
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Find in topic
INTRODUCTION
Diagnosis and management of face and brow presentations will be reviewed here. Other cephalic malpresentations are discussed separately. (See "Occiput posterior position" and "Occiput transverse position" .)
Prevalence — Face and brow presentation are uncommon. Their prevalences compared with other types of malpresentations are shown below [ 1-9 ]:
● Occiput posterior – 1/19 deliveries
● Breech – 1/33 deliveries
To continue reading this article, you must sign in . For more information or to purchase a personal subscription, click below on the option that best describes you:
- Medical Professional
- Resident, Fellow or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
Print Options

- Physician Physician Board Reviews Physician Associate Board Reviews CME Lifetime CME Free CME MATE and DEA Compliance
- Student USMLE Step 1 USMLE Step 2 USMLE Step 3 COMLEX Level 1 COMLEX Level 2 COMLEX Level 3 96 Medical School Exams Student Resource Center NCLEX - RN NCLEX - LPN/LVN/PN 24 Nursing Exams
- Nurse Practitioner APRN/NP Board Reviews CNS Certification Reviews CE - Nurse Practitioner FREE CE
- Nurse RN Certification Reviews CE - Nurse FREE CE
- Pharmacist Pharmacy Board Exam Prep CE - Pharmacist
- Allied Allied Health Exam Prep Dentist Exams CE - Social Worker CE - Dentist
- Point of Care
- Free CME/CE
Delivery, Face and Brow Presentation
Introduction.
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common presentation in term labor is the vertex, where the fetal neck is flexed to the chin, minimizing the head circumference.
Face presentation – an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations. [1] [2] [3]
In brow presentation, the neck is not extended as much as in face presentation, and the leading part is the area between the anterior fontanelle and the orbital ridges. Brow presentation is considered the rarest of all malpresentation with a prevalence of 1 in 500 to 1 in 4000 deliveries. [3]
Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow presentation. These risk factors may be related to either the mother or the fetus. Maternal risk factors are preterm delivery, contracted maternal pelvis, platypelloid pelvis, multiparity, previous cesarean section, black race. Fetal risk factors include anencephaly, multiple loops of cord around the neck, masses of the neck, macrosomia, polyhydramnios. [2] [4] [5]
These malpresentations are usually diagnosed during the second stage of labor when performing a digital examination. It is possible to palpate orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, anterior fontanelle and face can be palpated except for the mouth and the chin. Brow presentation can then be further described based on the position of the anterior fontanelle as frontal anterior, posterior, or transverse.
Diagnosing the exact presentation can be challenging, and face presentation may be misdiagnosed as frank breech. To avoid any confusion, a bedside ultrasound scan can be performed. [6] The ultrasound imaging can show a reduced angle between the occiput and the spine or, the chin is separated from the chest. However, ultrasound does not provide much predicting value in the outcome of the labor. [7]
Anatomy and Physiology
Register for free and read the full article, learn more about a subscription to statpearls point-of-care.
Before discussing the mechanism of labor in the face or brow presentation, it is crucial to highlight some anatomical landmarks and their measurements.
Planes and Diameters of the Pelvis
The three most important planes in the female pelvis are the pelvic inlet, mid pelvis, and pelvic outlet.
Four diameters can describe the pelvic inlet: anteroposterior, transverse, and two obliques. Furthermore, based on the different landmarks on the pelvic inlet, there are three different anteroposterior diameters, named conjugates: true conjugate, obstetrical conjugate, and diagonal conjugate. Only the latter can be measured directly during the obstetric examination. The shortest of these three diameters is obstetrical conjugate, which measures approximately 10.5 cm and is a distance between the sacral promontory and 1 cm below the upper border of the symphysis pubis. This measurement is clinically significant as the fetal head must pass through this diameter during the engagement phase. The transverse diameter measures about 13.5cm and is the widest distance between the innominate line on both sides.
The shortest distance in the mid pelvis is the interspinous diameter and usually is only about 10 cm.
Fetal Skull Diameters
There are six distinguished longitudinal fetal skull diameters:
- Suboccipito-bregmatic: from the center of anterior fontanelle (bregma) to the occipital protuberance, measuring 9.5 cm. This is the presenting diameter in vertex presentation.
- Suboccipito-frontal: from the anterior part of bregma to the occipital protuberance, measuring 10 cm
- Occipito-frontal: from the root of the nose to the most prominent part of the occiput, measuring 11.5cm
- Submento-bregmatic: from the center of the bregma to the angle of the mandible, measuring 9.5 cm. This is the presenting diameter in face presentation where the neck is hyperextended.
- Submento-vertical: from the midpoint between fontanelles and the angle of the mandible, measuring 11.5cm
- Occipito-mental: from the midpoint between fontanelles and the tip of the chin, measuring 13.5 cm. It is the presenting diameter in brow presentation.
Cardinal Movements of Normal Labor
- Neck flexion
- Internal rotation
- Extension (delivers head)
- External rotation (Restitution)
- Expulsion (delivery of anterior and posterior shoulders)
Some of the key movements are not possible in the face or brow presentations.
Based on the information provided above, it is obvious that labor will be arrested in brow presentation unless it spontaneously changes to face or vertex, as the occipito-mental diameter of the fetal head is significantly wider than the smallest diameter of the female pelvis. Face presentation can, however, be delivered vaginally, and further mechanisms of face delivery will be explained in later sections.
Indications
As mentioned previously, spontaneous vaginal delivery can be successful in face presentation. However, the main indication for vaginal delivery in such circumstances would be a maternal choice. It is crucial to have a thorough conversation with a mother, explaining the risks and benefits of vaginal delivery with face presentation and a cesarean section. Informed consent and creating a rapport with the mother is an essential aspect of safe and successful labor.
Contraindications
Vaginal delivery of face presentation is contraindicated if the mentum is lying posteriorly or is in a transverse position. In such a scenario, the fetal brow is pressing against the maternal symphysis pubis, and the short fetal neck, which is already maximally extended, cannot span the surface of the maternal sacrum. In this position, the diameter of the head is larger than the maternal pelvis, and it cannot descend through the birth canal. Therefore the cesarean section is recommended as the safest mode of delivery for mentum posterior face presentations.
Attempts to manually convert face presentation to vertex, manual or forceps rotation of the persistent posterior chin to anterior are contraindicated as they can be dangerous.
Persistent brow presentation itself is a contraindication for vaginal delivery unless the fetus is significantly small or the maternal pelvis is large.
Continuous electronic fetal heart rate monitoring is recommended for face and brow presentations, as heart rate abnormalities are common in these scenarios. One study found that only 14% of the cases with face presentation had no abnormal traces on the cardiotocograph. [8] It is advised to use external transducer devices to prevent damage to the eyes. When internal monitoring is inevitable, it is suggested to place monitoring devices on bony parts carefully.
People who are usually involved in the delivery of face/ brow presentation are:
- Experienced midwife, preferably looking after laboring woman 1:1
- Senior obstetrician
- Neonatal team - in case of need for resuscitation
- Anesthetic team - to provide necessary pain control (e.g., epidural)
- Theatre team - in case of failure to progress and an emergency cesarean section will be required.
Preparation
No specific preparation is required for face or brow presentation. However, it is essential to discuss the labor options with the mother and birthing partner and inform members of the neonatal, anesthetic, and theatre co-ordinating teams.
Technique or Treatment
Mechanism of Labor in Face Presentation
During contractions, the pressure exerted by the fundus of the uterus on the fetus and pressure of amniotic fluid initiate descent. During this descent, the fetal neck extends instead of flexing. The internal rotation determines the outcome of delivery, if the fetal chin rotates posteriorly, vaginal delivery would not be possible, and cesarean section is permitted. The approach towards mentum-posterior delivery should be individualized, as the cases are rare. Expectant management is acceptable in multiparous women with small fetuses, as a spontaneous mentum-anterior rotation can occur. However, there should be a low threshold for cesarean section in primigravida women or women with large fetuses.
When the fetal chin is rotated towards maternal symphysis pubis as described as mentum-anterior; in these cases further descend through the vaginal canal continues with approximately 73% cases deliver spontaneously. [9] Fetal mentum presses on the maternal symphysis pubis, and the head is delivered by flexion. The occiput is pointing towards the maternal back, and external rotation happens. Shoulders are delivered in the same manner as in vertex delivery.
Mechanism of Labor in Brow Presentation
As this presentation is considered unstable, it is usually converted into a face or an occiput presentation. Due to the cephalic diameter being wider than the maternal pelvis, the fetal head cannot engage; thus, brow delivery cannot take place. Unless the fetus is small or the pelvis is very wide, the prognosis for vaginal delivery is poor. With persistent brow presentation, a cesarean section is required for safe delivery.
Complications
As the cesarean section is becoming a more accessible mode of delivery in malpresentations, the incidence of maternal and fetal morbidity and mortality during face presentation has dropped significantly. [10]
However, there are still some complications associated with the nature of labor in face presentation. Due to the fetal head position, it is more challenging for the head to engage in the birth canal and descend, resulting in prolonged labor.
Prolonged labor itself can provoke foetal distress and arrhythmias. If the labor arrests or signs of fetal distress appear on CTG, the recommended next step in management is an emergency cesarean section, which in itself carries a myriad of operative and post-operative complications.
