
PEOP Model: Fundamentals in OT Practice
- Mandy Chamberlain MOTR/L
By our very nature and the influence of our educational background, occupational therapists have to take a wholesome approach in therapeutic intervention. This means looking beyond the patient or client’s medical limitations and considering outside-of-the-box barriers and enablers related to occupational success. One of the dozen theoretical models that OTs learn in school that provides a basis for such a mindset is the Person-Environment-Occupation Performance or PEOP Model .
In this post, we will give a basic overview of what the PEOP model entails, give a PEOP example so you can understand how it is applied in occupational therapy practice and then talk a little bit about the pros and cons of the model.
Overview: What is PEOP?
The first thing to understand is that the PEOP model of occupational therapy (Christiansen and Baum, 1985) and the PEO model (Law et al., 1996) are not synonymous. Although both models have some similarities, PEOP holds to a handful of different principles.
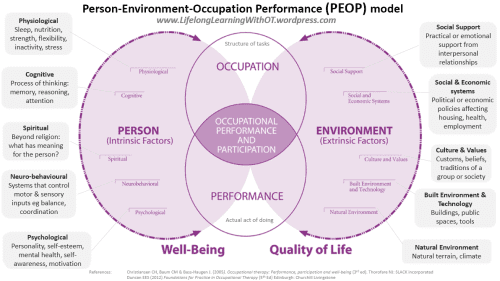
The PEOP model highlights occupational performance as its key feature, which is made up of three interacting components (ach of their detailed characteristics which are listed in the previous image):
- person (client),
- environment, and
- occupation (i.e. activity, role, or task)
Inevitably, environmental factors will impact a person for better or for worse which determines the occupational performance outcome. If there is a healthy interaction between the person and their environment, then the person will experience success and improved well-being in occupational performance (Baum et al., 2015).
Since its original development in 1985, several revisions have been made to make PEOP more client-centered. This means that through a collaborative and supportive relationship between the client and the practitioner, the client’s needs and goals are highly vocalized and used in personal narrative form to determine the course of therapeutic care.
PEOP Model Example
Confused yet?
Below, we have created a practical case study in which the PEOP model is applied to see how it can be applied in practice:
Diana is a 54-year old patient who was admitted for a short hospital stay following a ground-level fall. She was attempting to transfer from her powered wheelchair to her bed at home when she slipped, resulting in a minor left shoulder fracture. After her hospital stay, she was admitted to a skilled nursing facility for further rehabilitation. She also has primary-progressive multiple sclerosis. Although she can stand for brief periods to perform transfers, she relies heavily on her powered wheelchair to get around at home and in the community. Diana’s priority goal is to get her left shoulder stronger so she can still perform her own transfers safely at home.
Through a comprehensive evaluation and collaborative conversations, Diana’s OT can identify factors in all three components of Diana’s overall occupational performance:
Environment
Social support:.
Diana lives at home with her husband, who is retired and acts as her primary caregiver. However, her husband is aging and frail and struggles with physically helping Diana get around. She has two children who live out of state and rarely visit her.
Social and economic systems:
Diana has been medically involved in the healthcare system for many years. She has Medicare A, Medicare B, and a supplemental HMO insurance plan.
Culture and values:
Diana strongly values her own independence. She is also a devout catholic who attends church on a regular basis.
Built environment and technology:
Diana lives in a single-level townhome and owns a wheelchair ramp, a powered wheelchair, a shower chair, a transfer board, a walker, a fall alert home system, and a toilet riser. She also has grab bars installed throughout her home.
Natural environment:
Diana and her husband live in a city in the U.S. with easy access to flat terrain with sidewalks and other wheelchair accessible surfaces.
Physiological:
Due to MS, Diana fatigues easily and has overall low muscle tone and body strength. The nature of her left shoulder fracture limits her range of motion and strength in upper extremity use.
Diana has experienced some mild memory deficits within the last few years.
Diana regularly attends catholic services and goes to bible study as often as possible.
Neuro-behavioral:
Due to MS, Diana has reduced sitting and standing balance as well as decreased sensation in her feet.
Psychological:
Although Diana is highly motivated to participate in therapy, she does have clinical depression.
After examining all of Diana’s unique environmental and personal factors, she, with the help of her OT, can create a tailored intervention plan to help her meet her functional transfer goals.
Pros to PEOP
- The emphasis on a client-centered approach allows the patient or client to develop goals for themselves based on their individual wants and needs.
- The comprehensive model lists out a wide array of factors that many OTs (especially new therapists) may not otherwise consider in intervention.
- It’s a very top-down approach, which takes the focus away from the client’s medical barriers and acknowledges both limitations and enablers in the client’s overall occupational performance.
PEOP Model Limitations
- According to the authors Christiansen and Baum (2015), there is currently no assessment tool that measures outcomes based on the PEOP model. So OTs are on their own using other tools to obtain relevant client information.
- Like a number of therapeutic models, PEOP could use additional evidence-based research to better support its principles in clinical practice.
We have also discussed a number of other occupational therapy models throughout the website including the Biopsychosocial Model here.

Baum, C. M., Christiansen, C. H., & Bass, J. D. (2015). The Person-Environment-Occupation- Performance (PEOP) model. In C. H. Christiansen, C. M. Baum, & J. D. Bass (Eds.), Occupational therapy: Performance, participation, and well-being (4th ed., pp. 49-56). Thorofare, NJ: SLACK Incorporated.
Occupation Models: PEOP (Person-Environment-Occupation Performance) (2015). Lifelong Learning in OT. https://lifelonglearningwithot.wordpress.com/tag/peop-model/ . Viewed on January 30, 2020.
Post by Meredith D. Chandler, OTR/L, Freelance Content Writer and Mandy Chamberlain MOTR/L
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

Learn👇 how to write OT goals that WON’T be denied & make treatment planning easier!
Medbridge promo code: FLOURISH for $150 off unlimited CEUs

OccupationalTherapy.com promo code: FLOURISH13 & get 1 extra month FREE of unlimited CEUs
- Privacy Overview
- Strictly Necessary Cookies
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
Case Studies for Contemporary OT Practice
Already purchased? Please sign in to view.
Do you need to re-use or reproduce this work?
current document all documents
Advanced search
Table of Contents
- Table of Contents v 6
Remember login
Enable two-factor authentication codes.
Forgot password
Please log in to view your account information. Don't have any account? You can register for one now.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Occupational Therapy Case Study

- identified the PICO components of your patient scenario,
- formulated a clinical question,
- found an appropriate article to answer your question,
- and critically appraised the article.
Now, it’s time to apply what you’ve learned to your patient.
For an accessible version of this activity, please refer to our document Step 4: Apply – Accessible Case Studies .
Evidence-Based Practice Copyright © by Various Authors - See Each Chapter Attribution is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.

You are here
Case study template.
- Occupational Therapy - Case Study Guidelines
QMU Occupational Therapy - Case Study Guidelines
Case Study Guidelines
Introduction
This is a brief guide to the content of a case study. The individual selected for case study may be considered in terms of an Occupational Therapy Model/ Approach to practice and also the wider environments and networks that play a role in a person’s life.
This guide is created with an individual in mind but may also be used for a group, community or population that you have worked with. RCOT have an interesting case study template: Royal Collage of Occupational Therapy which they used for one of their influencing campaigns. You may find it useful if you are presenting work you have done with a group, community or population rather than an individual service user.
Mandatory for all case studies
Anonymity and confidentiality of the service user(s), service provider and all staff involved must be maintained through out the case study . You are advised to use pseudonyms, delete the name of service and any geographical locations.
Consider how your case study will demonstrate or include the points below:
- Identify a main focus (why are you writing this, what do you want to learn from this?)
- Wider context - How does this impact on the OT process?
- Service user involvement – How did you facilitate them to work in partnership with you? What was important to them?
- Critical engagement - Rationales for choices/ decisions made throughout the OT process must be detailed, and include a balanced critique (i.e. pro’s and con’s)
- Evidence - Support your work with literature and other resources available to you i.e. reading, useful placement resources, theory, policy and other documents
- How will you present your case study to your team? Consider different media (PowerPoint, video diary, photo’s, end products).
- Consider facilitating the person to present their case with you.

