Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- New editors
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 52, Issue 6
- A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
This article has a correction. Please see:
- Correction: A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults - October 01, 2020
- Robert W Morton 1 ,
- Kevin T Murphy 1 ,
- Sean R McKellar 1 ,
- Brad J Schoenfeld 2 ,
- Menno Henselmans 3 ,
- Eric Helms 4 ,
- Alan A Aragon 5 ,
- Michaela C Devries 6 ,
- Laura Banfield 7 ,
- James W Krieger 8 ,
- http://orcid.org/0000-0002-1956-4098 Stuart M Phillips 1
- 1 Department of Kinesiology , McMaster University , Hamilton , Canada
- 2 Department of Health Sciences , Lehman College of CUNY , Bronx , New York , USA
- 3 Bayesian Bodybuilding , Gorinchem , Netherlands
- 4 Sport Performance Research Institute New Zealand, AUT University , Auckland , New Zealand
- 5 California State University , Northridge , California , USA
- 6 Department of Kinesiology , University of Waterloo , Waterloo , Canada
- 7 Health Sciences Library , McMaster University , Hamilton , Canada
- 8 Weightology, LLC , Issaquah , Washington , USA
- Correspondence to Dr Stuart M Phillips, Department of Kinesiology, McMaster University, 1280 Main Street, West Hamilton, Ontario, Canada; phillis{at}mcmaster.ca

Objective We performed a systematic review, meta-analysis and meta-regression to determine if dietary protein supplementation augments resistance exercise training (RET)-induced gains in muscle mass and strength.
Data sources A systematic search of Medline, Embase, CINAHL and SportDiscus.
Eligibility criteria Only randomised controlled trials with RET ≥6 weeks in duration and dietary protein supplementation.
Design Random-effects meta-analyses and meta-regressions with four a priori determined covariates. Two-phase break point analysis was used to determine the relationship between total protein intake and changes in fat-free mass (FFM).
Results Data from 49 studies with 1863 participants showed that dietary protein supplementation significantly (all p<0.05) increased changes (means (95% CI)) in: strength—one-repetition-maximum (2.49 kg (0.64, 4.33)), FFM (0.30 kg (0.09, 0.52)) and muscle size—muscle fibre cross-sectional area (CSA; 310 µm 2 (51, 570)) and mid-femur CSA (7.2 mm 2 (0.20, 14.30)) during periods of prolonged RET. The impact of protein supplementation on gains in FFM was reduced with increasing age (−0.01 kg (−0.02,–0.00), p=0.002) and was more effective in resistance-trained individuals (0.75 kg (0.09, 1.40), p=0.03). Protein supplementation beyond total protein intakes of 1.62 g/kg/day resulted in no further RET-induced gains in FFM.
Summary/conclusion Dietary protein supplementation significantly enhanced changes in muscle strength and size during prolonged RET in healthy adults. Increasing age reduces and training experience increases the efficacy of protein supplementation during RET. With protein supplementation, protein intakes at amounts greater than ~1.6 g/kg/day do not further contribute RET-induced gains in FFM.
- hypertrophy
- performance. leucine
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
https://doi.org/10.1136/bjsports-2017-097608
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Resistance exercise training (RET) in combination with dietary protein supplementation is a common practice, in athletes and recreational exercisers alike, with the aim of enhancing RET-induced gains in muscle mass and strength. Recognised as a potent antisarcopenic stimulus, protein supplementation has also been advocated for ageing persons participating in RET. Despite a large volume of work in this area, narrative reviews 1–5 and even meta-analyses 6–12 yield conflicting results as to the actual effectiveness of protein supplementation to enhance RET-mediated gains in muscle mass and strength. This lack of agreement on the efficacy of protein supplementation 6–12 is likely due to the use of divergent study inclusion criteria and inclusion of subjects with differing: ages, training statuses, total protein intakes, protein sources and protein doses. Thus, an evidence-based answer to the main question of the efficacy of protein supplementation, while previously reported, 7 now appears to be controversial. 4
We conducted a meta-analysis that was more inclusive in nature than previous meta-analyses 6–12 to provide a broad, systematic and evidence-based assessment on whether protein supplementation can augment changes in relevant RET outcomes. We used meta-regression to evaluate the impact of important potentially mediating covariates that were decided a priori to the meta-analysis. The present meta-analysis includes more than double the number of studies and participants than the largest published comprehensive meta-analysis on protein supplementation during RET to date. 7ST1
We also undertook an additional rational, mechanism-based analysis that had the aim of answering the following question: is there a protein intake beyond which protein supplementation ceases to provide a measurable benefit in increasing muscle mass during RET? To answer this question, we recognised that the process of muscle protein synthesis (MPS), as the primary determinant of muscle hypertrophy, 13 shows a saturable dose-response relationship with increasing protein intake. 14 Since measures of MPS show good agreement with hypertrophy 13 we theorised that the effect of daily protein intake on RET-induced changes in muscle mass would show a dose-responsive relationship but that this would ultimately plateau.
Inclusion criteria
Any randomised controlled trials (RCTs) that combined a RET and protein supplement intervention were considered for this meta-analysis. Trials had to be at least six weeks in duration, participants had to be performing RET at least twice per week, and at least one group had to be given a protein supplement that was not co-ingested with other potentially hypertrophic agents (eg, creatine, β-HMB, or testosterone-enhancing compounds). Only trials with humans who were healthy and not energy-restricted were accepted. Manuscripts had to be original research (not a review or conference abstract) and be written in English.
Search strategy
A systematic search of the literature was conducted (LB) in Medline, Embase, CINAHL and SportDiscus, current to January 2017 (see online supplementary appendix 1 ). As appropriate, a combination of keywords and subject headings was used for the following concepts: protein supplementation and resistance training or muscle strength. The original search yielded 3056 studies. Any overlooked trials were identified by consulting other reviews and meta-analyses on the subject and were added in manually (17 studies). After deduplication and screening for inclusion criteria, 155 articles were independently read/reviewed by three authors (RWM, KTM and SRM). A total of 49 RCTs were selected for inclusion in this meta-analysis ( figure 1 ).
Supplementary Appendix 1
- Download figure
- Open in new tab
- Download powerpoint
PRISMA flow chart.
Data extraction
Predetermined relevant variables from each included study were gathered independently by three investigators (RWM, KTM and SRM). Relevant variables included those regarding the study design, details of the RET intervention, participant characteristics, protein supplement information, placebo/control information, performance outcomes, body composition outcomes and any other notable information (eg, sources of bias/conflict of interest). Where data were not presented in table or text and authors could not be reached, data were extracted using WebPlotDigitizer (Web Plot Digitizer, V.3.11. Texas, USA: Ankit Rohatgi, 2017) or calculated from baseline values and/or percentage change. Where there were any discrepancies between the three reviewers the manuscripts were revisited by all reviewers (RWM, KTM and SRM) and agreed on by discussion. We also conducted a post hoc reassessment of 10 randomly selected studies and compared the extracted results. 15 Coder drift was <10% in all cases for each investigator and inter-rater (RWM, KTM and SRM) reliability was excellent (>95%).
A total of 58 different body composition and 66 performance outcomes were extracted from the final 49 studies. 16–64 Primary outcomes were limited and amalgamated to include two different performance outcomes and four different body composition outcomes based on those most commonly reported in the 49 RCTs. Performance outcomes were: one-repetition-maximum strength (1RM; measured by any 1RM strength test) and maximum voluntary contraction (MVC; measured by both isokinetic and/or isometric contractions using a dynamometer with any muscle group/action). Body anthropometric and composition outcomes included: total body mass (TBM; measured by any scale); fat-free mass (FFM) and bone-free mass (or lean mass if FFM was not available; FFM; measured by dual-energy X-ray absorptiometry (DXA), hydrodensitometry, or whole-body air plethysmography (BodPod)); fat mass (FM; measured by DXA, hydrodensitometry and/or BodPod); muscle fibre cross-sectional area (CSA; measured in any fibre subtype (I, IIa, and/or IIx) obtained from either vastus lateralis and/or latissimus dorsi biopsies using microscopy); and mid-femur whole muscle CSA (mid-femur CSA, measured by MRI and/or CT).
Data syntheses
When data were reported in different units (eg, pounds vs kilograms) the data were converted to metric units. In all analyses the comparator group received an identical RET intervention but was non-supplemented or placebo-supplemented. If a study included a protein-supplemented group, a non-supplemented control group and a placebo-supplemented control group that were all part of the RET intervention, the protein-supplemented and placebo-supplemented groups were retrieved. If a study had multiple time points, only the preintervention and postintervention outcomes were retrieved. Where the change in SD (ΔSD) was available it was collected alongside the preintervention and postintervention SD. Where ΔSD was not reported, the correlation coefficient (corr) for each primary outcome was calculated according to the Cochrane Handbook for Systematic Reviews of Interventions : 65
and the ΔSD was then calculated as:
The change in mean (ΔMean) and ΔSD were calculated for each condition and uploaded to RevMan (Review Manager (RevMan), V.5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). Where studies had more than one protein-supplemented group (eg, soy and whey), measure of MVC (eg, isokinetic and isometric) or measure of 1RM (eg, bench press and leg press) the ΔMean and ΔSD were independently calculated and later combined, unless otherwise stated, using the RevMan calculator (Review Manager (RevMan), V.5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
Meta-analyses
Random-effects meta-analyses were performed in RevMan (Review Manager (RevMan), V.5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) on the change in each outcome. Effect sizes are presented as mean difference (MD) with means±SD and 95% CIs for 1RM, TBM, FFM, FM, fibre CSA and mid-femur CSA and as standardised mean difference (SMD) and 95% CIs for MVC because it had multiple outcomes presented on non-comparable scales (eg, N and Nm).
Heterogeneity and risk of bias
Heterogeneity was assessed by χ 2 and I 2 and significance was set at p<0.05. The internal validity of each study was determined by domain-based evaluation to quantify risk of bias for each study 65 and was independently performed by three investigators (RWM, KTM and SRM). The data included in the meta-analyses were restricted to studies with less than three reported high or unclear risk domains (predominately due to reported conflicts of interest and lack of blinding investigators and/or participants; (see online supplementary appendix 2 )). Funnel plots were visually inspected to determine publication bias. Multiple sensitivity analyses were performed to determine if any of the results were influenced by the studies that were removed.
Supplementary Appendix 2
Meta-regression.
In an effort to understand the sources of heterogeneity meta-regressions were performed on 1RM, FFM and fibre CSA because they were statistically significant, had considerable unexplained heterogeneity ( I 2 ) and had a sufficient number of studies (≥10). Meta-regression was used instead of subgroup analyses to allow for the use of continuous covariates and to allow for the inclusion of more than one covariate at a time. Four covariates were chosen a priori to be included in our meta-regression: baseline protein intake (g/kg/day), postexercise protein dose (g), chronological age and training status because there is evidence that baseline protein intake, 66 protein dose, 14 age 67 and training status 68 could influence the efficacy of protein supplementation; summarised here. 4 5 These covariates were meta-regressed individually and together in a random-effects meta-regression model using Stata (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, Texas, USA). The random-effects meta-regression used residual restricted maximum likelihood to measure between-study variance (τ 2 ) with a Knapp-Hartung modification as recommended. 69 When all four covariates were analysed together permutation tests were performed (n=1000) to address the issue of multiple testing by calculating adjusted p values. 70 Additional covariates were identified and individually analysed post hoc to further explore the unexplained variance of the effect of protein supplementation during RET on changes in 1RM and FFM. Continuous covariates were: MD in the change in protein intake (g/day), MD in the total relative protein intake (g/kg/day), number of repetitions/set, number of sets/exercise, number of exercises/session, number of sessions/week, number of weeks and total RET volume in kg: repetitions/set × sets/exercise × exercises/session × sessions/week × intervention duration in weeks. Categorical variables were: protein supplement source (whey vs soy), sex (male vs female), type (dietary-supplement vs RET-supplement), whole-body RET (whole-body RET vs not whole-body RET) and RET supervision (supervised vs not supervised). Protein supplement source was limited to soy and whey because there were few study groups that were provided either a casein (n=3 21 59 60 ) or pea (n=1 22 ) protein supplement exclusively.
Subgroup analyses
Subgroup analyses were performed in RevMan (Review Manager (RevMan), V.5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). Subgroup analyses were performed on changes in FFM and 1RM with training status (untrained vs trained) as the subgroup to generate forest plots and neatly present training status as a categorical variable. Subgroup analyses were also performed on changes in FFM with age categorised into subgroups (old (>45 years) and young (<45 years)) to be presented below for the interested reader.
Break point analysis
To investigate the influence of protein intake as a continuous variable on individual study arms (as opposed being limited to MDs between groups in a meta-regression) linear and segmental regressions on the change in FFM (measured by DXA) were plotted against daily and baseline protein intake. Linear and segmental regressions were performed using GraphPad Prism (V.6, GraphPad Software, La Jolla, California, USA) to determine models of best fit as has been previously done in acute tracer trials measuring MPS. 14 Where segmental regression was the preferred model the slope of the second line was set to zero to determine the break point (biphasic regression). Each group from each study that presented daily or baseline protein intake with changes in FFM from DXA was included. Significance was set at p<0.05 and data for the break point is presented as mean (95% CI).
Participant characteristics
Participant details and outcomes are presented elsewhere (see online supplementary table 1 . A total of 49 studies from 17 countries met the inclusion criteria ( figure 1 ). There were 10 studies in resistance-trained participants and 14 study groups in exclusively female participants. Publications ranged from 1962 to 2016. There was a total of 1863 participants (mean±SD; 35±20 years).
Supplementary Table 1
Ret characteristics.
The RET characteristics are also presented elsewhere (see online supplementary table 1) . The RET interventions lasted from 6 weeks to 52 weeks (13±8 weeks) performing RET between 2 days and 5 days per week (3±1 days/week) with between 1 to 14 exercises per session (7±3 exercises/session), 1 to 12 sets per exercise (4±2 sets/exercise) and anywhere between 3 to 25 repetitions per set (9±4 repetitions/set). Four studies used just lower-body RET, two studies used just knee extensor RET, one study used elbow flexor RET only, and two studies used one lower-body and one upper-body exercise only.
Protein supplementation
Details regarding the experimental (protein supplementation) and control (placebo- or no-supplement) groups are presented elsewhere (see online supplementary table 2) . A range of 4 g to 106 g of protein was supplemented per day to the protein group (36±30 g/day; young: 42±32 g/day; old: 20±18 g/day) with a range of 5 g to 44 g of protein supplemented postexercise on training days (24±11 g; young: 24±12 g; old: 23±10 g). Twenty-three conditions supplemented with whey protein, 3 with casein protein, 6 with soy protein, 1 with pea protein, 10 with milk or milk protein, 7 with whole food (eg, beef, yogurt, between-meal snack) and 13 with non-specific protein blends or blends containing multiple protein sources (eg, whey, casein, soy and egg). In 40 studies the participants consumed part or all of their daily protein supplement after their RET sessions. In 36 studies with 48 different conditions authors reported either total (g/day) or relative (g/kg/day or %kcal/day) daily protein intake preintervention and/or postintervention. There was an increase in daily protein intake in the protein group (mean±SD; range: 23±41 g/day; −25 g/day to 158 g/day; p=0.004) and no change in the control group (1±14 g/day; −17 g/day to 40 g/day; p=0.83) such that the change in daily protein intake was significantly greater in the protein group (p=0.01). Relative daily protein intake (g/kg/day) increased in the protein group (pre: 1.4±0.4, post: 1.8±0.7, Δ: 0.3±0.5 g/kg/day, p=0.002) and did not change in the control group (pre: 1.4±0.3, post: 1.3±0.3, Δ: −0.02±0.1 g/kg/day, p=0.48) such that there was a greater change in the protein group (p<0.001). Daily energy intake (kcal/day) was gathered from 23 studies with 29 conditions and did not change with the prolonged RET and protein supplementation nor was it significantly different between the protein or control groups (Δ protein group: 50±293 kcal/day, Δ control group: 70±231 kcal/day, p=0.71).
Supplementary Table 2
Significant heterogeneity was found for changes in 1RM (χ 2 =53.49, I 2 =33%, p=0.003) and fibre CSA (χ 2 =30.97, I 2 =68%, p=0.0006). Nine studies were removed based on risk of bias 17 18 25 26 50 63 (see online supplementary appendix 2 ) or publication bias assessment 24 32 64 (see online supplementary figure 1 ). In particular, four studies were removed from 1RM, 17 26 32 50 four from TBM, 17 18 63 64 three from FM, 17 18 63 five from FFM, 17 18 24 63 64 three from MVC 25 26 50 and one from fibre CSA. 50
Supplementary Figure 1
Sensitivity analyses.
Sensitivity analysis was performed with the nine high-risk studies mentioned above included in the outcomes they were removed from to determine if their removal changed any of the results. The inclusion of those studies did not influence the difference in means or significance in 1RM, TBM, FFM or mid-femur CSA; however, when Mitchell et al 50 was included in the fibre CSA assessment the effect of protein supplementation (310 µm 2 (51, 570), p=0.02) was eliminated (153 µm 2 (−137, 443), p=0.30). This is likely due to the small number of studies that included muscle biopsies but may warrant caution when interpreting the effect of protein supplementation on changes fibre CSA during RET. In no instance did fixed-effect meta-analysis deliver a different magnitude of effect or significance compared with random-effect meta-analysis.
Protein supplementation during prolonged RET significantly improved gains in 1RM strength (MD: 2.49 kg (0.64, 4.33), p=0.01; figure 2 ) but had no effect on MVC (SMD: 0.04 (-0.09, 0.16), p=0.54). Protein supplementation did not have a significant effect on changes in TBM (MD: 0.11 kg (−0.23, 0.46), p=0.52) but improved changes in FFM (MD: 0.30 kg (0.09, 0.52), p=0.007; figure 3 ), FM (MD: −0.41 kg (−0.70,–0.13), p=0.005), fibre CSA (MD: 310 µm 2 (51, 570), p=0.02; see online supplementary figure 2 : panel A) and mid-femur CSA (MD: 7.2 mm 2 (0.20, 14.30), p=0.04; see online supplementary figure 2 : panel B) during prolonged RET.
Supplementary Figure 2
Forest plot of the results from a random-effects meta-analysis shown as mean difference with 95% CIs on one-repetition-maximum (1 RM; kg) in untrained and trained participants. For each study, the circle represents the mean difference of the intervention effect with the horizontal line intersecting it as the lower and upper limits of the 95% CI. The size of each circle is indicative of the relative weight that study carried in the meta-analysis. The rhombi represent the weighted untrained, trained and total group’s mean difference. Total: 2.49 kg (0.64, 4.33), p=0.01, untrained: 0.99 kg (−0.27, 2.25), p=0.12 and trained: 4.27 kg (0.61, 7.94), p=0.02.
Forest plot of the results from a random-effects meta-analysis shown as mean difference with 95% CIs on lean or fat-free mass (FFM; kg) in untrained and trained participants. For each study, the circle represents the mean difference of the intervention effect with the horizontal line intersecting it as the lower and upper limits of the 95% CI. The size of each circle represents the relative weight that study carried in the meta-analysis. The rhombi represent the weighted untrained, trained and total group’s mean difference. Total: 0.30 kg (0.09, 0.52) p=0.007, untrained: 0.15 kg (−0.02, 0.31), p=0.08 and trained: 1.05 kg (0.61, 1.50), p<0.0001.
Meta-regression.
The results from the full model meta-regressions are presented in table 1 . When combined, baseline protein intake, protein dose, age and training status did not explain any of the variance in the changes in 1RM (15 studies, 1216 subjects, p=0.77) or FFM (15 studies, 642 participants, p=0.12). There were insufficient observations (<10) when all covariates were compared with the changes in fibre CSA.
- View inline
Meta-regression output
Univariate meta-regressions on changes in 1RM and FFM following prolonged RET are also presented in table 1 . None of our covariates explained any of the heterogeneity of protein supplementation’s effect on changes in 1RM: baseline protein intake (21 studies, 814 participants, p=0.59), age (27 studies, 802 participants, p=0.78), training status (28 studies, 858 participants, p=0.40) and post-exercise protein dose (23 studies, 589 participants, p=0.13). In contrast, when the ability of protein supplementation to affect changes in FFM was evaluated with univariate meta-regressions, the postexercise protein dose was the only covariate that did not influence the efficacy of protein supplementation on changes in FFM (20 studies, 793 participants, p=0.25) whereas baseline protein intake (22 studies, 988 participants, p=0.045; see online supplementary figure 3 : panel A), age (25 studies, 1033 participants, p=0.02; figure 4 ) and training status (26 studies, 1089 participants, p=0.03) all influenced the effect of protein supplementation. When the effect of protein supplementation on changes in FFM was evaluated with age stratified into two subgroups the difference between old (>45; 67±7 years; MD: 0.06 (-0.14, 0.26)) and young (<45; 24±4 years; MD: 0.55 (0.30, 0.81)) participants remained significant (χ 2 =8.71, I 2 =89%, p=0.003). There were no covariates that explained any of the variance in the change in fibre CSA following RET: age (10 studies, 474 participants, I 2 =65%, Adj. R 2 =-3%, p=0.50), baseline protein intake (8studies, 384 participants, I 2 =43%, Adj. R 2 =-44%, p=0.84), postexercise protein dose (10 studies, 270 participants, I 2 =77%, Adj. R 2 =-38%, p=0.92) and training status (11 studies, 586 participants, I 2 =71%, Adj. R 2 =-24%, p=0.94).
Supplementary Figure 3
Random-effects univariate meta-regression between age and the mean difference in fat-free mass (FFM) between groups. Each circle represents a study and the size of the circle reflects the influence of that study on the model (inversely proportionate to the SE of that study). The regression prediction is represented by the solid line (−0.01 kg (−0.02,–0.00), p=0.02).
Additional univariate meta-regressions are presented in elsewhere (see online supplementary table 3 ). Only whether the RET was whole-body (27 studies, including only 4 studies that were not whole-body RET, I 2 =2%, Adj. R 2 =76%, p=0.01) or supervised (28 studies, I 2 =5%, Adj. R 2 =58%, p=0.047) explained part of the variance in the effectiveness of protein supplementation on changes in 1RM. No other covariates explained any of the variance associated with the efficacy of protein supplementation on changes in 1RM or FFM.
Supplementary Table 3
Biphasic regression (42 study arms, 723 participants) explained more variation than a linear regression between the change in FFM and daily protein intake (break point=1.62 (1.03, 2.20) g/kg/day, slope=1.75, R 2 =0.19, df=36) and is presented as a segmental regression despite not being statistically significant (p=0.079; figure 5 ) When plotting the change in FFM against baseline protein intake, linear regressions explained significantly more variance than biphasic regressions in both young (slope=−1.54 g/kg/day, R 2 =0.17, df=34) and old (slope=0.16 g/kg/day, R 2 =0.04, df=14) participants with a statistically significant difference between age groups (p=0.042; see online supplementary figure 3 : panel D).
Segmental linear regression between relative total protein intake (g/kg body mass/day) and the change in fat-free mass (ΔFFM) measured by dual energy X-ray absorptiometry. Each circle represents a single group from a study. Dashed arrow indicates the break point=1.62 g protein/kg/day, p=0.079. Solid arrow indicates 95% CI, (1.03 to 2.20).
This is the largest meta-analysis on interventions including dietary protein supplementation with muscle and strength-related outcomes during prolonged RET to date. Our main finding was that dietary protein supplementation augmented RET-induced increases in 1RM strength ( figure 2 ) and FFM ( figure 3 ). For changes in FFM, dietary protein supplementation was more effective in resistance-trained individuals ( table 1 and figure 3 ), less effective with increasing chronological age ( table 1 and figure 4 ) and did not increase beyond total protein intakes of ~1.6 g/kg/day ( figure 5 ). Our data show dietary protein supplementation is both sufficient and necessary to optimise RET adaptations in muscle mass and strength.
Previous meta-analyses 6–12 have reached varying conclusions when examining the impact of protein supplementation on changes in lean mass or FFM and 1RM strength during RET. The discrepancies are likely a consequence of differing study inclusion criteria. For example, previous meta-analyses have included only trained participants, 8 only older adults, 9 11 supplements containing more than just protein, 8 10 only one source of protein, 8 12 shorter RET interventions, 10 12 frail/sarcopenic participants 7 9 11 and/or participants who were energy-restricted. 6 7 12 Previously, the largest comprehensive meta-analysis to date on protein supplementation during RET included 22 studies and 680 participants 7 and did show a significant effect of protein supplementation on RET-stimulated gains in strength and FFM. In agreement with this previous report, 7 and strengthening the conclusion of that same report by including 49 studies and 1863 participants, we show that protein supplementation augmented gains in FFM and strength with RET.
The average RET-induced increase, with all measures of 1RM included, was 27 kg (mean±SD; 27±22 kg 22 32 ). Notably, dietary protein supplementation augmented the increase in 1RM strength by 2.49 kg (9%; figure 2 ; see online supplementary figure 4 ), which strongly suggests that the practice of RET is a far more potent stimulus for increasing muscle strength than the addition of dietary protein supplementation. None of our covariates (age, training status, postexercise protein dose or baseline protein intake) influenced the efficacy of protein supplementation on changes in 1RM strength. Improving performance of a specific task (eg, the 1RM of an exercise) is predominately determined by the practice of that task. 71 Though protein supplementation may slightly augment changes in 1RM (~9%), which may be important for those competing in powerlifting or weightlifting, it is pragmatic to advocate that if an increase in 1RM is the objective of an RET programme, a sufficient amount of work and practice at or around the 1RM is far more influential than protein supplementation.
Supplementary Figure 4
Muscle mass.
In addition to increasing changes in muscle strength, RET alone (≥6; 13±8 weeks) resulted in an increase in FFM (1.1±1.2 kg), an increase in fibre CSA (808±) and an increase in mid-femur CSA (52±30 mm 2 ). Dietary protein supplementation augmented the increase in FFM by 0.30 kg (27%; figure 3 ; see online supplementary figure 4 ), fibre CSA by 310 µm 2 (38%; see online supplementary figure 2 : panel A) and mid-femur CSA by 7.2 mm 2 (14%; see online supplementary figure 2 : panel B). The postexercise protein dose did not affect the efficacy of protein supplementation on RET-induced changes in FFM whereas training status (positive), age (negative) and baseline protein intake (positive) did. Relative to untrained participants, resistance-trained participants have a smaller potential for muscle growth 72 and an attenuated postexercise muscle protein turnover. 73 As a result, we speculate that trained persons may have less ‘degrees of freedom’ to change with RET and therefore have a greater need for protein supplementation to see increases in muscle mass. Our thesis is supported by the observation of a more consistent impact of protein supplementation on gains in FFM in resistance-trained individuals than in novice trainees ( figure 3 ).
Older individuals are anabolically resistant 74 and require higher per-meal protein doses to achieve similar rates of MPS, the primary variable regulating changes in skeletal muscle mass, 75 compared with younger participants. 14 The average supplemental daily protein dose given to older participants was surprisingly low (20±18 g/day); thus, it is perhaps not surprising that we did not find that older individuals were responsive to protein supplementation ( figure 4 ). Though age did not affect the RET-induced change in fibre CSA, the negative effect age had on changes in FFM leads us to speculate that even though exercise sensitises muscle to the effect of protein ingestion, 3 older persons have an increased need for higher protein intakes to optimally respond to this effect and see gains in FFM. 76
It has been theorised that the increased deviation from normal protein intake (g/kg/day) will positively affect the RET-induced gains in FFM. 77 Contrary to this thesis, we found that a higher prestudy protein intake actually resulted in a greater effect of protein supplementation on changes in FFM ( table 1 ); however, this was likely driven by the lower mean baseline protein intake (old: 1.2±0.2 g/kg/day, young: 1.5±0.4 g/kg/day) and daily protein dose (old: 20±18 g/day, young: 42±32 g/day) in the studies that included older participants (see online supplementary figure 3 : panel B and D). Indeed, a sensitivity analysis that did not include older (>45; 65±14 years) versus younger (<45; 24±4 years) individuals found that baseline protein intake had no effect on the efficacy of protein supplementation in young individuals (see online supplementary figure 3 , panel C). In an unadjusted meta-regression analysis, a higher baseline protein intake in young individuals actually attenuated the change in FFM (see online supplementary figure 3 , panel D).
A goal of this meta-analysis was to deliver evidence-based recommendations that could be readily translated. A crucial point is that even though the mean baseline protein intake for the 1863 participants was ~1.4 g protein/kg/day, which is 75% greater than the current US/Canadian recommended dietary allowance (RDA), 78 an average supplementation of ~35 g protein/day still augmented RET-stimulated gain in FFM ( figure 3 ) and 1RM strength ( figure 2 ). Thus, consuming protein at the RDA of 0.8 g protein/kg/day appears insufficient for those who have the goal of gaining greater strength and FFM with RET. This conclusion is emphasised for older men 79 and women 80 81 wishing to obtain strength and gain lean mass with RET and protein supplementation.
A recent retrospective analysis showed a ‘breakpoint’ for the stimulation of MPS when ingesting an isolated protein source at 0.24 g protein/kg and 0.40 g protein/kg in younger and older participants, respectively. 14 Given the observation of a dose-responsive relationship between protein intake and MPS 82–85 and the fact that MPS is aligned with muscle hypertrophy, 13 we elected to use an identical two-segment regression approach between total daily protein intake and changes in FFM ( figure 5 ) as has been done for changes in protein dose and MPS. 14 Here we provide significant insight (using 42 study arms including 723 young and old participants with protein intakes ranging from 0.9 g protein/kg/day to 2.4 g protein/kg/day) by reporting an unadjusted plateau in RET-induced gains in FFM at 1.62 g protein/kg/day (95% CI: 1.03 to 2.20). These results are largely in congruence with previous narrative reviews that comment on the optimal nutritional strategies to augment skeletal muscle adaptation during RET. 3 86 Given that the CI of this estimate spanned from 1.03 to 2.20, it may be prudent to recommend ~2.2 g protein/kg/d for those seeking to maximise resistance training-induced gains in FFM. Though we acknowledge that there are limitations to this approach, we propose that these findings are based on reasonable evidence and theory and provide a pragmatic estimate with an incumbent error that the reader could take into consideration.
Although the present analysis provides important and novel data, there are limitations that we acknowledge. First, the lack of RET research in older individuals has led to inconclusive recommendations from previous meta-analyses specifically focusing on older individuals. 9 11 Indeed, in this manuscript there were only 13 studies that met our inclusion criteria in older (>45 years) individuals and only six of those studies reported baseline protein intakes with changes in FFM. In addition, only four studies 27 29 33 45 in older individuals had participants that consumed what we consider to be close to optimal total protein intake (~1.2 g/kg/day to 1.6 g/kg/day) in non-exercising adults 5 . Furthermore, only two studies 23 30 in older individuals provided a postexercise supplemental protein dose that we consider to be close to optimal (~35–40 g) to stimulate FFM accretion in elderly individuals. 76 Given that older adults require more protein per day, 79–81 consume less protein per day 87 and that dietary protein ingestion and RET are effective strategies to maintain muscle mass and function with age, 67 future RET research should focus on using higher protein doses (or potentially higher leucine), larger sample sizes and longer interventions in ageing populations. Second, we included a variety of additional covariates into univariate meta-regressions to elucidate the variables that may modify whether protein supplementation affects RET-induced changes in muscle mass and strength. Such an approach is generally considered to be hypothesis generating. The only significant findings we found were that if the RET sessions were whole-body (adjusted R 2 =76%, p=0.01) or supervised (adjusted R 2 =58%, p=0.047), protein supplementation was more effective at augmenting changes in 1RM. No variable affected changes in FFM (see online supplementary table 3 ). Given the relatively small effect that protein supplementation has on changes in FFM and 1RM, clearly other variables as a component of RET programmes are of much greater importance. Our meta-analyses also only included studies with participants that were at or above their energy requirements, which may have omitted the significant impact protein has during periods of weight loss with RET. 88 Lastly, we found that the postexercise protein dose did not affect the efficacy of protein supplementation on RET-induced changes in FFM. Our analysis, and those from others, 6 leads us to conclude that the specifics of protein supplementation (eg, timing, postexercise protein dose or protein source) play a minor, if any, role in determining RET-induced gains in FFM and strength over a period of weeks. Instead, our results indicate that a daily protein intake of ~1.6 g/kg/day, separated into ~0.25 g/kg doses, 14 is more influential on adaptive changes with RET, at least for younger individuals.
Dietary protein supplementation augments changes in muscle mass and strength during prolonged RET. Protein supplementation is more effective at improving FFM in young or resistance-trained individuals than in older or untrained individuals. Protein supplementation is sufficient at ~1.6 g/kg/day in healthy adults during RET. Based on limited data we observed no overtly apparent sex-based differences but acknowledge that far less work has been done in women than men. This analysis shows that dietary protein supplementation can be, if protein intake is less than 1.6 g protein/kg/day, both sufficient and necessary to optimise RET-induced changes in FFM and 1RM strength. However, performance of RET alone is the much more potent stimulus, accounting, at least according to this meta-analysis, for a substantially greater portion of the variance in RET-induced gains in muscle mass and strength.
Summary box
There is no consensus on the efficacy of protein supplementation during prolonged resistance exercise training (RET).
Novel findings
Dietary protein supplementation augments changes in fat-free mass (FFM, (0.30 kg (0.09, 0.52), p=0.007) and one-repetition-maximum strength (2.49 kg (0.64, 4.33), p=0.01) during prolonged RET.
Dietary protein supplementation during RET is more effective at increasing changes in FFM in resistance-trained individuals (0.75 kg (0.09, 1.40), p=0.03) and less effective in older individuals (−0.01 kg (−0.02,–0.00), p=0.02).
Protein supplementation beyond a total daily protein intake of ~1.6 g/kg/day during RET provided no further benefit on gains in muscle mass or strength.
Acknowledgments
SMP thanks the Canada Research Chairs, Canadian Institutes for Health Research, and the Natural Science and Engineering Research Council of Canada for their support during the completion of this work.
- Dideriksen K ,
- Reitelseder S ,
- Lockwood CM ,
- Morton RW ,
- McGlory C ,
- Phillips SM
- Rasmussen BB
- Phillips SM ,
- Chevalier S ,
- Schoenfeld BJ ,
- Aragon AA ,
- Cermak NM ,
- de Groot LC , et al
- Naclerio F ,
- Larumbe-Zabala E
- Umpierre D , et al
- Nissen SL ,
- Thomas DK ,
- Saunders DH , et al
- Miller PE ,
- Alexander DD ,
- Libardi CA , et al
- Churchward-Venne TA ,
- Witard O , et al
- Valentine J
- Andersen LL ,
- Tufekovic G ,
- Zebis MK , et al
- Antonio J ,
- Ellerbroek A ,
- Silver T , et al
- Peacock CA ,
- Ellerbroek A , et al
- Arnarson A ,
- Gudny Geirsdottir O ,
- Ramel A , et al
- Babault N ,
- Le Ruyet P , et al
- Deley G , et al
- Bemben MG ,
- Witten MS ,
- Carter JM , et al
- DiSilvestro RA ,
- Babaknia A , et al
- Barrera G ,
- de la Maza P , et al
- Chilibeck PD ,
- Davidson KS , et al
- Campbell WW ,
- Young VR , et al
- Candow DG ,
- Smith-Palmer T , et al
- Facci M , et al
- Carter JM ,
- Bemben DA ,
- Knehans AW , et al
- Coburn JW ,
- Housh TJ , et al
- Williams AD ,
- Stathis CG , et al
- O’Connell SL ,
- Mundell NL , et al
- Deibert P ,
- Solleder F ,
- König D , et al
- Knehans AW ,
- Bemben DA , et al
- Erskine RM ,
- Fletcher G ,
- Hanson B , et al
- Rahbek SK ,
- Vendelbo MH , et al
- Hartman JW ,
- Wilkinson SB , et al
- Costa PB , et al
- Hoffman JR ,
- Ratamess NA ,
- Kang J , et al
- Tranchina CP , et al
- Kovanen V ,
- Selänne H , et al
- Mero AA , et al
- Tannerstedt J ,
- Apolzan JW ,
- Gerrard DE , et al
- Tarnopolsky MA , et al
- Kerksick CM ,
- Rasmussen CJ ,
- Lancaster SL , et al
- Leenders M ,
- Verdijk LB ,
- Van der Hoeven L , et al
- Malek MH , et al
- Mitchell CJ ,
- Oikawa SY ,
- Ogborn DI , et al
- Vandoni M ,
- Ottobrini S , et al
- Hofmann M , et al
- Aagaard P ,
- Kadi F , et al
- Pacelli Q ,
- Cancellara P , et al
- Pacelli QF ,
- Neri M , et al
- Rankin JW ,
- Goldman LP ,
- Puglisi MJ , et al
- Borack MS ,
- Markofski MM , et al
- Rozenek R ,
- Long S , et al
- Snijders T ,
- Smeets JS , et al
- Jonkers RA ,
- Gleeson BG , et al
- Gómez AL , et al
- Weisgarber KD ,
- Hartz KK , et al
- Willoughby DS ,
- Higgins JPT ,
- Gorissen SH ,
- Horstman AM ,
- Franssen R , et al
- Cederholm T , et al
- Pasiakos SM ,
- McLellan TM ,
- Lieberman HR
- Higgins JP ,
- Thompson SG
- Harbord RM ,
- Buckner SL ,
- Jessee MB ,
- Mattocks KT , et al
- Wilkinson DJ ,
- Mitchell WK , et al
- Staron RS ,
- Pennings B , et al
- Rennie MJ ,
- Wackerhage H ,
- Spangenburg EE , et al
- Holwerda AM ,
- Phillips SM , et al
- Schlicker S ,
- Yates AA , et al
- Chapman K ,
- Elango R , et al
- McCabe GP ,
- Owens J , et al
- Robinson MJ ,
- Fry JL , et al
- Burd NA , et al
- Pennings B ,
- de Lange A , et al
- Breen L , et al
- Van Loon LJ
- ↵ U.S. Department of Agriculture ARS . Nutrient intakes from food and beverages: mean amounts consumed per individual, by gender and age . What We Eat In America 2014 : NHANES , 2011:12 .
- Longland TM ,
- Mitchell CJ , et al
Contributors RWM, BJS, MH, EH, AAA, MCD, JWK and SMP contributed to the conception and design of the study. RWM, BJS, MH, EH, AAA, MCD, LB, JWK and SMP contributed to the development of the search strategy. LB conducted the systematic search. RWM, KTM and SRM completed the acquisition of data. RWM and SMP performed the data analysis. All authors assisted with the interpretation. RWM and SMP were the principal writers of the manuscript. All authors contributed to the drafting and revision of the final article. All authors approved the final submitted version of the manuscript.
Competing interests SMP has received grant support, travel expenses, and honoraria for presentations from the US National Dairy Council. This agency has supported trials reviewed in this analysis.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement All data are available in the submitted manuscript or as supplementary files.
Read the full text or download the PDF:
Effects of protein supplements on muscle damage, soreness and recovery of muscle function and physical performance: a systematic review
Affiliation.
- 1 Military Nutrition Division, US Army Research Institute of Environmental Medicine (USARIEM), Natick, MA, 01760-5007, USA.
- PMID: 24435468
- DOI: 10.1007/s40279-013-0137-7
Background: Protein supplements are frequently consumed by athletes and recreationally-active individuals, although the decision to purchase and consume protein supplements is often based on marketing claims rather than evidence-based research.
Objective: To provide a systematic and comprehensive analysis of literature examining the hypothesis that protein supplements enhance recovery of muscle function and physical performance by attenuating muscle damage and soreness following a previous bout of exercise.
Data sources: English language articles were searched with PubMed and Google Scholar using protein and supplements together with performance, exercise, competition and muscle, alone or in combination as keywords.
Study selection: Inclusion criteria required studies to recruit healthy adults less than 50 years of age and to evaluate the effects of protein supplements alone or in combination with carbohydrate on performance metrics including time-to-exhaustion, time-trial or isometric or isokinetic muscle strength and markers of muscle damage and soreness. Twenty-seven articles were identified of which 18 dealt exclusively with ingestion of protein supplements to reduce muscle damage and soreness and improve recovery of muscle function following exercise, whereas the remaining 9 articles assessed muscle damage as well as performance metrics during single or repeat bouts of exercise.
Study appraisal and synthesis methods: Papers were evaluated based on experimental design and examined for confounders that explain discrepancies between studies such as dietary control, training state of participants, sample size, direct or surrogate measures of muscle damage, and sensitivity of the performance metric.
Results: High quality and consistent data demonstrated there is no apparent relationship between recovery of muscle function and ratings of muscle soreness and surrogate markers of muscle damage when protein supplements are consumed prior to, during or after a bout of endurance or resistance exercise. There also appears to be insufficient experimental data demonstrating ingestion of a protein supplement following a bout of exercise attenuates muscle soreness and/or lowers markers of muscle damage. However, beneficial effects such as reduced muscle soreness and markers of muscle damage become more evident when supplemental protein is consumed after daily training sessions. Furthermore, the data suggest potential ergogenic effects associated with protein supplementation are greatest if participants are in negative nitrogen and/or energy balance.
Limitations: Small sample numbers and lack of dietary control limited the effectiveness of several investigations. In addition, studies did not measure the effects of protein supplementation on direct indices of muscle damage such as myofibrillar disruption and various measures of protein signaling indicative of a change in rates of protein synthesis and degradation. As a result, the interpretation of the data was often limited.
Conclusions: Overwhelmingly, studies have consistently demonstrated the acute benefits of protein supplementation on post-exercise muscle anabolism, which, in theory, may facilitate the recovery of muscle function and performance. However, to date, when protein supplements are provided, acute changes in post-exercise protein synthesis and anabolic intracellular signaling have not resulted in measureable reductions in muscle damage and enhanced recovery of muscle function. Limitations in study designs together with the large variability in surrogate markers of muscle damage reduced the strength of the evidence-base.
Publication types
- Research Support, U.S. Gov't, Non-P.H.S.
- Systematic Review
- Bicycling / physiology
- Dietary Carbohydrates / administration & dosage
- Dietary Proteins / administration & dosage*
- Dietary Supplements*
- Exercise / physiology*
- Muscle Fatigue / physiology*
- Muscle, Skeletal / injuries*
- Muscle, Skeletal / physiology
- Myalgia / prevention & control*
- Physical Education and Training
- Resistance Training
- Running / physiology
- Weight-Bearing
- Dietary Carbohydrates
- Dietary Proteins

