tools, 5 results in a structured approach to assessing the rigour of studies being reviewed. 3 Approaches to data synthesis for quantitative studies may include a meta-analysis (statistical analysis of data from multiple studies of similar designs that have addressed the same question), or findings can be reported descriptively. 6 Methods applicable for synthesising qualitative studies include meta-ethnography (themes and concepts from different studies are explored and brought together using approaches similar to qualitative data analysis methods), narrative summary, thematic analysis and content analysis. 7 Table 1 outlines the stages undertaken for a published review that summarised research about parents’ experiences of living with a child with a long-term condition. 8
- View inline
An example of rapid evidence assessment review
In summary, the type of literature review depends on the review purpose. For the novice reviewer undertaking a review can be a daunting and complex process; by following the stages outlined and being systematic a robust review is achievable. The importance of literature reviews should not be underestimated—they help summarise and make sense of an increasingly vast body of research promoting best evidence-based practice.
- ↵ Centre for Reviews and Dissemination . Guidance for undertaking reviews in health care . 3rd edn . York : CRD, York University , 2009 .
- ↵ Canadian Best Practices Portal. http://cbpp-pcpe.phac-aspc.gc.ca/interventions/selected-systematic-review-sites / ( accessed 7.8.2015 ).
- Bridges J , et al
- ↵ Critical Appraisal Skills Programme (CASP). http://www.casp-uk.net / ( accessed 7.8.2015 ).
- Dixon-Woods M ,
- Shaw R , et al
- Agarwal S ,
- Jones D , et al
- Cheater F ,
Twitter Follow Joanna Smith at @josmith175
Competing interests None declared.
Read the full text or download the PDF:
- Search Menu
- Sign in through your institution
- Advance articles
- Themed Collections
- Editor's Choice
- Ilona Kickbusch Award
- Supplements
- Author Guidelines
- Submission Online
- Open Access Option
- Self-Archiving Policy
- About Health Promotion International
- Editorial Board
- Advertising and Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, supplementary material, authorship contributions, acknowledgements, data availability.
- < Previous
Unleashing the potential of Health Promotion in primary care—a scoping literature review
- Article contents
- Figures & tables
- Supplementary Data
Adela Bisak, Martin Stafström, Unleashing the potential of Health Promotion in primary care—a scoping literature review, Health Promotion International , Volume 39, Issue 3, June 2024, daae044, https://doi.org/10.1093/heapro/daae044
- Permissions Icon Permissions
The purpose of this study is to gain a better understanding of the role and extent of health promotion lifestyle interventions targeting adults in primary care, and especially those who are considered overall healthy, i.e. to study the outcomes of research applying salutogenesis. We performed a literature review, with three specific aims. First, to identify studies that have targeted the healthy population in intervention within the primary health care field with health promotion activities. Second, to describe these interventions in terms of which health problems they have targeted and what the interventions have entailed. Third, to assess what these programs have resulted in, in terms of health outcomes. This scoping review of 42 studies, that applied salutogenesis in primary care interventions shows that health promotion targeting healthy individuals is relevant and effective. The PRISMA-ScR guidelines for reporting on scoping review were used. Most interventions were successful in reducing disease-related risks including CVD, CVD mortality, all-cause mortality, but even more importantly success in behavioural change, sustained at follow-up. Additionally, this review shows that health promotion lifestyle interventions can improve mental health, even when having different aims.
This article describes the importance of including healthy individuals in health promotion activities, applying salutogenesis, as there are significant positive health outcomes effects if they participate in health interventions.
The study amplifies that the prevention paradox should always be considered when designing health promotion interventions.
This article shows that the greatest effects when targeting healthy individuals are found in lower all-cause mortality and CVD risks, mainly because these programs manage to lead to long-lasting lifestyle changes.
Health Promotion is, according to Nutbeam and Muscat (2021 , p. 1580), ‘[…] the process of enabling people to increase control over, and to improve their health’. This process entails a comprehensive approach to change on all levels, from structures to individuals, improving health mainly through addressing the social determinants of health.
Whereas the most overarching processes are initiated on a structural level through global and national health policies ( Cross et al ., 2020 ), health promotion strategies are also widely employed in health interventions targeting individuals. It could entail smoking cessation programs, weight loss programs and adolescent alcohol use, just to mention some common health outcome target areas ( Green et al. , 2019 ). Even when deploying health promotion strategies at a national policy level, it is not uncommon that the programs designed to target individuals and groups are more inspired by pathogenesis, rather than salutogenesis ( Nutbeam and Muscat, 2021 ).
A widespread strategy in the latter programs is that individuals are screened for a need to receive an intervention, so-called secondary or indicated prevention programs, where those who report a riskier lifestyle, or test worse on psychometric or biometric indicators are eligible for receiving the intervention, and those not having the same risks are excluded from the program on the premise that they are, based on study protocol definitions, healthy individuals.
Based on the principles of salutogenesis, this is a somewhat inappropriate approach. Within the strategy of health promotion, it is assumed that all people, no matter their level of risk, would find feedback on their health valuable. Those in need of change should receive the necessary resources and tools to change, whereas those who do not have to change should have their lifestyles positively reinforced. In addition, the prevention paradox ( Rose, 1981 ) postulates that it is important to address the majority, as there will be plenty of adverse health outcomes stemming from them. In conventional indicated prevention programs, attention to those who are non-eligible for interventions is, thus, often completely disregarded.
One common arena for such programs is primary health care. There is a wide range of evidence-based programs that have shown efficacy in reducing the health risks among those who have the riskiest lifestyles in relation to, e.g. alcohol use ( Beyer et al ., 2019 ), smoking ( Cantera et al ., 2015 ), depression ( Bortolotti et al ., 2008 ), diabetes ( Galaviz et al ., 2018 ) and cardiovascular diseases ( Álvarez-Bueno et al. , 2015 ). The at-risk groups vary across the different diseases, but a vast majority of patients targeted in the above studies were identified after screening as non-eligible to participate in the intervention in question. From this follows that a large number of individuals do not receive any substantial health information, nor are their health outcomes measured as they are not included in the intervention. From a health promotion perspective, this seems like a lost opportunity. Additionally, this raises the question of whether a healthy population is systematically disadvantaged compared to those individuals at high risk, which might point to some less-known health inequities or disparities ( Braveman, 2006 ) present in primary care.
In order to gain a better understanding of the effects of health promotion as an overall approach, and to understand the implications of the prevention paradox, it would be pertinent to include the non-eligible group in both the feedback loop—mainly offering them structured positive reinforcement—and to subsequently measure their health and attributed lifestyles.
The purpose of this study is to gain a better understanding of the role and extent of health promotion lifestyle interventions targeting adults in primary care, especially those who are considered overall healthy. More precisely we aim to assess to what extent health promotion practices in primary care address healthy individuals, not only those who need to undergo a lifestyle change. In order to do so, we performed a literature review, with three specific aims. First, to identify studies that have only targeted the healthy population, or healthy population in addition to high-risk group in intervention within the primary health care field with health promotion activities. Second, to describe these interventions in terms of which health problems they have targeted and what the interventions have entailed. Third, to assess what the initiatives published in the research literature have resulted in terms of health outcomes.
Due to the width of the topic and study designs we chose to perform a scoping review, with the aim of summarizing and disseminating previous research and identifying research gaps in the literature ( Arksey and O’Malley, 2005 ). The search process was iterative and non-linear, reflecting upon the results from the literature search at each stage and then repeating steps where necessary to cover the literature more comprehensively ( Arksey and O’Malley, 2005 ).
A few terms demand some further definition within the scope of this review . Healthy individual is a fluid term varying across different studies and contexts, yet it is a key concept in this particular study. The term involves those without chronic disease, who are indicated as not being of an elevated risk of developing a disease linked to the health outcome they have been screened for, but they could very well be at risk for diseases beyond the scope of the study they have been examined within. Primary health care may in this review indicates different types of settings from the most common one relating to general practitioners and family doctors to occupational medicine or periodical work-related health check-ups but also dental health care. Health promotion interventions in this study are understood as interventions that aim to keep people healthy longer, by providing positive feedback in relation to current and new health behaviours, rather than controlling health status by medication use.
Search strategy
The search was done across two databases PubMed and Embase, by combining different strings related to keywords ‘health promotion’ and ‘primary care’, while the rest of the strings varied, more specific search queries are available in Supplementary Appendix A . The search was conducted during June and July 2023 and consisted of publications dated between July 2008 and July 2023 (i.e. the last 15 years). Additional studies were identified manually from references of the included articles and by ‘See all similar articles’ option in PubMed and ‘similar records’ in Embase. The article titles were scanned from databases, followed by screening titles and abstracts through the Covidence software, and then finally the full articles were read. Results were filtered for adult humans, defined as age 18–75, abstracts being available and the studies were authored in English.
Articles were included if (i) the population consisted of working-age adults, (ii) the population included those screened as healthy within a whole sample followed by an intervention or interventions ideally at follow-up, (iii) the study focused on primary prevention (iv) the study focused on lifestyle interventions, (v) the study examined lifestyle-related behaviours. Exclusion criteria for papers were (i) focused on children—below the age of 18 or elderly, (ii) addiction behaviours, (iii) excluding healthy individuals from intervention after screening or using them exclusively in the control group, (iv) using only high-risk population as healthy, (v) promoting only mental health, (vi) secondary prevention, (vii) screening is the only intervention, (viii) reviews and study protocols.
After full-text screening, the data charting process for reviewing, sorting and documenting information ( Arksey and O’Malley, 2005 ) was done using Covidence, Data Extraction version 2 recommended for scoping reviews. The Data Extraction Template included columns for article title, author, country in which the study was conducted, methods (aim, design, population description, inclusion and exclusion criteria) intervention description, outcome measures, relevant results, follow-up (yes/no), study setting (primary care, worksite/occupational, population-based), study category (lifestyle, physical activity and diet, cardiovascular disease, alcohol consumption) and a field for additional notes where needed.
Due to great inconsistencies between studies in the design, populations and outcomes, critical appraisal of individual sources of evidence—an optional step in PRISMA-ScR ( Tricco et al ., 2018 ) guideline list was not done, although concerning research aim it would be useful for assessing the quality of evidence. Although exclusion/inclusion criteria were respected, what was considered as ‘healthy’, ‘middle-’ or ‘high-risk population’ differed significantly in studies, due to differences in definition of terms. Moreover, this decision was made as the AMSTAR tool would not be an adequate choice due to the inclusion of a non-randomized design, and although the AMSTAR 2 tool could potentially be used, this review also included several economic evaluations and follow-ups ( Supplementary Table S1 for more details), or indicators differing highly across studies.
For the synthesis of results ( Tricco et al ., 2018 ), the studies were grouped by the type of the outcome—disease, i.e. CVD or lifestyle/behaviour: physical activity and diet or alcohol consumption. Furthermore, the studies were summarized by setting, risk group and follow-up. None of the systematic reviews with similar research aims were detected during the search.
The selection of sources of evidence ( Tricco et al ., 2018 ) was done as described: 353 references were imported for screening, 72 duplicates were removed, 268 studies were screened against title and abstract during which 198 studies were excluded while 69 studies were assessed for full-text eligibility, when 27 studies were excluded: 12 for wrong intervention, 8 for wrong patient population, 4 for wrong study design 1 was not in English, 1 for wrong indication and 1 for wrong setting, after which 42 studies were included. PRISMA of full screening is found in Figure 1 .

PRISMA of full screening strategy.
Lifestyle interventions
A summary of the study setting, samples and the main outcomes of the 42 studies analysed in this scoping review is presented in Supplementary Table S1 .
In general, the intervention studies analysed here had different main strategies, including: individually tailored programs ( Doumas and Hannah, 2008 ; Gram et al ., 2012 ; Watson et al ., 2015 ) risk-based, group-based ( Recio-Rodriguez et al ., 2016 ) or mixed variants ( Matano et al ., 2007 ; Matzer et al ., 2018 ).
Cardiovascular health
We found several different lifestyle interventions targeting CVD risk. There were a set of programs that addressed physical activity in the workplace, which significantly reduced the CVD risk in healthy participants adhering to the program ( Gram et al ., 2012 ; Dalager et al ., 2016 ; Eng et al ., 2016 ; Biffi et al ., 2018 ). In primary care, an observational study by Journath et al . (2020) , showed an association between healthy participant participation in a CVD prevention programme promoting physical activity and a healthy lifestyle with lower risk of CV events (12%), CV mortality (21%) and all-cause mortality (17%) after 20 years of follow-up.
Similarly, we found interventions in primary care settings that led to changes in physical activity and dietary patterns among all participants—not only those at high risk of CVD morbidity and mortality. These studies described generally decreased CVD risks ( Richardson et al ., 2008 ; Buckland et al ., 2009 ; Nguyen et al ., 2012 ; Gibson et al ., 2014 ; Bo et al ., 2016 ; Lidin et al ., 2018 ; Lingfors and Persson, 2019 ), CVD-related mortality ( Blomstedt et al ., 2011 ; Persson et al ., 2015 ; Jeong et al ., 2019 ) and all-cause mortality ( Blomstedt et al ., 2015 ; Bo et al ., 2016 ; Bonaccio et al ., 2019 ).
In a prospective observational study on healthy individuals and those with CVD conducted by Lidin et al . (2018) , the prevalence within the sample at risk of CVD decreased significantly at 12-month follow-up by 15%. In several studies, the changes in health behaviours among the participants showed to be sustained in follow-ups conducted after intervention discontinuation ( Buckland et al ., 2009 ; Gibson et al ., 2014 ; Baumann et al ., 2015 ; Blomstedt et al ., 2015 ; Lidin et al ., 2018 ), while some cardiovascular risk factors, such as salty diets and smoking, showed evidence of significant decrease in a relatively short period ( Nguyen et al ., 2012 ).
Physical activity and diet
In interventions addressing physical activity and diet, it was evident that healthy individuals were more likely to adhere to physical activity interventions ( Dalager et al ., 2016 ; Biffi et al ., 2018 ; Jeong et al ., 2019 ) compared to those with a disease. One community-based walking intervention ( Yang and Kim, 2022 ) affected not only the level of physical activity significantly but also a positive overall change towards a health-promoting lifestyle and decreased perceived stress. Similarly, several mental health measures including general mental health ( Oude Hengel et al ., 2014 ), anxiety and depression ( Gibson et al ., 2014 ) and stress ( Lingfors et al ., 2009 ; Matzer et al ., 2018 ) in participants improved during interventions and at follow-up when targeting physical activity and diet.
Additionally, concerning physical activity and diet outcomes, there were a higher feasibility of uptake among participants in health promotion programs compared to those only receiving standard care in primary care ( Lingfors et al ., 2009 ; Zabaleta-Del-Olmo et al ., 2021 ). Anokye et al. (2014) argued that brief advice intervention was more effective—leading to 466 QALYs gained, compared to standard care—implying greater cost-effectiveness.
Healthier lifestyles were also maintained at the follow-up. Reduction in risk factors was found to be sustained in follow-ups at 12 months ( Gibson et al ., 2014 ) or improvements in dietary outcomes over 5 years ( Baumann et al ., 2015 ), and sustained lower blood pressure over 6 years ( Eng et al ., 2016 ).
Several interventions promoting physical activity in primary care settings showed significant results in increasing it in all patients, not only in those with chronic disease diagnosis ( Robroek et al ., 2010 ; Gram et al ., 2012 ; Hardcastle et al ., 2012 ; Viester et al ., 2015 ; Byrne et al ., 2016 ; Dalager et al ., 2016 ; Eng et al ., 2016 ; Recio-Rodriguez et al ., 2016 ; Biffi et al ., 2018 ; Matzer et al ., 2018 ; Yang and Kim, 2022 ), and similar patterns were also found concerning a change towards a healthier diet ( Lingfors et al ., 2009 ; Wendel-Vos et al ., 2009 ; Robroek et al ., 2010 ; Baumann et al ., 2015 ; Viester et al ., 2015 ; Bo et al ., 2016 ; Byrne et al ., 2016 ; Kosendiak et al ., 2021 ).
There was disagreement among the above studies in relation to the effectiveness of these interventions among healthy individuals. For example, in the case of implementing a Mediterranean diet, one report argued that a healthy diet should be prioritized, indicating significant hazard ratios (HR) of attaining a Mediterranean diet for all-cause mortality (HR = 0.83), CV mortality (HR = 0.75) and CV events (HR = 0.79) among low-risk individuals ( Bo et al ., 2016 ). Others, however, claimed that there was no evidence of healthier participants being more susceptible to changes in physical activity and diet ( Robroek et al ., 2010 ).
Alcohol consumption
Interventions aimed at decreasing alcohol consumption were divided between those being most effective in high-risk drinkers ( Doumas and Hannah, 2008 ; Kirkman et al ., 2018 ), and both moderate and low-risk drinkers ( Matano et al ., 2007 ). These interventions were, at large, seen as cost-saving ( Watson et al ., 2015 ) and feasible in primary care ( Neuner-Jehle et al ., 2013 ). Some studies found a sustained decrease in alcohol consumption in those adhering to the interventions, compared to the control groups at 1 ( Pemberton et al ., 2011 ) and 4 months after the intervention ( Kirkman et al ., 2018 ), whereas others failed to find a significant difference between groups.
Intervention setting
The interventions took place in primary care settings, though these were either in community-based or occupational settings. The findings suggested that there were some discrepancies between these different settings.
When it comes to a community-based setting, the difference is made between interventions conducted on a sample of those visiting primary health care or a sample representative for a population of one community—town, or region. Primary care community-based studies tended to either include participants who were primary care visitors with a long follow-up period, or interventions conducted in primary care clinic centres with a shorter follow-up period, most often using experimental design, sampling individuals living in the community that did not necessarily had an intention to seek care ( Richardson et al ., 2008 ; Hardcastle et al ., 2012 ; Nguyen et al ., 2012 ; Grunfeld et al ., 2013 ; Baumann et al ., 2015 ; Bo et al ., 2016 ; Lidin et al ., 2018 ; Zabaleta-Del-Olmo et al ., 2021 ).
Overall, the community-based studies were conducted on a sample representative for a population of a smaller community ( Kosendiak et al ., 2021 ; Yang and Kim, 2022 ), region ( Lingfors et al ., 2009 ; Wendel-Vos et al ., 2009 ; Gibson et al ., 2014 ; Persson et al ., 2015 ; Bonaccio et al ., 2019 ; Jeong et al ., 2019 ; Lingfors and Persson, 2019 ; Journath et al ., 2020 ) or a country ( Buckland et al ., 2009 ; Blomstedt et al ., 2011 ; Neuner-Jehle et al ., 2013 ), often followed by a longer follow-up period. Finally, some studies were evaluations of previous interventions ( Richardson et al ., 2008 ; Anokye et al ., 2014 ).
Worksite interventions comprised of different occupational roles, often including several of those in the same sample ( Eng et al ., 2016 ), or segmenting based on how physically active the occupation was, e.g. office workers ( Dalager et al ., 2016 ), construction workers ( Gram et al ., 2012 ; Oude Hengel et al ., 2014 ; Viester et al ., 2015 ), sailors ( Hjarnoe and Leppin, 2013 ), farmers ( van Doorn et al ., 2019 ) or simply more active individuals ( Biffi et al ., 2018 ). This had the implication that approaches to intervention differed widely across the studies.
Several interventions were conducted online using a web-based interface, while others were in a professional setting ( Matano et al ., 2007 ; Doumas and Hannah, 2008 ; Robroek et al ., 2010 ; Pemberton et al ., 2011 ; Khadjesari et al ., 2014 ) or in some cases community-based ( Recio-Rodriguez et al ., 2016 ; Kirkman et al ., 2018 ).
Categorization of risk among participants
Many studies applied specific risk criteria based on the participants’ morbidity risks: including groups of low, middle, high risk ( Persson et al ., 2015 ; Bo et al ., 2016 ; Lingfors and Persson, 2019 ), low and high risk ( Baumann et al ., 2015 ), middle and high risk ( Gibson et al ., 2014 ). While some did not distinguish between risk groups ( Wendel-Vos et al ., 2009 ; Blomstedt et al ., 2011 ; Byrne et al ., 2016 ; Journath et al ., 2020 ). In some studies, however, the protocol included mixed populations of those who were healthy and those who had a chronic disease ( Anokye et al ., 2014 ; Bonaccio et al ., 2019 ). Finally, different studies came up with their own meaning of ‘healthy individual’ or ‘healthy population’ based on the health problem they addressed, i.e. having a sedentary lifestyle or high alcohol consumption. Other criteria for being a part of a healthy population were having a high risk for a disease, one or several risks but not the disease itself, or being above a reference value without having a diagnosis.
Ethical implications of healthy controls
Some interventions were screening-result-based, meaning that there was a difference in the treatment of those with good health and those with some complications. In other words, although not excluding healthy individuals, the study protocol included healthy individuals partially receiving full treatment, in the intervention. Studies that excluded those who were healthy from the sample after screening or used them as a control group were excluded from this review. However, some included studies had a healthy control group. Overall, the studies included in this review did not discuss the ethical implications of including healthy populations as controls, or when that was the case, the ethical impact of excluding healthy participants from an intervention.
This scoping review speaks not only of the role and extent of health promotion for healthy individuals in primary care but also of the importance and effects it has on population health. The results showing the association of lifestyle interventions with CVD risk show great implications for future use in primary care, different contexts and feasibility. Physical activity interventions were additionally found to be related to some improvements in mental health.
Interventions aimed at alcohol consumption were found successful in decreasing the amount of drinking sustainably, while the main discussion was based on whether they should be aimed at high-risk only, or at middle- and low-risk drinkers as well, due to mixed results in said groups. The majority of interventions were based in a worksite setting, meaning that this context might be useful for tackling the issue. This approach showed that outcomes might be beneficial even when not reaching the primary goal. Examples of this are findings showing that although not reducing CVD risk, changes in health behaviours were sustained in follow-up ( Baumann et al ., 2015 ), less drastic changes decreasing CVD risk in the healthy population ( Buckland et al ., 2009 ) and beneficial effects of physical activity intervention on worker’s health without an overall increase in physical activity ( McEachan et al ., 2011 ). Finally, in most cases, as mentioned, changes in health behaviours were associated with changes in CVD risk.
Some interventions showed that health promotion benefits could be even bigger ( Bo et al ., 2016 ) or that adherence is higher in healthy participants ( Dalager et al ., 2016 ; Biffi et al ., 2018 ; Jeong et al ., 2019 ), while other authors disagree ( Robroek et al ., 2010 ). This could be traced to the topic of prioritising primary care for healthy, versus only those at high risk/ already with a disease—secondary care approach according to this review definitions. Designing interventions only for high-risk can make them less successful in healthy participants, as displayed in a study by Blomstedt et al . (2011) where self-rated health decreased in 21% of the good baseline health participants at the 10-year follow-up. Furthermore, from the Rose’s (1981) term of prevention paradox—a great benefit for the population can be almost non-existent for an individual, while if we only focus on high-risk cases, many individuals at low-risk can mean worse health outcomes compared to a small number at high-risk ( Rose, 2001 ). In other words, by focusing only on high-risk population, the downsides are care that can be less efficient, less feasible, more expensive and lead to worse health outcomes. This choice should not be exclusive, as excluding either populations can cause ethical concerns. However, this article gives priority to early prevention, by health promotion for healthy individuals in primary care. Additionally, if it is shown that ‘ Systems based on primary care have better population health, health equity, and health care quality, and lower health care expenditure… ’ ( Stange et al. , 2023 ), different treatment of those who are currently healthy presents an obstacle worth mentioning for achieving health equity in primary care. Furthermore, the role of promoting health to healthy populations and their inclusion in interventions is crucial for improving population health in the future.
Articles focusing on smoking cessation, alcoholism, substance misuse interventions were excluded from this scoping review as they represent addictions and are therefore different from lifestyle interventions. Originally, oral health and dental care interventions were to be included, but there were not enough studies matching the scoping review inclusion requirements.
As expected, the process of finding articles appropriate for inclusion was challenging. Even when the inclusion criteria, at first glance, were satisfied, most studies we came across had excluded healthy participants from the sample after screening for being asymptomatic or not having enough risk factors. They were, however, often a part of a control group, and usually received standard care or no care at all. This approach puts healthy individuals in a vulnerable position, by not addressing their needs to change lifestyles that eventually could contribute to an early death or becoming unwell. Our findings suggest that interventions that include healthy individuals could improve quality of life and health status both at the population and individual levels.
Due to studies using different risk criteria, as well as including many study designs and topics, it was hard to make general conclusions. Nevertheless, as a scoping review, we mapped the area of research by identifying the gaps in the evidence base, and summarizing and disseminating research findings ( Arksey and O’Malley, 2005 ), instead of appraising the quality of evidence in different studies.
Concerning the above, a big research gap was detected in studies focusing on, or even including healthy populations. Furthermore, there is a lack of a coherent or comprehensive methodology in assessing the effects of what is considered health promotion, which calls for a more specific approach and a clear definition of the term. Additionally, the question of intervention staff skills should be raised. Is it necessary that health promotion interventions should be conducted by clinically trained professionals or, innovatively, by staff trained in the topic at hand when possible? Another aspect that is important to problematize is whether it is ethical to exclude healthy individuals in health promotion intervention studies even if they would benefit from participating if included? Furthermore, if healthy individuals are systematically discriminated ( Braveman, 2006 ), receive worse treatment and have the risk of worse health outcomes in the future, it is critical to include them in interventions for achieving better health of populations. This has great practical implications for primary care. Similarly, from a cost-benefit perspective, research should address if excluding healthy individuals might affect the cost-effectiveness of health promotion interventions.
An apparent limitation within this review is the culturally uniform sample of studies. Most studies that we were able to identify were a result of research in the global north, with a strong emphasis on either North America or the EU. Only two studies were from less affluent settings in Southeast Asia ( Nguyen et al ., 2012 ; Bo et al ., 2016 ). Given that the findings suggest that these interventions are cost-effective and do not require substantial investments, these programs could have great potential in low-resource settings if more systematically researched.
This scoping review of 42 studies applying salutogenesis in primary care interventions shows that health promotion targeting healthy individuals is relevant and effective. Most interventions were successful in reducing disease-related risks including CVD, CVD mortality, all-cause mortality, but even more importantly success in behavioural change, sustained at follow-up. Additionally, this review shows that health promotion lifestyle interventions can improve mental health, even when having different aims.
Supplementary material is available at Health Promotion International online.
A.B. performed the literature search, performed most of the data analysis and was the major contributor in writing the Methods and Results sections of the manuscript. M.S. formulated the research questions and scope of the study. He gave considerable input to the data analysis, gave input on all sections of the study—including writing and editing—and was the main author of the Introduction and Discussion. Both authors read and approved the final manuscript.
We would like to express our gratitude to Maria Björklund, librarian, at the Faculty of Medicine Library, Lund University at CRC in Malmö, who assisted us in the literature search.
A.B.’s contribution was in part funded by a scholarship she received from the Faculty of Medicine and in part by internal funds at the Division of Social Medicine and Global Health, Lund University, the latter also funded M.S.’s contribution.
The data underlying this article are available in the article and in its online supplementary material.
Álvarez-Bueno , C. , Cavero-Redondo , I. , Martínez-Andrés , M. , Arias-Palencia , N. , Ramos-Blanes , R. and Salcedo-Aguilar , F. ( 2015 ) Effectiveness of multifactorial interventions in primary health care settings for primary prevention of cardiovascular disease: a systematic review of systematic reviews . Preventive Medicine , 76 , S68 – S75 .
Google Scholar
Anokye , N. K. , Lord , J. and Fox-Rushby , J. ( 2014 ) Is brief advice in primary care a cost-effective way to promote physical activity ? British Journal of Sports Medicine , 48 , 202 – 206 .
Arksey , H. and O’Malley , L. ( 2005 ) Scoping studies: towards a methodological framework . International Journal of Social Research Methodology , 8 , 19 – 32 .
Baumann , S. , Toft , U. , Aadahl , M. , Jørgensen , T. and Pisinger , C. ( 2015 ) The long-term effect of screening and lifestyle counseling on changes in physical activity and diet: the Inter99 Study—a randomized controlled trial . The International Journal of Behavioral Nutrition and Physical Activity , 12 , 33 .
Beyer , F. R. , Campbell , F. , Bertholet , N. , Daeppen , J. B. , Saunders , J. B. , Pienaar , E. D. et al. . ( 2019 ) The Cochrane 2018 review on brief interventions in primary care for hazardous and harmful alcohol consumption: a distillation for clinicians and policy makers . Alcohol and Alcoholism (Oxford, Oxfordshire) , 54 , 417 – 427 .
Biffi , A. , Fernando , F. , Adami , P. E. , Messina , M. , Sirico , F. , Di Paolo , F. et al. . ( 2018 ) Ferrari corporate wellness program: results of a pilot analysis and the ‘Drag’ impact in the workplace . High Blood Pressure & Cardiovascular Prevention , 25 , 261 – 266 .
Blomstedt , Y. , Emmelin , M. and Weinehall , L. ( 2011 ) What about healthy participants? The improvement and deterioration of self-reported health at a 10-year follow-up of the Västerbotten Intervention Programme . Global Health Action , 4 , 5435 .
Blomstedt , Y. , Norberg , M. , Stenlund , H. , Nyström , L. , Lönnberg , G. , Boman , K. et al. . ( 2015 ) Impact of a combined community and primary care prevention strategy on all-cause and cardiovascular mortality: a cohort analysis based on 1 million person-years of follow-up in Västerbotten County, Sweden, during 1990-2006 . BMJ Open , 5 , e009651 .
Bo , S. , Ponzo , V. , Goitre , I. , Fadda , M. , Pezzana , A. , Beccuti , G. et al. . ( 2016 ) Predictive role of the Mediterranean diet on mortality in individuals at low cardiovascular risk: a 12-year follow-up population-based cohort study . Journal of Translational Medicine , 14 , 91 .
Bonaccio , M. , Di Castelnuovo , A. , Costanzo , S. , De Curtis , A. , Persichillo , M. , Cerletti , C. et al. ; Moli-sani Study Investigators . ( 2019 ) Impact of combined healthy lifestyle factors on survival in an adult general population and in high-risk groups: prospective results from the Moli-sani Study . Journal of Internal Medicine , 286 , 207 – 220 .
Bortolotti , B. , Menchetti , M. , Bellini , F. , Montaguti , M. B. and Berardi , D. ( 2008 ) Psychological interventions for major depression in primary care: a meta-analytic review of randomized controlled trials . General Hospital Psychiatry , 30 , 293 – 302 .
Braveman , P. ( 2006 ) Health disparities and health equity: concepts and measurement . Annual Review of Public Health , 27 , 167 – 194 .
Buckland , G. , González , C. A. , Agudo , A. , Vilardell , M. , Berenguer , A. , Amiano , P. et al. . ( 2009 ) Adherence to the Mediterranean diet and risk of coronary heart disease in the Spanish EPIC cohort study . American Journal of Epidemiology , 170 , 1518 – 1529 .
Byrne , D. W. , Rolando , L. A. , Aliyu , M. H. , McGown , P. W. , Connor , L. R. , Awalt , B. M. et al. . ( 2016 ) Modifiable healthy lifestyle behaviors: 10-year health outcomes from a health promotion program . American Journal of Preventive Medicine , 51 , 1027 – 1037 .
Cantera , C. M. , Puigdomènech , E. , Ballvé , J. L. , Arias , O. L. , Clemente , L. , Casas , R. et al. . ( 2015 ) Effectiveness of multicomponent interventions in primary healthcare settings to promote continuous smoking cessation in adults: a systematic review . BMJ Open , 5 , e008807 .