Copyright © 2024 OccupationalTherapy.com - All Rights Reserved
Pediatric Case Study: Child with ADHD
Nicole quint, dr.ot, otr/l.
- Early Intervention and School-Based
To earn CEUs for this article, become a member.
unlimit ed ceu access | $129/year
Attention deficit hyperactivity disorder (adhd).
Hello everyone. Today, we are going to be talking about attention deficit hyperactivity disorder. I consider this to be under the umbrella of "invisible diagnoses." This population has a special place in my heart because it is very easy to misconstrue some of the challenges that they have as intentional and behavior-based, and therefore, sometimes they get a bad rap. Thus, I am always happy to help kids with ADHD.
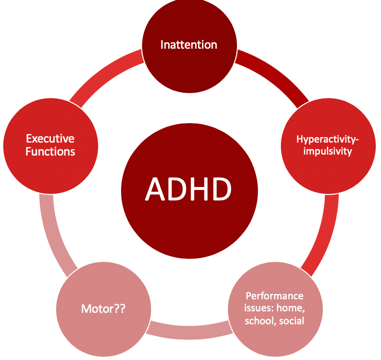
Figure 1. Overview of ADHD.
Individuals with ADHD have a lot of challenges that affect their occupational participation and performance. I think most of us are very comfortable with the idea that inattention, hyperactivity, and impulsivity are the hallmarks, but what sometimes can get lost is the idea that executive functions are very much affected by impulsivity. Motor issues are also often involved with kids with ADHD and are not always considered. In fact, there is a lot of evidence to support that the motor needs of these kids often go unaddressed. Typically, these kids come to us when parents or schools have major concerns about their behavior. Therefore, this tends to be where everyone focuses their attention. Oftentimes, the motor issues then fly under the radar and do not get addressed. The cool thing is that motor interventions can be the means to make some really significant changes for these kids, particularly in the area of executive function. There is a win-win situation when we address the motor issues. Lastly, they tend to also have performance issues not only in their home environment but also in their school and social environments as well.
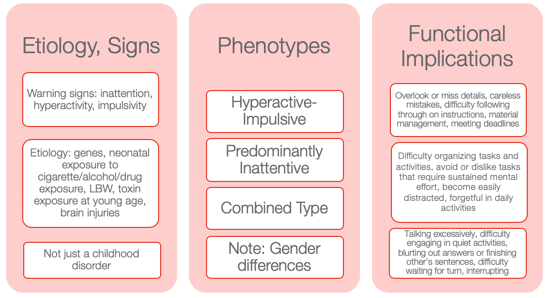
Figure 2. Other information from the NIMH Information Resource Center (2020).
I wanted to provide some information to help you to appreciate how diverse ADHD is. Many might still use ADD when we are talking about the children who have an inattentive type as it seems to make more sense. However, that is not how it is defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM–5).
Etiology and Signs
The etiology and the signs are inattention, hyperactivity, and impulsivity. We also know there is a genetic predisposition to this. Neonatal exposure to cigarettes, alcohol, and drugs can also lead to ADHD. Low birth weight and toxin exposure are some of the environmental elements. ADHD can also be the result of a brain injury. This is not just a childhood disorder, and people do not grow out of it. In fact, the symptoms can actually get worse as life gets harder as one gets older. Adults who have ADHD can have some significant struggles, particularly if they do not know that they have ADHD or if it was never addressed.
There are three phenotypes: hyperactive-impulsive type, predominantly inattentive type, and a combination type. I think the hyperactive-impulsive type is the picture most people have when they think of ADHD. Then, we have the predominantly inattentive type. These are the daydreamers or the individuals that jump from one thought to the next. They have a really hard time staying focused for long. Lastly, there is the combined type. This is where we see both elements of inattention and hyperactivity and/or impulsivity. I think it is really important to also appreciate gender differences. You can see very different types of ADHD in girls versus boys. Boys obviously tend to be of the hyperactive-impulsive type, but even the inattentive type can be a little different. Girls, who have ADHD, tend to be talkative and a little more anxious. They definitely have a different predisposition as opposed to the boys. Thus, it might be the same diagnosis but look very different between the genders.
Functional Implications
Functional implications become extremely important. These are individuals who tend to overlook or miss details. They might make careless mistakes. They have difficulty following through with directions at school. Material management can become very challenging especially dealing with paperwork. They can miss deadlines and have a hard time keeping track of and prioritizing tasks. These are some of the higher-level executive functions. You might also see an avoidance or an expressed dislike of tasks that require a significant amount of sustained mental effort. They might tell you it is too hard, and they might feel very overwhelmed. They become very easily distracted by anything. The use of electronics adds to the issue. They can be forgetful in daily activities, talk excessively, have difficulty engaging in quiet activities, and tend to blurt out answers or finish others' sentences. Often, the perception is they are interrupting and being rude. They may have difficulty waiting for their turn or interrupt during someone else's turn. These are examples of impulsive behaviors. We will talk more about this when we get to executive functions.
Differential Diagnosis Between ADHD and SPD
- A high rate of comorbidity between SMD and ADHD
- ADHD and SMD
- Both at risk for limited participation in many aspects of daily life
- ADHD slightly worse attention scores than SMD
- Tactile, taste/smell, and movement sensitivity, visual-auditory sensitivity; behavioral manifestations of sensory systems
- Exaggerated electrodermal responses to sensory stimulation, thus increased risk of sympathetic “fight or flight” reactions
(Miller et al., 2012; Yochman et al., 2013)
Sometimes, kids who have ADHD also have some sensory issues. You may wonder, "Do they have just ADHD by itself?" This is probably one of the most common questions I get when working with kids with ADHD whether it is from teachers, other therapists, or from parents. Next, we are going to be talking about a child who has straight ADHD. However, for a few minutes, I want to talk about the whole idea of differential diagnosis between ADHD and SPD and how this all fits together. There is a very high comorbidity between sensory modulation disorder and ADHD. When I am referring to sensory modulation disorder, I am using the Lucy Jane Miller nosology. Sensory modulation disorder refers to the over-responsive, under-responsive, and/or craving of sensory input. For both ADHD and sensory modulation disorder, you will see that these diagnoses are both at risk for limited participation. These are kids who will not participate in certain activities because the sensory input is too much or overwhelming for them. ADHD will have slightly worse attention scores than SMD when you complete a formal attention test like the Test of Everyday Attention. However, you will see the same kind of impulsive behaviors.
Those with sensory modulation disorders tend to have difficulty with tactile, taste, smell, and movement sensitivities. You might also see some visual-auditory sensitivity so there are some behavioral manifestations that come of that. They might become stressed related to fears of vestibular or other movement input. They might also dislike certain noises or touch.
They found in the research that sensory modulation dysfunction, not ADHD , will have an exaggerated electrodermal response to sensory stimulation. This means that they have an increased risk of sympathetic activation which is the fight-or-flight, freeze/faint reactions, and meltdowns. When you have a child with meltdowns, you want to investigate if they have sensory modulation dysfunction right away. And, if you have a child with ADHD who does not have a history of meltdowns, that is a really good sign of your initial hypothesis. While this alone does not mean that they do not a sensory modulation dysfunction, chances are that they do not. Additionally, they might have dyspraxia or a discrimination disorder.
This is just a brief summary of how this all comes to play with an ADHD diagnosis and possible comorbidities.
Case Introduction: Jeremy (Age 9, ADHD, Combined Type)
- He lives with his mother and older sister in SFH and goes to his father’s house on the weekend (divorced)
- He is in the 4th grade and has an IEP for OHI
- Strengths: funny, good at math, helps the family to take care of pets, watches WWE with father, loves dogs, likes to play board games (Monopoly, Sorry)
- School concerns: material management, organization, completing tasks or losing work , impulsive, social difficulties (short-lived relationships, fights), “lacks self-control” and “messy”, underperforming and sometimes seems “lost”
- Family concerns: Fights with a sibling, sleep difficulties, messy room, messy notebooks, and backpack, loses things, avoids homework, resists bedtime, difficult to wake in the morning and slow with routine , poor hygiene
- Jeremy’s goal: make friends, be able to find his schoolwork, have good friends, be better at kickball and wrestling
Jeremy is nine, and his diagnosis is ADHD, combined type. I have a feeling Jeremy is probably similar to a lot of the kids you see. I know I have seen a lot of these types of kids. He lives with his mother and older sister in a single-family home and goes to his father's house on the weekend because of a divorce. He is in the fourth grade, is eligible for an IEP because of an OHI (other health impairment), and is eligible for special education services because of his diagnosis of ADHD.
I always like to start with strengths with all kids, especially ADHD because these kids can have a really hard time with confidence and self-esteem. They also get blamed for their behaviors. For his strengths, he is funny, good at math, and he likes to help take care of his pets at home. He likes to watch wrestling, World Wrestling Federation (WWF) with his father, loves dogs, and loves to play board games. He is really good at Monopoly and Sorry.
At school, he had challenges with material management, organization, completing tasks, and not losing work. These last two are highlighted as we are going to focus on that. He is impulsive, and he has social difficulties. His teacher described his relationships as short-lived. He would have a friend, and then all of a sudden, they were not friends anymore. She also reported that he lacked self-control, was messy, and thought he underperformed. And, she felt like he always seemed lost. When they were going through the instructions or going through something, he was always looking at his peer's work or looking confused while he was trying to figure out what was going on.
The family had some concerns about his fighting with a sibling, significant sleep difficulties, a messy room, messy notebooks and backpack, and that he would often lose things. He also avoided his homework and resisted bedtime. As a result, it was very difficult to wake him up in the morning, and he was slow with his AM routine. His mom said that he also had an impulsive way of performing hygiene tasks. For example, he would brush his teeth in two seconds and say he was done. Everything was quick and impulsive. This is very typical for boys with this type of ADHD.
His goals were to make friends and find his school work. He said it was very stressful to always feel like he was losing his school work. He was motivated to do well in school. He did not just want to make friends, but he wanted to have good friends. He also wanted to be better at kickball because that is what the kids played at recess and in PE. He also wanted to be better at wrestling as not only did he like to watch with his dad, but he also liked to wrestle with him.
I want to go back to the highlighted areas in my list: completing tasks, losing work, and difficulty waking in the morning. These are the areas we are going to focus on.
Assessments
Assessments are one of the most challenging things for people because they are often under a time crunch, and the reports are difficult to write up and are time-consuming. However, it is really important with these kids as it gives us a full perspective on where they are having challenges. Knowing that he has "ADHD combined type" does not really tell us about his occupational performance and participation. We want to really get all that information. I like to be pretty thorough, and I will scatter assessments throughout my time with them to try to get a good idea. Again, I really like to check out their motor skills. I have kids that are superstars in sports, but I will still find out that there are some motor problems.
Typically, the motor challenges with ADHD have to do with bilateral coordination, dexterity, and those kinds of things. They might be good at some things, like basketball or baseball, but this does not mean that they are good at fine manipulation. Thus, it is really important to find out where they are. Figure 3 shows a summary of the assessments I did with Jeremy.
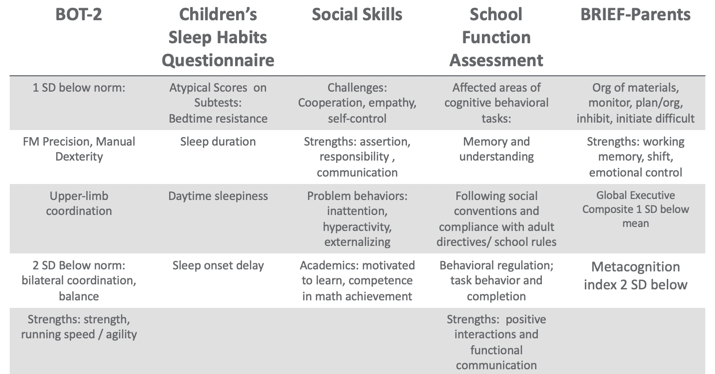
Figure 3. Assessment results.