Protein is an essential macronutrient, but not all food sources of protein are created equal, and you may not need as much as you think. Learn the basics about protein and shaping your diet with healthy protein foods.
Jump to: – What is protein? – How much protein do I need? – It’s all about the protein “package” – Research on protein and human health – Protein foods and the planet – The bottom line: choosing healthy protein foods – [Quiz] Test your protein knowledge!
What Is Protein?
Protein is found throughout the body—in muscle, bone, skin, hair, and virtually every other body part or tissue. It makes up the enzymes that power many chemical reactions and the hemoglobin that carries oxygen in your blood. At least 10,000 different proteins make you what you are and keep you that way.
Protein is made from twenty-plus basic building blocks called amino acids. Because we don’t store amino acids, our bodies make them in two different ways: either from scratch, or by modifying others. Nine amino acids—histidine, isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan, and valine—known as the essential amino acids, must come from food.
How Much Protein Do I Need?
The National Academy of Medicine recommends that adults get a minimum of 0.8 grams of protein for every kilogram of body weight per day, or just over 7 grams for every 20 pounds of body weight . [1]
- For a 140-pound person, that means about 50 grams of protein each day.
- For a 200-pound person, that means about 70 grams of protein each day.
The National Academy of Medicine also sets a wide range for acceptable protein intake—anywhere from 10% to 35% of calories each day. Beyond that, there’s relatively little solid information on the ideal amount of protein in the diet or the healthiest target for calories contributed by protein. In an analysis conducted at Harvard among more than 130,000 men and women who were followed for up to 32 years, the percentage of calories from total protein intake was not related to overall mortality or to specific causes of death. [2] However, the source of protein was important.
“Pure” protein, whether derived from plant or animal foods, probably has similar effects on health, although the mix of amino acids can have health implications. Some proteins found in food are “complete,” meaning they contain all twenty-plus types of amino acids needed to make new protein in the body. Others are incomplete, lacking one or more of the nine essential amino acids, which our bodies can’t make from scratch or from other amino acids. Animal-based foods (meat, poultry, fish, eggs, and dairy foods) tend to be good sources of complete protein, while plant-based foods (fruits, vegetables, grains, nuts, and seeds) often lack one or more essential amino acid. Those who abstain from eating animal-based foods can eat a variety of protein-containing plant foods each day in order to get all the amino acids needed to make new protein, and also choose to incorporate complete plant proteins like quinoa and chia seeds .
It’s important to note that millions of people worldwide, especially young children, don’t get enough protein due to food insecurity. The effects of protein deficiency and malnutrition range in severity from growth failure and loss of muscle mass to decreased immunity , weakening of the heart and respiratory system, and death.
However, it’s uncommon for healthy adults in the U.S. and most other developed countries to have a deficiency, because there’s an abundance of plant and animal-based foods full of protein. In fact, many in the U.S. are consuming more than enough protein, especially from animal-based foods. [3]
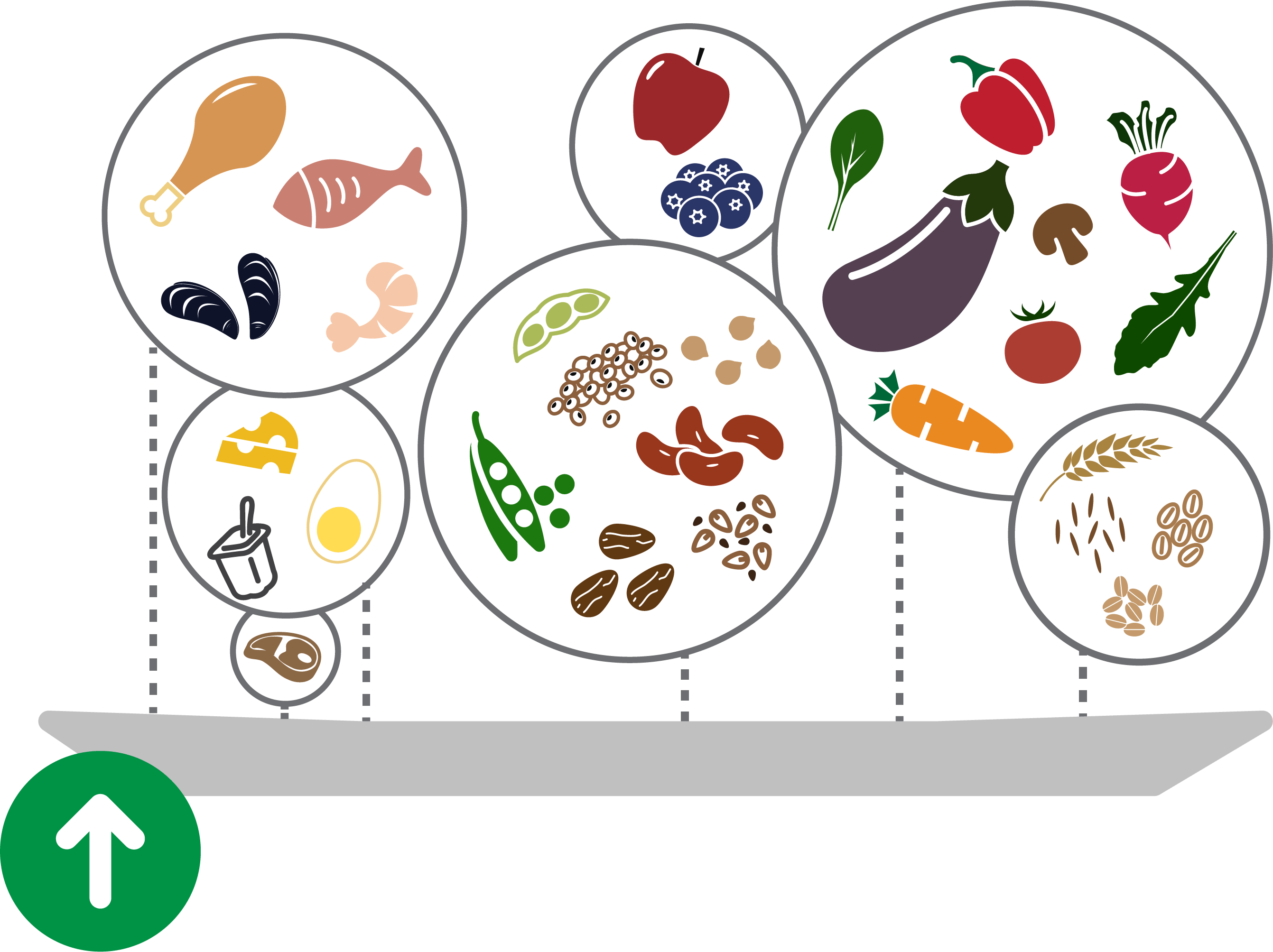
It’s All About the Protein “Package”
When we eat foods for protein, we also eat everything that comes alongside it: the different fats, fiber, sodium, and more. It’s this protein “package” that’s likely to make a difference for health.
The table below shows a sample of food “packages” sorted by protein content, alongside a range of components that come with it.
![research on protein supplementation table comparing protein packages Food /[Category] Protein (g) Saturated Fat (g) Mono-unsaturated Fat (g) Poly-unsaturated Fat (g) ALA (g) Marine Omega-3 Fats (g) Fiber (g) Sodium (mg) Sirloin steak, broiled (4oz) [Red Meat] 33 4.6 4.9 0.4 0.4 0 0 66 Sockeye salmon, grilled (4oz) [Seafood] 30 1.1 2.1 1.5 0.3 1.0 0 104 Chicken, thigh, no skin (4oz) [Poultry] 28 2.7 3.9 2.0 0.1 0.1 0 120 Ham steak (4oz) [Red Meat] 22 1.6 2.2 0.5 0.5 0 0 1,439 Lentils (1 cup, cooked) [Legumes] 18 0.1 0.1 0.3 0.3 0 15 4 Milk (8oz) [Dairy] 8 3.1 1.4 0.2 0.3 O0 0 115 Almonds, dry roasted, unsalted (1oz) [Nuts] 6 1.2 9.4 3.4 0 0 3.1 1](https://www.hsph.harvard.edu/nutritionsource/wp-content/uploads/sites/30/2018/11/Screen-Shot-2018-11-08-at-3.52.40-PM.png)
To call out a few examples:
- A 4-ounce broiled sirloin steak is a great source of protein—about 33 grams worth. But it also delivers about 5 grams of saturated fat .
- A 4-ounce ham steak with 22 grams of protein has only 1.6 grams of saturated fat, but it’s loaded with 1,500 milligrams worth of sodium .
- 4 ounces of grilled sockeye salmon has about 30 grams of protein, naturally low in sodium, and contains just over 1 gram of saturated fat. Salmon and other fatty fish are also excellent sources of omega-3 fats , a type of fat that’s especially good for the heart.
- A cup of cooked lentils provides about 18 grams of protein and 15 grams of fiber , and it has virtually no saturated fat or sodium.

What about protein powders?
Research on protein and health.
Available evidence indicates that it’s the source of protein (or, the protein “package”), rather than the amount of protein, that likely makes a difference for our health. You can explore the research related to each disease in the tabs below, but here’s the evidence-based takeaway: eating healthy protein sources like beans, nuts, fish, or poultry in place of red meat and processed meat can lower the risk of several diseases and premature death.
Research conducted at the Harvard Chan School of Public Health has found that eating even small amounts of red meat—especially processed red meat—on a regular basis is linked to an increased risk of heart disease and stroke , and the risk of dying from cardiovascular disease or any other cause. [4-6] Conversely, replacing red and processed red meat with healthy protein sources such as beans, soy foods, nuts, fish, or poultry seems to reduce these risks. One of the reasons why plant sources of protein are related to lower risk of cardiovascular disease compared to protein from red meat and dairy is because of the different types of fat in these protein packages. Plant-based protein sources are more unsaturated, which lowers LDL cholesterol—an established risk factor for heart disease. Also, plant sources contain no cholesterol . Other factors are likely to contribute to the lower risk, but this is a key factor.
- Processed red meat was even more strongly linked to dying from cardiovascular disease—and in smaller amounts: every additional 1.5 ounce serving of processed red meat consumed each day (equivalent to one hot dog or two strips of bacon) was linked to a 20% increase in the risk of cardiovascular disease death.
- Cutting back on red meat could save lives: the researchers estimated that if all the men and women in the study had reduced their total red and processed red meat intake to less than half a serving a day, one in ten cardiovascular disease deaths would have been prevented.
- In another study of 43,000 men that looked at both amount and sources of protein found that intake of total protein was minimally associated with heart disease risk, but intake of protein from red meat was associated with higher risk. [7]
- The study included data from 36 randomized controlled trials involving 1,803 participants. The researchers compared people who ate diets with red meat with people who ate more of other types of foods (i.e. chicken, fish, carbohydrates, or plant proteins such as legumes, soy, or nuts), looking at blood concentrations of cholesterol, triglycerides, lipoproteins, and blood pressure—all risk factors for cardiovascular disease.
- Researchers found that when diets with red meat were compared with all other types of diets combined, there were no significant differences in total cholesterol, lipoproteins, or blood pressure, although diets higher in red meat did lead to higher triglyceride concentrations than the comparison diets.
- However, researchers found that diets higher in high-quality plant protein sources such as legumes, soy, and nuts resulted in lower levels of both total and LDL (“bad”) cholesterol compared to diets with red meat.
In terms of the amount of protein consumed, there’s evidence that eating a relatively high-protein diet may be beneficial for the heart, as long as the protein comes from a healthy source.
- A 20-year prospective study of over 80,000 women found that those who ate low-carbohydrate diets that were high in plant-based sources of fat and protein had a 30%lower risk of heart disease compared with women who ate high-carbohydrate, low-fat diets. [8] However, eating a low-carbohydrate diet high in animal fat or protein did not offer such protection.
- Further evidence of the heart benefits of eating healthy protein in place of carbohydrate comes from a randomized trial known as the Optimal Macronutrient Intake Trial for Heart Health (OmniHeart). A healthy diet that replaced some carbohydrate with healthy protein (or healthy fat) did a better job of lowering blood pressure and harmful low-density lipoprotein (LDL) cholesterol than a higher carbohydrate diet. [9]
- Similarly, the “EcoAtkins” weight loss trial compared a low-fat, high -carbohydrate, vegetarian diet to a low-carbohydrate vegan diet that was high in vegetable protein and fat. Though weight loss was similar on the two diets, study participants on the high protein diet saw improvements in blood lipids and blood pressure. [10]
- Of course, occasionally a study will generate headlines because it found the opposite result. For example, one study of Swedish women who ate low-carbohydrate, high-protein diets had higher rates of cardiovascular disease and death than those who ate lower-protein, higher-carbohydrate diets. [11] But the study, which assessed the women’s diets only once and then followed them for 15 years, did not look at what types of carbohydrates or what sources of protein these women ate. That was important because most of the women’s protein came from animal sources.
Again, the source of protein matters more than protein quantity when it comes to diabetes risk. Eating more red meat predicts a higher risk of type 2 diabetes, while consuming nuts, legumes, and poultry is related to lower risk.
- A 2011 study found that people who ate diets high in red meat, especially processed red meat, had a higher risk of type 2 diabetes than those who rarely ate red or processed meat. [12] For each additional serving a day of red meat or processed red meat that study participants ate, their risk of diabetes rose 12% and 32%, respectively. Investigators also found that replacing a serving of red meat with one serving of nuts, low-fat dairy products, or whole grains each day was associated with an estimated 16% to 35% lower risk of type 2 diabetes.
- A related study also found that people who started eating more red meat than usual were had a 50% higher risk of developing type 2 diabetes during the next four years, and researchers also found that those who reduced red meat consumption had a 14% lower risk of type 2 diabetes over a 10-year follow-up period. [13]
- How meat is cooked may also affect type 2 diabetes risk . In a study that tracked the health of over 289,000 men and women, researchers found that individuals who most frequently ate red meats and chicken cooked at high temperatures were 1.5 times more likely to develop type 2 diabetes, compared to those who ate the least. There was also an increased risk of weight gain and developing obesity in the frequent users of high-temperature cooking methods, which may have contributed to the development of diabetes. Of note, this research demonstrated that cooking methods might contribute to diabetes risk beyond the effects of meat consumption alone. [14] Learn more about this study .
- More evidence that the source of protein matters comes from a 20-year study that looked at the relationship between low-carbohydrate diets and type 2 diabetes in women. Low-carbohydrate diets that were high in vegetable sources of fat and protein were associated with a lower risk of type 2 diabetes. [15] But low-carbohydrate diets that were high in animal sources of protein or fat did not show this benefit.
- For type 1 diabetes (formerly called juvenile or insulin-dependent diabetes), proteins found in cow’s milk have been implicated in the development of the disease in babies with a predisposition to the disease, but research remains inconclusive. [16,17]
When it comes to cancer, once again, the source of protein seems to matter more than quantity.
- In the Nurse’s Health Study and the Health Professionals Follow-Up Study, every additional serving per day of red meat or processed red meat was associated with a 10% and 16% higher risk of cancer death, respectively. [5]
- Conclusions were primarily based on the evidence for colorectal cancer . Data also showed positive associations between processed meat consumption and stomach cancer , and between red meat consumption and pancreatic and prostate cancer .
- A 2014 study also found a link between high consumption of red meat during adolescence and premenopausal breast cancer, while higher intakes of poultry, nuts, and legumes were associated with lower risk. Using data on the health of 89,000 women (aged 24 to 43) followed over a 20-year period, researchers found a 22% higher risk of breast cancer in those who ate 1.5 servings of red meat per day while in high school, compared to those who only had one serving per week. Each additional daily serving of red meat seemed to increase the risk of breast cancer by another 13%. [19]
- How meat is cooked may also have implications for cancer risk. High-temperature grilling creates potentially cancer-causing compounds in meat, including polycyclic aromatic hydrocarbons and heterocyclic amines. Learn about tips for healthy grilling.
- In 2016, researchers reviewed protein intakes of more than 131,000 women and men from the Nurses’ Health Study and Health Professionals Follow-up Study. After tracking their diets for up to 32 years, the authors found that a higher intake of red meat, especially processed versions (sausage, bacon, hot dogs, salami), was linked to a modestly higher risk of death, while a higher protein intake from plant foods carried a lower risk. [2] Learn more about this study .
- Digesting protein releases acids into the bloodstream, which the body usually neutralizes with calcium and other buffering agents. As a result, early research theorized that eating lots of protein requires a lot more calcium – which may be pulled from bone. A 2009 systematic review found that this doesn’t appear to happen. [20]
The same healthy protein foods that are good choices for disease prevention may also help with weight control. Again, it’s the source of protein that matters.
- Those who ate more red and processed meat over the course of the study gained more weight, about one extra pound every four years, while those who ate more nuts over the course of the study gained less weight, about a half pound less every four years.
- A subsequent detailed analysis of this cohort also found that eating red meat, chicken with skin, and regular cheese was associated with greater weight gain. Yogurt, peanut butter, walnuts and other nuts, chicken without skin, low-fat cheese, and seafood was associated with less weight gain. [22]
- Another study showed that eating around one daily serving of beans, chickpeas , lentils or peas can increase fullness, which may lead to better weight management and weight loss. [23]
There’s no need to go overboard on protein. Though some studies show benefits of high-protein, low-carbohydrate diets in the short term (such as the paleo diet ), avoiding fruits and whole grains means missing out on healthful fiber, vitamins, minerals, and other phytonutrients.
- Specific proteins in food and the environment are involved in food allergies, which are overreactions of the immune system (take gluten and celiac disease , for example).
- Medical journals are also full of reports linking allergic responses to specific protein sources with a variety of conditions (breathing problems, chronic digestive issues, etc.). Eggs, fish, milk, peanuts, tree nuts, and soybeans cause allergic reactions in some people.
- Individuals diagnosed with certain diseases (such as kidney and liver disease) need to monitor their protein intake according to their physician’s guidelines.
- You may have also heard that the use of antibiotics in the production of animal-based foods has contributed to the emergence of “superbugs,” or strains of bacteria resistant to currently available antibiotics. In 2016, the FDA announced a voluntary program to limit the routine use of antibiotics in food production (such as giving antibiotics to healthy animals to help them grow faster). [24] As a consumer, you may want to find products “raised without antibiotics” if you plan on eating meat. Some companies feature this language on the packaging, others don’t.

