
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death
Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
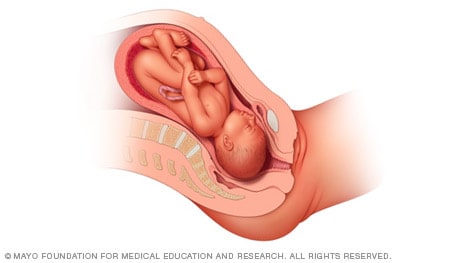
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Your baby in the birth canal
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between their head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Alternative Names
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal

Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Review Date 11/10/2022
Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems
- Monday, May 20, 2024
- Nursing Article
4 Key Steps of the Leopold Maneuver for Accurate Fetal Positioning
The Leopold Maneuver is a fundamental examination technique used to assess fetal presentation, position, and size during pregnancy . It has been widely employed as a routine prenatal assessment tool by obstetricians and midwives for over a century. The technique involves a series of four maneuvers that allow the examiner to palpate the maternal abdomen and identify the fetal presentation and position.
In this article, we will explore the history, purpose, benefits, and limitations of the Leopold Maneuver , as well as provide a step-by-step guide on how to perform the examination. We will also discuss the importance of the Leopold Maneuver in prenatal care, common issues that may arise during the examination , and the role of the procedure in diagnosing fetal position.
Table of Contents
Definition of the Leopold Maneuver
The Leopold maneuver is a four-step procedure used by healthcare professionals to assess the fetal presentation, fetal lie, and fetal position . This technique involves feeling the abdomen, identifying the location of the fetal back, and palpating the fetal head, buttocks, and limbs to determine their position within the uterus .
History of the Leopold Maneuver
The Leopold maneuver was first described in 1899 by Christian Gerhard Leopold , a German obstetrician. Since then, it has become a standard procedure in obstetrics worldwide. Over the years, the technique has undergone several modifications to make it more accurate and reliable.
Importance of Leopold Maneuver in Obstetrics
The Leopold maneuver is a vital tool in assessing fetal presentation, lie, and position. The information obtained from this technique helps healthcare professionals determine the best mode of delivery and anticipate potential complications during labor and delivery. It also assists in identifying multiple gestations and abnormal fetal presentations , ensuring the safe delivery of the baby.
Purpose and Benefits of the Leopold Maneuver
Assessment of fetal presentation.
The Leopold maneuver is used to determine fetal presentation, which refers to the part of the fetus that enters the maternal pelvis first. The most common fetal presentation is the cephalic presentation, where the baby is head-down. However, other presentations, such as breech or transverse, require special attention during labor and delivery. The Leopold maneuver helps healthcare professionals determine the fetal presentation to prepare for the most optimal delivery for both the mother and baby.
Estimating Fetal Weight
During the Leopold maneuver, healthcare professionals can estimate fetal weight by palpating the mother’s abdomen. This information is crucial in assessing fetal growth and development and determining the need for intervention or delivery in cases where the fetus is too large or too small.
Identifying Fetal Lie and Attitude
The Leopold maneuver also helps healthcare professionals identify fetal lie and attitudes. Fetal lie refers to the orientation of the fetus in the uterus , while fetal attitude refers to the position of the fetus’s head and limbs in relation to its body . Accurate identification of fetal lie and attitudes is essential in preparing for safe and successful delivery.
Step-by-Step Guide on Performing the Leopold Maneuver
Preparing the Patient for the Examination
Before beginning the Leopold maneuver, the mother should empty her bladder, lie down, and relax her abdominal muscles. The healthcare professional should wash their hands and warm them before beginning the examination.
Step 1: Identification of the Fundus

Palpation of the fundus: The first maneuver is also called Fundal Grip . The healthcare professional palpates the uppermost part of the uterus (fundus) to determine the fetal lie, presentation, and engagement . The healthcare professional should identify the position of the fundus, which is the top of the uterus, by palpating the abdomen with both hands. The fundus is usually located near the navel.
Your Findings Should Be Recorded as, Head : round, more mobile Breach : Large, nodular mass
Step 2: Identification of the Fetal Back

Palpation of the sides of the uterus : The second maneuver is also called Umbilical Grip . The healthcare professional palpates the sides of the uterus to determine the fetal presentation and position . The healthcare professional should identify the location of the fetal back by feeling a smooth, firm, and long surface on one side of the uterus.
Your Findings Should Be Recorded as,
Back : Hard, resistant structure, directed anteriorly, posteriorly, or transversely Fetal Extremities : Numerous small irregular mobile parts
Step 3: Identification of the Fetal Part occupying the Pelvic Inlet

Palpation of the fetal parts : This maneuver is also known as the first Pawlik Grip . The healthcare professional palpates the fetal parts to determine the fetal position and engagement . The healthcare professional should identify the fetal part occupying the pelvic inlet by palpating the lower abdomen . Depending on the fetal presentation, this could be the fetal head or buttocks.
When the head has descended, can feel the anterior shoulder or the space created by the neck from the head.
- Palpate the lower abdomen to identify the presenting part of the fetus (e.g., “The fetal buttocks are presenting at the inlet.”)
- Note the position of the presenting part in relation to the mother’s pelvis (e.g., “The presenting part is in a transverse lie.”)
Step 4: Identification of the Fetal Part in the Pelvic Cavity

Palpation of the pelvic inlet : This maneuver is also known as the second Pawlik Grip . The healthcare professional palpates the pelvic inlet to determine fetal engagement . Finally, the healthcare professional should identify the fetal part in the pelvic cavity . This could be the fetal head, buttocks, or limbs.
Not engaged: Movable mass is felt
Engaged : Fixed mass is felt
Importance of the Leopold Maneuver in Prenatal Care
Identification of abnormal fetal presentation.
The Leopold maneuver is crucial in identifying abnormal fetal presentations , such as breech or transverse, which require special attention during labor and delivery to ensure the safety of both the mother and baby.
Assessment of Fetal Growth and Development
The Leopold maneuver provides healthcare professionals with vital information about fetal growth and development and helps them anticipate potential complications during labor and delivery.
Identification of Multiple Gestations
The Leopold maneuver is an essential tool in identifying multiple gestations to ensure appropriate prenatal care and delivery planning for mothers carrying more than one baby.
Common Issues and Solutions During the Leopold Maneuver
The Leopold maneuver is an obstetric examination technique used to assess fetal presentation, position, and engagement. However, performing this maneuver can be challenging due to various factors. Here are some common issues and solutions during the Leopold maneuver.
Difficulty in Assessing the Fetal Presentation
One common issue during the Leopold maneuver is difficulty in identifying fetal presentation . This can happen when the fetal presentation is not well defined or when there are multiple fetuses. To solve this issue, the examiner should carefully palpate the abdomen and try to differentiate between the fetal parts.
Difficulties in Identifying the Fetal Parts
Another common issue during the Leopold maneuver is difficulty in identifying fetal parts . This can happen when the fetus is in an atypical position or when there are fetal anomalies. To solve this issue, the examiner should use various techniques such as ultrasound or auscultation to guide them in identifying the fetal parts.
Confounding Factors that May Affect the Examination
There are confounding factors that may affect the accuracy of the Leopold maneuver, including obesity, polyhydramnios, fetal anomalies, and fetal movements . These factors can make it more challenging to perform the Leopold maneuver accurately. To solve this issue, examiners should try to minimize these factors or use additional examination techniques to confirm fetal presentation and position.
The Role of the Leopold Maneuver in Diagnosing Fetal Position
The Leopold maneuver is a crucial examination technique for diagnosing fetal position, and it plays a significant role in obstetric care. Here are some important factors to consider when using the Leopold maneuver to diagnose fetal position.
Importance of Diagnosing Fetal Position
Diagnosing fetal position is essential for obstetricians and midwives to ensure safe delivery. By knowing the fetal position, they can anticipate any potential complications during delivery and prepare accordingly. This can help minimize the risk of fetal distress, maternal injury, and other delivery-related complications .
Accuracy of Leopold Maneuver in Diagnosing Fetal Position
The Leopold maneuver is an accurate technique for diagnosing fetal position, with a sensitivity of up to 84%. It is a non-invasive and cost-effective method that can be performed by most healthcare providers. Therefore, it is widely used in obstetric care to diagnose fetal position.
Limitations of the Leopold Maneuver in Diagnosing Fetal Position
However, the Leopold maneuver has some limitations in diagnosing fetal position. It may not be accurate in identifying fetal presentation in cases of multiple pregnancies, fetal anomalies, or when the fetus is in an atypical position . Additionally, the examiner’s experience and skill level can also affect the accuracy of the Leopold maneuver.
Complications
The Leopold maneuver is generally considered a safe and non-invasive examination, but as with any medical procedure, there are potential complications that can occur. Some possible complications of the Leopold maneuver include:
- Discomfort: The Leopold maneuver can cause some discomfort or mild pain for the patient, especially if the examiner is pressing too hard or manipulating the fetus in a way that causes discomfort.
- False results: In some cases, the Leopold maneuver can produce false results, which can lead to incorrect decisions about delivery options or interventions. This can occur if the fetus is in an unusual position or if the examiner is inexperienced or unable to accurately interpret the results of the exam.
- Fetal distress: In rare cases, the Leopold maneuver can cause fetal distress or other complications, such as premature labor or rupture of the amniotic sac. This can occur if the examiner is too forceful or aggressive during the exam or if the fetus is in a vulnerable position.
- Infection: While the Leopold maneuver is a non-invasive exam, there is still a small risk of infection if the examiner does not follow proper hygiene protocols, such as washing their hands before and after the exam.
Nurse’s Responsibilities
The Leopold maneuver is a technique used by healthcare professionals, including nurses, to assess the position of a fetus in the mother’s uterus. As a nurse, your responsibilities during Leopold maneuvers include:
- Explaining the procedure to the patient: Before performing the Leopold maneuver, it is important to explain the procedure to the patient and ensure that they understand what will happen during the exam. This can help reduce anxiety and improve the patient’s overall experience.
- Preparing the patient: Before performing the exam, you will need to ensure that the patient is positioned correctly and that their clothing is adjusted to allow access to their abdomen. You may also need to provide a drape or cover for modesty.
- Assisting the healthcare provider: During the Leopold maneuver, you may be asked to assist the healthcare provider by holding the patient’s abdomen or providing support as needed. You may also need to help position the patient to allow for optimal access to the uterus.
- Monitoring the patient: As the Leopold maneuver can cause some discomfort or pain for the patient, it is important to monitor their vital signs and overall comfort level throughout the exam. If the patient experiences any discomfort or pain, you may need to provide comfort measures, such as adjusting their position or providing pain relief medication.
- Documenting the exam: After the Leopold maneuver, it is important to document the results of the exam in the patient’s medical record. This includes noting the fetal presentation, position, and engagement, as well as any other relevant information.
- Providing patient education: Following the exam, you may need to provide the patient with education about the results of the exam, as well as any next steps that may be needed. This can include discussing delivery options, potential complications, and follow-up appointments.
What is the Leopold Maneuver?
The Leopold Maneuver is a manual examination technique used by obstetricians and midwives to assess the fetal presentation, position, and size during pregnancy. The technique involves a series of four maneuvers that allow the examiner to palpate the maternal abdomen and identify the fetal presentation and position.
How is the Leopold Maneuver performed?
The Leopold Maneuver involves four maneuvers, which are performed in sequence. The first maneuver involves palpating the fundus to determine the location of the fetal head or buttocks. The second maneuver involves identifying the location of the fetal back. The third maneuver involves palpating the lower abdomen to identify the presenting part of the fetus. The fourth maneuver involves determining fetal descent and engagement.
What is the purpose of the Leopold Maneuver?
The purpose of the Leopold Maneuver is to assess the fetal presentation, position, and size during pregnancy. The examination can provide valuable information to obstetricians and midwives to ensure the health and safety of both the mother and the baby. The Leopold Maneuver can help identify abnormal fetal presentation, and multiple gestations, and estimate fetal weight.
Can the Leopold Maneuver be performed at home?
No, the Leopold Maneuver is a medical examination technique that should only be performed by trained healthcare professionals, such as obstetricians or midwives. It requires specialized knowledge, training, and experience to perform the examination accurately.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.
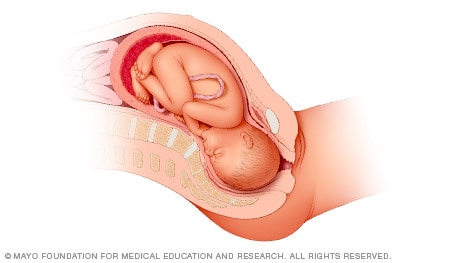
Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.
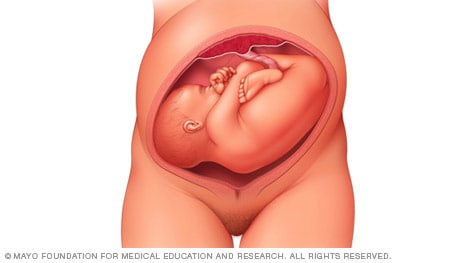
Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

