Essay Sample on Why I Want to Be A Nurse
Nursing is a rewarding and challenging career that has the power to make a real difference in people’s lives. Whether your motivation is to help others, attain financial freedom, or both, writing a “Why I Want To Be A Nurse” essay is an excellent opportunity to express your passion and commitment to the field.
In this article, we’ll explore the reasons why you might want to become a nurse and provide you with helpful tips and inspiration for writing a powerful and persuasive essay .

Why I Want to Be A Nurse (Free Essay Sample)
Nursing is a career that offers a unique combination of hands-on care and emotional support to those in need. There are many reasons why someone might choose to become a nurse, including:
The Empathy and Altruism of Nursing
I have a strong desire to help people and hope to become a nurse. I think nursing is the best way for me to make a difference in other people’s lives because it combines my natural empathy and desire to help people. Nursing gives me a chance to positively touch people’s lives, which has always attracted me to the thought of doing so.
I saw the beneficial effects that nurses may have on people’s life as a child. I have always been moved by the kindness and concern they have for their patients. The small gestures of kindness, like holding a patient’s hand or speaking encouraging words, have always touched me. I think nurses have a special power to change people’s lives and leave a lasting impression, and I want to contribute to that.
Additionally, I think that becoming a nurse is a great and selfless job. To provide for their patients and ensure they are secure and comfortable, nurses put their own needs on hold. I absolutely respect this kind of dedication to helping others, and I aim to exhibit it in my own nursing career.
The Economic Benefits of Nursing
The financial stability that comes with being a nurse is one of the reasons I wish to pursue this career. Nursing is a field that is in high demand, which translates to a wealth of job opportunities and competitive salaries. This profession offers the chance for a stable income, which makes it a good choice for people who want to secure their financial future.
Nursing not only gives economic freedom but also a flexible work schedule that promotes a healthy work-life balance. Many nurses can choose to work part-time or in a variety of places, such as clinics, hospitals, and schools..
A Love for the Science and Art of Nursing
To succeed in the unique field of nursing, one must have both artistic talent and scientific knowledge. This mix is what initially drew me to the thought of becoming a nurse. The human body and its mechanisms have always captivated me, and I enjoy learning about the science that underpins healthcare. But nursing requires more than just a scientific knowledge of the body. It also requires an artistic understanding of the patient and their needs.. Nursing is a demanding and fulfilling job since it combines science and art, which is why I’m drawn to it.
I saw as a child the effect nurses had on patients and their families. Their compassion and understanding have motivated me to seek a profession in nursing because they frequently offer comfort and help in the hardest of situations. My enthusiasm for the science and art of nursing will undoubtedly help me to have a good influence on other people’s lives. I want to work as a nurse and improve the lives of the people I take care of, whether it be by giving medication, educating patients, or just being a reassuring presence.
Continuous Professional Development in Nursing
I think the nursing industry is dynamic and always changing, which gives people a lot of chances to learn and grow. I would have the chance to continuously advance my knowledge and abilities in this sector if I choose to become a nurse. In turn, this would enable me to better care for my patients and stay abreast of professional developments.
There are several different nursing specialties available as well. There are many options, including critical care, pediatrics, gerontology, and surgical nursing. Because of the variety of disciplines available, nurses have the chance to develop their interests and find their niche.
I am certain that a career in nursing will provide me the chance to pursue my passion for healthcare while also allowing me to grow professionally.
Nursing is a fulfilling and noble career that offers a mix of hands-on care, emotional support, and professional growth. I am inspired by the positive impact nurses have on patients and their families and aim to offer my own empathy and compassion. The nursing industry is constantly changing, providing ample opportunities for growth and job prospects with financial stability. The ultimate reward in a nursing career is the satisfaction of making a difference in people’s lives.
Tips for Writing A Compelling Why I Want To Be A Nurse Essay
Now that you understand the reasons why someone might want to become a nurse, it’s time to learn how to write a compelling essay. Here are some tips and strategies to help you get started:
Create an Outline
Before you start writing, it’s important to identify the main points you’ll discuss in your essay. This will help you stay organized and make your essay easier to read.
Start with an Attention-grabbing Introduction
Your introduction is your chance to make a good first impression and engage the reader. Start with a hook that captures the reader’s attention, such as a surprising statistic or personal story .
Be Specific and Personal
Rather than making general statements about why you want to become a nurse, be specific and personal. Share your own experiences, motivations, and passions, and explain why nursing is the right career choice for you.
Highlight your Skills and Qualifications
Nursing is a demanding and complex profession that requires a wide range of skills and qualifications. Be sure to highlight your relevant skills, such as compassion, communication, and problem-solving, and explain how they make you a good fit for the nursing field.
Related posts:
- The Great Gatsby (Analyze this Essay Online)
- Pollution Cause and Effect Essay Sample
- Essay Sample on How Can I Be a Good American
- The Power of Imaging: Why I am Passionate about Becoming a Sonographer
Improve your writing with our guides

Youth Culture Essay Prompt and Discussion
Why Should College Athletes Be Paid, Essay Sample

Reasons Why Minimum Wage Should Be Raised Essay: Benefits for Workers, Society, and The Economy
Get 15% off your first order with edusson.
Connect with a professional writer within minutes by placing your first order. No matter the subject, difficulty, academic level or document type, our writers have the skills to complete it.
100% privacy. No spam ever.

- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
- Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring
Seeing Myself in the Future as a Nurse, Essay Example
Pages: 1
Words: 380
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
This week’s lessons took me to a whole new picture of seeing myself in the future as a nurse who does not only assists doctors and provides care for the sick ones, but as an individual capable of changing matters, capable of improving the lives of communities that are stricken by particularly devastating situations in life. I have fully been aware of the fact that nursing as a career changes the life of the nurse; however, It is only now that I have seen the broader scope of this life-changing course of living. As for a fact, I have created several other goals in my life to make my nursing career more affective towards others’ welfare and I do hope that in the future, I would be able to relive these conditions of personal and professional development and be of great use to the society.
Learning about more than one effective and remarkable nurse in history, I have learned that there is more to nursing than simply assisting and caring for the sick. Becoming a machine of change requires one to be creative, innovative and determined enough to make sure that the changes do occur. Noticeably, I have now realized that as a learning nurse, I do have the capacity to impact more lives and bring in more possible forms of transformation that could make the world a better place to live in. I personally feel for those in remote areas who may not have access to good medical attention and medical supplies that they need. This is why I do have a goal of making a difference –how do I reach such goals? I do look forward to the coming weeks to establish my plans more and find a better way to make sure that this condition of realization does occur in the near future. I do look forward to learning more about what nursing is and how it could change the world depending on how I view the situation that surrounds me and how it could relate to the value of nursing that is being developed within me. More lessons are to be learned and I know that all these would help me build a better me with a much better purpose in life and in my chosen career.
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Arrangements for Late Submission With the Coaches, Capstone Project Example
Understanding the New Student, Essay Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Pages: 4
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371

How to Write an Essay about Why You Want to Become a Nurse

If you’re eager to write an essay about why you want to become a nurse, then you’ve arrived at the right tutorial!
An essay about why you want to enter the nursing profession can help to communicate your passion, commitment, and the values that led you to choose this career. In this tutorial, I’ll show you how to write such an essay in five easy steps. We’ll also build a sample essay so you can visualize how to implement these steps.
Ready to get started?
Step 1. Plan the word count for your essay’s paragraphs.
The first step to effective essay writing is planning the word count for each of your paragraphs. It’s a simple way to ensure balance in your essay and make your writing process smoother.
Every essay should have the following sections:
- The introductory paragraph
- Three body paragraphs
- The concluding paragraph
So, if you want a 300-word essay, you can distribute the 300 words across five paragraphs this way:
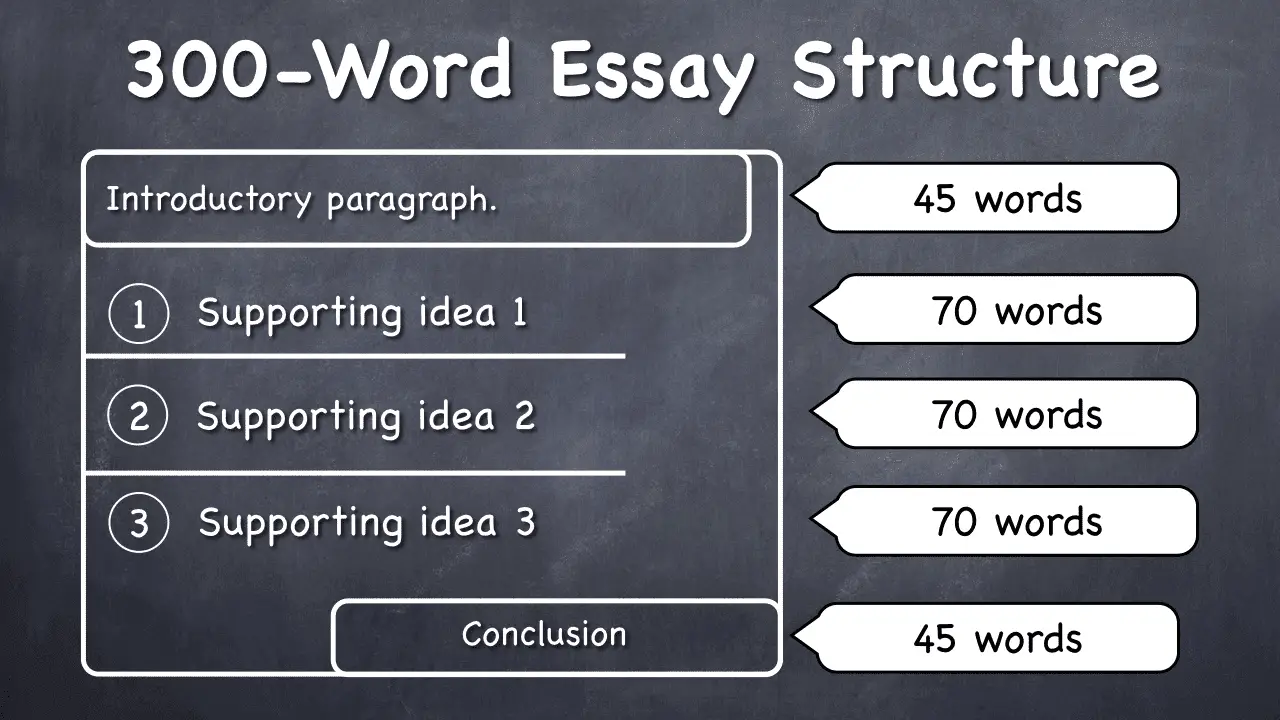
That’s all you need for your essay — five nice paragraphs.
Step 2. Formulate your central idea and supporting points.
This step involves deciding on the central idea that will guide your essay. This involves reflecting on why you want to become a nurse. What has led you to this decision?
For instance, are you compassionate and patient? Do you find joy in helping others? Are you inspired by a close relative who is a nurse? Do you have a desire to work in healthcare?
Whatever the reasons, these will serve as your thesis statement or your essay’s main idea.
Let’s take this as our main idea for our example essay: “My desire to become a nurse is driven by my innate compassion, a significant personal experience, and a desire to contribute to healthcare.”
Next, using the Power of Three, we can divide this main idea into three supporting points.
The Power of Three is a structure that can help you frame your body paragraphs effectively.
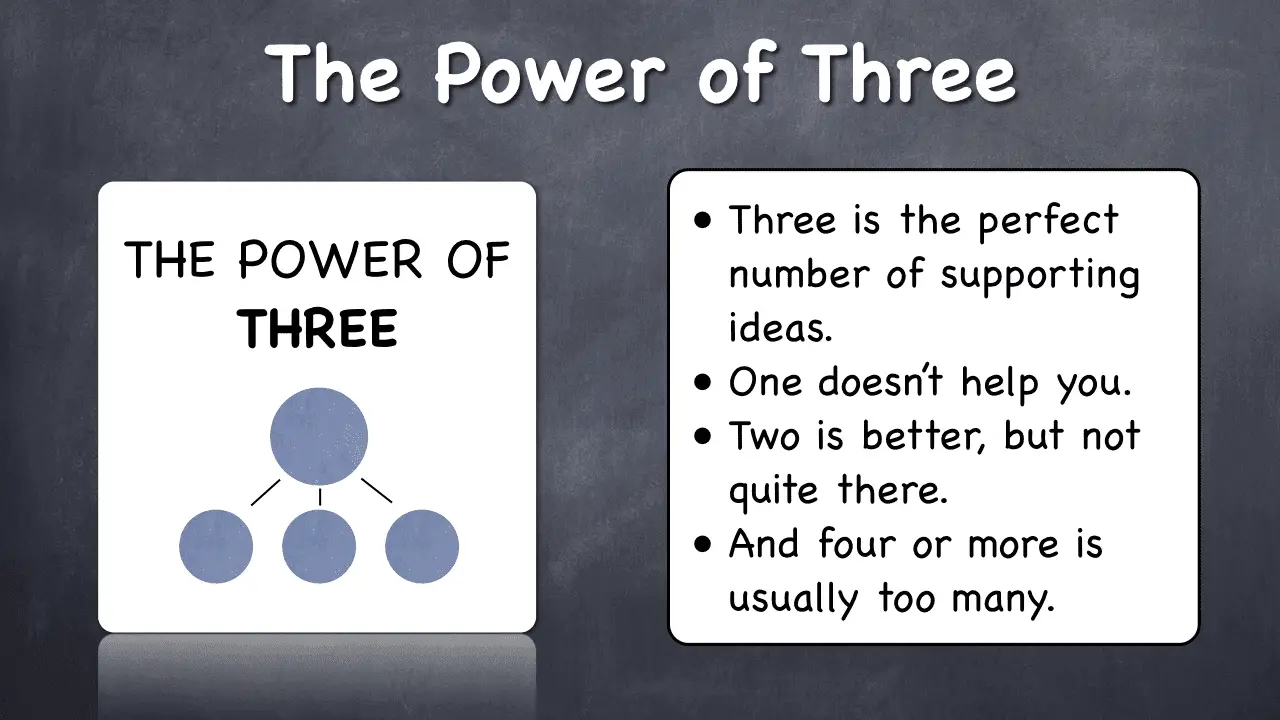
Here’s how it works for our sample essay. We’ll use three reasons for someone’s desire to become a nurse:
- Compassion is at the core of my personality.
- A personal experience influenced my decision to become a nurse.
- A desire to contribute to healthcare.
Now we have our foundation for writing our essay. Let’s move to the next step!
Step 3. Write the introductory paragraph.
To write an introductory paragraph , follow this diagram:
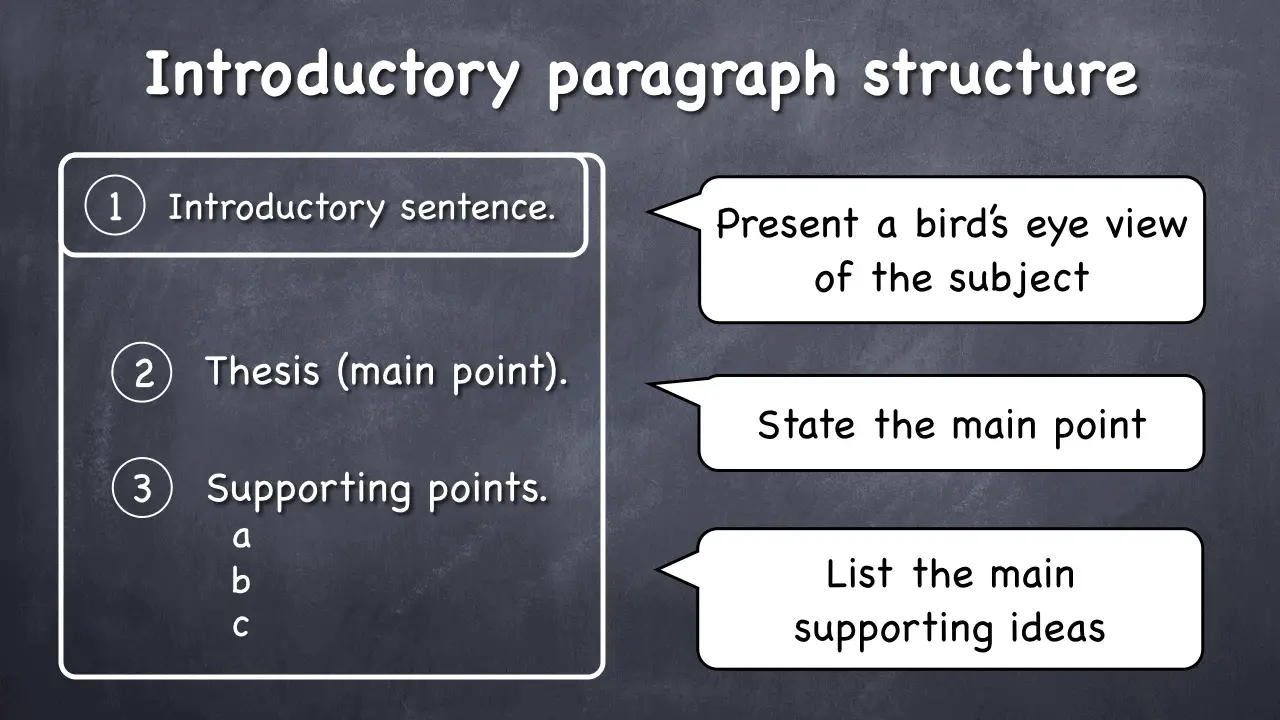
Your introduction should contain an opening sentence to set the context of your essay. Next, include your thesis statement and your three supporting points.
Here’s an example:
Introductory Paragraph
“The nursing profession is one that requires compassion, resilience, and a dedication to the service of others. My aspiration to become a nurse is fueled by my natural compassion, a pivotal personal experience, and a deep-rooted desire to contribute to healthcare. My compassion enables me to care for patients empathetically, my personal experience has provided me a profound understanding of patient needs, and my desire to contribute to healthcare constantly motivates me to pursue this path.”
Notice that the introductory paragraph transitions from general to specific, starting with an introduction, followed by the thesis and three supporting points.
Step 4. Write the body paragraphs.
Our essay will contain three body paragraphs, discussing our supporting points.
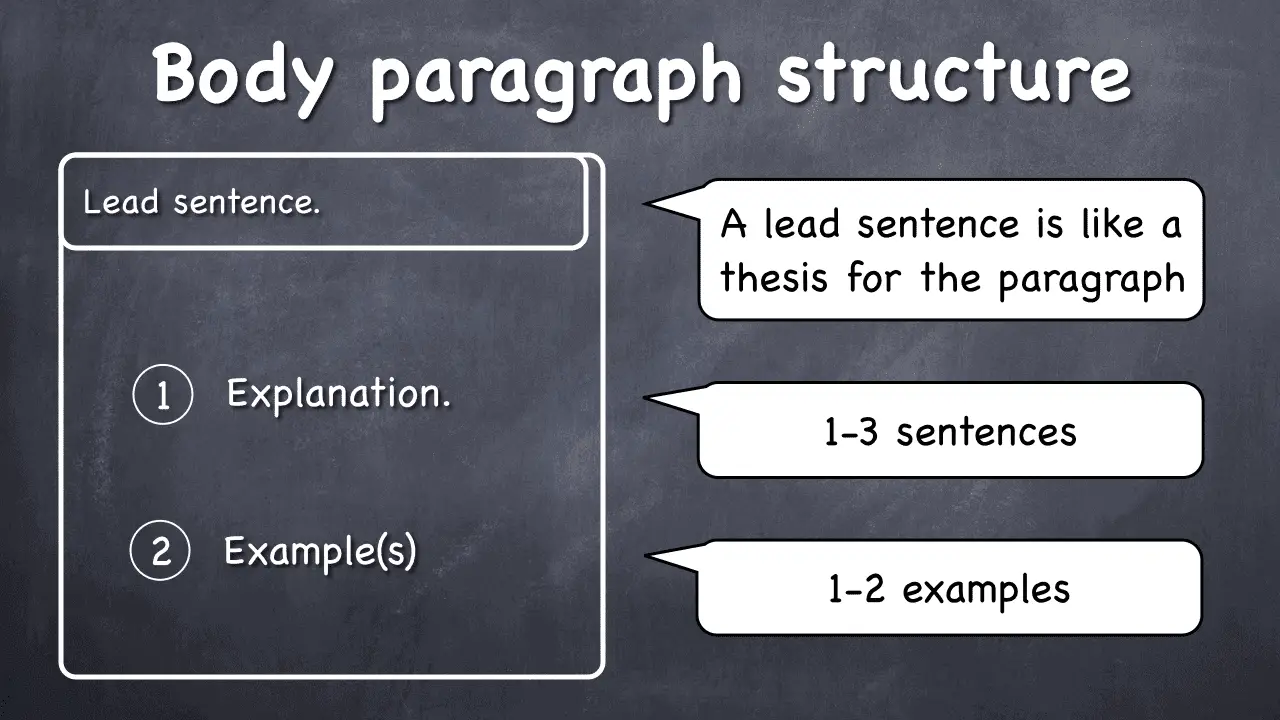
Each body paragraph begins with a topic sentence summarizing the main point of the paragraph, followed by a detailed explanation and examples. Let’s write our body paragraphs.
Paragraph 1
“Compassion is at the core of my personality, driving my aspiration to become a nurse. It allows me to form connections with patients, understanding their needs and providing empathetic care. I have always found satisfaction in helping others, which I believe will aid in providing quality nursing care to my patients.”
Note that the topic sentence gives the context for the entire paragraph. The subsequent sentences explain the supporting point, and the rest provides an illustration.
Paragraph 2
“A personal experience profoundly influenced my decision to become a nurse. A close family member was hospitalized for a long period, and I observed the exceptional care provided by the nurses, which brought comfort not just to the patient, but to our entire family. This experience demonstrated the positive impact nurses can have on patients and their families, inspiring me to join this noble profession.”
Paragraph 3
“My desire to contribute to healthcare is another driving factor behind my aspiration to become a nurse. The healthcare field is constantly evolving, and I yearn to be a part of the progress, enhancing patient care and healthcare delivery. I want to utilize my skills and knowledge to improve the health outcomes of my patients, contributing to the larger healthcare framework.”
Each body paragraph follows the structure mentioned above, starting with the topic sentence, followed by an explanation and an example.
Excellent! Now, let’s move on to the final step.
Step 5. Write the concluding paragraph.
The easiest way to write a concluding paragraph is to paraphrase the points you’ve already mentioned in the introductory paragraph. Don’t just copy it! Instead, look at your introductory paragraph and write the conclusion based on it.
Here’s how to do this for our sample essay:
“The nursing profession demands compassion, resilience, and a commitment to improving healthcare. My aspiration to become a nurse stems from my innate compassion, a life-changing personal experience, and a strong desire to contribute to healthcare. My compassion forms the basis for providing empathetic care, my personal experience highlights the crucial role nurses play, and my commitment to healthcare propels me to continuously strive for better patient care.”
By paraphrasing the points made in the introductory paragraph, writing the concluding paragraph becomes a straightforward task.
And that’s it! I hope you find this tutorial useful and feel more prepared to write your essay about why you want to become a nurse.
Tutor Phil is an e-learning professional who helps adult learners finish their degrees by teaching them academic writing skills.
Recent Posts
How to Write an Essay about Why You Deserve a Job
If you're preparing for a job application or interview, knowing how to express why you deserve a role is essential. This tutorial will guide you in crafting an effective essay to convey this...
How to Write an Essay about Why You Want to Do Something
If you're exploring ways to pen down an essay on why you want to do something, you've come to the right tutorial! Writing an essay about your motivations can be an excellent opportunity to express...
How to Write a Nursing Essay with a Quick Guide