New research highlight: Red meat and diabetes risk
Protein foods and the planet.

To give you an idea, this “scorecard” from the World Resources Institute illustrates the differing GHG emissions per gram of protein from both animal and plant-based protein foods. [25] Making just one pound (454 grams) of lamb generates five times more GHGs than making a pound of chicken and around 30 times more than making a pound of lentils. [26] In the U.S. alone, beef accounts for 36% of all food-related GHG emissions. [27] Beyond emissions, it’s also important to note that food production places an enormous demand upon our natural resources, as agriculture is a major contributor to deforestation, species extinction, and freshwater depletion and contamination.
Bottom Line
Protein is a key part of any diet. The average person needs about 7 grams of protein every day for every 20 pounds of body weight. Because protein is found in an abundance of foods, many people can easily meet this goal. However, not all protein “packages” are created equal. Because foods contain a lot more than protein, it’s important to pay attention to what else is coming with it. That’s why the Healthy Eating Plate encourages choosing healthy protein foods.
Building off this general guidance, here are some additional details and tips for shaping your diet with the best protein choices:
- Legumes: lentils , beans (adzuki, black, fava, chickpeas /garbanzo, kidney, lima, mung, pinto etc.), peas (green, snow, snap, split, etc.), edamame/soybeans (and products made from soy : tofu, tempeh, etc.), peanuts.
- Nuts and Seeds: almonds , pistachios, cashews, walnuts, hazelnuts, pecans, hemp seeds, squash and pumpkin seeds, sunflower seeds, flax seeds, sesame seeds, chia seeds .
- Whole Grains: kamut, teff, wheat, quinoa , rice , wild rice, millet, oats , buckwheat,
- Other: while many vegetables and fruits contain some level of protein, it’s generally in smaller amounts than the other plant-based foods. Some examples with higher protein quantities include corn, broccoli, asparagus, brussels sprouts , and artichokes.
Prioritize hearty and savory plant-based preparations
- Generally, poultry (chicken, turkey, duck) and a variety of seafood ( fish , crustaceans, mollusks) are your best bet. Eggs can be a good choice, too.
- If you enjoy dairy foods , it’s best to do so in moderation (think closer to 1-2 servings a day; and incorporating yogurt is probably a better choice than getting all your servings from milk or cheese ).
- Red meat —which includes unprocessed beef, pork, lamb, veal, mutton, and goat meat—should be consumed on a more limited basis. If you enjoy red meat, consider eating it in small amounts or only on special occasions.
- Processed meats , such as bacon, hot dogs, sausages, and cold cuts should be avoided. Although these products are often made from red meats, processed meats also include items like turkey bacon, chicken sausage, and deli-sliced chicken and ham. (Processed meat refers to any meat that has been “transformed through salting, curing, fermentation, smoking, or other processes to enhance flavor or improve preservation.” [18])
Looking to reduce red and processed meats, but unsure where to start? Here are a few approaches to cutting-back while keeping your meals satiating and flavorful. Simply find your “starting point” and move forward with the strategies that work for you:
Eat a little less red meat, any way you can
Swap out red meat for healthier meats
Consume less meat, enjoy more variety
Test your protein knowledge.
Ready to see how much you know about protein and healthy protein foods? Try this 10 question quiz to find out:
- National Academies of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) .
- Song M, Fung TT, Hu FB, Willett WC, Longo VD, Chan AT, Giovannucci EL. Association of animal and plant protein intake with all-cause and cause-specific mortality. JAMA internal medicine . 2016 Oct 1;176(10):1453-63.
- Fehrenbach KS, Righter AC, Santo RE. A critical examination of the available data sources for estimating meat and protein consumption in the USA. Public health nutrition . 2016 Jun;19(8):1358-67.
- Bernstein AM, Sun Q, Hu FB, Stampfer MJ, Manson JE, Willett WC. Major dietary protein sources and risk of coronary heart disease in women. Circulation . 2010 Aug 31;122(9):876-83.
- Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Stampfer MJ, Willett WC, Hu FB. Red meat consumption and mortality: results from 2 prospective cohort studies. Archives of internal medicine . 2012 Apr 9;172(7):555-63.
- Bernstein AM, Pan A, Rexrode KM, Stampfer M, Hu FB, Mozaffarian D, Willett WC. Dietary protein sources and the risk of stroke in men and women. Stroke . 2011 Jan 1:STROKEAHA-111.
- Preis SR, Stampfer MJ, Spiegelman D, Willett WC, Rimm EB. Dietary protein and risk of ischemic heart disease in middle-aged men–. The American journal of clinical nutrition . 2010 Sep 29;92(5):1265-72.
- Halton TL, Willett WC, Liu S, Manson JE, Albert CM, Rexrode K, Hu FB. Low-carbohydrate-diet score and the risk of coronary heart disease in women. New England Journal of Medicine . 2006 Nov 9;355(19):1991-2002.
- Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, Charleston J. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA . 2005 Nov 16;294(19):2455-64.
- Jenkins DJ, Wong JM, Kendall CW, Esfahani A, Ng VW, Leong TC, Faulkner DA, Vidgen E, Greaves KA, Paul G, Singer W. The effect of a plant-based low-carbohydrate (“Eco-Atkins”) diet on body weight and blood lipid concentrations in hyperlipidemic subjects. Archives of internal medicine . 2009 Jun 8;169(11):1046-54.
- Lagiou P, Sandin S, Lof M, Trichopoulos D, Adami HO, Weiderpass E. Low carbohydrate-high protein diet and incidence of cardiovascular diseases in Swedish women: prospective cohort study. BMJ . 2012 Jun 26;344:e4026.
- Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC, Hu FB. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis–. The American journal of clinical nutrition . 2011 Aug 10;94(4):1088-96.
- Pan A, Sun Q, Bernstein AM, Manson JE, Willett WC, Hu FB. Changes in red meat consumption and subsequent risk of type 2 diabetes mellitus: three cohorts of US men and women. JAMA internal medicine . 2013 Jul 22;173(14):1328-35.
- Pan A, Sun Q, Bernstein AM, Manson JE, Willett WC, Hu FB. Changes in red meat consumption and subsequent risk of type 2 diabetes mellitus: three cohorts of US men and women. JAMA internal medicine . 2013 Jul 22;173(14):1328-35.
- Halton TL, Liu S, Manson JE, Hu FB. Low-carbohydrate-diet score and risk of type 2 diabetes in women–. The American journal of clinical nutrition . 2008 Feb 1;87(2):339-46.
- Åkerblom HK, Vaarala O, Hyöty H, Ilonen J, Knip M. Environmental factors in the etiology of type 1 diabetes. American journal of medical genetics . 2002 May 30;115(1):18-29.
- Vaarala O, Ilonen J, Ruohtula T, Pesola J, Virtanen SM, Härkönen T, Koski M, Kallioinen H, Tossavainen O, Poussa T, Järvenpää AL. Removal of bovine insulin from cow’s milk formula and early initiation of beta-cell autoimmunity in the FINDIA pilot study. Archives of pediatrics & adolescent medicine . 2012 Jul 1;166(7):608-14.
- Bouvard V, Loomis D, Guyton KZ, Grosse Y, El Ghissassi F, Benbrahim-Tallaa L, Guha N, Mattock H, Straif K. Carcinogenicity of consumption of red and processed meat. The Lancet Oncology . 2015 Dec 1;16(16):1599-600.
- Farvid MS, Cho E, Chen WY, Eliassen AH, Willett WC. Adolescent meat intake and breast cancer risk. International journal of cancer . 2015 Apr 15;136(8):1909-20.
- Darling AL, Millward DJ, Torgerson DJ, Hewitt CE, Lanham-New SA. Dietary protein and bone health: a systematic review and meta-analysis–. The American journal of clinical nutrition . 2009 Nov 4;90(6):1674-92.
- Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. New England Journal of Medicine . 2011 Jun 23;364(25):2392-404.
- Smith JD, Hou T, Ludwig DS, Rimm EB, Willett W, Hu FB, Mozaffarian D. Changes in intake of protein foods, carbohydrate amount and quality, and long-term weight change: results from 3 prospective cohorts–. The American journal of clinical nutrition . 2015 Apr 8;101(6):1216-24.
- Li SS, Kendall CW, de Souza RJ, Jayalath VH, Cozma AI, Ha V, Mirrahimi A, Chiavaroli L, Augustin LS, Blanco Mejia S, Leiter LA. Dietary pulses, satiety and food intake: A systematic review and meta‐analysis of acute feeding trials. Obesity . 2014 Aug;22(8):1773-80.
- Food and Drug Administration. FDA’s Strategy on Antimicrobial Resistance – Questions and Answers. https://www.fda.gov/animalveterinary/guidancecomplianceenforcement/guidanceforindustry/ucm216939.htm . Accessed on 11/6/2018.
- World Resources Institute. Protein Scorecard. https://www.wri.org/resources/data-visualizations/protein-scorecard . Accessed on 11/6/2018.
- Culinary Institute of America and Harvard T.H. Chan School of Public Health. Menus of Change: 2016 Annual Report. http://www.menusofchange.org/
- Heller MC, Keoleian GA. Greenhouse gas emission estimates of US dietary choices and food loss. Journal of Industrial Ecology . 2015 Jun;19(3):391-401.
- Guasch-Ferré M, Satija A, Blondin S, Janiszewski M, Emlen E, O’Connor L, Campbell W, Hu F, Willett W, Stampfer M. Meta-Analysis of Randomized Controlled Trials of Red Meat Consumption in Comparison With Various Comparison Diets on Cardiovascular Risk Factors. Circulation . 2019 Apr 1;139(15):1828-45. *Disclosures: Dr. Hu has received research support from the California Walnut Commission. Dr. Campbell reported receiving research support from the National Institutes of Health (T32 Fellowship for Lauren O’Connor), the American Egg Board – The Egg Nutrition Center, The Beef Checkoff Program, The National Dairy Council, The Pork Checkoff Program, and the Barilla Group. Dr. Campbell also reported serving on the 2015 Dietary Guidelines Advisory Committee. Dr. Satija is an employee of Analysis Group, Inc. The other authors declare no conflicts.
Terms of Use
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.
Building muscle isn't that easy. But consuming protein the right way is critical

Summer's just around the corner and it's starting to get warm. That means a lot of people will be flocking to the gym or spend our time exercising outdoors.
We want the strength and stamina to work and play hard, and the confidence to enter a room and feel good about our appearance.
Though aerobic exercise and physical fitness are paramount, the food we eat to fuel such activity matters even more. A balanced diet helps with everyday health and function, but protein is the nutrient required for muscle maintenance and growth .
What is protein?
Proteins are complex molecules made up of smaller building blocks called amino acids . All together, they make up a macronutrient that's vital for cell growth and repair − working to improve function, structure and regulation of one's organs and one's body tissue.
Protein targets muscle tissue growth and development especially. "Amino acids are the main building block for muscle," explains Walter Willett, MD, professor of epidemiology and nutrition at Harvard T. H. Chan School of Public Health. "Basically, our digestive system pulls apart the building blocks in the proteins that we eat, and our body reassembles these building blocks into muscle."
Is creatine safe? The supplement is popular with athletes, but should you take it?
Why does protein help with muscle growth?
Such growth occurs, in part, because muscle tissue "is made of protein fibers," explains Loren Fishman, MD, a professor of physical medicine and rehabilitation at Columbia University and the medical director of Manhattan Physical Medicine and Rehabilitation. He says when protein fibers slide past each other, they cause one's muscles to contract. "The reason consuming protein in food is so important is because muscle contraction always damages these sliding protein fibers and you need to consume protein in your diet to repair and replace them," he says. That repair and replacement can lead to muscle growth and expansion.
How much protein should I eat to gain muscle?
The Dietary Guidelines for Americans ' recommended daily allowance is 0.8 grams of protein per kilogram of one's body weight. That means a person weighing 160 pounds should eat about 57 grams of protein each day.
But that amount should be higher when muscle growth and development is the goal. "We must consume about 10% of our calories as protein to maintain our muscles, and just a little bit more than this will be enough to gain muscle," advises Willett. He says most people get adequate protein for muscle growth from a healthy diet because protein-rich foods are abundant. Protein is common in animal products such as beef, pork, chicken and fish, plus seeds and nuts , beans and lentils, and it is also present in dairy products such as milk, yogurt , cheese and eggs .
Through regular consumption of such foods, "almost everyone gets enough protein to gain muscle ," explains Willett. "However, just eating more protein won’t lead to gains in muscle, we need to work for that." Physical activities that contribute to muscle growth include resistance training such as weightlifting or the use of exercise bands, plus any repetitive movement that targets specific muscle groups. "Remember, we only add to the muscles that we use," Willett says, "so climbing stairs or riding a bike will help build up our thighs but won’t do anything for muscles in our arms."
In other words, "loading up on steak and cheese will give us lots of protein," Willett says, but if we fail to also target a variety of muscle groups through proper workout routines and resistance training, we aren't likely to achieve the results we're seeking.
Children and adults are gobbling supplements. Do you know the risks?
Among some population groups, it’s not unusual to down four or more vitamins or supplements every day, new research shows

Americans spend billions of dollars every year on dietary supplements that claim to promote almost every aspect of our health. But how much do you know about the supplements you’re taking?
A recent government study found that nearly 60 percent of adults take vitamins, minerals, fish oil, herbal capsules, melatonin, probiotics and other types of dietary supplements. While most people used just one or two supplements — multivitamins and vitamin D were the two most popular products — it was not uncommon for people to report using three, four or more supplements at a time.
Among some parts of the population, it’s not unusual to down a handful of vitamins or supplements every day. About 15 percent of adults said they used four or more dietary supplements. Among older adults, the number reporting multi-supplement use is even higher — about 25 percent of adults 60 or older use four or more. About 35 percent of children and adolescents used dietary supplements, and nearly 10 percent of children between 2 and 5 years old were given two or more dietary supplements.
Experts say that vitamin and mineral supplements are generally safe when taken in small to moderate doses, like the amounts found in a basic multivitamin. Dietary supplements can be beneficial for pregnant women and for people with nutrient deficiencies and other health conditions. A clinical trial earlier this year found that for people who are 60 and older, taking a daily multivitamin helped to slow memory loss. Other studies have found that probiotic supplements can help with gastrointestinal disorders such as irritable bowel syndrome.
But taking supplements comes with risks, and for many healthy adults, it’s not always clear from research that the benefits outweigh the risks.
Get Well+Being tips straight to your inbox

In fact, some randomized trials have found that assigning people to take supplements with large doses of beta-carotene, selenium, and vitamins A, C, and E actually increased mortality rates. Rigorous clinical trials have also failed to support the hype around vitamin D, finding that people who were assigned to take the popular supplement did not develop lower rates of cardiovascular disease, cancer or bone fractures despite widespread marketing claims to the contrary.
Supplements don’t follow the same rules as drugs
Many people assume that the Food and Drug Administration tests supplements for safety. But that’s not how it works .
“Dietary supplements enter the market before there’s any real review of them by the FDA,” said Amy B. Cadwallader, the director of regulatory and public policy development at the United States Pharmacopeia, a nonprofit organization that examines the quality of drugs, food and dietary supplements.
Under federal law, companies are allowed to operate on the honor system. The FDA’s role in regulating supplements mostly involves trying to make sure products are safe and accurately labeled after they have already entered the marketplace.
Are you getting what you paid for?
In the United States, companies sell an estimated 90,000 dietary supplements, representing a roughly $50 billion industry . As a result, some experts say, consumers who buy supplements can’t always be sure that they are getting what they paid for. Studies of melatonin , fish oil , probiotics , ginkgo biloba , and other supplements have found that the doses and compounds listed on their labels are often not what are found in their bottles.
- In one study in the journal Pediatric Research , researchers tested 16 probiotic supplements and found that only one of them contained the specific bacterial strains listed on its label.
- In another study , researchers tested 30 dietary supplements that claimed to strengthen immune health and found that 17 of the products were “misbranded.” These supplements either lacked key ingredients listed on their labels — such as vitamin B12, garlic extract, ginger root and folate — or they contained a variety of unlisted ingredients.
- One study by the FDA estimated that the agency is notified of less than 1 percent of all adverse events linked to supplement use. Another study by the federal government estimated that injuries caused by supplements are responsible for about 23,000 emergency room visits each year.
Howard Luks, an orthopedic surgeon and sports medicine specialist in New York, said he routinely encounters patients who worry about potential side effects from medications but have no problem taking 10 or 20 supplements that they heard about from health influencers on social media. He said that many people who lost trust in public health authorities during the pandemic have turned to social media influencers for health advice.
“They view supplements as being holistic, natural, and therefore not potentially harmful for them,” he said.
In one case study published in March, doctors in New Jersey described a 76-year-old woman who went to an emergency room after experiencing heart palpitations, dizziness and fainting episodes. It turned out she had been taking black cohosh, an herbal supplement often used to treat hot flashes. A few days after stopping the supplement, her heartbeat returned to normal, and her other symptoms disappeared.
In another recent case , a 47-year-old woman in Houston suffered jaundice and liver damage after taking a supplement containing a blend of probiotics and herbal extracts. The case report noted that dietary supplements account for about 20 percent of drug-induced liver injuries nationwide.
How to shop smarter for supplements
Here are some tips when buying supplements.
Look for third-party certifications: The United States Pharmacopeia, or USP, vets dietary supplements to ensure they are meeting high standards for factors such as purity and potency. USP has a voluntary program through which companies can have their supplements and facilities routinely tested and examined. Companies that meet the organizations high standards are allowed to use a black and yellow “USP Verified” logo on their products. You can find them using the product-finder search tool on USP’s website. NSF is another independent group that tests and reviews dietary supplements. You can look for the blue and white “NSF” logo on your supplements or go to the group’s website to look up products.
Do your homework. Consumerlab.com is an independent laboratory that tests dietary supplements to see if they contain the ingredients and doses listed on their labels. The company publishes reports with their findings on a wide variety of supplements, which you can access on their website for a fee.
Talk to your doctor or pharmacist . Many people don’t realize that a lot of supplements and medications use the same metabolic pathways and that they can cause dangerous side effects when you combine them, said Michael Schuh, an assistant professor of pharmacy, family medicine and palliative medicine at the Mayo Clinic in Florida.
Vitamins E and K, ginseng, ginkgo biloba, resveratrol, turmeric and CoQ10 for example can interact with blood thinning medications. Vitamin C can interact with statins, niacin, estrogen, warfarin and chemotherapy drugs. St. John’s wort can make antidepressants and birth control pills less effective.
“We see it with a lot of supplements,” Schuh said. “Even something like resveratrol from grape skins: When you take it in concentrated form, it can interact with a lot of medications.”
Do you have a question about healthy eating? Email [email protected] and we may answer your question in a future column.
Read more from Well+Being
Well+Being shares news and advice for living well every day. Sign up for our newsletter to get tips directly in your inbox.
Diabetes, air pollution and alcohol consumption could be the biggest risk factors for dementia .
Dairy vs. plant milk : Which is better?
Why is my gas so smelly ? Gender, diet and plane rides can play a role.
Quitting can be a superpower that helps your mental health. Here’s how to quit smarter .
Our relationships with pets can be strong and uncomplicated.

- health-fitness
ICMR warns against protein supplements: All about the potential health risks

ICMR guidelines on protein powder
Potential health risks to know if consuming protein supplements.
Protein-rich hummus made with roasted chana: A Weight loss friendly alternative
Foods that are high in protein content
- Lean meats: Chicken breast, turkey, and lean cuts of beef provide high-quality protein with low fat content.
- Fish: Salmon, tuna, and other fatty fish are not only rich in protein but also omega-3 fatty acids, beneficial for heart health.
- Eggs: A complete protein source, eggs offer versatility and nutrients like vitamins B12 and D.
- Dairy: Greek yogurt, cottage cheese, and milk are rich in protein and calcium for bone health.
- Legumes: Beans, lentils, and chickpeas are plant-based protein sources, also high in fiber and micronutrients.