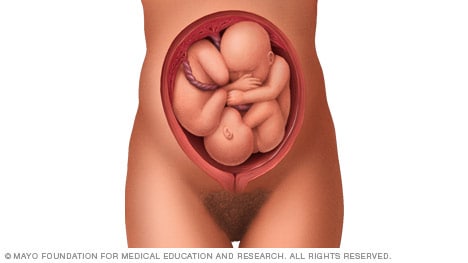
Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.
If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.
- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Delivery, face and brow presentation.
Julija Makajeva ; Mohsina Ashraf .
Affiliations
Last Update: January 9, 2023 .
- Continuing Education Activity
Face and brow presentation is a malpresentation during labor when the presenting part is either the face or, in the case of brow presentation, it is the area between the orbital ridge and the anterior fontanelle. This activity reviews the evaluation and management of these two presentations and explains the role of the interprofessional team in managing delivery safely for both the mother and the baby.
- Describe the mechanism of labor in the face and brow presentation.
- Summarize potential maternal and fetal complications during the face and brow presentations.
- Review different management approaches for the face and brow presentation.
- Outline some interprofessional strategies that will improve patient outcomes in delivery cases with face and brow presentation issues.
- Introduction
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common presentation in term labor is the vertex, where the fetal neck is flexed to the chin, minimizing the head circumference.
Face presentation – an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations. [1] [2] [3]
In brow presentation, the neck is not extended as much as in face presentation, and the leading part is the area between the anterior fontanelle and the orbital ridges. Brow presentation is considered the rarest of all malpresentation with a prevalence of 1 in 500 to 1 in 4000 deliveries. [3]
Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow presentation. These risk factors may be related to either the mother or the fetus. Maternal risk factors are preterm delivery, contracted maternal pelvis, platypelloid pelvis, multiparity, previous cesarean section, black race. Fetal risk factors include anencephaly, multiple loops of cord around the neck, masses of the neck, macrosomia, polyhydramnios. [2] [4] [5]
These malpresentations are usually diagnosed during the second stage of labor when performing a digital examination. It is possible to palpate orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, anterior fontanelle and face can be palpated except for the mouth and the chin. Brow presentation can then be further described based on the position of the anterior fontanelle as frontal anterior, posterior, or transverse.
Diagnosing the exact presentation can be challenging, and face presentation may be misdiagnosed as frank breech. To avoid any confusion, a bedside ultrasound scan can be performed. [6] The ultrasound imaging can show a reduced angle between the occiput and the spine or, the chin is separated from the chest. However, ultrasound does not provide much predicting value in the outcome of the labor. [7]
- Anatomy and Physiology
Before discussing the mechanism of labor in the face or brow presentation, it is crucial to highlight some anatomical landmarks and their measurements.
Planes and Diameters of the Pelvis
The three most important planes in the female pelvis are the pelvic inlet, mid pelvis, and pelvic outlet.
Four diameters can describe the pelvic inlet: anteroposterior, transverse, and two obliques. Furthermore, based on the different landmarks on the pelvic inlet, there are three different anteroposterior diameters, named conjugates: true conjugate, obstetrical conjugate, and diagonal conjugate. Only the latter can be measured directly during the obstetric examination. The shortest of these three diameters is obstetrical conjugate, which measures approximately 10.5 cm and is a distance between the sacral promontory and 1 cm below the upper border of the symphysis pubis. This measurement is clinically significant as the fetal head must pass through this diameter during the engagement phase. The transverse diameter measures about 13.5cm and is the widest distance between the innominate line on both sides.
The shortest distance in the mid pelvis is the interspinous diameter and usually is only about 10 cm.
Fetal Skull Diameters
There are six distinguished longitudinal fetal skull diameters:
- Suboccipito-bregmatic: from the center of anterior fontanelle (bregma) to the occipital protuberance, measuring 9.5 cm. This is the presenting diameter in vertex presentation.
- Suboccipito-frontal: from the anterior part of bregma to the occipital protuberance, measuring 10 cm
- Occipito-frontal: from the root of the nose to the most prominent part of the occiput, measuring 11.5cm
- Submento-bregmatic: from the center of the bregma to the angle of the mandible, measuring 9.5 cm. This is the presenting diameter in face presentation where the neck is hyperextended.
- Submento-vertical: from the midpoint between fontanelles and the angle of the mandible, measuring 11.5cm
- Occipito-mental: from the midpoint between fontanelles and the tip of the chin, measuring 13.5 cm. It is the presenting diameter in brow presentation.
Cardinal Movements of Normal Labor
- Neck flexion
- Internal rotation
- Extension (delivers head)
- External rotation (Restitution)
- Expulsion (delivery of anterior and posterior shoulders)
Some of the key movements are not possible in the face or brow presentations.
Based on the information provided above, it is obvious that labor will be arrested in brow presentation unless it spontaneously changes to face or vertex, as the occipito-mental diameter of the fetal head is significantly wider than the smallest diameter of the female pelvis. Face presentation can, however, be delivered vaginally, and further mechanisms of face delivery will be explained in later sections.
- Indications
As mentioned previously, spontaneous vaginal delivery can be successful in face presentation. However, the main indication for vaginal delivery in such circumstances would be a maternal choice. It is crucial to have a thorough conversation with a mother, explaining the risks and benefits of vaginal delivery with face presentation and a cesarean section. Informed consent and creating a rapport with the mother is an essential aspect of safe and successful labor.
- Contraindications
Vaginal delivery of face presentation is contraindicated if the mentum is lying posteriorly or is in a transverse position. In such a scenario, the fetal brow is pressing against the maternal symphysis pubis, and the short fetal neck, which is already maximally extended, cannot span the surface of the maternal sacrum. In this position, the diameter of the head is larger than the maternal pelvis, and it cannot descend through the birth canal. Therefore the cesarean section is recommended as the safest mode of delivery for mentum posterior face presentations.
Attempts to manually convert face presentation to vertex, manual or forceps rotation of the persistent posterior chin to anterior are contraindicated as they can be dangerous.
Persistent brow presentation itself is a contraindication for vaginal delivery unless the fetus is significantly small or the maternal pelvis is large.
Continuous electronic fetal heart rate monitoring is recommended for face and brow presentations, as heart rate abnormalities are common in these scenarios. One study found that only 14% of the cases with face presentation had no abnormal traces on the cardiotocograph. [8] It is advised to use external transducer devices to prevent damage to the eyes. When internal monitoring is inevitable, it is suggested to place monitoring devices on bony parts carefully.
People who are usually involved in the delivery of face/ brow presentation are:
- Experienced midwife, preferably looking after laboring woman 1:1
- Senior obstetrician
- Neonatal team - in case of need for resuscitation
- Anesthetic team - to provide necessary pain control (e.g., epidural)
- Theatre team - in case of failure to progress and an emergency cesarean section will be required.
- Preparation
No specific preparation is required for face or brow presentation. However, it is essential to discuss the labor options with the mother and birthing partner and inform members of the neonatal, anesthetic, and theatre co-ordinating teams.
- Technique or Treatment
Mechanism of Labor in Face Presentation
During contractions, the pressure exerted by the fundus of the uterus on the fetus and pressure of amniotic fluid initiate descent. During this descent, the fetal neck extends instead of flexing. The internal rotation determines the outcome of delivery, if the fetal chin rotates posteriorly, vaginal delivery would not be possible, and cesarean section is permitted. The approach towards mentum-posterior delivery should be individualized, as the cases are rare. Expectant management is acceptable in multiparous women with small fetuses, as a spontaneous mentum-anterior rotation can occur. However, there should be a low threshold for cesarean section in primigravida women or women with large fetuses.
When the fetal chin is rotated towards maternal symphysis pubis as described as mentum-anterior; in these cases further descend through the vaginal canal continues with approximately 73% cases deliver spontaneously. [9] Fetal mentum presses on the maternal symphysis pubis, and the head is delivered by flexion. The occiput is pointing towards the maternal back, and external rotation happens. Shoulders are delivered in the same manner as in vertex delivery.
Mechanism of Labor in Brow Presentation
As this presentation is considered unstable, it is usually converted into a face or an occiput presentation. Due to the cephalic diameter being wider than the maternal pelvis, the fetal head cannot engage; thus, brow delivery cannot take place. Unless the fetus is small or the pelvis is very wide, the prognosis for vaginal delivery is poor. With persistent brow presentation, a cesarean section is required for safe delivery.
- Complications
As the cesarean section is becoming a more accessible mode of delivery in malpresentations, the incidence of maternal and fetal morbidity and mortality during face presentation has dropped significantly. [10]
However, there are still some complications associated with the nature of labor in face presentation. Due to the fetal head position, it is more challenging for the head to engage in the birth canal and descend, resulting in prolonged labor.
Prolonged labor itself can provoke foetal distress and arrhythmias. If the labor arrests or signs of fetal distress appear on CTG, the recommended next step in management is an emergency cesarean section, which in itself carries a myriad of operative and post-operative complications.
Finally, due to the nature of the fetal position and prolonged duration of labor in face presentation, neonates develop significant edema of the skull and face. Swelling of the fetal airway may also be present, resulting in respiratory distress after birth and possible intubation.
- Clinical Significance
During vertex presentation, the fetal head flexes, bringing the chin to the chest, forming the smallest possible fetal head diameter, measuring approximately 9.5cm. With face and brow presentation, the neck hyperextends, resulting in greater cephalic diameters. As a result, the fetal head will engage later, and labor will progress more slowly. Failure to progress in labor is also more common in both presentations compared to vertex presentation.
Furthermore, when the fetal chin is in a posterior position, this prevents further flexion of the fetal neck, as browns are pressing on the symphysis pubis. As a result, descend through the birth canal is impossible. Such presentation is considered undeliverable vaginally and requires an emergency cesarean section.
Manual attempts to change face presentation to vertex, manual or forceps rotation to mentum anterior are considered dangerous and are discouraged.
- Enhancing Healthcare Team Outcomes
A multidisciplinary team of healthcare experts supports the woman and her child during labor and the perinatal period. For a face or brow presentation to be appropriately diagnosed, an experienced midwife and obstetrician must be involved in the vaginal examination and labor monitoring. As fetal anomalies, such as anencephaly or goiter, can contribute to face presentation, sonographers experienced in antenatal scanning should also be involved in the care. It is advised to inform the anesthetic and neonatal teams in advance of the possible need for emergency cesarean section and resuscitation of the neonate. [11] [12]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Julija Makajeva declares no relevant financial relationships with ineligible companies.
Disclosure: Mohsina Ashraf declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Makajeva J, Ashraf M. Delivery, Face and Brow Presentation. [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. [Am J Obstet Gynecol MFM. 2020] Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. Bellussi F, Livi A, Cataneo I, Salsi G, Lenzi J, Pilu G. Am J Obstet Gynecol MFM. 2020 Nov; 2(4):100217. Epub 2020 Aug 18.
- Review Sonographic evaluation of the fetal head position and attitude during labor. [Am J Obstet Gynecol. 2022] Review Sonographic evaluation of the fetal head position and attitude during labor. Ghi T, Dall'Asta A. Am J Obstet Gynecol. 2022 Jul 6; . Epub 2022 Jul 6.
- Stages of Labor. [StatPearls. 2024] Stages of Labor. Hutchison J, Mahdy H, Hutchison J. StatPearls. 2024 Jan
- Leopold Maneuvers. [StatPearls. 2024] Leopold Maneuvers. Superville SS, Siccardi MA. StatPearls. 2024 Jan
- Review Labor with abnormal presentation and position. [Obstet Gynecol Clin North Am. ...] Review Labor with abnormal presentation and position. Stitely ML, Gherman RB. Obstet Gynecol Clin North Am. 2005 Jun; 32(2):165-79.
Recent Activity
- Delivery, Face and Brow Presentation - StatPearls Delivery, Face and Brow Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
PATHOGENESIS AND RISK FACTORS
● The fetus does not fully occupy the pelvis, thus allowing a fetal extremity room to prolapse. Predisposing factors include early gestational age, multiple gestation, polyhydramnios, or a large maternal pelvis relative to fetal size [ 2,3 ].
● Membrane rupture occurs when the presenting part is still high, which allows flow of amniotic fluid to carry a fetal extremity, umbilical cord, or both toward the birth canal.
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).
Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Presentation and position of baby through pregnancy and at birth
9-minute read
If you are concerned about your baby’s movements, contact your doctor or midwife for advice immediately.
- If you baby is in a breech presentation, your doctor may recommend trying a technique called an external cephalic version to try and move your baby while they are still in the uterus for an easier birth.
What does presentation and position mean?
Presentation refers to the part of your baby’s body that is facing downwards in the direction of the birth canal.
Position refers to where your baby’s occiput (the bottom part of the back of their head) is in relation to your body.
If your baby is in a breech presentation , then position refers to where your baby’s sacrum (lower back) is in relation to your body.
People — including medical professionals — sometimes use these terms incorrectly. Sometimes when speaking about babies in breech presentation, the word ‘position’ will be used to refer to their presentation. For example, you may read information or hear people say ‘breech position’ instead of ‘breech presentation’.
What are the different types of presentation my baby could be in during pregnancy and birth?
Most babies present headfirst, also known as cephalic presentation. Most babies that are headfirst will be vertex presentation. This means that the crown of their head sits at the opening of your birth canal.
In rare cases, your baby can be headfirst but in face or brow presentation, which may not be suitable for vaginal birth.