Ever felt the blank-page panic when assigned a nursing essay? Wondering where to start or if your words will measure up to the weight of your experiences? Fear not, because today, we're here to guide you through this process.
Imagine you're at your favorite coffee spot, armed with a cup of motivation (and maybe a sneaky treat). Got it? Great! Now, let's spill the secrets on how to spin your nursing tales into words that not only get you that A+ but also tug at the heartstrings of anyone reading. We've got your back with nursing essay examples that'll be your inspiration, an outline to keep you on the right path, and more!
What Is a Nursing Essay
Let's start by dissecting the concept. A nursing essay serves as a focused exploration of a specific aspect of nursing, providing an opportunity for students to demonstrate their theoretical knowledge and its practical application in patient care settings.
Picture it as a journey through the challenges and victories of a budding nurse. These essays go beyond the classroom, tackling everything from tricky ethical dilemmas to the impact of healthcare policies on the front lines. It's not just about grades; it's about proving, 'I'm ready for the real deal.'
So, when you read or write a nursing essay, it's not just words on paper. It's like looking into the world of someone who's about to start their nursing career – someone who's really thought about the ins and outs of being a nurse. And before you kick off your nursing career, don't shy away from asking - write my essay for me - we're ready to land a professional helping hand.
How to Start a Nursing Essay
When you start writing a nursing essay, it is like gearing up for a crucial mission. Here's your quick guide from our nursing essay writing service :

Choosing Your Topic: Select a topic that sparks your interest and relates to real-world nursing challenges. Consider areas like patient care, ethical dilemmas, or the impact of technology on healthcare.
Outline Your Route : Plan your essay's journey. Create a roadmap with key points you want to cover. This keeps you on track and your essay on point.
Craft a Strong Thesis: Assuming you already know how to write a hook , kick off your writing with a surprising fact, a thought-provoking quote, or a brief anecdote. Then, state your main argument or perspective in one sentence. This thesis will serve as the compass for your essay, guiding both you and your reader through the rest of your writing.
How to Structure a Nursing Essay
Every great essay is like a well-orchestrated performance – it needs a script, a narrative that flows seamlessly, capturing the audience's attention from start to finish. In our case, this script takes the form of a well-organized structure. Let's delve into the elements that teach you how to write a nursing essay, from a mere collection of words to a compelling journey of insights.

Nursing Essay Introduction
Begin your nursing essay with a spark. Knowing how to write essay introduction effectively means sharing a real-life scenario or a striking fact related to your topic. For instance, if exploring patient care, narrate a personal experience that made a lasting impression. Then, crisply state your thesis – a clear roadmap indicating the direction your essay will take. Think of it as a teaser that leaves the reader eager to explore the insights you're about to unfold.
In the main body, dive into the heart of your essay. Each paragraph should explore a specific aspect of your topic. Back your thoughts with examples – maybe a scenario from your clinical experience, a relevant case study, or findings from credible sources. Imagine it as a puzzle coming together; each paragraph adds a piece, forming a complete picture. Keep it focused and let each idea flow naturally into the next.
Nursing Essay Conclusion
As writing a nursing essay nears the end, resist the urge to introduce new elements. Summarize your main points concisely. Remind the reader of the real-world significance of your thesis – why it matters in the broader context of nursing. Conclude with a thought-provoking statement or a call to reflection, leaving your reader with a lasting impression. It's like the final scene of a movie that leaves you thinking long after the credits roll.
Nursing Essay Outline
Before diving into the essay, craft a roadmap – your outline. This isn't a rigid skeleton but a flexible guide that ensures your ideas flow logically. Consider the following template from our research paper writing service :
Introduction
- Opening Hook: Share a brief, impactful patient care scenario.
- Relevance Statement: Explain why the chosen topic is crucial in nursing.
- Thesis: Clearly state the main argument or perspective.
Patient-Centered Care:
- Definition: Clarify what patient-centered care means in nursing.
- Personal Experience: Share a relevant encounter from clinical practice.
- Evidence: Integrate findings from reputable nursing literature.
Ethical Dilemmas in Nursing Practice
- Scenario Presentation: Describe a specific ethical challenge faced by nurses.
- Decision-Making Process: Outline steps taken to address the dilemma.
- Ethical Frameworks: Discuss any ethical theories guiding the decision.
Impact of Technology on Nursing
- Current Trends: Highlight technological advancements in nursing.
- Case Study: Share an example of technology enhancing patient care.
- Challenges and Benefits: Discuss the pros and cons of technology in nursing.
- Summary of Key Points: Recap the main ideas from each section.
- Real-world Implications: Emphasize the practical significance in nursing practice.
- Closing Thought: End with a reflective statement or call to action.
A+ in Nursing Essays Await You!
Ready to excel? Let us guide you. Click now for professional nursing essay writing assistance.
Nursing Essay Examples
Here are the nursing Essay Examples for you to read.
Writing a Nursing Essay: Essential Tips
When it comes to crafting a stellar nursing essay, a few key strategies can elevate your work from ordinary to exceptional. Here are some valuable tips from our medical school personal statement writer :

Connect with Personal Experiences:
- Approach: Weave personal encounters seamlessly into your narrative.
- Reasoning: This not only adds authenticity to your essay but also serves as a powerful testament to your firsthand understanding of the challenges and triumphs in the nursing field.
Emphasize Critical Thinking:
- Approach: Go beyond describing situations; delve into their analysis.
- Reasoning: Nursing essays are the perfect platform to showcase your critical thinking skills – an essential attribute in making informed decisions in real-world healthcare scenarios.
Incorporate Patient Perspectives:
- Approach: Integrate patient stories or feedback into your discussion.
- Reasoning: By bringing in the human element, you demonstrate empathy and an understanding of the patient's experience, a core aspect of nursing care.
Integrate Evidence-Based Practice:
- Approach: Support your arguments with the latest evidence-based literature.
- Reasoning: Highlighting your commitment to staying informed and applying current research underscores your dedication to evidence-based practice – a cornerstone in modern nursing.
Address Ethical Considerations:
- Approach: Explicitly discuss the ethical dimensions of your topic.
- Reasoning: Nursing essays provide a platform to delve into the ethical complexities inherent in healthcare, showcasing your ability to navigate and analyze these challenges.
Balance Theory and Practice:
- Approach: Connect theoretical concepts to real-world applications.
- Reasoning: By bridging the gap between theory and practice, you illustrate your capacity to apply academic knowledge effectively in the dynamic realm of nursing.
Highlight Interdisciplinary Collaboration:
- Approach: Discuss collaborative efforts with other healthcare professionals.
- Reasoning: Acknowledging the interdisciplinary nature of healthcare underscores your understanding of the importance of teamwork – a vital aspect of successful nursing practice.
Reflect on Lessons Learned:
- Approach: Conclude with a thoughtful reflection on personal growth or lessons from your exploration.
- Reasoning: This not only provides a satisfying conclusion but also demonstrates your self-awareness and commitment to continuous improvement as a nursing professional.
As we wrap up, think of your essay as a story about your journey into nursing. It's not just about getting a grade; it's a way to share what you've been through and why you want to be a nurse.
Imagine the person reading it – maybe a teacher, a future coworker, or someone starting their nursing journey. They're trying to understand your passion and why you care about nursing.
So, when you write, remember it's more than just an assignment. It's your chance to show why nursing matters to you. And if you ever need help – there's always support from our essay writer online .
Ready to Excel in Your Nursing School Essay?
Order now and experience the expertise of our professional writers!
How to Write a Nursing Essay?
How can a nursing essay effectively address ethical considerations, what are some examples of evidence-based practices in nursing essays.

Daniel Parker
is a seasoned educational writer focusing on scholarship guidance, research papers, and various forms of academic essays including reflective and narrative essays. His expertise also extends to detailed case studies. A scholar with a background in English Literature and Education, Daniel’s work on EssayPro blog aims to support students in achieving academic excellence and securing scholarships. His hobbies include reading classic literature and participating in academic forums.

is an expert in nursing and healthcare, with a strong background in history, law, and literature. Holding advanced degrees in nursing and public health, his analytical approach and comprehensive knowledge help students navigate complex topics. On EssayPro blog, Adam provides insightful articles on everything from historical analysis to the intricacies of healthcare policies. In his downtime, he enjoys historical documentaries and volunteering at local clinics.
Related Articles
.webp)

Nursing Scholarship Essay Example
Home » Nursing Scholarship Essay Example
Wow! I never thought I would have my own scholarship , but this opportunity has come to fruition and I plan to use every dollar for the good of nursing. It is wonderful to be able to give back to the nursing profession, and it humbles me to be a part of this year’s recipient’s journey. I have been there, and nursing school is incredibly tough. To be able to ease the stress of that journey for a nurse pursuing his or her BSN is an honor !
I want to tell you why I believe scholarships are so important.
You always hear people talking about “nurse burnout”. Well, it is a real thing. Retirement is also a real thing. And the nursing shortage is a real thing . Therefore, we want and we need more nurses in this profession. I, personally, had to take out over $40,000 in student loans when I went to school, so I completely understand the need for scholarship and outside opportunities to fund your dreams. I want to live in a scholastic world where money does not stop one selfless human being from pursuing the most trusted profession in the world. Scholarships are super important to ensure that we can build up our profession with nurses for the future.
I would like to share an example of the Nurse Kelley Scholarship essay that I have written. It is completely true, and hopefully, this nursing scholarship essay example will give you a good idea of what we are looking for in a submission.
There are many reasons someone might choose to go into the nursing profession. Maybe they “want to help people”. Maybe they love math and science. Maybe they want to give back to their community. Maybe their mom was a nurse. Whatever the reason may be, for most of us, it’s different. I chose to go into nursing because of a personal experience that I had when I was young. I lost my biological father to colon cancer, and I wanted to be a caring support system for other families going through what we did. The strange thing about the many reasons people choose nursing, is that somehow, we are all still very connected in this choice.
You see, nursing is a profession where you have to take care of complete strangers, and we have signed on to do this for life.
Nursing is so incredibly unique and selfless in that what we do every single day is care for people who are at their most vulnerable moments, and we often times do it while missing something in our life that means something to us. We constantly sacrifice for our patients. We constantly give while barely taking. The most important thing to remember is that we don’t mind. That’s what makes us different. We know what we have gotten ourselves into, and we love doing it. There is a special place in a nurse’s heart that draws them to the type of work that we do. And it brings us all together, our binding character trait.
I think I can say now that I guess my reason for going into nursing is a combination of everyone’s reason. They may spark from different experience, but we are intertwined in our methodology for career choice through our heart for others. I am PROUD to be a nurse!
I want to remind any nurse reading this that nursing will continue to choose you throughout your career. It is so funny how nursing just pulls you out of your everyday life as if to say, “nope, you don’t get to be a civilian today, you’re still a nurse”! I’ll give you an example. Four days after I was crowned Miss Colorado I was driving in my crown and sash away from an appearance as a car flipped over on our interstate and started on fire. Of course, I pulled over. A fireman also pulled over (that special place in our hearts, other service industry members have that too!), and we collectively (after removing the crown and sash) helped pull this man from his car and start working on him. It was wild. I remember shaking my head thinking, “thanks a lot, nursing”, and then giggling. How lucky I am to have been chosen by this profession!
Nursing is the best. It will be a part of you forever.
Congratulations on making this choice for your career. You won’t regret it.
All my love,
Nurse Kelley
Related Posts:
- Meet Our 2019 Scholarship Winner!
- 6 Tips to Avoid Travel Nurse Burnout
- Wanderly 2018 Roundup: Our 12 Favorite Blog Posts
- The Top 6 Nursing Interview Tips
- 10 Questions Nurses Should Ask in a Job Interview
- Advocacy In Nursing
Leave a Reply Cancel reply
You must be logged in to post a comment.
- MEMBER DIRECTORY
- Member Login
- Publications
- Clinician Well-Being
- Culture of Health and Health Equity
- Fellowships and Leadership Programs
- Future of Nursing
- U.S. Health Policy and System Improvement
- Healthy Longevity
- Human Gene Editing
- U.S. Opioid Epidemic
- Staff Directory
- Opportunities
- Action Collaborative on Decarbonizing the U.S. Health Sector
- Climate Communities Network
- Communicating About Climate Change & Health
- Research and Innovation
- Culture of Health
- Fellowships
- Emerging Leaders in Health & Medicine
- Culture & Inclusiveness
- Digital Health
- Evidence Mobilization
- Value Incentives & Systems
- Substance Use & Opioid Crises
- Reproductive Health, Equity, & Society
- Credible Sources of Health Information
- Emerging Science, Technology, & Innovation
- Pandemic & Seasonal Influenza Vaccine Preparedness and Response
- Preventing Firearm-Related Injuries and Deaths
- Vital Directions for Health & Health Care
- NAM Perspectives
- All Publications
- Upcoming Events
- Past Events
- MEMBER HOME

The Future of Nursing 2020-2030
The future of nursing 2020-2030: charting a path to achieve health equity, a consensus study from the national academy of medicine.