Cross , R. , Foster , S. , O’Neil , I. , Rowlands , S. , Warwick-Booth , L. and Woodall , J . ( 2020 ) Health Promotion: Global Principles and Practice . CABI , Wallingford .
Google Preview
Dalager , T. , Justesen , J. B. , Murray , M. , Boyle , E. and Sjøgaard , G. ( 2016 ) Implementing intelligent physical exercise training at the workplace: health effects among office workers—a randomized controlled trial . European Journal of Applied Physiology , 116 , 1433 – 1442 .
Doumas , D. M. and Hannah , E. ( 2008 ) Preventing high-risk drinking in youth in the workplace: a web-based normative feedback program . Journal of Substance Abuse Treatment , 34 , 263 – 271 .
Eng , J. Y. , Moy , F. M. and Bulgiba , A. ( 2016 ) Impact of a workplace health promotion program on employees’ blood pressure in a public university . PLoS One , 11 , e0148307 .
Galaviz , K. I. , Weber , M. B. , Straus , A. , Haw , J. S. , Narayan , K. V. and Ali , M. K. ( 2018 ) Global diabetes prevention interventions: a systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose . Diabetes Care , 41 , 1526 – 1534 .
Gibson , I. , Flaherty , G. , Cormican , S. , Jones , J. , Kerins , C. , Walsh , A. M. et al. . ( 2014 ) Translating guidelines to practice: findings from a multidisciplinary preventive cardiology programme in the west of Ireland . European Journal of Preventive Cardiology , 21 , 366 – 376 .
Gram , B. , Holtermann , A. , Søgaard , K. and Sjøgaard , G. ( 2012 ) Effect of individualized worksite exercise training on aerobic capacity and muscle strength among construction workers—a randomized controlled intervention study . Scandinavian Journal of Work Environment & Health , 38 , 467 – 475 .
Green , J. , Cross , R. , Woodall , J. and Tones , K. ( 2019 ) Health Promotion: Planning & Strategies , 4th edition. Sage , London .
Grunfeld , E. , Manca , D. , Moineddin , R. , Thorpe , K. E. , Hoch , J. S. , Campbell-Scherer , D. et al. ; BETTER Trial Investigators . ( 2013 ) Improving chronic disease prevention and screening in primary care: results of the BETTER pragmatic cluster randomized controlled trial . BMC Family Practice , 14 , 175 .
Hardcastle , S. , Blake , N. and Hagger , M. S. ( 2012 ) The effectiveness of a motivational interviewing primary-care based intervention on physical activity and predictors of change in a disadvantaged community . Journal of Behavioral Medicine , 35 , 318 – 333 .
Hjarnoe , L. and Leppin , A. ( 2013 ) Health promotion in the Danish maritime setting: challenges and possibilities for changing lifestyle behavior and health among seafarers . BMC Public Health , 13 , 1 – 12 .
Jeong , S. W. , Kim , S. H. , Kang , S. H. , Kim , H. J. , Yoon , C. H. , Youn , T. J. et al. . ( 2019 ) Mortality reduction with physical activity in patients with and without cardiovascular disease . European Heart Journal , 40 , 3547 – 3555 .
Journath , G. , Hammar , N. , Vikström , M. , Linnersjö , A. , Walldius , G. , Krakau , I. et al. . ( 2020 ) A Swedish primary healthcare prevention programme focusing on promotion of physical activity and a healthy lifestyle reduced cardiovascular events and mortality: 22-year follow-up of 5761 study participants and a reference group . British Journal of Sports Medicine , 54 , 1294 – 1299 .
Khadjesari , Z. , Freemantle , N. , Linke , S. , Hunter , R. and Murray , E. ( 2014 ) Health on the web: randomised controlled trial of online screening and brief alcohol intervention delivered in a workplace setting . PLoS One , 9 , e112553 .
Kirkman , J. J. L. , Leo , B. and Moore , J. C. ( 2018 ) Alcohol consumption reduction among a web-based supportive community using the hello Sunday morning blog platform: observational study . Journal of Medical Internet Research , 20 , e196 .
Kosendiak , A. , Felińczak , A. and Szymańska-Chabowska , A. ( 2021 ) The role of physical training in the prevention of cardiovascular disease in a population of healthy people . The Journal of Sports Medicine and Physical Fitness , 61 , 844 – 850 .
Lidin , M. , Hellénius , M. L. , Rydell-Karlsson , M. and Ekblom-Bak , E. ( 2018 ) Long-term effects on cardiovascular risk of a structured multidisciplinary lifestyle program in clinical practice . BMC Cardiovascular Disorders , 18 , 59 .
Lingfors , H. and Persson , L. -G. ( 2019 ) All-cause mortality among young men 24–26 years after a lifestyle health dialogue in a Swedish primary care setting: a longitudinal follow-up register study . BMJ Open , 9 , e022474 .
Lingfors , H. , Persson , L. G. , Lindström , K. , Bengtsson , C. and Lissner , L. ( 2009 ) Effects of a global health and risk assessment tool for prevention of ischemic heart disease in an individual health dialogue compared with a community health strategy only results from the Live for Life health promotion programme . Preventive Medicine , 48 , 20 – 24 .
Matano , R. A. , Koopman , C. , Wanat , S. F. , Winzelberg , A. J. , Whitsell , S. D. , Westrup , D. et al. . ( 2007 ) A pilot study of an interactive web site in the workplace for reducing alcohol consumption . Journal of Substance Abuse Treatment , 32 , 71 – 80 .
Matzer , F. , Nagele , E. , Lerch , N. , Vajda , C. and Fazekas , C. ( 2018 ) Combining walking and relaxation for stress reduction—a randomized cross-over trial in healthy adults . Stress and Health , 34 , 266 – 277 .
McEachan , R. R. C. , Lawton , R. J. , Jackson , C. , Conner , M. , Meads , D. M. and West , R. M. ( 2011 ) Testing a workplace physical activity intervention: a cluster randomized controlled trial . International Journal of Behavioral Nutrition and Physical Activity , 8 , 29 .
Neuner-Jehle , S. , Schmid , M. and Grüninger , U. ( 2013 ) The ‘Health Coaching’ programme: a new patient-centred and visually supported approach for health behaviour change in primary care . BMC Family Practice , 14 , 100 .
Nguyen , Q. N. , Pham , S. T. , Nguyen , V. L. , Weinehall , L. , Wall , S. , Bonita , R. et al. . ( 2012 ) Effectiveness of community-based comprehensive healthy lifestyle promotion on cardiovascular disease risk factors in a rural Vietnamese population: a quasi-experimental study . BMC Cardiovascular Disorders , 12 , 56 .
Nutbeam , D. and Muscat , D. M. ( 2021 ) Health promotion glossary 2021 . Health Promotion International , 36 , 1578 – 1598 .
Oude Hengel , K. M. , Bosmans , J. E. , Van Dongen , J. M. , Bongers , P. M. , Van der Beek , A. J. and Blatter , B. M. ( 2014 ) Prevention program at construction worksites aimed at improving health and work ability is cost-saving to the employer: results from an RCT . American Journal of Industrial Medicine , 57 , 56 – 68 .
Pemberton , M. R. , Williams , J. , Herman-Stahl , M. , Calvin , S. L. , Bradshaw , M. R. , Bray , R. M. et al. . ( 2011 ) Evaluation of two web-based alcohol interventions in the U.S. military . Journal of Studies on Alcohol and Drugs , 72 , 480 – 489 .
Persson , L. G. , Lingfors , H. , Nilsson , M. and Mölstad , S. ( 2015 ) The possibility of lifestyle and biological risk markers to predict morbidity and mortality in a cohort of young men after 26 years follow-up . BMJ Open , 5 , e006798 .
Recio-Rodriguez , J. I. , Agudo-Conde , C. , Martin-Cantera , C. , González-Viejo , M. N. , Fernandez-Alonso , M. D. C. , Arietaleanizbeaskoa , M. S. et al. ; EVIDENT Investigators . ( 2016 ) Short-term effectiveness of a mobile phone app for increasing physical activity and adherence to the Mediterranean diet in primary care: a randomized controlled trial (EVIDENT II study) . Journal of Medical Internet Research , 18 , e331 .
Richardson , G. , van Woerden , H. C. , Morgan , L. , Edwards , R. , Harries , M. , Hancock , E. et al. . ( 2008 ) Healthy hearts—a community-based primary prevention programme to reduce coronary heart disease . BMC Cardiovascular Disorders , 8 , 18 .
Robroek , S. J. , Brouwer , W. , Lindeboom , D. , Oenema , A. and Burdorf , A. ( 2010 ) Demographic, behavioral, and psychosocial correlates of using the website component of a worksite physical activity and healthy nutrition promotion program: a longitudinal study . Journal of Medical Internet Research , 12 , e44 .
Rose , G. ( 1981 ) Strategy of prevention: lessons from cardiovascular disease . British Medical Journal , 282 , 1847 – 1851 .
Rose , G. ( 2001 ) Sick individuals and sick populations . International Journal of Epidemiology , 30 , 427 – 432; discussion 433 .
Stange , K. C. , Miller , W. L. and Etz , R. S. ( 2023 ) The role of primary care in improving population health . The Milbank Quarterly , 101 , 795 – 840 .
Tricco , A. C. , Lillie , E. , Zarin , W. , O’Brien , K. K. , Colquhoun , H. , Levac , D. et al. . ( 2018 ) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation . Annals of Internal Medicine , 169 , 467 – 473 .
van Doorn , D. , Richardson , N. , Osborne , A. and Blake , C. ( 2019 ) The impact of a workplace cardiovascular health screening programme ‘Farmers have hearts’ on health behaviour change among Irish farmers . Work , 63 , 113 – 123 .
Viester , L. , Verhagen , E. A. , Bongers , P. M. and van der Beek , A. J. ( 2015 ) The effect of a health promotion intervention for construction workers on work-related outcomes: results from a randomized controlled trial . International Archives of Occupational and Environmental Health , 88 , 789 – 798 .
Watson , H. , Godfrey , C. , McFadyen , A. , McArthur , K. , Stevenson , M. and Holloway , A. ( 2015 ) Screening and brief intervention delivery in the workplace to reduce alcohol-related harm: a pilot randomized controlled trial . International Journal of Nursing Studies , 52 , 39 – 48 .
Wendel-Vos , G. C. , Dutman , A. E. , Verschuren , W. M. , Ronckers , E. T. , Ament , A. , van Assema , P. et al. . ( 2009 ) Lifestyle factors of a five-year community-intervention program: the Hartslag Limburg intervention . American Journal of Preventive Medicine , 37 , 50 – 56 .
Yang , S. and Kim , H. ( 2022 ) Effects of a walking exercise-focused health promotion program for middle-aged women in the Korean community . International Journal of Environmental Research and Public Health , 19 , 14947 .
Zabaleta-Del-Olmo , E. , Casajuana-Closas , M. , López-Jiménez , T. , Pombo , H. , Pons-Vigués , M. , Pujol-Ribera , E. et al. . ( 2021 ) Multiple health behaviour change primary care intervention for smoking cessation, physical activity and healthy diet in adults 45 to 75 years old (EIRA study): a hybrid effectiveness-implementation cluster randomised trial . BMC Public Health , 21 , 2208 .
Supplementary data
| Month: | Total Views: |
|---|---|
| May 2024 | 290 |
| June 2024 | 194 |
Email alerts
Citing articles via.
- Recommend to Your Librarian
- Journals Career Network
Affiliations
- Online ISSN 1460-2245
- Print ISSN 0957-4824
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 03 June 2024
The impact of long-term care interventions on healthcare utilisation among older persons: a scoping review of reviews
- Nur Zahirah Balqis-Ali 1 ,
- Suhana Jawahir 1 ,
- Yee Mang Chan 2 ,
- Amanda Wei-Yin Lim 3 ,
- Ummi Wahidah Azlan 1 ,
- Sal Sabila Mohd Shaffie 1 ,
- Weng Hong Fun 1 &
- Shaun Wen Huey Lee 4 , 5
BMC Geriatrics volume 24 , Article number: 484 ( 2024 ) Cite this article
190 Accesses
Metrics details
As the ageing population grows, the demand for long-term care (LTC) services will rise, concurrently amplifying healthcare utilisation. This review aims to examine and consolidate information on LTC interventions that influence healthcare utilisation among older persons.
A scoping review was performed through a systematic search in PubMed, EBSCO CINAHL, EBM Reviews - Cochrane Database of Systematic Reviews, Embase, APA PsycInfo, EBM Reviews - Health Technology Assessment, and EBM Reviews - NHS Economic Evaluation Database. Systematic reviews with meta-analyses published between 1 January 2010 and 2 June 2022 among older persons aged 60 and above were included. The characteristics of LTC interventions were mapped to the World Health Organization (WHO) Healthy Ageing Framework. The effect sizes of healthcare utilisations for LTC interventions were recalculated using a random-effects model. The methodological quality was assessed with the AMSTAR-2 checklist, while the quality of evidence for each association was evaluated using GRADE.
Thirty-seven meta-analyses were included. The most prominent domain of the healthy ageing framework was managing chronic conditions. One hundred twelve associations between various LTC interventions and healthcare utilisations were identified, with 22 associations impacting healthcare utilisation. Four interventions were supported by suggestive or convincing evidence. Preventive home visits were found to reduce hospital admission (OR: 0.73, 95% CI: 0.59, 0.91, p = 0.005), caregiver integration during discharge planning (OR: 0.68, 95% CI: 0.57, 0.81, p < 0.001), and continuity of care (OR: 0.76, 95% CI: 0.61, 0.95, p = 0.018) reduced hospital readmission, and perioperative geriatric interventions reduced the length of hospital stay (MD: -1.50, 95% CI: -2.24, -0.76, p < 0.001). None of the associations impacted emergency department visits, medication use, and primary care utilisations with convincing evidence. Most reviews received low methodological quality.
The findings suggest that LTC interventions could benefit from transitioning to a community-based setting involving a multidisciplinary team, including carers. The spectrum of services should incorporate a comprehensive assessment to ensure continuous care.
Peer Review reports
Population ageing is a global phenomenon, with the number of older persons projected to double from 771 million in 2022 to 1.6 billion in 2050 [ 1 ]. Low—and middle-income countries (LMICs) are projected to experience the most significant change, with nearly 80% of the world’s population over 60 living in LMICs by 2050 [ 2 ]. This demographic shift is expected to transform societies across many spectrums, impacting healthcare systems, social welfare programs, economic productivity, and family structures [ 3 ].
As the older population continues to increase, there will be a corresponding rise in the demand for long-term care (LTC) services, encompassing home and community-based care, healthcare monitoring, rehabilitation, and therapy services. These services are defined as those that safeguard older persons’ intrinsic capacities and functional ability, ensuring they align with their fundamental rights, basic freedoms, and human dignity [ 4 , 5 ]. As the healthcare system shifts away from being disease-based and evolves towards holistic and comprehensive care, the importance of LTC services in supporting older persons becomes increasingly acknowledged and emphasised [ 6 ]. In response, the World Health Organization (WHO) identified a need to promote health, prevent disease, maintain intrinsic capacity, and enable the functional ability of older persons by ensuring access to LTC [ 5 ]. The WHO has developed a public health framework for healthy ageing comprising three domains: health services, LTC, and environments [ 7 ]. These domains encompass various aspects of healthcare, such as preventing chronic conditions, facilitating early detection and control, reversing or mitigating declines in capacity, managing advanced chronic conditions, and promoting capacity-enhancing behaviours.
Evidence suggests that diminished functional ability in older persons correlates with increased utilisation of healthcare services, leading to higher treatment costs and a greater likelihood of institutionalisation [ 8 , 9 , 10 ]. Despite some progress in the formal delivery of LTC services in many LMICs, family members or caregivers continue to shoulder the bulk of LTC needs [ 6 ]. Thus, there exists a pressing need to integrate LTC into health systems delivery to ensure that services are readily accessible to support and prevent functional decline among older persons [ 11 ]. The WHO has developed guiding frameworks and models to facilitate the seamless integration of LTC into health system policies, promoting accessibility and efficacy in care delivery [ 12 ]. However, incorporating an effective LTC system is complex, often involving commitments across diverse care settings. In many LMICs, policymakers encounter the challenge of aligning LTC within broader health system perspectives, usually contending with limited resources and conflicting priorities [ 13 , 14 ]. Therefore, it is crucial to identify, map, and summarise the global LTC interventions and services for older persons while considering their influence on healthcare utilisation.
While substantial evidence exists regarding the effectiveness of various LTC interventions [ 15 , 16 , 17 , 18 ], there are conflicting findings. To our knowledge, few studies have mapped the characteristics of LTC interventions [ 19 , 20 ], but the impact of LTC interventions on healthcare utilisation is unknown. Owing to the abundance of knowledge on LTC interventions, we augmented and advanced the existing knowledge through a comprehensive scoping review focused on systematic reviews with meta-analyses. The primary objective is to examine and consolidate information on LTC interventions that influence healthcare utilisation among older persons. These findings are pivotal in guiding policy development, particularly in identifying and prioritising LTC services that positively contribute to the healthcare system and improve the overall care for older persons.
A scoping review was reported based on the methodological framework for scoping studies by Arksey and O’Malley [ 21 ] and Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) guidelines [ 22 ]. The research protocol was registered as part of a more extensive study (Trial registration: NMRR-21-467-58076) and in the Open Science Framework (OSF) [ 23 ]. Due to the extent of the study scope and search, the study was amended from an umbrella review to a scoping review. While an umbrella review typically addresses a narrower research question, often focusing on specific interventions or outcomes [ 24 ], the current study encompasses a broader range of both interventions and outcomes. Therefore, it was determined that a scoping review would be a more appropriate methodology based on the research focus.
The scoping review specifically targeted systematic reviews accompanied by meta-analyses, delineated as articles explicitly identified as such in their title, abstract, or methods section. This allows the examination of a range of heterogeneous interventions that could be aggregated to assess and quantify their collective impact on healthcare utilisation. To provide a comprehensive overview of interventions considered in the meta-analysis, individual trials not pooled into meta-analyses in the articles were retained in this study.
Stage 1: identifying the research question
The scoping review aimed to address the following question: What insights does the existing systematic review with meta-analyses offer regarding the impact of LTC interventions on healthcare utilisation among older persons?
Stage 2: identifying relevant studies
A systematic search was performed on the following databases: PubMed, EBSCO CINAHL Plus, Cochrane Database Systematic Review, Embase, APA PsychINFO, EBM Reviews - Health Technology Assessment, and EBM Reviews - NHS Economic Evaluation Database. The search included Medical Subject Headings (MeSH) terms supplemented with a search of reference lists from identified studies (Additional file 1). The initial search occurred in November 2021, with three updated searches in June 2022, May 2023, and April 2024.
Stage 3: study selection
Inclusion criteria.
Studies were eligible for inclusion if they were: a) Systematic reviews with meta-analyses encompassing Randomised Controlled Trials (RCTs) and observational studies investigating both single and multi-component LTC interventions or services; b) included older persons aged 60 years and above; c) targeted interventions or services in any setting, including home, community, healthcare facility, nursing homes or residential aged care facility; d) reported on health service utilisation as an outcome; and e) published between January 2010 and June 2022 in English. This study defined LTC as a wide range of interventions and services, such as managing chronic geriatric conditions, rehabilitation, palliation, promotion, and preventative services [ 25 ]. The search was limited to the year 2010 onwards to allow for the identification of recent evidence. As the aim of this study was to support health systems planning, only healthcare service utilisation reported from a health systems perspective was included, such as a) Hospital utilisation, b) Emergency department (ED) utilisation, c) Medication utilisation, and d) Primary care utilisation [ 26 ].
Exclusion criteria
Studies were excluded if: a) they included a disease-specific population; b) the target participants were not exclusively older persons and included a mixture of younger (below 60 years old) and older persons; c) reported outcomes focused exclusively on caregivers and/or health providers; d) reported on patient outcomes such as health-related quality of life; and e) focused exclusively on outcome measures for economic evaluation.
Screening and selection process
The selected studies were exported to a reference manager (EndNote X9) and deduplicated. Two reviewers independently screened the citation titles and abstracts for inclusion. The full text of the identified articles was retrieved and screened against the inclusion/exclusion criteria by another two independent reviewers. Any disagreements were resolved by consensus with a third reviewer.
Stage 4: charting the data
Two pairs of reviewers then independently extracted the included studies using a standardised, pre-piloted data extraction form. The extracted information included study demographics, information related to primary studies included in the review, and LTC interventions/services. Summary findings were recorded in Excel Microsoft Office 365 (Additional file 2).
Data synthesis and analysis
The results of the study were first described narratively. The LTC interventions were given a code based on the objective of the intervention in preventing or managing older persons’ intrinsic capacities or functional abilities. The coded LTC interventions were then mapped into several domains according to the WHO Healthy Ageing Framework [ 7 ], namely prevention activities, detection and control activities, management of chronic diseases, promotion and support of capacity-enhancing behaviours, ensuring a dignified late life, removing barriers to participation, and compensation for the loss of capacity by three independent reviewers. If needed, two other reviewers discussed any discrepancies and disagreements regarding the adjudication.
Interventions were then grouped into the four primary outcomes: hospital, emergency department, medication, and primary care utilisations and subdivided into separate domains. Hospital utilisation was further split into hospital admission, hospital readmission, length of stay or bed days. Emergency department (ED) utilisation was divided into ED visit, ED revisit, and length of stay. Medication utilisation refers to the number of drug use, and primary care utilisation refers to the number of visits.
Values extracted from all articles were reanalysed to standardise the findings, considering that various articles reported results in different units of measurement. Values were extracted across all interventions mentioned in the articles, irrespective of their inclusion in either meta-analyses or standalone analyses within the article. Trials from separate meta-analyses with similar intervention characteristics were analysed together unless the setting or follow-up duration differed. Redundant trials across different meta-analyses were removed, except in several situations whereby different values were extracted differently from the same trials. This discrepancy could arise from varying definitions of the outcomes among the authors or possibly from some authors reaching out to the primary author for supplementary data. The intervention durations were reclassified into four categories: less than six months, 7–12 months, 13–24 months, and 25–36 months for all outcomes. Consequently, the pooled interventions reported may deviate from the classification utilised in the original article. An illustration of the process flow is depicted in Additional File 3.
Due to the heterogeneity of included articles, RCTs and observational studies were analysed separately. Each association of long-term intervention with healthcare utilisations was reported in mean difference (MD) or odds ratio (OR) with a corresponding 95% confidence interval (CI) using the random-effects model, given the heterogeneity in design between and within studies [ 27 ]. The analysis was repeated using a fixed-effect model as a sensitivity analysis to investigate whether the method contributed to the observed high heterogeneity. When data from the articles were insufficient for reanalysis, we tried to contact the authors to gain the data. However, in cases where authors were not contactable, the data was extracted from the result as reported or marked as not reported (NR) when the data was unavailable. All statistical analyses were conducted with Stata version 14.0 (Stata Corp, College Station, TX, USA).
Assessment of methodological quality
Two independent reviewers assessed the methodological quality of the included studies using the A Measurement Tool to Assess Systematic Reviews-2 (AMSTAR-2) checklist [ 28 ]. The index rates the quality of the studies based on seven critical and nine non-critical domains. Studies were rated high, moderate, low, and critically low quality. To aid in interpreting results, we assessed the quality of evidence of each outcome using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) [ 29 ]. The quality of evidence was evaluated based on five domains, including a) risk of bias in individual studies b), inconsistency c), indirectness d), imprecision, and e) publication bias, subsequently classified as high, moderate, low, or very low quality. The quality ratings assigned to the evidence indicate the level of assurance in the accuracy of the estimated effects [ 30 ].
Stage 5: collating, summarising, and reporting the results
All results were collated and summarised. The LTC interventions and their impacts on healthcare utilisation were presented.
Ethics considerations
This scoping review was part of a more extensive study, ‘Simulation of Long-Term Care for Elderly in Malaysia’ (MyLTC, Trial registration number: NMRR-21-467-58076). The MyLTC protocol was approved by the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia. The study was conducted by Good Clinical Practice guidelines and the Declaration of Helsinki.
The initial search identified 3,350 records, with 3,056 records screened after deduplication. Fifty-one full-text articles were screened, and 26 articles were selected after exclusion. An additional 11 studies were sourced from the reference list search. A total of 37 articles were included in this review (Fig. 1 ). The reasons for exclusion are provided in Additional File 4.
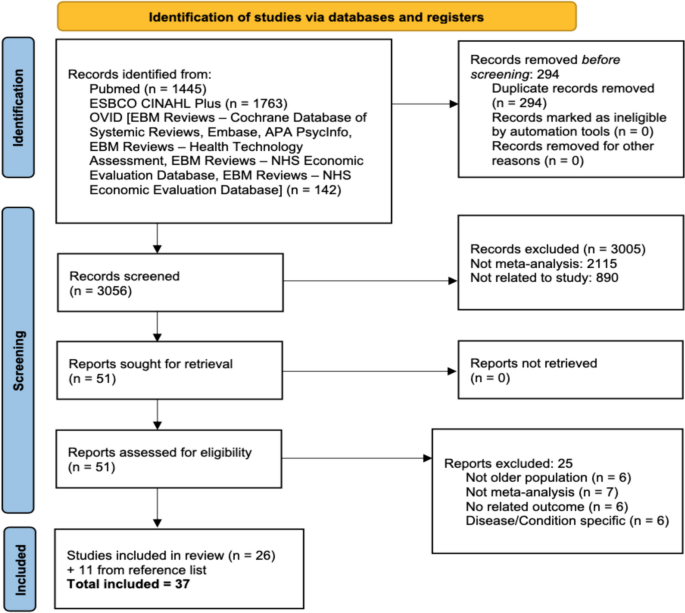
PRISMA 2020 flow diagram
Characteristics and methodological quality of articles exploring associations of long-term care interventions with healthcare utilisations for older persons
Of the 37 articles included, 17 were RCTs or cluster RCTs, while the remaining were mixed study designs. The median and interquartile range (IQR) for the number of studies per article was 17 [ 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ]. The sample sizes ranged from 811 to the largest, involving 108,838 participants, with a median (IQR) of 9,679 (3,976 − 18,992). The duration of follow-up varies between studies, with the shortest follow-up within one week and the longest over 60 months. A total of 82 outcomes across all articles were identified. The most studied outcomes reported were hospital readmission ( n = 19, 23.2%) and hospital admission ( n = 18, 21.9%).
Most articles were rated either low or critically low in the methodological assessment using AMSTAR-2 (Table 1 and Additional file 5). This was mainly due to methodological issues, including the need for more justification for excluding individual studies and a lack of assessment regarding publication bias and its potential impact. The descriptive characteristics of the 37 eligible articles are provided in Table 1 .
Characteristics and mapping of long-term care interventions to the healthy ageing Framework
Altogether, 37 LTC interventions were included in the analysis (Table 2 ). Although various interventions share similar names, they were implemented in distinct settings, yielded diverse outcomes, featured varying durations of outcomes follow-up, or engaged different providers, warranting separate descriptions. No overlap of intervention from the same meta-analyses was identified.
Most interventions involved multidisciplinary teams or coordination, with only six interventions among a single healthcare professional [ 37 , 42 , 45 , 50 , 52 , 67 ]. The most common settings were community-based or involved transfer back to the community following discharge from the hospital, including the older person’s home, with 17 interventions. Nine interventions were set in long-term care institutions [ 31 , 44 , 45 , 51 , 52 , 55 , 58 , 64 , 65 ], with the remaining in hospitals or in mixed settings. The most common type of intervention was the Comprehensive Geriatric Assessment (CGA) ( n = 8, 23.5%). However, the intervention was applied across various settings, delivered by different teams of healthcare professionals, and had different follow-up durations. Mapping to the WHO Healthy Ageing Framework revealed that 11 interventions focused on managing chronic conditions [ 31 , 42 , 44 , 45 , 49 , 52 , 53 , 55 , 58 , 64 , 67 ], ten supported capacity enhancement [ 37 , 41 , 46 , 51 , 56 , 59 , 62 , 63 , 65 , 66 ], eight were on early detection and control [ 33 , 35 , 36 , 38 , 39 , 40 , 43 , 60 ], six were to promote capacity enhancement [ 32 , 47 , 48 , 50 , 57 , 61 ], and one each for prevention of chronic conditions [ 54 ] and compensation of capacity [ 34 ].
Associations between long-term care interventions with healthcare utilisations among older persons
One hundred and twelve associations were reported between LTC interventions and healthcare utilisations, mostly on hospital utilisation ( n = 86, 76.8%). Seventeen associations were reported on ED utilisation, six on medication utilisation and three on primary care service utilisation (Additional file 6). Twenty-two out of the 112 associations (19.6%) were statistically significant (Table 3 ). The GRADE reporting for all associations is reported in Additional File 7.
Hospital utilisation
Altogether, 35 associations discussed hospital admission (Additional file 6). Six associations (17.1%) reflected a significant reduction in the risk of hospital admission among older persons. The associations mapped to five interventions: Deprescribing interventions [ 64 ], community-based aged care [ 47 ], preventive home visits [ 48 ], CGA implemented in a community setting [ 33 ], and medication review by pharmacists in Long-term Care Facility (LTCF) [ 52 ]. Three of the five significant interventions were implemented in the community-based setting (community-based aged care [ 47 ], preventive home visits [ 48 ], and CGA implemented in a community setting [ 33 ]). Among these five interventions, only preventive home visits at 7–12 months follow-up (OR: 0.73, 95% CI: 0.59, 0.91, p = 0.005) received a moderate GRADE quality of evidence rating [ 48 ], with all other interventions rated either low or very low quality.
For hospital readmission, there were 32 associations (Additional file 6). Eight associations (25%) from six interventions were significantly associated with hospital readmission. All six interventions involved implementation in a community setting or a transfer back into the community following discharge from the hospital [ 41 , 47 , 51 , 56 , 63 , 65 ]. Six associations were found to reduce hospital readmission, with only one intervention, caregiver integration during discharge planning at 1–6 months follow-up (OR: 0.68, 95% CI: 0.57, 0.81, p < 0.001), had high-quality evidence [ 51 ]. This intervention included 13 studies with a low heterogeneity. Another intervention found to have a moderate quality of evidence in reducing hospital readmission was continuity of care at a 7–12 months follow-up (OR: 0.76, 95% CI: 0.61, 0.95, p = 0.018) [ 41 ]. The other two interventions representing four associations with low and very low-quality evidence were integrating primary healthcare in aftercare [ 63 ] and transitional care programs for community-dwelling older persons [ 56 ]. The remaining two interventions increased the odds or risk of hospital readmissions among older persons (transitional care programs for long-term care facility residents [ 65 ] and community-based aged-care interventions [ 47 ]). However, both interventions received low and very low-quality evidence.
There were 17 associations regarding the outcome of length of stay (Additional file 6). Three associations (17.6%) from three interventions demonstrated significant reductions in the length of hospital stay [ 43 , 54 , 59 ]. All interventions were implemented in a hospital setting. Perioperative geriatric interventions at a 12-month follow-up, which involved twelve studies, were the only intervention with a moderate quality of evidence (MD: -1.50, 95% CI: -2.24, -0.76, p < 0.001) and low heterogeneity (32.7%) [ 54 ]. The remaining two interventions, early support discharge [ 59 ] and CGA, were implemented in the ward and had low or very low-quality evidence and high or moderate heterogeneity.