Finally, due to the nature of the fetal position and prolonged duration of labor in face presentation, neonates develop significant edema of the skull and face. Swelling of the fetal airway may also be present, resulting in respiratory distress after birth and possible intubation.
Clinical Significance
During vertex presentation, the fetal head flexes, bringing the chin to the chest, forming the smallest possible fetal head diameter, measuring approximately 9.5cm. With face and brow presentation, the neck hyperextends, resulting in greater cephalic diameters. As a result, the fetal head will engage later, and labor will progress more slowly. Failure to progress in labor is also more common in both presentations compared to vertex presentation.
Furthermore, when the fetal chin is in a posterior position, this prevents further flexion of the fetal neck, as browns are pressing on the symphysis pubis. As a result, descend through the birth canal is impossible. Such presentation is considered undeliverable vaginally and requires an emergency cesarean section.
Manual attempts to change face presentation to vertex, manual or forceps rotation to mentum anterior are considered dangerous and are discouraged.
Enhancing Healthcare Team Outcomes
A multidisciplinary team of healthcare experts supports the woman and her child during labor and the perinatal period. For a face or brow presentation to be appropriately diagnosed, an experienced midwife and obstetrician must be involved in the vaginal examination and labor monitoring. As fetal anomalies, such as anencephaly or goiter, can contribute to face presentation, sonographers experienced in antenatal scanning should also be involved in the care. It is advised to inform the anesthetic and neonatal teams in advance of the possible need for emergency cesarean section and resuscitation of the neonate. [11] [12]
Gardberg M,Leonova Y,Laakkonen E, Malpresentations--impact on mode of delivery. Acta obstetricia et gynecologica Scandinavica. 2011 May; [PubMed PMID: 21501123]
Tapisiz OL,Aytan H,Altinbas SK,Arman F,Tuncay G,Besli M,Mollamahmutoglu L,Danışman N, Face presentation at term: a forgotten issue. The journal of obstetrics and gynaecology research. 2014 Jun; [PubMed PMID: 24888918]
Zayed F,Amarin Z,Obeidat B,Obeidat N,Alchalabi H,Lataifeh I, Face and brow presentation in northern Jordan, over a decade of experience. Archives of gynecology and obstetrics. 2008 Nov; [PubMed PMID: 18283473]
Bashiri A,Burstein E,Bar-David J,Levy A,Mazor M, Face and brow presentation: independent risk factors. The journal of maternal-fetal [PubMed PMID: 18570114]
Shaffer BL,Cheng YW,Vargas JE,Laros RK Jr,Caughey AB, Face presentation: predictors and delivery route. American journal of obstetrics and gynecology. 2006 May; [PubMed PMID: 16647888]
Bellussi F,Ghi T,Youssef A,Salsi G,Giorgetta F,Parma D,Simonazzi G,Pilu G, The use of intrapartum ultrasound to diagnose malpositions and cephalic malpresentations. American journal of obstetrics and gynecology. 2017 Dec; [PubMed PMID: 28743440]
Ghi T,Eggebø T,Lees C,Kalache K,Rozenberg P,Youssef A,Salomon LJ,Tutschek B, ISUOG Practice Guidelines: intrapartum ultrasound. Ultrasound in obstetrics [PubMed PMID: 29974596]
Benedetti TJ,Lowensohn RI,Truscott AM, Face presentation at term. Obstetrics and gynecology. 1980 Feb; [PubMed PMID: 7352081]
Ducarme G,Ceccaldi PF,Chesnoy V,Robinet G,Gabriel R, [Face presentation: retrospective study of 32 cases at term]. Gynecologie, obstetrique [PubMed PMID: 16630740]
Cruikshank DP,Cruikshank JE, Face and brow presentation: a review. Clinical obstetrics and gynecology. 1981 Jun; [PubMed PMID: 7307363]
Domingues AP,Belo A,Moura P,Vieira DN, Medico-legal litigation in Obstetrics: a characterization analysis of a decade in Portugal. Revista brasileira de ginecologia e obstetricia : revista da Federacao Brasileira das Sociedades de Ginecologia e Obstetricia. 2015 May; [PubMed PMID: 26107576]
. Intrapartum care for healthy women and babies. 2022 Dec 14:(): [PubMed PMID: 32212591]
Use the mouse wheel to zoom in and out, click and drag to pan the image
Having a C-Section (Cesarean Section)
Medical review policy, latest update:, what is a c-section , what are the reasons for a c-section, read this next, what happens during a c-section, preparation and anesthesia, incision and delivery, meeting your baby, what are possible c-section complications, can i have an elective c-section, what is the typical c-section recovery time, c-section recovery tips.
What to Expect When You’re Expecting , 5th edition, Heidi Murkoff. WhatToExpect.com, Breech Position: What It Means if Your Baby is Breech , February 2021. WhatToExpect.com, Heart Conditions During Pregnancy , December 2020. WhatToExpect.com, Fetal Macrosomia , April 2020. WhatToExpect.com, How Does Gestational Diabetes (GD) Affect Your Pregnancy and Baby? , December 2020. WhatToExpect.com, Placenta Previa , April 2019. WhatToExpect.com, Preeclampsia: Symptoms, Risk Factors and Treatments , April 2019. WhatToExpect.com, Vaginal Birth After Cesarean (VBAC) , November 2018. WhatToExpect.com, Inducing Labor: What Happens When You’re Induced? , April 2019. WhatToExpect.com, Medications to Manage Labor Pain , September 2018. WhatToExpect.com, Giving Birth by Vaginal Delivery , April 2021. WhatToExpect.com, Forceps Delivery , April 2020. WhatToExpect.com, Episiotomy , April 2019. WhatToExpect.com, Postpartum Bleeding (Lochia) , February 2020. WhatToExpect.com, C-section Scars: Care Basics During and After Healing , November 2020. WhatToExpect.com, Postpartum Recovery Timeline , March 2021. Mayo Clinic, C-Section , June 2020. Mayo Clinic, Repeat C-Sections: Is There a Limit? , June 2020. American College of Obstetricians and Gynecologists, Cesarean Birth , June 2020. American College of Obstetricians and Gynecologists, Cesarean Delivery on Maternal Request , January 2019. Centers for Disease Control and Prevention, Births – Method of Delivery , March 2021. March of Dimes, Having a C-Section , October 2018. Kids Health Nemours, Cesarean Sections (C-Sections) , February 2017. Icahn School of Medicine at Mount Sinai, Going Home After a C-Section , August 2018. Human Reproduction, A Population-based Cohort Study of the Effect of Caesarean Section on Subsequent Fertility , June 2014.
Jump to Your Week of Pregnancy
Trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Pan Afr Med J
Management of face presentation, face and lip edema in a primary healthcare facility case report, Mbengwi, Cameroon
Nzozone henry fomukong.
1 Microhealth Global Medical Centre, Mbengwi, Cameroon
2 Department of Medicine and Surgery, Faculty of Health Sciences University of Buea, Buea, Cameroon
Ngouagna Edwin
Mandeng ma linwa edgar, ngwayu claude nkfusai.
3 Department of Microbiology and Parasitology, Faculty of Science, University of Buea, Buea, Cameroon
4 Cameroon Baptist Convention Health Services (CBCHS), Yaoundé, Cameroon
Yunga Patience Ijang
5 Department of Public Health, School of Health Sciences, Catholic University of Central Africa, Box 1110, Yaoundé, Cameroon
Joyce Shirinde
6 School of Health Systems and Public Health, Faculty of Health Sciences, University of Pretoria Private Bag X323, Gezina, Pretoria, 0001, Pretoria, South Africa
Samuel Nambile Cumber
7 Institute of Medicine, Department of Public Health and Community Medicine (EPSO), University of Gothenburg, Box 414, SE - 405 30 Gothenburg, Sweden
8 Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
Face presentation is a rare obstetric event and most practitioners will go through their carriers without ever meeting one. Face presentation can be delivered vaginally only if the foetus is in the mentum anterior position. More than half of the cases of face presentation are delivered by caesarean section. Newborn infants with face presentation usually have severe facial oedema, facial bruising or ecchymosis. These syndromic facial features usually resolved within 24-48 hours.
Introduction
Face presentation is a rare unanticipated obstetric event characterized by a longitudinal lie and full extension of the foetal head on the neck with the occiput against the upper back [ 1 - 3 ]. Face presentation occurs in 0.1-0.2% of deliveries [ 3 - 5 ] but is more common in black women and in multiparous women [ 5 ]. Studies have shown that 60 per cent of face presentations have one or more of the following risk factors: small fetus, large fetus, high parity, previous caesarean section (CS), contracted pelvis, fetopelvic disproportion, cord around the neck multiple pregnancy, hypertensive disorders of pregnancy, polyhydramnios, uterine or nuchal cord anomaly. But 40 per cent of face presentations occur with none of these factors [ 6 , 7 ]. A vaginal birth at term is possible only if the fetus is in the mentum anterior position. More than half of cases of face presentation are delivered by caesarean section [ 4 ]. Newborn infants with face presentation usually have severe facial edema, facial bruising or ecchymosis [ 8 ]. Repeated vaginal examination to assess the presenting part and the progress of labor may lead to bruises in the face as well as damage to the eyes.
Patient and observation
Case presentation: a 21 year old primigravida at 40 weeks gestation from the last normal menstrual period referred to our facility for prolonged second stage of labor after visiting two health centres. She labored for a total of 14hrs, membrane ruptured spontaneously 12hrs before referral. Amniotic fluid was documented by midwife to be clear. She attended antenatal clinics in Mbengwi health centre 5 times, was diagnosed of hepatitis B during antenatal consultations, received no treatment. She did not do any ultrasound due to financial constraints. On examination, she was healthy, in painful distress, blood pressure 131/76mmhg, pulse 85 beats/min, temperature 37.2 o C SPO2 98%. On abdominal exams, uterus was gravid, fundal height 35cm, lie longitudinal, fetal heart rate 137bpm, cephalic presentation, engaged 2/5, with moderate contractions of 2 in 10 minutes. On vaginal examination, cervix was fully dilated, membranes ruptured, presenting part was face, mentum anterior. The conclusion made was mento-anterior face presentation ( Figure 1 ). Paturient was counseled, labor was augmented with 1 amp of oxytocin in 500ml of glucose 5% and started at 10drops/mins. Ten minutes later she delivered a male baby with Apgar score 6/10, 8/10 on the first and fifth minute. The baby weighed 3.2kg, length was 50cm, and head circumference was 41cm. Syndromic facial appearance with marked edema at the baby's lips, face and scalp was evident and he had bruising on the right nasolabial groove and right cheeks ( Figure 2 ). Physical examination of the infant's respiratory system, cardiovascular system, and his abdominal examination were normal, as was his neurological examination. Placenta was delivered by controlled cord traction 5mins later with all cotyledons. Delivery was complicated by a second degree perineal tear. Perineal tear was repaired with absorbable suture under local anaesthesia. Estimated blood lost was 350ml. baby received Hepatitis B immunoglobulins, hepatitis B vaccine and vitamin K were administered to the baby. 24 hours later, facial swellings resolved ( Figure 3 ), baby breast feeds well. Baby and mother were discharged on day 3 postpartum all fine.

