

What Should You Do When Your Judgment Is Impaired?
When your ability to act in your best interests is compromised, you need a plan..
Posted November 22, 2013

There’s a supreme irony here. If your judgment is temporarily impaired, then—now afflicted with such a deficit—how could you possibly know it was impaired? And realistically, how could you even be expected to act prudently in a state where cautiousness or circumspection may totally elude you?
These are tough questions. But still, it’s unquestionably true that at one time or another all of us have found ourselves in such an untenable situation. In fact, if you look at some of the worst decisions you’ve ever made, did you not make them when your common sense was, well, “offline”? Times when you just couldn’t access the knowledge or past experience that, doubtless, would have let you know that you were about to step on a land mine—or fall headfirst over a precipice? In other words, there are various circumstances when you should have known better than to say or do something that almost certainly would get you into trouble. But in that crucial instant, you didn’t . . . or couldn’t.
So how can you avoid the pitfalls that your momentarily “logged off” mind may topple you into (as in, “What in the world were you thinking of when you did that?!”)?
The first thing to do is determine your personal risk factors for such a lapse in judgment. Traditional twelve-step programs for addiction —each in their own way focusing on what can catapult an individual back into their dysfunctional behavior—employs the term HALT to abort the downwards progression. This useful acronym alludes to the four main threats to maintaining abstinence from one’s drug of choice. That is, it’s essential for the addict to be mindful of the contingencies most commonly linked to losing control and resorting, yet again, to one’s particular addiction. So, to “unpack” the acronym, the “H” in HALT stands for getting too Hungry, the “A” for becoming too Angry, the “L” for feeling too Lonely, and the “T” for being in a state of fatigue—that is, too Tired.

In such situations, it’s crucial to mindfully “halt” (or stop in your tracks), and to contemplate what’s going on inside yourself. For when you’re in any of these negative states, you’re at increased risk for relapsing back into your addiction (whether it’s related to a substance, activity, or an unhealthy, harmful relationship). In such hazardous moments, recovering addicts are advised to immediately get in touch with their sponsor or another program member, or to go to a 12-step meeting—and, if possible, both .
But the great majority of us aren’t members of a 12-step program—either because the religious dogma usually attached to it doesn’t much appeal to us, or (more likely) because our problems don’t really pertain to addiction. Still, the HALT model, even though it doesn’t address all the problematic situations we’re vulnerable to, represents a good starting point. If we can become more aware of just what mental or emotional states put us at risk for acting foolishly, recklessly, or otherwise ill-advisedly, we may be able to avoid doing something we’ll later regret. Consequently, it’s helpful to make a list of what—for us personally—exemplify cues or clues that we’re in danger of acting contrary to our best interests. And then to determinedly revisit this list with sufficient frequency that it enters our head almost automatically before our judgment becomes so clouded that it’s no longer to be trusted.
For this self-protective internal mechanism to work, we need to maintain at least a glimmer of self-recognition when we’re in a mental—or emotional —state that threatens to vex us with sudden amnesia for our well-memorized (i.e., overlearned) catalog of cautions. Which is to say that we have to be on guard for those times, people, and places when our optimal cerebral functioning may become compromised. Situations in which our higher neo-cortical operations are beginning to falter and our far more primitive reptilian (or "dinosaur") brain is on the verge of taking over.
Of course, if in such cases we have a “back up,” we’re that much more likely to withstand any internal pressure to act contrary to our better judgment. So you might think of giving a copy of your list of hazardous situations to a trusted friend, spouse, or parent(s), or in certain instances, your son or daughter. If your emotions are so strong that they’re beginning to overwhelm you—if you’re well on your way to tumbling down your own private rabbit hole—then there’s a good chance that the other person, forewarned of your susceptibilities and “authorized” to act on your behalf, can catch you before you fall. Similar to sponsors in 12-step programs, they might prevent you from doing something that could return to haunt you.

So, once you’re able to identify the precipitants (or “usual suspects”) of past imprudences or indiscretions, it’s wise to let trusted others know about them. And your vulnerability may go well beyond your being in a state of excess hunger, anger , loneliness , or tiredness. In fact, if you’re in any heightened emotional state, your ability to accurately evaluate your situation will be weakened. For example, if you’re extremely anxious you may be tempted to avoid dealing with something that’s critical to handle, or to do something impulsive that could make matters much worse. If you’re overcome with anger, you may be sorely tempted to verbally strike out at someone, which could do irreparable damage to the relationship—or maybe get you fired. And if you’re depressed to the point of being suicidal , without altering your catastrophic thoughts or talking to someone who can offer you sympathy and reassurance, your very life may be at stake.
It’s now established scientific fact that emotions must come into play if you’re to intelligently decide among various alternatives, or be sufficiently motivated to take action on things affecting your welfare. And your emotions, at least those experienced to a mild or moderate degree, typically guide your behavior in positive ways. But whenever your emotions are so pronounced—and stressful —that they literally preempt your rational mind, you need to “retreat” to your list, stopping (or “halting”) yourself in your mental/emotional tracks. Then you can work on productively modifying your negatively distorted self-talk . Or, if that’s no longer feasible, contact a friend or engage in a distracting activity that will lessen your anxiety , anger, guilt , depression , humiliation , or shame .
Finally, if your problems are related to an addiction and you’re about to succumb to your drug of choice, or are already “under the influence,” you need to access something deep inside yourself to circumvent further craving or use—or get in touch with an understanding, compassionate person or professional to help you better cope with your temporary crisis. At times when you can no longer trust yourself, you need to have enough “sanity” left to reach out to another whom you can trust.

Remember, it’s okay to make mistakes. That’s inevitable, and it’s also how you learn to do better next time. But it’s less acceptable to continue to make the same mistakes once you’ve learned what caused them initially. So when your judgment is beginning to go south, look to your list to locate the origin of its degradation. Then do what’s needed to reverse direction.
NOTE: If you think any of the ideas in this piece might be of interest to others, please consider sending them the link. If, additionally, you’d like to explore other posts I’ve done for Psychology Today , click here .
© 2013 Leon F. Seltzer, Ph.D. All Rights Reserved.
---I invite readers to join me on Facebook , and to follow my miscellaneous musings on Twitter .

Leon F. Seltzer, Ph.D. , is the author of Paradoxical Strategies in Psychotherapy and The Vision of Melville and Conrad . He holds doctorates in English and Psychology. His posts have received over 53 million views.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Identifying and managing cognitive impairment
What is it.
Cognitive impairment refers to an individual having memory and thinking problems. The person may have difficulty with learning new things, concentrating, or making decisions that affect their daily life. The most common causes of cognitive impairment among older people are dementia and delirium. 1
Dementia is a general term used to describe a form of cognitive impairment that is chronic, generally progressive and occurs over a period of months to years. It can affect memory, language, perception, personality and cognitive skills. 2
Delirium is an acute disturbance of attention and cognition where the patient experiences confusion. It is temporary and is a symptom of an underlying issue. 3 Delirium is often overlooked or misdiagnosed in the hospital setting. 4
Depression is not just low mood or feeling sad, but a serious condition that needs treatment. Its symptoms can mimic those associated with cognitive impairment and it is often overlooked or misdiagnosed.
Why is it important?
- In the hospital environment almost 30 per cent of older people have cognitive impairment. 5
- malnutrition
- dehydration
- hospital-acquired pressure injuries
- developing incontinence
- medication issues.
- These risks often lead to an increased hospital stay 6,7 and poorer outcomes for older people.
- Screening and early recognition is vital as the first presentation of cognitive impairment can occur during hospital admission. 5
- Ten to 15 per cent of older people have delirium at admission, and a further five to 40 percent are estimated to develop it during their hospital stay. Patients with dementia have double the risk of developing delirium. 5
- The hospital environment can increase levels of distress and disorientation experienced by people with cognitive impairment. This can put older people at risk and be distressing for staff, carers and family.
- If unrecognised, cognitive impairment can increase the likelihood that an older person will end up in a premature placement rather than return home.
How can you care for people with cognitive impairment?
All hospital staff have a shared role in caring for patients with cognitive impairment. Best practice informs us that all patients over the age of 65 should be screened for cognitive impairment at the first point of contact with the health service, and when they transition to another area in the hospital. It is vital that this screening is documented in the patient’s medical record, and that the patient’s premorbid state is taken into account.
Screen and assess patients with cognitive impairment
- Recognise the different characteristics of delirium and dementia and rule out the possibility of depression.
- It is vital that the all patients with a delirium are thoroughly investigated for the underlying cause so it can be treated.
- Abbreviated Mental Test (AMT)
- Standardised Mini-Mental State Examination (SMMSE)
- Clock Drawing Test (CDT).
- resistance to care
- screaming/calling out/agitation
- withdrawal.
- Always check your observations with the person’s family or carer to ascertain if these BPSD symptoms are long standing or new. This will assist in developing an intervention plan and in forming a diagnosis.
- If the patient is displaying signs of agitation, consider whether they may need to go to the toilet, if they are hungry or are in pain.
Actively engage patients and families in all aspects of their care plan
Families and carers offer a wealth of expertise and can often suggest care strategies to minimise risk of functional decline and the person’s level of distress.
- Involve the family and carer in the care planning process and provide them with written information about cognitive and memory difficulties.
- Establish the patient’s pre-morbid cognitive status. This will help you to determine intervention strategies.
- Be mindful that a diagnosis can be quite confronting for the individual and their family and carer.
- Screen the patient’s carer and family for carer stress and refer to appropriate inpatient and outpatient support services such as the Social Work team, Alzheimer’s Victoria and Carers Victoria.
- Communicate clearly by using the strategies outlined in the Improving communication factsheet.
- introduce yourself
- always use the patient’s name when addressing them
- make sure you have eye contact at all times
- remain calm and talk in a matter-of-fact way
- keep sentences short and simple
- give time for a response
- take the time to explain what you are going to do and why you are doing it
- focus on one instruction at a time
- repeat yourself – don't assume you have been understood
- don’t offer too many choices.
- Encourage the patient and family and carer to discuss advance care planning with each other and the care team. See Advance care planning factsheet for more information.
Respond to the needs of a patient with cognitive impairment
- make every effort to reduce the number of times a patient transfers between wards
- reduce stimulation
- use diversional strategies such as engaging in a one-on-one conversation
- situate the patient within sight of the nursing station
- make sure the call bell is within the patient’s reach
- involve the family and carers in providing direct care.
- Engage in intentional rounding (carrying out regular checks with the patient at set intervals). Assist the patient with eating, drinking, pain relief, ambulation, regular toileting and repositioning (as required).
- Some hospitals place the cognitive impairment identifier (cii) , the information about me form, and a universal falls symbol above a patient’s bed, which acts as a communication tool to all staff.
- Improving the environment for older people in health services: an audit tool
- Dementia Enabling Environment Principles.
Monitor and evaluate a patient’s ongoing care
- Document all interventions, and in conjunction with family and staff monitor whether they have been successful.
- between nursing shifts
- within interdisciplinary care planning meetings
- when the patient transfers to another area of the health service.
All healthcare organisations and clinicians must practice in alignment with the National Safety and Quality Health Service Standards.
1. Milisen K, Braes T, Fick DM & Foreman MD 2006, ‘Cognitive Assessment and Differentiating the 3 Ds (Dementia, Depression, Delirium)’, Nursing Clinics of North America, 41(3):1-22.
2. Australian Institute of Health and Welfare 2012, Dementia in Australia , Australian Institute of Health and Welfare, Canberra, Australia.
3. Clinical Epidemiology and Health Service Evaluation Unit, Melbourne Health 2006, Clinical Practice Guidelines for the Management of Delirium in Older People . Report to Australian Health Ministers’ Advisory Council.
4. Inouye S, Foreman M, Mion L, Katz K & Cooney L. 2001, ‘Nurses' recognition of delirium and its symptoms – Comparison of nurse and researcher ratings’, Archives of Internal Medicine, 160(20):2467-2473.
5. Travers C, Byrne G, Pachana N, Klein K & Gray L. 2013, ‘Prospective observational study of dementia and delirium in the acute hospital setting’, Internal Medicine Journal, 43(3):262-269.
6. Australian Institute of Health and Welfare 2013, Dementia care in hospitals: costs and strategies , Australian Institute of Health and Welfare, Canberra, Australia.
7. Bail K, Berry H, Grealish L, Draper B, Karmel R, Gibson D & Peut A 2013, ‘Potentially preventable complications of urinary tract infections, pressure areas, pneumonia, and delirium in hospitalised dementia patients: retrospective cohort study’, BMJ Open, 3(6):2770.
Identifying and managing cognitive impairment fact sheet for clinicians
Reviewed 05 October 2015
- Hospitals & health services
- Public hospitals in Victoria
- Patient care
- Ambulance and patient transport
- Non-emergency patient transport
- Non-emergency patient transport review
- NEPT legislation and clinical practice protocols
- Non-emergency patient transport licensing
- NEPT licensing fees
- NEPT services information and guidance
- First Aid Services
- First aid licences
- First aid services information and guidance
- First aid service fees
- Victorian State Trauma System
- Acute medicine
- Emergency care
- Surgical services
- Better at Home
- Critical care
- Hospital in the Home
- Virtual care (Telehealth)
- Perinatal and reproductive services
- Rehabilitation and complex care
- Renal health
- Renal services in Victoria
- Funding for renal services
- Different approaches to haemodialysis
- Specialist clinics
- Access to non-admitted services
- Minimum referral information
- Communication toolkit
- Integrated care
- HealthLinks: Chronic Care
- Community Health Integrated Program (CHIP) guidelines
- Service coordination in Victoria
- Victorian integrated care online resources
- Specialist clinics programs
- Specialist clinics reform
- Specialty diagnostics, therapeutics and programs
- Older people in hospital
- End of life and palliative care in Victoria
- Voluntary assisted dying
- Quality, safety and service improvement
- Planned surgery recovery and reform program
- Digital Health
- Roadmap and Maturity Model
- Standards and guidelines
- Policies and frameworks
- Health Information Sharing Legislation Reform
- My Health Record
- Public hospital accreditation in Victoria
- Credentialing for senior medical staff in Victoria
- Clinical risk management
- Preventing infections in health services
- Healthy choices
- Victorian Perinatal Data Collection
- Rural health
- Improving Access to Primary Care in Rural and Remote Areas Initiative
- Rural x-ray services
- Rural health regions and locations
- Rural and regional medical director role
- Victorian Patient Transport Assistance Scheme
- Rural and isolated practice registered nurses
- Urgent care in regional and rural Victoria
- Private health service establishments
- Private hospitals
- Day procedure centres
- Mobile health services
- Fees for private health service establishments in Victoria
- Design resources for private health service establishments
- Professional standards in private health service establishments
- Legislation updates for private health service establishments
- Complaints about private health service establishments
- Cosmetic procedures
- Guideline for providers of liposuction
- Private hospital funding agreement
- Boards and governance
- About health service boards in Victoria
- Information and education
- Education resources for boards
- Sector leadership
- Data, reporting and analytics
- Health data standards and systems
- Funding, performance and accountability
- Statements of Priorities
- Performance monitoring framework
- Integrity governance framework and assessment tool
- Pricing and funding framework
- Patient fees and charges
- Fees and charges for admitted patients
- Non-admitted patients - fees and charges
- Other services
- Planning and infrastructure
- Sustainability in Healthcare
- Medical equipment asset management framework
- Health system design, service and infrastructure planning
- Complementary service and locality planning
- Primary & community health
- Primary care
- Community pharmacist pilot
- EOI - Victorian Community Pharmacist Statewide Pilot
- Victorian Community Pharmacist Statewide Pilot – Resources for pharmacists
- Emergency Response Planning Tool
- Working with general practice
- Victorian Supercare Pharmacies
- NURSE-ON-CALL
- Priority Primary Care Centres
- Local Public Health Units
- Community health
- Community health services
- Community health pride
- Registration and governance of community health centres
- Community Health Directory
- Community Health Program in Victoria
- Community health population groups
- Dental health
- Access to public dental care services
- Victoria's public dental care fees
- Victoria's public dental care waiting list
- Dental health for SRS residents
- Dental health program reporting
- Smile Squad school dental program
- Maternal and Child Health Service
- Nursery Equipment Program
- Maternal and Child Health Service Framework
- Maternal and Child Health Service resources
- Child Development Information System
- Early parenting centres
- Maternal Child and Health Reporting, Funding and Data
- Baby bundle
- Sleep and settling
- Maternal and Child Health Workforce professional development
- Aboriginal Maternal and Child Health
- Public Dental and Community Health Program funding model review
- Public health
- Women's Health and Wellbeing Program
- Inquiry into Women's Pain
- Inquiry into Women's Pain submissions
- Support groups and programs
- About the program
- Victorian Women's Health Advisory Council
- Cemeteries and crematoria
- Cemetery trust member appointments
- Cemetery search
- Cemeteries and crematoria complaints
- Exhumations
- Governance and finance
- Cemetery grants
- Interments and memorials
- Land and development
- Legislation governing Victorian cemeteries and crematoria
- Cemeteries and crematoria publications
- Repatriations
- Rights of interment
- Medicines and Poisons Regulation
- Patient Schedule 8 treatment permits
- Schedule 8 MDMA and Schedule 8 psilocybine
- Schedule 9 permits for clinical trials
- Documents and forms to print or download
- Legislation and Approvals
- Frequently Asked Questions - Medicines and Poisons Regulation
- Health practitioners
- Licences and permits to possess (& possibly supply) scheduled substances
- Medicinal cannabis
- Pharmacotherapy (opioid replacement therapy)
- Recent updates
- Environmental health
- Improving childhood asthma management in Melbourne's inner west
- Climate and weather, and public health
- Environmental health in the community
- Environmental health in the home
- Environmental health professionals
- Face masks for environmental hazards
- Human health risk assessments
- Lead and human health
- Per- and poly-fluoroalkyl substances (PFAS)
- Pesticide use and pest control
- Food safety
- Information for community groups selling food to raise funds
- Food businesses
- Food safety information for consumers
- Food regulation in Victoria
- Food safety library
- Food allergens
- Introducing Standard 3.2.2A: Food safety management tools
- Immunisation
- Respiratory syncytial virus (RSV) immunisation
- Seasonal influenza vaccine
- Immunisation schedule and vaccine eligibility criteria
- Ordering vaccine
- Immunisers in Victoria
- Immunisation provider information
- Cold chain management
- Adverse events following immunisation reporting
- Vaccine error management
- Vaccination for infants and children
- Vaccination for adolescents
- Vaccination program for adults
- Vaccination for special-risk groups
- Immunisation resources order form
- Victorian coverage rates for Victoria
- Infectious diseases guidelines & advice
- Infection control guidelines
- Disease information and advice
- Advice to the cruise industry: reporting infections
- Notifiable infectious diseases, conditions and micro-organisms
- Notification procedures for infectious diseases
- Infectious diseases surveillance in Victoria
- Germicidal ultraviolet light
- Protecting patient privacy in Victoria
- Population health systems
- Evidence and evaluation
- Health promotion
- Health status of Victorians
- Municipal public health and wellbeing planning
- Population screening
- Cancer screening
- Conditions not screened
- Improving outcomes in under-screened groups
- Infant hearing screening
- Newborn bloodspot screening
- Prenatal screening
- Screening registers
- Preventive health
- Type 2 diabetes and cardiovascular disease prevention
- Eye health promotion
- Injury prevention
- Healthy eating
- Oral health promotion
- Physical activity
- Sexual health
- Sex worker health
- Decriminalisation of sex work
- Automatic mutual recognition
- Domestic smoke detectors
- Lasers, IPL and LED devices for cosmetic treatments and beauty therapy
- Victoria's regulatory framework for radiation
- Radiation newsletter
- Tobacco reforms
- Tobacco reform legislation and regulations
- E-cigarettes and vaping
- Quitting smoking and vaping
- Smoke-free and vape-free areas
- Building entrances
- Children's indoor play centres
- Public hospitals and health centres
- Children's recreational areas
- Playground equipment
- Skate parks
- Swimming pools
- Under-age sporting events
- Enclosed workplaces
- Government buildings
- Learning environments
- Outdoor dining
- Outdoor drinking areas
- Patrolled beaches
- Train platforms and bus and tram shelters
- Under-age music or dance events
- Tobacco and e-cigarette retailers
- Making a report or complaint
- Resources and factsheets
- Alternative water supplies
- Aquatic facilities
- Blue-green algae (cyanobacteria)
- Drinking water in Victoria
- Legionella risk management
- Private drinking water
- Recreational water use and possible health risks
- Water fluoridation
- Chief Health Officer
- About the Chief Health Officer
- Chief Health Officer publications
- Health alerts and advisories
- Mental health
- Mental Health and Wellbeing Act 2022
- Mental Health and Wellbeing Act 2022 Handbook
- Community information
- Mental Health and Wellbeing Act 2022 in your language
- About Victoria's mental health services
- Area-based services
- Statewide and specialist mental health services
- Mental Health Community Support Services
- Support and intervention services
- Language services - when to use them
- Access to mental health services across areas
- Transport for people in mental health services
- Practice and service quality
- Medical Treatment Planning and Decisions Act
- Service quality
- Specialist responses
- Mental health and wellbeing reform
- Reform activity updates
- Priority areas
- Latest news
- Working with consumers and carers
- Consumer and carer engagement
- Consumer and Carer Experience Surveys
- Family support and crisis plans
- Consumer and carer financial support
- Supporting children whose parents have a mental illness
- Supporting parents with a mental illness
- Prevention and promotion
- Early intervention in mental illness
- Mental health promotion in Victoria
- Suicide prevention in Victoria
- Priorities and transformation
- Supporting the social and emotional wellbeing of Aboriginal and Torres Strait Islander Victorians
- National mental health strategy
- Rights and advocacy
- Making a complaint about a mental health service
- Chief Psychiatrist
- About the Chief Psychiatrist
- Principles in the Mental Health and Wellbeing Act and the Chief Psychiatrist's guidelines
- Obligations under the Mental Health and Wellbeing Act 2022
- Reporting a failure to comply with the Mental Health and Wellbeing Act 2022
- Governance and committees
- Reporting obligations for clinical mental health and wellbeing services
- Mental health and wellbeing support
- Making a complaint and seeking advocacy
- Second psychiatric opinion and process of review by Chief Psychiatrist
- Office of the Chief Psychiatrist's reform activities and news
- Oversight of forensic mental health and wellbeing services
- Resources and reports
- Chief psychiatrist guidelines
- Chief Mental Health Nurse
- About Victoria's Chief Mental Health Nurse
- Best practice
- Reducing restrictive interventions
- Research and reporting
- Mental health performance reports
- Reporting requirements and business rules for clinical mental health services
- Alcohol & drugs
- Alcohol and other drug treatment services
- Overview of Victoria's alcohol and drug treatment system
- Pathways into alcohol and other drugs treatment
- Prevention and harm reduction
- Medically supervised injecting room
- Victoria's Take-Home Naloxone Program
- Community-based AOD treatment services in Victoria
- Residential treatment services
- Mildura statewide alcohol and drug residential treatment service
- Drug rehabilitation plan
- Hospital-based services
- Forensic services
- Pharmacotherapy treatment
- Services for Aboriginal people
- Services for young people
- Statewide and specialist services
- Compulsory treatment
- Family and peer support
- Public intoxication reform
- New public intoxication response services
- Policy, research and legislation
- Alcohol and drug research and data
- Legislation governing alcohol and other drug treatment
- Alcohol and other drug service standards and guidelines
- Alcohol and other drug client charter and resources
- Alcohol and other drug treatment principles
- Service quality and accreditation
- Alcohol and other drug program guidelines
- Maintenance pharmacotherapy
- Specialist Family Violence Advisor capacity building program in mental health and alcohol and other drug services - Victoria
- Alcohol and other drug workforce
- Learning and development
- Alcohol and other drug workforce Minimum Qualification Strategy
- Workforce data and planning
- Funding and reporting for alcohol and other drug services
- Funding of alcohol and other drugs services in Victoria
- Reporting requirements and business rules for alcohol and other drug services
- Drug alerts
- 25C-NBOMe and 4-FA sold as '2C-B'
- Novel stimulants sold as MDMA, cocaine or speed
- Protonitazene sold as ketamine
- High potency benzodiazepine tablets
- MDMA adulterated with PMMA
- 25B-NBOH sold as powdered 'LSD'
- Green 'UPS' pills containing N-ethylpentylone (no MDMA)
- N-ethylpentylone in cocaine
- Ageing & aged care
- Supporting independent living
- Low cost accommodation support programs
- Personal Alert Victoria
- Dementia services
- Victorian Aids and Equipment Program
- Residential aged care services
- Public sector residential aged care services
- Safety and quality in public sector residential aged care
- Physical and social environments
- Emergency preparedness in residential aged care services
- My Aged Care assessment services
- Home and Community Care Program for Younger People
- HACC data reporting
- HACC PYP fees policy and schedule of fees
- Wellbeing and participation
- Age-friendly Victoria
- Healthy ageing
- Seniors participation
- Dementia-friendly environments
- Designing for people with dementia
- Maintaining personal identity
- Personal enjoyment
- Interior design
- Dining areas, kitchens and eating
- Bedrooms and privacy
- Gardens and outdoor spaces
- Assistive technology
- Staff education and support
- Strategies, checklists and tools
- Our Strategic Plan 2023-27
- Our organisation
- Our secretary
- Leadership charter
- Our services
- Our vision and values
- Specialist offices
- Senior officers in health
- Human Research Ethics Committee (HREC)
- Gifts, benefits and hospitality policy
- Information Asset Register
- Health legislation
- Health legislation overview
- Health Complaints legislation
- Health Records Act
- Human Tissue Act 1982
- Public Health and Wellbeing Act 2008
- Voluntary Assisted Dying Act
- Victoria's pandemic management framework
- Independent Pandemic Management Advisory Committee
- Pandemic Order Register
- Our ministers
- Our role in emergencies
- State Health Emergency Response Arrangements
- Emergency type
- Department's responsibilities in emergencies
- Health services’ responsibilities in emergencies
- Aboriginal employment
- Current vacancies
- Employment programs for students and graduates
- Rise program
- Inclusion and diversity at the Department of Health
- Health workforce
- Working in health
- Information sharing and MARAM
- Child Safe Standards
- Regulatory functions
- Reviews of decisions
- Victorian Public Healthcare Awards
- Aboriginal healthcare workers
- Mental health workforce
- Lived and living experience workforces
- Engaging with lived and living experience workforces
- Our workforce, our future
- Nursing and midwifery
- Free nursing and midwifery study
- Additional funding for nursing and midwifery positions
- Becoming a nurse or midwife
- Undergraduate nursing and midwifery scholarships
- Undergraduate student employment programs
- Nursing and midwifery graduates
- Nursing and midwifery graduate sign-on bonus
- Working as a nurse or midwife
- Enrolled nurse to registered nurse transition scholarships
- Support for new nurse practitioners
- Postgraduate scholarships for nurses and midwives
- Nurse practitioners
- Returning to nursing or midwifery
- Refresher pathway for nurses and midwives
- Re-entry pathway scholarships for nurses and midwives
- Nursing and midwifery - legislation and regulation
- Nursing and midwifery program - health sector
- Allied health workforce
- Education and training
- Enterprise agreements
- Worker health and wellbeing
- Working with us
- Grants and programs
- Freedom of Information
- Part II - Information Statements
- Procurement policies
- Protective markings
- Health and medical research
- Sponsorship application information
- Publications
- Annual reports
- Fact sheets
- Strategies, plans and charters
- Policies, standards and guidelines
- Research and reports
- Forms and templates
- Communities
- Designing for Diversity
- Vulnerable children
- Vulnerable children - responsibilities of health professionals
- Identifying and responding to children at risk
- Pathway to good health for children in care
- Older people
- Aboriginal health
- Improving health for Victorians from culturally and linguistically diverse backgrounds
- Asylum seeker and refugee health in Victoria
- News and media hub
- Media releases
- Health alerts
- Feedback and complaints
- Make a payment
- Fees, charges and penalties subject to automatic indexation
- Our campaigns
In this topic
- Providing best care fact sheet
- Improving communication fact sheet
- Comprehensive assessment fact sheet
- Cognitive impairment fact sheet
- Multimorbidity fact sheet
- Preventing adverse events fact sheet
- Interdisciplinary approach fact sheet
- Evidence-based practice fact sheet
- Advance care planning fact sheet
- Transitions fact sheet
In this section
- Cognition case study
- Dementia case study
- ICOP initiatives - Cognition
More information
- Dementia Enabling Environment Principles External Link
- NSQHS Standards External Link
- Consumer fact sheet – Mind and mood in hospital External Link
- Dementia Australia External Link
- Carers Victoria External Link
- Cognitive Impairment Identifier External Link
Share this page
- Facebook , opens a new window
- X (formerly Twitter) , opens a new window
- LinkedIn , opens a new window
- Patient Care & Health Information
- Diseases & Conditions
- Mild cognitive impairment (MCI)
Mild cognitive impairment (MCI) is the stage between the expected decline in memory and thinking that happens with age and the more serious decline of dementia. MCI may include problems with memory, language or judgment.
People with MCI may be aware that their memory or mental function has "slipped." Family and close friends also may notice changes. But these changes aren't bad enough to impact daily life or affect usual activities.
MCI may increase the risk of dementia caused by Alzheimer's disease or other brain disorders. But some people with mild cognitive impairment might never get worse. And some eventually get better.
Products & Services
- A Book: Day to Day: Living With Dementia
- A Book: Mayo Clinic on Alzheimer's Disease
- A Book: Mayo Clinic on Healthy Aging
The brain, like the rest of the body, changes with age. Many people notice they become more forgetful as they age. It may take longer to think of a word or to recall a person's name.
If concerns with mental function go beyond what's expected, the symptoms may be due to mild cognitive impairment (MCI). MCI may be the cause of changes in thinking if:
- You forget things more often.
- You miss appointments or social events.
- You lose your train of thought. Or you can't follow the plot of a book or movie.
- You have trouble following a conversation.
- You find it hard to make decisions, finish a task or follow instructions.
- You start to have trouble finding your way around places you know well.
- You begin to have poor judgment.
- Your family and friends notice any of these changes.
If you have MCI , you also may experience:
- Depression.
- A short temper and aggression.
- A lack of interest.
When to see a doctor
Talk to your health care provider if you or someone close to you notices you're having problems with memory or thinking. This may include trouble recalling recent events or having trouble thinking clearly.
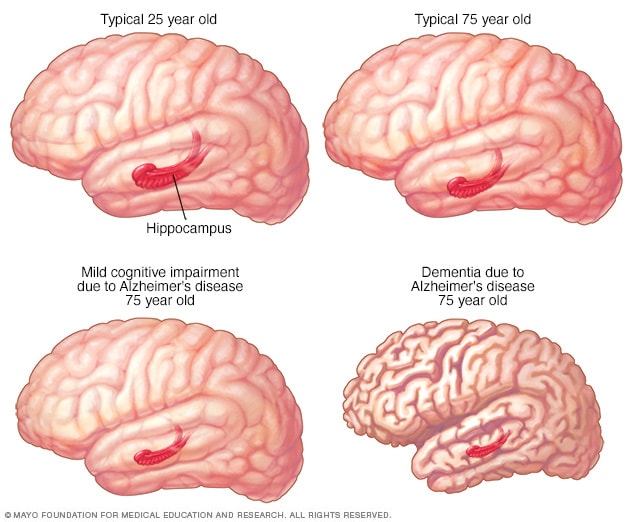
- Changes in brain structure with MCI and Alzheimer's disease
Some changes in brain structure — such as the decrease in size of the brain's memory center (hippocampus) — are typical with aging. However, this reduction in size is greater in those with mild cognitive impairment and even more dramatic in people with Alzheimer's disease.
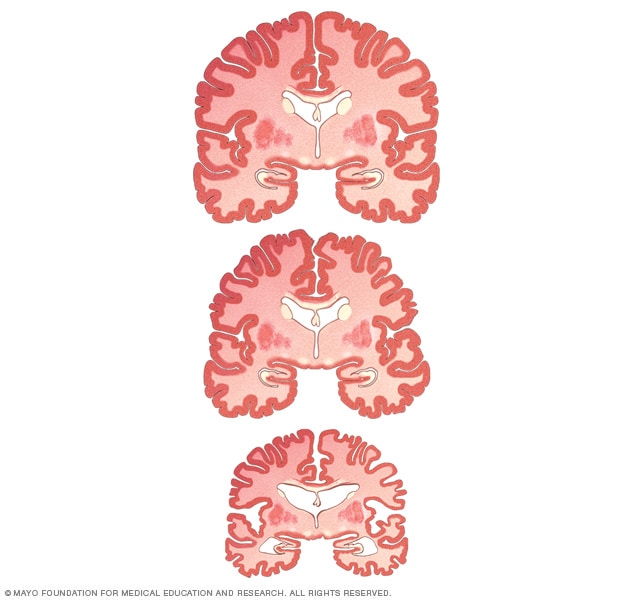
- Brain shrinkage in MCI and Alzheimer's disease
Dementia causes the brain to lose mass, especially in critical areas. Note the difference in size between a healthy brain (top), a mild cognitive impairment brain (middle) and an Alzheimer's disease brain (bottom).
There's no single cause of mild cognitive impairment (MCI), although MCI may be due to early Alzheimer's disease. There's no single outcome for the disorder. Symptoms of MCI may remain stable for years. Or MCI may progress to Alzheimer's disease dementia or another type of dementia. In some cases, MCI may improve over time.
MCI often involves the same types of brain changes seen in Alzheimer's disease or other forms of dementia. In MCI , those changes occur at a lesser degree. Some of these changes have been seen in autopsy studies of people with MCI .
These changes include:
- Clumps of beta-amyloid protein, called plaques, and tangles of tau proteins that are seen in Alzheimer's disease.
- Microscopic clumps of a protein called Lewy bodies. These clumps are associated with Parkinson's disease, dementia with Lewy bodies and some cases of Alzheimer's disease.
- Small strokes or reduced blood flow through brain blood vessels.
Brain-imaging studies show that the following changes may be associated with MCI :
- Decreased size of the hippocampus, a brain region important for memory.
- Increased size of the brain's fluid-filled spaces, known as ventricles.
- Reduced use of glucose in key brain regions. Glucose is the sugar that's the main source of energy for cells.
Risk factors
The strongest risk factors for MCI are:
- Increasing age.
- Having a form of a gene known as APOE e4 . This gene also is linked to Alzheimer's disease. But having the gene doesn't guarantee that you'll have a decline in thinking and memory.
Other medical conditions and lifestyle factors have been linked to an increased risk of changes in thinking, including:
- High blood pressure.
- High cholesterol.
- Obstructive sleep apnea.
- Lack of physical exercise.
- Low education level.
- Lack of mentally or socially stimulating activities.
Complications
People with MCI have an increased risk — but not a certainty — of developing dementia. Overall, about 1% to 3% of older adults develop dementia every year. Studies suggest that around 10% to 15% of people with MCI go on to develop dementia each year.
Mild cognitive impairment can't be prevented. But research has found some lifestyle factors may lower the risk of getting MCI . Studies show that these steps may help prevent MCI :
- Don't drink large amounts of alcohol.
- Limit exposure to air pollution.
- Reduce your risk of a head injury.
- Don't smoke.
- Manage health conditions such as diabetes, high blood pressure, obesity and depression.
- Practice good sleep hygiene and manage any sleep problems.
- Eat a healthy diet full of nutrients. Include fruits and vegetables and foods low in saturated fats.
- Stay social with friends and family.
- Exercise at a moderate to vigorous intensity most days of the week.
- Wear a hearing aid if you have hearing loss.
- Stimulate your mind with puzzles, games and memory training.
Mild cognitive impairment (MCI) care at Mayo Clinic
- Knopman DS, et al. Alzheimer disease. Nature Reviews. Disease Primers. 2021; doi:10.1038/s41572-021-00269-y.
- Jankovic J, et al., eds. Alzheimer disease and other dementias. In: Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Sept. 21, 2022.
- Zhuang L, et al. Cognitive assessment tools for mild cognitive impairment screening. Journal of Neurology. 2021; doi:10.1007/s00415-019-09506-7.
- What is mild cognitive impairment? National Institute on Aging. https://www.nia.nih.gov/health/what-mild-cognitive-impairment. Accessed Sept. 21, 2022.
- Mild cognitive impairment (MCI). Alzheimer's Association. https://www.alz.org/alzheimers-dementia/what-is-dementia/related_conditions/mild-cognitive-impairment. Accessed Sept. 21, 2022.
- Lewis JE, et al. The effects of twenty-one nutrients and phytonutrients on cognitive function: A narrative review. Journal of Clinical and Translational Research. 2021; doi:10.18053/jctres.07.202104.014.
- Kellerman RD, et al. Alzheimer's disease. In: Conn's Current Therapy 2022. Elsevier; 2022. https://www.clinicalkey.com. Accessed Sept. 21, 2022.
- Ferri FF. Mild cognitive impairment. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Sept. 21, 2022.
- Petersen RC, et al. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018; doi:10.1212/WNL.0000000000004826.
- Budson AE, et al. Subjective cognitive decline, mild cognitive impairment and dementia. In: Memory Loss, Alzheimer's Disease, and Dementia. 3rd ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Sept. 21, 2022.
- Cognitive impairment in older adults: Screening. U.S. Preventive Services Task Force recommendation statement. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cognitive-impairment-in-older-adults-screening. Accessed Sept. 21, 2022.
- Levenson JL, ed. Dementia. In: The American Psychiatric Association Publishing Textbook of Psychosomatic Medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2019. https://psychiatryonline.org. Accessed Sept. 21, 2022.
- Livingston G, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet. 2020; doi:10.1016/S0140-6736(20)30367-6.
- Cummings J, et al. Alzheimer's disease drug development pipeline: 2022. Alzheimer's and Dementia. 2022; doi:10.1002/trc2.12295.
- Memory, forgetfulness and aging: What's normal and what's not? National Institute on Aging. https://www.nia.nih.gov/health/memory-forgetfulness-and-aging-whats-normal-and-whats-not. Accessed Sept. 26, 2022.
- Ami T. Allscripts EPSi. Mayo Clinic. April 21, 2022.
- Alzheimer's disease research centers. National Institute on Aging. https://www.nia.nih.gov/health/alzheimers-disease-research-centers#minnesota. Accessed Sept. 26, 2022.
- About the Alzheimer's Consortium. Arizona Alzheimer's Consortium. https://azalz.org/about/#institutes. Accessed Sept. 26, 2022.
- Shi M, et al. Impact of anti-amyloid-β monoclonal antibodies on the pathology and clinical profile of Alzheimer's disease: A focus on aducanumab and lecanemab. Frontiers in Aging and Neuroscience. 2022; doi:10.3389/fnagi.2022.870517.
- Graff-Radford J (expert opinion). Mayo Clinic. Sept. 30, 2022.
- HABIT program orientation
Associated Procedures
News from mayo clinic.
- Maximize memory function with a nutrient-rich diet June 19, 2023, 01:40 p.m. CDT
- Mayo Clinic Q and A: Memory loss July 07, 2022, 01:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Jump to navigation
Find What You Need Get targeted resources quickly!