- 1 Center for Health and Human Performance, Rutgers University, New Brunswick, NJ, United States
- 2 Department of Health and Human Performance, Nova Southeastern University, Davie, FL, United States
- 3 Department of Kinesiology and Health, Rutgers University, New Brunswick, NJ, United States
There is robust evidence which shows that consuming protein pre- and/or post-workout induces a significant rise in muscle protein synthesis. It should be noted, however, that total daily caloric and protein intake over the long term play the most crucial dietary roles in facilitating adaptations to exercise. However, once these factors are accounted for, it appears that peri-exercise protein intake, particularly in the post-training period, plays a potentially useful role in terms of optimizing physical performance and positively influencing the subsequent recovery processes for both resistance training and endurance exercise. Factors that affect the utility of pre- or post-workout feeding include but are not necessarily limited to: training status (e.g., novice vs. advanced, or recreational vs. competitive athlete), duration of exercise, the number of training sessions per day, the number of competitive events per day, etc. From a purely pragmatic standpoint, consuming protein post-workout represents an opportunity to feed; this in turn contributes to one's total daily energy and protein intake. Furthermore, despite recent suggestions that one does not “need” to consume protein during the immediate (1 h or less) post-training time frame, it should be emphasized that consuming nothing offers no advantage and perhaps even a disadvantage. Thus, based on performance and recovery effects, it appears that the prudent approach would be to have athletes consume protein post-training and post-competition.
Introduction
Dietary protein plays a critical role in countless physiological processes in the body. The current Recommended Dietary Allowance (RDA) for healthy individuals is 0.8 g/kg/day ( 1 ). It is increasingly evident, however, that protein intake of at least 1.4–1.6 g/kg/day ( 2 ) would be more appropriate for active individuals attempting to optimize training adaptations. In an effort to meet this threshold, protein supplements are often consumed. In 2015, protein powder sales were valued at 4.7 billion U.S. dollars and were second only to sport drinks in the sports nutrition market ( 3 ). The popularity of protein supplements is likely influenced by the claims of increased muscle mass, increased fat loss, improved performance, and improved markers of recovery.
To date several meta-analyses, reviews, and systematic reviews have attempted to quantify and clarify these claims, but with mixed results ( 2 , 4 – 7 ). However, these efforts are complicated by the fact that the populations studied included trained and untrained, healthy normal weight, overweight or obese individuals, as well as injured, movement impaired, and those with metabolic or other diseases states. Additionally, the emphasis of recent reviews has been largely on impacts on muscle protein synthesis (MPS), hypertrophy, and body composition, with most of the outcomes pertaining solely to resistance training ( 2 , 4 – 7 ). Performance and recovery effects have been given secondary consideration at best, and these are areas that would be of particular interest to most athletes or athletic individuals.
Furthermore, performance and recovery outcomes, as well as physiological adaptations, are unique to the modality of training primarily employed. Anaerobic training refers to short bouts of high intensity movements which are often interspersed with longer recovery periods between efforts, with two of the most popular applications being resistance training or interval training ( 8 ). On the other hand, aerobic or endurance training refers to exercise bouts that primarily rely on oxidative phosphorylation and can last from minutes to hours ( 9 ). This latter type of training has received almost no consideration in recent protein reviews. Whether engaging in resistance or endurance training, protein supplementation may have the potential to enhance or complement exercise-induced physiological responses. The purpose of this review is to examine these potential performance and recovery applications of protein supplementation for both resistance and endurance training, with emphasis placed on studies utilizing various “peri-exercise” supplementation protocols within ~60 min pre- or post-training in healthy, exercising individuals.
Protein Supplementation and Resistance Training
A recent comprehensive review by Jager et al. ( 2 ) identified a number of key issues related to protein intake in healthy, exercising individuals. Of particular note, the importance of protein intake during and around a training session for recovery and performance appears to be dependent on total daily protein intake, as well as presence or absence of an energy deficit. While findings do support the effect of post-exercise protein intake on increases in fat free mass (FFM), individuals consuming adequate daily calories and a minimum daily protein intake of 1.6 g/kg may not see any added benefit of immediate post-training protein consumption on muscular strength ( 2 ). However, Morton et al. ( 7 ) suggested that the strength (and hypertrophy) effects of additional post-resistance training protein supplementation may be greater in those with previous resistance training experience and that the magnitude of this effect is somewhat mitigated with aging. Furthermore, it is important to note that resistance-trained individuals in a caloric deficit require significantly more protein to offset any potential loss of lean body mass, with optimal daily protein intake for these individuals potentially being in the range of 2.3–3.1 g/kg FFM ( 10 ). While this recommendation increases total caloric intake from protein, resulting in the necessity to decrease energy intake from fat and carbohydrate, protein appears to have unique characteristics, and overfeeding with protein has been shown to have no negative effects on body composition in trained individuals ( 11 ). Similarly, healthy, older adults also require a greater quantity of total daily protein (0.61 g/kg FFM) compared to their younger counterparts (0.25 g/kg FFM) ( 12 ). Additionally, as a percentage of total daily energy intake, older adults must increase the contribution from protein due to decreases in energy intake, as well as protein's ability to attenuate sarcopenia by increasing muscle hypertrophy, subsequently maintaining or increasing muscular strength and power ( 13 ).
It has previously been demonstrated that ingestion of milk-based protein following a damaging eccentric resistance protocol helps to attenuate the expected decrements in strength and repeated sprint ability from 24 to 72 h following the bout ( 14 – 16 ). Recently, a group of researchers found that whey protein can facilitate muscle recovery following an intense isotonic exercise bout as well and that it is more than just an issue of caloric replacement ( 17 ). They compared the effects of a whey protein supplement (25 g protein, 2.5 g fat, and 3 g CHO) to a calorie-equated carbohydrate drink (32.5 g CHO) in resistance-trained young men performing an acute, total body resistance training protocol, and assessed performance variables at 10- and 24-h post-exercise. A moderate beneficial effect on acute anaerobic power and strength was found in the group that consumed the protein supplement, suggesting that there may have been improvements in rate of recovery over those who consumed the carbohydrate drink ( 17 ). This is particularly notable given that the subjects were already habitually consuming 1.9 g/kg/d of protein and may hold particular relevance for athletes engaging in high-intensity, explosive sports.
It has been suggested that protein quality may have an effect on both acute and chronic adaptations to exercise ( 2 , 18 , 19 ). Protein quality is a measure of a given protein source's ability to provide adequate quantities of the essential amino acids required for protein synthesis ( 20 ). Additionally, leucine, a branched-chain amino acid (BCAA), has been shown to be a prerequisite stimulator of skeletal MPS, which is critical for both the recovery and adaptive processes following a training bout ( 21 ). Given some of the favorable outcomes seen with ingestion of certain complete proteins, particularly milk-based and, more specifically, whey proteins ( 2 ), questions have been raised about the possible application of other protein sources that may be lower in leucine content. Two recent investigations have studied the effects of the quality of a post-exercise protein source on performance and recovery ( 22 , 23 ). Each of these studies took a unique approach to determining the differences in physiological changes following exercise and protein supplementation. Fabre et al. ( 22 ) compared the effects of 20 g of whey protein, 10 g of whey protein plus 10 g of casein protein, and 4 g of whey protein plus 16 g of casein protein consumed post-exercise in 31 recreationally resistance-trained males. Following 9 weeks of resistance training 4 days per week, no differences in changes in body composition, muscular strength, or muscular endurance were found, suggesting all three protein supplements were equally effective. When comparing 16 g of beef protein, 18 g of whey protein, and a calorie-equated carbohydrate drink consumed post-resistance training 3 days per week for 8 weeks in 42 recreationally resistance-trained males, no differences in changes in body composition, muscle thickness, or performance variables were found ( 23 ). One limitation of each of these studies is that they failed to control for total daily energy and macronutrient intake; therefore, subjects may have already been consuming adequate total daily calories and protein so the additional protein, regardless of its source, failed to result in any additional improvements in performance or body composition.
While most protein supplement resistance training studies have used a “post-exercise” administration protocol, it is possible that timing effects extend to the entire peri-workout period. Schoenfeld et al. ( 24 ) examined the effects of consuming 25 g of hydrolyzed whey protein immediately prior to a resistance training session with a 3-h fast post-exercise vs. consuming the same quantity and source of protein immediately following the same training session after having fasted for 3 h in 21 resistance-trained males. All subjects were consuming a 500-kcal surplus and 1.8 g/kg of protein daily. No differences in changes in body composition or one-rep max back squat or bench press were found between the groups after the 8-week intervention. Along with the findings from other studies ( 22 , 23 , 25 ), these data support the idea that protein intake post-workout may not be critical as long as protein is consumed prior to training or total daily protein intake is adequate. However, this does not preclude the possibility that pre- and post-exercise supplementation would be even more beneficial depending on dose.
To interpret the disparate effects of protein supplementation on resistance training performance, a few issues should be taken into account. The training stimulus must be adequate to result in strength improvement, regardless of protein timing, total protein intake, or nutritional status. Protein supplementation by individuals participating in ineffective resistance training programs will be less impactful. The beginning training status of individuals also appears to play a significant a role in any potential benefit seen as a result of protein consumption on strength, hypertrophy, and body composition ( 7 ). While the main focus of this paper is the healthy, trained individual, it is worth noting that protein supplementation for novice individuals may not confer any additional benefit above and beyond that of the training intervention ( 5 ). However, as training status increases, so does the potential effect of protein supplementation for improving performance and recovery.
Alternatively, Reidy and Rasmussen ( 6 ) have proposed the existence of a “protein paradox” wherein well-trained individuals may require less dietary protein due to the increased efficiency of protein turnover in this population. However, it should be noted that this is speculative and has not been fully substantiated by the available research, particularly for performance-related outcomes. Even taking this into account, one factor that appears to be just as important as total daily protein intake in well-trained individuals is the utilization of a specific protein dosing strategy based on body weight or FFM. Additionally, Thomson et al. ( 12 ) showed that healthy, older adults may also benefit from a higher protein intake in addition to a protein dosing strategy to adequately stimulate MPS. Thus, the appropriate timing or pacing of protein intake throughout the day may optimize results from resistance training ( 26 ). While recent critical or meta-analytic reviews have argued that protein timing is inconsequential after accounting for total protein intake ( 6 , 27 ), there are two factors that must be taken into account when considering these conclusions. First, very few “timing” studies have actually been conducted. In most cases, the studies were not designed to compare time of administration, but rather type or quantity of nutrient (or placebo) ingested post-exercise. Second, only a few of the included studies used trained subjects. Most employed novice exercisers. One of the studies that has found a benefit of protein timing ( 28 ) was conducted in experienced resistance-trained males. Again, this may lend credence to the notion that training status matters when considering protein supplementation strategies. Additionally, it should be noted that strength improvements not reaching statistical significance may prove to be significant in areas of individual competition or performance. Very few studies have actually utilized highly trained individuals or athletes, so translating the current findings to this population should be done with caution. Finally, it is worth noting that several studies have shown the addition of carbohydrate and creatine monohydrate to a protein supplement, typically whey protein, results in greater strength and hypertrophy improvements from resistance training programs ( 26 ). Though a detailed discussion of these other macronutrients is beyond the scope of this review, these results do point to an overall “nutrient” impact as well as possible synergistic effects.
Perhaps a driving factor in performance (i.e., strength or power) improvements with peri-workout protein supplementation could be enhanced recovery, which would potentially translate to enhanced capacity for an increased training load stimulus. Recovery from exercise has been measured through many different methods in previous research. Delayed onset muscle soreness (DOMS), which is defined as an aching pain in a given muscle following a novel exercise bout, has been measured subjectively ( 29 ). Though the cause of DOMS is multifaceted and tied to a cascade of events linked to muscle damage, it is not necessarily an indicator of the magnitude of muscle damage and, therefore, cannot be used by itself to determine muscular recovery and adaptations from exercise ( 29 ). Specific biomarkers and MPS rates appear to be the most efficient and widely used methods of objectively determining muscle breakdown, recovery, and adaptation from exercise. Acute elevations of cortisol and creatine kinase (CK) are two biological indicators of muscle damage and the subsequent recovery processes that can be measured through blood sample analysis ( 30 , 31 ). Post-exercise muscle biopsies can be used to determine rates of MPS, which directly measure the magnitude of the recovery process immediately following exercise ( 32 ).
West et al. ( 17 ) measured recovery variables following a total-body resistance training session and found that those subjects who consumed a whey protein supplement (25 g protein, 2.5 g fat, and 3 g CHO) had lower rates of whole body protein breakdown, while those who consumed a carbohydrate supplement (32.5 g CHO) actually had higher rates of whole body protein synthesis. The protein group, however, appeared to improve whole body net protein balance over 24 h post-exercise. As noted previously, the subjects were already consuming 1.9 g/kg/d protein, so additional protein through supplementation may have been less impactful. Interestingly, there was no difference between total body net protein balance between the groups. It should be noted that whole body protein synthesis is not necessarily a reflection of skeletal muscle protein synthesis ( 33 ). Kim et al. ( 33 ) discovered that net protein (whole body) balance was superior with a 70 vs. 40 g dose consumed prior to a resistance-training protocol. However, no differences were found in muscle protein synthesis between the 40 and 70 g dose. Thus, one must not conflate measures of whole body protein metabolism with those of skeletal muscle.
Nevertheless, the recovery of muscle function has been demonstrated in other studies ( 15 , 16 ) of milk protein supplementation after eccentric exercise, perhaps due to myofibrillar protein remodeling. The results of these studies further support the idea that protein consumed post-exercise is crucial for maximizing rates of protein synthesis in skeletal muscle. The effect on total body protein balance, however, is still a bit unclear. Carbohydrates have been shown to have a protein sparing effect, therefore the combination of protein and carbohydrate to decrease rates of muscle protein breakdown (MPB) and increase rates of MPS may be the best strategy for shifting total body protein balance to the net anabolic side ( 34 ), even if carbohydrate itself does not necessarily enhance MPS ( 35 , 36 ). This may partially explain the benefits of the milk supplement used by Cockburn et al. ( 15 ) and Cockburn and Stevenson ( 16 ) as it also contained carbohydrate. Perhaps there is a synergistic effect.
In addition to the investigations discussed earlier regarding post-exercise protein quality and training adaptations, Burd et al. ( 25 ) also measured markers of recovery through protein synthesis. The researchers collected muscle biopsies and measured rates of MPS following resistance training. In the 0–2 h post-exercise window, the group that consumed 30 g of protein in the form of skim milk expressed higher rates of MPS than the group that consumed 30 g of protein from beef ( 25 ). However, rates of MPS in the 2–5 h post-exercise window did not differ. This may be explained by the rate of digestion and absorption of these protein sources. Protein from dairy, specifically the whey portion, appears to be absorbed faster, and elicit a faster MPS response than beef.
The difference between whole egg and protein-equated egg white consumption post-exercise was also studied recently ( 37 ). The researchers measured rates of MPS through muscle biopsies and found that the group that consumed the whole egg exhibited higher rates of MPS. One limitation to this study was the lack of control for total calories and macronutrients. The whole egg treatment consisted of 18 g of protein, 17 g of fat, and 223 kcal, while the egg white treatment consistent of 18 g of protein, 0 g of fat, and only 73 kcal ( 37 ). While the discrepancy in calories between treatment groups may have impacted total daily calories, thus impacting MPS, one cannot ignore the possibility of the role that differences in macronutrients may play.
Lastly, a 2017 investigation looked at the differences between protein-equated native whey protein, whey protein concentrate, and milk ( 38 ). Native whey protein is produced through the filtration of raw milk, while whey protein concentrate is a byproduct of cheese production. Native whey protein consists of undenatured proteins and has a higher leucine content ( 38 ). Each treatment consisted of ~20 g of protein, ~6 g of fat, and ~40 g of carbohydrates but contained 2.7, 2.2, and 2.0 g of leucine, respectively. The supplements were ingested immediately after and again 2 h post-exercise following a moderate intensity lower body resistance training session. Results showed higher blood amino acids concentrations in native whey and whey protein concentrate than in milk. MPS was elevated in the whey protein condition from 1 to 3 h post, while it was elevated 1–5 h post in the native whey condition. There was no difference in MPS 1–5-h post-workout between native whey and whey protein concentrate, though MPS was higher from 1 to 5 h post-workout in the native whey condition compared to milk ( 38 ). Collectively, these data support that whey protein, regardless of its levels of processing (i.e., native whey protein vs. whey protein concentrate), increase MPS by similar magnitudes that are greater than those of milk alone. How this translates to long-term differences remains to be determined.
Protein Supplementation and Endurance Training
While the majority of the literature regarding the effects of protein intake on performance has focused on anaerobic activities, more recent work has examined its role on endurance activities, but this has mostly been absent from the most recent reviews. Similar to resistance training, the impact appears to be at least somewhat dependent on the presence or absence of other nutrients, particularly carbohydrate. A 2010 systematic review and meta-analysis compared 11 studies investigating the effects of consumption of protein and carbohydrate vs. consumption of carbohydrate alone during a bout of cycling on performance during a subsequent bout of cycling ( 39 ). Across the 11 studies, consumption of protein and carbohydrate resulted in an average improvement of 9% in performance (defined as time to exhaustion and time trial performance) compared to consumption of carbohydrate alone ( 39 ). To investigate if the increased caloric intake due to inclusion of protein was responsible for this improved performance, a further analysis of isocarbohydrate and isocaloric conditions was performed. Examination of isocarbohydrate conditions yielded a 10.5% improvement in overall performance, while isocaloric conditions resulted in 3.4% improvement ( 39 ), suggesting that the improvements due to protein inclusion were not simply due to increased calories. When considering only those studies measuring performance by time trial (3), improvements were not statistically significant. However, studies utilizing time to exhaustion protocols (8) did result in statistically significant improvements. It is worth noting that in all studies showing statistically significant improvement, whey protein was the source of protein utilized, though differences between concentrate vs. isolate were not quantified. Again, it is prudent to highlight that performance improvements not reaching statistical significance may have clinical or practical relevance, specifically for athletes. For example, a 1% improvement in performance would have been the difference in winning the Gold Medal instead of the Silver Medal in the men's marathon in the 2016 Olympic Games in Rio. Therefore, even seemingly “trivial” differences do indeed have a significant effect on performance and outcomes at the elite level.
When discussing the impact of protein on performance, it is imperative to include the impact that protein may have on glycogen replenishment and subsequent exercise performance. Standard discussions of glycogen replenishment focus solely on carbohydrate consumption. Recommendations for adequate post-exercise carbohydrate consumption are to consume 0.6–1.0 g/kg carbohydrate within 30 min of cessation of exercise and again every 2 h for the next 4–6 h ( 40 , 41 ). Carbohydrate consumption of 1.2 g/kg every 30 min over 3.5 h also resulted in maximal glycogen replenishment ( 41 , 42 ). In cases of suboptimal post-exercise carbohydrate consumption, the addition of protein can improve glycogen replenishment and decrease symptoms of muscle damage ( 43 ). Practical applications of standard post-exercise carbohydrate consumption recommendations may be limited in real world situations. Moreover, athletes training multiple times daily may have fewer opportunities to consume recovery meals or have an elevated need for “rapid” recovery, including rehydration, to facilitate the subsequent training session. Beyond just glycogen replenishment aspects, it has also been shown that the presence of protein in rehydration beverages can enhance intestinal fluid uptake, aiding in rehydration ( 44 ) and that BCAA consumption during endurance exercise may improve time trial performance and peak power output while improving markers of immune health ( 45 ) and attenuate serotonin levels, subsequently resulting in a delay of central fatigue ( 46 ).
A systematic review by Pasiakos et al. ( 5 ) investigated the relationship between protein, muscle function, and recovery. The authors included studies that measured markers of muscle damage followed by a test of physical performance or muscle function. Populations of the review included healthy individuals with daily dietary protein intake at or above the current RDA of 0.8 g/kg per day. While some of the endurance exercise studies included showed decreases in markers of muscle damage, such as CK, or decreases in muscle soreness in groups consuming protein after initial exercise bout ( 47 – 49 ), many did not ( 50 – 52 ). This may have resulted from the inclusion of studies utilizing both trained and untrained subjects, as well as individuals consuming suboptimal daily protein intakes. Despite the reduced plasma CK levels and muscle soreness, consumption of protein did not result in improvements in subsequent performance measures when repeat performance was tested < 24 h following the initial bout. This evidence suggests that plasma CK levels, perceived level of muscle soreness, and muscle function may only be modestly related or perhaps utilizing a single method of measure paints an inadequate picture of recovery due to individual variability ( 5 ). Without additional studies to clarify these relationships, developing guidelines based on these markers as representing recovery may be ill-advised. Individuals must be cautious when attempting to measure recovery from exercise based on these metrics alone. For example, a recent study of 20 high-level soccer players tested the effects of a milk protein concentrate supplement (80% casein and 20% whey) compared to an isocaloric carbohydrate-containing placebo on high intensity running performance, knee extensor and flexor strength, and antioxidative capacity over the course of a 1-week in-season microcycle consisting of two games separated by 2 days ( 53 ). On game days (days 1 and 4), the supplement was consumed immediately post-, 3 h post-, and 6 h post-match in three different doses of 25, 30, and 25 g, respectively, resulting in a total of 80 g. On training days (days 2, 3, 5, and 6), 20 g of the supplement was consumed with breakfast. High intensity running performance, measured as distance covered at speeds >19 km/h, was greater during the last 15 min of game two following protein supplementation. Additionally, knee extensor concentric strength recovered quicker after the first game following protein supplementation. Endogenous antioxidant concentrations were greater following game two only in the protein-supplemented condition. Though soccer is a “power-endurance” sport rather than simply an endurance sport, these findings hold relevance for understanding the impact of protein intake on recovery and repeated performance in actual athletes.
Since 2014, additional work investigating the impact of protein consumption on biochemical markers of metabolic status, physiological fatigue, and recovery in endurance-trained athletes has been performed ( 54 ). For 5 weeks, elite or experienced marathon runners received either 33.5 g/day of whey protein or maltodextrin 30 min following the completion of each training session leading up to a race covering marathon distance. Blood samples were collected to assess biochemical markers of metabolism, muscle damage, and fatigue and took place prior to beginning the intervention, 1 day following the marathon, and 1 week following the marathon. These markers included CK, lactate dehydrogenase (LDH), AST, and ALT. Runners who supplemented with whey protein displayed decreased AST and ALT compared to maltodextrin-supplemented runners. CK and LDH, biochemical indicators of muscle damage, were significantly greater in the maltodextrin group post-marathon compared to the whey protein-supplemented group. Elevations in CK and LDH were still significant 1-week post-marathon in the maltodextrin group compared to the whey protein group ( 54 ). The whey protein group also showed significantly decreased triglycerides (TG) and total cholesterol (TC) compared to the maltodextrin group post-marathon. The maltodextrin group actually showed increased TC levels. Only the whey protein group showed significant decreases in LDL post-marathon and at 1 week post-marathon ( 54 ). The authors suggested that the decrease in TC seen in whey-supplemented runners may indicate that cholesterol was more efficiently converted to steroid hormones, resulting in improved physiological recovery and adaptations from the strenuous exercise bout. One week post-marathon, most biomarkers of damage and stress were still significantly lower in the whey protein group compared to the maltodextrin group ( 54 ). In addition to the more favorable biomarker profiles in the protein supplemented group, performance in the 12-min run/walk test was also greater in the whey protein-supplemented group 1-week post-marathon. Together, these results indicate that whey protein supplementation during marathon preparation and recovery, and that the supplement aids in attenuating metabolic and muscular damage. Daily dietary assessments were not included in this study ( 54 ), thus limiting possible practical applications or recommendations. As we have addressed previously, caloric deficit or daily protein consumption <1.4–1.6 g/kg may potentiate the effect of peri-workout protein consumption on recovery and subsequent performance. Further studies are necessary to elucidate the potential contribution of peri-workout whey protein ingestion on makers of muscle damage, recovery, and subsequent performance measures in endurance athletes.
In real-world sport performance situations, recovery and performance must be evaluated in the context of an accumulated effect. The ability to train consistently while remaining healthy is critical for continued progression and optimal performance. Endurance athletes in particular are at increased risk for upper respiratory tract infections ( 55 ). Factors contributing to this increased risk may include reduced immune function through low circulation of certain T-lymphocytes, especially during periods of increased volume and/or intensity of training. A diet providing a daily protein intake of 3 g/kg, including 60 g/day of casein protein, has been shown to be sufficient in returning circulating immune cell levels to those seen during lighter training periods, while a diet providing a daily protein intake 1.5 g/kg did not result in enhanced immune cell levels ( 56 , 57 ). Kephart et al. ( 45 ) have also found this beneficial effect on the immune system to extend to BCAA supplementation in doses of 12 g/d in trained cyclists.
Additionally, Rowlands et al. ( 58 ) found that consumption of ~64 g protein over 3 h following intense endurance exercise resulted in gene expression favorable for improving substrate, specifically fatty acid, mobilization and mitochondrial proteins for oxidation, especially in the electron transport chain. Post-exercise consumption of protein at levels thought to maximally stimulate MPS would potentially not have this same impact. Post-exercise protein consumption affects other systems and pathways and should not be considered only in terms of stimulating MPS. As further evidence of this notion, Levenhagen et al. ( 59 ) demonstrated that 10 g of casein protein enhanced MPS following 60 min of moderate intensity endurance exercise. Although this supplementation protocol stimulated MPS, subjects were found to be in negative whole-body protein balance. Because prolonged bouts of endurance exercise (i.e., >2 h) result in considerable oxidation of amino acids, specifically leucine, and intense or prolonged bouts of endurance exercise result in hypoxia-mediated small intestinal injury, negative whole-body protein balance may be common in endurance athletes ( 60 – 62 ). Because of this, protein requirements and recommendations for endurance athletes must consider more than MPS, especially since short-term increases in MPS do not fully explain the dynamics of long-term whole-body net protein balance and various training adaptations.
Conclusions and Future Direction
Overall, total daily energy and protein intake over the long term play the most crucial dietary roles in facilitating adaptations to exercise. However, once these factors are accounted for, it appears that peri-exercise protein intake plays a potentially useful role in optimizing physical performance and positively influencing the subsequent recovery processes. Challenges surround the definition of “performance” and the appropriate metrics by which to measure it based on desired outcomes. Difficulties also arise in attempting to define and quantify the concept of recovery. Additionally, both performance and recovery must be viewed in context depending on whether the emphasis is an immediate, short-term effect (i.e., 24 h or less) or a long-term training response.
It should also be noted that protein timing, whether it is pre-, during, or post-workout, is often framed within the context of bodybuilding (i.e., the singular goal of increasing skeletal muscle mass). It is evident that to use such a narrow frame of reference ignores the potential utility of protein timing within the context of endurance events (i.e., running, cycling, rowing, swimming, triathlon, etc.), as well as the vast majority of individual and team sports in which skeletal muscle hypertrophy is not a pre-eminent concern. For instance, if one competes in a weight-class sport (e.g., boxing, mixed martial arts, weightlifting, powerlifting, etc.), gains in body weight or lean body mass are often avoided; otherwise, the individual athlete would need to compete in a heavier weight class. In these situations, protein timing in particular may serve a useful role in recovery.
Translating research into practical application requires differentiation between novice or trained individuals, healthy normal weight or healthy overweight individuals, special populations, or those with certain metabolic or disease states. Here, we specifically focus on healthy, exercising individuals and limit our conclusions to these individuals. It is important moving forward that the study populations used are appropriate for the goals of the study and desired applications. For example, it is of little use to have a sample of recreationally-trained individuals if the goal is to understand performance in high-level athletes.
Though protein-containing meals result in increase of MPS on their own, as does resistance training, the timing of ingestion of protein around exercise further enhances this increase of MPS ( 63 , 64 ). It is worth noting that an upper limit for this acute dosing has not really been established, though there is evidence that 40 g of protein stimulates MPS to a greater degree than 20 g following whole-body resistance training ( 65 ). A dose higher than this, however, has not been included using the same timing paradigm. In reality, the “ideal” amount of peri-exercise protein consumption depends on many factors, including total caloric intake, total daily protein intake, training status of the individual, age of the individual, FFM, type of protein consumed, type and amount of other nutrients consumed, and the composition and timing of the most recent pre-training meal.
Much attention has been given to daily protein consumption and thresholds that must be met for peri-training protein consumption to exert additional benefit (>1.6–2.2 g/kg/d). As such, pre-, intra-, and post-training nutrient consumption present additional opportunities for athletes to contribute to their daily protein intake total and can be viewed in the context of ways to meet these “larger” daily needs by optimizing intake.
With regard to endurance exercise, protein consumption during exercise may not confer an immediate ergogenic benefit, especially when carbohydrate consumption is adequate. It may, however, aid in delaying central fatigue, reducing MPB, and contributing to a more positive, whole-body nitrogen balance. Additionally, protein consumption in and around intense or prolonged endurance activity may aid in reduction of upper respiratory tract infection incidence and improved immune system function. It may also aid in upregulating gene expression of proteins necessary for improving bioenergetic pathways. The impact of this on subsequent training sessions should not be dismissed and is an important part of improving performance.
The effect of protein consumption on resistance training is highly dependent on many variables not related to protein. The combination of peri-training protein consumption with inadequate or ineffective resistance training protocols will not maximize improvements in strength or hypertrophy. Resistance training protocol interventions must be of adequate intensity, volume, and frequency with an emphasis on progressive overload to produce results. Additionally, adequate training interventions coupled with calorie-restricted nutrition protocols may require increased protein intake of 2.3–3.1 g/kg FFM to yield desired improvements in strength, hypertrophy, or maintenance of FFM ( 10 ). Consideration must also be made for the age of resistance-trained individuals, as older adults require protein intake over and above that of their younger counterparts to receive the same benefits noted above ( 66 ).
In order to fully understand the role of protein (or any substrate for that matter) on performance, the practical application beyond the contrived training or recovery interventions presented must be addressed. Daily training schedules of athletes require an ongoing ability to recover and perform. As an example, most of the studies included in this area utilized a training protocol that took ~3–4 h per week, typically in moderately-trained individuals. For comparative purposes, a competitive athlete may spend 3–10 times this amount of time training per week (if not more). For this reason, the “window” for recovery should be considered to encompass each and every hour between training and competition. Protein dosing strategies need to take this into account. This becomes even more apparent when considering that the uniform distribution of protein throughout the day results in greater MPS than an uneven distribution even when total daily protein intake is equal ( 67 ). Arciero et al. ( 64 ) demonstrated the combination of resistance training and consumption of 4–6 meals per day containing 20–40 g of protein per meal resulted in positive changes in body composition and physical performance. These results suggest that the pattern of daily protein ingestion may also impact results from resistance training protocols and provides further evidence that we must look beyond the few hours following training to determine the impact that protein may have on performance and recovery. Further evidence in support of extending the “recovery window” concept are results from nighttime protein ingestion studies. Madzima et al. ( 68 ) found that consumption of 30 g of casein, 30 g of whey, or 33 g of carbohydrate 30 min prior to sleep resulted in increased resting energy expenditure and improved VO 2 the following morning. While no statistically significant changes were observed between groups, protein groups trended toward greater increases when compared to the carbohydrate group while morning fat oxidation was greatest in the casein supplemented group.
Taken together, these data demonstrate the need for a more comprehensive view and methods of measuring recovery. Increased sensitization of muscle to protein and nutrients for 24–72 h following training coupled with multiple weekly training sessions results in an on-going state of recovery. Because of this, we need to begin considering this longer stimulus window as an opportunity to maximize feeding, rather than as a reason why immediate post-workout ingestion may not be particularly important. In other words, consuming nothing post-workout would be an unwise strategy if the goal is to potentially optimize the adaptive response to exercise training.
Overall, there appears to be no adaptive advantage to avoiding protein intake in the peri-workout period. Stimulation of MPS in the acute period following training may not result in improvements in strength, hypertrophy, body composition, or performance without deliberate implementation of additional strategies during the prolonged recovery period. As such, this much broader view should be considered with regard to future investigations.
Author Contributions
JA and SA conceived the topic. HC, MA, JA, and SA wrote the paper.