About the Study
An expert committee will extend the vision for the nursing profession into 2030 and chart a path for the nursing profession to help our nation create a culture of health, reduce health disparities, and improve the health and well-being of the U.S. population in the 21st century. The committee will consider newly emerging evidence related to the COVID-19 global pandemic and include recommendations regarding the role of nurses in responding to the crisis created by a pandemic.
The committee will examine the lessons learned from the Future of Nursing Campaign for Action as well as the current state of science and technology to inform their assessment of the capacity of the profession to meet the anticipated health and social care demands from 2020 to 2030.
In examining current and future challenges, the committee will take into account the dramatically changed context and the rapidly deployed changes in clinical care, nurse education, nursing leadership, and nursing-community partnerships as a result of the pandemic. The committee will consider:
- The role of nurses in improving the health of individuals, families, and communities by addressing social determinants of health and providing effective, efficient, equitable, and accessible care for all across the care continuum, as well as identifying the system facilitators and barriers to achieving this goal.
- The current and future deployment of all levels of nurses across the care continuum, including in collaborative practice models, to address the challenges of building a culture of health.
- System facilitators and barriers to achieving a workforce that is diverse, including gender, race, and ethnicity, across all levels of nursing education.
- The role of the nursing profession in assuring that the voice of individuals, families and communities are incorporated into design and operations of clinical and community health systems.
- The training and competency-development needed to prepare nurses, including advanced practice nurses, to work outside of acute care settings and to lead efforts to build a culture of health and health equity, and the extent to which current curriculum meets these needs.
- The ability of nurses to serve as change agents in creating systems that bridge the delivery of health care and social needs care in the community.
- The research needed to identify or develop effective nursing practices for eliminating gaps and disparities in health care.
- The importance of nurse well-being and resilience in ensuring the delivery of high quality care and improving community health.
- The role of nurses in response to emergencies that arise due to natural and man-made disasters and the impact on health equity.
In developing its recommendations for the future decade of nursing in the United States, the committee will draw from domestic and global examples of evidence-based models of care that address social determinants of health and help build and sustain a culture of health. Join the conversation using #FutureofNursing2030 on Twitter!
In 2009, the Robert Wood Johnson Foundation partnered with the Institute of Medicine to produce The Future of Nursing: Leading Change, Advancing Health , which set a vision for nursing in 2020. The authoring committee produced a set of recommendations for the field of nursing and it provided a blueprint for improving nurse education; ensuring that nurses can practice to the full extent of their education and training; providing opportunities for nurses to assume leadership positions; and improving data collection for policymaking and workforce planning.
A variety of current and emerging issues influence the field of nursing, from ongoing health care reform and integration of new technologies to patient-centered care to respect for the profession and its expertise, merit exploration and consideration in setting national priorities for the next ten years. Additionally, nurses serve in many community settings; therefore, the nursing profession is well-positioned to serve an important role in implementing the Robert Wood Johnson Foundation’s vision for a culture of health.
The Future of Nursing 2020-2030 Webinar Series | Day 4:Diversifying the Nursing Workforce to Advance Health Equity August 11, 2021 | Webinar
The Future of Nursing 2020-2030 Webinar Series | Day 3: Fully Supporting Nurses’ Well-Being to Advance Health Equity August 4, 2021 | Webinar
The Future of Nursing 2020-2030 Webinar Series | Day 2: Lifting Practice Barriers and Designing Better Payment Models to Expand the Contributions of Nurses July 21, 2021 | Webinar
The Future of Nursing 2020-2030 Webinar Series | Day 1: An Overview of Nursing’s Role in Addressing Health Equity June 29, 2021 | Webinar
Report Release Webinar: The Future of Nursing 2020-2030 May 11, 2021 | Webinar
Nursing’s Role in Health Equity, Public Health Emergencies, and COVID-19 – Critical Issues for The Future of Nursing 2020-2030 August 20, 2020 | Webinar
Future of Nursing 2020-2030 Town Halls
- Chicago – June 7, 2019 Twitter Chat #1
- Philadelphia – July 24, 2019 Twitter Chat #2
- Seattle – August 7, 2019 Twitter Chat #3
Public Session for the Committee on the Future of Nursing March 20, 2019 | Washington, DC & Webcast
Technical Panel and Discussion November 20, 2019 | Webinar
Robert Wood Johnson Foundation
Board on Health Care Services, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine
- Suzanne Le Menestrel, Study Director
- Jennifer Flaubert, Program Officer
- Adrienne Formentos, Research Associate
- Tochi Ogbu-Mbadiugha, Senior Program Assistant
National Academy of Medicine
- Susan Hassmiller, Senior Scholar in Residence and Advisor to the President on Nursing at the National Academy of Medicine
- Ashley Darcy-Mahoney, Distinguished Nurse Scholar-in-Residence
Contact us at [email protected]
Join Our Community
Sign up for nam email updates.
Writing Tips for Nursing School Students

- Nursing School Writing Types
- Writing a Nursing Essay
- Citations Guide
- Common Writing Mistakes
- Writing Resources
Are you ready to earn your online nursing degree?

Writing is an essential skill nurses should achieve proficiency in early in their career. It is a crucial part of the profession, as nurses need to be able to effectively communicate with patients, families, and other healthcare professionals.
While verbal communication also plays a vital role in nursing, being able to write well builds the nurse’s ability to provide better care.
Being able to accurately detail a patient’s personal history, symptoms, and diagnosis allows for the execution of a precise treatment plan that is clearly communicated to all parties involved, both professional and personal.
From registered nurses to clinical nurses and beyond, being able to communicate effectively and efficiently is a critical soft skill that will help nurses in any role increase their ability to treat their patients.
This guide provides an overview of the types of writing nurses will experience throughout their educational training. Utilize the following tips and tricks to help strengthen your writing skills, which will ultimately help in the development of transferable career skills .
Types of Writing Nurses Will Do in School
Personal statements for nursing school.
Nursing schools want candidates who meet academic and professional requirements. They also want a candidate who demonstrates a sincere passion for patient care and individual connections. You should always craft a personal statement, even when the application doesn’t explicitly require one. Personal statements allow you to describe your goals, characteristics, credentials, volunteer work, and meaningful life experiences. A well-crafted essay can help you stand out among other qualified applicants. And, as with any piece of writing, you must take the time to revise.
In your personal statement, you should portray yourself as determined and empathetic, with characteristics, goals, work ethic, and healthcare philosophy that align with a program’s values. Some nursing schools ask for a general personal statement, while others require a specific prompt. Colleges commonly ask students to describe a hardship they overcame, a difficult task they accomplished, or a professional goal they hope to achieve through the program. Many schools also ask students to detail previous experiences in healthcare. You may decide to write about how you connect with patients or how you provide practical and emotional support to loved ones.
You will also encounter writing prompts during examinations, including standardized tests like the GRE or MCAT, nursing school entrance exams , and course-specific evaluations. You may also take exams to get state licensure or professional certification. In most of these instances, you will need to write one or several long-form essays. Proper planning is key. Though you won’t know what specific prompt the test will require, you can expect certain common topics. You can search online or use study guides to determine which prompts usually appear on each test.
On test day, you should begin by creating an outline that lists three main points in response to the prompt. Using these points, work backwards to write a central thesis to guide the essay’s structure. Review what you’ve written to ensure that the essay actually responds to the prompt at hand. Be sure to leave time to correct spelling, grammar, and stylistic errors.
Research Papers
Like essays, research papers follow a long-form structure. Unlike an essay, which heavily relies on the writer’s point of view, a research paper presents an in-depth investigation of a topic using data, expert opinions, and insights. While an essay evaluates general critical thinking and writing skills, a research paper tests your knowledge, research skills, and original contributions. Research papers also allow you to prove you understand what has been argued and discovered about a topic. Research papers, especially at the graduate and doctoral levels, require independent research and analyses. These papers sometimes take months or years to complete.
To write a successful research paper, you should pick a topic relevant to your interests and the nursing field. Possibilities include elderly care challenges, patient safety and ethics, mental health treatment and regulations in the U.S., and nursing shortages and possible solutions. Whatever your choice, you must plan accordingly. Advanced papers such as dissertations may require funding or help from professors. Research papers often consist of the following sections: abstract, introduction, literature review, methods, results, discussion, conclusion, and references. You should keep this general structure in mind as you prepare notes and outlines.
How Do You Write a Nursing Essay?
In nursing school, essay writing includes academic papers, personal narratives, and professional compositions. You should become familiar with each of the five major forms below. There are many similarities between these essay types, such as an overarching thesis and a supportive, logical structure. You should support claims with factual, statistical, anecdotal, and rhetorical evidence. However, each form requires distinct skills to achieve specific results.
Comparative
Cause and effect, citations guide for nursing students.
Citations allow readers to know where information came from. By citing sources, you avoid plagiarizing or stealing another person’s ideas, research, language, and analyses. Whether intentional or unintentional, plagiarism is one of the most egregious errors one can make. Consequences for plagiarism include automatic course failure, disciplinary actions from the university, and even legal repercussions. You should take special care to ensure you properly cite sources.
American Psychological Association (APA) Style
APA is the most commonly used style among natural scientists, social scientists, educators, and nurses. Like other citation styles, APA emphasizes clarity of font style, font size, spacing, and paragraph structure. APA citations focus on publication date, and in most cases, the date comes right after the author’s name. This order makes the style particularly useful for scientists, who value new research and updates on current findings. For more information on APA style, visit this official website .
(Author and year of publication, page number) “Punishment, then, will tend to become the most hidden part of the penal process” (Foucault, 1977, p. 9).
Chicago Manual of Style (CMS)
CMS (also known as CMOS or, simply, Chicago) features two citation systems, the notes and bibliography, and the author and date. This style is used primarily by historians, who place high importance on a text’s origin. The notes and bibliography include a superscript number with a corresponding footnote or endnote. Scientific professionals use the author and date citation, a generic parenthetical system with similarities to other citation styles. The CMS official website provides additional information, including changes to citation systems in the current edition.
“Punishment, then, will tend to become the most hidden part of the penal process”. 1 1. Michel Foucault, trans. Alan Sheridan, Discipline and Punish: The Birth of the Prison (New York: Pantheon Books, 1977), 9.
(Author and year of publication, page number) “Punishment, then, will tend to become the most hidden part of the penal process” (Foucault 1977, 9).
Modern Language Association (MLA) Format
MLA format traces its history to 1951 when it was first published as a thin booklet. Today, MLA is the primary format used by academics and professionals in humanities, English, literature, media studies, and cultural studies. To adapt to the rapid growth of new mediums over the past few decades, MLA updates its citation system. Visit the MLA Style Center for in-depth information on new guidelines and ongoing changes. In general, in text citations consist of author and page number, or just page number if the author’s name appears in the text.
(Author and page number) “Punishment, then, will tend to become the most hidden part of the penal process” (Foucault 9).
Associated Press (AP) Style
Published in 1952, the original AP Stylebook was marketed to journalists and other professionals related to the Associated Press. AP now stands as the go-to style for professionals in business, public relations, media, mass communications, and journalism. AP style prioritizes brevity and accuracy. The style includes specific guidelines regarding technological terms, titles, locations, and abbreviations and acronyms. Unlike the previous styles, AP does not use parenthetical or in-text citations. Rather, writers cite sources directly in the prose. For more information, including style-checking tools and quizzes, visit the Associated Press Stylebook .
In the book, “Discipline and Punish: The Birth of the Prison,” first published in English in 1977, philosopher Michel Foucault argues that “Punishment, then, will tend to become the most hidden part of the penal process”.
Which Style Should Nursing Students Use?
Because nurses rely on scientific terms and information, professionals in the field usually use APA style. Regardless of the purpose and specific genre of your text, you should always strive for concise, objective, and evidenced-based writing. You can expect to learn APA style as soon as you enroll in a major course. However, you should also prepare to learn other styles as part of your academic training. For example, freshman composition classes tend to focus on MLA guidelines.
Common Writing Mistakes Students Make
Active vs. passive voice.
Active and passive voice represent two different ways to present the same piece of information. Active voice focuses on the subject performing an action. For example, the dog bites the boy. This format creates clear, concise, and engaging writing. Using active voice, nurses might write, I administered patient care at 11:00. Passive voice, on the other hand, focuses on the object of the sentence or the action being performed. For example, the boy was bitten by the dog. A passive sentence is usually one that contains the verb “to be.” Using passive voice, you might write, patient care was administered at 11:00.
Professionals in the sciences often use passive voice in their writing to create an objective tone and authorial distance. Passive voice can prioritize specific terms, actions, evidence, or research over the writer’s presence. Additionally, nurses use passive voice because it is usually clear that the reported thoughts, actions, and opinions come from them. However, you must also learn how to use active voice.
Punctuation
There are 14 punctuation marks in the English language, each with multiple and sometimes overlapping uses. Additionally, certain punctuation marks only make sense in highly specific and nuanced grammatical instances. To master punctuation, you must learn through practice, particularly by revising your own writing.
For example, colons and semicolons are often used interchangeably, when they actually serve distinct purposes. Generally used before itemized lists, colons stand in for the phrases “here is what I mean” or “that is to say.” For example, I am bringing three things to the picnic: applesauce, napkins, and lemonade. Semicolons separate two independent clauses connected through topic or meaning. For example, It was below zero; Ricardo wondered if he would freeze to death. Comma splices, which create run on sentences, are another common mistake. You can identify a comma splice by learning the differences between an independent and dependent clause.
Grammar refers to the rules of a particular language system. Grammar determines how users can structure words and form sentences with coherent meaning. Aspects include syntax (the arrangement of words to convey their mutual relations in a sentence) and semantics (how individual words and word groups are understood). Unless you major in writing, literature, etymology, or another related field, you generally won’t examine English grammar deeply. Through years of cognitive development and practice, native users implicitly understand how to effectively employ the language.
Distinct grammatical systems exist for each language and, sometimes, even within a single language. For example, African American Vernacular English uses different syntactic rules than General American English. You should learn grammatical terms and definitions. Common errors include subject/verb agreement, sentence fragments, dangling modifiers, and vague or incorrect pronoun usage. Hasty writers can also misuse phonetically similar words (your/you’re, its/it’s, and there/their/they’re).
Writing Resources for Nursing Students
Apa style central, reviewed by:.

Shrilekha Deshaies, MSN, RN
Shri Deshaies is a nurse educator with over 20 years of experience teaching in hospital, nursing school, and community settings. Deshaies’ clinical area of expertise is critical care nursing and she is a certified critical care nurse. She has worked in various surgical ICUs throughout her career, including cardiovascular, trauma, and neurosurgery.
Shri Deshaies is a paid member of our Healthcare Review Partner Network. Learn more about our review partners here .
Page last reviewed November 30, 2021
Whether you’re looking to get your pre-licensure degree or taking the next step in your career, the education you need could be more affordable than you think. Find the right nursing program for you.
You might be interested in

HESI vs. TEAS Exam: The Differences Explained
Nursing schools use entrance exams to make admissions decisions. Learn about the differences between the HESI vs. TEAS exams.

10 Nursing Schools That Don’t Require TEAS or HESI Exam

For Chiefs’ RB Clyde Edwards-Helaire, Nursing Runs in the Family
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030; Flaubert JL, Le Menestrel S, Williams DR, et al., editors. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington (DC): National Academies Press (US); 2021 May 11.