Impaired Cognition: Frequently Asked Questions

What Is Cognition?
Cognition is another word for thinking and the process that describes how we understand and interact with the world. Cognition also describes how the brain perceives and expresses experiences.
What Is Meant by Impaired Cognition?
When a person is diagnosed with impaired cognition, it means their skills and abilities may have diminished or disappeared as a result of a medical problem. There are special names for some of these impairments; for example, an impairment in language skills that makes it hard for people to speak or understand speech is called aphasia.
How Is Cognition Affected by Brain Injury?
ince a brain injury can occur in any part of the brain, any thinking abilities may be affected. This could include attention, communication, visual perception (the ability to understand what is seen) and memory. Very often, the parts of the brain located toward the front of the skull are most severely damaged. Typical impairments due to injury in this area include:
- Problems with attention, concentration and organization
- Difficulty remembering things that happened since the injury
- Lack of awareness of your behavior or how others see you
- Appearing inconsiderate, selfish, and not caring how others feel or just not being aware of how you make other people feel.
What is “Minimal Consciousness?”
People who are minimally conscious are more awake than someone in a deep coma, but they may actually have little awareness of their surroundings. They may open their eyes and look around the room, but not respond to what they see or hear in the room. Minimally conscious people may benefit by having things to think about; for example, having visitors, talking to them, having the television on, or reading aloud. While none of the following activities has been proven to help recovery, they could be used to assist the individual to get started:
- It may help for the minimally conscious person to start using different senses again, so talking to them or playing music is a reasonable thing to do
- Gentle touching or holding hands
- Having sweet smelling flowers in the room
- Playing recorded messages from family or friends
- Using complex stimuli such as audiobooks or television usually is not helpful.
- When around a minimally conscious patient, avoid speaking as if they are not there and cannot hear you.
How Does Brain Injury Affect Actions and Feelings?
Sometimes brain injuries damage the part of the brain that controls emotional expression. As a result, people may become angry much more easily and their anger may be much more forceful. Often, people with this problem feel embarrassed after an angry outburst because they know their reaction was inappropriate. Other people may laugh or cry at inappropriate times because of the same problem. Doctors describe this lack of control of emotions with a number of terms including “emotional lability” or “affective dysregulation.” People may also act before they think and may do and say things they would never have done or said before. Such behavior is sometimes described as “impulsivity” or “disinhibition.”
How Long Does It Take to Recover From a Brain Injury?
Recovery time depends on the severity of the injury. If someone was unconscious for less than 30 minutes, the recovery usually occurs within three months. If a person was unconscious for more than 24 hours, recovery may take up to a year. Recovery is usually most rapid in the days and weeks immediately after an injury (improvements can often be noticed from one day to another). Then, recovery slows down and improvements may not be noticeable unless compared month to month.
What is the Definition of Recovery?
Rehabilitation helps people to recover but recovery may not mean completely returning to the way things were before the injury. One way to think of recovery is that the person with the injury (impairment) has acknowledged that there is a change, has learned how to do things differently or compensate for problems, and has decided to do as much in life as they can. It means enjoying life as much as possible and feeling good as a person while being aware of one's limitations. It also means feeling valuable to others. It does not mean being exactly the same as before the injury. Recovery is an ongoing process, and after all, everybody changes over time. It has always been very difficult to predict the amount of recovery someone has after brain injury. When a serious injury results in unconsciousness for a long time, there are usually some lasting effects, but it is hard to predict how much they might interfere with normal life. Depending upon how severe the injury, the effects and changes to life can be permanent. In less severe cases, some functions may recover, while others remain weak, such as short–term memory. Either way, recovery can take a long time. At some point, it becomes hard to know if improvement comes from brain recovery or just learning to do things differently.
What Can Help with Recovery from Brain Injury?
Most important is to work at recovery rather than just sit around and wait for improvements to happen.
- Therapies are essential, even after leaving the hospital.
- Keep to a routine and stay active. Think of the brain as a muscle; it will weaken if it is not exercised.
- Look for ways to stimulate thinking. Games, puzzles, reading and performing everyday tasks that offer mental challenge can be useful.
- Focus on doing only one thing at a time.
- Try to strike a balance between doing too little and too much. Go slowly and set realistic goals for the things that you used to do.
Which Activities Could Interfere with Recovery?
These chemicals have direct effects on the brain and can impair judgment and put a person at risk for further injury. Be careful when using them, if at all, and consult with your doctor if you have questions about any particular substance.
- Avoid risky activities like extreme sports that could cause another brain injury.
What about Returning to Work, School, or Driving?
Work (or school) and driving involve very complex behaviors. Some of these activities can be resumed as soon as a person becomes aware of their limitation, has mastered some techniques to make up for weaknesses, and has realistic goals. Limitations due to the injury may, however, present difficulties. Doctors and therapists will have advice on these matters.
Driving can be very dangerous if there are impairments that affect vision, reflexes or problem solving. A special driving evaluation may be necessary.
How Can I Talk to Me Children About Brain Injury?
Children need to know some basic things about brain impairment; for example people with brain injuries may act confused or have trouble remembering or talking about things. Remind your children that a brain impaired person is not ”retarded”, ”stupid” or ”child like” even if other adults use those labels. Find out your child's questions. If you do not have answers, check with a trusted professional to help you find the appropriate response.
How Does a Brain Injury Affect Family?
A brain injury can be scary and confusing, resulting in a number of family reactions. Many of these reactions are understandable, but not helpful. For example:
- Treating the person with brain injury like a child or a baby
- Feeling angry at the person with the impairment because of a sense that they were somehow responsible for what happened
- Disagreeing and arguing about what is best for the individual
- There may be times when some family members are upset and even withdraw from family contact. With patience and time, hopefully they will come to a better understanding of the injury and re–establish contact.
Brain impairments can make family members feel personally vulnerable, frustrated and misunderstood. Like any other serious family problem, it is not always possible to agree about what to do, but it is important to listen to different points of view and treat others with respect and kindness.
What Should I Do If My Family Member with Brain Injury Has Problems with Anger and Becomes Violent?
Sometimes people have difficulty with emotional control after brain injury and this can include having a short temper. Family members need to learn different ways to respond to someone with a brain injury who is easily angered.
- The best way to deal with violence is to learn how to prevent it. Watch for patterns or triggers that set off the person with brain injury; try to avoid responses that only make anger build.
- Remain calm. It is usually not helpful to argue logically when a person with brain injury has become upset.
- Try diversion or redirection in any form. This takes away the irritation and allows the person time to calm down.
- Try to avoid physical restrictions and allow the person (within limits) to freely express themselves physically and verbally.
- If the situation becomes physically violent or threatening, direct appeals for calm can be tried, but may not have the desired effect. In extreme situations, where physical restraint seems necessary, try to have a phone available and numbers to call (such as the doctor or police) for quick, efficient use. Do not try to handle these situations alone.
- If anger control is a chronic problem, ask your doctor about the possibility of medications to help manage the behavior.
Additional Resources
American Stroke Assc., 888-4-STROKE
Brain Injury Assc., 703-236-6000
Gronwall, D, Wrightson, P, and Waddell, P., 1999. Head Injury: The Facts: A guide for families and care-givers. Oxford Press.
National Stroke Assc, 800-STROKES
Osborn, Claudia, 1998. Over My Head: A doctor's own story of head injury from the inside looking out, Andrews McMeel Publishing
Stoler, D and Hill, BA Coping with Mild Traumatic Brain Injury Avery Press, 1998
- Add new comment
Comments (2)
Please remember, we are not able to give medical or legal advice. If you have medical concerns, please consult your doctor. All posted comments are the views and opinions of the poster only.
Anonymous replied on Tue, 04/26/2016 - 7:19pm Permalink
Some of us who have a tbi never recover. Mild medium or severe brain injury doesn't matter . Every brain is different there is no true time line for recovery . There are milestones that are used as gauges.
Anonymous replied on Tue, 08/13/2013 - 9:54am Permalink

This program is made possible in part by a grant from the Bob Woodruff Foundation, which is dedicated to ensuring that impacted post-9/11 veterans, service members, and their families are thriving long after they return home.
BrainLine is a national service of WETA-TV, the flagship PBS station in Washington, D.C.
BrainLine, WETA Public Television 3939 Campbell Ave. Arlington, VA 22206 E-mail | Phone: 703.998.2020
© 2023 WETA All Rights Reserved | Contact Us
Healthdirect Free Australian health advice you can count on.
Medical problem? Call 1800 022 222. If you need urgent medical help, call triple zero immediately
healthdirect Australia is a free service where you can talk to a nurse or doctor who can help you know what to do.
Cognitive impairment
5-minute read
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
- Cognitive impairment is not an illness, but it can signal other medical conditions.
- Signs of cognitive impairment can include memory loss, mood swings and behavioural changes.
- There are ways to treat and prevent cognitive impairment and its complications
What is cognitive impairment?
Cognitive impairment is when you have problems remembering things and solving problems. Cognitive impairment is not an illness. It can be caused by many conditions.
You may struggle with:
- remembering things
- paying attention
- speaking or understanding
- recognising people, places or things
- experiencing new places and situations — you may become overwhelmed
Cognitive impairment can come and go. This is often called delirium . Delirium can be a sign of serious medical problems.
Cognitive impairment can go from mild to severe.
What are the symptoms of cognitive impairment?
If someone you know has cognitive impairment, you may notice:
- they sometimes feel confused , agitated or distressed
- a change in their speech or behaviours
- that they struggle to finish their daily tasks
What causes cognitive impairment?
There are many causes of cognitive impairment. Some causes of short-term or reversible cognitive impairment are:
- head injury
- anxiety or depression
- recreational use of alcohol and/or drugs
- vitamin deficiency
- dehydration
- reactions to medicines
Some causes of cognitive impairment that lasts forever are:
- brain injury
- intellectual disability
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
When should I see my doctor?
If you, or someone you know is showing signs of cognitive impairment, see your doctor. They can help find out the cause, rule out any serious conditions, and help arrange treatment.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is cognitive impairment diagnosed?
To work out if you have cognitive impairment, your doctor might ask questions to test your:
- concentration
- understanding
They may also ask your family or carers questions. This is because they may have noticed changes in your behaviour over time. Doctors may also examine you, and do more tests to try to find the cause.
How is cognitive impairment treated?
Treatment will depend on what is causing your cognitive impairment. Exercise, healthy sleep and relaxation techniques may also help. You may find familiar objects comforting.
Not every older person has cognitive impairment. But cognitive impairment is more common in older people.
What are the complications of cognitive impairment?
People who have delirium and confusion have a higher chance of falls and injuries . It’s important to avoid dangerous activities like driving.
Can cognitive impairment be prevented?
Sometimes, cognitive impairment can be prevented.
A doctor can give advice on preventing cognitive impairment. They can also refer you for more help, such as:
- physiotherapy
- occupational therapy
For people with long-term cognitive impairment, there are ways to prevent delirium, confusion and other complications.
Resources and Support
You can learn more about cognitive impairment on the Caring for Cognitive Impairment website .
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with 24 hours a day, 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: November 2022
Search our site for
- Mini Mental State Examination
Need more information?
These trusted information partners have more on this topic.
Top results
Mild Cognitive Impairment | Dementia Australia
Memory loss has long been accepted as a normal part of ageing. Recently there has been increasing recognition that some people experience a level of memory loss greater than that usually experienced with ageing, but without other signs of dementia. This has been termed Mild Cognitive Impairment (MCI). As MCI has only recently been defined, there is limited research on it and there is much that we do not yet understand.
Read more on Dementia Australia website

Homelessness | Dementia Australia
Homelessness and dementia There are significant numbers of people in the homeless population with cognitive impairment, including dementia.
Are aged care workers required to have dementia training? | Dementia Australia
An estimated two-thirds of Australians living in residential aged care live with moderate to severe cognitive impairment, so what are the requirements for dementia specific training for aged care workers?
Cognitive screening and assessment | Dementia Australia
Cognitive screening and assessment Why is an assessment for cognitive impairment and dementia so important? It is because an early diagnosis means early access to support, information and medication. There is no single definitive test for diagnosing dementia. Assessment will account for behavioural, functional and psychosocial changes, together with radiological and laboratory tests. The assessment process may take three to six months to achieve.
Planning: early stages | Dementia Australia
Helping someone at the early stages of losing capacity Many of the people who are losing capacity have mild cognitive impairment or are in the early stage of dementia. While each person’s experience will be different, it will be a challenging and confronting time for most people. The person losing capacity may not be aware of this happening to them. They may be confused, resentful or angry about this being suggested. Alternatively, they could be aware of it happening and respond with a range of emotions – such as acceptance, depression, confusion, anger or grief.
Cognitive Impairment and Dementia in Practice
Cognitive Issues in Practice
Read more on palliAGED website

Commission cognitive impairment resources - All Events
These resources will help you gain a better understanding of caring for people with cognitive impairment
Read more on Australian Commission on Safety and Quality in Health Care website

Cognitive impairment and COVID-19 | Australian Commission on Safety and Quality in Health Care
During COVID-19, people with cognitive impairment may be further disoriented by the use of personal protective equipment (PPE) and find instructions such as social distancing hard to follow. There may be restrictions on family and carers who are usually there to support them.
My Healthcare Rights - A guide for people with cognitive impairment | Australian Commission on Safety and Quality in Health Care
This resource describes what to expect when going to hospital, information about informed consent and what to do if something doesn't go to plan. The Easy English version of this guide is available here
Changes in thinking and memory - Cancer Council Victoria
You may notice changes in the way you think and remember information. This is called cancer-related cognitive impairment, 'cancer fog' or 'chemo brain'.
Read more on Cancer Council Victoria website

Dementia and chronic conditions series toolkit | Dementia Australia
There is increasing evidence that a number of different chronic conditions are associated with the development of cognitive impairment and dementia.The Dementia and Chronic Condi
Cognitive Impairment and Dementia - Synthesis
Cognitive Issues - Synthesis
Delirium Awareness and Cognitive Impairment | Ausmed
When any person, particularly an older adult, accesses a healthcare service, there is a need for health professionals to not only treat their prioritising health concerns but also recognise and treat any other comorbidities they may have concurrently (or consequently) developed during their stay. One such comorbidity that may occur during a hospital stay is delirium. Any patient who has had surgery, is in pain, has moved beds multiple times or is dehydrated is at risk of delirium.
Read more on Ausmed Education website

Myalgic Encephalomyelitis and Chronic Fatigue Syndrome | NHMRC
Overview ME/CFS is a complex and debilitating condition, characterised by profound fatigue following exertion (not relieved by sleep or rest), unrefreshing sleep and cognitive impairment. Secondary symptoms may include gastrointestinal disorders, muscle and joint pain and immune impairments. Post exertional malaise (PEM) is suggested as a cardinal feature of ME/CFS.1, 2
Read more on NHMRC – National Health and Medical Research Council website

Risk Screening: What is it? | Ausmed
Risk screening is the process of identifying clients who may be at risk of harm and then minimising any risks that have been recognised. Risk screening can assist in the early detection of potential harm to clients and ensure that care is delivered safely, effectively and appropriately.
The Dementia Guide | Dementia Australia
The Dementia Guide is an important resource for any person impacted by any form of dementia, of any age. The Dementia Guide can help anyone learn about dementia and the treatments, support and services available.
Dementia language guidelines | Dementia Australia
The purpose of this paper is to promote the consistent use of appropriate, inclusive and non stigmatising language when talking or writing about dementia and people living with dementia.
Purposeful activities for people with dementia: a resource | Dementia Australia
Purposeful Activities for Dementia is a Montessori-based professional development and education resource developed for aged care and dementia care staff and carers.This resource is part
Dementia Learning Guide | Dementia Australia
Explore a wide range of tools and programs for organisations and staff supporting people living with dementia.
Healthdirect Australia is not responsible for the content and advertising on the external website you are now entering.
Healthdirect 24hr 7 days a week hotline
24 hour health advice you can count on
1800 022 222
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
Support for this browser is being discontinued
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Call our 24 hours, seven days a week helpline at 800.272.3900

- Professionals

- Younger/Early-Onset Alzheimer's
- Is Alzheimer's Genetic?
- Women and Alzheimer's
- Creutzfeldt-Jakob Disease
- Dementia with Lewy Bodies
- Down Syndrome & Alzheimer's
- Frontotemporal Dementia
- Huntington's Disease
- Mixed Dementia
- Normal Pressure Hydrocephalus
- Posterior Cortical Atrophy
- Parkinson's Disease Dementia
- Vascular Dementia
- Korsakoff Syndrome
- Traumatic Brain Injury (TBI)
- Know the 10 Signs
- Difference Between Alzheimer's & Dementia
- 10 Steps to Approach Memory Concerns in Others
- Medical Tests for Diagnosing Alzheimer's
- Why Get Checked?
- Visiting Your Doctor
- Life After Diagnosis
- Stages of Alzheimer's
- Earlier Diagnosis
- Part the Cloud
- Research Momentum
- Our Commitment to Research
- TrialMatch: Find a Clinical Trial
- What Are Clinical Trials?
- How Clinical Trials Work
- When Clinical Trials End
- Why Participate?
- Talk to Your Doctor
- Clinical Trials: Myths vs. Facts
- Can Alzheimer's Disease Be Prevented?
- Brain Donation
- Navigating Treatment Options
- Lecanemab Approved for Treatment of Early Alzheimer's Disease
- Aducanumab Discontinued as Alzheimer's Treatment
- Medicare Treatment Coverage
- Donanemab for Treatment of Early Alzheimer's Disease — News Pending FDA Review
- Questions for Your Doctor
- Medications for Memory, Cognition and Dementia-Related Behaviors
- Treatments for Behavior
- Treatments for Sleep Changes
- Alternative Treatments
- Facts and Figures
- Assessing Symptoms and Seeking Help
- Now is the Best Time to Talk about Alzheimer's Together
- Get Educated
- Just Diagnosed
- Sharing Your Diagnosis
- Changes in Relationships
- If You Live Alone
- Treatments and Research
- Legal Planning
- Financial Planning
- Building a Care Team
- End-of-Life Planning
- Programs and Support
- Overcoming Stigma
- Younger-Onset Alzheimer's
- Taking Care of Yourself
- Reducing Stress
- Tips for Daily Life
- Helping Family and Friends
- Leaving Your Legacy
- Live Well Online Resources
- Make a Difference
- Daily Care Plan
- Communication and Alzheimer's
- Food and Eating
- Art and Music
- Incontinence
- Dressing and Grooming
- Dental Care
- Working With the Doctor
- Medication Safety
- Accepting the Diagnosis
- Early-Stage Caregiving
- Middle-Stage Caregiving
- Late-Stage Caregiving
- Aggression and Anger
- Anxiety and Agitation
- Hallucinations
- Memory Loss and Confusion
- Sleep Issues and Sundowning
- Suspicions and Delusions
- In-Home Care
- Adult Day Centers
- Long-Term Care
- Respite Care
- Hospice Care
- Choosing Care Providers
- Finding a Memory Care-Certified Nursing Home or Assisted Living Community
- Changing Care Providers
- Working with Care Providers
- Creating Your Care Team
- Long-Distance Caregiving
- Community Resource Finder
- Be a Healthy Caregiver
- Caregiver Stress
- Caregiver Stress Check
- Caregiver Depression
- Changes to Your Relationship
- Grief and Loss as Alzheimer's Progresses
- Home Safety
- Dementia and Driving
- Technology 101
- Preparing for Emergencies
- Managing Money Online Program
- Planning for Care Costs
- Paying for Care
- Health Care Appeals for People with Alzheimer's and Other Dementias
- Social Security Disability
- Medicare Part D Benefits
- Tax Deductions and Credits
- Planning Ahead for Legal Matters
- Legal Documents
- ALZ Talks Virtual Events
- ALZNavigator™
- Veterans and Dementia
- The Knight Family Dementia Care Coordination Initiative
- Online Tools
- Asian Americans and Pacific Islanders and Alzheimer's
- Native Americans and Alzheimer's
- Black Americans and Alzheimer's
- Hispanic Americans and Alzheimer's
- LGBTQ+ Community Resources for Dementia
- Educational Programs and Dementia Care Resources
- Brain Facts
- 50 Activities
- For Parents and Teachers
- Resolving Family Conflicts
- Holiday Gift Guide for Caregivers and People Living with Dementia
- Trajectory Report
- Resource Lists
- Search Databases
- Publications
- Favorite Links
- 10 Healthy Habits for Your Brain
- Stay Physically Active
- Adopt a Healthy Diet
- Stay Mentally and Socially Active
- Online Community
- Support Groups
Find Your Local Chapter
- Any Given Moment
- New IDEAS Study
- Bruce T. Lamb, Ph.D., Chair
- Christopher van Dyck, M.D.
- Cynthia Lemere, Ph.D.
- David Knopman, M.D.
- Lee A. Jennings, M.D. MSHS
- Karen Bell, M.D.
- Lea Grinberg, M.D., Ph.D.
- Malú Tansey, Ph.D.
- Mary Sano, Ph.D.
- Oscar Lopez, M.D.
- Suzanne Craft, Ph.D.
- RFI Amyloid PET Depletion Following Treatment
- About Our Grants
- Andrew Kiselica, Ph.D., ABPP-CN
- Arjun Masurkar, M.D., Ph.D.
- Benjamin Combs, Ph.D.
- Charles DeCarli, M.D.
- Damian Holsinger, Ph.D.
- David Soleimani-Meigooni, Ph.D.
- Donna M. Wilcock, Ph.D.
- Elizabeth Head, M.A, Ph.D.
- Fan Fan, M.D.
- Fayron Epps, Ph.D., R.N.
- Ganesh Babulal, Ph.D., OTD
- Hui Zheng, Ph.D.
- Jason D. Flatt, Ph.D., MPH
- Jennifer Manly, Ph.D.
- Joanna Jankowsky, Ph.D.
- Luis Medina, Ph.D.
- Marcello D’Amelio, Ph.D.
- Marcia N. Gordon, Ph.D.
- Margaret Pericak-Vance, Ph.D.
- María Llorens-Martín, Ph.D.
- Nancy Hodgson, Ph.D.
- Shana D. Stites, Psy.D., M.A., M.S.
- Walter Swardfager, Ph.D.
- ALZ WW-FNFP Grant
- Capacity Building in International Dementia Research Program
- ISTAART IGPCC
- Alzheimer’s Disease Strategic Fund: Endolysosomal Activity in Alzheimer’s (E2A) Grant Program
- Imaging Research in Alzheimer’s and Other Neurodegenerative Diseases
- Zenith Fellow Awards
- National Academy of Neuropsychology & Alzheimer’s Association Funding Opportunity
- Part the Cloud-Gates Partnership Grant Program: Bioenergetics and Inflammation
- Pilot Awards for Global Brain Health Leaders (Invitation Only)
- Robert W. Katzman, M.D., Clinical Research Training Scholarship
- Funded Studies
- How to Apply
- Portfolio Summaries
- Supporting Research in Health Disparities, Policy and Ethics in Alzheimer’s Disease and Dementia Research (HPE-ADRD)
- Diagnostic Criteria & Guidelines
- Annual Conference: AAIC
- Professional Society: ISTAART
- Alzheimer's & Dementia
- Alzheimer's & Dementia: DADM
- Alzheimer's & Dementia: TRCI
- International Network to Study SARS-CoV-2 Impact on Behavior and Cognition
- Alzheimer’s Association Business Consortium (AABC)
- Global Biomarker Standardization Consortium (GBSC)
- Global Alzheimer’s Association Interactive Network
- International Alzheimer's Disease Research Portfolio
- Alzheimer’s Disease Neuroimaging Initiative Private Partner Scientific Board (ADNI-PPSB)
- Research Roundtable
- About WW-ADNI
- North American ADNI
- European ADNI
- Australia ADNI
- Taiwan ADNI
- Argentina ADNI
- WW-ADNI Meetings
- Submit Study
- RFI Inclusive Language Guide
- Scientific Conferences
- AUC for Amyloid and Tau PET Imaging
- Make a Donation
- Walk to End Alzheimer's
- The Longest Day
- RivALZ to End ALZ
- Ride to End ALZ
- Tribute Pages
- Gift Options to Meet Your Goals
- Founders Society
- Fred Bernhardt
- Anjanette Kichline
- Lori A. Jacobson
- Pam and Bill Russell
- Gina Adelman
- Franz and Christa Boetsch
- Adrienne Edelstein
- For Professional Advisors
- Free Planning Guides
- Contact the Planned Giving Staff
- Workplace Giving
- Do Good to End ALZ
- Donate a Vehicle
- Donate Stock
- Donate Cryptocurrency
- Donate Gold & Sterling Silver
- Donor-Advised Funds
- Use of Funds
- Giving Societies
- Why We Advocate
- Ambassador Program
- About the Alzheimer’s Impact Movement
- Research Funding
- Improving Care
- Support for People Living With Dementia
- Public Policy Victories
- Planned Giving
- Community Educator
- Community Representative
- Support Group Facilitator or Mentor
- Faith Outreach Representative
- Early Stage Social Engagement Leaders
- Data Entry Volunteer
- Tech Support Volunteer
- Other Local Opportunities
- Visit the Program Volunteer Community to Learn More
- Become a Corporate Partner
- A Family Affair
- A Message from Elizabeth
- The Belin Family
- The Eliashar Family
- The Fremont Family
- The Freund Family
- Jeff and Randi Gillman
- Harold Matzner
- The Mendelson Family
- Patty and Arthur Newman
- The Ozer Family
- Salon Series
- No Shave November
- Other Philanthropic Activities
- Still Alice
- The Judy Fund E-blast Archive
- The Judy Fund in the News
- The Judy Fund Newsletter Archives
- Sigma Kappa Foundation
- Alpha Delta Kappa
- Parrot Heads in Paradise
- Tau Kappa Epsilon (TKE)
- Sigma Alpha Mu
- Alois Society Member Levels and Benefits
- Alois Society Member Resources
- Zenith Society
- Founder's Society
- Joel Berman
- JR and Emily Paterakis
- Legal Industry Leadership Council
- Accounting Industry Leadership Council
Find Local Resources
Let us connect you to professionals and support options near you. Please select an option below:
Use Current Location Use Map Selector
Search Alzheimer’s Association

Make an Impact in the Fight to End Alzheimer's
What is dementia.
Dementia is a general term for loss of memory, language, problem-solving and other thinking abilities that are severe enough to interfere with daily life. Alzheimer's is the most common cause of dementia. Subscribe to E-News to learn how you can help those affected by Alzheimer's.
About dementia
- Risk and prevention
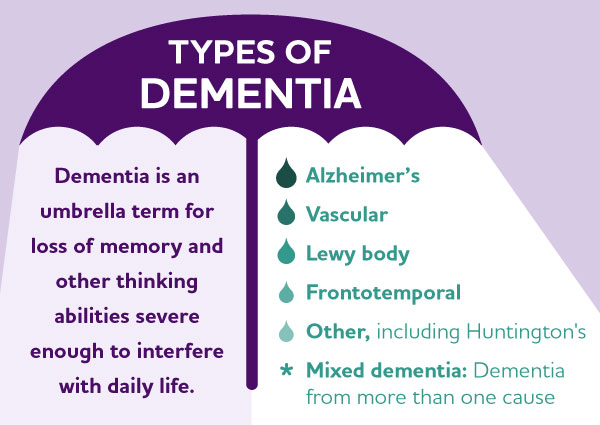
Know the 10 signs
Find out how typical age-related memory loss compares to early signs of Alzheimer's and other dementias.
Symptoms and signs of dementia
Signs of dementia can vary greatly. Examples include problems with:
- Short-term memory.
- Keeping track of a purse or wallet.
- Paying bills.
- Planning and preparing meals.
- Remembering appointments.
- Traveling out of the neighborhood.
Dementia symptoms are progressive, which means that the signs of cognitive impairment start out slowly and gradually get worse over time, leading to dementia. If you or someone you know is experiencing memory difficulties or other changes in thinking skills, don't ignore them. See a doctor soon to determine the cause. Professional evaluation may detect a treatable condition. And even if symptoms suggest dementia, early diagnosis allows a person to get the maximum benefit from available treatments and provides an opportunity to volunteer for clinical trials or studies . It also provides time to plan for the future. Learn more: 10 Warning Signs , Stages of Alzheimer's
Dementia is caused by a variety of diseases that cause damage to brain cells. This damage interferes with the ability of brain cells to communicate with each other. When brain cells cannot communicate normally, thinking, behavior and feelings can be affected.
The brain has many distinct regions, each of which is responsible for different functions (for example, memory, judgment and movement). When cells in a particular region are damaged, that region cannot carry out its functions normally.

Take our free e-learning course
Understanding Alzheimer's and Dementia outlines the difference between Alzheimer's and dementia, symptoms, stages, risk factors and more.
While most changes in the brain that cause dementia are permanent and worsen over time, thinking and memory problems caused by the following conditions may improve when the condition is treated or addressed:
- Depression.
- Medication side effects.
- Excess use of alcohol.
- Thyroid problems.
- Vitamin deficiencies.
Diagnosis of dementia
Dementia help and support are available.
- Call our 24/7 Helpline: 800.272.3900
- See our caregiving information for Alzheimer’s and dementia caregivers
- Locate a support group in your community
Donate to fight Alzheimer's
The first survivor of Alzheimer's is out there, but we won't get there without you.
Dementia treatment and care
Treatment of dementia depends on its cause. In the case of most progressive dementias, including Alzheimer's disease, there is no cure, but two treatments — aducanumab (Aduhelm®) and lecanemab (Leqembi®) — demonstrate that removing beta-amyloid, one of the hallmarks of Alzheimer’s disease, from the brain reduces cognitive and functional decline in people living with early Alzheimer’s. (Aducanumab will be discontinued on Nov. 1, 2024. Please connect with your provider on treatment options.) Others can temporarily slow the worsening of dementia symptoms and improve quality of life for those living with Alzheimer's and their caregivers. The same medications used to treat Alzheimer's are among the drugs sometimes prescribed to help with symptoms of other types of dementias . Non-drug therapies can also alleviate some symptoms of dementia.
Ultimately, the path to effective new treatments for dementia is through increased research funding and increased participation in clinical studies. Right now, volunteers are urgently needed to participate in clinical studies and trials about Alzheimer's and other dementias. Learn more: Medications for Memory Loss , Alternative Treatments for Alzheimer's
Dementia risk and prevention
Sprint for discovery.
New research shows there are things we can do to reduce the risk of mild cognitive impairment and dementia.
Learn more: Brain Health
Keep Up With Alzheimer’s News and Events
The alzheimer’s association is in your community., learn how alzheimer’s disease affects the brain..
Take the Brain Tour
Don't just hope for a cure. Help us find one.

Cognitive impairment
About cognitive impairment.
Cognitive impairment in hospital is often associated with adverse outcomes, such as falls. For some people with cognitive impairment and for their carers and families, a hospital stay can be a negative experience. Staff may struggle to provide the right care in the absence of appropriate education and training.
The first step to making a person’s stay safer is to understand the different forms of cognitive impairment, the people who are at risk, and what steps can be taken to reduce harm.
Cognitive impairment:
- Impedes communication, attention, memory, thinking and problem solving
- Means a person may not be able to carry out tasks or be unable to recognise people or objects
- Can be temporary or permanent
- Will affect what the person can understand and how they relate to others and interpret the environment.
Understanding what each person is experiencing will help you to communicate with that person and provide the right care.
Cognitive impairment can affect us all. People with cognitive impairment may be our patients, our parents, our loved ones, or us.
Common conditions associated with cognitive impairment
Dementia and delirium are the two most common forms of cognitive impairment among older people admitted to hospital. While they are not a normal part of getting old, these conditions commonly affect older people. As our population ages, the number of people with delirium and dementia in hospital will increase.
Dementia causes progressive cognitive impairment, affecting memory, judgement, language and the ability to perform everyday tasks. Alzheimer’s disease is the most common type of dementia. Dementia is predominately a disorder related to age but can affect people younger than 65 years old. This is known as younger onset dementia.
Delirium is an acute disturbance of consciousness, attention and cognition that tends to fluctuate during the course of the day. It can be a treatable medical emergency. Delirium is common in hospitals but is often not detected or is misdiagnosed. Delirium can be treated if diagnosed early and even prevented with the right care following a hospital admission.People with dementia are at a greater risk of developing delirium.
People may also be cognitively impaired due to either:
- An acquired brain injury
- A stroke, or
- An intellectual disability.
Any form of cognitive impairment needs to recognised, understood and acted on.
Further information is available on the Caring for cognitive impairment website .
Improving Mi Practices
- The IMP Advantage
- All Courses
- Training for Behavioral Health Professionals
- Who We Serve
- In Memoriam: Alyson Rush Tarrant
- Autism Spectrum Disorders
- Assertive Community Treatment (ACT)
- Benefit-to-Work (B2W)
- Clubhouse - Psychosocial Rehabilitation (PSR)
- Co-Occurring Disorders
- Cognitive Abilities and Intervention Strategies (CAIS) - Beyond Behavior
- Cognitive Behavioral Therapy (CBT)
- Diagnostic & Statistical Manual of Mental Disorders (DSM-5)
- Dialectical Behavior Therapy (DBT)
- Family Psychoeducation (FPE)
- Individual Placement & Support
- Infants & Children (IC)
- Intellectual & Developmental Disabilities (IDD)
- Lesbian, Gay, Bisexual, Transgender, & Queer (LGBTQ+)
- Motivational Interviewing (MI)
- Older Adults (OA)
- Pain Management (PM)
- Person-Centered Planning (PCP)
- Self-Determination in Long-Term Care (SLC)
- Substance Use Disorder (SUD)
- Trauma and the Brain (TBI)
- Trauma-Informed Care (TIC)
- Veterans (V)
- Workplace Essentials (WE)
- Working With Community Partners
- Additional Resources
- Advisory Groups
- Encyclopedia
- Supplementary Videos
- What's New?
- Support / Contact
- Create an Account
Impaired Judgement
Definition:.
Impaired judgement is a medical condition that results in a person not being able to make good decisions because of an underlying medical problem, environmental factors, diet, or drugs and alcohol .
The Mayo Clinic notes that many people with impaired judgement suffer from mild cognitive impairment, which also causes impairment in memory, language and thinking skills.
ORIGINAL RESEARCH article
Impaired reasoning and problem-solving in individuals with language impairment due to aphasia or language delay.