Utilisation of emergency department
ED utilisation was found to have 17 associations (Additional file 6). Three associations (17.6%) from three interventions significantly reduced ED utilisation. Two were on ED visits (community-based case management [ 49 ] and CGA implemented in a community setting [ 33 ]), and one was on the length of ED stay (transitional care programs for long-term care facility residents [ 65 ]). However, all three interventions were found to have either low or very low-quality evidence.
Utilisation of medications and prescriptions
The outcome of drug use had six associations (Additional file 6). Only one association (16.7%) from an intervention, anti-microbial stewardship at a 12-month follow-up, significantly reduced the number of drugs used among older persons (MD: -0.47, 95% CI: -0.87, -0.07, p = 0.02) [ 58 ]. However, this association was graded as having very low quality and high heterogeneity.
Utilisation of primary care
Three associations were found for the outcome of primary care visits (Additional file 6). One association (33.3%) from an intervention was statistically significant. A community-based aged care intervention increased the number of visits (RR: 1.43, 95% CI: 1.11, 1.18, p: 0.002) [ 47 ]. The quality of evidence was found to be very low.
Sensitivity analysis
The re-analysis of associations with high heterogeneity using a fixed-effect model did not significantly alter the associations between the intervention and the outcome measured.
Thirty-seven meta-analyses were included in the study, comprising 112 associations between various LTC interventions and healthcare utilisations. Four of the 22 statistically significant associations were supported by suggestive or convincing evidence and remarked as either high or moderate quality of evidence. These associations include four different LTC interventions: preventive home visits were found to reduce hospital admission [ 48 ], caregiver integration during discharge planning [ 51 ], and continuity of care [ 41 ], reduced hospital readmission, and perioperative geriatric interventions [ 54 ] reduced the length of hospital stay. There was no convincing evidence on the association between LTC and ED, medication and primary care utilisation.
Mapping the LTC interventions to the WHO Healthy Ageing Framework revealed that the most extensive domain explored was managing chronic conditions (11 out of 37 interventions), followed by support of capacity enhancement (9 out of 37 interventions). These findings fit well with the aims of the healthy ageing framework, whereby both domains were crucial in preventing substantial loss of capacity among older persons [ 7 ]. However, it represents opportunities or a need to explore services in other domains, facilitating the evidence-based implementation of more comprehensive LTC services. This is essential for supporting health systems in meeting the evolving needs of the ageing population, ensuring that older persons receive high-quality and coordinated care for their well-being. Most interventions were found to be implemented in a community setting or involved a transfer back into the community following discharge from the hospital. This finding aligns with other evidence emphasising that while LTC services can be implemented in various settings, a community-based approach offers the most benefit to older persons [ 7 , 19 , 68 ]. However, this finding could also be due to the exclusion of interventions among disease-specific conditions, which may have been more extensively implemented in hospital or institutional-based settings. Therefore, future comparisons and discussions should consider the contextual factors of LTC implementations, including the specific settings in which they occur.
Most interventions involved multidisciplinary teams of various health, social care, and community-based providers, supporting findings and recommendations elsewhere [ 7 , 20 ]. Indeed, the involvement of relevant providers in caring for and providing LTC services for older persons is essential in ensuring that all their needs are adequately assessed and addressed in an integrated and coordinated approach [ 12 , 68 ]. CGA emerged as the most common intervention recurring across all meta-analyses. It signifies the importance of a thorough clinical and psychological evaluation and the presence of support evaluation in delivering care to older persons [ 69 ]. However, since this review identified interventions labelled as ‘long-term care’, it could also suggest that CGA was among the most developed LTC interventions that have been assessed and evaluated across multitudes of different outcomes, including healthcare utilisations, which highlights future research opportunities for evaluating other LTC interventions that were less explored.
This review found suggestive evidence that preventive home visits [ 48 ] reduced the likelihood of hospital admission among older persons. The service was provided by a multidisciplinary team offering comprehensive care, including assessment of health and support needs, referral to relevant care providers, medication review, and rehabilitation at the older person’s home [ 48 ]. The approach ensures early detection of diseases and conditions, improves access to care, and offers a large spectrum of services that are otherwise not provided during routine care [ 70 ]. The finding reciprocates a recent umbrella review reporting that home visits were favourable in reducing hospital admission frequency [ 71 ]. As debated in the review, the definitions and components of what constituted ‘home visits’ vary across studies and warrant further evaluation. Nevertheless, the heterogeneity for this intervention was found to be low in this study [ 72 ].
Caregiver integration during discharge planning had convincing evidence in reducing hospital readmission [ 51 ]. The service included linking caregivers to external or community resources, preparing written care plans, performing caregiver assessment, medication reconciliation, and iterative teaching sessions in providing care, all planned and executed during the discharge process of older persons from the hospital. Discharge planning implies a comprehensive plan was prepared based on the anticipated healthcare needs of the older persons [ 73 ]. Including caregivers in the discharge planning enhanced the care by delegating part of the responsibilities to the person managing the patient [ 74 ]. Similarly, continuity of care upon discharge from the hospital was found to have suggestive evidence in reducing hospital readmission [ 41 ]. Early hospital readmissions are often due to insufficient recognition of a patient’s needs, leading to unaddressed issues and poor management at home [ 75 ]. Ensuring that care is continued primarily through care coordination between hospital and primary healthcare providers means the underlying disease that caused the earlier hospital admission is appropriately managed. A recurrent episode requiring further hospitalisation (readmission) is thus prevented [ 41 ]. The overarching idea was that to reduce hospital readmission, there was a need for a comprehensive assessment and identification of an older person’s health and other requirements within the hospital setting before discharge. This process involves crafting a detailed, coordinated care plan that includes caregivers and other healthcare providers, ensuring a smooth transition and effective ongoing care management post-discharge.
Perioperative geriatric interventions, defined as any program aiming to enhance clinical outcomes of older persons having surgeries performed, was the only intervention with suggestive evidence of reducing the length of stay in hospital [ 54 ]. The interventions mitigate the increased risk associated with surgeries by customising care to the specific needs of the patients, potentially preventing functional decline and related complications [ 54 ]. No convincing LTC intervention was found to influence ED, drug use, and primary care utilisation. This could be due to the limited number of studies that evaluated these outcomes, warranting future research.
Implications for practice and future research
This scoping review offers an extensive summary across meta-analyses on existing LTC interventions that impacted healthcare utilisations. Since the scope of this study covers the general older population, the findings may be beneficial for policymakers looking to implement LTC interventions at a macro rather than disease-specific level. The review found a few effective LTC interventions in reducing healthcare utilisations. Nevertheless, from the health systems point of view, it provides insights for potential interventions that could alleviate the strain on healthcare systems, exacerbated by the increasing prevalence of non-communicable diseases (NCDs) and age-related functional disabilities [ 76 ]. It also means future research may be directed towards exploring the impact of more and newer LTC interventions towards healthcare utilisations. The limited number of existing studies assessing the impact of LTC interventions on healthcare utilisation may partly explain the little evidence found through this study. Still, it also suggests that LTC interventions could have broader positive effects on various other outcomes, including individual well-being, mortality, clinical outcomes, and functional limitations, which were not within the scope of the current study. Despite the small number of effective LTC interventions found, the overall picture suggests that LTC interventions need to move away from hospital or institution-based implementations to the community or older persons’ homes. Such a move offers integrated, person-centred care at the place most comfortable for the older person, increasing adherence to care [ 77 ]. Comprehensive assessment identifying all aspects of the needs of older persons while being hospitalised, coupled with a properly documented detailed discharge plan, which includes roles of carers and other professionals that will continue the care upon discharge, is crucial in ensuring older persons’ well-being, hence impacting the subsequent healthcare utilisation.
Limitations
This scoping review has several limitations. The search strategy relied on interventions labelled ‘long-term care’ or other terms referring to LTC interventions. While the keywords postulated in the study covered as comprehensive LTC interventions as possible, more interventions may have served LTC functions but were not labelled as such. While the study covers multiple outcomes related to healthcare utilisations, more outcomes existed that were not included in the current review. For example, preventable hospitalisation, preventable ED visits, and time to hospitalisation were among various related outcomes not included in the present review. While the inclusion of meta-analysis in our review offers a comprehensive overview of the outcomes’ direction and strength across different interventions, it is essential to acknowledge the diversity in implementation, contextual backgrounds, and settings of various other interventions, making it impossible for studies to pool and analyse all existing interventions. As a result, while our current review encompasses broad LTC interventions for older persons analysed within a systematic review with meta-analysis, it is essential to recognise that a wealth of additional evidence available could offer further insights into practical strategies for reducing healthcare utilisation among this population. The review also did not directly assess the quality of individual primary studies included in each meta-analysis but instead relied on the assessment reported by the authors. A further limitation was that we did not perform subgroup analysis (for example, by age groups, sex, and location where the intervention was delivered) due to the lack of data for grading the quality evidence for most interventions.
The findings of this study suggest LTC interventions could benefit from transitioning to a community-based setting, involving a multidisciplinary team including the carers that offer a large spectrum of services fulfilling various needs of older persons, incorporate comprehensive and holistic assessment plan, and include a detailed discharge plan that ensures integrated, coordinated and continuous care is achieved. However, the current evidence pertains to hospital utilisation, with more research needed to identify interventions impacting other healthcare utilisations. Nevertheless, the present findings offer insights into effective LTC interventions that may be considered for implementation by policymakers at a macro level.
Availability of data and materials
The data analysed for this review is part of the ‘Simulation of Long-Term Care for Elderly in Malaysia’ (MyLTC) study and belongs to the Ministry of Health Malaysia. Requests for the data can be obtained from the Principal Investigator, Dr Fun Weng Hong, through email: [email protected] with permission from the Director-General of Health, Malaysia.
Abbreviations
A Measurement Tool to Assess Systematic Reviews-2
Comprehensive Geriatric Assessment
Confidence interval
Emergency department
Grading of Recommendations, Assessment, Development, and Evaluations
Interquartile range
Low- and middle-income countries
- Long-term care
Long-term Care Facility
Mean difference
Medical Subject Headings
Medical Research and Ethics Committee
Non-communicable diseases
Not reported
Open Science Framework
Preferred Reporting Items for Systematic Review and Meta-analyses
Randomised Controlled Trials
World Health Organization
United Nations Department of Economic and Social Affairs, Population Division. World Population Prospects 2022: Summary of Results. New York; 2022.
World Health Organization. Ageing and health 2022 [ https://www.who.int/news-room/fact-sheets/detail/ageing-and-health .
European Commission. European Commission Report on the Impact of Demographic Change. 2020.
Kane RA, Kane RL, Ladd RC. The heart of long term care. USA: Oxford University Press; 1998.
Book Google Scholar
World Health Organization. Decade of healthy ageing: baseline report. 2021.
Google Scholar
World Health Organization. Long-term care financing: lessons for low-and middle-income settings: brief 1: drivers of the demand for long-term care. 2024.
Beard JR, Officer A, De Carvalho IA, Sadana R, Pot AM, Michel J-P, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–54.
Article PubMed Google Scholar
Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161(21):2602–7.
Article CAS PubMed Google Scholar
Miller EA, Weissert WG. Predicting elderly people’s risk for nursing home placement, hospitalization, functional impairment, and mortality: a synthesis. Med care Res Rev. 2000;57(3):259–97.
Palladino R, Tayu Lee J, Ashworth M, Triassi M, Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing. 2016;45(3):431–5.
Article PubMed PubMed Central Google Scholar
Tessier L, de Wulf N, Momose Y. Long-term care in the context of population ageing: A rights-based approach to universal coverage: ILO Working Paper. Geneva: International Labour Office; 2022.
Brodsky J, Habib J, Hirschfeld M. Key policy issues in long-term care. Geneva: World Health Organization; 2003.
Feng Z. Global convergence: aging and long-term care policy challenges in the developing world. J Aging Soc Policy. 2019;31(4):291–7.
World Health Organization. Long-term care financing: lessons for low-and middle-income settings: brief 2: decisions about population coverage of long-term care. 2024.
Abbott RA, Whear R, Thompson-Coon J, Ukoumunne OC, Rogers M, Bethel A, et al. Effectiveness of mealtime interventions on nutritional outcomes for the elderly living in residential care: a systematic review and meta-analysis. Ageing Res Rev. 2013;12(4):967–81.
Cao Py Z, Qh X, Mz K, Ln XL. The effectiveness of exercise for fall prevention in nursing home residents: a systematic review meta-analysis. J Adv Nurs. 2018;74(11):2511–22.
Frost R, Belk C, Jovicic A, Ricciardi F, Kharicha K, Gardner B, et al. Health promotion interventions for community-dwelling older people with mild or pre-frailty: a systematic review and meta-analysis. BMC Geriatr. 2017;17:1–13.
Article Google Scholar
Giné-Garriga M, Roqué-Fíguls M, Coll-Planas L, Sitjà-Rabert M, Salvà A. Physical exercise interventions for improving performance-based measures of physical function in community-dwelling, frail older adults: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95(4):753–69. e3.
Arias-Casais N, Thiyagarajan JA, Perracini MR, Park E, Van den Block L, Sumi Y, et al. What long-term care interventions have been published between 2010 and 2020? Results of a WHO scoping review identifying long-term care interventions for older people around the world. BMJ Open. 2022;12(1):e054492.
Bayly J, Bone AE, Ellis-Smith C, Yaqub S, Yi D, Nkhoma KB, et al. Common elements of service delivery models that optimise quality of life and health service use among older people with advanced progressive conditions: a tertiary systematic review. BMJ Open. 2021;11(12):e048417.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Reviews. 2015;4(1):1–9.
Balqis-Ali NZ, Jawahir S, Mohd Shaffie SS, Azlan UW, Fun WH, Chan YM, Lim AWY, Lee SWH. The impact of long-term care interventions on healthcare utilisation among older persons: A scoping review of meta-analyses [Internet]. OSF; 2024. [Available from: https://www.osf.io/sjfzn ].
Aromataris E, Fernandez RS, Godfrey C, Holly C, Khalil H, Tungpunkom P. Methodology for JBI umbrella reviews. Joanna Briggs Institute Reviewers’ Manual. Australia: The Joanna Briggs Institute; 2014.
World Health Organization. Rebuilding for sustainability and resilience: strengthening the integrated delivery of long-term care in the European Region. Copenhagen: World Health Organization, Regional Office for Europe; 2022.
Arueira Chaves L, de Serio S, dos Santos D, Rodrigues Campos M, Luiza VL. Use of health outcome and health service utilization indicators as an outcome of access to medicines in Brazil: perspectives from a literature review. Public Health Rev. 2019;40(1):1–20.
Dettori JR, Norvell DC, Chapman JR. Fixed-effect vs random-effects models for meta-analysis: 3 points to consider. Global Spine J. 2022;12(7):1624–6.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008–4008.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6.
Almutairi H, Stafford A, Etherton-Beer C, Flicker L. Optimisation of medications used in residential aged care facilities: a systematic review and meta-analysis of randomised controlled trials. BMC Geriatr. 2020;20(1):1–19.
Beswick AD, Gooberman-Hill R, Smith A, Wylde V, Ebrahim S. Maintaining independence in older people. Reviews Clin Gerontol. 2010;20(2):128–53.
Briggs R, McDonough A, Ellis G, Bennett K, O'Neill D, Robinson D. Comprehensive Geriatric Assessment for community‐dwelling, high‐risk, frail, older people. Cochrane Database Syst Reviews. 2022;5(5):CD012705.
Cochrane A, Furlong M, McGilloway S, Molloy DW, Stevenson M, Donnelly M. Time‐limited home‐care reablement services for maintaining and improving the functional independence of older adults. Cochrane Database Syst Rev. 2016;10(10):CD010825.
Conroy SP, Stevens T, Parker SG, Gladman JR. A systematic review of comprehensive geriatric assessment to improve outcomes for frail older people being rapidly discharged from acute hospital:‘interface geriatrics’. Age Ageing. 2011;40(4):436–43.
Deschodt M, Flamaing J, Haentjens P, Boonen S, Milisen K. Impact of geriatric consultation teams on clinical outcome in acute hospitals: a systematic review and meta-analysis. BMC Med. 2013;11:1–13.
Deschodt M, Laurent G, Cornelissen L, Yip O, Zuniga F, Denhaerynck K, et al. Core components and impact of nurse-led integrated care models for home-dwelling older people: a systematic review and meta-analysis. Int J Nurs Stud. 2020;105:103552.
Ekdahl A, Sjöstrand F, Ehrenberg A, Oredsson S, Stavenow L, Wisten A, et al. Frailty and comprehensive geriatric assessment organized as CGA-ward or CGA-consult for older adult patients in the acute care setting: a systematic review and meta-analysis. Eur Geriatr Med. 2015;6(6):523–40.
Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9(9):CD006211.
Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553.
Facchinetti G, D’Angelo D, Piredda M, Petitti T, Matarese M, Oliveti A, et al. Continuity of care interventions for preventing hospital readmission of older people with chronic diseases: a meta-analysis. Int J Nurs Stud. 2020;101:103396.
Forster A, Young J, Lambley R, Langhorne P. Medical day hospital care for the elderly versus alternative forms of care. Cochrane Database Syst Rev. 2008;(4):CD001730.
Fox MT, Persaud M, Maimets I, O’Brien K, Brooks D, Tregunno D, et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc. 2012;60(12):2237–45.
Hill-Taylor B, Walsh K, Stewart S, Hayden J, Byrne S, Sketris IS. Effectiveness of the STOPP/START (Screening Tool of older persons’ potentially inappropriate Prescriptions/Screening tool to alert doctors to the right treatment) criteria: systematic review and meta‐analysis of randomized controlled studies. J Clin Pharm Ther. 2016;41(2):158–69.
Lee JK, Slack MK, Martin J, Ehrman C, Chisholm-Burns M. Geriatric patient care by US pharmacists in healthcare teams: systematic review and meta‐analyses. J Am Geriatr Soc. 2013;61(7):1119–27.
Lowthian JA, McGinnes RA, Brand CA, Barker AL, Cameron PA. Discharging older patients from the emergency department effectively: a systematic review and meta-analysis. Age Ageing. 2015;44(5):761–70.
Luker JA, Worley A, Stanley M, Uy J, Watt AM, Hillier SL. The evidence for services to avoid or delay residential aged care admission: a systematic review. BMC Geriatr. 2019;19:1–20.
Mayo-Wilson E, Grant S, Burton J, Parsons A, Underhill K, Montgomery P. Preventive home visits for mortality, morbidity, and institutionalization in older adults: a systematic review and meta-analysis. PLoS ONE. 2014;9(3):e89257.
Poupard N, Tang CY, Shields N. Community-based case management does not reduce hospital admissions for older people: a systematic review and meta-analysis. Aust Health Rev. 2019;44(1):83–92.
Spiers G, Matthews F, Moffatt S, Barker R, Jarvis H, Stow D, et al. Impact of social care supply on healthcare utilisation by older adults: a systematic review and meta-analysis. Age Ageing. 2019;48(1):57–66.
Rodakowski J, Rocco PB, Ortiz M, Folb B, Schulz R, Morton SC, et al. Caregiver integration during discharge planning for older adults to reduce resource use: a metaanalysis. J Am Geriatr Soc. 2017;65(8):1748–55.
Sadowski CA, Charrois TL, Sehn E, Chatterley T, Kim S. The role and impact of the pharmacist in long-term care settings: a systematic review. J Am Pharmacists Association. 2020;60(3):516–24 e2.
Tecklenborg S, Byrne C, Cahir C, Brown L, Bennett K. Interventions to reduce adverse drug event-related outcomes in older adults: a systematic review and meta-analysis. Drugs Aging. 2020;37:91–8.
Thillainadesan J, Yumol MF, Hilmer S, Aitken SJ, Naganathan V. Interventions to improve clinical outcomes in older adults admitted to a surgical service: a systematic review and meta-analysis. J Am Med Dir Assoc. 2020;21(12):1833–43. e20.
Wallerstedt SM, Kindblom JM, Nylén K, Samuelsson O, Strandell A. Medication reviews for nursing home residents to reduce mortality and hospitalization: systematic review and meta-analysis. Br J Clin Pharmacol. 2014;78(3):488–97.
Weeks LE, Macdonald M, Martin-Misener R, Helwig M, Bishop A, Iduye DF, et al. The impact of transitional care programs on health services utilization in community-dwelling older adults: a systematic review. JBI Evid Synthesis. 2018;16(2):345–84.
Wong KC, Wong FKY, Yeung WF, Chang K. The effect of complex interventions on supporting self-care among community-dwelling older adults: a systematic review and meta-analysis. Age Ageing. 2018;47(2):185–93.
Crespo-Rivas JC, Guisado-Gil AB, Peñalva G, Rodríguez-Villodres Á, Martín-Gandul C, Pachón-Ibáñez ME, et al. Are antimicrobial stewardship interventions effective and safe in long-term care facilities? A systematic review and meta-analysis. Clin Microbiol Infect. 2021;27(10):1431–8.
Williams S, Morrissey A-M, Steed F, Leahy A, Shanahan E, Peters C, et al. Early supported discharge for older adults admitted to hospital with medical complaints: a systematic review and meta-analysis. BMC Geriatr. 2022;22(1):302.
O’Shaughnessy Í, Robinson K, O’Connor M, Conneely M, Ryan D, Steed F, et al. Effectiveness of acute geriatric unit care on functional decline, clinical and process outcomes among hospitalised older adults with acute medical complaints: a systematic review and meta-analysis. Age Ageing. 2022;51(4):afac081.
Lin I, Glinsky J, Dean C, Graham P, Scrivener K. Effectiveness of home-based exercise for improving physical activity, quality of life and function in older adults after hospitalisation: a systematic review and meta-analysis. Clin Rehabil. 2022;36(9):1170–85.
Van Grootven B, Flamaing J, Dierckx de Casterlé B, Dubois C, Fagard K, Herregods MC, et al. Effectiveness of in-hospital geriatric co-management: a systematic review and meta-analysis. Age Ageing. 2017;46(6):903–10.
Li R, Geng J, Liu J, Wang G, Hesketh T. Effectiveness of integrating primary healthcare in aftercare for older patients after discharge from tertiary hospitals—a systematic review and meta-analysis. Age Ageing. 2022;51(6):afac151.
Kua C-H, Mak VS, Lee SWH. Health outcomes of deprescribing interventions among older residents in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(3):362–72. e11.
Birtwell K, Planner C, Hodkinson A, Hall A, Giles S, Campbell S, et al. Transitional care interventions for older residents of long-term care facilities: a systematic review and meta-analysis. JAMA Netw Open. 2022;5(5):e2210192–e.
Tomlinson J, Cheong V-L, Fylan B, Silcock J, Smith H, Karban K, et al. Successful care transitions for older people: a systematic review and meta-analysis of the effects of interventions that support medication continuity. Age Ageing. 2020;49(4):558–69.
Lee SWH, Mak VSL, Tang YW. Pharmacist services in nursing homes: a systematic review and meta-analysis. Br J Clin Pharmacol. 2019;85(12):2668–88.
Tamiya N, Noguchi H, Nishi A, Reich MR, Ikegami N, Hashimoto H, et al. Population ageing and wellbeing: lessons from Japan’s long-term care insurance policy. Lancet. 2011;378(9797):1183–92.
Parker SG, McCue P, Phelps K, McCleod A, Arora S, Nockels K, et al. What is comprehensive geriatric assessment (CGA)? An umbrella review. Age Ageing. 2018;47(1):149–55.
Rosenberg T. Acute hospital use, nursing home placement, and mortality in a frail community-dwelling cohort managed with Primary Integrated Interdisciplinary Elder Care at Home. J Am Geriatr Soc. 2012;60(7):1340–6.
Eltaybani S, Kawase K, Kato R, Inagaki A, Li C-C, Shinohara M, et al. Effectiveness of home visit nursing on improving mortality, hospitalization, institutionalization, satisfaction, and quality of life among older people: umbrella review. Geriatr Nurs. 2023;51:330–45.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Craven E, Conroy S. Hospital readmissions in frail older people. Reviews Clin Gerontol. 2015;25(2):107–16.
Family Caregiver Alliance. Caregiver assessment: principles, guidelines and strategies for change: report from a National Consensus Development Conference. San Francisco; 2006.
Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374(16):1543–51.
Holmes W. Projecting the need for and cost of long-term care for older persons. 2021.
Sanerma P, Miettinen S, Paavilainen E, Åstedt-Kurki P. A client-centered approach in home care for older persons–an integrative review. Scand J Prim Health Care. 2020;38(4):369–80.
Download references
Acknowledgements
We thank the Director-General of Health, Ministry of Health Malaysia, for permission to publish this review.
This review was part of a more extensive study, ‘Simulation of Long-Term Care for Elderly in Malaysia (MyLTC)’ (Trial registration: NMRR-21-467-58076). The MyLTC study is funded by the Ministry of Health Malaysia (NIH/800-3/2/1 Jilid 8 (35), Warrant number: 91000050). Part of the funding was used to support the conduct of this review.
Author information
Authors and affiliations.
Institute for Health Systems Research, National Institutes of Health, Ministry of Health, Shah Alam, Selangor, Malaysia
Nur Zahirah Balqis-Ali, Suhana Jawahir, Ummi Wahidah Azlan, Sal Sabila Mohd Shaffie & Weng Hong Fun
Institute for Public Health, National Institutes of Health, Ministry of Health, Shah Alam, Selangor, Malaysia
Yee Mang Chan
Institute for Clinical Research, National Institutes of Health, Ministry of Health, Shah Alam, Selangor, Malaysia
Amanda Wei-Yin Lim
School of Pharmacy, Monash University Malaysia, Subang Jaya, Selangor, Malaysia
Shaun Wen Huey Lee
School of Pharmacy, Taylor’s University Lakeside Campus Malaysia, Subang Jaya, Selangor, Malaysia
You can also search for this author in PubMed Google Scholar
Contributions
NZB, YMC, SJ, and AL contributed to the early conception and study design. NZB, YMC, SJ, AL, WHF, and SWHL conceived and designed the review. NZB, YMC, SJ, AL, UWA, and SMS performed the review. SWHL provided technical advice on data extraction and analysis. NZB, YMC, SJ, AL, UWA, SMS and WHF analysed and interpreted the data. NZB, YMC, SJ, AL, UWA, SMS, WHF, and SWHL contributed to the writing and reviewing of the manuscript.
Corresponding author
Correspondence to Suhana Jawahir .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. search strategy , additional file 2. template for extraction record, additional file 3. flowchart for reanalysing extracted values, additional file 4. excluded articles, additional file 5. amstar-2 assessment of all included studies, 12877_2024_5097_moesm6_esm.docx.
Additional file 6. Summary of associations between long-term care interventions with hospital utilisation among older persons
Additional file 7. GRADE assessment for significant associations
Additional file 8. prior checklist, 12877_2024_5097_moesm9_esm.docx.
Additional file 9. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Balqis-Ali, N.Z., Jawahir, S., Chan, Y.M. et al. The impact of long-term care interventions on healthcare utilisation among older persons: a scoping review of reviews. BMC Geriatr 24 , 484 (2024). https://doi.org/10.1186/s12877-024-05097-9
Download citation
Received : 07 March 2024
Accepted : 20 May 2024
Published : 03 June 2024
DOI : https://doi.org/10.1186/s12877-024-05097-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Older persons
- Healthcare utilisation
- Scoping review
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 03 September 2021
A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward
- Abukari Kwame 1 &
- Pammla M. Petrucka 2
BMC Nursing volume 20 , Article number: 158 ( 2021 ) Cite this article
389k Accesses
170 Citations
97 Altmetric
Metrics details
Providing healthcare services that respect and meet patients’ and caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns, beliefs, and contextual variables. Achieving patient-centered care and communication in nurse-patient clinical interactions is complex as there are always institutional, communication, environmental, and personal/behavioural related barriers. To promote patient-centered care, healthcare professionals must identify these barriers and facitators of both patient-centered care and communication, given their interconnections in clinical interactions. A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice.
Peer Review reports
Providing healthcare services that respect and meet patients’ and their caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thus constituting patient-centered care. Care is “a feeling of concern for, or an interest in, a person or object which necessitates looking after them/it” [ 1 ]. The Institute of Medicine (IOM) noted that to provide patient-centered care means respecting and responding to individual patient’s care needs, preferences, and values in all clinical decisions [ 2 ]. In nursing care, patient-centered care or person-centered care must acknowledge patients’ experiences, stories, and knowledge and provide care that focuses on and respects patients’ values, preferences, and needs by engaging the patient more in the care process [ 3 ]. Healthcare providers and professionals are thus required to fully engage patients and their families in the care process in meaningful ways. The IOM, in its 2003 report on Health Professions Education , recognized the values of patient-centered care and emphasized that providing patient-centered care is the first core competency that health professionals’ education must focus on [ 4 ]. This emphasis underscored the value of delivering healthcare services according to patients’ needs and preferences.
Research has shown that effective communication between patients and healthcare providers is essential for the provision of patient care and recovery [ 5 , 6 , 7 , 8 ]. Madula et al. [ 6 ], in a study on maternal care in Malawi, noted that patients reported being happy when the nurses and midwives communicated well and treated them with warmth, empathy, and respect. However, other patients said poor communication by nurses and midwives, including verbal abuse, disrespect, or denial from asking questions, affected their perceptions of the services offered [ 6 ]. Similarly, Joolaee et al. [ 9 ] explored patients’ experiences of caring relationships in an Iranian hospital where they found that good communication between nurses and patients was regarded as “more significant than physical care” among patients.
According to Boykins [ 10 ], effective communication is a two-way dialogue between patients and care providers. In that dialogue, both parties speak and are listened to without interrupting; they ask questions for clarity, express their opinions, exchange information, and grasp entirely and understand what the others mean. Also, Henly [ 11 ] argued that effective communication is imperative in clinical interactions. He observed that health and illness affect the quality of life, thereby making health communication critical and that the “intimate and sometimes overwhelming nature of health concerns can make communicating with nurses and other healthcare providers very challenging” [ 11 ]. Furthermore, Henly [ 11 ] added that patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns. Given the prevalence of face-to-face and device-mediated communications and interactions in healthcare settings, we must explore and clarify who, what, where, when, why, and how interactions with individuals, families, and communities are receiving care and health services [ 11 ].
The value of effective communication in nurse-patient clinical interactions cannot be overemphasized, as “research has shown that communication processes are essential to more accurate patient reporting and disclosure” [ 12 ]. Respectful communication between nurses and patients can reduce uncertainty, enhance greater patient engagement in decision making, improve patient adherence to medication and treatment plans, increase social support, safety, and patient satisfaction in care [ 12 , 13 ]. Thus, effective nurse-patient clinical communication is essential to enhancing patient-centered care and positive care outcomes.
Patient-centered communication, also known as person-centered communication or client-centered communication, is defined as a process that invites and encourages patients and their families to actively participate and negotiate in decision-making about their care needs, as cited in [ 7 ]. Patient-centered communication is crucial in promoting patient-centered care and requires that patients and their caregivers engage in the care process. As McLean [ 14 ] observed, patient-centered care can be enhanced through patient-centered communication by valuing patients’ dignity and rights. Through open communication and collaboration, where information and care plans are shared among care providers, patients, and their families, care provision becomes patient-centered [ 14 ].
Given the interconnected nature of patient-centered care and communication, we must identify the barriers and enablers of patient-centered care and communication and proposed efficient ways to enhance that because patient-centered communication is essential in achieving patient-centered care. Our aim in this paper is to identify the barriers and facilitators of patient-centered care and communication and propose and present a patient-centered care and communication continuum (PC4) Model to explain how patient-centered care can be enhanced in nurse-patient clinical interactions. As Grant and Booth argued, critical reviews are often used to present, analyse, and synthesized research evidence from diverse sources, the outcome of which is a hypothesis or a model as an interpretation of existing data to enhance evidence-based practice [ 15 ]. Thus, this critical literature review study explores the questions: what are the barriers and facilitators of patient-centered care and how can patient-centered care be enhanced through effective clinical communication?