Using the BOT, I found that Jeremy was one standard deviation below the norm in fine motor, precision, and manual dexterity, which was not surprising. He was two standard deviations below the norm in bilateral coordination and balance. However, his overall strength, running speed, and agility were fine.
There are many great tools out there for sleep including free ones. One of my favorites is the Sleep Habits Questionnaire. It is free online. It is great because it uncovers behaviors regarding going to bed, sleep duration, daytime sleepiness, and sleep onset delay. Many kids with ADHD have an overactive thinking process which then causes a sleep latency problem. It is hard for them to settle their brain and get to sleep. They also might have difficulty with sleep duration and not get enough sleep or good quality of sleep. If their arousal level is still high at night, it' is hard to get them to calm down and want to go to bed, especially if they are very disorganized in their thinking. This questionnaire gives you good information. Our results with Jeremy found that had bedtime resistance, sleep duration, daytime sleepiness, and sleep onset delays that were all atypical scores.
I also did a social skills assessment with him because his goal was to make friends, and school indicated that he had a hard time with solid friendships. I like to have a social-emotional learning perspective, and the more I know about a child's emotional intelligence, the better. We want these kids to be successful in their social interactions because that affects their whole life. With the Social Skills Improvement System (SSIS) Rating Scales, I found challenges with cooperation, empathy, and self-control. His strengths included assertion, responsibility, and communication. Under "problem behaviors", I found inattention, hyperactivity, and some externalizing behaviors. With his diagnosis, this all seems to fit. For academics, he was motivated to learn and had competence in math achievement. We already knew he had strengths in math.
I also did the School Function Assessment. I love this tool. There is one section that is a little dated as it talks about a floppy disk or something, but the other information on there is fantastic. This is especially true if you have kids who have a hard time following rules, social conventions, and material management. You can give it to the teacher, and they can score that. I found that Jeremy had some affected areas with memory and understanding, following social conventions, and compliance with adult directives and school rules. Additionally, he had some behavioral regulation issues, and task behavior and completion were difficult for him. His strengths included positive interactions and functional communication. Communication is strong for him,= which is a good thing.
The BRIEF (Behavior Rating Inventory of Executive Function) is an executive function tool that I did that with his parents. What we found was that the organization of materials, monitoring, planning and organization, inhibition, and initiation were difficult for him. His strengths were his working memory. Additionally, cognitive shifting and emotional control were also strong. However, his global executive composite was one standard deviation below the mean which means that he was low in everything. While it was not devastatingly low, he was below the average in everything. He struggled the most in metacognition, and that was two standard deviations below the norm. Thinking about his own thinking was a struggle for him.
From an observation standpoint, I also got a video from him mom of his AM routine so I could see what that looked like. He was in slow motion, very tired, not wanting to do the routine, and his performance was of low quality, I would put it, writing examples from school, because sometimes you'll see that the handwriting is indicative kind of the brain and the body not matching up, the brain going a little faster than the body. And so I also had a homework video watching him kind of resist homework. And then I did ocular motor testing, checked his tracking, convergence, divergence, and saccades and those kinds of things. Because there is a correlation between having some difficulties with that sometimes. But he actually was fine, and that wasn't a complaint from parents. So I just wanted to make sure it wasn't an issue that we were missing. So that gave me a lot of information.
Research Implications: Assessment
This is information about some of the research implications regarding the assessment process and kind of why I chose the tools that I chose and why I recommend a comprehensive one.
- Motor: Children with parent-reported motor issues received more PT than those with teacher-reported motor issues (risk)/undertreated motor problems in children with ADHD (due to behavioral factors in referral); HW difficulties; higher ADHD and lower motor proficiency scores reported more sleep problems (Papadopoulos et al., 2018)
- Sleep: Sleep deficits negatively affect inhibitory control (Cremone-Caira et al., 2019); Difficulties initiating and maintaining sleep 25-50% in ADHD (Corkum et al., 1998); Prevalence of sleep disorders 84.8 % affecting QoL (Yurumez & Gunay Kilic, 2013)
- EF: Motor skills and EF related (Pan et al., 2015); boys with ADHD have lower EF abilities than typical peers on both performance-based and parent report tools, thus combo is recommended (Sgunibu et al., 2012)
- Social: Children with ADHD 50% lower odds of sports participation than children with asthma with higher incidences of screen time (Tanden et al., 2019); childhood ADHD associated with obesity (Kim et al., 2011); underlying lack of interpersonal empathy (Cordier et al., 2010); Playfulness indicators: ADHD group “typical” with some difficult items but difficulty with basic skills (sharking) (Wilkes-Gillan et al., 2014); seek green outdoor settings at a higher rate (Taylor & Kuo, 2011)
For motor, Papadopoulos and his group (2018) found that there is some difficulty with handwriting. They also reported the higher ADHD and lower motor proficiency scores, the more sleep problems. The fact that Jeremy had sleep problems made me want to look at his motor skills for this reason. This is another interesting one. Children with parent-reported motor issues received more PT than those with teacher-reported motor issues. The fact that we listen to the parents more than the teachers about motor issues is important to consider. Under-treated motor problems in children with ADHD are really due to a behavioral focus so that is why it tends to get missed.
Sleep deficits negatively affect inhibitory control (Cremone-Caira et al., 2019). If we know that these kids have inhibition issues, we need to help them get some sleep. Poor sleep is only reinforcing their challenges and making it worse. They found that there were difficulties initiating and maintaining sleep at a rate of 20 to 50% of kids with ADHD (Corkum et al., 1998). Now, granted, that was 20 years ago, but they have replicated that since. And, if you have a sleep disorder, there is an 84.8% chance that it is negatively affecting your quality of life (Yurumez & Gunay Kilic, 2013).
Motor skills and executive functions are related. If you have some motor difficulties, it is going to influence your executive function ability (Pan et al., 2015). Boys with ADHD have lower executive function ability than typical peers on both performance-based and parent report tools, thus, it is really important that you use a combination of both performance and parent report tools (Sgunibu et al., 2012).
Children with ADHD are 50% less likely to participate in sports than children with asthma (Tanden et al., 2019). I find that amazing. Kids with ADHD also have a higher incidence of screen time usage, and we know that that is always a challenge (Tanden et al., 2019). Childhood ADHD is also associated with obesity. Hence, if you are not doing anything physical and you are sitting there watching your computer or playing video games, and you are impulsive, you are more likely to be obese (Kim et al., 2011). An underlying lack of interpersonal empathy can be something that you often see in ADHD. This affects social abilities and participation and success (Cordier et al., 2010). There are also playfulness indicators. An ADHD group might score as "typical" with some difficult play criteria, but then have more difficulty with basic items (Wilkes-Gillan et al., 2014). Their play may be developmentally out of whack. Again, they might be okay with some high-level types of behaviors, but then when it comes to something simple like taking turns or sharing, they cannot do it. Sometimes we have to go back and practice these rudimentary skills. This might be why they are struggling socially because they are having problems with age-inappropriate items. Lastly, these kids with ADHD really seek green outdoor settings at a higher rate (Taylor & Kuo, 2011). It would be interesting to monitor how outside time might influence their performance on assessments.
EF and Self-Regulation Connection
- Inhibitory control
- Cognitive/mental flexibility
- Working memory
Can these kids self-regulate? When they cannot, it does not work out well for them in school or at home, and it does not work out well in terms of social abilities. When they become adults, they have trouble keeping and maintaining a job. This is the definition of EF.
Some of you might be very familiar with this definition, but it is also quite complicated. This is how we remember information, filter distractions, resist impulses, and sustain attention during an activity that is also goal-directed. While we also adjust our plan as needed to avoid frustration in the process. That is a lot of working parts. Many times, you see people refer to executive functions like an air traffic controller of information and materials. These are the "big 3."
This is how we remember information, filter distractions, resist impulses, and sustain attention during an activity that is goal-directed while adjusting our plan as necessary and avoiding frustration!
Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., Howerter, A., & Wager, T. D. (2000). The unity and diversity of executive functions and their contributions to complex "frontal lobe" tasks: A latent variable analysis, Cognitive Psychology, 41 , 49-100.
- Impulse Control
- socially acceptable (Olson, 2010)
- Ability to store, update and manipulate /process information over short periods of time (Best & Miller, 2010)
- “Limited-capacity information-processing system” (Roman et al., 2015)
- Verbal, visuospatial, and coordinating central executive
- Ability to think flexibly and shift perspective and approaches easily, critical to learning new ideas (different perspectives)
- Switching between two or more mental sets with each set containing several tasks rules
- Feedback related (unlike inhibition) (Best & Miller, 2010)
All these things are important, but the three basic dimensions are inhibitory control, which develops first around four years of age, cognitive and mental flexibility, and working memory. Mental flexibility is the result of inhibitory control and working memory working together. If you have a problem with inhibition or working memory, or both, you are going to have problems with cognitive flexibility. The flip side of that would be rigidity. It is also being able to shift your thinking in the moment back and forth. The flip side of that would be to be stuck. Working memory is the ability to use your memory functionally. It is very important to know that we only have a very limited amount of memory capacity, and it is all we have. I like to call my working memory my suitcase. You have to make sure you pack the right things in there for the trip that you are going on. If you pack your suitcase for Fiji and you are going to Alaska, you are going to be on the beach with boots and a parka and be miserable. It is really important that we pull in the information that we need. This takes sustained attention. If you cannot sustain your attention, you are not going to capture the right memories. And again, if there are problems with inhibitory control or impulse control, this is going to be challenging. Impulse control is controlling yourself in the moment. If I can string those together, now I have more self-regulation ability. Again, these are the big three: inhibition, working memory, and cognitive flexibility and shifting.