- 1 VA Northern California Health Care System, Martinez, CA, USA
- 2 Palo Alto University, Palo Alto, CA, USA
- 3 Center for Mind and Brain, University of California, Davis, Davis, CA, USA
- 4 National Research University Higher School of Economics, Moscow, Russian Federation
The precise nature of the relationship between language and thought is an intriguing and challenging area of inquiry for scientists across many disciplines. In the realm of neuropsychology, research has investigated the inter-dependence of language and thought by testing individuals with compromised language abilities and observing whether performance in other cognitive domains is diminished. One group of such individuals is patients with aphasia who have an impairment in speech and language arising from a brain injury, such as a stroke. Our previous research has shown that the degree of language impairment in these individuals is strongly associated with the degree of impairment on complex reasoning tasks, such as the Wisconsin Card Sorting Task (WCST) and Raven’s Matrices. In the current study, we present new data from a large group of individuals with aphasia that show a dissociation in performance between putatively non-verbal tasks on the Wechsler Adult Intelligence Scale (WAIS) that require differing degrees of reasoning (Picture Completion vs. Picture Arrangement tasks). We also present an update and replication of our previous findings with the WCST showing that individuals with the most profound core language deficits (i.e., impaired comprehension and disordered language output) are particularly impaired on problem-solving tasks. In the second part of the paper, we present findings from a neurologically intact individual known as “Chelsea” who was not exposed to language due to an unaddressed hearing loss that was present since birth. At the age of 32, she was fitted with hearing aids and exposed to spoken and signed language for the first time, but she was only able to acquire a limited language capacity. Chelsea was tested on a series of standardized neuropsychological measures, including reasoning and problem-solving tasks. She was able to perform well on a number of visuospatial tasks but was disproportionately impaired on tasks that required reasoning, such as Raven’s Matrices and the WAIS Picture Arrangement task. Together, these findings suggest that language supports complex reasoning, possibly due to the facilitative role of verbal working memory and inner speech in higher mental processes.
Introduction
To what extent is thought dependent on language? This question has been pondered by philosophers and scientists alike for millenia. When asked about the nature of thinking, Socrates stated: “The soul when thinking appears to me to be just talking" ( Jowett, 1892 , p. 252). Many individuals echo this same subjective experience of an internal dialog that often accompanies their thoughts ( Hurlburt, 1990 ; Hurlburt and Heavey, 2001 ; Carruthers, 2002 ), but how can we objectively study the relationship between language and thought? A number of efforts to address this question experimentally have made use of data from a range of sources, including animals, young children, healthy adults, and language-impaired individuals ( Watson, 1920 , 1924 ; Piaget, 1967 ; Kertesz and McCabe, 1975 ; Vygotsky, 1978 ; Hjelmquist, 1989 ; Hurlburt, 1990 ; Halford et al., 1998 ; Hermer-Vazquez et al., 1999 ; Kinsbourne, 2000 ; Varley and Siegal, 2000 ; Kuczaj and Hendry, 2003 ; Wheeler, 2004 ; Machery, 2005 ; Clark, 2006 ; Penn et al., 2008 ; Carpendale et al., 2009 ; for a review, see Perrone-Bertolotti et al., 2014 ). In the current paper, we focus on the role that language plays in reasoning and problem-solving in particular. First, we review prior work in this area from a range of sources and then describe our current research focused on studying the relationship between language and reasoning in individuals with varying degrees of language impairment.
Evidence from a number of animal studies clearly demonstrate remarkable reasoning and problem-solving abilities in non-human species ( Blaisdell et al., 2006 ; Taylor et al., 2009 ; Smirnova et al., 2015 ), but it is argued that such abilities have reached a higher level in humans ( Premack, 1983 , 2007 ; O’Brien and Opie, 2002 ; Penn et al., 2008 ). Since abstract, symbolic language reaches its apex in humans as well, it has been suggested that these abilities are causally related, that is, our language system facilitates logical reasoning in some way ( Sokolov, 1968/1972 ; Premack, 1983 ; Carruthers, 2002 ; O’Brien and Opie, 2002 ; Bermudez, 2003 ; Gentner, 2003 ; Kuczaj and Hendry, 2003 ; Goel and Dolan, 2004 ). Interestingly, it has been shown that chimpanzees who receive language-training have superior reasoning and problem-solving skills compared to language-naïve chimpanzees ( Premack, 1983 ), supporting the notion that representational language facilitates advanced reasoning.
Data from children also suggest that language plays an important role in thought and reasoning ( Behrend et al., 1989 ; Gentner and Loewenstein, 2002 ; Gentner, 2003 ; Loewenstein and Gentner, 2005 ; Lidstone et al., 2012 ). Vygotsky (1978 , 2012 ) argued that young children first use overt speech to work through problems in conjunction with elders, then learn to speak to themselves privately while working through problems on their own, and eventually internalize that overt speech into private, covert speech while problem-solving. Piaget also believed that children’s private speech supported thinking and was related to the development of reasoning ability ( Piaget, 1926 , 1967 ). Young children verbalize overtly when performing cognitively demanding tasks, but by 14–17 years of age, children report using an inner speech strategy ( Winsler and Naglieri, 2003 ). Experimental evidence for these ideas comes from studies showing that problem-solving performance in children is associated with the use of private speech: Fernyhough and Fradley (2005) showed that the use of self-regulating statements in children correlated with performance on the Tower of London puzzle task (see also Winsler et al., 2009 ). Similarly, it has been shown that children exhibit increased self-directed and private speech when performing a difficult task and that children who exhibit more self-directed speech are better able to solve problems ( Berk and Garvin, 1984 ; Berk, 1986 ; Behrend et al., 1989 ; Winsler et al., 1997 ). Finally, others such as Hermer-Vazquez et al. (1999) have shown that children’s ability to perform a problem-solving task involving spatial orientation is related to their level of language competence (but see Learmonth et al., 2008 ).
Other work has approached the study of the relationship between language and reasoning by assessing cognitive functioning in individuals with varying degrees of language impairment ( Kinsbourne, 2000 ; Varley and Siegal, 2000 ). A series of findings have shown that individuals with aphasia (an impairment in language due to brain injury) show deficits in reasoning and problem-solving (e.g., Weinstein and Teuber, 1957 ; Piercy, 1964 ; De Renzi et al., 1966 ; Archibald et al., 1967 ; Basso et al., 1973 ; Edwards et al., 1976 ; Borod et al., 1982 ; Larrabee, 1986 ; Hjelmquist, 1989 ; Hamsher, 1991 ; Baldo et al., 2005 , 2010 ; but see Kinsbourne and Warrington, 1963 ; Basso et al., 1973 ). Moreover, a large number of these studies have shown that the degree of aphasia severity is correlated with the level of cognitive impairment ( De Renzi et al., 1966 ; Archibald et al., 1967 ; Edwards et al., 1976 ; Borod et al., 1982 ; Larrabee, 1986 ; Vilkki, 1988 ; Baldo et al., 2005 , 2010 ; but see Basso et al., 1973 ; Helm-Estabrooks, 2002 ). In particular, individuals with severe comprehension deficits such as those with Wernicke’s aphasia appear to be especially impaired on problem-solving and reasoning tasks ( Kertesz and McCabe, 1975 ; Hjelmquist, 1989 ; Baldo et al., 2005 ), a finding not simply explained by a failure to understand task instructions.
In our work, we have examined the role of language in reasoning by comparing large groups of stroke patients with and without aphasia on standardized tests of non-verbal reasoning and problem-solving. Such tests require the ability to recognize/represent a problem, use available information to test possible solutions, and monitor the veracity of those solutions. By “non-verbal,” we refer to the fact that these tasks do not require a spoken response and have no/minimal language comprehension requirements. For example, Baldo et al. (2005) tested 41 right and left hemisphere stroke patients with a wide range of aphasia severity on the Wisconsin Card Sorting Test (WCST; Heaton et al., 1993 ) and showed that problem-solving performance was significantly related to the degree of patients’ language impairment. Interestingly, performance was most strongly related to patients’ comprehension scores in particular, suggesting that core language processes are most important for successful problem-solving. In an effort to establish discriminant validity (i.e., to show that the relationship between language scores and performance on the WCST was not simply a matter of overall cognitive impairment), we also showed that there was no relationship between patients’ language scores and performance on Block Design, a non-verbal test of visuospatial functioning that is minimally dependent on reasoning. This dissociation reinforces the idea that individuals with aphasia, particularly those with core language impairments, have difficulty on tasks involving reasoning that are not explained by a general cognitive impairment.
Similarly, we have shown that aphasic individuals also exhibit poor performance on another test of non-verbal reasoning, Raven’s Coloured Progressive Matrices ( Baldo et al., 2010 ). Importantly, there was a significant interaction in performance on this test such that individuals with aphasia were disproportionately impaired on Raven’s items that required relational reasoning relative to those items that only required visual-pattern completion (see Figure 1 for examples; Bunge et al., 2005 ; Crone et al., 2009 ). Again, the specificity of these findings bolster the conclusion that decrements in reasoning in particular are associated with language impairment following stroke, rather than such deficits being part of a more general cognitive impairment.
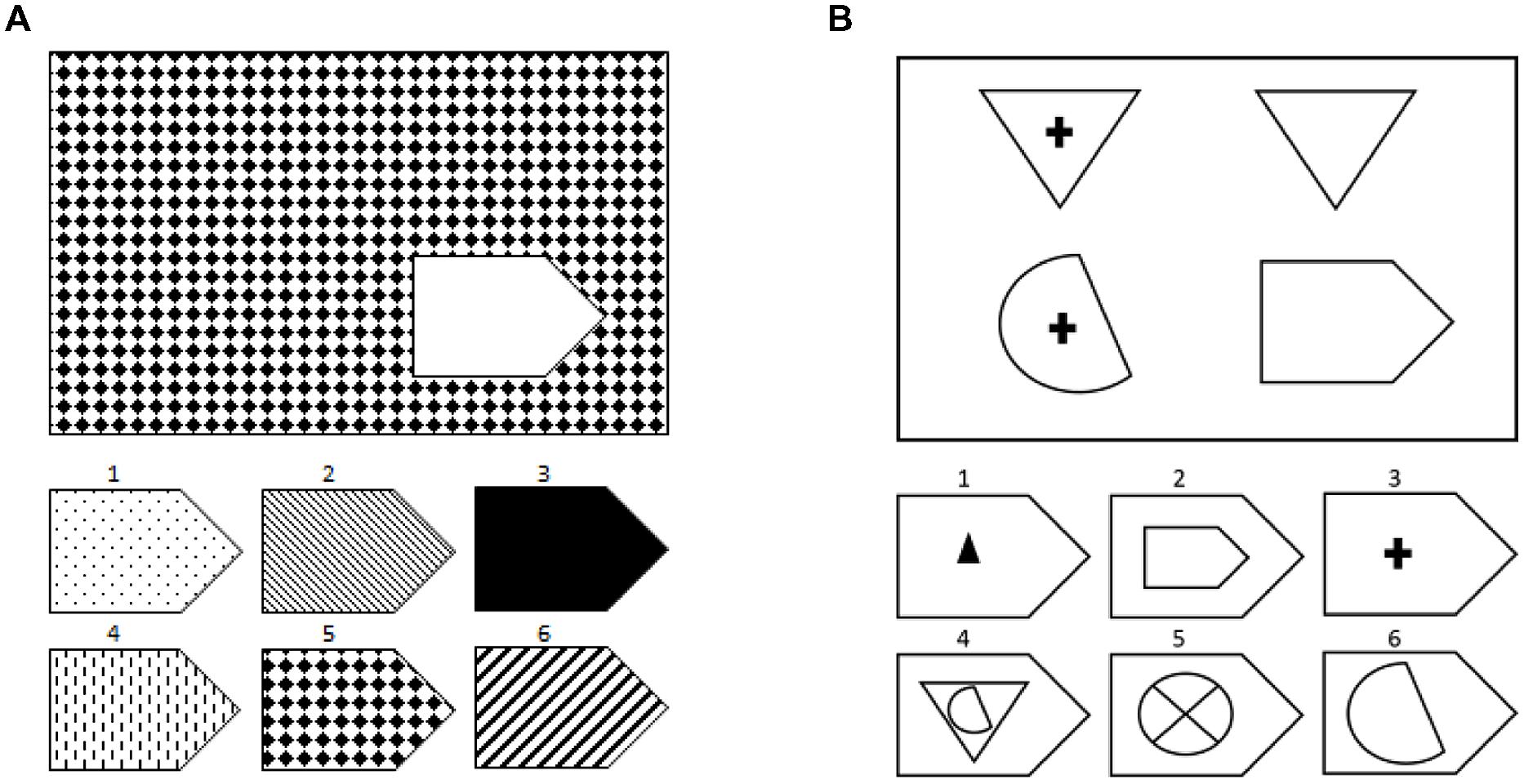
FIGURE 1. Examples of the types of problems on Raven’s Matrices: (A) visual-pattern completion and (B) relational reasoning. These are not actual items from the test due to copyright issues and to maintain test security.
In the current paper, we sought to extend our previous findings by testing the relationship between aphasia severity and reasoning using a series of putatively non-verbal tasks from a commonly administered instrument, the Wechsler Adult Intelligence Scale (WAIS; Experiment 1A). We also sought to replicate and extend our previous findings with the WCST in a larger and more homogeneous patient sample that included left hemisphere-injured patients only (Experiment 1B). Rather than focus solely on aphasia subtypes, which can be problematic due to the multi-dimensional nature of these syndromes ( Caramazza and McCloskey, 1988 ; Coltheart, 2004 ), we also assessed the relationship between reasoning performance and specific language sub-processes (e.g., auditory comprehension, repetition). In the second part of this paper, we describe findings from a unique individual whose language impairment derives not from aphasia but from the fact that she was not exposed to language until the age of 32 due to an unaddressed hearing loss (Experiment 2). Together, these data provide further insights into the close relationship between language and reasoning.
Experiment 1A: Reasoning Performance in Aphasic Individuals on the WAIS
In a further effort to understand the role of language in reasoning, we conducted an analysis of aphasic patients’ performance on the Picture Completion and Picture Arrangement subtests of the WAIS-R and WAIS-III ( Wechsler, 1981 , 1997 ). These standardized tasks were chosen for comparison because they both require visual perception and attention with no/minimal language or motor requirements, but differ with respect to the amount of reasoning required ( Ryan and Paolo, 2001 ; Tulsky et al., 2003 ). A previous study ( Varley, 1998 ) used the Picture Arrangement task as a measure of causal reasoning in aphasia and reported that one of the two aphasic individuals tested showed impaired performance; however, there was concern that visual impairments could have contributed to performance. Given these equivocal results, it was of interest to compare performance on the Picture Arrangement task to performance on the Picture Completion task, which also involves visual perception and attention but a smaller reasoning component. Also, we analyzed performance from a large sample of well-characterized left hemisphere patients with a range of language disturbance and no known visual disturbance. Our prediction was that aphasic individuals would be disproportionately impaired on the more reasoning-intensive Picture Arrangement task, relative to Picture Completion and that patients’ comprehension scores would be most strongly correlated with performance.
Participants
A retrospective analysis was performed on data from 60 individuals (17 female) in our database who met strict inclusion/exclusion criteria: history of a single left hemisphere stroke, at least 6 months post-stroke (to ensure that behaviors had stabilized), native English-speaking (by age 5), right-handed, 8 th grade education or higher, and no prior neurologic or severe psychiatric history. The determination of language impairment was made with the Western Aphasia Battery (WAB; Kertesz, 1982 , 2006 ), which also provides scores for language sub-processes (fluency, comprehension, naming, etc.) as well as an aphasia subtype diagnosis (i.e., Broca’s, Wernicke’s, conduction aphasia, etc.). Individuals that score above the cut-off for normal language on the WAB (93.7 out of 100 points possible) are considered non-aphasic according to the WAB manual and norms. Based on this cut-off, our sample included 37 individuals with aphasia and 23 non-aphasic individuals. The aphasic individuals included 17 individuals with anomic aphasia, nine with Broca’s aphasia, five with conduction aphasia, five with Wernicke’s aphasia, and one individual who was unclassifiable. Patients’ mean age ± SD was 61.7 ± 11.0 years for the aphasic individuals and 59.6 ± 10.9 years for non-aphasic individuals; mean education was 14.6 ± 2.3 years for the aphasic individuals and 15.8 ± 3.0 years for non-aphasic individuals; mean months post-stroke was 44.4 ± 46.9 months for aphasic individuals and 41.7 ± 48.3 months for non-aphasic individuals; and mean lesion volume was 136.1cc ± 71.6 for aphasic individuals and 31.5cc ± 29.0 for non-aphasic individuals. Finally, the aphasic group included eight women and the non-aphasic group included six women.
Materials and Procedures
Participants were administered the Picture Completion and Picture Arrangement subtests from the WAIS-R or WAIS-III. The Picture Completion task requires examinees to point to something missing in a series of drawings of increasing difficulty (e.g., a number missing from a keypad). The Picture Arrangement task requires examinees to rearrange a series of pictures so that they tell a story, like the tiles in a comic strip (e.g., a series of pictures showing different stages of people cooking a meal). While both tasks require visuo-spatial perception and attention, the Picture Arrangement task puts a greater burden on reasoning ability ( Varley, 1998 ; Tulsky et al., 2003 ). The tasks were administered and scored in the standard manner according to the WAIS manual. Because the data were collected over a period of years, some participants were administered the Picture Completion and Picture Arrangement subtests from the WAIS-R and others, the WAIS-III. In order to combine data from the WAIS-R and WAIS-III, scores were adjusted according to Gläscher et al. (2009) , which involved converting the WAIS-R raw scores to WAIS-III raw scores by adding the mean difference to each subtest (-0.4 for Picture Completion and -0.6 for Picture Arrangement). Last, we also analyzed data from the Benton Face Recognition Task ( Benton et al., 1983 ) for these 60 individuals. The Benton Face Recognition Task is a visuo-perceptual task in which examinees are asked to point to which of six faces on the bottom of the page is the same person as the face on top. Despite being called a face recognition task, it is simply a face-matching task involving non-famous faces with no delay.
An analysis of covariance (ANCOVA) was used to compare aphasic and non-aphasic individuals’ raw scores on the different tasks with age, years of education, months post-stroke, and lesion volume included as covariates. Partial correlation coefficients (two-tailed) were computed to relate reasoning performance to WAB subtest scores for speech fluency, object naming, repetition, and auditory comprehension, with the same nuisance factors as control variables. The WAB fluency score is a rating from 0 to 10 of an individual’s spontaneous speech based on fluency of speech, grammatical competence, and paraphasic errors; the WAB naming subtest involves naming a series of 20 physically presented items (e.g., ball, cup); the WAB repetition subtest requires examinees to repeat 15 items that include single words, phrases, and sentences; and the WAB auditory comprehension score is based on yes/no questions, single-word recognition (both physical object-word matching and picture-word matching), and sequential commands.
As predicted, the ANCOVA showed that aphasic individuals performed significantly poorer than non-aphasic individuals on the Picture Arrangement task, F (1,54) = 6.25, p = 0.04 ( M ± SD = 34.8 ± 21.7% vs. 60.8 ± 22.3%, respectively), but the groups did not differ statistically on the Picture Completion task (49.0 ± 19.1% vs. 68.5 ± 14.6%, respectively), F (1,54) = 1.51, p = 0.24 (see Figure 2 ), controlling for age, education, months post-stroke, and lesion volume. Again, these results suggest that language impairment is related to reduced performance on tasks that place a greater demand on reasoning ability, even when that task does not require any overt language production. As in our previous work, the most severely language-compromised individuals in the sample, those with Wernicke’s aphasia, had the numerically lowest performance on the Picture Arrangement (reasoning) task. In keeping with this result and similar to our previous findings, partial correlations revealed significant relationships between scores on the Picture Arrangement task and comprehension, r (58) = 0.27, p = 0.04, as well as repetition, r (58) = 0.28, p = 0.03, but not with naming or fluency ( p s > 0.05). The same pattern held true when we repeated the partial correlation analyses with the sub-sample of aphasic individuals only, with comprehension and repetition alone showing marginally significant correlations of 0.33 ( p = 0.07) and 0.32 ( p = 0.08), respectively. With respect to normative cut-offs based on age-adjusted norms provided by the WAIS manual, 13.5% of the aphasic individuals performed in the significantly impaired range on the Picture Arrangement task (age-adjusted scale score of 4 or lower) but only a single individual in the non-aphasic subgroup. On the Picture Completion task, 18.9% of aphasic individuals performed in the significantly impaired range and none of the non-aphasic individuals.
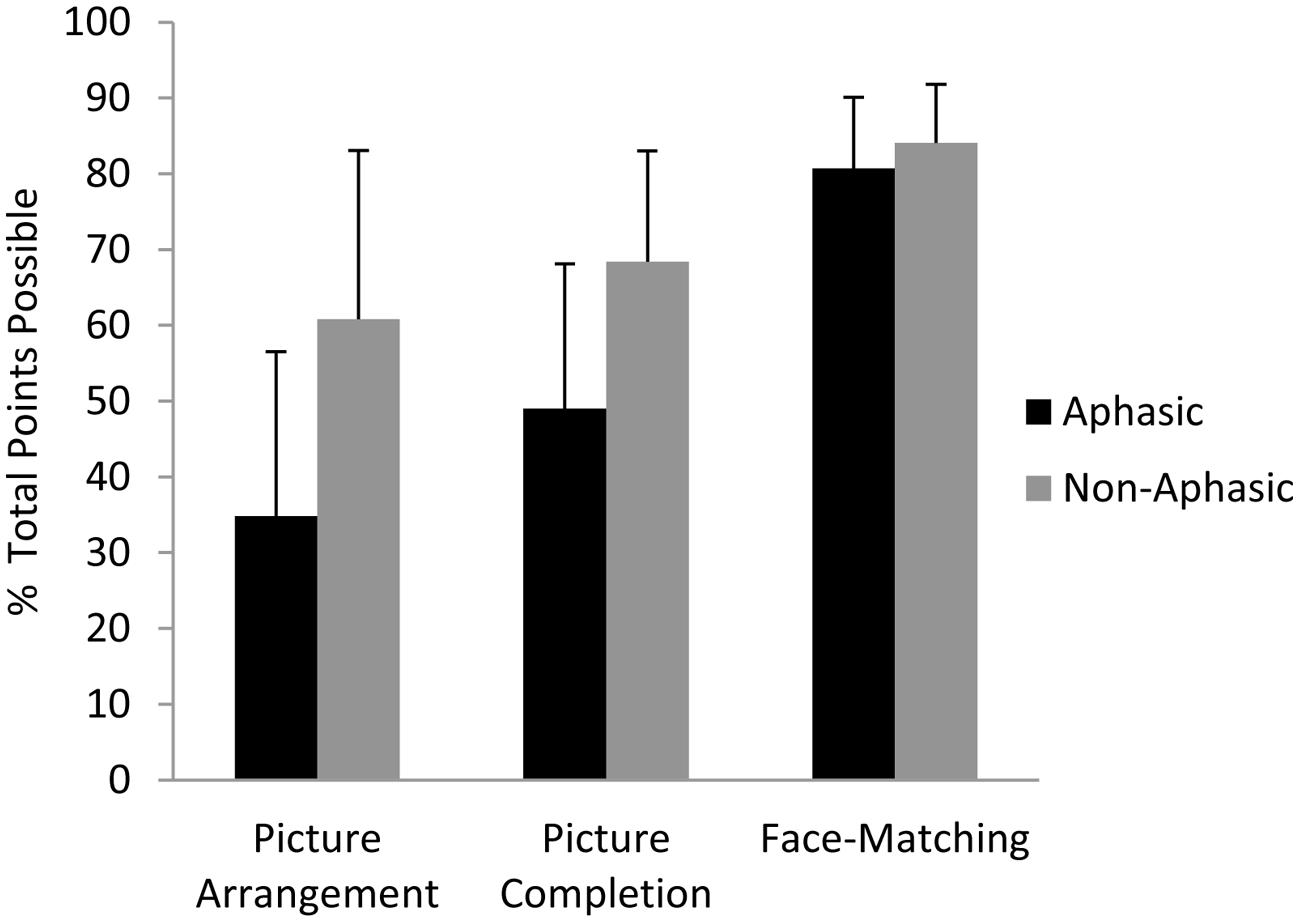
FIGURE 2. Performance of aphasic and non-aphasic stroke patients on the WAIS Picture Completion and Picture Arrangement subtests, and the Benton Face Recognition (Matching) Task. The raw data (number of points attained on each task) were converted to a percentage of total points possible for each task in order to compare the results across tasks. Standard deviation bars are shown.
As can be seen in Figure 2 , aphasic individuals exhibited numerically (though not statistically) poorer performance than non-aphasic individuals on the Picture Completion task as well. For this reason, we additionally analyzed performance from these same 60 individuals on another standardized test of visuospatial functioning that does not involve reasoning, the Benton Face Recognition Task. On this more purely visual-perceptual task, aphasic and non-aphasic individuals performed comparably as revealed by ANCOVA, F (1,54) = 0.72, p = 0.40 ( M ± SD = 81 ± 9.4% vs. 84 ± 7.7%, respectively; see Figure 2 ).
These findings are consistent with the notion that language facilitates reasoning. Specific correlations between problem-solving performance and comprehension and repetition further suggest that core language processes (as opposed to output processes such as fluency and naming) are most strongly related to performance. It should be emphasized that poor performance cannot simply be explained by individuals with severe language impairments misunderstanding the task, as they are able to demonstrate their understanding of task instructions in the initial trials, before it becomes more difficult. In the Discussion, we explore potential explanations of the observed relationship between compromised core language and impaired reasoning as they relate to the supportive role of inner speech and working memory.
Experiment 1B: WCST Performance in Individuals with Aphasia
We previously showed that performance on the WCST, a standardized measure of problem-solving and reasoning, was impaired in aphasic individuals and also correlated with a number of critical language variables ( Baldo et al., 2005 ). However, our paper included a relatively small sample and a heterogeneous group of both right and left hemisphere patients. Therefore, we sought to replicate our previous findings in a larger sample of patients whose lesions were restricted to the left hemisphere, in order to confirm our previous findings of a relationship between language impairment and problem-solving performance.
A retrospective data analysis was conducted on data from 81 chronic left hemisphere stroke patients from our database (23 female) who met the same strict inclusion/exclusion criteria described above in Experiment 1A. Seventeen of these patients were also included in Baldo et al. (2005) . Based on the WAB, 35 patients were non-aphasic (i.e., scored within normal limits) and 46 patients were aphasic. This latter group included 20 individuals with anomic aphasia, 12 with Broca’s aphasia, seven with conduction aphasia, two with transcortical sensory aphasia, and five with Wernicke’s aphasia. Patients’ mean age ± SD was 60.6 ± 11.6 years for the aphasic individuals and 60.5 ± 10.3 years for non-aphasic individuals; mean education was 14.3 ± 2.7 years for the aphasic individuals and 15.3 ± 2.8 years for non-aphasic individuals; mean months post-stroke was 48.5 ± 50.5 months for aphasic individuals and 44.7 ± 53.2 months for non-aphasic individuals; and mean lesion volume was 126.2cc ± 67.1 in aphasic individuals and 35.1cc ± 43.6 in non-aphasic individuals. Finally, the aphasic group included 12 women and the non-aphasic group included 11 women.
The WCST requires examinees to match test cards with different arrays of 1–4 items (e.g., two triangles) drawn in different colors to one of four key cards with similar arrays. Participants are not told how to match the test cards to the key cards but are provided with feedback from the examiner ( correct or incorrect ) after each move. Unbeknownst to the examinee, the examiner repeatedly changes the sorting category after a set number of trials, and the examinee must recognize this switch and modify their sorting behavior based on the feedback. As an indication of adequate comprehension of task instructions, only a single individual with Wernicke’s aphasia was unable to sort at least 1 category.
Aphasic and non-aphasic individuals’ raw scores were compared with an ANCOVA using age, years of education, months post-stroke, and lesion volume as covariates as above. In addition, individuals’ praxis subtest scores from the WAB were included as an extra covariate to ensure that poor performance was not related to ideomotor apraxia ( Basso et al., 1981 ; a subset of 10 individuals in the sample scored below 80% correct on the praxis subtest). Partial correlation coefficients (two-tailed) were computed with the same nuisance factors, in order to test the relationship between problem-solving performance on the WCST and language processes including speech fluency, naming, repetition, and auditory comprehension.
Confirming our 2005 findings, the left hemisphere stroke patients with aphasia performed poorly on the WCST, completing an average of just 2.6 out of 6 possible category sorts ( SD = 2.1), compared to non-aphasic left hemisphere stroke patients who completed an average of 4.4 out of 6 category sorts ( SD = 1.9). An ANCOVA confirmed that this difference was significant, F (1,64) = 4.16, p = 0.04, correcting for age, education, praxis, and months post-onset. The size of patients’ lesions, another potential confound, was available for 79 of the patients and did not change the results when included as an additional covariate.
As in our previous studies, aphasic individuals with the most severe comprehension deficits, those with Wernicke’s and transcortical sensory aphasia, were particularly impaired and were the only subgroups significantly impaired relative to the non-aphasic group, Dunnett’s T3 (equal variances not assumed), p s < 0.001 (see Figure 3 ). As shown, individuals with milder comprehension impairments (i.e., Broca’s, anomic, and conduction aphasia) performed in the moderately impaired range on the WCST task. Since aphasia subtypes can be problematic as they are multi-determined syndromes, we also analyzed WCST performance in relation to specific language subprocesses as measured by the WAB, including speech fluency, auditory comprehension, repetition, and naming. Partial correlations revealed that overall performance on the WCST based on the number of categories sorted was significantly related to auditory comprehension alone, r (65) = 0.46, p < 0.001. The same was true when the partial correlation analyses were repeated using data from only the aphasic individuals rather than the entire sample: only auditory comprehension significantly correlated with WCST performance, r (37) = 0.41, p = 0.01.
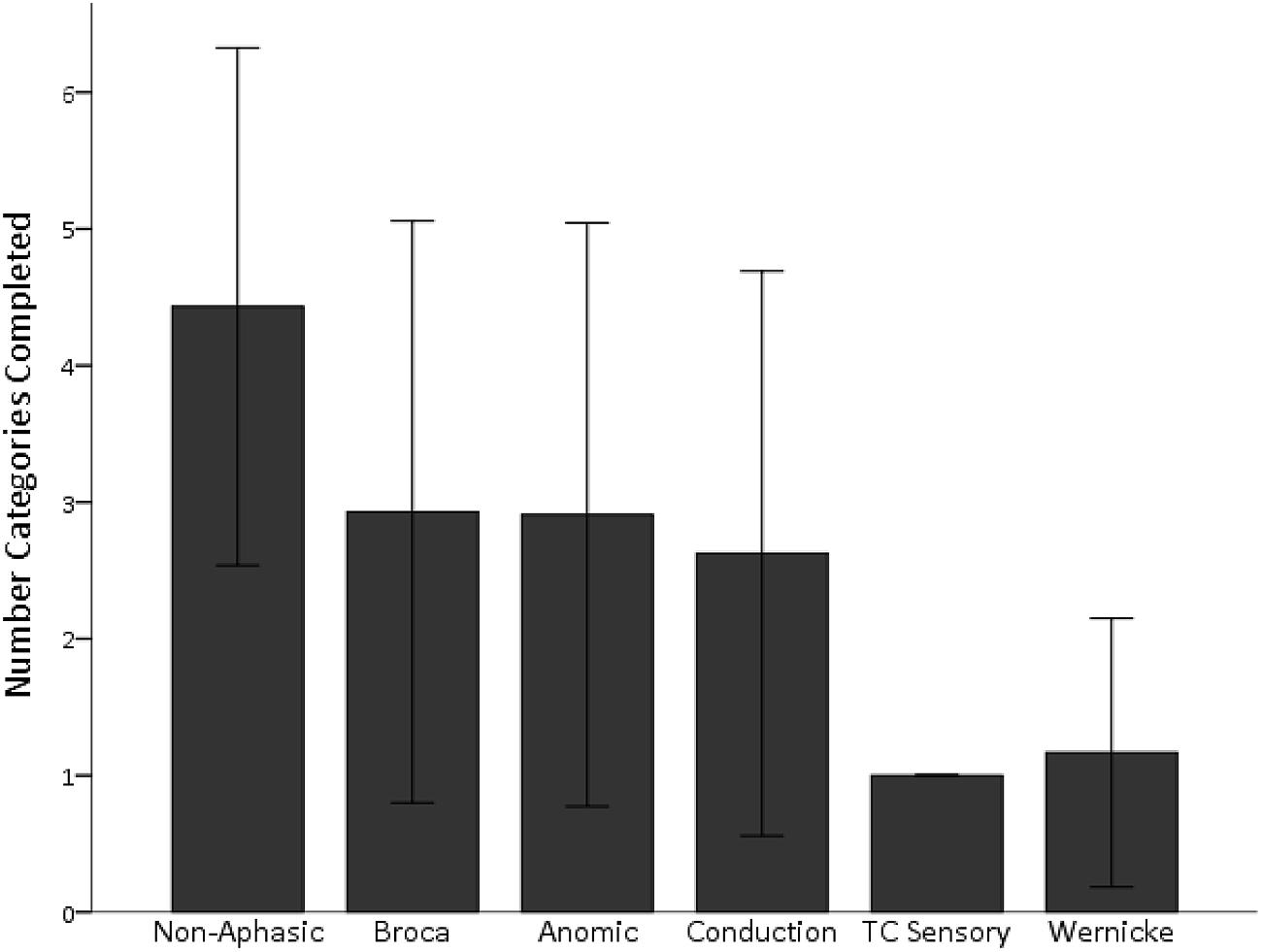
FIGURE 3. Wisconsin Card Sorting Task (WCST) performance is shown for the number of categories completed, based on aphasia subtype. Individuals with severe comprehension deficits (Wernicke’s and TC Sensory aphasia) sorted the fewest number of categories on the WCST. Performance in individuals with milder deficits overlapped with that of non-aphasic individuals. TC Sensory, transcortical sensory aphasia. Standard deviation bars are shown.
These new findings on the WCST reinforce our previous work showing that many individuals with aphasia exhibit difficulties on putatively non-verbal problem-solving tasks and thus suggest a relationship between the presence of language deficits and the degree of impairment in problem-solving capacity. Furthermore, individuals with the most severe language impairments (those with transcortical sensory and Wernicke’s aphasia) performed worse overall, and correlational data showed a significant relationship between comprehension scores and problem-solving performance. These latter findings again suggest that core language processes (as opposed to production processes such as fluency) are most significantly related to problem-solving performance.
In short, we have conducted a series of large-scale studies comparing reasoning/problem-solving in aphasic vs. non-aphasic individuals that suggest a supportive role of language in these abilities. Although concerns about potentially confounding factors such as lesion size and overall cognitive impairment were addressed, one could still argue that brain-injured individuals are not the ideal population for addressing the issue of language and cognition. Thus, we now turn to complementary data obtained from a healthy adult with a severely restricted language capacity.
Experiment 2: Reasoning in a Deaf Individual with Impaired Language
Another way to examine the role that language plays in reasoning and problem-solving is by assessing cognition in healthy individuals with compromised language abilities. This can happen, for example, in deaf individuals who are not exposed to language until they are older ( Siegal et al., 2001 ; Morgan and Kegl, 2006 ). One of the authors (ND) has worked with such an individual (pseudonym “Chelsea”) who had an untreated, congenital hearing loss and was not exposed to language or any formal education until the age of 32. In Experiment 2, we describe Chelsea’s performance on non-verbal measures of reasoning in comparison to her performance on other cognitively demanding tasks that do not involve reasoning. Data from this unique individual parallel findings in aphasic individuals and offer additional insights into the role that language plays in reasoning and problem-solving.
Data were collected from a single case whose pseudonym is “Chelsea,” as well as her parents and two sisters who served as controls. Chelsea was born with a severe to profound sensorineural hearing loss that went unaddressed due to being raised in a rural setting with limited resources ( Dronkers, 1987 ; Glusker, 1987 ; Glusker et al., 1990 ; Curtiss, 2014 ). Her mother had a viral illness while pregnant with Chelsea that is associated with congenital deafness, but a definitive cause of her sensorineural hearing loss was not established. She was raised in a supportive home with her parents and six siblings, and she functioned normally according to family report: carrying out household chores, taking care of younger siblings, etc. As an infant/toddler, she achieved all developmental milestones at a normal rate and at a pace similar to her siblings (e.g., sitting, crawling, standing, walking, etc.), with the exception of language. According to family report, there were no home-signs used to communicate with Chelsea, but rather she relied on pointing, gestures, and miming to indicate her needs. Home visits and videotapes of the family interacting with Chelsea (without researchers present) confirmed the apparent lack of any home-signing system (see Curtiss, 2014 ).
At the age of 32, Chelsea was evaluated by a number of medical providers and was fitted with bilateral hearing aids that allowed her to hear speech for the first time. She started receiving instruction in both spoken English and Signing Exact English by a licensed speech pathologist. CT and MRI as well as EEG studies conducted at the time were all normal. The neurologist who evaluated her over several sessions reported that she showed no evidence of neurologic disabilities except for a single neurologic sign of mild hyperreflexia on the left side ( Glusker et al., 1990 and personal communication).
After being fitted with bilateral hearing aids, Chelsea gradually began acquiring spoken and receptive language, and she achieved a good command of the English lexicon (i.e., production and comprehension of single words; Curtiss, 2014 ). However, her ability to process syntax, both in production and comprehension, was extremely limited. Not surprisingly, she was difficult to understand and converse with. Examples of Chelsea’s spontaneous speech are provided in Table 1 . In contrast, she demonstrated relatively preserved pragmatics, including normal body language, prosody, facial expressions, gesture, etc. ( Dronkers, 1987 ; Dronkers et al., 1998 ; Curtiss, 2014 ). Curtiss (2014) concluded that Chelsea’s case provides clear evidence that there exists a critical period for acquiring grammar but not for acquiring other aspects of language such as the lexicon, which continues to grow in Chelsea’s case.
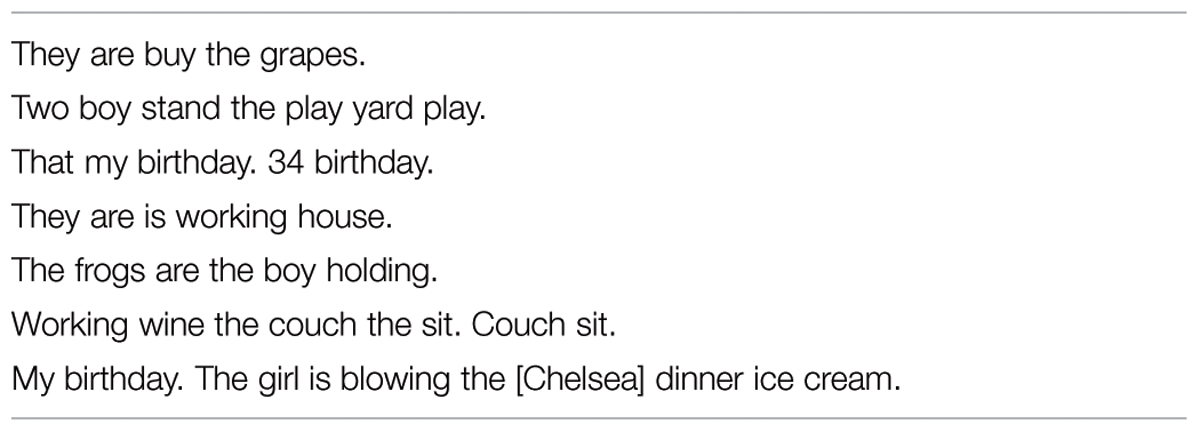
TABLE 1. Examples of Chelsea’s spontaneous speech.
Cognitive performance data from Chelsea’s parents and two sisters are also reported here for comparison. Her mother and father were tested at ages 52 and 62, and had 6th and 9th grade educations, respectively. While not as restricted in their schooling as Chelsea, her parents’ performance offers an informative comparison. Her two sisters were tested at ages 33 and 36, and had 12 and 13 years of education, respectively.
Chelsea was administered Raven’s Coloured Progressive Matrices and the WAIS-R Performance subtests at several time points from age 32–41. Raven’s Coloured Progressive Matrices includes a series of 36 non-speeded trials in which examinees have to point to 1 of 6 visual patches that best completes a visual pattern or sequence. She was also administered the WAIS-R Performance subtests, which represent the putatively non-verbal portion of the WAIS and are the preferred means of assessing intellectual functioning in hearing-impaired individuals ( Braden, 1992 ). The subtests include Picture Completion, Picture Arrangement, Block Design, Object Assembly, and Digit-Symbol. As described above, the WAIS-R Picture Completion task involves identifying a missing object in a picture, and the Picture Arrangement task involves rearranging a series of pictures so that they tell a story. Block Design requires examinees to rearrange red and white colored cubes to match a pattern printed in a stimulus book, and performance is based on both speed and accuracy. Object Assembly is a series of jigsaw puzzles that begin with very simple ones and get progressively harder. Last, the Digit-Symbol test involves speeded writing of symbols that correspond to numbers provided in a legend at the top of the page.
Serving as controls, Chelsea’s parents and two of her sisters were also administered the WAIS-R and Raven’s Matrices at a single time point that occurred between Chelsea’s 2nd and 3rd testing sessions. Her family was administered the Raven’s Standard Progressive Matrices, a more advanced version for adults whereas Chelsea was administered a simpler version, the Raven’s Coloured Progessive Matrices, which is administered to children. The data described below for all testing are presented as percentiles based on age-corrected, published norms.
Consistent with our findings in aphasic individuals, Chelsea showed a large discrepancy in performance between the Picture Completion and Picture Arrangement subtests of the WAIS-R. This discrepancy is even more striking in Chelsea than in the aphasic individuals: her performance on the Picture Completion task ranged from the average to high average range across five different administrations, while her performance on the Picture Arrangement task was consistently in the impaired range (based on age-adjusted WAIS-R norms; see Figure 4 ). Importantly, she was able to solve the first item on the Picture Arrangement task, indicating that she understood the task instructions. Furthermore, her poor performance on the Picture Arrangement task was not explained by exceeding time limits on the task, as she rearranged the cards (incorrectly) with time to spare. In contrast to Chelsea’s performance, her parents’ and two sisters’ scores were all in the average to high average range on both of these tasks.
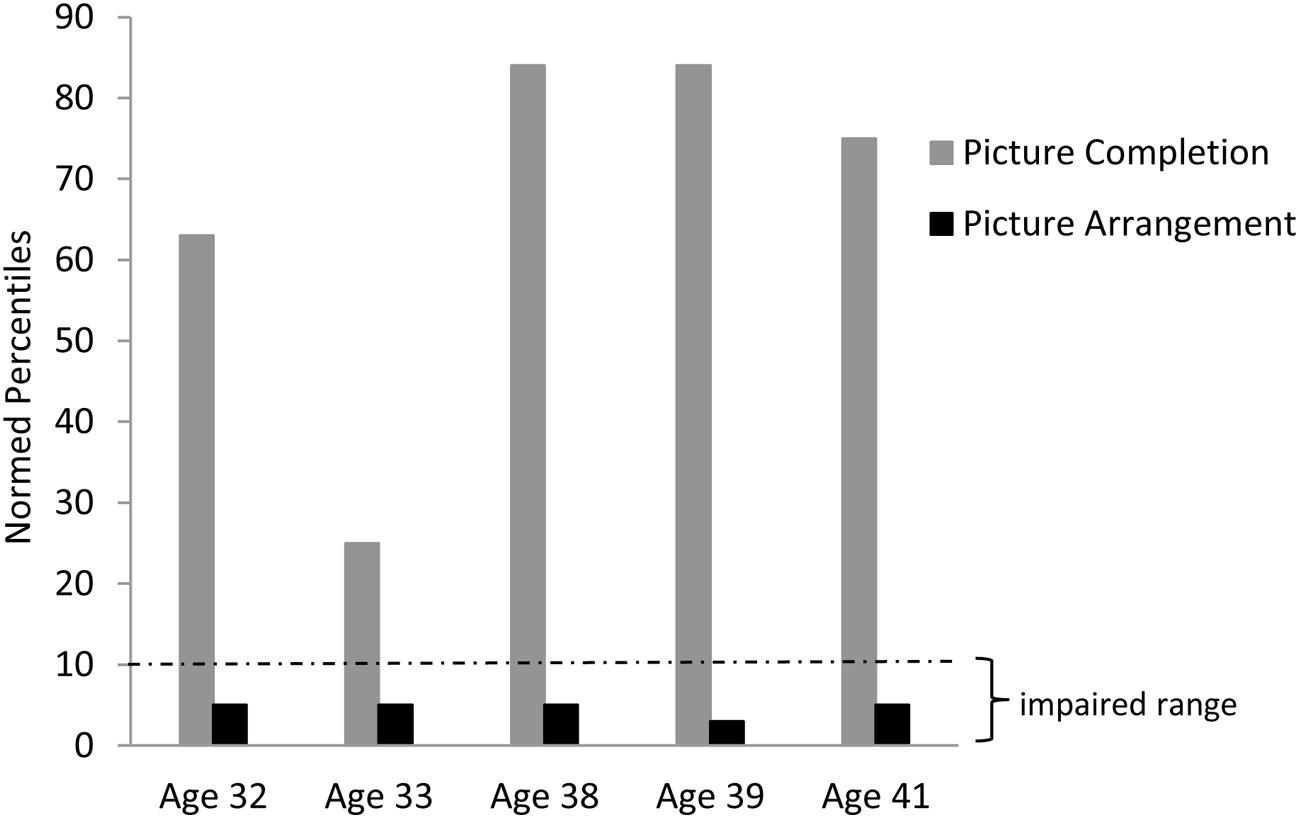
FIGURE 4. Chelsea’s discrepant performance on the WAIS-R Picture Completion vs. Picture Arrangement tasks across several different testing sessions.
Chelsea performed in the average to high average range on two other non-verbal WAIS-R subtests that are less dependent on reasoning, Block Design and Object Assembly. Like the Picture Arrangement and Completion tasks, these subtests also require visual perceptual processing and attention as well as a manual response. On the other non-verbal subtest of the WAIS-R, the Digit-Symbol test, Chelsea initially performed in the impaired range as it requires speeded writing with a pencil, to which she was not accustomed, but by the last administration, she performed in the average range. This striking contrast in Chelsea’s performance across WAIS-R subtests lends further support to the idea that language competence is related to reasoning performance; if Chelsea’s poor performance were due to her lack of formal education or some other general cognitive impairment, one would expect to see consistently impaired performance across all WAIS subtests.
Chelsea was also tested on the Raven’s Coloured Progressive Matrices at four different time-points. Similar to findings in the aphasic individuals described above, Chelsea performed in the impaired range on this test. Figure 5 shows her performance in relation to that of her two sisters and parents who all performed in the normal range based on normative percentiles. Importantly, just as with our findings in aphasic individuals described above, Chelsea showed a dissociation across different types of Raven’s items, correctly solving 100% of items requiring visual-pattern completion but only 20% of those requiring relational reasoning.
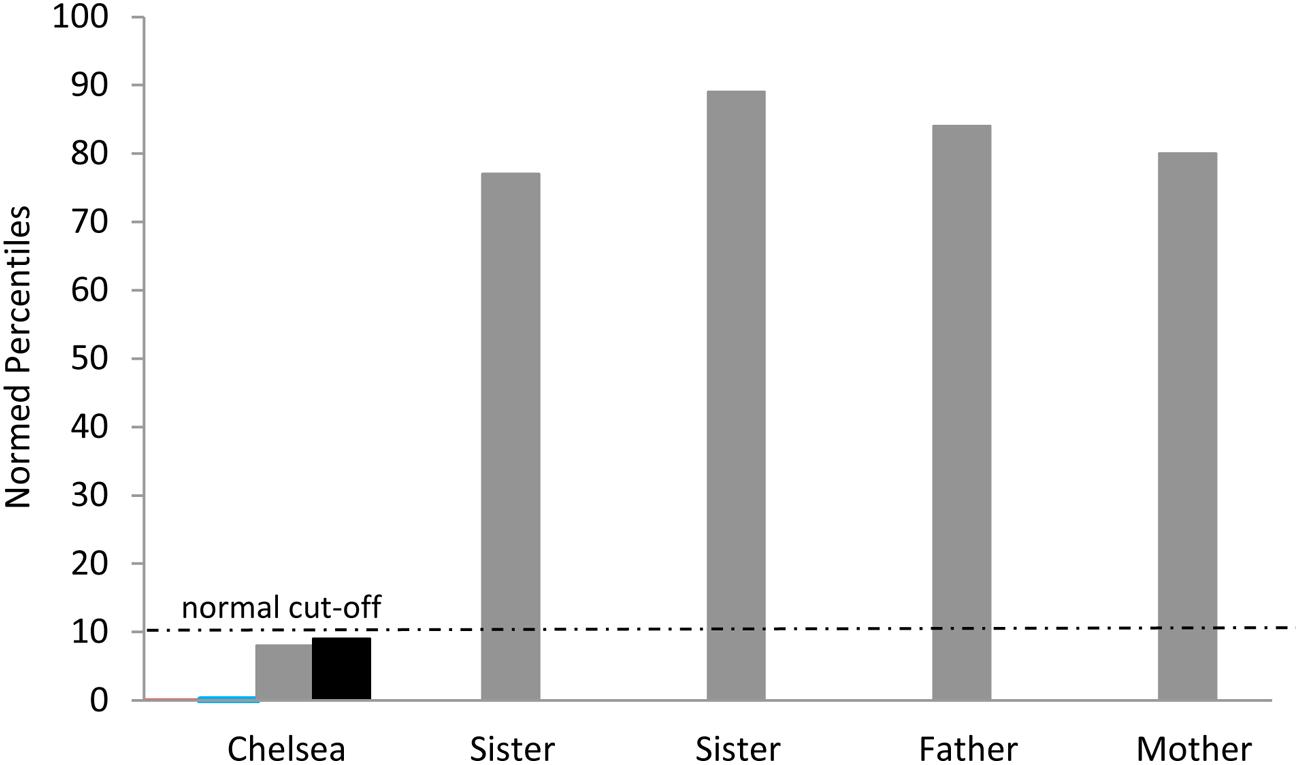
FIGURE 5. Chelsea’s performance on Raven’s Coloured Progressive Matrices at four different time points (normed percentiles ranged from <0.01 -9th percentile) and her family’s performance on a single administration of Raven’s Standard Matrices. Note that Chelsea’s scores on the first two administrations are difficult to see since they approach the x-axis at 0. The normal cut-off at the 10th percentile is shown.
In summary, Chelsea, a congenitally deaf individual with poor language skills, showed disproportionately impaired performance on standardized neuropsychological tasks that involved reasoning. Based on her pattern of performance as well as a comparison with other family members who also had limited educational backgrounds, we conclude that her impaired reasoning skills may be in part due to her restricted language abilities.
In this paper, we have argued that there is a close relationship between language competence and the ability to reason and problem-solve. We have come to this conclusion based on our own work and the work of others showing that individuals with impaired language, particularly those with core language deficits (i.e., impaired comprehension and disordered language output), exhibit diminished performance on tests of reasoning and problem-solving ( Piercy, 1964 ; De Renzi et al., 1966 ; Borod et al., 1982 ; Larrabee, 1986 ; Hjelmquist, 1989 ; Hamsher, 1991 ; Baldo et al., 2005 , 2010 ). Specifically, we described data from a series of studies in which we compared the performance of aphasic (i.e., language-impaired) and non-aphasic stroke patients on a variety of reasoning and problem-solving tasks, such as the WCST and non-verbal subtests of the WAIS. In these analyses, the aphasic group as a whole was disproportionately impaired on reasoning tasks relative to the non-aphasic group, but the two groups showed comparable performance on other cognitively demanding tasks that did not involve reasoning. In the second part of the paper, we described complementary findings from a case of a healthy individual with delayed exposure to language due to an unaddressed congenital deafness. She, too, exhibited marked impairment on tasks of reasoning that stood in stark contrast to her ability to perform in the average to high average range on numerous cognitive tasks that did not involve reasoning. Taken together, these data are highly suggestive of an important role for language in reasoning and problem-solving.
Our findings in language-impaired individuals are consistent with previous studies in non-human animals and children that also suggest an association between language and reasoning. With respect to animal research, studies have shown that language-training in non-human primates facilitates problem-solving performance ( Premack, 1983 , 2007 ). Thompson et al. (1997) further showed that this facilitation is likely due to the learned ability of these animals to associate a token with an abstract relation, much like language provides us with words that can singly represent other propositional knowledge. In studies with children, it has been shown that the level of language competence and the use of private speech are directly related to problem-solving performance ( Berk and Garvin, 1984 ; Berk, 1986 ; Winsler et al., 1997 ; Hermer-Vazquez et al., 1999 ; Fernyhough and Fradley, 2005 ; Carpendale et al., 2009 ). Vygotsky (1978 , 2012 ) championed this idea that language plays a role in children’s development of reasoning skills: initially overt speech and dialoguing with elders is used to work through problems and is later internalized and becomes covert or inner speech. Before him, Piaget (1967) believed that language, while not critical for most stages of development, did play a role in formal operations when abstract reasoning emerges. In support of this idea, performance on Piagetian tasks involving formal operations is impaired in language-delayed individuals, while performance on tasks involving concrete operations is relatively intact ( Furth, 1966 ; Furth and Youniss, 1971 ; Twilling, 1984 ). This dissociation between concrete and formal operations was also exhibited by Chelsea, the deaf individual with language impairment described above.
If we accept the idea that language facilitates problem-solving and reasoning in some way, this still leaves the question: what is the mechanism underlying this relationship? The answer to this question remains elusive and was not the focus of our investigations reported above, but a number of data points are instructive. First, prior work from our group and others have shown that articulatory suppression in healthy individuals (e.g., vocalizing nonsense syllables or irrelevant speech while doing a task) is disruptive to performance on reasoning/problem-solving tasks, suggesting that some form of verbal mediation (e.g., talking to oneself) facilitates reasoning and problem-solving ( Hermer-Vazquez et al., 1999 ; Baldo et al., 2005 ; Wallace et al., 2009 ; Lidstone et al., 2010 ; but see Learmonth et al., 2008 ; Bek et al., 2010 ; Forgeot d’Arc and Ramus, 2011 ). Importantly, control conditions with non-verbal distraction (e.g., tapping a rhythm) are much less disruptive, showing that the effect is specific to verbal disruption, not a general disruption of attention or some other process. Furthermore, as in children, it has been shown that when healthy adults think out loud on a reasoning task, performance can improve (see Fox and Charness, 2010 ). Such studies in healthy individuals provide a causal link between language and reasoning.
In keeping with this idea, Sokolov (1968/1972 ) described studies in which individuals doing mental arithmetic and repeating words had recordable muscle activity in the articulators (e.g., tongue, lips, etc.), suggesting that such inner speech is literally that—covert vocalization. More recent studies measuring muscular activity show incredible specificity: when participants silently read the letter “P,” muscular activity was detected in their lips and when they silently read the letter “T,” muscular activity was detected in their tongue ( McGuigan and Dollins, 1989 ; but see discussion below regarding dissociations of covert and overt speech). Sokolov concluded: “Inner speech emerges as a rather intricate phenomenon, where thought and language are bound in a single, indissoluble complex acting as the speech mechanism of thinking” (p. 1; also see Clark, 2006 ). Similarly, Carruthers (2002) echoes this notion: “Central cognition may also deploy the resources of the language system to generate representations of natural language sentences (in “inner speech”), which can similarly be of use in a variety of conceptual reasoning tasks” (p. 658).
A more systematically studied concept that can be invoked to explain the role of verbal mediation or inner speech is verbal working memory ( Baddeley and Logie, 1999 ; Baddeley, 2000 ; Al-Namlah et al., 2006 ; Marvel and Desmond, 2012 ; Perrone-Bertolotti et al., 2014 ). It may be that this mechanism underlies successful problem-solving performance, as it provides a real-time rehearsal and updating of relevant information that can provide cognitive flexibility on reasoning and problem-solving tasks ( Jonides, 2000 ; Emerson and Miyake, 2003 ; Carpendale et al., 2009 ). Verbal working memory may also facilitate problem-solving/reasoning by focusing attention and supporting self-cueing and self-monitoring ( Clark, 2005 ; Unsworth and Engle, 2007 ; Forgeot d’Arc and Ramus, 2011 ). Verbal working memory, as measured by tasks such as repetition, is impaired in many aphasic individuals ( Brown, 1975 ; Goodglass, 1992 ; Kohler et al., 1998 ; Baldo et al., 2012 ), and we have shown that patients’ repetition scores correlate with the percent of perseverative errors on the WCST and performance on Raven’s Matrices ( Baldo et al., 2005 , 2010 ).
In our current findings described above, repetition impairment, along with comprehension impairment, was related to poor performance on the Picture Arrangement (reasoning) task, although comprehension alone was most strongly related to performance on the WCST. Moreover, we also found that individuals with transcortical sensory aphasia (who have impaired comprehension but relatively preserved repetition) were greatly impaired in their reasoning performance, suggesting that core language (rather than simple repetition) is most strongly related to reasoning performance. By “core language,” we refer to the ability to both formulate and comprehend meaningful language. That is, while posterior patients with Wernicke’s/transcortical sensory aphasia (and global aphasics as well) are defined in part based on their poor comprehension, they also have a corresponding inability to produce meaningful language. Presumably, this limited ability to produce meaningful, overt language is paralleled by a limited ability to produce meaningful inner speech, a supposition which has only just recently begun to be tested more systematically (see Fama et al., 2014 ; Hayward et al., 2014 , discussed below). Our speculation is that disordered inner speech is central to the reasoning performance decrements we observe in many language-impaired individuals. Such suppositions need to be explored in future studies to assess the extent to which inner speech is disordered in different aphasic subgroups and demonstrate how this relates to impaired reasoning ( Kinsbourne, 2000 ).
Interesting insights on the role of inner speech in reasoning come from Jill Bolte Taylor, the neuroanatomist who suffered a left hemisphere stroke and later recounted her subjective experiences ( Taylor, 2008 ; Morin, 2009 ). Taylor describes a striking loss of inner speech that accompanied her aphasia and negatively impacted her ability to reason and think through problems:
The most notable difference between my pre- and post-stroke cognitive experience was the dramatic silence that had taken residency inside my head. I just didn’t think in the same way. Communication with the external world was out. Language with linear processing was out. But thinking in pictures was in (pp. 75–76).
A similar parallel between overt and covert language loss in aphasia has also been described in other case studies of severe aphasia ( Lecours and Joanette, 1980 ; Kertesz, 1988 ).
In contrast, individuals whose aphasia is more related to production deficits (e.g., Broca’s aphasia, anomic aphasia) appear to retain some capacity to generate inner speech, which might explain their residual reasoning ability. Although difficult to study, evidence for this capacity comes from two recent studies that assessed inner speech and the tip-of-the-tongue phenomenon in a group of aphasic individuals who had primarily output production deficits ( Fama et al., 2014 ; Hayward et al., 2014 ). In Fama et al. (2014) , 82% of the aphasic individuals reported hearing the words they wanted in their head but being unable to articulate them. Both Fama et al. (2014) and Hayward et al. (2014) reported anatomical and functional dissociations that mirrored the patients’ self-reports, such as fMRI activity in brain regions associated with phonological access (in left superior temporal cortex) when patients had this subjective experience. Single cases with such a dissociation between inner speech and overt language capacity have also been reported ( Lecours and Joanette, 1980 ; Hanley and McDonnell, 1997 ).
Findings from the current study stand in seeming contrast to a handful of smaller case studies that have concluded that language is not critical for reasoning. For example, Varley and Siegal (2000) reported a case study of an individual with agrammatic aphasia who was trained to understand and then pass a theory of mind (perspective-taking) test. Another study by this group ( Bek et al., 2010 ) tested five individuals with aphasia on a spatial-landmark conjunction task used previously to show the reliance of such tasks on language ( Hermer-Vazquez et al., 1999 ). They found that language was not critical for performance, but they also concluded that such tasks are likely “assisted by” language (p. 656), consistent with our position. Last, Apperly et al. (2006) showed that a severely aphasic individual was able to pass first- and second-order false belief (theory of mind) tasks, again concluding that grammar is not a requisite for such performance.
One likely explanation for differing conclusions about the role of language in reasoning between our work and others’ is a difference in the types of patients investigated. What we refer to as “severe aphasia” is a syndrome in which patients have core language deficits: they cannot generate meaningful language, they are far below chance on simple word-picture matching tasks, and they have difficulty understanding simple sentences. In the case studies described above, the use of the term “severe aphasia” refers to primarily agrammatic patients who are well above chance on basic language tasks such as single word-picture matching vs. our severely aphasic patients who score in the very impaired range on such tasks. Our studies also include individuals with severe agrammatism, and these individuals do relatively well on our reasoning tasks. We believe they do well because their core language is less impaired and they may thus possess relatively preserved inner speech (see discussion of overt vs. covert speech above). In our opinion, the individuals who provide the best test of the role of language in reasoning are patients with severe, core language impairments who have an inability to generate meaningful language (e.g., individuals with chronic Wernicke’s aphasia) and who likely have disordered inner speech. These types of patients are more rare (relative to agrammatic patients), and it has taken many years to be able to analyze data from a group of such individuals.
Another explanation for the different conclusions reached by previous case studies of language and reasoning is the types of tasks employed. Most of these previous case studies focused on theory of mind/perspective-taking tasks, whereas we have focused on standardized neuropsychological tasks of reasoning and problem-solving like the WCST. Interestingly, in Apperly et al. (2006) , the individual with severe aphasia who was able to perform false belief tasks was greatly impaired on executive functioning tests that included the WCST. Similarly, Varley (1998) reported impaired performance on the WAIS Picture Arrangement (reasoning) task in a fluent aphasic patient who was able to pass theory of mind tasks. These dissociations suggest that the two types of tasks likely tap distinct functions. False-belief tasks, including theory of mind, do not require the same degree of planning, self-monitoring, and online processing as the standardized neuropsychological tasks used to test reasoning and problem-solving in our studies described above. It is perhaps for this reason that performance on these latter types of tasks is more strongly related to language ability.
At the same time, a number of other studies on theory of mind in children and in delayed language learners have shown that performance is related to language competence ( de Villiers and Pyers, 2002 ; Hale and Tager-Flusberg, 2003 ; Schick et al., 2007 ; Pyers and Senghas, 2009 ; see de Villiers, 2007 ; Carpendale et al., 2009 for reviews). In an interesting experimental paper, theory of mind performance was shown to be disrupted in adults under conditions of articulatory suppression (verbal shadowing) but not tapping ( Newton and de Villiers, 2007 ). However, there is debate as to the precise nature of the role that language competence plays in theory of mind tasks ( de Villiers, 2007 ). Although we have not collected data on theory of mind tasks with our aphasic patients, our case study described above, Chelsea, was tested on a spatial perspective-taking task that involved minimal verbal instructions and required a simple pointing response. She was able to understand the task and comply with instructions when asked to point to the picture that matched the visual scene in front of her. However, she failed when asked to point to the picture that matched the scene in front of the examiner (who sat to her side). Given her excellent spatial skills on tasks such as the WAIS Block Design and Object Assembly subtests, this poor performance was more likely due to her inability to take another’s perspective but could also have been due to her impaired language-understanding. A similar problem arises when attempting to test aphasic individuals on theory of mind tasks: the instructions themselves necessitate a minimal level of language competence, even when the task is visually presented. To the extent that a patient can understand the instructions on a theory of mind task, even a visually presented one, likely indicates that their language is not completely impaired. Indeed, it would be impossible for us to successfully convey instructions for theory of mind tasks to the severely aphasic individuals that were most impaired on our reasoning tasks described above.
To ensure that we did not overlook any “exceptional” cases in our large datasets, we inspected our data for single individuals demonstrating a dissociation between core language and reasoning, that is, individuals with a severe impairment in comprehension/lexical-semantics such as those with Wernicke’s aphasia who nonetheless showed preserved reasoning. On the WCST problem-solving task, 70% of patients were able to sort between 2 and 6 categories (out of a possible 6) and not a single patient with severe language impairment was among this group. All of the individuals with Wernicke’s or transcortical sensory aphasia (i.e., patients with severe core language impairments) sorted 0–1 categories. On the WAIS Picture Arrangement task, 9 of the top 10 performers were non-aphasic (within normal limits on the WAB language battery), with the 10th patient being an individual with mild anomic aphasia. There was one individual with Wernicke’s aphasia who scored 70% correct on the task (moderately impaired), and the other three individuals with Wernicke’s aphasia were in the bottom 10 performers. In contrast, many of the Broca’s/agrammatic individuals in our study were able to perform well on both the WCST and Picture Arrangement tasks (exceptions were those Broca’s/agrammatic individuals with more severe comprehension deficits), similar to the previous case studies of agrammatic aphasia. Thus, we would concur with previous studies suggesting an independence of grammar and reasoning (e.g., Varley and Siegal, 2000 ), but suggest that core language processes such as those most typically affected in Wernicke’s aphasia play an important role in reasoning. As suggested above, further work is needed to further explore these dissociations among different aphasic subgroups.
It should be noted that we are not claiming here that intelligence, or thought more generally, is necessarily dependent on language (also see Carruthers, 2012 ). Rather, we restrict our claims to higher-level reasoning/problem-solving, that is, the kind of thought normally facilitated by verbal mediation or inner speech ( Sokolov, 1968/1972 ; Carruthers, 2002 ; Evans, 2008 ). This distinction has been made by Evans (2008) who contrasts a heuristic, quick and dirty system that “rapidly contextualize[s] problems with prior knowledge and belief” vs. a slow and serial system that is engaged during “conscious effortful analytic reasoning” (p. 261). He argues that the former is a non-verbal system that we share with other animals, while the latter system is dependent on language and is unique to humans.
Nor are we making the claim that language is absolutely indispensable to reasoning—we have rather argued throughout this paper that language can “facilitate” and is “supportive” of higher-level reasoning capacity. Even Ratliff and Newcombe (2008) who were skeptical of the original Hermer-Vazquez et al. (1999) shadowing study on reasoning and language reported that the original findings hold up to a certain degree. They concluded that, although language may not be “crucial” to reasoning, it is “helpful.” Similarly, Forgeot d’Arc and Ramus (2011) showed that verbal shadowing impaired performance overall on a non-verbal task involving belief attribution but that performance was still above chance. Although they felt their data supported the idea that belief attribution is independent from language, they also concluded that language acts as “an additional tool to keep relevant information in short-term memory” (p. 984). Similarly, Varley (2014) concluded that “language resources may often be deployed to scaffold performance on a range of problems” by way of supporting short- and long-term memory (p. 242). Again, this is consistent with the idea that language can serve a facilitatory role in online processes that support reasoning performance.
Finally, we are not suggesting that the use of inner speech and language to support reasoning is somehow predetermined; it is apparently a learned phenomenon ( Vygotsky, 2012 ) that can vary across individuals. Interesting cross-cultural research has also shown that the use of inner speech, while facilitatory for non-verbal reasoning in European–Americans (healthy individuals), can be disruptive for non-verbal reasoning in East Asian–American participants on particular tasks ( Kim, 2002 ). This finding makes the intriguing prediction that reasoning performance in East Asian patients with aphasia would not show a similar pattern of disruption as in our current study which included predominantly European–American patients. We are currently investigating this prediction with a cross-linguistic study of aphasia in collaboration with colleagues in Taiwan. It is likely that the degree to which language is invoked to support reasoning within and across cultures depends on the type of task involved (e.g., supportive strategies for particular tasks in one culture may be more visual-spatial while in another, more verbal). More experimental work in this intriguing area of investigation is clearly needed.
Brain imaging studies have also provided novel insights into the relationship between language/inner speech and cognition (for a review, see Girbau, 2007 ; Morin and Hamper, 2012 ). Consistent with our findings, Pillay et al. (2014) found that posterior brain regions overlapping with Wernicke’s area, including the left posterior superior temporal gyrus and inferior parietal cortex, were most closely related to pre-articulatory phonological access (what they and others have used as a stand-in for inner speech). However, some recent functional imaging studies in healthy individuals have suggested that language areas can dissociate from higher-level cognitive processes ( Monti et al., 2007 ; Willems et al., 2010 ; Fedorenko et al., 2011 ). In our work, we have shown that lesions involving language areas in the left hemisphere (most consistently, left posterior temporal cortex) are associated with decreased performance on reasoning and problem-solving tasks ( Baldo et al., 2005 , 2010 ). In Baldo et al. (2010) , we found a dissociation between brain regions associated with performance on the visual-pattern completion items on Raven’s Matrices vs. performance on the relational reasoning items: the former was associated with visual association regions in left inferior temporo-occipital cortex and the latter, with left posterior middle and superior temporal cortex (a critical language zone). Still, caution is warranted in drawing strong conclusions from lesion data as there is also the possibility that distinct but overlapping networks underlie language and reasoning processes in the brain ( Kertesz, 1988 ; Baldo et al., 2010 ).
In short, a range of philosophical inquiries and experimental evidence supports the idea that language and reasoning are highly inter-dependent. Further experimental investigations of this relationship are needed in order to establish more evidence for a causal role of language in reasoning ( Varley, 2014 ), especially with respect to the putative role that inner speech plays as a mediating mechanism. We conclude here with an elegant description by O’Brien and Opie (2002) of the relationship between language and cognition:
Natural language thereby becomes a powerful cognitive tool… one that can regulate the sequencing of thought, via the constant interplay between networks that encode linguistic signals and those that encode thoughts… Such causal loops catch up language and thought in a tight web of mutual influence that extends our cognitive capacities well beyond those of infra-verbal organisms (p. 327).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This material is based on work supported in part by the U.S. Department of Veterans Affairs, Office of Research & Development Rehabilitation R&D and CSR&D Programs, NIH/NINDS 5 P01 NS040813, NIH/NIDCD 5 R01 DC00216, and a subsidy granted to the National Research University Higher School of Economics, by the Government of the Russian Federation for the implementation of the Global Competitiveness Program. The contents reported within do not represent the views of the Department of Veterans Affairs or the United States Government. All of the research described herein was carried out in a manner consistent with the Helsinki Declaration. Written consent was obtained from all study participants, and the study was approved by the local Institutional Review Board. We would like to thank Christine Chiarello, Catherine O’Connor, Susan Curtiss, and Peter Glusker for their work in evaluating the case of Chelsea. We would like to thank Lisa LeJeune for her assistance with data compilation. We would also like to thank our lab colleagues as well as two reviewers for their feedback on earlier versions of this paper. Finally, we would like to thank all of the research volunteers who took part in our studies.
Al-Namlah, A. S., Fernyhough, C., and Meins, E. (2006). Sociocultural influences on the development of verbal mediation: private speech and phonological recoding in Saudi Arabian and British samples. Dev. Psychol. 42, 117–131. doi: 10.1037/0012-1649.42.1.117
PubMed Abstract | CrossRef Full Text | Google Scholar
Apperly, I. A., Samson, D., Carroll, N., Hussain, S., and Humphreys, G. (2006). Intact first-and second-order false belief reasoning in a patient with severely impaired grammar. Soc. Neurosci. 1, 334–348. doi: 10.1080/17470910601038693
Archibald, Y. M., Wepman, J. M., and Jones, L. V. (1967). Nonverbal cognitive performance in aphasic and nonaphasic brain-damaged patients. Cortex 3, 275–294. doi: 10.1016/S0010-9452(67)80017-0
CrossRef Full Text | Google Scholar
Baddeley, A. (2000). The episodic buffer: a new component of working memory? Trends Cogn. Sci. 4, 417–423. doi: 10.1016/S1364-6613(00)01538-2
Baddeley, A. D., and Logie, R. H. (1999). “Working memory: the multiple component model,” in Models of Working Memory: Mechanisms of Active Maintenance and Executive Control , eds A. Miyake and P. Shah (New York, NY: Cambridge University Press), 28–61.
Google Scholar
Baldo, J. V., Bunge, S. A., Wilson, S. M., and Dronkers, N. F. (2010). Is relational reasoning dependent on language? A voxel-based lesion symptom mapping study. Brain Lang. 113, 59–64. doi: 10.1016/j.bandl.2010.01.004
Baldo, J. V., Dronkers, N. F., Wilkins, D., Ludy, C., Raskin, P., and Kim, K. (2005). Is problem solving dependent on language? Brain Lang. 92, 240–250. doi: 10.1016/j.bandl.2004.06.103
Baldo, J. V., Katseff, S., and Dronkers, N. F. (2012). Brain regions underlying repetition and auditory-verbal short-term memory deficits in aphasia: evidence from voxel-based lesion symptom mapping. Aphasiology 26, 338–354. doi: 10.1080/02687038.2011.602391
Basso, A., Capitani, E., Luzzatti, C., and Spinnler, H. (1981). Intelligence and left hemisphere disease: the role of aphasia, apraxia, and size of lesion. Brain 104, 721–734. doi: 10.1093/brain/104.4.721
Basso, A., De Renzi, E., Faglioni, P., Scotti, G., and Spinnler, H. (1973). Neuropsychological evidence for the existence of cerebral areas critical to the performance of intelligence tasks. Brain 96, 715–728. doi: 10.1093/brain/96.4.715
Behrend, D. A., Rosengren, K., and Perlmutter, M. (1989). A new look at children’s private speech: the effects of age, task difficulty, and parent presence. Int. J. Behav. Dev. 12, 305–320. doi: 10.1177/016502548901200302
Bek, J., Blades, M., Siegal, M., and Varley, R. (2010). Language and spatial reorientation: evidence from severe aphasia. J. Exp. Psychol. Learn. Mem. Cogn. 36, 646–658. doi: 10.1037/a0018281
Benton, A. L., Sivan, A. B., Hamsher, K., Varney, N. R., and Spreen, O. (1983). Contribution to Neuropsychological Assessment. New York, NY: Oxford University Press.
Berk, L. E. (1986). Relationship of elementary school children’s private speech to behavioral accompaniment to task, attention, and task performance. Dev. Psychol. 22, 671–680. doi: 10.1037/0012-1649.22.5.671
Berk, L. E., and Garvin, R. A. (1984). Development of private speech among low-income Appalachian children. Dev. Psychol. 20, 271–286. doi: 10.1037/0012-1649.20.2.271
Bermudez, J. L. (2003). Thinking without Words. Oxford: Oxford University Press.
Blaisdell, A. P., Sawa, K., Leising, K. J., and Waldmann, M. R. (2006). Causal reasoning in rats. Science 311, 1020–1022. doi: 10.1126/science.1121872
Borod, J. C., Carper, M., and Goodglass, H. (1982). WAIS Performance IQ in aphasia as a function of auditory comprehension and constructional apraxia. Cortex 18, 199–210. doi: 10.1016/S0010-9452(82)80003-8
Braden, J. P. (1992). Intellectual assessment of deaf or hard-of-hearing people: a quantitative and qualitative research synthesis. School Psych. Rev. 21, 82–94.
Brown, J. W. (1975). The problem of repetition: a study of “conduction” aphasia and the “isolation” syndrome. Cortex 11, 37–52. doi: 10.1016/S0010-9452(75)80019-0
Bunge, S. A., Wendelken, C., Badre, D., and Wagner, A. D. (2005). Analogical reasoning and prefrontal cortex: evidence for separable retrieval and integration mechanisms. Cereb. Cortex 15, 239–249. doi: 10.1093/cercor/bhh126
Caramazza, A., and McCloskey, M. (1988). The case for single-patient studies. Cogn. Neuropsychol. 5, 517–527. doi: 10.1080/02643298808253271
Carpendale, J., Lewis, C., Susswein, N., and Lunn, J. (2009). “Talking and thinking: the role of speech in social understanding,” in Private Speech, Executive Function, and the Development of Verbal Self-Regulation , eds J. I. M. Carpendale, C. Lewis, N. Susswein, and J. Lunn (Cambridge: Cambridge University Press), 83–94.
Carruthers, P. (2002). The cognitive functions of language. Behav. Brain Sci. 25, 657–674. doi: 10.1017/S0140525X02000122
Carruthers, P. (2012). “Language in cognition,” in The Oxford Handbook of Philosophy of Cognitive Science , eds E. Margolis, R. I. Samuels, and S. P. Stich (Oxford: Oxford University Press).
Clark, A. (2005). Word, niche and super-niche: how language makes minds matter more. Theoria 20, 255–268.
Clark, A. (2006). Language, embodiment, and the cognitive niche. Trends Cogn. Sci. 10, 370–374. doi: 10.1016/j.tics.2006.06.012
Coltheart, M. (2004). PALPA: what next? Aphasiology 18, 181–183. doi: 10.1080/02687030344000526
Crone, E. A., Wendelken, C., Van Leijenhorst, L., Honomichl, R. D., Christoff, K., and Bunge, S. A. (2009). Neurocognitive development of relational reasoning. Dev. Sci. 12, 55–66.
Curtiss, S. (2014). The effects of late age at exposure to language on language performance and evidence for the modularity of language and mind. UCLA Work. Papers Linguist. 18, 115–146.
De Renzi, E., Faglioni, P., Savoiardo, M., and Vignolo, L. A. (1966). The influence of aphasia and of the hemispheric side of the cerebral lesion on abstract thinking. Cortex 2, 399–420. doi: 10.1016/S0010-9452(66)80017-5
de Villiers, J. (2007). The interface of language and theory of mind. Lingua 117, 1858–1878. doi: 10.1016/j.lingua.2006.11.006
de Villiers, J. G., and Pyers, J. E. (2002). Complements to cognition: a longitudinal study of the relationship between complex syntax and false-belief-understanding. Cogn. Dev. 17, 1037–1060. doi: 10.1016/S0885-2014(02)00073-4
Dronkers, N. (1987). Chelsea’s cognitive and neuropsychological status. Paper Presented at the Orton Dyslexia Society Annual Meeting , San Francisco, CA.
Dronkers, N. F., Ludy, C. A., and Redfern, B. B. (1998). Pragmatics in the absence of verbal language: descriptions of a severe aphasic and a language-deprived adult. J. Neurolinguist. 11, 179–190. doi: 10.1016/S0911-6044(98)00012-8
Edwards, S., Ellams, J., and Thompson, J. (1976). Language and intelligence in dysphasia: are they related? Int. J. Lang. Commun. Disord. 11, 83–94. doi: 10.3109/13682827609011295
Emerson, M. J., and Miyake, A. (2003). The role of inner speech in task switching: a dual-task investigation. J. Mem. Lang. 48, 148–168. doi: 10.1016/S0749-596X(02)00511-9
Evans, J. S. B. (2008). Dual-processing accounts of reasoning, judgment, and social cognition. Annu. Rev. Psychol. 59, 255–278. doi: 10.1146/annurev.psych.59.103006.093629
Fama, M., Snider, S., Hayward, W., Friedman, R., and Turkeltaub, P. (2014). “I know it but I can’t say it: clarifying the subjective experience of inner speech in aphasia,” in Proceedings of the Frontiers in Psychology Conference Abstract: Academy of Aphasia – 52nd Annual Meeting , Miami, FL.
Fedorenko, E., Behr, M. K., and Kanwisher, N. (2011). Functional specificity for high-level linguistic processing in the human brain. Proc. Natl. Acad. Sci. U.S.A. 108, 16428–16433. doi: 10.1073/pnas.1112937108
Fernyhough, C., and Fradley, E. (2005). Private speech on an executive task: relations with task difficulty and task performance. Cogn. Dev. 20, 103–120. doi: 10.1016/j.cogdev.2004.11.002
Forgeot d’Arc, B., and Ramus, F. (2011). Belief attribution despite verbal interference. Q. J. Exp. Psychol. 64, 975–990. doi: 10.1080/17470218.2010.524413
Fox, M. C., and Charness, N. (2010). How to gain eleven IQ points in ten minutes: thinking aloud improves Raven’s Matrices performance in older adults. Aging Neuropsychol. Cogn. 17, 191–204. doi: 10.1080/13825580903042668
Furth, H. G. (1966). Thinking without Language: Psychological Implications of Deafness. New York, NY: Free Press.
Furth, H. G., and Youniss, J. (1971). Formal operations and language. A comparison of deaf and hearing adolescents. Int. J. Psychol. 6, 49–64. doi: 10.1080/00207597108247297
Gentner, D. (2003). “Why we’re so smart,” in Language in Mind , eds D. Gentner and S. Goldin-Meadow (Cambridge: MIT Press).
Gentner, D., and Loewenstein, J. (2002). “Relational language and relational thought,” in Language, Literacy, and Cognitive Development: The Development and Consequences of Symbolic Language , eds E. Amsel and J. R. Byrnes (Mahwah, NJ: Lawrence Erlbaum Associates), 87–120.
Girbau, D. (2007). A neurocognitive approach to the study of private speech. Span. J. Psychol. 10, 41–51. doi: 10.1017/S1138741600006302
Gläscher, J., Tranel, D., Paul, L. K., Rudrauf, D., Rorden, C., Hornaday, A., et al. (2009). Lesion mapping of cognitive abilities linked to intelligence. Neuron 61, 681–691. doi: 10.1016/j.neuron.2009.01.026
Glusker, P. (1987). Chelsea. Paper Presented at the Orton Dyslexia Society Annual Meeting , San Francisco, CA.
Glusker, P., Curtiss, S., Dronkers, N., Howard, F., Moilanen, N., Neville, H., et al. (1990). Primary language acquisition in a deaf adult: the Chelsea Project. Paper Presented at the 1990 Biennial Conference of the Orton Society , San Francisco, CA.
Goel, V., and Dolan, R. J. (2004). Differential involvement of left prefrontal cortexin inductive and deductive reasoning. Cognition 93, B109–B121. doi: 10.1016/j.cognition.2004.03.001
Goodglass, H. (1992). “Diagnosis of conduction aphasia,” in Conduction Aphasia , ed. S. E. Kohn (Hillsdale, NJ: Lawrence Earlbaum Associates).
Hale, C. M., and Tager-Flusberg, H. (2003). The influence of language on theory of mind: a training study. Dev. Sci. 6, 346–359. doi: 10.1111/1467-7687.00289
Halford, G. S., Wilson, W. H., and Phillips, S. (1998). Processing capacity defined by relational complexity: implications for comparative, developmental, and cognitive psychology. Behav. Brain Sci. 21, 803–831. doi: 10.1017/S0140525X98001769
Hamsher, K. (1991). “Intelligence and aphasia,” in Acquired Aphasia , 2nd Edn, ed. M. Sarno (San Diego, CA: Academic Press).
Hanley, J. R., and McDonnell, V. (1997). Are reading and spelling phonologically mediated? Evidence from a patient with a speech production impairment. Cogn. Neuropsychol. 14, 3–33.
Hayward, W., Fama, M. E., Sullivan, K. L., Snider, S. F., Lacey, E. H., Friedman, R. B., et al. (2014). “Inner speech in people with aphasia,” in Proceedings of the Frontiers in Psychology Conference Abstract: Academy of Aphasia – 52nd Annual Meeting , Miami, FL.
Heaton, R. K., Chelune, G. J., Talley, J. L., Kay, G. G., and Curtis, C. (1993). Wisconsin Card Sorting Test (WCST) Manual Revised and Expanded. Odessa, FL: Psychological Assessment Resources.
Helm-Estabrooks, N. (2002). Cognition and aphasia: a discussion and a study. J. Commun. Disord. 35, 171–186. doi: 10.1016/S0021-9924(02)00063-1
Hermer-Vazquez, L., Spelke, E. S., and Katsnelson, A. S. (1999). Sources of flexibility in human cognition: dual-task studies of space and language. Cogn. Psychol. 39, 3–36. doi: 10.1006/cogp.1998.0713
Hjelmquist, E. K. (1989). Concept formation in non-verbal categorization tasks in brain-damaged patients with and without aphasia. Scand. J. Psychol. 30, 243–254. doi: 10.1111/j.1467-9450.1989.tb01087.x
Hurlburt, R. T. (1990). Sampling Normal and Schizophrenic Inner Experience. Berlin: Springer Science & Business Media.
Hurlburt, R. T., and Heavey, C. L. (2001). Telling what we know: describing inner experience. Trends Cogn. Sci. 5, 400–403. doi: 10.1016/S1364-6613(00)01724-1
Jonides, J. (2000). “Mechanisms of verbal working memory revealed by neuroimaging studies,” in Perception, Cognition, and Language: Essays in Honor of Henry and Lila Gleitman , eds H. Gleitman, L. R. Gleitman, and B. Landau (Cambridge, MA: MIT Press).
Jowett, A. (1892). The Dialogues of Plato. New York, NY: Macmillan and Co.
Kertesz, A. (1982). Western Aphasia Battery. New York, NY: Grune & Stratton.
Kertesz, A. (1988). “Cognitive function in severe aphasia,” in Thought Without Language , ed. L. Weiskrantz (Oxford: Clarendon Press).
Kertesz, A. (2006). Western Aphasia Battery-Revised. San Antonio, TX: Harcourt Assessment.
Kertesz, A., and McCabe, P. (1975). Intelligence and aphasia: performance of aphasics on Raven’s coloured progressive matrices (RCPM). Brain Lang. 2, 387–395. doi: 10.1016/S0093-934X(75)80079-4
Kim, H. S. (2002). We talk, therefore we think? A cultural analysis of the effect of talking on thinking. J. Pers. Soc. Psychol. 83, 828–842.
Kinsbourne, M. (2000). Inner speech and the inner life. Brain Lang. 71, 120–123. doi: 10.1006/brln.1999.2229
Kinsbourne, M., and Warrington, E. K. (1963). Jargon aphasia. Neuropsychologia 1, 27–37. doi: 10.1016/0028-3932(63)90010-1
Kohler, K., Bartels, C., Herrmann, M., Dittmann, J., and Wallesch, C.-W. (1998). Conduction aphasia—11 classic cases. Aphasiology 12, 865–884. doi: 10.1080/02687039808249456
Kuczaj, S. A., and Hendry, J. L. (2003). “Does language help animals think?,” in Language in Mind , eds D. Gentner and S. Goldin-Meadow (Cambridge, MA: MIT Press).
Larrabee, G. J. (1986). Another look at VIQ-PIQ scores and unilateral brain damage. Int. J. Neurosci. 29, 141–148. doi: 10.3109/00207458608985644
Learmonth, A. E., Newcombe, N. S., Sheridan, N., and Jones, M. (2008). Why size counts: children’s spatial reorientation in large and small enclosures. Dev. Sci. 11, 414–426. doi: 10.1111/j.1467-7687.2008.00686.x
Lecours, A., and Joanette, Y. (1980). Linguistic and other psychological aspects of paroxysmal aphasia. Brain Lang. 10, 1–23. doi: 10.1016/0093-934X(80)90034-6
Lidstone, J. S., Meins, E., and Fernyhough, C. (2010). The roles of private speech and inner speech in planning during middle childhood: evidence from a dual task paradigm. J. Exp. Child Psychol. 107, 438–451. doi: 10.1016/j.jecp.2010.06.002
Lidstone, J. S., Meins, E., and Fernyhough, C. (2012). Verbal mediation of cognition in children with specific language impairment. Dev. Psychopathol. 24, 651–660. doi: 10.1017/S0954579412000223
Loewenstein, J., and Gentner, D. (2005). Relational language and the development of relational mapping. Cogn. Psychol. 50, 315–353. doi: 10.1016/j.cogpsych.2004.09.004
Machery, E. (2005). Concepts are not a natural kind ∗ . Philos. Sci. 72, 444–467. doi: 10.1086/498473
Marvel, C. L., and Desmond, J. E. (2012). From storage to manipulation: how the neural correlates of verbal working memory reflect varying demands on inner speech. Brain Lang. 120, 42–51. doi: 10.1016/j.bandl.2011.08.005
McGuigan, F. J., and Dollins, A. B. (1989). Patterns of covert speech behavior and phonetic coding. Pavlov. J. Biol. Sci. 24, 19–26.
PubMed Abstract | Google Scholar
Monti, M. M., Osherson, D. N., Martinez, M. J., and Parsons, L. M. (2007). Functional neuroanatomy of deductive inference: a language-independent distributed network. Neuroimage 37, 1005–1016. doi: 10.1016/j.neuroimage.2007.04.069
Morgan, G., and Kegl, J. (2006). Nicaraguan sign language and theory of mind: the issue of critical periods and abilities. J. Child Psychol. Psychiatry 47, 811–819. doi: 10.1111/j.1469-7610.2006.01621.x
Morin, A. (2009). Self-awareness deficits following loss of inner speech: Dr. Jill Bolte Taylor’s case study. Conscious. Cogn. 18, 524–529. doi: 10.1016/j.concog.2008.09.008
Morin, A., and Hamper, B. (2012). Self-reflection and the inner voice: activation of the left inferior frontal gyrus during perceptual and conceptual self-referential thinking. Open Neuroimag. J. 6, 78–89. doi: 10.2174/1874440001206010078
Newton, A. M., and de Villiers, J. G. (2007). Thinking while talking: adults fail nonverbal false-belief reasoning. Psychol. Sci. 18, 574–579. doi: 10.1111/j.1467-9280.2007.01942.x
O’Brien, G., and Opie, J. (2002). Radical connectionism: thinking with (not in) language. Lang. Commun. 22, 313–329. doi: 10.1016/S0271-5309(02)00010-1
Penn, D. C., Holyoak, K. J., and Povinelli, D. J. (2008). Darwin’s mistake: explaining the discontinuity between human and nonhuman minds. Behav. Brain Sci. 31, 109–130. doi: 10.1017/S0140525X08003543
Perrone-Bertolotti, M., Rapin, L., Lachaux, J. P., Baciu, M., and Loevenbruck, H. (2014). What is that little voice inside my head? Inner speech phenomenology, its role in cognitive performance, and its relation to self-monitoring. Behav. Brain Res. 261, 220–239. doi: 10.1016/j.bbr.2013.12.034
Piaget, J. (1926). The Language and Thought of the Child. New York, NY: Harcourt, Brace & Company.
Piaget, J. (1967). Six Psychological Studies , trans. D. Elkind and A. Tenzer. New York, NY: Random House, 53.
Piercy, M. (1964). The effects of cerebral lesions on intellectual function: a review of current research trends. Br. J. Psychiatry 110, 310–352. doi: 10.1192/bjp.110.466.310
Pillay, S. B., Stengel, B. C., Humphries, C., Book, D. S., and Binder, J. R. (2014). Cerebral localization of impaired phonological retrieval during rhyme judgment. Ann. Neurol. 76, 738–746. doi: 10.1002/ana.24266
Premack, D. (1983). Animal cognition. Annu. Rev. Psychol. 34, 351–362. doi: 10.1146/annurev.ps.34.020183.002031
Premack, D. (2007). Human and animal cognition: continuity and discontinuity. Proc. Natl. Acad. Sci. U.S.A. 104, 13861–13867. doi: 10.1073/pnas.0706147104
Pyers, J. E., and Senghas, A. (2009). Language promotes false-belief understanding evidence from learners of a new sign language. Psychol. Sci. 20, 805–812. doi: 10.1111/j.1467-9280.2009.02377.x
Ratliff, K. R., and Newcombe, N. S. (2008). Is language necessary for human spatial reorientation? Reconsidering evidence from dual task paradigms. Cogn. Psychol. 56, 142–163.
Ryan, J. J., and Paolo, A. M. (2001). Exploratory factor analysis of the WAIS-III in a mixed patient sample. Arch. Clin. Neuropsychol. 16, 151–156. doi: 10.1093/arclin/16.2.151
Schick, B., De Villiers, P., De Villiers, J., and Hoffmeister, R. (2007). Language and theory of mind: a study of deaf children. Child Dev. 78, 376–396. doi: 10.1111/j.1467-8624.2007.01004.x
Siegal, M., Varley, R., and Want, S. C. (2001). Mind over grammar: reasoning in aphasia and development. Trends Cogn. Sci. 5, 296–301. doi: 10.1016/S1364-6613(00)01667-3
Smirnova, A., Zorina, Z., Obozova, T., and Wasserman, E. (2015). Crows spontaneously exhibit analogical reasoning. Curr. Biol. 25, 256–260. doi: 10.1016/j.cub.2014.11.063
Sokolov, A. N. (1968/1972). Inner Speech and Thought , trans. G. T. Onischenko. New York, NY: Plenum.
Taylor, A. H., Hunt, G. R., Medina, F. S., and Gray, R. D. (2009). Do New Caledonian crows solve physical problems through causal reasoning? Proc. R. Soc. B Biol. Sci. 276, 247–254. doi: 10.1098/rspb.2008.1107
Taylor, J. B. (2008). My Stroke of Insight: A Brain Scientist’s Personal Journey. London: Penguin.
Thompson, R. K., Oden, D. L., and Boysen, S. T. (1997). Language-naive chimpanzees (Pan troglodytes) judge relations between relations in a conceptual matching-to-sample task. J. Exp. Psychol. Anim. Behav. Process. 23, 31–43.
Tulsky, D. S., Saklofske, D. H., Chelune, G., Heaton, R. K., Ivnik, R. J., Bornstein, R., et al. (2003). Clinical Interpretation of the WAIS-III and the WMS: Practical Resources for Mental Health Professional. San Diego, CA: Academic Press.
Twilling, L. S. (1984). Formal Operational Thinking in Deaf and Hearing Adolescents: And Its Relationship to Language Background, Math Skills and Reading Skills. Ph.D. thesis, University of California, Berkeley, CA.
Unsworth, N., and Engle, R. W. (2007). The nature of individual differences in working memory capacity: active maintenance in primary memory and controlled search from secondary memory. Psychol. Rev. 114, 104–132. doi: 10.1037/0033-295X.114.1.104
Varley, R. (1998). “Aphasic language, aphasic thought: an investigation of propositional thinking in an a-propositional aphasic,” in Language and Thought: Interdisciplinary Themes , eds P. Carruthers and J. Boucher (Cambridge: Cambridge University Press), 128–145.
Varley, R. (2014). Reason without much language. Lang. Sci. 46, 232–244. doi: 10.1016/j.langsci.2014.06.012
Varley, R., and Siegal, M. (2000). Evidence for cognition without grammar from causal reasoning and ‘theory of mind’ in an agrammatic aphasic patient. Curr. Biol. 10, 723–726. doi: 10.1016/S0960-9822(00)00538-8
Vilkki, J. (1988). Problem solving deficits after focal cerebral lesions. Cortex 24, 119–127. doi: 10.1016/S0010-9452(88)80020-0
Vygotsky, L. (1978). Interaction between learning and development. Read. Dev. Child. 23, 34–41.
Vygotsky, L. S. (2012). Thought and Language. Cambridge, MA: MIT Press.
Wallace, G. L., Silvers, J. A., Martin, A., and Kenworthy, L. E. (2009). Brief report: further evidence for inner speech deficits in autism spectrum disorders. J. Autism Dev. Disord. 39, 1735–1739. doi: 10.1007/s10803-009-0802-8
Watson, J. B. (1920). Is thinking merely action of language mechanism? Br. J. Psychol. Gen. 11, 87–104. doi: 10.1111/j.2044-8295.1920.tb00010.x
Watson, J. B. (1924). The place of kinaesthetic, visceral and laryngeal organization in thinking. Psychol. Rev. 31, 339–347.
Wechsler, D. (1981). Wechsler Adult Intelligence Scale-Revised. San Antonio, TX: The Psychological Corporation.
Wechsler, D. (1997). Wechsler Adult Intelligence Scale , 3rd Edn. San Antonio, TX: The Psychological Corporation.
Weinstein, S., and Teuber, H. L. (1957). Effects of penetrating brain injury on intelligence test scores. Science 125, 1036–1037. doi: 10.1126/science.125.3256.1036
Wheeler, M. (2004). Is language the ultimate artefact? Lang. Sci. 26, 693–715. doi: 10.1002/nbm.1585
Willems, R. M., De Boer, M., De Ruiter, J. P., Noordzij, M. L., Hagoort, P., and Toni, I. (2010). A dissociation between linguistic and communicative abilities in the human brain. Psychol. Sci. 21, 8–14. doi: 10.1177/0956797609355563
Winsler, A., Diaz, R. M., and Montero, I. (1997). The role of private speech in the transition from collaborative to independent task performance in young children. Early Child. Res. Q. 12, 59–79. doi: 10.1016/S0885-2006(97)90043-0
Winsler, A., Fernyhough, C., and Montero, I. (eds). (2009). Private Speech, Executive Functioning, and the Development of Verbal Self-Regulation. Cambridge: Cambridge University Press, 3–41.
Winsler, A., and Naglieri, J. (2003). Overt and covert verbal problem-solving strategies: developmental trends in use, awareness, and relations with task performance in children aged 5 to 17. Child Dev. 74, 659–678. doi: 10.1111/1467-8624.00561
Keywords : reasoning, problem-solving, aphasia, language delay, deafness, thought, language, inner speech
Citation: Baldo JV, Paulraj SR, Curran BC and Dronkers NF (2015) Impaired reasoning and problem-solving in individuals with language impairment due to aphasia or language delay. Front. Psychol. 6:1523. doi: 10.3389/fpsyg.2015.01523
Received: 08 May 2015; Accepted: 22 September 2015; Published: 26 October 2015.
Reviewed by:
Copyright © 2015 Baldo, Paulraj, Curran and Dronkers. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Juliana V. Baldo, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
American English
Cognitive Impairment, Adult
Cognitive Impairment (Adult Inpatient)
Clinical description.
- Care of the hospitalized patient experiencing impairment related to cognitive skills that include attention, memory, orientation, judgment, reasoning, problem-solving and executive functioning with reasonable potential for improvement.
Key Information
- Language and culture may affect results of standardized assessment tools. Choose tools appropriate for the patient to provide the most accurate cognitive assessment.
- Hospitalization and illness stress cognitive abilities and exacerbate dysfunctional behaviors.
- It is important to identify and address safety concerns related to cognitive dysfunction, such as medication adherence, decision-making capacity, safety with functional mobility tasks and wandering.
Clinical Goals
Optimal Cognitive Function
- Education: Overview
- Education: Self-Management
- Education: When to Seek Medical Attention
Correlate Health Status
Correlate health status to:
- history, comorbidity
- age, developmental level
- sex, gender identity
- baseline assessment data
- physiologic status
- response to medication and interventions
- psychosocial status, social determinants of health
- barriers to accessing care and services
- health literacy
- cultural and spiritual preferences
- safety risks
- family interaction
- plan for transition of care
Cognitive Impairment
Signs/symptoms/presentation.
- concentration poor
- difficulty learning or following instructions
- disorientation
- distractibility
- forgetfulness
- impulsive behavior
- irritability
- judgment impaired
- memory impaired
- problem-solving ability altered
- reasoning ability impaired
- word-finding difficulty
Problem Intervention
Optimize cognitive function.
- Assess cognitive function using a standardized tool to establish baseline and identify areas of deficit.
- Establish rapport and trust; utilize unhurried and calm approach.
- Utilize clear communication; address patient by name, speak slowly with simple directions and gestures; provide time for patient response, listen carefully and maintain eye contact.
- Provide environmental adaptations to support cognitive function and safety; consider sensory exposure, hearing ability and distractions.
- Establish familiarity using a structured routine congruent with home schedule, when possible, such as family presence, consistent caregiver, sleep and meal schedule, toileting schedule.
- Provide conducive environment for sleep, such as uninterrupted sleep times and light therapy.
- Optimize nutrition and fluid intake; encourage and offer fluid intake frequently and assist with meal set-up and feeding if needed.
- Encourage multimodal physical activity, exercise and complementary interventions, such as mind-body exercise; consider combined exercise and cognitive activity.
- Implement cognitive remediation or restorative techniques, such as training in direct attention, occupation, activity-based and functional communication strategies.
Associated Documentation
- Environment Familiarity/Consistency
- Self-Care Promotion
- Sensory Stimulation Regulation
CPG-Specific Education Topics
risk factors
signs/symptoms
Self-Management
assistive/adaptive devices
cognitive support measures
home safety
provider follow-up
rehabilitation therapy
When to Seek Medical Attention
unresolved/worsening symptoms
General Education Topics
General education.
admission, transition of care
orientation to care setting, routine
advance care planning
diagnostic tests/procedures
diet modification
opioid medication management
oral health
medication management
pain assessment process
safe medication disposal
tobacco use, smoke exposure
treatment plan
Safety Education
call light use
equipment/home supplies
fall prevention
harm prevention
infection prevention
MDRO (multidrug-resistant organism) care
personal health information
resources for support
- (2019). Lazaro, R. T.; Reina-Guerra, S. G.; Quiben, M (Eds.), Umphred's Neurological Rehabilitation . St. Louis: Elsevier. [Expert/Committee Opinion]
- Austrom, M. G.; Boustani, M.; LaMantia, M. A. Ongoing medical management to maximize health and well-being for persons living with dementia. The Gerontologist. 2018;58(S1), S48-S57. doi:10.1093/geront/gnx147 Source [Review Articles]
- Bahar-Fuchs, A.; Martyr, A.; Goh, A. M.; Sabates, J.; Clare, L.. Cognitive training for people with mild to moderate dementia. Cochrane Database of Systematic Reviews. 2019;3(3) doi:10.1002/14651858 [Systematic Review]
- Basak, C.; Qin, S.; O'Connell, M. A. Differential effects of cognitive training modules in healthy aging and mild cognitive impairment: A comprehensive meta-analysis of randomized controlled trials. Psychology and Aging. 2020;35(2), 220-249. doi:10.1037/pag0000442 Source [Meta-analysis]
- Brandt, Å.; Jensen, M. P.; Søberg, M. S.; Andersen, S. D.; Sund, T. Information and communication technology-based assistive technology to compensate for impaired cognition in everyday life: A systematic review. Disability and Rehabilitation: Assistive Technology. 2020;15(7), 810-824. doi:10.1080/17483107.2020.1765032 Source [Systematic Review]
- Brenes, G. A.; Sohl, S.; Wells, R. E.; Befus, D.; Campos, C. L.; Danhauer, S. C.. The effects of yoga on patients with mild cognitive impairment and dementia: A scoping review. American Journal of Geriatric Psychiatry. 2019;27(2), 188-197. doi:10.1016/j.jagp.2018.10.013 [Review Articles,Expert/Committee Opinion,Core Curriculum,Position Statements,Practice Bulletins]
- Bruderer-Hofstetter, M.; Rausch-Osthoff, A. K.; Meichtry, A.; Münzer, T.; Niedermann, K. Effective multicomponent interventions in comparison to active control and no interventions on physical capacity, cognitive function and instrumental activities of daily living in elderly people with and without mild impaired cognition–a systematic review and network meta-analysis. Ageing Research Reviews. 2018;45, 1-14. doi:10.1016/j.arr.2018.04.002 [Metasynthesis,Meta-analysis,Systematic Review]
- Cicerone, K. D.; Goldin, Y.; Ganci, K.; Rosenbaum, A.; Wethe, J. V.; Langenbahn, D. M.; Malec, J. F.; Bergquist, T. F.; Kingsley, K.; Nagele, D.; Trexler, L.; Fraas, M.; Bogdanova, Y.; Harley, J. P. Evidence-based cognitive rehabilitation: Systematic review of the literature from 2009 through 2014. Archives of Physical Medicine and Rehabilitation. 2019; doi:10.1016/j.apmr.2019.02.011 [Review Articles,Expert/Committee Opinion,Core Curriculum,Position Statements,Practice Bulletins]
- Dauwan, M.; Begemann, M. J.; Slot, M. I.; Lee, E. H.; Scheltens, P.; Sommer, I. E. Physical exercise improves quality of life, depressive symptoms, and cognition across chronic brain disorders: a transdiagnostic systematic review and meta-analysis of randomized controlled trials. Journal of Neurology. 2019;, 1-25. doi:10.1007/s00415-019-09493-9 [Metasynthesis,Meta-analysis,Systematic Review]
- Demurtas, J.; Schoene, D.; Torbahn, G.; Marengoni, A.; Grande, G.; Zou, L.; et al. Physical activity and exercise in mild cognitive impairment and dementia: An umbrella review of intervention and observational studies. Journal of the American Medical Directors Association. 2020;21(10), 1415-1422. doi:10.1016/j.jamda.2020.08.031 Source [Systematic Review]
- Dequanter, S.; Gagnon, M. P.; Ndiaye, M. A.; Gorus, E.; Fobelets, M.; Giguère, A.; et al . The effectiveness of E-health solutions for ageing with cognitive impairment: A systematic review. The Gerontologist. 2020;, 1-22. doi:10.1093/geront/gnaa065 Source [Systematic Review]
- D’Rozario, A. L.; Chapman, J.; Phillips, C. L.; Palmer, J. R.; Hoyos, C. M.; Mowszowski, L.; et al. Objective measurement of sleep in mild cognitive impairment: A systematic review and meta-analysis. Sleep Medicine Reviews. 2020;52, 1-17. doi:10.1016/j.smrv.2020.101308 Source [Meta-analysis,Systematic Review]
- Erickson, K. I.; Hillman, C.; Stillman, C. M.; Ballard, R. M.; Bloodgood, B.; Conroy, D. E.; Macko, R.; Marquez, D. X.; Petruzzello, S. J.; Powell, K. E. Physical Activity, Cognition, and Brain Outcomes: A Review of the 2018 Physical Activity Guidelines. Medicine and Science in Sports and Exercise. 2019;51(6), 1242-1251. doi:10.1249/MSS.0000000000001936 [Metasynthesis,Meta-analysis,Systematic Review]
- Fazio, S.; Stocking, J.; Kuhn, B.; Doroy, A.; Blackmon, E.; Young, H. M.; Adams, J. Y. How much do hospitalized adults move? A systematic review and meta-analysis. Applied Nursing Research. 2020;51, 1-10. doi:10.1016/j.apnr.2019.151189 Source [Meta-analysis,Systematic Review]
- Fogg, C.; Griffiths, P.; Meredith, P.; Bridges, J.. Hospital outcomes of older people with cognitive impairment: an integrative review. International Journal of Geriatric Psychiatry. 2018;33(9), 1177-1197. doi:10.1002/gps.4919 [Review Articles]
- Gates, N. J.; Vernooij, R. W.; Di Nisio, M.; Karim, S.; March, E.; Martinez, G.; et al. Computerised cognitive training for preventing dementia in people with mild cognitive impairment. Cochrane Database of Systematic Reviews. 2019;(3), 1-121. doi:10.1002/14651858.CD012279.pub2 [Meta-analysis,Systematic Review]
- Gulanick, M.; Myers, J. L. (2017). Nursing care plans: Diagnoses, interventions and outcomes . St. Louis: Mosby, Elsevier. [Review Articles,Expert/Committee Opinion,Core Curriculum,Position Statements,Practice Bulletins]
- Haugen, N.; Galura, S. (2020). Ulrich and Canale's Nursing Care Planning Resource-E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health . St. Louis: Saunders, Elsevier. [Review Articles,Expert/Committee Opinion,Core Curriculum,Position Statements,Practice Bulletins]
- He, W.: Wang, M.; Jiang, L.; Li, M.; Han, X. Cognitive interventions for mild cognitive impairment and dementia: An overview of systematic reviews. Complementary Therapies in Medicine. 2019;47, 1-10. doi:10.1016/j.ctim.2019.102199 Source [Meta-analysis,Systematic Review]
- Hwang, A. B.; Boes, S.; Nyffeler, T.; Schuepfer, G. Validity of screening instruments for the detection of dementia and mild cognitive impairment in hospital inpatients: A systematic review of diagnostic accuracy studies. PloS One. 2019;14(7) doi:10.1371/journal.pone.0219569 Source [Metasynthesis,Meta-analysis,Systematic Review]
- Kim, O.; Pang, Y.; Kim, J. H. The effectiveness of virtual reality for people with mild cognitive impairment or dementia: a meta-analysis. BMC Psychiatry. 2019;19(1), 219. doi:10.1186/s12888-019-2180 [Metasynthesis,Meta-analysis,Systematic Review]
- Kruse, C. S.; Fohn, J.; Umunnakwe, G.; Patel, K.; Patel, S. Evaluating the Facilitators, Barriers, and Medical Outcomes Commensurate with the Use of Assistive Technology to Support People with Dementia: A Systematic Review Literature. Healthcare . 2020;8(3), 278-322. doi:10.3390/healthcare8030278 Source [Systematic Review]
- Lai, X.; Wen, H.; Li, Y.; Lu, L.; Tang, C. The Comparative Efficacy of Multiple Interventions for Mild Cognitive Impairment in Alzheimer's Disease: A Bayesian Network Meta-Analysis. Frontiers in Aging Neuroscience. 2020;12(121), 1-12. doi:10.1155/2020/3620534 Source [Meta-analysis]
- Law, L. L. F.; Barnett, F.; Yau, M. K.; Gray, M. A. Effects of combined cognitive and exercise interventions on cognition in older adults with and without cognitive impairment: A systematic review. Ageing Research Reviews. 2014;(15), 61-75. [Metasynthesis,Meta-analysis,Systematic Review]
- Leong, R. L.; Cheng, G. H. L.; Chee, M. W.; Lo, J. C. The effects of sleep on prospective memory: A systematic review and meta-analysis. Sleep Medicine Reviews. 2019; doi:10.1186/s12888-019-2180-x [Metasynthesis,Meta-analysis,Systematic Review]
- Li, W.; Wang, Q.; Du, S.; Pu, Y.; Xu, G. Acupuncture for mild cognitive impairment in elderly people: Systematic review and meta-analyses. Medicine. 2020;99(39) doi:10.1097/MD.0000000000022365 Source [Meta-analysis,Systematic Review]
- Liang, J. H.; Xu, Y.; Lin, L.; Jia, R. X.; Zhang, H. B.; Hang, L. Comparison of multiple interventions for older adults with Alzheimer disease or mild cognitive impairment: A PRISMA-compliant network meta-analysis. Medicine. 2018;97(20) doi:10.1097/MD.0000000000010744 Source [Metasynthesis,Meta-analysis,Systematic Review]
- Loprinzi, P. D.; Blough, J.; Ryu, S.; Kang, M. Experimental effects of exercise on memory function among mild cognitive impairment: systematic review and meta-analysis. The Physician and Sports Medicine. 2019;47(1), 21-26. doi:10.1080/00913847.2018.1527647 [Metasynthesis,Meta-analysis,Systematic Review]
- Mamo, S. K.; Reed, N. S.; Price, C.; Occhipinti, D.; Pletnikova, A.; Lin, F. R.; Oh, E. S. Hearing loss treatment in older adults with cognitive impairment: A systematic review. Journal of Speech, Language, and Hearing Research. 2018;61(10), 2589-2603. doi:10.1044/2018_JSLHR-H-18-0077 Source [Systematic Review]
- Miotto, E. C.; Batista, A. X.; Simon, S. S.; Hampstead, B. M. Neurophysiologic and cognitive changes arising from cognitive training interventions in persons with mild cognitive impairment: a systematic review. Neural Plasticity. 2018;2018, 1-14. doi:10.1155/2018/7301530 Source [Systematic Review]
- Naef, R.; Ernst, J.; Burgi, C.; Petry, H.. Quality of acute care for persons with cognitive impairment and their families: a scoping review. International Journal of Nursing Studies. 2018;85, 80-89. doi:10.1016/j.ijnurstu.2018.05.006 [Review Articles,Systematic Review]
- National Institute for Health and Care Excellence (NICE). (2018). Dementia: Assessment, management and support for people living with dementia and their carers . Source [Quality Measures,Clinical Practice Guidelines]
- Oliva, H. N. P.; Machado, F. S. M.; Rodrigues, V. D.; Leão, L. L.; Monteiro-Júnior, R. S. The effect of dual-task training on cognition of people with different clinical conditions: An overview of systematic reviews. IBRO Reports. 2020;9, 24-31. doi:10.1016/j.ibror.2020.06.005 Source [Review Articles,Systematic Review]
- O’Caoimh, R.; Mannion, H.; Sezgin, D.; O’Donovan, M. R.; Liew, A.; Molloy, D. W. Non-pharmacological treatments for sleep disturbance in mild cognitive impairment and dementia: A systematic review and meta-analysis. Maturitas. 2019;127, 82-94. doi:10.1016/j.maturitas.2019.06.007 Source [Meta-analysis,Systematic Review]
- Patnode, C. D.; Perdue, L. A.; Rossom, R. C.; Rushkin, M. C.; Redmond, N.; Thomas, R. G.; Lin, J. S.. (2020, Feb). Screening for cognitive impairment in older adults: an evidence update for the U. S. preventative services task force . (Report No. 19-05257-EF-1)Rockvile, MD: Agency for Healthcare Research and Quality (US). Source [Position Statements]
- Pendleton, H. M.; Schultz-Krohn, W. (2018). Pedretti's occupational therapy: Practice skills for physical dysfunction . St. Louis: Elsevier. [Review Articles,Expert/Committee Opinion,Core Curriculum,Position Statements,Practice Bulletins]
- Petersen, R. C.; Lopez, O.; Armstrong, M. J.; Getchius, T. S.; Ganguli, M.; Gloss, D.; Gronseth, G. S.; Marson, D.; Pringsheim, T.; Day, G. S.; Sager, M.; Stevens, J.; Rae Grant, A. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018, Jan;90(3), 126-135. doi:10.1212/WNL.000000000000482 [Quality Measures,Clinical Practice Guidelines]
- Reilly, J. C.: Houghton, C. The experiences and perceptions of care in acute settings for patients living with dementia: A qualitative evidence synthesis. International Journal of Nursing Studies. 2019;96, 82-90. doi:10.1016/j.ijnurstu.2019.04.018 Source [Review Articles]
- Reuben, D. B.; Herr, K. A.; Pacala, J. T.; Pollock, B. G.; Potter, J. F.; Semla, T. P. (2017). Geriatrics at your fingertips 2017 . (pp.73-79). New York: American Geriatrics Society. [Review Articles,Expert/Committee Opinion,Core Curriculum,Position Statements,Practice Bulletins]
- Russell-Williams, J.; Jaroudi, W.; Perich, T.; Hoscheidt, S.; El Haj, M.; Moustafa, A. A. Mindfulness and meditation: Treating cognitive impairment and reducing stress in dementia. Reviews in the Neurosciences. 2018;29(7), 791-804. doi:10.1515/revneuro-2017-0066 [Review Articles,Expert/Committee Opinion,Core Curriculum,Position Statements,Practice Bulletins]
- Sehn, L. F. B.: Schuch, F. B.: Firth, J.: de Souza Stigger, F. Effects of physical exercise on cognitive function of older adults with mild cognitive impairment: A systematic review and meta-analysis. Archives of Gerontology and Geriatrics. 2020;89, 1-10. doi:10.1016/j.archger.2020.104048 Source [Meta-analysis,Systematic Review]
- Song, D.; Doris, S. F.; Li, P. W.; Lei, Y. The effectiveness of physical exercise on cognitive and psychological outcomes in individuals with mild cognitive impairment: A systematic review and meta-analysis. International Journal of Nursing Studies. 2018;79, 155-164. doi:10.1016/j.ijnurstu.2018.01.002 [Metasynthesis,Meta-analysis,Systematic Review]
- Swearingen, P. L.; Wright, J. (2019). All-in-One Nursing Care Planning Resource-E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health . Philadelphia: Elsevier Health Sciences. [Review Articles,Expert/Committee Opinion,Core Curriculum,Position Statements,Practice Bulletins]
- Wang, Y. Q.; Jia, R. X.; Liang, J. H.; Li, J.; Qian, S.; Li, J. Y.; et al . Effects of non‐pharmacological therapies for people with mild cognitive impairment. A Bayesian network meta‐analysis. International Journal of Geriatric Psychiatry. 2020;35(6), 591-600. doi:10.1002/gps.5289 Source [Meta-analysis]
- Yang, H. L.; Chan, P. T.; Chang, P. C.; Chiu, H. L.; Hsiao, S. T. S.; chu, H.; Chou, K. R. Memory-focused interventions for people with cognitive disorders: A systematic review and meta-analysis of randomized controlled studies. International Journal of Nursing Studies. 2017;78, 44-51. doi:10.1016/j.ijnurstu.2017.08.005 [Metasynthesis,Meta-analysis,Systematic Review]
- Yang, J.; Zhang, L.; Tang, Q.; Wang, F.; Li, Y.; Peng, H.; et al . Tai Chi is effective in delaying cognitive decline in older adults with mild cognitive impairment: Evidence from a systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine. 2020;2020, 1-11. doi:10.1155/2020/3620534 Source [Meta-analysis,Systematic Review]
- Yang, Q.; Tian, C.; Tseng, B.; Zhang, B.; Huang, S.; Jin, S.; et al. Gait change in dual-task as a behavioral marker to detect mild cognitive impairment in the elderly-A systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation. 2020;101(10), 1818-1821. doi:10.1016/j.apmr.2020.05.020 Source [Meta-analysis,Systematic Review]
- Zhang, H.; Huntley, J.; Bhome, R.; Holmes, B.; Cahill, J.; Gould, R. L.; et al. Effect of computerised cognitive training on cognitive outcomes in mild cognitive impairment: A systematic review and meta-analysis. BMJ Open. 2019;9(8), 1-10. doi:10.1136/bmjopen-2018-027062 Source [Meta-analysis,Systematic Review]
- Zhou, X. L.; Wang, L. N.; Wang, J.; Zhou, L.; Shen, X. H . Effects of exercise interventions for specific cognitive domains in old adults with mild cognitive impairment: A meta-analysis and subgroup analysis of randomized controlled trials. Medicine. 2020;99(31), 1-11. doi:10.1097/MD.0000000000020105 Source [Meta-analysis]
- Zou, L.; Loprinz, P. D.; Yeung, A. S.; Zeng, N.; Huang, T. The beneficial effects of mind-body exercises for people with mild cognitive impairment: A systematic review with meta-analysis. Archives of Physical Medicine and Rehabilitation. 2019; doi:10.1016/j.apmr.2019.03.009 Source [Metasynthesis,Meta-analysis,Systematic Review]
Clinical Practice Guidelines represent a consistent/standardized approach to the care of patients with specific diagnoses. Care should always be individualized by adding patient specific information to the Plan of Care.
- About Elsevier
- Accessibility Policy
- Terms and conditions
- Privacy policy
- Cookie settings
Cookies are used by this site. To decline or learn more, visit our cookie notice .
Copyright © 2024 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.
- Skip to navigation
- Skip to main content
- Skip to footer
EAF/SWS Login
- News & Media
- Complaints & Report Abuse
- Available support
- Your rights and responsibilities
- Employer Toolkit
- Intermediary Toolkit