An earlier version of this study was submitted as part of author AK’s doctoral comprehensive exams in February 2021. An interdisciplinary doctoral committee recommended many of the included literature and the questions explored in this study based on the current discourse of patient-centered care advocated for in many healthcare facilities and in recognition of the universal healthcare access objective of the health sustainable development goal. Additional searches for literature were conducted between September and November 2020 using keywords such as barriers and facilitators of nurse-patient interaction, patient-centered care, patient-centered communication , and nurse-patient communication . Databases searched included CINAHL, PubMed, Medline, and Google Scholar. Included studies in this critical review were empirical research on nurse-patient interactions in different care settings published in English and open access. All relevant articles were read, and their main findings relevant to our review questions were identified and organized into themes and subthemes discussed in this paper. Other published studies were read, and together with those that addressed the review question, a model was developed regarding how to enhance patient-centered care through effective communication.
Barriers to Patient-Centered Care and Communication
Nurses constitute a significant workforce of care providers whose practices can severely impact care outcomes (both positive and negative). Nurses spend much time with patients and their caregivers. As a result, positive nurse-patient and caregiver relationships are therapeutic and constitute a core component of care [ 9 , 13 ]. In many instances, nurses serve as translators or patients’ advocates, in addition to performing their primary care duties. Although good nurse-patient relationships positively impact nurse-patient communication and interaction, studies have shown that several factors impede these relationships with significant consequences on care outcomes and quality [ 6 , 16 , 17 ]. Thus, these barriers limit nurses’ and other care providers’ efforts to provide healthcare that meets patients’ and caregivers’ needs. We categorize the barriers to patient-centered care and communication into four kinds: institutional and healthcare system-related, communication-related, environment-related, and personal and behaviour-related barriers. Although these barriers are discussed in separate subheadings, they are interlinked in complex ways during clinical practice.
Institutional and Healthcare System Related Barriers
Many barriers to providing patient-centered care and communication during nurse-patient interactions emanate from healthcare institutional practices or the healthcare system itself. Some of these factors are implicated in healthcare policy or through management styles and strategies.
Shortage of nursing staff, high workload, burnout, and limited-time constituted one complex institutional and healthcare system-level barrier to effective care delivery [ 18 , 19 ]. For instance, Loghmani et al. [ 20 ] found that staffing shortages prevented nurses from having adequate time with patients and their caregivers in an Iranian intensive care unit. Limitations in nursing staff, coupled with a high workload, led to fewer interactions between nurses, patients, and caregivers. Similarly, Anoosheh et al. [ 16 ] found that heavy nursing workload was ranked highest as a limiting factor to therapeutic communication in nurse-patient interactions in Iran.
In a study on communication barriers in two hospitals affiliated with Alborz University of Medical Sciences, Norouzinia et al. [ 21 ] found that shortage of nurses, work overload, and insufficient time to interact with patients were significant barriers to effective nurse-patient interactions. Similar factors are identified as barriers to nurse-patient communication and interactions in other studies [ 13 , 16 , 18 ]. For instance, Amoah et al. [ 16 ] reported that nursing staff shortage and high workload were barriers to patient-centered care and therapeutic communication among Ghanaian nurses and patients. Amoah and colleagues reported a patient’s statement that:
[B]ecause there are few nurses at the ward, sometimes you would want a nurse to attend to you, but he or she might be working on another patient, so in such case, the nurse cannot divide him or herself into two to attend to you both [ 16 ].
Nurses and patients and their caregivers have noted that limited time affects nurse-patient interactions, communication, and care quality. Besides, Yoo et al. [ 22 ] reported that limited visiting hours affected communications between caregivers and nurses in a tertiary hospital in Seoul, Korea. Since the caregivers had limited time to spend with patients, they had little knowledge about the intensive care unit and distrusted the nurses.
Although nursing staff shortage is a significant barrier to patient-centered care and communication that healthcare institutions and managers must know, some healthcare scholars have critique nurses’ complaints of time limitation. For instance, McCabe [ 7 ] argued that the quality of nurse-patient interactions is what matters and not the quantity of time spent with patients and their caregivers. McCabe maintained that “spending long periods with patients does not always result in positive nurse-patient relationships” [ 7 ]. He argued that implementing patient-centered care does not require additional time; hence, nurses’ perceptions of being too busy cannot excuse poor therapeutic communication during clinical interactions. Instead, nurses are encouraged to develop self-awareness, self-reflection, and a commitment to ensuring that patients receive the needed care.
Another institution-related barrier to patient-centered care and communication is the healthcare system’s emphasis on task-centered care. Care providers are more focused on completing care procedures than satisfying patients’ and caregivers’ needs and preferences. This barrier to patient-centered care and communication is acknowledged in several studies [ 7 , 14 , 20 , 22 , 23 ]. For example, McLean [ 14 ] studied dementia care in nursing homes in the United States. She found that patient-centered care and communication in one nursing home (Snow I) were severely affected when nurses, physicians, and care managers focused on completing tasks or observing care and institutional routines to the detriment of satisfying patients’ care needs. However, in the other care home (Snow II), patient-centered care was enhanced as nurses, physicians, and the care home managers focused on addressing patients’ needs and values rather than completing care routines and tasks.
Similarly, Yoo and colleagues [ 22 ] observed that nurse-patient communication was affected when the ICU nurses placed urgency on completing tasks linked directly to patients’ health (e.g., stabilizing vital signs) than communicating to addressed patients’ specific needs. This evidence shows that when nurses are more task-focused, patients and caregivers are treated as bodies and objects, on which medical and care practices must be performed to restore health. Research has shown that when nurses focus on task-oriented care, it becomes hard to provide holistic care to patients or teach and communicate with patients even when nurses are less busy [ 20 ].
Nursing managers and their management styles can affect patient-centered care and communication. Studies have revealed that the management styles that nursing managers implement can either facilitate or impede patient-centered care [ 14 , 22 ]. When nurse managers orient their nursing staff towards task-centered care practices, it affects nurse-patient interaction and communication. Moreover, when nurse managers fail to address their staff’s mental health needs and personal challenges, it influences how nurses attend to patients’ care needs. For example, nurses have indicated that nurse-patient communication is affected when nurse managers are unsupportive or unresponsive to their needs [ 20 ].
In a study exploring nursing and midwifery managers’ perspectives on obstacles to compassion giving and therapeutic care across 17 countries, Papadopoulos et al. [ 24 ] discovered that nurses and midwifery managers’ characteristics and experiences could facilitate or impede compassion and therapeutic interactions in nursing care. Negative personal attitudes, including selfishness, arrogance, self-centeredness, rudeness, lack of leadership skills, the desire for power, and feelings of superiority among nurses and midwifery managers, were obstacles to compassion building. The study further showed that managers who emphasize rules, tasks, and results do not prioritize relationship-building and see their staff as workers rather than team members [ 24 ]. Therefore, nurse managers and care administrators must monitor nurse-patient interaction and communication to address nurses’ concerns and support them, especially in resource-constrained and high patient turnover contexts [ 25 , 26 ].
Communication-Related Barriers
Effective communication is essential to providing patient-centered care. Studies have shown that poor communication between care providers and patients and their caregivers affects care outcomes and perceptions of care quality [ 7 , 16 , 27 , 28 ]. A consistent communication-related barrier in nurse-patient interaction is miscommunication, which often leads to misunderstandings between nurses, patients, and their families [ 20 ]. Other communication-related barriers include language differences between patients and healthcare providers [ 6 , 16 , 27 ], poor communication skills, and patients’ inability to communicate due to their health state, especially in ICU, dementia, or end-of-life care contexts [ 13 , 22 ]. For instance, in their maternity care study, Madula et al. [ 6 ] noted that language barriers significantly affected effective communication between nurses/midwives and expectant mothers. A patient in their study indicated that although many nurses were polite and communicated well, some nurses had challenges communicating with patients in the Chitumbuka language, which affected those nurses’ ability to interact effectively with patients [ 6 ].
Furthermore, Norouzinia et al. [ 21 ] asserted that effective communication could not be established when nurses and patients have a language difference. Moreover, the meanings of certain non-verbal communication acts (e.g., head nodding, eye gaze, touch) can invoke different interpretations across different cultures, which could impede the interactions between patients and nurses. Even in healthcare contexts where nurses and patients speak the same language, “differences in vocabulary, rate of speaking, age, background, familiarity with medical technology, education, physical capability, and experience can create a huge cultural and communication chasm” between nurses and patients [ 12 ]. In ICU and other similar care settings, nurses find it difficult to effectively communicate with patients because the mechanical ventilators made it hard for patients to talk [ 22 ].
To overcome the communication-related barriers, healthcare institutions must make it a responsibility to engage translators and interpreters to facilitate nurse-patient interactions where a language barrier exists. Moreover, nurses working in ICU and other similar settings should learn and employ alternative forms of communication to interact with patients.
Environment-Related Barriers
The environment of the care setting can impact nurse-patient communication and the resulting care. Thus, “good health care experiences start with a welcoming environment” [ 29 ]. Mastors believed that even though good medicine and the hands working to provide care and healing to the sick and wounded are essential, we must not “forget the small things: a warm smile, an ice chip, a warm blanket, a cool washcloth. A pillow flipped to the other side and a boost in bed” [ 29 ]. The environment-related barriers are obstacles within the care setting that inhibit nurse-patient interaction and communication and may include a noisy surrounding, unkept wards, and beds, difficulties in locating places, and navigating care services. Noisy surroundings, lack of privacy, improper ventilation, heating, cooling, and lighting in specific healthcare units can affect nurse-patient communication. These can prevent patients from genuinely expressing their healthcare needs to nurses, which can subsequently affect patient disclosure or make nursing diagnoses less accurate [ 13 , 18 , 21 ]. For instance, Amoah et al. [ 16 ] revealed that an unconducive care environment, including noisy surroundings and poor ward conditions, affected patients’ psychological states, impeding nurse-patient relationships and communication. Moreover, when care services are not well-coordinated, new patients and their caregivers find it hard to navigate the care system (e.g., locating offices for medical tests and consultations), which can constrain patient-centered care and communication.
Reducing the environment-related barriers will require making the care setting tidy/clean, less noisy, and coordinating care services in ways that make it easy for patients and caregivers to access. Coordinating and integrating care services, making care services accessible, and promoting physical comfort are crucial in promoting patient-centered care, according to Picker’s Eight Principles of Patient-Centered Care [ 30 ].
Personal and Behaviour Related Barriers
The kind of nurse-patient relationships established between nurses and patients and their caregivers will affect how they communicate. Since nurses and patients may have different demographic characteristics, cultural and linguistic backgrounds, beliefs, and worldviews about health and illnesses, nurses’, patients’, and caregivers’ attitudes can affect nurse-patient communication and care outcomes. For instance, differences in nurses’ and patients’ cultural backgrounds and belief systems have been identified as barriers to therapeutic communication and care [ 12 , 13 , 21 ]. Research shows that patients’ beliefs and cultural backgrounds affected their communication with nurses in Ghana [ 16 ]. These scholars found that some patients refused a blood transfusion, and Muslim patients refused female nurses to attend to them because of their religious beliefs [ 16 ]. Further, when nurses, patients, or their caregivers have misconceptions about one another due to past experiences, dissatisfaction about the care provided, or patients’ relatives and caregivers unduly interfere in the care process, nurse-patient communication and patient-centered care were affected [ 16 , 21 ].
Similarly, nurse-patient communication was affected when patients or caregivers failed to observe nurses’ recommendations or abuse nurses due to misunderstanding [ 20 ], while patients’ bad attitudes or disrespectful behaviours towards nurses can inhibit nurses’ ability to provide person-centered care [ 31 ]. The above-reviewed studies provided evidence on how patients’ and caregivers’ behaviours can affect nurses’ ability to communicate and deliver patient-centered care.
On the other hand, nurses’ behaviours can also profoundly affect communication and care outcomes in the nurse-patient dyad. When nurses disrespect, verbally abuse (e.g., shouting at or scolding), and discriminate against patients based on their social status, it affects nurse-patient communication, care outcomes, and patient disclosure [ 6 , 32 ]. For instance, Al-Kalaldeh et al. [ 18 ] believe that nurse-patient communication is challenged when nurses become reluctant to hear patients’ feelings and expressions of anxiety. When nurses ignore patients’ rights to share ideas and participate in their care planning, such denials may induce stress, discomfort, lack of trust in nurses, thereby leading to less satisfaction of care [ 18 ].
Furthermore, when nurses fail to listen to patients’ and caregivers’ concerns, coerce patients to obey their rules and instructions [ 16 , 17 , 20 ], or fail to provide patients with the needed information, nurse-patient communication and patient-centered care practices suffer. To illustrate, in Ddumba-Nyanzia et al.‘s study on communication between HIV care providers and patients, a patient remarked that: “I realized no matter how much I talked to the counselor, she was not listening. She was only hearing her point of view and nothing else, [and] I was very upset” [ 17 ]. This quote indicates how care provider attitudes can constrain care outcomes. Due to high workload, limited time, poor remunerations, and shortage of personnel, some nurses can develop feelings of despair, emotional detachment, and apathy towards their job, which can lead to low self-esteem or poor self-image, with negative consequences on nurse-patient interactions [ 13 , 18 ].
Given the significance of effective communication on care, overcoming the above personal and behaviour related barriers to patient-centered care and communication is crucial. Nurses, patients, and caregivers need to reflect on the consequences of their behaviours on the care process. Thus, overcoming these barriers begins with embracing the facilitators of patient-centered care and communication, which we turn to in the next section.
Facilitators of patient-centered care and communication
Patient-centered care and communication can be facilitated in several ways, including building solid nurse-patient relationships.
First, an essential facilitator of patient-centered care and communication is overcoming practical communication barriers in the nurse-patient dyad. Given the importance of communication in healthcare delivery, nurses, patients, caregivers, nursing managers, and healthcare administrators need to ensure that effective therapeutic communication is realized in the care process and becomes part of the care itself. Studies have shown that active listening among care providers is essential to addressing many barriers to patient-centered care and communication [ 7 , 13 ]. Although handling medical tasks promptly in the care process is crucial, the power of active listening is critical, meaningful, and therapeutic [ 22 ]. By listening to patients’ concerns, nurses can identify patients’ care needs and preferences and address their fears and frustrations.
Another facilitator of patient-centered care is by understanding patients and their unique needs [ 25 ], showing empathy and attending attitudes [ 7 , 13 ], expressing warmth and respect [ 22 ], and treating patients and caregivers with dignity and compassion as humans. For instance, McCabe [ 7 ] noted that attending, which obligates nurses to demonstrate that they are accessible and ready to listen to patients, is a patient-centered care process; a fundamental requirement for nurses to show genuineness and empathy, despite the high workload. Showing empathy, active listening, respect, and treating patients with dignity are core to nursing and care, and recognized in the Code of Ethics for Nurses [ 33 ], and further emphasized in the ongoing revision of the Code of Ethics for nurses [ 34 ].
Besides, engaging patients and caregivers in the care process through sharing information, inviting their opinion, and collaborating with them constitutes another facilitator of patient-centered care and communication. When patients and caregivers are engaged in the care process, misunderstandings and misconceptions are minimized. When information is shared, patients and caregivers learn more about their health conditions and the care needed. As McLean [ 14 ] argued, ensuring open communication between care providers and patients and their families is essential to enhancing patient-centered care. Conflicts ensue when patients or their families are denied information or involvement in the care process. As a result, the Harvard Medical School [ 30 ] identified patient engagement, information sharing, and nurse-patient collaboration during care as essential patient-centered care principles.
Finally, health policy must be oriented towards healthcare practices and management to facilitate patient-centered care and communication. These policies, at a minimum, can involve changes in management styles within healthcare institutions, where nurse managers and healthcare administrators reflect on nursing and care practices to ensure that the Code of Ethics of Nurses and patients’ rights are fully implemented. Resource constraints, staff shortages, and ethical dilemmas mainly affect care practices and decision-making. Nonetheless, if patients are placed at the center of care and treated with dignity and respect, most of the challenges and barriers of patient-centered care will diminish. Empowering practicing nurses, equipping them with interpersonal communication skills through regular in-service training, supporting them to overcome their emotional challenges, and setting boundaries during nurse-patient interactions will enhance patient-centered care practices.
In line with the above discussion, Camara et al. [ 25 ] identify three core dimensions that nurses, patients, and caregivers must observe to enhance patient-centered care: treating the patient as a person and seeing the care provider as a person and a confidant. Regarding the first dimension, care providers must welcome patients, listen to them, share information with them, seek their consent, and show them respect when providing care. The second dimension requires that the healthcare provider be seen and respected as a person, and negative perceptions about care providers must be demystified. According to Camara et al. [ 25 ], care providers must not overemphasize their identities as experts but rather establish good relationships with patients to understand patients’ personal needs and problems. Lastly, patients and caregivers must regard care providers as confidants who build and maintain patients’ trust and encourage patients’ participation in care conversations. With this dimension, patients and caregivers must know that nurses and other care providers have the patient at heart and work to meet their care needs and recovery process.
Camara et al.‘s [ 25 ] three dimensions are essential and position patients, their caregivers, and nurses as partners who must engage in dialogic communication to promote patient-centered care. As a result, effective communication, education, and increased health literacy among patients and caregivers will be crucial in that direction.
Enhancing Patient-Centered Care and Communication: A Proposed Model
Nursing care practices that promote patient-centered communication will directly enhance patient-centered care, as patients and their caregivers will actively engage in the care process. To enhance patient-centered communication, we propose person-centered care and communication continuum (PC4) as a guiding model to understand patient-centered communication, its pathways, and what communication and care practices healthcare professionals must implement to achieve person-centered care. In this PC4 Model, we emphasize the person instead of the patient because they are a person before becoming a patient. Moreover, the PC4 Model is supposed to apply to all persons associated with patient care; thus, respect for the dignity of their personhood is crucial.
Although much is written about patient-centered communication in the healthcare literature, there is a gap regarding its trajectory and what communication content enhances patient-centered communication. Also, little is known about how different clinical discourse spaces influence communication and its content during nurse-patient clinical interactions. Using evidence from Johnsson et al. [ 3 ], Murira et al. [ 23 ], and Liu et al. [ 35 ], among other studies, we outline the components of the PC4 Model and how different discourse spaces in the clinical setting and the content of communication impact patient-centered care and communication.
The proposed PC4 Model in this paper has three unbounded components based on the purpose of and how communication is performed among care providers, patients, and their caregivers. Figure 1 illustrates the PC4 Model, its features, and trajectory.
A Person-Centered Care and Communication Continuum (PC4 Model)
Task-Centered Communication
At the lowest end of the PC4 Model is task-centered communication. Here, the care provider’s role is to complete medical tasks as fast as possible with little or no communication with the patient and their caregivers. Patients and caregivers are treated as bodies or objects whose disease symptoms need to be studied, identified, recorded, treated, or cured. As Johnsson et al. [ 3 ] observed, communication content at this stage is mainly biomedically oriented, where nurses and other healthcare professionals focus on the precise medical information (e.g., history taking, medical examination, test results, medication, etc.) about the patient. With a task-centered orientation, nurses make journal entries about their patients’ disease state and ensure that treatment plans, diagnostic tests, and medical prescriptions are completed. Communication at this stage is often impersonal or rigid (see [ 23 ] for details). Care providers may address patients and their caregivers by using informal attributes (e.g., bed 12, the woman in the red shirt, card 8, etc.), thereby ignoring patients’ and caregivers’ personal and unique identities. Patients’ and caregivers’ nonverbal communication signs are mostly overlooked.
Motivations for task-centered communication can be attributed to time limitation, high workload, and staff shortage, thereby pushing nurses and other care providers to reach as many patients as possible. Moreover, the healthcare system’s orientation towards and preference for biomedically-focused care seems to favour task-centered communication [ 7 , 14 ].
Depending on the clinical discourse space under which patient-provider interactions occur, different forms of communication are employed. Clinical discourse spaces can be public (e.g., in the ward, patient bedside), private (e.g., consulting rooms, medical test labs, nurse staff station, etc.), or semi-private (e.g., along the corridor) [ 35 ]. In these clinical discourse spaces, nurse-patient communication can be uninformed (patients or caregivers are not informed about patients’ care conditions or why specific data and routines are performed). It can be non-private (others can hear what the nurse and patient are talking about) or authoritative (care providers demonstrate power and control and position themselves as experts) [ 23 ]. Finally, in task-centered communication, healthcare providers often use medical jargon or terminologies [ 3 ] since the goal of communication is not to engage the patient in the process. Usually, patients or their caregivers are not allowed to ask questions, or their questions get ignored or receive superficial, incomprehensible responses.
Process-Centered Communication
Process-centered communication is an intermediate stage on the continuum, which could slip back into the task-centered or leap forward into person-centered communication. Through process-centered communication, care providers make an effort to know patients and their caregivers as they perform care routines. Care providers ask patients or their caregivers questions to understand the care conditions but may not encourage patients or caregivers to express their thoughts about their care needs. Patients and caregivers are recognized as persons with uniques care needs but may not have the agency to influence the care process. Care providers may chit-chat with patients or their caregivers to pass the time as they record patients’ medical records or provide care. Unlike task-centered communication, there is informative and less authoritative communication between nurses and patients and their caregivers. The goal of process-centered communication could be a mixture of instrumental and relational, with less display of power and control by nurses.
Person-Centered Communication
This is the highest point of the PC4 Model, where patient-centered care is actualized. At this stage of the communication continuum, patients and caregivers are treated as unique persons with specific care needs and are seen as collaborators in the care process. As McLean [ 14 ] observed, caregiving becomes a transactional relationship between the care provider and receiver at the person-centered stage of the continuum. The care itself becomes intersubjective, a mutual relational practice, and an ongoing negotiation for care providers and receivers [ 14 ].
The content of communication at this stage of the continuum is both “personal” and “explanatory” [ 3 ]. Nurses and other healthcare providers create meaningful relationships with patients and their caregivers, understand patients’ concerns, needs, and problems, use open-ended questions to encourage patients or caregivers to express their thoughts and feelings about the care situation. Nurses and other healthcare professionals explain care routines, patients’ health conditions, and management plans in lay language to patients and caregivers through person-centered communication. Accomplishing this level includes employing alternative forms of communication to meet the needs of intensive care unit patients, deaf patients, and ventilated and intubated patients. For instance, it has been shown that “deaf people […] frequently do not have access to clear and efficient communication in the healthcare system, which deprives them of critical health information and qualified health care” [ 36 ]. Empathetic communication practices, including active listening, showing genuine interest in patients’ care, and respect and warmth, become a significant part of nursing care [ 3 , 7 , 14 , 22 ].
Different communication strategies are employed based on the care situation and context. Chit-chatting, as a form of personal communication [ 3 ], use of humor as a communication strategy [ 7 , 8 ], and even maintaining silence [ 28 ] are essential in enhancing person-centered care and communication. Both care providers and patients or their caregivers use relationship-building and -protecting humor (see [ 28 ] for details) to address difficult situations in the care process.
Implications of the PC4 Model for Nursing Practice
Given the values of effective communication in nurse-patient interactions and care outcomes, nurses and other healthcare providers must ensure that they develop therapeutic relationships with patients, their families, and caregivers to promote person-centered care and communication. Achieving that begins with knowing and reflecting on the barriers of therapeutic communication and ways to minimize them. The PC4 Model draws nurses and all healthcare providers’ attention to patient-centered care pathways and how effective communication is necessary. Healthcare professionals, including nurses, must be aware of how their communication orientation–––either oriented toward completing tasks, following care processes or toward addressing patients’ and their caregivers’ needs––can impact patient-centered care. Healthcare providers must observe the care context, patients’ unique situations, their non-verbal language and action, and whether they belong to historically marginalized groups or cultures.
Mastors [ 29 ] has offered healthcare providers some guidance to reflect on as they communicate and interact with patients and caregivers. Thus, (a) instead of asking patients, “What’s the matter?“ care providers must consider asking them, “What’s important to you?“ With this question, the patient is given a voice and empowered to contribute to their own care needs. Care providers should (b) check with patients in the waiting room to update patients whose waiting time has been longer than usual, based on the care context. They should also (c) try to remember their conversations with patients to build on them during subsequent interactions. This continuity can be enhanced by nurse managers reexamining how they deploy care providers to patients. The same nurse can be assigned to the same patients for the duration of the patient’s stay to help patients feel valued and visible [ 29 ].
Knowledge of cultural competence, sensitivity, humility, and interpersonal communication skills will help achieve and implement the PC4 Model. As Cuellar [ 37 ] argues, “[h]umility is about understanding and caring for all people [and] being empathetic.“ Cultural competence is a “dynamic process of acquiring the ability to provide effective, safe, and quality care to the patients through considering their different cultural aspects” [ 38 ]. The concept of cultural competence entails “cultural openness, awareness, desire, knowledge and sensitivity” during care [ 39 ]. It demands that care providers respect and tailor care to align with patients’ and caregivers’ values, needs, practices, and expectations, based on care and moral ethics and understanding [ 39 ]. Active listening and showing compassion as therapeutic relationship-building skills are essential, and continuous education and mentorship will be crucial to developing these skills among healthcare providers.
We invite qualitative and quantitative studies, especially on language use and communication strategies, to explore and evaluate the PC4 Model. Providing in-depth and experiential data on ways to increase its effectiveness as a tool to guide healthcare providers is highly desired. More knowledge can support healthcare providers in offering evidence-based patient-centered care in different healthcare settings and units.
Conclusions
Effective communication is an essential factor in nurse-patient interactions and a core component of nursing care. When communication in the nurse-patient dyad is patient-centered, it becomes therapeutic. It allows for trust and mutual respect in the care process, thereby promoting care practices that address patients’ and caregivers’ needs, concerns, and preferences. We have identified the barriers and facilitators of patient-centered care and communication and proposed a person-centered care and communication continuum (PC4 Model) to demonstrate how patient-centered communication intersects with patient-centered care.
Availability of data and materials
Not applicable.
Abbreviations
Intensive Care Unit
Institution of Medicine
Person-Centered Care and Communication Continuum
Etheredge HR. “Hey sister! Where’s my kidney?“ Exploring ethics and communication in organ transplantation in Gauteng, South Africa, Ph.D. dissertation, Johannesburg. University of the Witwatersrand; 2015.
Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. National Academy Press; 2001.
Johnsson A, Wagman P, Boman A, Pennbrant S. What are they talking about? Content of the communication exchanges between nurses, patients and relatives in a department of medicine for older people: An ethnographic study. J Clin Nurs. 2018 Apr;27(7–9):e1651-9. doi: https://doi.org/10.1111/jocn.14315 .
Long KA. The Institute of Medicine report on health professions education: A bridge to quality. Policy Polit Nurs Pract. 2003 Nov;4(4):259–62. doi: https://doi.org/10.1177/1527154403258304 .
Crawford T, Candlin S, Roger P. (2017). New perspectives on understanding cultural diversity in nurse-patient communication. Collegian, 2017 Feb 1;24(1):63 – 9. https://doi.org/10.1016/j.colegn.2015.09.001 .
Madula P, Kalembo WF, Yu H, Kaminga CA. Healthcare provider-patient communication: A qualitative study of women’s perceptions during childbirth. Reprod Health. 2018 Dec;15(135):1–10. https://doi.org/10.1186/s12978-018-0580-x .
McCabe C. Nurse-patient communication: An exploration of patients’ experiences. J Clin Nurs. 2004 Jan;13(1):41–9.
Schöpf AC, Martin GS, Keating MA. Humor as a communication strategy in provider-patient communication in a chronic care setting. Qual Health Res. 2017 Feb;27(3):374–90. doi: https://doi.org/10.1177/1049732315620773 .
Joolaee S, Joolaei A, Tschudin V, Bahrani N, Nikbakht NA. Caring relationship: the core component of patients’ rights practice as experienced by patients and their companions. J Med Ethics Hist Med. 2010;3(4):1–7.
Google Scholar
Boykins AD. Core communication competences in patient-centered care. The ABNF J. 2014 Apr 1;25(2):40 – 5.
Henly SJ. Health communication research for nursing science and practice. Nurs Res [Editorial] 2016:257–8. doi: https://doi.org/10.1097/NNR.0000000000000171 .
Ruben BD. Communication theory and health communication practice: The more things change, the more they stay the same. Health Commun. 2016 Jan 2;31(1):1–11. doi: https://doi.org/10.1080/10410236.2014.923086 .
Bello P. Effective communication in nursing practice: A literature review. BSc Nursing Thesis. Arcada; 2017. Available at https://core.ac.uk/download/pdf/84798372.pdf Accessed 20 Jan 2021.
McLean A. The person in dementia: A study of nursing home care in the US. Toronto, University of Toronto Press; 2007.
Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libraries J. 2009;26:91–108. Doi: https://doi.org/10.1111/j.1471-1842.2009.00848.x .
Article Google Scholar
Amoah KMV, Anokye R, Boakye SD, Acheampong E, Budu-Ainooson A, Okyere E, Kumi-Boateng G, Yeboah C, Afriyie OJ. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nurs. 2019 Dec;18(4)1–8. https://doi.org/10.1186/s12912-019-0328-0 .
Ddumba-Nyanzia I, Kaawa-Mafigiria D, Johannessen H. Barriers to communication between HIV care providers (HCPs) and women living with HIV about childbearing: A qualitative study. Patient Educ Couns. 2016 May 1:99(5):754–9. https://doi.org/10.1016/j.pec.2015.11.023 .
Al-Kalaldeh M, Amro N, Qtait M. Barriers to effective nurse-patient communication in the emergency department. Emerg Nurse. 2021 Mar 2;29(2). doi: https://doi.org/10.7748/en.2020.e1969 .
Sethi D, Rani MK. Communication barrier in health care setting as perceived by nurses and patient. Int J Nurs Educ 2017 Oct. 2016;9(4):30. doi: https://doi.org/10.5958/j.2320-8651.2.1.001 .
Loghmani L, Borhani F, Abbaszadeh A. Factors affecting the nurse-patients’ family communication in intensive care unit of Kerman: A qualitative study. J Caring Sci. 2014 Mar;3(1):67–2. doi: https://doi.org/10.5681/jcs.2014.008 .
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2016 Jun;8(6):65–4. https://doi.org/10.5539/gjhs.v8n6p65 .
Yoo HJ, Lim OB, Shim JL. Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study. PLoS One. 2020 Jul 9;15(7):e0235694. https://doi.org/10.1371/journal.pone.0235694 .
Murira N, Lützen K, Lindmark G, Christensson K. Communication patterns between healthcare providers and their clients at an antenatal clinic in Zimbabwe. Health Care Women Int. 2003 Feb 1;24(2):83 – 2. https://doi.org/10.1080/07399330390170060 .
Papadopoulos I, Lazzarino R, Koulouglioti C, Aagard M, Akman O, Alpers L-M, Apostolara P, Araneda Bernal J, Biglete-Pangilinan S, Eldar-Regev O, Gonzalez-Gil MT, Kouta C, Zorba A. Obstacles to compassion-giving among nursing and midwifery managers: An international study. Int Nurs Rev. 2020 Aug;11:1–13.
Camara BS, Belaid L, Manet H, Kolie D, Guilard E, Bigirimana T, Delamou A. What do we know about patient-provider interactions in sub-Saharan Africa? A scoping review. Pan Afr Med J. 2020;88(88):1–13. doi: https://doi.org/10.11604/pamj.2020.37.88.24009 .