Men-tum anterior face presentation

Bruising, marked lip and facial edema

Baby 24 hours later with all syndromic facial features resolved
Ethics : informed consent: written informed consent was obtained from the patient's parents for the publication of this case report.
Face presentation is a rare obstetric event and most practitioner will go through their carriers without ever meeting one [ 3 ]. We presented a case of face presentation noticed in the delivery room on digital examination in a patient with no risk factors. In a poor resource setting as ours where ultrasound is not readily available, this event is often scary and confusing to most midwives and nurses. This may prompt repeated vaginal exams for confirmation of presentation. This intend will lead to bruising of the baby's face and delay effective management [ 8 ]. Exact knowledge about the fetal position and level is important for providing the correct management of this malpresentation. When face presentation is diagnosed, around 60% of cases are in the mentum anterior position, 25% are mentum posterior and 15% are mentum transverse [ 5 ]. The patient presented the most common form of face presentation (mentum anterior). Labor was augmented, vaginal delivery was attempted and successfully conducted. Facial bruising, lip and face edema are very common complication of face presentation. These complications usually resolve within 24-48 hours [ 9 , 10 ] in this case facial edema completely resolved within 24hours ( Figure 3 ) and baby breastfeed well.
Repeated vaginal exams should be avoided when presenting part is unsure. Vaginal delivery should be attemped only on mentum anterior face presentation, in other cases, emergency ceserian section should be performed. Syndromic facial features in babies born from face presentation resolve completely within 24-48 hours.
Competing interests
The authors declare no competing interests.
Acknowledgements
We thank the participant of this study.
Authors’ contributions
NHF, NE, MMLE, NCN, YPI, FB, JS and SNC conceived the case series, assisted with the study design and participant enrollment, designed the study protocol and collected the data. NE, MMLE, NCN and SNC assisted in interpretation of results and wrote the manuscript. All authors read and approved the final manuscript.
- Patient Care & Health Information
- Tests & Procedures
Cesarean delivery (C-section) is used to deliver a baby through surgical incisions made in the abdomen and uterus.
Planning for a C-section might be necessary if there are certain pregnancy complications. Women who have had a C-section might have another C-section. Often, however, the need for a first-time C-section isn' clear until after labor starts.
If you're pregnant, knowing what to expect during and after a C-section can help you prepare.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- A Book: Obstetricks
Why it's done
Health care providers might recommend a C-section if:
- Labor isn't progressing normally. Labor that isn't progressing (labor dystocia) is one of the most common reasons for a C-section. Issues with labor progression include prolonged first stage (prolonged dilation or opening of the cervix) or prolonged second stage (prolonged time of pushing after complete cervical dilation).
- The baby is in distress. Concern about changes in a baby's heartbeat might make a C-section the safest option.
- The baby or babies are in an unusual position. A C-section is the safest way to deliver babies whose feet or buttocks enter the birth canal first (breech) or babies whose sides or shoulders come first (transverse).
- You're carrying more than one baby. A C-section might be needed for women carrying twins, triplets or more. This is especially true if labor starts too early or the babies are not in a head-down position.
- There's a problem with the placenta. If the placenta covers the opening of the cervix (placenta previa), a C-section is recommended for delivery.
- Prolapsed umbilical cord. A C-section might be recommended if a loop of umbilical cord slips through the cervix in front of the baby.
- There's a health concern. A C-section might be recommended for women with certain health issues, such as a heart or brain condition.
- There's a blockage. A large fibroid blocking the birth canal, a pelvic fracture or a baby who has a condition that can cause the head to be unusually large (severe hydrocephalus) might be reasons for a C-section.
- You've had a previous C-section or other surgery on the uterus. Although it's often possible to have a vaginal birth after a C-section, a health care provider might recommend a repeat C-section.
Some women request C-sections with their first babies. They might want to avoid labor or the possible complications of vaginal birth. Or they might want to plan the time of delivery. However, according to the American College of Obstetricians and Gynecologists, this might not be a good option for women who plan to have several children. The more C-sections a woman has, the greater the risk of problems with future pregnancies.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Like other types of major surgery, C-sections carry risks.
Risks to babies include:
- Breathing problems. Babies born by scheduled C-section are more likely to develop a breathing issue that causes them to breathe too fast for a few days after birth (transient tachypnea).
- Surgical injury. Although rare, accidental nicks to the baby's skin can occur during surgery.
Risks to mothers include:
- Infection. After a C-section, there might be a risk of developing an infection of the lining of the uterus (endometritis), in the urinary tract or at the site of the incision.
- Blood loss. A C-section might cause heavy bleeding during and after delivery.
- Reactions to anesthesia. Reactions to any type of anesthesia are possible.
- Blood clots. A C-section might increase the risk of developing a blood clot inside a deep vein, especially in the legs or pelvis (deep vein thrombosis). If a blood clot travels to the lungs and blocks blood flow (pulmonary embolism), the damage can be life-threatening.
- Surgical injury. Although rare, surgical injuries to the bladder or bowel can occur during a C-section.
Increased risks during future pregnancies. Having a C-section increases the risk of complications in a later pregnancy and in other surgeries. The more C-sections, the higher the risks of placenta previa and a condition in which the placenta becomes attached to the wall of the uterus (placenta accreta).
A C-section also increases the risk of the uterus tearing along the scar line (uterine rupture) for women who attempt a vaginal delivery in a later pregnancy.
How you prepare
For a planned C-section, a health care provider might suggest talking with an anesthesiologist if there are medical conditions that might increase the risk of anesthesia complications.
A health care provider might also recommend certain blood tests before a C-section. These tests provide information about blood type and the level of the main component of red blood cells (hemoglobin). The test results can be helpful in case you need a blood transfusion during the C-section.
Even for a planned vaginal birth, it's important to prepare for the unexpected. Discuss the possibility of a C-section with your health care provider well before your due date.
If you don't plan to have more children, you might talk to your health care provider about long-acting reversible birth control or permanent birth control. A permanent birth control procedure might be performed at the time of the C-section.
What you can expect
Before the procedure.
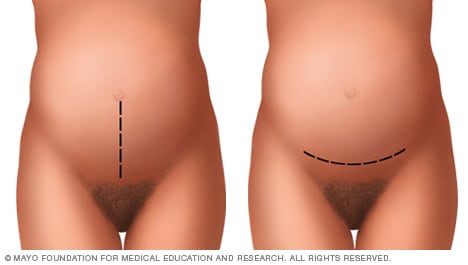
- Abdominal incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. The abdominal incision is made first. It's either a vertical incision between your navel and pubic hair (left) or, more commonly, a horizontal incision lower on your abdomen (right).
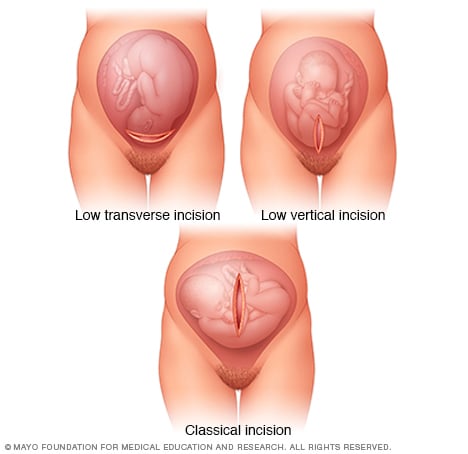
- Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
A C-section can be done in various ways. But most C-sections involve these steps:
- At home. Your health care provider might ask you to shower at home with an antiseptic soap the night before and the morning of your C-section. Don't shave your pubic hair within 24 hours of your C-section. This can increase the risk of a surgical site infection. If your pubic hair needs to be removed, it will be trimmed by the surgical staff just before surgery.
- At the hospital. Your abdomen will be cleansed. A thin tube (catheter) will likely be placed into your bladder to collect urine. An intravenous line will be placed in a vein in your hand or arm to provide fluid and drugs, including antibiotics to prevent infection.
Anesthesia. Most C-sections are done under regional anesthesia, which numbs only the lower part of your body. This allows you to be awake during the procedure. Common choices include a spinal block and an epidural block.
Some C-sections might require general anesthesia. With general anesthesia, you won't be awake during the birth.
During the procedure
A doctor makes surgical incisions in the abdomen and the uterus to deliver the baby.
- Abdominal incision. The doctor makes an incision in the abdominal wall. It's usually done horizontally near the pubic hairline. Or the doctor might make a vertical incision from just below the navel to just above the pubic bone.
- Uterine incision. The uterine incision is then made — usually horizontally across the lower part of the uterus (low transverse incision). Other types of uterine incisions might be used depending on the baby's position within the uterus and whether there are complications, such as placenta previa or preterm delivery.
- Delivery. The baby will be delivered through the incisions. The doctor clears the baby's mouth and nose of fluids, then clamps and cuts the umbilical cord. The placenta is then removed from the uterus, and the incisions are closed with sutures.
If you have regional anesthesia, you're likely to be able to hold the baby shortly after delivery.
After the procedure
A C-section usually requires a hospital stay for 2 to 3 days. Your health care provider will discuss pain relief options with you.
Once the anesthesia begins to wear off, you'll be encouraged to drink fluids and walk. This helps prevent constipation and deep vein thrombosis. Your health care team will monitor your incision for signs of infection. The bladder catheter will likely be removed as soon as possible.
You can start breastfeeding as soon as you're ready, even in the delivery room. Ask your nurse or a lactation consultant to teach you how to position yourself and support your baby so that you're comfortable. Your health care team will select medications for your post-surgical pain with breastfeeding in mind.
When you go home
During the C-section recovery process, discomfort and fatigue are common. To promote healing:
- Take it easy. Rest when possible. Try to keep everything that you and your baby need within reach. For the first few weeks, don't lift more than 25 pounds.
- Use recommended pain relief. To soothe incision soreness, your health care provider might recommend a heating pad and pain medications that are safe for breastfeeding women and their babies. These include ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others).
- Wait to have sex. To prevent infection, wait at least six weeks to have sex and don't put anything in your vagina after your C-section.
- Wait to drive. If you're taking narcotics for pain relief, it might take 1 to 2 weeks before you can comfortably apply brakes and twist to check blind spots.
Check your C-section incision for signs of infection. Pay attention to any symptoms. Contact your health care provider if:
- Your incision is red, swollen or leaking discharge
- You have a fever
- You have heavy bleeding
- You have worsening pain
If you have severe mood swings, loss of appetite, overwhelming fatigue and lack of joy in life shortly after childbirth, you might have postpartum depression. Contact your health care provider if you think you might be depressed, especially if your symptoms don't go away, you have trouble caring for your baby or completing daily tasks, or you have thoughts of harming yourself or your baby.
The American College of Obstetricians and Gynecologists recommends that postpartum care be ongoing. Have contact with your health care provider within three weeks after delivery. Within 12 weeks after delivery, see your health care provider for a postpartum evaluation.
During this appointment your health care provider likely will check your mood and emotional well-being, discuss contraception and birth spacing, review information about infant care and feeding, talk about your sleep habits and issues related to fatigue and do a physical exam, including a pap smear if it's due. This might include a check of your abdomen, vagina, cervix and uterus to make sure you're healing well.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
- FAQs: Cesarean birth. The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/cesarean-birth. Accessed Feb. 19, 2022.
- AskMayoExpert. Cesarean delivery. Mayo Clinic; 2021.
- Gabbe SG, et al., eds. Cesarean delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Feb. 19, 2022.
- C-section. American Society of Anesthesiologists. https://www.asahq.org/madeforthismoment/preparing-for-surgery/procedures/c-section/. Accessed Feb. 19, 2022.
- Berghella V. Cesarean delivery: Preoperative planning and patient preparation. https://www.uptodate.com/contents/search. Accessed Feb. 24, 2022.
- Berghella V. Cesarean delivery: Postoperative issues. https://www.uptodate.com/contents/search. Accessed Feb. 24, 2022.
- American College of Obstetricians and Gynecologists' Committee on Obstetric Practice. Committee Opinion No. 736: Optimizing postpartum care. Obstetrics & Gynecology. 2018; doi:10.1097/AOG.0000000000002633.
- American College of Obstetricians and Gynecologists' Committee on Obstetric Practice. Committee Opinion No. 761: Caesarian delivery on maternal request. Obstetrics & Gynecology. 2019; doi:10.1097/AOG.0000000000003006.
- Conjoined twins
- C-section recovery
- Fetal macrosomia
- Placenta accreta
- Placenta previa
- Placental abruption
- Preeclampsia
- Pregnancy and obesity
- Repeat C-sections
- Spina bifida
- Video: Cesarean section
- Doctors & Departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Face Presentation
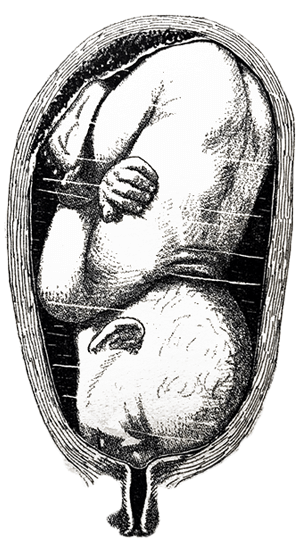
Pictoral Midwifery, Comyns Berkely, 4th Edition. 1941
Face it. We have a lot to learn about fetal positioning. The old paradigm is fetal positions are random. The new paradigm is that babies match the space available.
Face and brow presentations occur when baby’s spine extended until the head is shifted back so baby’s face comes through the pelvis first.
Baby may settle in a face or brow presentation before labor or they may become a face or brow presentation, usually when a posterior baby has it’s chin pushed further up by the pelvic floor during descent.
A baby who is in a face-first or forehead-first position often started as an extended (chin up) occiput posterior or occiput transverse position. Coming down on to the pelvic floor with the forehead leading then “converted” this baby’s head to the face first position.
The baby’s face may be bruised for a couple days after the birth. The brow presentation may cause a redness but only occasionally will cause a bruise.
Mobility of the pelvis and the freedom of maternal movements often help bring the face-first baby down through the pelvis with good strong, uterine surges.
But not always. Sometimes the labor can’t move baby down. Cesareans are more common, but a portion of the higher surgical rate is because time is not given to the mother to begin or continue labor, or to be out of bed for this labor. Monitoring becomes important. Expect a bit of an unusual heart rate to contraction pattern seen in these labors.
- When is Breech an Issue?
- Belly Mapping® Breech
- Flip a Breech
- When Baby Flips Head Down
- Breech & Bicornuate Uterus
- Breech for Providers
- What if My Breech Baby Doesn't Turn?
- Belly Mapping ®️ Method
- After Baby Turns
- Head Down is Not Enough
- Sideways/Transverse
- Asynclitism
- Oblique Lie
- Left Occiput Transverse
- Right Occiput Anterior
- Right Occiput Posterior
- Right Occiput Transverse
- Left Occiput Anterior
- OP Truths & Myths
- Anterior Placenta
- Body Balancing
What makes labor easier for a face-first baby and you?
Balance the body and the baby will thank you by curling into position to aim, not their face, but the crown of their head.
Flexion is physiological. So support physiology and the baby will change their position. We may need a little physics.