If your baby is in a breech presentation, their feet or bottom will be closest to your birth canal. The 3 most common types of breech presentation are:
- frank or extended breech — where your baby’s legs are straight up in front of their body, with their feet up near their face
- complete or flexed breech — where your baby is in a sitting position with their legs crossed in front of their body and their feet near their bottom
- footling breech — where one or both of your baby’s feet are hanging below their bottom, so the foot or feet are coming first
Read more on breech presentation .
What are the different positions my baby could be in during pregnancy and birth?
If your baby is headfirst, the 3 main types of presentation are:
- anterior – when the back of your baby’s head is at the front of your belly
- lateral – when the back of your baby’s head is facing your side
- posterior – when the back of your baby’s head is towards your back

How will I know what presentation and position my baby is in?
Your doctor or midwife can usually work out your baby’s presentation by feeling your abdomen. They may also double check it with a portable ultrasound. Your baby’s presentation is usually checked around 36 weeks .
Your doctor or midwife will also confirm your baby’s head position in labour by examining your belly and using an ultrasound , and they may also do a vaginal examination . During the vaginal examination they are feeling for certain ridges on your baby’s head called sutures and fontanelles that help them work out which way your baby is positioned.
What is the ideal presentation and position for baby to be in for a vaginal birth?
For a vaginal birth, your baby will ideally be headfirst with the back of their head at the front of your belly, also known as being in the anterior position. This position is best for labour and birth since it means that the smallest part of your baby’s head goes down the birth canal first.

When does a baby usually get in the ideal presentation and position for birth?
Your baby will usually be in a headfirst position by 37 weeks of pregnancy. Around 3 in every 100 babies will be in breech presentation after 37 weeks.
Your baby’s position can change with your contractions during labour as they move down the birth canal, so their exact position can change during labour.
What are my options if baby isn't in the ideal presentation or position for a vaginal birth?
If your baby is in a breech presentation, your doctor may recommend a technique called an external cephalic version (ECV) to try and move your baby while they are still in the uterus . An ECV involves your doctor using their hands to apply pressure on your belly and help turn your baby to a headfirst position. It has a 1 in 2 chance of success and is a safe option in most pregnancies.
There is no evidence to show that alternative therapies, such as exercises, acupuncture or chiropractic treatments, help your baby change from a breech presentation to headfirst.
If your baby remains breech, your doctor may discuss having a breech vaginal birth. Not all doctors and hospitals offer this option. They may also suggest you birth your baby with a planned caesarean section .
If your baby’s presentation is headfirst but the position of your baby’s head is not ideal for labour, it can lead to a longer labour, and potential complications . The position of your baby’s head will often change as your labour progresses. If it doesn’t, sometimes you can still give birth without assistance, or you may need your doctor to help turn your baby’s head or help your birth with a vacuum or forceps .
Any procedure or decision for a type of birth will only go ahead with your consent . You will be able to discuss all the options with your doctor, and based on your preferences for yourself and your baby’s safety, make a decision together .
Resources and support
The Royal Australian and New Zealand College of Obstetrics and Gynaecology has a factsheet about the options available to you if your baby is in a breech presentation at the end of your pregnancy .
Mercy Perinatal has information on external cephalic version (ECV) safety and benefits if your baby is in a breech presentation at the end of your pregnancy.
The Women’s Hospital has information about the different presentations and positions your baby could be in, and how it can affect your birthing experience.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: October 2023

Related pages
External cephalic version (ecv), malpresentation, breech pregnancy, search our site for.
- Foetal Version
- Breech Presentation
Need more information?
Top results
Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
ECV is a procedure to try to move your baby from a breech position to a head-down position. This is performed by a trained doctor.
Having a baby
The articles in this section relate to having a baby – what to consider before becoming pregnant, pregnancy and birth, and after your baby is born.
Anatomy of pregnancy and birth - pelvis
Your pelvis helps to carry your growing baby and is tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Planned or elective caesarean
There are important things to consider if you are having a planned or elective caesarean such as what happens during and after the procedure.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.

Obstetric and Newborn Care I
10.02 key terms related to fetal positions.
a. “Lie” of an Infant.
Lie refers to the position of the spinal column of the fetus in relation to the spinal column of the mother. There are two types of lie, longitudinal and transverse. Longitudinal indicates that the baby is lying lengthwise in the uterus, with its head or buttocks down. Transverse indicates that the baby is lying crosswise in the uterus.
b. Presentation/Presenting Part.
Presentation refers to that part of the fetus that is coming through (or attempting to come through) the pelvis first.
(1) Types of presentations (see figure 10-1). The vertex or cephalic (head), breech, and shoulder are the three types of presentations. In vertex or cephalic, the head comes down first. In breech, the feet or buttocks comes down first, and last–in shoulder, the arm or shoulder comes down first. This is usually referred to as a transverse lie.
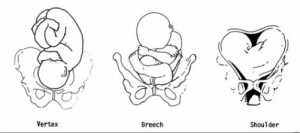
(2) Percentages of presentations.
(a) Head first is the most common-96 percent.
(b) Breech is the next most common-3.5 percent.
(c) Shoulder or arm is the least common-5 percent.
(3) Specific presentation may be evaluated by several ways.
(a) Abdominal palpation-this is not always accurate.
(b) Vaginal exam–this may give a good indication but not infallible.
(c) Ultrasound–this confirms assumptions made by previous methods.
(d) X-ray–this confirms the presentation, but is used only as a last resort due to possible harm to the fetus as a result of exposure to radiation.
c. Attitude.
This is the degree of flexion of the fetus body parts (body, head, and extremities) to each other. Flexion is resistance to the descent of the fetus down the birth canal, which causes the head to flex or bend so that the chin approaches the chest.
(1) Types of attitude (see figure 10-2).
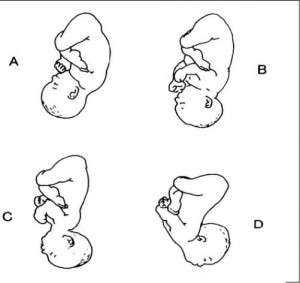
(a) Complete flexion. This is normal attitude in cephalic presentation. With cephalic, there is complete flexion at the head when the fetus “chin is on his chest.” This allows the smallest cephalic diameter to enter the pelvis, which gives the fewest mechanical problems with descent and delivery.
(b) Moderate flexion or military attitude. In cephalic presentation, the fetus head is only partially flexed or not flexed. It gives the appearance of a military person at attention. A larger diameter of the head would be coming through the passageway.
(c) Poor flexion or marked extension. In reference to the fetus head, it is extended or bent backwards. This would be called a brow presentation. It is difficult to deliver because the widest diameter of the head enters the pelvis first. This type of cephalic presentation may require a C/Section if the attitude cannot be changed.
(d) Hyperextended. In reference to the cephalic position, the fetus head is extended all the way back. This allows a face or chin to present first in the pelvis. If there is adequate room in the pelvis, the fetus may be delivered vaginally.
(2) Areas to look at for flexion.
(a) Head-discussed in previous paragraph, 10-2c(1).
(b) Thighs-flexed on the abdomen.
(c) Knees-flexed at the knee joints.
(d) Arches of the feet-rested on the anterior surface of the legs.
(e) Arms-crossed over the thorax.
(3) Attitude of general flexion. This is when all of the above areas are flexed appropriately as described.
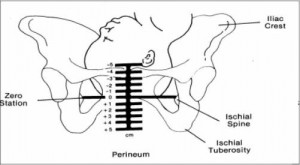
d. Station.
This refers to the depth that the presenting part has descended into the pelvis in relation to the ischial spines of the mother’s pelvis. Measurement of the station is as follows:
(1) The degree of advancement of the presenting part through the pelvis is measured in centimeters.
(2) The ischial spines is the dividing line between plus and minus stations.
(3) Above the ischial spines is referred to as -1 to -5, the numbers going higher as the presenting part gets higher in the pelvis (see figure10-3).
(4) The ischial spines is zero (0) station.
(5) Below the ischial spines is referred to +1 to +5, indicating the lower the presenting part advances.
e. Engagement.
This refers to the entrance of the presenting part of the fetus into the true pelvis or the largest diameter of the presenting part into the true pelvis. In relation to the head, the fetus is said to be engaged when it reaches the midpelvis or at a zero (0) station. Once the fetus is engaged, it (fetus) does not go back up. Prior to engagement occurring, the fetus is said to be “floating” or ballottable.
f. Position.
This is the relationship between a predetermined point of reference or direction on the presenting part of the fetus to the pelvis of the mother.
(1) The maternal pelvis is divided into quadrants.
(a) Right and left side, viewed as the mother would.
(b) Anterior and posterior. This is a line cutting the pelvis in the middle from side to side. The top half is anterior and the bottom half is posterior.
(c) The quadrants never change, but sometimes it is confusing because the student or physician’s viewpoint changes.
NOTE: Remember that when you are describing the quadrants, view them as the mother would.
(2) Specific points on the fetus.
(a) Cephalic or head presentation.
1 Occiput (O). This refers to the Y sutures on the top of the head.
2 Brow or fronto (F). This refers to the diamond sutures or anterior fontanel on the head.
3 Face or chin presentation (M). This refers to the mentum or chin.
(b) Breech or butt presentation.
1 Sacrum or coccyx (S). This is the point of reference.
2 Breech birth is associated with a higher perinatal mortality.
(c) Shoulder presentation.
1 This would be seen with a transverse lie.
2. Scapula (Sc) or its upper tip, the acromion (A) would be used for the point of reference.
(3) Coding of positions.
(a) Coding simplifies explaining the various positions.
1 The first letter of the code tells which side of the pelvis the fetus reference point is on (R for right, L for left).
2 The second letter tells what reference point on the fetus is being used (Occiput-O, Fronto-F, Mentum-M, Breech-S, Shoulder-Sc or A).
3 The last letter tells which half of the pelvis the reference point is in (anterior-A, posterior-P, transverse or in the middle-T).