Kwame A, Petrucka PM. Communication in nurse-patient interaction in healthcare settings in sub-Saharan Africa: A scoping review. Int J Afr Nurs Sci. 2020 Jan 1;12:100198. https://doi.org/10.1016/j.ijans.2020.100198 .
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009 Jun;56(2):243–9.
Vuković M, Gvozdenović BS, Stamatović-Gajić B, Ilić M, Gajić T. Development and evaluation of the nurse quality of communication with patient questionnaire. Srp Arh Celok Lek. 2010;138(1–2):79–4. doi: https://doi.org/10.2298/SARH1002079V .
Article PubMed Google Scholar
Mastors P. (2018). What do patients want, need, and have the right to expect? Nurs Adm Q. 2018 Jul 1;42(3):192-8. doi: https://doi.org/10.1097/NAQ.0000000000000297 .
Harvard Medical School. The Eight Principles of Patient Centered Care; 2015 Nov 18. Available from OneView: https://www.oneviewhealthcare.com/the-eight-principles-of-patient-centered-care/ Accessed 28 Dec 2020.
White J, Phakoe M, Rispel LC. ‘Practice what you preach’: Nurses’ perspectives on the Code of Ethics and Service Pledge in five South African hospitals. Glob Health Action. 2015 Dec 1;8(1):26341. https://doi.org/10.3402/gha.v8.26341 .
Kruger L-M, Schoombee C. The other side of caring: abuse in a South African maternity ward. J Reprod Infant Psychol. 2010 Feb 1;28(1):84–101. doi: https://doi.org/10.1080/02646830903294979 .
International Council of Nurses. ICN Code of Ethics for Nurses; 2012. Available from www.icn.ch/images/stories/documents/about/icncode_english.pdf . Accessed 20 Dec 2020.
Stievano A, Tschudin V. The ICN code of ethics for nurses: A time for revision. Nurs Health Policy Perspect. 2019 Jun;66(2):154–6.
Liu W, Manias E, Gerdtz M. Medication communication during ward rounds on medical wards: Power relations and spatial practices. Health 2012 Mar. 2012;17(2):113–34. doi: https://doi.org/10.1177/1363459312447257 .
Hoglind TA. Healthcare language barriers affect deaf people, too. 2018 Oct 11. Retrieved from Boston University [BU] School of Public Health: Available from https://www.bu.edu/sph/news/articles/2018/healthcare-language-barriers-affect-deaf-people-too/ Accessed 15 Jan 2021.
Cuellar NG. Humility. A concept in cultural sensitivity. JTranscult Nurs [Editorial]. 2018 Apr 26; 29(4):317. https://doi.org/10.1177/1043659618772384 .
Sharifi N, Adib-Hajbaghery M, Najafi M. Cultural competence in nursing: A concept analysis. Int J Nurs Stud. 2019 Nov 1;99(103386):1–8. https://doi.org/10.1016/j.ijnurstu.2019.103386 .
Henderson S, Horne M, Hills R, Kendall E. Cultural competence in healthcare in the community: A concept analysis. Health Soc Care Community. 2018 Jul;26(4):590–603. doi: https://doi.org/10.1111/hsc.12556 .
Download references
Acknowledgments
We express our gratitude to the first author’s doctoral committee members for their valuable comments, suggestions, and critique of an earlier version of this paper. We are also grateful to the anonymous reviewers for the insightful comments and suggestions that have helped us improve the study’s quality.
Authors' information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan, interested in patients' rights in nurse-patient clinical communications and interactions in the hospital setting. He holds two Master of Philosophy degrees in Indigenous Studies and English Linguistics. Abukari's research interests include language use in social interaction, health communication, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is a professor in Nursing and has international research experience with many of her graduate students from Africa, Asia, and the Caribbean. Pammla has published extensively in the field of nursing. Her research interests are vast, including child and maternal health, Indigenous peoples' health, global health, and vulnerable populations, with extensive experiences in qualitative research and indigenous research methodologies. Pammla is co-editor of the BMC Nursing journal and a reviewer for many other academic journals.
The authors have not received any funding for the conduct, preparation, and publication of this paper.
Author information
Authors and affiliations.
College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Abukari Kwame
College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Pammla M. Petrucka
You can also search for this author in PubMed Google Scholar
Contributions
Both authors conceived the topic. PMP recommended the literature, AK searched and added more sources, and drafted the paper. PMP reviewed the paper for intellectual content. Both AK and PMP read and approved the final version.
Corresponding author
Correspondence to Abukari Kwame .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kwame, A., Petrucka, P.M. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs 20 , 158 (2021). https://doi.org/10.1186/s12912-021-00684-2
Download citation
Received : 05 May 2021
Accepted : 18 August 2021
Published : 03 September 2021
DOI : https://doi.org/10.1186/s12912-021-00684-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient-centered care
- Therapeutic communication
- Nurse-patient interactions
- Clinical discourse space
- Patient-centered care and communication continuum
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 29 May 2024
The implementation of person-centred plans in the community-care sector: a qualitative study of organizations in Ontario, Canada
- Samina Idrees 1 ,
- Gillian Young 1 ,
- Brian Dunne 2 ,
- Donnie Antony 2 ,
- Leslie Meredith 1 &
- Maria Mathews 1
BMC Health Services Research volume 24 , Article number: 680 ( 2024 ) Cite this article
409 Accesses
2 Altmetric
Metrics details
Person-centred planning refers to a model of care in which programs and services are developed in collaboration with persons receiving care (i.e., persons-supported) and tailored to their unique needs and goals. In recent decades, governments around the world have enacted policies requiring community-care agencies to adopt an individualized or person-centred approach to service delivery. Although regional mandates provide a framework for directing care, it is unclear how this guidance is implemented in practice given the diversity and range of organizations within the sector. This study aims to address a gap in the literature by describing how person-centred care plans are implemented in community-care organizations.
We conducted semi-structured interviews with administrators from community-care organizations in Ontario, Canada. We asked participants about their organization’s approach to developing and updating person-centred care plans, including relevant supports and barriers. We analyzed the data thematically using a pragmatic, qualitative, descriptive approach.
We interviewed administrators from 12 community-care organizations. We identified three overarching categories or processes related to organizational characteristics and person-centred planning: (1) organizational context, (2) organizational culture, and (3) the design and delivery of person-centred care plans. The context of care and the types of services offered by the organization were directly informed by the needs and characteristics of the population served. The culture of the organization (e.g., their values, attitudes and beliefs surrounding persons-supported) was a key influence in the development and implementation of person-centred care plans. Participants described the person-centred planning process as being iterative and collaborative, involving initial and continued consultations with persons-supported and their close family and friends, while also citing implementation challenges in cases where persons had difficulty communicating, and in cases where they preferred not to have a formal plan in place.
Conclusions
The person-centred planning process is largely informed by organizational context and culture. There are ongoing challenges in the implementation of person-centred care plans, highlighting a gap between policy and practice and suggesting a need for comprehensive guidance and enhanced adaptability in current regulations. Policymakers, administrators, and service providers can leverage these insights to refine policies, advocating for inclusive, flexible approaches that better align with diverse community needs.
Peer Review reports
The community-care sector facilitates the coordination and administration of in-home and community-based health and social services. Community-care services include supports for independent living, residential services, complex medical care, and community-participation services to support personal and professional goals (e.g., education, employment, and recreation-based supports) [ 1 ]. There is substantial heterogeneity in the clinical and demographic characteristics of the community-care population, including individuals with physical and developmental disabilities, and complex medical needs [ 2 ]. We refer to the individuals served by these organizations as ‘persons-supported’ in line with person-first language conventions [ 3 , 4 ].
In recent decades, governments across the world have enacted policies requiring community-care agencies to adopt an individualized or person-centred approach to service delivery [ 5 , 6 , 7 , 8 ]. Person-centred care encompasses a broad framework designed to direct care delivery, as opposed to a singular standardized process. In the context of community-care, person-centred planning refers to a model of care provision in which programs and services are developed in collaboration with persons-supported and tailored to their unique needs and desired outcomes [ 9 , 10 ].
In Ontario, Canada, community-care services are funded by the Ministry of Health (MOH) and the Ministry of Children, Community and Social Services (MCCSS). Service agreements between these ministries and individual agencies can be complex and contingent on different factors including compliance with a number of regulatory items and policies [ 7 , 11 ]. MOH provides funding for health-based services including in-home physiotherapy, respiratory therapy, and personal support services, among several others. MOH funds Home and Community Care Support Services (HCCSS), a network of organizations responsible for coordinating the delivery of in-home and community-based care in the province. MCCSS funds social service agencies including those providing community participation and residential support for people with intellectual and developmental disabilities (IDDs).
Several tools and resources have been developed to aid organizations in providing person-centred care and organizations may differ in their use of these tools and their specific approach. Although regional mandates provide a framework for directing care delivery, it is unclear how this guidance is implemented in practice given the diversity and range of organizations within the sector. In addition, as noted by a recent scoping review, there is limited literature on the implementation process and impact of person-centred planning on individual outcomes [ 12 ]. Using a pragmatic, qualitative, descriptive approach [ 13 ], we outline how community-care organizations enact a person-centred approach to care and the factors that shape their enactment. By describing existing practices in the context of the community-care sector, we aim to provide insight on how to optimize care delivery to improve outcomes and inform current policy. This study is part of a larger, multi-methods project examining the implementation of person-centred care plans in the community-care sector. This project encompasses qualitative interviews with representatives from different community-care organizations, as well as staff and persons-supported at a partner community-care organization. This paper focuses on analyzing data from interviews with representatives from different community-care organizations.
We conducted semi-structured interviews with administrators from community-care organizations in Southwestern Ontario (roughly the Ontario Health West Region) between October 2022 and January 2023. We included community-care organizations funded by MOH or MCCSS. We excluded organizations that did not provide services in Southwestern Ontario. We identified eligible organizations and participants by searching online databases, including community resource lists, as well as through consultation with members of the research team.
We used maximum variation sampling [ 14 ], to recruit participants from organizations with a wide range of characteristics including location (i.e., urban, rural), organization type (i.e., for-profit, not-for-profit), and types of services provided (e.g., residential, recreation, transportation, etc.) We contacted eligible organizations via email, providing them with study information and inviting them to participate. We recruited until the data reached saturation, defined as the point at which there was sufficient data to enable rigorous analysis [ 14 , 15 ].
In each interview, we asked participants about their organization’s approach to developing and updating individual service agreements or person-centred care plans, and the supports and barriers (e.g., organizational, funding, staffing, etc.) that facilitate or hinder the implementation of these plans (Supplementary Material 1 : Interview Guide). We also collected information on relevant participant and organizational characteristics, including participant gender, position, years of experience, organization location, type (i.e., for-profit, not-for-profit), services offered, years in operation, and client load. The interviews were approximately one hour in length and conducted virtually via Zoom (Zoom Video Communications Inc.) or by telephone. The interviews were audio-recorded and transcribed verbatim. Interviewer field notes were also used in data analysis.
We analyzed the data thematically [ 16 ]. The coding process followed a collaborative and multi-step approach. Initially, three members of the research team independently reviewed and coded a selection of transcripts to identify key ideas and patterns in the data, and form a preliminary coding template. We then met to consolidate individual coding efforts. We compared coding of each transcript, resolving conflicts through discussion and consensus. In coding subsequent transcripts and through a series of meetings, we worked together to finalize the codebook to reflect more analytic codes. We used the finalized template to code all interview transcripts in NVivo (QSR International), a software designed to facilitate qualitative data analysis. We refined the codebook on an as-needed basis by incorporating novel insights gleaned from the coding of additional transcripts, reflecting the iterative nature of the analysis.
We increased the robustness of our methodology by pre-testing interview questions, documenting interview and transcription protocols, using experienced interviewers, and confirming meaning with participants in interviews [ 14 , 15 , 16 ]. We kept detailed records of interviews, field notes, and drafts of the coding template. We made efforts to identify negative cases and provided rich descriptions and illustrative quotes [ 17 ]. We included individuals directly involved in the administration of community-care services on our research team. These individuals provided important context and feedback at each stage of the research process.
This study was approved by the research ethics board at Western University. We obtained informed consent from participants prior to the onset of interviews. We maintained confidentiality through secure storage of interview data (e.g., audio recordings), password-protection of sensitive documents, and the de-identification of transcripts.
Positionality
The authors represent a multidisciplinary team of researchers, clinicians, and community-care leaders. The community-care leaders and clinicians on our team provided key practical expertise to inform the development of interview questions and the analysis of study findings.
We interviewed administrators across 12 community-care organizations in Southwestern Ontario. The sample included representatives from seven organizations that received funding from MCCSS, three organizations that received funding from MOH, and two organizations that received funding from both MCCSS and MOH (Table 1 ). Eleven organizations were not-for-profit, one was a for-profit agency. The organizations provided care in rural ( n = 3), urban ( n = 4), or both rural and urban populations ( n = 5). Seven of the 12 participants were women, nine had been working with their organization for more than 11 years, and all had been working in the community-care sector for more than 12 years (Table 2 ).
We identified three key categories or processes relating to organizational characteristics and their impact on the design and delivery of person-centred care plans: (1) organizational context, (2) organizational culture, and (3) the development and implementation of person-centred care plans.
Organizational context
Organizational context refers to the characteristics of persons-supported, and the nature of services provided. Organizational context accounts for the considerable heterogeneity across organizations in the community-care sector and their approach to person-centred care plans.
Populations served
The majority of organizations included in the study supported individuals with IDDs: “all of the people have been identified as having a developmental disability. That’s part of the eligibility criteria for any funded developmental service in Ontario.” [P10]. Participants described how eligibility was ascertained through the referral process: “ the DSO [Developmental Services Ontario] figures all of that out and then refers them to us .” [P08]. These descriptions highlighted a common access point for publicly-funded adult developmental services in the province. Accordingly, these organizations were primarily funded by MCCSS. Other organizations focused on medically complex individuals including those with acquired brain injuries or those unable to access out-patient services due to physical disabilities: “the typical reason for referral is going to be around a physical impairment… But, with this medically complex population, you’re often seeing comorbidities where there may be some cognitive impairment, early dementia.” [P04]. In these organizations, eligibility and referral were usually coordinated by HCCSS. These insights highlighted the diverse characteristics of community-care populations, emphasizing the need to consider both physical and cognitive health challenges in care provision approaches.
Services offered
The characteristics of persons-supported informed the context of care and the type of services offered by the organization. The different dimensions of services offered within this sector include social and medical care, short and long-term care provision, in-home and community-care, and full and part-time care.

Nature of care: social vs. medical
Many organizations serving individuals with IDDs employed a holistic, psychosocial model of care, designed to support all areas of an individual’s life including supports for independent-living, and community-based education, employment, and recreation services to support personal and professional goals: “we support people in their homes, so residential supports. We also support people in the community, to be a part of the community, participate in the community and also to work in the community.” [P06]. These descriptions reflect a comprehensive approach to care, aiming to address needs within and beyond residential settings to promote active participation within the broader community. In contrast, some organizations followed a biomedical model of care, designed to support specific health needs: “We provide all five therapies… physiotherapy, occupational therapy, speech, social work, and nutrition. In some locations we provide visiting nursing, at some locations shift nursing. We have some clinic-nursing… and we provide personal support and home-making services in a number of locations as well.” [P04]. These organizations adopted a more clinically-focused approach to care. In either instance, the care model and the nature of services offered were largely determined by an organization’s mandate including which gaps they aimed to fill within the community. Many organizations described providing a mixture of social and medical care for individuals with complex needs. However, the implementation of care plans could be impacted by the lack of integration between social and medical care sectors, as some participants spoke to the importance of “[integrating] all of the different healthcare sector services… [including] acute care and public health and home and community care and primary care, and mental health and addictions.” [P04].
Duration of care: short-term vs. long-term
The duration of care also varied based on the needs of persons-supported. Organizations serving individuals with IDDs usually offered support across the lifespan: “We support adults with developmental disabilities and we support them from 18 [years] up until the end of their life.” [P06]. Some organizations provided temporary supports aimed at addressing specific health needs: “For therapies – these are all short-term interventions and typically they’re very specific and focused on certain goals. And so, you may get a referral for physiotherapy that is authorized for three visits or five visits” [P04], or crisis situations (e.g., homelessness): “Our services are then brought in to help provide some level of support, guidance, stabilization resource, and once essentially sustainability and positive outcomes are achieved—then our services are immediately withdrawn.” [P12]. One organization employed a model of care with two service streams, an initial rehabilitation stream that was intended to be short-term and an ongoing service stream for individuals requiring continuing support.
In-home vs. community-based care
Many organizations provided in-home care and community-based supports, where residential supports were designed to help individuals lead independent lives, and community-based supports encouraged participation in community activities to further inclusion and address personal and professional goals. One participant spoke about the range of services offered in the home and community:
“There’s probably two big categories of [services we offer]: community support services—so that includes things like adult day programs, assisted living, meals on wheels, transportation, friendly visiting … and things like blood pressure clinics, exercise programs… and then on the other side we do home care services. In the home care basket, we provide personal support, and we also provide social work support.” [P05].
Likewise, another participant spoke in further detail on the types of services that allow individuals to live independently within their homes, or in community-based residential settings (e.g., long-term care facilities):
“We provide accommodation supports to about 100 people living in our community—which means that we will provide support to them in their own homes. So, anywhere from an hour a week to 24 hours a day. And that service can include things from personal care to home management to money management, cooking, cleaning, and being out and about in communities—so community participation. We also provide supports for about 50 people living in long-term care facilities and that is all community participation support. So, minus the last 2 and a half years because of the pandemic, what that means is that a person living in a long-term care facility with a developmental disability can have our support to get out and about for 2 or 3 hours a week, on average.” [P10].
Full-time vs. part-time support
The person-supported’s needs also determined whether they would receive care within their homes and if they would be supported on a full-time (i.e., 24 h a day, 7 days a week) or part-time basis:
“ It really does range from that intensive 24- hour/7 day a week support, which we actually do provide that level of intense support in the family home, if that’s needed. And then, all the way through to just occasional advocacy support and phone check-in.” [P01].
Organizational Culture
Organizational culture was described as a key influence in the development and implementation of person-centred care plans. The culture of the organization includes their perceptions, attitudes and beliefs surrounding persons-supported; their model of care provision; as well as their willingness to evolve and adapt service provision to optimize care delivery.
Perceptions, attitudes, and beliefs regarding persons-supported
Participants described their organization’s view of persons-supported, with many organizations adopting an inclusionary framework where persons-supported were afforded the same rights and dignities as others in the community. This organizational philosophy was described as being deeply intertwined with an organization’s approach to personalizing programs and services:
“…an organization needs to be able to listen to the people who are receiving the service… and support them, to learn more, figure out, articulate, whatever it is, the service or the supports that they need in order to get and move forward with their life.” [P10].
The focus on the person-supported, their needs, likes, and dislikes, was echoed across organizations, with an emphasis on the impact of “culture and trying to embed for each person who delivers service the importance of understanding the individual.” [P05]. Participants also described their organization’s approach to allowing persons-supported to take risks, make mistakes, and live life on their own terms:
“You have to go and venture out and take some [risks]… We try to exercise that philosophy - people with disabilities should have the same rights and responsibilities as other people in the community. Whether that’s birthing or education, getting a job, having a house they can be proud of, accessing community supports, whether that be [a] library or community centre, or service club, whatever that is.” [P03].
Model of care provision
The model of care provision was heavily influenced by the organization’s values and philosophy. Several organizations employed a flexible model of care where supports were developed around the needs, preferences, and desired outcomes of the person-supported:
“…if we don’t offer [the program they want], we certainly build it. Honestly, most of our programs were either created or built by someone coming to us [and] saying ‘I want to do this with my life,’ or …‘my son would like to do art.’” [P02].
Although there were similarities in models across the different organizations, one participant noted that flexibility can be limited in the congregate care setting as staff must tend to the needs of a group as opposed to an individual:
“Our typical plan of operation outside of the congregate setting is we design services around the needs of the person. We don’t ask them to fit into what we need, we build services for what they need. Within the congregate care setting, we have a specific set of rules and regulations for safety and well-being of the other people that are here.” [P11].
Evolving service orientation
In organizations serving individuals with IDDs, many described shifting from program-based services to more individualized and community-based supports: “The goal was always to get people involved in their community and build in some of those natural supports … [we] are looking to support people in their own communities based on their individual plans.” [P07]. One participant described this model as a person-directed approach as opposed to person-centred, citing the limitations of program-based services in meeting individual needs:
“[Persons-supported] couldn’t [do] what they wanted because they were part of a bigger group. We would listen to the bigger group, but if one person didn’t want to go bowling … we couldn’t support them because everybody had to go bowling.” [P06].
The focus on individualized support could potentially lead to increased inclusion for persons-supported in their communities:
“… people go to Tim Horton’s, and if they go every day at 9 they probably, eventually will meet other people that go at 9 o’clock and maybe strike up a conversation and get to know somebody and join a table … and meet people in the community.” [P02].
By creating routines centred on individual preferences, the person-supported becomes a part of a community with shared interests and values.
Person-centred care plans
Community-care organizations enacted a person-centred approach by creating person-centred care plans for each person-supported. Although all participants said their organization provided person-centred services, there was considerable variation in the specific processes for developing, implementing, and updating care plans.
Developing a person-centred care plan
The development of a care plan includes assessment, consultation, and prioritization. The initial development of the care plan usually involved an assessment of an individual’s needs and goals. Participants described agency-specific assessment processes that often incorporated information from service referrals: “ In addition to the material we get from the DSO [Disability Services Ontario] we facilitate the delivery of an intake package specifically for our services. And that intake package helps to further understand the nature and needs of an individual.” [P12]. Agency-specific assessment processes differed by the nature of services provided and the characteristics of the population. However, most organizations included assessments of “not only physical functioning capabilities, but also cognitive.” [P01]. Assessment also included an appraisal of the suitability of the organization’s services. In instances where persons-supported were seeking residential placements or independent-living support, organizations assessed their ability to carry out the activities of daily living:
“[Our internal assessment] is an overview of all areas of their life. From, ‘do they need assistance with baking, cooking, groceries, cleaning, laundry? Is there going to be day program opportunities included in that residential request for placement? What the medical needs are?’” [P02].
In contrast, the person-supported’s community-based activities were primarily informed by their interests and desired outcomes: “We talk about what kinds of goals they want to work on. What kind of outcomes we’re looking for…” [P06].
The development of the care plan also included a consultation phase, involving conversations with the person-supported, their family members, and potentially external care providers: “We would use the application information, we’d use the supports intensity scale, but we’d also spend time with the person and their connections, their family and friends, in their home to figure out what are the kinds of things that this person needs assistance with.” [P10]. Participants described the person-supported’s view as taking precedence in these meetings: “We definitely include the family or [alternate] decision-maker in that plan, but the person-supported ultimately has the final stamp of approval.” [P08]. Many participants also acknowledged the difficulty of identifying and incorporating the person-supported’s view in cases where opinions clash and the person-supported has difficulty communicating and/or is non-verbal: “Some of the people we support are very good at expressing what they want. Some people are not. Some of our staff are really strong in expressing what they support. …And some of the family members are very strong. So you have to be very careful that the [person-supported] is not being lost in the middle of it.” [P06].
Participants also noted that some persons-supported preferred not to have a care plan:
“Some of the people say ‘I hate [the plans] I don’t want to do them’…. we look at it in a different way then. We’ll use graphic art, we’ll use video, we’ll think outside the box to get them to somehow—because at the end of the day when we’re audited by MCCSS every [person-supported] either has to have [a plan]… or there has to be [an approval of] why it wasn’t completed.” [P02].
Plan development may also include a prioritization process, particularly in cases where resources are limited. A person-supported’s goals could be prioritized using different schemas. One participant noted that “the support coordinator takes the cue from the person-supported - … what they’ve identified as ‘have to have’ and ‘nice to have’. … because the ‘have to haves’ are prioritized.” [P09]. Likewise, the person-supported’s preference could also be identified through “[an] exercise, called ‘what’s important for and what’s important to .’” [P06]. This model, based on a Helen Sanderson approach [ 18 ], was described as being helpful in highlighting what is important to the person-supported, as opposed to what others (i.e., friends, family, staff, etc.) feel is important for them.
Several organizations updated care plans throughout the year, to document progress towards goals, adapt to changing needs and plan for future goals: “We revisit the plan periodically through the year. And if they say the goal is done, we may set another goal.” [P06]. Organizations may also change plans to adapt to the person-supported’s changing health status or personal capacity.
Implementing a person-centred care plan
The implementation of care plans differed based on the nature of services provided by the organization. The delivery of health-based or personal support services often involved matching the length and intensity of care with the individual’s needs and capacity:
“Sometimes that is a long time, sometimes it’s a short time, sometimes it’s an intervention that’s needed for a bit, and then the person is able to function.” [P05].
In contrast, the delivery of community-based services involved matching activities and staff by interests: “[if] a person-supported wants to go out and be involved in the music community, then we pull the staff pool in and match them up according to interest.” [P06].
Broad personal goals were broken down into smaller, specific activities. For example, one participant described their organization’s plan in helping a person-supported achieve his professional goal of securing employment:
“[The person-supported] said ‘Okay, I want a job.’ So for three weeks he was matched up with a facilitator. They came up with an action plan in terms of how to get a job, what kind of job he’s looking for, where he wants to go, where he wants to apply, how to conduct an interview. And after three weeks he got a job.” [P09].
Organizations that provided residential services focused on developing independent-living skills. One participant described their organization’s plan to empowering persons-supported by allowing them to make their own financial decisions:
“If one month they’re looking after their own finances, and they’ve overspent. Well, maybe we help them out with a grocery card or something and say ‘okay, next month how are you going to do this?’ [The person-supported may say], ‘well, maybe I’ll put so much money aside each week rather than doing a big grocery shop the first week and not having enough money left at the end of the month.’” [P03].
The participant noted that “a tremendous amount of learning [happens] when a person is allowed to [take] risks and make their own decisions.” [P03].
Likewise, participants representing organizations that provided residential services described tailoring care to the persons-supported’s sleeping schedule and daily routine:
“We develop a plan and tweak it as we go. With [the person-supported] coming to the home, what worked well was, we found that he wanted to sleep in, so we adjusted the [staff] time. We took a look at his [medication] times in the morning… and [changed] his [medication] times. We found that he wanted to sleep [until] later in the day, so he would get up at 10 o’clock, so then instead of having breakfast, lunch, and supper he would just have a bigger brunch. Just really tailoring the plan around the person-supported, and it’s worked out well.” [P08].
These examples highlight how organizational context and culture influence how organizations operationalize person-centred care plans; the same individual may experience different approaches to care and engage in different activities depending on the organization they receive services from.
In this paper, we described key elements of the person-centred planning process across different community-care organizations in Southwestern Ontario. We also identified that the context and culture of an organization play a central role in informing the process by which services are personalized to an individual’s needs. These findings shed light on the diversity of factors that influence the implementation of person-centred care plans and the degree to which organizations are able to address medical and social needs in an integrated fashion. They also inform future evaluations of person and system-related outcomes of person-centred planning.
There are regulations around individualizing services delivered by community-care organizations, whereby care providers must allow persons-supported to participate in the development and evaluation of their care plans. HCCSS or MOH-funded services are largely focused on in-home rehabilitation or medical care. In contrast, MCCSS-funded organizations often focus on developing independent living skills or promoting community participation, thus highlighting the role of the funding agency in determining organizational context as well as the nature of services and personalization of care plans.
We also identified organizational culture as a key influence in the person-centred planning process. In previous reports, organizational culture, and specifically the way in which staff perceive and view persons-supported and their decision-making capabilities can impact the effective delivery of person-centred care [ 19 ]. Staff support, including their commitment to persons-supported and the person-centred process, has been regarded as one of the most powerful predictors of positive outcomes and goal attainment in the developmental services sector [ 20 , 21 ]. Moreover, in order to be successful, commitment to this process should extend across all levels of the organization, be fully integrated into organizational service delivery, and be reflected in organizational philosophy, values and views of persons-supported [ 22 , 23 , 24 ].
MCCSS mandates that agencies serving individuals with IDDs develop an individual service plan (ISP) for each person-supported, one “that address[es] the person’s goals, preferences and needs.” [ 7 ]. We reference ISPs as person-centred care plans, as is in line with the view of participants in interviews. There are a series of checklists designed to measure compliance with these policies, and the process is iterative, with mandated annual reviews of care plans and active participation by the person-supported [ 25 ]. In our study, the agencies funded by MCCSS adhered to the general framework outlined by these regulations and informed service delivery accordingly. However, participants also described areas for improvement with respect to the implementation of these policies in practice. These policies, while well-intentioned, may imply a one-size-fits-all approach and appear more as an administrative exercise as opposed to a meaningful endeavor designed to optimize care. Participants spoke about individuals who preferred not to have an ISP, and how that in and of itself is a person-centred approach, respecting the person’s wishes. Additionally, we heard about how the goal-setting process may not be realistic as it can be perceived as unnatural to have goals at each point in one’s life. Moreover, participants noted challenges in implementing person-centred care in shared residential settings (e.g., group homes) or in cases where persons-supported had difficulty communicating.
Prior research indicates that individuals living in semi-independent settings fare better across several quality-of-life measures relative to individuals living in group homes, including decreased social dissatisfaction, increased community participation, increased participation in activities of daily living, and increased empowerment [ 26 ]. Furthermore, a recent study by İsvan et al. (2023) found that individuals living in the community (e.g., own home, family home, or foster home) exhibit greater autonomy in making everyday and life decisions, and greater satisfaction with their inclusion in the community [ 27 ]. These findings may be indicative of a reduced focus on person-centred care plan development and implementation in congregate care settings, where limited staff capacity can make it difficult to tend to the needs of everyone in the home. However, poor outcomes may also be explained by potentially more complex health challenges or more severe disability in persons-supported living in congregate care settings. The challenges described in our study are consistent with calls to improve the quality of care provided in residential group home settings [ 28 , 29 ].
In line with our findings, previous literature also describes challenges in implementing person-centred planning for individuals who have difficulty communicating or are non-verbal [ 19 , 30 , 31 , 32 ]. Communication has also been identified as a barrier to patient-centred care for adults with IDDs in healthcare settings [ 33 , 34 ]. Other reports have identified a need for increased training and awareness of diverse communication styles (including careful observation of non-verbal cues) to aid staff in including persons-supported in the development of care plans [ 35 , 36 , 37 ]. Importantly, these methods take substantial time which is often limited, and compounded by staffing shortages that are widespread across the sector [ 38 ]. Similar barriers were identified in interviews with staff and persons-supported at a partner community-care agency within our larger project [ 39 ]; other papers from the project examine strategies used by the organization to overcome these barriers.
Limitations
The findings from this study should be interpreted in the context of the following limitations. There is a risk for social desirability bias, whereby participants may feel pressure to present their care plan process in a more positive light due to societal norms and expectations [ 40 ]. Additionally, the experiences and views of community-care organizations may vary by region and organization type (i.e., for-profit vs. not-for-profit). In this study, we limited participation to agencies providing services in Southwestern Ontario and we were only able to interview one for-profit agency, despite concerted recruitment efforts. Consequently, we may not have fully captured how financial pressures, or different contextual and cultural components of an organization impact their implementation of care plans.