I already explained these, but I want you to appreciate what the research says. Inhibition requires an arbitrary rule to be held in your mind while you are inhibiting one response to produce an alternative response, which is typically the one that is more socially acceptable. Working memory is storing, updating, and manipulating information over short periods of time. It has a limited capacity, and it is verbal and visuospatial. Then, for cognitive shifting and flexibility, there are two pieces to it. It is being open and being able to shift. Here is what is interesting. Cognitive flexibility and shifting respond really well to internal feedback. You can actually start to observe things and gain some insight and make changes. Why that is important is because inhibition does not get better from internal feedback. It only gets better from external feedback. Think about someone you know who interrupts a lot because they are impulsive. They see that they do it and do not change because no one has said anything to them. It requires external feedback for them to say, "Oh, I'm doing it wrong." We do not have this internal mechanism to change our impulsivity. We cannot assume these kids will figure it out and fix it, because they will not. We have to be very stern and to the point and say, "You're doing it wrong. This is why it's wrong and here's what you need to do instead." This is the key. Figure 4 is an executive function cheat sheet.
(Cooper-Kahn & Dietzel, 2008)
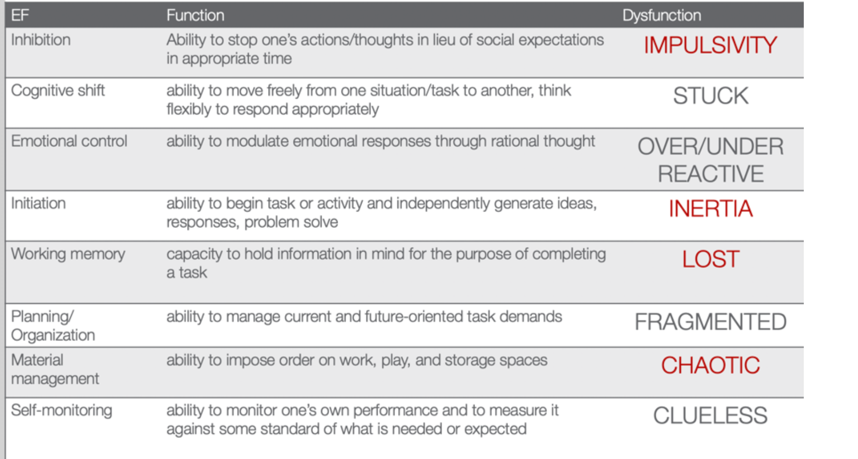
Figure 4. EF cheat sheet.
This is from Cooper-Kahn and Dietzel (2008). They tell you the executive function, what the function is, and then the end dysfunction. For inhibition, the dysfunction is impulsive. If you cannot cognitively shift, you can get stuck. If you do not have emotional control, you are going to be over or under-reactive. If you cannot initiate a task, you are stuck in inertia. If you do not have a good working memory, you are lost. If you cannot plan and organize, you are fragmented. If you cannot manage your materials, you are chaotic. And then, if you cannot self-monitor, you are clueless. The red ones are those that Jeremy struggled with. He was impulsive, had inertia, was lost, and chaotic. He was also a little fragmented and had a difficult time with organization. However, these four things were his biggest challenges.
Review of Evidence-based Interventions for Case
One of the objectives is to talk about evidence and how we are going to use the evidence to support our intervention. I focused on motor, social, executive functions, and sleep. These are the things that were assessed that also had evidence for different intervention strategies (see Figure 5).
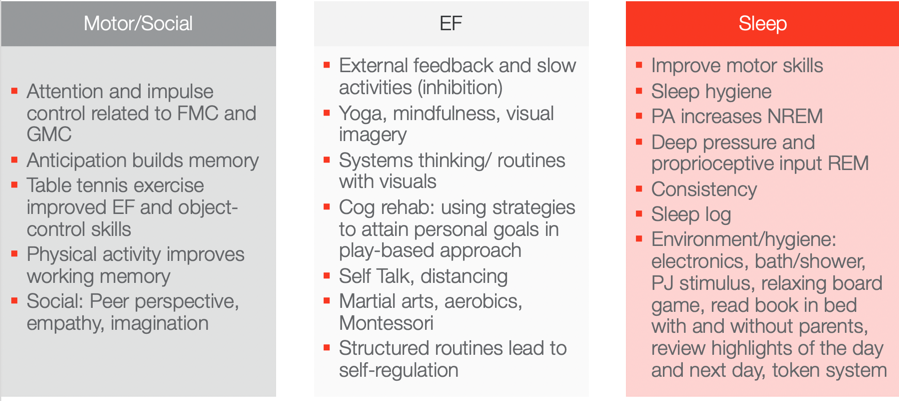
Figure 5. Evidence-based interventions ((Hui Tseng, et al., 2004; Hahn-Markowitz et al., 2016; Washington University, n.d.; Diamond & Lee, 2011; White & Carlson, 2016; Winsler et al., 2009; Marjorek et al., 2004; Kuhn & Floress, 2008; Frike et al, 2006; Keshavarzi et al., 2014).
Motor/Social Categories
Let's look at the motor and social categories. What is really interesting is that attention and impulse control are related to fine motor and gross motor coordination. If we can work on coordination, we can also increase attention and impulse control. This is killing two birds with one stone in Jeremy's case. I do not know who is familiar with Hebbian's law, but it says is that the (brain) cells that fire together wire together. One of the ways to do that is through the concept of anticipation. Anticipation builds memory capacity and will improve working memory. Anticipation is a context, and you can basically put anticipation in anything. With turn-taking, there is anticipation. If there is a competition, there is anticipation among the competitors. If you know you are going to be called on, there is anticipation. If you are playing a game where something might jump out, there is anticipation. These are just a few examples of where you can build in anticipation. If you can add that into your activities, you can build memory capacity. Another study looked at how table tennis exercises improved executive function and object control skills. Table tennis does not require a lot of heavy-duty cardio and it is not a tiring exercise, but it requires a lot of hand-eye coordination and sustained attention. I think this is a really good occupation-based strategy to improve executive function and object control. Physical activity also improves working memory. I have had tons of success with kids doing physical activity both in therapy and at home to improve their working memory. Some of the social strategies that work really for kids, and we will talk about a few in a little bit, is taking a peer's perspective and working on empathy and imagination. These things were really shown to be effective ways to change someone's social success.
Executive Function
For executive function, you have to give them external feedback. You have to tell them when they are being impulsive, and then you have to tell them how to fix it. These are kids who are on a very fast, impulsive temporal context. I talk to them about the hare versus the turtle. I tell them to be more like the turtle. Yoga, mindfulness, and visual imagery are other strategies. Yoga and mindfulness are occupations, and you can incorporate visual imagery into any occupation. They are so effective especially living in a very stressful, fast-paced society. There is self-distancing involved which we know also helps with the social skills for these kids. Systems thinking and routines with visuals are other options. The more visuals we use, the better for these kids. If we can give them visual imagery, it helps. Here is an example of systems thinking. You have family coming over for Thanksgiving dinner. There are 17 people coming and three courses. Each dish takes this long and I need these ingredients for each. Additionally, these dishes all cook at different times so they come out at the right time. This is systems thinking. As a strategy, I gather my recipes and my materials and then put them in order for which ones I have to cook first and for how long. I form a little assembly line of what I am going to do. We can use this type of strategy for kids who struggle with material management and organization. It can be a game-changer. Other ideas include self-talk, martial arts, aerobics, and Montessori. I do not know if anyone has any experience with a Montessori approach. One of the reasons why it is effective is because Montessori uses self-distancing activities. Telling the kids what you want them to do instead of what you do not want them to do really works. It also includes structured routines that lead to self-regulation.
The last section shows that motor skills, as well as sleep hygiene, can improve sleep. Physical activity actually increases non-REM sleep. Deep pressure and proprioceptive can increase REM sleep. A sleep log is actually evidence-based as well. Shortly, I am going to describe a routine that works with kids that is evidence-based. All of these things here you can use as your evidence-based toolkit to work with kids with ADHD.
Case Study Application- Improve ADLs
Top-down analysis.
Jeremy's goal is to have a timely morning routine which involves waking up, dressing, brushing teeth, and packing a backpack. This is a top-down analysis in Figure 6.
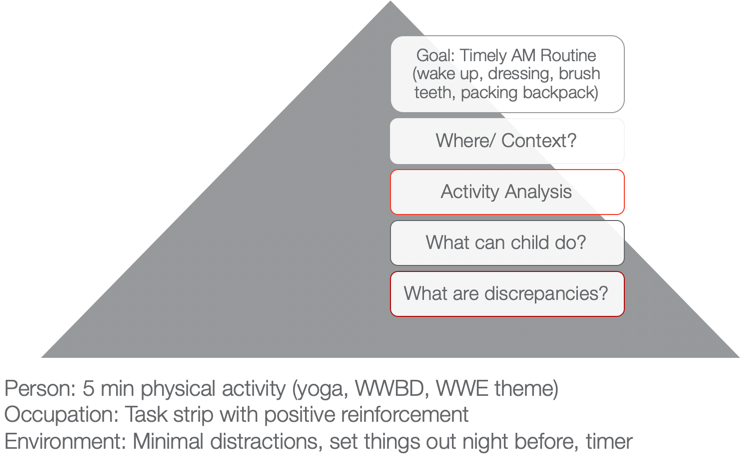
Figure 6. Example of a top-down analysis for ADL routine.
When we use a top-down approach, we are starting with the actual occupation and the goal is to look at where this happens and in what context. I want you to think about where that would happen. In Jeremy's case, it is his bedroom and bathroom. Activity analysis is the bread and butter of OTs. His routine consists of waking up, dressing, brushing his teeth, and packing a backpack. During this analysis, we want to see what he can do and what he cannot do. What are some of your thoughts? Here are some answers from our audience:
- Being aware of time during all tasks/Using a timer. You are seeing a discrepancy between time awareness, time estimation, time monitoring, and time management. I would agree with you that he probably has a hard time all of those.
- Packing the backpack. We know that he is sleepy in the morning and he has a difficult time staying organized. This is especially true if he is half asleep or stressed in the morning.
- Finding his folders. Folders can be elusive sometimes to these kids, so that is a great point. Folders can be found in very strange places.
- Hygiene/organization. Even in hygiene, it is important to make sure that they are organized.
I used a PEO or person-occupation-environment perspective here. We started with some physical activity in the morning to help him to wake up. We did yoga. I asked, "What would Batman do?" He was a big Batman guy. We did some self-distancing by him coming up with strategies for Batman. Or, we used a wresting theme. These activities helped him to be more alert and be able to increase his attention.
We also used a task strip with positive reinforcement to help him see what he needed to do. Visuals can be very helpful for these kids.
Then, we used minimal distractions. We set things out the night before and used that visual so he could match things. We also devised a place where his folders could go. This all might seem trivial, but it really matters for this type of kid. The timer helps as well. You can make it a game.
Activities to Improve ADLs
- Focus on physical activity, motor skills with automaticity and incorporate aspects of yoga to increase sustained attention and memory
- Visual supports and routine with structure
- Self-talk and self-distancing strategies
- Positively reward
To improve ADLs, the key is to focus on physical activity and motor skills with the goal of automaticity. For example, we can incorporate yoga to increase sustained attention and memory. As we talked about earlier, visual supports and structured routines are other great ideas. I cannot emphasize enough the idea of self-talk. This helps with self-regulation and impulsivity on a lower level. The ability to "self-talk" should be pretty solid for kids around the age of seven, but the kids that we are talking about lack this skill. Self-distancing, or having them give strategies to someone other than themselves, is also great. Let them problem-solve and talk it through for someone else, like Batman or John Cena. This way they do not feel like they are picking on themselves or feeling pressured to figure it out for themselves. They are figuring out for someone else, and this strategy is evidence-based. We often forget to positively reward these kids. I like to do something like time with mom and dad, I develop short-term and long-term rewards with mom and dad. For example, Jeremy wanted a wrestling figure for his long term reward. But on a daily basis, he got wrestling bucks and that bought time to wrestle with dad on the weekends.
Case Study Application- Finish a Task with Necessary Supplies
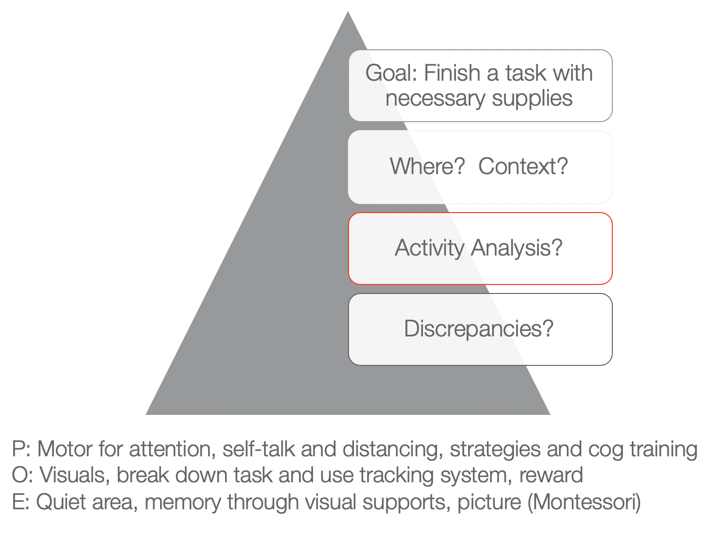
Figure 7. Example of a top-down analysis for finishing a task with necessary supplies.
The next goal is to finish a task with the necessary supplies. You can fill in whatever task that he needed to do like homework, hygiene, or whatever it was with the necessary supplies. Typically, he would start something and then not have all the supplies he needed. He would then run to go get something and then lose track of what he was doing. Activities would not get done and then there would be a mess. We want to know when this would happen and the context. What is required of that activity, and then what can he do versus what he cannot do? Those are the discrepancies.
As I stated a few moments ago, he tends to not have the needed materials. That is the first issue right out of the gate. And because he is impulsive, he starts doing something else. Eventually, he does not finish anything due to a lack of persistence and distractibility. From a personal standpoint, we could work on using motor tasks for increased attention. We know that fine motor and gross motor tasks are going to help. We could also look at using coordination tasks, self-talk, and distancing. Cognitive training is also evidence-based. Can they start to use a checklist or something to create a better strategy?
Then, from an occupation standpoint, again we can use visuals and break down the task. We can also use a tracking system that we are going to go over in just a second.
From an environmental aspect, we can encourage the use of quiet areas to help with sustained attention and better memory. Here we can also use some visual supports or a Montessori approach. "This is what the task is supposed to look like when I am finished." If we have a task, what does the end result look like so that the person knows? And even better, what are the supplies pictured so I know what I have to get first, and then I know what the end result should look like. That is super helpful for someone who is so disorganized when putting materials together.
Activities for Completing Tasks
- Inhibition: Self-talk, slowing down, self-distancing, external feedback
- WM: physical activity
- Attention: physical activity
- Using environmental strategies and visuals to support
- Behavioral: task breakdown, positive reinforcers
- Occupation-based is imperative!
We want to use occupation-based tasks, but we want them to be fun and let the child make a choice. When things are getting easier, we can then move toward less preferred tasks. For example, we do not want to start with homework.