Conflict of Interest Statement
SA is on the Advisory Panel for Dymatize. JA is the CEO of the International Society of Sports Nutrition—an academic non-profit that receives grants in part from companies that sell dietary protein.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer CK declared a past co-authorship with several of the authors SA and JA to the handling Editor.
1. USDA. “ 2015–2020 Dietary Guidelines for Americans, 8th edn ” (2015).
2. Jager R, Kerksick CM, Campbell BI, Cribb PJ, Wells SD, Skwiat TM, et al. International society of sports nutrition position stand: protein and exercise. J Int Soc Sports Nutr. (2017) 14:20. doi: 10.1186/s12970-017-0177-8
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Statista. The Statistics Portal. (2018). Available: Available online: https://www.statista.com/statistics/727930/sports-nutrition-market-size-by-product-us/ (Accessed January 15:2018).
4. Cermak NM, Res PT, de Groot LC, Saris WH, van Loon LJ. Protein supplementation augments the adaptive response of skeletal muscle to resistance-type exercise training: a meta-analysis. Am J Clin Nutr. (2012) 96:1454–64. doi: 10.3945/ajcn.112.037556
5. Pasiakos SM, Lieberman HR, McLellan TM. Effects of protein supplements on muscle damage, soreness and recovery of muscle function and physical performance: a systematic review. Sports Med. (2014) 44:655–70. doi: 10.1007/s40279-013-0137-7
6. Reidy PT, Rasmussen BB. Role of ingested amino acids and protein in the promotion of resistance exercise–induced muscle protein anabolism. J Nutr. (2016) 146:155–83. doi: 10.3945/jn.114.203208
7. Morton RW, Murphy KT, McKellar SR, Schoenfeld BJ, Henselmans M, Helms E, et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br J Sports Med . (2017) 52:376–84. doi: 10.1136/bjsports-2017-097608
8. Haff GG, Triplett NT. Essentials of Strength Training and Conditioning. Champaign, IL: Human Kinetics (2016).
Google Scholar
9. McArdle WD, Katch FI, Katch VL. Exercise Physiology: Nutrition, Energy, and Human Performance. Philadelphia, PA: Lippincott, Williams, and Wilkins (2014).
10. Helms ER, Zinn C, Rowlands DS, Brown SR. A systematic review of dietary protein during caloric restriction in resistance trained lean athletes: a case for higher intakes. Int J Sport Nutr Exerc Metab. (2014) 24:127–38. doi: 10.1123/ijsnem.2013-0054
11. Antonio J, Peacock CA, Ellerbroek A, Fromhoff B, Silver T. The effects of consuming a high protein diet (4.4 g/kg/d) on body composition in resistance-trained individuals. J Int Soc Sports Nutr. (2014) 11:19. doi: 10.1186/1550-2783-11-19
12. Thomson RL, Brinkworth GD, Noakes M, Buckley JD. Muscle strength gains during resistance exercise training are attenuated with soy compared with dairy or usual protein intake in older adults: a randomized controlled trial. Clin Nutr. (2016) 35:27–33. doi: 10.1016/j.clnu.2015.01.018
CrossRef Full Text | Google Scholar
13. Volpi E, Campbell WW, Dwyer JT, Johnson MA, Jensen GL, Morley JE, et al. Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? J Gerontol A Biol Sci Med Sci. (2013) 68:677–81. doi: 10.1093/gerona/gls229
14. Cockburn E, Hayes PR, French DN, Stevenson E, St Clair Gibson A. Acute milk-based protein-CHO supplementation attenuates exercise-induced muscle damage. Appl Physiol Nutr Metab. (2008) 33:775–83. doi: 10.1139/H08-057
15. Cockburn E, Stevenson E, Hayes PR, Robson-Ansley P, Howatson G. Effect of milk-based carbohydrate-protein supplement timing on the attenuation of exercise-induced muscle damage. Appl Physiol Nutr Metab. (2010) 35:270–7. doi: 10.1139/H10-017
16. Cockburn E, Bell PG, Stevenson E. Effect of milk on team sport performance after exercise-induced muscle damage. Med Sci Sports Exerc. (2013) 45:1585–92. doi: 10.1249/MSS.0b013e31828b7dd0
17. West DWD, Abou Sawan S, Mazzulla M, Williamson E, Moore DR. Whey protein supplementation enhances whole body protein metabolism and performance recovery after resistance exercise: a double-blind crossover study. Nutrients (2017) 9:735. doi: 10.3390/nu9070735
18. Tang JE, Phillips SM. Maximizing muscle protein anabolism: the role of protein quality. Curr Opin Clin Nutr Metab Care (2009) 12:66–71. doi: 10.1097/MCO.0b013e32831cef75
19. Hulmi JJ, Lockwood CM, Stout JR. Effect of protein/essential amino acids and resistance training on skeletal muscle hypertrophy: a case for whey protein. Nutr Metab. (2010) 7:51. doi: 10.1186/1743-7075-7-51
20. Millward DJ, Layman DK, Tome D, Schaafsma G. Protein quality assessment: impact of expanding understanding of protein and amino acid needs for optimal health. Am J Clin Nutr. (2008) 87:1576S−81S. doi: 10.1093/ajcn/87.5.1576S
21. Garlick PJ. The role of leucine in the regulation of protein metabolism. J Nutr. (2005) 135:1553S−6S. doi: 10.1093/jn/135.6.1553S
22. Fabre M, Hausswirth C, Tiollier E, Molle O, Louis J, Durguerian A, et al. Effects of postexercise protein intake on muscle mass and strength during resistance training: is there an optimal ratio between fast and slow proteins? Int J Sport Nutr Exerc Metab. (2017) 27:448–57. doi: 10.1123/ijsnem.2016-0333
23. Naclerio F, Larumbe-Zabala E, Ashrafi N, Seijo M, Nielsen B, Allgrove J, et al. Effects of protein-carbohydrate supplementation on immunity and resistance training outcomes: a double-blind, randomized, controlled clinical trial. Eur J Appl Physiol. (2017) 117:267–77. doi: 10.1007/s00421-016-3520-x
24. Schoenfeld BJ, Aragon A, Wilborn C, Urbina SL, Hayward SE, Krieger J. Pre- vs. post-exercise protein intake has similar effects on muscular adaptations. PeerJ (2017) 5:e2825. doi: 10.7717/peerj.2825
25. Burd NA, Gorissen SH, van Vliet S, Snijders T, van Loon LJ. Differences in postprandial protein handling after beef compared with milk ingestion during postexercise recovery: a randomized controlled trial. Am J Clin Nutr. (2015) 102:828–36. doi: 10.3945/ajcn.114.103184
26. Naclerio F, Larumbe-Zabala E. Effects of whey protein alone or as part of a multi-ingredient formulation on strength, fat-free mass, or lean body mass in resistance-trained individuals: a meta-analysis. Sports Med. (2016) 46:125–37. doi: 10.1007/s40279-015-0403-y
27. Schoenfeld BJ, Aragon AA, Krieger JW. The effect of protein timing on muscle strength and hypertrophy: a meta-analysis. J Int Soc Sports Nutr. (2013) 10:53. doi: 10.1186/1550-2783-10-53
28. Cribb PJ, Hayes A. Effects of supplement timing and resistance exercise on skeletal muscle hypertrophy. Med Sci Sports Exerc. (2006) 38:1918–25. doi: 10.1249/01.mss.0000233790.08788.3e
29. Nosaka K, Newton M, Sacco P. Delayed-onset muscle soreness does not reflect the magnitude of eccentric exercise-induced muscle damage. Scand J Med Sci Sports (2002) 12:337–46. doi: 10.1034/j.1600-0838.2002.10178.x
30. Pyne DB. Exercise-induced muscle damage and inflammation: a review. Aust J Sci Med Sport (1994) 26:49–58.
PubMed Abstract | Google Scholar
31. Kraemer WJ, Ratamess NA. Hormonal responses and adaptations to resistance exercise and training. Sports Med. (2005) 35:339–61. doi: 10.2165/00007256-200535040-00004
32. Dreyer HC, Fujita S, Cadenas JG, Chinkes DL, Volpi E, Rasmussen BB. Resistance exercise increases AMPK activity and reduces 4E-BP1 phosphorylation and protein synthesis in human skeletal muscle. J Physiol. (2006) 576:613–24. doi: 10.1113/jphysiol.2006.113175
33. Kim IY, Schutzler S, Schrader A, Spencer HJ, Azhar G, Ferrando AA, et al. The anabolic response to a meal containing different amounts of protein is not limited by the maximal stimulation of protein synthesis in healthy young adults. Am J Physiol Endocrinol Metab. (2016) 310:E73–80. doi: 10.1152/ajpendo.00365.2015
34. Davies CTM, Halliday D, Millward DJ, Rennie MJ, Sutton JR. Glucose inhibits CO2 production from leucine during whole-body exercise in man. J Physiol. (1982) 332:40P−1P.
35. Koopman R, Beelen M, Stellingwerff T, Pennings B, Saris WH, Kies AK, et al. Coingestion of carbohydrate with protein does not further augment postexercise muscle protein synthesis. Am J Physiol Endocrinol Metab. (2007) 293:E833–42. doi: 10.1152/ajpendo.00135.2007
36. Staples AW, Burd NA, West DW, Currie KD, Atherton PJ, Moore DR, et al. Carbohydrate does not augment exercise-induced protein accretion versus protein alone. Med Sci Sports Exerc. (2011) 43:1154–61. doi: 10.1249/MSS.0b013e31820751cb
37. van Vliet S, Shy EL, Sawon SA, Beals JW, West DWD, Skinner SK, et al. Consumption of whole eggs promotes greater stimulation of postexercise muscle protein synthesis than consumption of isonitrogenous amounts of egg whites in young men. Am J Clin Nutr. (2017) 106:1401–12. doi: 10.3945/ajcn
38. Hamarsland H, Nordengen AL, Nyvik Aas S, Holte K, Garthe I, Paulsen G, et al. Native whey protein with high levels of leucine results in similar post-exercise muscular anabolic responses as regular whey protein: a randomized controlled trial. J Int Soc Sports Nutr. (2017) 14:43. doi: 10.1186/s12970-017-0202-y
39. Stearns RL, Emmanuel H, Volek JS, Casa DJ. Effects of ingesting protein in combination with carbohydrate during exercise on endurance performance: a systematic review with meta-analysis. J Strength Cond Res. (2010) 24:2192–202. doi: 10.1519/JSC.0b013e3181ddfacf
40. Jentjens RL, van Loon LJ, Mann CH, Wagenmakers AJ, Jeukendrup AE. Addition of protein and amino acids to carbohydrates does not enhance postexercise muscle glycogen synthesis. J Appl Physiol. (2001) 91:839–46. doi: 10.1152/jappl.2001.91.2.839
41. Jentjens R, Jeukendrup AE. Determinants of post-exercise glycogen synthesis during short-term recovery. Sports Med. (2003) 33:117–44. doi: 10.2165/00007256-200333020-00004
42. van Loon LJ, Saris WH, Kruijshoop M, Wagenmakers AJ. Maximizing postexercise muscle glycogen synthesis: carbohydrate supplementation and the application of amino acid or protein hydrolysate mixtures. Am J Clin Nutr. (2000) 72:106–11. doi: 10.1093/ajcn/72.1.106
43. McLellan TM, Pasiakos SM, Lieberman HR. Effects of protein in combination with carbohydrate supplements on acute or repeat endurance exercise performance: a systematic review. Sports Med. (2014) 44:535–50. doi: 10.1007/s40279-013-0133-y
44. Leiper JB. Intestinal water absorption–implications for the formulation of rehydration solutions. Int J Sports Med. (1998) 19(Suppl. 2):S129–32. doi: 10.1055/s-2007-971977
45. Kephart WC, Wachs TD, Mac Thompson R, Brooks Mobley C, Fox CD, McDonald JR, et al. Ten weeks of branched-chain amino acid supplementation improves select performance and immunological variables in trained cyclists. Amino Acids (2016) 48:779–89. doi: 10.1007/s00726-015-2125-8
46. Blomstrand E. Amino acids and central fatigue. Amino Acids (2001) 20:25–34. doi: 10.1007/s007260170063
47. Romano-Ely BC, Todd MK, Saunders MJ, Laurent TS. Effect of an isocaloric carbohydrate-protein-antioxidant drink on cycling performance. Med Sci Sports Exerc. (2006) 38:1608–16. doi: 10.1249/01.mss.0000229458.11452.e9
48. Rowlands DS, Rossler K, Thorp RM, Graham DF, Timmons BW, Stannard SR, et al. Effect of dietary protein content during recovery from high-intensity cycling on subsequent performance and markers of stress, inflammation, and muscle damage in well-trained men. Appl Physiol Nutr Metab. (2008) 33:39–51. doi: 10.1139/H07-136
49. Valentine RJ, Saunders MJ, Todd MK, St Laurent TG. Influence of carbohydrate-protein beverage on cycling endurance and indices of muscle disruption. Int J Sport Nutr Exerc Metab. (2008) 18:363–78. doi: 10.1123/ijsnem.18.4.363
50. Cermak NM, Solheim AS, Gardner MS, Tarnopolsky MA, Gibala MJ. Muscle metabolism during exercise with carbohydrate or protein-carbohydrate ingestion. Med Sci Sports Exerc. (2009) 41:2158–64. doi: 10.1249/MSS.0b013e3181ac10bf
51. Breen L, Tipton KD, Jeukendrup AE. No effect of carbohydrate-protein on cycling performance and indices of recovery. Med Sci Sports Exerc. (2010) 42:1140–8. doi: 10.1249/MSS.0b013e3181c91f1a
52. Ferguson-Stegall L, McCleave EL, Ding ZP, Doerner PG, Wang B, Liao YH, et al. Postexercise carbohydrate-protein supplementation improves subsequent exercise performance and intracellular signaling for protein synthesis. J Strength Cond Res. (2011) 25:1210–24. doi: 10.1519/JSC.0b013e318212db21
53. Poulios A, Fatouros IG, Mohr M, Draganidis D, Deli CK, Papanikolaou K, et al. Post-game high protein intake may improve recovery of football-specific performance during a congested game fixture: results from the PRO-FOOTBALL study. Nutrients (2018) 10:10040494. doi: 10.3390/nu10040494
54. Huang WC, Chang YC, Chen YM, Hsu YJ, Huang CC, Kan NW, et al. Whey protein improves marathon-induced injury and exercise performance in elite track runners. Int J Med Sci. (2017) 14:648–54. doi: 10.7150/ijms.19584
55. Gleeson M. Immune function in sport and exercise. J Appl Physiol. (2007) 103:693–9. doi: 10.1152/japplphysiol.00008.2007
56. Witard OC, Turner JE, Jackman SR, Tipton KD, Jeukendrup AE, Kies AK, et al. High-intensity training reduces CD8+ T-cell redistribution in response to exercise. Med Sci Sports Exerc. (2012) 44:1689–97. doi: 10.1249/MSS.0b013e318257d2db
57. Witard OC, Turner JE, Jackman SR, Kies AK, Jeukendrup AE, Bosch JA, et al. High dietary protein restores overreaching induced impairments in leukocyte trafficking and reduces the incidence of upper respiratory tract infection in elite cyclists. Brain Behav Immun. (2014) 39:211–9. doi: 10.1016/j.bbi.2013.10.002
58. Rowlands DS, Thomson JS, Timmons BW, Raymond F, Fuerholz A, Mansourian R, et al. Transcriptome and translational signaling following endurance exercise in trained skeletal muscle: impact of dietary protein. Physiol Genomics (2011) 43:1004–20. doi: 10.1152/physiolgenomics.00073.2011
59. Levenhagen DK, Carr C, Carlson MG, Maron DJ, Borel MJ, Flakoll PJ. Postexercise protein intake enhances whole-body and leg protein accretion in humans. Med Sci Sports Exerc. (2002) 34:828–37. doi: 10.1097/00005768-200205000-00016
60. Breen L, Philp A, Witard OC, Jackman SR, Selby A, Smith K, et al. The influence of carbohydrate-protein co-ingestion following endurance exercise on myofibrillar and mitochondrial protein synthesis. J Physiol. (2011) 589:4011–25. doi: 10.1113/jphysiol.2011.211888
61. van Wijck K, Lenaerts K, van Loon LJ, Peters WH, Buurman WA, Dejong CH. Exercise-induced splanchnic hypoperfusion results in gut dysfunction in healthy men. PLoS ONE (2011) 6:e22366. doi: 10.1371/journal.pone.0022366
62. Moore DR, Camera DM, Areta JL, Hawley JA. Beyond muscle hypertrophy: why dietary protein is important for endurance athletes. Appl Physiol Nutr Metab. (2014) 39:987–97. doi: 10.1139/apnm-2013-0591
63. Areta JL, Burke LM, Ross ML, Camera DM, West DW, Broad EM, et al. Timing and distribution of protein ingestion during prolonged recovery from resistance exercise alters myofibrillar protein synthesis. J Physiol. (2013) 591:2319–31. doi: 10.1113/jphysiol.2012.244897
64. Arciero PJ, Ives SJ, Norton C, Escudero D, Minicucci O, O'Brien G, et al. Protein-pacing and multi-component exercise training improves physical performance outcomes in exercise-trained women: the PRISE 3 study. Nutrients (2016) 8:332. doi: 10.3390/nu8060332
65. Macnaughton LS, Wardle SL, Witard OC, McGlory C, Hamilton DL, Jeromson S, et al. The response of muscle protein synthesis following whole-body resistance exercise is greater following 40 g than 20 g of ingested whey protein. Physiol Rep. (2016) 4:e12893. doi: 10.14814/phy2.12893
66. Moore DR, Churchward-Venne TA, Witard O, Breen L, Burd NA, Tipton KD, et al. Protein ingestion to stimulate myofibrillar protein synthesis requires greater relative protein intakes in healthy older versus younger men. J Gerontol A Biol Sci Med Sci. (2015) 70:57–62. doi: 10.1093/gerona/glu103
67. Mamerow MM, Mettler JA, English KL, Casperson SL, Arentson-Lantz E, Sheffield-Moore M, et al. Dietary protein distribution positively influences 24-h muscle protein synthesis in healthy adults. J Nutr. (2014) 144:876–80. doi: 10.3945/jn.113.185280
68. Madzima TA, Panton LB, Fretti SK, Kinsey AW, Ormsbee MJ. Night-time consumption of protein or carbohydrate results in increased morning resting energy expenditure in active college-aged men. Br J Nutr. (2014) 111:71–7. doi: 10.1017/S000711451300192X
Keywords: protein, athlete, endurance, strength, nutrient timing
Citation: Cintineo HP, Arent MA, Antonio J and Arent SM (2018) Effects of Protein Supplementation on Performance and Recovery in Resistance and Endurance Training. Front. Nutr . 5:83. doi: 10.3389/fnut.2018.00083
Received: 23 May 2018; Accepted: 23 August 2018; Published: 11 September 2018.
Reviewed by:
Copyright © 2018 Cintineo, Arent, Antonio and Arent. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shawn M. Arent, [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 08 May 2024
Major AlphaFold upgrade offers boost for drug discovery
- Ewen Callaway
You can also search for this author in PubMed Google Scholar
An AlphaFold3 model of a bacterial enzyme bound to a chemical. Credit: Isomorphic Labs
Since the powerhouse artificial intelligence (AI) tool AlphaFold2 was released in 2021, scientists have used the protein-structure-prediction model to map one of our cells’ biggest machines, discover drugs and chart the universe of every known protein.
Despite such successes, John Jumper — who leads AlphaFold’s development at Google DeepMind in London — is regularly asked whether the tool can do more. Requests include the ability to predict the shape of proteins that contain function-altering modifications, or their structure alongside those of DNA, RNA and other cellular players that are crucial to a protein’s duties. “I would say ‘no, you can’t put that into AlphaFold’,” Jumper says. “I would rather solve their problems.”
What’s next for AlphaFold and the AI protein-folding revolution
The latest version of AlphaFold, described on 8 May in Nature 1 , aims to do just that — by giving scientists the ability to predict the structures of proteins during interactions with other molecules. But whereas DeepMind made the 2021 version of the tool freely available to researchers without restriction, AlphaFold3 is limited to non-commercial use through a DeepMind website.
Frank Uhlmann, a biochemist at the Francis Crick Institute in London who gained early access to AlphaFold3, has been impressed with its capabilities. “This is just revolutionary,” he says. “It’s going to democratize structural-biology research.”
Another revolution
“Revolutionary” is how many scientists have described the impact of AlphaFold2 on biology since it was unleashed 2 ( the first version 3 , released in 2020, was good, but not game-changing, Jumper has said). The AI predicts a protein’s structures from its amino-acid sequence, often with startling accuracy that is on par with that of experimental methods.
A freely available AlphaFold database holds the predicted structure of nearly every known protein. The availability of the AlphaFold2 code has also allowed other researchers to easily build on it: an early hack enabled the prediction of interactions between multiple proteins, a capability included in an update to AlphaFold2.
Jumper’s ennui over explaining AlphaFold’s inability to predict other aspects of a protein’s ecosystem stems from their importance: protein modifications, such as the addition of a phosphate molecule, can allow cells to respond to external cues, an infection, for instance, and set off a chain of events in response. Interactions with DNA, RNA and other chemicals are essential to many proteins’ duties.
Real-world examples of these interactions are readily available in the Protein Data Bank (PDB), a repository of experimentally determined structures that is the foundation of AlphaFold’s capabilities. An ideal tool would be able to predict structures of a protein alongside its accessories, says Jumper. “We want to solve the whole PDB.”
Major upgrade
To create AlphaFold3, Jumper, DeepMind chief executive Demis Hassabis and their colleagues made large changes to its predecessor: the latest version depends less on information about proteins related to a target sequence, for instance. AlphaFold3 also uses a type of machine-learning network — called a diffusion model — that is used by image-generating AIs such as Midjourney. “It’s a pretty substantial change,” says Jumper.
AlphaFold’s new rival? Meta AI predicts shape of 600 million proteins
AlphaFold3, the researchers found, substantially outperforms existing software tools at predicting the structure of proteins and their partners. For instance, scientists — especially those interested in finding new drugs — have conventionally used ‘docking’ software to physically model how well chemicals bind to proteins (usually with help from the proteins’ experimentally determined structures). AlphaFold3 proved superior to two docking programs, as well as to another AI-based tool called RoseTTAFold All-Atom 4 .
Uhlmann’s team has used AlphaFold3 to predict the structure of DNA-interacting proteins involved in copying the genome, a step that is essential to cell division. Experiments in which proteins are mutated to alter such interactions suggest that the predictions were usually spot on, Uhlmann says. “It’s an amazing discovery tool,” he adds.
“The structure-prediction performance of AlphaFold3 is very impressive,” says David Baker, a computational biophysicist at the University of Washington in Seattle. It’s better than RoseTTAFold All-Atom, which his team developed 4 , he adds.
Restricted access
Unlike RoseTTAFold and AlphaFold2, scientists will not be able to run their own version of AlphaFold3, nor will the code underlying AlphaFold3 or other information obtained after training the model be made public. Instead, researchers will have access to an ‘AlphaFold3 server’, on which they can input their protein sequence of choice, alongside a selection of accessory molecules.

How AlphaFold can realize AI’s full potential in structural biology
Uhlmann likes what he has so far seen of the server, which he says is simpler and quicker than the version of AlphaFold2 that he has access to at his institute. “You upload it and 10 minutes later, you’ve got the structures,” he says. For most scientists, “the server is really going to smash it. Everybody can do it.”
Access to the AlphaFold3 server, however, is limited. Scientists are currently restricted to 10 predictions a day, and it is not possible to obtain structures of proteins bound to possible drugs.
Isomorphic Labs, a DeepMind spin-off company in London, is using AlphaFold3 to develop drugs, both through its own pipeline and with other pharmaceutical companies. “We have to strike a balance between making sure that this is accessible and has the impact in the scientific community as well as not compromising Isomorphic’s ability to pursue commercial drug discovery,” says Pushmeet Kohli, DeepMind’s head of AI science and a study co-author.
Because of the restriction on modelling protein interactions with possible drugs, “I can’t see it having the impact AlphaFold2 had”, says Brian Shoichet, a pharmaceutical chemist at the University of California, San Francisco, who has been using AlphaFold structures to hunt for therapeutic candidates.
Sergey Ovchinnikov, an evolutionary biologist at the Massachusetts Institute of Technology in Cambridge, had hoped to develop a web version of AlphaFold3, as he and his colleagues have done for AlphaFold2 shortly after its code was released. But based on the ample information provided in the latest Nature paper, it shouldn’t take long for other teams to create their own versions, he says. “I would expect open-source solutions before the end of the year.”
doi: https://doi.org/10.1038/d41586-024-01383-z
Abramson, J. et al. Nature https://doi.org/10.1038/s41586-024-07487-w (2024).
Article Google Scholar
Jumper, J. et al. Nature 596 , 583–589 (2021).
Article PubMed Google Scholar
Senior, A. W. et al. Nature 577 , 706–710 (2020).
Krisha, R. et al. Science https://doi.org/10.1126/science.adl2528 (2024).
Download references
Reprints and permissions
Related Articles

- Structural biology
- Machine learning
- Drug discovery
Structural mechanism of angiogenin activation by the ribosome
Article 08 MAY 24
Accurate structure prediction of biomolecular interactions with AlphaFold 3

Structural pharmacology and therapeutic potential of 5-methoxytryptamines

The US Congress is taking on AI —this computer scientist is helping
News Q&A 09 MAY 24

Who’s making chips for AI? Chinese manufacturers lag behind US tech giants
News 03 MAY 24

Discovery of potent small-molecule inhibitors of lipoprotein(a) formation

UTIs make life miserable — scientists are finding new ways to tackle them
News 02 MAY 24
Faculty Positions at the Center for Machine Learning Research (CMLR), Peking University
CMLR's goal is to advance machine learning-related research across a wide range of disciplines.
Beijing, China
Center for Machine Learning Research (CMLR), Peking University
Faculty Positions at SUSTech Department of Biomedical Engineering
We seek outstanding applicants for full-time tenure-track/tenured faculty positions. Positions are available for both junior and senior-level.
Shenzhen, Guangdong, China
Southern University of Science and Technology (Biomedical Engineering)
Southeast University Future Technology Institute Recruitment Notice
Professor openings in mechanical engineering, control science and engineering, and integrating emerging interdisciplinary majors
Nanjing, Jiangsu (CN)
Southeast University
Staff Scientist
A Staff Scientist position is available in the laboratory of Drs. Elliot and Glassberg to study translational aspects of lung injury, repair and fibro
Maywood, Illinois
Loyola University Chicago - Department of Medicine
W3-Professorship (with tenure) in Inorganic Chemistry
The Institute of Inorganic Chemistry in the Faculty of Mathematics and Natural Sciences at the University of Bonn invites applications for a W3-Pro...
53113, Zentrum (DE)
Rheinische Friedrich-Wilhelms-Universität
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

- WEB STORIES New
- ENTERTAINMENT
- CAREER & CAMPUS
- INFOGRAPHICS
- ISL 2023-24

- Manorama Online
- Manorama News TV
- ManoramaMAX
- Radio Mango
- Subscription

ICMR asks Indians to avoid protein supplements: Why?
New Delhi: The Indian Council of Medical Research has urged to avoid protein supplements for building body mass and has recommended restricting salt intake, minimising sugar and ultra-processed foods and reading information on food labels to make informed and healthy food choices. The Hyderabad-based National Institute of Nutrition (NIN) under the apex health research body released revised 'Dietary Guidelines for Indians (DGIs)' to meet the requirements of essential nutrients and prevent non-communicable diseases (NCDs).
Why avoid protein powders? The DGIs have been drafted by a multi-disciplinary committee of experts led by Dr Hemalatha R, Director, ICMR-NIN and have undergone several scientific reviews. Seventeen guidelines have been listed in it. In the DGIs, the NIN stated that prolonged intake of large amounts of protein powders or consumption of high protein concentrate has been associated with potential dangers such as bone mineral loss and kidney damage. It also stated that sugar should be less than 5 per cent of total energy intake and a balanced diet should provide not more than 45 per cent calories from cereals, and millets and up to 15 per cent of calories from pulses, beans and meat.
The rest of the calories should come from nuts, vegetables, fruits and milk. Total fat intake should be less than or equal to 30 per cent energy, the guidelines said. Due to the limited availability and high cost of pulses and meat, a significant proportion of the Indian population relies heavily on cereals, resulting in poor intake of essential macronutrients (essential amino acids and essential fatty acids) and micronutrients, it stated.

Snake fruit: Did you know it has these nutritional benefits?

West Nile fever in Kerala: Precautions, causes, symptoms, treatment and more
What causes the maximum diseases in India? Low intake of essential nutrients can disrupt metabolism and increase the risk of insulin resistance and associated disorders from a young age. Estimates show that 56.4 per cent of the total disease burden in India is due to unhealthy diets, it said. Healthy diets and physical activity can reduce a substantial proportion of coronary heart disease (CHD) and hypertension (HTN) and prevent up to 80 per cent of type 2 diabetes."A significant proportion of premature deaths can be averted by following a healthy lifestyle," it said, adding that the upsurge in the consumption of highly processed foods laden with sugars and fats, coupled with reduced physical activity and limited access to diverse foods, aggravated micronutrient deficiencies and obesity.
- Weight loss

Mother's Day: Why some moms can't connect with their newborns

Buttermilk with chia seeds: Boost gut, cardiac health with this amazing drink

Are sleep wrinkles temporary? How to avoid them?