Cognition – Managing problem solving, thinking, attention and memory at work
Cognitive and thinking skills.
Cognitive or thinking skills can be hard for people if their disability affects the way their brain processes information, for example, people with intellectual disabilities, acquired brain injuries, specific learning disabilities, autism spectrum disorders, psychiatric disorders, dementia or other neurological conditions. Poor cognitive and thinking skills can lead to stress, social withdrawal and poor work performance. This can cause people to feel frustrated with themselves and others, become overwhelmed and easily confused when trying to learn new information. As a result, people can withdraw from others and underperform in their role at work.
The processes affected by cognitive or thinking skills include critical thinking, problem solving, attention, concentration and memory, organisation and planning. These processes and some suggested workplace solutions and adjustments are provided below.
Original and creative thinking
Original or creative thinking means the ability to question the common way of doing things and form new ideas or approaches to solve a problem or meet a need. It involves higher-level brain functioning, incorporating the use of intuition, making unusual connections or associations, imagination, objectivity and the willingness to take risks.
Workplace adjustments and solutions
- fostering a friendly, open work environment, where verbal and written input from workers regarding operations, work processes and methods is valued and encouraged
- establishing a buddy program with a co-worker to provide mentoring and prompting for workers with a cognitive impairment
Problem Solving
Problem solving is the ability to find answers to problems using an organised thought process.
Critical thinking
Critical thinking refers to the mental process of analysing information accurately, precisely, comprehensively and without bias. Both problem solving and critical thinking involve gathering of information, defining the issue and breaking it down into smaller sections to action through to an outcome or solution.
- prompts, reminders and checklists can assist people with problem solving as they can be used to assess the situation and provide information about the problem, such as what has been done, when and what is next
- aids like graphic organisers can help people with problem solving. These enable the removal of most of the words and focus on connections or links between ideas using only key words and images. This allows people to look at the whole problem as well as the interrelated smaller issues. Graphic organisers have many names including visual maps, mind mapping, and visual organisers.
Attention, concentration and remembering work tasks
Attention is the process of selectively concentrating thinking on one aspect or task whilst ignoring other things, so thinking in an intended direction. The ability to maintain attention and concentration to focus on learning new information and/or focus on carrying out tasks and activities is a general work requirement across all industries.
The ability to remember work tasks and activities is also a necessary requirement across workplaces.
It is important to recognise that difficulty maintaining attention/concentration or remembering can be related to disability and that understanding and support at work should be made available. Memory issues in particular can affect job performance and safety in the workplace.
Workplace solutions and adjustments
- avoid or eliminate distractions and do not multitask as this will divide attention
- break down job tasks into small steps and use visual prompts for each step to assist with refocus and continuation with tasks
- use a pin-up board/white board to display task flow charts
- use ‘to do’ lists which can be ticked off as completed to help with tracking actions
- schedule regular breaks to accommodate a reduced attention span
- schedule the early part of the working day for ‘attention demanding’ tasks or activities, with less demanding tasks scheduled later in the day
- rotate between tasks to increase interest
- establish a buddy program with a co-worker to provide extra support and encouragement to keep on task
- establish a set work routine to make it easier to remember and allow time to adjust if the routine alters
- minimise potential distractions to concentration, for example, partition off the workspace, have a workstation away from other colleagues and reduce noise or other distracting factors
- incorporate the use of acronyms and mnemonics which can be short poems or sayings used to remember information
- foster a healthy lifestyle for workers, for example, be conscious of stress levels in the workplace, encourage physical fitness and, if food or meals are provided, make healthy foods available
There are also different aids and products that can help prompt memory:
- clocks, watches and timers with built-in prompts
- colour coding
- electronic organisers
Organising, planning and managing time
Difficulties associated with organisation, planning and the ability to effectively judge and manage time can adversely affect job performance, as they are important skills for efficiency and effectiveness in the workplace. The ability to prepare and organise daily work requirements or tasks provides structure or a semblance of order to each working day and can reduce stress levels. Examples include not being prepared at meetings, poor punctuality due to lack of travel planning or limited reliability as an employee.
- establish a buddy system with a co-worker to provide extra support and guidance
- various organising and timing devices are available including calendars, watches and timers with prompts
Support Services
For all cognition deficits, other supports such as job coaches, skills trainers and mentors can assist people with problem solving and critical thinking skill development in the workplace. Strategies may include role playing, reviewing information with the employee or presenting information in a way that is more easily understood, such as through Easy English translation. A cognition and communication specialist, such as a speech pathologist, may be helpful in identifying any barriers through an assessment.
Specialist employment agencies who provide coaching and support on the job for people with disability may be able to assist a person to learn how to problem solve at work. Find a provider near you.
Related Links
Dementia Australia Autism Awareness Australia Brain Injury Australia
Last updated: 21 May 2024 - 1:27pm
Need more help?
Contact a JobAccess Advisor by phoning 1800 464 800 or fill our our enquiry form .
Connection denied by Geolocation Setting.
Reason: Blocked country: Russia
The connection was denied because this country is blocked in the Geolocation settings.
Please contact your administrator for assistance.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How Poor Judgment Can Be a Sign of Early Dementia
Poor judgment is one of the hallmarks of Alzheimer’s disease . In fact, while a typical symptom of early stages of Alzheimer’s is short-term memory loss , poor judgment can sometimes precede memory loss.
Poor judgment refers to the inability to make appropriate decisions. If your relative has Alzheimer's or another type of dementia, they might be unable to evaluate the different factors that should be considered when making a decision. Looking ahead to the possible outcome of behavior or choice may also be a challenge, as is considering abstract ideas vs. concrete ideas.
Poor judgment in Alzheimer's is not just one questionable decision, but rather a pattern of clearly inappropriate decisions or actions. Here are a few examples of poor judgment in Alzheimer’s disease and other kinds of dementia.
Safety/Danger Recognition
Your loved one recently fell and broke their hip . They had surgery and fortunately came through that well. However, they are not able to accurately assess their safety limits. At times, they clearly seem to have forgotten the restrictions regarding weight bearing. However, even when reminded, they still express an uncharacteristic desire to disregard this important medical advice. They may keep trying to get up and walk. Even the fact that it hurts doesn’t stop them from trying to get up out of the chair.
Another scenario that demonstrates an inability to recognize danger is one in which your loved one wanders away from the house and tries to walk across a very busy street during rush hour. They are not able to assess the traffic to determine that it's too busy to cross the street at this time.
Even though you’ve told your father he can’t give away money anymore, he continues to fall for get-rich-quick scams and phony prize offers. You’ve tried explaining that he needs his money to pay for the groceries and the home health aide who comes to help him shower. You've even put a note in his checkbook reminding him of this. Regardless, he continues to write checks and give away money that he needs, or even money that he doesn't have.
Social Interaction
Perhaps your husband has always been an outgoing, friendly man. Now, however, he doesn't seem to know when to stop. Yesterday, you took him out to lunch and he was so flirty with the waitress that everyone was uncomfortable. The waitress ended up trading tables with another server because she wasn't sure how to react to him.
Personal Grooming and Hygiene
Your sister, who was diagnosed with Alzheimer's a year ago, doesn't spend any time on her appearance anymore. She always had her hair nicely styled, and now she rarely seems to wash or comb it. When you remind her that it's a special occasion, it doesn't seem to make a difference. You also notice that she could benefit from a bath or shower more frequently.
Even if it’s the middle of a cold, snowy winter day, your wife with Alzheimer’s might try to go outside dressed in shorts and a t-shirt. When you suggest a change of clothes, she appears irritated and continues to try to wander out the door.
This is an area that can be difficult to address. However, if you’re uncomfortable riding with your loved one as he drives, that’s a pretty clear sign that he shouldn’t be driving anymore. Perhaps he can’t judge the distance from his car to the next one anymore, or he’s not able to discern how fast he should be driving on the expressway.
Driving requires the use of multiple aspects of our brains, and as the symptoms of Alzheimer's progress, these abilities continue to decrease. (If driving is questionable for your loved one, you can request a driving evaluation specialist to assess his safety and ability.)
A Word From Verywell
While it can be worrisome and even frustrating to see these signs of poor judgment in your loved one, it may be helpful as you cope to consider that there may be a reason for these behaviors that are beyond their control. An evaluation by a physician can help rule out reversible causes of memory loss , and treatment can begin if it appears that dementia is the cause of these judgment problems.
Capucho PHFV, Brucki SMD. Judgment in mild cognitive impairment and Alzheimer's disease . Dement Neuropsychol . 2011;5(4):297-302. doi:10.1590/S1980-57642011DN05040007
Alzheimer's Association. Home safety .
National Institute on Aging. Managing money problems in Alzheimer's disease .
Daily Caring. 9 Ways to handle Alzheimer's and sexually inappropriate behavior .
National Institute on Aging. Bathing, dressing, and grooming: Alzheimer's caregiving tips .
National Institute on Aging. Driving safety and Alzheimer's disease .
By Esther Heerema, MSW Esther Heerema, MSW, shares practical tips gained from working with hundreds of people whose lives are touched by Alzheimer's disease and other kinds of dementia.
Impaired Thought Processes & Cognitive Impairment Nursing Care Plan and Management