Case Study Application: Social
- Involve a peer or sibling
- Play-based model:
- Capture intrinsic motivations (WWE)
- Empathy focus
- Arrange the environment to foster mutually enjoyable social interaction and imagination
- Teaching social play language and reading expressive body language (can use dogs and their behavior)
- Incorporate parents and coach them so they can coach outside of therapy
(Cordier et al., 2009; Wilkes-Gillan et al., 2016)
There is a play-based model that is evidence-based. They recommend involving a peer or sibling. This play-based model focuses on intrinsic motivation. With Jeremy, we could do wrestling. We could focus on empathy. It is important to arrange the environment so that it is mutually enjoyable. We need to teach social play language and reading expressive body language. The evidence was interesting as it said to use dogs because it could help the child start to read behaviors. Dogs are a little bit easier than people. Jeremy loves dogs so that would work. You could then incorporate parents in order to coach him outside of therapy. They found that to be very successful.
Case Study Application: Sleep
- Turn off electronics 2 hours prior
- Hot bath or shower
- PJs prepped
- Boardgame in room
- Read in bed (parents, then alone
- Highlights with organizer, feelings
- Token reward system
- Flexibility on weekends
- Sleep logs are evidence-based
- Physical activity during day imperative
(Kuhn & Floress, 2008; Fricke et al., 2006)
For sleep, this is the protocol that is highly recommended for these kids. You should turn electronics off two hours prior. Do not shoot the messenger. I know that is really easier said than done. Another protocol is to have the child take a hot bath or shower. They need to have their pajamas prepared. It is a stimulus that can help them progress through the routine. They can do a board game in the room. Another activity is reading in bed. It can start out with the parents reading and then progress to the child reading alone. They can also organize their thoughts and feelings throughout the day. It will help the brain calm down. A token reward system is another great strategy. Make sure to incorporate flexibility on the weekends. It is ok. Sleep logs are evidence-based. And again, physical activity during the day really works.
Systems and Organization
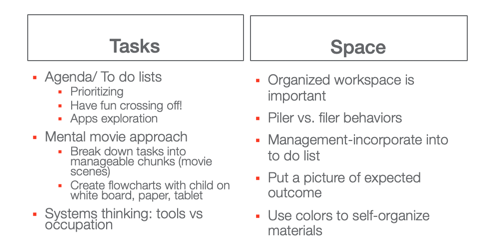
This information is what we already talked about, but I wanted to give you a good resource as well in Figure 8.
Great resource: https://www.understood.org/~/media/040bfb1894284d019bf78ac01a5f1513.pdf
Figure 8. Systems and organization examples.
I like the idea of a mental movie approach. If they are piler and not a filer, we have to appreciate that and try to use things that can help them. This may be an accordion folder or something like that.
Self-Monitoring: GOAL Attainment Scaling
This is the idea of a Goal Attainment Scale (see Figure 9). It is a strategy to identify changes in academic and social behavior. It creates habits and routines.
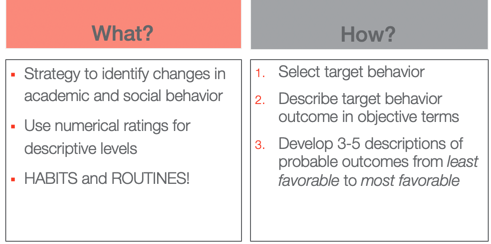
Figure 9. Goal Attainment Scale overview.
The way that you do it is you select the target behavior. You describe that behavior outcome in objective terms and then you develop three to five (I typically use five) descriptions of probable outcomes from least favorable to most favorable.
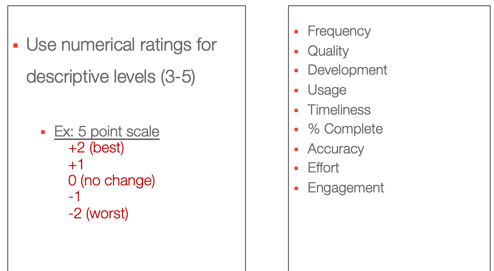
Figure 10. Numerical ratings for the Goal Attainment Scale.
These are some options that you can use, frequency, quality, usage, percent complete.
- Frequency (Never–Sometimes–Very Often–Almost Always–Always)·
- Quality (Poor–Fair–Good–Excellent)·
- Development (Not Present–Emerging–Developing–Accomplished–Exceeding)·
- Usage (Unused–Inappropriate Use–Appropriate Use–Exceptional Use)·
- Timeliness (Late–On-Time–Early)·
- Percent complete (0%–25%–50%–75%–100%)·
- Accuracy (Totally Incorrect–Partially Correct–Totally Correct)·
- Effort (Not Attempted–Minimal Effort–Acceptable Effort–Outstanding Effort)·
- Amount of Support Needed (Totally Dependent–-Extensive Assistance–Some Assistance–Limited Assistance–Independent)·
- Engagement (None–Limited–Acceptable–Exceptional)
This is what the five looks like. You have two choices. You can do a baseline here at zero or the baseline at minus two where that is the worst with no change. Or, you can start at their baseline here at two and only go up. If they cannot handle seeing that they went down, you might choose that option instead. We do not want any negative things causing them anxiety. I have also listed the actual ratings. Here is the example for our friend Jeremy in Figure 11.
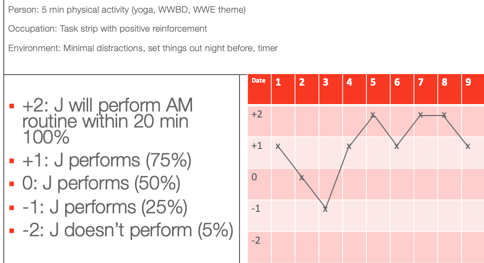
Figure 11. GAS scale example for Jeremy.
He wanted to perform his AM routine within 20 minutes according to his mom. On the first date, he was a +1, which is he did only 75% within 20 minutes. On Day 2, he had 50% of his stuff done within 20 minutes. Day three, he had only 25% done. On four, he was back up to 75%. Day five, he did everything in 20 minutes. Day six, he was back to 75%. And then you see on days seven and eight, he actually met his goal. And on day nine, he almost met his goal. Once you plot the dates you have a graph. This shows change over time and whether or not things are working. You can also do this at home to capture the change in a more specific and sensitive way. On that note, we focused on time.
Thanks for joining me today. I hope you find the information helpful. Feel free to reach out to me if you have any questions.
Best, J. R., & Miller, P. H. (2010). A developmental perspective on executive function. Child Development, 81 (6), 1641-1660.
Cremone-Caira, A., Root, H., Harvey, E. A., McDermott, J. M., & Spencer, R. M. (2019). Effects of sleep extension on inhibitory control in children with ADHD: A pilot study. Journal of Attention Disorders , 1087054719851575.
Corkum, P., Tannock, R., & Moldofsky, H. (1998). Sleep disturbances in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 37 , 637-646.
Cordier, R., Bundy, A., Hocking, C., & Einfeld, S. (2010). Empathy in the play of children with attention deficit hyperactivity disorder. OTJR: Occupation, Participation, and Health, 30 (3), 122-132.
Diamond, A. (2012). Activities and programs that improve children’s executive functions. Current Directions in Psychological Science, 21 (5), 335-341.
Levanon-Erez, N., Cohen, M., Traub Bar-Ilan, R., & Maeir, A. (2017). Occupational identity of adolescents with ADHD: A mixed methods study. Scandinavian journal of occupational therapy, 24 (1), 32-40.
Hahn-Markowitz, J., Berger, I., Manor, I., & Maeir, A. (2016). Efficacy of cognitive-functional (Cog-Fun) occupational therapy intervention among children with ADHD: An RCT. Journal of Attention Disorders , 1087054716666955.
Faber Taylor, A., & Kuo, F. E. (2011). Could exposure to everyday green spaces help treat ADHD? Evidence from children's play settings. Applied Psychology: Health and Well‐Being, 3 (3), 281-303.
Fricke L, Mitschke A, Wiater A, Lehmkuhl G. 2006. A new treatment program for children with sleep disorders – concept, practicability, and first empirical results. Prax Kinderpsychol Kinderpsychiatr 55 :141–154.
Keshavarzi, Z., Bajoghli, H., Mohamadi, M. R., Salmanian, M., Kirov, R., Gerber, M., ... & Brand, S. (2014). In a randomized case–control trial with 10-years olds suffering from attention deficit/hyperactivity disorder (ADHD) sleep and psychological functioning improved during a 12-week sleep-training program. The World Journal of Biological Psychiatry, 15 (8), 609-619.
Kuhn BR, Floress MT. (2008). Nonpharmacological interventions for sleep disorders in children. In Ivanenko A, ed. Sleep and psychiatric disorders in children and adolescents . New York, NY: Informa Healthcare USA Inc. pp 261–278.
Majored, M., Tüchelmann, T., & Heusser, P. (2004). Therapeutic Eurythmy—movement therapy for children with attention deficit hyperactivity disorder (ADHD): a pilot study. Complementary therapies in Nursing and Midwifery, 10 (1), 46-53.
Pan, C. Y., Tsai, C. L., Chu, C. H., Sung, M. C., Huang, C. Y., & Ma, W. Y. (2019). Effects of physical exercise intervention on motor skills and executive functions in children with ADHD: A pilot study. Journal of Attention Disorders, 23 (4), 384-397.
Papadopoulos, N., Stavropoulos, V., McGinley, J., Bellgrove, M., Tonge, B., Murphy, A., ... & Rinehart, N. (2019). Moderating effect of motor proficiency on the relationship between ADHD symptoms and sleep problems in children with attention deficit hyperactivity disorder–combined type. Behavioral Sleep Medicine, 17 (5), 646-656.
Tandon, P. S., Sasser, T., Gonzalez, E. S., Whitlock, K. B., Christakis, D. A., & Stein, M. A. (2019). Physical activity, screen time, and sleep in children with ADHD. Journal of Physical Activity and Health, 16 (6), 416-422.
Toplak, M. E., West, R. F., & Stanovich, K. E. (2017). The assessment of executive functions in attention-deficit/hyperactivity disorder: Performance-based measures versus ratings of behavior.
Tseng, M. H., Henderson, A., Chow, S. M., & Yao, G. (2004). Relationship between motor proficiency, attention, impulse, and activity in children with ADHD. Developmental Medicine and Child Neurology, 46 (6), 381-388.
Wilkes-Gillan, S., Bundy, A., Cordier, R., Lincoln, M., & Chen, Y. W. (2016). A randomised controlled trial of a play-based intervention to improve the social play skills of children with attention deficit hyperactivity disorder (ADHD). PLOS one, 11 (8), e0160558
Yürümez, E., & Kılıç, B. G. (2016). Relationship between sleep problems and quality of life in children with ADHD. Journal of Attention Disorders, 20 (1), 34-40.
Quint, N. (2020). Pediatric case study: Child with ADHD. OccupationalTherapy.com, Article 5145 . Retrieved from http://OccupationalTherapy.com