The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity.
- Hardcopy Version at National Academies Press
9 Nurses Leading Change
Minister to the world in a way that can change it. Minister radically in a real, active, practical, and get your hands dirty way. —Chimamanda Ngozi Adichie, author
As demonstrated by the COVID-19 pandemic, nurses at every level and across all settings are positioned to lead. Nurses can lead teams, promote community health, advocate for systems change and health policy, foster the redesign of nursing education, and advance efforts to achieve health equity. Even so, educational institutions and health systems can better prepare and empower new and practicing nurses, including licensed practical nurses, registered nurses, advanced practice registered nurses, and those with doctoral degrees to develop and grow in leadership roles. To this end, it will be necessary to place more intentional focus on providing models and opportunities for the emergence of more diverse nurse leaders who can reflect the people and families they care for and can mentor and serve as role models for underrepresented students.
Creating a future in which opportunities to optimize health are more equitable will require disrupting the deeply entrenched prevailing paradigms of health care, which in turn will require enlightened, diverse, courageous, and competent leadership. The seminal Institute of Medicine report Crossing the Quality Chasm: A New Health System for the 21st Century ( IOM, 2001 ) calls for broad and sweeping transformation of the health care system in order to improve the quality of care. It identifies six aims for improvement that define quality health care: to provide care that is safe, effective, patient-centered, timely, efficient, and equitable ( IOM, 2001 ). The Institute for Healthcare Improvement (IHI) has found that progress on health equity has lagged behind that on the other five aims, calling it “the forgotten aim” of health care ( Feely, 2016 ). The Crossing the Quality Chasm report emphasizes the importance of leadership in achieving the six aims, noting that leaders have a wide variety of roles and responsibilities that include
creating and articulating the organization’s vision and goals, listening to the needs and aspirations of those working on the front lines, providing direction, creating incentives for change, aligning and integrating improvement efforts, and creating a supportive environment and a culture of continuous improvement that encourages and enables success. ( IOM, 2001 , p. 137)
It must be emphasized that having this type of leadership only at the top of an organization or initiative is not enough. Rather, leadership is needed at multiple levels to “provide clear strategic and sustained direction and a coherent set of values and incentives to guide group and individual actions” ( IOM, 2001 , p. 137) and to ensure that health equity is a strategic priority at every level ( Feely, 2016 ).
This chapter focuses on how nurse leaders can, and do, address social determinants of health (SDOH) and health equity in all settings and all nursing roles. It begins by articulating how nurses are well suited to lead in such efforts, and then outlines the committee’s vision for nursing leadership specific to these challenges in the future. Next is a discussion of the competencies that will enhance nurses’ ability to lead effective change. Finally, the chapter explores ways to help achieve the committee’s vision for nursing leadership through training and leadership development specific to advancing an agenda of greater health equity.
- NURSES LEADING IN HEALTH EQUITY
Nurses have a rich history of both advocacy and the provision of holistic care that includes meeting social needs of individuals and focusing on SDOH. As presented in this report, there are numerous examples illustrating how nurses are already working effectively as leaders on equity issues across a variety of settings. If nurses are to build on this rich tradition, it will not be enough for them to see themselves as leaders; the organizations that employ them will have to provide them with ample opportunities, resources, and mentorship to fully realize their leadership potential. This is the case even for nurses who are self-employed, who can benefit from opportunities provided by the external systems around them.
Nursing’s Focus on Social Determinants
Nurses have always been key to the health and well-being of individuals and communities, but a new generation of nurse leaders is now needed—one that recognizes the importance of SDOH and diversity and is able to use and build on the increasing evidence base supporting the link between SDOH and health status. Today’s nurses are called on to lead in the development of effective strategies for improving the nation’s health ( Lathrop, 2013 ; Ogbolu et al., 2018 ) with due attention to the needs of the most underserved individuals, neighborhoods, and communities and the crucial importance of advancing health equity.
Leadership can be defined as a process of social influence that maximizes the efforts of others toward achievement of a goal ( Kruse, 2013 ). Leaders set direction, build an inspiring vision, press for change, and create new ways of thinking and doing. Nurses as a professional group manifest many of the characteristics of strong leadership—including courage, humility, caring, compassion, intelligence, empathy, awareness, and accountability—that are essential to leading the way on health equity ( Shapiro et al., 2006 ). In addition to their deep understanding of how health intersects with SDOH ( Olshansky, 2017 ), they have a holistic view of people across systems and settings, they are active listeners, they establish therapeutic relationships, and they practice person-centered care. Increasingly, nurses are serving as innovators and codesigners of health care in their roles in the public health and health care systems ( Jouppila and Tianen, 2020 ), and by continuing to learn and apply improvement and innovation skills, will be able to help create new care models for the decade ahead. Given the wide range of settings and roles in which nurses at all levels serve (see Chapter 1 ), their leadership in this regard can have broad and far-reaching impacts on equity in health and health care.
THE COMMITTEE’S VISION FOR NURSING LEADERSHIP
Implementing change to address SDOH and advance health equity will require the contributions of nurses in all roles and all settings, and recognition that no one nurse can successfully implement change without the collaboration of others. Clinical nurses manage the nursing care of patients and coordinate care, making decisions and communicating with families and other health care professionals. These nurses can influence clinical practice environments and local organizational culture, as well as organizational processes and policies, often working with members of other health care disciplines. Public health and school nurses and other community-based nurses engage with the community to identify and address individual- and community-level needs, often working with professionals from other disciplines and sectors. Some nurses serve on boards, manage organizations, direct programs, and have direct responsibility for developing policies and practices. Nurses leading community organizations often lead team members and partner with community members and organizations in other sectors. Nurses serving on health care boards can exert leadership influence on the organization’s policies and structures while not leading day-to-day organizational operations. Still other nurses work with but outside the health care system, advocating for and working toward public- and private-sector policies and structures that can have positive impacts on health and well-being. These nurses (e.g., a public health nurse advocating for more equitable transportation policy) may lead individuals and organizations as part of a multidisciplinary, multisector coalition. And nurses with formal leadership roles, such as nurse managers, chief executive officers (CEOs), and deans, can use their positions to establish organizational cultures and implement practices that advance health equity. In addition to collaboration among members of the nursing profession and across other disciplines and sectors, the creation of enduring change requires the involvement of individuals and community members. Rather than a more hierarchal system of leadership, collaborative leadership assumes that everyone involved has unique contributions to make and that constructive dialogue and joint resources are needed to achieve ongoing goals ( Eckert et al., 2014 ).
Each of the various leadership roles described above involves different skills and responsibilities, as shown in the framework for nurse leadership in Table 9-1 . It is important to note that an individual nurse may lead in multiple areas of this framework and can lead in both formal and informal capacities. While some nursing positions (e.g., CEO, dean, nurse manager) entail more explicit leadership responsibilities, all nurses can lead according to their own interests, capacities, and opportunities. For example, a staff nurse who has no official leadership position in the workplace can lead others by modeling behaviors that promote a culture of diversity, equity, and inclusion, and can also lead beyond health care through involvement in political advocacy. As noted earlier, fulfillment of this potential will require support, encouragement, mentorship, and advancement opportunities, with nurses operating to the full scope of their education, training, and expertise.
A Framework for Nurse Leadership.
The subsections below detail the leadership roles nurses can play at the four levels shown in Table 9-1 : leading self, leading others, leading health care, and leading beyond health care. Nurses engaging in each of these leadership levels are important to advancing health equity. Together, the various roles at these four levels constitute the committee’s vision for nursing leadership.
Leading Self
Before nurses can lead others, they need to be able to lead themselves. To address SDOH, nurses need to understand and acknowledge how social determinants affect them personally, and to be aware of implicit biases that may influence the decisions they make and the outcomes of the people and communities they serve. They must understand and manage their own emotional responses, invest in their own physical and mental health, serve as role models for others, and continue their personal and professional development. Nurses can lead at this level by advocating for themselves and others in the workplace, functioning as effective team players, and developing coping and self-care skills ( NASEM, 2020 ).
Part of leading oneself is seeing oneself as a leader and viewing leadership as an integral part of one’s role. One barrier to effective leadership is that not all nurses see themselves in this way or have the bandwidth to take on or understand what leadership entails ( Dyess et al., 2016 ; Sherman, 2019 ). Given the right environment and support, however, nurses can overcome these barriers. (See Chapter 7 for further discussion of implicit bias and Chapter 10 for further discussion of self-care.)
Leading Others
In the pursuit of health equity, nurses have the opportunity to lead others, including other nurses, students, health care professionals, staff, community members, and partners. Leading others may occur in a wide range of contexts, including working with clinical nurse managers, community organization leaders, nurses engaging in policy development, and educators and research teams. Leading and managing effective teams requires building and maintaining trusting relationships among team members, communicating effectively, and supporting each team member. In this role, nurses can leverage and actively promote diversity within their teams and create an atmosphere of equity, inclusion, innovation, support, and growth. As team leaders, they can use their position to motivate and empower others to work to identify and address social in addition to health care needs, take action on health equity, and provide the tools and resources needed to do so.
One example of nurses leading others in pursuit of health equity is Cultivando Juntos, a community wellness program aimed at helping farmworkers live longer, healthier lives ( Berger, 2019 ). Two nursing students designed the program, which has expanded to include a biostatistician, a postdoctoral fellow, and undergraduate nursing students. The team meets with local Hispanic farmworkers to discuss their health and well-being and to conduct demonstrations on cooking healthy food. Baseline and longitudinal data are collected across the program to track progress on outcomes that include HgbA1c and lipid levels and body mass index ( Berger, 2019 ). This program is an example of nurses leading others by bringing multiple sectors together to engage with a community in order to address the community’s needs.
Nurses Leading Health Care
Nurses lead in numerous ways within health care, both in health care organizations and beyond their organizational boundaries. Within an organization, nurses can assess the organization’s readiness to address issues of equity and recommend related improvement. For example, a staff nurse on an inpatient unit can advocate for incorporating an assessment tool that can systematically collect data on SDOH within the electronic health record. Or a nursing director within a health care organization can engage other leaders, as well as members of the community, in initiating a healthy foods program within the hospital and connecting with related community-based agencies. Nurses can also identify and disseminate best and evidence-based practices to ensure equitable health care services within departments and across patient populations, improving and sustaining a supportive culture of care for both staff and those they serve, and advocate for policy changes that address population health and SDOH at the organizational and public policy levels. Nurses leading at higher levels within health care, such as nurse CEOs, chief nursing officers (CNOs), and chief operating officers, can work collaboratively with their organization to set direction and develop a vision and strategies for advancing organization-wide goals that include the drive for greater health equity through engagement with SDOH to meaningfully impact communities served by the health system. Successful organizational leaders can span boundaries between disciplines and sectors in an inclusive way to create meaningful, respectful, and sustainable partnerships to address issues of health equity. For example, public health nurse leaders can bring together representatives of the community served along with leaders from other sectors, including health care, transportation, housing, and food security, to address community needs (see the section below on leading multisector partnerships).
Nurses also have the capacity to lead in health care more broadly. For example, a nurse can seek to influence SDOH by working with a specialty organization such as the National Black Nurses Association, which focuses on the professional development of Black nurses and the delivery of culturally competent care, or serve as a leader for the Council of Public Health Nursing Organizations (CPHNO) or the National Rural Health Association. Many nurses also serve on boards of health care organizations, where they can provide their unique perspective on health-related issues facing individuals, families, and communities ( Harper and Benson, 2019 ). And nurses can serve as leaders in a variety of interprofessional contexts within health care; an example is a nurse researcher leading a multiorganizational research team. In each of these contexts and roles, nurses can share nursing’s perspective and expertise while collaborating with others to address health disparities, SDOH, and health equity.
Leading Beyond Health Care
Nurses have myriad opportunities to lead entirely outside the traditional boundaries of health care, in both the public and private sectors. In the public sector, they can lead through positions in local, state, and national government organizations, such as departments of human services, public health, and education. Nurses can be appointed to senior government positions or stand for election to political office, positions in which they can use their expertise and voice to advocate for policy change in the areas of SDOH and health equity. Applying her expertise, U.S. House of Representatives member Lauren Underwood, a registered nurse, discussed the disproportionate health and economic impacts of COVID-19 on communities of color, particularly Black Americans, in a Committee on Education and Labor virtual hearing in June 2020, calling these disparities “the pandemic inside this pandemic.” 1 She also sponsored a number of bills to eliminate disparities, such as H.R. 6142, 2 focused on maternal health outcomes among minority populations.
A number of other nurses serve in state legislatures, the U.S. Congress, state and federal executive branch positions, and national and state commissions and committees. Nurse leaders also can bring nursing perspective and expertise to private organizations. For example, Microsoft employs a CNO, and AARP has been served by several nurse CEOs. Nurses can facilitate and convene multisector partnerships, leading efforts to disseminate and implement interventions aimed at improving population health, and can engage communities and partners through local, regional, and national networks. Just as nurses serve as board members within health care, they can also serve on boards for programs or organizations that are outside of health care but have impact on health. The Nurses on Boards Coalition works to create opportunities for nurses to participate in a wide range of boards outside of health care, from boards of local schools or places of worship to those of Fortune 500 companies and large international corporations ( Harper and Benson, 2019 ). In the next 10 years, nurse leaders in these types of positions can become drivers for change within their communities by advocating for social change and health equity, and bringing nursing’s perspective to organizational and public policy-making discussions.
- LEADERSHIP COMPETENCIES FOR ADVANCING HEALTH EQUITY
While nurses’ specific leadership roles vary depending on the focus of their work, the setting in which they work, and the people whom they lead, there are certain skills and competencies on which all nurse leaders need to draw as they work to advance health equity by creating a vision and culture of equity, putting the necessary structures and supports in place, and working both within and across boundaries to achieve the vision of health for all. The committee identified eight skills and competencies that are essential for nurse leadership in nearly every setting, which are described in turn below:
- visioning for health equity,
- leading multisector partnerships,
- leading change,
- innovating and improving,
- teaming across boundaries,
- creating a culture of equity,
- creating systems and structures for equity, and
- mentoring and sponsoring.
Visioning for Health Equity
In all types of work, a leader is responsible for articulating a vision, setting direction and goals, and developing clear expectations for individuals and teams. Nurse leaders are no exception, whether the vision they create is for providing quality patient care in a clinic, meeting the needs of a community, setting the direction and goals for an organization or company, or redesigning the nation’s health care system. In the context of this report, nurse leaders at all levels and in all settings can work collectively with others to develop and communicate a clear and compelling vision for a future state of greater health equity. The creation of a vision for greater health equity can be squarely rooted in existing data demonstrating profound differences in care quality and health outcomes among people of color compared with their White counterparts ( Betancourt et al., 2017 ).
The most effective visions are a shared product ( Boyatzis et al., 2015 ). Nurse leaders can articulate ideas for a vision, and develop a shared vision by working collaboratively with others. Fully understanding the needs, hopes, and aspirations of a community or population is critical to achieving an effective shared vision ( Kouzes and Posner, 2009 ). To this end, nurse leaders can engage in dialogue with community members, whether that community consists of patients in a clinical setting; a subpopulation such as juveniles in the justice system; or residents of a neighborhood, city, or state. Regardless of the specific target community, this engagement requires a nurse leader to apply such skills as listening, acknowledging, and collaborating in order to create trusted relationships that are needed to build community-centric, community-informed solutions to complex health and social needs. Additionally, data collection and analysis to identify, assess, and prioritize opportunities for advancing health equity is essential ( Wesson et al., 2019 ).
Nurses can work with communities to identify and address their needs in a number of ways, including collecting and analyzing data, leading community meetings, presenting at city council meetings, and working to implement and evaluate strategies for eliminating health disparities. One established mechanism in which nurse leaders can engage is community health needs assessments, which are a statutory requirement for nonprofit hospitals (see Chapter 4 for a fuller description). Ensuring that these needs assessments explicitly target health disparities and prioritize SDOH and that they are conducted with input from members of the community on which they focus are examples of the considerations nurses can advance while helping to align community needs with culturally sensitive and relevant resources. Nurse leaders in both health care systems and public health (the entities involved in developing these needs assessments) can use these data to develop nurse-led and other innovative solutions for meeting the identified needs ( Swider et al., 2017 ).
Leading Multisector Partnerships
Strategic partnerships involving a broad range of stakeholders are essential to address factors that perpetuate structural inequities in health and health care ( NASEM, 2017 ). In the Framework for Achieving Health Equity of IHI, developing partnerships with community organizations is identified as one of the framework’s fundamental elements ( Laderman and Whittington, 2016 ). Nurses are skilled in working on and leading clinical teams. However, the role of the interprofessional health team is evolving beyond individual clinical encounters and extending beyond the walls of health care systems into the communities where people live ( NASEM, 2019a ; Pittman, 2019 ). Multisector models involving innovative interprofessional collaboration among, for example, police, emergency services, the legal system, housing, and public works and the health care system are showing promise and demonstrating positive health outcomes for underserved populations ( Hardin and Mason, 2020 ).
The ability to develop and lead multisector partnerships is critical to achieving health equity for a number of reasons ( NASEM, 2017 ). First, community needs are complex and wide-ranging, and necessarily involve actors from multiple sectors (e.g., employment services, education transportation, health). Collaboration across sectors is essential to break down existing silos that are counterproductive to improving health and health care ( NAM, 2017 ). Second, collaboration among partners introduces “more expertise and knowledge than what resides in any one stakeholder group” ( Wakefield, 2018 ), and multisector partnerships can leverage unique skills and resources from multiple stakeholders (e.g., faith leaders, philanthropists, researchers). Third, working with community partners can help nurses reach underserved populations, including the homeless, recent immigrants, and non-English-speaking families. Fourth, multisector partnerships increase a community’s capacity to make sustainable changes by bringing energy, expertise, and perspectives from multiple arenas. Fifth, multisector partnerships can simultaneously address upstream, midstream, and downstream SDOH and ensure alignment of efforts across these levels. Finally, bringing people together from multiple sectors can facilitate and encourage creative approaches; the intersections across boundaries are “where the promise of innovation lies” ( Pittman, 2019 , p. 27). As Johansson (2004 , p. 2) puts it, “When you step into an intersection of fields, disciplines, or cultures, you can combine existing concepts into a large number of extraordinary new ideas.”
It is important for multisector partnerships to be formal, structured, and collaborative relationships ( Siegel et al., 2018 ) in which partners have mutual respect for one another, and time and attention are devoted to maintaining those relationships ( Chandra et al., 2016 ). Trust among partners is also essential for a collaborative relationship, and once established, can serve as a foundation for future collaborations ( Wakefield, 2018 ). Nurses leading and engaged in multisector partnerships can help ensure that collaborative efforts are based on an understanding that health is a value shared among all partners ( Erickson et al., 2017 ; Mason et al., 2019 ; Realized Worth, 2018 ).
Nurses need to be able to build partnerships that include a focus on integrating clinical and nonclinical services and ensuring access to health and human services. Collaborative multisector efforts are common in the work of public health nurse leaders, and their experience and expertise can inform new approaches. Nurses currently have limited opportunities to learn from such efforts working in traditional health care systems. There is a need to start providing nurses with substantial exposure to experiences that involve developing and maintaining effective cross-sector partnerships, rather than what is often quite limited observational experience in public health and other social services settings.
While nurses have long worked at the intersection of individuals, families, other health professionals, social workers, educators, and others to improve health, more nurses will increasingly need to apply and expand this skill set to participating in or leading community-engaged multisector partnerships. The Crossing the Quality Chasm report ( IOM, 2001 ) calls for health care leaders to invest in their nursing workforce to enable nurses to achieve their full potential as individuals, team members, and leaders. Going forward, then, there is an expanding need to build and engage teams that reach beyond health care to include other sectors. Just as working in health care teams represented a “fundamental shift” in perspective in 2001 ( IOM, 2001 , p. 139), so, too, working across health and social sectors for the benefit of individuals and communities will require a fundamental shift in perspective, resources, and academic preparation.
Leading Change
Reducing disparities and achieving health equity will require nurse leaders to be skilled in leading change. To be effective, these efforts will need to be anchored in the theoretical constructs of change management and occur at multiple levels, within clinical practice, organizations, communities, populations, health authorities, and nations ( Browne et al., 2018 ). Evidence suggests that health care leaders are knowledgeable about disparities and what can be done to eliminate them, but that a number of barriers to successful change exist ( Betancourt et al., 2017 ). These barriers, including a lack of leadership buy-in, competing organizational priorities, existing culture, and ineffective execution, can be addressed through effective change management ( Betancourt et al., 2017 ). Effective change management requires that individuals learn and apply new behaviors and skills, as well as lead and collaborate with others in driving change within and outside of the organizations where they work. Empirically based interventions to drive change that can reduce health disparities include developing a vision for change (as discussed above), aligning executive support, engaging a coalition of committed stakeholders, setting expectations, establishing clear goals and a plan for change, anchoring change in the existing culture, measuring progress, iterating as needed, and communicating status reports and results ( Betancourt et al., 2017 ). Nurses at all levels can exert substantial influence on SDOH by using their experience and knowledge to engage in such change management efforts.
Innovating and Improving
Changing the prevailing health care paradigm to address SDOH and advance health equity will require innovation. The U.S. Department of Commerce’s Advisory Committee on Measuring Innovation in the 21st Century Economy defines innovation as the “design, invention, development, and/or implementation of new or altered products, services, processes, systems, organizational structures, or business models for the purpose of creating new value” ( ESA, 2007 ). For the complex work of eliminating disparities and impacting SDOH, knowledge and skill in innovation will be an important competency for nurses. Nurse leaders can facilitate the creation of innovative approaches by challenging the status quo, breaking down traditional barriers to change, teaching and encouraging team members to solve problems using design thinking, identifying best practices, and facilitating the translation and adoption of new ideas.
Virtually all nurses have opportunities to innovate by developing new ideas for improving health and translating these ideas into practice and policy. Over the past several years, nurse-designed and nurse-led innovations addressing SDOH among underserved populations have increasingly appeared in the literature. As described in Chapter 4 , for example, nurses in the Netherlands developed and implemented Buurtzorg, an innovative nurse-led, nurse-run organization of self-managed teams that provide home care to individuals in their neighborhoods (Monsen and de Blok, 2013 ). Similarly, the SOAR (Supporting Older Adults at Risk) program reimagined how to prepare and support frail older adults in the transition back to their homes following a hospital admission. The program addresses issues of transportation, nutrition, and medication access ( IHI, 2018 ).
Yet, while some nurses are already leading efforts focused on health equity in their work settings and communities, this focus is not consistent across the profession. It is a leader’s responsibility to create an environment that allows for innovation ( IOM, 2000 ). Leaders can provide a forum for continual innovation in and testing of strategies for improving population health and health equity, and ensure that their organization is flexible and able to adapt to those changes ( IOM, 2001 ). For example, leaders of front-line health teams can encourage team members to share their own observations and ideas for improving patient health and facilitate the transfer of new ideas across professional boundaries ( IOM, 2001 ). Likewise, nurse leaders working in the community or in multisector partnerships can encourage communication and collaboration without regard for traditional boundaries and recognize that innovative ideas can surface from an array of individuals across sectors, such as those working in aging-related services or Medicaid managed care organizations.
Nurses have a rich tradition of working creatively to solve problems and improve the quality of care in clinical settings ( Thomas et al., 2016 ), and these experiences and skills can apply to efforts designed to address SDOH. These types of initiatives require systematic, continuous, data-driven, and rigorous processes of assessment, innovation, implementation, evaluation, and diffusion or translation of the evidence or best practices into tangible strategies or policies for improving population health. For example, IHI’s Model for Improvement for quality improvement initiatives uses a Plan-Do-Study-Act (PDSA) cycle that involves planning exactly how the intervention will be implemented; implementing it; studying whether and how it is being conducted; and then acting to either adapt it, adopt it as a standard practice, collect more data, or abandon it ( IHI, 2020 ). This model has been used with great success in the clinical setting. Transforming Care at the Bedside (TCAB), was one such model using the PDSA cycle. A partnership between the Robert Wood Johnson Foundation and IHI, TCAB created learning collaboratives at the front lines of care on medical-surgical units that engaged nurses and other front-line staff in generating and testing ideas that led to processes and practices that improved the efficiency, safety, and satisfaction of care. 3 This process has the potential to be equally successful in addressing SDOH and health equity ( IHI, 2020 ).
Teaming Across Boundaries
As nurses work within and across organizations to address SDOH and advance health equity, they will need the skills to develop, engage, and lead cross-boundary teams. Cross-boundary teaming is a strategy for driving innovation that engages diverse stakeholders and subject-matter experts to expand the range of views and ideas on which teams can draw ( Edmondson and Harvey, 2018 ). In cross-boundary teams, individuals work across knowledge boundaries. Teams are diverse in expertise, knowledge, and educational background, characterized by deep-level differences or what Edmondson and Harvey call “knowledge diversity” (p. 3480).
Addressing SDOH and advancing health equity will require a cross-boundary team approach that includes not only people from different disciplines and sectors but also individuals and organizations from within the community. Regardless of the composition of the team, the cross-boundary team leader will need to support each team member, balance the use of resources, facilitate communication, and ensure the team’s effectiveness. A leader’s job is to “optimize the performance of teams that provide various services in pursuit of a shared set of aims” ( IOM, 2001 ). Evidence suggests that high-performing team members listen to one another and show sensitivity to feelings and needs ( Duhigg, 2016 ). To support the team and optimize its performance, a nurse leader will need to work to help its members achieve their full potential, both individually and collectively. This investment may include providing support and time for self-care, providing access to and time for ongoing professional development, and supporting individuals as they seek higher levels of education and responsibility. Facilitating nurses’ well-being and self-care is one particularly important way in which nurse leaders can support and optimize cross-boundary teams (see Chapter 10 on the importance of facilitating nurse well-being).
Creating a Culture of Equity
Nurse leaders in many positions of authority, including academic leaders ( DeWitty and Murray, 2020 ), journal editors ( Villarruel and Broome, 2020 ), educators ( Graham et al., 2016 ), and managers ( ANA, 2018 ), can act to call out and dismantle racism. To advance equity in society, nursing needs first to work to create a culture of equity within the profession itself. Nursing has a history of racism that continues to impact the experiences of nursing faculty, nurses in practice, communities, and patients ( DeWitty and Murray, 2020 ; Iheduru-Anderson, 2020a ; Villarruel and Broome, 2020 ; Waite and Nardi, 2019 ; Whitfield-Harris et al., 2017 ). The nursing profession’s substantive and sustained attention is required to address and eliminate racism in nursing and in broader organizations where nurses work. Waite and Nardi (2019 , p. 20) call on nurse leaders to “urge their colleagues and students to characterize, name, contest, and transform the norms, traditions, structures, and establishments that preserve White supremacy through continued effects of American colonialism.” Over the past few years, the nursing literature, including statements issued by national nursing organizations, has reflected increased attention to these issues.
Nurse leaders must acknowledge existing disparities and facilitate open, honest, and respectful discussions about factors that drive disparities (Oruche, and Zapolski, 2020 ; Purtzer and Thomas, 2019 ) and the challenges staff face as they engage in this work within organizations and with communities. It will be essential for these discussions to include opportunities for and support of the expression of patient and community perspectives ( NASEM, 2017 ). Specific strategies for promoting equity and inclusion include (1) creating safe spaces to engender trust and open communication; (2) reassessing recruitment and advancement processes; (3) examining and redesigning equity policies, procedures, and practices; (4) requiring a diverse pool of applicants for applicant selection; (5) moving from mentorship to sponsorship, which focuses on protégé advancement; (6) creating an infrastructure to monitor and track progress with development programs; and (7) dismantling racism, including applying an equity lens to all practices ( Fitzsimmons and Peters-Lewis, 2021 ). Nurse leaders need to set an example of inclusion and confront negative and toxic cultural norms in nursing, such as bullying and in-fighting ( Kaiser, 2017 ). Nurse leaders need to be knowledgeable about and able to lead others in cultural humility and culturally competent practices, which are critical for reducing health disparities and improving access to high-quality health care ( Powell, 2016 ).
In a recent analysis of six models of cultural competence, Botelho and Lima (2020) argue that existing approaches to the delivery of culturally appropriate care may assist with cultural respect, but tend to oversimplify patients’ cultural experiences and overlook the complexities associated with power dynamics ( Botelho and Lima, 2020 ). They propose the practices of not only cultural humility but also relational ethics 4 to facilitate cross-cultural work. To practice cultural humility, clinicians relinquish their role as experts in a culturally diverse world where power imbalances exist and embrace an attitude characterized by constant questioning, openness, self-awareness, absence of ego, and self-reflection and -critique, willingly interacting with diverse individuals. Practicing with cultural humility can foster mutual empowerment, respect, partnerships, optimal care, and lifelong learning ( Foronda et al., 2016 , p. 213). (See Chapter 7 for further discussion of cultural humility.)