The person-centred planning process in community-care organizations is largely informed by the characteristics of the population served and the nature of services offered (i.e., organizational context). This process usually involves initial and continued consultations with persons-supported to tailor plans to their specific needs and desired outcomes. There are ongoing challenges in the implementation of person-centred planning, including a need for increased adaptability and clarity in current regulations. In some areas, there may be benefit to incorporating nuance in the application of policies (e.g., in cases where a person-supported does not want to have a formal plan in place). In other areas, it may be helpful to have increased guidance on how to optimize care delivery to improve outcomes (e.g., in cases where a person-supported has difficulty communicating, or is residing in a group home). Policymakers, administrators, and service providers can leverage these insights to refine policies, advocating for inclusive, flexible approaches that better align with diverse community needs.
Data availability
The datasets generated and analyzed in the current study are not publicly available to maintain participant confidentiality, however access may be granted by the corresponding author upon reasonable request.
Abbreviations
Acquired Brain Injury
Disability Services Ontario
Home and Community Care Support Services
Intellectual and Developmental Disabilities
Individual Service Plan
Ministry of Children, Community and Social Services
Ministry of Health
Purbhoo D, Wojtak A. Patient and family-centred home and community care: realizing the opportunity. Nurs Leadersh Tor Ont. 2018;31(2):40–51.
Article PubMed Google Scholar
Lin E, Balogh RS, Durbin A, Holder L, Gupta N, Volpe T et al. Addressing gaps in the health care services used by adults with developmental disabilities in Ontario. ICES. 2019 [cited 2023 Aug 30]. https://www.ices.on.ca/publications/research-reports/addressing-gaps-in-the-health-care-services-used-by-adults-with-developmental-disabilities-in-ontario/
American Psychological Association. APA Guidelines for Assessment and Intervention with Persons with Disabilities: (502822022-001). 2022 [cited 2023 Aug 30]; http://doi.apa.org/get-pe-doi.cfm?doi=10.1037/e502822022-001
Dunn DS, Andrews EE. Person-first and identity-first language: developing psychologists’ cultural competence using disability language. Am Psychol. 2015;70(3):255–64.
Burke C. Building a stronger system for people with developmental disabilities: a six-month progress report from Commissioner Courtney Burke. New York Office for People with Developmental Disabilities; 2011. https://opwdd.ny.gov/system/files/documents/2019/12/6_month_progress_report_0.pdf
Government of Manitoba. Agency service coordination manual: 5.1 person-centred planning. 2021. https://www.gov.mb.ca/fs/clds/asc-manual/pubs/5.1-person-centred-planning.pdf
Government of Ontario. Services and supports to promote the social inclusion of Persons with Developmental Disabilities Act, 2008. 2008 [cited 2023 Aug 30]. https://www.ontario.ca/laws/regulation/100299#:~:text=O.-,Reg.,and other relevant clinical assessments
State of Michigan. Person Centered Planning.pdf. 2018.
O’Brien CL, O’Brien J. The origins of person-centered planning: a community of practice perspective.
Sanderson H. Person Centred Planning. York, Joseph Rowntree Foundation; 2000.
Government of Ontario. Ontario.ca. 2019 [cited 2023 Sep 4]. Connecting Care Act, 2019: Home and Community Care Services. https://www.ontario.ca/laws/regulation/220187#BK17
Dong M. Examining individualized participatory approaches to care for individuals with intellectual and developmental disabilities. University of Western Ontario; 2023. https://ir.lib.uwo.ca/etd/9517
Doyle L, McCabe C, Keogh B, Brady A, McCann M. An overview of the qualitative descriptive design within nursing research. J Res Nurs. 2020;25(5):443–55.
Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. SAGE; 2014. p. 305.
Berg BL. Qualitative research methods for the social sciences: 2nd ed. Bostan, MA: Allyn and Bacon; 1995. p. 421.
Google Scholar
Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis. SAGE; 2012. p. 321.
Yin RK. Case study research design and methods. 5th ed. Thousand Oaks, CA: SAGE; 2014. p. 282.
Helen Sanderson Associates. Helen Sanderson Associates. [cited 2023 Oct 31]. Sorting important to/for. http://helensandersonassociates.co.uk/person-centred-practice/person-centred-thinking-tools/sorting-important-tofor/
Hughes CA. The benefits and barriers to person centered planning for adults with developmental disabilities. [Saint Paul, Minnesota, USA]: St. Catherine University; 2013. https://sophia.stkate.edu/msw_papers/191
Heller T, Miller AB, Hsieh K, Sterns H. Later-life planning: promoting knowledge of options and choice-making. Ment Retard. 2000;38(5):395–406.
Article CAS PubMed Google Scholar
Ratti V, Hassiotis A, Crabtree J, Deb S, Gallagher P, Unwin G. The effectiveness of person-centred planning for people with intellectual disabilities: a systematic review. Res Dev Disabil. 2016;57:63–84.
Kaehne A, Beyer S. Person-centred reviews as a mechanism for planning the post-school transition of young people with intellectual disability. J Intellect Disabil Res. 2014;58(7):603–13.
Parley FF. Person-centred outcomes: are outcomes improved where a person-centred care model is used? J Learn Disabil. 2001;5(4):299–308.
Article Google Scholar
Sanderson H, Thompson J, Kilbane J. The emergence of person-centred planning as evidence‐based practice. J Integr Care. 2006;14(2):18–25.
Government of Ontario. Ministry of Children, Community and Social Services. Developmental service (DS) compliance inspection: indicator list. 2021 [cited 2023 Sep 4]. https://www.mcss.gov.on.ca/documents/en/mcss/developmental/EN_DS_Indicator_List.pdf
Stancliffe RJ, Keane S. Outcomes and costs of community living: a matched comparison of group homes and semi-independent living. J Intellect Dev Disabil. 2000;25(4):281–305.
İsvan N, Bonardi A, Hiersteiner D. Effects of person-centred planning and practices on the health and well-being of adults with intellectual and developmental disabilities: a multilevel analysis of linked administrative and survey data. J Intellect Disabil Res. 2023 [cited 2023 Sep 4]; https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/jir.13015
Office of the Auditor General of Ontario. 3.10: residential services for people with developmental disabilities. 2014. https://www.auditor.on.ca/en/content/annualreports/arreports/en14/310en14.pdf
Office of the Auditor General of Ontario. 1.10 residential services for people with developmental disabilities. 2016. https://www.auditor.on.ca/en/content/annualreports/arreports/en16/v2_110en16.pdf
Robertson J, Emerson E, Hatton C, Elliott J, McIntosh B, Swift P, et al. Person-centred planning: factors associated with successful outcomes for people with intellectual disabilities. J Intellect Disabil Res JIDR. 2007;51(Pt 3):232–43.
Everson JM, Zhang D, Person-Centered Planning. Characteristics, inhibitors, and supports. Educ Train Ment Retard Dev Disabil. 2000;35(1):36–43.
Claes C, Van Hove G, Vandevelde S, van Loon J, Schalock RL. Person-centered planning: analysis of research and effectiveness. Intellect Dev Disabil. 2010;48(6):432–53.
Stringer K, Terry AL, Ryan BL, Pike A. Patient-centred primary care of adults with severe and profound intellectual and developmental disabilities. Can Fam Physician. 2018;64(Suppl 2):S63–9.
PubMed PubMed Central Google Scholar
Badcock E, Sakellariou D. Treating him… like a piece of meat: poor communication as a barrier to care for people with learning disabilities. Disabil Stud Q. 2022 [cited 2023 Sep 4];42(1). https://dsq-sds.org/index.php/dsq/article/view/7408
Mansell J, Beadle-Brown J. Person-centred planning or person-centred action? Policy and Practice in Intellectual Disability Services. J Appl Res Intellect Disabil. 2004;17(1):1–9.
Bigby C, Frawley P. Social work practice and intellectual disability: working to support change. Bloomsbury Publishing; 2018. p. 253.
Taylor JE, Taylor JA. Person-centered planning: evidence-based practice, challenges, and potential for the 21st century. J Soc Work Disabil Rehabil. 2013;12(3):213–35.
Zijlstra R, Vlaskamp C, Buntinx W. Direct-care staff turnover: an indicator of the quality of life of individuals with profound multiple disabilities. Eur J Mental Disabil. 2001;(22):39–55.
Canadian Institutes of Health Research (CIHR), CIHR-Institute of Health Services and Policy Research (CIHR-IHSPR) and partners. Evidence brief booklet: quadruple aim & equity catalyst grants. 2024 [cited 2024 Apr 2]. https://face2face.events/wp-content/uploads/2024/01/Evidence-Brief-Booklet-Quadruple-Aim-and-Equity-EN.pdf
Bergen N, Labonté R. Everything is perfect, and we have no problems: detecting and limiting social desirability bias in qualitative research. Qual Health Res. 2020;30(5):783–92.
Download references
Acknowledgements
The authors thank Ruth Armstrong, from PHSS - Medical & Complex Care in Community, for her valuable feedback and support throughout the research process.
This research was funded by the Canadian Institutes of Health Research. The funding agency had no role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Family Medicine, Schulich School of Medicine & Dentistry, Western University, 1151 Richmond St, London, ON, N6A 5C1, Canada
Samina Idrees, Gillian Young, Leslie Meredith & Maria Mathews
PHSS - Medical & Complex Care in Community, 620 Colborne St, London, ON, N6B 3R9, Canada
Brian Dunne & Donnie Antony
You can also search for this author in PubMed Google Scholar
Contributions
S.I. conducted the interviews, developed the coding template, coded the data, thematically analyzed the data, and prepared the manuscript. G.Y. helped develop the coding template, and reviewed and approved the final manuscript. B.D. and D.A. helped conceptualize the study, aided in the interpretation and analysis of study findings, and reviewed and approved the final manuscript. L.M. coordinated research activities, aided in the interpretation and analysis of study findings, and reviewed and approved the final manuscript. M.M. conceptualized the study, supervised its implementation, and was a major contributor in reviewing and editing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Maria Mathews .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the research ethics board at Western University. We obtained informed consent from participants prior to the onset of interviews.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Idrees, S., Young, G., Dunne, B. et al. The implementation of person-centred plans in the community-care sector: a qualitative study of organizations in Ontario, Canada. BMC Health Serv Res 24 , 680 (2024). https://doi.org/10.1186/s12913-024-11089-7
Download citation
Received : 14 February 2024
Accepted : 08 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1186/s12913-024-11089-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Person-centred planning
- Community-based care
- Integrated care
- Social services
- Health services
- Organizational culture
- Qualitative study
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 04 June 2024
What are medical students taught about persistent physical symptoms? A scoping review of the literature
- Catie Nagel 1 ,
- Chloe Queenan 1 &
- Chris Burton 1
BMC Medical Education volume 24 , Article number: 618 ( 2024 ) Cite this article
133 Accesses
Metrics details
Persistent Physical Symptoms (PPS) include symptoms such as chronic pain, and syndromes such as chronic fatigue. They are common, but are often inadequately managed, causing distress and higher costs for health care systems. A lack of teaching about PPS has been recognised as a contributing factor to poor management.
The authors conducted a scoping review of the literature, including all studies published before 31 March 2023. Systematic methods were used to determine what teaching on PPS was taking place for medical undergraduates. Studies were restricted to publications in English and needed to include undergraduate medical students. Teaching about cancer pain was excluded. After descriptive data was extracted, a narrative synthesis was undertaken to analyse qualitative findings.
A total of 1116 studies were found, after exclusion, from 3 databases. A further 28 studies were found by searching the grey literature and by citation analysis. After screening for relevance, a total of 57 studies were included in the review. The most commonly taught condition was chronic non-cancer pain, but overall, there was a widespread lack of teaching and learning on PPS. Several factors contributed to this lack including: educators and learners viewing the topic as awkward, learners feeling that there was no science behind the symptoms, and the topic being overlooked in the taught curriculum. The gap between the taught curriculum and learners’ experiences in practice was addressed through informal sources and this risked stigmatising attitudes towards sufferers of PPS.
Faculties need to find ways to integrate more teaching on PPS and address the barriers outlined above. Teaching on chronic non-cancer pain, which is built on a science of symptoms, can be used as an exemplar for teaching on PPS more widely. Any future teaching interventions should be robustly evaluated to ensure improvements for learners and patients.
Peer Review reports
Persistent Physical Symptoms (PPS) are symptoms which are disproportionate to currently recognised pathology and are common in all fields of medicine. The term encompasses single symptoms such as pain, dizziness or fatigue, and established syndromes including fibromyalgia and irritable bowel syndrome. It is increasingly understood that PPS arise from complex interactions between the brain and body [ 1 , 2 ]. While historically terms such as “medically unexplained symptoms” have been in common use, most symptoms can actually be explained [ 3 ] and PPS is a more acceptable term to patients [ 4 ].
PPS are common and present to nearly every medical specialty. They represent the primary reason for presentation in around 45% of general practice consultations and between 30 and 70% of presentations to neurology, gynaecology, and rheumatology outpatient clinics [ 5 ]. People with PPS suffer unduly in a medical system that is predisposed to ‘body part medicine,’ [ 6 ] resulting in what Balint referred to as the “collusion of anonymity.” [ 7 ] In other words, patients who pass from specialist to specialist, without any doctor taking full responsibility for holistic care. Patients with PPS consult more frequently [ 8 ] and tend to have a higher rate of referral to secondary care [ 9 ]. This is costly, both in financial terms and in terms of the emotional work for patients and clinicians [ 10 , 11 ]. Patients with PPS often have a poor experience of the health system and can be left feeling marginalised and even stigmatised [ 12 ].
Doctors find it difficult to consult and manage patients with persistent physical symptoms [ 8 ]. The absence of a common language of explanation to reconcile patients’ lived experience with doctors’ biomedical models, is particularly problematic [ 13 ]. It is plausible that difficulties may arise, or be perpetuated by, issues in each of the three domains of learning: cognitive (knowledge), psychomotor (skills) and affective (attitudes) [ 14 ].
The shifting perspectives, particularly around “medically unexplained symptoms” may account for historical uncertainty, however recent adoption of more consistent language and underlying models of symptoms mean that a common curriculum should be possible [ 15 ]. It is the authors’ experience that little teaching and learning at the undergraduate level has previously taken place on this topic. We wanted to find out if this was still the case, by reviewing the current medical education literature.
We carried out a scoping review with narrative synthesis following the approach of Arksey & O’Malley [ 16 ]. The PRISMA-ScR guidelines were used to structure reporting [ 17 ].
Research questions
The aim of the review was to explore the published literature regarding undergraduate medical teaching and learning on persistent physical symptoms. The specific research questions were:
What teaching and learning on persistent physical symptoms has been described for medical undergraduates?
What teaching methods have been used and how have these been evaluated?
Search strategy
We used a Population, Concept, and Context (PCC) framework to structure a systematic search. The population was undergraduate medical students, the concept was persistent physical symptoms, and the context was teaching and learning. A variety of synonyms were used in order to be inclusive, given the constant evolution of terms for persistent physical symptoms. We used adjacency searching and truncation methods in order to broaden the search as widely as possible and to account for different spellings of words or use of phrases across the international context. Search concepts were then combined using Boolean operators. No date range was used, so all studies before 31 March 2023 were included. Inclusion criteria were: studies relating to the teaching and learning of Persistent Physical Symptoms; medical students included in the population; available in the English language. Exclusion criteria were: studies about cancer or terminal pain without the inclusion of other forms of chronic or persistent pain; population not including medical students; letters to the editor, and papers which were not available in the English language. See Table 1 for the full search strategy.
Sources of evidence
Two authors searched for published literature in MEDLINE, PsycINFO, and Web of Science. Additionally, we searched Google and Google Scholar in order to include any grey literature or sources that had not been picked up by the previous search method. We employed citation analysis, by following backward citations from included papers and analysed the citations of any existing literature reviews.
Study selection
We used a two-stage screening process to identify eligible papers: first at title and abstract level and then at full text. This method was undertaken separately by two reviewers.
Literature reviews were excluded to avoid duplicated representation of primary data, but citations in these reviews were analysed to ensure consistent inclusion of studies and to check for any additional sources.
Charting the data: summary and synthesis
Summary findings for each full text article were charted to determine the most relevant items for extraction. This was an iterative process given the high degree of heterogeneity between the studies. Charting was conducted by two reviewers independently. Discrepancies in charting and data extraction were discussed in review meetings and a consensus was reached regarding which data to include for analysis.
Reviewers extracted descriptive data including: country of origin, whether the study was experimental or observational, the characteristics of the study participants, and whether any teaching intervention was evaluated. Other study characteristics were noted, such as the symptom or syndrome represented, as well as the type of study or intervention.
The expectation was that there would be a lack of teaching and learning on the subject of persistent physical symptoms. For this reason, the scoping review aimed to capture the greatest breadth of studies, rather than exclude studies based on quality criteria. If a teaching intervention was used, we did look at whether this was evaluated using a validated tool.
Following the extraction of descriptive data, a narrative synthesis was undertaken to identify other key findings. An inductive, iterative approach was taken in order to identify themes relating back to the research question. Manual coding was undertaken by two authors independently, followed by a discussion with all authors to arrive at an interpretation of the findings.
Search strategy, study selection, and data extraction
Searches identified 1390 unique titles. Studies were limited to English language and human participants, leading to 274 being excluded. First stage screening excluded a further 1080 studies. It was not possible to retrieve one study and six were excluded on full text. Ten further records were identified through a grey literature search using Google and Google Scholar and 18 were found through citation searching, three of which were from a previous literature review [ 15 ]. This resulted in 57 publications for inclusion in the review. See the PRISMA flow diagram in Fig. 1 for a summary of these findings.
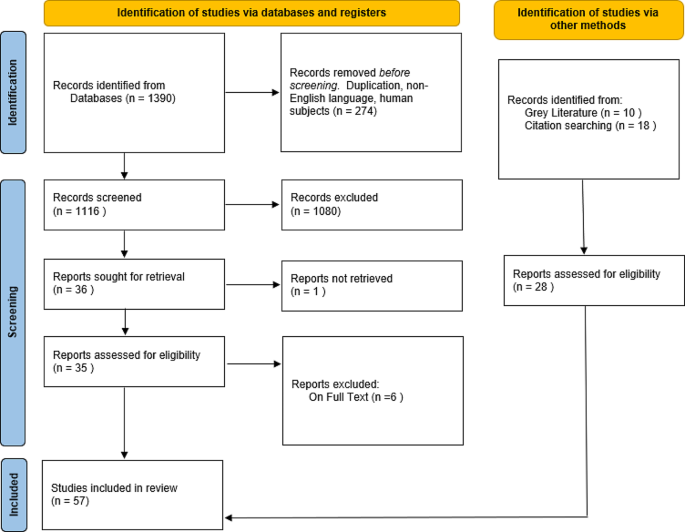
PRISMA Diagram
Adapted from Page MJ, et al. [ 17 ]
Descriptive analysis
Study types.
The studies included for review were highly heterogeneous in their nature. 15/57 (26%) studies employed a teaching intervention, with the remaining either being observational or qualitative. 8/57 (14%) studies described or evaluated the teaching curriculum, 13/57 (22%), included an assessment of the current level of learner knowledge. 9/57 (16%) used qualitative methods with learners and 6/57 (11%) with medical educators. One literature review on assessing knowledge, perceptions and attitudes to pain was found [ 15 ]. The citations of this review were checked and the three new sources [ 18 , 19 , 20 ] were included for review. Sources within this literature review that did not meet the eligibility criteria were excluded. The findings of the review itself were noted for congruity, but not formally analysed.
Study characteristics
23/57(40%) of studies took place in USA and 13/57 (23%) in the UK. Six studies took place in Scandinavia and four in Canada, four in Australia and one in New Zealand, India, and Nigeria respectively. Some studies were based in more than one country e.g. Australia and New Zealand [ 21 ]. Publication dates ranged from 1992 to 2022. See Table 2 for a summary of the descriptive data.
Teaching and learning methods
A wide range of teaching and learning methods were discussed in the literature. These are fully described in Table 3 , but included lectures, workshops, reflective practice, and forum theatre.
Evaluation of teaching studies
Four studies used validated tools to assess learner attitudes towards patients with PPS, but only one used such a tool to evaluate a teaching intervention [ 22 ]. Morris, Rankin, and Briggs used the HC-PAIRS attitudinal questionnaire to assess learner attitudes towards patients with chronic low back pain [ 18 , 23 , 24 ]. Whereas Friedberg et al. [ 22 ] used the Chronic Fatigue Syndrome Attitudes Test (CFSAT) and paired t-test to analyse learner attitudes before and after a teaching intervention. The remaining educational interventions either did not use a validated tool for evaluation or were not formally evaluated. See Table 3 for more details.
Thematic synthesis
All studies identified a lack of teaching about persistent physical symptoms (PPS) at undergraduate level. The narrative synthesis identified four themes: An awkward problem, an absence of science, being easily overlooked, and a hidden curriculum.
An awkward problem
PPS was consistently viewed as an awkward problem. Medical educators and learners found it difficult to understand, particularly when referring to the symptoms as ‘unexplained.’ Some educators described PPS as too complex or too confusing, even ‘dangerous’ to introduce at an undergraduate level and stated the need to focus on the easily ‘explainable.’ [ 25 ] Chronic non-cancer pain was the dominant condition represented in the literature, but despite theoretical concepts of chronic pain being more established, learners found the subject challenging, even ‘unpleasant.’ [ 26 , 27 ].
The absence of science
Four studies highlighted that learners infer patients with PPS have ‘no science’ behind their symptoms. In the study by Vasanthy [ 28 ], clinical role models in Kerala were found to have a ‘nihilistic’ attitude towards people with fibromyalgia and regarded the condition as benign and unimportant. This finding was echoed by UK studies [ 29 , 30 , 31 ] where the impact of a lack of teaching and negative role modelling was evident:
“You can’t really train someone for it because there is no science behind it” [ 30 ].
One final year medical student stated that fibromyalgia was “not a medical issue” intimating that it had no place in the taught curriculum [ 29 ]. Learners understood the need to be supportive and for good communication, but only as a way of achieving relational congruence, not epistemic congruence [ 8 ]. Terminology may be important and in one study learners’ attitudes towards PPS varied depending on the diagnostic label [ 32 ]. As an example, learners thought that people with myalgic encephalopathy were less likely to recover than those with chronic fatigue syndrome [ 32 ].
Easily overlooked
Even without the overt attitudinal barriers described in some studies, PPS as a topic is overlooked in undergraduate medical education. The most common barrier was an already overloaded teaching curriculum [ 25 , 33 ]. PPS was not deemed a priority area by educational leaders and [ 33 ] even when they recognised its importance, they cited a lack of ownership of the topic and a lack of coordination between teaching specialties as a barrier to implementing teaching. This was in contrast to chronic non-cancer pain teaching which usually did have clear ownership by pain specialists and established interdisciplinary relationships [ 34 ]. The experience of learners in the clinical setting was that they were shielded from patients with PPS or directed towards patients with other more easily defined clinical problems [ 28 ].
Stigma and the hidden curriculum
Given the vacuum of formal teaching, learners were taking on stigmatised messages about sufferers of PPS, frequently from role models in the clinical placement setting. Stenhoff and colleagues described a cycle of negativity created by the lack of teaching on the subject of chronic fatigue, which resulted in negative behaviour by clinical role models, in turn perpetuating negative attitudes in the next generation of learners [ 31 ]. Whilst learners recognised the problematic nature of the attitudes towards people with PPS, they lacked the tools to challenge negative stereotypes [ 29 , 30 , 35 ]. Learners experienced a mismatch between formal teaching on the topic and their experience on placement, where these conditions were frequently encountered. They addressed the gap by seeking information about PPS from informal sources, such as their own or their families’ experiences or from the internet [ 36 ]. This lack of explicit teaching and the influence of informal sources has been termed by some authors as the ‘hidden curriculum’ [ 29 , 30 , 31 , 36 ] and this has had a significant impact on learners’ attitudes towards people suffering with PPS.
Suggestions for improvement: relationship to domains of learning
The findings of the narrative synthesis map onto Bloom’s revised three domains of learning [ 14 ].
Knowledge (cognitive)
A number of studies demonstrate success in teaching on the topic of chronic non-cancer pain. Teaching interventions tended to include a foundation of knowledge such as teaching on pain mechanisms, pharmacology, and pain management [ 37 , 38 ]. Such theory-driven interventions led to improved scores on assessment [ 39 ]. Methods of teaching should be considered in the explicitly taught curriculum. Authors recommended an integrated approach [ 40 , 41 ] and one which drew on the skills and knowledge from a variety of disciplines [ 37 , 42 ]. Curriculum mapping was recommended by Howman et al. [ 33 ] in order to identify ways in which this integration could be implemented. The need for an holistic approach which emphasises the importance of empathy [ 41 ] and the biopsychosocial was also widely recognised [ 43 , 44 , 45 , 46 ]. Learners cited a lack of assessment as an indicator that PPS was either unimportant or uncommon [ 29 , 33 ] and therefore any teaching intervention should include assessment in order to drive learning and engagement.
Skills (psychomotor)
Learners valued the addition of skills-based teaching and engaged best with teaching that was experiential [ 47 ] and included either patients with PPS or simulated patients [ 45 , 48 , 49 ]. In one study the focus of the teaching was on interactive, practical teaching for emotionally demanding consultations and the skills taught in such a programme could be transferable to the PPS context [ 49 ]. Approaches to help learners find a common language of explanation [ 13 ] will not only bridge the epistemic gap between clinicians and patients [ 8 ], but should give learners greater confidence and satisfaction in consultations where PPS are the focus.
Attitudes (affective) and the role of reflection
Reflection is a key transferable skill that graduates should acquire as part of their undergraduate training [ 50 ]. Both learners and educators voiced a great deal of anxiety regarding teaching and managing patients with PPS. Some authors utilised reflective logs and visual art as a way of teaching about chronic pain [ 51 ] and learners valued the deep insights provided by this method. Skills in reflection might help to ameliorate the negative emotions felt by learners, especially if combined with a taught framework that helps them understand concepts such as internal bias and cognitive dissonance [ 52 ].
Summary of main findings
This review found that teaching on persistent physical symptoms in undergraduate medical education is inconsistent and incomplete. We identified four important themes: an awkward problem, the absence of science, easily overlooked, and the hidden curriculum. Mapping these to teaching and learning domains provides a coherent framework for undergraduate teaching of these common conditions. Where teaching does take place, this is more frequently on the topic of chronic non-cancer pain. A number of studies have demonstrated improved knowledge [ 39 ], skills [ 49 ], and attitudes [ 51 ] as a result of this teaching [ 34 , 47 ], but high quality evaluation of such teaching and learning is lacking.
Strengths and limitations
This scoping review has addressed a gap in the literature. By undertaking a search of three databases, the grey literature, and citation analysis, a wide range of sources were included for initial screening. Two researchers independently undertook the search strategy before comparing findings which has helped to ensure a robust and systematic approach. Narrative synthesis was undertaken by three researchers, one with expertise in the field of persistent physical symptoms.
The majority of the studies identified were from the USA and UK. Papers that were not accessible in English were excluded, which may explain this finding. Where teaching and learning evaluations had taken place, this was on a small scale usually within one institution. Only one study [ 22 ] used a validated tool to evaluate the efficacy of the teaching intervention.
Implications for practice, policy, and research
There is a lack of teaching on PPS in undergraduate medical education. As a result, medical graduates are ill-equipped to recognise, consult for, and manage this group of conditions. Given the prevalence of PPS across medical specialties this is a priority area that needs to be addressed, whilst acknowledging the barriers that exist to implementation.
The solutions offered up in the literature include the need to consider whole-person care, in order to avoid fragmentation and the “collusion of anonymity” [ 7 ] described above. For this reason, teaching on PPS should be integrated into the core curriculum and draw on a variety of disciplines.
A better understanding of the science behind PPS [ 1 , 2 ] is needed for both educators and learners. There is also a need to move learners beyond reductionist models of communication skills towards more theory-driven approaches of person-centredness, as identified by Bansal [ 53 ]. We need to convey to learners that skilled communication is not about platitudes, but can make a difference to recovery and addresses the current epistemic gap between clinicians and their patients [ 8 , 13 ].
Future educational research should focus on the most effective methods to improve the knowledge base of both educators and students and how best to evaluate the success of future teaching interventions. Skills in person-centred communication and explanation [ 3 ] need to be taught, alongside those in reflection and challenging prejudice.
We identified four important themes which underpin the challenges of teaching medical undergraduates about persistent physical symptoms. Educational faculties need to find ways to integrate teaching into current programmes and work around the existing barriers to successful implementation and evaluation of teaching about these common and limiting conditions. Examples of successful teaching on chronic non-cancer pain were found in the literature. These tended to articulate the science behind symptoms and often included experiential elements. Such examples should be used to inform an approach for teaching about other forms of PPS. Importantly, robust evaluation that accounts for the complexity of the taught environment is needed to ensure our teaching is making a difference, both for our learners and the patients they will go on to encounter.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
Henningsen P, et al. Persistent physical symptoms as Perceptual Dysregulation: a Neuropsychobehavioral Model and its clinical implications. Psychosom Med. 2018;80(5):422–31.
Article Google Scholar
Burton C et al. Functional somatic disorders: discussion paper for a new common classification for research and clinical use BMC Medicine, 2020;18(1).
Morton L, et al. A taxonomy of explanations in a general practitioner clinic for patients with persistent medically unexplained physical symptoms. Patient Educ Couns. 2017;100(2):224–30.
Picariello F, Ali S, Moss-Morris R, Chalder T. The most popular terms for medically unexplained symptoms: the views of CFS patients. J Psychosom Res. 2015;78(5):420–6.
Haller H, Cramer H, Lauche R, Dobos G. Somatoform disorders and medically unexplained symptoms in primary care. Deutsches Ärzteblatt international, 2015.
Oldham J. Reform reform: an essay by John Oldham. BMJ: Br Med J. 2013;347:f6716.
Balint M. The doctor, his patient and the illness . 2000, Edinburgh: Edinburgh: Churchill Livingstone, 2000.
Johansen M-L, Risor MB. What is the problem with medically unexplained symptoms for GPs? A meta -synthesis of qualitative studies. Patient Educ Couns. 2017;100(4):647–54.
Verhaak PFM. Persistent presentation of medically unexplained symptoms in general practice. Fam Pract. 2006;23(4):414–20.
Mcgorm K, et al. Patients repeatedly referred to secondary care with symptoms unexplained by organic disease: prevalence, characteristics and referral pattern. Fam Pract. 2010;27(5):479–86.
Barsky AJ, Orav EJ, Bates DW. Somatization increases medical utilization and costs Independent of Psychiatric and Medical Comorbidity. Arch Gen Psychiatry. 2005;62(8):903.
Polakovská L, Řiháček T. What is it like to live with medically unexplained physical symptoms? A qualitative meta-summary. Psychology & Health. 2021:pp. 1–17.
Salmon P. Conflict, collusion or collaboration in consultations about medically unexplained symptoms: the need for a curriculum of medical explanation. Patient Educ Couns. 2007;67(3):246–54.
Anderson L. A taxonomy for learning, teaching, and assessing: a revision of Bloom’s . Pearson new international ed. 2014, Harlow, Essex: Pearson.
Ung A, Salamonson Y, Hu W, Gallego G. Assessing knowledge, perceptions and attitudes to pain management among medical and nursing students: a review of the literature. Br J Pain. 2016;10(1):8–21.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Page MJ et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, 2021:p. n71.
Briggs AM, et al. Low back pain-related beliefs and likely practice behaviours among final-year cross-discipline health students. Eur J Pain. 2013;17(5):766–75.
Murinson BB, et al. A new program in pain medicine for medical students: integrating core curriculum knowledge with emotional and reflective development. Pain Med. 2011;12(2):186–95.