Nicole Quint has been an occupational therapist for over 15 years, currently serving as an Associate Professor in the Occupational Therapy Department at Nova Southeastern University, teaching in both the Masters and Doctoral programs. She provides outpatient pediatric OT services, specializing in children and adolescents with Sensory Processing Disorder and concomitant disorders. She also provides consultation services for schools, professional development, and special education services. She provides continuing education on topics related to SPD, pediatric considerations on the occupation of sleep, occupational therapy and vision, reflective therapist, executive functions, leadership in occupational therapy and social emotional learning.
Related Courses
Evidence-based approaches: a pediatric perspective of the occupation of sleep, course: #6204 level: intermediate 2 hours, pediatric case study: child with oculomotor and perceptual challenges, course: #4536 level: intermediate 1 hour, from meltdowns to an occupation-centered approach for self-regulation and management, course: #6106 level: intermediate 2 hours, course: #4577 level: intermediate 1 hour, motor skill acquisition for optimal occupational performance, course: #3747 level: introductory 1 hour.
Our site uses cookies to improve your experience. By using our site, you agree to our Privacy Policy .
This site uses essential cookies. We'd also like to set additional cookies . | Manage preferences
Call for more information and costs or if you are enquiring for yourself or a family member you can use our online cost guide for individuals.
A Professional’s Guide to Sensory Impairment