Creating Systems and Structures for Equity
Nurse leaders at all levels and in all settings can help create systems and structures that promote equity and do not unintentionally exacerbate inequalities through unintended incentives. For example, working midstream (see Chapter 2 ), a nurse leader who oversees a home visiting program can educate around the concept of equitable care and establish expectations of nurses that encourage the provision of equitable care, including meeting social needs, rather than orienting nursing’s interventions to the volume of visits they make ( IOM, 2001 ). A nurse leader who manages an organization can develop organization-wide policies that put equity at the forefront of the staff’s work, and ensure that the provision of services does not exacerbate existing inequalities. Upstream, a nurse leader can influence government policy by advocating for policies that improve equity, such as a city transportation policy that prioritizes traditionally underserved rather than higher-income neighborhoods, or by highlighting exposure to noise pollution and associated health impacts related to building low-income housing near railroad tracks.
The goal of health equity is more likely to be achieved when it becomes deeply ingrained in official systems and structures and becomes inherent in a cultural shift that includes inner reflections on bias and structural racism ( Chin, 2020 ), rather than being pursued through one-off initiatives or well-intentioned efforts that are not formalized. Systems and structures are never neutral—they either entrench or dismantle existing health inequities. Nurse leaders have a responsibility to advocate for and build systems that promote equitable health for all.
Mentoring and Sponsoring
The transformation toward a health system that is more equitable and just will require explicit preparation of and support for future nurse leaders in multiple settings ( AACN, 2016 ). A key strategy for achieving this goal is mentorship and sponsorship of the next generation of nurses and nurse leaders. Mentoring is critical across the trajectory of nurses’ professional lives, particularly as they take on new and increasingly complex leadership roles ( Vitale, 2018 ). Given the overarching need for nurse leaders with expertise and commitment to achieving equity in health and health care, and given the need for more nurses with expertise in such priority areas as care for the aging, maternal mortality, mental and behavioral health, rural health, and public health (see Chapter 3 ), mentoring is critical to building and supporting the next generation of nurses.
Mentoring is associated with positive benefits, including professional development, greater skills, a better fit with one’s choice of specialty, and greater life–work balance ( Disch, 2018 ). In mentoring new nurses in the application of concepts related to health equity or in needed specialty areas as identified above, nurses with experience can encourage collaboration among nurses of different ages and at different professional development stages. In general, a lack of support and mentoring by senior nurses has negative impacts on well-being and workforce turnover ( IOM, 2011 ), and mentoring is therefore a critical part of building capacity in the profession and of mitigating the loss of knowledge and experience that results when retiring nurses leave the profession.
A particularly critical role for nurse leaders is mentoring nurses from traditionally underrepresented communities to build a more diverse nursing workforce and increase the number of nurses from underrepresented groups in leadership positions ( Phillips and Malone, 2014 ). Mentoring is a critical component of recruiting, supporting, and advancing nurses of color through the ranks of leadership ( DeWitty and Murray, 2020 ; Iheduru-Anderson, 2020b ; Whitfield-Harris et al., 2017 ). As discussed in Chapter 3 , diversity in the nursing workforce—and in nursing leadership in particular—is essential to achieving health equity. There are relatively few nurses of color in leadership positions, particularly in more senior executive positions ( Phillips and Malone, 2014 ; Schmieding, 2000 ). A 2019 National Academies report on increasing the number of professionals of color in science, technology, engineering, and mathematics found that structured mentorship programs in minority-serving institutions 5 can improve leadership diversity in nursing and the health care field generally ( NASEM, 2019b ). One such effort is being led by the Center to Champion Nursing in America (CCNA) in its convenings of mentor training programs with historically Black colleges and universities (HBCUs). CCNA will continue to convene mentoring programs in Hispanic- and American Indian–serving nursing schools as well ( CCNA, 2020 ).
Serving as a sponsor becomes even more critical than mentoring when a more active role is required to help nurses rise in leadership ranks ( Williams and Dawson, 2021 ). The expectations of a sponsor include being a staunch advocate for career advancement for the protégé, including making assignments and connecting the protégé to key decision makers while keeping her or him protected from negative influences. Sponsors take advantage of the organizations and people in their sphere to present their protégés in the most positive light, with the goal of career advancement. This more active approach has been shown to be especially helpful in helping nurses of color rise in the leadership ranks ( Beckwith et al., 2016 ).
ACHIEVING THE COMMITTEE’S VISION OF NURSE LEADERSHIP
As previously noted, many nurse leaders are currently focused on incorporating equity into their work. To achieve the committee’s vision, however, a significant investment in broader and deeper development of nurse leadership will be needed. New and established nurse leaders—at all levels and in all settings—are needed to lead change that results in meeting social needs, eliminating health disparities, addressing SDOH, and ultimately achieving equity in health and health care, with the aim of improved health for all individuals and communities. Nurse leaders need to both develop and expand the leadership competencies described in this chapter, and implement strategies targeted to achieving diversity among nurse leaders. Nurse leadership competencies and knowledge can be developed through approaches that encompass education, fellowships, and nursing organizations, as discussed below.
Increasing Diversity in Nurse Leadership
Diverse leaders can serve as particularly important role models, provide guidance and mentoring for other nurses, influence the allocation of resources, and shape policies aimed at eliminating inequities ( Phillips and Malone, 2014 ). The prior The Future of Nursing report identifies the need for a renewed focus on diversity in nursing, calling for the development of novel education models that promote respect for diversity along a number of dimensions, such as race, ethnicity, geography, background, and personal experiences ( IOM, 2011 ). Even when nurse leaders hold similar positions, salary disparities are seen among racial and ethnic groups. Among nurse leaders with the highest salaries (ranging from clinical staff to C-suite executives), only 11 percent are Black, compared with 27 percent who are Asian American, 25 percent who are Hispanic, and 21 percent who are White. Not only are few Black nurses in positions of leadership at all, but even fewer advance to careers as nurse executives ( Iheduru-Anderson, 2020a ; Jefferies et al., 2018 ).
Understanding and addressing the reasons for the diversity gap in nursing leadership is essential. The existing literature identifies racism as a significant factor ( Iheduru-Anderson, 2020a ). Nursing’s roots in the United States have been shaped within the context of colonialism, a history that has influenced the makeup of the profession’s leaders ( Waite and Nardi, 2019 ). As discussed earlier, acknowledging and addressing how racism has been internalized and how it has manifested within the field, including in the advancement of nurses of color, is key ( Brathwaite, 2018 ; Waite and Nardi, 2019 ). Other barriers include stereotyping; a lack of career development opportunities ( Carroll, 2020 ); a lack of mentorship ( Ihederu-Anderson, 2020b ); inadequate support systems; isolation; the perception of being overlooked for positions in contrast to White counterparts ( Kolade, 2016 ); and the cultural taxation or diversity tax ( Gewin, 2020 ), characterized by the role assigned to the ethnic representative of a group involving the expectation that this individual will provide unofficial diversity consultation. 6
Numerous innovative programs aimed at cultivating diversity in nursing leadership have been developed and implemented. A number of these programs target nurses early in the trajectory of development (in prebaccalaureate or baccalaureate programs), while others are aimed at later stages of professional growth. Examples of programs focused on early leadership training include EMBRACE (Engaging Multiple communities of BSN [bachelor of science in nursing] students in Research and Academic Curricular Experiences), which was developed to provide comprehensive experiences in research and leadership for undergraduate students of color who are underrepresented in nursing, and the Duke University School of Nursing’s Making a Difference program ( Carter et al., 2015 ; Stacciarini and McDaniel, 2019 ). Likewise, the University of North Dakota has a program called Recruitment & Retention of American Indians into Nursing (RAIN), which provides academic support and assistance to American Indian nursing students, from prenursing programs through doctoral education ( UND, 2020 ). (See Chapter 7 for further discussion of recruiting and supporting underrepresented students.) To fully support the goal of diversity in nurse leadership, such programs will need to be evaluated and scaled.
Nursing Education, Fellowships, and Certificates
While nursing school curricula often include some information about public health, SDOH, and health equity, they do not always prepare students to engage fully with and serve as leaders on these issues. Nursing education traditionally has emphasized the development of clinical skills over leadership and management skills ( Joseph and Huber, 2015 ). As discussed in Chapter 7 , the American Association of Colleges of Nursing’s (AACN’s) Essentials 7 provides an outline for the necessary curriculum content and expected competencies for graduates of baccalaureate, master’s, and doctor of nursing practice (DNP) programs. Introducing the concept of health equity in school is a necessary first step in professional role development and leadership, but nurses also need to take every opportunity to supplement their preparation through continuing education.
A number of fellowships support education in leadership skills with a focus on health equity and community health. 8 Nearly all of these fellowships are interdisciplinary, bringing together professionals from multiple sectors, including health care, business, community organizing, education, and the law. These types of fellowships present opportunities for nurses to grow their leadership skills, to collaborate and innovate with professionals from multiple disciplines and sectors, and to develop and implement projects within their areas of interest that relate directly to achieving health equity. In addition to equity-specific fellowships, a wide variety of fellowships available for nurses are focused on general leadership skills that can be transferred to any area and any setting, including addressing SDOH and pursuing health equity.
One fellowship specifically for nurses and focused on equity is the Environmental Health Nurse Fellowship, which trains nurses to work with communities to address environmental health threats. In 2019, the Alliance of Nurses for Healthy Environments (ANHE) launched this fellowship to focus on environmental health equity and justice and on the disproportionate impact of environmental conditions on underserved groups. The 30 fellows, all of whom are nurses, work with mentors to help communities identify environmental needs and build support for community-driven solutions ( ANHE, 2019 ).
The Global Nursing Leadership Institute 9 (GNLI) fellowship, sponsored by the International Council of Nurses and supported by the Burdett Trust for Nursing, is available to nurses worldwide. This fellowship is focused on policy leadership, with a special emphasis on strengthening political and policy understanding and influence. Its framework includes in-depth work on the United Nations’ Sustainable Development Goals, which reflect multiple SDOH. The focus of 2020 was on health disparities in the context of the COVID-19 pandemic.
Many certificate programs in the United States can help nurses develop leadership skills that can be leveraged to lead work in equity in health and health care. Examples include the Health Equity Certificate at the University of Pittsburgh School of Public Health 10 and the Graduate Certificate in Health Equity at the Vanderbilt University Medical Center. 11
The Role of Nursing Organizations
Most professional nursing organizations recognize and specifically call out leadership as an essential competency for nurses in all settings ( NAHN, 2020 ; NCEMNA, 2020 ; NLN, 2005 ; Quad Council, 2018 ). These organizations offer leadership courses, resources, and support, most pertaining to leadership in general rather than leadership on health equity, for current and aspiring nurse leaders. Nursing organizations also have undertaken specific initiatives to develop and support nurse leaders that include content related to equity in health and health care. Examples include the following: (1) the American Public Health Association Public Health Nursing Section, with the vision of advancing social justice and equity to achieve population health for all 12 ; (2) the Future of Nursing: Campaign for Action, with the vision of working toward an America in which everyone can live a healthier life, supported by nurses as essential partners in providing care and promoting health equity and well-being 13 ; (3) the Black Coalition Against COVID-19, 14 an interprofessional multisector coalition, co-led by the National Black Nurses Association, focused on urgently mobilizing and coordinating all available community assets in a collaborative effort with the government of Washington, DC; and (4) the National Coalition of Ethnic Minority Nurse Associations (NCEMNA), which stands as a unified force advocating for equity and justice in nursing and health care for ethnic minority populations. 15 In addition, professional associations offer nurses an opportunity to build leadership competencies by leading within the association. While some nursing associations are small and others large, each can offer nurses an opportunity to meet other nurses, join boards and workgroups, and help guide the association’s direction, especially toward the goals germane to this report.
Nursing associations that are organized around a racial or ethnic identity may offer a particularly good opportunity for underrepresented nurses to hone their leadership skills. The NCEMNA is an umbrella organization of five national ethnic nurse associations: the Asian American/Pacific Islander Nurses Association, the National Alaska Native American Indian Nurses Association, the National Association of Hispanic Nurses (NAHN), the National Black Nurses Association, and the Philippine Nurses Association of America. One of the five strategic goals of the NCEMNA is to “promote ethnic minority nurse leadership in areas of health policy, practice, education and research” through the implementation of leadership development and mentorship programs ( NCEMNA, 2020 ).
- CONCLUSIONS
All nurses have the capability to lead and engage in meaningful roles in addressing SDOH and health equity, with their specific roles and functions depending on individual interests, capacities, and opportunities.
Conclusion 9-1: Nurse leaders at every level and across all settings can strengthen the profession’s long-standing focus on social determinants of health and health equity to meet the needs of underserved individuals, neighborhoods, and communities and to prioritize the elimination of health inequities.
Given that social determinants that affect health exist largely outside of the health care system (e.g., poverty, literacy, housing, transportation, and food security), addressing SDOH and eliminating health disparities will require collaboration and partnership among a broad group of stakeholders. Public health nurses have a long history of working collaboratively to meet social needs and address SDOH, and their experiences can be used as models for other nurses seeking to work collaboratively across sectors.
Conclusion 9-2: Achieving health equity will require multisector collaboration, and nurse leaders can participate in and lead these efforts. Conclusion 9-3: Many community and public health nurse leaders have expertise and experience in leading cross-sector partnerships to meet social needs and address social determinants of health, and their expertise can be leveraged to inform the broader nursing profession in both practice and education.
Racism and discrimination are deeply entrenched in U.S. society and its institutions, and the nursing profession is no exception. Nurse leaders have an important role to play in acknowledging the history of racism within the profession and in moving forward to dismantle structural racism and mitigate the effects of discrimination and implicit bias on health. Role modeling listening, engagement, and inclusivity within and outside of nursing will be necessary to foster trust and achieve needed change. A critical part of these efforts will be building a more diverse nursing workforce and supporting these nurses in their pursuit of and success in leadership roles.
Conclusion 9-4: Nurse leaders have a responsibility to address structural racism, cultural racism, and discrimination based on identity (e.g., sexual orientation, gender), place (e.g., rural, urban), and circumstances (e.g., disability, mental health condition) within the nursing profession and to help build structures and systems at the societal level that address these issues to promote health equity. Conclusion 9-5: A critical role for nurse leaders is mentoring and sponsoring nurses from traditionally underrepresented communities in order to build a more diverse nursing workforce and increase the number of underrepresented nurses in leadership positions.
- AACN (American Association of Colleges of Nursing). Advancing healthcare transformation: A new era for academic nursing. 2016. [April 8, 2021]. https://www .aacnnursing .org/Portals/42/Publications /AACNNew-Era-Report.pdf .
- AACN. The essentials: Core competencies for professional nursing education: Final draft. 2021. [April 16, 2021]. https://www .aacnnursing .org/Portals/42/AcademicNursing /pdf/Essentials-Final-Draft-2-18-21 .pdf?ver=hNeCl7OjgamIA9sHgDi _Yw %3d%3d×tamp=1613742420447 .
- ANA (American Nurses Association). Position Statement. 2018. [April 8, 2021]. The nurse’s role in addressing discrimination: Protecting and promoting inclusive strategies in practice settings, policy, and advocacy. https://www .nursingworld .org/~4ab207/globalassets /practiceandpolicy /nursingexcellence /ana-position-statements /social-causes-and-health-care /the-nurses-role-in-addressingdiscrimination.pdf .
- ANHE (Alliance of Nurses for Healthy Environments). ANHE environmental health nurse fellowship: 2019–2020 cohort. 2019. [April 8, 2021]. https://envirn .org/anhe-fellowship .
- Beckwith AL, Carter DR, Peters T. The underrepresentation of African American women in executive leadership: What’s getting in the way? Journal of Business Studies Quarterly. 2016; 7 (4):115–134.
- Berger MW. Penn Today. Oct 23, 2019. [April 8, 2021]. Cultivando Juntos takes shape in Kennett Square. https://penntoday .upenn .edu/news/cultivando-juntos-takes-shape-kennett-square .
- Bergum V, Dossetor JB. Relational ethics: The full meaning of respect. Hagerstown, MD: University Publishing Group; 2005.
- Betancourt JR, Tan-McGrory A, Kenst KS, Phan TH, Lopez L. Organizational change management for health equity: Perspectives from the disparities leadership program. Health Affairs (Millwood). 2017; 36 (6):1095–1101. [ PubMed : 28583969 ]
- Botelho MJ, Lima CA. From cultural competence to cultural respect: A critical review of six models. Journal of Nursing Education. 2020; 59 (6):311–318. doi: 10.3928/01484834-20200520-03. [ PubMed : 32497232 ]
- Boyatzis RE, Rochford K, Taylor SN. The role of the positive emotional attractor in vision and shared vision: Toward effective leadership, relationships, and engagement. Frontiers in Psychology. 2015; 6 :670. [ PMC free article : PMC4439543 ] [ PubMed : 26052300 ]
- Brathwaite B. Black, Asian and minority ethnic female nurses: Colonialism, power and racism. British Journal of Nursing. 2018; 27 (5):254–258. [ PubMed : 29517323 ]
- Browne AJ, Varcoe C, Ford-Gilboe M, Nadine Wathen C, Smye V, Jackson BE, Wallace B, Pauly B, Herbert CP, Lavoie JG, Wong ST, Blanchet Garneau A. Disruption as opportunity: Impacts of an organizational health equity intervention in primary care clinics. International Journal for Equity in Health. 2018; 17 (1):154. [ PMC free article : PMC6161402 ] [ PubMed : 30261924 ]
- Carroll D. Diversity: Lack of African American presence in nursing leadership. DNP qualifying manuscripts. 2020; 45 [April 15, 2021]; https://repository .usfca .edu/dnp_qualifying/45 .
- Carter BM, Powell DL, Derouin AL, Cusatis J. Beginning with the end in mind: Cultivating minority nurse leaders. Journal of Professional Nursing. 2015; 31 (2):95–103. [ PubMed : 25839948 ]
- CCL (Center for Creative Leadership). Executive nurse fellows program, outcome and competency chart. Princeton, NJ: Robert Wood Johnson Foundation; 2010.
- CCNA (Center to Champion Nursing in America). Campaign for Action. 2020. [June 7, 2021]. Mentoring for better health. https: //campaignforaction .org/resource/mentoring-for-better-health .
- Chandra A, Miller CE, Acosta JD, Weilant S, Trujillo M, Plough A. Drivers of health as a shared value: Mindset, expectations, sense of community, and civic engagement. Health Affairs. 2016; 35 (11):1959–1963. [ PubMed : 27834233 ]
- Chin M. BMJ Quality and Safety. 2020. Advancing health equity in patient safety: A reckoning, challenge, and opportunity. Epub ahead of print. doi: 10.1136/bmjqs-2020-012599. [ PMC free article : PMC8627426 ] [ PubMed : 33376125 ]
- DeWitty VP, Murray TA. Influence of climate and culture on minority faculty retention. Journal of Nursing Ethics. 2020; 59 (9):483–484. [ PubMed : 32865579 ]
- Disch J. Rethinking mentoring. Critical Care Medicine. 2018; 46 (3):437–441. [ PubMed : 29474324 ]
- Duhigg D. The New York Times Magazine. Feb 25, 2016. [April 8. 2021]. What Google learned from its quest to build the perfect team. https://www .nytimes.com /2016/02/28/magazine /what-googlelearned-from-its-quest-to-build-the-perfect-team.html .
- Dyess SM, Sherman RO, Pratt B, Chiang-Hanisko L. Growing nurse leaders: Their perspectives on nursing leadership and today’s practice environment. Online Journal for Issues in Nursing. 2016; 21 (1) [April 9, 2021]; http://ojin .nursingworld .org/MainMenuCategories /ANAMarketplace /ANAPeriodicals/OJIN /TableofContents/Vol-21-2016 /No1-Jan-2016 /Articles-Previous-Topics /Growing-Nurse-Leaders.html . [ PubMed : 27853273 ]
- Eckert R, West M, Altman D, Steward K, Pasmore B. Delivering a collective leadership strategy for health care. Greensboro, NC: Center for Creative Leadership and Kings Fund; 2014.
- Edmondson AC, Harvey J-F. Cross-boundary teaming for innovation: Integrating research on teams and knowledge in organizations. Human Resource Management Review. 2018; 28 (4):347–360.
- Erickson J, Milstein B, Schafer L, Pritchard KE, Levitz C, Miller C, Cheadle A. ReThink Health and the Center for Community Health and Evaluation. 2017. [April 8, 2021]. Progress along the pathway for transforming regional health: A pulse check on multi-sector partnerships. https://www .rethinkhealth .org/wp-content /uploads/2017/03/2016-Pulse-Check-Narrative-Final.pdf .
- ESA (Economics and Statistics Administration, U.S. Department of Commerce). Innovation measurement. Federal Register. 2007; 72 (71):18627. [April 8, 2021]; https://www .govinfo.gov /content/pkg/FR-200704-13 /pdf/07-1827.pdf .
- Feely D. Equity: The forgotten aim? Institute for Healthcare Improvement Blog. Aug 11, 2016. [April 8, 2021]. http://www .ihi.org/communities /blogs/equity-the-forgotten-aim .
- Fitzsimmons MJ, Peters-Lewis A. Voice of Nursing Leadership. American Organization for Nursing Leadership; Mar 1, 2021. [April 8, 2021]. Creating more diverse C-suites: From intention to outcomes. https://www .aonl.org /news/voice/mar-2021 /creating-more-diverse-csuite-from-intention .
- Foronda C, Baptiste DL, Reinholdt MM, Ousman K. Cultural humility: A concept analysis. Journal of Transcultural Nursing. 2016; 27 (3):210–217. [ PubMed : 26122618 ]
- Gewin V. The time tax put on scientists of colour. Nature. 2020; 583 (7816):479–481. [ PubMed : 32647354 ]
- Graham CL, Phillips SM, Newman SD, Atz TW. Baccalaureate minority nursing students perceived barriers and facilitators to clinical education practices: An integrative review. Nursing Education Perspective. 2016; 37 (3):130–137. [ PubMed : 27405193 ]
- Hardin L, Mason DJ. Lessons from complex care in a COVID-19 world. JAMA Health Forum. 2020; 1 (7):e200908.
- Harper KJ, Benson LS. The importance and impact of nurses serving on boards. Nursing Economics. 2019; 37 (4):209–212.
- Iheduru-Anderson KC. Journal of Professional Nursing. 2020a. The white/black hierarchy institutionalizes White supremacy in nursing and nursing leadership in the United States. Epub ahead of print. doi: 10.1016/j.profnurs.2020.05.005. [ PubMed : 33867099 ]
- Iheduru-Anderson K. Barriers to career advancement in the nursing profession: Perceptions of Black nurses in the United States. Nursing Forum. 2020b; 55 (4):664–677. [ PMC free article : PMC7689724 ] [ PubMed : 32643168 ]
- IHI (Institute for Healthcare Improvement). Institute for Healthcare Improvement Blog. Oct 23, 2018. [April 8, 2021]. How “flipped” discharge can help your largest patient population. http://www .ihi.org/communities /blogs/how-flipped-discharge-can-help-your-largest-patient-population .
- IHI. Science of improvement: How to improve. 2020. [April 8, 2021]. http://www .ihi.org/resources /Pages/HowtoImprove /ScienceofImprovementHowtoImprove.aspx .
- IOM (Institute of Medicine). Exploring innovation and quality improvement in health care micro-systems: A cross-case analysis. Washington, DC: National Academy Press; 2000. [ PubMed : 25057555 ]
- IOM. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. [ PubMed : 25057539 ]
- IOM. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press; 2011. [ PubMed : 24983041 ]
- Jefferies K, Goldberg L, Aston M, Tomblin Murphy G. Understanding the invisibility of black nurse leaders using a black feminist poststructuralist framework. Journal of Clinical Nursing. 2018; 27 (15–16):3225–3234. [ PubMed : 29752837 ]
- Johansson F. The Medici effect: Breakthrough insights at the intersection of ideas, concepts & cultures. Boston, MA: Harvard Business School Press; 2004.
- Joseph ML, Huber DL. Clinical leadership development and education for nurses: Prospects and opportunities. Journal of Healthcare Leadership. 2015; 7 :55–64. [ PMC free article : PMC5740995 ] [ PubMed : 29355179 ]
- Jouppila T, Tiainen T. Health Environments Research & Design Journal. 2020. Nurses’ participation in the design of an intensive care unit: The use of virtual mock-ups. doi: 10.1177/1937586720935407. [ PubMed : 32672071 ]
- Kaiser JA. The relationship between leadership style and nurse-to-nurse incivility: Turning the lens inward. Journal of Nursing Management. 2017; 25 (2):110–118. [ PubMed : 27896878 ]
- Kolade FM. The lived experience of minority nursing faculty: A phenomenological study. Journal of Professional Nursing. 2016; 32 (2):107–114. [ PubMed : 27000195 ]
- Kouzes JM, Posner BZ. To lead, create a shared vision. Harvard Business Review. 2009; 87 (1):20–21.
- Kruse K. What is leadership? Forbes. Apr 9, 2013. [April 8, 2021]. https://www .forbes.com /sites/kevinkruse/2013 /04/09/what-is-leadership /?sh=98657e85b90c .
- Laderman M, Whittington J. A framework for improving health equity. Healthcare Executive. 2016; 31 (3):82–85. [ PubMed : 27319115 ]
- Lathrop B. Nursing leadership in addressing the social determinants of health. Policy, Politics, & Nursing Practice. 2013; 14 (1):41–47. [ PubMed : 23793135 ]
- Mason DJ, Martsolf GR, Sloan J, Villarruel A, Sullivan C. Making health a shared value: Lessons from nurse-designed models of care. Nursing Outlook. 2019; 67 (3):213–222. [ PubMed : 30755319 ]
- Monsen KA, de Blok J. Buurtzorg: Nurse-led community care. Creative Nursing. 2013; 19 (3):122–127. [ PubMed : 24400466 ]
- NAHN (National Association of Hispanic Nurses). About NAHN. 2020. [April 8, 2021]. https://nahnnet .org/about .
- NAM (National Academy of Medicine). Vital directions for health and health care. 2017. [April 8, 2021]. (Discussion Paper Series). https://nam .edu/initiatives /vital-directions-for-health-and-health-care /vital-directions-for-health-health-care-discussion-papers .
- NASEM (National Academies of Sciences, Engineering, and Medicine). Communities in action: Pathways to health equity. Washington, DC: The National Academies Press; 2017. [ PubMed : 28418632 ]
- NASEM. Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health. Washington, DC: The National Academies Press; 2019a. [ PubMed : 31940159 ]
- NASEM. Minority serving institutions: America’s underutilized resource for strengthening the STEM workforce. Washington, DC: The National Academies Press; 2019b.
- NASEM. Educating health professionals to address the social determinants of mental health: Proceedings of a workshop. Washington, DC: The National Academies Press; 2020. [ PubMed : 33180403 ]
- NCEMNA (National Coalition of Ethnic Minority Nurse Associations). History. 2020. [April 8, 2021]. https://ncemna .org/history .
- NLN (National League for Nursing). NLN core competencies for academic nurse educators. 2005. [April 8, 2021]. http://www .nln.org/professional-development-programs /competencies-for-nursing-education /nurse-educator-core-competency .
- Ogbolu Y, Scrandis DA, Fitzpatrick G. Barriers and facilitators of care for diverse patients: Nurse leader perspectives and nurse manager implications. Journal of Nursing Management. 2018; 26 (1):3–10. [ PubMed : 29076628 ]
- Olshansky EF. Social determinants of health: The role of nursing. American Journal of Nursing. 2017; 117 (12):11. [ PubMed : 29189220 ]
- Oruche UM, Zapolski TCB. The role of nurses in eliminating health disparities and achieving health equity. Journal of Psychosocial Nursing and Mental Health Services. 2020; 58 (12):2–4. [ PMC free article : PMC8827216 ] [ PubMed : 33238019 ]
- Phillips JM, Malone B. Increasing racial/ethnic diversity in nursing to reduce health disparities and achieve health equity. Public Health Reports. 2014; 129 (Suppl 2):45–50. [ PMC free article : PMC3863700 ] [ PubMed : 24385664 ]
- Pittman P. Activating nursing to address unmet needs in the 21st century. Princeton, NJ: Robert Wood Johnson Foundation; 2019.
- Pollard C. What is the right thing to do: Use of a relational ethic framework to guide clinical decision-making. International Journal of Caring Sciences. 2015; 8 (2):362–368.
- Powell DL. Social determinants of health: Cultural competence is not enough. Creative Nursing. 2016; 22 (1):5–10. [ PubMed : 29669640 ]
- Purtzer MA, Thomas JJ. Intentionality in reducing health disparities: Caring as connection. Public Health Nursing (Boston, Mass.). 2019; 36 (3):276–283. [ PMC free article : PMC6482073 ] [ PubMed : 30790330 ]
- Quad Council (Quad Council Coalition Competency Review Task Force). Community/public health nursing [C/PHN] competencies. 2018. [April 8, 2021]. https://www .cphno.org /wp-content/uploads /2020/08/QCC-C-PHN-COMPETENCIES-Approved_2018 .05.04_Final-002.pdf .
- Realized Worth. Multi-sector partnerships—The key to a brighter future? 2018. [April 8, 2021]. https://www .realizedworth .com/2018/07/07 /multi-sector-partnerships-the-key-to-a-brighter-future .
- Schmieding NJ. Minority nurses in leadership positions: A call for action. Nursing Outlook. 2000; 48 (3):120–127. [ PubMed : 10870020 ]
- Shapiro ML, Miller J, White K. Community transformation through culturally competent nursing leadership: Application of theory of culture care diversity and universality and tri-dimensional leader effectiveness model. Journal of Transcultural Nursing. 2006; 17 (2):113–118. [ PubMed : 16595398 ]
- Sherman RO. A new generation of nurse leaders. Nurse Leader. 2019; 17 (4):276–277.
- Siegel B, Erickson J, Milstein B, Pritchard KE. Multisector partnerships need further development to fulfill aspirations for transforming regional health and well-being. Health Affairs. 2018; 37 (1):30–37. [ PubMed : 29309220 ]
- Stacciarini JR, McDaniel AM. Embrace: Developing an inclusive leadership program with and for undergraduate nursing students. Journal of Professional Nursing. 2019; 35 (1):26–31. [ PubMed : 30709461 ]
- Swider SM, Levin PF, Reising V. Evidence of public health nursing effectiveness: A realist review. Public Health Nursing. 2017; 34 (4):324–334. [ PubMed : 28295536 ]
- Thomas TW, Seifert PC, Joyner JC. Registered nurses leading innovative changes. Online Journal of Issues in Nursing. 2016; 21 (3):3. [ PubMed : 27856917 ]
- UND (University of North Dakota). Recruitment & retention of American Indians into nursing. 2020. [April 8, 2021]. https://cnpd .und.edu/rain .
- Villarruel AM, Broome ME. Beyond the naming: Institutional racism in nursing. Nursing Outlook. 2020; 68 (4):375–376. [ PMC free article : PMC7473708 ] [ PubMed : 32896302 ]
- Vitale TR. Nurse leader mentorship. Nursing Management. 2018; 49 (2):8–10. [ PubMed : 29381531 ]
- Waite R, Nardi D. Nursing colonialism in America: Implications for nursing leadership. Journal of Professional Nursing. 2019; 35 (1):18–25. PMID: 30709460. doi: 10.1016/j.profnurs.2017.12.013. [ PubMed : 30709460 ]
- Wakefield M. The next era of regulation: Partnerships for change. Journal of Nursing Regulation. 2018; 9 (1):4–10.
- Wesson DE, Lucey CR, Cooper LA. Building trust in health systems to eliminate health disparities. Journal of the American Medical Association. 2019; 322 (2):111–112. [ PubMed : 31173060 ]
- Whitfield-Harris L, Lockhart JS, Zoucha R, Alexander R. The lived experience of black nurse faculty in predominantly white schools of nursing. Journal of Transcultural Nursing. 2017; 28 (6):608–615. [ PubMed : 28826318 ]
- Williams E, Dawson M. Voice of Nursing Leadership. American Hospital Association; Mar, 2021. [June 7, 2021]. Cultivating diversity in nursing leadership: Role of the sponsors. https://www .aonl.org /news/voice-of-nursing-leadership .
The full committee hearing is available at https://edlabor .house .gov/hearings/inequities-exposed-how-covid-19-widened-racial-inequities-in-education-health-and-the-workforce- (accessed April 8, 2021).
See https://www .congress .gov/bill/116th-congress /house-bill/6142?q= %7B%22search%22%3A %5B%22Black+Maternal+Health+Momnibus+Act %22%5D%7D&s=1&r=1 (accessed April 8, 2021).
See http://www .ihi.org/Engage /Initiatives/Completed /TCAB/Pages/default.aspx for more information about TCAB (accessed April 8, 2021).
Relational ethics is defined in health care as actions that take place within relationships and consider the existence of the other (i.e., patient, nurse) ( Bergum and Dossetor, 2005 ). Core tenets include mutual respect, engagement, embodied knowledge, environment, and uncertainty; the most important tenet is mutual respect ( Pollard, 2015 ).
Institutions serving people of color are commonly defined in two distinct categories: historically Black colleges and universities and tribal colleges and universities (NASEM, 2019).
Cultural taxation refers to the phenomenon whereby faculty who are individuals of color are asked routinely to take on extra, uncompensated work to address a lack of diversity in their institutions.
The February 2021 final draft ( AACN, 2021 ) is available at https://www .aacnnursing .org/Portals/42/AcademicNursing /pdf/Essentials-Final-Draft-2-18-21 .pdf?ver=hNeCl7OjgamIA9sHgDi _Yw %3d%3d×tamp=1613742420447 (accessed April 8, 2021).
See, for example, the Atlantic Fellows for Health Equity at The George Washington University Health Workforce Institute, the Diversity and Health Equity Fellowship of the American Hospital Association, and the Robert Wood Johnson Foundation’s Health Policy Fellows and Culture of Health Leaders programs.
See https://www .icn.ch/what-we-do /projects/global-nursing-leadership-institutetm-gnli (accessed April 8, 2021).
See https://catalog .upp.pitt .edu/preview_program .php?catoid=73&poid =23709&returnto=6375 (accessed April 8, 2021).
See https://www .vumc.org /healthequity/graduate-certificate-health-equity (accessed April 8, 2021).
See https://www .apha.org /apha-communities/member-sections /public-health-nursing (accessed June 7, 2021).
See https: //campaignforaction.org/about (accessed June 7, 2021).
See https: //blackcoalitionagainstcovid.org (accessed June 7, 2021).
See https://ncemna .org/about (accessed June 7, 2021).
- Cite this Page National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030; Flaubert JL, Le Menestrel S, Williams DR, et al., editors. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington (DC): National Academies Press (US); 2021 May 11. 9, Nurses Leading Change.
- PDF version of this title (5.6M)
In this Page
- THE COMMITTEE’S VISION FOR NURSING LEADERSHIP
- ACHIEVING THE COMMITTEE’S VISION OF NURSE LEADERSHIP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Nurses Leading Change - The Future of Nursing 2020-2030 Nurses Leading Change - The Future of Nursing 2020-2030
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Home — Essay Samples — Life — Nurse — Career Choice: My Dream To Become A Nurse
Career Choice: My Dream to Become a Nurse
- Categories: Nurse Why I Want To Be A Nurse
About this sample