This disease makes you appear drunk without drinking: Know more

Is your sedentary job increasing your lower belly fat? Try active sitting and transportation

Taking shade under teak trees in summer can be risky: Here's why

- India Today
- Business Today
- Reader’s Digest
- Harper's Bazaar
- Brides Today
- Cosmopolitan
- Aaj Tak Campus
- India Today Hindi
Restrict sugar, salt, avoid protein supplements: ICMR's new dietary guidelines
Icmr has released a new set of dietary guidelines, saying that around 56.4% of the total disease burden in india is because of unhealthy diet habits. .
Listen to Story

- Around 56.4% of the total disease burden in India is because of unhealthy diet habits, says ICMR
- Get fatty acid intake from nuts, oilseeds and seafood instead of cooking oil, as per ICMR's new dietary guidelines
- The research body urged people to "avoid protein supplements" for building body mass
The Indian Council of Medical Research (ICMR) released a set of dietary guidelines for Indians on Wednesday.
According to the guidelines to meet the requirements of essential nutrients and prevent noncommunicable diseases in the country, around 56.4% of the total disease burden in India is because of unhealthy diet habits.
The National Institute of Nutrition (NIN) under the apex health research body, that revised the guidelines after 13 years, said that healthy diets and physical activity can reduce a substantial proportion of coronary heart disease (CHD) and hypertension (high blood pressure) and prevent up to 80% of type 2 diabetes.
"A significant proportion of premature deaths can be averted by following a healthy lifestyle," it said.

- Fazheng Yu 1 ,
- Xiaoxu Wang 2 ,
- Honglin Ren 1 ,
- Jiang Chang 1 na1 ,
- Jian Guo 1 ,
- Zhaoqi He 1 ,
- Ruoran Shi 1 ,
- Xueyu Hu 1 ,
- Yuanyuan Jin 1 ,
- Shiying Lu 1 ,
- Yansong Li 1 ,
- Zengshan Liu 1 &
- Pan Hu ORCID: orcid.org/0000-0002-2045-3694 1
Ulcerative colitis (UC) is a serious health problem with increasing morbidity and prevalence worldwide. The pathogenesis of UC is complex, currently believed to be influenced by genetic factors, dysregulation of the host immune system, imbalance in the intestinal microbiota, and environmental factors. Currently, UC is typically managed using aminosalicylates, immunosuppressants, and biologics as adjunctive therapies, with the risk of relapse and development of drug resistance upon discontinuation. Therefore, further research into the pathogenesis of UC and exploration of potential treatment strategies are necessary to improve the quality of life for affected patients. According to previous studies, Lactobacillus paracasei Jlus66 (Jlus66) reduced inflammation and may help prevent or treat UC.
We used dextran sulfate sodium (DSS) to induce a mouse model of UC to assess the effect of Jlus66 on the progression of colitis. During the experiment, we monitored mouse body weight, food and water consumption, as well as rectal bleeding. Hematoxylin-eosin staining was performed to assess intestinal pathological damage. Protein imprinting and immunohistochemical methods were used to evaluate the protein levels of nuclear factor-kappa B (NF-κB), mitogen-activated protein kinase (MAPK), and tight junction (TJ) proteins in intestinal tissues. Fecal microbiota was analyzed based on partial 16S rRNA gene sequencing.
Jlus66 supplementation reduced the degree of colon tissue damage, such as colon shortening, fecal occult blood, colon epithelial damage, and weight loss. Supplementation with Jlus66 reduced DSS-induced upregulation of cytokine levels such as TNF-α, IL-1β, and IL-6 ( p < 0.05). The NF-κB pathway and MAPK pathway were inhibited, and the expression of TJ proteins (ZO-1, Occludin, and Claudin-3) was upregulated. 16S rRNA sequencing of mouse cecal contents showed that Jlus66 effectively regulated the structure of the intestinal biota.
In conclusion, these data indicate that Jlus66 can alter the intestinal biota and slow the progression of UC, providing new insights into potential therapeutic strategies for UC.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
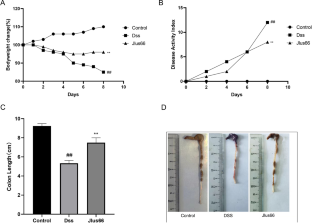
Data availability
The datasets used and analysed in this current study are available from the corresponding author upon reasonable request.
Abbreviations
Ulcerative Colitis
Dextran Sulfate Sodium
Haematoxylin and Eosin
Tumor Necrosis Factor
Interleukin
Glyceraldehyde-3-phosphate dehydrogenase
Colony Forming Unit
Alcian Blue-Periodic Acid Schif
Nuclear Factor-Kappa B
Mitogen-Activated Protein Kinase
Lee CH et al (2023) Animal models of inflammatory bowel disease: novel experiments for revealing pathogenesis of colitis, fibrosis, and colitis-associated colon cancer. Intestinal Res 21(3):295–305
Article Google Scholar
Wang GQ et al (2019) The ameliorative effect of a strain with good adhesion ability against dextran sulfate sodium-induced murine colitis, vol 10. Food & Function, pp 397–409. 1
Celiberto LS et al (2018) Inflammatory bowel disease and immunonutrition: novel therapeutic approaches through modulation of diet and the gut microbiome. Immunology 155(1):36–52
Article CAS PubMed PubMed Central Google Scholar
Shen W, Durum SK (2010) Synergy of IL-23 and Th17 cytokines: New Light on Inflammatory Bowel Disease. Neurochem Res 35(6):940–946
Article CAS PubMed Google Scholar
Yue YS et al (2024) Lycopene ameliorated DSS-Induced colitis by improving epithelial barrier functions and inhibiting the Escherichia coli Adhesion in mice. Journal of Agricultural and Food Chemistry
Faith JJ et al (2013) The Long-Term Stability of the human gut microbiota. Science 341(6141):44–
Article CAS Google Scholar
Joo MK et al (2024) Regulation of colonic neuropeptide Y expression by the gut microbiome in patients with ulcerative colitis and its association with anxiety- and depression-like behavior in mice. Gut Microbes, 16(1)
Neufeld SFM et al (2024) Adolescence, the Microbiota-Gut-Brain Axis, and the Emergence of Psychiatric disorders. Biol Psychiatry 95(4):310–318
Xie YS et al (2024) Apple polyphenol extract ameliorates sugary-diet-induced depression-like behaviors in male C57BL/6 mice by inhibiting the inflammation of the gut-brain axis, vol 15. Food & Function, pp 2939–2959. 6
Harris KG, Chang EB (2018) The intestinal microbiota in the pathogenesis of inflammatory bowel diseases: new insights into complex disease. Clin Sci 132(18):2013–2028
Huttenhower C, Kostic AD, Xavier RJ (2014) Inflammatory bowel disease as a model for translating the Microbiome. Immunity 40(6):843–854
Wang C et al (2024) The roles of different strains in alleviating DSS-induced ulcerative colitis and related functional genes. Food & Function
Ao TX et al (2024) Ameliorative effect of bound polyphenols in mung bean coat dietary fiber on DSS-induced ulcerative colitis in mice: the intestinal barrier and intestinal flora. Food & Function
Cheng N et al (2024) Schisandra Chinensis Bee Pollen ameliorates colitis in mice by modulating gut microbiota and regulating Treg/Th17 Balance. Foods, 13(4)
Rocha CS et al (2012) Anti-inflammatory properties of dairy lactobacilli. Inflamm Bowel Dis 18(4):657–666
Hudson LE et al (2017) Gleaning insights from fecal microbiota transplantation and probiotic studies for the Rational Design of Combination Microbial therapies. Clin Microbiol Rev 30(1):191–231
Article PubMed Google Scholar
Stofilová J et al (2017) Cytokine production and in rat model of colitis in response to LS/07. Biomed Pharmacother 94:1176–1185
Choi SH et al (2019) CAU1055 ameliorates inflammation in lipopolysaccharide-induced RAW264.7 cells and a dextran sulfate sodium-induced colitis animal model. J Dairy Sci 102(8):6718–6725
Kim MH et al (2018) -derived Extracellular vesicles protect atopic Dermatitis Induced by-derived Extracellular vesicles. Allergy Asthma Immunol Res 10(5–6):516–532
Ye HQ et al (2017) Effect of a novel potential probiotic Jlus66 isolated from fermented milk on nonalcoholic fatty liver in rats. Food Funct 8(12):4539–4546
Ji YY et al (2021) Ameliorates cognitive impairment in high-fat induced obese mice insulin signaling and neuroinflammation pathways, vol 12. Food & Function, pp 8728–8737. 18
Shi K et al (2024) The protective effect of Okanin on colitis induced by dextran sulfate sodium in mice. Food Bioscience, 57
Wang YY et al (2018) Potential of ZDY2013 and WBIN03 in relieving colitis by gut microbiota, immune, and anti-oxidative stress. Can J Microbiol 64(5):327–337
Shi RR et al (2023) Protective effect of subsp. SC-5 on Dextran Sulfate Sodium-Induced Colitis in mice. Foods, 12(4)
Ung V et al (2014) Real-life treatment paradigms Show Infliximab is cost-effective for management of Ulcerative Colitis. Clin Gastroenterol Hepatol 12(11):1871–U351
Hu RJ et al (2021) -derived extracellular vesicles maintain intestinal immune homeostasis against lipopolysaccharide-induced inflammatory responses in broilers. J Anim Sci Biotechnol, 12(1)
Li M et al (2017) -derived extracellular vesicles enhance host immune responses against Vancomycin-resistant enterococci. BMC Microbiol, 17
Schulz-Kuhnt A et al (2024) ATP citrate lyase (ACLY)-dependent immunometabolism in mucosal T cells drives experimental colitis in vivo. Gut
Li C et al (2024) Enocyanin alleviates experimental colitis and restores gut microbiota homeostasis as functional foods. Food Bioscience, 57
Ruffolo C et al (2010) Subclinical intestinal inflammation in patients with Crohn’s Disease following Bowel Resection: a smoldering fire. J Gastrointest Surg 14(1):24–31
Figueredo CM et al (2017) Activity of inflammatory bowel disease influences the expression of cytokines in gingival tissue. Cytokine 95:1–6
Yamamoto-Furusho JK (2018) Inflammatory bowel disease therapy: blockade of cytokines and cytokine signaling pathways. Curr Opin Gastroenterol 34(4):187–193
Kai Y et al (2005) Colitis in mice lacking the common cytokine receptor γ chain is mediated by IL-6-producing CD4T cells. Gastroenterology 128(4):922–934
Yu M et al (2018) Aryl Hydrocarbon receptor activation modulates intestinal epithelial barrier function by maintaining tight Junction Integrity. Int J Biol Sci 14(1):69–77
Günzel D, Fromm M (2012) Claudins and other tight Junction proteins. Compr Physiol 2(3):1819–1852
Oshima T, Miwa H (2016) Gastrointestinal mucosal barrier function and diseases. J Gastroenterol 51(8):768–778
Jiang N et al (2020) Andrographolide derivative AL-1 reduces intestinal permeability in dextran sulfate sodium (DSS)-induced mice colitis model. Life Sci, 241
Vendrig JC, Fink-Gremmels J (2012) Intestinal barrier function in neonatal foals: options for improvement. Vet J 193(1):32–37
Mohamed SS et al (2021) Effect of the standard herbal preparation, STW5, treatment on dysbiosis induced by dextran sodium sulfate in experimental colitis. Bmc Complement Med Ther, 21(1)
Zou LJ et al (2019) Identification of microRNA transcriptome reveals that miR-100 is involved in the renewal of porcine intestinal epithelial cells. Sci China-Life Sci 62(6):816–828
Zhang F et al (2019) The Impact of on the Gut Microbiota of Mice with DSS-Induced Colitis Biomed Research International, 2019
Shang LJ et al (2021) Core altered microorganisms in Colitis Mouse Model: a Comprehensive Time-Point and Fecal Microbiota Transplantation Analysis. Antibiotics-Basel, 10(6)
Seo B et al (2024) Strain-specific anti-inflammatory effects of strain KBL1027 in koreans. Probiotics and Antimicrobial Proteins
Zang ZZ et al (2024) Study on the ameliorative effect of honeysuckle on DSS-induced ulcerative colitis in mice. J Ethnopharmacol, 325
Download references
This work was supported by the National Key Research and Development Program of China (No.2023YFD1801000) and the Interdisciplinary Integration and Innovation Project of JLU (No. JLUXKJC2021ZY08).
Author information
Fazheng Yu, Xiaoxu Wang, Honglin Ren and Jiang Chang contributed equally to this work.
Authors and Affiliations
State Key Laboratory for Diagnosis and Treatment of Severe Zoonotic Infectious Diseases, Key Laboratory for Zoonosis Research of the Ministry of Education, Institute of Zoonosis, College of Veterinary Medicine, Jilin University, Changchun, 130062, China
Fazheng Yu, Honglin Ren, Jiang Chang, Jian Guo, Zhaoqi He, Ruoran Shi, Xueyu Hu, Yuanyuan Jin, Shiying Lu, Yansong Li, Zengshan Liu & Pan Hu
Institute of Special Animal and Plant Sciences of Chinese Academy of Agricultural Sciences, Changchun, Jilin, 130112, China
Xiaoxu Wang
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Pan Hu .
Ethics declarations
Ethical approval.
All experimental procedures were performed according to the guidelines of Animal Investigation Ethics Committee in Jilin University (No. SY202010004). They were therefore performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Competing interest
No competing financial interests exist.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Yu, F., Wang, X., Ren, H. et al. Lactobacillus paracasei Jlus66 relieves DSS-induced ulcerative colitis in a murine model by maintaining intestinal barrier integrity, inhibiting inflammation, and improving intestinal microbiota structure. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03419-6
Download citation
Received : 06 June 2023
Accepted : 29 April 2024
Published : 11 May 2024
DOI : https://doi.org/10.1007/s00394-024-03419-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lactobacillus paracasei
- Intestinal biota
- Find a journal
- Publish with us
- Track your research
Does your gut need a reset?
Do you want to start feeling better?
- Work With Us
- Shop Solutions
- Meet Dr. Ruscio Why patients choose Dr. Ruscio, DC
- Our Virtual Clinic Get on the clear path to feeling better
- Research & Scientific Review Board Experts in the health and wellness space
- Contact Dr. Ruscio How can we help you?
- Blog Helpful articles to improve your health
- Podcast Conversations with health and nutrition experts Login
- Videos Practical health advice straight from Dr. Ruscio, DC
- Get the Book Read "Healthy Gut Healthy You" by Dr. Ruscio
- Free Guides Read "Healthy Gut Healthy You" by Dr. Ruscio
- Gut Health & Digestion
- Nutritional Support
- Energy & Vitality
- Antimicrobials, Immune & Inflammatory Support
- Best Sellers
- SHOP ALL PRODUCTS
- Work With Us Get started and complete the online application
- Our Process Simple steps with transparent pricing
- Published Science Insightful science-based articles we've written
- Client Success Stories "I loved my doctor's simple approach."
- Free Discovery Call Schedule a 15 min. meeting to ask questions
- Thyroid Course Take control of your thyroid health today
- Client Shop Login Login Become a Patient
- Client Portal Login Login
- Practitioner Login Login
Evidence Based
This article is based on scientific evidence, written by experts and fact checked by experts.
Our team of licensed nutritionists and dietitians strive to be objective, unbiased, honest and to present both sides of the argument.
This article contains scientific references. The numbers in the parentheses (1, 2, 3) are clickable links to peer-reviewed scientific papers.
The 6 Best Gut Health Supplements
Written by Dr. Ruscio on May 9, 2024
Unpacking Which Research-Backed Supplements Are Worth Their Salt to Address Your Gut Challenges
- The Best Supplements for Gut Health |
- Supplements Geared Toward Specific Gut Health Conditions |
- Start Simply |
Gut health sits at the center of overall health and well-being. Nearly every nutrient our body needs comes to us through the foods we eat, and we rely heavily on our gut microbiome to break down and assimilate those nutrients. When digestive function begins to degrade, so too do other systems and processes that help our bodies and health thrive.
If you’ve been experiencing digestive health symptoms like bloating, constipation, diarrhea, cramping, or indigestion, it’s likely time to start thinking about some diet shifts and possibly gut health supplements. If you’ve been experiencing seemingly unrelated symptoms like skin irruptions (acne, rash, rosacea), brain fog, mood changes, unexplained fatigue or headaches, or even sudden hormonal changes, then improving your gut health should be prioritized.
When it comes to finding the best gut health supplements, some support overall gut health and can benefit a wide variety of people. Others target specific issues like leaky gut, small intestinal bacterial overgrowth (SIBO), irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and other gut challenges that could be causing some of the more disparate symptoms.
Let’s take a look at what I consider the best gut health supplements based on thorough research and my own clinical experience. I’ll start with the ones that are our top picks in the clinic for overall gut health and then drill down into those that may improve more specific gut issues.
The Best Supplements for Gut Health
The supplements I’ll list below have varying amounts of evidence to back up their efficacy for gut health and human health generally. I’ve listed them in order, starting with the one with the most research and clinical evidence
You’ll notice in the sections below that certain nutrients on this list, like vitamin D for example, are better obtained through means other than supplementation. That doesn’t mean there’s never a reason to supplement. I’ll dive deeper into details in the sections where it’s relevant.
The best supplements for improving overall gut health include:
I don’t mean to imply that it’s time to buy every last one of these today. You might find that one or two work great to noticeably improve your digestive system function. A more scientific and cost-effective approach is to start one at a time and be methodical with a gut-healing protocol . After I go through these, I’ll also share a few more targeted supplements for specific gut situations.
1. Probiotics
Probiotics are almost always the first supplement I reach for when it comes to addressing anything gut-related. The health benefits of probiotics can hardly be understated when considering the abundant research supporting their efficacy. Probiotics introduce good bacteria and fungi into your microbiome to provide a host of health benefits that reach far beyond gut-related symptoms. Benefits of probiotics include [ 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 ]
- Correcting dysbiosis
- Improving leaky gut
- Reducing immune system activation
- Anti-inflammatory properties
- Reducing visceral hypersensitivity
- Improving motility
- Improving bowel movements and regularity
- Treating infections like SIBO , Giardia, and vaginal Candida (yeast infection)
- Reducing antibiotic-related digestive side effects like diarrhea
- Improving inflammation-related mood and cognition issues like anxiety, depression, and brain fog through the gut-brain axis
High-quality research shows that probiotics are consistently better than placebos at improving leaky gut, reducing inflammation, increasing beneficial bacteria and biodiversity, and correcting dysbiosis [ 2 ]. Each of these conditions is linked to all manner of health challenges, so correcting at the gut level has far-reaching benefits across the whole picture of your health.
Probiotics are an excellent treatment for common gut ailments like IBS, IBD, constipation, and for preventing the side effects of antibiotic treatments [ 1 , 6 , 9 , 10 , 11 ]. Low biodiversity in the gut microbiome has been associated with mood issues like anxiety and depression, IBS and IBD symptoms, as well as decreased immune function.
This isn’t to say that taking a daily probiotic will cure every ailment you have, but it’s a key ingredient to improving certain health issues at the root cause. By taking a daily supplement and adding probiotic-rich foods like sauerkraut, kimchi, kefir, kombucha, and plain yogurt to your diet, you will be consistently adding those beneficial microbes into your gut bacteria ecosystem, improving the microbial diversity in your gut, and giving yourself the best chance at getting on top of your health challenges.
How to Choose A Probiotic
Probiotic supplements come in serving sizes of billions—sometimes trillions—of live bacteria and fungi in each capsule or packet. The best probiotics offer a wide variety of probiotic strains and species. Based on observation in my clinic, I recommend including all three categories into one formula for maximum impact . The three types and my recommended dosing are below.
Dosing by Type of Probiotic :