In Labor with a Face or Brow Presentation
Back baby up!
Forward-leaning Inversion with a jiggle of the buttocks right through 1-2 contractions often backs baby up so they can tuck their chin. Then they can aim into the pelvis with an easier position.

Shake the Apples in Forward-leaning Inversion with hands
A little effort can make labor a lot easier!
Only after baby’s crown is first, then do Side-lying Release in labor.
Before Labor with a face or brow presentation
Face presentation may reflect a psoas/pelvic floor imbalance with a collapse in the front body.
Free the piriformis, strengthen the buttocks, lengthen the hamstrings, squat for lengthening the pelvic floor, don’t worry about strengthening the pelvic floor right now. Alignment, walking, stabilizing and lengthening will tone the pelvic floor. Use it by breathing with your whole body.
Before labor, it’s safe to do Side-lying Release when baby’s face-first head isn’t in the pelvis yet.
Free the way
The psoas is the upper guide, the pelvic floor is the lower guide. release spasms and lengthen both.
Make room for the baby by releasing muscles that spasm, lengthen ligaments that are shortened, and support the abdominal muscles by attending to the muscles that interact with them, don’t go directly to the front first.

Contact to Listing Owner

Cesarean Delivery (C-section): How to Prepare and What to Expect

What is a C-section?
- What are the reasons that you may need a primary cesarean delivery?
When should my planned c-section be scheduled?
How should i prepare for a c-section, what should i expect on the day of my cesarean section, what should i expect during surgery.
- What is a stat C-section?
What happens after the c-section is over?
One day after your c/section.
- I’m Home, Now What?
Babies are born through either the vagina or via a C-section. A C-section describes when a baby is born through an incision in your abdomen and uterus. Cesarean deliveries are major surgery.
According to the Centers for Disease Control and Prevention, cesarean sections (c-sections) account for 32% of births in the US . Your doctor may recommend a C-section before you go into labor or after your labor has started ( 8 ).
Your first C-section is called a primary C-section. C/sections occurring for the second time or greater are called secondary C-sections.
What are the reasons that you may need a cesarean delivery?
- Failure to make progress during labor – your labor may not be progressing as it should. The slow progress may indicate that your baby may not fit through your pelvis.
- Concern for fetal well-being. If the monitoring shows the baby may be struggling in utero, this is called a non-reassuring status of the baby.
- Breech Positioning. When your baby is not coming out head first, this is called fetal malpresentation or breech.
- Multiple Pregnancies. Pregnancies with twins or more are called multi-fetal pregnancies.
- Fibroids obstructing the birth canal.
- Maternal Infection. Some infections in the mom can travel to the baby through the birth canal, such as herpes or HIV, which can preclude an attempt at vaginal birth.
- Placental Problems
- Very Large Baby. If your doctor suspects that your baby is too large, this is called macrosomia. Macrosomic babies can get stuck in the birth canal.
- Maternal Medical Conditions. Concern that continuing your pregnancy places your health at significant risk. In addition, pushing can aggravate some heart conditions.
- Elective Repeat C/sections- you and your doctor decide to deliver your baby by C-section because you have had a previous C-section or other uterine surgery.
- Maternal Request- while rare, some women may request a C-section, choosing to avoid labor. C/sections performed without a medical reason are not recommended. Vaginal deliveries are a much safer way to have a baby. Cesarean deliveries based on maternal requests are discouraged (7) .
The timing of your scheduled repeat C-section will vary according to each medical situation. Your doctor will try to deliver your baby as close to 39 weeks gestation as possible. Thirty-nine weeks gestation is one week before your due date. However, it may not be safe to wait until 39 weeks. In some cases, your doctor may recommend delivery earlier. For instance, if you have severe preeclampsia, your doctor will deliver no later than 34 weeks . If you have chronic hypertension , your baby will likely be born at 38 weeks or sooner. Patients who would like a trial of labor after C-section may be allowed to go past 39 weeks in the hopes that spontaneous labor may occur. Your surgeon will schedule your C-section according to you and your baby’s personalized needs.
Your doctor will try to deliver your baby as close to 39 weeks gestation as possible. On your due date you are 40 weeks pregnant. Thirty-nine weeks gestation is one week before your due date.
Treat Your Anemia
One of the most important ways to prepare for your surgery well in advance is to correct your anemia. Take your prenatal vitamins along with any iron supplements your doctor may have prescribed. Avoid taking iron pills within two hours of taking any dairy or antacids. Calcium and antacids will not allow your body to absorb the iron. You will not see results. Taking your iron supplement with citric acid or vitamin c will help your body absorb the iron and boost your response.
One of the most important ways to prepare for your surgery is to treat your anemia.
Sign Informed Consent
Before your C-section, you will have an office visit with your doctor to discuss the surgery and sign the surgical consent forms. Write down your questions in advance of your visit. Bring your birth partner or a close friend with you to take notes and ask questions.
Do Not Eat or Drink Eight Hours Before Surgery
Do not eat or drink anything after midnight, the night before your surgery. You may take your medicines with small sips of water. If you have diabetes, your doctor may advise you NOT to take your diabetic medicines since you will not eat.
Get a good night’s rest before surgery. Having to care for a baby immediately after having a C-section will be exhausting. Rest up to avoid a sleep deficit right before your surgery.
Do Not Shave for One Week
Do not attempt to shave your pubic area. Home shaving can cause tiny nicks in the skin and increase your risk of infection. You will be shaved in the hospital using surgical clippers.
Surgical Prep
Your hospital may have your shower with surgical soap before you arrive.
In the days leading up to your surgery, be sure to ramp up your self-care routine. Read, take hot baths, relax, surround yourself with positivity. Having surgery is one of life’s great stressors. Be sure to do all you can to keep your mind at ease. You will meet your baby in the best state of mind possible.
- You will likely have an early morning start to your day. Be prepared to arrive at the hospital at least two hours before your scheduled C-section.
- Start your IV.
- Draw blood work.
- Place the baby on the monitor.
- Provide antacid to neutralize stomach acid just in case you throw up during surgery.
- Shave the area around your pubic bone.
- You will sign consent forms for surgery if you haven’t done so already.
- The anesthesia team will assess you and take a history. Your anesthesiologist will discuss the type of anesthesia planned and the associated risks.
- If your baby is preterm, you will meet the neonatal intensive care unit (NICU) team. The NICU team is a diverse team of healthcare professionals who care for babies born early. They will inform you and your partner of what to expect.
- Once everything is ready, your nurse will walk you to the operating room.
In the C/Section Operating Room:
- Your team performs a surgical pause. A surgical pause, or time out, is where your team will have you identify yourself and the intended procedure.
- Your anesthesiologist will perform regional anesthesia to numb you from the waist down.
- A nurse will place wraps on your legs that will blow up intermittently to prevent blood clots from developing.
- A catheter will be inserted into your bladder to drain urine. Keeping your bladder drained reduces the risk of injury during surgery.
- Antibiotics are given in your IV to help prevent infection.
- Your nurse will surgically cleanse your abdomen.
- Your surgeon will place sterile drapes. Sterile drapes help to prevent infection and shields you from seeing your surgery.
- Your arms will be outstretched to the sides and strapped to prevent injury.
- Your doctor will do a test to make sure that your anesthesia is working before beginning the c-section.
- Another timeout or surgical pause takes place before surgery starts. A surgical pause is when your team pauses to identify the patient, the planned procedure, and any concerns.
You may feel the pressure of your surgeon’s hands, but you will not feel the pain of an incision. You may also feel some pressure as the baby is being born. You may become nauseated. If so, let your anesthesia team know. They will give you medicine to relieve nausea.
At the time your baby is being born, your partner may stand up and take pictures. Most hospitals prohibit the use of video recordings of the surgery and only permit still photos. When the baby is at the warmer, your partner can record video.
Some hospitals have both a transparent and opaque drape between you and the surgeons. In that case, your surgeon may lower the opaque drape so you can see the birth of your baby. Not everyone will want to have this experience. You and your doctor will decide. Your doctor may also hold the baby up for you to glimpse your baby above the drape.
After stabilizing the baby, they will be swaddled and brought to you for you and your partner to enjoy. The baby nurse and your partner will escort your baby to the recovery room, where you will later join them.
Most C-sections last about an hour. Your first C-section will be the fastest. The time lengthens with each C-section as more scar tissue develops after each surgery.
What is an Emergency (Stat) C/Section?
If an emergency occurs with you or your baby, your doctor may recommend an emergency C-section. The medical term for an emergency C-section is a stat C-section. The most common fetal indication for stat C-sections is fetal distress. If the fetal monitoring suggests that your baby is not receiving enough oxygen, your doctor will recommend an emergency C-section.
Maternal indications for emergency C-section are more varied. Maternal hemorrhage or heavy vaginal bleeding is a common reason for requiring emergency delivery.
Indications for Emergency C/section
- Fetal Distress
- Umbilical Cord Prolapse
- Placental Abruption
- Maternal Hemorrhage
- Maternal Seizures
With a stat C-section, the staff moves very quickly. There is a race against the clock to prevent loss of oxygen that may lead to fetal brain damage. Prompt delivery is required. A key reason you sign a C-section consent when you first arrive at the hospital is to avoid the loss of valuable time in case an emergency C-section is required. While seeing all the staff move so speedily around you can be scary for you and your family, rest assured, this is best for you and your baby.
For a stat C-section, you may require general anesthesia if you do not have an epidural . There will not be enough time to administer regional anesthesia. With general anesthesia, you’re asleep. Your anesthesiologist places a tube in your throat, which is attached to a machine that helps you breathe. Unfortunately, this means you will not be awake for the actual birth of your baby. Your support person will not be allowed in the operating room if you receive general anesthesia. You and your partner will see your beautiful baby in the recovery room.
With a stat C-section, the staff moves very quickly. There is a race against the clock to prevent loss of oxygen that may lead to fetal brain damage. Prompt delivery is required.
- If your baby does not need NICU care, you will be able to hold your newborn when you get to the recovery room.
- Your team will monitor your temperature, blood pressure, urine output, vaginal bleeding, and pain level.
- Your nurse will massage your uterus intermittently to ensure you are not bleeding excessively.
- As the anesthesia begins to wear off, you will be able to start wiggling your toes. Sensation will gradually return, starting in your feet and moving upward.
- As the feeling returns, you will begin to notice pain and numbness around your incision. Your team will make sure the pain medications keep you comfortable before taking you to the postpartum room.
- Don’t be surprised at the speed of your recovery. You will be allowed to start eating shortly after surgery.
- You are allowed to get out of bed with assistance either a few hours after surgery or the following morning.
- A nurse or tech will remove your bladder catheter and encourage you to urinate the morning after surgery.
- Studies show that walking within four hours after delivery and for at least ten minutes four times a day makes your body recover faster. Early walking causes your intestines to get back to normal faster and decrease the chance of developing a blood clot in your vein. Early ambulation also reduces your risk of respiratory infection. Gentle walking is an essential part of your recovery.
- Expect discomfort the first few times you get up. Some pain is normal, but it will continue to improve daily.
If not already done, your nurse or tech will remove the bladder catheter. She will assist you out of bed to the bathroom to attempt urination. If you have an incisional dressing, you may remove it during your shower. Removal during the shower will reduce your discomfort from the tape pulling on your skin.
Your doctor will switch your pain medicines from IV to pills. Don’t forget that you may need to request pain pills. Your nurse will not give them automatically. Using a breathing tool called an incentive spirometer will encourage your body to take deep breaths, which helps prevent lung infection. You will be encouraged to walk. Walking goes a long way in preventing multiple complications and boost recovery.
Don’t forget that you may need to request pain pills. Your nurse may not give them automatically.
I’m Home, Now What?
- Barring any complications, you can anticipate a discharge from the hospital anywhere from two to four days after your C-section.
- If you can stay on top of the pain, it will be easier to get around, and you can care for yourself and your baby better. A good regimen is to alternate non-opioid pain medicine with opioids regularly. So, alternate your ibuprofen with percocet or lortab. After a few days, you will be able to limit your opioid use to nighttime only and eventually phase them out altogether. Discuss this with your physician.
- Deep breathing and coughing exercises are essential to prevent lung infections after surgery. Take a slow deep breath, trying to fill your lungs with air. Hold it for two seconds and then slowly release the air, forcing out every last bit at the end. Try to do a few of these every hour for the first four days you are home. Holding a pillow against your incision as you breathe or cough makes it more tolerable.
- You may notice that the swelling in your feet and hands worsens when you get home. You received a lot of IV fluids in the hospital, so be patient, drink a lot of water, elevate your feet as much as you can. The swelling will gradually improve. If you notice excessive facial swelling with headaches or visual changes, contact your doctor.