Words: 525 |
Published: Dec 16, 2021
Words: 525 | Page: 1 | 3 min read
Works Cited:
- Hemphill, T. A., & Syagnik, B. (2017). What is a GMO and why should you care? A Brief Review. Biotech Patent News, 1(1), 8-13. doi: 10.1080/24749508.2017.1285867
- “What Is a GMO?” Non-GMO Project. (n.d.). https://www.nongmoproject.org/gmo-facts/what-is-gmo/
- Network, K. H. (2019, October 15). What are genetically modified (GM) plants? How are they made?
- “U.S. Food and Drug Administration.” (2022, March 18). Genetically Engineered Foods. https://www.fda.gov/food/food-new-plant-varieties/genetically-engineered-foods
- “The Truth About GMOs.” Institute for Responsible Technology. (n.d.). https://www.responsibletechnology.org/gmo-education/
- GMO OMG. (2013). Directed by Jeremy Seifert. United States: Compeller Pictures.
- “Going against GMO’s.” Food & Water Watch. (n.d.).
- Faber, S. (2017). Labeling of genetically modified foods: The consumer’s right to know. Journal of Food Law & Policy, 13, 45-75.
- Cassidy, E. S., West, P. C., Gerber, J. S., & Foley, J. A. (2013). Redefining agricultural yields: from tonnes to people nourished per hectare. Environmental Research Letters, 8(3), 034015.
- Kimbrell, A. (2009). The Monsanto menace: Why genetically modified crops may be harmful to your health. Harvard Law & Policy Review, 3, 293-312.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof. Kifaru
Verified writer
- Expert in: Life