You may also want to simplify the process by trying my Triple Therapy Probiotic Powder Sticks , which contain the proportions of all three categories above.
Key Point: Probiotics are the most researched gut-supportive supplement available and have been shown to improve all manner of gut challenges. Combine two or three categories for maximum impact.
2. Glutamine
Glutamine is the most abundant free amino acid in human blood and the main energy source for intestinal cells [ 12 ]. Studies suggest that it may reduce inflammation and leaky gut by supporting the integrity of tight junctions in the intestinal lining [ 12 , 13 , 14 , 15 ].
In the case of leaky gut, those tight junctions become less tight and more permeable, allowing partially digested food and sometimes harmful bacteria out of the intestine and into the bloodstream. When this happens, it can set off a cascade of inflammatory reactions, sometimes leading to an overactive immune system and compromised immune health. When compared to placebo, glutamine was shown to reduce leaky gut and improve IBS symptoms to a large degree [ 13 ].
How to Dose Glutamine
While our bodies make glutamine, it can sometimes still be useful to supplement it for additional gut support. When supplementing glutamine, you’ll likely see a label that says “L-glutamine,” as that is the type found most often in foods and supplements. Research suggests that a daily intake of about 15 grams of glutamine per day may reduce leaky gut and improve IBS symptoms by as much as 80% [ 13 ].
If you’re looking for a supplement, you’ll likely see dosages anywhere from 500mg to 5000mg per serving. You’ll want to check with your healthcare provider, nutritionist, or registered dietitian to determine an ideal dosage for you based on your diet and other particulars of your health.
My product Gut Rebuild Nutrients contains 1500 mg, which is a great supplement to add to a diet rich in dietary sources of glutamine like beef, poultry, pork, dairy products, raw spinach, and cabbage.
Key Point: Glutamine may reduce leaky gut and gut inflammation.
3. Curcumin
Curcumin is an anti-inflammatory, antioxidant compound found in the culinary spice turmeric. It’s what makes turmeric and curry yellow and has been used medicinally in India for at least 4,000 years [ 16 ]. Curcumin may block inflammatory pathways and reduce oxidative stress. Oxidative stress occurs when there are more free radicals than antioxidants in the body, leading to cell damage over time, including cells in the digestive tract [ 16 ].
Human studies have found that curcumin can benefit IBS and IBD symptoms, has the potential to help eradicate H. pylori infection, and is better than a placebo at reducing gut pain, diarrhea, constipation, and indigestion [ 17 , 18 ]. An in vitro study suggests it has the potential to reduce leaky gut as well [ 19 ]. Curcumin also stimulates bile and supports healthy digestion of fats [ 20 ].
In the clinic, many patients have noticed that taking 1–2 tablespoons of turmeric or 500–1,000 mg of supplemental curcumin daily improves their gut health.
Key Point: Curcumin is an anti-inflammatory, antioxidant compound that may benefit those with those with a range of gut issues.
4. Butyrate
Healthy gut bacteria actually create the short-chain fatty acid butyrate when they digest the fiber we eat [ 21 ]. Even though your gut bacteria make butyrate, you can also supplement it.
(Side note: Without the live microorganisms in our gut, we wouldn’t be able to digest fiber at all.)
Researchers found that those with digestive issues like IBS and IBD have lower butyrate levels than healthy people with healthy gut function [ 22 , 23 ]. Based on these findings, it would theoretically make sense that supplementing butyrate may improve those issues, and the research actually bears this out, although results are mixed within the category of IBD.
A large 2022 study of 2,990 IBS patients were all treated with butyrate (no placebo group). After 3 months, 99.7% of them had improvements, and 94% said they would continue using butyrate after the study. Patients saw improvements in abdominal pain, gas, diarrhea, constipation, urgency, nausea, and quality of life after 3 months [ 21 ].
Ulcerative colitis patients may not benefit from butyrate, based on current research, but it shows promising results for increasing long-term remission rates for other IBD patients like those with Crohn’s disease [ 24 , 25 , 26 ].
How to Supplement Butyrate
Butyrate may be safely taken as a supplement to help address symptoms of IBS, Crohn’s disease, traveler’s diarrhea, and diverticulitis flares [ 21 , 22 , 26 , 27 , 28 , 29 , 30 ].
As a supplement, it’s safe and well-tolerated at dosages between 300 mg to 4 g/day for up to a year [ 21 , 26 , 28 , 29 , 30 ].
Key Point: Butyrate is produced by gut bacteria, but supplementing may still benefit those with GI symptoms, although we need more research.
5. Vitamin D
Vitamin D is a key component in immune system regulation, metabolizing calcium, the growth and development of cells, and bone health [ 31 , 32 , 33 ]. Low vitamin D levels may contribute to obesity, malnutrition, autoimmunity, and gastrointestinal, liver, and kidney diseases [ 34 ].
When it comes to gut support, early evidence suggests that vitamin D may help regulate gut microbiota. However, the most consistent findings on this front were when vitamin D was obtained through sun exposure rather than supplementation [ 35 , 36 , 37 , 38 , 39 , 40 ].
As you may have guessed from my previous sentence, the most ideal way to obtain vitamin D is to make it yourself through sun exposure —as long as you’re careful not to get burned [ 41 ]. Through safe sun exposure, your skin actually synthesizes the correct amount of vitamin D your body needs to optimize all the functions vitamin D facilitates.
That being said, your location on the globe, your skin tone, and your ability to be outside enough during peak sunshine may not allow you to get your full dose of sunshine every day. In this case, you’ll want to supplement.
Take a look at this chart to determine where you fall based on skin type and geography.
Table 1. Each skin phototype (lightest to darkest skin), response to UV, cancer risk, SED (amount of UV required to burn), and time in the sun at each UV Index level before burning [ 42 , 43 , 44 , 45 ].
More work needs to be done to clearly define the gut health benefits of vitamin D, but the early research is promising.
How to Choose a Vitamin D Supplement
The most bioavailable form of vitamin D is vitamin D3. Look for labels that say D3 [ 46 ]. Studies at the NIH have found that vitamin K and vitamin D have a synergistic effect when taken together, so it makes sense to find one that contains both [ 47 ]. Additionally, a 2020 meta-analysis of 8 randomized controlled trials found that combining the two significantly increased bone mineral density in people [ 48 ].
Key Point: Vitamin D may help regulate gut microbiota. It’s ideal to get your vitamin D from sunlight; however, if you need to supplement, choose a vitamin D3 that also includes vitamin K2.
6. Collagen
Collagen is the most abundant protein in the body. It’s found in the bone matrix, muscle tissue, tendons, ligaments, and cartilage, and it’s the reason so many functional doctors and holistic practitioners recommend drinking bone broth to support gut health [ 49 ].
Evidence for using collagen to support human gut health is thin, but animal and in vitro cell studies show interesting findings for what’s possible. Animal studies have shown collagen may improve dysbiosis, reduce inflammation, and increase short-chain fatty acid production [ 50 , 51 , 52 ].
Cell studies suggest collagen may have the potential to reduce leaky gut and inflammation, and increase short-chain fatty acid production [ 51 , 53 , 54 ]. This brings us back to butyrate—collagen may support your body’s production of more butyrate.
In the clinic, I’ve seen improvements when patients include collagen powder in their diet—increased energy and decreased fatigue. Collagen is a protein, so adding it to your diet as an additional protein source can also be really beneficial to your overall health. It’s also been shown to support skin health and reduce fine lines and wrinkles when ingested (not topically) [ 55 ].
How to take Collagen
Collagen comes in powder form and can be added to smoothies, soups, or even whisked into your morning coffee for a morning protein boost. It’s an animal product sourced from cows, pigs, or fish, so isn’t suitable for vegetarians. Your body makes collagen, but adding high-quality protein into your diet and shooting for 30 grams per meal, is a great goal to boost collagen production for your overall health. Collagen supplementation can help you achieve that goal. Most collagen supplements recommend around 10 grams/day, but up to 40 grams appears to be well-tolerated for most people.
If you want to make your own collagen-rich bone broth , using the most cartilaginous parts of a chicken is the easiest (and, in my opinion, the most delicious) way to go—chicken feet and wings work best.
Key Point: Collagen may reduce leaky gut and inflammation. It’s also a great source of protein and may improve skin health.
Supplements Geared Toward Specific Gut Health Conditions
After the top six I listed above, there are a few others I’d like to mention for their potential efficacy in addressing specific gut conditions. Here they are:
- Hydrochloric Acid (HCl)
Herbal Antimicrobials
- Oral Fecal Microbiota Transplant (FMT) or “Microbiome Pills”
Berberine is a plant compound often used for improving metabolic health and lowering inflammation. It also has antimicrobial effects.
While there’s little research to support berberine for addressing gut health, what’s available is promising and worth investigating. A fairly large randomized controlled trial found that berberine may be effective at treating IBS symptoms, including diarrhea, abdominal pain, bowel urgency, anxiety, and depression [ 56 ]. These findings are encouraging for future research on berberine’s effects on SIBO, since SIBO and IBS tend to go hand in hand. A new clinical trial is underway comparing berberine’s efficacy to that of rifaxamin, the gold standard for treating SIBO with antibiotics [ 57 ].
It’s also worth noting that berberine may lower blood glucose, which means it could cause hypoglycemia in some people, so talk to your healthcare provider before starting this one.
Key Point: Berberine may be effective in treating IBS symptoms, including urgency, anxiety, and depression.
Hydrochloric Acid
HCl, or hydrochloric acid, is made in the stomach when the brain tells the stomach you’re about to eat. Its purpose is to break down protein, increase nutrient absorption, enhance digestion in the small intestine, and defend against pathogens.
If you’re dealing with upper GI symptoms, HCl could be a good solution to consider. Risk factors are low if you don’t already have an ulcer, and you can easily run an at-home assessment to determine whether you’ll benefit from it.
Upper GI issues that HCl may improve include:
- Indigestion
- Feeling full quickly
- Difficulty digesting animal protein
How to Use HCl
You can look for Betaine HCl at your local health foods store or grab a bottle here . For our patients in the clinic, we recommend starting with one capsule 15 minutes prior to each meal. If they don’t experience any relief with just one pill after two to three days, we’ll often have them increase to two capsules before each meal. Some may eventually work up to as many as four capsules to find the ideal dose.
A good rule of thumb in our experience is that if patients see improved symptoms, it’s safe to assume that their body needs supplemental HCl. If there’s no change after two weeks, we’ll recommend they stop taking it and try another avenue.
If you decide to try HCl on your own or, preferably, with a practitioner’s help, be sure to stop taking HCl right away if you feel any burning in your esophagus or stomach after taking it.
Key Point: HCl may be beneficial for those experiencing upper GI issues like burping, indigestion, and reflux.
Herbal antimicrobials are used for dysbiosis and certain gut infections. Curcumin (mentioned in the first section for general gut health) can offer some antimicrobial benefits, especially in combination with other herbs. Other herbal antimicrobials may include oregano oil, boswellia, wormwood, peppermint oil, and STW 5 (Iberogast), although this isn’t an exhaustive list.
Herbal antimicrobials can be effective against:
- IBS symptoms [ 58 , 59 , 60 , 61 , 62 , 63 ]
- IBD [ 64 , 65 , 66 , 67 , 68 ]
- Parasites [ 69 , 70, 71 ]
- Bacterial infections [ 72 , 73 , 74 , 75 , 76 ]
- Diarrhea [ 77 , 78 ]
- Inflammation [ 59 , 79 , 80 ]
- SIBO (Ruscio Institute clinical trial)
Always use herbal antimicrobials with the guidance of a knowledgeable healthcare professional. People with compromised immunity should take extra caution. Just because herbal antimicrobials are natural doesn’t mean they aren’t potent and can’t cause problems if used incorrectly. We also don’t know if they might eventually contribute to antimicrobial resistance if used too frequently and unnecessarily [ 81 ].
Key Point: Herbal antimicrobials are intended for those with symptoms of gut dysbiosis and should only be taken under the guidance of a healthcare professional.
The reason fiber is listed here in this section rather than in the top six supplements above is because fiber is best consumed in the foods we eat rather than through supplements [ 82 , 83 , 84 ]. I see the best results when our patients work in five servings of fiber-rich food per day. This amounts to about 25-30 grams of fiber per day. It’s also true that certain gut conditions specifically require a deliberate reduction in fiber as part of the treatment protocol, like SIBO. SIBO protocol calls for a low-FODMAP diet, which may impact your total fiber intake. If you focus on low-FODMAP veggies, you may still be able to reach that 25-30 gram goal.
That being said, you might want to try fiber supplements if your diet is low in fiber and you have constipation, diarrhea, high cholesterol, and high blood glucose [ 85 ]. Fiber may aid in lowering blood glucose and cholesterol levels. This type of supplement is meant only for brief, temporary use rather than as an ongoing solution to gut challenges [ 86 ].
The best fiber to choose is dependent on your goals and needs. Based on available research, psyllium husk seems to be the most effective at lowering blood glucose and cholesterol [ 85 ]. Use the recommended dosing on the label as your eventual goal dose, but don’t stop there. I usually have my patients who may benefit from supplemental fiber start with a ½-teaspoon and then slowly work their way up to three full teaspoons over the course of a few weeks to help reduce any potential side effects.
Risks of Fiber Supplementation
Fiber supplements, especially higher doses, may cause a number of mild GI side effects for people who have IBS, such as:
- Diarrhea [ 87 ]
- Constipation [ 87 ]
- Nausea and vomiting [ 87 ]
- Difficulty swallowing [ 87 ]
- Back pain [ 87 ]
- Fatigue [ 87 ]
- Flatulence and gas [ 87 ]
- Heartburn [ 87 ]
- Pelvic pain [ 87 ]
- Joint pain [ 87 ]
- Bloating [ 88 ]
- Sense of fullness [ 89 ]
People who are malnourished, sick, very young, or very old, or people with impacted bowels or who can’t tolerate the side effects should avoid supplemental fiber [ 86 ].
Key Point: Fiber is best consumed in the diet, but supplements may benefit some. Those with IBS have a greater risk of experiencing negative symptoms.
Oral FMT or “Microbiome Pills”
FMT stands for fecal microbiota transplants. Yes, poop pills. These capsules are filled with matter from the GI tracts of healthy people and are used to introduce live, beneficial bacteria to someone with signs of gut imbalance or poor gut health.
FMT research has shown it is effective for treating:
- Recurrent Clostridium difficile infections [ 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 ]
- Inflammatory bowel disease (IBD) [ 92 , 97 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 ]
- Irritable bowel syndrome (IBS) [ 109 , 110 , 111 , 112 ]
- Diarrhea [ 110 , 112 , 113 ]
- Bloating [ 113 ]
- Abdominal pain [ 113 ]
- Constipation [ 97 ]
- Small intestinal bacterial overgrowth (SIBO) [ 114 ]
Risks of FMT
The risks of this treatment are low beyond the slight “ick” factor. Side effects may include mild bloating, abdominal pain, diarrhea, and constipation, but generally resolve on their own [ 115 ]. That being said, this is a newer intervention, and you should try it only after other treatment options fail.
If you go with FMT pills, it is vital to make sure you only source them from reputable sources. Two people reportedly died after using fecal samples from donors who were not properly screened for intestinal pathogens [ 116 ]. Please don’t ever follow DIY instructions that describe how to take someone else’s poop and introduce it into your own body.
Key Point: FMT is a new intervention that may improve a number of gut issues. This intervention should always be explored under medical supervision.
Start Simply
I’ve given you a LOT of information here. Instead of feeling overwhelmed with the array of potential supplements, start by adding a probiotic and probiotic foods into your daily routine. There are endless dietary supplements on the market making claims about what’s effective for gut health, but the one with absolutely rock-solid research to back its efficacy is probiotics.
The most important thing in choosing supplements is to buy from a reputable company. That’s because the FDA doesn’t regulate supplements the way they regulate pharmaceuticals. Look for the Truth in Labeling logo or other evidence of third-party testing, and ensure that the ingredients underneath the nutrition facts don’t’ include anything you’re allergic to before you buy.
From there, if you’re not experiencing relief, you can make your way down the list of the top six I listed here. Importantly, your diet is a huge factor in your gut health, and supplementation will only go so far if you’re not giving your body the correct inputs. If you’d like to explore on your own, check out my book Healthy Gut, Healthy You . If you’d like more support on your gut health journey, we’d love to help. Reach out to our clinic to set up a consultation.
The Ruscio Institute has developed a range of high-quality formulations to help our patients and audience. If you’re interested in learning more about these products, please click here . Note that there are many other options available, and we encourage you to research which products may be right for you.
➕ References
- Zhang T, Zhang C, Zhang J, Sun F, Duan L. Efficacy of Probiotics for Irritable Bowel Syndrome: A Systematic Review and Network Meta-Analysis. Front Cell Infect Microbiol. 2022 Apr 1;12:859967. DOI: 10.3389/fcimb.2022.859967. PMID: 35433498 . PMCID: PMC9010660.
- Zheng Y, Zhang Z, Tang P, Wu Y, Zhang A, Li D, et al. Probiotics fortify intestinal barrier function: a systematic review and meta-analysis of randomized trials. Front Immunol. 2023 Apr 24;14:1143548. DOI: 10.3389/fimmu.2023.1143548. PMID: 37168869 . PMCID: PMC10165082.
- Zhong C, Qu C, Wang B, Liang S, Zeng B. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth: A Meta-Analysis and Systematic Review of Current Evidence. J Clin Gastroenterol. 2017 Apr;51(4):300–11. DOI: 10.1097/MCG.0000000000000814. PMID: 28267052 .
- Besirbellioglu BA, Ulcay A, Can M, Erdem H, Tanyuksel M, Avci IY, et al. Saccharomyces boulardii and infection due to Giardia lamblia. Scand J Infect Dis. 2006;38(6–7):479–81. DOI: 10.1080/00365540600561769. PMID: 16798698 .
- Mollazadeh-Narestan Z, Yavarikia P, Homayouni-Rad A, Samadi Kafil H, Mohammad-Alizadeh-Charandabi S, Gholizadeh P, et al. Comparing the Effect of Probiotic and Fluconazole on Treatment and Recurrence of Vulvovaginal Candidiasis: a Triple-Blinded Randomized Controlled Trial. Probiotics Antimicrob Proteins. 2023 Oct;15(5):1436–46. DOI: 10.1007/s12602-022-09997-3. PMID: 36198994 . PMCID: PMC9534588.
- Fernández-Alonso M, Aguirre Camorlinga A, Messiah SE, Marroquin E. Effect of adding probiotics to an antibiotic intervention on the human gut microbial diversity and composition: a systematic review. J Med Microbiol. 2022 Nov;71(11). DOI: 10.1099/jmm.0.001625. PMID: 36382780 .
- Musazadeh V, Zarezadeh M, Faghfouri AH, Keramati M, Jamilian P, Jamilian P, et al. Probiotics as an effective therapeutic approach in alleviating depression symptoms: an umbrella meta-analysis. Crit Rev Food Sci Nutr. 2023;63(26):8292–300. DOI: 10.1080/10408398.2022.2051164. PMID: 35348020 .
- Lv T, Ye M, Luo F, Hu B, Wang A, Chen J, et al. Probiotics treatment improves cognitive impairment in patients and animals: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2021 Jan;120:159–72. DOI: 10.1016/j.neubiorev.2020.10.027. PMID: 33157148 .
- Zhang X-F, Guan X-X, Tang Y-J, Sun J-F, Wang X-K, Wang W-D, et al. Clinical effects and gut microbiota changes of using probiotics, prebiotics or synbiotics in inflammatory bowel disease: a systematic review and meta-analysis. Eur J Nutr. 2021 Aug;60(5):2855–75. DOI: 10.1007/s00394-021-02503-5. PMID: 33555375 .
- Zhang C, Jiang J, Tian F, Zhao J, Zhang H, Zhai Q, et al. Meta-analysis of randomized controlled trials of the effects of probiotics on functional constipation in adults. Clin Nutr. 2020 Oct;39(10):2960–9. DOI: 10.1016/j.clnu.2020.01.005. PMID: 32005532 .
- Šola KF, Vladimir-Knežević S, Hrabač P, Mucalo I, Saso L, Verbanac D. The effect of multistrain probiotics on functional constipation in the elderly: a randomized controlled trial. Eur J Clin Nutr. 2022 Dec;76(12):1675–81. DOI: 10.1038/s41430-022-01189-0. PMID: 35927504 . PMCID: PMC9708599.
- Camilleri M, Vella A. What to do about the leaky gut. Gut. 2022 Feb;71(2):424–35. DOI: 10.1136/gutjnl-2021-325428. PMID: 34509978 . PMCID: PMC9028931.
- Zhou Q, Verne ML, Fields JZ, Lefante JJ, Basra S, Salameh H, et al. Randomised placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome. Gut. 2019 Jun;68(6):996–1002. DOI: 10.1136/gutjnl-2017-315136. PMID: 30108163 . PMCID: PMC9549483.
- Mottaghi A, Yeganeh MZ, Golzarand M, Jambarsang S, Mirmiran P. Efficacy of glutamine-enriched enteral feeding formulae in critically ill patients: a systematic review and meta-analysis of randomized controlled trials. Asia Pac J Clin Nutr. 2016;25(3):504–12. DOI: 10.6133/apjcn.092015.24. PMID: 27440684 .
- Wang H, Zhang C, Wu G, Sun Y, Wang B, He B, et al. Glutamine enhances tight junction protein expression and modulates corticotropin-releasing factor signaling in the jejunum of weanling piglets. J Nutr. 2015 Jan;145(1):25–31. DOI: 10.3945/jn.114.202515. PMID: 25527658 .
- Hatcher H, Planalp R, Cho J, Torti FM, Torti SV. Curcumin: from ancient medicine to current clinical trials. Cell Mol Life Sci. 2008 Jun;65(11):1631–52. DOI: 10.1007/s00018-008-7452-4. PMID: 18324353 . PMCID: PMC4686230.
- Atefi M, Darand M, Entezari MH, Jamialahmadi T, Bagherniya M, Sahebkar A. A systematic review of the clinical use of curcumin for the management of gastrointestinal diseases. Adv Exp Med Biol. 2021;1291:295–326. DOI: 10.1007/978-3-030-56153-6_18. PMID: 34331698 .
- Lopresti AL, Smith SJ, Rea A, Michel S. Efficacy of a curcumin extract (Curcugen TM ) on gastrointestinal symptoms and intestinal microbiota in adults with self-reported digestive complaints: a randomised, double-blind, placebo-controlled study. BMC Complement Med Ther. 2021 Jan 21;21(1):40. DOI: 10.1186/s12906-021-03220-6. PMID: 33478482 . PMCID: PMC7818735.
- Wang J, Ghosh SS, Ghosh S. Curcumin improves intestinal barrier function: modulation of intracellular signaling, and organization of tight junctions. Am J Physiol, Cell Physiol. 2017 Apr 1;312(4):C438–45. DOI: 10.1152/ajpcell.00235.2016. PMID: 28249988 . PMCID: PMC5407015.
- Prasad S, Aggarwal BB. Turmeric, the golden spice: from traditional medicine to modern medicine. In: Benzie IFF, Wachtel-Galor S, editors. Herbal medicine: biomolecular and clinical aspects. 2nd ed. Boca Raton (FL): CRC Press/Taylor & Francis; 2011. PMID: 22593922 .
- Lewandowski K, Kaniewska M, Karłowicz K, Rosołowski M, Rydzewska G. The effectiveness of microencapsulated sodium butyrate at reducing symptoms in patients with irritable bowel syndrome. Prz Gastroenterol. 2022 Jan 18;17(1):28–34. DOI: 10.5114/pg.2021.112681. PMID: 35371361 . PMCID: PMC8942000.
- Sun Q, Jia Q, Song L, Duan L. Alterations in fecal short-chain fatty acids in patients with irritable bowel syndrome: A systematic review and meta-analysis. Medicine (Baltimore). 2019 Feb;98(7):e14513. DOI: 10.1097/MD.0000000000014513. PMID: 30762787 . PMCID: PMC6408019.
- Zhuang X, Li T, Li M, Huang S, Qiu Y, Feng R, et al. Systematic Review and Meta-analysis: Short-Chain Fatty Acid Characterization in Patients With Inflammatory Bowel Disease. Inflamm Bowel Dis. 2019 Oct 18;25(11):1751–63. DOI: 10.1093/ibd/izz188. PMID: 31498864 .
- Jamka M, Kokot M, Kaczmarek N, Bermagambetova S, Nowak JK, Walkowiak J. The Effect of Sodium Butyrate Enemas Compared with Placebo on Disease Activity, Endoscopic Scores, and Histological and Inflammatory Parameters in Inflammatory Bowel Diseases: A Systematic Review of Randomised Controlled Trials. Complement Med Res. 2021;28(4):344–56. DOI: 10.1159/000512952. PMID: 33352566 .
- Vernero M, De Blasio F, Ribaldone DG, Bugianesi E, Pellicano R, Saracco GM, et al. The Usefulness of Microencapsulated Sodium Butyrate Add-On Therapy in Maintaining Remission in Patients with Ulcerative Colitis: A Prospective Observational Study. J Clin Med. 2020 Dec 4;9(12). DOI: 10.3390/jcm9123941. PMID: 33291846 . PMCID: PMC7762036.
- Di Sabatino A, Morera R, Ciccocioppo R, Cazzola P, Gotti S, Tinozzi FP, et al. Oral butyrate for mildly to moderately active Crohn’s disease. Aliment Pharmacol Ther. 2005 Nov 1;22(9):789–94. DOI: 10.1111/j.1365-2036.2005.02639.x. PMID: 16225487 .
- Staudacher HM, Rossi M, Kaminski T, Dimidi E, Ralph FSE, Wilson B, et al. Long-term personalized low FODMAP diet improves symptoms and maintains luminal Bifidobacteria abundance in irritable bowel syndrome. Neurogastroenterol Motil. 2022 Apr;34(4):e14241. DOI: 10.1111/nmo.14241. PMID: 34431172 .
- Banasiewicz T, Krokowicz Ł, Stojcev Z, Kaczmarek BF, Kaczmarek E, Maik J, et al. Microencapsulated sodium butyrate reduces the frequency of abdominal pain in patients with irritable bowel syndrome. Colorectal Dis. 2013 Feb;15(2):204–9. DOI: 10.1111/j.1463-1318.2012.03152.x. PMID: 22738315 .
- Krokowicz L, Kaczmarek BF, Krokowicz P, Stojcev Z, Mackiewicz J, Walkowiak J, et al. Sodium butyrate and short chain fatty acids in prevention of travellers’ diarrhoea: a randomized prospective study. Travel Med Infect Dis. 2014 Apr;12(2):183–8. DOI: 10.1016/j.tmaid.2013.08.008. PMID: 24063909 .
- Krokowicz L, Stojcev Z, Kaczmarek BF, Kociemba W, Kaczmarek E, Walkowiak J, et al. Microencapsulated sodium butyrate administered to patients with diverticulosis decreases incidence of diverticulitis–a prospective randomized study. Int J Colorectal Dis. 2014 Mar;29(3):387–93. DOI: 10.1007/s00384-013-1807-5. PMID: 24343275 . PMCID: PMC3936115.
- Morris AL, Mohiuddin SS. Biochemistry, Nutrients. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. PMID: 32119432.
- Sizar O, Givler A. Vitamin D Deficiency. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2018. PMID: 30335299 .
- Papadimitriou DT. The big vitamin D mistake. J Prev Med Public Health. 2017 Jul;50(4):278–81. DOI: 10.3961/jpmph.16.111. PMID: 28768407 . PMCID: PMC5541280.
- Rasheed H, Mahgoub D, Hegazy R, El-Komy M, Abdel Hay R, Hamid MA, et al. Serum ferritin and vitamin d in female hair loss: do they play a role? Skin Pharmacol Physiol. 2013 Feb 20;26(2):101–7. DOI: 10.1159/000346698. PMID: 23428658 .
- Bosman ES, Albert AY, Lui H, Dutz JP, Vallance BA. Skin exposure to narrow band ultraviolet (UVB) light modulates the human intestinal microbiome. Front Microbiol. 2019 Oct 24;10:2410. DOI: 10.3389/fmicb.2019.02410. PMID: 31708890 . PMCID: PMC6821880.
- Conteville LC, Vicente ACP. Skin exposure to sunlight: a factor modulating the human gut microbiome composition. Gut Microbes. 2020 Sep 2;11(5):1135–8. DOI: 10.1080/19490976.2020.1745044. PMID: 32339065 . PMCID: PMC7524261.
- De Pessemier B, Grine L, Debaere M, Maes A, Paetzold B, Callewaert C. Gut-Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions. Microorganisms. 2021 Feb 11;9(2). DOI: 10.3390/microorganisms9020353. PMID: 33670115 . PMCID: PMC7916842.
- Bellerba F, Muzio V, Gnagnarella P, Facciotti F, Chiocca S, Bossi P, et al. The Association between Vitamin D and Gut Microbiota: A Systematic Review of Human Studies. Nutrients. 2021 Sep 26;13(10). DOI: 10.3390/nu13103378. PMID: 34684379 . PMCID: PMC8540279.
- Waterhouse M, Hope B, Krause L, Morrison M, Protani MM, Zakrzewski M, et al. Vitamin D and the gut microbiome: a systematic review of in vivo studies. Eur J Nutr. 2019 Oct;58(7):2895–910. DOI: 10.1007/s00394-018-1842-7. PMID: 30324342 .
- Pham VT, Fehlbaum S, Seifert N, Richard N, Bruins MJ, Sybesma W, et al. Effects of colon-targeted vitamins on the composition and metabolic activity of the human gut microbiome- a pilot study. Gut Microbes. 2021;13(1):1–20. DOI: 10.1080/19490976.2021.1875774. PMID: 33615992 . PMCID: PMC7899684.
- Grigalavicius M, Moan J, Dahlback A, Juzeniene A. Vitamin D and ultraviolet phototherapy in Caucasians. J Photochem Photobiol B, Biol. 2015 Jun;147:69–74. DOI: 10.1016/j.jphotobiol.2015.03.009. PMID: 25846579 .
- Salvadori G, Lista D, Burattini C, Gugliermetti L, Leccese F, Bisegna F. Sun exposure of body districts: development and validation of an algorithm to predict the erythemal ultra violet dose. Int J Environ Res Public Health. 2019 Sep 27;16(19). DOI: 10.3390/ijerph16193632. PMID: 31569692 . PMCID: PMC6801664.
- Table 4, Ultraviolet (UV) Index Levels – The Surgeon General’s Call to Action to Prevent Skin Cancer – NCBI Bookshelf [Internet]. [cited 2023 Jul 18]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK247164/table/skincancer.t4/
- UV Index Scale | US EPA [Internet]. [cited 2023 Jul 18]. Available from: https://www.epa.gov/sunsafety/uv-index-scale-0
- Lucas RM, Neale RE, Madronich S, McKenzie RL. Are current guidelines for sun protection optimal for health? Exploring the evidence. Photochem Photobiol Sci. 2018 Dec 5;17(12):1956–63. DOI: 10.1039/c7pp00374a. PMID: 29904757 .
- Balachandar R, Pullakhandam R, Kulkarni B, Sachdev HS. Relative Efficacy of Vitamin D2 and Vitamin D3 in Improving Vitamin D Status: Systematic Review and Meta-Analysis. Nutrients. 2021 Sep 23;13(10). DOI: 10.3390/nu13103328. PMID: 34684328 . PMCID: PMC8538717.
- van Ballegooijen AJ, Pilz S, Tomaschitz A, Grübler MR, Verheyen N. The Synergistic Interplay between Vitamins D and K for Bone and Cardiovascular Health: A Narrative Review. Int J Endocrinol. 2017 Sep 12;2017:7454376. DOI: 10.1155/2017/7454376. PMID: 29138634 . PMCID: PMC5613455.
- Kuang X, Liu C, Guo X, Li K, Deng Q, Li D. The combination effect of vitamin K and vitamin D on human bone quality: a meta-analysis of randomized controlled trials. Food Funct. 2020 Apr 30;11(4):3280–97. DOI: 10.1039/c9fo03063h. PMID: 32219282 .
- Paul C, Leser S, Oesser S. Significant amounts of functional collagen peptides can be incorporated in the diet while maintaining indispensable amino acid balance. Nutrients. 2019 May 15;11(5). DOI: 10.3390/nu11051079. PMID: 31096622 . PMCID: PMC6566836.
- Axarlis K, Daskalaki MG, Michailidou S, Androulaki N, Tsoureki A, Mouchtaropoulou E, et al. Diet Supplementation with Fish-Derived Extracts Suppresses Diabetes and Modulates Intestinal Microbiome in a Murine Model of Diet-Induced Obesity. Mar Drugs. 2021 May 11;19(5). DOI: 10.3390/md19050268. PMID: 34064922 . PMCID: PMC8151984.
- Rahabi M, Salon M, Bruno-Bonnet C, Prat M, Jacquemin G, Benmoussa K, et al. Bioactive fish collagen peptides weaken intestinal inflammation by orienting colonic macrophages phenotype through mannose receptor activation. Eur J Nutr. 2022 Jan 8; DOI: 10.1007/s00394-021-02787-7. PMID: 34999930 . PMCID: PMC9106617.
- Mei F, Duan Z, Chen M, Lu J, Zhao M, Li L, et al. Effect of a high-collagen peptide diet on the gut microbiota and short-chain fatty acid metabolism. J Funct Foods. 2020 Dec;75:104278. DOI: 10.1016/j.jff.2020.104278 .
- Chen Q, Chen O, Martins IM, Hou H, Zhao X, Blumberg JB, et al. Collagen peptides ameliorate intestinal epithelial barrier dysfunction in immunostimulatory Caco-2 cell monolayers via enhancing tight junctions. Food Funct. 2017 Mar 22;8(3):1144–51. DOI: 10.1039/c6fo01347c. PMID: 28174772 .
- Larder CE, Iskandar MM, Kubow S. Gastrointestinal digestion model assessment of peptide diversity and microbial fermentation products of collagen hydrolysates. Nutrients. 2021 Aug 7;13(8). DOI: 10.3390/nu13082720. PMID: 34444880 . PMCID: PMC8401164.
- Al-Atif H. Collagen supplements for aging and wrinkles: A paradigm shift in the fields of dermatology and cosmetics. Dermatol Pract Concept. 2022 Feb;12(1):e2022018. DOI: 10.5826/dpc.1201a18. PMID: 35223163 . PMCID: PMC8824545.
- Chen C, Tao C, Liu Z, Lu M, Pan Q, Zheng L, et al. A Randomized Clinical Trial of Berberine Hydrochloride in Patients with Diarrhea-Predominant Irritable Bowel Syndrome. Phytother Res. 2015 Nov;29(11):1822–7. DOI: 10.1002/ptr.5475. PMID: 26400188 .
- Guo H, Lu S, Zhang J, Chen C, Du Y, Wang K, et al. Berberine and rifaximin effects on small intestinal bacterial overgrowth: Study protocol for an investigator-initiated, double-arm, open-label, randomized clinical trial (BRIEF-SIBO study). Front Pharmacol. 2023 Feb 15;14:1121435. DOI: 10.3389/fphar.2023.1121435. PMID: 36873985 . PMCID: PMC9974661.
- Hawrelak JA, Wohlmuth H, Pattinson M, Myers SP, Goldenberg JZ, Harnett J, et al. Western herbal medicines in the treatment of irritable bowel syndrome: A systematic review and meta-analysis. Complement Ther Med. 2020 Jan;48:102233. DOI: 10.1016/j.ctim.2019.102233. PMID: 31987249 .
- Tan N, Gwee KA, Tack J, Zhang M, Li Y, Chen M, et al. Herbal medicine in the treatment of functional gastrointestinal disorders: A systematic review with meta-analysis. J Gastroenterol Hepatol. 2020 Apr;35(4):544–56. DOI: 10.1111/jgh.14905. PMID: 31674057 .
- Khanna R, MacDonald JK, Levesque BG. Peppermint oil for the treatment of irritable bowel syndrome: a systematic review and meta-analysis. J Clin Gastroenterol. 2014 Jul;48(6):505–12. DOI: 10.1097/MCG.0b013e3182a88357. PMID: 24100754 .
- Alammar N, Wang L, Saberi B, Nanavati J, Holtmann G, Shinohara RT, et al. The impact of peppermint oil on the irritable bowel syndrome: a meta-analysis of the pooled clinical data. BMC Complement Altern Med. 2019 Jan 17;19(1):21. DOI: 10.1186/s12906-018-2409-0. PMID: 30654773 . PMCID: PMC6337770.
- Black CJ, Yuan Y, Selinger CP, Camilleri M, Quigley EMM, Moayyedi P, et al. Efficacy of soluble fibre, antispasmodic drugs, and gut-brain neuromodulators in irritable bowel syndrome: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(2):117–31. DOI: 10.1016/S2468-1253(19)30324-3. PMID: 31859183 .
- Mahboubi M. Therapeutic Potential of Zataria multiflora Boiss in Treatment of Irritable Bowel Syndrome (IBS). J Diet Suppl. 2019;16(1):119–28. DOI: 10.1080/19390211.2017.1409852. PMID: 29333891 .
- Rahimi R, Nikfar S, Abdollahi M. Induction of clinical response and remission of inflammatory bowel disease by use of herbal medicines: a meta-analysis. World J Gastroenterol. 2013 Sep 14;19(34):5738–49. DOI: 10.3748/wjg.v19.i34.5738. PMID: 24039370 . PMCID: PMC3769914.
- Ng SC, Lam YT, Tsoi KKF, Chan FKL, Sung JJY, Wu JCY. Systematic review: the efficacy of herbal therapy in inflammatory bowel disease. Aliment Pharmacol Ther. 2013 Oct;38(8):854–63. DOI: 10.1111/apt.12464. PMID: 23981095 .
- Omer B, Krebs S, Omer H, Noor TO. Steroid-sparing effect of wormwood (Artemisia absinthium) in Crohn’s disease: a double-blind placebo-controlled study. Phytomedicine. 2007 Feb;14(2–3):87–95. DOI: 10.1016/j.phymed.2007.01.001. PMID: 17240130 .
- Krebs S, Omer TN, Omer B. Wormwood (Artemisia absinthium) suppresses tumour necrosis factor alpha and accelerates healing in patients with Crohn’s disease – A controlled clinical trial. Phytomedicine. 2010 Apr;17(5):305–9. DOI: 10.1016/j.phymed.2009.10.013. PMID: 19962291 .
- Langhorst J, Wulfert H, Lauche R, Klose P, Cramer H, Dobos GJ, et al. Systematic review of complementary and alternative medicine treatments in inflammatory bowel diseases. J Crohns Colitis. 2015 Jan;9(1):86–106. DOI: 10.1093/ecco-jcc/jju007. PMID: 25518050 .
- Mueller MS, Runyambo N, Wagner I, Borrmann S, Dietz K, Heide L. Randomized controlled trial of a traditional preparation of Artemisia annua L. (Annual Wormwood) in the treatment of malaria. Trans R Soc Trop Med Hyg. 2004 May;98(5):318–21. DOI: 10.1016/j.trstmh.2003.09.001. PMID: 15109558 .
- Priotto G, Kabakyenga J, Pinoges L, Ruiz A, Eriksson T, Coussement F, et al. Artesunate and sulfadoxine-pyrimethamine combinations for the treatment of uncomplicated Plasmodium falciparum malaria in Uganda: a randomized, double-blind, placebo-controlled trial. Trans R Soc Trop Med Hyg. 2003 Jun;97(3):325–30. PMID: 15228253 .
- Force M, Sparks WS, Ronzio RA. Inhibition of enteric parasites by emulsified oil of oregano in vivo. Phytother Res. 2000 May;14(3):213–4. DOI: 10.1002/(sici)1099-1573(200005)14:3<213::aid-ptr583>3.0.co;2-u. PMID: 10815019 .
- Ghitea TC, El-Kharoubi A, Ganea M, Bimbo-Szuhai E, Nemeth TS, Ciavoi G, et al. The Antimicrobial Activity of Origanum vulgare L. Correlated with the Gastrointestinal Perturbation in Patients with Metabolic Syndrome. Molecules. 2021 Jan 8;26(2). DOI: 10.3390/molecules26020283. PMID: 33429991 . PMCID: PMC7827761.
- Shayegh S, Rasooli I, Taghizadeh M, Astaneh SDA. Phytotherapeutic inhibition of supragingival dental plaque. Nat Prod Res. 2008 Mar 20;22(5):428–39. DOI: 10.1080/14786410701591739. PMID: 18404563 .
- Hu Q, Peng Z, Li L, Zou X, Xu L, Gong J, et al. The Efficacy of Berberine-Containing Quadruple Therapy on Helicobacter Pylori Eradication in China: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Front Pharmacol. 2019;10:1694. DOI: 10.3389/fphar.2019.01694. PMID: 32116685 . PMCID: PMC7010642.
- Wang F, Feng J, Chen P, Liu X, Ma M, Zhou R, et al. Probiotics in Helicobacter pylori eradication therapy: Systematic review and network meta-analysis. Clin Res Hepatol Gastroenterol. 2017 Sep;41(4):466–75. DOI: 10.1016/j.clinre.2017.04.004. PMID: 28552432 .
- Singh A, Daing A, Dixit J. The effect of herbal, essential oil and chlorhexidine mouthrinse on de novo plaque formation. Int J Dent Hyg. 2013 Feb;11(1):48–52. DOI: 10.1111/j.1601-5037.2012.00556.x. PMID: 22583681 .
- Yu M, Jin X, Liang C, Bu F, Pan D, He Q, et al. Berberine for diarrhea in children and adults: a systematic review and meta-analysis. Therap Adv Gastroenterol. 2020 Oct 23;13:1756284820961299. DOI: 10.1177/1756284820961299. PMID: 33149763 . PMCID: PMC7586028.
- Di Pierro F, Bertuccioli A, Giuberti R, Saponara M, Ivaldi L. Role of a berberine-based nutritional supplement in reducing diarrhea in subjects with functional gastrointestinal disorders. Minerva Gastroenterol Dietol. 2020 Mar;66(1):29–34. DOI: 10.23736/S1121-421X.19.02649-7. PMID: 32283882 .
- Beba M, Djafarian K, Shab-Bidar S. Effect of Berberine on C-reactive protein: A systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2019 Oct;46:81–6. DOI: 10.1016/j.ctim.2019.08.002. PMID: 31519292 .
- Lockyer S, Corona G, Yaqoob P, Spencer JPE, Rowland I. Secoiridoids delivered as olive leaf extract induce acute improvements in human vascular function and reduction of an inflammatory cytokine: a randomised, double-blind, placebo-controlled, cross-over trial. Br J Nutr. 2015 Jul 14;114(1):75–83. DOI: 10.1017/S0007114515001269. PMID: 26051429 .
- Purssell E. Antimicrobials. In: Hood P, Khan E, editors. Understanding pharmacology in nursing practice. Cham: Springer International Publishing; 2020. p. 147–65. DOI: 10.1007/978-3-030-32004-1_6 .
- Wagenaar CA, van de Put M, Bisschops M, Walrabenstein W, de Jonge CS, Herrema H, et al. The effect of dietary interventions on chronic inflammatory diseases in relation to the microbiome: A systematic review. Nutrients. 2021 Sep 15;13(9). DOI: 10.3390/nu13093208. PMID: 34579085 . PMCID: PMC8464906.
- White N. A Guide to Recommending Fiber Supplements for Self-Care. Am J Lifestyle Med. 2020 Dec;14(6):589–91. DOI: 10.1177/1559827620947375. PMID: 33117099 . PMCID: PMC7566180.
- Dahl WJ, Stewart ML. Position of the academy of nutrition and dietetics: health implications of dietary fiber. J Acad Nutr Diet. 2015 Nov;115(11):1861–70. DOI: 10.1016/j.jand.2015.09.003. PMID: 26514720 .
- McRorie JW, McKeown NM. Understanding the Physics of Functional Fibers in the Gastrointestinal Tract: An Evidence-Based Approach to Resolving Enduring Misconceptions about Insoluble and Soluble Fiber. J Acad Nutr Diet. 2017;117(2):251–64. DOI: 10.1016/j.jand.2016.09.021. PMID: 27863994 .
- Muir J. An overview of fiber and fiber supplements for irritable bowel syndrome. Gastroenterol Hepatol (N Y). 2019 Jul;15(7):387–9. PMID: 31391809 . PMCID: PMC6676347.
- Nagarajan N, Morden A, Bischof D, King EA, Kosztowski M, Wick EC, et al. The role of fiber supplementation in the treatment of irritable bowel syndrome: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2015 Sep;27(9):1002–10. DOI: 10.1097/MEG.0000000000000425. PMID: 26148247 .
- Christodoulides S, Dimidi E, Fragkos KC, Farmer AD, Whelan K, Scott SM. Systematic review with meta-analysis: effect of fibre supplementation on chronic idiopathic constipation in adults. Aliment Pharmacol Ther. 2016 Jul;44(2):103–16. DOI: 10.1111/apt.13662. PMID: 27170558 .
- Bliss DZ, Savik K, Jung H-JG, Whitebird R, Lowry A. Symptoms associated with dietary fiber supplementation over time in individuals with fecal incontinence. Nurs Res. 2011 Jun;60(3 Suppl):S58-67. DOI: 10.1097/NNR.0b013e3182186d8c. PMID: 21543963 . PMCID: PMC3400503.
- Tun KM, Hsu M, Batra K, Lo C-H, Laeeq T, Vongsavath T, et al. Efficacy and Safety of Fecal Microbiota Transplantation in Treatment of Clostridioides difficile Infection among Pediatric Patients: A Systematic Review and Meta-Analysis. Microorganisms. 2022 Dec 12;10(12). DOI: 10.3390/microorganisms10122450. PMID: 36557703 . PMCID: PMC9781859.
- Yang L, Li W, Zhang X, Tian J, Ma X, Han L, et al. The evaluation of different types fecal bacteria products for the treatment of recurrent Clostridium difficile associated diarrhea: A systematic review and network meta-analysis. Front Surg. 2022 Jul 20;9:927970. DOI: 10.3389/fsurg.2022.927970. PMID: 36468073 . PMCID: PMC9709817.
- Cheng F, Huang Z, Li Z, Wei W. Efficacy and safety of fecal microbiota transplant for recurrent Clostridium difficile infection in inflammatory bowel disease: a systematic review and meta-analysis. Rev Esp Enferm Dig. 2022 Sep;114(9):543–9. DOI: 10.17235/reed.2022.8814/2022. PMID: 35510325 .
- Vaughn BP, Fischer M, Kelly CR, Allegretti JR, Graiziger C, Thomas J, et al. Effectiveness and safety of colonic and capsule fecal microbiota transplantation for recurrent Clostridioides difficile infection. Clin Gastroenterol Hepatol. 2022 Sep 17; DOI: 10.1016/j.cgh.2022.09.008. PMID: 36126907 .
- Wang J-G, Liang Q, Dou H-H, Ou Y. The global incidence of adverse events associated with fecal microbiota transplantation in children over the past 20 years: A systematic review and meta-analysis. J Gastroenterol Hepatol. 2022 Nov;37(11):2031–8. DOI: 10.1111/jgh.15996. PMID: 36066910 .
- Park S-H, Lee J-H, Kim J-S, Kim TJ, Shin J, Im JH, et al. Fecal microbiota transplantation can improve cognition in patients with cognitive decline and Clostridioides difficile infection. Aging (Albany NY). 2022 Aug 16;14(16):6449–66. DOI: 10.18632/aging.204230. PMID: 35980280 . PMCID: PMC9467396.
- Song YN, Yang DY, Veldhuyzen van Zanten S, Wong K, McArthur E, Song CZ, et al. Fecal Microbiota Transplantation for Severe or Fulminant Clostridioides difficile Infection: Systematic Review and Meta-analysis. J Can Assoc Gastroenterol. 2022 Feb;5(1):e1–11. DOI: 10.1093/jcag/gwab023. PMID: 35118227 . PMCID: PMC8806043.
- Li Y, Zhang T, Sun J, Liu N. Fecal Microbiota Transplantation and Health Outcomes: An Umbrella Review of Meta-Analyses of Randomized Controlled Trials. Front Cell Infect Microbiol. 2022 Jun 27;12:899845. DOI: 10.3389/fcimb.2022.899845. PMID: 35832379 . PMCID: PMC9271871.
- Nicholson MR, Alexander E, Ballal S, Davidovics Z, Docktor M, Dole M, et al. Efficacy and Outcomes of Faecal Microbiota Transplantation for Recurrent Clostridioides difficile Infection in Children with Inflammatory Bowel Disease. J Crohns Colitis. 2022 Jun 24;16(5):768–77. DOI: 10.1093/ecco-jcc/jjab202. PMID: 34788420 . PMCID: PMC9228903.
- Kedia S, Virmani S, K Vuyyuru S, Kumar P, Kante B, Sahu P, et al. Faecal microbiota transplantation with anti-inflammatory diet (FMT-AID) followed by anti-inflammatory diet alone is effective in inducing and maintaining remission over 1 year in mild to moderate ulcerative colitis: a randomised controlled trial. Gut. 2022 Dec;71(12):2401–13. DOI: 10.1136/gutjnl-2022-327811. PMID: 35973787 .
- Wei Z-J, Dong H-B, Ren Y-T, Jiang B. Efficacy and safety of fecal microbiota transplantation for the induction of remission in active ulcerative colitis: a systematic review and meta-analysis of randomized controlled trials. Ann Transl Med. 2022 Jul;10(14):802. DOI: 10.21037/atm-22-3236. PMID: 35965832 . PMCID: PMC9372650.
- Huang C, Huang Z, Ding L, Fu Y, Fan J, Mei Q, et al. Fecal microbiota transplantation versus glucocorticoids for the induction of remission in mild to moderate ulcerative colitis. J Transl Med. 2022 Aug 12;20(1):354. DOI: 10.1186/s12967-022-03569-3. PMID: 35962454 . PMCID: PMC9373544.
- Tan X-Y, Xie Y-J, Liu X-L, Li X-Y, Jia B. A Systematic Review and Meta-Analysis of Randomized Controlled Trials of Fecal Microbiota Transplantation for the Treatment of Inflammatory Bowel Disease. Evid Based Complement Alternat Med. 2022 Jun 26;2022:8266793. DOI: 10.1155/2022/8266793. PMID: 35795291 . PMCID: PMC9251102.
- El Hage Chehade N, Ghoneim S, Shah S, Chahine A, Mourad FH, Francis FF, et al. Efficacy of Fecal Microbiota Transplantation in the Treatment of Active Ulcerative Colitis: A Systematic Review and Meta-Analysis of Double-Blind Randomized Controlled Trials. Inflamm Bowel Dis. 2023 May 2;29(5):808–17. DOI: 10.1093/ibd/izac135. PMID: 35766805 .
- Seth AK, Jain P. Fecal microbiota transplantation for induction of remission, maintenance and rescue in patients with corticosteroid-dependent ulcerative colitis: a long-term follow-up real-world cohort study. Intest Res. 2022 Apr;20(2):251–9. DOI: 10.5217/ir.2021.00069. PMID: 35124952 . PMCID: PMC9081992.
- Haifer C, Paramsothy S, Kaakoush NO, Saikal A, Ghaly S, Yang T, et al. Lyophilised oral faecal microbiota transplantation for ulcerative colitis (LOTUS): a randomised, double-blind, placebo-controlled trial. Lancet Gastroenterol Hepatol. 2022 Feb;7(2):141–51. DOI: 10.1016/S2468-1253(21)00400-3. PMID: 34863330 .
- Green JE, Davis JA, Berk M, Hair C, Loughman A, Castle D, et al. Efficacy and safety of fecal microbiota transplantation for the treatment of diseases other than Clostridium difficile infection: a systematic review and meta-analysis. Gut Microbes. 2020 Nov 9;12(1):1–25. DOI: 10.1080/19490976.2020.1854640. PMID: 33345703 . PMCID: PMC7757860.
- Zhou S, Cui Y, Zhang Y, Zhao T, Cong J. Fecal microbiota transplantation for induction of remission in Crohn’s disease: a systematic review and meta-analysis. Int J Colorectal Dis. 2023 Mar 8;38(1):62. DOI: 10.1007/s00384-023-04354-4. PMID: 36882658 .
- Feng J, Chen Y, Liu Y, Lin L, Lin X, Gong W, et al. Efficacy and safety of fecal microbiota transplantation in the treatment of ulcerative colitis: a systematic review and meta-analysis. Sci Rep. 2023 Sep 3;13(1):14494. DOI: 10.1038/s41598-023-41182-6. PMID: 37661203 . PMCID: PMC10475461.
- Tkach S, Dorofeyev A, Kuzenko I, Sulaieva O, Falalyeyeva T, Kobyliak N. Fecal microbiota transplantation in patients with post-infectious irritable bowel syndrome: A randomized, clinical trial. Front Med (Lausanne). 2022 Oct 20;9:994911. DOI: 10.3389/fmed.2022.994911. PMID: 36341232 . PMCID: PMC9631772.
- Huang H-L, Zhu J-Q, Yang L-S, Wu Q, Shou D-W, Chen H-T, et al. Fecal Microbiota Transplantation Combined with a Low FODMAP Diet for the Treatment of Irritable Bowel Syndrome with Predominant Diarrhea. Oxid Med Cell Longev. 2022 Sep 21;2022:5121496. DOI: 10.1155/2022/5121496. PMID: 36187337 . PMCID: PMC9519354.
- El-Salhy M, Winkel R, Casen C, Hausken T, Gilja OH, Hatlebakk JG. Efficacy of fecal microbiota transplantation for patients with irritable bowel syndrome at three years after transplantation. Gastroenterology. 2022 Jun 13; DOI: 10.1053/j.gastro.2022.06.020. PMID: 35709830 .
- Guo Q, Lin H, Chen P, Tan S, Wen Z, Lin L, et al. Dynamic changes of intestinal flora in patients with irritable bowel syndrome combined with anxiety and depression after oral administration of enterobacteria capsules. Bioengineered. 2021 Dec;12(2):11885–97. DOI: 10.1080/21655979.2021.1999374. PMID: 34923901 . PMCID: PMC8810103.
- Wang YZ, Xiao FF, Xiao YM, Li XL, Hu H, Hong K, et al. Fecal microbiota transplantation relieves abdominal bloating in children with functional gastrointestinal disorders via modulating the gut microbiome and metabolome. J Dig Dis. 2022 Aug;23(8–9):482–92. DOI: 10.1111/1751-2980.13135. PMID: 36208299 .
- Xu F, Li N, Wang C, Xing H, Chen D, Wei Y. Clinical efficacy of fecal microbiota transplantation for patients with small intestinal bacterial overgrowth: a randomized, placebo-controlled clinic study. BMC Gastroenterol. 2021 Feb 6;21(1):54. DOI: 10.1186/s12876-021-01630-x. PMID: 33549047 . PMCID: PMC7866462.
- Gupta S, Allen-Vercoe E, Petrof EO. Fecal microbiota transplantation: in perspective. Therap Adv Gastroenterol. 2016 Mar;9(2):229–39. DOI: 10.1177/1756283X15607414. PMID: 26929784 . PMCID: PMC4749851.
- Park S-Y, Seo GS. Fecal microbiota transplantation: is it safe? Clin Endosc. 2021 Mar 30;54(2):157–60. DOI: 10.5946/ce.2021.072. PMID: 33827154 . PMCID: PMC8039753.
➕ Links & Resources
Further Reading:
- Revolting or Revolutionary? A Guide to Fecal Transplant Pills
- The 8 Best Supplements for Bloating | 2024
Need help or would like to learn more? View Dr. Ruscio’s, DC additional resources
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!
Transform your health
Every product is science-based, validated by real-world use, and personally vetted by Dr. Ruscio, DC.
A personal trainer shared the 2 popular fitness supplements that she would never take
- Personal trainer Hayley Madigan isn't against supplements but there are some common ones she avoids.
- Madigan told Business Insider why she doesn't use products including energy drinks and protein bars.
- There's no one-size-fits-all approach to taking supplements.