(b) Each presenting part has the possibility of six positions. They are normally recognized for each position–using “occiput” as the reference point.
1 Left occiput anterior (LOA).
2 Left occiput posterior (LOP).
3 Left occiput transverse (LOT).
4 Right occiput anterior (ROA).
5. Right occiput posterior (ROP).
6 Right occiput transverse (ROT).
(c) A transverse position does not use a first letter and is not the same as a transverse lie or presentation.
1 Occiput at sacrum (O.S.) or occiput at posterior (O.P.).
2 Occiput at pubis (O.P.) or occiput at anterior (O.A.).
(4) Types of breech presentations (see figure10-4).
(a) Complete or full breech. This involves flexion of the fetus legs. It looks like the fetus is sitting in a tailor fashion. The buttocks and feet appear at the vaginal opening almost simultaneously.
A–Complete. B–Frank. C–Incomplete.
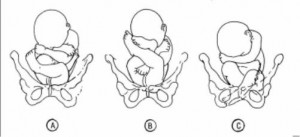
(b) Frank and single breech. The fetus thighs are flexed on his abdomen. His legs are against his trunk and feet are in his face (foot-in-mouth posture). This is the most common and easiest breech presentation to deliver.
(c) Incomplete breech. The fetus feet or knees will appear first. His feet are labeled single or double footing, depending on whether 1 or 2 feet appear first.
(5) Observations about positions (see figure 10-5).
(a) LOA and ROA positions are the most common and permit relatively easy delivery.
(b) LOP and ROP positions usually indicate labor may be longer and harder, and the mother will experience severe backache.
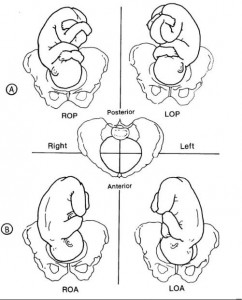
(c) Knowing positions will help you to identify where to look for FHT’s.
1 Breech. This will be upper R or L quad, above the umbilicus.
2 Vertex. This will be lower R or L quad, below the umbilicus.
(d) An occiput in the posterior quadrant means that you will feel lumpy fetal parts, arms and legs (see figure 10-5 A). If delivered in that position, the infant will come out looking up.
(e) An occiput in the anterior quadrant means that you will feel a more smooth back (see figure 10-5 B). If delivered in that position, the infant will come out looking down at the floor.
Distance Learning for Medical and Nursing Professionals
Labour and Delivery Care Module: 8. Abnormal Presentations and Multiple Pregnancies
Study session 8 abnormal presentations and multiple pregnancies, introduction.
In previous study sessions of this module, you have been introduced to the definitions, signs, symptoms and stages of normal labour, and about the ‘normal’ vertex presentation of the fetus during delivery. In this study session, you will learn about the most common abnormal presentations (breech, shoulder, face or brow), their diagnostic criteria and the required actions you need to take to prevent complications developing during labour. Taking prompt action may save the life of the mother and her baby if the delivery becomes obstructed because the baby is in an abnormal presentation. We will also tell you about twin births and the complications that may result if the two babies become ‘locked’ together, preventing either of them from being born.
Learning Outcomes for Study Session 8
After studying this session, you should be able to:
8.1 Define and use correctly all of the key words printed in bold . (SAQs 8.1 and 8.2)
8.2 Describe how you would identify a fetus in the vertex presentation and distinguish this from common malpresentations and malpositions. (SAQs 8.1 and 8.2)
8.3 Describe the causes and complications for the fetus and the mother of fetal malpresentation during full term labour. (SAQ 8.3)
8.4 Describe how you would identify a multiple pregnancy and the complications that may arise. (SAQ 8.4)
8.5 Explain when and how you would refer a woman in labour due to abnormal fetal presentation or multiple pregnancy. (SAQ 8.4)
8.1 Normal and abnormal presentations
8.1.1 vertex presentation.
In about 95% of deliveries, the part of the fetus which arrives first at the mother’s pelvic brim is the highest part of the fetal head, which is called the vertex (Figure 8.1). This presentation is called the vertex presentation . Notice that the baby’s chin is tucked down towards its chest, so that the vertex is the leading part entering the mother’s pelvis. The baby’s head is said to be ‘well-flexed’ in this position.
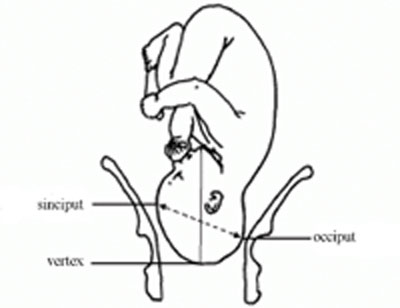
During early pregnancy, the baby is the other way up — with its bottom pointing down towards the mother’s cervix — which is called the breech presentation . This is because during its early development, the head of the fetus is bigger than its buttocks; so in the majority of cases, the head occupies the widest cavity, i.e. the fundus (rounded top) of the uterus. As the fetus grows larger, the buttocks become bigger than the head and the baby spontaneously reverses its position, so its buttocks occupy the fundus. In short, in early pregnancy, the majority of fetuses are in the breech presentation and later in pregnancy most of them make a spontaneous transition to the vertex presentation.
8.1.2 Malpresentations
You will learn about obstructed labour in Study Session 9.
When the baby presents itself in the mother’s pelvis in any position other than the vertex presentation, this is termed an abnormal presentation, or m alpresentation . The reason for referring to this as ‘abnormal’ is because it is associated with a much higher risk of obstruction and other birth complications than the vertex presentation. The most common types of malpresentation are termed breech, shoulder, face or brow. We will discuss each of these in turn later. Notice that the baby can be ‘head-down’ but in an abnormal presentation, as in face or brow presentations, when the baby’s face or forehead (brow) is the presenting part.
8.1.3 Malposition
Although it may not be so easy for you to identify this, the baby can also be in an abnormal position even when it is in the vertex presentation. In a normal delivery, when the baby’s head has engaged in the mother’s pelvis, the back of the baby’s skull (the occiput ) points towards the front of the mother’s pelvis (the pubic symphysis ), where the two pubic bones are fused together. This orientation of the fetal skull is called the occipito-anterior position (Figure 8.2a). If the occiput (back) of the fetal skull is towards the mother’s back, this occipito-posterior position (Figure 8.2b) is a vertex malposition , because it is more difficult for the baby to be born in this orientation. The good thing is that more than 90% of babies in vertex malpositions undergo rotation to the occipito-anterior position and are delivered normally.
You learned the directional positions: anterior/in front of and posterior/behind or in the back of, in the Antenatal Care Module, Part 1, Study Session 3.
Note that the fetal skull can also be tilted to the left or to the right in either the occipito-anterior or occipito-posterior positions.