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 968 words
2 pages / 933 words
3 pages / 1217 words
4 pages / 1642 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Nurse
In today's fast-paced healthcare environment, the impact of nurse shortages is becoming increasingly evident. The shortage of qualified nurses not only affects the quality of patient care but also places a significant strain on [...]
Leadership in nursing is a critical component of healthcare delivery, influencing patient outcomes, nurse performance, job satisfaction, and the overall quality of care. This essay explores the significance of leadership in [...]
Nursing, to me, is more than just a profession; it is a calling, a commitment, and a profound expression of compassion and care. In this essay, I will delve into what nursing means to me personally and the significant impact it [...]
Nursing as a profession is rooted in the nurturing and care of individuals, families, and communities to achieve optimal health. The development of a professional identity is crucial for nurses as it impacts patient care, career [...]
Why do you want to become a nurse? When being asked such question I would respond that Nurse Practitioner is a great occupation for me because it satisfies my personality, interests, and values. I took two personality tests and [...]
Nursing practice especially in terms of registered nurse (RN) practice should address the aspects of person-centered care along with evidence based practice in order to include the elements of preventative, curative, formative, [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Nursing Profession: The Vision for the Future Essay
Vision fitness in relation to the recommendations in the iom report, two action steps to promote the vision.
My vision for the future of nursing is to make the profession more personalized and have inclusivity of new ideas which embrace innovation and legacy. Again, there is a need to ensure that all parties involved in the provision of care work as a team. Such collaboration enables innovations and change in healthcare for a better outcome which is an aspect that covers the mental, physical, and emotional aspects of patients and nurses (Hassmiller, 2022). Healthcare workers must strike to create an environment that enables them to provide care efficiently.
My vision fits with set recommendations in the IOM based on how a nurse should increase collaboration and teamwork at the professional level. Since the vision set requires multidisciplinary action and approach, it is appropriate to settle the cooperation by dealing with all probable challenges (Maughan & Bergren, 2021). However, the set vision creates the practice of highly standardized legislation, thus providing confidence and support on methods that act across the nation in executing IOM recommendation(s) reports.
Integration of nursing, which is set in the vision, fits in the IOM recommendation based on the practice set and technology that provides patients exemplary care and support. Nurses must show their particular interaction to bear on more responsibilities that coincide with employment and patient population, as the outcome forecast will only advocate for success (Maughan & Bergren, 2021). On other levels, the agreed vision ensures that nurses continue with the approach of IOM report recommendation in the manner of how they prevail in some trusted professions. The interaction level of the vision creates a diverse representation of the population that execute change towards various interaction, either emotionally or mentally.
The vision fits establishment recommendations based on how nurses help bridge the gap between access and coverage in a routine of increasing level that creates complex care for a wide range of patients. The future of these visions enables full economic value, which makes a valuable contribution towards evidence-based practice and settling of realized features. The outcome of this issue allows for future role change, which reduces the rate of infection in patients and facilitates transition (Bergren & Maughan, 2021). The vision increases the autonomy of the nursing profession, which is an issue that improves work conditions.
Vision set creates the scope of practice and professional tension, which undermines how nursing professionals provide for a change in advanced care. Nursing students must ensure that all set roles in the future of nursing have the ability and interactive respect to make more extraordinary verdicts in the care of different patients. It is an issue that allows for an ideal outcome that deserves better working conditions in the future, as there are no limits. To emphasize this, there is a need for wellness levels and better nurse-to-patient ratios (Bergren & Maughan, 2021). The other aspect is the expansion of opportunities and acceptance of the future of nursing, which is bedside nursing, based on the IOM report’s recommendation.
The two action steps I plan to promote this vision vary depending on the set representation level and its professional setup. One of these action steps is to gain knowledge on matters of culture, which is an issue that creates change. The other step is ensuring nurse interaction has a set of motivations with the patients who collaborate with involved parties. These action steps allow for advancement in nursing interaction on both medical and diagnosis interventions, such as the set of practice-based evidence.
Bergren, M. D., & Maughan, E. D. (2021). The Future of nursing 2020–2030: School nursing research. The Journal of School Nursing , 37 (5), 321-322.
Hassmiller, S. B. (2022). The future of nursing 2020-2030: Charting a path to achieve health equity. Washington, DC: The National Academies Press.
Maughan, E. D., & Bergren, M. D. (2021). Future of nursing 2030: The future is bright for school nursing. NASN School Nurse , 36 (5), 248-251.
- The Future of Nursing in the United States
- Continued Professional Development
- Transforming Nursing Profession and Services
- Medication Errors Among Nursing Students
- Statistical Analysis of East Austen Community Health Problem
- Social Media: The Use in Nursing
- Illness Theories: Nightingale's Environment Nursing and Mishel's Uncertainty
- Incorporating a Holistic Approach to Nursing
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, August 12). Nursing Profession: The Vision for the Future. https://ivypanda.com/essays/nursing-profession-the-vision-for-the-future/
"Nursing Profession: The Vision for the Future." IvyPanda , 12 Aug. 2023, ivypanda.com/essays/nursing-profession-the-vision-for-the-future/.
IvyPanda . (2023) 'Nursing Profession: The Vision for the Future'. 12 August.
IvyPanda . 2023. "Nursing Profession: The Vision for the Future." August 12, 2023. https://ivypanda.com/essays/nursing-profession-the-vision-for-the-future/.
1. IvyPanda . "Nursing Profession: The Vision for the Future." August 12, 2023. https://ivypanda.com/essays/nursing-profession-the-vision-for-the-future/.
Bibliography
IvyPanda . "Nursing Profession: The Vision for the Future." August 12, 2023. https://ivypanda.com/essays/nursing-profession-the-vision-for-the-future/.