Watt-Watson J, et al. An integrated undergraduate pain curriculum, based on IASP curricula, for six Health Science Faculties. Pain. 2004;110(1):140–8.
Shipton EE, et al. Pain medicine content, teaching and assessment in medical school curricula in Australia and New Zealand. Volume 18. BMC Medical Education; 2018:1.
Friedberg F, Sohl SJ, Halperin PJ. Teaching medical students about medically unexplained illnesses: a preliminary study. Med Teach. 2008;30(6):618–21.
Morris H, Ryan C, Lauchlan D, Field M. Do medical student attitudes towards patients with chronic low back pain improve during training? A cross-sectional study. BMC Med Educ. 2012;12(1):10.
Rankin L, Fowler CJ, Stålnacke B-M, Gallego G. What influences chronic pain management? A best–worst scaling experiment with final year medical students and general practitioners. Br J Pain. 2019;13(4):214–25.
Joyce E, et al. Training tomorrow’s doctors to explain ‘medically unexplained’ physical symptoms: an examination of UK medical educators’ views of barriers and solutions. Patient Educ Couns. 2018;101(5):878–84.
Corrigan C, et al. What can we learn from First-Year Medical Students’ perceptions of Pain in the primary care setting? Pain Med. 2011;12(8):1216–22.
Wilson JF, et al. Medical students’ attitudes toward pain before and after a brief course on pain. Pain. 1992;50(3):251–6.
Vasanthy B, Parameswaran Nair VC. Fibromyalgia: perspective of patients, medical students and professionals. Journal of evidence based Medicine and Healthcare. J Evid Based Med Healthc. 2018;5(34):2463–7.
Silverwood V et al. ‘If it’s a medical issue I would have covered it by now’: learning about fibromyalgia through the hidden curriculum: a qualitative study. BMC Med Educ, 2017;17(1).
Shattock L, et al. They’ve just got symptoms without science’: medical trainees’ acquisition of negative attitudes towards patients with medically unexplained symptoms. Patient Educ Couns. 2013;91(2):249–54.
Stenhoff AL, Sadreddini S, Peters S, Wearden A. Understanding medical students’ views of chronic fatigue syndrome: a qualitative study. J Health Psychol. 2015;20(2):198–209.
Jason LA, et al. Evaluating attributions for an illness based upon the name: chronic fatigue syndrome, myalgic Encephalopathy and Florence Nightingale Disease. Am J Community Psychol. 2002;30(1):133–48.
Howman M, et al. Teaching about medically unexplained symptoms at medical schools in the United Kingdom. Med Teach. 2012;34(4):327–9.
Vargovich AM, et al. Difficult conversations: Training Medical students to assess, educate, and treat the patient with Chronic Pain. Acad Psychiatry. 2019;43(5):494–8.
Yon K, et al. Improving teaching about medically unexplained symptoms for newly qualified doctors in the UK: findings from a questionnaire survey and expert workshop. BMJ Open. 2017;7(4):e014720.
Emorinken A, et al. Assessment of Undergraduate Medical Students Knowledge and Awareness of Fibromyalgia. J Evol Med Dent Sci. 2022;11(5):551–6.
Comer L. Content analysis of chronic pain content at three undergraduate medical schools in Ontario. Can J Pain. 2017;1(1):75–83.
Kolber BJ, Janjic JM, Pollock JA, Tidgewell KJ. Summer undergraduate research: a new pipeline for pain clinical practice and research. BMC Med Educ, 2016;16(1).
Weiner DK, et al. E-Learning Module on Chronic Low Back Pain in older adults: evidence of Effect on Medical Student Objective Structured Clinical Examination performance. J Am Geriatr Soc. 2014;62(6):1161–7.
Pöyhiä R, Niemi-Murola L, Kalso E. The outcome of pain related undergraduate teaching in Finnish medical faculties. Pain. 2005;115(3):234–7.
Murinson BB, et al. Recommendations for a New Curriculum in Pain Medicine for Medical students: toward a Career distinguished by competence and Compassion. Pain Med. 2013;14(3):345–50.
Morley-Forster P et al. Mitigating the risk of opioid abuse through a balanced undergraduate pain medicine curriculum. J Pain Res, 2013:p. 791.
Wojtowicz AA, et al. Perceptions of clinical training in biopsychosocial treatment of pediatric functional abdominal pain: a survey of medical students. Clin Pract Pediatr Psychol. 2020;8:37–44.
Google Scholar
Dwyer CPM-P, Phoebe E, Durand H, Gormley EM, Slattery BW, Harney OM, MacNeela P, McGuire BE. Factors influencing the application of a Biopsychosocial Perspective in Clinical Judgement of Chronic Pain: interactive management with medical students. Pain Physician. 2017;20(6):E951–60.
Ali N, Thomson DI. A comparison of the knowledge of chronic pain and its management between final year physiotherapy and medical students. Eur J Pain. 2009;13(1):38–50.
Tauben DJ, Loeser JD. Pain Education at the University of Washington School of Medicine. J Pain. 2013;14(5):431–7.
Stevens DL, et al. Medical students retain pain assessment and management skills long after an experiential curriculum: a controlled study. Pain. 2009;145(3):319–24.
Bradner M, et al. Chronic non-malignant pain: it’s complicated. Clin Teach. 2019;16(5):530–2.
Baessler F, et al. Are we preparing future doctors to deal with emotionally challenging situations? Analysis of a medical curriculum. Patient Educ Couns. 2019;102(7):1304–12.
GMC, Outcomes for Graduates . 2018.
Lempp H, Potter J, Petit P, Hester J. Exploring chronic pain with patients: medicine meets art. Med Educ. 2010;44(11):1139–40.
Syed M. Black box thinking: marginal gains and the secrets of high performance. London: John Murray; 2016.
Bansal A, et al. Optimising planned medical education strategies to develop learners’ person-centredness: A realist review. Medical Education, 2021.
Turner GH, Weiner DK. Essential components of a Medical Student Curriculum on Chronic Pain Management in older adults: results of a modified Delphi process. Pain Med. 2002;3(3):240–52.
Niemi-Murola L, et al. Training medical students to manage a chronic pain patient: both knowledge and communication skills are needed. Eur J Pain. 2006;10(2):167–167.
Saypol B, Schmulson DD. A review of three educational projects using interactive theater to improve physician-patient communication when treating patients with irritable bowel syndrome. Rev Esp Enferm Dig. 2015;107(5):268–73.
Bradshaw YS, et al. Deconstructing one Medical School’s Pain Curriculum: II. Partnering with medical students on an evidence-guided redesign. Pain Med. 2017;18(4):664–79.
Leeds FS, et al. A patient-narrative Video Approach to Teaching Fibromyalgia. J Med Educ Curric Dev. 2020;7:238212052094706.
Gadde U, et al. Implementing an interactive introduction to complementary medicine for chronic Pain Management into the Medical School Curriculum. MedEdPORTAL. 2020;16(1):11056.
Campbell WI. What do medical-students know about chronic pain and its management. Ulster Med J. 1992;61(2):139–43.
Chibnall JT, Tait RC, Ross LR. J Behav Med. 1997;20(3):257–71.
Niemi-Murola L, Nieminen JT, Kalso E, Pöyhiä R. Medical undergraduate students’ beliefs and attitudes toward pain - how do they mature? Eur J Pain. 2007;11(6):700–6.
Amber KT, Brooks L, Chee J, Ference TS. Assessing the perceptions of Fibromyalgia Syndrome in United States among Academic Physicians and Medical students: where are we and where are we headed? J Musculoskelet Pain. 2014;22(1):13–9.
Amber KT, Brooks L, Ference TS. Does Improved confidence in a Disease relate to increased knowledge? Our experience with medical students: table 1. Pain Med. 2014;15(3):483–4.
Adillón C, Lozano È, Salvat I. Comparison of pain neurophysiology knowledge among health sciences students: a cross-sectional study. BMC Res Notes, 2015. 8(1).
Argyra E, et al. How does an undergraduate Pain Course Influence Future Physicians’ awareness of Chronic Pain concepts? A comparative study. Pain Med. 2015;16(2):301–11.
Briggs EV, et al. Current pain education within undergraduate medical studies across Europe: advancing the provision of Pain Education and Learning (APPEAL) study. BMJ Open. 2015;5(8):e006984.
Hollingshead NA et al. Examining influential factors in providers’ chronic pain treatment decisions: a comparison of physicians and medical students. BMC Med Educ, 2015. 15(1).
Rankin L, Stålnacke B-M, Fowler CJ, Gallego G. Differences in Swedish and Australian medical student attitudes and beliefs about chronic pain, its management, and the way it is taught. Scandinavian J Pain. 2018;18(3):533–44.
Cristóvão I, Reis-Pina P. O Ensino Da Dor Crónica em Portugal: as Perspectivas Dos Estudantes De Medicina E dos internos do Ano Comum. Acta Med Port. 2019;32(5):338.
Gustafsson Sendén M, Renström EA. Gender bias in assessment of future work ability among pain patients – an experimental vignette study of medical students’ assessment. Scandinavian J Pain. 2019;19(2):407–14.
Lechowicz K, et al. Acute and Chronic Pain Learning and Teaching in Medical School—An observational cross-sectional study regarding Preparation and Self-confidence of clinical and Pre-clinical Medical Students. Medicina. 2019;55(9):533.
Storrar A, Rayment D, Mallam E. 47 undergraduate teaching and perceptions of functional neurological disorders. Members’ POSTER abstracts. BMJ Publishing Group Ltd; 2019.
Muirhead N, Muirhead J, Lavery G, Marsh B. Medical School Education on myalgic encephalomyelitis. Medicina. 2021;57(6):542.
Simons J, et al. Disorders of gut-brain interaction: highly prevalent and burdensome yet under‐taught within medical education. United European Gastroenterology Journal, 2022.
Lambson R. Chronic fatigue syndrome: where do your views lie? An experience from a UK Medical Student. Int J Med Students. 2015;3(2):117–8.
Raber I, et al. Qualitative Assessment of Clerkship Students’ perspectives of the topics of Pain and Addiction in their preclinical curriculum. Acad Psychiatry. 2018;42(5):664–7.
Rice K, et al. Medical trainees’ experiences of Treating People with Chronic Pain: a lost opportunity for Medical Education. Acad Med. 2018;93(5):775–80.
Sallay V, et al. Medical educators’ experiences on medically unexplained symptoms and intercultural communication—an expert focus group study. Volume 22. BMC Medical Education. 2022;1.
Download references
Acknowledgements
Not applicable.
CN is undertaking an In Practice Fellowship which has been funded by the NIHR (Reference number NIHR301019). This is an educational award and does not fund direct research costs.
Author information
Authors and affiliations.
Primary Care Research Group, Division of Population Health, School of Medicine, University of Sheffield, Regent Court, 30 Regent Street, S1 4DA, Sheffield, UK
Catie Nagel, Chloe Queenan & Chris Burton
You can also search for this author in PubMed Google Scholar
Contributions
Chris Burton: review and editing (equal); formal analysis (supporting). Catie Nagel: Conceptualisation (lead); Methodology (lead); writing – original draft (lead); formal analysis (lead); writing – review and editing (lead). Chloe Queenan: review and editing (supporting); formal analysis (supporting).
Corresponding author
Correspondence to Catie Nagel .
Ethics declarations
Ethics approval and consent to participate, authors’ information, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nagel, C., Queenan, C. & Burton, C. What are medical students taught about persistent physical symptoms? A scoping review of the literature. BMC Med Educ 24 , 618 (2024). https://doi.org/10.1186/s12909-024-05610-z
Download citation
Received : 03 November 2023
Accepted : 27 May 2024
Published : 04 June 2024
DOI : https://doi.org/10.1186/s12909-024-05610-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Scoping review
- Narrative synthesis
- Undergraduate
- Persistent physical symptoms
- Medically unexplained symptoms
- Chronic pain
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Practical considerations of remote care in thoracic aortopathy in india.

1. Introduction
- Geographical Challenges: India’s vast and diverse geography includes many remote areas with limited healthcare access. In India, there is a significant disparity in healthcare resources between urban and rural areas ( Figure 1 A). Telemedicine can bridge these gaps by offering virtual consultations and medical services, reducing the need for long-distance travel, and improving healthcare accessibility [ 5 ].
- Financial Constraints: Many Indians face financial barriers to quality healthcare. Telemedicine provides a cost-effective alternative to in-person consultations, eliminating travel expenses and hospital visits and making healthcare more affordable and accessible from home [ 6 ].
- Healthcare Density: India faces challenges in healthcare density, especially in rural areas, with around 9 doctors per 10,000 inhabitants. Telemedicine optimizes existing healthcare resources by connecting patients remotely with healthcare providers, extending services to underserved populations, and easing the burden on urban healthcare facilities [ 2 ].
- Improved Health Outcomes: Telemedicine facilitates early diagnosis, timely intervention, and continuity of care, improving health outcomes by preventing complications, reducing hospitalizations, and enhancing patient well-being, which is crucial in managing India’s significant burden of non-communicable diseases [ 7 ].
- Public Health Benefits: Telemedicine supports public health initiatives like disease surveillance, outbreak management, and health education. Digital technologies enable healthcare authorities to monitor trends, disseminate information, and deliver preventive care efficiently, aiding disease prevention and population health management.
3.1. Long-Term Management of Thoracic Aortopathy
- Regular monitoring and surveillance: Lifelong monitoring using echocardiography, CT angiography, or MRI to assess disease progression and detect complications like dissection or rupture. Patients with thoracic aortopathy require continuous monitoring to detect any changes in aortic size or morphology and identify complications such as dissection, rupture, or aneurysm formation. Imaging studies such as echocardiography, computed tomography (CT) angiography, or magnetic resonance imaging (MRI) are typically performed at regular intervals as determined by the patient’s specific condition and risk factors [ 1 ].
- Blood pressure management: Strict control of blood pressure is essential for preventing further dilation of the aorta and reducing the risk of aortic dissection or rupture. Patients are often prescribed antihypertensive medications to maintain blood pressure within a target range, and lifestyle modifications such as dietary changes, regular exercise, and stress reduction techniques may also be recommended [ 16 ].
- Medication management: Depending on the underlying cause of thoracic aortopathy and the presence of associated conditions, patients may require long-term medication therapy. This may include medications to lower blood pressure, such as beta-blockers or angiotensin-converting enzyme (ACE) inhibitors, as well as medications to reduce the risk of blood clots or manage other cardiovascular risk factors.
- Genetic counseling and screening: Patients with hereditary forms of thoracic aortopathy, such as Marfan syndrome, Loeys-Dietz syndrome, or familial thoracic aortic aneurysm and dissection (FTAAD), may benefit from genetic counseling and screening for family members. Identifying individuals at risk allows for early detection, surveillance, and intervention to prevent or delay the onset of aortic complications [ 17 ].
- Lifestyle modifications: Encouraging healthy lifestyle habits is important for overall cardiovascular health and can help reduce the progression of thoracic aortopathy. Patients should be advised to maintain a balanced diet low in sodium and saturated fats, engage in regular physical activity, achieve and maintain a healthy weight, avoid tobacco products, and limit alcohol consumption.
- Avoidance of high-impact activities: Patients with thoracic aortopathy are typically advised to avoid activities that may increase the risk of aortic dissection or rupture, such as heavy lifting, strenuous exercise, or contact sports. Low-impact activities such as walking, swimming, or cycling may be recommended instead [ 18 ].
- Surgical intervention: In certain cases, surgical intervention may be necessary to repair or replace the diseased portion of the aorta, particularly if there is evidence of significant dilation, dissection, or impending rupture. Surgical options may include open surgical repair or minimally invasive endovascular procedures, depending on the patient’s specific anatomy and comorbidities.
- Psychosocial support: Living with a chronic condition such as thoracic aortopathy can be challenging, both physically and emotionally. Patients may benefit from access to psychosocial support services, such as counseling, support groups, or online resources, to help cope with the psychological impact of the disease and improve their overall quality of life [ 19 ].
3.2. Benefits of Remote Care in Thoracic Aortopathy [ 3 , 20 ]:
3.3. challenges and considerations of remote care in thoracic aortopathy [ 3 , 20 , 21 ]:, 4. discussion, 5. limitations, 6. future directions, 7. conclusions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Isselbacher, E.M.; Preventza, O.; Hamilton Black Iii, J.; Augoustides, J.G.; Beck, A.W.; Bolen, M.A.; Braverman, A.C.; Bray, B.E.; Brown-Zimmerman, M.M.; Chen, E.P.; et al. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2022 , 80 , e223–e393. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Karan, A.; Negandhi, H.; Hussain, S.; Zapata, T.; Mairembam, D.; De Graeve, H.; Buchan, J.; Zodpey, S. Size, composition and distribution of health workforce in India: Why, and where to invest? Hum. Resour. Health 2021 , 19 , 39. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Castaneda, P.R.; Duffy, B.; Andraska, E.A.; Stevens, J.; Reschke, K.; Osborne, N.; Henke, P.K. Outcomes and safety of electronic consult use in vascular surgery. J. Vasc. Surg. 2020 , 71 , 1726–1732. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Telemedicine, W. World Health Organization Unpublished Document, WHO/DGO/98.01, A Health Telematics Policy: In Support of the WHO’s Health-for-All Strategy for Global Health Development, Report of the WHO Group Consultation on Health Telematics, 11–16, December, Geneva, 1997 ; World Health Organization: Geneva, Switzerland, 1997. [ Google Scholar ]
- Kasthuri, A. Challenges to Healthcare in India—The Five A’s. Indian J. Community Med. 2018 , 43 , 141–143. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ghia, C.; Rambhad, G. Implementation of equity and access in Indian healthcare: Current scenario and way forward. J. Mark. Access Health Policy 2023 , 11 , 2194507. [ Google Scholar ] [ CrossRef ]
- Nethan, S.; Sinha, D.; Mehrotra, R. Non Communicable Disease Risk Factors and their Trends in India. Asian Pac. J. Cancer Prev. 2017 , 18 , 2005–2010. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- CAGR. Available online: https://www.insights10.com/report/india-telemedicine-market-analysis/ (accessed on 6 April 2024).
- Chronicle, D. Available online: https://www.deccanchronicle.com/lifestyle/health-and-wellbeing/130923/the-state-of-telemedicine-in-india.html (accessed on 6 April 2024).
- eSanjeevani. Press Information Bureau, New Delhi. A Big Win for Digital India: Health Ministry’s ‘eSanjeevani’ Telemedicine Service Records 2 Lakh Tele-Consultations. 2020. Available online: https://pib.gov.in/PressReleasePage.aspx?PRID=1646913 (accessed on 6 April 2024).
- Adams, J.G.; Walls, R.M. Supporting the Health Care Workforce During the COVID-19 Global Epidemic. Jama 2020 , 323 , 1439–1440. [ Google Scholar ] [ CrossRef ]
- Grewal, N.; Girdauskas, E.; Idhrees, M.; Velayudhan, B.; Klautz, R.; Driessen, A.; Poelmann, R.E. Structural abnormalities in the non-dilated ascending aortic wall of bicuspid aortic valve patients. Cardiovasc. Pathol. Off. J. Soc. Cardiovasc. Pathol. 2023 , 62 , 107478. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Grewal, N.; Dolmaci, O.; Jansen, E.; Klautz, R.; Driessen, A.; Poelmann, R.E. Thoracic aortopathy in Marfan syndrome overlaps with mechanisms seen in bicuspid aortic valve disease. Front. Cardiovasc. Med. 2023 , 10 , 1018167. [ Google Scholar ] [ CrossRef ]
- Dolmaci, O.B.; Driessen, A.H.G.; Klautz, R.J.M.; Poelmann, R.; Lindeman, J.H.N.; Grewal, N. Comparative evaluation of coronary disease burden: Bicuspid valve disease is not atheroprotective. Open Heart 2021 , 8 , e001772. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shetty, V.; Shetty, D.; Grewal, N. Acute aortic syndromes in India: The need for a nationwide program to increase awareness. Indian Heart J. 2021 , 74 , 76–78. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dolmaci, O.B.; El Mathari, S.; Driessen, A.H.G.; Klautz, R.J.M.; Poelmann, R.E.; Lindeman, J.H.N.; Grewal, N. Are Thoracic Aortic Aneurysm Patients at Increased Risk for Cardiovascular Diseases? J. Clin. Med. 2022 , 12 , 272. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Paterick, T.E.; Humphries, J.A.; Ammar, K.A.; Jan, M.F.; Loberg, R.; Bush, M.; Khandheria, B.K.; Tajik, A.J. Aortopathies: Etiologies, genetics, differential diagnosis, prognosis and management. Am. J. Med. 2013 , 126 , 670–678. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Monda, E.; Verrillo, F.; Rubino, M.; Palmiero, G.; Fusco, A.; Cirillo, A.; Caiazza, M.; Guarnaccia, N.; Mauriello, A.; Lioncino, M.; et al. Thoracic Aortic Dilation: Implications for Physical Activity and Sport Participation. Diagnostics 2022 , 12 , 1392. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Breel, J.S.; de Klerk, E.S.; Strypet, M.; de Heer, F.; Hermanns, H.; Hollmann, M.W.; Eberl, S. What Really Matters to Survivors of Acute Type A Aortic Dissection-A Survey of Patient-Reported Outcomes in the Dutch National Aortic Dissection Advocacy Group. J. Clin. Med. 2023 , 12 , 6584. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chen, A.J.; Yeh, S.L.; Delfin, D.; Hoal, G.; Barron, N.; Riedinger, T.; Kashanijou, N.; Lieland, J.; Bickel, K.; O’Connell, J.B.; et al. Telemedicine and Vascular Surgery: Expanding Access and Providing Care Through the COVID-19 Pandemic. Am. Surg. 2022 , 88 , 2561–2564. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kuwabara, A.; Su, S.; Krauss, J. Utilizing Digital Health Technologies for Patient Education in Lifestyle Medicine. Am. J. Lifestyle Med. 2020 , 14 , 137–142. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lin, J.C.; Crutchfield, J.M.; Zurawski, D.K.; Stevens, C. Implementation of a virtual vascular clinic with point-of-care ultrasound in an integrated health care system. J. Vasc. Surg. 2018 , 68 , 213–218. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Solimini, R.; Busardò, F.P.; Gibelli, F.; Sirignano, A.; Ricci, G. Ethical and Legal Challenges of Telemedicine in the Era of the COVID-19 Pandemic. Medicina 2021 , 57 , 1314. [ Google Scholar ] [ CrossRef ] [ PubMed ]
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Grewal, N.; Idhrees, M.; Velayudhan, B.; Klautz, R.J.M.; Grewal, S. Practical Considerations of Remote Care in Thoracic Aortopathy in India. J. Clin. Med. 2024 , 13 , 3327. https://doi.org/10.3390/jcm13113327
Grewal N, Idhrees M, Velayudhan B, Klautz RJM, Grewal S. Practical Considerations of Remote Care in Thoracic Aortopathy in India. Journal of Clinical Medicine . 2024; 13(11):3327. https://doi.org/10.3390/jcm13113327
Grewal, Nimrat, Mohammed Idhrees, Bashi Velayudhan, Robert J. M. Klautz, and Simran Grewal. 2024. "Practical Considerations of Remote Care in Thoracic Aortopathy in India" Journal of Clinical Medicine 13, no. 11: 3327. https://doi.org/10.3390/jcm13113327
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Role of Magnesium in the Intensive Care Unit and Immunomodulation: A Literature Review
Affiliations.
- 1 Santa Croce and Carle Hospital, Department of Emergency and Critical Care, 12100 Cuneo, Italy.
- 2 Division of Anesthesiology, Department of Anesthesiology, Intensive care and Emergency Medicine, Ospedale Regionale di Lugano, 69000 Lugano, Switzerland.
- 3 Department of Medicine and Surgery, University of Milan-Bicocca, 20900 Monza, Italy.
- 4 Department of Prehospital Emergency Medicine, ASL TA, Italian Society of Prehospital Emergency Medicine (SIS 118), 74121 Taranto, Italy.
- 5 Department of Neurology, Fondazione IRCCS San Gerardo dei Tintori, School of Medicine and Surgery, Milan Center for Neuroscience, University of Milano-Bicocca, 20900 Monza, Italy.
- PMID: 37376511
- PMCID: PMC10304084
- DOI: 10.3390/vaccines11061122
Both the role and the importance of magnesium in clinical practice have grown considerably in recent years. Emerging evidence suggests an association between loss of magnesium homeostasis and increased mortality in the critical care setting. The underlying mechanism is still unclear, but an increasing number of in vivo and in vitro studies on magnesium's immunomodulating capabilities may shed some light on the matter. This review aims to discuss the evidence behind magnesium homeostasis in critically ill patients, and its link with intensive care unit mortality via a likely magnesium-induced dysregulation of the immune response. The underlying pathogenetic mechanisms, and their implications for clinical outcomes, are discussed. The available evidence strongly supports the crucial role of magnesium in immune system regulation and inflammatory response. The loss of magnesium homeostasis has been associated with an elevated risk of bacterial infections, exacerbated sepsis progression, and detrimental effects on the cardiac, respiratory, neurological, and renal systems, ultimately leading to increased mortality. However, magnesium supplementation has been shown to be beneficial in these conditions, highlighting the importance of maintaining adequate magnesium levels in the intensive care setting.
Keywords: critical care; immunomodulation; infections; magnesium.
PubMed Disclaimer
Conflict of interest statement
The authors declare no conflict of interest.
Similar articles
- Feeding the critically ill obese patient: a systematic review protocol. Secombe P, Harley S, Chapman M, Aromataris E. Secombe P, et al. JBI Database System Rev Implement Rep. 2015 Oct;13(10):95-109. doi: 10.11124/jbisrir-2015-2458. JBI Database System Rev Implement Rep. 2015. PMID: 26571286
- Magnesium and stress. Cuciureanu MD, Vink R. Cuciureanu MD, et al. In: Vink R, Nechifor M, editors. Magnesium in the Central Nervous System [Internet]. Adelaide (AU): University of Adelaide Press; 2011. In: Vink R, Nechifor M, editors. Magnesium in the Central Nervous System [Internet]. Adelaide (AU): University of Adelaide Press; 2011. PMID: 29920004 Free Books & Documents. Review.
- Hypomagnesemia in critically ill medical patients. Limaye CS, Londhey VA, Nadkart MY, Borges NE. Limaye CS, et al. J Assoc Physicians India. 2011 Jan;59:19-22. J Assoc Physicians India. 2011. PMID: 21751660
- Effects of magnesium, phosphate, or zinc supplementation in intensive care unit patients-A systematic review and meta-analysis. Vesterlund GK, Jensen TS, Ellekjaer KL, Møller MH, Thomsen T, Perner A. Vesterlund GK, et al. Acta Anaesthesiol Scand. 2023 Mar;67(3):264-276. doi: 10.1111/aas.14186. Epub 2023 Jan 6. Acta Anaesthesiol Scand. 2023. PMID: 36562170 Review.
- Magnesium supplementation and the potential association with mortality rates among critically ill non-cardiac patients. Dabbagh OC, Aldawood AS, Arabi YM, Lone NA, Brits R, Pillay M. Dabbagh OC, et al. Saudi Med J. 2006 Jun;27(6):821-5. Saudi Med J. 2006. PMID: 16758043
- The Impact of Chronic Magnesium Deficiency on Excitable Tissues-Translational Aspects. Stanojević M, Djuricic N, Parezanovic M, Biorac M, Pathak D, Spasic S, Lopicic S, Kovacevic S, Nesovic Ostojic J. Stanojević M, et al. Biol Trace Elem Res. 2024 May 6. doi: 10.1007/s12011-024-04216-2. Online ahead of print. Biol Trace Elem Res. 2024. PMID: 38709369 Review.
- Wacker W.E.C., Parisi A.F. Magnesium Metabolism. N. Engl. J. Med. 1968;278:712–717. doi: 10.1056/NEJM196803282781306. - DOI - PubMed
- Yunes P., Mojtaba M., Atabak N., Mohammad R.G., Mohammad A., Mohammad S., Arezoo A., Seyyed M.R., Amirhossein S. The role of magnesium sulfate in the intensive care unit. EXCLI J. 2017;16:464–482. - PMC - PubMed
- Mazur A., Maier J.A.M., Rock E., Gueux E., Nowacki W., Rayssiguier Y. Magnesium and the inflammatory response: Potential physiopathological implications. Arch. Biochem. Biophys. 2007;458:48–56. doi: 10.1016/j.abb.2006.03.031. - DOI - PubMed
- Tam M., Gómez S., González-Gross M., Marcos A. Possible roles of magnesium on the immune system. Eur. J. Clin. Nutr. 2003;57:1193–1197. doi: 10.1038/sj.ejcn.1601689. - DOI - PubMed
- Cascella M., Vaqar S. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2023. Hypermagnesemia. - PubMed
Publication types
- Search in MeSH
Grants and funding
Linkout - more resources, full text sources.
- Europe PubMed Central
- PubMed Central

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Online First
- Assessing health outcomes: a systematic review of electronic patient-reported outcomes in oncology
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1880-5731 Mikel Urretavizcaya 1 ,
- Karen Álvarez 2 ,
- Olatz Olariaga 1 ,
- Maria Jose Tames 1 ,
- Ainhoa Asensio 1 ,
- Gerardo Cajaraville 1 ,
- http://orcid.org/0000-0002-8986-0247 Ana Cristina Riestra 1 , 3
- 1 Pharmacy Department , Onkologikoa , San Sebastian , País Vasco , Spain
- 2 Pharmacy Department , Nuestra Senora de la Candelaria University Hospital , Santa Cruz de Tenerife , Canarias , Spain
- 3 Medicine Department , University of Deusto , Bilbao , País Vasco , Spain
- Correspondence to Mikel Urretavizcaya, Pharmacy Department, Onkologikoa, San Sebastian, País Vasco, Spain; urretabizkaia.mikel{at}gmail.com
Purpose This study investigates the clinical impact of electronic patient-reported outcome (ePRO) monitoring apps/web interfaces, aimed at symptom-management, in cancer patients undergoing outpatient systemic antineoplastic treatment. Additionally, it explores the advantages offered by these applications, including their functionalities and healthcare team-initiated follow-up programmes.
Methods A systematic literature review was conducted using a predefined search strategy in MEDLINE. Inclusion criteria encompassed primary studies assessing symptom burden through at-home ePRO surveys in adult cancer patients receiving outpatient systemic antineoplastic treatment, whenever health outcomes were evaluated. Exclusion criteria excluded telemedicine-based interventions other than ePRO questionnaires and non-primary articles or study protocols. To evaluate the potential bias in the included studies, an exhaustive quality assessment was conducted, as an additional inclusion filter.
Results Among 246 identified articles, 227 were excluded for non-compliance with inclusion/exclusion criteria. Of the remaining 19 articles, only eight met the rigorous validity assessment and were included for detailed examination and data extraction, presented in attached tables.
Conclusion This review provides compelling evidence of ePRO monitoring’s positive clinical impact across diverse cancer settings, encompassing various cancer types, including early and metastatic stages. These systems are crucial in enabling timely interventions and reducing communication barriers, among other functionalities. While areas for future ePRO innovation are identified, the primary limitation lies in comparing clinical outcomes of reviewed articles, due to scale variability and study population heterogeneity. To conclude, our results reaffirm the transformative potential of ePRO apps in oncology and their pivotal role in shaping the future of cancer care.