This is the first article in our new series of CPD insights. Read this professional's guide on sensory impairment to learn more about the functional impacts and strategies to avoid clients becoming invisible.
Case Study: Static Seating

A road traffic accident left Jane heavily reliant on her husband and children for physical assistance. Following a seating assessment a static chair tailored to Jane's clinical needs was trialled and selected, allowing her to feel more able, independent and comfortable within her home.
Case Study: Training

In this article Louise describes how she used training as part of her treatment programme with Rob during his rehabilitation following significant orthopaedic trauma. The case study brings to life how training can be an invaluable tool in a the rehabilitation journey.
Case Study: Functional rehabilitation
Following a car accident and resulting leg injuries, Wendy found simple household tasks challenging. Here we explore how Wendy and her OT undertook a functional OT assessment of her abilities, and found real-world solutions to help her increase her independence.
Case Study: Neurological rehabilitation

In this case study Lucas has sustained an head injury resulting in multiple impairments including cognitive and some physical difficulties. Here we can see how an OT can help with neuro rehabilitation using a goal centred approach.
Case Study: Paediatric Moving & Handling

Jack experienced a brain injury at birth, resulting in complex physical and cognitive disabilities including wheelchair dependence. This case study highlights how an OT assessed his needs then trained his parents on correct moving and posture for Jack.
Vocational Rehabilitation in practice: Simon's story

In this case study we learn how structure and routine combined with anxiety and fatigue management techniques can support the transition back to work following accident or illness.
Case study in making homes accessible: George’s story

In this case study we meet George and his family, an OT Practice client that needed home modifications after discharge from a rehabilitation setting. Caroline Pomeroy analyses the collaboration between statutory and private therapists with respect to the solutions that were implemented for George and his family.
A journey to regaining hand function: Phil’s story

This case study follows the progress of Phil who experienced an extensive hand injury at work. It highlights the emotional, physical and practical consequences a client may experience when faced with hand trauma.
Assistive technology brought to life

This case study tells the story of Hannah, one of our clients at The OT Practice. Referred by her case manager, Hannah and her OT worked together to ensure that assistive technology was used practically and appropriately to achieve her goals of independence. Hannah has kindly agreed to allow us to share her story
View articles by topic
- Industry news
- Professional guides
- Press release
- Our clients
- Daily Living Skills
- Military charities
- Royal Visit
- Fatigue management
- Networking event
- Assistive technology
- Remote Services
- Catrin Pugh
- Educational Series for Charities
- Returning to work
- Clinical governance
- Psychological trauma
- pain-management
- Workplace assessments
- Paediatrics
- Financial management
- Educational Needs
- Mental Health
- Disabled Facilities Grant (DFG)
- Speech and Language
- Recruitment
Problems we solve
- Access in & out of the home
- Balance & coordination
- The work place
- Getting out & about
- Seating & wheelchairs
- Memory problems
- Organisation skills
- Planning activities
- Moving around the home
- Fine motor skills
- Handwriting
- Self care skills
- Complex needs
- Gross motor skills
- Cooking & household activities
- Personal care & dressing
- Standing & self-support
- Mobility & falls
Conditions we treat
- Brain injury
- Motor Neurone Disease
- Multiple Sclerosis
- Attention Deficit Hyperactivity Disorder (ADHD)
- Amputations
- Developmental delay
- Sensory Processing Disorder
- Spinal injury
- Learning difficulties
- Scar management
Manage your cookie preferences.
You can learn more about the cookies we set in our cookie policy .
Essential cookies
These cookies are essential for the website to function and are always on.
Analytics Cookies
These cookies are used to collect information about how visitors use our site.
Profile Cookies
Whilst we do not show advertising on our site, we may collect data to sign-post our services elsewhere.

Occupational Therapy Pediatric Case Study Examples
Select the pediatric case for study, review child's diagnosis and medical history, set up an initial meeting with the child and parents or guardians, prepare a detailed initial assessment plan, conduct initial assessment on physical, cognitive and emotional capabilities of the child, record observations during the initial assessment, evaluate child's clinical reports, develop an occupational therapy treatment plan based on findings, approval: treatment plan.
- Develop an occupational therapy treatment plan based on findings Will be submitted
Prepare necessary therapy materials and equipment
Conduct therapy sessions.
- 1 Sensory integration activities
- 2 Fine motor skill exercises
- 3 Hand-eye coordination games
- 4 Social skills building exercises
- 5 Cognitive tasks
Monitor and record the child's progress during each therapy session
Provide feedback and recommendations to parents or guardians, regularly update the treatment plan based on child's progress, re-evaluate the child's capabilities periodically, prepare a comprehensive final report based on case study, approval: final report.
- Prepare a comprehensive final report based on case study Will be submitted
Discuss final report and future recommendations with parents or guardians
Final Report and Future Recommendations - {{form.Meeting_Date}}
We are pleased to share the comprehensive final report on {{form.Child_Name}} 's occupational therapy case study. The report highlights the assessment findings, progress, and specific recommendations for future interventions.
We kindly request your presence at a scheduled meeting on {{form.Meeting_Date}} to discuss the report and address any questions or concerns you may have. Your active participation is essential in shaping the child's therapy journey.
We look forward to fruitful and collaborative discussions.
Best regards,
The Occupational Therapy Team
Close the case study
Take control of your workflows today., more templates like this.

- Collections
Fostering the discussion of planetary health in occupational therapy and physiotherapy
Introduction: Occupational therapists and physiotherapists aim to promote health, prevent various diseases and help people in their rehabilitation processes. So far, there is a paucity of understanding of the big picture of how the new paradigm of planetary health (PH) is connected to the education and practice of these professionals. Methods: This research aimed to address this gap by investigating and deploying a bibliometric analysis to elucidate the pivotal role of occupational therapists and physiotherapists in addressing PH challenges. The ultimate goal is to construct a comprehensive framework crosschecking the bibliometric analysis and the collection of 10 case studies selected by experts to outline how best practices in occupational therapy and physiotherapy, related to the three pillars of sustainability and the UN's Sustainable Development Goals (SDGs), can contribute to increasing PH. Results: The bibliometric analysis revealed four major research strands: 1) enhancing patient care and quality of life; 2) integrating sustainability in health care and rehabilitation; 3) professional development and clinical competence; and 4) evidence-based practice and quality improvement. Moreover, further temporal analysis revealed how the topic evolved, from advancing evidence-based practice and clinical effectiveness, exploring the strengthening of health care and person-centred practices, to connecting the topic to aspects also predicted by the SDGs, such as integrating environmental and climate concerns in therapy and addressing psychological and self-care impacts on health. The case studies confirmed this trend, and a framework of PH in occupational therapy and physiotherapy through the lens of the SDGs was developed to support future research and practitioners in advancing this research field. Conclusions: Occupational therapists and physiotherapists are essential players in public health and can integrate sustainability at every level of practice, from using resources during therapy sessions to advocating for more sustainable lifestyles.
Impact and Reach

Additional statistics for this dataset are available via IRStats2 .
If Altmetric statistics are available for this item, they will be visible below.
Repository staff only
Main navigation
- Clinical Education
- Initiatives
- Alumni/Events
- Professional Development
- Registration
- Travel Grants
Daniel Nguyen: Faculty Lecturer and Occupational Therapist Working in Long-term, Geriatric Care, and Return to Work

- Add to calendar
- Tweet Widget
Daniel Nguyen, erg., completed his MSc (Applied) in Occupational Therapy in 2012. Since that time, he has worked in geriatric care in several long-term care settings within the CIUSSS Ouest-de-l’ile de Montreal, supervised 19 OT students, and is currently working in return-to-work. He has been a faculty lecturer at the School of Physical and Occupational Therapy since 2018.
As part of our Question-and-Answer series to showcase the McGill Occupational Therapy program and illustrate the diversity of the profession, Daniel recently answered these questions.
How did you decide on OT as a career choice?
When I applied out of CEGEP, I was looking for a career in health care which was practical and hands-on, and I didn’t know too much about the profession, it just seemed like an interesting option. It was during my clinical placements, especially my placement at Villa Medica Hospital where I realized the important, and positive, impact we have on a client’s recovery process and their personal life. I remember being surprised that I was able to apply much of the learning we had done in class right into the clinic! It made me reflect on the impact of our decisions in improving other peoples’ conditions and how important participation was in one’s quality of life. That professional objective, to maintain that for our clients, is so important but the broadness of it also makes it difficult to describe in words alone.
What are some of the skills you feel make a great OT?
Being an active listener with a genuine interest in other people is important. OT practice is very client centered, so you may encounter the same condition or problem and even the same environment but completely different issues just because it's a different client with different personal needs.
Another key characteristic is to be interested in problem solving. We learn anatomy, physiology, and pathology of different conditions but there is no guidebook to solving every problem and each issue is different from person to person. In my current work, I help healthcare workers who are going through mental health issues that have led them to take time off work. Each work environment is different, everyone has different life experiences and stressors affecting them so helping them build up their skills to get back to work, identifying strategies to cope with different stressors combined with the right intervention plans during their return-to-work timeline requires creative problem solving.
Just to give you a few examples, my interventions in my current practice have ranged from helping a client develop strategies to dial in their day to day schedule at home in preparation for their return to work, deal with an overloaded Outlook inbox to role-playing and strategies on how to navigate workplace discussion to avoid sensitive topics.
Finally, a holistic view is important. I’ve heard one of my colleagues say that the OT’s superpower is their activity analysis. OTs are skilled at instantly breaking down a specific activity in multiple components and seeing how all these components interact with each other. To understand how personal systems and environmental components affect the participation in an activity, that's a very specific OT skill.
How would you describe OT to someone?
I usually explain that OTs answer three fundamental questions. When observing a client, we ask ourselves: What can’t they do, why can't they do it and what can we do about it? That's it.
If for example, you meet a client with carpal tunnel syndrome (CTS) who has difficulties at their office job. Your first part would be to identify which tasks are affected by the CTS. In this case, typing on the keyboard could be an answer to the first question of what they can’t do. Then we ask ourselves the reasons why the client can’t type. This will be identified through our different assessment tools. In this case, we could measure multiple factors such as range of motion, endurance, strength, fine motor dexterity, body positioning, office set-up, the type of keyboard, potential accommodations in the workspace, the relationship that the client has with their employer that could affect the implementation of said accommodations, etc. Finally, we ask ourselves what we, as OTs, do about it, which would be to develop a treatment plan to manage the symptoms, improve on the physical limitations that have been assessed and make recommendations on optimizing the office area so that in the end, the client performs their task in a more efficient and satisfactory manner.
Why did you choose McGill University?
I am born and raised in Montreal and had always attended school in French. Although I spoke both English and French, I wanted the opportunity to learn in English at the University Level.
Any advice for someone deciding on a career in OT?
I would advise them to get a good understanding of what OT is and the role of an OT from multiple health care professionals. OT is a very broad and holistic program and having a better understanding of it when going into the program will help you contextualise what you are learning and imagine what kind of practice you may see yourself doing later. You also have to enjoy anatomy, physiology and learning about the development through the lifespan.
Do you have questions about OT?
Please feel free to contact daniel.nguyen2 [at] mcgill.ca (subject: Question%20regarding%20OT%20program%20or%20profession%20from%20OT%20webpage%20) (Daniel via email.)
Department and University Information
School of physical & occupational therapy.