8.2 Causes and consequences of malpresentations and malpositions
In the majority of individual cases it may not be possible to identify what caused the baby to be in an abnormal presentation or position during delivery. However, the general conditions that are thought to increase the risk of malpresentation or malposition are listed below:
Multiple pregnancy is the subject of Section 8.7 of this study session. You learned about placenta previa in the Antenatal Care Module, Study Session 21.
- Abnormally increased or decreased amount of amniotic fluid
- A tumour (abnormal tissue growth) in the uterus preventing the spontaneous inversion of the fetus from breech to vertex presentation during late pregnancy
- Abnormal shape of the pelvis
- Laxity (slackness) of muscular layer in the walls of the uterus
- Multiple pregnancy (more than one baby in the uterus)
- Placenta previa (placenta partly or completely covering the cervical opening).
If the baby presents at the dilating cervix in an abnormal presentation or malposition, it will more difficult (and may be impossible) for it to complete the seven cardinal movements that you learned about in Study Sessions 3 and 5. As a result, birth is more difficult and there is an increased risk of complications, including:
You learned about PROM in Study Session 17 of the Antenatal Care Module, Part 2.
- Premature rupture of the fetal membranes (PROM)
- Premature labour
- Slow, erratic, short-lived contractions
- Uncoordinated and extremely painful contractions, with slow or no progress of labour
- Prolonged and obstructed labour, leading to a ruptured uterus (see Study Sessions 9 and 10 of this Module)
- Postpartum haemorrhage (see Study Session 11)
- Fetal and maternal distress, which may lead to the death of the baby and/or the mother.
With these complications in mind, we now turn your attention to the commonest types of malpresentation and how to recognise them.
8.3 Breech presentation
In a b reech presentation , the fetus lies with its buttocks in the lower part of the uterus, and its buttocks and/or the feet are the presenting parts during delivery. Breech presentation occurs on average in 3–4% of deliveries after 34 weeks of pregnancy.
When is the breech position the normal position for the fetus?
During early pregnancy the baby’s bottom points down towards the mother’s cervix, and its head (the largest part of the fetus at this stage of development) occupies the fundus (rounded top) of the uterus, which is the widest part of the uterine cavity.
8.3.1 Causes of breech presentation
You can see a transverse lie in Figure 8.7 later in this study session.
In the majority of cases there is no obvious reason why the fetus should present by the breech at full term. In practice, what is commonly observed is the association of breech presentation at delivery with a transverse lie earlier in the pregnancy, i.e. the fetus lies sideways across the mother’s abdomen, facing a sideways implanted placenta. It is thought that when the placenta is in front of the baby’s face, it may obstruct the normal process of inversion, when the baby turns head-down as it gets bigger during the pregnancy. As a result, the fetus turns in the other direction and ends in the breech presentation. Some other circumstances that are thought to favour a breech presentation during labour include:
- Premature labour, beginning before the baby undergoes spontanous inversion from breech to vertex presentation
- Multiple pregnancy, preventing the normal inversion of one or both babies
- Polyhydramnios: excessive amount of amniotic fluid, which makes it more difficult for the fetal head to ‘engage’ with the mother’s cervix (polyhydramnios is pronounced ‘poll-ee-hy-dram-nee-oss’. Hydrocephaly is pronounced ‘hy-droh-keff-all-ee’)
- Hydrocephaly (‘water on the brain’) i.e. an abnormally large fetal head due to excessive accumulation of fluid around the brain
- Placenta praevia
- Breech delivery in the previous pregnancy
- Abnormal formation of the uterus.
8.3.2 Diagnosis of breech presentation
On abdominal palpation the fetal head is found above the mother’s umbilicus as a hard, smooth, rounded mass, which gently ‘ballots’ (can be rocked) between your hands.
Why do you think a mass that ‘ballots’ high up in the abdomen is a sign of breech presentation? (You learned about this in Study Session 11 of the Antenatal Care Module.)
The baby’s head can ‘rock’ a little bit because of the flexibility of the baby’s neck, so if there is a rounded, ballotable mass above the mother’s umbilicus it is very likely to be the baby’s head. If the baby was ‘bottom-up’ (vertex presentation) the whole of its back will move of you try to rock the fetal parts at the fundus (Figure 8.3).
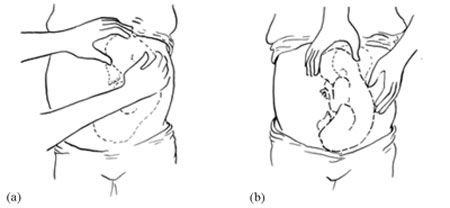
Once the fetus has engaged and labour has begun, the breech baby’s buttocks can be felt as soft and irregular on vaginal examination. They feel very different to the relatively hard rounded mass of the fetal skull in a vertex presentation. When the fetal membranes rupture, the buttocks and/or feet can be felt more clearly. The baby’s anus may be felt and fresh thick, dark meconium may be seen on your examining finger. If the baby’s legs are extended, you may be able to feel the external genitalia and even tell the sex of the baby before it is born.
8.3.3 Types of breech presentation
There are three types of breech presentation, as illustrated in Figure 8.4. They are:
- Complete breech is characterised by flexion of the legs at both hips and knee joints, so the legs are bent underneath the baby.
- Frank breech is the commonest type of breech presentation, and is characterised by flexion at the hip joints and extension at the knee joints, so both the baby’s legs point straight upwards.
- Footling breech is when one or both legs are extended at the hip and knee joint and the baby presents ‘foot first’.
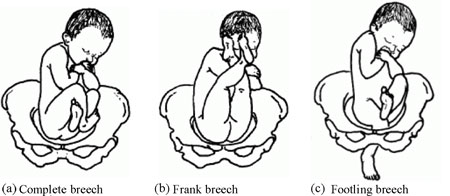
8.3.4 Risks of breech presentation
Regardless of the type of breech presentation, there are significant associated risks to the baby. They include:
- The fetal head gets stuck (arrested) before delivery
- Labour becomes obstructed when the fetus is disproportionately large for the size of the maternal pelvis
- Cord prolapse may occur, i.e. the umbilical cord is pushed out ahead of the baby and may get compressed against the wall of the cervix or vagina
- Premature separation of the placenta (placental abruption)
- Birth injury to the baby, e.g. fracture of the arms or legs, nerve damage, trauma to the internal organs, spinal cord damage, etc.
A breech birth may also result in trauma to the mother’s birth canal or external genitalia through being overstretched by the poorly fitting fetal parts.
Cord prolapse in a normal (vertex) presentation was illustrated in Study Session 17 of the Antenatal Care Module, and placental abruption was covered in Study Session 21.
What will be the effect on the baby if it gets stuck, the labour is obstructed, the cord prolapses, or placental abruption occurs?
The result will be hypoxia , i.e. it will be deprived of oxygen, and may suffer permanent brain damage or die.
You learned about the causes and consequences of hypoxia in the Antenatal Care Module.
8.4 Face presentation
Face presentation occurs when the baby’s neck is so completely extended (bent backwards) that the occiput at the back of the fetal skull touches the baby’s own spine (see Figure 8.5). In this position, the baby’s face will present to you during delivery.
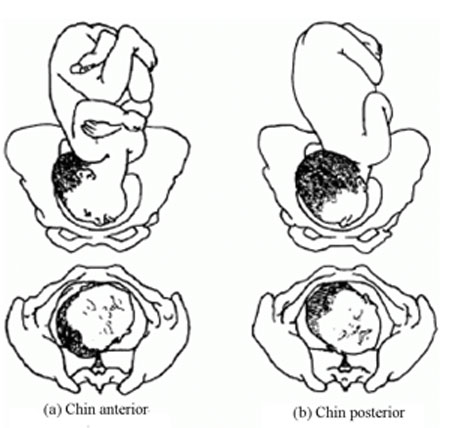
Refer the mother if a baby in the chin posterior face presentation does not rotate and the labour is prolonged.
The incidence of face presentation is about 1 in 500 pregnancies in full term labours. In Figure 8.5, you can see how flexed the head is at the neck. Babies who present in the ‘chin posterior’ position (on the right in Figure 8.5) usually rotate spontaneously during labour, and assume the ‘chin anterior’ position, which makes it easier for them to be born. However, they are unlikely to be delivered vaginally if they fail to undergo spontaneous rotation to the chin anterior position, because the baby’s chin usually gets stuck against the mother’s sacrum (the bony prominence at the back of her pelvis). A baby in this position will have to be delivered by caesarean surgery.
8.4.1 Causes of face presentation
The causes of face presentation are similar to those already described for breech births:
- Laxity (slackness) of the uterus after many previous full-term pregnancies
- Multiple pregnancy
- Polyhydramnios (excessive amniotic fluid)
- Congenital abnormality of the fetus (e.g. anencephaly, which means no or incomplete skull bones)
- Abnormal shape of the mother’s pelvis.
8.4.2 Diagnosis of face presentation
Face presentation may not be easily detected by abdominal palpation, especially if the chin is in the posterior position. On abdominal examination, you may feel irregular shapes, formed because the fetal spine is curved in an ‘S’ shape. However, on vaginal examination, you can detect face presentation because:
- The presenting part will be high, soft and irregular.
- When the cervix is sufficiently dilated, you may be able to feel parts of the face, such as the orbital ridges above the eyes, the nose or mouth, gums, or bony chin.
- If the membranes are ruptured, the baby may suck your examining finger!
But as labour progresses, the baby’s face becomes o edematous (swollen with fluid), making it more difficult to distinguish from the soft shape you will feel in a breech presentation.
8.4.3 Complications of face presentation
Complications for the fetus include:
- Obstructed labour and ruptured uterus
- Cord prolapse
- Facial bruising
- Cerebral haemorrhage (bleeding inside the fetal skull).
8.5 Brow presentation

In brow presentation , the baby’s head is only partially extended at the neck (compare this with face presentation), so its brow (forehead) is the presenting part (Figure 8.6). This presentation is rare, with an incidence of 1 in 1000 deliveries at full term.
8.5.1 Possible causes of brow presentation
You have seen all of these factors before, as causes of other malpresentations:
- Lax uterus due to repeated full term pregnancy
- Polyhydramnios
8.5.2 Diagnosis of brow presentation
Brow presentation is not usually detected before the onset of labour, except by very experienced birth attendants. On abdominal examination, the head is high in the mother’s abdomen, appears unduly large and does not descend into the pelvis, despite good uterine contractions. On vaginal examination, the presenting part is high and may be difficult to reach. You may be able to feel the root of the nose, eyes, but not the mouth, tip of the nose or chin. You may also feel the anterior fontanel, but a large caput (swelling) towards the front of the fetal skull may mask this landmark if the woman has been in labour for some hours.
Recall the appearance of a normal caput over the posterior fontanel shown in Figure 4.4 earlier in this Module.
8.5.3 Complications of brow presentation
The complications of brow presentation are much the same as for other malpresentations:
- Cerebral haemorrhage.
Which are you more likely to encounter — face or brow presentations?
Face presentation, which occurs in 1 in 500 full term labours. Brow presentation is more rare, at 1 in 1,000 full term labours.
8.6 Shoulder presentation
Shoulder presentation is rare at full term, but may occur when the fetus lies transversely across the uterus (Figure 8.7), if it stopped part-way through spontaneous inversion from breech to vertex, or it may lie transversely from early pregnancy. If the baby lies facing upwards, its back may be the presenting part; if facing downwards its hand may emerge through the cervix. A baby in the transverse position cannot be born through the vagina and the labour will be obstructed. Refer babies in shoulder presentation urgently.

8.6.1 Causes of shoulder presentation
Causes of shoulder presentation could be maternal or fetal factors.
Maternal factors include:
- Lax abdominal and uterine muscles: most often after several previous pregnancies
- Uterine abnormality
- Contracted (abnormally narrow) pelvis.
Fetal factors include:
- Preterm labour
- Placenta previa.
What do ‘placenta previa’ and ‘polyhydramnios’ indicate?
Placenta previa is when the placenta is partly or completely covering the cervical opening. Polyhydramnios is an excess of amniotic fluid. They are both potential causes of malpresentation.
8.6.2 Diagnosis of shoulder presentation
On abdominal palpation, the uterus appears broader and the height of the fundus is less than expected for the period of gestation, because the fundus is not occupied by either the baby’s head or buttocks. You can usually feel the head on one side of the mother’s abdomen. On vaginal examination, in early labour, the presenting part may not be felt, but when the labour is well progressed, you may feel the baby’s ribs. When the shoulder enters the pelvic brim, the baby’s arm may prolapse and become visible outside the vagina.
8.6.3 Complications of shoulder presentation
Complications include:
- Trauma to a prolapsed arm
- Fetal hypoxia and death.
Remember that a shoulder presentation means the baby cannot be born through the vagina; if you detect it in a woman who is already in labour, refer her urgently to a higher health facility.
8.7 Multiple pregnancy
In this section, we turn to the subject of multiple pregnancy , when there is more than one fetus in the uterus. More than 95% of multiple pregnancies are twins (two fetuses), but there can also be triplets (three fetuses), quadruplets (four fetuses), quintuplets (five fetuses), and other higher order multiples with a declining chance of occurrence. The spontaneous occurrence of twins varies by country : it is lowest in East Asia n countries like Japan and China (1 out of 1000 pregnancies are fraternal or non-identical twins), and highest in black Africans , particularly in Nigeria , where 1 in 20 pr egnancies are fraternal twins. In general, compared to single babies, multiple pregnancies are highly associated with early pregnancy loss and high perinatal mortality, mainly due to prematurity.
8.7.1 Types of twin pregnancy
Twins may be identical (monozygotic) or non-identical and fraternal (dizigotic). Monozygotic twins develop from a single fertilised ovum (the zygote), so they are always the same sex and they share the same placenta . By contrast, dizygotic twins develop from two different zygotes, so they can have the same or different sex, and they have separate placenta s . Figure 8.8 shows the types of twin pregnancy and the processes by which they are formed.

8.7.2 Diagnosis of twin pregnancy
On abdominal examination you may notice that:
- The size of the uterus is larger than the expected for the period for gestation.
- The uterus looks round and broad, and fetal movement may be seen over a large area. (The shape of the uterus at term in a singleton pregnancy in the vertex presentation appears heart-shaped rounder at the top and narrower at the bottom.)
- Two heads can be felt.
- Two fetal heart beats may be heard if two people listen at the same time, and they can detect at least 10 beats different (Figure 8.6).
- Ultrasound examination can make an absolute diagnosis of twin pregnancy.