- Patient Reported Outcomes
- Adverse Drug Reaction Reporting Systems
- Antineoplastic agents
- MEDICAL ONCOLOGY
- Quality of Life
- Outcome Assessment, Health Care
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. As this study is a systematic review, no new data were generated or analysed. All data used in this review are publicly available in the cited sources, and the comprehensive list of references is provided in the manuscript. The authors confirm that they had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
https://doi.org/10.1136/ejhpharm-2023-004072
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Read the full text or download the PDF:
- Case report
- Open access
- Published: 27 May 2024
A rare incidence of severe dermatological toxicities triggered by concomitant administration of all-trans retinoic acid and triazole antifungal in patients with acute promyelocytic leukemia: a case series and review of the literature
- Aisha Jamal ORCID: orcid.org/0000-0001-5022-7498 1 , 3 ,
- Rafia Hassam 1 ,
- Qurratulain Rizvi 1 ,
- Ali Saleem 1 ,
- Anum Khalid 2 &
- Nida Anwar 1
Journal of Medical Case Reports volume 18 , Article number: 261 ( 2024 ) Cite this article
482 Accesses
2 Altmetric
Metrics details
All-trans retinoic acid (ATRA) is an indispensable part of the treatment of acute promyelocytic leukemia (APL). Although, mild cutaneous toxicities like mucocutaneous xerosis, rash, and pruritus are well reported, ATRA associated severe dermatological toxicities are extremely rare. ATRA is primary metabolized by cytochrome P450 (CYP450) enzyme system, and triazole antifungals are notorious for their strong inhibitory effect on CYP450.
Case presentation
Three Asian APL patients experienced rare ATRA-induced severe dermatological toxicities: exfoliative dermatitis (ED) in cases 1 and 2, and necrotic scrotal ulceration in case 3. Both case 1 (33-year-old female), and case 2 (28-year-old male) landed in emergency department with dehydration, generalized skin erythema and xerosis during their induction chemotherapy. Both of these patients also developed invasive aspergillosis and required concomitant triazole antifungals during their chemotherapy. For ED, intravenous fluids and broad-spectrum antibiotics were started along with application of local emollients to prevent transdermal water loss. Although their general condition improved but skin exfoliation continued with complete desquamation of palms and soles. Dermatology was consulted, and clinical diagnosis of ED was established. Discontinuation of ATRA resulted in complete resolution of ED. Case 3 (15-year-old boy) reported two blackish mildly tender scrotal lesions during induction chemotherapy. He also had mucocutaneous candidiasis at presentation and was kept on triazole antifungal. Local bacterial & fungal cultures, and serological testing for herpes simplex virus were reported negative. Despite adequate local care and optimal antibiotic support, his lesions persisted, and improved only after temporary discontinuation of ATRA. After a thorough literature review and considering the temporal association of cutaneous toxicities with triazole antifungals, we speculate that the concomitant use of triazole antifungals inhibited the hepatic metabolism of ATRA, resulting in higher serum ATRA concentration, and markedly accentuated cutaneous toxicities in our patients.
By highlighting this crucial pharmacokinetic interaction, we want to caution the fellow oncologists to be mindful of the inhibitory effect of triazole antifungals on CYP450. We propose using a non-myelosuppressive combination of ATRA and arsenic trioxide for management of APL hence, obliterating the need of prophylactic antifungals. However, in the event of invasive fungal infection (IFI), we suggest using alternative class of antifungals.
Peer Review reports
Acute promyelocytic leukemia (APL) is a rare and potentially curable subtype of acute myeloid leukemia (AML), accounting for 5–8% of AML cases [ 1 ]. Genetically, APL is characterized by reciprocal translocation t(15:17) (q22;q11–12), with consequent fusion of promyelocytic (PML) gene on chromosome 15q22 to retinoic acid receptor-alpha (RAR-alpha) gene on chromosome 17q21. The resultant fusion oncoprotein, PML-RARA, induces transcriptional repression, chromatin condensation, maturation arrest, and accumulation of abnormal promyelocytes [ 2 ]. Advent of all-trans retinoic acid (ATRA) has revolutionized the treatment landscape of APL, and along with the backbone of anthracycline based chemotherapy, it is considered to be the standard of care for APL patients. Combination treatment with ATRA plus anthracycline based chemotherapy achieves an overall complete remission and cure rate of 95% and 80% respectively, rendering ATRA indispensable in the management of APL [ 3 ].
ATRA, an active metabolite of vitamin A, belongs to a class of retinoids. Although retinoids are well known for their dermatological side effects like xerosis, xerostomia, erythema, pruritis, and exfoliation; severe dermatological side effects of ATRA, especially in the dosage pertinent to APL (45 mg/m 2 ), are rare. So far, only a single case of exfoliative dermatitis (ED) and a few cases of scrotal ulceration have been reported in literature [ 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ]. We, here in, report a case series of three patients with serious and rare ATRA associated dermatological complications. We have also discussed upon the potentially precipitating pharmacokinetic interactions, as well as the detailed clinical course and management of our patients as simply withholding ATRA can jeopardize the outcome of this potentially curable malignant disorder.
In all three patients, ATRA was started as soon as abnormal promyelocytes were documented on peripheral smear/bone marrow aspirate examination (Figs. 1 , 2 , 3 ). Diagnosis was further confirmed through cytogenetic analysis as well as PML-RARA detection by polymerase chain reaction. Additionally, in all three patients, chemotherapeutic treatment was instituted according to European APL protocol, based on their risk-group classification.

Exfoliative dermatitis &Onychomadesis (CASE 1). a Peripheral smear. b Bone marrow aspirate. c Desquamation of soles. d Desquamation of palms. e Dry exfoliation of feet and shins. f Onychomadesis
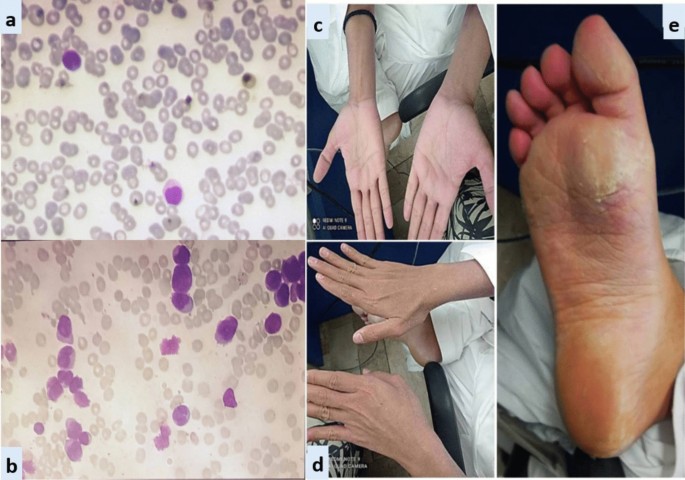
Exfoliative dermatitis (CASE 2). a Peripheral smear. b Bone marrow aspirate. c and d Erythema and scaling of hands. e Cutaneous desquamation of soles
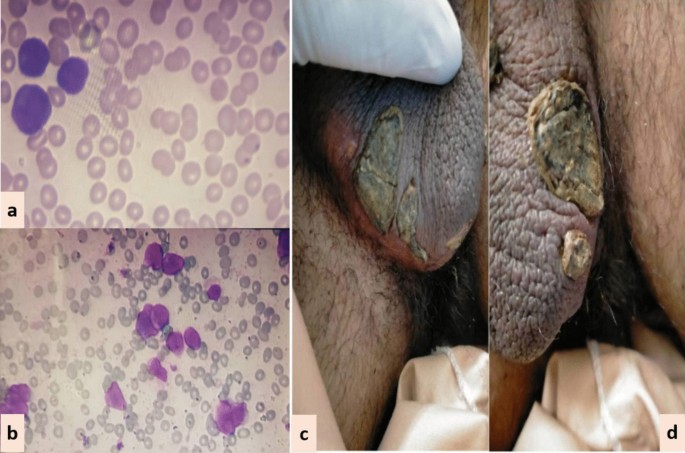
Scrotal lesions (CASE 3). a Peripheral smear. b Bone marrow aspirate. c and d Necrotic scrotal lesions with black eschar
Case 1: A 33-year-old Asian female presented in ER with history of fever, heavy menstrual bleeding and rash all over body. Induction chemotherapy and steroid prophylaxis was promptly started to prevent differentiation syndrome (DS). On Day-10 of induction chemotherapy, she developed high grade fever, cough and shortness of breath. High-resolution computerized tomography (HRCT) showed randomly scattered discrete nodular opacities with surrounding ground glass haze in both lung fields, suggestive of invasive fungal infection (IFI). Voriconazole was immediately started along with broad-spectrum antibiotics. She improved over the following 72 hour, and was discharged from hospital on Day-17. Subsequently, she landed in emergency department on Day-23 with severe dehydration, shivering, tachycardia, generalized skin erythema and discoloration of nail beds. Intravenous fluids and broad-spectrum antibiotics were started along with application of local emollients to prevent transdermal water loss. Over the next 24-36 hour, her general condition was stabilized however; skin exfoliation continued with complete desquamation of palms and soles (Fig. 1 ). Dermatology was consulted, and a clinical diagnosis of onychomadesis and exfoliative dermatitis (ED) was made. A review of her clinical case demonstrated no apparent cause for ED except for a rare association with ATRA. However, considering the curative potential of ATRA, it was continued till Day-28 as per protocol. Her skin condition gradually resolved over next 10–14 days after discontinuation of ATRA. She had recurrence of similar skin condition upon re-exposure to ATRA in her consolidation chemotherapeutic cycles, however, the exfoliation was mild and patchy that responded well to good oral hydration and local skin emollients.
Case 2: A 28-year-old Asian male presented in the out-patient clinic with the history of generalized weakness, high-grade-fever, productive cough and bruises over body. On examination, he had multiple ecchymosis and petechiae with coarse crepitations involving right-middle and left-lower lung fields. He was promptly started on broad-spectrum antibiotics. Additionally, as per protocol, induction chemotherapy and dexamethasone prophylaxis was also instituted. His fever and cough remained unresponsive despite broad-spectrum antibiotics. Voriconazole was instituted upon the identification of IFI on HRCT findings. By day-10, coagulopathy was normalized, and clearance of abnormal promyelocytes was documented by Day-18. On Day-20, he complained of skin dryness, itching and scaling; physical examination revealed generalized xerosis and erythema (Fig. 2 ). Despite aggressive skin care, generalized skin exfoliation, most pronounced on palms and soles, ensued. Clinical diagnosis of ED was established after obtaining dermatological consultation. However, in view of his clinical stability, ATRA was continued. Bone marrow aspirate on Day-28 showed morphological remission. Recurrence of erythema and exfoliation was documented during consolidation phase of chemotherapy, but the condition was responsive to local emollients and oral hydration.
Case 3: A 15-year-old Asian male presented in the out-patient clinic with complains of high-grade-fever, muco-cutaneous bleeding and pancytopenia. On presentation, patient was febrile and had oral thrush. After sending his baseline tests he was taken on broad-spectrum antibiotics and triazole antifungal (itraconazole). After completion of induction chemotherapy, patient was discharged with bi-weekly follow-ups.On Day15, he reported two blackish, mildly tender scrotal lesions with minimal serous discharge (Fig. 3 ). Antibiotic cover for soft tissue infection was commenced along with local wound care with topical steroids and antibiotics. He had no sign of systemic infection/sepsis. Local bacterial & fungal cultures and serological testing for herpes simplex virus were reported negative. Despite adequate local care and optimal antibiotic support, his lesions showed no sign of healing, and two new lesions were developed. Lesion biopsy for histopathological evaluation was declined by the patient. Keeping the rare but reported occurrence of ATRA-induced scrotal ulceration and fournier's gangrene; ATRA was transiently withheld for ten days and the lesions started to regress. However, considering the indispensable role of ATRA in APL, it was reinstituted. Scrotal lesions persisted without any worsening. ATRA was stopped after completion of protocol. Complete resolution of scrotal lesions was documented over the following two weeks. Afterwards, he received two cycles of consolidation chemotherapy, but no recurrence was reported.
Discussion and conclusion
The antineoplastic role of ATRA remains indispensable in the curative management of APL. It is considered a relatively safe drug with a well-known toxicity profile. Commonly reported adverse events include DS, pseudotumor-cerebri, hypertriglyceridemia, transaminitis, and headache. Although, mild cutaneous toxicities like muco-cutaneous xerosis, photosensitivity, rash, pruritus and sweet’s syndrome are well reported, severe dermatological toxicities are rarely reported in literature [ 18 , 19 ]. In this case series, we have discussed three cases of ATRA-induced rare dermatological complications in APL.
Case 1 and 2 developed ED during remission induction phase of chemotherapy. Literature review revealed only a single reported occurrence of ATRA-induced ED in APL by YonelIpek et al. [ 4 ]. ED is a potentially life-threatening cutaneous manifestation that is characterized by diffuse skin erythema and scaling. Various underlying disorders can trigger its onset through a complex interplay of inflammatory cytokines and phagocytes. In contrast to our cases, the case reported by Yonel Ipek et al. developed xerosis in consolidation phase, which akin to our cases started after two weeks of ATRA exposure and rapidly deteriorated to generalized erythroderma and scaling. In both cases, discontinuation of ATRA resulted in complete resolution of ED.
In case 3, we have reported ATRA-induced necrotic scrotal ulceration. Literature review revealed that over the last two decades, a total of twenty cases of ATRA-induced scrotal ulceration have been reported. Histopathological evaluation of these lesions revealed atypical granulocytic infiltration, pointing towards the possible etiological role of differentiated APL cells in the pathogenesis. Most of these cases, including ours, developed genital-lesions almost after two weeks of ATRA exposure and remained unresponsive to local and systemic antibiotics. ATRA had to be halted in most of the cases to prevent progression to fournier’s gangrene [ 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ].
Scattered over the span of three years and considered in isolation, it was not initially apparent to us that all three cases had one striking similarity: concomitant use of ATRA and triazole antifungals. ATRA is primary metabolized by cytochrome P450 enzyme system. Triazole antifungals are notorious for their strong inhibitory effect on CYP450 enzyme system, resulting in supra-therapeutic drug levels and toxicity [ 20 , 21 , 22 ].
Potentiation of serum ATRA levels by inhibition of CYP450 system was first explored by Rigas et al. [ 23 ]. This study reported 1.8 times higher serum concentration of ATRA with concomitant use of ketoconazole. Since then a number of cases have reported the augmentation of ATRA-induced toxicities due to this pharmacokinetic interaction. Concomitant use of ATRA and triazole antifungals that is voriconazole and posaconazole has been implicated to cause severe hypercalcemia [ 24 , 25 , 26 , 27 ]. Similarly, combination with fluconazole has been reported to cause severe neurotoxicity and nephrotoxicity [ 28 , 29 ].
Considering the temporal association of dermatological complications with triazole antifungals in our patients, we speculate that the concomitant use of triazole antifungals inhibited the metabolism of ATRA, resulting in higher serum concentrations and markedly accentuated cutaneous toxicities. A study further strengthening our hypothesis was conducted by Kurzrock et al. to evaluate the maximum tolerable dose of ATRA in myelodysplastic syndrome. The study reported severe dose-limiting cutaneous toxicities, such as generalized desquamation and genital ulceration, at doses > 150 mg/m 2 /day, compared to mild xerosis and erythema in the dose range of 45–100 mg/m 2 /day. Akin to our cases, the study reported complete resolution of cutaneous toxicities within 1–2 weeks of ATRA discontinuation [ 30 ].
Another important point is the recurrence of ED in both case 1 and 2 during their consolidation chemotherapy cycles, whereas recurrent scrotal ulceration was not documented in case 3. The most likely explanation is the continuation of voriconazole as secondary prophylaxis in patients with invasive fungal infections (IFI) (case 1 and 2), whereas itraconazole was discontinued after remission induction in case 3. This once again underscores the pharmacokinetic potentiation of ATRA-induced cutaneous toxicities by triazole antifungals. An important limitation of our study is that, due to the unavailability of serum voriconazole testing, we couldn’t document serum voriconazole levels, something that could provide valuable insights into the effect of serum azole levels on the severity of cutaneous manifestations.
By highlighting this crucial pharmacokinetic interaction and its potentially severe implications, we urge our fellow oncologists to remain vigilant regarding the inhibitory effects of triazole antifungals on the metabolism of ATRA. We propose the use of a non-myelosuppressive combination of ATRA and arsenic trioxide for APL, thereby eliminating the need for prophylactic antifungals. In the case of invasive fungal infections (IFI), we recommend considering alternative classes of antifungals. However, if triazole antifungals are deemed unavoidable, we suggest close monitoring for potential side effects and implementing prophylactic measures as clinically necessary.
Availability of data and materials
Data sharing is not applicable to this manuscript as no datasets were generated or analyzed during the current study.
Abbreviations
Acute promyelocytic leukemia
All-trans retinoic acid
Cytochrome P450
Differentiation syndrome
- Exfoliative dermatitis
High-resolution computerized tomography
Invasive fungal infections
Promyelocytic leukemia-retinoic acid receptor alpha
Yilmaz M, Kantarjian H, Ravandi F. Acute promyelocytic leukemia current treatment algorithms. Blood Cancer J. 2021;11:123.
Article PubMed PubMed Central Google Scholar
Lo-Coco F, Ammatuna E. The biology of acute promyelocytic leukemia and its impact on diagnosis and treatment. Hematology. 2006;2006:156–61.
Article Google Scholar
Lo-Coco F, Avvisati G, Vignetti M, Thiede C, Orlando SM, Iacobelli S, et al . Retinoic acid and arsenic trioxide for acute promyelocytic leukemia. N Engl J Med. 2013;369:111–21.
Article CAS PubMed Google Scholar
Ipek Y, Hulya D, Melih A. Disseminated exfoliative dermatitis associated with all-transretinoic Acid in the treatment of acute promyelocytic leukemia. Case Rep Med. 2012;2012:236174–236174.
Mori A, Tamura S, Katsuno T, Nishimura Y, Itoh T, Saheki K, et al . Scrotal ulcer occurring in patients with acute promyelocytic leukemia during treatment with all-trans retinoic acid. Oncol Rep. 1999;6:55–8.
CAS PubMed Google Scholar
Charles KS, Kanaa M, Winfield DA, Reilly JT. Scrotal ulceration during all-trans retinoic (ATRA) therapy for acute promyelocytic leukaemia. Clin Lab Haematol. 2000;22:171–4.
Pavithran K, Arjun R, Aruna R, Thomas M. Scrotal ulceration during induction therapy of acute promyelocytic leukemia with ATRA. Am J Hematol. 2004;75:260–1.
Article PubMed Google Scholar
Fukuno K, Tsurumi H, Goto H, Oyama M, Tanabashi S, Moriwaki H. Genital ulcers during treatment with ALL-trans retinoic acid for acute promyelocytic leukemia. Leuk Lymphoma. 2003;44:2009–13.
Mourad YA, Jabr F, Salem Z. Scrotal ulceration induced by all-trans retinoic acid in a patient with acute promyelocytic leukemia. Int J Dermatol. 2005;44:68–9.
Shimizu D, Nomura K, Matsuyama R, Matsumoto Y, Ueda K, Masuda K, et al . Scrotal ulcers arising during treatment with all-trans retinoic acid for acute promyelocytic leukemia. Internal Med (Tokyo, Japan). 2005;44:480–3.
Lee HY, Ang AL, Lim LC, Thirumoorthy T, Pang SM. All-trans retinoic acid-induced scrotal ulcer in a patient with acute promyelocytic leukaemia. Clin Exp Dermatol. 2010;35:91–2.
Tazi I, Rachid M, Quessar A, Benchekroun S. Scrotal ulceration following all-trans retinoic Acid therapy for acute promyelocytic leukemia. Indian J Dermatol. 2011;56:561–3.
Schmutz JL, Trechot P. Tretinoin and scrotal ulceration. Ann Dermatol Venereol. 2012;139:588–9.
Al Huneini M, Wasim F, Al Farsi K, Al-Khabori M, Al KS. Genital ulcer development in patients with acute promyelocytic leukaemia treated with all-trans retinoic Acid: a case series. Oman Med J. 2013;28:207–9.
Tajima K, Sagae M, Yahagi A, Akiba J, Suzuki K, Hayashi T, et al . Scrotum exfoliative dermatitis with ulcers associated with treatment of acute promyelocytic leukemia with all-trans retinoic acid [Rinsho ketsueki]. Jpn J Clin Hematol. 1998;39:48–52.
CAS Google Scholar
Drago MJ, Kim BS, Bennett D, Elder D, Rosenbach M. All-trans-retinoic acid-induced scrotal ulcers in a patient with acute promyelocytic leukemia. Cutis. 2013;91:246–7.
PubMed Google Scholar
Sutherland J, Kempton CL, Curry MA. Continuation of all-trans retinoic acid despite the development of scrotal ulcerations in a black male. J Oncol Pharmacy Pract. 2015;21:393–5.
Article CAS Google Scholar
Sun GL. Treatment of acute promyelocytic leukemia (APL) with all-trans retinoic acid (ATRA): a report of five-year experience. Zhonghua Zhong Liu Za Zhi [Chin J Oncol]. 1993;15:125–9.
BC Cancer Agency Cancer Drug Manual. Tretinoin. February 2014. Available from: http://www.bccancer.bc.ca/drug-database-site/Drug%20Index/Tretinoin_monograph_1Feb2014.pdf . Accessed 27 Sept 2023.
McSorley LC, Daly AK. Identification of human cytochrome P450 isoforms that contribute to all-trans-retinoic acid 4-hydroxylation. Biochem Pharmacol. 2000;60:517–26.
Brüggemann RJM, Alffenaar J-WC, Blijlevens NMA, Billaud EM, Kosterink JGW, Verweij PE, et al . Clinical relevance of the pharmacokinetic interactions of azole antifungal drugs with other coadministered agents. Clin Infect Dis. 2009;48:1441–58.
Bellmann R, Smuszkiewicz P. Pharmacokinetics of antifungal drugs: practical implications for optimized treatment of patients. Infection. 2017;45:737–79.
Article CAS PubMed PubMed Central Google Scholar
Rigas JR, Francis PA, Muindi JR, Kris MG, Huselton C, DeGrazia F, et al . Constitutive variability in the pharmacokinetics of the natural retinoid, all-trans-retinoic acid, and its modulation by ketoconazole. J Natl Cancer Inst. 1993;85:1921–6.
Bennett MT, Sirrs S, Yeung JK, Smith CA. Hypercalcemia due to all trans retinoic acid in the treatment of acute promyelocytic leukemia potentiated by voriconazole. Leuk Lymphoma. 2005;46:1829–31.
Cordoba R, Ramirez E, Lei SH, Lopezdela Guia A, Sanjurjo MJ, Carcas AJ, et al . Hypercalcemia due to an interaction of all-trans retinoic acid (ATRA) and itraconazole therapy for acute promyelocytic leukemia successfully treated with zoledronic acid. Eur J Clin Pharmacol. 2008;64:1031–2.
Yozgat AK, Akçabelen Y, Unal Y, Yaralı N. Hypercalcemia due to concomitant use of all trans retinoic acid and voriconazole. Hematol Transfusion Cell Therapy. 2020;42:73.
Afacan Ozturk HB, Albayrak M, Maral S, Reis Aras M, Yilmaz F, Akyol P, et al . Hypercalcemia associated with the interaction between all trans retinoic acid and posaconazole in an acute promyelocytic leukemia case. J Oncol Pharm Pract. 2021;27:2027–9.
Vanier KL, Mattiussi AJ, Johnston DL. Interaction of all-trans-retinoic acid with fluconazole in acute promyelocytic leukemia. J Pediatr Hematol Oncol. 2003;25:403–4.
Yarali N, Tavil B, Kara A, Ozkasap S, Tunç B. Acute renal failure during ATRA treatment. Pediatr Hematol Oncol. 2008;25:115–8.
Kurzrock R, Estey E, Talpaz M. All-trans retinoic acid: tolerance and biologic effects in myelodysplastic syndrome. J Clin Oncol. 1993;11:1489–95.
Download references
Acknowledgements
This research did not receive any specific grant from funding agencies in public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Section of Malignant Haematology, National Institute of Blood Disease and Bone Marrow Transplantation, Karachi, Pakistan
Aisha Jamal, Rafia Hassam, Qurratulain Rizvi, Ali Saleem & Nida Anwar
Research and Development, National Institute of Blood Disease and Bone Marrow Transplantation, Karachi, Pakistan
Anum Khalid
Department of Clinical Haematology, National Institute of Blood Diseases and Bone Marrow Transplantation, Plot # Special D-3, Block-6, (Across Railway Line), P.E.C.H.S, Karachi, Pakistan
Aisha Jamal
You can also search for this author in PubMed Google Scholar
Contributions
Aisha Jamal: Conceptualization, writing-original draft, writing-review & editing. Rafia Hassam: Conceptualization, writing-original draft. Qurratulain Rizvi: Writing-review & editing. Ali Saleem: Data curation, writing—review & editing. Anum Khalid: Writing—review &editing. Nida Anwar: Writing—review & editing.
Corresponding author
Correspondence to Aisha Jamal .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the ethics committee of National Institute of Blood Disease & Bone Marrow Transplantation, Karachi, Pakistan. The patient’s consent was obtained for publication of case.
Consent for publication
Written informed consent was obtained from the patients for publication of this case report and any accompanying images. Written informed consent was obtained from the patient’s legal guardian(s) for publication of this case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jamal, A., Hassam, R., Rizvi, Q. et al. A rare incidence of severe dermatological toxicities triggered by concomitant administration of all-trans retinoic acid and triazole antifungal in patients with acute promyelocytic leukemia: a case series and review of the literature. J Med Case Reports 18 , 261 (2024). https://doi.org/10.1186/s13256-024-04577-1
Download citation
Received : 19 December 2023
Accepted : 01 May 2024
Published : 27 May 2024
DOI : https://doi.org/10.1186/s13256-024-04577-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pharmacokinetic drug interaction
- Necrotic scrotal ulceration
- All-trans retinoic acid toxicity
- Triazole anti-fungal
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
This paper identifies the core dimensions of integrated care based on a review of previous literature on the topic. Methodology: The research reviewed literature evidence from the peer-reviewed and grey literature. It focused on reviewing research articles that had specifically developed frameworks on integrated care and/or set out key elements ...
This review focuses on the concept of care, a concept that has never been more popular as a focus of study. It undertakes a critical review, motivated by the breadth of the field and the lack of coherence and linkages across a diverse literature. The review concentrates first on organizing and reviewing the literature in terms of key focus and ...
Literature describing nursing care (concepts and theories on nursing care) Abstracts, discussion articles, non-research articles, systematic reviews, anecdotal reports or editorials, conference proceedings, dissertations and concept analysis ... The findings of this integrative literature review are important in terms of developing research ...
A systematic review of the primary care literature was carried out, restricted to English language journals reporting original research or systematic reviews. Studies published between 2003 and July 2008 were searched in MEDLINE, Embase, Cochrane Library, CINAHL, King's Fund Database, IDEAS Database, and EconLit. Eighty-five studies were ...
Kinley J, Froggatt K, Bennett MI. The effect of policy on end-of-life care practice within nursing care homes: a systematic review. Palliat Med. 2013;27:209-20. Article PubMed Google Scholar Kuhlmann AS, Gavin L, Galavotti C. The integration of family planning with other health services: a literature review.
The Patient Perspective of Quality Care: A Literature Review. January 2019. The George Washington University Undergraduate Review 2 (Spring 2019) DOI: 10.4079/2578-9201.2 (2019).10. Authors ...
The systematic review of the literature in health and social care has a differ-ent focus. It aims to contribute to clinical practice through an assessment of the efficacy of a particular health care intervention and, with the emphasis on evidence-based practice, has become increasingly important. A basic overview
Nursing care planning is an essential part of nursing practice that provides the framework for patient care (Can & Erol, 2012). Quality of information in nursing care plans includes completeness, content and accuracy as essential characteristics. ... A scoping review of the literature was conducted (2019) across PubMed, CINAHL, Embase and ...
Implementing evidence into practice requires nurses to identify, critically appraise and synthesise research. This may require a comprehensive literature review: this article aims to outline the approaches and stages required and provides a working example of a published review. Literature reviews aim to answer focused questions to: inform professionals and patients of the best available ...
A formal literature review is an evidence-based, in-depth analysis of a subject. There are many reasons for writing one and these will influence the length and style of your review, but in essence a literature review is a critical appraisal of the current collective knowledge on a subject. Rather than just being an exhaustive list of all that ...
The purpose of this article was to investigate the outcome measures developed and used in palliative care. The paper involved a literature review of published research. Many of the reviewed papers concluded similarly that there was lack of good quality evidence on which to base conclusions. More high quality evidence is needed to compare the ...
The aim of this systematic review was examine the available literature related to nursing documentation and care plans, in relation to the impacts of using standardised nursing language. Methods The electronic databases of Medline and Cumulative Index to Nursing and Allied Health Literature were searched using predetermined search strategy.
Critical care is a unique specialised area of practice; critical care clinicians should, wherever possible, promote and use evidence-based practice. Nurse researchers and clinicians often use literature reviews to support their practice or justify research projects. With an overwhelming volume of evidence (new and old) available, literature reviews act as a librarian, filtering through ...
Adela Bisak, Martin Stafström, Unleashing the potential of Health Promotion in primary care—a scoping literature review, Health Promotion International, Volume 39, Issue 3, June 2024, daae044, ... We performed a literature review, with three specific aims. First, to identify studies that have targeted the healthy population in intervention ...
Thus, through a comprehensive review of the extant literature, this study presents a critique of the health information system for healthcare to supplement the gap created as a result of the lack of an in-depth outlook of the current health information system from a holistic slant. ... Although several authors identified the unique disposition ...
As the ageing population grows, the demand for long-term care (LTC) services will rise, concurrently amplifying healthcare utilisation. This review aims to examine and consolidate information on LTC interventions that influence healthcare utilisation among older persons. A scoping review was performed through a systematic search in PubMed, EBSCO CINAHL, EBM Reviews - Cochrane Database of ...
A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice. ... Thus, this critical literature review study explores the ...
Background Person-centred planning refers to a model of care in which programs and services are developed in collaboration with persons receiving care (i.e., persons-supported) and tailored to their unique needs and goals. In recent decades, governments around the world have enacted policies requiring community-care agencies to adopt an individualized or person-centred approach to service ...
Persistent Physical Symptoms (PPS) include symptoms such as chronic pain, and syndromes such as chronic fatigue. They are common, but are often inadequately managed, causing distress and higher costs for health care systems. A lack of teaching about PPS has been recognised as a contributing factor to poor management. The authors conducted a scoping review of the literature, including all ...
Background: Thoracic aortopathy includes conditions like aortic aneurysms and dissections, posing significant management challenges. In India, care delivery is complicated by geographic vastness, financial constraints, and healthcare resource disparities. Telemedicine and digital health technologies offer promising solutions. Methods: A comprehensive review of literature and clinical ...
Role of Magnesium in the Intensive Care Unit and Immunomodulation: A Literature Review Vaccines (Basel). 2023 Jun 20;11(6):1122. doi: 10.3390/vaccines11061122. ... This review aims to discuss the evidence behind magnesium homeostasis in critically ill patients, and its link with intensive care unit mortality via a likely magnesium-induced ...
Conclusion This review provides compelling evidence of ePRO monitoring's positive clinical impact across diverse cancer settings, encompassing various cancer types, including early and metastatic stages. These systems are crucial in enabling timely interventions and reducing communication barriers, among other functionalities. While areas for future ePRO innovation are identified, the ...
Despite adequate local care and optimal antibiotic support, his lesions persisted, and improved only after temporary discontinuation of ATRA. After a thorough literature review and considering the temporal association of cutaneous toxicities with triazole antifungals, we speculate that the concomitant use of triazole antifungals inhibited the ...