Effective nursing care planning and management is important for patients with impaired thought process or cognitive impairment as they aim to promote safety, optimize functioning, and enhance quality of life for these individuals. Get to know the nursing assessment , nursing diagnosis , and interventions for patients with cognitive impairment or impairment in their thought processes.
Table of Contents
What is cognitive impairment, nursing problem priorities, nursing assessment, nursing diagnosis, nursing goals, 1.1. assessing the client’s cognitive abilities, 1.2. determining the etiology of cognitive decline, 2. managing cognitive decline, 3. advocating for the client’s safety, 4. improving client communication, 5. providing interventions to improve nutrition and hydration, recommended resources, references and sources.
Impairment in cognition describes an individual with altered perception and cognition that interferes with daily living. The alteration can result in cognitive and perceptual deficits, including difficulty concentrating, organizing thoughts, and communicating effectively. Disturbances in thought processes can be caused by various conditions, such as mental illness , substance abuse , brain injury , or medication side effects.
Mild cognitive impairment (MCI) exceeds the normal, expected changes related to age. The defining element of MCI, according to Ronald C. Petersen, is a single sphere of slowly progressive cognitive impairment that is not attributable to motor or sensory deficits and to which other areas of involvement may eventually be added before social or occupational impairment supervenes (Mehta & Chawla, 2019).
The focus of nursing management is to reduce impairment in thinking and promote reality orientation. Often, confusion in older adults is erroneously attributed to aging. Confusion in an older adult can be caused by a single factor or multiple factors such as depression , dementia , medication side effects, or metabolic disorders. Depression causes impaired thinking in older adults more frequently than dementia .
Disturbances in thought process can be caused by various factors including psychiatric disorders, neurological conditions, substance abuse , medication side effects, and systemic illnesses affecting the brain. Here are some factors that may cause cognitive impairment:
Physical changes
- Head injuries
- Malnutrition
Biochemical changes
- Medications
- Substance abuse
Psychological conflicts
- Emotional changes
- Mental disorders
Maturational
- Late-life depression
Situational (Personal, Environmental)
- Abuse (physical, sexual, mental)
- Childhood trauma
Nursing Care Plans and Management
Caring for clients with cognitive impairment presents unique challenges that require a comprehensive and individualized approach. Nursing care plans involve a systematic process of assessment , diagnosis, planning , implementation , and evaluation . They are tailored to the specific needs and abilities of each client, recognizing that cognitive impairment varies in its presentation and progress. Management of these clients focuses not only on medical interventions but also on creating a supportive and nurturing environment that fosters a sense of security, engagement, and comfort .
The following are the nursing priorities for clients with cognitive impairment:
- Client safety. Cognitive impairment can affect balance and coordination , increasing the risk of falls. These clients may also wander and become disoriented, leading to risks to safety.
- Communication. Cognitive impairment can impair communication skills, leading to frustration and isolation .
- Impaired activities of daily living (ADLs). Cognitive impairment often affects the client’s ability to perform ADLs independently.
- Nutrition and hydration. cognitive impairment can lead to forgetfulness or difficulty eating and drinking independently. Prioritizing adequate nutrition and hydration to prevent malnutrition and dehydration is essential.
Common signs and symptoms of cognitive impairment or disturbed thought process may include memory loss, confusion, disorientation , difficulty concentrating, impaired judgment, language difficulties, changes in behavior or personality, and problems with problem-solving and decision-making abilities. The following signs and symptoms characterize cognitive impairment:
- Memory impairment. Significant difficulty in retaining new information or recalling previously learned information.
- Cognitive disorientation. Altered perception of time, place, and person, often resulting in confusion about surroundings and events.
- Impaired attention and concentration. Difficulty focusing, sustaining attention, and staying engaged in activities.
- Executive dysfunction. Challenges in planning, organizing, and executing complex tasks result in difficulties with problem-solving and decision-making .
- Aphasia. Language impairments involve difficulties with speech production, comprehension, or word finding.
- Changes in behavior and personality. Observable alterations in mood, emotions, social interactions, or impulse control.
- Apraxia. Difficulty performing purposeful movements or using objects correctly despite intact motor function.
- Agnosia. Inability to recognize or identify objects, people, or familiar sensory stimuli.
- Disrupted visuospatial abilities. Impairments in perceiving and interpreting spatial relationships, depth perception, or object recognition.
- Psychomotor disturbances. Changes in motor activity, such as agitation, restlessness, or slowed movements.
Nursing diagnosis is a critical step in providing effective care to clients with cognitive disorders. This process involves a systematic assessment and analysis of the client’s condition, which helps the nurse identify the client’s unique nursing care needs. It is essential to maintain open communication with the client and their caregivers to ensure that care plans are client-centered and responsive to changing needs and preferences.
The following are the common goals and expected outcomes:
- The client will maintain reality orientation and communicate clearly with others
- The client will recognize changes in thinking/behavior.
- The client will recognize and clarify possible misinterpretations of the behaviors and verbalization of others.
- The client will identify situations that occur before hallucinations /delusions.
- The client will use coping strategies to deal effectively with hallucinations/delusions.
- The client will participate in unit activities.
- The client will express delusional material less frequently.
- The client will appropriately interact and cooperate with staff and peers in a therapeutic community setting.
Nursing Interventions and Actions
Nursing interventions are crucial in supporting clients with cognitive impairment or disturbed thought processes by ensuring their safety, facilitating effective communication, promoting cognitive functioning, and enhancing their overall well-being and quality of life.
1. Assessing for Cognitive Impairment
Nursing assessment is crucial for clients with cognitive impairment or disturbed thought processes as it helps identify their specific needs, tailor care interventions, and monitor changes in cognitive function, allowing for individualized and effective care.
1. Assess attention span/distractibility and ability to make decisions or problem-solving. This determines the ability of the client to participate in planning/executing care. Attention span can be measured by asking the client to repeat increasingly lengthy strings of information, such as digit sequences, sentences, or spatial locations. A reduced attention span may explain poor performance across a number of domains like language memory due to limited processing.
2. Assist with testing/reviewing results and evaluating mental status according to age and developmental capacity. This is to assess the degree of impairment. The prevalence of mild cognitive impairment increases with age, with a prevalence of 10% in those aged 70 to 79 years and 25% in those aged 80 to 89 years. Clients with mild cognitive impairment may often present with vague and subjective symptoms of declining cognitive performance, which may be difficult to distinguish from the typical performance decline in healthy older adults.
3. Interview significant others (SOs) or caregivers to determine the client’s usual thinking ability, changes in behavior, length of time the problem has existed, and other pertinent information. This is to provide a baseline for comparison. The Alzheimer’s Association released guidelines, including an algorithm, to help clinicians in the primary care setting detect cognitive impairment and determine whether referral or further testing is required, and this includes the use of structured cognitive assessment tools for clients and their significant others or informants.
4. Perform periodic neurological/behavioral assessments, as indicated, and compare with baseline. Early recognition of changes promotes proactive modifications to the plan of care. Few clients have undergone baseline testing before the onset of impairment, therefore the healthcare professional will have to determine whether a particular score represents a significant change from the client’s presumed baseline. Such determinations are not exact, and serial testing eventually will be needed to establish whether the client’s cognitive function is improving, staying stable, or progressing to full-blown clinical dementia .
5. Assess the severity of the level of impairment. Cognitive impairment can be mild, severe, or anything in between. With mild impairment, there are changes in cognitive functions, but the client can still do their everyday activities. Severe levels of impairment, such as dementia, can lead to a point where the client is incapable of living independently because of the inability to plan and carry out regular tasks and apply judgment.
6. Utilize screening tools for the client’s cognitive abilities. There are various screening tools used by clients, families, and healthcare providers to assess the client’s cognitive abilities. Short Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE), Dementia Severity Rating Scale (DSRS), AD-8, and General Practitioner Assessment of Cognition (GPCOG) can be used to gather information from caretaker/ family members . The Mini-Mental State Examination (MMSE) is used for the evaluation of clients with Alzheimer disease because of its main focus on testing memory.
1. Identify factors present [acute/chronic brain syndrome (recent stroke , Alzheimer’s disease ), brain injury or increased intracranial pressure, anoxic event, acute infections, malnutrition, sleep or sensory deprivation, chronic mental illness ( schizophrenia )]. Identifying the factors present is important to know the causative/contributing factors. Mood disorders, medical illnesses, and medications may affect cognition in such a way that a client will meet the criteria for mild cognitive impairment. Nonamnestic forms of MCI may be caused by cerebrovascular disease, Lewy body dementia, Parkinson disease, frontotemporal dementias, atypical Alzheimer disease, or no specific underlying pathology.
2. Determine alcohol/other drug use. Drugs can have direct effects on the brain, or have side effects, dose-related effects, and/or cumulative effects that alter thought patterns and sensory perception. Cognitive alterations and deficits that are observed in substance use disorders contribute directly and indirectly to the overall tremendous public health burden that these disorders place on society. The typical cognitive domains contributing to this understanding of addiction are attention, response inhibition, decision-making , and working memory (Ramey & Regier, 2018).
3. Assess dietary intake/ nutritional status . This helps in identifying contributing factors. A high salt diet has been independently linked to an increased risk of cerebrovascular disease and dementia. Therefore, dietary salt, although not currently identified as one of the risk factors targeted for the prevention of dementia, may also contribute to cognitive impairment (Ramey & Regier, 2018).
4. Review laboratory values for abnormalities such as metabolic alkalosis, hypokalemia , anemia , elevated ammonia levels, and signs of infection . Monitoring laboratory values aids in identifying contributing factors. However, no specific laboratory studies are indicated for cognitive impairment. Most practitioners perform at least a basic workup to rule out treatable conditions that may cause dementia, such as thyroid disease and cobalamin deficiency.
5. Assess for signs of a depressive disorder. Depressive disorders are prevalent in older adults, who frequently exhibit vague somatic symptoms and anxiety and report an inability to concentrate and poor memory. Depression may certainly be accompanied by cognitive dysfunction that abates with successful treatment of the depression.
Research in other populations with chronic conditions suggests that disease management, especially the performance of self-management behaviors like healthy diets and exercise, may be influenced by the way that an individual views the nature and cause of a disease or its symptoms. Healthcare professionals agree that, even as disease-modifying pharmacological treatments become available, lifestyle modifications will be required to stabilize or reverse the course of cognitive impairment (Kim et al., 2022).
1. Assist with treatment for underlying problems, such as anorexia , brain injury/increased intracranial pressure, sleep disorders, and biochemical imbalances. Cognition/thinking often improves with treatment/correction of medical/psychiatric problems. Correcting (to the extent possible) any sensory and motor manifestations compounding the cognitive symptoms is important for minimizing their impact on cognitive impairment.
2. Reorient to time/place/person, as needed. The inability to maintain orientation is a sign of deterioration. Accordingly, a multi-component family reorientation strategy has recently been proposed to achieve better outcomes. Family reorientation messages refer to the use of family members’ voices in orienting clients to reality, providing a familiar, reassuring comfort , and assisting in counteracting inattention , and disorganized thinking in addition to memory and perceptual disturbances (Elcokany & Ahmed, 2019).
3. Have the client write their name periodically; keep this record for comparison and report differences. These are important measures to prevent further deterioration and maximize the level of function. The act of rewriting one’s name engages cognitive functions such as memory, fine motor skills, and concentration. Regular cognitive stimulation can help slow down the progression of cognitive decline and improve overall brain function.
4. Present reality concisely and briefly and do not challenge illogical thinking. Avoid vague or evasive remarks. Delusional clients are extremely sensitive about others and can recognize insincerity. Evasive comments or hesitation reinforces mistrust or delusions. Validation therapy is a technique used for older adults who are confused. The focus is on the emotional aspect of the communication. It does not reinforce incorrect perceptions but focuses on validating the client’s feelings (Ernstmeyer & Christman, 2021).
5. Be consistent in setting expectations, enforcing rules, and so forth. Clear, consistent limits provide a secure structure for the client. Predictability is often reassuring for clients with cognitive impairment, as it reduces confusion and anxiety, contributing to a sense of stability. Clear boundaries can prevent confusion and frustration that might lead to agitation or challenging behavior.
6. Reduce provocative stimuli, negative criticism, arguments, and confrontations. This is to avoid triggering fight/flight responses. Negative stimuli or criticism can trigger agitation and challenging behaviors in clients with cognitive impairment. This can include verbal outbursts, physical aggression, or withdrawal . By minimizing provocative stimuli, these reactions can be prevented, creating a calmer and safer environment.
7. Do not flood the client with data regarding his or her past life. Individuals who are exposed to painful information from which the amnesia is providing protection may decompensate even further into a psychotic state. Memories, especially if they involve significant life events or traumatic experiences, can evoke strong emotions. To cope with the flood of information, some clients may withdraw from social interactions, preferring to isolate themselves to avoid emotional turmoil.
8. Identify specific conflicts that remain unresolved, and assist the client in identifying possible solutions. Unless these underlying conflicts are resolved, any improvement in coping behaviors must be viewed as only temporary. Conflict can cause stress and anxiety. By resolving conflicts, clients experience emotional relief and a sense of calm, contributing to their overall emotional well-being. Additionally, engaging in conflict resolution exercises the brain’s problem-solving abilities.
9. Recognize and support the client’s accomplishments (projects completed, responsibilities fulfilled, or interactions initiated). Recognizing the client’s accomplishments can lessen anxiety and the need for delusions as a source of self-esteem . This is especially crucial for clients with cognitive impairments who may face challenges in completing tasks. Recognition of their accomplishments helps them feel valued and competent. Positive feedback also triggers the release of neurotransmitters like dopamine , which can improve the client’s mood and emotional state.
10. Teach the client to intervene, using thought-stopping techniques, when irrational or negative thoughts prevail. Thought-stopping involves using the command “stop!” or loud noise (such as hand clapping) to interrupt unwanted thoughts. This noise or command distracts the individual from the undesirable thinking that often precedes undesirable emotions or behaviors. However, research has found that if the thought is stopped without replacing it with a more positive one, negative thoughts tend to increase. Thought-m is more about noticing these thoughts and then gently redirecting the mind to a more helpful, positive one (Fritscher, 2022).
11. Encourage the client to engage in regular physical activity and exercise. Physical activity and exercise are beneficial for brain health, according to a growing body of evidence. In a prospective study, it was suggested that engaging in moderate exercise of any frequency in midlife or late life was associated with reduced odds of having cognitive impairment. According to one study, aerobic exercise was associated with a slight improvement in cognition.
12. Assist in identifying ongoing treatment needs/rehabilitation programs for the individual. This measure is essential to maintain gains and continue progress if able. Social isolation can be minimized through referral to senior community centers or a day treatment program. Cognitive retraining and rehabilitative strategies offer considerable promise in cognitive impairment and are being explored.
13. Identify problems related to aging that are remediable and assist the client in seeking proper assistance/access to resources. These encourage problem-solving to improve conditions rather than accept the status quo. Many experts suggest that mentally challenging activities, such as crossword puzzles and brain teasers, may be helpful for clients. Such exercises should be kept to a level of difficulty that is reasonable for the client.
14. Assist the client and SO in developing a plan of care when problems are progressive/long-term. Advanced planning addressing home care, transportation, assistance with care activities, support and respite for caregivers, enhance management of patients in a home setting. Several studies have focused on the importance of including caregivers in interventions, especially those caring for clients with dementia, and since having a cognitive impairment often affects the entire family, it is important to include relatives in the process of interventions (Stigen et al., 2021).
15. Encourage smoking cessation. It was found that young cigarette smokers experienced significant impairment in cognitive function compared to nonsmokers. Cigarette smoking affects cognitive abilities and can trigger demonstrable abnormalities in brain neurocognition (Riaz et al., 2021).
16. Refer to community resources (e.g., daycare programs, support groups, drug/alcohol rehabilitation, and mental health treatment programs). These measures are necessary to promote wellness. Cognitive impairment, such as Alzheimer disease and dementia, can create havoc not only in the client but also in the family, friends, and the community. Therefore, management encompasses the role of the healthcare providers, clients, family and friends, and also policymakers. Healthcare policymakers must explore policy changes and initiatives that will increase support, expand, research, and ultimately improve the quality of life for people with cognitive impairment and their families (Dhakal & Bobrin, 2023).
17. Perform sensory stimulation as recommended. Sensory stimulation is considered one of the therapeutic tools used to prevent cognitive impairments. Its main goal is to provide a similar environment that is close to the real world which cognitively stimulates critically ill clients in a safe and controlled manner. Using auditory stimulation as a non-pharmacological intervention can avoid sensory deprivation that could slow down the client’s recovery. A family member’s voice can grasp the client’s attention without much effort.
18. Refer the client for occupational therapy as appropriate. Occupational therapy can help facilitate the client’s cognitive functioning to enhance occupational performance, self-efficacy, participation, and perceived quality of life. Research showed that ten sessions of occupational therapy improved the daily functioning of clients with dementia and diminished the burden of care on their primary caregivers.
Environmental barriers in the home environment can compromise the performance of everyday occupations and modifying the environment is a common compensatory intervention to enhance independent living.
1. Provide safety measures (e.g., side rails , padding, as necessary; close supervision, seizure precautions), as indicated. It is always necessary to consider the safety of the client. The physical home environment is altered based on the needs of the client who lives and performs occupations in the home with an aim to enable occupational performance. However, the occupational therapist also needs to be aware of how many environmental modifications can be done before the environment becomes unfamiliar to the client.
2. Schedule structured activities and rest periods. This provides stimulation while reducing fatigue . Activities that challenge the brain, such as puzzles or memory games, can help maintain cognitive abilities and slow down the progression of cognitive impairment. Some individuals may become overstimulated, therefore, proper rest can provide a break to prevent sensory overload and promote a sense of calm.
3. Maintain a pleasant and quiet environment and approach clients in a slow and calm manner. A client may respond with anxious or aggressive behaviors if startled or overstimulated. A calm and positive environment fosters a sense of security. Clients with cognitive impairment may already feel disoriented or confused; creating a pleasant environment can help establish a stable and secure atmosphere.
4. Refrain from forcing activities and communications. Clients may feel threatened and may withdraw or rebel. Feeling overwhelmed or distressed can lead to agitation or even aggressive behavior. The client might express their frustration physically or verbally, especially if they are unable to communicate their feelings effectively.
5. Encourage the use of assistive devices as recommended. The use of assistive devices is also a means to increase occupational performance. This is described as the ‘traditional way’ of working in community service when providing occupational therapy.
6. Consider the use of assistive technology. Innovative Assistive Technology (IAT) is an important tool for maintaining independence and quality of life for community-living older adults with cognitive impairment. IAT includes sensor-based surveillance and monitoring systems, mobile technology such as wearable fall detectors, and activity bracelets as well as tablets with health information or alarm functions (Thordardottir et al., 2019).
Communication has been defined as a context-dependent construct, which is closely related to well-being and distinct from functional linguistic skills of an individual. The verbal content strongly declines in the course of dementia, whereas non-verbal relationship channels can be preserved for a longer time (Schnabel et al., 2019).
1. Use validated instruments to assess the client’s communication needs. The CODEM instrument, an observational tool to assess Communication Behavior in Dementia, considers both the verbal content and the non-verbal relationship aspect inherent in communication behavior. CODEM allows communication resources and deficits of acutely ill older clients to be detected at different stages of the communication process. This may enable the healthcare team to accommodate their communication behavior in a specific manner leading to more efficient and enriching social interactions.
2. Use touch cautiously, notably if thoughts reveal ideas of persecution. Clients who are suspicious may perceive touch as threatening and may respond with aggression. When appropriate, touch provides comfort for clients. It provides sensory stimulation to avoid sensory deprivation and demonstrates caring and warmth. It is important to assess the client’s reaction to touch before implementing therapeutic gentle touch.
3. Use the techniques of consensual validation and seeking clarification when communication reflects an alteration in thinking. (Examples: “Could you clarify what you mean?” or “I’m not quite following, could you please explain?”) These techniques reveal to the client how others are perceiving him or her, while the responsibility for not understanding is accepted by the nurse. Consensual validation acknowledges the client’s feelings and experiences, validating their emotions. Seeking clarification ensures that both the caregiver and the client have a clear understanding of the communication.
4. Engage the client in one-to-one activities at first, then activities in small groups, and gradually activities in larger groups. A distrustful client can best deal with one person initially. The gradual introduction of others when the client can tolerate is less threatening. Ideally, the activities should be interactive rather than passive, and they should be administered in a fashion that does not cause excessive frustration. If the activity is not enjoyable or stimulating for the client, it is unlikely to offer much cognitive benefit.
5. Encourage the client to verbalize true feelings. Avoid becoming defensive when angry feelings are directed at him or her. Verbalization of feelings in a non-threatening environment may help the client come to terms with long-unresolved issues. Establishing a therapeutic relationship based on trust by sitting at the level of the client and engaging in eye contact shows an attitude of caring and compassion while maintaining the dignity of the client.
6. Encourage the client to participate in resocialization activities/groups when available. This is to maximize the level of function. A study showed certain activities lower the risk of mild cognitive impairment in cognitively normal clients older than 70 years. These included playing games, reading magazines, being engaged in crafts, computer use, and social activities. Among these, being social and using computers were shown to reduce the risk of MCI the most in clients.
7. Recommend the use of information and communication technologies. According to a study regarding the use of ICTs in the daily life of clients with cognitive impairment, popular devices included telephones or mobile and smartphones, smart TVs, and tablets, as well as desktops and laptops. Clients perceive ICTs as useful because these could improve feelings of belongingness, support interaction with loved ones, and allow the client to be engaged in hobbies, passions, or daily activities. Clients can stay connected to children, siblings, and others with whom they have a close relationship, even without interactive conversation (Blok et al., 2020).
Cognitive decline is particularly feared among people because of the possibility of losing self-sufficiency and the need to depend on others. Therefore, people should be made aware that cognitive impairment can be largely prevented with a long life proper nutrition, and a healthy lifestyle.
1. Provide a nutritionally well-balanced diet, incorporating the client’s preferences as much as possible. Encourage the client to eat. Provide a pleasant environment and allow sufficient time to eat. These enhance intake and general well-being. A study found that the risk of developing MCI is lower in clients who consume a Mediterranean diet, which is high in vegetables and unsaturated fats.
2. Encourage the intake of dietary supplements as prescribed. A randomized study involving older adults diagnosed with cognitive impairment determined that dietary supplementation with an oily emulsion of DHA-phospholipids containing melatonin and tryptophan yielded significant improvements in several measures of cognitive function as compared with supplementation with the placebo.
3. Provide foods rich in folate, vitamin E, and fatty acids. Folate has been studied as a solitary intervention; cognitive improvement in general intelligence, attention span, and visuospatial metrics within six months has been reported in mild cognitive impairment. Two other large studies examined the effect of vitamin E on the progression rate of Alzheimer disease and showed slower functional decline with a focus on the ADL. Omega-3 fatty acids are credited with anti-inflammatory and neuroprotective properties that can cause slower cognitive decline, less agitation, and lower depression scores (Vlachos & Scarmeas, 2019).
4. Recommend the use of olive oil and natural flavorings such as garlic and curcumin. Olive oil is a staple of the Mediterranean diet and is a natural product rich in oleic acid. It has been associated with beneficial effects on human health which is attributable to its composition that gives its antioxidant and anti-inflammatory properties. Garlic also exhibits antioxidant properties that may have protective actions against neurotoxic effects (Dominguez et al., 2021).
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition) Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ! Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch.
- Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing Our comprehensive guide on how to create and write diagnostic labels. Includes detailed nursing care plan guides for common nursing diagnostic labels.
Resources to further your research about cognitive impairments:
- Blok, M., van Ingen, E., de Boer, A. H., & Slootman, M. (2020, March). The use of information and communication technologies by older people with cognitive impairments: from barriers to benefits. 104 .
- Butler, R., & Katona, C. (Eds.). (2019). Seminars in Old Age Psychiatry . Cambridge University Press.
- Dhakal, A., & Bobrin, B. D. (2023, February 14). Cognitive Deficits – StatPearls . NCBI.
- Dominguez, L. J., Veronese, N., Vernuccio, L., Catanese, G., Inzerillo, F., Salemi, G., & Barbagallo, M. (2021). Nutrition, Physical Activity, and Other Lifestyle Factors in the Prevention of Cognitive Decline and Dementia . Nutrients , 13 (11).
- Elcokany, N. M., & Ahmed, F. R. (2019). Effect of family reorientation messages on delirium prevention among critically ill patients . Journal of Nursing Education and Practice , 9 (10).
- Fritscher, L. (2022, April 19). 3 Thought Stopping Techniques . Verywell Mind.
- Kim, H., Sereika, S. M., Albert, S. M., Bender, C. M., & Lingler, J. H. (2022). Do Perceptions of Cognitive Changes Matter in Self-Management Behaviors Among Persons With Mild Cognitive Impairment? The Gerontologist , 62 (4).
- Mehta, S., & Chawla, J. (2019, April 22). Mild Cognitive Impairment: Practice Essentials, Overview, Pathophysiology . Medscape Reference.
- Ramey, T., & Regier, P. S. (2018, December). Cognitive impairment in substance use disorders . CNS Spectrums .
- Riaz, T., Murtaza, G., Arif, A., Mahmood, S., Sultana, R., Al-Hussain, F., & Bashir, S. (2021, June 2). Nicotine smoking is associated with impaired cognitive performance in Pakistani young people . NCBI.
- Santisteban, M. M., & Iadecola, C. (2018). Hypertension, dietary salt and cognitive impairment . Journal of Cerebral Flow & Metabolism , 38 (12).
- Schnabel, E.-L., Wahl, H.-W., Penger, S., & Haberstroh, J. (2019). Communication behavior of cognitively impaired older inpatients. Zeitschrift fur Ferontologie und Geriatrie , 52 (4).
- Stigen, L., Bjørk, E., & Lund, A. (2021). Occupational Therapy Interventions for Persons with Cognitive Impairments Living in the Community . Occupational Therapy in Health Care .
- Thordardottir, B., Fänge, A. M., Lethin, C., Gatta, D. R., & Chiatti, C. (2019, March). Acceptance and Use of Innovative Assistive Technologies among People with Cognitive Impairment and Their Caregivers: A Systematic Review . Assistive Technology Innovations in Neurological Conditions , 2019 .
- Vlachos, G. S., & Scarmeas, N. (2019). Dietary interventions in mild cognitive impairment and dementia . Dialogues in Clinical Neuroscience , 21 (1).
1 thought on “Impaired Thought Processes & Cognitive Impairment Nursing Care Plan and Management”
Your notes are amazing
Leave a Comment Cancel reply
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Integr Neurosci
Emotion and cognition interactions in PTSD: a review of neurocognitive and neuroimaging studies
Jasmeet p. hayes.
1 National Center for PTSD, VA Boston Healthcare System, Boston, MA, USA
2 Department of Psychiatry, Boston University School of Medicine, Boston, MA, USA
Michael B. VanElzakker
3 Department of Psychology, Tufts University, Medford, MA, USA
4 Department of Psychiatry, The Massachusetts General Hospital, Boston, MA, USA
Lisa M. Shin
Posttraumatic stress disorder (PTSD) is a psychiatric syndrome that develops after exposure to terrifying and life-threatening events including warfare, motor-vehicle accidents, and physical and sexual assault. The emotional experience of psychological trauma can have long-term cognitive effects. The hallmark symptoms of PTSD involve alterations to cognitive processes such as memory, attention, planning, and problem solving, underscoring the detrimental impact that negative emotionality has on cognitive functioning. As such, an important challenge for PTSD researchers and treatment providers is to understand the dynamic interplay between emotion and cognition. Contemporary cognitive models of PTSD theorize that a preponderance of information processing resources are allocated toward threat detection and interpretation of innocuous stimuli as threatening, narrowing one's attentional focus at the expense of other cognitive operations. Decades of research have shown support for these cognitive models of PTSD using a variety of tasks and methodological approaches. The primary goal of this review is to summarize the latest neurocognitive and neuroimaging research of emotion-cognition interactions in PTSD. To directly assess the influence of emotion on cognition and vice versa, the studies reviewed employed challenge tasks that included both cognitive and emotional components. The findings provide evidence for memory and attention deficits in PTSD that are often associated with changes in functional brain activity. The results are reviewed to provide future directions for research that may direct better and more effective treatments for PTSD.
Introduction
Stress and anxiety serve the important functions of preparing an individual to meet the demands of everyday life and increasing the chance for survival. It is therefore not surprising that arousing and emotionally salient stimuli readily capture attention and have a powerful influence on how information is processed, encoded, stored, and retrieved. However, extreme levels of stress can have a devastating effect on healthy functioning. Nowhere is this demonstrated more clearly than in psychiatric disorders such as posttraumatic stress disorder (PTSD). PTSD develops after exposure to terrifying and life threatening events and is characterized by intense reliving of the traumatic event through disruptive memories and nightmares, avoidance of reminders of the event, and hypervigilance toward potential threats in the environment. These hallmark symptoms involve alterations to cognitive processes such as memory, attention, planning, and problem solving, underscoring the impact that emotion has on cognitive functioning.
Influential cognitive theories of PTSD emphasize the interaction between emotion and cognition in contributing to the symptoms of PTSD. These theories contend that psychopathology arises when emotional stress alters cognitive networks that process information about perception, meaning, and action responses toward executing goals (Lang, 1977 ; Foa and Kozak, 1986 ; Chemtob et al., 1988 ). In PTSD, networks representing information about fear become highly elaborated and accessible, which has implications for encoding and retrieval of information. For instance, an elaborated fear structure may lower one's capacity to process non-threat related information, leading to attentional bias toward potential threats in the environment (Chemtob et al., 1988 ). Furthermore, nodes of the fear network representing threat arousal may predispose an individual to interpret even innocuous stimuli as threatening. Intrusive memories result from spreading activation of the threat arousal node to related threat nodes, while nodes representing opposing alternatives become inhibited.
In this review, we summarize the latest research examining the dynamic interplay between emotions and cognitive processes in PTSD. We begin with an overview of the criteria that must be met for a PTSD diagnosis. Next, we separately review studies that examine the effect of emotion on cognitive functions and those that examine the effect of top-down cognitive control processes on emotion, following this useful distinction put forth by Dolcos et al. ( 2011 ). Finally, we provide a summary of the reviewed literature and discuss open questions in the field. To directly assess emotion-cognition interactions in PTSD, we focus our review on studies employing a challenge task in which both emotional and neutral stimuli were presented. Such studies may lend themselves to better reproduce conditions in everyday life in which emotions influence task performance. Other recent papers have comprehensively reviewed studies that employed only neutral stimuli (i.e., Aupperle et al., 2012b ) or have examined the brain under task-free conditions in PTSD (i.e., Engdahl et al., 2010 ; Georgopoulos et al., 2010 ; Daniels et al., 2012 ).
Clinical definition of PTSD
As outlined in the current Diagnostic and Statistical Manual (DSM-IV-TR), PTSD develops after exposure to a Criterion A1 event, defined as involving actual or threatened death, serious injury, or threat to one's physical integrity (American Psychiatric Association, 2000 ). To meet Criterion A1, the individual must have been directly involved in the traumatic event, witnessed the event, or learned about the death or serious injury of a family member or close friend. The individual must have responded to the traumatic event with intense fear, helplessness, or horror (referred to as Criterion A2) although future conceptualizations of PTSD may omit this criterion (Friedman et al., 2011 ). The symptoms of PTSD can be broadly divided into three symptom clusters, B, C, and D. Symptom cluster B involves persistent and unwanted recollections of the traumatic event, intrusive memories of the event, and dissociative flashbacks. The individual re-experiences the event despite being removed from the traumatic situation and context. These symptoms can be frightening and highly disruptive of activities of daily living. Cluster C involves persistent avoidance of people, places, and activities that serve as reminders of the traumatic event, emotional numbing, difficulty experiencing a full range of emotions, and diminished expectations of one's ability to lead a long, fulfilling life. Finally, symptom cluster D involves symptoms of hyperarousal including difficulty with sleep, irritability and anger, poor concentration, hypervigilance, and exaggerated startle response. The symptoms of PTSD must be present for more than one month and cause significant distress or impairment in social and occupational functioning in order to differentiate the disorder from transient and acute stress reactions. The typical course of PTSD begins with the development of symptoms within 6 months of the onset of the traumatic event, although delays in symptom occurrence can occur. Individuals whose symptoms persist for more than 3 months are diagnosed with chronic PTSD, which is associated with a host of poor health outcomes, including heart disease, obesity, alcohol abuse, and lowered perceptions of general health (Dobie et al., 2004 ; Hoge et al., 2007 ; Boscarino, 2008 ).
The prevalence rate of PTSD is estimated to be 7–8% in the general population (Kessler et al., 1995 ) although prevalence estimates have varied depending on the type of trauma exposure and demographic characteristics. For instance, prevalence rates are higher among individuals exposed to military combat, ranging between 12–20% (Hoge et al., 2004 ; Dohrenwend et al., 2006 ; Tanielian and Jaycox, 2008 ).
Emotional effects on cognitive function
Memory and learning, explicit memory.
Decades of emotional memory research in healthy individuals suggests that emotional information tends to be remembered better than neutral information (Christianson, 1992 ; Kensinger, 2007 ). However, the extent to which emotion provides a facilitating effect on memory encoding and retrieval in PTSD is unclear. Cognitive models of PTSD predict that patients remember emotional information better due to a bias toward (Chemtob et al., 1988 ) or difficulty disengaging from (Chemtob et al., 1999 ) threat-related information, which may lead to greater resources applied to processing and encoding emotional information. A variety of behavioral and neuroimaging memory paradigms have been employed to examine the extent to which patients with PTSD remember emotional information better than neutral information in comparison to healthy or trauma-exposed controls. Consistent with the notion that emotion enhances memory, there is evidence for a memory advantage in patients vs. controls for negative threat information (Vrana et al., 1995 ; McNally et al., 1998 ; Golier et al., 2002 ; Paunovic et al., 2002 ). In these studies, word lists were presented with either incidental or intentional encoding instructions and participants were subsequently instructed to recall as many words as they could from the lists. Results showed that patients either remembered more emotional words than controls or that memory performance for emotional vs. neutral words improved to a greater extent than controls.
However, memories are often subject to a wide range of distortions and biases that impact accurate recollection (Schacter, 1999 ). One of the most controversial topics in the field of traumatic stress is that of the accuracy of recovered memories, prompting PTSD researchers to examine how memory for negative and traumatic information fares in false memory paradigms such as the Deese–Roediger–McDermott (DRM) paradigm (Roediger and McDermott, 1995 ). In the DRM paradigm, participants are presented with a list of words that are semantically related to a critical non-presented word (lure). The critical lure is often falsely remembered as being previously presented on subsequent recall and recognition tests and may reflect gist-based encoding rather than encoding of specific details (Brainerd and Reyna, 2002 ). In PTSD, two of the three DRM studies employing verbal lists indeed reported greater false alarms to critical lures in patients with PTSD than control participants (Bremner et al., 2000 ; Brennen et al., 2007 ). However, a third study employing the DRM paradigm did not report greater false alarms in patients (Zoellner et al., 2000 ). It is unclear why these studies found differential effects, although it is possible that the false memory effect is more likely to be elicited when trauma-specific material, as opposed to generally negative material, is presented. Studies employing paradigms other than the DRM but including trauma-specific material have reported greater false alarms in PTSD (Hayes et al., 2011 ) or a bias in making memory decisions about trauma-specific information (Litz et al., 1996 ).
Negative arousal can alter the type of information that is encoded and retrieved. Neurohormones including norepinephrine and cortisol play a critical role in the fear and stress response by mobilizing the body's response to the stressor via the hypothalamus-pituitary-adrenal axis (HPA) and amygdala, among several other key regions. Norepinephrine has been shown to facilitate emotional memory (for a review see Ferry et al., 1999 ). However, emotional memory may not be uniformly enhanced during high levels of arousal. For example, individuals exposed to highly arousing negative material show a narrowing of attention (Easterbrook, 1959 ), referred to as “tunnel memory,” in which the central objects and features of a scene are better remembered than peripheral background (Christianson et al., 1991 ). A recent study examined the extent to which patients with PTSD showed this memory trade-off effect (i.e., greater memory for negative items vs. backgrounds) in comparison to a trauma-exposed control group and a healthy unexposed group (Mickley Steinmetz et al., 2012 ). The findings showed that the PTSD and the healthy non-trauma exposed group exhibited a greater memory trade-off effect for emotional items than the trauma-exposed-no-PTSD group. Although further research is required, these results suggest that patients with PTSD do not exhibit greater tunnel memory than healthy control participants.
Distortions in memory have been observed during autobiographical retrieval in PTSD. Autobiographical memories represent personally experienced recollections and knowledge about oneself (Conway and Pleydell-Pearce, 2000 ) and may be key in understanding the accessibility and completeness of traumatic memories (McNally et al., 1994 ). Two experimental studies have shown that during the recollection of personal past events, individuals with PTSD tend to recall personal memories with very few details and very little specificity (McNally et al., 1994 , 1995 ). This “overgeneral memory” effect is thought to result from inadequate search of memory during retrieval, perhaps due to rumination, avoidance, and impairment in executive capacity (Williams et al., 2007 ). However, the difficulty with retrieving detailed personal information does not appear to be specific to traumatic memories but extends to neutral and positive events.
Research on the neural underpinnings emotion and memory suggests that the benefit of emotion on memory occurs in part via interactions between the amygdala and hippocampus. According to the modulation hypothesis , emotional events are remembered better than neutral events due to the amygdala's influence on other medial temporal lobe structures including the hippocampus (McGaugh et al., 1996 ). Support for the modulation hypothesis has been reported in humans using fMRI, showing greater activity in the amygdala and hippocampus for successfully remembered vs. forgotten emotional memories (Dolcos et al., 2004 ). However, a key question is whether medial temporal lobe structures interact in PTSD as the modulation hypothesis would predict. Whereas the majority of imaging studies have shown increased amygdala activity in PTSD (Pissiota et al., 2002 ; Shin et al., 2004a , 2005 ), studies of hippocampal activity have been mixed, showing either an increase (Shin et al., 2004b ; Thomaes et al., 2009 ) or decrease in PTSD (Bremner et al., 2003 ; Astur et al., 2006 ). To examine the role of the amygdala and hippocampus in emotional memory formation in PTSD, researchers have employed the subsequent memory paradigm, in which neural activity is measured at encoding for items that are probed for memory success after a delay. Differences in encoding activity for successfully remembered and forgotten material is evaluated to identify brain regions subserving successful memory operations (Paller and Wagner, 2002 ). Hayes et al. ( 2011 ) reported reduced amygdala and hippocampal activity during successful memory encoding of trauma-related material in patients with PTSD. In this study, patients with PTSD produced greater false alarms for trauma-specific negative information, suggesting that the reduced medial temporal lobe activity may underlie memory distortions. However, Brohawn et al. ( 2010 ) reported enhanced hippocampal activity in patients with PTSD during encoding of emotional items relative to controls and Dickie et al. ( 2008 ) reported greater activity in both the amygdala and hippocampus for remembered vs. forgotten stimuli (a control group was not included in this study and therefore comparisons were made within the PTSD group). Two major differences may explain the discrepant results among studies. In the latter two studies, there were no behavioral differences in memory performance between patients and controls or between emotional and neutral information, and general negative stimuli were used whereas Hayes and colleagues used trauma-specific combat stimuli in recent war veterans. Therefore, although these studies report mixed results, the findings may provide more support for the notion that false memory, and associated decreases in neural signal in the amygdala and hippocampus, is elicited primarily for trauma-specific information in PTSD.
In summary, the research findings of explicit memory performance in PTSD are decidedly complex. The evidence suggests that recall of gist-based negative information may be enhanced in PTSD, whereas information about specific details and contextual information appears to be diminished. This is consistent with the notion that cognitive resources may be preferentially allocated to process threat information at the expense of neutral or non-threat related information. An important consideration is whether memory alterations occur for all types of emotional information or only for trauma-specific information. Although there are mixed findings in this regard, overall there is stronger evidence that false memories are elicited mainly for trauma-specific information. Research regarding the neural correlates of memory in PTSD is still in its infancy, but the abnormalities observed in the amygdala and hippocampus suggests that the symptoms of PTSD are associated with disturbances in memory encoding and retrieval.
Fear conditioning
Pavlovian fear conditioning and extinction has been a fruitful model of fear memory in PTSD. Fear conditioning paradigms involve the repeated presentation of a neutral conditioned stimulus (CS) such as an auditory tone or a colored light, followed immediately by an aversive unconditioned stimulus (US) such as a finger shock. Extinction of the fear memory occurs when the CS is subsequently and repeatedly presented in the absence of the US. This experimental paradigm models a crucial aspect of emotion-cognition interactions in PTSD: individuals with PTSD repeatedly show elevated fear responses to trauma reminders, even when those reminders occur in a safe context (i.e., a film portraying combat). Some researchers see a parallel between this clinical phenomenon and a failure of fear extinction or fear extinction recall (e.g., Pitman, 1988 ).
Early in the PTSD fear conditioning and extinction literature, fear responsivity was quantified as physiological responses such as skin conductance responsivity and heart rate. In line with the enhanced effect of emotion on explicit declarative memory discussed above, physiological studies have demonstrated that, relative to controls, individuals with PTSD show evidence of enhanced fear conditioning (Orr et al., 2000 ). This may represent a pre-existing vulnerability. Severity of PTSD symptoms and the PTSD-linked personality trait of behavioral inhibition have been correlated with facilitated eyeblink conditioning (Myers et al., 2012 ). Furthermore, fear extinction studies have demonstrated impaired safety signal learning (Orr et al., 2000 ; Peri et al., 2000 ), a possible mechanism for the intractability of fear responses to reminders of a trauma decades past. A more recent study measuring skin conductance responses in identical twins discordant for Vietnam combat exposure provided evidence that deficits in fear extinction recall are an acquired characteristic of PTSD and not a familial risk factor (Milad et al., 2008 ).
In general, neuroimaging studies of healthy individuals have found activation of amygdala and dorsal anterior cingulate cortex (dACC) during fear conditioning, and activation of ventral medial prefrontal cortex (vmPFC) structures during fear extinction and extinction recall (reviewed in VanElzakker et al., 2012 ). The first imaging study of fear conditioning in PTSD compared a fear acquisition condition, in which a picture of a blue square was paired with shock, to a control condition, in which participants were shocked randomly without a CS, and found that women with childhood sexual abuse-related PTSD had greater dACC and left amygdala activation than healthy women with no history of abuse (Bremner et al., 2005 ). During extinction of the blue square-shock association, the PTSD group had less activation in vmPFC structures than the comparison group.
More recently, a series of studies compared fMRI responses between individuals with PTSD and trauma-exposed healthy control participants at each stage of a two-day fear conditioning and extinction paradigm. The authors reported that the PTSD group had increased amygdala responsivity to the UC (shock) relative to trauma-exposed control group (Linnman et al., 2011 ). During late conditioning and early extinction, after the CS had been associated with the US and still signaled threat, the PTSD group showed increased dACC activation, relative to the control group. Presentation of the CS during late extinction learning, when the CS should no longer have signaled danger, also led to relatively increased amygdala and dACC responses and relatively decreased vmPFC activation in the PTSD group. Furthermore, on the second day of the paradigm, during early extinction recall, the PTSD group showed vmPFC hypoactivation and dACC hyperactivation (Milad et al., 2009 ; Rougemont-Bücking et al., 2011 ) (Figure (Figure1 1 ).