- Don’t forget that although common, a cesarean section is major surgery, and you have to take care of yourself, too. Accept help with cooking, cleaning, and child care. Don’t try to do it all yourself.
Persistent heavy lifting places stress on the wound and can lead to your incision opening up. You must avoid heavy lifting for four to six weeks after surgery to minimize stress on the healing wound.
- Use an abdominal binder to help you feel more stabilized as your incision and muscles heal. Don’t try to use your abs to transition from lying to sitting. Roll to your side and use your arms to push yourself up instead.
- Your incision might look a little pink and swollen when you get home. Call your doctor for signs of infection such as drainage, redness, fever, chills, or foul odor from the wound. Numbness and tingling around the incision are normal and will get better with time.
- Heavy lifting and lifting from a squatting position increase your intra-abdominal pressure, which then pushes against the wound. Increased pressure against your wound can cause it to open up. Ask your doctor what weight limit is appropriate for you. For some, it may be anywhere from 10-15 lbs. Some surgeons recommend avoiding lifting anything heavier than the baby. Persistent heavy lifting places stress on the wound and can lead to surgical complications. You must avoid heavy lifting for four to six weeks to minimize stress on the healing wound.
- Do not drive if you are taking narcotics. If you do, you will be driving under the influence. You should put off driving until you can turn your body quickly without hesitation. You will need to be able to turn your head and body and move your legs without pain. Give yourself a minimum of two weeks after surgery before attempting to drive. You may slowly increase aerobic activities, depending on your level of discomfort.
- Resume sexual intercourse when vaginal discharge stops, and you feel ready. Remember to use contraception because you can still ovulate unexpectedly and get pregnant in the postpartum period, although it is less likely.
Do not drive if you are taking narcotics. Give yourself a minimum of two weeks after surgery before attempting to drive.
Lastly, remember that recovery from surgery is a process, so be patient and enjoy your time with your new baby.
Written by: Lisa Ann Shephard, MD | Editor: Dayna Smith MD | Reviewed: July 30, 2021 | Copyright: myObMD Media, 2021
- Caughey AB, Wood SL, Macones GA, et al. Guidelines for intraoperative care in cesarean delivery: Enhanced Recovery After Surgery Society Recommendations (Part 2). Am J Obstet Gynecol . 2018;219(6):533-544. doi:10.1016/j.ajog.2018.08.006.
- Lockley S, Demitry A. Enhanced recovery for obstetric surgery (EROS): an effective and proactive new ethos for managing low-risk elective caesarean sections. BJOG. 2018; 125 (55–55) doi:https://doi.org/10.1016/j.ijoa.2020.03.003.
- Lockley S, Demitry A, Cherot E. Enhanced recovery program reduces length of stay & improves value for patients undergoing elective cesarean section. Obstet Gynecol. 2018; 131 (107S–107S) doi:https://doi.org/10.1016/j.ijoa.2020.03.003.
- Macones G, Caughey A, Wood S, etal. Guidelines for postoperative care in cesarean delivery: Enhanced Recovery After Surgery (ERAS) Society recommendations (part 3)(2019) American Journal of Obstetrics and Gynecology, 221(3), pp. 247.e1-247.e9 Accessed 09/01/2020 from https://www.ajog.org/article/S0002-9378(19)30572-1/fulltext.
- Tita AT, Landon MB, Spong CY, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med . 2009;360(2):111-120. doi:10.1056/NEJMoa0803267.
- Wilson RD, Caughey AB, Wood SL, et al. Guidelines for Antenatal and Preoperative care in Cesarean Delivery: Enhanced Recovery After Surgery Society Recommendations (Part 1). Am J Obstet Gynecol . 2018;219(6):523.e1-523.e15. doi:10.1016/j.ajog.2018.09.015.
- American College of Obstetrics and Gynecology (ACOG), Cesarean Birth, Frequently Asked Questions, FAQ 006, Published May 2018, Last Reviewed June 2020.
- Sung, Sharon, Mahdy Heba. Review: Cesarean Section, Stat Pearls Publishing, 2021 Jan Apr 25. PMID: 31536313, Bookshelf ID NBK546707 .
Search for More Women’s Health Information
Myobmd media, llc.
1700 Northside Drive Suite A7, Unit # 5252 Atlanta, GA 30318
(833) 569-6263
- Health Calculators
- Advertise With Us
- Privacy Policy
Recent Articles
- Demystifying Depression: Breaking the Stigma and Unraveling The Complexities
- From Restless to Restful: Exploring the Causes and Treatment of Insomnia
- Decoding Anxiety: Unraveling the Origins, Varieties, and Steps Towards Well-Being
Copy short link
Stay in the know.
Face Presentation and Birth Injury
Normally, children are born head-first with the chin tucked towards the chest (vertex presentation). In a face presentation, the chin is not tucked and the neck is hyperextended. This can inhibit the engagement of the head and complicate the labor process. In some cases, a baby in face presentation can be delivered vaginally, but in other cases vaginal delivery is difficult and dangerous. Face presentation increases the risk of facial edema, skull molding, breathing problems (due to tracheal and laryngeal trauma), prolonged labor, fetal distress, spinal cord injuries, permanent brain damage, and neonatal death. Usually, medical staff conduct a vaginal examination to determine the position of the baby. If they suspect an abnormal presentation, they can confirm with an ultrasound and take action to properly handle the delivery of a baby in the face presentation. This includes additional monitoring and in some cases requires a C-Section. Because ventilation issues are more common in babies with face presentation, staff should be ready to intubate immediately after delivery (1).
Risk factors and causes of face presentation
Conditions that may increase the likelihood of a face presentation include the following (1, 2, 3, 4):
- Prematurity
- Very low birth weight
- Fetal macrosomia (large baby)
- Cephalopelvic disproportion, or CPD (a mismatch in size between the mother’s pelvis and the baby’s head)
- Anencephaly (a birth defect in which the baby is missing part of the brain and skull)
- Severe hydrocephalus with enlargement of the head
- Anterior neck mass
- Multiple nuchal cords (umbilical cord wrapped around baby’s neck more than once)
- Maternal pelvis abnormalities
- Maternal obesity
- Multiparity (the mother has previously given birth)
- Polyhydramnios (too much amniotic fluid)
- Previous cesarean delivery
Diagnosing face presentation
Face presentation is diagnosed late in the first or second stage of labor by vaginal examination. The distinctive facial features of the chin, mouth, nose, and cheekbones can be felt. Face presentation is sometimes confused with breech presentation (because both are characterized by soft tissues with an orifice), which is why it is imperative that a very skilled physician be present during any potentially risky delivery or malpresentation . Diagnosis can be confirmed by an ultrasound, which reveals a deflexed/hyperextended neck (1).
Face presentation and delivery
There are three types of face presentation:
- Mentum anterior (MA) . In this position, the chin is facing the front of the mother, and will be the presenting part of the face. Babies in mentum anterior position are usually delivered vaginally, although in some cases a C-section may be necessary.
- Mentum posterior (MP) . In this position, the chin is facing the mother’s back. The baby’s head, neck, and shoulders enter the pelvis at the same time, and the pelvis is usually not large enough to accommodate this (however, the baby may spontaneously rotate into mentum anterior position) . Typically, a C-section is indicated, but there are certain circumstances under which vaginal delivery may be attempted (e.g. the mother is multiparous, the infant in face presentation is relatively small compared to her other children, fetal monitoring is reassuring, and the baby is progressing in labor). Regardless, the medical team should be prepared to perform a prompt C-section if there are any complications.
- Mentum transverse (MT) . In this position, the baby’s chin is facing the side of the birth canal. Doctors may recommend a trial of labor under certain circumstances, but they should promptly proceed to a C-section if there are issues. If labor is progressing and the fetal heart monitor is reassuring when face presentation is present, physician intervention may not be necessary since many MP and MT positions convert to MA. Oxytocin (Pitocin) augmentation may be used in a face presentation with a normal fetus and abnormally slow progress, as long as fetal heart rate patterns remain reassuring (although there are certain risks associated with this drug, including uterine tachysystole ). Of course, in any face presentation, if progress in dilation and descent ceases despite adequate contractions, delivery must occur by C-section.
There is an increased risk of trauma to the baby when the face presents first, and the physician should not internally manipulate (try to rotate) the baby. In addition, the physician must not use vacuum extractors or manual extraction (grasping the baby with hands) to pull the baby from the uterine cavity. Furthermore, midforceps ( forcep extraction when the baby’s station is above +2 cm, but the head is engaged) should never be used. Outlet forceps should only be used by experienced physicians who understand the circumstances under which this is appropriate (1).
Abnormalities of the fetal heart rate occur more frequently with face presentation. In one study, 59% of infants in face presentation had variable heart decelerations, and 24% had late decelerations. Of the babies who were born live, 37% had 1-minute Apgar scores lower than 7, and 13% had 5-minute Apgar scores lower than 7. The majority of the low 5-minute Apgar scores were babies that had been in mentum posterior position (5).
For these reasons, it is crucial that babies are continuously monitored during labor, ideally with an external heart monitoring device. An internal device may cause facial or eye injuries if improperly placed. If internal monitoring is needed, the electrode should be cautiously placed over a bony structure such as the forehead, jaw or cheekbone to minimize the risk of trauma (1).
It is always critical that doctors obtain a mother’s informed consent , which means discussing delivery options (vaginal, C-section, enhanced with oxytocin, etc.) with her and explaining the potential risks and benefits of each. Failure to do so constitutes negligence.
Complications and side effects of face presentation
Complications associated with face presentation include the following:
- Prolonged labor
- Facial trauma
- Facial edema (fluid build up in the face, often caused by trauma)
- Skull molding (abnormal head shape that results from pressure on the baby’s head during childbirth)
- Respiratory distress /difficulty in ventilation due to airway trauma and edema
- Spinal cord injury
- Abnormal fetal heart rate patterns
- Low Apgar score
A baby may be at increased risk of complications if forceps or oxytocin are used during labor. Forceps can cause traumatic injury to the head, and oxytocin can deprive a baby of oxygen due to uterine tachysystole/hyperstimulation (strong, frequent contractions). Hyperstimulation increases pressure on the blood vessels in the womb, which can deprive the baby of oxygen-rich blood.
Trauma to the head and decreased oxygenation can cause permanent brain damage, such as hypoxic-ischemic encephalopathy (HIE) and cerebral palsy (CP) , as well as fetal deaths.
Our team is here to help.
Call ABC Law Centers today to secure your child’s care and reclaim their future.
Standards of care, medical malpractice, and face presentation
Informed consent must be given during all medical procedures. This means that when a mother has a baby with face presentation, she must be given the option of a C-section versus a vaginal birth. One of the reasons a mother may opt for a C-section is to avoid the extensive facial bruising/trauma that is common in babies with face presentation. In addition to thoroughly explaining the risks and benefits of each type of delivery method, the physician must explain and obtain consent from the mother if forceps or oxytocin are used.
Because there are many complications associated with face presentation, it is essential that the baby be closely monitored and that delivery is handled by a physician with experience in this area. Furthermore, the physician must quickly proceed to a C-section delivery if there are any signs of fetal distress , labor is not progressing, or the baby fails to convert (rotate) to MA position. In addition, once a face presentation is diagnosed, the physician must check for pelvic adequacy. When the pelvis is inadequate (contracted/small), a C-section is recommended (1).
Since respiratory problems can occur in babies with face presentation, equipment and staff to perform intubation of the baby (placement of a breathing tube) should be readily available at the time of delivery.
Failure to follow any of these standards of care is negligence. If this negligence results in injury to the baby, it is medical malpractice .
Trusted birth injury attorneys
If your baby has HIE, cerebral palsy, periventricular leukomalacia (PVL), developmental delays , a seizure disorder , or any other birth injury , we may be able to help. Unlike other firms, the attorneys at ABC Law Centers (Reiter & Walsh, P.C.) focus solely on birth injury cases and have been helping children throughout the nation since 1997. During your free legal consultation, our attorneys will discuss your case with you, determine if negligence caused your loved one’s injuries, identify the negligent party, and discuss your legal options with you. Moreover, you pay nothing throughout the entire legal process unless we win or favorably settle your case.
“Reiter and Walsh goes above and beyond the norm in getting their clients the best possible results. Each client is treated with respect and compassion, and they are truly sensitive to what it means to help a family whose child has been injured.” -Client review from 11/23/2015
- Free Case Review
- Available 24/7
- No Fee Unless We Win
Featured Videos
Testimonial from keziah’s family, posterior position, hypoxic-ischemic encephalopathy (hie).
Featured Testimonial
What Our Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on . ABC Law Centers was just that.
Helpful resources
More about our firm.
- Meet our birth injury attorneys
- Meet our in-house medical staff
- Verdicts and settlements
- Testimonials
- Julien, S., Lockwood, C. J., & Barss, V. A. (2014). Face and brow presentations in labor. Up to date.
- Duff, P. (1981). Diagnosis and management of face presentation. Obstetrics and gynecology, 57(1), 105-112.
- S. BHAL NJ DAVIES T. CHUNG, P. (1998). A population study of face and brow presentation. Journal of Obstetrics and Gynaecology, 18(3), 231-235.
- Shaffer, B. L., Cheng, Y. W., Vargas, J. E., Laros Jr, R. K., & Caughey, A. B. (2006). Face presentation: predictors and delivery route. American journal of obstetrics and gynecology, 194(5), e10-e12.
- Benedetti, T. J., Lowensohn, R. I., & Truscott, A. M. (1980). Face presentation at term. Obstetrics and gynecology, 55(2), 199-202.
The above information is intended to be an educational resource. It is not meant to be, and should not be interpreted as, medical advice.
Over $350 Million Recovered
In Verdicts, Settlements, & Judgements
$4.75 Million
$3.9 Million
$5.85 Million
Awards & Memberships
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
How your twins’ fetal positions affect labor and delivery