How to Write a Nursing Reflective Essay (Guide for Nurse Students)

If you are a nursing or medicine student, you are aware that you will come across or have already come across assignments requiring you to write a nursing reflection essay. At first, such a task always appears challenging, but given the understanding of the steps, things flat out, and you can write reflective essays and get better grades.
Reflective practice is highly encouraged in nursing. Reflection entails making sense of situations, events, actions, and phenomena in the workplace.
As a nursing student, you will be asked to write a reflective essay on your clinical placement, practicum, shadowing experience, shadow health DCE activities, personal nursing philosophy, why you want to become a nurse, nursing program, ethical dilemma, knowledge, skills, and abilities, systems, and processes.
The easiest way to complete the reflective essay assignment is by first determining what reflective writing entails, its significance, its steps, and some of the best tips that form the core of this ultimate guide.
Basics of Reflective Writing in Nursing
Reflective writing is an analytical writing practice where the writer describes a real or imaginary event, scene, phenomenon, occurrence, or memory, including their takeaway. It entails the critical analysis of an experience, including recording how it has impacted you and what you intend to do with the new knowledge or how to act when such an occurrence recurs.
As you document the encounter, you can use first-person pronouns and write subjectively and objectively. This means that you can decide to either use personal experiences alone or support these experiences using citations from scholarly sources.
When writing a reflective essay in nursing, you must recount the events and give critical detail of how the events shaped your knowledge acquisition. Reflection helps nursing students develop skills in self-directed learning, which is directly associated with high motivation and improved quality of care .
In most cases, reflection occurs on what went well and what went wrong. It could be a successful operation, a thank you note from a patient, a patient who regained their health faster, or a new nursing care plan that worked. However, it can also be about adverse events such as death, postoperative complications, death of an infant at birth, dissatisfied patient, medical error, or a failed procedure.
As a nursing student, when you learn to reflect on situations, you grow to become a professional nurse who diligently does their noble duty.
When writing a reflective essay, you begin by setting the scene (explaining what, where, how, and who-the situation), detailing how you felt (emotional state), why it happened (making sense of the situation), critical review and development of insights, a note on what was learned, and strategies to address future recurrence.
Your professor may ask you to write a nursing reflective paper about various topics in your course or your experience working in a group, how you solved a problem, a healthcare issue, or clinical practice. Consider the following example of a reflective statement in nursing; in my clinical practices, I realized I focused more on the technical aspects but failed to explain what it was doing to improve their health. I would like to understand more about listening to patience and their concerns to better care for them.
As you will notice later, these reflective stages are structured into different reflective models and frameworks that we will explore in-depth. So, with the understanding of what comprises reflective writing and its importance in nursing, let's now get solid on the structure.
Related Reading:
- Philosophy of Nursing Example.
- Ideas and topics for nursing capstone or project papers
- How to write a SOAP note paper
- Top nursing debate topics
- Nursing Theories and Theorists.
Structure of a Reflective Essay in Nursing
A reflective essay is an analytical writing piece describing and evaluating encounters or experiences. When asked to write one, you should know that an excellent reflective essay consists of different parts, just like a typical academic essay. It comprises the cover or title page, introduction, body paragraphs, conclusions, and a references page.
The title page contains information about the assignment. If you are writing the reflective essay in APA, include these on the title page:
- Title of the reflective essay
- Course code and name
- Instructors name
- Name of your institution
- Date of submission
When writing in Harvard format, the title or the cover page will consist of the following:
- Title of the essay in title case and the page number (upper right margin),
- Title of the essay in CAPS,
- Name of class or course,
- Name of the instructor,
- Name of your school,
- City and state where your school is located and,
- The date of submission.
Introduction
The introduction begins with an attention grabber or a hook sentence to attract readers' attention. It should then explain the essay's purpose and signpost the ideas that will come later in the essay. The introduction also has a thesis statement at the end of the paragraph- the last sentence. The thesis is concise, clear, and relatable and should reflect your position.
Body Paragraphs
The body paragraphs of a reflective essay can be three or more, depending on the length of the essay. Essentially, the body comprises 80% of the total word count.
The first paragraph is where you describe the situation, including the events, why they occurred, how they occurred, and those involved.
The second paragraph entails your personal feelings or reaction to the situation and how it made you feel.
The third paragraph can include making sense of the situation. You have to think about why things happened the way they did. You should also critically review and develop insights based on the situation. Finally, think of the factors that could have influenced the situation.
The next paragraph should explain how the event or situation will change your practice, approach, decisions, perspective, or perception. This is where you evaluate the experience by detailing the knowledge and skills you took from the experience.
The last body paragraph should entail a critical reflection on the learning opportunities. First, describe the situation and what it made you learn. Next, elaborate on how you intend to make yourself better poised to address such situations.
Mostly, you should structure the body of your essay as per the preferred nursing reflective model.
After everything else falls into place, you need to summarize the information you presented in the essay. Then, finally, restate your thesis and have a call to action to bring a sense of closure to your readers.
Steps for Writing a Nursing Reflection Essay � The Guide
When assigned to write a reflective essay for your nursing class, here are the surefire steps to get you to success.

Read the instructions
The first step after receiving an assignment is to begin reading the instructions. as you read, note what your instructor or professor expects in the paper you will submit for marking.
Reading instructions helps you to get informed on the scope of the paper, word count, number of references and pages, and the formatting style to use.
Besides, you also get to plan your paper with the deadline highlighted in the instructions.
You need to get a conducive environment where you can start writing.
The first step of writing is to brainstorm about situations during your clinical hours when you were shadowing a Nurse Practitioner or one you have read about.
Assess whether the situation or scenario you have thought, encountered, or chosen can help you write a reflective essay that meets the requirements.
Research and Plan
After choosing a scenario, the next step is researching the best reflective model.
You can use your class text, the instructions, the college library, course readings, and online nursing journals to get articles and resources with information about specific reflective models.
Select the best reflective model and take notes on the steps it entails.
As you research, write down notes on how to address your paper based on your selected framework or model of reflection . Additionally, research nursing journal articles with information you can use when critically analyzing a situation.
Plan how you will handle the paper as well. For instance, as you research, develop a thesis statement that grounds your entire paper, then draft an outline on how to develop the thesis.
Write an Outline
Outlining is a crucial aspect of writing. It helps you envision how you will meet the objective of writing a reflective essay. As an essential part of the essay writing process, outlining helps create a good flow of ideas and can come in handy in helping you overcome writer's block. Your outline should comprise the following:
- The hook or attention grabber
- Thesis statement
- Main points of each body paragraph (topic sentence, evidence, examples, illustrations, etc.)
- Conclusion (restated thesis and call-to-action)
With the outline done, you should take a break and resume writing your first draft of the nursing reflection essay. Writing with an outline helps avoid mistakes and also helps you write faster.
Describe the Experience
Once you have identified the relevant experience, begin describing it chronologically.
Describe the experience that prompted you to consider nursing your ideal career goal. Think of this experience's key elements, such as the setting, patient demographics, and significant events that impacted you.
Show how these events changed your perspective on life. Ensure you are as descriptive as possible to paint a clear picture for readers.
Consider the following questions to come up with a good description:
- What happened?
- Was there someone involved? If yes, what part did they play?
- Where did the event take place?
- What actions did you take?
Set the context of this experience by giving relevant background information. Ensure you are objective and pay attention to the facts.
Provide a Reflection
Talk about your feelings and thoughts concerning the particular experience you went through. You have to be honest and open up about your initial expectations and challenges you faced at each stage of the experience. The following questions can help you come up with a good reflection:
- What was I trying to achieve?
- What prompted me to act the way I did?
- Are there any consequences for my actions? If yes, what are they?
- How did I feel about this event as it was happening?
- How did those around me react to it?
- How do I know how those around me felt about it?
Analyze the Experience
Description of an experience is essential, but so is analysis. You have to move beyond the surface and give a critical analysis of your experience.
State your actions, and your overall experience will give insights into your experience. Think of how the experience has impacted your actions, feelings, and thoughts.
Give an Evaluation
Evaluate the skills and knowledge you got from the experience. Show how you can apply these skills and knowledge in your nursing practice. Also, state the actions and interventions you took during the nursing experience.
State whether you achieved the desired outcome and if there are any specific areas that you need to improve on.
Talk about how you built or improved skills like communication, teamwork, and critical thinking.
As you evaluate the experience, identify what you believe to be your strengths and weaknesses in the nursing experience. What have you learned from the experience? State the areas where you excelled and what abilities contributed to your success.
Talk about how those you were with during the clinical experience complimented you. Similarly, acknowledge your weaknesses.
What kind of mistakes did you make, and how did you improve them? Talk about the tasks that drain you most during the experience.
Illustrate Learning
Demonstrate elements of deeper thought and reflection levels. This is a great point to include nursing theories in your reflection essay to support analysis of your experience.
Relate your experiences to the theoretical frameworks you were taught in class. This is effective learning and will demonstrate your ability to apply knowledge to real-life nursing situations.
Doing this will also show that you can effectively deduce different things from observations made during the reflection process.
Ensure you also demonstrate a change in perspective, as this will prove that you learned something from the experience.
Write Your Conclusion
Conclude by summarizing your points and highlighting the lessons learned.
The lessons you reached as part of your reflection should support your overall conclusion.
Also, restate your thesis statement.
Come Up with an Action Plan
Now that you have learned from your reflection develop an action plan for future nursing practice.
This part should contain all the details you have learned and actions needed to improve when faced with a similar situation. Consider the following questions:
- What would I change if faced with a similar situation?
- How can I develop the necessary skills needed to face this situation?
- How can I act differently in a similar situation?
Ensure you identify areas to improve and set realistic goals to enhance your nursing skills. Discuss how you intend to seek additional education, training, or mentorship to address your shortcomings.
Finally, end the essay with a happy note so readers know you learned something from the experiences.
Proofread, Edit, and Polish
After doing your first draft, take a break to relax and get out of the writing mood - it helps you to become objective.
You can then resume reading out loud to yourself, make necessary tweaks, and ensure that every part you include meets the rubric requirements.
Edit for grammar, punctuation, tenses, voice, spelling, and use of language. You should also proofread the essay to adhere to the style, organization, and presentation requirements.
Ensure that all the in-text citations are accounted for in the reference list and are up-to-date. You are good to go when you have an essay that meets all the instructions.
Finally, you can submit the paper for grading.
Writing is not everyone's cup of tea. For that reason, you can hire a nursing reflection essay writer from our website to assist you in crafting a top-grade paper. In addition, we have nursing writers whose forte is writing various nursing papers.
Choosing the suitable Reflective Model or Framework
As you can see above, many reflective models are used for your reflective essay. We have not exhaustively listed and expounded on all of them. Other reflective models and frameworks you can also consider when writing a reflective essay in nursing include:
- Bouds Reflective Model
- Brookfield Reflective Model
- Pender's Health Promotion Model
- Roper Logan and Tierney Model
- Driscoll Reflective Model
- The Johari window model
Note that most nursing instructors will often suggest the models they prefer for you to use in your essay.
For example, in most nursing reflective essays. Whichever the case, readily available information expands on each model to make it easier to write a reflection essay on a specific aspect of nursing education or practice.
Read the assignment rubric and instructions to understand the specific model. If it is unclear, ask for clarification from your instructor early enough.
Tips for Writing a Good Nursing Reflective Essay
As you try to figure out how to write a nursing reflective essay, keep the following tips in mind.
Choose the Right Topic
If the instructions from your professors involve choosing a topic for the reflective essay, you must select one that is meaningful to you.
This will ensure you can easily write and easily develop relevant elements about the topic. Therefore, take time to pick a topic that you find interesting.
As you write, ensure you stay on topic, whether sharing a one-off event or a recurrent story.
Use the Right Tone
A reflective essay is more personal, unlike other types of academic essays. This means you don't need a strict or formal tone.
Since this is about your experiences, use personal pronouns such as I and Me.
Be Vulnerable
You must be extremely vulnerable to learn how to write a reflective essay in nursing.
Be open about your thoughts, feelings, and beliefs about something you went through that sparked an interest in nursing.
It's okay to share mistakes or things you did wrong that eventually led you to this career path.
Choose the Right Focus
A reflection essay is all about narrating your experience during the nursing experience.
While including other people in your experience is okay, please let them not be the center of your reflection.
This is your essay, so you should be the focus of attention.
Keep it Brief
A good nursing reflection essay should be between 300 and 800 consciously written words. Because of this length, you must only write relevant information about your reflection. Refrain from lengthy reflections, as they make it difficult to pass your points across.
Convey Your Information Wisely
Even though a nursing reflection essay is about your personal experiences, it doesn't mean you should reveal everything about yourself. Ask yourself whether something is appropriate before including it in your paper.
Mistakes to Avoid When Writing a Reflection Essay in Nursing
A good reflection essay involves reflecting on your nursing studies and practices throughout school and career to demonstrate your competence. For this reason, there are certain mistakes you should be aware of when writing an essay.
Not including a Personal Story
Like food tastes bland without salt, so does a reflection essay without a personal story. At the center of a reflection essay is You. This means the essay should focus on your personal story that led you to want a nursing career. A lot of times, students miss out on this instead of talking about their story. You need more than just the personal qualities you think will be a great fit for the nursing program; you must also share a story that shows how well you contributed to nursing care.
Failing to Share Your Experience
You will lose points when you fail to include nursing-related experiences in your reflection essay. Mentioning that you want to be a nurse is great, but failing to show specific events that led to the desire will cost you a great point.
Plagiarizing Your Essay
Plagiarism is a serious academic offense because it is considered taking other people's ideas and using them as your own without crediting the author. So, provide relevant citations and references for any ideas that aren't your own. Also, an AI will not write your essay as a human writer would.
Related Readings:
- How to write a student nurse resume with no experience.
- PICOT examples and guides
Sample of a Nursing Reflective Essay
The following is a sample of a nursing Reflective essay using Gibb's Model of Reflection. Use this sample to guide you when writing your own.
Introduction Communication is an important element in healthcare practice as it determines patient satisfaction and treatment outcomes. This essay will focus on reflecting on an experience I went through with a 40-year-old diabetic patient who also had a foot infected with an ulcer. When I approached the patient to sign the consent form, I noticed that he wasn't happy because of the news given to him about his health. I concluded that there must be a communication dilemma. I will reflect on the experience using Gibb's Model of Reflection. Using this model, I will identify and discuss the actions taken to resolve the issue. Description This incident happened a few months ago when I was working as a wound nurse in a Methodist hospital in my hometown. I was part of a care team handling the case of a 40-year-old male patient with diabetes and an infected diabetic foot ulcer. After careful examination, a team comprising various specialists concluded that his leg needed amputation below the knee. After making this decision, the team left, and I was asked to give the patient a consent form to sign. When I came back from retrieving the form, I noticed the patient looked sorrowful because of the news given to him. Feelings As soon as I saw the patient, I knew what he was going through. He perceived the situation to be irreparable, but I wasn't sure whether to console the patient or not. I was powerless and couldn't imagine what he was going through. At the same time, I was startled that the team left without showing any compassion. They could have handled the situation more delicately. I, on the other hand, could have relayed the information better. I wasn't sure whether my approach would be acceptable or appropriate. Evaluation I always go back to that particular situation and wonder whether I could have acted better. The situation helped me better understand the importance of good communication in patient care, particularly in therapeutic care. Before the incident, I didn't acknowledge the role of nurses play in caring for patient's emotional needs. I realized nurses must show compassion and console patients in their low moments. Analysis Most healthcare professionals do not know how to deliver bad news to patients. They find the process extremely challenging and always feel psychologically unprepared. This has a negative impact on patients and could lead to bad health outcomes. Furthermore, how information is relayed could impact a patient's adherence to treatment. Because of these effects, multiple protocols and approaches were developed to help with communicating bad news to patients. One of the approaches that was proposed is emotion-centered. This proposes that a healthcare provider acknowledges how sad the patient is and builds a professional relationship based on empathy and sympathy. Action Plan I now understand the essence of communicating bad news with compassion. The experience allowed me to look closely at different aspects of my professional development that needed more improvement. Thus, I plan to be more empathetic and speak up in support of patient's emotional and psychological well-being, especially when presented with traumatic news about their health. Additionally, I now understand I am not powerless when dealing with a sorrowful patient. I believe I have learned from my experience, and I'm not able to communicate well with patients any more. Conclusion The experience allowed me to value good communication in nursing and the need to incorporate it into daily nurse-patient interaction. Nurses must learn how to deliver bad news and manage patient's sorrow. This has been and will continue to be my biggest priority in patient care. References Street Jr, R. L., Makoul, G., Arora, N. K., & Epstein, R. M. (2009). How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient education and counselling, 74(3), 295-301. Buckman, R. (1992). Breaking bad news: why is it still so difficult? BMJ: British Medical Journal, 304(6842), 886. Ptacek, J. T., & Eberhardt, T. L. (1996). Breaking bad news: a review of the literature. The Journal of the American Medical Association, 276(6), 496-502.
Writing is not everyone's cup of tea. For that reason, you can hire a nursing reflection essay writer from NurseMyGrade to assist you in crafting a top-grade paper. In addition, we have nursing writers whose forte is writing various nursing papers. Just place an order , and we will get back to you ASAP.
Struggling with
Related Articles

Critical Appraisal or Article Critique Guide for Nursing Students

Best Topics and Ideas for an Epidemiology Paper
How to Do a Nursing Concept Analysis Paper and score an A
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
Home / Essay Samples / Life / Career Goals / Setting My Career Goals in Nursing: Aspirations for My Future
Setting My Career Goals in Nursing: Aspirations for My Future
- Category: Life , Profession
- Topic: Career Goals , Nurse
Pages: 1 (622 words)
Views: 1943
- Downloads: -->
--> ⚠️ Remember: This essay was written and uploaded by an--> click here.
Found a great essay sample but want a unique one?
are ready to help you with your essay
You won’t be charged yet!
Passion Essays
Pilot Essays
Internship Essays
Adversity Essays
Pediatrician Essays
Related Essays
We are glad that you like it, but you cannot copy from our website. Just insert your email and this sample will be sent to you.
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Your essay sample has been sent.
In fact, there is a way to get an original essay! Turn to our writers and order a plagiarism-free paper.
samplius.com uses cookies to offer you the best service possible.By continuing we’ll assume you board with our cookie policy .--> -->