Neural correlates of extinction recall in PTSD. During early extinction recall, participants with PTSD showed hypoactivation in bilateral ventromedial prefrontal cortex (vmPFC) and hippocampus and hyperactivation in dorsal anterior cingulate cortex (ACC) relative to the trauma-exposed normal control (TENC) group. CS + E = stimulus that was extinguished; CS + U = stimulus that was not extinguished. Adapted with permission from Figure 3; Milad et al. ( 2009 ).
These results provide a neurobiological basis to the characteristic unrelenting strength of trauma memories in PTSD patients (re-experiencing) and the mechanisms of associative learning between trauma and the environmental cues that later serve as triggers for intrusive memories. The simple fear conditioning model of PTSD does not explain aspects of the disorder such as emotional responses other than fear, neuroendocrine dysfunction, or many of the more complex cognitive deficits discussed elsewhere in this review. However, it has been a valuable model of PTSD in that the functional neurocircuitry abnormalities in this disorder point to enhanced conditioning responses during trauma, as well as deficits in fear extinction and extinction recall after the trauma has passed.
Implicit memory
Implicit memory refers to memory for encoded items that are not associated with conscious recollection. Perceptual priming is a type of implicit memory in which prior exposure to a stimulus leads to subsequent facilitated perception of this stimulus. Intrusive memories in PTSD are often triggered by sensory cues that individuals experienced right before or during their traumatic event. Thus, several studies have examined the hypothesis that there is enhanced perceptual priming for trauma-related cues. Early PTSD priming studies used word-stem completion tasks and either failed to find evidence that individuals with PTSD have enhanced priming for trauma-related words (McNally and Amir, 1996 ) or found only weak evidence (Amir et al., 1996 ). Using a more sensitive word-stem completion protocol, Michael et al. ( 2005 ) found that participants with assault-related PTSD showed preferential priming for assault-related words more than general threat or neutral words, relative to the control group who had experienced assault but did not have PTSD. However, there may be an important reason for the inconsistent findings in word-stem priming studies: words prime conceptual or semantic trauma reminders while the cues that trigger re-experiencing in PTSD tend to be perceptual or sensory. Therefore, perceptual stimuli such as pictures may be more appropriate priming stimuli than conceptual stimuli such as words.
A two-part study utilizing a blurred picture paradigm reported that individuals with PTSD and acute stress disorder (ASD) identified more blurred trauma-related pictures than blurred neutral pictures (see Figure Figure2), 2 ), and that this processing advantage for trauma-related pictures correlated positively with severity of PTSD symptoms, dissociative symptoms, and re-experiencing symptoms, as well as with self-reports of fear levels and perceptual processing during the actual traumatic experience (Kleim et al., 2012 ). A follow-up study of the individuals with ASD demonstrated that the initial processing advantage for trauma-related pictures predicted a diagnosis of PTSD 6 months post-trauma.