Twin fetal presentation – also known as the position of your babies in the womb – dictates whether you'll have a vaginal or c-section birth. Toward the end of pregnancy, most twins will move in the head-down position (vertex), but there's a risk that the second twin will change position after the first twin is born. While there are options to change the second twin's position, this can increase the risk of c-section and other health issues. Learn about the six possible twin fetal presentations: vertex-vertex, vertex-breech, breech-breech, vertex-transverse, breech-transverse, and transverse-transverse – and how they'll impact your delivery and risks for complications.
What is fetal presentation and what does it mean for your twins?
As your due date approaches, you might be wondering how your twins are currently positioned in the womb, also known as the fetal presentation, and what that means for your delivery. Throughout your pregnancy, your twin babies will move in the uterus, but sometime during the third trimester – usually between 32 and 36 weeks – their fetal presentation changes as they prepare to go down the birth canal.
The good news is that at most twin births, both babies are head-down (vertex), which means you can have a vaginal delivery. In fact, nearly 40 percent of twins are delivered vaginally.
But if one baby has feet or bottom first (breech) or is sideways (transverse), your doctor might deliver the lower twin vaginally and then try to rotate the other twin so that they face head-down (also called external cephalic version or internal podalic version) and can be delivered vaginally. But if that doesn't work, there's still a chance that your doctor will be able to deliver the second twin feet first vaginally via breech extraction (delivering the breech baby feet or butt first through the vagina).
That said, a breech extraction depends on a variety of factors – including how experienced your doctor is in the procedure and how much the second twin weighs. Studies show that the higher rate of vaginal births among nonvertex second twins is associated with labor induction and more experienced doctors, suggesting that proper delivery planning may increase your chances of a vaginal birth .
That said, you shouldn't totally rule out a Cesarean delivery with twins . If the first twin is breech or neither of the twins are head-down, then you'll most likely have a Cesarean delivery.
Research also shows that twin babies who are born at less than 34 weeks and have moms with multiple children are associated with intrapartum presentation change (when the fetal presentation of the second twin changes from head-down to feet first after the delivery of the first twin) of the second twin. Women who have intrapartum presentation change are more likely to undergo a Cesarean delivery for their second twin.
Here's a breakdown of the different fetal presentations for twin births and how they will affect your delivery.
Head down, head down (vertex, vertex)
This fetal presentation is the most promising for a vaginal delivery because both twins are head-down. Twins can change positions, but if they're head-down at 28 weeks, they're likely to stay that way.
When delivering twins vaginally, there is a risk that the second twin will change position after the delivery of the first. Research shows that second twins change positions in 20 percent of planned vaginal deliveries. If this happens, your doctor may try to rotate the second twin so it faces head-down or consider a breech extraction. But if neither of these work or are an option, then a Cesarean delivery is likely.
In vertex-vertex pairs, the rate of Cesarean delivery for the second twin after a vaginal delivery of the first one is 16.9 percent.
Like all vaginal deliveries, there's also a chance you'll have an assisted birth, where forceps or a vacuum are needed to help deliver your twins.
Head down, bottom down (vertex, breech)
When the first twin's (the lower one) head is down, but the second twin isn't, your doctor may attempt a vaginal delivery by changing the baby's position or doing breech extraction, which isn't possible if the second twin weighs much more than the first twin.
The rates of emergency C-section deliveries for the second twin after a vaginal delivery of the first twin are higher in second twins who have a very low birth weight. Small babies may not tolerate labor as well.
Head down, sideways (vertex, transverse)
If one twin is lying sideways or diagonally (oblique), there's a chance the baby may shift position as your labor progresses, or your doctor may try to turn the baby head-down via external cephalic version or internal podalic version (changing position in the uterus), which means you may be able to deliver both vaginally.
Bottom down, bottom down (breech, breech)
When both twins are breech, a planned C-section is recommended because your doctor isn't able to turn the fetuses. Studies also show that there are fewer negative neonatal outcomes for planned C-sections than planned vaginal births in breech babies.
As with any C-section, the risks for a planned one with twins include infection, loss of blood, blood clots, injury to the bowel or bladder, a weak uterine wall, placenta abnormalities in future pregnancies and fetal injury.
Bottom down, sideways (breech, transverse)
When the twin lowest in your uterus is breech or transverse (which happens in 25 percent of cases), you'll need to have a c-section.
Sideways, sideways (transverse, transverse)
This fetal presentation is rare with less than 1 percent of cases. If both babies are lying horizontally, you'll almost definitely have a C-section.
Learn more:
- Twin fetal development month by month
- Your likelihood of having twins or more
- When and how to find out if you’re carrying twins or more
Was this article helpful?
28 weeks pregnant with twins