- Academic Integrity
- Athletics and Recreation
- Counselling Services
- Health Sciences Calendar
- Ombudsperson
- P&OT Undergraduate Society (POTUS)
- Psychiatric Services
- Student Information
- Student Rights and Responsibilities
- Graduate and Post-Graduate Calendar
- Graduate rehabilitation science society (GRSS)
- Life Sciences Library
- McGill Writing Centre
- PGSS Insurance
- The WELL Office : Wellness Enhanced Lifelong Learning
- Association of Canadian Occupational Therapy University Programs
- Canadian Association of Occupational Therapists
- Canadian Council of Physiotherapy University Programs
- Canadian Physiotherapy Association
- CRIR Website
- Ordre des ergothérapeutes du Québec
- Ordre professionnel de la physiothérapie du Québec
- REPAR Website

IMAGES
VIDEO
COMMENTS
Occupational therapy theories/models: List initial occupational theories or models that might guide the occupational therapy process: • Person-Environment-Occupation (PEO) (Case-Smith & O'Brien, 2015, p. 31): o Focus on child's performance and the environmental influences that enable a child's engagement and participation in activities
1) Name, validate and prioritize occupational performance issues. 2) Where would you look for more information on your client? Stage #2: 1) Select theoretical approach(es), both generic and specific, clearly give a rationale for your choice(s). Stage #3: 1) Identify occupational performance components and environmental conditions
The first thing to understand is that the PEOP model of occupational therapy (Christiansen and Baum, 1985) and the PEO model (Law et al., 1996) are not synonymous. Although both models have some similarities, PEOP holds to a handful of different principles. The PEOP model highlights occupational performance as its key feature, which is made up ...
Case Study 2 Background Mary, aged 74, was referred to occupational therapy following treatment for breast cancer, which was now in remission. Her illness and associated treatment had resulted in her becoming weak and deconditioned. Her GP therefore made a referral to community therapies for a Physiotherapy intervention to
Case Studies. The case studies listed below cover some of the common questions or challenges occupational therapists may face in their practice. Use them to test your understanding of Practice Standards, guide discussions with your colleagues, and reflect on your own practice. If you've experienced a professional challenge or situation you ...
Abstract: Realistic case studies are a critical part of occupational therapy education to strengthen students' clinical reasonings skills, challenge their assumptions and biases, and expose them to the complexities of real clients. Case Studies for Contemporary Occupational Therapy Practice comprises 40 case studies across eight practice settings.
This case study intends to use PEOP to explore and reflect on an occupational therapy assessment, intervention and formulation of recommendations. Image 1. Summary of the Case to be applied. Vincent is a 79-year-old gentleman, widowed 5 years ago and has a diagnosis of Parkinson's Disease (PD). He has recently moved from his long-term home ...
Occupational Therapy Case Study. A 55-year-old man with rheumatoid arthritis is referred to you for occupational therapy to help decrease pain in his wrists to help regain function. You have been utilizing wrist splints for quite some time in treating rheumatoid arthritis patients, but wonder if there are other occupational therapy ...
her Masters of Science in Occupational Therapy. She plans to graduate in December 2013 and hopes to start practicing soon thereafter. Case studies within the medical field are used to perform "an in-depth study of a single unit" (Gerring, 2004). In most cases this unit is the client and a particular condition.
The strength of case study methodology is its flexibility to capture the complexity of the phenomenon under study and take into account the context in which it is situated (Hyett et al., 2014; Stake, 1995).As a result, case studies are well suited to exploring a variety of complex research questions such as the development and evaluation of programs, interventions, and theories (Baxter & Jack ...
Case report of a child with sensory integration dysfunction. GRETCHEN DAHL REEVES Medical College of Ohio at Toledo, School of Allied Health, Department of Occupational Therapy, Toledo, Ohio 43614-5803, USA. Abstract: This case report describes a 6-year-old boy with delays in fine motor skills, low frustration level, poor eating behaviour, low ...
Occupational Therapy Case Study. In the past case studies and activities you have: identified the PICO components of your patient scenario, formulated a clinical question, found an appropriate article to answer your question, and critically appraised the article. Now, it's time to apply what you've learned to your patient.
Royal College of Occupational Therapists. Phoenix House. 106-114 Borough High Street. London SE1 1LB. 020 3141 4600. [email protected]. Connect with us.
This qualitative case study research (Thomas, Citation 2015) supported construction of a case that is both exemplary - as a good example of occupational therapy - and instrumental in facilitating readers' in depth understanding (Simons, Citation 2009) with the aim of bringing the case to life.
Case Study Guidelines. Introduction. This is a brief guide to the content of a case study. The individual selected for case study may be considered in terms of an Occupational Therapy Model/ Approach to practice and also the wider environments and networks that play a role in a person's life. This guide is created with an individual in mind ...
Realistic case studies are a critical part of occupational therapy education to strengthen students' clinical reasonings skills, challenge their assumptions and biases, and expose them to the complexities of real clients. Case Studies for Contemporary Occupational Therapy Practice comprises 40 case studies across eight practice settings. Read ...
This course focuses on a case study for a 9-year-old male with ADHD experiencing occupational challenges in education, ADL, IADL, and social participation. 5145 OccupationalTherapy.com Article ... Example of a top-down analysis for finishing a task with necessary supplies. ... Scandinavian journal of occupational therapy, 24(1), 32-40.
Case Studies Occupational Therapy Case Studies We are delighted to share with you some successful stories from our occupational therapy team regarding specific conditions and disorders that many people are faced with, and organisations may need to accomodate for. Our work helps people of all ages with all kinds of physical, mental or.
In a case study, an occupational therapist described her experience providing interventions from an occupation-centered approach (Skubik-Peplaski, Howell, & Harrison, 2014). The authors reported a ...
Assistive technology brought to life. This case study tells the story of Hannah, one of our clients at The OT Practice. Referred by her case manager, Hannah and her OT worked together to ensure that assistive technology was used practically and appropriately to achieve her goals of independence. Hannah has kindly agreed to allow us to share her ...
This client centered case study is an example of good practice, which reveals the possibility of achieving a higher level of occupational performance and to increase self-esteem for individuals with depression. We chose to present an exemplifying case-study of occupational therapy (OT) application in an adult patient with depression and hypoacusis by using the narrative interview method.
Aim: To consider the use of case study research in contributing to the. occupational therapy evidence base. Material and methods: A critical discussion of the current state of evidence-based. practice in occupational therapy and exploration of a viable approach to case. study research is used.
1. Select the pediatric case for study. Review child's diagnosis and medical history. Set up an initial meeting with the child and parents or guardians. Prepare a detailed initial assessment plan. Conduct initial assessment on physical, cognitive and emotional capabilities of the child. Record observations during the initial assessment.
In addition, RTs from different professions, such as occupational therapy (OT) and physiotherapy (PT), ... • Use of case studies and examples to stimulate reflection. Ease of navigation: Limit number of clicks and support scrolling. 40 • Drop down (accordion) menus which show extra information with a single click. ...
Occupational Justice The patient with Autism Spectrum Disorfer speaks out to advocate for classmates with Autism Spectrum Disorfer. For a complete description of each component and examples of each, refer to the Occupational Therapy Practice Framework: Domain and Process (4th ed.). Resources American Occupational Therapy Association. (2020).
The case studies confirmed this trend, and a framework of PH in occupational therapy and physiotherapy through the lens of the SDGs was developed to support future research and practitioners in advancing this research field. Conclusions: Occupational therapists and physiotherapists are essential players in public health and can integrate ...
DEI Toolkit Case Studies; Transgender and gender-diverse resources; Coding & Billing Resources. Medicare Fee Schedule Calculator; Caregiver training services; ... Occupational therapy can help clients, groups, and communities to manage physical and mental health needs, develop healthy and effective daily routines to promote well-being, and ...
Daniel Nguyen, erg., completed his MSc (Applied) in Occupational Therapy in 2012. Since that time, he has worked in geriatric care in several long-term care settings within the CIUSSS Ouest-de-l'ile de Montreal, supervised 19 OT students, and is currently working in return-to-work. He has been a faculty lecturer at the School of Physical and Occupational Therapy since 2018.
The case study in this chapter pulls together the main suggestions I have made for understanding clients' identities, establishing a respectful relationship, conducting a culturally responsive assessment, making a culturally responsive diagnosis, and implementing culturally responsive therapies. In this case, the therapies included a systems intervention involving the whole family, an ...
The previous two chapters illustrated how case formulation is applied in specific cases, with an emphasis on Stages 1 and 2, respectively. Stage 3 is the process formulation stage. This chapter provides examples of case formulations mapped out in chart form with five clients whose conditions are typical of those with whom we work in emotion-focused therapy (EFT). Each of the problems in the ...