Personal trainer Hayley Madigan knows that certain supplements can help her feel and perform at her best.
But, there are others that Madigan, 34, would never take.
More than half of US adults take supplements , according to the American Medical Association, and the market is set to be worth about $308 billion worldwide by 2028, up from $191 billion in 2020, according to Statista.
But experts say that we should aim to get the nutrients our bodies need from food. While supplements, such as protein powders and creatine, may be particularly useful for those who are active like Madigan, not everyone needs to take them. And some can even leave us feeling worse than we did before. If you're not sure what supplements you might need, speak to your doctor.
Madigan, who's based in Portsmouth, UK, told Business Insider why she avoids products including energy drinks and pre-workout supplements.
Madigan avoids energy drinks and pre-workout supplements
It's not uncommon to see people going into the gym sipping energy and pre-workout drinks , but not everyone gets on well with them.
Madigan used to take pre-workout supplements, which are different to regular energy drinks because they also contain ingredients designed to increase workout performance, to boost her energy.
Related stories
But Madigan said she steers clear of high-caffeine supplements like these as they tend to make her energy levels crash and make her feel anxious and unwell, she said.
"I found that I was crashing after the pre-workout had worn off and it had a tendency to make me feel more tired," Madigan said. "So now I train in the morning and tend to use my morning coffee instead of pre-workout."
Madigan is not the only personal trainer to have stopped taking pre-workout supplements. Celebrity trainer Luke Worthington previously told BI he made the same decision after realizing he was working out when he should have been resting.
Protein bars often contain artificial sweeteners
While protein bars can be a convenient way to eat more protein, they're often highly processed and contain various artificial ingredients. Research suggests that ultra-processed foods are linked to a range of health problems, including cardiovascular diseases, type 2 diabetes, cancer, and obesity. They can also have a more immediate negative effect on someone's health if they are sensitive to certain ingredients.
"I also don't have protein bars anymore as the artificial sweeteners in them were causing havoc with my stomach and digestion," Madigan said. "I prefer to add in more 'real food' as opposed to having too many artificial supplements throughout the day."
Studies suggest that eating too many artificial sweeteners can lead to gas and bloating, while research on rodents indicates that they could harm "good" gut bacteria.
Everyone is different
It may be tempting to try supplements we see others taking, but there's no one-size-fits-all approach, as each of us has different requirements.
Vitamin B12 helps keep our body's blood and nerve cells healthy. Madigan thought she might need to take a supplement if she wasn't getting enough through her diet (it's found in foods such as meat, fish, eggs, and dairy). But a blood test showed that she had naturally high levels, so she doesn't need to, she said.
Watch: All the differences between Red Bull in the US and the UK
- Main content

IMAGES
VIDEO
COMMENTS
Protein supplementation and resistance training. A recent comprehensive review by Jager et al. identified a number of key issues related to protein intake in healthy, exercising individuals.Of particular note, the importance of protein intake during and around a training session for recovery and performance appears to be dependent on total daily protein intake, as well as presence or absence ...
Among protein supplements, those containing BCAA are rising in popularity among consumers and have attracted the attention of the sports nutrition industry. ... Grand View Research, Inc. Protein Supplements Market Analysis by Raw Material, by Source, by Product, by Distribution Channel, Bay Application, and Segment Forecasts, 2014-2025 ...
Therefore, additional research is warranted to determine to what extent protein supplementation may facilitate a more rapid recovery of muscle performance after an acute bout of resistance exercise. Thus, in the present study, we employed a crossover design, controlled diet, and conducted a battery of tests to assess the recovery of exercise ...
Background: Protein supplements are frequently consumed by athletes and recreationally active adults to achieve greater gains in muscle mass and strength and improve physical performance. Objective: This review provides a systematic and comprehensive analysis of the literature that tested the hypothesis that protein supplements accelerate gains in muscle mass and strength resulting in ...
Protein supplementation often refers to increasing the intake of this particular macronutrient through dietary supplements in the form of powders, ready-to-drink shakes, and bars. ... Exercise & Sport Nutrition Lab, Human Clinical Research Facility, Department of Health & Kinesiology, College Station, TX, USA. PMID: 38626029
The limited understanding of the impact of protein supplementation for resistance EIMD management in females should be addressed by conducting high-quality research with females or both sexes.
Protein supplements are widely consumed by athletes, recreationally active adults, and soldiers [1-4], who generally believe that combining the consumption of protein supplements with exercise will promote gains in lean mass, resulting in improved physical performance [2, 5].This belief is based on information typically obtained from coaches, teammates, advertising, and family or friends [1 ...
These protein supplements have varying pros and cons associated with them, which are often overlooked by the public. This review aims to assimilate existing studies and form a consensus regarding the benefits and disadvantages of protein supplementation. The purported health benefits of protein supplementation have led to overuse by both adults ...
Protein supplementation stimulated bacterial amino acid metabolism (90% amino-acid synthesis functions enriched with IP versus 13% in CP group (p < 0.01)). ... Research was performed in accordance ...
Objective We performed a systematic review, meta-analysis and meta-regression to determine if dietary protein supplementation augments resistance exercise training (RET)-induced gains in muscle mass and strength. Data sources A systematic search of Medline, Embase, CINAHL and SportDiscus. Eligibility criteria Only randomised controlled trials with RET ≥6 weeks in duration and dietary protein ...
Protein supplements are important to maintain optimum health and physical performance, particularly in athletes and active individuals to repair and rebuild their skeletal muscles and connective tissues. ... A total of 19 eligible original research articles were included that investigated the effect of SP supplementation on muscle adaptations ...
Background: Protein supplements are frequently consumed by athletes and recreationally-active individuals, although the decision to purchase and consume protein supplements is often based on marketing claims rather than evidence-based research. Objective: To provide a systematic and comprehensive analysis of literature examining the hypothesis that protein supplements enhance recovery of ...
Protein supplementation alone or combined with resistance training has been proposed to be effective in counteracting age-related losses of ... when combined with whey protein supplementation. Future research and innovation efforts should focus on improving long-term compliance to heavy-resistance exercise in healthy older adults to obtain ...
Purpose of Review The purpose of this review is to provide background on the present literature regarding the utility and effectiveness of protein supplements, including protein source and nutrient timing. Recent Findings In the setting of adequate dietary protein consumption, research suggests some benefit particularly in sport or exercise activities. Summary Protein supplements command a ...
This narrative review critically examines the current research on the health implications of whey protein (WP) supplementation, with a focus on potential risks and adverse effects. WP, commonly consumed for muscle building and weight loss, has been associated with various health concerns. ... The consumption of protein supplements grows ...
Learn more about protein powders and other workout supplements. Research on Protein and Health. Available evidence indicates that it's the source of protein (or, the protein "package"), rather than the amount of protein, that likely makes a difference for our health. You can explore the research related to each disease in the tabs below ...
Human Food and Protein Supplements: 2.1.1. Soy protein. Most plant-based meat alternatives have soy protein as their main component. ... and further research and development is needed to optimize the processes and make it economically feasible on a large scale.
The study aimed to determine the phenolic content and antioxidant capacity of five protein supplements of plant origin. The content and profile of phenolics were determined using the UHPLC-DAD-MS method, while antioxidant capacity (ABTS and DPPH assays) and total phenolic content (TPC) were evaluated using spectrophotometric tests. In the analyzed proteins, twenty-five polyphenols were ...
Protein targets muscle tissue growth and development especially. "Amino acids are the main building block for muscle," explains Walter Willett, MD, professor of epidemiology and nutrition at ...
In fact, some randomized trials have found that assigning people to take supplements with large doses of beta-carotene, selenium, and vitamins A, C, and E actually increased mortality rates ...
ICMR and NIN guidelines caution against protein supplements due to various risks like kidney damage, dehydration, and nutrient imbalances. In the 148 page guidelines, the ICMR has warned against ...
There is robust evidence which shows that consuming protein pre- and/or post-workout induces a significant rise in muscle protein synthesis. It should be noted, however, that total daily caloric and protein intake over the long term play the most crucial dietary roles in facilitating adaptations to exercise. However, once these factors are accounted for, it appears that peri-exercise protein ...
Since the powerhouse artificial intelligence (AI) tool AlphaFold2 was released in 2021, scientists have used the protein-structure-prediction model to map one of our cells' biggest machines ...
New Delhi: The Indian Council of Medical Research has urged to avoid protein supplements for building body mass and has recommended restricting salt intake, minimising sugar and ultra-processed foods and reading information on food labels to make informed and healthy food choices. The Hyderabad ...
The research body urged people to "avoid protein supplements" for building body mass The Indian Council of Medical Research (ICMR) released a set of dietary guidelines for Indians on Wednesday. According to the guidelines to meet the requirements of essential nutrients and prevent noncommunicable diseases in the country, around 56.4% of the ...
Summarizing the results of literature analysis on frailty/sarcopenia since 2014, research results have consistently reported that protein supplementation or high-protein diet in elderly subjects suppresses the sarcopenia/frailty indicators (muscle mass and muscle strength loss) and increases muscle fiber production (Table 4).
Interestingly, supplementation with Jlus66 restored DSS-induced TJ protein expression. Therefore, Jlus66 may play an important role in maintaining the mechanical barrier of the intestinal mucosa. Intestinal dysbacteriosis is an important factor in inducing UC, and microorganisms may lead to the destruction of the intestinal mucosal barrier or ...
2. Glutamine. Glutamine is the most abundant free amino acid in human blood and the main energy source for intestinal cells [].Studies suggest that it may reduce inflammation and leaky gut by supporting the integrity of tight junctions in the intestinal lining [12, 13, 14, 15].In the case of leaky gut, those tight junctions become less tight and more permeable, allowing partially digested food ...
Beans are high in protein and stave off snack cravings Nico Schnico for BI "If you want to take a supplement, take about 80 black beans a day," Buettner said.
Personal trainer Hayley Madigan knows that certain supplements can help her feel and perform at her best. But, there are others that Madigan, 34, would never take. More than half of US adults take ...