32 weeks pregnant with twins

36 weeks pregnant with twins

24 weeks pregnant with twins

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Cleveland Clinic. Fetal Positions for Birth: https://my.clevelandclinic.org/health/articles/9677-fetal-positions-for-birth Opens a new window [Accessed July 2021]
Mayo Clinic. Fetal Presentation Before Birth: https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/multimedia/fetal-positions/sls-20076615?s=7 Opens a new window [Accessed July 2021]
NHS. Giving Birth to Twins or More: https://pubmed.ncbi.nlm.nih.gov/29016498/ Opens a new window [Accessed July 2021]
Science Direct. Breech Extraction: https://www.sciencedirect.com/topics/medicine-and-dentistry/breech-extraction Opens a new window [Accessed July 2021]
Obstetrics & Gynecology. Clinical Factors Associated With Presentation Change of the Second Twin After Vaginal Delivery of the First Twin https://pubmed.ncbi.nlm.nih.gov/29016498/ Opens a new window [Accessed July 2021]
American Journal of Obstetrics and Gynecology. Fetal presentation and successful twin vaginal delivery: https://www.ajog.org/article/S0002-9378(04)00482-X/fulltext [Accessed July 2021]
The Journal of Maternal-Fetal & Neonatal Medicine. Changes in fetal presentation in twin pregnancies https://www.tandfonline.com/doi/abs/10.1080/14767050400028592 Opens a new window [Accessed July 2021]
Reviews in Obstetrics & Gynecology. An Evidence-Based Approach to Determining Route of Delivery for Twin Gestations https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3252881/ Opens a new window [Accessed July 2021]
Nature. Neonatal mortality and morbidity in vertex–vertex second twins according to mode of delivery and birth weight: https://www.nature.com/articles/7211408 Opens a new window [Accessed July 2021]
Cochrane. Planned cesarean for a twin pregnancy: https://www.cochrane.org/CD006553/PREG_planned-caesarean-section-twin-pregnancy Opens a new window [Accessed July 2021]
Kids Health. What Is the Apgar Score?: https://www.kidshealth.org/Nemours/en/parents/apgar0.html Opens a new window [Accessed July 2021]
American Journal of Obstetrics & Gynecology. Neonatal mortality in second twin according to cause of death, gestational age, and mode of delivery https://pubmed.ncbi.nlm.nih.gov/15467540/ Opens a new window [Accessed July 2021]
Lancet. Planned cesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group https://pubmed.ncbi.nlm.nih.gov/11052579/ Opens a new window [Accessed July 2021]
Cleveland Clinic. Cesarean Birth (C-Section): https://my.clevelandclinic.org/health/treatments/7246-cesarean-birth-c-section Opens a new window [Accessed July 2021]
St. Jude Medical Staff. Delivery of Twin Gestation: http://www.sjmedstaff.org/documents/Delivery-of-twins.pdf Opens a new window [Accessed July 2021]

Where to go next


Meredith’s Labor and Delivery
Which character will you worry about the most this summer? There’s April, who recently accepted Matthew’s proposal, yet we can see that she still may harbor feelings for Jackson (watching someone almost blow up in a bus can do that). Meanwhile, despite Owen’s protests, Cristina walked away from him, knowing that she can never fulfill his dreams of having children. The last conversation between Callie and Arizona broke my heart so completely that I don’t even know how to approach it. And Richard… Goodness, what the heck is going to happen to poor Richard Webber? At least the lights came back on, right? Can you believe we performed surgery on Meredith… In the DARK?!
Why did Meredith need a C-section again? Meredith needed a C-section due to her baby’s presentation – the way that the baby was coming down through the birth canal. Typically, babies present head-first, specifically with the crown of the head leading and therefore resting their chin on their chest. However, in Meredith’s case, Dr. Ryan detected a “face presentation” – the baby’s head extended backward, so that his head rested on his upper back. Face presentation can be diagnosed during labor when the doctor, while examining the mother, can feel the baby’s eyes, nose, mouth, or chin. Depending on the severity of the flexion of the neck, the baby can still be delivered vaginally. However, Meredith’s baby specifically had a mento-posterior face presentation, which means that his chin pointed further back and his neck could not extend any further without additional complications. After McBaby was delivered and whisked away, why did Meredith suddenly start to bleed uncontrollably? As Shane worked to close up Meredith’s uterus, he and Heather saw additional bleeding in the abdomen. As they explored further, Meredith looked over and noticed that blood had started to come from her IV sites – a frightening sign that she was in DIC, or disseminated intravascular coagulation. DIC means that small blood clots have formed throughout the entire body’s blood vessels. These clots can impede blood flow to organs and cause them to malfunction, but the even bigger problem is that since the clotting factors have been used up, the blood starts flowing uncontrollably. All of this bleeding becomes extremely serious and life-threatening. When Meredith fell down the stairs in Episode 923, she sustained an injury to her spleen, which began to actively bleed once she started the labor and delivery process, which then caused the DIC process to start. However, a variety of conditions can lead to overactive clotting factors and DIC such as: • Some types of snakebites. • Some types of bacterial, viral, or fungal infection. • Surgery and trauma. • Cancer. • Serious complications of pregnancy and childbirth. Treatment for DIC varies according to the specific cause, but in Meredith’s case, Shane and Heather needed to replenish the depleted fluids, immediately find the source of the bleeding and quickly control it. After making an incision into the abdomen, Shane isolated the spleen as the source of the bleeding. How are these injuries repaired? In the past, doctors handled splenic injuries by always performing splenectomies, or surgeries to remove the spleen. Doctors felt that assessing the injuries remained difficult and did not believe that the spleen healed well. However now, due to better diagnostic technologies, the treatment differs depending on the grade of the splenic injury. For example, Grades I and II may only involve minor tears to the organ and only require a brief hospitalization and observation. In these situations, the patients typically stay in the Intensive Care Unit while their blood and fluid levels are closely monitored and replaced. But Grades III and IV, which could be characterized by more serious lacerations or complete rupture, would necessitate surgery. Surgeons have the option of accessing the spleen by creating several small incisions in the abdomen (laparoscopic surgery) and inserting a camera to help excise the spleen. However, due to the emergent nature of Meredith’s splenic injury, Shane completely opened her abdomen in order to gain immediate visualization. In several cases, surgeons try to avoid removing the entire spleen and will only do a partial splenectomy. But when the patient’s bleeding cannot be controlled, such as Meredith, the safer decision remains to be a complete splenectomy. Studies have found that people can survive without the spleen, but doctors know that the spleen does play a role in fighting infection and therefore may recommend certain protective measures in the future, such as certain vaccinations. For more information on Disseminated Intravascular Coagulation, please visit the following link: http://www.nhlbi.nih.gov/health/health-topics/topics/dic/
Follow Grey's Anatomy:

- Share full article
Advertisement
Supported by
Guest Essay
Jamie Raskin: How to Force Justices Alito and Thomas to Recuse Themselves in the Jan. 6 Cases