8.7.3 Consequences of twin pregnancy
Women who are pregnant with twins are more prone to suffer with the minor disorders of pregnancy, like morning sickness, nausea and heartburn. Twin pregnancy is one cause of hyperemesis gravidarum (persistent, severe nausea and vomiting). Mothers of twins are also more at risk of developing iron and folate-deficiency anaemia during pregnancy.
Can you suggest why anaemia is a greater risk in multiple pregnancies?
The mother has to supply the nutrients to feed two (or more) babies; if she is not getting enough iron and folate in her diet, or through supplements, she will become anaemic.
Other complications include the following:
- Pregnancy-related hypertensive disorders like pre-eclampsia and eclampsia are more common in twin pregnancies.
- Pressure symptoms may occur in late pregnancy due to the increased weight and size of the uterus.
- Labour often occurs spontaneously before term, with p remature delivery or premature rupture of membranes (PROM) .
- Respiratory deficit ( shortness of breath, because of fast growing uterus) is another common problem.
Twin babies may be small in comparison to their gestational age and more prone to the complications associated with low birth weight (increased vulnerability to infection, losing heat, difficulty breastfeeding).
You will learn about low birth weight babies in detail in the Postnatal Care Module.
- Malpresentation is more common in twin pregnancies, and they may also be ‘locked’ at the neck with one twin in the vertex presentation and the other in breech. The risks associated with malpresentations already described also apply: prolapsed cord, poor uterine contraction, prolonged or obstructed labour, postpartum haemorrhage, and fetal hypoxia and death.
- Conjoined twins (fused twins, joined at the head, chest, or abdomen, or through the back) may also rarely occur.
8.8 Management of women with malpresentation or multiple pregnancy
As you have seen in this study session, any presentation other than vertex has its own dangers for the mother and baby. For this reason, all women who develop abnormal presentation or multiple pregnancy should ideally have skilled care by senior health professionals in a health facility where there is a comprehensive emergency obstetric service. Early detection and referral of a woman in any of these situations can save her life and that of her baby.
What can you do to reduce the risks arising from malpresentation or multiple pregnancy in women in your care?
During focused antenatal care of the pregnant women in your community, at every visit after 36 weeks of gestation you should check for the presence of abnormal fetal presentation. If you detect abnormal presentation or multiple pregnancy, you should refer the woman before the onset of labour.
Summary of Study Session 8
In Study Session 8, you learned that:
- During early pregnancy, babies are naturally in the breech position, but in 95% of cases they spontaneously reverse into the vertex presentation before labour begins.
- Malpresentation or malposition of the fetus at full term increases the risk of obstructed labour and other birth complications.
- Common causes of malpresentations/malpositions include: excess amniotic fluid, abnormal shape and size of the pelvis; uterine tumour; placenta praevia; slackness of uterine muscles (after many previous pregnancies); or multiple pregnancy.
- Common complications include: premature rupture of membranes, premature labour, prolonged/obstructed labour; ruptured uterus; postpartum haemorrhage; fetal and maternal distress which may lead to death.
- Vertex malposition is when the fetal head is in the occipito-posterior position — i.e. the back of the fetal skull is towards the mother’s back instead of pointing towards the front of the mother’s pelvis. 90% of vertex malpositions rotate and deliver normally.
- Breech presentation (complete, frank or footling) is when the baby’s buttocks present during labour. It occurs in 3–4% of labours after 34 weeks of pregnancy and may lead to obstructed labour, cord prolapse, hypoxia, premature separation of the placenta, birth injury to the baby or to the birth canal.
- Face presentation is when the fetal head is bent so far backwards that the face presents during labour. It occurs in about 1 in 500 full term labours. ‘Chin posterior’ face presentations usually rotate spontaneously to the ‘chin anterior’ position and deliver normally. If rotation does not occur, a caesarean delivery is likely to be necessary.
- Brow presentation is when the baby’s forehead is the presenting part. It occurs in about 1 in 1000 full term labours and is difficult to detect before the onset of labour. Caesarean delivery is likely to be necessary.
- Shoulder presentation occurs when the fetal lie during labour is transverse. Once labour is well progressed, vaginal examination may feel the baby’s ribs, and an arm may sometimes prolapse. Caesarean delivery is always required unless a doctor or midwife can turn the baby head-down.
- Multiple pregnancies are always at high risk of malpresentation. Mothers need greater antenatal care, and twins are more prone to complications associated with low birth weight and prematurity.
- Any presentation other than vertex after 34 weeks of gestation is considered as high risk to the mother and to her baby. Do not attempt to turn a malpresenting or malpositioned baby! Refer the mother for emergency obstetric care.
Self-Assessment Questions (SAQs) for Study Session 8
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 8.1 (tests Learning Outcomes 8.1, 8.2 and 8.4)
Which of the following definitions are true and which are false? Write down the correct definition for any which you think are false.
A Fundus — the ‘rounded top’ and widest cavity of the uterus.
B Complete breech — where the legs are bent at both hips and knee joints and are folded underneath the baby.
C Frank breech — where the breech is so difficult to treat that you have to be very frank and open with the mother about the difficulties she will face in the birth.
D Footling breech — when one or both legs are extended so that the baby presents ‘foot first’.
E Hypoxia — the baby gets too much oxygen.
F Multiple pregnancy — when a mother has had many babies previously.
G Monozygotic twins — develop from a single fertilised ovum (the zygote). They can be different sexes but they share the same placenta.
H Dizygotic twins — develop from two zygotes. They have separate placentas, and can be of the same sex or different sexes.
A is true. The fundus is the ‘rounded top’ and widest cavity of the uterus.
B is true. Complete breech is where the legs are bent at both hips and knee joints and are folded underneath the baby.
C is false . A frank breech is the most common type of breech presentation and is when the baby’s legs point straight upwards (see Figure 8.4).
D is true. A footling breech is when one or both legs are extended so that the baby presents ‘foot first’.
E is false . Hypoxia is when the baby is deprived of oxygen and risks permanent brain damage or death.
F is false. Multiple pregnancy is when there is more than one fetus in the uterus.
G is false. Monozygotic twins develop from a single fertilised ovum (the zygote), and they are always the same sex , as well as sharing the same placenta.
H is true. Dizygotic twins develop from two zygotes, have separate placentas, and can be of the same or different sexes.
SAQ 8.2 (tests Learning Outcomes 8.1 and 8.2)
What are the main differences between normal and abnormal fetal presentations? Use the correct medical terms in bold in your explanation.
In a normal presentation, the vertex (the highest part of the fetal head) arrives first at the mother’s pelvic brim, with the occiput (the back of the baby’s skull) pointing towards the front of the mother’s pelvis (the pubic symphysis ).
Abnormal presentations are when there is either a vertex malposition (the occiput of the fetal skull points towards the mother’s back instead towards of the pubic symphysis), or a malpresentation (when anything other than the vertex is presenting): e.g. breech presentation (buttocks first); face presentation (face first); brow presentation (forehead first); and shoulder presentation (transverse fetal).
SAQ 8.3 (tests Learning Outcomes 8.3 and 8.5)
- a. List the common complications of malpresentations or malposition of the fetus at full term.
- b. What action should you take if you identify that the fetus is presenting abnormally and labour has not yet begun?
- c. What should you not attempt to do?
- a. The common complications of malpresentation or malposition of the fetus at full term include: premature rupture of membranes, premature labour, prolonged/obstructed labour; ruptured uterus; postpartum haemorrhage; fetal and maternal distress which may lead to death.
- b. You should refer the mother to a higher health facility – she may need emergency obstetric care.
- c. You should not attempt to turn the baby by hand. This should only be attempted by a specially trained doctor or midwife and should only be done at a health facility.
SAQ 8.4 (tests Learning Outcomes 8.4 and 8.5)
A pregnant woman moves into your village who is already at 37 weeks gestation. You haven’t seen her before. She tells you that she gave birth to twins three years ago and wants to know if she is having twins again this time.
- a. How would you check this?
- b. If you diagnose twins, what would you do to reduce the risks during labour and delivery?
- Is the uterus larger than expected for the period of gestation?
- What is its shape – is it round (indicative of twins) or heart-shaped (as in a singleton pregnancy)?
- Can you feel more than one head?
- Can you hear two fetal heartbeats (two people listening at the same time) with at least 10 beats difference?
- If there is access to a higher health facility, and you are still not sure, try and get the woman to it for an ultrasound scan.
- Be extra careful to check that the mother is not anaemic.
- Encourage her to rest and put her feet up to reduce the risk of increased blood pressure or swelling in her legs and feet.
- Be alert to the increased risk of pre-eclampsia.
- Expect her to go into labour before term, and be ready to get her to the health facility before she goes into labour, going with her if at all possible.
- Get in early touch with that health facility to warn them to expect a referral from you.
- Make sure that transport is ready to take her to a health facility when needed.
Except for third party materials and/or otherwise stated (see terms and conditions ) the content in OpenLearn is released for use under the terms of the Creative Commons Attribution-NonCommercial-Sharealike 2.0 licence . In short this allows you to use the content throughout the world without payment for non-commercial purposes in accordance with the Creative Commons non commercial sharealike licence. Please read this licence in full along with OpenLearn terms and conditions before making use of the content.
When using the content you must attribute us (The Open University) (the OU) and any identified author in accordance with the terms of the Creative Commons Licence.
The Acknowledgements section is used to list, amongst other things, third party (Proprietary), licensed content which is not subject to Creative Commons licensing. Proprietary content must be used (retained) intact and in context to the content at all times. The Acknowledgements section is also used to bring to your attention any other Special Restrictions which may apply to the content. For example there may be times when the Creative Commons Non-Commercial Sharealike licence does not apply to any of the content even if owned by us (the OU). In these stances, unless stated otherwise, the content may be used for personal and non-commercial use. We have also identified as Proprietary other material included in the content which is not subject to Creative Commons Licence. These are: OU logos, trading names and may extend to certain photographic and video images and sound recordings and any other material as may be brought to your attention.
Unauthorised use of any of the content may constitute a breach of the terms and conditions and/or intellectual property laws.
We reserve the right to alter, amend or bring to an end any terms and conditions provided here without notice.
All rights falling outside the terms of the Creative Commons licence are retained or controlled by The Open University.
Head of Intellectual Property, The Open University

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Lie, Presentation, Position, Attitude and Denominator
Published by Annabel McCoy Modified over 5 years ago
Similar presentations
Presentation on theme: "Lie, Presentation, Position, Attitude and Denominator"— Presentation transcript:
Malposition of the fetal head By dr. sallama kamel
The mechanism of normal labour By Dr. sallama kamel
Anatomy of normal pelvis & Fetal skull
Definition: Childbirth is the period from the onset of regular uterine contractions until expulsion of the placenta..
MECHANISM OF LABOUR (NORMAL & ABNORMAL)
Chapter 22: processes and stages of labor and birth
Antenatal care X iu Xiu Jiang. Terms Fetal lie Fetal lie the relationship of the long axis of the fetus to that of the mother. the relationship of the.
MALPRESENTATION &MALPOSITION.
Abnormal labor Li Ruzhi Ob&Gy Hospital, Fudan University.
Leopold’s - Abdominal Palpation for Fetal Position
DR. AHMED ABDULWAHAB Assistant Professor, Consultant OBGYN Department

Pregnancy and labor at fetal malpresentations and abnormal pelvis
Process and Stages of Labor and Birth Chapter 17.
Malpresentaton and Breech presentation. Definitions Position The relationship of a defined area on the presenting part to the mother’s pelvis (Denominator)
ABNORMAL PRESENTATIONS: SINCIPUT, BROW, FACE

MECHANISM OF LABOUR Lateefa Al Dakhyel FRCSC, FACOG Assistant professor & consultant Obstetric & gynecology department Collage of medicine King Saud University.
Abdominal Palpation for Fetal Position

Malpresentaion.
Giving Birth Chapter 17.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.