Performance on an implicit memory task (blurred picture paradigm). Patients with PTSD identified more trauma-related blurred images than neutral images. No difference between trauma-related and neutral pictures was observed for the No PTSD group. This figure was created from the data supplied in Table 3; Kleim et al. ( 2012 ).
Blurred picture paradigms have also been used to demonstrate enhanced perceptual priming in healthy, trauma-unexposed individuals for neutral pictures that were associated with violent stories, and an association between enhanced perceptual priming and trait dissociation (Ehlers et al., 2006 ; Michael and Ehlers, 2007 ). In addition, “re-experiencing” (operationalized as sensory memories imbued with a sense of immediacy) was associated with greater priming, and that re-experiencing was reduced by asking participants to write about the stories and relate them to their personal lives, which the authors argued was a model of elaboration of traumatic memories during clinical therapy. Future studies may replicate these findings in participants with PTSD.
In a recent fMRI study of trauma-unrelated emotional priming, Mazza et al. ( 2012 ) administered a subliminal affective priming task to 10 individuals with earthquake-related PTSD and to 10 healthy controls. In this task, the subliminal (150 ms) presentation of emotional faces was immediately followed by the supraliminal (1850 ms) presentation of neutral pictures (Chinese ideographs), which were later rated as pleasant or unpleasant. Individuals with PTSD were more likely than controls to rate the ideographs that followed negative facial expressions as negative, and less likely than controls to rate the ideographs that followed positive facial expressions as pleasant, suggesting a propensity in PTSD for priming of threat-related cues. Furthermore, during the contrast between negative facial expression primes and the baseline fixation dot, individuals with PTSD had significantly greater BOLD responses in left amygdala and right insular cortex, relative to controls.
In summary, some priming studies demonstrate enhanced perceptual priming for threat-associated cues in both individuals with PTSD and in healthy populations. The enhanced priming for threat cues may be associated with hyperactivity of amygdala and insular cortex in PTSD. Future studies should more systematically investigate differences in conceptual vs. perceptual priming. The propensity for enhanced perceptual priming of these cues, combined with the facilitated conditioning and attenuated fear extinction recall discussed previously, may be a powerful combination in both the etiology and maintenance of PTSD.
Attention and working memory
Attention bias.
In individuals with PTSD, trauma-related memories intrude into consciousness and are difficult to ignore. In addition, reminders of traumatic events can capture attention and evoke distress and anxiety. Some researchers have hypothesized that in PTSD, attention is involuntarily biased toward stimuli that are threatening, leading to a disruption of ongoing cognitive activities. Researchers have attempted to study attention biases in the laboratory using several different paradigms: the emotional Stroop (also known as the “modified Stroop”), the dot probe paradigm, and the emotional oddball paradigm.
In the emotional Stroop, researchers ask participants to view (on a computer screen or on printed cards) words of varying emotional salience and to name the color of the words while ignoring their meaning. The researchers record the time it takes for participants to name the colors of different types of words (e.g., trauma-related words, neutral words, positive words). Delays in color naming (i.e., Stroop interference) occur when the meaning of a particular category of words is closely related to the participants' psychopathology and thus attracts attention despite efforts to the contrary.
Several studies in the literature have reported increased response times for trauma-related words relative to neutral words (and/or other types of words) in individuals with PTSD compared to trauma-exposed comparison participants without PTSD (e.g., McNally et al., 1990 ; Foa et al., 1991 ; Cassiday et al., 1992 ; Thrasher et al., 1994 ; Bryant and Harvey, 1995 ; Kaspi et al., 1995 ; Vrana et al., 1995 ; Beck et al., 2001 ; El Khoury-Malhame et al., 2011a ). Furthermore, measures of trauma-related Stroop interference have been shown to positively correlate with PTSD symptom severity (McNally et al., 1990 ; Cassiday et al., 1992 ; Paunovic et al., 2002 ; Fleurkens et al., 2011 ). Stroop interference in PTSD appears to be specific to trauma-related material, although some studies have reported interference to other types of emotional stimuli (Litz et al., 1996 ; Paunovic et al., 2002 ). Increased interference for trauma-related words in PTSD may not occur outside of conscious awareness, as this effect has not been consistently demonstrated with masked stimulus presentations (McNally et al., 1996 ; Paunovic et al., 2002 ) but see also (Harvey et al., 1996 ). Importantly, however, some studies have failed to replicate the finding of greater interference for trauma-related words in PTSD (e.g., Freeman and Beck, 2000 ; Devineni et al., 2004 ; Wittekind et al., 2010 ) see also (Kimble et al., 2009 ).
Two functional neuroimaging studies have attempted to examine the brain circuits that may mediate emotional Stroop interference in PTSD (Shin et al., 2001 ; Bremner et al., 2004 ). Both studies reported that the rostral anterior cingulate cortex (rACC) was less activated during trauma-related vs. control Stroop conditions in individuals with PTSD compared to trauma-exposed individuals without PTSD. One of the studies also found greater activation in the dACC in PTSD during trauma-related vs. generally negative Stroop conditions (Shin et al., 2001 ). Rostral ACC activation may be required to effectively ignore the trauma-related information in the service of completing the color-naming (or word-counting) task at hand. When the rACC is not functioning normally, increased activation of the dACC may be required in order to facilitate task performance. Interpretation of these imaging findings within the framework of earlier behavioral findings in the literature is somewhat limited by the fact that response times in the neuroimaging studies were either not measured (Bremner et al., 2004 ) or did not show significant group differences (Shin et al., 2001 ) probably due to small sample sizes.
Although a useful tool for investigating the nature of intrusive cognitions in PTSD, the emotional Stroop is limited in that it cannot be used to determine whether individuals with PTSD have increased attentional engagement to trauma-related stimuli or delayed disengagement from them. The dot probe task (sometimes called the attentional deployment task, the visual probe task, or the probe detection task) represents an improvement over the Stroop task in that it can measure the direction of attentional bias (e.g., toward or away from trauma-related stimuli) as opposed to merely assessing the existence of interference, and can also use pictorial stimuli, reducing the need for semantic processing (MacLeod et al., 1986 ). In the dot probe task, two stimuli (e.g., one trauma-related and one neutral) are briefly shown on either side of a screen. The participant responds when a target probe then appears in the location previously occupied by one of the stimuli. Attentional bias toward trauma-related stimuli would result in faster reaction time during those trials in which the probe replaces the trauma-related stimulus.
Dot probe studies in PTSD have reported mixed findings. Some studies have found bias toward trauma or threat-related stimuli in PTSD (Bryant and Harvey, 1997 ; Dalgleish et al., 2001 , 2003 ; Fani et al., 2012 ), while others reported an association between PTSD and a bias away from trauma or threat (Pine et al., 2005 ; Fani et al., 2011 ). Still others have failed to find significant attentional bias differences between PTSD and two control groups, consisting of healthy individuals and a group of recent trauma survivors that included both individuals with and without ASD (Elsesser et al., 2004 , 2005 ).
A recent fMRI study of the dot probe task presented angry (threat-related) and happy and neutral (threat-unrelated) faces to female survivors of multiple traumas who either did or did not have PTSD (Fani et al., 2012 ). Within the PTSD group but not within the control group, bias toward threatening faces correlated positively with activation in the dACC and insula, as well as the parietal lobe, caudate and the medial frontal, precentral and parahippocampal gyri. However, there were no response time differences between the two groups, indicating no consistent bias toward or away from threat.
Time since trauma may be an important factor in these inconsistencies. There is evidence that, under immediate acute stress conditions, individuals under threat have a bias away from threat-related stimuli, which predicts later PTSD symptoms (Wald et al., 2011 ). One series of studies tested this explicitly, under unique circumstances. During the Israeli military operation against Gaza (Operation Cast Lead) Israeli civilians near the border experienced a predictable increase in danger from retaliatory rocket attacks. The immediacy of danger increased as a function of proximity to border areas, allowing for quantification of threat. Using a dot probe task adapted for Hebrew, researchers found that individuals under greatest imminent threat had an attentional bias away from threat-related words (e.g., DEAD) compared to neutral words (e.g., DATA) (Bar-Haim et al., 2010 ). Individuals who were more than 40 km from the border and not within rocket range showed attention bias toward threat-related words. PTSD and depression symptoms also increased as a function of threat, and state anxiety was highest among individuals who lived within 10 km of the border and thus had 15 s or less to seek shelter when they heard warning sirens. One year after the conflict, attentional bias away from threat during the acute stressor predicted PTSD symptoms (Wald et al., 2011 ). The process by which attentional bias away from threat during an acute stressor putatively transforms to attentional bias toward threat in PTSD may be related to the “rebound effect” discussed below in the section concerning thought suppression.
Attentional bias toward threat in PTSD could reflect either difficulty disengaging from threat-related stimuli or facilitated engagement of such stimuli. A study of healthy individuals that related attentional mechanisms to subclinical PTSD symptoms provided indirect evidence that attentional bias toward threat in PTSD reflects difficulty disengaging as opposed to facilitated engagement (Bardeen and Orcutt, 2011 ). Interestingly, difficulty disengaging from threatening stimuli has been associated with the 5-HTTLPR serotonin transporter gene polymorphism (Beevers et al., 2009 ). Children's 5-HTTLPR short allele significantly moderated the relationship between maternal criticism and the children's attentional bias for angry faces, but not happy or sad faces, in a dot probe task (Gibb et al., 2011 ). This same polymorphism may predict poor response to cognitive-behavioral therapy in PTSD (Bryant et al., 2010 ). Furthermore, an fMRI study of a related attentional task called the detection of target (DOT) paradigm demonstrated that amygdala activation in PTSD patients, but not in healthy controls, correlated with attentional bias toward threatening faces and words (El Khoury-Malhame et al., 2011b ). Future studies can better elucidate the relationships among time since trauma, serotonin function in the amygdala, and attentional processes in PTSD.
The emotional oddball paradigm has proved to be useful in demonstrating attention bias in PTSD. In this task, infrequent target stimuli are interspersed with frequent standard stimuli and infrequent distractor emotional stimuli. The task requires participants to inhibit their prepotent response to frequent standard and distractor stimuli in order to identify the target stimuli accurately. Patients with PTSD are impaired in identifying neutral targets, which may be a consequence of attention bias to distracting, potentially threat-related information (Pannu Hayes et al., 2009 ). Furthermore, event-related potential (ERP) studies have shown that during processing of threat stimuli, an enhanced P3 amplitude response is observed in patients with PTSD, which is thought to reflect heightened attention toward those stimuli (Attias et al., 1996 ; Stanford et al., 2001 ). More recently, fMRI studies using the emotional oddball paradigm demonstrated that PTSD symptomatology was associated with greater activity in the dorsolateral prefrontal cortex and vmPFC for threat stimuli (Pannu Hayes et al., 2009 ), accompanied by a reduction in dorsolateral prefrontal cortex activity for target, non-threat stimuli (Morey et al., 2008 ; Pannu Hayes et al., 2009 ). These studies provide a neural marker for threat bias in PTSD that is characterized by heightened activity in putative attention and emotion circuitry for potentially threatening information and dysfunction in attention circuitry during goal-relevant target identification.
Anticipation of an impending negative stimulus may influence attention allocation and subsequent cognitive performance. Researchers have examined whether women exposed to intimate partner violence show alterations in attention performance and neural circuitry while anticipating a negative visual stimulus (Simmons et al., 2008 ; Aupperle et al., 2012a ). One particular study with a large sample size (41 women with PTSD and 34 healthy controls) examined the neural correlates of negative and positive anticipation embedded within a continuous performance task (Aupperle et al., 2012a ). Results indicated that patients with PTSD showed greater activity in the insula and less activity in the dorsolateral prefrontal cortex than controls during anticipation of negative events. Furthermore, greater activity in the dorsolateral and ventrolateral prefrontal cortex was associated with better performance on an attention switching task (i.e., the Color–Word Interference Inhibition/Switching subtest of the Delis–Kaplan Executive Function System) and a digit symbol test. These intriguing results may suggest that engaging the lateral prefrontal cortex in the face of anticipatory threat supports cognitive performance, possibly through an inhibitory mechanism.
In summary, a majority of studies have found evidence for attentional bias effects in PTSD. Although the findings are mixed, there appears to be growing evidence that the attentional bias reflects difficulty disengaging from, rather than facilitated detection of, negative stimuli. Collectively, the brain regions consistently active during tasks of negative attention in PTSD include the dACC, amygdala, insula, with mixed findings of the vmPFC. The aforementioned regions have previously been associated with emotional reactivity, perhaps underlying privileged processing of negative images in PTSD.
Working memory
Working memory is often defined as the maintenance and manipulation of information in a temporary memory store (Baddeley, 1992 ). Importantly, working memory has a limited capacity, suggesting that individuals can track and work with a small amount of information at a given time. An implication of this limited capacity store is that interference from distracting stimuli can reduce an individual's ability to maintain goal-relevant information. The interference of distracting stimuli, such as intrusive thoughts and trauma memories seems to be a particular difficulty in PTSD and may underlie the hallmark symptom of difficulty with concentration. Working memory deficits in patients with PTSD have been demonstrated using both verbal and visual stimuli. Schweizer and Dalgleish ( 2011 ) reported poorer working memory performance in patients vs. trauma-exposed controls on a verbal sentence task, in which participants were instructed to remember words presented following trauma-related or neutral sentences. Consistent with the idea that trauma-related material is particularly disruptive to working memory performance, memory was worse for words presented after trauma vs. neutral sentences. Working memory difficulty was observed in both participants with a current diagnosis of PTSD and individuals with a lifetime history of PTSD.
Neuroimaging studies investigating the impact of emotional distraction on working memory have suggested that hyperactivity in an emotional processing network (including regions such as the amygdala, ventrolateral prefrontal cortex, and medial prefrontal cortex) and hypoactivity in a dorsal executive function processing network (including regions such as the dorsolateral prefrontal cortex and parietal cortex) underlies impaired maintenance of information in working memory as a result of emotional distraction (Dolcos and McCarthy, 2006 ). This model was supported in an fMRI studying examining working memory in PTSD. Morey et al. ( 2009 ) showed that patients with PTSD had poorer memory performance when both neutral and trauma-specific distracters were presented during the working memory delay in comparison to a trauma-exposed control group. Furthermore, this fMRI study showed disrupted activity in the dorsal executive function network during the working memory delay in PTSD that could explain the diminished performance. An interesting outcome of this study is that performance was disrupted for both trauma-specific and neutral distracters, perhaps providing evidence for generalized hypervigilance.
Decision-making and reward processing
Individuals make decisions in part based on motivational influences, weighing the rewards and costs that may result from each option. On one end of the spectrum, seeking immediate positive rewards is associated with the psychopathology of addiction disorders (Bechara et al., 2002 ) while on the other end of the spectrum, lack of reward seeking is associated with depressive disorders (Pizzagalli et al., 2008 ). In PTSD, numbing symptoms including loss of pleasure in activities and loss of the ability to experience positive emotions may suggest altered processing of positive rewards. Consistent with this notion, patients with PTSD are less satisfied with rewards than controls (Hopper et al., 2008 ) and expend less effort to obtain positive rewards (Elman etal., 2005 ). Thus, it follows that patients with PTSD may have altered decision-making capacity if the drive to achieve positive rewards is reduced.
Neuroimaging studies in healthy individuals have supported the notion of a putative reward circuit that includes the ventral striatum, ventral pallidum, orbital frontal cortex, and anterior cingulate. Two studies have examined the neural correlates of decision-making and reward in PTSD, both providing evidence for reduced capacity for positive reward in PTSD. Sailer et al. ( 2008 ) showed that the nucleus accumbens (part of the ventral striatum) was less active in patients with PTSD than controls during processing of positive gains. Behaviorally, patients with PTSD were slower in learning how to maximize their gains in a monetary gain/loss paradigm. Although speculative, it is possible that reduced reward processing in PTSD may have negatively influenced patients' motivation in learning the task. Similarly, PTSD patients showed reduced activity in the striatum during gains vs. losses of a monetary task in another study (Elman et al., 2009 ). Interestingly, striatal activity for gains vs. losses was negatively correlated with CAPS items “loss of interest in significant activities” and “feelings of detachment/estrangement.”
Cognitive control of emotion and treatment effects
When distressing events occur during the course of the lifespan, individuals often engage in various strategies to manage and cope with negative emotions. In doing so, they can change their emotional experience of the stimulus, and also change how the emotional stimulus affects their cognitive performance. Individuals can exercise control of emotion for the desired effect; they can engage in cognitive reappraisal to improve affect, or conversely, amplify negative affect (Dillon et al., 2007 ). Furthermore, cognitive control strategies can be used to improve memory performance (Hayes et al., 2010 ) or suppress unwanted memories (Depue et al., 2007 ). Such deliberate modulation of emotion serves to manage distractions in the face of otherwise debilitating affect and helps individuals to remain focused on goal-directed behaviors. In treating psychopathology, cognitive-behavioral interventions often instruct patients to exercise greater control of emotion through thought challenging exercises and promoting alternative ways of thinking about a negative situation (Resick and Schnicke, 1993 ). Preliminary evidence suggests that these types of interventions not only reduce symptoms, but also improve cognitive performance (Sutherland and Bryant, 2007 ).
In PTSD, experimental work investigating the cognitive control of emotion has examined whether patients can purposely forget negative information. Some researchers have suggested that patients with PTSD have an enhanced ability to forget information, which may explain amnesia for important details of their traumatic event. This idea, mainly evolving out of the child sexual abuse literature, suggests that repeat trauma survivors with PTSD cope during their trauma by dissociating from their surroundings and disengaging attention from the event, sometimes leading to amnesia for large stretches of time (Terr, 1991 ). This avoidant coping style may manifest in adulthood by increased ability to forget new information presented in an experimental setting (McNally et al., 1998 ). Alternatively, others have suggested that intrusive memories arise from the failure of inhibitory processes to curb distracting and aversive memories (Zwissler et al., 2011 ).
One frequently used paradigm to examine this issue is the directed forgetting task, which examines deliberate attempts to control memory performance. In this task, participants are instructed to either remember or forget words presented in a list. Subsequently, participants attempt to recall and/or recognize all the words that were presented in the list regardless of whether they were to-be-remembered or to-be-forgotten. The “standard directed forgetting effect” refers to the behavioral outcome showing greater remembering for items presented during the remember condition than the forget condition. The task is often adapted for study of PTSD by including general emotional or trauma-specific words. Two studies that examined directed forgetting of trauma-relevant information in PTSD failed to show between group differences among PTSD and control participants (McNally et al., 1998 ; Zoellner et al., 2003 ). However, these studies and others have demonstrated differences between groups for non-trauma emotional and/or neutral stimuli. Specifically, patients fail to show the standard directed forgetting effect either due to difficulty forgetting to-be-forgotten items (Zoellner et al., 2003 ; Cottencin et al., 2006 ) or decreased performance in the remember condition (McNally et al., 1998 ; Zwissler et al., 2011 ). Taken together, the directed forgetting literature provides little evidence that patients with PTSD adopt an avoidant coping style that results in enhanced forgetting of negative information. Rather, a general inhibitory control mechanism may be impaired evidenced by poorer performance for non-threat related items.
A separate literature has emerged examining the effects of actively suppressing one particular thought. Unlike directed forgetting paradigms, thought suppression is less concerned with recall and recognition memory performance but rather the frequency with which thoughts arise following instructions to suppress them. Wegner and colleagues demonstrated that when participants were instructed to initially suppress a thought, they went on to think about it to a greater extent than if they were initially allowed to let the thought enter consciousness, referred to as a “rebound effect” (Wegner et al., 1987 ). Two studies have shown that patients with PTSD have more trauma-related thoughts after a thought suppression period than trauma-exposed controls (Shipherd and Beck, 1999 , 2005 ) (see Figure Figure3). 3 ). In another study that instructed participants to suppress neutral information, combat veterans with PTSD had greater combat-trauma related intrusions during attempts to suppress thoughts about a “white bear” than combat veterans without PTSD (Aikins et al., 2009 ). These studies suggest that attempts at thought suppression might in fact be associated with greater frequency of trauma-related cognitions in PTSD.

Performance on a thought suppression task. (A) Patients with PTSD reported more trauma-related (i.e., motor vehicle accident, MVA) thoughts after engaging in thought suppression, showing a “rebound” effect. ( B ) Participants did not show a rebound effect for neutral thoughts. Reproduced with permission from Shipherd and Beck ( 2005 ).
Other forms of cognitive control include emotion regulation strategies, in which participants are instructed to change their natural response to a stimulus. Gross and colleagues have shown that individuals can engage in thought-change strategies, such as cognitive reappraisal, to deliberately reduce negative affect (Gross, 1998 ). Most studies examining emotion regulation in PTSD have used self-report measures to examine the frequency with which these different strategies are used and whether they are associated with greater or reduced frequency of trauma symptoms. However, there appears to be only one paper to date that has directly manipulated emotion regulation strategies in PTSD (New et al., 2009 ). This fMRI study compared sexual assault victims with and without PTSD on an emotion regulation task. Participants were shown negative photos and instructed to down-regulate their emotional response to the picture (diminish condition), enhance their negative response, or maintain their current response to the picture. Behavioral results showed that the healthy control group was able to diminish negative affect to a greater extent than the PTSD group whereas no group difference was observed in the enhance condition. Imaging results showed that the control group recruited greater prefrontal cortex activity across superior and middle frontal gyri for both the diminish and enhance conditions, which may suggest that controls engage in cognitive control to a greater extent than patients with PTSD.
Psychosocial treatment interventions may benefit patients by teaching them the cognitive control skills necessary to manage their symptoms, thereby reducing the detrimental effect of strong negative emotion on cognitive performance. Alternatively, drug therapies may directly affect neural circuitry and consequently blunt the effect of emotion on cognitive function. A few studies have examined the extent to which therapy improves cognitive function in PTSD. Although the evidence is limited, there is a small body of data that supports the effectiveness of therapy on normalizing cognitive function in certain domains in patients. Sutherland and Bryant ( 2007 ) reported improved autobiographical memory specificity in PTSD after treatment. Two studies have reported improved emotional Stroop performance in patients relative to controls after psychosocial intervention (El Khoury-Malhame et al., 2011a ; Thomaes et al., 2012 ). Finally, Putman et al. ( 2007 ) reported a reduction in color naming response times to masked fearful vs. neutral facial expressions after a 40 mg dose of hydrocortisone (vs. placebo) in highly anxious men. Although this study did not include individuals with PTSD, its findings seem to call for examining the effect of glucocorticoids on emotional Stroop interference in PTSD, especially given that the administration of glucocorticoids has been associated with symptomatic improvement (e.g., Surís et al., 2010 ) and a reduction of fear responses in this disorder (e.g., Jovanovic et al., 2011 ; Miller et al., 2011 ), but see also (Grossman et al., 2006 ). Other studies, however, have not found effects of treatment on emotional Stroop measures in PTSD (Devineni et al., 2004 ; Taylor et al., 2006 ). Clearly, additional research is necessary to examine what types of treatments may confer benefits in cognitive function to individuals with PTSD.
Summary and future directions
The literature summarized here provides strong support for the privileged processing of emotionally charged information in PTSD. A key question is whether emotional information facilitates or interferes with cognitive processing. In other words, does PTSD confer advantages in cognitive performance given that emotional stimuli are often processed with greater efficiency than neutral stimuli? Over the span of different study paradigms, there appears to be a trade-off in cognitive performance as cognitive models of PTSD predict; although fear learning, perceptual priming, and recall memory for negative items are sometimes enhanced in PTSD, this advantage comes at the expense of processing other types of information. For example, task-irrelevant emotional information slows processing of goal-directed activity and interferes with memory and learning of neutral information. Furthermore, extinction learning and learning of safety cues is often impaired, memory for specific, detailed information is often poor, and patients with PTSD may be more prone to falsely remembering novel information. Deficits in cognitive control and emotion regulation may be exacerbated by the impact of emotion on cognitive function.
Neuroimaging studies have uncovered several key brain regions that may underlie the emotional bias effects observed in PTSD. Across studies, activity appears to be altered in the anterior cingulate cortex, vmPFC, amygdala, hippocampus, insula, and lateral prefrontal cortex. Findings from quantitative meta-analyses of the neural correlates of PTSD have confirmed the importance of these regions in PTSD (Etkin and Wager, 2007 ; Hayes et al., 2012 ; Simmons and Matthews, 2012 ). A recent meta-analysis of imaging studies in PTSD showed that the amygdala and mid-ACC is hyperactive, whereas lateral and medial prefrontal cortex is hypoactive in PTSD for negative emotional stimuli vs. neutral and positive stimuli (Figure (Figure4). 4 ). A neurocircuitry model of PTSD posits that dysfunction of the vmPFC prefrontal cortex results in failure to inhibit an overactive amygdala, leading to an exaggerated fear response and impaired fear extinction learning (Rauch et al., 2006 ). Hippocampal dysfunction may be related to impairment in processing contextual information (Rauch et al., 2006 ; Hayes et al., 2011 ). The dACC, anterior insula, and amygdala, among other regions, comprise a putative “salience network” that processes information of personal relevance and is hyperresponsive in individuals with anxiety (Seeley et al., 2007 ). Researchers have posited that, in PTSD, hyperresponsivity of salience network regions and hyporesponsivity in putative regions important for cognitive control and working memory underlie greater distribution of processing resources in favor of potentially threatening stimuli even when neutral information is goal-relevant (Morey et al., 2009 ; Pannu Hayes et al., 2009 ; Hayes et al., 2012 ).