By Jamie Raskin
Mr. Raskin represents Maryland’s Eighth Congressional District in the House of Representatives. He taught constitutional law for more than 25 years and was the lead prosecutor in the second impeachment trial of Donald Trump.
Many people have gloomily accepted the conventional wisdom that because there is no binding Supreme Court ethics code, there is no way to force Associate Justices Samuel Alito and Clarence Thomas to recuse themselves from the Jan. 6 cases that are before the court.
Justices Alito and Thomas are probably making the same assumption.
But all of them are wrong.
It seems unfathomable that the two justices could get away with deciding for themselves whether they can be impartial in ruling on cases affecting Donald Trump’s liability for crimes he is accused of committing on Jan. 6. Justice Thomas’s wife, Ginni Thomas, was deeply involved in the Jan. 6 “stop the steal” movement. Above the Virginia home of Justice Alito and his wife, Martha-Ann Alito, flew an upside-down American flag — a strong political statement among the people who stormed the Capitol. Above the Alitos’ beach home in New Jersey flew another flag that has been adopted by groups opposed to President Biden.
Justices Alito and Thomas face a groundswell of appeals beseeching them not to participate in Trump v. United States , the case that will decide whether Mr. Trump enjoys absolute immunity from criminal prosecution, and Fischer v. United States , which will decide whether Jan. 6 insurrectionists — and Mr. Trump — can be charged under a statute that criminalizes “corruptly” obstructing an official proceeding. (Justice Alito said on Wednesday that he would not recuse himself from Jan. 6-related cases.)
Everyone assumes that nothing can be done about the recusal situation because the highest court in the land has the lowest ethical standards — no binding ethics code or process outside of personal reflection. Each justice decides for him- or herself whether he or she can be impartial.
Of course, Justices Alito and Thomas could choose to recuse themselves — wouldn’t that be nice? But begging them to do the right thing misses a far more effective course of action.
The U.S. Department of Justice — including the U.S. attorney for the District of Columbia, an appointed U.S. special counsel and the solicitor general, all of whom were involved in different ways in the criminal prosecutions underlying these cases and are opposing Mr. Trump’s constitutional and statutory claims — can petition the other seven justices to require Justices Alito and Thomas to recuse themselves not as a matter of grace but as a matter of law.
The Justice Department and Attorney General Merrick Garland can invoke two powerful textual authorities for this motion: the Constitution of the United States, specifically the due process clause, and the federal statute mandating judicial disqualification for questionable impartiality, 28 U.S.C. Section 455. The Constitution has come into play in several recent Supreme Court decisions striking down rulings by stubborn judges in lower courts whose political impartiality has been reasonably questioned but who threw caution to the wind to hear a case anyway. This statute requires potentially biased judges throughout the federal system to recuse themselves at the start of the process to avoid judicial unfairness and embarrassing controversies and reversals.
The constitutional and statutory standards apply to Supreme Court justices. The Constitution, and the federal laws under it, is the “ supreme law of the land ,” and the recusal statute explicitly treats Supreme Court justices as it does other judges: “Any justice, judge or magistrate judge of the United States shall disqualify himself in any proceeding in which his impartiality might reasonably be questioned.” The only justices in the federal judiciary are the ones on the Supreme Court.
This recusal statute, if triggered, is not a friendly suggestion. It is Congress’s command, binding on the justices, just as the due process clause is. The Supreme Court cannot disregard this law just because it directly affects one or two of its justices. Ignoring it would trespass on the constitutional separation of powers because the justices would essentially be saying that they have the power to override a congressional command.
When the arguments are properly before the court, Chief Justice John Roberts and Associate Justices Amy Coney Barrett, Neil Gorsuch, Ketanji Brown Jackson, Elena Kagan, Brett Kavanaugh and Sonia Sotomayor will have both a constitutional obligation and a statutory obligation to enforce recusal standards.
Indeed, there is even a compelling argument based on case law that Chief Justice Roberts and the other unaffected justices should raise the matter of recusal on their own, or sua sponte. Numerous circuit courts have agreed with the Eighth Circuit that this is the right course of action when members of an appellate court are aware of “ overt acts ” of a judge reflecting personal bias. Cases like this stand for the idea that appellate jurists who see something should say something instead of placing all the burden on parties in a case who would have to risk angering a judge by bringing up the awkward matter of potential bias and favoritism on the bench.
But even if no member of the court raises the issue of recusal, the urgent need to deal with it persists. Once it is raised, the court would almost surely have to find that the due process clause and Section 455 compel Justices Alito and Thomas to recuse themselves. To arrive at that substantive conclusion, the justices need only read their court’s own recusal decisions.
In one key 5-to-3 Supreme Court case from 2016, Williams v. Pennsylvania, Justice Anthony Kennedy explained why judicial bias is a defect of constitutional magnitude and offered specific objective standards for identifying it. Significantly, Justices Alito and Thomas dissented from the majority’s ruling.
The case concerned the bias of the chief justice of Pennsylvania, who had been involved as a prosecutor on the state’s side in an appellate death penalty case that was before him. Justice Kennedy found that the judge’s refusal to recuse himself when asked to do so violated due process. Justice Kennedy’s authoritative opinion on recusal illuminates three critical aspects of the current controversy.
First, Justice Kennedy found that the standard for recusal must be objective because it is impossible to rely on the affected judge’s introspection and subjective interpretations. The court’s objective standard requires recusal when the likelihood of bias on the part of the judge “is too high to be constitutionally tolerable,” citing an earlier case. “This objective risk of bias,” according to Justice Kennedy, “is reflected in the due process maxim that ‘no man can be a judge in his own case.’” A judge or justice can be convinced of his or her own impartiality but also completely missing what other people are seeing.
Second, the Williams majority endorsed the American Bar Association’s Model Code of Judicial Conduct as an appropriate articulation of the Madisonian standard that “no man can be a judge in his own cause.” Model Code Rule 2.11 on judicial disqualification says that a judge “shall disqualify himself or herself in any proceeding in which the judge’s impartiality might reasonably be questioned.” This includes, illustratively, cases in which the judge “has a personal bias or prejudice concerning a party,” a married judge knows that “the judge’s spouse” is “a person who has more than a de minimis interest that could be substantially affected by the proceeding” or the judge “has made a public statement, other than in a court proceeding, judicial decision or opinion, that commits or appears to commit the judge to reach a particular result.” These model code illustrations ring a lot of bells at this moment.
Third and most important, Justice Kennedy found for the court that the failure of an objectively biased judge to recuse him- or herself is not “harmless error” just because the biased judge’s vote is not apparently determinative in the vote of a panel of judges. A biased judge contaminates the proceeding not just by the casting and tabulation of his or her own vote but by participating in the body’s collective deliberations and affecting, even subtly, other judges’ perceptions of the case.
Justice Kennedy was emphatic on this point : “It does not matter whether the disqualified judge’s vote was necessary to the disposition of the case. The fact that the interested judge’s vote was not dispositive may mean only that the judge was successful in persuading most members of the court to accept his or her position — an outcome that does not lessen the unfairness to the affected party.”
Courts generally have found that any reasonable doubts about a judge’s partiality must be resolved in favor of recusal. A judge “shall disqualify himself in any proceeding in which his impartiality might reasonably be questioned.” While recognizing that the “challenged judge enjoys a margin of discretion,” the courts have repeatedly held that “doubts ordinarily ought to be resolved in favor of recusal.” After all, the reputation of the whole tribunal and public confidence in the judiciary are both on the line.
Judge David Tatel of the D.C. Circuit emphasized this fundamental principle in 2019 when his court issued a writ of mandamus to force recusal of a military judge who blithely ignored at least the appearance of a glaring conflict of interest. He stated : “Impartial adjudicators are the cornerstone of any system of justice worthy of the label. And because ‘deference to the judgments and rulings of courts depends upon public confidence in the integrity and independence of judges,’ jurists must avoid even the appearance of partiality.” He reminded us that to perform its high function in the best way, as Justice Felix Frankfurter stated, “justice must satisfy the appearance of justice.”
The Supreme Court has been especially disposed to favor recusal when partisan politics appear to be a prejudicial factor even when the judge’s impartiality has not been questioned. In Caperton v. A.T. Massey Coal Co. , from 2009, the court held that a state supreme court justice was constitutionally disqualified from a case in which the president of a corporation appearing before him had helped to get him elected by spending $3 million promoting his campaign. The court, through Justice Kennedy, asked whether, quoting a 1975 decision, “under a realistic appraisal of psychological tendencies and human weakness,” the judge’s obvious political alignment with a party in a case “poses such a risk of actual bias or prejudgment that the practice must be forbidden if the guarantee of due process is to be adequately implemented.”
The federal statute on disqualification, Section 455(b) , also makes recusal analysis directly applicable to bias imputed to a spouse’s interest in the case. Ms. Thomas and Mrs. Alito (who, according to Justice Alito, is the one who put up the inverted flag outside their home) meet this standard. A judge must recuse him- or herself when a spouse “is known by the judge to have an interest in a case that could be substantially affected by the outcome of the proceeding.”
At his Senate confirmation hearing, Chief Justice Roberts assured America that “judges are like umpires.”
But professional baseball would never allow an umpire to continue to officiate the World Series after learning that the pennant of one of the two teams competing was flying in the front yard of the umpire’s home. Nor would an umpire be allowed to call balls and strikes in a World Series game after the umpire’s wife tried to get the official score of a prior game in the series overthrown and canceled out to benefit the losing team. If judges are like umpires, then they should be treated like umpires, not team owners, fans or players.
Justice Barrett has said she wants to convince people “that this court is not comprised of a bunch of partisan hacks.” Justice Alito himself declared the importance of judicial objectivity in his opinion for the majority in the Dobbs v. Jackson Women’s Health Organization decision overruling Roe v. Wade — a bit of self-praise that now rings especially hollow.
But the Constitution and Congress’s recusal statute provide the objective framework of analysis and remedy for cases of judicial bias that are apparent to the world, even if they may be invisible to the judges involved. This is not really optional for the justices.
I look forward to seeing seven members of the court act to defend the reputation and integrity of the institution.
Jamie Raskin, a Democrat, represents Maryland’s Eighth Congressional District in the House of Representatives. He taught constitutional law for more than 25 years and was the lead prosecutor in the second impeachment trial of Donald Trump.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .

IMAGES
VIDEO
COMMENTS
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common ...
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.. In brow presentation, the neck is moderately arched so that the brow presents first.. Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor.
The vast majority of fetuses at term are in cephalic presentation. Approximately 5 percent of these fetuses are in a cephalic malpresentation, such as occiput posterior or transverse, face ( figure 1A-B ), or brow ( figure 2) [ 1 ]. Diagnosis and management of face and brow presentations will be reviewed here.
With persistent brow presentation, a cesarean section is required for safe delivery. Complications. As the cesarean section is becoming a more accessible mode of delivery in malpresentations, the incidence of maternal and fetal morbidity and mortality during face presentation has dropped significantly.
Cesarean section is a fetal delivery through an open abdominal incision (laparotomy) and an incision in the uterus (hysterotomy). The first cesarean documented occurred in 1020 AD, and since then, the procedure has evolved tremendously.[1] It is now the most common surgery performed in the United States, with over 1 million women delivered by cesarean every year. The cesarean delivery rate ...
In a brow presentation, the fetal head is midway between full flexion (vertex) and hyperextension (face) along a longitudinal axis. The presenting portion of the fetal head is between the orbital ridge and the anterior fontanel. The face and chin are not included. The frontal bones are the point of designation and can present (as with the ...
A C-section, or cesarean section, is the surgical delivery of a baby through incisions in the abdomen and uterus. A C-section is typically only recommended in medically necessary cases, such as in some high-risk pregnancies or when the baby is in the breech position and can't be flipped before labor begins. You may hear the following terms used ...
A total of 61 women who met the study criteria were diagnosed with face presentation in labor; for 55 of the women, follow-up data were available for analysis. Cases of face presentation were abstracted from a cohort of 40,598 cases, which gave an incidence rate of 1 in 666. Preterm delivery, birth weight <2500 g, and maternal obesity were more ...
Introduction. Face presentation is a rare unanticipated obstetric event characterized by a longitudinal lie and full extension of the foetal head on the neck with the occiput against the upper back [1-3].Face presentation occurs in 0.1-0.2% of deliveries [3-5] but is more common in black women and in multiparous women [].Studies have shown that 60 per cent of face presentations have one or ...
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. Cesarean section or C-section is the surgical delivery of a baby through a cut (incision) made in the mother's abdomen and uterus.
C-Section. A C-section (or cesarean birth) is a surgical procedure used to deliver a baby when a vaginal delivery can't be done safely. A C-section can be planned ahead of time or performed in an emergency. It carries more risk than a vaginal delivery, with a slightly longer recovery period.
C-section: Cesarean delivery — also known as a C-section — is a surgical procedure used to deliver a baby through incisions in the mother's abdomen and uterus.
In most cases, a face presentation birth shouldn't be attempted vaginally. A C-section is the safer alternative. But this depends on several factors, such as the type of face presentation. That's what we'll look at next. Types of Face Presentation. These are the three main types of face presentation: Mentum Anterior (Chin First) Presentation.
Face presentation may reflect a psoas/pelvic floor imbalance with a collapse in the front body. Free the piriformis, strengthen the buttocks, lengthen the hamstrings, squat for lengthening the pelvic floor, don't worry about strengthening the pelvic floor right now. Alignment, walking, stabilizing and lengthening will tone the pelvic floor.
With a stat C-section, the staff moves very quickly. There is a race against the clock to prevent loss of oxygen that may lead to fetal brain damage. Prompt delivery is required. A key reason you sign a C-section consent when you first arrive at the hospital is to avoid the loss of valuable time in case an emergency C-section is required.
Informed consent must be given during all medical procedures. This means that when a mother has a baby with face presentation, she must be given the option of a C-section versus a vaginal birth. One of the reasons a mother may opt for a C-section is to avoid the extensive facial bruising/trauma that is common in babies with face presentation.
Twin fetal presentation - also known as the position of your babies in the womb - dictates whether you'll have a vaginal or c-section birth. Toward the end of pregnancy, most twins will move in the head-down position (vertex), but there's a risk that the second twin will change position after the first twin is born.
Some breech births can happen vaginally, but there are risks. The risks of a vaginal breech birth include: Injuries to your baby's legs or arms such as dislocated or broken bones. Your baby's head can get stuck or trapped. Umbilical cord problems. The umbilical cord can flatten or twist during delivery.
Face presentation can be diagnosed during labor when the doctor, while examining the mother, can feel the baby's eyes, nose, mouth, or chin. Depending on the severity of the flexion of the neck, the baby can still be delivered vaginally. However, Meredith's baby specifically had a mento-posterior face presentation, which means that his chin ...
"Nurturing Roots, Growing Futures: Combining Policies and Partnerships for Urban Resilience and Transformation"
Local, state, and federal government websites often end in .gov. Commonwealth of Pennsylvania government websites and email systems use "pennsylvania.gov" or "pa.gov" at the end of the address.
Justices Alito and Thomas face a groundswell of appeals beseeching them not to participate in Trump v. United States , the case that will decide whether Mr. Trump enjoys absolute immunity from ...