14 Practical Tips to Improve Your Presentation Skills
- The Speaker Lab
- May 11, 2024
Table of Contents
Ever felt complete dread and fear at the thought of stepping up to deliver a presentation? If so, you’re not alone. The fear of public speaking is more common than you might think, but with the right presentation skills , it’s a hurdle that can be overcome.
In this article, we’ll help you master basic confidence-building techniques and conquer advanced communication strategies for engaging presentations. We’ll explore how body language and eye contact can make or break your connection with your audience; delve into preparation techniques like dealing with filler words and nervous habits; discuss tailoring content for different audiences; and much more.
Whether you’re prepping for job interviews or gearing up for big presentations, being prepared is key. With adequate practice and the proper attitude, you can crush your speech or presentation!
Mastering the Basics of Presentation Skills
Presentation skills are not just about speaking in front of a crowd. It’s also about effective communication, audience engagement, and clarity. Mastering these skills can be transformative for everyone, from students to corporate trainers.
Building Confidence in Presentations
Becoming confident when presenting is no small feat. But fear not. Even those who feel jittery at the mere thought of public speaking can become masters with practice and patience. Just remember: stage fright is common and overcoming it is part of the process towards becoming an effective presenter.
Taking deep breaths before you start helps calm nerves while visualizing success aids in building confidence. Also, know that nobody minds if you take a moment to gather your thoughts during your presentation—everybody minds more if they cannot understand what you’re saying because you’re rushing.
The Role of Practice in Enhancing Presentation Skills
In line with old wisdom, practice indeed makes perfect, especially when improving presentation skills. Consistent rehearsals allow us to fine-tune our delivery methods like maintaining eye contact or controlling body language effectively.
You’ll learn better control over filler words through repeated drills. Plus, the extra practice can help you troubleshoot any technical glitches beforehand, saving you the sudden panic during your actual presentations.
Remember that great presenters were once beginners too. Continuous effort will get you there sooner rather than later.
Find Out Exactly How Much You Could Make As a Paid Speaker
Use The Official Speaker Fee Calculator to tell you what you should charge for your first (or next) speaking gig — virtual or in-person!
Body Language and Eye Contact in Presentations
The effectiveness of your presentation can hinge on more than just the words you say. Just as important is your body language .
Impact of Posture on Presentations
Your posture speaks volumes before you utter a word. Standing tall exudes confidence while slouching could signal nervousness or lack of preparation.
If there’s one lesson to take away from our YouTube channel , it’s this: good presenters know their message but great ones feel it through every fiber (or muscle) of their being. The audience can sense that energy when they see open body language rather than crossed arms.
Maintaining Eye Contact During Your Presentation
Eyes are often called windows to the soul for a reason. They’re communication powerhouses. Making eye contact helps build trust with your audience members and keeps them engaged throughout your speech.
Avoid staring at note cards or visual aids too much as this might give an impression that you’re unprepared or uncertain about your chosen topic. Instead, aim to maintain eye contact between 50% of the time during presentations. This commonly accepted “50/70 rule” will help you exhibit adequate confidence to your audience.
If stage fright has gotten a hold on you, take deep breaths before you start speaking in order to stay calm. Make sure that fear doesn’t disrupt your ability to maintain eye-contact during presentations.
If body language and eye contact still feel like a lot to manage during your big presentation, remember our golden rule: nobody minds small mistakes. It’s how you handle questions or mishaps that truly makes a difference—so stay positive and enthusiastic.
Preparation Techniques for Successful Presentations
Presentation skills are like a craft that requires meticulous preparation and practice. Aspects like visual aids and time management contribute to the overall effectiveness of your delivery.
The first step towards delivering an impactful presentation is research and organization. The content should be well-researched, structured logically, and presented in simple language. This will make sure you deliver clear messages without any room for misinterpretation.
Dealing with Filler Words and Nervous Habits
Nervous habits such as excessive use of filler words can distract from your message. Luckily, there are plenty of strategies that can address these issues. For instance, try taking deep breaths before speaking or using note cards until fluency is achieved. In addition, practice regularly to work on eliminating these verbal stumbling blocks.
Avoiding Distractions During Presentations
In a digital age where distractions abound, maintaining focus during presentations has become an even more crucial part of the preparation process. This video by motivational speaker Brain Tracy provides insights on how one could achieve this level of focus required for effective presentations.
Maintaining Confidence Throughout Your Presentation
Confidence comes from thorough understanding of the chosen topic combined with regular practice sessions before the big day arrives. Make use of note cards or cue cards as needed but avoid reading from them verbatim.
Taking control over stage fright starts by arriving early at the venue so that you familiarize yourself with the surroundings, which generally calms nerves down considerably. So next time you feel nervous before a big presentation, remember—thorough preparation can make all the difference.
Engaging Your Audience During Presentations
Connecting with your audience during presentations is an art, and mastering it can take your presentation skills to the next level. Making the message conveyed reach an emotional level is essential, not just conveying facts.
Understanding Your Target Audience
The first step towards engaging your audience is understanding them. Tailor the content of your presentation to their needs and interests. Speak in their language—whether that be professional jargon or everyday slang—to establish rapport and ensure comprehension.
An effective presenter understands who they’re speaking to, what those individuals care about, and how best to communicate complex ideas understandably.
Making Complex Information Understandable
Dense data or complicated concepts can lose even the most interested listener if presented ineffectively. Breaking your key points down into manageable chunks helps maintain attention while promoting retention. Analogies are especially useful for this purpose as they make unfamiliar topics more relatable.
Audience Participation & Questions: A Two-Way Street
Incorporating opportunities for audience participation encourages engagement at another level. It allows listeners to become active participants rather than passive receivers of knowledge.
Consider techniques like live polls or interactive Q&A sessions where you invite questions from attendees mid-presentation instead of saving all queries until the end.
This gives you a chance not only engage but also address any misunderstandings right on spot.
- Treat each question asked as an opportunity—it’s evidence someone has been paying attention. Even challenging questions should be welcomed as they demonstrate an engaged, thoughtful audience.
- Encourage participation. It can be as simple as a show of hands or the use of interactive technologies for live polling during your presentation. This keeps your audience active and invested in the content.
Remember, your presentation isn’t just about putting on a show—it’s about meaningful interaction.
Free Download: 6 Proven Steps to Book More Paid Speaking Gigs in 2024
Download our 18-page guide and start booking more paid speaking gigs today!
Presentation Skills in Specific Contexts
Whether you’re nailing your next job interview, presenting an exciting marketing campaign, or delivering insightful educational content, the context matters. Let’s take a look.
The Art of Job Interviews
A successful job interview often hinges on effective communication and confidence. Here, the target audience is usually small but holds significant influence over your future prospects. Body language plays a crucial role; maintain eye contact to show sincerity and interest while open body language communicates approachability.
Bullet points summarizing key experiences are also helpful for quick recall under pressure. This allows you to present your chosen topic with clarity and positive enthusiasm without relying heavily on note or cue cards.
Pitching in Public Relations & Marketing
In public relations (PR) and marketing contexts, presentations need to capture attention quickly yet hold it long enough to deliver key messages effectively. Visual aids are valuable tools here—they help emphasize points while keeping the audience engaged.
Your aim should be highlighting presentation benefits that resonate with potential clients or partners, making them feel as though ignoring such opportunities would mean missing out big time.
Educational Presentations
An educational setting demands its own unique set of presentation skills where deep understanding trumps flashy visuals. You must make complex information understandable without oversimplifying essential details—the use of analogies can be beneficial here.
Keeping the audience’s attention is critical. Encourage questions and participation to foster a more interactive environment, enhancing learning outcomes for all audience members.
Tips for Becoming a Great Presenter
No single method is suitable for everyone when it comes to speaking in public. However, incorporating continuous improvement and practice into your routine can make you an exceptional presenter.
Tailor Your Presentation to Your Audience
Becoming an excellent speaker isn’t just about delivering information; it’s also about making a connection with the audience. So make sure that you’re taking setting, audience, and topic into consideration when crafting your presentation. What works for one audience may not work for another, so be sure to adapt your presentation styles according to the occasion in order to be truly effective.
The Power of Practice
The art of mastering public speaking skills requires practice —and lots of it . To become a great presenter, focus on improving communication skills through practice and feedback from peers or mentors. Try to seek feedback on every speech delivered and incorporate those pointers in your future presentations. Over time, this cycle of delivery-feedback-improvement significantly enhances your ability to connect with audiences and convey ideas effectively.
If you’re looking for examples of good speakers, our speech breakdowns on YouTube provide excellent examples of experienced presenters who masterfully utilize speaking techniques. Analyzing their strategies could give you great ideas for enhancing your own style.
Finding Your Style
A crucial part of captivating any audience lies in how you deliver the message rather than the message itself. Developing a unique presentation style lets you stand out as an engaging speaker who commands attention throughout their talk. Through — you guessed it — practice, you can develop a personal presentation style that resonates with listeners while showcasing your expertise on the chosen topic.
Your body language plays a pivotal role here: open gestures communicate confidence and enthusiasm towards your subject matter, two qualities essential for keeping audiences hooked. Similarly, using vocal variety adds dynamism to speeches by emphasizing points when needed or creating suspense during storytelling parts of your talk.
Cultivating Passion & Enthusiasm
Showcasing genuine passion for the subject helps keep listeners engaged throughout even lengthy presentations. Sharing stories related to the topic or expressing excitement about sharing knowledge tends to draw people in more than mere data recitation ever could.
Recognize that everybody is distinctive; don’t expect identical results from every speaker. The path to becoming a great presenter involves recognizing your strengths and working tirelessly on areas that need improvement.
FAQs on Presentation Skills
What are good presentation skills.
Good presentation skills include a clear message, confident delivery, engaging body language, audience understanding, and interaction. They also involve effective preparation and practice.
What are the 5 steps of presentation skills?
The five steps of presenting include: planning your content, preparing visual aids if needed, practicing the delivery aloud, performing it with confidence, and finally post-presentation reflection for improvements.
What are the 5 P’s of presentation skills?
The five P’s stand for Preparation (researching your topic), Practice (rehearsing your talk), Performance (delivering with confidence), Posture (standing tall), and Projection (using a strong voice).
What are your presentation skills?
Your personal set of abilities to deliver information effectively is what we call your presentation skill. It can encompass public speaking ability, clarity in speech or writing as well as visual communication talent.
Mastering presentation skills isn’t an overnight process, but practice and perseverance will put you well on your way to becoming an effective speaker.
You’ve learned that confidence plays a crucial role in effective presentations, so take deep breaths, make eye contact, and keep your body language open. As always, preparation is key. Tackle filler words head-on and get comfortable with visual aids for impactful storytelling.
Remember the importance of audience engagement — it’s all about understanding their needs and tailoring your content accordingly. This way, complex information turns into digestible insights.
Above all else: practice! After all, nothing beats experience when it comes to improving public speaking abilities.
- Last Updated: May 9, 2024

Explore Related Resources
Learn How You Could Get Your First (Or Next) Paid Speaking Gig In 90 Days or Less
We receive thousands of applications every day, but we only work with the top 5% of speakers .
Book a call with our team to get started — you’ll learn why the vast majority of our students get a paid speaking gig within 90 days of finishing our program .
If you’re ready to control your schedule, grow your income, and make an impact in the world – it’s time to take the first step. Book a FREE consulting call and let’s get you Booked and Paid to Speak ® .
About The Speaker Lab
We teach speakers how to consistently get booked and paid to speak. Since 2015, we’ve helped thousands of speakers find clarity, confidence, and a clear path to make an impact.
Get Started
Let's connect.
Copyright ©2023 The Speaker Lab. All rights reserved.
Cutting sugar cane stalks, not burning them, could make money, Belle Glade officials told