Meta-analysis of functional neuroimaging studies in PTSD. Across various task designs, the amygdala and mid-ACC are hyperactive in PTSD whereas the lateral and medial prefrontal cortex are hypoactive for negative emotional stimuli vs. neutral and positive stimuli. Areas of hyperactivation in PTSD (PTSD > Control) are shown in yellow and areas of hypoactivation in PTSD (Control > PTSD) are shown in blue. AMY = amygdala, IFG = inferior frontal gyrus, L = left, mid-ACC = mid anterior cingulate cortex, R = right, vmPFC = ventromedial prefrontal cortex. Reproduced from Hayes et al. ( 2012 ).
As reviewed in this paper, our understanding of emotion-cognition interactions in PTSD has progressed tremendously over the last two decades and neuroimaging research has identified pathways involved in the effect of emotion on cognition. However, a number of key questions need to be further examined to gain a better understanding of how emotion affects cognitive function in PTSD. An important consideration is the extent to which individual differences and moderating factors impact the development of PTSD. There is some evidence that deficits in configural cue processing and lower IQ precede the development of PTSD (Gilbertson et al., 2007 ; Vasterling et al., 2002 ). Further research is necessary to determine whether impairment in other cognitive processes precede trauma exposure and, conversely, the extent to which cognitive control and emotion regulation capacity prior to trauma exposure can offer resilience.
Currently, little is known regarding the neurobiology of cognitive control in PTSD. Surprisingly few studies have examined the neural correlates of deliberate attempts to control emotions. As reviewed above, there is presently only one neuroimaging study investigating emotion regulation in PTSD (New et al., 2009 ). This area needs to be developed to further examine whether impairment in the cognitive control of emotions is a PTSD symptom-maintaining factor and whether neural abnormalities during top-down regulation of emotion represents a useful biomarker for the diagnosis of PTSD. Moreover, further examination of the interplay between medial temporal lobe structures and the prefrontal cortex is necessary to better understand control processes during emotional memory encoding and retrieval. In healthy individuals, prefrontal cortex activity is associated with deep semantic encoding that supports improved recall of emotional memories (Ritchey et al., 2011 ), as well as suppression of aversive memories that reduces recall (Depue et al., 2007 ). However, less is known regarding the extent to which patients with PTSD can engage critical prefrontal cortex regions to influence the memorability of emotional stimuli.
Another emerging area of research is using drug therapies to manipulate emotion-cognition interactions. Norepinephrine has been shown to enhance emotional memory whereas adrenergic receptor blockers such as propranolol compromise the enhancing effect that emotional arousal has on memory (Cahill et al., 1994 ). Cerebrospinal norepinephrine levels are elevated in chronic PTSD (Geracioti et al., 2001 ) and research regarding the effectiveness of adrenergic blockers in preventing PTSD is underway. Although preliminary results have not yielded strong evidence to recommend the use of propronolol for the prevention of PTSD (Pitman et al., 2002 ; Vaiva et al., 2003 ; Hoge et al., 2012 ), further research is necessary to determine the precise time window in which such drug therapies may be useful (Cain et al., 2012 ). Furthermore, additional research is required to examine whether these drugs impact specific types of memory (e.g., explicit vs. implicit memory, autobiographical vs. memory for general negative events, central vs. peripheral details).
Finally, a very important area that is understudied is the commonalities or specificity of cognitive alterations in PTSD vs. other comorbidities such as depression, traumatic brain injury, and attention deficit and hyperactivity disorder. In many cases, cognitive abnormalities are observed across different mood and anxiety disorders. For example, overgeneral autobiographical memory is also a characteristic of individuals diagnosed with depression. Although many studies of PTSD focus on the fear and anxiety based symptoms such as hypervigilance, it is possible that many of these cognitive deficits are related to the dysphoria and maladaptive appraisals that are often observed in PTSD. In fact, in recognition of these common symptoms, the proposed changes to the current diagnosis of PTSD for DSM-V may add a fourth symptom cluster of “negative alterations in cognitions and mood” (Friedman et al., 2011 ). Furthermore, a movement toward dimensional classification of symptoms that are shared among disorders is gaining momentum (Ofrat and Krueger, 2012 ). It is therefore important to understand the similarities and differences in emotion-cognition interactions between PTSD and other comorbidities to better determine the origin of and potential treatments for PTSD.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors were supported by grants from the National Institute of Mental Health (K23 MH084013 awarded to Jasmeet P. Hayes and 5R01MH054636 awarded to Lisa M. Shin) and a National Defense Science and Engineering Graduate Fellowship (awarded to Michael B. VanElzakker). These funding sources had no further role in the interpretation of the findings, writing of the paper, or approval of the paper.
- Aikins D. E., Johnson D. C., Borelli J. L., Klemanski D. H., Morrissey P. M., Benham T. L., et al. (2009). Thought suppression failures in combat PTSD: a cognitive load hypothesis . Behav. Res. Ther . 47 , 744–751 10.1016/j.brat.2009.06.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders . 4th Edn Text Revision. Washington DC: American Psychiatric Association [ Google Scholar ]
- Amir N., McNally R. J., Wiegartz P. S. (1996). Implicit memory bias for threat in post-traumatic stress disorder . Cognit. Ther. Res . 20 , 625–635 [ Google Scholar ]
- Astur R. S., St Germain S. A., Tolin D., Ford J., Russell D., Stevens M. (2006). Hippocampus function predicts severity of post-traumatic stress disorder . Cyberpsychol. Behav . 9 , 234–240 10.1089/cpb.2006.9.234 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Attias J., Bleich A., Furman V., Zinger Y. (1996). Event-related potentials in post-traumatic stress disorder of combat origin . Biol. Psychiatry 40 , 373–381 10.1016/0006-3223(95)00419-X [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aupperle R. L., Allard C. B., Grimes E. M., Simmons A. N., Flagan T., Behrooznia M., et al. (2012a). Dorsolateral prefrontal cortex activation during emotional anticipation and neuropsychological performance in posttraumatic stress disorder . Arch. Gen. Psychiatry 69 , 360–371 10.1001/archgenpsychiatry.2011.1539 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aupperle R. L., Melrose A. J., Stein M. B., Paulus M. P. (2012b). Executive function and PTSD: disengaging from trauma . Neuropharmacology 62 , 686–694 10.1016/j.neuropharm.2011.02.008 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baddeley A. (1992). Working memory . Science 255 , 556–559 10.1126/science.1736359 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bardeen J. R., Orcutt H. K. (2011). Attentional control as a moderator of the relationship between posttraumatic stress symptoms and attentional threat bias . J. Anxiety Disord . 25 , 1008–1018 10.1016/j.janxdis.2011.06.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bar-Haim Y., Holoshitz Y., Eldar S., Frenkel T. I., Muller D., Charney D. S., et al. (2010). Life-threatening danger and suppression of attention bias to threat . Am. J. Psychiatry 167 , 694–698 10.1176/appi.ajp.2009.09070956 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bechara A., Dolan S., Hindes A. (2002). Decision-making and addiction (part II): myopia for the future or hypersensitivity to reward? Neuropsychologia 40 , 1690–1705 10.1016/j.bandc.2007.05.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beck J. G., Freeman J. B., Shipherd J. C., Hamblen J. L., Lackner J. M. (2001). Specificity of Stroop interference in patients with pain and PTSD . J. Abnorm. Psychol . 110 , 536–543 [ PubMed ] [ Google Scholar ]
- Beevers C. G., Wells T. T., Ellis A. J., McGeary J. E. (2009). Association of the serotonin transporter gene promoter region (5-HTTLPR) polymorphism with biased attention for emotional stimuli . J. Abnorm. Psychol . 118 , 670–681 10.1037/a0016198 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boscarino J. (2008). A prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: implications for surveillance and prevention . Psychosom. Med . 70 , 668–676 10.1097/PSY.0b013e31817bccaf [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brainerd C., Reyna V. (2002). Fuzzy-trace theory and false memory . Curr. Dir. Psychol. Sci . 11 , 164 10.1006/jecp.1998.2472 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bremner J. D., Shobe K. K., Kihlstrom J. F. (2000). False memories in women with self-reported childhood sexual abuse: an empirical study . Psychol. Sci . 11 , 333–337 [ PubMed ] [ Google Scholar ]
- Bremner J. D., Vermetten E., Schmahl C., Vaccarino V., Vythilingam M., Afzal N., et al. (2005). Positron emission tomographic imaging of neural correlates of a fear acquisition and extinction paradigm in women with childhood sexual-abuse-related post-traumatic stress disorder . Psychol. Med . 35 , 791–806 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bremner J. D., Vermetter E., Vythilingam M., Afzal N., Schmahl C., Elzinga B., et al. (2004). Neural correlates of the classic color and emotional stroop in women with abuse-related posttraumatic stress disorder . Biol. Psychiatry 55 , 612–620 10.1016/j.biopsych.2003.10.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bremner J. D., Vythilingam M., Vermetten E., Southwick S. M., McGlashan T., Staib L. H., et al. (2003). Neural correlates of declarative memory for emotionally valenced words in women with posttraumatic stress disorder related to early childhood sexual abuse . Biol. Psychiatry 53 , 879–889 10.1016/S0006-3223(02)01891-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brennen T., Dybdahl R., Kapidzic A. (2007). Trauma-related and neutral false memories in war-induced posttraumatic stress disorder . Conscious. Cogn . 16 , 877–885 10.1016/j.concog.2006.06.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brohawn K. H., Offringa R., Pfaff D. L., Hughes K. C., Shin L. M. (2010). The neural correlates of emotional memory in posttraumatic stress disorder . Biol. Psychiatry 68 , 1023–1030 10.1016/j.biopsych.2010.07.018 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bryant R. A., Felmingham K. L., Falconer E. M., Pe Benito L., Dobson-Stone C., Pierce K. D., et al. (2010). Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder . Biol. Psychiatry 67 , 1217–1219 10.1016/j.biopsych.2010.03.016 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bryant R. A., Harvey A. G. (1995). Processing threatening information in posttraumatic stress disorder . J. Abnorm. Psychol . 104 , 537–541 [ PubMed ] [ Google Scholar ]
- Bryant R. A., Harvey A. G. (1997). Attentional bias in posttraumatic stress disorder . J. Trauma. Stress 10 , 635–644 [ PubMed ] [ Google Scholar ]
- Cahill L., Prins B., Weber M., McGaugh J. L. (1994). Beta-adrenergic activation and memory for emotional events . Nature 371 , 702–704 10.1038/371702a0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cain C. K., Maynard G. D., Kehne J. H. (2012). Targeting memory processes with drugs to prevent or cure PTSD . Expert Opin. Investig. Drugs 21 , 1323–1350 10.1517/13543784.2012.704020 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cassiday K. L., McNally R. J., Zeitlin S. B. (1992). Cognitive processing of trauma cues in rape victims with post-traumatic stress disorder . Cognit. Ther. Res . 16 , 283–295 [ Google Scholar ]
- Chemtob C., Roitblat H. L., Hamada R. S., Carlson J. G., Twentyman C. T. (1988). A cognitive action theory of post-traumatic stress disorder . J. Anxiety Disord . 2 , 253–275 [ Google Scholar ]
- Chemtob C. M., Roitblat H. L., Hamada R. S., Muraoka M. Y., Carlson J. G., Bauer G. B. (1999). Compelled attention: the effects of viewing trauma-related stimuli on concurrent task performance in posttraumatic stress disorder . J. Trauma. Stress 12 , 309–326 10.1023/A:1024728626505 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Christianson S. A. (1992). Emotional stress and eyewitness memory: a critical review . Psychol. Bull . 112 , 284–309 [ PubMed ] [ Google Scholar ]
- Christianson S. Ã., Loftus E. F. (1991). Remembering emotional events: the fate of detailed information . Cogn. Emot . 5 , 81–108 [ Google Scholar ]
- Conway M. A., Pleydell-Pearce C. W. (2000). The construction of autobiographical memories in the self-memory system . Psychol. Rev . 107 , 261–288 [ PubMed ] [ Google Scholar ]
- Cottencin O., Vaiva G., Huron C., Devos P., Ducrocq F., Jouvent R., et al. (2006). Directed forgetting in PTSD: a comparative study versus normal controls . J. Psychiatr. Res . 40 , 70–80 10.1016/j.jpsychires.2005.04.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dalgleish T., Moradi A. R., Taghavi M. R., Neshat-Doost H. T., Yule W. (2001). An experimental investigation of hypervigilance for threat in children and adolescents with post-traumatic stress disorder . Psychol. Med . 31 , 541–547 [ PubMed ] [ Google Scholar ]
- Dalgleish T., Taghavi R., Neshat-Doost H., Moradi A., Canterbury R., Yule W. (2003). Patterns of processing bias for emotional information across clinical disorders: a comparison of attention, memory, and prospective cognition in children and adolescents with depression, generalized anxiety, and posttraumatic stress disorder . J. Clin. Child Adolesc . 32 , 10–21 10.1207/S15374424JCCP3201_02 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Daniels J. K., Bluhm R. L., Lanius R. A. (2012). Intrinsic network abnormalities in posttraumatic stress disorder: research directions for the next decade . Psychol. Trauma . [Epub ahead of print]. 10.1037/a0026946 [ CrossRef ] [ Google Scholar ]
- Depue B., Curran T., Banich M. (2007). Prefrontal regions orchestrate suppression of emotional memories via a two-phase process . Science 317 , 215–219 10.1126/science.1139560 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Devineni T., Blanchard E. B., Hickling E. J., Buckley T. C. (2004). Effect of psychological treatment on cognitive bias in motor vehicle accident-related posttraumatic stress disorder . J. Anxiety Disord . 18 , 211–231 10.1016/S0887-6185(02)00247-5 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dickie E., Brunet A., Akerib V., Armony J. (2008). An fMRI investigation of memory encoding in PTSD: influence of symptom severity . Neuropsychologia 46 , 1522–1531 10.1016/j.neuropsychologia.2008.01.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dillon D. G., Ritchey M., Johnson B. D., LaBar K. S. (2007). Dissociable effects of conscious emotion regulation strategies on explicit and implicit memory . Emotion 7 , 354–365 10.1037/1528-3542.7.2.354 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dobie D., Kivlahan D., Maynard C., Bush K., Davis T., Bradley K. (2004). Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment . Arch. Intern. Med . 164 , 394–400 10.1001/archinte.164.4.394 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dohrenwend B., Turner J., Turse N., Adams B., Koenen K., Marshall R. (2006). The psychological risks of Vietnam for US veterans: a revisit with new data and methods . Science 313 , 979 10.1126/science.1128944 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dolcos F., Iordan A. D., Dolcos S. (2011). Neural correlates of emotion-cognition interactions: a review of evidence from brain imaging investigations . J. Cogn. Psychol . 23 , 669–694 10.1080/20445911.2011.594433 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dolcos F., LaBar K. S., Cabeza R. (2004). Interaction between the amygdala and the medial temporal lobe memory system predicts better memory for emotional events . Neuron 42 , 855–863 10.1016/S0896-6273(04)00289-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dolcos F., McCarthy G. (2006). Brain systems mediating cognitive interference by emotional distraction . J. Neurosci . 26 , 2072–2079 10.1523/JNEUROSCI.5042-05.2006 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Easterbrook J. A. (1959). The effect of emotion on cue utilization and the organization of behavior . Psychol. Rev . 66 , 183–201 [ PubMed ] [ Google Scholar ]
- Ehlers A., Michael T., Chen Y. P., Payne E., Shan S. (2006). Enhanced perceptual priming for neutral stimuli in a traumatic context: a pathway to intrusive memories? Memory 14 , 316–328 10.1080/09658210500305876 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- El Khoury-Malhame M., Lanteaume L., Beetz E. M., Roques J., Reynaud E., Samuelian J. C., et al. (2011a). Attentional bias in post-traumatic stress disorder diminishes after symptom amelioration . Behav. Res. Ther . 49 , 796–801 10.1016/j.brat.2011.08.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- El Khoury-Malhame M., Reynaud E., Soriano A., Michael K., Salgado-Pineda P., Zendjidjian X., et al. (2011b). Amygdala activity correlates with attentional bias in PTSD . Neuropsychologia 49 , 1969–1973 10.1016/j.neuropsychologia.2011.03.025 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elman I., Ariely D., Mazar N., Aharon I., Lasko N. B., Macklin M. L., et al. (2005). Probing reward function in post-traumatic stress disorder with beautiful facial images . Psychiatry Res . 135 , 179–183 10.1016/j.psychres.2005.04.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elman I., Lowen S., Frederick B. B., Chi W., Becerra L., Pitman R. K. (2009). Functional neuroimaging of reward circuitry responsivity to monetary gains and losses in posttraumatic stress disorder . Biol. Psychiatry 66 , 1083–1090 10.1016/j.biopsych.2009.06.006 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elsesser K., Sartory G., Tackenberg A. (2004). Attention, heart rate, and startle response during exposure to trauma-relevant pictures: a comparison of recent trauma victims and patients with posttraumatic stress disorder . J. Abnorm. Psychol . 113 , 289–301 10.1037/0021-843X.113.2.289 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elsesser K., Sartory G., Tackenberg A. (2005). Initial symptoms and reactions to trauma-related stimuli and the development of posttraumatic stress disorder . Depress. Anxiety 21 , 61–70 10.1002/da.20047 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Engdahl B., Leuthold A. C., Tan H. R., Lewis S. M., Winskowski A. M., Dikel T. N., et al. (2010). Post-traumatic stress disorder: a right temporal lobe syndrome? J. Neural Eng . 7 , 066005 10.1088/1741-2560/7/6/066005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Etkin A., Wager T. D. (2007). Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia . Am. J. Psychiatry 164 , 1476–1488 10.1176/appi.ajp.2007.07030504 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fani N., Bradley-Davino B., Ressler K. J., McClure-Tone E. B. (2011). Attention bias in adult survivors of childhood maltreatment with and without posttraumatic stress disorder . Cognit. Ther. Res . 35 , 57–67 [ Google Scholar ]
- Fani N., Tone E. B., Phifer J., Norrholm S. D., Bradley B., Ressler K. J., et al. (2012). Attention bias toward threat is associated with exaggerated fear expression and impaired extinction in PTSD . Psychol. Med . 42 , 533–543 10.1017/S0033291711001565 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ferry B., Roozendaal B., McGaugh J. L. (1999). Role of norepinephrine in mediating stress hormone regulation of long-term memory storage: a critical involvement of the amygdala . Biol. Psychiatry 46 , 1140–1152 10.1016/S0006-3223(99)00157-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fleurkens P., Rinck M., van Minnen A. (2011). Specificity and generalization of attentional bias in sexual trauma victims suffering from posttraumatic stress disorder . J. Anxiety Disord . 25 , 783–787 10.1016/j.janxdis.2011.03.014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Foa E. B., Feske U., Murdock T. B., Kozak M. J., McCarthy P. R. (1991). Processing of threat-related information in rape victims . J. Abnorm. Psychol . 100 , 156–162 [ PubMed ] [ Google Scholar ]
- Foa E. B., Kozak M. J. (1986). Emotional processing of fear: exposure to corrective information . Psychol. Bull . 99 , 20–35 [ PubMed ] [ Google Scholar ]
- Freeman J. B., Beck J. G. (2000). Cognitive interference for trauma cues in sexually abused adolescent girls with posttraumatic stress disorder . J. Clin. Child Psychol . 29 , 245–256 10.1207/S15374424jccp2902_10 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Friedman M. J., Resick P. A., Bryant R. A., Brewin C. R. (2011). Considering PTSD for DSM 5 . Depress. Anxiety 28 , 750–769 10.1002/da.20767 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Georgopoulos A. P., Tan H. R., Lewis S. M., Leuthold A. C., Winskowski A. M., Lynch J. K., et al. (2010). The synchronous neural interactions test as a functional neuromarker for post-traumatic stress disorder (PTSD): a robust classification method based on the bootstrap . J. Neural Eng . 7 , 016011 10.1088/1741-2560/7/1/016011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Geracioti T., Jr., Baker D., Ekhator N., West S., Hill K., Bruce A., et al. (2001). CSF norepinephrine concentrations in posttraumatic stress disorder . Am. J. Psychiatry 158 , 1227–1230 10.1176/appi.ajp.158.8.1227 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gibb B. E., Johnson A. L., Benas J. S., Uhrlass D. J., Knopik V. S., McGeary J. E. (2011). Children's 5-HTTLPR genotype moderates the link between maternal criticism and attentional biases specifically for facial displays of anger . Cogn. Emot . 25 , 1104–1120 10.1080/02699931.2010.508267 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gilbertson M., Williston S., Paulus L., Lasko N., Gurvits T., Shenton M., et al. (2007). Configural cue performance in identical twins discordant for posttraumatic stress disorder: theoretical implications for the role of hippocampal function . Biol. Psychiatry 62 , 513–520 10.1016/j.biopsych.2006.12.023 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Golier J. A., Yehuda R., Lupien S. J., Harvey P. D., Grossman R., Elkin A. (2002). Memory performance in Holocaust survivors with posttraumatic stress disorder . Am. J. Psychiatry 159 , 1682–1688 10.1176/appi.ajp.159.10.1682 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gross J. J. (1998). Antecedent and response-focused emotion regulation: divergent consequences for experience, expression, and physiology . J. Pers. Soc. Psychol . 74 , 224–237 [ PubMed ] [ Google Scholar ]
- Grossman R., Yehuda R., Golier J., McEwen B., Harvey P., Maria N. S. (2006). Cognitive effects of intravenous hydrocortisone in subjects with PTSD and healthy control subjects . Ann. N.Y. Acad. Sci . 1071 , 410–421 10.1196/annals.1364.032 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Harvey A. G., Bryant R. A., Rapee R. M. (1996). Preconscious processing of threat in posttraumatic stress disorder . Cognit. Ther. Res . 20 , 613–623 [ Google Scholar ]
- Hayes J. P., Hayes S. M., Mikedis A. M. (2012). Quantitative meta-analysis of neural activity in posttraumatic stress disorder . Biol. Mood Anxiety Disord . 2 , 9 10.1186/2045-5380-2-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hayes J. P., LaBar K. S., McCarthy G., Selgrade E., Nasser J., Dolcos F., et al. (2011). Reduced hippocampal and amygdala activity predicts memory distortions for trauma reminders in combat-related PTSD . J. Psychiatr. Res . 45 , 660–669 10.1016/j.jpsychires.2010.10.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hayes J. P., Morey R. A., Petty C. M., Seth S., Smoski M. J., McCarthy G., et al. (2010). Staying cool when things get hot: emotion regulation modulates neural mechanisms of memory encoding . Front. Hum. Neurosci . 4 : 230 10.3389/fnhum.2010.00230 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoge C., Terhakopian A., Castro C., Messer S., Engel C. (2007). Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans . Am. J. Psychiatry 164 , 150–153 10.1176/appi.ajp.164.1.150 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoge C. W., Castro C. A., Messer S. C., McGurk D., Cotting D. I., Koffman R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care . N. Engl. J. Med . 351 , 13–22 10.1056/NEJMoa040603 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoge E. A., Worthington J. J., Nagurney J. T., Chang Y., Kay E. B., Feterowski C. M., et al. (2012). Effect of acute posttrauma propranolol on PTSD outcome and physiological responses during script-driven imagery . CNS Neurosci. Ther . 18 , 21–27 10.1111/j.1755-5949.2010.00227.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hopper J. W., Pitman R. K., Su Z., Heyman G. M., Lasko N. B., Macklin M. L., et al. (2008). Probing reward function in posttraumatic stress disorder: expectancy and satisfaction with monetary gains and losses . J. Psychiatr. Res . 42 , 802–807 10.1016/j.jpsychires.2007.10.008 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jovanovic T., Phifer J. E., Sicking K., Weiss T., Norrholm S. D., Bradley B., et al. (2011). Cortisol suppression by dexamethasone reduces exaggerated fear responses in posttraumatic stress disorder . Psychoneuroendocrino 36 , 1540–1552 10.1016/j.psyneuen.2011.04.008 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaspi S. P., McNally R. J., Amir N. (1995). Cognitive processing of emotional information in posttraumatic stress disorder . Cognit. Ther. Res . 19 , 433–444 [ Google Scholar ]
- Kensinger E. A. (2007). Negative emotion enhances memory accuracy . Curr. Dir. Psychol. Sci . 16 , 213 10.1162/jocn.2007.19.11.1872 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kessler R. C., Sonnega A., Bromet E., Hughes M., Nelson C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey . Arch. Gen. Psychiatry 52 , 1048–1060 10.1001/archpsyc.1995.03950240066012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kimble M., Frueh B. C., Marks L. (2009). Does the modified Stroop effect exist in PTSD? Evidence from dissertation abstracts and the peer reviewed literature . J. Anxiety Disord . 23 , 650–655 10.1016/j.janxdis.2009.02.002 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kleim B., Ehring T., Ehlers A. (2012). Perceptual processing advantages for trauma-related visual cues in post-traumatic stress disorder . Psychol. Med . 42 , 173–181 10.1017/S0033291711001048 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lang P. J. (1977). Physiological assessment of anxiety and fear , in Behavioral Assessment: New Directions in Clinical Psychology , eds Cone J. D., Hawkins R. P. (New York, NY: Brunner/Mazel; ), 178–195 [ Google Scholar ]
- Linnman C., Zeffiro T. A., Pitman R. K., Milad M. R. (2011). An fMRI study of unconditioned responses in post-traumatic stress disorder . Biol. Mood Anxiety Disord . 1 , 8 10.1186/2045-5380-1-8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Litz B. T., Weathers F. W., Monaco V., Herman D. S., Wulfsohn M., Marx B., et al. (1996). Attention, arousal, and memory in posttraumatic stress disorder . J. Trauma. Stress 9 , 497–520 [ PubMed ] [ Google Scholar ]
- MacLeod C., Mathews A., Tata P. (1986). Attentional bias in emotional disorders . J. Abnorm. Psychol . 95 , 15–20 [ PubMed ] [ Google Scholar ]
- Mazza M., Catalucci A., Mariano M., Pino M. C., Tripaldi S., Roncone R., et al. (2012). Neural correlates of automatic perceptual sensitivity to facial affect in posttraumatic stress disorder subjects who survived L'Aquila earthquake of April 6, 2009 . Brain Imaging Behav . 6 , 374–386 10.1007/s11682-012-9151-x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McGaugh J. L., Cahill L., Roozendaal B. (1996). Involvement of the amygdala in memory storage: interaction with other brain systems . Proc. Natl. Acad. Sci. U.S.A . 93 , 13508–13514 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McNally R. J., Amir N. (1996). Perceptual implicit memory for trauma-related information in post-traumatic stress disorder . Cogn. Emot . 10 , 551–556 [ Google Scholar ]
- McNally R. J., Amir N., Lipke H. J. (1996). Subliminal processing of threat cues in posttraumatic stress disorder? J. Anxiety Disord . 10 , 115–128 [ Google Scholar ]
- McNally R. J., Kaspi S. P., Riemann B. C., Zeitlin S. B. (1990). Selective processing of threat cues in posttraumatic stress disorder . J. Abnorm. Psychol . 99 , 398–402 [ PubMed ] [ Google Scholar ]
- McNally R. J., Lasko N. B., Macklin M. L., Pitman R. K. (1995). Autobiographical memory disturbance in combat-related posttraumatic stress disorder . Behav. Res. Ther . 33 , 619–630 10.1016/0005-7967(95)00007-K [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McNally R. J., Litz B. T., Prassas A., Shin L. M., Weathers F. W. (1994). Emotional priming of autobiographical memory in post-traumatic stress disorder . Cogn. Emot . 8 , 351–367 [ Google Scholar ]
- McNally R. J., Metzger L. J., Lasko N. B., Clancy S. A., Pitman R. K. (1998). Directed forgetting of trauma cues in adult survivors of childhood sexual abuse with and without posttraumatic stress disorder . J. Abnorm. Psychol . 107 , 596–601 [ PubMed ] [ Google Scholar ]
- Michael T., Ehlers A. (2007). Enhanced perceptual priming for neutral stimuli occurring in a traumatic context: two experimental investigations . Behav. Res. Ther . 45 , 341–358 10.1016/j.brat.2006.03.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Michael T., Ehlers A., Halligan S. L. (2005). Enhanced priming for trauma-related material in posttraumatic stress disorder . Emotion 5 , 103–112 10.1037/1528-3542.5.1.103 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mickley Steinmetz K. R., Scott L. A., Smith D., Kensinger E. A. (2012). The effects of trauma exposure and posttraumatic stress disorder (PTSD) on the emotion-induced memory trade-off . Front. Integr. Neurosci . 6 : 34 10.3389/fnint.2012.00034 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Milad M. R., Gold A. L., Shin L. M., Handwerger K., Lasko N., Orr S. P., et al. (2008). Neuroimaging correlates of impaired extinction memory in PTSD . Biol. Psychiatry 63 , 178S. [ Google Scholar ]
- Milad M. R., Pitman R. K., Ellis C. B., Gold A. L., Shin L. M., Lasko N. B., et al. (2009). Neurobiological basis of failure to recall extinction memory in posttraumatic stress disorder . Biol. Psychiatry 66 , 1075–1082 10.1016/j.biopsych.2009.06.026 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miller M. W., McKinney A. E., Kanter F. S., Korte K. J., Lovallo W. R. (2011). Hydrocortisone suppression of the fear-potentiated startle response and posttraumatic stress disorder . Psychoneuroendocrino 36 , 970–980 10.1016/j.psyneuen.2010.12.009 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morey R. A., Dolcos F., Petty C. M., Cooper D. A., Hayes J. P., LaBar K. S., et al. (2009). The role of trauma-related distractors on neural systems for working memory and emotion processing in posttraumatic stress disorder . J. Psychiatr. Res . 43 , 809–817 10.1016/j.jpsychires.2008.10.014 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morey R. A., Petty C. M., Cooper D. A., LaBar K. S., McCarthy G. (2008). Neural systems for executive and emotional processing are modulated by symptoms of posttraumatic stress disorder in Iraq War veterans . Psychiat. Res . 162 , 59–72 10.1016/j.pscychresns.2007.07.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Myers C. E., Vanmeenen K. M., McAuley J. D., Beck K. D., Pang K. C., Servatius R. J. (2012). Behaviorally inhibited temperament is associated with severity of post-traumatic stress disorder symptoms and faster eyeblink conditioning in veterans . Stress 15 , 31–44 10.3109/10253890.2011.578184 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- New A. S., Fan J., Murrough J. W., Liu X., Liebman R. E., Guise K. G., et al. (2009). A functional magnetic resonance imaging study of deliberate emotion regulation in resilience and posttraumatic stress disorder . Biol. Psychiatry 66 , 656–664 10.1016/j.biopsych.2009.05.020 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ofrat S., Krueger R. F. (2012). How research on the meta-structure of psychopathology aids in understanding biological correlates of mood and anxiety disorders . Biol. Mood Anxiety Disord . 2 , 13 10.1186/2045-5380-2-13 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Orr S., Metzger L., Lasko N., Macklin M., Peri T., Pitman R. (2000). De novo conditioning in trauma-exposed individuals with and without posttraumatic stress disorder . J. Abnorm. Psychol . 109 , 290–298 [ PubMed ] [ Google Scholar ]
- Paller K. A., Wagner A. D. (2002). Observing the transformation of experience into memory . Trends Cogn. Sci . 6 , 93–102 10.1016/S1364-6613(00)01845-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pannu Hayes J., LaBar K. S., Petty C. M., McCarthy G., Morey R. A. (2009). Alterations in the neural circuitry for emotion and attention associated with posttraumatic stress symptomatology . Psychiatry Res . 172 , 7–15 10.1016/j.pscychresns.2008.05.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Paunovic N., Lundh L. G., Ost L. G. (2002). Attentional and memory bias for emotional information in crime victims with acute posttraumatic stress disorder (PTSD) . J. Anxiety Disord . 16 , 675–692 [ PubMed ] [ Google Scholar ]
- Peri T., Ben-Shakhar G., Orr S. P., Shalev A. Y. (2000). Psychophysiologic assessment of aversive conditioning in posttraumatic stress disorder . Biol. Psychiatry 47 , 512–519 [ PubMed ] [ Google Scholar ]
- Pine D. S., Mogg K., Bradley B. P., Montgomery L., Monk C. S., McClure E., et al. (2005). Attention bias to threat in maltreated children: implications for vulnerability to stress-related psychopathology . Am. J. Psychiatry 162 , 291–296 10.1176/appi.ajp.162.2.291 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pissiota A., Frans O., Fernandez M., von Knorring L., Fischer H., Fredrikson M. (2002). Neurofunctional correlates of posttraumatic stress disorder: a PET symptom provocation study . Eur. Arch. Psychiatry Clin. Neurosci . 252 , 68–75 10.1007/s004060200014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pitman R. K. (1988). Post-traumatic stress disorder, conditioning, and network theory . Psychiat. Ann . 18 , 182–189 [ Google Scholar ]
- Pitman R. K., Sanders K. M., Zusman R. M., Healy A. R., Cheema F., Lasko N. B., et al. (2002). Pilot study of secondary prevention of posttraumatic stress disorder with propranolol . Biol. Psychiatry 51 , 189–192 [ PubMed ] [ Google Scholar ]
- Pizzagalli D. A., Iosifescu D., Hallett L. A., Ratner K. G., Fava M. (2008). Reduced hedonic capacity in major depressive disorder: evidence from a probabilistic reward task . J. Psychiatr. Res . 43 , 76–87 10.1016/j.jpsychires.2008.03.001 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Putman P., Hermans E. J., Koppeschaar H., van Schijndel A., van Honk J. (2007). A single administration of cortisol acutely reduces preconscious attention for fear in anxious young men . Psychoneuroendocrino 32 , 793–802 10.1016/j.psyneuen.2007.05.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rauch S. L., Shin L. M., Phelps E. A. (2006). Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research - past, present, and future . Biol. Psychiatry 60 , 376–382 10.1016/j.biopsych.2006.06.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Resick P., Schnicke M. (1993). Cognitive Processing Therapy for Rape Victims: A Treatment Manual . Newbury Park, CA: Sage Publications [ Google Scholar ]
- Ritchey M., LaBar K. S., Cabeza R. (2011). Level of processing modulates the neural correlates of emotional memory formation . J. Cogn. Neurosci . 23 , 757–771 10.1162/jocn.2010.21487 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roediger H., McDermott K. (1995). Creating false memories: remembering words not presented in lists . J. Exp. Psychol. Learn. Mem. Cogn . 21 , 803–814 [ Google Scholar ]
- Rougemont-Bücking A., Linnman C., Zeffiro T. A., Zeidan M. A., Lebron-Milad K., Rodriguez-Romaguera J., et al. (2011). Altered processing of contextual information during fear extinction in PTSD: an fMRI study . CNS Neurosci. Ther . 17 , 227–236 10.1111/j.1755-5949.2010.00152.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sailer U., Robinson S., Fischmeister F. P. S., Konig D., Oppenauer C., Lueger-Schuster B., et al. (2008). Altered reward processing in the nucleus accumbens and mesial prefrontal cortex of patients with posttraumatic stress disorder . Neuropsychologia 46 , 2836–2844 10.1016/j.neuropsychologia.2008.05.022 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schacter D. L. (1999). The seven sins of memory: insights from psychology and cognitive neuroscience . Am. Psychol . 54 , 182–203 [ PubMed ] [ Google Scholar ]
- Schweizer S., Dalgleish T. (2011). Emotional working memory capacity in posttraumatic stress disorder (PTSD) . Behav. Res. Ther . 49 , 498–504 10.1016/j.brat.2011.05.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Seeley W. W., Menon V., Schatzberg A. F., Keller J., Glover G. H., Kenna H., et al. (2007). Dissociable intrinsic connectivity networks for salience processing and executive control . J. Neurosci . 27 , 2349–2356 10.1523/JNEUROSCI.5587-06.2007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shin L. M., Orr S. P., Carson M. A., Rauch S. L., Macklin M. L., Lasko N. B., et al. (2004a). Regional cerebral blood flow in the amygdala and medial prefrontal cortex during traumatic imagery in male and female Vietnam veterans with PTSD . Arch. Gen. Psychiatry 61 , 168–176 10.1001/archpsyc.61.2.168 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shin L. M., Shin P. S., Heckers S., Krangel T. S., Macklin M. L., Orr S. P., et al. (2004b). Hippocampal function in posttraumatic stress disorder . Hippocampus 14 , 292–300 10.1002/hipo.10183 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shin L. M., Whalen P. J., Pitman R. K., Bush G., Macklin M. L., Lasko N. B., et al. (2001). An fMRI study of anterior cingulate function in posttraumatic stress disorder . Biol. Psychiatry 50 , 932–942 [ PubMed ] [ Google Scholar ]
- Shin L. M., Wright C. I., Cannistraro P. A., Wedig M. M., McMullin K., Martis B., et al. (2005). A functional magnetic resonance imaging study of amygdala and medial prefrontal cortex responses to overtly presented fearful faces in posttraumatic stress disorder . Arch. Gen. Psychiatry 62 , 273–281 10.1001/archpsyc.62.3.273 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shipherd J., Beck J. (2005). The role of thought suppression in posttraumatic stress disorder . Behav. Ther . 36 , 277–287 [ Google Scholar ]
- Shipherd J. C., Beck J. G. (1999). The effects of suppressing trauma-related thoughts on women with rape-related posttraumatic stress disorder . Behav. Res. Ther . 37 , 99–112 10.1016/S0005-7967(98)00136-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Simmons A. N., Matthews S. C. (2012). Neural circuitry of PTSD with or without mild traumatic brain injury: a meta-analysis . Neuropharmacology 62 , 598–606 10.1016/j.neuropharm.2011.03.016 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Simmons A. N., Paulus M. P., Thorp S. R., Matthews S. C., Norman S. B., Stein M. B. (2008). Functional activation and neural networks in women with posttraumatic stress disorder related to intimate partner violence . Biol. Psychiatry 64 , 681–690 10.1016/j.biopsych.2008.05.027 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stanford M. S., Vasterling J. J., Mathias C. W., Constans J. I., Houston R. J. (2001). Impact of threat relevance on P3 event-related potentials in combat-related post-traumatic stress disorder . Psychiatry Res . 102 , 125–137 10.1016/S0165-1781(01)00236-0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Surís A., North C., Adinoff B., Powell C., Greene R. (2010). Effects of exogenous glucocorticoid on combat-related PTSD symptoms . Ann. Clin. Psychiatry 22 , 274–279 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sutherland K., Bryant R. (2007). Autobiographical memory in posttraumatic stress disorder before and after treatment . Behav. Res. Ther . 45 , 2915–2923 10.1016/j.brat.2007.08.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tanielian T., Jaycox L. H. (2008). Invisible wounds of War: Psychological and Cognitive Injuries, their Consequences, and Services to Assist Recovery . Santa Monica, CA: RAND Corporation [ Google Scholar ]
- Taylor F. B., Lowe K., Thompson C., McFall M. M., Peskind E. R., Kanter E. D., et al. (2006). Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder . Biol. Psychiatry 59 , 577–581 10.1016/j.biopsych.2005.09.023 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Terr L. C. (1991). Childhood traumas: an outline and overview . Am. J. Psychiatry 148 , 10–20 [ PubMed ] [ Google Scholar ]
- Thomaes K., Dorrepaal E., Draijer N., de Ruiter M., Elzinga B., van Balkom A., et al. (2009). Increased activation of the left hippocampus region in Complex PTSD during encoding and recognition of emotional words: a pilot study . Psychiatry Res . 171 , 44–53 10.1016/j.pscychresns.2008.03.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thomaes K., Dorrepaal E., Draijer N., de Ruiter M. B., Elzinga B. M., van Balkom A. J., et al. (2012). Treatment effects on insular and anterior cingulate cortex activation during classic and emotional Stroop interference in child abuse-related complex post-traumatic stress disorder . Psychol. Med . [Epub ahead of print]. 10.1017/S0033291712000499 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thrasher S. M., Dalgleish T., Yule W. (1994). Information processing in post-traumatic stress disorder . Behav. Res. Ther . 32 , 247–254 10.1016/0005-7967(94)90119-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vaiva G., Ducrocq F., Jezequel K., Averland B., Lestavel P., Brunet A., et al. (2003). Immediate treatment with propranolol decreases posttraumatic stress disorder two months after trauma . Biol. Psychiatry 54 , 947–949 10.1016/S0006-3223(03)00412-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- VanElzakker M. B., Staples L. K., Shin L. M. (2012). The neurocircuitry of fear and PTSD , in Sleep and Combat-Related Post-Traumatic Stress Disorders , eds Vermetten E., Pandi-Perumal T. N. S. R., Kramer M. (New York, NY: Springer-Verlag; ) (In press). [ Google Scholar ]
- Vasterling J. J., Duke L. M., Brailey K., Constans J. I., Allain A. N., Jr., Sutker P. B. (2002). Attention, learning, and memory performances and intellectual resources in Vietnam veterans: PTSD and no disorder comparisons . Neuropsychology . 16 , 5–14 [ PubMed ] [ Google Scholar ]
- Vrana S. R., Roodman A., Beckham J. C. (1995). Selective processing of trauma-relevant words in posttraumatic stress disorder . J. Anxiety Disord . 9 , 515–530 [ Google Scholar ]
- Wald I., Shechner T., Bitton S., Holoshitz Y., Charney D. S., Muller D., et al. (2011). Attention bias away from threat during life threatening danger predicts PTSD symptoms at one-year follow-up . Depress. Anxiety 28 , 406–411 10.1002/da.20808 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wegner D. M., Schneider D. J., Carter S. R., White T. L. (1987). Paradoxical effects of thought suppression . J. Pers. Soc. Psychol . 53 , 5–13 [ PubMed ] [ Google Scholar ]
- Williams J., Barnhofer T., Crane C., Hermans D., Raes F., Watkins E., et al. (2007). Autobiographical memory specificity and emotional disorder . Psychol. Bull . 133 , 122–148 10.1037/0033-2909.133.1.122 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wittekind C. E., Jelinek L., Kellner M., Moritz S., Muhtz C. (2010). Intergenerational transmission of biased information processing in posttraumatic stress disorder (PTSD) following displacement after World War, I. I . J. Anxiety Disord . 24 , 953–957 10.1016/j.janxdis.2010.06.023 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zoellner L. A., Foa E. B., Brigidi B. D., Przeworski A. (2000). Are trauma victims susceptible to “false memories”? J. Abnorm. Psychol . 109 , 517–524 [ PubMed ] [ Google Scholar ]
- Zoellner L. A., Sacks M. B., Foa E. B. (2003). Directed forgetting following mood induction in chronic posttraumatic stress disorder patients . J. Abnorm. Psychol . 112 , 508–514 [ PubMed ] [ Google Scholar ]
- Zwissler B., Hauswald A., Koessler S., Ertl V., Pfeiffer A., Wohrmann C., et al. (2011). Memory control in post-traumatic stress disorder: evidence from item method directed forgetting in civil war victims in Northern Uganda . Psychol. Med . 1 , 1–9 10.1017/S0033291711002273 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
How We Use Abstract Thinking
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
MoMo Productions / Getty Images
- How It Develops
Abstract thinking, also known as abstract reasoning, involves the ability to understand and think about complex concepts that, while real, are not tied to concrete experiences, objects, people, or situations.
Abstract thinking is considered a type of higher-order thinking, usually about ideas and principles that are often symbolic or hypothetical. This type of thinking is more complex than the type of thinking that is centered on memorizing and recalling information and facts.
Examples of Abstract Thinking
Examples of abstract concepts include ideas such as:
- Imagination
While these things are real, they aren't concrete, physical things that people can experience directly via their traditional senses.
You likely encounter examples of abstract thinking every day. Stand-up comedians use abstract thinking when they observe absurd or illogical behavior in our world and come up with theories as to why people act the way they do.
You use abstract thinking when you're in a philosophy class or when you're contemplating what would be the most ethical way to conduct your business. If you write a poem or an essay, you're also using abstract thinking.
With all of these examples, concepts that are theoretical and intangible are being translated into a joke, a decision, or a piece of art. (You'll notice that creativity and abstract thinking go hand in hand.)
Abstract Thinking vs. Concrete Thinking
One way of understanding abstract thinking is to compare it with concrete thinking. Concrete thinking, also called concrete reasoning, is tied to specific experiences or objects that can be observed directly.
Research suggests that concrete thinkers tend to focus more on the procedures involved in how a task should be performed, while abstract thinkers are more focused on the reasons why a task should be performed.
It is important to remember that you need both concrete and abstract thinking skills to solve problems in day-to-day life. In many cases, you utilize aspects of both types of thinking to come up with solutions.
Other Types of Thinking
Depending on the type of problem we face, we draw from a number of different styles of thinking, such as:
- Creative thinking : This involves coming up with new ideas, or using existing ideas or objects to come up with a solution or create something new.
- Convergent thinking : Often called linear thinking, this is when a person follows a logical set of steps to select the best solution from already-formulated ideas.
- Critical thinking : This is a type of thinking in which a person tests solutions and analyzes any potential drawbacks.
- Divergent thinking : Often called lateral thinking, this style involves using new thoughts or ideas that are outside of the norm in order to solve problems.
How Abstract Thinking Develops
While abstract thinking is an essential skill, it isn’t something that people are born with. Instead, this cognitive ability develops throughout the course of childhood as children gain new abilities, knowledge, and experiences.
The psychologist Jean Piaget described a theory of cognitive development that outlined this process from birth through adolescence and early adulthood. According to his theory, children go through four distinct stages of intellectual development:
- Sensorimotor stage : During this early period, children's knowledge is derived primarily from their senses.
- Preoperational stage : At this point, children develop the ability to think symbolically.
- Concrete operational stage : At this stage, kids become more logical but their understanding of the world tends to be very concrete.
- Formal operational stage : The ability to reason about concrete information continues to grow during this period, but abstract thinking skills also emerge.
This period of cognitive development when abstract thinking becomes more apparent typically begins around age 12. It is at this age that children become more skilled at thinking about things from the perspective of another person. They are also better able to mentally manipulate abstract ideas as well as notice patterns and relationships between these concepts.
Uses of Abstract Thinking
Abstract thinking is a skill that is essential for the ability to think critically and solve problems. This type of thinking is also related to what is known as fluid intelligence , or the ability to reason and solve problems in unique ways.
Fluid intelligence involves thinking abstractly about problems without relying solely on existing knowledge.
Abstract thinking is used in a number of ways in different aspects of your daily life. Some examples of times you might use this type of thinking:
- When you describe something with a metaphor
- When you talk about something figuratively
- When you come up with creative solutions to a problem
- When you analyze a situation
- When you notice relationships or patterns
- When you form a theory about why something happens
- When you think about a problem from another point of view
Research also suggests that abstract thinking plays a role in the actions people take. Abstract thinkers have been found to be more likely to engage in risky behaviors, where concrete thinkers are more likely to avoid risks.
Impact of Abstract Thinking
People who have strong abstract thinking skills tend to score well on intelligence tests. Because this type of thinking is associated with creativity, abstract thinkers also tend to excel in areas that require creativity such as art, writing, and other areas that benefit from divergent thinking abilities.
Abstract thinking can have both positive and negative effects. It can be used as a tool to promote innovative problem-solving, but it can also lead to problems in some cases:
- Bias : Research also suggests that it can sometimes promote different types of bias . As people seek to understand events, abstract thinking can sometimes cause people to seek out patterns, themes, and relationships that may not exist.
- Catastrophic thinking : Sometimes these inferences, imagined scenarios, and predictions about the future can lead to feelings of fear and anxiety. Instead of making realistic predictions, people may catastrophize and imagine the worst possible potential outcomes.
- Anxiety and depression : Research has also found that abstract thinking styles are sometimes associated with worry and rumination . This thinking style is also associated with a range of conditions including depression , anxiety, and post-traumatic stress disorder (PTSD) .
Conditions That Impact Abstract Thinking
The presence of learning disabilities and mental health conditions can affect abstract thinking abilities. Conditions that are linked to impaired abstract thinking skills include:
- Learning disabilities
- Schizophrenia
- Traumatic brain injury (TBI)
The natural aging process can also have an impact on abstract thinking skills. Research suggests that the thinking skills associated with fluid intelligence peak around the ages of 30 or 40 and begin to decline with age.
Tips for Reasoning Abstractly
While some psychologists believe that abstract thinking skills are a natural product of normal development, others suggest that these abilities are influenced by genetics, culture, and experiences. Some people may come by these skills naturally, but you can also strengthen these abilities with practice.
Some strategies that you might use to help improve your abstract thinking skills:
- Think about why and not just how : Abstract thinkers tend to focus on the meaning of events or on hypothetical outcomes. Instead of concentrating only on the steps needed to achieve a goal, consider some of the reasons why that goal might be valuable or what might happen if you reach that goal.
- Reframe your thinking : When you are approaching a problem, it can be helpful to purposefully try to think about the problem in a different way. How might someone else approach it? Is there an easier way to accomplish the same thing? Are there any elements you haven't considered?
- Consider the big picture : Rather than focusing on the specifics of a situation, try taking a step back in order to view the big picture. Where concrete thinkers are more likely to concentrate on the details, abstract thinkers focus on how something relates to other things or how it fits into the grand scheme of things.
Abstract thinking allows people to think about complex relationships, recognize patterns, solve problems, and utilize creativity. While some people tend to be naturally better at this type of reasoning, it is a skill that you can learn to utilize and strengthen with practice.
It is important to remember that both concrete and abstract thinking are skills that you need to solve problems and function successfully.
Gilead M, Liberman N, Maril A. From mind to matter: neural correlates of abstract and concrete mindsets . Soc Cogn Affect Neurosci . 2014;9(5):638-45. doi: 10.1093/scan/nst031
American Psychological Association. Creative thinking .
American Psychological Association. Convergent thinking .
American Psychological Association. Critical thinking .
American Psychological Association. Divergent thinking .
Lermer E, Streicher B, Sachs R, Raue M, Frey D. The effect of abstract and concrete thinking on risk-taking behavior in women and men . SAGE Open . 2016;6(3):215824401666612. doi:10.1177/2158244016666127
Namkoong J-E, Henderson MD. Responding to causal uncertainty through abstract thinking . Curr Dir Psychol Sci . 2019;28(6):547-551. doi:10.1177/0963721419859346
White R, Wild J. "Why" or "How": the effect of concrete versus abstract processing on intrusive memories following analogue trauma . Behav Ther . 2016;47(3):404-415. doi:10.1016/j.beth.2016.02.004
Williams DL, Mazefsky CA, Walker JD, Minshew NJ, Goldstein G. Associations between conceptual reasoning, problem solving, and adaptive ability in high-functioning autism . J Autism Dev Disord . 2014 Nov;44(11):2908-20. doi: 10.1007/s10803-014-2190-y
Oh J, Chun JW, Joon Jo H, Kim E, Park HJ, Lee B, Kim JJ. The neural basis of a deficit in abstract thinking in patients with schizophrenia . Psychiatry Res . 2015;234(1):66-73. doi: 10.1016/j.pscychresns.2015.08.007
Hartshorne JK, Germine LT. When does cognitive functioning peak? The asynchronous rise and fall of different cognitive abilities across the life span . Psychol Sci. 2015;26(4):433-43. doi:10.1177/0956797614567339
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."

IMAGES
VIDEO
COMMENTS
Mild cognitive impairment (MCI) happens when you experience a slight — but noticeable — decline in mental abilities compared to others your age. Mental abilities include: Memory. Reasoning and judgment. Planning and completing complex tasks. You may notice the decline in your abilities, or a loved one might. But the changes aren't severe ...
The first thing to do is determine your personal risk factors for such a lapse in judgment. Traditional twelve-step programs for addiction —each in their own way focusing on what can catapult an ...
Dementia is a general term used to describe a form of cognitive impairment that is chronic, generally progressive and occurs over a period of months to years. It can affect memory, language, perception, personality and cognitive skills. 2. Delirium is an acute disturbance of attention and cognition where the patient experiences confusion.
Mild cognitive impairment (MCI) is the stage between the expected decline in memory and thinking that happens with age and the more serious decline of dementia. MCI may include problems with memory, language or judgment. People with MCI may be aware that their memory or mental function has "slipped." Family and close friends also may notice ...
When a person is diagnosed with impaired cognition, it means their skills and abilities may have diminished or disappeared as a result of a medical problem. There are special names for some of these impairments; for example, an impairment in language skills that makes it hard for people to speak or understand speech is called aphasia.
Cognitive impairment is when you have problems remembering things and solving problems. Cognitive impairment is not an illness. It can be caused by many conditions. You may struggle with: remembering things. paying attention. speaking or understanding. recognising people, places or things. experiencing new places and situations — you may ...
Judgment can be defined as the capacity to make decisions after careful consideration of available information, contextual factors, possible solutions and probable outcomes. It is intimately linked with the process of problem solving and decision-making, and these terms are often used interchangeably in the neuropsychological literature. 1.
Dementia symptoms trigger a decline in thinking skills, also known as cognitive abilities, severe enough to impair daily life and independent function. They also affect behavior, feelings and relationships. Alzheimer's disease accounts for 60-80% of cases. Vascular dementia, which occurs because of microscopic bleeding and blood vessel blockage ...
Challenges in planning or solving problems. This includes changes in an individual's ability to develop and follow a plan or work with numbers. For example, they may have trouble following a familiar recipe or keeping track of monthly bills. They may have difficulty concentrating and take much longer to do things than they did before.
Cognitive impairment: Impedes communication, attention, memory, thinking and problem solving. Means a person may not be able to carry out tasks or be unable to recognise people or objects. Can be temporary or permanent. Will affect what the person can understand and how they relate to others and interpret the environment.
Cognitive constructs that overlap with judgment include everyday problem solving, everyday decision making, ... may uncover specific circumstances or cognitive processes that contribute to poor judgment. For example, some patients may show an impaired ability to organize information while others may have trouble generating solutions, initiating ...
Definition: Impaired judgement is a medical condition that results in a person not being able to make good decisions because of an underlying medical problem, environmental factors, diet, or drugs and alcohol. The Mayo Clinic notes that many people with impaired judgement suffer from mild cognitive impairment, which also causes impairment in ...
Evidence from a number of animal studies clearly demonstrate remarkable reasoning and problem-solving abilities in non-human species (Blaisdell et al., 2006; Taylor et al., 2009; Smirnova et al., 2015), but it is argued that such abilities have reached a higher level in humans (Premack, 1983, 2007; O'Brien and Opie, 2002; Penn et al., 2008).
When learning something new, analyzing a problem, or making a decision, recognizing the emotional context is often important. However, insufficient sleep impedes the ability to properly process the emotional component of information. Impaired Judgment: In some cases, this
Deficits in executive function and problem-solving are greater in depressed individuals with a history of suicide attempts or even suicidal ideation compared with depressed controls. 90 Impaired decision making, reflected in poor performance in the Iowa Gambling Task (IGT), which is designed to mimic complex and uncertain decision making, is ...
Optimize Cognitive Function. Assess cognitive function using a standardized tool to establish baseline and identify areas of deficit. Establish rapport and trust; utilize unhurried and calm approach. Utilize clear communication; address patient by name, speak slowly with simple directions and gestures; provide time for patient response, listen ...
Cognition - Managing problem solving, thinking, attention and memory at work Cognitive and thinking skills. Cognitive or thinking skills can be hard for people if their disability affects the way their brain processes information, for example, people with intellectual disabilities, acquired brain injuries, specific learning disabilities, autism spectrum disorders, psychiatric disorders ...
Adolescents differ from adults in the way they behave, solve problems, and make decisions. There is a biological explanation for this difference. Studies have shown that brains continue to mature and develop throughout childhood and adolescence and well into early adulthood. Scientists have identified a specific region of the brain called the ...
Abstract. Dementia is characterized by a decline in memory, language, problem-solving and in other cognitive domains that affect a person's ability to perform everyday activities and social functioning. It is consistently agreed that cognitive impairment is an important risk factor for developing functional disabilities in patients with dementia.
Poor judgment is one of the hallmarks of Alzheimer's disease. In fact, while a typical symptom of early stages of Alzheimer's is short-term memory loss, poor judgment can sometimes precede memory loss. Poor judgment refers to the inability to make appropriate decisions. If your relative has Alzheimer's or another type of dementia, they ...
Common signs and symptoms of cognitive impairment or disturbed thought process may include memory loss, confusion, disorientation, difficulty concentrating, impaired judgment, language difficulties, changes in behavior or personality, and problems with problem-solving and decision-making abilities. The following signs and symptoms characterize ...
These hallmark symptoms involve alterations to cognitive processes such as memory, attention, planning, and problem solving, underscoring the impact that emotion has on cognitive functioning. Influential cognitive theories of PTSD emphasize the interaction between emotion and cognition in contributing to the symptoms of PTSD.
Abstract thinking is a skill that is essential for the ability to think critically and solve problems. This type of thinking is also related to what is known as fluid intelligence, or the ability to reason and solve problems in unique ways. Fluid intelligence involves thinking abstractly about problems without relying solely on existing knowledge.