The practice of cutting off the tough outer husks of sugar cane stalks as an alternative to burning them off in pre-harvest fires has been adopted almost everywhere the crop is grown.
Known as "green harvesting," it has become part of the production process for sugar industries in Brazil, Australia, Zimbabwe, Belize, Thailand, India and in the Glades, Belle Glade resident Steve Messam told Belle Glade city commissioners this week.
Used in U.S. Sugar's fields bordering a Walmart in Clewiston as well as in Florida Crystal's fields where sugar labeled organic is grown, the method, Messam said, turns the “trash” on the sugar-cane stalks into “treasure,” including fuel, biodegradable products ... and jobs.
More: Burning sugar cane pollutes communities of color in Palm Beach County. Brazil shows another way.
“If you can do it in some fields, you can do it in more fields,” he said during Monday's commission meeting. “It’s a win for the environment, a win for industry, and a win for the economy.”
'We want to present a solution'
Messam is a local pastor, businessman and member of the “ Stop the Burn ” campaign, an effort that for seven years has worked to draw attention to the harmful effects to health and property that the industry’s eight months of preharvest fires each year inflict on the community.
Last year a long-term study led by researchers at Florida State University showed that pollution released by the smoke shortens the lives of people living near fires. Soot that falls from the sky in the wake of the fires settles on the cars, homes and property of Glades residents who have come to call it “Black Snow.”
Those effects and what Stop the Burn calls the failure of Palm Beach County officials to address them have been the subject of protest rallies by the campaign.
More: Sugar cane fire pollution kills up to three South Floridians yearly, study finds
The focus of this presentation was the good that doing things differently could bring to the community. It included a list of companies interested in working with the industry to turn the “trash” into profitable products.
“We don’t just want to highlight the problem,” Messam said. “We want to present a solution.”
Belle Glade Mayor Steve Wilson, who lobbied in Tallahassee for a law to prevent people most harmed by smoke from sugar cane fires from suing the industry, said he appreciated that.
What he hadn’t liked, he added, was “the negativity” of some of the Stop the Burn campaign’s arguments, which, he said, included discussion of studies saying that smoke from sugar-cane fires was “causing people to die.”
“That’s not the case,” said Wilson, who added that he had never seen the FSU study that linked one to six premature deaths a year in South Florida to breathing air polluted by sugar cane fire smoke.
“It isn’t untrue,” Messam assured him. Wilson accepted Messam’s offer to send him the study.
More: Why Palm Beach County's health department hasn't sounded the alarm on sugar-cane burning
One Belle Glade commissioner says 'We can do it here' on green harvesting; another says it will cost jobs
Commissioner Mary Ross Wilkerson, who has served on the city body since 2009, said she, too, had been a critic of the Stop the Burn campaign until recently, when she learned that green harvesting is already in use in the Glades.
“I also heard it cost jobs. Green harvesting doesn’t cost jobs,” she said. “I had to see it for myself. We can do it here.”
Commissioner Zayteck Marin, elected in March 2023, however, argued that green harvesting would cost jobs and more. Paging through reams of notes, she referred repeatedly to the sugar industry with the pronoun “we,” and noted that with a husband who works for a sugar company, she feels a part of it as well.
The cost of expanding green harvesting, she said, would necessitate massive layoffs.
While saying that workers depending on those jobs “can’t just pick up and leave,” Marin also asserted that green harvesting would drive workers from the community, leaving their homes up for grabs.
“It’s all about gentrification,” she said, predicting: “Palm Beachers are going to come for land, to build things we can’t afford.”
All of that cost and loss were unnecessary, she said, noting that all sugar cane fires require a permit, which would not be granted if smoke from the fires presented a threat.
Permits are not granted, Messam noted, when prevailing winds will blow the smoke and ash east toward whiter and wealthier communities.
Post/ProPublica investigation The smoke comes every year. Sugar companies say the air is safe.
'To move into the future by improving the quality of life'
“I’m hoping a dialogue between the industry and those companies and even our group will follow this,” Messam said. “In almost seven years, we have yet to get a meeting with anyone in the industry.”
A Florida Crystals representative responded to a request for comment with an email noting that the company has used the method to harvest its organic sugar cane for 30 years.
"In addition to the food products we make, Florida Crystals uses the plant fiber to produce renewable energy to power our operations," the company's statement said. "Our biomass renewable energy facility, operational since 1996, is one of the largest of its kind in the country with additional renewable electricity sold to Florida’s power grid. We also use our fiber to make sustainable molded fiber tableware products. The tableware business was developed after many years of research and includes an eco-friendly, proprietary process and has resulted in a major investment in the Glades communities over the past eight years."
U.S. Sugar, which uses green harvesting in fields bordering the Walmart in Clewiston, did not respond to a request for comment.
Messam says he believes making the most of green harvesting would be in keeping with Belle Glade’s mission statement, which he quoted at the start of his presentation:
“To move into the future by improving the quality of life and promoting growth through economic diversification and development of human and natural resources while providing a safe and healthy environment.”
“Why not,” Messam said, “allow the Glades to be the Silicone Valley of green energy?”
Antigone Barton is a reporter with The Palm Beach Post. You can reach her at [email protected] . Help support our work: Subscribe today .
Advertisement
Who Was President Ebrahim Raisi of Iran?
Mr. Raisi had been seen as a possible successor to Ayatollah Ali Khamenei as supreme leader, the highest political and religious position in the Islamic republic.
- Share full article

By Emma Bubola
- Published May 19, 2024 Updated May 20, 2024, 4:41 a.m. ET
Ebrahim Raisi, 63, a hard-line religious cleric, was elected president of Iran in 2021. In his tenure as president, he oversaw a strategy to expand his country’s regional influence — backing militant proxies across the Middle East, expediting the country’s nuclear program and bringing Iran to the brink of war with Israel.
But in the same period, Iran experienced some of its largest antigovernment protests in decades and a severe economic downturn driven by international sanctions and high unemployment.
Mr. Raisi’s background
Mr. Raisi, born in the eastern city of Mashhad in 1960 to a devoutly religious family, was swept up in the fervor of Iran’s Islamic Revolution, which toppled the country’s monarchy in 1979.
As a religious scholar in Iran’s theocratic government and a protégé of Ayatollah Khamenei, Mr. Raisi climbed the ranks of the judiciary, serving as a prosecutor in several cities.
After being named Iran’s top judge, he was believed to have been part of a small committee that ordered the executions of thousands of political dissidents in 1988.
Accused of decades of human rights violations, Mr. Raisi had been the subject of punishing sanctions by the United States.
His presidency
During Mr. Raisi’s presidency, Iran faced large antigovernment protests after the death of a young Kurdish woman, Mahsa Amini, in police custody. The authorities responded with a brutal crackdown that included killings and executions.
Tehran has also continued its uranium-enrichment program and has gone ahead with its ballistic missile program .
A yearslong shadow war with Israel burst into the open last month after Iran launched a salvo of hundreds of missiles and drones at Israel. That attack resulted from escalating tensions between the two countries after Hamas, an Iranian-backed militant group, raided Israel on Oct. 7.
In the same period, Iran has also emerged as Russia’s trusted foreign supplier of military drones . Last year Iran made a deal with Saudi Arabia and restored diplomatic relationships.
Emma Bubola is a Times reporter based in London, covering news across Europe and around the world. More about Emma Bubola

COMMENTS
Presentation refers to the part of the fetus's body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way. Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput ...
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
The next step in the assessment of the fetus consists of determining the position of the presenting part. This is a description of the relation of the presenting part of the fetus to the maternal pelvis. In the case of a longitudinal lie with a vertex presentation, the occiput of the fetal calvarium is the landmark used to describe the position.
compound presentation—when any other part presents along with the fetal head; Related obstetrical terms Attitude. Definition: Relationship of fetal head to spine: flexed, (this is the normal situation) neutral ("military"), extended. hyperextended; Position. Relationship of presenting part to maternal pelvis based on presentation.
The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet. ... This is called cephalic presentation. This position makes it easier and safer for your baby to pass through the birth canal. Cephalic ...
Palpate the lower abdomen to identify the presenting part of the fetus (e.g., "The fetal buttocks are presenting at the inlet.") Note the position of the presenting part in relation to the mother's pelvis (e.g., "The presenting part is in a transverse lie.") Step 4: Identification of the Fetal Part in the Pelvic Cavity
Fetal presentation and position During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Presentation. This describes that part on the fetus lying over the inlet of the pelvis or at the cervical os. Point of Reference or Direction. This is an arbitrary point on the presenting part used to orient it to the maternal pelvis [usually occiput, mentum (chin) or sacrum]. Position.
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Face presentation - an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations. [1] [2] [3]
Compound presentation is a fetal presentation in which an extremity presents alongside the part of the fetus closest to the birth canal. The majority of compound presentations consist of a fetal hand or arm presenting with the head [ 1 ]. This topic will review the pathogenesis, clinical manifestations, diagnosis, and management of this ...
The Trusted Provider of Medical Information since 1899
The vertex presentation describes the orientation a fetus should be in for a safe vaginal delivery. It becomes important as you near your due date because it tells your pregnancy care provider how they may need to deliver your baby. Vertex means "crown of the head.". This means that the crown of the fetus's head is presenting towards the ...
Presentation refers to which part of your baby's body is facing towards your birth canal. Position refers to the direction your baby's head or back is facing. Your baby's presentation will be checked at around 36 weeks of pregnancy. Your baby's position is most important during labour and birth.
Breech Presentations. Breech presentation happens when your little one's feet or buttocks are in position to be delivered first, and make up just under 5 percent of all pregnancies. Your provider will likely order an ultrasound toward the end of your pregnancy if they suspect your baby is in a breech position.
presentation, in childbirth, the position of the fetus at the time of delivery. The presenting part is the part of the fetus that can be touched by the obstetrician when he probes with his finger through the opening in the cervix, the outermost portion of the uterus, which projects into the vagina. In nearly all deliveries the presenting part ...
(b) Each presenting part has the possibility of six positions. They are normally recognized for each position-using "occiput" as the reference point. 1 Left occiput anterior (LOA). 2 Left occiput posterior (LOP). 3 Left occiput transverse (LOT). 4 Right occiput anterior (ROA). 5. Right occiput posterior (ROP). 6 Right occiput transverse ...
8.1 Normal and abnormal presentations 8.1.1 Vertex presentation. In about 95% of deliveries, the part of the fetus which arrives first at the mother's pelvic brim is the highest part of the fetal head, which is called the vertex (Figure 8.1).This presentation is called the vertex presentation.Notice that the baby's chin is tucked down towards its chest, so that the vertex is the leading ...
1 Lie, Presentation, Position, Attitude and Denominator. 2 Lie The lie refers to the relationship of the longitudinal axis of the fetus to long axis of maternal spine. Lie - 1.Vertical or Longitudinal (99.5%) 2.Transverse 3.Oblique. 3 Lie Longitudinal:- when long axis of the foetus corresponds to the long axis of the mother.
Take a positive approach. Practice your delivery. Use nonverbal communication. Create visuals. End strongly. 1. Ask for guidance. Before developing your presentation, ask the hiring manager for any clarification you may need. First, read and review all the instructions you received about the presentation.
Whether you're nailing your next job interview, presenting an exciting marketing campaign, or delivering insightful educational content, the context matters. Let's take a look. The Art of Job Interviews. A successful job interview often hinges on effective communication and confidence.
Summary: The program manager, as program team coordinator, is responsible for leading the extended cross-functional program team to ensure real-time sharing of information and team cohesion around common objectives. The program manager is responsible for delivering the Program objectives through the Safran PROMPT process, managing program performance, risks, product configuration and ...
The State Hygienic lab (SHL) celebrated Medical Laboratory Professionals Week or Lab week on April 15-19th 2024, to show appreciation to its hardworking staff. It is a week where laboratorians and all lab staff take a break from the demands of the job to participate in fun activities and events. The
Known as "green harvesting," it has become part of the production process for sugar industries in Brazil, Australia, Zimbabwe, Belize, Thailand, India and in the Glades, Belle Glade resident Steve ...
Mr. Raisi has been seen as a possible successor to Ayatollah Ali Khamenei as supreme leader, the highest political and religious position in the Islamic republic. By Emma Bubola Ebrahim Raisi, 63 ...